Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/47/17. The contractual start date was in December 2018. The final report began editorial review in July 2019 and was accepted for publication in September 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Andrew Booth is a member of the National Institute for Health Research (NIHR) Health Services and Delivery Research Funding Board and the NIHR Systematic Reviews Advisory Group, and is Convener of the Cochrane Qualitative and Implementation Methods Group.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Chambers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Parts of this report have been reproduced from Chambers et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The impact of reconfiguration of health services is important to commissioners, providers, patients and the public. Currently in the English NHS, programmes of service reconfiguration are being proposed at a local level by Sustainability and Transformation Partnerships, involving collaboration of all relevant stakeholders. Some of the proposed reconfigurations will increase travel time and/or distance for patients to reach their nearest hospital or other urgent and emergency care (UEC) facility.
Many communities value their local UEC services and perceive that planned or proposed changes could worsen outcomes for patients, particularly for those requiring emergency medical or obstetric care. Commissioners and service providers need evidence regarding the impacts of reconfiguration not only on patient outcomes, but also for the wider health-care system. For example, commissioners may have questions about effects on other provisions, such as ambulance and community-based services. Providers may face difficulties in staffing other services if they are no longer providing emergency care. A systematic review of evidence relating to outcomes for patients following service reconfigurations that change the time/distance to the nearest UEC facility is needed to examine whether or not the available evidence supports or refutes the belief that such reconfiguration is harmful. Furthermore, evidence on the broader relationships between distance to an emergency care facility, morbidity/mortality and health system outcomes is needed to inform evidence-based decision-making.
The recently completed closED study2 analysed data from five locations where emergency departments (EDs) were downgraded between 2009 and 2011. Although the authors found no evidence of an impact on mortality, despite patients having to travel further to access an emergency facility, there was evidence of an effect on the system, with the finding of an increased burden on emergency care providers. This systematic review will set the closED findings in the context of the wider international literature. A review of this topic will also contribute to evidence regarding the delivery of services in rural and coastal areas, which is a priority for the Health Services and Delivery Research (HSDR) programme.
Chapter 2 Review methods
Research questions and aims
The aim of this systematic review was to identify, appraise and synthesise existing research evidence regarding the outcomes and impacts of service reconfigurations that have the effect of increasing the time and/or distance for patients to reach an UEC facility. A list of potentially time-sensitive conditions requiring treatment at a UEC facility was developed in advance (see Inclusion and exclusion criteria). The list prioritised conditions more likely to be affected by service reconfiguration or requiring a decision whether or not to travel further to reach a more specialist facility. However, this list was not intended to be exhaustive.
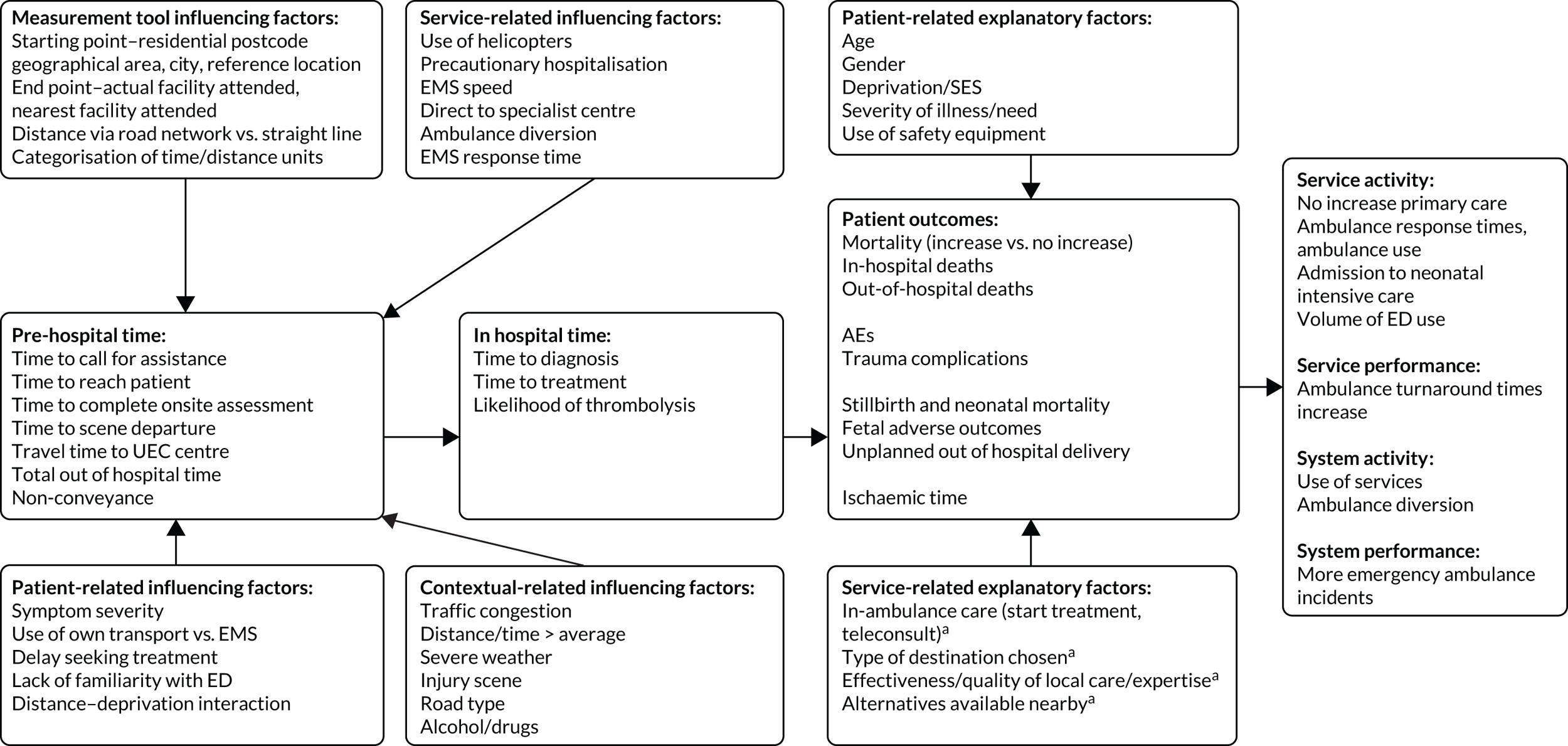
We also aimed to examine the available evidence regarding associations between distance to an UEC facility and outcomes for patients and services, together with factors that may influence (moderate or mediate) these associations. A moderating factor was defined as one that may directly alter the relationship (e.g. weather/climate). A mediating factor was defined as one that acts indirectly and may help to explain the relationship (e.g. patient age, acting indirectly by influencing the patient’s risk status). Mitigating factors were those that could potentially reduce the influence of other factors on outcomes (e.g. starting treatment in the ambulance rather than at the hospital).
In our synthesis of the identified factors, we also used the terminology of ‘influencing factors’ (which influenced outcomes via travel time) and ‘explanatory factors’ (which influenced outcomes directly). These factors were broadly classified as patient related, context related or service related.
The research questions were as follows:
-
What is the evidence regarding effects on patients of service reconfigurations that increase the time/distance to an UEC facility?
-
What is the evidence regarding associations between time/distance from an UEC facility and outcomes for patients requiring UEC?
-
What is the evidence regarding effects on the health system of service reconfigurations that have the effect of increasing the time/distance to an UEC facility?
-
What factors might mediate, moderate or mitigate the effects of increased distance to an UEC facility on patient outcomes and/or the health-care system?
Literature search and screening
A comprehensive literature search was conducted in February 2019. The search was developed on MEDLINE and utilises diverse medical subject heading (MeSH) and free-text terms. The search comprised four broad facets: (1) emergency care, (2) rural or island services, (3) service reconfiguration and (4) potentially relevant emergency conditions. The search was limited to papers from 2000 to February 2019 and in English. The MEDLINE search was translated to the other databases. The following databases were searched:
-
MEDLINE via OvidSP (1946–present).
-
EMBASE via Ovid (1974–present).
-
Cochrane Database of Systematic Reviews via Wiley Online Library (2003–present).
-
Cochrane Central Register of Controlled Trials via Wiley Online Library
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature) via EBSCOhost (1981–present).
-
HMIC (Health Management Information Consortium) via OpenAthens (1983–present).
-
Web of Science (Science Citation Index and Social Sciences Citation Index; Clarivate Analytics, Philadelphia, PA, USA).
All of the references were imported into EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] and then automatic and manual deduplication was conducted.
The MEDLINE search is provided in Appendix 1 with details of how the different facets of the search were combined.
Additionally, a search was conducted for current reviews of telehealth. The search was conducted on the databases listed above and was limited to 2009–19 and research published in English. After deduplication, there were 550 references. The MEDLINE search strategy is provided in Appendix 1.
Citation-tracking of the included reconfiguration studies was performed on Web of Science and Google Scholar (Google Inc., Mountain View, CA, USA) in April 2019. Web of Science identified 52 new references and Google Scholar identified 63.
Given the diffuse nature of the topic and the associated terminology, the reference lists of all included articles were manually screened to identify additional studies.
Search results were stored in a reference manager system (EndNote X8.2) and imported into EPPI-Reviewer software (Evidence for Policy and Practice Information and Co-ordinating Centre, University of London, London, UK) for screening, data extraction and quality assessment. The search results were screening against the inclusion criteria by one reviewer, with a 10% sample screened by a second reviewer. Uncertainties were resolved by discussion among the review team.
Inclusion and exclusion criteria
Population
The population was adults or children with conditions that required emergency treatment including, but not limited to, acute myocardial infarction (AMI), stroke, major trauma, severe exacerbations of asthma, chronic obstructive pulmonary disease or complications during pregnancy and the neonatal period. In practice, included studies included data on any patient wishing to access an UEC facility.
Intervention
Studies looking at changes to the delivery of health-care services (service reconfiguration) that may have an effect on the time or distance for patients to access an UEC facility were included. The review included reconfigurations that have an effect on access to any UEC services including ambulance services, maternity services and hospital EDs. The review also included studies evaluating changes to service delivery that aim to mitigate negative effects of living at a distance from an UEC facility. These included, for example, new forms of services providing UEC at the scene, such as first responders or specialist centre retrieval services.
Given the substantial volume of research on telemedicine/telehealth, particularly for patients living in rural areas, we decided not to conduct a review of this literature. To contextualise the evidence identified, however, we provide a brief narrative summary of key review-level evidence in this field.
Comparison
-
Studies comparing outcomes in groups of people travelling different distances/times to receive UEC, or
-
studies comparing outcomes before and after a service reconfiguration that has an effect on time/distance to UEC. Studies with no comparator were included if they met the other inclusion criteria.
Outcomes
Any outcomes for patients were included, including mortality/morbidity, travel time by ambulance or private care, or other perceived or measured effects, as well as outcomes or impacts on the health-care system such as non-transportation, emergency admissions, increase or decrease in contacts/service use. Transportation by helicopter as an outcome was excluded because of its limited applicability in the UK (not funded by the NHS and, therefore, any findings would not be relevant to commissioners).
Setting
The setting was the UK and other developed countries with relevant health-care systems. Absolute travel distances and density of population (which will affect distribution and density of health-care facilities) were also taken into account in assessing applicability of findings to the UK. In particular, studies of ‘remote’ health care from countries such as Australia were fully considered for relevance.
Study design
Scoping work undertaken for this review found two types of relevant studies.
-
Studies of changes to travel distances/times/outcomes following changes to the health-care system (designated ‘reconfiguration studies’). These studies are generally of observational or experimental design including before-and-after/longitudinal, cohort, case–control, or randomised designs.
-
Studies reporting the relationship between distance and outcome for particular groups of patients in a particular health system/setting without an actual change to service delivery (‘association studies’).
The initial scoping also identified a third group of studies that used population-level data to examine associations between population mortality/morbidity and distance to the nearest hospital. The review is investigating immediate access to UEC, thus studies that only provided data for whole populations rather than particular groups of patients were excluded.
Any identified mixed-methods or qualitative studies that reported perceived effects on patients or services of reconfigurations that increased time/distance to UEC were included.
Other inclusion criteria
-
Literature published since 2000.
-
Literature published in English.
-
Grey literature in the form of service evaluations or reports from the UK.
Other exclusion criteria
-
Studies that describe reconfigurations or initiatives without providing any quantitative or qualitative data.
-
Conceptual papers and projections of possible future developments.
-
Studies conducted in low- or middle-income country health systems.
-
Theses, conference abstracts, articles in professional magazines, books and book chapters.
Data extraction and quality/strength of evidence assessment
We extracted and tabulated key data from the included studies, including study design, population/setting, results and key limitations. The full data extraction template is provided in Appendix 2. Data extraction was performed by one reviewer, with a 10% sample checked for accuracy and consistency.
Quality (risk-of-bias) assessment was undertaken using The Joanna Briggs Institute Checklist for Quasi-Experimental Studies. This nine-question checklist was chosen because of its relative simplicity and because the questions are applicable to a wide range of non-randomised study designs. Quality assessment was performed by one reviewer with a 10% sample checked for accuracy and consistency. Details of the quality assessment tool can be found at http://joannabriggs.org/research/critical-appraisal-tools.html (accessed 1 November 2019).
Evidence synthesis
We performed a narrative synthesis structured around the prespecified research questions and outcomes. The included primary studies were classified into three groups (i.e. reconfiguration, association and mitigation studies) corresponding to the prespecified research questions. We first described the characteristics of the groups as a whole. We then summarised the results in terms of the types of patients included (e.g. general UEC population, AMI, trauma, etc.), again considering reconfiguration, association and mitigation studies separately. Further analyses examined the results in terms of setting to assess the relevance of the evidence as a whole to the UK health-care system and to rural as against urban and suburban settings. Given the current background of changes to services in the UK NHS, we also summarised information from the studies about how health systems implemented service reconfigurations and subsequent adaptations to increased travel distances/times affecting emergency medical services (EMS) vehicles as well as patients’ own transport.
Mediating, moderating and mitigating factors identified by study authors were extracted from included studies and used to populate a logic model incorporating effects on patient outcomes via time to access UEC (‘influencing factors’) and directly (‘explanatory factors’).
Summary tables were generated from extracted data using the reporting function of the EPPI-Reviewer program. The overall strength of evidence was assessed using a previously described method. 3 Evidence was rated as ‘stronger’, ‘weaker’, ‘inconsistent’ or ‘very limited’ based on study numbers and design. Specifically, ‘stronger evidence’ represented generally consistent findings in multiple studies with a comparator group design or comparative diagnostic accuracy studies; ‘weaker evidence’ represented generally consistent findings in one study with a comparator group design and several non-comparator studies or multiple non-comparator studies; ‘very limited evidence’ represented an outcome reported by a single study; and finally, ‘inconsistent evidence’ represented an outcome where < 75% of studies agreed on the direction of effect. All studies included in the review were included in the analysis of overall strength of evidence.
Public and patient involvement
We had input from our Evidence Synthesis Centre Public Advisory Group during all stages of the review. In the early stages, a meeting was convened to outline the topic of the review and to seek input regarding the questions and focus from a patient and public perspective. There was considerable interest in this topic among group members, and discussion regarding the high profile nature of this area and importance to members of the public. In particular, the experiences of local reconfigurations were described and discussed, and challenges for individual patients when reconfigurations occurred, particularly where travelling was not straightforward, and there were limitations in available transport options. This input provided the team with valuable insights into the concerns and worries of local communities, and highlighted the need to consider potential impacts on differing local communities. Our group members emphasised that distance and travelling time were very different concepts, with traffic conditions and road networks of key importance in time to access UEC, which focused the team on carefully examining the nature of the measurements used within the identified literature. The group also highlighted the potentially positive impacts on the health-care system of reducing ease of access to care, in terms of reducing unnecessary use of accident and EDs, which provided the team with an important area to consider when examining the literature.
Towards the final stages of the review, a further meeting was convened to examine the emerging results, and to consider the findings in regard to key messages for members of the public, and implications for the health-care system. At this meeting the key results were presented by a member of the team. There was considerable discussion regarding the applicability of the findings to the UK system, with members of the group wishing for greater information regarding the country of origin of the evidence underpinning the findings. There was consensus that it was important that in our reporting, we highlighted where evidence came from countries with very different health-care systems, or very different geography to the UK as this could be crucial to interpreting the findings. This input was therefore very helpful to the team in consideration of interpretation of the findings. Members also emphasised that it should be made clear where there was insufficient evidence available and uncertainty, as this was important for members of the public to be aware of. This input informed our reporting, and will be considered during future dissemination activities. At this meeting members also drafted the Plain English summary to be included in the final report.
Registration and outputs
The protocol was registered as PROSPERO CRD42019123061 and is also available via the HSDR programme website (www.journalslibrary.nihr.ac.uk/programmes/hsdr/164717/; accessed 16 May 2019).
Chapter 3 Review results
Results of the literature search
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram (Figure 1) details the study selection process.
FIGURE 1.
The PRISMA flow diagram. Adapted from Chambers et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. This figure includes minor additions and formatting changes to the original text.
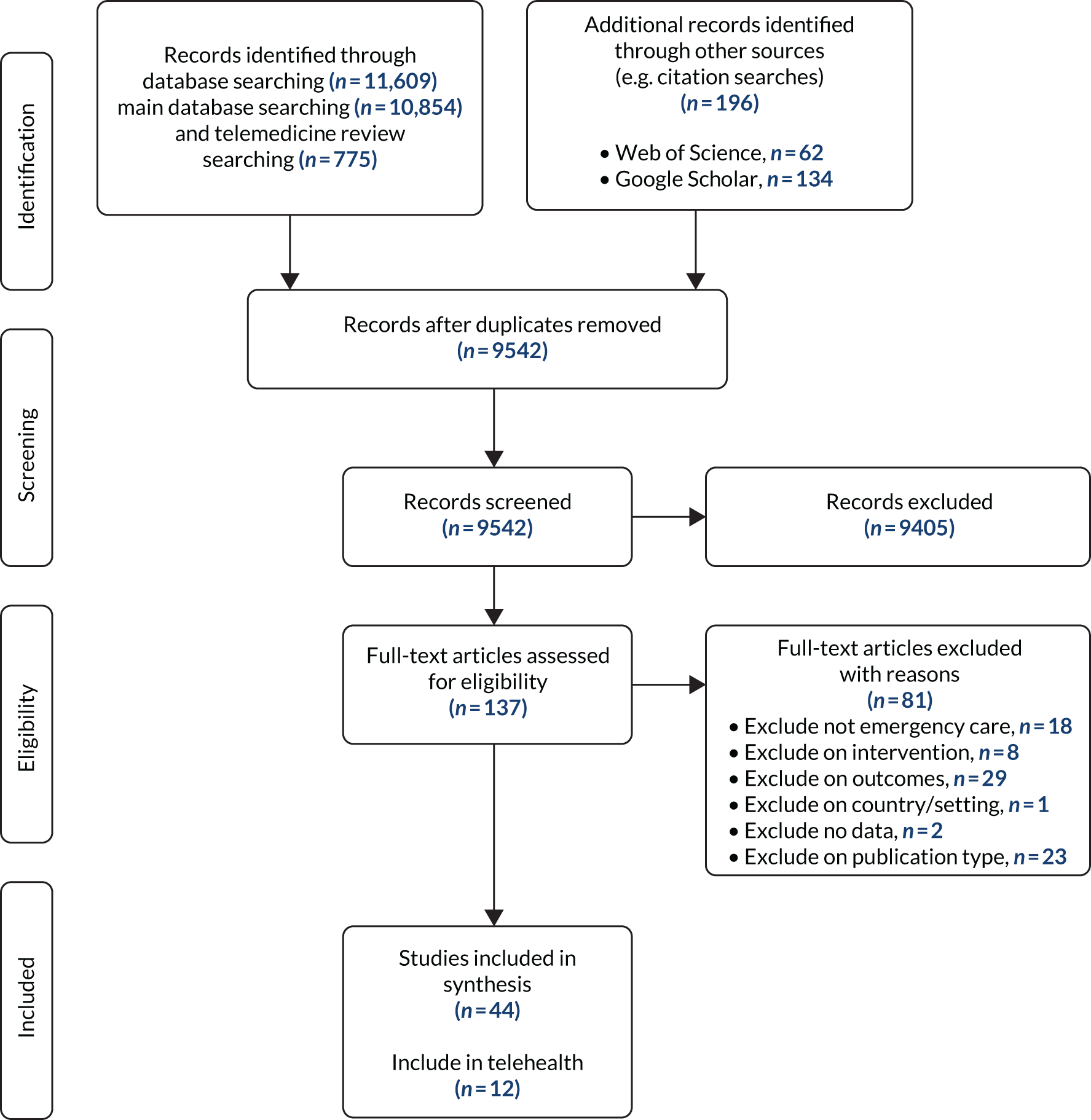
After deduplication of the searches from the different databases, there were 8870 references from the main database search and 550 from the telemedicine/telehealth search. Citation searching of Web of Science identified 52 new references and Google Scholar identified 63 new references.
