Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/195/02. The contractual start date was in January 2016. The final report began editorial review in January 2019 and was accepted for publication in October 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Vaughan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background and rationale
The rising number of older patients with multiple chronic conditions and/or more complex needs is considered to be one of the most pressing problems facing the NHS. 1 Although these patients receive the most resource-intensive care, their problems are less likely to be accurately diagnosed and they have more adverse outcomes than other age groups. 2–5 The emerging consensus is that current models of hospital care, which are heavily based around specialists delivering disease-specific care, serves these patients poorly, as it is often fragmented and poorly co-ordinated. A revival of medical generalism has been suggested to provide better and more cost-effective care. 6–10
On paper, this appears to be an excellent suggestion. However, it is based on the pervasive assumptions that what is meant by ‘medical generalism’ is clearly understood, that the patients who would benefit most from a revival of medical generalism have been identified and that current service models are uniform, well-delineated and that changing these will result in better outcomes. The reality is that there is a paucity of evidence and clinical consensus on which to base new models of medical generalism. As noted in the Australian ‘2020’ review, the policy discourse is heavily dominated by opinion and commentary. 11 Here, we will review the evidence across each of these aspects of the debate, professional, service model and patient need, beginning with the core driver of the debate, patient need.
Patients and generalism
Patient demography has been changing rapidly over the past two decades. The population is becoming older, with one in six people the UK now aged > 65 years. The latest projections have this figure doubling to around 19 million people by 2050. Within this total, the number of very old people is expected to grow even faster, with the number of those aged > 80 years set to reach 8 million by 2050. This group of the ‘oldest old’ are the biggest consumers of health and social services. 12 Almost 75% of those aged > 65 years have multiple chronic medical conditions,13 whereas 25–50% of those aged > 85 years are thought to have a frailty syndrome as a result of the general decline in their physical and psychological reserves. 14
The rising number of patients with comorbidities or complex disease is not confined to those aged > 65 years. A recent Scottish study15 found that around one-quarter of patients have two or more morbidities and that, although the presence of multimorbidity increases with age, the absolute number of comorbid patients is largest among those aged < 65 years. 15 Other studies have found that there are associations between multimorbidity and increased risk of mortality, disability, poor quality of life and adverse drug events. 16,17 Patients with multiple comorbidities also have substantially higher rates of general practice consultation, experience less continuity of care and are more dissatisfied with the care that they receive. 18
It is then, perhaps, not entirely unexpected that there has been a sharply rising demand for unscheduled medical care, with the number of English hospital admissions increasing by 2 million patients per year over the last 6 years. 19 These patterns of demographic change and the accompanying rise in health-care usage have led to calls for the whole system of medicine to be realigned with the needs of this patient population. 8,20 However, the impact of the changing patterns of age and disease on secondary care is not fully understood. Recent work by the Nuffield Trust, for example, found that there were 60% more hospital admissions than could be accounted for by the ageing population. 21 There is also an increasingly compelling body of evidence that poor outcomes for patients are more directly the result of poor processes of care contained within a model, rather than the model itself. Misdiagnosis is increasingly held at the international level to be the commonest cause of potentially preventable deaths,22–24 with adverse events relating to diagnostic errors being associated with the highest mortality rate. 25 Although National Confidential Enquiry into Patient Outcome and Death (NCEPOD) reports have made clear that errors in processes of care antecede poor outcomes for most patients,26,27 there is a suggestion that the higher rates of morbidity and mortality suffered during hospital admissions by patients with complex disease are a result of their being, as a group, more susceptible to the impacts of below-average care than their less comorbid counterparts. 28 It also worth noting that there have been no high-quality studies relating to the secondary care of multimorbid patients and that a recent systematic review found very little evidence for primary care interventions in this group. 29
To our knowledge, the acceptability of generalist care to patients is yet to explored, a key consideration given that patients value and actively seek specialist care. 30
Professional concepts of generalism
The professional discourse around ‘generalism’ over the last few decades has suffered owing to the lack of a clear definition of what generalism actually is. This has hampered intelligent debate and has contributed to the lack of evidence on the benefits (or otherwise) of generalism and consensus on which to base change. 31 The Australian ‘2020’ review11 of generalism proposed a ‘continuum of generalism’ that used three overlapping dimensions to define a philosophy of practice: ‘ways of being, ways of knowing and ways of doing’. 11 A more recent review by the Royal College of Physicians and Surgeons of Canada31 argued for a clear delineation between the frequently conflated concepts of ‘generalism’ and ‘generalist’. They proposed that ‘generalism’ should be seen as a philosophy within medicine:
Generalism is a philosophy of care that is distinguished by a commitment to the breadth of practice within each discipline and collaboration with the larger health care team in order to respond to patient and community needs.
Royal College of Physicians and Surgeons of Canada31
The term ‘generalist’ should be used to refer to a subset of physicians who possess a unique group of competencies:
Generalists are a specific set of physicians and surgeons with core abilities characterized by a broad-based practice. Generalists diagnose and manage clinical problems that are diverse, undifferentiated, and often complex. Generalists also have an essential role in co-ordinating patient care and advocating for patients.
Royal College of Physicians and Surgeons of Canada31
Discussions of generalism have, almost invariably, been set alongside and reactive to shifts in the nature of ‘specialism’. Since the emergence of modern concepts of physiology and pathology in the late 19th century, there has been a tension between those who provide a broad scope of services to their patients and those who are specialists with a restricted range of expertise, usually focused on a single organ. 32 Although generalism dominated for much of the early 20th century, medical and technical advances have led to an almost continuous increase in the number of and variety of specialties and subspecialties, with 60 specialties now recognised in the UK and 80 specialties and a further 120 subspecialties recognised in the USA. 33 In parallel with these changes, concerns have been expressed about the increasing complexity of clinical services, rising costs and the fragmentation of care for patients. 34
In the mid-1990s, the debate between generalists and specialists became particularly heated. 35–37 The ‘overspecialised’ American physician workforce was seen as a threat to the provision of affordable, equitable and high-quality health care. 38,39 The resulting flurry of research noted that although generalist was often defined solely in terms of being ‘not specialism’,33 generalists had a strong sense of professional identity. 36 They were usually the first point of contact for the patient in their care pathway, were skilled at diagnosing illness and were able to provide comprehensiveness and continuity of care. 40,41 Contrary to the notion of generalists as ‘failed specialists’, they were found to have a better knowledge base, which was maintained for longer, than their specialist counterparts. 42,43 There was evidence of better outcomes for selected patient groups of receiving specialist care, such as the treatment of myocardial infarction by cardiologists,44,45 depression by psychiatrists,46 acquired immunodeficiency syndrome (AIDS) by infectious diseases experts47 and some rheumatic conditions by rheumatologists. 48 However, generalist care was found to match or outperform specialist care in other areas. 49,50 More importantly, variations in quality of care between individual generalists and between individual specialists were often found to be larger than the variations between generalists and specialists as groups. 36
In the USA, policy-makers at the time interpreted the evidence to be in favour of increasing the number of medical graduates entering postgraduate training programmes in general internal medicine (GIM). 38,39 The response to this has been the advent of new forms of generalism. In the USA, ‘hospitalism’ focuses on the delivery of inpatient care that was previously provided by specialists or family physicians, whereas acute internal medicine, developed in the UK, provides the initial assessment and management of patients during the first 72 hours of hospital inpatient stay or in the acute ambulatory setting. 51 Despite the arrival of newer specialties that focus on generalist-type care, this has failed to shift the balance towards generalists in the overall medical workforce, with the eclipse of the traditional general physician who could provide care across the whole patient pathway and across a broad range of settings.
Initially, the gradual fading away of the general physician was not mourned, but there have been increasingly urgent calls for the revival of general medicine in the last 5 years. 6–8,52,53 Almost entirely this has been fuelled by the perceived gap between models of care and the needs of patients, leading to the concept of the generalist being both idealised and reimagined with little or no reference to either current models of care or ‘traditional’ general medicine. 11,54 However, although there is a strong policy and professional consensus about the importance of the generalist and generalism,8 it is the branches of medicine that are more generalist, such as acute internal medicine and geriatrics, that are experiencing some of the greatest difficulties recruiting staff. 55 These are also specialties that tend to contribute the most to the acute medical take. 56
Attempts to fill the space that was once occupied by general medicine has led to suggestions that acute physicians should extend their scope of practice beyond the first 72 hours of care,57 whereas the British Society of Geriatrics has suggested that all geriatricians should consider themselves as generalist physicians, rather than confining themselves to caring for patients with diseases relating to ageing and degeneration. 58
Service models and generalism
Until the early 1990s, the bulk of secondary care in the UK was delivered by general physicians. Unscheduled medical patients were admitted by the medical team on the day and remained under the care of the admitting general physician on a general medical ward until their discharge or referral to a specialist service; follow-up care was also frequently the responsibility of the admitting general medical team. 59,60
Alongside the evidence that certain patient groups fare better when cared for by specialists rather than generalists, a large number of observational studies reported that poor outcomes, particularly mortality, reduced as patient number increased. 61–66 These findings added weight to the NHS policy drive that was to reconfigure services in hospitals and centralise them across regions, shifting patients from generalist to specialist services and closing or merging smaller hospitals. 67 The underlying evidence and the assumptions around these drives towards centralisation are now being questioned. There is a recognition that much of the research that examines the relationships between health outcomes and numbers did not take sufficient account of the effects of differences in patient case mix or the additional resources that are often attached to specialist services. 36,68–70 Furthermore, mergers of hospitals have failed to produce gains in efficiency or save costs. 71,72
By the early 2000s, it was becoming clear that these changes were having an impact on the ‘front door’ of hospitals and the assessment of the acutely sick medical patient. The loss of the general medical beds meant that patients were being boarded for long periods in emergency departments (EDs)73 or being admitted directly to inappropriate beds in other parts of the hospital. 74 This, coupled with the erosion of the traditional medical ‘on take’ system,59,60 led to the development of acute medical units (AMUs) in Scotland. These units are designed to improve patient safety by cohorting newly admitted patients in a highly resourced, purpose-built space. 75 Although the initial studies demonstrated that there was a benefit to this,76 AMUs did not become widespread until the 4-hour waiting time ED target was introduced in 2004. It is now estimated that > 95% of acute hospitals in the UK have an AMU.
These twin drivers, the increasing specialisation of the medical workforce and the introduction of AMUs, have transformed the landscape of medical secondary care. Many factors have needed to be aligned with the new models of care,77,78 including:
-
consultant working patterns
-
undergraduate medical education
-
junior and middle-grade postgraduate training
-
the configuration and staffing of hospital wards
-
patient pathways
-
patterns of referral and investigation.
To our knowledge, there has been no wholescale evaluation of the impact of AMUs. The systematic review76 of AMUs in 2009 found that although studies on the introduction of AMUs all reported that there were positive improvements in patient and/or hospital-related outcomes, only nine studies from six hospitals were found. 76 Although guidelines do exist for the structure of and the processes contained in an AMU,79 several smaller studies have found that these are not uniformly adhered to and that the variability between AMUs may account for the differences in outcomes for patients and hospitals alike. 80,81 Concerns have been raised that although AMUs do benefit some patients, they disadvantage those patients with more complex needs by increasing the fragmentation of care, with nearly 30% of physicians considering that care in their own institutions lacks continuity. 82
There is also a perception that management of the ‘acute take’ has become more onerous since the introduction of the AMU as a result in the loss of traditional ‘on take’ teams, driving further flight from generalist work. 83 The proportion of all consultant physicians who committed to the acute medical take fell from > 40% in 2012 to 33% in 2017/18, with the participation of consultants from the four largest specialties (geriatric medicine, respiratory medicine, endocrinology and diabetes mellitus, gastroenterology and hepatology) dropping from > 80% to < 60% over the same period. 84 To the knowledge of the research team, there is only one hospital in England that continues to operate a traditional ‘consultant of the take’ model of general medicine.
Despite their rapid spread, AMUs are not ubiquitous in the NHS. Around 5% of hospitals appear to have systems where patients are seen in the ED by acute physicians who act in a generalist-type role, before being triaged to specialty teams without a stay on an AMU. Explorations of unscheduled emergency care suggest that most hospitals operate some type of hybrid model, deploying medical staff across the ED and the AMU,85 although this has never been systematically investigated.
The increasing use of dedicated ambulatory care and frailty services to provide locations to assess the acutely sick medical patient, something that was encouraged by national policy guidance,86 also has significant consequences for the generalist medical workforce in hospitals. In common with the AMU, there are a wide variety of approaches in providing and staffing these services and little formal evaluation. 87 However, in most hospitals the medical leadership for these services comes from doctors who have more generalist skills, while the medical wards are generally led by specialists. 87
Why smaller hospitals?
From this overview of the literature, it is clear that there are a number of gaps in the evidence that need to be addressed. There is a lack of clarity around the meaning of ‘generalism’ in medicine, which has consequences for the professional identity and the role of the ‘general physician’. There is a paucity of information about the current models of care in England and the balance of care offered by generalists and specialists. Furthermore, there has not been an assessment of the impact of the wholescale changes driven by the increase in specialist care and the advent of a variety of services dedicated to the assessment of the acutely unwell patient. There has also been little exploration of what the case mix of patients presenting acutely to hospitals actually is and what the needs of patients actually are.
It is the intention of this study to begin to fill-in these gaps in the evidence base and in particular concentrate on generalist care in smaller hospitals. The rationale for the focus on smaller hospitals is that:
-
A recent study88 suggests that the tensions in the wider health-care service around generalist care versus specialist care are concentrated in smaller hospitals.
-
As a group, smaller hospitals provide care for nearly half of all medical patients. 88
-
The patient populations are older, more vulnerable and have more complex needs in smaller hospitals and, hence, could be considered to require more ‘general medical’ than specialist-type care. 88
-
The trends towards subspecialty care have affected smaller hospitals significantly. With the shift of services to larger sites, smaller hospitals are often left struggling to balance inpatient services and the need to hit targets for outpatient specialist clinics and procedures. 89,90
-
Smaller hospitals are financially constrained and understaffed, with mismatches between service capacity and workload and difficulties in innovating services. 91
In short, smaller hospitals are an ideal microcosm in which to investigate what the needs of patients are, how well these needs are being met by different models of medical generalism and what medical generalism means to medical and other staff.
Chapter 2 Overview of methods
Design
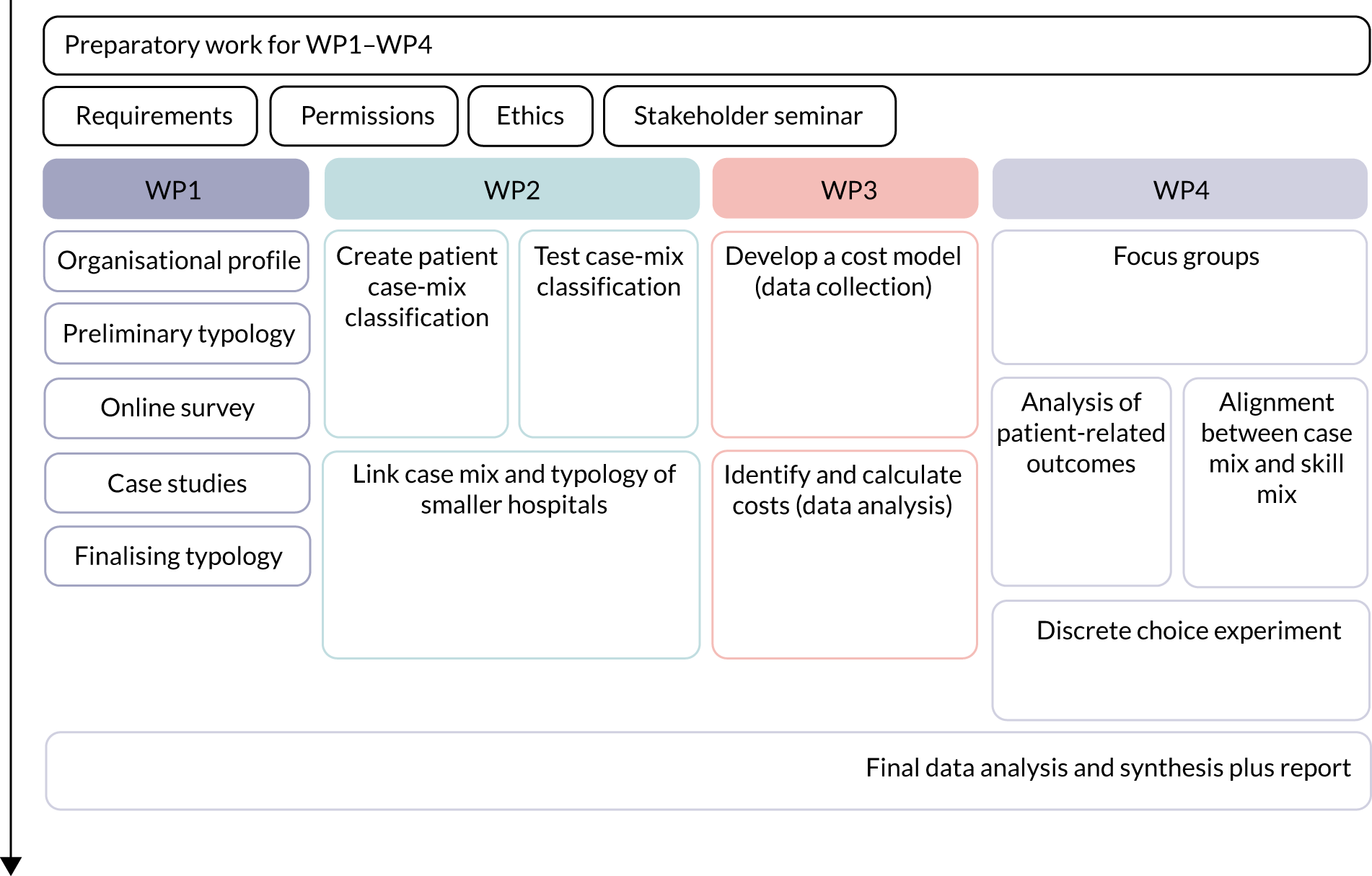
This study used a mixed-methods approach with five work packages (WPs) executed over four phases. The first WP used a variety of methods to map and characterise the models of medical generalism used in smaller English hospitals with a view to create a typology. The second WP used qualitative techniques to create a case-mix classification that identified patients who might benefit from generalist care and used this classification to describe and compare workload, resource utilisation and outcomes between hospitals and models of care. An assessment of the degree of alignment between the patient case mix and the medical generalist skill mix in smaller hospitals was also performed. The third WP explored the economic costs of the different models of generalist care. The fourth WP assessed the strengths and weaknesses of the different models of care using qualitative and semiquantitative approaches from patient, professional and service perspectives. The final WP, which ran across all four phases of the study, drew the results together into an overarching analysis and synthesis. The overall approach to the study allowed for both induction (data-driven generalisation) and deduction (theory-driven exploration of hypotheses), with each stage of the study able to inform the next. The aims and the methods of each WP are outlined in Table 1 and the design of the study is represented in Figure 1.
| Work package | Aims/research question | Methods/data source |
|---|---|---|
| WP1: describing models of medical generalism in smaller hospitals |
|
|
| WP2: understanding the case mix of generalist medical care in smaller hospitals |
|
|
| WP3: investigating the economic costs |
|
|
| WP4: understanding the strengths and weaknesses of current models of medical generalism |
|
|
| WP5: analysis and synthesis |
|
FIGURE 1.
Scheme of the study design.
Study design
Integration between the qualitative and quantitative components of the study was built into the design, which allowed us to robustly test and explore several underpinning hypotheses:
-
that the models of care deployed by hospitals would be shaped equally by theoretical considerations about medical generalism and the resources available to them, making size an important determinant of the model
-
that performance of the models of care would be dependent, at least partially, on an alignment between the hospital’s case mix and the available skill mix
-
that medical generalism provides a solution to the problem of rising numbers of patients with complex and/or multimorbid disease
-
that different models of care would carry cost implications.
Where these hypotheses were not upheld, the design allowed us to explore other potential explanatory factors and generate alternative theories.
Definition of smaller hospital
NHS Improvement (formerly Monitor) previously defined ‘smaller hospitals’ in England as providers with an operating revenue (income) of < £300M in the 2012/13 financial year. 88 This definition was adopted and updated to apply to the 2015/16 financial year.
Conceptual framework
Models of care in hospitals in England are not currently mapped with any level of detail. The literature suggests that medical generalist care has been driven by three main paradigms:92
-
general medical care as the default for all medical patients, unless/until a patient is referred to a specialist service
-
general medical care provided in response to patient needs
-
general medicine providing the ‘work left undone’ by specialists.
However, maps of pathways of emergency care suggest that the organisation of the care of acutely unwell patients tends to be parsed around the pragmatics of deploying available medical, nursing and other staff either on the AMU (where present) or on the downstream medical wards. Subsequently, systems of triage often reflect attempts to manage workload, rather than theoretical considerations. 93 This study attempted to bridge this gap between the theoretical aspects and the pragmatic aspects of general medical care.
Our theoretical framework of medical generalism was built on the Australian ‘2020’ conceptual model of generalism. 11 The resulting conceptual model views ‘ways of being’ (ontological frame), ‘ways of knowing’ (epistemological frame) and ‘ways of doing’ (practical frame) as a continuum that captures the attributes of ‘generalism’. 11 This sits with Abbott’s work,94 which considers that professional ways of working are ‘ecologically driven’ and situated in the context of actors, tasks, locations and the relationships between these. We, therefore, considered that hospital generalists and their ways of working are therefore not only ideologically or theoretically driven but also ‘ecologically’ determined by the locations in which they work, the tasks they are required to perform and the relationships between these and the professional identity and attributes of physicians. Our theoretical framework, therefore, addressed medical generalism in hospitals through three different perspectives:
-
the patient’ perspective – the needs of the patient and the tasks required to meet these
-
the ‘professional’ perspective – in particular, the knowledge and skills of the professional
-
the ‘service’ perspective – the context of the hospital in which they work, including their deployment, the configuration of beds and the allocation of resources.
This framework informed theoretical explorations of the essential dimensions of generalism in the English hospital context. We sought also to define and understand the duties and responsibilities of the general physician, the boundaries between generalist and specialist care and what is considered to constitute the ‘general medical patient’. These explorations were used to inform the body of the study, before being refined as part of the final study analysis.
Patient and public involvement
We were strongly committed through this project to active and meaningful patient and public involvement (PPI) and have been assisted throughout by the Engagement Team of the North-West London Collaboration for Leadership in Health Research and Care (CLAHRC) and the patient involvement unit of the Royal College of Physicians (RCP). The original proposal was developed in conjunction with two experienced patient representatives. The Study Steering Committee was led by a lay chairperson, with second PPI representative offering further input. A group of seven PPI representatives were recruited and then trained, using a co-design approach, to join the research team on the case study visits, review the coding of the patient focus groups and provide comment on findings. For this reason, the study has been heavily influenced by the patient voice in its shaping, the collection of qualitative data and the interpretation of overall findings.
Research ethics and other approvals
The case study visits were given a favourable opinion by the Yorkshire and The Humber – Leeds East Research Ethics Committee on 17 August 2016 (16/YH/0361) and final approval was granted by the Health Research Authority on 9 October 2016 (IRAS Project ID 191393).
A data-sharing agreement between NHS Digital and the Nuffield Trust for the purposes of this study was made on 9 March 2017 (NHS Digital reference DARS-NIC-384572-J7P6Y-v6.5).
Ethics approval for the discrete choice experiment (DCE) was granted by the joint chairperson of the University College London Research Ethics Committee on 8 May 2018 (Project ID 13187/001).
Changes to the protocol
The following changes to the original protocol were made:
-
In WP1, information on models of care was to be collected using two separate methods: telephone interview and online survey. The experience that was gained since the original proposal suggested that gathering information on models of care using online tools is problematic, so instead the decision was made to use telephone interviews for all sites. Interviews were conducted in three rounds.
-
In WP1, case study site selection was to occur at two time points: (1) after the telephone interviews and (2) after the online survey. Instead, case study selection occurred after each round of telephone interviews.
-
The case study interviews and the staff focus groups were to be analysed independently, in WP2 and WP4, respectively. However, as both methods collected information relevant to each of the WPs, it was decided to abandon this distinction and analyse all of the qualitative material in both WPs.
The following minor deviations from the protocol were made:
-
A single framework was intended to be used for the analysis of the case studies for WP1. Instead, the complexity of the material meant that the use of multiple separate frameworks was more pragmatic and allowed for better comparisons.
-
Testing of the typology was to be carried out using an expert consensus group convened for that sole purpose. We instead used a range of existing groups, including the New Cavendish Group, the steering group and the panel used to test the case-mix classification. This meant that the typology was tested on a wider group of clinicians and managers on more occasions, over a longer time period, ensuring its robustness.
-
The Day of Care Survey (DCS) was included as an additional means by which the efficiency of models of care could be measured. However, we found that all hospitals were suffering from high numbers of delayed transfers of care (DToCs), meaning that inappropriate care was more often the result of shortfalls in local social provision rather than being related to the model of care. As a result, we did not use the results of the DCS as initially intended.
-
The descriptive analysis of workforce was to include specialist procedural and outpatient work. As this work varied markedly at the level of individual consultants, it was not possible to obtain sufficiently accurate information to include in the analysis.
-
The aims of WP2 have been altered to more accurately represent the work carried out. Notably, the assessment of the alignment between case mix and skill mix originally formed part of WP4. It was felt that this sat more naturally with WP2 and has been reported as such.
-
In WP3 we had planned to run a hospital-level cost analysis exploring the relationship between total staffing costs and hospital characteristics. We were unable to obtain data on total staffing costs. Rather than using total operating revenue as the dependent variable, which is an imperfect measure, we elected to forgo this analysis.
-
In WP3 we were unable to compare characteristics of smaller hospitals in our survey to all small hospitals (as we did not have analogous data for the latter) and consequently we were unable to investigate systematic differences between responders and non-responders and adjust for any differences using selection bias methods.
-
In WP4, a Delphi-style assessment of the alignment of case mix versus skill mix was to be performed. However, as there was no evidence of any relationship between hospital case mix and case mix, it was decided that this analysis would not provide any further useful information.
-
In WP4, responses to the DCE were to be analysed by subgroups. There were insufficient responses from managers for this to be meaningful but we did undertake analyses for the other two subgroups (hospital doctors, patients and public).
-
In WP4, the patient volunteer group was to assist with the coding of the patient focus groups. This was collectively thought to be too time-consuming by the volunteers, so they were asked to comment on the final analysis of the coding. One volunteer provided feedback.
-
The patient volunteer group was to provide comments on the final draft report. Time constraints did not permit this, although the Plain English summary was circulated to the lay members of the Study Steering Committee.
-
An open space was organised to obtain further PPI input into the study; this was cancelled owing to a lack of expressed interest despite heavy advertising.
Chapter 3 Concepts of medical generalism
Objectives
In this chapter, we describe our initial explorations of medical generalism. We conducted a literature review and held two stakeholder workshops to clarify the understanding of medical generalism and how this is currently enacted in the English NHS. As this took place outside the WPs and acted as necessary context for the rest of the study, we describe the methods and findings separately here.
Methods and analysis
Overview of methods
We conducted a systematised literature review with the aim of providing context for our discussion around the patient, public and professional views of medical generalism in the acute setting (see Appendix 1 and Report Supplementary Material 1). We were particularly interested any definitions or paradigms of medical generalism underpinning current models of care in the UK.
Two stakeholder workshops were undertaken to explore how theories of medical generalism influence models of care.
Initial development of theoretical models of acute care
The literature review failed to find any consistent or shared definitions of generalism or what constitutes a generalist, with a profound separation between any theoretical models of medical generalism and how these are enacted within clinical practice. It was hoped that with the construction of this study this divide would be crossed, by devising a classification scheme for typology that was primarily based on the realities of day-to-day service delivery but informed by an understanding of how theories of medical generalism shape the ways of working and influence decision-making about patient care.
To explore how the theories of medical generalism might influence models of care, we convened two typology workshops (10 June 2016 and 14 November 2016). The first workshop was designed to explore with both medical generalists and medical specialists the boundaries between disciplines, the approaches to triage and how one judges how ‘generalist’ a medical service actually is. The second workshop was designed to explore the contexts in which models of care operate and which aspects of the wider system are driving them. As the aims of the two meetings were different, participants in the first group consisted of generalist physicians, as well as representatives from subspecialty societies (such as rheumatology and neurology); participants in the second workshop were selected for their ability to provide insights into the workings of either smaller hospitals and/or insight into service configuration at a national level.
At each workshop, group discussions were facilitated by Louella Vaughan, Candace Imison and Anne Marie Rafferty. Whole-group discussions were recorded and transcribed verbatim. Additional notes were taken by team members to capture smaller group discussions. Data were discussed by the team on consecutive occasions, with attention paid to emerging themes and points of divergence. All quotes extracted have been fully anonymised.
Workshop 1
At workshop 1, the participants were asked to engage in a series of group exercises. For each, background information was provided and participants were asked to discuss a series of questions. The topics of interest were:
-
Potential dimensions of investigation for use in the construction of the typology.
-
Useful definitions of medical generalism.
-
Capturing models of service.
-
The rules for triage – what does a ‘general medical patient’ look like?
-
What does a ‘good’ medical service look like?
-
To what extent can whole pathways of care be characterised as ‘generalist’ or ‘specialist’?
Workshop 2
At the second workshop participants were asked to engage in a series of linked group exercises, which were based around the drawing of ‘Rich pictures’. Rich pictures are a tool developed by Checkland95 as part of soft systems methodology to capture the complexity, nuance and multiple perspectives that often characterise complex human systems. 95 Groups were first asked to draw a picture of the operations and processes that characterise the emergency/acute medicine pathway. They were then asked to consider what the key drivers of the pathway at the hospital and the external landscape-level (such as staffing, finances and policy directives) were and to indicate where and how these influence the pathways. For the final round, participants were asked to consider what underlies positive and negative experiences of the system from the perspectives of staff and patients.
Findings
Theoretical models of medical generalism
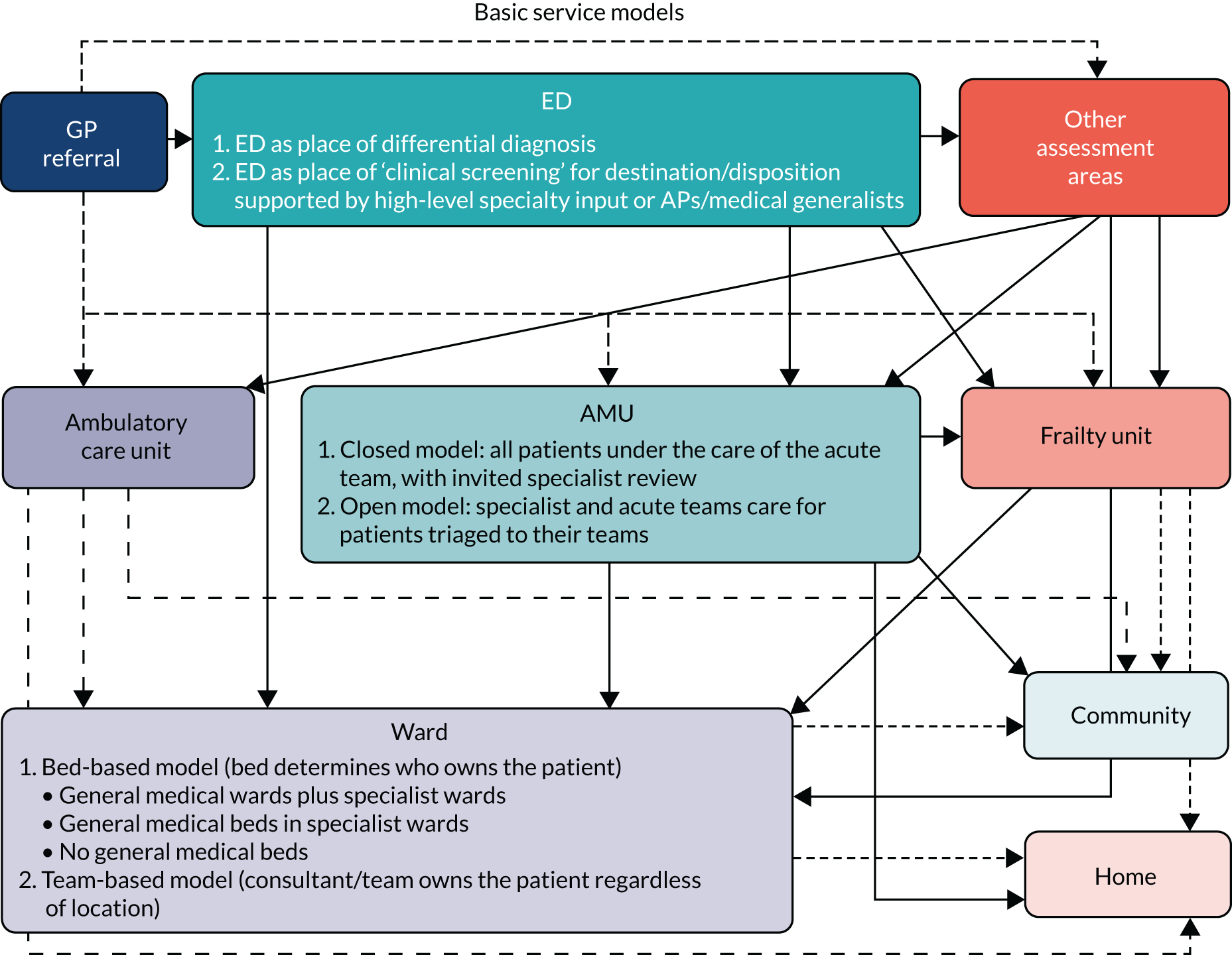
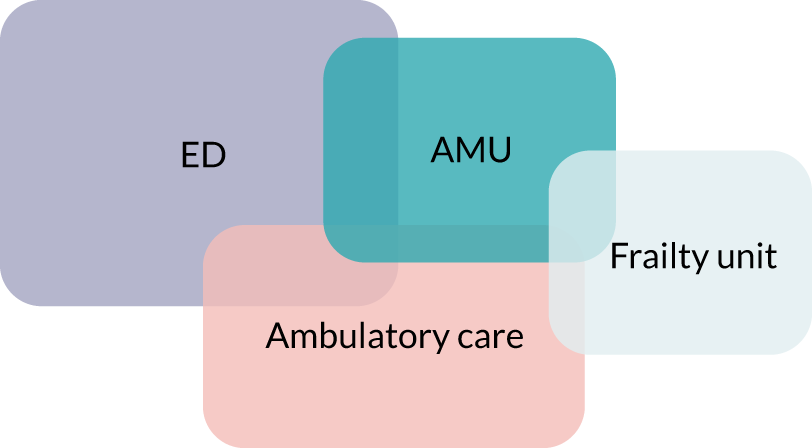
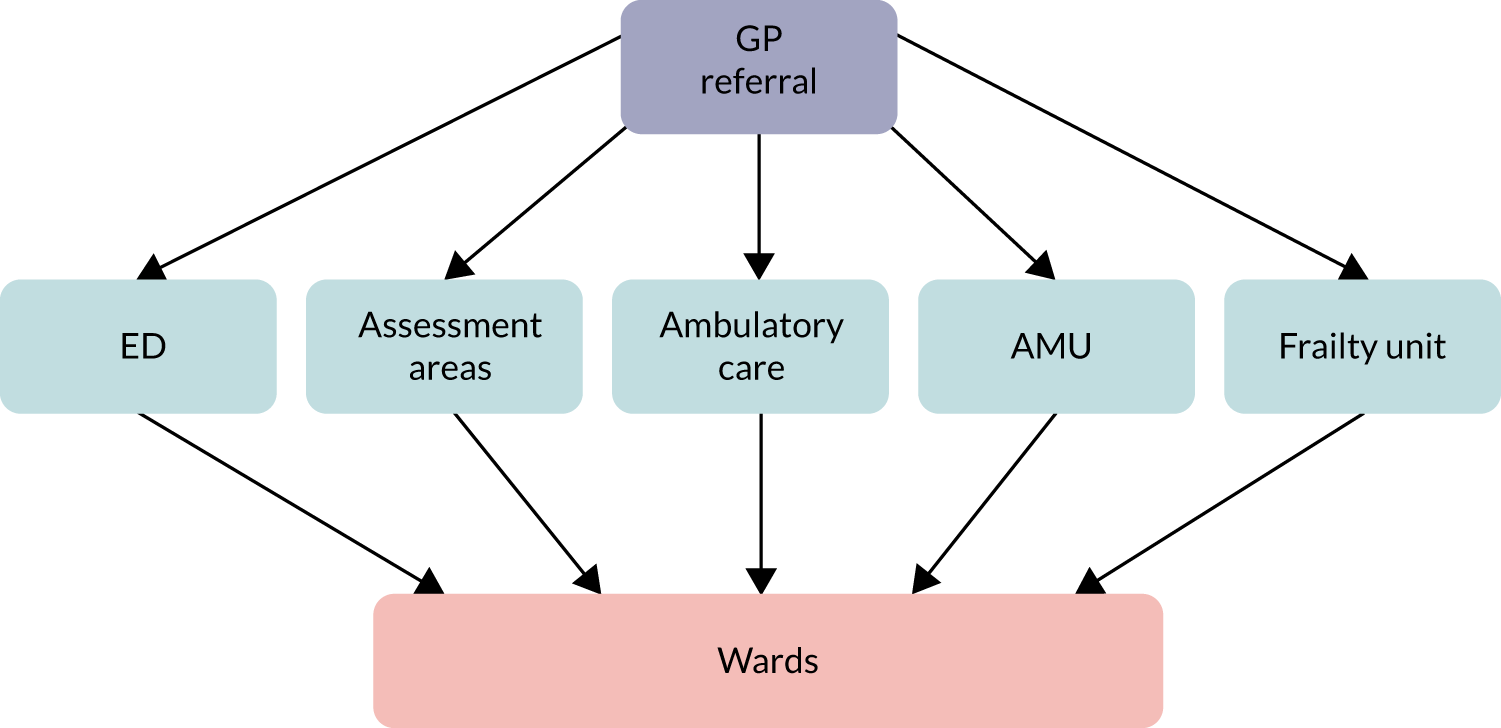
The first workshop was useful in honing the theoretical construction of the emergency and acute medicine pathway. The team had initially assumed that patients would pass in a relatively uniform way between the ED, the AMU and the downstream medical wards (Figure 2). Intelligence from the participants suggested that models have become substantially more complex over the past 2–3 years, with the spread of services such as ambulatory/emergency care and frailty services, which has led to revision of the model (Figure 3).
FIGURE 2.
Assumed basic service model for the delivery of emergency/acute care.
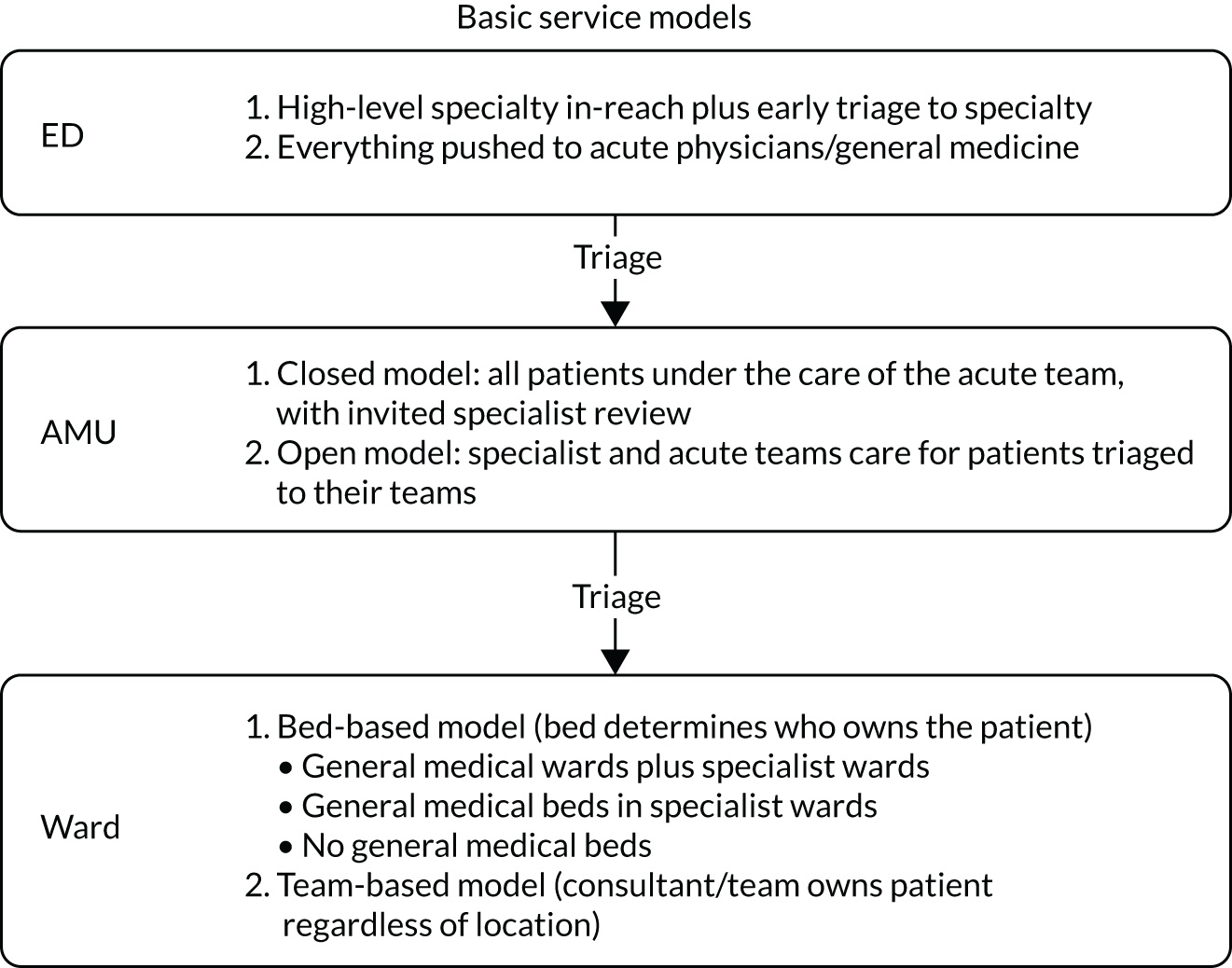
FIGURE 3.
Revised service model (v3.0) for the delivery of emergency/acute care. AP, acute physicians; GP, general practice.
There was no consensus among participants, however, on how to characterise either the system components or the whole system as specialist or generalist.
The views expressed in the workshop confirmed that, rather than attempting to explore both service issues and professional issues in the telephone interviews, these should concentrate on capturing systems and processes of care, whereas the case studies should explore in more depth the issues that relate to professional identity and hospital culture.
Professional aspects of medical generalism
The first workshop also focused on professional aspects of medical generalism: who are the general physicians and what are their attributes? The following key themes emerged from the discussion.
Complex definitions
There was general agreement with the primary underlying assumption of the study: that more ‘generalists’ are required to meet the needs of the growing numbers of multimorbid patients. However, participants agreed that there was no universal definition of general medicine, that it was unclear which doctors deliver generalist care and that it was unclear what might actually constitute generalist care. Indeed, it was argued that attempting to nail down definitions may be counter-productive for the purposes of the study. The boundaries between specialist and generalist practice emerged as permeable and partially located at the level of the individual doctor, rather than being neatly and consistently drawn at system level:
General physicians have the use the expertise they have from where they recognise that they can manage the problem and when they recognise they can’t manage the problem they find someone who can.
Workshop participant
A complex mosaic of overlapping factors that might constitute the general physician as a professional emerged and are shown in Figure 4.
FIGURE 4.
The general physician as a professional: identified factors.
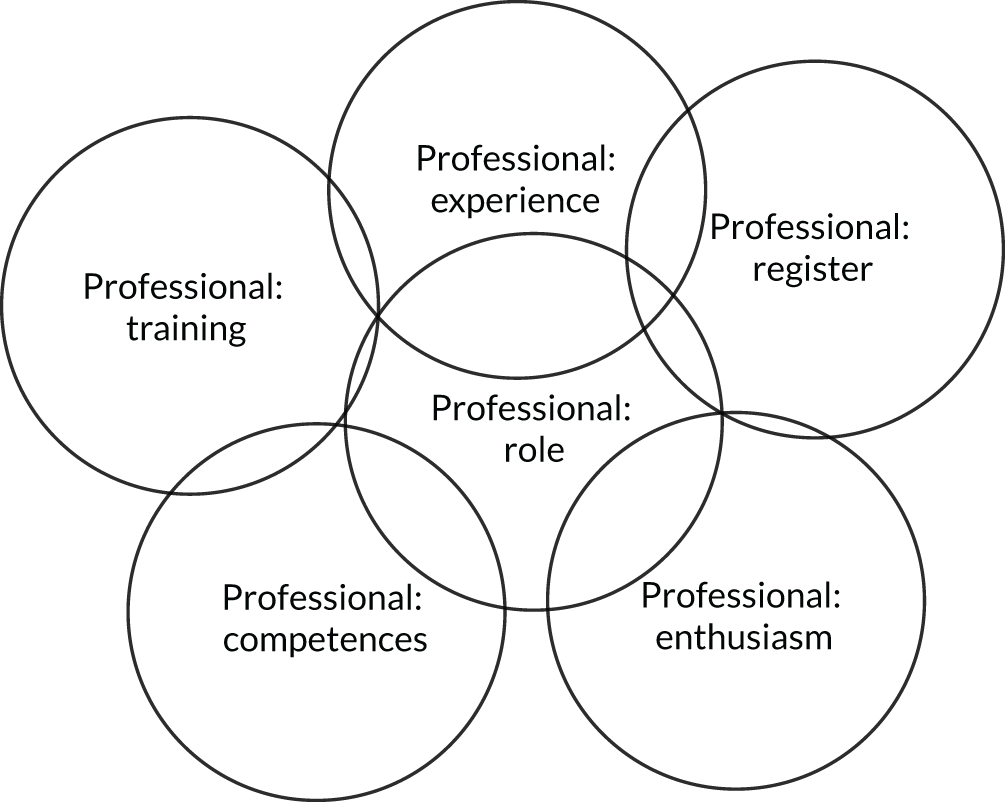
Skills versus role versus identity
Participants drew distinctions between the skills required to be an effective general physician, the role of the general physician in providing care and the extent to which a consultant identified as being a general physician.
The skills and competencies that were required were considered to be a function of training, which were sanctioned by general medical council certification, as well as maintenance over time:
You may have had the ticket for general medicine . . . but what is at issue is people’s skills atrophy.
Workshop participant
The role of the general physician was considered to be determined largely by service needs, particularly the acute medical take and the provision of downstream care to ‘general medical patients’:
Modern general medicine largely is . . . the first 2 or 3 days for young and non-frail people or in the deeper wards it is generally older people with complex needs.
Workshop participant
The distinctions between skills and role were repeatedly emphasised, given that the role of the general physician was heavily context driven and was dependent on factors such as type of organisation (teaching vs. non-teaching), location in the hospital (AMU vs. ward) and the case mix:
So what people’s training is and what their skillset is, is one thing, but what their actual role is, is another.
Workshop participant
We have been talking a lot about roles and training which actually defines a general physician whereas general medicine is what you actually practice, it’s the medicine that you actually do.
Workshop participant
Moreover, the skills of general medicine were not seen to be professionally contained. Although many specialists might no longer explicitly act as general physicians, that is they no longer contribute to the medical take or look after general medical inpatients, they were still capable of providing generalist care to their specialist patients:
If you are a neurologist who has a patient who comes in with hypertension . . . [that makes you someone] who is practising general medicine even if you are not a general physician.
Workshop participant
The split between skills and role was also seen to be a by-product of the nature of training as a physician in the UK. With standalone GIM training being almost completely replaced by dual accreditation in both a specialty and GIM over the past two decades, virtually all younger physicians have specialist skills and generalist skills and competencies and are capable of adopting more than one clinical role. This duality of medical training alongside the gradual disappearance of consultant physicians without a specialty was also considered to play a major role in the fact that although many doctors practised general medicine, they no longer primarily identified themselves as general physicians:
There aren’t many doctors left who would call themselves [general physicians] . . . they might say ‘I’m a consultant in geriatrics and general medicine or chest and general medicine’. But there aren’t many doctors left who call themselves a general physician when they are describing what they do.
Workshop participant
The degree to which consultants self-identified as a generalist or a specialist emerged partially as a function of the degrees to which professional and personal satisfaction were derived from the different roles. Notably, satisfaction with meeting the needs of patients and a diagnostic challenge were associated with general medicine, whereas prestige and advancement were attached to specialist medicine:
We get a different buzz out of [general medicine] . . . It’s the job satisfaction that you get from doing general medicine.
Workshop participant
Your specialty consumes you. Your ability to distinguish yourself, become famous and all that sort of stuff depends largely on how you perform in your specialty.
Workshop participant
The profound aversion that some specialists feel towards practice as a general physician, particularly in the context of the acute take, was also commented on:
Some people are doing [the acute take] . . . [it] is their idea of hell so they are not going to do it well if they are not committed to it.
Workshop participant
The cases of acute medicine and geriatrics
Participants touched on the issues of whether or not the specialties of acute medicine and geriatrics were fully generalist in nature. This was considered of relevance given that neither discipline routinely provides care across the whole patient pathway, with acute medicine focusing on the first 3 days of inpatient care and geriatrics focussing on the wards. Although it was agreed that both specialties provide generalist care, the group was split on whether or not either specialty could be considered to be a branch of general medicine. The nature of the debate highlighted that ‘true’ general physicians were capable of meeting the broadest spectrum of patient needs, regardless of their location of practice or their point in the patient journey:
In our hospital, [geriatrics] is aged-based and therefore by definition actually our care services are offering general medicine to those over the age of 75 is a specialist service.
Workshop participant
Conclusions
These findings suggested that the study team should refrain from imposing hard definitions of what constituted generalist practice for the purposes of the study. Instead, attempts should be made to explore further the boundaries between generalism and specialism and the contexts of practice.
