Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/52/40. The contractual start date was in March 2016. The final report began editorial review in November 2018 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Scott Weich reports grants from the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme during the conduct of the study and reports that he is employed by Sheffield University, which receives grant funding from NIHR. He also reports other from NIHR Health Technology Assessment (HTA) outside the submitted work (i.e. membership of the HTA Clinical Evaluation and Trials Board and has been reimbursed for expenses only). Helen Parsons reports grants from NIHR during the conduct of the study. Graham Moon reports grants from NIHR and grants from Economic and Social Research Council during the conduct of the study. Patrick Keown reports grants from the NIHR HSDR programme during the conduct of the study and is a full-time NHS consultant working with patients who are detained under the Mental Health Act (Great Britain. Mental Health Act. London: The Stationery Office; 2007), including patients subject to community treatment orders.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Weich et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Community treatment orders: a global phenomenon
As a result of deinstitutionalisation of mental health care in many parts of the world, services for people with serious mental disorders have moved from hospital to community settings. This has resulted in legal frameworks allowing for compulsory outpatient treatment. Originating in North America and Australia, and now present in > 75 jurisdictions, these frameworks take different forms in different places. This is highlighted by their different names that include ‘involuntary outpatient commitment’, ‘assisted outpatient treatment’, ‘supervised discharge’, ‘compulsory community treatment’ and ‘compulsory ambulatory treatment’. 1 In England, the name used most commonly is ‘community treatment order’ (CTO) and this term is used throughout the rest of this report. In some places, CTOs are initiated only by courts, whereas elsewhere (as in England), they remain a matter exclusively for health and social care providers, albeit within a framework prescribed by statute and subject to legal review. There are also differences between countries in the organisation and funding of mental health services, including separation of inpatient from community mental health teams (MHTs) and variations in the nature and availability of care for people with serious mental disorders. Making general statements about CTOs is, therefore, problematic.
A common literature has, nevertheless, developed, aiming to establish the appropriateness and, particularly, the effectiveness of CTOs. 2–7 This literature emphasises that, although being widely used, CTOs remain controversial. In part, this is because patients and carers often, although not always, see them as coercive and mainly concerned with medication adherence. 8–11 Unsurprisingly, this has raised fears that they damage therapeutic relationships. 12,13 Such concern has come to particular prominence in recent years with the advent of the United Nations Convention on the Rights of Persons with Disabilities. 14,15
This disquiet around coercion has been heightened by conflicting research evidence about the effectiveness of CTOs. 16 Although some studies have found positive outcomes for patients, others have not. In response, clinicians, researchers and government bodies have called for its use to be reconsidered. 17,18 Obviously, such calls also have resonance in the light of ever increasing demands for financial efficiency in health service delivery. There is, therefore, a clear need for new research on CTOs. 19
Community treatment orders in England
In England, CTOs were initiated through provision in the Mental Health Act (MHA) (2007)20 for patients detained in hospital to continue treatment in the community following discharge, under specific conditions. Under Section 20A of the MHA (2007),20 such patients may subsequently be recalled to hospital for assessment and, if appropriate, detained for further treatment. The CTO states the conditions that the patient is required to meet once discharged from hospital. CTOs were first introduced in England in November 2008.
To be eligible for a CTO, a patient must be detained in hospital under the MHA on a Section that allows for compulsory treatment. The most common inpatient treatment orders are Sections 3 and 37, the former being a civil order and the latter a forensic, court-imposed equivalent for mentally ill offenders. At CTO initiation (the point of discharge from inpatient care) there are two mandatory conditions, namely that the person subject to a CTO makes themselves available for assessment for its renewal and that (where necessary) they are seen by an approved second opinion appointed doctor (SOAD) for the purposes of assessing the proposed treatment plan should the patient lack capacity in respect of their treatment. Discretionary conditions can also be specified, which most often include treatment (i.e. medication) adherence and engagement with services (e.g. attending appointments with professionals). CTOs do not permit compulsory (i.e. forcible) treatment in the community,21 but those who default from these conditions may, as already stated, be recalled to hospital for assessment by the responsible clinician if there are grounds to suspect deterioration in their mental health and/or risk to the patient or others. Where this assessment indicates the need for further treatment, the CTO is revoked, and the original hospital treatment order applies.
There were two specific motivations for introducing CTOs in England:2 to reduce ‘revolving door’ admissions associated with non-adherence with care by a small group of patients, and to allow treatment in the least restrictive setting, in accordance with the Human Rights Act (1988). 22 Although it was originally envisaged that around 10% of eligible patients would be placed on CTOs in England, the figure is currently closer to 30%. 23 As more CTOs have tended to be issued than are ended each year, the number of patients who are subject to CTOs has increased over time. In 2016–17, the latest year for which data are available, almost 5000 new CTOs were issued (and perhaps more, given potential under-reporting),24 compared with 4361 in 2015–16. 25
These trends should be seen in the context of increasing numbers of compulsory hospital admissions in England over the past two decades or longer. There were 63,622 compulsory civil admissions to hospital (i.e. excluding forensic orders via the criminal justice system) under the MHA in England in 2015–16 (the last year before reporting processes changed). 24 This represented an increase of 47% in the decade since 2005–6, and an 8% increase on the previous year. 25
Community treatment orders: previous research
Patterns of use
Unlike compulsory inpatient admission, there has been relatively little research on patterns of use for CTOs. In England, routine administrative data sources suggest that the use varies between demographic groups: for example, in 2016–17 rates of CTO use for males (11.4 per 100,000 population) were almost twice the rate for females (6.6 per 100,000 population), and the rate for black and black British people (60.1 per 100,000 population) was almost nine times the rate for those of white people (6.8 per 100,000 population). 24 Strong patterning on the basis of ethnic characteristics has also recently been found in Western Australia. 26 Few studies have, however, moved beyond the univariate demographic profiles given in routine statistics or considered how these relate to other patient characteristics, such as clinical need. One recent exception in terms of the latter is work in Victoria, Australia, where CTO patients were found to have greater clinical need on the basis of Health of the Nation Outcome Scales (HoNOS). 27
Routine administrative data also suggest that significant spatial variation in CTO use, either between geographical areas and/or service providers. The former is perhaps seen most clearly at a national scale with Australia, New Zealand and some parts of the USA having much higher rates (40–60 per 100,000 of the population) than Canada and New York (around 2 per 100,000 population),28 with England being low to moderate at about 10 per 100,000. 29 There are, however, variations within national jurisdictions, as Australian data emphasises, with estimated rates of CTO use varying between 30 per 100,000 in Tasmania to almost 100 per 100,000 in Victoria. 30 In England, routine statistics suggest significant differences between service providers,25 a point emphasised by recent research exploring these data. 29,31 Again, however, little attempt has been made to relate spatial variations in CTO use to patient demographic or clinical characteristics, or, indeed, to the characteristics of the areas or service providers themselves.
Association with patient outcomes
Much of the existing literature on CTOs has focused on associations with patient outcomes. Following the traditional hierarchy of evidence, the results of the three randomised controlled trials (RCTs) conducted to date (comprising a total sample of 749 patients) have come to assume special prominence. 5
The first two of these trials were conducted in the late 1990s in the USA: one in New York32 and the other in North Carolina. 33,34 Both of the US trials evaluated court-imposed ‘outpatient commitment’ and both excluded patients with a history of violence. Neither trial reported significant differences over 12 months in health service or patient-related outcomes, including re-admission to hospital, compliance with medication or social functioning. 5 Results from the North Carolina trial were more positive, but mostly for a specific patient subgroup: hospital re-admissions and total hospital bed-days were reduced for psychotic patients on longer-term CTOs (≥ 180 days) who received intensive community treatments. 33 Patients on CTOs also showed a reduced rate of violent behaviour and were less likely to be victims of crime over 12 months in the North Carolina study. 34
A third trial has been conducted more recently based on CTOs in England, the Oxford Community Treatment Order Evaluation Trial (OCTET), comprising 333 patients followed up over 36 months. 14 The original main study arising from this trial found that CTOs did not demonstrate improved outcomes on re-admission rates and time spent in hospital over 12 months. 35 A number of additional studies arising from the trial have now been published, including two studies based on longer-term follow-up data and another based on a subgroup analysis. 36–38 These found no evidence of benefits accruing over 36 to 48 months or on a larger number of secondary outcomes, including symptoms, social functioning, substance misuse and a broad range of social/welfare outcomes. In addition, recent work based on CTO recalls over time has been used to counter the suggestion that the original study found negative outcomes because clinicians were not yet familiar enough with CTO regimes for them to be used effectively. 39
The evidence from RCTs has, therefore, demonstrated relatively few benefits for patients. As several commentators have noted, however, RCTs of CTOs face particular ethical and practical challenges that limit their utility. In critically appraising the two US trials, Kisely et al. 3 highlighted small sample sizes, the court-imposed nature of compulsory community treatment and the exclusion of patients with a history of violence.
Although the least prone of the three trials to bias,5 the OCTET trial in England also experienced several methodological limitations, including the involuntary nature of the control condition, high rates of non-participation and patients moving between trial arms after randomisation. 40–42 To comply with ethics standards, the control condition involved Section 17 leave, which is itself a form of compulsory care. In the light of these difficulties, it has been suggested that RCTs may be less suited to evaluating complex mental health interventions such as CTOs. 43
A number of observational studies of CTOs have also been conducted. After excluding uncontrolled studies, this observational research is characterised by matched cohort designs and before-and-after studies, with outcomes generally (but not invariably) assessed over 2 years or less. The results of these studies are more positive overall, with several showing benefits for CTO patients.
Early work in Australia centred on large-scale, population-based data from the states of Victoria and Western Australia. Although the Victorian work showed some positive effects in terms of reduced mortality for those receiving CTOs (a 14% reduction in the probability of non-injury related death and a 24% reduction per day on CTOs for injury related death), findings for key measures such as re-admissions and length of stay were more mixed. 44–46 West Australian work, meanwhile, reported a reduction in bed-days among those placed on CTOs (19.16 days less per episode of hospitalisation), as well as reduced mortality. 47–49 More recent work from New South Wales has suggested a delay in rehospitalisation for CTO patients [incidence rate ratio = 1.47, 95% confidence interval (CI) 1.36 to 1.58]50 whereas the latest work from Victoria has found reduced hospital stays [10.4 fewer days per inpatient episode (INPATEP)], lower rate of mortality (9% less for any cause and 20% less for non-injury) and marginally better quality-of-life scores. 27,51
In North America, a number of studies have used long-term routine administrative data from the New York Office of Mental Health. These have shown a reduced likelihood of re-admission plus increased use of community mental health services for those receiving CTOs, especially when CTOs were implemented for longer (≥ 6 months). 52 Such population studies have also shown more favourable forensic outcomes in terms of fewer arrests. 53 Early work comparing a Canadian province (Nova Scotia) without CTOs to an Australian state (Western Australia) with CTOs showed reduced inpatient stays in the latter,54 and more recent Canadian findings based on a province (Quebec) with CTOs suggest that CTO patients experienced better physical health and reduced mortality. 55
By contrast, there has been only one observational study of CTO outcomes in the UK, an uncontrolled before-and-after study based in Scotland. 56 This absence is particularly surprising given the rich source of administrative data available, as highlighted above in Patterns of use.
Evidence relating to the outcomes of CTOs is, therefore, complex. Discrepant findings may highlight the importance of local context. Together with evidence of variation in use, such findings suggest potential differences between people and places in both the operation and the effects of CTOs.
Financial implications
The NHS is operating in an increasingly resource constrained environment. Mental health services in particular have been stretched thin with 40% of mental health trusts experiencing reductions in income through 2013–15. 57 Consequently, bed occupancy in inpatient facilities is frequently above recommended levels placing increased strain on community services. When considering the impact of CTOs on service usage, it is imperative to consider the implications that such changes may have on scarce resources.
There is scant evidence surrounding the cost implications and cost-effectiveness of CTOs both internationally and in England. Only the OCTET trial has addressed the question of cost-effectiveness of CTOs. 35 It found no difference in health and social care costs, and no difference in outcomes between CTO and non-CTO groups. For all participants, the biggest cost driver was mental health hospitalisation (> 85%). As noted earlier, the findings of this trial are to be treated with caution. Although observational studies have examined impacts on service use,44–52,54,55 they have not extended their analysis to consider the implications of changes in service use on cost to health care services. There is little evidence linking the use of CTOs with NHS spending in England.
Rationale for the current study
CTOs are a well-established, yet controversial, global phenomenon. Significant differences in the particular legal frameworks through which they have come about makes it difficult to generalise findings across jurisdictions. There is, therefore, a continuing need for country-specific research.
Review of the broader literature shows two particular lacunae that should drive such efforts. First, patterns of use are understudied, particularly with regard to the independent contribution of demographic and clinical characteristics of patients subject to CTOs. Greater consideration also needs to be given to understanding variations in patterns of use between geographical areas and between service providers, and the degree to which these are associated with, or modified by, patient characteristics.
Second, undertaking RCTs of CTOs has proven inordinately challenging, and the difficulty of applying this methodology to such a complex intervention is likely to preclude further efforts. On one level, these difficulties are technical in nature and relate to the ethical and practical problems associated with randomising patients with serious mental disorders to experimental intervention. There is the inevitable unblinding of participants and clinicians, as well as the impossibility of disentangling the effects of legal compulsion from the vigilance and intensive level of care associated with CTO implementation. 1 RCTs are not well-suited to the evaluation of complex, multicomponent interventions aimed at changing patient and/or clinician behaviour within social and community contexts, such as CTOs.
Thus, rather than privileging a method designed to estimate singular ‘average treatment effects’,58 what is required is an approach to evaluation that is capable of capturing the variation and difference that is likely to arise when interventions centre on human agency and depend on the contexts in which they are situated. One way of achieving this is through robust population-based observational studies. Crucially, in the case of England, there have been no such studies to date.
Aims and objectives of the current study
In light of the above, the present study used routine clinical and administrative data to analyse variations in the use of CTOs and their association with patient outcomes in England. 16,59 Given the ever-increasing need to ensure health service resources are used effectively, we also modelled the health-care cost implications of these variations. More specifically, the study used data collected over 4 years from the Mental Health Services Data Set (MHSDS) to:
-
examine variation in the use of CTOs between patients, local areas and service providers
-
estimate associations between the use of CTOs and a selection of key patient outcomes
-
explore variation in these associations between patients, places and providers, establishing when, where and for whom CTOs may be effective
-
estimate the health-care costs associated with CTOs.
Chapter 2 Methods
Study overview and design
The study was based on a multilevel secondary analysis of annual, routinely collected, administrative data from providers of secondary mental health care services in England during 2011–15. These data were augmented by linkage to an external database recording the deaths of those patients who used these services based on national death registration.
Ethical and governance approvals
Ethics approval for the study was obtained from Warwick Medical School Biomedical Research Ethics Committee on 12 August 2015 (reference REGO-2015-1623). The data used in the study contained confidential patient-level information and the research team were granted access to anonymised data by the NHS Digital (NHSD) Data Access and Advisory Group. All data analyses took place through the Secure Research Service (SRS) for accredited researchers provided by the Office for National Statistics (ONS) at their safe setting in Titchfield. The Economic and Social Research Council (ESRC)’s Administrative Data Research Network (ADRN) oversaw and facilitated these arrangements.
Data source
The primary data source for this study was the MHSDS, formerly known as the Mental Health and Learning Disabilities Data Set (MHLDS) and before that as the Mental Health Minimum Data Set (MHMDS). 60 The MHSDS is collated, analysed and owned by NHSD, previously known as the NHS Health and Social Care Information Centre (HSCIC) and now known as NHS Digital.
Brief overview of the Mental Health Services Data Set
The MHSDS is a mandatory data return for all providers of NHS-funded mental health services. It is a patient-level, output-based, secondary uses data set that aims to deliver robust, comprehensive, nationally consistent and comparable person-based information on children, young people and adults who are in contact with mental health services. It supports a variety of secondary use functions, such as commissioning, clinical audit, research, service-planning, inspection and regulation, monitoring government policies and legislation, local and national performance management and benchmarking, and national reporting and analysis.
The MHSDS provides data on a wide range of secondary and tertiary mental health services, including those provided in hospitals, outpatient clinics and in the community (where the majority of people in contact with these services are treated). It brings together key information from adult and children’s mental health, learning disabilities or autism spectrum disorder, Children and Young People’s Improving Access to Psychological Therapies programme (CYP-IAPT) and early intervention care pathways that have been captured on clinical systems as part of patient care.
Although still not problem free, systems for MHSDS data collection, collation and curatorship have improved dramatically since the data set’s original inception. This has been reflected most recently in the decision for MHSDS returns to supplant KP90 returns as the official national statistics source for uses of the MHA. 24
The MHSDS is a large and complex data set. This study used annual ‘sensitive’ extracts from MHSDS for 2011–12, 2012–13, 2013–14 and 2014–15, with the period between 1 April 2011 and 31 March 2015 being referred to, hereafter, as ‘the study period’. Sensitive extracts cover uses of the MHA 1983 and include periods of time when service users were subject to a section of the MHA, on a CTO, or recalled to hospital while on a CTO.
Figure 1 provides a schematic representation of the structure of the MHSDS based on one hypothetical patient’s case history.
FIGURE 1.
Schematic representation of the structure of the MHSDS based on one hypothetical patient’s case history. a, Within MHMDS, the acronym ‘SCT’, supervised community treatment, is used to refer to CTO episodes. DAYATT, number of attendances at day treatment facilities; MHAEVENT, Mental Health Act event episodes; PROVSPELL, Hospital Provider Spell episodes.
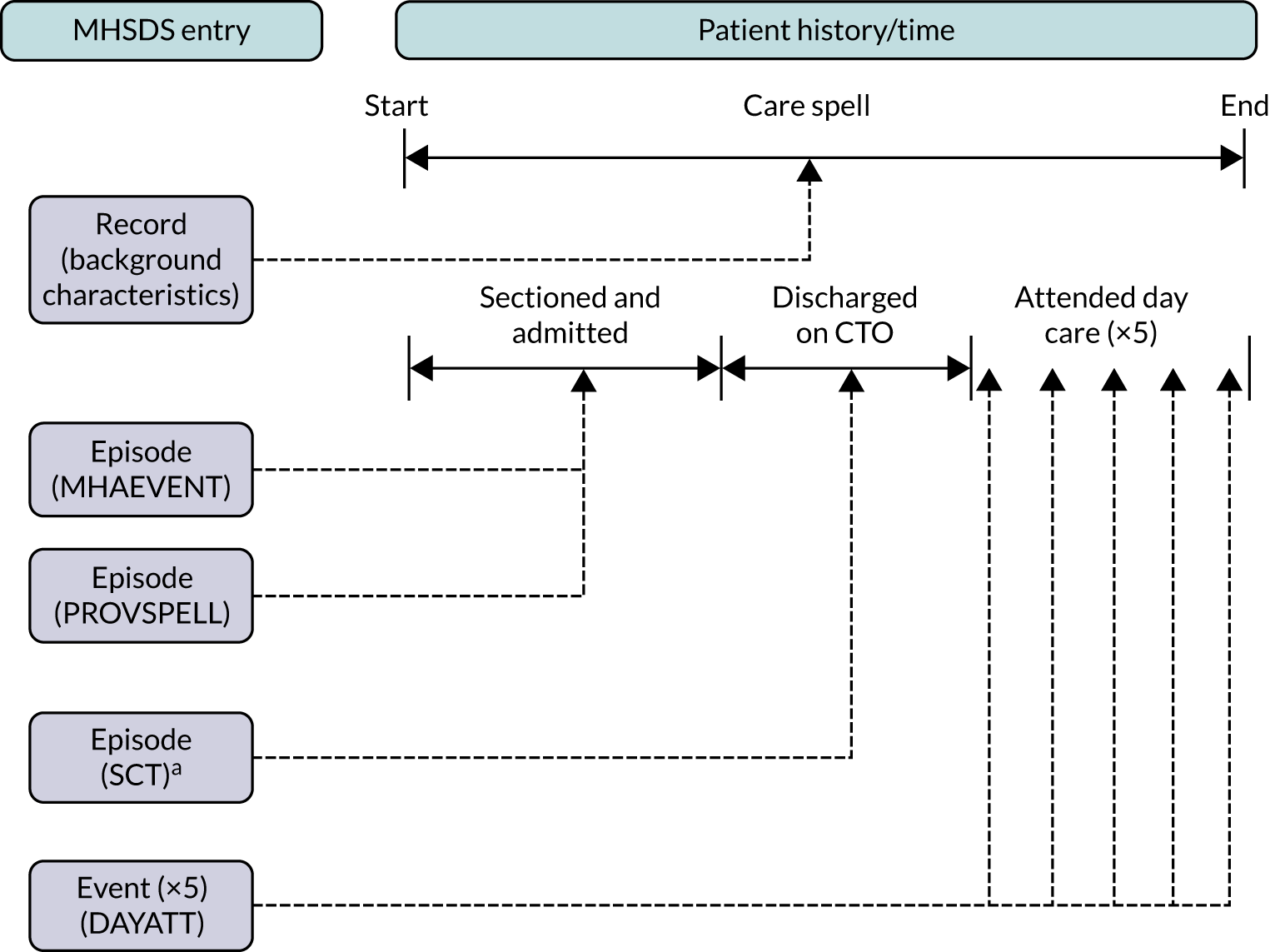
As can be seen, annual extracts (downloads to prespecified formats) are structured around care spells – periods of complete continuous care delivered to patients by a care provider. Care spells consist of episodes and events. Episodes are elements of care delivered over extended periods of time. Events are elements of care delivered at specific moments in time. Care spells also have records associated with them that provide key ‘background’ information about the patient receiving a care spell (e.g. sociodemographic characteristics, area of residence) as well as details of the organisation providing it.
Every care spell has a unique identifier (ID) that is present on all episodes, events and records relating to it. Although most patients have only one care spell in any particular year, care spells (and, therefore, care spell IDs) can extend over > 1 year.
Each patient has a unique person ID that is present on all records, episodes and events relating to them. Person IDs can, therefore, be used to link records, episodes and events for patients across all years and all care spells.
Periods of time during which patients are subject to a section of the MHA, admitted to hospital or placed on a CTO constitute episodes. These episodes formed the main data source for the present study. Within MHMDS, the first two are referred to as Mental Health Act event (MHAEVENT) and Hospital Provider Spell (PROVSPELL) episodes. PROVSPELL episodes start at the time a patient is admitted to hospital and end at the time they are discharged from hospital. Time spent receiving treatment under a CTO is referred to in these records as supervised community treatment (SCT) episodes, SCT being the name of the overall legal framework allowing the use of CTOs in England. For the sake of consistency, we use the name CTO for these episodes in this report (see Figure 1).
Since 2011, the dates on which specific care spells start and end, together with the episodes and events that comprise them, have been included. These dates can, therefore, be used together with the unique patient ID code to determine the duration and timing of CTO use and hospital admissions for individual patients.
The patient ID code also facilitates the linkage of MHSDS data with external data sources. In the present study, this was used to link patient records to the ONS Mortality Database to ascertain patient deaths during the study period. Access to, and linkage of, these data sets was facilitated by the ESRC’s ADRN.
Defining the study cohort
The study cohort initially consisted of any patient who, at some point during the study period, had been subject to a section of the MHA (1983) that made them eligible for a CTO on discharge from compulsory admission to hospital. In MHSDS, this was defined by patients with a MHAEVENT episode with a legal status classification code that related to one of the following: Section 3, 37, 47, 48 or 45a (all without ‘restrictions’ where applicable). On this basis, the initial study cohort comprised 69,490 patients.
Defining community treatment order status
The initial study cohort was categorised on the basis of CTO status as follows:
-
‘Ever on a CTO’ – patients who had at least one MHAEVENT episode coded with an eligible section and at least one CTO episode during the study period (n = 15,095).
-
‘Never on a CTO’ – patients who had at least one MHAEVENT episode coded with an eligible section but no CTO episodes during the study period (n = 54,395).
Separate analysis of CTO episodes revealed an additional 3464 patients who, during the study period, had at least one CTO episode but no eligible MHAEVENT episodes. As these patients had CTO episodes, they were included in the ‘ever on a CTO’ group, giving a cohort of 72,954 patients: 18,559 as ‘ever on a CTO’ and 54,395 as ‘never on a CTO’.
Geographical and spatial identifiers
Records in each annual extract included information about where patients lived and where they received health care for care spells that were open within that year. Several geographical or spatial levels are identified in the MHSDS. In terms of variation in the use and effectiveness of CTOs, the local area in which patients lived and the provider from whom they received specialist secondary mental health care are of most relevance. Further information about the operationalisation of these in the current study is given in the following sections.
Local area of residence
Lower-layer super output areas (LSOAs) are a set of stable geographical areas developed to facilitate estimation and dissemination of census data and neighbourhood statistics by England’s national statistics office. 61 Originally developed for the 2001 Census, modifications were made to their boundaries in the light of population change for the 2011 Census. More recent 2011 LSOA boundaries have only been used in MHSDS data since 2017. Accordingly, this study’s data were based on 2001 LSOAs. In 2001, there were 34,378 LSOAs across England (n = 32,482) and Wales (n = 1896), with a LSOA typically including 672 households and 1614 residents. Equivalent spatial units were also developed in Scotland and Northern Ireland.
For those patients in the ‘ever on a CTO’ group, the LSOA given in the record for the year of the care spell relating to their first SCT episode was used. For patients in the ‘never on a CTO’ group, the LSOA given in the record for the year of the care spell at the end of their first eligible MHAEVENT episode was used.
Using this approach, LSOA identifiers were missing for 2415 patients. Further analysis found: 1154 of these had one LSOA code in records in other years and these were used, 478 had more than one LSOA code in records in other years and the earliest available was used, and 783 had no LSOA codes in records in any other year. Although the majority of these 783 respondents were ‘never on a CTO’ (95.1%), not all of them were, and given their small number as a proportion of the sample overall, they were removed. This left a study sample of 72,171 patients from 23,481 LSOAs in 2001.
