Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/196/04. The contractual start date was in September 2016. The final report began editorial review in March 2019 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sharon Spooner and Kath Checkland work as general practitioners in the English NHS. Ruth McDonald, Sharon Spooner and Kath Checkland are employed by the Centre for Primary Care and Health Services Research, which is part-funded by National Institute for Health Research (NIHR) School for Primary Care Research (SPCR) funding. Ruth McDonald and Kath Checkland’s posts were part-funded by NIHR Greater Manchester Collaborations for Leadership in Applied Health Research and Care (CLAHRC) funding until September 2019. Kath Checkland's salary is part-funded by the NIHR Policy Research Unit in the Health and Care System and Commissioning. During the study, Ruth McDonald was joint principal investigator for the Policy Research Programme (PRP)-funded research Evaluation of strategies for supporting innovation in the NHS to improve quality and efficiency. Kath Checkland was principal investigator for the NIHR PRP-funded national evaluation of the Vanguard for New Care Models programme. Sharon Spooner’s NIHR grants during this period were for An investigation of the scale, scope and impact of skill mix change in primary care (Health Services and Delivery Research 17/08/25); An investigation into the career intentions and training experiences of newly qualified general practitioners (NCITE) (NIHR SPCR); An investigation of factors which are associated with successful transitions from GP Specialty Training Programmes to long-term careers in NHS general practice (FIT2GP) (NIHR SPCR); and An investigation of the factors behind the training choices of junior doctors which result in inadequate recruitment to general practice careers (FACSTiM) (NIHR SPCR).
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by McDonald et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction and background
In England, most general practitioners (GPs) are based in general practices, which are, mostly, small professional partnerships independent of other general practices. However, recent decades have seen successive organisational reforms encouraging GPs from different practices to collaborate,1–10 particularly (but not exclusively) in relation to commissioning care for NHS patients. In addition to collaborating to commission care and provide out-of-hours services, GPs have started to come together to create new provider collaborations between practices. 11 These new organisational forms are sometimes referred to as GP federations, defined by the Royal College of General Practitioners (RCGP) as groups of practices and primary care teams that work together, sharing responsibility for the development and delivery of high-quality, patient-focused services for their local populations. 12 In 2010, the RCGP, in conjunction with various organisations, published a primary care federations toolkit12 that includes advice, evidence, case studies and other resources intended to help practices navigate the changing organisational landscape.
General practitioner federations vary in scope, geographical reach and organisational form, from loose alliances of a small number of local practices to much larger organisations,11 some of which have been established as limited companies. Potential benefits of federations might include efficiencies of scale and scope, strengthening capacity to deliver services outside hospital (by either direct provision or contracting) and improving local integration. 12 Federations might also present many challenges including balancing the ways of working, autonomy and identity of individual practices with the requirements of more centralised and standardised procedures that interorganisational collaboration implies. Federations are substantially different from the traditional partnership model; however, little is known about how federations are working in practice and the implications of different organisational forms for the organisation of primary care.
The changing context of English general practice
The context for this report is England, as responsibility for health-care policy was fully devolved to Scotland, Wales and Northern Ireland in 1999. 13 Thereafter, health-care policy increasingly diverged across the four nations.
General practice as a profession
Traditionally, GPs in practices have enjoyed a high degree of autonomy with regard to their clinical practice. 14 As generalists, their professional identity narrative is based on a biographical approach to medical care,14 emphasising a ‘patient-centred’ approach to the patient consultation,15 although this aspiration is not necessarily matched by the reality. 16 This patient-centred narrative traditionally helped GPs to maintain clinical autonomy and control14 and involved GPs incorporating a range of diverse elements (e.g. time, organisation, knowledge of the patient, financial considerations) into their decision-making process. However, this idiosyncratic approach to decision-making, reflecting high levels of individual discretion, has been constrained over time by the state, peers, pharmacists, nurses and patients. 17,18 Furthermore, over time, there has been an increasing acceptance by GPs of the legitimacy of scrutiny and accountability in relation to their work. 19
The growth of and support for evidence-based medicine by professional elites has been described as justifying professional autonomy, legitimising GPs’ decisions on the basis of their access to this knowledge. Yet there is a tension between the preservation of the powers of the profession as a collective and the ability of individual practitioners to exercise clinical discretion. 14,18 As we discuss further in the following section, various initiatives have contributed to a move away from individualised decision-making and towards a more standardised and collaborative way of working. 19
General practice collaborative working: a recent history
These developments build on a rich, layered history of collaborative working and network arrangements in UK and English general practice. The first formalised initiative of note occurred in the form of Medical Audit Advisory Groups (MAAGs) in the late 1980s, which saw groups of practices in particular geographical areas working together to audit care across their patch and share best practice. 2,20 Evidence from attempts elsewhere to incorporate peer review and audit21 provided encouragement for those seeking to introduce greater conformity and co-operation within and between practices. 22 In the early 1990s, in the context of the creation of the internal market and the split between the purchasing and providing of care,23 general practitioner fundholding (GPFH) was introduced. This voluntary scheme allowed practices access to a portion of secondary and community care budgets to purchase certain services for their patients (e.g. various inpatient and outpatient services), with any surpluses generated available for reinvestment in the practices for patient benefit. 24 In many cases, groups of practices worked together in consortia or multifund groups to purchase care under the scheme. Total purchasing pilots,25 introduced in 1995, built on aspects of the GPFH model and allowed groups of practices to, in theory, purchase all secondary and community care for their patient population with the budget delegated to them by the Health Authority (which retained statutory responsibility for the spending).
In parallel with these developments in care commissioning, out-of-hours co-operatives (or GP co-operatives) emerged as a notable form of networked primary care provision in response to heightened pressures associated with delivering care out of hours. 6 GP co-operatives involved groups of practices coming together, often formally as a non-profit organisation, and jointly developing processes to provide out-of-hours services to all patients in their combined geographical area. A variety of models was employed, but common practices involved the use of a central telephone triage function and patient access ‘hubs’ in convenient locations.
In 1997, following a change in government, GPFH and MAAGs were formally abolished. The policy language used to describe the acquisition of care shifted from ‘purchasing’ to ‘commissioning’. A small number of GP commissioning pilots were launched to test different commissioning models. These were predicated on collaborative working between local clinicians to commission secondary and community care and included a role for public stakeholders. The pilots ran for 2 years but were superseded by Primary Care Groups (PCGs). These new organisations were intended to extend GP involvement in commissioning further than ever before. Each typically covered a patient population of 50,000–100,000 and it was compulsory for general practices to join one (although there was some flexibility in terms of their level of involvement). Within 3 years, however, all PCGs had evolved into primary care trusts (PCTs) and the level of GP involvement in these new, more autonomous organisations was significantly curtailed.
The emergence of the more managerially focused PCTs was one reason why, by the mid-2000s, collaborative activities between general practices had begun to wane significantly. 26 Other factors are also of importance in explaining this trend. Changes to payment mechanisms also meant that collective provision of additional services across more than one practice became more difficult, with the new general medical services (GMS) contract of 2004 supporting the individual provision by practices of what were called ‘Local Enhanced Services’. 27 This did not provide a straightforward mechanism for remunerating practices for offering additional services to patients beyond those registered on their practice list, and was associated with the disappearance of many GP co-operatives. By 2004, it was clear that collaborative activity between practices and engagement in the commissioning and collective provision of services had declined. 26 To remedy this, and to re-engage GPs in commissioning services, practice-based commissioning (PBC)28 was introduced in 2005. GP consortia formed, each becoming established as a subcommittee of a local PCT, and were allocated an indicative budget.
The refreshed role for GPs working collaboratively to commission care was a feature of a broader set of measures, including increased choice of providers for patients and the introduction of Payment by Results contracts (so funding would ‘follow the patient’). GPs were seen as key to fulfilling an aspiration to help create a more efficient system in which services were more local to patients and better suited to their needs. Like with GPFH, any profits realised from clinical commissioning could be reinvested by consortia for patient benefit. A review of GPs’ involvement in commissioning in the English NHS between 1991 and 2010 concluded that this focused on activities closest to general practice, such as prescribing, and developing general practice and community health services. There was little evidence that GPs’ involvement in commissioning had improved the delivery of secondary care services or overall outcomes. 8 This does not suggest that GP groups have been able to make meaningful system-wide change, despite working together, albeit in forms that differ from GP federations. By 2010, many consortia were considering formalising structures and relationships and developing formal provider organisations, using a variety of organisational forms such as Community Interest Companies. At around the same time, GP provider federations began to be promoted by organisations such as the RCGP,29 and many of these had a focus on collective provision by general practices.
In 2012, clinical commissioning and collaborative working between general practices became even more firmly established in the structure and operation of the English NHS in the form of Clinical Commissioning Groups (CCGs). These GP-led, compulsory membership organisations were allocated responsibility for around two-thirds of the total English NHS budget and charged with commissioning most secondary and community care. In their establishment, CCGs were initially afforded considerable flexibility when forming their geographical footprint and general practice composition, which, in many cases, reflected previous working arrangements relating to PBC and other prior collaborative arrangements. Initially, due to concerns about conflicts of interest, CCGs did not have a role in commissioning primary care services from their members, but, over time, this has been relaxed, with an increasing number taking on delegated responsibility for this function from NHS England. Through this co-commissioning of primary care, many CCGs have opted to reintroduce various incentives and peer audit processes developed through PBC to foster closer working between GPs. 30
Pressures on primary medical care and renewed support for collaborative working
The move towards creating and joining GP federations has taken place in the context of significant pressures on general practice in England. 31,32 These include rising patient demand in general practice and other NHS and social care sectors, NHS budgetary constraints, increasing expectations concerning quality and reduction of variations in general practice, and recruitment and retention issues. The recruitment and retention issues have been exacerbated, in the context of an ageing workforce, by incentives for GPs to retire early, created by tax changes affecting their pensions. 33 This has also happened during a period when traditional general practices have felt under threat from non-GP-owned private companies tendering to provide general practice services. 34 This was enabled with the ‘alternative provider of medical services’ (APMS)34 NHS contract route introduced in 2004 to increase capacity and broaden the range of providers of primary medical care, and subsequent ‘any willing provider’ and ‘any qualified provider’ policies.
Over the last decade or so, policy-makers have encouraged ‘primary care at scale’ working, viewing this as a solution to the problems in primary care. 35 (We use the term ‘at scale’ to cover arrangements that involve practices working together, which could include, but is not limited to, working in federations). Another policy strand has focused on new models of care, which included 50 ‘vanguards’36 focused on delivering the NHS Five Year Forward View. 37 Some of these involve new ways of working, with the intention being to bring together providers to collaborate on improving and integrating services. Other initiatives are aimed at helping an overburdened general practice, through policies such as funding pharmacists to work in general practices. 38 These three strands have existed alongside each other, rather than being integrated to focus on joining up potential solutions. Another initiative, Primary Care Home, developed by the National Association of Primary Care,39 aims to strengthen and redesign primary care, bringing together a range of health and social care professionals. The Primary Care Home initiative is cited as informing the new policy of encouraging and incentivising practices to work together across a geographical footprint in primary care networks (PCNs). 40 This is a complex policy, which we will return to in the discussion. However, it is noteworthy that, in their early stages, PCNs are being expected to address issues relating to extended access and broadening workforce skill mix.
There is, therefore, an array of policies directed towards the development of at-scale working in primary care. The intention is for practices to work collaboratively to provide enhanced care for their local community. Although policy-makers have acknowledged the need to expand the primary care workforce,35 they have also imposed targets for increasing access to general medical practice, adding to existing pressures on GPs and practice staff more generally. Furthermore, the emphasis on new collaborative structures implicitly assumes that structural reorganisation will go a long way to solving the problems, which leads to GPs leaving the profession and workforce shortages more generally. It also assumes the existence of sufficient knowledge, skills and human resources (HR), which will be required to staff these new structures. Although collaborative organisational forms offer the potential to strengthen the workforce,41–43 this would require substantial time and resources. Bringing together organisations that face problems may have an intuitive appeal but may not produce the desired results in a context of workforce shortages and rising expectations. 44 Although there are widespread perceptions that there has been a transfer of responsibilities from secondary to primary care, with practices expected to undertake tasks previously performed in secondary care, there has been no associated shift in resources or significant disinvestment in secondary care provision. This may act as an incentive for practices to come together to provide and draw on support, but it also raises questions about the capacity of practices to actively participate in emerging organisations, as well as the resource implications of doing so.
Furthermore, GP federations operate within a broader health system characterised by perverse and conflicting incentives and a range of diverse organisations involved in the provision and commissioning of health and social care services. This places significant constraints on their ability to engage in system-wide change. 8,45 In these circumstances, collaboration or at-scale working may begin to resemble an intrinsically idealistic46 solution that exists independently of a problem, becoming attached to it when a policy window presents an opportunity for this to happen. 47 Yet policies are likely to fail when these are formulated in denial of their contextual reality. 46 The collapse of federations and failures to deliver contracted services48–50 in a challenging context suggest that federating is, therefore, not a universal panacea.
In response to the pressures affecting the NHS more generally, NHS England has proposed a significant shift in the way that services are commissioned and provided, with integration between primary, secondary and community care services. 40,51 As part of the Five Year Forward View,37 NHS England divided England into 44 footprints, bringing together NHS, local authority and other health and care organisations to collaboratively determine the future of their health and care system. The systems were required to produce 5-year sustainability and transformation plans, intended to be place-based plans for the health and social care within their footprint. Subsequently, as NHS England has placed greater emphasis on system-wide working and integration, their name and nature have changed. In March 2017, these 44 systems were renamed sustainability and transformation partnerships (STPs),35 with their role being to enable services to be delivered in a more co-ordinated way, to decide system-wide priorities and to plan, collectively, how to improve citizens’ health. In some areas, STPs have evolved to form an integrated care system (ICS), involving even closer collaboration. In an ICS, NHS organisations, in partnership with local councils and others, take collective responsibility for managing resources, delivering NHS standards and improving the health of the population they serve. 51
The NHS Long Term Plan40 places great emphasis on integration and states that, by April 2021, ICSs will cover the whole of England, growing out of the current network of STPs. GPs working collaboratively will be a key element of these new arrangements. There is, however, little evidence that integrated care initiatives, comprising interorganisational collaborations and/or mergers, have reduced service use or produced cost savings. 52,53
In March 2017, NHS England announced that practices were to be encouraged to work together in networks serving populations of at least 30,000 to 50,000. 35 Following on from this, the 2018 planning guidance for the NHS54 emphasised actively encouraging every practice to be part of a local PCN, with the goal of ensuring complete geographically contiguous population coverage of PCNs by the end of 2018/19, serving populations of at least 30,000 to 50,000. The NHS Long Term Plan40 added more detail on proposals for PCNs. It promised new investment to fund expanded community multidisciplinary teams aligned with new PCNs based on neighbouring general practices that work together typically covering 30,000–50,000 people. A set of multiyear contract changes will result in individual practices in a local area entering into a network [Directed Enhanced Service (DES)] contract as an extension of their existing contract, and have a designated single fund through which all network resources will flow. 40 (DES contracts involve additional services that GPs can choose to provide to their patients and that are financially incentivised by NHS England). PCNs will have a single clinical director, appointed from local general practices, and will be represented on the ICS partnership board. Their focus will be on population health management and on the provision of a wider variety of services in the community. The ‘network contract’ will bring together existing ‘enhanced’ services across a network area and will fund the appointment of new types of clinical workers (e.g. physiotherapists, pharmacists) across the network. Community services will be more closely aligned with networks, to support the provision of integrated care to defined geographical populations. Practices were required to join a network, and those unable to do this on a voluntary basis would be assigned to a network by NHS England. Importantly, it is envisaged that network practices will be geographically contiguous in their coverage. Networks had to be formed by July 2019. 40 Approaching the deadline, it was reported that 99% of practices were participating, with only 25 practices (of about 7000 practices nationally) actively deciding not to participate. 55
Primary care networks are different from federations, the latter being ‘bottom-up’ organisations. Although the terms network and federation have been used interchangeably on some occasions (e.g. General Practice Forward View38), the central policy of PCN creation, although allowing some local freedom, is fairly prescriptive in terms of the likely size of PCNs, their role and the need for a geographically consistent footprint. Therefore, federations, as they were not developed in response to an NHS England policy direction, have much greater freedom. However, the creation of PCNs in a landscape where federations have existed for some time raises questions about the ways in which these different types of organisations interact and develop over time.
Lessons from the literature
When considering successive waves of collaboration in primary care together, it becomes clear how influential previous arrangements have been in shaping local responses to, and the form of, subsequent arrangements. 56 For example, the legacies of specific local partnerships and networking footprints associated with MAAGs, GP co-operatives and GPFH can been seen expressed in the political dynamics of PCGs or the delineation of sub-CCG ‘neighbourhoods’. 57
Research also identifies a number of other issues of particular importance to networked arrangements in primary care:
-
General practitioners tend to work together most successfully when they have some agency over deciding with whom they collaborate and how they do so. 58,59
-
Successful collaborations tend to be in response to or focused on issues of particular salience to GPs and their everyday work. 26
-
Sufficient trust between parties is of crucial importance to successful collaborations – this can take time and effort to establish or build.
-
Historic issues between individuals and groups can mediate the success of this process. 60
A recent systematic review of new forms of large-scale general practice provider collaborations in England61 (see Appendix 1 for more detail) found that larger scale could contribute positively to sustainability in general practice through standardised processes and operational efficiency, maximising income, enhancing the workforce and deploying technology. However, it highlighted the significant levels of leadership and resources needed to create, develop and maintain these organisations. The quality of relationships with commissioners and local providers was found to be an important influence on the extent to which the GP organisations could go beyond the provision of core services.
Networks in health care
There is a literature that is concerned with organisational forms (called variously alliances, partnerships, networks and collaborations) in relation and as a response to problems facing public service provision. We use the term ‘network’ here for simplicity’s sake. Studies focusing on public services suggest that networks are particularly effective in tackling ‘wicked problems’62,63 and are able to respond rapidly to a changing environment. 64,65
Ferlie et al. 41 suggest that public networks with strong professions are characterised by a relatively benign ‘post bureaucratic’ style. This chimes with much of the literature on networks, which contrasts them with hierarchical, bureaucratic organisational forms. 66 Various commentators identify networks as embodiments of heterarchy that overcome weaknesses of hierarchical forms of organisation. 67–69 However, this raises questions about how and to what extent heterarchical and hierarchical forms interact in the context of formal organisations, such as federations, as well as the nature, location and mechanisms of accountability in these network forms. 70
Network structures and practices can vary widely, but Ferlie et al. 41 identify six continua to classify network forms, which are as follows: (1) the extent of complexity in the context; (2) mandated, hybrid or organic networks; (3) the extent of resourcing (including dedicated staffing time); (4) the extent to which roles, structures and governance are formalised; (5) the number and variety of stakeholder groups and the internal power balance; and (6) shared and accepted norms underpinning decision-making processes and management skills, which could enable collective decision-making or shared learning to occur.
Complexity of context
Smaller scale and simpler settings ‘have been identified as being “less challenging” ’,41 although to say that contexts are less complex because they are ‘simpler’ is a somewhat tautological explanation. ‘The dimension of “complexity” might include such indicators as: scale; the size of the population affected; challenging geography; extent of social deprivation or multi culturalism; number of teaching hospitals; degree of behaviour change sought’41 (contains information licensed under the Non-Commercial Government Licence v2.0.).
Mandatory/hybrid/organic
Federations are bottom-up organisations and they are not mandated. One consequence of this may be to exacerbate inequalities, with only the more capable practices entering into at-scale working arrangements. Furthermore, voluntary participation means that even these well-placed practices may fall far short of implementing recommended behaviours if they involve managing clinical and financial risk. 71
Mandating collaborative working among health-care providers in a ‘top-down’ manner can provide a stimulus to develop new relationships. 72 However, this is likely to result in clinician disengagement compared with collaborations that emerge organically. 73,74 (It is worth mentioning that Guthrie et al. 45 found that distinctions between mandated and voluntary networks may overstate the extent to which these represent a dichotomy. Furthermore, they observed that, over time, initial advantages and disadvantages relating to the voluntary/mandated status of networks became less well defined as the mandated networks they studied matured.)
Degree of resourcing
Most commentators agree that organisations find autonomy preferable to dependence, but that they may sacrifice some of this to gain access to increased resources. Theories that focus on resource acquisition75–77 suggest that, by forming collaborative alliances, organisations will gain access to a wider range or volume of resources and/or capacity than would otherwise be the case. This may not be enough, however, to motivate organisations to actively engage in participation. 78–81 In the context of workforce shortages, whereby federations are successful in gaining access to resources, this may involve attracting staff from neighbouring federations, as the overall availability of care staff is fixed or limited in the short term at least. There is also the issue of who controls resources in federations, which we return to later.
The extent to which roles, structures and governance are formalised
Provan and Kenis82 see tensions arising from the need to maintain a stable and sustainable formal structure and avoiding bureaucratic hierarchical processes, which risk destroying the intent and purpose of the form and alienating network members. Informal and more flexible arrangements may be easier for smaller networks,72 but larger networks may be more able to influence the local health economy, bear financial risks and manage the administrative requirements of regulation. 81 There is no clear consistent relationship between the size of health-care organisations and their performance,72 but smaller collaborations may be able to exercise greater performance management accountability. 83 The size of the population needed to manage clinical risks and associated costs is another consideration, which depends on the range of services for which the organisation is responsible and the pre-existing health of the population. 11,53,84
According to Provan and Kenis,82 networks face tensions between the need for internal and external legitimacy and between the need for administrative efficiency and inclusive decision-making. These have implications for governance arrangements. Developing a governance structure that is both stable and flexible requires ongoing monitoring of structural mechanisms and procedures, and a willingness to make changes when necessary. 82 A perception of organisational legitimacy82 is important. For example, if practices wish to bid for resources, they may appear to have greater legitimacy to external funders if they are collaborating as part of a group than if they are bidding as individual entities. The building of trust with external stakeholders and members has been seen as important, as this has implications for autonomy. 81 Perceived trust has been shown to be linked to achievement of goals and increased interactions. 85 O’Leary and Blomgren Bingham78 suggest that, although organisations may relinquish control over some aspects of organisational business, they may develop new sources of autonomy, linked to new forms of power.
We might expect that governance structures are designed to meet the functions of the network. However, Shortell and Addicott86 suggest that governance structures are not necessarily designed with a clear definition of network functions in mind. Instead, new organisational forms emerge in response to problems associated with existing forms, and functions are worked out later, based on activities that these new forms can enable. They also suggest that governance through networks requires leadership, rather than authority, as well as ‘bargaining, negotiation, guidance and facilitation’. 86 These new organisational forms are characterised by high-risk interdependent relationships, which require accountability mechanisms that clearly locate responsibility for actions and allow for the exercise of professional judgment. 70
Provan and Kenis82 hypothesise that, as networks develop, their governance arrangements will tend to shift from relatively participative, democratic, egalitarian forms to more centralised, brokered, formal governance. These formal arrangements may go some way to addressing concerns about accountability of network forms. 70 Collaborative forms, especially where these are not mandated, offer the potential to exercise greater control over professionals,19,41,87 with a more hierarchical structure helping to focus network activities on their strategic goals. 70 Of course, even where formal structures and processes exist, we cannot assume that they are necessarily followed to the letter, so it is important to go beyond the formal structures to understand how governance is manifest in practice.
With regard to networks involving general practices, Sheaff et al. 52 highlight that accountability operates by concertive control, ‘legitimation of collective decisions by appeal either to an organisational culture or to technical knowledge; and as a last resort expulsion of non-compliant members’; ‘members or partners monitor each other’s work and through peer pressure prevent shirking’ (contains information licensed under the Non-Commercial Government Licence v2.0.). Concertive control involves workers reaching a consensus about how to manage their work, and collaborating to develop the means of their own control. 88 This results in a shift from management to workers controlling themselves in a way that constrains organisation members more tightly than under traditional bureaucratic control, relying for its effectiveness on close working within teams of peers. This raises questions about the feasibility and effectiveness of this approach in federations, which comprise large numbers of staff from a range of groupings and member organisations. The issue of compliance and accountability may be important when federations seek to standardise processes and meet key performance indicators. However, GP federations also need to engage member practices, especially because, in many cases, they are reliant on them for their existence, and hierarchical governance can leave individual GPs feeling alienated. 89 Furthermore, in some cases, practices have a choice of federations and participation is not mandated in a top-down manner.
In terms of governance and ownership, Pettigrew et al. 72 suggest that non-hierarchical and hierarchical organisations are likely to bring about change through different internal mechanisms. They are likely to have different organisational goals and require different levers to maximise performance. 52 However, this dichotomy ignores the fact that change may be best achieved using a combination of top-down and bottom-up mechanisms. 90
With regard to specific governance issues, conflicts of interest can emerge when providers also act as commissioners of services, which could happen if/when GPs sell their practice to a larger group. 91,92 According to Pettigrew et al. ,72 this could also pose the risk of creating an organisation that becomes ‘too big to fail’,72 thereby needing public funds to bail it out. 93,94
The number and variety of stakeholder groups and internal power balance
Federations operate within a broader landscape populated by a range of stakeholders and influenced by a collection of regulatory and other policies and mechanisms. Their activities and fortunes will be subject to the constraints imposed on them by local and national policy-makers, which may distort their purpose and practices. 95–97 In addition, the divergent performance frameworks characterising organisations and stakeholders within health economies act to inhibit collaboration. 98
Studies that have examined networks involving groups of people from different types of organisations have identified power differentials, among other things, as inhibiting network progress. 98,99 Specialists, particularly hospital surgeons and hospital physicians, enjoy an elevated status compared with GPs,98 GPs being dubbed the ‘subalterns’ of medicine. 100 This means that the views of hospital surgeons and hospital physicians are likely to prevail, regardless of any formal arrangements ostensibly embodying parity across network members. 41,97,99 Federations are composed of practices as opposed to more diverse groups of stakeholders. However, within practices hierarchies exist based on professional status and practice ownership, resulting in power asymmetries, which may be reproduced in collaborative ventures. These power differentials are also likely to inhibit lay and service user representatives involved.
With regard to lay and/or service user input into networks, in many cases this is reported as being absent or limited,41,45 although this is not always the case. Sheaff et al. 52 suggest that service user involvement in voluntary networks will be more extensive, but also more uneven, than in mandated networks. They describe public and patient participation being used as an ‘add on’ to networks, after the networks’ main function and membership were established. They specify two necessary conditions for extensive and influential involvement of users in health networks: users (1) dominate the co-ordinating body and (2) are integral to the network’s core process.
Shared and accepted norms underpinning decision-making processes and management skills that could enable collective decision-making or shared learning to occur
A number of studies emphasise the importance of a shared vision of purpose, trusting relationships and good leadership, in particular the importance of clinical–managerial hybrid leaders with ‘soft’ skills. 11,41,45,52,101 Boundary-spanning roles and the ‘capacity to hold multiple perspectives within the federation’102 are also seen as contributing to network effectiveness. 41,45 In part, these roles are necessary because of the absence of formal authority and power over staff and/or resources in a context of diverse network membership. In these circumstances, networks rely on co-operation and co-ordination, rather than a strong mandate and/or statutory status. 41,45
With regard to effective network processes, it is advisable to avoid too strong a focus on business-dominated meetings. This means that networks should create opportunities for network members to come together to exchange ideas and influence decisions. 41
In the networks literature, the distinction between the terms ‘leader’ and ‘manager’ is not always clear. However, heroic leadership11 is seen as unsustainable, with leadership by small teams (‘duos and trios’41) viewed as preferable to a highly individualistic approach. Many of the positive attributes of managers and/or leaders (e.g. ability to combine soft and ‘hard’ approaches to management,41 span boundaries,41 draw on social capital,52 communicate effectively43) in networks might plausibly be applied to managers and leaders in organisations more generally.
Several authors highlight the importance of culture,52 with some suggesting that an ‘inclusive organisational culture’43 is a key feature of effective networks. This is defined in one study as involving widespread engagement and participation. 43 However, it could be argued that this is an aspect of a management or leadership style, rather than being a ‘culture’ that is shared by all members. General practice has been described as predominantly characterised by a clan culture. 103 However, at the level of the individual practice there is no discernible relationship between culture and performance,103 which raises questions about the mechanisms by which culture is assumed to be influential at a network level. A pragmatic and widely used definition of culture as ‘the way we do things around here’104 raises questions about who ‘we’ are in the context of federations. Furthermore, a shared culture will take time to evolve. For federations in their early stages of development and where practices are members of organisations whose members may have little involvement with the central authority function of the federation, it is not clear how useful the notion of a shared culture would be. In addition, if practices work together at the subfederation level, then they may develop shared ways of relating and acting, which are different from, but not necessarily incompatible with, those of the federation. Rather than exploring the extent to which there is a shared federation culture, therefore, it may be more useful to examine the degree to which members are encouraged to and do engage with the federation and how this influences their attitudes and behaviours. Sheaff et al. 105 suggested that ‘network macroculture’ can be used to manage the formation and operation of health networks, but acknowledge that the main limitation of their argument is the absence of a standardised definition of (network or organisational) ‘culture’ and the existence of > 100 dimensions of ‘organisational culture’. It may be preferable, therefore, to describe structures and processes, and to use this in providing explanations, rather than to invoke ‘culture’, with all its problematic connotations. Regarding inclusive communication and engagement style, this issue can be explored without recourse to concepts such as culture, which may not be helpful in federations, particularly in their early stages of development.
Meta-organisations
As discussed, the term network has been used to denote a broad and diverse range of organisational forms, leading some to suggest that it has been used to describe far too many phenomena. 106 Networks have been contrasted with meta-organisations (MOs)107 and federations resemble MOs. An advantage of using the term MO is that the organisational form is clearly defined and this definition is very applicable to federations. According to MO theorists, there are large and significant differences between networks and MOs. 107–109 Networks are often based on differences (different types of organisations such as hospitals and primary care organisations), with the network providing opportunities for interactions that bring mutual advantages:
The collaboration itself is based on trust and reciprocity – on the assumption that those included in the network give, and that they receive in return. In most meta-organizations, on the other hand, the members take similarities as their starting point and there are efforts to clarify and manifest these similarities in making decisions about common rules. [. . .] Networks among organizations are embedded in a set of other social relationships (Thompson 2003: 144), and their boundaries are blurred [. . .] Meta-organizations, on the other hand, create boundaries between themselves and the world around them. They make decisions about who is a member and who is not. Instead of being embedded, meta-organizations strive to create autonomy and distinctions.
Ahrne and Brunsson107
Meta-organisation relationships are characterised by disembeddedness, as staff in the different member organisations may not meet in person. Instead, the foundation for creating trust is the MO’s striving towards similarity and shared status among its members, whereas network participants may develop trust via face-to-face interaction. Networks are viewed as less hierarchical than traditional organisational forms, but MOs are hierarchical in nature:
They possess an authoritative centre called a board, management, government, leadership, or some such term; and the people who comprise these units have the right to issue commands and rules prescribing their members’ actions [. . .] The right to enforce compliance with commands and rules requires organization; such rights do not exist outside organizations.
Ahrne and Brunsson107
Traditional forms of organising rely on hierarchical mechanisms to control and co-ordinate the activities of organisational employees,110,111 yet the members of MOs are not individual employees but organisations. 107 Although organisational employees are relatively dispensable, MOs are dependent on certain organisations being willing to join. This dependence of MOs on its member organisations to constitute its organisational identity contrasts with individual-based organisations, in which skill sets, as opposed to recruitment of certain individuals, are much more likely to influence the search for organisational members. 107 Combined with the important fact that MO membership is voluntary, this contributes to relations of interdependence, which are very different from those characterising both traditional organisations and networks. In MOs, member organisations retain their identity and a high degree of autonomy. 107,109 There is a potential tension, therefore, between the MO’s requirement for a degree of authority to organise its members and each member organisation’s need to organise itself.
There may be financial costs to member organisations that contribute to the central authority function, but often these costs are not high relative to members’ turnover. MO theory suggests that free-riding will be low because the benefits of membership relative to costs make membership attractive. However, this also means that organisations may join because they do not wish to be left out of the MO, rather than from a genuine interest in the MO’s purpose and activities. This contrasts with network studies that often depict members as actively engaged, even if they are, at times, constrained by power asymmetries in the network. Furthermore, whereas studies of networks have emphasised the danger that the network will be captured by powerful stakeholders, MO theory highlights the threat to the MO central authority from its member organisations. Combined with the absence of mandatory membership (unlike mandated networks and PCNs, which contain strong incentives to comply) the result can be that MOs become organisations for the weak, rather than the strong. 107 MOs are viewed as aiming for 100% membership and monopoly strengthens their position, yet competition can be a feature of the MO landscape, whereas this is usually absent in network contexts. However, as we elaborate on later, we suggest that competition for members between MOs can also have strengths, insofar as members being able to make an active choice between options can enhance legitimacy and compliance.
A key aspect of the attraction of MOs for individual organisations is strength in numbers far beyond that enjoyed by individual organisations. As part of this process, MOs can be seen as creating a protected zone,112 restricting the influence of other, at times more hostile, organisations outside the MO. This explicit rationale may mean that they are less vulnerable to pressures from the external environment than health networks. ‘Fear of the future’113 as an explicit driver for federation formation also suggests that to understand MOs we should, rather than asking what they are for, try to understand what it is that they are against. It also highlights the importance of emotion in motivating federation creation, whereas many network studies focus on rational, instrumental aspects neglecting the emotional dimension. In addition, although (implicit) support for the creation of a protected zone may be seen as a goal around which member organisations can coalesce, this does not imply collective support for all MO policies.
It has been suggested that MOs have specific characteristics, such as the need for member approval of decisions and development of an elitist identity, which make them prone to avoiding risk and uncertainty. 114 However, another view is that MOs encourage the development of organisational capabilities for sustainable innovation, by virtue of their ability to combine multiple stakeholders with reporting and accountability mechanisms. 115
Despite the emphasis on similarity, MO member organisations are characterised by dissimilarity (for federations all members are practices), but practices differ markedly in many respects. 116 To survive, MOs must manage differences between members and between the MO and its members. This involves continually having to balance their own identities (e.g. small-town GP federation) with those of its members (e.g. small-street practice). Members join MOs because they feel weaker without membership. The diverse membership of MOs means that they face trade-offs in terms of standardisation versus local freedom. 102 Furthermore, within MOs we would expect to see an avoidance of top-down directives, as these involve an element of constraint and inflexibility, thereby curbing member autonomy. 107 If MOs are to introduce and enforce clear rules, then it is easier to do this at their inception. 107 They may employ staff (‘direct’ resources), but they may also draw on ‘indirect’ resources,117 relying on staff from member organisations to undertake some of the MO’s work. Although the latter may cost less and involve staff who understand the local member context, it runs the risk that those staff will prioritise their employing organisation over the MO.
With regard to service users, the formation of a MO is aimed at reducing what members perceive as disorder, thereby increasing predictability and control, for themselves and their customers as well as other interested parties. We would not necessarily expect customers (or, in the NHS, patients or service users) to be involved in a MO’s activities, therefore, but they should be beneficiaries of the new more stable environment that the MO strives to create. 107
The foregoing provides useful and important lessons, as well as raising questions about how and to what extent these apply to federations working in practice today and the implications of these different organisational forms for the organisation of primary care.
Aims
The aims of the research were to:
-
provide a wide-ranging and in-depth exploration of GP federations in England
-
strengthen the evidence base on the organisation and management of general practice for the twenty-first century.
The second of these aims was based on an assumption that GP federations would endure for several years. However, recent policy announcements about PCNs raise questions about the future role of federations. Furthermore, PCNs are very different from federations in many respects and are still in the early stages of development, which makes it difficult, at this stage, to discern how these two organisational forms will interact with each other.
Research questions
This research focus was intended to allow us to provide answers to the following questions:
-
Managing practice processes – how does federation affect the way practices organise themselves internally, and which governance arrangements best enhance practices’ ability to work co-operatively with others?
-
Workforce – how does federating affect the way practices use their staff, skill mix, etc., and what impact does federating have on the general practice workforce?
-
Innovations in practices and interface with health-care and social care stakeholders – to what extent and how is the federation enabling or inhibiting integration with community and social care?
In addition to asking these ‘how’ and ‘to what extent’ questions, we also sought to provide answers that explain why these things happen in the way they do at each of the study sites.
Structure of the report
In Chapter 2, we describe the methods used in our study, as well as outlining changes to the original protocol and reasons for these changes. Chapter 3 contains in-depth descriptions of the case study sites and compares their differing approaches. It also draws out key drivers influencing relationships, events and attitudes at those sites. In Chapter 4, we explore the ways in which federation members worked together, as well as using the Improving Access to General Practice (IAGP)38 policy as a tracer issue to compare and contrast the ways in which the case study sites approached the requirement to increase access by 1 October 2018. Chapter 5 examines the working relationships between federations and a range of stakeholders in their environment. Chapter 6 synthesises and discusses the findings of the empirical chapters (see Chapters 3–5) using concepts from literature on MOs and networks to extrapolate beyond the detail of individual sites. Finally, Chapter 7 presents implications for policy and practice.
Chapter 2 Methods
Study design
There is a growing interest in the topic of general practices working together,61 with various researchers seeking to add to the knowledge on this topic. We designed this study to be different from, but also complementary to, other approaches that emphasise large-scale data collection via surveys118 and/or that focus on federations, which may be more developed than is typical, nationally. 13
We used a qualitative comparative case study design that was longitudinal in nature. We chose this approach because we envisaged that it was not possible to quantify the impact of changes on health (proxy) outcomes, given the diverse objectives of federations and the evolving nature of the organisations concerned. This design was appropriate to our research aims and research questions outlined in Chapter 1, as it enabled us to examine organisational process over time. It also allowed for an element of induction to identify aspects that had not been reported in previous studies. We planned for 200 interviews during the study (i.e. approximately 50 per case), including repeat interviews to capture development over time when indicated. This was because federations comprise large numbers of organisations, which employ a variety of staff types and include GP partner owners. In addition, we expected that federations would interact with other organisations (e.g. NHS trusts, local authorities) and we planned to interview staff from those external organisations too, as well as interviewing patients. As there was already a large literature on collaborative working and networks in health generally, it was also important to provide sufficient detail from case study sites to enable readers to make judgements about the extent to which federations did or did not resemble networks already described in the literature. This meant that observation was a key aspect of the design, as it was important to watch interactions and events generally, as opposed to relying on retrospective accounts.