Contexts of models of care
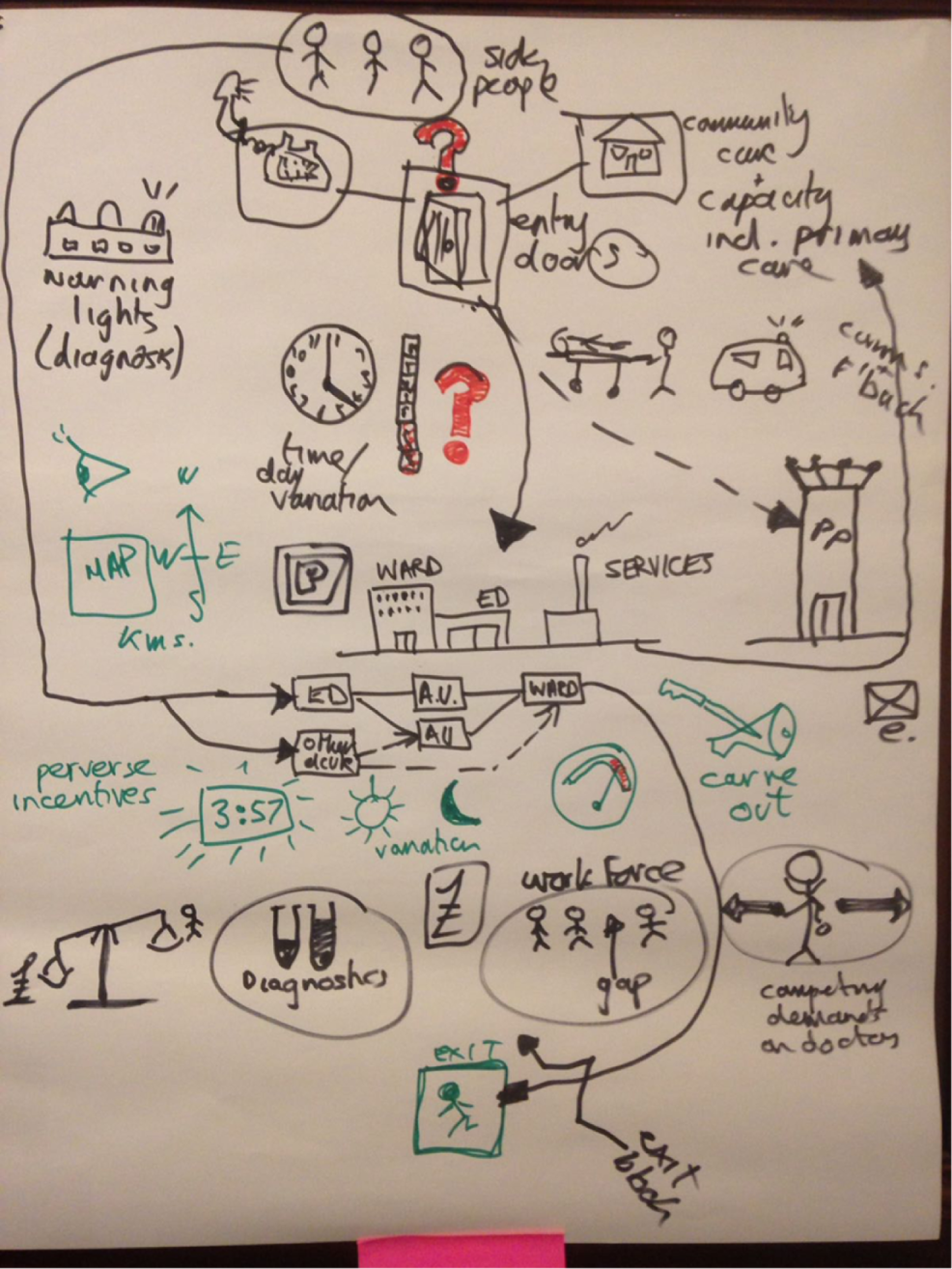
The second workshop explored the extent to which the emergency and acute medicine pathway is shaped by factors at multiple levels. Examples of the resulting rich pictures are given in Figures 5 and 6.
FIGURE 5.
Rich picture produced for workshop 2, example 1.
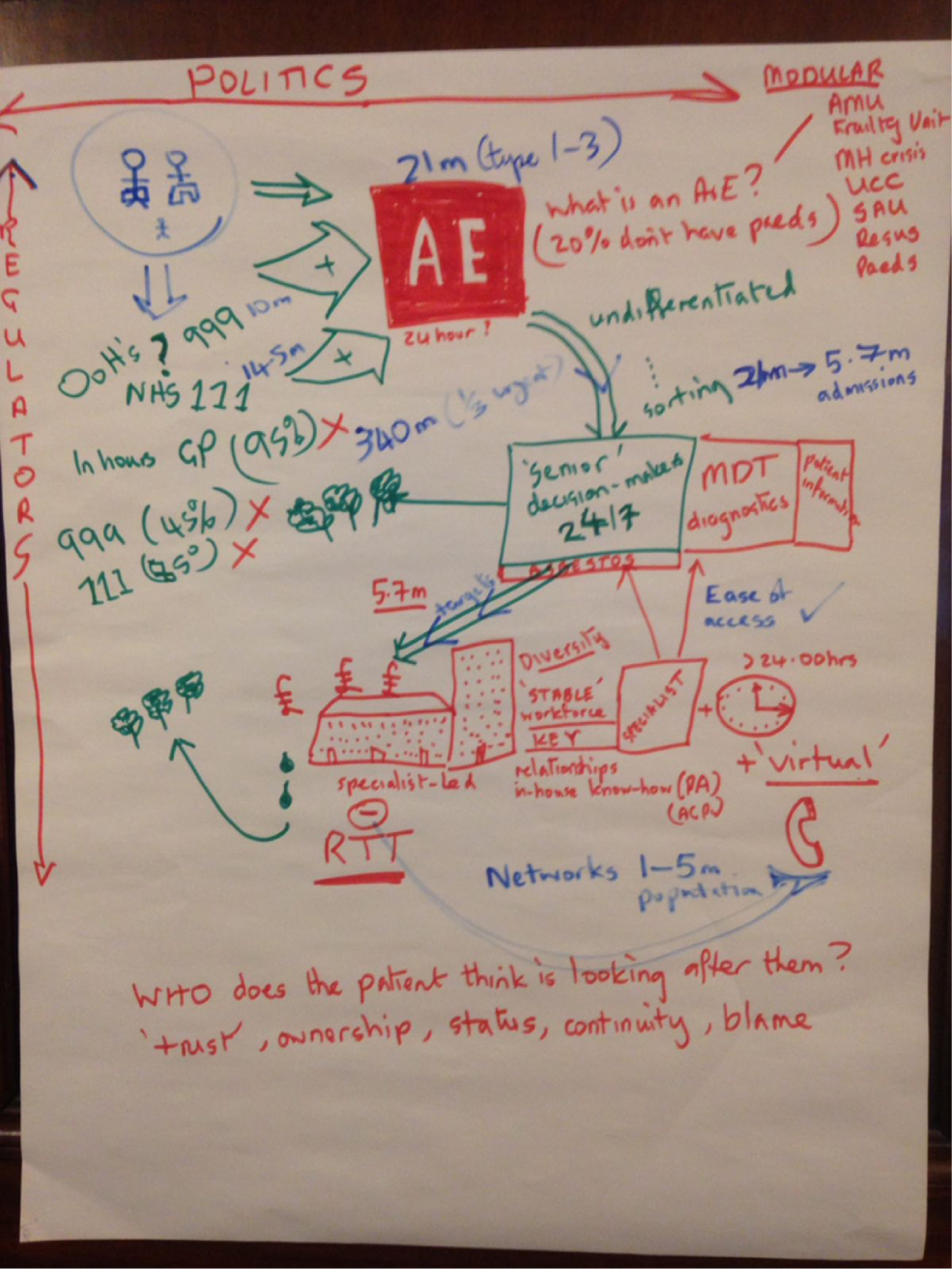
FIGURE 6.
Rich picture produced for workshop 2, example 2.
Factors at the hospital level
The factors at the hospital level that were thought to have a major influence on the shape of models of care included the:
-
capacity of the hospital, as well as individual services (such as the ED)
-
size and skills of the hospital workforce
-
access to diagnostics, in terms of both hardware and staffing
-
access to allied health-care services
-
financial position of the hospital
-
provision of ‘turnaround’ services at the front door
-
level of consultant cover, especially at weekends
-
‘carve out’ versus streaming allocations at the front door (siloed working vs. allocation of patients to appropriate flows)
-
slickness of transfers between clinical areas
-
organisational culture
-
relationships between clinicians, especially between specialists and generalists.
Factors at the regional level
The factors at regional level that were thought to have a major influence on the shape of models of care included the:
-
geography, especially the time to the next ED
-
number, capacity and quality of local general practice (GP) services
-
ease of access to and the quality of out-of-hours services
-
capacity and quality of local ambulance services, especially paramedical teams with the ability to treat onsite rather than transfer
-
presence and use of networked services
-
social care provision
-
integration with community services
-
relationships with relevant Clinical Commissioning Group (CCGs) and local authorities.
Factors at the national/policy level
The national policy and regulatory frameworks were thought be critical in informing almost every aspect of care in smaller organisations. Key policies and factors included:
-
the 4-hour target
-
24/7 consultant working
-
the review and recommendations of the Care Quality Commission (CQC)
-
Health Education England’s attitudes towards training in smaller organisations
-
directives from NHS England (NHSE) and NHS Improvement (NHSI) on acute service provision.
Other factors
The question of ‘who owns the patient’ and the associated issues around trust, ownership, status, continuity and blame were seen as important drivers of clinician and system behaviour.
Conclusions
These findings pointed to models of care shaped by numerous factors at multiple levels, with interactions between each level. At one end, individual hospitals were located in a complex regulatory and policy environment, which influenced almost every aspect of service provision. At the other end, the cultural, organisational and behavioural factors moulded services in hospitals. This suggests that models of care cannot be considered as independent of the contexts in which they sit and that the study would need to take account of these factors in the conduct of the research.
Chapter 4 Describing models of medical generalism in smaller hospitals
Objectives
In this chapter, we describe the models of medical generalism used in smaller hospitals and recount the creation of a typology of the different models of care. We then explore the models of generalism through case studies and other methods, with a focus on the medical workforce, their roles, skill mix and the boundaries between specialist care and generalist care.
Methods
Overview of methods
We outline here the methods used; a fuller description is contained in Appendix 2.
This study aimed to explore medical generalism through the perspectives of the patient, the professional and the service. WP1 was designed primarily to define and explore the service perspective, as well as elements of the professional perspective, namely how doctors define and experience medical generalist work.
We used a multistep approach to investigate models of care in smaller hospitals and understand how and why these models of care are deployed. This was carried out by:
-
identifying and creating organisational profiles of all smaller trusts in England (n = 69)
-
undertaking telephone surveys of all smaller trusts that agreed to participate in the study (n = 48 trusts; 50 hospital sites) with a view to map processes of medical care across the acute/emergency pathway
-
creating a typology of the models of medical generalism used by smaller hospitals, based on the telephone surveys
-
carrying out case study visits (n = 11) to examine in more detail the similarities and differences between main models of care identified by the typology and to evaluate the broader contexts in which the models of care sit, as well as the definitions, boundaries and meanings of medical generalism as theoretical concepts and lived experiences
-
undertaking a descriptive analysis of workforce, combining data obtained from the interviews and case studies with national workforce data from NHS Digital.
We considered the service perspective in two ways. First, we considered that the emergency and acute medicine pathway could be considered a closed system, boundaried by the patient’s presentation to and discharge from hospital, and therefore amenable to a general systems approach, which seeks to define and understand systems in terms of the functions and processes of each component within systems and the relationships between these. 96 Emergency and acute medicine pathways have also undergone radical change over the past two decades, with the introduction of AMUs, ambulatory care and the maturing of emergency medicine as a specialty. 76,97,98 It was therefore considered that emergency and acute medicine pathways in individual organisations were the result of serial rounds of innovation and improvement, mediated by contextual factors at multiple levels. 99 The Consolidated Framework for Improvement Research was adopted so as to better conceptualise and explore how and why hospitals operationalise their services and the contexts in which these services exist, particularly at the levels of the team provider, hospital and external landscape/policy. 100
Identification of smaller hospitals
NHS Improvement (formerly Monitor) has previously defined ‘smaller hospitals’ in England as providers with an operating revenue (income) of < £300M in the 2012/13 financial year. 88 Of the 142 general acute trusts, 75 of these in the 2012/13 financial year were found to fit into this category. Following review of financial information for 2015/16, six trusts were removed from the sample on the grounds that their operating revenues now exceeded that which might be expected from natural growth and were likely the result of major service reconfiguration. This left a sample of 69 smaller hospitals in England. This definition captures trusts that are predominantly single site, minimising the problem of attempting to distinguish Hospital Episode Statistics (HES) data at the hospital level in multisite trusts. It also ensures that there is a reasonable geographical distribution of sites, including hospitals in urban, provincial and rural settings.
Organisational profiles
Organisational profiles were constructed for all smaller trusts (n = 69) from a combination of publicly available data (e.g. trust and CQC reports) and hospital-level data that were collected by Monitor88 (later NHSI) and the Health and Social Care Information Centre (HSCIC), now known as NHS Digital.
Exploring models of care in smaller hospitals
Semistructured telephone interviews were used to gather data on the models of medical generalism deployed in smaller hospitals. Guides for the semistructured telephone interviews were constructed, following the work of Reid et al. ,101 to explore the following:
-
hospital department characteristics across the emergency and acute medicine pathway (ED, AMU, ambulatory care, frailty services, downstream wards and any other relevant spaces)
-
local triage rules for determining patient journeys
-
construction of the acute medical take
-
cover of the downstream medical wards
-
networking arrangements.
Constructing the typology
As discussed in Appendix 3, the marked differences between organisations with regard to almost every aspect of service delivery across the emergency and acute medicine pathway made meaningful classification and comparison of the models of care difficult.
The classification scheme that was ultimately adopted focused on the AMU and the downstream wards, the components of the system through which the majority of patients with medical conditions flow. The classification also limited the analysis to the categories that best express splits between generalist medicine and specialist medicine:
-
AMU – unit openness (closed/partial/open)
-
AMU – patterns of consultant working [acute physician dominant (APD), mixed, specialist dominant (SpD)]
-
wards – unit openness (closed/partial/open)
-
wards – patterns of ward distribution within the hospital (some designated general medical wards, SpD wards only).
Using this scheme, distinct models were visible for the AMUs and the wards. However, there were still no consistent relationships between the models used on AMUs and the models used on the downstream wards. For this reason, some aspects of the analysis have been carried out using the typologies of AMUs and wards separately.
Analysis
Full details of the analysis can be found in Appendix 2.
Case studies: investigating the typology
The purpose of the case studies was threefold:
-
to examine in more detail the operational aspects, such as the processes of care and staffing, with particular reference to the similarities and differences between models of care
-
to evaluate the contexts in which the models of care sit at provider team, hospital and external landscape/policy level
-
to explore concepts of medical generalism and how these may relate to the development and deployment of the different models of care.
Case studies were chosen so as to explore the different models of care that emerged from the typology. Care was taken to ensure that there was appropriate representation of trusts according to geographical location (urban vs. rural), size (small vs. ‘smallest’) and case mix. Three pairs of adjacent trusts were chosen, providing an opportunity to explore the contribution of external landscape and case mix to model development.
Case study visits were conducted over 1–2 days and involved the following activities:
-
Semistructured interviews with key clinical, managerial and nursing staff. Topics included processes of care and triage, past and present organisational strategies, local networking arrangements, tensions between generalists and specialist workloads.
-
Mapping patient flows by ‘walking’ through the emergency and acute medicine patient journeys. 102
-
DCSs103 that allow insight into the appropriateness of inpatient care.
-
Observations, with particular interest in unwritten rules, that influence how patients pass the emergency and acute medicine pathway.
-
Staff focus groups (at half of the sites), exploring themes around processes of care, organisational culture and views of medical generalism.
-
Document review, with a particular interest in standard operating policies for the AMU and downstream wards.
The case study interview guides and other materials can be found in Report Supplementary Material 2.
Testing the typology
There were two concerns about the typology: (1) whether or not clinicians and managers would recognise the models described and (2) whether or not the typology would be sufficiently pragmatic, as opposed to theoretical and abstracted, to be useful. To this end, the typology was presented, in various stages of development, for expert consideration by convened groups of senior managers and clinicians. It was presented twice to the New Cavendish Group and to the expert convened to look at case mix (see Chapter 5). It was also iteratively reviewed by the Study Steering Committee.
Construction of case studies
Case studies for each site were constructed, which were supplemented by material from the telephone survey and publicly available data such as trust annual reports. The studies aimed to combine detailed information about the processes of care at the unit level, while also providing contextual information about the hospital’s internal and external environments. Sankey diagrams, which depict flow through systems, were constructed for each organisation (Density Design Research Lab, Milan, Italy, URL: https://rawgraphs.io).
Framework analysis
Five separate sets of coding frameworks were used for all of the material generated by the case studies and relevant portions of the telephone surveys:
-
models of care – descriptions of mechanics of care were grouped by system component
-
the Consolidated Framework for Implementation Research (CFIR),100 which explores the contexts in which systems exist through five major domains – intervention characteristics, outer setting, inner setting, characteristics of the individuals involved and the process of implementation
-
medical generalism and specialism
-
smaller hospitals
-
workforce.
‘Pattern matching logic’ was used to look for emerging themes, with an emphasis on convergent and divergent evidence between data sources. 103 An iterative approach was taken, with regular discussions used to confirm important themes and guide further rounds of analysis.
Day of Care Survey
The DCS was analysed according to methods described elsewhere. 104
Findings
For ease of reading, the findings are presented in the following way:
-
We describe the key characteristics of the 69 trusts that were included in the study.
-
We describe the key characteristics of the 50 hospitals that participated in the telephone interviews.
-
We provide an overview of Emergency and Acute Medicine pathways in smaller hospitals in England.
-
We present the typology.
-
We relate the typology to the demographics of the study hospitals.
-
We provide an outline of the case study organisations.
-
We describe the factors, based on the case studies, that shape model development.
-
We explore the definitions and meanings of general medicine.
-
We provide a description of the workforce deployed by the study organisations.
Description of participation
Table 2 describes the participation of NHS staff in the study.
| Activity | Number of NHS staff participants |
|---|---|
| Telephone interviews (48 trusts) | 57 |
| Site A | |
| Staff interviews | 7 |
| Staff focus group | 7 |
| Walk around | 2 |
| Site B | |
| Staff interviews | 8 |
| Staff focus group | 10 |
| Walk around | 4 |
| Site C | |
| Staff interviews | 4 |
| Walk around | 1 |
| Site D | |
| Staff interviews | 7 |
| Staff focus group | 5 |
| Walk around | 3 |
| Site E | |
| Staff interviews | 5 |
| Staff focus group | 8 |
| Walk around | 3 |
| Site F | |
| Staff interviews | 6 |
| Staff focus group | 8 |
| Walk around | 4 |
| Site G | |
| Staff interviews | 7 |
| Walk around | 2 |
| Site H | |
| Staff interviews | 5 |
| Staff focus group | 9 |
| Walk around | 2 |
| Site I | |
| Staff interviews | 5 |
| Walk around | 5 |
| Site J | |
| Staff interviews | 5 |
| Walk around | 1 |
| Site K | |
| Total staff interviews | 5 |
| Total walk around | 4 |
| Total participants | 199 |
What do smaller acute hospitals in England look like?
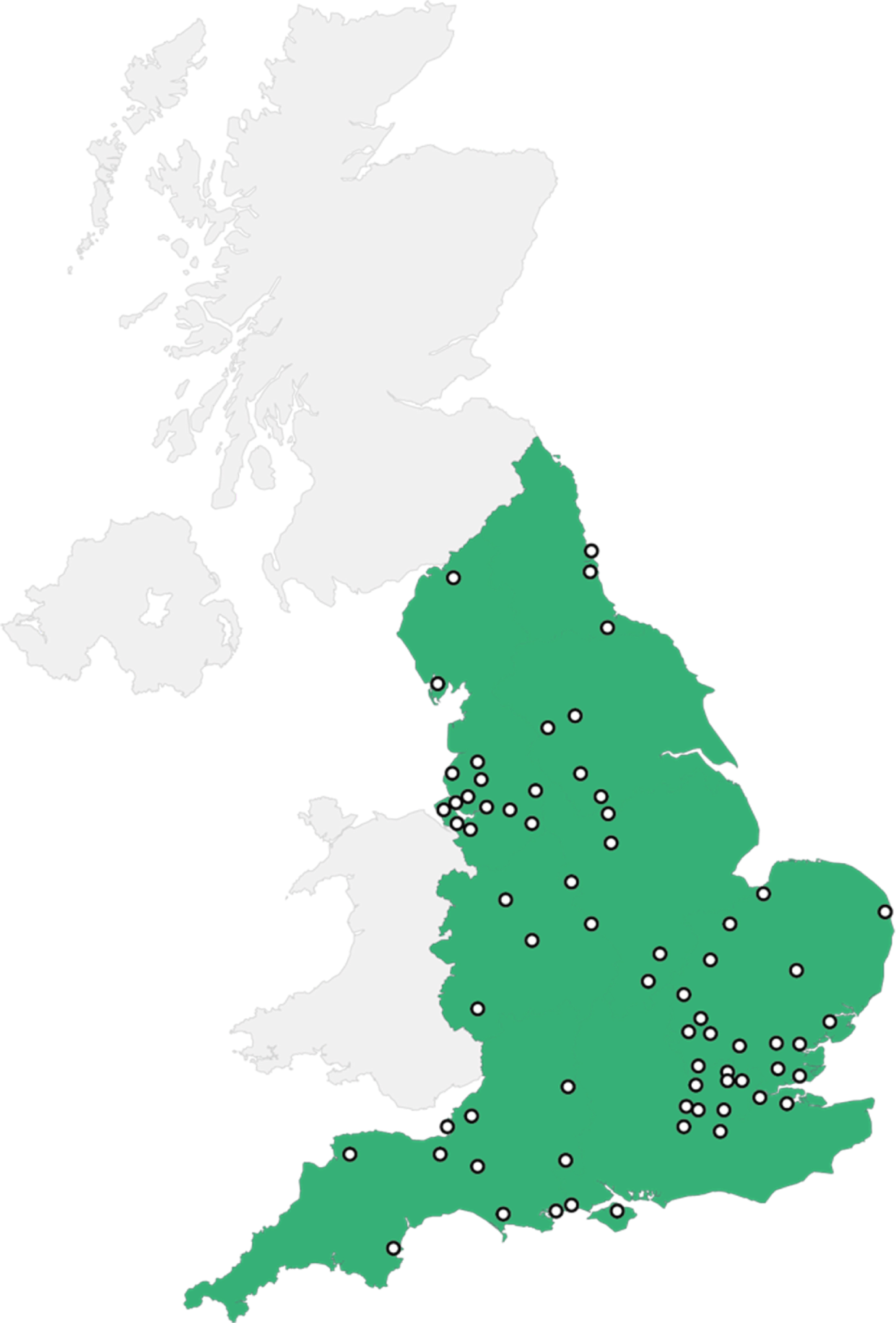
Using the definition of ‘smaller’ equating to an operating revenue of < £300M per annum,88 we identified 69 smaller trusts in England in 2015/16. Six of these trusts had more than one acute site. The geographical distribution of trusts is shown in Figure 7. Organisational profiles, detailing the number of beds, catchment population, distance to the next ED, ED attendances, medical admissions and CQC ratings, are given in Report Supplementary Material 3.
FIGURE 7.
Geographical distribution of the smaller hospitals in England.
Characteristics of the participating trusts
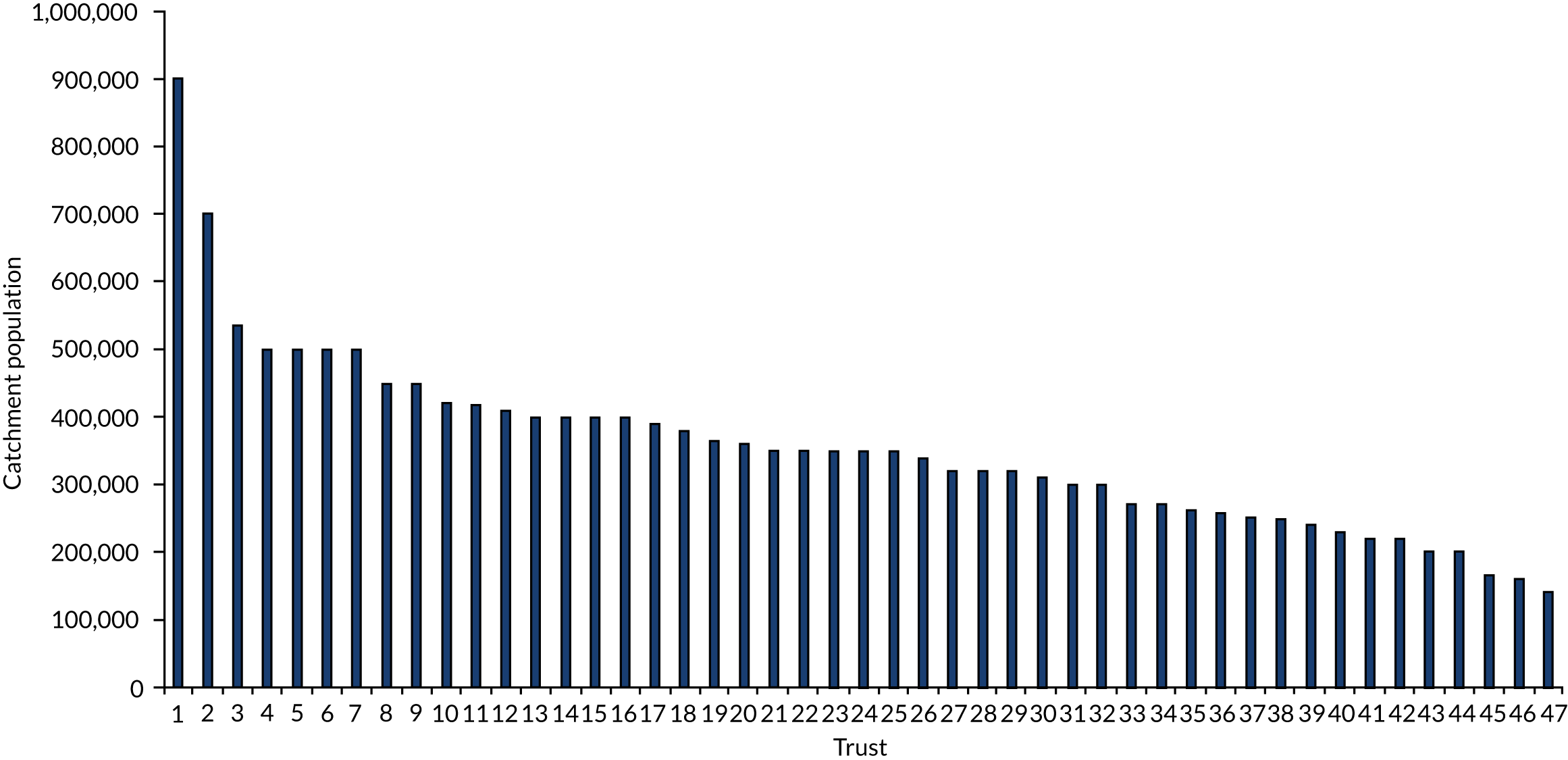
In total, 48 trusts, with 50 hospitals, agreed to participate in the study (including 70% of all smaller hospitals). The average population served by these was 300,000 people, compared with an average of 54,000 people for a ‘general hospital’ elsewhere in the European Union. The catchment populations varied from 140,000 to just over 500,000 (Figure 8), of which only 17 trusts had catchment populations of under 300,000. The average distance to the next nearest acute hospital was 17 miles; four hospitals were > 30 miles to their closest neighbour. The majority of hospitals were located in urban or well-populated rural areas.
FIGURE 8.
Trusts by catchment population.
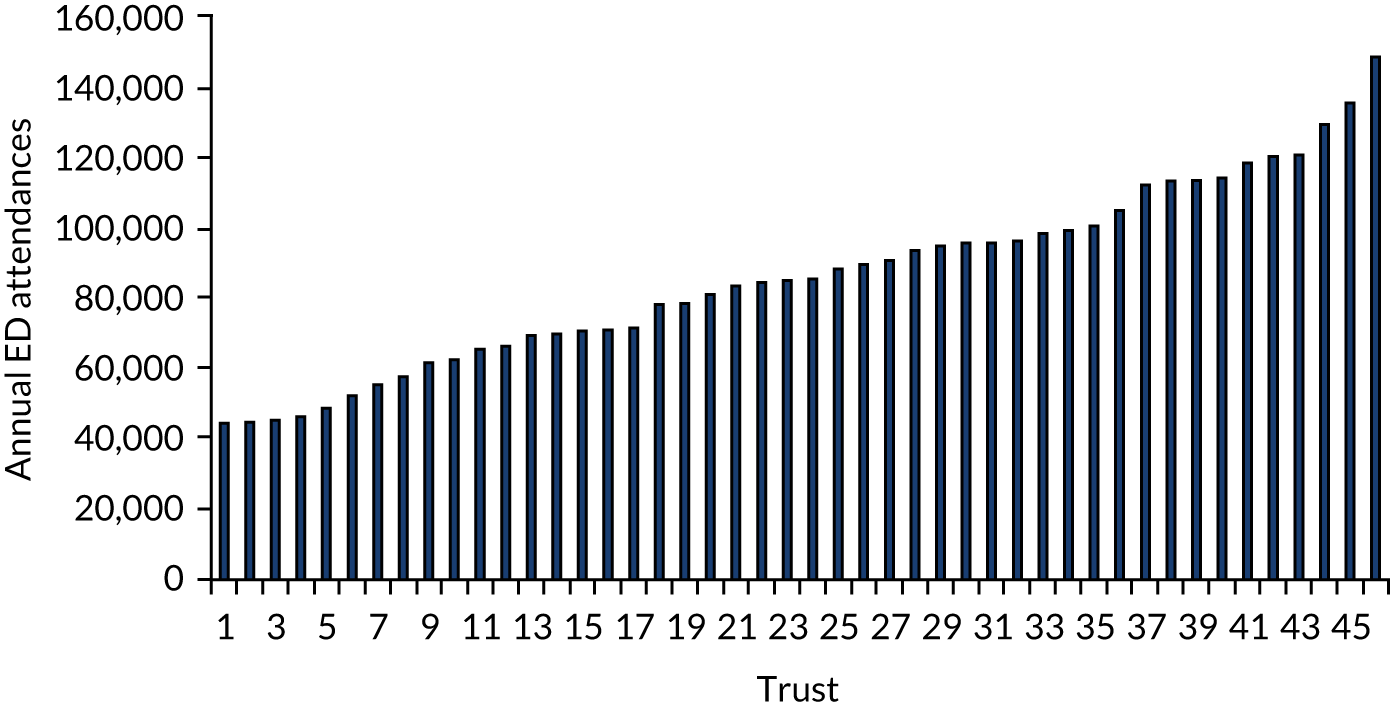
There was wide variation in the level of ED activity across the sites, from just over 40,000 attendances per annum to nearly 150,000 attendances (Figure 9).
FIGURE 9.
Annual ED attendances 2015/16 by trust.
Overview of models of acute medical care in smaller hospitals in England
The raw results of the telephone interviews are in Report Supplementary Material 4. These results have been the basis for two publications. 67,87
A system in flux
The original structure of the study had assumed that systems were in evolution but had stability in their underlying structures and degrees of coherence, with similarities between dominant models of care. However, the telephone interviews found that no two hospitals employed models of care that were similar across the three main components of the emergency and acute medicine pathway (ED, AMU and downstream wards). All of the organisations, with the exception of two, described major organisational change to emergency and acute medicine services within the last 12 months, with some engaged in a near frenzy of reorganisation and expansion of acute services. Many of the organisations also reported their usual systems and processes of care being overwhelmed at points either by spikes in patient demand or by external pressures to meet centrally mandated targets. Interviewees frequently framed their responses as ‘we should do A, but now we usually do B and we are planning to move to C’. All organisations, with the exception of one, declined to submit standard operating policies for analysis on the grounds of redundancy.
Although this flux in itself led to problems for interviewees to describe the systems in which they work, this was compounded by the fact that many organisations did not appear to have a coherent vision for the whole emergency and acute medicine pathway and that most interviewees, despite being selected on the basis of seniority, tended to be siloed within their own divisions with limited insight into other parts of the system. Almost all interviewees had to seek help from colleagues to answer all of the survey questions; some had managers from other departments join the telephone interviews.
Variation at every level
Our stakeholder engagement had suggested that emergency and acute medicine pathways in England have changed markedly over the past 5 years, with the expansion of ambulatory/emergency care and the introduction of frailty units (see Figure 3).
The reality did not quite match this theorised model. Although all hospitals by definition had an ED and downstream wards, there was marked variability in the numbers and types of other emergency and acute medicine components between hospitals (Table 3).
| Component of emergency/acute care | Percentage of hospitals (%) |
|---|---|
| AMU | 100 |
| Ambulatory care unit | 96 |
| Frailty unit | 56 |
| GP assessment area | 26 |
| Other assessment area | 41 |
Within each of these areas, there was marked variability between organisations with respect to the size, function(s) and, for certain components, criteria for accepting patients.
The relationships between these components of the system also varied markedly. Most organisations had a mosaic of services at the front door (e.g. ED, ambulatory care and GP assessment), all providing some form of primary assessment function, with patients moving from these areas to the AMU and then to the downstream wards. In other organisations, there were two discernible trends: towards either ‘acute hub’ or ‘hyperstreaming’ models of care. The acute hub, as suggested by the Future Hospital Commission,8 looks to co-locate and streamline all services with a primary assessment function into a single ‘hub’ (Figure 10). Although no hospital had fully achieved this, four hospitals reported moving towards this.
FIGURE 10.
Schematic of the acute hub model of emergency/acute care.
By contrast, ‘hyperstreaming’ models had moved the bulk of the work outside the ED into a series of parallel places of assessment (Figure 11). Seventeen hospitals reported having more than four places for the initial assessment of patients, with one organisation reporting eight.
FIGURE 11.
Schematic of the ‘hyperstreaming’ model of emergency/acute care.
Although this schematic shows the AMU in parallel, the rules for where patients should proceed varied by organisation, with some hospitals requiring all patients to pass also through the AMU and others allowing patients, after primary assessment (regardless of location), to be admitted directly to a ward. Other organisations conceded that patient flow through the system was wholly contingent on the availability of ward beds.
Highly complex systems
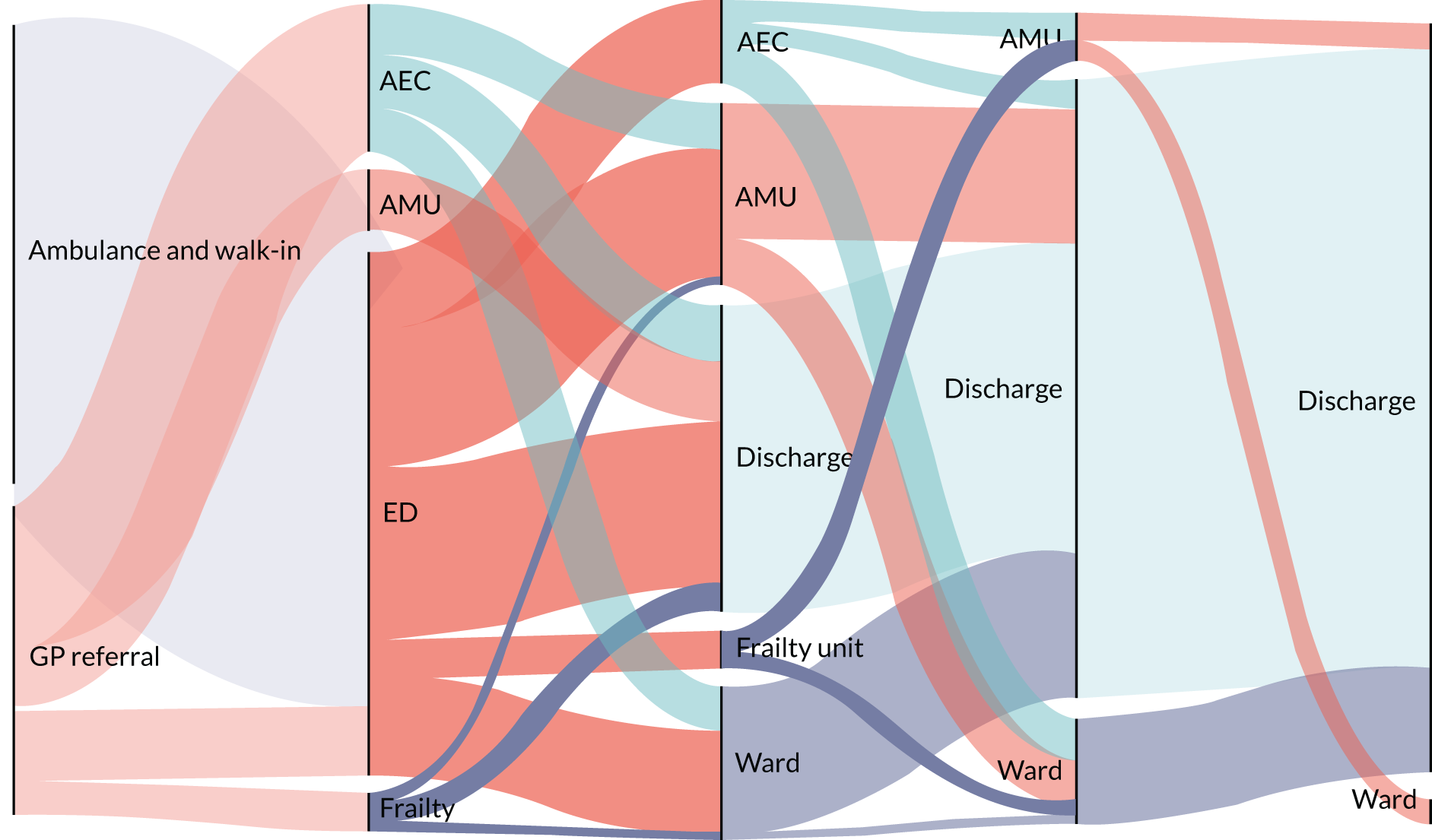
The result of the multiplication and the diversity of services at the front door has resulted in highly complex flows through the emergency and acute medicine pathway. Figure 12 shows the Sankey flows for a smaller rural hospital with 350 beds (Sankey flows for all case studies are given in Report Supplementary Material 5). Patients usually undergo multiple moves, through up to five different components of the system before finally being discharged. Considering that each move between the different components (denoted by the solid black lines) will be accompanied by a change of treating team, this visualises the fragmentation and complexity of the emergency and acute medicine pathway used in many hospitals.
FIGURE 12.
Sankey flow diagram of emergency/acute care at a 350-bed rural hospital.
Typology of models of medical generalism
The intention was to define and classify the degree to which each component of the emergency and acute medicine pathway was generalist or specialist, and then use this to form a judgement of how generalist or specialist the whole system of medical care in each organisation was. However, because of the extreme complexity and variability at almost every level, this was not feasible (see Appendix 3).
The RCP defines general medical work in two ways: (1) participating in the unselected acute medical take and (2) the care of general medical patients on the ward. 105 Therefore, we decided to focus on the patterns of consultant working on the AMU and the medical wards and the issue of who looks after the general medical patient: the generalist or the specialist? Our initial analysis of the data found that ‘ownership’ of a patient by a named consultant had the potential to occur at three specific time points in the patient journey: admission, first morning post admission and change of geographical location (predominantly the move from the AMU to the downstream wards). At each of these points, patient ownership could be considered a function of:
-
patterns of the contribution of medical consultants to the acute take (specialist vs. generalist)
-
patterns of the contribution of medical consultants to the post-take (specialist vs. generalist)
-
patterns of the contribution of medical consultants to ward work.
In all organisations, the patterns of work were also determined by the degree of permeability of the boundaries between the different components of the system, that is whether the service delivery unit is ‘closed’, with all patients within that space cared for by a single clinical team, or the service delivery units are ‘open’, with the allocated consultant caring for the patient regardless of their geographical location.
The other factor that emerged from the interviews as a key organising principle for medical work was the arrangement of downstream wards. Two dominant patterns were observed. Hospitals either had some wards designated as being ‘general medical’ or had all wards designated as being ‘specialty’.
It is acknowledged that the determination of whether a patient should be cared for by a generalist or a specialist is partly a function of the needs of the individual patient. However, the unwritten rules at each hospital for labelling patients were not visible in the telephone interviews, and so this dimension was not included in the creation of the typology. The issue of which patients were considered to be generalist was explored during the case study visits (see The general medical patient).
Acute medical units: definitions of generalist and specialist models of care
Two categories were chosen to classify the generalist nature of AMUs: the permeability of boundaries (Table 4) and the patterns of contribution of the medical consultants to the acute take (Table 5), a schematic of which is given in Figure 13.
| Type | Definition | Descriptive code | Type code |
|---|---|---|---|
| Closed | All patients on the AMU are under the care of the acute medical team | Clos | A1 |
| Partial | Most patients remain under the care of the acute medical team, with the exception of a small number of specific patients. This applies to models where one or two groups of patients routinely have their care transferred to a specialist team (e.g. care of a patient with myocardial infarction is routinely carried out by cardiology) | Part | A2 |
| Open | Newly admitted patients initially remain under the care of the acute medical team but are then triaged to a specialist team, which may include general or acute medicine | Open | A3 |
| Type | Definition | Descriptive code | Type code |
|---|---|---|---|
| APD | Acute physicians provide the majority of input into the acute take. SAG contribution is limited to acute take on the weekends and/or overnight on-call. This does not include models where the SAG are physically present in the evening | APD | B1 |
| Mixed | SAG consultants make a regular contribution to the acute take across the whole working week | Mix | B2 |
| SpD | SAGs provide the majority of input into the acute take | SpD | B3 |
FIGURE 13.
Schematic for the patterns of consultant working on the AMU.
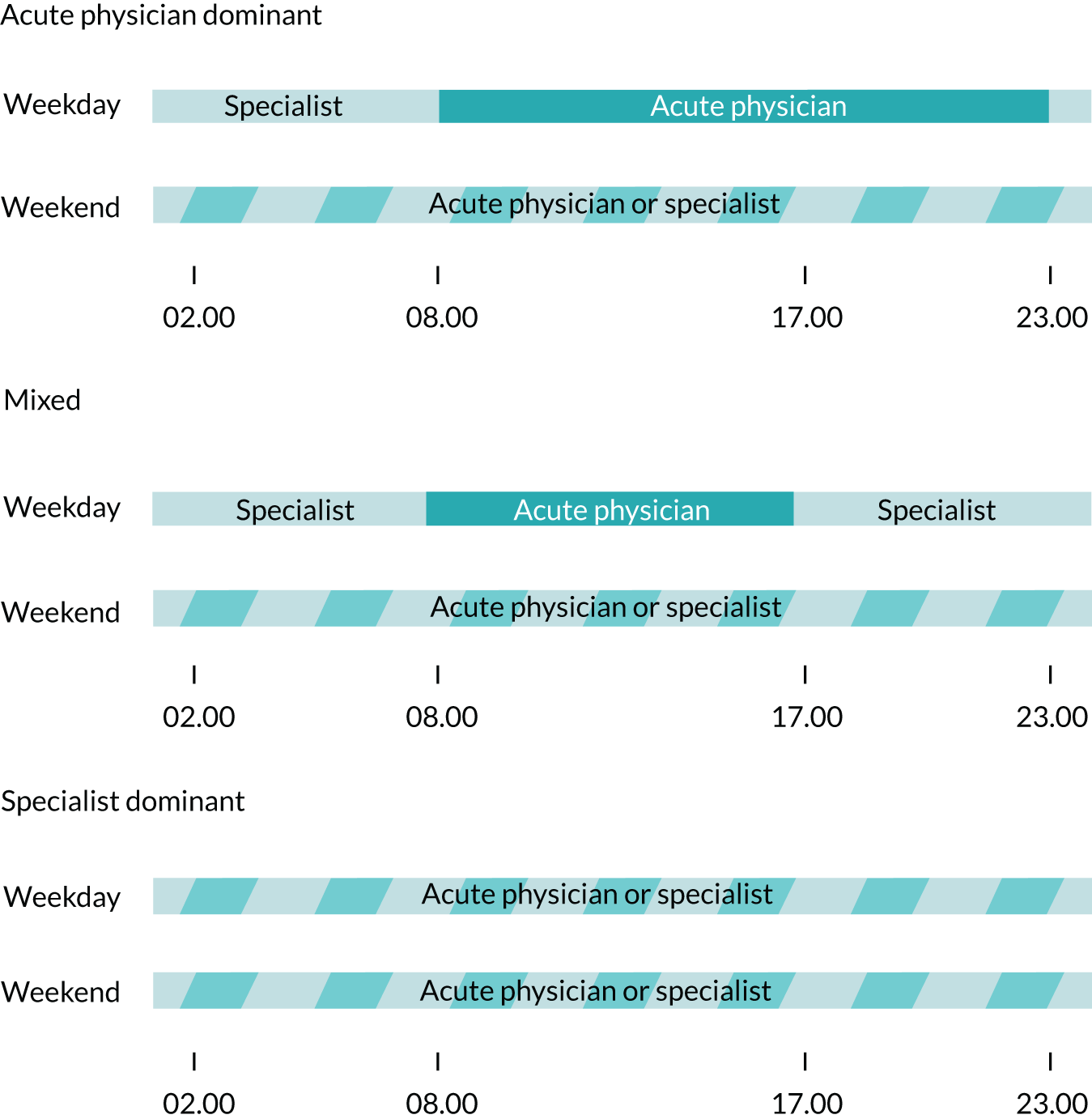
These definitions come with a number of important caveats:
-
They are based on usual patterns of care, rather than behaviour in exceptional circumstances (such as a patient belonging to a specialist consultant needing to remain on a closed AMU owing to nursing needs).
-
They do not capture all transfers of patient care between individual consultants, only those when the care has the potential to change from being generalist to specialist.
-
The closed/openness of an AMU ignores the issue of who leads the acute medical team at any point in time.
As all patients on a closed AMU will remain under the care of a single physician who co-ordinates their care, these units can be considered to be the most generalist. Conversely, the system operating in open units, commonly known as ‘take triage’ (patients are assigned or ‘triaged’ to specialty services as part of the admitting process), were specifically created to bring specialists as close to the front door as possible, rather than patients being assigned to specialist teams only at the point of transfer to the wards. 106
Prior to the fieldwork, it was assumed the balance between acute physicians and specialists and generalists would correlate with how generalist the unit was in its approach to patient care. Although during the course of the fieldwork it held that hospitals with an APD model viewed their care as being more generalist, hospitals with SpD models often viewed themselves as being highly generalist.
Downstream wards: definitions of generalist and specialist models of care
Two categories were chosen to classify the generalist nature of downstream medical wards: (1) the permeability of their geographical boundaries (Table 6) and (2) whether or not any wards were labelled as ‘general medical’ as opposed to all medical wards in a hospital being labelled as ‘specialty’ (Table 7).
| Type | Definition | Descriptive code | Type code |
|---|---|---|---|
| Closed | All patients on a given ward are cared for by a single team based on that ward. Transfers between wards necessitates a change of team | Clos | C1 |
| Partial | Most patients on a ward belong under the care of the ward team, with the exception of a small number of patients who belong under the care of other specialty teams | Part | C2 |
| Open | Patients belong to named consultants, rather than ward-based teams. Transfers between wards do not necessitate a change of team | Open | C3 |
| Type | Definition | Descriptive code | Type code |
|---|---|---|---|
| General medical wards | Wards that were explicitly designated as ‘general medical’ and/or wards where admittance was based around criteria other than medical specialty need, e.g. short-stay wards, medically fit for discharge wards, slow stream wards and rehabilitation wards | GMW | D1 |
| Specialty wards | All medical wards are allocated to a given specialty | SpW | D2 |
These definitions contain a number of important caveats:
-
They are based on usual patterns of care, rather than behaviour in exceptional circumstances.
-
They do not capture all transfers of patient care between individual consultants, only those when the care has the potential to change from being generalist to specialist.
Closed wards were considered as more specialist, whereas open wards were considered more generalist. Hospitals with some general medicine wards were considered to be more generalist than their counterparts with specialty wards only.
Classifying hospitals according to the typology
In total, 48 hospitals could be classified; two sites could not be categorised with sufficient accuracy. A total of 25 models were identified as being in use in the 48 organisations; the descriptive and numerical codes used to assist with the analysis can be found in Appendix 3.
The distribution of models of care is given in Table 8.
| AMU | Downstream wards | ||||||
|---|---|---|---|---|---|---|---|
| C1 D1 | C1 D2 | C2 D1 | C2 D2 | C3 D1 | C3 D2 | Total | |
| A1 B1 | 3 | 2 | 2 | 1 | 8 | ||
| A1 B2 | 1 | 3 | 3 | 1 | 8 | ||
| A1 B3 | 3 | 1 | 4 | ||||
| A2 B1 | 3 | 2 | 1 | 6 | |||
| A2 B2 | 4 | 3 | 2 | 4 | 13 | ||
| A2 B3 | 1 | 1 | |||||
| A3 B1 | 1 | 2 | 1 | 4 | |||
| A3 B2 | 1 | 2 | 3 | ||||
| A3 B3 | 1 | 1 | |||||
| Total | 12 | 13 | 7 | 13 | 2 | 1 | 48 |
There were no more than four hospitals using any one type of AMU or ward model, with eight hospitals operating models not used by any other organisation.
Testing the typology
The typology was reviewed on several occasions by both clinicians and managers. The standard response was that, although aspects of the typology were complicated, it did capture the critical differences between the most common ways of working across the acute/emergency care pathway and was clinically meaningful.
Are models of care contingent?
An underlying premise of this study was that hospitals would be consistent in their approaches to generalism across the whole of the patient care pathway, and that this would be visible in the relationships between different aspects of care within service units and between different system components. The relationships between the different AMU and ward categories are given in Appendix 4. Statistical analysis found no relationships between the overall models of care used on the AMU and the wards (p = 0.21). No relationships were found between the open/closed nature and the patterns of consultant working for either the AMUs (p = 0.40) or the wards (p = 0.49).
Although there was no consistent approach to models of care, some patterns were apparent:
-
Closed and partially open AMUs were more common than their open counterparts.
-
Acute medical units that relied on acute physicians (APD and Mix; see Table 5) were more common than SpD models.
-
Closed and partially open wards were more common than their open counterparts.
-
Only nine hospitals with a partial/open AMU (out of 28) had any form of general medicine ward.
Do hospital characteristics affect models of care?
It was hypothesised that hospital characteristics, particularly size, would be a factor in determining the model of care that was used, with smaller hospitals thought to be more likely to adopt a more generalist approach to care. As the models of care in the AMU and the wards were found to be independent and not contingent, as had been theorised, we also considered the AMU and the ward models separately.
There was no overall relationship between any measure of hospital size (i.e. bed number, ED presentations, emergency medical admissions or operating revenue) and overall, AMU and ward models of care (see Appendix 4).
However, a number of trends were observed:
-
The AMUs of the three smallest hospitals were all closed and APD.
-
There were no open AMUs in rural areas.
-
No hospital with < 400 beds used an open model of AMU.
-
There was a trend for partial/open AMUs in urban city areas.
-
All models of AMU were seen in towns.
-
Most hospitals used closed or partial models on their wards. The three hospitals that deployed open models were all middle-sized.
Outline of case study organisations
In total, 13 hospitals were approached for case study fields. One hospital declined, and pressures owing to reconfiguration prevented a visit being arranged at another hospital. The final selection of case studies (n = 11) by typology is shown in Table 9.
| Site | AMU type | Ward type |
|---|---|---|
| A | A2 B2 | C1 D1 |
| B | A1 B1 | C2 D1 |
| C | A1 B3 | C1 D1 |
| D | A1 B3 | C3 D2 |
| E | A1 B2 | C2 D2 |
| F | A3 B2 | C2 D2 |
| G | A1 B2 | C2 D2 |
| H | A2 B1 | C3 D1 |
| I | A2 B1 | C2 D2 |
| J | A2 B1 | C1 D2 |
| K | A2 B1 | C1 D1 |
All common models were explored during the field work. Three models were not represented, but these were relatively rare. The A2B1 model was over-represented, but this allowed for potentially better urban–rural comparisons to be made. Geographically, the very far north of England was under-represented. However, the interviews suggested that hospitals in this location were struggling with recruitment issues and that the models of care were highly unstable.