Although the vast majority of the included LSOAs or equivalents were in England (n = 23,285, 99.2%), a small number were in Wales (n = 168, 0.7%), Scotland (n = 18, 0.08%) and Northern Ireland (n = 6, 0.03%). The number of patients distributed across English and Welsh LSOAs or Scottish and Northern Irish equivalents were 71,740 (99.4%), 309 (0.4%), 18 (0.02%) and 6 (< 0.01%) respectively. In addition, a very small number of patients (n = 98, 0.14%) were recorded with ‘pseudo-LSOAs’ indicating other jurisdictions of residence rather than local areas (i.e. ‘Northern Ireland’, Channel Islands, Isle of Man and ‘Scotland’). These patients, and their ‘pseudo-LSOAs’ (n = 4, 0.02%), were retained.
Given the sample size and the fine scale of geographical disaggregation, a high percentage of LSOAs contained only one patient. To ensure stable models, it was, therefore, necessary to use middle-layer super output areas (MSOAs), rather than LSOAs. MSOAs are aggregations of LSOAs; in 2001 there were 7194 MSOAs across England (n = 6781) and Wales (n = 413). To facilitate the use of data reflecting local area characteristics contemporaneous with the period covered by the MHSDS data, it was decided that 2011 MSOAs should be used rather than 2001 MSOAs. In 2011, there were 7201 MSOAs across England (n = 6791) and Wales (n = 410), with a MSOA typically including 3245 households and 7787 residents.
Using lookup tables provided by the UK Data Service,62 a two-step process was followed. First, 2001 LSOAs were linked to 2011 LSOAs. Second, 2011 LSOAs were then aggregated to 2011 MSOAs. Following this work, the cohort of 72,171 patients were linked to a total of 6841 2011 MSOAs, 6708 of which were in England and 132 in Wales, with the number of patients in the two countries remaining the same as before (71,740 and 309 respectively). All those patients (n = 122) residing in other constituent parts of the UK (i.e. Scotland, Northern Ireland, Channel Islands and Isle of Man) were assigned to a single pseudo-MSOA, as LSOA to MSOA lookup tables are specific to England and Wales.
Provider trust
The provider organisation code was present for all care spells for all patients because it is automatically derived at the time of data submission. The same process for selecting provider trusts was used as for selecting local area of residence. Hence, for those patients in the ‘ever on a CTO’ group, the provider given in the record for the year of the care spell relating to their first CTO episode was used. For patients in the ‘never on a CTO’ group, the provider given in the record for the year of the care spell at the end of their first eligible MHAEVENT episode was used. In total, this resulted in 77 provider trusts, 67 of which were NHS providers and 10 of which were independent sector providers. Six of the NHS provider trusts recorded in the data were no longer active, and data relating to these were assigned to the 61 active providers based on organisational change information available on these trusts’ websites.
Outcome variables
Two sets of outcome variables were used in the current study – one relating to the use of CTOs and another relating to the association between the use of CTOs and patient outcomes. Summary details of the variables used in each are given in the following sections. Further details about all outcome variables used in the study are provided in Strategies for analysis.
Variation in the use of community treatment orders between patients, places and service providers
The primary outcome variable for the analysis of the use of CTOs was based on the binary categorisation of patients as ‘ever on a CTO’ or ‘never on a CTO’, as defined earlier. A secondary outcome in this part of the analysis was the time in days that ‘ever on a CTO’ patients had been subject to CTOs over the entire study period.
Association between the use of community treatment orders and patient outcomes
The association between the use of CTOs and patient outcomes was assessed according to three outcomes: re-admission, total time in admission and mortality.
Re-admission was defined in two ways: first, by categorising patients according to whether or not they were admitted after becoming eligible for a CTO (whether or not placed on one) and, second, the time between becoming eligible for a CTO (whether or not placed on one) and the start of the first, if any, subsequent period of hospital admission (i.e. time to re-admission). Total time in admission was defined as the total period of time that a patient spent in hospital between becoming eligible for a CTO (whether or not placed on one) and the end of the study period (or the date of death if they had died during the study period). Mortality was defined on an all-cause basis, with patients categorised as either having died during the study period or not.
For data quality reasons, we could not distinguish the cause of admission for the two admission-based patient outcomes just described. Although CTO episodes have a variable giving the reason for the termination of a CTO, this had high levels of missing data. Separate episodes recording supervised community treatment recalls were similarly affected by high rates of erroneous or missing data. Accordingly, we could not differentiate between recall, revocation and other types of admission.
Explanatory variables and data linkage
Explanatory variables related to patient- and local area-level characteristics. Owing to time constraints, and the findings from previous research on other aspects of compulsory treatment,63 no variables were included at provider trust level. Although patient-level characteristics were available entirely within the MHSDS, local area-level characteristics were included through linkage to the Department of Communities and Local Government Index of Multiple Deprivation (IMD). The following sections provide further details of each.
Patient-level variables: sociodemographic characteristics
Data on the sociodemographic characteristics of patients were obtained from the same records referred to in the section on geographical and spatial identifiers. Thus, for patients in the ‘ever on a CTO’ group, the record for the year of the care spell relating to their first SCT episode was used, whereas for patients in the ‘never on a CTO’ group, the record for the year of the care spell at the end of their first eligible MHAEVENT episode was used. Three sociodemographic characteristics were considered: gender, age and ethnicity. Information for age was complete for all 72,171 patients, whereas for gender and ethnicity the level of missing data was low: gender was missing for 395 patients (0.5%) and ethnicity was missing for 880 patients (1.2%). Although several other sociodemographic individual-level variables were present (e.g. employment status, accommodation status), they were not included because of high levels of missing data.
Patient-level variable: clinical characteristics
Data on the clinical characteristics of patients were obtained from an additional type of episode recorded in MHMDS – Payment by Results (PbR) Care Cluster episodes. These episodes reflect each period that a patient is assigned to a PbR Care Cluster (derived from clinician assessment using the HoNOS for PbR) assessment. 64
To avoid misclassification (e.g. due to clinical presentations changing over time and/or with age), the highest care cluster recorded in the years up to and including each patient’s ‘index year’ was used, (i.e. for patients in the ‘ever on a CTO’ group, this was the year of the care spell relating to their first SCT episode, whereas for patients in the ‘never on a CTO’ group, it was the year of the care spell at the end of their first eligible MHAEVENT episode). Care cluster information was less complete than age, sex and ethnicity and was missing for 5211 patients (7.2%).
Patients were grouped as follows according to their highest care cluster code: group 1 (non-psychotic): codes 0 to 9; group 2 (less severe psychotic): codes 10, 11, 14 and 15; group 3 (severe psychotic): codes 12, 13, 16 and 17; group 4 (cognitive impairment): codes 18 to 21; and group 5 (missing): no codes present.
Local area-level variable: neighbourhood deprivation
Neighbourhood deprivation was measured using the English Indices of Deprivation 2015. 65 These are based on 37 separate indicators at 2011 LSOA level and are used to calculate the IMD 2015. These indicators reflect seven distinct domains of deprivation: income; employment; health and disability; education, skills and training; crime; housing and services; and living environment. Only the overall summary IMD 2015 score was used here. To produce IMD 2015 scores for 2011 MSOAs, IMD 2015 scores for 2011 LSOAs were population weighted according to 2011 LSOA population counts based on the lookup tables referred to earlier and averages calculated across the LSOAs within each MSOA. Those patients living in Wales, Scotland, Northern Ireland, the Channel Islands and the Isle of Man (n = 431; 0.6%) were assigned a missing value for IMD 2015. A categorical variable for the IMD score for each MSOA was then created by dividing the score into quintiles, with the least deprived quintile serving as the reference category.
Strategies for analysis
Because the overarching aims of the study were to examine variation between patients, places and service providers in CTO use, and to estimate associations between CTO use and patient outcomes, all of the analyses conducted centred on the use of multilevel models (MMs). The actual form and type of MM used was, however, different in different analyses, depending on the response variable being studied. The next section gives a brief overview of multilevel modelling in general before subsequent sections outline the specific type of MM used in each part of the study. Table 1 presents a summary of the models/type of analysis outlined in these sections. All MMs were estimated using the MLwIN software package (MLwiN v2.22, Centre for Multilevel Modelling, Bristol, UK), whereas SPSS (SPSS v24, IBM Corp, New York, USA) was used for data preparation and the Kaplan–Meier survival analysis.
| Study focus | Response | Type of model/analysis |
|---|---|---|
| Use of CTOs |
‘Ever on a CTO’ (denoted by a ‘1’) or ‘never on a CTO’ (denoted by a ‘0’) Time subject to CTOs (days) |
|
| Association between the use of CTOs and patient outcomes |
Time to re-admission (days/90-day period) Rate of re-admission (90-day period) |
|
| Total time in admission (days) |
|
|
| Mortality (0,1) |
|
|
| Association between the use of CTOs and health-care costs | Cost (£) |
|
Multilevel models
Multilevel models are widely used for analysing hierarchically clustered data. 66 They provide a statistical framework where the complex structure of real-world settings in which patients live and use mental health services can be considered of substantive interest (i.e. they permit models that mirror the structure of the data). Importantly, they allow variation in the response variable to be apportioned to the appropriate level as well as providing measures of association with characteristics at each level.
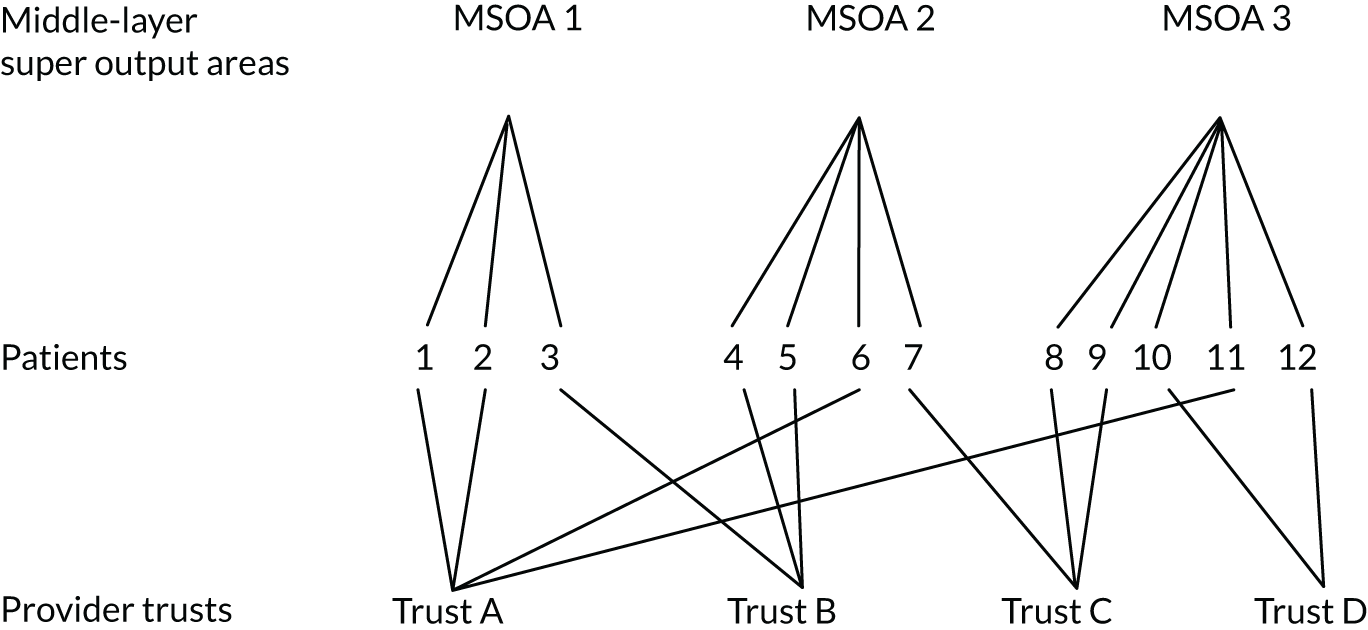
As outlined earlier, there are three distinct levels at which variation might occur: between patients, between the local areas in which patients live (MSOAs) and between the settings in which mental health services are delivered to patients (provider trusts). These levels do not, however, nest neatly within each other. Although patients nest within MSOAs, MSOAs do not nest within provider trusts, because patients residing in the same MSOA may receive services from different provider trusts. This produces what is known as a cross-classified data structure. 67 This is illustrated schematically in Figure 2. Such structures can be handled through the use of cross-classified multilevel models (CCMMs).
FIGURE 2.
An illustration of cross-classified multilevel data. Reproduced from Weich et al. 68 This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/.
Cross-classified multilevel models cannot, however, be estimated for all types of response variable. Accordingly, conventional two-level hierarchical MMs based on either patients within MSOAs or patients within provider trusts were used as well as CCMMs based on all three levels.
The most basic MM, whether hierarchical or cross-classified, is the null or empty model. This model estimates the total variance in the response variable without the inclusion of any explanatory variables. This variance is apportioned to each level of the model such that it equals the sum of the variances at each level. Further models, sometimes known as random-intercepts models, can then be developed that attempt to account for this variation by including explanatory variables at each level in the model. These types of models acknowledge that the average relationship (i.e. the regression intercept) between an outcome and any one explanatory variable may differ across different provider trusts and local areas. A final type of model, random-slope or fully random models, can also be estimated in which the effect of one or more explanatory variables is allowed to vary across higher-level settings. These types of models allow the gradient relationship (i.e. the regression slope) between the outcome and any one explanatory variable to vary across different provider trusts or areas.
Variation in the use of community treatment orders between patients, places and service providers
‘Ever on a CTO’ versus ‘never on a CTO’
The main analysis of the use of CTOs used CCMMs with a logit link function to model the binary response of ‘ever on a CTO’ (denoted by a ‘1’) or ‘never on a CTO’ (denoted by a ‘0’) for the study sample as a whole. The binary outcome was defined by a continuous latent variable and patient-level variance standardised to the logistic variance of π2/3 = 3.29. 66 Variances at each level were summed, allowing the proportion of (unexplained) variation, the variance partition coefficient (VPC), to be calculated at each level.
Median odds ratios (MORs) were calculated. 69 MORs can be conceptualised as the increased odds that would result from comparing two randomly chosen persons with the same covariates, one from a lower ‘rate’ service provider or local area where the models are over-predicting the outcome (i.e. there is a negative residual, see Residuals), the other from a higher ‘rate’ service provider or local area where the models are underpredicting the outcome (i.e. there is a positive residual, see Residuals). They are computed with the formula:(1)MOR=exp[√(2×VH)×0.6745],where VH is the relevant higher-level variance term and 0.6745 is the 75th centile of the cumulative distribution function of the normal distribution with mean 0 and variance 1. If the MOR is 1, there is no difference in the likelihood that the two randomly chosen people, one in the low ‘rate’ service provider or local area, the other in the ‘high rate’ service provider or local area, have the outcome (i.e. there is no variation between higher-level settings); where there is a considerable difference in the likelihood, the MOR is large (i.e. there is significant variation between higher-level settings).
Markov chain Monte Carlo (MCMC) estimation methods were used to estimate all of the CCMMs in this part of the analysis, with 1 million iterations being completed to ensure Raftery–Lewis and Brooks–Draper diagnostic conditions were satisfied. 70,71
Odds ratios (ORs) with 95% credible intervals (CrIs) are reported to show the size and significance of the effect of covariates in these models. MORs are directly comparable to these ORs.
Time spent on community treatment orders
A subsidiary analysis of the subset of ‘ever on a CTO’ patients was also carried out. This used a negative binomial link function to model the total time in days (consisting of either single or multiple SCT episodes) these patients had been subject to CTOs over the entire study period. As MCMC methods have not yet been developed for models with this link function and iterative generalised least squares methods have to transform cross-classified models into constrained nested models, conventional two-level hierarchical MMs of either patients within provider trusts or patients within MSOAs were used for this analysis. 70
To take into account the varying amounts of time that patients were ‘at risk’ of being placed on a CTO, an offset variable was included. This was calculated as the number of days from the start of a patient’s first CTO episode to the end of the study period, or, if they had died during the study period, to the date of death. As a result of including this variable, these models estimated the rate of CTO use per day (i.e. the likelihood, on any given day, that a patient would be on a CTO) rather than the absolute number of days that an individual spent on CTOs. 72 Accordingly, results for covariates in these models are given as rate ratios (RRs) with 95% CIs.
Following recent methodological developments in respect of multilevel analyses of rates/count data, median rate ratios (MRRs) were used to assess the VPC for these models. MRRs are equivalent to MORs for binary response data, with the resultant values interpretable in the same way (i.e. if the MRR is 1, there is no variation in the rate between higher-level settings, whereas if the MRR is large, there is significant variation in the rate between higher-level settings), and are calculated using the same formula (see Equation 1). 72
Residuals
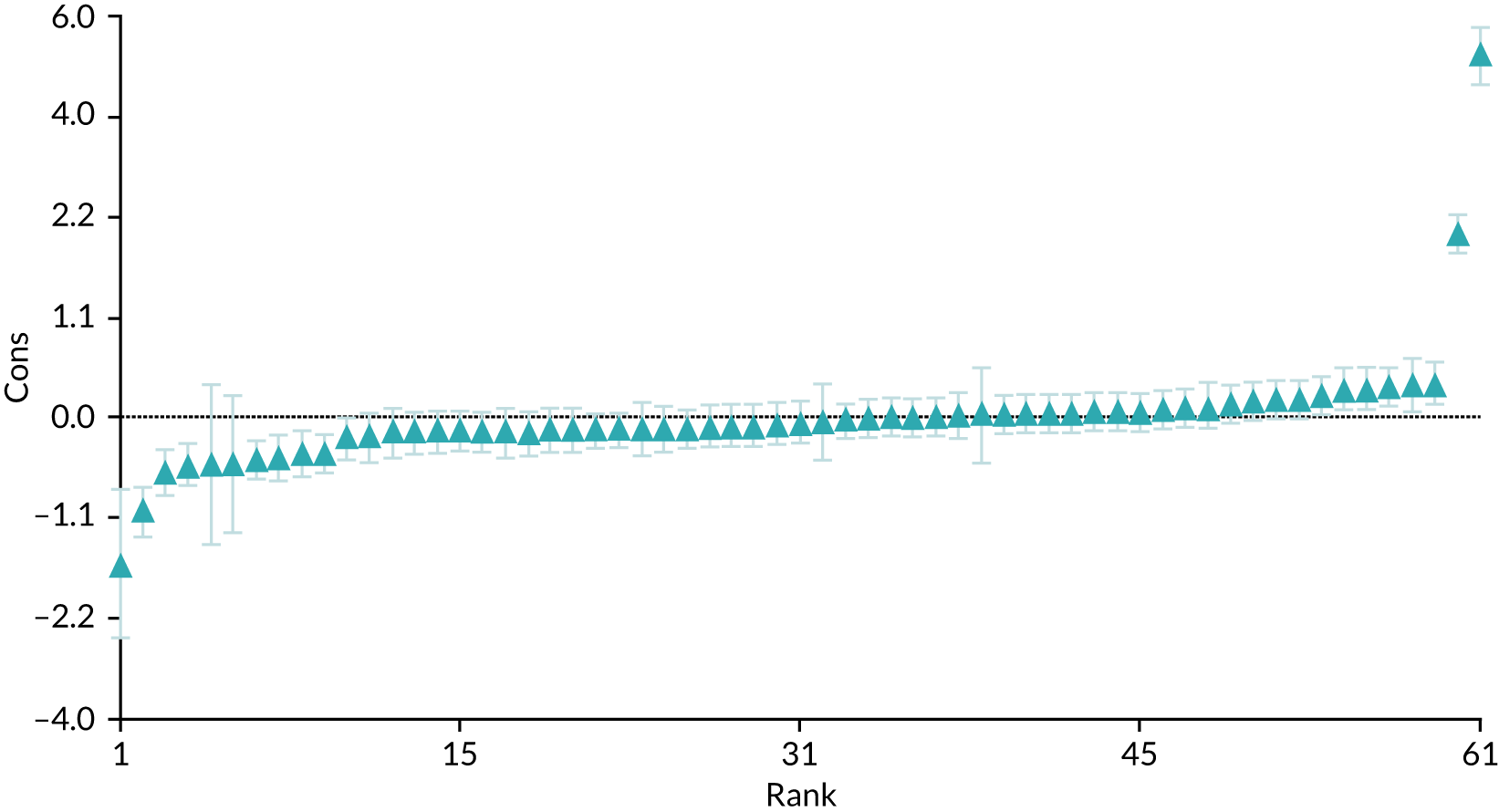
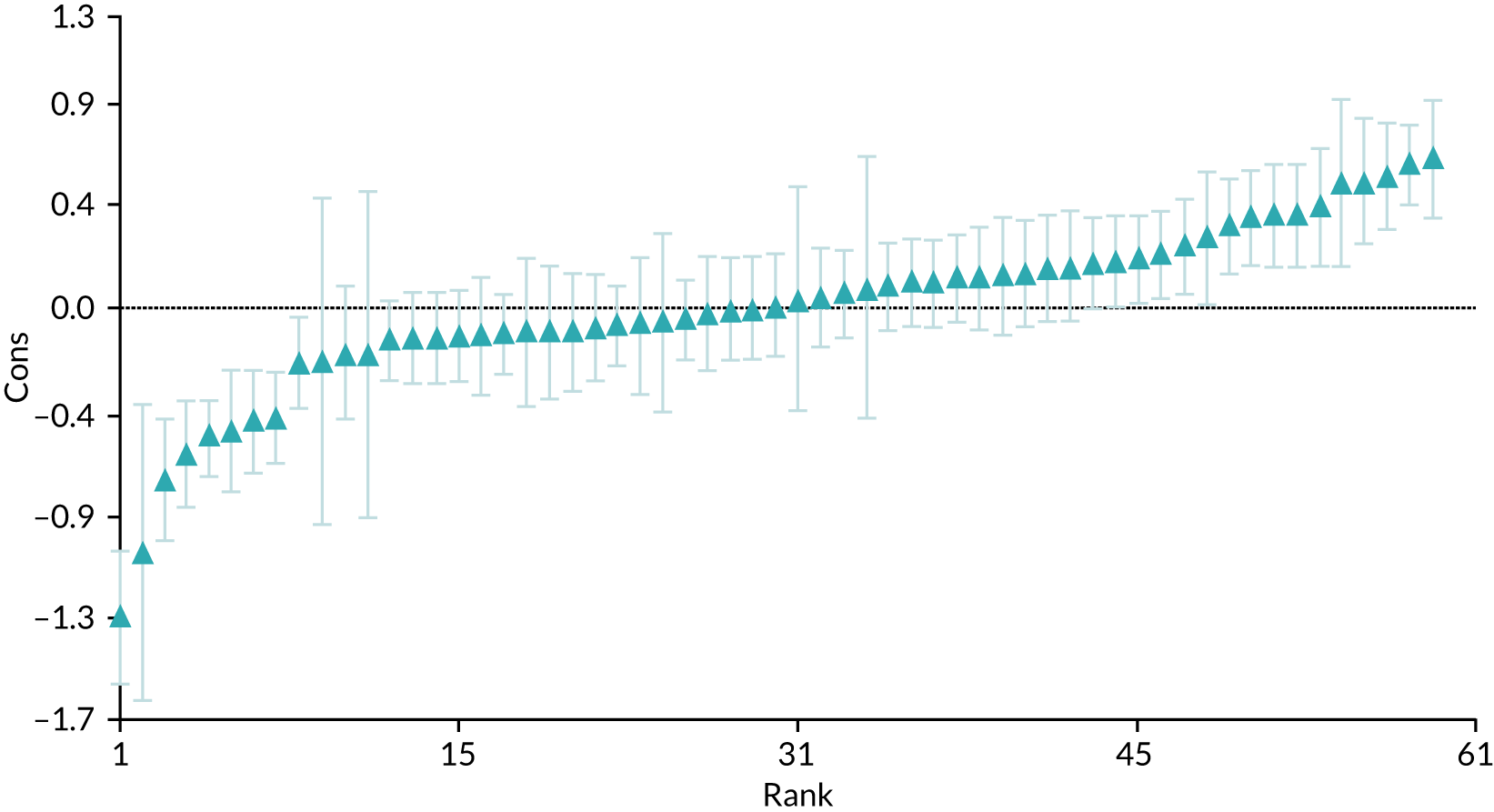
After estimating each model in the two analyses just described, we examined provider trust-level residuals to identify variation in CTO use between service settings. A residual at provider trust level is the difference between the actual (observed) value of the response and the value predicted by the (covariate-adjusted) model. Positive residuals indicate that the model is underpredicting the value (i.e. that a provider trust has a value above the average for all trusts combined) whereas negative residuals indicate that the model is overpredicting the value (i.e. that a provider trust has a value below the average for all trusts combined). Residual results are presented graphically using caterpillar plots that show the raw residual for each provider trust in rank order as a point estimate together with 95% CI error bars (see Figure 4). Upper and lower CIs were obtained by multiplying the standard error of each residual by 1.96 and adding and subtracting this value from each estimate respectively.
Associations between the use of community treatment orders and patient outcomes
To examine associations between the use of CTOs and patient outcomes, a subset of the full study sample was created consisting of a treatment group (‘CTO’) selected from those ‘ever on a CTO’, and a matched control group (‘non-CTO’), selected from those ‘never on a CTO’.
The treatment group consisted of patients who had been subject to a single CTO episode that had started and finished during the study period. These patients were selected as they had complete information for the start and finish dates of CTO episodes. The matched control group consisted of patients who had at least one MHAEVENT episode coded with an eligible section that had finished during the study period but who had no CTO episodes during the study period.
To prevent bias arising from secular changes in clinical practice, control group patients were frequency-matched to treatment group patients on the basis of the time at which both types of patient were discharged from hospital [i.e. the start date of CTO episodes for CTO (treatment group) patients and the end date of MHAEVENT episodes for non-CTO (control group) patients]. In this way, these dates represent the ‘index event’ for patients in each arm of the study.
Mental Health Act event episodes for control group patients were randomised and a window of ± 42 days around the CTO start dates was applied. Three MHAEVENT episode matches per CTO episode were allowed. Where there was more than one match for a control group patient, one was chosen at random. A wider range of matching variables would have led to considerable difficulties in achieving adequate matches, resulting in a much smaller sample size and reduced external validity. The window of ± 42 days was applied as it provided the best trade-off in terms of closeness in time to the index event and sample size requirements. Using this window enabled us to achieve the approximate 3 : 1 ratio between non-CTO and CTO patients in the final sample.
