Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/11. The contractual start date was in November 2018. The final report began editorial review in August 2019 and was accepted for publication in November 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Raine et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Objectives
-
To conduct a rapid scoping exercise to identify existing reviews on workplace-based interventions to promote health and well-being.
-
To produce a descriptive map of the extent and nature of the available research evidence, and assess the scope for further evidence synthesis work.
Chapter 2 Background
The health and well-being of staff working in the NHS is a significant and long-standing issue in UK health care. In 2019, NHS England reported that in the NHS the sickness absence rate (4%) is higher than in both other public sector organisations (2.9%) and the private sector (1.9%); the cost of sickness absence of NHS staff has been estimated at £2.4B. 1 In addition to having financial implications for the NHS through levels of sickness absence, there is strong evidence linking staff health and well-being with quality of care, safety and patient outcomes/experience. 2–5 More broadly, the NHS has a responsibility to protect the health of all its employees. 6 The NHS constitution makes a pledge to support staff in maintaining their health, well-being and safety. 7 Guidance produced by the Health and Safety Executive also addresses staff well-being, including work-related stress (e.g. Health and Safety Executive8).
Consistent with the situation in other occupational sectors, data reveal that musculoskeletal and mental health conditions are major causes of ill health and sickness absence among NHS staff. The Boorman review found that musculoskeletal disorders account for almost half of all sickness absence in the NHS. 9 Findings from the 2017 NHS staff survey revealed that 26% of respondents experienced musculoskeletal problems as a result of work activities in the previous 12 months. 10 A large proportion of musculoskeletal disorders cases result in long-term absence. 6
Approximately one-third of sickness absence in the NHS is a consequence of mental health issues. 11 The 2017 NHS staff survey found that 38% of all staff, and 49% of individuals working in ambulance trusts, had felt unwell because of work-related stress in the last 12 months. 12 As a professional group, doctors experience high levels of mental health problems and have one of the highest suicide rates. 4 The existence of a bi-directional relationship between mental and physical health is well recognised, and evidence suggests that poor mental well-being can negatively affect lifestyle behaviours. For example, a study conducted by the Nursing Standard of 3500 nurses, midwives and health-care assistants in the UK reported that workplace stress had a negative impact on the diet of 60% of respondents. 13
Health professionals, and nurses in particular, have been encouraged to promote healthy lifestyle choices among patients. 14 Emphasis has been placed on staff taking responsibility for their own health and acting as a positive role model for engaging in healthy behaviours. 15 Notably, a number of recent UK studies found that a large proportion of health-care staff do not themselves meet public health guidance in relation to healthy lifestyle behaviours including consumption of fruit and vegetables,16,17 consumption of fats,16 consumption of sugars,16 physical activity16,17 and alcohol consumption;17 for example, Mittal et al. 16 reported that 83% of all staff did not eat the recommended five or more portions of fruit or vegetables per day. Similarly, Schneider et al. 17 found that 68% of nurses, 53% of other health-care professionals and 82% of unregistered care workers (including nursing auxiliaries and assistants) did not eat five or more portions of fruit or vegetables daily. They also reported that 46% of nurses, 49% of other health-care professionals and 44% of unregistered care workers did not meet physical activity guidelines. 17 These figures for physical activity are consistent with the proportion reported by Mittal et al. 16 for all staff (44%). In addition, the proportion of UK health-care workers who reported being overweight or obese in four recent studies ranged from 44% to 69%. 14,16,18,19
Schneider et al. 17 raised concerns about the potential impact of nurses’ low personal adherence to public health guidance in relation to healthy lifestyles on their health promotion work with patients and its effectiveness. Furthermore, Kyle et al. 14 highlighted an increased risk of both musculoskeletal and mental health conditions from having excess body weight, which, as highlighted earlier, are leading causes of ill health and sickness absence among NHS staff.
The negative influence that organisational-level factors can have on the lifestyle behaviours of health-care staff has been highlighted in past UK studies; for example, 51% of the hospital staff who responded in the study by Mittal et al. 16 indicated that long working hours impeded their ability to stay fit. Furthermore, in the Nursing Standard study reported by Keogh,13 79% of respondents indicated that eating a healthy meal while at work was made difficult by a lack of breaks. Over half (56%) of respondents also reported that inadequate staff levels had a negative impact on their food choices. 13
Findings from the 2017 NHS staff survey showed that 15% of all staff, and around one-third (34%) of employees at ambulance trusts, had experienced physical violence from patients, relatives or the public in the previous 12 months. In addition, over one-quarter of all staff (28%) and nearly half of the staff at ambulance trusts (47%) also suffered harassment, bullying or abuse from patients, relatives, or members of the public in the last 12 months. Just under one-quarter of all staff (24%) experienced harassment, bullying or abuse from other members of staff. 12
The importance of improving the health and well-being of NHS staff has repeatedly been recognised in government and NHS England publications published within the last 10 years. The NHS Long Term Plan1 re-emphasises the key role that employers have in supporting staff to remain healthy, and provides a clear commitment to the continued promotion of positive physical and mental well-being among the NHS workforce. This includes reducing the level of violence and abuse experienced by staff.
Over a number of years, there have been various initiatives to improve the health and well-being of NHS staff. On a national level, the NHS Healthy Workforce Programme was established in 2016 to identify best practice in relation to promoting staff health. The focus within the programme was on the implementation of employer-led health and well-being initiatives as well as creating organisational practices and culture that are supportive of staff health. 11
The NHS Health and Wellbeing Framework20 introduced in 2018 was informed by the findings and learning from the NHS Healthy Workforce Programme. 6 The framework document includes guidance and actionable steps to enable all NHS providers to plan and implement a staff health and well-being strategy. 21 There is a focus within the framework on promoting healthy lifestyles in addition to addressing mental health and musculoskeletal health. Health and well-being interventions incorporated into the framework comprise prevention-/self-management-focused approaches (e.g. physical activity classes) and more targeted forms of support such as weight loss services, health checks, addiction support, counselling and physiotherapy. An accompanying diagnostic tool enables organisations to carry out self-assessment against the Health and Wellbeing Framework. 21
The NHS Staff and Learners’ Mental Wellbeing Commission report22 published in 2019 by Health Education England reviewed evidence of good practice in relation to organisational policies within NHS organisations that had made mental health and well-being of staff and learners a priority. A number of recommendations were made to improve support, including ensuring the provision of tailored in-house mental health support and signposting to clinical help.
A Commissioning for Quality and Innovation (CQUIN) payment was introduced in 2016 in order to provide financial incentives for NHS providers to support staff health and well-being. Payment is dependent on (1) the introduction of workplace health and well-being initiatives, with a particular focus on physical activity, and improving support for mental health and musculoskeletal issues, (2) encouraging healthier food choices and (3) increasing staff uptake of the influenza vaccination. 11
The York Health Services and Delivery Research Evidence Synthesis Centre was asked by NHS England to identify evidence relevant to the promotion of healthy lifestyles among NHS staff. For this piece of work, the term ‘NHS staff’ was conceptualised broadly as any individual working for the organisation in any post.
Chapter 3 Methods
Scoping and mapping of the evidence
This rapid scoping and mapping exercise was undertaken to provide a high-level overview of the available evidence from existing reviews and reviews of reviews (RoRs). The objective was to classify the evidence in terms of broad descriptive characteristics and it was not intended that the findings from the reviews or RoRs would be extracted, evaluated and synthesised.
Although we did not aim to conduct a full systematic review, aspects of systematic review research methodology were applied, wherever possible, to maintain the rigour, transparency and reproducibility of the mapping process.
Identification of evidence
Database searches were undertaken to identify systematic reviews about health and well-being at work. Results were limited by publication date (2000 to January/February 2019). No language or geographical limits were applied. The following databases were searched:
-
Cochrane Database of Systematic Reviews (CDSR)
-
Database of Abstracts of Reviews of Effects (DARE)
-
HTA database
-
Epistemonikos
-
Health Evidence
-
Database of Promoting Health Effectiveness Reviews (DoPHER)
-
PROSPERO
-
MEDLINE
-
Business Source Premier.
The search strategies are provided in Appendix 1. Searches were limited to the year 2000 onwards to maximise the relevance of the evidence identified.
Once it became apparent that database searches had identified a large number of potentially relevant reviews, it was decided not to undertake supplementary searching of specific websites to identify any additional relevant publications or grey literature.
Selection procedure
A sample of title and abstracts were initially pilot screened by two reviewers independently and their decisions compared. On achieving at least 90% agreement, the remaining title and abstracts were screened against the selection criteria by one reviewer only. If there was uncertainty regarding the eligibility of any record, it was discussed with a second reviewer. Records without an abstract were screened on title only.
It had been intended that the full text of potentially relevant reviews would be retrieved and screened for inclusion, but because of the large number identified, this was not practical within the available time frame. A pragmatic post-protocol decision was taken to adjust the approach and select reviews for inclusion in the evidence map based on information in the title and abstracts of records only. However, the full text of all RoRs identified during the selection process was retrieved in order to conduct a more detailed examination of these publications.
Selection criteria
Records were screened for potential inclusion against the following selection criteria:
-
Population – adult employees (aged ≥ 18 years) in any occupational setting and in any role. Any reviews focusing solely on self-employed workers or including participants from other settings (e.g. school students) were not eligible for inclusion.
-
Interventions – any intervention aimed at promoting or maintaining physical or mental health and well-being (however conceptualised). Interventions could also be focused on early intervention and reducing the incidence or symptoms of common mental health conditions (stress, anxiety or depression) among staff. Reviews of interventions addressing violence against staff, workplace bullying or harassment were also eligible for inclusion. Occupational health interventions and those aimed at returning employees to work after absence were considered beyond the scope of the review. Occupational health interventions were conceptualised as those with a predominate focus on promoting safer working environments and practices, and reducing injuries and workplace health risks.
Interventions could be either or both (1) individual-level interventions, for example, initiatives focused on individual behaviour modification, (2) organisational-level interventions aimed at modifying the workplace environment, culture or ethos.
-
Outcomes – any outcome related to the effectiveness of interventions. Relevant outcomes could include, (but were not limited to) staff satisfaction, sickness absence, mental resilience, staff uptake of flu vaccination, lifestyle choices (smoking rates, alcohol consumption, physical activity levels, sedentary behaviour, dietary behaviour), coping skills, symptom reduction, levels of violence against staff and levels of bullying. Reviews could also report on outcomes related to the implementation of initiatives.
-
Study design – any form of evidence synthesis including systematic reviews of effectiveness, systematic reviews of implementation, meta-analyses, qualitative reviews or realist reviews. Reviews could include primary studies of any design or other reviews (i.e. RoRs).
All RoRs also met the following additional study design criteria: authors (1) searched at least two sources, and (2) reported inclusion/exclusion criteria. One of the sources searched must have been a named database. Other acceptable sources were conducting internet searches, hand-searching journals, citation searches, reference checking, contacting other authors.
It was stated in the protocol that all forms of evidence synthesis would have to meet the two criteria above to be included in the map; however, as the full text of reviews was not retrieved, this stipulation could not be implemented. In most cases, there was insufficient detail reported in title and abstracts alone to complete an assessment.
Data extraction
For each included review, data on key characteristics were extracted from titles and abstracts into a spreadsheet, including type of document, focus of the review, intervention type (where identifiable), population(s) and whether the review had a primary focus on effectiveness, costs/cost-effectiveness or implementation. A sample of reviews were extracted independently by two reviewers to ensure consistency of coding and decisions compared. Once there was a high level of agreement, data extraction was conducted by one reviewer.
For the included RoRs, data on key characteristics were also extracted by one reviewer. In addition, comments by the RoRs’ authors reflecting on the included evidence were noted. One reviewer checked to ensure that relevant reviews reported in the RoRs had been identified in the searches and included in the mapping of the evidence. Data extraction was not checked by a second reviewer, which represents another post-protocol change necessitated by the large number of relevant publications identified and the limited time available.
Summary of post-protocol changes
As indicated previously, it was necessary for the review team to make the following post protocol changes:
-
No supplementary searching of specific websites was conducted to identify any additional relevant publications or grey literature.
-
Reviews and meta-analyses (RMAs) were selected for inclusion in the evidence map based on information in the title and abstracts only.
-
It was not possible to assess whether or not RMAs were conducted using a systematic methodology.
-
Data extraction was not checked by a second reviewer.
Synthesis
Data from the spreadsheet were imported into the software package IBM SPSS Statistics version 25(IBM Corporation, Armonk, NY, USA) and descriptive statistics for key characteristics generated (counts and percentages). Data from the reviews and RoRs were then used to produce a map and descriptive summary of the evidence. This provided an overview of the extent and nature of the current evidence base relevant to promoting healthy lifestyles in NHS staff. Reviews and RoRs were grouped by topic focus (e.g. lifestyle behaviour, mental health, violence/bullying) and briefly described.
External engagement
This mapping work was conducted for NHS England, which was consulted at the start and end of the process. The research team initially received a very brief outline of the topic area of interest via the National Institute for Health Research (NIHR). A teleconference with NHS England and NIHR colleagues was subsequently held to establish the goals and scope of the work. Based on this discussion, the research team produced a review protocol, conducted the mapping exercise and produced an interim report for NHS England.
Following the submission of the interim report, a second teleconference was held between the York research team, NHS England and NIHR in order to discuss the interim results, conclusions and scope for further evidence synthesis work. During this teleconference, the York research team gave a presentation of key findings and answered any questions arising. On the basis of this discussion, no additional evidence synthesis work was requested from the research team. Three regional medical directors at NHS England were involved over the course of the work. Owing to the rapid and responsive nature of the work, patient or public representatives were not asked to be involved.
Chapter 4 Results
In total, 9622 search results were downloaded and imported into a reference management software package. After deduplication there was a total of 8241 unique records. In total, we identified 408 potentially relevant reviews of workplace-based interventions focused on the health and well-being of staff. The flow of literature through the review is shown in Figure 1.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart.
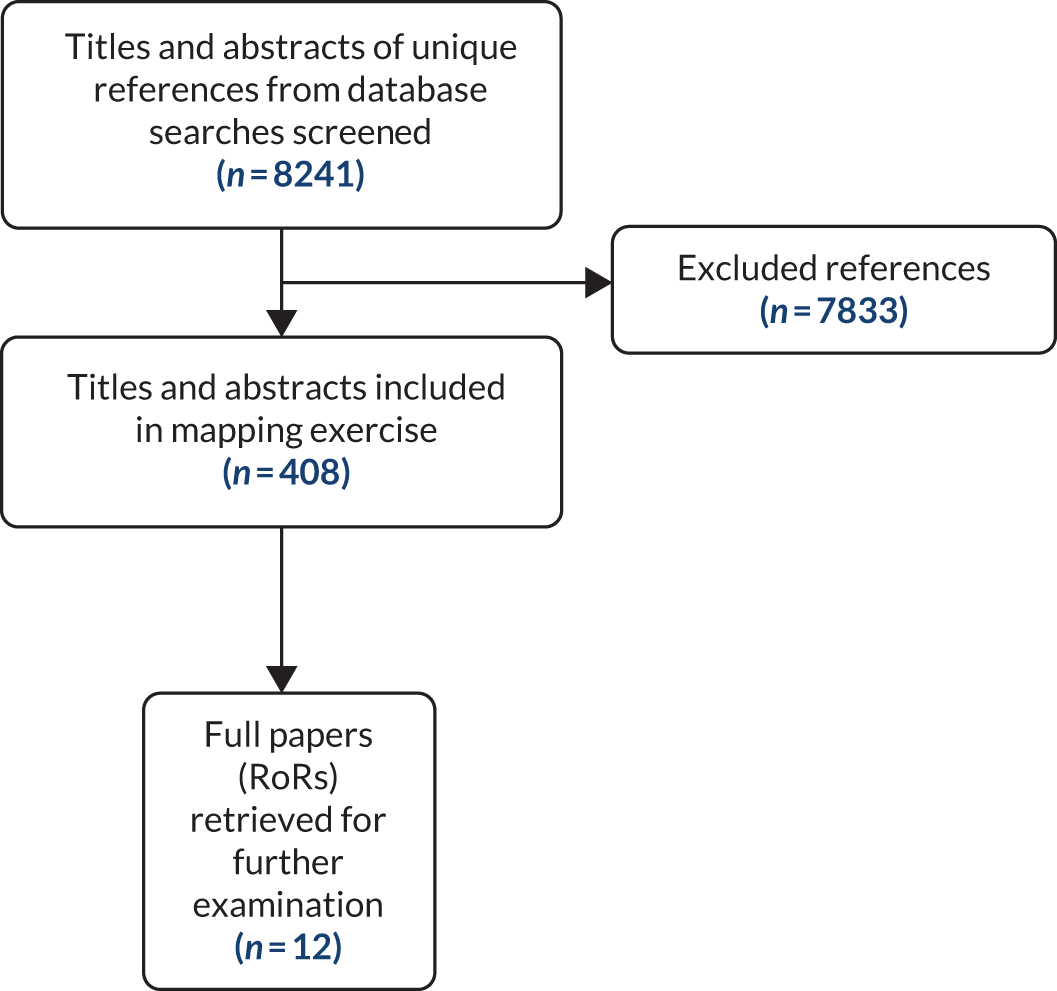
Figure 2 shows the different types of publications identified from the scoping searches of key databases.
FIGURE 2.
Type of publication (n = 408). NICE, National Institute for Health and Care Excellence.
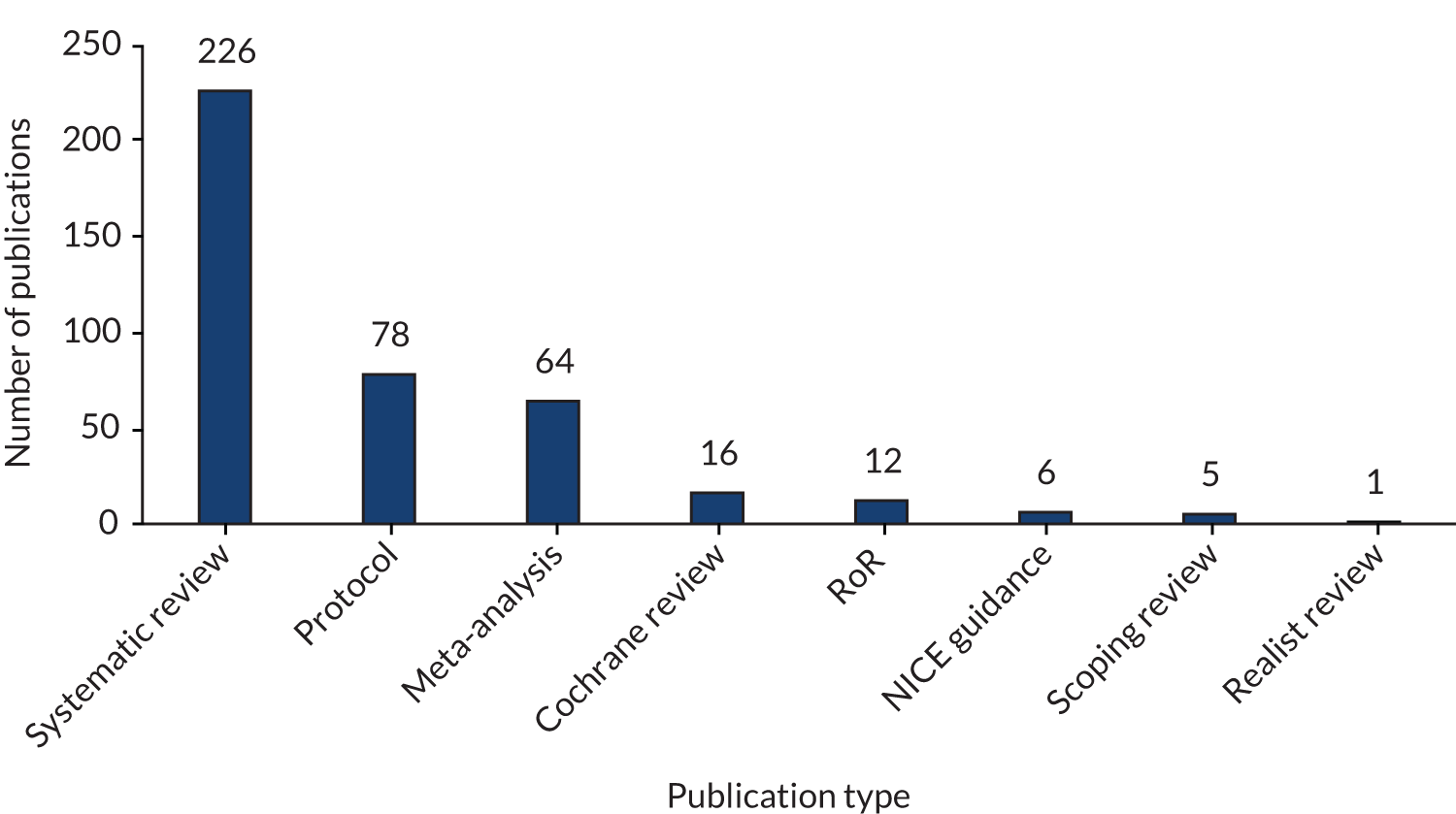
Results are presented below by the following categories of publication type: RoRs; Cochrane reviews; National Institute for Health and Care Excellence (NICE) guidance; a merged grouping of systematic reviews, scoping reviews, realist reviews, and meta-analyses, which has been labelled as ‘reviews and meta-analyses’ (RMAs); and protocols.
‘Reviews of reviews’
It can be seen from Figure 2 that there is a sizeable number of existing RoRs (n = 12). These have examined the effectiveness of workplace interventions targeting both physical and mental health. Two reviews addressed interventions focused on employees in the health sector. 23,24 The primary topic addressed in each of the 12 RoRs is outlined below:
General health and lifestyles/mixed physical and mental health
-
Health promotion and primary prevention, including interventions focused on stress, physical activity, nutrition and smoking. 25
-
Smoking cessation. 26
-
‘Healthy lifestyles’ focused on physical activity, healthy weight and good nutrition. 27
-
‘Workplace health programmes’ for improving both physical and mental health. This review addressed implementation issues as well as effectiveness. 28
-
Organisational-level interventions in the ‘health sector’ to improve health. 23
-
Physical activity. 29
-
Dietary change. 30
Mental health
-
Stress management with a particular emphasis on preventing common mental health disorders (anxiety and depression). 31
-
Mental health including stress management and the prevention of psychological disorders. 32
-
Common mental disorders (depression and anxiety). 33
-
Interventions to prevent mental health problems and absenteeism. 34
-
Physician burnout (including medical students and residents). 24
A more detailed description of the 12 RoRs is provided in Review of reviews: full-text scoping.