Three pairs of neighbouring organisations were also chosen for comparison, to allow for better exploration of the impact of both geography and local health economy on the model of care (Table 10).
| Type | Comparator site 1 | Comparator site 2 |
|---|---|---|
| Urban: inner | A1 B3 C3 D2 | A2 B1 C1 D2 |
| Urban: periphery | A1 B2 C2 D2 | A2 B2 C1 D1 |
| Rural | A2 B1 C2 D2 | A2 B1 C3 D1 |
The key characteristics of the case study sites are shown in Table 11. Full descriptions of the case studies can be found in Report Supplementary Material 6. Sankey diagrams demonstrating the flow of hospital sites through the emergency and acute medicine pathways are presented in Report Supplementary Material 5.
| Site | Location | Population covered (rounded to nearest 50,000 people) | Distance to nearest A&E (rounded to 5 miles) | Size status | Operating revenue 2016–17 (£M) | Approximate number of beds (rounded to nearest 50) | Hyper acute services (e.g. trauma, stroke, primary coronary intervention) | Number of CCGs (main contracts) | Number of CCGs in partnership (related party transactions) | Integrated trust (Y/N) | Vanguard site (Y/N) | Case mix (%) | ED attendances 2016–17 (rounded to nearest 1000) | Emergency admissions 2016–17 (rounded to nearest 1000) | CQC rating (correct from January 2018) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Rural: town in sparse settings | 300,000 | 15 | Small | 200–250 | 550 | Trauma unit, hyper acute stroke unit | 2 | 3 | Y | N | 61.70 | 80,000–90,000 | 30,000–40,000 | Good |
| B | Rural: town in sparse settings | 200,000 | 20 | Smallest | 100–150 | 350 | Major trauma unit, hyper acute stroke unit | 2 | 3 | N | Y | 40,000–50,000 | 20,000–30,000 | Requires improvement | |
| C | Urban: town | 300,000 | 10 | Small | 200–250 | 500 | Designated trauma centre, hyper acute stroke care | 3 | 8 | N | N | 61.70 | 120,000–130,000 | 30,000–40,000 | Requires improvement |
| D | Urban: city | 250,000 | 5.0 | Small | 250–300 | 500 | Level 1 trauma centre | 1 | 8 | Y | N | 46.70 | 110,000–120,000 | 20,000–30,000 | Good |
| E | Rural: town | 700,000 | 25 | Small | 250–300 | 650 | Trauma unit, hyper acute stroke unit | 2 | 5 | N | N | 62.80 | 100,000–110,000 | 30,000–40,000 | Good |
| F | Coastal | 500,000 | 10 | Small | 200–250 | 650 | Designated trauma unit, acute stroke unit | 1 | 2 | N | N | 60.80 | 70,000–80,000 | 30,000–40,000 | Requires improvement |
| G | Urban: town | 350,000 | 10.0 | Small | 200–250 | 500 | Trauma unit | 1 | 8 | N | N | 60.20 | 110,000–120,000 | 30,000–40,000 | Requires improvement |
| H | Rural: town | 900,000 | 15 | Small | 200–250 | 400 | Designated trauma unit, acute stroke unit | 1 | 8 | Y | Y | 60.50 | 40,000–50,000 | 15,000–20,000 | Good |
| I | Rural: town in sparse settings | 200,000 | 10 | Smallest | 150–200 | 400 | Trauma unit, acute stroke unit | 1 | 3 | N | N | 60.10 | 50,000–60,000 | 20,000–30,000 | Requires improvement |
| J | Urban: city | 500,000 | 0 | Small | 250–300 | 300 | Designated trauma unit | 2 | 6 | Y | N | 55.50 | 90,000–100,000 | 15,000–20,000 | Good |
| K | Urban: town | 550,000 | 15 | Small | 250–300 | 700 | Designated trauma unit, hyper acute stoke unit, primary coronary unit | 2 | 11 | N | N | 57.30 | 90,000–100,000 | 30,000–40,000 | Good |
Correlation between interviews and case study visits
There were two major discrepancies between the description of the models of care given in the telephone interviews and those that were observed during the field work. In the case of hospital A, the whole patient pathway had been changed during the intervening 6 months. Hospital K was classified as an A2 B2, but was operating an A3 B1 model.
For all other sites, the overall models of care observed agreed with the telephone interview descriptions.
Similarities and differences within models of care
One of the purposes of the case studies was to assess the extent to which the typology accurately captured the critical differences between models of care. We found that AMUs varied substantially more within categories than wards. Subtleties of consultant working, particularly continuity of care, and the ways in which different functions (e.g. primary assessment and ongoing care) were distributed within the components of the system accounted for the main differences within models of care.
Consultant working
Although the overall patterns of consultant working between organisations with the same models were consistent, there were important differences in aspects of how the consultants worked, especially on the AMU. For example, having a large cadre of acute physicians and a closed/mixed unit (implying heavy consultant presence) did not ensure that there was daily consultant review of patients nor any continuity of care. Indeed, the norm was for patients to receive a single ‘post-take’ review, with the predominance of care then being delivered by junior and middle-grade staff. For take triage models (open AMUs), continuity of care was entirely dependent on whether specialist services arranged consultant working as ‘specialist of the day’ or ‘specialist of the week’.
The category of AMU consultant working also failed to adequately characterise one of the A2 B1 models visited. At hospital H, one acute physician ran the AMU almost single-handedly, providing 16 professional activities of input per week, with methods of working not seen in any other organisation.
Function and capacity
The functions that were provided by any front-door service component in the ambulatory/emergency care pathway could include:
-
gatekeeping/triage, that is directing and/or controlling access to other services
-
primary assessment
-
initial management
-
secondary assessment, including specialist opinion
-
ongoing management
-
other services, for example ‘hot clinics’ (urgent outpatient review) and ambulatory care.
The variation in the distribution of these services was explored in the interviews. However, the number, functions and capacity of any service component in the ambulatory pathway had a knock-on effect on the delivery of care on the AMU. The work on the AMU in hospitals B and D was limited to secondary assessment and ongoing management, despite other aspects of the system being entirely different: hospital B had six locations for the primary assessment of patients, whereas hospital D provided all primary assessments and initial management through its ED.
The speed at which different functions could be provided to patients also varied substantially from hospital to hospital, and was not contingent on model of care. Some units could access same-day specialist opinions despite being closed, whereas others had to submit formal requests for these, resulting in substantial delays in waiting for a review.
The differences between wards were much less marked. Indeed, almost all of the specialty wards were run in a uniform fashion, the only significant variation being the length of time spent by individual consultants on the ward. The organisation of the general medical wards, however, varied markedly from organisation to organisation. One organisation claimed to be running open generalist wards (hospital H); although this was technically true, the wards had reverted from being specialty wards to open generalist wards because of substantial problems with flow. All other generalist wards varied in nature from organisation to organisation. Most generalist wards were short stay, although the criteria for entry, consultant cover and expected length of stay (LOS) were different for each unit. Hospitals B and K ran wards for patients awaiting discharge, but whereas hospital B was a multidisciplinary team-led unit, hospital K had a specific consultant assigned. Regardless of these differences, the presence of generalist-type wards was reported as affecting the case mix of the remaining specialist wards.
Coherence of models of care
As with the interviews, the extent that models of care could be presented as coherent models across the whole emergency and acute medicine pathway varied. Staff in four hospitals viewed their models of care in this way: hospitals D, H, J and K. Hospitals F and I identified as having a clear approach to care on the AMU, but not across the whole system.
Hospitals that viewed their models of care as a coherent whole all operated different models of care, which does not match the assumption that coherent whole systems of care should all look the same. Staff all viewed their models of care as unique, and as an expression of their organisations’ overall commitment to serving the needs of the local community. Notably, all four organisations had stable leadership at both hospital level and team level [i.e. chief executive officers (CEOs) and key service leads had been in place for > 5 years], and all had substantially invested in programmes to imbed quality improvement and/or cultural change into their organisation.
Factors influencing model development
For the purposes of the discussions that follow, interviewees will be identified only by their level of seniority and whether their role is medical, managerial or nursing. Where quotes are taken from the focus groups and identification of individuals was not possible, the quotes will be cited as ‘focus group participant’ (FGP). Representative analysis by hospital site is presented in Report Supplementary Material 7.
Although mentioned during the telephone interviews, the case studies allowed for exploration of the factors that influenced model development from clinical, managerial and nursing perspectives.
The most striking finding was that no hospital felt that their model of care was ideal and many viewed their model as being much less than ideal. A symptom of this was the almost frenetic activity reported in remodelling components of the system, from tweaks to hospital processes to major capital spend on AMUs, EDs and ambulatory infrastructures:
They’re continuously designing and redesigning.
Senior clinical manager
Models were also highly negotiated and contingent on a series of internal and external factors.
Hospital-level factors
Hospital size and location
The size of the hospital was viewed as the single most important characteristic in determining the model of care used. For most, being small implied the use of a more generalist model by default, with specialism being more of a characteristic of larger organisations:
So there is something different about a small hospital, isn’t there, which is why we’re all working here because we like the DGH [district general hospital], because we are inherently a bit more generalist.
FGP
Generalism was also viewed as being inherently collaborative by many interviewees, with connections drawn between the co-operative working that is fostered in smaller organisations and the desirability of a generalist approach to care:
It’s probably less of an issue at a small district general hospital, compared with your city centre royal hospitals and your teaching hospitals in terms of generalism, partly because there’s more interface between people on the corridor.
FGP
Interviewees drew connections between the size and location of the hospitals and the perceived needs of the local population, who were viewed as being older with complex comorbidities and, hence, more likely to benefit from a generalist approach to their care. They also viewed medical staff who were working in isolated locations as needing a broader skill-set, which lends itself to more generalist ways of working.
The size of the organisation was also consistently linked with the ability to implement change and ‘getting things to work properly’:
In a big hospital, you can quite easily avoid doing something because you won’t see people . . . whereas here, it’s not big enough that you don’t bump into someone and go ‘Ah! I will try to catch you with that’.
Senior non-clinical manager
Medical staffing
The workforce was viewed as a critical factor in developing and sustaining models of care. Only three hospitals considered that they had a workforce to match demand (D, F and K). All other hospitals considered their workforce shortages to be so severe that they affected performance and posed a potential threat to patient safety:
If we had five acute physicians in the trust as a starting position, around which to build a team, I think whichever model we use would work really well.
Senior clinical manager
Most organisations aspired to change their models of care entirely, with most wishing to have their acute take led by acute physicians and to implement better frailty/care of the elderly services, with many larger organisations desiring a move to a take triage model. Instead, the inability to recruit and retain staff left organisations with models that they felt were second best.
The corollary of the inability to recruit was a reliance on locum staff, which was seen as further negatively affecting the ability to change model of care:
There are challenges with using so many locums because you run into challenges with consistency and leadership, particularly when you’re wanting to embed improvements, it becomes quite a challenge if the majority of your consultant staff are transient.
Senior clinical manager
Hospitals with substantial workforce shortages reported extreme difficulties in recruitment. Not only did poor staffing limit the desirability of a consultant post at an organisation, but the increased burden on those remaining made them, in turn, more likely to seek employment elsewhere, exacerbating the staff shortages further.
Beyond the size of the workforce, the viability and acceptance of a model of care was strongly linked with having the right type of staff, in terms of skills, approaches to work and personal character. This was true, especially for hospitals that were operating more generalist models:
People seem fairly committed to the business of working in a small DGH . . . so I think it attracts a certain kind of person who wants to do this type of work, which helps.
Senior doctor
Consultant behaviour
Issues with workforce shortages were exacerbated by negative consultant behaviours. Two particular patterns occurred across organisations, which appeared to affect the model.
The first issue was specialist staff refusing to participate in the acute take, thereby ‘withdrawing’ their services from the front door. This was more common in large organisations that had sufficient staff to support the aspiration towards separate on-call for specialties, or in those organisations that were moving towards regional networked approaches for interventional work. Withdrawal of individual or groups of specialists from the acute take was considered to increase the pressure on those still participating in the on-call, which drives further flight, resulting in a ‘spiral of doom’ (Figure 14).
FIGURE 14.
Schematic of the ‘spiral of doom’.
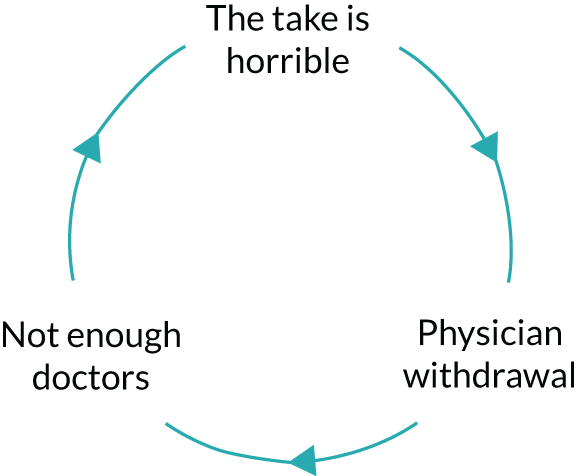
The second phenomenon described we have termed 'fortressing', which was where staff actively limited their workload by tightly patrolling service boundaries. This was more often seen in organisations with more geographical places for the parallel processing of patients, and tended to occur when services were shoe-horned into small or otherwise inappropriate spaces. Hospitals B and E, for example, both moved from providing consult-type geriatric services (where roving teams reviewed all of the referred patients across the hospital) to frailty units, with a limited number of beds. The result was that rather than 15–30 patients having specialist input, the number of patient contacts was limited by the number of unit beds (6 and 10 beds, for hospitals B and E, respectively). This phenomenon was also seen in other places including the AMU at hospital E, where the acute physicians insisted that each of the four ‘sides’ of the AMU (10 beds per side) required its own consultant each day, and hospital B, where the cardiologists refused to provide input into patients not on their ward:
It was an attempt to get them to take ownership of their own area and to react to the needs of the service. And, unfortunately, what happened was that they took ownership of their own well-being and made it quite easy for themselves.
Senior clinical manager
Instances of fortressing and flight behaviours were not isolated. Instead, attempts had been made by clinicians to employ these strategies at least once at every organisation, with fortressing being described as present at four sites and flight at five sites. Although such behaviours were usually presented by consultants as rational responses to their increasing work pressures, they effectively created artificial workforce shortages. Moreover, these behaviours caused ripples throughout the rest of the consultant body, with other groups of specialists then attempting to deploy similar strategies. The end result, almost invariably, was a consultant body where relationships could be described as fragmented at best and openly hostile at worst:
[When] there were two of them on who were sharing the bulk – it was fine . . . I don’t think [specialist staff] loved it and embraced it, but I don’t think they were hating the concept of coming down [to the AMU]. Since the acute physicians retrenched into the aberrant model of looking after themselves, they all are really quietly pissed off because they’re coming on at four o’clock to an oncoming battlefield.
Senior clinical manager
Resistance to flight and fortressing was frequently discussed by senior managers. Managers in organisations where flight and fortressing had occurred were usually regretful that matters had been allowed to develop in that way. In organisations where the behaviour had been resisted, managers remained vigilant about their possible return.
Staffing strategy
Although most organisations had coherent strategies for the recruitment and retention of nurses, this was not the case for consultant staff. Instead, this was led by the demands that were placed on specialist services, particularly by outpatient and interventional targets, and the ability for clinical leads to build effective business cases for additional staff. In turn, imbalances across the organisation in terms of the capacity to deliver specialist care on both the AMU and the wards were visible, again limiting the organisation’s innovate with models.
Where recruitment strategies did exist, these tended to focus on international recruitment or ‘golden handshakes’ for new consultants, rather than ensuring that the whole hospital had a consultant workforce that matched the hospital’s overall needs. The exceptions to this were hospitals D and K, which both had long-term strategies at the whole-hospital level for service provision, and consultant recruitment and retention. It is notable that neither of these hospitals had unfilled posts.
Leadership
Leadership was important at two levels: clinical leadership and executive management.
It was striking the extent to which individual clinicians acted as the architects of systems. In three out of the four hospitals with well-articulated models of model, the structure of the models of care could be considered a direct expression of the ethos and beliefs of clinical leaders:
And, within that governance for the department, again, I’ve tried to structure that incredibly similar to the way what I see the process in urgent care running.
Senior clinical manager
The championing of models of care, especially more generalist models, was also viewed as important in persuading colleagues to continue to support and sustain the models:
[Name withheld] appears to run the place . . . [they’re] fantastic.
Senior clinical manager
By contrast, executive management was constructed as either enabling or inhibiting models of care, rather than being directly responsible for their architecture. Management was viewed as particularly important when the relationships between clinical staff and executives were characterised as distant, poorly collaborative or where the aims of the executives and the clinicians did not align. Problematic relationships were often linked to the derailment of change and the creation of dissatisfaction among staff:
At the top, there’s an extraordinarily siloed thinking . . . all they’re interested in is what they’re accountable for . . . So you go tell them something they don’t want to hear and they don’t listen to it . . . you flag [matters] up and you’re essentially hauled into the office and told off.
Senior clinical manager
Hospitals where the ‘business of the front door’ and meeting the needs of the local community were seen as organisational priorities, were more likely to invest in front-door services, such as the ED and AMU, and create space for model innovation.
Attitudes of the executive towards behaviours such as withdrawal from the acute take and fortressing varied from organisation to organisation. Some organisations seemed unable to tackle poor consultant behaviour, whereas others refused to condone it. Other organisations successfully negotiated with their consultant staff, either by offering generous additional payments for the specialty on-call service or by demanding improved day-time services (e.g. same-day interventions) in exchange for less onerous on-call.
External factors
External factors were less frequently mentioned as a determinant of model of care and were usually seen as negative or inhibitory rather than as a positive influence. There were few direct external drivers of model, but a number of external factors exerted substantial indirect pressures on systems and, hence, on models of care.
Externally-set targets
Concern around ED performance, as measured by the 4-hour target, was the chief external driver of model of care. The response of many hospitals was to create or enlarge places of parallel for primary assessment, such as AMUs, frailty units and ambulatory care. In turn, increasing the patient flow through these areas drove a search for alternative models of care. Anxiety about performance was also linked with poor managerial behaviours and the creation of an unsatisfactory working environment.
Central bodies
Recommendations from central bodies, particularly NHSI and NHSE, to implement ambulatory care, frailty units, GP streaming and other service components had major impacts at the whole-system level, markedly changing the distributions of work and staffing around the system. Hospitals responded to these external pressures by frequently setting up new services in relative haste, shoe-horning new services into inappropriate spaces and relying on existing staff to take on additional roles (recruitment being difficult). The spreading of staff across a wider geographical area, alongside a perceived increase in workload, was a critical factor in fortressing and other negative consultant behaviours, which, in turn, made existing models of care more fragile (see Consultant behaviour). Where multiple new services were being implemented, this was not always carried out in a co-ordinated fashion, with improvements often falling under different managerial divisions; the result of this was increasing fragmentation of the patient journey.
Relationships with NHSI and NHSE were also seen as problematic and as a driver of perverse behaviours:
Do you know Ben Elton’s bin: the thing about the bin? It’s a student house and you’ve got a bin and ‘What do you do when the bin gets full?’ ‘Get a second bin’. But they were given hell [by NHSI] because, the next thing, you’ve got two bins.
Senior clinical manager
Guidelines and recommendations
Only one organisation (site J) reported explicitly organising their AMU according to the RCP’s recommendations for acute medicine. 79 Other organisations aspired to the ‘acute-hub’ model that was outlined in the RCP’s Future Hospital Commission, but felt unable to implement this because of the central drive towards multiple places of parallel processing. 8 Negative views about the national-level recommendations for service provision were frequent and the consensus was that models of care developed in larger organisations were rarely suitable for use in smaller ones.
Clinical commissioning groups and local authorities
The role of CCGs in funding and supporting aspects of models of care was viewed as highly significant, and relationships between the hospitals and the CCGs were usually characterised as difficult. Multiple accounts were given of CCGs withdrawing funds for key components of acute services, such as rapid assessment or frailty services, with little or no notice, which ratcheted-up the pressure on fragile services. During one visit, the CCG had reneged the previous day on its agreement about tariffs for ambulatory care, which had halted the opening of a multi-million pound, purpose-built facility. Hospitals dealing with multiple CCGs reported substantially more problems than organisations with a less complex local environment:
It’s a very simple system . . . because we’ve got a single CCG and a single council basically. So we’ve got good relationships with them.
Senior clinical manager
Most hospitals reported that the funding crisis for social care had resulted in a substantial and sustained negative impact, increasing the number of DToCs. The problems posed by ‘bed blocking’ were seen in some cases as overwhelming the acute care system:
We’re, ultimately, powerless and whatever else. We’re limited as to what we could actually do. We’ve done everything we can.
FGP
Sustainability and transformation plans
Virtually all of the organisations viewed themselves as under threat of closure as part of local sustainability and transformation plans (STPs). Some places viewed this as being a major inhibition to any form of change to services, beyond those demanded by NHSI and NHSE. Others continued to cautiously invest and innovate, albeit still expressing marked concerns about the future:
We worry too much as a small organisation about the big takeover . . . and that sometimes does stop, it does stop some change and development and I’m really surprised that over the past 5 or 6 years we’ve invested.
Senior manager
The threat of closure was also seen as a major impediment to consultant recruitment, with potential employees unlikely to commit to a job that may not exist in the near future.
Other indirect influences on model of care
A range of other factors appear to influence models of care in less direct but still important ways:
-
Change in hospital case mix – all organisations reported an increase in the number of frail elderly patients. Although attempts to improve care for this group of patients had been universally made, two hospitals had changed their model of care in response to this. One had instituted a parallel ‘elderly care’ take and the other was in the process of ‘right-sizing’ its downstream wards.
-
Geography – the distance between individual service components, particularly the ED and the AMU, was a major factor in determining the distribution of medical work across the system.
-
Junior medical staff – all hospitals reported severe shortages of junior-grade and middle-grade staff. Although this did not directly affect the patterns of consultant working, this was seen a major threat to the stability of models, with most organisations seeking alternative types of staff to augment the junior-grade and middle-grade rosters.
-
Surgical services – the reorganisation of local surgical services, independent of STPs, was considered to affect the arrangement and even sustainability of medical services.
-
Relationships with other hospitals – the quality of the relationships with neighbouring hospitals, particularly referral centres, was considered important in shaping local services. Movements towards networked regional services were generally seen as positive, although some viewed this as having potentially negative impacts, through loss of income and reducing the attractiveness of specialty jobs with an interventional component.
The development of models of care as a ‘journey’
Virtually all of the organisations described the development of their models of care as being a dynamic process taking place over a period of many years. In many places, development of models was evolutionary, but some described episodes of revolutionary change that were usually prompted by a change in clinical or executive leadership. In all cases, the ‘journey’ was shaped by the size, skill-set and co-operativeness of the available consultant workforce. This, in turn, was influenced by a whole constellation of other factors exerting influence at various points, sometimes being the catalyst to force change, other times influencing change already under way. This led to a sense, in most organisations, of change (and hence model of care) being reactive rather than carefully planned and executed.
Day of Care Surveys
The DCS is a validated tool that captures the appropriateness of inpatient care and the reasons for delays in discharge of patients. 103 It had been theorised that there would be a relationship between the performance of the model of care and the appropriateness of inpatient care, as measured by the DCS. It was appreciated that a snapshot of care on a single day was not a perfect basis for comparison, but it was intended that this would supplement data obtained elsewhere and inform comparisons of models of care.
Data were collected by local teams. Despite training, there was substantial variation in the quality and consistency of data recorded, not only between sites but between wards in single hospitals.
The number of patients receiving inappropriate care ranged from 2% to 45%, with nine organisations having more than one-fifth of their inpatient medical beds occupied by patients who could be better cared for elsewhere. The overall reported rates of patients receiving inappropriate care were similar to the official NHS figures for DToCs (Figure 15). 107,108
FIGURE 15.
Number of DToCs compared with the DCS.
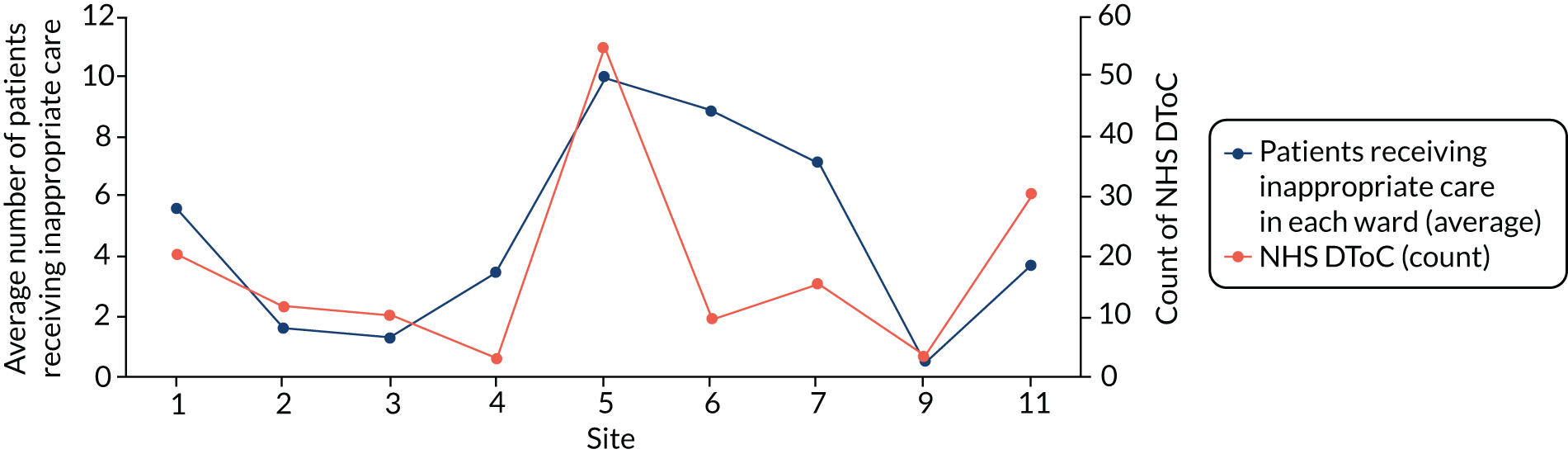
These data confirmed reports that changes to social care provision had resulted in models of care breaking down. Given that the number of patients receiving inappropriate care was more likely to be a factor of the state of local care than the model of care, no further analysis was undertaken.
Medical generalism: definitions, meanings and attitudes
The limited literature suggested that models of medical care would be driven by three main paradigms:92
-
General medical care as the default for all medical patients unless/until referral to a specialist.
-
General medical care provided in response to patient need.
-
General medical care provided the ‘work left undone’ by the specialists.
As a corollary of this, we expected to find a limited number of meanings attached to the concept of medical generalism and that these would be broadly shared across hospitals and between physicians.
Instead, we found a plethora of meanings and it was not uncommon for multiple and sometimes contradictory meanings to be held simultaneously by a given individual. This appeared to be a function of the fact that most clinicians to whom we spoke were dual-accredited in both a specialty and general medicine, and usually had both clinical and managerial roles. Opinions, rather than being consistent, arose from the persona or ‘hat’ worn by the interviewee in response to any given question. Moreover, medical generalism was almost always framed in pragmatic terms, such as the general medical patient, practising as a ‘generalist’ physician or the models of medical generalism, rather than as a distinct concept or discipline. The subtle tensions between the loci of medical generalism (patient, clinician or system) contributed substantially to the complexity and multiplicity of meanings. Still, a number of consistent sets of themes arose.
The general medical patient
Medical generalism was most frequently framed in terms of ‘the general medical patient’. There was a universally held assumption that virtually all patients started out as general medical patients at the point of admission to the hospital (i.e. during the process of the acute take). Patients were then sorted into the categories of ‘general medicine’ or ‘specialty’ at any one of a series of time points: the first review by a senior medical decision-maker (registrar or consultant), the post-take review, the triage meeting, the point of specialty review or the discharge from the AMU to a downstream medical ward.
Positive definitions of the general medical patient were framed around their age, frailty, number and type of comorbidities, deprivation and social circumstances of the patient. However, definitions were not fixed and varied both within and between organisations. This, in turn, stemmed from the complexity and fluidity of these concepts themselves. That there is no clear or universally accepted definition of ‘frailty’ was frequently touched on:
Those frail elderly and the complex comorbid patients who aren’t necessarily elderly. I mean, it’s always difficult, how do you define ‘elderly’? I’ve always felt that we should have a biological definition rather than a chronological definition of who requires elderly care.
Senior doctor
Patients with intersections of needs, particularly if social needs were dominant, were almost universally seen as belonging to general medicine, regardless of other aspects of definitions:
Sometimes [the patients] haven’t got any acute medical problems, so it’s more regarding their social circumstances or families not coping with their care at home because of all the chronic comorbidities they’ve got.
Senior doctor
However, more frequently the general medical patient was framed in a negative sense, predominantly owing to them not having an easily definable, organ-based reason for their admission:
[General medical patients] don’t come in neat little packages of ‘I’ve got a gastroenterology problem’ or ‘I’ve got a cardiology problem’.
Senior manager
However, even in patients with organ-based disease, decisions around which patients were the preserve of the specialists varied and were dependent on factors such as the commonness of the disease, disease severity and expected LOS, with patients with an expected LOS of < 2 days usually remaining under the care of the acute physicians:
The one specialty that puzzles me is respiratory. Is it a specialty or is it a general thing? On the one hand, I think that 40% of the general medical take you could, if you wished, classify it as ‘respiratory’ – COPD [chronic obstructive pulmonary disorder], pneumonia or whatever. On the other hand, the number of people who actually need a specialist respiratory opinion is relatively small.
Senior clinical manager
The capacity of the specialists to provide care was also a factor in drawing boundaries. For example, in one organisation the lone cardiologist was always off-site on a Wednesday, meaning that patients who would be otherwise assigned to his care would remain under the acute team on that day. Capacity, in turn, was at least partially determined by the attitudes of individual clinicians towards service provision. Two organisations had only one respiratory physician; although in both of the hospitals this resulted in patients with chronic obstructive pulmonary disorder (COPD) and pneumonia consistently being labelled as ‘general medicine’, in one organisation the respiratory physician provided a daily round to all patients with respiratory conditions, regardless of their location, and in the other organisation, patients were cared for by teams other than the respiratory team with no additional specialist input.
Specialty patients were also relabelled as ‘general medicine’ when they were unable to be placed on the base ward of their team in partial and closed-ward models. Hence, a patient with a respiratory problem would be regarded as ‘general medical’ if placed on a gastroenterology ward. This also applied to patients if a particular specialty service was not available at the hospital; for example, almost all patients with neurological or renal problems became ‘general medicine’ by default:
If you’re in a gastro[enterology] ward, you’ll be looked after by a gastro[enterology] consultant: you may have a respiratory problem but you’ll be looked after by a gastro[enterology] consultant. If you then move wards and end up on a cardiology ward, you’ll then be looked after by a cardiologist. So we’ve got care, at the moment that is based on location of patient as opposed to patient need.
Senior clinical manager
Diagnostic uncertainty was viewed as problematic. As one of the tasks expected of the AMU was to assign a diagnostic label to the patient, those patients who left the AMU without a clear diagnosis were viewed as also general medical by default:
There are always patients where it could be anything . . . you are always going to get patients who fall through the cracks.
Senior doctor
Other negative definitions of the general medical patient could be considered as hostile, with the general medical patients being characterised as ‘the least interesting cases’ or ‘the ones that that we are stuck with’.
Labels were rarely assigned in a consistent fashion, even in single organisations. Most organisations attempted to sort the specialist from generalist patients clinically, with labels being assigned by either the take consultant or the take registrar; in one organisation, sorting was carried out by senior nursing staff on the AMU. Formal sets of rules were rarely used. Instead, there were often loose sets of understandings about what might be specialist (e.g. troponin-positive, anginal-type chest pain being the preserve of cardiology), along with calibrations for personal opinions of the assigning clinician and the knowledge of the receiving clinician’s capacity and preferences. However, pressures in the system meant that patients were often moved ‘to the next available bed’ without labels being formally assigned:
It depends upon the geriatrician.
Senior clinical manager
We’ve got some specialist ward areas that may or may not have specialty patients and gen[eral] med[ical] patients on them. We do have a gen[eral] med[ical] ward that’s called something else but, essentially, delivers the general medical service.
Senior clinical manager
The general physician
As with the general medical patient, definitions and meanings around the general physician were inconsistent and fluid. Importantly, few doctors characterised themselves as being solely general physicians, with discussions instead framed around acting as a ‘generalist’, which was one of a series of roles that a consultant physician could adopt:
When we’re ‘on’ each of gets rids of our regular hat . . . and all our other roles are cancelled for that day.
Senior doctor
Three factors emerged as defining the generalist role:
-
the place of working, with front-door working being predominantly generalist
-
the type of care delivered, with primary assessment and initial management functions being predominantly generalist
-
the label attached to the patient, with consultants adopting the generalist role when delivering care to a patient labelled as ‘general medical’ (regardless of place).
That these three factors were highly intermingled and difficult to disentangle was reflected in the fact that no interviewee articulated a consistent view of what constituted a generalist or generalism. However, it was apparent that the generalist skill-set required by the acute take was fundamentally different from that for managing patients on the downstream wards.
Distinctions between generalism and specialism were drawn on the basis of the skills and training of individuals, where older physicians or those with longer periods of training were more likely to identify with the role of the general physician than their younger colleagues, who had straight-through dual-specialty training. Notably, younger consultants did not dispute their ability to manage the take, but rather struggled with the needs of complex medical patients requiring ongoing care:
I wasn’t trained to look after these sorts of patients. It’s not the job I [trained for]. Even before I started here as a consultant it was already different.
Senior doctor
Although the acute physicians were considered to be generalists by their colleagues, the ability to provide competent care to patients, regardless of their location or their needs, was considered to be clear point of distinction between acute physicians and those who identified as ‘true’ general physicians.
Opinion was split as to whether or not geriatricians were ‘generalists’. As geriatrics was considered to be need-based rather than organ-based, it was viewed as some as being entirely generalist. Others thought that their training equipped them to care for a specific group of patients:
Geriatricians more than any other profession bring together the knowledge base that encourages and foster more generic identification of needs outside disciplinary-focussed care.
Senior clinical manager
I would not call a geriatrician a generalist. I’d call them a Geriatrician.
Senior doctor
Some viewed the essence of generalist working as being co-operative and collaborative, and focused on the co-ordination of care:
My tagline is that your role as a general physician is to make everyone else do their job, because it literally feels like you’re going down to the playground and dragging people to come home early to do scopes, to offer opinions, to get their arse into gear and actually do the job they applied to do.
Senior doctor
Systems as generalist or specialist
In discussions about generalism and specialism being properties of models of care or systems, there was a clear split between organisations who identified as having coherent models of care and organisations who did not identify as having coherent models of care. Interviewees from the former readily identified their organisations as being ‘generalist’, regardless of the model of care. Hospital K was one of the largest hospitals in the sample and operated a take triage system, properties otherwise associated with specialism, but it viewed itself as being highly generalist on the grounds that the acute work was equally divided among specialties on a daily basis. Interviewees at other organisations were able to locate their hospitals along a spectrum of ‘more generalist’, ‘hybrid’ or ‘more specialist’, but on prompting only. Clinicians at the smallest hospitals were more likely to identify their systems as ‘generalist’, regardless of the model of care.
Descriptive analysis of workforce
A descriptive analysis of the workforce data that were obtained throughout WP1, supplemented with NHS Digital workforce data,109 was undertaken.
Originally, this was intended to include the balance of work of specialists across the acute take, the wards, the outpatients and procedural work. However, we found that job plans were highly individualised and that it was not possible to obtain readily analysable data at the hospital level. Hence, this has not been included.
Here we present the key findings. More detail can be found in Report Supplementary Material 8, Section 8.
Staffing as a major challenge
A key finding of the telephone interviews was the scale of the staffing challenge that was faced by trusts. Staffing problems for junior medical staff are severe, described to us as a ‘nightmare’. Nearly all of the hospitals that were surveyed were dependent on locum staff to support their senior medical rotas. Proportional dependence on locum staff seemed to be greatest in the smallest hospitals.
Hospitals were trying to address these problems using a variety of means, including redesigning job roles, changing skill mix, offering recruitment incentives including ‘golden handshakes’ and international recruitment. However, the scale of the challange meant that few of the case study sites had fully addressed these problems. The capacity to recruit can be affected by the location and the dynamics within some clinical teams, in some cases acting as either a deterrent or an enabler.
Variation
There were stark variations in the number of medical staff, and non-medical staff in advanced roles, who were working within each of the medical specialties. For example, the number of respiratory physicians varied from one to 16 and the number of staff in elderly care medicine ranged from zero to 14. This variation is not fully explained by the size of a hospital, the number of patients or the case mix of patients (see Chapter 5).
In addition, there is nearly a three-fold variation in the number of junior medical staff per consultant, with the medical specialties going from 0.9 junior medical staff per consultant to 2.75 junior medical staff per consultant.
Balance between generalist and specialists
Most trusts had a comparatively low number of consultant medical ‘generalists’, including general medicine, acute physicians and geriatricians. Only five hospitals had > 60% ‘generalist’ doctors, as shown in Figure 16. The balance was different for junior medical staff.
FIGURE 16.
Percentage of generalist and specialist consultants by trust, smallest to largest.
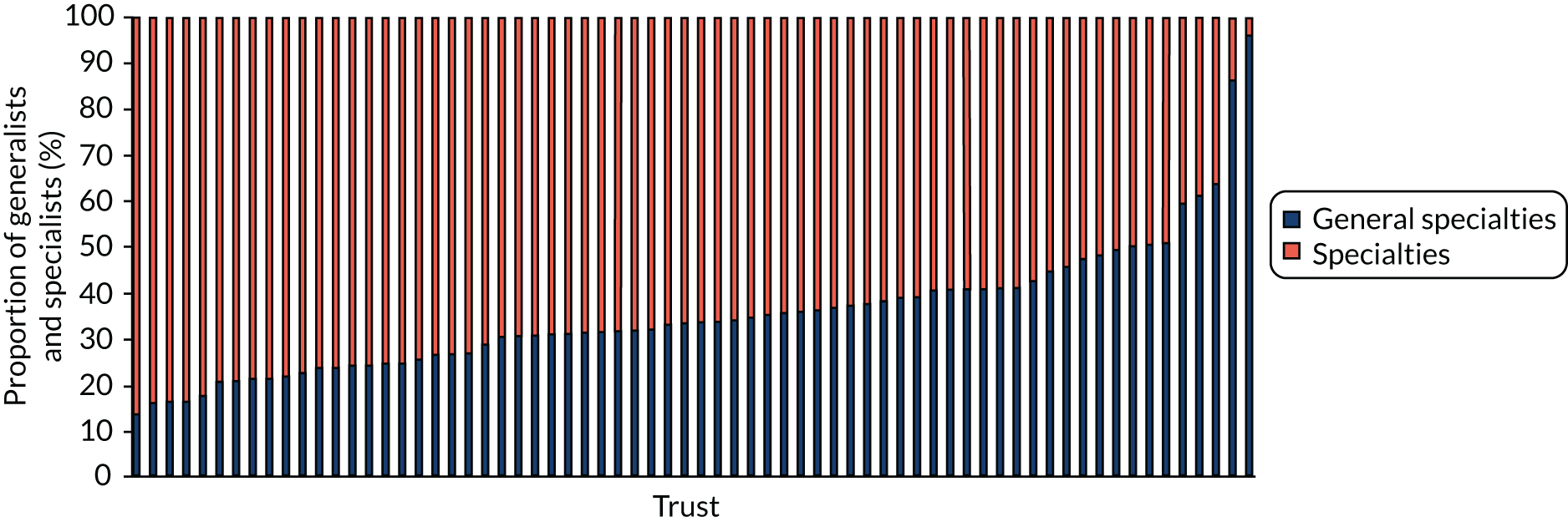
Management of the acute take
The number of consultants supporting the medical on-call rota varied significantly. On-call cover included specialists from respiratory medicine (90% of sites), geriatric medicine (84% of sites), endocrinology and diabetes (86% of sites) and acute medicine (65% of sites). A number of specialties have started to withdraw from the on-call rota. Some sites have insisted that their specialists do take part in the medical on-call rota.
Staffing ambulatory/emergency care
Ambulatory/emergency care was a service where generalists rather than specialists took the lead. Acute physicians provided clinical leadership for 75% of the ambulatory care services. In other sites this was provided by the ED, or exceptionally by specialty physicians.
Staffing the acute medical unit
The AMU was also a service where generalists rather than specialists took the lead. In 90% of sites an acute physician provided medical leadership for the AMU. The number of acute physicians employed by sites varied significantly. Many places had very few acute physicians in post (five or less), with heavy AMU commitments. One site had no acute physicians, preferring a model in which specialists provide cover to the AMU.
Ward responsibilities
Ward-based care was specialty led. In the majority of cases, patients would be managed by the specialist medical team responsible for their ward and would be reliant on the host ward calling in the appropriate advice. Only 12% of sites had specialists managing patients, irrespective of their location.
Outpatient and other commitments
We did not explore outpatient and other commitments in depth. It was clear from the interviews that there were some medical specialties for which the competing demands between inpatient work and outpatient work were a problem. The most notable was gastroenterology.
Support from other clinical staff
Increasingly, trusts are deploying staff in advanced non-medical roles; however, there was significant variation in the number of these non-medical roles across hospital sites (Figure 17).
FIGURE 17.
Maximum and average number of advanced non-medical roles by specialty.
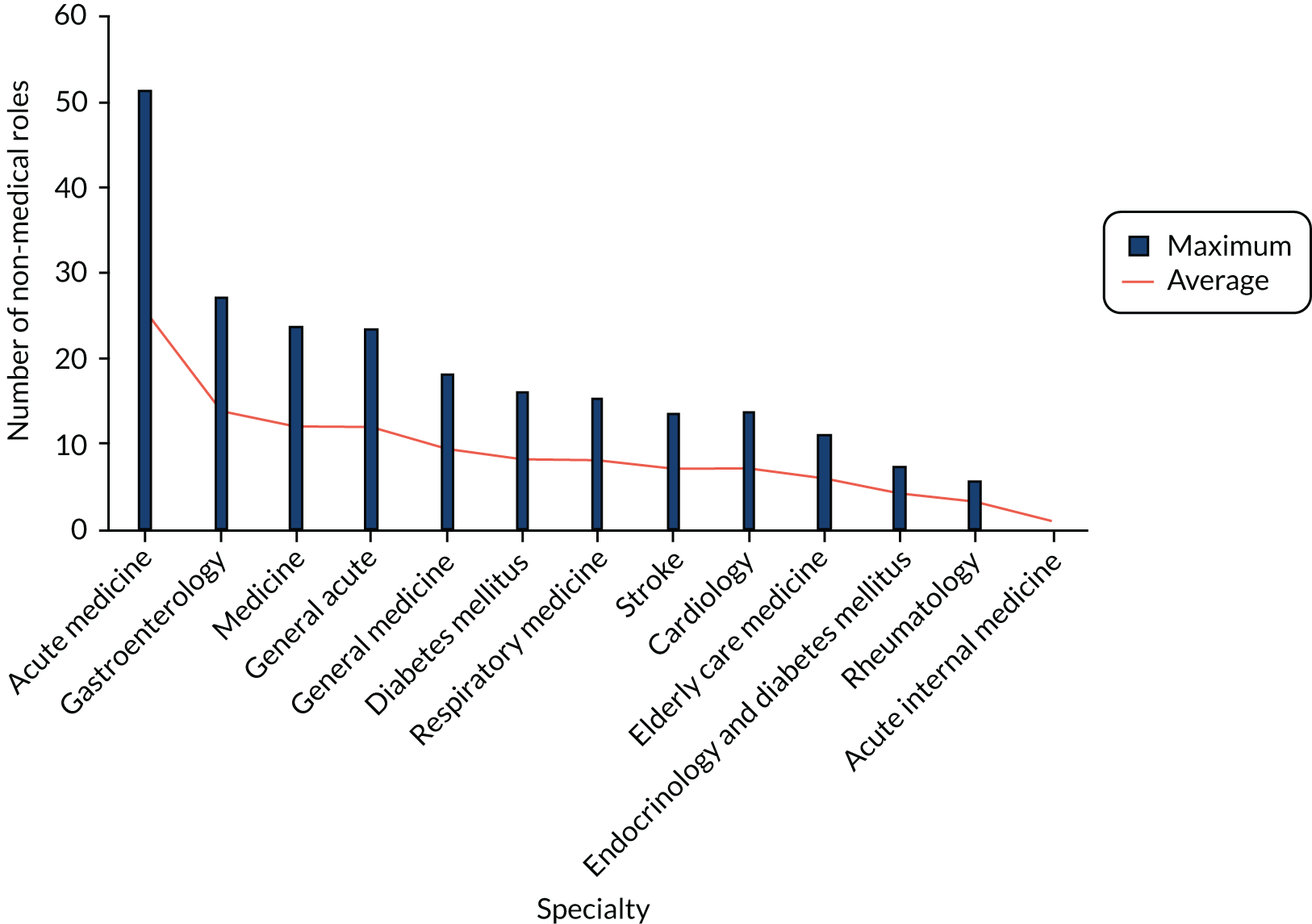
Summary
We found that emergency/acute care in smaller hospitals in England, rather than being uniform and predictable, was highly variable, complex and fluid, with patients frequently following fragmented pathways of care across multiple system components. The staffing of hospitals was highly variable, with most organisations reporting significant staff shortages. This made construction of a typology using a system approach difficult; instead, we focused on patterns of consultant working on the AMUs and the downstream wards. We were able to classify 48 hospitals according to the typology. We found 25 different models of care, with no more than four hospitals operating any one model of care and eight hospitals operating unique models of care. Generalist models of care were more common in very small and rural hospitals; beyond this, there were no associations found between models of care and other factors such as hospital size, number of emergency admissions or hospital location. Patterns of work in AMUs varied more than working on downstream wards. Telephone and case study interviews found that models of care were shaped by complex constellations of interacting factors of multiple levels. Important factors included hospital size and location, the ability to retain and recruit staff, organisational culture and leadership, and often competing policy imperatives. Negative consultant behaviours, such as ‘flight from the front door’ and ‘fortressing’, emerged as highly problematic. Models were also highly reactive, rather than proactive, and there were marked differences between models as conceived and models as enacted. Where there was evidence of strategic planning, this tended to be driven by single individuals operating at the service level, who were hindered or enabled by other factors at the hospital level. Hospitals with the most stable and mature models of care were those that planned at higher levels, had clear strategic aims to meet local community needs and fostered a collaborative working environment. We did not find any consistent definitions of, or boundaries between, generalist and specialist working, beyond a rough consensus that a limited number of patient groups with specific disease processes should belong to specialists. Instead, there was often a substantial distance between what clinicians thought systems of care should look like and their enaction. Within systems, there was evidence of the boundaries of medical working being almost constantly negotiated and renegotiated.
Chapter 5 Exploring case mix of acute medical care in smaller hospitals
Introduction
To compare different service models, account needs to be taken of possible differences in the types of patients treated, so we need some way to describe and compare the case mix of different hospitals. Therefore, the aims of this element of the study were to:
-
create a case-mix classification that identifies patients who may benefit from generalist care and use this to describe and compare workload, resource utilisation and outcomes between hospitals and models of care
-
assess the degree of alignment between patient case mix and medical generalist skill mix in smaller hospitals.
There are a number of case-mix descriptors that have been applied in UK hospital settings, ranging from classifications of disease110 or procedures, to more complex approaches that use a range of patient-level variables to identify homogenous patient groups,111 such as health-care resource groups (HRGs)112 and adjusted clinical groups,113 various risk-scoring methods114–116 and models to predict hospital admission. 117 Case-mix descriptors typically group together episodes of care that are mutually exclusive and exhaustive, so that they cover all cases. In creating such schemes, there is inevitably a degree of compromise, often driven by the limitations of the available data. 118
For this study, we needed a system whereby patients were grouped in ways that were representative of workload in generalist medical care. The need to compare case mix across hospitals meant having to rely on existing data sets that were common to many hospitals; the obvious candidate was HES. 119 The HES cover all English NHS hospitals and are based on summary electronic records from individual consultant episodes, which can be linked across hospital spells and across patient histories (using pseudonymised identifiers). The ability to link over time means that the analysis can exploit information about prior hospital activity before an admission spell, as well as track subsequent events, such as re-admission. Although the data sets have faults,120,121 these are the only data sets that allow consistent comparison across hospitals. The HES data set records individual episodes of care that can be linked into spells of admission and longer patient histories.
For the definition of case mix there are a number of options that we could have adopted. The use of standardised diagnostic classifications in the form of International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10),122 and therapeutic procedure coding has been the standard in HES. In addition, in the UK we have a system of case-mix classification that is used for hospital funding, which is based on HRGs. 123 The problem with using these classification schemes for this study was that:
-
they used a large number of groups (e.g. 10,000 ICD-10 codes, 2782 HRGs124), which meant many groups had few cases and were more difficult to use as descriptors of activity
-
health-care resource groups and procedure codes also included elements of the treatment received, so could be influenced by hospital treatment choices
-
they were not considered clinically meaningful in describing the case mix for acute generalist medical care.
Therefore, we required a case-mix descriptor that:
-
was tailored to the requirement to describe general medical workload and smaller hospitals
-
had a manageable number of categories
-
was considered clinically relevant
-
captured broadly similar care processes – as indicated by the ability to ‘explain’ patterns of bed use
-
was comprehensive in that it captured all cases.
The following sections briefly describe the work to derive the case-mix descriptor and its application to look at acute inpatient emergency medical workload in smaller hospitals. More details are available in Report Supplementary Material 8.
Overview of methods
Creating and testing the classification
In brief, creating and testing the classification followed the following stages:
-
defining a working data set of 1.9 million care episodes based on acute medical emergencies that were admitted under the care of a defined set of treatment specialties
-
creating an initial classification of broad diagnostics groups that sought to identify high-number common cases
-
testing the affect of a range of secondary diagnostic characteristics and prior history variables
-
working with a group of clinicians to test the face validity of the groups and use their input to refine the scheme
-
finalising the model and comparing the explanatory power in terms of the reduction in variance in length of stay, including a comparison to HRGs.
Describing inpatient case mix in acute medicine
The case-mix classification was then used to describe case mix at the hospital level, in terms of the number of episodes of care within a given time period, the number of admitting spells and the total bed-days. We also estimated the average number of admissions on any single day (based on average episodes of care per day) and estimated the number of beds occupied by any one case type. Other features of episodes were also noted, including the proportion of short-stay cases, where stays lasted 0 or 1 day, and the proportion of patients aged > 75 years.
We undertook a range of analyses to explore:
-
Changes in case mix over time (see Report Supplementary Material 8, Section 5). Changes over time were examined by using the data for successive years, from 2012–13 to 2017–18.
-
Differences in case mix between providers (see Report Supplementary Material 8, Section 4). Each of the 69 hospitals had its own profile of case types; however, we can also summarise similarities and differences into single metrics, such as the proportion of cases falling into the most common case-mix groups (CMGs). We also calculated some measures of case-mix complexity based on weighting activity in each case-mix group by the overall average stay length.
-
Differences in underlying admission rates at the population level (see Report Supplementary Material 8, Section 4). We undertook this analysis to assess the degree of variation in the underlying needs for acute emergency medical care between geographic areas. 125 To do this, we used data from all hospitals at the hospital-spell level. The analyses used data from 2017–18 and related those to ONS population estimates from 2016126 of 326 local authority areas.
-
Differences in average LOS in hospitals (see Report Supplementary Material 8, Section 5.5). We compared the aggregated LOS at the hospital level with the impact of case mix on this value. This used a technique advocated by Fetter et al. 111 in their original paper on the creation of HRGs, which was based on a technique described by Kitagawa. 127
-
Pathways through the hospital (see Report Supplementary Material 8, Section 6). The analysis of the consistency of treatment specialties for the case types explored handovers between specialties within a given spell of care, focusing on a small number of tracer conditions. The pathways of care were defined using spell-level data from all of the smaller hospitals in the cohort. Pathways of care for individual trusts were examined to consider the extent to which they were similar or different from the pattern exhibited across the set of smaller hospitals as a whole.
Chapter 7 describes the patterns of mortality and re-admission that are associated with case-mix groups and explore the relationship to hospital typology.
Comparing the case mix according to organisation of general medical services
For this we looked at two key features:
-
The differences in case mix associated with acute medical typology (see Report Supplementary Material 8, Section 9). We looked for a major difference in case mix associated with the hospital typologies that were identified in Chapter 4. We considered a range of basic descriptors, including number of cases, lengths of stay and case-mix complexity.
-
The relationship between inpatient case mix and medical skill mix (see Report Supplementary Material 8, Section 9). In this section, we looked at whether or not there are observable relationships between the numbers of ‘specialist consultants’ within a hospital and the mix of cases seen in acute medical workload, using information on the medical workforces from NHS Digital. We used a variety of tests to explore the relationships for the overall proportion of generalists and four specialty groups: respiratory medicine, cardiology, gastroenterology and care of the elderly.
