Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/154/09. The contractual start date was in July 2016. The final report began editorial review in July 2019 and was accepted for publication in January 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Mike Crawford is Director of the College Centre for Quality Improvement at the Royal College of Psychiatrists (2011 to present) and was a member of the National Institute for Health Research Health Technology Assessment General Committee (2018–19). He also reports that Imperial College London has received other research grants from the National Institute for Health Research and other funding bodies. Alan Quirk and Chloe Hood work at the Royal College of Psychiatrists (London, UK) and oversee the National Audit of Dementia, since 2013 and 2008 respectively. Peter Crome is chairperson of the Steering Group for the National Audit of Dementia and has been on the Health Technology Assessment Primary Care, Community and Preventive Interventions Panel and Health Technology Assessment Prioritisation Committee A (Out of Hospital) (2014–19). He also reports that University College London has received other research grants from the National Institute for Health Research and other funding bodies. Sophie Staniszewska has been on the following committees: Health Services and Delivery Research Associate Board Members (2012–17); and Health Services and Delivery Research Researcher Led – Associate Board Members and INVOLVE Board (2005–12). She also reports that University of Warwick has received other research grants from the National Institute for Health Research and other funding bodies. Kate Seers was a member of the Health Services and Delivery Research Commissioning Board (Researcher Led) (2010–18). She also reports that University of Warwick has received other research grants from the National Institute for Health Research and other funding bodies.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Sanatinia et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Context
The number of people living with dementia is increasing and it is expected that > 1 million people in the UK will have dementia by 2021. 1,2 The number of people with dementia who are admitted to acute hospitals is also increasing, with an estimated one in four beds occupied by a person with dementia at any one time. 3,4 People with dementia are more than twice as likely to be admitted to hospital than those without this condition. 5 Admission to hospital is rarely due to cognitive impairment. Most people with dementia have coexisting physical health conditions6 and admissions to hospital are precipitated by acute problems, such as hip fractures, stroke, urinary tract and respiratory infections. 7,8 In addition to higher rates of admission, people with dementia also spend longer in hospital once they are admitted and have higher rates of readmission once they are discharged. 9,10
Admission to hospital is very difficult for people with dementia. 7 Loss of contact with familiar surroundings and people, and disruption of regular routines, can be unsettling for patients and give rise to anxiety and agitation. 11,12 In one study,13 consisting of 230 inpatients with dementia in two acute hospitals in London, 57% of patients displayed signs of aggression and 35% of patients had significant anxiety during the course of their admission. 13 Problems that people with dementia may have in communicating their needs to staff may lead to poor pain management, which further increases the likelihood of agitated behaviour. 14 The likelihood of delirium, falls and other adverse events is also higher among inpatients who have dementia than those who do not. 3,15
Quality of care received by inpatients with dementia
Concerns have repeatedly been expressed about the quality of inpatient care that people with dementia receive. 16–19 Inquiries into poorly performing hospitals have highlighted the mismanagement of frail elderly people with dementia. 20 In its thematic review of the quality of care received by people with dementia in 2014, the Care Quality Commission reported that over half of hospitals had variable or poor practice when assessing the needs of people with dementia. 21 It also found variable or poor practice regarding staff knowledge and understanding of dementia in over half of hospitals. 21 Carers of people with dementia have reported dissatisfaction with the quality of care that people receive. 22
In an online survey of 570 carers of people with dementia, almost 60% of people felt that the person with dementia was not treated with dignity or understanding while in hospital. 7 A national audit of treatment received by people with dementia in general hospitals in England and Wales found that many people do not receive a comprehensive assessment of their needs and that carers are not sufficiently involved at the time of the admission or when planning for discharge from hospital. 23
Qualitative research conducted in acute inpatient settings has explored factors that influence the quality of care that people with dementia receive. Semistructured interviews with nurses working in a general hospital in southern Sweden identified a lack of time and other resources needed to care for people with dementia. 24 Nursing staff reported that they did not have the knowledge or skills to manage behavioural problems associated with dementia, leading to frustration and use of force and neglect in an effort to manage such problems. 24 Qualitative interviews with staff working on general medical and surgical wards in a general hospital in Queensland, Australia, revealed that nurses tended to focus on the safety of people with dementia, which led to an emphasis on monitoring patients at the expense of efforts to maintain their dignity and well-being. 25 In their literature review of the state of care of older people in general hospitals, Dewing and Dijk15 conclude that available evidence suggests that prioritisation of acute care for physical health conditions often means that staff do not deliver person-centred dementia care. 15
Concerns have also been expressed about the length of time people with dementia remain in hospital. It has been argued that failure to assess and respond to the needs of inpatients with dementia can lead to longer length of stay. 3,26 Follow-up studies have shown that, even when demographic and clinical conditions of patients are accounted for, people with dementia may stay in hospital for twice as long as those who do not have this condition. 10 Identifying steps that hospitals could take to avoid lengthy admissions of people with dementia has the potential to improve both the clinical outcomes and the cost of care for people with dementia.
Efforts to improve the quality of care that people with dementia receive
Concerns about poor health outcomes and negative experiences of inpatient care among people with dementia have promoted the development of a range of different policies and practices aimed at improving the quality of care that people receive. These efforts include better training for staff,27 deployment of specialist nurses,28 the expansion of mental health liaison teams29 and specialist units. 30–32 Although studies based in single wards or hospitals have shown that it may be possible to improve patient and carer experience and physical and mental health outcomes,30,31,33 there is very little understanding of the impact that efforts to improve quality of care at a national level have on the quality of care that people with dementia receive.
Specialist units have been designed to try to better meet the needs of inpatients with cognitive impairment. 34,35 Available evidence suggests that such units may increase carer satisfaction and reduce the incidence of adverse events, but may not have an impact on mortality or length of admission. 30,31,36 However, the vast majority of people with dementia who are admitted to an acute hospital are admitted to general medical and surgical wards, and there is limited evidence about what staff on these wards can do to ensure that people with dementia receive high-quality care.
Over the last 20 years, a number of hospitals have set up specialist posts in an effort to improve the quality of inpatient care that people with dementia receive. 37 Specialist nurses, such as those deployed in Cambridge,28 helped hospitals develop policy and practice guidelines, and trained and supported colleagues working on inpatient wards. In a survey of 75 dementia specialist nurses working in the UK, Griffiths et al. 38 reported that people working in these roles undertook a broad range of activities, including efforts to prevent adverse events, supporting successful and timely discharge of patients, and reducing the use of antipsychotic medications. 38 In a parallel scoping literature review, the team identified a number of interventions that may reduce the length of stay and rate of readmission of people with dementia, but did not find direct evidence for the impact of dementia nurse specialists on patient outcomes. 39
Regarding psychiatric liaison services, research into the impact of a service, which was set up to deliver ‘rapid assessment, interface and discharge’ in an acute hospital in Birmingham, used data from a matched sample of historical controls to calculate the impact of the service. 40 Although the mean age of referrals to the service was 65.7 years, only 18% of people referred to the team had dementia. The team found that length of stay of patients referred to the service was shorter than those of matched patients before the introduction of the service, raising the possibility that psychiatric liaison services can assist in facilitating the discharge of older adults with mental health conditions, including dementia. 41 National mental health policy published in England in 2014, called for all acute hospitals to have access to liaison mental health teams that include expertise in psychiatry of older adults by 2021. 42
The National Audit of Dementia
The National Audit of Dementia (NAD) was established in 2008 to provide comparative data on the quality of care that people with dementia receive from acute hospitals in England and Wales. The audit is funded by the Healthcare Quality Improvement Partnership (HQIP) on behalf of the NHS England and the Welsh Government. To date, there have been three rounds of data reporting, in 2011, 2013 and 2017. 8,23,43 The 2017 audit, combined a retrospective audit of clinical data obtained from case notes with a survey of carers of people with dementia who had been admitted to acute hospitals. Clinical data included information about whether or not assessment of patients had been conducted in accordance with national guidelines, as well as information about length of stay. In addition to this audit, leads in each hospital completed an ‘organisational checklist’, which quantified aspects of the organisation and delivery of care for people with dementia (e.g. involvement of senior managers in reviewing the care of people with dementia and the deployment of specialist dementia nurses).
The third round of the NAD generated benchmarked data for each hospital in England and Wales, which was used by local commissioners, providers and users of services to identify poor performance and support efforts to improve the quality of care they provide. 8 Although the audit was not designed to generate or test hypotheses about factors that influence the quality of care delivered to inpatients with dementia, data from the audit provides a rich source information about both the processes and the outcomes of care that inpatients with dementia receive. A secondary analysis of data from the second round of the audit found differences in the quality of assessment of patients according to the type of ward they were treated on. 44 However, data from the audit have not been used to examine the impact of the organisation and delivery of general hospital services on the length of stay or carer-rated quality of care for people with dementia.
Chapter 2 Research objectives
The overall aim of the study was to identify aspects of the organisation and delivery of general hospital acute care that are associated with better-quality care and shorter length of stay for people with dementia, and to understand how the organisation and delivery of hospital services influences the quality of care that people receive. To meet this aim, our objectives were to:
-
identify factors that are associated with higher quality of assessment, shorter length of admission and better carer-rated experience of care for inpatients with dementia
-
understand how aspects of organisational form and function of services impact on the quality of care that inpatients with dementia receive
-
examine how contextual factors, including organisational culture, can support and/or impede the delivery of effective care to inpatients with dementia
-
synthesise data on factors that may improve the quality of care for people with dementia, to make recommendations for commissioners, providers and users of acute inpatient services about the optimal organisation and delivery of inpatient services for people with dementia.
Although there is a considerable body of evidence that the quality and availability of community-based services has a significant impact on the length of stay and quality of care that inpatients with dementia receive, this study was designed to focus only on those factors that are under the direct control of those working in acute inpatient settings.
Aim of patient and carer involvement in the study
We set out to work closely with patients and carers throughout every stage of the study. A patient and a carer representative were members of the Project Management Group and patients and carers were also members of the Stakeholder Reference Group. Through working closely with patients and carers, we aimed to ensure that the study properly considered the experiences of people with dementia and their carers, and generated relevant and appropriate outputs that could improve patient and carer experience.
Chapter 3 Scoping review of the literature
Prior to the start of the study, we undertook a scoping review of the literature. We did not aim to systematically review the literature, as a comprehensive review of factors that affect the quality of care received by inpatients with dementia had already been published. 15 Instead, we aimed to identify any important new research that had been published following this review, to help guide the selection of items from the audit, which were to be included in the secondary analysis of data, and to inform the development of questions for the topic guide for the qualitative component of the study.
Dewing and Dijk15 searched electronic databases [PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE and PsycINFO] for papers on the acute care of older people with dementia in general hospitals, which were written in English and published between 2007 and 2013. They chose 2007 as the start date for their review, so as not to duplicate work already undertaken by Moyles et al. 45 who conducted an earlier review. Dewing and Dijk retrieved 278 papers, of which 53 met their inclusion criteria (written in English, published between 2007 and 2013, with a clear focus on care of older people with dementia in acute settings). In their narrative synthesis of data from these papers on factors affecting quality of inpatient care for people with dementia, Dewing and Dijk15 identified the following seven themes.
Care environment
Inpatient care on acute wards was generally considered unsuitable for people with dementia, because of the busy environment, the lack of familiar surroundings and personal objects, and too little or too much contact with staff. People with mild dementia who are able to discuss their experience of acute care described being ignored and being surrounded by noise and busy surroundings. 46,47
Cultures of care
Concerns expressed that senior managers often underestimate the needs of people with dementia. Front-line staff report inadequate training and a lack of time to spend with patients.
Attitudes
Observational evidence suggests that positive nursing attitudes have a positive effect on care and that attitudes of nurses may vary according to the type of ward people that are treated on (with nurses on medical wards tending to have more positive attitudes than those on surgical wards). There is also some evidence that the attitudes of front-line staff can have an impact on their willingness to use a person-centred approach.
Challenges for people with dementia as an acute patient
People with dementia experience disruption in their routines. ‘Challenging’ behaviours may be a response to a patient trying to assert control over a changing environment.
Challenges for carers
Descriptive accounts of how an admission to hospital can add to a carer’s physical and emotional exhaustion. 19 Evidence suggests that some staff find carers demanding and disruptive, which may further impede the delivery of effective care and discharge from hospital. 48
Challenges for staff
Clinical staff have reported feeling overwhelmed when having to deal simultaneously with medical emergencies and with ‘challenging behaviours’ of people with dementia. 48 Staff express concerns about not having adequate training to meet the demands of people with dementia. 25
Service models
Dewing and Dijk15 highlighted a number of service-level interventions that have aimed to improve the quality of inpatient care that people with dementia receive and concluded that mental health liaison services and specialist roles vary considerably, making it difficult to generalise findings from single-site studies; a number of studies have examined the impact of staff training; and several studies have found short-term improvements in knowledge and increased confidence in caring for people with dementia, but longer-term outcomes have not been examined.
To update this review, we searched two electronic databases [Web of Knowledge and Google Scholar (Google Inc., Mountain View, CA, USA)] from January 2013 to April 2016, using the search terms related to ‘dementia/cognitive impairment’, ‘acute hospital care/general hospital’ and ‘quality of care/length of stay/experience of care/safety’. We included:
-
papers that reported the results of observational studies and described the quality of acute care for people with dementia, and experimental studies that tested the impact of interventions aimed at improving it
-
papers that were published after December 2012 and were written in English
-
papers that used a full range of research methods, including quantitative, qualitative and mixed-methods studies.
We excluded:
-
papers that focused on care received by people with dementia outside acute care settings
-
opinion pieces and non-peer-reviewed publications.
The initial search generated > 17,677 papers. Examination of titles and abstracts of these papers led to 68 full-text articles being assessed for possible inclusion in the review. The main reason for excluding papers was that they did not examine acute care for people with dementia. Twelve of these 68 papers focused on factors influencing the quality of inpatient acute care that people with dementia receive. Details of these 12 papers are provided in Table 1. We started our analysis of the data by summarising the key features of the included papers and tabulating their results to identify patterns across different studies. We then grouped the papers together, based on the themes that Dewing and Djik used in their previous review. 15 Throughout this process, we attempted to find evidence that supported or challenged the results of Dewing and Djik’s review,15 as well as attempting to identify any aspects of the organisation and delivery of services that influenced the quality of acute care for people with dementia that the Dewing and Djik review15 did not report.
| Study | Study type | Study setting (country, clinical setting) | Study sample | Main aims | Main findings |
|---|---|---|---|---|---|
| Banks et al.49 | Mixed-methods study | 113 health professionals from 14 NHS boards in Scotland | 78 nurses, 10 occupational therapists and 25 allied health professionals (physiotherapists, dieticians, one consultant physician) | To assess the impact of training new ‘dementia champions’ on staff perceptions, knowledge and understanding of dementia, and their ability to foster innovative practice | The training programme was judged to be effective and transferable to other staff groups, including community settings, etc. |
| Connolly and O’Shea50 | Case study | Discharge data from all acute hospitals in Ireland during 2010 | 6702 discharges for which there was a diagnosis of dementia | To identify measures to improve the experience of those with dementia in acute hospitals and reduced length of stay | Those with a dementia diagnosis had a longer inpatient stay than those without. Explanations for this were suggested by the authors |
| Goldberg et al.51 | Qualitative case study | Large hospital in the East Midlands region of UK | Field notes were analysed, and 360 hours of observations conducted from MMHU and standard care wards | To compare and contrast behaviours of staff and patients on each of the wards, to explain the link between structure, process and reported outcomes | MMHU offered distinctively different care, although good practice remained difficult to sustain |
| Griffiths et al.39 | Narrative literature review | Various | 71 papers included, mainly from Europe and North America | To identify the potential benefits of dementia specialist nursing and to inform the implementation of roles to support people with dementia during hospital admission | A skilled dementia specialist nurse can make a positive difference to the quality of care offered to those with dementia, but only if the role is clearly defined and they are permitted to work with patients and carers for a significant proportion of their time |
| Hynninen et al.52 | Qualitative study | Four surgical wards of a Finnish university hospital | Seven people with dementia and five close relatives | To describe the care of older people with dementia on surgical wards from the perspective of patients and their close relatives | Treatment of people with dementia in hospital improved when close relatives were involved in care planning |
| Hynninen et al.53 | Qualitative study | A surgical ward at a Finnish university hospital | 19 nursing staff and nine physicians | To describe the care of older people with dementia in surgical wards from the viewpoint of the nursing staff and physicians | Nursing staff believed that caring for people with dementia was physically and mentally demanding. Physicians and nursing staff had different views about patients’ challenging behaviour |
| Ibrahim et al.54 | Narrative literature review | Various | Papers mainly from Europe and North America | To examine domains of treatment effectiveness, burden of care, quality of life, and patient autonomy and capacity | Options identified for improving how limitations of care orders can be implemented more successfully at individual, organisational and societal levels |
| McPherson et al.55 | Qualitative study | Three inpatient dementia wards in UK | Qualitative interviews with 10 front-line nurses and health-care assistants | To explore the experiences of managing work pressures in the NHS when caring for older adults with dementia | Value-based recruitment is insufficient to deliver a high quality of care. Further attention should be paid to creating a culture of staff reliance and self-care |
| Scerri et al.56 | Qualitative study | Two geriatric hospitals in Malta | 33 care workers working in a geriatric hospital and 10 family members of patients with dementia | To explore the quality of inpatient dementia care | Five care processes identified: (1) role of other patients on the ward, (2) providing quality time, (3) providing care in time, (4) going the extra mile and (5) attending to needs with a human touch |
| Surr et al.57 | Case study | One NHS trust in the North of England | 40 acute hospital staff working in clinical roles (90% of whom were nurses) |
To evaluate a specialist training programme for acute hospital staff to deliver more person-centred care Impact on self-reported attitudes and behaviour was assessed 4 months later |
Positive change noted on all outcome measures following completion of intermediate training. Significant positive effect found on ‘approaches to dementia’ measure, but not in staff experiences and ‘caring efficacy’, after the foundation training |
| Whittamore et al.58 | Randomised trial | General wards and a specialist MMHU in a general hospital in England | 600 cognitively impaired individuals aged ≥ 65 years and 488 related caregivers | To identify patient and caregiver characteristics associated with caregiver dissatisfaction with hospital care of cognitively impaired elderly adults | Dissatisfaction was associated with carer strain and their response to behavioural and psychological symptoms of the patient, but was lower among those admitted to the MMHU |
| Yevchak et al.59 | Mixed-methods case study (in the context of a RCT) | Three clinical sites: an academic centre, a regional trauma centre and a regional medical centre in the USA | Acute care staff, including registered nurses, nursing assistants and other staff |
To determine whether or not there are differences in nursing rounds across three diverse settings, with regard to number and staff attendance To assess barriers to and facilitators of conducting nurse-led rounds |
A unit champion was present on 64% of all nursing rounds in each site, the only obstacle to their presence being ‘busy on the unit’ Barriers to care that were identified via qualitative research were ‘busy on the unit’, ‘lack of awareness’ and ‘no study patients’ |
Summary of the results of the scoping literature review
Care environment
Lack of privacy, including the impact of noise, was regarded by service users and their families as a significant issue that compromised patients’ basic care on occasions, as well as their sense of identity and self-esteem. 51 Organised activities were regarded as contributing to the creation of a homely and comfortable environment conducive to quality care. 51,57 Basic safety and cleanliness, as well as other inexpensive but effective touches, were identified as important in making the patient feel more comfortable, which, in turn, were believed to ameliorate fear and anxiety. 57
Cultures of care
The frenetic nature of activity on the ward, combined with a sense of professional abnegation of responsibility, were viewed as barriers to assessing the mental health needs of the patients. 52 Staff felt as if there was insufficient time to care for patients, resulting in a focus on task management.
Patients were often excluded from decision-making, which, aside from leading to inaccurate judgement calls in relation to patients’ needs, led to a fractured caring relationship with professionals. 54
Attitudes
The resilience of staff to manage their workloads was significantly undermined by the lack of organisational training, access to pastoral and professional support, and time for emotional processing. 56 When person-centred training had been offered to staff, positive changes in approach to work were observed, in terms of a professional’s approach both to their work and to the patients. 59
Challenges for people with dementia as an acute patient
Lack of consultation with patients often made them feel frustrated, which had an impact on their ability to function in a non-aggressive way on the ward. 54 Patients often coped better when they were able to access family support, instead of relying entirely on staff, particularly in circumstances when the family felt welcomed and were provided with feedback as to how to manage the care needs and welfare of the patient. 57 Patients often felt insecure without family support and missed them. 39
Challenges for carers
Carers’ dissatisfaction was found to be mostly associated with discharge planning, clinical management and poor communication. When patients were treated on specialist medical and mental health units, carers were less dissatisfied. 58 Carers who were allowed to become more involved with their loved one while they were a patient helped bridge the difficulties in communication about welfare needs between patient and staff. This was even more beneficial when visiting hours were flexible and staff were not rotating frequently. Greater consistency in staffing was viewed as improving rapport between patients and staff. 57 When carers were not involved appropriately, this led to significant strains, especially around discharge planning. Care diaries, family meetings and routine engagement by staff (including consultants overseeing a patient’s care)39 with family members were all considered helpful and inexpensive methods to achieve a joined-up experience of care for patients and their family. 52
Challenges for staff
Nursing staff on surgical wards reported that providing care for patients with dementia was demanding and that they felt that they did not have the skills needed to effectively manage challenging behaviour. 53 The importance of assessing capacity and knowing how to manage care in consultation with the patient was highlighted in the research undertaken by Ibrahim et al. 54 The ability of staff to identify and manage delirium was considered a barrier to the assessment of capacity. 49,50 Staff reported wanting to have better information about what community-based services they can involve or refer people on to. 50 In their analysis of qualitative comments from front-line staff working with people with dementia, Banks et al. 49 reported that some staff had positive experiences of using patient-held documents. These documents summarise a person’s history, cultural and family background, and their preferences.
Service models
Specialist nurse involvement improves patient experience and outcomes, in terms of both cost and delivery of specialist care. Specialist nurses can also assist in training other staff and thus enhance the general levels of skills and care afforded to patients with dementia. 55 The dementia champions training programme was also assessed to lead to positive changes in confidence, aptitude and work satisfaction in staff dealing with patients who have dementia. 56
Unit champions were considered to promote the welfare of patients, particularly if they had a strong interest in gerontology, and were prepared to act in a mediation-type role between staff, patients, family support and administrative leadership. 59
Specialist units were found to provide more consistent and enduring attention to a patient’s mental health needs, despite a need to concentrate more time to basic physical health care,51 which was enhanced even more so if the patient was cared for on a specialist mental health ward. 52
The results of the scoping review of the literature provided additional evidence to support the roles that the ward environment, staffing levels and staff training, and supervision and support for staff and carer involvement play in the quality of inpatient care that people with dementia receive. We also found, largely qualitative, evidence supporting the deployment of specialist nurses and patient-held records. The results of the scoping review led to our decision to include the deployment of specialist staff and the availability of personal information as items in our secondary analysis of quantitative data from the NAD. We also enquired about these elements of care in the subsequent qualitative case studies.
Chapter 4 Methodology
We used a mixed-methods approach to examine factors associated with the delivery of high-quality acute care for people with dementia. The study consisted of two work packages: a secondary analysis of data from the third round of the NAD (work package 1), followed by nested comparative case studies of hospitals and wards that provide the most and least effective care using a ‘realist’ approach (work package 2). This ‘sequential’ approach to mixed-methods research has been recommended as a means of understanding the significance of quantitative associations between interventions and outcomes, and has been used to develop a better understanding of how, and in what circumstances, positive outcomes of interventions can be delivered. 60,61
We used the results of the scoping review of the literature to help select items for inclusion in the quantitative analysis in work package 1 and the development of topic guides used in work package 2.
Work package 1
Work package 1 consisted of a secondary analysis of data, primarily from the third round of the NAD. 8 We obtained data for work package 1 from the Royal College of Psychiatrists’ (RCPsych’s) Centre for Quality Improvement. We applied, via the HQIP’s Data Access Request Group, for access to password-protected copies of two databases that contained the results of the case note audit and the carer survey. Neither database contained any identifiable data, such as name or contact details of patients or carers. Hospital names were replaced by codes.
Data on provision of psychiatric liaison services were not collected in the third round of the audit. We therefore used data from the second national survey of liaison psychiatry services for working-age adults and for older adults in England, which was conducted by Peninsula College of Medicine and Dentistry, on behalf of NHS England. 62 The two sources of data were linked using the name of the hospital. The survey was limited to acute hospitals in England that had an emergency department at the time when the survey was conducted.
Study setting and sample
The setting for the study was acute hospitals in England and Wales. We analysed data from all acute hospitals that took part in the third round of the NAD. Overall, 203 hospitals were asked to take part in the audit and 200 (98.5%) participated. Each hospital that took part in the audit was asked to submit anonymised data on a consecutive sample of at least 50 people (and a maximum of 100 people) admitted to the hospital from 1 April 2016. To be eligible to take part in the audit, patients had to have been given a diagnosis of dementia and to have been in hospital for ≥ 72 hours. Case notes were identified by hospitals using a list of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, codes for dementia. When patients had more than one admission during the data collection period, data from the first admission only were used.
Data collection methods
Each hospital that took part in the audit was asked to collect and submit five different sets of data:
-
a hospital-level organisational checklist
-
a retrospective case note audit of at least 50 sets of patient records
-
an examination of the availability of personal information on 10 people with dementia
-
a survey of carers of people with dementia
-
a staff survey.
Data from the first four sets of data were included in this analysis. Data from the staff survey were not included.