Cochrane reviews
Out of the 16 Cochrane reviews identified,35–50 eight were targeted at general health, physical health or lifestyle behaviour. This included reviews related to improving physical activity through the use of pedometers,37 decreasing sitting time at work,46 sex risk behaviour and preventing human immunodeficiency virus (HIV) infection,43 and smoking cessation. 36 The latter review examined the effectiveness, costs and cost-effectiveness of smoking cessation interventions. 36 Strategies to improve the implementation of workplace-based policies/practices aimed at lifestyle behaviours (diet, physical activity, obesity, tobacco use and alcohol use) have also been examined in a Cochrane review. The effectiveness and cost-effectiveness of such strategies were also assessed as secondary outcomes. 50
Four Cochrane reviews examined the effectiveness of interventions to prevent or reduce workplace stress/burnout, two of which were focused on health-care workers. 45,49 One other review that was also focused on the well-being of health-care personnel, reported on the psychological effects of making changes to the physical workplace environment, although only one primary study met the authors’ inclusion criteria. 48 One Cochrane review on the prevention of workplace bullying was identified. In addition, there are Cochrane reviews of interventions addressing sleepiness and sleep disorders among shift workers; the effects of flexible working interventions on the health and well-being of employees and their families; breastfeeding support at work; alertness and mood in daytime workers; and absenteeism among workers with inflammatory arthritis.
National Institute for Health and Care Excellence guidance
The National Institute for Health and Care Excellence has produced evidence-based guidance on a number of workplace health issues including the promotion of mental well-being,51 physical activity52 and encouraging employees to stop smoking. 53
Reviews and meta-analyses
Workplace settings
In total, 296 reviews (systematic reviews/scoping/realist reviews) and meta-analyses were identified, which focused on primary studies with 23 different groups of workers. For a full list of all 23 population groups/workplace settings in the 296 RMAs, see Appendix 2, Table 13. The largest proportion of RMAs had a focus on generic ‘workplace’ interventions, and did not state a specific target group of workers (n = 155, 52%). There were 31 RMAs focused on primary studies with nurses of all types, and a similar number were focused on ‘health-care’ workers (n = 28). A further 36 RMAs had a specific focus on other groups of health-care workers, and these are shown in Table 1. Out of the 296 RMAs identified, a total of 95 (32%) focused on individuals working in a health-care setting in some capacity. Among RMAs not focused on health care, the groups of workers most frequently studied were individuals who work shifts (n = 9), those based in offices (n = 7) and female workers (n = 7).
| Staff groups | Number of RMAs |
|---|---|
| Nurses | 31 |
| ‘Health-care’ staff | 28 |
| Staff working in mental health care | 8 |
| Medical students | 7 |
| Doctors | 7 |
| Nurses/nursing students | 4 |
| Nursing students | 3 |
| Emergency medical service personnel | 3 |
| Midwives/obstetricians and midwives | 2 |
| Doctors/medical students | 1 |
| Health-care students/professionals | 1 |
Health focus of reviews and meta-analyses
The primary health focus of each review or meta-analysis was categorised into seven broad groupings: lifestyles, general health/health promotion, mental health, physical health, work relationships, general work and ‘other’ health-related interventions. As the grouping of RMAs was based on information in titles and abstracts only, it should not be considered a definitive categorisation of health focus. It is also important to recognise that there is potentially considerable overlap between some of the groups depending on the specific aims of interventions, and particularly the general health/health promotion and lifestyles categories.
Figure 3 shows the primary health focus of the 296 identified RMAs. In order to retain pertinent information, RMAs have been separated into those that had a specific focus on health-care settings (health care focused) and those that did not (non-health care focused). However, it should be recognised that some of the RMAs without a health-care focus could, depending on the inclusion criteria applied, have also potentially included primary studies conducted with staff in health-care settings. A full bibliographic list for the 296 RMAs by primary health focus and setting is provided in Appendix 3.
FIGURE 3.
Primary focus of RMAs (n = 296).
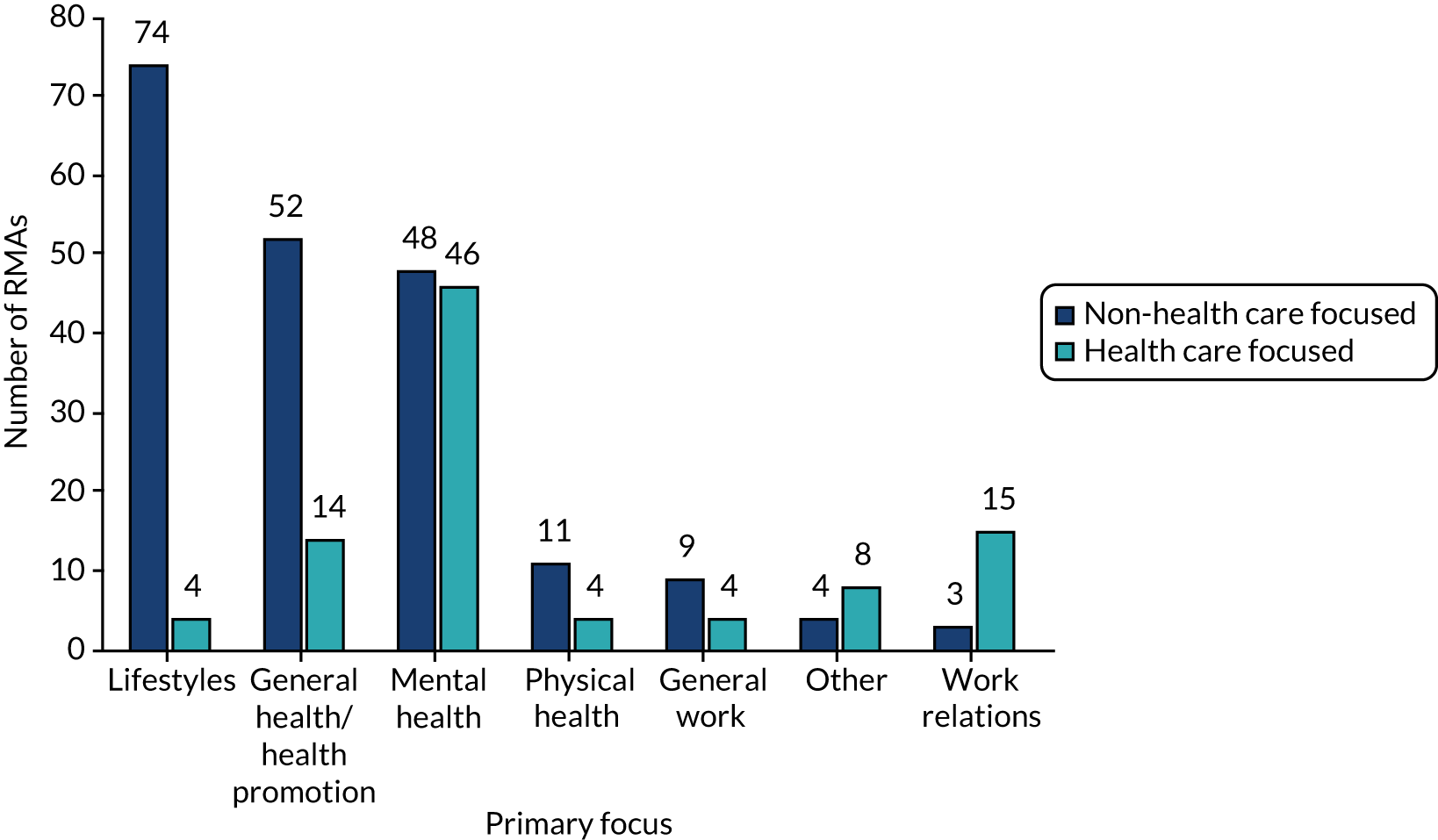
Lifestyles
In total, 78 out of the 296 RMAs addressed lifestyles and lifestyle behaviour, of which four were focused on staff in health-care settings. As Table 2 reveals, the largest proportion of the non-health-care focused RMAs addressed physical activity, sedentary behaviour or sitting time (n = 29). Five RMAs included interventions that examined both physical activity and/or dietary behaviour/nutrition. It can also be seen from Table 2 that a total of 22 non-health-care-focused RMAs were on obesity/weight status (n = 11), general diet/nutrition (n = 7), fruit and vegetable consumption (n = 3) or dietary behaviours and adiposity (n = 1). A further nine RMAs addressed smoking cessation or employees’ smoking behaviour. The four RMAs related to health-care staff were focused on physical activity and/or dietary behaviour (n = 2), weight status (n = 1) and dietary behaviour (n = 1). Of these four RMAs, two were focused on nurses and two on a broad grouping of ‘health-care’ staff.
| Health focus | Number of RMAs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Physical activity/sedentary/sitting time | 29 | 0 |
| Obesity/weight | 11 | 1 |
| Smoking cessation | 9 | 0 |
| Diet/nutrition | 7 | 1 |
| Physical activity/diet/nutrition | 5 | 2 |
| Alcohol | 3 | 0 |
| Fruit/vegetable consumption | 3 | 0 |
| Diabetes | 2 | 0 |
| Substance use | 2 | 0 |
| Dietary behaviours/adiposity | 1 | 0 |
| Physical activity/diet/weight | 1 | 0 |
| Substance use and HIV-risk behaviours | 1 | 0 |
| Total | 74 | 4 |
In terms of interventions, it was possible to determine from information provided in the abstracts that at least 12 of the non-health-care-focused RMAs had included both individual- and organisational-level interventions. These addressed weight status (n = 5); physical activity, sedentary behaviour or sitting time (n = 3); alcohol (n = 1); smoking (n = 1); physical activity/diet/weight (n = 1); and diet/nutrition (n = 1). It was not possible to make a similar determination for the four RMAs conducted in health-care settings.
Eight lifestyle RMAs (seven non-health care focused and one health care focused) examined organisational-level interventions or policies only. The one health-care-based review was commissioned by Public Health England to examine the evidence on environmental (choice architecture) interventions to increase the purchase and consumption of healthier food and drinks by NHS staff. 54
Interventions evaluated in six other RMAs (all non-health care focused) were aimed at reducing sedentary behaviour in office workers through desk-based changes such as the use of active workstations, and cycle and treadmill desks.
Among the 74 non-health-care-focused RMAs, one had a primary focus on the costs and financial return of worksite programmes aimed at improving various lifestyle behaviours rather than effectiveness. Furthermore, four other RMAs (addressing physical activity and smoking) focused primarily on implementation and process-related issues.
General health/health promotion
The scoping searches identified 66 RMAs that were concerned with general health promotion or interventions to promote the health and well-being of workers in broad terms. Of this total, 14 had a specific focus on health-care staff.
The most common intervention type that was identified among the 52 non-health-care-focused RMAs was various forms of ‘workplace health promotion programmes’ (n = 18). Other specific types of intervention that were also identified included:
-
alterations to the jobs or work patterns of employees; for example, changing shift patterns, task restructuring, increasing employee control and job redesign (n = 5)
-
organisational-level interventions including improving the social or psychosocial work environment (n = 4)
-
digital-/technology-based interventions (n = 2)
-
mentoring, training or support (n = 2).
One of the 14 RMAs of general health promotion in health-care settings was commissioned by the Department of Health and Social Care in the UK and examined whole-system approaches to improving the health and well-being of health-care workers. 55
Where a specific intervention type could be determined, three out of the other 13 health-care-focused RMAs addressed alterations to jobs or work patterns. Other RMAs examined clinical supervision; mentoring, training and support; Schwartz Center Rounds; exercise interventions to promote both physical and mental health; and health promotion programmes to improve behavioural health-risk factors. Table 3 provides details of the specific groups of staff that were the target population in the 14 health-care-focused RMAs.
| Staff groups | Number of RMAs |
|---|---|
| Nurses | 7 |
| Health-care workers | 3 |
| Medical students | 2 |
| Doctors | 1 |
| Mental health-care workers | 1 |
Reviews and meta-analyses of general health/well-being were largely focused on effectiveness outcomes, but several had a primary aim of evaluating the costs and economic impact of worksite health promotion programmes. One RMA focused solely on process issues and the factors that influence the implementation of workplace health promotion interventions. Similarly, one RMA, focused on health-care staff, examined barriers to promoting the health and well-being of Brazilian health-care workers.
Mental health issues
In total, 94 RMAs had a focus on mental health issues. Notably, almost half of all RMAs focused on health-care staff were related to mental health (n = 46, 49%). The largest proportion of RMAs (38/94) comprised primary studies that were aimed at improving psychological health or well-being outcomes (non-health care focused, n = 23; health care focused, n = 15). The remaining 56 RMAs had a primary focus on more specific mental health issues, and these are shown in Table 4. The majority of the 56 RMAs concerned interventions targeting stress and/or burnout among workers (n = 39). Stress and burnout-related interventions were a particular focus of RMAs in health-care settings (26/31). In addition, nine of the RMAs on stress and/or burnout were based on primary studies with nurses.
| Focus | Number of RMAs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Stress | 8 | 11 |
| Burnout | 5 | 12 |
| Compassion fatigue/secondary traumatic stress/vicarious traumatisation | 0 | 2 |
| Stress/burnout | 0 | 2 |
| Compassion fatigue | 1 | 1 |
| Coping/resilience | 0 | 1 |
| Depression | 6 | 1 |
| Stress/burnout/depression/suicide | 0 | 1 |
| Anxiety | 1 | 0 |
| Depression/anxiety | 1 | 0 |
| PTSD | 1 | 0 |
| Suicide prevention | 2 | 0 |
| Total | 25 | 31 |
It is likely that a number of the issues in Table 4 were also outcomes of interest in at least some of the 38 broad RMAs of mental health interventions in the workplace. Consequently, the table potentially underestimates the frequency with which issues have been addressed in RMAs.
Eleven mental health-related RMAs had an identifiable focus on mindfulness-/meditation-based interventions (health care focused, n = 6; non-health care focused, n = 5). Four addressed digital or web-based interventions including apps (applications). In addition, two RMAs examined the effectiveness of physical activity interventions to improve mental health outcomes. It was further possible from the abstracts to determine that 19 other RMAs included both individual and organisational-level interventions. In terms of outcomes, nearly all RMAs synthesised evidence in relation to the effectiveness of interventions; however, one had a primary focus on the financial return and cost-effectiveness of mental health interventions in the workplace, and another examined process-related outcomes in workplace stress management intervention studies. Finally, one review reviewed workplace guidelines to prevent, detect and manage mental health issues.
Physical health issues
Fifteen RMAs addressed a number of other issues related to the physical health of the workforce, and these are shown in Table 5. The largest group (8/15 RMAs) was focused on issues around fatigue, sleep, sleepiness, insomnia and alertness, particularly among shift workers. Interventions included changing shift patterns and length, napping, restorative breaks, fatigue training and other non-pharmacological measures. Three RMAs had a specific focus on reducing cardiovascular risk, one of which evaluated lifestyle-targeted interventions. Another addressed internet-based cardiovascular wellness and prevention programmes.
| Focus | Number of RMAs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Sleep/fatigue | 4 | 4 |
| Cardiovascular risk | 3 | 0 |
| Cervical cancer screening | 1 | 0 |
| Headaches | 1 | 0 |
| Hearing difficulties | 1 | 0 |
| HIV/tuberculosis | 1 | 0 |
| Total | 11 | 4 |
Work relations
Eighteen RMAs were related to violence, bullying or other unacceptable behaviour in the workplace. Fifteen RMAs were focused on health-care settings, 12 of which addressed violence/aggression prevention or management. The other three health-care-focused RMAs addressed bullying, violence and/or incivility. Approximately half (n = 8) involved interventions conducted with nursing staff, and two focused solely on nurses working in emergency departments. Some of the health-care-focused RMAs evaluated specific forms of interventions including de-escalation techniques training and aggression management programmes. The prevention of bullying, incivility or unprofessional behaviour was the focus of three RMAs of non-health-care settings.
General work issues
Table 6 shows the primary focus of 13 RMAs that addressed general work issues. It can be seen that an equal number of RMAs were related to sickness absence (n = 4) and absenteeism (n = 4), and a further two had a focus on presenteeism. Three of these 11 RMAs examined the role of physical activity in reducing sickness absence, absenteeism or presenteeism. Two health-care-focused RMAs synthesised evidence on the effectiveness of interventions and strategies to support student well-being during their transition to becoming qualified nurses.
| Focus | Number of RMAs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Sickness absence | 3 | 1 |
| Absenteeism | 3 | 1 |
| Transition to work | 0 | 2 |
| Presenteeism | 1 | 0 |
| Presenteeism and mental health | 1 | 0 |
| Work ability | 1 | 0 |
| Total | 9 | 4 |
Other health-related issues
Four RMAs of workplace interventions aimed to promote or support breastfeeding. Eight RMAs were also identified that addressed influenza vaccination among health-care workers. Five examined interventions to improve vaccination uptake and two focused on implementation issues. This included exploring factors that may influence the success of strategies to increase uptake, as well as exploring the views and experiences of health-care staff. One other review investigated both barriers to health-care staff getting vaccinated and components of effective programmes.
Review protocols
The scoping searches identified 78 protocols for reviews, of which 19 had a health-care focus and 59 did not. A bibliographic list of all 78 protocols is provided in Appendix 3. As Table 7 details, approximately 83% (65/78) were published on PROSPERO or elsewhere from 2016 onwards.
| Year of publication | Number of protocols | |
|---|---|---|
| Non-health care focused | Health care focused | |
| 2009 | 0 | 1 |
| 2010 | 1 | 0 |
| 2013 | 0 | 3 |
| 2014 | 2 | 0 |
| 2015 | 3 | 3 |
| 2016 | 8 | 3 |
| 2017 | 19 | 4 |
| 2018 | 25 | 5 |
| 2019 | 1 | 0 |
| Total | 59 | 19 |
The two protocols from 2014 were registered on PROSPERO, and the records indicate that both have been completed. One examined environmental interventions for changing the eating behaviours of employees, and the other evaluated the effectiveness of height-adjustable desks for decreasing sedentary behaviour among office workers. Both these reviews were included in the current evidence map. The status of reviews relating to the other 11 protocols published between 2009 and 2015 is unclear.
The status of reviews based on the more recent protocols published since the end of 2015 is also currently unknown. Nonetheless, the focus of the 65 protocols (53 non-health care focused and 12 health care focused) that were published between 2016 and 2019 is shown in Table 8.
| Focus | Number of protocols | |
|---|---|---|
| Non-health care focused | Health care focused | |
| General health/health promotion | 14 | 4 |
| Mental health and well-being | 12 | 2 |
| Physical activity/sedentary/sitting | 10 | 0 |
| Cardiovascular health | 4 | 0 |
| Alcohol | 2 | 0 |
| Breastfeeding | 2 | 0 |
| Absenteeism and presenteeism | 1 | 0 |
| Depression (prevention) | 1 | 0 |
| Dietary behaviour | 1 | 0 |
| Musculoskeletal problems | 1 | 0 |
| Physical activity/diet/sleep | 1 | 0 |
| Resilience | 1 | 0 |
| Self-confidence | 1 | 0 |
| Sleep/fatigue | 1 | 0 |
| Work/life balance | 1 | 0 |
| Violence/aggression | 0 | 5 |
| Violence/harassment/bullying | 0 | 1 |
| Total | 53 | 12 |
Approximately half of the non-health-care-focused protocols were related to general health and well-being or lifestyle-related behaviours, such as physical activity, sedentary behaviour, sitting time, dietary behaviour and alcohol consumption. These protocols have targeted effectiveness, financial outcomes or process-related outcomes including:
-
digital [mhealth (mobile health)] interventions to promote physical activity and reduce sedentary behaviour
-
return on investment for workplace chronic disease prevention programmes
-
factors influencing the implementation of interventions to improve workplace health and well-being.
The largest number of health-care-focused protocols (6/12) were on the prevention of violence or bullying/harassment. Two protocols published recently (2018) focused on the effectiveness of general health and lifestyle interventions. One aimed to synthesise evidence on the effectiveness of interventions to improve the health and well-being of hospital staff, with a specific focus on nutrition, physical activity, stress and musculoskeletal interventions. The other was targeted at improving the health risk of nurses using behavioural and/or educational interventions. Finally, two other health-care-related protocols were published in 2018, which addressed the following issues:
-
health, well-being and support interventions for UK ambulance service personnel
-
use of technology to provide social or emotional support to nurses.
Review of reviews: full-text scoping
The full texts of all 12 RoRs were retrieved and key characteristics examined in greater depth. 23–34 The reviews were published between 2009 and 2019, seven of which had been published since 2016. There was variation between the RoRs in terms of focus, interventions and outcomes; therefore, the RoRs have been described individually below. Table 9 shows the main focus of the reviews.
| Focus | Number of RoRs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Lifestyle | 3 | 0 |
| General health/health promotion | 3 | 1 |
| Mental health | 4 | 1 |
| Total | 10 | 2 |
Workplace settings
Only two RoRs explicitly stated that they had a health-care focus. One RoR evaluated interventions to improve mental health by reducing physician burnout. 24 The other evaluated interventions that facilitate sustainable jobs and have a positive impact on the health of workers in health-sector workplaces. However, the included RMAs evaluated interventions in a range of workplace settings, only some of which were in the health sector. 23
The remaining RoRs reported little information on workplace setting. Some did incorporate RMAs that included staff in the health sector; however, other workplace settings were included and findings were not reported separately.
Health focus of reviews of reviews
Lifestyles
Three RoRs addressed lifestyles and lifestyle behaviours but each evaluated different interventions. 26,29,30 None of the RoRs was explicitly set in a health-care sector. The RoRs were published from 2013 to 2019 and included RMAs published from 1994 to 2017. The main focus of the RoRs are listed in Table 10.
| Focus | Number of RoRs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Dietary change | 1 | 0 |
| Physical activity | 1 | 0 |
| Smoking cessation | 1 | 0 |
| Total | 3 | 0 |
Schliemann and Woodside30
The most recent RoR,30 published in 2019, included 21 RMAs and evaluated the effectiveness of dietary workplace interventions. However, authors reported that only one component of a workplace intervention had to be dietary and, therefore, RMAs also reported other components that were largely general wellness programmes (e.g. physical activity, smoking cessation, alcohol use). As well as reporting effects on dietary behaviour, such as fruit and vegetable consumption, some environmental aspects (e.g. catering policies, healthy choices, labelling healthy options) were reported together with economic outcomes (e.g. absenteeism, productivity and health-care costs). In their discussion section, authors reported a lack of consistency across the results due to variation of the RMAs and the included primary studies. They noted many of the outcomes were self-reported rather than objectively measured and there were a lack of process evaluations.
Jirathananuwat and Pongpirul29
One RoR published in 201729 included 11 RMAs and aimed to categorise interventions into factors that could optimise improvements in physical activity in the workplace. The factors were classified as enabling (e.g. information, self-motivation, programme training), predisposing (e.g. instrument resources such as pedometers), reinforcing (e.g. incentives, social support), policy regulatory (e.g. organisational action) and environmental development (e.g. break rooms, signage). The interventions addressed multiple health behaviours of which promoting physical activity was just one part; others included diet, stress management, weight control and smoking cessation. Workplaces included health service, government, industry, factory, educational and private sectors, but results were not reported separately for the health-service settings.
Fishwick et al.26
A RoR evaluating smoking cessation was published in 201326 and included six RMAs. The journal article also included a summary of a systematic review of relevant published qualitative literature, two case studies and findings from an expert focus group. Interventions included workplace cessation programmes (including behavioural, self-help and pharmacological) as well as legislative smoking bans. Specific workplace settings were not described by the RoR authors. Outcomes included rates of cessation, abstinence, quit rates and costs.