We made a number of changes to our initial design, as we explain in the following section.
Key changes to the initial design
Case selection
We intended to undertake a national mapping exercise of federations and to include a non-federation case study site. Appendix 2 explains why we did not undertake these.
We planned to select four case studies to reflect a range of types of organisations, defined according to their form and function. In addition to one non-federation case study, we planned to select:
-
a set of general practices with collaborative arrangements but without a significant provider function (sharing back-office functions, staff or premises)
-
the creation of a provider entity separate to, but owned by, general practices
-
a formal merger of general practices into a super-practice.
This was based on our understanding of the landscape at the time of the bid. In addition, we were keen to avoid sites where federations were participating in other qualitative studies and those involved in national large-scale change initiatives, such as NHS vanguards, as overlapping initiatives involving the same practices would make it difficult to tease out the specific impact of the federation. We planned to use the mapping exercise to inform the selection of sites, but this was abandoned after several months. However, during this process, a staff member at one federation expressed an interest for their organisation to be included. This site partially met the criteria for category 1 above. It did not share back-office functions, but it did have a management team. We also recruited a site that intended to create a provider entity as described in point 2 above. An additional site was committed to standardising systems across practices in a way that differed from the other sites. It did not formally merge practices, but it did obtain registration with the Care Quality Commission (CQC), which meant pooling risk insofar as it was accountable to the CQC for the performance of all member practices. The other site was evolving from an informal collaborative organisation to one involved in bidding for contracts and providing new services.
All the sites were federations with a central authority function. Box 1 summarises key features of each.
-
One provider for CQC purposes, developing centralised systems for finance, payroll and intranet, and aiming to pool staff and share risk across the federation.
-
Bidding for service contracts, but without shared functions across practices.
-
Federation with provider entity created to run small number of practices and joint vehicle to deliver community health services with a local trust.
-
No significant provider function; less developed compared with other sites.
In all cases, we observed changes over time as goals, tactics and organisational forms underwent a process of evolution and adaptation. We explain more about these processes of evolution and adaptation in our empirical sections in Chapters 3 and 4. Therefore, rather than seeking to understand federation forms in terms of a snapshot at a point in time, we traced their ongoing journeys in the context of an evolving external environment.
The selection of sites was a more pragmatic and opportunist process than originally intended. We did not include a super-practice, but, based on our telephone survey, these are relatively rare. Furthermore, by selecting cases that had some features in common (e.g. employment of a management function, formal agreements), we were able to explore differences in processes and outcomes and the factors influencing these in terms other than differences in organisational forms. We also envisaged that factors such as whether or not there were other federations in the same geographical footprint competing to recruit member practices might influence events.
Case study data collection and analysis
Following four organisations over time enabled us to understand how federations were emerging and operating and allowed us to produce early lessons to inform their future development. To protect the identity of the sites, we use pseudonyms, which are indicative of the findings and of the broader characterisation of each site. These are Expanding, Embedded, Struggling and Small. We chose ‘Expanding’ because this site increased its membership over time and expanded its geographical coverage. ‘Embedded’ reflects the embedded nature of the federation, with close links to the CCG and no competing federations in its geographical footprint. The other two pseudonyms reflect the fact that Struggling experienced difficulties during the fieldwork that were much greater than those at the other sites and Small was chosen because of the size of the federation generally and, in particular, in relation to the other sites. We elaborate on this in Chapter 3. We also use pseudonyms in the vignettes included in Appendix 3 featuring individuals at case study sites.
Data collection
We used qualitative methods to explore the stated aims of federations and the mechanisms by which such aims were intended to be achieved, as well as assessing progress against these aims. Other foci included the perceptions of member practices, their motivations for joining, the mechanisms by which practices were working together within the federation, enabling and constraining factors regarding establishment and operation of the federation, and the impact on the constituent practices (in the widest possible sense, including practical impacts on their work and impacts on practice identity). We interviewed staff to explore the creation of the federation and its history and context, how the federation was intended to achieve its aims, as well as views on progress towards these aims. We recognised, from our earlier work and the literature, the difficulty in assessing the performance of federations,60 in part because of the different goals of different federations and the tendency for goals to shift in the light of changes in the wider policy environment. Nonetheless, we examined performance claims by federations, seeking to understand the mechanisms underlying any claimed benefits. In addition, we explored patient perceptions in our case study sites using interviews and focus groups.
Data collection involved attending and observing meetings and conducting documentary analysis in case study sites. We identified the meetings where federation leaders came together and focused, in all sites, on board meetings and other meetings of federation leaders. As time went on, we also observed meetings relating to IAGP, as well as any events to which the broader membership was invited [i.e. annual general meetings (AGMs) and open forums]. In total, 139 meetings were observed (Expanding, n = 43; Embedded, n = 28; Struggling, n = 39; and Small, n = 29), equating to almost 320 hours of observation (Table 1). In terms of documents, we examined business plans, shareholder agreements and documentation relating to governance structures and processes. These enabled us to gain an understanding of the formal structures and processes of the federation at each site.
| Site | Type and number of meeting observed | Total (n) | |||
|---|---|---|---|---|---|
| Federation | Federation services | Practice | Other | ||
| Federation A (Expanding) |
|
|
|
One strategy | 43 |
| Federation B (Embedded) |
|
IAGP was covered during other meetings |
|
|
28 |
| Federation C (Struggling) |
|
|
One CCG Patient consultation | – | 39 |
| Federation D (Small) |
|
Two IAGP |
|
|
29 |
| Total (n) | 77 | 25 | 29 | 8 | 139 |
Field notes taken during observation of meetings were added to at the earliest opportunity following the end of the meeting. These were typed in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) documents by the observing researcher to enable easy access for analysis by core research team members. Interviews (n = 205) were conducted with a range of stakeholders and were digitally recorded and transcribed verbatim (Table 2). We used a standard interview schedule, but varied the questions according to the role and background of the interviewee. In some cases, the questions were informed by observations undertaken prior to interview. In addition, the patient members of the advisory group helped to inform the interview topic guide, as well as the data collection and analysis more generally. We expected that federation activities would affect a range of different staff (for example, standardisation of software and/or documentation may result in changes for clinicians, managerial and administrative staff). We therefore aimed to interview a range of different types of staff and included a range of practices for staff interviews. Selection of interviewees was, in part, informed by the aims and activities of the federation, but, as a minimum, we aimed to interview clinicians (doctors, both partners and salaried GPs and nurses), practice managers (PMs), administrative staff and local providers (hospital and/or community). We interviewed patients and carers in a targeted way, namely we used the plans and activities of federations to identity potential impacts on patients, and chose relevant respondents. However, we also interviewed patients to ascertain their views and priorities in relation to their health care, comparing these with those of the federation.
| Site | Interviewee type (n) | Total interviews (n) | |||||
|---|---|---|---|---|---|---|---|
| Clinicians | PMs | Federation staff | Patients | CCG | Other | ||
| Federation A | 17 | 5 | 11 | 9 | 1 | 2 | 45 |
| Federation B | 22 | 9 | 6 | 21 | 3 | 7 | 68 |
| Federation C | 23 | 5 | 2 | 7 | 3 | 3 | 43 |
| Federation D | 12 | 5 | 8 | 8 | 3 | 4 | 40 |
| National perspectives | 9 | ||||||
| Total | 74 | 24 | 27 | 45 | 10 | 16 | 205 |
Data collection time scales
We started our observations of meetings at the first two sites (Expanding and Struggling) in December 2016, and we commenced observations of meetings at the other two sites (Embedded and Small) in April 2017. All observation had ceased by the end of November 2018, although two interviews were conducted in January 2019. We lost access at one site (Struggling) where our meeting observations ceased in September 2017, but we conducted a small number of interviews at the site after that date that enabled us to fill in gaps in our knowledge of their story.
Data analysis
Owing to the need to capture events at federations as they were unfolding, we concentrated initially on data collection, with analysis comprising regular team meetings to discuss researchers’ experiences and reflections. After several months, we constructed a coding framework drawing on themes arising from the data. We used some of the concepts from the literature on GP working at scale, organisational networks, MOs and organisational behaviour to inform our understanding of the data. This literature also helped provide a focus for data collection. This was an iterative process, with periods of researchers coding independently, interspersed with regular meetings and discussion to address areas of disagreement to obtain consensus. We used NVivo 11 (QSR International, Warrington, UK) to code data and this process helped to identify initial themes. Having identified relevant first-order codes, we conducted further analyses to refine what was a large number of codes to consolidate findings in a smaller number of second-order codes, which, although grounded in the data, reflect a higher level of abstraction. This process was aimed at providing generalisable lessons beyond the immediate cases.
After the initial 4 months focusing on data collection, we undertook data collection and analysis concurrently. In addition to observations recorded and reflected on, and interview transcripts, we used documentary analysis and relevant quantitative data produced and discussed in these settings to provide understanding, seeking out systematic relationships and patterns. We have attempted to reflect this in the presentation of data. Rather than insert short extracts from meeting notes, we use vignettes, based on observation and interviews, to convey key aspects of context, activities and interaction. Owing to their length, they are included in Appendix 3. We do use quotations from interviews in the main body of the report.
Ethics approval
We received ethics approval from the South East Scotland NHS Research Ethics Committee. As part of this process, we used generic job titles to describe individuals’ roles and, in some cases, to alter certain contextual details to preserve anonymity. We also did not quote directly from minutes of meetings to avoid the possibility that doing so would enable the individuals and/or organisations to be identified.
Conclusion
For each federation, we produced an in-depth description of organisational form, processes and activities, factors that influenced events and actions and a description of the extent to which ‘success’ (in terms of its stated aims) was achieved. We compared sites to look at common and site-specific factors to generate wider learning. We also examined the ways in which, and extent to which, the federations were involved in responding to the IAGP policy. We discuss this in more detail in Chapter 4, but before that, in Chapter 3, we provide detailed information on each of the case study sites.
Chapter 3 Case study sites: an in-depth discussion
Introduction
Federations differed in a number of respects. In this chapter, we draw on our observations, documentary analysis and interviews to describe formal structures and processes. We also discuss the findings in relation to the ways in which these evolved over time, and compare the formal arrangements with the day-to-day realities of how these worked in practice. As MOs, each federation had their own ‘central authority function. By central authority we mean a combination of structures and processes for making decisions and, when relevant, holding member organisations to account.
We found that a number of factors were important in influencing events at each site. These were the styles adopted by federations, historical context, the relationship between the federation and the CCG, the extent of competition between federations locally, money, size and geography, and leadership and management.
In this chapter, we aim to provide sufficient detail to convey the activities and processes in which federations participated. At the same time, word constraints and the need to protect the identities of our sites mean that we have been selective in what follows.
The characteristics in Table 3 are based on the position at the start of the fieldwork. We use rounding to avoid identification of sites.
| Characteristic | Federation | |||
|---|---|---|---|---|
| Expanding | Embedded | Struggling | Small | |
| Size (n organisations) | 40 | 50 | 90 | < 10 |
| Size (n patients) | 330,000 | 335,000 | 500,000 | 90,000 |
| Competition for members | Yes | No | No | Yes |
| Local geography | Predominantly urban | Predominantly urban | Predominantly urban | Rural and urban |
| Deprivation | Above average | Above average | Above average | Below average |
| Single local authority | Yes | Yes | Yes | No |
These characteristics remained unchanged throughout, apart from changes to membership, which we describe in more detail in the following sections.
Site A: Expanding
History and geography
The federation was based in a largely urban area, in a major conurbation. At the start of the fieldwork, federation practices were located in one CCG, in which there was a history of working together in a number of geographical ‘localities’. In 2014, in the context of growing pressures and vulnerability, GP partners in two separate localities began discussing closer working and, in response, the CCG funded a series of ‘working-at-scale’ workshops, providing venues and facilitation consultants with influential key GPs invited to participate. During this period, the General Practice Forward View38 was published. In interviews, the founding board members were keen to highlight that their discussions around setting up the federation were clarified by the publication, rather than being a knee-jerk reaction to it.
Expanding had competition for members from three other local federations, two of which had expanded nationally. Their co-existence meant that the city’s CCG was keen not to be seen to favour any one GP federation, so initial support was limited to start-up workshops. During our fieldwork, the federation expanded its operations into a second geographical area, which was more rural in nature.
The majority of practices in the city had previously been involved in a provider collaboration that had ceased to exist. In terms of other forms of collaborative working, there was an existing ‘locality alliance’ situated within the federation itself. Before the federation began to bid to deliver services, the locality alliance had previously successfully bid alone to deliver services.
Core aims
Expanding aimed to help practices to retain their autonomy, providing leadership and support, and enable the delivery of high-quality care. As part of this process, it attempted to provide efficient centralised processes and systems to reduce the operational burden on practices. These included a single CQC registration, accounting and payroll, intranet system and staffing solutions. To facilitate this aim, all constituent practices were expected to convert to using these standard systems and related software as part of the joining process.
Structure, governance and decision-making
Structure
The federation formally commenced in November 2015, as an overarching umbrella organisation under which all the constituent practices retained their individual GP partnerships, ensuring their autonomy and the preservation of their individual GMS contracts.
Expanding was set up as a traditional partnership, with each partner being equal and having one vote at partner, or other, events. A detailed deed of partnership was drawn up by a legal firm and governed the rights and responsibilities of constituent practices. GP partners from member practices retained their income and autonomy with regard to the running of their practices. Two GP partners from the board were added to each of the constituent practice’s local partnership agreement, to protect smaller single- or two-handed practices from closure.
Governance
A transitional board was tasked with establishing the federation over a 6-month period (May–November 2015). Nominations were then sought from within the federation for the full board, and the election process was contracted to, and overseen by, an independent organisation. Partners were asked to vote for directors; the candidate securing the most votes was appointed chairperson of the board of directors.
Board of directors
The board of directors comprised seven directors (including the board chairperson); the board also included three non-voting officers: a part-time managing director (MD), a full-time chief operating officer (COO) and a full-time finance director (FD), all of whom were salaried. The board was chaired by a GP partner and, initially, all board directors were GP partners from constituent practices.
In May 2017, two additional directors were co-opted onto the board to represent constituent practices from the new second area.
In addition, a PM, who had previously had a non-voting role as a HR advisor during the ‘transition’ board, joined the board in December 2017, following competitive interview.
Central team
Day-to-day work and roll-out of the standard systems and processes to constituent practices were undertaken by a central team, which was under the direction of the three non-voting board officers. These officers formed the management team, which met weekly with the board chairperson.
Governance team
The governance team met fortnightly to oversee data collated centrally from the practices and reviewed complaints and compliments as part of the process of ensuring adherence to standardised policies and processes. Members were a GP from the board who was responsible for governance, the project manager responsible for governance from the central team and a practice nurse from one of the constituent practices.
Decision-making
The board were authorised to make strategic decisions, with each director holding one vote in elections. During the observation period, decisions were made by discussion rather than formal voting within the board. Board meetings were held monthly and were live-streamed for access by partners. GP partners and PMs were invited to attend, although only one GP partner and PM attended during our observation period.
Any variation in the partnership deed, approval of accounts or dissolution of the board had to be approved by the partners with a special resolution via a partners’ meeting. Partners’ meeting approval was necessary for change in directorships to be announced and new nominations to be sought for board positions. Elections were held by postal vote from individual partners within the federation to allow maximum involvement, including those unable to attend partners’ events.
Monthly informal board meetings were held as a closed meeting 2 weeks ahead of the formal board meetings. The former were used to collate and discuss ideas and strategies, as well as to finalise information to be shared with partners at the formal board meetings. The board chairperson met weekly with the MD to discuss strategic direction and approaches from practices wishing to join the federation.
Membership and recruitment
Expanding began within a single CCG and it intended to recruit practices in this CCG area. Board members were each allocated a geographical area (not necessarily their practice area) to recruit ‘non-constituent’ practices via (1) providing a point of contact and (2) reporting feedback on the federation and other federations.
The board discussed many strategies to encourage more practices to join the federation and the central team supported these aspirations by identifying more lucrative practices (e.g. list size, locality, previous contact with the federation) that could be approached first. However, growth in membership failed to meet that required to offset running costs.
The initial growth strategy to focus on recruiting local CCG practices in the city changed following an approach by a group of nine practices in another much more rural (second) area some distance from the CCG boundary. This resulted in six of these practices joining in May 2017.
Business model and finance
Subscriptions paid by constituent practices were expected to cover the cost of the board and central team. The central team expected to bid for and win contracts to deliver services, which would then generate an operating profit through at-scale delivery, which would be shared among its partners.
Practices contributed a £2-per-patient charge (payable annually) based on their registered patient list size. Initially, half the payment was described as a ‘levy’ or joining fee and the remainder a ‘subscription’. Practices that opted out of joining after paying the initial levy were not reimbursed. There was an expectation that, over time, the federation would generate profits, which would be redistributed among the practices according to list size.
The set-up and running costs of centralised systems was an issue for the federation. This, along with failure to meet the projected membership growth, meant that Expanding operated at a deficit for the first 2 years. GP board members were reimbursed for 3 hours per week, and the chairpersons for 6 hours per week, which reflected their additional workload. In April 2017 in response to the financial deficit, the MD reduced his input from 3 to 2 days for a 6-month trial period. This was accepted by the board, reluctantly, and subsequently continued at this level. In September 2017, the chairperson was appointed to the STP board.
Progress towards achieving aims
Centralisation and standardisation were considered key to increasing efficiency and quality as part of a process of sharing good practice and reducing duplication of work at practice level. This was also intended to enable the federation to bid for funds, either on behalf of practices or to co-ordinate practices to deliver services themselves. As outlined in Core aims, this strategy included a single CQC registration, accounting and payroll, intranet system and staffing solutions.
Care Quality Commission
The process of registering the federation as the new provider with the CQC was complex, as the CQC had not previously dealt with an application for a single organisation with so many sites. This single CQC registration was a disincentive to leaving the federation, as reversing this process was both time-consuming and costly at practice level.
Intranet
Practices were required to use an intranet system where practice staff uploaded a wide range of data (staffing numbers and cost, patient complaints, significant events, family and friends reporting) and federation policies. Anonymised results of benchmarking exercises proved popular; practices were allocated a unique code, allowing self-identification.
Payroll
A company was appointed for a period of 2 years to transfer staff from their employing practice over to the federation’s employment. Future plans for the federation included harmonising pay and terms for new staff being employed centrally by the federation. In a federation survey, practices expressed dissatisfaction with the payroll service provider; in August 2018, the board agreed to retender the service with an agreement that the existing provider could terminate early once a new provider was found.
Accounting
Among the original federation practices, four practices failed to comply with adoption of the centralised accounting system (one maintaining only paper records), which meant that the finance team had to run accounts manually. Despite legal requirements in the deeds of agreement to adopt these central requirements, there were no adverse consequences for a small number of practices not adopting these systems. Instead, staff from the federation operated in a supportive manner to help these practices move towards the transition.
Staffing solutions
With many practices experiencing difficulties recruiting and retaining clinical and non-clinical staff, the federation began working with a staffing solutions company from August 2016. Staff with spare capacity were encouraged to register availability to support other practices and a local solution was developed as part of this process.
Delivering new services
Over time, the federation was able to bid successfully to provide services. This led to a much more stable financial position.
Building local capacity
Funding was secured and distributed across the federation’s localities to accelerate the development of locality working.
Roles and relationships
Engagement with members
Board members were conscious that, to retain practices in the federation, it was important to maintain formal engagement with them as part of the process of communication and to demonstrate value for money.
Two events for GP partners were held each year, with over half the practices being represented by one or more partners. The federation held a parallel partner event in May 2018 in the more rural second area, to which they invited other non-member local practices. The two board partners from the second area also ran their own engagement events for local partners from the six practices they represented.
Expanding’s project involved helping vulnerable organisations by securing agreement to add doctors from other member organisations to their business contracts. This meant that there was a commitment by these organisations to cover absences, when such absences jeopardised the survival of small practices, even though the immediate benefits affected only some smaller organisations, with larger ones taking on risk. Importantly, rather than encouraging members to look to the federation centre, this created a structure of interdependence among member organisations. This approach also underpinned a series of peer-to-peer networks for different types of staff from member organisations, whose creation Expanding initiated, but whose ongoing operational activities were managed by their members. This context of interdependence also made it easier to recruit new doctors. Expanding’s approach did not involve attempting to arbitrate with regard to the competing ‘orders of worth’119,120 or attempting a compromise involving trade-offs, as a way of obtaining consensus. Instead, because problems were interdependent, making ranking difficult, Expanding pursued an approach that attempted to solve different problems simultaneously. A combination of new structures and rational and value-based arguments, as well as tapping into members’ fears, contributed to new norms of risk-sharing and interdependence.
Communication
The chairperson initially e-mailed an update to all GP partners following the formal board meetings, but, aware that these were not being read, from October 2017 he also circulated a short video outlining highlights from the meeting and featuring different board members. The COO sent weekly (and then fortnightly) newsletters compiled by the central office via the intranet system, which tended to focus on the operational side of the federation’s activities. Active construction,102 as opposed to merely ‘translation’,121 was a key feature of communication with members. In a context of diversity of membership, different member organisations in federations face different problems. For example, smaller organisations were vulnerable to closure in cases of prolonged sickness absence, but this was not an issue confronting larger practice organisations. Some member organisations were struggling with what they perceived as internal factors (e.g. their small size or inadequate premises) and others focused on external issues (e.g. increasing patient demands and a nationwide shortage of doctors). This federation, in common with Embedded, actively constructed problems to garner collective support for action. In both federations (Expanding and Embedded) the problem was constructed using three different arguments to resonate with the diversity of opinion in the membership. First, if some organisations were seen to be failing, then this would undermine the case for preserving traditional ways of organising primary medical care across the whole system, not just for those organisations. Second, organisation closure would result in the allocation of their patients to other member organisations, whose staff were already overstretched. In addition, a third threat invoked by MO leaders was the risk that, under such circumstances, policy-makers would move to open up primary medical care to limited companies, whose motives were shareholder profit rather than patient care. This combined threats to business with a strong moral and emotional appeal, tapping into the public service ethos of member organisations. 118 These approaches combined rational (business-oriented concerns) and value-based (pro-social) aspects when engaging in dialogue with member organisations. Importantly, these might both be seen as top-down responses to bottom-up concerns.
Internal roles and relationships
Practice managers were relied on to implement changes required to systems at practice level, but PM meetings were not well attended. Therefore, the federation employed a full-time deputy operations director to work with PMs, providing one-to-one support to practices in rolling out these changes.
Owing to his professional role and experience, the MD had links to many influential people in the local health economy, as well as links with the CCG chairperson, as they previously worked together.
Most of the board directors had roles in other organisations, including clinical leads for a CCG and acute trust, a local medical committee (LMC), the RCGP and the Academic Health Sciences Network.
External relationships
Clinical Commissioning Group
The city CCG was felt by the federation to not be taking a lead on helping deliver new models of care, and so the federation saw their role as acting to fill that void. The chairperson of the CCG, however, was very supportive of the federation and attended and spoke at member events. CCG reorganisation meant that, during the fieldwork, the federation’s relationship with the CCG changed as leadership changed in the new unified CCG.
Sustainability and transformation partnership
With links to the wider health economy, the federation was very aware of (possibly from the MD’s connections with acute trusts, which tended to be at the heart of STPs), and able to provide input into, the STP integrated care programme. Previous relationships between the acute trust, the community, the CCG and the local authority had not always been harmonious. A ‘refreshed’ primary care-focused STP, following changes to STP leadership and federation input, was reported.
Changes over time
The federation evolved from an organisation initially focused on its own local area to one expanding into a second area. This was prompted by requests from outside, rather than the federation actively seeking expansion in this way. However, the financial situation and changing views over time contributed to a revised approach to membership.
The desire to increase membership led to some discussion and disagreement about whether or not local practices with poor CQC ratings should be permitted to join. The MD argued that helping practices was part of their objectives, and this view received sufficient support from federation members to enable them to proceed on this basis. Thereafter, the federation was keen to limit the level of support it provided to practices and much stricter criteria were applied to potential new practices located outside the initial area.
In April 2017, the board discussed charging smaller practices a higher subscription, as, historically, smaller practices utilised more central office team time than larger practices. This proposal was not adopted and the ‘standard’ subscription was maintained.
In autumn 2017, the federation was approached by a large group practice from a more distant geographical location, which considered leaving their own federation to join this federation. Their inclusion would have brought the federation closer to their break-even point in terms of income needed to support the existing team, but issues related to distance would have made this less attractive than recruitment of local practices. The group practice subsequently remained with their original federation.
There were many challenges throughout the establishment and evolution of the federation. The majority of the central team had previously worked in acute trusts or CCG commissioning, which led to them experiencing a steep learning curve around general practices. This may, in part, have explained their reliance on outside consultants, some of whom did not always provide sound advice. Inaccurate advice on value-added tax (VAT) from a national body stopped some dispensing practices in the new location from joining, because of perceived losses and VAT implications of being part of the larger organisation. Many consultants realised the need for additional advice and support but provided this in terms of existing independent general practices rather than having knowledge of what new rules would arise in these emergent federation organisations. As a consequence, some guidance evolved over time and workaround solutions were adopted in the interim period.
Although the federation was primarily established to support the delivery of general practice at scale, the push towards STPs and general practice involvement meant that this became a major part of its work. The federation, along with other federations and individual practices, became part of a GP provider group, represented at many board levels within the STP. A memorandum of understanding, signed in 2018, meant that the GP federation would participate on an equal footing with hospital trusts at the STP programme board. This was an important development as it provided further representation for the federation as potential providers during key meetings.
As latecomers to the federation, the six rural practices from the second area were able to learn from the federation’s STP bid experience. The MD, along with the COO, attended some STP meetings in the second area, and an amended version of the city STP area bid formed the basis for a submission to the STP in the second area, which was co-ordinated by their CCG.
The federation was able to win smaller bids (e.g. to provide sexual health services) before bidding for and delivering improved access to primary medical care for > 60 practices. This, however, created a challenge in co-ordinating and delivering services including non-constituent practices with which the federation did not have an existing relationship. We report on this further in Chapter 4.
Site B: Embedded
History and geography
This federation occupied the same footprint as the CCG, which covered a largely urban area. There was a strong history of general practices working together, with around 70% of the city’s GPs collaborating in the 1990s as part of a non-fundholder initiative. General practices had operated for many years in a number of ‘clusters’, comprising groups of compatible practices rather than strict geographical boundaries, so local links between these practices were already present and ongoing prior to the creation of the federation.
In February 2015, local GP leaders and managers began discussing developing closer working collaboration between practices with the CCG. Workforce shortages and a large number of single-handed practices created fears about the future viability of general practice in the city; 30–40 practices were invited to an initial event, hosted by the CCG, to discuss this. Following the meeting, the CCG engaged and funded a local independent consultancy, which specialised in ‘integrating services’, to help facilitate the process of federation creation, and stepped back to avoid ongoing commissioner/provider conflict of interest. A series of monthly workshops then followed, during which attendees discussed various models of collaboration and agreed which best suited their needs. During these workshops, governance was discussed and one GP partner was approached with the suggestion that he stand for chairperson of the board. A shadow board was elected in January 2016 with the chairperson being proposed by the consultancy lead and unanimously elected by the shadow board members. The shadow board continued to meet weekly until the full board was established in July 2016.
Core aims
Initially, Embedded was established to support practices to:
-
aid and improve practice resilience by developing support in HR, practice management, policies, administration, etc.
-
provide a strong and influential voice for general practices as policy-makers and enable leaders to drive change in the NHS locally
-
identify and win new work and funding, recognising that individual practices did not have the capacity to do so
-
develop the readiness of, and provide support to, practices for a revised contract from the CCG for ‘any qualified provider’ services. This would allow practices to provide additional services to other practices/areas using in-house skills to generate additional income for the practice.
Structure, governance and decision-making
Structure
Embedded was established as a limited company by shares in April 2016, with all member practices being equal shareholders. Each member practice held one ‘A’ voting (£100) share and a number of ‘B’ shares (£0.10) equal to the number of registered patients.
Governance
Board of directors
The company was managed by a board of eight elected representatives (four GPs and four PMs) from member practices, along with three co-opted positions for individuals representing nursing, the lay perspective and a salaried GP. Nominations for the role of board directors were sought from partners in the member practices, many of whom had been part of the initial shadow board. The election process was managed by the independent consultancy. The federation board was established and began meeting monthly from July 2016; this moved to bimonthly from October 2017. The shareholders’ agreement required that one-third of the board members must step down in the third year, but would be eligible for re-election subject to a maximum of three terms.
Senior management team
The day-to-day running of the company was via a senior management team (SMT). Members were the board chairperson (a GP) reimbursed for 1 day per week, the board secretary (a GP) and board treasurer (a PM), reimbursed half a day per week each, and the company’s COO. The COO was a PM with experience in NHS information technology (IT) systems and practice consultancy experience who was recruited initially for an interim role in March 2016 for 3 days per week, but then became a permanent employee of the federation. The SMT met formally each fortnight, with much of the work led by the COO, supported by a small central office team. The COO and board chairperson also met most weeks to discuss opportunities for funding and collaborations as they arose. The shareholder’s agreement stated that only one SMT member was permitted to step down each year, to preserve continuity.
Central office team
Initially, there were two part-time central office posts (COO and an office manager), although additional roles were created during the observation period and filled mainly by PMs from member practices, who were reimbursed centrally for their input. Staff joining the organisation tended to take on responsibility for specific projects as project leads, supported by the COO. Largely led by the COO, this team approach freed up COO time to actively seek out new opportunities on behalf of member practices and to co-ordinate bid submissions on their behalf.
Decision-making
The SMT tended to do much of the planning and developing of ideas, which were then conveyed to the board. The project leads reported directly to the COO and were also invited to attend the SMT meetings to present progress around certain projects as required. The board met monthly; formal agendas and papers were circulated to board members ahead of meetings. The COO and one of the board GP members developed a red–amber–green rating system of project reporting. Reports were subsequently presented in this format as board papers, with only red items being discussed in detail, and amber items noted. This change reflected the need to ensure that the board focused on strategic oversight rather than day-to-day operational issues.
There were few disagreements at the board meetings because SMT meetings were used to work up project plans with assistance from the federation office team ahead of presentation at board meetings. The board tended to discuss items until a consensus was reached and very rarely relied on formal voting. Voting did occur outside the board meetings by e-mail when the COO requested board input around new streams of work that the federation could be involved in that required quick responses; agreement to these was secured, without exception.
Embedded held AGMs in the evenings after regular surgery hours, which GPs and PMs from member practices attended. In 2017, representatives from around 75% of member practices attended and were given promotional information about the newly updated website. Similar levels of representation were observed at the 2018 meeting. AGMs demonstrated the federation’s achievements and offered updates on future projects, as well as asking for members’ views. Formal voting for motions put forward by the board were held at these meetings, as well as through postal ballots.
Membership and recruitment
The high level of involvement from practices during the federation’s initial workshop phase meant that practices had already discussed the federation model they wished to adopt, their priorities and funding of the model. Therefore, the model adopted reflected a consensus about members’ needs locally. As a result the federation received more expressions of interest to join than the founding members had anticipated.
Business model and finance
The CCG provided the federation with £70,000 of ‘organisational development monies’ for each of the first 3 years (2016–19) to assist with set-up costs. Initially, the federation also received staff support from a local development organisation funded by the NHS local area team and the LMC. CCG support allowed a cautious and emergent approach to staffing, meaning the federation employed additional staff when there was certainty of funding.
Annual subscriptions were paid by member practices and based on £0.50 per registered patient per quarter. As the federation began to bid for and win contracts, it moved towards becoming more financially self-sustaining. The federation’s success in winning bids generated income both in terms of management fees for running services on behalf of non-member practices and by selling products that they developed to other CCGs (e.g. training). Income generated from projects and support from the CCG meant that both the ongoing board and central team costs were covered and that subscriptions were reduced. The COO and board secretary were keen to reduce visible profits to minimise VAT and corporation tax.
Progress towards achieving aims
Projects
By March 2017, Embedded had won two contracts totalling around £100,000. In July 2016, a CCG local incentive scheme was launched to incentivise practices to improve quality and access. The specification and funding model selected had been developed in collaboration with the LMC and federation. This provided the federation with its first set of projects collaborating with a community health provider, and co-ordinating those practices that wished to provide the offer with those wanting other practices to provide it on their behalf. The ‘virtual hub’ was created, allowing those practices that were not providing all of these services themselves to access services provided from another practice within the federation.
Initial work around system interoperability allowed referrals from practices using different clinical systems to be centrally co-ordinated from a ‘referral hub’, which became an important forerunner to the IAGP work (discussed in Chapter 4).
Other non-clinical CCG tenders were also successfully bid for, including (1) workforce, (2) general practice resilience and (3) workflow optimisation (via the document hub system).
Workforce
Embedded was awarded £60,000 to help look at recruitment issues. An application was developed to help staff with capacity to volunteer to work at other practices. This also facilitated intercharging between practices, reducing the administrative burden on PMs or finance managers. A further initiative funded receptionist signposting training to ensure that patients contacting the practice could be seen by the person most appropriate for their needs. The federation also bid successfully for the NHS England clinical pharmacists in general practice scheme, which provided a tapered contribution towards employment costs over 3 years. Bidding for this scheme as a federation enabled greater affordability and the sharing of staff between smaller practices.
General practice resilience
The CCG provided £5000 in funding from their share of the national allocation to all practices for work related to building general practice resilience. (This fund was intended to provide support to help practices to become more sustainable and resilient, in the context of present and future challenges. 38) Rather than contract separately with each practice, the federation received funding on behalf of its membership practices. This reduced the burden on practices and the CCG team. A small amount of unused funding was used to centrally fund PM development. A further £5000 in funding was awarded to each of the 11 ‘vulnerable’ practices.
Workflow optimisation
The federation appointed a company to train PMs, enabling them to understand and process the majority of paperwork, leaving only those items that required GP action. The federation oversaw the roll-out of this training, including the nomination of GP champions in each practice.
Roles and relationships
Engagement with members
Despite good uptake from practices in the city, ongoing engagement with practices was difficult initially. Changes to the website and recruitment of communications staff helped to improve communication with member practices, although this required ongoing effort. The federation had targets for engagement; progress against these targets was monitored on a regular basis.
Internal roles and relationships
Many of the individuals who were instrumental in the set-up of the federation became board directors by election, notably because of their high profile among city GPs.
As a former LMC role holder, the chairperson of the board was well known locally, respected and considered to be hard-working. The board secretary was a business manager from one of the largest ‘university’ practices in the city, for which the CCG lead was a senior partner. Along with the board secretary’s financial background, the partners at this practice also held an APMS contract for another university practice in another city, which enabled comparisons to be made with tenders arising in a different CCG.
As the federation set-up was aimed at, and subsequently comprised, ‘local leaders’, some had roles in other organisations, such as the CCG (as non-commissioning GPs; importantly, this meant that there was no conflict of interest in being both commissioner and provider of primary care services), LMC, RCGP, local hospitals and as out-of-hours providers. This enabled the federation to have a good awareness of opinions, events and personalities in other parts of the health system, developing relationships over time with others, such as community health-care and urgent care providers, which facilitated the delivery of contracts.
The SMT acknowledged the role of PMs in the success of the federation, particularly in relation to the volume of work required from PMs and their role in practice engagement.
External relationships
Other federations
The federation had little direct local competition for members and the federation had no plans to extend outside their CCG area. There was competition between the adjacent federations for involvement and leadership at the new STP provider level. One federation in this group was previously funded as a vanguard site and their clinical chairperson was appointed as the clinical lead for the STP primary care provider group, but other federations felt that they should be equal partners in delivering primary care services. To increase ‘provider voice’, the STP board appointed four GPs with provider roles in addition to those already representing the four CCGs as commissioners. At a regional level, a ‘learning federation of GP federations’ was set up following discussions between the chairperson of Embedded and the consultant who initially advised them during formation. During these meetings, federation chairpersons and COOs shared experiences and offered solutions to common issues.
Clinical Commissioning Group
From the outset, the federation’s relationship with the CCG appeared to be a constructive one. Because Embedded was coterminous with the CCG boundary, it was not embroiled in competition for members or cross-boundary issues that might otherwise have complicated its relationship with the CCG. Lack of competition from other federations, along with the high proportion of practices that were members, made it easier for the CCG to communicate with the federation. The CCG and LMC had previously held joint meetings and a federation board member was invited to attend part of this now ‘triumvirate’ meeting, representing the federation as providers at meetings. The federation aspired to be the ‘go-to’ organisation that the CCG would contact when looking to commission new services and there was ongoing evidence of this during our observations. At SMT meetings, the federation chairperson reported back on regular meetings he had with the COO of the federation and the CCG Primary Care Chairperson and team.
Sustainability and transformation partnership
Although the STP leadership board included representatives from the constituent CCGs, county and council representatives and mental health and hospital representatives, there were no primary care providers present. Two GPs from the federation’s board attended clinical cabinet meetings, but questioned whether or not they had seats at the ‘right table’, that is were able to ‘represent primary care [providers]’. The federation was termed a ‘partner organisation’ and became more involved from July 2017 when it became part of the ‘collaboration of GP providers’, which represented three of the largest GP federations in the area, which were established to develop a unified plan that could be presented to STP leaders. GPs felt that the hospitals dominated the local health and social care economy and that their voices needed to be heard and that Embedded helped to fulfil that role. There was some dissatisfaction that, although the federation’s local CCG wanted them to be involved in the STP discussions, they did not fund their attendance at STP-related meetings. The importance of this representation was deemed so great that costs were borne by the federation itself.