A senior member of staff at each hospital was asked to complete the organisational checklist. The checklist consisted of 42 questions on topics including collection and reporting of data to the executive board; staff training; carer engagement; environmental review; the collection of personal information about patients with dementia; and food provision. The audit team asked for the member of staff who completed the organisational checklist to be aware of how senior managers and front-line staff aimed to support people with dementia, and that they consulted with colleagues in the hospital to ensure that the information they provided was accurate. Data were entered by staff in each hospital via a secure online survey portal.
Hospital staff were asked to enter data extracted from clinical records for between 50 and 100 patients with dementia. This approach meant that larger hospitals with greater numbers of admissions could submit more data if they chose to. The case note audit covered 36 items, including the person’s admission, their assessment, use of personal information, care planning and delivery, and the discharge process. Data were submitted by audit leads from each hospital, with input from colleagues from audit departments, junior doctors and dementia champions. Data from patient records were entered by staff in each hospital via a secure online survey portal.
Staff at each participating hospital were also asked to examine the extent to which personal information on people with dementia was available to front-line clinical staff. To establish this, the audit lead at each hospital was asked to select three acute adult wards with the highest admissions of patients with dementia. They were then asked to identify 10 patients with dementia on these wards and to check whether a personal information document (e.g. the Alzheimer’s Society’s This is Me document63) was present at the bedside or in the patients’ clinical notes.
A median of 10 patients were checked per site. Of the patients checked at each site, a mean average of 49% had a personal information document present. This ranged from 0% to 100% of patients checked.
The carer questionnaire was developed specifically for the NAD by staff at the Patient Experience Research Centre at Imperial College London. The questionnaire consisted of 10 items, out of which eight were ranked high in terms of relevance to the care of people with dementia, by a panel of carers. The panel thought that all carers and family members who might visit people with dementia would answer these questions. The questionnaire also incorporated the Friends and Family Test question for validation and comparison,64 and a final question, added at the suggestion of the audit reference group, on support provided by the hospital to the carer. Paper versions of the carer questionnaire were distributed by staff to both paid and family carers visiting patients during June to September 2016. Questionnaires were returned directly to the audit team at the RCPsych. Carers could also complete an online version of the questionnaire, which was publicised via social media and on posters displayed around participating hospitals. The questionnaire did not include personal identifiable information and could not be linked to individual patients. All tools used in the audit were piloted by 10 hospitals in 2015 and changes made prior to the full audit in 2016.
Data for the second national survey of liaison psychiatry services for working-age adults and for older adults in England were collected between 14 January 2015 and 30 April 2015.
The team conducting this survey contacted liaison psychiatry teams at all acute trusts in England that included an emergency department. Data were returned on 179 hospitals in England. 62 The questionnaire included 27 items, covering the composition of teams and the hours that the liaison service covered.
Outcome measures
We set out to examine factors influencing three aspects of the quality of acute care that people with dementia receive: (1) length of admission, (2) carer-rated quality of care and (3) quality of patient assessment. The date of a patient’s admission and discharge from hospital was included in the case note audit. We used this to calculate the length of admission for each patient.
We used scores on carer-rated quality of care for each hospital, which had been calculated for the third round of the NAD. This score was derived from responses carers made to a single item, ‘overall, how would you rate the care received by the person you look after during the hospital stay?’, which could be rated excellent, very good, good, fair or poor. The maximum rating for a hospital was 100 (awarded if all carers rated the hospital as excellent) and the minimum rating for a hospital was 0 (if all carers rated the hospital poor). Details of how carer responses were used to calculate the aggregate hospital score can be found at URL: www.rcpsych.ac.uk/improving-care/ccqi/national-clinical-audits/national-audit-of-dementia/nad-reports-and-resources (accessed 18 March 2020).
We used data from the case note audit records to assess the quality of assessment that each patient received. 44 Each patient was given a score of between 0 and 7, according to whether or not seven components of a high-quality assessment had been conducted (mobility, nutritional status, pressure ulcer risk assessment, continence needs, presence of any pain, a structured assessment of functioning and assessment of delirium). These seven items were selected because they are included in the guidelines produced by the British Geriatrics Society. 65 Failure to assess these aspects of health care have also been shown to be associated with the likelihood of early readmission to hospital of people with dementia. 33,66
Predictor variables
We used a three-stage process to generate a list of predictor variables for work package 1. We selected these variables from those assessed in the dementia audit and survey of psychiatric liaison services. In the first stage, we used data from our scoping review of the literature and from our previous research examining factors associated with the quality of assessment of people with dementia who are admitted to acute hospital beds,44 to draw a long list of items that we judged could influence one or more of our three study outcomes. We presented this long list to the Project Management Group and Stakeholder Reference Group for their views (see Patient and carer involvement). This generated a short list of variables paired with each outcome. Having examined the distribution and frequency of these measures, we noted that in some instances there was very little variation and excluded any predictor variables that were present or absent in > 90% of hospitals. In all instances, variables were excluded from the analysis because they were nearly always present. A list of these variables is provided in Appendix 1. The final list of variables included in the main analysis is presented in Tables 2–4.
| Predictor variable | Source of data | Audit item |
|---|---|---|
| Type of ward | Case note audit | Q5 |
| Primary diagnosis | Case note audit | Q6 |
| Discharge planning within 24 hours of admission | Case note audit | Q34 |
| Evidence of discussing discharge with carers | Case note audit | Q29b |
| Executive board reviews delayed discharge | Organisational checklist | Q2b |
| Evidence of discussing discharge with consultant responsible for the patient | Case note audit | Q29c |
| Dementia specialist nurse | Organisational checklist | Q6 |
| Social worker or other designated person | Organisational checklist | Q34 |
| Dementia care pathway/bundle | Organisational checklist | Q1 |
| Liaison hours | Liaison survey | Q21 |
| Older adult consultant | Liaison survey | Q14 |
| Demographic variable | ||
| Age of the patient | Case note audit | Q1 |
| Gender of the patient | Case note audit | Q2 |
| Ethnicity of the patient | Case note audit | Q3 |
| Predictor variablea | Source of data | Audit item |
|---|---|---|
| Evidence of discussing discharge with carers | Case note audit | Q29b |
| Social worker or other designated person | Organisational checklist | Q34 |
| Strategy or plan for carer engagement (e.g. triangle of care) | Organisational checklist | Q7 |
| Hospital provides finger food for people with dementia | Organisational checklist | Q35 |
| 24-hour food service | Organisational checklist | Q36 |
| Carer visit at any time (carer passport) | Organisational checklist | Q13 |
| Availability of personal information (mini audit) | Organisational checklist | Q16 |
| Carer received notice of discharge (< 24 hours and ≥ 24 hours) | Case note audit | Q35 |
| Documented assessment of carer needs prior to discharge | Case note audit | Q36 |
| Care assessment contains section dedicated to information from carer | Case note audit | Q22 |
| Demographic variables (patient) | ||
| Age of the patient | Case note audit | Q1 |
| Gender of the patient | Case note audit | Q2 |
| Ethnicity of the patient | Case note audit | Q3 |
| Demographic variable (carer) | ||
| Gender of the carer | Carer survey | Q1 |
| Age of the carer | Carer survey | Q2 |
| Ethnicity of the carer | Carer survey | Q3 |
| Predictor variable | Source of data | Audit item |
|---|---|---|
| Type of ward | Case note audit | Q5 |
| Length of stay | Case note audit | Q11 |
| Dementia care pathway in place | Organisational checklist | Q1 |
| Dementia champion (at directorate level) | Organisational checklist | Q5 |
| Dementia specialist nurse | Organisational checklist | Q6 |
| Liaison hours | Liaison survey | Q21 |
| Older adult liaison psychiatry consultant | Liaison survey | Q14 |
| Primary diagnosis | Case note audit | Q6 |
| Demographic variable | ||
| Age of the patient | Case note audit | Q1 |
| Gender of the patient | Case note audit | Q2 |
| Ethnicity of the patient | Case note audit | Q3 |
Carer-rated quality of care was measured at the hospital level; therefore, all variables needed to be aggregated at hospital level. We were therefore unable to include primary diagnosis and type of ward in this analysis.
Data management and analysis
A number of the predictor variables included large numbers of categories with small numbers of patients in them. To simplify the analysis, we combined some categories prior to data analysis. When possible, we used categories that were developed by the audit team. Case notes included > 100 descriptions of primary diagnosis. These were grouped together in 11 categories, such that myocardial infarction was combined with other vascular conditions, and kidney and urological conditions were grouped together. Ethnicity was not well recorded in the case notes. The majority of the sample were recorded as white or white British (82.1%) and 12.4% of the sample were recorded as ‘other’. Less than 2% of records indicated other ethnicities (black/black British 1.2%, Asian/Asian British 1.9%, Chinese 0.1% and mixed 0.1%). We therefore combined these groups with ‘other’ to create a dichotomous variable white and white British, or black, Asian and minority ethnic (BAME).
We used univariate tests to conduct preliminary analysis of the relationship between dependent variables (length of admission, carer-rated quality of care and quality of assessment of patient needs) and patient-level (age, gender, presenting complaint), ward-level (type of ward) and hospital-level (access to liaison mental health services, deployment of specialist dementia nurses, etc.) predictor variables. Further exploratory analyses were carried out to look at which combinations of these exploratory variables could best explain the variations in dependent variables.
Given the nested structure of the data (patients within hospitals), the final analysis was carried out using hierarchical models. 67,68 Traditional regression methods were not deemed appropriate because they assume independent observations. For instance, measurements taken from patients in the same hospital can no longer be assumed to be independent (i.e. they are correlated). Hierarchical models take this into account to draw valid statistical inferences. 69 Using hierarchical modelling made it possible to compare hospitals in terms of patient outcomes. This was achieved by testing cross-level interactions, which combine the effects of explanatory variables at the patient and hospital level. Interactions between explanatory variables within each level were also tested.
Using this methodology, we combined the information across hospitals with patient-level information to identify predictors that may have an impact on length of admission and quality of assessment of needs. Unlike length of admission and quality of assessment, which were measured at the patient level, carer-rated quality of care was measured at the hospital level. Therefore, for this analysis, variables that were not at the hospital level were aggregated. Multiple linear regression was used for this analysis.
Patient-level scores on quality of assessment were not continuous; they were ordered categorical variables, ranging from 0 (no items completed) to 7 (all items completed). We therefore used ordered logistic regression applied to hierarchical models to analyse these data. Most patients (n = 9260, 91.6%) had a score of ≥ 5 on this measure. We therefore collapsed the seven categories to create a variable with four categories: 0 (zero to four items completed), 1 (five items completed), 2 (six items completed) and 3 (seven items completed).
All data were analysed using statistical packages Stata® (version 13; StataCorp LP, College Station, TX, USA) and SPSS 23 (IBM Corporation, Armonk, NY, USA).
The outcome measure, length of admission, was skewed so transformation of data on length of admission was required. For the outcome measure, we excluded all those who died during their admission from all analyses, including the sensitivity analyses.
Sensitivity analysis
In addition to examining factors associated with mean length of stay among the entire audit sample (excluding those who died during their admission to hospital), we conducted two sensitivity analyses. In the first of these, we repeated the analysis in a subsample of people who were admitted to hospital with fracture of the hip and related injuries. In the second, we restricted the analysis to the 50% of hospitals that had higher carer-rated quality of care.
By limiting the sample to those with hip injuries we sacrificed study power, but aimed to provide a more precise estimate of the association between practice and outcomes, by reducing confounding resulting from differences in case mix across study sites. 70 We selected hip injuries for this analysis following consultation with front-line clinicians and other stakeholders, as it is prevalent among people admitted to acute hospitals with dementia and because they are relatively easy to diagnose. 26,70
We conducted a sensitivity analysis among the hospitals that were in the top half of carer-rated quality of care because of concerns from members of our Stakeholder Reference Group that hospitals could achieve shorter average lengths of stay by discharging patients prematurely. We therefore wanted to check that any factors assorted with shorter lengths of stay were not at the cost of low carer-rated satisfaction.
Work package 2
Work package 2 consisted of six comparative case studies of dementia care in acute hospitals. Hospitals were sampled to include pairs of hospitals that organise and deliver care in a similar way, but which achieve different outcomes. The overarching aim of this study was to identify aspects of organisation and delivery of general hospital services associated with the three key outcomes measured for the third round of the NAD: (1) carer-rated experience of care, (2) length of stay and (3) quality of assessment.
Theory development: a ‘twin-track’ approach
To optimise the contribution of work package 2 to the study, we designed and implemented a ‘twin-track’ approach to theory development. 71
Track A: qualitative exploration of factors associated with patient outcomes
In parallel with a realist evaluation [see Track B: theory testing and refinement (realist evaluation)], we explored factors associated with patient outcomes in work package 1. For example, we found that initiation of discharge planning within the first 24 hours of admission was associated with shorter length of stay. In work package 2, we were interested in finding out how and why that might be the case.
Track B: theory testing and refinement (realist evaluation)
We conducted a realist evaluation of the delivery of acute care for people with dementia. 72,73 Realist research design employs no single standard ‘formula’, other than producing a clear theory of programme mechanisms, contexts and outcomes, and then using appropriate empirical measures and comparisons. We considered the most effective approach for this study to be a comparative case study design. The selection of hospitals, methods and research questions was theory driven (i.e. driven by the research team’s theory for how interventions for improving dementia care bring about change and how organisational culture shapes the response of hospital staff).
At the outset of the study, we developed programme theories for aspects of dementia care assessed by the NAD (see Appendix 2). These theories were informed by the results of our scoping review of the literature and results from earlier rounds of the audit and, thus, summarise our initial thinking about how aspects of hospital care, such as dementia-friendly food provision, can make a difference in favourable contexts to outcomes, such as carer-rated quality of care.
Realist evaluation can be used to test theory for how change occurs (if the evaluators already have a fairly well-developed theory) or to formulate and develop theory through a more exploratory approach. 72 We considered our programme theories to be only moderately well developed, so after testing the theories in the main 18-month phase of fieldwork in four hospitals, we sought to refute or refine them in a second 4-month phase of fieldwork in two additional hospitals. By interviewing staff and carers in contrasting hospitals, we sought to understand better why something that can work well in one context may make little difference in another.
Over the course of the fieldwork period we progressively focused data collection and analysis on two main context–mechanism–outcome (CMO) configurations. We chose to do this because it became apparent very early on in the fieldwork that attempting to address all CMO configurations associated with the delivery of care to this patient group would result in an unacceptably superficial research report. The two CMO configurations selected for in-depth analysis were chosen because they had emerged as key issues for interviewees and were considered by them to be areas that were amendable to quality improvement.
Work package 2 thus has two distinct analytic foci: exploring the nature of the relationship between specific predictor variables and outcomes (track A), and testing and refining programme theories in the context of a realist evaluation (track B).
This is reflected in the design of the data collection and data management tools, which have clearly demarcated sections for each track of the study. It is also reflected in the approach we adopted for analysing the qualitative data, which involved asking distinctly different analytic questions of the same data set. 74 These two tracks were then brought together in the discussion.
Selection of case study sites
Case study sites were selected from hospitals participating in the NAD. We thought that there was likely to be a complex relationship between service organisation and delivery, experience of care and length of stay, so hospitals were carefully chosen for detailed case study analysis based on their capacity to (1) provide insights into this relationship, and (2) provide a better understanding of what works for whom and under what circumstances.
We had planned to use data from work package 1 to help select the first four case study sites. However, time constraints required us to select the first site before the results of the third round of the NAD had become available. Our selection of the first hospital was based on its performance in previous rounds of the audit and other intelligence, which led us to predict (correctly) that it would score comparatively highly in relation to carer-rated quality of care. Findings from interim analysis of the qualitative data from this first site clearly demonstrated that, despite lack of governance infrastructure, this hospital scored highly on carer-rated quality of care. After discussions with the project working group it was decided that governance score should be chosen as the other main criterion for selecting sites. This would provide the opportunity to explore how and why governance infrastructure might or might not result in desirable patient outcomes and whether or not there are some other organisational and/or contextual factors that lead to high-quality care.
When the audit results subsequently became available, we reviewed those results alongside other data sources, such as Care Quality Commission reports, and undertook telephone interviews with key stakeholders, before selecting three further hospitals. A paired sampling approach was used to help us understand similarities and differences between sites (Table 5).
| Site | Governance audit score | Carer-rated quality of care |
|---|---|---|
| 1 | Low | High |
| 2 | High | Low |
| 3 | Low | Low |
| 4 | High | High |
| 5 | Average | Not available |
| 6 | High | Average |
Members of the Project Management Group and Stakeholder Reference Group informed us about hospitals that had put measures in place to reduce length of stay. We were also interested in collecting data from hospitals that were geographically different from our four main study sites, which were all in London or the South East/West. Selecting two additional study sites in the south-west and north of England allowed us to test our theories in hospitals with different characteristics to the first four study sites.
Our sampling approach resulted in the inclusion of hospitals with differing levels of performance. We define good performance or ‘outcome’ in realist evaluation terms, as comparatively positive carer-rated experiences of care plus shorter admissions. It also resulted in the inclusion of hospitals operating in differing contextual conditions for delivering good-quality acute care for people with dementia, including key components in the organisation and delivery of care identified through the third round of the NAD, such as adequate staffing levels and access to liaison mental health services.
Data sources
At each hospital we conducted in-depth interviews and assembled documentary evidence at three key organisational ‘levels’ relating to the quality of care: (1) clinical governance, (2) middle management and (3) the staff–patient interface.
In-depth interviews
The main source of data was in-depth interviews, with a total of 56 staff and seven carers. The interviews were undertaken by the lead researcher and two managers from the NAD, who had been trained in qualitative interviewing.
Aim
Following Pawson75 and Manzano,76 our interviews were theory driven, in that they were designed to inspire, validate, falsify or modify our hypotheses about how dementia care programmes and interventions work (track B), while in parallel exploring with participants their views on factors associated with patient outcomes (track A). 75,76
Inclusion criteria for staff interviews
-
Aged ≥ 18 years.
-
Experience of working directly or indirectly with patients with dementia in acute hospital settings.
-
Willingness to provide written informed consent to take part in an interview.
-
Agreement that the interview is digitally recorded.
Sampling strategy
The associations found in work package 1 guided our plans for data collection in work package 2. Most of the associations we found in work package 1 related to the way that staff and managers organised services. After discussions with the Project Management Group, it was decided that the main focus of data collection in work package 2 should be on interviewing a wide range of managers and front-line staff. This was because it seemed unlikely that carers would have direct experience of the decisions that hospital staff made about the organisation of the service. Staff members were purposively sampled to include a mix of those with professional and non-professional backgrounds (nursing, medical, professions allied to medicine, nursing assistants), and a mixture of junior and senior staff, including those who hold management responsibilities and those who do not. We also sought to interview staff who had specific responsibility for overseeing care for people with dementia, such as a dementia ‘champion’, a specialist dementia nurse and a member of the trust board who is responsible for care of people with dementia.
The carers who took part were identified, with support from staff, and approached for their consent to be interviewed.
Topic guides
Following Manzano’s guiding principles76 for realist interviews, we produced separate topic guides for staff (see Appendix 3) and carers (see Appendix 4). The guides were drafted by the study team and presented to the Project Advisory Group, which included a patient and a carer, for their comments. The guides were designed to be used flexibly to allow researchers to be responsive to issues raised by participants.
Interview procedure
All interviews were conducted using a topic guide. With consent, the interviews were digitally recorded and transcribed, or handwritten notes were made during the interview and subsequently typed up as a fieldnote.
After each interview, the researcher noted reflections that might be analytically useful, along with two or three high-level bullets about interview content, to help with navigating managed data later. The researcher also carefully documented sampling characteristics. All this information was collated in a central location [a Microsoft Excel® spreadsheet (Microsoft Corporation, Redmond, WA, USA)] and updated after each interview, to give the research team a good sense of the sample as it developed.
Staff and carer participants were offered a choice over whether they would like to be interviewed face to face at the NHS participating site, over the telephone or by video chat. Carers were also given the option of being interviewed at a place of their convenience, for example in their home.
Documentary evidence
We obtained and studied documentary data prior to visits to case study sites. This included data from recent Care Quality Commission reports, which were examined to identify any areas of achievement or concern about care for frail elderly patients in the hospital. We also asked each hospital to provide policy documents relevant to care of frail elderly patients, including (when available) their dementia care pathway, service-level agreements for the mental health liaison service and policy on the management of vulnerable patients. Other documents included work unit guidelines, any information provided to staff regarding working with frail elderly, guidance in relation to working with carers, and assessment and treatment protocols.
None of the documents was subjected to any form of content or discourse analysis. Rather, the documents were gathered to familiarise the researcher with the context and information derived from them was fed into interview questions as appropriate.
Data management and analysis
Data management
We had 62 interviews transcribed in full by an external transcribing agency. One interviewee did not consent to their interview being recorded, so for that interview the researcher took notes and typed them up later.
We coded the transcripts in NVivo Pro 11 (QSR International, Warrington, UK), using the final version of the coding scheme shown in Appendix 5. The coding scheme reflects the study’s twin-track approach, with the first part of it being used to code data for the realist evaluation and second part for track A.
We incorporated a framework approach, which involved creating a case and theme-based matrix in NVivo, and systematically summarising the data into relevant cells. 77 The aim was to ensure that no data were lost in the process of condensing them into a more manageable, summarised form, and the end result was a series of populated matrices that could be viewed in multiple configurations. After the first few interviews had been summarised, we reflected on how the framework was working and revised it.
Managing data in this way made it easier to identify patterns in the data and then interrogate the data to explain them. Doing this in NVivo made it possible to maintain links to the raw data.
Data analysis
We analysed data using a thematic analysis approach to detect the most salient patterns from a realist perspective. 78 The analysis and write-up focused on the relationship between service organisation and delivery, experience of care, carer involvement and length of stay. We addressed questions such as:
-
What hinders hospitals from performing as well as other similar hospitals?
-
How do hospitals operating with minimal governance infrastructure manage to deliver good-quality care?
-
Why do certain predictors, such as discharge planning in the first 24 hours of admission, lead to shorter length of stay?
The lead researcher met regularly with the research team throughout the fieldwork process to share and reflect on what had been observed, which fed into theory development.
Patient and carer involvement
With support from the team co-ordinating the NAD, we co-opted members of the Audit Advisory Group to comment on the methods and results of this study. Throughout the report, we refer to this group as the Stakeholder Reference Group. We took this approach because the Advisory Group was an established group of people with relevant expertise who provided and used acute care for people with dementia. Members of the group were already engaged in discussing the quality of care that people with dementia receive while in hospital, and they were aware of and interested in this study. We added a regular item on the agenda of the Advisory Group to discuss the design of this study and discuss emerging findings. In addition to this, a patient and a carer representative on the Project Management Group provided a range of comments and suggestions about the design and conduct of the study. Recommendations of patients and carers on these two groups were used to:
-
select which predictor variables to include in work package 1 from among the long list that we initially developed
-
help us develop the content of the topic guides that we used in work package 2
-
help us to interpret the results of the findings of the study.
In addition to this, Gemma Zafarani (carer representative) helped us prepare this report and write the lay summary for the study.
Ethics issues
We received approval for the secondary analysis of data from the National Clinical Audit and Patient Outcomes Programme from the HQIP prior to the start of work package 1 (reference HQIP162). We obtained ethics approval for work package 2 from the proportionate review subcommittee of the South West – Frenchay Research Ethics Committee prior to the start of data collection for work package 2 (reference 17/SW/0038).
All clinicians, managers and carers were provided with written and verbal information about the study before being asked if they were willing to take part in the study. Only those people who provided written informed consent were interviewed.
Changes to the study protocol
In work package 1, data on access to mental health liaison services at acute hospitals in England and Wales were not collected in the third round of the NAD. However, we were able to access data on the provision of liaison mental health services in England from a separate survey, conducted by the University of Plymouth on behalf of NHS England (see Work package 1).
Although we were able to collect data on the type of ward that patients were admitted to, we were unable to obtain accurate information on the identity of the ward. This meant that our original plan to conduct three-level modelling (patients within wards within hospitals) was not possible. Instead, we used a two-level model of patients in hospitals.
For work package 2, we originally proposed collecting data from ‘up to 15’ hospitals. However, feedback from the commissioning board was that these plans were overambitious and we were encouraged to reduce the number of case study sites. Following discussions within the Project Management Group, we modified our original plans and focused, initially, on collecting data from four sites, adding two further hospitals following an initial analysis of data, which suggested that we needed to capture more data from carers of people with dementia.
We originally proposed analysing qualitative data from work package 2 purely from a realist perspective. This approach proved helpful for developing an understanding of the CMOs of particular ‘programmes’ operating in hospitals (e.g. staff training). To optimise the contribution of the qualitative component to the study, we used a ‘twin-track’ approach to theory development. In parallel with a realist evaluation, we used a broader thematic approach to analyse data arising from associations identified in work package 1 (see Work package 2 for details).