General health/health promotion
Four RoRs had a more general health focus;23,25,27,28 one of which evaluated interventions aimed at improving the health of health-sector employees, although RMAs in a non-health-care setting were also included. 23 RoRs were published between 2010 and 2016 and included RMAs published between 1997 and 2014. The main focus of the RoRs is listed in Table 11.
| Focus | Number of RoRs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Workplace health programmes for both physical and mental health | 1 | 0 |
| Organisational level to improve health | 0 | 1 |
| ‘Healthy lifestyles’ (physical activity, weight and nutrition) | 1 | 0 |
| Health promotion and primary prevention | 1 | 0 |
| Total | 3 | 1 |
Brunton et al.28
The Department of Health and Social Care (UK) commissioned a report, published in 2016,28 to understand whether or not workplace health programmes are effective for improving health and business outcomes and to identify characteristics that potentially influence their success. As well as a RoR, the authors included research on stakeholders’ views and experiences and a summary of key workplace health policy documents. Although the RoR identified a large number of RMAs (n = 106), the authors chose to include only those providing pooled effects sizes (n = 24). Interventions were multicomponent including education, exercise, counselling, screening, change to company regulations or policy, and risk assessments. Health-related outcomes included body mass index, diabetes risk, stress and physical activity. Business outcomes included absenteeism and related costs, health-care costs and productivity. The RoR authors did not report details of the types of workplace included in the RMAs. They did report that interventions differed across varying types of workplace making it difficult to judge the applicability of interventions to other settings. They also commented that physical activity interventions predominated and there were few data on other public health topics. Costs were rarely evaluated and few RMAs reported on the follow-up of interventions, therefore, making it difficult to assess the sustainability of the interventions.
Haby et al.23
One RoR23 published in 2016 (containing 14 RMAs) evaluated interventions to facilitate sustainable jobs and promote the health of workers in health-sector workplaces. However, the included RMAs evaluated interventions in a range of workplace settings, only some of which were in the health sector. Interventions included flexible work arrangements, compressed working week and task restructuring. Reported outcomes varied widely between RMAs and included disease incidence and prevalence, health-service use, and health and socioeconomic inequalities. Authors commented that interventions were not well described, which made it difficult to fully understand important factors such as delivery of the intervention and whether it was supported by employees or managers.
Schröer et al.27
A RoR published in 201427 included 15 RMAs and evaluated interventions promoting healthy lifestyles, preventing disease and reducing health-care costs. Physical activity and/or dietary interventions at the individual and/or organisational level were assessed. Details of workplaces and employees were not described in the RoR. Outcomes of interest were weight, physical activity and nutritional, together with some limited economic data. The authors reported a lack of consistency in the findings, and noted that few outcomes were evaluated long term.
Goldgruber and Aherns25
A RoR conducted in 201025 with 17 RMAs focused on the effectiveness of workplace health promotion and primary prevention interventions. The authors did not report details of workplace settings. The interventions targeted stress reduction, physical activity and nutrition, organisational development, smoking cessation, as well as ergonomics and back pain. Multiple outcomes were reported including psychosocial, physical and mental health, and economic indicators.
Mental health
Five RoRs focused on mental health,24,31–34 one of which evaluated interventions aimed at health-care staff. 24 RoRs were published between 2009 and 2016 and included RMAs published between 1996 and 2016. The main focus of the RoRs are listed in Table 12.
| Focus | Number of RoRs | |
|---|---|---|
| Non-health care focused | Health care focused | |
| Physician burnout (including medical students, residents and fellows) | 0 | 1 |
| Common mental health disorders (anxiety and depression) | 1 | 0 |
| Prevention of mental health problems and absenteeism | 1 | 0 |
| Mental health including stress management and prevention of psychological disorders | 1 | 0 |
| Stress management | 1 | 0 |
| Total | 4 | 1 |
Kalani et al.24
Reductions in physician burnout was the focus of one RoR published in 201824 with four RMAs. Participants included medical students, interns, physicians, residents and fellows. One of the three RMAs also included nurses. Most of the interventions were at an individual level including counselling, support groups and mindfulness. Organisational-level interventions included duty standards, shift-work staffing and change in workload. The authors commented that there were conflicting findings across RMAs at both individual and organisational level. It was suggested by the review authors that this could be owing to primary studies including different groups of physicians or other mediating or moderating factors that were not investigated. Sample sizes were also reported to be small in some primary studies and interventions differed across reviews.
Joyce et al.33
Workplace interventions for common mental health disorders were the focus of a RoR published in 201633 containing 20 RMAs. Interventions were aimed at primary, secondary and tertiary prevention, but details of workplace settings were not reported. Primary prevention interventions aimed to reduce the onset of a condition as well as reducing the impact of related risk factors; for example, through increasing employee control, physical activity and workplace health promotion. Secondary prevention interventions aimed to identify early symptoms and risk factors to reduce progression and included screening, counselling, stress management programmes and post-trauma debriefing. Tertiary prevention interventions aimed to provide therapy and rehabilitation to those formally diagnosed with a mental health condition and included cognitive–behavioural therapy, exposure therapy and medication. Outcomes included changes in physical activity, symptom reduction and occupational outcomes (e.g. sickness absence). The authors commented that few RMAs explored the impact of interventions on work-related aspects such as absenteeism and presenteeism.
Wagner et al.34
A RoR also published in 201634 and including 14 RMAs aimed to determine the level of evidence supporting mental health interventions relating to work outcomes such as absenteeism, productivity and cost. Workplace settings varied widely, where reported. Interventions also varied and many were multicomponent. Others included cognitive–behavioural therapy, exercise and injury prevention.
Dalsbø et al.32
Workplace interventions for employees’ mental health was the subject of a RoR published in 201332 in Norwegian with an English summary. Only three RMAs were included. Employees included health-care workers, law enforcement officers as well as ‘all employees’ in workplace settings. Interventions included stress management, mental image training and flexible working. Outcomes were stress, mental strain, self-image, quality of sleep and alertness. The RoR authors commented that no outcomes were reported for productivity, absence, sick leave, costs or adverse events.
Bhui et al.31
A synthesis of evidence on the effectiveness of different workplace stress management interventions was the focus of a RoR published in 2012,31 which included 23 RMAs. Interventions varied and included those at the individual (e.g. stress management, cognitive–behavioural therapy, relaxation, mindfulness) and organisational level (e.g. wellness programmes, support groups, problem-solving committees, work redesign). However, details of workplaces were not reported by the RoR authors. Outcomes were anxiety, depression and absenteeism. Authors reported that interventions differed in their components, mode of delivery and whether they targeted individuals or organisations. This made it difficult to compare benefits from any single intervention across a number of primary studies both within a RMA and across RMAs. Furthermore, outcomes of anxiety and depression were measured in different ways and there was not always clarity within RMAs as to which outcomes were included in meta-analyses. It was also reported that although many RMAs appeared to be reviewing the same evidence, they did not all identify the same primary studies and, therefore, did not always reach the same conclusions.
Further details about the characteristics of the 12 RoRs are provided in Appendix 4, Table 14.
Chapter 5 Discussion and conclusions
Summary of process
This evidence map provides a descriptive overview of the extent and nature of the available research evidence relevant to the promotion of healthy lifestyles among NHS staff. It was conducted to meet the requirements of NHS England, which was consulted at the start and end of the mapping process. It was not the aim of this piece of work to extract, evaluate and synthesise findings from individual publications.
In total, the title and abstracts of over 8000 records were screened and 408 potentially relevant publications were identified. Such a large number of potentially relevant reviews meant that it was necessary to map reviews based on details provided in titles and abstracts rather than on the full text of publications.
Summary of key findings
Workplace interventions targeting health and well-being, including the promotion of healthy lifestyle behaviours, have been reviewed extensively in the literature. Existing reviews have largely addressed effectiveness, but some have focused primarily on cost-effectiveness and/or implementation.
Evidence relating to a broad range of physical and mental health issues was identified across 12 RoRs and 312 other reviews, including 16 potentially relevant Cochrane reviews, published since 2000. Cochrane reviews are systematic reviews that are recognised to be methodologically rigorous and have high standards of reporting. Furthermore, there exists NICE guidance addressing multiple issues of potential relevance. NICE public health guidance is developed through a rigorous process and is based on the best available evidence in relation to effectiveness and cost-effectiveness. 56 In addition to published reviews of all types, RoRs and NICE guidance, protocols for a further 65 potentially relevant reviews were published between 2016 and 2019.
In terms of the health issues addressed in publications, some differences were identified between reviews that had a specific focus on health-care settings (health care focused) and ones that did not (non-health care focused). In total, 144 RMAs addressed aspects of lifestyle or general health/health promotion. Out of the 144 RMAs, most (n = 126, 88%) were non-health care focused. Furthermore, approximately 63% of all non-health-care RMAs addressed lifestyle and general health/health promotion (n = 126/201). In comparison, lifestyle and general health/health promotion reviews/meta-analyses constituted a relatively small proportion of all health-care-focused RMAs (19%, n = 18/95). The largest proportion of health-care-focused RMAs addressed mental health issues (n = 46/95), and stress and burnout in particular (n = 26/46).
Physical activity, sedentary behaviour or sitting time was the issue most commonly addressed in lifestyle-focused RMAs. In total, 37 RMAs were identified that addressed physical activity/sedentary behaviour/sitting time either as the sole focus of a review or in combination with other issues such as diet and nutrition. Multiple RMAs also examined the effectiveness of physical activity interventions to improve broader outcomes including those related to mental health, sickness absence and presenteeism.
Sixty seven out of the 95 health-care-focused RMAs involved a specific group of workers. However, the roles and settings examined were quite limited in scope, and nearly all RMAs were focused on nurses of various types, nursing students, doctors, medical students or staff working in mental health settings.
On a general level, it is unclear to what extent findings from reviews of studies conducted in non-health-care settings or in other countries are generalisable to the NHS workforce. There could be factors specific to UK health-care settings that impact on the ability of staff to adopt healthier behaviours, which limit the generalisability of findings from existing reviews; for example, differing organisational structures and practices, or the working conditions of staff. Most reviews are likely to have synthesised international evidence, and some may have drawn conclusions that are broadly generalisable across countries. Others could have taken local context into consideration when interpreting findings from primary studies.
Several publications identified in the scoping searches were commissioned by agencies in the UK. One RoR and one other review were commissioned by the Department of Health and Social Care. 28,55 A third review was conducted on behalf of Public Health England. 54 The RoR by Brunton et al. 28 examined workplace health programmes for improving health and business outcomes in any occupational setting. In contrast, the two reviews by Al-Khudairy et al. 54 and Brand et al. 55 included approaches to promoting health or health-related behaviour among health-care staff. The study by Al-Khudairy et al. 54 evaluated environmental level interventions to promote healthier food and drink choices. Brand et al. reviewed interventions to improve the health of health-care workers that adopted a whole-system approach. A considerable number of other reviews have also evaluated organisational-level interventions, or a combination of both individual and organisational-level interventions. Evidence on the effectiveness of interventions that integrate workplace health promotion and occupational health and safety activities has also been evaluated; for example, integrated ‘Total Worker Health’ programmes.
Multiple reviews were identified that focused on the same broad health issue, and in the case of physical activity, obesity and stress/burnout in particular, a large number of potentially relevant RMAs were mapped. It is possible, therefore, that there was considerable overlap in the primary studies included across RMAs (i.e. the same primary studies being included in multiple RMAs), which increases the potential for bias. If an in-depth synthesis were to be conducted on a subset of the evidence, it would be important to assess the extent of overlap in primary studies included across reviews.
A more in-depth examination was conducted of the 12 RoRs. These focused predominantly on evidence of effectiveness, with little information reported on costs or the delivery of interventions. Review questions, inclusion criteria and included publications differed across RoRs. There was also variation within individual RoRs in terms of interventions assessed, outcomes and length of follow-up (most were short term). It is worth noting that 5 of the 12 RoRs were over 5 years old (at the time of inclusion), and several RoRs, regardless of their publication date, included reviews from before 2000. This could have implications for the current relevance of some of the findings reported. The same issue could also apply to the RMAs in the evidence map as some may have included primary studies that were conducted prior to 2000.
Limitations of the scoping and mapping review
A pragmatic search strategy was developed for this mapping exercise, which was designed to identify key reviews related to the promotion of health and well-being in all types of workplace settings. It involved searching six databases with a primary focus on indexing evidence reviews. A more focused search of two other databases was also conducted specifically to identify additional reviews of interventions in health-care settings only. Although the search process was extensive and clearly effective at identifying relevant publications, the strategy used may not have identified every potentially relevant review; however, this is not a significant concern given the very large number of publications that were identified. Any reviews that the searches failed to capture would not have impacted significantly on the broad results of this evidence map.
Including publications in the evidence map based only on information in titles and abstracts should be recognised as a limitation. Without examining the full text of publications, it was not possible to verify that all reviews met the inclusion criteria. It also prevented a definitive determination being made about the health focus of reviews, and little detail was reported in title and abstracts about the specific type of intervention being examined. In addition, some of the reviews included in the map may not have been conducted in a systematic way; for example, a proportion may have been non-systematic literature review style publications, which are potentially at a high risk of bias and have poorer reliability.
Implications for additional synthesis work
The current mapping exercise was conducted on behalf of NHS England shortly after the introduction in 2018 of the NHS Health and Wellbeing Framework. 20 The framework exists to enable NHS providers to develop a staff health/well-being strategy, and it has a key focus on promoting both healthy lifestyles and positive mental health. The framework was the product of a multiorganisation collaboration and incorporated ‘best practice, research and insights’. 21
In addition, NICE has produced evidence-based public health guidance on a number of relevant issues. These were not examined in depth for the mapping exercise, but the guidance documents are appropriate for all employers, including the NHS. NICE routinely reviews its guidance and produces updates as required. Information provided on the NICE website indicates, for example, that:
-
The guidance on workplace smoking cessation was last checked in 2014 and no major evidence that would affect the recommendations was identified. 53
-
The guidance on promoting physical activity in the workplace was last checked in January 2019. It was assessed as still being largely relevant, but an update is being planned for 2021 to incorporate evidence on sit-stand desks. 57
-
The guidance on mental well-being at work was last checked in March 2018, and NICE is planning to update some recommendations in order to incorporate new evidence around certain issues including the effectiveness of educational and well-being interventions at an organisational level; the effectiveness of specific interventions such as mindfulness, cognitive–behavioural therapy and stress management. 58
The review team is doubtful that further evidence synthesis work at this stage would be of value to NHS England and add substantially to the existing knowledge base. Additional synthesis work may be useful if it addressed an identifiable need, and it was possible to identify one of the following:
-
A specific and focused research question arising from the current evidence map. It may then be appropriate to focus on a smaller number of reviews only, and provide a more thorough and critical assessment of the available evidence.
-
A specific gap in the literature (i.e. an issue not addressed by existing reviews or guidance). It may then be possible to undertake further literature searching and conduct a new evidence review; for example, the limited number of reviews focused specifically on groups of health-care staff other than doctors, nurses or medical/nursing students could indicate a potential research gap.
Conducting a ‘meta-review’ of evidence would not be appropriate as there was a considerable degree of heterogeneity between RoRs, for example in terms of focus and interventions.
Acknowledgements
We would like to thank NHS England colleagues for their input and feedback over the course of this piece of work.
Contributions of authors
Gary Raine (https://orcid.org/0000-0002-0354-0518) (Research Fellow, Evidence Synthesis) drafted the protocol and carried out study selection, data extraction, and write up of the report.
Sian Thomas (https://orcid.org/0000-0003-0917-0068) (Research Fellow, Evidence Synthesis) carried out study selection, data extraction, and write up of the report.
Mark Rodgers (https://orcid.org/0000-0002-5196-9239) (Research Fellow, Evidence Synthesis) contributed to the write up of the report.
Kath Wright (https://orcid.org/0000-0002-9020-1572) (Information Specialist) conducted all searching, wrote the search sections of the report and commented on the draft report.
Alison Eastwood (https://orcid.org/0000-0003-1079-7781) (Professor, Research) oversaw the project, contributed advice and expertise and commented on all drafts of the report.
All authors commented on the protocol.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- NHS England . The NHS Long Term Plan 2019.
- Boorman S. NHS Health and Well-Being: Final Report 2009.
- Department of Health and Social Care . NHS Health &Amp; Well-Being Improvement Framework 2011.
- Royal College of Physicians . Work and Wellbeing in the NHS: Why Staff Health Matters to Patient Care 2015.
- Sizmur S, Raleigh V. The Risks to Care Quality and Staff Wellbeing of an NHS System Under Pressure. Oxford: Picker Institute Europe; 2018.
- NHS England . NHS Staff Health &Amp; Wellbeing: CQUIN 2017–19 Indicator 1 Implementation Support 2018.
- NHS England . The NHS Constitution: The NHS Belongs to Us All 2015.
- Health and Safety Executive (HSE) . Tackling Work-Related Stress Using the Management Standards Approach: A Step-by-Step Workbook 2017.
- Boorman S. NHS Health and Well-Being: Interim Report 2009.
- NHS Survey Coordination Centre . NHS Staff Survey 2017 – National Weighted Data 2018. www.nhsstaffsurveys.com/Page/1064/Latest-Results/2017-Results/ (accessed 10 January 2019).
- NHS England . NHS Staff Health and Wellbeing: CQUIN Supplementary Guidance 2016. https://doi.org/10.1136/bmj.i4023.
- NHS Survey Coordination Centre . NHS Staff Survey 2017: National Briefing 2018.
- Keogh K. Eat Well, Nurse Well survey reveals stress at work leads to poor diets. Nurs Stand 2014;29. https://doi.org/10.7748/ns.29.8.7.s2.
- Kyle RG, Wills J, Mahoney C, Hoyle L, Kelly M, Atherton IM. Obesity prevalence among healthcare professionals in England: a cross-sectional study using the Health Survey for England. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018498.
- Malik S, Blake H, Batt M. How healthy are our nurses? New and registered nurses compared. Br J Nurs 2011;20:489-96. https://doi.org/10.12968/bjon.2011.20.8.489.
- Mittal T, Clegnorn C, Cade J, Barr S, Grove T, Bassett P, et al. A cross-sectional survey of cardiovascular health and lifestyle habits of hospital staff in the UK: do we look after ourselves?. Eur J Prev Cardiol 2018;25:543-50. https://doi.org/10.1177/2047487317746320.
- Schneider A, Bak M, Mahoney C, Hoyle L, Kelly M, Atherton I, et al. Health-related behaviours of nurses and other healthcare professionals: a cross-sectional study using the Scottish health survey. J Adv Nurs 2019;75:1239-51. https://doi.org/10.1111/jan.13926.
- Bakhshi S, Sun F, Murrells T, While A. Nurses’ health behaviours and physical activity-related health-promotion practices. Br J Community Nurs 2015;20:289-96. https://doi.org/10.12968/bjcn.2015.20.6.289.
- Kyle RG, Neall RA, Atherton IM. Prevalence of overweight and obesity among nurses in Scotland: a cross-sectional study using the Scottish Health Survey. Int J Nurs Stud 2016;53:126-33. https://doi.org/10.1016/j.ijnurstu.2015.10.015.
- NHS England . Workforce Health and Wellbeing Framework 2018. www.nhsemployers.org/-/media/Employers/Publications/Health-and-wellbeing/NHS-Workforce-HWB-Framework_updated-July-18.pdf (accessed 10 January 2019).
- NHS Employers . NHS Health and Wellbeing Framework 2018. www.nhsemployers.org/your-workforce/retain-and-improve/staff-experience/health-and-wellbeing/the-way-to-health-and-wellbeing/health-and-wellbeing-framework (accessed 20 December 2018).
- Health Education England . NHS Staff and Learners’ Mental Wellbeing Commission 2019.
- Haby MM, Chapman E, Clark R, Galvão LA. Interventions that facilitate sustainable jobs and have a positive impact on workers’ health: an overview of systematic reviews. Rev Panam Salud Publica 2016;40:332-40.
- Kalani SD, Azadfallah P, Oreyzi H, Adibi P. Interventions for physician burnout: a systematic review of systematic reviews. Int J Prev Med 2018;9. https://doi.org/10.4103/ijpvm.IJPVM_255_18.
- Goldgruber J, Ahrens D. Effectiveness of workplace health promotion and primary prevention interventions: a review. J Public Health 2010;18:75-88. https://doi.org/10.1007/s10389-009-0282-5.
- Fishwick D, Carroll C, McGregor M, Drury M, Webster J, Bradshaw L, et al. Smoking cessation in the workplace. Occup Med 2013;63:526-36. https://doi.org/10.1093/occmed/kqt107.
- Schröer S, Haupt J, Pieper C. Evidence-based lifestyle interventions in the workplace – an overview. Occup Med 2014;64:8-12. https://doi.org/10.1093/occmed/kqt136.
- Brunton G, Dickson K, Khatwa M, Caird J, Oliver S, Hinds K, et al. Developing evidence informed, employer-led workplace health. London: Department of Health Reviews Facility; 2016.
- Jirathananuwat A, Pongpirul K. Promoting physical activity in the workplace: a systematic meta-review. J Occup Health 2017;59:385-93. https://doi.org/10.1539/joh.16-0245-RA.
- Schliemann D, Woodside JV. The effectiveness of dietary workplace interventions: a systematic review of systematic reviews. Public Health Nutr 2019;22:942-55. https://doi.org/10.1017/S1368980018003750.
- Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health 2012;2012. https://doi.org/10.1155/2012/515874.
- Dalsbø TK, Thuve Dahm K, Austvoll-Dahlgren A, Knapstad M, Gundersen M, Merete Reinar L. Workplace-based Interventions for Employees’ Mental Health. Oslo: Knowledge Centre for the Health Services at the Norwegian Institute of Public Health (NIPH); 2013.
- Joyce S, Modini M, Christensen H, Mykletun A, Bryant R, Mitchell PB, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med 2016;46:683-97. https://doi.org/10.1017/S0033291715002408.
- Wagner SL, Koehn C, White MI, Harder HG, Schultz IZ, Williams-Whitt K, et al. Mental health interventions in the workplace and work outcomes: a best-evidence synthesis of systematic reviews. Int J Occup Environ Med 2016;7:1-14. https://doi.org/10.15171/ijoem.2016.607.
- Abdulwadud OA, Snow ME. Interventions in the workplace to support breastfeeding for women in employment. Cochrane Database Syst Rev 2012;10. https://doi.org/10.1002/14651858.CD006177.pub3.
- Cahill K, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev 2014;2. https://doi.org/10.1002/14651858.CD003440.pub4.
- Freak-Poli RL, Cumpston M, Peeters A, Clemes SA. Workplace pedometer interventions for increasing physical activity. Cochrane Database Syst Rev 2013;4. https://doi.org/10.1002/14651858.CD009209.pub2.
- Gillen PA, Sinclair M, Kernohan WG, Begley CM, Luyben AG. Interventions for prevention of bullying in the workplace. Cochrane Database Syst Rev 2017;1. https://doi.org/10.1002/14651858.CD009778.pub2.
- Hoving JL, Lacaille D, Urquhart DM, Hannu TJ, Sluiter JK, Frings-Dresen MH. Non-pharmacological interventions for preventing job loss in workers with inflammatory arthritis. Cochrane Database Syst Rev 2014;11. https://doi.org/10.1002/14651858.CD010208.pub2.