All titles and abstracts were screened by one of the review team with a subset (about 10%) of the titles and abstracts being screened by two reviewers. Any queries were resolved by discussion. A similar process was followed for final decisions on inclusion/exclusion based on full-text documents. Calculation of the kappa coefficient demonstrated good agreement between reviewers [K = 0.729, 95% confidence internal (CI) 0.542 to 0.916]. Studies were excluded at the full-text stage for a variety of reasons (e.g. they covered access to services generally and not emergency care in particular; the intervention was not relevant, e.g. public access defibrillators; or the study discussed changes to services without relating outcomes to travel time or distance).
Characteristics of included studies
We included 44 publications in the review, reporting 43 unique studies. Of these, 12 evaluated the effects of an intervention or change to the health-care system (reconfiguration studies); 30 examined associations between travel distance or time and outcomes in the absence of a specific intervention (association studies); and two evaluated interventions to mitigate the effects of being at distance from an emergency care facility (mitigation studies).
Reconfiguration studies
Table 1 summarises the basic characteristics of the included reconfiguration studies. Six of the included studies were conducted in the USA, with just two2,4 being from the UK. The remaining studies were conducted in other European countries; there were no studies in this group from Canada, Australia or New Zealand.
| First author and year of publication | Country | Study design | Condition | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|---|---|
| Avdic 20165 | Other Europe (Sweden) | Controlled observational (analysis of linked administrative data sets) | Acute MI | Hospital ED | Administrative registers obtained from the Swedish National Board of Health and Welfare (hospitalisations and deaths) | Approximately 374,000 events | 21 years (1990–2010) |
| Combier 20136 | France (Burgundy region) | Uncontrolled observational (before–after study) | Obstetric/neonatal complications | Obstetric unit | Hospital discharge summary data for all deliveries from 22 weeks’ gestation in the region’s maternity units | 111,001 deliveries | 10 years (2000–9) |
| El Sayed 20127 | USA | Uncontrolled observational (before–after study) | General emergency care | Hospital ED | Routinely collected EMS and ED data | 5338 EMS transports; 21,685 ED visits | 3 months (June 1 to August 26 2010) |
| Hansen 20118 | Other Europe (Denmark) | Uncontrolled observational (before–after study) | General emergency care | Hospital ED | Danish National Person Registry including all Danish residents | 21,000 residents of Viborg county (2300 from Morso) | 7 years (1997 – 2003) |
| Hsia 20129 | USA (CA) | Controlled observational (cohort) | General emergency care: acute MI, stroke, sepsis and asthma/COPD | Hospital ED | California Office of Statewide Health and Planning Development database, combined with information on ED closures by year between 1999 and 2009 | 785,385, of whom 67,577 (8.6%) experienced an increase in distance to ED care as a result of an ED closure | 11 years (1999 – 2009) |
| Hsia 201410 | USA | Other (cross-sectional comparison of existing data sets, compared at T1 and T2 10 years later) | Major trauma: acute trauma aged ≥ 20 years | Specialist centre: trauma unit | Database of trauma centres open at T1 and 10 years later at T2. Patient discharge database. Household demographic database | 266,023 had no increased drive time, 5122 had increased drive time | Compared 1999 with 2009 |
| Knowles 20182 | UK | Controlled observational (interrupted time series) | General emergency care | Hospital ED | ONS, HES, ambulance dispatch records | Unable to locate, refers to areas only | 2 years pre closure and 2 years post closure |
| Mustonen 201711 | Other Europe [Finland (Vantaa, Finland’s third-largest city, with approximately 182,000 inhabitants)] | Controlled observational (controlled before–after study) | General emergency care | Other: whole UEC system, including other primary care EDs, office-hour primary care, secondary care EDs and private primary care | Electronic health records plus monthly mortality statistics by age groups | Unclear (34,000 inhabitants in area with ED closure) | 4 years (February 2004 to December 2007) |
| Roberts 20144 | UK (England only) | Uncontrolled observational (national data on distance travelled to emergency care plus three case studies of local reconfiguration) | General emergency care | Hospital ED | Hospital Episode Statistics plus data on ED attendances from every major (type 1) ED in England | 13 million ED attendances and 5.4 million emergency admissions (2011/12) | 10 years (2001/2 to 2011/12) |
| Shen 201212 | USA | Controlled observational (difference in difference approach) | Acute MI | Hospital ED | American hospital annual survey, database for California hospitals, Medicare claims | Unclear | 4 years before change to 4 years after change to ED access |
| Shen 201613 | USA | Controlled observational | Acute MI | Hospital ED | Medicare records, cost provider systems | 1.35 million patients | 90-day mortality reported in this paper |
| Yaghoubian 200814 | USA [CA (Los Angeles county)] | Uncontrolled observational (interrupted time series) | Major trauma | Specialist centre: trauma centre | Patient records from prospectively collected database (Trauma and Emergency Medicine Information System) | 14,996 | 9 years 2 months (January 1997 to 1 March 2006) |
Six of the included studies focused on ED reconfiguration, providing data on patients with many different types of emergency conditions. Three looked specifically at patients with AMI requiring access to percutaneous coronary interventions (PCI). Two studies examined the effects of service changes involving specialist trauma centres and one looked at the effects of maternity unit closures in France (see Table 1).
The studies used a variety of observational designs, with before–after and cohort designs being most common. Knowles et al. 2 and Mustonen et al. 11 were the only studies with independent control sites where no reconfiguration had taken place.
Association studies
The largest group of association studies focused on AMI (10 studies), followed by trauma and maternity (seven studies each). Four studies examined general populations and three dealt with stroke [including one study also included in the myocardial infarction (MI) group15]. One study included people with ruptured abdominal aortic aneurysms (AAAs).
Six studies were derived from UK settings. These included two studies of stillbirth risk and travel time in Cumbria;16,17 studies of risk and travel time for life-threatening conditions18 and specifically for MI19 and for ruptured aortic aneurysms;20 and a study of the relationship between distance and social deprivation as influences on ED attendance. 21 Other studies were conducted in the USA, Canada, Japan and various European countries. Most studies used a cohort or cross-sectional design with comparisons between distance or time categories and no separate control group. Sample size and study duration varied substantially between studies, with the largest covering whole-country populations, for example Switzerland or the Netherlands. Tables 2–5 summarise the study characteristics.
| First author and year of publication | Country | Study design | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|---|
| Andersson 201922 | USA | Controlled observational (cohort) | Hospital ED | Blue Cross Blue Shield of Michigan Cardiovascular Consortium registry | 27,205 (25,927 primary PCI, 1278 pharmacoinvasive) | 7 years (January 2010 to December 2016) |
| Balamurugan 201623 | USA (AR) | Controlled observational {cohort [cross-sectional (authors’ terminology)]} | Hospital ED: PCI-capable hospital | All death certificates with AMI as underlying cause of death | 14,027 | 5 years (2008–12) |
| Balamurugan 201824 | USA (AR) | Controlled observational {cohort [cross-sectional (authors’ terminology)]} | Hospital ED: hospitals with and without continuous PCI capability | Arkansas Department of Health data on deaths and hospital discharges associated with AMI | 15,514 (4613 deaths, 10,901 discharges) | 2 years (2012–13) |
| Berlin 201615 | Switzerland | Controlled observational (cohort) | Hospital ED: hospitals classified as acute, acute with ED, central and university | Swiss National Cohort study: population of Switzerland at the time of the 2000 census | Total 4.5 million; 19,301 AMI and 21,931 stroke deaths | 8 years (December 2000–December 2008) |
| Bussières 201825 | Canada | Controlled observational (cohort) | Specialist centre: tertiary cardiology centre | Patients with STEMI transported to a tertiary cardiology centre for PCI | 880 | 9.5 years (January 2006 to June 2017) |
| Di Domenicantonio 201626 | Other Europe (Italy) | Controlled observational (cohort) | Hospital ED | Routinely collected anonymised data from regional health information system | 3608 | 4 years 11 months (January 2009 to November 2013) |
| Langabeer 201527 | USA (WY) | Uncontrolled observational (cohort) | Specialist centre | Data on patients with STEMI undergoing primary PCI in 10 Wyoming hospitals | 395 | 21 months (January 2013 to September 2014) |
| Postma 201428 | The Netherlands | Controlled observational (field triage in an ambulance with direct travel to a PCI centre vs. referral to a spoke centre and then travel to a PCI centre) | Specialist centre: PCI centre | Database of patients registered on the project | 4149 | 6 years |
| Svensson 200329 | Other Europe (Sweden) | Controlled observational (urban versus rural populations) | Other: ambulance | Data collection during study (unclear) | 64 in urban areas, 90 in rural areas, 148 received thrombolysis prehospital | Unclear recruitment 16 months |
| Wei 200819 | UK (Tayside, Scotland) | Uncontrolled observational (cohort) | Hospital ED | Hospital discharge data for patients resident in Tayside who experienced a first MI between 1994 and 2003 | 10,541 | 10 years (January 1994 to December 2003) |
| First author and year of publication | Study design | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|
| Durkin 200530 | Uncontrolled observational | Hospital ED | Wisconsin Crash Outcome Data Evaluation System database | Study covered 10 years during which there were 1,365,642 car crashes on roads in Wisconsin. 3,612,898 people were involved in the collisions and 654,920 were reported as potentially injured | 10 years (1992–2001) |
| Gomez 201031 | Uncontrolled observational (retrospective cohort) | Specialist centre: trauma centre | Ontario Trauma Register | 3486 | Retrospective, 1 year of data |
| Gonzalez 200932 | Other (cross-sectional comparison of data from two sources) | Other: emergency medical service (presumably ambulances) | Patient care reports and police crash reports | 45,763 | 2 years |
| Jarman 201833 | Other (cross-sectional comparison of data) | Specialist centre (trauma centre) | Data provided by EMS companies and trauma centres, geocoding of injury locations, 1-year period | 16,082 aged ≥ 18 years | 1 year (January to December 2015) |
| Lee 201834 | Uncontrolled observational (development of random-effects probit model) | Hospital ED | 2016 Fatality Analysis Reporting System data | 20,100 observations; 13 excluded during modelling process due to missing values | Not specified |
| Lerner 200335 | Uncontrolled observational (retrospective review of data from convenience sample of medical records) | Hospital ED | Patient records from trauma centre’s trauma registry for patients who had been transported to hospital by an ambulance or helicopter from January 1993 to October 1996 | 2925 records that met the study criteria. 2410 of these patients had complete time data and were not in cardiac arrest. Further exclusion led to 1877 records suitable for analysis | January 1993–October 1996, 46 months |
| McCoy 201336 | Uncontrolled observational | Hospital ED | Trauma registry at a university teaching hospital | 19,167 cases were included in analysis | 14 years (1996–2009) |
| First author and year of publication | Country | Study design | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|---|
| Dummer 200416 | UK (Cumbria) | Uncontrolled observational (cohort) | Obstetric unit: for stillbirth, all hospitals with a maternity facility were included | Cumbrian Births Database covering years 1950–93 | 283,668 live births; 4325 stillbirths; 4889 infant deaths (birth to 1 year) | 44 years (1950 to 1993) |
| Engjom 201737 | Other Europe (Norway) | Uncontrolled observational (retrospective cohort) | Obstetric unit: units and out of hospital births. Unplanned birth rather than designated emergency care | Medical birth registry of Norway and statistics Norway | Travel data available for 646,898 births | Data from 10-year period |
| Featherstone 201638 | USA | Other (cross-sectional) | Obstetric unit: level III neonatal intensive care unit | Birth and death and hospital records | Number of participants (2030) | Data for 2 years |
| Grzybowski 201139 | Canada (BC) | Uncontrolled observational (cohort) | Maternity services with caesarean section capability | British Columbia Perinatal Health Programme | 49,402 women/newborns (only singleton pregnancies included) | 4 years (April 1 2000 to March 31 2004) |
| Parker 200017 | UK (West Cumbria) | Uncontrolled observational (cohort) | Obstetric unit: all maternity services | Database of Cumbrian births | 77,995 live births; 1234 stillbirths | 40 years (1950 to 1989) |
| Pilkington 201440 | France | Other (cross-sectional) | Obstetric unit: maternity unit | French national registry | 14,860 neonatal deaths, 6,202,918 live births | Data from 7 years |
| Ravelli 201141 | The Netherlands | Uncontrolled observational | Obstetric unit | Netherlands Perinatal Registry | 751,926 term singleton births | 7 years (2000 to 2006) |
| First author and year of publication | Country | Study design | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|---|
| General population studies | ||||||
| Murata 201342 | Other non-Europe (Japan) | Other (cross-sectional) | Other: unclear whether or not it relates to UEC, refers to in-hospital mortality only | Ministry of Health’s disease database, distance from Diagnosis Combination database | 108,314 | Data from 1 year (2008) |
| Nicholl 200718 | UK (England) | Uncontrolled observational (cohort) | Hospital ED | Ambulance patient report forms and patients’ ED notes | 10,315 | 5 years (1997 to 2001) |
| Rudge 201321 | UK | Uncontrolled observational | Hospital ED: type one EDs – consultant-led 24-hour service with resuscitation facilities and designated A&E reception area. 21 sites included | Database of ED visits (records of attendance) made by residents of the region | 1,413,363 visits | 1 year (2006–7) |
| Stroke studies | ||||||
| Acharya 201143 | USA | Controlled observational (retrospective cohort) | Hospital ED | Patients admitted to Barnes Jewish Hospital in St Louis with a diagnosis of stroke | 330 | 2 years (January 2006 to December 2007) |
| Berlin 201615 | Switzerland | Controlled observational (cohort) | Hospital ED: hospitals classified as acute, acute with ED, central and university | Swiss National Cohort study: population of Switzerland at the time of the 2000 census | Total 4.5 million; 19,301 AMI and 21,931 stroke deaths | 8 years (December 2000–December 2008) |
| Leyden 201144 | Australia (SA) | Uncontrolled observational (retrospective review case note) | Hospital ED: many patients presented to hospitals without stroke units. Specialist centre acute stroke unit | Electronic data repositories and other prospective clinical registries | 157 patients with 158 cases of thrombolysis during the study period | 2 years (1 October 2007–30 September 2009) |
| Ruptured AAA study | ||||||
| Souza 200520 | UK (West Sussex) | Uncontrolled observational (cohort) | Hospital ED | Hospital admission and death certification data | 515 | 3 years 9 months (January 1996 to September 1999) |
Mitigation studies
We identified two studies that met our inclusion criteria and provided evidence regarding interventions that might mitigate the effects of being at a distance from an ED (Table 6). The interventions evaluated were first a specialist stroke ambulance and second a co-ordinated state-wide initiative to improve care for rural patients experiencing an AMI. These two studies represented contrasting approaches to mitigation. The specialist stroke ambulance study45 was performed in an urban setting (in Berlin) and the intervention appeared to be of value in reducing time to thrombolysis for patients located within 18 minutes’ travel time from the ambulance base, making its relevance to more rural areas uncertain. The Wyoming intervention of co-ordination between hospitals and other health-care providers covered a largely rural state with long distances between UEC facilities. 46 The study reported a reduction in total ischaemic time following introduction of the new system.
| First author and year of publication | Country | Study design | Condition | UEC facility | Sample source | Sample size | Length of study |
|---|---|---|---|---|---|---|---|
| Koch 201645 | Germany (Berlin) | Experimental (secondary analysis of PHANTOM-S study, which is a clinical trial) | Stroke | Other: specialty stroke ambulance | Data from the PHANTOM-S trial | Patients in the PHANTOM-S trial. 530 patients received intravenous thrombosis. 200 patients received specialised stroke ambulance care; 330 patients were cared for by conventional emergency medical service | 21 months (1 May 2011–31 January 2013) |
| Langabeer 201646 | USA (WY) | Uncontrolled observational (before–after study) | Acute MI (ST elevation MI) | Specialist centre: hospital with PCI capability | National Cardiovascular Data Registry submissions for patients undergoing PCI at four hospitals in Wyoming and seven in neighbouring states | 889 (206 pre intervention; 123 baseline; 560 post intervention) | Length of study [2 years (2013–14)] |
A study of public access defibrillators47 was fully considered for eligibility as being potentially mitigating. However, in the final analysis this study was excluded on the grounds that survival of out-of-hospital cardiac arrest was unlikely to be affected by distance to the ED.
We examined the use of telehealth as a potentially mitigating intervention by means of a separate review of systematic reviews (see Chapter 4).
Risk-of-bias assessment
Results of the risk-of-bias assessment are presented in Tables 21–23 (see Appendix 3). Many of the studies were inherently at high risk of bias because of lack of an independent control group. In the reconfiguration group, the most common design was before–after and only four studies compared outcomes between settings with and without changes in distance/time. 2,5,9,11 Association studies generally used a cohort or cross-sectional design (see Table 2).
With regard to each question on the evaluation tool, the following comments can be made about the overall quality of the included literature. Most of the included studies were clear about the temporal relationship of the variables of interest (i.e. which was the ‘cause’ and which the ‘effect’; Q1), although the issue was sometimes confused by the use of linked data sets. Similarity between populations being compared (Q2) varied across the studies, with some being clinically heterogeneous. Similarly, it was often unclear whether comparison groups were being treated similarly other than the intervention or exposure of interest (Q3). This was related to differences over time as well as to studies recruiting clinically diverse populations. Absence of a separate independent control group (Q4) was noted in most of the studies and similarly few studies carried out measurements at multiple time points before and after an intervention or exposure (interrupted time series design; Q5). Completeness of follow-up (Q6) did not show a clear pattern across studies; this question was not applicable for studies with measurement at a single time point. Most studies measured outcomes in a standard (Q7) and reliable (Q8) way, although again some exceptions were identified. Statistical analysis (Q9) was judged to be appropriate with the exception of one study. 42 However, as with all observational studies, the possibility of unmeasured confounders affecting the results could not be ruled out.
Results by condition
For each condition, the reconfiguration studies are considered first, followed by the association studies, concluding with an overall summary for each group.