Changes over time
A history of collaborative working between practices and respect for federation GP leaders facilitated the federation in representing the voice of general practice locally. Initially, the federation was keen to influence the local health economy as providers rather than as commissioners. However, the federation was seen to support a blurring of boundaries between commissioning and provider functions, which was reflected when changes were made to the shareholder agreement following discussion at the AGM in 2018. Outlawing participation in bodies established by the CCG, it was agreed, would limit the extent of the federation’s impact.
An extraordinary general meeting was held in March 2017 to discuss plans to provide extended access to general practice. In November 2017, the federation’s bid to provide extended access from hub ‘centres’ with an anticipated start date of 1 April 2019 was successful. We discuss this further in Chapter 4.
By late 2017, Embedded had moved to a larger central base to house the growing central team. This move facilitated work on additional projects’ delivery of the extended access service. In early spring 2018, the federation was asked by the CCG to bid for a caretaker contract on behalf of a failing practice. This would strengthen general practice locally by helping make practices more viable and ensuring that bids were not won by ‘private providers’. In April 2018, the federation was awarded an APMS ‘caretaker’ contract role for 12 months. After coming under the federation’s care, patient feedback improved and numbers of registered patients were increasing.
Site C: Struggling
History and geography
This federation occupied the same footprint as the CCG and covered a largely urban area. Although those involved in the CCG saw advantages in commissioning general contracts with a single organisation, others viewed this shared footprint as an indication of the conflicted interests of the federation and its lack of independence from the CCG.
Struggling was initiated through discussions between the CCG and LMC about the best way to deal with the challenges facing general practice (e.g. rising demand, constraints on funding, complexity), which were causing concern for all practices. In addition, the large number of small and single-handed practices in the area, which were thought to be especially vulnerable to these challenges, was an added worry. A core group of four individuals developed the federation: two GPs both with CCG roles, one GP who was also the LMC secretary and an external organisational consultant. There was also substantial input from other members of the CCG, as well as the local authority.
Core aims
The core aim when Struggling was established was to provide ‘higher quality services’ in general practice and promote ‘greater integration’ between primary care and other sectors. Concrete objectives at the outset were to establish a provider organisation and tender for substantial provider contracts, use bulk procurement and other efficiency-gaining activity, pursue quality improvement through development of enhanced services and tackle workforce supply issues (through direct employment of staff on behalf of practices and development of a locum bank).
Structure, governance and decision-making
Structure
Struggling was established in early 2015 as a private company limited by shares, with each member practice holding one share. It was a social enterprise, with a formal commitment for any surplus monies to be reinvested. There was a formal membership agreement outlining the rights and responsibilities of each shareholding practice.
Governance
Struggling had a board of directors, with a management team supporting the work of the board. Member practices elected directors, as well as approving any change in directorship.
In addition, there was a federation governing body, comprising one representative per shareholding practice, intended to meet annually or whenever there were significant issues to discuss. These might include entering into major contracts of work, changes to directorship, purchase or disposal of assets or other major financial issues or plans, and major structural changes to the organisation (mergers, transfers, etc.). This body was not mentioned in any of the meetings we observed and never met during our fieldwork.
Board of directors
This initially comprised three GP directors [chairperson, chief executive officer (CEO) and clinical director] and two PMs. There were two co-opted directors: the LMC secretary, who had been instrumental in the development of the federation, and the head of the city council; throughout data collection, the former attended only one meeting and the latter attended none. Another GP was invited to attend meetings in August 2017, and had attended two meetings by the time data collection ended. The CEO, chairperson and clinical director were all from the south or central CCG footprint, and they had been keen to involve someone from the north for some time; this was one of the motivating factors in inviting this GP. His practice was also very well regarded by both patients and health professionals in the area, and several of the practice partners had CCG roles or sat on neighbourhood committees. He was invited initially on a trial basis, with a view to the potential for creating an additional director post to accommodate him in the future.
Management team
All members of the board were also members of the management team, which met on a weekly basis, with every fourth meeting scheduled as a board meeting (in practice, they were held less frequently). In addition, the CCG paid for a full-time general manager (GM) and an administrator for 12 months. Following this period, the GM left because there were insufficient funds for her to be retained, and the relatively junior administrator took on the role of GM. Other attendees at the management meeting were invited on an ad hoc basis. These included partners or potential partners in projects (e.g. pharmaceutical companies, other providers), external consultants and other paid support (e.g. accountants). Attendance at these meetings was variable, often either the chairperson or CEO would not be present or be late, and often the GPs had to leave the meeting after the first hour or so.
Decision-making
From the outset, concerns were raised by both members and potential members that the day-to-day conduct of Struggling was not in keeping with its formal governance arrangements. The close connection between it and the CCG, particularly the period of time when there was overlapping membership between the CCG and federation boards, had raised concerns among GPs in the area about conflicts of interest (the chairperson, CEO and clinical director had all previously held CCG positions). In some cases, these concerns led to formal requests to the CCG to publish information about procurement processes that had involved Struggling (e.g. procurement of the APMS contracts). Some of the decisions taken by the board (such as pursuing the community services contract, see Progress towards achieving aims) also raised concerns among members, some of whom felt that this should have been a matter for formal consultation with the governing body. These perceived shortcomings led to Struggling’s governance being described by one partner provider as ‘murky’, who also claimed that the directors did not fully understand their own governance arrangements. Similar views were also held by both member and non-member GPs and by CCG members. We observed a degree of informality in the manner in which Struggling operated, involving a lack of rigorous attention to formal organisational processes and procedures (e.g. project management, priority setting, documentation and bookkeeping).
The regular meeting schedule was hampered by the other commitments of the directors. Meetings often required more time than the 1 or 2 hours that directors could give, and workload in the intervening period often exceeded directors’ capacity. Consequently, meeting agendas were often dominated by one or two of several priorities, with little progress made between meetings. However, Struggling had insufficient resources at its disposal to be able to design a sustainable solution to this issue. Furthermore, there was little to indicate that the federation leaders saw this state of affairs as problematic.
Membership and recruitment
All but two of the practices in this area were members of the federation. The two non-members were one GMS practice and one APMS that was run by a third-sector provider. When the federation was established, there had been 12 APMS practices in the area operated by the same private provider. However, between 2016 and 2017, these were retendered: six of them were taken on by a joint venture, involving Struggling in partnership with a local community trust; three were taken by a third-sector provider; and three were taken by one of the Struggling member practices, which bid against Struggling for the contracts (see Progress towards achieving aims).
The large number of small and single-handed practices, some of which were also among the poorest-performing practices nationwide, was one of the challenges faced by Struggling. Although this lay behind its core aim to improve clinical quality across the region, some GPs in the region were concerned that having all practices in the same federation would undermine this aim.
Business model and finance
All joining practices paid a one-off £0.20 per-patient fee to join Struggling, with the intention that this represented a loan to be paid back to practices by the federation out of future surpluses.
Beneath the formal aims of the federation, there existed differences of opinion among the board concerning aims and the means according to which they might be pursued. These differences largely lay between the chairperson and CEO (see Roles and relationships), who embodied very different approaches to general practice (traditional versus ‘corporate’), relating to philosophies of what general practice, and the federation, ought to be.
In addition, the lack of tangible achievements was acknowledged regularly in management meetings with all directors recognising that members felt that Struggling had not done anything concrete for them.
Money was a significant challenge facing Struggling. This was, in part, because of the very low cost of membership at the beginning. In 2016, the CCG invested approximately £70,000 in the federation, which paid for the GM and administrator posts for 1 year. All of the directors worked for free from the outset and, as of September 2017, there were still substantial debts owed to outgoing directors for their unpaid labour.
Owing to the challenges faced with the CCG relationship (see Clinical Commissioning Group) and problems associated with their two largest contracts (see Changes over time), Struggling could not afford to invest in the infrastructure that could support them to win contracts and grow. Without substantial external investment or profitable contracts, it was difficult to see Struggling becoming financially sustainable.
Progress towards achieving aims
Struggling’s approach, which was based on establishing a provider vehicle, meant that it needed to pursue and win contracts to achieve sustainability. It had some early successes, including securing wave one funding from the NHS England pharmacy pilots scheme. It also formed two partnerships to pursue substantial provider contracts: one with the local authority and a local NHS foundation trust established to tender for the community services contract, and the second an alliance with the same foundation trust to tender for the APMS contracts (see History and geography). They had success, with these ventures winning the community services contract and six of the APMS contracts. These were awarded at similar times, in mid-2016, with both of them set to ‘go live’ in April 2017. Planning and mobilising around these two contracts therefore took up the vast majority of Struggling’s time from this point on. However, both these contracts caused substantial problems and, as of September 2017, their accumulated value to Struggling, in terms of becoming an established provider, generating a surplus income or building credibility as an organisation, was very limited (see Changes over time).
Roles and relationships
Engagement with members
As noted above, there was a perceived mismatch between formal roles and procedures in Struggling and everyday practice. One example was a distinct lack of formal engagement with member practices throughout the data collection period. This was acknowledged among the board of directors, with the CEO and one of the PMs regularly complaining of the need for better engagement. This was also acknowledged by members, who felt ill informed and excluded from decision-making. Instead of formal processes, there were a handful of GPs who were trusted by the chairperson and/or the CEO, and with whom informal discussions of plans would often take place and be reported back to board and management meetings. In addition, board members each sat on various committees (PM meetings, community services board) and used these as a forum for discussion and dissemination, as well as the LMC meetings, at which the chairperson was a prominent voice and the LMC secretary an advocate for Struggling.
As part of an attempt to improve engagement, Struggling planned a marketplace event to which all practices were invited. The first, in July 2017, was well attended and the LMC secretary spoke about the worsening situation for general practice and the need, therefore, to work at scale, selling this as a necessary evil, rather than highlighting positive aspects. The chairperson stated that the federation had started to engage with practices to look at the issues that were important to them, but acknowledged that this was a work in progress. He mentioned the APMS success and a planned magazine, as well as conversations with local NHS providers and providing ‘medical leadership’. Rather than demonstrating tangible benefits or support tailored to the immediate needs of member practices, he went on to present NHS England’s 10 High Impact Actions for Primary Care,122 published in November 2016. These are ways of working that have been shown to release clinician time and improve care for patients. Struggling did not offer specific help, instead supporting the view that practices should help themselves by implementing some of these actions. This was in sharp contrast to the concrete examples of federation activity that had improved the experience of member practices given at member meetings in Expanding and Embedded. He then encouraged the audience of busy staff to volunteer to give some of their free time to the federation, which may have felt like adding insult to injury for those assembled in the room.
Another formal attempt at engagement came through the magazine, which was proposed and established by one of the PMs, disseminating information and generating a monthly income via advertising revenues. The first issue was scheduled for July 2017, but as of September 2017 nothing had materialised, and sufficient advertising revenue had not been raised to support its production.
Internal roles and relationships
As outlined, a large part of the success and failure of Struggling appeared to reside with two key individuals: the chairperson and CEO. They were very different personalities with different philosophies of general practice. The latter expressed disappointment that Struggling was not generating large surpluses to supplement practice income, especially as he had encouraged GPs to join the federation based on this assumption. In contrast, the chairperson’s concerns appeared to relate to the long-term best interests of the city and its residents. The chairperson was responsible for a substantial part of the federation’s attempt to develop and maintain relationships with potential partners, and represented it in discussions of STPs, accountable care systems and other multipartner plans. In contrast, the CEO was very outspoken at meetings but did not appear to get particularly involved in federation activity. This became a serious issue when there were open talks about replacing the CEO with someone who could commit the time the role needed. However, given the financial situation, it was not clear how Struggling could attract the right person to such a role, as everyone on the board had been unpaid throughout their tenure. Differences of opinion between the CEO and the chairperson concerning the role and focus of the federation did not tend to lead to open discussion on the topic. The lack of concrete action meant that, during the period of fieldwork observations, these differences could peacefully co-exist, without having to be explicitly confronted. When differences were aired, this often concerned the manner in which Struggling should (or should not) be working with other organisations to achieve their goals, with the chairperson advocating an open and collaborative outlook and the CEO adopting a much more guarded stance. Time constraints in or around meetings in which to work through these issues led to ongoing challenges managing external relationships (see External relationships) and also meant that projects with potential partners were very often stalled in the early stages of development.
Practice managers held formal roles in Struggling. The roles of the two PMs were quite different, given their contrasting experience and knowledge. PM1 had been an NHS PM based in the same practice for many years, and so had a stock of local knowledge. She often played a ‘reality-checking’ role, laying out what would be required operationally for something to happen. She also played a very active role in the mobilisation of the APMS contracts over to the new provider company that was established by Struggling in partnership with a community foundation trust.
Practice manager 2 had much less experience in the NHS, but was sought, in large part, because the board felt that they lacked ‘business acumen’. PM2 was instrumental in developing a strategy around income generation; this involved smaller projects that could be pursued for a ‘quick win’ to boost cash flow. He has also pushed for greater engagement with members, and attempted to bring these two aims together by establishing the magazine.
The directors did not feel that Struggling was at risk of competition for members from other organisations; compared with neighbouring federations in other CCGs, directors saw Struggling as the most developed. However, a competitive threat emerged through the APMS procurement process from within Struggling’s own membership, from a large group practice, which had merged with several other practices to form a super-practice with a list size of approximately 50,000 patients, holding a near monopoly over the city centre population it served. The principal partner of this practice was the outgoing clinical director for Struggling. Following his departure from the board, his practice bid against the federation for three of the APMS contracts and won two of them. This came as a great surprise to Struggling and there were fears among all directors that the practice might desire further expansion, was likely to be a competitive threat on future contracts and might also want to establish its own federation. Struggling did not make any formal changes regarding this practice (i.e. seek to formally exclude them from the federation); however, the CEO regularly expressed distrust of the practice and all of the federation directors expressed caution about entering into specific projects or even discussions with members of this practice. Existing committees on which directors sat (e.g. LMC, practice leads’ meeting, PMs’ forum) were forums for gathering intelligence about what other practices were doing and could lead to possible projects being discussed, with this large practice regularly featuring in these informal discussions among directors.
External relationships
Clinical Commissioning Group
In spite of the fact that the CCG was heavily involved in the early development of Struggling, and the chairperson and CEO both moved across from CCG roles, the relationship with the CCG was not a productive one and it worsened over time. This was in large part due to personal differences between the CEO and the CCG. The CEO stated many times in meetings that he did not trust many of the people occupying CCG roles and believed that the CCG had a particular agenda regarding the federation and what it should be doing. He therefore continually warned against getting too involved in CCG-initiated projects. Somewhat ironically, the external perspective, from some GPs in the region, was that Struggling and the CCG were too close, occupying the same footprint and with almost the same membership; the view of some GPs was that this represented an irreconcilable conflict of interest.
Other providers
Relationships with other providers and potential partners often fell into the same pattern as the CCG relationship, with the chairperson and CEO at odds as to whether or not Struggling should seek to partner with particular organisations, or hold discussions about potential projects with particular individuals. Furthermore, as noted above, when Struggling had entered into formal relationships with outside parties (the community services contract and the APMS contract), these had progressed with very mixed results.
Nevertheless, Struggling attempted to develop and maintain partnership links with other organisations, while potentially competing against them to tender for services. There were two acute provider trusts in the local health economy, which were potential partners in several smaller ventures. The directors feared that these providers would control the emerging STP agenda, and so were motivated to establish and maintain friendly relations with them. At the same time, they could also be in competition with them for provider contracts. The view of the chairperson was that the long-term relationship was the most important thing, and that smaller contracts might have to wait until a city-wide provider partnership had become more formalised. The CEO, meanwhile, held an ambivalent attitude about involvement with the acute trusts. He wanted to see income generated and also believed that pursuing projects with acute providers might be a way to gain influence. However, he was also cautious of what he perceived to be the ulterior motives of potential partners. This mistrust was deemed a significant problem for Struggling by the other directors, the CCG and federation members. The result was that many projects stalled, with the chairperson and CEO, in their different ways, uncertain about how best to balance short- and long-term goals.
The community services contract played a significant role in terms of a provider partnership. The contract had been taken away from the joint venture in which Struggling was involved owing to a decision taken by NHS Improvement, over-ruling the CCG decision to continue with the contract as awarded. The subsequent procurement exercise lasted around 6 months, during which different combinations of providers partnered with each other to bid for the contract and it was unclear to the board which organisational relationships were worth investment of time and effort. Once procurement had been settled, the CCG established a provider alliance involving all the major providers in the area, and Struggling held two seats on this board, alongside acute, community and specialist trusts; the local authority; and the out-of-hours provider. This board was established by the CCG with the intention of bringing providers together to strategically direct provision across the region, leaving the CCG free to focus on commissioning. According to a CCG manager, it represented a significant opportunity for Struggling because, through it, the CCG were asking them to represent all the practices in the region. This same manager started attending the weekly meetings of Struggling, and described a healthy relationship developing between the CCG, the federation and other providers for a time. However, the CCG wanted Struggling to obtain formal approval from its members to be their representative and collective voice through this forum. This sparked a disagreement between the CEO, who was unwilling to do this, and the chairperson. Subsequently, the chairperson resigned from Struggling.
Changes over time
The core aims were reviewed in June 2017. The most significant change to the strategy was prompted by the community services contract being taken away from the partnership in which Struggling was involved, several months after it was awarded to them. The circumstances surrounding this were not made explicit and were beyond the control of Struggling. Furthermore, many members had not fully supported the decision to bid for this contract in the first place. Some thought that this had distracted Struggling from the core aim of supporting and developing general practice. In the chairperson’s view, the management and delivery of community services was central to this aim. He claimed that the community contract was more important than the federation itself, which reflected his prioritisation of what he saw as the longer-term interests of the city. However, it appeared that not everyone on the board (the CEO), the federation (member general practices) or the region (non-member general practices) agreed with this assessment. Therefore, Struggling not only wasted time and effort but also suffered reputational damage through their pursuit of this contract.
The APMS contract was, therefore, the only substantial provider contract held by Struggling and faced significant problems. The company established to manage the contract was seen by many as a top-heavy and essentially conflicted organisation, with too many directors and potentially competing agendas. As soon as the community services bid fell through, the foundation trust, which was a partner in both the community services bid and the APMS practices contract, became very disengaged from this contract, and started reneging on many of the things it had agreed to do, or attaching additional fees to things that were formerly part of the original agreement. When the service went live in April 2017, it was almost immediately reported to the CCG for failing to provide a doctor in one of the practices and, by September 2017, the company faced a bleak financial forecast.
Struggling was subsequently awarded a contract from the CCG to provide an extended hours pilot in collaboration with the local out-of-hours provider. Although this small and brief NHS provider contract could have increased their chances of success when bidding for future contracts, neither the piloted service model nor the partnership was viewed as a success by the CCG or the out-of-hours provider.
As noted in Other providers, Struggling failed to get a mandate from their member practices to represent them collectively, as requested by the CCG. It was speculated by individuals in the CCG and in Struggling’s member practices that this was the result of the fundamental disagreement between the chairperson and CEO about the purpose of the federation and the appropriate means for pursuing this. In June 2018, following the chairperson’s resignation, members concerned about the values of the organisation called an extraordinary general meeting of the board of governors for August 2018. Strong feelings of mistrust emerged towards the CEO and his capacity to lead the organisation in a direction that most members would support. Rather than wait for a federation that would represent them, a large number of practices formed groups and bid successfully for funding to work at scale, in a defined geographical footprint, but on a sub-CCG scale.
Site D: Small
History and geography
This federation was located in a CCG footprint that covered a mixture of urban and rural environments where, for CCG purposes, practices formed groups in three localities. The federation comprised some of the practices in the city centre and rural areas to the north of the city, spanning two (i.e. central and northern) of the three CCG localities. Unlike the central practices, the northern rural practices were mostly dispensing practices. The area covered by Small was much more affluent than those of the other three federations.
Prior to 2012, although some practices had been involved in PBC, beyond this there had been no recent history of joint working across general practice. There was no reported collaboration between primary and secondary care, and board members indicated that the local hospital trust had a reputation for being very difficult to work with. In early 2012, a GP who had been involved in PBC and had a LMC role was asked by the CCG clinical chairperson to talk to representatives of the hospital trust about setting up front-of-house GP premises. Following that, he convened a meeting of the practice leads from the six or seven practices in the vicinity of the hospital and that grew into thinking about a wider federation of which he subsequently became chairperson. A few months later, a Commissioning Support Unit (CSU) representative spoke to the LMC about the NHS Five Year Forward View37 and general practice at scale, which prompted the chairperson to seek a wider conversation involving other practices. There was some hope that there would be a CCG-wide federation, but this did not happen, owing to different views and agendas. In 2013, a group of several GPs who were keen to pursue working at scale met, with membership of this steering group dwindling over time. Fears about the future sustainability of general practice and the attraction of safety in numbers meant that two of these GPs continued to meet and became the driving force for establishing the federation.
Core aims
The core aims were to ensure high-quality care and the sustainability of member practices. This would be achieved by developing a supportive federation, helping practices to take control of their futures and remain independent, but providing access to development opportunities afforded by working at scale.
Structure, governance and decision-making
Structure
Small formed as a legal entity in July 2014, being established as a private limited company issuing a £0.01 share to the chairperson as an expedient measure.
The federation board periodically discussed options concerning changing the legal status of their organisation (such as limited company and limited liability partnership models); changes would have implications for accountability and governance. However, the issue was deferred and it was agreed in June 2018 that having more time to evolve and experience the changing landscape would be helpful before making decisions about this.
Governance
Board of directors
Small’s board had three executive and three non-executive director positions, in addition to the chairperson. Board members could hold office for a 3-year term, with an option to stand again if they wished. They needed to be proposed and seconded and then approved by members at the AGM. The federation’s clinical director post was filled by a GP who had worked in the area for many years. The other board directors were a FD and a director of operations, both of whom were also PMs whose practices received sessional payments for their input. A patient representative was appointed to the board in 2017 after a formal interview process. However, she was not replaced when she resigned after 1 year because of health and family issues.
The frequency of meetings changed from monthly to quarterly in 2017. This was due to an increasing awareness of the board workload, the need to get practices more engaged with the federation, a perception that practices should be involved in agreeing priorities as well as implementing agreed activities, a need for more transparency and accountability concerning federation activity and the costs of remunerating board members and running the federation more generally. Board members’ remuneration also changed, at this time, from one session per week to being project based, with agreed sessional activity.
Member organisation leads
Each of the member practices nominated a lead GP to represent their views at member organisation leads’ (MOLs’) meetings. These meetings were described, at the start of data collection, as ‘dysfunctional’ and were held sporadically. Observation of one of these meetings in April 2017 saw board members challenged on a number of issues including a failure to engage more closely with member practices. In addition, attendees complained about a mismatch between their priorities and those of the board. The views expressed at this meeting may have contributed to the changes to governance agreed at the June board meeting (described above), putting MOLs in the driving seat. This revised role for MOLs resulted in changes to the way that the meeting worked. Starting in the summer of 2017, MOL meetings became regular monthly events and included a GP partner from each member practice, and often also a PM. There was also a declared emphasis on keeping formal records of meetings and sharing these minutes to promote greater transparency and accountability.
In spring 2016, one of the PMs who had been working with Small filled a newly created post of CEO. This was initially for 2 days per week from April, and subsequently increased to 3 days in November. He had presented the business plan and related priorities at the April 2017 MOL meeting, which had not had a good reception. The poor financial position of the federation meant that this person was employed on a rolling monthly contract and the post was abolished after he left in June 2017.
Revised governance structure
In June 2018, a revised governance structure was formally agreed. This was intended to reflect the new way in which the board was working following changes agreed in 2017. The board’s oversight role and duties entailed managing the federation by:
-
setting the overall strategic direction in the context of NHS priorities
-
regularly monitoring performance against objectives
-
providing effective stewardship by ensuring value for money, financial control and financial planning.
In addition, a proposed structure was agreed that involved the creation of subcommittees of the board to cover finance and performance, quality and safety, workforce and development, and estates and technology, and meeting every 6–8 weeks. There was a planned audit committee, which would meet every 6 months, and a remuneration committee, which would meet annually.
The revised governance structure included an increased allocation of 104 hours per annum for the clinical director, as well as 48 hours for the chairperson, reflecting the workload related to these posts. In part, this demonstrates the growing workload associated with new projects. However, this intended structure had not begun to be implemented by the completion of the fieldwork, nor had routine functions of minute-taking or appointment of an administrative contact been resolved.
Decision-making
During MOL meetings, during which key decisions were made, the approach was to ask each person in turn for their opinion to enable every practice representative to give their views. A member of each practice had to be present for the AGM to be quorate and all practices were usually represented at MOL meetings.
Membership and recruitment
This was the smallest of the case study federations, initially comprising 10 member practices with around 96,000 patients. Approximately half of the federation practices’ patient population were registered with one large practice in the city, which was formed when six practices merged during 2016–17. The initial board chairperson was a partner at this practice.
One practice left in 2018, citing discontent at the failure of Small to make faster progress, and unfairness about the time invested by some practices compared with others. In March 2018, the chairperson (from the large practice) announced that their practice had applied to join the local ‘predatory’ federation (see External relationships) and a due diligence process was under way as part of their application to join that federation. The decision was prompted by the CCG’s expressed intention to move towards a locality-based commissioning model. This process of leaving the federation could be delayed by the due diligence processes. However, the federation chairperson stood down in April 2018 and a replacement chairperson from another of the member practices was appointed on a temporary basis before being elected unopposed at the subsequent AGM.
Business model and finance
As a one-off joining fee, practices contributed £0.50 per patient, plus £1.50 of the £5 per-patient ‘PMS [Personal Medical Services] premium’ funding that they all received in 2014. The CSU provided funds for management consultancy in the early phase of development and a pharmaceutical company provided £10,000.
Business objectives for 2016/17 covered a range of issues. Training and research objectives were reported as having been achieved in the business plan produced for 2017–20. However, objectives concerning co-ordination of back-office functions and adherence to best practice (e.g. in Quality and Outcomes Framework targets) were taking longer to progress. The 2017/18 clinical objectives concerned ensuring that patients could have timely access to primary care services. This would involve extended access and the federation would undertake to provide this. Financial objectives included establishing independent regular income to support board and related federation activity. In addition, working with the CCG to identify gain-share models was a key component of their anticipated income. An objective of working together to share resources and build economies of scale was also included. No detail was provided on how these objectives would be achieved.
Data collection started in April 2017, when the financial position was worse than projected and causing stress during the MOL meeting. By November 2017, funds were sufficient to meet only 1 month’s expenses. However, there was hope for an improvement to the financial position, owing mainly to income due from other sources, in particular the prescribing scheme (PS) project (described in Progress towards achieving aims).
Progress towards achieving aims
The partners representing member practices viewed themselves as having shared values and a consultative and collaborative approach to federation working. They contrasted their approach with what was referred to as another ‘predatory’ local federation (see External relationships). The very large practice had been formed as a result of merging a number of struggling city area practices, and several smaller member practices expressed an interest in pooling back-office functions and working in a more joined-up way. However, pooling risk and income has implications for autonomy, and practices with no staff recruitment problems had much less appetite for giving up existing independent practice arrangements. Although most federation members expressed no desire to grow the organisation in terms of size, some were interested in federation models that entailed working in a more merged way. Small’s original chairperson had had discussions with one of these organisations, on behalf of the large merged practice, where he was a partner, because they were struggling with the poor relationships with neighbouring practices. He proposed that Small’s northern practices should consider merging, because this had resolved issues at his own practice. Despite the two camps (those leaning towards merger and those seeking to retain their independent practice status), these differences did not cause tensions. The focus on specific projects and being adaptive in a changing environment meant that discussions and decisions about this issue could be, and were, deferred on an ongoing basis.
Small successfully negotiated the PS project with the CCG on behalf of its members. The PS involved meeting specific prescribing-related key performance indicators to receive financial rewards for reinvestment. The PS was described as a ‘no brainer’ that would save money and provide a source of income to enable sustainability. Without this, it was difficult to see how the federation would have been able to continue, other than by relying on unpaid volunteers. Another incentive scheme involving GPs providing more information with referrals added modest support to federation expenses and practice income.
Roles and relationships
Engagement with members
Engagement with member practices was initially reported as patchy. Resentment was expressed at MOL meetings about the large merged practice ‘doing its own thing’ and not collaborating with the others. However, the regular MOL meetings and a more strategic role for the board resulted in greater involvement from member practices. In addition, the federation initially held ‘time-out’ events during which practices were closed for an afternoon and all staff in federation practices came together to focus on training.
Internal roles and relationships
Practice managers were formally involved to varying degrees. The original plan was for PMs at all member practices to contribute 10% of their time to developing and running the federation. Several PMs were allocated responsibilities for certain areas, whereas others took responsibility for work streams, such as procurement, training, research and data quality. Over time, it became apparent that some PMs were contributing more and were more engaged with the federation than others.
At the large merged practice, a CEO, who had led the practice merger, oversaw the organisation. This individual lived outside the region and used well-developed networks to act as a boundary spanner, bringing knowledge from elsewhere to discussions and the decision-making process at MOL meetings. Having space to think beyond the immediate operational issues meant that this individual often explained the wider and longer-term importance of issues under discussion at the MOL meetings. Although not a clinician, this individual appeared to command the respect and trust of the MOLs.
Small’s FD was from a traditional practice management background and drew on prior experience but was less aware of making strategic decisions about future directions in a changing landscape. For example, whereas the FD recommended the reappointment of the existing accountancy firm, the CEO suggested an alternative firm, which was more in tune with the changing needs of general practice organisations, as well as being cheaper and of higher quality. Despite their very different styles, the two individuals worked well together leading the negotiations around the PS with the CCG, and together they established contractual terms for the PS, which would also apply to other federations signing up to it in future.
External relationships
Other federations
There was one other relevant local federation whose members were located mainly in the city centre. Board members described this federation as ‘aggressive’ and ‘predatory’ and suggested that this federation had a history of taking over practices, poaching staff across the city and offering high salaries but then moving people off NHS pension entitlements. Small’s board GPs expressed their disapproval of what they considered to be a very different philosophy to their own and some discontented practices had left the other federation to join Small. There was increasing pressure from the CCG for general practices to collaborate at locality level, which raised questions about whether or not federations should be based on a locality footprint. However, federation members preferred to join with like-minded people, which would not preclude working across a locality footprint with non-federation members, if required. Like-minded appeared to be based on negative views and experiences regarding the leaders of the ‘predatory’ federation. There had also been an attempt (driven by some GPs) to form a local clinical federation that would give a stronger, unified, general practice voice across the whole CCG, driven by a need to respond to the transformation agenda. The clinical federation was created as a legal entity in September 2016 and most practices in the CCG agreed to sign up. However, the clinical federation was officially dissolved in May 2017, for reasons including a lack of dedicated posts/resources, lack of clarity regarding roles and differences in approach between and within practices. The CCG had set up a new Local Enhanced Service (i.e. a local scheme of additional services provided by GPs in response to local needs and priorities). The clinical federation developed shared clinical protocols and jointly purchased new equipment, and appeared to be moving towards contracting with general practice as a single provider organisation across the area, but lack of a cohesive approach contributed to its demise.
Clinical Commissioning Group
Relationships were complicated by the clash between the CCG’s desire for localities, based on geography, and the federation’s approach to membership, based on like-minded practices. Various federation members had contacts at the CCG, with whom they would liaise on relevant issues, reporting to MOL and board meetings. Individual relations were cordial, but CCG announcements about preferred locality models, which sent the large group practice to investigate joining another federation, created anxiety for federation members, especially as this had come as a surprise. In terms of the CCG’s approach to communicating with general practice more generally, given the diversity of views across the CCG footprint, instead of one or two people being able to represent general practice as a whole, federation members felt that a member of each federation needed to be at CCG-organised meetings to defend their interests. The issue of engaging with stakeholders such as the CCG was a point of discussion at federation meetings. Initially, GP board members expressed resentment and frustration about the number of meetings they were expected to attend, although, over time, MOLs became fairly sympathetic to this, recognising that they would need to participate.
Changes over time
After the initial phase of establishing the federation as a legal entity and agreeing a rationale, Small shifted to become a more project-based organisation. The changes to governance structures and the revised role of the MOL meeting in 2017 seemed to be a turning point, with practice leads becoming more engaged in the decision-making process. Greater emphasis was placed on bottom-up input via the MOL group, which had representation from each member organisation. The MOL functions were strengthened and this was intended to move from a communication forum to being the driving force for Small’s activities. On paper, at least, efforts were being made to create structures and promote norms of lateral co-ordination, giving voice to the diverse organisations comprising the federation, but simultaneously placing an obligation on members to participate more actively in federation processes. This development was motivated in large part by what the original federation chairperson viewed as a dysfunctional MOL group, which complained about problems, expecting the federation to solve these on their behalf. Under these new arrangements, the MOL group was to take responsibility for decision-making and implementation. Rather than viewing the new rules as either constraining or empowering, these can be viewed as offering the potential to do both. However, the arrival of the new chairperson meant that, although MOLs became more involved in decision-making, the meetings were largely reactive, rather than MOLs driving change in a proactive manner. Initial concerns about money diminished following the success of the PS, which was rolled forward into 2018/19. For a long time, there was no intention to engage in tendering to provide services. However, the issue of ensuring extended access to meet the October 2018 deadline signalled a change in approach from small-scale projects to generate revenue to taking a more strategic view of the future of general practice. This meant competing for services as part of a process of seeking to secure control over the environment in which federation practices operated in the medium and longer term.
The departure of the chairperson during 2018, together with the need to create shares for all member practices, meant that changes were made to the shareholding arrangements. It was agreed at the AGM in June 2018 that all practices would hold a £1 share, whereas the sole shareholder had been the chairperson prior to this. The original shareholding reflected a pragmatic and expedient measure, and the intention was to put this on a more formal footing, reflecting the equal stakes each practice had in the federation. However, it was many months before this was actioned owing to the heavy reliance on staff employed by member practices, who had little time to do this.
The distinction between small practices, keen to pool functions and reduce their vulnerability, and larger practices with different goals surfaced at meetings, but the new chairperson dealt with these by narrowing the scope of the discussion to focus on the PS. Her position as a partner in a large practice, which had no problems recruiting staff, partly due to its location in an affluent and picturesque area, appeared to influence her attitude. Disinclined to take on risk for her medical practice, she habitually deferred discussions about sharing staff and merging functions.
In terms of the PS, dispensing practices were not inclined to change their prescribing approach as this would reduce income from dispensing medication for their practice. Most of the work to generate savings was undertaken by the single very large practice, yet the money was shared between all practices based on patient numbers, rather than effort. Little time was spent on scrutiny of performance and there was no discussion of non-compliant practices. The large practice was reluctant to leave and join the competing ‘predatory’ federation, with whose members it had more in common in terms of geography and patient characteristics, owing to distrust of that federation. This distrust was compounded when, having approached the ‘predatory’ federation, it was informed that, as a latecomer, its membership status would not be on an equal footing with original members. This suggests that its apparent commitment to Small was based on distrust of the alternative and a defensive reaction to the threat it was perceived as posing, rather than solely a positive commitment to Small.
Comparing and contrasting sites’ approaches
All the sites developed formal structures and governance processes and all were engaged in initiatives intended to generate income. All sites used a mixture of direct and indirect resources as a means of conducting federation business, but at Small this changed to a complete reliance on direct resources. There were also differences in terms of the obligations of member organisations. In only one site, Expanding, were directives designed and introduced, which had a substantive impact on the working processes of member organisations. These working processes had major implications for interdependence. At all sites, member organisations felt pressured in a context of rising workload and staff shortages. Expanding’s response was to attempt to reduce the operational burden on members, but in a way that had major implications for dependency relationships in the MO. It promised to provide efficient, centralised processes and systems relating to accounting and payroll, the intranet system and staffing solutions. To facilitate this, all member organisations were required to switch to using the standard federation systems and related software as a condition of membership. This approach was agreed in the early stages of formation with the decision made by a small number of Expanding’s board and executive team members. This formed part of the offer to prospective joiners, so that they had to accept these terms, or choose not to join. There were other competing federations in the area, which meant that prospective members did have a degree of choice. This may have reduced the potentially negative effects associated with directives in MOs. 107 Initial members endorsed the central team’s decisions, but the process can be viewed as one of hierarchical decision-making, albeit in a context of responding to member concerns. Furthermore, this decision was taken after a number of relatively large and important organisations had decided to join. This is likely to have had a ‘threshold effect’,107 facilitating recruitment but also making membership of competing federations less attractive. At the same time, this top-down requirement allowed member organisations to benefit from the production of shared information, which enabled them to begin to understand how they compared with other member organisations. Compliance was not achieved overnight, but it was monitored and discussed on an ongoing basis. It is easier for existing members to break MO rules than for relatively recent joiners to do so,107 but considerable support was provided when member organisations needed this. New member organisations, which achieved compliance quickly, raised the possibility of sanctions for non-compliance. After protracted discussions, it was agreed that this would be undesirable. By the end of the fieldwork, all but four member organisations were fully compliant, with these four working towards compliance.
In Expanding, vulnerable practices were supported by adding doctors from other member organisations to their business contracts. This meant that there was a commitment to cover absences when such absences jeopardised the survival of small practices. This was presented as an opportunity and a triumph of partnership, even though the immediate benefits were for some smaller practices only, with larger ones taking on risk. The willingness of member organisations to accept a degree of risk may be because membership goes beyond self-interested aspects of the federation to include a normative element. In Expanding, there was a high degree of engagement with the STP process, reflecting its expansive gaze in terms of geography and timelines. The ‘bigger picture’ perspective adopted by the federation meant that it engaged in formal collaboration with other stakeholders in the broader STP footprint, as part of a process of attempting to create the future, rather than merely responding to it when the time came. This meant that, early on, it recognised the importance of investing time and money in activities to support members, in a proactive manner. Rather than seeking to solve their immediate problems, the federation’s attention to national policy goals and direction enabled it to work with member organisations to bid for central funding to facilitate them to work at the subfederation level within a defined geographical footprint to develop their capacity to support each other.