- Joyce K, Pabayo R, Critchley JA, Bambra C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev 2010;2. https://doi.org/10.1002/14651858.CD008009.pub2.
- Kuster AT, Dalsbø TK, Luong Thanh BY, Agarwal A, Durand-Moreau QV, Kirkehei I. Computer-based versus in-person interventions for preventing and reducing stress in workers. Cochrane Database Syst Rev 2017;8. https://doi.org/10.1002/14651858.CD011899.pub2.
- Naghieh A, Montgomery P, Bonell CP, Thompson M, Aber JL. Organisational interventions for improving wellbeing and reducing work-related stress in teachers. Cochrane Database Syst Rev 2015;4. https://doi.org/10.1002/14651858.CD010306.pub2.
- Ojo O, Verbeek JH, Rasanen K, Heikkinen J, Isotalo LK, Mngoma N, et al. Interventions to reduce risky sexual behaviour for preventing HIV infection in workers in occupational settings. Cochrane Database Syst Rev 2011;12. https://doi.org/10.1002/14651858.CD005274.pub3.
- Pachito DV, Eckeli AL, Desouky AS, Corbett MA, Partonen T, Rajaratnam SM, et al. Workplace lighting for improving alertness and mood in daytime workers. Cochrane Database Syst Rev 2018;3. https://doi.org/10.1002/14651858.CD012243.pub2.
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2015;4. https://doi.org/10.1002/14651858.CD002892.pub5.
- Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Pedisic Z. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev 2018;12. https://doi.org/10.1002/14651858.CD010912.pub5.
- Slanger TE, Gross JV, Pinger A, Morfeld P, Bellinger M, Duhme AL, et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst Rev 2016;8. https://doi.org/10.1002/14651858.CD010641.pub2.
- Tanja-Dijkstra K, Pieterse ME. The psychological effects of the physical healthcare environment on healthcare personnel. Cochrane Database Syst Rev 2011;1. https://doi.org/10.1002/14651858.CD006210.pub3.
- van Wyk BE, Pillay-Van Wyk V. Preventive staff-support interventions for health workers. Cochrane Database Syst Rev 2010;3. https://doi.org/10.1002/14651858.CD003541.pub2.
- Wolfenden L, Goldman S, Stacey FG, Grady A, Kingsland M, Williams CM, et al. Strategies to improve the implementation of workplace-based policies or practices targeting tobacco, alcohol, diet, physical activity and obesity. Cochrane Database Syst Rev 2018;11. https://doi.org/10.1002/14651858.CD012439.pub2.
- NICE . Mental Wellbeing at Work 2009.
- NICE . Physical Activity in the Workplace 2008.
- NICE . Smoking: Workplace Interventions 2007.
- Al-Khudairy L, Uthman OA, Walmsley R, Johnson S, Oyebode O. Choice architecture interventions to improve diet and/or dietary behaviour by healthcare staff in high-income countries: a systematic review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-023687.
- Brand SL, Thompson Coon J, Fleming LE, Carroll L, Bethel A, Wyatt K. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0188418.
- NICE . Developing NICE Guidelines: The Manual 2014.
- NICE . 2019 Exceptional Surveillance of Physical Activity in the Workplace (NICE Guideline PH13) 2019. www.nice.org.uk/guidance/ph13/resources/2019-exceptional-surveillance-of-physical-activity-in-the-workplace-nice-guideline-ph13-6661547533/chapter/Surveillance-decision?tab=evidence (accessed April 2019).
- NICE . Surveillance Report 2018 – Mental Wellbeing at Work (2009) (NICE Guideline PH22) 2018. www.nice.org.uk/guidance/ph22/resources/surveillance-report-2018-mental-wellbeing-at-work-2009-nice-guideline-ph22-4787140141/chapter/Surveillance-decision?tab=evidence (accessed April 2019).
Appendix 1 Search strategy
The search strategies used for the literature search are reproduced below.
Cochrane Database of Systematic Reviews
Via The Cochrane Library.
Search date: 29 January 2019.
Records retrieved: 76.
Search strategy
-
ID Search
-
#1 MeSH descriptor: [Workplace] explode all trees
-
#2 (workplace*):ti,ab,kw OR (worksite*):ti,ab,kw (Word variations have been searched)
-
#3 MeSH descriptor: [Occupational Health] explode all trees
-
#4 ((work* or employment) near/6 “health promot*”):ti,ab,kw (Word variations have been searched)
-
#5 MeSH descriptor: [Health Promotion] explode all trees
-
#6 MeSH descriptor: [Work] explode all trees
-
#7 MeSH descriptor: [Employment] explode all trees
-
#8 #5 and (#6 or #7)
-
#9 #1 or #2 or #3 or #4 or #7
Database of Abstracts of Review of Effects
Via the Centre for Reviews and Dissemination website at www.crd.york.ac.uk/CRDWeb/HomePage.asp.
Search date: 29 January 2019.
Health Technology Assessment database
Via the Centre for Reviews and Dissemination website at www.crd.york.ac.uk/CRDWeb/HomePage.asp
Search date: 29 January 2019.
Search strategy
-
DARE ((workplace):TI OR (worksite):TI) and ((Systematic review:ZDT and Bibliographic:ZPS) OR (Systematic review:ZDT and Abstract:ZPS)) FROM 2000 TO 2019 (60)
-
DARE ((work) AND (health promotion)) and ((Systematic review:ZDT and Bibliographic:ZPS) OR (Systematic review:ZDT and Abstract:ZPS)) FROM 2000 TO 2019 (50)
-
HTA (workplace):TI OR (worksite):TI IN HTA FROM 2000 TO 2019 (3)
-
HTA work):TI OR (health promotion):TI IN HTA FROM 2000 TO 2019 (36)
-
DARE & HTA MeSH Descriptor Workplace AND Mesh Descriptor Health Promotion (58)
Epistemonikos
Via the website at www.epistemonikos.org/.
Search date: 29 January 2019.
Records retrieved: 392.
Search strategy
(advanced_title_en:(health promotion AND work) OR advanced_abstract_en:(health promotion AND work)) OR advanced_title_en:(workplace) OR advanced_title_en:(worksite) [Filters: protocol=no, classification=systematic-review, min_year=2000, max_year=2019]
Additional searches were conducted on 14 February 2019 as described below.
Search 1
(title:((title:(“Occupational health”) OR abstract:(“Occupational health”))) OR abstract:((title:(“Occupational health”) OR abstract:(“Occupational health”)))) AND (title:(doctor OR doctors OR clinician OR clinicians OR physician OR physicians OR nurse OR nurses OR dentist OR dentists) OR abstract:(doctor OR doctors OR clinician OR clinicians OR physician OR physicians OR nurse OR nurses OR dentist OR dentists)) 47 records
Search 2
(title:(workers OR workplace OR workplaces OR worksite OR worksites OR employment OR employees OR “job satisfaction”) OR abstract:(workers OR workplace OR workplaces OR worksite OR worksites OR employment OR employees OR “job satisfaction”)) 97 records
Restricted to 2000 to 2019. Broad synthesis category.
Search 3
(title:(workers OR workplace OR workplaces OR worksite OR worksites OR employment OR employees OR “job satisfaction”) OR abstract:(workers OR workplace OR workplaces OR worksite OR worksites OR employment OR employees OR “job satisfaction”)) 4206 records
Restricted to 2000 to 2019. Broad synthesis category.
Health Evidence
Via the website at www.healthevidence.org/.
Search date: 29 January 2019.
Records retrieved: 159.
Search strategy
| ID | Number of hits | Search terms |
|---|---|---|
| #11 | 0 | (workplace or worksite) AND Limit: Date = Published from 2019 to 2019 |
| #10 | 17 | (workplace or worksite) AND Limit: Date = Published from 2018 to 2018 |
| #9 | 20 | (workplace or worksite) AND Limit: Date = Published from 2017 to 2017 |
| #8 | 14 | (workplace or worksite) AND Limit: Date = Published from 2016 to 2016 |
| #7 | 21 | (workplace or worksite) AND Limit: Date = Published from 2015 to 2015 |
| #6 | 22 | (workplace or worksite) AND Limit: Date = Published from 2014 to 2014 |
| #5 | 16 | (workplace or worksite) AND Limit: Date = Published from 2013 to 2013 |
| #4 | 22 | (workplace or worksite) AND Limit: Date = Published from 2012 to 2012 |
| #3 | 9 | (workplace or worksite) AND Limit: Date = Published from 2011 to 2011 |
| #2 | 18 | (workplace or worksite) AND Limit: Date = Published from 2010 to 2010 |
| #1 | 274 | (workplace or worksite) |
Database of promoting health effectiveness reviews
Via the website at https://eppi.ioe.ac.uk/webdatabases4/Intro.aspx?ID = 9.
Search date: 29 January 2019.
Records retrieved: 307.
Two search strategies were used.
Search 1
| Search # | Search | Number of hits |
|---|---|---|
| 1 | Freetext (Title): work | 75 |
| 2 | Freetext (Title): workplace | 97 |
| 3 | Freetext (Title): worksite | 55 |
| 4 | 1 OR 2 OR 3 | 221 |
Search 2
| Search # | Search | Number of hits |
|---|---|---|
| 5 | Freetext (All but Authors): workplace | 117 |
| 6 | Freetext (All but Authors): worksite | 89 |
| 7 | 5 OR 6 | 246 |
MEDLINE (via OVID)
Search date: 7 February 2019.
Records retrieved: 3063.
Database: Ovid MEDLINE® ALL < 1946 to 05 February 2019>.
Search strategy
-
1 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers).ti,ab. (695)
-
2 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers).ti,ab. (7035)
-
3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers).ti,ab. (26,580)
-
4 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers).ti,ab. (33,594)
-
5 (health employees or health practitioners or health professionals or health staff or health workforce or health workers).ti,ab. (62,452)
-
6 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers).ti,ab. (21,254)
-
7 (medical students or medical undergraduates).ti,ab. (32,692)
-
8 (nurse$ or nursing or doctor$ or physician$ or midwi$).ti,ab. (853,683)
-
9 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 (977,641)
-
10 Mental Health/ or Anxiety/ or Occupational Stress/ or Burnout/ or Bullying/ (107,669)
-
11 Lifestyle/ or Exercise/ or Diet/ or Obesity/ or Overweight/ (429,256)
-
12 exp Substance-Related Disorders/ or Smoking/ or Alcoholism/ (386,075)
-
13 Sick Leave/ or Absenteeeism/ or Occupational Health/ or Influenza Vaccines/ or Workplace Violence/ (57,885)
-
14 10 or 11 or 12 or 13 (950,112)
-
15 9 and 14 (51,674)
-
16 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (6)
-
17 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (72)
-
18 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (84)
-
19 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (164)
-
20 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (16)
-
21 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (medical students or medical undergraduates)).ti,ab. (110)
-
22 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (2048)
-
23 ((wellbeing or well-being or wellness or health promot$ or health check$) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (20)
-
24 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 (2505)
-
25 (sick$ adj3 (leave or absence) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (4)
-
26 (sick$ adj3 (leave or absence) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (14)
-
27 (sick$ adj3 (leave or absence) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (13)
-
28 (sick$ adj3 (leave or absence) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (5)
-
29 (sick$ adj3 (leave or absence) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (1)
-
30 (sick$ adj3 (leave or absence) adj3 (medical students or medical undergraduates)).ti,ab. (0)
-
31 (sick$ adj3 (leave or absence) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (155)
-
32 (sick$ adj3 (leave or absence) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (10)
-
33 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (197)
-
34 ((flu vaccinat$ or influenza vaccinat$) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (3)
-
35 ((flu vaccinat$ or influenza vaccinat$) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (186)
-
36 ((flu vaccinat$ or influenza vaccinat$) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (151)
-
37 ((flu vaccinat$ or influenza vaccinat$) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (20)
-
38 ((flu vaccinat$ or influenza vaccinat$) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (7)
-
39 ((flu vaccinat$ or influenza vaccinat$) adj3 (medical students or medical undergraduates)).ti,ab. (14)
-
40 ((flu vaccinat$ or influenza vaccinat$) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (173)
-
41 ((flu vaccinat$ or influenza vaccinat$) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (13)
-
42 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 (550)
-
43 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (15)
-
44 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (287)
-
45 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (611)
-
46 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (6280)
-
47 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (178)
-
48 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (medical students or medical undergraduates)).ti,ab. (608)
-
49 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (12,284)
-
50 ((anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (76)
-
51 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 (19,671)
-
52 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (5)
-
53 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (120)
-
54 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (130)
-
55 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (359)
-
56 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (36)
-
57 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (medical students or medical undergraduates)).ti,ab. (208)
-
58 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (3065)
-
59 ((healthy eating or diet or nutrition or obesity or overweight or exercise or physical activity or sedentary behavi$ or lifestyle) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (21)
-
60 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 (3887)
-
61 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (NHS employees or NHS practitioners or NHS professionals or NHS staff or NHS workforce or NHS workers)).ti,ab. (0)
-
62 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (healthcare employees or healthcare practitioners or healthcare professionals or healthcare staff or healthcare workforce or healthcare workers)).ti,ab. (46)
-
63 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (health care employees or health care practitioners or health care professionals or health care staff or health care workforce or health care workers)).ti,ab. (105)
-
64 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (health employees or health practitioners or health professionals or health staff or health workforce or health workers)).ti,ab. (241)
-
65 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (medical employees or medical practitioners or medical professionals or medical staff or medical workforce or medical workers)).ti,ab. (31)
-
66 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (medical students or medical undergraduates)).ti,ab. (247)
-
67 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (nurse$ or nursing or doctor$ or physician$ or midwi$)).ti,ab. (2040)
-
68 ((smoking or tobacco or alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$) adj3 (hospital employees or hospital practitioners or hospital professionals or hospital staff or hospital workforce or hospital workers)).ti,ab. (48)
-
69 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 (2654)
-
70 *Health Personnel/ (23,667)
-
71 (wellbeing or well-being or wellness or health promot$ or health check$).ti. (27,028)
-
72 (anxiety or depressed or depression or mental health or stress or burnout or bullying or harass$ or violence or violent$).ti. (418,265)
-
73 (healthy eating or diet or nutrition or exercise or physical activity or sedentary behavi$ or lifestyle or obesity or overweight).ti. (338,587)
-
74 (alcoholism or alcohol abus$ or alcohol addict$ or alcohol drink$ or alcohol misus$ or drug abus$ or drug addict$ or drug misus$ or smoking or tobacco).ti. (117,867)
-
75 (sick$ leave or sick$ absence or absenteeism or flu vaccinat$ or influenza vaccinat$).ti. (7982)
-
76 (back adj2 pain).ti. (17,183)
-
77 71 or 72 or 73 or 74 or 75 or 76 (909,277)
-
78 70 and 77 (2526)
-
79 15 or 24 or 33 or 42 or 51 or 60 or 69 or 78 (74,491)
-
80 (systematic$ adj2 review$).ti,ab. (146,640)
-
81 meta-analysis as topic/ (16,702)
-
82 meta-analytic$.ti,ab. (6342)
-
83 meta-analysis.ti,ab,pt. (145,685)
-
84 metanalysis.ti,ab. (181)
-
85 metaanalysis.ti,ab. (1491)
-
86 meta analysis.ti,ab. (120,969)
-
87 meta-synthesis.ti,ab. (704)
-
88 metasynthesis.ti,ab. (272)
-
89 meta synthesis.ti,ab. (704)
-
90 meta-regression.ti,ab. (6211)
-
91 metaregression.ti,ab. (564)
-
92 meta regression.ti,ab. (6211)
-
93 (synthes$ adj3 literature).ti,ab. (2860)
-
94 (synthes$ adj3 evidence).ti,ab. (8651)
-
95 integrative review.ti,ab. (2383)
-
96 data synthesis.ti,ab. (10,216)
-
97 (research synthesis or narrative synthesis).ti,ab. (2374)
-
98 (systematic study or systematic studies).ti,ab. (10,981)
-
99 (systematic comparison$ or systematic overview$).ti,ab. (3005)
-
100 evidence based review.ti,ab. (1852)
-
101 comprehensive review.ti,ab. (12,741)
-
102 critical review.ti,ab. (14,551)
-
103 quantitative review.ti,ab. (629)
-
104 structured review.ti,ab. (740)
-
105 realist review.ti,ab. (239)
-
106 realist synthesis.ti,ab. (166)
-
107 pooled analysis.ti,ab. (7300)
-
108 or/80-107 (303,757)
-
109 review.pt. (2,477,929)
-
110 medline.ab. (100,321)
-
111 pubmed.ab. (90,896)
-
112 cochrane.ab. (67,385)
-
113 embase.ab. (72,406)
-
114 cinahl.ab. (22,305)
-
115 psyc?lit.ab. (913)
-
116 psyc?info.ab. (27,151)
-
117 (literature adj3 search$).ab. (51,438)
-
118 (database$ adj3 search$).ab. (50,418)
-
119 (bibliographic adj3 search$).ab. (2221)
-
120 (electronic adj3 search$).ab. (18,711)
-
121 (electronic adj3 database$).ab. (24,199)
-
122 (computeri?ed adj3 search$).ab. (3365)
-
123 (internet adj3 search$).ab. (2894)
-
124 included studies.ab. (18,879)
-
125 (inclusion adj3 studies).ab. (13,809)
-
126 inclusion criteria.ab. (72,125)
-
127 selection criteria.ab. (27,992)
-
128 predefined criteria.ab. (1770)
-
129 predetermined criteria.ab. (970)
-
130 (assess$ adj3 (quality or validity)).ab. (69,431)
-
131 (select$ adj3 (study or studies)).ab. (59,357)
-
132 (data adj3 extract$).ab. (53,494)
-
133 extracted data.ab. (12,362)
-
134 (data adj2 abstracted).ab. (4848)
-
135 (data adj3 abstraction).ab. (1489)
-
136 published intervention$.ab. (157)
-
137 ((study or studies) adj2 evaluat$).ab. (166,265)
-
138 (intervention$ adj2 evaluat$).ab. (9967)
-
139 confidence interval$.ab. (365,701)
-
140 heterogeneity.ab. (146,219)
-
141 pooled.ab. (77,750)
-
142 pooling.ab. (11,003)
-
143 odds ratio$.ab. (239,017)
-
144 (Jadad or coding).ab. (167,100)
-
145 or/110-144 (1,284,446)
-
146 109 and 145 (222,997)
-
147 review.ti. (413,989)
-
148 147 and 145 (116,759)
-
149 (review$ adj4 (papers or trials or studies or evidence or intervention$ or evaluation$)).ti,ab. (166,288)
-
150 108 or 146 or 148 or 149 (506,309)
-
151 letter.pt. (1,015,413)
-
152 editorial.pt. (481,572)
-
153 comment.pt. (752,482)
-
154 151 or 152 or 153 (1,694,614)
-
155 150 not 154 (494,494)
-
156 exp animals/ not humans/ (4,544,871)
-
157 155 not 156 (481,921)
-
158 79 and 157 (3336)
-
159 limit 158 to yr=“2000 -Current” (3063)
Business Source Premier (via EBSCOhost)
Search date: 7 February 2019.
Records retrieved: 711.
Search strategy
| # | Query | Number of hits |
|---|---|---|
| S19 | S6 OR S8 OR S10 OR S12 OR S14 OR S16 OR S18 | 714 |
| S18 | S1 AND S4 AND S17 | 44 |
| S17 | TX “back pain” | 7819 |
| S16 | S1 AND S4 AND S15 | 119 |
| S15 | TX smoking or tobacco or alcoholism or “alcohol abus*” or “alcohol addict*” or “alcohol drink*” or “alcohol misus*” or “drug abus*” or “drug addict*” or “drug misus*” | 443,257 |
| S14 | S1 AND S4 AND S13 | 310 |
| S13 | TX “healthy eating” or diet or nutrition or obesity or overweight or exercise or “physical activity” or “sedentary behavi*” or lifestyle | 797,679 |
| S12 | S1 AND S4 AND S11 | 661 |
| S11 | TX anxiety or depressed or depression or “mental health” or stress or burnout or bullying or harass* or violence or violent* | 979,468 |
| S10 | S1 AND S4 AND S9 | 6 |
| S9 | TX “flu vaccinat*” or “influenza vaccinat*” | 3366 |
| S8 | S1 AND S4 AND S7 | 114 |
| S7 | TX ( sick* N3 (leave or absence) ) OR TX absenteeism | 39,270 |
| S6 | S1 AND S4 AND S5 | 295 |
| S5 | TX (wellbeing or well-being or wellness or “health promot*” or “health check*”) | 243,733 |
| S4 | S2 OR S3 | 62,535 |
| S3 | TI ( “NHS employees” or “NHS practitioners” or “NHS professionals” or “NHS staff” or “NHS workforce” or “NHS workers” ) OR TI ( “hospital employees” or “hospital practitioners” or “hospital professionals” or “hospital staff” or “hospital workforce” or “hospital workers” ) OR TI ( “healthcare employees” or “healthcare practitioners” or “healthcare professionals” or “healthcare staff” or “healthcare workforce” or “healthcare workers” ) OR TI ( “health care employees” or “health care practitioners” or “health care professionals” or “health care staff” or “health care workforce” or “health care workers” ) OR TI ( “health employees” or “health practitioners” or “health professionals” or “health staff” or “health workforce” or “health workers” ) OR TI ( “medical employees” or “medical practitioners” or “medical professionals” or “medical staff” or “medical workforce” or “medical workers” ) OR TI ( “medical students” or “medical undergraduates” ) OR TI ( “nurse* or nursing or doctor* or physician* or midwi*) | 34,129 |
| S2 | DE “MEDICAL personnel” OR DE “DENTAL personnel” OR DE “ENGLISH language -- Conversation & phrase books (for medical personnel)” OR DE “HEALTH practitioners” OR DE “HEALTH services administrators” OR DE “HOSPITAL personnel” OR DE “MENTAL health personnel” OR DE “NURSES” OR DE “PHYSICIANS” OR DE “PODIATRISTS” | 37,984 |
| S1 | TI “systematic review” OR TI meta-analysis OR TX ( review N3 (research or comprehensive or integrated or structured or realist or evidence) ) OR TX ( synthesis N3 (research or comprehensive or integrated or structured or realist or evidence) ) OR TI ( review AND (research or comprehensive or integrated or structured or realist or evidence) ) | 136,990 |
PROSPERO
Via website at www.crd.york.ac.uk/prospero/.
Search date: 30 January 2019.
Records retrieved: 357.