General urgent and emergency care
Of the nine studies of general UEC populations, five focused on adults only. 2,7,9,18,42 Four studies included data on patients of all ages,4,8,11,21 but only one reported separate data for adults and children. 21
Reconfiguration studies
Six studies evaluated the effects of reconfigurations that increased distance to the ED for general UEC populations. One study9 differed from the others in that it involved subgroups of people with specific conditions (i.e. MI, stroke, sepsis, asthma or chronic obstructive pulmonary disease) rather than general populations of people attending the ED. Details of the methods and findings of the studies are summarised in Table 7.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| El Sayed 20127 | Large city/city region (Boston, MA, USA) |
Intervention ED closure or relocation Boston Medical Center: two EDs merged into one Comparator Earlier time period 6 weeks before vs. 6 weeks after closure |
Hospital ED | Travel time: not measured directly but EMS turn round time was an outcome | Other: EMS turn round times, ED volumes and transport volumes | The closure of one ED resulted in a statistically significant increase in turnaround times and a significant decrease in ED volume with no change in EMS volumes |
| Hansen 20118 | Mixed (municipality of Morso in Viborg county, mid-Jutland) |
Intervention ED closure or relocation. Hospital ED was reduced to a daytime emergency clinic in 2000 and closed in September 2002 Comparator Earlier time period. Study covers period before-and-after ED closure |
Hospital ED | Direct distance: nearest alternative hospitals reported to be 30 km away |
Hospital admissions Other: ED visits; use of alternative services, e.g. GP consultations |
Emergency services at neighbouring hospitals (up to 40 km away) were able to compensate in part for a decrease in local provision |
| Hsia 20129 | Other: whole US state (CA) |
Intervention ED closure or relocation Comparator Baseline distance to nearest ED for patient’s year of admission was compared with that for 1999 |
Hospital ED | Actual travel distance: driving distance | Mortality: inpatient mortality | < 10% of patients experienced an increase in distance to the nearest ED and the majority of increases were < 1 mile. These small increases were not associated with increased inpatient mortality for time-sensitive conditions |
| Knowles 20182 | Mixed: five intervention areas. Time to nearest ED typically varied from 0 to 20 minutes |
Intervention ED closure or relocation. Closure or downgrade Comparator No intervention. Control areas |
Hospital ED | Travel time: the ED which was used most for incidents within each area was designated as the destination. Time from scene of the incident using department for transport travel time to designated ED |
Mortality Morbidity Hospital admissions Other: A&E attendance |
No reliable evidence of adverse effect on mortality from ED closure. Effects vary between sites. Potentially negative effects might be offset by other factors. Ambulance services may experience greater burden |
| Mustonen 201711 | Urban/suburban |
Intervention ED closure or relocation. Closure of small suburban primary care ED (June 2005) Comparator No intervention. Neighbouring city (Espoo) without ED closure |
Other: whole UEC system, including other primary care EDs, office-hour primary care, secondary care EDs and private primary care | Direct distance: distance from centre of district of residence to alternative facilities |
Mortality: secondary outcome, from monthly mortality statistics Other: visits to different types of health facilities before and after the intervention |
ED closure can be used to direct patients to use other parts of the health system. The study confirmed a negative correlation between distance to the ED and levels of ED use by local people. The availability of secondary care ED services protected against the risk of increased mortality following closure of a primary care ED |
| Roberts 20144 | Other: whole country (England) |
Intervention ED closure or relocation. Evaluated in case studies Comparator Earlier time period |
Hospital ED | Direct distance | Hospital admissions | Where an ED is closed or downgraded, the direct impact on the local population can be large, in some cases doubling the distance that they travel for emergency admissions. However, the national impact of these changes is small. There has only been a small increase in average home-to-hospital distances since 2001/2: from 8.3 to 8.7 km. However, there is a subset of mostly rural areas where the distances are much further than average |
Five of the studies reported at least some data on patient outcomes (including hospital admissions) associated with ED reconfiguration or closure. 2,4,8,9,11 Two of these were controlled studies2,11 and two were from UK settings. 2,4 The three studies that reported on mortality2,9,11 found no evidence of increased mortality rates associated with ED reconfiguration. A limitation of this evidence is the fact that one study measured only inpatient mortality9 and another only documented mortality as a secondary outcome. 11
The other main patient outcome reported in these studies was hospital admissions, reported in three studies. 2,4,8 Hansen et al. 8 found a reduction in hospital inpatient admissions in a municipality where the ED changed from 24-hour to daytime only and then closed, requiring residents to travel further to use ED services. However, this reduction was only seen in women and its clinical significance was unclear. In the UK ClosED study, there was no consistent effect on emergency admissions. 2 The study found some evidence of a decrease in emergency admissions and admissions considered potentially avoidable, but this was not considered statistically reliable. In their case studies of reconfiguration in the English NHS, Roberts et al. 4 presented limited data on emergency admissions. In Burnley, these admissions remained broadly constant despite an increased distance to the nearest ED, while in Kent emergency admissions increased in areas where new facilities were introduced. The limited evidence from these studies makes it difficult to draw firm conclusions about the effect of ED reconfigurations on hospital admissions.
Most studies also reported health system outcomes. The most short term of the included studies7 reported on the effects of closure of an ED in Boston, MA, USA, on a neighbouring ED. This study only measured outcomes related to the ambulance service for 6 weeks before and after the closure. There was a significant increase in ambulance turnaround times (time the ambulance is out of service and unable to respond to another call) and a decrease in the volume of patients attending the remaining ED but no change in the volume of patients transported by EMS vehicles. Further research would be needed to assess whether or not these changes were sustained in the longer term. In the UK, Knowles et al. 2 found evidence of an increased burden on ambulance services (increased activity, e.g. increases in emergency ambulance incidents) following closure or downgrading of EDs, reflecting increases in the distances patients had to be transported to reach the nearest ED.
Knowles et al. 2 found no consistent effects of ED closure or downgrading on UEC attendance. There was some indication of a decrease in attendances on average across the sites studied but this was not considered statistically reliable. A similar pattern (statistically unreliable evidence of a decrease) was found for attendances by patients who were discharged without treatment or further investigation. 2
Two studies in Scandinavian countries investigated patients’ use of alternative services following closure of a local ED. Hansen et al. 8 (Denmark) found that patients used services located up to 40 km away. The authors noted that free access to ambulance services and high levels of car ownership meant that distance was not a serious barrier to people accessing urgent or emergency care. Similarly, in Finland the availability of alternative secondary care ED facilities was considered to protect against any risk of increased mortality following closure of a local primary care ED. 11 This study reported a negative relationship between distance and ED use by local residents, suggesting that ED closure can be used to encourage patients to access other more appropriate services.
Overall, the reconfigurations evaluated in these studies had relatively small effects on travel times/distance and hence few negative effects on outcomes for patients were reported in the studies that evaluated them. However, even in a relatively small country such as England, there are localities where travel distances are considerably longer than average and where service reconfigurations might be expected to have most impact. Furthermore, general populations of people attending an ED include many people with less time-sensitive conditions who, by definition, are at lower risk of being negatively affected by increased travel times. Effects on health system outcomes varied across studies and settings but the included studies did not suggest that ED closure or reconfiguration causes significant problems for neighbouring services. There was, however, evidence of an impact on local ambulance services, as highlighted by El Sayed et al. 7 and Knowles et al. 2
Association studies
Only three included studies examined the association between travel times and outcomes in UEC populations not restricted by condition (Table 8). Two of these involved patients with diverse but serious conditions,18,42 whereas the third examined all visits to EDs in the West Midlands region of England. 21
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Murata 201342 | Mixed (whole of Japan) |
Intervention None Comparator Not applicable |
Other: unclear whether or not it relates to UEC, only refers to in-hospital mortality | Direct distance: GIS data to estimate distance an ambulance had to travel | Mortality | Distance by ambulance to hospital affects mortality for acute conditions |
| Nicholl 200718 | Mixed (Berkshire, Derbyshire, Essex and West Midlands, including urban, mixed and rural areas) |
Intervention None Comparator Distance/time categories 0–10, 11–20 and > 21 km |
Hospital ED | Direct distance: distance from incident scene to hospital | Mortality: survival to discharge | Increased distance to hospital appears to be associated with increased risk of death. Results suggest that a 10-km increase in straight-line distance is associated with around a 1% absolute increase in mortality |
| Rudge 201321 | Mixed (population living in West Midlands) |
Intervention None Comparator Not applicable |
Hospital ED: type one EDs – consultant-led 24-hour service with resuscitation facilities and designated A&E reception area. 21 sites included | Actual travel distance: units of geography were lower level super outputs (small neighbourhoods), km from hospital measured for people from each of these units using residential postcode. Used GIS software and calculated shortest road distance for each population area | Other: deprivation and distance, A&E attendance | Distance to ED and patterns of usage is modified by levels of deprivation. Proximity to a MIU reduces ED usage for those at greater distance from an ED |
Nicholl et al. 18 and Murata et al. 42 both focused on in-hospital mortality and both found an association between distance to hospital and mortality risk. Nicholl et al. 18 looked at people transported by ambulance who were considered to have a potentially life-threatening condition. Distances travelled ranged from 0 to 58 km (median 5 km). Increased risk of death was expressed as an odds ratio (OR) (1.02 per km, 95% CI 1.01 to 1.03 per km). 18 Murata et al. 42 expressed the association between distance and mortality as a correlation coefficient (R). Values of R for AMI and brain infarction (stroke) were 0.315 (p < 0.01) and 0.233 (p < 0.001), respectively. 42 The studies differed in their populations of interest: Nicholl et al. 18 studied people with life-threatening conditions whereas Murata et al. 42 focused more broadly on ‘acute diseases’ and included people with non-emergency conditions, such as pneumonia. The small number of studies and differences in populations and statistical methods make it difficult to gain an overall estimate of the strength of the association.
The study by Rudge et al. 21 examined the association between distance and ED attendance, an important health system outcome, and the influence of socioeconomic circumstances on this association. This study analysed data on over 1.4 million ED visits in the West Midlands during the financial year 2007–8. The authors’ regression model indicated that ED attendance declines with distance by 1.5% (95% CI 1.2% to 1.8%) for adults and 2.2% (95% CI 1.7% to 2.6%) for children. Levels of ED attendance increased with increasing socioeconomic deprivation. ED attendance was also affected by proximity to a minor injury unit (MIU), suggesting that provision of MIUs can modify ED attendance. ED attendance was more sensitive to increased distance in deprived neighbourhoods compared with less deprived areas. This large single study adds to the findings of studies in the reconfiguration group2,8,11 by assessing the role of deprivation in the complex relationship between distance and ED attendance in the general UEC population.
Acute myocardial infarction
Reconfiguration studies
Two studies, reported in three publications, investigated the effects of reconfigurations or closures that increased travel distance on outcomes for patients with AMI,5,12,13 and Table 9 summarises these studies. The two papers by Shen and Hsia12,13 appear to use the same data, and the 2016 paper13 may be considered as an update to the 2012 publication,12 although the later paper does not cite the earlier one.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Avdic 20165 | Other: whole country (Sweden) |
Intervention ED closure or relocation. Sixteen emergency hospital closures between 1990 and 2010 Comparator No intervention Compares areas with and without closures |
Hospital ED |
Direct distance Actual travel distance Travel time |
Mortality: includes out-of-hospital mortality as well as in-hospital mortality | The results provide some evidence that geographical access to health care has at least a short-term impact on the quality of emergency care. Ambulance services should be properly prepared for changes in the distance patients need to travel for emergency care |
| Shen 201212 | Mixed (appears to be data for AMI patients for the whole of the USA) |
Intervention ED closure or relocation Comparator Earlier time period |
Hospital ED | Actual travel distance: driving time from residential postcode to the nearest ED |
Mortality Morbidity: whether patient received percutaneous transluminal coronary angioplasty |
Increases in driving time of < 10 minutes have a small effect on mortality, with effect greater for those who have longer travelling distances before the change. For those with increases in driving times of < 30 minutes adverse effects tend to be temporary. Increases in driving time of > 30 minutes have an adverse effect on mortality in both the short and long term |
| Shen 201613 | Mixed |
Intervention ED closure or relocation Comparator Earlier time period |
Hospital ED | Actual travel distance: driving time |
Mortality Morbidity: likelihood of percutaneous transluminal coronary angioplasty or thrombolytic treatment |
Increased travel of > 10 minutes is associated with increased AMI mortality |
All of the publications reported some negative effects of increased travel distance on mortality of patients with AMI. Avdic5 compared areas of Sweden with and without ED closures over the period 1990–2010. Overall, there was an increase in mortality of approximately 2 percentage points for each extra 10 km of travel distance. The effect was driven by out-of-hospital deaths and was most pronounced in the first year after an ED closure. This led the author to suggest that ambulance services in particular need to be prepared for the impact of ED closures.
Shen and Hsia in their two publications12,13 analysed data on driving times and outcomes associated with ED closures in the whole of the mainland USA. The first paper12 covered the period 1996–2005. The majority of the study population (89.2%) did not experience any increase in driving time to the nearest ED during the study period. There was a small increase in mortality associated with small increases in driving time (up to 10 minutes), the effect being strongest for those with limited access to hospitals at baseline (e.g. in rural or mountainous areas). Increases in driving time of > 30 minutes were associated with increased long-term (up to 1 year) mortality rates, although increases of this magnitude only affected 0.2% of the study population. Most changes were relatively short term and mortality rates 3 years after ED closure were generally similar to those before the closure.
The later publication from these authors13 analysed similar data for the period 2001–11. This publication presented information on increases in absolute mortality risk. Patients whose driving time increased by 10–30 minutes had an increased risk of 90-day mortality by 1.6 percentage points (95% CI 0.53 to 2.67 percentage points) and 1-year mortality by 2.05 percentage points (95% CI 0.96 to 3.14 percentage points). Corresponding figures for those with > 30 minutes longer driving time were 6.58 percentage points (95% CI 2.49 to 10.68 percentage points) and 6.52 percentage points (95% CI 1.69 to 11.35 percentage points), respectively. The authors noted that 6.58 percentage points represented a 30% relative increase in 90-day mortality in this population.
Association studies
Ten included studies (Table 10) explored the relationship between ED distance and MI outcomes in the absence of reconfiguration. Of these, eight reported the presence of an association and two reported unclear findings. Six studies investigated mortality alone or in combination with other outcomes. Other main outcomes related to travel time or distance were type of treatment strategy, adverse events during transportation and total ischaemic time (time from symptom onset to start of treatment, which was evaluated in two studies). All the studies used a cohort-type design.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Andersson 201922 | Other: all 47 non-federal hospitals in Michigan |
Intervention None Comparator Distance/time categories: travel time ≤ 1 hour vs. > 1 hour |
Hospital ED | Travel time: time from home zip code to PCI-capable hospital zip code estimated using Google Maps | Other: type of treatment strategy (primary PCI or pharmacoinvasive) | The great majority of patients with STEMI had timely access to a suitable hospital and were treated by primary PCI |
| Balamurugan 201623 | Other: whole US state (AR) |
Intervention None Comparator Distance/time categories |
Hospital ED PCI-capable hospital |
Direct distance: geodesic distance Travel time: driving time |
Mortality | AMI mortality increases with increasing driving time to the nearest PCI-capable hospital |
| Balamurugan 201824 | Other: whole US state (AR) |
Intervention None Comparator Distance/time categories |
Hospital ED Hospitals with and without continuous PCI capability | Direct distance | Mortality | A higher risk of AMI deaths was associated with health-care system factors, especially distance to nearest hospital and hospitals’ ability to deliver PCI, even after adjusting for individual and environmental factors |
| Berlin 201615 | Other: whole country |
Intervention None Comparator Distance/time categories: highest vs. lowest quintile of driving time |
Hospital ED Hospitals classified as acute, acute with ED, central and university |
Direct distance Travel time: driving time |
Mortality | The increasing MI mortality with increasing driving time to the nearest university hospital but not to other types of hospital reflects a complex situation influenced by many factors along the care pathway |
| Bussières 201825 | Rural Chaudière-Appalaches and Québec City regions, QC, Canada |
Intervention None Comparator Distance/time categories |
Specialist centre Tertiary cardiology centre | Travel time | Morbidity: clinical adverse events, classified as important or minor | Transport time is not associated with clinical adverse events in rural STEMI patients transported by basic life support paramedics |
| Di Domenicantonio 201626 | Mixed: Lazio region of Italy |
Intervention None Comparator Distance/time categories |
Hospital ED | Travel time | Mortality: mortality within 30 days of PCI | Travel time affects survival after PCI for patients treated in line with current guidance |
| Langabeer 201527 | Rural |
Intervention None Comparator Distance/time categories: compares transfer vs. direct arrival at PCI hospital |
Specialist centre | Direct distance | Other: total ischaemic time (time from symptom onset to treatment) | There is a need to focus on improving transitions between referral and receiving centres and to enhance co-ordination between services in US rural settings |
| Postma 201428 | Mixed: < 90 km from the PCI centre |
Intervention Mitigation: field triage in an ambulance or referral via a spoke centre for assessment. Some ambulances equipped with field triage equipment and highly trained paramedics who performed an ECG and this was interpreted by a computerised algorithm. If a diagnosis of STEMI was made the ambulance went directly to a specialist centre Comparator Alternative intervention: triage in an ambulance and direct travel to centre, compared with travel to and then referral from a spoke centre |
Specialist centre: PCI centre | Actual travel distance: patient residence postcode and travel time via a motorway to PCI centre | Morbidity: total ischaemic time | Residential distance is only weakly associated with ischaemic time if patients are transported directly to PCI centres after triage in an ambulance, rather than being assessed in a spoke centre |
| Svensson 200329 | Mixed: urban and more sparsely populated rural areas |
Intervention Pre-hospital ECG carried out by ambulance crew and results transmitted to a physician who went through a checklist before thrombolysis was performed Comparator Not applicable |
Other: ambulance | Travel time: compared travel time between large populations (> 90,000 inhabitants) defined as urban with smaller populations defined as rural |
Mortality Morbidity Other: time intervals – 911 call, ambulance arrival, EEG transmission, departure, arrival, start of thrombolysis. Clinical signs – heart rate, blood pressure, rhythm, treatment complications, medications |
Pre-hospital ECG should be recorded and if required pre-hospital thrombolysis carried out by trained ambulance personnel |
| Wei 200819 | Mixed: appears to include both urban and rural areas (rurality indicated by postcode) |
Intervention None Comparator Distance/time categories |
Hospital ED |
Direct distance: calculated from grid references of postcodes for home and hospital Travel time |
Mortality | Distance between home and hospital may predict mortality in patients experiencing a first AMI. This association was found both before-and-after hospitalisation. The findings provide support for policies that locate services for AMI closer to where patients live |
Two studies by Balamurugan et al. ,23,24 set in Arkansas, USA, analysed data on AMI cases from 2008 to 2012 and from 2012 to 2013, respectively. The earlier study23 focused exclusively on the relationship between driving time to the nearest PCI-capable hospital and MI mortality. Mortality risk in patients from the neighbourhoods with the longest driving distances were 26% higher than those with the shortest distances after adjusting for a range of confounding factors. For comparison with UK studies, the median geodesic distance (shortest path) and driving time were 12.8 miles [interquartile range (IQR) 3.6–30.1 miles] and 28.3 minutes (IQR 9.6–58.7 miles), respectively. This compares with a median distance of 5 km (3.1 miles) in a typical UK study. 18 The second study by these authors24 looked at patients who survived to discharge as well as those who died and considered a range of factors affecting mortality risk, including comparing hospitals with and without a continuous PCI capability. The authors found a 9.2% increase in the odds of death for every 10 miles of additional distance to the nearest hospital (with or without continuous PCI capability) (OR 1.092, 95% CI 1.009 to 1.181). Admission to a hospital without continuous PCI capability was the other factor associated with increased odds of death (OR 1.64, 95% CI 1.15 to 2.34).
A large national cohort study in Switzerland (4.5 million participants and > 19,000 AMI deaths over 8 years) also found an association between driving time to hospital and risk of mortality from AMI. 15 The association was strongest for driving time to a university hospital [hazard ratio (HR) for highest vs. lowest quintile 1.19 (95% CI 1.10 to 1.30) for men and 1.10 (95% CI 1.01 to 1.20) for women aged > 65 years)]. This study also examined stroke mortality as discussed below (see Stroke).
A smaller study (3608 patients) in Italy looked at patients with ST elevation myocardial infarction (STEMI) who underwent PCI between 2009 and 2013. 26 The authors defined system delay on treatment (PCI) as travel time to hospital plus door-to-balloon time (DTBT) within the hospital. Among those with ≤ 90 minutes of symptom delay, in line with current guidelines, travel time above the median (14 minutes) was associated with significantly higher odds of 30-day mortality (OR 2.46, 95% CI 1.25 to 4.86). There was a significant interaction between travel time and DTBT, such that patients with DTBT below the median only experienced a survival benefit if travel time was also below the median.
ST-elevation MI was also the focus of a small study by Svensson et al. 29 in Sweden, who evaluated treatment with a thrombolytic agent (reteplase) in the ambulance before hospital admission. The median interval between the onset of symptoms and the start of thrombolysis was 1 hour 44 minutes in urban areas versus 2 hours 14 minutes in rural areas (p = 0.03). Median time of transport from the scene of the incident to hospital was 17 vs. 33 minutes. There was no difference between the urban and rural groups in 30-day mortality but the rural patients had more symptoms of heart failure. One-year mortality was higher in the rural patients (17 vs. 5%; p = 0.02).
The only UK study in this group was performed by Wei et al. 19 in Tayside, Scotland. They analysed data on 10,541 patients with AMI between 1994 and 2003. Survivors were followed for a median of 3.2 years. After adjustment for known risk factors, distance from home to hospital was associated with risk of death before arrival at the hospital and after discharge but not with death in hospital. Compared with < 3 miles, ORs for pre-hospital death were 2.05 (95% CI 1.00 to 4.21) for > 9 miles and 1.46 (95% CI 1.09 to 1.95) for 3–9 miles. The corresponding adjusted HRs for death during follow-up were 1.90 (95% CI 1.19 to 3.02) and 1.27 (95% CI 0.96 to 1.68).
In summary, all of the studies that evaluated mortality found a positive association between increasing travel time/distance and increased mortality following AMI. Variation in populations, settings, statistical methods and length of follow-up make it difficult to estimate an overall effect measure, as discussed further in Strength of evidence.