Further details of the methodology are given in Report Supplementary Material 8.
Summary findings
Basic case-mix classification
The case-mix classification was derived from a data set covering 1.9 million records from acute medical specialties in a subset of 69 smaller hospitals. The final classification consisted of 82 base CMGs, most of which were defined in terms of diagnostic criteria. The nine groups that described cancer workload were created on a more complex basis by combining information regarding prior episodes of care, treatment recorded and cancer diagnoses.
In addition to the base CMGs, additional flags were created to split these, where necessary, according to:
-
A frailty flag. In our analysis of reduction in variance we had found that applying a basic flag indicating potential ‘frailty’ proved better than age at explaining differences in the LOS and was also felt to be more clinically meaningful. There are a number of approaches to measuring frailty. 128–131 We tested two alternatives,132,133 which produced similar results. We opted for the one that had slightly higher reductions in variance.
-
A procedure flag. One of the issues raised in our workshops was that the clinical perception of a patient often revolves around whether or not there was some procedure undertaken, usually diagnostic. Empirically, this was seen to be a large influence on resource use.
-
Cancer as a secondary diagnosis. One of the problems raised by our clinical groups was the challenge of distinguishing what were the most important diagnoses influencing care. We used the principal diagnosis to drive our schemes, although we recognised that in some cases that could potentially be misleading, such as a patient admitted with pneumonia but who also has lung cancer. Sometimes the principal diagnosis may not be the most important one influencing treatment and care. This was felt to be particularly problematic for people with a cancer diagnosis. Therefore, we added a flag to see if any of the secondary diagnostic field include cancer, as this might be driving an atypical pattern of resource use.
If all variables were used, there were a total of 328 permutations, which is still less than the number of HRGs. Table 12 summarises the reduction in variance in LOS that was associated with different combinations of variables. The descriptive analysis predominantly used the diagnostic groupings at the episode level, with secondary variables being used for sensitivity testing. For some analyses of overall hospital length of stay, we used classifications based on the first episode of the hospital spell.
| Description | Groups | Reduction in variance (%) |
|---|---|---|
| CMGs diagnostic groups | 82 | 12.1 |
| CMGs plus flag for secondary diagnoses | 161 | 13.0 |
| CMGs plus flag for procedure yes/no | 164 | 23.0 |
| CMGs plus flag for age > 75 years split | 164 | 15.9 |
| CMGs plus flag for frailty (Nuffield) | 164 | 20.2 |
| CMGs plus flag for frailty (Imperial) | 164 | 17.9 |
| CMGs plus flags for procedure plus frailty (Nuffield) | 328 | 30.8 |
| HRGs | 969 | 28.6 |
Case-mix episodes in acute medicine
Table 13 summarises the 25 most common base CMGs seen across the subset of 69 smaller hospitals. Figure 18 relates these conditions to the use of occupied beds (average of average across the 69 hospitals). There was a high concentration of cases in a relatively small number of diagnostic groups. The most common grouping J3 Pneumonia (aspiration) and LRTI and pneumonitis due to solids and liquids accounts for 12% of all cases and approximately 16% of all bed-days. Approximately 80% of all care episodes and 75% of all bed-days fall into just 31 groups (full details can be found in Report Supplementary Material 8). Table 13 also includes estimates of the typical number of admissions per day linked to that group, and the estimated number of beds that might be occupied on any one day.
| Case-mix group | Number of episodes | Percentage of cases | Percentage of bed-days | Beds (average beds per day per smaller hospital) | Admissions (beds in the average smaller hospital divided by 365) |
|---|---|---|---|---|---|
| J3 Pneumonia (aspiration) and LRTI and pneumonitis due to solids and liquids | 233,311 | 11.9 | 16.26 | 43.2 | 9.3 |
| N3 Other genitourinary and retention of urine | 102,558 | 5.2 | 7.39 | 19.6 | 4.1 |
| R1 Pain in throat and chest | 94,436 | 4.8 | 0.90 | 2.4 | 3.7 |
| J4 Chronic lung disease including COPD | 90,467 | 4.6 | 4.34 | 11.5 | 3.6 |
| I8 Conduction disorder, tachycardia arrhythmias atrial fibrillation and abnormalities of heart beat | 66,612 | 3.4 | 2.18 | 5.8 | 2.6 |
| R4 Signs/symptoms not elsewhere classified | 59,427 | 3.0 | 1.67 | 4.4 | 2.4 |
| M1 Joints | 56,788 | 2.9 | 2.26 | 6.0 | 2.3 |
| I9 Heart failure and pulmonary oedema | 53,876 | 2.8 | 4.13 | 11.0 | 2.1 |
| G4 Transient ischaemic attacks and dizziness and giddiness | 52,549 | 2.7 | 1.16 | 3.1 | 2.1 |
| I3 Acute myocardial infarction | 50,620 | 2.6 | 2.65 | 7.0 | 2.0 |
| I10 Cerebrovascular haemorrhages/stroke/cerebral infarction | 50,452 | 2.6 | 5.89 | 15.7 | 2.0 |
| R2 Skin and cellulitis | 50,333 | 2.6 | 2.69 | 7.1 | 2.0 |
| T1 Poisoning | 42,955 | 2.2 | 0.71 | 1.9 | 1.7 |
| A1 Intestinal infections and nausea and vomiting | 42,185 | 2.2 | 1.81 | 4.8 | 1.7 |
| R3 Abnormalities of gait and mobility | 42,098 | 2.2 | 2.53 | 6.7 | 1.7 |
| S1 Head injury | 41,836 | 2.1 | 1.26 | 3.4 | 1.7 |
| K6 Other digestive and dysphagia | 40,153 | 2.1 | 1.59 | 4.2 | 1.6 |
| N1 Acute kidney disease and chronic kidney disease | 40,078 | 2.1 | 2.50 | 6.6 | 1.6 |
| A2 Septicaemia | 38,580 | 2.0 | 2.84 | 7.5 | 1.5 |
| G3 Migraine and headache | 31,797 | 1.6 | 0.46 | 1.2 | 1.3 |
| K2 Crohn’s disease and other intestinal diseases | 31,230 | 1.6 | 1.64 | 4.4 | 1.2 |
| K1 Oesophagitis and ulcers of the digestive system and gastritis | 29,979 | 1.5 | 0.96 | 2.6 | 1.2 |
| J8 Other respiratory and haemorrhage from respiratory passages and cough and abnormalities of breathing | 26,657 | 1.4 | 0.74 | 2.0 | 1.1 |
| G2 Epilepsy and convulsions, not elsewhere classified | 26,189 | 1.3 | 0.89 | 2.4 | 1.0 |
| E5 Volume depletion and other fluid disorders | 26,057 | 1.3 | 1.23 | 3.3 | 1.0 |
| Total | 1,954,933 | 100 | 100 | 266 | 78 |
FIGURE 18.
Approximate use of occupied beds for acute emergency medical admissions (excluding short stay) for 2017/18. Full codes and code titles are presented in Table 13. LRTI, lower respiratory tract infection.
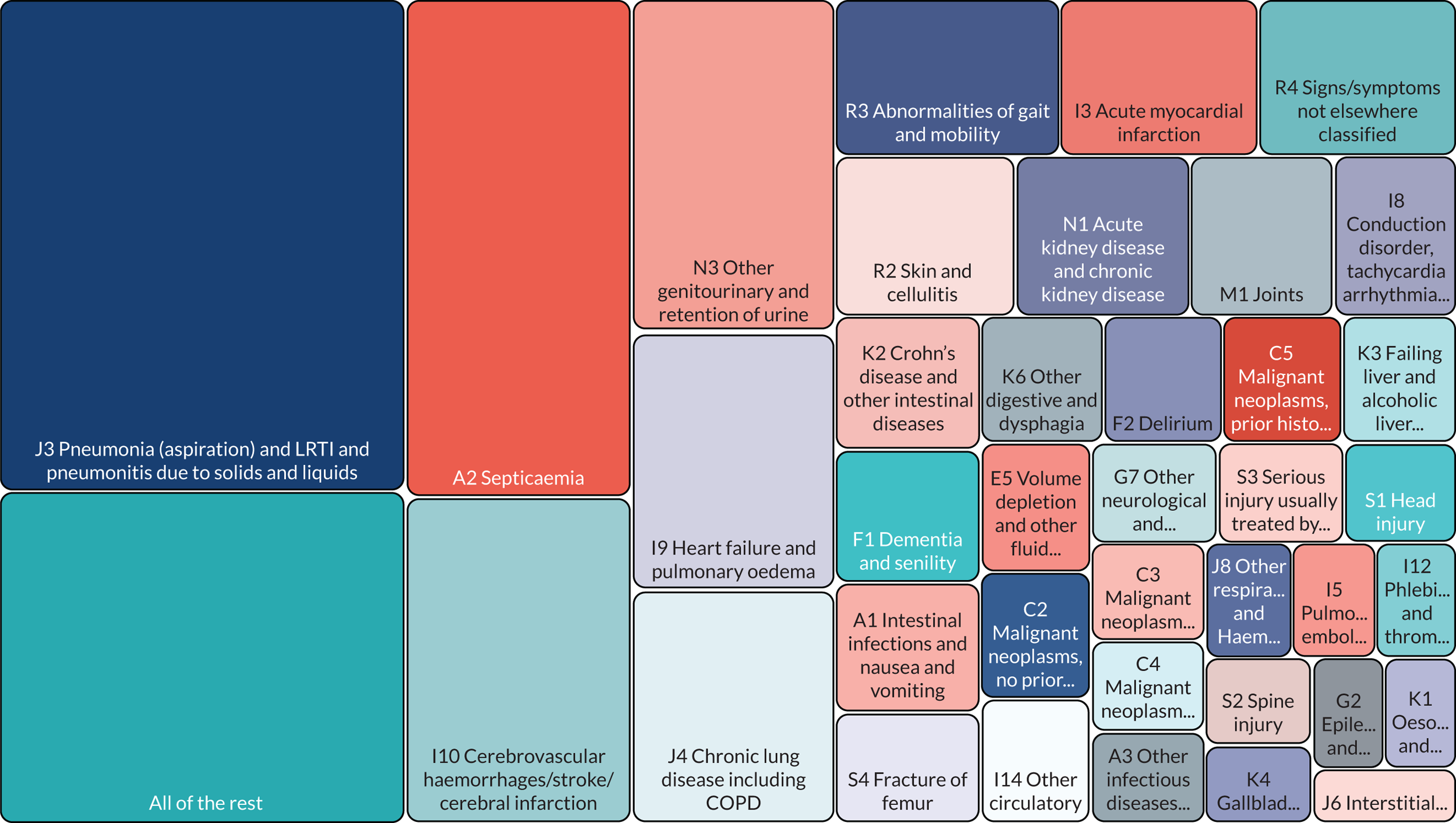
An average across all 69 hospitals suggests that the acute emergency medical caseload in a typical smaller hospital consists of:
-
78 episodes per day
-
266 occupied beds at any one time
-
145 occupied beds were short stays of < 2 days
-
121 occupied beds were longer stays (≥ 2 days).
In total, 27% of cases had some form of procedure and 31% of cases had an indication of frailty. Around 51% of all cases had neither a procedure nor a frailty flag. The presence of either a frailty flag or a procedure was associated with much longer lengths of stay. For example, for the simplest cases (i.e. no frailty flag or procedure) the average episode length was 1.8 days, whereas for the 8.6% of cases which had both a frailty flag and a procedure, the average episode length was 9.1 days. The average length of episode for cases with a secondary cancer diagnosis was longer than cases with no cancer diagnoses, but less than for episodes with a primary diagnosis of cancer.
In exploring the characteristics of the case-mix grouping, we looked at the level of variability between geographic areas and the extent to which such variability might be explained by local demographic factors (see Report Supplementary Material 8). At the CMG level, the groups with the least variability [standard deviation (SD) < 0.26] represent groups in which the underlying incidence of the disease was more constant and less influenced by differences in disease prevalence, the accessibility of services or the vagaries of hospital recording systems. Although some groups that varied considerably are clearly linked with differences in local population needs, such as sickle cell disease, others are harder to explain.
Changes in case mix over time
Overall, there was a 26% increase in the total number of emergency medical episodes between 2012–13 and 2017–18, from 1,703,783 cases to 2,155,126 cases; the average yearly increase in the number of episodes was 5% (range 4–6%). There was a 19% increase in the total number of spells across a comparable time-period. The number of short-stay episodes (0–1 days) increased by 34% and the number of long-stay episodes by 18%.
Length of stay declined at both episode level and spell level between 2012–13 and 2017–18. Average episode-level LOS declined by 0.71 days, from 4.12 days to 3.41 days. Average spell-level LOS fell by 0.73 days, from 6.52 days to 5.79 days. Table 14 shows the total number of episodes, spells and LOS, by year.
| Year | Total number of episodes | Number of short-stay cases | Total number of episodes (excludes short-stay episodes) | Bed-days | Average episode-level stay | Average episode-level LOS (excluding short stays) |
|---|---|---|---|---|---|---|
| 2012–13 | 1,703,783 | 924,983 | 778,800 | 7,019,586 | 4.1 | 7.5 |
| 2013–14 | 1,766,171 | 968,274 | 797,897 | 7,082,346 | 4.0 | 7.4 |
| 2014–15 | 1,868,511 | 1,023,029 | 845,482 | 7,193,767 | 3.9 | 7.2 |
| 2015–16 | 1,954,933 | 1,091,738 | 863,195 | 7,291,900 | 3.7 | 7.1 |
| 2016–17 | 2,057,845 | 1,152,778 | 905,067 | 7,490,556 | 3.6 | 7.0 |
| 2017–18 | 2,155,126 | 1,237,581 | 917,545 | 7,348,980 | 3.4 | 6.7 |
| Increase | 26% | 34% | 18% | 5% | –17% | –11% |
Some groups showed a particularly large change in LOS, including septicaemia and pneumonia, most probably related to coding practices. A few groups decreased in number, with the most marked changes in absolute terms for I2 Angina pectoris and dyspepsia, R1 Pain in throat and chest and G4 Transient ischaemic attacks and dizziness and giddiness. Some of these changes in presentation, such as for cardiovascular conditions, may be the results of deliberate changes in the referral pathways for selected conditions.
Analysis of changes in the distribution of case types at individual trust level showed that of the 69 hospital trusts, only three showed significant changes in their case-mix distribution over time (p < 0.01 was used to allow for multiple tests across 69 trusts). Although the case mix in diagnostic terms remained fairly stable, there were other indications of changes during this period. A number of groups showed a marked increase in cases aged > 74 years, despite the fact that the average age remained fairly consistent across the time period. The proportion of cases flagged as ‘frail’ also increased from 2015–16 to 2017–18.
Differences in acute medical inpatient case mix between trusts
We used a number of approaches to summarise the case-mix complexity within an individual hospital. One approach was to study the proportion of cases that fell into the 10 or 20 most common CMGs. Table 15 summarises the results, showing the trusts with highest and lowest values. Homerton University Hospital NHS Foundation Trust appears to be an outlier, which was a result of a high number of cases in one particular group (D2 Sickle cell disorders). If Homerton University Hospital NHS Foundation Trust is excluded, the proportion of cases falling in the top 20 CMGs shows little variation: the range is from 65% in Poole Hospital NHS Foundation Trust to 70% in Burton Hospitals NHS Foundation Trust.
| HES code and trust | Top 10 CMGs (%) | Top 20 CMGs (%) |
|---|---|---|
| RQX Homerton University Hospital NHS Foundation Trust | 34.6 | 55.8 |
| RD3 Poole Hospital NHS Foundation Trust | 40.0 | 65.4 |
| RKE Whittington Health (The Whittington Hospital NHS Trust) | 40.4 | 62.7 |
| RDE Colchester Hospital University NHS Foundation Trust | 40.9 | 65.2 |
| RAS The Hillingdon Hospitals NHS Foundation Trust | 41.3 | 63.4 |
| RBL Wirral University Teaching Hospital NHS Foundation Trust | 41.4 | 64.8 |
| RGN Peterborough and Stamford Hospitals NHS Foundation Trust | 41.6 | 67.7 |
| RA2 Royal Surrey County Hospital NHS Foundation Trust | 41.6 | 65.2 |
| RA3 Weston Area Health NHS Trust | 48.0 | 70.4 |
| RC9 Luton and Dunstable University Hospital NHS Foundation Trust | 48.1 | 68.8 |
| RAX Kingston Hospital NHS Foundation Trust | 48.5 | 68.9 |
| RE9 South Tyneside NHS Foundation Trust | 48.7 | 68.1 |
| RFR The Rotherham NHS Foundation Trust | 49.5 | 69.4 |
| RNA The Dudley Group NHS Foundation Trust | 49.7 | 70.0 |
| RNQ Kettering General Hospital NHS Foundation Trust | 50.6 | 69.0 |
| RJF Burton Hospitals NHS Foundation Trust | 51.2 | 69.7 |
The consequences of differences in a case-mix profile can also be expressed in terms of the affect of different case types on the demand for beds. We applied a simple case mix-specific weighting based on the ratio of the group average length of episode to the hospital-specific case mix, to calculate an expected number of bed-days that arise from the particular mix of cases. Values of this ratio greater than 1 indicate a case-mix profile that is expected to require more beds than average, and in these terms, be more complex. Note that this approach does not equate to a measure of complexity in clinical terms, for example acuity, risk of death or costs.
The results suggest that when a simple diagnostic standardisation is used, the complexity ratio ranges from 0.92 to 1.14, and most hospitals sit within a range of ± 5% of the average. Overall, these results indicate that there is relatively little variation. Table 16 shows the hospitals at either end of this range.
| HES code and trust | Episodes | Length of episode | Bed needs complexity |
|---|---|---|---|
| RQX Homerton University Hospital NHS Foundation Trust | 21,245 | 3.2 | 0.92 |
| RAS The Hillingdon Hospitals NHS Foundation Trust | 15,423 | 4.3 | 0.92 |
| RC9 Luton and Dunstable University Hospital NHS Foundation Trust | 37,422 | 3.3 | 0.94 |
| RBT Mid Cheshire Hospitals NHS Foundation Trust | 32,936 | 3.0 | 0.94 |
| RJ6 Croydon Health Services NHS Trust | 34,710 | 3.0 | 0.95 |
| RA3 Weston Area Health NHS Trust | 15,468 | 3.7 | 1.07 |
| RTK Ashford and St Peter’s Hospitals NHS Foundation Trust | 21,941 | 4.2 | 1.09 |
| RDD Basildon and Thurrock University Hospitals NHS Foundation Trust | 26,538 | 5.5 | 1.09 |
| RLQ Wye Valley NHS Trust | 19,378 | 3.9 | 1.09 |
| RGP James Paget University Hospital NHS Foundation Trust | 18,726 | 4.3 | 1.11 |
| R1F Isle of Wight NHS Trust | 9726 | 5.5 | 1.14 |
Differences in average length of stay in hospitals
The average length of stay in hospital is best summarised in terms of the whole spell length rather than individual episodes of care. The unstandardised average lengths of stay in 2017–18 across all hospitals was 5.2 days and ranged from 8.4 days (Isle of Wight NHS Trust) and 8.1 days (East Cheshire NHS Trust) to 2.8 days (Torbay and South Devon NHS Foundation Trust) and 2.55 days (Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust). The proportion of short-stay episodes had a strong effect on average stay lengths. Figure 19 shows that the average length of stay excluding the short-stay cases was usually around 2–3 days longer.
FIGURE 19.
Average length of stay of spell with (vertical) and without (horizontal) short-stay cases (data from 2017/18).
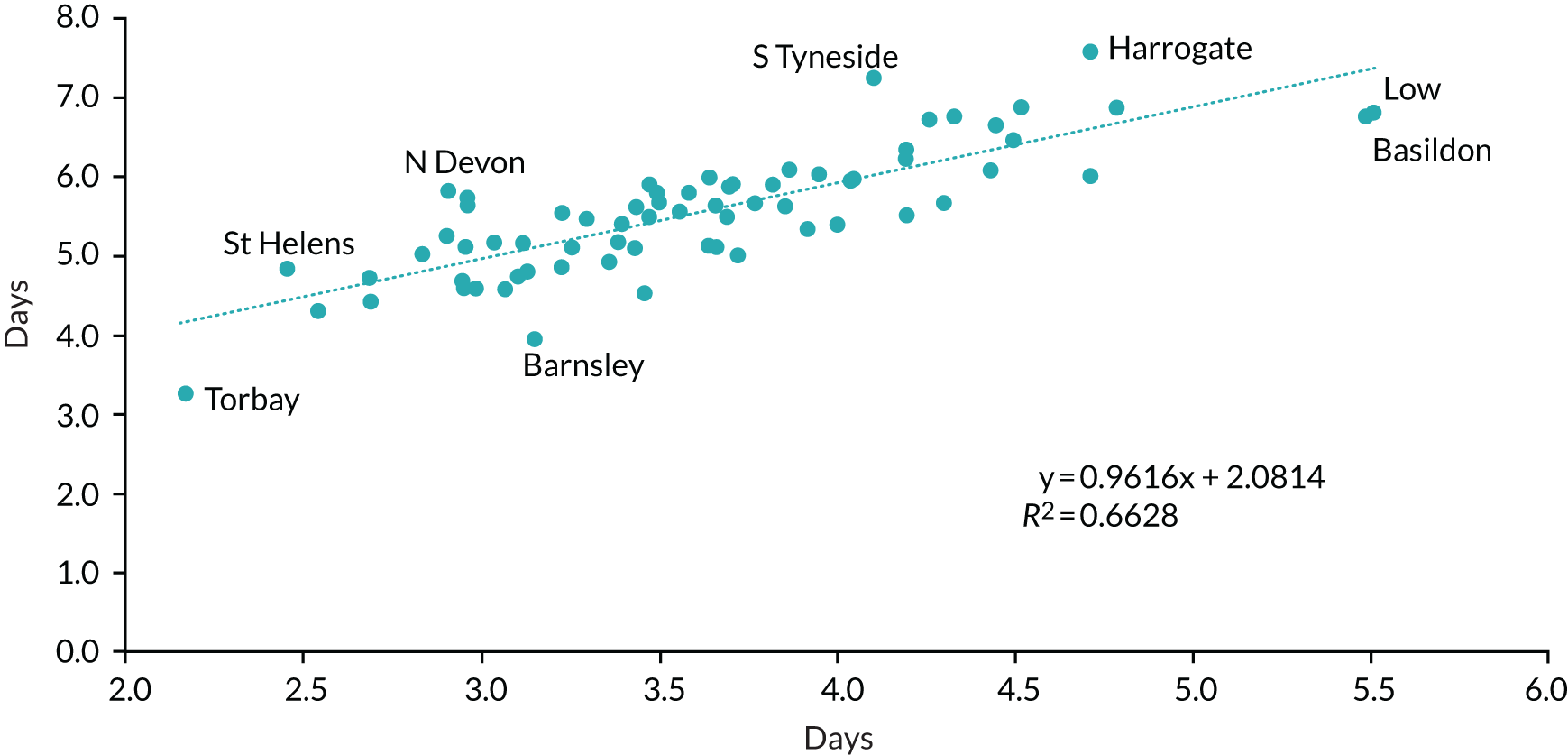
To quantify the effects of case mix on the aggregated length of stay, we split the differences in the group-average LoS into three components: (1) the effects of case mix, (2) the effect of within case-type stay length and (3) the interaction between these (see Report Supplementary Material 8). For this analysis we also included frailty flags to indicate something about patients whose prior history indicated greater needs, which, in turn, may be a reflection of stay length.
Table 17 summarises findings for the hospitals that had the longest and shortest average LOS. It appears that in most of the hospitals, the within case-type LOS effect is greater than the case mix itself; hospitals tend to exhibit lower than average stay length across all or most case types. For most of these hospitals, the case-mix elements are also negative in effects – indicating that these hospitals have slightly fewer than expected case types where you might expect a longer LOS, that is a less demanding (in bed terms) case mix. The exceptions are Southend University Hospital NHS Foundation Trust (where the case mix is more demanding) and Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust where there is little effect due to LOS.
| Hospital | Length of stay (days) | Difference from group mean | Owing to case mix | Owing to length of stay | Interaction |
|---|---|---|---|---|---|
| Shortest stay length | |||||
| RAJ Southend University Hospital NHS Foundation Trust | 4.36 | –0.88 | 0.47 | –0.98 | –0.45 |
| RQX Homerton University Hospital NHS Foundation Trust | 4.33 | –0.91 | –0.32 | –0.25 | –0.29 |
| RFS Chesterfield Royal Hospital NHS Foundation Trust | 4.30 | –0.94 | 0.08 | –0.88 | –0.15 |
| RDZ The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust | 4.26 | –0.97 | –0.83 | –0.02 | 0.07 |
| RBN St Helens and Knowsley Hospitals NHS Trust | 4.26 | –0.98 | –0.17 | –0.64 | –0.14 |
| RRF Wrightington, Wigan and Leigh NHS Foundation Trust | 4.19 | –1.05 | 0.04 | –0.98 | –0.07 |
| RCX The Queen Elizabeth Hospital, King’s Lynn, NHS Foundation Trust | 4.14 | –1.10 | –0.38 | –0.54 | 0.03 |
| RBT Mid Cheshire Hospitals NHS Foundation Trust | 4.01 | –1.23 | –0.22 | –0.97 | 0.01 |
| RJF Burton Hospitals NHS Foundation Trust | 3.93 | –1.30 | –0.34 | –0.94 | 0.17 |
| RA9 Torbay and South Devon NHS Foundation Trust | 2.80 | –2.43 | –0.44 | –1.76 | 0.15 |
| Longest stay length | |||||
| R1F Isle of Wight NHS Trust | 8.41 | 3.17 | 1.23 | 2.34 | –0.39 |
| RJN East Cheshire NHS Trust | 8.07 | 2.83 | 0.77 | 1.94 | 0.17 |
| RLT George Eliot Hospital NHS Trust | 7.27 | 2.04 | 0.99 | 1.13 | –0.08 |
| RLQ Wye Valley NHS Trust | 7.04 | 1.80 | 0.36 | 1.47 | –0.02 |
| RTP Surrey and Sussex Healthcare NHS Trust | 6.65 | 1.42 | 0.69 | 0.77 | 0.03 |
| RJR Countess of Chester Hospital NHS Foundation Trust | 6.55 | 1.32 | 0.10 | 1.21 | 0.00 |
| RD8 Milton Keynes University Hospital NHS Foundation Trust | 6.52 | 1.28 | 0.64 | 0.71 | –0.03 |
| RNZ Salisbury NHS Foundation Trust | 6.46 | 1.23 | –0.03 | 1.36 | –0.09 |
| RA3 Weston Area Health NHS Trust | 6.46 | 1.23 | 0.65 | 0.81 | –0.14 |
| RVY Southport and Ormskirk Hospital NHS Trust | 6.36 | 1.12 | 0.00 | 1.24 | –0.02 |
Looking at the hospitals where the average length of episode is longer than elsewhere (see Table 17), it seems that the case-mix element is more marked in these hospitals, with effects on average lengths of stay of plus 1.2 days at the Isle of Wight NHS Trust and plus 0.99 days at George Eliot Hospital NHS Trust. However, the LOS effect was generally large and positive and, in most cases, greater in magnitude than the case-mix effect. Therefore, the implication is that although these hospitals may have a case mix that would suggest longer lengths of stay, the stay lengths within groups are still longer than average. This was a relatively small difference compared with the lengths of stay within case types.
Figure 20 shows the effect of the two elements plotting the size of each element for each hospital moving from shortest to longest LOS. Figure 20 shows that as you move from shortest to longest stay length hospitals, the case-mix elements generally stay in a band of ± 0.5 days; however, the LOS element swings more dramatically and is clearly far more important in ‘explaining’ differences in the aggregate stay lengths. Aside from the extremes, there are some trusts that appear atypical in that they have a positive case-mix effect but negative lengths of stay – these are Ashford and St Peter’s Hospitals NHS Foundation Trust, Mid Essex Hospital Services NHS Trust and Southend University Hospital NHS Foundation Trust.
FIGURE 20.
The LOS and case-mix components for individual hospitals standardised using CMG and frailty (sorted by aggregate average LOS: longest LOS on right).
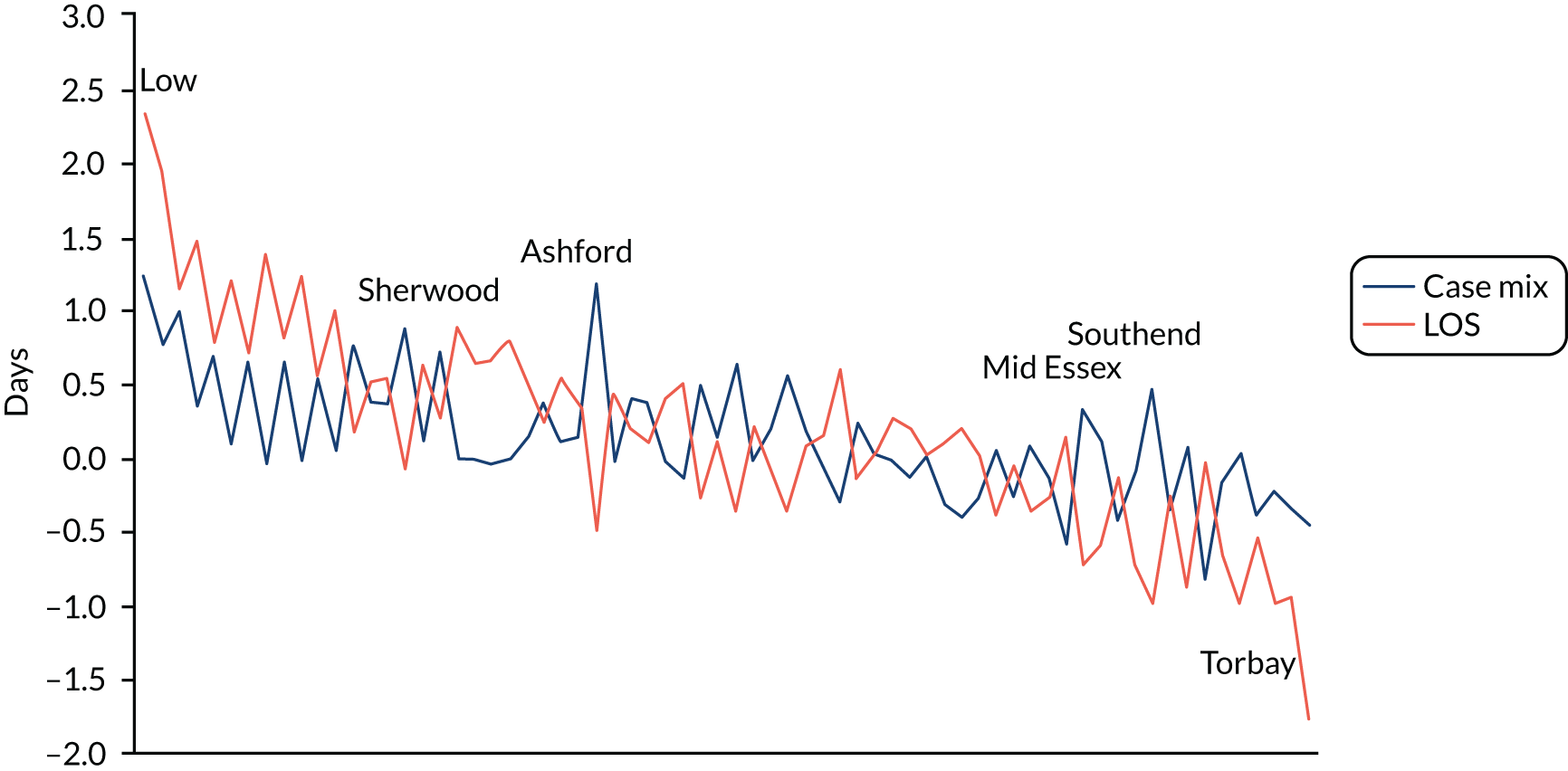
Pathways through the hospital
Tracer conditions were selected to test and document pathways of care on the basis of sufficient case number and clinical knowledge of pathway variation. Analysis of pathways of care at an overall level showed that for all of our tracer conditions, the most common pathway of care was a single episode spell under general medicine. The results also show, as might be expected, that where patients are treated under geriatric medicine, average lengths of stay tended to be longer, most likely a result of more complex case presentation and/or increased levels of frailty as individuals age.
We suggest that there are three key points to note:
-
There was heterogeneity in the pathways within the same basic diagnostic group.
We noted that there were no simple patterns describing the specialties within a diagnostics group. As an example, Table 18 shows the most common patterns for one CMG, I9 Heart failure and pulmonary oedema. Across all of the groups that we looked at, there was considerable variation in the pathways adopted (see Report Supplementary Material 8, Section 6). At a trust level, on average, 41% (range 15–95%) of spells for I9 Heart failure and pulmonary oedema were managed under ‘other pathways’, that is they were not categorised under the top five pathways of care.
| Pathway | General medical treatment specialties | Episode 1 (average episode length) (days) | Episode 2 (average episode length) (days) | Number of spells | Average LOS | Average patient age (years) | Percentage of patients classified as frail (%) |
|---|---|---|---|---|---|---|---|
| 1 | General medicine | 2.80 | 6334 | 2.80 | 78 | 27 | |
| 2 | General medicine – general medicine | 2.02 | 5.64 | 3427 | 7.66 | 80 | 38 |
| 3 | General medicine – cardiology | 2.06 | 8.04 | 3155 | 10.10 | 76 | 28 |
| 4 | General medicine – geriatric medicine | 2.06 | 8.52 | 1626 | 10.59 | 86 | 52 |
| 5 | Cardiology | 7.66 | 1202 | 7.66 | 74 | 24 |
-
There were large differences in patterns of bed use linked with the pathways.
Table 18 shows that patients seen in a single care episode in general medicine had an average LOS approximately 5 days shorter than any of the other top five pathways of care. This would fit with a model whereby short-stay patients were retained under the acute physician along with some other patients who are kept on the AMU for clinical reasons (e.g. infection control). There are indications of patient differences linked to the pathway; for example, the average patient age was highest (86 years) under pathway 4 (general medicine – geriatric medicine) and was lowest (74 years) under pathway 5, where patients received a single episode of care under cardiology.
-
There were large differences between trusts in the range of pathways.
When we examined the patterns at trust level, it became apparent that even within trusts the distribution of different pathways was complex. Figure 21 summarises the pathways used in different trusts for chronic lung disease and COPD, looking at the most common six pathways, with the remainder categorised as ‘other pathways’. Spells falling under ‘other pathways’ ranged between 6% in Rotherham NHS Foundation Trust and 91% in Royal Surrey County Hospital NHS Foundation Trust.
FIGURE 21.
Differences between trusts in pathways used for J4 Chronic lung disease, including COPD: trusts with the five highest and five lowest percentages of spells managed under other pathways.
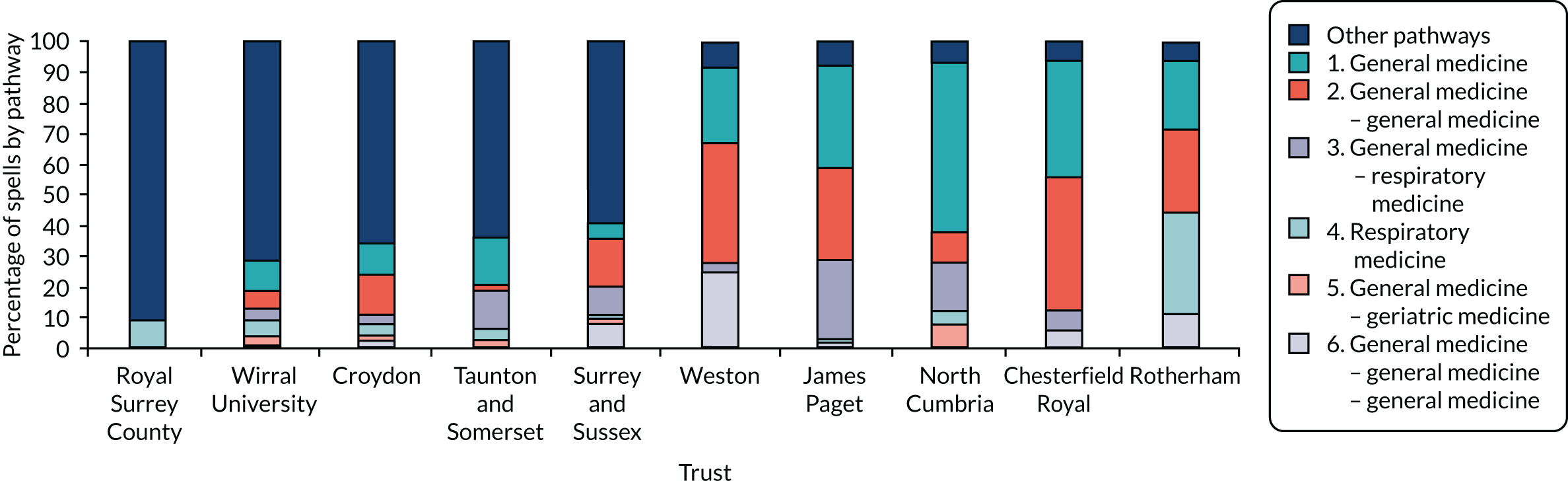
Differences in case mix associated with acute medical typology
We compared the case-mix characteristics of hospitals classified using the four attributes of the typology (described in Chapter 7) to test for any major differences between hospital subtypes. The analysis was based on a subset of 46 hospitals for which we had a typology and data on case mix from HES. Table 19 summarises some basic characteristics of the hospitals according to the four dimensions in our typology.
| Typology | Number of trusts | Proportion short-stay cases (%) | Length of episode (all cases) | Length of episode (excluding short stay) | Percentage of patients aged > 74 years (%) | Case-mix complexity | % frail hosp avg (%) |
|---|---|---|---|---|---|---|---|
| AMU1: openness | |||||||
| Closed | 18 | 56.8 | 3.2 | 5.0 | 47.7 | 1.02 | 32.29 |
| Open | 8 | 54.9 | 3.5 | 5.5 | 50.2 | 1.02 | 34.96 |
| Partial | 20 | 56.2 | 3.3 | 5.3 | 46.7 | 1.01 | 34.18 |
| AMU2: dominant physician | |||||||
| APD | 17 | 57.6 | 3.2 | 5.2 | 49.7 | 1.03 | 32.50 |
| Mix | 24 | 55.0 | 3.4 | 5.3 | 47.8 | 1.01 | 34.08 |
| Specialist physician dominant | 5 | 57.7 | 3.1 | 4.9 | 41.8 | 0.96 | 34.82 |
| Ward1: openness | |||||||
| Closed | 23 | 57.0 | 3.3 | 5.3 | 47.2 | 1.02 | 34.00 |
| Open | 3 | 58.9 | 3.3 | 5.6 | 41.3 | 0.96 | 29.61 |
| Partial | 19 | 55.1 | 3.3 | 5.1 | 48.8 | 1.01 | 33.28 |
| Ward2: ward focus | |||||||
| General medicine | 20 | 56.9 | 3.3 | 5.4 | 48.3 | 1.01 | 33.81 |
| Specialist ward | 26 | 55.7 | 3.3 | 5.1 | 47.2 | 1.01 | 33.39 |
| Total | 46 | 56.2 | 3.3 | 5.2 | 1.00 | 34.0 | |
Overall, there were no major differences in terms of the proportion of short-stay cases, the case-mix complexity (bed use) and the proportion of ‘frail’ patients across the types of model. There were some exceptions in which there were small differences. For example, the episode length was slightly longer for the small number of open AMU hospitals and the proportion of cases in the top CMG was slightly higher. There were also tiny differences in the proportion of older people, suggesting a more typical case mix; however, these differences were small.
Relationship between inpatient case mix and medical skill mix
In this section we looked at whether or not there was an observable relationship between the number of ‘specialist consultants’ within a hospital and the mix of cases seen in the acute medical workload (see Report Supplementary Material 8, Section 8). Chapter 5 provides an overview of skill mix. Note that in this analysis we separated the numbers of very short-stay patients from the longer stay patients, as these patients would in most cases be associated with AMU care only. This analysis was undertaken for four specialist consultant subtypes: respiratory medicine, cardiology, gastroenterology and elderly care medicine, and took into account the number of patients with a frailty flag. We also examined the proportion of frail cases and the number of generalists in acute medical staffing.
Overall, the analysis did not find a relationship between the case mix and the widely different patterns of medical staffing. The two examples below demonstrate these results (see Report Supplementary Material 8, Section 8, for further details).
Respiratory medicine
Although the number of consultants in respiratory medicine in the hospitals ranged from zero to 16, there was no clear link between the number of respiratory medicine consultants and the proportion of patients (excluding short stays) in the seven key CMGs who were linked with respiratory medicine (Figure 22).
FIGURE 22.
Percentage of spells in respiratory CMGs vs. the number of respiratory medicine consultants.
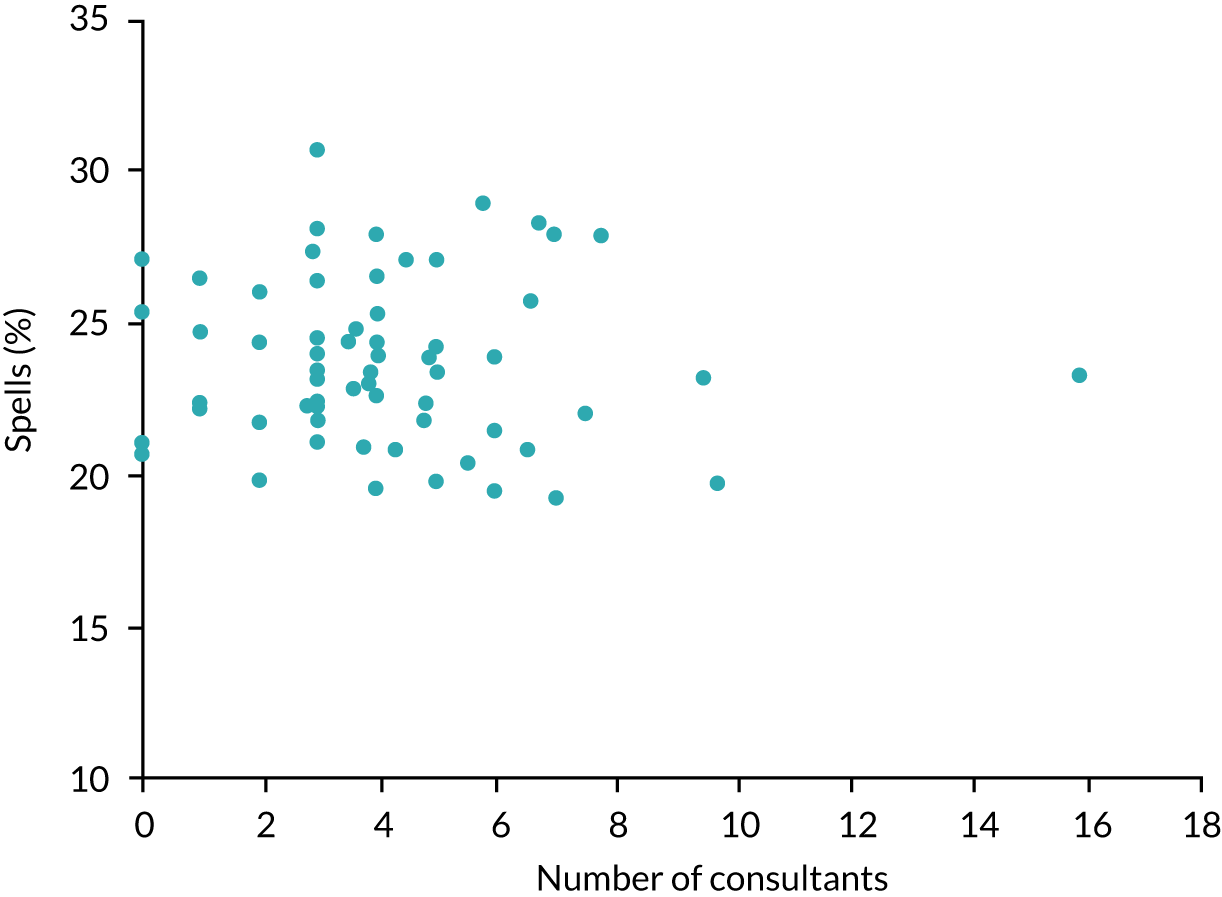
Geriatrics and frailty
We compared the prevalence of the frailty flag with the number of consultants in geriatrics (care of the elderly). At trust level, the proportion of cases flagged as at risk of frailty showed quite a large range from 14.4% to 39% of spells, and these equated to between 30% and 66% of acute medical bed-days. As shown in Figure 23, although the number of consultants described as geriatricians/elderly care medicine varied from zero to over 14, there was no relationship between this number and the proportion of admitting spells where the patient has been flagged as frail (or potentially frail).
FIGURE 23.
Percentage of spells flagged as frail vs. the percentage of consultant geriatricians in overall medical consultant workforce.
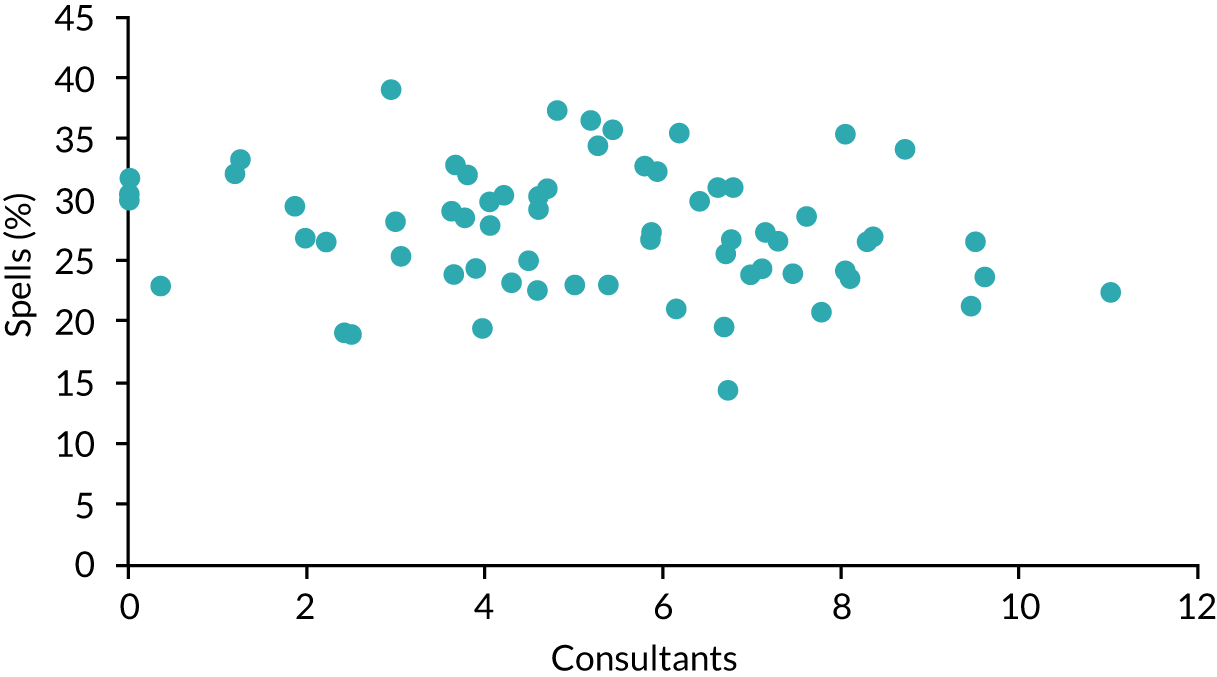
Conclusions
Developing a new classification
As part of this study, we have developed a new classification scheme to capture the case-mix dimension in relation to acute medical emergency inpatient care in small- to medium-sized hospitals. At its simplest, the classification scheme can operate on one level, driven by clusters of diagnoses, but these can be augmented by other information. It is worth noting that, for our general acute medical caseload, the resulting scheme outperforms HRGs (which has many more groups) in terms of the reduction in variance in lengths of stay. It also has a more manageable number of groups and allows flexibility in use.
The resulting classification seems to demonstrate validity in a number of ways:
-
The recognition of certain diagnostic categories in describing the overall case mix fitted with the clinical perception of what constitutes key elements in the workload.
-
Where differences in case mix exist, they seem to fit with expected patterns. For instance, prehospital triage will influence admissions for some specialist care (e.g. stroke).
-
The scheme identifies expected differences in specific hospitals – for example, the importance of D2 Sickle cell disorders in a hospital such as the Homerton or differences between neighbouring hospitals such as Harrogate and Airedale.
-
The scheme explains differences in the length of stay and the incremental benefits of including measures such as ‘frailty’ or process measures such as the presence of a procedure.
The scheme, like many other case-mix descriptors, does have limitations:
-
A reliance on existing computerised data sets means that the scheme is at the mercy of variable hospital information systems. Moreover, as we have observed, coding practices change over time, which can interfere with studies of change.
-
The level of clinical detail is limited to standard diagnostic and procedure coding schemes. Similarly, the level of detail on the care process is limited – we cannot say which patients went to an intensive care unit or a frailty unit.
-
The scheme does not deal with ambulatory care, which is of increasing importance, and could not use newly emerging emergency care data sets. Once established, these new data sets would help to develop the approach. We feel that this is a major weakness, which is driven by the lack of information about outpatient care.
-
Although the observed reduction in variance was better than HRGs when the full classification was applied, and produced values typically in line with the case-mix groupings, it still reaches only 30% of variance explained. This leaves a lot of unexplained variation in lengths of stay, which may be related to dimensions of case mix that we cannot measure with the data to hand.
Perhaps most importantly, the classification provided a more sophisticated way to use information about the same person, linked over time134,135 within the hospital spell or between hospital spells. One of the major constraints in case-mix classifications is the depth of information usually available and, therefore, it is important to make the best use of it by linking data between episodes. The ability to make better use of existing information is now possible through better computing power and data sets. It enables a better approach to case-mix descriptors that can use information about prior events to classify a patient on admission. In this case, we looked at the prior diagnoses linked to frailty or previous admissions for cancer. Basic descriptors of case mix were first used in hospital planning and finance over 30 years ago,136 and they have remained largely the same as static cross-sections of activity at one point in time;112 as we have shown, there is scope to do better than this.
What does this tell us about acute medical case mix in small- to medium-sized hospitals?
We have looked at acute medical emergency case mix from 6 years of data across 69 NHS trusts, a total of over 10 million patient episodes. The most striking features of our analysis were:
-
The differences in acute emergency medical case mix between hospitals (with a few exceptions) are not that large – whether within our subset of smaller hospitals or across larger hospitals. The profile of acute medical emergencies across hospitals has more in common than it has differences. Therefore, we concluded that the myriad of different organisational forms for dealing with these are probably not a result of underlying differences in the presenting cohort of patients.
-
There are large differences in bed use that cannot be explained by case mix. We noted that when using standard weighting, expected bed needs per cases varied by a small amount only (±10%) compared with the twofold to threefold differences in the average LOS.
-
We did note the importance of short-stay cases in shaping the overall average lengths of stay. This is hardly a surprising finding but we also noted that across all cases, hospitals with a higher number of cases had shorter lengths of stay. The significance in terms of the resource use of short-stay cases is an indication of the way hospital practice is changing137,138 and presents a challenge for traditional approaches to describe hospital case mix and activity.
-
Overall, we found that case mix was less important than within-hospital effects as an explanation of differences in aggregated LOS. The implication is that there are many different ways in which hospitals are managing throughput in the hospital and it is these options that drive the efficient use of one of the most critical of hospital resources, available beds. It is important to note that bed use and lengths of stay are highly imperfect as measures of efficiency, and even worse as markers of outcomes. However, it can reflect something important about how hospitals are run, and more work is urgently needed to understand this better.
-
For selected case types there was huge variability in the pathways taken through hospitals. The variability in pathways was in some cases linked to subsets of patients within diagnostic groups, which may reflect the limited depth of the information we had. Overall, the impression was that for a given diagnostic category, the range of specialties employed within a hospital spell was extremely variable.