Search strategy
| ID | Search terms | Number of hits |
|---|---|---|
| #1 | (employees AND (health OR wellbeing)): TI, KW, RQ, SM | 21 |
| #2 | (employees AND (health OR well-being)): TI, KW, RQ, SM | 21 |
| #3 | (staff AND (health OR wellbeing)): TI, KW, RQ, SM | 92 |
| #4 | (staff AND (health OR well-being)): TI, KW, RQ, SM | 95 |
| #5 | (employment AND (health OR wellbeing)): TI, KW, RQ, SM | 32 |
| #6 | (employment AND (health OR well-being)): TI, KW, RQ, SM | 31 |
| #7 | (workplace): TI, KW, RQ, SM | 168 |
| #8 | (worksite): TI, KW, RQ, SM | 9 |
| #9 | MeSH DESCRIPTOR workplace EXPLODE ALL TREES | 148 |
| #10 | MeSH DESCRIPTOR Occupational Health EXPLODE ALL TREES | 67 |
| #11 | #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 | 357 |
Appendix 2 List of population groups/workplace settings
| Population group/workplace setting | Number of reviews |
|---|---|
| Workplace | 155 |
| Nursesa | 31 |
| ‘Health-care’ staff | 28 |
| Shift workers | 9 |
| Mental health care | 8 |
| Medical students | 7 |
| Office-based workers | 7 |
| Women | 7 |
| Doctors | 7 |
| Otherb | 6 |
| Nurses/nursing students | 4 |
| Employees with conditions | 3 |
| Emergency medical services | 3 |
| Male | 3 |
| Managers/supervisors | 3 |
| Nursing students | 3 |
| Older workers | 3 |
| Public sectorc | 3 |
| Midwives/obstetricians/midwives | 2 |
| Doctors/medical students | 1 |
| University and college staff | 1 |
| Workers (Latin American) | 1 |
| Health-care students and professionals | 1 |
Appendix 3 Reviews and meta-analyses, and protocols included in the evidence map
Lifestyles
Non-health care focused (n = 74)
Abraham C, Graham-Rowe E. Are worksite interventions effective in increasing physical activity? A systematic review and meta-analysis. Health Psychol Rev 2009;3:108–144.
Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med 2006;43:291–305.
Allan J, Querstret D, Banas K, de Bruin M. Environmental interventions for altering eating behaviours of employees in the workplace: a systematic review. Obes Rev 2017;18:214–26. https://doi.org/10.1111/obr.12470
Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med 2009;37:340–57. https://doi.org/10.1016/j.amepre.2009.07.003
Archer WR, Batan MC, Buchanan LR, Soler RE, Ramsey DC, Kirchhofer A, Reyes M. Promising practices for the prevention and control of obesity in the worksite. Am J Health Promot 2011;25:e12–26. https://doi.org/10.4278/ajhp.090421-QUAN-144
Ausburn TF, LaCoursiere S, Crouter SE, McKay T. Review of worksite weight management programs. Workplace Health Saf 2014;62:122–6. https://doi.org/10.3928/21650799-20140219-06
Barbato DL, Sancini A, Caciari T, Rosati MV, Tomei G, Tomei F. [Dietary intervention programs in the workplace: an effective prevention strategy.] G Ital Med Lav Ergon 2010;32(Suppl. 4):100–3.
Becker I, Wallmann-Sperlich B, Rupp R, Bucksch J. [Workplace interventions to reduce sedentary behavior: A systematic review]. Gesundheitswesen 2019;81:606–14.
Bell K, McCullough L, DeVries K, Greaves L, Jategaonkar N. NICE Rapid review. Workplace Policies and Interventions for Smoking Cessation. Vancouver, BC: British Columbia Centre of Excellence for Women’s Health; 2006.
Bell K, Richardson L, McCullough L, Greaves L. Workplace Interventions to Promote Smoking Cessation. Vancouver, BC: British Columbia Center of Excellence for Women’s Health; 2006.
Benedict MA, Arterburn D. Worksite-based weight loss programs: a systematic review of recent literature. Am J Health Promot 2008;22:408–16. https://doi.org/10.4278/ajhp.22.6.408
Brinkley A, McDermott H, Munir F. What benefits does team sport hold for the workplace? A systematic review. J Sports Sci 2017;35:136–48. https://doi.org/10.1080/02640414.2016.1158852
Brown SA, García AA, Zuñiga JA, Lewis KA. Effectiveness of workplace diabetes prevention programs: A systematic review of the evidence. Patient Educ Couns 2018;101:1036–50.
Burnhams NH, Musekiwa A, Parry C, London L. A systematic review of evidence-based workplace prevention programmes that address substance abuse and HIV risk behaviours. Afr J Drug Alcohol Stud 2013;12:1–22.
Cairns JM, Bambra C, Hillier-Brown FC, Moore HJ, Summerbell CD. Weighing up the evidence: a systematic review of the effectiveness of workplace interventions to tackle socio-economic inequalities in obesity. J Public Health 2015;37:659–70. https://doi.org/10.1093/pubmed/fdu077
Cao C, Liu Y, Zhu W, Ma J. Effect of active workstation on energy expenditure and job performance: a systematic review and meta-analysis. J Phys Act Health 2016;13:562–71. https://doi.org/10.1123/jpah.2014-0565
Carroll C, Rick J, Leaviss J, Fishwick D, Booth A. A qualitative evidence synthesis of employees’ views of workplace smoking reduction or cessation interventions. BMC Public Health 2013;13:1095. https://doi.org/10.1186/1471-2458-13-1095
Chau JY, der Ploeg HP, van Uffelen JG, Wong J, Riphagen I, Healy GN, et al. Are workplace interventions to reduce sitting effective? A systematic review. Prev Med 2010;51:352–6. https://doi.org/10.1016/j.ypmed.2010.08.012
Chu AH, Ng SH, Tan CS, Win AM, Koh D, Müller-Riemenschneider F. A systematic review and meta-analysis of workplace intervention strategies to reduce sedentary time in white-collar workers. Obes Rev 2016;17:467–81. https://doi.org/10.1111/obr.12388
Commissaris DA, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes LLj, Hendriksen IJ. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scand J Work Environ Health 2016;42:181–91. https://doi.org/10.5271/sjweh.3544
Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med 2009;37:330–9. https://doi.org/10.1016/j.amepre.2009.06.008
Cook A, Teleni L, Allman-Farinelli M. Are workplaces an appropriate setting for nutrition promotion? A systematic review. Obes Rev 2014;15:T7:S32.11.
Cook R, Schlenger W. Prevention of substance abuse in the workplace: review of research on the delivery of services. J Prim Prev 2002;23:115–42.
Demou E, MacLean A, Cheripelli LJ, Hunt K, Gray CM. Group-based healthy lifestyle workplace interventions for shift workers: a systematic review. Scand J Work Environ Health 2018;44:568–84. https://doi.org/10.5271/sjweh.3763
Dugdill L, Brettle A, Hulme C, McCluskey S, Long AF. A Review of Effectiveness of Workplace Health Promotion Interventions on Physical Activity and What Works in Motivating and Changing Employees’ Health Behaviour; London: NICE; 2007.
Ferreira ML, Sartes LMA. Interventions carried out in the workplace for the use of drugs: systematic review. Psicol ciênc prof 2015;35:96–110.
Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ 2002;325:188.
Flahr H, Brown WJ, Kolbe-Alexander TL. A systematic review of physical activity-based interventions in shift workers. Prev Med Rep 2018;10:323–31. https://doi.org/10.1016/j.pmedr.2018.04.004
Geaney F, Kelly C, Greiner BA, Harrington JM, Perry IJ, Beirne P. The effectiveness of workplace dietary modification interventions: a systematic review. Prev Med 2013;57:438–47. https://doi.org/10.1016/j.ypmed.2013.06.032
Hadgraft NT, Brakenridge CL, Dunstan DW, Owen N, Healy GN, Lawler SP. Perceptions of the acceptability and feasibility of reducing occupational sitting: review and thematic synthesis. Int J Behav Nutr Phys Act 2018;15:90. https://doi.org/10.1186/s12966-018-0718-9
Hafez D, Fedewa A, Moran M, O’Brien M, Ackermann R, Kullgren JT. Workplace interventions to prevent type 2 diabetes mellitus: a narrative review. Curr Diab Rep 2017;17:9. https://doi.org/10.1007/s11892-017-0840-0
Hendren S, Logomarsino J. Impact of worksite cafeteria interventions on fruit and vegetable consumption in adults: a systematic review. Int J Workplace Health Manag 2017;10:134–52.
Hutchinson AD, Wilson C. Improving nutrition and physical activity in the workplace: a meta-analysis of intervention studies. Health Promot Int 2012;27:238–49. https://doi.org/10.1093/heapro/dar035
Jensen JD. Can worksite nutritional interventions improve productivity and firm profitability? A literature review. Perspect Public Health 2011;131:184–92. https://doi.org/10.1177/1757913911408263
Knowlden A, Ickes MJ, Sharma M. Systematic analysis of tobacco treatment interventions implemented in worksite settings. J Subst Abuse 2014;19:283–94.
Kolar C, von Treuer K. Alcohol misuse interventions in the workplace: A systematic review of workplace and sports management alcohol interventions. Int J Ment Health Addict 2015;13:563–83.
Lassen AD, Fagt S, Lennernäs M, Nyberg M, Haapalar I, Thorsen AV, et al. The impact of worksite interventions promoting healthier food and/or physical activity habits among employees working ‘around the clock’ hours: a systematic review. Food Nutr Res 2018;62. https://doi.org/10.29219/fnr.v62.1115
Lee NK, Roche AM, Duraisingam V, Fischer J, Cameron J, Pidd K. A systematic review of alcohol interventions among workers in male-dominated industries. J Mens Health 2014;11:53–63.
Leeks KD, Hopkins DP, Soler RE, Aten A, Chattopadhyay SK, Task Force on Community Preventive Services. Worksite-based incentives and competitions to reduce tobacco use. A systematic review. Am J Prev Med 2010;38(Suppl. 2):263–74. https://doi.org/10.1016/j.amepre.2009.10.034
MacDonald B, Janssen X, Kirk A, Patience M, Gibson AM. An integrative, systematic review exploring the research, effectiveness, adoption, implementation, and maintenance of interventions to reduce sedentary behaviour in office workers. Int J Environ Res Public Health 2018;15:E2876.
MacEwen BT, MacDonald DJ, Burr JF. A systematic review of standing and treadmill desks in the workplace. Prev Med 2015;70:50–8. https://doi.org/10.1016/j.ypmed.2014.11.011
Mackenzie K, Such E, Norman P, Goyder E. The development, implementation and evaluation of interventions to reduce workplace sitting: a qualitative systematic review and evidence-based operational framework. BMC Public Health 2018;18:833. https://doi.org/10.1186/s12889-018-5768-z
Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol 2014;19:149–80. https://doi.org/10.1111/bjhp.12052
Malińska M. [Effectiveness of physical activity intervention at workplace.] Med Pr 2017;68:277–301.
Mehta S, Dimsdale J, Nagle B, Holub CK, Woods C, Barquera S, Elder JP. Worksite interventions: improving lifestyle habits among Latin American adults. Am J Prev Med 2013;44:538–42. https://doi.org/10.1016/j.amepre.2013.01.015
Neuhaus M, Eakin E, Straker L, Owen N, Dunstan D, Reid N, et al. A systematic review and meta-analysis of the effectiveness of activity-permissive workstations to reduce sedentary time in office workers. J Sci Med Sport 2014;18:e126–e7.
Ni Mhurchu C, Aston LM, Jebb SA. Effects of worksite health promotion interventions on employee diets: a systematic review. BMC Public Health 2010;10:62. https://doi.org/10.1186/1471-2458-10-62
Ojo SO, Bailey DP, Chater AM, Hewson DJ. The Impact of Active Workstations on Workplace Productivity and Performance: A Systematic Review. Int J Environ Res Public Health 2018;15:E417.
Penalvo JL, Micha R, Smith JD, Rehm CD, Bishop E, Onopa JA, et al. Do worksite wellness programs improve dietary behaviors and adiposity? A systematic review and meta-analysis. Circulation 2017;135:AMP005.
Pereira MJ, Coombes BK, Comans TA, Johnston V. The impact of onsite workplace health-enhancing physical activity interventions on worker productivity: a systematic review. Occup Environ Med 2015;72:401–12. https://doi.org/10.1136/oemed-2014-102678
Podrekar N, Kozinc Ž, Šarabon N. Effects of cycle and treadmill desks on energy expenditure and cardio-metabolic parameters in sedentary workers: review and meta-analysis. Int J Occup Saf and Ergon 2018:1–34.
Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med 2003;13:106–17. https://doi.org/10.1097/00042752-200303000-00008
Proper KI, Staal BJ, Hildebrandt VH, van der Beek AJ, van Mechelen W. Effectiveness of physical activity programs at worksites with respect to work-related outcomes. Scand J Work Environ Health 2002;28:75–84.
Robroek SJ, van Lenthe FJ, van Empelen P, Burdorf A. Determinants of participation in worksite health promotion programmes: a systematic review. Int J Behav Nutr Phys Act 2009;6:26. https://doi.org/10.1186/1479-5868-6-26
Rudolph S, Göring A, Padrok D. [Physical activity in the context of workplace health promotion: a systematic review on the effectiveness of software-based in contrast to personal-based interventions]. Gesundheitswesen 2019;81:866–80.
Rueff A, Logomarsino J. Increasing fruit and vegetable intake among manufacturing workers. Int J Workplace Health Manag 2016;9:32–45.
Ryde GC, Gilson ND, Burton NW, Brown WJ. Recruitment rates in workplace physical activity interventions: characteristics for success. Am J Health Promot 2013;27:e101–12. https://doi.org/10.4278/ajhp.120404-LIT-187
Sandercock V, Andrade J. Evaluation of worksite wellness nutrition and physical activity programs and their subsequent impact on participants’ body composition. J Obes 2018;2018:1035871. https://doi.org/10.1155/2018/1035871
Shaw AM, Wootton SA, Fallowfield JL, Allsopp AJ, Parsons EL. Environmental interventions to promote healthier eating and physical activity behaviours in institutions: a systematic review. Public Health Nutr 2019;22:1518–31. https://doi.org/10.1017/S1368980018003683
Smedslund G, Fisher KJ, Boles SM, Lichtenstein E. The effectiveness of workplace smoking cessation programmes: a meta-analysis of recent studies. Tob Control 2004;13:197–204.
Sorensen G, Linnan L, Hunt MK. Worksite-based research and initiatives to increase fruit and vegetable consumption. Prev Med 2004;39(Suppl. 2):94–100. https://doi.org/10.1016/j.ypmed.2003.12.020
Steyn NP, Parker W, Lambert EV, McHiza Z. Nutrition interventions in the workplace: evidence of best practice. South Afr J Clin Nutr 2009;22:111–17.
Tam G, Yeung MPS. A systematic review of the long-term effectiveness of work-based lifestyle interventions to tackle overweight and obesity. Prev Med 2018;107:54–60.
Taylor N, Conner M, Lawton R. The impact of theory on the effectiveness of worksite physical activity interventions: a meta-analysis and meta-regression. Health Psychol Rev 2012;6:33–73.
Taylor WC, Suminski RR, Das BM, Paxton RJ, Craig DW. Organizational culture and implications for workplace interventions to reduce sitting time among office-based workers: a systematic review. Front Public Health 2018;6:263. https://doi.org/10.3389/fpubh.2018.00263
Tew GA, Posso MC, Arundel CE, McDaid CM. Systematic review: height-adjustable workstations to reduce sedentary behaviour in office-based workers. Occup Med 2015;65:357–66. https://doi.org/10.1093/occmed/kqv044
To QG, Chen TT, Magnussen CG, To KG. Workplace physical activity interventions: a systematic review. Am J Health Promot 2013;27:e113–23. https://doi.org/10.4278/ajhp.120425-LIT-222
van Dongen JM, Proper KI, van Wier MF, van der Beek AJ, Bongers PM, van Mechelen W, van Tulder MW. Systematic review on the financial return of worksite health promotion programmes aimed at improving nutrition and/or increasing physical activity. Obes Rev 2011;12:1031–49. https://doi.org/10.1111/j.1467-789X.2011.00925.x
Verweij LM, Coffeng J, van Mechelen W, Proper KI. Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obes Rev 2011;12:406–29. https://doi.org/10.1111/j.1467-789X.2010.00765.x
Vuillemin A, Rostami C, Maes L, Van Cauwenberghe E, Van Lenthe FJ, Brug J, et al. Worksite physical activity interventions and obesity: a review of European studies (the HOPE project). Obes Facts 2011;4:479–88. https://doi.org/10.1159/000335255
Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ 2002;325:188.
Webb G, Shakeshaft A, Sanson-Fisher R, Havard A. A systematic review of work-place interventions for alcohol-related problems. Addiction 2009;104:365–77. https://doi.org/10.1111/j.1360-0443.2008.02472.x
Weerasekara YK, Roberts SB, Kahn MA, LaVertu AE, Hoffman B, Das SK. Effectiveness of workplace weight management interventions: a systematic review. Curr Obes Rep 2016;5:298–306. https://doi.org/10.1007/s13679-016-0205-z
Wong JY, Gilson ND, van Uffelen JG, Brown WJ. The effects of workplace physical activity interventions in men: a systematic review. Am J Mens Health 2012;6:303–13. https://doi.org/10.1177/1557988312436575
Health care focused (n = 4)
Al-Khudairy L, Uthman OA, Walmsley R, Johnson S, Oyebode O. Choice architecture interventions to improve diet and/or dietary behaviour by healthcare staff in high-income countries: a systematic review. BMJ Open 2019;9:e023687. https://doi.org/10.1136/bmjopen-2018-023687
Kelly M, Wills J. Systematic review: what works to address obesity in nurses? Occup Med 2018;68:228–38. https://doi.org/10.1093/occmed/kqy038
Power BT, Kiezebrink K, Allan JL, Campbell MK. Effects of workplace-based dietary and/or physical activity interventions for weight management targeting healthcare professionals: a systematic review of randomised controlled trials. BMC Obes 2014;1:23. https://doi.org/10.1186/s40608-014-0023-3
Torquati L, Pavey T, Kolbe-Alexander T, Leveritt M. Promoting Diet and Physical Activity in Nurses. Am J Health Promot 2017;31:19–27. https://doi.org/10.4278/ajhp.141107-LIT-562
General health/health promotion
Non-health care focused (n = 52)
Aust B, Ducki A. Comprehensive health promotion interventions at the workplace: experiences with health circles in Germany. J Occup Health Psychol 2004;9:258–70. https://doi.org/10.1037/1076-8998.9.3.258
Bambra C, Egan M, Thomas S, Petticrew M, Whitehead M. The psychosocial and health effects of workplace reorganisation. 2. A systematic review of task restructuring interventions. J Epidemiol Community Health 2007;61:1028–37.
Bambra C, Gibson M, Sowden AJ, Wright K, Whitehead M, Petticrew M. Working for health? Evidence from systematic reviews on the effects on health and health inequalities of organisational changes to the psychosocial work environment. Prev Med 2009;48:454–61. https://doi.org/10.1016/j.ypmed.2008.12.018
Bambra CL, Whitehead MM, Sowden AJ, Akers J, Petticrew MP. Shifting schedules: the health effects of reorganizing shift work. Am J Prev Med 2008;34:427–34. https://doi.org/10.1016/j.amepre.2007.12.023
Bambra C, Whitehead M, Sowden A, Akers J, Petticrew M. ‘A hard day’s night?’ The effects of compressed working week interventions on the health and work-life balance of shift workers: a systematic review. J Epidemiol Community Health 2008;62:764–77.
Buchberger B, Heymann R, Huppertz H, Friepörtner K, Pomorin N, Wasem J. The effectiveness of interventions in workplace health promotion as to maintain the working capacity of health care personal. GMS Health Technol Assess 2011;7:Doc06. https://doi.org/10.3205/hta000097
Carvalho AFS, Dias EC. Health promotion in the workplace: a systematic review of the literature. Rev Bras Promoç Saúde (Impr) 2012;25:116–26.
Chapman LS. Meta-evaluation of worksite health promotion economic return studies: 2012 update. Am J Health Promot 2012;26:TAHP1–TAHP12. https://doi.org/10.4278/ajhp.26.4.tahp
Cloostermans L, Bekkers MB, Uiters E, Proper KI. The effectiveness of interventions for ageing workers on (early) retirement, work ability and productivity: a systematic review. Int Arch Occup Environ Health 2015;88:521–32.
Cooklin A, Joss N, Husser E, Oldenburg B. Integrated approaches to occupational health and safety: a systematic review. Am J Health Promot 2017;31:401–12. https://doi.org/10.4278/ajhp.141027-LIT-542
Cox A, Hillage J, Fletcher L, Marvell R, Willson S, Miller L, et al. The Effectiveness and Cost-effectiveness of Methods of Protecting and Promoting the Health of Older Workers. Evidence Review for Research Question 1. Brighton: Institute for Employment Studies; 2014.
Daniels K, Gedikli C, Watson D, Semkina A, Vaughn O. Job design, employment practices and well-being: a systematic review of intervention studies. Ergonomics 2017;60:1177–96. https://doi.org/10.1080/00140139.2017.1303085
Daniels K, Watson D, Gedikli C. Well-being and the social environment of work: a systematic review of intervention studies. Int J Environ Res Public Health 2017;14:E918.
Dos Santos NC, Santos LS, Camelier FWR, Maciel RRBT, Portella DDA. Technologies applied to occupational health promotion: a systematic review. Rev bras med trab 2017;15:113–22.
Egan M, Bambra C, Thomas S, Petticrew M, Whitehead M, Thomson H. The psychosocial and health effects of workplace reorganisation. 1. A systematic review of organisational-level interventions that aim to increase employee control. J Epidemiol Community Health 2007;61:945–54.
Engbers LH, van Poppel MN, Chin A Paw MJ, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med 2005;29:61–70.
Feltner C, Peterson K, Palmieri Weber R, Cluff L, Coker-Schwimmer E, Viswanathan M, Lohr KN. The effectiveness of Total Worker Health interventions: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med 2016;165:262–9. https://doi.org/10.7326/M16-0626
Grossmeier J, Terry PE, Anderson DR, Wright S. Financial impact of population health management programs: reevaluating the literature. Popul Health Manag 2012;15:129–34. https://doi.org/10.1089/pop.2010.0086
Hillage J, Holmes J, Rickard C, Marvell R, Taskila T, Bajorek Z, et al. Workplace Policy and Management Practices to Improve the Health of Employees. Evidence Review 2 (Effectiveness of Organisational Interventions that Aim to Support Line Managers to Enhance the Wellbeing of the People They Manage). Brighton: Institute for Employment Studies; 2014.
Hillage J, Holmes J, Rickard C, Marvell R, Taskila T, Bajorek Z, et al. Workplace Policy and Management Practices to Improve the Health of Employees. Evidence Review 1 (Effectiveness of Interventions Taken by Supervisors That Could Enhance the Wellbeing of the People They Manage). Brighton: Institute for Employment Studies; 2014.
Howarth A, Quesada J, Silva J, Judycki S, Mills PR. The impact of digital health interventions on health-related outcomes in the workplace: A systematic review. Digit Health 2018;4:2055207618770861. https://doi.org/10.1177/2055207618770861
Jacobs JC, Yaquian E, Burke SM, Rouse M, Zaric G. The economic impact of workplace wellness programmes in Canada. Occup Med 2017;67:429–34. https://doi.org/10.1093/occmed/kqx075
Janer G, Sala M, Kogevinas M. Health promotion trials at worksites and risk factors for cancer. Scand J Work Environ Health 2002;28:141–57.