Turning to other outcomes, Langabeer et al. 27 and Postma et al. 28 related distance to total ischaemic time [i.e. time from symptom onset to start of treatment (in hospital)]. For patients with STEMI undergoing PCI in the study by Langabeer et al. ,27 total ischaemic time and travel distance were higher for patients who were transferred to a different hospital to receive PCI than for those who did not need to be transferred. However, over the whole sample, distance was not significantly associated with total ischaemic time. A similar finding was reported by Postma et al. 28 for STEMI patients undergoing PCI in the Netherlands: a longer distance from home to hospital was associated with longer total ischaemic time in patients referred for PCI from a non-PCI ‘spoke’ hospital but not for those transported by ambulance directly to the PCI centre.
The PCI must be performed promptly for optimum results (90 minutes for first-contact patients and 2 hours for transferred patients). 22 Andersson et al. 22 analysed data on > 27,000 patients who underwent PCI for STEMI in Michigan, USA, between 2010 and 2016. They examined the relationship between transport time to a PCI-capable hospital and choice of treatment (reperfusion) strategy, comparing primary PCI with a drug therapy strategy. Use of the latter decreased during the study period and overall 95% of patients received primary PCI. However, the study demonstrated a clear relationship with distance as primary PCI was used in 97% of patients living < 1 hour from the hospital but only 48% of those with estimated transport times over an hour. Clinical outcomes did not differ significantly between the two strategies.
Transport to hospital involves a risk of adverse events causing a patient’s condition to deteriorate. Bussières et al. 25 studied patients with STEMI who were transported to a PCI centre by paramedics in a rural part of Québec, Canada. Increased transport time (comparing 0–14, 15–30 and > 30 minutes) was not associated with an increased risk of clinical adverse events during transport, but patient age was identified as a significant risk factor in this study.
In summary, most of the included studies suggest that increased distance or travel time is associated with increased risk of mortality for patients with MI (some studies specifically recruited those with STEMI). Transfer between hospitals may increase risk by lengthening delays in starting treatment (increased total ischaemic time) and time to reach hospital may influence the choice of treatment strategy. However, the one study that looked at adverse events during transport found no evidence of a link to transport time. 25
Mitigation studies
Improved co-ordination of services may improve quality of care for patients in rural areas and mitigate the effect of being at a distance from an ED or specialist centre. A before–after study by Langabeer et al. 46 evaluated an initiative in the rural US state of Wyoming and reported increased use of primary PCI and reduced total ischaemic time for patients with STEMI (see also the study by Svensson et al. 29 discussed above under Association studies, involving pre-hospital electrocardiogram (ECG) and administration of a thrombolytic agent in the ambulance).
The role of telehealth as a mitigation intervention is discussed in Chapter 4.
Trauma
Reconfiguration studies
Two included studies dealt with reconfigurations affecting trauma care,10,14 and both looked at the closure of trauma centres in California, USA, and their impact on remaining centres (Table 11). The earlier study, by Yaghoubian et al. ,14 covered Los Angeles County, whereas Hsia et al. 10 analysed data for non-federal trauma centres across the whole state. The time periods covered by the studies also differed (1997 to 2006 for Yaghoubian et al. ,14 and 1999 to 2009 for Hsia et al. 10). Nevertheless, there is likely to be a degree of overlap in the data, which should be taken into account in interpreting the results.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Hsia 201410 | Mixed: California state, excluded those resident > 100 miles away from nearest trauma centre and those out of state |
Intervention ED closure or relocation. During the time period three level I and II adult trauma centres closed. Average drive time after closures was 47 minutes for those who were affected by a closure and 34 minutes for those who were not Comparator Earlier time period. Closure of units comparing 10 years prior |
Specialist centre: trauma unit | Travel time: drive time to nearest trauma centre from patient’s residential postcode. Excluded patients who did not go to nearest centre | Mortality: inpatient mortality | While rates of trauma mortality declined overall in a 10-year period, people living in areas with longer driving time had increased risk (21% higher) of mortality as an inpatient following trauma unit closures compared with those who had experienced no change. Those with reduced driving time had reduced risk (17%) of mortality compared with those experiencing no change |
| Yaghoubian 200814 | Large city/city region: Los Angeles |
Intervention ED closure or relocation. Closure of level I trauma centre Comparator Earlier time period. Compares 1997–2005 (before closure) with March 1 2005–March 1 2006 (after closure) |
Specialist centre: trauma centre | Travel time |
Mortality Morbidity: injury severity score and complication rate Other: patient volume |
Closure of a level I trauma centre was associated with significant increases in patient volume and injury severity and a slight increase in paramedic transport times. However, complication rate was unchanged and adjusted mortality rates improved |
Both studies identified short-term effects on patient outcomes following trauma centre closures. Yaghoubian et al. 14 reported increases in monthly patient volume and injury severity in the year after closure. However, after adjusting for injury severity, the mortality rate was lower in the post-closure period than before and the complication rate was unchanged. 14 The authors attributed the relatively favourable outcomes to increased experience resulting from the increased number of patients attending the centre. Importantly, this study also reported on changes to the staffing and organisation of the trauma centre that are also likely to have contributed to successful adaptation to increased demand. Changes included addition of a dedicated nurse practitioner, four surgery residents and an additional trauma attending physician. The resident trauma staff were reorganised into three smaller teams with a view to distributing patient care more evenly. Advances in critical care during the study period were also likely to have played a role in improving outcomes. 14
The state-wide study by Hsia et al. 10 was distinctive in that the authors were able to identify (based on postal codes) patients whose travel times were affected or unaffected by trauma centre closures. The key finding of the study was that odds of inpatient mortality were significantly higher for patients with increased driving time compared with those experiencing no change (OR 1.21, 95% CI 1.04 to 1.40). The increased odds of death was even more pronounced in the 2 years after a closure (OR 1.29, 95% CI 1.11 to 1.51). By contrast, patients whose driving distance to a trauma centre decreased during the study period had lower odds of death compared with the ‘no change’ group (OR 0.83, 95% CI 0.75 to 0.92). These differences in outcomes were observed against the background of an overall decrease in trauma mortality in California during the study period. 10
The results of these two studies suggest that reconfiguration in the form of trauma centre closures may negatively affect outcomes for patients with potentially life-threatening trauma. This effect may be mitigated by improved quality of care and more efficient organisation of services in remaining centres but these centres are likely to experience increased demand and possibly an increase in the proportion of more severely injured patients. This evidence comes from the USA, where services are largely delivered by private providers in an insurance-based system. The English NHS has an organised system of major trauma networks and lower trauma centre capacity than the USA, which makes reconfiguration involving trauma centres unlikely.
Association studies
Seven studies examined the association between distance/time and outcomes for trauma patients in the absence of reconfiguration (Table 12). Most studies used a cohort design and all were conducted in North America (six in the USA and one in Canada). The majority of included studies found a clear association between distance to a trauma centre and outcomes (primarily mortality) for trauma patients. 30–34 These studies were performed in rural or mixed settings (often covering a large area such as the whole of a US state) and used a variety of distance/time measures (see Table 12).
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Durkin 200530 | Mixed: state of Wisconsin |
Intervention None Comparator Not applicable |
Specialist centre: trauma centre | Direct distance: distance between crash site and level I/II trauma centre |
Mortality Morbidity Hospital admissions |
Disparity in traffic injury case fatality across the state of Wisconsin needs to address to improve outcome for people living in counties distant from level I/II trauma centre |
| Gomez 201031 | Rural: 90% of area considered rural, 15% of people at least 60 miles from the nearest physician |
Intervention None Comparator Not applicable |
Specialist centre: trauma centre | Travel time: land transport time from place of injury to nearest trauma centre |
Mortality Other: type of injury, patient characteristics |
Pre-hospital deaths were twice as likely among those in rural areas, and also dying in an ED department (rather than other hospital department) was more likely for those from areas with limited trauma care |
| Gonzalez 201032 | Mixed: 75% rural, 25% urban. Rural defined by density of population rather than distance |
Intervention None Comparator Not applicable |
Other: emergency medical service (presumably ambulances) | Travel time EMS response time | Mortality | Increased pre-hospital time is associated with higher rates of mortality |
| Jarman 201833 | Mixed: state of Maryland. Mean distance to nearest trauma centre was 9.9 miles and mean pre-hospital time 64.6 minutes. Authors refer to it being a small state |
Intervention None Comparator Not applicable |
Specialist centre: trauma centre |
Direct distance: Euclidean distance between incident scene and nearest trauma centre Travel time: number of minutes from initial emergency call to trauma centre arrival |
Mortality: included patients dying at scene or in transit Other: characteristics of the trauma centre, patient demographics |
Increased distance to the nearest trauma centre was associated with increased mortality. This was independent of prehospital time suggesting that distance is associated with mortality independent of time. Odds of death highest for patients in transportation areas (e.g. highways). Age and income differences |
| Lee 201834 | Mixed |
Intervention None Comparator Not applicable |
Hospital ED | Travel time: T1 crash reporting – time from when the crash happened to notification to EMS. T2 reporting-scene arrival interval – time from notification to EMS to EMS arrival at the crash site. T3 Scene-hospital interval – time from EMS arrival to arrival at hospital (this also includes time to extract patients and provide first aid treatment and moving them to EMS vehicle) |
Mortality Morbidity: injury severity Other: difference in EMS times due to urban or rural location |
EMS differ according to urban/rural location and road functional classification. Reporting scene arrival and scene–hospital arrival and various factors have a significant effect on traffic injury severity |
| Lerner 200335 | Large city/city region: New York, NY, USA, adult regional trauma centre serving 8 counties in western New York |
Intervention None Comparator Not applicable |
Hospital ED | Travel time: total out of hospital time | Mortality | Total out-of-hospital time was not associated with adult trauma patient mortality |
| McCoy 201336 | Large city/city region |
Intervention None Comparator Not applicable |
Hospital ED | Travel time: scene time (time of arrival of first EMS responding vehicle on scene to time leaving the scene). Transport time (time leaving the scene to vehicle arrival at the receiving hospital) | Mortality: non-conveyance/treatment at scene | This study observed increased odds of mortality among patients with penetrating trauma if scene time was greater than 20 minutes. Findings would need to be proved in an external data set |
Only two studies did not find an association between distance/time and outcomes. In the study by Lerner et al. ,35 the time measure was total out-of-hospital time rather than travel time per se. A possible explanation suggested by the authors is that more severely injured patients were prioritised for rapid transport to hospital, leading to those with less severe injuries and a higher probability of survival spending more time in reaching the hospital. In an urban setting, McCoy et al. 36 found no association between transport time and mortality for patients with either blunt or penetrating trauma. The authors suggested this may be because patients transported to trauma centres have higher survival rates than those taken to other facilities despite longer transport times.
Maternity
Reconfiguration studies
Only one study from the reconfiguration group examined reconfiguration affecting maternity services. 6 In the largely rural region of Burgundy, France, the number of maternity units decreased from 20 to 15 between 2000 and 2009. Mean estimated journey time to the nearest maternity unit increased from 21 to 24 minutes and the maximum time increased from 61 to 72 minutes. The study found that a travel time of ≥ 30 minutes was associated with an increased risk of fetal heart rate anomalies, meconium-stained amniotic fluid, unplanned out-of-hospital births and pregnancy-related hospitalisation. Odds of perinatal death were increased for those travelling furthest (≥ 46 minutes) but the number of deaths was small and the CIs of the OR were wide (OR 1.86, 95% CI 0.69 to 5.01).
A limitation of this study was that it did not distinguish between areas with and without maternity closures. As such, it was primarily measuring the association between travel time and outcomes rather than the effect of increased travel times following closure of the nearest unit.
Association studies
In addition to the Combier et al. 6 study, seven studies examined associations between travel time to maternity units and maternal or perinatal outcomes (Table 13). Three studies found evidence of an association, including large national cohort studies from Norway37 and the Netherlands. 41 The third study to find an association was conducted in rural British Columbia, Canada,39 and the long travel times involved make the findings less applicable to the UK setting.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Dummer 200416 | Rural |
Intervention None Comparator Distance/time categories |
Obstetric unit: for stillbirth, all hospitals with a maternity facility were included | Travel time | Mortality: stillbirths and infant deaths, categorised as early neonatal (0–6 days), neonatal (0–27 days), and post neonatal (28 days to 1 year) | There was no evidence to suggest that living further from hospitals increased the risk of infant death or stillbirth in Cumbria. Lack of recent data means that the findings should not be used to support centralisation of services |
| Engjom 201737 | Mixed: national cohort of births |
Intervention None Comparator Not applicable |
Obstetric unit: units and out of hospital births. Unplanned birth rather than designated emergency care | Travel time: minimum time obeying speed limits from the geographic zone residential postcode was in, to nearest obstetric institution. Grouped into under 1 hour, 1–2 hours and over 2 hours |
Mortality: peripartum mortality Other: unplanned birth outside an institution, in a basic care institution or in an emergency obstetric and newborn care institution |
Increased travel time is associated with increased risk of out of institution births, and out of institution birth is associated with increased risk of peripartum mortality |
| Featherstone 201638 | Mixed: South Carolina state 50% of mothers travelled < 30 minutes, 23% between 30 minutes and 1 hour and 20% > 1 hour |
Intervention None Comparator No intervention |
Obstetric unit: level III neonatal intensive care unit | Travel time: travel time in minutes from mother’s postcode address to delivery hospital in categories of under 30, 30–59 and over one hour. Used a programme (ARCGIS) to calculate time | Mortality | Causes of death in very low birthweight infants are not related to time to care, but may be associated with other maternal, neonatal or service factors |
| Grzybowski 201139 | Rural: women residing outside the main urban and suburban areas of British Columbia were included |
Intervention None Comparator Distance/time categories |
Obstetric unit: maternity services with caesarean section capability | Travel time |
Mortality: perinatal mortality Hospital admissions: admission to neonatal ICU Other: various newborn and maternal outcomes, including caesarean section, induction of labour and out-of-hospital birth |
Rural women who have to travel long distances to access maternity services have increased rates of adverse perinatal outcomes |
| Parker 200017 | Rural |
Intervention None Comparator Distance/time categories |
Obstetric unit: all maternity services | Direct distance | Mortality: stillbirth | There was no significant increase in stillbirth risk with distance to maternity services after adjusting for year of birth, father’s social class and birth order |
| Pilkington 201440 | Mixed: all of France |
Intervention None Comparator Not applicable |
Obstetric unit: maternity unit | Actual travel distance: municipality where mother resided to a maternity unit using major regional road networks | Mortality: stillbirth, neonatal and out of hospital deaths | While stillbirth rates appeared to increase for those closest to and furthest from maternity units, this association was no longer apparent following adjustment for sociodemographic factors. Mortality was not associated with distance after adjustment. Distance was still associated with the risk of out of hospital births and, therefore, risk of mortality |
| Ravelli 201141 | Other: whole country |
Intervention None Comparator Distance/time categories |
Obstetric unit | Travel time |
Mortality: combined mortality during labour or in the neonatal period Morbidity: ‘adverse outcome’ (combined end point of mortality and/or 5-minute Apgar score < 4, and/or transfer of a newborn to a neonatal intensive care unit at birth) |
A driving time from home to hospital of 20 minutes or more is associated with an increased risk of mortality and adverse outcomes in women at term in the Netherlands. These findings should be considered in plans for the centralisation of obstetric care |
By contrast, two publications from Cumbria found no evidence of an association between distance to hospital and risk of stillbirth. 16,17 It appears that there is some overlap of data between these two publications, with the later report16 covering a longer time period and a larger population (the whole of Cumbria compared with West Cumbria in the earlier publication). Although from a UK setting, these studies are of limited value because the included date range is unlikely to reflect current practice and service delivery. A further study from the USA that found no evidence of an association looked specifically at very low birth weight infants (500–1499 g). 38 The authors noted that in this study a high proportion of neonatal deaths occurred within 24 hours of birth and were likely to be related to factors other than access to care.
Finally, a study by Pilkington et al. 40 examined data for the whole of France for the period 2001–8. In contrast to the Combier et al. 6 study from Burgundy, these authors found that women living closer to a maternity unit had a higher risk of neonatal mortality. They attributed this to many maternity units being located in socioeconomically deprived areas where the risk of poor outcomes is likely to be higher.
In summary, the findings of the review for maternity and neonatal populations were inconclusive. The relationship between distance and outcomes varied between studies, reflecting differences in populations and settings as well as possible changes over time.
Stroke
Reconfiguration studies
None of the reconfiguration studies looked solely at patients with stroke. Hsia et al. 9 presented results by condition for a variety of UEC conditions. Patients with stroke who experienced an increase in distance to the nearest ED did not have higher in-hospital mortality compared with those who experienced no increase.
Association studies
Three association studies reported data for patients with stroke (Table 14). 15,43,44 Acharya et al. 43 and Leyden et al. 44 both focused on timely receipt of thrombolytic therapy as a major outcome and both concluded that patients living further from stroke units or hospitals with appropriate facilities were less likely to receive thrombolytic therapy. The Swiss National Cohort study reported by Berlin et al. 15 analysed data on stroke deaths. In comparison with the situation with MI (reported in the MI section of this chapter, see Acute myocardial infarction), the relationship between mortality risk and driving time to a university hospital was less pronounced for stroke; the results varied for different age and sex groups and also by the type of statistical model used.
| First author and year of publication | Setting | Intervention and comparator | UEC facility | Distance measure | Outcomes | Headline findings |
|---|---|---|---|---|---|---|
| Acharya 201143 | Mixed: St Louis City and St Louis County, MO, USA |
Intervention None Comparator Distance/time categories: study compares group living closest to the hospital (first quintile, group A) with the remainder of the cohort (group B) |
Hospital ED | Actual travel distance: ‘best route’ from patient’s home to hospital ED | Other: arrival within 3 hours of stroke onset; receipt of thrombolytic treatment | Patients living close to the hospital are more likely to receive thrombolytic therapy for stroke than those living further away. The difference is not explained by differences in time taken to reach the hospital |
| Berlin 201615 | Other: whole country (Switzerland) |
Intervention None Comparator Distance/time categories: highest vs. lowest quintile of driving time |
Hospital ED: hospitals classified as acute, acute with ED, central and university |
Direct distance Travel time: driving time |
Mortality | The increasing MI mortality with increasing driving time to the nearest university hospital but not to other types of hospital reflects a complex situation influenced by many factors along the care pathway. For stroke mortality, the association with university hospital driving time was less pronounced than for MI mortality. Mortality did not show a clear incremental pattern with increasing driving time |
| Leyden 201144 | Mixed: SA, Australia |
Intervention None: coincided with opening of an acute stroke unit Comparator Not applicable |
Hospital ED: many patients presented to hospitals without stroke units Specialist centre: acute stroke unit |
Direct distance: longitude and latitude co-ordinates were used to calculate distance between postcode of each patient and the stroke unit closest to them using the haversine formula |
Mortality Morbidity: intracranial haemorrhage Hospital admissions Other: thrombolysis administration Rate of thrombolysis by distance from stroke unit |
Poor access to acute stroke units in rural and urban locations means that a large proportion of the population in South Australia are not receiving thrombolysis |
The review thus provides inconsistent evidence on the relationship between distance and mortality for patients with stroke. There is limited evidence from two studies suggesting that more distant patients are less likely to receive prompt thrombolytic therapy.
Mitigation study
The only included mitigation study evaluated the effectiveness of a specialist stroke ambulance in an urban setting (Berlin) and concluded that benefits from reduced time to thrombolysis justify a specialist ambulance up to a travel time of 18 minutes. 45
The role of telehealth as a mitigation intervention is discussed in Chapter 4.
Other conditions
One included study looked at the relationship between travel time and survival for patients with a ruptured AAA, which is a condition with a high pre-hospital mortality rate. 20 This study in West Sussex, England, found no relationship between travel time and mortality risk. After adjustment for confounders, the OR for survival associated with a 10-minute increase in estimated travel time to the nearest hospital was 0.97 (95% CI 0.70 to 1.34), the wide CI suggesting uncertainty about the true effect. The study authors noted that earlier studies (mainly dating from outside the search period for this review) had found a relationship; they suggested that such studies were biased by the omission of deaths that occurred before reaching hospital. 20 Given that Souza et al. 20 published their study in 2005, the possible impact of changes in management of ruptured AAA should be taken into account in interpreting the study results.