-
The rise in activity for these acute medical cases seems especially high; although partly explained by increasing numbers of short stays, this is not wholly the case. Over the past 5 years, hospitals seem to have squeezed 20% more patients through the available beds.
What’s the link between the case mix and the organisation of acute medical care?
In this section, we have looked in cross-section at two key issues: (1) the typology describing arrangements in AMUs and wards and (2) the differences in the skill mix of medical consultants.
As Chapter 4 notes, there are major differences in the way acute medical services are organised; however, we were unable to see any strong relationships between the case types treated and these organisational factors. There was a weak relationship between the size of the hospital and the case mix, but otherwise no relationships were found between case mix and the organisation of care. Whatever is driving models of care in hospitals, it is not the case mix that presents to them.
With regard to medical skill mix, there are large differences between hospitals. Our analyses looked at a number of selected specialist areas (cardiology, respiratory medicine, gastroenterology and elderly care) and found no relationships between the number of consultants in these areas and the number of cases admitted to diagnostic groups linked to these specialties. Once again, the conclusion is that whatever is driving differences in the mix of consultant specialties in a hospital, does not seem to be the acute medical workload.
Understanding hospital activity
Some of the analyses that we have undertaken have been new and innovative ways of looking at characterising current hospital activity, for example the use of linked data over time and breaking down constituent care episodes within a hospital spell; much of what we have carried out is the type of basic case-mix analyses that has been common for many years. This suggests that there is still untapped potential to exploit HES data further to look at models of service delivery and support better ways of understanding and reimbursing care. This is symptomatic of a wider problem that our ability to analyse data has not grown to match the massive expansion in the data available, and there is a shortfall in the analytical capability required to support decision-making.
Chapter 6 Investigating the economic costs
Introduction
There is little or no previous research examining the association between models of generalist and models of specialist staffing in small hospitals and their costs. There is some evidence from outside the UK that generalist models of care in hospitals reduce the length of hospital stay and costs,41,139 but this evidence may not be applicable to small hospitals in the UK setting. We conducted a review of the PubMed database (www.ncbi.nlm.nih.gov/pubmed/) using the search terms ‘(generalism OR generalist) AND hospital AND costs AND (small or smaller)’ (date of search 8 October 2018) and identified 109 publications. None of these compared generalist models of care with specialist models of care. Therefore, we conducted a de novo cost analysis to examine generalist and specialist staffing models in small hospitals and NHS costs. The aim was to investigate the association between staffing models and patient-level costs.
Materials and methods
Overview of approach
We explored the relationship between the hospital staffing model and the patient-level costs by using costed emergency admissions data from the 2015–16 HES database119 for the 43 smaller hospitals from our survey. We constructed a data set that contained spell-, patient- and hospital-level variables, including staffing model typology, and regressed the spell-level cost variable against the medical generalism typology variables plus covariates.
Data and variables
Sample
We identified all emergency admissions/spells at 43 smaller hospitals (full data were not available for seven hospitals) from our survey in the 2015–16 HES database (716,547 spells in total). We dropped 41 observations with missing sex data and 9452 observations with missing cost data, giving a final sample of 707,054 spells. In analyses including data on the proportion of medical staff who were generalist, the total number of spells was 677,159.
Dependent variables
We costed emergency admissions/spells at the 43 smaller hospitals from our survey in the 2015/16 HES database using 2015/16 local trust-specific (i.e. not national) NHS reference costs based on 2017/18 HRG codes140 (2015/16 reference costs are reported using 2017/18 HRGs). The costs were adjusted for unavoidable geographical variations in costs using the market forces factor [payments index, all elements (staff, medical and dental London weighting, buildings, land, ‘other’)], to produce a data set of spell-level costs that varied by hospital and HRG, which also accounted for unavoidable cost differences between hospitals.
Independent variables
Our independent variables were a mixture of hospital-, spell- and patient-level variables. Our main hospital-level variables of interest were the medical staffing typology variables described in Chapter 7. There were four categorical variables that were labelled AMU1, AMU2, Ward1 and Ward2, which were categorised as follows:
-
AMU1 – AMU is ‘closed’, ‘open’ or ‘partial’ (three categories).
-
AMU2 – AMU is ‘acute physician dominant’, ‘mixed’ or ‘specialist physician dominant’ (three categories).
-
Ward1 – wards are ‘closed’, ‘open’ or ‘partial’ (three categories).
-
Ward2 – wards are ‘general medical wards’ or ‘specialist wards’ (two categories).
In addition, we also included a variable that quantified the proportion of the medical staff in each hospital who were generalists. This was calculated as the total full-time equivalent (FTE) number of generalists among the medical staff of the hospital in 2017/18, divided by the total FTE number of medical staff (2017/18). Given the skewness of this variable, from the continuous variable we created a binary categorical variable describing whether or not the proportion of the medical staff in each hospital who were generalists was > 0.5 (two categories: ‘no’ and ‘yes’); we plotted the proportion of the medical staff in each hospital who were generalists and 0.5 was a natural break in the distribution (see Report Supplementary Material 9, Figure 1). We also experimented with using the mean value as the break in the distribution (0.412) and 0.6, and the results were qualitatively the same. We also included the following hospital-level variables, which were derived from our survey:
-
population covered by hospital (number)
-
distance to nearest ED (miles)
-
trust operating revenue in 2015/16 (£M)
-
approximate number of beds at the main hospital site in 2017/18 (number)
-
number of ED attendances per annum in 2015/16 (number)
-
number of emergency admissions per annum in 2015/16 (number)
-
urban/rural indicator for the location of the hospital (six categories: ‘coastal’, ‘island’, ‘rural – town’, ‘rural – town in sparse settings’, ‘urban – city’, ‘urban – town’)
-
hospital size status in 2016/17 (three categories: ‘> small’, ‘small’, ‘smallest’)
-
trust CQC rating as of January 2018 (three categories: ‘good’, ‘inadequate’, ‘requires improvement’).
We also included the following spell- and patient-level variables that were available from the HES database or were created using HES data specifically for this study (see Chapter 5 for further details):
-
patient age in years (continuous variable)
-
patient sex (categorical variable – ‘male’, ‘female’)
-
patient ethnic group [categorical variable – ‘British (white)’, ‘Irish (white)’, ‘any other white background’, ‘white and black Caribbean (mixed)’, ‘white and black African (mixed)’, ‘white and Asian (mixed)’, ‘any other mixed background’, ‘Indian (Asian or Asian British)’, ‘Pakistani (Asian or Asian British)’, ‘Bangladeshi (Asian or Asian British)’, ‘any other Asian background’, ‘Caribbean (black or black British)’, ‘African (black or black British)’, ‘any other black background (other ethnic group)’, ‘any other ethnic group’, ‘not stated’, ‘not’]
-
admission source [categorical variable – ‘the usual place of residence’, ‘temporary place of residence when usually resident elsewhere’, ‘penal establishment, court or police station/police custody suite’, ‘NHS other hospital provider: high security psychiatric accommodation in an NHS hospital provider’, ‘NHS other hospital provider: ward for general patients or the younger physically disabled or A&E (accident and emergency) department’, ‘NHS other hospital provider: ward for maternity patients or neonates’, ‘NHS other hospital provider: ward for patients who are mentally ill or have learning disabilities’, ‘NHS run care home’, ‘local authority residential accommodation’, ‘local authority foster care’, ‘babies born in or on the way to hospital’, ‘non-NHS (other than local authority) run care home’, ‘non-NHS (other than local authority) run nursing home’, ‘non-NHS run hospital’, ‘non-NHS (other than local authority) run hospice’, ‘ not applicable’, ‘not known’]
-
urban/rural indicator for patient’s small area of residence (categorical variable – ‘urban – sparse’, ‘town and fringe – sparse’, ‘village – sparse’, ‘hamlet and isolated dwelling – sparse’, ‘urban – less sparse’, ‘town and fringe – less sparse’, ‘village – less sparse’, ‘hamlet and isolated dwelling – less sparse’)
-
whether or not the patient died in the hospital (categorical variable – ‘no’, ‘yes’)
-
case-mix groups (categorial variable – 82 categories; see Chapter 5)
-
frailty flag (categorial variable – ‘no’, ‘yes’; see Chapter 5)
-
procedure flag (categorial variable – ‘no’, ‘yes’; see Chapter 5)
-
secondary cancer flag (categorial variable – ‘no’, ‘yes’; see Chapter 5).
Analysis
We regressed spell-level costs against medical staffing typology (the four categorical variables, all included in the same regression model), controlling for spell-, patient- and hospital-level variables (patient age, patient sex, patient ethnic group, admission source, urban/rural indicator for patient’s small area of residence, whether or not the patient died in the hospital, case-mix group, frailty flag, procedure flag, secondary cancer flag); the population covered by hospital (number); distance to nearest ED (miles); trust operating revenue in 2015/16 (£M); approximate number of beds at the main hospital site; number of ED attendances per annum; number of emergency admissions per annum; urban/rural indicator for the location of the hospital; hospital size status; and trust CQC rating.
The cost data are skewed (see Figure 24) and to account for this we used a generalised linear model with gamma family and log link, which have been recommended for regression analyses of skewed cost data. 141 We also considered using log-normal, Gaussian, inverse Gaussian and negative-binomial distributions, but the gamma model gave the best fit in terms of residual plots and the Akaike information criterion. We adjusted for clustering at the hospital level in all of the regression models. Results of the regression are presented as predictive margins, which give the mean cost per spell in each category of the medical generalism typology, controlling for the covariates and accounting for data skewness. We run two versions of the regression models, one (model 1) not including the proportion of the medical staff in each hospital who were generalists (given that this variable is available only for 41/43 hospitals) and the other including this variable (model 2). We also ran similar models, but dropped low-cost spells (dropping the lowest cost 1% of spells and dropping spells that did not involve an overnight stay).
Results
Hospital-level characteristics
Hospital-level characteristics are presented in Tables 20–22. In terms of the medical staffing typology, the modal categories were: AMU1 partial, AMU2 mixed, Ward1 closed and Ward2 specialist ward (see Table 20). The mean proportion of the medical staff in each hospital who were generalists was 0.412 (range 0.223–0.833; see Table 21). Most hospitals were in ‘urban – town’ locations, were a ‘small’ size, were rated as ‘requires improvement’ in terms of their CQC rating and fewer than half of their medical staff were generalists (see Table 22).
| Typology | Number of hospitals (N = 43), n (%) |
|---|---|
| AMU1 | |
| Closed | 17 (40) |
| Open | 8 (19) |
| Partial | 18 (42) |
| AMU2 | |
| APD | 17 (40) |
| Mixed | 22 (51) |
| Specialist physician dominant | 4 (9) |
| Ward1 | |
| Closed | 23 (53) |
| Open | 3 (7) |
| Partial | 17 (40) |
| Ward2 | |
| General medical ward | 18 (42) |
| Specialist ward | 25 (58) |
| Characteristic | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Population covered by hospital (n) | 352,093 | 142,159 | 140,000 | 900,000 |
| Distance to nearest ED (miles) | 15 | 8 | 2 | 45 |
| Trust operating revenue in 2015/16 (£M) | 226 | 54 | 112 | 326 |
| Approximate number of beds at the main hospital site in 2017/18 (n) | 515 | 154 | 236 | 887 |
| Number of ED attendances per annum in 2015/16 (n) | 86,326 | 26,554 | 44,727 | 149,398 |
| Number of emergency admissions per annum in 2015/16 (n) | 28,298 | 9834 | 11,652 | 51,712 |
| Total FTE number of generalists among the medical staff in 2017/18 (n)a | 43.5 | 18.3 | 15.6 | 85.6 |
| Total FTE number of medical staff in 2017/18 (n)a | 106.4 | 32.5 | 49.3 | 196.4 |
| Proportion of the medical staff in each hospital who were generalists (proportion)a | 0.412 | 0.145 | 0.223 | 0.833 |
| Characteristic | Number of hospitals (N = 43) |
|---|---|
| Urban/rural indicator for the location of the hospital | |
| Coastal | 3 |
| Island | 1 |
| Rural – town | 12 |
| Rural – town in sparse settings | 7 |
| Urban – city | 5 |
| Urban – town | 15 |
| Hospital size status in 2016/17 | |
| Larger than small | 6 |
| Small | 26 |
| Smallest | 11 |
| Trust CQC rating as of January 2018 | |
| Good | 19 |
| Inadequate | 1 |
| Requires improvement | 23 |
| Proportion of the medical staff in each hospital who were generalistsa | |
| ≤ 0.5 | 34 |
| > 0.5 | 7 |
Spell-level analysis
The distribution of costs per spell are shown in Figure 24. Across the 707,054 costed spells, the mean cost per spell was £2445 (SD £2921) and median cost per spell was £1624 [interquartile range (IQR) £437–3414]. The 1st and 99th percentile costs per spell were £168 and £13,809, respectively. We explored the lowest cost spells in further detail. For spells with at least one overnight stay (507,655 observations), the mean cost per spell was £3170 (SD £3033) and the median cost was £2530 (IQR £1051–4161) (see Report Supplementary Material 9, Figure 3). For spells with no overnight stay (199,399 observations), the mean cost per spell was £592 (SD £1413) and the median cost was £396 (IQR £301–507). Four hospitals accounted for 70% of the 1% lowest cost spells and three case-mix groups accounted for over half of the 1% lowest cost spells (‘pain in throat and chest’, ‘sickle cell disorders’, ‘poisoning’; see Report Supplementary Material 9, Table 5).
FIGURE 24.
Distribution of cost per spell values (707,054 observations). Mean cost per spell: £2445 (SD £2921). Median cost per spell: £1624 (IQR £437–3414). The 10th and 90th percentile costs per spell: £302 and £5695. 5th and 95th percentile costs per spell: £246 and £7718. The 1st and 99th percentile costs per spell: £168 and £13,809.
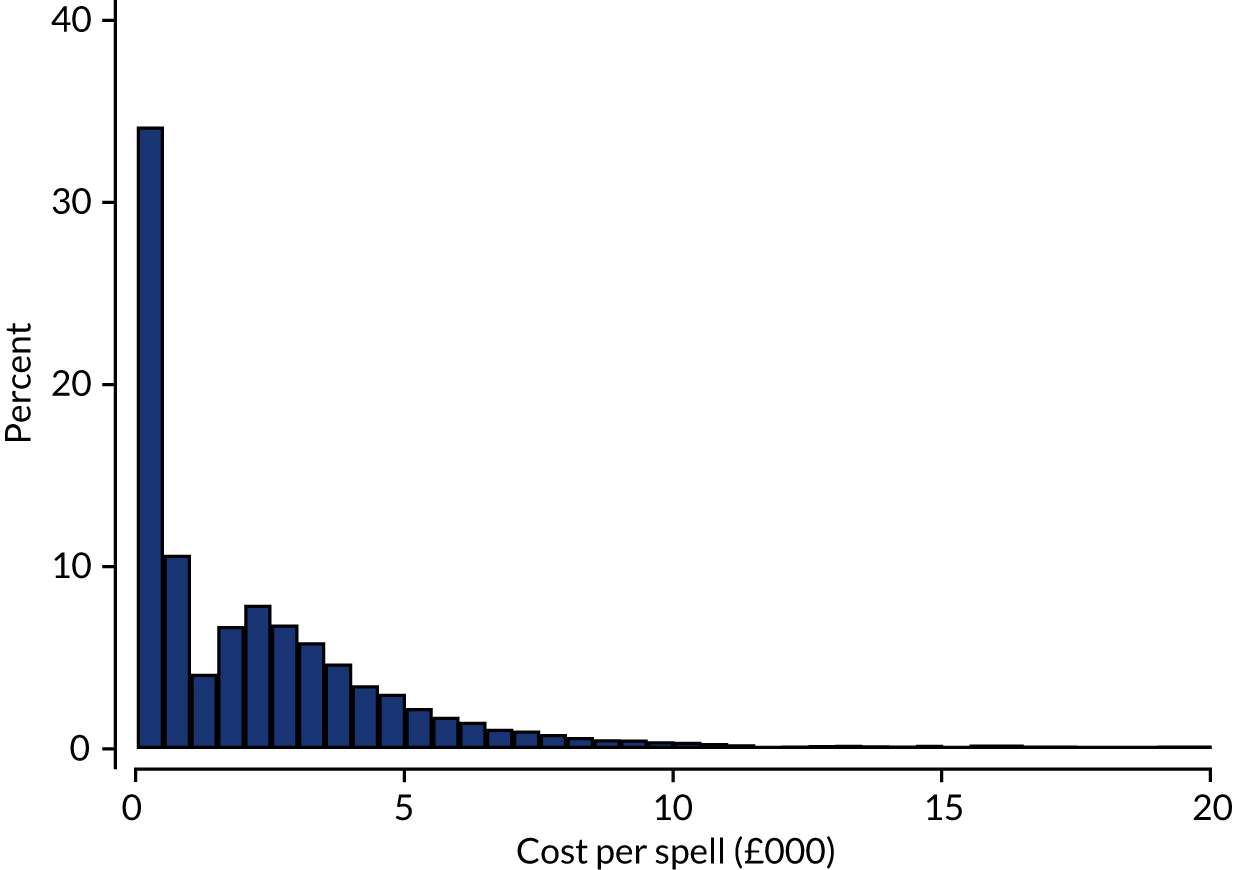
Unadjusted mean (SD) and median (IQR) costs per spell by selected categorical variables are shown in Report Supplementary Material 9, Table 7. By inspection, unadjusted costs per spell do not seem to vary appreciably by medical staffing typology or the proportion of the medical staff in each hospital who were generalists. ‘Fracture of femur’ was the case-mix group with the highest median cost per spell, and ‘sickle cell disorders’ were the least costly. In addition, spells involving a procedure incurred higher median costs on average than those not involving a procedure; spells involving frail patients incurred higher costs than those not involving frail patients; spells for patients with secondary cancer incurred higher costs than spells for patients who did not have secondary cancer. There was considerable variation in the median cost per spell by trust (median values ranged from £361 to £3137).
Results of the regression models (models 1 and 2) are shown in Table 23. Based on the predictive margins and 95% CIs around these, there is no significant variation in cost per spell depending on whether the AMU is ‘open’, ‘closed’ or ‘partial’ (AMU1), whether the AMU is ‘acute physician dominant’, ‘specialist physician dominant’ or ‘mixed’ (AMU2) and whether the ward is a ‘general medical ward’ or ‘specialist ward’ (Ward2). There is some evidence that if the ward is ‘open’ it has significantly lower mean costs per spell than if it is ‘closed’ or ‘partial’ (Ward1), that is the 95% confidence interval (CI) around the predictive margin for the ‘open’ category does not overlap those of the other categories. Similar results are obtained for both model 1 and model 2. In model 2 we also controlled for the proportion of the medical staff in each hospital who were generalists > 0.5; adjusted costs for this variable were similar in the ‘no’ and ‘yes’ categories.
| Typology | Model 1a | Model 2b | ||||
|---|---|---|---|---|---|---|
| Predictive margin | Standard error | 95% CI | Predictive margin | Standard error | 95% CI | |
| AMU1 | ||||||
| Closed | 2649 | 119 | 2417 to 2882 | 2681 | 156 | 2376 to 2987 |
| Open | 2712 | 213 | 2295 to 3129 | 2679 | 229 | 2230 to 3129 |
| Partial | 2377 | 85 | 2210 to 2543 | 2347 | 91 | 2168 to 2527 |
| AMU2 | ||||||
| APD | 2498 | 130 | 2244 to 2752 | 2524 | 132 | 2266 to 2782 |
| Mixed | 2593 | 92 | 2414 to 2773 | 2553 | 93 | 2371 to 2735 |
| Specialist physician dominant | 2481 | 148 | 2191 to 2770 | 2470 | 157 | 2163 to 2777 |
| Ward1 | ||||||
| Closed | 2656 | 145 | 2371 to 2941 | 2656 | 147 | 2368 to 2945 |
| Open | 1779 | 169 | 1447 to 2111 | 1674 | 215 | 1252 to 2096 |
| Partial | 2530 | 83 | 2368 to 2691 | 2526 | 122 | 2286 to 2766 |
| Ward2 | ||||||
| General medical ward | 2599 | 142 | 2320 to 2877 | 2562 | 147 | 2274 to 2851 |
| Specialist ward | 2507 | 80 | 2350 to 2664 | 2509 | 85 | 2343 to 2676 |
| Proportion of medical staff who are generalist | ||||||
| ≤ 0.5 | 2553 | 95 | 2366 to 2740 | |||
| > 0.5 | 2421 | 193 | 2043 to 2798 | |||
| Observations | 707,054 | 677,159 | ||||
| AIC | 17.09774 | 17.08068 | ||||
| BIC | –8987515 | –8576559 | ||||
The following covariates were also included in models (but not reported):
-
case-mix groups
-
procedure flag
-
frailty flag
-
secondary cancer flag
-
patient age
-
patient gender
-
patient ethnic group
-
admission source
-
urban/rural indicator for patient’s small area of residence
-
whether or not the patient died in hospital
-
population covered by hospital
-
hospital distance to nearest A&E
-
trust operating revenue
-
approximate number of beds on main hospital site
-
hospital A&E attendances 2015/16
-
hospital emergency admissions 2015/16
-
urban/rurality indicator
-
hospital size
-
the CQC rating.
Standard errors were adjusted for clustering at hospital level.
The association between selected covariates and the adjusted mean cost per spell are shown in Report Supplementary Material 9, Table 8. As with the unadjusted analyses, ‘fracture of femur’ is the highest cost spell and now ‘calculus of kidney or urinary tract’ is the lowest cost spell. As with the unadjusted figures (see above), spells involving a procedure were more costly than those that did not; spells involving frail patients were more costly than those that did not; spells involving patients with secondary cancer were more costly than those that did not. Adjusted costs per spell do not seem to vary by whether or not the patient died in the hospital, conditional on the other variables included in the models.
When low-costs spells were removed, there was some evidence that the significantly lower costs for patients treated on ‘open’ wards remain, and that the trends with regard to the medical staffing typology variables were similar to the main analysis described above (see Report Supplementary Material 8, Table 4).
Conclusions
Summary of main results
In this study, we investigated the relationship between medical staffing typology in small hospitals and health-care costs. We found that costs did not vary by characteristics of the AMU (whether it was open, closed or partial; whether it was APD, specialist physician dominant, or mixed), by whether the wards were general medical wards or specialist wards and by the proportion of medical staff in the hospital who were generalist. There was some evidence that costs were lower in open wards compared with those that were closed or partial, but the reasons for this finding were unclear. It could be due to chance, as there were only three hospitals from our sample of 43 that were in this category (see Table 20). It might also be a true effect and one hypothesis is that ‘open’ wards facilitate continuity of care in a way in the hospital that ‘closed’ or ‘partial’ wards do not. 142 Further research to understand the reasons for this finding would be beneficial.
Strengths and limitations
This study provides, to our knowledge, the first quantitative analysis exploring the association between models of medical staffing in small hospitals in the UK and health-care costs. The analysis was undertaken using a large, comprehensive data set accounting for hospital variation in resource utilisation and unit costs, including a range of covariates to control for differences in patient case mix between hospitals. The medical staffing typology variables were derived from comprehensive assessments undertaken as part of the present study.
There are several limitations. Our costs are based on trust-level unit costs and rely on hospital recording of resource use, which may be inaccurate. In addition, we cannot exclude the possibility that unobserved confounding factors might affect the observed relationship between staffing typology and spell-level costs.
Chapter 7 Strengths and weaknesses of models of care
Objectives
In this chapter, we describe the strengths and weaknesses of current models of medical generalism from patient, professional and service perspectives.
Overview of methods
As work in this package was conducted independently by three different teams, the methods and the findings will be presented together for each component of work. The main methods used to assess strengths and weaknesses included:
-
staff interviews and staff focus groups to explore the lived experiences of staff working in smaller hospitals and their attitudes towards models of care
-
patient and carer focus groups to explore the lived experiences of patients and their carers and their attitudes towards models of care
-
a DCE to examine and quantify the relative importance of the different attributes of medical generalism and the preferences of patients and health-care professionals
-
an exploration of the impact of models of care on other outcomes, such as mortality and re-admissions
It should be noted that as medical professionals almost invariably discussed models of care as ‘more generalist’ or ‘more specialist’, we have used these terms to guide the analysis, rather than linking responses to the typology.
Strengths and weaknesses: staff interviews and focus groups
Overview
The aim of the staff focus groups was to explore the lived experiences of health-care professionals who were working in each of the different models of care and their attitudes towards generalism. The original intention was to conduct focus groups for one of each of the different models of care expected to emerge from the typology. As there were more models of care than anticipated, sites for focus groups were chosen to explore the more common models of care, as well as those that appeared novel. Given that the interviews with staff conducted as part of case study visits contained substantial data regarding the topics of interest, the protocol was amended to include the interviews from all study sites in the analysis.
Methods
Participants for the focus groups were recruited via the site liaison officer (see Appendix 2). Informed consent was obtained. The focus groups were moderated by Louella Vaughan and Candace Imison; other team members recorded non-verbal communication and other interactions. Prompts were used to facilitate discussions around the staff’s experiences of providing care, especially in a smaller hospital, and the competing demands of generalist and specialist care and the boundaries between these. The groups were then presented with a simplified version of the main models of care and asked to discuss where they thought their hospital might fit in the typology and whether or not the perceived strengths and weaknesses of models of care were a property of the model or the hospital in which it was located. The focus group guide can be found in Report Supplementary Material 4.
Given that the staff interviews also contained rich material on the perceived strengths and weaknesses of the models, the protocol was changed to permit analysis of these, alongside the focus groups. Analysis was conducted as outlined in Chapter 4.
Overview of the findings
Two assumptions underpinned this WP: (1) that models and systems of care would heavily influence the lived experiences of staff and (2) that staff would have defined views of the strengths and weaknesses of the models and systems in which they worked. Instead, we found that staff found it difficult to discuss models and systems of care and instead tended to focus on the experience of working at a smaller hospital. Moreover, explorations of lived experiences were almost solely discussed in terms of the extent to which clinicians felt that their own workloads were manageable and whether or not their training equipped them for generalist working. In Chapter 4, we noted that staff were more able to relate to systems as sitting along a spectrum from ‘more general’ to ‘less general’; therefore, what follows here is framed around that spectrum, rather than relating findings to the typology. We also touch on views of the hyperstreaming model of care (see The hyperstreaming model of care), as this was viewed by staff as affecting the system and patients in unique ways.
Strengths of the generalist approach
The main strengths of a generalist approach were framed around its ability to meet the needs of the local population and improve patient care.
Supporting case mix
Generalist models were seen as aligning closely with the case mix of smaller and/or rural hospitals, in which patient populations were likely to be older and/or have complex comorbidities:
For a hospital like this to continue to thrive, it has to be dealing with the general everyday medicine, which is just basically people being general physicians, whether they’re geriatricians or rheumatologists or whatever.
Senior clinical manager
Generalism was also seen by many as a ‘patient model and not a disease model’ and, thus, was able to deliver holistic care to all patients and better meet their needs:
You can see patients as whole and you’re treating them as a whole, and that’s what they want.
Senior doctor
Supporting continuity of care
Generalist models of care were seen as reducing the number of handovers between teams and supporting continuity of care:
I am definitely an advocate of the generalist approach . . . it makes it a lot simpler and it’s generally often better for patients . . . they don’t feel like they’re being pushed from one specialty to another.
Senior clinical manager
Helping to reduce length of stay
The ability of generalist models to meet patient needs and support continuity of care was widely held to contribute to reducing the length of stay.
Weakness of the generalist approach
A weakness of generalist approaches was that they were seen as delaying the delivery of specialist care to the cohort of patients who had specific organ-based problems:
I think that the downside is that when you then have to refer to a specialist you can build in sometimes a 1 to 2 days of delay for that specialist input.
FGP
Strengths of the specialist approach
Specialist approaches were seen to support the best evidence-based care for specific conditions that are associated with higher short-term mortality, such as myocardial infarction or gastrointestinal bleeding:
So a patient with a respiratory problem will get a better outcome and a shorter length of stay and lower mortality and morbidity if looked after by a respiratory consultant . . . there has been good evidence to say, ‘the earlier you get your specialist involved . . . the better your outcome’.
Senior clinical manager
Patients were also noted at times to have preferences for specialist care and to have an expectation that this should be provided regardless of the size of the organisation:
It can be a bit devastating when you’re doing a consultant ward round and the patient just says ‘Well, I only want to see the cardiologist . . . I was promised I’d see a cardiologist’.
Senior clinical manager
Weaknesses of the specialist approach
Consultant skills may not match patient need
Specialist approaches were seen by many as less able to meet the needs of complex comorbid patients who were using smaller hospitals:
I wasn’t trained to look after these sorts of [complex comorbid] patients.
FGP
Resource intensive
As specialist approaches imply a larger and more diverse consultant body, they were seen as being difficult to implement and costly to deliver in smaller organisations:
We couldn’t run this organisation with highly specialised doctors . . . because we haven’t got the resources to then provide the general medical support that patients need . . . we couldn’t manage our cohort of patients.
FGP
Generalist patients as less important
Highly negative attitudes were frequently expressed towards ‘general medical patients in specialty beds’ by both clinical and nursing staff. From a medical perspective, these patients were frequently seen as displacing patients who had specialist needs. This was viewed as having two key effects: (1) it created the need for the specialist team to review patients on other wards, hence increasing their workload and (2) it disrupted the flow of the ward rounds, with teams needing to switch from specialist to generalist mode:
The consultants don’t like to go off their base ward to look at patients.
FGP
Nurses commented that the number of ‘general medical patients’ with complex needs on their specialty wards had substantially increased over recent years without any increase in the nursing allocation. The increased burden on nurses was seen as an underlying problem with the recruitment and retention of staff:
I’d say mine [nurses] are less satisfied, I think they’re finding it very hard with the complexity of the patients that are being admitted, they’re acutely unwell . . . The patients who are coming up to the wards are very sick, but they also have complex social needs as well, so they tend to stay longer.
FGP
This combination of factors led to staff admitting that these patients frequently received less than optimal care.
Problems with a dichotomised approach
A recurring theme was that highly dichotomised approaches to care were in themselves unhelpful and that the key to improving care lay not in changing models of care along the lines of more generalist or more specialist, but rather in improving collaboration between consultants within a single organisation:
I would like to not see that model of a specialist sat over there somewhere behind 12 beds, ‘these are mine’. I would like to see them here, right next to me, go ‘yes, let’s have a look at this patient’.
Senior doctor
Thinking about generalist and specialist care in smaller hospitals . . . actually all hospitals . . . we need to work as one service rather than split services with barriers in between.
FGP
The hyperstreaming model of care
The hyperstreaming model of care involves having multiple services at the front door, such as ambulatory care and frailty units, which can provide the same functions of the first assessment and initial management of unselected patients with medical needs (see Overview of models of acute medical care in smaller hospitals in England). This emerged as a distinct model of care in the interviews and case studies, with unique strengths and weaknesses.
The main strength of this model was in decongesting the ED by moving patients elsewhere in the system. This was seen as essential in helping organisations to achieve the 4-hour target, as well as in reducing admissions and improving flow through the system. It was also seen as providing patients, particularly the elderly, with better care environments.
Staff, however, described the model as having a number of flaws. Substantial problems were created through the stretching of limited staff across highly dispersed geographic areas. The inherent complexity and the dispersed geography meant that it was difficult for managers to have an operational overview of the system and to respond to variations in demand. Being off the ‘ED clock’ in parallel assessment areas meant that patients frequently experienced delays in receiving care and that less urgency was described in the running of these units in comparison with EDs. Moves between different areas were more common than might be expected and often difficult to carry out, leading to fragmentation and discontinuity of care. In the case of patients who were moved between areas, the standard practice of reclerking patients with each transfer also led to substantial duplication of work across the system. It was rare for all of the system components to sit within the same managerial structures, with little thought given to how the individual areas might interact at the system level or how the burgeoning complexity ought to be managed.
The strengths and weaknesses of smaller hospitals
Most staff found it difficult, if not impossible, to divorce their experiences of models of care from the overall hospital context. This was particularly the case in smaller organisations, where generalism was seen to be the natural default model of care. Hence, strengths and weaknesses of models of care were more often than not coterminous with the strengths and weaknesses of the smaller hospital. Notably, strengths were almost always framed as properties of the hospital, whereas weaknesses, with the exception of a relative lack of resources, were referred to in the context of the increasing external expectations to deliver the same standards of quality and to meet the same requirements of bigger teaching hospitals, while negotiating a treacherous political landscape. It was striking the extent to which particular characteristics were viewed as both positive and negative features of a smaller hospital. For this reason, results will be presented by characteristic, rather than as lists of respective strengths and weaknesses.
Hospital culture
Issues around culture were considered to be amplified in smaller hospitals. Smaller size was thought to inherently enhance face-to-face communication, in turn fostering trust, friendlier relationships and collaborative working. Given that most staff lived locally and that the hospital was highly likely to be the care provider to their families was thought to translate into a deeper collective commitment to performance and the continuing existence of the hospital.
However, in some cases, smaller hospitals were likened to an ‘island’, in the sense of being unwelcoming to newcomers and being reliant on old strategies rather than being open to innovation:
I think culture is a massive barrier . . . there is a belief that we can’t do any of these things because they’re really hard, so we’re just not going to do them . . . I think this organisation hasn’t made some of those difficult decisions in the past and now it needs to.
Senior manager
Leadership
Many respondents drew connections between the size of their organisations, culture and the visibility and accessibility of senior management. There was a perception that smaller trusts had fewer tiers of management, making senior executives more directly accountable. Staff in smaller organisations more frequently reported feeling supported and listened to, while the direct involvement of senior leaders in improvement projects hastened their implementation:
The [executive leaders] are very approachable and interested and keen to learn . . . helpful and want to allow people to lead their clinical services the way they know how.
Senior clinical manager
Poor leadership was held to be more damaging in smaller organisations. Negative behaviours were thought more likely to have a direct impact on staff and weak or inaccessible leadership was thought to hinder change, derail innovation and even jeopardise the survival of the hospital:
But the way [the executive] went about it was absolutely wrong, so no consultation, no stakeholder engagement, no taking people on a journey, very much a dictatorial approach to life. So you know the best way of showing you who is the boss here, we’ll just resist your change and we’ll make it fail.
Senior manager
Multiprofessional working
A perceived strength of a number of trusts was the level of formal service integration and the presence of highly evolved multidisciplinary services. The inability of smaller organisations to recruit consultants and gaps in the middle-grade rosters had led to some highly innovative programmes for the recruitment and training of advanced practitioners from a wide variety of backgrounds. The intimate nature of working in smaller organisations meant that these newer types of practitioners were reported to quickly integrate into existing teams, strengthening the delivery of care. However, concerns were expressed by junior staff that the use of advanced practitioners limited their own opportunities, increasing dissatisfaction with the smaller hospital as a training environment.
Interfaces with community services
Many respondents pointed to the unique capability of smaller organisations to establish strong connections with community services. At one hospital, the CEO visited every local general practice each year to listen to concerns and take on views as to how services might be improved. Such relationships were not just doctor-to-doctor, but crossed all aspects of health and social care provision:
One of the over-riding benefits of it being a small hospital and a mixture of small teams is that between those small teams all of them have different networks within the community and within the hospital and in that context, sharing that open, flexible outlook as a team has made it much easier in creating interfaces . . . So I think there’s benefits all round small teams. Small hospitals have it much easier.
Senior doctor
However, close relationships between the hospital and the community services sometimes shaded into dependence, hindering a trust’s ability to be self-sufficient and respond to change and, therefore, leaving it potentially vulnerable to changes in community provision.
Vulnerability to external pressures
All trusts reported that their external environments had become substantially more difficult to navigate, with the need to adapt, often very quickly, to policy changes, external reviews (such as by the CQC), funding gaps, withdrawal of community and social services and a whole raft of other external issues. Most respondents felt that smaller organisations were substantially more vulnerable to these external threats, in that they had fewer resources, in terms of revenue, capital and workforce, and narrower margins for error than their larger counterparts:
With more people, let’s say, then you can kind of ‘rob Peter to pay Paul’ a bit. Here we haven’t got that . . . and it doesn’t take much to destabilise something that’s going really, really well.
Senior clinical manager
The risk that you’re exposed to as an NHS organisation are amplified the smaller that you are . . . Those sorts of things are out of our control yet we get held accountable to them and that is very difficult for us as a smaller organisation.
Senior clinical manager
For some, the very nature of the smaller hospital implied a constant questioning of their overall sustainability and the near inevitability of a merger or hospital closure. In others, existential threats were a motivation to create a strong identity and ensure that the hospital became utterly essential in meeting the needs of the local community:
The advantage is that adversity is a resource. You have to do things differently, you have to work well. We’re not a world class centre as some of the London hospitals . . . so we have to do it in different ways.
Senior manager
Management of workload and experiences of training
Discussions of medical generalism were substantially influenced by the personal preferences and attitudes of clinicians, which appeared to be heavily informed by the extent to which clinicians felt that their own workloads were manageable and whether or not their training equipped them for generalist working.
In hospitals where the ‘horrendousness versus frequency’ of general medical working was able to be managed, clinicians were substantially more likely to express positive attitudes towards medical generalism or to tolerate generalist working, despite that they may experience greater satisfaction from specialty working:
We just accept that as a respiratory physician . . . I may have to accept an elderly patient with complex geriatric-type problems and I’ve just to suck that up and deal with it because it’s a DGH . . . I think that most people get that.
Senior clinical manager
Instances in which the insufficient workforce meant that consultants were struggling to meet the targets for specialty outpatients or the delivery of interventional services, or the medical take was considered to be busy, generalist work was considered an unnecessary burden with consultants actively seeking to withdraw. Some argued that generalist work was ‘deskilling’ and that the task of staying sufficiently up-to-date in two specialties was difficult given the service demands:
The problem is, you know, on-call weekends are so busy that it’s just exhausting, physically and mentally exhausting.
FGP
Current models of training were seen as being particularly important in shaping attitudes towards general medicine. Experiences and role-modelling appeared integral to the shaping of future attitudes, both positive and negative:
The thing I’d enjoyed most about my training was being on-call and looking after people . . . when they’re so unwell.
Senior clinical manager
Generally speaking, these days, the physicians I think are trained to see themselves as specialists . . . the trainees see the general medicine as drudgery that they have to do.
Senior doctor
Conclusions
Both generalist and specialist models of care were seen as having advantages and disadvantages. More generalist models were seen as a more natural fit for smaller organisations. Of note, perceptions of models of care were difficult to disentangle from staff’s views of working in smaller organisations. Positive aspects of smaller hospitals, such as an enjoyable working environment, were located as being properties of the organisation, whereas negative aspects were more often attributed to external factors. Perceptions of workload and experiences of training were also critical in informing doctors’ opinions of models of care.
Patient and carer focus groups
Patient and carer focus groups were conducted to gain a better understanding of how patients and their carers experience models of care.
Methods
Patient focus groups were held at the same hospitals as the staff focus groups. Recruitment differed for the patient focus groups, with advertising material being distributed across a number of channels, including local patient and Healthwatch groups. Participants were paid in-line with Involve guidelines143 Focus groups were conducted in the same way as the staff groups and informed consent was gained for all participants. Topic guides and other materials can be found in Report Supplementary Material 4. Participants were first asked to recount their experiences of specialist and/or generalist care; they were then presented with outlines of the more generalist and more specialist models of care and asked to discuss how this might lead to different outcomes for different groups of patients. A discussion of how care might be better delivered in smaller organisations, such as the use of networks, was facilitated. Analysis was conducted by a single team member (HC) using pattern-matching logic searching for convergent and divergent themes. This was then reviewed by two senior team members (LV and CI).
Description of participation
Five patient and carer focus groups were held. The typology of the organisations and the number of participants is given in Table 24.
| Focus group | AMU type | Ward type | Number of participants |
|---|---|---|---|
| 1 | A2 B2 | C1 D1 | 4 |
| 2 | A1 B1 | C2 D2 | 7 |
| 3 | A1 B3 | C1 D1 | 1 |
| 4 | A1 B2 | C2 D2 | 4 |
| 5 | A2 B1 | C3 D1 | 1 |
Findings
Further details of the findings are presented in Appendix 5.
Patients expressed an overall preference for specialist care, although when pressed, participants could see that patients with complex needs may be better cared for by generalists and that specialist care may not be universally possible in the context of the smaller hospital. Moreover, it was considered that the overall quality of care given by local hospitals was more important than the actual model of care.
There was an overall perception that specialist care was the gold standard of treatment. However, the choice between a generalist and a specialist clinician was seen by some as a matter of personal preference, rather than as a choice between superior and inferior options. For others, the overall quality performance of the hospital seemed a more significant factor than the role profile of individual clinicians, and as long as they were satisfied with the hospital, they did not see a need to express a preference for a specialist or a generalist clinician. Some wished that the local hospital could deliver that standard of care universally, yet it was tacitly understood that expert care for ‘more obscure, difficult things’ may involve a transfer to a tertiary organisation:
Our age group, that grew up with the NHS just coming and the doctors were all powerful. If they told you to do something, you didn’t think ‘do I want a specialist or a generalist?’.
FGP
Some participants were reluctant to support the notion of generalist roles being a preferred option in secondary care. Only when pressed were certain respondents able to accept that there could be a benefit in seeing a generalist clinician when a patient had five or six things wrong under different specialties. Where respondents were able to acknowledge a role for care co-ordination by a generalist clinician, more than one respondent appeared to view that this co-ordinating role should belong to their general practitioner rather than a hospital doctor:
. . . it comes down to the GP [general practitioner] who knows you and knows you as a person – she should be able to discern whether it needs just solely a cardiologist or a general physician that would take it on a broader level.
FGP
However, geriatric care was the one area where most respondents saw a potential benefit of a generalist role in secondary care, particularly where patients had dementia. As one respondent put it:
If they’re presented with half a dozen different doctors, they usually don’t understand what it’s all about and it’s confusing. They get conflicting messages and it’s not good care. Particularly for the elderly I think you need one person.
FGP
However, these views were not universal, and one participant expressed a preference for specialist care, even when presented with the hypothetical situation of being an older patient with multiple complex conditions.
Conclusion
Overall, patients expressed preferences for specialist care, which was viewed as being the ‘gold standard’. However, most were prepared to accept that generalism was useful for patients with complex comorbid disease. The overall quality of care at any hospital was considered to be more important than the type of doctor delivering the care.
Discrete choice experiment
Introduction
We conducted a DCE144 to examine preferences between different workforce models in small hospitals. The aim was to quantify the preferences of hospital doctors, managers, patients and carers for different workforce models; the relative importance of different attributes of these models; and how the preferences vary between different stakeholders.
A DCE is a quantitative technique for eliciting individual preferences. Based on the assumptions that a service model can be described by its characteristics (attributes) and that individuals’ valuations of the model depend on the levels of these characteristics, it uncovers how individuals value selected attributes of a service model by asking them to state their choice over different hypothetical alternatives. This allows the attributes of a service to be evaluated, as well as the trade-off that individuals are willing to make between attributes of said service.
Ethics approval for this study was granted by the joint chairperson of the University College London Research Ethics Committee on 8 May 2018 (project ID 13187/001). International best practice guidelines for DCE were followed for study design and analysis. 145
Materials and methods
Sampling and recruitment
The DCE responses were obtained from three groups: (1) hospital doctors who were involved in the care of patients with acute medical conditions (n = 173); (2) members of public, including patients and carers (n = 20); and (3) managers in the hospitals that admit patients with acute medical conditions (n = 9). Data were collected by online anonymised surveys.
Hospital doctors who were working at organisations that admit patients with acute medical conditions were recruited via the RCP president’s e-bulletin, the Contact, Help, Advice and Information Network (CHAIN) mailing list, the National Institute for Health Research (NIHR) CLAHRC North Thames newsletter, the Nuffield Trust newsletter and the Nuffield Trust mailing list for this project. The public sample was recruited through a number of routes: Twitter (Twitter, Inc., San Francisco, CA, USA; URL: www.twitter.com) accounts of the Patient Voices charity (Landbeach, UK), The Patients’ Association (Harrow, UK), Healthwatch England, Iwantgreatcare (Charlbury, UK), Healthtalk (Dipex Charity, Oxford, UK), UK Health Radio (London, UK), NHS Choices, The Health Foundation (London, UK), the CHAIN mailing list, the NIHR CLAHRC North Thames newsletter, the Nuffield Trust newsletter, and the Nuffield Trust mailing list for this project. Managers were recruited via the Nuffield Trust newsletter, the Nuffield Trust mailing list for this project, the New Cavendish Group and the CHAIN mailing list.
Potential participants were sent an e-mail inviting them to participate, containing a weblink to the online survey. When clicking on the weblink, they were provided with detailed information about the study that also explained what their participation would entail. They were asked to click to another webpage to access the survey and were informed that by filling in the survey they consented to take part in the study. They were also told that their responses were given anonymously, so it would not be possible to withdraw consent after returning the questionnaire. They were also told that they did not have to take part if they did not want to.
Attributes and attribute levels
The key attributes and levels used in the DCE that described different models of medical generalism were identified using the typology developed during WP1. Attributes were constructed to capture the differences between the different models of medical generalism. These were derived from multiple sources, including outcomes from WP1 and WP2, early analyses of other components of WP4, the emerging theoretical framework and the literature review.
Feedback on early versions of the DCE was obtained from several sources: members of the study expert panel, which was convened as part of WP2, members of the Study Steering Committee and the patient volunteers involved in WP1. Following this, we identified four attributes most likely to be important to respondents and characterise different models of medical staffing in small hospitals: (1) the role of doctors in ED, (2) the type of doctors in the AMU, (3) the organisation of hospital wards and (4) the total cost of patient stay in the hospital (see Figure 24). The levels of each attribute were based on the quantitative data collected during the survey in WP1, the descriptive analysis of workload in WP2 and the input from the Study Steering Committee members, which included relevant clinical and academic experts. Three of the attributes were selected to have two levels and the remaining attribute had four levels. Descriptions were developed for each of the attributes to help participants understand the nature of each attribute that they were being asked to consider (see Report Supplementary Material 9).
Questionnaire design
In the DCE, respondents were asked to choose their preferred option from a series of pairwise choices, that is in which of two fictitious hospitals would they prefer to be admitted to, or, in the case of hospital doctors or managers, would they prefer to work for. Each hospital was described by a unique combination of different levels of the attributes (see Report Supplementary Material 9, Figures 1 and 2, for examples of DCE questions). We did not include an opt-out or ‘neither’ option, assuming that people with acute conditions requiring an emergency admission are unlikely to choose not to be admitted to one of the available hospitals, and that hospital doctors and managers are unlikely to choose not to work.
The number of potential combinations of attributes with three two-level attributes and one four-level attribute is 32 combinations (23 × 41). With two options to choose from in each choice question, this gives a possible 992 choices (32 × 31). To reduce the number of choices to a manageable number, a fractional design was applied using the –dcreate– command in Stata® (StataCorp LP, College Station, TX, USA),146 which creates efficient designs for DCEs using the modified Fedorov algorithm. The choice set was reduced to eight scenarios, which was thought to be a manageable number for participants to consider. To check consistency in the answers, the first choice set was included twice, as the first and as the last scenario, so that each respondent was expected to make nine pairwise choices. Overall, three versions of the DCE questionnaire (one version for patients, one for hospital doctors and one version for managers) were used.
The questionnaire also included a question that asked respondents to rank the four attributes according to their overall importance, from one (most important) to four (least important). Information on demographic, socioeconomic and hospital-related experience was also collected (see Report Supplementary Material 9).
The questionnaire was piloted by four PPI representatives who were identified from the project mailing list and six health professionals who participated in the project expert panel meeting. This resulted in minor improvements to the wording of the questionnaire being made.
Data analysis
Descriptive statistics for the characteristics of the participants who completed the questionnaire were computed. Responses to the ranking questions were presented graphically and we measured inter-rater agreement using kappa statistics. 147
The DCE data were analysed using a conditional logit regression model, where the outcome was hospital preference (A or B) and the variables in the equation were the individual attributes. We did not include a constant term. We ran the model on the whole sample, as well as stratifying participants by the three subgroups. For the doctors’ subgroup, comparative analyses were also performed for participants who characterised themselves as specialists or generalists, and by their area of residence (urban/rural), main clinical specialty (geriatric medicine/acute internal medicine) and age (< 50 years/≥ 50 years). We tested for differences in preferences between the groups by comparing the coefficients for each group using chi-squared tests.
The specification of the total cost attribute also allowed marginal rates of substitution (MRS) with respect to the costs to be computed. The MRS allow direct assessment of how much of one attribute participants are willing to trade for one unit of another attribute and, therefore, enables a comparison of different attributes on a common scale. We calculated the MRS values using the ‘total cost of patient stay in the hospital’ attribute as the denominator, so that participants’ preferences and the trade-offs could be compared on a common value scale in terms of ‘willingness to pay’ for each attribute.
In addition, we used the regression analysis results to calculate the predicted probabilities of choosing a model of staffing with attribute levels corresponding to the most and least preferred options according to the observed outcomes. Specifically, we compared the probability that a respondent would choose a hypothetical ‘least preferred’ scenario, which was defined as doctors in the ED referring patients to specialists, acute/general medicine doctors in AMU, mixed-condition hospital wards and the cost of £4000 per patient stay, with various alternative scenarios.
In each of these alternative scenarios the following potential characteristics were added individually and then jointly:
-
costs of £3500 per patient stay
-
costs of £3000 per patient stay
-
costs of £2500 per patient stay
-
doctors diagnose and treat patients in the ED
-
doctors with expert knowledge in specific clinical areas in the AMU
-
condition-specific hospital wards
-
combination of doctors diagnose and treat patients in the ED, doctors with expert knowledge in specific clinical areas in AMU and condition-specific hospital wards.
In scenarios 4–6, the cost of £4000 per patient stay was chosen as the baseline, as these models require more staffing to operate.
All analyses were undertaken using the software package Stata 13.1.
Results
Respondents’ characteristics
In total, 214 responses were received between June and August 2018 (182 responses from hospital doctors, 23 from members of the public and nine from managers). DCE questions were completed in full by 173 hospital doctors, 20 members of the public and nine managers. It was not possible to estimate a response rate for each group because the survey was sent via multiple overlapping distribution routes using convenience sampling and snowball sampling techniques. The analysis was a complete-case analysis using these respondents’ answers only.
Of the 173 doctors, 78 were female (45.1%) compared with 17 (85.0%) of the patients and public sample (N = 20), and five (55.6%) of the sample of managers (N = 9). Mean ages were 47, 52 and 49 years, respectively. In total, 17 of the patients and public sample (85.0%) had a degree, nine (45.0%) patients were full-time employed at the time of the survey. In the samples of doctors (N = 173) and managers (N = 9), most respondents were working full time: 138 (79.8%) and 8 (88.9%), respectively. A total of 68 (39.3%) doctors classified themselves as ‘generalist with some specialism’, 13 (7.5%) as ‘pure generalist’, 15 (8.7%) as ‘pure specialist’ and 67 (38.7%) as ‘specialist with some generalism’. There were doctors from 17 different specialties, the biggest group being geriatric medicine (n = 84, 48.6%), followed by acute internal medicine (n = 15, 8.7%) and gastroenterology and hepatology (n = 10, 5.8%). In the managers’ sample (N = 9), there were representatives from finance (n = 1, 11.1%), human resources (n = 2, 22.2%), clinical management (n = 1, 11.1%) and operational management (n = 4, 44.4%).
Among the sample of doctors, 68 (39.3%) were resident in urban areas, compared with seven (35.0%) of the patients and public sample and two (22.2%) of the sample of managers. From all three groups, there was a mix of respondents across different regions of England, with only three (1.8%), two (10.0%) and one (11.1%) respondents from London among doctors, patients and public and managers, respectively. Some of the respondents had been admitted to a hospital in the past year: seven (4.0%) doctors and two (10.0%) of the patients and public sample.