Kahn-Marshall JL, Gallant MP. Making healthy behaviors the easy choice for employees: a review of the literature on environmental and policy changes in worksite health promotion. Health Educ Behav 2012;39:752–76. https://doi.org/10.1177/1090198111434153
Kaspin LC, Gorman KM, Miller RM. Systematic review of employer-sponsored wellness strategies and their economic and health-related outcomes. Popul Health Manag 2013;16:14–21. https://doi.org/10.1089/pop.2012.0006
Knight C, Patterson M, Dawson J. Building work engagement: a systematic review and meta-analysis investigating the effectiveness of work engagement interventions. J Organ Behav 2017;38:792–812. https://doi.org/10.1002/job.2167
Kuoppala J, Lamminpää A, Husman P. Work health promotion, job well-being, and sickness absences – a systematic review and meta-analysis. J Occup Environ Med 2008;50:1216–27. https://doi.org/10.1097/JOM.0b013e31818dbf92
Lerner D, Rodday AM, Cohen JT, Rogers WH. A systematic review of the evidence concerning the economic impact of employee-focused health promotion and wellness programs. J Occup Environ Med 2013;55:209–22. https://doi.org/10.1097/JOM.0b013e3182728d3c
Meng L, Wolff MB, Mattick KA, DeJoy DM, Wilson MG, Smith ML. Strategies for Worksite Health Interventions to Employees with Elevated Risk of Chronic Diseases. Saf Health Work 2017;8:117–29. https://doi.org/10.1016/j.shaw.2016.11.004
Micucci S, Thomas H. The Effectiveness of Multi-faceted Health Promotion Interventions in the Workplace to Reduce Chronic Disease. Effective Public Health Practice Project. Dundas: Public Health and Community Services Department; 2007.
Montano D, Hoven H, Siegrist J. A meta-analysis of health effects of randomized controlled worksite interventions: does social stratification matter? Scand J Work Environ Health 2014;40:230–4.
Montano D, Hoven H, Siegrist J. Effects of organisational-level interventions at work on employees’ health: a systematic review. BMC Public Health 2014;14:135. https://doi.org/10.1186/1471-2458-14-135
Neil-Sztramko SE, Pahwa M, Demers PA, Gotay CC. Health-related interventions among night shift workers: a critical review of the literature. Scand J Work Environ Health 2014;40:543–56. https://doi.org/10.5271/sjweh.3445
Nestler K, Witzki A, Rohde U, Rüther T, Tofaute KA, Leyk D. Strength training for women as a vehicle for health promotion at work. Dtsch Arztebl Int 2017;114:439–46. https://doi.org/10.3238/arztebl.2017.0439
Nielsen K, Nielsen MB, Ogbonnaya C, Känsälä M, Saari E, Isaksson K. Workplace resources to improve both employee well-being and performance: a systematic review and meta-analysis. Work & Stress 2017;31:101–20.
Osilla KC, Van Busum K, Schnyer C, Larkin JW, Eibner C, Mattke S. Systematic review of the impact of worksite wellness programs. Am J Manag Care 2012;18:e68–81.
Parks KM, Steelman LA. Organizational wellness programs: a meta-analysis. J Occup Health Psychol 2008;13:58–68. https://doi.org/10.1037/1076-8998.13.1.58
Pelletier KR. A review and analysis of the clinical- and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1998–2000 update. Am J Health Promot 2001;16:107–16. https://doi.org/10.4278/0890-1171-16.2.107
Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: update VI 2000–2004. J Occup Environ Med 2005;47:1051–8.
Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: update VII 2004–2008. J Occup Environ Med 2009;51:822–37. https://doi.org/10.1097/JOM.0b013e3181a7de5a
Pelletier KR. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: update VIII 2008 to 2010. J Occup Environ Med 2011;53:1310–31. https://doi.org/10.1097/JOM.0b013e3182337748
Plat MJ, Frings-Dresen MH, Sluiter JK. A systematic review of job-specific workers’ health surveillance activities for fire-fighting, ambulance, police and military personnel. Int Arch Occup Environ Health 2011;84:839–57. https://doi.org/10.1007/s00420-011-0614-y
Plotnikoff R, Collins CE, Williams R, Germov J, Callister R. Effectiveness of interventions targeting health behaviors in university and college staff: a systematic review. Am J Health Promot 2015;29:e169–87.
Poscia A, Moscato U, La Milia DI, Milovanovic S, Stojanovic J, Borghini A, et al. Workplace health promotion for older workers: a systematic literature review. BMC Health Serv Res 2016;16(Suppl. 5):329. https://doi.org/10.1186/s12913-016-1518-z
Reed JL, Prince SA, Elliott CG, Mullen KA, Tulloch HE, Hiremath S, et al. Impact of workplace physical activity interventions on physical activity and cardiometabolic health among working-age women: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2017;10:e003516.
Riedel JE, Lynch W, Baase C, Hymel P, Peterson KW. The effect of disease prevention and health promotion on workplace productivity: a literature review. Am J Health Promot 2001;15:167–91. https://doi.org/10.4278/0890-1171-15.3.167
Rojatz D, Merchant A, Nitsch M. Factors influencing workplace health promotion intervention: a qualitative systematic review. Health Promot Int 2017;32:831–9. https://doi.org/10.1093/heapro/daw015
Rongen A, Robroek SJW, van Lenthe FJ, Burdorf A. Workplace health promotion: a meta-analysis of effectiveness. Am J Prev Med 2013;44:406–15.
Soler RE, Leeks KD, Razi S, Hopkins DP, Griffith M, Aten A, et al. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med 2010;38(Suppl. 2):237–62. https://doi.org/10.1016/j.amepre.2009.10.030
Stiehl E, Shivaprakash N, Thatcher E, Ornelas IJ, Kneipp S, Baron SL, Muramatsu N. Worksite health promotion for low-wage workers: a scoping literature review. Am J Health Promot 2018;32:359–73. https://doi.org/10.1177/0890117117728607
Torp S, Eklund L, Thorpenberg S. Research on workplace health promotion in the Nordic countries: a literature review, 1986-2008. Glob Health Promot 2011;18:15–22. https://doi.org/10.1177/1757975911412401
Whybrow D, Jones N, Greenberg N. Promoting organizational well-being: a comprehensive review of trauma risk management. Occup Med 2015;65:331–6. https://doi.org/10.1093/occmed/kqv024
Health care focused (n = 14)
Addo MA, Stephen AI, Kirkpatrick P. Acute mental health/psychiatric nurses’ experiences of clinical supervision in promoting their wellbeing in their workplace: a systematic review. JBI Libr Syst Rev 2012;10(Suppl. 56):1–16.
Brand SL, Thompson Coon J, Fleming LE, Carroll L, Bethel A, Wyatt K. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PLOS ONE 2017;12:e0188418. https://doi.org/10.1371/journal.pone.0188418
Chan CW, Perry L. Lifestyle health promotion interventions for the nursing workforce: a systematic review. J Clin Nurs 2012;21:2247–61. https://doi.org/10.1111/j.1365-2702.2012.04213.x
Fibbins H, Ward PB, Watkins A, Curtis J, Rosenbaum S. Improving the health of mental health staff through exercise interventions: a systematic review. J Ment Health 2018;27:184–91. https://doi.org/10.1080/09638237.2018.1437614
Häggman-Laitila A, Romppanen J. Outcomes of interventions for nurse leaders’ well-being at work: a quantitative systematic review. J Adv Nurs 2018;74:34–44. https://doi.org/10.1111/jan.13406
Harris JD, Staheli G, LeClere L, Andersone D, McCormick F. What effects have resident work-hour changes had on education, quality of life, and safety? A systematic review. Clin Orthop Relat Res 2015;473:1600–8.
King A, Long L, Lisy K. Effectiveness of team nursing compared with total patient care on staff wellbeing when organizing nursing work in acute care wards: a systematic review. JBI Database System Rev Implement Rep 2015;13:128–68. https://doi.org/10.11124/jbisrir-2015-2428
Letvak S. We cannot ignore nurses’ health anymore: a synthesis of the literature on evidence-based strategies to improve nurse health. Nurs Adm Q 2013;37:295–308. https://doi.org/10.1097/NAQ.0b013e3182a2f99a
Li H, Shao Y, Xing Z, Li Y, Wang S, Zhang M, et al. Napping on night-shifts among nursing staff: a mixed-methods systematic review. J Adv Nurs 2019;75:291–312. https://doi.org/10.1111/jan.13859
Raj KS. Well-being in residency: a systematic review. J Grad Med Educ 2016;8:674–84. https://doi.org/10.4300/JGME-D-15-00764.1
Reinhardt EL, Fischer FM. [Barriers to interventions aimed at promoting the health of health care workers in Brazil.] Rev Panam Salud Publica 2009;25:411–17.
Romppanen J, Häggman-Laitila A. Interventions for nurses’ well-being at work: a quantitative systematic review. J Adv Nurs 2017;73:1555–69. https://doi.org/10.1111/jan.13210
Taylor C, Xyrichis A, Leamy MC, Reynolds E, Maben J. Can Schwartz Center Rounds support healthcare staff with emotional challenges at work, and how do they compare with other interventions aimed at providing similar support? A systematic review and scoping reviews. BMJ Open 2018;8:e024254. https://doi.org/10.1136/bmjopen-2018-024254
Wilson G, Larkin V, Redfern N, Stewart J, Steven A. Exploring the relationship between mentoring and doctors’ health and wellbeing: a narrative review. J R Soc Med 2017;110:188–97. https://doi.org/10.1177/0141076817700848
Mental health
Non-health care focused (n = 48)
Abdin S, Welch RK, Byron-Daniel J, Meyrick J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: a systematic review. Public Health 2018;160:70–6.
Ahola K, Toppinen-Tanner S, Seppanen J. Interventions to alleviate burnout symptoms and to support return to work among employees with burnout: systematic review and meta-analysis. Burnout Research 2017;4:1–11.
Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Educ Couns 2010;78:184–90. https://doi.org/10.1016/j.pec.2009.04.008
Bartlett L, Martin A, Neil AL, Memish K, Otahal P, Kilpatrick M, Sanderson K. A systematic review and meta-analysis of workplace mindfulness training randomized controlled trials. J Occup Health Psychol 2019;24:108–26. https://doi.org/10.1037/ocp0000146
Bellón J, Conejo-Cerón S, Cortés-Abela C, Pena-Andreu JM, García-Rodríguez A, Moreno-Peral P. Effectiveness of psychological and educational interventions for the prevention of depression in the workplace: a systematic review and meta-analysis. Scand J Work, Environ Health 2019;45:324–32.
Bergerman L, Corabian P, Harstall C. Effectiveness of Organizational Interventions for the Prevention of Stress in the Workplace. Edmonton, AB: Institute of Health Economics; 2009.
Carolan S, Harris PR, Cavanagh K. Improving employee well-being and effectiveness: systematic review and meta-analysis of web-based psychological interventions delivered in the workplace. J Med Internet Res 2017;19:e271. https://doi.org/10.2196/jmir.7583
Caulfield N, Chang D, Dollard MF, Elshaug C. A review of occupational stress interventions in Australia. Int J Stress Manag 2004;11:149–66.
Chu AH, Koh D, Moy FM, Müller-Riemenschneider F. Do workplace physical activity interventions improve mental health outcomes? Occup Med 2014;64:235–45. https://doi.org/10.1093/occmed/kqu045
Corbière M, Shen J, Rouleau M, Dewa CS. A systematic review of preventive interventions regarding mental health issues in organizations. Work 2009;33:81–116. https://doi.org/10.3233/WOR-2009-0846
Czabała C, Charzyńska K, Mroziak B. Psychosocial interventions in workplace mental health promotion: an overview. Health Promot Int 2011;26(Suppl. 1):i70–84. https://doi.org/10.1093/heapro/dar050
Dietrich S, Deckert S, Ceynowa M, Hegerl U, Stengler K. Depression in the workplace: a systematic review of evidence-based prevention strategies. Int Arch Occup Environ Health 2012;85:1–11. https://doi.org/10.1007/s00420-011-0634-7
Doki S, Sasahara S, Matsuzaki I. Psychological approach of occupational health service to sick leave due to mental problems: a systematic review and meta-analysis. Int Arch Occup Environ Health 2015;88:659–67.
Furlan AD, Gnam WH, Carnide N, Irvin E, Amick BC, DeRango K, et al. Systematic review of intervention practices for depression in the workplace. J Occup Rehabil 2012;22:312–21. https://doi.org/10.1007/s10926-011-9340-2
Gayed A, Milligan-Saville JS, Nicholas J, Bryan BT, LaMontagne AD, Milner A, et al. Effectiveness of training workplace managers to understand and support the mental health needs of employees: a systematic review and meta-analysis. Occup Environ Med 2018;75:462–70. https://doi.org/10.1136/oemed-2017-104789
Graveling RA, Crawford JO, Cowie A, Vohra S. A Review of Workplace Interventions That Promote Mental Wellbeing in the Workplace. Edinburgh: Institute of Occupational Medicine; 2008.
Hamberg-van Reenen HH, Proper KI, van den Berg M. Worksite mental health interventions: a systematic review of economic evaluations. Occup Environ Med 2012;69:837–45. https://doi.org/10.1136/oemed-2012-100668
Hanisch SE, Twomey CD, Szeto AC, Birner UW, Nowak D, Sabariego C. The effectiveness of interventions targeting the stigma of mental illness at the workplace: a systematic review. BMC Psychiatry 2016;16:1. https://doi.org/10.1186/s12888-015-0706-4
Heckenberg R, Wright B, Kent S. Do workplace-based mindfulness meditation programs alter physiological indicators of stress? A systematic review and meta-analysis. J Psychosom Res 2018;114:62–71.
Hua Y, Dai J. [Studies on occupational stress intervention in workplaces abroad: a systematic review.] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2015;33:759–64.
Hunter C, Verreynne M-L, Pachana N, Harpur P. The impact of disability-assistance animals on the psychological health of workplaces: a systematic review. Human Resource Management Review 2019;29:400–17.
Ivandic I, Freeman A, Birner U, Nowak D, Sabariego C. A systematic review of brief mental health and well-being interventions in organizational settings. Scand J Work Environ Health 2017;43:99–108. https://doi.org/10.5271/sjweh.3616
Janssen M, Heerkens Y, Kuijer W, van der Heijden B, Engels J. Effects of mindfulness-based stress reduction on employees’ mental health: a systematic review. PLOS ONE 2018;13:e0191332. https://doi.org/10.1371/journal.pone.0191332
Kröll C, Doebler P, Nüesch S. Meta-analytic evidence of the effectiveness of stress management at work. Eur J Work Organ Psychol 2017;26:677–693.
Lee NK, Roche A, Duraisingam V, Fischer JA, Cameron J. Effective interventions for mental health in male-dominated workplaces. Ment Health Rev 2014;19:237–50.
Luken M, Sammons A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther 2016;70:7002250020p1–7002250020p10. https://doi.org/10.5014/ajot.2016.016956
Maricuţoiu LP, Sava FA, Butta O. The effectiveness of controlled interventions on employees’ burnout: a meta-analysis. Journal of Occup Organ Psychol 2016;89:1–27.
Martin A, Sanderson K, Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health 2009;35:7–18.
McLeod J. The effectiveness of workplace counselling: a systematic review. Counsell Psychother Res 2010;10:238–48.
Milner A, Page K, Spencer-Thomas S, Lamotagne AD. Workplace suicide prevention: a systematic review of published and unpublished activities. Health Promot Int 2015;30:29–37. https://doi.org/10.1093/heapro/dau085
Moreno-Peral P, Conejo-Cerón S, Rubio-Valera M, Fernández A, Navas-Campaña D, Rodríguez-Morejón A, et al. Effectiveness of psychological and/or educational interventions in the prevention of anxiety: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 2017;74:1021–9. https://doi.org/10.1001/jamapsychiatry.2017.2509
Murta SG, Sanderson K, Oldenburg B. Process evaluation in occupational stress management programs: a systematic review. Am J Health Promot 2007;21:248–54. https://doi.org/10.4278/0890-1171-21.4.248
Nexø MA, Kristensen JV, Grønvad MT, Kristiansen J, Poulsen OM. Content and quality of workplace guidelines developed to prevent mental health problems: results from a systematic review. Scand J Work Environ Health 2018;44:443–57. https://doi.org/10.5271/sjweh.3731
Nigatu YT, Huang J, Rao S, Gillis K, Merali Z, Wang J. Indicated prevention interventions in the workplace for depressive symptoms: a systematic review and meta-analysis. Am J Prev Med 2019;56:e23–e33.
Perski O, Grossi G, Perski A, Niemi M. A systematic review and meta-analysis of tertiary interventions in clinical burnout. Scand J Psychol 2017;58:551–61. https://doi.org/10.1111/sjop.12398
Pomaki G, Franche RL, Murray E, Khushrushahi N, Lampinen TM. Workplace-based work disability prevention interventions for workers with common mental health conditions: a review of the literature. J Occup Rehabil 2012;22:182–95. https://doi.org/10.1007/s10926-011-9338-9
Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. J Occup Health Psychol 2008;13:69–93. https://doi.org/10.1037/1076-8998.13.1.69
Rohlf VI. Interventions for occupational stress and compassion fatigue in animal care professionals: a systematic review. Traumatology 2018;24:10.1037/trm0000144
Seymour L, Grove B. Workplace Interventions for People with Common Mental Health Problems. London: British Occupational Health Research Foundation; 2005.
Slemp GR, Jach HK, Chia A, Loton DJ, Kern ML. Contemplative interventions and employee distress: a meta-analysis. Stress Health 2019;35:227–55. https://doi.org/10.1002/smi.2857
Stergiopoulos E, Cimo A, Cheng C, Bonato S, Dewa CS. Interventions to improve work outcomes in work-related PTSD: a systematic review. BMC Public Health 2011;11:838. https://doi.org/10.1186/1471-2458-11-838
Stratton E, Lampit A, Choi I, Calvo RA, Harvey SB, Glozier N. Effectiveness of eHealth interventions for reducing mental health conditions in employees: a systematic review and meta-analysis. PLOS ONE 2017;12:e0189904. https://doi.org/10.1371/journal.pone.0189904
Tan L, Wang MJ, Modini M, Joyce S, Mykletun A, Christensen H, Harvey SB. Preventing the development of depression at work: a systematic review and meta-analysis of universal interventions in the workplace. BMC Med 2014;12:74. https://doi.org/10.1186/1741-7015-12-74
Tsutsumi A. Development of an evidence-based guideline for supervisor training in promoting mental health: literature review. J Occup Health 2011;53:1–9.
van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. The benefits of interventions for work-related stress. Am J Public Health 2001;91:270–6.
von Hofe I, Latza U, Lönnfors S, Muckelbauer R. [Online health services for the prevention of stress-associated psychological impairments at the workplace.] Gesundheitswesen 2017;79:144–52. https://doi.org/10.1055/s-0042-100618
Wan Mohd Yunus WMA, Musiat P, Brown JSL. Systematic review of universal and targeted workplace interventions for depression. Occup Environ Med 2018;75:66–75. https://doi.org/10.1136/oemed-2017-104532
Witt K, Milner A, Allisey A, Davenport L, LaMontagne AD. Effectiveness of suicide prevention programs for emergency and protective services employees: a systematic review and meta-analysis. Am J Ind Med 2017;60:394–407. https://doi.org/10.1002/ajim.22676
Health care focused (n = 46)
Bercier ML. Interventions That Help the Helpers: A Systematic Review and Meta-analysis of Interventions Targeting Compassion Fatigue, Secondary Traumatic Stress and Vicarious Traumatization in Mental Health Workers. 2013; No. 3566519. Available from ProQuest Dissertations & Theses A&I (1416424184).
Bercier ML, Maynard BR. Interventions for secondary traumatic stress with mental health workers: a systematic review. Res Soc Work Pract 2015;25:81–9.
Burton A, Burgess C, Dean S, Koutsopoulou GZ, Hugh-Jones S. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress Health 2017;33:3–13. https://doi.org/10.1002/smi.2673
Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ 2017;9:294–301. https://doi.org/10.4300/JGME-D-16-00372.1
Carrieri D, Briscoe S, Jackson M, Mattick K, Papoutsi C, Pearson M, Wong G. ‘Care Under Pressure’: a realist review of interventions to tackle doctors’ mental ill-health and its impacts on the clinical workforce and patient care. BMJ Open 2018;8:e021273. https://doi.org/10.1136/bmjopen-2017-021273
Chen D, Sun W, Liu N, Wang J, Guo P, Zhang X, Zhang W. Effects of nonpharmacological interventions on depressive symptoms and depression among nursing students: a systematic review and meta-analysis. Complement Ther Clin Pract 2019;34:217–28.
Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev 2017;6:144. https://doi.org/10.1186/s13643-017-0526-3
Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: a systematic review. Int J Environ Res Public Health 2016;13:E618. https://doi.org/10.3390/ijerph13060618
Dharmawardene M, Givens J, Wachholtz A, Makowski S, Tjia J. A systematic review and meta-analysis of meditative interventions for informal caregivers and health professionals. BMJ Support Palliat Care 2016;6:160–9. https://doi.org/10.1136/bmjspcare-2014-000819
Dreison KC, Luther L, Bonfils KA, Sliter MT, McGrew JH, Salyers MP. Job burnout in mental health providers: a meta-analysis of 35 years of intervention research. J Occup Health Psychol 2018;23:18–30. https://doi.org/10.1037/ocp0000047
Duhoux A, Menear M, Charron M, Lavoie-Tremblay M, Alderson M. Interventions to promote or improve the mental health of primary care nurses: a systematic review. J Nurs Manag 2017;25:597–607. https://doi.org/10.1111/jonm.12511
Edwards D, Burnard P. A systematic review of stress and stress management interventions for mental health nurses. J Adv Nurs 2003;42:169–200.
Elliott KE, Scott JL, Stirling C, Martin AJ, Robinson A. Building capacity and resilience in the dementia care workforce: a systematic review of interventions targeting worker and organizational outcomes. Int Psychogeriatr 2012;24:882–94. https://doi.org/10.1017/S1041610211002651
Friganović A, Kovačević I, Ilić B, Žulec M, Krikšić V, Grgas Bile C. Healthy settings in hospital – how to prevent burnout syndrome in nurses: literature review. Acta Clin Croat 2017;56:292–8. https://doi.org/10.20471/acc.2017.56.02.13
Galbraith ND, Brown KE. Assessing intervention effectiveness for reducing stress in student nurses: quantitative systematic review. J Adv Nurs 2011;67:709–21. https://doi.org/10.1111/j.1365-2648.2010.05549.x
Gilbody S, Cahill J, Barkham M, Richards D, Bee P, Glanville J. Can we improve the morale of staff working in psychiatric units? A systematic review. J Ment Health 2006;15:7–17.
Gillman L, Adams J, Kovac R, Kilcullen A, House A, Doyle C. Strategies to promote coping and resilience in oncology and palliative care nurses caring for adult patients with malignancy: a comprehensive systematic review. JBI Database System Rev Implement Rep 2015;13:131–204. https://doi.org/10.11124/jbisrir-2015-1898
Guillaumie L, Boiral O, Champagne J. A mixed-methods systematic review of the effects of mindfulness on nurses. J Adv Nurs 2017;73:1017–34. https://doi.org/10.1111/jan.13176
Hill RC, Dempster M, Donnelly M, McCorry NK. Improving the wellbeing of staff who work in palliative care settings: a systematic review of psychosocial interventions. Palliat Med 2016;30:825–33. https://doi.org/10.1177/0269216316637237
Lavenberg JG, Williams K. Interventions to Reduce Stress Among Nurses Caring For Patients With Sickle Cell Disease. Philadelphia, PA: Center for Evidence-based Practice; 2014.