Summary of reconfiguration studies
Most of the included reconfiguration studies reported on changes in mortality rates following reconfiguration (Table 15). For studies of general UEC populations, there was no evidence that reconfiguration resulting in increased travel time/distance affected mortality rates. This was classed as stronger evidence being derived from studies with control groups. By contrast, there was evidence of increased risk from studies restricted to patients with AMI. Evidence for other conditions was inconsistent or very limited and none of the included studies looked at stroke patients specifically (although people with stroke were an identifiable subgroup in the study by Hsia et al. 9).
| Population | Relevant studies (first author and year of publication) | Evidence statement | Strength of evidence | Comments |
|---|---|---|---|---|
| General UEC |
Hsia 20129 = Mustonen 201711 = Knowles 20182 = |
No effect of reconfiguration on mortality | Stronger | Interpret as no evidence of an effect |
| AMI |
Avdic 20165 – Shen 201212 – Shen 201613 – |
Increased mortality risk following reconfiguration | Stronger? | |
| Trauma |
Hsia 201410 – Yaghoubian 200814 + |
Unclear effect on mortality risk following reconfiguration | Inconsistent | |
| Maternity | Combier 20136 = | Insufficient evidence | Very limited |
Evidence on health system outcomes was inconsistent (Table 16), reflecting the diverse outcomes and settings included. El-Sayed et al. 7 identified some short-term negative effects on EMS systems following closure of an ED in Boston, MA, USA. More significantly, the closED study in the UK (England) identified some evidence of increased pressure on ambulance services in areas where an ED had been closed or downgraded, including an increase in emergency ambulance incidents. 2 Across England as a whole, distances travelled to access emergency care increased only slightly between 2001/2 and 2011/12. 4 Case studies analysed by Roberts et al. 4 demonstrate how reconfigurations affects travel distances and hospital admissions in specific local contexts.
| Population | Relevant studies (first author and year of publication) | Evidence statement | Strength of evidence | Comments |
|---|---|---|---|---|
| General UEC |
El-Sayed 20127 – Hansen 20118 = Knowles 20182 – Mustonen 201711 = Roberts 2014 ?4 |
Effects on health system outcomes vary between studies depending on the specific outcome and setting | Inconsistent |
Summary of association studies
The association studies found evidence that increased travel time or distance is associated with increased mortality risk for the AMI and trauma populations, whereas for maternity the evidence was inconsistent (Table 17). Where evidence was classified as ‘weaker’, this reflects the absence of true control groups but the large size of some of the studies and plausibility of the association are additional supporting factors. There was also weaker evidence of an association from two studies of patients with a range of conditions typically requiring emergency care. 18,42
| Population | Relevant studies (first author and year of publication) | Evidence statement | Strength of evidence | Comments |
|---|---|---|---|---|
| General UEC |
Nicholl et al. 200718 – Murata 201342 +/– |
Evidence of a relationship for most conditions | Weaker | |
| AMI |
Balamurugan 201623 – Balamurugan 201824 – Berlin 201615 – Di Domenicantonio 201626 – Wei 200819 – |
Evidence of a relationship | Weaker | |
| Trauma |
Durkin 200530 – Gomez 201031 – Jarman 201833 – Lerner 200335 = McCoy 201336 +/– |
Evidence of a relationship | Weaker | |
| Maternity |
Dummer 200416 = Engjom 201737 – Featherstone 201638 = Grzybowski 201139 – Parker 200017 = Pilkington 201440 + Ravelli 201141 – |
Relationship varies between studies/settings | Inconsistent | Grzybowski 201139 limited relevance to UK |
| Ruptured aneurysm | Souza 200520 = | Insufficient evidence | Very limited |
Other outcomes (Table 18) were reported in smaller numbers of studies. Although evidence for these outcomes was inconsistent for patients with AMI, weaker but consistent evidence was found for adverse maternity outcomes and access to thrombolysis for stroke patients being influenced by distance from specialist services.
| Population | Relevant studies (first author and year of publication) | Evidence statement | Strength of evidence | Comments |
|---|---|---|---|---|
| General UEC | Rudge 201321 – | Evidence from a single UK study that attendance at ED is influenced by socioeconomic deprivation as well as distance | Very limited | |
| Acute MI |
Andersson 201922 = Bussières 201825 = Langabeer 201527 +/– Postma 201428 +/– Svensson 200329 – |
Inconsistent evidence for association between travel time and non-mortality outcomes | Inconsistent | |
| Trauma | Lee 201834 – | Evidence from one study of an association between travel time and morbidity | Very limited | |
| Maternity |
Engjom 201737 – Grzybowski 201139 – |
Evidence of a relationship between travel time and adverse outcomes other than mortality | Weaker | |
| Stroke |
Acharya 201143 – Leyden 201144 – |
Evidence that patients living closer to a hospital are more likely to receive thrombolysis | Weaker |
Quantitative estimates of the relationship between travel distance or time and mortality risk are summarised in Table 19. Studies varied widely in their methodology. In particular, authors calculated either an effect measure per unit of distance (e.g. 10 miles or 10 km) or between different distance categories (e.g. highest vs. lowest quintile). This, together with the variety of different outcomes measured (e.g. in-hospital mortality, 30-day mortality or mortality at various follow-up points) makes it difficult to pool outcomes across studies.
| First author and year of publication | Outcome | Population | Effect estimate |
|---|---|---|---|
| Balamurugan 201623 | Mortality during study period? | AMI | 26% higher absolute risk for areas with longest vs. shortest driving times (RR 1.11 vs. 0.88) |
| Balamurugan 201824 | Mortality (in hospital) | AMI | OR 1.092/10 miles (95% CI 1.009 to 1.181) |
| Berlin 201615 | Mortality during the study period | AMI | HR 1.19 (95% CI 1.10 to 1.30) for men and 1.10 (95% CI 1.01 to 1.20) for women (highest vs. lowest quintile) |
| Di Domenicantonio 201626 | 30-day mortality | STEMI | OR 2.46 (95% CI 1.25 to 4.86) for travel time above vs. below median (14 minutes) |
| Dummer 200416 | Infant mortality | Maternity | All ORs close to 1 |
| Durkin 200530 | Hospital mortality? | Trauma | RR 1.87 (95% CI 1.77 to 1.97) for 11–79 miles vs. < 10 miles to trauma centre; 1.57 (95% CI 1.50 to 1.63) for ≥ 30 miles vs. < 30 miles |
| Engjom 201737 | Unplanned birth outside institution | Maternity | Adjusted RR 5.3 (95% CI 5.0 to 5.8) for 1 to 2 hours and 7.2 (6.3 to 8.2) for > 2 hours vs. 1 hour or less |
| Featherstone 201638 | Neonatal mortality | Maternity | Adjusted ORs not significant for 30–59 and > 60 minutes vs < 30 minutes |
| Gomez 201031 | Mortality in ED | Trauma | Adjusted OR 3.5 (95% CI 2.5 to 4.9) for > 1 hour vs. < 1 hour to trauma centre (note the high rate of deaths before reaching hospital) |
| Grzybowski 201139 | Perinatal mortality | Maternity | Adjusted OR 3.17 (95% CI 1.45 to 6.95) for > 4 hours to services vs. local services |
| Jarman 201833 | Injury mortality (at scene, en route or in hospital) | Trauma | 8% increase in odds of death for every 5 miles to nearest trauma centre (OR 1.08, 95% CI 1.01 to 1.15) |
| Lerner 200335 | Injury mortality (at scene, en route or in hospital) | Trauma | Total out-of-hospital time not a predictor of mortality (OR 0.987, 95% CI 0.97 to 1.00) |
| McCoy 201336 | Hospital mortality | Trauma | Penetrating trauma: OR for transport time ≥ 20 minutes was 0.40 (95% CI 0.14 to 1.19); value for 10–19 minutes was 0.64 (95% CI 0.35 to 1.15). No association for blunt trauma |
| Murata 201342 | Mortality (data from administrative databases) | General UEC (various conditions) | Correlation between transport distance and mortality per 100,000. R2 = 0.315 for acute MI, 0.398 for brain infarction, 0.112 for subarachnoid haemorrhage and 0.233 for pneumonia |
| Nicholl 200718 | Mortality (in hospital) | General UEC (life-threatening conditions) | OR 1.02 per km, 95% CI 1.01 to 1.03 per km |
| Parker 200017 | Stillbirth | Maternity | No significant increase in risk with increased distance to nearest and second nearest hospital (p = 0.85 and 0.11, respectively) |
| Pilkington 201440 | Fetal and neonatal mortality | Maternity | Fetal and neonatal mortality rates were highest in women living < 5 km from a maternity unit. In adjusted models, long distance to a maternity unit had no impact on overall mortality but women living closer to a maternity unit had a higher risk of neonatal mortality (RR 0.91 for 5–15 km vs. < 5 km) |
| Ravelli 201141 | Intrapartum and neonatal mortality | Maternity | OR 1.17 (95% CI 1.002 to 1.46) for travel time ≥ 20 minutes vs. < 20 minutes |
| Shen 201613 | Mortality (90 days) | AMI | 6.58 percentage points increase for > 30 minutes more driving time |
| Shen 201212 | Mortality (long-term) | AMI | 180-day and 1-year mortality rates increased by 5 percentage points for those with > 30 minute increase in driving time |
| Souza 200520 | Mortality (at scene, en route or in hospital) | Ruptured AAA | Adjusted OR for survival per 10-minute increase in travel time 0.97 (95% CI 0.70 to 1.34) |
| Wei 200819 | Mortality during study period | AMI |
Pre-hospital Adjusted OR 2.05 (95% CI 1.00 to 4.21) for > 9 miles and 1.46 (1.09 to 1.95) for 3–9 miles compared with < 3 miles After hospitalisation Adjusted HR 1.90 (95% CI 1.19 to 3.02) and 1.27 (95% CI 0.96 to 1.68) In-hospital Adjusted OR 0.95 (95% CI 0.45 to 2.03) and 1.02 (95% CI 0.66 to 1.58) (no difference) |
As an example, two studies from the UK18,19 used different distance measures (km vs. distance categories in miles) and measured mortality at different time points, as well as studying different populations (general life-threatening conditions vs. AMI). Qualitatively, the increase in risk with distance appears greater for the AMI population, but interpretation is complicated by the fact that differences between distance categories were statistically significant for pre-hospital and follow-up mortality but not for deaths in hospital. 19 There was more uniformity in UK-based maternity studies, but these were conducted by the same research team in broadly the same setting16,17
Summary of mitigation studies
The two included mitigation studies provide very limited evidence for the effectiveness of improved service co-ordination for STEMI in a US rural setting46 and of a specialist stroke ambulance in an urban setting. 45
Results by setting
UK versus international
Possible limitations to the relevance of international evidence to the UK setting need to be taken into account in interpreting the study findings and this topic will be addressed in Chapter 5.
Only two of the 12 reconfiguration studies were conducted in the UK (see Tables 1 and 2). Despite this, UK studies provided the larger part of the evidence related to mortality risk for this patient group following service reconfiguration. Other reconfiguration studies came from western European countries (i.e. Sweden, France, Denmark and Finland) and the USA (six studies). In terms of specific conditions, all the reconfiguration studies of patients with AMI and trauma came from the USA, which differs considerably from the UK in size and health system organisation.
Turning to association studies, the UK was relatively well represented in studies of general UEC populations (two out of three) with included studies covering mortality18 and effects of distance on ED attendance. 21 By contrast, only 1 out of 10 studies on AMI came from the UK (Scotland). 19 All of the included studies on trauma came from the USA (six studies) or Canada (one study).
Maternity was one area where there was a suggestion of a difference between UK and non-UK studies, with two linked studies from Cumbria16,17 finding no evidence of a link between distance to hospital and neonatal death, in contrast to a number of international studies. There was one UK study of ruptured aortic aneurysm, providing the very limited evidence on this condition included in the review. 20
Some European health systems place particular emphasis on pre-hospital diagnosis and triage, for example by doctors working alongside paramedics. We did not include any studies of this type of model in relation to distance, but differences in service organisation should be taken into account when assessing study applicability to the UK context.
There were no included UK studies for stroke or for mitigation interventions other than telehealth.
Urban versus rural
The effects of service reconfiguration and the relationship between distance/time and outcomes may differ between rural and urban areas. Some studies included in the review focused on the needs of rural areas whereas others compared outcomes between rural and urban areas.
None of the reconfiguration studies of general UEC populations was conducted in specifically rural settings but several covered whole countries or US states, including both urban and rural areas. Roberts et al. 4 analysed data for England as a whole and highlighted areas where distances travelled to access emergency care were considerably higher than the national average. Unfortunately, the detailed data on distances travelled in this report were accompanied by limited outcome data from a few case studies, making it difficult to draw firm conclusions about rural versus urban differences. The closED study also included sites in diverse areas of England but discussion of issues specific to rural areas was limited. 2 Reconfiguration studies for AMI and trauma also mainly covered large areas and provided limited information specific to rural settings.
Combier et al. 6 reported on the impact of maternity unit closures in a largely rural part of France. Closure of a number of units between 2000 and 2009 was associated with increases in mean (21 to 24 minutes) and maximum (61 to 72 minutes) estimated journey times. Increased travel time was associated with increased risk of various adverse outcomes (see Maternity). By contrast, two studies of births in a rural English county (Cumbria) found no evidence of an increase in risk of perinatal death associated with increased distance to hospital. 16,17 This UK evidence should be interpreted cautiously because of the length of time since the data were collected but advances in perinatal care in recent years give no reason to suspect that the situation is likely to have changed. The only other specifically rural study included (conducted in British Columbia, Canada) is likely to be of limited relevance to UK settings because of the large distances involved. 39 The overall evidence for distance to maternity units in rural areas may thus be classified as ‘inconsistent’.
Much of the evidence from association studies of patients with AMI relates to rural areas, including US states that are mainly rural such as Arkansas23,24 and Wyoming,27 and a rural region of Québec, Canada. 25 This evidence was again inconsistent in terms of presence versus absence of an association.
The only UK study in the MI association studies group was conducted in Tayside, Scotland, by Wei et al. 19 This study found an association between distance and mortality (including both pre-hospital and follow-up mortality). In addition, the authors classified patients’ home addresses into eight rurality categories based on postcode data. The results suggested that outcomes may be influenced by rurality as well as distance per se. The study authors noted that the rurality code may be a surrogate measure of different patient behaviour in different geographical settings (i.e. people in rural areas may behave differently in terms of reacting to symptoms and seeking help).
For trauma patients, a number of studies covering rural or mixed areas of the USA (often whole states) found associations between mortality risk and distance to hospital (generally a trauma centre rather than a normal ED). 30–33 The exception was a study by Lerner et al. 35 in New York state, which found that total out-of-hospital time was not associated with mortality risk. There were no UK studies in this group and the evidence should be interpreted with this in mind.
Finally, three studies of stroke patients conducted in mixed settings shed some light on urban–rural differences. Two studies focused on timely receipt of thrombolysis. In St Louis city and St Louis county, Missouri (USA), patients living further from the hospital were less likely to receive thrombolysis, but the difference was not explained by differences in time taken to reach the hospital. 43 The others suggested that other factors such as type of transport to the hospital or patient awareness of available services may have been important. In a study in South Australia, access to thrombolysis was described as poor in both urban and rural areas. 44 In the report of the Swiss National Cohort study, the authors speculated on possible differences between rural and urban populations, including lower awareness of stroke symptoms and more reliance on helicopter transport in rural areas. 15
In summary, factors other than increased distance to hospital that may affect the relationship with outcomes have been tentatively identified in a few studies. Only a few studies have focused on UK rural populations or compared rural and urban populations.
Health system context and implementation of service changes
All of the studies included in the reconfiguration group mentioned the context in which changes to services are implemented and the need for planning and co-operation to minimise the impact on patients. However, only six of them provided any substantial information. Broader implications for health services are considered in Chapter 5 (see Implications for service delivery).
The closED study authors sought information about relevant service changes through a documentary analysis of material from NHS trusts, ambulance trusts and commissioning organisations (clinical commissioning groups and primary care trusts). 2 No information on how the health service planned for the impact of ED closures or downgrading was obtained from either NHS annual reports or ambulance service sources. Data analysed in the study suggested that ambulance services made changes in anticipation of ED closures as increases in average journey times were lower than expected. The authors identified understanding the processes used by health-care providers and commissioners to minimise adverse effects of implementing service reorganisation as a priority for future research. The study also called for improved consistency of recording and coding of routine data.
In the context of the UK NHS, the case studies provided by Roberts et al. 4 provided examples of UEC reconfigurations carried out in England and their effect on travel times. However, there was no background information on the rationale for and implementation of the changes.
Some additional evidence came from non-UK studies. The most detailed information was reported by Yaghoubian et al. 14 in their before–after study of a trauma centre closure. Changes made in anticipation of increased patient numbers included additional staffing and changes to team organisation. Increased experience and background improvements in care were identified as factors that supported an improvement in adjusted mortality rates in the post-closure period. A ‘mature’ regional trauma system ensured that remaining trauma centres were able to handle additional patients.
In another study from the USA, El-Sayed et al. 7 commented on the importance of early notification of a planned ED closure and ‘continuous and dynamic co-operation’ between hospital and EMS administrations in minimising the impact on EMS services.
In addition to early planning, there was evidence of health systems adapting during the first few years after a reconfiguration. Avdic5 noted that the effect of ED closures on AMI mortality was only statistically significant for the first year, attributing this to attempts to compensate for increased travel distance by, for example, increased investment in emergency services or greater use of preventative care. Shen and Hsia12 identified a 4-year transition period after which outcomes were similar to the pre-reconfiguration period.
Moderating and mediating factors
Key moderating and mediating factors extracted from included studies are summarised in Figure a in relation to patient and health system outcomes. Not all relevant studies are included in the figure, but fuller details of influencing and explanatory factors extracted from included studies are presented in Appendix 4, Table 24.
A point not stressed elsewhere in this report is the influence of measurement factors on the reported travel time/distance to hospital. The included studies differed in their methodological approach according to the availability of data. For example, data on the exact location of incidents were often not available and the patient’s residential postcode or similar was used instead. Studies also differed in whether they measured direct distance to a UEC facility or attempted to assess distance or time using the actual road network.
Patient-related and context-related influences on pre-hospital time identified in Figure a were often found in similar forms in multiple studies. In particular, optimal deployment of EMS services and the choice between use of private or ambulance transport can substantially influence the time taken to reach hospital. Service-related factors that influence outcomes for patients range from pre-hospital initiation of treatment to the range and location of specialist facilities available. These can potentially mitigate the effects of travelling further for emergency care.
Included studies have also evaluated impacts of service changes on broader health system activity and performance, including primary care11 and alternative UEC facilities8 as well as indicators of ambulance service quality. 2
Chapter 4 Narrative overview of systematic reviews of telehealth to support urgent and emergency care
Systematic reviews of telehealth interventions in UEC settings were identified by a search of seven databases. The search was conducted in February 2019 and limited to studies published in 2009 or later. Further details can be found in Chapter 2 (see Literature search and screening) and a sample search strategy is provided in Appendix 1. In selecting reviews for inclusion, we accepted reviews of telehealth as defined by the review authors and we did not exclude reviews on the basis of methodological quality. We have also followed authors’ practice regarding the use of ‘telehealth’, ‘telemedicine’ and similar terms.