Chapter 5 Results: work package 1
Two hundred (98.5%) of 203 acute hospitals in England and Wales took part in the third round of the audit. All 200 hospitals submitted an organisational checklist. Data from the clinical records of 10,106 patients were also submitted and 4688 carer questionnaires were received. A summary breakdown of the number of participating hospitals and data submission is provided in Table 6.
| Audit tool/questionnaire | Hospitals participating, n | Data received, n | Average per hospital, n | Range per hospital |
|---|---|---|---|---|
| Organisational checklist | 200 | 200 | N/A | N/A |
| Case note audit | 196 | 10,106 | 52 | 22–99 |
| Carer questionnaire | 197 | 4688 | 24 | 1–104 |
| Liaison psychiatry | 176 | 176 | N/A | N/A |
Data on predictor (explanatory) variables extracted from the organisational checklists submitted by the 200 hospitals are presented in Table 7.
| Predictor variable | Number | Percentage |
|---|---|---|
| Executive board reviews delayed discharge | ||
| Yes | 63 | 31.5 |
| No | 137 | 68.5 |
| Dementia specialist nursea | ||
| Yes | 64 | 32 |
| No | 136 | 68 |
| Dementia care pathway/bundle | ||
| Yes | 121 | 60.5 |
| No | 26 | 13 |
| In development | 53 | 26.5 |
| Dementia champion at directorate level | ||
| Yes | 164 | 82 |
| No | 35 | 17.5 |
| In development | 1 | 0.5 |
| Social worker or other designated person | ||
| Yes | 152 | 76 |
| No | 48 | 24 |
| Strategy or plan for carer engagement | ||
| Yes | 153 | 76.5 |
| No | 47 | 23.5 |
| Hospital provides finger food for people with dementia | ||
| Every day/4–6 days | 133 | 66.5 |
| Sandwich or wraps only | 167 | 33.5 |
| 24-hour food service | ||
| Yes (full range/simple food supply) | 166 | 83 |
| No | 34 | 17 |
| Carer visit at any time (carer passport) | ||
| Yes | 177 | 88.5 |
| No | 23 | 11.5 |
Data from the case note audit
Of the 200 hospitals that took part in the audit, 152 (76%) submitted data from the recommended minimum of 50 case notes and 186 (93%) submitted data from at least 40 sets of case notes. Demographic and clinical details of patients who were included in the audit sample are presented in Table 8 and data on predictor variables extracted from the case note audit are presented in Table 9. The youngest patient in the audit was 34 years and the oldest was 108 years.
| Predictor variable | Number | Percentage or SD |
|---|---|---|
| Age (years) (n = 10,096) | ||
| Mean | 84.3 | 7.9 |
| Gender | ||
| Male | 4052 | 40.1% |
| Female | 6054 | 59.9% |
| Ethnicity | ||
| White | 8274 | 81.9% |
| BAME | 1622 | 16% |
| Not documented | 210 | 2.1% |
| Specialty of the ward | ||
| Cardiac | 248 | 2.5% |
| Care of the elderly/complex care | 4125 | 40.8% |
| Critical care | 23 | 0.2% |
| General medical | 2397 | 23.7% |
| Nephrology | 52 | 0.5% |
| Obstetrics/gynaecology | 41 | 0.4% |
| Oncology | 22 | 0.2% |
| Orthopaedics | 906 | 9.0% |
| Stroke | 457 | 4.5% |
| Surgical | 686 | 6.8% |
| Other medical | 1000 | 9.9% |
| Other | 136 | 1.3% |
| Unknown | 13 | 0.1% |
| Primary diagnosis (n = 10,048) | ||
| Respiratory | 2005 | 19.8 |
| Fall | 1346 | 13.3 |
| Urinary/renal | 906 | 9.0 |
| Hip fracture/dislocation/other fractures/trauma | 886 | 8.8 |
| Sepsis | 635 | 6.3 |
| Delirium/confusion/cognitive impairment | 1204 | 11.9 |
| Gastrointestinal | 595 | 5.9 |
| Cardiac/vascular/chest pain | 518 | 5.1 |
| Stroke + neurological | 750 | 7.4 |
| Other | 1239 | 12.3 |
| Missing | 22 | 0.2 |
| Predictor variable | Number | Percentage |
|---|---|---|
| Carer received notice of discharge (n = 7385) | ||
| < 24 hours | 1446 | 14.3 |
| 24 hours | 899 | 8.9 |
| 25–48 hours | 1090 | 10.8 |
| > 48 hours | 1902 | 19.7 |
| No notice at all | 35 | 0.3 |
| No carer, family or friend | 129 | 1.3 |
| Not documented | 1786 | 17.7 |
| Patient specified information to be withheld | 3 | 0.0 |
| Could not contact | 5 | 0.0 |
| Missing | 2721 | 26.9 |
| Evidence of discussing discharge with carer (n = 7385) | ||
| Yes | 5628 | 55.7 |
| No | 1359 | 13.4 |
| N/A | 398 | 3.9 |
| Missing | 2721 | 26.9 |
| Evidence of discussing discharge with consultant (n = 7385) | ||
| Yes | 5529 | 54.7 |
| No | 1856 | 25.1 |
| Missing | 2721 | 26.9 |
| Care assessment contained a section dedicated to collecting information from a carer or next of kin | ||
| Yes | 5759 | 57.0 |
| No | 4347 | 43.0 |
| Discharge planning initiated within 24 hours of admission (n = 7385) | ||
| Yes | 2499 | 24.7 |
| No | 2791 | 27.6 |
| N/Aa | 2095 | 20.7 |
| Missing | 2721 | 26.9 |
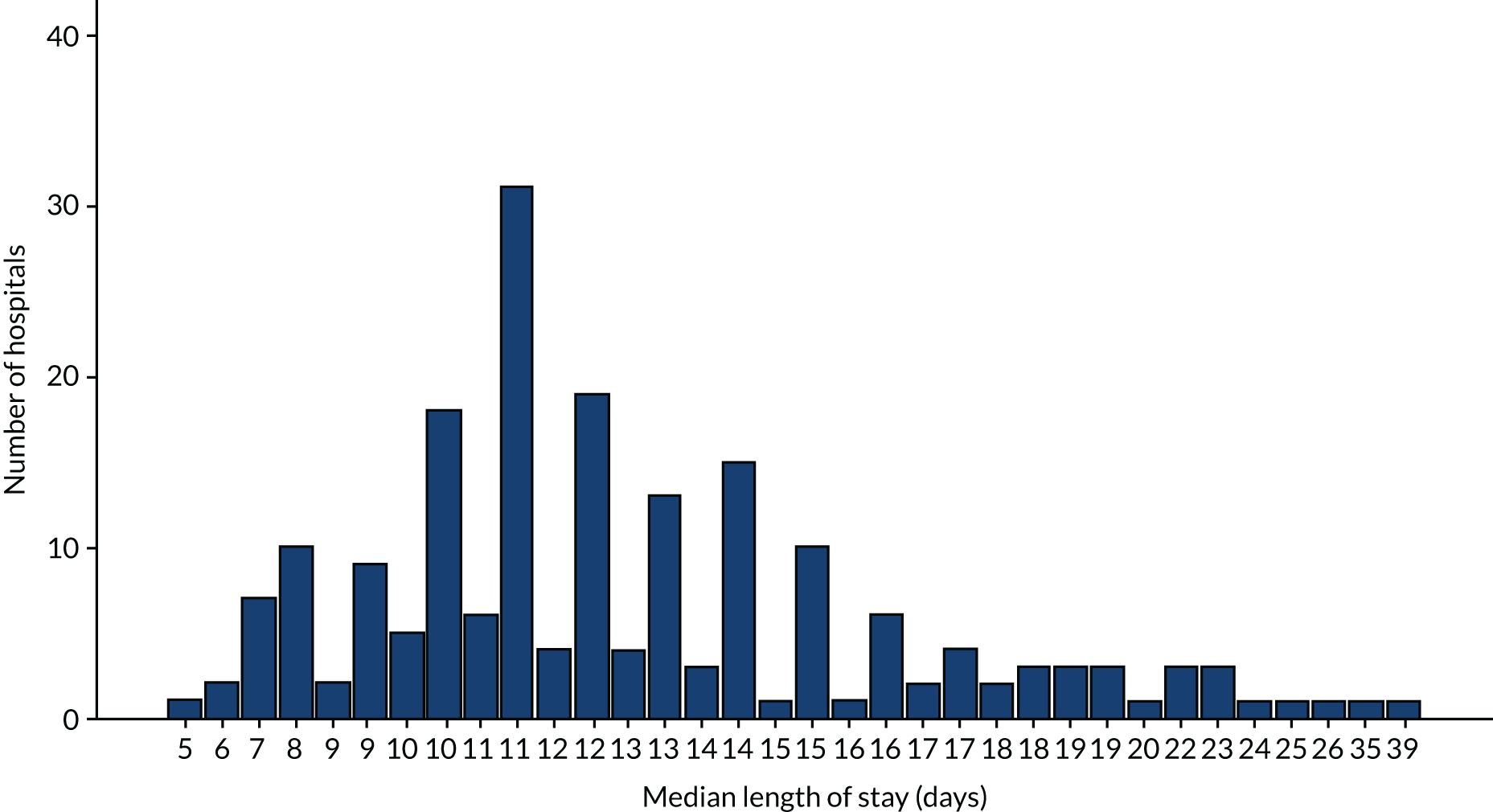
Valid data on length of stay were recorded for 10,105 patients. Variation in length of stay is illustrated in Figure 1. The median length of stay was 12 days [interquartile range (IQR) 6–23 days]. As seen in Figure 2, the median length of stay varied between different hospitals, ranging from 5 to 39 days (IQR 10–14 days).
FIGURE 1.
Length of inpatient stay among 10,105 patients in the case note audit.
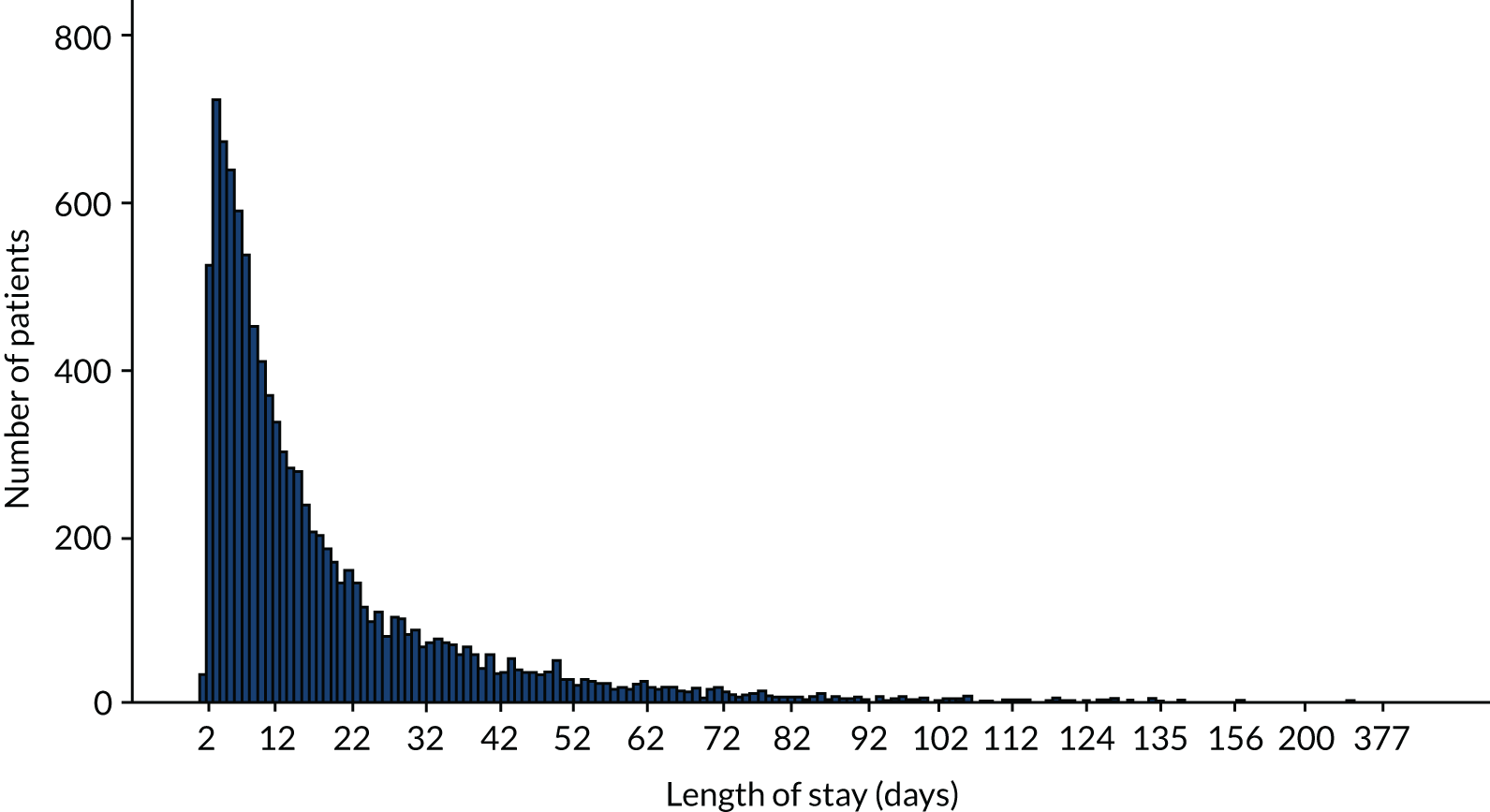
FIGURE 2.
Median length of stay of people with dementia at 200 hospitals in England and Wales.
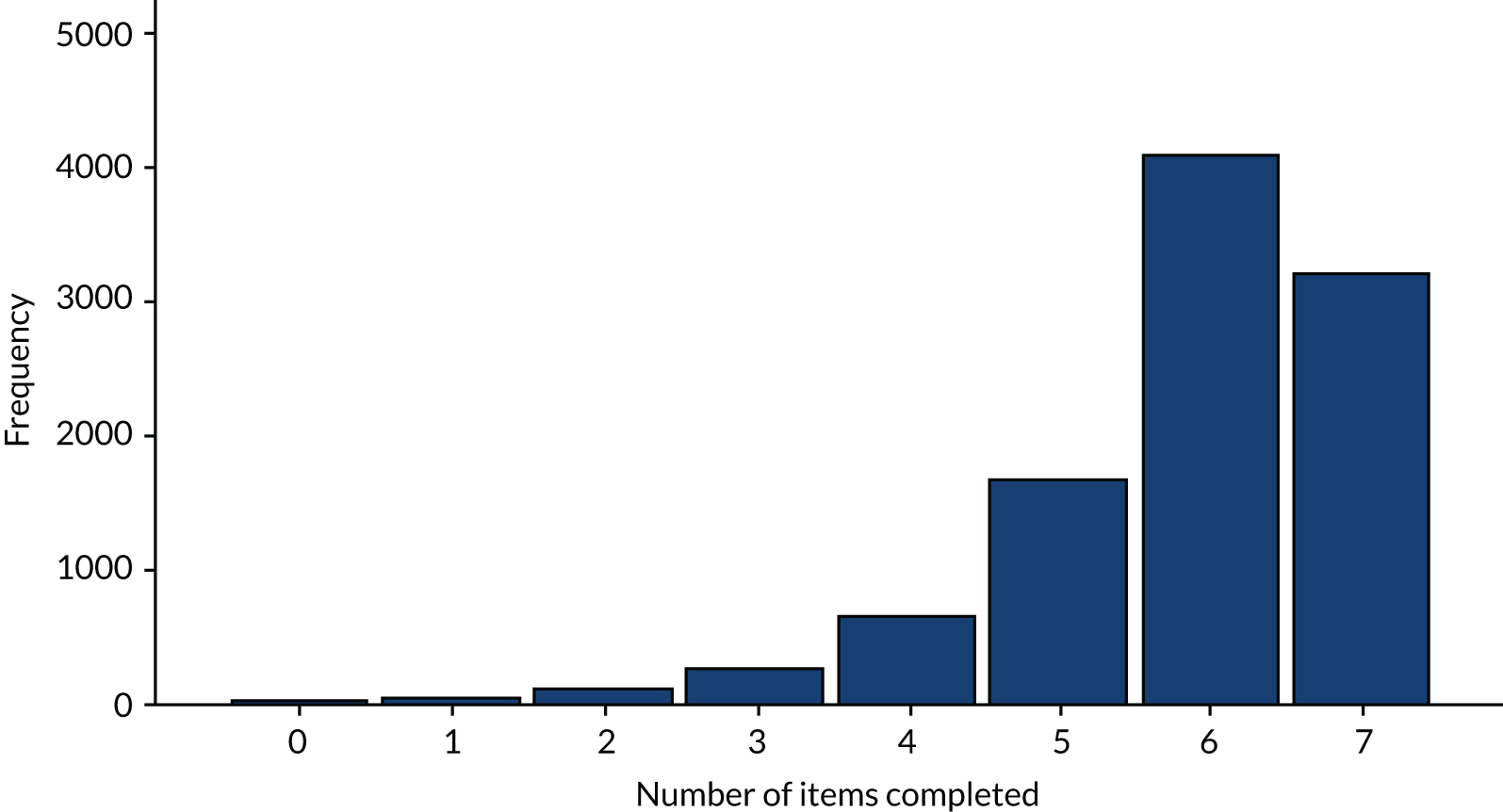
Data on quality of assessment were recorded for all 10,106 (100%) patients in the audit. Variation in the quality of assessment of patients is illustrated in Figure 3. The median number of items of assessment that were completed for each patient was six (n = 4093, 40.50%) and ranged from zero (n = 26, 3.0%) to seven (n = 3210, 31.8%).
FIGURE 3.
Number of items of assessment completed in 10,106 (100%) patient records.
Carer-rated quality of care
In total, 197 hospitals returned a total of 4688 carer questionnaires. Demographic characteristics of the carers who took part in the survey are presented in Table 10.
| Variable | Number | Percentage |
|---|---|---|
| Age (years) | ||
| 18–24 | 48 | 1.0 |
| 25–34 | 135 | 2.9 |
| 35–44 | 259 | 5.5 |
| 45–54 | 753 | 16.1 |
| 55–64 | 1200 | 25.6 |
| 65–74 | 965 | 20.6 |
| 75–84 | 891 | 19.4 |
| ≥ 85 | 343 | 4.0 |
| Missing | 94 | 2.0 |
| Gender | ||
| Male | 1418 | 30.2 |
| Female | 3168 | 67.6 |
| Other | 4 | 0.1 |
| Missing | 98 | 2.1 |
| Ethnicity | ||
| White | 4102 | 87.5 |
| BAME | 410 | 8.7 |
| Prefer not to say | 124 | 2.6 |
| Missing | 52 | 1.1 |
Forty-eight hospitals returned fewer than 10 carer questionnaires and data from these hospitals were excluded from subsequent analysis. Among the 149 hospitals that returned useable data from the survey, the median aggregate score for carer satisfaction was 72.3, ranging from a minimum score of 21.8 to a maximum score of 93.3 (mean 71.84, standard deviation 10.14).
Liaison psychiatry data
Data for the 2015 audit of psychiatric liaison services were returned by teams serving 176 of the 200 hospitals that took part in the dementia audit. Data submitted on the two predictor variables we used in our analysis are presented in Table 11. Six of the 176 teams did not provide information about the hours of operation of the liaison service and seven did not provide information about whether or not the liaison service included an old age consultant psychiatrist.
| Predictor variable | Number | Percentage |
|---|---|---|
| Liaison hours | ||
| No service | 3 | 1.5 |
| Part time (< 40 hours/week) | 1 | 0.5 |
| Working hours (40 hours/week) | 3 | 1.5 |
| Extended hours (> 40 hours/week) | 72 | 36.0 |
| 24 hours | 91 | 45.5 |
| Missing | 30 | 15.0 |
| Team includes a specialist old age psychiatrist | ||
| Yes | 83 | 41.5 |
| No | 86 | 43.0 |
| Missing | 31 | 15.5 |
Factors associated with average length of stay
Association between explanatory variables and mean length of stay are presented in Table 12. Univariate associations were found between length of stay and the primary diagnosis of the patient, the type of ward the patient was treated on and the ethnicity of the patient, with BAME patients tending to have shorter admissions to hospital. When there was documented evidence that discussions with carers had taken place prior to discharge, the average length of stay was higher. When there was documented evidence that discussions had taken place with the patient’s consultant prior to discharge, the average length of stay was also higher. Patients whose records indicated that discharge planning had been initiated within 24 hours of admission had, on average, shorter lengths of stay in hospital.
| Predictor variable | Estimated effect | 95% CI | p-value |
|---|---|---|---|
| Patient age (n = 8817) | 0.0005 | –0.0018 to 0.0028 | 0.665 |
| Patient gender (base: male) (n = 8817) | |||
| Female | 0.0181 | –0.0188 to 0.055 | 0.337 |
| Patient ethnicity (base: white) (n = 8638) | |||
| BAME | –0.067 | –0.1225 to –0.0112 | 0.019 |
| Ward type (base: care of the elderly) (n = 8807) | |||
| Cardiac | –0.4553 | –0.5705 to –0.3401 | < 0.0001 |
| Other | –0.6204 | –0.7792 to –0.4616 | < 0.0001 |
| Critical care | –0.0777 | –0.5571 to 0.4016 | 0.751 |
| General medical | –0.326 | –0.3758 to –0.2769 | < 0.0001 |
| Nephrology | –0.1999 | –0.4538 to 0.0540 | 0.123 |
| Obstetrics/gynaecology | –0.2412 | –0.5156 to 0.0333 | 0.085 |
| Oncology | –0.1058 | –0.4694 to 0.2580 | 0.569 |
| Orthopaedics | 0.0301 | –0.0354 to 0.0955 | 0.368 |
| Stroke | –0.0651 | –0.1580 to 0.0279 | 0.170 |
| Surgical | –0.4090 | –0.4826 to –0.3354 | < 0.0001 |
| Other medical | –0.361 | –0.4262 to –0.2974 | < 0.0001 |
| Primary diagnosis (base: respiratory) (n = 8798) | |||
| Other | 0.1066 | 0.0416 to 0.1716 | 0.001 |
| Fall | 0.2624 | 0.1989 to 0.3259 | < 0.0001 |
| Urinary/renal | 0.0069 | –0.064 to 0.0783 | 0.850 |
| Hip fracture/trauma | 0.4249 | 0.3524 to 0.4974 | < 0.0001 |
| Sepsis | 0.1108 | 0.0251 to 0.1965 | 0.011 |
| Delirium/confusion/cognitive impairment | 0.3068 | 0.2413 to 0.3722 | < 0.0001 |
| Gastrointestinal | –0.1364 | –0.2198 to –0.0529 | 0.001 |
| Cardiac/vascular/chest pain | –0.0245 | –0.1136 to 0.0645 | 0.590 |
| Stroke/neurological | 0.1825 | 0.1032 to 0.2617 | < 0.0001 |
| Discharge planning within 24 hours (base: no) (n = 7384) | |||
| Yes | –0.1850 | –0.2368 to –0.1348 | < 0.0001 |
| Not applicable | 0.1140 | 0.0592 to 0.17024 | < 0.0001 |
| Discussion of discharge plan with carer (base: no) (n = 7384) | |||
| Yes | 0.3596 | 0.3120 to 0.4072 | < 0.0001 |
| Discussion of discharge with consultant (base: no) (n = 8817) | |||
| Yes | 0.2644 | 0.2142 to 0.3147 | < 0.0001 |
| Executive board reviews delayed discharges (base: no) (n = 8817) | |||
| Yes | –0.0355 | –0.1180 to 0.0468 | 0.396 |
| Hospital deploys dementia nurse specialists (base: no) (n = 8817) | |||
| Yes | 0.0274 | –0.1097 to 0.0550 | 0.513 |
| Social worker or other designated person (base: no) (n = 8817) | |||
| Yes | 0.0338 | –0.0574 to 0.1251 | 0.466 |
| Hospital has dementia care pathway/bundle (base: no) (n = 8817) | |||
| Yes | 0.0451 | –0.0766 to 0.1668 | 0.466 |
| In development | 0.0033 | –0.1300 to 0.1366 | 0. 961 |
| Liaison hours (base: 24 hours) | |||
| No service | 0.9619 | –0.1939 to 0.3863 | 0.514 |
| Part time (< 40 hours) | 0.1726 | –0.0851 to 0.4303 | 0.188 |
| Extended hours (> 40 hours) | 0.0330 | –0.0462 to 0.1121 | 0.412 |
| Liaison service includes old age psychiatrist (base: no) | |||
| Yes | –0.0450 | –0.1221 to 0.0314 | 0.245 |
The results of the multivariate analysis are presented in Table 13. All risk factors were included in the initial full-effects model. This model is reduced by excluding stepwise non-significant effects. The model presented here is the model with the significant effects only. In the multivariate model, the ethnicity of the patient influenced length of stay, with BAME patients spending less time in hospital. As in the univariate analysis, both primary diagnosis and ward type were associated with length of stay, such that patients treated for respiratory conditions had shorter lengths of stay than patients with other conditions, and patients treated on care of the elderly wards tended to have longer admissions than patients admitted to general medical and surgical wards.
| Predictor variable | Interactionsa | Estimated effect (95% CI) | p-value |
|---|---|---|---|
| Patient age | –0.003 (–0.005 to 2.19) | 0.052 | |
| Patient ethnicity (base: white) | |||
| BAME | –0.066 (–0.13 to –0.002) | 0.043 | |
| Ward type (base: care of the elderly) | |||
| Cardiac | –0.33 (–0.47 to –0.19) | < 0.001 | |
| General medical | –0.28 (–0.33 to –0.22) | < 0.001 | |
| Orthopaedics | –0.16 (–0.26 to –0.05) | 0.003 | |
| Surgical | –0.32 (–0.41 to –0.23) | < 0.001 | |
| Other medical | –0.26 (–0.33 to –0.18) | < 0.001 | |
| Other | –0.56 (–0.74 to –0.37) | < 0.001 | |
| Primary diagnosis (base: respiratory) | |||
| Fall | 0.24 (0.17 to 0.32) | < 0.001 | |
| Orthopaedic | 0.39 (0.27 to 0.50) | < 0.001 | |
| Delirium/confusion | 0.25 (0.18 to 0.33) | < 0.001 | |
| Other | 0.13 (0.05 to 0.20) | 0.001 | |
| Discharge planning within 24 hours of admission: yes vs. no | –0.24 (–0.29 to –0.18) | < 0.001 | |
| Executive board reviews delayed discharge: yes vs. no | –0.08 (–0.17 to 0.006) | 0.069 | |
| Evidence of discussing discharge with carers: yes vs. no | 0.26 (0.21 to 0.32) | < 0.001 | |
| Evidence of discussing discharge with consultant responsible for patient’s care | In hospitals with old age liaison psychiatrist | ||
| Yes | –0.039 (–0.12 to 0.05) | 0.367 | |
| No | –0.15 (–0.03 to –0.26) | 0.012 | |
We found further evidence that patients whose records indicated that discharge planning had been initiated within the first 24 hours of their admission had shorter average lengths of stay. When discussions with carers were recorded in case notes, patients had a longer average length of stay. We found an interaction between whether or not the hospital had a specialist old age psychiatrist as part of the mental health liaison service and documented evidence of discussion of the discharge with the responsible consultant. In hospitals in which there was a specialist old age psychiatrist, shorter lengths of stay were found in the records of patients when there had not been a discussion with the responsible consultant, but not found when such a discussion had been documented in the patient’s records. There was a non-statistically significant trend towards patients having shorter average lengths of stay in hospitals when trust boards regularly reviewed delayed discharges.