Lee HF, Kuo CC, Chien TW, Wang YR. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl Nurs Res 2016;31:100–10. https://doi.org/10.1016/j.apnr.2016.01.001
Li C, Yin H, Zhao J, Shang B, Hu M, Zhang P, Chen L. Interventions to promote mental health in nursing students: a systematic review and meta-analysis of randomized controlled trials. J Adv Nurs 2018;74:2727–41. https://doi.org/10.1111/jan.13808
Li H, Zhao M, Shi Y, Xing Z, Li Y, Wang S, et al. The effectiveness of aromatherapy and massage on stress management in nurses: a systematic review. J Clin Nurs 2019;28:372–85. https://doi.org/10.1111/jocn.14596
Lomas T, Medina JC, Ivtzan I, Rupprecht S, Eiroa-Orosa FJ. A systematic review of the impact of mindfulness on the well-being of healthcare professionals. J Clin Psychol 2018;74:319–55. https://doi.org/10.1002/jclp.22515
McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: is there hope? Fam Med 2008;40:626–32.
McNamara K, Meaney S, Campillo ISL, Greene R, O’Donoghue K. An evaluation of the effectiveness of available support systems for obstetricians and midwives when dealing with workplace adversity; a systematic review. BJOG: An International Journal of Obstetrics and Gynaecology 2017;124:134–5.
Medland J, Howard-Ruben J, Whitaker E. Fostering psychosocial wellness in oncology nurses: addressing burnout and social support in the workplace. Oncol Nurs Forum 2004;31:47–54. https://doi.org/10.1188/04.ONF.47-54
Mimura C, Griffiths P. The effectiveness of current approaches to workplace stress management in the nursing profession: an evidence based literature review. Occup Environ Med 2003;60:10–15.
Morgan P, Simpson J, Smith A. Health care workers’ experiences of mindfulness training: a qualitative review. Mindfulness 2014;6:1–15.
Morse G, Salyers MP, Rollins AL, Monroe-DeVita M, Pfahler C. Burnout in mental health services: a review of the problem and its remediation. Adm Policy Ment Health 2012;39:341–52. https://doi.org/10.1007/s10488-011-0352-1
Nowrouzi B, Lightfoot N, Larivière M, Carter L, Rukholm E, Schinke R, Belanger-Gardner D. Occupational stress management and burnout interventions in nursing and their implications for healthy work environments: a literature review. Workplace Health Saf 2015;63:308–15. https://doi.org/10.1177/2165079915576931
Panagioti M, Panagopoulou E, Bower P, Lewith G, Kontopantelis E, Chew-Graham C, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195–205. https://doi.org/10.1001/jamainternmed.2016.7674
Pospos S, Young IT, Downs N, Iglewicz A, Depp C, Chen JY, et al. Web-based tools and mobile applications to mitigate burnout, depression, and suicidality among healthcare students and professionals: a systematic review. Acad Psychiatry 2018;42:109–20. https://doi.org/10.1007/s40596-017-0868-0
Regehr C, Glancy D, Pitts A, LeBlanc VR. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis 2014;202:353–9. https://doi.org/10.1097/NMD.0000000000000130
Silva-Junior JS. Preventing occupational stress in healthcare workers. São Paulo Med J 2016;134:92. https://doi.org/10.1590/1516-3180.20161341T1
Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health 2008;34:169–78.
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry 2013;37:158–64. https://doi.org/10.1176/appi.ap.12010003
Stewart W, Terry L. Reducing burnout in nurses and care workers in secure settings. Nurs Stand 2014;28:37–45. https://doi.org/10.7748/ns2014.04.28.34.37.e8111
van der Riet P, Levett-Jones T, Aquino-Russell C. The effectiveness of mindfulness meditation for nurses and nursing students: an integrated literature review. Nurse Educ Today 2018;65:201–11.
Walsh AL, Lehmann S, Zabinski J, Truskey M, Purvis T, Gould NF, et al. Interventions to prevent and reduce burnout among undergraduate and graduate medical education trainees: a systematic review. Acad Psychiatry 2019;43:386–95. https://doi.org/10.1007/s40596-019-01023-z
Wasson LT, Cusmano A, Meli L, Louh I, Falzon L, Hampsey M, et al. Association between learning environment interventions and medical student well-being: a systematic review. JAMA 2016;316:2237–52. https://doi.org/10.1001/jama.2016.17573
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272–81.
Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for physician burnout: a systematic review. Open Med 2018;13:253–63. https://doi.org/10.1515/med-2018-0039
Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry 2015;39:47–54. https://doi.org/10.1007/s40596-014-0197-5
Wright EM, Matthai MT, Warren N. Methods for alleviating stress and increasing resilience in the midwifery community: a scoping review of the literature. J Midwifery Womens Health 2017;62:737–45. https://doi.org/10.1111/jmwh.12651
Zhang Y, Qian Y, Wu J, Wen F, Zhang Y. The effectiveness and implementation of mentoring program for newly graduated nurses: a systematic review. Nurse Educ Today 2016;37:136–44. https://doi.org/10.1016/j.nedt.2015.11.027
Physical health
Non-health care focused (n = 11)
Aneni EC, Roberson LL, Maziak W, Agatston AS, Feldman T, Rouseff M, et al. A systematic review of internet-based worksite wellness approaches for cardiovascular disease risk management: outcomes, challenges and opportunities. PLOS ONE 2014;9:e83594. https://doi.org/10.1371/journal.pone.0083594
Coughlin SS, Caplan LS, Lawson HW. Cervical cancer screening in the workplace. Research review and evaluation. AAOHN J 2002;50:32–9.
Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W. Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease – a systematic review. Scand J Work Environ Health 2010;36:202–15.
Gussenhoven AH, Jansma EP, Goverts ST, Festen JM, Anema JR, Kramer SE. Vocational rehabilitation services for people with hearing difficulties: a systematic review of the literature. Work 2013;46:151–64. https://doi.org/10.3233/WOR-131743
Lardon A, Girard MP, Zaïm C, Lemeunier N, Descarreaux M, Marchand AA. Effectiveness of preventive and treatment interventions for primary headaches in the workplace: a systematic review of the literature. Cephalalgia 2017;37:64–73. https://doi.org/10.1177/0333102416636096
Pilcher JJ, Lambert BJ, Huffcutt AI. Differential effects of permanent and rotating shifts on self-report sleep length: a meta-analytic review. Sleep 2000;23:155–63.
Richter K, Acker J, Adam S, Niklewski G. Prevention of fatigue and insomnia in shift workers-a review of non-pharmacological measures. EPMA J 2016;7:16. https://doi.org/10.1186/s13167-016-0064-4
Ruggiero JS, Redeker NS. Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol Res Nurs 2014;16:134–42. https://doi.org/10.1177/1099800413476571
Short MA, Agostini A, Lushington K, Dorrian J. A systematic review of the sleep, sleepiness, and performance implications of limited wake shift work schedules. Scand J Work Environ Health 2015;41:425–40. https://doi.org/10.5271/sjweh.3509
Wolkow A, Netto K, Aisbett B. The effectiveness of health interventions in cardiovascular risk reduction among emergency service personnel. Int Arch Occup Environ Health 2013;86:245–60. https://doi.org/10.1007/s00420-013-0854-0
Yassi A, O’Hara LM, Lockhart K, Spiegel JM. Workplace programmes for HIV and tuberculosis: a systematic review to support development of international guidelines for the health workforce. AIDS Care 2013;25:525–43. https://doi.org/10.1080/09540121.2012.712668
Health care focused (n = 4)
Barger LK, Runyon MS, Renn ML, Moore CG, Weiss PM, Condle JP, et al. Effect of fatigue training on safety, fatigue, and sleep in emergency medical services personnel and other shift workers: a systematic review and meta-analysis. Prehosp Emerg Care 2018;22:58–68. https://doi.org/10.1080/10903127.2017.1362087
James FO, Waggoner LB, Weiss PM, Patterson PD, Higgins JS, Lang ES, Van Dongen HPA. Does implementation of biomathematical models mitigate fatigue and fatigue-related risks in emergency medical services operations? a systematic review. Prehosp Emerg Care 2018;22:69–80. https://doi.org/10.1080/10903127.2017.1384875
Martin-Gill C, Barger LK, Moore CG, Higgins JS, Teasley EM, Weiss PM, et al. Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: a systematic review and meta-analysis. Prehosp Emerg Care 2018;22:47–57. https://doi.org/10.1080/10903127.2017.1376136
Nejati A, Shepley M, Rodiek S. A review of design and policy interventions to promote nurses’ restorative breaks in health care workplaces. Workplace Health Saf 2016;64:70–7. https://doi.org/10.1177/2165079915612097
Work relations
Non-health care focused (n = 3)
Escartín J. Insights into workplace bullying: psychosocial drivers and effective interventions. Psychol Res Behav Manag 2016;9:157–69. https://doi.org/10.2147/PRBM.S91211
Hodgins M, MacCurtain S, Mannix-McNamara P. Workplace bullying and incivility: a systematic review of interventions. Int J Workplace Health Manag 2014;7:54–72.
Tricco AC, Rios P, Zarin W, Cardoso R, Diaz S, Nincic V, et al. Prevention and management of unprofessional behaviour among adults in the workplace: a scoping review. PLOS ONE 2018;13:e0201187. https://doi.org/10.1371/journal.pone.0201187
Health care focused (n = 15)
Anderson KK, Jenson CE. Violence risk-assessment screening tools for acute care mental health settings: literature review. Arch Psychiatr Nurs 2019;33:112–19.
Anderson L, FitzGerald M, Luck L. An integrative literature review of interventions to reduce violence against emergency department nurses. J Clin Nurs 2010;19:2520–30. https://doi.org/10.1111/j.1365-2702.2009.03144.x
Armstrong N. Management of nursing workplace incivility in the health care settings: a systematic review. Workplace Health Saf 2018;66:403–10. https://doi.org/10.1177/2165079918771106
Bambi S, Guazzini A, De Felippis C, Lucchini A, Rasero L. Preventing workplace incivility, lateral violence and bullying between nurses a narrative literature review. Acta Biomed 2017;88:39–47. https://doi.org/10.23750/abm.v88i5-S.6838
Blackstock S, Salami B, Cummings GG. Organisational antecedents, policy and horizontal violence among nurses: an integrative review. J Nurs Manag 2018;26:972–91. https://doi.org/10.1111/jonm.12623
Heckemann B, Zeller A, Hahn S, Dassen T, Schols JM, Halfens RJ. The effect of aggression management training programmes for nursing staff and students working in an acute hospital setting. A narrative review of current literature. Nurse Educ Today 2015;35:212–19. https://doi.org/10.1016/j.nedt.2014.08.003
Kynoch K, Wu CJ, Chang AM. The effectiveness of interventions in the prevention and management of aggressive behaviours in patients admitted to an acute hospital setting: a systematic review. JBI Libr Syst Rev 2009;7:175–233.
Kynoch K, Wu CJ, Chang AM. Interventions for preventing and managing aggressive patients admitted to an acute hospital setting: a systematic review. Worldviews Evid Based Nurs 2011;8:76–86. https://doi.org/10.1111/j.1741-6787.2010.00206.x
Martinez AJ. Managing workplace violence with evidence-based interventions: a literature review. J Psychosoc Nurs Ment Health Serv 2016;54:31–6. https://doi.org/10.3928/02793695-20160817-05
Morphet J, Griffiths D, Beattie J, Velasquez Reyes D, Innes K. Prevention and management of occupational violence and aggression in healthcare: a scoping review. Collegian 2018;25:621–32.
Pich J, Kable, A. Patient-related violence against nursing staff working in the emergency department: a systematic review. JBI Library of Systematic Reviews 2011;9:1–22.
Price O, Baker J, Bee P, Lovell K. Learning and performance outcomes of mental health staff training in de-escalation techniques for the management of violence and aggression. Br J Psychiatry 2015;206:447–55. https://doi.org/10.1192/bjp.bp.114.144576
Runyan CW, Zakocs RC, Zwerling C. Administrative and behavioral interventions for workplace violence prevention. Am J Prev Med 2000;18(Suppl. 4):116–27.
Stagg SJ, Sheridan D. Effectiveness of bullying and violence prevention programs. AAOHN J 2010;58:419–24. https://doi.org/10.3928/08910162-20100916-02
Strong BL, Shipper AG, Downton KD, Lane WG. The effects of health care-based violence intervention programs on injury recidivism and costs: a systematic review. J Trauma Acute Care Surg 2016;81:961–70. https://doi.org/10.1097/TA.0000000000001222
General work issues
Non-health care focused (n = 9)
Amlani NM, Munir F. Does physical activity have an impact on sickness absence? A review. Sports Med 2014;44:887–907. https://doi.org/10.1007/s40279-014-0171-0
Brown HE, Gilson ND, Burton NW, Brown WJ. Does physical activity impact on presenteeism and other indicators of workplace well-being? Sportsmedicine (Auckland, NZ) 2011;41:249–62
Cancelliere C, Cassidy JD, Ammendolia C, Côté P. Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health 2011;11:395. https://doi.org/10.1186/1471-2458-11-395
López Bueno R, Casajús Mallén JA, Garatachea Vallejo N. Physical activity as a tool to reduce disease-related work absenteeism in sedentary employees: a systematic review. Rev Esp Salud Publica 2018;92:e201810071.
Oakman J, Neupane S, Proper KI, Kinsman N, Nygård CH. Workplace interventions to improve work ability: a systematic review and meta-analysis of their effectiveness. Scand J Work Environ Health 2018;44:134–46. https://doi.org/10.5271/sjweh.3685
Odeen M, Magnussen LH, Maeland S, Larun L, Eriksen HR, Tveito TH. Systematic review of active workplace interventions to reduce sickness absence. Occup Med 2013;63:7–16. https://doi.org/10.1093/occmed/kqs198
Richardson LJ. A meta-analytic review of programs designed to combat workplace absenteeism. 2014; No. 3625046. Available from ProQuest Dissertations & Theses A&I (1554718148).
Vargas-Prada S, Demou E, Lalloo D, Avila-Palencia I, Sanati KA, Sampere M, et al. Effectiveness of very early workplace interventions to reduce sickness absence: a systematic review of the literature and meta-analysis. Scand J Work Environ Health 2016;42:261–72. https://doi.org/10.5271/sjweh.3576
Williams-Whitt K, White MI, Wagner SL, Schultz IZ, Koehn C, Dionne CE, et al. Job demand and control interventions: a stakeholder-centered best-evidence synthesis of systematic reviews on workplace disability. Int J Occup Environ Med 2015;6:61–78. https://doi.org/10.15171/ijoem.2015.553
Health care focused (n = 4)
Blanca-Gutiérrez JJ, Jiménez-Díaz Mdel C, Escalera-Franco LF. [Effective interventions to reduce absenteeism among hospital nurses.] Gac Sanit 2013;27:545–51. https://doi.org/10.1016/j.gaceta.2012.09.006
Edwards D, Hawker C, Carrier J, Rees C. The effectiveness of strategies and interventions that aim to assist the transition from student to newly qualified nurse. JBI Libr Syst Rev 2011;9:2215–323.
Edwards D, Hawker C, Carrier J, Rees C. A systematic review of the effectiveness of strategies and interventions to improve the transition from student to newly qualified nurse. Int J Nurs Stud 2015;52:1254–68. https://doi.org/10.1016/j.ijnurstu.2015.03.007
Larun L, Dalsbø TK, Hafstad E, Reinar LM. Effects of Interventions for Prevention of Sick Leave and Disability for Health Personnel. Oslo: Knowledge Centre for the Health Services, Norwegian Institute of Public Health; 2014.
Other health-related issues
Non-health care focused (n = 4)
Dinour LM, Szaro JM. Employer-based programs to support breastfeeding among working mothers: a systematic review. Breastfeed Med 2017;12:131–41. https://doi.org/10.1089/bfm.2016.0182
Hilliard ED. A review of worksite lactation accommodations: occupational health professionals can assure success. Workplace Health Saf 2017;65:33–44.
Hirani SA, Karmaliani R. Evidence based workplace interventions to promote breastfeeding practices among Pakistani working mothers. Women Birth 2013;26:10–16. https://doi.org/10.1016/j.wombi.2011.12.005
Kim JH, Shin JC, Donovan SM. Effectiveness of workplace lactation interventions on breastfeeding outcomes in the United States: an updated systematic review. J Hum Lact. 2019;35:100–13.
Health care focused (n = 8)
Dada YM. Evidence-based health care worker influenza vaccination program. Minneapolis, MN: Walden University; 2014.
Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection 2006;34:142–7. https://doi.org/10.1007/s15010-006-5109-5
Hollmeyer H, Hayden F, Mounts A, Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses 2013;7:604–21. https://doi.org/10.1111/irv.12002
Lorenc T, Marshall D, Wright K, Sutcliffe K, Sowden A. Seasonal influenza vaccination of healthcare workers: systematic review of qualitative evidence. BMC Health Serv Res 2017;17:732. https://doi.org/10.1186/s12913-017-2703-4
Lytras T, Kopsachilis F, Mouratidou E, Papamichail D, Bonovas S. Interventions to increase seasonal influenza vaccine coverage in healthcare workers: A systematic review and meta-regression analysis. Hum Vaccin Immunother 2016;12:671–81. https://doi.org/10.1080/21645515.2015.1106656
Pitts SI, Maruthur NM, Millar KR, Perl TM, Segal J. A systematic review of mandatory influenza vaccination in healthcare personnel. Am J Prev Med 2014;47:330–40. https://doi.org/10.1016/j.amepre.2014.05.035
Rashid H, Yin JK, Ward K, King C, Seale H, Booy R. Assessing interventions to improve influenza vaccine uptake among health care workers. Health Aff 2016;35:284–92. https://doi.org/10.1377/hlthaff.2015.1087
Schmidt S, Saulle R, Di Thiene D, Boccia A, La Torre G. Do the quality of the trials and the year of publication affect the efficacy of intervention to improve seasonal influenza vaccination among healthcare workers?: Results of a systematic review. Hum Vaccin Immunother 2013;9:349–61.
Review protocols
Non-health care focused (n = 59)
Aboagye E, Kwak L, Grimani A. The impact of worksite nutrition and physical activity interventions on productivity, work performance and work ability: a systematic review. PROSPERO 2017:CRD42017081837. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017081837 (accessed 9 March 2020).
Anthony L. Identifying work-life balance interventions for the public sector: a systematic review. PROSPERO 2018:CRD42018117145. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018117145 (accessed 9 March 2020).
Backhaus T. Mental health promotion in workplace settings: a systematic literature review of economic evaluation studies. PROSPERO 2016:CRD42016037703. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016037703 (accessed 9 March 2020).
Baid D, Finkelstein E, Patnaik D. Tranter E. Is there a return on investment for chronic disease prevention programmes in the workplace? A systematic review of the literature. PROSPERO 2018:CRD42018090630. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018090630 (accessed 9 March 2020).
Bailey C, Hill B, Hills A, Venn A, Teede H, Skouteris H, et al. Preconception, pregnancy and postpartum health and well-being interventions in the workplace: a systematic review. PROSPERO 2018:CRD42018116435. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018116435 (accessed 9 March 2020).
Berkman L, Kubzansky L, Kelly EL, Sianoja M, Johnson S. An exploration of workplace interventions intended to improve the psychosocial, job-related, eudaimonic, and/or work-family well-being of workers 18 and over: protocol for a systematic review. PROSPERO 2018:CRD42018084007. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018084007 (accessed 9 March 2020).
Brakenridge C, Healy G, Dunstan D, Owen N, Lawler S. Factors perceived to influence workplace sitting time: thematic synthesis of qualitative findings. PROSPERO 2017:CRD42017081880. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017081880 (accessed 9 March 2020).
Brierley M, Smith L, Bailey D, Chater A. Effectiveness of sedentary behaviour workplace interventions on cardiometabolic risk markers: a systematic review. PROSPERO 2017:CRD42017072427. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017072427 (accessed 9 March 2020).
Buckingham S, Williams AJ, Morrissey K, Price L, Harrison J. Mobile health interventions to promote physical activity and reduce sedentary behaviour in the workplace: a systematic review. PROSPERO 2017:CRD42017058856. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017058856 (accessed 9 March 2020).
Burn N, Maguire N, Weston K, Weston M, Atkinson G. Workplace exercise interventions: a systematic review and meta-analysis. PROSPERO 2017:CRD42017057498. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017057498 (accessed 9 March 2020).
Burrell J, Baker F, Allen C. Resilience factors in employees: a systematic review of the capacities and strategies that employees use to strengthen their resilience in the workplace. PROSPERO 2018:CRD42018117788. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018117788 (accessed 9 March 2020).
Court A. The effects of exposure to natural light in the workplace on the health and productivity of office workers: a systematic review protocol. JBI Library of Systematic Reviews 2010;8:1–19.
Czuba K, Oliver F, Vandal A, Kayes N. Workplace interventions to improve work-related psychosocial outcomes and reduce turnover of support workers in residential aged care: a systematic review. PROSPERO 2017:CRD42017059007. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017059007 (accessed 9 March 2020).
Dagnan D, Eastlake L, Jackson I. Systematic review of staff based interventions and support systems to improve the well-being of staff that provide care to people with intellectual disabilities. PROSPERO 2016:CRD42016037234. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016037234 (accessed 9 March 2020).
Daniels K, Hogg M, Nayani R, Tregaskis O, Watson D. Factors influencing the implementation of workplace health and wellbeing interventions. PROSPERO 2019:CRD42019119656. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42019119656 (accessed 9 March 2020).
Engelen L, Chau J, Jeyapalan D, Mackey M. Systematic review of the state of the art of the physical and mental effects of activity based working. PROSPERO 2016:CRD42016043659. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016043659 (accessed 9 March 2020).
Engelen L, Ochs K. Active design and healthy behaviour and wellbeing: a systematic review. PROSPERO 2016:CRD42016048165. URL: www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016048165 (accessed 9 March 2020).
Fereday R, Bosworth C, Charalampous M. How effective are workplace mindfulness-based interventions (MBIs) at improving common mental disorders and reducing absenteeism? PROSPERO 2018:CRD42018092112. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018092112 (accessed 9 March 2020).
Foster H. Lactation in the workplace: a systematic review of worksite-based policies, programs to improve breastfeeding outcomes of working women. PROSPERO 2017:CRD42017052662. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017052662 (accessed 9 March 2020).
Grande AJ, Fuga M, Ayres NO. Chair massage for adults in the workplace: systematic review. PROSPERO 2017:CRD42017077413. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017077413 (accessed 9 March 2020).
Gray K, Springer A, Taylor W, VonVille H. Increasing physical activity in the workplace: a systematic review. PROSPERO 2017:CRD42017054844. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017054844 (accessed 9 March 2020).
Grimani A, MacGillivray S, Newnam S. The impact of workplace mental health interventions on work-related outcomes: a systematic review. PROSPERO 2018:CRD42018093812. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018093812 (accessed 9 March 2020).