In contrast, at Embedded, a surplus was distributed to member practices, reducing their membership fees, rather than investing in a development fund for the future. This meant that member organisations received funds, providing a positive benefit in the immediate present, but this approach also meant that less time was spent on encouraging the growth and capacity of groups of member organisations at the subfederation level. In Embedded, there was a history of joint working between health and social care across a number of Local Delivery Groups. These footprints could form the basis of new PCNs, but, at the federation level, there was limited discussion of this issue because the focus had been much more on establishing and maintaining the federation and supporting member practices. In addition, as part of its supportive approach, at Embedded, the federation stepped in, acting as a ‘caretaker’ by assuming responsibility when a medical practice failed and no other local doctors were interested in running it. Furthermore, in a context of unequal provision between practices in the city, the federation also agreed with the CCG and some member practices that they would offer additional services to patients across the city to ensure that all patients covered by the federation received a minimum standard of care. This was welcomed by member organisations because it expanded service provision and enabled practices to refer to these new services. Rather than creating expectations of practices, its approach was focused on supporting them by attempting to solve the immediate problems they faced.
In Struggling, at a meeting of all members, the chairperson focused almost entirely on threats to the well-being of the city’s residents, with little concrete action on tackling the problems faced by member practices.
In Small, a new chairperson dealt with the issue of vulnerable practices by narrowing the scope of the federation in terms of her steering of discussions. Her position as a partner in a large practice, which had no problems recruiting staff, partly owing to its location in an affluent and picturesque area, appeared to influence this attitude. Disinclined to take on risk for her medical practice, she deferred discussions about sharing staff and merging functions, whenever these arose. Instead, the focus was on the PS. Most of the work was undertaken by the very large practice, yet savings were shared between all practices, based on patient numbers rather than effort. The reliance on indirect resources meant that there was little time for scrutiny and almost no discussion of non-compliant practices.
Comparing sites: what drives differences?
The different styles adopted by federations (ranging from clear expectations to change systems as a condition of membership to arrangements that involved much more distant relationships and little engagement) were important in explaining the activities and structures that characterised federations. We elaborate on this further in Chapter 4. In addition, there are a number of other factors that explain differences between the sites. It is clear that the historical context of each of the federations was different and had implications for what followed. The extent to which there had been prior experience of general practices working together varied between sites, as did the prior relationship between practices and the CCG. Although federations could not change the historical context, there were several other factors over which they had varying degrees of influence, which acted as important drivers influencing the operation of GP federations. These were the relationship between the federation and the CCG, the extent of competition between federations locally, money, size and geography, and leadership and management.
Comparing the four sites, Embedded appears to have enjoyed the strongest relationship with the CCG. This is partly reflected in the degree of financial support given to the federation by the CCG. It is also evidenced by the CCG’s transparent approach to discussing forthcoming tenders enabling Embedded to be ‘tender ready’ when these were announced. The size of the federation, with a relatively large number of practices in one compact geographical area was also helpful. Therefore, the income generated from member practices was substantial relative to Small and Struggling. Unlike in Expanding, there were no costs incurred in travelling relatively long distances to conduct federation business in regions outside the core federation footprint. The income generated from members was important symbolically in terms of signalling their commitment and support. This contrasts markedly with Struggling, where income was non-recurrent and represented loans rather than a membership fee. Furthermore, the money facilitated capacity-building, enabling the evolution of a federation workforce adapting to its external environment. In terms of leadership and management, the fact that the chairperson of Embedded was a well-known and respected GP in the federation footprint appeared to help consolidate member support. Colleagues described him as ‘intelligent and articulate’ and recognised that he used his own experience but, importantly, canvassed others to ensure that the federation provided what its membership required to sustain general practice. In addition, the COO had a background in practice management and organisational development. This provided a good understanding of the issues faced by general practice and, importantly, meant that she had developed relationships with many PMs around operational issues.
Offering some degree of contrast, Expanding’s CCG was characterised by a different approach and the relationship, although still functional, was not as close as with Embedded. This appeared to relate, in part, to competitive tensions in the region. When Expanding was first established, there were other existing GP federations in the area. This contributed to an approach within Expanding to develop their own business model as something different from what was already on offer. It also appeared to make the CCG much more guarded about pushing particular projects towards Expanding, or otherwise acting in a manner that might be construed as favouring one federation over another. Partway through data collection, the CCG started working with neighbouring CCGs through ‘Joint Committees in Common’ across larger STP commissioning footprints. Although this appeared to reinforce the formal nature of the relationships, it opened up opportunities for federations to come together to represent general practice provider organisations. The constituent CCGs remained as formal entities, but staffing changes affected ongoing relationships between the federation and the CCG. The influence of money as a key driver in Expanding’s activities was illustrated by their desire to grow the federation to cover running costs. Money was also linked to the issue of leadership and management, as the recruitment of a very senior and relatively expensive MD was based on the availability of a particular individual with relevant skills, knowledge and local networks. The MD’s experience of operating in a high-level, strategic role was unusual compared with the experience of other federation managers. Expanding was the only federation to employ a person in this role, albeit part-time, this reducing as the other two officers, the COO and FD, who, like the MD, had substantial experience in the acute sector, were recruited. The COO, in addition, had some programme management and primary care integration experience. As more people were required to deliver the requirements for the federation in Expanding, there was a reliance on agency staff, although short-term contracts meant that there was a loss of learning in some areas. This contrasts with Embedded, where staff joined the central team in a part-time capacity, increasing hours as required and being transferred onto new projects once they arose.
In terms of size, the population covered by practices in Expanding was very similar to Embedded. However, it was much more dispersed, as the membership comprised two discrete geographical areas. This had cost implications. Rurality was a particular issue for one of the geographical areas in Expanding, which made working together more difficult. Attempts to provide similar levels of engagement across federations meant that board members had to travel long distances, adding to the time lost from clinical work. Unequal density of practices involved in the federation made it difficult to develop consistent approaches locally: issues and interests of dispensing practices had not been encountered previously in the city practices.
Of the four sites, Struggling appeared to have the least productive relationship with the CCG. The business model with which Struggling proceeded was not dissimilar to Embedded: pursuing contracts as a means to generating income and developing a portfolio. However, the differences in the relationship with the CCG were an important factor here. Struggling did not take up pieces of work suggested by the CCG, but rather went for two much more ambitious provider contracts, both of which created substantial problems for them. Our data indicate that the struggles faced in this site stem, in part, from the poor relationship with the CCG, combined with the degree to which the fortunes of the federation appeared to be very dependent on two individuals. The personalities involved and, in particular, the perception of the CEO as being out of step with the views of the rank-and-file membership were very important in explaining why events unfolded as they did. Money, particularly the lack of it, was a key factor explaining Struggling’s relatively poor performance. Unlike the other federations, which had several sources of income, Struggling was reliant on winning big contracts, with no plan B in the event that these failed to materialise.
Although the relationship with the CCG in Small was not as bad as in Struggling, it was complicated by the CCG’s focus on its own internal problems. The CCG’s relatively poor performance on key indicators resulted in much greater external scrutiny of its management and operations generally. In addition, the existence of more than one GP federation within the CCG footprint meant that the CCG had to spread its efforts at engagement across all three federations. Relationships between Small and one of the other federations were poor, and Small decision-makers were critical of any behaviour on the part of the CCG that they perceived to be favouring the other federation. The CCG’s approach, focusing commissioning around localities, was problematic insofar as Small’s membership crossed the locality boundaries and overlapped with one of the other federations. However, there were clear difference between the two (urban and rural) localities in terms of health needs and service provision. These were seen by a number of people, including some federation personnel, as supporting a configuration based on localities rather than a shared ethos. Leadership issues were important: participants described personality clashes between GP leaders in the central locality as the reason for the failure to create a unifying single federation for the locality. When one of these central locality GPs stood down as federation chairperson, his replacement, a GP from a northern locality, was much less inclined to favour practice mergers. Furthermore, the former’s involvement with the CCG and his strategic focus contrasted with his successor’s greater focus on local operational issues. As with all the federations, money was very important for a number of reasons. At one point, the federation looked as though it could not continue as a result of the absence of resources to enable it to remain a going concern. It had been forced to let its CEO go and it was only at the 11th hour that the success of the initiatives to generate income managed to turn its fortunes around. Size was important because the federation needed sufficient members to generate the overhead to fund staff. This meant that, despite the mismatch between the rural and urban practices, it was heavily reliant on the large urban practice, which generated much of the income for redistribution to member practices, to provide central funding. Small’s size meant that income from membership fees was low and, following the CEO’s departure, it was totally reliant on indirect resources, which led to staff prioritising the business of their host organisation. This meant that its governance and accountability processes were weak in terms of implementation of formal structures and procedures.
More generally, being based in a relatively affluent area was cited by some participants as historically having cushioned practices from issues associated with high levels of deprivation and struggles to recruit staff. Although not enjoying the economies of scale of larger federations, the small size was beneficial in that it enabled engagement and discussion in a way that was very different from the other sites, where the number of practices was much larger. There was also less attention paid to selling the benefits of membership to members both at the AGM and MOL meetings than at some of the other sites. This is understandable because member practices were all part of the MOL decision-making process in a way that did not occur in any of the other federations.
Conclusion
This chapter has provided in-depth descriptions of the cases, including formal structures and processes and the operational realities of these. We also compared sites identifying drivers, which explain some of the differences between the sites. Chapter 4 expands on this, examining in more detail how staff at the sites worked together.
Chapter 4 Working together
Introduction
In this chapter, we examine in more detail the issues facing the federations, focusing mainly on interaction and relationships with members, as well as discussing the views of clinicians and PMs. We describe complex and varied motivations of GPs and PMs regarding membership, as well as contrasting approaches to the IAGP policy. We describe three types of activity for managing interdependence: directing, engineering and co-producing. We also describe an emerging typology for categorising federation styles and use this to categorise each of the federations.
Motivations for joining the federation
Much of the information in Chapter 3 was derived from observations of meetings and interviews with members of the federation central authority. Among those interviewees and meeting attendees, fear of the future and a feeling that things could not continue as they were provided an impetus for action. With regard to motivation for federation membership, views of general practice as being under threat and of GPs being fearful of the future were universally shared. These were motivators for joining, but a variety of reasons and expectations of the federation were mentioned in interviews. These included the appeal of a collective voice, a sense that federating was the ‘direction of travel’ and that it would be advantageous to join rather than be left out, and a need to build security and resilience to ‘future-proof’ general practice. We discuss these issues further in the following sections.
Vulnerability and collective strong voice
General practitioners (each identified by site and a numerical identifier, e.g. ‘Struggling, 15’) spoke about the initial attraction of ‘strength in numbers’ and the associated power and authority this could bring, enabling them to cope under growing pressure in a context where they felt very vulnerable:
. . . sit at the same table and talk with the same power [as a foundation trust] . . . that then enables you . . . when so much more of the direction of care is going to be out in the community, it’s going to have to be, that all seems entirely appropriate that you’re going to need someone to deliver that care.
GP, Struggling, 15
. . . a collective voice . . . empowering the discussions that occur within a health community, around a whole range of things. It’s one of the things that primary care lacks, because individual general practices are relatively tiny, and there’s an awful lot of them, so you can’t listen to all of them.
GP, Embedded, 39
Linked to this motivation was self-preservation, as this GP from a small practice explained:
We just thought that if some problem arises . . . We took it as a precautionary measure . . . If something goes wrong, you’ve got a backup.
GP, Embedded, 33
Motivations of self-preservation were not exclusive to those from small practices, however, as the following quotation illustrates:
If the federation fails and a lot of those practices go under, then those patients then end up coming onto someone else’s doorstep, which is probably yours. Which, from a self-interest point of, that actually it’s trying to prevent a catastrophe.
GP, Struggling, 15
Direction of travel and fear of missing out
For some GPs, federating was viewed as the obvious next step for general practice and it was preferable to be involved in this process and any decision-making early on:
. . . for me, anyway, there was a certain amount of ‘it’s something that we’re all going to have to do, it’s the future’ . . .
GP, Struggling, 20
Some GPs had been motivated to join because of a sense of urgency that they might be missing out in some way if they did not sign up:
I guess one of the anxieties was . . . if we weren’t involved with something, what were we missing out on?
GP, Small, 17
However, one GP stated that, with hindsight, it would have been more advantageous to wait and observe what the federation actually achieved, rather than joining right at the start and making the financial commitment:
[Joining late] was the right thing, in my opinion, because what we paid initially for 1 or 2 years . . . nothing happened with that money.
GP, Embedded, 33
In contrast, a GP from Struggling, where the financial commitment was small, explained that involvement was considered to be low risk, with little personal sacrifice:
Well, my perception personally is that it’s always better to be involved in conversation than out. And actually, you’ve got nothing to lose. If you throw yourself in there and try and direct it and have a say within that as well, even better.
GP, Struggling, 15
Realisation of benefits
Several GP interviewees expressed frustration at what they considered to be a lack of progress by their federation. Some attributed this to an absence of clear vision and strong leadership at the outset. Others felt that the benefits for members of joining had been overstated. Several were more ambivalent about a lack of tangible benefit and expressed a feeling that, over time, potential benefits may be gradually realised. In their discussions of these benefits, the three key areas discussed by GPs were return on investment, impact on workload and improvement of standards.
Return on investment
Return on investment was a greater concern for the Expanding and Embedded GPs, perhaps because, in these two sites, an ongoing financial commitment was required. Several interviewees from these sites expressed frustration about a perceived lack of return on investment:
I think the amount of money that we’ve invested . . . we haven’t had a great return . . . [it] still seems to be quite limited.
GP, Expanding, 22
We ask ourselves, ‘what are we getting in return for the shares that we have?’ . . . And at the moment, I struggle to count a single one for a practice like ours.
GP, Embedded, 34
There was a perception among some GPs that the work of the federation could be more financially beneficial for smaller practices or those struggling with resources and/or performance levels. For example, one GP felt that the investments made by the federation had been directed towards practices with greater needs:
. . . the schemes they put in haven’t been relevant to our practice . . . to be fair . . . they have invested in receptionist training and triage and stuff like that. [But] for our particular practice it didn’t make sense, we do a lot of that anyway.
GP, Embedded, 22
A GP partner from a small practice in Embedded, whose practice did not have the resource or space to be an IAGP provider, also stated that their return on investment had been ‘very good, so far’ (GP, Embedded, 32) owing to the federation’s support with improving access provision. In contrast, however, another Embedded GP from a different small practice had felt unsupported by the federation regarding their request for help arranging cover for their practice during half-day closing (‘the [federation] had been unable to do these types of things’; GP, Embedded, 33), and had independently arranged this with local practices instead. This GP appreciated that, as the small practices had differing needs, the federation was not able to solve all of their issues.
Some practices appeared to take a more pragmatic approach, balancing the savings over the costs, which varied according to practice size. In Expanding, PMs were very aware of the impact of federation membership, as they were often the people at practice level dealing with the switch to new standardised systems for finance and payroll:
. . . we have to pay our [subscription] money, but we have had quite a lot out, because we’re not paying [licences] for the accounts or the wages and we’re not paying the accountant anymore.
PM, Expanding, 15
However, changes in government policy diminished the benefits of membership:
A lot of the things that were selling points, originally, didn’t come to fruition, because they said, ‘well, you’ll only have to pay a fraction of your CQC costs’. But then the government decides that they’re going to refund them . . . So, that was one area, we were going to save £6000 or £7000 there, but actually we haven’t because we’ve got them back anyway, without joining.
GP who did not join, Expanding, 13
When GPs raised questions at AGMs, these tended to relate to immediate pressures and practice operational problems. One GP, when interviewed, was relatively unusual in criticising their own practice, which chose not to join the federation, for being too ‘focused on the transactional part’ (Embedded, C39) and not enough on the strategic view and aims of the federation. However, the fact that they had held CCG and PCT roles and had retired by the time they were interviewed may explain this perspective. At Struggling, one GP, who also occupied a CCG role, expressed frustration about the failure of the federation to help practices work together:
It’s been more about ‘how can we make this a successful business organisation?’, rather than ‘how can we federate in the true sense or collaborate to support collaboration?’ . . . There’s loads of things that we want to do . . . would be really good to be able to say ‘we want to collectively employ an immunisation nurse . . . can the fed[eration] help us to do the technical bit of that?’ To help us to work together more effectively.
GP, Struggling, 20
Impact on workload
The impact on workload was described most acutely by GPs from Expanding, and mostly in relation to the effect that the federation’s centralisation approach had had on practice management workload. This is perhaps understandable, because Expanding was the only site that required practices to modify their systems and behaviours. Mixed opinions were expressed by GPs from this site about whether this approach had reduced or adversely affected workload:
. . . managing all the paying of the staff and things like that was going to be a big help for the practice, but . . . it’s all gone back to really old-fashioned software to do the wages that no-one was using anymore. So, it’s been a big headache.
GP, Expanding, 29
The most positive things have been from the management and admin[istration] side of things. And our practice manager had a lot of positive things to say about how it has changed her workload and things like that.
GP, Expanding, 34
Comments were made by PMs about the difficulties in adopting new systems and the lack of reimbursement for some tasks, which they felt compelled to undertake in their own time:
. . . I don’t think they quite realise how much work they gave the practice managers . . . I understand why they’re doing it, everything’s centralised . . . but once you get used to it, it’s fine.
PM, Expanding, 15
At Expanding and Small, the tight time scale for implementing the IAGP policy meant that PMs often had to work additional hours without being reimbursed for this:
. . . I’m having to absorb work within my core hours and then pick up my core hour work at home . . . We have to launch [IAGP], we’ve got no choice . . . and whether I’m funded to do it or not is irrelevant, it just needs to get done . . .
PM, Expanding, 31
Furthermore, at Small, because the model was based on PMs giving 10% of their time, there were impacts on their workload. For several PMs, this input was important and valuable, although the workload and related effort was not evenly distributed across practices, which did not go unnoticed:
I know in one or two cases, the [Small] board have spoken to the partners of the respective practices where that’s been the case, but there hasn’t always been a great improvement . . . we accept it a little bit, I suppose . . . in any team, you’re probably always going to get those that end up being carried a little bit.
PM, Small, 09
Improving standards
The aim of improving practice performance standards and failure to achieve this was mainly raised by GPs from Struggling:
. . . one of the hopes of the federation was that it would raise standards within general practice and that hasn’t been the case.
GP, Struggling, 06
There was a perception among GPs who saw their practices as performing well that the federation, rather than tackling poor performance and recognising that some practices in the area were unsustainable, acted to maintain the status quo:
. . . this is sometimes where I’m worried that the federation might be a little bit of a blocker, is that if there’s unsustainable practices, businesses, that are running things there, and they’re not changing . . . if it offers that resilience without being progressive and without encouraging people to be dynamic and make changes, then it actually keeps us in a bit of a status quo for too long.
GP, Struggling, 15
There were mixed feelings in Expanding on the benefits of supporting weaker practices that might join the federation. The MD and several board members expected centralised systems to play a role in improving the quality of practices by providing data not available previously:
. . . we will probably have the first-ever database that allows us to link elements of practice, things like quality measurements, you know, CQC ratings, with, you know, what per cent of drawings did they take, for instance . . . So, we can put in place all the things that get you a high rating.
MD, Expanding, 02
. . . So, for me, if there’s a bigger need elsewhere, then we should be helping, and that was one of the ethos of [the federation] that attracted us, is the whole support and, you know, trying to bring up the standards of general practice throughout [the city], not just choice practices.
Board GP, Expanding 12
However, opinions differed between member practices about the desirability of this approach:
Why should a strong unit pay the same levy as a weaker unit which receives all the support from [the federation]? . . . What am I getting for my money? Why should I fund another practice which runs into trouble?
GP, Expanding, 11
What is the federation’s contribution?
The perceived lack of progress led several GP interviewees to question what it actually meant to be part of a federation, as well as the federation’s unique contribution as an organisation. Some felt that their federation’s achievements could have been accomplished via another existing alliance or organisation:
. . . it’s given us access to the integrated care work, which had to be through a large organisation. But, actually, if we didn’t have [the federation], there would have been a number of other large organisations we could have done it through, potentially easier and potentially without a top slice to [the federation] too.
GP, Expanding, 22
The same GP felt that the federation became a substitute for the CQC inspection team, although they acknowledged that there were other benefits of federation membership:
. . . [the single CQC registration is] we’ve traded people that we didn’t know observing us and seeing how we’re doing for people that we do know doing the same thing . . . I’m unconvinced it’s going to make life very much easier for us. The thing that might make things a bit easier for us is we’re getting slightly better systems for doing it like [intranet system]; that is quite useful.
GP, Expanding, 22
Several GPs from Struggling questioned what membership of the federation actually meant, relating this to a lack of collective identity due to the all-inclusive membership and absence of any ongoing financial commitment from members:
. . . you have got . . . [large number of] practices, which are not bound by anything really. So, it’s difficult to actually grasp what the local federation means apart from they have got a large number of practices that have, sort of, signed up that have just carried on doing their own thing.
GP, Struggling, 06
. . . in reality [the federation] doesn’t exist in any tangible form.
GP, Struggling, 11
Lack of awareness and understanding of the federation among practice staff, salaried GPs and locums was also said to be widespread across sites:
Well, in our practice, the [federation] is a completely alien concept to the team on the front line. So, my partners know of the [federation], because we have paid to be the members, but . . . the rest of us, don’t necessarily know what we are getting out of it.
GP, Embedded, 34
I don’t think it’s making a lot of difference; however, I think if you took it away they [GP members] would notice. They don’t think they would, but I think they would . . . with the [prescribing incentive scheme] they couldn’t have done that without [Small] because they wouldn’t have been organised . . . I think they would notice if it wasn’t there, but they might not necessarily have a very good word to say [about it].
Non-executive director, Small, 29
Ongoing commitment
The lack of progress and lack of materialisation of promised benefits had led some GPs to question their commitment to the federation. A decision for a practice to join the federation does not mean that, at an individual level, members of the practice are committed to it.
Some GPs were initially attracted to joining the federation owing to their alignment with its perceived goals and values. These GPs tended to be more concerned with the transformational potential of the federation rather than the transactional. One GP from Small explained that they rejected the idea of joining another federation in the area owing to a perceived misalignment of values:
Our values didn’t match those of that federation at that time. And being very patient-driven, you know . . . is it going to benefit our patients? And if it’s not, then we’ll stop there . . . it wasn’t really an option to join another federation . . .
GP, Small, 17
Gradually, however, this commitment began to evaporate. The practice felt that the federation did not have the ‘transformational leadership’ and solid foundation to achieve these goals, resulting in the practice’s departure from Small. This suggests that, for some practices, a shared ethos alone may be insufficient to retain their commitment. Despite the perception of strength in numbers, several GPs concluded that, with the benefit of hindsight, bigger was not always better. Smaller groupings of general practices, with which they shared similar goals and values, might be preferable:
I would probably argue for a more elite grouping of like-minded practices, I think that would work better . . . if you’re members with everybody, you’ve got to be able to have a choice and be able to partner with organisations who share your values. And that you respect and that you think are going to be working with the same goals . . .
GP, Struggling, 15
As described in Return on investment, the financial contribution made by general practices at each site varied. At Expanding, switching to the single CQC registration and centralised systems raised the costs of exiting the federation:
I think they’re so integrated now, it would be quite difficult for them to leave. So, they’ve got their pound value back in the back-office stuff and the other pound is their investment in the development of the organisation they’re part of. I think they’ve got that now.
Board GP, Expanding, 06
For those paying ongoing subscriptions (members of Expanding and Embedded), the financial costs of membership were higher than for the other two sites, and, for some, this led to greater ongoing scrutiny of the benefit–cost ratio:
So we’ve got a certain degree of sunk cost in [Expanding] and now isn’t necessarily the time just to pull it out, although I do have that conversation relatively regularly with my partner.
GP, Expanding, 22
Looking at the extended hours access [IAGP] is, I think, a feasible direct impact initiative . . . that will provide appointments and take pressure off practices . . . it’s going to, hopefully, work well for the city as a whole. And we’ll actually start to see value for money there.
GP, Embedded, 31
General practitioners from Struggling also described a situation whereby the financial costs of membership were considered to be low and, therefore, the benefits of membership were viewed to outweigh this cost. Being a whole-city federation, there was also little viable alternative. Some GPs felt that this type of commitment and a lack of financial ‘buy-in’ had led to apathy among members:
. . . if you were asked to pay regularly, I think . . . maybe that would encourage people to engage more, but that doesn’t happen.
GP, Struggling, 06
Decisions by member organisations may be based on fear of the future, as opposed to a shared positive commitment by all individuals involved in member organisations. Furthermore, power asymmetries in member organisations mean that decisions to join federations do not necessarily reflect a collective practice viewpoint. It has been suggested that, in a context of diversity, collaborating on projects, rather than arguing about philosophical differences, brings ‘practical coherence’,123 inculcating confidence, self-efficacy and accountability in participants. The IAGP policy presented an opportunity for the federations to engage member organisations in a concrete project; we elaborate on this in the following section.
Improving Access to General Practice
Improving Access to General Practice required the provision of access to GP services, including at evenings and weekends. A decision was taken by NHS England to move the timetable for implementation forward by 6 months, at relatively short notice. This meant that commissioners and GP federations had to work quickly, attempting to get some kind of service together in time. Embedded and Expanding managed to win contracts and provide services in accordance with these. In contrast, Small did not submit a bid. The CCG chose to commission services on a locality basis. This meant that there were two tender exercises, one for each of the localities; therefore, the tender cut across the internal boundaries of Small. Small collaborated on service provision with ‘Big’, a large federation operating in a number of geographical sites. Big submitted a successful bid for one locality with Small’s support, but its bid for the other locality was unsuccessful and this contract was won by the other competing ‘predatory’ federation. At Struggling, no bid was forthcoming and another service provider was awarded the contract. Table 4 summarises the contrasting situations at each site.
| Policy | Federation | |||
|---|---|---|---|---|
| Expanding | Embedded | Struggling | Small | |
| IAGP provision |
|
|
|
|
The IAGP policy raised issues of risk and commitment in all sites, although less so in Embedded, where the federation managed the process centrally and practices were not required to undertake additional work for IAGP delivery. At Struggling, the federation was asked to demonstrate member support and commitment and its reluctance to seek this from its membership meant that no bid was submitted. In all sites, the wisdom of both the IAGP policy and the federation’s engagement with it was questioned. Many GPs in each federation voiced their opposition, and several also had issues with the relationship of risk and effort to reward. IAGP was considered a somewhat risky undertaking in all sites. However, in each of the three sites that went ahead with provision, the risk of not being involved outweighed the perceived problems associated with IAGP. Yet we cannot interpret this as meaning that member practices were committed to the service and happy to share the risk associated with delivery.
The decision to bid or partner with a bidder at each of these three sites raises questions about what exactly we might view the federations as committing to, and, linked to that, what constitutes commitment more generally in the context of federations. The predatory federation competing with Small, which won the contract for central locality, required its members to commit to staffing the service. No such commitment was required from Small members. At Embedded, there was little apparent deliberation regarding the need for IAGP and the central role of the federation in implementing it was supported by members. Expanding organised an evening event aimed at recruiting staff for its IAGP service, as opposed to expecting existing members to staff IAGP sessions. However, it worked at the subfederation level with groupings of practices that took on responsibility for delivery in their locality, albeit in collaboration with the federation central authority.
Key drivers
We suggest that some of the drivers identified in Chapter 3 were important in explaining the different approaches to co-ordinating IAGP that we observed in our sites. For the most part, the analysis focused on three of these four sites, because (as outlined in Chapter 2, Study design, Key changes to the initial design, Data collection time scales) we were unable to continue our observations in one of the sites (Struggling).
Relationship with, and approach of, Clinical Commissioning Groups
This was an important factor in explaining how and why the federations approached the issue in the ways that they did. We discuss this issue further in Chapter 5, but focus here on its implications for internal working in relation to IAGP. In Embedded, the long-standing productive relationship with the CCG meant that IAGP had been on the federation’s radar for a considerable time. The chairperson and the COO held regular discussions with the CCG about it, anticipating the announcement of the procurement process. Several years earlier, the CCG had funded a small number of practices to pilot providing additional GP and nurse appointments at weekends. Some practices, therefore, had first-hand experience of delivering this type of service, although a decline in funding gradually reduced this provision. Embedded had an advantage because their CCG had awarded them the contract for IAGP, many months earlier than in the other sites.
The process of tendering involved the COO drawing up the service specifications in collaboration with the CCG. The SMT took the IAGP bid work forward themselves, bringing only decisions about staffing models, which affected projected income, back for board discussion.
At Expanding, the more formal relationship with the CCG meant that, although federation staff had been aware that the procurement was approaching, there was much less open communication between the CCG and the federation than in Embedded. This meant that mismatches could be observed between the formal requirements of the contract (e.g. start dates) and the provision plans of the federation, miscommunication regarding reimbursement and instances when the CCG appeared not to be forthcoming with information to support the development of the service.
Individuals in the CCG voiced concerns about the ability of the federation to establish an operable service in time, and some federation members felt that they were being put under an excessive degree of scrutiny by the CCG.
As outlined in Chapter 3, the locality approach had already prompted concerns from the large group practice in Small (in the central locality), which had led to the resignation of the chairperson. Although the relationship with the CCG was neither strained nor particularly close, the CCG was keen to encourage a joined-up approach to the delivery of IAGP. The pre-existing tensions between Small and the other federation covering the central locality meant that collaborative working across the locality was not seen as a good option. The other federation was not trusted and was viewed as predatory. Federation members feared that, if a collaborative bid was successful, the other federation would try to take over and not involve Small in a meaningful way. Frustration was expressed in Small about the CCG’s approach of forcing them into locality working. The demands of locality working and the fact that Small lacked experience in bidding for or providing something of the scale required for the IAGP service were important drivers in them choosing to partner with an external federation (we include more detail in Competition for members and Size and geography). Concerns about the reliability of the CCG in transferring payment for contracts, and evidence that the CCG was trying to micromanage the contract, were discussed at MOL meetings in the run-up to the launch of the service.
Competition for members
The presence or absence of other competing federations was also a significant theme emerging from our data on IAGP. Significantly, this appears to have shaped attitudes towards the provision of IAGP at each site, as well as the manner in which information and knowledge relevant to the organisation of IAGP was passed between organisations. In Embedded, there was a lack of real competition, in terms of the presence of either other federations or large group practices within their own membership. There appeared to be collegiate relations with the other federations that existed in the same STP as Embedded, which meant that knowledge and information appeared to pass between these federations. Because one of their neighbouring federations was a vanguard site, this appears to have been a useful source of information on how to provide an IAGP service (extended hours).
In Expanding, IAGP was a more complex undertaking, in part because of the existence of competing federations with which Expanding had overlapping boundaries. The IAGP contract complicated these boundaries, requiring Expanding to provide IAGP services to non-members’ patients. The presence of several different federations created further boundaries relating to sharing information and knowledge about plans and progress. In spite of the fact that there were neighbouring federations with IAGP services already established, a key senior staff member was reluctant to be seen to be learning from their experiences. The result was that board and IAGP working group members were advised against seeking information, as this might negatively affect the federation’s reputation. When Expanding tried to use the CCG as a conduit for obtaining such information, the CCG refused and suggested that the federations talk to each other. The federation sought the experience of a neighbouring GP federation that was aligned to the new merged CCG, but, being outside their own area, were unlikely to be competing for practice members.
At Small, the locality-based contract required by the CCG complicated Small’s overlapping boundaries with a neighbouring federation. The poor relationships that existed between Small and the neighbouring federation meant that they did not want to collaborate on IAGP. The CCG decision to award the IAGP contract for the central locality to the other local general practice gave rise to further animosity between Small and the neighbouring federation, with both Small and Big questioning the veracity of the information the neighbouring federation had supplied to secure the bid, and both expecting delivery to become very problematic in practice. Although there was very little in the way of information-sharing between Small and the neighbouring federation, one of the staff at Small, in initiating a search for outside help, indicated their willingness to learn from others. The national federation sought to capitalise on this by encouraging open communication between the different localities with which they operated the IAGP service.
Money
Money was an important issue in all sites, with opinions voiced in both Expanding and Small about the lack of potential income-generation in the contract, and also tensions faced by both these sites relating to transition and mobilisation costs and whether or not the CCG would pay for this. At Expanding, having to provide services for non-members involved a series of negotiations with board members about the appropriate manner in which to involve and charge non-members. Initially, the board communicated its intention to charge non-member practices a percentage from any surplus to cover infrastructure costs, because federation members had already contributed via their membership fees. However, there was disagreement about this. One board member warned others that treating non-federation practices differently could risk alienating them, which could affect the number of patients they were providing services to and potentially make some of the smaller hubs non-viable. This charge was subsequently removed and a revised memorandum of understanding proposed a one-off levy for non-member practices from the per-patient funding to be retained centrally, with all shares of any profit to then be distributed among members and non-members equally.
In Small, some GPs, who were not particularly supportive of the idea of providing the IAGP service in the first place, cited the lack of money as potentially problematic. When Big came on board, the finance conversation shifted in tone, with the CEO of Big appearing willing to spend money when it was necessary, while also being keen to establish standard practices across different localities from which they could derive economies of scale. She suggested that Small might be able to share workforce with one of these other regions, which, although in the same county, was many miles away; individuals in Small considered this too far. This prompted some concerns in Small that Big was more focused on efficiency than had first appeared to be the case.
Embedded was unusual among our cases in that money did not seem to be a significant issue. This perhaps relates to what has already been said about the good relationship with the CCG, in this specific case evidenced by the CCG’s willingness to support the IAGP service set-up and mobilisation costs. It also relates to the fact that Embedded had only one hub to manage, across a dense, urban footprint, which contrasts markedly with the situation in Expanding and Small.
Size and geography
Operating across a large footprint, Expanding had to provide multiple hubs to facilitate easy access for patients to comply with the IAGP contract.
For Small, the footprint to be covered by the northern locality contract was complex, because the rural nature of the landscape meant that, unlike in Embedded, there was no obvious single centre in which to locate a hub and the population density was much lower than in the other sites. Because, in population terms, patient numbers were relatively small, the central running costs of IAGP would consume a much greater share of income than in the other sites, leaving less money for staffing the service. Locating hubs as close as possible to urban centres with a larger pool of potential staff would increase the chances of attracting staff. However, the rural setting meant that it made more sense to establish a hub some distance from urban centres, based on patient location. Two hubs were chosen and the more remote one experienced staffing difficulties from the outset. The relatively small size of the federation, which had helped maintain cohesion in focusing on the prescribing project, meant that members felt daunted by the larger and more complex IAGP project.
Embedded appeared the least affected by issues related to their size, owing to their coterminous footprint with the CCG, the lack of any formal internal divisions, such as non-members or competing federations within the same footprint, and their geography.
Leadership and management
The issue of leadership and management in a relatively large federation, with practices dispersed across a large area, raises questions about the nature of the relationship between the centre and member practices. At Expanding, the central authority had hoped that practices would come forward with their own blueprints for operating their hub. However, these local plans were not always forthcoming. Although the differing needs of each hub area had been discussed during an initial workshop, many member practices were expecting a top-down approach similar to other centralised ‘roll-outs’, for example intranet and finance systems.
At Small, leaders and managers questioned their own ability to organise around such an undertaking, and this was a key factor in initiating their partnership with the national federation. With the former chairperson having departed, the experience of the senior staff was limited to local operational issues. This lack of experience and the sudden entry into partnership with a much larger organisation raised issues for several members of Small about the ‘professional’ nature of their own federation. This was particularly evident in the light of the fact that they should now expect to be under a much greater degree of scrutiny, from the CCG as a major contract provider, but also as a provider of IAGP, which remained a contentious political subject more widely, with individual services being scrutinised for evidence of robust and transparent organisational processes. This raised questions of additional costs concerning governance mechanisms and processes in the context of a small organisation, with no capacity to spread these over a large membership and income base.
Embedded’s senior team were also more experienced in dealing with local, operational matters than more strategic system-wide issues. But their close relationship with the CCG and previous experience at implementing local projects meant that they were well placed to deliver on their IAGP contract.
To some extent, some of the drivers listed above were beyond the control of the federation. However, the ways in which the federation central authority responded to challenges and opportunities varied between sites, and this is something over which they have greater control. These differences were indicative of the different styles adopted by federations more generally, as we discuss in the following sections.
Working together: managing interdependence
Federation-working involved managing interdependence in relation to both the internal and external context. Based on our data, we conceptualised federation activities in terms of three broad categories for managing interdependence: directing, engineering and co-producing. Directing involves high levels of control and co-producing reflects contexts in which, for various reasons, controlling approaches are not pursued and/or are likely to fail. This entails working with groups or organisations to develop shared approaches based on relevant knowledge rather than hierarchical status. Engineering is somewhere between the two, with federations playing a key role in facilitating the creation of structures and processes aimed at developing lateral relationships. Rather than federations choosing one type of activity for managing interdependence, in some cases these processes were used in combination.
Directing
If MOs are to introduce and enforce clear rules, then it is easier to do this at their inception. 107 At all sites, there were directives aimed at protecting members. The formal governance systems and directives, including regulations about voting rights and processes, were described in Chapter 3.
Directives explicitly constraining members
Only in Expanding were directives designed and introduced that had a substantive impact on the working processes of member organisations. These had major implications for interdependence. The requirement of member organisations to switch to using the standard federation systems as a condition of membership was agreed in the early stages of formation. The decision was made by a small number of board and executive team members and formed part of the offer to prospective joiners, so that they had to accept these terms or choose not to join. The existence of other competing federations in the area, which meant prospective members did have a degree of choice, may have reduced the potentially negative effects associated with directives. 107 Rather than relying on trust or ‘concertive control’,52,88 enabling ‘value-based normative rules’88 to constrain actions, it used regular monitoring by the central authority and a non-negotiable requirement as part of its hierarchical approach.
In Embedded, the approach appeared to be one of a supportive relationship with member organisations. This meant recognising their pressurised workload and avoiding introducing rules that might add to their burden.
At Small, participation in the federation prescribing initiative involved adherence to rules about prescribing medication, which would require effort, in return for financial rewards; all MOLs agreed to participate. There was little time for scrutiny and no discussion of non-compliant practices, with the result that, in many cases, doctors ignored the rules. Similarly, revised structures placing obligations on member organisations were not implemented in the manner intended, meaning that member organisations were not constrained by federation rules.