Sensitivity analysis
We conducted two sensitivity analyses in which we restricted the analysis to subsamples of (1) patients who were admitted with hip fractures or trauma and (2) hospitals that scored above the median carer satisfaction ratings. The results of these analyses are presented in Tables 14 and 15.
| Predictor variable | Interactionsa | Estimated effect (95% CI) | p-value |
|---|---|---|---|
| Ward type (base: care of the elderly) | |||
| Orthopaedics | 0.46 (0.25 to 0.66) | < 0.001 | |
| Surgical | 0.34 (0.04 to 0.65) | 0.29 | |
| Other medical | NS | ||
| Other (non-medical) | 1.34 (0.31 to 2.36) | 0.011 | |
| Executive board reviews delayed discharge | Age | ||
| Yes | –0.02 (–0.04 to –0.005) | 0.010 | |
| No | 0.01 (–0.00 to 0.20) | 0.102 | |
| Evidence of discussing discharge with carers: yes vs. no | 0.41 (0.27 to 0.55) | < 0.001 | |
| Discharge planning within 24 hours of admission: yes vs. no | –0.38 (–0.55 to –0.21) | < 0.001 | |
| Ethnicity | Gender: female vs. male | ||
| BAME | –0.51 (–0.85 to –0.18) | 0.003 | |
| White | –0.06 (–0.23 to 0.11) | 0.474 | |
| Dementia specialist nurse | Gender: female vs. male | ||
| Yes | –0.47 (–0.75 to –0.20) | 0.001 | |
| No | –0.11 (–0.32 to 0.11) | 0.33 |
| Predictor variable | Interactionsa | Estimated effect (95% CI) | p-value |
|---|---|---|---|
| Ward type (base: care of the elderly) | |||
| Cardiac | –0.40 (–0.64 to –0.16) | 0.001 | |
| General medical | –0.28 (–0.38 to –0.19) | < 0.001 | |
| Orthopaedics | –0.23 (–0.40 to –0.06) | 0.008 | |
| Surgical | –0.39 (–0.53 to –0.25) | < 0.001 | |
| Other medical | –0.37 (–0.49 to –0.25) | < 0.001 | |
| Other (non-medical) | –0.57 (–0.86 to –0.28) | < 0.001 | |
| Primary diagnosis (respiratory) | |||
| Fall | 0.30 (0.18 to 0.41) | < 0.001 | |
| Hip fracture/trauma | 0.50 (0.31 to 0.67) | < 0.001 | |
| Cardiac/vascular | 0.21 (0.04 to 0.39) | 0.019 | |
| Delirium/confusion | 0.31 (0.18 to 0.43) | < 0.001 | |
| Other | 0.18 (0.05 to 0.30) | 0.006 | |
| Evidence of discussing discharge with carers | Gender of the patient: female vs. male | ||
| Yes | 0.005 (–0.07 to 0.08) | 0.901 | |
| No | –0.20 (–0.34 to –0.05) | 0.008 | |
| Discharge planning within 24 hours of admission | Old age liaison psychiatrist consultant: yes vs. no | ||
| Yes | –0.29 (–0.46 to –0.11) | 0.002 | |
| No | –0.07 (–0.25 to 0.11) | 0.425 | |
| Social worker or other designated person | Old age liaison psychiatrist consultant: yes vs. no | ||
| Yes | –0.04 (–0.19 to 0.12) | 0.645 | |
| No | –0.41 (–0.66 to –0.16) | 0.002 | |
| Evidence of discussing discharge with consultant responsible for patient’s care: yes vs. no | 0.13 (0.04 to 0.22) | 0.005 | |
Among the restricted sample of patients admitted to hospital with hip injuries, fewer associations were found with average length of stay. Patients whose records included documented evidence of discussion of discharge with carers had longer periods of time in hospital, and patients who had documented evidence of discharge planning being initiated within 24 hours of their admissions spent less time in hospital. Shorter lengths of stay were seen among women from BAME communities, but not among men from these communities. We also found evidence that when the hospital deployed dementia nurse specialists, female patients had shorter average periods of time in hospital.
In the subsample of data from 74 hospitals with high carer-rated satisfaction with care, associations between length of stay and primary diagnosis, and length of stay and ward type, were still seen. Among female patients, there was evidence of shorter admissions to hospital among those for whom there was no documented evidence of discussion with carers about the patient’s discharge. When liaison teams included a specialist old age psychiatrist, shorter lengths of stay were seen when discharge planning had been initiated within the first 24 hours and in hospitals in which patients did not have a designated social worker.
Factors associated with carer-rated quality of care
Association between explanatory variables and mean carer-rated quality of care are presented in Table 16. In the univariate analysis we present the associations between the outcome(s) and each of the predictor variables, without adjusting for the other variables. The only univariate association found was between carer-rated quality of care and carer gender: hospitals with a higher proportion of male carers had higher carer-rated quality of care scores. A non-statistically significant trend was found between higher carer-rated quality of care and greater use of systems for keeping a record of personal information on patients (p = 0.057).
| Predictor variable | Estimated effect | 95% CI | p-value |
|---|---|---|---|
| Carer age (n = 149) | 0.4464 | –3.0949 to 3.9878 | 0.25 |
| Carer gender (base: female) (n = 149) | |||
| Male | –18.3579 | –33.0811 to –3.6347 | 0.015 |
| Carer ethnicity (base: white) (n = 149) | |||
| BAME | –0.0173 | –13.3729 to 13.3384 | 0.998 |
| Patient age (n = 147) | –0.1272 | –1.3350 to 1.0804 | 0.835 |
| Patient gender (base: female) (n = 147) | |||
| Male | –10.8474 | –30.1876 to 8.4928 | 0.269 |
| Patient ethnicity (base: white) (n = 147) | |||
| BAME | 1.8410 | –5.3939 to 9.0759 | 0.50 |
| Personal information collection (mini-audit) per cent had information (n = 148) | 0.0510 | –0.0015 to 0.1035 | 0.057 |
| Care assessment contains section dedicated to collecting info from the carer (n = 147) | 0.54849 | –4.4870 to 5.5839 | 0.830 |
| Evidence of discussing discharge with carers (n = 147) | 3.296335 | –7.7608 to 14.3535 | 0.557 |
| Carer received notice of discharge (proportion of ‘>24 hours’ out of those documented) (n = 147) | 6.5550 | –3.6083 to 16.7183 | 0.204 |
| Documented assessment of carer needs prior to discharge (n = 147) | 4.0628 | –10.907 to 5.1529 | 0.480 |
| Carer visit at any time (n = 149) | –1.8326 | –7.2970 to 3.6318 | 0.509 |
| Social worker or other designated person (n = 149) | –0.0289 | –3.8067 to 3.7488 | 0.988 |
| Food available 24 hours (n = 149) | 0.5655 | –3.5926 to 4.7236 | 0.788 |
| Finger food availability (every day/4–6 days) (n = 149) | –3.0561 | –6.4192 to 0.30696 | 0.075 |
| Strategy for carer in place (base: no) | |||
| Yes | –0.9028 | –5.0064 to 3.2009 | 0.664 |
The results of the multivariate analysis are presented in Table 17. Variables that had no impact on average carer-rated quality of care were excluded from the model. As can be seen in Table 17, hospitals in which there was a carer strategy in place had lower overall carer-rated quality of care scores. We also found a non-statistically significant trend towards hospitals that had care assessments containing a section dedicated to collecting information from the carer, having lower carer-rated quality of care scores [mean difference –3.94, 95% confidence interval (CI) –8.36 to 0.47; p = 0.08].
| Predictor variable | Interactionsa | Estimated effect (95% CI) | p-value |
|---|---|---|---|
| Strategy for carer in place: yes vs. no | –3.83 (–3.89 to –6.61) | 0.021 | |
| Care assessment contains section dedicated to collecting info from the carer | –3.94 (–8.36 to 0.47) | 0.08 | |
| Finger food availability | Social worker/designated person: yes vs. no | ||
| Yes | –7.27 (–11.36 to –3.18) | 0.001 | |
| No | 5.137 (0.56 to 9.71) | 0.028 | |
| Food available 24 hours | Carer gender: proportion of female carers | ||
| Yes | –108.22 (–177.79 to –38.65) | 0.003 | |
| No | –143.66 (–219.53 to –67.78) | < 0.001 | |
| Yes vs. no | 35.44 (29.13 to 41.74) | 0.015 | |
| Food available 24 hours | Patient ethnicity: proportion of BAME | ||
| Yes | –21.71 (–34.29 to –9.13) | 0.001 | |
| No | 1.99 (–16.63 to 20.61) | 0.833 | |
| Evidence of discussing discharge with carers | Carer gender: proportion of female carers | ||
| 0.2 | –89.47 (–142.22 to –36.72) | 0.001 | |
| 0.3 | –71.88 (–114.63 to –29.13) | 0.001 | |
| 0.4 | –54.29 (–87.29 to –21.30) | 0.001 | |
| 0.5 | –36.71 (–60.48 to –12.93) | 0.003 | |
| 0.6 | –19.12 (–35.19 to –3.05) | 0.020 | |
| 0.7 | –1.54 (–14.46 to 11.39) | 0.814 | |
| 0.8 | 16.05 (–1.03 to 33.13) | 0.065 | |
| 0.9 | 33.64 (8.49 to 58.79) | 0.009 | |
| Personal information collection (mini-audit) per cent who had information | Patient ethnicity: proportion of BAME | ||
| 0.05 | 0.06 (0.01 to 0.11) | 0.027 | |
| 0.10 | 0.07 (0.03 to 0.12) | 0.002 | |
| 0.15 | 0.09 (0.04 to 0.13) | < 0.001 | |
| 0.20 | 0.10 (0.06 to 0.15) | < 0.001 | |
| 0.25 | 0.12 (0.07 to 0.16) | < 0.001 | |
| 0.30 | 0.14 (0.09 to 0.18) | < 0.001 | |
| Personal information collection (mini-audit) per cent who had information | Carer ethnicity: proportion of BAME | ||
| 0.02 | 0.06 (0.01 to 0.11) | 0.003 | |
| 0.04 | 0.07 (0.03 to 0.12) | 0.001 | |
| 0.06 | 0.09 (0.04 to 0.13) | < 0.001 | |
| 0.08 | 0.10 (0.06 to 0.15) | < 0.001 | |
| 0.1 | 0.12 (0.07 to 0.16) | < 0.001 | |
| 0.12 | 0.14 (0.09 to 0.18) | < 0.001 | |
| 0.14 | 0.09 (0.04 to 0.13) | < 0.001 | |
| 0.16 | 0.10 (0.06 to 0.15) | < 0.001 | |
| 0.18 | 0.12 (0.07 to 0.20) | < 0.001 | |
| 0.20 | 0.14 (0.07 to 0.21) | < 0.001 | |
| Carer received discharge notice (25–48 hours vs. > 48 hours) | Carer age (years) | ||
| 35–44 | –67.71 (–113.41 to –22.02) | 0.004 | |
| 45–54 | –39.87 (–67.31 to –12.43) | 0.005 | |
| 55–64 | –12.02 (–23.03 to –1.01) | 0.033 | |
| 65–74 | 15.82 (1.94 to 29.70) | 0.026 | |
| 75–84 | 43.66 (12.57 to 74.77) | 0.006 |
We also found a number of statistically significant interactions:
-
As the proportion of female carers increases, carer-rated satisfaction is lower in hospitals that do not have food available 24 hours per day.
-
The impact of discussing discharge with carers in hospitals varies according to the gender of carers at the hospital, such that discussions with carers are associated with higher levels of satisfaction when there are more female carers of patients at the hospital.
-
Collection of personal information is associated with higher satisfaction in areas in which there are more patients from BAME backgrounds.
-
Greater discharge notice is associated with greater satisfaction in hospitals with a higher proportion of younger carers.
Factors associated with quality of patient assessment
Association between explanatory variables and quality of patient assessment are presented in Table 18. Univariate associations were found between quality of patient assessment and the age of the patient, with older patients having a higher-quality assessment. Patients who spend longer in hospital were also noted to have a higher-quality assessment, whereas patients from BAME backgrounds had lower-quality assessments. Higher-quality assessments were seen in hospitals that deploy dementia nurse specialists. The quality of assessment was higher on care of the elderly wards than in other types of wards, and higher in those presenting with falls, hip injuries, cognitive impairment and gastrointestinal problems than those presenting with respiratory problems.
| Predictor variable | Estimated effect | 95% CI | p-value |
|---|---|---|---|
| Patient age (n = 10,096) | 0.0079 | 0.0031 to 0.0127 | 0.001 |
| Length of stay (days) (n = 10,105) | 0.0155 | 0.0135 to 0.0175 | < 0.0001 |
| Patient gender (base: male) (n = 10,106) | |||
| Female | 0.01007 | –0.0664 to 0.0865 | 0.796 |
| Patient ethnicity (base: white) (n = 9896) | |||
| BAME | –0.2424 | –0.3636 to –0.1211 | < 0.0001 |
| Hospital has dementia care pathway/bundle (base: no) (n = 10,106) | |||
| Yes | 0.4542 | –0.0325 to 0.9409 | 0.067 |
| In development | 0.3941 | –0.1406 to 0.9288 | 0.149 |
| Dementia champion at directorate level (base: no) (n = 10,106) | |||
| Yes | 0.3326 | –0.0781 to 0.7432 | 0.112 |
| In development | 0.4617 | –1.7119 to 2.6353 | 0.677 |
| Hospital deploys dementia specialist nurse (base: no) (n = 10,106) | |||
| Yes | 0.3572 | 0.0255 to 0.6889 | 0.035 |
| Ward type (base: care of the elderly) (n = 10,093) | |||
| Cardiac | –0.8213 | –1.0678 to –0.5749 | < 0.0001 |
| Critical care | –0.5973 | –1.3592 to 0.1646 | 0.124 |
| General medical | –0.4402 | –0.5476 to –0.3327 | < 0.0001 |
| Nephrology | –0.2719 | –0.8117 to 0.2679 | 0.324 |
| Obstetrics/gynaecology | –0.2480 | –0.8322 to 0.3362 | 0.405 |
| Oncology | –0.8009 | –1.5991 to –0.0026 | 0.049 |
| Orthopaedics | 0.0044 | –0.1398 to 0.1487 | 0.952 |
| Stroke | –0.2064 | –0.3924 to –0.0205 | 0.030 |
| Surgical | –0.8832 | –1.0410 to –0.7255 | < 0.0001 |
| Other medical | –0.6008 | –0.7390 to –0.4626 | < 0.0001 |
| Other | –0.8660 | –1.2089 to –0.5232 | < 0.0001 |
| Diagnosis (base: respiratory) (n = 10,084) | |||
| Fall | 0.4170 | 0.2827 to 0.5514 | < 0.0001 |
| Urinary/renal | 0.1265 | –0.0257 to 0.2788 | 0.103 |
| Hip fracture/dislocation/other fractures | 0.5793 | 0.4248 to 0.7338 | < 0.0001 |
| Sepsis | 0.1053 | –0.0668 to 0.2775 | 0.230 |
| Delirium/confusion/cognitive impairment | 0.6106 | 0.4693 to 0.7519 | < 0.0001 |
| Gastrointestinal | –0.3550 | –0.5299 to –0.1801 | < 0.0001 |
| Cardiac/vascular/chest pain | –0.1634 | –0.3466 to 0.0197 | 0.080 |
| Stroke/neurological | 0.1376 | –0.0227 to 0.2979 | 0.092 |
| Other | 0.0613 | –0.0742 to 0.1968 | 0.375 |
| Liaison hours (base: 24 hours) (n = 8640) | |||
| No service | 0.1270 | –1.1356 to 1.3895 | 0.844 |
| Part time (< 40 hours) + normal working hours (40 hours) | –0.5420 | –1.6447 to 0.5607 | 0.335 |
| Extended hours (> 40 hours) | 0.0513 | –0.2925 to 0.3952 | 0.770 |
| Liaison service includes old age psychiatrist (base: no) | |||
| Yes | 0.1960 | –0.1397 to 0.5318 | 0.253 |
Results of the multivariate analysis of factors associated with the quality of assessment are presented in Table 19. Unlike length of stay and carer-rated quality of care, quality of assessment is not a continuous outcome and the normality assumption is therefore not valid. Its values are ordered categories so the statistical methodology used in the analysis is ordered logistic regression applied to hierarchical models. We present only the final model, which consists of only the explanatory variables and predictors that had a significant effect on quality of assessment. Significant effects were observed for the following variables: ward type, age of patients, length of stay, dementia champion at directorate level and deployment of dementia specialists. There was also an interaction effect between length of stay and the deployment of dementia specialist nurses.
| Predictor variable | Interactionsa | Estimated effect (95% CI) | OR | p-value |
|---|---|---|---|---|
| Age of patient (in years) | 0.0045 (–0.0004 to 0.0094) | 1.004 | 0.070 | |
| Ward type (base: care of the elderly) | ||||
| Cardiac | –0.56 (–0.82 to –0.29) | 0.57 | < 0.001 | |
| General medical | –0.30 (–0.41 to –0.19) | 0.74 | < 0.001 | |
| Oncology | –0.71 (–1.51 to 0.10) | 0.49 | 0.085 | |
| Orthopaedics | –0.25 (–0.45 to –0.06) | 0.77 | 0.011 | |
| Surgical | –0.70 (–0.86 to –0.53) | 0.49 | < 0.001 | |
| Other medical | –0.43 (–0.57 to –0.29) | 0.64 | < 0.001 | |
| Other | –0.72 (–1.06 to –0.38) | 0.49 | < 0.001 | |
| Primary diagnosis (base: respiratory) | ||||
| Fall | 0.29 (0.15 to 0.42) | 1.32 | < 0.001 | |
| Hip fracture | 0.49 (0.28 to 0.70) | 1.64 | < 0.001 | |
| Delirium/confusion | 0.47 (0.33 to 0.61) | 1.59 | < 0.001 | |
| Dementia champion at directorate level: yes vs. no | 0.39 (–0.03 to 0.81) | 1.47 | 0.071 | |
| Length of stay | Dementia specialist nurse | |||
| Yes | 0.17 (0.01 to 0.021) | 1.017 | < 0.001 | |
| No | 0.022 (0.018 to 0.024) | 1.021 | < 0.001 | |
| Difference between the rates of increase: yes vs. no | 0.021 | |||
| Dementia specialist nurse: yes vs. no | Length of stay: average of 20 days | 0.38 (–0.04 to 0.72) | 1.47 | 0.029 |
Interpreting associations identified in work package 1
In keeping with the design of this mixed-methods study, we used data from work package 1 to develop the content of the semistructured interviews used in work package 2. Feedback from stakeholders, including patients and carers, on the Project Management Group and Stakeholder Reference Group, raised queries about the meaning of some of the associations that we found. Members of the groups were especially interested in the relationship between trust boards and front-line staff on factors that supported effective discharge planning and on why the data appeared to suggest that hospitals that had policies in place aimed at improving carer engagement appeared to have lower levels of carer satisfaction. Members of the groups discussed the possibility that such measures could raise carer expectations, which could lead to lower satisfaction with care. These suggestions and comments fed into the collection and analysis of qualitative data in work package 2 (see Chapter 6).
Chapter 6 Results: work package 2
In this chapter we will present findings from the analysis of the qualitative interviews with staff working in acute hospitals and family carers in the six study sites. As described in Chapter 4, we present the findings in two main sections: the first section (track A) is a thematic exploration of key associations between outcomes of interest and predictor variables found in work package 1; and the second section (track B) presents a realist evaluation account of two areas of interest (carer involvement and staff dementia training).
In total, we conducted 63 interviews in six study sites, comprising seven carers and 56 staff.
The characteristics of the participants we interviewed are presented in Tables 20 and 21.
| Study ID | Gender | Role |
|---|---|---|
| Site 1 | ||
| 1ST001 | Female | Consultant nurse: older adult |
| 1ST002 | Male | Consultant geriatrician |
| 1ST003 | Female | Consultant geriatrician |
| 1ST004 | Female | Clinical nurse specialist: older adult |
| 1ST005 | Female | Sister: acute medical unit |
| 1ST006 | Female | Senior nurse: acute medical unit |
| 1ST007 | Female | Deputy sister: older adult ward |
| 1ST008 | Female | Clinical nurse specialist: orthopaedics |
| 1ST009 | Female | Nurse educator |
| 1ST010 | Female | Clinical nurse specialist |
| 1ST011 | Male | Nursing assistant: acute medical unit |
| 1ST012 | Female | Staff nurse |
| 1ST013 | Female | Staff nurse |
| 1ST014 | Female | Nursing assistant |
| 1ST015 | Female | Senior nurse manager |
| Site 2 | ||
| 2ST001 | Female | Dementia specialist nurse |
| 2ST002 | Female | Staff nurse |
| 2ST003 | Female | Deputy ward manager |
| 2ST004 | Female | Ward manager |
| 2ST005 | Female | Staff nurse |
| 2ST006 | Female | Senior nursing manager |
| 2ST007 | Female | Ward manager |
| 2ST008 | Female | Staff nurse: care of the elderly ward |
| 2ST009 | Female | Ward administrator |
| 2ST010 | Female | Consultant geriatrician |
| 2ST011 | Female | Senior medical manager |
| Site 3 | ||
| 3ST001 | Male | Older adult consultant |
| 3ST002 | Female | Staff nurse: care of the elderly ward |
| 3ST003 | Female | Ward manager |
| 3ST004 | Male | Clinical nurse specialist |
| 3ST005 | Female | Clinical nurse specialist |
| 3ST006 | Female | Carer support worker (CSW) |
| 3ST007 | Female | Carer support worker (CSW) |
| 3ST008 | Female | Carer support worker (CSW) |
| 3ST009 | Female | Senior carer support worker (CSW) |
| 3ST010 | Female | Clinical sister |
| 3ST011 | Female | Senior nursing manager |
| 3ST012 | Female | Senior nursing manager |
| 3ST013 | Female | Senior medical manager |
| Site 4 | ||
| 4ST001 | Female | Research nurse |
| 4ST002 | Female | Staff nurse |
| 4ST003 | Male | Senior manager |
| 4ST004 | Female | Research nurse |
| 4ST005 | Female | Consultant geriatrician |
| 4ST006 | Female | Research nurse |
| 4ST007 | Male | Research nurse |
| 4ST008 | Female | Research nurse |
| 4ST009 | Female | Dementia co-ordinator |
| 4ST010 | Female | Dementia co-ordinator |
| 4ST011 | Male | Dementia co-ordinator |
| 4ST012 | Female | Dementia co-ordinator |
| Site 5 | ||
| 5ST001 | Male | Consultant physician |
| 5ST002 | Female | Operational lead |
| 5ST003 | Female | Occupational therapist |
| Site 6 | ||
| 6ST001 | Female | Dementia specialist |
| 6ST002 | Female | Educator |
| Study ID | Gender | Relationship to the patient |
|---|---|---|
| Site 1 | ||
| 1CA001 | Female | Daughter |
| Site 2 | ||
| 2CA001 | Female | Wife |
| Site 3 | ||
| 3CA001 | Female | Wife |
| 3CA002 | Female | Daughter |
| 3CA003 | Female | Daughter |
| 3CA004 | Female | Daughter |
| 3CA005 | Female | Daughter |
Track A: qualitative exploration of factors associated with patient outcome
In our qualitative interviews, we explored some of the associations found between the outcomes of interest and predictor variables in work package 1. In this section, we provide a thematic interpretation of associations found in the work package 1 quantitative data analyses, to explain some of the quantitative data trends.
Length of stay
The associations found between outcome measure ‘length of stay’ and predictor variables are described as follows. As presented in Chapter 5, in the primary multivariate analyses, these associations were:
-
shorter average length of stay and documented evidence that discharge planning is initiated within 24 hours of admission
-
shorter stays and executive boards reviewing delayed discharge for people with dementia (the effect is borderline)
-
longer stays and carer involvement in discharge planning.
Each of these associations were explored in our interviews. Here, we present the findings and use direct quotes to put these findings into context. To ensure anonymity and identity protection, the participant identifiers accompanying direct quotes will be restricted to the participating site, whether they are carers or staff and participant number (e.g. 3ST012 indicates that the participant is a member of staff from site number three and recorded as participant number 12 in this site).
How documented evidence of discharge planning initiated within 24 hours of admission can impact on length of stay
The results from the secondary analysis of audit data suggested that the length of stay was shorter for patients who had their discharge planning initiated within the first 24 hours of admission than for those for whom the discharge planning was not initiated. This was explored further in the subsequent qualitative interviews with staff. The emergent themes were (1) level of complexity, (2) multidisciplinary and/or cross-organisational communication, (3) accountability, (4) too early and futile, (5) putting off making difficult decisions and (6) strategies for reducing length of stay.