This matched subsample was used for the analysis of the three patient outcomes defined earlier (re-admission, total time in admission and mortality) as well as the analysis of the health-care costs associated with CTOs. The following sections provide further detail about each of these outcomes and outline the way in which each was analysed. Once again, these methods centre on the use of MMs, although the same set of covariates was used as in the work analysing the use of CTOs (i.e. gender, age, ethnicity, care cluster group and local area deprivation), the modelling strategy was slightly different. First, an additional covariate was included indicating patients’ treatment status (i.e. CTO or non-CTO). Second, rather than estimate ‘null’ models with no covariates, models with only the treatment status covariate were estimated. In this way, the models provided an estimate of the effect of CTOs on patient outcomes before and after adjusting for the effect of other covariates.
Re-admission
For patients who were categorised as being re-admitted after the date of their index event, time to re-admission was calculated as the number of days from each patient’s index event (i.e. the start date of CTO episodes for treatment group patients and the end date of MHAEVENT episodes for control group patients) to the first day of the first re-admission as recorded by the first PROVSPELL episode after the index event date. Those patients who were not re-admitted after their index event were (right) censored, with the time to censorship calculated as the number of days from each patient’s index event (as for those re-admitted) to the last day of the study period. For patients who died during the study period, the time of censorship was the date of death. As all PROVSPELL episodes had start dates, there was no need to impute missing data for this outcome variable.
Two methods of analysis were used: Kaplan–Meier survival analyses were undertaken to provide a description of times to re-admission for the two study groups, and discrete-time survival analyses were used to identify the association of CTO use with re-admission, independent of the effect of other covariates. 73 Both analyses take account of censoring (i.e. those patients who were not re-admitted before the end of the study period).
In the Kaplan–Meier analyses, the survival function for the probability of being re-admitted by a certain time period was estimated for each study group. Plots of these functions were then produced showing the proportion of each study group who had not been re-admitted (i.e. who had survived by remaining out of hospital) at each time point. Although it is not possible to take account of the type of patients in the two groups or the multilevel structure in this type of analysis, it shows whether or not the hazard remains proportional over time for the two groups.
Discrete-time MMs were used to take account of the type of patients in each group and hence to estimate the independent effect of CTO use on re-admission, while adjusting also for the nested (and clustered) nature of the data. 73 In using this approach, patients were categorised as being re-admitted or not (i.e. censored) in terms of 90-day periods based on the times to re-admission or censorship described above. This interval was chosen to balance between detail and aggregation. 74
To undertake discrete-time analysis, the data have to be structured so that the number of time periods before re-admission or censoring is nested within individual patients. A hypothetical example of the data restructuring required is given in Appendix 1. To extend this to a multilevel framework, time periods or patients are then situated within higher level contexts (i.e. provider trusts and local areas in this case).
The advantage of a multilevel approach to discrete-time analysis here is that it allows us to examine the degree of variation in the rate of re-admission between provider trusts and local areas. It also ensures that estimates are adjusted for autocorrelation and can ‘borrow strength’ from where there is the greatest amount of information (i.e. the provider trusts with the largest sample size).
A logit formulation was used for these models in which the observed response was being re-admitted (coded 1) or not (coded 0), with the data structure consisting of four levels in total: time periods, patients, MSOAs and provider trusts. The logit of being re-admitted was then modelled as a function of time, t, with a set of terms representing the passage of each 90-day time period and a set of covariates (including one denoting CTO treatment status). The inclusion of time accounted for the underlying hazard of re-admission (i.e. the probability of being re-admitted in a 3-month period), while the other parameters then estimated the independent effect of each covariate on the hazard. Interaction terms were also included to assess whether or not the underlying hazard of re-admission varied according to treatment status.
Random effects were estimated showing the variation in the rate of re-admission between MSOAs and provider trusts, respectively, after taking account of time and covariates. There were no random effects showing variation between patients, as the response is an absorbing end state (i.e. time to first re-admission) rather than a repeated event. 74 MORs were calculated as outlined earlier to assess the degree of (unexplained) variation at each higher spatial level (MSOAs and trusts), whereas ORs with 95% CrIs show the size and significance of the effect of covariates. In addition, MCMC estimation methods were used, with 100,000 iterations being completed to ensure that Raftery–Lewis and Brooks–Draper diagnostic conditions were satisfied for key parameters. 70,71
Total time in admission
For those patients who were re-admitted after their index event, the total time spent in admission was calculated by using patient ID codes to link subsequent PROVSPELL episodes and cumulating the number of days between the start and end dates of each.
PROVSPELL episodes record ‘a continuous period of inpatient care under a single Hospital Provider starting with a hospital admission and ending with discharge from hospital’ (information from NHS Digital, licensed under the current version of the Open Government Licence). 75 Additionally, two other types of episodes within MHSDS record information connected with hospital admissions:76 INPATEPs that are ‘a continuous period of care for a patient under the responsibility of a consultant or nurse’ (information from NHS Digital, licensed under the current version of the Open Government Licence)75 and ward stay within hospital provider spell (WARDSTAYS) episodes that are ‘a record for each stay of a patient on a ward during an inpatient stay’ (information from NHS Digital, licensed under the current version of the Open Government Licence). 75 Given this, the latest end date for either of these episodes was used to impute any missing PROVSPELL end dates where they were later than the start dates of PROVSPELL episodes with missing end dates.
A value for the total time in admission, in days, was derived for each patient. For those not admitted after their index event or who had a missing end date on their only/last PROVSPELL episode that could not be imputed, the value was zero. Meanwhile, for those admitted after their index event and who had at least one PROVSPELL episode with an end date, or an end date that could be imputed, it was non-zero.
The total time in admission (days) was then modelled using a negative binomial link. As described earlier for models of time subject to CTOs, multilevel MCMC methods are not available for this link function and so conventional two-level hierarchical MMs of patients within provider trusts were used.
To take account of the different amounts of time that patients were ‘at risk’ of admission, an offset variable was included. This was calculated as the number of days between a patient’s index event and the end of the study period, with two exceptions: where patients died during the study period, this was calculated to the date of death, whereas for those patients who had an admission but who had a missing only/last PROVSPELL end date that could not be imputed, it was calculated to the start date of that PROVSPELL episode.
As with the models of time subject to CTOs, owing to the inclusion of the offset variable, these models estimated the rate of admission per day (i.e. the likelihood, on any given day, that a patient would be in hospital) rather than the absolute number of days a patient spent in hospital. As a result, the effects of covariates are given as RRs with 95% CIs, whereas MRRs were used to assess the VPC, (i.e. to indicate the magnitude of variation occurring between MSOAs and provider trusts, respectively). 72
Mortality
As outlined earlier, data from the ONS Mortality Database was linked to MHSDS patient records through the unique patient ID code. Consequently, it was possible to identify those patients in the study cohort who had died during the study period. To help ensure patient confidentiality, only the month and year of death were available.
Using this information, three-level CCMMs of patients within MSOAs and provider trusts and with a logit link function were used to model the binary response of ‘having died in the study period’ (denoted by a ‘1’) or ‘not having died in the study period’ (denoted by a ‘0’). The patient-level variance, VPC and MORs were all handled as in the main analysis of the use of CTOs, as were the MCMC estimation methods, whereas ORs with 95% CrIs are reported to show the size and significance of the effect of covariates.
Variation in the associations between the use of community treatment orders and patient outcomes
In order to examine variation in the association between the use of CTOs and patient outcomes, models were estimated in which the covariate for treatment status was allowed to vary across provider trusts, producing what are known as random-slopes or fully random models.
In these models, the effect for treatment status on patient outcome is not, therefore, fixed (i.e. uniform) across all provider trusts, but can be different in different trusts. Crucially, this difference is not estimated through the inclusion of a set of separate ‘dummy’ variables, one for each trust, but through the addition of an extra variance and covariance term at provider trust level. This formulation brings a number of benefits, most particularly the ability for information about the association between CTO use and patient outcomes to be shared so that the estimates of variation ‘borrow strength’ from where there is the greatest amount of information (i.e. the provider trusts with the largest sample size).
Association between community treatment orders and health-care costs
The matched subsample was also used to examine the associations between the use of CTOs and health-care costs for patients. As outlined earlier (see Association between the use of community treatment orders and patient outcomes), the treatment group comprised those patients who had been subject to a single CTO episode that had started and finished during the study period, whereas the control group had at least one MHAEVENT episode with an eligible section, but had no CTO episodes.
The key cost driver associated with this population group is mental health hospitalisation. 35 Consequently, the analysis of costs associated with the use of CTOs focused on the burden of inpatient admission. To estimate the costs associated with CTO vs non-CTO we measured the health-care resource used by both groups, and then attached unit costs to calculate total cost, before assessing difference in costs between the two groups. The primary resource use in this study was days in inpatient admission, whereas the unit cost for each admission day was sourced from the Personal and Social Services Research Unit (PSSRU) Costs of health and social care 2017. 77
The PSSRU unit cost used was sourced from the NHS reference cost data for ‘per bed-day’ mental health care clusters. 77 This unit cost was used because costing was reliant on the output of the prior total admission data analysis. Costs were estimated using the output of the hierarchical MMs with the negative binomial link model used for the total admission analysis, and consequently the results on which the costs were estimated are at an aggregated level. Given this, the average PSSRU unit cost was chosen (Table 2).
| Activity | Additional resources | Resource use | Unit cost per hour or contacta (£) | Cost per CTO patient over 1 year (£) |
|---|---|---|---|---|
| Increased visits by community MHT | One extra visit from MHT per 3 months for 6 months | Two extra MHT visits | 248 | 496 |
| MHRT | Social circumstances report prepared by CC. 4–6 hours report writing time. Meeting lasts 1–2 hours, every 6–12 months, attended by three public panel members, CC and consultant psychiatrist | Report writing: | ||
| CC – 5 hours | 43 | 430.10c | ||
| Meeting: | ||||
| CC – 1.5 hours | 43 | 129.03c | ||
| Consultantb – 1.5 hours | 109 | 327.07c | ||
| Panel: (N/A) | N/A | N/A | ||
| SOAD Review | Independent senior psychiatrist: 2 hours for SOAD and 1 hour travel time | Consultantb – 3 hours | 109 | 65.4d |
| Admin time: 2 hours | Admin – 2 hours | N/Ae | N/A | |
| Capacity assessment and consent to treat forms | Approximately 30–60 minutes of consultant time in total | Consultantb – 45 minutes | 109 | 81.75 |
| Additional cost per CTO patient over 1 year | 1529.35 | |||
There is additional burden associated with delivering CTOs including increased visits by community MHTs, mental health review tribunals (MHRTs), increased chance of SOAD assessment; and clinician time completing capacity assessment and consent to treat forms. In consultation with two experienced psychiatrists who implement CTOs (SW and PK), the incremental burden of each of these activities relating to CTO patients was also estimated. This was an iterative process to identify all of the elements of burden associated with the implementation of CTOs and the resource use associated with each. PSSRU Unit costs77 were attached to these to create a fixed cost associated with the implementation of a CTO.
Three analyses were conducted: (1) the primary analyses focused solely on the costs associated with time in inpatient admission between CTO and non-CTO patients, (2) a secondary analysis included the incremental burden of CTO use in addition to inpatient admission data to assess the difference in cost when accounting for the extra burden of CTO implementation and (3) a final sensitivity analysis considered only severe psychotic patients.
To examine difference in cost of inpatient admission between CTO and non-CTO groups, results from the time in admission models described earlier were used (see Total time in admission). Estimates from these models were exponentiated to give mean daily rates of admission. These were multiplied by a period of risk (365 days) to give the total number of days in admission per year. Unit costs were attached to derive cost estimates for patients in both CTO and non-CTO groups. Results are presented as mean costs with associated 95% CIs.
Chapter 3 Results
Use of community treatment orders and description of the final study sample
Preliminary descriptive work showed that 19,084 patients had experienced one or more of a total of 45,500 CTO episodes during the study period. Although the largest group of patients had experienced only one CTO episode in this period (n = 7664, 40.2%), a small but not insignificant number were recorded as having had 5 or more CTO episodes (n = 1,958, 10.3%) during the study period. Of the 45,500 recorded CTO episodes, 2965 (6.5%) episodes lasted ≤ 1 week and 1123 (5.9%) patients only had episodes that lasted ≤ 1 week.
After removing patients with erroneous dates and missing geographical information, preliminary analysis of the use of CTOs by provider trust showed clear differences in the likelihood of being on a CTO between patients (n = 69,832) receiving care from NHS providers (n = 61), and patients (n = 2339) receiving care from independent sector providers (n = 10). Although 18,388 (26.3%) patients were ‘ever on a CTO’ among the former, only 133 (5.7%) patients were among the latter. In the light of this, and given that independent providers are likely to operate in different ways from NHS trusts (for instance by providing specialist or tertiary services only), the decision was made to remove independent sector providers from the study sample.
Table 3 shows the sociodemographic, clinical and area of residence characteristics for the resulting final study sample of patients (n = 69,832) receiving care from NHS provider trusts (n = 61) by treatment status (‘ever on a CTO’ vs. ‘never on a CTO’). As can be seen, ‘ever on a CTO’ patients were more likely to be male, aged < 65 years, of minority ethnic origin (particularly black), belong to the ‘severe psychotic’ care cluster group and live in more deprived areas.
| Characteristic | Treatment status | |
|---|---|---|
| ‘Ever on a CTO’ (N = 18,388), n (%) | ‘Never on a CTO’ (N = 51,444), n (%) | |
| Gender | ||
| Male | 11,400 (62.0) | 26,231 (51.0) |
| Female | 6978 (37.9) | 24,843 (48.3) |
| Missing | 10 (< 0.1) | 370 (0.7) |
| Age (years) | ||
| < 18 | 62 (0.3) | 315 (0.6) |
| 18–35 | 6727 (36.6) | 14,334 (27.9) |
| 36–64 | 9864 (53.6) | 22,639 (44.0) |
| ≥ 65 | 1735 (9.4) | 14,156 (27.5) |
| Ethnicity | ||
| White | 11,998 (65.2) | 40,114 (78.0) |
| Mixed | 632 (3.4) | 1066 (2.1) |
| Asian | 1563 (8.5) | 3189 (6.2) |
| Black | 3389 (18.4) | 4521 (8.8) |
| Other | 700 (3.8) | 1886 (3.7) |
| Missing | 106 (0.6) | 668 (1.3) |
| Care cluster group | ||
| 1: non-psychotic | 1019 (5.5) | 5511 (10.7) |
| 2: less severe psychotic | 4841 (26.3) | 14,986 (29.1) |
| 3: severe psychotic | 11,544 (62.8) | 18,916 (36.8) |
| 4: cognitive impairment | 466 (2.5) | 8064 (15.7) |
| 5: missing | 518 (2.8) | 3967 (7.7) |
| MSOA deprivation (least to most)a | ||
| First quintile | 1365 (7.4) | 6113 (11.9) |
| Second quintile | 2170 (11.8) | 7656 (14.9) |
| Third quintile | 3162 (17.2) | 9046 (17.6) |
| Fourth quintile | 5016 (27.3) | 12,396 (24.1) |
| Fifth quintile | 6661 (36.2) | 15,938 (31.0) |
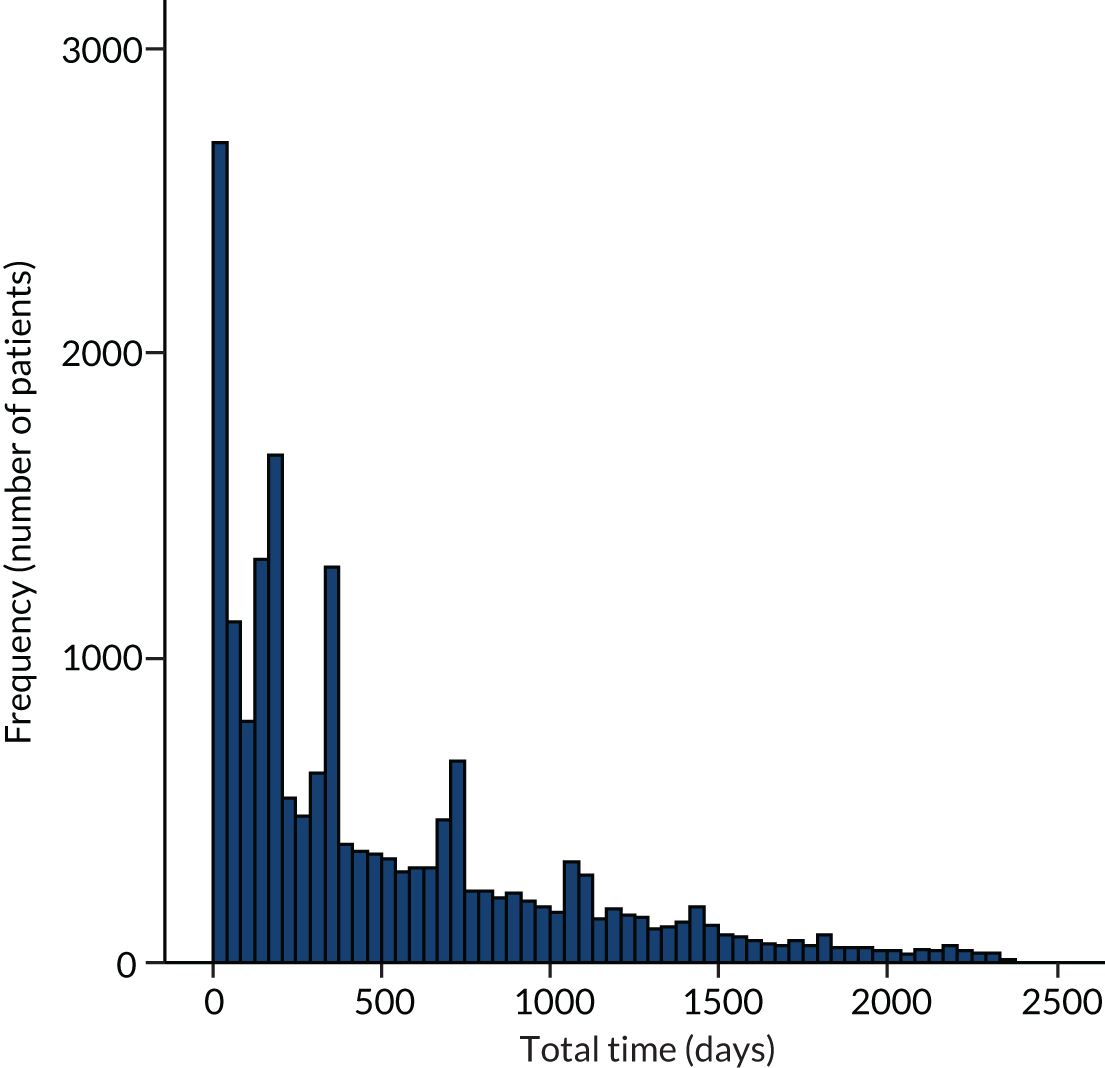
Figure 3 shows the distribution of the total time, in days, during the study period that ‘ever on a CTO’ patients (n = 18,388) were subject to CTOs. As can be seen, the distribution (mean = 498.2, standard deviation = 507.2) is considerably overdispersed owing to the tail of ‘ever on a CTO’ patients who were subject to CTOs for long periods of time.
FIGURE 3.
Distribution of the total time during the study period that ‘ever on a CTO’ patients in the final study sample (n = 18,388) were subject to CTOs.
Variation in the use of community treatment orders between patients, places and services (aim 1)
‘Ever on a CTO’ versus ‘never on a CTO’
Initial comparison of NHS provider trusts revealed large variation in the likelihood of eligible patients being on a CTO, which was due to the presence of two outlier trusts. Although the likelihood of being ‘ever on a CTO’ ranged from 0% to 37.3% across 59 of the 61 NHS provider trusts (with an average of 21.4%), the proportion of eligible patients who were subject to CTOs was 82.8% and 98.6% in the other two trusts. Under the terms of use agreed with the NHS Data Access and Advisory Group, we are not able to name these, or any other, service providers.
The results of CCMMs based on patients, MSOAs and provider trusts for the binary response of ‘ever on a CTO’ (1) and ‘never on a CTO’ (0) are shown in Table 4.
| Characteristic | Patient and MSOA-level covariates, all provider trustsa | Patient and MSOA-level covariates, excluding outlier trustsb | |
|---|---|---|---|
| Patient level, OR (95% CrI) | |||
| Gender (vs. male) | |||
| Female | 0.70 (0.67 to 0.73) | 0.69 (0.66 to 0.72) | |
| Age (vs. < 18 years) | |||
| 18–35 years | 1.20 (0.89 to 1.65) | 1.33 (0.94 to 1.97) | |
| 36–64 years | 1.21 (0.89 to 1.66) | 1.33 (0.94 to 1.97) | |
| ≥ 65 years | 0.61 (0.44 to 0.84) | 0.66 (0.46 to 0.98) | |
| Ethnicity (vs. white) | |||
| Mixed | 1.27 (1.13 to 1.43) | 1.32 (1.17 to 1.49) | |
| Asian | 1.06 (0.98 to 1.15) | 1.07 (0.99 to 1.16) | |
| Black | 1.43 (1.33 to 1.53) | 1.46 (1.36 to 1.57) | |
| Other | 0.79 (0.71 to 0.89) | 0.77 (0.69 to 0.87) | |
| Missing | 0.59 (0.46 to 0.74) | 0.50 (0.38 to 0.65) | |
| Care cluster group (vs. non-psychotic) | |||
| Less severe psychotic | 1.61 (1.47 to 1.77) | 1.72 (1.56 to 1.90) | |
| Severe psychotic | 3.76 (3.45 to 4.11) | 4.14 (3.77 to 4.55) | |
| Cognitive impairment | 0.42 (0.36 to 0.48) | 0.39 (0.34 to 0.46) | |
| Missing | 1.04 (0.91 to 1.20) | 1.09 (0.95 to 1.26) | |
| MSOA level | |||
| Deprivation (vs. least deprived),c OR (95% CrI) | |||
| Second quintile | 1.02 (0.92 to 1.12) | 1.01 (0.92 to 1.12) | |
| Third quintile | 1.10 (1.00 to 1.21) | 1.09 (0.99 to 1.20) | |
| Fourth quintile | 1.13 (1.03 to 1.24) | 1.12 (1.02 to 1.23) | |
| Fifth quintile | 1.13 (1.03 to 1.24) | 1.11 (1.02 to 1.22) | |
| Characteristic | Null model, all provider trustsa | Patient and MSOA-level covariates, all provider trustsa | Patient and MSOA-level covariates, excluding outlier trustsb |
| Unexplained variance (SE) | |||
| Patient | 3.29 | 3.29 | 3.29 |
| MSOA | 0.27 (0.02) | 0.20 (0.02) | 0.21 (0.02) |
| Provider trust | 1.13 (0.23) | 1.01 (0.21) | 0.15 (0.04) |
| % unexplained variance, VPC (95% CrI) | |||
| Patient | 70.18 | 73.14 | 90.01 |
| MSOA | 5.82 (5.14 to 6.53) | 4.47 (3.80 to 5.18) | 5.80 (4.95 to 6.70) |
| Provider trust | 24.00 (16.10 to 35.56) | 22.39 (15.14 to 32.81) | 4.19 (2.65 to 6.43) |
| MOR (95% CrI) | |||
| MSOA | 1.83 (1.77 to 1.90) | 1.68 (1.62 to 1.75) | 1.71 (1.64 to 1.78) |
| Provider trust | 3.43 (2.74 to 4.48) | 3.21 (2.61 to 4.10) | 1.58 (1.44 to 1.76) |
The null model, Table 4, shows that although most variation in the use of CTOs occurred between patients (70.2%), there was a significant amount of variation between MSOAs (5.8%) and between provider trusts (24.0%). When patient- and MSOA-level covariates were included in the model, the amount of variation between MSOAs and provider trusts was reduced slightly to 4.5% and 22.4%, respectively.
Analysis of the provider trust-level residuals from this second model confirmed the existence of two dominant outliers where the use of CTOs was considerably more common than that for other provider trusts, and substantially beyond that predicted by the types of patients and places (MSOAs) that they served (Figure 4). In these two trusts, the prevalence of ‘ever on a CTO’ predicted by the model that took account of patient and MSOA-level covariates was 97.7% and 71.1% respectively, whereas across the other trusts this ranged from 1.2% to 18.5%.
A third model excluding these two provider trusts, showed much less variation between the remaining providers (4.2%), with the amount of variation between MSOAs being slightly greater (5.8%). The influence of the two outlier trusts was confirmed on examining the provider trust-level residuals from this third model (Figure 5). As can be seen, however, there were still a number of remaining providers at both tails of the distribution where levels of CTO use differed significantly from the overall average (i.e. where the CI around their point estimate does not straddle the dotted horizontal line is the overall average). In total, 15 provider trusts had rates of CTO use that were significantly higher than the overall average, and nine had rates that were significantly lower.