Internalising directives from the external environment
As outlined in Chapter 3, Expanding proposed, and member agreement was secured for, switching to a single CQC registration in the name of the federation, rather than each member organisation being registered with the national regulator. This provided a degree of protection for organisations that found the regulatory process challenging. It also created an expectation that members would engage in open communication with the federation and maximise efforts to comply with the regulator’s rules. Furthermore, as Expanding was, for regulatory purposes, one provider organisation, poor performance at any one of the many member sites would reflect badly on all member organisations and threaten their ability to practise. This, combined with the switch to the federation’s centralised systems, created additional incentives to remain with the federation:
So we’ve got a certain degree of sunk cost in [Expanding] and now isn’t necessarily the time just to pull it out, although I do have that conversation relatively regularly with my partner.
GP, Expanding, 22
The willingness of members to comply with these expectations, which involved sharing risk, signified a high degree of commitment to the process. Following implementation, some member organisations expressed disappointment, but this appeared to be based on an assumption that the federation would undertake functions that only the member organisations could complete. At Expanding, the approach was one of creating pluricentric, as opposed to merely unicentric,124 relationships. Although the latter is likely to encourage a dependency on the federation central authority, the former is based on interdependence.
Engineering interdependence
A process of creating a protected zone,112 restricting the influence of other more hostile organisations outside the MO, was evident to varying degrees at federation sites. The move at Expanding to co-ordinate the regulatory process can be seen as an example of protecting member organisations in this way. In doing so, it created expectations of members and exposed them to risk-sharing in a way that increases interdependence.
In all sites, the diversity of membership meant that different member organisations in federations faced different problems. Some member organisations were struggling with what they perceived as internal factors (e.g. their small size or inadequate premises) and others focused on external issues (e.g. increasing patient demands and a nationwide shortage of doctors). This would involve member organisations developing solutions by working together in some configuration, reflecting a high degree of interdependence. However, in the early stages of federation evolution, structures to facilitate lateral communication and co-ordination were absent or, at best, underdeveloped, and where problems were resolved, federation responses were more top down in nature.
At Embedded, this top-down response consisted of the federation stepping in to act as a ‘caretaker’, assuming responsibility when a medical practice failed and other member organisations were not willing to take on its management. A similar approach was reflected in its response to a problem of unequal service provision between practices in the city. The federation agreed with some member organisations that they would offer additional services to patients across the city to ensure that all patients covered by the federation received a minimum standard of care. Member organisations welcomed this because it expanded service provision and enabled practices to refer to these new services. Importantly, however, it did not extend to offering meaningful support to help organisations struggling to meet minimum standards. In particular, it encouraged dependence on the federation, rather than facilitating direct collaboration among member organisations to improve peer learning and build their capacity. This strategy resonated with Embedded’s approach to the IAGP policy. Rather than asking member organisations to work together on this, the federation managed the process and arranged a central location for these services, to which it also relocated its headquarters. This minimised the degree of interdependence and reinforced unicentric relationships.
In contrast, Expanding’s project involved helping vulnerable organisations by securing agreement to add doctors from other member organisations to their business contracts. This meant that there was a commitment by these organisations to cover absences, when such absences jeopardised the survival of small practices, even though the immediate benefits were for some smaller organisations only, with larger ones taking on risk. Importantly, rather than encouraging members to look to the federation central authority, this created a structure of interdependence among member organisations. This approach also underpinned a series of peer-to-peer networks for different types of staff from member organisations whose creation the federation central authority initiated but whose ongoing operational activities were managed by their members. This context of interdependence also made it easier to recruit new doctors. A combination of new structures and both rational and value-based arguments, in a threatening context, contributed to new relationships of risk-sharing and interdependence.
In response to the IAGP policy, Expanding worked with groups of organisations at the subfederation level to support them to deliver this. As part of the process, these member organisations were required to collaborate with non-federation organisations and were exposed to the requirements and processes of working in a cross-cutting manner with external bodies. Not all of these groups were equally capable of responding in the manner encouraged by the federation, so that variable amounts of support were required. But the overall approach reinforced the existing policies and structures intended to promote lateral co-ordination and peer learning rather than dependence on the federation central authority. Furthermore, organisations at the subfederation level possessed valuable local knowledge, which was essential for designing services at their local level. They brought this to discussions with each other and with the central federation authority, which was itself on a steep learning curve.
Struggling did not bid for IAGP, but, like Embedded, it took on the running of some vulnerable practices. This was beset with difficulty, as a failure to engineer structures and processes to meaningfully engage the wider federation membership meant that, from the outset, staff shortages made fulfilling the contractual obligations for these organisations difficult. This meant reproducing the same problems that it had set out to solve. Ultimately, towards the end of our study, the collaborative vehicle created to manage the contracts and service provision gave notice that it could no longer do this.
Meanwhile, in Small, the fact that a new chairperson was elected unopposed following the resignation of the founding chairperson reflected the lack of appetite for taking on such roles among the relatively small membership pool. The problem of member organisation vulnerability was dealt with by narrowing the scope of the federation rather than engineering structures and processes to increase lateral interdependence. This was not a formal decision but, rather, resulted from the way in which the chairperson enacted her role. The chairperson’s position as a partner in a large organisation, which had fewer problems recruiting staff, partly owing to its location in an affluent and picturesque area, appeared to influence this attitude. Previously, when the practice had experienced problems with staffing, it had solved these by internal reorganisation, and this may have contributed to the chairperson’s approach. Although the formal structures and goals of the federation remained unchanged, the chairperson’s resistance to risk-sharing meant that she deferred discussions about pooling staff and merging functions whenever these arose. A reliance on indirect resources meant that the formal processes of minute-taking and accountability more generally were neglected, making it easy to defer discussion and decisions indefinitely.
Co-producing interdependence
The environment in which federations operated was characterised by a number of hierarchical relationships with external bodies, which had implications for federation interactions and interdependence activities. We discuss this in relation to external organisations in more detail in Chapter 5. In terms of internal relationships, at the subfederation level in Expanding, Embedded and Struggling, historically, groups of member organisations had operated as networks in the context of various initiatives to improve patient care. Some of these had coalesced around a shared geographical footprint and/or a common set of values and interpersonal compatibilities. The existence of productive lateral relationships between these member organisations, together with high levels of expertise in relation to their domains, meant that these groups represented a potential challenge to the federation central authority. The existence of these groups, some of which had the capacity to undertake things the federation was doing, did not act as a barrier to recruitment. In Expanding, the federation encouraged collaboration at the subfederation level, supporting groups of member organisations to bid successfully for national resources to develop lateral co-ordination mechanisms to build their capacity. In the context of a changing national policy environment, placing heavy emphasis on PCNs, these sort of subfederation-level groups of organisations were seen as key to delivering new ways of working, underpinned by collaborative relationships with organisations external to them. Having encouraged their development, by working with subfederation groupings to influence the external environment, the federation was faced with having to adapt to this changing environment, which threatened its future, but created opportunities for new ways of interacting:
We still provide member services . . . But we also provide support with developing the PCNs. So you could see it as an opportunity or threat but we’ve got to get our heads around that . . . It’s in the early stages . . . We’ve been able to influence that . . .
Director of Strategy, Expanding, A02 – second interview
This policy has implications for all federations, but Expanding was the only one actively engaging with the process and influencing relationships to create opportunities in the brave new world of PCNs.
Central authority leadership and management
The range of approaches to managing interdependency (summarised in Table 5) reflected differences in federation central authority member skills and experiences. At all sites, there were individuals who acted as boundary spanners, and, in all sites, the lead GP had experience of undertaking a range of roles outside the practice. At Small, the new chairperson was very different in this respect, which may have contributed to their focus on protecting their practice as opposed to promoting the goals of the federation.
| Aspect | Federation | |||
|---|---|---|---|---|
| Expanding | Embedded | Struggling | Small | |
| Relationships | MD (hybrid) and chairperson held regular meetings | Close-knit small SMT | CEO and chairperson held divergent views | Chairperson had a strong influence |
| Structures | Hands-on board and informal board meetings, peer support structures, subfederation groupings | Board rubber-stamping | Weekly operational meeting: big overlap with board | Board and MOL big overlap. Board members from single locality |
| Temporal focus | Medium and long term | Short to medium term | Divergent views | Short term |
| Spatial focus | System wide | Local | Divergent views | Local |
| Proactivity | Highly proactive | Responsive and sometimes proactive | Passive | Passive/reactive |
Clinicians were key players in terms of board and management arrangements more generally at all sites. At Expanding, the close relationship and regular meetings between the MD and the chairperson41 appeared to be effective in generating ideas and action related to furthering federation goals. Expanding’s MD was a hybrid clinician manager, no longer practising as a doctor, with wide experience of operating at a strategic level. Their extensive knowledge and network of contacts in the wider health system was unusual, compared with that of other federation managers. In addition, rather than solely focusing on business meetings, Expanding held regular informal board meetings to develop ideas and to help build a team spirit. The MD, chairperson and some of the other GPs were very experienced at ‘wearing two hats’. 102 Furthermore, rather than leaving to chance the ability of board members to shift perspectives, their structures ensured that GPs developed this skill by requiring GP board members to act as a representative for a locality that was not their own. Embedded sought to bring PMs onto the board and to encourage them to act as representatives, but they played a largely symbolic part, owing to the board’s ‘rubber-stamping’ function status.
Expanding and Embedded appeared to have the most effective approaches to leadership and management, if we judge effectiveness in terms of the ability to bid for and deliver services. At Embedded, the chairperson and COO worked closely together. In addition, a relatively tight-knit, small SMT, comprising clinicians and managers, enabled decisions to be made relatively quickly and flexibly, with the board playing a much more rubber-stamping role than at other sites. Having a COO who was also a PM meant that they possessed valuable contextual knowledge that enabled a realistic grasp of time scales and workload for projects. Embedded’s chairperson was well respected and locally well networked, but the fact that a neighbouring federation was involved in a vanguard initiative meant that the vanguard federation’s chairperson took a more strategic and system-wide role, representing primary care across the wider footprint at the STP level. These factors may also have contributed to a focus on short-term goals and a failure to work on a more system-wide basis.
Many studies41,52 examining networks in health stress the importance of leadership and management communication in engaging members. The MO literature suggests that it is important to go beyond translation (i.e. recontextualising knowledge to render its meaning comprehensible to the receiver121) to actively construct102 problems in a way that aims to garner collective support for action. In Expanding and Embedded, this approach helped with the progression of engineering and co-producing new structures and processes. It also assisted with acceptance of directives at Expanding. Here and in Embedded, the problem was constructed using three different arguments to resonate with the diversity of opinion within the membership. First, if some organisations were seen to be failing, then this would undermine the case for preserving traditional ways of organising primary medical care across the whole system, not just for those organisations. Second, organisation closure would result in the allocation of their patients to other member organisations, whose staff were already overstretched. In addition, a third threat invoked by federation leaders was the risk that, under such circumstances, policy-makers would move to open up primary medical care to limited companies, whose motives would be shareholder profit rather than patient care. This combined threats to business with a strong moral and emotional appeal, tapping into the public service ethos of member organisations. 118 These approaches combined ‘rational’ (business-oriented concerns) and value-based (pro-social) aspects when engaging in dialogue with member organisations. They also tapped into fears by emphasising threats in a way that resonated with member concerns and fears.
Communication took various forms, with member views encouraged; although few members accessed Expanding’s live-streamed meetings, this live streaming symbolically reflected a commitment to transparency and member involvement. Furthermore, at Expanding, in addition to initiating member events and soliciting ideas and concerns from members, risk-sharing, collective responsibility for provision of services and accessing comparative data prompted communication between member organisations, as well as between the centre and the members, in a manner resembling a multilogue125 rather than a dialogue.
In response to the IAGP national policy and to the threat of practice closure, Embedded acted to protect its practices. Its approach can be characterised as one that is low level in terms of control over members, as it asks very little of member practices. It also appeared to be motivated by a well-intentioned desire to be responsive to member organisations. In this sense, it resonates with concepts from the parenting styles literature. 126 This characterises relationships using the dimensions of control and responsiveness. Our findings also suggest that approaches can be categorised in terms of the degree to which federations are passive, reactive or proactive. Rather than responsiveness, which might convey a static and dyadic127 approach to relationships, we suggest that our concept of ‘system proactivity’ is more appropriate for classifying approaches to the management of interdependence. This signifies the extent to which federations are proactive in working across a broader system, reflecting the range of spatial and temporal contexts in which relationships of interdependence are played out. In our study, a high degree of system proactivity was indicative of a federation’s ability to both grasp the significance of external organisations and take an expansive view with regard to spatiotemporal horizons, as both were key to the federation’s long-term survival.
Using these dimensions (control and system proactivity), we identified three MO styles – neglectful, authoritative and indulgent – that corresponded to our sites. None of our sites was classified as authoritarian, our fourth style, which involves high levels of control and low levels of system proactivity. This is not necessarily surprising, as this seems less likely to occur in MOs owing to the structure of interdependence, which places limits on the powers of even strong MO central authorities.
Conclusions
Our data suggest that GPs’ motivations for joining federations are complex and nuanced. Fear appears to be a powerful driver in terms of motivating action, but it does not necessarily translate into collective goals. Trust did not feature heavily in explanations and accounts, but mistrust (of the CEO at Struggling and the ‘predatory’ federation at Small) appeared to be powerful influences driving actions. This suggests that emotions are powerful influences on participation in federations, but to go beyond membership to more active forms of participation depends on the approach adopted by the federation central authority. Although key drivers help explain differences between sites, the approach of the central federation appears to be the most important thing in terms of influencing events.
Chapter 5 Working with others
Introduction
In this chapter, we examine the experiences of the federations as they work with other organisations outside the federation, as well as exploring the views and attitudes of staff from those organisations with which federations interact. Federations cannot issue directives to external organisations over which they have no control, yet managing interdependence in relation to these organisations is important for the federation to achieve its goals. In Chapter 4, we described processes by which federations ‘co-produced’ interdependence in their organisations. Here, we examine this co-production involving external organisations. We also discuss patient perspectives. We then draw on findings to present a typology of federation style.
Working with Clinical Commissioning Groups
In Chapters 3 and 4, we highlighted the importance of the relationship with the CCG in influencing developments in federations. In the CCG interviews, we explored what staff expected from federations, as well as working relationships with them. From the perspective of individuals in CCGs in each of the sites, there was a great deal of consistency about the purpose of federating, which tended to cut across four overlapping categories: sustainability (making general practice sustainable in the face of an increasing workload and decreasing funds), quality (reducing variation between practices, developing more proactive quality models), scale (working at scale, across a locality or population) and representation (representing general practice, giving voice to general practice in interaction with more established providers). A common theme was the perception that general practice comprises a number of silos, and that this was something that must be addressed to enable new models of care:
I was hopeful that the federation and the business plan would really start to focus on how do we start to shape what the skill mix might look like, the workforce and for practices to think differently about how they deliver things, because every single day we have [total number of practices] silo organisations who are all delivering [total number of practices] things, [total number of practices] times.
CCG Manager, Struggling, 09
Liaising with federations was also seen as making life easier for commissioners, although this assumes that those federations can speak on behalf of member practices. The following two quotations illustrate the contrasting situations of Embedded and Struggling in this respect:
[Embedded] are good in that they have got off the ground, they have got their mechanism, they have got a track record, they are linking all the practices together . . . I know that if I go and talk to [Embedded] I have covered [a high percentage] of my [total number of practices] practices and [Embedded], because they are, by nature, forward thinking, so they have got off their backsides and done this themselves, they are very responsive, they are strategic, they get where it’s going, they have already moved away from an individual practice viewpoint and thinking collective general practice.
CCG Manager, Embedded, 36
I’m not sure [CEO’s] approach isn’t going to cut it with practices for much longer . . . they mistrust him . . . there needs to be a leadership conversation at the fed[eration] . . . our colleagues that deliver traditional general practice aren’t going to be comfortable trusting an organisation with him at the head.
CCG GP, Struggling, 08
As outlined in Chapter 3, the degree of support provided by CCGs to federations varied between sites. In part, this reflected the novel and uncertain nature of these emerging organisational forms:
Is it the commissioner’s responsibility to help these provider bodies develop, and get off the ground, and get into a position where they can hold contracts? . . . On one hand, the CCG very much had this strategy, of, actually we want to develop general practice, because our whole strategic view is that we want to shift stuff into out of hospital, and we want general practice to lead that. But, on the other hand, we don’t give any kind of organisational development support to any other provider body.
Commissioning Manager, Small, 02
In the two sites without competing federations, it was easier for the CCG to justify support, although this was not always unproblematic:
They put a plan together as a group of GPs and they said, right, but it’s not going to go anywhere unless it gets an injection of money . . . They met with our governing body, put a proposal together of how they would move forward with a request for some funding. That was granted . . . on the basis that it would be around supporting them with legal advice and things like that.
Commissioning Manager, Embedded, 24
We’ve got no money, as a commissioner, and when we did support the fed[eration], in terms of their infrastructure, all we got was Freedom of Information requests from [a local member of parliament]. [The CEO and chairperson] had just come off our governing body and it looked like jobs for the boys, because that’s exactly what it was, with absolutely the best motives.
CCG GP, Struggling, 08
Clinical Commissioning Groups also varied in the extent to which they attempted to influence events and the future direction in each of the sites. At Expanding, where the CCG underwent a number of reorganisations and staff changes during the study, the CCG’s role was one of relative detachment, although it did provide funding early on for working-at-scale workshops. Subsequently, it agreed to reimburse the costs of federation staff in recognition of their work on the CCG’s integrated care plan. CCG staff were very aware of the need to avoid trying to curtail GP autonomy in a way that would alienate them. In the context of competing federations, the CCG did not endorse any particular model, but was aware of the potential impact on GP autonomy of the different models:
. . . with the [Expanding] model, you kind of maintained your practice autonomy, with [Big] you’re kind of signing it over . . . That loss of autonomy, that loss of the ability for a practice to make its decisions within its own practice was something that people were quite worried about.
GP CCG role, Expanding, 09
At Small, the LMC suggested that competing federations weakened GPs’ ability to protest, but there were no attempts to unite around specific issues, despite GPs agreeing that the CCG approach was to attempt to ‘pick off’ individual practices, suggesting that they were out of step with their colleagues elsewhere in the CCG.
In Expanding and Small, where there were competing federations, CCGs also used the IAGP process to some extent to encourage GPs from different groupings, as well as practices not in a federation, to work together by constructing tenders based on geographical footprints as opposed to federation practices. In Small, the configuration of federations was identified early on by the CCG as likely to perpetuate existing problems:
. . . there are still challenges because GPs don’t see themselves as a locality, they still see themselves as separate federations.
CCG Nurse Manager, Small, 05
The CCG’s insistence on commissioning on a locality footprint was instrumental in pushing Small’s very large city-based practice to seek to leave the federation and join the ‘predatory’ federation. This would have succeeded had it not been for the predatory federation’s insistence on a two-tier membership, which penalised newcomers. Although relationships with some individuals at the CCG were relatively cordial, Small members generally regarded the CCG as inefficient in terms of processing payments and providing advice and information; however, they acknowledged that high levels of turnover and staff shortages were a key contributory factor here.
From this CCG manager’s point of view, the existence of federations crossing geographical boundaries need not be a barrier to PCN development. However, the ability to develop PCNs with an already overstretched workforce was likely to prove a more significant obstacle:
. . . federations . . . probably came out of more of a rationalising back-office services and efficiencies in the business-end of practices. Whereas the PCN agenda has probably come more out of the population health-type agenda. And the two don’t necessarily need to align . . . But I think it’s hard to do that when you’re so caught up in the pressure of the day job and the demand. What general practice desperately needs more than anything, I think, is some headspace: some space to take a step back from where they are, to reassess how they can work differently and collaboratively.
CCG Manager, Small, 02 – second interview
In Struggling, the failure of the federation to command widespread GP support resulted in its demise. However, groups of practices came together to form networks and bid for resources to help develop these. Most bids were successful, but in two cases, where the network’s population was not located in a single defined geographical area, they were not:
The unsuccessful bids, were mosaics . . . So [federation CEO’s] got a network of his practices . . . they’re scattered all over the city, and that was his network . . . the two that didn’t get the network, with the NHS England funding, were the mosaic ones. They also cover some of the most deprived areas in the city, which has left the CCG with a significant problem . . . You take [large, well-organised practice grouping], and they are way on with it, it’s brilliant what they’re doing. And you don’t want to hold them back. However, we can’t change everything to fit their [mosaic] model, when over there, there’s this scattergun approach to how practices are organising themselves, and a real risk to delivery of patient outcomes.
CCG GP, Struggling, 34
This quotation illustrates the dilemmas facing CCGs attempting to negotiate choices around configurations of GP groupings in a way that focuses on place, but does not ride roughshod over existing successful groupings that are not place-based to the same extent.
A model that encompasses PCNs, nested within a supportive federation, might have benefits whereby the federation is able to provide central support to the PCN process. At Expanding, the federation had begun a piece of work to develop networks based on a set of local geographical footprints, but also informing the STP process more widely. It was, therefore, much more proactive than the other sites and took a much more expansive view with regard to spatiotemporal horizons:
We’ve used our extended access network to be the . . . sensible place to start, and I have done this within [Expanding] and also led a conversation across the wider health economy . . . What the profession needs [is] resilience across, within and between practices. And, I think, that’s the scaffolding on which you then look to improve care at the interfaces, so towards the community with traditional health and social care etc. . . . If you’ve got an extended-access hub, you’ve already got a shared patient database or registered list that’s shared, you’ve got data-sharing agreements and then you’ve got a geographic component . . . the system wants PCNs but it needs to make sense of the jigsaw that all kind of matches up. So, that’s the piece of work that I’m helping the system [STP level] with as well.
Federation chairperson, Expanding 07-2
The emphasis on resilience echoes the previous comment about headspace, as well as illustrating how PCNs might develop in a nurturing umbrella federation, where one exists, rather than ignoring existing organisational forms. This issue was causing federation board members to consider how changes might fit with existing structures, as well as the purpose of the federation overall:
We still provide member services . . . But we also provide support with developing the PCNs. So you could see it as an opportunity or threat but we’ve got to get our heads around that . . . the next stage is then working with them in building up the PCNs across the patch . . . What added value are we providing? . . . It’s in the early stages . . . We’ve been able to influence that. So there isn’t going to be any major conflict between what they see as a development [of] networks and we do . . .
Director of Strategy, Expanding, A02 – second interview
In contrast, successive CCG reorganisation at Expanding’s host CCG was seen as having ultimately led to improved relationships:
We were struggling to get much recognition with the old CCG. They still preferred to communicate with individual practices rather than with [the federation]. So we kept getting cut out of the loop. So it’s loads better now.
Director of Strategy, Expanding, A02 – second interview
At Expanding, CCG managers reported some concerns about the lack of a place-based network arrangement; however, they also appeared relatively relaxed about the pace of change with regard to this:
I don’t think we could have done extended access without it [the federation]; I think in terms of resilience it’s absolutely vital. So, I think the only downside of all of this is that the boundaries don’t match the CCG boundaries; I would see, over time, the GP providers coming together more and more, at least to talk as a set of providers with a single voice, and this is going to allow us to create some sort of integrated care system over time.
CCG Manager (clinical), Expanding, 37
The quotation above suggests that, rather than attempting to coerce GPs to organise around geographical footprints and/or to work more collaboratively as federations, the CCG is relatively relaxed, expecting that this will happen in an organic way over time.
Working with other providers and local authority staff
Local trusts
The activities in which federations were engaged meant that interactions with acute trusts did not feature heavily in federation meetings. In all sites, acute trusts were perceived by federation board members as a huge drain on the local health economy, with an uneven and unfair balance of power, limiting what federations could achieve. At Small, an initiative to recruit two health-care assistants via the local trust led to delays owing to the trust’s competing pressures, as well as its lengthy recruitment process. This left federation staff expressing frustrations, with some GPs reluctant to collaborate with the trust again.
In Embedded, relations with the local community health services provider were generally very good and the federation spent time on one project trying to establish a joint approach. Ultimately, circumstances unrelated to relationships meant that the project did not come to fruition, but all involved agreed that they would be keen to work together in the future. As outlined in Chapter 4, Struggling had entered into a collaborative arrangement with a local community services provider to submit a successful bid, although the decision was subsequently overturned because of concerns about the community trust involved. In the early stages of our fieldwork, Struggling had also started discussions with the smallest of their local acute trusts about collaborating, as this hospital manager explained:
I think it’s easier to get something done when there’s fewer players to agree it with . . . there are quite a lot of GPs in [city] who’d much rather just work with their mates and feel that that would be a better way of doing something than being forced to work in a geographical footprint . . . [CEO]’s Mr. Entrepreneur . . . But [chairperson] is a big-hearted visionary . . . if you ever want to be inspired, there’s no better person to talk to than [chairperson]. But the problem with a lot of visionaries, unless they get the right people around them, they’re not very good at translating it into stuff.
Acute trust manager, Struggling, 17
The quotation above illustrates the importance of leadership and management issues and the reputations of federation leaders in relation to expectations and interaction with potential partners. As discussed in Chapter 4, Struggling’s lack of resources made it difficult to take on concrete projects and pay for staff. A chairperson whose skills did not relate to implementation made taking on specific projects difficult.
Local authorities
The sites differed with respect to the extent of federation/local authority joint working. At Expanding, where the chairperson occupied a key position in the STP committee structure, this was helpful in developing relationships with other stakeholders. However, concerns were expressed by public health staff about the mismatch between the configuration of federation practices and networks based on geographical footprints:
The federations aren’t geographically based . . . they’re worried about being taken over by an accountable care organisation . . . through the STP, the community trust, the mental health trust, and the acute hospitals, and the GPs, are meant to be working together, and moving from a competitive marketplace to a sort of co-ordinated patient-centred system . . . I think the problem is, there’s such a pressure on budgets that it pushes everyone . . . we’ve got to command and control, very close monitoring of everything, moving away from that sort of partnership stuff that we were trying to develop in the last couple of years . . .
Public health consultant, Expanding, 38
This quotation reflects tensions between, on the one hand, groupings based on place, and, on the other hand, those based on practices that want to work together because of shared values or compatible personalities, which resonates with the previous quotations from CCG staff. The issue of top-down ‘command and control’ approaches and the potential harm that these can cause to potential collaborations also echoes concerns reported earlier in this chapter.
Although STP processes enabled some staff at federation sites to interact with stakeholders to discuss strategic direction, in Small, the STP was almost never mentioned in meetings and a CCG manager described how, for the CCG, a focus on its internal difficulties, as well as the acute trust deficit, meant that the CCG was not as engaged in the STP process as it might be. At one meeting organised by the CCG for the Small practices in the rural locality, a public health consultant presented data on local health indicators as part of a process of initiating a dialogue about these. However, there was a long way to travel in terms of developing this relationship, particularly when the federation’s priorities were IAGP and the PS, on which it was hugely reliant for its income. Furthermore, as the federation covered two localities, this was not a federation-wide conversation. The public health consultant, quoted below, had a good, if distant, relationship with one of the Small board GPs and suggested that their retirement would be a real loss to the system. The issue of local authority budget cuts and primary care picking up services also reared its head:
. . . we’re facing really, really difficult troubling times . . . you can’t overspend, legally, but something is going to have to give . . . we would really like a public health approach to be embedded into GPs’ practice . . . in future, if we keep getting the cuts that we’re getting, we might have to have conversations . . . what can we do . . . if not enough money provided to local authorities, you know, can the NHS step in? . . . And if GPs were organised and to be able to, kind of, collectively offer services in primary care, that would probably be really helpful.
Public health consultant, Small, 33
These comments reflect the importance of personal relationships, particularly in the absence of structures to bring people together, but they also reflect the risks of collaboration in the context of budget cuts. In the city area of Small, the local authority was taking steps to work more closely with health organisations; this included a joint appointment to a role intended to bridge gaps between health and local government, as well as local liaison workers. However, these staff interacted with the fledgling PCNs in operation in the city areas of the CCG, rather than at federation level:
. . . the [PCN] steering group . . . I’ve been to a couple of the meetings to talk about things where it’s important to kind of open the door to primary care homes. An example would be the council plan includes the development of major new housing developments . . . because I’m a bit of an ambassador for both organisations, I went with a colleague from the council to talk about the development arrangements.
Assistant Director, City Council, Small, 39
They were talking about ‘oh, if only we had a resource for our pre-diabetic patients’, and I said ‘well, have you heard about these community health champions?’ They just looked flabbergasted . . . I mean, I was originally invited to their meetings to help them connect with the community over child obesity, but really it tends to be a much wider connection now.
Local authority worker, Small, 40
The experiences of this staff member suggest that PCNs can be helpful in bringing together practice staff and other relevant stakeholders. However, the example also illustrates the need for better co-ordination at a senior level, if collaboration between local authority and health staff is to achieve its potential. Progress often appeared to rely on committed individuals and luck, rather than on structures and processes to co-produce structures and processes for connecting strategic decisions (e.g. the employment of local authority liaison workers) with the operational aspects of these policies on the ground.
At Embedded, the public health consultant liaising with the federation was very positive about the relationship:
It’s refreshing to work with a group of people who are so keen to get on.
Local authority public health consultant, Embedded, 60
However, efforts to collaborate with the local authority led to frustrations on the part of federation GPs, owing to the lengthy approval process that involved elected members and council staff.
Other federations
In Struggling and Embedded, there were no competing federations. At Expanding, some board members had travelled to speak to other federations at their invitation, being seen as a good example from which to learn. They were also mentioned by one of the GPs at a Small meeting as offering a good model, although this was a GP from a small and vulnerable practice who was keen to move towards having more centralised support. In Embedded, the cordial relationships with neighbouring federations, one of which had been a vanguard site, provided an opportunity to meet as part of a collaborative group to share learning and advice. This was unusual because, at all sites, despite federations often facing common problems, there was little interaction between federations in a way that would facilitate shared learning. In some cases, this may have been due to a defensive approach, but it is also likely to relate to constraints on capacity, as well as a focus on reactive, rather than proactive, activities.
At Small, working with Big as part of the IAGP contract meant that Big had ultimate responsibility for service delivery. This relationship also had the potential to start to change the ways in which Small worked in relation to IAGP, but also more generally. For example, although the CEO of Big stated that ‘local is king’, suggesting a high degree of freedom for Small, she also sent a list of roles that Small should think about creating and filling, including Caldicott guardian, senior information risk owner and head of emergency planning. Small had to agree standard sets of competences for clinical staff serving in frontline IAGP roles. This process revealed huge variations between and within practices in, for example, what sets of activities health-care assistants were qualified to carry out. This was aimed at ensuring that patients from across the locality, regardless of their registered practice, would experience a standardised service at IAGP consultations. The CEO of Big also suggested that it would make sense for Small to grasp this opportunity to learn from Big and to ‘harmonise’ (not standardise, as she said that she did not like that term) systems and competences across Small in the way Big had done, rather than just for IAGP sessions. In addition to the need to increase transparency and create robust governance mechanisms as a result of IAGP income flowing through the books, these suggestions encouraged discussion about becoming a more ‘professional’ organisation. However, a combination of establishing and sustaining services in the context of a looming deadline and the fact that there were no dedicated staff employed by Small to take things forward meant that, in the short term, there was no action taken on the more challenging of these suggestions, namely the ‘harmonisation’ aspects. Longer term, the fact that the chairperson was very resistant to processes that might threaten practice autonomy or lead towards merger might also prevent such developments.
A meeting convened by the LMC in October 2018, covering the CCG in which Small was located, brought together representatives from practices in the CCG to discuss working together at scale. Two members of one of the city-based Small practices were present, as were several staff from the ‘predatory’ federation practices too. The LMC representative suggested that divisions between practices based on personal differences meant that general practice across the CCG was losing out, compared with other CCGs in which GPs joining one big federation added to their strength. However, several of the GP attendees were less keen to talk about feuds across federations, suggesting that collaborating as part of a PCN was the way to bring practices to work together. Some practice staff had started to work on developing a PCN to focus on local population health. When a report of the meeting was fed back subsequently at the next MOL meeting, the two GPs present from the central locality said that they were aware of and interested in participating in their PCN, but that the meetings were arranged by non-clinicians and, therefore, were at times when they could not attend. This was the first mention of PCNs at any of the Small meetings we attended. This is perhaps not surprising, given the absence of a PCN in the rural areas where many northern-locality Small practices were located. The view from the ‘predatory’ federation GP who was actively involved in the PCN process suggested that collaborating as part of a PCN might help in moving beyond feuds based on egos. This is understandable because city practices in Small, in population health terms, had much more in common with the practices in the ‘predatory’ city federation than with the rural practices that occupy all the seats on Small’s board. However, there were no attempts by Small, as a federation, at collaborative working to facilitate PCN development owing to the mistrust by some in Small of the ‘predatory’ federation and a focus on issues concerning the rural, as opposed to the city, practices of the federation.
Co-producing interdependence
The environment in which federations operated was characterised by a number of hierarchical relationships. This meant that they were faced with a degree of uncertainty and interdependence related to their formal and informal position in the larger system. We would expect federations, as is the case with other organisations,75 to attempt to actively create their environment, by seeking to shape it. Federations could not simply impose structures on this external landscape, but instead had to work as part of a process of co-production, especially as many external organisations held positions above them in the hierarchy. Expanding’s collaborative project with the national regulator (CQC) discussed in Chapters 2–4 is one example of working outside the vertical hierarchy to develop shared approaches based on relevant knowledge, rather than hierarchical status. Despite its position relatively low down in the hierarchy, Expanding was also able to exert influence at senior levels of the hierarchy, because its chairperson had cultivated a relationship with NHS England. The federation’s proactive efforts to promote and raise its profile had resulted in it appearing on the radar of relevant national policy-making bodies. This helped to develop relationships, with Expanding increasingly being regarded as a trusted source of advice and information. These relationships also provided opportunities for Expanding to lobby as part of its process of shaping the external environment. In addition to the national context, the fact that federations were part of a regional system, with a strategic planning body (STP) operating at a level above them, had consequences for the development of plans across this broader regional footprint. Despite a financial deficit, the federation invested time and effort in ensuring that it was represented at the STP level. This involved a proactive approach convincing the STP of the need for representation of primary care doctors and the co-creation of structures to facilitate this. Paying attention to developing these relationships wherein status was based on knowledge, rather than formal hierarchical location, meant that it positioned itself to help to create the future,75 rather than merely respond to it.
These examples and those discussed earlier in this chapter demonstrate why other organisations, beyond federation members, have an interest in the formation and continued existence of a MO. 107 In our sites, we found that, to varying degrees, other organisations offered encouragement for federation formation and opportunities for collaborative working. In particular, the local CCG, which allocated resources for primary health care and entered into contracts with the federation member organisations, was an important body in this respect. Federations offered the potential to simplify relationships by representing members in discussions with CCGs. We found that CCG capacity and attitudes towards federations varied between sites. Embedded’s relationship with its CCG was close and co-operative. The CCG had contributed resources to help establish the federation; this was facilitated, in part, by the absence of other competing federations. Whenever it was minded to consider developing new primary care medical services, the CCG approached the federation, which responded with enthusiasm. The approach at Embedded was much more reactive than at Expanding; relational embeddedness128,129 was important here. This interacted with a degree of experiential embeddedness (i.e. ‘the propensity to anchor information gathering and operations within the problems’ relevant context’121) to constrain the way in which the context, and therefore relevance, was perceived. The federation’s view appeared to be based on historical relationships and contexts, which prevented it from perceiving the changing environment and the longer term and broader system-level aspects of the context, which were both highly relevant to the issues it faced. During the study, Embedded was forced to change its constitution when a valued board member decided to join a CCG committee. The decision to recommend the constitutional change to the federation membership was the subject of protracted discussion among board and SMT members, many of whom were against the proposal. This view was based on historical principal/agent contractual relationships, as opposed to the important role of federation knowledge in shaping future service planning and delivery. Eventually, an agreement was reached to support the change. Yet the fact that the federation had initially designed its constitution to ensure a clear boundary between itself and the CCG was indicative of its failure to recognise the CCG’s strategic role in the health economy and the advantages to the federation of developing lateral relationships, which were not solely focused on immediate contractual issues.
As outlined in Chapter 3, Comparing sites: what drives differences?, Expanding and Small, where competition for members existed between federations, had more distant relationships with the CCGs than Embedded had with their CCG. The absence of such competition at Struggling did not guarantee cordial relationships with the CCG, which were instead characterised by mutual distrust and acrimony. Struggling’s failure to implement its governance processes, which meant that meetings were not formally minuted and meetings with the membership did not take place, exacerbated the situation. At Small, relationships were hampered by a combination of reliance on indirect resources, which meant that it was always in reactive, rather than proactive, mode, and a relationship with a CCG whose focus was on its own internal problems. At Expanding, the absence of a close relationship with the CCG meant that generating income was a slow process. To fund central costs, the federation board took a calculated risk and ran a financial deficit for a lengthy period. This was a matter of ongoing concern and discussion at board meetings, although, ultimately, the federation’s approach resulted in a financially stable position.
Embedded’s close relationship with its CCG meant that it focused on maintaining a productive collaboration, which resulted in income generation, enabling recruitment of staff to the central federation team. Its concentration on relationships with the CCG and its desire to protect member organisations meant that it did not prioritise capacity-building within those organisations. Although collaborative alliances had existed at the subfederation level prior to the creation of the federation, these had been neglected since then. Indicative of its short-term focus and desire to please members, its financial surplus was distributed to member practices, rather than invested in a development fund for the future. Nor did it invest time in STP relationship building, preferring instead to focus at an operational level on issues of immediate concern. However, it did build links with neighbouring federations and developed a ‘buddy’ relationship with a ‘successful’ federation. This created opportunities for learning, but posed risks too, owing to the elitist identity of the successful federation, which was led by a charismatic doctor whose style was acknowledged to be top down. The fact that the successful federation had (1) received additional funding as part of a national initiative to encourage collaborative working across health organisations and (2) relatively low levels of economic disadvantage may also have limited the potential for cross-federation learning.