Level of complexity
Most staff believed that discharge planning within the first 24 hours of admission for patients who do not have complex needs could usually ensure timely discharge. Factors such as having a listed next of kin at the time of admission would facilitate gauging whether or not the patients are at their baseline (before admission) cognitive function and have an impact on the decisions that the clinical team would make about the treatment trajectory. This would have a direct impact on the quality of assessment and lead to a smooth and timely discharge. However, some staff were unsure about the value of early discharge planning for patients with more complex needs. Although staff spoke about planning an expected discharge date on admission, there were clear differences between hospitals that have and hospitals that do not have strategies in place for early identification of complexities, needs and planning:
When they come in we just put an expected date of discharge, so we plan ahead . . . So we put that and then as days go by we find that, no, this patient won’t be able to go back to their home or usual environment because their condition has deteriorated. Or we think that if they go home with a package of care they might not be able to open the door for the carers when they come in, they might wonder, So we can’t just say OK we’re sending them home . . .
2ST004
In hospitals with higher scores for carer-rated quality of care, staff strongly believed that established multidisciplinary team meetings will lead to a smooth and timely discharge, as issues are identified early. Having this infrastructure in place means that complexity would not stop staff planning the discharge. Staff in other hospitals were explicit about how they might not always start the discharge planning straight away due to foreseen complexities:
I have a patient who let’s say has a pneumonia. I know that they’ll need maybe four days of IV [intravenous] antibiotics or maybe two days of IV antibiotics, but I think it might take four days to wean them off the oxygen. Would I start thinking about discharge explicitly then? No, I wouldn’t. Should I? Probably.
5ST001
Multidisciplinary and/or cross-organisational communication
In some hospitals there are daily meetings with multidisciplinary teams, in which patients with complex needs are identified early on, and an estimated discharge date and plan is allocated to each patient, regardless of their level of complexity. It emerged that hospitals that hold daily multidisciplinary team meetings are more likely to achieve the intended discharge date, as complex needs are identified early on and attempts are made to facilitate timely discharge. Most patients with complex needs also require support from social services and community care providers. In hospitals in which there is an established link with community services and regular meetings with a Clinical Commissioning Group (CCG), issues are flagged up early on and plans are made accordingly, which ultimately leads to a timelier discharge:
Yes. I mean it might be that the transfer care nurse thinks: I don’t know where we’re going with this. So, what happens in here is there is a daily meeting between myself, someone from the local authority and someone from the CCG. And the transfer care nurses will bring that patient to that meeting, and then cross organisation will come up with a plan and then a solution. And if we can’t find one we’ll escalate. We have got two escalation policies as well. So, we’ve got that cross-organisational working right from the beginning, which will hopefully unblock the patient as well.
5ST002
Accountability
In further interviews, the issue of accountability was raised. Daily review meetings mean that challenging discharge issues will become apparent and a member of staff will need to take the responsibility for resolving this issue and be required to report back the following day:
It’s very clear who owns the delayed transfer and what we’re waiting for. So, it could be something as simple as package of care being delayed. So, that immediately goes to the person that’s responsible for that package of care and they will come back the next day to say: OK, that’s what we’ve sorted, and this is when it can start. It doesn’t get hung over or rolled over, so it is about the accountability and the ownership.
3ST013
Too early and is futile
We sought to explore the reasons why, in some circumstances, discharge planning does not start in the first 24 hours of admission and if staff working in acute hospitals believed that this would contribute to longer stays. Staff reported that for complex patients, factors such as the availability of care homes that can provide enhanced care for patients with complex needs play a significant role in discharge. Others commented that early discharge planning is futile and would not have an impact on the length of stay because there are too many unknown factors involved in the recovery of a patient with dementia. In addition, in many circumstances, the existing care package would no longer be suitable at the time of discharge:
I think this whole concept of, as soon as somebody comes in, you need to be thinking about discharge, and that’s something that I have been taught since I started nursing years ago, I just think it’s the most unrealistic thing . . . there’s actual discharge planning, which, for acute older people who are unwell, it’s really hard to do, and there’s so many factors, and I think planning for discharge on the day, I just don’t know how realistic it is . . .
1ST004
Putting off making difficult decisions
One of the emerging themes from interviews was the belief that working out where a patient with dementia lies on the spectrum of needs is one of the most complicated assessments that staff need to make. This complexity leads to many staff putting off making the decision about a discharge date. Various staff members might conduct a thorough assessment at the time of admission, which includes information required for a safe, organised discharge. However, the information is not always used in a systematic way to initiate discharge planning, so sometimes the work done, which contributes to discharge planning, is thus invisible:
. . . in my sort of first assessment I have a lot to assess for a patient with a broken hip, the sort of getting them ready for surgery and so on. And a lot of the information I gather is useful in future discharge planning, but it’s not recorded in those terms . . . So, in a sense discharge planning has started. I’ve discovered how far they can walk, how many carers they have, how bad their dementia is, and what led to their fall. All of these things contribute to a healthy organised discharge, but they don’t go in a discharge planning box.
4ST005
Most staff agreed that hospitals are not the best environment for a patient with dementia and that patients will benefit from an early discharge. However, staff believed that patients with complex needs might not necessarily fit the existing dementia pathways. In these circumstances, staff would end up spending unnecessary time to try to ‘fit a patient in a box’ (existing dementia pathways), which leads to longer stays.
Strategies for reducing length of stay
During interviews with staff, we became aware of new strategies that hospitals have used to reduce length of stay for patients with dementia. A few hospitals in England had adopted the strategy of trying to avoid assessing patients’ needs while they are in hospital. The rationale is that patients might present very differently in unfamiliar environments, and that they adapt and implement better coping skills when discharged. The system is tier based, which means that depending on the severity and complexity of patients’ presentation, hospitals adopt one of three approaches: discharge to (1) home with no additional package of care or assessment, (2) home with a plan for assessment at home after discharge, or (3) an intermediate care provider with a plan for assessment after discharge.
How executive boards reviewing delayed discharge for people with dementia can impact on length of stay
One of the findings from work package 1 was that patients in hospitals for which an executive board reviews delayed discharge had shorter stays, on average. We explored this further in our qualitative interviews with staff working in acute hospitals, focusing on how decisions made at board level are implemented on individual wards. The emergent themes were (1) identification of recurrent patterns of delayed discharge, (2) co-operative working compared with micromanagement and (3) external factors.
Identification of recurrent patterns of delayed discharge
Staff in various hospitals shed light on this matter. Regular executive board reviews mean that delays are flagged up, and issues that need to be discussed are escalated and negotiated with local authorities when patients are waiting for a care package.
Review of delayed discharge provides the opportunity for finding patterns of recurrent situations that lead to long hospital stays. Staff believed that very often lengthy stays are due to local policies (e.g. when the CCG refuses to commission intermediate care or divert enough resources to care support agencies).
Some councils require assessments to be performed by multiple organisations. For example, in some areas, council-run nursing homes require a full assessment to be conducted, despite one having already been performed by the multidisciplinary teams at hospital:
And unless senior members are aware of patterns across their hospital of recurrent causative situations then they can’t really address those. And I can get frustrated by something that I see recur but if it’s just my ward I’ve only ever got, you know, three examples to give . . . it doesn’t carry so much weight. Whereas, I think if the Chief Executive rings up the Chief Exec [Executive] of the CCG and says, look, here’s a major issue we have, it trickles down to some potential effect.
4ST005
Cooperative working compared with micromanagement
Staff said that in circumstances when there is no representation of ward-level staff at the board meetings, the reviews might be a source of contention. Some senior dementia leads were explicit about difficult conversations they have had with executive boards when early discharge had not been deemed in a patient’s best interest. These senior staff believed that executive board involvement is only effective when there is a co-operative working relationship in place, and members of the board are fully aware of and in agreement with the memorandum of understanding:
Micromanagement is not really of use because they’ll fixate on one thing without having a background knowledge on it. But, actually there are at least within the senior level, people who understand the process and are able to put the challenge into the community support services, etc. But I’m not sure that the board are the right people for that.
3ST012
External factors
Staff believed that executive board review would not have a huge impact in circumstances in which the delay is caused by factors out of the board’s control (e.g. when family members are taking a long time to choose a care home for their relative):
I think it’s good that they [executive board] have an awareness, but it doesn’t always make things happen quicker . . . say for example [with] family having to pick a home and they’re a self-funding patient. Sometimes the issues are that the family take as long as they may need. So sometimes those meetings don’t always help to speed up. But if there are issues like maybe someone is waiting for package of care, they can then escalate it appropriately . . . maybe.
3ST003
Other factors that lead to longer patient stay include socially isolated patients who do not have family members living nearby, which means that staff need to organise more social care on discharge. Staff mentioned that if during admission it transpires that a patient’s needs have reached a level where they need an assessment to determine if they qualify for NHS-funded care, this most likely would delay discharge, as the process of continuing care health-care assessment takes a long time to complete:
Well I think although the care here is good, hospital is never a good place for somebody with dementia and being back in their own home as quickly as possible is always going to be the thing that, in the long run, will lead to better outcomes. But there are quite a lot of older people living in this area who are quite socially isolated, which means that their need for input from social care is much more, because they don’t even have somebody who will go and buy them a pint of milk.
1ST003
How carer involvement in discharge planning can impact on length of stay
One of the findings from work package 1 was that involving carers in discharge planning is associated with longer admissions for patients with dementia. We explored this finding in our interviews with staff and carers. We also presented these findings to the Project Management Group. Staff and some members of the Project Management Group told us that the reason for this association could be that the longer the patient stays in hospital, the more likely they are to have documented evidence of carer involvement. This association was explored further in our interviews with staff and carers, to understand if, why and when carers might be obstructive to a timely discharge. It emerged that, in most cases, family carers are aware that hospitals are not the best environment for someone with dementia:
I have seen it because the family have got strong views about somebody, about their level of dementia or what they can and can’t do. But I’ve also seen it being very supportive where people are like, yes, we know this or really pushing to get the person out . . . They don’t want them in hospital. They want them in an environment where they will be cared for with taking into consideration their dementia for a long-term . . . so, it works both ways.
3ST012
However, in circumstances when family members have unrealistic expectations, or when hospitals fail to involve family members meaningfully from the outset, it is more likely that involving carers will lead to longer patient stays. In situations when family carers think that they are unheard by health and social care professionals in the community, and/or when family carers are exhausted and see a hospital stay as respite, they might dispute discharge plans, which results in a longer stay:
The only thing I was a bit disappointed with was when they kept saying that they couldn’t put her in the rehab, because I think she came home too early, really, me personally, but that’s just I don’t think she was ready to come home. I still don’t. Even now she’s not right. That’s probably just a part of more the dementia than the . . . Like you say, the physical side of it, even now she’s mending OK.
3CA005
In more complex cases, patients might deteriorate during their hospital stay, and the assessments performed in hospital require the family carers to make some significant changes to their homes to make it safe for their relative with dementia. These changes take time and, in some circumstances, it puts a lot of pressure on family carers, and might result in disputes over the time of discharge among different members of a family and/or with hospital:
You probably expect the length of stay to be extended a little bit. But part of that could be driven by family members not wanting their parents to be discharged home sooner despite them being well enough to go home. There’re sometimes other complex issues in the background. Certainly, even family dynamics, if families don’t talk to you, certainly if there’s two or three different people who agree, disagree about care that can cause problems in itself because they’ll disagree on what would be best for their parent or relative as to where they should be going.
1ST002
Carer-rated quality of care
As detailed in work package 1 results (see Chapter 5), we found that hospitals in which there is a strategy for carer involvement in place have lower carer-rated quality of care scores. We found a borderline significant association between hospitals in which the care assessment contained a section dedicated to collecting information from the carer and having lower carer-rated quality-of-care scores. In hospitals with higher proportions of patients and carers from BAME communities, we found that levels of carer-rated quality of care was higher when there was greater availability of personal information about patients in documents, such as This is Me. 63
In our qualitative interviews we sought to explore the reasons why carer satisfaction may be lower in hospitals when there appeared to be more evidence of organisational efforts to involve carers. Factors that might explain this association include raising expectations and not delivering what was promised, whereas early planning, clear communication and consistency were things staff could do to help manage carers’ expectations.
Interviews with front-line staff and managers suggested that carer involvement could also be a source of contention and may lead to certain challenges. In circumstances in which staff obtain information from carers, but do not address their concerns, the collection of such information could adversely impact the carer-rated quality of care, as care will be perceived as not having been delivered up to expectations:
If someone says oh she likes going for walks outside, or she doesn’t like to eat this or that. We can’t take people outside realistically, there is not enough staff to give care on the wards, let alone to take someone out and walk with someone outside. And the food that’s available is limited by what’s on the menu. And now with health and safety there is sometimes governing what people can bring in, etc. So sometimes you can ask for a lot of information, but you can’t necessarily do what you would like to do with it.
4ST006
Interviews with carers also highlighted that collecting information that is not fully followed through could potentially lead to carers’ dissatisfaction with care provision:
Mum tended to eat with that little spoon, don’t like the big one going in, and I said to them can you feed her with the little spoon because she doesn’t like that big one going in. I even got about 20 out of McDonald’s and leave them up there, but when I come up, they still were feeding her with the big silver one.
1CA001
Staff believed that discharge arrangement is an area that is most likely to be the source of family carer dissatisfaction. Although staff make efforts to involve carers in discharge planning, they can only advise other parties involved (e.g. social services) and are not necessarily in control of what happens, which might be perceived as not delivering what was promised:
I think it makes us a little bit tentative, to say that the person can definitely go home with four times a day care, or they can definitely go to a care home, because although we are going to give information to the social worker, we are not the decision-maker in that situation. I think that makes communication slightly more difficult.
2ST007
Some family carers might be seen by staff to be obstructive to the discharge process, as they prefer their family members to stay longer in the hospital for various reasons. Disagreements about time of discharge will lead to carer dissatisfaction.
Carers also commented on the importance of clear communication during their relative’s hospital stay. Carers spoke of the many occasions where they had felt that they were left in the dark by staff about the progress of their relative’s illness, and commented on how they would have appreciated a more structured and frequent communication:
If you see where I’m coming from . . . an update for dementia patients would be brilliant, because you can’t go to your relative and say, what did the doctor say to you today? Because they can’t know . . . they wouldn’t be able to tell you.
3CA001
To minimise subsequent conflicts and manage carers’ expectations, hospitals have put some measures in place. Staff believed that envisaging potential problems early on means that meetings are arranged with the relatives to discuss the discharge plan. Staff were adamant that in these meetings they would make it clear to relatives that although they will continue to address the family’s concerns, hospitals will progress with the discharge, as the plan is based on the offer from the commissioners:
. . . unfortunately, a lot of it is the expectations of carers, and it’s the expectations that we can’t always deliver. Because obviously the system can’t deliver what sometimes, what they want . . . we will offer them all the support to manage that message [discharge plan], but ultimately that is the message that we have to give.
5ST002
Staff believed that, in some cases, patients do not require the level of care their relatives might ask for. Although these disagreements might lead to some very difficult conversations, engaging carers early on and keeping them informed could minimise the contentions.
Lack of consistency was something else that was considered to contribute to carer dissatisfaction. In some hospitals, there are designated members of staff whose role is to liaise with carers and to ensure that all staff members are fully aware of the hospital policy and discharge strategy. Barriers include when hospitals have staff shortages and need to employ agency staff who might not be fully aware of the strategies and discharge plans for any individual patient.
This feedback contrasted with examples that staff gave of when use of documents, such as This is Me,63 which contain details about a person’s background and important events, people and places from their life, had supported the delivery of better care:
And things like how people eat and drink as well, having that written down, because if you are vegetarian and you keep getting delivered meat and you haven’t got the ability to communicate that, then staff just goes, she’s off her food, she’s not eating and drinking. Well actually it’s because you keep giving her the wrong food, or somebody delivers like a really milky cup of tea with no sugar and someone likes it strong with three sugars, we assume it’s because she’s off her food and drink, well actually you just made her a really bad cup of tea. It’s nothing to do with anything else. So, it does help having that written down.
1ST004
Indeed, staff offered us many tangible examples on how ensuring that staff have access to personal information can lead to better-quality care for patients with dementia. For example, in situations in which a patient is distressed and might mention a family member, if staff are aware who and what the patient is talking about, they can comfort the patient and reassure them. Staff believed that having this information not only reassures patients and calms them, but also lowers the level of anxiety in staff who otherwise would not know how to react and what to do to calm the patient:
We are using This is Me. Some people I’ve spoken to have said, God, this is amazing because my dad gets car sick and, there’s never a space to tell anybody that. Because he gets transport home, because there might be an issue, and I can actually write it down. But then again, if you’ve done it all and then people are not taking any notice of it that must be really annoying.
2ST001
Track B: theory testing and refinement (realist evaluation)
In this section we present CMO configurations for two main areas: (1) staff dementia training and (2) carer involvement. As described in Chapter 4, our choice was guided by, and based on, the richness of data collected from the first three study sites. In the subsequent interviews and in further sites, we refined our theories. As described in Chapter 4, CMO configuration is a theory or hypothesis about how a particular mechanism works in a specific context to lead to an outcome.
Staff training
One of the recurrent themes from the interviews with staff was the importance of dementia-specific training for staff who provide care for patients with dementia. Staff members unanimously believed that dementia training plays an important role in ensuring good-quality care. Staff education in dementia care has the potential to make a significant impact on the quality of dementia care provision, as it enables staff to realise that they can be flexible in their approach to deliver care in a more individually appropriate manner.
We now present some CMO configurations that explain how, why and under what circumstances dementia-specific training can lead to higher-quality care and shorter inpatient stays.
Example 1
When training material includes ‘simulation sessions’, in which trainees are encouraged to feel what it must be like for patients with dementia (context), this gives trainees insight into experience and perspective of patients with dementia (mechanism 1), and would enable them to empathise with and be more aware of the difficulties that patients with dementia experience (mechanism 2); this leads to staff providing more person-centred, dignified and humane care (outcome):
You put a headset on, dark room [for a simulation session]. I cried my eyes out afterwards. So, I couldn’t believe that people live like that. And that’s the part of it that you don’t realise. So, when you’re put in their shoes it just makes me want to help them even more.
3ST009
Example 2
Assuming that there is enough training available for staff, in hospitals in which there is an in-house educational training lead or dementia specialist nurse (context), they monitor how taught materials are put in practice by role modelling best practice (mechanism 1) and they also provide short ad hoc sessions when gaps in knowledge and practice are identified (mechanism 2); this leads to providing a more consistent care (outcome 1) and reduction in unnecessary lengthy stays (outcome 2):
What makes a difference is when, there’s always a question about implementing what you learn in a classroom into practice, and that bridge has always been difficult in every aspect of nursing.
1ST004
That’s the only way I can see, from being in this for a long time, that you can really influence the quality of care . . . by me modelling best practice, asking the questions, oh, I think he’s got dementia, shall we find out? I know he’s got dementia, should we put a This is Me up? Or walking past saying, oh he’s got a This is Me, can you put the Forget Me Not up? And just reminding staff, it takes a long time and it is hard work and you take two steps forward, 10 steps back sometimes.
1ST004
Example 3
When dementia training is delivered to a wide range of staff working with patients with dementia, including volunteers, hostesses and ward clerks (context 1), and when the training material addresses practical issues, such as how to deal with challenging situations (context 2), this upskills the professionals and other staff and makes them feel confident in dealing with challenging situations (mechanism), which ultimately leads to person-centred, individualised and consistent care provision (outcome):
But it’s things like the housekeeping staff, people that bring and take the food away, the people that clean and change the beds. Now, you know, it’s all very well for all the nursing staff and all the doctors to be fully aware of what to do with dementia, but if, you know . . . One occasion I was there for lunch, a chap brought his food, on a red tray, which is supposed to signify that he needs help, and put it in front of him. He must have come back not more than 5, 10 minutes later, and he said, have you finished? And I was a bit stressed that day, and I said, I’m sorry, but does it look like he’s finished, you know, he hasn’t even started. So, I feel that had I not been there, that tray would have just gone, and he would not have got any food.
3CA004
Example 4
In hospitals in which training is delivered using real-life scenarios and reflective practice (context), this enables staff to come together and openly talk about challenges that they have faced, and realise they are not alone with these experiences and that others face the same sort of challenges (mechanism 1), which helps to alleviate professional anxiety and guilt they may feel about ‘not ideal’ and ‘task-oriented’ practice that they have carried out (mechanism 2), which leads to providing more dignified, humane care for patients with dementia (outcome):
You can teach people in the classroom but actually what is the benefit if you can’t relate what you’ve learnt to real-life practice? So, what we do in the training is we do a lot of reflection about things that have happened in the past and then we talk about how we could have done those situations differently. And then I’ll go to the wards and work with nursing assistants.
1ST009
Carer involvement
Carer involvement comprises various strategies that hospitals might adopt to actively involve family carers in different stages of patient stay in acute settings, from admission through to discharge planning. Overall, staff believed that having family carers on board will lead to providing better quality of care for patients with dementia. Presence of family carers allows patients to settle, as they are better able to make patients feel at home by following the routines the patients are used to.
Staff also spoke about difficulties when there is no family carer or relative present who can advocate for the patient and be consulted on various issues. Lack of family carers also means that hospitals need to organise more social care for patients on discharge.
In the subsequent series of CMO configurations, we elaborate on how, and why, carer involvement strategies might lead to positive outcomes.
Example 1
In hospitals in which carers are allowed to be present or stay on the wards, and be more involved in providing care to patients (context), it allows patient to be more settled and makes the hospital environment more familiar (mechanism 1), making them more likely to co-operate with attempts to give them medication, and ensure that they eat and drink well (mechanism 2), which leads to faster recovery (outcome 1), timely discharge planning (outcome 2) and better quality of care (outcome 3):
They fairly soon realised that he wasn’t terribly keen on the monotony of hospital food. There again, someone with dementia, you ask them what they want for lunch, they’re going to give you a random answer. When it comes, they don’t want it. And he got rather tired of baked potatoes and baked beans. More than one ward staff actually asked, can you bring something in to try and tempt him, because he lost over 2 stones. I think that’s quite significant.
2CA001
Example 2
In hospitals in which there is clear communication between staff and family carers (context), this ensures that family carers understand the progression of their family member’s dementia (mechanism) and have realistic expectations (mechanism), which leads to a higher carer-rated quality of care (outcome 1) and timely discharge planning (outcome 2):
And sometimes the patient doesn’t need what they [carers] want. So, it can lead to quite difficult complex situations. But what we find is, if we’re engaged with carers from the beginning keep them informed, it does minimise that conflict.
5ST002
Example 3
In circumstances when there is a lack of carer or family involvement (context), this makes it difficult for staff to find out information about patients, including their medical history, normal functional level and cognitive baseline (mechanism), which can lead to patients being kept in hospital for longer than they need to be (outcome):
We will try and engage carers. We had one gentleman that was really agitated at night and wouldn’t settle down. But once we’d spoken to his carers, they told us that he always liked to check the doors and windows were locked before he went to bed. So, the staff let him get up, he went and checked all the windows and doors and he just went to bed. So that’s the difference about getting their involvement. This gentleman could have been really close to being sedated because he was getting very agitated, very upset, putting himself at the risk of falls, but that one simple thing, because of the information and engagement with carers, actually meant that he didn’t fall . . .
3ST011
Organisational and contextual factors
One of the emergent themes across interviews was the focus on organisational culture and contextual factors that enable staff to provide more dignified and humane care for patients with dementia. Based on our findings, we have compiled a list of factors (derived from the qualitative interviews) that appear to influence the culture of care for people with dementia in acute hospitals, such as culture/attitudes and resources (e.g. staffing, recruitment and retention).
Culture and attitudes
An organisational culture that encourages and supports staff to be flexible in delivering patient-centred care fosters a certain degree of autonomy. This provides staff with a degree of freedom whereby they can use their discretion and show flexibility in applying the ‘rules’, which leads to patients receiving more individualised and dignified care.
In better-performing hospitals, senior clinical staff are seen and present on the wards, and encourage more junior staff to ask questions when dealing with complex scenarios. Senior staff champion a culture of ‘it is OK not to know everything’ about dementia and encourage front-line staff to ask for help or second medical opinions. Furthermore, in situations when things go wrong, there is a culture in which the responsibility is shared, rather than adopting a ‘punitive approach’. This means that mistakes are learned from and used to improve care provision:
I think it’s a really fine line . . . what I’ve tried to do is foster a way of working that when things go wrong we ask ourselves the difficult questions, but when actually, if I found that I was in that position I would’ve made exactly the same decision I will say it, regardless of what other people think we should be saying. So, actually, I remember we had a pressure ulcer on one of our older people’s wards and I went through and said I can see you’ve done everything, actually, is there anything else you think they could’ve done that could’ve protected this patient? No. Well, then I think this is unavoidable. And we need to recognise that. You carry on doing what you’re doing. Don’t be disheartened. I can’t see what else you would’ve done. Because, there can be a culture of fear where people think, like, just because something goes wrong that somebody’s made a mistake. Sometimes things go wrong. As long as we’re honest about that and we’re challenging, and we don’t accept the unacceptable, then we can create a culture that says OK, we will have a difficult conversation, but at the end of that difficult conversation, if we’ve done the right thing, then I will stand behind you, 100%.
1ST015
Staff believed that people choose nursing because they genuinely care about others. However, constant heavy workloads might lead people to temporarily lose touch with the human side of their jobs and become very ‘task orientated’ to achieve the targets:
You see different people every day. You come across one or two who have genuine empathy, I suppose is the best word, others who . . . I don’t know if it’s they’re rather more concerned with the hours they have to work. It is difficult, I do sympathise greatly with a lot of their situation, but nevertheless, this is a very special place for people, and they know that emotions are generally high, and people are very much more concerned than they might be in a different situation.