Simple attribute ranking
The responses to the ranking question that was posed before the DCE questions were examined (Report Supplementary Material 9, Figure 3 graphically displays the responses for each of the three groups separately). Attributes are ranked by the likelihood of being selected as the ‘most important’ factor. The kappa statistic overall was 0.2234; it was 0.2236, 0.2593 and 0.1481 for doctors, patients and the public, and managers, respectively, representing ‘fair’ agreement among rankers in most cases. 148
Using this method of ranking, the type of doctors in the AMU is ranked highly in each sample, except for managers, and the total cost is consistently considered to be the least important factor by each group. We observe some differences between groups: patients and public appear to consider the role of doctors in the ED to be the second-most important, whereas hospital doctors consider the organisation of hospital wards to be the second-most important.
Discrete choice experiment analysis
The regression results for all groups combined and by subgroups are shown in Report Supplementary Material 9.
Given the small sample size of the managers’ subgroup (n = 9), we do not discuss the results for this subgroup any further and instead focus on the results for the doctors and the public and patients subgroups. Both the doctors and the patient and public subgroups prefer that in the ED, doctors diagnose and treat patients instead of referring them to specialists; they also prefer that the AMU is run by specialists compared with generalists, and that there are condition-specific hospital wards compared with mixed wards for follow-up care. All subgroups prefer lower levels of total cost per patient stay. There were no statistically significant differences in preferences between the doctors and the patients and public subgroups (all p > 0.1).
The MRS show the relative importance of each attribute by enabling the comparison of different attributes on a common scale. Overall, doctors’ willingness to pay was higher than the patients and public. Doctors were willing to pay £2469 for ED doctors to work on patients instead of triaging them to specialists, whereas patients and public were willing to pay £1123 for this. Doctors were willing to pay £4609 for AMUs to be run by specialists with expert knowledge in specific clinical areas, instead of specialists in acute/general medicine with broad knowledge in most clinical areas; patients and public were willing to pay £2827. Finally, doctors were willing to pay £6545 for patients with specific conditions to be treated on specialist wards instead of on mixed wards, in which patients with a variety of conditions are treated on the same ward; patients and public were willing to pay £2797 for this. These MRS values reflect the ranking of attributes that can be derived from combining the estimated coefficient for each attribute and the range of levels. According to this ranking, for doctors the most important attribute was organisation of hospital wards (range 1.44), followed by the type of doctors in the AMU (range 1.01) and the role of doctors in the ED (range 0.55). For patients and public, the most important attribute was the type of doctors in the AMU (range 1.66), followed up by the organisation of hospital wards (range 1.64) and, finally, the role of doctors in the ED (range 0.66). 149
Further subgroup analyses were conducted, stratifying the doctors’ sample by role (generalist/specialist), age (< 50 years/≥ 50 years old), area of residence (rural/urban) and specialty (geriatric medicine specialists and acute internal medicine specialists). The results are presented in Report Supplementary Material 9. We observed significant differences in the preferences between generalists and specialists, in particular the trade-off between the types of doctors in the AMU is higher for specialists, as well as the trade-off between different types of the organisation of the hospital ward. Doctors who were working in geriatric medicine preferred hospitals in which the AMU was run by specialists, whereas for those working in acute internal medicine, this attribute was not statistically important (this could be due to the small sample size, n = 15). There were significant differences in the preferences for the organisation of hospital wards by age: for doctors aged < 50 years it was more important to work in a hospital with specialist hospital wards than for doctors aged ≥ 50 years.
The probability that respondents would choose a hospital with particular attribute levels compared with a least preferred model of staffing is presented in Report Supplementary Material 9. Compared with a hospital in which doctors in the ED refer patients to specialists, there are acute/general medicine doctors in AMU, there are mixed-condition hospital wards and there is a cost of £4000 per patient stay, respondents were more likely to choose a hospital in which doctors diagnose and treat patients in the ED (holding the rest of the attributes constant), a hospital in which the AMU is run by doctors with expert knowledge in specific clinical areas (holding the rest of the attributes constant) and a hospital in which there are condition-specific hospital wards (holding the rest of the attributes constant). If a hospital had all of these changes in the attributes, at the expense of having the largest cost, £4000 per patient stay, defined as the ‘best case scenario’, the probability that respondents would prefer to work or to be admitted to this hospital reached 95% and 98%, respectively.
Conclusions
Summary of the main results
In this study we explored the preference of hospital doctors, patients and public and managers for different workforce models using a DCE. We found that responses were consistent between the hospital doctors and the patients and public; both prefer that in the ED doctors diagnose and treat patients compared with referring them to specialists, that the AMU is run by specialists rather than generalists, and that there are condition-specific hospital wards compared with mixed wards for follow-up care. Both groups prefer lower levels of total cost per patient stay, and there were no statistically significant differences in preferences between these two groups.
Strengths and limitations
This study provides, to our knowledge, the first evaluation of individual preferences with respect to workforce models in small hospitals. We used a DCE that allowed the evaluation of the attributes of a service that respondents would prefer to receive and the trade-offs they are willing to make between these attributes. The analysis was carried out with responses from over 200 participants. Content validity of the DCE was obtained by grounding the attributes and levels included in the experiment on careful construction of the typology conducted during this study. The questionnaire was carefully tested and revised during piloting.
We acknowledge several limitations, the main limitation being the limited sample size for the patient and public and manager subgroups. In particular, the number of responses from the latter was very small and, therefore, meaningful analyses were not possible. In addition, DCEs elicit hypothetical choices and, therefore, might lack external validity if individuals do not make the same choices in real-life situations. The representativeness of the sample responding to the questionnaire might be limited, as the generalisability of the findings depends on individuals elsewhere having similar preferences. Although the selection of attributes included in the DCE was carefully considered, we acknowledge that there might be other factors affected by workforce models that are not included in our analysis that may also be considered important for individuals; however, the number of attributes that can be included in a DCE exercise is limited.
Exploratory analysis of patient-related outcomes
In this study, we wanted to explore measures that could be derived from routinely available data and to test the value in helping to evaluate different models of medical generalism. Our analysis focused on two measures in particular: mortality and re-admission. Full details of the analysis can be found in Report Supplementary Material 10.
Mortality rates
The measurement and use of mortality rates following a hospital admission has been the subject of considerable debate in the UK over the past few years. 150–152 Our position is that some examination of what happens to patients in terms of survival is essential in a modern health service, with survival being the most basic of outcome measures. However, to come to conclusions about what is driving differences in mortality rates between clinicians, services, hospitals and areas, additional evidence is required, and there is a danger of jumping to conclusions too quickly. In this study, our concerns were establishing whether or not we could observe crude differences in mortality between hospitals and whether or not these could be linked to patterns of consultant working.
The analysis of mortality considered both in-hospital mortality, as recorded in 2015/16 HES data for the smaller hospitals cohort, and out-of-hospital mortality. Overall, the analysis of mortality was limited by the time frame for which corresponding out-of-hospital mortality data were available (up to August 2015 only). Therefore, the analysis focused on 12-week survival of patients who were admitted between 1 April 2015 and 31 May 2015.
Observations
Within our 3-month follow-up period we studied 151,430 patients who were admitted to hospital, of whom 16,130 (10.7%) died within 3 months. Of these, 7587 patients (5.0%) died in the first week after admission, 38% of whom died in hospital (Table 25).
| Survival (weeks) | Frequency (n) | Cumulative per cent who died | Per cent of deaths that were in hospital |
|---|---|---|---|
| 0 | 7587 | 5.0 | 38.9 |
| 1 | 1235 | 5.8 | 9.7 |
| 2 | 1043 | 6.5 | 12.6 |
| 3 | 987 | 7.2 | 11.9 |
| 4 | 841 | 7.7 | 11.3 |
| 5 | 773 | 8.2 | 11.3 |
| 6 | 731 | 8.7 | 13.1 |
| 7 | 681 | 9.2 | 9.3 |
| 8 | 666 | 9.6 | 9.8 |
| 9 | 589 | 10.0 | 9.5 |
| 10 | 530 | 10.3 | 10.0 |
| 11 | 467 | 10.7 | 8.8 |
| Total in 3 months | 16,130 | 10.7 | 24.0 |
Deaths were concentrated in a relatively small number of case-mix groups: 15 groups accounted for 70% of all deaths. This is not surprising, as although there are many different health problems and underlying diseases that might exist in an individual, there are a few common reasons that predominate as the final cause of death, especially in the acute hospital setting. It is probably the case that the information derived from diagnostic codes in these final episodes of care does not capture the underlying clinical complexity of an individual. Therefore, caution should be used in interpreting the quality of care provided or the avoidablity of the final outcome.
The crude death rates showed a three-fold range from 5% to 15%, although the variability was less when standardising for differences in age and sex. This was further reduced when the diagnostic CMG grouping was used to standardise between trusts (see Report Supplementary Material 11). However, few of these differences appeared to be statistically different from the group averages at the 1% level. This could arise from a number of reasons, including different recording systems for the denominator and differences in the presenting patients that are not captured in the diagnostic standardisation. It is worth noting that routinely used hospital indicators, such as the HSMR or the SHMI, include more sophisticated risk adjustment.
Re-admissions
The occurrence of an emergency re-admission has been widely used for some time as an indication of the quality of hospital care. Some health systems, including the NHS, have looked at ways to penalise hospitals that show high rates of emergency re-admission, on the basis that these are a result of a lapse in the quality of care. However, there are a number of studies that suggest that the reasons for an emergency re-admission are more complex and that, at most, only about 30% of emergency re-admissions could be related to lapses in the quality of care in the index episode. 137 For example, re-admission may be a fact of life for people with some types of chronic disease, with the rates of emergency re-admission giving a small glimpse of longer disease trajectories.
We were interested in the degree of variation between case types and between hospitals in the observed re-admission rates to see whether or not these could be related to the approach to medical generalism. The analysis of re-admission was based on emergency re-admissions following one of 1.2 million admission spells in 2015/16. We looked at three different time periods following the discharge date:
-
re-admission within 30 days
-
re-admissions within 90 days
-
re-admissions within 365 days.
The proportion of episodes leading to re-admission was fairly high at 14% after 30 days and 29% after 365 days (Table 26). Given that these are acute medical cases, it is perhaps not surprising that these re-admission rates are slightly higher than those recorded for a wider set of index episodes; for example, for the same year, Friebel et al. 153 observed a 30-day re-admission rate of 12.7% based on all emergency admissions.
| Time period | Re-admissions (n) | Re-admissions rate |
|---|---|---|
| Within 30 days | 168,807 | 14.1% |
| Within 90 days | 266,944 | 22.3% |
| Within 365 days | 350,097 | 29.3% |
Re-admission rates at the trust level show some variation between hospitals. For example, 30-day re-admission rates were highest at the Homerton (25%), which is probably linked to the high incidence of sickle cell problems in the admissions. A few other trusts showed crude 30-day re-admission rates of 15–17%.
Links between outcome measures and hospital characteristics
To look at the relationships between these outcome measures and the characteristics of the way hospitals organised acute medical work, we used the typologies that were described in Chapter 7. In this section, the mortality was derived from in-hospital deaths; this was necessary to increase the number of cases that could be examined.
In developing the models, we sought to test the association between an outcome model and hospital subtypes, standardising for a range of covariates that could influence the outcome. These included:
-
Information about the patients, including case-mix markers of frailty.
-
Characteristics of the provider hospital, including size and CQC rating.
-
Characteristics of the local area, including a measure of deprivation, markers of urban/rural areas and the distance to hospital.
The models were developed in parallel with the economic models described in Chapter 6, and used logistic regression throughout with a wide range of covariates. Standard errors were adjusted for clustering at the hospital level. For each outcome we present two models, one including percentage of medical staff who are generalist > 0.5 and one not including it [the proportion (%) of medical staff who are generalist are not available for all hospitals, so the sample size is smaller].
Results
Table 27 summarises the model results when looking at in-hospital mortality. There was little difference in the adjusted probability of in-hospital mortality for all of the typology subtypes, and the 95% CIs overlap. Therefore, we conclude that there is no detectable association between the models used to organise acute medical care and the observed mortality rates, when a series of additional covariates are included. Both the models that include and the models that exclude the proportion of medical staff who were generalist produced the same results.
| Typology | Model 1a | Model 2b | ||||
|---|---|---|---|---|---|---|
| Adjusted probability | Standard error | 95% CI | Adjusted probability | Standard error | 95% CI | |
| AMU1 | ||||||
| Closed | 0.020 | 0.001 | 0.018 to 0.022 | 0.019 | 0.002 | 0.016 to 0.022 |
| Open | 0.020 | 0.002 | 0.016 to 0.023 | 0.020 | 0.002 | 0.016 to 0.024 |
| Partial | 0.020 | 0.001 | 0.018 to 0.021 | 0.020 | 0.001 | 0.018 to 0.022 |
| AMU2 | ||||||
| APD | 0.019 | 0.001 | 0.016 to 0.021 | 0.019 | 0.001 | 0.017 to 0.022 |
| Mixed | 0.020 | 0.001 | 0.018 to 0.022 | 0.020 | 0.001 | 0.018 to 0.022 |
| Specialist physician dominant | 0.022 | 0.001 | 0.019 to 0.025 | 0.022 | 0.002 | 0.018 to 0.025 |
| Ward1 | ||||||
| Closed | 0.019 | 0.001 | 0.017 to 0.020 | 0.019 | 0.001 | 0.017 to 0.020 |
| Open | 0.018 | 0.002 | 0.013 to 0.022 | 0.020 | 0.004 | 0.012 to 0.027 |
| Partial | 0.022 | 0.002 | 0.019 to 0.025 | 0.021 | 0.002 | 0.018 to 0.024 |
| Ward2 | ||||||
| General medical ward | 0.020 | 0.001 | 0.017 to 0.023 | 0.020 | 0.001 | 0.017 to 0.023 |
| Specialist ward | 0.020 | 0.001 | 0.018 to 0.021 | 0.019 | 0.001 | 0.018 to 0.021 |
| Proportion of medical staff who are generalists > 0.5 | ||||||
| No | 0.020 | 0.001 | 0.018 to 0.021 | |||
| Yes | 0.020 | 0.002 | 0.017 to 0.024 | |||
| Observations | 699,792 | 670,182 | ||||
| Pseudo R2 value | 0.202 | 0.202 | ||||
We also note that although a lot of predictor variables were included in the models, the overall adjusted R2 value was 0.202, which indicates that only 20% of the variability in mortality was accounted for by these variables. Therefore, there is a lot of variation linked to other factors. For each of the typology categories, the adjusted probabilities of in-hospital CIs overlap as shown in Table 27.
The same approach was used to look at emergency re-admission rates for 30, 90 and 365 days. Table 28 shows the results for the model based on 30-day re-admissions. Once again, there were no discernible differences between hospital subtypes and re-admission rates at 30 days. The pseudo R2 value for this model was lower than that for mortality, which indicates that there are higher levels of uncertainty about what drives differences in re-admission rates.
| Typology | Model 1a | Model 2b | ||||
|---|---|---|---|---|---|---|
| Adjusted probability | Standard error | 95% CI | Adjusted probability | Standard error | 95% CI | |
| AMU1 | ||||||
| Closed | 0.146 | 0.002 | 0.142 to 0.150 | 0.145 | 0.002 | 0.140 to 0.149 |
| Open | 0.139 | 0.004 | 0.132 to 0.146 | 0.138 | 0.004 | 0.131 to 0.146 |
| Partial | 0.142 | 0.002 | 0.139 to 0.146 | 0.143 | 0.002 | 0.140 to 0.147 |
| AMU2 | ||||||
| APD | 0.143 | 0.003 | 0.138 to 0.147 | 0.141 | 0.002 | 0.136 to 0.145 |
| Mixed | 0.144 | 0.002 | 0.141 to 0.147 | 0.144 | 0.001 | 0.141 to 0.147 |
| Specialist physician dominant | 0.144 | 0.004 | 0.136 to 0.153 | 0.143 | 0.005 | 0.134 to 0.152 |
| Ward1 | ||||||
| Closed | 0.140 | 0.002 | 0.136 to 0.144 | 0.139 | 0.002 | 0.135 to 0.143 |
| Open | 0.154 | 0.007 | 0.140 to 0.168 | 0.158 | 0.008 | 0.142 to 0.175 |
| Partial | 0.147 | 0.001 | 0.144 to 0.150 | 0.146 | 0.002 | 0.143 to 0.149 |
| Ward2 | ||||||
| General medical ward | 0.140 | 0.002 | 0.136 to 0.143 | 0.140 | 0.002 | 0.136 to 0.145 |
| Specialist ward | 0.146 | 0.002 | 0.142 to 0.150 | 0.145 | 0.002 | 0.141 to 0.148 |
| Proportion of medical staff who are generalists > 0.5 | ||||||
| No | 0.143 | 0.001 | 0.140 to 0.145 | |||
| Yes | 0.142 | 0.004 | 0.135 to 0.150 | |||
| Observations | 707,054 | 677,159 | ||||
| Pseudo R2 value | 0.066 | 0.066 | ||||
Similar results were observed for models looking at 90-day and 365-day re-admissions (not shown).
Covariates that were also included in models but not reported were the:
-
case-mix groups
-
procedure flags
-
frailty flags
-
secondary cancer flags
-
patient age
-
patient gender
-
patient ethnic group
-
admission source
-
urban/rural indicator for patient’s small area of residence
-
population covered by hospital
-
hospital distance to nearest ED
-
trust operating revenue
-
approximate number of beds on main hospital site
-
hospital ED attendances 2015–16
-
hospital emergency admissions 2015–16
-
urban/rurality indicator
-
hospital size
-
CQC rating.
Standard errors were adjusted for clustering at hospital level.
Discussion
The analyses covered in this section have been exploratory and were designed to test for any large-scale impacts that might be present and help to inform more detailed modelling. We noted that:
-
The severity of illness that was present on these cases that meant a relatively large proportion of these patients died within 3 months, and even within the first week.
-
Re-admission was a common phenomenon and for many patients acute medical episodes are just one element of a much longer and more complex disease trajectory.
-
Although there can be some large differences in crude mortality rates between trusts, many of these differences are reduced using simple standardisation methods. There are, however, some residual values that look atypical and would merit further investigation.
-
For the acute medical caseload, a relatively small number of the diagnostic categories can be used to capture the majority of deaths. This suggests that comparisons between providers using this standardisation should be treated with some cautions, as there will be other factors, not captured in the information we have, that may influence these local rates.
-
Despite building complex models we could not detect any difference between the way acute medical services were organised and the outcomes in terms of in-hospital mortality rates or emergency re-admission after 30, 90 or 365 days.
The biggest limitation in our analysis, and our greatest challenge, has been obtaining permission to use the relevant data sets, despite that our organisation held these data for other projects. Throughout the course of this project, the national requirements on information governance have been subject to constant flux that has meant that it proved impossible, despite our very best endeavours, to obtain the data that we wanted. For this study it meant that the information on out-of-hospital mortality was limited to a relatively short window. Therefore, for some analyses, we restricted ourselves to in-hospital mortality only.
The implication of our findings is that the organisation of acute medical services does not have a dramatic impact on some basic outcome measures, such as mortality and re-admissions. Any claims otherwise should be treated with caution. It also suggests that explanation of the benefits or disbenefits need to consider other factors, such as process measures for staff continuity, or explore other outcomes.
Chapter 8 Discussion
Summary of findings
Generalist and specialist models of care
At its conception, the key underpinning assumptions of this study were that smaller hospitals used a limited number of clearly defined models of care, which could be classified along a spectrum of generalist to specialist and would be amenable to a systems analysis approach. Instead, we found that no two hospitals operated identical systems of care and that systems were resistant to classification and comparison. This necessitated a switch in approach, so instead we concentrated on the two main locations of medical general working: the AMU and the downstream medical wards. We categorised AMUs according to patterns of consultant working (APD, SpD or mixed), whether or not units were heavily boundaried and the subsequent patterns of patient ‘ownership’ by medical teams (closed, open or partial). Downstream wards were similarly classified by their degree of closed/openness, as well as how hospitals labelled wards and distributed patients across them (general medical wards, specialty wards).
Classification of the 48 hospitals for which we had sufficient data revealed that there were 25 different models of care in operation. Correlation of the organisational profiles with the typology found that there were more generalist models of care in smaller organisations (< 300 beds). Beyond this, there were no associations found between models of care and other factors, such as hospital size, number of emergency admissions or hospital location. Patterns of working in AMUs varied more than patterns of working on downstream wards.
We further found that there were two trends in terms of arranging care at the front door. The ‘acute hub’ model looked to co-locate services with a primary assessment function into a single ‘hub’, whereas the ‘hyperstreaming’ model saw the bulk of the primary assessment work move out of the ED and into a series of parallel locations, such as ambulatory care, frailty units and other assessment units.
The telephone interviews and case study visits found that most models of care, however defined or arranged, were highly unstable and in an almost constant state of flux, with usual processes of care frequently breaking down in the face of internal and external pressures.
Patient perspective
Review of over 10 million acute medical emergency episodes of care at 69 NHS trusts over 6 years confirmed a rising demand in smaller hospitals. Overall, there was a 26% increase in the total number of episodes between 2012–13 and 2017–18, with an average yearly increase of 5%.
Analysis of the case mix for the same patient cohort found that most patients had conditions that could be considered to be largely amenable to generalist care. There was a high concentration of cases from relatively few diagnostic groups, with over 80% of episodes and 75% of bed-days falling into 31 groups; 31% of patients had a frailty indicator. Overall, there were more similarities than differences with regard to case mix across hospitals, the exception being smaller hospitals in urban areas.
There was no correlation between the case mix of hospitals and the skill mix of the medical staff within them. Telephone interviews and the case studies revealed that although attempts were made to meet patient need at the service level, such as the introduction of frailty teams or units, care was rarely orientated around patient need at the hospital level.
The DCE found that patients have a weak preference for specialist care. This was confirmed by the patient and carer focus groups, although participants indicated that the quality of care at their local hospital was more important than what type of consultants provided care, and acknowledged that smaller hospitals cannot necessarily be expected to provide highly specialist services.
Service perspective
Smaller hospitals have responded to the challenge of rising admissions by improving flow through their systems. Between 2012–13 and 2016–17 the number of episodes of care rose by 26% but the number of occupied bed-days rose by only 5%. The extra activity was accommodated by a reduction in the length of stay and an increase in short-stay cases. There was a three-fold difference between hospitals in terms of the shortest (2.8 days) and longest (8.41 days) average LOS.
Neither the model of care, as defined by the typology, nor the case mix accounted for the variability in the average LOS between hospitals (no associations were significant at p < 0.5). There were also no detectable associations between the models of care and the observed in-patient mortality rates or re-admissions at 30, 90 and 365 days. These findings imply that other factors acting at the hospital level are the critical determinants of outcomes. There were no significant differences in the costs of the models of care.
Telephone and case study interviews found that models of care were shaped by complex constellations of factors that interacted at multiple levels. Predominant among these were hospital size and location; the ability to retain and recruit staff; organisational culture and leadership; and often competing policy imperatives. Models tended to be highly reactive, rather than proactive. Where there was evidence of strategic planning, this tended to be driven by single individuals operating at the service level who were hindered or enabled by other factors at the hospital level. Hospitals with the most stable and mature models of care were those that planned at higher levels, had clear strategic aims to meet local community need and fostered collaborative working environments.
The work on pathways found that the journeys of patients with similar conditions through the emergency and acute medicine system varied markedly both within and between organisations. The telephone interviews and case study visits corroborated these findings. The interviews also found that systems were frequently overwhelmed by demand, leading to differences between models as conceived and models in action. It was also found that staff frequently adjusted the pathways of patient care according to complex calculations that were based on instinct, experience and intimate knowledge of their hospital system.
Both more generalist and more specialist models of care were viewed as having significant advantages and disadvantages by hospital staff. Overall, more generalist models were thought to be more appropriate models of care for smaller organisations. Staff viewed the size of the hospital as being a more powerful explanatory category for almost all aspects of service delivery and outcomes than the model of care per se.
Professional perspective
The qualitative work found that the preference of doctors for generalist or specialist working was contingent on the hospital environment and the heaviness of the burden of generalist working. Experiences of training were also important, with preferences for generalism being associated with longer periods of training; younger specialists frequently felt poorly equipped to care for older complex patients.
Although the majority of consultants who were interviewed accepted generalist working as an inevitable consequence of working in a smaller hospital, we found patterns of behaviours, particularly ‘flight from the front door’ and ‘fortressing’, whereby consultants actively sought to limit their exposure to generalist working and regulate their own workloads. These behaviours were viewed as highly destabilising and their presence was correlated with more negative views of organisational culture and leadership.
The preferences for withdrawal from participation in front-door services and for working only as a specialist were expressed more strongly in the DCE.
Smaller hospitals
Although this study was constructed primarily as an exploration of aspects of care within hospitals, it rapidly emerged that systems of care could not be divorced from their contexts. Staff considered their smaller hospitals to be categorically distinct from larger teaching organisations and ‘smallness’ to be the most powerful explanatory category of their experiences of delivering care.
The idea that smaller hospitals might be categorically distinct was supported by the explorations of case mix, which found that there were more similarities than differences across all 69 organisations. The exception to this was the few smaller hospitals in urban areas.
Most smaller hospitals viewed themselves as being under genuine existential threat, being understaffed, being under-resourced and almost constantly battered by ‘system shocks’, to the point where positive change was extremely difficult to enact. Although we did not measure resilience or any other measure of organisational climate, hospitals with skilled, stable leadership teams who had invested long term in cultural change were associated with environments that staff viewed as desirable to work in and more stable systems of care.
Concepts of medical generalism
No clear or consistent definitions of medical generalism were found in the literature. Instead, the term emerged as slippery and frequently negatively defined, for example as ‘the work left undone’ or a ‘gap’ to be bridged. Moreover, there was a major schism between the constructions of medical generalism as a philosophy of care or a discipline within medical practice, and the way generalist practice was enacted, especially where generalism was viewed as the solution to a particular problem within health care.
These inconsistencies and gaps were reflected in what we saw in practice. Although there was a broad consensus about which patients should belong to specialists, we did not find any consistent definitions in use nor was there any real agreement about the boundaries between specialism and generalism. Instead, there was often a substantial distance between what clinicians and managers thought systems of care should look like and the enaction of these systems of care. Within systems, there was evidence of the boundaries of medical working being almost constantly negotiated and renegotiated.
Doctors enjoyed generalist working more in systems that were geared to meeting patient need, regardless of the location of the patient or the label allocated to them, and where work was shared in ways that were transparent, equitable and collaborative. Some clinicians viewed these ways of working as being the definition of ‘true generalism’.
Discussion of key findings
The mapping of emergency and acute medical services
To the knowledge of the authors, this was the first systematic attempt to map and compare emergency and acute services for medically unwell patients across the whole patient pathway in English hospitals.
This study revealed that emergency and acute medicine services were highly complex. National surveys of the acute care of specific conditions154,155 and research on emergency services125 have noted marked variability in the structures of acute care in England and the journeys followed by patients. However, the increasing complexity of front-door services in England has been most clearly highlighted by the annual Society for Acute Medical Benchmarking Audit (SAMBA),156 which also found an increasing array of parallel front-door services, with patients following highly fragmented pathways through systems, with multiple handovers, before arriving at a definitive place of care.
This contrasts with Reid’s survey on Scottish hospitals,101 where it was noted that although 65.5% of hospitals had ‘acute medical work’ happening outside the AMU, the only other locations for work were the ED and the downstream medical wards. By contrast, we found that 100% of hospitals had some form of the same work taking place outside the AMU and the ED, with most hospitals providing multiple parallel geographic spaces for the primary assessment of patients. This underlines the impact of central policy drivers that have sought to move acute work out of the ED in English hospitals.
The emergence of models of care
We expected that the establishment of models of care with hospitals would follow logical pathways, with a conscious choice of a coherent model thought to be suited to the hospital, planned execution and subsequent evaluation of implementation. Instead, we found that models were heavily contingent, driven by policy imperatives, hastily executed and rarely systematically evaluated. They were frequently cobbled together and the result of negotiations and compromises, which were based on available staff and resources. Models that were presented initially in the interviews and case studies as being stable were revealed as actually being fluid, dynamic and frequently overwhelmed by the combination of demand and inherent fragility. These findings point to the tension between the presentation of change within health-care systems as being ordered and planned, and the actuality of systems as being emergent and dependent. 157 Moreover, models of care, in many cases, were so tightly bound to their contexts that staff were unable to articulate models of care as independent artefacts.
This is particularly problematic in the NHS, given the implicit assumptions that components of care, such as EDs, AMUs and ambulatory care, are independent of microlevel factors and an increasingly top-down driven model of change. Moreover, although individual studies of AMUs and ambulatory care units have been found to produce better outcomes for certain groups of patients, the evidence base remains limited and there has been very little or no study of their impact at the system level. 76,97,158 The implication is that there is a major gap between the theoretical understandings of context, and its importance in the diffusion of innovation, and the non-linearity of complex systems159,160 and the reality of how this is conceived and enacted within the NHS at multiple levels.
The other gap that emerged from the interviews was the lack of capacity within smaller organisations for the rapid change that is demanded of them at almost every level: financial, managerial, geographical, staffing and other resources. Such pressures led to organisations ‘making do’ to meet external expectations, rather than embarking on programmes of sustained change.
Patterns of presentations and admission to hospitals
Patterns of presentations of acute disease across first-world countries are highly similar, with a predominance of cardiovascular and respiratory disease. 161–163 However, there have been few systematic attempts to identify how patient care might be better organised at the system level according to disease state. Kellett and Deane’s164 efforts to categorise medical admissions to a single hospital in Ireland similarly found that most of the acute work could be accounted for by relatively few conditions and was amenable to a generalist approach to care, with near complete overlap of the top 20 conditions between their cohort and ours. 164 The similarities between these two studies, despite geographical and temporal distance, suggest that acute medical work in smaller hospitals is predictable and that services should be able to be better matched to demand.
Despite similarities in patterns of presentation, patterns of admission to hospital were found to have changed over time, with increasing numbers of short-stay presentations, and found to exhibit marked variation between organisations. This is in line with other studies that have suggested that thresholds for admission have fallen in England over time165 and that admission appears contingent on other factors, such as the structure of front-door hospital services and consultant preference. 125,166
Association between outcomes and models of care and case mix
Variations in the quality of outcomes are a key concern to health-care professionals and policy-makers alike. Despite decades of research, consensus has not yet been unreached around the boundaries between ‘warranted’ and ‘unwarranted’ variation, and to what extent unwarranted variation is driven by differences in the underlying demographics of patients, by differences between organisations and their delivery of services or by the performance of individual clinicians. 167–169
A key finding of this study was that variations in LOS and other outcomes were not explained by either the typology or the case mix, implying that other hospital-level factors were responsible. We first discuss aspects of case mix and models of care with regard to other literature and the implications of our findings, and second explore the other potential explanatory factors.
Case mix and outcomes
The routine measurement of acute hospital case mix has become a common theme in systems of funding and reimbursement of hospitals, as well as in comparative assessments of performance. 111,170,171 Fundamental to this is the idea that differences in the mix of patients have implications for the likely use of resources and models of care offered in a single institution, and that measurement of and adjustment for case mix is a prerequisite for meaningful comparisons between hospitals with different patient populations. 172–174
The use of case-mix systems as a tool to explore within hospital organisations is less developed and there is little published work that looks specifically at the case mix in acute medicine, although some research has been carried out in the hospitalist setting in the USA. 175 This is despite the identification of case mix as a critical priority for service development. 176
Our study found that the differences in acute emergency medical case mix between hospitals were not that large. The large differences in bed use could, therefore, not be explained by case mix. We noted that when using standard weighting, expected bed needs per cases varied only by a small amount (± 10%) in comparison with the twofold to threefold difference in average LOS.
Although this study fits with other research that suggests that hospital-level factors other than case mix account for variations in LOS,138,168,177 it sits less well with studies that suggest that differences in case mix at least partially account for differences in outcomes between larger urban hospitals and smaller rural hospitals. 178,179 We did find that smaller hospitals in London were outliers with regard to case mix, but it should also be considered that the hospitals in this study were larger (all over 300 beds) and less rural than their international counterparts.
Acute medical unit models of care and outcomes
The prevailing ethos is that interventions early in the patient pathway account for differences in both patient-level and hospital-level outcomes. However, we did not find evidence that the organisation of care on AMUs had an impact on outcomes, although we were able to look at only a limited range of indicators.
In addition, the only aspect of care that we were able to examine in any depth was patterns of consultant working. We viewed the patterns as sitting along a spectrum of more generalist to more specialist. At one end there is the model that is widely considered to be the gold-standard model, whereby AMUs are closed, with all patients being cared for by a single physician working in a generalist capacity. 180 At the other end are open units, with ‘take triage’ specialist models, which are premised on studies showing that earlier specialist input improves outcomes for patients with specific conditions, such as myocardial infarction181 and COPD,182 and further driven by concerns that specialists working intermittently on AMUs have difficulty in maintaining the skills required for the safe management of the medical take. 183,184 We found that there were no significant differences between outcomes for the generalist and take triage models of care with regard to LOS (3.2 days vs. 3.5 days, respectively) or for the probability of mortality or re-admission.
These findings sit with a growing body of evidence that patterns of consultant working as a whole are less important than other factors at the system level. The dominant hypothesis that patterns of consultant care impact on morbidity and mortality, is largely based on the consistent association between levels of consultant input and poor patient outcomes in morbidity and mortality reviews. 155 One study81 of outcomes on AMUs found that longer periods of consultant presence were associated with lower mortality. However, more recent studies have begun to challenge this. Aldridge et al. 185 found that there was no difference in weekend mortality between high intensity and low intensity patterns of consultant working, whereas two other studies failed to find improvements in patient outcomes following the introduction of 7-day consultant working for acute services. 166,186 These studies used non-commensurate ways of measuring consultant working, yet they support the finding that although patterns of consultant working may contribute to high-quality care, the association with hard outcomes remains weak and there is little evidence to guide best practice.
Ward models of care and outcomes
Given that only half of all acutely unwell medical patients ever reach the downstream wards, the finding that the organisation of care has minimal impact on outcomes is perhaps not unexpected. Moreover, although we found differences in the organisation of wards at the hospital level, with some hospitals having generalist wards, overall we found that the majority of patients were cared for on closed wards by a single consultant at any given point in time. This homogeneity is probably explained by long-standing safety concerns around ‘safari ward rounds’90 and ‘boarding’,187 and the management of patients in inappropriate clinical spaces.
Although there was no difference in the LOS between the open model and the closed model, the economic costs were lower in the three hospitals that had open downstream wards. This may be accounted for by differences in continuity of care. Although closed wards may imply more continuity, we found that the reverse was true. In a system with closed wards, every movement of a patient necessitates a change of consultant. Moreover, specialty consultants tend to rotate through closed specialty wards on a weekly or even daily basis, making discontinuity of care the norm. This contrasts with open models, where consultants follow patients regardless of their location in the hospital, thereby increasing continuity. Continuity is less well-studied in hospitals, but is associated with better outcomes for patients in primary care settings. 188
Models of care and hospital size
The statistical analysis of HES data did not consider hospital size in relation to outcomes. However, the qualitative work found that smaller hospitals tended to use more generalist models, whereas take triage models, which require a larger consultant body to support them, were found in larger organisations only. It is possible that any theoretical benefits of take triage models were cancelled out by their use in organisations that were too small to optimally execute them. This implies that there may be a threshold effect with regard to models of care and that smaller hospitals need different solutions from larger ones.
Models of care as emergent systems
An explanation for the failure to find differences in outcomes between models of care is the finding that models of care could not be considered to be independent of the organisations in which they sit, but were rather more emergent than planned and could be considered to be ‘ecological artefacts’ of a range of hospital-related factors, such as staffing, resources, attitudes and behaviours, while also being heavily influenced by external policy imperatives. Moreover, we found that systems of care were not uniformly executed but actually varied in a highly dynamic and fluid fashion, which went beyond breaking down in the face of demand, but rather operated on a daily basis in response to hospital, ward and staffing circumstances according to a complex calculus. This notion of systems as being emergent and/or ecological is fundamental to concepts in Soft Systems Engineering95 and is well recognised in the general field of organisational research. 189,190 These concepts have yet to widely penetrate research in health-care systems. If models and pathways of care are not uniform and static, but rather are highly dynamic and variable, as suggested by this and a handful of other studies,177,191,192 then more sophisticated approaches than are currently deployed are required to understand and improve the execution of models of care. It also suggests that prescriptions for improving care at macro level are much less likely to be successful.
Culture and consultant behaviour
The qualitative work strongly suggests that culture should be considered as an important explanatory category for differences in hospital performance. Although we did not use formal measurements of culture, mature and coherent models of care were found only in organisations with stable leadership and seemingly healthy organisational culture. This view of culture as being of over-riding importance is congruent with the Francis Report193 and other explorations of system success and failure within the NHS. 194,195 However, we found several aspects of culture that are worth further consideration.
Improvements in organisational culture within the NHS are consistently framed around leadership and management,196,197 which was affirmed by the interviews. However, two other factors emerged as being important determinants. The first of these was a sense of mission. Organisations that saw their purpose as being to meet the needs of their local communities, and were fully committed to managing the ‘business’ of the front door, were more likely to have staff who were willing to share the burden of the acute work. The second related factor was the importance of harnessing the more informal and friendly environment that emerged naturally from organisational size and geography to foster collaborative working practices. In most cases, although not all, hospitals in which we found these attitudes and behaviours had invested in the long term in a variety of long-term programmes of staff development and culture change.
Organisational studies within the NHS have also tended to focus on the internal climate and management; however, we found that the most difficult challenges were reported as external factors. This is supported by recent work from Dixon–Woods et al. ,198 which noted the highly populated regulatory environment in the UK and the extent to which this distracts from the delivery of care. More importantly, a systematic review199 of studies of organisations that were struggling to improve care, found that although ‘system shock’, an event that detracts from the day-to-day running of the organisation, was less commonly reported than other factors, such as poor organisational culture or inadequate infrastructure, its effects were more severe, difficult to overcome and lingered for unexpectedly long periods of time. 199 This suggests that the efforts directed towards improving models of care may be futile unless the turbulence that many smaller hospitals are facing can be calmed.
We observed a number of negative consultant behaviours, which were capable of undermining the sustainability of the staffing and, hence, models of care within smaller hospitals. Disruptive behaviour in the medical context is usually described in the literature as acts of aggression, such as incivility or bullying,200,201 or as withdrawal from the emotional labour of doctoring, such as the exhibition of uncaring attitudes towards patients and colleagues. 202,203 Instead, two relatively novel yet pervasive behaviours were described by staff: ‘fortressing’ and ‘flight from the front door’.
Both behaviours have effectively been described before. The increasing preference for specialists to work within their own disciplines has been well documented by the RCP’s annual census reports. 105 Siloing and protectionist approaches to work are considered to be a common feature of NHS systems204 and competition to withdraw has been found in ethnographic studies of medical team working. 205 The negative impacts of these are usually framed in the context of fragmented or less-safe care for patients. However, we found that both ‘flight’ and ‘fortressing’ were highly deleterious through the creation of artificial workforce shortages and discontent among colleagues, shifting the behaviours from preferences for patterns of working to forms of service disruption or even sabotage. 206
Both the organisational management and the medical behavioural literature associate disruptive behaviours with organisational culture and leadership,207–209 findings consistent with this study. The medical literature has focused on burnout as another explanatory factor, particularly in doctors working in acute settings. 210,211 This was not explored in this study, although negative experiences of generalist work were common and associated with desire to withdraw from generalist work.
Other factors
Interviews found a whole range of factors, acting at every point in the patient journey, which were elsewhere described as having an impact on outcomes: increasing patient demand with subsequent ED overcrowding,212 differences in provision of front-door services,125 shortages of nursing staff,213 access to diagnostics214 and changes to health and social care provision. 215 The extent to which any or all of these factors contributed to the hospital-level outcomes was unknowable from the study design.
The utility of the approach to typology
It had been assumed that a systems approach would be the most appropriate method to explore, classify and compare systems. However, the degree of variation between organisations was such that the degree of similarity between organisations at whole-system level was minimal. Mapping of AMUs was recently carried out by Reid et al. 101 in Scotland, which found that full description of the models of care required 12 structural and staffing categories, alongside seven patterns of consultant working216 in a smaller sample (n = 29), again with little overlap between organisations. This matches our experience of finding systems approaches useful for the understanding of acute medical care, but not for their comparison because of the marked degree of variability.
An alternative way to manage this variability would have been to construct regression models to identify which aspects of the emergency and acute medicine system affected outcomes. However, the initial stakeholder workshops clearly indicated that it was difficult enough to identify whole systems of care as being generalist or specialist, without trying to pin down constituent factors in the same way. Moreover, this study was constructed as being exploratory, rather than definitive, and the spectrum of more generalist to more specialist still provided a useful framework for the mixed methods nature of the research.
The chief weakness of the typology was the assumption that AMU models of care in which specialists worked as generalists would be more specialist than AMUs that were predominantly staffed by acute physicians. Instead, specialists who worked as generalists were frequently adamant that they were the ‘true generalists’. Hence, AMUs are better categorised as being generalist or specialist according to their degree of openness.
Supporting and sustaining smaller hospitals
Interviewees were virtually united in the view that smaller organisations felt different from their larger counterparts. Although it was not a principal focus of the study, a number of findings are likely to be immediately useful in improving care in smaller hospitals, some of which have already been presented. 67
Are smaller hospitals different?
The design of this study did not seek to compare smaller hospitals with larger hospitals. However, we did find that smaller hospitals as group shared more similarities than differences. The case mix showed much less variation than expected between hospitals, with a few exceptions. Generalist working was more likely to be found in much smaller organisations. Staff were united in their views that working in smaller hospitals was qualitatively different from that of working in larger teaching hospitals, in terms of both the medicine practised and the environment. Both positive and negative behaviours and attitudes were thought to spread more quickly throughout smaller organisations; flat hierarchical structures and open leadership styles were appreciated by staff. Smaller organisations suffered from similar problems, struggling to balance external exigencies with the demands of improving care while lacking sufficient staff and having fewer resources. Most strikingly, however, was the extent to which staff identified with their organisations as ‘District General Hospitals’ (DGH), a term which has almost completely fallen out of use across the NHS.
It is an accepted truism that, in organisational research in the business setting, smaller organisations are different from their larger counterparts, requiring different sets of leadership, managerial, communication and relational styles for success. 217,218 These sets of considerations can be seen as underpinning Bonham-Carter’s 1969 report219 of the functions of DGHs. However, the trend over the past decade within the NHS has been to frame solutions to the multitude of problems which it faces (leadership, culture, unwarranted variation) generically. The naming of ‘viable smaller hospitals’ as a priority in the Five Year Forward View programme of NHS reform signalled change,220 but we still found that smaller organisations struggled to implement policies, directives and practices that were geared towards larger hospitals. This suggests that a return to treating smaller hospitals as a separate unique category within the NHS, particularly given the continuing pervasiveness of the DGH identity, may be a route to improving care within them.
Constructing appropriate models of care
The qualitative work found that models of care were highly influenced by central directives and mediated by available staffing and resources, rather than being consciously constructed to match the needs of the local patient population. There was very little strategic planning at the whole hospital level, with decisions about consultant recruitment and deployment frequently sitting at departmental level rather than the divisional or board levels. As a result, there was no relationship found between patient need and consultant skill mix at the hospital level.
We did not find any significant differences in outcomes for the different models of care. Moreover, the finding that models were emergent suggests that wholesale model change is unlikely to produce substantial benefits. The results instead suggest that aiming for a deep understanding of local patient need, looking for gaps in consultant skill mix at the whole hospital level and evolving existing models are likely to be more fruitful. Importantly, the finding that most case mix could be considered as amenable to generalist approaches suggests that there is a threshold below which take triage models are unlikely to function. This should encourage hospitals to focus on developing appropriate models for their circumstances rather than seeking to emulate much larger organisations.
Training of doctors
The training of doctors and the extent to which they felt comfortable managing the current patient case mix emerged as an important theme in the interviews. There was virtually a generational split between the older doctors who had experienced longer periods of training, often with considerable periods in smaller hospitals, and the younger consultants who often had only 2 years of training in general (internal) medicine alongside specialist training, mostly in the context of larger teaching organisations. Moreover, although consultants of all ages spoke of the pressures of the acute take, it was the complex, older patients on the downstream wards that the younger consultants struggled with most. Both the stress of the acute take and the feelings of being unable to deliver adequate care were major factors in driving flight into specialty and the withdrawal of labour across the whole emergency and acute medicine pathway.
Surveys of specialty trainees have noted the perceived inadequacy of GIM training in its current form,221 something that the Shape of Training review222 proposed to rectify. However, the proposed changes have focused on broadening the trainees’ exposure to patients with multimorbid illness early in training (Senior House Officer equivalent) and on acute illnesses. 223 This does not seem fully to address the management of more complex patients across the whole of their hospital stay. Moreover, this training in the care of older, multimorbid patients is likely to be delivered by consultants who feel less well-equipped to provide care themselves for this group than the previous generation. Alongside this has been the trend to move trainees out of smaller organisations, despite research suggesting that doctors prefer to work in the types of organisations in which they train. The logical outcome of these two policies is that workforce shortages in smaller hospitals are likely to worsen rather than improve.
Meeting patient and carer expectations
We found that patients and carers tend to view specialist types of care as being the ‘gold standard’. However, at the same time, there were acknowledgements that smaller hospitals could not be expected to deliver the same care as larger hospitals and that the overall quality of care provided by a hospital was more important than the type of doctor or service delivering the care.
The fact that these findings should contain a degree of cognitive dissonance is congruent with the literature. A study224 of patient experience on AMUs in England found little variance between organisations, with perceptions of care being associated more with patient-level factors. From the perspective of generalist versus specialist care, the limited research has found that patients are happy with generalist care, so long as access to specialists, when required, is quick and easy. 225 Studies of preferences for the provision of rural care echo this: patients strongly prefer services to be local, so long as it is backed up by tertiary care. 226–228 Watson et al. ’s study229 of preferences of a patient population in rural Scotland found that patients wished for cutting-edge services to be provided locally.
These findings suggest that patients may find generalist models of care acceptable, despite the overall preference for specialist services, so long as they are constructed to meet patient needs, are of high quality and are backed by robust networked services.
Assessment of underpinning assumptions
This study proceeded from four underpinning assumptions:
-
that the models of care deployed by hospitals would be shaped equally by theoretical considerations about medical generalism and the resources available to them, making size an important determinant of the model
-
that performance of models of care would be dependent, at least partially, on an alignment between the hospital’s case mix and the available skill mix
-
that medical generalism provides a solution to the problem of rising numbers of patients with complex and/or multimorbid disease
-
that different models of care would carry cost implications.
Although we did find that size appears to be an important determinant of the model of care, we found that resources, especially staffing, and policy imperatives were more important than theoretical considerations about the benefits of generalism. Indeed, we found that most hospitals were running models that they thought were ‘second best’.
We found no difference in the performance of models of care with regard to outcomes or costs. We also found that staffing was highly variable, with no relationship to size or case mix.
Medical generalism may well provide a solution to the problem of rising numbers of patients in smaller hospitals with complex and/or multimorbid disease. The current models of generalist medical care appear to be more suited to the smaller hospital environment, with no difference in outcomes from more specialist models. However, consultants providing care in generalist models need to be equipped with appropriate skills and experience, and hospitals within which the models sit need to create the right circumstances in which generalist models can thrive, while fostering and supporting collaborative working.
Theoretical considerations of medical generalism
The theoretical framework for this study drew heavily on two sources: the Australian ‘2020’ conceptual model of generalism, which views ‘ways of being’ (ontological frame), ‘ways of knowing’ (epistemological frame) and ‘ways of doing’ (practical frame) as a continuum that captures the attributes of ‘generalism’,11 and Abbott’s work,94 which considers professional ways of working as being ‘ecologically’ driven and situated in the context of actors, tasks, location and the relationships between these.
The 2020 theoretical model of generalism is framed in a positive sense, while still acknowledging the slipperiness of defining a complex nexus of attributes that shift from clinician to clinician. However, the broader literature is full of inconsistencies around the definitions, purposes and advantages of generalism. In particular, there is a chasm between the construction of generalism as a philosophy or way of being and the way that it is enacted in a health-care system, in which it is often presented in a negative sense: ‘the work left undone’ or ‘bridging the gaps’ between fragmented services.
These inconsistencies and gaps were reflected in what we saw in practice. There were no consistent sets of definitions or boundaries around what constituted generalism at any level: system, patient or doctor. Instead, these were permeable and were constantly negotiated and renegotiated. Moreover, there was a substantial difference between what clinicians and what managers thought systems should look like and their reality.
We did find that two of the attributes of generalism (‘ways of knowing’ and ‘ways of being’) were framed positively by medical staff, but ‘ways of being’ emerged as contingent. The desire to identify as a ‘generalist’ was not so much dependent on knowledge, skills or the actual work required, but rather on doctors’ daily experiences of work and the sense of satisfaction derived from this. This in itself was frequently influenced by the individual’s sense of the workload, both in terms of it being manageable by the individual and in terms of the collective sense of it being transparently and equitably shared.
Abbott’s ‘system of professions’ provides a further theoretical lens through which to view these findings. 94,230 As well as work being ecological, professions are defined by their jurisdiction over sets of activities and the capacity to resist or head-off inter-professional competition. The dynamics between specialists and generalists that were found in this study revealed a negotiated order of relationships, which were contingent on a series of internal and external factors. Moreover, specialists and generalists frequently operated with different sets of priorities and logic models for their work, with there being an inherent tension between specialty consultants being recruited to meet the demands of their own departments and the hospital’s need for those with generalist skills to deal with the problems of the ‘front door’, and the enlarging penumbra of services coalescing around the ED and the 4-hour target (e.g. AMUs, ambulatory care, frailty units). Logic would suggest that doctors should be deployed according to case mix and patient need, but this was not found to be the case. Moreover, clinicians and managers found it difficult to articulate models of care and we found little evidence of data being used to plan service configurations and, hence, workload.
Instead, models of care were characterised by heterogeneity and ‘fuzzy logic’,231 which were driven predominantly by service pressures and human factors, such as willingness to flex roles and operate collaboratively. Equally, behaviours could flip in specialists through withdrawal from generalist work, both on the AMU and on the downstream wards, and the fortressing of services. Therefore, whereas Abbott230 found that professional conflicts were usually drawn around the control and domination of territory, we found that disputes within smaller hospitals were more often characterised by retreat and vacating of territory.
The fluid nature of the label ‘medical general’ and the dynamic nature of how this was applied to doctors, patients and systems could be seen as positive, in terms of the wearing of multiple hats or being adaptive to circumstances, or negative, in the sense that the label was more often applied to breaches of classificatory boundaries. The dynamic nature of the negotiation of boundaries and identities between doctors was also reflective of the multidirectionality expressed in Abbott’s230 argument, which claimed that professional jurisdiction is not a uniform or unidirectional process, but can move in different directions at the same time. This argument derives from an analysis of work content, which many traditional sociologists of professions have tended to overlook, focusing instead on the view from 35,000 feet. This articulates well and helps to explain why models of care tend to be emergent and, hence, why the morphology of generalist and specialist care is not a clear binary but something which is constantly on the move and in flux.
Within this messiness of generalism, we did find doctors who were attempting to redefine what it should mean, looking back towards generalism not as a category for defining work, but rather as an approach, or even philosophy, of work: work that was shared, transparent and collaborative and geared towards meeting patient need regardless of labels, location within the system or professional boundaries.
This begs the question of whether or not the categories of generalist and specialist are useful labels for ongoing division of hospital work. However, any genuine change would require a fundamental rethinking of the needs of patients, how care in hospitals is delivered and the making of medical identity. Not carrying this out, however, risks a profound mismatch between future service demands and the willingness of doctors to deliver this.