Hadley S, Tudor-Edwards R. Bryning L Global review of the cost-benefit and or cost-effectiveness of mental health interventions in the workplace. PROSPERO 2018:CRD42018096826. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018096826 (accessed 9 March 2020).
Hengel KO, Coenen P, Robroek S, Boot C, Van Lenthe F, Van der Beek A, et al. Socioeconomic differences in reach, compliance and effectiveness of lifestyle interventions among workers: protocol for an individual participant meta-analysis and the separate equity-specific re-analysis of each study PROSPERO 2018:CRD42018099878. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018099878 (accessed 9 March 2020).
Krishnamoorthy Y, Eliyas SK, Sarveswaran G, Sakthivel M. The effectiveness of workplace interventions for reducing alcohol consumption: a systematic review and meta-analysis. PROSPERO 2018:CRD42018116343. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018116343 (accessed 9 March 2020).
Kuehnl A, Rehfuess E, von Elm E, Nowak D, Glaser J. Human resource management training of supervisors for improving health and well-being of employees. PROSPERO 2015:CRD42015016987. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015016987 (accessed 9 March 2020).
Kwan SC, Imai H, Sakamoto R. A systematic review on the effects of active commuting on cardiovascular health. PROSPERO 2018:CRD42018094312. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018094312 (accessed 9 March 2020).
Lee A. Efficacy of mobile apps in improving psychological well-being in the workplace: a systematic review. PROSPERO 2017:CRD42017067821. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017067821 (accessed 9 March 2020).
Lock M, Dollman J, Post D, Eston R, Parfitt G. Efficacy of theory-driven workplace physical activity interventions: a systematic literature review. PROSPERO 2017:CRD42017056615. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017056615 (accessed 9 March 2020).
Loitz CC, Potter RJ, Walker JL, McLeod NC, Johnston NJ. The effectiveness of workplace interventions to increase physical activity and decrease sedentary behaviour in adults: protocol for a systematic review. Syst Rev 2015;4:178.
Lyssenko L, Hahn C, Kleindienst N, Bohus M, Ostermann M, Vonderlin R. A systematic review of mindfulness-based interventions in occupational settings. PROSPERO 2015:CRD42015019282. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015019282 (accessed 9 March 2020).
Merida MJ, Saldaña MR, Abellan MV, Monroy AM, Cordero RDD, Luque RM, et al. Effectiveness of workplace health promotion in workers’ health: Systematic review and meta-analysis. PROSPERO 2018:CRD42018103825. URL: www.crd.york.ac.uk/prospero/display_record.php?RecordID=103825 (accessed 9 March 2020).
Merom D, Gebel K, Sweeting J, Stanaway F, Ding D, Mumu S. Physical activity worksite interventions delivered to older employees: a systematic review, PROSPERO 2018:CRD42018084863. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018084863 (accessed 9 March 2020).
Micklitz K,Wong G, Howick J. Workplace mindfulness-based programs for mental health: a realist review. PROSPERO 2018:CRD42018086280. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018086280 (accessed 9 March 2020).
Moreno-Peral P, Bellón JÁ. Effectiveness of psychological and/or educational interventions to prevent depression at work place: a systematic review and meta analysis. PROSPERO 2017:CRD42017055728. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017055728 (accessed 9 March 2020).
Muir S, Silva S, Woldegiorgis M, Rider H, Meyer D, Jayawardana M. Predictors of engagement and successful outcomes in workplace health and exercise programs targeting physical activity: a systematic review. PROSPERO 2017:CRD42017074358. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017074358 (accessed 9 March 2020).
Mulchandani R, Chandrasekaran AM, Goenka S, Agrawal A, Panniyammakal J, Prabhakaran D, et al. Effect of workplace physical activity interventions on the cardio-metabolic health of working adults: systematic review and meta-analysis. PROSPERO 2018:CRD42018094436. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018094436 (accessed 9 March 2020).
Murawski B, Hodder R, Hope K, Reilly K, Jackson R, Sutherland R, et al. The effectiveness of interventions on improving the dietary, physical activity and sleep behaviours of school and childcare staff: a systematic review of the evidence. PROSPERO 2018:CRD42018107750. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018107750 (accessed 9 March 2020).
Murtagh MJ, Yarker J, Lewis R. To explore the prevalence, effectiveness and impact of self-confidence training interventions in the workplace. A systematic review. PROSPERO 2018:CRD42018099715. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018099715 (accessed 9 March 2020).
Neez E, De Wilt E, Pentafragka E, Chan A. Costs and benefits of workplace wellness programs in Europe: a systematic review. PROSPERO 2018:CRD42018091972. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018091972 (accessed 9 March 2020).
Nielsen MB, Christensen JR. A systematic review of exercise adherence workplace interventions. PROSPERO 2016:CRD42016039542. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016039542 (accessed 9 March 2020).
Oliver M. A systematic review of psychological, wellbeing or emotional benefits of interventions in office-centred workplaces which take place away from the desk during designated break times. PROSPERO 2017:CRD42017054114. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017054114 (accessed 9 March 2020).
Parry SP, Coenen P, OSullivan PB, Maher CG, Straker LM. Workplace interventions for increasing standing or walking for preventing musculoskeletal symptoms in sedentary workers. Cochrane Database of Systematic Reviews 2017.
Pham CT, Nguyen TV, Phung TD, Cordia C. Constraints and barriers to implementing workplace health promotion programs in low-and middle-income countries. PROSPERO 2017:CRD42017081181. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017081181 (accessed 9 March 2020).
Querstret D, de Bruin M, Allan J, Banas K. Environmental interventions for altering eating behaviours of employees in the workplace: a systematic review and meta-analysis. PROSPERO 2014:CRD42014015200. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014015200 (accessed 9 March 2020).
Rivera MP, Tew G, McDaid C. Height-adjustable workstations to reduce sedentary behaviour in office-based workers. PROSPERO 2014:CRD42014008723. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014008723 (accessed 9 March 2020).
Ryde G, Gorely T. A realist review of workplace sedentary behaviour interventions. 2016:CRD42016038299. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016038299 (accessed 9 March 2020).
Sands C, Aguiar E, Tudor-Locke C. Best practices for using wearable technologies to promote workplace physical activity: a systematic review. PROSPERO 2018:CRD42018102059. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018102059 (accessed 9 March 2020).
Sköld MB, Tork MB, Schlünssen V, Andersen LL. Psychosocial effects of workplace exercise: Protocol for a systematic review. PROSPERO 2018:CRD42018099556. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018099556 (accessed 9 March 2020).
Smith SA, Lake AA, Summerbell C, Araujo-Soares V, Hillier-Brown F. The effectiveness of workplace dietary interventions: protocol for a systematic review and meta-analysis. Syst Rev 2016;5:20.
Smoktunowicz E, Rogala A, Cieslak R, Benight CC, Yeager C, Michalak N, et al. Effectiveness of web- and mobile-based interventions for stress, job burnout, and depression in the workplace setting: systematic review with meta-analysis. PROSPERO 2017:CRD42017052712. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017052712 (accessed 9 March 2020).
Solà R, Tarro L, Llauradó E, Hermoso P, Ulldemolins G. Workplace interventions for improving production, employee performance, presenteeism, and absenteeism. PROSPERO 2018:CRD42018094083. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018094083 (accessed 9 March 2020).
Souza F, Rezende J, Lima D, Santos AC. Effects of labor gymnastics on workers’ health: a systematic review protocol. PROSPERO 2017:CRD42017084750. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017084750 (accessed 9 March 2020).
Tang X, Patterson P, Reidlinger D, Bishop J, MacKenzie-Shalders K. Workplace interventions for supporting breastfeeding: a systematic review. PROSPERO 2018:CRD42018103009. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018103009 (accessed 9 March 2020).
Thompson A, Pearce G, Grant C, Hands A, Cox V. Which objectively measured interventions designed to disrupt sitting time and increase physical activity in the workplace are effective in the medium to long term?: a meta-analysis. PROSPERO 2018:CRD42018016977. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018016977 (accessed 9 March 2020).
Ulloa A, Robbins R, Vieira D. Sleep interventions in the workplace: implications for public health and policy. PROSPERO 2016:CRD42016037748. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016037748 (accessed 9 March 2020).
Wanjau M, Zapata-Diomedi B, Veerman L. Health promotion at the workplace setting: a systematic review of effectiveness and sustainability of current practice in low and middle income countries. PROSPERO 2018:CRD42018110853. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018110853 (accessed 9 March 2020).
Watterson J, Gabbe B, Dietze P, Romero L, Rosenfeld JV. Workplace intervention programs for decreasing alcohol use in Military personnel. PROSPERO 2017:CRD42017076155. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017076155 (accessed 9 March 2020).
Westenhöfer J, Buchcik J, Borutta J. Mental health promotion at the workplace. PROSPERO 2018:CRD42018088603.. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018088603 (accessed 9 March 2020).
Health care focused (n = 19) (accessed 9 March 2020).
Blake H, Batt M, Khunti K. Effectiveness of lifestyle health promotion interventions for nurses: a systematic review. PROSPERO 2018:CRD42018098642. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018098642 (accessed 9 March 2020).
Bolton K, Fraser P, Worley V. Describing interventions aimed to improve health of staff in a hospital setting: a systematic review. PROSPERO 2018:CRD42018096797. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018096797 (accessed 9 March 2020).
Botha E, Gwin T, Purpora C. The effectiveness of mindfulness based programs in reducing stress experienced by nurses in adult hospital settings: a systematic review of quantitative evidence protocol. JBI Database System Rev Implement Rep 2015;13:21–9.
Clark L, Fida R, Skinner J, Murdoch J, Rees N, Williams J, et al. The health, well-being and support interventions for UK ambulance service personnel: a systematic evidence map 1998–2018. PROSPERO 2018:CRD42018104659. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018104659 (accessed 9 March 2020).
Cooper A, Ferreira N, Slesser M. A systematic review of interventions to improve the wellbeing of staff employed in forensic settings. PROSPERO 2016:CRD42016033524. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016033524 (accessed 9 March 2020).
Hills DJ, Ross HM, Pich J, Hill AT, Dalsbø TK, Riahi S, et al. Education and training for preventing and minimising workplace aggression directed toward healthcare workers. Cochrane Database of Systematic Reviews 2015.
Iqbal S, Fearns N, Gillanders D. The impact of training in nursing or care homes on stress and burnout in healthcare workers: a systematic review. PROSPERO 2013:CRD42013004017. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013004017 (accessed 9 March 2020).
Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: a review of empirical studies of mindfulness-based stress reduction (MBSR). Complement Ther Clin Pract 2009;15:61–6.
Lamothe J. Social support in the context of workplace violence: a systematic review. PROSPERO 2016:CRD42016039660. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016039660 (accessed 9 March 2020).
Leonard G, Smith S, Cupples M, Tully M. A systematic review of the effectiveness of physical activity interventions in health care professionals. PROSPERO 2013:CRD42013004855. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42013004855 (accessed 9 March 2020).
Murray M, Murray L, Donnelly M. Systematic review protocol of interventions to improve the psychological well-being of general practitioners. Syst Rev 2015;4:117.
Okubo CVC, Martins JT. Effectiveness of interventions in reducing occupational violence between health workers: systematic review and meta-analysis. PROSPERO 2018:CRD42018111383. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018111383 (accessed 9 March 2020).
Siemieniuk R, Coleman B, Al-Den A, Shafinaz S, Bornstein S, Goodliffe L, et al. Program factors associated with success in vaccinating healthcare workers against influenza. PROSPERO 2013:CRD42013006122. URL: www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42013006122 (accessed 9 March 2020).
Spelten E, Thomas B, O’Meara PF, Maguire BJ, FitzGerald D, Begg SJ. Organisational interventions for preventing and minimising aggression directed toward healthcare workers by patients and patient advocates. Cochrane Database of Systematic Reviews 2017. 10.1002/14651858.Cd012662 (accessed 9 March 2020).
Strauss C, Cavanagh K, Jones F, Strohmaier S, Mundy T, O’Hanlon P. A systematic review and meta-analysis of randomised controlled trials of mindfulness-based interventions for healthcare staff. PROSPERO 2016:CRD42016051773. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016051773 (accessed 9 March 2020).
Webster N, Oyebode J, Jenkins C, Smythe A. Using technology to support the social and emotional wellbeing of nurses: a scoping review protocol. J Adv Nurs 2018;26:26.
Xiong P, Yin M, Sui X, Hall B. Intervention after workplace violence among healthcare workers: a systematic review. PROSPERO 2017:CRD42017060509. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017060509 (accessed 9 March 2020).
Yip KK. Effectiveness of workplace violence preventive intervention among psychiatric nurses: a systematic review. PROSPERO 2017:CRD42017073269. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017073269 (accessed 9 March 2020).
Zucal G, Legere L, Jacob G. Violence, harassment, and bullying: prevention and management in healthcare workplaces. 2nd edn. PROSPERO 2017:CRD42017074158. URL: www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017074158 (accessed 9 March 2020).
Appendix 4 Characteristics of reviews of reviews
|
First author, year of publication Country of publication Title Aim/objective |
Number of included reviews Country and year of publication of included reviews |
Review designs Designs of primary studies |
Population | Interventions | Outcomes | Review authors’ comments on evidence |
|---|---|---|---|---|---|---|
| Lifestyles | ||||||
|
Schliemann, 201930 UK The effectiveness of dietary workplace interventions: a systematic review of systematic reviews To summarise findings of systematic reviews that distinctively report dietary intervention components and their effects on diet-, health- and economic-related outcomes in the workplace setting |
n = 21 Described as American or Western Europe 1996–2017 |
Systematic reviews including three that were also meta-analyses Not explicitly reported but appears to include RCTs, non-RCTs, and uncontrolled studies |
Adults | Workplace interventions of which one component had to be dietary. Other interventions included general wellness programmes (e.g. physical activity, smoking, alcohol use). Most interventions targeted multiple health behaviours of which diet was one | Dietary behaviour (e.g. fruit/vegetable intake), weight loss, environmental aspects, economic related (e.g. absenteeism, productivity, health-care costs) |
Only four reviews were diet only, others were general workplace wellness programmes focusing on multiple health behaviours Lack of consistency across results due to heterogeneity of reviews (and included studies) Environmental interventions should also be included Many outcomes were self-report; there was a lack of process evaluations Improvements in diet could be linked to dietary interventions but conclusion for health and economic measures limited Recommendations that interventions and messages should be tailored to the study population and adapted to the requirements of each workplace to increase effectiveness. Should have longer-term evaluations |
|
Jirathananuwat, 201729 Thailand/USA Promoting physical activity in the workplace: a systematic meta-review To classify and describe interventions to promote physical activity in the workplace |
n = 11 NR 2009–14 |
Systematic reviews, meta-analyses, systematic reviews including meta-analyses Unclear but could include RCTs, quasi-experimental or observational studies |
Workplaces included health service, government, company/workplace/industry, factory, educational institution, private sector | Interventions aimed to change multiple behaviours and included nutrition/dietary programmes, stress (mental health) management programmes, weight control programmes and smoking cessation programmes | Review aim was to classify rather than evaluate: sought to identify intervention factors including enabling (e.g. information delivery, self-motivation or programme training), predisposing (e.g. instrument resources such as pedometers), reinforcing (e.g. incentive, social support), policy regulatory (e.g. organisational action) and environmental development (e.g. break rooms, signage) | Interventions aimed to change multiple behaviours so were not exclusively focused on physical activity |
|
Fishwick, 201326 UK Smoking cessation in the workplace To summarise the evidence on smoking cessation interventions in the workplace |
n = 6 NR 1994–2010 |
Systematic review and/or meta-analysis Unclear but included controlled studies, and some evaluating cost-effectiveness |
Workplace | Legislative smoking bans; workplace cessation programmes including behavioural interventions, self help, pharmacological; and non-workplace cessation programmes | Rates of cessation, abstinence, quit; also costs | Findings on cost-effectiveness were mixed |
| General health promotion | ||||||
|
Brunton, 201628 UK Developing evidence-informed, employer-led workplace health To understand whether or not workplace health programmes are effective for improving health and business outcomes, and to identify the characteristics of workplace health programmes that are thought to influence their success |
n = 24 (gave pooled effect size. Overall 106 reviews identified but only those with a pooled effect size were included in the synthesis) International (countries not stated) 2001–13 |
Systematic reviews Trials and outcome evaluations |
Workplace | Multicomponent, education, exercise, counselling, screening, medical/assistance devices, access to resources, changes to company regulations or policy, risk assessment and participatory research |
Health including mental health, stress, weight management Financial/business including absenteeism and related costs; health-care costs, job satisfaction, job stress, productivity |
Interventions differed across varying types of workplace making it difficult to judge the generalisability of interventions to other settings Physical activity and mental health interventions predominated, whereas other public health topics, such as healthy eating, cancer prevention and cardiovascular risk reduction were rarely seen There is very little evaluation of costs across studies There was a lack of follow-up in interventions, which limits the amount of information available concerning the sustainability of workplace health interventions |
|
Haby, 201623 Mexico/Brazil Interventions that facilitate sustainable jobs and have a positive impact on workers’ health: an overview of systematic reviews To identify interventions that facilitate sustainable jobs and have a positive impact on the health of workers in health-sector workplaces |
n = 14 Described as developed or developing. Included mainly ‘developed countries’ 1997–2014 |
Systematic reviews RCTs (individuals or clusters); quasi-RCTs; controlled before-and-after studies; interrupted time series; and analytic observational studies (cohort, case–control, and cross-sectional studies). Economic evaluations were eligible but none were found |
Health-sector workplace | Occupational health and safety; precarious employment/production system rationalisation (e.g. downsizing, temporary work); flexible work arrangements; shift work – organisational level; task restructuring; employee participation – organisational level; professional nursing practice; paying for performance to improve the delivery of health interventions; and in-work tax credits for families | Various including disease incidence, prevalence and burden; mortality; morbidity; symptoms and signs of disease; health service use; quality of care; health-related costs; and health inequalities, including by gender, age, socioeconomic status, area of residence, etc. |
To be included, systematic reviews had to report health outcomes, precluding reviews that only reported changes in environmental, economic, or peace and security outcomes Interventions were poorly described making it difficult to understand how interventions were implemented and whether or not managers were supportive of the interventions |
|
Schröer, 201427 Germany Evidence-based lifestyle interventions in the workplace – an overview To summarise the effectiveness of different workplace health interventions for promoting healthy lifestyle, preventing diseases and reducing health-care costs |
n = 15 Australia, Belgium, Denmark, France, the Netherlands, the USA and the UK 2007–12 |
Systematic reviews Experimental (including RCTs) and non-experimental designs were included |
Workplace | Physical activity and/or dietary interventions at individual and/or organisational levels | Weight, physical activity and nutritional outcomes and some economic data |
There was a lack of consistency in findings Some reviews mentioned poor-quality primary studies Short-term outcomes Few employee characteristics reported Many outcomes were self-reported |
|
Goldgruber, 201025 Germany Effectiveness of workplace health promotion and primary prevention interventions: a review Effectiveness of health promotion and primary prevention interventions in the workplace |
n = 17 (including two Cochrane reviews, one on occupational health and one on smoking cessation) Australia, Finland, the Netherlands, Norway, the USA and the UK 2004–8 |
Systematic reviews and/or meta-analyses Multiple including RCTs, experimental and non-experimental |
Workplace | Stress, physical activity and nutrition; organisational development; smoking, and ergonomics and back pain | Multiple (mainly individual) psychosocial, health (physical and mental); economic (absenteeism); ergonomic; health-risk indicators | One of the challenges with multimodal interventions is that it is not obvious which components in what frequency should be applied |
| Mental health | ||||||
|
Kalani, 201824 Iran Interventions for physician burnout: a systematic review of systematic reviews To evaluate interventions to reduce physician burnout |
n = 4 NR 2008–16 |
Reviews and systematic reviews Experimental (including RCTs) and non-experimental designs were included |
Medical students, interns, physicians, residents and fellows. One review also includes nurses |
Most were individual level (e.g. counselling, support groups, mindfulness) Organisational-level interventions included pass/fail grading; duty standards, shift working staffing; change in workload |
Reduction in burnout |
Conflicting findings across reviews for individual- and organisational-level interventions. This may be as a result of individual primary studies including different groups of physicians but being considered as one group by a review, or other mediating or moderating factors not investigated Sample sizes were limited in some of the primary studies included in reviews Differing interventions across reviews |
|
Joyce, 201633 Australia/Norway Workplace interventions for common mental disorders: a systematic meta-review To evaluate the effectiveness of workplace mental health interventions |
n = 20 (includes six Cochrane reviews) Australia, Canada, Finland, the Netherlands, the USA and the UK 2001–12 |
Described as reviews Unclear |
Workplace | Primary prevention interventions included increasing employee control, physical activity and workplace health promotion. Secondary prevention interventions included screening, counselling, stress management programmes and post-trauma debriefing. Tertiary prevention interventions included cognitive–behavioural therapy, exposure therapy and medication | Multiple including employee control, increasing physical activity, symptom reduction | In most of the included reviews ‘the impact the interventions had on work-related aspects such as absenteeism, presenteeism and productivity remained relatively unexplored’ |
|
Wagner, 201634 Canada Mental health interventions in the workplace and work outcomes: a best-evidence synthesis of systematic reviews To determine the level of evidence supporting mental health interventions as valuable to work outcomes |
n = 14 NR 2001–2 |
Systematic reviews NR |
Workplace | Multiple including multicompoment interventions, therapy, cognitive–behavioural therapy, exercise, injury prevention | Absenteeism, productivity and cost |
Broad range of interventions from being handed a pamphlet to therapy Variation in populations, interventions and outcomes |
|
Dalsbø, 201332 Norway Workplace-based interventions for employees’ mental health To systematically review the research about the effects of workplace-based interventions |
n = 3 (all are Cochrane reviews) 2009–10 |
Systematic reviews RCTs, non-RCTs, controlled before and after |
In the included reviews were health-care workers, law enforcement officers as well as ‘all employees’ in workplace settings | Stress management, mental image training, flexible working | Stress, mental strain, self-image, quality of sleep, alertness | Reviews did not include outcomes such as function, productivity, absence, disability, sick leave, costs and adverse events |
|
Bhui, 201231 UK A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism To identify the key findings and gaps in the literature on the effectiveness of different stress management interventions for preventing anxiety and depression as the main cause of absenteeism |
n = 23 NR 1996–2011 |
Systematic reviews NR |
Workplace |
Individual including stress management, cognitive–behavioural therapy, relaxation, massage, personal skills training, mindfulness Organisational including comprehensive wellness programmes, support groups, problem-solving committees, work redesign |
Anxiety, depression, and absenteeism |
Interventions differed by their components, mode of delivery and whether they targeted individuals or organisations making it difficult for all of the reviews to compare benefits from any single intervention across a number of studies There were many different outcome measures for assessing anxiety and depression, and many proxy measures of mental health, sometimes without clarity about which outcomes were used in the meta-analyses Although many reviews appeared to be reviewing the same evidence, the reviews did not all identify the same primary studies and, therefore, did not always reach the same conclusions |
List of abbreviations
- HIV
- human immunodeficiency virus
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- RMAs
- reviews and meta-analyses
- RoR
- review of reviews