2CA001
In hospitals with high ratings on quality of care, we found evidence that there is a culture that leaders are frequently seen on the wards and can identify when staff find it overwhelming to provide ‘compassionate care’. Staff had different views on whether or not compassion is innate, and if and to what extent staff can be taught how to practise compassion or dignity. However, most agreed that there are simple measures that can be incorporated into everyday practice that do not require any extra resources. For example, language used on a ward has a huge impact on how staff relate to patients. Using patients’ first names in staff meetings and ward rounds instead of referring to them by their diagnosis or their characteristic behaviour (e.g. ‘Mr Wanderer’) makes staff more aware and in touch with the human side of their jobs; and is a reminder for staff that there is a person behind the disease who needs care. Furthermore, it helped if senior staff champion a culture that encourages more junior staff to ask questions when dealing with complex scenarios:
Ideally, anybody with dementia, regardless of what’s wrong with them, should go to a dementia ward, but that isn’t what happens. Because then the team that works on that ward, even if they don’t know your particular individual, have a far better understanding of dementia. But sometimes it was just basic compassion that was missing, because if somebody is making no sense when they talk to you, and they look ancient when you look at them, then even if you don’t know for sure they’ve got dementia, it’s quite a, you know, a logical conclusion to come to.
3CA004
Carers who we interviewed also pointed out the potential difficulties of communication with a patient with dementia and emphasised the significance of compassionate care when dealing with patients with dementia:
So, you shouldn’t be taking what a person with dementia says on face value, . . . And I know they have to explain what they’re doing, but it would be, right, sir, we’re going to reinsert your catheter for you, right? Firstly, he doesn’t know what reinsert means. Secondly, he doesn’t know what a catheter is. Thirdly, he doesn’t know where you’re going to put it. So, he’d sort of nod at you, and say, yes, so they think, right, he knows what we’re talking about – in they’d go, and he’d scream the place down . . . I had one doctor, registrar, describing him as aggressive – I said, no, my dad’s not aggressive, never has been aggressive, he’s the most placid person you would ever want to meet. I said, what he was, was frightened. I said, if you were doing that to a two-year-old, and they started screaming, would you call them aggressive? You wouldn’t, you’d just say, poor little frightened child. And that’s exactly what he was at that point. And I think it’s just a lack of understanding, that . . . I can understand that they might not know exactly how to handle each individual, but we were there, saying he’s got advanced dementia, that wasn’t good enough really . . .
3CA004
Resources (staffing, recruitment and retention)
Adequate staffing level was mentioned by many staff as one of the most important factors in enabling staff to provide high-quality care. Some were explicit about the challenges that they face in delivering high-quality care when there are staff shortages:
If I’m honest, we have a recruitment problem. So, to really understand what the care needs are we need to spend quite a lot of time with the individual patients and we probably haven’t got the time to do that because the turnover of patients is quite fast . . . I mean, part of it is taking time to discuss if there are relatives and friends coming in. We’ll eventually use patient passports and that obviously will help, but I’m not sure how frequently they’re completing the individual patient passports, if I’m honest.
2ST010
It emerged that in hospitals with higher scores on carer-rated quality of care, specific attention is paid to the recruitment process, in which challenges and details about working with patients with dementia is explicitly discussed in the interviews with candidates for nursing jobs. Staff believed that these strategies would increase the likelihood of recruiting people who are willing and ready to work with patients with dementia. Awareness of potential difficulties means that they are more likely to stay and carry on working on the wards. This was further supported when staff spoke about problems with temporary workers:
One of the barriers for us is our staffing levels . . . I never want to make that an excuse, but I can’t deny it. We’ve got up to about 30% vacancy of nurses on our wards. So, we’re using an awful lot of agency and temporary staff. So, are they consistent with your processes and your pathways? No! If you’ve only got one trained substantive member and you’ve got at best two other trained, you’re really struggling on a ward of 26. So, for me, there’s something around temporary staffing use and making sure that they’re aware of what our expectations of them are . . .
3ST013
It also emerged that in better-performing hospitals there is a culture that focuses on individual staff members’ strengths and this would be considered when allocating more sensitive tasks, such as one-to-one patient observation, so that tasks are fitted to personalities. In such a culture, senior staff recognise and thank front-line staff for their hard work during challenging times. Not surprisingly, hospitals in which staff feel valued and supported have a good record of staff retention, which leads to patients receiving more consistent and personalised care:
I mean a lot of our nurses here we’re lucky they have stayed here for quite a long time now and, you know, we are quite good at retaining our staff. I think there’s something about valuing your staff and investing in them as well and making sure that they are supported, and they know they can turn to you when things are difficult. And that’s kind of coming from leadership I think really.
1ST007
Chapter 7 Discussion
In this section we summarise the results of our secondary analysis of data from the NAD and the analysis of qualitative data from high- and poor-performing trusts. This is followed by an integrated summary of the study findings, drawn from both quantitative and qualitative elements of the study. We conclude with a series of recommendations for services and future research in this field.
This study started with a scoping review of the literature and the results are discussed with reference to previous research on the quality of acute care delivered to people with dementia. In developing our recommendations and conclusions, we have incorporated feedback from a range of stakeholders who commented on the findings of the study. These stakeholders include patient and carer representatives on the Stakeholder Reference Group.
The aim of this study was to identify factors that are associated with higher quality of care and shorter length of admission to hospital for people with dementia. Although a range of factors outside the control of staff working in acute hospitals have an important bearing on these outcomes, our focus was on steps that managers and clinicians working in general hospitals can take to provide better care for people with dementia.
Summary of findings
Through conducting a secondary analysis of data from the third round of the NAD and collecting qualitative data from staff and carers of people with dementia, we aimed to examine how the organisation and delivery of hospital services influence the quality of care that people with dementia receive. We focused our quantitative analysis on two outcomes of care (length of stay and carer-rated experience) and one process (quality of assessment that patients receive). The results of the secondary analysis of audit data indicate that the amount of time that people with dementia spend in hospital varies according to the ward that they are treated on and their primary diagnosis. People admitted to specialist wards for older adults and those with hip fractures and other fall-related conditions spent longer in hospital. Length of stay was associated with ethnicity, with white patients having longer admissions than those from BAME communities. We found that patients spent longer in hospital when discussions with a carer about discharge had been documented in the patient’s notes. Among patients for whom there was no evidence of discussion about discharge with a medical consultant, we found evidence of shorter lengths of stay among patients admitted to hospitals that had a psychiatric liaison service that included a specialist in old age psychiatry. We also found a non-statistically significant association between shorter average length of stay and hospitals in which trust boards reviewed delayed discharge of people with dementia.
Results of the sensitivity analyses generally supported the findings of the main analysis of data from the total sample. Among people presenting with hip injuries and fractures, we found evidence that shorter lengths of stay among people from BAME backgrounds were more pronounced among women with dementia than among men. We found lower average lengths of admission among female patients in hospitals reporting that they employ at least one full-time dementia specialist nurse for every 300 admissions of people with dementia per year. In hospitals that received better than average carer-rated quality of care, we found a statistically significant association between discussing discharge with consultant and longer lengths of stay. In hospitals in which the liaison psychiatric team included a specialist in old age psychiatry, we found shorter lengths of stay among those for whom discharge planning was started within 24 hours of admission.
Regarding carer-rated quality of care, the results of this analysis are more difficult to interpret because we were not able to link carer-rated experience with the care received by individual patients. We found that hospitals with lower carer-rated experience of care were more likely to have developed a formal strategy for carer engagement. Case notes of patients in hospitals with lower carer-rated quality of care were, on average, more likely to include a section dedicated to information collected from carers. We found a range of statistically significant interactions between the demographic characteristics of carers at the hospital and other predictor variables. Discussing discharge with carers was associated with better carer experience in hospitals with higher proportions of female carers, but lower levels of carer experience in hospitals with lower proportions of female carers. Providing carers with < 48 hours notice of a patient’s discharge was associated with lower levels of carer-rated quality of care in hospitals with younger carers, but higher levels of carer experience in hospitals with a greater proportion of older carers. In hospitals with a greater proportion of female carers and carers from BAME backgrounds, higher levels of carer-rated experience were seen in those hospitals making finger food available to patients 24 hours a day.
Regarding the quality of patient assessment, we found that older patients were more likely to have a higher quality of assessment of their health and social functioning, as were patients admitted to the care of the elderly wards. Patients who had a longer length of stay were more likely to have a high-quality assessment; this was especially the case in hospitals employing greater numbers of specialist dementia nurses. A trend towards higher-quality assessments being completed in hospitals that had deployed dementia champions at a directorate level did not attain statistical significance.
We were able to explore possible explanations for some of these associations through the collection and analysis of qualitative data from staff working in hospitals and from the carers of people with dementia. We also used these interviews to explore aspects of the organisation and the delivery of acute care that may have an impact on the quality of care that people with dementia receive.
Staff working in acute hospitals emphasised the importance of early discharge planning and described how the complexity of the needs of some people with dementia can make it difficult to keep a focus on discharge planning and how daily multidisciplinary team meetings in which people are assigned specific tasks can help to maintain this focus. Although most executive boards routinely review delayed discharges, less than one-third specifically review delayed discharges among people with dementia. 8 Trusts that do review delayed discharges among people with dementia may be more likely to identify problems in the provision of intermediate and step-down health and social care services, which may prevent timely discharge of people with dementia.
There was widespread recognition of the important role that carers can play in supporting people with dementia during an inpatient stay, both through helping staff recognise and prevent the development of behavioural and emotional problems, and by their presence on the ward. Although most staff and carers are keen to minimise the length of inpatient stay of people with dementia, there are also times when staff and carers have different views about how long a person needs to remain in hospital. Staff working in acute hospitals told us that it was important to give carers clear information at an early stage of an admission about what hospital services could and could not provide, to avoid raising expectations that could not be met.
Dementia-specific training was repeatedly raised by staff from a range of different backgrounds as an essential component of efforts to raise the quality of care that people with dementia receive. There was a consensus that dementia training needed to be a mandatory part of the continuing professional development of all staff working in acute hospitals. Simulation sessions, in which staff are given opportunities to experience what it might be like to have dementia, were especially valued. To be effective, staff told us that training needed be followed up with ongoing practical support from senior staff and that opportunities are required for people to talk openly about the challenges that they face. Front-line staff considered dementia nurse specialists who used a ‘hands-on approach’ as particularly helpful.
Integrated summary of findings
Discharge planning
The factor that had the greatest bearing on length of stay was whether or not discharge planning was initiated within 24 hours of admission. Discharge planning involved setting a planned discharge date, identifying tasks that needed be taken to achieve the planned discharge date and assigning staff who would be responsible for working to complete these tasks. Although it has long been recognised that early discharge planning is helpful,79,80 our analysis of data from the audit allowed us to quantify this, and the qualitative data we analysed suggested factors that support and impede effective discharge planning for people with dementia. A coefficient of –0.24 is equivalent to an average length of stay that is 27% lower among people whose discharge planning was initiated within 24 hours of their admission to hospital. The association in the subsample of people admitted with hip fracture and associated problems was greater, equivalent to a 46% reduction in length of stay. With an average length of stay of 12 days, this amounts to about 3 days per patient across the group as a whole and 5.5 days per patient admitted with hip fracture. With > 100,000 people with dementia admitted to hospital per year, the impact of increasing the use of early discharge planning for people with dementia is considerable. In some instances, we found that staff believed that early discharge planning would not be needed because the patient’s needs were not sufficiently complex. In other instances, staff felt that the patient’s presentation was too complex to make early discharge planning a useful exercise. In wards in which early discharge planning appeared to be most effective, named staff were allocated the task of keeping track of the discharge planning process and there were established processes for raising concerns with more senior staff when plans were off track, so that additional resources could be provided. The results of this study suggest that more could be done to ensure that discharge planning for inpatients with dementia is initiated within 24 hours of the person’s admission to hospital.
Reviewing delayed discharges among people with dementia
Although most trust boards routinely review delayed discharges, data from the NAD suggest that only one-third of trusts specifically review delayed discharges among people with dementia. 8 The association we found between length of stay and trust board reviews was not statistically significant. However, a strong trend emerged with people with dementia spending, on average, 1 day less in those hospitals in which trust boards regularly reviewed delayed discharges of people with dementia. In our sensitivity analysis of patients admitted with hip fractures and related conditions, the association between trust boards reviewing delayed discharges and shorter length of stay attained statistical significance for older patients. Qualitative data from senior managers and front-line staff suggested that the response that trust boards make to this process is important, with staff reporting greatest benefit from trusts that use data to identify gaps in the provision of community services and have discussions with local commissioners to try to ensure that these are filled. With plans in England for strengthening co-operation between health and social care services via the development of sustainability and transformation plans, and the development of accountable care organisations, the value of reviewing delayed discharges among people with dementia is likely to increase. 81 In the meantime, an increase in the proportion of trusts that specifically review delayed discharge among people with dementia could help shorten the amount of time that these patients spend in hospital, and having someone in this meeting who understood what happened on the ward was seen as important.
Involving carers of people with dementia
Interviews with staff and carers of people with dementia highlighted the important role that the presence of carers on wards can play in helping patients feel more settled, while also supporting nutrition, hydration and adherence to treatment. In this way, carers can help reduce the incidence of challenging behaviour and may be able to minimise the likelihood of complications arising, which can increase the length of the patient’s admission. 82 In discussions with members of the Stakeholder Reference Group, carers highlighted practical barriers that reduce the presence of carers on the wards, including restrictions on visiting times, parking fees and the availability of alternative forms of transport, especially for elderly carers.
Carers of people with dementia also play an important role in helping to ensure that hospital staff are aware of the patient’s needs. Communication with carers needs to take place at an early stage of the admission. Our finding that patients whose records included evidence of discussion with carers about discharge spent longer in hospital supports the views of both carers and staff, who told us that, if communication with carers does not start until discharge is being arranged, then new concerns, which could have been addressed earlier in the patient’s admission, may be raised.
The collection of information from carers seems unlikely, by itself, to improve the quality of care that people with dementia receive in hospital. Indeed, analysis of data from the audit suggested that hospitals had lower levels of carer-rated quality of care when a greater proportion of case notes had information recorded following discussions with carers. Data collected from carers and feedback from our Stakeholder Reference Group highlighted difficulties that can arise when carers are asked about patient needs or preferences but then find that these are not met. When discussion with carers starts soon after the admission to hospital, there is greater opportunity for these to be acted on. There is also the potential for needs or concerns to be raised, which staff in hospitals are unable to meet. For instance, acute hospitals may not be able to reverse reductions in health and functioning that are a result of health problems precipitating the admission to hospital. Early discussions with carers may help to ensure that carers have realistic expectations about what can and cannot be achieved during the hospital admission. 19 Some hospital staff may also have existing beliefs about what carers want and have concerns that this could slow down the discharge process. However, interviews with carers and staff suggest that many carers are aware of the reasons why prolonged lengths of stay of people with dementia should be avoided, and that other carers will better appreciate the need for a timely discharge when these issues are discussed.
Our finding of lower levels of carer-rated quality of care at hospitals that reported having a carer strategy in place was unexpected. In response to this unexpected finding, members of the audit team conducted a simple univariate analysis of the relationship between carer-rated quality of care and whether or not hospitals reported having a carer strategy over all four rounds of the audit. This confirmed that in each of the first three rounds (2010/11, 2012/13 and 2015/16), hospitals with a carer strategy had lower levels of carer-rated quality of care. However, in the fourth round of the audit, for which data were collected in April–May 2018, the relationship changed, with hospitals with a carer strategy in place having higher levels of carer-rated quality of care. We do not know the reasons for this change. It is possible that there was a delay between the development of a carer strategy and implementing the strategy in practice. Therefore, any positive impact on carer-rated quality of care would have taken time to appear. An alternative explanation is that hospitals that were the first to develop carer strategies did so in response to negative feedback from carers.
Availability of personal information
We found some evidence from our analysis of audit data that the degree to which wards ensured that staff had access to personal documents, such as This is Me,63 was associated with improved carer-rated experience of care. This attained statistical significance in hospitals that had a greater proportion of patients and carers from BAME backgrounds. Interviews with front-line staff generated multiple examples of when access to personal information had enabled them to comfort an anxious or distressed patient. If efforts to reduced distress and agitation are successful, they have the potential to reduce the amount of time that people with dementia stay in hospital. 83 Staff also highlighted the role that access to personal information plays in helping colleagues feel more confident that there are things they can do or say that may help calm a patient if they become agitated.
These documents were developed in response to evidence highlighting the value that people with dementia place on a personal approach to their care. 84,85 There is evidence from the NAD that hospitals have successfully taken steps to improve staff access to personal information;8 however, there is still marked variation in practice across hospitals and between wards in the same hospital. Our data emphasise the importance of making these documents a central component of the resources that staff use to help to improve the quality of care that patients with dementia receive.
Specialist staff and teams
One of the key areas of enquiry in this study was the role that specialist staff might play in improving the quality of care that people with dementia receive. In the third round of the NAD, > 80% of hospitals reported that they employed a dementia champion at a directorate level and just under one-third reported that, in keeping with Royal College of Nursing guidance, they employed at least one full-time dementia specialist nurse for every 300 admissions of people with dementia per year. 86 Data from the second annual survey of liaison psychiatry in England62 showed that just over half (53%) of mental health liaison teams were providing a 24-hour service and that 49% had a specialist in old age psychiatry as part of their team. Accounts of discussions with specialist staff did not feature widely in the qualitative interviews we conducted with managers and front-line clinicians, and were absent from interviews with carers of people with dementia. However, indications of the impact of specialist staff were found in our secondary analysis of audit data. In the main multivariate analysis of factors associated with length of stay, patients generally had shorter admissions in hospitals in which the mental health liaison team included a specialist old age psychiatrist. This association reached statistical significance for patients for whom there was no record of discussions about discharge with a medical consultant. In the subanalysis of factors associated with length of stay in the hospitals that had higher ratings for carer satisfaction, we found evidence of lower average lengths of stay in hospitals that had teams with an old age psychiatrist when there was no record of discussions about discharge with a social worker. In the subanalysis of factors associated with length of stay in the hospitals among people treated for hip fractures and related complaints, we found evidence of lower average lengths of stay among female patients in hospitals that employed higher numbers of dementia specialist nurses. We also found some evidence that quality of assessments of patients with dementia was higher in hospitals that deployed at least one dementia specialist nurse per every 300 admissions of people with dementia per year. Although these data provide some evidence to support the role that specialist staff play in delivering high-quality inpatient care to people with dementia,28 previous studies have reported that most people with dementia do not have direct input from specialist staff. 87 The high prevalence of dementia among people in general hospitals highlights the need for all staff to develop expertise in the assessment and treatment of people with dementia. 88 In a recent systematic review of effective dementia training programmes, authors highlight (among other factors) the importance of supporting staff in applying taught materials in clinical practice and providing dementia-specific guidelines. 89
Hospital culture
A central finding from the qualitative interviews we conducted was how the culture of hospitals can have an impact on the quality of care that people with dementia receive. Changing the culture of any organisation is a considerable task that can take time to achieve. 90,91 It is also influenced by resources and may prove especially challenging at times of financial restraint. We have highlighted some of the factors that appear to have a bearing on hospital culture in Chapter 6, Organisational and contextual factors, including attitudes, staffing, recruitment and retention. Although staffing levels require funding, other components, such as adopting a flexible approach and encouraging delivery of compassionate and person-centred care, may be possible with existing resources. The role of ward managers and other senior staff appears to be particularly important in creating an environment in which solely ‘task-oriented’ practice is discouraged and front-line staff are encouraged to use a flexible approach to delivering patient-centred care. Identifying individual strengths in staff, allocating tasks that are compatible with their abilities and acknowledging staff for their hard work are among factors that lead to higher rates of staff retention. Previous research has highlighted that hospitals in which staff are given the permission to adapt clinical care to patient needs and in which person-centred care is encouraged by senior managers, can provide better dementia care. 92
Strengths and limitations
By using data from the third round of the NAD we were able to analyse data on the quality of inpatient care for people with dementia from 203 (98.5%) of all hospitals in England and Wales. This means that our results could be generalisable to hospitals across the country. Levels of completeness of data collected at hospitals were high for most variables, and included complete data on length of stay and organisational data from 200 hospitals. People with lived experience of dementia and caring for people with dementia helped us select items for including in the analysis and interpreting. We used qualitative interviews with staff and carers of people with dementia from six hospitals in England, to help interpret these findings and examine other factors that support the delivery of effective inpatient services for people with dementia. By selecting hospitals based on their performance in the audit, we were able not only to examine the meaning of associations we observed in work package 1, but were also able to explore contextual factors that influence the impact that components of care have on the service that patients receive.
The study also had a number of limitations that need to be considered when interpreting the study findings. The audit was limited to people who were admitted to hospital in April and May of 2016, had a diagnosis of dementia recorded by the clinical team and had an admission that lasted ≥ 3 days. Not all people with dementia who are admitted to hospital have this recorded and many patients are discharged prior to 72 hours. The findings of our secondary analysis of audit data cannot be generalised to people with dementia who have only short admissions to hospital.
Data on the provision of mental health liaison services were not collected as part of the audit and we had to rely on a parallel audit of these services. Data from 31 (15.5%) services were missing, increasing the possibility of type II errors in our analysis of the impact of liaison mental health services on the quality of inpatient care received by people with dementia.
All data from the audit are observational, which makes it difficult to ascertain whether or not the associations between the variables are causal. For instance, our finding of an association between longer lengths of stay when there was documented evidence of discussing discharge with carers could be because discussions with carers led to the identification of additional needs that took longer to treat. An alternative explanation is that the longer a patient spends in hospital, the more likely there is to be documented evidence of a discussion with a carer. We attempted to reduce the likelihood of these alternative explanations by including risk factors for longer lengths of stay in our multivariate analysis. We also used a qualitative approach to explore potential explanations for quantitative associations in work package 2. This qualitative component of the study provided additional evidence to support a causal link between involving carers in discussions about discharge and length of stay, but we cannot be certain that this or any of the other associations we found are causal.
As a secondary analysis of data from an audit that had been completed, we were not able to examine the influence of factors that may have an impact on our outcomes but were not in the audit. We were also unable to examine the impact of factors that were excluded from the analysis, as there was insufficient variation across hospitals to conduct a meaningful analysis. So, for instance, it is possible that using an evidence-based tool that takes account of the needs of people with dementia for establishing ward staffing levels is associated with changes in length of stay or carer-rated satisfaction with care. However, > 98% of hospitals that took part in the audit reported that they were using such a tool and we were therefore unable to explore the impact that this approach may have on study outcomes. Similarly, access to intermediate care for people with dementia and the deployment of dementia champions on wards may have had an impact on study outcomes, but we were unable to examine this. A full list of variables we were unable to include in our analysis can be found in Appendix 1.
As we analysed data from an audit, we relied on the quality of information that was submitted to the audit team. If staff indicated in the organisational survey that they had adopted a process, we included this information in our analysis without knowing whether or not the process, such as reviewing delayed discharge among people with dementia, was being fully implemented. Similarly, if staff failed to document an assessment that they conducted or a discussion with a consultant or carer that had taken place, we could not include this in our analysis. Discussions with front-line staff provided some reassurance that it was very unlikely that specific assessments or consultations would take place without these being recorded in the patient’s notes; however, it is likely there were occasions when this happened, and this type of error will have reduced the likelihood of our finding associations between predictor variables and the outcomes that we examined.
The reliability of data submitted to the audit was examined by the audit team. Hospitals were asked to ‘double’ enter data from their first five cases using an independent rater, and 163 hospitals submitted data on 806 ‘pairs’ of records. A report on the results of this exercise can be found on the website for the NAD [URL: www.rcpsych.ac.uk/improving-care/ccqi/national-clinical-audits/national-audit-of-dementia/nad-reports-and-resources/data-tables (accessed 21 February 2020)]. The reliability of data collected in the audit was higher for demographic characteristics of the patient (mean kappa 0.83, IQR 0.74–0.97) than it was for components of patient assessment (mean kappa 0.61, IQR 0.51–0.71) or for whether or not aspects of the discharge planning process had been completed (mean kappa 0.55, IQR 0.48–0.61). Reliability was higher for length of stay, for which there was complete agreement in 694 (86%) of 806 cases, and ratings varied by only 1 day in 68 (61%) of the remaining 112 cases.
Regarding work package 2, although we were able to interview a diverse range of staff in terms of seniority level, professional background, years of experience and designated dementia roles, we cannot rule out the possibility that staff working in other hospitals have different views. As described in Chapter 4, our selection criteria for hospitals was to choose pairs of matching hospitals with high and low scores on carer-rated quality of care, with and without governance infrastructure (including other factors such as deployment of specialist staff) in place. We conducted additional interviews at two further sites to refine our programme theories. Although the six study sites were geographically distributed across England, we cannot rule out the possibility that staff and carers in other parts of the country could have provided further or alternative explanations for the associations we found in our analysis of audit data.
The main limitation of this component of the study was the absence of patient voices and the limited number of data we obtained from carers of people with dementia. Although the interviews we conducted with carers provided us with helpful insight into their experience of care received by their family member, it is possible that other carers would have provided additional insights or had different views.
A number of previous studies have examined the experiences of people with dementia who are admitted to acute hospitals. 85,93,94 These provide important data about the value placed by inpatients with dementia on maintaining their identity, on the attentiveness of staff and on shared decision-making. The focus for this study was understanding the relationship between the organisation and delivery of acute care, and the length of stay and quality of care that patients receive. Although people with mild and moderate dementia in acute hospitals would have been able to provide an account of their experience of care, we judged that they may have limited awareness of the steps that hospitals may be taking to try to assure and improve the quality of care they received. This may be especially true for some of the organisational-level interventions that we examined, such as whether or not the trust board reviewed delayed discharges among people with dementia, or whether or not the local mental health liaison team included a specialist in old age psychiatry. Indeed, our interviews with carers supported this hypothesis. Carers were able to comment on the overall quality of care received by their spouse or relative, and discussed the importance of factors such as visiting times and arrangements for discharge planning. However, other aspects of the organisation and delivery of care within the hospital were largely absent from their accounts and carers did not report having direct contact with dementia nurse specialists or mental health liaison teams. Nearly all the qualitative data we collected were cross-sectional. Although we did go back to some key informants to sense-check emerging findings and fill in some gaps in the data, it may have been helpful to obtain a longitudinal account from stakeholders, especially when hospitals had recently introduced changes aimed at improving the quality of care that people with dementia received.