Quantity and scope of included reviews
We included 12 systematic reviews published between 2010 and 2019. Seven of the reviews were published in 2017 or later. Four reviews dealt with ‘telestroke’, two dealt with trauma care and the remainder with a variety of other telehealth applications. Table 20 summarises the basic characteristics of the included reviews.
| First author and year of publication | Review objectives | Search date | Included studies | Headline findings |
|---|---|---|---|---|
| Telestroke reviews | ||||
| Baratloo 201848 | To assess the effect of telemedicine on treatment times and clinical outcomes of acute stroke care | May 2017 | 26 | Telemedicine significantly reduced onset to door and hospital stay durations without increasing mortality or symptomatic intracranial haemorrhage |
| Hubert 201449 | To analyse recent advances in the field of telemedicine for acute stroke, with a focus on pre-hospital management | May 2014 | 25 | Studies of pre-hospital management (n = 9) showed that stroke recognition can start at the dispatch emergency call, important clinical information can be electronically transmitted to hospitals before admission and acute treatment such as thrombolysis can be initiated if ambulances are suitably equipped |
| Johansson 201050 | To assess the feasibility, acceptability and treatment delivery reliability of telemedicine systems in acute stroke management | November 2008 | 18 | Telemedicine systems can be safe, feasible and acceptable and are associated with increased delivery of thrombolytic therapy |
| Rubin 201351 | To conduct a systematic review of the published literature on telemedical consultation for acute stroke evaluation and management | July 2012 | 145 | Telestroke technology is part of mainstream clinical practice in North America and internationally. More recent studies (n = 13) have evaluated telestroke in pre-hospital settings |
| Trauma reviews | ||||
| Eder 201852 | To provide a comprehensive overview of telemedicine applications in pre-hospital trauma care | March 2018 | 15 (including six simulation studies) | Evidence regarding effectiveness is still limited |
| Lewis 201253 | To offer a systematic review of the literature on telemedicine for the management of acute phase injuries | December 2010 | 31 | Potential benefits include lower travelling expenses, enhanced continuity of care and increased access to specialists in underserved and rural areas. Barriers to wider adoption remain |
| Other reviews | ||||
| Brunetti 201754 | To measure the effect of pre-hospital ECG triage by telemedicine on time to treatment in patients with STEMI | May 2016 | 11 | In a meta-analysis, relative reduction in time to treatment using telemedicine was around 40%. Absolute reduction was correlated with control group time to treatment, suggesting benefit was greatest in those travelling further for treatment |
| du Toit 201955 | To identify how telehealth has been used to assist in management of non-critical conditions in rural and remote EDs and summarise the outcomes | December 2017 | 15 | Telehealth was predominantly used for remote consultation by nurses with limited local medical support. Teleconsultation altered diagnosis or management in 18–66% of consultations. Transfers were increased but unnecessary transfers were reduced |
| Gattu 201656 | To review current literature relating to telemedicine in paediatric emergency medicine | Not reported | Unclear | Use of telemedicine in paediatric emergency medicine is limited by a lack of evidence, with most published studies coming from a few centres in the USA and Europe |
| Marsh-Feiley 201857 | To assess the literature regarding telesonography (ultrasound) in emergency medicine | February 2017 | 28 | Feasibility of telesonography was supported by multiple studies. There was evidence of clinical utility in remote and low resource settings. Diagnostic accuracy was slightly reduced by image transmission. There was a need for better study design and reporting |
| Rogers 201758 | To assess the efficacy and implementation challenges of telemedicine systems in ambulances | December 2016 | 23 | Telemedicine feasible and effective in reducing treatment times with high diagnostic accuracy. There was a lack of high-quality implementation research |
| Winburn 201859 | To systematically review published research on the use of telehealth in pre-hospital emergency care | April 2017 | 68 | The majority of included studies involved stroke or acute cardiovascular care. The use of telehealth in pre-hospital settings remains limited and there are opportunities for wider diffusion. Understanding of incentives and barriers to telehealth adoption a priority for research |
Summary of review findings
Stroke reviews
Three of the four included reviews of telehealth for stroke were essentially descriptive or mapping reviews with a narrative synthesis of included studies. 49–51 The review by Hubert et al. 49 was particularly relevant to our review because of its focus on pre-hospital applications. The authors concluded that use of telehealth technology to transmit information from the ambulance to hospital and to allow early initiation of treatment can help to mitigate the effects of distance from a hospital ED or stroke unit.
The review by Baratloo et al. 48 used meta-analysis of 26 studies (6605 patients) to quantify the effect of telehealth care on time to treatment and other relevant outcomes. The authors found no statistical difference between telehealth care and standard care groups for in-hospital mortality, 90-day mortality, symptomatic intracranial haemorrhage or favourable clinical outcome (at discharge or 90 days later). Telehealth technology was associated with a reduction in onset to door time [mean difference (MD) –10.4 minutes, 95% CI –14.79 to –0.01 minutes) and duration of hospital stay. Onset to treatment time was significantly reduced in a fixed-effect model but not in a random-effects model, suggesting an influence of heterogeneity on the findings. Although based largely on observational studies, this meta-analysis provides some further support for telehealth care as a mitigation intervention.
Trauma reviews
Two narrative synthesis reviews looked at the role of telehealth in the management of trauma patients. 52,53 The more recent review focused specifically on pre-hospital trauma care. 52 The authors identified telemedical assistance by real-time telemetry and telemedical pre-hospital notification as complementary applications of the technology but concluded that evidence of effectiveness in this setting remains limited.
Pre-hospital reviews
Two reviews focused on pre-hospital applications of telehealth generally rather than specific conditions. 58,59 One review dealt specifically with the use of the technology in ambulances. 58 Overlap of included studies between the two reviews was low. Despite some promising findings, both studies identified barriers to uptake of telehealth in this setting and emphasised the need for high-quality research into understanding barriers to wider uptake and promoting effective implementation.
Specific telehealth technologies
Two reviews looked at telehealth-care-assisted ultrasound (telesonography)57 and pre-hospital triage by transmission of electrocardiographic data to support management of patients with STEMI. 54 The telesonography review concluded that the intervention was feasible and potentially useful in remote settings, but the quality of research was generally poor. 57
Brunetti et al. 54 performed a meta-analysis of 11 non-randomised studies (7552 patients). Pre-hospital triage by telemedicine was associated with a significant reduction in time to treatment compared with control groups [relative reduction of 40% (95% CI 33% to 48%) in a random-effects model and 38% (95% CI 37% to 39%) in a fixed-effect model]. There was a strong correlation between absolute reduction in time to treatment and time to treatment in the control group (R2 = 0.83). This was based on an exploratory analysis (metaregression) but the correlation remained significant after correction for age, gender and sample size. This correlation suggests that people experiencing a longer time to treatment may benefit most from the use of telemedicine to aid triage, supporting the role of this technology to mitigate the impact of being at a distance from a suitable treatment facility.
Other reviews
Other included reviews provided evidence that telehealth care can be used in rural and remote locations with limited clinical support and reduce unnecessary transfers of patients with non-critical conditions;55 and that evidence for the technology in paediatric emergency care is relatively limited outside specialist centres. 56
Summary
The included systematic reviews synthesise a large body of research on telehealth care for UEC conditions, particularly stroke. Most reviews have involved narrative synthesis, including identifying barriers to uptake of the technology and priorities for better research. Meta-analyses suggest that telehealth technologies can reduce time to treatment for people with stroke48 and STEMI54 by allowing initiation of treatment before arriving at the hospital and/or by transmitting clinical data to clinicians at the receiving hospital.
Chapter 5 Discussion and conclusions
Main findings
This systematic review addressed the effect of increasing distance to UEC on patient and health system outcomes by looking at two main groups of studies. In relation to the first research question (What is the evidence regarding effects on patients of service reconfigurations which increase the time/distance to an UEC facility?), the reconfiguration studies found no evidence that increasing travel time or distance increased mortality risk for general populations of patients attending UEC facilities. There was some evidence from studies that were restricted to patients with AMI of an increased risk of mortality, whereas evidence for other conditions was inconsistent or very limited.
The association studies addressed the second research question (What is the evidence regarding associations between time/distance from an UEC facility and outcomes for patients requiring UEC?). These studies found evidence of an association between distance and mortality for general, AMI and trauma populations, whereas evidence for maternity was inconsistent. Pregnant women differ from other populations requiring emergency care in that their period of highest risk is finite and predictable. In some health systems, primarily those with potentially very long travel distances or times, this risk can be mitigated by the option of temporary relocation closer to a specialist unit. 6,39
Telehealth care is clearly the most important intervention for mitigating the effects of distance from specialist emergency care. Because of the large volume of available research, we performed a narrative overview of recent systematic reviews (see Chapter 4). Telehealth technology mitigates distance effects by facilitating access to clinical expertise and/or by speeding up treatment, as demonstrated in two meta-analyses. 48,54 Although we did not formally assess the quality of the included reviews, review quality was clearly variable and most of the reviews used a mapping or narrative synthesis approach. Telehealth is most strongly established as an intervention for timely treatment of stroke patients. 51 Telehealth technology in pre-hospital settings is relatively new and included reviews have identified a range of barriers to adoption and questions about how best to implement the technology. 58,59 None of the systematic reviews focused on cost-effectiveness, which has been a barrier to the adoption of telehealth in some UK settings.
Much of the research included in our review comes from non-UK settings and we have endeavoured to keep applicability in mind throughout. Absolute distances and times of travel vary within countries, including the UK, but large countries such as the USA, Canada and Australia are likely to have longer travel times/distances on average outside urban areas. This is also true for some of the Scandinavian countries where travel times can be long as the population is centred in fewer areas, meaning that remote communities have less access to UEC.
Several included studies suggest that the effects of service reconfiguration on outcomes, particularly patient outcomes, may be short-lived, with health systems adapting to the new situation over a few years. In the study by Avdic,5 effects of ED closures on AMI mortality were statistically significant only for the first year after closure, while Shen and Hsia12 identified a 4-year transition period. Some studies reported on efforts by health-care commissioners and providers to mitigate the effects of reconfiguration. Avdic5 mentioned increased investment in both emergency service provision and prevention although the study did not evaluate whether or not these actually occurred. A hospital in Boston, USA, provided early notice of its intention to close an ED and worked closely with EMS providers to minimise the effect on the EMS system in the city. 7 Yaghoubian et al. 14 also in the USA, reported on changes in trauma centre staffing and organisation to prepare for the closure of a nearby centre. The limited insights provided by these studies emphasise the need for greater understanding of how health service stakeholders prepare for the system-wide impacts of changes that require patients to travel further for treatment, as also mentioned by Knowles et al. 2
We identified a large number of potential mediating, moderating and mitigating factors (see Figure a and Appendix 4). The extent to which these factors occur and their amenability to modification by health system interventions is highly variable. Most of the included studies adjusted for the influence of common moderators and mediators in their statistical analysis, which provides reasonable confidence in the observed associations between travel distance/time and patient outcomes. However, an influence of confounding factors not allowed for in authors’ analyses and statistical models cannot be ruled out.
Service reconfigurations are often supported by decision-makers on the grounds that increased patient volume and/or specialisation in a smaller number of UEC facilities will increase the quality of patient care overall. This review did not directly address the relationship between volume and outcomes, which has been the subject of a large volume of research. However, one included study14 attributed successful adaptation to a trauma centre closure partly to staff gaining experience from treating more patients during the study period. We also note that there is substantial evidence for the benefits of transporting patients with stroke or severe trauma to specialist centres, often bypassing nearer non-specialist facilities. Studies included in this review identified benefits of transport to a PCI-capable hospital for patients with AMI, particularly STEMI. 22–24
Interpretation of the findings of included studies should be guided by the quality and strength of the included evidence. We have assessed risk of bias at the level of the individual study and overall strength of evidence for key findings using a scheme successfully employed in previous reviews. Many of the included studies were judged to be at relatively high risk of bias because of their observational design and the absence of an independent control group in many cases. On the positive side, most studies acknowledged and attempted to adjust for the influence of confounding factors and some were large and/or long term. Furthermore, studies using routinely collected data may reflect real clinical practice more accurately than those involving carefully selected and knowingly recruited research participants. In view of this uncertainty, we have been relatively conservative in assessing the overall strength of evidence for effects and associations (see Tables 15–18).
Strengths and limitations
This systematic review was undertaken by an experienced team including both methodological and topic experts. We followed a protocol developed in collaboration with the National Institute for Health Research (NIHR) HSDR programme team as the review was designed in part to help clarify research priorities. The protocol was registered prospectively with the PROSPERO database of systematic review protocols (registration number CRD42019123061).
We performed a thorough search for published literature dating back to 2000 supplemented by citation-tracking of key studies and reference list checking of all included studies. This was clearly worthwhile as six included studies were identified by reference list checking and three by citation-tracking.
Resource constraints meant that we abbreviated the review process by using a single reviewer to perform study selection, quality assessment and data extraction, with checking of a 10% sample by a second member of the review team. This may be considered a limitation when measured against the gold standard of double independent performance of these stages but analysis of study selection revealed a high level of agreement among three reviewers. Although there is a risk of some errors or subjective assessments, we do not believe that these would have influenced the review’s main findings and conclusions.
The coverage of telehealth by an overview of relevant systematic reviews was partly determined by the limited available resources but we believe the decision was justified by the 12 largely recent systematic reviews included. The included reviews provide a thorough overview of this heavily researched field, using a mixture of quantitative (including meta-analysis) and narrative synthesis. It was encouraging that the reviews covered aspects of the implementation of telehealth58 as well as reviews of intervention effectiveness.
A strength of the review is that we approached the research question from two different angles, represented by the reconfiguration and association groups of studies. The reconfiguration studies address a dynamic situation where change to services has actually happened, while the association studies take a more static approach, examining how distance to UEC influences outcomes in a particular setting. Both groups of studies represent substantial bodies of research using different study designs and with largely complementary results. In the narrative synthesis, we considered these groups of studies (together with the mitigation and telehealth studies) separately but also assessed the body of evidence as a whole in relation to relevance to the UK and to rural settings. We have summarised the overall strength of evidence from the two main groups of studies using a published framework that we hope will be helpful for decision-makers needing a quick overview (see Tables 15–18).
We extracted details of moderating and mediating factors from the included studies, as summarised in Figure a. Figure a includes both factors that influence travel time and those that influence patient outcome (either alone or through interaction with time/distance). The figure is not comprehensive and the relative importance of different factors will vary between settings. In spite of this, the information in the figure and related appendix (see Appendix 4) may be of value to decision-makers by helping them to identify service factors that can be modified to enable faster access to treatment and potentially better outcomes.
The relationship between distance/time to emergency care and patient outcomes is clearly a complex one. The diverse measurement methods and outcomes in the included studies meant that we were unable to perform any meta-analyses to estimate pooled outcome measures across studies. Although this may be considered a limitation of the review, we did not have meta-analysis as one of our predefined objectives and any estimate would only be meaningful in the absence of major clinical and/or statistical heterogeneity. The summary table of association studies (see Table 19) illustrates the wide range of measures used in included studies and allows readers to identify studies relevant to their population and setting of interest.
Implications for service delivery
Timely and equitable access to UEC is important to all population groups in both urban and rural settings. Ensuring such access requires commissioners and providers of health services to work effectively together, informed by their understanding of the evidence and data relevant to their local context. As many of the studies included in this review demonstrate, the relationship between time or distance and outcomes is influenced by many factors, including patient characteristics, clinical care, geography and infrastructure.
Studies included in this review provide insight into issues that decision-makers may wish to consider and act on when reconfiguration that may affect access to UEC is under consideration. For England, Roberts et al. 4 identified the following considerations for planners: size of population served, availability of specialist centres (e.g. for trauma, stroke), availability of workforce, organisation of training and whether or not there are sufficient ‘support facilities’. The authors also pointed out the need for political decisions at the national and local level about which services are affordable.
Empirical studies of the effects of ED closures and reconfigurations have provided insights into how change can be managed to minimise any adverse effects on patients or the stability of the wider health and care system. El-Sayed et al. 7 noted the importance of early notification of planned closure and ‘continuous and dynamic co-operation’ between hospital and EMS administrations. Yaghoubian et al. 14 prepared for closure of a nearby trauma centre by putting in place additional staffing and changes to team organisation. A strong regional trauma system also helped to ensure that remaining trauma centres were able to accommodate additional patients.
Several included studies suggest that the effects of increased travel distance/time on outcomes may be temporary, lasting 1 or a few years. The research suggests that health services may be able to minimise the transition period by measures such as investment in EMS5 and by providing capacity elsewhere before any closures take place. 12 Studies also suggest that the scale of any changes in distance or time is important and small changes may have a minimal impact on outcomes at the population level. 4,9 Service design needs to take into account the effects of distance on outcomes but also allow for the fact that rural and remote areas are less densely populated than towns and cities, resulting in lower demand/need for services. The benefits to individuals of having services located close by have to be balanced against overall population benefits that may accrue from centralisation of services and concentration of expertise at selected sites.
Another approach to handling increased distance to UEC facilities is through new service delivery models. This review has identified a number of different models that decision-makers may wish to consider. In the maternity setting, some health-care systems provide the option for women from more remote regions to travel to a more central facility for a short period before the expected date of delivery. 6 Service models based on telehealth have been extensively researched, as covered in Chapter 4. For example, telehealth technologies may enable EDs in rural and remote areas to be run on a ‘hub-and-spoke’ model, with less critical emergencies being handled by nurses with remote clinical support. 55 The use of telehealth in ambulances allows service models based on early initiation of diagnosis and/or treatment by paramedics as well as triage to divert less seriously ill patients away from EDs when clinically appropriate. 52,58,59 However, barriers remain to the widespread adoption of telehealth technology in some settings. Other mitigation interventions, including improved co-ordination between services,46 are discussed in the relevant sections of Chapter 3 (see Mitigation studies).
Some service models that may be of interest to decision-makers fell outside the scope of this review (e.g. air ambulance services) or were excluded after full consideration (e.g. public access defibrillators). We did not identify any evaluations of community first responders, although this service is available in many parts of the UK. Descriptions of the service suggest that first responders may be of most value for conditions such as cardiac arrest for which distance to the nearest UEC facility is unlikely to influence survival.
Although increased distance to UEC is generally discussed in terms of possible risks, included studies also suggested some potential benefits to patients and the health system. EDs may close or be downgraded for reasons to do with quality of care,2,9 potentially encouraging patients to use superior services. Reconfiguration of services may encourage EDs and other centres to organise their work more efficiently and a greater volume of patients may enable staff to improve the quality of the care they deliver through increased experience. 14 This aspect is reflected most clearly in the increasing trend to transport patients to specialist centres, especially for stroke and trauma, rather than to closer but less specialised facilities.
Two studies from Scandinavia provide further insights into the effects of UEC service reconfigurations on the wider health and care system. In Denmark, Hansen et al. 8 reported that EDs up to 40 km away were able to compensate, at least in part, for closure of a local ED. However, the authors noted that this was dependent on free and rapid access to ambulance services and high levels of car ownership. A controlled before–after study in Finland reported that closure of a local primary care ED decreased use of ED services in nearby areas without increasing use of other office-hour services. 11 The authors concluded that distance is an important influence on ED attendance and ED closure can be used to encourage patients to access care via other routes. Differences between the primary care-based ED system in Finland and that of the UK should be taken into account when considering this evidence.
Despite these caveats, the review provides some evidence that closing EDs may reduce self-presentation at an ED by patients who could be treated elsewhere. The relationship between distance and ED attendance in the UK was studied by Rudge et al. ,21 who found that the availability of a MIU nearby reduced ED use by those living at a distance from an ED. This suggests that if alternatives can be put in place, there will not necessarily be a commensurate increase in workload for an ED if a neighbouring ED closes. Effects on patient flow could be taken into account at an early stage of planning for possible service reconfigurations.
Studies included in this review illustrate the importance of up-to-date research and evidence to inform decision-making. An example is the care of patients with AMI, where PCI is now the therapy of choice in most regions. This implies the need for health systems to monitor the long-term effects of service reconfigurations as they become mature and to account for other innovations which may ultimately offset any disadvantages from having to travel further.
There is a consistent message from both UK and international research about the importance of considering the EMS implications of planned service changes. 2,7,34 EMS staff cover the whole catchment area of a specialist service, meaning that increased travel distances result in increased job cycle times and more resources needed to maintain the same response to demand. The challenge for decision-makers is how to fund and staff the service while also using EMS staff in a wider variety of roles (e.g. treating more patients at the scene rather than transporting them to hospital).
Health services need to ensure that increases in time or distance to UEC are not associated with increased health inequity. A large UK study suggested that there may be a risk of this. 21 Rudge et al. 21 found that ED attendance decreased as distance to the nearest ED increased but the effect was more notable in deprived areas than less deprived ones. Mustonen et al. 11 also emphasised the importance of ensuring that UEC services are not located far away from socially deprived areas.
Finally, although the focus of this review is on UEC and other health services, actions taken elsewhere can influence distance/time to UEC and hence outcomes for patients. Examples include improvements to road networks and associated factors, such as junctions and lighting, as well as regulations surrounding alcohol and drug use by drivers (which, in turn, affect actual consumption).
Implications for research
We have identified the following implications for further research.
There is a need for further time series analyses along the lines of the closED study2 to examine the longer-term effects of service reconfigurations on the whole UEC system and to take into account the impact of other service and technological changes over time. Although such studies should ideally be controlled, uncontrolled time series also have some value and are easier to organise.
Research is needed to better understand how local and regional health systems plan for and adapt to increases in travel distance/time. As suggested by other researchers,2 this could take the form of qualitative research and/or documentary analysis. The current programme of service reconfiguration provides opportunities for prospective studies in a range of different settings. Research should aim to capture the perspectives of a range of different stakeholders including health professionals, managers in both commissioner and provider organisations and the general public.