Limitations
Implications of sampling strategy
The Monitor report’s88 definition of smaller organisations was based on operating revenues of trusts, not hospitals. We were aware that a different sample would have emerged if we had used hospital size (either by beds or by ED attendances) as the inclusion criteria. We are also aware that we achieved a response rate of only 70% for the telephone interviews and purposively sampled for the case study visits, which introduced the possibility of selection bias at several points in the study. The strengths of this approach were that we looked at a broader range of organisations by size and location than if we had used other criteria. Even within this sample, we still found more similarities than differences between the case mix, and the qualitative work reached saturation in terms of themes, although we still may have missed some of the more unusual examples.
Dynamic nature of models of care
The original study design had assumed that systems were in evolution rather than revolution, with the quantitative comparisons between models of care to encompass a period of 5–6 years. Where revolution did exist, we had assumed that change would be easy to locate and amenable to capture using interrupted time series analysis. Instead, we found models of care that were highly unstable and changing rapidly, with staff frequently unable to pinpoint the exact dates of change. To reduce the likelihood of hospitals switching categories within the typology entirely, we limited the time frame to 1–2 years for some analyses. However, we are aware of at least one organisation switching models within this time frame, and the possibility of others, which limits the reliability and reproducibility of the results.
A priori assumptions about medical generalism
The study was predicated on a number of a priori assumptions about medical generalism and systems of medical care. We had assumed that the demarcations between generalism and specialism would be clearer and more universally agreed, with a limited number of well-defined models of care in operation, meaning that a systems approach would offer a mechanism for understanding and comparing organisations and their structures. The structure of the study, with its iterative approach to the emerging data, meant that we were able to adopt different frameworks for analysis in response to this. This does, however, mean that our conclusions are not definitive, but should rather be considered the starting point for further work.
Narrow scope of analysis
The framing of this study around medical generalism has led to a focus on doctors, particularly at consultant level, and the nature of doctoring. The original intention had been to explore generalism at the system level, which would have naturally encompassed other types of staff, particularly nurses and allied health staff, who are essential to the delivery of high-quality care. These voices were captured through the course of the study, although the analysis has been necessarily limited, owing to the complexity and scope of the material. Even when discussing issues around doctors and doctoring, the focus on generalism and smaller hospitals means that we may have missed other important factors, especially with regard to what influences the shape of work.
No comparisons with larger hospitals
The design of this study did not allow for comparisons between smaller organisations and larger organisations. Although the evidence suggests that smaller hospitals are distinct, this cannot be confirmed without a similar exploration of urban teaching organisations.
Interview focus of the case studies
The case studies did not include extensive non-participant observation or immersion and so we relied heavily on direct accounts and experiences of the systems. To have included this type of research would have been time-consuming and would have reduced the number of case studies that could have been completed in the time that was available. We tried to compensate for this by using the ‘walk around’ method of mapping the patient journey, talking to a broad range of staff across multiple departments and using patient volunteers to provide an additional perspective.
Lack of patient voice
This study was planned to have extensive PPI input at every stage. However, we found it difficult to recruit for the patient and carer focus groups, with some groups being very small with one or two participants only, and the open space event was cancelled because of a lack of interest. This does leave a sense of not having adequately captured patient voices. However, the analysis of the focus groups rapidly reached saturation of themes and there was broad agreement across organisations, both with the results of the DCE and with the general literature. This reassured us that while we may have missed unique perspectives, the overall views presented are very likely representative.
Representativeness of the discrete choice experiment and the response rate
The DCEs are based on preselected attributes and elicit hypothetical responses. We acknowledge that there may have been other factors affecting workforce models that were not included in the DCE, which limits the external validity in real life situations. The number of responses was also limited, meaning that the findings may not be generalisable to larger groups of doctors, patients or managers.
Uncertainty around economic costs
The hospital-level economic analysis was severely limited by the lack of data on hospital staffing costs, while the small number of observations meant that adjusted analyses controlling for observed characteristics between hospitals were not possible. For the spell-level analyses, costs were based on trust-level costs that may be inaccurate.
Generalisability, transferability and reflexivity
This study was carried out in England using qualitative data from 2015 to 2018 and quantitative data from 2012 to 2018. Comparisons of the English acute care system with those of other countries suggests that it differs markedly, even within the rest of the UK. 67,101,232 This limits the generalisability of certain aspects of the qualitative and quantitative work. However, the findings regarding the increasing complexity of medical systems, the challenges posed by the changing needs of patients, the division of medical labour and the identity of the doctor are likely to be relevant internationally.
The research team was highly diverse in its composition, including practising clinicians, and spanned multiple organisations rather than being solely located within a university. The intention of the study was always to produce results that would be directly applicable to clinicians, managers and policy-makers within the NHS and, hence, was heavily informed by clinical and health policy perspectives, rather than taking a strictly sociological stance. Furthermore, it was not bound to a single frame of reference and was bolstered by the integration of PPI into most aspects of the research, including its direct conduct.
Conclusions
Implications for health care
-
National strategies to identify and remove unwarranted variation in the surgical and procedural realm have been successful in reducing cost and improving efficiency. 233 However, such strategies rely on an established evidence base and shared understanding of best practices. In this study, models were emergent and dependent on complex constellations of local factors, rather than driven by an evidence base or theoretical considerations. No model of care emerged as being better than any other, with outcomes appearing dependent on other hospital-level factors and the suggestion that the size and staffing of hospitals may affect their ability to implement standardised models. Furthermore, the ‘system shock’ of external political imperatives frequently undermined the ability of hospitals to enact change. This suggests that a ‘one size fits all’ approach may be less appropriate to guide best practice with regard to emergency and acute medicine in smaller hospitals. Empowering and enabling organisations to understand how to adapt their staff model to the local case mix and the requirements imposed by how their local microsystems operate, may be a more productive approach to improving patient care.
-
Overall, the cohort of smaller hospitals shared more commonalities than differences, with both organisations and staff seeing themselves as having an identity distinct from their larger counterparts. This suggests that treating smaller hospitals as a separate, unique category within the NHS and supporting their specific needs may be an effective strategy in ensuring their survival and improving patient care.
-
There was substantial variability in pathways of care for specific conditions and their relationships with LOS, both within and between organisations. This suggests that understanding pathways and improving flow for specific groups of patients may be more efficient than a wholescale change in the model of care.
-
Workforce gaps at the middle grade and consultant level were found to be a major problem across nearly all organisations. This suggests that there is a particular need for best practices around recruitment and retention to be identified and disseminated, with hospitals encouraged to shift to strategically planning their consultant workforce at the hospital level. With regard to the training and distribution of middle-grade doctors, the study suggests the imbalances in workforce distribution and improving training experiences outside major urban areas may need to be readdressed to ensure that there is an adequate workforce in both the short term and the long term.
-
The remit of the Shape of Training review7 was to look at potential reforms to the structure of postgraduate medical education and training across England to meet the needs of the increasingly older and multimorbid patient population. This includes management of patients across traditional inpatient–outpatient boundaries in integrated care systems. The evidence supports the contention that the current generation of consultants is not as well equipped as it ought to be in dealing with a generalist patient population. However, the finding that preferences for generalism were associated with long periods of training suggests that Shape of Training’s7 recommendations may still not be sufficient to produce a consultant workforce not only capable of, but willing to care for an ageing population.
-
‘Fortressing’ and ‘flight behaviours’, whereby consultants actively sought to limit generalist working and regulate their workloads, emerged as a significant issue in this study, undermining the stability of emergency and acute medicine systems and creating artificial workforce shortages. The creation of more collaborative working environments, with the transparent and equitable sharing of work across the consultant body, is likely to reduce incentives for consultants to withdraw from generalist working. Alternative ways of providing consultant cover out-of-hours for relatively rare interventions, such as regional networks, need to be urgently explored.
-
The advent of integrated care systems offers an opportunity for the reimagining of the organisation of care across regions and between multiple providers. Much of the work to date has explored how specialists might better support community-based services. 8 This study suggests that rethinking how specialists might better support generalists in smaller hospitals and reshaping the boundaries between generalists and specialists might be equally useful. The same understanding of the local case mix, the demand for acute services and the organisational mechanics required for improving care at the hospital level, could also provide a platform for innovations in models of care that are based around skill mix, multisite working, networks for the delivery of specialist advice and interventional care, and standardising and smoothing pathways between providers and across systems.
Recommendations for further research
-
Mapping and understanding models of emergency and acute care across the whole of the NHS, including an exploration of the relationship of models of care with patient and hospital-level outcomes, and the models of care and the organisations in which they sit.
-
Studies on the deployment of the medical workforce across the NHS as a whole and within individual hospitals, and the relationships between workforce, models of care and measures of hospital culture. This should include an exploration of how skills gaps in doctoring impact on and are compensated for by others, particularly nursing and allied health staff.
-
Development of more sophisticated methodologies, particularly those of a rapid nature, to deal with the marked variation seen in health-care systems and testing of specific organisational and contextual factors that help or hinder system improvements.
-
Applied research into how more refined case-mix analyses may allow organisations to make better choices around the configurations of services, model future services and monitor subsequent change.
-
Better understanding of medical work, the decisions around its distribution, how this translates into differences in patient journeys and impacts on outcomes for both the patients and the system.
-
Analysis of what skills, experience and expertise are required to provide excellent care for complex comorbid patients and how the undergraduate and postgraduate curricula should be structured to ensure that the next generation of doctors is fully equipped to meet the challenges of the changing patient need.
-
Further research into what constitutes satisfying work for doctors and other health-care professionals, the relationship between work environment and both positive and negative physician behaviours and how hospitals environments can be shaped to support this.
-
Better understanding of how smaller hospitals might meet the needs of their local populations, recruit and retain appropriate staff and be supported to provide high-quality care.
-
Better understanding and further exploration of the costs attached to different models of care, particularly the nuances around the patterns of deployment of consultant staff.
Final conclusions
This study sought to examine the hypothesis that medical generalism may provide a way to deal with the rising numbers of patients who are complex and/or have multiple comorbidities, particularly in smaller hospitals. We found that the case mix of smaller hospitals was dominated by patients, with presentations likely to be amenable to generalist approaches to care. Although generalist models of care appeared a more natural fit for smaller organisations, there was no evidence in our study to suggest that any particular model of care produced better outcomes for patients. The willingness of medical staff to work in generalist ways was dependent on their training and their lived experiences of working within organisations. This suggests that matching hospital staff to meet patient need and the creation of more collaborative working environments is more likely to improve care than changing models. Therefore, although medical generalism may provide a way of caring for an ageing population, the delivery of high-quality care will be possible only if the right conditions are created to support generalist working, both within individual organisations and across the NHS as a whole.
Acknowledgements
Contributions of project team members
Helen Crump (former Fellow, Health Policy) analysed the patient and carer focus group material.
Matt Gaskins (former Researcher, Health Policy) assisted with the telephone interviews.
Rachel Hutchings (Researcher, Health Policy) assisted with the project management; conducted the literature review and wrote the relevant portion of the appendices; and assisted extensively with the preparation and presentation of the first draft.
Claudia Leone (Researcher, Health Policy) acted as project manager and conducted the primary framework analyses of the qualitative material, contributed to the workforce analyses, oversaw the literature review and contributed to the interpretation of the study.
Silvia Lombardo (former Researcher, Health Policy) collected data for and prepared the organisational and workforce profiles, and assisted with the telephone interviews and the case study visits.
Silvia Machaquiero (former Researcher, Health Policy) was the chief project manager for the study; assisted with the preparation of the study protocol and other materials; acted as principal liaison for the PPI portions of the study; helped with the conduct of the telephone interviews and the field work; and helped with the coding and preparation of the qualitative materials for analysis.
Alasdair MacDonald (Consultant Physician, Acute and General Medicine) assisted with the case study visits.
Danielle Nimmons (former Academic Placement, Health Policy) assisted with the telephone interviews, case study visits and the typology analysis.
Paul Smith (former Research Analyst, Data Analytics) assisted with the development of the case-mix classification; assisted with the preparation of key data sets; carried out the sensitivity testing and comparisons of different approaches to the data sets; and carried out the analysis of national data sets and estimation of population-based admission rates.
Louise Taylor (former Academic Placement) assisted with the coding and preparation of the qualitative materials for analysis; performed the analysis of the DCS; and created the Sankey diagrams.
Contributions of others
Study Steering Committee
We would like to thank David Steel for his most excellent chairing of the Study Steering Committee and the support he has offered to the study team over the past 3 years.
We would like to thank the members of the Study Steering Committee who offered support and advice and assisted with the evaluation and interpretation of the content and progress of the study: Mrs. Marilyn Frampton (Governor, Kingston Hospital NHS Foundation Trust), Professor Karen Bloor (University of York), Professor Mary Boulton (Oxford Brookes University), Professor Tim Evans (NHS England), Professor Hugh Gravelle (University of York), Dr Jonathan Howes (Yeovil District Hospital), Dr Alasdair MacDonald (Launceston General Hospital), Dr Cliff Mann (NHS England), Professor Jane Sandall (King’s College London) and Dr David Ward (Hinchingbrooke Hospital).
We would like to note the sad passing of Professor Tim Evans in November 2018, shortly after the submission of this manuscript. Professor Evans' forensic eye was critical to the shaping of aspects of this work from its inception to completion. For this, and other acts of kindness, we are deeply grateful.
Patient and public involvement
We would like to thank our patient volunteers for their contributions to the conduct and interpretation of the case studies: Kenneth Greenfield, Joanna Parker, Frank Rust, Linda Samuels, Keith Spurr, Jenny Stiling and Malcolm Watson.
We would like to thank David Steel and Marilyn Frampton, also members of the Study Steering Committee, for providing a public and patient perspective on the design, findings and interpretation of the study.
We would like to thank Rachel Matthews (Patient and Public Engagement and Involvement Theme Lead, Northwest London CLAHRC), Rachel Downing and Francine Beadsworth (both formerly of the RCP) for their assistance with planning and executing the PPI engagement with the patient volunteers.
Other Nuffield Trust staff
We would like to thank the following Nuffield Trust staff.
Nigel Edwards (Chief Executive Officer) for his support of this project from its inception to completion.
April McMullen (former Team Assistant) for her administrative assistance with the qualitative portions of the study and ensuring that the case study visits were well organised.
Ben Willbond (Deputy Director, Finance and IT) for his oversight of the finances and data governance.
Rowan Dennison (Editorial and Content Manager), Meilir Jones (Comment Editor) and Paul Kirkup (Digital Officer) for their extensive assistance with the preparation of the final document and other publications relating to this study.
Leonora Merry (Deputy Director of Communications) and the rest of the Communications Team for their support in the production of and promotion of other publications relating to this study.
Eilis Keeble (Research Analyst), Theo Georghiou (Senior Research Analyst) and Sarah Scobie (Deputy Director of Research) for supporting the quantitative work.
Sophie Castle-Clarke (Senior Fellow) for support with the production of the final document.
Rachel Bleach for ongoing administrative support.
The New Cavendish Group
We would like to thank the members of The New Cavendish Group for their interest in and support of this project.
Participation in the study
We would like to thank all those who participated in the study. This study would not have been possible without your willingness to share your experiences and opinions openly and honestly. We are particularly appreciative of those who, despite working in highly pressured environments, assisted with the organisation and conduct of the case study visits.
Project website
www.nuffieldtrust.org.uk/research/acute-medical-care-in-england-findings-from-a-survey-of-smaller-acute-hospitals (accessed 11 November 2020).
Contributions of authors
Louella Vaughan (https://orcid.org/0000-0002-7626-0779) (Senior Clinical Research Fellow, Health Services Research) designed and led the study; oversaw and contributed to the conduct and analysis of the qualitative material; provided clinical insight into the qualitative and economic analyses; and was responsible for all portions of the first draft of the study that are not outlined below.
Martin Bardsley (https://orcid.org/0000-0002-9853-6019) (Senior Fellow, Data Analytics) contributed to the original study design, led the quantitative work, wrote the relevant parts of the first draft and contributed to the management and interpretation of the study.
Derek Bell (https://orcid.org/0000-0002-9944-1097) (Professor of Acute Medicine, Healthcare Systems) brought expertise on emergency and acute care.
Miranda Davies (https://orcid.org/0000-0003-1217-4836) (Senior Research Analyst, Data Analytics) worked on the development of the case-mix classification; created and analysed the key quantitative data sets; led the work on the patient pathways and changes over time; and assisted with the drafting of the relevant portions of the first draft.
Andrew Goddard (https://orcid.org/0000-0002-0130-7966) (President of the Royal College of Physicians, Medical Workforce) brought expertise on medical workforce and professionalism and contributed to the interpretation of the study.
Candace Imison (https://orcid.org/0000-0002-2576-2111) (Director of Policy, Health Policy) contributed to the original study design; led the workforce aspects of the study; conducted the primary analysis of the case study interviews; assisted with the case study visits and the analysis of the qualitative material; wrote the relevant parts of the first draft; and contributed to the management and interpretation of the study.
Mariya Melnychuk (https://orcid.org/0000-0003-4992-1612) (Research Associate, Health Economics) assisted the economic analysis; prepared, conducted and analysed the discrete experiment; wrote the relevant parts of the first draft and contributed to the interpretation of the study.
Stephen Morris (https://orcid.org/0000-0002-5828-3563) (Professor of Health Economics, Health Economics) contributed to the original study design, oversaw the DCE, conducted the economic analysis, wrote the relevant parts of the first draft and contributed to the management and interpretation of the study.
Anne Marie Rafferty (https://orcid.org/0000-0003-1010-6581) (Professor of Nursing Policy, Workforce and Health Policy) brought expertise on concepts of professionalism and aspects of workforce; wrote the portion of the first draft relating to the theoretical implications and contributed to the interpretation of the study.
Publications
Imison C, Vaughan L. Acute Medical Care in England: Findings from a Survey of Smaller Acute Hospitals [slide set resource]. London: Nuffield Trust; 2018. URL: www.nuffieldtrust.org.uk/research/acute-medical-care-in-england-findings-from-a-survey-of-smaller-acute-hospitals
Vaughan L, Edwards N, Imison C, Collins B. Rethinking Acute Medical Care in Smaller Hospitals. London: Nuffield Trust; 2018. URL: www.nuffieldtrust.org.uk/research/rethinking-acute-medical-care-in-smaller-hospitals (accessed 4 June 2020).
Data-sharing statement
We shall make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Cracknell R. The Ageing Population. London: House of Commons Library Research; 2007.
- Sinha SK, Bessman ES, Flomenbaum N, Leff B. A systematic review and qualitative analysis to inform the development of a new emergency department-based geriatric case management model. Ann Emerg Med 2011;57:672-82. https://doi.org/10.1016/j.annemergmed.2011.01.021.
- Foot C, Harrison T. How to Improve Cancer Survival: Explaining England’s Relatively Poor Rates. London: The King’s Fund; 2011.
- Lyon C, Clark DC. Diagnosis of acute abdominal pain in older patients. Am Fam Physician 2006;74:1537-44.
- Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C, et al. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med 2010;17:284-92. https://doi.org/10.1111/j.1553-2712.2009.00658.x.
- Brindle D. Guiding Patients Through Complexity: Modern Medical Generalism. Report of an Independent Commission for the Royal College of General Practitioners and The Health Foundation 2011. www.health.org.uk/publication/guiding-patients-through-complexity-modern-medical-generalism (accessed July 2018).
- Greenaway D. Shape of Training: Securing the Future of Excellent Patient Care. London: General Medical Council; 2013.
- Future Hospital Commission . Future Hospital: Caring for Medical Patients 2013. www.rcplondon.ac.uk/projects/outputs/future-hospital-commission (accessed July 2018).
- Jenkins PF, Thompson CH, MacDonald AB. What does the future hold for general medicine?. Med J Aust 2011;195:49-50. https://doi.org/10.5694/j.1326-5377.2011.tb03192.x.
- Kirthi V, Temple RM, Patterson LJ. Inpatient care: should the general physician now take charge?. Clin Med 2012;12:316-19. https://doi.org/10.7861/clinmedicine.12-4-316.
- Gunn J, Naccarella L, Palmer V, Kokanovic R, Pope C, Lathlean J. What is the Place of Generalism in the 2020 Primary Care Team?. Canberra, ACT: Australian Primary Health Care Research Institute; 2007.
- Robineau D. Ageing Britain: Two-Fifths of NHS Budget Is Spent on Over-65s 2016. www.theguardian.com/society/2016/feb/01/ageing-britain-two-fifths-nhs-budget-spent-over-65s (accessed July 2018).
- Salive ME. Multimorbidity in older adults. Epidemiol Rev 2013;35:75-83. https://doi.org/10.1093/epirev/mxs009.
- British Geriatrics Society . Fit For Frailty Part 1 – Consensus Best Practice Guidance for the Care of Older People Living in the Community and Outpatient Settings 2014.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. https://doi.org/10.1016/S0140-6736(12)60240-2.
- Paddison CA, Saunders CL, Abel GA, Payne RA, Campbell JL, Roland M. Why do patients with multimorbidity in England report worse experiences in primary care? Evidence from the General Practice Patient Survey. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006172.
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 2005;294:716-24. https://doi.org/10.1001/jama.294.6.716.
- Cowling TE, Soljak MA, Bell D, Majeed A. Emergency hospital admissions via accident and emergency departments in England: time trend, conceptual framework and policy implications. J R Soc Med 2014;107:432-8. https://doi.org/10.1177/0141076814542669.
- Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition – multimorbidity. JAMA 2012;307:2493-4. https://doi.org/10.1001/jama.2012.5265.
- Smith P, McKeon A, Blunt I, Edwards N. NHS Hospitals Under Pressure: Trends in Acute Activity up to 2022. London: Nuffield Trust; 2014.
- Hogan H, Healey F, Neale G, Thomson R, Vincent C, Black N. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual Saf 2012;21:737-45. https://doi.org/10.1136/bmjqs-2011-001159.
- James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 2013;9:122-8. https://doi.org/10.1097/PTS.0b013e3182948a69.
- Graber ML, Trowbridge R, Myers JS, Umscheid CA, Strull W, Kanter MH. The next organizational challenge: finding and addressing diagnostic error. Jt Comm J Qual Patient Saf 2014;40:102-10. https://doi.org/10.1016/S1553-7250(14)40013-8.
- Baines RJ, Langelaan M, de Bruijne MC, Asscheman H, Spreeuwenberg P, van de Steeg L, et al. Changes in adverse event rates in hospitals over time: a longitudinal retrospective patient record review study. BMJ Qual Saf 2013;22:290-8. https://doi.org/10.1136/bmjqs-2012-001126.
- Anderson CI, Nelson CS, Graham CF, Mosher BD, Gohil KN, Morrison CA, et al. Disorganized care: the findings of an iterative, in-depth analysis of surgical morbidity and mortality. J Surg Res 2012;177:43-8. https://doi.org/10.1016/j.jss.2012.05.007.
- Vlayen A, Verelst S, Bekkering GE, Schrooten W, Hellings J, Claes N. Incidence and preventability of adverse events requiring intensive care admission: a systematic review. J Eval Clin Pract 2012;18:485-97. https://doi.org/10.1111/j.1365-2753.2010.01612.x.
- Findlay GP, Shotton H, Kelly K, Mason M. Time To Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation As a Result of an In-Hospital Cardiorespiratory Arrest 2012. www.ncepod.org.uk/2012report1/downloads/CAP_fullreport.pdf (accessed July 2018).
- Cooper H, Findlay G, Goodwin APL, Gough MJ, Lucas SB, Mason DG, et al. Caring to the End? A Review of the Care of Patients Who Died in Hospital Within Four Days of Admission 2009. www.ncepod.org.uk/2009report2/Downloads/DAH_report.pdf (accessed July 2018).
- Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012;345. https://doi.org/10.1136/bmj.e5205.
- Fusco M, Buja A, Furlan P, Casale P, Marcolongo A, Baldovin T, et al. Older adults in emergency department: management by clinical severity at triage. Ann Ig 2014;26:409-17. https://doi.org/10.7416/ai.2014.2000.
- Royal College of Physicians and Surgeons of Canada . Report of the Generalism and Generalist Task Force 2013. www.royalcollege.ca/rcsite/educational-initiatives/generalism-medical-education-e (accessed July 2018).
- Porter R. The Greatest Benefit to Mankind: A Medical History of Antiquity to the Present. New York, NY: Harper Collins; 1997.
- General Medical Council . Specialties, Sub-Specialties and Progression Through Training: The International Perspective 2011. www.gmc-uk.org/-/media/documents/specialties-subspecialties-and-progression-through-training---the-international-perspective-45500662.pdf (accessed July 2018).
- Starr P. The Social Transformation of American Medicine: The Rise of a Sovereign Profession and the Making of a Vast Industry. New York, NY: Basic Books; 2008.
- Moore GT. The case of the disappearing generalist: does it need to be solved?. Milbank Q 1992;70:361-79. https://doi.org/10.2307/3350064.
- Donohoe MT. Comparing generalist and specialty care: discrepancies, deficiencies, and excesses. Arch Intern Med 1998;158:1596-608. https://doi.org/10.1001/archinte.158.15.1596.
- Harrold LR, Field TS, Gurwitz JH. Knowledge, patterns of care, and outcomes of care for generalists and specialists. J Gen Intern Med 1999;14:499-511. https://doi.org/10.1046/j.1525-1497.1999.08168.x.
- Rivo ML. Internal medicine and the journey to medical generalism. Ann Intern Med 1993;119:146-52. https://doi.org/10.7326/0003-4819-119-2-199307150-00009.
- Nasca TJ, Mohn K, Wright R. Physician manpower reform: an analysis of the effects of the COGME Fourth Report on internal medicine residency positions. Council on Graduate Medical Education. Am J Med 1994;97:317-22. https://doi.org/10.1016/0002-9343(94)90297-6.
- Cave DG. Analyzing the content of physicians’ medical practices. J Ambul Care Manage 1994;17:15-36. https://doi.org/10.1097/00004479-199407000-00006.
- Greenfield S, Nelson EC, Zubkoff M, Manning W, Rogers W, Kravitz RL, et al. Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA 1992;267:1624-30. https://doi.org/10.1001/jama.1992.03480120062034.
- Carline JD, Inui TS, Larson EB, LoGerfo JP, Ramsey PG. The knowledge base of certified internists. Relationships to training, practice type, and other physician characteristics. Arch Intern Med 1989;149:2311-13. https://doi.org/10.1001/archinte.1989.00390100115025.
- Ramsey PG, Carline JD, Inui TS, Larson EB, LoGerfo JP, Norcini JJ, et al. Changes over time in the knowledge base of practicing internists. JAMA 1991;266:1103-7. https://doi.org/10.1001/jama.1991.03470080073032.
- Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med 1994;331:1136-42. https://doi.org/10.1056/NEJM199410273311707.
- Schreiber TL, Elkhatib A, Grines CL, O’Neill WW. Cardiologist versus internist management of patients with unstable angina: treatment patterns and outcomes. J Am Coll Cardiol 1995;26:577-82. https://doi.org/10.1016/0735-1097(95)00214-O.
- Gerber PD, Barrett J, Barrett J, Manheimer E, Whiting R, Smith R. Recognition of depression by internists in primary care: a comparison of internist and ‘gold standard’ psychiatric assessments. J Gen Intern Med 1989;4:7-13. https://doi.org/10.1007/bf02596483.
- Kitahata MM, Koepsell TD, Deyo RA, Maxwell CL, Dodge WT, Wagner EH. Physicians’ experience with the acquired immunodeficiency syndrome as a factor in patients’ survival. N Engl J Med 1996;334:701-6. https://doi.org/10.1056/NEJM199603143341106.
- Ward MM, Leigh JP, Fries JF. Progression of functional disability in patients with rheumatoid arthritis. Associations with rheumatology subspecialty care. Arch Intern Med 1993;153:2229-37. https://doi.org/10.1001/archinte.1993.00410190069009.
- Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and specialties. Results from the medical outcomes study. JAMA 1995;274:1436-44. https://doi.org/10.1001/jama.1995.03530180030026.
- Strauss MJ, Conrad D, LoGerfo JP, Hudson LD, Bergner M. Cost and outcome of care for patients with chronic obstructive lung disease. Analysis by physician specialty. Med Care 1986;24:915-24. https://doi.org/10.1097/00005650-198610000-00005.
- Joint Royal College of Physicians Training Board . Specialty Training Curriculum for Acute Internal Medicine 2012. www.jrcptb.org.uk/specialities/acute-medicine (accessed July 2018).
- The World Health Organization . The World Health Report 2008 - Primary Health Care (Now More Than Ever 2008. www.who.int/whr/2008/en/ (accessed July 2018).
- Julian K, Riegels NS, Baron RB. Perspective: Creating the next generation of general internists: a call for medical education reform. Acad Med 2011;86:1443-7. https://doi.org/10.1097/ACM.0b013e3182303a32.
- Firth J. The future of general medicine. Clin Med 2014;14:354-6. https://doi.org/10.7861/clinmedicine.14-4-354.
- Royal College of Physicians . 2016–17 Census (UK Consultants and Higher Specialty Trainees 2017. www.rcplondon.ac.uk/projects/outputs/2016-17-census-uk-consultants-and-higher-specialty-trainees (accessed July 2018).
- Dewhurst N. 10th college of physicians lecture: the challenges of reinventing medical generalism in the 21st century. Ann Acad Med Singap 2013;42:708-11.
- Wachter B. Acute Physicians: Hospitalists Bounded by Time and Space n.d. https://thehospitalleader.org/acute-physicians-hospitalists-bounded-by-time-and-space/ (accessed August 2018).
- Banerjee J, Conroy S. Quality care for older people with urgent and emergency care needs - the Silver Book. London: British Geriatrics Society; 2012.
- Mather HM. Royal College of Physicians Trainees Committee . The Royal College of Physicians specialist registrar shift survey. Hosp Med 2002;63:429-31. https://doi.org/10.12968/hosp.2002.63.7.1989.
- Gordon F. Shift work for specialist registrars in acute medicine: more questions than solutions. Clin Med 2002;2:41-2. https://doi.org/10.7861/clinmedicine.2-1-41.
- Barbash GI, White HD, Modan M, Diaz R, Hampton JR, Heikkila J, et al. Outcome of thrombolytic therapy in relation to hospital size and invasive cardiac services. The Investigators of the International Tissue Plasminogen Activator/Streptokinase Mortality Trial. Arch Intern Med 1994;154:2237-42. https://doi.org/10.1001/archinte.1994.00420190141016.
- Hillner BE, Smith TJ, Desch CE. Hospital and physician volume or specialization and outcomes in cancer treatment: importance in quality of cancer care. J Clin Oncol 2000;18:2327-40. https://doi.org/10.1200/JCO.2000.18.11.2327.
- Jones J, Rowan K. Is there a relationship between the volume of work carried out in intensive care and its outcome?. Int J Technol Assess Health Care 1995;11:762-9. https://doi.org/10.1017/S0266462300009193.
- Oei TT, Dulai GS, Gralnek IM, Chang D, Kilbourne AM, Sale GA. Hospital care for low-risk patients with acute, nonvariceal upper GI hemorrhage: a comparison of neighboring community and tertiary care centers. Am J Gastroenterol 2002;97:2271-8. https://doi.org/10.1111/j.1572-0241.2002.05981.x.
- Bardach NS, Zhao S, Gress DR, Lawton MT, Johnston SC. Association between subarachnoid hemorrhage outcomes and number of cases treated at California hospitals. Stroke 2002;33:1851-6. https://doi.org/10.1161/01.str.0000019126.43079.7b.
- Ward MM. Hospital experience and mortality in patients with systemic lupus erythematosus: which patients benefit most from treatment at highly experienced hospitals?. J Rheumatol 2002;29:1198-206.
- Vaughan L, Imison C, Edwards N, Collins B. Rethinking Acute Medical Care in Smaller Hospitals. London: Nuffield Trust; 2018.
- Nuffield Institute for Health . Hospital Volume and Health Care Outcomes, Costs and Patient Access 1996. www.york.ac.uk/media/crd/ehc28.pdf (accessed July 2018).
- Rosenblatt RA, Hart LG, Baldwin LM, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care?. JAMA 1998;279:1364-70. https://doi.org/10.1001/jama.279.17.1364.
- Jelinek M. Spectrum bias: why generalists and specialists do not connect. Evid Based Med 2008;13:132-3. https://doi.org/10.1136/ebm.13.5.132.
- Gaynor M, Laudicella M, Propper C. Can governments do it better? Merger mania and hospital outcomes in the English NHS. J Health Econ 2012;31:528-43. https://doi.org/10.1016/j.jhealeco.2012.03.006.
- Barratt H, Harrison DA, Fulop NJ, Raine R. Factors that influence the way communities respond to proposals for major changes to local emergency services: a qualitative study. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0120766.
- Cooke MW, Wilson S, Halsall J, Roalfe A. Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J 2004;21:575-6. https://doi.org/10.1136/emj.2004.015081.
- Proudlove NC, Gordon K, Boaden R. Can good bed management solve the overcrowding in accident and emergency departments?. Emerg Med 2003;20:149-55. https://doi.org/10.1136/emj.20.2.149.
- Bell D, Skene H, Jones M, Vaughan L. A guide to the acute medical unit. Br J Hosp Med 2008;69:M107-9. https://doi.org/10.12968/hmed.2008.69.Sup7.30432.
- Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 2009;21:397-40. https://doi.org/10.1093/intqhc/mzp045.
- Federation of Medical Royal Colleges . Acute Medicine: The Physician’s Role: Proposals for the Future. A Working Party Report of the Federation of Medical Royal Colleges 2000.
- Dowdle JR. Acute medicine: past, present, and future. Emerg Med J 2004;21:652-3. https://doi.org/10.1136/emj.2003.012211.
- Acute Medicine Taskforce . Acute Medical Care: The Right Person, In The Right Setting – First Time 2007. www.acutemedicine.org.uk/wp-content/uploads/2014/04/RCP-Acute-Medicine-Task-Force-Report.pdf (accessed July 2018).
- Ward D, Potter J, Ingham J, Percival F, Bell D. Acute medical care. The right person, in the right setting--first time: how does practice match the report recommendations?. Clin Med (Lond) 2009;9:553-6. https://doi.org/10.7861/clinmedicine.9-6-553.
- Bell D, Lambourne A, Percival F, Laverty AA, Ward DK. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0061476.
- Royal College of Physicians . Hospitals on the Edge? The Time For Action 2015. www.rcplondon.ac.uk/guidelines-policy/hospitals-edge-time-action (accessed July 2018).
- Chaudhuri E, Mason NC, Logan S, Newbery N, Goddard AF. The Medical Registrar: Empowering the Unsung Heroes of Patient Care. London: Royal College of Physicians; 2013.
- Trudgill N. Census of Consultant Physicians and Higher Specialty Trainees 2017–18. London: Royal College of Physicians; 2018.
- Seccombe A, Kennedy A, Holland M, Subbe C. The SAMBA highlights increasing complexity of acute medical systems. Br J Hosp Med 2018;79:4-5. https://doi.org/10.12968/hmed.2018.79.1.4.
- NHS Improvement . Rapid Improvement Guides for Urgent and Emergency Care 2016. https://improvement.nhs.uk/resources/rapid-improvement-guides-urgent-and-emergency-care/ (accessed October 2018).
- Imison C, Vaughan L. Acute Medical Care in England: Findings From a Survey of Smaller Acute Hospitals. London: The Nuffield Trust; 2018.
- Monitor . Facing the Future: Smaller Acute Providers 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/320075/smalleracuteproviders-report.pdf (accessed April 2017).
- Watson R, Crump H, Imison C, Currie C, Gaskins M. Emergency General Surgery: Challenges and Opportunities. London: Nuffield Trust; 2016.
- Appleby J, Boyle S, Devlin N, Harley M, Harris A, Locock L, et al. Sustaining Reductions in Waiting Times: Identifying Successful Strategies. London: The King’s Fund; 2004.
- Ham C, Berwick D. Organising Care at the NHS Front Line. Who is Responsible?. London: The King’s Fund; 2017.
- Royal College of Physicians and Surgeons of Canada . Generalism: Achieving a Balance With Specialization. A White Paper Prepared for the Royal College of Physicians and Surgeons of Canada, Future of Medical Education in Canada 2011.
- NHS England . Transforming Urgent and Emergency Care Services in England. Urgent and Emergency Care Review. End of Phase 1 Report 2013. www.nhs.uk/NHSEngland/keogh-review/Documents/UECR.Ph1Report.Appendix%201.EvBase.FV.pdf (accessed July 2018).
- Abbott A. Linked Ecologies: States and universities as environments for professions. Sociological Theory 2005;23:245-74. https://doi.org/10.1111/j.0735-2751.2005.00253.x.
- Checkland P. Systems Thinking, Systems Practice. Hoboken, NJ: John Wiley & Sons; 1981.
- von Bertalanffy L. General Systems Theory. Foundations, Development, Applications. New York, NY: George Braziller; 1968.
- Lasserson DS, Harris C, Elias T, Bowen J, Clare S. What is the evidence base for ambulatory care for acute medical illness?. Acute Med 2018;17:148-53.
- Benger JR, Hassan TB. Emergency medicine in the UK: the future is bright!. Emerg Med J 2007;24:748-9. https://doi.org/10.1136/emj.2007.046953.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-50.
- Reid LEM, Prestsch U, Jones MC, Lone NI, Weir CJ, Morrison Z. The acute medical unit model: a characterisation based upon the National Health Service in Scotland. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0204010.
- Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. BMJ 2010;341. https://doi.org/10.1136/bmj.c4078.
- Sinkovics N, Cassell C, Cunliffe AL, Grandy G. The SAGE Handbook of Qualitative Business and Management Research Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2018.
- Reid E, King A, Mathieson A, Woodcock T, Watkin SW. Identifying reasons for delays in acute hospitals using the Day-of-Care Survey method. Clin Med 2015;15:117-20. https://doi.org/10.7861/clinmedicine.15-2-117.
- Gordon H. Focus on Physicians. Census of Consultant Physicians and Higher Specialty Trainees 2016–17. London: Royal College of Physicians; 2017.
- The Health Foundation . Shine: Improving the Value of Local Healthcare Services. How Healthcare Teams Took on the Challenge to Improve Quality While Reducing the Cost of Services 2014.
- NHS England . Delayed Transfers of Care Data 2016–17 n.d. www.england.nhs.uk/statistics/statistical-work-areas/delayed-transfers-of-care/2016-17-data/ (accessed 4 September 2020).
- NHS England . Delayed Transfers of Care Data 2017–18 n.d. www.england.nhs.uk/statistics/statistical-work-areas/delayed-transfers-of-care/delayed-transfers-of-care-data-2017-18/ (accessed 4 September 2020).
- NHS Digital . NHS Workforce Statistics, September 2017, Provisional Statistics n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics/nhs-workforce-statistics-september-2017-provisional-statistics (accessed 4 September 2020).
- World Health Organization . WHO International Classification of Diseases, 11th Revision (ICD-11) 2018. www.who.int/classifications/icd/en/ (accessed August 2017).
- Fetter RB, Shin Y, Freeman JL, Averill RF, Thompson JD. Case mix definition by diagnosis-related groups. Med Care 1980;18:1-53.
- NHS Digital . National Casemix Office n.d. https://digital.nhs.uk/services/national-casemix-office (accessed August 2017).
- Weiner JP, Starfield BH, Lieberman RN. Johns Hopkins Ambulatory Care Groups (ACGs) . A case-mix system for UR, QA and capitation adjustment. HMO Pract 1992;6:13-9.
- Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg 1999;16:9-13. https://doi.org/10.1016/S1010-7940(99)00134-7.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. https://doi.org/10.1097/00003246-198510000-00009.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. https://doi.org/10.1016/0021-9681(87)90171-8.
- Billings J, Georghiou T, Blunt I, Bardsley M. Choosing a model to predict hospital admission: an observational study of new variants of predictive models for case finding. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003352.
- Bardsley M, Coles J, Jenkins L. DRGs and Health Care: The Management of Case-mix. Oxford, UK: Oxford University Press; 1989.
- NHS Digital . Hospital Episode Statistics Data Dictionary n.d. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics/hospital-episode-statistics-data-dictionary (accessed October 2018).
- Spencer SA, Davies MP. Hospital episode statistics: improving the quality and value of hospital data: a national internet e-survey of hospital consultants. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2012-001651.
- Spencer SA. Hospital Episode Statistics: Improving the Quality and Value of Hospital Data. London, UK: Academy of Medical Royal Colleges; 2011.
- World Health Organization (WHO) . International Statistical Classification of Diseases and Related Health Problems n.d. https://icd.who.int/browse10/2016/en (accessed 4 September 2020).
- NHS Digital . Emergency Care Data Set (ECDS) n.d. https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-sets/emergency-care-data-set-ecds (accessed November 2017).
- NHS Digital . HRG4+ 2017 18 Local Payment Grouper n.d. https://digital.nhs.uk/services/national-casemix-office/downloads-groupers-and-tools/payment-hrg4-2017-18-local-payment-grouper (accessed November 2017).
- O’Caithain A, Knowles E, Turner J, Maheswaran R, Goodacre S, Hirst E, et al. Explaining variation in emergency admissions: a mixed-methods study of emergency and urgent care systems. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02480.
- Office for National Statistics . National and Local Authority Level Population Estimates 2016. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/methodologies/nationalandlocalauthoritylevelpopulationestimates (accessed October 2018).
- Kitagawa EM. Components of a difference between two rates. J Am Stat Assoc 1955;50:1168-94. https://doi.org/10.2307/2281213.
- Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci 2007;62:722-7. https://doi.org/10.1093/gerona/62.7.722.
- Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146-56. https://doi.org/10.1093/gerona/56.3.m146.
- British Geriatrics Society . Frailty: What’s It All About? 2018. www.bgs.org.uk/resources/frailty-what%E2%80%99s-it-all-about (accessed 23 October 2018).
- Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016;45:353-60. https://doi.org/10.1093/ageing/afw039.
- Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 2018;391:1775-82. https://doi.org/10.1016/S0140-6736(18)30668-8.
- Soong J, Poots AJ, Scott S, Donald K, Woodcock T, Lovett D, et al. Quantifying the prevalence of frailty in English hospitals. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-008456.
- Jutte DP, Roos LL, Brownell MD. Administrative record linkage as a tool for public health research. Annu Rev Public Health 2011;32:91-108. https://doi.org/10.1146/annurev-publhealth-031210-100700.
- Bardsley M. Understanding patterns of complex care: putting the pieces together. J Health Serv Res Policy 2012;17:195-6. https://doi.org/10.1258/jhsrp.2012.012110.
- Street A, Maynard A. Activity based financing in England: the need for continual refinement of payment by results. Health Econ Policy Law 2007;2:419-27. https://doi.org/10.1017/S174413310700429X.
- Blunt I, Bardsley M, Dixon J. Trends in Emergency Admissions in England 2004–2009: Is Greater Efficiency Breeding Inefficiency?. London: Nuffield Trust; 2010.
- Wittenberg R, Sharpin L, McCormick B, Hurst J. The ageing society and emergency hospital admissions. Health Policy 2017;121:923-8. https://doi.org/10.1016/j.healthpol.2017.05.007.
- Peterson MC. A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clin Proc 2009;84:248-54. https://doi.org/10.1016/S0025-6196(11)61142-7.
- Department of Health . Reference Costs 2015–16 2016. https://webarchive.nationalarchives.gov.uk/20200506094432/https://www.gov.uk/government/publications/nhs-reference-costs-2015-to-2016 (accessed October 2018).
- Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 2004;9:197-204. https://doi.org/10.1258/1355819042250249.
- Jung B, Cho KH, Lee DH, Kim S. The effects of continuity of care on hospital utilization in patients with knee osteoarthritis: analysis of Nationwide insurance data. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2951-y.
- NIHR Involve . Payment and Recognition for Public Involvement n.d. www.invo.org.uk/resource-centre/payment-and-recognition-for-public-involvement/ (accessed 29 August 2020).
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. PharmacoEconomics 2008;26:661-77. https://doi.org/10.2165/00019053-200826080-00004.
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403-13. https://doi.org/10.1016/j.jval.2010.11.013.
- Hole A. DCREATE: Stata Module to Create Efficient Designs for Discrete Choice Experiments 2015. https://econpapers.repec.org/RePEc:boc:bocode:s458059 (accessed February 2017).
- Altman DG. Practical Statistics for Medical Research. Boca Raton, FL: CRC Press; 1990.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Hauber AB, González JM, Groothuis-Oudshoorn CG, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR conjoint analysis good research practices task force. Value Health 2016;19:300-15. https://doi.org/10.1016/j.jval.2016.04.004.
- Hogan H, Zipfel R, Neuburger J, Hutchings A, Darzi A, Black N. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015;351. https://doi.org/10.1136/bmj.h3239.
- Jarman B, Pieter D, van der Veen AA, Kool RB, Aylin P, Bottle A, et al. The hospital standardised mortality ratio: a powerful tool for Dutch hospitals to assess their quality of care?. Qual Saf Health Care 2010;19:9-13. https://doi.org/10.1136/qshc.2009.032953.
- Bottle A, Jarman B, Aylin P. Strengths and weaknesses of hospital standardised mortality ratios. BMJ 2010;342. https://doi.org/10.1136/bmj.c7116.
- Friebel R, Hauck K, Aylin P, Steventon A. National trends in emergency readmission rates: a longitudinal analysis of administrative data for England between 2006 and 2016. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020325.
- George PM, Stone RA, Buckingham RJ, Pursey NA, Lowe D, Roberts CM. Changes in NHS organization of care and management of hospital admissions with COPD exacerbations between the national COPD audits of 2003 and 2008. QJM 2011;104:859-66. https://doi.org/10.1093/qjmed/hcr083.
- National Confidential Enquiry into Patient Outcome and Death . Themes and Recommendations Common to All Hospital Specialties 2018.
- Ala L, Cooksley T, Cozens T, Duckitt R, Hislop R, Holland M, et al. SAMBA17 Report. Against the Clock – Time for Patients 2018. www.acutemedicine.org.uk/wp-content/uploads/2017/12/Society-for-Acute-Medicine-Benchmarking-Audit-2017-National-Report.pdf (accessed July 2018).
- Essén A, Lindblad S. Innovation as emergence in healthcare: unpacking change from within. Soc Sci Med 2013;93:203-11. https://doi.org/10.1016/j.socscimed.2012.08.035.
- Reid LEM, Crookshanks AJF, Jones MC, Morrison ZJ, Lone NI, Weir CJ. How is it best to deliver care in acute medical units? A systematic review. QJM 2017. https://doi.org/10.1093/qjmed/hcx161.
- Plsek P. Complexity and the Adoption of Innovation in Health Care. Washington DC, USA: National Institute for Health Care Management; 2003.
- Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.8775.
- Lowthian JA, Curtis AJ, Cameron PA, Stoelwinder JU, Cooke MW, McNeil JJ. Systematic review of trends in emergency department attendances: an Australian perspective. Emerg Med J 2011;28:373-7. https://doi.org/10.1136/emj.2010.099226.
- Mockel M, Searle J, Muller R, Slagman A, Storchmann H, Oestereich P, et al. Chief complaints in medical emergencies: do they relate to underlying disease and outcome?. Eur J Emerg Med 2013;20:103-8. https://doi.org/10.1097/MEJ.0b013e328351e609.
- Burt CW, McCaig LF. Trends in hospital emergency department utilization: United States, 1992–99. Vital Health Stat 2001;150:1-34.
- Kellett J, Deane B. The diagnosis and co-morbidity encountered in hospital practice of acute internal medicine. Eur J Intern Med 2007;18:467-73. https://doi.org/10.1016/j.ejim.2007.02.019.
- National Audit Office . Emergency Admissions to Hospital. Managing the Demand 2015.
- Meacock R, Sutton M. Elevated mortality among weekend hospital admissions is not associated with adoption of seven day clinical standards. EMJ 2018;35:108-13. https://doi.org/10.1136/emermed-2017-206740.
- Wennberg J, Gittelsohn A. Small area variations in health care delivery. Science 1973;182:1102-8. https://doi.org/10.1126/science.182.4117.1102.
- Gutacker N, Bloor K, Bojke C, Walshe K. Should interventions to reduce variation in care quality target doctors or hospitals?. Health Policy 2018;122:660-6. https://doi.org/10.1016/j.healthpol.2018.04.004.
- Appleby J, Raleigh V, Frosini F, Bevan G, Gao H, Lyscom T. Variations in Health Care: The Good, The Bad and The Inexplicable. London: The King’s Fund; 2011.
- Hornbrook MC. Techniques for assessing hospital case mix. Annu Rev Public Health 1985;6:295-324. https://doi.org/10.1146/annurev.pu.06.050185.001455.
- Söderlund N. Product definition for healthcare contracting: an overview of approaches to measuring hospital output with reference to the UK internal market. J Epidemiol Community Health 1994;48:224-31. https://doi.org/10.1136/jech.48.3.224.
- Guo P, Dzingina M, Firth AM, Davies JM, Douiri A, O’Brien SM, et al. Development and validation of a casemix classification to predict costs of specialist palliative care provision across inpatient hospice, hospital and community settings in the UK: a study protocol. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020071.
- Tsan L, Davis C, Langberg R, Pierce JR. Quality indicators in the Department of Veterans Affairs nursing home care units: a preliminary assessment. Am J Med Qual 2007;22:344-50. https://doi.org/10.1177/1062860607303291.
- Mesterton J, Lindgren P, Ekenberg Abreu A, Ladfors L, Lilja M, Saltvedt S, et al. Case mix adjustment of health outcomes, resource use and process indicators in childbirth care: a register-based study. BMC Pregnancy Childbirth 2016;16. https://doi.org/10.1186/s12884-016-0921-0.
- Goodwin JS, Lin YL, Singh S, Kuo YF. Variation in length of stay and outcomes among hospitalized patients attributable to hospitals and hospitalists. J Gen Intern Med 2013;28:370-6. https://doi.org/10.1007/s11606-012-2255-6.
- James NJ, Hussain R, Moonie A, Richardson D, Waring WS. Patterns of admissions in an acute medical unit: priorities for service development and education. Acute Med 2012;11:74-80.
- van de Vijsel AR, Heijink R, Schipper M. Has variation in length of stay in acute hospitals decreased? Analysing trends in the variation in LOS between and within Dutch hospitals. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1087-6.
- Steinwald B, Dummit LA. Hospital case-mix change: sicker patients or DRG creep?. Health Aff 1989;8:35-47. https://doi.org/10.1377/hlthaff.8.2.35.
- Engineer LD, Winters BD, Weston CM, Zhang A, Sharma R, Bass E, et al. Hospital characteristics and the agency for healthcare research and quality inpatient quality indicators: a systematic review. J Healthc Qual 2016;38:304-13. https://doi.org/10.1097/JHQ.0000000000000015.
- Appleby J, Buckingham H, Dayan M, Edwards N, Imison C, Palmer W, et al. Doomed to Repeat? Lesson from the History of NHS Reform. London: Nuffield Trust; 2018.
- Hartz A, James PA. A systematic review of studies comparing myocardial infarction mortality for generalists and specialists: lessons for research and health policy. J Am Board Fam Med 2006;19:291-302. https://doi.org/10.3122/jabfm.19.3.291.
- Price LC, Lowe D, Hosker HS, Anstey K, Pearson MG, Roberts CM. the Royal College of Physicians Clinical Effectiveness Evaluation Unit (CEEu) . UK National COPD Audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax 2006;61:837-42. https://doi.org/10.1136/thx.2005.049940.
- Harbord M. Why I don’t want to continue practising general medicine and delivering the acute ‘take’. Future Hosp J 2016;3:70-1. https://doi.org/10.7861/futurehosp.3-1-70.
- Conway R, O’Riordan D, Silke B. Consultant volume, as an outcome determinant, in emergency medical admissions. QJM 2013;106:831-7. https://doi.org/10.1093/qjmed/hct119.
- Aldridge C, Bion J, Boyal A, Chen YF, Clancy M, Evans T, et al. Weekend specialist intensity and admission mortality in acute hospital trusts in England: a cross-sectional study. Lancet 2016;388:178-86. https://doi.org/10.1016/S0140-6736(16)30442-1.
- Vaughan L, Machaqueiro S, Gaskins M, Imison C. The London Quality Standards: A Case Study in Changing Clinical Care. London: Nuffield Trust; 2017.