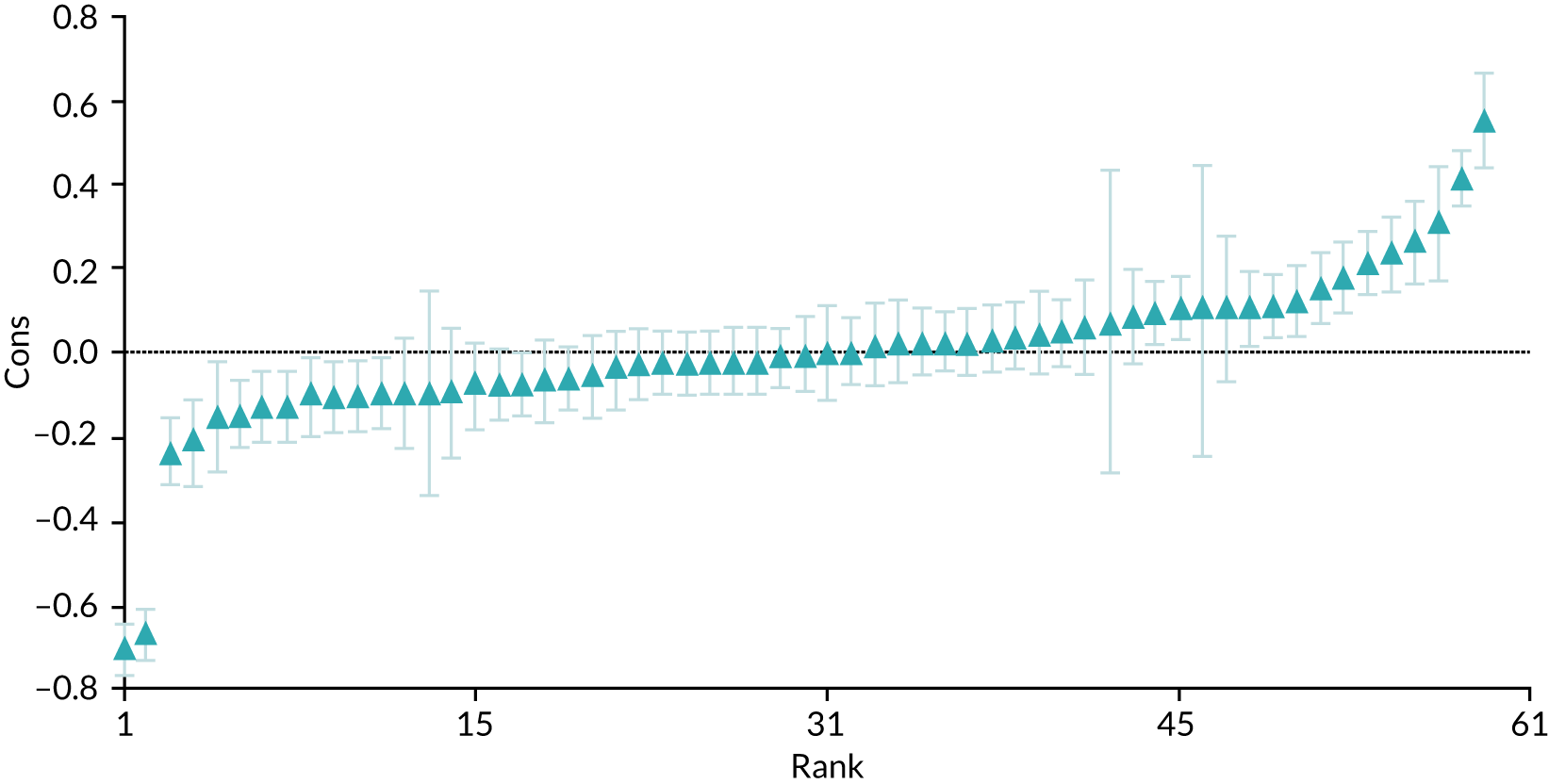
Excluding the two outlier provider trusts from the models did not have a marked effect on the estimates of the associations between CTO use and either patient or neighbourhood characteristics. As a result, tests for association between CTO use and patient characteristics were based on the results for all patients (i.e. Table 4). These results are shown graphically in Figure 6, where the vertical line for an OR of 1 relates to the reference category for each patient and local area characteristic.
FIGURE 6.
‘Ever on a CTO’ versus ‘never on a CTO’, by group category.
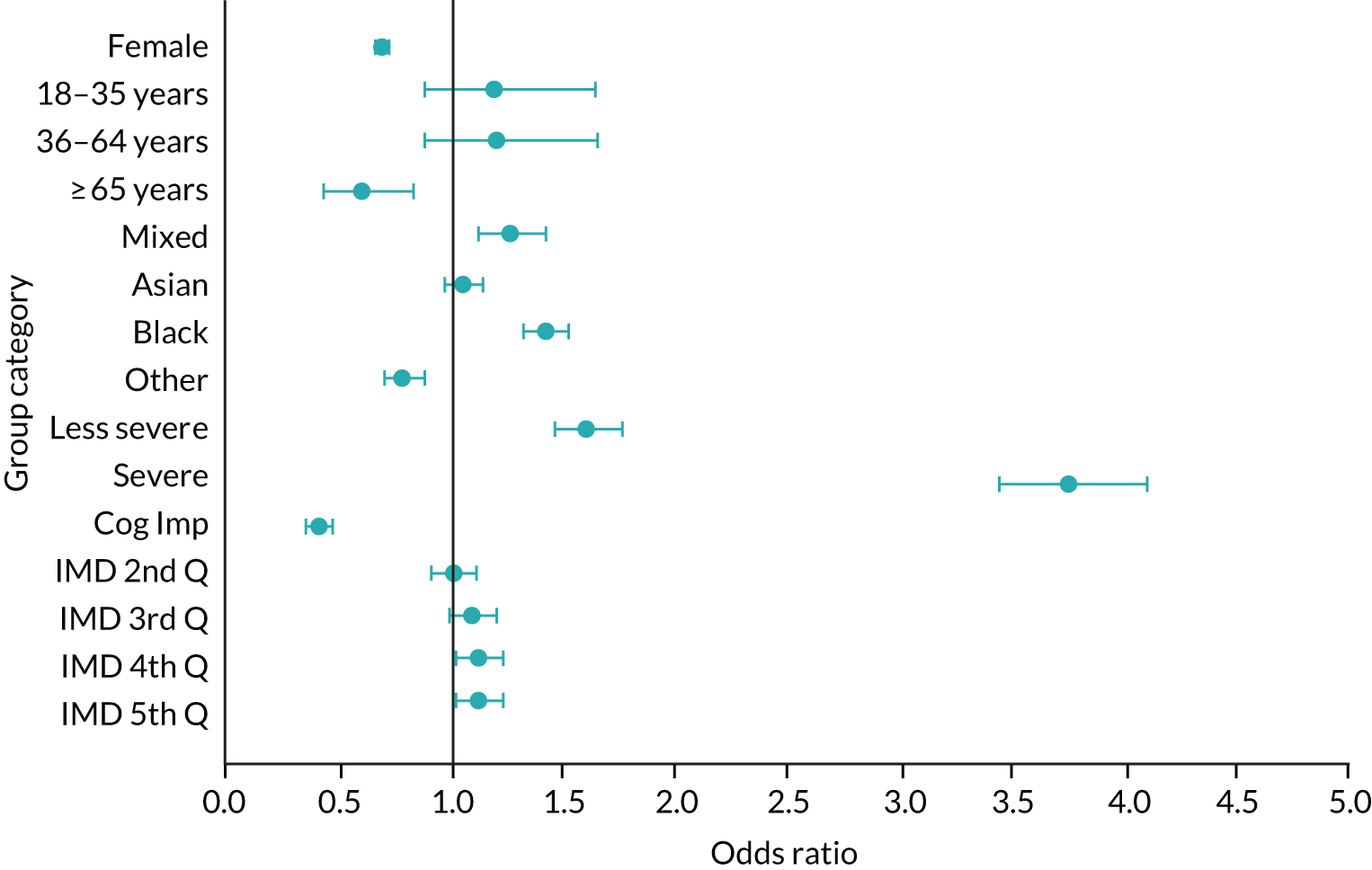
As can be seen, women had lower odds of being on CTOs than men (OR 0.70, 95% CrI 0.67 to 0.73). Patients aged ≥ 65 years were the least likely to be on CTOs (OR 0.61, 95% CrI 0.44 to 0.84) compared with those of other ages, all of whom were not significantly different from each other. Black patients had a significantly higher rate of CTO use than the white reference group (OR 1.43, 95% CrI 1.33 to 1.53) as did patients of mixed ethnicity (OR 1.27, 95% CrI 1.13 to 1.43). The largest associations were with care cluster grouping, with those in the ‘severe psychotic’ group (group 3) being almost four times more likely to be on a CTO than the ‘non-psychotic’ reference group (OR 3.76, 95% CrI 3.45 to 4.11).
At MSOA level, being on a CTO was associated with socioeconomic deprivation in a manner that suggested a dose–response relationship. ORs for being on a CTO rose to a peak of 1.13 (95% CrI 1.03 to 1.24) for those living in MSOAs in the top two (most deprived) quintiles compared with those living in the least deprived areas. Taking account of socioeconomic deprivation did not, however, substantially reduce the variation between MSOAs, and this was particularly true when the two outlier provider trusts were excluded (see Table 4).
Time subject to community treatment orders
An analysis of the total time, in days, that ‘ever on a CTO’ patients were subject to CTOs over the whole study period was also carried out. As the distribution of these times was substantially overdispersed owing to a small number of patients being on CTOs for much longer periods of time than the rest, a negative binomial link function was used. As outlined earlier (see Chapter 2, Strategies for analysis), CCMMs cannot be estimated for this link function as MCMC methods have not yet been developed. Accordingly, a series of two-level hierarchical MMs were estimated in which variation between provider trusts and between MSOAs was considered separately rather than simultaneously. Table 5 shows the results for models based on patients within provider trusts, whereas Table 6 shows the results for models based on patients within MSOAs.
| Characteristic | Model with patient and MSOA-level covariatesa | |
|---|---|---|
| Patient level, RR (95% CI) | ||
| Gender (vs. male) | ||
| Female | 0.93 (0.92 to 0.95) | |
| Age (vs. < 18 years) | ||
| 18–35 years | 1.13 (0.99 to 1.29) | |
| 36–64 years | 1.20 (1.05 to 1.37) | |
| ≥ 65 years | 1.23 (1.08 to 1.41) | |
| Characteristic | Null modela | Model with patient and MSOA-level covariatesa |
| Ethnicity (vs. white) | ||
| Mixed | 1.01 (0.97 to 1.05) | |
| Asian | 0.97 (0.95 to 1.00) | |
| Black | 1.02 (1.00 to 1.05) | |
| Other | 0.96 (0.92 to 1.00) | |
| Missing | 0.86 (0.78 to 0.94) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 1.13 (1.09 to 1.17) | |
| Severe psychotic | 1.22 (1.18 to 1.26) | |
| Cognitive impairment | 1.10 (1.04 to 1.16) | |
| Missing | 1.28 (1.21 to 1.35) | |
| MSOA level | ||
| Deprivation (vs. least deprived),b RR (95% CI) | ||
| Second quintile | 0.99 (0.95 to 1.02) | |
| Third quintile | 0.99 (0.96 to 1.02) | |
| Fourth quintile | 0.99 (0.95 to 1.02) | |
| Fifth quintile | 0.98 (0.95 to 1.01) | |
| Unexplained variance (SE) | ||
| Provider trust | 0.04 (0.01) | 0.04 (0.01) |
| MRR (95% CI) | ||
| Provider trust | 1.26 (1.20 to 1.31) | 1.25 (1.20 to 1.30) |
| Characteristic | Model with patient and MSOA-level covariatesa | |
|---|---|---|
| Patient level, RR (95% CI) | ||
| Gender (vs. male) | ||
| Female | 0.93 (0.91 to 0.94) | |
| Missing | 0.95 (0.67 to 1.34) | |
| Age (vs. < 18 years) | ||
| 18–35 years | 1.14 (0.99 to 1.33) | |
| 36–64 years | 1.23 (1.06 to 1.43) | |
| ≥ 65 years | 1.23 (1.06 to 1.43) | |
| Characteristic | Null modela | Model with patient and MSOA-level covariatesa |
| Ethnicity (vs. white) | ||
| Mixed | 1.01 (0.96 to 1.06) | |
| Asian | 0.94 (0.91 to 0.97) | |
| Black | 1.01 (0.99 to 1.04) | |
| Other | 0.89 (0.85 to 0.93) | |
| Missing | 0.82 (0.73 to 0.91) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 1.19 (1.15 to 1.24) | |
| Severe psychotic | 1.34 (1.29 to 1.39) | |
| Cognitive impairment | 1.10 (1.03 to 1.17) | |
| Missing | 1.36 (1.27 to 1.44) | |
| MSOA level | ||
| Deprivation (vs. least deprived),b RR (95% CI) | ||
| Second quintile | 0.96 (0.91 to 1.01) | |
| Third quintile | 0.97 (0.92 to 1.01) | |
| Fourth quintile | 0.98 (0.93 to 1.02) | |
| Fifth quintile | 1.01 (0.97 to 1.06) | |
| Unexplained variance (SE) | ||
| MSOA | 0.10 (0.004) | 0.10 (0.004) |
| MRR (95% CI) | ||
| MSOA | 1.43 (1.41 to 1.45) | 1.43 (1.41 to 1.45) |
All of the models in Tables 5 and 6 included an offset variable to take account of the differing amounts of time (in days) that ‘ever on a CTO’ patients were ‘at risk’ of being on a CTO. As a result, it is the proportion of an ‘ever on a CTO’ patient’s time at risk that is spent on CTOs that was modelled, rather than the absolute number of days they spent on CTOs. In this way, estimates from these models give the rate of CTO use per day (i.e. the likelihood, on any given day, that a patient would be on a CTO), with higher daily rates indicating a greater incidence of days on CTOs. When exponentiated, these estimates result in RRs, that have the same interpretation as ORs but for rates rather than odds.
As can be seen, estimates of between-provider and between-neighbourhood variation remained statistically significant after taking account of patient and neighbourhood characteristics, with variation in the daily rate of CTO use appearing to be greater between MSOAs (MRR 1.43, 95% CI 1.41 to 1.45) than between provider trusts (MRR 1.25, 95% CI 1.20 to 1.30). It is important to remember, though, that variances were estimated separately here, not simultaneously as in the CCMMs reported in the previous section.
Provider trust-level residuals for the model in Table 5 are shown in Figure 7. The two outlying trusts reported in the previous section were also unusual here, though less prominently so, appearing this time with the largest negative residuals (i.e. with their patients spending less time subject to CTOs, on average, than the mean for all trusts). There were also a number of other provider trusts at both tails of the distribution that were significantly different from the overall average (shown again by the horizontal line). In total, 13 provider trusts were significantly higher than the overall average and 12 were significantly lower.
As estimates of the effect of patient and area characteristics were similar when they were included in the model of patients within provider trusts and the model for patients within MSOAs, respectively, only the results from the model in Table 5 are shown graphically in Figure 8. The vertical line for a RR of 1 relates to the same reference categories for patient and local area characteristic as in Figure 6.
FIGURE 8.
Time subject to CTOs for ‘ever on a CTO’ patients, by group category.
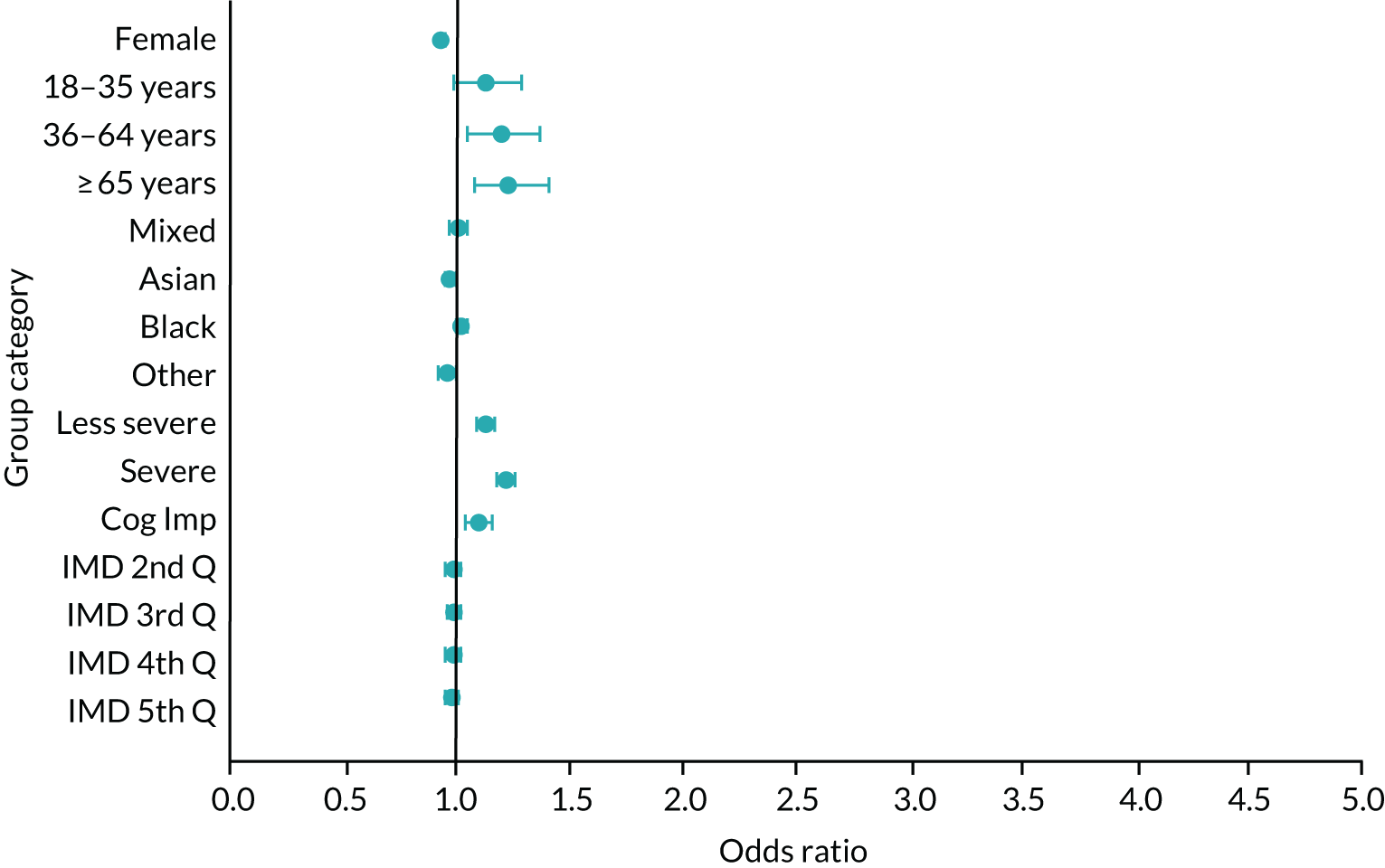
As can be seen, women were subject to a lower rate of CTO use per day than men (RR 0.93, 95% CI 0.92 to 0.95) and people aged 36–64 and ≥ 65 years were subject to a higher rate than people of other ages (RR 1.20, 95% CI 1.05 to 1.37 and RR 1.23, 95% CI 1.08 to 1.41, respectively). Although black people experienced a higher rate of CTO use per day than any other ethnic group, the effect size was not large or significant (RR 1.02, 95% CI 1.00 to 1.05). In terms of care cluster group, the largest effect size was for those in the severe psychosis category (RR 1.22, 95% CI 1.18 to 1.26). All of the effect sizes for socioeconomic deprivation at MSOA-level were small and non-significant.
Comparing Figure 8 with Figure 6 we find a noticeable difference. The likelihood of being on a CTO is strongly patterned across a range of patient characteristics, with some groups of patients being much more likely than others to be on a CTO (see Figure 6). By contrast, the degree of patterning is much reduced for the time that CTO patients spend on CTOs, with no patient groups (as characterised by the covariates available in our data set) spending particularly longer or shorter periods of time on CTOs, although some are still statistically significantly different from others (see Figure 8).
Associations between use of community treatment orders and patient outcomes (aim 2)
Description of the matched subsample
As described earlier (see Chapter 2, Strategies for analysis), analyses of associations between the use of CTOs and patient outcomes were conducted using a matched subsample. This was drawn from the final study sample of patients in NHS provider trusts and comprised:
-
Treatment group (‘CTO’) – patients who had been subject to a single CTO episode that had started and finished during the study period.
-
Matched control group (‘non-CTO’) – patients who had at least one MHAEVENT episode coded with an eligible section that had finished during the study period but who had no CTO episodes during the study period.
The final matched sample comprised 6329 treatment group (CTO) patients and 16,842 control group (non-CTO) patients. The sociodemographic, clinical and area of residence characteristics of the patients in these two groups are shown in Table 7. As with the main study sample, CTO patients were more likely than non-CTO patients to be male, aged < 65 years, of minority ethnic origin (particularly black), belong to the ‘severe psychotic’ care cluster group and live in more deprived areas (Table 7).
| Characteristic | Matched subsample | |
|---|---|---|
| Treatment status | ||
| CTO (N = 6329), n (%) | Non-CTO (N = 16,842), n (%) | |
| Gender | ||
| Men | 3726 (58.9) | 8555 (50.8) |
| Female | 2593 (41.0) | 8260 (49.0) |
| Missing | 10 (0.2) | 27 (0.2) |
| Age (years) | ||
| < 18 | 32 (0.5) | 67 (0.4) |
| 18–35 | 2354 (37.2) | 4867 (28.9) |
| 36–64 | 3262 (51.5) | 7669 (45.5) |
| ≥ 65 | 681 (10.8) | 4239 (25.2) |
| Ethnicity | ||
| White | 4015 (63.4) | 13,064 (77.6) |
| Mixed | 226 (3.6) | 357 (2.1) |
| Asian | 576 (9.1) | 1079 (6.4) |
| Black | 1140 (18.0) | 1602 (9.5) |
| Other | 311 (4.9) | 544 (3.2) |
| Missing | 61 (1.0) | 196 (1.2) |
| Care cluster group | ||
| Non-psychotic | 478 (7.6) | 1951 (11.6) |
| Less severe psychotic | 1917 (30.3) | 4982 (29.6) |
| Severe psychotic | 3531 (55.8) | 6784 (40.3) |
| Cognitive impairment | 236 (3.7) | 2450 (14.5) |
| Missing | 167 (2.6) | 675 (4.0) |
| MSOA deprivation (least to most)a | ||
| First quintile | 474 (7.5) | 1903 (11.3) |
| Second quintile | 804 (12.7) | 2436 (14.5) |
| Third quintile | 1165 (18.4) | 2911 (17.3) |
| Fourth quintile | 1714 (27.1) | 4110 (24.4) |
| Fifth quintile | 2165 (34.2) | 5398 (32.1) |
Figure 9 shows the distribution of the total time, in days, during the study period that the CTO patients were subject to CTOs. As before (see Figure 3), the distribution is considerably over dispersed owing to the tail of patients subject to CTOs for long periods of time, although the mean (197.7 compared with 498.2) and standard deviation (222.6 compared with 507.2) are much reduced.
FIGURE 9.
Distribution of the total time during the study period that CTO patients in the matched subsample (n = 6329) were subject to CTOs.
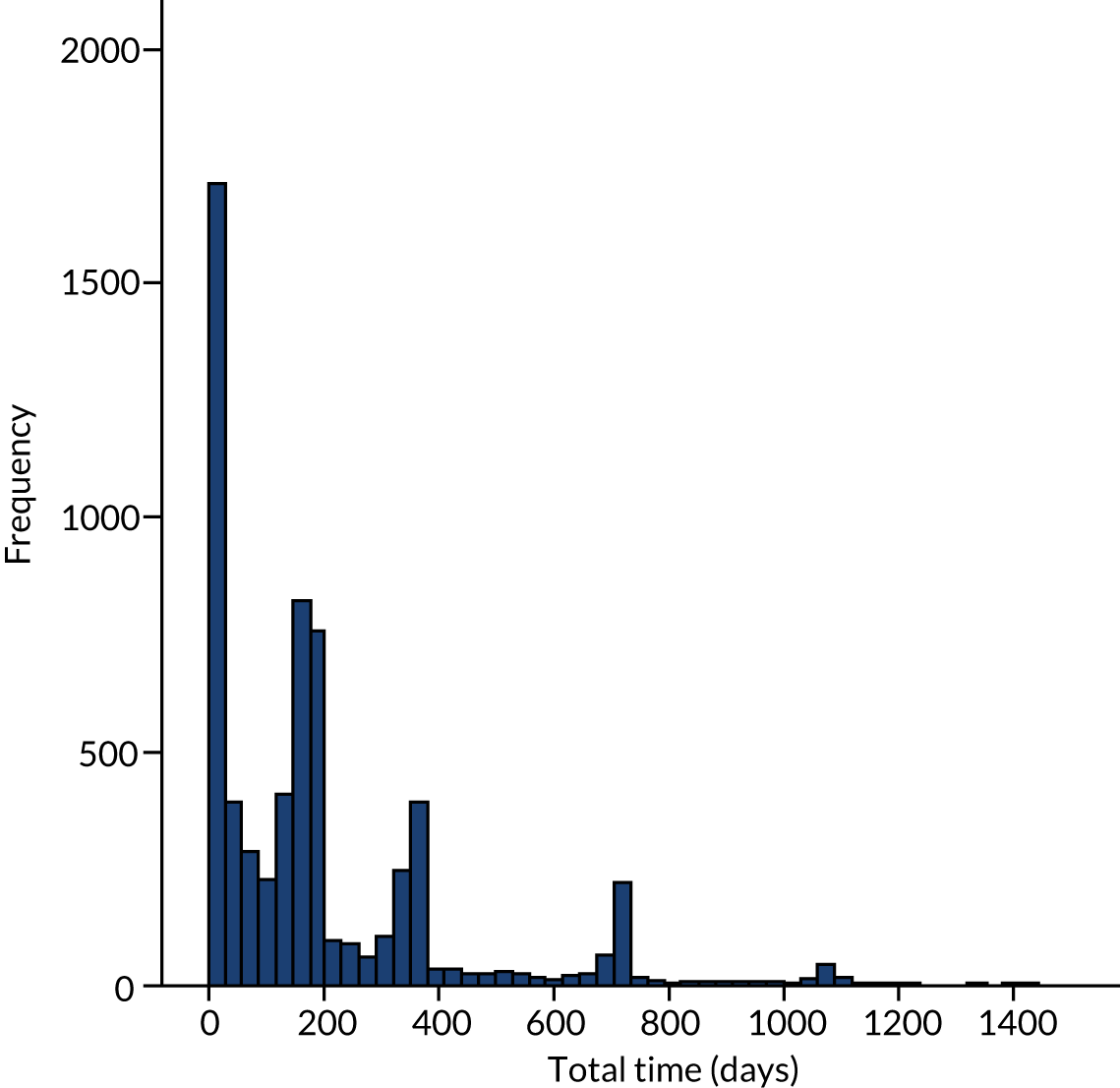
Three patient outcomes were studied: re-admission, total time in admission and mortality. Results for each outcome based on all NHS provider trusts now follow.