Data analysis is needed to address uncertainty about how risk increases with distance/time within the range relevant to UK urban and rural populations. This could involve analysis of existing data or new research to ascertain whether or not the findings of earlier studies18,19 remain valid with current road conditions and technology.
Analysis of routine data to examine whether UEC reconfigurations reduce overall demand for ED care or merely displace demand to other parts of the health-care system. Data can also be used to examine the nature and extent of variation between different localities with a view to reducing unnecessary variation and improving overall quality of care.
Research is needed to assess patient outcomes other than mortality and hospital admission/length of stay. This could include effects of service reconfiguration on families who may incur additional social and financial costs because of increased travel distance/time to visit patients.
Public attitudes to reconfiguration and involvement in decision-making were outside the scope of this review. Nevertheless, it is clear that proposals to reconfigure UEC services are often opposed by local communities based on concerns that increased travel distance/time may increase the risk of adverse outcomes. Further research would be valuable to understand public attitudes to risk and preferences for different alternatives. Research could involve a variety of methods including consultation via citizens’ assemblies or similar.
Conclusions
This systematic review found no evidence that service changes that increased average travel time or distance increased mortality risk for general populations of patients attending UEC facilities. There was some evidence of an increased risk from studies restricted to patients with AMI, whereas evidence for other conditions was inconsistent or very limited. Studies that examined the association between distance and outcomes in the absence of reconfiguration found evidence of an association between distance and mortality for general, AMI and trauma populations, whereas evidence for maternity was inconsistent. The relatively low quality of much of the research suggests that findings should be interpreted cautiously. In particular ‘no evidence of increased risk’ does not necessarily mean ‘evidence of no increase in risk’, as the finding could be overturned by further research in the future.
Empirical studies of the effects of ED closures and reconfigurations have provided insights into how change can be managed to minimise any adverse effects on patients or the stability of the wider health and care system. Important factors include early notification and discussion of planned changes, co-operation between different stakeholders, and appropriate changes to staffing and organisation of the workforce. Several included studies suggest that the effects of increased travel distance/time on outcomes may be temporary, lasting one or a few years. Health-care services may be able to minimise the transition period by measures such as investment in EMS and by providing capacity elsewhere before any closures take place.
There is a consistent message from both UK and international research about the importance of considering the EMS implications of planned service changes. We also found evidence that people in more deprived areas were less willing/able to travel to attend an ED. This suggests that consideration should be given to ensuring that UEC services are not located far away from socially deprived areas.
Research priorities include work to examine the longer-term effects of service reconfigurations on the whole UEC system and to better understand how local and regional health-care systems plan for and adapt to increases in travel distance/time.
Acknowledgements
We thank Dr Daniel Mason (Sheffield Clinical Commissioning Group) for reading and commenting on some sections of the draft report. We also thank the members of the Sheffield Evidence Synthesis Centre Public Advisory Group for their contributions.
Contributions of authors
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) (Research Fellow in Public Health) was involved in the project co-ordination, study selection, data extraction, quality assessment and report writing.
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) (Research Associate in Health Economics and Decision Science) was involved in information retrieval, study selection, data extraction, quality assessment and report writing.
Susan K Baxter (https://orcid.org/0000-0002-6034-5495) (Senior Research Fellow in Public Health) was involved in the protocol development, study selection and report writing, and she co-ordinated the patient and public involvement meeting.
Janette Turner (https://orcid.org/0000-0003-3884-7875) (Reader in Emergency and Urgent Care Research) provided topic expert advice and was involved in the report writing.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) (Reader in Evidence-Based Information Practice) was involved in information retrieval, study selection and report writing.
All authors commented on drafts of the protocol and report.
Chambers D, Cantrell A, Baxter S, Turner J, Booth A. Effects of service changes affecting distance/time to access urgent and emergency care facilities on patient outcomes: a systematic review. BMC Medicine 2020;18:117.
Publication
Chambers D, Cantrell A, Baxter S, Turner J, Booth A. Effects of service changes affecting distance/time to access urgent and emergency care facilities on patient outcomes: a systematic review. BMC Medicine 2020;18:117.
Data-sharing statement
Any additional data not included in this report and its appendices are available on request. All queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Chambers D, Cantrell A, Baxter S, Turner J, Booth A. Effects of service changes affecting distance/time to access urgent and emergency care facilities on patient outcomes: a systematic review. BMC Medicine 2020;18. https://doi.org/10.1186/s12916-020-01580-3.
- Knowles E, Shephard N, Stone T, Bishop-Edwards L, Hirst E, Abouzeid L, et al. Closing five Emergency Departments in England between 2009 and 2011: the closED controlled interrupted time-series analysis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06270.
- Chambers D, Cantrell AJ, Johnson M, Preston L, Baxter SK, Booth A, et al. Digital and online symptom checkers and health assessment/triage services for urgent health problems: systematic review. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027743.
- Roberts A, Blunt I, Bardsley M. Focus On: Distance From Home to Emergency Care. London: The Health Foundation and Nuffield Trust; 2014.
- Avdic D. Improving efficiency or impairing access? Health care consolidation and quality of care: Evidence from emergency hospital closures in Sweden. J Health Econ 2016;48:44-60. https://doi.org/10.1016/j.jhealeco.2016.02.002.
- Combier E, Charreire H, Le Vaillant M, Michaut F, Ferdynus C, Amat-Roze JM, et al. Perinatal health inequalities and accessibility of maternity services in a rural French region: closing maternity units in Burgundy. Health Place 2013;24:225-33. https://doi.org/10.1016/j.healthplace.2013.09.006.
- El Sayed M, Mitchell PM, White LF, Rubin-Smith JE, Maciejko TM, Obendorfer DT, et al. Impact of an emergency department closure on the local emergency medical services system. Prehosp Emerg Care 2012;16:198-203. https://doi.org/10.3109/10903127.2011.640418.
- Hansen KS, Enemark U, Foldspang A. Health services use associated with emergency department closure. J Health Serv Res Policy 2011;16:161-6. https://doi.org/10.1258/jhsrp.2010.010100.
- Hsia RY, Kanzaria HK, Srebotnjak T, Maselli J, McCulloch C, Auerbach AD. Is emergency department closure resulting in increased distance to the nearest emergency department associated with increased inpatient mortality?. Ann Emerg Med 2012;60:707-15 e4. https://doi.org/10.1016/j.annemergmed.2012.08.025.
- Hsia RY, Srebotnjak T, Maselli J, Crandall M, McCulloch C, Kellermann AL. The association of trauma center closures with increased inpatient mortality for injured patients. J Trauma Acute Care Surg 2014;76:1048-54. https://doi.org/10.1097/TA.0000000000000166.
- Mustonen K, Kantonen J, Kauppila T. The effect on the patient flow in local health care services after closing a suburban primary care emergency department: a controlled longitudinal follow-up study. Scand J Trauma Resusc Emerg Med 2017;25. https://doi.org/10.1186/s13049-017-0460-3.
- Shen YC, Hsia RY. Does decreased access to emergency departments affect patient outcomes? Analysis of acute myocardial infarction population 1996–2005. Health Serv Res 2012;47:188-210. https://doi.org/10.1111/j.1475-6773.2011.01319.x.
- Shen YC, Hsia RY. Association between emergency department closure and treatment, access, and health outcomes among patients with acute myocardial infarction. Circulation 2016;134:1595-7. https://doi.org/10.1161/CIRCULATIONAHA.116.025057.
- Yaghoubian A, Lewis RJ, Putnam BA, De Virgilio C. Impact on patient outcomes after closure of an adjacent trauma center. Am Surg 2008;74:930-4.
- Berlin C, Panczak R, Hasler R, Zwahlen M. Swiss National Cohort Study Group . Do acute myocardial infarction and stroke mortality vary by distance to hospitals in Switzerland? Results from the Swiss National Cohort Study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013090.
- Dummer TJ, Parker L. Hospital accessibility and infant death risk. Arch Dis Child 2004;89:232-4. https://doi.org/10.1136/adc.2003.030924.
- Parker L, Dickinson HO, Morton-Jones T. Proximity to maternity services and stillbirth risk. Arch Dis Child Fetal Neonatal Ed 2000;82:F167-8. https://doi.org/10.1136/fn.82.2.F167.
- Nicholl J, West J, Goodacre S, Turner J. The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J 2007;24:665-8. https://doi.org/10.1136/emj.2007.047654.
- Wei L, Lang CC, Sullivan FM, Boyle P, Wang J, Pringle SD, et al. Impact on mortality following first acute myocardial infarction of distance between home and hospital: cohort study. Heart 2008;94:1141-6. https://doi.org/10.1136/hrt.2007.123612.
- Souza V, Strachan D. Relationship between travel time to the nearest hospital and survival from ruptured aortic aneurysm: record linkage study. J Public Health 2005;27:165-70. https://doi.org/10.1093/pubmed/fdi001.
- Rudge GM, Mohammed MA, Fillingham SC, Girling A, Sidhu K, Stevens AJ. The combined influence of distance and neighbourhood deprivation on emergency department attendance in a large English population: a retrospective database study. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0067943.
- Andersson HB, Seth M, Gurm HS, Bates ER. Pre-hospital Transport times and outcomes after different reperfusion strategies for ST-elevation myocardial infarction. Am J Cardiol 2019;123:375-81. https://doi.org/10.1016/j.amjcard.2018.10.015.
- Balamurugan A, Delongchamp R, Im L, Bates J, Mehta JL. Neighborhood and acute myocardial infarction mortality as related to the driving time to percutaneous coronary intervention-capable hospital. J Am Heart Assoc 2016;5. https://doi.org/10.1161/JAHA.115.002378.
- Balamurugan A, Phillips M, Selig JP, Felix H, Ryan K. Association between system factors and acute myocardial infarction mortality. South Med J 2018;111:556-64. https://doi.org/10.14423/SMJ.0000000000000853.
- Bussières S, Bégin F, Leblanc PA, Tanguay A, Paradis JM, Hébert D, et al. Clinical adverse events in prehospital patients with ST-elevation myocardial infarction transported to a percutaneous coronary intervention centre by basic life support paramedics in a rural region. CJEM 2018;20:857-64. https://doi.org/10.1017/cem.2018.383.
- Di Domenicantonio R, Cappai G, Sciattella P, Belleudi V, Di Martino M, Agabiti N, et al. The tradeoff between travel time from home to hospital and door to balloon time in determining mortality among STEMI patients undergoing PCI. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0158336.
- Langabeer JR, Prasad S, Seo M, Smith DT, Segrest W, Owan T, et al. The effect of interhospital transfers, emergency medical services, and distance on ischemic time in a rural ST-elevation myocardial infarction system of care. Am J Emerg Med 2015;33:913-16. https://doi.org/10.1016/j.ajem.2015.04.009.
- Postma S, Dambrink JH, de Boer MJ, Gosselink AT, Ottervanger JP, Koopmans PC, et al. The influence of residential distance on time to treatment in ST-elevation myocardial infarction patients. Neth Heart J 2014;22:513-19. https://doi.org/10.1007/s12471-014-0599-8.
- Svensson L, Karlsson T, Nordlander R, Wahlin M, Zedigh C, Herlitz J. Safety and delay time in prehospital thrombolysis of acute myocardial infarction in urban and rural areas in Sweden. Am J Emerg Med 2003;21:263-70. https://doi.org/10.1016/S0735-6757(03)00040-8.
- Durkin M, McElroy J, Guan H, Bigelow W, Brazelton T. Geographic analysis of traffic injury in Wisconsin: impact on case fatality of distance to level I/II trauma care. WMJ 2005;104:26-31.
- Gomez D, Berube M, Xiong W, Ahmed N, Haas B, Schuurman N, et al. Identifying targets for potential interventions to reduce rural trauma deaths: a population-based analysis. J Trauma 2010;69:633-9. https://doi.org/10.1097/TA.0b013e3181b8ef81.
- Gonzalez RP, Cummings GR, Phelan HA, Mulekar MS, Rodning CB. Does increased emergency medical services prehospital time affect patient mortality in rural motor vehicle crashes? A statewide analysis. Am J Surg 2009;197:30-4. https://doi.org/10.1016/j.amjsurg.2007.11.018.
- Jarman MP, Curriero FC, Haut ER, Pollack Porter K, Castillo RC. Associations of distance to trauma care, community income, and neighborhood median age with rates of injury mortality. JAMA Surg 2018;153:535-43. https://doi.org/10.1001/jamasurg.2017.6133.
- Lee J, Abdel-Aty M, Cai Q, Wang L. Effects of emergency medical services times on traffic injury severity: A random effects ordered probit approach. Traffic Inj Prev 2018;19:577-81. https://doi.org/10.1080/15389588.2018.1468889.
- Lerner EB, Billittier AJ, Dorn JM, Wu YW. Is total out-of-hospital time a significant predictor of trauma patient mortality?. Acad Emerg Med 2003;10:949-54. https://doi.org/10.1197/S1069-6563(03)00313-0.
- McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban Level I trauma center. Ann Emerg Med 2013;61:167-74. https://doi.org/10.1016/j.annemergmed.2012.08.026.
- Engjom HM, Morken NH, Høydahl E, Norheim OF, Klungsøyr K. Increased risk of peripartum perinatal mortality in unplanned births outside an institution: a retrospective population-based study. Am J Obstet Gynecol 2017;217. https://doi.org/10.1016/j.ajog.2017.03.033.
- Featherstone P, Eberth JM, Nitcheva D, Liu J. Geographic Accessibility to health services and neonatal mortality among very-low birthweight infants in South Carolina. Matern Child Health J 2016;20:2382-91. https://doi.org/10.1007/s10995-016-2065-2.
- Grzybowski S, Stoll K, Kornelsen J. Distance matters: a population based study examining access to maternity services for rural women. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-147.
- Pilkington H, Blondel B, Drewniak N, Zeitlin J. Where does distance matter? Distance to the closest maternity unit and risk of foetal and neonatal mortality in France. Eur J Public Health 2014;24:905-10. https://doi.org/10.1093/eurpub/ckt207.
- Ravelli AC, Jager KJ, de Groot MH, Erwich JJ, Rijninks-van Driel GC, Tromp M, et al. Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG 2011;118:457-65. https://doi.org/10.1111/j.1471-0528.2010.02816.x.
- Murata A, Matsuda S. Association between ambulance distance to hospitals and mortality from acute diseases in Japan: national database analysis. J Public Health Manag Pract 2013;19:E23-8. https://doi.org/10.1097/PHH.0b013e31828b7150.
- Acharya AB, Nyirenda JC, Higgs GB, Bloomfield MS, Cruz-Flores S, Connor LT, et al. Distance from home to hospital and thrombolytic utilization for acute ischemic stroke. J Stroke Cerebrovasc Dis 2011;20:295-301. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.12.009.
- Leyden JM, Chong WK, Kleinig T, Lee A, Field JB, Jannes J. A population-based study of thrombolysis for acute stroke in South Australia. Med J Aust 2011;194:111-15. https://doi.org/10.5694/j.1326-5377.2011.tb04191.x.
- Koch PM, Kunz A, Ebinger M, Geisler F, Rozanski M, Waldschmidt C, et al. Influence of distance to scene on time to thrombolysis in a specialized stroke ambulance. Stroke 2016;47:2136-40. https://doi.org/10.1161/STROKEAHA.116.013057.
- Langabeer JR, Smith DT, Cardenas-Turanzas M, Leonard BL, Segrest W, Krell C, et al. Impact of a rural regional myocardial infarction system of care in Wyoming. J Am Heart Assoc 2016;5. https://doi.org/10.1161/JAHA.116.003392.
- Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM. Potential impact of public access defibrillators on survival after out of hospital cardiopulmonary arrest: retrospective cohort study. BMJ 2002;325. https://doi.org/10.1136/bmj.325.7363.515.
- Baratloo A, Rahimpour L, Abushouk AI, Safari S, Lee CW, Abdalvand A. Effects of telestroke on thrombolysis times and outcomes: a meta-analysis. Prehosp Emerg Care 2018;22:472-84. https://doi.org/10.1080/10903127.2017.1408728.
- Hubert GJ, Müller-Barna P, Audebert HJ. Recent advances in TeleStroke: a systematic review on applications in prehospital management and stroke unit treatment or telestroke networking in developing countries. Int J Stroke 2014;9:968-73. https://doi.org/10.1111/ijs.12394.
- Johansson T, Wild C. Telemedicine in acute stroke management: systematic review. Int J Technol Assess Health Care 2010;26:149-55. https://doi.org/10.1017/S0266462310000139.
- Rubin MN, Wellik KE, Channer DD, Demaerschalk BM. A systematic review of telestroke. Postgrad Med 2013;125:45-50. https://doi.org/10.3810/pgm.2013.01.2623.
- Eder PA, Reime B, Wurmb T, Kippnich U, Shammas L, Rashid A. Prehospital telemedical emergency management of severely injured trauma patients. Methods Inf Med 2018;57:231-42. https://doi.org/10.1055/s-0039-1681089.
- Lewis ER, Thomas CA, Wilson ML, Mbarika VW. Telemedicine in acute-phase injury management: a review of practice and advancements. Telemed J E Health 2012;18:434-45. https://doi.org/10.1089/tmj.2011.0199.
- Brunetti ND, De Gennaro L, Correale M, Santoro F, Caldarola P, Gaglione A, et al. Pre-hospital electrocardiogram triage with telemedicine near halves time to treatment in STEMI: A meta-analysis and meta-regression analysis of non-randomized studies. Int J Cardiol 2017;232:5-11. https://doi.org/10.1016/j.ijcard.2017.01.055.
- du Toit M, Malau-Aduli B, Vangaveti V, Sabesan S, Ray RA. Use of telehealth in the management of non-critical emergencies in rural or remote emergency departments: A systematic review. J Telemed Telecare 2019;25:3-16. https://doi.org/10.1177/1357633X17734239.
- Gattu R, Teshome G, Lichenstein R. Telemedicine applications for the pediatric emergency medicine: a review of the current literature. Pediatr Emerg Care 2016;32:123-30. https://doi.org/10.1097/PEC.0000000000000712.
- Marsh-Feiley G, Eadie L, Wilson P. Telesonography in emergency medicine: a systematic review. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0194840.
- Rogers H, Madathil KC, Agnisarman S, Narasimha S, Ashok A, Nair A, et al. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed J E Health 2017;23:707-17. https://doi.org/10.1089/tmj.2016.0248.
- Winburn AS, Brixey JJ, Langabeer J, Champagne-Langabeer T. A systematic review of prehospital telehealth utilization. J Telemed Telecare 2018;24:473-81. https://doi.org/10.1177/1357633X17713140.
Appendix 1 Search strategies
Main database search example search strategy from MEDLINE
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily <1946 to February 05, 2019>.
Search strategy
-
*Emergency Service, Hospital/ (37,159)
-
*Emergency Medical Services/ (28,356)
-
*Emergency Medicine/ (9491)
-
(emergency adj2 service*).ab,ti. (15,026)
-
‘emergency care’.ab,ti. (7936)
-
‘urgent care’.ab,ti. (1763)
-
‘emergency department* ‘.ab,ti. (79,373)
-
‘accident and emergency’.ab,ti. (4515)
-
casualty.ab,ti. (5181)
-
*Ambulances/ (3459)
-
ambulance$.ab,ti. (9514)
-
‘Transportation of Patients’/ (8960)
-
or/1-12 (153,712)
-
Rural Health Services/ (11,879)
-
(rural$ or island$).ab,ti. (203,994)
-
14 or 15 (206,752)
-
13 or 16 (356,779)
-
((service$ or health or department$ or deliver$) adj3 (clos$ or chang$ or reorganis$ or merg$ or reconfigur$ or relocat$ or restructur$)).ab,ti. (33,564)
-
health facility closure/or health facility merger/or health facility moving/ (7163)
-
Health Services Accessibility/ (67,829)
-
distance.ab,ti. (207,028)
-
access$.ab,ti. (450,752)
-
Time Factors/(114,3527)
-
(time$ adj2 travel$).ab,ti. (3348)
-
or/18-24 (1,840,113)
-
17 and 25 (49,092)
-
Myocardial Infarction/(159,731)
-
myocardial infarction.ab,ti. (166,461)
-
MI.ab,ti. (42,299)
-
heart attack$.ab,ti. (5148)
-
Stroke/(88,836)
-
stroke.ab,ti. (213,756)
-
major trauma.ab,ti. (3231)
-
ASTHMA/ (119,387)
-
asthma attack$.ab,ti. (2337)
-
(asthma adj3 exacerbation$).ab,ti. (6461)
-
Pulmonary Disease, Chronic Obstructive/ (35,064)
-
chronic obstructive pulmonary disease$.ab,ti. (42,822)
-
copd.ab,ti. (40,387)
-
Pregnancy Complications/ (86,598)
-
pregnancy complication$.ab,ti. (5384)
-
Emergency Treatment/ (10,211)
-
*EMERGENCIES/ (12,339)
-
*Acute Disease/ (8158)
-
or/27-44 (745,351)
-
26 and 45 (5124)
-
limit 46 to (English language and yr = ‘2000 -Current’) (3960)
Search step 13 combines the different terms and synonyms for the concept Emergency Care using OR.