Reflections on patient and carer involvement
This study benefited from the contribution of people with dementia and carers of people with dementia. As active members of both the study’s Project Management Group and the Stakeholder Reference Group, people with lived experience helped determine the content and focus of the study, and the interpretation of study findings. By working with the Steering Group for the NAD, we were able to obtain helpful feedback from a range of people with mild dementia and from carers of people with dementia throughout the study. One of the advantages of working with this existing group was that they were already familiar with the data we were analysing, and they were keen to develop learning from the audit process to which they had already contributed. As a well-established group that has a culture of actively valuing contributions from people with lived experience, patient and carer members of the group had the confidence to comment on a question plan for the study and how the data would be interpreted. For instance, the initial response of some service providers to our finding of an inverse association between the collection of information from carers and lower satisfaction with carer, was that hospitals that promoted this may have done so in response to negative feedback from carers. However, carer members of the group raised the possibility that collecting information from carers could increase expectations and lead to dissatisfaction of the carer if the suggestions were not acted on.
Dementia is a progressive condition and some of the patients involved in this study at the start were not able to contribute throughout the study period. However, because the Steering Group for the NAD had strong links with a range of voluntary sector organisations, we were able to ensure that people with lived experience contributed to each stage of the study, even if people attending each meeting varied.
During the course of this study, a number of clinical and academic staff that were involved had personal experiences of supporting a relative or friend with dementia during an inpatient admission. These experiences will also have influenced the contributions that people made to the study and support the notion that dementia is, increasingly, ‘everybody’s business’. 95
Chapter 8 Conclusions
Implications for services
The results of this study have identified key modifiable actions that staff in acute hospitals could take in an effort to improve the quality of care and reduce the length of stay of people with dementia. These include making every effort to initiate discharge planning within 24 hours for all patients with dementia who are admitted to hospital. It is important for named staff to co-ordinate these plans and be supported by more senior staff when barriers are identified that could lead to delayed discharge. Trust and health boards could review delayed discharges among people with dementia in an effort to identify trends and patterns of delayed discharge that indicate problems in the wider health and social care system. It might be helpful if senior hospital staff work with local authorities and other providers of social care services to identify priorities for strengthening support for people with dementia in the community.
Staff on hospital wards could communicate with carers at an early stage following the admission of a person with dementia. Contact with carers would provide an opportunity to ensure that additional concerns and needs are identified, that information that can assist with the delivery of personalised care is collected and shared with all those working with the patient, and that carers have realistic expectations about what can and cannot be achieved during the hospital admission. Hospital managers could identify ways to increase the availability of personal documents for people with dementia on wards, so that staff have the knowledge they need to help reduce anxiety and to try to calm patients who become agitated.
It is important that all staff in hospitals are trained in the assessment and management of dementia. Training could incorporate simulation, in which staff are given opportunities to experience what it might be like to have dementia. It would be helpful for front-line staff to receive ongoing support from senior staff and have opportunities to talk openly about the challenges they face. Ward managers and other senior staff should consider creating an environment in which solely ‘task-oriented’ practice is discouraged and in which staff are encouraged to use a flexible approach to delivering patient-centred care.
The work of mental health liaison teams may be enhanced by employing staff specialised in the assessment and treatment of people with dementia.
Future research
We did not collect data directly from people with dementia who are admitted to acute hospitals in this study. Previous research that has involved interviewing people with dementia during an acute admission has highlighted the importance of involving people in decisions and the delivery of person-centred care. However, greater knowledge is needed of the experience of people with dementia who are treated in acute hospital settings. Future research that tests new initiatives aimed at improving inpatient care could ensure that the perspectives of people with dementia are captured.
Reducing the need for inpatient admission
Although there are a variety of steps that staff at acute hospitals can take to improve the quality of care and decrease the length of stay of people with dementia, their implementation will not overcome the inherent challenges associated with caring for people with memory problems in an unfamiliar environment, surrounded by people who do not know them well. During the course of this research, we became aware of initiatives that acute hospitals are developing to try to prevent admission to hospital of people with dementia. These include steps taken in emergency departments to divert people from an admission, by strengthening community-based support, services and technologies that aim to treat acute conditions in a person’s home. Future research could identify and describe the CMOs of policies and practices that support the delivery of acute care for people with dementia in the community, and avoid an admission to hospital.
Ethnic minority differences in acute care for people with dementia
Our findings that both the length of stay and the quality of assessment of people with dementia from ethnic minority backgrounds differed from those of other patients was unexpected. The qualitative data we collected were not sufficient to fully explain reasons for these differences. Demographic changes in Britain mean that the numbers of people from BAME communities with dementia will rise in the coming years and steps need to be taken to ensure that all patients with dementia receive high-quality inpatient care. Further research using both qualitative and quantitative methods could examine associations between ethnicity and the quality of inpatient care that people with dementia receive.
Carer involvement
Not all people admitted to hospital have an informal carer who is able to support the care of a person with dementia during their admission to hospital, but a substantial minority do. There is increasing recognition of the support that carers provide to people with dementia during an admission to hospital, but there has been little research into how the role of carers on wards can be strengthened and supported. The age, occupation, health and proximity of carers have an impact on their ability to provide care for their loved ones. It is important that future research considers how carers who are able and willing to contribute to the acute care of people with dementia can be better supported. This could include training and support for carers to co-produce aspects of inpatient care. Our finding of a negative correlation between having a carer strategy and carer satisfaction was not fully explicated. We believe that this would benefit from further research, with a focus on the relationship between intention, execution and organisational culture.
In summary, we recommend future research examines the following areas:
-
Identifying the CMOs of policies to deliver acute care for people with dementia in the community.
-
Exploring associations between ethnicity and the quality of inpatient care that people with dementia receive.
-
Exploring the relationship between hospitals having a carer strategy and levels of carer satisfaction, with a focus on relationships between intention, execution and organisational culture.
-
Examining how carers who are able and willing to contribute to acute care of people with dementia can be supported.
-
Investigating methods for enhancing carer involvement by co-producing optimal care packages and co-delivering dementia training for staff.
Furthermore, we recommend that future rounds of NAD consider collecting data on the median length of stay as one of the key outcome measures, due to the marked variation across hospitals. We also recommend collecting information on carer-rated quality of care and the presence of a personal information document, and to explore their associations with length of stay.
Acknowledgements
We would like to thank all the managers, clinicians and carers of people with dementia who agreed to be interviewed and provided the qualitative data for the study. We also acknowledge the valuable contribution made by our collaborators: Daphne Wallace (retired psychiatrist with lived experience), Amy Claringbold (Trial Manager, Imperial College London) and Chloe Snowdon (Deputy Programme Manager, RCPsych) who assisted with the collection of the qualitative data; Rachael Owen who assisted with the management of the qualitative data; Jasmin Keeble (Research Fellow, RCPsych) who assisted with the analysis of the qualitative data; and William Lee, for providing advice and support on the analysis of data from the second national survey of mental health liaison services.
We are grateful to patients and carers and other members of the Stakeholder Reference Group, including Nicci Gerrard (carer representative, John’s Campaign), Sue Pierlejewski (carer representative), Hilary Doxford (Alzheimer’s Society Ambassador), Jayne Goodrick (carer representative) and Chris Roberts (Alzheimer’s Society Ambassador).
Contributions of authors
Rahil Sanatinia (https://orcid.org/0000-0002-3466-4644) (Research Fellow, Health Services Research) was lead researcher, assisted with the analysis of quantitative data, led the collection, analysis and write-up of the qualitative component of the study and prepared the final report.
Mike J Crawford (https://orcid.org/0000-0003-3137-5772) (Professor of Mental Health Research) was chief investigator and oversaw all aspects of the study.
Alan Quirk (https://orcid.org/0000-0002-7255-856X) (Senior Programme Manager, Health Services Research) contributed to the design of work package 2, supported the collection and analysis of qualitative data, and contributed to the write-up of this report.
Chloe Hood (https://orcid.org/0000-0001-7550-3428) (Programme Manager, NAD) facilitated the analysis of qualitative data, contributed to the collection and analysis of qualitative data, and contributed to the write-up of this report.
Fabiana Gordon (https://orcid.org/0000-0002-5827-0017) (Senior Research Associate, Medical Statistics) led the analysis of quantitative data and contributed to the write-up of this report.
Peter Crome (https://orcid.org/0000-0001-6299-6091) (Professor of Geriatric Medicine, Academic Geriatrics) chaired the Stakeholder Reference Group, and contributed to the interpretation of the results and to the write-up of this report.
Sophie Staniszewska (https://orcid.org/0000-0002-7723-9074) (Professor of Health Research, Care Experience) advised on the methods used to collect and analyse qualitative data, and contributed to the interpretation of the results and to the write-up of this report.
Gemma Zafarani (https://orcid.org/0000-0003-4570-6480) (Carer) contributed to the interpretation of the results and to the write-up of this report.
Sara Hammond (https://orcid.org/0000-0002-3640-7203) (Honorary Research Assistant) led the scoping review, and contributed to the interpretation of the results and to the write-up of this report.
Alistair Burns (https://orcid.org/0000-0002-9837-0645) (Professor of Old Age Psychiatry, Dementia) advised on the methods and contributed to the write-up of this report.
Kate Seers (https://orcid.org/0000-0001-7921-552X) (Professor of Health Research) contributed to the design of work package 2, advised on the methods used to collect and analyse qualitative data, and contributed to the interpretation of the results and to the write-up of this report.
Data-sharing statement
All available data can be obtained by contacting the corresponding author. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. The data generated in the qualitative component are not suitable for sharing beyond those contained within the report. Further information can be obtained from the corresponding author. Applications for access to data from the third round of the NAD should be made to the HQIP. Details of the process for obtaining these data are available at URL: www.hqip.org.uk/national-programmes/accessing-ncapop-data/#.W-7gS0ca7oo (accessed February 2020).
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Health Service Ombudsman . Care and Compassion? Report of the Health Service Ombudsman on Ten Investigations into NHS Care of Older People 2011.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005;366:2112-17. https://doi.org/10.1016/S0140-6736(05)67889-0.
- Mukadam N, Sampson EL. A systematic review of the prevalence, associations and outcomes of dementia in older general hospital inpatients. Int Psychogeriatr 2011;23:344-55. https://doi.org/10.1017/S1041610210001717.
- Department of Health and Social Care (DHSC) . Living Well With Dementia: A National Dementia Strategy. Putting People First 2009.
- Maslow K. How Many Hospital Patients have Dementia? Improving Hospital Care for People with Dementia. New York, NY: Springer; 2006.
- Schubert CC, Boustani M, Callahan CM, Perkins AJ, Carney CP, Fox C, et al. Comorbidity profile of dementia patients in primary care: are they sicker?. J Am Geriatr Soc 2006;54:104-9. https://doi.org/10.1111/j.1532-5415.2005.00543.x.
- Alzheimer’s Society . Fix Dementia Care: Hospitals 2016.
- Royal College of Psychiatrists . National Audit of Dementia Care in General Hospitals 2016–2017: Third Round of Audit Report 2017.
- Holmes J, House A. Psychiatric illness predicts poor outcome after surgery for hip fracture: a prospective cohort study. Psychol Med 2000;30:921-9. https://doi.org/10.1017/s0033291799002548.
- King B, Jones C, Brand C. Relationship between dementia and length of stay of general medical patients admitted to acute care. Australas J Ageing 2006;25:20-3. https://doi.org/10.1111/j.1741-6612.2006.00135.x.
- Nolan L. Caring for people with dementia in the acute setting: a study of nurses’ views. Br J Nurs 2007;16:419-22. https://doi.org/10.12968/bjon.2007.16.7.23245.
- Department of Health and Social Care . Everybody’s Business: Integrated Mental Health Services for Older Adults. A Service Development Guide 2005.
- Sampson EL, White N, Leurent B, Scott S, Lord K, Round J, et al. Behavioural and psychiatric symptoms in people with dementia admitted to the acute hospital: prospective cohort study. Br J Psychiatry 2014;205:189-96. https://doi.org/10.1192/bjp.bp.113.130948.
- Morrison RS, Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage 2000;19:240-8. https://doi.org/10.1016/S0885-3924(00)00113-5.
- Dewing J, Dijk S. What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia 2016;15:106-24. https://doi.org/10.1177/1471301213520172.
- Alzheimer’s Society . Counting the Cost. Caring for People With Dementia on Hospital Wards 2009.
- NHS Confederation . Acute Awareness: Improving Hospital Care for People With Dementia 2010.
- House of Commons All-party Parliamentary Group on Dementia . The £20 Billion Question: An Enquiry into Improving Lives Through Cost-Effective Dementia Services 2011.
- Jurgens FJ, Clissett P, Gladman JR, Harwood RH. Why are family carers of people with dementia dissatisfied with general hospital care? A qualitative study. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-57.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013.
- Care Quality Commision . Cracks in the Pathway: People’s Experiences of Dementia Care As They Move Between Care Homes and Hospitals 2014.
- Bradshaw LE, Goldberg SE, Schneider JM, Harwood RH. Carers for older people with co-morbid cognitive impairment in general hospital: characteristics and psychological well-being. Int J Geriatr Psychiatry 2013;28:681-90. https://doi.org/10.1002/gps.3871.
- Young J, Hood C, Gandesha A, Souza R. National Audit of Dementia Care in General Hospitals 2012–13: Second Round Audit Report and Update 2013.
- Eriksson C, Saveman BI. Nurses’ experiences of abusive/non-abusive caring for demented patients in acute care settings. Scand J Caring Sci 2002;16:79-85. https://doi.org/10.1046/j.1471-6712.2002.00061.x.
- Moyle W, Borbasi S, Wallis M, Olorenshaw R, Gracia N. Acute care management of older people with dementia: a qualitative perspective. J Clin Nurs 2011;20:420-8. https://doi.org/10.1111/j.1365-2702.2010.03521.x.
- Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. https://doi.org/10.1192/bjp.bp.108.055335.
- Gandesha A, Souza R, Chaplin R, Hood C. Adequacy of training in dementia care for acute hospital staff. Nurs Older People 2012;24:26-31. https://doi.org/10.7748/nop2012.05.24.4.26.c9070.
- Elliot R, Adams J. The creation of a dementia nurse specialist role in an acute general hospital. J Psychiatr Ment Health Nurs 2011;18:648-52. https://doi.org/10.1111/j.1365-2850.2011.01771.x.
- Holmes J, Montana C, Powell G, Hewison J, House A, Mason J, et al. Liaison Mental Health Services for Older People: A Literature Review, Service Mapping and In-Depth Evaluation of Service Models. Southampton: National Institute for Health Research Service Delivery and Organisation programme; 2010.
- Goldberg SE, Bradshaw LE, Kearney FC, Russell C, Whittamore KH, Foster PE, et al. Care in specialist medical and mental health unit compared with standard care for older people with cognitive impairment admitted to general hospital: randomised controlled trial (NIHR TEAM trial). BMJ 2013;347. https://doi.org/10.1136/bmj.f4132.
- Lai CK, Yeung JH, Mok V, Chi I. Special care units for dementia individuals with behavioural problems. Cochrane Database Syst Rev 2009;4. https://doi.org/10.1002/14651858.CD006470.pub2.
- Arthur A, Wilson E, Hale J, Forsythe A, Seymour J. Environments for Care at End of Life: Evaluation of The King’s Fund Enhancing the Healing Environment Programme. Nottingham: University of Nottingham; 2010.
- Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d6553.
- Harwood RH, Porock D, King N, Edwards G, Hammond S, Howe L, et al. Development of a Specialist Medical and Mental Health Unit for Older People in an Acute General Hospital. Nottingham: University of Nottingham; 2010.
- Nichols JN, Heller KS. Windows to the heart: creating an acute care dementia unit. J Palliat Med 2002;5:181-92. https://doi.org/10.1089/10966210252785187.
- Zieschang T, Dutzi I, Müller E, Hestermann U, Grünendahl K, Braun AK, et al. Improving care for patients with dementia hospitalized for acute somatic illness in a specialized care unit: a feasibility study. Int Psychogeriatr 2010;22:139-46. https://doi.org/10.1017/S1041610209990494.
- Dewing J, Traynor V. Admiral nursing competency project: practice development and action research. J Clin Nurs 2005;14:695-703. https://doi.org/10.1111/j.1365-2702.2005.01158.x.
- Griffiths P, Bridges J, Sheldon H. Scoping the Role of the Dementia Nurse Specialist in Acute Care. Southampton: Centre for Innovation and Leadership in Healthcare, University of Southampton; 2012.
- Griffiths P, Bridges J, Sheldon H, Thompson R. The role of the dementia specialist nurse in acute care: a scoping review. J Clin Nurs 2015;24:1394-405. https://doi.org/10.1111/jocn.12717.
- Tadros G, Salama R, Kingston P, Mustafa N, Johnson E, Pannell R, et al. Impact of an integrated rapid response psychiatric liaison team on quality improvement and cost savings: the Birmingham RAID model. Psychiatrist 2013:4-10. https://doi.org/10.1192/pb.bp.111.037366.
- Singh I, Ramakrishna S, Williamson K. The rapid assessment interface and discharge service and its implications for patients with dementia. Clin Interv Aging 2013;8:1101-8. https://doi.org/10.2147/CIA.S36398.
- NHS England . Five Year Forward View 2014.
- Young J, Hood C, Woolley R, Gandesha A, Souza R. Report of the National Audit of Dementia Care in General Hospitals 2011.
- Souza R, Gandesha A, Hood C, Chaplin R, Young J, Crome P, et al. Quality of care for people with dementia in general hospitals: national cross-sectional audit of patient assessment. Clin Med 2014;14:490-4. https://doi.org/10.7861/clinmedicine.14-5-490.
- Moyle W, Olorenshaw R, Wallis M, Borbasi S. Best practice for the management of older people with dementia in the acute care setting: a review of the literature. Int J Older People Nurs 2008;3:121-30. https://doi.org/10.1111/j.1748-3743.2008.00114.x.
- Cowdell F. The care of older people with dementia in acute hospitals. Int J Older People Nurs 2010;5:83-92. https://doi.org/10.1111/j.1748-3743.2010.00208.x.
- Cowdell F. Care of older people with dementia in an acute hospital setting. Nurs Stand 2010;24:42-8. https://doi.org/10.7748/ns2010.02.24.23.42.c7551.
- Gladman J, Porock D, Griffiths A, Clissett P, Harwood RH, Knight A, et al. Better Mental Health: Care of Older People With Cognitive Impairment in General Hospitals: Final Report 2012.
- Banks P, Waugh A, Henderson J, Sharp B, Brown M, Oliver J, et al. Enriching the care of patients with dementia in acute settings? The dementia champions programme in Scotland. Dementia 2014;13:717-36. https://doi.org/10.1177/1471301213485084.
- Connolly S, O’Shea E. The impact of dementia on length of stay in acute hospitals in Ireland. Dementia 2015;14:650-8. https://doi.org/10.1177/1471301213506922.
- Goldberg SE, Whittamore KH, Pollock K, Harwood RH, Gladman JR. Caring for cognitively impaired older patients in the general hospital: a qualitative analysis of similarities and differences between a specialist medical and mental health unit and standard care wards. Int J Nurs Stud 2014;51:1332-43. https://doi.org/10.1016/j.ijnurstu.2014.02.002.
- Hynninen N, Saarnio R, Isola A. Treatment of older people with dementia in surgical wards from the viewpoints of the patients and close relatives. J Clin Nurs 2015;24:3691-9. https://doi.org/10.1111/jocn.13004.
- Hynninen N, Saarnio R, Isola A. The care of older people with dementia in surgical wards from the point of view of the nursing staff and physicians. J Clin Nurs 2015;24:192-201. https://doi.org/10.1111/jocn.12669.
- Ibrahim JE, MacPhail A, Winbolt M, Grano P. Limitation of care orders in patients with a diagnosis of dementia. Resuscitation 2016;98:118-24. https://doi.org/10.1016/j.resuscitation.2015.03.014.
- McPherson S, Hiskey S, Alderson Z. Distress in working on dementia wards – a threat to compassionate care: a grounded theory study. Int J Nurs Stud 2016;53:95-104. https://doi.org/10.1016/j.ijnurstu.2015.08.013.
- Scerri A, Innes A, Scerri C. Discovering what works well: exploring quality dementia care in hospital wards using an appreciative inquiry approach. J Clin Nurs 2015;24:1916-25. https://doi.org/10.1111/jocn.12822.
- Surr CA, Smith SJ, Crossland J, Robins J. Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: a repeated measures study. Int J Nurs Stud 2016;53:144-51. https://doi.org/10.1016/j.ijnurstu.2015.09.009.
- Whittamore KH, Goldberg SE, Bradshaw LE, Harwood RH. Medical Crises in Older People Study Group. Factors associated with family caregiver dissatisfaction with acute hospital care of older cognitively impaired relatives. J Am Geriatr Soc 2014;62:2252-60. https://doi.org/10.1111/jgs.13147.
- Yevchak AM, Fick DM, McDowell J, Monroe T, May K, Grove L, et al. Barriers and facilitators to implementing delirium rounds in a clinical trial across three diverse hospital settings. Clin Nurs Res 2014;23:201-15. https://doi.org/10.1177/1054773813505321.
- Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: SAGE Publications Ltd; 2017.
- Crawford MJ, Weaver T, Rutter D, Sensky T, Tyrer P. Evaluating new treatments in psychiatry: the potential value of combining qualitative and quantitative research methods. Int Rev Psychiatry 2002;14:6-11.
- Barrett J, Aitken P, Lee W. Report of the 2nd Annual Survey of Liaison Psychiatry in England. Report. 2015.
- Alzheimer’s Society . This Is Me n.d. www.alzheimers.org.uk/sites/default/files/2019-03/Alzheimers-Society_NEW_This-is-me-booklet_190318.pdf (accessed 24 February 2020).
- NHS England . Friends and Family Test Data 2013. www.england.nhs.uk/statistics/statistical-work-areas/friends-and-family-test/friends-and-family-test-data/ (accessed 18 November 2019).
- Martin F. Comprehensive Assessment of the Frail Older Patient. London: British Geriatrics Society; 2010.
- Ellis G, Langhorne P. Comprehensive geriatric assessment for older hospital patients. Br Med Bull 2004;71:45-59. https://doi.org/10.1093/bmb/ldh033.
- Tom A, Bosker TASRJ, Bosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Thousand Oaks, CA: SAGE Publications Ltd; 1999.
- Hox J. Quantitative Methodology Series. Multilevel Analysis Techniques and Applications. Mahwah, NJ: Lawrence Erlbaum Associates; 2002.
- Goldstein H. Multilevel Statistical Models. London: Edward Arnold; 1995.
- Kessner DM, Kalk CE. A Strategy for Evaluating Health Services. Washington, DC: Institute of Medicine, National Academy of Sciences; 1973.
- Silverman D. Interpreting Qualitative Data: Methods for Analyzing Talk, Text and Interaction. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Pawson R, Tilley N. Realistic Evaluation. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Pawson R. The Science of Evaluation: A Realist Manifesto. Thousand Oaks, CA: SAGE Publications Ltd; 2013.
- Miller G, Fox KJ, Silverman D. Qualitative Research: Theory, Method and Practice. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Pawson R. Theorizing the interview. Br J Sociol 1996:295-314. https://doi.org/10.2307/591728.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Ritchie J, Spencer L. Qualitative data analysis for applied policy research. Qual Res Companion 2002;573:305-29.
- Joffe H, Harper J. Qualitative Research Methods in Mental Health and Psychotherapy: A Guide for Students and Practitioners. London: Wiley-Blackwell; 2012.
- Styrborn K. Early discharge planning for elderly patients in acute hospitals – an intervention study. Scand J Soc Med 1995;23:273-85. https://doi.org/10.1177/140349489502300409.
- National Institute for Health and Care Excellence (NICE) . Emergency and Acute Medical Care in Over 16s: Service Delivery and Organisation 2018.
- NHS England . NHS Long Term Plan 2019.
- Douglas-Dunbar M, Gardiner P. Support for carers of people with dementia during hospital admission. Nurs Older People 2007;19:27-30. https://doi.org/10.7748/nop2007.10.19.8.27.c6269.
- Saravay SM, Kaplowitz M, Kurek J, Zeman D, Pollack S, Novik S, et al. How do delirium and dementia increase length of stay of elderly general medical inpatients?. Psychosomatics 2004;45:235-42. https://doi.org/10.1176/appi.psy.45.3.235.
- Clissett P, Porock D, Harwood RH, Gladman JR. The challenges of achieving person-centred care in acute hospitals: a qualitative study of people with dementia and their families. Int J Nurs Stud 2013;50:1495-503. https://doi.org/10.1016/j.ijnurstu.2013.03.001.
- Bridges J, Flatley M, Meyer J. Older people’s and relatives’ experiences in acute care settings: systematic review and synthesis of qualitative studies. Int J Nurs Stud 2010;47:89-107. https://doi.org/10.1016/j.ijnurstu.2009.09.009.
- Royal College of Nursing . Specialist Nurses: Changing Lives, Saving Money 2010.
- Timmons S, O’Shea E, O’Neill D, Gallagher P, de Siún A, McArdle D, et al. Acute hospital dementia care: results from a national audit. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0293-3.