Re-admission
In the treatment group, 36.9% (n = 2335) of CTO patients were recorded as being admitted to hospital after their index event. The remaining 3994 (63.1%) CTO patients were not re-admitted to hospital during the study period and were, therefore, censored at the end of the study period (or, date of death, if applicable, whichever was earliest).
In the control group, 35.6% (n = 5999) of non-CTO patients were re-admitted during the study period and 64.4% (n = 10,843) were censored at the end of the study period (or date of death, if applicable, whichever was earliest).
Based on Kaplan–Meier estimates, the mean time to re-admission was 967.0 days (95% CI 951.4 to 982.6 days) for CTO patients and 957.9 days (95% CI 948.1 to 967.7 days) for non-CTO patients. Thus, although CTO patients had a slightly longer time on average to re-admission (9.1 days), the overlapping CIs suggested that there was little difference in the two groups in terms of average time to re-admission.
These results took no account, however, of patient or local area characteristics. To do this, a series of discrete-time models were estimated. To facilitate this approach, times to re-admission/censoring were grouped into 90-day periods, with time to censoring (i.e. for those not re-admitted to hospital during the study period) being defined as the interval between a patient’s index event from CTO start (CTO group) or discharge from hospital (non-CTO group) to the end of the study period or, for those who died during the study period, the date of death. A Kaplan–Meier survival plot based on these time periods is shown in Figure 10 and indicates a high degree of similarity in re-admission over time between the two groups.
FIGURE 10.
Survival (time to re-admission) curves for the two treatment groups based on 90-day periods.
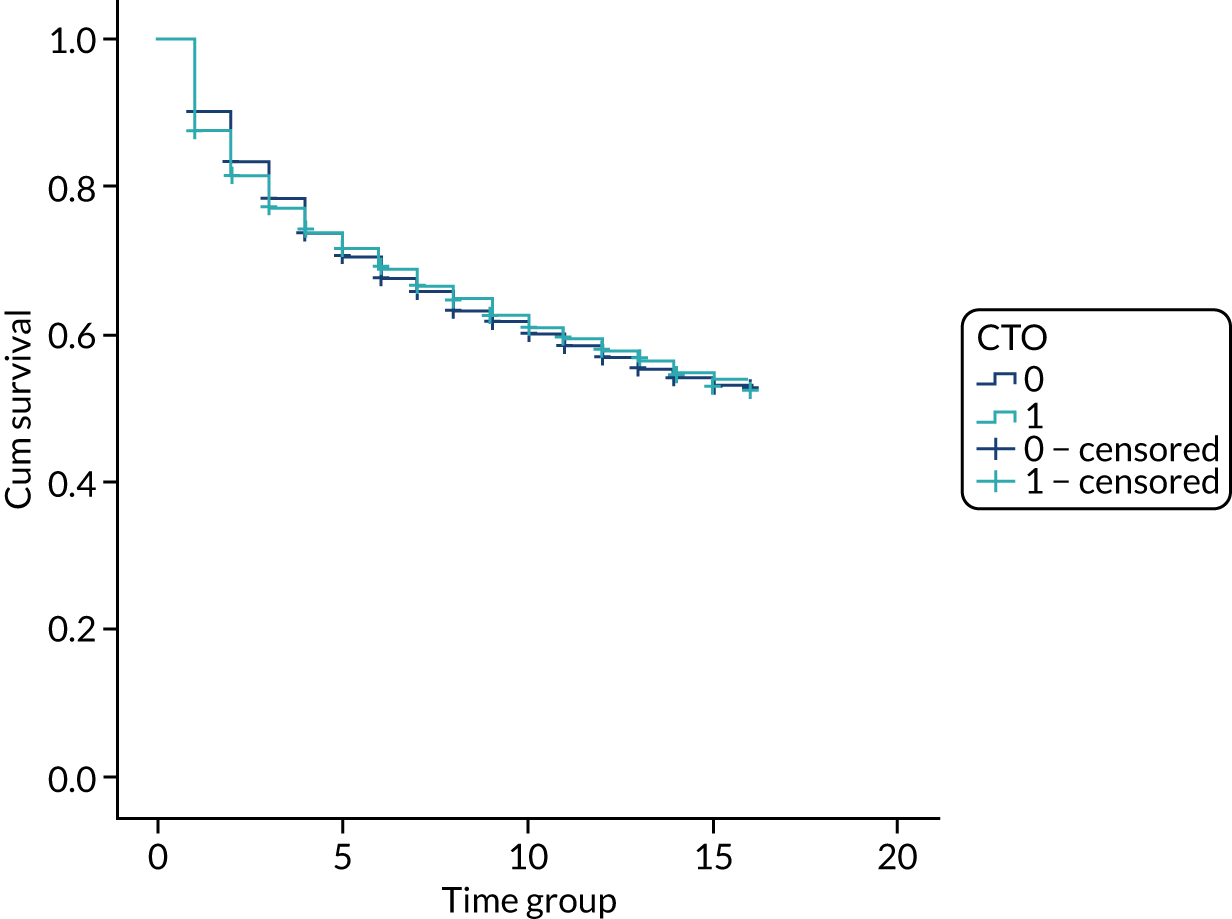
As discrete-time models are particularly computationally intensive (i.e. take several days to run) when estimated as CCMMs using MCMC methods in MLwiN, a series of single-level discrete-time models were first estimated in SPSS. These showed that there was no significant interaction between treatment status and time period, (i.e. the hazard profile over time was similar for each treatment group). Interaction terms between treatment status and care cluster group were, however, statistically significant, and so these were included in a four-level CCMM (in MLwiN).
The results for discrete-time CCMMs are shown in Table 8. Taking the model with time periods and treatment status only (Table 8), results showed the rate of re-admission reduced over time. Because interaction terms between time period and treatment status were not required, this reduction is the same for each treatment group and is shown graphically in Figure 11.
| Characteristic | Model with time period and treatment status covariate onlya | Model with time period, treatment status, patient and MSOA covariatesa |
|---|---|---|
| Period level, OR (95% CrI) | ||
| Time period (vs. period 1) | ||
| Period 2 | 0.66 (0.62 to 0.70) | 0.66 (0.62 to 0.71) |
| Period 3 | 0.51 (0.47 to 0.55) | 0.51 (0.47 to 0.55) |
| Period 4 | 0.45 (0.42 to 0.49) | 0.45 (0.42 to 0.49) |
| Period 5 | 0.37 (0.33 to 0.40) | 0.37 (0.33 to 0.40) |
| Period 6 | 0.34 (0.31 to 0.38) | 0.34 (0.31 to 0.38) |
| Period 7 | 0.30 (0.27 to 0.33) | 0.30 (0.27 to 0.33) |
| Period 8 | 0.28 (0.25 to 0.31) | 0.28 (0.24 to 0.31) |
| Period 9 | 0.24 (0.21 to 0.28) | 0.24 (0.21 to 0.28) |
| Period 10 | 0.23 (0.19 to 0.26) | 0.23 (0.19 to 0.26) |
| Period 11 | 0.23 (0.19 to 0.27) | 0.23 (0.19 to 0.27) |
| Period 12 | 0.22 (0.19 to 0.27) | 0.22 (0.19 to 0.27) |
| Period 13 | 0.24 (0.19 to 0.29) | 0.24 (0.19 to 0.29) |
| Period 14 | 0.17 (0.13 to 0.23) | 0.17 (0.13 to 0.23) |
| Period 15 | 0.19 (0.14 to 0.26) | 0.20 (0.14 to 0.27) |
| Period 16 | 0.12 (0.07 to 0.21) | 0.13 (0.07 to 0.21) |
| Patient level, OR (95% CrI) | ||
| Treatment status (vs. non-CTO) | ||
| CTO | 1.12 (1.06 to 1.18) | 0.90 (0.75 to 1.08) |
| Gender (vs. male) | ||
| Female | 1.08 (1.03 to 1.13) | |
| Age (vs. < 18 years) | ||
| 18–35 years | 1.22 (0.89 to 1.69) | |
| 36–64 years | 0.99 (0.72 to 1.37) | |
| ≥ 65 years | 0.75 (0.54 to 1.05) | |
| Ethnicity (vs. white) | ||
| Mixed | 1.01 (0.88 to 1.16) | |
| Asian | 0.83 (0.76 to 0.91) | |
| Black | 0.94 (0.87 to 1.02) | |
| Other | 0.78 (0.69 to 0.89) | |
| Missing | 0.89 (0.70 to 1.12) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 0.79 (0.72 to 0.86) | |
| Severe psychotic | 0.89 (0.82 to 0.97) | |
| Cognitive impairment | 0.39 (0.35 to 0.45) | |
| Missing | 0.22 (0.17 to 0.28) | |
| Patient-level interactions, ORs (95% CrI) | ||
| CTO*Less severe psychotic | 1.08 (0.89 to 1.30) | |
| CTO*Severe psychotic | 1.09 (0.91 to 1.31) | |
| CTO*Cognitive Impairment | 2.16 (1.55 to 3.00) | |
| CTO*Missing Care cluster group | 2.53 (1.66 to 3.86) | |
| MSOA level | ||
| Deprivation (vs. least deprived),b OR (95% CrI) | ||
| Second quintile | 1.06 (0.96 to 1.17) | |
| Third quintile | 1.16 (1.05 to 1.27) | |
| Fourth quintile | 1.09 (0.99 to 1.19) | |
| Fifth quintile | 1.17 (1.07 to 1.28) | |
| Unexplained variance (SE) | ||
| MSOA | 0.03 (0.01) | 0.03 (0.01) |
| Provider trust | 0.03 (0.01) | 0.02 (0.01) |
| MOR (95% CrI) | ||
| MSOA | 1.22 (1.15 to 1.30) | 1.21 (1.05 to 1.30) |
| Provider trust | 1.21 (1.15 to 1.27) | 1.18 (1.14 to 1.24) |
FIGURE 11.
Rate of re-admission (log-odds) by 90-day period and treatment status.
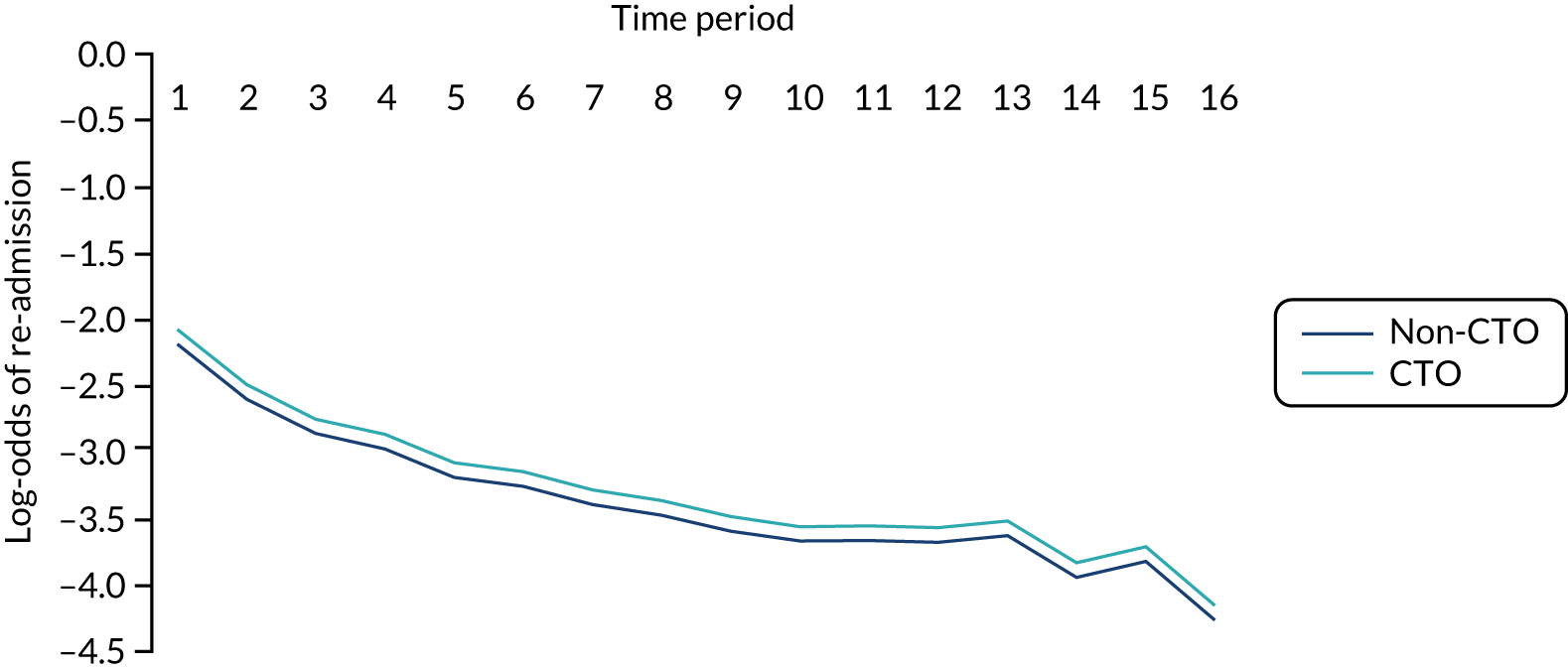
The results from this model also showed that, when the multilevel structure was recognised, CTO patients were estimated as having a slightly overall greater rate of re-admission than non-CTO patients before taking account of patient and local area characteristics (OR 1.12, 95% CrI 1.06 to 1.18). Although this appears to contradict the results of the Kaplan–Meier analysis, differences can be expected given that the estimates of MMs adjust for autocorrelation and have a cluster-specific interpretation (i.e. they relate to the typical community) rather than a population-averaged interpretation (i.e. they relate to the average across all communities). 78
Taking the model with other covariates included (Table 8), we see first that the estimates for time periods were virtually the same, thus the hazard profile shown in Figure 11 remained unchanged after taking account of other patient and local area characteristics. Because interaction terms between treatment status and care cluster group were included in this model, the interpretation of the effect of treatment status on the rate of re-admission is not straightforward as it is different for different care cluster groups. Figure 12 uses the relevant terms to show these differential effects graphically. As can be seen, although there was a suggestion that the rate of re-admission was lower for CTO patients in the non-psychotic, less severe psychotic and severe psychotic care cluster groups than for the non-CTO patients in these groups, the effects were small (and non-significant). However, the rate of re-admission was significantly higher for CTO patients in the cognitive impairment care cluster group than for the non-CTO patients in that group.
FIGURE 12.
Rate of re-admission (probability) by treatment status and care cluster group.
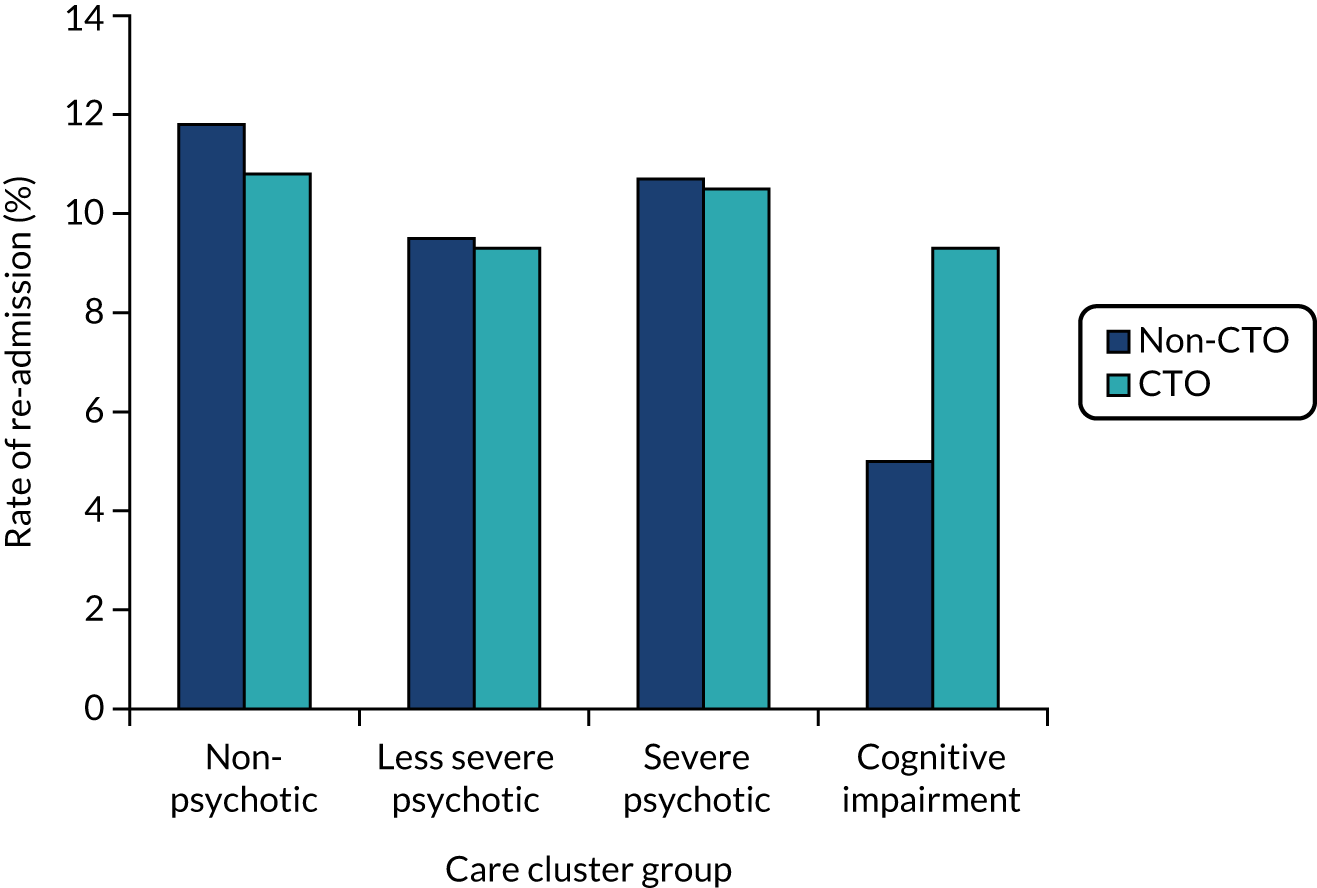
In terms of other patient and local area characteristics, women had a slightly higher rate of re-admission than men (OR 1.08, 95% CrI 1.03 to 1.13) and Asian patients had a lower rate than white patients (OR 0.83, 95% CrI 0.76 to 0.91). There was no clear patterning on the basis of local-area deprivation, although the rate was significantly higher in the third and fifth quintiles.
There was significant variation between both MSOAs and provider trusts in the rate of re-admission, even after taking account of all patient and local area characteristics, with the former being slightly greater (MOR 1.21, 95% CrI 1.05 to 1.30 vs. MOR 1.18, 95% CrI 1.14 to 1.24 respectively).
Total time in admission
In the treatment group (CTO), 35.0% (n = 2216) of patients were recorded as having at least one hospital admission of known duration (i.e. the end date was present or could be imputed), with each of these patients having, on average, two admissions. In the control group (non-CTO), 33.7% (n = 5674) of patients were recorded as having at least one hospital admission of known duration (i.e. the end date was present or could be imputed), with each of these patients having, on average 2.2 admissions. A small number of patients (325 non-CTO patients and 119 CTO patients) had PROVSPELL episodes (i.e. admission end dates) that could not be imputed.
For all patients in each treatment group (i.e. not just those who had admissions), the average total time in admission across the study period was 54.4 days (standard deviation 144.3 days) for the CTO group, and 46.9 days (standard deviation 120.2 days) for the non-CTO group. CTO patients, therefore, spent 7.5 days longer in admission on average across the study period than non-CTO patients. It should be noted that the median value for the total time in admission was zero for both groups, as the majority of patients were not admitted to hospital during the study period.
Table 9 presents the results of two, two-level hierarchical MMs of patients within provider trusts based on all 61 NHS provider trusts for the total time in admission. As with time subject to CTOs in the previous section, total time in admission was substantially overdispersed with most patients having short periods of time in admission, whereas a small number had considerably longer periods. Accordingly, a negative binomial link function was used and hierarchical MMs rather than CCMMs were applied. An offset variable was, again, included to take account of time ‘at risk’. Thus, the outcome modelled was the rate of admission per day (i.e. the likelihood of being in hospital on any given day), with higher daily rates indicating a greater total time in admission. As before, when exponentiated, these estimates resulted in RRs.
| Characteristic | Model with treatment status covariate onlya | Model with treatment status, patient and MSOA covariatesa |
|---|---|---|
| Patient level, RR (95% CI) | ||
| Treatment status (vs. non-CTO) | ||
| CTO | 1.34 (1.24 to 1.44) | 1.20 (1.10 to 1.30) |
| Gender (vs. male) | ||
| Female | 0.94 (0.88 to 1.00) | |
| Age (vs. ≤ 18 years) | ||
| 18–35 years | 0.98 (0.60 to 1.59) | |
| 36–64 years | 0.78 (0.47 to 1.25) | |
| ≥ 65 years | 0.62 (0.37 to 1.02) | |
| Ethnicity (vs. white) | ||
| Mixed | 1.01 (0.83 to 1.25) | |
| Asian | 0.82 (0.72 to 0.94) | |
| Black | 0.96 (0.86 to 1.07) | |
| Other | 0.68 (0.57 to 0.81) | |
| Missing | 0.68 (0.50 to 0.93) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 0.78 (0.70 to 0.88) | |
| Severe psychotic | 0.96 (0.87 to 1.08) | |
| Cognitive impairment | 0.54 (0.46 to 0.62) | |
| Missing | 0.36 (0.30 to 0.44) | |
| MSOA level | ||
| Deprivation (vs. least deprived)b | ||
| Second quintile | 1.06 (0.93 to 1.20) | |
| Third quintile | 1.12 (0.98 to 1.26) | |
| Fourth quintile | 1.02 (0.91 to 1.14) | |
| Fifth quintile | 1.11 (0.98 to 1.24) | |
| Unexplained variance (SE) | ||
| Provider trust | 0.04 (0.01) | 0.03 (0.01) |
| MRR (95% CI) | ||
| Provider trust | 1.27 (1.19 to 1.34) | 1.24 (1.15 to 1.31) |
As can be seen, CTO patients had a significantly higher daily rate of admission (RR 1.34, 95% CI 1.24 to 1.44) than non-CTO patients before taking account of patient and local area characteristics. Although this was reduced adjusting for these characteristics, their daily rate of admission remained significantly higher (RR 1.20, 95% CI 1.10 to 1.30) than those not subject to CTOs.
A model that included interactions between treatment status and care cluster group was also estimated. These additional terms were not statistically significant and did not improve the fit of the model and are not reported here. As a result, what follows is based on the model in Table 9, with treatment status, patient and MSOA covariates.
At patient-level, Asian patients (RR 0.82, 95% CI 0.72 to 0.94) had a lower daily rate of time in hospital than white patients, whereas patients in the less severe psychosis (RR 0.78, 95% CI 0.70 to 0.88) or cognitive impairment (RR 0.54, 95% CI 0.46 to 0.62) care cluster groups had lower daily rates than patients in the non-psychotic group. RRs for patients in the severe psychotic group, meanwhile, were not significantly different from the non-psychotic group (RR 0.96, 95% CI 0.87 to 1.08). There was no significant patterning on the basis of gender, age or local area deprivation.
There was significant variation in the daily rate of admission between all NHS provider trusts, even after taking account of all patient and local area characteristics (MRR 1.24, 95% CI 1.15 to 1.31), with the effect size being greater than any of these characteristics.
As this outcome was likely to have the greatest impact in terms of treatment costs, a sensitivity analysis based on the 59 provider trusts that remained after the two outliers were excluded was conducted. Results for this analysis are provided in Appendix 2. They did not show any marked differences from the results for all provider trusts.
The fixed part estimates of the model in Table 9, with treatment status, patient and MSOA covariates were used to obtain predictions of each patient’s daily rate of admission. Using these, the average number of days in hospital per year, based on all patients, was 27.1 days (95% CI 26.9 to 27.2 days) for those on CTOs and 20.5 days (95% CI 20.4 to 20.6 days) for those not on CTOs. The corresponding figures based on severe psychotic patients only, the care cluster group most likely to be on CTOs, were 29.7 days (95% CI 29.5 to 29.8 days) and 24.4 days (95% CI 24.3 to 24.5 days).