Search step 16 combines the different terms for the concept of rural or Island health care using OR.
Search step 17 combines the Emergency Care and Rural health-care terms terms using OR.
Search step 25 combines the different terms for services changes and distance using OR.
Search step 26 combines steps 17 and 25 together using AND.
Search step 45 combines the terms for different emergency medical conditions relevant to the review using OR.
Search step 46 combines steps 26 and 45 together using AND.
Search step 47 limits the search to English Language and the date range 2000–February 2019.
Medline search strategy for telehealth systematic reviews
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily <1946 to February 26, 2019>.
Search strategy
-
*Emergency Service, Hospital/ (37,180)
-
*Emergency Medical Services/ (28,364)
-
*Emergency Medicine/ (9491)
-
(emergency adj2 service*).ab,ti. (15,051)
-
‘emergency care’.ab,ti. (7943)
-
‘urgent care’.ab,ti. (1770)
-
‘emergency department* ‘.ab,ti. (79,539)
-
‘accident and emergency’.ab,ti. (4520)
-
casualty.ab,ti. (5186)
-
*Ambulances/ (3461)
-
ambulance$.ab,ti. (9527)
-
‘Transportation of Patients’/ (8963)
-
or/1-12 (153,926)
-
Rural Health Services/ (11,881)
-
(rural$ or island$).ab,ti. (204,324)
-
14 or 15 (207,084)
-
13 or 16 (357,319)
-
Telemedicine/ (18,867)
-
telemedicine.ab,ti. (8924)
-
telehealth.ab,ti. (3205)
-
ehealth.ab,ti. (1981)
-
mobile health.ab,ti. (2334)
-
health mobile.ab,ti. (73)
-
mhealth.ab,ti. (2052)
-
telemonitoring.ab,ti. (1249)
-
‘*telemonitoring’.kw. (221)
-
18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 (26,790)
-
17 and 27 (3689)
-
meta analysis.mp,pt. (157,721)
-
review.pt. (2,484,004)
-
search:.tw. (402,770)
-
29 or 30 or 31 (2,777,183)
-
28 and 32 (445)
-
limit 33 to (English language and yr = ‘2009 -Current’) (307)
The search used the main search up to search line 17.
Search line 27 combines the different terms for telemedicine using OR.
Search line 28 combines search line 17 and 27 using AND.
Search lines 29–32 are McMasters Reviews filter Medline best balance of sensitivity and specificity (URL: https://hiru.mcmaster.ca/hiru/HIRU_Hedges_MEDLINE_Strategies.aspx).
The McMasters Reviews filter is then combined with search line 28 to find reviews of the use of telemedicine in Emergency Care.
In search line 34 the search is limited to English-language papers and the years 2009–February 2019.
Text in this appendix is reproduced from Chambers et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text.
Appendix 2 Data extraction template
-
Study ID
-
Reference Author year {#EN citation} (e.g. {Jones, 2016 #1999}).
-
-
Country
-
UK
-
Netherlands
-
France
-
Germany
-
Spain
-
Switzerland
-
Other Europe Specify in info box
-
USA
-
Canada
-
Australia
-
New Zealand
-
Other non-Europe Specify in info box
-
Multiple countries
-
Unclear/not reported
-
Not applicable Use for systematic reviews.
-
-
Study design
-
Experimental
-
Controlled observational
-
Uncontrolled observational
-
Qualitative
-
Mixed methods
-
Systematic review
-
Other Add brief details in info box.
-
-
Type of setting Where population of interest live
-
Rural
-
Remote
-
Coastal
-
Mixed
-
Urban/suburban
-
Large city/city region
-
Other Specify in info box
-
Unclear/not reported.
-
-
Population/condition
-
General emergency care
-
AMI
-
Stroke
-
Asthma/chronic obstructive pulmonary disease
-
Major trauma
-
Obstetric/neonatal complications
-
Other Add details in ‘info’ box.
-
-
Sample source Source from which data were derived, e.g. local audit; national primary care database; hospital records etc.
-
Data source.
-
-
Sample size
-
Number of participants.
-
-
Intervention
-
ED closure or relocation Add details in ‘info’ box
-
Obstetric unit closure or relocation
-
Centralisation of services
-
Mitigation Intervention aims to mitigate effect of being far away from a UEC facility. Add details in ‘info’ box
-
None Study evaluates relationship of distance and outcomes in the absence of reconfiguration.
-
-
Comparator
-
Alternative intervention
-
Earlier time period
-
Baseline
-
Not applicable.
-
-
Type of UEC facility
-
Hospital ED
-
Specialist centre e.g. major trauma centre, specialist stroke unit)
-
Obstetric unit
-
Other Add details in ‘info’ box.
-
-
Distance/time measure
-
Direct distance Distance ‘as the crow flies’
-
Actual travel distance
-
Travel time.
-
-
Type of transport
-
Ambulance/other EMS vehicle
-
Private car
-
Public transport
-
Helicopter Normally excluded.
-
-
Outcomes assessed
-
Mortality
-
Morbidity Add brief details in ‘info’ box
-
Hospital admissions Includes avoided admissions/re-admissions
-
Non-conveyance/treatment at scene
-
Qualitative
-
Other Only if main or important outcome.
-
-
Length/period of study
-
Length of study.
-
-
Logic model factors
-
Influencing factors Factors affecting time
-
Explanatory factors Factors affecting patient (and hence health-care system) outcomes.
-
-
Summary of key results
-
Results.
-
-
Key conclusions
-
Conclusions.
-
-
Limitations
-
Identified limitations Identified by author or obvious before QA.
-
Italic text is a note or instruction about how to complete that part of the data extraction.
Text in this appendix is reproduced from Chambers et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text.
Appendix 3 Risk-of-bias tables
| First author and year of publication | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| Avdic 20165 | Yes | Yes | Unclear | Yes | Yes | Yes: registers covered whole population | Yes | Yes | Yes |
| Combier 20136 | Yes | Unclear | Unclear | No | No | Yes | Yes | Yes | Yes |
| El Sayed 20127 | Yes | Yes | Yes | No | Yes | Not applicable: system rather than patient outcomes | Yes | Yes | Yes |
| Hansen 20118 | Yes | Yes | Yes | No | No | Not applicable: health system outcomes | Yes | Yes | Yes |
| Hsia 20129 | Yes | Yes | Unclear: possible changes over time | Yes | No | Unclear | Yes | Yes | Yes |
| Hsia 201410 | No association between data sets | No: Table 1 appears to show significant differences (p < 0.001) before–after in several patient group characteristics in those having further to travel post closure. Included all trauma patients. While the study did have a sizeable number of exclusions, the participant group was still considerably heterogeneous | No | No: compares pre and post reconfiguration | No | Not applicable: compares different populations at different time points | Yes | Yes | Yes |
| Knowles 20182 | Yes | No: heterogeneous population of those attending EDs | No | Yes: control sites | No | Not applicable | Yes | Yes | Yes |
| Mustonen 201711 | Yes | Yes | Yes | Yes | No | Not applicable: health system outcomes | Yes | Yes | Yes |
| Roberts 20144 | Yes: in case studies | Yes | Yes | No | Yes | Not applicable | Yes | Yes | Not applicable: only descriptive data presented |
| Shen 201212 | No: association using modelling of data sets | Yes: all AMI patients | Unclear: all had AMI so may be similar across comparator communities | No | No | Not applicable | Yes | No: model estimated effects | Yes |
| Shen 201613 (same study as other Shen and Hsia paper12) | No: complex associational data, 30-day, 90-day and 1-year mortality | Yes: all AMI patients so potentially similar | Unclear: potentially as all AMI patients may have been receiving similar care | No | No | Not applicable | Yes | Yes | Yes |
| Yaghoubian 200814 | Yes | Unclear | Yes | No | Yes | Unclear | Yes | Yes | Yes |
| First author and year of publication | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| Acharya 201143 | Yes | Unclear | Yes | No | No | Yes | Yes | Yes | Yes |
| Andersson 201922 | Yes | Unclear | No: received different treatment but treatment was the outcome so not relevant to validity | No | No | Yes | Yes | Yes | Yes |
| Balamurugan 201623 | Yes | Unclear | Yes | No | No | Yes | Yes | Yes | Yes |
| Balamurugan 201824 | Yes | Unclear | Yes | No | No | Yes | Yes | Yes | Yes |
| Berlin 201615 | Yes | Unclear | Unclear | No | Not applicable | Yes | Yes | Yes | Yes |
| Bussières 201825 | Yes | Unclear | Yes | No | No | Yes | Yes | Unclear: authors’ own classification | Yes |
| Di Domenicantonio 201626 | Yes | Unclear | Yes | No | No | Unclear: about 8% not included in travel time analysis | Yes | Yes | Yes |
| Dummer 200416 | Yes | Unclear | No: changes likely during period of the study | No | No | Yes: appears to be, though not explicitly stated (‘all’ births and stillbirths included) | Yes | Yes | Yes |
| Durkin 200530 | Yes | Yes | No | No | Not applicable | Yes | Yes | Yes | Yes |
| Engjom 201737 | No: association between different sets of data | No: heterogeneous population of births | Unclear: heterogenous, but potentially all receiving similar maternity care | No | No | Not applicable | Not applicable | Yes | Yes |
| Featherstone 201638 | No: association between patient records and travel time | Yes: all very low birthweight infants | Unclear: all similar condition so potentially were receiving similar maternity care | No | No | Not applicable | Not applicable | Yes | Yes |
| Gomez 201031 | No: association between two sets of data over time (trends) | No: heterogeneous population – deaths from trauma | Not applicable | No | No | Not applicable | Not applicable | Yes | Yes |
| Gonzalez 200932 | No: association between several sets of data | Unclear: paper does not provide detail of patient characteristics in the two groups, potentially heterogeneous populations | No | No: compares rural and urban area patients | No | Not applicable: single time point | Yes | Yes | Yes |
| Grzybowski 201139 | Yes | Yes | Unclear | No | No | Yes | Yes | Yes | Yes |
| Jarman 201833 | No: associations between different sets of data | No: the study details and analyses participant characteristics and effect on outcomes | No | No | No | Not applicable | Yes | Yes | Yes |
| Langabeer 201527 | Yes | Unclear | Yes | No | No | Unclear | Yes | Unclear: patient reported time of symptom onset | Yes |
| Lee 201834 | Yes | Yes | Yes | No | Not applicable | Not applicable | Yes | Yes | Yes |
| Lerner 200335 | Yes | Yes | Yes | No | Not applicable | Not applicable | Yes | Yes | Yes |
| Leyden 201144 | Yes | Yes | Yes | No | Not applicable | Unclear | Yes | Yes | Yes |
| McCoy 201336 | Yes | Yes: all trauma patients but comparison between blunt and penetrating trauma | Unclear: all trauma patients but comparison between blunt and penetrating trauma | No | Not applicable | Yes | Yes | Yes | Yes |
| Murata 201342 | No: association between two sets of data | No: different conditions | No | No | No | Not applicable | Yes | No: used inpatient data for disease type, so unknown whether used ambulance transport to arrive in hospital | No: association between people in hospital for acute disease and ambulance distance, not known whether were an emergency admission |
| Nicholl 200718 | Yes | Unclear: differences in Rapid Emergency Medicine Score | Unclear: possible changes over time | No | No | Yes | Yes | Yes | Yes |
| Parker 200017 | Yes | Yes | Unclear | No | No | Yes | Yes | Yes | Yes |
| Pilkington 201440 | No: association between two databases | No: heterogeneity in terms of cause of neonatal death | Unclear: similar condition so potentially similar maternity care | No | No | Not applicable | Yes | Yes | Yes |
| Postma 201428 | No: association between distance and ischaemic time | Yes: all STEMI so potentially similar | Unclear: same condition so potentially were receiving similar care | No: compared two types of transportation | No | Not applicable | Yes | Yes | Yes |
| Ravelli 201141 | Yes | Unclear | Unclear | No | No | Yes | Yes | Yes | Yes |
| Rudge 201321 | No: association between attendance data and population demographics | No: study explores how different participant characteristics may affect demand | No: heterogeneous population | No | No | Not applicable | Yes | Yes | Yes |
| Souza 200520 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes |
| Svensson 200329 | No: unclear association between treatment, hospital admission and 30-day and 1-year outcomes | Yes: similar condition STEMI and same treatment | Unclear: same condition so potentially same treatment/care | No | No | Not applicable | Yes | Yes | Yes |
| Wei 200819 | Yes | Unclear | Yes | No | No: post exposure only | Yes | Yes | Yes | Yes |
| First author and year of publication | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 |
|---|---|---|---|---|---|---|---|---|---|
| Koch 201645 | Yes | Yes | Yes | No | Not applicable | Not applicable | Yes | Yes | Yes |
| Langabeer 201646 | Yes | Yes | Yes | No | No | No: 889 vs. 703 | Yes | Unclear | Yes |
Appendix 4 Moderating and mediating factors
| First author and year of publication | Influencing factors | Explanatory factors | Outcomes | Impacts (longer term) |
|---|---|---|---|---|
| Acharya 201143 | Symptom severity (P) | More severe symptoms → fast tracking | Receipt of specialist treatment (thrombolysis); timely arrival at hospital | |
| Andersson 201922 |
Traffic delays Bad weather |
Access to PCI-capable hospital (geographic) (S) | Choice of treatment strategy | |
| Avdic 20165 | Increased pre-hospital mortality | Mortality | ||
| Investment in EMS (S) | Reduced impact of reconfiguration | |||
| Balamuguran 201623 | Travel distance and time above national average (C) |
Socioeconomic factors (C) Co-ordinated health system response (S) |
Mortality | |
| Balamuguran 201824 | Travel time using EMS (S) | PCI capability (S) | Mortality | |
| Berlin 201615 | Use of helicopter transport (S) |
Higher early mortality (stroke) Higher long-term mortality (MI) |
Mortality | |
| Roberts 20144 | Distance from home (trauma) | Distance travelled | ||
| Bussières 201825 |
EMS service model/quality (S) Patient age (P) |
Adverse events | Long-term morbidity/mortality | |
| Combier 20136 | Maternity unit closure? | Perceived link between volume and outcomes (S) |
Maternity unit closure Distance travelled |
|
| Precautionary hospitalisation (S) | Minimal travel time for ‘distant’ patients | Distance travelled | ||
| Di Domenicantonio 201626 |
EMS transport (S) Direct transport to PCI centres (S) |
In-hospital delays (S) | Mortality | |
| Dummer 200416 | Maternity unit closure | Distance travelled | ||
| Durkin 200530 | Use of safety equipment (P); patient age (P) | Mortality | ||
| El-Sayed 20127 | Ban on ambulance diversion (S) | Co-ordination between services (S) | Short-term EMS outcomes | |
| Engjom 201737 | Winter conditions (C) | Unplanned OOH births | Mortality | |
| Featherstone 201638 |
Ethnicity (P) Access to level III hospital (S) |
Travel time | ||
|
Gestational age (P) Admission to ICU |
Neonatal mortality | |||
| Gomez 201031 | Rural vs. urban setting |
Patient age and sex (P) Injury severity (pre-hospital death) |
Trauma mortality | |
| Gonzalez 200932 | On-scene time (longer in rural settings) | Injury severity | Trauma mortality | |
| Grzybowski 201139 |
Mountainous terrain; severe weather (C) Precautionary hospitalisation (S) |
Precautionary hospitalisation? | OOH birth (1–2 hours vs. over 2 hours) | |
| Hansen 20118 | Distance to nearest ED (C) | Access to free ambulance services (S) and own car | Use of alternative health services | |
| Hsia 20129 |
Use of private transport rather than EMS (P) Delay in seeking treatment (stroke) (P) |
Closures affected a minority and alternatives were available nearby (S) Travel time could be short relative to waiting time (S) EDs that closed could be those providing poorer care (S) |
Travel time Mortality |
|
| Hsia 201410 | Trauma centre closure | Socioeconomic status | Inpatient mortality | Up to 2 years after closure |
| Jarman 201833 | Injury severity (mainly mild) |
Type of injury Location of injury (residential vs. non-residential) (C) Type of hospital (S) Age (P) Socioeconomic status (P) |
Trauma mortality | |
| Knowles 20182 |
Increased travel time if using own transport (P) Lack of familiarity with location of ED following reconfiguration (P) |
New services or diversion to more effective services (S) Urgent care centres provide continuity for less severe conditions (S) Use of non-conveyance by ambulance staff (S) |
Mortality Travel times Service use |
2 years before-and-after reconfiguration |
| Koch 201645 | Availability of stroke ambulance (S) | Time to treatment | ||
| Langabeer 201527 |
Patient transfer (S) EMS transport faster (P/S) |
Gender (shorter in men) (P) | Ischaemic time | |
| Langabeer 201646 | Focus on reducing medical contact to treatment time (S) | Organisational/individual relationships |
Ischaemic time Use of PCI |
|
| Lee 201834 |
Type of road Urban vs. rural area |
Crash type; ‘violation’; age; location; lighting conditions; alcohol/drugs (P/C) | Injury severity | Mortality |
| Lerner 200335 | Total OOH time (not correlated with mortality) |
Patient age (P) Clinical status or Injury Severity Score |
Mortality | |
| Leyden 201144 | Distance from stroke unit vs. other hospital |
Contraindications (P) Type of hospital |
Receipt of thrombolysis | |
| McCoy 201336 | Time at scene (S) | Type of injury (blunt vs. penetrating) | Mortality | |
| Murata 201342 | None identified | None identified | ||
| Mustonen 201711 | Access to alternative services |
Service use Mortality |
||
| Nicholl 200718 | Ambulance response times (S/C) | Injury severity | Mortality | |
| Parker 200017 | Closure of some small local units (S) |
Improvements in care Social class Birth order |
Stillbirth | |
| Pilkington 201440 | Location of maternity units | Social deprivation | Mortality (fetal/neonatal) | |
| Postma 201428 | Ambulance triage, direct transport to specialist centre (S) | Total ischaemic time | ||
| Ravelli 201141 | Advance referral if needing specialist care (S) |
Risk status (P) Gestation time Ethnicity |
Neonatal mortality Adverse outcomes |
|
| Rudge 201321 | Distance-social deprivation interaction | ED attendance | ||
| Shen 201212 |
Patient age (P) Death en route to hospital |
Mortality | ||
| Shen 201613 | Availability of technology (does not mitigate closure effects) | |||
| Souza 200520 |
Severity of illness (P) Narrow range of travel times because of nature of area |
Selection bias or confounding may explain false-positive results | ||
| Svensson 200329 | Ambulance response time (S) |
Staff training (S) Treatment begun pre-hospital (S) |
Heart failure symptoms | 1-year mortality |
| Wei 200819 |
Patient delay (P) Ambulance response time (S) |
Place of residence (P) |
Thrombolysis Pre-hospital mortality |
Follow-up mortality |
| Yaghoubian 200814 |
Additional staff (S) Reorganisation of teams (S) Regional trauma system (S) Increased experience and improved treatments over time (S) |
Injury severity Complications Mortality |
List of abbreviations
- AAA
- abdominal aortic aneurysm
- AMI
- acute myocardial infarction
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- DTBT
- door-to-balloon time
- ECG
- electrocardiogram
- ED
- emergency department
- EMS
- emergency medical services
- HR
- hazard ratio
- HSDR
- Health Services and Delivery Research
- IQR
- interquartile range
- MD
- mean difference
- MI
- myocardial infarction
- MIU
- minor injury unit
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PCI
- percutaneous coronary intervention
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-analyses
- STEMI
- ST elevation myocardial infarction
- UEC
- urgent and emergency care