- Featherstone K, Northcott A, Harden J, Harrison Denning K, Tope R, Bale S, et al. Refusal and resistance to care by people living with dementia being cared for within acute hospital wards: an ethnographic study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07110.
- Surr CA, Gates C, Irving D, Oyebode J, Smith SJ, Parveen S, et al. Effective dementia education and training for the health and social care workforce: a systematic review of the literature. Rev Educ Res 2017;87:966-1002. https://doi.org/10.3102/0034654317723305.
- Patterson M, G, Nolan M, Rick J, Brown J, Adams R, et al. From Metrcos to Meaning: Culture Change and Quality Links Between Staff and Older Peoples’ Hospital Experiences of Acute Hospital Care for Older People. Southampton: National Institute for Health Research Service Delivery and Organisation programme; 2011.
- Nicholson C, Morrow EM, Hicks A, Fitzpatrick J. Supportive care for older people with frailty in hospital: an integrative review. Int J Nurs Stud 2017;66:60-71. https://doi.org/10.1016/j.ijnurstu.2016.11.015.
- Handley M, Bunn F, Goodman C. Dementia-friendly interventions to improve the care of people living with dementia admitted to hospitals: a realist review. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-015257.
- Reilly JC, Houghton C. The experiences and perceptions of care in acute settings for patients living with dementia: a qualitative evidence synthesis. Int J Nurs Stud 2019;96:82-90. https://doi.org/10.1016/j.ijnurstu.2019.04.018.
- Petry H, Ernst J, Steinbrüchel-Boesch C, Altherr J, Naef R. The acute care experience of older persons with cognitive impairment and their families: a qualitative study. Int J Nurs Stud 2019;96:44-52. https://doi.org/10.1016/j.ijnurstu.2018.11.008.
- National Institute for Health and Care Excellence (NICE), Social Care Institute for Excellence . Dementia: Supporting People With Dementia and Their Carers in Health and Social Care 2006.
Appendix 1 List of predictor variables excluded
| Predictor variable | Source of data | Audit question number | Proportion of hospitals reporting them (%) |
|---|---|---|---|
| Named person/identified team with overall responsibility for complex needs discharge | Organisational checklist | 32 | 95.5 |
| Access to intermediate care for people with dementia | Organisational checklist | 30 | 92.5 |
| Dementia working group in place | Organisational checklist | 9 | 93.5 |
| Evidence-based tool is used for establishing ward staffing levels | Organisational checklist | 11 | 98.5 |
| Formal system for gathering personal information | Organisational checklist | 16 | 98.5 |
| Protected mealtimes | Organisational checklist | 12 | 98.0 |
| Dementia champion at ward level | Organisational checklist | 5a | 93.5 |
Appendix 2 DemCARE initial programme theories
Outcomes
-
Comprehensive assessment.
-
Length of stay.
-
Patient experience of care (as rated by carers).
Dementia-friendly environments
Hypothesised impact of dementia-friendly environments on all three outcomes (Table 23):
By reducing agitation due to unsuitable furnishings, noise, etc., a dementia friendly environment will improve patient experience of care (as rated by carers) and other outcomes.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Environmental review |
Funding available to improve environment in response to review findings Age of hospital (harder to make changes to older wards) |
Completion of a structured review of the physical environment, which can be done across the whole hospital, parts of it, or elder care wards only. (NAD also asked how hospitals responded to the results, e.g. ‘implemented changes’ through to ‘planned actions but no funding available’) | Reduction of agitation due to unsuitable furnishings, noise, etc. | Carer-rated patient experience of care and other outcomes |
(Note, the measure of this in the NAD is whether an ‘environmental review’ has been carried out, but this will only make a difference to the dementia friendliness of the environment if the results of the review had been acted on. If considered important, this could be checked in the case study visits.)
Dementia-friendly food provision
Hypothesised impact of dementia-friendly food provision on length of stay (Table 24):
By encouraging better nutrition and hydration, dementia-friendly food provision (particularly finger food and 24-hour food availability) will help patients recover faster, resulting in shorter stays in hospital.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Mealtimes uninterrupted by clinical activity | Hospital policy | Patients not removed from ward when meals are served (e.g. for medical procedures, physiotherapy) | Faster recovery, through patients not missing set meals |
Length of stay Carer-rated patient experience of care (note, this aspect of care is of great concern to carers, so it is likely to be noticed) |
| Sociable mealtimes |
Ratio of staff to people with additional needs at mealtimes Number of carers and volunteers available to assist patients at mealtimes Space on ward for people to sit together |
Programmes vary but might include:
|
Faster recovery, through social cues at mealtimes and encouraging increased food and drink intake |
Length of stay Carer-rated patient experience |
| Finger food availability | Choice and quality of finger food | Food made available at mealtimes that is easy to eat by people who can no longer use cutlery (e.g. cut up fruit, chicken nuggets) | Faster recovery, through reducing patients’ dependency on others to eat and drink |
Length of stay Carer-rated experience of care |
| 24-hour food availability |
Facilities on ward for staff to make food available outside mealtimes (e.g. kitchen with toaster) Budget for food [e.g. soup, cake (on some wards staff bring in their own food for patients)] |
Food made available between meals by staff (note, not vending machines) | Faster recovery, through patients not missing meals for whatever reason (e.g. patient asleep at mealtime, mealtime interrupted by clinical activity) |
Length of stay Carer-rated experience of care |
Hypothesised impact on carer-rated experience:
By encouraging better nutrition and hydration, dementia-friendly food provision will improve patient experience of care (as rated by carers). (Note, this is an aspect of care which is of great concern to carers, so when it is done well, or not done well, it is likely to be noticed.)
Dementia training for staff
Hypothesised impact of dementia training for staff on carer-rated experience (Table 25):
Through staff communicating to patients and observing carers that they have good awareness of the needs of people with dementia, dementia awareness training will improve carer-rated patient experience.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Dementia awareness training |
Form and content of training [e.g. per cent of e-learning (which NAD respondents complained about) vs. face to face] Training budget |
Training to raise awareness of the needs of people with dementia | Staff communicating to patients (and observing carers), such that they demonstrate that they have good awareness of the needs of people with dementia | Carer-rated patient experience |
Staff with designated dementia roles
Hypothesised impact of staff with designated dementia roles on carer-rated experience (Table 26):
By leading and implementing dementia care in a hospital, the dementia lead supported by dementia champions and dementia working groups will improve all four outcomes.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Dementia specialist nurses | Ratio of dementia specialist nurses to number of admissions of people with dementia and hospital size | Consultant nurse specialist in dementia | Better overall quality of care, through the nurse supervising the workings of the care pathway from assessment to discharge | All outcomes |
| Dementia lead |
Level of support from other staff with designated dementia roles Support from chief executive/trust board |
Dementia lead, supported by other staff with designated dementia roles | Better overall quality of care, through having someone leading on the development and implementation of the care pathway, including getting resources in place for effective delivery | All outcomes |
| Dementia champions | Mix of champions across hospital [it is better to have champions from different levels and occupations, e.g. HCAs, head of directorate, nurses, allied health professionals] | ‘Go-to’ person with a comparatively high level of dementia knowledge, for peer support. Usually at ward level and usually a nurse | Better overall quality of care, through staff receiving advice from champions on aspects of essential care (e.g. how to encourage eating and how to distract someone who wants to leave) | All outcomes |
| Dementia working group in place |
Breadth and quality of representation Frequency of meetings Extent and quality of group’s engagement with hospital processes |
Working group, typically made up of staff with designated dementia roles (above) and representatives from local charities (e.g. Alzheimer's Society), carer groups, general practitioners, etc. | Better overall quality of care, through the group informing the development and implementation of the care pathway (e.g. giving feedback on what is not working and why) | All outcomes |
Dementia-specific care
Hypothesised impact of dementia-specific care on length of stay (Table 27):
By prompting the development and implementation of an action plan to improve carer engagement including in the discharge planning process, self-assessment via the triangle of care tool will reduce length of stay for patients with dementia.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Triangle of care self-assessment tool | Translation services (to facilitate communication with carers who need this) | Hospital self-assessment and production of an action plan to improve carer engagement | Better involvement of carers in decision-making, including discharge planning |
Length of stay Carer-rated patient experience |
| Alerts/symbols to highlight dementia patients to staff in hospital |
Staff awareness of the scheme Staff training (i.e. so that they know what to do when they see the symbol) |
Visual reminders to staff of which patient have dementia (e.g. symbol at bedside, on patient’s wristband or in their notes) | Dementia-specific care provided to those who need it | Care- rated patient experience |
Hypothesised impact on carer-rated experience (1):
By prompting the development and implementation of an action plan to improve carer engagement including in the discharge planning process, self-assessment via the triangle of care tool will improve carer-rated experience.
Hypothesised impact on carer-rated experience (2):
By giving staff visual reminders of which patients have dementia, dementia-specific care in the form of alerts like This is Me will make them aware that the patient might need different or additional forms of help, which carers will notice.
Better involvement of carers
Hypothesised impact of better carer involvement on carer-rated experience (Table 28):
By having an ID [identification] scheme that allows carers to visit at any time, better involvement of carers via the Carer’s Passport Scheme will improve carer-rated experience.
| Programme | Context: key influences | Programme content/resources | Mechanisms: the anticipated ‘triggers’ | Outcomes: anticipated and desired outcomes |
|---|---|---|---|---|
| Carer passport scheme |
Subsidy scheme for carers to facilitate 24/7 visiting (e.g. meals, parking) Availability of overnight facilities for carers |
ID scheme to allow carers 24/7 access | Better representation of patient’s needs, via advocacy and/or quality checking by their carer | Carer-rated patient experience |
Appendix 3 Topic guide for staff and managers
Cover notes for researchers
Aims and objectives
We are conducting qualitative case studies of dementia care in general hospitals. Hospitals have been sampled to include pairs of hospitals that organise and deliver care in a similar way, but which achieve different outcomes. The overarching aim of this study is to identify aspects of organisation and delivery of general hospital services associated with three key outcomes measured by the National Audit of Dementia (NAD):
-
patient experience for people with dementia (as rated by their carers)
-
the length of stay that people with dementia have in hospital
-
comprehensive assessment of people with dementia.
At each case study site, we are aiming to undertake strategic interviews with those who have an oversight of dementia care in their hospital. These interviews will help shape the content and nature of subsequent interviews at the case study site and are an opportunity to understand any changes since NAD data collection (2016). The specific aims of these are to:
-
identify things participants think their hospital is doing (or not doing), which in their view make a difference to the quality of dementia care in the hospital
-
understand the rationale and theory underpinning these ‘programmes’ [i.e. how they think it makes a difference to outcomes listed above (carer-rated experience of care; length of stay; comprehensive assessment)]
-
explore explanations underpinning predictors of outcome (from work package 1).
‘Twin-track’ approach
We want to do a realist evaluation and look at what works for whom and what leads to better outcomes for people with dementia in general hospitals. Our initial programme theories are summarised in a separate document, which should be referred to in Approach to optimising acute care for patients with dementia (20 minutes). These theories summarise how the research team, informed by existing literature and learning from NAD, think certain aspects of hospital care – for example, dementia-friendly food provision – make a difference, in favourable contexts, to outcomes such as carer-rated quality of care. The point of the research is to test and refine those theories by talking with people responsible for delivering and receiving care. By interviewing people in different, contrasting hospitals, we expect to be able to find out why something that works well in one context (e.g. dementia champions), may not appear to make much of a difference in another.
We also want to explore factors found to ‘predict’ certain outcomes in our secondary analysis of NAD data.
In interviews, then, we are focusing on testing and refining programme theories and exploring why certain things predict certain outcomes.
Use of topic guide
The topic guide includes prompts and probes for researchers, rather than fully formed questions. The guide is designed to be used flexibly to allow researchers to be responsive to issues raised by participants. Responses to questions will be probed fully, with researchers asking ‘why’ throughout. (See comment above.)
Introduction (5 minutes)
Aim
To explain the research, answer any questions and ensure informed consent.
-
Introduce self.
-
Purpose: brief explanation of DemCARE and purpose of this interview.
-
We want to understand what makes a difference to:
-
patient experience for people who have dementia (as rated by their carers)
-
the length of stay people with dementia have in general hospitals
-
comprehensive assessment of people who have dementia.
-
-
We would like to explore:
-
the hospital approach to dementia care
-
the rationale of this approach to dementia care
-
any key changes in dementia care in acute hospital since the last year (when NAD data were collected)
-
who else we should speak to from their hospital.
-
-
-
Explain voluntary nature.
-
Interested in views and experiences: no right or wrong answers.
-
Confidentiality and anonymity: everything is confidential, might use quotations in written reports, not possible to identify individuals.
-
Recording: would like to audio-record with permission, data stored in accordance with the Data Protection Act.
-
Timings: reiterate start and finish times.
-
Any questions?
Start recording: record verbal consent.
Participant background and context (5 minutes)
Aim
To establish rapport, help participant feel at ease and gain important background information.
Professional background
-
Briefly explore professional background (what do they do, how long for, length of time working in current hospital/setting).
-
Explore any dementia-specific experience (training, role, champion, old age specialism).
Time dependent.
Hospital context
-
Briefly explore hospital make-up and demographic (what specialist wards or treatment centres for elderly people and those with dementia).
Exploring recent developments
-
Explore how similar or different dementia care is in the hospital now compared with a year ago.
-
Map what (if anything) has changed and why.
-
In your experience, what sorts of things for a patient with dementia are likely to make a difference to the outcomes of their stay in hospital? (Start openly then probe: financial situation, social support, health condition, other. )
-
What characteristics in the way staff work with patients with dementia help to create better outcomes (e.g. quicker discharge)? What makes a difference?
-
Can you think of any external factors that can support or impede the delivery of effective care? (Start openly then probe: onwards health care, local social services, other.)
-
Other contextual factors? (Start openly then probe: beds, staff experience, dementia training, organisational culture, other.)
Approach to optimising acute care for patients with dementia (20 minutes)
Aim
To explore what dementia care looks like in the acute hospital and identify priority areas.
Identifying relevant programme and subprogramme theories
Activity by programme theory
Map what they do in relation to relevant key programme theory categories (Table 29).
| Programme | Subprogramme | Potential outcome(s) |
|---|---|---|
| Dementia-friendly environment | Environmental review | Carer-rated patient care |
| Nutrition | Protected mealtimes |
Length of stay Carer-rated patient care |
| Sociable mealtimes |
Length of stay Carer-rated patient care |
|
| Finger food |
Length of stay Carer-rated patient care |
|
| Snacks |
Length of stay Carer-rated patient care |
|
| Dementia training | Dementia awareness training | Carer-rated patient care |
| Designated dementia roles | Dementia specialist nurse |
Length of stay Carer-rated patient care Comprehensive assessment |
| Dementia lead |
Length of stay Carer-rated patient care Comprehensive assessment |
|
| Dementia champions |
Length of stay Carer-rated patient care Comprehensive assessment |
|
| Dementia working group |
Length of stay Carer-rated patient care Comprehensive assessment |
|
| Dementia-specific care | Triangle of care self-assessment tool |
Length of stay Carer-rated patient care |
| Involvement of carers | Carer’s passport | Carer-rated patient care |
Refer to programme theory prompt sheet.
Formalised versus ‘just happens’
-
Explore how far dementia care is formalised and defined versus ‘just happens’: how far is it shaped by wider hospital and trust policies and the broader context.
-
For each programme identified, probe in depth on:
-
Why they think this makes a difference?
-
How they think this makes a difference?
-
How do you think [programme X, Y, Z] has had an impact on how staff deal with patients with dementia?
-
How do you think this programme has affected the way staff work as a team?
-
Has the programme affected your relationships with colleagues in other hospital departments and social services?
-
Can you think of any other intended or unintended outcomes of the programme for patients with dementia and their carers?
-
-
-
Explore which subprogrammes have made the biggest difference to the quality of dementia care in their hospital.
-
Explore obstacles to implementing the programmes (contextual factors) and how these can be or have been overcome.
Absent programmes
-
Identify what (if anything) they think they should be doing, but currently are not or cannot do (and why).
Exploring predictors (20 minutes – or less – judge by interview until now)
Aim
To explore explanations underpinning predictors of outcome (from work package 1).
Overall approach to optimising dementia care
-
Shared understanding of terms. [Briefly reiterate (from introduction) that our focus is on comprehensive assessment, length of stay, carer-rated quality of care (briefly explain that our definition of carer-rated quality of care is informed by NAD and show the handout).]
-
Explore any other outcomes they think should feature in high-quality dementia care.
-
Most important ‘thing’ (intervention/policy/programme).
-
Explore what they think is the most important ‘thing’ the acute hospital does to optimise care for people with dementia, in relation to:
-
comprehensive assessment
-
length of stay
-
carer-rated quality of care.
-
-
-
For each ‘thing’ identified, probe in depth on:
-
Why they think this makes a difference?
-
How they think this makes a difference?
-
-
Explore any links between predictors and outcomes (Table 30), go through each in turn, probe on:
-
how far this seems unusual or surprising
-
extent to which they think it is true of their own hospital
-
any explanations (i.e. why is there this link).
-
| Outcome | Predictor |
|---|---|
| Length of stay | Shorter stays when discharge planning is initiated within 24 hours of admission |
| Longer stays if involving carers in discharge planning | |
| Shorter stays when executive board reviews delayed discharge (the effect is borderline) | |
| Carer-rated quality of care | Higher carer-rated quality of care when hospitals do not have a strategy or plan for carer engagement (e.g. triangle of care) |
| Lower carer-rated quality of care when there is more information about the care and communication needs of the person with dementia recorded in case note (collects information from carer) | |
| Comprehensive assessment | More comprehensive assessment as age increases |
| Dementia champion at directorate level leads to more comprehensive assessment |
Conclusion and wind down (5 minutes)
Aim
Give a chance to add anything else and wind down.
Check whether there is anything else to add, that should be kept in mind for remaining interviews.
Stop recording.
-
Wind down.
-
Reassure about confidentiality.
-
Check whether or not there are any questions (when recorder is off).
-
Check if they want to be informed of findings of the study (note e-mail address if they do).
Appendix 4 Topic guide for carers
Aims and objectives
The aim of this study is to . . .
This will involve finding out your views on the care the person you look after has received while they have been in hospital.
Introduction
Aim
To introduce the research and set the context for the discussion.
-
Introduce self and Imperial College London/RCPsych.
-
Introduce the study: who is it for, what is it about?
-
Talk through the key points:
-
purpose of the interview
-
length of the interview
-
voluntary nature of participation and right to withdraw
-
reasons for recording the interview.
-
-
Confidentiality, and how findings will be reported.
-
Check for any questions they have.
-
Start recording, then ask:
-
what relationship the interviewee has to the person they look after/care for (e.g. spouse or partner)
-
whether or not they regard themselves as one of the person’s main carers
-
how they would like the person they care for to be referred to (e.g. ‘your husband/wife’, ‘the person you care for’).
-
Section 1: experience of care
Aim
To explore carers’ views and experiences of the quality of care, things they think may have influenced care quality and how those things have made a difference.
-
Overall, how would you rate the quality of care received by [the person you look after] during their stay in hospital? (Start openly then probe, eliciting examples when possible.)
-
Staff:
-
well informed and understood person’s needs
-
treated person with respect
-
kept you informed (e.g. about progress)
-
involved you/person as much as you wanted in care decisions
-
asked you about person’s needs for care planning
-
other.
-
-
-
In your experience, what things may have influenced the quality of care [the person you look after] has received? (Start openly then probe for contextual factors and dementia care programmes/interventions, eliciting examples where possible. )
-
How do you think those things have made a difference?
Section 2: length of stay
Aim
To explore carers’ views on length of stay, things they think may have influenced this and how those things have made a difference.
-
What are your views on how long [the person you care for] is expected to stay in hospital? (Start openly then probe, eliciting examples when possible: too long/too short, other.)
-
In your experience, what things may have influenced their length of stay here? (Start openly then probe for contextual factors and dementia care programmes/interventions, eliciting examples when possible. )
-
How do you think those things have made a difference?
Section 3: discharge planning
Aim
To explore carers’ views on discharge planning, things they think may have influenced this and how those things have made a difference. (Establish if they are aware of any discharge planning; if not, skip to next section. )
-
Overall, how would you rate the discharge planning process? (Start openly then probe, eliciting examples when possible: involved in decisions, other. )
-
In your experience, what things may have influenced discharge planning? (Start openly then probe for contextual factors and dementia care programmes/interventions, eliciting examples when possible. )
-
How do you think those things made a difference?
Section 4: other outcomes
Aim
To explore carers’ views on other outcomes that they perceive to be important, things they think may have influenced those outcomes and how those things have made a difference. (Ask these questions about each outcome. )
-
Overall, how would you rate [outcome X, Y, Z]? (Start openly then probe, eliciting examples when possible. )
-
In your experience, what things may have influenced [this outcome]? (Start openly then probe for contextual factors and dementia care programmes and interventions, eliciting examples when possible. )
-
How do you think those things made a difference?
At the end of the interview
-
Thank participant for taking part in an interview.
-
Provide reassurance about confidentiality.
-
Check if they want to be informed of findings.
-
Check whether or not they have any questions.
Appendix 5 DemCARE coding frame in NVivo
1.1 Programme: environment
-
1.1.1 Description.
-
1.1.2 Impact.
-
1.1.3 How.
-
1.1.4 Context, facilitators, barriers.
-
1.1.5 Miscellaneous.
1.2 Programme: food provision
-
1.2.1 Description.
-
1.2.2 Impact.
-
1.2.3 How.
-
1.2.4 Context, facilitators, barriers.
-
1.2.5 Miscellaneous.
1.3 Programme: staff training
-
1.3.1 Description.
-
1.3.2 Impact.
-
1.3.3 How.
-
1.3.4 Context, facilitators, barriers.
-
1.3.5 Miscellaneous.
1.4 Programme: designated dementia roles
-
1.4.1 Description.
-
1.4.2 Impact.
-
1.4.3 How.
-
1.4.4 Context, facilitators, barriers.
-
1.4.5 Miscellaneous.
1.5 Programme: dementia-specific care
-
1.5.1 Description.
-
1.5.2 Impact.
-
1.5.3 How.
-
1.5.4 Context, facilitators, barriers.
-
1.5.5 Miscellaneous.
1.6 Programme: carer involvement
-
1.6.1 Description.
-
1.6.2 Impact.
-
1.6.3 How.
-
1.6.4 Context, facilitators, barriers.
-
1.6.5 Miscellaneous.
1.7 Other programmes
-
1.7.1 Description.
-
1.7.2 Impact.
-
1.7.3 How.
-
1.7.4 Context, facilitators, barriers.
-
1.7.5 Miscellaneous.
2.1 Predictors: dementia champion at directorate level
-
2.1.1 Description.
-
2.1.2 Impact on comprehensiveness of assessment.
-
2.1.3 Impact on other outcomes.
-
2.1.4 How impacts on comprehensiveness of assessment.
-
2.1.5 How impacts on other outcomes.
-
2.1.6 Context, facilitators, barriers.
2.2 Predictors: discharge planning within 24 hours
-
2.2.1 Description.
-
2.2.2 Impact on length of stay.
-
2.2.3 Impact on other outcomes.
-
2.2.4 How impacts on length of stay.
-
2.2.5 How impacts on other outcomes.
-
2.2.6 Context, facilitators, barriers.
2.3 Predictors: increasing age
-
2.3.1 Description.
-
2.3.2 Impact on comprehensiveness of assessment.
-
2.3.3 Impact on other outcomes.
-
2.3.4 How impacts on comprehensiveness of assessment.
-
2.3.5 How impacts on other outcomes.
-
2.3.6 Context, facilitators, barriers.
2.4 Predictors: information about care and communication needs in case notes
-
2.4.1 Description.
-
2.4.2 Impact on carer-rated quality of care.
-
2.4.3 Impact on other outcomes.
-
2.4.4 How impacts on carer-rated quality of care.
-
2.4.5 How impacts on other outcomes.
-
2.4.6 Context, facilitators, barriers.
2.5 Predictors: carer involvement in discharge planning
-
2.5.1 Description.
-
2.5.2 Impact on length of stay.
-
2.5.3 Impact on other outcomes.
-
2.5.4 How impacts on length of stay.
-
2.5.5 How impacts on other outcomes.
-
2.5.6 Context, facilitators, barriers.
2.6 Predictors: hospital does not have strategy or plan for carer engagement
-
2.6.1 Description.
-
2.6.2 Impact on carer-rated quality of care.
-
2.6.3 Impact on other outcomes.
-
2.6.4 How impacts on carer-rated quality of care.
-
2.6.5 How impacts on other outcomes.
-
2.6.6 Context, facilitators, barriers.
2.7 Predictors: executive board reviews delayed discharges
-
2.7.1 Description.
-
2.7.2 Impact on length of stay.
-
2.7.3 Impact on other outcomes.
-
2.7.4 How impacts on length of stay.
-
2.7.5 How impacts on other outcomes.
-
2.7.6 Context, facilitators, barriers.
2.8 Other predictors
-
2.8.1 Description.
-
2.8.2 Impact on other predictor.
-
2.8.3 How impacts on other predictors.
-
2.8.4 Context, facilitators, barriers.
3.1 Organisational factors
-
3.1 Culture.
-
3.2 Resources.
-
3.3 Staffing.
-
3.4 Recruitment and retention.
List of abbreviations
- BAME
- black, Asian and minority ethnic
- CCG
- Clinical Commissioning Group
- CI
- confidence interval
- CMO
- context–mechanism–outcome
- HQIP
- Healthcare Quality Improvement Partnership
- IQR
- interquartile range
- NAD
- National Audit of Dementia
- NIHR
- National Institute for Health Research
- RCPsych
- Royal College of Psychiatrists
- SD
- standard deviation