Mortality
In total, 98.4% (n = 22,799) of patients in the matched subsample could be linked to the ONS mortality database. Of these patients, 2143 (9.4%) were recorded as having died during the study period. The 1.6% (n = 372) of patients whose records could not be linked to mortality data were not concentrated in any particular provider trust or care cluster and did not appear to differ in these respects from those whose records were linked. Table 10 shows the distribution of deaths in the study period according to treatment status; as can be seen, 280 (4.5%) CTO patients died during the study period, whereas 1863 (11.2%) non-CTO patients died. Table 11 shows the distribution of cause of death by treatment status.
| Treatment status | Died in study period, n (%) | Total |
|---|---|---|
| Non-CTO | 1863 (11.2) | 16,577 |
| CTO | 280 (4.5) | 6222 |
| Totala | 2143 (9.4) | 22,799 |
| Cause of death (ICD-10 block code)a | Treatment status | |
|---|---|---|
| CTO, n (%) | Non-CTO, n (%) | |
| A–D (infectious/neoplasm/blood) | 29 (10.4) | 214 (11.5) |
| E (endocrine) | 10 (3.6) | 23 (1.2) |
| F (mental/behavioural) | 19 (6.8) | 401 (21.5) |
| G (nervous system) | 12 (4.3) | 237 (12.7) |
| I (circulatory system) | 63 (22.5) | 374 (20.1) |
| J (respiratory system) | 50 (17.9) | 254 (13.6) |
| K–M (digestive/skin/muscular) | 11 (3.9) | 83 (4.5) |
| N–W (genitourinary/perinatal/congenital/other) | 19 (6.8) | 112 (6.0) |
| X–Y (external causes) | 61 (21.8) | 144 (7.7) |
| All causesb | 274 | 1842 |
Owing to small numbers, the analysis of mortality was conducted on an all-cause basis. Results for CCMMs based on patients, MSOAs and provider trusts for the binary response of ‘died in study period’ (1) and ‘stayed alive in study period’ (0) are shown in Table 12. As can be seen, CTO patients were much less likely to die than non-CTO patients, particularly before (OR 0.37, 95% CrI 0.32 to 0.43) (Table 12), but also after taking account of patient and local characteristics including age, gender, ethnicity and care cluster group (OR 0.69, 95% CrI 0.60 to 0.81) (see Table 12, Model with treatment status, patient and MSOA covariates). A model with interaction effects between treatment status and care cluster group was also estimated but the additional terms were non-significant and did not improve the fit of the model (results not reported here). As a result, the remainder of the discussion relating to Table 12 is based on the results from the model with treatment status, patient and MSOA covariates.
| Characteristic | Model with treatment status covariate onlya | Model with treatment status, patient and MSOA covariatesa |
|---|---|---|
| Patient level, OR (95% CrI) | ||
| Treatment status (vs. non-CTO) | ||
| CTO | 0.37 (0.32 to 0.43) | 0.69 (0.60 to 0.81) |
| Gender (vs. male) | ||
| Female | 0.72 (0.65 to 0.79) | |
| Age (vs. < 18 years) | ||
| 18–35 years | 0.96 (0.31 to 3.71) | |
| 36–64 years | 2.95 (0.95 to 11.36) | |
| ≥ 65 years | 13.65 (4.39 to 52.40) | |
| Ethnicity (vs. white) | ||
| Mixed | 0.68 (0.40 to 1.10) | |
| Asian | 0.67 (0.50 to 0.89) | |
| Black | 0.67 (0.53 to 0.85) | |
| Other | 0.92 (0.66 to 1.25) | |
| Missing | 1.15 (0.74 to 1.73) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 0.64 (0.53 to 0.77) | |
| Severe psychotic | 0.82 (0.69 to 0.98) | |
| Cognitive impairment | 2.05 (1.71 to 2.46) | |
| Missing | 2.18 (1.66 to 2.85) | |
| MSOA level | ||
| Deprivation (vs. least deprived),b OR (95% CrI) | ||
| Second quintile | 0.87 (0.72 to 1.04) | |
| Third quintile | 1.01 (0.84 to 1.20) | |
| Fourth quintile | 0.92 (0.77 to 1.09) | |
| Fifth quintile | 0.98 (0.83 to 1.17) | |
| Unexplained variance (SE) | ||
| Patient | 3.29 | 3.29 |
| MSOA | 0.37 (0.06) | 0.02 (0.02) |
| Provider trust | 0.15 (0.04) | 0.02 (0.01) |
| % unexplained variance: VPC (95% CrI) | ||
| Patient | 86.44 | 98.86 |
| MSOA | 9.64 (6.54 to 13.08) | 0.51 (0.03 to 1.83) |
| Provider trust | 3.91 (2.29 to 6.31) | 0.63 (0.09 to 1.50) |
| MOR (95% CrI) | ||
| MSOA | 2.02 (1.79 to 2.27) | 1.16 (1.04 to 1.33) |
| Provider trust | 1.57 (1.41 to 1.77) | 1.18 (1.07 to 1.30) |
As predicted, there was a clear association between age and likelihood of death, with the latter being highest among those aged ≥ 65 years (OR 13.65, 95% CrI 4.39 to 52.40). There was also a higher likelihood of death among patients with cognitive impairment (OR 2.05, 95% CrI 1.71 to 2.46). Women had a lower likelihood of death compared with men (OR 0.72, 95% CrI 0.65 to 0.69). Patients in all of the main ethnic minority groups had a lower likelihood of death compared with white patients. There was no significant association with care cluster group or local area deprivation.
There was substantial variation between provider trusts and, particularly, between MSOAs before taking account of patient and local area characteristics (MOR 1.57, 95% CrI 1.41 to 1.77, and MOR 2.02, 95% CrI 1.79 to 2.27, respectively). After taking account of these characteristics, however, this association was considerably reduced (MOR 1.18, 95% CrI 1.07 to 1.30, and MOR 1.16, 95% CrI 1.04 to 1.33, respectively), although it may be that this lack of variation is due to the comparatively small number of deaths in the subsample.
Variation in associations between use of community treatment orders and patient outcomes (aim 3)
In the previous section, the effect of treatment status was estimated as a fixed-part effect (i.e. it was estimated across the sample as a whole and was not allowed to vary between provider trusts or local areas). This was based on an implicit assumption that the association between treatment status and each of the patient outcomes was the same in all areas, and for all provider trusts. The effect of treatment status on a patient outcome may, however, be different in different places (i.e. it may vary between areas and between provider trusts). For example, in some provider trusts, CTO patients may spend more time in hospital than non-CTO patients, whereas in other provider trusts they may spend less.
This variation can be investigated by allowing the effect of treatment status to vary across higher-level settings. In MMs, this is done by estimating the effect of treatment status in both the fixed and the random parts of the model. Although the fixed-part estimate gives the ‘average’ association across all settings, the random-part estimate gives the degree of variation around this average between settings. As outlined earlier (see Chapter 2, Strategies for analysis), such models are known as ‘fully random’ MMs and involve the estimation of an additional variance term, together with an additional covariance term as there are now two variance terms (one for each treatment group in effect).
Owing to time limitations with regard to time to first admission analyses (i.e. computing overheads for discrete-time models) and data limitations with regards to mortality analyses (i.e. few patient deaths), fully random MMs were estimated only for total time in admission. Table 13 shows the results based on all NHS provider trusts. Given the results reported earlier for this outcome (see Table 8), no interaction effects were considered and the only new terms were the two additional parameters relating to the unexplained variance at provider trust-level referred to earlier (see Chapter 2, Strategies for analysis).
| Characteristic | Model with treatment status, patient and MSOA covariatesa |
|---|---|
| Patient level, RR (95% CI) | |
| Treatment status (vs. non-CTO) | |
| CTO | 1.22 (1.09 to 1.36) |
| Gender (vs. male) | |
| Female | 0.94 (0.88 to 1.00) |
| Age (vs. ≤ 18 years) | |
| 18–35 years | 0.98 (0.60 to 1.54) |
| 36–64 years | 0.78 (0.48 to 1.21) |
| ≥ 65 years | 0.63 (0.38 to 0.98) |
| Ethnicity (vs. white) | |
| Mixed | 1.02 (0.84 to 1.24) |
| Asian | 0.82 (0.72 to 0.93) |
| Black | 0.96 (0.87 to 1.08) |
| Other | 0.69 (0.59 to 0.82) |
| Missing | 0.69 (0.51 to 0.94) |
| Care cluster group (vs. non-psychotic) | |
| Less severe psychotic | 0.78 (0.70 to 0.87) |
| Severe psychotic | 0.96 (0.85 to 1.06) |
| Cognitive impairment | 0.53 (0.46 to 0.62) |
| Missing | 0.36 (0.30 to 0.44) |
| MSOA level | |
| Deprivation (vs. least deprived),b RR (95% CI) | |
| Second quintile | 1.06 (0.94 to 1.20) |
| Third quintile | 1.12 (0.98 to 1.26) |
| Fourth quintile | 1.02 (0.91 to 1.14) |
| Fifth quintile | 1.10 (0.98 to 1.23) |
| Provider-level: unexplained variance (SE) | |
| Non-CTO variance | 0.02 (0.01) |
| Non-CTO/CTO covariance | 0.00 (0.01) |
| CTO variance | 0.06 (0.03) |
The first thing to note about Table 13 is that none of the three terms relating to the random part (unexplained variance) of the model at provider trust-level are large or substantially greater than two times their standard error (i.e. they are unlikely to be statistically significant). It would appear, therefore, that there is little variation in the effect of treatment status between provider trusts. This was confirmed by calculating the Wald statistic, a joint chi-squared test, for the addition of the two new terms (Wald statistic = 4.837, 2 degrees of freedom; p = 0.09).
It should also be noted that the estimate and standard error for the overall ‘fixed’ effect of treatment status (CTO) at patient level (RR 1.22, 95% CI 1.09 to 1.36) was broadly unchanged compared with the corresponding value in the model with time period, treatment status, patient and MSOA covariates in Table 9 (RR 1.20, 95% CI 1.10 to 1.30). Such evidence suggests that this estimate was accurate and reliable.
A sensitivity analysis based on the 59 trusts that remained after the two outliers were excluded was conducted for this part of the study. Results for this analysis are given in Appendix 3. They supported the estimated ‘fixed’ effect of treatment status and confirmed that, if there was any variation, it related to the two outlier trusts rather than the remaining majority.
Association between community treatment orders and health-care costs (aim 4)
As described previously, the analysis of associations between the use of CTOs and health-care costs used the matched subsample consisting of 6329 patients in the treatment group (CTO) and 16,842 in the control group (non-CTO).
The time in admission per year, and the associated health-care costs for both the CTO and the non-CTO group are presented in Table 14. For those within the treatment (CTO) group there was a higher daily rate of admission compared with those in the control group. Consequently, over a 1-year period the treatment group was predicted to spend on average 27.1 days in admission compared with 20.5 days in the control group. This increase is reflected in the costs associated with inpatient admission with those who are subject to a CTO being estimated at £10,941.53 (95% CI £10,876.14 to £11,006.93) compared with £8272.51 (95% CI £8233.53 to £8311.48) per year for the non-CTO group. Thus, the mean difference was £2669.03 (95% CI £2592 to £2745.15).
| All patientsa | Estimate | 95% CI |
|---|---|---|
| Non-CTO patients | ||
| Mean daily rates | 0.0561 | 0.0558 to 0.0564 |
| Number of days in admission in 1-year period | 20.5 | 20.4 to 20.6 |
| Cost of days in admission in 1-year period per patient (£) | 8272.51 | 8233.53 to 8311.48 |
| CTO patients | ||
| Mean daily rates | 0.0742 | 0.0738 to 0.0746 |
| Number of days in admission in 1-year period | 27.1 | 26.9 to 27.2 |
| Cost of days in admission in 1-year period per patient (£) | 10,941.53 | 10,876.14 to 11,006.93 |
| Cost of admission in 1 year including extra administrative burden (£) | 12,470.88 | 12,405.49 to 12,536.28 |
There are extra administrative burdens associated with implementing CTOs as outlined in Table 2 (see Chapter 2). This includes the cost of increased MHT visits, tribunals, SOAD assessments and the completion of other formal, legal and administrative tasks associated with implementing CTOs. In this analysis, an extra fixed annual cost (£1529.35) associated with CTO implementation was attached to those patients who were subject to a CTO (see Table 2). The result of this is a further increase in cost for those who received a CTO to £12,470.88 (95% CI £12,405.49 to £12,536.28) per year compared with the £8272.51 (95% CI £8233.53 to £8311.48) in the control group (see Table 14). This further increased the difference in costs between the two groups.
A supplementary subgroup analysis considered only those patients in the severe psychotic care cluster group (as the group most likely to be subject to a CTO). As shown in Table 15, the severe psychotic patients typically had higher inpatient costs than the rest of the sample. In terms of comparisons between the two treatment groups, the results were consistent with main results. Again, average costs were higher within the CTO group, with the average cost being £11,988.50 (95% CI £11,920.89 to £12,056.11) compared with £9850.33 (95% CI £9809.27 to £9891.38).
| Severe psychotic patients onlya | Estimate | 95% CI |
|---|---|---|
| Non-CTO severe psychotic patients | ||
| Mean daily rates | 0.0668 | 0.0665 to 0.0671 |
| Number of days in admission in 1-year period | 24.4 | 24.3 to 24.5 |
| Cost of days in admission in 1-year period per patient (£) | 9850.33 | 9809.27 to 9891.38 |
| CTO severe psychotic patients | ||
| Mean daily rates | 0.0813 | 0.0808 to 0.0818 |
| Number of days in admission in 1-year period | 29.7 | 29.5 to 29.8 |
| Cost of days in admission in 1-year period per patient (£) | 11,988.50 | 11,920.89 to 12,056.11 |
In summary, we found that patients in the CTO group had consistently higher rates of admission and consequently higher admission costs than the non-CTO group.
Chapter 4 Stakeholder involvement
Purpose
The project team believe that stakeholder engagement is a necessary part of any effective research in health and social care. To ensure that the engagement was a productive experience for the research team and the stakeholders we engaged, we were guided by INVOLVE’s National Standard for Public Involvement (see Appendix 4). 79 The standards provide a framework for reflecting on and improving the purpose, quality and consistency of public involvement in research. They describe the building blocks for good public involvement and provide a baseline of expectations. This helps the public know what to expect when involved in research, and researchers know what needs to be done.
Involvement events were held to support the research project in several ways: to share preliminary findings of the research with interested stakeholders; to provide the research team with broader insights into some of the initial findings; and to identify further questions that might be addressed either through further examination of the existing data or by further, future research. The overarching purpose of these events was consultative and to assist the study team in the conduct, interpretation and dissemination of the research.
Meetings and people
We ran two involvement events. The first meeting was held in Sheffield and was attended by a range of mental health professionals and the second, held in London, was for people with lived experience of being on a CTO or for people caring for someone with such experience.
Sheffield event for mental health professionals
The first event took place in Sheffield on 2 May 2018, at Fulwood House, the headquarters and training base for Sheffield Health and Social Care NHS Foundation Trust. The event, which formed part of the monthly Regional Grand Round programme for South Yorkshire, was attended by a range of mental health clinicians, service managers and other health and social care professionals working in South Yorkshire and North Derbyshire. Many of those attending (including consultant psychiatrists) had extensive experience of caring for and treating patients subject to CTOs. Approximately 70 staff attended the half-day event that included presentations from four members of the research team, a plenary question and answer session, small group discussions, feedback and a final summary. The event was chaired by Scott Weich.
The discussions covered the following topics: the benefits of CTOs, possible disadvantages of CTOs, reasons for geographic variation in rates and duration of use, and alternative options for reducing compulsory detentions.
London event for service users and carers
The second event took place in London, at the Mental Health Foundation (MHF)’s main office on 19 July 2018. The format was based on learning from previous public and patient involvement events facilitated by the MHF in response to feedback from service users and carers about how to make such events accessible, and also in line with the INVOLVE standards 1–4 that consider accessibility (both physical access and the use of accessible language with timely and appropriate communications throughout the engagement process). The format included provision of summary materials in advance; a mid-morning start time to allow comfortable travel times; refreshment breaks and lunch provided; travel arranged on people’s behalf and out-of-pocket expenses settled on the day if requested. This sometimes required direct one-to-one support for participants, tailoring the practical support to each individual to ensure that they had support needs met both in advance and on the day. This was delivered by MHF staff with considerable experience of face-to-face work with those who have used mental health services but were less familiar with academic research.
The event was attended by 10 people who had either been subject to a CTO or provided informal care (as a family member or friend) to someone who had (two people had both of these experiences). People were recruited through existing MHF networks and most participants had previously participated in research as members of service user and carer reference groups (and knew each other either through this research or through their own support networks). Some were new to involvement in research. The majority (seven) were based in London with three people travelling from Hampshire. The group was balanced in terms of gender (six male, four female) and had a degree of ethnic diversity (seven white British, one Asian British, two black British).
The half-day event was chaired by David Crepaz-Keay and included presentations from three members of the research team and covered the following topics: the history and scope of CTOs; trends in rates of detention; an overview of the study and its predecessor; and the study’s initial findings, including rates and variations in the use of CTOs. The presentations were followed by whole group facilitated discussions based on three questions, namely:
-
What are your experiences of CTOs?
-
What do you think about the study findings?
-
What do you think might help to reduce rates of detention?
The agenda was approached with a degree of flexibility to ensure that contributors had an opportunity to articulate broader views before returning the focus directly to the research questions and interim findings. This meant that the discussion was wide ranging and prompted much thought that extended beyond the remit of the research but enhanced the experience for individual participants.
Emergent themes: professionals
A number of key themes emerged from the discussion that followed the presentation of interim study findings, which included thoughts on the benefits and disadvantages of CTOs, thoughts about why there was such a degree of variation between provider trusts and what might help to reduce rates of admission to hospital.
Benefits of community treatment orders
Access to services or resources
Some professionals reported that follow-up services from their community teams were more readily available to former inpatients who were subject to CTOs; others concurred that the care of patients on CTOs was prioritised. Additionally, clinicians felt that they were more accountable for patients on CTOs and, therefore, paid much greater attention to the needs of these patients. Overall, the view was that CTOs made it more likely that patients would get the services that they needed.
Adherence to treatment and reduction of re-admissions
Many professionals agreed that CTOs increased the likelihood that patients would adhere to prescribed treatments and thought that for some patients this increased adherence would reduce the likelihood of relapse and re-admission. Others thought that any reductions in re-admissions among the CTO group may directly result from the fact that they were more likely to get support after discharge from hospital than the non-CTO group. Most agreed that CTOs were more likely to be helpful where there was access to good-quality community resources.
Disadvantages of community treatment orders
Some of the perceived disadvantages of CTOs reflected a different perspective on the advantages outlined above.
Community treatment orders may distort or restrict access to services/resources
Some participants felt that the existence of CTOs and the priority given to patients subject to them meant that there was little left for patients not subject to them. This could lead to CTOs being used as a way of accessing services rather than for the purpose intended.
Increase perceived coercion/may damage relationships
The power of recall to hospital was seen by some professionals as a potential threat and, therefore, something that may actively harm the therapeutic relationship. Some professionals also thought that CTOs encouraged defensive practice and reduced incentives to take positive risks, which may mean some patients were on medication for longer than was necessary.
Problems with recall
There were two different concerns expressed that related to either recall or re-admission to hospital. Some people found it difficult to find available beds when recall was required under the terms of a CTO; they noted that the existence of a CTO did not, in itself, guarantee that a bed was available if recall was indicated. Some also thought that CTOs encouraged earlier discharge than was appropriate.
May pathologise or mask social issues
Some concern was expressed that there were examples of clear social causes of distress (e.g. housing or debt issues) that were being treated as clinical issues. Therefore, CTOs, with their emphasis on medication adherence, may be distracting from measures to address social care needs.
Takes time and resources to apply
Some found the CTO process was a bureaucratic burden and took time that could be spent on other things, including direct patient care.
Reasons for geographic variations in use of community treatment orders
Most professionals expressed surprise at the geographic variation in the use of and duration of use of CTOs across the country, particularly to the extent observed in the course of the study. The following possibilities were proposed:
-
Variation in use or duration of CTOs might be associated with the availability of community-based health or social care services.
-
Use of CTOs (particularly to facilitate early discharge) might be associated with bed numbers and/or bed occupancy rates.
-
Variation in CTO use might be associated with clinical or socioeconomic differences between the populations served.
-
Variation in CTO use might reflect differences between clinical teams and/or trusts in the perceptions of and/or attitudes towards risk.
Ways to reduce compulsory admissions
The consultation event concluded with an invitation to participants to reflect on the wider issue of rising rates of compulsory admission under the MHA, and to consider actions to address this. Most professionals expressed concern at the continuing rise in rates of compulsory admissions and greater concern was expressed at the rising proportion of inpatients who were detained under section compared with informal patients. Many thought that this was making inpatient settings less therapeutic for all patients and more challenging for staff to manage.
Most professionals considered that compulsory detention was necessary under some circumstances but identified several ways that the need might be reduced.
One proposed approach was stronger integration of health and social care that would enable people to get rapid appropriate support in their own homes, either before admission became necessary or as part of a discharge process. Participants also reflected on the need to see care in holistic, rather than purely medical terms.
A number of people suggested that closer collaboration with local police could be valuable, so that mental health needs would be considered and addressed more quickly without the need for formal detention. In many places, there has been a policy change that ensured that those detained on Section 136 are assessed in health-based settings rather than at police stations. This may have contributed to more Section 136 detentions being converted to inpatient detentions.
Emergent themes: service users and carers
Service users and carers described their personal experiences of CTOs. A number of themes emerged following the presentation of interim study findings, which included both positive and negative views on CTOs, thoughts about why there was such a degree of variation between provider trusts and what might help to reduce rates of admission to hospital.
Experiences of community treatment orders
One theme that emerged, and was striking, was that many participants were not entirely familiar with the rationale for, and workings of CTOs, even if they had been subject to them. When people had been subject to a CTO, they had often been confused about what they could and could not do as a result, and particularly what the consequences might be of discontinuing medication. It was also evident that most participants did not understand what they needed to do to be released from a CTO.
There was some difference in views between service users and carers about whether CTOs were a good or bad thing. Where carers thought that the medication was effective and that the person they cared for had a tendency to withdraw from medication after discharge from hospital, they thought that CTOs may encourage longer medication use that they saw as beneficial. Similarly, where people who had been detained patients saw CTOs as a way of spending less time in hospital, they favoured CTOs over extended detention.
Participants had a variety of experiences of CTOs. They were generally perceived as an increased form of control (i.e. coercion), which was definitely not welcome. Most people also thought that CTOs had an adverse impact on relationships with staff. Some people thought that good therapeutic relationships led to care and treatment that was agreed by both clinician and patient and that this agreement made the coercion associated with CTOs unnecessary. Other people described how relationships had been damaged by the threat of compulsion that CTOs carried.
One person gave a very detailed description of her experience of CTOs. She described them as counter-therapeutic (in her experience) and something that prevented her from managing her medication in the way she found most effective. The group broadly agreed that CTOs ‘assume’ that medication compliance is ‘right’ and did not seem to offer flexibility or choice that some people highlighted as important in getting the right treatment. Most participants thought that the availability, accessibility and quality of community support was much more important to recovery than CTOs.
Responses to research findings
The complicated nature of both the research and its findings was reflected in the participants’ reaction to the interim findings. Most of the service user or carer participants were not used to quantitative analysis and so the presentation and interpretation of interim results provided an opportunity to explore ways of making the complicated findings more accessible to wider audiences.
Participants were interested in the research findings and some were surprised by the range of differences in the use of CTOs, in particular by provider trusts that used them in nearly all discharge procedures. In these areas, people thought it showed that services were not responding to individual need. Others were less surprised and had experience of receiving different approaches from different psychiatrists and thought it was likely that psychiatrists’ views (and uses) of CTOs would vary.
Participants also raised a number of questions, including whether or not CTOs were more effective if they were used for longer, whether or not people on CTOs received more or better services, and whether or not CTOs cost money or took up time that could be used for other things.
Ways of reducing compulsory admission
Possible explanations for rising rates of detention
Participants were not surprised that rates of compulsory admission had increased and were continuing to increase over time. Some thought this was attributable to a fear of dangerousness, some that it was a result of a ‘medication first’ attitude to dealing with distress, and some that it related directly to cuts in resources elsewhere and the distress caused by reforms to the benefits system.
Suggestions for reducing compulsory admissions
The following suggestions were offered as potential ways of reducing compulsory admission:
-
More support for carers, who are having to spend more time on providing care at personal financial cost, and at a cost to their own mental and physical health, particularly as they got older.
-
Quicker access to crisis services, so that people could get help when they needed it – before compulsory detention became necessary.
-
More day facilities to reduce the isolation people experience during the day.
-
More choices of and alternative approaches to medication, which might also encourage those who are put off from seeking help if they think medication is all they will be offered.
-
Support with financial and housing difficulties, including problems with neighbours and experience of discrimination. These are often issues that might ‘tip people over the edge’ and into a crisis that may lead to compulsory admission.
Conclusions
Stakeholder engagement adds significant value to research but needs to be done well to ensure that there are benefits to both the research and to those who engage with it, particularly those who are service users or informal carers. This engagement was led by a co-investigator with direct experience of using mental health services (including formal detention but not CTOs) and supported by MHF staff with experience of engaging service users and carers in similar projects. Every effort was made to apply INVOLVE standards and the feedback received from those who engaged was positive.
We were struck by the similarities in the responses of the two distinct stakeholder groups to the interim research findings. Both groups were surprised by the extent of the geographic variation in the rates of CTO use; both could see that CTO use could be beneficial under some circumstances but may lead to an over reliance on purely medication-orientated treatment. Both groups were also concerned that there were insufficient resources to support people in their own homes, both prior to admission and post discharge, and thought that this may contribute to rising admission rates.
There were also some notable differences between the groups. The professional group understood the concept and practice of CTOs well, but remained ambivalent about their benefit and found it difficult to weigh the positive benefits that were seen with some patients against the administrative burden and over-reliance on medication that came with them. It was clear that, in some cases, professionals used CTOs because, without them, very little was on offer to meet broader patient needs.
The service users and carers were much less clear about how CTOs operated and what they actually meant in terms of the consequences of non-compliance. They clearly highlighted a need for a more careful explanation of the restrictions they were bound by and what happened in the case of breaches.
The events also highlighted that it is both important and difficult to communicate complicated findings from sophisticated analysis to interested but non-technical audiences.
Chapter 5 Discussion and conclusions
Overview of the study
Community treatment orders were introduced to England in November 2008. They allow certain patients detained in hospital with serious mental disorders to continue treatment in the community following discharge under specific conditions. Although well-established, there has been little research into patterns of use and evidence from outcome studies, both in England and other countries, has been mixed. In the light of this, the present study used routine clinical and administrative data to analyse variations in use and associations with patient outcomes and health-care costs.
The four main aims of the study were to:
-
examine variation in the use of CTOs between patients, local areas and service providers
-
estimate associations between the use of CTOs and key patient outcomes
-
explore variation in these associations between patients, places and service providers
-
estimate the health-care costs associated with CTOs.
We set out to achieve these aims through multilevel statistical analysis of 4 years of data (between 2011/12 and 2014/15) from the MHSDS, a routine administrative data set that records all specialist NHS-funded mental health treatment activity in England. We addressed the first research aim by describing the frequency and distribution of CTO use across all study years and, for those patients who had ‘ever’ been on a CTO, the amount of time they had been subject to CTOs over the 4 years. The second and third research aims were addressed by estimating associations between CTO use and three patient outcomes: re-admission, total time in admission and mortality. The final research aim was addressed by estimating the mental health treatment costs, and the costs of inpatient admission in particular, over a 1-year period, together with the costs associated with the administration and oversight of CTOs.
Although the first research aim was considered using data from the full study sample, the second, third and fourth aims were addressed using a subset of patients who had only been on a CTO once and a temporally matched sample of patients who had never been on a CTO.