Federation central authority style: a typology
Table 6 summarises the different approaches to managing interdependence and their effects. Drawing on our findings in Chapters 3–5, we illustrate our typology of federation styles in Figure 1.
| Activity | Federation | |||
|---|---|---|---|---|
| Expanding | Embedded | Struggling | Small | |
| Directing |
|
|
|
Formal rules regarding prescribing initiative. Little monitoring. No action regarding non-compliance. Absence of compliance norms. Choice of federations |
| Engineering |
|
Multiple rationales to reflect member diversity. Avoids tensions associated with member diversity. Ongoing dialogue. Interdependence relatively low | Diversity not an issue owing to disconnect with membership level. Monologue. Interdependence relatively low | Narrow scope of problem definition in response to member diversity. No shared responsibility in practice. Constrained dialogue. Interdependence relatively low |
| Co-producing |
|
Focus on federation and lateral relationships with CCG. Mainly short-term member protection, but some proactivity | Disconnect between CEO focused on local short-term horizons and chairperson focused on system-level strategic goal | Uniscalar. Short-term thinking |
| Effect of above | Encourages lateral/pluricentric relationships and shared norms. Norms of dependence and interdependence | Encourages unicentric relationships and shared norms of dependence on central authority | Distant relationship with members. Absence of norms of dependence and interdependence | Congenial relationships, but limited dependence and interdependence |
FIGURE 1.
Federation styles.
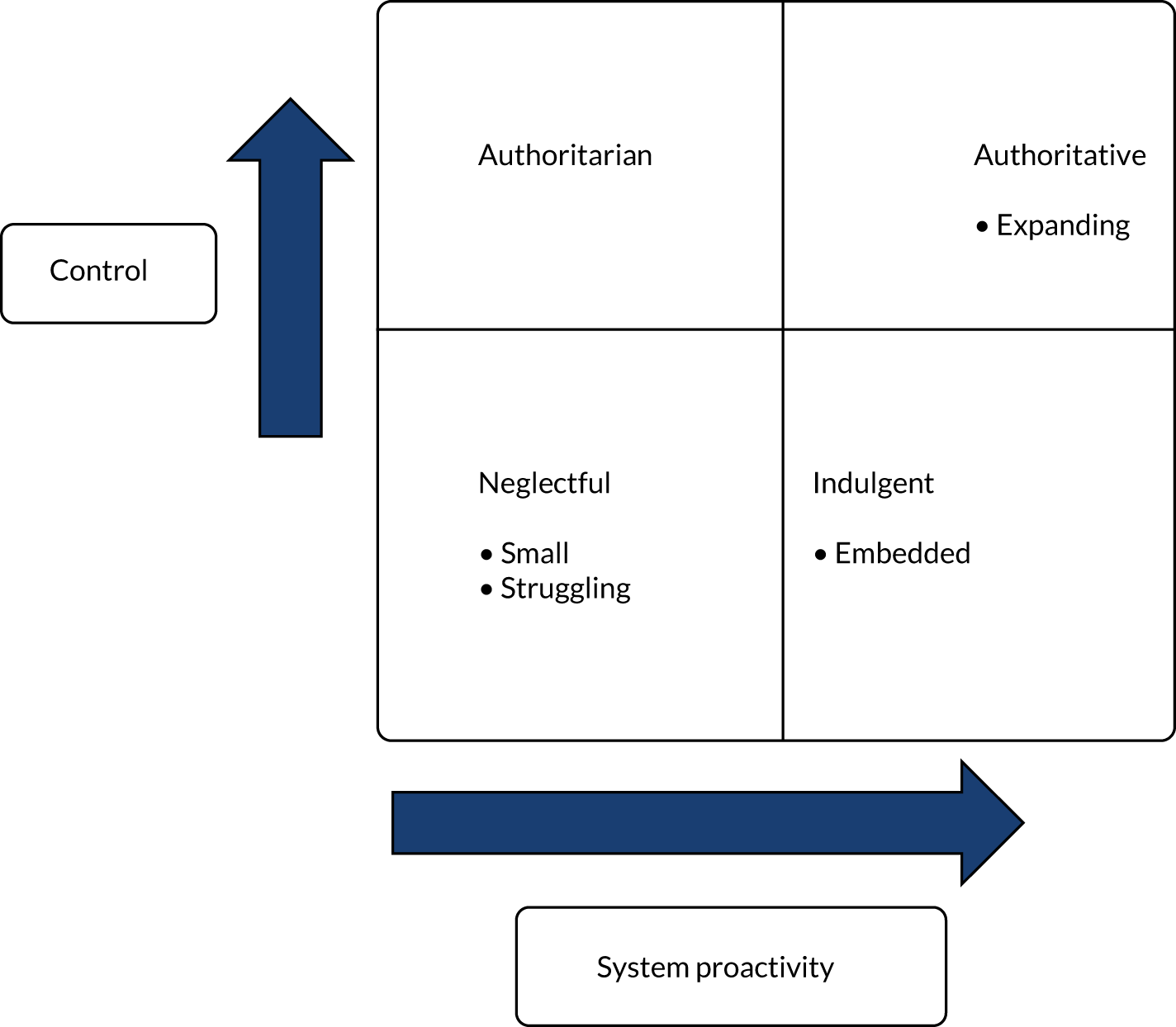
Working with patients
In Chapter 3, we described how, for the most part, the federations did not prioritise patient input. This did not appear to be a result of their relatively embryonic status, as the issue was almost never mentioned unless federation members were asked about it in interviews. We interviewed members of practice patient participation groups (PPGs) and, beyond this, individual patients at each of our sites to ascertain their views and opinions in relation to both federations and primary medical care services more generally. We also interviewed three staff from local Healthwatch organisations.
We found that, generally, patients knew little or nothing about their federations, or about the concept of federations more generally. Some patients confused federations with mergers and moves towards large group practices, which, in some cases, were seen as inconveniencing patients:
I’m just aware of the surgery being the surgery.
Patient, Embedded, 46
One interviewee stated that they would expect, from their role collating health and social care data, to know if their own practice was part of a GP federation. Following this interview, we discovered that their practice was part of a federation, yet they were unaware of this.
Despite many federation staff saying that they had informed their patients, very few had done this ahead of joining the federation and certainly not in consultation with patients. We found that this communication with patients tended to be at the PPG level, which often was not cascaded further. One PPG member, however, spoke of his role in producing a PPG newsletter, which was made available to patients more widely. Another board GP updated patients via infrequent updates at PPG meetings:
. . . our PPG periodically, once every 6 to 12 months, will have a section to say ‘what’s [the federation] doing that might influence you?’ But, it’s fairly lightweight, because there isn’t much. They all perceive . . . the patient sees the practice, the practice sees [the locality] and [the locality] sees [the federation].
Board GP, Expanding, 06
Federation staff and patients themselves both felt that patients would need to be informed only if the federation led to changes in the way their health care was delivered:
. . . most of the people that I speak to . . . they’re possibly more interested in the smooth running of the practice and probably not why it’s smooth running.
Patient and PPG member, Embedded, 16
Therefore, co-producing structures and processes for managing interdependence did not extend to including patients. This resonates with the view of MOs as helping to stabilise the environment for consumers, rather than involving them in their internal processes. 107 At the start of the federating process, most general practices were focused on organisational development and felt that patients would not detect any difference in their usual experience at their general practice. Despite this, some interviewees thought that patient involvement in them would be a good thing in principle:
I mean, in principle, I think it would be a good idea for patients to be more involved . . . to contribute the kind of patient view and the patient experience, because I think that’s something that often gets overlooked when all decisions are made based on, kind of, the organisational level and the organisational processes.
Patient, Embedded, 44
Embedded was the only federation that held a patient consultation event seeking views from the invited PPG chairpersons on the development of the new IAGP service ahead of its launch. However, the service provided did not appear to reflect the opinions expressed at that event. In part, this was because the people who had time to act as PPG chairpersons were more interested in accessing GP services during the day than at evenings and weekends. Furthermore, most patients we interviewed focused on access to services, rather than wishing to be involved in federation development per se:
. . . availability of appointments, time taken between making an appointment and getting one, and probably a feeling of not being ever so important . . .
Patient and PPG member, Embedded, 18
Among those interviewed, patients with some awareness of new services provided by GP federations tended to be those who had used the recently developed IAGP services:
. . . I’ve got a really bad earache, and she said ‘well, we’ve got a new thing [IAGP] in place’, which I haven’t heard about it before . . . I think they should have told us about it before. I mean, I don’t know how they would’ve done it . . . God knows how long it’s been there for.
Patient, Embedded, 44
In Embedded, where receptionist signposting had been implemented across practices led by the federation, some patients found this helpful and understood the reasons behind it, but others were less pleased:
. . . I’m not particularly fond . . . of people asking me for an awful lot of details about anything I might rung [sic] up the doctor for . . . It’s probably a good idea if it’s done well, but if it ties up the phone . . . people are going to be much longer on the phone, aren’t they?
Patient and PPG Member, Embedded, 16
Only one federation, Small, had a patient representative at board level. Her role included liaising with PPGs in each of the member practices and helping them to grow their membership and be more representative of patient demographics, but also providing a direct wider patient voice back to the federation:
I contacted all the PPGs for the surgeries involved with [federation] and I went to their meetings . . . There was only, I think, two of the groups that were aware [of the federation] . . . [I] fed back to them and also asked them if there was anything that they felt were issues that needed covering and things like that. It was general questions about how it would work . . . why was there a need for this and worried was it because GPs were failing . . . [me] reassuring people that it was no, nothing like that . . . It wasn’t about closing surgeries down . . . It was about a support network and making sure that GPs were managing well.
Board patient representative, Small, 03
As reported in Chapter 3, when she resigned because of ill health, her role was not filled.
Federations did, to varying degrees, win contracts to provide services to patients, in some cases in partnership with other providers. These are listed in Table 7. However, patients were not generally aware of the federation role in providing these.
| Site | Services |
|---|---|
| Expanding | IAGP |
| Sexual health | |
| Embedded | IAGP |
|
|
| Smoking cessation | |
| ‘Caretaker’ contract (one general practice) | |
| Struggling | Six general practice contracts (note: with foundation trust provider), but gave notice to terminate contract |
| Small | IAGP (note: with contract held by another federation) |
Conclusions
For GP federations attempting to work with other organisations, collaboration appeared to bring both challenges and opportunities.
Among our case study sites, we observed highly motivated professionals, in many cases such people contributed effort above and beyond their job requirements for the greater good. However, building sustainable collaborative relationships cannot rely on an assumption of limitless goodwill on the part of already overstretched professionals. With regard to the creation and development of PCNs in one site, which would involve working with non-federation practices, there appeared to be an appetite for this among at least some of the general medical practice workforce. Progress was being made on establishing this, based on a bottom-up enthusiasm, as opposed to national or local mandates. Our interviewees acknowledged the damage that can be done by mandating approaches, as these risk losing the goodwill linked to local voluntarism.
There were clear tensions also between working collaboratively using a place-based approach and collaboration based on shared values and ethos. PCNs present additional challenges because these potentially involve multisite practices being split across a number of PCNs. Given the costs of participation, in terms of time and commitment, this is likely to present obstacles, which will add to the tasks to be tackled by an overstretched workforce. The findings illustrate the problem of GP capacity in relation to available time to devote PCN development, and comments from interviewees reflect the need for ‘headspace’, which was in very scarce supply in our sites. They also highlight the potential role that federations can play in supporting the development of PCNs, as well as existing structures and relationships that may provide foundations on which PCNs can build.
Issue of capacity and resources were not confined to federations, with factors such as staff turnover, commissioner reorganisations and local authority budget cuts all influencing relationships in our case study sites. In an evolving policy landscape, federations also had to work within national guidance, although, as discussed in Chapter 4, this was not always readily available. Furthermore, effective working with other organisations at local or national level requires a common understanding of the evolving landscape. Examples of commissioning organisations bypassing federations and national bodies not being sufficiently geared up to deal with federations suggest that the process of collaborative working is not merely one of primary medical care adapting, but requires flexibility and adaptation on the part of local and national actors too.
This means that there are issues that are beyond the control of the federation. However, the federation central authority style was both highly influential and much more under its own influence.
Chapter 6 Discussion
Introduction
In this chapter, we discuss the study’s main findings. We also outline the strengths and limitations of the research. We developed a typology, classifying federation styles in relation to the central federation authority using two dimensions: (1) control over member organisations and (2) system proactivity. Using this, we classified one site (Expanding) as authoritative, as it was high on both dimensions. Two sites (Struggling and Small) were classified as neglectful, being low on both control and system proactivity. One site (Embedded), was low on control and more proactive than the neglectful sites, adopting what we classified as an indulgent approach. We draw on this typology when discussing the findings in this chapter in relation to the research questions.
Findings
Research questions
-
Managing practice processes: how does federation affect the way practices organise themselves internally, and which governance arrangements best enhance practices’ ability to work co-operatively with others?
-
Workforce: how does federating affect the way practices use their staff, skill mix etc., and what impact does federating have on the general practice workforce?
-
Innovations in practices and interface with health and social care stakeholders: to what extent and how is the federation is enabling or inhibiting integration with community and social care?
Managing practice processes
With regard to the effect of federations on internal ways of working, we found substantial impacts in only one site. In this ‘authoritative’ site, we observed a shift to standardised systems and centralised procedures, involving a great deal of effort for member practices, as well as for central federation staff. This also had implications for relationships of interdependence and raised the costs of exiting the federation. Competition between federations to attract members in this site and one other meant that potential members had a broader range of choice than members in the other sites. The ability to make an active choice may have made it easier for the authoritative-style site to make demands of its members and for member organisations to agree to comply with these. Most practices at the federation moved to these new ways of working and could see the benefit either in the short or longer term. The central CQC registration process at this site also had implications for member practices. One of the (neglectful) sites struggled to make progress and to command the active support of its membership. However, at the other three sites, training and development organised by the federation was well received and the evidence suggests that this enabled staff to improve internal processes.
In addition, it is important to note that, at the authoritative site, changes to practice processes did not require changes in clinical practice. Furthermore, most of the burden involved in complying with federation directives fell to non-clinical staff. We cannot make assumptions, therefore, about whether or not compliance would be achieved so readily if directives attempt to constrain clinical autonomy.
Fear of the future113 and a sense of strength in numbers acted as motivations for initial federation formation and for practices to become members. As MOs, federation member organisations share a similarity that constitutes an important part of their identity. It also means that (as observed in some of our sites) federations may lack a specific and shared focus. In all but the authoritative site, we found that a shared ideology at an abstract level, although important, was insufficient to promote action when this involved risk-sharing among practices. Linked to this, we suggest that federations are not necessarily designed with a clear definition of their functions in mind. 86 Instead, these new organisational forms emerged in response to fears and problems. Enthusiasm for federating, based on shared problem-recognition, did not always translate into collective support for a preferred solution. This may explain why we did not find more substantial changes in relation to practice processes.
Furthermore, capacity was a major issue at all of our sites. Federations were created, in part, as a response to workload pressures and, paradoxically, it was only by GPs and other practice staff taking on additional work that federations were able to sustain themselves; although, in two sites, the recruitment of federation staff helped ease the burden. Often federations relied on a small number of key individuals, but there were limits to how thinly they could spread themselves across federation business. Capacity in relation to a range of non-clinical (e.g. management, leadership, financial, HR) knowledge and skills was variable and, at times, lacking, but expensive to provide.
Governance
At all sites, processes were introduced that were intended to ensure the accountability of the federation central authority to the broader federation membership. In terms of governance, formal structures evolved over the fieldwork period as federations adapted to a changing environment and perceived needs. There was diversity with regard to the form of legal entity chosen by federations, but this did not appear to explain differences between them with regard to processes and outcomes.
Federations, as MOs, are not loose network structures governed by ‘orchestration’ or ‘co-ordination’52 mechanisms. As organisations, they all had a central authority function, which occupied a hierarchical position at the top of the organisation, on paper at least. The federation central authority was dependent on member organisations, which, in turn, depended on it and was also dependent on external organisations in the environment. We conceptualised federation approaches to managing interdependence in terms of three types of activity: directing, engineering and co-producing. Directing involves high levels of control and co-producing reflects contexts in which, for various reasons, controlling approaches are not pursued and/or are likely to fail. Engineering is somewhere between the two, with MOs playing a key role in facilitating the development of structures and processes aimed at developing lateral relationships.
Federations tended to avoid directives backed up with monitoring and accountability of practices to the central authority in all but the authoritative site. In this site, a more hierarchical approach was combined with activities to empower groups at the subfederation level. This combination of control and increasing the capacity of groups that could challenge the centre was associated with successful outcomes, in terms of bidding for contracts and preparing the ground for PCN development. This suggests that, rather than viewing MOs as making a trade-off between a weak centre and strong membership or vice versa, the ongoing negotiation of tensions between the centre and groups at the subfederation level can have a positive influence on processes and outcomes. This implies that the tendency in the MO and network literatures to conceptualise power as a zero-sum game130 is not helpful in this context.
Concerns have been expressed about the nature of accountability to external stakeholders in network forms70 of organisation. With regard to the external environment, a federation’s ability to construct itself as an efficient hierarchy, which can be trusted to deliver on its promises, is important in obtaining funding from and developing relationships with external organisations. Our federations, as MOs with a central authority, had clear lines of accountability in relation to external stakeholders. At the same time, the internal environment in which the federation can be seen to speak for its diverse and strong membership, capitalising on this diversity, is also helpful in conveying to external organisations that the federation is not merely an empty shell, lacking legitimacy. 82 This appeared to contribute to external legitimacy, but did not necessarily compromise internal legitimacy. In the indulgent site, the ability of the federation central authority to deliver services without making demands on practices meant that internal legitimacy was not threatened or diminished. At the two neglectful sites, internal legitimacy was an issue, although this did not arise from a conflict with external legitimacy. In one case, weak internal legitimacy was a major obstacle to progress, and this contributed to reduced external legitimacy. In the other case, practices were able to flout a key federation agreement, with this behaviour going unchallenged by the federation central authority. At the authoritative site, systems to monitor progress and to ensure accountability of member organisations were in place, in a way that was absent in the other sites.
In all of our federations, there were groupings of practices, engaged to varying degrees in collaborative working, below the level of the federation. However, the authoritative federation was different from the other sites in the way it sought to engineer structures to facilitate lateral communication and interdependence. These structures involved a relatively high degree of risk-sharing, as well as peer support networks and the development of capacity at subfederation (locality) level. Obtaining a central CQC registration helped as part of a process of creating a protected zone112 for member organisations, enabling the federation to exercise greater control over its environment. At the same time, this also involved practices in compliance with federation directives.
This site, where standardised processes were introduced and some aspects of work (e.g. CQC registration) were centralised, contrasts with our other cases, where there were no challenges to practice autonomy. At the indulgent site, the federation was responsive to member concerns and fears, but not demanding, with few rules set for member practices. Providing support for member organisations by creating a protected zone shielding them from pressures is understandable. However, the lack of expectation raises questions about what, if anything, practices contribute beyond a relatively low-cost membership fee. In addition, this approach may detract from building capacity at the locality level, as practices may rely on the federation, rather than other local practices, for help and support. At our other two (neglectful) sites, the federations were more distant and there were no (or limited) attempts to create expectations of members. This lack of expectation is understandable in the context of an overstretched workforce. However, it also means that staff in member organisations were often remote and uninformed in relation to the activities of their federation, despite attempts to encourage greater engagement.
Federations constructed rules and policies as part of their process of evolving in response to internal demands and those of the external environment. Gaps in knowledge were identified, which needed to be filled. Some of this knowledge related to national or local NHS rules and guidelines, but there were also issues relating to legal and financial aspects of governing enterprises. In some cases, federation staff sought clarity from relevant bodies. When this was forthcoming, they were able to apply it, in some cases, using flexible interpretation to achieve their goals. There were instances when guidance was not forthcoming and/or was contradictory. This meant that federations had to make assumptions and/or were forced to wait for this to appear. In a rapidly changing context characterised by a high degree of novelty and uncertainty, it may be that existing rules are no longer suited to the context, or that federations that obey those rules are held back in their attempts to achieve legitimate objectives.
With regard to non-NHS-related knowledge, federations grappled with issues such as shareholding and the most appropriate legal vehicle to adopt, with these issues becoming more complex as federations won contracts to provide services. Disincentives to accumulate surpluses, for example, reduced federations’ ability to focus on longer-term resource requirements and stability. This raises questions about the extent to which federations should operate according to commercial accounting and taxation rules, and the disincentives contained therein, which may inhibit federation growth and development. Linked to this, there is also the issue that federations seeking advice from legal and financial professionals were incurring costs in doing so, in the absence of a free and independent central resource. Although circumstances were different at each site, there were also common issues, which highlights the need to avoid reinventing wheels at each federation.
Federations could not simply impose structures on this external landscape, but instead had to work as part of a process of co-production, especially because many external organisations held positions above them in the hierarchy. The authoritative site’s collaborative project with the CQC is one example of working outside the vertical hierarchy to develop shared approaches based on relevant knowledge, rather than hierarchical status. Despite its position relatively low down in the hierarchy, the federation was also able to exert influence at senior levels of the hierarchy, owing to its having cultivated a relationship with NHS England. The federation’s proactive efforts to promote and raise its profile had resulted in it appearing on the radar of relevant national policy-making bodies. This helped to develop relationships, with the federation increasingly being regarded as a trusted source of advice and information. These relationships also provided opportunities to lobby as part of its process of shaping the external environment. Despite a financial deficit, the federation invested time and effort in ensuring that it was represented at the STP level. This involved a proactive approach convincing the STP of the need for the representation of primary care doctors and the co-creation of structures to facilitate this. Paying attention to developing these relationships, wherein ranking was based on knowledge, rather than formal hierarchical status, meant that it positioned itself to help to create the future,77 rather than merely respond to it.
Workforce
We found evidence that federation initiatives were helping with recruitment issues in two sites (authoritative and indulgent). In addition, solutions to avoid reliance on external locums, supporting resilience for practices, as well as consistency for patients, were implemented at these sites. At one site (authoritative), the move to add partners to contracts also provided support for practices, which felt themselves to be especially vulnerable to practice closure in the event of GP sickness. Here, non-GP partners were transferred from their employing practice over to the federation’s employment and pharmacists were also employed by the federation. However, hopes of standardising pay and terms and conditions across these staff were not achieved in the projected time scale because of the wide variation of salary and roles. Federating meant that, in some sites, there were central federation staff who could provide advice and support, but for many of the senior GPs who actively participated in federation meetings and activities their overall workload increased. In addition, IAGP, as opposed to federating itself, influenced discussions about workforce and raised issues about workforce ‘harmonisation’ across practices, but did not result in immediate changes in response to these.
The ability of federations to assist with recruitment problems, although a positive finding, raises questions about the overall benefit to general practice, given that federations are all fishing in the same staff pool. Furthermore, the many hours of time required from lead GPs and some PMs, raises an issue of sustainability. Although federations did not rely on highly individualised forms of leadership, they did involve small teams of dedicated staff, with heavy workloads, running on goodwill. Moving from one individual to reliance on several does not necessarily result in sustainability, particularly when the overall context in which federations are located is characterised by scarcity, instability and growing demands to participate in other forms of collaborative ventures.
Innovations in practices and interface with health and social care stakeholders
With regard to innovations in practices and particularly the interface with health and social care stakeholders, generally, progress in our sites was slower than federation leaders had anticipated. In part, this was because, in some cases, partner organisations’ systems and processes took much longer than those of member practices and the federation itself.
There were mixed experiences in relation to working with others outside the federation. In addition to being disappointed at the pace of change of large and bureaucratic organisations, some federation staff were conscious of the constraints on local authority budgets, which could adversely affect local health contexts. During our fieldwork, federations negotiated changing relationships with local commissioners. Uncertainty about the extent to which commissioners and federations should be collaborators was a feature of the landscape. Commissioner reorganisation and restructuring were reported as adding to this uncertainty in some sites, although, in one site, revised arrangements were reported as improving relationships and opportunities for collaboration.
Explaining the findings
Based on themes arising from the data, we identified key drivers influencing events and opinions in our sites. These were competition for members between federations (if any), relationship with the CCG, money, history, leadership and management, and size and geography; these interacted in a dynamic way. The fact that the context was one of GP scarcity relative to workload acted to make these factors particularly salient, so that, even when financial resources were available, it was not always easy to find staff to cover for those undertaking federation, as opposed to practice, work.
These drivers resonate with findings from previous research,13,41,52,56,72 although the issue of competition between networks (and between MOs) is a relatively unexplored topic. Whether or not federations had competition for members was an important factor influencing events. Where competition existed, this gave prospective member organisations a choice. It may also have helped the authoritative site’s ability to make demands on practices, because members were freely choosing from at least two alternatives to join and to accept the conditions of membership.
Leadership and management has received considerable attention in the literature41,52,72 but it merits further discussion here, especially as this appeared to be highly influential in relation to federation style (e.g. authoritative) and the approach to managing interdependence. Federation style also seemed to be the most significant factor in terms of explaining events and outcomes in our sites. Leadership and management issues were important in a number of ways. First, lead GPs and some other staff at all sites were endowed with social capital (due to having held roles previously that brought them into contact with stakeholders outside their practice), which helped in terms of interactions and the boundary-spanning activities required by their roles. Second, in one case (the authoritative site), a senior manager who was formerly a clinician was able to perform a clinical/hybrid manager role, with their clinical status conferring legitimacy among clinicians. In addition, their extensive experience of strategic, system-wide health-care management was not present among central authority staff at other sites. This experience may also have contributed to the more system-wide and proactive approach adopted by the federation central authority, as well as its focus on accountability mechanisms and relatively hierarchical approach.
Many of the positive attributes of managers and/or leaders identified in the literature on GP collaborations and public sector networks (e.g. ability to combine soft and hard approaches to management,41 span boundaries,41 draw on social capital,52 communicate effectively43) in networks might plausibly be applied to managers and leaders in organisations more generally. Our findings did not contradict these earlier studies. A novel contribution of this research is the identification of activities for managing interdependence and classification of federation styles. In terms of explaining the differences between sites in their approach to these, we identified differences in terms of leadership and management capabilities, beyond the exceptional experience of a senior hybrid manager at the authoritative site. Lead GPs at all sites were used to ‘wearing different hats’, but in only one site (authoritative) did the structure encourage the development of perspective-shifting skills and experience via the mechanism of board members representing groups of practices that do not include their own. In addition, care was taken to ensure that meetings were timetabled that were not focused on immediate business,41 but instead enabled the development of ideas and provided mechanisms for peer support.
Although boundary spanners and clinical/hybrid managers occupied senior positions at all sites, at the authoritative site the close relationship between the chairperson and the clinical/hybrid manager, and the timetabling of regular meetings between them, constituted a productive ‘duo’41 facilitating the development of ideas and activities. However, the absence of senior staff members with practice management experience at this site may have contributed to unrealistic expectations about time scales for compliance with new systems and processes. In contrast, at another site (indulgent), the COO’s background as a PM and the inclusion of another PM in the SMT was very important for enabling the delivery of contracts within budgets and time scales. But it may have contributed to the more operational and short-term perspective observed at that site.
Decisions about the type and quantity of staff time required reflected the views of senior clinicians and managers at each site. Money was influential in decisions about this, although the authoritative site ran a deficit for most of the fieldwork period, in contrast with other sites where affordability was a key criterion. Having dedicated staff time has been associated with positive progress in health networks. 41 Federations may employ staff (‘direct’ resources), but they may also draw on dedicated staff time using ‘indirect’ resources, relying on staff from member organisations to undertake some of the MO’s work. In those sites that relied on indirect resources, balancing the federation with the practice workload was a struggle. This was a lower-cost option and involved staff who understood the local member context. However, in practice, those staff prioritised their employing organisation over the federation work. At the indulgent site, the practices employing senior PMs who were members of the SMT were paid for their federation work and these PMs were sufficiently senior to ensure that they were able to contribute to the federation as agreed.
Effective communication by leaders is seen as important for networks (and for traditional organisations). 41,43 Our research suggests that avoiding neutral or bland messages is important to tap into emotions of staff in member organisations. Active construction,102 as opposed to merely ‘translation’,121 was a key feature of communication with members in two sites. This capitalised on staff fears and mobilised threats to help retain member support. These negative aspects combined with positive messages that demonstrated achievements of the federation to reinforce the benefits of federation membership and achievements.
Leadership and management roles and governance structures were formalised at all sites, but processes, rather than formal structures, appeared to be more important in explaining events and outcomes. Ferlie et al. 41 discuss the importance of shared norms and the ‘presence of a shared ideology or set of values’41 (contains information licensed under the Non-Commercial Government Licence v2.0.) as being important for network cohesion. In one neglectful site, a mismatch between the CEO’s perceived values and those of the membership more generally led to dissatisfaction with the federation. This was a key factor in the failure of the federation to achieve its aims. At the other neglectful site, member representatives were split on whether the practices should be working together more closely to support each other or merely working in collaboration on initiatives that would provide benefits to individual practices. Although a shared ideology at an abstract level was present in documentation, the lack of detail about this obscured the reality, which was a schism in relation to the future direction and focus of the federation. However, although shared underpinning values were common to the other sites, these were expressed in vague terms and the diverse motivations and expectations of members raises questions about what exactly was shared in relation to ideology. Furthermore, the absence of leadership behaviours that challenge a vague shared ideology may be necessary to sustain membership, but this is not necessarily sufficient to guarantee active engagement.
Federation success and failure
If we judge success in terms of the federation continuing to function and to win tenders for service delivery, we can see that some approaches (authoritative and indulgent) were more successful than others. In our neglectful cases, at the time the fieldwork ceased, in one site, the future of the federation was at risk and, in the other, member organisations had come together at the subfederation level to form alternative collaborative arrangements, bypassing the federation completely. In the two successful cases, federations employed hierarchical processes and systems to get things done, albeit in the context of being accountable to member practices. However, in only one case were these used to promote pluricentric, as opposed to merely unicentric, relationships.
At the neglectful site that combined rural and urban practices, the interests of rural dispensing practices were not well aligned with those of other practices. In addition, the complicated geographical footprint, arising from the federation’s comprising ‘like-minded’ practices with different populations, demographic make-up and acute providers, meant that working together was more meaningful at the subfederation level, with little progress made on working collaboratively across the federation footprint. This state of affairs was also influenced by the CCG, which was keen to encourage working across locality rather than federation footprints.
The existing literature on health networks stresses the negative effect of power asymmetries on collaborative working. 41,52,97,99 GPs as subalterns of medicine100 are often disadvantaged in cross-sector networks involving hospital doctors. However, federations as MOs comprise member organisations characterised by similarities as opposed to differences. In theory, member organisations have equal standing, although some larger, well-resourced organisational members may be better able to challenge the MO central authority than others. We found that power struggles between members or between groups of members and the central authority was less of an issue than in studies of networks. However, that may be because many of these concern diverse groups of stakeholders. For MOs, a key concern is passive membership,107 with members joining because costs are low relative to potential benefits and a fear of missing out on benefits. This might explain why a fear of the future113 motivates practices to join, but it does not mean that staff in member organisations want to take on work or change organisational behaviours and processes as part of their membership.
Furthermore, much of the literature concerning network forms and MOs appears to conceptualise power as a zero-sum game. 107 Rather than viewing federation power relationships in terms of trade-offs between the federation and its membership or between more or less powerful actors in the federation, our study suggests that conceptualising power as being derived from different sources and operating in different domains is a more useful approach. Strengthening lateral relationships and building membership capacity can be of great assistance to the federation in its dealings with external organisations, as well as its internal operations. Comparing federations in our study, we suggest that a federation’s strength can be enhanced by its ability to build capabilities in its member organisations. At our authoritative site, the power of groupings at the subfederation level was increased as part of a process of lateral collaboration engineered by the federation.
The network literature often identifies national targets as having a negative influence, distorting network activities. 41,97,99 The requirement to respond to the IAGP policy placed staff under pressure, but it also provided a concrete project123 around which federations could mobilise. This created an opportunity to generate income to support the federation central authority. At the authoritative site, IAGP encouraged the development of lateral communication and co-ordination at subfederation level. This strengthened groups at this level that could present a potential challenge to the federation central authority. Therefore, targets were not wholly negative, but, instead, had a double-edged aspect. Targets were voluntary, insofar as federations were not required to submit bids for IAGP contracts. However, there were strong (mainly non-financial) incentives to do so. This did not involve federation managers in using a combination of hard/soft management approaches with national targets to coerce members into action. Nor were federations ‘overwhelmed’131 by national targets. Instead, IAGP helped as part of a process of creating a protected zone for member organisations, enabling the federation to exercise greater control over its environment.
Previous research has highlighted the importance of trusting relationships in network forms of organisations (and in traditional organisations). 41,43,52,72 Perceived trust has been shown to be linked to the achievement of goals and increased interactions. 85 From a MO perspective, MO relationships are characterised by disembeddedness, as staff in the different member organisations may not meet in person. Instead, the foundation for creating trust is the MO’s striving towards similarity and shared status among its members, whereas network participants may develop trust via face-to-face interaction. Elections for board GPs meant that these individuals had a degree of legitimacy and tended to possess social capital prior to being elected. Yet most organisations had agreed to join before elections took place. Rather than strong feelings of trust in individuals or systems, we may interpret this as demonstrating a degree of faith in the idea of federating, at least in the early stages of formation and evolution. The absence of members’ ‘skin in the game’, with little asked of member practices (as in three of our sites), may make it relatively easy to sustain membership in the absence of mistrust. Distrust, however, was a strong influence in two of our case study sites. This contributed to the failure of the membership to support the federation in one site, and, in another, it sustained a messy geographical footprint due to the distrust on the part of some urban practices of the urban federation in their footprint.
We might consider that all of our federations were failures with regard to service user involvement in their structures and processes. Our federations did not meet Sheaff et al. ’s52 conditions for meaningful service user involvement. Furthermore, federations, for the most part, did not set out to actively involve service users, instead suggesting that stabilising service provision should mean that patients would not notice any difference to the status quo. This is in line with the formation of a MO being aimed at reducing what members perceive as disorder, thereby increasing predictability and control, for themselves and their customers, as well as other interested parties. 107 Therefore, following MO theory, we would not necessarily expect customers (or, in the NHS, patients or service users) to be involved in the MO’s activities, but they should be beneficiaries of the new, more stable environment that the MO strives to create. Such a perspective may be a cause for concern and be perceived as unduly paternalistic, especially as the absence of service user input was not viewed as something to rectify once the federation had dealt with immediate concerns and issues.
Strengths and limitations of the study
This study had a number of limitations. We focused in an in-depth manner on case study sites, which meant that we were able to include only four federations in the research. We found a high degree of variation between sites, and we are aware that even more variation exists. Furthermore, we initially planned to use a maximum variation approach, but subsequently decided to exclude vanguard sites because it would be difficult to isolate federating from vanguard effects. The result was that we may have excluded federations that are more active in changing local services, models of care and interorganisational relationships.
In addition, although we interviewed patients, as most were unaware of federations they generally had little to say on the subject. Where federations had made changes to services, we did ask patients about these, although their experience and knowledge of them was limited. Because we lost access to Struggling, we were unable to observe all of the meetings we had planned to attend, although, by continuing to interview individuals in the CCG, member practices and other stakeholders in the area, we did manage to compile a data set from which to draw robust conclusions.
Furthermore, at the time of the study, GP federations were still at an early stage in development. Roles within them and their external relationships with commissioners were still forming and substantial changes in service models had not occurred. Therefore, this study may tend to understate what GP federations may eventually achieve. Federations are bottom-up organisations with a central authority function, with membership being on a voluntary basis. They differ from both primary care provider networks, which are top down, mandated or at least strongly incentivised by central policy-makers, and loosely coupled networks, which lack hierarchical structures. This will limit what lessons may be learnt for other types of non-federation primary care provider collaborations.
We followed the ‘action’ in relation to observation of meetings, which meant that most of our data were concerned with interactions and events involving organisational elites, as opposed to rank-and-file GPs. With regard to the GPs, this meant that we were reliant mostly on interviews, as opposed to observations, including of these GPs, to gather data on federations. It may be that, when responding to questions about reasons for joining federations, GPs felt required to justify affiliations, providing explanations suggesting a more considered, rational and logical process than was the case.
The study strengths include the rich observational data from each site, which enabled us to provide an in-depth understanding of events and processes, as well as key drivers. In addition, we interviewed a range of stakeholders, some of whom were interviewed more than once to provide a longitudinal perspective on events. Another strength is that we avoided sites that had already been included in researching at-scale working, conveying a range of experiences and capabilities. This helped us to identify the factors contributing to poor performance, in addition to those enabling sustainability.
Conclusions
These findings chime with existing literature, which highlights the potential of at-scale working to produce benefits and emphasises the need for realistic expectations concerning time scales. 11,72 Two of our federations were able to respond to the IAGP policy, winning contracts for service provision. They also helped alleviate recruitment problems and were successful in bidding for and delivering new services for patients. The provision of staff training was appreciated by the staff involved. The findings also resonate, in many respects, with existing literature in relation to problems and challenges facing networks in health care.
The literature describes the need for trade-offs in a number of areas (e.g. voluntary versus mandatory approaches, larger and smaller size). 72 Based on our data, an important trade-off appears to be the balance to be struck between providing support to solve problems for practices and facilitating their ability to work to support themselves and others. Linked to this, although the former may be quicker, it may not build capacity within member organisations. This suggests that there are trade-offs between short-term quick fixes and a focus on longer-term goals. The evidence also highlights the potential for conflicts of interest and the need for realistic time scales, and our findings support this.
In addition, although existing literature emphasises the need for clear and realistic goals,11 our data suggest that, given diverse expectations and interests of member practices, some fluidity enabling these to co-exist peacefully in the minds of members may be necessary to hold relationships together, especially in the initial stages of federation formation. Furthermore, in our sites, a degree of flexibility and willingness to adapt to circumstances in a changing environment was helpful, even when it resulted in changes to goals.