For all analyses, we only included patients who had been treated at NHS provider trusts. MSOAs were used to operationalise the local area in which patients lived. Four key patient characteristics were considered in each analysis: gender, age, ethnicity and diagnostic/illness severity as indicated by means of PbR care clusters. Local area characteristics were considered in terms of a single multidimensional measure of deprivation.
Summary of main findings
Variation in the use of community treatment orders (aim 1)
Our first aim was to examine variation in the use of CTOs between patients, local areas and service providers. We began by estimating null or ‘empty’ MMs to assess the total degree of variation at each of these levels. Next, we estimated models with covariates to show how this variation related to patient and local area characteristics, and the effects of adjusting for these variables on higher-level variation in the use of CTOs. Provider-level residuals from these models were then examined to identify service providers where variation did not relate to these characteristics.
‘Ever on a CTO’ versus ‘Never on a CTO’
Although most variation in whether a patient had ‘ever’ or ‘never’ been on a CTO was observed between patients, there was also significant independent variation in this outcome between provider trusts and between local areas. Most of the between-provider trust variation appeared to arise from substantially different practice in a small number of trusts. Although one provider trust was recorded as making no use of CTOs, the most significant difference concerned two trusts where there appeared to be almost universal use of CTOs for all eligible patients. These trusts were also characterised by a substantial proportion (75–80%) of the 1123 patients who only had CTO episodes that lasted a week or less during the study period. The reasons for this are unclear but may reflect guidance in the Mental Health Code of Practice,80 which advises use of CTOs for leave of absence from the ward for > 7 days.
To illustrate the effect of these outliers (for which we are confident that the data are real and not artefactual), we note that 24.0% of the total variation in CTO use occurred at provider trust-level when they were included, and just over 4% when they were excluded. When the outliers were removed, however, variation in CTO use between provider trusts was still statistically significant. There was a tail of providers where CTO use was either significantly above (n = 15; 25.4%) or below (n = 9; 15.3%) the average.
Approximately 5–6% of variation in CTO use was observed between local areas (MSOAs). Although local area deprivation was found to be associated with the use of CTOs, it did not account for a significant proportion of variation between local areas. The association between local area deprivation and the use of CTOs appeared to follow a dose–response relationship whereby CTO use increased with the level of deprivation.
Variation in the use of CTOs between provider trusts and local areas remained after taking account of a number of significant associations at patient level. The most significant individual level association was with diagnostic/illness severity category (as indicated by PbR care clusters). Those in the ‘less severe psychotic’ group were more than one and a half times more likely, and those in the ‘severe psychotic’ group almost four times more likely than non-psychotic patients to be on CTOs.
Associations between CTO use and other patient characteristics were also found. Women were much less likely to be on CTOs than men (OR 0.70, 95% CrI 0.67 to 0.73) and black patients were more likely to be on CTOs than white patients, although the difference was not as marked as that found recently for compulsory admission (OR 1.43, 95% CrI 1.33 to 1.53). 63 As the current study was able to take account of diagnosis/illness severity as well as local area deprivation, there are better grounds for thinking that the associations estimated here constitute independent ethnic and gender effects.
Time subject to community treatment orders
There was also statistically significant variation between providers and between local areas (MSOAs) in the time patients were subject to CTOs. In terms of the former, there was a tail of providers where the time subject to CTOs was either significantly above (n = 13; 21.7%) or significantly below (n = 14; 23.3%) the average.
The most significant association with time subject to CTOs was with PbR care cluster, with patients in the ‘severe psychotic’ group having the highest rate of CTO use per day (RR 1.22; 95% CI 1.18 to 1.26). Apart from age and gender, all other patient and local neighbourhood characteristics were characterised by small, non-significant effects. Associations with patient and local area characteristics were, therefore, much smaller for the time patients were subject to CTOs than whether patients had ‘ever’ or ‘never’ been subject to CTOs.
Association between community treatment orders and patient outcomes (aim 2)
The second aim of the study was to examine the association between the use of CTOs and patient outcomes. To achieve this, we estimated MMs with a single covariate denoting treatment status (CTO vs. non-CTO). We then estimated models with additional covariates denoting other patient and local area characteristics to establish the independent effect of treatment status. We also considered the degree of variation between local areas and provider trusts in each outcome before and after taking account of patient and local area characteristics. Three patient outcomes were studied: re-admission, total time in admission and mortality.
Re-admission
Slightly more CTO patients were re-admitted than non-CTO patients (36.9% compared with 35.6%). Although Kaplan–Meier estimates suggested that CTO patients had a slightly longer time on average to re-admission (9.1 days) than non-CTO patients, overlapping CIs together with the results of more robust discrete-time MMs, suggested that the rate of re-admission over time was very similar for the two groups overall.
Models with interaction terms between treatment status and care cluster group suggested that CTO patients in the non-psychotic, less severe psychotic and severe psychotic patients care cluster groups had a lower rate of re-admission than non-CTO patients in the same groups, but the effects were small and non-significant. The rate of re-admission was significantly higher for CTO patients in the cognitive impairment care cluster group than non-CTO patients in the same group. Women had a slightly higher rate of re-admission than men and Asian patients had a lower rate than white patients. There were no statistically significant associations with age or local area deprivation.
There was significant variation between both service providers and local areas in the rate of re-admission after taking account of patient- and local area-level characteristics. The degree of variation was slightly greater at local area rather than service provider level (MOR 1.21, 95% CrI 1.05 to 1.30, and MOR 1.18, 95% CrI 1.14 to 1.24, respectively).
Total time in admission
Over the study period, CTO patients spent 7.5 days longer, on average, in admission than non-CTO patients. Models of total time in admission included an offset variable to take account of the varying amounts of time (in days) patients were ‘at risk’ of admission. As a result, estimates from these models constituted daily rates rather than numbers of days. CTO patients had a significantly higher daily rate of admission than non-CTO patients after taking account of other patient and local area characteristics (RR 1.20, 95% CI 1.10 to 1.30). The effect of CTOs on the daily rate of admission did not differ according to PbR care cluster group.
The daily rate of admission was lower for Asian patients (RR 0.82, 95% CI 0.72 to 0.94) and for patients in the less severe psychotic (RR 0.78, 95% CI 0.70 to 0.88) or cognitive impairment (RR 0.54, 95% CI 0.46 to 0.62) care cluster groups. There was no significant patterning in the daily rate of admission on the basis of age, gender or local area deprivation.
There was significant variation between service providers in the daily rate of admission (MRR 1.24, 95% CI 1.15 to 1.31). This variation could not be accounted for by patient and local area characteristics.
Using the estimated daily rate of admission, the average number of days in hospital per year, based on all patients, was estimated to be 27.1 days (95% CI 26.9 to 27.2 days) for those on CTOs and 20.5 days (95% CI 20.4–20.6 days) for those not on CTOs. The corresponding figures based on severe psychotic patients only were 29.7 days (95% CI 29.5 to 29.8 days) and 24.4 days (95% CI 24.3 to 24.5 days), respectively. These data were used to populate our health economic models.
Mortality
Community treatment order patients were much less likely to die than non-CTO patients, before (OR 0.37, 95% CrI 0.32 to 0.43) and after (OR 0.69, 95% CrI 0.60 to 0.81) taking account of other patient and local area characteristics. The effect of CTOs on the likelihood of death did not differ according to care cluster group. There was some variation between both service providers and local areas in mortality, although it was much reduced after taking account of patient and local area characteristics. It was not as substantial as for the other patient outcomes. This finding may be attributable to the small number of deaths in the subsample.
Although we considered that mortality might be lower in those subject to CTO (given increased contact with services), the size of the observed association was unexpected. The association remained after taking account of the major confounders of the association between CTO use and lower mortality. We adjusted our estimate of this association for age, gender and ethnicity. We also took account of care cluster because death was much more likely in those with organic disorders. We also adjusted for local area deprivation, although there was no clear association between this and mortality.
We believe that this finding may be subject to residual confounding and should be treated with caution. In particular, we note that we were unable to adjust these analyses for the effects of differences in physical health (including body mass index), comorbid physical disorders and differences in lifestyle factors, particularly smoking, drinking and use of recreational drugs. We were also unable to control for differences in prescription medication. Of these, we think that physical health, obesity and smoking were the most likely factors to confound the association with mortality. Although the non-CTO group may have included a greater number of patients with so-called ‘negative’, avolitional symptoms of schizophrenia, the fact that patients in both groups had all experienced episode of acute illness requiring admission to hospital subject to a compulsory treatment orders argues against this.
Among other potential between-group differences, we think it unlikely that medication adherence varied substantially between groups given that this is often addressed in patients on CTOs. Interestingly, there may be other potential unmeasured differences between groups that could have acted as negative confounders, increasing the advantage observed in the CTO group had we been able to adjust for them. For instance, the CTO group may have included a greater number of patients with treatment-refractory illnesses who may therefore have been prescribed higher doses of psychotropic drugs. We also think it is probable that the CTO group were more likely to have included patients with a history of alcohol and substance misuse.
Overall, we would argue that this finding needs to be taken seriously but treated with caution pending further investigation, replication and confirmation.
Variation in the association between community treatment orders and patient outcomes (aim 3)
The third aim of the study was to explore variation in the association between the use of CTOs and patient outcomes. We did this by estimating fully random MMs in which the effect for treatment status was not ‘fixed’ (i.e. the same) across all provider trusts but was ‘random’ (i.e. allowed to vary) at provider trust-level. Owing to computing and data restrictions, we only estimated these models for one patient outcome, total time in admission.
There was no evidence of significant variation between provider trusts in the effect of treatment status on total time in admission. Our results did, however, confirm the higher daily rate of admission for CTO patients than non-CTO patients.
Association between community treatment orders and health-care costs (aim 4)
Health-care costs for CTO patients were estimated to be greater than for non-CTO patients. For the most part, this was due to the longer period of time CTO patients spent in admission compared with non-CTO patients, although ‘one off’ administrative burdens associated with CTOs were also a factor. When both were taken into account, the estimated cost per year was £12,470.88 (95% CI £12,405.49 to £12,536.28) for CTO patients compared with £8272.51 (95% CI £8233.53 to £8311.48) for non-CTO patients. Thus, the mean difference was £2669.03 (95% CI £2592.89 to £2745.15). Although there were increased costs associated with CTO patients, there was a correspondingly lower rate of mortality than in non-CTO patients. Therefore, there is a possibility that CTOs could be cost-effective using conventional methods of economic evaluation that consider both cost and impact on lifetime health-related quality of life. However, we were unable to formally assess this owing to data limitations.
Strengths of the study
To our knowledge, this was the largest study of its kind in England, and the first to use complete national data on CTOs and other mental health service use. As such, there are no comparable studies of either the use of CTOs or their association with patient outcomes in England. Indeed, we believe this may even be the largest and most complete study of its kind in the world as it was based on a nationally representative data set covering every person who received, or was eligible to receive, CTOs within England.
Being based on routine clinical data, the samples included in our analyses were less restrictive than those of studies based on RCTs. Although we were unable to include independent sector providers, we included all patients discharged from NHS provider trusts who were eligible to be placed on a CTO. We did not exclude any particular patient groups (e.g. those who were at risk of suicide or violence to others). Patients on Restriction Orders are not eligible for a CTO and were therefore excluded. Furthermore, patients were categorised into clearly distinct treatment groups on the basis of what had actually happened to them. As the data were derived from routine clinical activity, it captured and reflected the full range of real world settings in which mental health services are delivered. Consequently, the results of the study are highly generalisable to England as a whole.
The large sample size ensured a high degree of precision in our estimates of variances and residuals. Furthermore, it ensured that it was possible to assess variations and differences across a range of patient subgroups, as well as consider interactions between them. A major reason for the large sample size was the use of 4 years of data. As well as giving advantages in terms of the precision of estimates, using data over this time period allowed us to study patient outcomes across a longer period of time than is possible in RCTs.
Using multilevel modelling techniques allowed us to consider variation across a highly complex, overlapping and intersecting series of geographies that reflected both local residential settings as well as service provider settings. This is the first study as far as we are aware that modelled variation in CTO use and its association with patient outcomes at several spatial scales simultaneously.
Limitations of the study
There were a number of limitations that need to be taken into account when interpreting the study findings. The most significant of these relate to the study design and especially the secondary analysis of a routine administrative data set. Such research is always reliant on variables that have been collected for other purposes and on the quality and completeness of the data.
Although the MHMDS is undoubtedly improving as a source of data for mental health research, it still has some significant weaknesses. First, although the data set contains a wide range of variables, high rates of missing data mean many of them cannot be used. This issue is most acute around variables recording background characteristics, particularly measures of individual social status, although it also applies to variables giving alternative measures of clinical need to those used here (e.g. HoNOS).
Second, historical problems with date recording meant that it was not possible to take account of patients’ previous clinical histories. Although this situation had improved greatly by the start of the study period adopted here, mitigating any substantial direct effects, it still prevented the use of data from before the study period to reflect prior service use.
Third, even when data fields were present, the information they contained could be erroneous and inconsistent. This was most noticeable with date sequences for individual patients where start and end dates were sometimes in conflict. Programing code was used to circumvent these problems, with dates being taken from elsewhere within the sequence or imputed from alternative data fields as outlined in the methods chapter.
Data quality and completeness issues, together with the large number of available data, meant that it was necessary to simplify the way in which the longitudinal dimension of the study was handled. Thus, although using 4 years of data allowed outcomes to be considered over a long period of time, some assumptions were necessary to make analysis strategies manageable. For instance, patients were allocated to the area of residence and care cluster group pertaining to the time of their index event although both characteristics were potentially dynamic.
Data issues also had an impact on the study sample that could be used in work analysing the association between patient outcomes and the use of CTOs. As two of the three outcome measures centred on date information, either as the duration of an event (i.e. period of time in hospital) or the specific timing of an event (i.e. occurrence of first re-admission), it was essential that this part of the study used data where we could be most certain about the quality of data relating to temporality. This necessitated the use of a subsample of CTO patients, those with one CTO episode that had started and finished during the study period, for which there was complete and unambiguous date information.
Although working with this subsample may have reduced the study’s representativeness, it amounted to more than one-third of CTO patients within the study sample as a whole and included patients who would almost certainly have gone on to have further CTO episodes. In addition, the first CTO episode can be thought of as being particularly significant in patient histories.
It should also be noted that we considered only the association between the use of CTOs and patient outcomes using a limited range of outcome measures. Although the health service usage measures investigated here are routinely used,81 other studies have considered the effectiveness of CTOs in terms of a much wider variety of outcomes, including social functioning and criminal justice outcomes.
Perhaps the single greatest limitation of observational research is confounding by indication because patients are not randomised to treatment groups. Hence, variables associated with the intervention (i.e. being on a CTO or not) may also be associated with the study outcome (i.e. being admitted to hospital or not). Although there is no way of eliminating the effect of this altogether, we attempted to control for the most obvious confounding variables statistically. As well as using a time-matched subsample for the work on outcomes, in effect a design approach to adjustment, we also included key co-variates in our models of the association between use of CTO and patient outcomes.
For statistical adjustment to be effective in dealing with confounding by indication, three requirements need to be met. First, all relevant determinants of the indications should be known. Second, data on confounding factors should be of sufficient quality to allow complete adjustment. Third, the sample size should be sufficient to allow for statistical modelling of many confounding variables. 82 Although the first requirement is a challenge for any observational study, the foregoing discussion of the MHSDS shows that the second requirement was a particular challenge, especially given the difficulties around adjusting for individual socioeconomic status and clinical need. In particular, we regret that missing data precluded the use of diagnosis as a covariate; care cluster was used instead as a proxy.
However, the large sample size did mean that the third requirement could, at least, be partly satisfied. Although far from ideal, the use of local area deprivation and care cluster code measures, together with basic sociodemographic characteristics, meant that a broader range of confounding factors were taken into account than is sometimes the case in this type of research. Nevertheless, it remains the case that the estimates of variation and association may still have been misestimated, and that our findings may have been due to residual confounding. We think that it is unlikely that this could have accounted for the largely negative study findings, but may have contributed to the association between CTO use and (reduced) mortality. However, the size of this association after adjusting for study covariates argues against this as the sole explanation for this finding.
Our economic analyses were also limited by data quality issues. These analyses, and the estimates of costs that they were based on, were limited to inpatient costs and estimates of the administrative costs associated with CTOs. Although this overlooked the costs associated with community treatment, these are minimised by inpatient costs. It is unlikely that the additional inpatient costs incurred by CTO patients would have been offset by reduced costs of community treatment; if anything, the opposite was more likely to be true.
Finally, despite the evident strength of multilevel modelling techniques, the complexity and size of some of the data sets meant that it was not always possible to estimate the full range of models. We did, therefore, have to be more selective than we would have liked.
User involvement
Two involvement events were held, one for people who had been subject to a CTO or had provided informal care to someone who had been, and another for an expert group of professionals involved in the delivery of mental health services. To ensure that the events were productive, INVOLVE’s National Standards for Public Involvement were followed.
Although there were similarities in the responses of the two groups to interim findings from the study, there were noticeable differences in their general responses to CTOs. The professional group understood the concept and practice of CTOs well, whereas service users and carers were much less clear about how a CTO operated and what it actually meant in terms of the consequences of non-compliance. Although carers could see the benefits of a CTO, as could service users when it had been an alternative to extended detention, professionals remained ambivalent in the light of the administrative burden and over-reliance on medication that came with it.
Clinical implications
Community treatment orders were (and remain) a controversial addition to the MHA (2007) since their introduction in England in 2008. 83 Evidence from qualitative research suggests that, whereas some patients (and to a greater degree, carers) see benefit in these orders (arising from more regular contact from services), they object to their coercive nature. Although many clinicians believe that CTOs improve outcomes through better treatment adherence, they are often ambivalent about the potential negative impact on therapeutic relationships.
It is clear from our research that there are differences in the ways that CTOs are used in different trusts, and this is something we need to understand better. We need to know why for instance, nearly all eligible patients in some trusts are placed on CTOs, and likewise why these orders are used over such short intervals in some places. It may be that CTOs are being used in some settings to cover leave (rather than Section 17 leave), or that they are being used to enable acute treatment to continue in the community where bed pressure is severe and/or where crisis services are stretched or indeed where being placed on a CTO brings with it additional resources, like a community care co-ordinator. To make matters more complex, in some places CTOs are instigated by inpatient doctors without the involvement of the community teams to whom patients are transferred on discharge. We think that it is highly likely, therefore, that the advantages (and disadvantages) of CTOs are highly context dependent.
Perhaps the most intriguing finding was the association between CTO and reduced mortality. We believe that it is too early to say whether this is a true effect or the result of some other explanation. But if it were to be the case that CTOs improved survival, this would be an extremely powerful argument for their continued (and even extended) use.
The results of this research are likely to sow further clinical and therapeutic uncertainty. Although many clinicians will be able to cite examples of patients who have remained well and out of hospital while on CTOs, our findings suggest that this is not true of the majority. Although further examination of the effects of CTOs in specific subgroups of patients is warranted, our findings are consistent with calls for more limits to their use in future.
Conclusions
Among a nationally representative sample of almost 70,000 patients in England who were eligible to be subject to CTOs over a 4-year period, we found that CTO use varied to a significant degree between patients, provider trusts and local areas. CTO use was not associated to a statistically significant degree with shorter time to re-admission or reduced time in hospital. Although admission rates and length of stay varied between provider trusts, we found no evidence of variation between services in the effectiveness of CTOs. Likewise, CTO use was not associated with reduced mental health treatment costs. Our findings are consistent with the results of the OCTET trial,35 and support the view that the use of CTOs in England is not effective in reducing future admissions or time spent in hospital. We provide preliminary evidence of an association between CTO use and reduced risk of death.
Recommendations for further research
Our results are likely to be seen as further evidence for the lack of effectiveness of CTOs, particularly in the light of impending changes in mental health legislation. However, there were clear benefits for some patients in some circumstances and it is important that these potential gains are not overlooked. This applies particularly to the association reported here between CTO use and reduced mortality. It is also possible that the limitations of the study (and especially the availability of data of sufficient quality) prevented us from identifying further groups of patients who might benefit from CTOs, including those who are on CTOs more than once and those with the largest numbers of previous admissions, and beyond the first re-admission after being subject to a CTO. This research therefore needs to be extended as well as replicated. There is a further need for greater clinical detail (including diagnosis, previous service use – especially admissions – and risk history including aggression, violence and self-harm) to enable better adjustment for confounding by indication.
The association between CTO use and reduced mortality in particular needs further investigation and replication over a longer period of time among all patients subject to CTOs, to allow subgroup analysis by cause of death, care cluster and other patient-, area- and service-level variables. The continuation of such analyses is vital, not least because longer follow-up and reduced right censoring would enable researchers to consider whether the mortality difference is a short-term time offset in a very high-risk group or a longer-term effect. We also recommend that other research designs are considered, including retrospective case-control studies, given the relatively small number of deaths in a sample such as ours. This recommendation is dependent on the availability and ease of access to longer-term longitudinal data and may not be possible immediately given historical MHSDS data quality issues, particularly prior to 2011–12. Any such approach is likely to be equally dependent on the quality and completeness of data on potential confounders, especially at the patient level.
Further exploration is also needed of the extreme variation in practice in the use of CTOs between provider trusts and particularly where almost all eligible patients are subject to these orders (and often for short periods). Further subgroup analyses are required to explore the potential benefits of CTOs in non-psychotic care clusters.
This research further highlights both the potential and the current challenges associated with the use of routine clinical data to answer important questions about the effectiveness and safety of health-care interventions. This is particularly important where interventions (like the use of CTOs) are ethically challenging, organisationally complex or highly context dependent, and where RCTs are unfeasible or unhelpful. Urgent investment is needed across the NHS, and especially in mental health services, to support the collection, curation and use of routine data, and to address issues of completeness, data quality and clinical- and service-level detail.
Finally, the user involvement and the overall findings indicate that a variety of methods, including qualitative work, is needed to explore the impacts of CTOs. This work needs to be extended to carers (and even to professionals) to provide a rounded view of their benefits as well as their drawbacks.
Acknowledgements
This work uses data provided by patients and collected by the NHS as part of their care and support and would not have been possible without access to these data. The National Institute for Health Research recognises and values the role of patient data, securely accessed and stored, both in underpinning and leading to improvements in research and care.
We acknowledge the assistance, support and guidance of the ESRC-funded ADRN in facilitating our use of the MHSDS and specifically the efforts of Kakia Chatsiou and Danielle Gomes at the University of Essex and Peter Smith, Emma White and Corine Driessens at the University of Southampton.
Data access was provided by the SRS at the ONS, Titchfield and we acknowledge the assistance, support and guidance of those responsible for this service, particularly the statistical support team.
The use of the ONS statistical data in this work does not imply the endorsement of the ONS in relation to the interpretation or analysis of the statistical data. This work uses research data sets that may not exactly reproduce National Statistics aggregates.
Sam Wilding of the University of Southampton kindly helped with data preparation for parts of the study.
We are grateful to Jo Ackerman for organising the service users and carers involvement event and to the MHF for hosting it.
We are grateful to Dr Abhijeeth Shetty and colleagues for organising the mental health service professionals involvement event and for Sheffield Health and Social Care NHS Foundation Trust for hosting it.
Contributions of authors
Scott Weich (https://orcid.org/0000-0002-7552-7697) was the Chief Investigator and guarantor of the research. He had overall responsibility for the design, delivery and interpretation of the study findings, as well as research governance and data security. He chaired project team meetings and attended (and co-led) user consultation events and is responsible for the final version of this report.
Craig Duncan (https://orcid.org/0000-0003-0687-5783) undertook the study analyses in relation to project aims 1–3, drafted interim and final study reports, contributed fully to the interpretation of the study findings and their reporting, and attended project team meetings.
Liz Twigg (https://orcid.org/0000-0003-0861-5248) provided multilevel statistical modelling expertise, and advised CD on data analysis, contributed to the management of the study, interpretation and analysis of results, the drafting of the study reports and attended project team meetings.
Orla McBride (https://orcid.org/0000-0003-3399-9466) provided expertise about the MHSDS and advised on data analysis, attended project team meetings, and contributed to the interpretation and reporting of study findings.
Helen Parsons (https://orcid.org/0000-0002-2765-3728) was the study statistician and advised on data analysis, attended project team meetings and contributed to the interpretation and reporting of study findings.
Graham Moon (https://orcid.org/0000-0002-7256-8397) contributed to the design of the study, led on data access, contributed to the interpretation and analysis of results, commented in detail on study reports and attended project team meetings.
Alastair Canaway (https://orcid.org/0000-0002-4270-6808) undertook the study analyses in relation to project aim 4, drafted interim and final study reports, contributed fully to the interpretation of the study findings and their reporting and attended project team meetings.
Jason Madan (https://orcid.org/0000-0003-4316-1480) provided health economics expertise and advised AC on data analysis, contributed to the management of the study, interpretation and analysis of results, the drafting of the study reports and attended project team meetings.
David Crepaz-Keay (https://orcid.org/0000-0003-3845-4721) was responsible for coordinating and leading the mental health service user consultation throughout the project, attended project team meetings, drafted the report of the service user involvement work and contributed to the interpretation and reporting of the study findings.
Patrick Keown (https://orcid.org/0000-0003-4727-5880), Swaran Singh (https://orcid.org/0000-0003-3454-2089) and Kamaldeep Bhui (https://orcid.org/0000-0002-9205-2144) contributed to the design of the study, commented on and contributed to the interpretation of results throughout the project, commented in detail on study reports and attended project team meetings.
Data-sharing statement
The data used in this study were obtained from the HSCIC (www.hscic.gov.uk), now known as NHS Digital. The agreements in place with the NHS Data Access and Advisory Committee for use of these data do not permit further distribution or sharing. Requests for the relevant data sets must be made directly to HSCIC. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- O’Brien AJ, McKenna BG, Kydd RR. Compulsory community mental health treatment: literature review. Int J Nurs Stud 2009;46:1245-55. https://doi.org/10.1016/j.ijnurstu.2009.02.006.
- Churchill R, Owen G, Singh S, Hotopf M. International Experiences of Using Community Treatment Orders. London: Institute of Psychiatry; 2007.