Chapter 7 Implications
This study was designed and conducted before the introduction of PCNs and our focus was on federations, which are different in important respects from PCNs. Nevertheless, recent policy statements place heavy emphasis on PCNs, and further guidance is emerging as we write. Since 1 July 2019, all but a handful of general practices in England have come together to form around 1300 PCNs. 132 However, many of these cover populations that far exceed the 30,000–50,000 population suggested in current guidance. 133
Our research suggests that PCN development may be able to build on existing subfederation (locality or neighbourhood) structures and relationships, rather than seeking to start with a blank sheet of paper. However, the PCN policy may also destabilise federations by placing additional demands on their member organisations and directly employed staff. Federation leaders were involved, to varying degrees, in collaboration and communication with various bodies (e.g. CCG, STP, NHS England), which added to pressures on their time. In the context of overlapping relationships of interdependence, the introduction of PCNs raises questions about how these new organisational forms will interact with the existing complex and crowded landscape of collaborative forms and relationships. Furthermore, the fact that PCNs are expected to be geographically contiguous in their coverage contrasts with the varied footprints of federations and poses a challenge for federations that are not geographically contiguous in their coverage.
In this context, and drawing on the previous chapters, we have developed a set of implications for three main audiences: those involved in primary care collaborations, policy-makers and researchers. This study has other implications for those seeking to create and sustain at-scale working, as we describe below.
Implications for those involved in local at-scale working
The typology of federation styles and the categorisation of activities for managing interdependencies that we developed could be used by federations as tools to inform planning and management. The tools will also be helpful for newly created PCNs, especially if there is an existing federation, in thinking through issues of control and system proactivity, as well as activities related to the management of interdependencies. With regard to activities related to the management of interdependencies, PCNs can use the categorisation of activities for managing interdependence as a starting point for mapping relationships, as well as for considering the division of tasks and responsibilities between federations and PCNs.
The two most effective approaches to federation management were very different from each other. One of these involved risk-sharing and required system changes at member practices. The other involved the federation central authority taking on work in order to protect practices from workload pressures. Federations (and PCNs) should consider the balance to be struck between supporting practices to solve short-term problems and creating expectations aimed at building members’ capacity to resolve issues for the longer term.
The ability to create expectations and for practices to meet these is limited by available resources. In a context of workforce shortage, federations are severely constrained with regard to the pace of progress. The introduction of PCNs places additional demands on practices and raises questions about the capacity of practices to respond to these.
In our sites, most members were not actively involved in federation business and projects. A realistic expectation is that, where collaborative forms require increases in the costs of membership (in terms of time and money), clinician involvement will not increase in the absence of offsetting resources. Linked to this, consideration should be given to the extent to which commitment (as opposed to merely membership) is required and the mechanisms for achieving this. As part of this process of securing commitment, it is important to create opportunities for communication and dialogue, and to be aware of the range of motivations for participation. Communications need to use a mix of positive (opportunities) and negative (threats) messages, which combine tangible benefits and resonate with both instrumental and emotional concerns.
Much of the literature on networks emphasises their flatter structures relative to traditional organisations. 106 However, these findings suggest that federations resemble MOs, with central authority functions and clear structures for accountability to members and external organisations. MOs are characterised by hierarchy, but rely on member support for their continued existence. In this study, hierarchical approaches were most effective at achieving results and this involved top-down directives in one case. If PCNs are to use directives to exercise control over members, then this is likely to be easier when these directives are formulated and agreed on early in the process of their creation.
Directives need to be backed up with monitoring and support from the federation central authority. Implementing the DES for PCNs40 is likely to require more formal governance mechanisms than those that exist in many federations. However, based on our research, understanding reasons for non-compliance is important and knee-jerk punitive approaches should be avoided. Furthermore, when organisations involve mandatory participation, consideration needs to be given to mechanisms that mitigate the potential negative effects of this.
National targets place constraints on organisations and have been reported as distorting network functioning. 131 Our research suggests that they should not be viewed in wholly negative terms, especially if they are voluntary and/or linked to positive incentives. They can provide opportunities for engaging members, particularly when these contribute to realising objectives that are salient to member interests and motivations. They can also provide a ‘concrete project’123 around which to build coherence and focus.
We found that the choice of legal organisational form and governance structure did not influence events at our sites. However, issues such as the distribution of risks and any relevant rewards and whether or not new members will have equal status with long-standing members were agreed early on. In addition, thought was given to incentives for non-member practices to collaborate when this was beneficial for the federation. Rather than viewing these issues as a ‘one-off’ exercise, it makes sense to keep structures and processes under review to be able to adapt to changes in the external (and at times internal) environment, when necessary. Furthermore, it is important to go beyond the design of governance mechanisms, to ensure robust mechanisms are in place to monitor compliance.
In addition to clinical/manager hybrids, it is essential to involve staff with practice management experience in the business of federations. In addition, it is important to attract individuals who are able to bring multiple perspectives,102 span boundaries41 and shift perspectives according to the context. 121 Rather than leaving this to chance, attention should be paid to developing mechanisms (e.g. board members representing practices that do not include their own, focused organisational development opportunities) aimed explicitly at doing this. 63 Small teams,41 as opposed to a reliance on ‘heroic’ individuals,13 will be a more effective and sustainable approach to organisational leadership and management. Moreover, for federation staff whose prior experience is unlikely to adequately equip them for performing new roles in a federation setting, thought needs to be given to their training and development needs and how best to meet them. It should be recognised that, even with this training, individuals will take time to develop skills requiring experiential learning. Bringing staff together to create peer support and learning opportunities requires dedicated resources. However, this was reported in very positive terms in our sites and was a very important part of the process of breaking down practice boundaries and creating a shared identity.
Having dedicated staff time is associated with effectiveness in networks. 41 The MO literature distinguishes between direct and indirect resources with regard to ‘dedicated’ time, with a lack of control being identified as a disadvantage of using indirect resources. We found detrimental effects of a reliance on indirect resources. Although this is a low-cost option, the disadvantages of this approach appeared to outweigh this advantage. However, the legal and financial implications of employing staff directly will need explicit attention.
Member practices and federations can make decisions more quickly and implement them more rapidly than other organisations in the health and social care landscape. At the same time, there is a balance to be struck between being flexible and open to opportunities and maintaining a coherent strategy, which reflects members’ long-term interests. It is important to recognise the time taken to build relationships with other stakeholders, as well as the, often lengthy, decision-making and implementation processes, which characterise many of the organisations with which federations seek to work. In addition, when federations are expected to collaborate with local authority bodies, whose budgets are being reduced, there is the potential for shifting costs and/or effort to primary care staff. Consideration should be given to the ways in which this risk can be minimised to avoid undermining collaboration between at-scale organisations and the local bodies with responsibility for social care and public health.
There is an expectation that at-scale working in PCNs will involve engagement with local communities,40 but this is no easy task. Patients and carers played little or no part in federation activities. Institutions or structures other than federations may be better placed to give patients and carers a strong voice52 in these circumstances.
Implications for policy-makers
A combination of positive incentives and fear helped mobilise federations to deliver IAGP. Although there was variable progress on other areas, federations can provide a supportive environment for practices. Where effective federation structures exist, it is important to avoid destabilising these as part of the PCN process. Linked to this, it would make sense to agree a division of labour between federations and PCNs to avoid duplication of tasks, especially given the context of workforce scarcity.
The NHS Long Term Plan40 implies a higher degree of compulsion in relation to at-scale working than was the case in our sites. However, the absence of compulsion meant that, in some sites, practice owners and staff were remote from the federation, with low levels of engagement. Compulsion may produce greater focus and more rapid change,72 but thought needs to be given to mechanisms that create positive incentives in order to mitigate the potential adverse effects of such compulsion.
The results of this study suggest that setting up standardised operating procedures, sharing records, managing staff performance collaboratively and agreeing objectives for different types of staff is not necessarily easy, and requires time as well as significant upfront investment. The tight timetable means that groups that have already established ways of working together will be at a significant advantage, and there is a danger that existing inequalities in service provision will be exacerbated. Furthermore, when this has been achieved at the federation level, then it makes sense to build on existing systems rather than dismantle them. Data requirements of effective at-scale working suggest that support is needed for enabling effective IT systems, which avoid the paper-based and resource-intensive ‘work-arounds’ that characterised the IAGP process.
Although we found some benefits related to competition between federations (i.e. offering choice, facilitating a more directive and focused approach), this competition can also present problems when it inhibits collaboration across geographical footprints. This study highlights tensions arising from collaboration based on a shared ethos, but not a collective geography. Linked to this, for large multisite practices, whose patients may be in more than one PCN, consideration needs to be given to the implications of participation in multiple PCNs.
In August 2019 NHS England and NHS Improvement published PCN Development Support – Guidance and Prospectus,134 which describes development domains for PCNs and outlines processes and funding for PCN development support and PCN clinical director support. Organisational development resources for at-scale working are very welcome, as we identified training needs among staff who were directly involved in federation business. Extending this beyond these staff is important for contributing to succession planning for at-scale organisations more generally. Enabling staff to come together is important for creating a shared identity beyond the individual practice. At the same time, creating opportunities for staff from different at-scale organisations to come together is also important to encourage networking and shared learning.
In addition, the creation of a central, but independent, facility to assist with legal, financial and HR queries to respond to a need identified in this study would be very welcome. As part of this process, it is important to appreciate that central resources should be facilitative and, when possible, avoid implying top-down mandates that attempt to constrain local freedoms.
Negotiating conflicts of interest consumed time and energy in our sites. The NHS Long Term Plan40 identifies rules and processes skewed to fostering competition as inhibiting enabling integration of care planning and delivery. Clear guidance would be helpful regarding changes to these rules, which facilitate more collaborative working involving at-scale organisations.
Motivations for federation membership were complex and variable, and ambition and progress varied hugely across the sites. This suggests that realistic expectations should not be based on organisations characterised by very keen and able staff. However, this also means that there is good potential for piloting initiatives in volunteer sites, to test new ideas, which may ultimately be adopted by others.
Implications for the consideration of the research community
The creation of PCNs implies a broad research agenda concerning the workings of these new organisational forms. Research examining PCNs will probably involve examining many of the issues we explored in relation to federations, such as governance mechanisms (on paper and in practice), workforce, innovations in practices and interface with health and social care stakeholders. In this section, we focus on research recommendations arising from this study, as opposed to PCN-related issues more generally.
Exploring the impact on federations of PCNs is a priority. As part of this process, there is a need to understand how and to what extent PCNs are affecting existing federations and other collaborative arrangements in an increasingly complex and crowded landscape.
This study identified factors that contributed to federation success and failure, which resonate with success factors identified in the existing literature. 41,43,52,58–60,72 However, the federation styles we identified offer an additional means of understanding factors contributing to success. Further research that tests the relationship between federation style and outcomes and enhances the understanding of federation style as an explanatory concept would add depth to the knowledge in this area.
Our research has methodological implications. In particular, because we found that new organisational forms emerged in response to problems, with functions worked out later,86 research should avoid a preoccupation with structures and focus on processes of interaction as part of managing relationships of interdependence. Our classification of activities for managing interdependence may be helpful in this case.
The nature and time scale of our research meant that quantitative assessment of impact was not part of the design. However, research would benefit from multimethod designs, which provide in-depth, longitudinal, qualitative and quantitative methods, to shed light on processes and impacts.
We found that emotion (e.g. fear and, in particular, feeling threatened and vulnerable) was important in motivating participation. This is a neglected topic in the existing MO and network literature, with the latter, although recognising the importance of values, often treating individuals as (pro-social) rational, instrumental beings, neglecting the emotional dimension. It would also be helpful to explore the issue of trust, which is linked to emotions and also features heavily in the network literature. This study suggests that the absence of mistrust and a perception of legitimacy may be sufficient to enable collaborative arrangements to make progress. According to MO theory, striving towards similarity and shared status among MO members ‘provides a foundation for creating trust in interaction that is characterized by disembeddedness’. 107 Research needs to explore how trust works in practice in MOs that comprise member organisations whose staff may have little or no contact with the MO central authority and/or other member organisations. Furthermore, as practices may be compelled to work with others in PCNs where distrust is present, research needs to explore whether or not, how and to what extent this obstacle is overcome.
The findings with respect to key drivers resonate with literature on networks in health contexts. 41,43,52,58–60,72 In addition, concepts from MO theory have been useful in helping to explain our findings, such as similarity and shared identity as a basis for MO formation, the likelihood of passive membership as a threat to the MO (as opposed to merely emphasising power struggles or free-riding), the distinction between direct and indirect resources, the desire to stabilise environments to increase predictability and control, and protected zones. 112 The concept of a protected zone applies to a federation seeking to control its environment. Included in this is the idea that, rather than involving patients in the federation’s internal processes, the federation staff aim to provide stability of provision for patients as part of the federation’s aim in creating a protected zone. This is a different approach to interacting with stakeholders such as customers and asking them to sit on committees/boards, which would be to involve them in internal processes. Yet there have been few applications of the MO concept in health-care contexts. The findings, which highlight the double-edged nature of both competition between MOs and of national targets, provided a contribution to the MO and network literatures, wherein these issues are either ignored or often treated as a malign influence. Furthermore, the findings also challenge the assumptions about trade-offs between internal and external legitimacy82 and the conception of power as a zero-sum game,130 which characterise these literatures. Research combining concepts from both MO and network theory that adopts a more nuanced view of power and top-down targets would help to contribute to both of these bodies of theory.
Conclusion
This study found evidence that federations can produce positive benefits but this takes time and effort. The approach of the federation central authority (authoritative, indulgent or neglectful) was highly influential in affecting processes and outcomes. However, progress against stated aims was much slower than expected and, in most cases, little was required of practices beyond payment of membership fees. In only one site were practices required to make changes to their internal processes, and these concerned changes to administrative functions rather than having implications for clinical autonomy. The creation of PCNs raises questions about the future of federations and whether or not and how general practice leaders can continue to spread themselves across an increasingly complex and demanding landscape.
Acknowledgements
We are very grateful to all participants who shared their views with us, many of whom allowed us to observe them in meetings. We are indebted to Damian Hodgson, Professor of Organisational Analysis at Alliance Manchester Business School, for his insight and intellectual input, particularly during the early stages of the research. Oz Gore, Lecturer in Innovation, Technology and Operations at Leicester School of Business, provided valuable input to data analysis during the early stages of the project; we are very grateful for his contribution. We offer particular thanks to members of the Study Advisory Group, whose combined lay, practitioner and academic expertise and input was invaluable.
Contributions of authors
Professor Ruth McDonald (https://orcid.org/0000-0002-3488-4209) was the chief investigator; she designed the study, collected and analysed data, provided supervisory support and co-wrote the report.
Dr Lisa Riste (https://orcid.org/0000-0003-2606-0717) collected and analysed data and co-wrote the report.
Dr Simon Bailey (https://orcid.org/0000-0001-9142-2791) was a co-investigator; he designed the study, collected and analysed data and co-wrote the report.
Dr Fay Bradley (https://orcid.org/0000-0002-0009-1470) analysed data and co-wrote the report.
Dr Jonathan Hammond (https://orcid.org/0000-0002-4682-9514) collected and analysed data and co-wrote the report.
Dr Sharon Spooner (https://orcid.org/0000-0001-6965-3673) was a co-investigator; she designed the study, contributed to the analysis and co-wrote the report.
Dr Rebecca Elvey (https://orcid.org/0000-0003-3754-4979) was a co-investigator; she designed the study, collected and analysed data and contributed to Chapter 3.
Professor Kath Checkland (https://orcid.org/0000-0002-9961-5317) was a co-investigator; she designed the study, contributed to the analysis and co-wrote the report.
Data-sharing statement
This is a qualitative study and the data format means that it is not possible to anonymise the data for sharing. Furthermore, access was granted and consent was given on the basis that only members of the study team would access the data. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Department of Health and Social Care . Working for Patients 1989.
- Humphrey C, Berrow D. Developing role of medical audit advisory groups. Qual Health Care 1993;2:232-8. https://doi.org/10.1136/qshc.2.4.232.
- Department of Health and Social Care (DHSC) . Primary Care Groups: Taking the Next Steps 1998.
- Mays N, Goodwin N, Killoran A, Malbon G. Total Purchasing: A Step Towards Primary Care Groups – National Evaluation of Total Purchasing Pilot Projects. London: The King’s Fund; 1998.
- Department of Health and Social Care . Practice-Based Commissioning: Engaging Practices in Commissioning 2004.
- Heaney D, Gorman D, Porter M. Self-recorded stress levels for general practitioners before and after forming an out-of-hours primary care centre. Br J Gen Pract 1998;48:1077-8.
- Coleman A, Checkland K, Harrison S, Dowswell G. Practice-Based Commissioning: Theory, Implementation and Outcome. Final Report 2009.
- Miller R, Peckham S, Coleman A, McDermott I, Harrison S, Checkland K. What happens when GPs engage in commissioning? Two decades of experience in the English NHS. J Health Serv Res Policy 2016;21:126-33. https://doi.org/10.1177/1355819615594825.
- SQW, Mott Macdonald . Prime Minister’s Challenge Fund: Improving Access to General Practice. First Evaluation Report – October 2015 n.d. www.england.nhs.uk/wp-content/uploads/2015/10/pmcf-wv-one-eval-report.pdf (accessed 10 July 2019).
- National Audit Office . Developing New Care Models Through NHS Vanguards 2018. www.nao.org.uk/report/developing-new-care-models-through-nhs-vanguards/ (accessed 10 July 2019).
- Rosen R, Kumpunen S, Curry N, Davies A, Pettigrew L, Kossarova L. Is Bigger Better? Lessons for Large-Scale General Practice. Research Report 2016.
- Imison C, Williams S, Smith J, Dingwall C. Toolkit to Support the Development of Primary Care Federations. London: The King’s Fund, Hempsons, Nuffield Trust; 2019.
- Greer S. Territorial Politics and Health Policy: UK Health Policy in Comparative Perspective. Manchester: Manchester University Press; 2009.
- Armstrong D. Clinical autonomy, individual and collective: the problem of changing doctors’ behaviour. Soc Sci Med 2002;55:1771-7. https://doi.org/10.1016/S0277-9536(01)00309-4.
- Baker R. Will the future GP remain a personal doctor?. Br J Gen Pract 1997;47:831-3.
- Dowrick C, May C, Richardson M, Bundred P. The biopsychosocial model of general practice: rhetoric or reality?. Br J Gen Pract 1996;46:105-7.
- Britten N. Prescribing and the defence of clinical autonomy. Sociol Health Illn 2001;23:478-96. https://doi.org/10.1111/1467-9566.00261.
- Cheraghi-Sohi C, Calnan M. Discretion or discretions? Delineating professional discretion: the case of English medical practice. Soc Sci Med 2013;96:52-9. https://doi.org/10.1016/j.socscimed.2013.07.011.
- McDonald R, Checkland K, Harrison S, Coleman A. Rethinking collegiality: restratification in English general medical practice 2004–2008. Soc Sci Med 2009;68:1199-205. https://doi.org/10.1016/j.socscimed.2009.01.042.
- Johnson R. Where have all the pennies gone? The work of Manchester Medical Audit Advisory Group. BMJ 1994;309:98-102. https://doi.org/10.1136/bmj.309.6947.98.
- Grol R, Mokkink H, Schellevis F. The effects of peer review in general practice. J R Coll Gen Pract 1988;38:10-3.
- Baker R, Samuel O. Quality assurance in general practice. Proc R Soc Edinb B Biol Sci 1993;101:123-41. https://doi.org/10.1017/S0269727000005704.
- Great Britain . The National Health Service and Community Care Act 1990 1990.
- Glennerster H. Implementing GP Fundholding: Wild Card or Winning Hand?. London: Open University Press; 1994.
- Goodwin N, Mays N, McLeod H, Malbon G, Raftery J. Evaluation of total purchasing pilots in England and Scotland and implications for primary care groups in England: personal interviews and analysis of routine data. BMJ 1998;317:256-9. https://doi.org/10.1136/bmj.317.7153.256.
- Miller R, Peckham S, Checkland K, Coleman A, McDermott I, Harrison S, et al. Clinical Engagement in Primary Care-led Commissioning: A Review of the Evidence. London: Policy Research Unit in Commissioning and the Healthcare System (PRUComm); 2012.
- Shekelle P. New contract for general practitioners. BMJ 2003;326:457-8. https://doi.org/10.1136/bmj.326.7387.457.
- Department of Health and Social Care (DHSC) . Practice-Based Commissioning: Engaging Practices in Commissioning 2004.
- Smith J, Holder H, Edwards N, Maybin J, Parker H, Rosen R, et al. Securing the Future of General Practice: New Models of Primary Care. London: Nuffield Trust; 2013.
- McDermott I, Warwick-Giles L, Gore O, Moran V, Bramwell D, Coleman A, et al. Understanding Primary Care Co-Commissioning: Uptake, Development, and Impacts (Final Report) 2018.
- Roland M, Everington S. Tackling the crisis in general practice. BMJ 2016;352. https://doi.org/10.1136/bmj.i942.
- Marchand C, Peckham S. Addressing the crisis of GP recruitment and retention: a systematic review. Br J Gen Pract 2017;67:e227-37. https://doi.org/10.3399/bjgp17X689929.
- Lawson N. GP Partnership Review: Final Report 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/770916/gp-partnership-review-final-report.pdf (accessed 10 July 2019).
- Heins E, Pollock AM, Price D. The commercialisation of GP services: a survey of APMS contracts and new GP ownership. Br J Gen Pract 2009;59:e339-43. https://doi.org/10.3399/bjgp09X472638.
- NHS England . Next Steps on the NHS Five Year Forward View n.d. www.england.nhs.uk/wp-content/uploads/2017/03/NEXT-STEPS-ON-THE-NHS-FIVE-YEAR-FORWARD-VIEW.pdf (accessed 10 July 2019).
- NHS England . New Care Models: Vanguards – Developing a Blueprint for the Future of NHS and Care Services 2016. www.england.nhs.uk/wp-content/uploads/2015/11/new_care_models.pdf (accessed 10 July 2019).
- NHS England . NHS Five Year Forward View 2014. www.england.nhs.uk/publication/nhs-five-year-forward-view/ (accessed 10 July 2019).
- NHS England . General Practice Forward View (GPFV) 2016. www.england.nhs.uk/publication/general-practice-forward-view-gpfv/ (accessed 10 July 2019).
- National Association of Primary Care . Primary Care Home n.d. https://napc.co.uk/primary-care-home/ (accessed 10 July 2019).
- NHS England . The NHS Long Term Plan 2019.
- Ferlie E, Fitzgerald L, McGivern G, Dopson S, Exworthy M. Networks in Health Care: A Comparative Study of their Management, Impact and Performance. NHS Service Delivery and Organisation Programme; 2010.
- Crump H, Edwards N. Provider Chains: Lessons From Other Sectors. London: The Nuffield Trust; 2014.
- Brown BB, Patel C, McInnes E, Mays N, Young J, Haines M. The effectiveness of clinical networks in improving quality of care and patient outcomes: a systematic review of quantitative and qualitative studies. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1615-z.
- Nelson PA, Bradley F, Martindale AM, McBride A, Hodgson D. Skill-mix change in general practice: a qualitative comparison of three ‘new’ non-medical roles in English primary care. Br J Gen Pract 2019;69:e489-98. https://doi.org/10.3399/bjgp19X704117.
- Guthrie B, Davies H, Greig G, Rushmer R, Walter I, Duguid A, et al. Delivering Health Care Through Managed Clinical Networks (MCNs): Lessons From the North. NHS Service Delivery and Organisation Programme; 2010.
- Fotaki M. Why do public policies fail so often? Exploring health policy-making as an imaginary and symbolic construction. Organization 2010;17:703-20. https://doi.org/10.1177/1350508410366321.
- Kingdon J. Agendas, Alternatives and Public Policies. New York, NY: Longman; 1995.
- Matthews-King A. GP practices lose ‘hundreds of thousands’ as federation goes bankrupt. Pulse 2016. www.pulsetoday.co.uk/hot-topics/stop-practice-closures/gp-practices-lose-hundreds-of-thousands-as-federation-goes-bankrupt/20033201.article (accessed 27 January 2020).
- Dunhill L. North by North West: what went wrong in Warrington?. Health Serv J 2018. www.hsj.co.uk/leadership/north-by-north-west-what-went-wrong-in-warrington/7023359.article (accessed 27 January 2020).
- Canter L. Recruitment crisis forces GP collaborative to hand back contracts on six practices. Pulse 2019. www.pulsetoday.co.uk/hot-topics/stop-practice-closures/recruitment-crisis-forces-gp-collaborative-to-hand-back-contracts-on-six-practices/20038204.article (accessed 27 January 2020).
- Ham C. Making Sense of Integrated Care Systems, Integrated Care Partnerships and Accountable Care Organisations in the NHS in England 2018. www.kingsfund.org.uk/publications/making-sense-integrated-care-systems (accessed 10 July 2019).
- Sheaff R, Childs S, Schofield J, Pickard S, Mannion R. Understanding Professional Partnerships and Non-Hierarchical Organisations. Final Report n.d. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1518-105_V01.pdf (accessed 10 July 2019).
- Bojke C, Gravelle H, Wilkin D. Is bigger better for primary care groups and trusts?. BMJ 2001;322:599-602. https://doi.org/10.1136/bmj.322.7286.599.
- NHS England, NHS Improvement . Refreshing NHS Plans for 2018 19 n.d. www.england.nhs.uk/wp-content/uploads/2018/02/planning-guidance-18-19.pdf (accessed 10 July 2019).
- Serle J. GPs to form 1,300 primary care networks. Health Serv J 2019. www.hsj.co.uk/service-design/gps-to-form-1300-primary-care-networks/7025432.article (accessed 29 November 2019).
- Coleman A, Checkland K, Harrison S, Hiroeh U. Local histories and local sensemaking: a case of policy implementation in the English National Health Service. Policy Politics 2010;38. https://doi.org/10.1332/030557309X462547.
- Hammond J. Health Policy, the Politics of Governance and Change: The Introduction of Clinical Commissioning Groups in Context 2015.
- Checkland K, Coleman A, McDermott I, Segar J, Miller R, Petsoulas C, et al. Primary care-led commissioning: applying lessons from the past to the early development of clinical commissioning groups in England. Br J Gen Pract 2013;63:e611-9. https://doi.org/10.3399/bjgp13X671597.
- Pickin DM, O’Cathain A, Fall M, Morgan AB, Howe A, Nicholl JP. The impact of a general practice co-operative on accident and emergency services, patient satisfaction and GP satisfaction. Fam Pract 2004;21:180-2. https://doi.org/10.1093/fampra/cmh213.
- Hodgson D, Anselmi L, Bailey S, Bower P, Checkland K, Elvey R, et al. NHS Greater Manchester Primary Care Demonstrator Evaluation. Manchester: Collaboration for Leadership in Applied Health and Care Research, Greater Manchester; 2015.
- Pettigrew LM, Kumpunen S, Mays N, Rosen R, Posaner R. The impact of new forms of large-scale general practice provider collaborations on England’s NHS: a systematic review. Br J Gen Pract 2018;68:e168-e177. https://doi.org/10.3399/bjgp18X694997.
- Ferlie E, McGivern G, Fitzgerald L, Dopson S, Bennett C. Public policy networks and ‘wicked problems’: a nascent solution?. Public Adm 2011;89:307-24. https://doi.org/10.1111/j.1467-9299.2010.01896.x.
- Rittel HWJ, Webber MM. Dilemmas in a general theory of planning. Policy Sci 1973;4. https://doi.org/10.1007/BF01405730.
- Edwards N. Clinical networks: advantages include flexibility, strength, speed, and focus on clinical issues. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7329.63.
- Edwards N, Fraser SW. Clinical Networks: A Discussion Paper. London: NHS Confederation; 2001.
- Flynn R, Williams G, Pickard S. Markets and Networks: Contracting in Community Health Services. Buckingham: Open University Press; 1996.
- Braithwaite J, Churruca K, Ellis L, Long J, Clay-Williams R, Damen N, et al. Complexity Science in Healthcare – Aspirations, Approaches, Applications, and Accomplishments: A White Paper 2017.
- Rouse W B. Health care as a complex adaptive system: implications for design and management. Bridge 2008;38:17-25.
- Stark D, DiMaggio P. The Twenty-first Century Firm: Changing Economic Organization in International Perspective. Princeton, NJ: Princeton University Press; 2001.
- Tuohy CH. Agency, contract and governance: shifting shapes of accountability in the health care arena. J Health Polit Policy Law 2003;28:195-21. https://doi.org/10.1215/03616878-28-2-3-195.
- Shortell SM, Ramsay PP, Baker LC, Pesko MF, Casalino LP. The characteristics of physician practices joining the early ACOs: looking back to look forward. Am J Manag Care 2018;24:469-74.
- Pettigrew LM, Kumpunen S, Rosen R, Posaner R, Mays N. Lessons for ‘large-scale’ general practice provider organisations in England from other inter-organisational healthcare collaborations. Health Policy 2019;123:51-6. https://doi.org/10.1016/j.healthpol.2018.10.017.
- Erens B, Wistow G, Mounier-Jack S, Douglas N, Jones L, Manacorda T, et al. Early Evaluation of the Integrated Care and Support Pioneers Programme: Interim Report 2015. https://researchonline.lshtm.ac.uk/2391580/1/Early%20evaluation%20of%20IC%20Pioneers%2C%20interim%20report.pdf (accessed 10 July 2019).
- Smith JA, Mays N. GP led commissioning: time for a cool appraisal. BMJ 2012;344. https://doi.org/10.1136/bmj.e980.
- Pfeffer J, Salancik G. The External Control of Organizations A Resource Dependence Perspective. New York, NY: Harper – Row; 1978.
- Dyer JH, Singh H. The relational view cooperative strategy and sources of interorganizational competitive advantage. Academ Manag Rev 1998;23:660-79. https://doi.org/10.2307/259056.
- Oliver C. Determinants of interorganizational relationships: integration and future directions. Academ Manag Rev 1990;15:241-65. https://doi.org/10.2307/258156.
- O’Leary R, Blomgren Bingham L. The Collaborative Public Manager: New Ideas for the Twenty-first Century. Washington, DC: Georgetown University Press; 2009.
- Thomson AM, Perry JL, Miller TK. Conceptualizing and measuring collaboration. J Public Adm Res Theory 2009;19:23-56. https://doi.org/10.1093/jopart/mum036.
- DiMaggio PJ, Powell W. The iron cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev 1983;48:147-60. https://doi.org/10.2307/2095101.
- Thomson AM, Perry JL, Thomson AM. Collaboration processes: inside the black box. Public Adm Rev 2006;66:20-32. https://doi.org/10.1111/j.1540-6210.2006.00663.x.
- Provan K, Kenis P. Modes of network governance: structure, management, and effectiveness. J Public Adm Res Theory 2008;8:229-52. https://doi.org/10.1093/jopart/mum015.
- Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable Care Organizations: the national landscape. J Health Polit Policy Law 2015;40:647-68. https://doi.org/10.1215/03616878-3149976.
- Greaves F, Millett C, Pape UJ, Soljak M, Majeed A. Association between primary care organisation population size and quality of commissioning in England: an observational study. Br J Gen Pract 2012;62:e46-54. https://doi.org/10.3399/bjgp12X616364.
- Chen B. Antecedents or processes? Determinants of perceived effectiveness of interorganizational collaborations for public service delivery. Int Public Manage J 2010;13:381-407. https://doi.org/10.1080/10967494.2010.524836.
- Shortell S, Addicott R, Ferlie E, Montgomery K, Pedersen A. The Oxford Handbook of Health Care Management. Oxford: Oxford University Press; 2016.
- Sheaff R, Marshall M, Rogers A, Roland M, Sibbald B, Pickard S. Governmentality by network in English primary healthcare. Soc Policy Adm 2004;38:89-103. https://doi.org/10.1111/j.1467-9515.2004.00378.x.
- Barker JR. Tightening the iron cage: concertive control in self-managing teams. Adm Sci Q 1993;38:408-37. https://doi.org/10.2307/2393374.
- Baker R, Willars J, McNicol S, Dixon-Woods M, McKee L. Primary care quality and safety systems in the English National Health Service: a case study of a new type of primary care provider. J Health Serv Res Policy 2014;19:34-41. https://doi.org/10.1177/1355819613500664.
- Pettigrew AM, Bedeian AG. Management Laureates: A Collection of Autobiographical Essays. Greenwich: JAI Press; 1998.
- Casalino LP, Chen MA, Staub CT, Press MJ, Mendelsohn JL, Lynch JT, et al. Large independent primary care medical groups. Ann Fam Med 2016;14:16-25. https://doi.org/10.1370/afm.1890.
- Checkland K, McDermott I, Coleman A, Perkins N. Complexity in the new NHS: longitudinal case studies of CCGs in England. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010199.
- Hawkes N. Two doctors are banned from acting as company directors after failing to pass on pension contributions. BMJ 2012;345. https://doi.org/10.1136/bmj.e8425.
- Dunn P, McKenna H, Murray R. Deficits in the NHS 2016. London: The King’s Fund; 2016.
- Addicott R, Ferlie E, McGivern G. Networks, organizational learning and knowledge management: NHS cancer networks. Public Money Manag 2006;26:87-94. https://doi.org/10.1111/j.1467-9302.2006.00506.x.
- Addicott R, McGivern G, Ferlie E. The distortion of a managerial technique? The case of NHS cancer networks. Br J Manag 2007;18:93-105. https://doi.org/10.1111/j.1467-8551.2006.00494.x.
- Currie G, Suhomlinova O. The impact of institutional forces upon knowledge sharing in the UK NHS: the triumph of professional power and the inconsistency of policy. Public Adm 2006;84:1-30. https://doi.org/10.1111/j.0033-3298.2006.00491.x.
- Addicott R, Ferlie E. Understanding power relationships in health care networks. J Health Organ Manag 2007;21:393-405. https://doi.org/10.1108/14777260710778925.
- Currie G, Grubnic S, Hodges R. Leadership in public services networks: antecedents, process and outcome. Public Adm 2011;89:242-64. https://doi.org/10.1111/j.1467-9299.2011.01931.x.
- Pringle R. Sex and Medicine, Gender, Power and Authority in the Medical Profession. Cambridge: Cambridge University Press; 1998.
- Checkland K, Coleman A, Segar J, McDermott I, Miller R, Wallace A, et al. Exploring the Early Workings of Emerging Clinical Commissioning Groups: Final Report 2012.
- Toubiana M, Oliver C, Bradshaw P. Beyond differentiation and integration: the challenges of managing internal complexity in federations. Organ Stud 2017;3:1013-37. https://doi.org/10.1177/0170840616670431.
- Hann M, Bower P, Campbell S, Marshall M, Reeves D. The association between culture, climate and quality of care in primary health care teams. Fam Pract 2007;24:323-9. https://doi.org/10.1093/fampra/cmm020.
- Deal TE, Kennedy AA. Corporate Cultures: The Rites and Rituals of Corporate Life. Reading, MA: Addison Wesley Publishing Company; 1982.
- Sheaff R, Benson L, Farbus L, Schofield J, Mannion R, Reeves D. Network resilience in the face of health system reform. Soc Sci Med 2010;70:779-86. https://doi.org/10.1016/j.socscimed.2009.11.011.
- Thompson G. Between Hierarchies and Markets – The Logic and Limit of Network Forms of Organization. Oxford: Oxford University Press; 2003.
- Ahrne G, Brunsson N. Meta-Organizations. Cheltenham: Edward Elgar; 2008.
- Berkowitz H, Dumez H. The concept of meta-organization: issues for management studies. Eur Manag Rev 2016;13:149-56. https://doi.org/10.1111/emre.12076.
- Berkowitz H, Bor S. Why meta-organizations matter: a response to Lawton et al. and Spillman. J Manag Inq 2018;27:204-11. https://doi.org/10.1177/1056492617712895.
- Blau PM, Scott WR. Formal Organizations. San Francisco, CA: Scott, Foreman; 1962.
- Weber M, Gerth HH, Mills CW. From Max Weber: Essays in Sociology. New York, NY: Oxford University Press; 1946.
- Ahrne G, Brunsson N, Seidl D. Resurrecting organization by going beyond organizations. Eur Manag J 2016;34:93-101. https://doi.org/10.1016/j.emj.2016.02.003.
- Hawkes N. Rise of the federation: how GPs are meeting the challenge of competition. BMJ 2014;348. https://doi.org/10.1136/bmj.g2155.
- Königa A, Schulteb M, Endersc A. Inertia in response to non-paradigmatic change: the case of meta-organizations. Res Policy 2012;41:1325-43. https://doi.org/10.1016/j.respol.2012.03.006.
- Berkowitz H. Meta-organizing firms’ capabilities for sustainable innovation: a conceptual framework. J Cleaner Production 2018;175:420-30. https://doi.org/10.1016/j.jclepro.2017.12.028.
- Checkland K. Understanding general practice: a conceptual framework developed from case studies in the UK NHS. Br J Gen Pract 2007;57:56-63.
- Bor S. A Theory of Meta-Organisation: An Analysis of Steering Processes in European Commission-Funded R–D ‘Network of Excellence’ Consortia 2014. http://hdl.handle.net/10138/144154 (accessed 27 January 2020).
- McDonald R. Market reforms in English primary medical care: medicine, habitus and the public sphere. Sociol Health Illn 2009;31:659-72. https://doi.org/10.1111/j.1467-9566.2009.01165.x.
- Boltanski L, Thévenot L. On Justification: Economies of Worth. Princeton, NJ: Princeton University Press; 2006.
- Stark D. The Sense of Dissonance. Accounts of Worth in Economic Life. Princeton, NJ: Princeton University Press; 2009.
- Valente M, Oliver C. Meta-organization formation and sustainability in sub-Saharan Africa. Organization Sci 2018;29:678-701. https://doi.org/10.1287/orsc.2017.1191.
- NHS England . General Practice Development Programme n.d. www.england.nhs.uk/gp/gpfv/redesign/gpdp/ (accessed 27 January 2020).
- Hedlund G, Rolander D, Bartlett C, Doz Y, Hedlund G. Managing the Global Firm. London: Routledge; 1990.
- Teisman GR, Tisma A. Complexere besluitvorming: een pluricentrisch perspectief op besluitvorming over ruimtelijke investeringen. Designing and Deciding: Development of an Decision Support System Based on the Case Study of the Landscape Transformation of the South Axes of Amsterdam 1992. https://pdfs.semanticscholar.org/daab/42b245a3c608e51d97b462357d0a7b318e10.pdf (accessed 27 January 2020).
- De la Mothe J, Paque G, De la Mothe J, Paque G. Evolutionary Economics and the New International Political Economy. Kent: Pinter Publishers; 1996.
- Baumrind D. Current patterns of parental authority. Dev Psychol 1971;4:1-103. https://doi.org/10.1037/h0030372.
- Thornberry T. Developmental Theories of Crime and Delinquency. New Brunswick, NJ: Transaction Publishers; 1997.
- Ebers M, Maurer I. Connections count: how relational embeddedness and relational empowerment foster absorptive capacity. Res Policy 2014;43:318-32. https://doi.org/10.1016/j.respol.2013.10.017.
- Uzzi B. Embeddedness in the making of financial capital: how social relations and networks benefit firms seeking financing. Am Sociol Rev 1999;64:481-505. https://doi.org/10.2307/2657252.
- Read J. Is power zero-sum or variable-sum? Old arguments and new beginnings. J Political Power 2012;5:5-31. https://doi.org/10.1080/2158379X.2012.659865.
- Pawa J, Robson J, Hull S. Building primary care practice networks to deliver better clinical care: a qualitative semi-structured interview study. Br J Gen Pract 2017;67:e764-74. https://doi.org/10.3399/bjgp17X692597.
- The King’s Fund . Primary Care Networks Explained 2019. www.kingsfund.org.uk/publications/primary-care-networks-explained (accessed 27 January 2020).
- Serle J. Revealed: 40 per cent of PCNs flout NHSE guidance on size. Health Serv J 2019. www.hsj.co.uk/service-design/revealed-40-per-cent-of-pcns-flout-nhse-guidance-on-size/7026193.article (accessed 27 January 2020).
- NHS England and NHS Improvement . PCN Development Support – Guidance and Prospectus 2019. www.healthylondon.org/wp-content/uploads/2018/10/PCN-Development-Support-Prospectus.pdf (accessed 27 January 2020).
- Cockman P, Dawson L, Mathur R, Hull S. Improving MMR vaccination rates: herd immunity is a realistic goal. BMJ 2011;343. https://doi.org/10.1136/bmj.d5703.
- Hull S, Chowdhury TA, Mathur R, Robson J. Improving outcomes for patients with type 2 diabetes using general practice networks: a quality improvement project in east London. BMJ Qual Saf 2014;23:171-6. https://doi.org/10.1136/bmjqs-2013-002008.
- Hull S, Mathur R, Lloyd-Owen S, Round T, Robson J. Improving outcomes for people with COPD by developing networks of general practices: evaluation of a quality improvement project in east London. NPJ Prim Care Respir Med 2014;24. https://doi.org/10.1038/npjpcrm.2014.82.
- Robson J, Hull S, Mathur R, Boomla K. Improving cardiovascular disease using managed networks in general practice: an observational study in inner London. Br J Gen Pract 2014;64:e268-74. https://doi.org/10.3399/bjgp14X679697.
- NHS England . General Practice Extended Access: September 2018 n.d. www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2018/11/GP-Extended-Access-Commentary-September-2018.pdf (accessed 27 January 2020).
- NHS England . Extended Access to General Practice n.d. www.england.nhs.uk/statistics/statistical-work-areas/extended-access-general-practice/ (accessed 27 January 2020).
- National Institute for Health and Care Excellence (NICE) . Stop Smoking Interventions and Services. NICE Guideline [NG92] 2018. www.nice.org.uk/guidance/ng92/chapter/Recommendations (accessed 28 January 2020).
Appendix 1 New forms of large-scale general practice provider collaborations in England
A recent systematic review of the literature on new forms of large-scale general practice provider collaborations in England concluded that ‘good-quality evidence of the impacts of “scaling up” general practice provider organisations in England is scarce’. 61 Only five studies met the inclusion criteria and four of these focused on developments in the same London borough. 135–138 These assessed the impact of an initiative by Tower Hamlets PCT in 2008/9 to incentivise collaboration to deliver packages of care in four clinical areas between 2009 and 2012 using funding of £10M, which was recycled from other initiatives. The PCT had also been one of the Integrated Care Pilots and later Integrated Care and Support Pioneer sites, and is often cited as a national leader in primary care; consequently, it might not be representative of general practice as a whole. In addition to identifying impacts on outcomes, the literature review identified useful lessons in relation to the process of working at scale. In particular, it noted that ‘[s]ubstantial financial investment was required’61 to establish the collaborations and associated interventions. Quality improved in the targeted areas, with a combination of standardised processes, federation-level incentives, IT-enabled performance dashboards and managers at the federation level said to be key contributory factors. The fifth study of a hierarchically organised chain of > 50 practices dispersed across England suggested that this organisational form ‘may be useful in standardizing policies and procedures, facilitating implementation of systems, and relieving clinical staff of administrative duties’. 89 The authors highlight three factors as being of interest: size and scale, hierarchical governance, and commercial imperatives. Although the first two were helpful in securing implementation of standardised policies and reducing the administrative burden on clinicians, there was some evidence of high staff turnover, with implications for continuity of care. In addition, the authors identified patient concerns relating to the tension between the goals of the commercial enterprise and public goals of service quality. Pettigrew et al. 61 also suggest that federations of existing practices should be investigated as these may reap the benefits of working at scale, but are less likely to clash with GP autonomy and may be better able to maintain continuity of care. In the Tower Hamlet examples, the sites included were actively involved in the delivery of clinical programmes and were financially incentivised to do so. The other case involved a large chain, with an explicitly corporate structure and ownership concentrated in the hands of a small number of individuals who had proactively pursued an explicitly commercial business venture. Although there is no such thing as a ‘typical’ federation, the literature raises questions about the extent to which these examples are representative of the English general practice landscape more generally, and the transferability of these lessons to it.
The systematic review was part of a larger piece of work exploring ‘large-scale general practice’. 11 It examined the factors influencing the evolution of these forms of organisation as well as their impact on staff, patients, the wider health economy and care quality. This combined data from large-scale surveys and four case studies, as well as a quantitative component aimed at assessing impacts on quality. The study found that nearly three-quarters of general practices were in some form of collaboration with other practices, with almost half of these being formed during 2014/15. It also found that larger scale could contribute positively to sustainability in general practice through standardised processes and operational efficiency, maximising income, enhancing the workforce and deploying technology. However, it highlighted the significant levels of leadership and resources needed to create, develop and maintain these organisations. Board accountability to member practices was key to building trust and engagement, but the style in which changes were implemented varied according to whether or not the central organisation held member practices’ contracts. When this was the case, a more directive approach to change, involving the executive team directing day-to-day operations, allocating additional resources and offering leadership support where needed, was in evidence. Elsewhere, a more concertive approach to change was implemented involving peer pressure and the offer of support from the central team.
Economies of scale enabled investment in staff, technology and support. In addition, the range of services offered in general practice was extended in case study sites, although service changes were mainly small-scale in nature. Patient views were mixed, but staff were largely positive. Working more collaboratively was valued, reducing professional isolation and providing rapid access to operational and clinical advice. Despite the routine use of quality improvement tools in case study sites, no marked differences in quality of care were observed compared with the national average.
The quality of relationships with commissioners and local providers influenced the extent to which the GP organisations could go beyond the provision of core services.
The authors recommended that large-scale general practice groups should invest time in agreeing the purpose, values and short- to medium-term organisational goals. Agreement should be reached on the extent to which the group wants to take on delivery of extended services. Investment in developing staff roles across practice boundaries and creating peer support and peer learning opportunities was also viewed as important. Consideration should be given to including quality improvement goals that are specific and measurable, as well as being consistent with local commissioning priorities. In addition to the aim of improving care, this will help build relationships with local CCGs and create a rationale for CCG investment in the organisation. Governance arrangements should be as simple as possible for delivering agreed goals, although groups should be prepared for them to become more complex as the organisation’s objectives develop. Linked to this, agreement should be reached on the level of decision-making authority given to the board that will best balance pace of change with maintaining member engagement. It is important to ensure that resources are available to achieve agreed goals and to be clear about the level of risk (in terms of investing resources) that members are willing to take in pursuit of these.
The authors recommend patient engagement to co-design services that address diverse needs and preferences. When organisations are seeking to establish extended services, the importance of establishing and maintaining collaborative relationships and shared goals with specialists is highlighted. Collaborative working to address population health needs and commissioning priorities is recommended and CCGs and national policy-makers are advised to have realistic expectations about the capacity of these new organisations and the pace of change required for new, high-quality and sustainable services to be developed. CCGs should also facilitate local discussions between patients, the public and other stakeholders about how these emerging organisations can contribute to the local health economy while minimising conflicts of interest.
Appendix 2 Changes to the initial design
Plans to construct a typology of federations based on national data
We started with a mapping exercise, which we anticipated would enable us to construct a national picture of the types of federations and their locations. We anticipated that this would add breadth to our analysis to enable comparison across a wider range of organisational forms. We also planned to use this to construct a typology of federations. However, as we prepared for this exercise, in July 2016, Rosen et al. 11 published their classification of general practice at-scale organisations using four categories: networks, federations, super-partnerships and multisite practice organisations. The variation between organisational forms was conceptualised using a spectrum ranging from ‘loose’ to ‘tight’ ties between members. For example, ‘networks’ embody loose ties and intangible objectives, lack an executive function and contracts are retained by member practices. In contrast, ‘multisite practice organisations’, at the other end of the spectrum, are characterised by tight ties, shared concrete objectives, employment of a management team and executive function, pooling of income and risk, and contracts being held by directors. Federations and super-partnerships lie between these extremes. The latter resemble a single organisation, with merged contracts and pooling of risk and reward.
In an attempt to map federation developments and provide a national picture, we used web searches and telephone calls to CCGs and LMCs to try to identify the names and locations of federations, as well as details such as number of federated practices and their number of registered patients. Using the telephone number given often resulted in local administrators struggling to identify the correct personnel. We also sent numerous e-mails in an attempt to gather relevant information. Although this approach occasionally resulted in correctly identifying a potential respondent, this was laborious and time-consuming. Furthermore, given the changing landscape, data collected in month 1 might be outdated within weeks. The benefits, in terms of the volume and quality of data collected, were dubious compared with the resources invested in this exercise. The study advisory group therefore suggested that we stopped our e-mail and telephone calls aimed at identifying all federations across England. This was because it was both time-consuming and difficult to obtain information, but also because, at this stage (month 7), we ascertained that information providing a national picture of GP federations and member practices was being collected elsewhere. Although not necessarily providing a comprehensive picture, NHS England collect and produce data identifying GP federations and member practices and make them available via NHS Digital. 54 The completion of a survey providing this information was a contractual requirement for general practices. The first collection took place during October 2016.
NHS England139 reported that, in response to the March 2018 survey, 5299 practices (representing 79.6% of the total number) were members of a group. This represented an increase of 9.3 percentage points since the previous data collection survey. The term group was defined as a collaboration of practices’ primary care services and their combined registered population. Federations were used as an example of a group.
The data are available on the NHS England website. 140
The data show each practice and the name of the ‘group’ of which it is member. However, this information does not enable us to compile a typology, because no information about the group beyond its name is provided.
Non-federation case study selection
We used in-depth case studies in four sites to collect and analyse the data that underpin the report. The selection of four case studies was a compromise between the breadth required to capture sufficient variation and the depth that we needed for detailed exploration. 56 We did initially plan to use a non-federation site to enable us to test out emerging findings and preliminary interpretations by comparing federation sites with the non-federation case study site. However, researching the absence of a federation raised a number of issues. Because federation formation was becoming increasingly common, its absence might imply that a site was, in relevant respects, untypical of general practice more generally, making it difficult to draw wider conclusions from this site. Furthermore, there would be no board and other federation-related meetings to attend. We could not ask questions about changes following the formation of the federation and other issues such as motivations and attitudes towards this emerging organisation. In addition, from our mapping work we had learned how diverse federations were in terms of organisational forms, scale and purpose. It made sense, therefore, to include as many federation sites as possible in our study, rather than a non-federation site, to increase learning; our advisory group supported this change in design.
Appendix 3 Vignettes
Working together: Improving Access to General Practice
The IAGP policy required the provision of access to GP services, including at evenings and weekends. A decision was taken by NHS England to move the timetable for implementation forward by 6 months, at relatively short notice. This meant that commissioners and GP federations had to work quickly, attempting to get some kind of service together in time. In what follows, we explore some of the issues raised by the IAGP policy and other problems facing the federations, to convey a greater understanding of the internal workings of each of them. In the vignettes that follow, pseudonyms have been used to preserve anonymity.
Working together vignette 1: Small – member organisation leads’ meeting
Meeting attendees had been discussing the issue of IAGP as the deadline for any bid was < 4 weeks away. The procurement process required bids for a locality, rather than federation, footprint. Queries raised by attendees included CQC registration for any proposed provider vehicle and costs associated with this, as well as ability to meet these from a small fixed pot. There was also an issue about shares and shareholding if practices from Central locality were not involved in a potential successful bid by Northern locality. This was seen as important as liability would rest with shareholders, but, also, any surplus would relate to shareholding status. David, a recently retired GP board member, made clear that, in terms of bidding for services, ‘this is completely different from GP contract stuff . . . and you’ve got to ensure it’s across all of your patch, you’ve got responsibility for this’. David acknowledged that IAGP was challenging, but asked ‘are you happy to let others do it?’.
An alternative was to bid in partnership with another organisation, sharing fixed costs. Lisa, the chief executive of the large merged practice in Central, suggested that others who were used to bidding would ‘walk all over us’. She had spoken to the CEO of Big, a much larger federation covering several regions of the country, the previous evening about a collaborative bid. Before this, Lisa had approached the local ‘predatory’ federation, but felt that their culture was so different from Small’s and that their attitude was that they were leading the bid and others would have to follow. Kate, a GP from a Central locality practice, expected to have ‘the square root of bugger all’ in terms of influencing that bid and said that they were being informed rather than engaged by the predatory federation.
Joe, a GP from a small practice in Central, asked about whether any of this would help in terms of funding to support back-office functions. He had already expressed the view that his patients would not use the service and later complained that, as a small practice, it was not in a position to influence anything. There was no expression of support for the new service and David, when asked, acknowledged that nobody thought that the service was a good idea, but, regardless, ‘the money’s going in there, so the appointments will be there for your patients’. ‘So’, David said, ‘if we look further ahead, urgent treatment centres are the next thing that’s going to come along. If you get the IAGP contract, you’re in pole position for bidding for these urgent treatment centres in the future, and if you don’t, then there’s a real issue’. He thought GMS could disappear, that these urgent care centre contracts ‘are going to be really important’ and this is the way the future’s going. Lisa explained that you could have the same people in multiple bids, so Small could be in more than one bid for the same service. Lisa also described various models for providing these services, which she had observed elsewhere in England. They both suggested that there would be little difficulty in staffing the new service, although it was not made explicit where the staff would be found for this.
The conversation then focused on partnering with external organisations locally and/or nationally. These organisations were described as sharing the NHS ethos and, therefore, consonant with Small’s underpinning beliefs. Andrew, whose concerns about being a small vulnerable practice mirrored those of Joe, suggested that perhaps a benefit of partnering with a much bigger federation would be that they might ‘also help us with the back-office stuff and related things that we can’t do without help’. Claire, the chairperson said that she was not comfortable talking about the future in terms of those back-office things; it was not a big issue for her practice. Kate supported the external partnering as ‘they’ll take the risk and then we could just be in a consultancy role’. After further discussions about logistics, a decision was taken to support a collaborative bid. This involved Claire going round the table and asking each attendee for their views. In one case, the GP lead was absent; his PM had spoken to him by telephone to ascertain his views. In all cases, there was support for a collaborative bid with an external partner for each of the two localities.
Although this vignette is concerned with decision-making in relation to the IAGP policy, it helps to illustrate a number of issues in Small more generally, and enables comparison with other sites. Unlike those sites, Small’s size meant that a representative from each practice was involved in the discussions and decision-making process at meetings. Consensus was reached without friction, but attendees had varying expectations about what entering into a partnership and being successful in bidding would entail. The divergence between smaller practices, keen to merge back-office functions, and larger ones, eager to retain control at practice level, did not disrupt the process nor did it create major divisions between members. The previous chairperson, whose own struggling practice had merged to become part of a much bigger practice, had been very keen on this approach for Small’s practices. However, Claire, whose large practice was located in a relatively affluent area and had no problems recruiting staff, was much less keen on this idea, and, as chairperson, was in a position to curtail discussion on this issue. This illustrates the impact that the varying interests and experience of individuals can have on federation processes and decisions in Small, but the issue applies more generally to all of our sites. David, as a recently retired partner, but still involved in the federation until autumn 2018, urged members to look ahead and sought to bring his views of likely changes in the landscape to the table. His background of having held CCG and other roles meant that he was well networked and experienced in adopting a proactive approach, outside the reactive process of seeing patients in his practice. He brought this ‘bigger picture’ perspective to meetings, as did Lisa, whose experience working in a range of sectors and cities and extensive network meant that, like David, she was able to act as a boundary spanner, bringing in contacts and ideas from outside the immediate area.
Discussions about issues such as CQC registration and shareholding highlighted the relative ignorance and lack of expertise concerning important topics. Often subjects were raised that were seen as important, but about which Small’s members lacked knowledge. These included issues relating to the IAGP policy such as indemnity arrangements for staff and the creation of wholly-owned subsidiaries to reflect the provision of services by locality as opposed to federation footprints, as well as more general matters such as the most appropriate organisational form to adopt and the implications of various shareholding arrangements. In our other sites too, federation staff grappled with issues that required knowledge outside their sphere of expertise. In the absence of any central resource for providing advice, staff expended valuable time and energy attempting to resolve issues, often reinventing the same wheel on the same issue. In addition to the lack of central resource, the fact that, in an evolving landscape, the organisations with which federations interacted lacked relevant knowledge exacerbated the problem. We return to the issue of interactions with external organisations in Vignette 3: smoking cessation in Embedded.
This vignette also illustrates how Small was forced to respond to activities in its external environment. The federation chairperson’s view that Small would provide a vehicle for mutual support and participation in a small number of collaborative projects such as the PS was at odds with those GP representatives from smaller practices who were interested in the potential for merging functions. However, at the same time, these practices had not joined Small to start to engage in bidding for new services, as their priority was to protect their vulnerable practices. Yet attendees were now changing their views about what the purpose of the federation should be. This was the case in Expanding and Embedded too, where issues of purpose and approach were fluid and emergent, rather than set in stone. In the case of the former, for example, admitting practices located at some distance from the local population footprint was a clear departure from the initial aims. At Embedded, for example, amendments were made to the constitution to reflect changes in the way it interacted with commissioners, which were indicative of a change in its perceived strategic role in the health economy. At Struggling, the competing perspectives of the CEO and chairperson were able to co-exist owing to the lack of concrete activities to necessitate a choice or trade-off between these, although the result was ultimately the demise of the federation.
The decision to bid, and subsequent success in one of the two bids, meant that much time and effort was expended by Small’s members based in one locality, such that the issue dominated Small’s agenda for many months. Furthermore, the departure of the original chairperson from the large central practice and their replacement by a GP from the northern locality meant that all board members were drawn from practices in the north. Attendance at practice leads’ meetings by central practices dipped at this point and the CEO of the large central practice e-mailed federation staff requesting that resources earmarked for centrally co-ordinated activities be released to practices. Her argument was that all of the work was being done by PMs and leads, and money earmarked for dedicated staff was no longer needed.
In contrast to Expanding and Embedded, Small did not directly employ staff following the departure of the CEO early on in our fieldwork, but instead drew on staff time from member organisations. Various issues (e.g. the processing of paperwork for the allocation of shares and the workload relating to taking minutes at meetings) remained unresolved for a lengthy period owing to the existing heavy workloads of staff who were unable to free up time for federation business.
The reliance on ‘indirect’ resources at Small also meant that the practice staff providing time to the federation were experienced in the day-to-day realities of practice life. Similarly, at Embedded, which deployed direct and indirect resources, the use of the indirect resources meant that the COO, who was instrumental in implementing new services, retained their PM role, albeit on a part-time basis. This contrasts with Expanding, where there was a heavy reliance on centrally employed senior non-clinical staff, who had no experience of working in practice settings. This may explain, in part, the mismatch between the centrally planned timetable for implementation of new centralised systems and the actual implementation, which took practices much longer than senior staff envisaged. At Struggling, the lack of centrally controlled resources meant that the organisation was heavily reliant on indirect resources, with busy staff expected to commit their time without reimbursement. Unlike in Small, where all practices were required to do this, at Struggling, very few practices were involved in this process, with the result that resource constraints inhibited activity. Furthermore, this enabled member practices to remain rather remote from the federation board, which was supposed to represent their views and interests.
Working together vignette 2: Expanding – informal board meeting
The need to make savings to reduce the deficit was discussed at each meeting, especially because membership (and hence income) growth consistently fell below target. Anne, the FD, worked full-time, alongside two assistants, to support the implementation of new finance system software across all member practices. Most had their own existing systems, and even those that had other versions of the system required by the federation were reluctant to migrate to a newer version. Jane, a GP who had recently joined the board from the second region, asked what was being done about practices that still had not installed the new software, given that this was a specific requirement of membership. Was the extra work these practices created being recharged to reflect the additional support they needed? Existing board members seemed less surprised that not all practices were compliant, having seen the time it took practices to agree to installation and the balance of ‘assisting’, with the sheer volume of work required to change systems in practices, some of which still used paper systems.
A debate followed as to whether these practices using additional central staff resource should be charged more or whether or not imposing sanctions on them might make them choose to leave. This issue had been raised previously at member events, particularly by representatives from larger practices who resented the time spent on practices that had chosen not to invest in newer systems themselves. The board had once discussed whether or not new practices should be limited to those over a certain size, or if a ‘small practice levy’ should be imposed to reflect the likely additional work they would require. The financial deficit, however, meant that Expanding could not afford to alienate, and risk losing, practices. Board members from the second region found this tolerant approach to non-compliant member practices difficult to believe as, during the pre-membership phase, all of their practices had changed over as requested in advance of their official joining date.
This vignette illustrates the issues grappled with at Expanding, where a financial deficit and competition between federations resulted in a relatively lenient approach to non-compliant practices. It may also be that a desire, more generally, to be an inclusive, as opposed to selective, organisation influenced the board’s approach. The fact that there were tensions relates to the membership conditions, which were much more exacting than those at our other sites, where member practices could be (semi-)detached from the organisation. Most Expanding practices were compliant at the point at which our fieldwork ended, and the close working and monitoring reduced the potential for free-riding in relation to this issue. In contrast, at Small, for example, although practices were required to achieve targets in relation to the federation PS, the vast majority of the work was done by the very large practice. The savings and CCG payment for this was distributed among practices based on population, as opposed to effort, so that a high degree of practice free-riding was in evidence. When the FD approached one practice about targets in the updated scheme, which would require all practices to be compliant on a specific measure, a GP at the practice said that they had no knowledge of the scheme and refused to comply. Although the FD was keen to follow this up with the senior partner at the practice, this was just one of many jobs on a long list, in addition to their PM role and other federation tasks, which took priority. This suggests that, although all practices are represented at the practice leads’ meeting, these lead GPs do not see their role as communicating and/or monitoring in relation to federation policy. Furthermore, because some of the measures had the potential to reduce income to dispensing practices, these practices refused to comply with these requirements. In an environment where there are no consequences for free-riding, this response is hardly surprising.
At Struggling, it was difficult to identify benefits of membership because the federation engaged in little, if any, concrete activity to support members. In Embedded, members appeared to have the best of all worlds, with benefits provided and little being required of member practices. For example, the federation negotiated contracts with the CCG for IAGP and other services, to which member practices could refer patients. It also took on a caretaker role for a failed practice whose patients would have otherwise been distributed among existing overstretched practices. Yet little was required of practices in terms of commitment to change processes or behaviours. This vignette also illustrates some of the issues raised by requiring commitment as opposed to involvement. In the case of involvement, it may be possible to minimise tensions and maintain the federation on a sustainable footing. However, at Small, where the federation was entirely reliant on income from prescribing savings, a failure to secure commitment, as opposed to merely membership, threatened to undermine the federation’s long-term financial viability.
The issue of practices that had recently joined Expanding and their parity at the board with original member practices also contrasts with the experiences of the large practice at Small, which planned to join the predatory federation in response to the CCG’s push for locality working. In that case, original members would be given preferential status, with new practices joining having a second tier and, therefore, inferior status. Although CCGs may be keen to encourage federations based on place, rather than personalities, federations that penalise newcomers are unlikely to facilitate this.
Vignette 3: smoking cessation in Embedded
In Embedded, local authority budget cuts resulted in the closure of the smoking cessation service it had previously funded. Following this decision, the CCG medicines management team asked GPs not to prescribe nicotine replacement therapy (NRT), because the National Institute for Health and Care Excellence guidance141 suggested that it should be used only in conjunction with the type of behavioural support provided by the smoking cessation service. The proposed service closure was a major source of concern for federation GPs and prompted Mike, one of the board GPs, to explore whether or not this could be offered within the new IAGP service that the federation had established.
Senior management team meetings had become the forum for discussing and working up ideas ahead of formal board meetings. Mike presented his idea explaining that some of the IAGP slots in the central hub could be used by the health advisors employed by smoking cessation services, avoiding redundancy and meeting patient demand. The cost was considerably lower than that of employing a sessional GP or nurse. Tim, who oversaw the federation’s finances, felt that it made perfect sense financially and avoided redundancies and loss of skills.
With SMT support, he spoke with the smoking cessation manager, public health colleagues and also the local CCG, clarifying what services were provided and whether or not and how some of this work could be transferred to the federation. Sue, the public health director, explained that she felt forced, reluctantly, to close down the service and make the health advisors redundant, but Mike’s discussions raised the possibility of some local authority resources being forthcoming. Nobody was sure what sum the local authority was willing or able to spend to contribute towards replacement services. John, from the CCG, supported the idea of using existing IAGP. Guidance was subsequently received from NHS England that IAGP sessions could not be used for smoking cessation, which threatened to derail the idea. It was agreed, therefore, that a generic term such as ‘health improvement’ would be used instead. Mike then produced a paper, which was presented at the next board meeting, where, previously, papers had always been readily accepted by the board.
Mike outlined the issues and how he felt that his solution could help, but Shona, a GP with a CCG role, was adamant that this represented the ‘thin end of the wedge’, stepping in to deliver a decommissioned service. Why wouldn’t the local authority make savings in other areas too and expect that to be funded and delivered elsewhere? Mike argued that, if the federation did not provide the service, then the work would fall back to individual GPs during consultations, which also created issues for the supply of NRT. Immediate supply was known to improve quit rates and central provision made this an easier option.
A debate followed and it was clear that neither party was likely to shift. Although this impasse represented a situation that could have been decided with a vote, many of the board members could appreciate both sides, so the chairperson suggested that people reflect on it further and he would then canvass opinion by e-mail. Over the ensuing period, discussions continued with public health staff who agreed, in principle, to contribute finances, ‘match funding’ those committed by the federation, although this would be for targeting high-risk groups rather than providing a universal service.
The process of agreeing funding was a lengthy one; ultimately, the decision was taken by the federation to deliver the service via the extended-hours clinic and to get on with implementing this rather than waiting for the local authority to complete its contracting process. Although this was too late to avoid redundancy of health advisors, the service was staffed by pharmacists whose previous workload in IAGP clinics had consisted mainly of medication reviews, for which uptake had been poor. The new service was launched and, months later, the local authority staff were finally approaching the stage of being ready to award the contract and related resources.
This vignette illustrates the ways in which federation staff had to respond to changes in their external environment and, in particular, some of the issues raised when working with other organisations. The unilateral decision taken by the local authority placed practices under enormous pressure and the CCG instructions sought to restrict GPs’ ability to prescribe, due, in part at least, to the financial implications. At the same time, none of the organisations involved considered smoking cessation to be a low priority. In addition, although much of the policy direction emphasises the need for GPs, as front-line professionals, to be involved in decisions about services aimed at improving local population health, central guidance appeared to over-ride this by outlawing smoking cessation sessions as part of IAGP in the way Mike suggested. Working collaboratively, over time, requires trust and a shared understanding of issues and priorities. However, in this case, the absence of a mechanism for this and the fact that budgets were not pooled meant that the local authority presented its closure decision almost as a fait accompli.
When the federation members started discussions, they were surprised at the length of the process, which appeared unnecessarily protracted:
Most things that happen in local authority, it’s slow, very, very slow-moving, so part of the reason why [the federation] went ahead and started to deliver a service was because they were understandably frustrated with . . . the speed at which we were moving . . . we needed to obtain approval for finance, for legal and from the relevant elected member. They went ahead and started a service . . . we always are very, very slow, but they’re not slow, they’re very, very motivated; they are the classic doers, they want to get on with things . . . It’s refreshing to work with a group of people who are so keen to get on.
LA PH consultant, Embedded, 60
Practices’ size and degree of control over governance mean that they are able to implement change quickly in contrast with NHS hospitals, CCGs and local authorities, for example. This mindset appeared to characterise federation staff views and left them feeling frustrated at the slow pace of progress, resulting in implementing the service without the formal processes being concluded. Similar frustrations were observed at Small, where the federation was actively encouraged to employ two health-care assistants via the acute trust. The funding was time limited for 2 years and, almost 1 year later, nobody was in post. A trust representative appeared at a Small meeting to apologise and explain that the reason for the delay was the trust’s competing pressures, as well as its lengthy recruitment process. From federation staff, the view was expressed repeatedly, at this and other meetings, that, if the staff appointed were employed by practices, the health-care assistants would have been in post within 3 months. Importantly, this served to actively discourage the federation from seeking to collaborate on any future projects:
I do remember some of the practice managers, some of the GPs, saying, just give us the money, we’ll go, we’ll recruit, we’ll make it happen. But it’s the trust, and the processes that they have to go through, and the amount of people that have to sanction it and sign it off . . . Here, if we were recruiting, I would look to recruit one health-care assistant for [name] surgery – job done.
Director of Operations, Small, 10, second interview
The decision by the local authority in Embedded to provide some financial support was not entirely based on building warm and cordial relationships, but instead on ‘playing hardball’, putting pressure on local authority staff:
We were basically saying ‘you want a smoking service, you can’t not provide any smoking services at all, otherwise you’re at risk of triggering an audit by the national public health team as to what you’re actually doing with your local authority public health budget’.
GP, Embedded, 05, second interview
A particularly committed GP demonstrated dogged determination to implement an innovative and workable solution to the problem created by the local authority decision, which illustrates the difference that particular individuals can have in these contexts.
The vignette also illustrates that federations may be required to work collaboratively, in a way that creates internal divisions, as well as working with external parties whose interests diverge. This is not merely a matter of negotiating the politics of local authority cuts and CCG prescribing budgets, but making choices, in this case about the wisdom of taking on work created by those cuts. Although differences of opinion among federation members can co-exist peacefully, when circumstances relating to these force a decision, tensions are likely to arise. Collecting ‘low-hanging fruit’ by focusing on issues that largely command consensus may help federations as they attempt to build membership and encourage participation and commitment. As discussed in Chapters 4 and 5, when disagreements arose (e.g. about bidding for new services as part of IAGP, whether or not to accept poorly performing practices), these tended to be resolved via discussion. Interaction with other organisations may act as a catalyst for change, but may also create tensions among federation members.
A further issue relates to the centrally determined rules to which federations and the organisations with which they interact are expected to adhere. In this case, a willingness to find a workable solution among the three sets of stakeholders meant that the NHS England instructions about the use of IAGP were interpreted flexibly. Standardised rules make no allowance for the fact that local contexts vary enormously, and in settings where local authorities withdraw smoking cessation resources, for example, abiding by rules, which assume such services are in place, may not be the most appropriate response. As discussed in Chapter 4, in Small and Expanding, CCGs abiding by what they saw as the rules of tender exercises for the IAGP process meant that the federation could not develop a close and collaborative relationship with the CCG in the way in which this happened in Embedded.
Vignette 4: a primary care network in Small
The next vignette is concerned with federation GPs interacting with members of another federation, as well as working with other stakeholders as part of a PCN. We draw on data collected at a meeting convened by the LMC in October 2018. This covered the CCG in which Small was located, which brought together representatives from practices in the CCG to discuss working together at scale. Two members of one of the city-based Small practices were present, and several staff from the ‘predatory’ federation practices were present too. The LMC representative suggested that divisions between practices based on personal differences meant that general practice across the CCG was losing out in contrast to other CCGs where GPs joining one big federation added to their strength. However, several of the GP attendees were less keen to talk about feuds across federations, suggesting that collaborating as part of a PCN was the way to bring practices to work together.
Frank, a GP whose practice was a member of the ‘predatory’ federation, mentioned the PCN. He asked ‘could that be a vehicle?’ And Jack, the LMC chairperson said that Sarah (a respected GP from the predatory federation and a GP representative at CCG level) was involved in the PCN and that seemed to be flavour of the month. Sarah had had very positive things to say, but Jack didn’t quite understand it. ‘What’s the reality on the ground?’ he asked. Frank said that, as a relative newcomer to the region, he was aware that there were lots of big egos. There’s lots of history and it’s going to be a while before certain practices are absolutely ‘knitted in’. Having said that, they’ve been meeting for about a year and trying to work in a unified way across practices. And that’s been a positive experience in terms of Improving Access to General Practice. The PCN has brought people to the table, got the voluntary sector and the hospital, which has always been a difficult and different beast, and the local authorities are now looking to buy into the proposal and participate in it.
Frank said ‘so we’ve got, at Townby, four GP practices in competition, but we need collaboration. The premises in each place are not really good enough. So if we take away the different organisations and look on a locality basis, we can start to break down the barriers. If we think about Practice 1, that’s got various different sites and different interactions. The implication was that some of the sites would be in one PCN and some might be in another. We’ve got no money, we’re doing it on love. It’s a big commitment, especially for the smaller practice. But, hopefully, the benefit is that we’re starting to align community services and to collaborate, get a feel for what [the city] could look like. It’s different for the rural practices. If we don’t get one federation, then maybe this would allow [the city] to concentrate on [the city] at least. It’s hard to think about [the city] and elsewhere within the CCG footprint in one group. So trying to get a giant federation may be not the best way’.
‘So’, Jack said, ‘there’s obviously lots of issues about turf wars and relationships, and it feels strange, but there’s also issues about rural practice’. One GP from a rural practice said ‘well, for us, it’s not about that we don’t want to work together’, and he talked about a warfarin contract where there have been benefits across rural practice and money attached to it. But, for him, it was more the imposition of a structure that doesn’t fit readily rural practices like his. And the examples of things that come out with it from NHSE [NHS England] don’t really fit, particularly where there’s no centre of population and there didn’t seem to be the necessary flexibility. ‘We’d like to be able to dip in and out as it suits us’.
Frank then talked about what they were doing with the PCN: ‘We got public health involved and they mapped our population and health issues. And then we had the £3-a-head money; we used that for mental health workers, enhanced primary care-based process. So we looked at the money on a population basis. And as long as we follow the steering group principles, we’ve got lots of control over how to distribute that money. And then it’s based on the needs of the area, so there’s local determination on this, which is not then about big practices seeming to suck up all the money. And in Townby, there are needs there, so you can see the potential to have a resource there where it’s needed’. Frank said that ‘it’s almost the opposite of what federations are doing, because they’re bringing people together to form bigger things. This [PCNs] is about deconstructing, getting practices to think, on an area basis, what is the form that would be good for that area?’. He repeated his earlier point about people and egos: ‘GPs shouldn’t let it fall just because somebody walks and starts throwing their dummy out of the pram’.
This vignette illustrates how some practice staff had started to work on developing a PCN to focus on local population health. For the LMC, the issue was primarily how best to represent the general practices, and it saw strength in numbers. In contrast, as Frank explained, PCNs are relatively small and they may cut across practices, where these have more than one site. During the meeting, the GM of the large practice in Small appeared to be largely unaware of the nature of these developments, even though the city had ‘six primary care home groupings, and the size of each of those population groupings is roughly between that magic 30,000 and 50,000 that people are quoting’ (Small CCG Manager, 38). When the GM fed back, subsequently, at the next practice leaders’ meeting, the two GPs present from the central locality said that they were aware of and interested in participating in their PCN, but that the meetings were arranged by non-clinicians and, therefore, at times when they could not attend. This was the first mention of PCNs at any of the Small meetings we attended. This is perhaps not surprising given the absence of a PCN in the rural areas where many northern locality Small practices were located. The view from the ‘predatory’ federation GP, which was actively involved in the PCN process, suggested that collaborating as part of a PCN might help in moving beyond feuds based on egos. This is understandable as city practices in Small, in population health terms, had much more in common with the practices in the ‘predatory’ federation than with the rural practices that occupy all the seats on Small’s board.
List of abbreviations
- AGM
- annual general meeting
- APMS
- alternative provider of medical services
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- COO
- chief operating officer
- CQC
- Care Quality Commission
- CSU
- Commissioning Support Unit
- DES
- Directed Enhanced Service
- FD
- finance director
- GM
- general manager
- GMS
- general medical services
- GP
- general practitioner
- GPFH
- general practitioner fundholding
- HR
- human resources
- IAGP
- Improving Access to General Practice
- ICS
- integrated care system
- IT
- information technology
- LMC
- local medical committee
- MAAG
- Medical Audit Advisory Group
- MD
- managing director
- MO
- meta-organisation
- MOL
- member organisation lead
- NRT
- nicotine replacement therapy
- PBC
- practice-based commissioning
- PCG
- Primary Care Group
- PCN
- Primary Care Network
- PCT
- primary care trust
- PM
- practice manager
- PPG
- patient participation group
- PS
- prescribing scheme
- RCGP
- Royal College of General Practitioners
- SMT
- senior management team
- STP
- sustainability and transformation partnership
- VAT
- value-added tax