- Kisely S, Campbell LA, Scott A, Preston NJ, Xiao J. Randomized and non-randomized evidence for the effect of compulsory community and involuntary out-patient treatment on health service use: systematic review and meta-analysis. Psychol Med 2007;37:3-14. https://doi.org/10.1017/S0033291706008592.
- Kisely SR, Campbell LA. Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev 2014;12. https://doi.org/10.1002/14651858.CD004408.pub4.
- Kisely S, Hall K. An updated meta-analysis of randomized controlled evidence for the effectiveness of community treatment orders. Can J Psychiatry 2014;59:561-4. https://doi.org/10.1177/070674371405901010.
- Maughan D, Molodynski A, Rugkåsa J, Burns T. A systematic review of the effect of community treatment orders on service use. Soc Psychiatry Psychiatr Epidemiol 2014;49:651-63. https://doi.org/10.1007/s00127-013-0781-0.
- Rugkåsa J. Effectiveness of community treatment orders: the international evidence. Can J Psychiatry 2016;61:15-24. https://doi.org/10.1177/0706743715620415.
- Newton-Howes G, Banks D. The subjective experience of community treatment orders: patients’ views and clinical correlations. Int J Soc Psychiatry 2014;60:474-81. https://doi.org/10.1177/0020764013498870.
- Canvin K, Rugkåsa J, Sinclair J, Burns T. Patient, psychiatrist and family carer experiences of community treatment orders: qualitative study. Soc Psychiatry Psychiatr Epidemiol 2014;49:1873-82. https://doi.org/10.1007/s00127-014-0906-0.
- Banks LC, Stroud J, Doughty K. Community treatment orders: exploring the paradox of personalisation under compulsion. Health Soc Care Community 2016;24:e181-e190. https://doi.org/10.1111/hsc.12268.
- O’Reilly R, Corring D, Richard J, Plyley C, Pallaveshi L. Do intensive services obviate the need for CTOs?. Int J Law Psychiatry 2016;47:74-8. https://doi.org/10.1016/j.ijlp.2016.02.038.
- Light E. The epistemic challenges of CTOs. Psychiatr Bull 2014;38:6-8. https://doi.org/10.1192/pb.bp.113.045732.
- Szmukler G. Is there a place for community treatment orders after the OCTET study?. Acta Psych Scand 2015;131:330-2. https://doi.org/10.1111/acps.12376.
- United Nations Commission for the Protection of Rights of Persons with Disabilities . Concluding Observations on the Initial Report of the United Kingdom of Great Britain and Northern Ireland (CRPD C GBR CO 1) 2017.
- Newton-Howes G, Ryan CJ. The use of community treatment orders in competent patients is not justified. Br J Psychiatry 2017;210:311-12. https://doi.org/10.1192/bjp.bp.116.193920.
- Kisely S, Molodynski A, Rugkåsa J, Burns T. Coercion in Community Mental Health Care: International Perspectives. Oxford: Oxford University Press; 2016.
- Rugkåsa J, Burns T. Community treatment orders: are they useful?. BJPsych Advances 2017;23:222-30. https://doi.org/10.1192/apt.bp.115.015743.
- Department for Health and Social Care (DHSC) . The Independent Review of the Mental Health Act: Interim Report 2018.
- Brophy L, Edan V, Gooding P, McSherry B, Burkett T, Carey S, et al. Community treatment orders: towards a new research agenda. Australas Psychiatry 2018;26:299-302. https://doi.org/10.1177/1039856218758543.
- Great Britain . Mental Health Act 2007.
- Care Quality Commission . Monitoring the Mental Health Act in 2016 17 2018. www.cqc.org.uk/sites/default/files/20190108_mhareport2017_amend_1.pdf (accessed 20 December 2019).
- Great Britain . The Human Rights Act 1988.
- House of Commons Health Committee . Post-Legislative Scrutiny of the Mental Health Act 2007: First Report of Session 2013–14 2013.
- NHS Digital . Mental Health Act Statistics, Annual Figures 2016 17 Experimental Statistics 2017. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-act-statistics-annual-figures/mental-health-act-statistics-annual-figures-2016-17-experimental-statistics (accessed 20 December 2019).
- NHS Digital . Inpatients Formally Detained in Hospitals Under the Mental Health Act 1983, and Patients Subject to Supervised Community Treatment: 2015 16 Annual Figures 2016. https://digital.nhs.uk/data-and-information/publications/statistical/inpatients-formally-detained-in-hospitals-under-the-mental-health-act-1983-and-patients-subject-to-supervised-community-treatment/inpatients-formally-detained-in-hospitals-under-the-mental-health-act-1983-and-patients-subject-to-supervised-community-treatment-2015-16-annual-figures (accessed 20 December 2019).
- Kisely S, Xiao J. Cultural and linguistic diversity increases the likelihood of compulsory community treatment. Schizophr Res 2018;197:104-8. https://doi.org/10.1016/j.schres.2017.12.005.
- Segal SP, Hayes SL, Rimes L. The utility of outpatient commitment: I. a need for treatment and a least restrictive alternative to psychiatric hospitalization. Psychiatr Serv 2017;68:1247-54. https://doi.org/10.1176/appi.ps.201600161.
- Lawton-Smith S. A Question of Numbers: The Potential Impact of Community-based Treatment Orders in England and Wales. London: The King’s Fund; 2005.
- Gupta S, Akyuz EU, Baldwin T, Curtis D. Community treatment orders in England: review of usage from national data. BJPsych Bull 2018;42:119-22. https://doi.org/10.1192/bjb.2017.33.
- Light E, Kerridge I, Ryan C, Robertson M. Community treatment orders in Australia: rates and patterns of use. Australas Psychiatry 2012;20:478-82. https://doi.org/10.1177/1039856212466159.
- Trevithick L, Carlile J, Nodiyal S, Keown P. Community treatment orders: an analysis of the first five years of use in England. Br J Psychiatry 2018;212:175-9. https://doi.org/10.1192/bjp.2017.51.
- Steadman HJ, Gounis K, Dennis D, Hopper K, Roche B, Swartz M, et al. Assessing the New York City involuntary outpatient commitment pilot program. Psychiatr Serv 2001;52:330-6. https://doi.org/10.1176/appi.ps.52.3.330.
- Swartz MS, Swanson JW, Wagner HR, Burns BJ, Hiday VA, Borum R. Can involuntary outpatient commitment reduce hospital recidivism?: findings from a randomized trial with severely mentally ill individuals. Am J Psychiatry 1999;156:1968-75. https://doi.org/10.1176/ajp.156.12.1968.
- Swanson JW, Swartz MS, Borum R, Hiday VA, Wagner HR, Burns BJ. Involuntary out-patient commitment and reduction of violent behaviour in persons with severe mental illness. Br J Psychiatry 2000;176:324-31. https://doi.org/10.1192/bjp.176.4.324.
- Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. Lancet 2013;381:1627-33. https://doi.org/10.1016/S0140-6736(13)60107-5.
- Burns T, Yeeles K, Koshiaris C, Vazquez-Montes M, Molodynski A, Puntis S, et al. Effect of increased compulsion on readmission to hospital or disengagement from community services for patients with psychosis: follow-up of a cohort from the OCTET trial. Lancet Psychiatry 2015;2:881-90. https://doi.org/10.1016/S2215-0366(15)00231-X.
- Vergunst F, Rugkåsa J, Koshiaris C, Simon J, Burns T. Community treatment orders and social outcomes for patients with psychosis: a 48-month follow-up study. Soc Psychiatry Psychiatr Epidemiol 2017;52:1375-84. https://doi.org/10.1007/s00127-017-1442-5.
- Rugkåsa J, Molodynski A, Yeeles K, Vazquez Montes M, Visser C, Burns T. OCTET Group . Community treatment orders: clinical and social outcomes, and a subgroup analysis from the OCTET RCT. Acta Psychiatr Scand 2015;131:321-9. https://doi.org/10.1111/acps.12373.
- Rugkåsa J, Yeeles K, Koshiaris C, Burns T. Recall of patients on community treatment orders over three years in the OCTET CTO cohort. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1102-4.
- Curtis D. OCTET does not demonstrate a lack of effectiveness for community treatment orders. Psychiatr 2014;38:36-9. https://doi.org/10.1192/pb.bp.113.044800.
- Mustafa FA. On the OCTET and supervised community treatment orders. Med Sci Law 2014;54:116-17. https://doi.org/10.1177/0025802413506898.
- Owen A, Sood L. OCTET does not prove community treatment orders are ineffective. Lancet Psychiatry 2015;2:373-5. https://doi.org/10.1016/S2215-0366(15)00116-9.
- Mustafa FA. Notes on the use of randomised controlled trials to evaluate complex interventions: community treatment orders as an illustrative case. J Eval Clin Pract 2017;23:185-92. https://doi.org/10.1111/jep.12699.
- Segal SP, Burgess PM. Effect of conditional release from hospitalization on mortality risk. Psychiatr Serv 2006;57:1607-13. https://doi.org/10.1176/ps.2006.57.11.1607.
- Segal SP, Burgess PM. The utility of extended outpatient civil commitment. Int J Law Psychiatry 2006;29:525-34. https://doi.org/10.1016/j.ijlp.2006.09.001.
- Segal SP, Burgess PM. Factors in the selection of patients for conditional release from their first psychiatric hospitalization. Psychiatr Serv 2006;57:1614-22. https://doi.org/10.1176/ps.2006.57.11.1614.
- Segal SP, Preston N, Kisely S, Xiao J. Conditional release in Western Australia: effect on hospital length of stay. Psychiatr Serv 2009;60:94-9. https://doi.org/10.1176/ps.2009.60.1.94.
- Kisely S, Preston N, Xiao J, Lawrence D, Louise S, Crowe E, et al. An eleven-year evaluation of the effect of community treatment orders on changes in mental health service use. J Psychiatr Res 2013;47:650-6. https://doi.org/10.1016/j.jpsychires.2013.01.010.
- Kisely S, Xiao J, Lawrence D, Jian L. Is the effect of compulsory community treatment on preventable deaths from physical disorders mediated by better access to specialized medical procedures?. Can J Psychiatry 2014;59:54-8. https://doi.org/10.1177/070674371405900110.
- Harris A, Chen W, Jones S, Hulme M, Burgess P, Sara G. Community treatment orders increase community care and delay readmission while in force: results from a large population-based study. Aust N Z J Psychiatry 2019;53:228-35. https://doi.org/10.1177/0004867418758920.
- Segal SP, Hayes SL, Rimes L. The utility of outpatient commitment: II. mortality risk and protecting health, safety, and quality of life. Psychiatr Serv 2017;68:1255-61. https://doi.org/10.1176/appi.ps.201600164.
- Swartz MS, Wilder CM, Swanson JW, Van Dorn RA, Robbins PC, Steadman HJ, et al. Assessing outcomes for consumers in New York’s assisted outpatient treatment program. Psychiatr Serv 2010;61:976-81. https://doi.org/10.1176/ps.2010.61.10.976.
- Gilbert AR, Moser LL, Van Dorn RA, Swanson JW, Wilder CM, Robbins PC, et al. Reductions in arrest under assisted outpatient treatment in New York. Psychiatr Serv 2010;61:996-9. https://doi.org/10.1176/ps.2010.61.10.996.
- Kisely S, Smith M, Preston NJ, Xiao J. A comparison of health service use in two jurisdictions with and without compulsory community treatment. Psychol Med 2005;35:1357-67. https://doi.org/10.1017/S0033291705004824.
- Nakhost A, Perry JC, Frank D. Assessing the outcome of compulsory treatment orders on management of psychiatric patients at 2 McGill University-associated hospitals. Can J Psychiatry 2012;57:359-65. https://doi.org/10.1177/070674371205700605.
- Taylor M, Macpherson M, Macleod C, Lyons D. Community treatment orders and reduced time in hospital: a nationwide study, 2007–2012. BJPsych Bull 2016;40:124-6. https://doi.org/10.1192/pb.bp.115.051045.
- The King’s Fund . Mental Health Under Pressure 2015. www.kingsfund.org.uk/sites/default/files/field/field_publication_file/mental-health-under-pressure-nov15_0.pdf (accessed December 2019).
- Subramanian SV, Kim R, Christakis NA. The ‘average’ treatment effect: a construct ripe for retirement. A commentary on Deaton and Cartwright. Soc Sci Med 2018;210:77-82. https://doi.org/10.1016/j.socscimed.2018.04.027.
- Johnson S. Can we reverse the rising tide of compulsory admissions?. Lancet 2013;381:1603-4. https://doi.org/10.1016/S0140-6736(13)60442-0.
- NHS Digital . Mental Health Services Data Set 2018. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-sets/mental-health-services-data-set (accessed December 2019).
- Office for National Statistics . Census Geography 2018. www.ons.gov.uk/methodology/geography/ukgeographies/censusgeography (accessed December 2019).
- UK Data Service . Census Boundary Data 2018. https://census.ukdataservice.ac.uk/get-data/boundary-data (accessed December 2019).
- Weich S, McBride O, Twigg L, Duncan C, Keown P, Crepaz-Keay D, et al. Variation in compulsory psychiatric inpatient admission in England: a cross-classified, multilevel analysis. Lancet Psychiatry 2017;4:619-26. https://doi.org/10.1016/S2215-0366(17)30207-9.
- NHS England . Mental Health Clustering Booklet v5.0, 2016 17 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/499475/Annex_B4_Mental_health_clustering_booklet.pdf (accessed December 2019).
- Ministry of Housing, Communities and Local Government . English Indices of Deprivation 2015. www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed 20 December 2019).
- Snijders TA, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. London: SAGE Publications Ltd; 2012.
- Fielding A, Goldstein H. Cross-Classified and Multiple Membership Structures in Models: An Introduction and Review. Research Report RR791 for DfES 2006.
- Weich S, Duncan C, Bhui K, Canaway A, Crepaz-Keay D, Keown P, et al. Evaluating the effects of community treatment orders (CTOs) in England using the Mental Health Services Dataset (MHSDS): protocol for a national, population-based study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-024193.
- Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol 2005;161:81-8. https://doi.org/10.1093/aje/kwi017.
- Browne WJ. MCMC Estimation in MLwiN v2.36. Bristol: Centre for Multilevel Modelling, University of Bristol; 2009.
- Spiegelhalter D, Best N, Carlin B, van der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc Series B Stat Methodol 2002;64:583-639. https://doi.org/10.1111/1467-9868.00353.
- Austin PC, Stryhn H, Leckie G, Merlo J. Measures of clustering and heterogeneity in multilevel Poisson regression analyses of rates/count data. Stat Med 2018;37:572-89. https://doi.org/10.1002/sim.7532.
- Steele F. Event History Analysis: A National Centre for Research Methods Briefing Paper. Bristol: Centre for Multilevel Modelling, University of Bristol; 2005.
- Feng Z, Jones K, Wang WW. An exploratory discrete-time multilevel analysis of the effect of social support on the survival of elderly people in China. Soc Sci Med 2015;130:181-9. https://doi.org/10.1016/j.socscimed.2015.02.020.
- NHS Digital . Mental Health Services Data Set n.d. www.datadictionary.nhs.uk/data_dictionary/messages/clinical_data_sets/data_sets/mental_health_services_data_set_fr.asp?shownav=1 (accessed 20 December 2019).
- Health and Social Care Information Centre . MHMDS v4.0 Specification 2011. https://digital.nhs.uk/data-and-information/information-standards/information-standards-and-data-collections-including-extractions/publications-and-notifications/standards-and-collections/dcb0011-mental-health-services-data-set (accessed 20 December 2019).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Steele F. Multilevel discrete-time event history models with applications to the analysis of recurrent employment transitions. Aust NZ J Stat 2011;53:1-20. https://doi.org/10.1111/j.1467-842X.2011.00604.x.
- INVOLVE . National Standards for Public Involvement 2018. www.invo.org.uk/posttypepublication/national-standards-for-public-involvement/ (accessed December 2019).
- Department of Health and Social Care (DHSC) . Code of Practice: Mental Health Act 1983 2015.
- Burns T, Kisely S, Rugkåsa J. Randomised controlled trials and outpatient commitment. Lancet Psychiatry 2017;4. https://doi.org/10.1016/S2215-0366(17)30442-X.
- Grobbee DE, Hoes AW. Confounding and indication for treatment in evaluation of drug treatment for hypertension. BMJ 1997;315:1151-4. https://doi.org/10.1136/bmj.315.7116.1151.
- NHS Digital . Community Treatment Orders ‘Don’t Reduce Psychiatric Readmissions’. 2013. www.nhs.uk/news/mental-health/community-treatment-orders-dont-reduce-psychiatric-readmissions/ (accessed 20 December 2019).
Appendix 1 Restructuring the data for discrete-time analysis
Typically, time-to-event data, like that used in the Kaplan–Meier analysis, are based on one record per patient (see table below).
| Person | Time_Group | Re-admission | Censored | CTO |
|---|---|---|---|---|
| 1 | 4 | 0 | 1 | 1 |
| 2 | 2 | 1 | 0 | 0 |
| 3 | 1 | 1 | 0 | 1 |
To conduct discrete-time analyses, these data have to be expanded to what is called a person-period file where the number of records per patient equals the number of time periods at which re-admission or censorship occurs (see table below).
| Person | Time_Group | Re-admission | Censored | CTO | t | y |
|---|---|---|---|---|---|---|
| 1 | 4 | 0 | 1 | 1 | 1 | 0 |
| 1 | 4 | 0 | 1 | 1 | 2 | 0 |
| 1 | 4 | 0 | 1 | 1 | 3 | 0 |
| 1 | 4 | 0 | 1 | 1 | 4 | 0 |
| 2 | 2 | 1 | 0 | 0 | 1 | 0 |
| 2 | 2 | 1 | 0 | 0 | 2 | 1 |
| 3 | 1 | 1 | 0 | 1 | 1 | 1 |
Thus, take person 1, who originally had one row of data showing that they were not re-admitted after being in the study for four time periods. After restructuring, person 1 now has four rows of data, with t going from 1 to 4, and the response variable y being 0 throughout, indicating they were not re-admitted while they were in the study. In contrast, person 2 who originally had one row of data showing they were re-admitted after their second time period in the study, after restructuring has two rows of data, with t going from 1 to 2 and the response variable y being 0 when t is 1 and then 1 when t is 2 as this is when they were re-admitted. Person 3 has only one row in the restructured data set with both t and y equal to 1 as they were re-admitted in their first time period. As can be seen, values for other explanatory variables relating to each person (e.g. CTO) are replicated for each row of that person’s data.
Appendix 2 Associations between use of community treatment orders and patient outcomes (aim 2)
Table 16 shows the results of models of total time in admission based on the 59 NHS provider trusts that remained after two outlier trusts were excluded. As with the corresponding analyses based on all NHS provider trusts, hierarchical models were used as the link function was negative binomial and an offset variable was included to take account of time ‘at risk’. Thus, what the model estimates are rates rather than direct counts, with a higher daily rate of admission indicating a greater total time in admission. As with all provider trusts, CTO patients had a higher daily rate of admission before taking account of patient and local area characteristics (RR 1.40, 95% CI 1.29 to 1.51) (see Table 16). Similarly, this reduced after taking account of these characteristics (RR 1.26, 95% CI 1.15 to 1.37) (see Table 16) but was still significant. Interaction effects between treatment status and care cluster group were non-significant and did not improve the fit of the model (results not reported here).
| Characteristic | Model with treatment status covariate onlya | Model with treatment status, patient and MSOA covariatesa |
|---|---|---|
| Patient level, RR (95% CI) | ||
| Treatment status (vs. non-CTO) | ||
| CTO | 1.40 (1.29 to 1.51) | 1.26 (1.15 to 1.37) |
| Gender (vs. male) | ||
| Female | 0.95 (0.89 to 1.02) | |
| Age (vs. < 18 years) | ||
| 18–35 years | 0.94 (0.56 to 1.53) | |
| 36–64 years | 0.74 (0.44 to 1.20) | |
| ≥ 65 years | 0.59 (0.36 to 0.98) | |
| Ethnicity (vs. white) | ||
| Mixed | 0.97 (0.79 to 1.21) | |
| Asian | 0.80 (0.70 to 0.93) | |
| Black | 0.95 (0.84 to 1.07) | |
| Other | 0.70 (0.58 to 0.85) | |
| Missing | 0.64 (0.46 to 0.89) | |
| Care cluster group (vs. non-psychotic) | ||
| Less severe psychotic | 0.77 (0.68 to 0.87) | |
| Severe psychotic | 0.93 (0.82 to 1.05) | |
| Cognitive impairment | 0.50 (0.43 to 0.59) | |
| Missing | 0.33 (0.27 to 0.41) | |
| MSOA level | ||
| Deprivation (vs. least deprived),b RR (95% CI) | ||
| Second quintile | 1.06 (0.93 to 1.22) | |
| Third quintile | 1.12 (0.98 to 1.26) | |
| Fourth quintile | 1.03 (0.91 to 1.17) | |
| Fifth quintile | 1.12 (0.99 to 1.26) | |
| Unexplained variance (SE) | ||
| Provider trust | 0.02 (0.01) | 0.02 (0.01) |
| MRR (95% CI) | ||
| Provider trust | 1.19 (1.12 to 1.25) | 1.17 (1.09 to 1.23) |
Associations with other patient and local area characteristics were the same as for all provider trusts, although people aged ≥ 65 years had a significantly lower daily rate of admission than people aged < 18 years (0.59, 95% CI 0.36 to 0.98). Patterns in the daily rate of admission across the 59 trusts were, therefore, very similar as across all 61 trusts.
Appendix 3 Variation in associations between use of community treatment orders and patient outcomes (aim 3)
Table 17 shows the results of fully random models of total time in admission based on the 59 NHS provider trusts that remained after two outlier trusts were excluded.
| Characteristic | Model with treatment status, patient and MSOA covariatesa |
|---|---|
| Patient level, RR (95% CI) | |
| Treatment status (vs. non-CTO) | |
| CTO | 1.26 (1.15 to 1.38) |
| Gender (vs. male) | |
| Female | 0.95 (0.89 to 1.02) |
| Age (vs. < 18) | |
| 18–35 years | 0.94 (0.56 to 1.54) |
| 36–64 years | 0.74 (0.44 to 1.21) |
| ≥ 65 years | 0.59 (0.36 to 0.98) |
| Ethnicity (vs. white) | |
| Mixed | 0.98 (0.79 to 1.22) |
| Asian | 0.80 (0.70 to 0.93) |
| Black | 0.95 (0.84 to 1.07) |
| Other | 0.70 (0.58 to 0.85) |
| Missing | 0.64 (0.47 to 0.90) |
| Care cluster group (vs. non-psychotic) | |
| Less severe psychotic | 0.77 (0.68 to 0.87) |
| Severe psychotic | 0.93 (0.83 to 1.05) |
| Cognitive impairment | 0.50 (0.43 to 0.59) |
| Missing | 0.33 (0.27 to 0.41) |
| MSOA level | |
| Deprivation (vs. least deprived),b RR (95% CI) | |
| Second quintile | 1.06 (0.93 to 1.22) |
| Third quintile | 1.11 (0.98 to 1.26) |
| Fourth quintile | 1.03 (0.91 to 1.16) |
| Fifth quintile | 1.12 (0.99 to 1.26) |
| Provider-level: unexplained variance (SE) | |
| Non-CTO variance | 0.02 (0.01) |
| Non-CTO/CTO covariance | 0.00 (0.01) |
| CTO variance | 0.02 (0.02) |
Although the overall ‘fixed’ effect of treatment status is broadly the same as when all provider trusts are considered (RR 1.26, 95% CI 1.15 to 1.38 compared with RR 1.22, 95% CI 1.09 to 1.36 for all provider trusts), the new CTO variance term reduced from 0.06 to 0.02 whereas the other variance and covariance terms stayed the same. This suggests that the small degree of variation in the treatment effect between provider trusts was related to the two outlier trusts rather than the remaining majority.
Appendix 4 INVOLVE’s National Standards for Public Involvement
Reproduced with permission from INVOLVE. 79 Copyright © all rights reserved 2020.
Standard 1: inclusive opportunities
We offer public involvement opportunities that are accessible and that reach people and groups according to research needs.
Standard 2: working together
We work together in a way that values all contributions, and that builds and sustains mutually respectful and productive relationships.
Standard 3: support and learning
We offer and promote support and learning that builds confidence and skills for public involvement in research.
Standard 4: communications
We use plain language for timely, two way and targeted communications, as part of involvement plans and activities.
Standard 5: impact
To drive improvement, we capture and share the difference that public involvement makes to research.
Standard 6: governance
We involve the public in our governance and leadership so that our decisions promote and protect the public interest.
List of abbreviations
- ADRN
- Administrative Data Research Network
- CCMM
- cross-classified multilevel model
- CI
- confidence interval
- CrI
- credible interval
- CTO
- community treatment order
- ESRC
- Economic and Social Research Council
- HoNOS
- Health of the Nation Outcome Scale
- HSCIC
- Health and Social Care Information Centre
- ID
- identifier
- IMD
- Index of Multiple Deprivation
- INPATEP
- inpatient episode
- LSOA
- lower-layer super output area
- MCMC
- Markov chain Monte Carlo
- MHA
- Mental Health Act
- MHAEVENT
- Mental Health Act event
- MHF
- Mental Health Foundation
- MHMDS
- Mental Health Minimum Data Set
- MHRT
- mental health review tribunal
- MHSDS
- Mental Health Services Data Set
- MHT
- mental health team
- MM
- multilevel model
- MOR
- median odds ratio
- MRR
- median rate ratio
- MSOA
- middle-layer super output area
- NHSD
- NHS Digital
- OCTET
- Oxford Community Treatment Order Evaluation Trial
- ONS
- Office for National Statistics
- OR
- odds ratio
- PbR
- Payment by Results
- PROVSPELL
- Hospital Provider Spell
- PSSRU
- Personal and Social Services Research Unit
- RCT
- randomised controlled trial
- RR
- rate ratio
- SCT
- supervised community treatment
- SOAD
- second opinion appointed doctor
- SRS
- Secure Research Service
- VPC
- variance partition coefficient