- McMurdo ME, Witham MD. Unnecessary ward moves. Age Ageing 2013;42:555-6. https://doi.org/10.1093/ageing/aft079.
- Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021161.
- Baum JAC, Shipilov AV. Sage Handbook for Organisational Studies. London: SAGE Publications Ltd; 2006.
- Tarandach R, Bartunek J, Woodman R, Pasmore W, Shani A. Research in Organisational Change and Development. Bingley: Emerald Group Publishing Limited; 2009.
- Duffield C, Roche M, Diers D, Catling-Paull C, Blay N. Staffing, skill mix and the model of care. J Clin Nurs 2010;19:2242-51. https://doi.org/10.1111/j.1365-2702.2010.03225.x.
- Martin GP, Kocman D, Stephens T, Peden CJ, Pearse RM. Inquiry. Pathways to professionalism? Quality improvement, care pathways, and the interplay of standardisation and clinical autonomy. Sociol Health Illn 2017;39:1314-29. https://doi.org/10.1111/1467-9566.12585.
- The Mid Staffordshire NHS Foundation Trust Public Inquiry . Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry 2013.
- National Advisory Group on the Safety of Patients in England . A Promise to Learn – A Commitment to Act 2013.
- Care Quality Commission . Opening the Door to Change: NHS Safety Culture and the Need to Change 2018.
- Department of Health and Social Care (DHSC) . Better Leadership for Tomorrow. NHS Leadership Review 2015.
- NHS Leadership Academy . Healthcare Leadership Model 2013. www.leadershipacademy.nhs.uk/wp-content/uploads/2014/10/NHSLeadership-LeadershipModel-colour.pdf (accessed October 2018).
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Vaughn VM, Saint S, Krein SL, Forman JH, Meddings J, Ameling J, et al. Characteristics of healthcare organisations struggling to improve quality: results from a systematic review of qualitative studies. BMJ Qual Saf 2018;28:74-8. https://doi.org/10.1136/bmjqs-2017-007573.
- Felblinger DM. Bullying, incivility, and disruptive behaviors in the healthcare setting: identification, impact, and intervention. Front Health Serv Manage 2009;25:13-2. https://doi.org/10.1097/01974520-200904000-00003.
- Petrovic MA, Scholl AT. Why we need a single definition of disruptive behaviour. Cureus 2018;10. https://doi.org/10.7759/cureus.2339.
- Khan A, Teoh KR, Islam S, Hassard J. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018720.
- Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: a meta-narrative review of the healthcare literature. Int J Nurs Stud 2017;69:9-24. https://doi.org/10.1016/j.ijnurstu.2017.01.003.
- Buchanan DA, Denyer D, Jaina J, Kelliher C, Moore C, Parry E, et al. How do they manage? A qualitative study of the realities of middle and front-line management work in health care. Health Serv Deliv Res 2013;1. https://doi.org/10.3310/hsdr01040.
- Caldwell K, Atwal A. The problems of interprofessional healthcare practice in hospitals. Br J Nurs 2003;12:1212-18. https://doi.org/10.12968/bjon.2003.12.20.11844.
- Harris LC, Ogbonna E. Exploring service sabotage: the antecedents, types and consequences of frontline, deviant, antiservice behaviors. J Serv Res 2002;4:163-83. https://doi.org/10.1177/1094670502004003001.
- British Medical Association . Workplace Bullying and Harassment of Doctors. A Review of Recent Research 2017.
- Chambers CNL, Frampton CMA, McKee M, Barclay M. ‘It feels like being trapped in an abusive relationship’: bullying prevalence and consequences in the New Zealand senior medical workforce: a cross-sectional study. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020158.
- Einarsen SV, Hoel H, Zapf D, Cooper CL. Bullying and Harassment in the Workplace: Developments in Theory, Research, and Practice, Second Edition. Boca Raton, FL: CRC Press; 2010.
- Bragard I, Dupuis G, Fleet R. Quality of work life, burnout, and stress in emergency department physicians: a qualitative review. Eur J Emerg Med 2015;22:227-34. https://doi.org/10.1097/MEJ.0000000000000194.
- Grocott HP, Bryson GL. The physician at risk: disruptive behaviour, burnout, addiction, and suicide. Can J Anaesth 2017;64:119-21. https://doi.org/10.1007/s12630-016-0782-z.
- Morley C, Unwin M, Petersen GM, Stankovich J, Kinsman L. Emergency department overcrowding: a systematic review of causes, consequences and solutions. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0203316.
- Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, et al. Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual Saf 2017;26:559-68. https://doi.org/10.1136/bmjqs-2016-005567.
- Hurlen P, Østbye T, Borthne AS, Gulbrandsen P. Does improved access to diagnostic imaging results reduce hospital length of stay? A retrospective study. BMC Health Serv Res 2010;10. https://doi.org/10.1186/1472-6963-10-262.
- Edwards N. What’s Behind Delayed Transfers of Care?. London: Nuffield Trust; 2017.
- Reid L, Rae R. Structures in AMUs – Qualitative and Quantitative n.d.
- Gray JH, Densten IL, Sarros JC. Size matters: organisational culture in small, medium, and large Australian organisations. J Small Bus Entrepreneurship 2003;17:31-46. https://doi.org/10.1080/08276331.2003.10593311.
- Meyer M. Size and the structure of organisations: a causal analysis. Am Soc Rev 1972;37:434-41. https://doi.org/10.2307/2093182.
- The Functions of the District General Hospital. Report of the Bonham-Carter Committee 1969.
- NHS England . Five Year Forward View 2014.
- Holdsworth D. Changes and challenges in cardiology training. BMJ 2012;345. https://doi.org/10.1136/bmj.e7269.
- Fuller G. Shape of training: a view from the specialties. Clin Med 2014;14:357-60. https://doi.org/10.7861/clinmedicine.14-4-357.
- Black D. The new UK internal medicine curriculum. Clin Med 2017;17:103-4. https://doi.org/10.7861/clinmedicine.17-2-103.
- Sullivan P, Bell D. Investigation of the degree of organisational influence on patient experience scores in acute medical admission units in all acute hospitals in England using multilevel hierarchical regression modelling. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-012133.
- Lewis CL, Wickstrom GC, Kolar MM, Keyserling TC, Bognar BA, Dupre CT, et al. Patient preferences for care by general internists and specialists in the ambulatory setting. J Gen Intern Med 2000;15:75-83. https://doi.org/10.1046/j.1525-1497.2000.05089.x.
- Droog E, Foley C, Healy O, Buckley C, Boyce M, McHugh S, et al. Perspectives on the underlying drivers of urgent and emergency care reconfiguration in Ireland. Int J Health Plann Manage 2018;33:364-79. https://doi.org/10.1002/hpm.2469.
- Wiseman V, Mooney G, Berry G, Tang KC. Involving the general public in priority setting: experiences from Australia. Soc Sci Med 2003;56:1001-12. https://doi.org/10.1016/S0277-9536(02)00091-6.
- Finlayson SR, Birkmeyer JD, Tosteson AN, Nease RF. Patient preferences for location of care: implications for regionalization. Med Care 1999;37:204-9. https://doi.org/10.1097/00005650-199902000-00010.
- Watson V, Carnon A, Ryan M, Cox D. Involving the public in priority setting: a case study using discrete choice experiments. J Public Health 2012;34:253-60. https://doi.org/10.1093/pubmed/fdr102.
- Abbott A. The System of Professions. An Essay on the Division of Expert Labour. Chicago, IL: University of Chicago Presss; 1988.
- Winter L, Kron T, Seising Rudolf. Views on Fuzzy Sets and Systems From Different Perspectives. Philosophy and Logic, Criticisms and Applications. Berlin: Springer; 2009.
- Rechel B, Džakula A, Duran A, Fattore G, Edwards N, Grignon M, et al. Hospitals in rural or remote areas: An exploratory review of policies in 8 high-income countries. Health Policy 2016;120:758-69. https://doi.org/10.1016/j.healthpol.2016.05.011.
- Briggs T. A National Review of Adult Elective Orthopaedic Services in England. Getting It Right First Time. London: British Orthopaedic Association; 2015.
- De Vaus D. Research Design in Social Research. London: SAGE Publications Ltd; 2001.
- Schmidt M. The Sankey Diagram in energy and material flow management. J Ind Ecol 2008;12:82-94. https://doi.org/10.1111/j.1530-9290.2008.00004.x.
- Huang C, Lu R, Iqbal U, Lin S, Nguyen P. A richly interactive exploratory data analysis and visualisation tool using electronic medical records. BMC Med Inform Decis Mak 2015;15. https://doi.org/10.1186/s12911-015-0218-7.
- NHS Elect . Directory of Ambulatory Emergency Care for Adults 2018.
- NHS Improvement . Ambulatory Emergency Care Guide: Same Day Acute Frailty Services 2018.
- Gnoli C. Phylogenetic classification. Knowl Org 2006;33:138-52.
Appendix 1 Literature review
This study was predicated on the notion that medical generalism may provide better outcomes for certain types of patients. Hence, it was essential to attempt to define and explore both concepts of medical generalism and their enaction in hospital practice, particularly in the UK setting.
The initial intention had been to perform a rapid systematic evaluation of the literature, with the results informing WP1. An initial search using the terms ‘general’ and ‘general medicine’ returned over 15,000 results. At this point, it became apparent that even a systematic rapid evaluation would be too resource-intensive and time-consuming to be practical. Instead, it was decided to conduct a systematised review. Although this method is less rigorous, the aim of the review was never to be definitive, but rather to pragmatically identify key themes and major studies, and, hence, was thought to be sufficient. The search terms used are given in Table 29.
| Search | Key words |
|---|---|
| 1 | Search ((medical generalism) AND medical generalist) NOT primary care |
| 2 | Search (hospitalist) AND generalist |
| 3 | Search ((hospitalist) AND generalist) AND specialist |
| 4 | Search ((((specialist) AND specialty) AND generalist) AND general med*) AND general physician |
| 5 | Search ((((general med*) AND special*) AND general physician) NOT general practi*) NOT primary care |
| 6 | Search (((acute take) AND acute med* take) AND general*) AND special* |
| 7 | Search (hospitalist) AND medical generalis* |
| 8 | Search (hospitalist) AND special* |
| 9 | Search (hospitalist) AND medical generalist |
| 10 | Search (generalism) AND rural hospital |
| 11 | Search (((medical generalism) AND medical generalist) NOT general practice) NOT general practitioner |
| 12 | Search ((((complex patient) AND comorbid*) AND generalis*) NOT general practitioner) NOT primary care |
| 13 | Search ((acute physician) AND geriatrician) AND specialist |
| 14 | Search (((((small* hospital) OR small* provider) OR rural hospital) OR remote hospital) AND medical generalis*) AND generalis* |
| 15 | Search ((medical generalism) NOT acute physician) AND general practi* |
| 16 | Search ((medical generalism) NOT general practi*) NOT primary care |
| 17 | Search (((future) AND medical generalism) NOT general practice) NOT primary care |
| 18 | Search ((acute physician) AND generalis*) AND complex* |
| 19 | Search (((medical generalis*) AND comorbidity) NOT general practi*) NOT primary care |
| 20 | Search ((role) AND medical generalis*) NOT general practi* |
| 21 | Search (((role) AND medical generalist) AND specialist) NOT general physician |
| 22 | Search (((role of the medical generalist) AND specialist) NOT general physician) NOT general practitioner |
Search strategy
Terms were searched for in the title and abstract, English-language text only and from the year 2000 onwards.
The databases that were searched included MEDLINE, Health Management Information Consortium, Social Sciences Citation Index, EMBASE and Web of Science.
The search was conducted by the University of Birmingham Library in November 2017.
Given the definitional problems around generalism, no strict inclusion criteria were used.
Criteria for exclusion for the review included:
-
language other than English
-
papers relating to non-hospital-based practice
-
papers relating to hospitalist-type models of specialist care.
Four reviewers working in pairs conducted the initial screening (Louella Vaughan, Claudia Leone, Louise Taylor, Rachel Hutchings); final assessment for eligibility was conducted by all four reviewers in regular team meetings. The results of the screening are shown in Figure 25. Two reviewers conducted the data extraction (Claudia Leone and Rachel Hutchings), which was again subjected to team review.
FIGURE 25.
Flow chart of literature review.
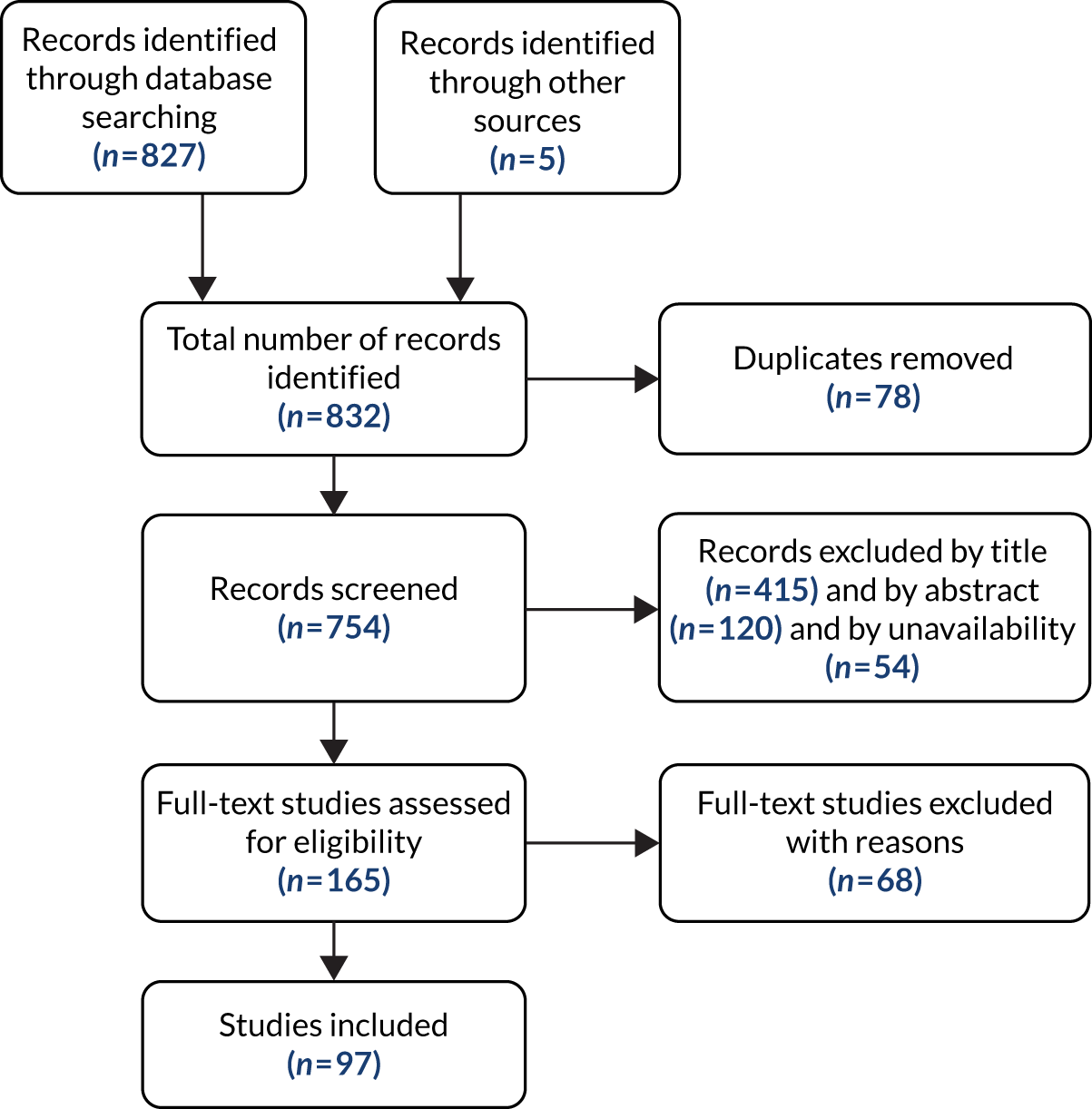
A summary of the studies included in the literature review can be found in Report Supplementary Material 1.
The literature review aimed to provide context for our discussion around the patient, public and professional views of medical generalism in the acute setting. We identified a series of themes from the literature, all highlighting that there is no consistent or shared definition of generalism, or what a ‘generalist’ is, with pieces suggesting that different attributes distinguish the generalist from the specialist. Some emphasised the practical aspects of the role, such as co-ordination and communication, but others focused on the more ethical or philosophical approach to the patient, such as the holistic approach which sees the person in their wider social context. For both of these aspects, these attributes demonstrated how important a generalist, or someone who adopts an approach that contains these qualities, is for addressing the demographic challenges facing health care today, that is older people with multimorbidity and different health and social care needs. Other key themes included the relevance of how a specialism is defined (i.e. whether the specialism is site-defined, such as an intensivist, or organ-defined, such as a cardiologist) and how this relates to the definition of generalism and the discussion of the role of generalism being to ‘bridge a gap’, but inconsistency as to what this gap was. Some argued it was the gap between the community and the hospital, therefore, emphasising the role of a generalist in providing continuity, whereas others suggested that it was the gap between the person’s medical experience and their social experience, therefore emphasising the role of a generalist in providing holistic and personalised care. The review of the literature also demonstrated that there are still negative perceptions of generalism and general medical patients. This has an impact on recruitment and on the work itself, with some reports suggesting that generalism was defined as work that does not fall neatly within another specialty. At the same time, there were also reports that held a negative view of specialism, viewing it as the antithesis to person-centred care.
Our review also explored the definitions of generalism used in an international context. To understand this better, we reviewed the definitions used by the various medical colleges in the USA, Australia, Canada, New Zealand and within Europe. The themes we identified here echoed the wider literature, with discussion heavily focused on the use of generalism as a pragmatic response to addressing particular demographic issues, such as an increasingly ageing and multimorbid population. In Canada, Australia and New Zealand especially, the constraints posed by rurality and geography were a key factor. Again, like the wider literature, what constituted generalism or the defining features of a generalist were inconsistent, with some approaches placing more recognition on the practical aspects of a generalist providing continuity and others recognising a more philosophical basis for generalism, which emphasised the holistic, person-centred approach taken to care. As with the wider literature, inconsistency around linguistics and terminology provided a constant source of confusion.
Appendix 2 Detailed methods for work package 1
Approach
This study aimed to explore medical generalism through the perspectives of the patient, the professional and the service. WP1 was designed primarily to define and explore the service perspective, as well as elements of the professional perspective, namely how doctors define and experience medical generalist work.
The initial plan was to use a two fold approach to define and understand models of care. The first was to use a ‘general systems’ approach to define the models of care in terms of their functions, processes and staffing that constituted each service delivery component of the emergency and acute medicine pathway (e.g. ED, AMU), which was based on the telephone surveys. This approach was also to be used to classify and organise the models of care into a typology. We then intended to use a framework approach to better understand the contexts in which these models operate at the team provider, the hospital and the external landscape/policy levels, which was based on data collected through fieldwork. It was intended that both approaches would be informed by theories of medical generalism and these relate to decision-making at individual patient and service levels, as explored in a series of workshops. It was hoped that this would result in a classification genuinely representative of models of care as defined by medical generalism.
This approach proved unexpectedly problematic in several ways.
First, although there was a clear consensus around the contextual factors that drive models of care, medical generalism emerged as being much more complex and multidimensional than had been suggested by review of the literature (see Appendix 1). There was also little agreement in which aspects of a model of care best captured the essence of generalism. This was mostly because the ‘hat’ that any doctor puts on is highly contingent and depends not only on the context in which the doctor is working (e.g. on call vs. a specialty clinic), but also on other intrinsic factors of the individual doctor such as education, training and personal preferences for ways of working. This meant that integrating medical generalism into every level of the analysis was not possible. Therefore, although we collected information pertaining to medical generalism across the whole WP, it was analysed using a separate framework.
Second, the approach, premised on review of the literature, assumed that most hospitals would operate models mostly similar to that described in the RCP’s guidelines on Acute Medical Units79 and that major innovations would have been described in the literature. Hence, there would be only a limited number of dominant models in operation. However, we found that models of care in English hospitals have been subject to almost relentless cycles of innovation and improvement, the combined result of edicts from the centre (such as the drive to introduce ambulatory/emergency care units by NHSI) and concerted efforts to meet targets (particularly the 4-hour target). 86,93 The result of this is that not only does each hospital employ an entirely unique model of care, but that care in many organisations could be described as being in a state of permanent flux.
These findings, plus those from the medical generalism workshops (see Chapter 3) meant that the original approach was not suitable for the material generated. Instead, we adopted a two-fold approach for considerations of service. We retained the General Systems Approach96 to the initial defining and understanding of models of care. The typology itself ultimately focused on the two components of the systems, the AMU and the downstream wards, through which medical inpatients flow, to limit the analysis to the categories that best expressed splits between generalist and specialist medicine (see Appendix 3). We adopted a second framework of analysis, the CFIR. 100 The CFIR considers that care in organisations is the result of innovation and improvement, mediated by contextual factors at multiple levels, particularly those of team provider, hospital and external landscape/policy. This approach would not only allow an understanding of how models of care come to be deployed as they are, but also help to explore why models of care are so different.
Identification of smaller hospitals
A report88 has previously defined ‘smaller hospitals’ in England as providers with an operating revenue (income) of under £300M in the 2012–13 financial year. 91 In that year, of the 142 general acute trusts, 75 trusts were found to fit into this category. Following review of financial information for 2015–16, six trusts were removed from the sample because their operating revenues now exceeded that which might be expected from natural growth, and were likely to be the result of a major service reconfiguration, including a hospital merger. This left a sample of 69 smaller hospitals in England. This definition captures trusts that are predominantly single site, which minimises the problem of attempting to distinguish HES data at the hospital level in multisite trusts. It also ensured that there was a reasonable geographical distribution of sites, including hospitals in urban, provincial and rural settings.
Organisational profiles
Organisational profiles were constructed for all smaller trusts (n = 69) from a combination of publicly available data (e.g. trust and CQC reports) and hospital-level data collected by Monitor88 (later NHS Improvement) and the HSCIC.
Exploring models of care in smaller hospitals
Semistructured telephone interviews were used to gather data on the models of medical generalism deployed in smaller hospitals. Guides for the semistructured telephone interviews were constructed, following the early work of Reid,101 to explore the following:
-
Hospital department characteristics of the ED, AMU and downstream wards of each hospital, and the ambulatory and frailty units where hospitals had these, including function, patterns of medical and advanced practitioner staffing, multidisciplinary team input, leadership and clinical pathways.
-
Local triage rules for determining how patients are moved between components of the system.
-
Construction of the acute medical take during the day, night and weekend and levels of consultant and junior doctor commitment.
-
Networking arrangements with other hospitals, in terms of both provision of urgent services to patients and medical staff working across multiple sites.
Invitations were sent in two tranches to the Chief Executive Officers of the 69 identified smaller trusts; the first tranche was sent to members of the New Cavendish Group, a learning network run by the Nuffield Trust for the CEOs of smaller trusts, and the second to the remainder. Following confirmation of participation, organisations were asked to nominate a contact person to arrange the interviews.
All interviews were conducted using two team members. The topic guides were iteratively revised to improve the clarity and flow of questions. Telephone and e-mail follow-up was used to clarify missing or potentially inaccurate data.
Data were transcribed into Excel® 2013 (Microsoft Corporation, Redmond, WA, USA) using the SurveyMonkey platform (www.surveymonkey.com; Palo Alto, CA, USA).
Constructing the typology
See Appendix 3 for the iterative approach taken to finalising the scheme for the typology.
Excel was used to construct a database of all hospitals against the typology. Interviews were independently reviewed by two team members (Louella Vaughan and Danielle Nimmons); conflicting results were resolved by consensus or through further clarification with the original interviewee. In two cases, there were insufficient data to fully classify the hospital according to the typology.
Case studies: investigating the typology
The purpose was of the case studies was three fold:
-
To examine in more detail the operational aspects, such as processes of care and staffing, with particular reference to similarities and differences between models of care.
-
To evaluate the contexts in which the models of care sit, at provider team, hospital and external landscape/policy level.
-
To explore concepts of medical generalism and how these may relate to the development and deployment of the different models of care.
Sampling strategy
The original intention was to undertake 2–3 case studies of each of the 4–5 different models of care expected to emerge from the typology. However, sites were primarily chosen because they were exemplars of the different AMU models. As there were fewer ward models, this approach captured most of them; only one site was selected explicitly on this basis. We sought to achieve appropriate representation of trusts according to geographical distribution (urban vs. rural), size (small vs. ‘smallest’) and case-mix.
To better explore the contribution of the external landscape and case-mix to the model development, we theorised that neighbouring organisations would probably be very alike in terms of case mix and probably similar in terms of regional political and other external pressures. We then included in our sample three pairs of adjacent trusts (one inner urban, one outer-urban and one rural), where each hospital employed different models of care.
Site recruitment
Recruitment took place in three rounds: after each round of the telephone interviews and then a final round after one hospital had declined to participate and another had failed to respond to the invitation. Initial invitations to participate in the case studies were made through either CEOs or medical directors (in cases where medical directors had been involved in the telephone interviews). Respondents were asked to nominate a study lead investigator, who could assist with co-ordinating study visits and obtaining local ethics approval.
Site visits
Each hospital site was visited over 1–2 days by between three and five team members and a lay researcher. Schedules were drawn up ahead of time, with local leads assisting with the recruitment of appropriate members of staff for the interviews and focus groups.
Interviews, observations and document reviews were carried out for each site. At half of the sites, separate focus groups were conducted for staff and patients. Topic and interview guides can be found in Report Supplementary Material 4.
Interviews
Three to five interviews were conducted with key clinical, managerial and nursing staff involved in the delivery of medical care. Care was taken to interview clinical staff working across the whole patient pathway (i.e. the ED, AMU and downstream medical wards and, where present, ambulatory care and frailty units). Informed consent was obtained from all interviewees. Interviews were semistructured and focused on the following:
-
The number and type of doctors contributing to the acute take and ward-based care. Where non-medical staff have extended roles, these were also documented.
-
Local definitions and systems used to triage between the ED, the AMU and the downstream wards.
-
Organisational workforce strategy.
-
Perceived tensions between generalist and specialist workloads.
-
Local networking arrangements.
-
Exploration of how and why current service models were implemented and plans for future change.
-
Experiences of facilitators and barriers to changes to services models.
-
Experiences of working in a smaller organisation.
Mapping patient flows
To better understand how patients moved between the different areas of the hospital and how transfers of care were managed, we mapped the possible journeys for medically unwell patients. 102 We had senior clinicians ‘walk’ the research team through each component and then describe how transfers of care were effected. This also allowed attention to be paid to the geographical layout of the hospital.
Day of Care Surveys
An adapted DCS was conducted at each site. A DCS is a validated tool that consists of 12 ‘severity of illness’ variables and 16 ‘service intensity’ variables to identify the appropriateness of inpatient care using ward visits and case record review. 103 The tool was adapted to identify whether a patient was labelled as a general medical or a specialty patient and whether or not the team caring for this patient was the most appropriate. The DCS was completed for medical wards only.
On some sites, the DCS was conducted by staff volunteers. On these occasions, brief training, written instructions and support from the research team were provided. On sites where insufficient staff were available, the clinical members of the research team completed the proformas with the assistance of senior ward staff, in a manner that preserved patient confidentiality.
Observations
At each site, a patient triage or handover meeting was observed. Of interest were the unwritten rules of triage that determined how patients pass along the acute/emergency care pathway.
Staff focus groups
At half of the sites, staff focus groups were conducted. Although these had been originally designed to explore the strengths and weaknesses of the different models of care (see Chapter 7), it was subsequently recognised that the material collected contained substantial information around processes of care, model development and other themes relevant to this WP. The protocol was subsequently amended to include the staff focus groups as part of this analysis.
Document review
Hospitals were asked to provide key documents for analysis, including consultant and middle-grade rosters for acute take and specialty on-call; standard operating procedures for the ED, AMU and downstream wards; and organisational workforce strategies for medicine and nursing.
Analysis
Walkarounds, interviews and focus groups were transcribed verbatim and organised using NVivo 11 (QSR International, Warrington, UK). Only one hospital provided documents for analysis. All others declined; either they did not have a standard operating procedure/policy or their existing policy no longer reflected actual practice. Data were then organised and analysed in a number of stages.
Construction of case studies
Case studies234 for each site were constructed from the data collected and field notes, supplemented by material from the telephone survey and publicly available data, such as trust annual reports. The studies aimed to combine detailed information about the processes of care at the unit level, while also providing contextual information about the hospital’s internal and external environments. Sankey diagrams, which were developed to depict proportionate flow through complex engineering systems235 and are increasingly being applied to health care,236 were constructed for each organisation (https://rawgraphs.io).
The study team attending the visit debriefed on multiple occasions after the case study visit. The first was conducted as soon as possible after the visit and team impressions were recorded to be included in the studies. The input of the lay researchers was particularly important, bringing a unique perspective. The draft write-ups were then reviewed collectively as a team: key points which marked organisations as being unique were decided in consensus fashion.
Framework analysis
Five separate sets of coding frameworks were used for all of the material generated by the case studies and relevant portions of the telephone surveys:
-
models of care – descriptions of mechanics of care were grouped by system component
-
the CFIR,100 which explores the contexts in which systems exist through five major domains – intervention characteristics, outer setting, inner setting, characteristics of the individuals involved and the process of implementation
-
medical generalism and specialism
-
smaller hospitals
-
workforce.
Each framework was separately coded by different members of the junior research team (Silvia Lombardo, Silvia Machaquiero, Louise Taylor and Claudia Leone) and then reviewed by senior members of the research team (LV, CI and AMR). ‘Pattern matching logic’237 was used to look for emerging themes, with emphasis on convergent and divergent evidence between data sources. An iterative approach was taken, with regular discussions (weekly among the WP1 team and monthly with the wider research team) being used to confirm important themes and guide further rounds of analysis.
The Day of Care Survey
The DCS was analysed according to methods described elsewhere. 103
Typology testing
The original intention was to convene an expert consensus group, with members drawn from the Study Steering Committee and relevant professional bodies, with the specific purpose of the group making a qualitative assessment of the typology and its generalisability.
Because of the difficulties in arriving at a final typology, we opted instead for using the New Cavendish Group and the Study Steering Committee to test the typology in an iterative fashion. The final typology was then presented as part of the workshop on case mix.
Descriptive analysis of workforce
A descriptive analysis of the workforce using data from the interviews and NHS Digital was carried out, looking in particular at the balance between generalist and specialist physicians.
Appendix 3 Constructing the typology
Although limited, the literature on models of ED, AMU and ward care suggests that clearly defined models of medical care are in use across England. Hence, the original intention was to use a system-based approach95,96 to describe each of the key components of the emergency/acute inpatient care pathway (ED, AMU, downstream wards as well as ambulatory/emergency care and frailty units, where they exist) and the relationships between these. Following the work of Reid et al. ,101 the interview guides for the telephone interviews were constructed to allow analysis of the following categories:
-
functions of the component, for example initial assessment, initial/onward/planned/higher-level care
-
footprint of the component, for example care areas and the resources contained within these
-
degree of permeability of the component’s boundaries, that is whether units are ‘closed’ (i.e. every patient on a unit is managed by a single clinical team) or ‘open’ (i.e. patients on a unit may be managed by more than one clinical team)1
-
patient population in terms of care requirements and LOS
-
consultant working patterns, including numbers and types of consultants, on-take and sessional work and duration of responsibility for patients
-
management of specialty patients
-
mechanisms for the triage and transfer of patients between clinical teams and wards
-
types of downstream wards, that is general medical wards, specialty wards and short-stay wards.
It was assumed that where the same models of care were used, this would be become apparent through similarities in properties of each component and the relationships between them. Furthermore, it was assumed that the relationships between some of the properties of the model and the relationships between the components would be contingent. For example, in hospitals with large numbers of acute physicians, the literature suggests that the AMUs in which they work will be closed, with the acute physicians responsible for the bulk of on the on-call work and having longer durations of responsibility for individual patients. 81
Although it was accepted that there would be nuances within individual systems, it was expected that 5–6 models would emerge from the classification. The plan was then to use the organisational profiles and the emerging theories of medical generalism to explore whether or not models of care were influenced by structural considerations, such as the size and location of the hospital, or by ideas around what constitutes best medical care in terms of the balance between generalist and specialist care.
These assumptions rapidly broke down in the face of the analysis. There was little or no consistency within components and no clear relationship between components, nor any evidence of contingency in any aspect of the system. Each and every hospital had an entirely individual model of care, with similarities between organisations being superficial, at best.
It was then decided to attempt a ‘phylogenetic’ classification of the models of care. Prior to 1990, the models of medical care were highly similar:
-
There were only two routes into the hospital – via the ED or direct referral by a general practitioner.
-
On a single take (which was usually 24 hours long), all patients were assigned to a single consultant (the ‘take’ consultant).
-
The bulk of patients remained under the care of the admitting consultant, regardless of their location within the hospital.
-
Specialist input was accessed through formal referral only.
-
The majority of consultants in a hospital made a contribution to this ‘general medical’ component of work, regardless of other specialty commitments.
The introduction of AMUs, ambulatory care units, frailty units and other ways of consultant working could, therefore, be considered to be a series of historical ‘innovations’,99 for each of which external standards now exist. 180,237,238 Therefore, it was theorised that models of care could be defined by the extent to which the underlying pathway has shifted from the ‘traditional’ model of care and the ‘maturity’ of each of the components when compared with external standards. The differences could be represented as branches on an ‘evolutionary’ tree. 239 A key advantage of phylogenetic classifications is that they trace the degree of similarity between categories of components and allow for multiple levels of analysis. On review of the interviews, it became apparent that hospitals did not adopt innovations at a smooth pace and that the enthusiasm for experimentation with various components of the system was heavily dependent on individual clinician preference. For example, one hospital with more traditional approaches to inpatient care had been persuaded to invest heavily in ambulatory services on appointment of a clinician who had previous experience in this area, whereas another with a ‘radical’ approach to inpatient care was yet to implement any type of frailty service because of a lack of interested geriatricians.
The systems approach was revisited, but with a view to identifying the critical categories where hospital care showed the most variation and where different approaches to medical generalism might be apparent. These categories included:
-
functions of the ED, including streaming, primary assessment and direct triage to specialties
-
functions of the AMU, including primary assessment, direct triage to specialties and short stay
-
average LOS on the ED and the AMU
-
open/closed nature of the AMU
-
consultant working patterns on the AMU and downstream wards
-
types of downstream wards
-
functions of the ambulatory care units, such as admission avoidance, hot clinics and ambulatory antibiotic services
-
number of general physicians and geriatricians versus the number of specialists employed.
Despite the reduction in the number of possible permutations, no two hospitals were found to be alike using this classification scheme.
Although we had been considering that models of medical generalism would be visible to the wider system level, it was decided to focus on the AMU and the downstream wards because these are the two components through which the majority of patients with medical conditions flow and to limit the analysis to the categories which best express splits between generalist and specialist medicine:
-
AMU – unit openness (closed/partial/open)
-
AMU – patterns of consultant working (acute physician only, APD mixed and SpD)
-
wards – unit openness (closed/partial/open)
-
wards – patterns of ward distribution (designated general medical wards, designated general medical wards and specialty wards, mixed wards and specialty wards only).
Using this scheme, distinct models were visible for the AMUs and the wards. However, the distribution of hospitals within the scheme was still extremely scattered and it was decided to further reduce the number of categories. As there were only a handful of AMUs that had no input from specialists, it was decided to fold this category into APD. As the pressures on the system meant that allocation rules for downstream wards were frequently ignored, it was considered that the presence of any wards considered to be generalist as opposed to specialist was a more reliable way of categorising downstream care.
This scheme resulted in 25 models of care being defined in 48 hospitals; however, there was still no consistent relationship between the models used on AMUs and the models used on downstream wards. For this reason, some aspects of the analysis are carried out using the typologies of AMUs and wards separately.
Assigning codes
In total, 48 interviews were conducted, which covered 50 hospital sites. For two hospital sites, the interview data were not sufficient to accurately define the model of care. Twenty-five different models of care were found in the 48 hospitals. To facilitate analysis, codes were assigned for overall AMU and ward models (Table 30).
| AMU | Wards | ||
|---|---|---|---|
| Assigned numerical code | Overall code | Assigned numerical code | Overall code |
| 1 | A1, B1 | 1 | E1, F1 |
| 2 | A1, B2 | 2 | E1, F2 |
| 3 | A1, B3 | 3 | E2, F1 |
| 4 | A2, B1 | 4 | E2, F2 |
| 5 | A2, B2 | 5 | E3, F1 |
| 6 | A3, B1 | 6 | E3, F2 |
| 7 | A3, D2 | ||
| 8 | A3, D3 | ||
Codes were also assigned for overall model. Rather than assigning codes by potential models (of which there are 54), codes were assigned by grouping together actual models that were found (Table 31).
| Overall code | Assigned numerical code |
|---|---|
| A1, B1, C1, D1 | 1 |
| A1, B1, C1, D2 | 2 |
| A1, B1, C2, D1 | 3 |
| A1, B1, C2, D2 | 4 |
| A1, B2, C1, D1 | 5 |
| A1, B2, C1, D2 | 6 |
| A1, B2, C2, D2 | 7 |
| A1, B2, C3, D1 | 8 |
| A1, B3, C1, D1 | 9 |
| A1, B3, C3, D2 | 10 |
| A2, B1, C1, D2 | 11 |
| A2, B1, C2, D2 | 12 |
| A2, B1, C3, D1 | 13 |
| A2, B1, C2, D2 | 14 |
| A2, B2, C1, D1 | 15 |
| A2, B2, C1, D2 | 16 |
| A2, B2, C2, D1 | 17 |
| A2, B2, C2, D2 | 18 |
| A2, B3, C1, D2 | 19 |
| A3, B1, C1, D1 | 20 |
| A3, B1, C2, D1 | 21 |
| A3, B1, C2, D2 | 22 |
| A3, B2, C1, D2 | 23 |
| A3, B2, C2, D2 | 24 |
| A3, B3, C2, D1 | 25 |
Appendix 4 Additional findings relating to the typology
Are models of care contingent?
An underlying premise of this study was that hospitals would be consistent in their approaches to generalism across the whole of the patient care pathway and that this would be visible in the relationship between different aspects of care within service units and between different system components. The relationships between the different AMU categories is demonstrated in Table 32 and the relationships between the different ward categories is shown in Table 33. Statistical analysis of the models of care was carried out using chi-squared test of independence.
Acute medical unit
| Code | APD/B1 | Mixed/B2 | SpD/B3 | Total |
|---|---|---|---|---|
| Closed/A1 | 8 | 8 | 4 | 20 |
| Partial/A2 | 6 | 13 | 1 | 20 |
| Open/A3 | 4 | 3 | 1 | 8 |
| Total | 18 | 24 | 6 | 48 |
Wards
| Code | GMW/D1 | SpW/D2 | Total |
|---|---|---|---|
| Closed/C1 | 12 | 13 | 25 |
| Partial/C2 | 7 | 13 | 20 |
| Open/C3 | 2 | 1 | 3 |
| Total | 21 | 27 | 48 |
There was no relationship found between the overall models of care used on the AMU and the overall models of care used on the wards [χ2 = 46.66; degrees of freedom (df) = 40; p = 0.21]. No relationships were found between the open/closed nature and the patterns of consultant working for either the AMUs (χ2 = 4.02; df = 4; p = 0.40) or the wards (χ2 = 1.45; df = 2; p = 0.49).
Do hospital characteristics have an impact on models of care?
It was hypothesised that hospital characteristics, particularly size, would be a factor in determining the model of care used, with smaller hospitals proposed as being more likely to have a more generalist approach to care. As the models of care in the AMU and the wards were found to be independent and not contingent, as had been theorised, we also considered the AMU and the ward models separately.
There was no consistent significant relationship between any measure of hospital size (bed number, ED presentations, emergency medical admissions or operating revenue) and overall, AMU and ward models of care. Figure 26 summarises the overall typology (types 1–25) against the number of beds.
FIGURE 26.
Typology summary score vs. number of hospitals beds.
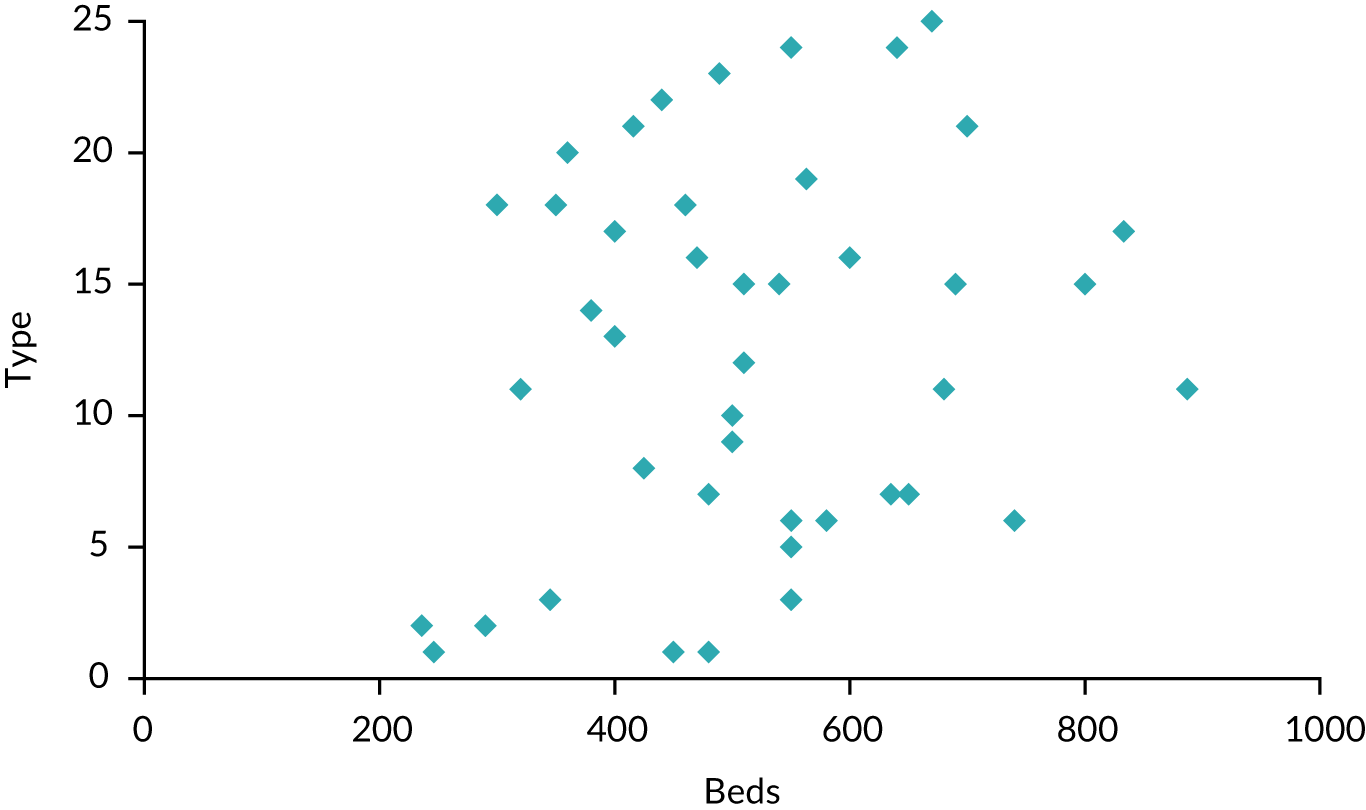
Table 34 shows the distribution of AMU type by hospital size. There was no significant relationship between the hospital size and the model of AMU (χ2 = 41.4, df = 40; p = 0.41); however, some differences were observed with regard to hospital size and the type of AMU:
-
the AMUs of the three smallest hospitals were all closed and APD
-
no hospital with < 400 beds used an open model of AMU.
| Hospital size (number of beds) | Assigned numerical code | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| < 300 | 3 | 3 | ||||||||
| 3–400 | 1 | 2 | 2 | 1 | 6 | |||||
| 400–500 | 2 | 2 | 1 | 3 | 2 | 1 | 11 | |||
| 500–600 | 1 | 3 | 2 | 1 | 2 | 1 | 1 | 11 | ||
| 600–700 | 2 | 1 | 2 | 1 | 1 | 7 | ||||
| > 700 | 1 | 1 | 2 | 1 | 5 | |||||
Table 35 shows the distribution of ward model by hospital size. There was no significant relationship between the ward model of care and the hospital size (χ2 = 30.7. df = 25; p = 0.20). Most hospitals used closed or partial models on their wards. The three hospitals that deployed open models were all middle sized.
| Hospital size (number of beds) | Assigned numerical code | Total | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| < 300 | 1 | 2 | 3 | ||||
| 300–400 | 1 | 1 | 1 | 3 | 6 | ||
| 400–500 | 2 | 3 | 1 | 3 | 2 | 11 | |
| 500–600 | 4 | 3 | 1 | 2 | 1 | 11 | |
| 600–700 | 1 | 2 | 1 | 3 | 7 | ||
| > 700 | 1 | 2 | 2 | 5 | |||
Table 36 shows the distribution of AMU type by geographic location. Although there were no consistent patterns between AMU type and geographical location (χ2 = 5.1, df = 10; p = 0.88), it is noticeable that there were no open AMUs in very rural areas and there was a slight preference for partial/open units in urban city areas. However, most types of models were seen in towns.
| Geographical location | AMU type | |||
|---|---|---|---|---|
| Closed | Partial | Open | Total | |
| Urban: city | 1 | 3 | 1 | 5 |
| Urban: town | 6 | 6 | 3 | 15 |
| Rural: town | 5 | 4 | 3 | 12 |
| Rural: sparse | 3 | 4 | 0 | 7 |
| Coastal | 1 | 1 | 1 | 3 |
| Island | 1 | 0 | 0 | 1 |
| Total | 17 | 18 | 8 | 43 |
Appendix 5 Patient and carer focus group findings
Results
Sample quotations are presented by theme in Table 37.
| Theme | Quote | Site |
|---|---|---|
| Generalist model vs. specialist model | No, I don’t think that’s a good idea at all . . . because you can have just a vague knowledge about everything or specific knowledge about one thing, I think that, for some things, is better. | A |
| . . . after my second stroke . . . I was referred to a specialist here and he said that the problem was that in my case that tablet is fine for most people but with my blood pressure they don’t know what can get through, and he said it’s the bane of my life, all I can suggest is you take a small aspirin every day and that may help. Now that specialist knowledge, I’m sure that a generalist wouldn’t necessarily be able to identify that . . . | B | |
| I have severe osteoarthritis and the last thing I want to do is see anyone generalist as they really don’t understand what’s going on, I can only see the top guy to be quite honest because what’s going on is so complex at the moment. I have no interest in seeing a generalist, I wouldn’t waste my time and there’s no point me seeing a specialist practitioner nurse because they don’t understand it either because of the detail. | E | |
| . . . if you have one and if they’ve got dementia and they come in and even if they’ve not got dementia, if you’ve got somebody that you can focus on and when they whooshed back the curtains and say hello Mr So and So, they automatically say hello Mrs Leigh and I say oh, it’s my doctor and straightway you can relate to that person and I think that you relax more, but if you’re going to have every Tom, Dick and Harry keep whooshing back the curtains you think what’s happening and you can get confused . . . | 6 | |
| Possibly because you could possibly miss out, if somebody is only dealing with, I go back to gastroenterology but they don’t know about bowel problems, then the two are linked but he may not fully know, also there may be other factors that that person has, other illnesses that contribute towards what is wrong with them, which might not be in his sphere of expertise and so therefore there is a potential that something is missed. | H | |
| Quality of hospital | I think one thing that’s well worth saying about this hospital is that the Chief Executive is a nurse, and that makes an enormous difference. You know, the Deputy Chief is a cardiologist, the Chief is a nurse, and it’s a very patient focussed place, and I think that’s very important. | A |
| Geriatric care | Yes, I think there’s a real problem with the elderly, particularly with elderly frail, because if they’re presented with half a dozen different doctors they usually don’t understand what it’s all about, and it’s confusing, they get conflicting messages, and it’s not good care. Particularly for the elderly I think you need one person and, just as you described, for the comorbidities they’re bringing in specialists of different types. | A |
| I think the people who are older when you’ve got a number of issues going on, you’ve got type 2 diabetes, you’ve got a skin cancer for instance, you’ve got some sort of lung issue. Here there is a view, longer term, being taken about moving towards a more general medical type approach because of what they noticed with patients over 65 with complex illnesses. | E | |
| I think if someone is elderly and they’ve got numerous things, it becomes good for the patient if they’ve just got one general person looking after them, because that person can become confused and has forgotten what they are seeing such and such a doctor for and what such and such a doctor has said. Separate doctors would be good if each of the doctors spoke to each other. | H | |
| . . . maybe care for the elderly for an elderly person, if they come in confused and not able to describe exactly what is wrong with them. | D | |
| Characteristics of smaller hospitals | I was thrombolysed and spent the night here, but I was told that I was very lucky that this particular consultant was here that day, because usually he’s at [other trust] and I could have ended up coming here and then being blue-lighted across to [other trust], so it was good that he was actually here and I was able to stay here, I appreciated that. | A |
| There is a growing partnership with this, the hospital and the University Hospital, and there is a thrombolysis service, but the consultant is frequently based at [another trust], and there is a sort of video link between the two. The problem is transport. | A | |
| I think the partnership business I think is absolutely crucial, you know, because we still want to retain our hospital, we want our A&E, we want access to really good regional services, and I think that is something that really should be pushed within the health service. You know, we can’t be Little Englanders, that’s not feasible. | A | |
| As an add-on to that, we equally don’t want just a few very large hospitals spread thinly, because then the patient, and if the patient has got to be in for a long period of time, isn’t going to have the same amount of visitors, which might be a thing that keeps them buoyant. So the smaller hospitals are useful for the less specialist care. | A | |
| But it’s when you’ve got to travel 40, 50, 60 miles to see a specialist and you’re critical. | B | |
| I think the larger hospital can be better in a lot of contexts because if you want to provide 24 hour care with specialist consultants then you’re going to need to have larger hospitals for the very fact that you’re going to need all those consultants to cover the shifts . . . With a small hospital it’s closer perhaps to the patient for travelling and particularly with somebody that’s elderly, but things can get missed with the out-patients. | F | |
| The facility is not there, if I’m in a smaller hospital for something like that, when it gets to a certain level then the person has got to be transferred out of here and especially if it’s an older person a one-step visit is better than multiple step visits, so that is the benefit of having a larger unit with more consultants in it specialising in that one item . . . | F | |
| Communication | You know, I think most of us would love to be able to go for good care to the specialist hospitals but expect that all the medical information transmits. It doesn’t always, I know. | A |
| Yes, I agree, I’ve got several health issues and I’m under several different specialists. Apart from communication they all treat me quite well, I’m quite happy with the treatment I’ve got, it’s just the length of time between specialists which is communication. | B | |
| I just think from personal experience, when I had my original stroke I spent 16 days in [one hospital] where the care was constant and I saw the same doctor all the time, and then I spent five weeks at [another hospital], the specialist stroke unit, but different doctors and that was a nightmare because you’ve got to start again. | B | |
| Individual suggestion | It might save emergency re-admissions going down that route rather than just seeing a specialist, you could emergency re-admissions down but you’d have to ensure the specialists are available, but I can see that as positive for the patient in reducing re-admission. | E |
The choice between a generalist and a specialist clinician was seen as a matter of personal preference rather than between a superior and an inferior option for several FGPs. For some respondents, the overall quality performance of the hospital seemed a more significant factor than the role profile of the individual clinician they would see, and as long as they were satisfied with the hospital, they did not see a need to express a preference for a specialist or a generalist. One participant expressed this as follows:
Our age group, that grew up with the NHS just coming and the doctors were all powerful. If they told you to do something, you didn’t think ‘do I want a specialist or a generalist?’.
That said, there was a perception among several participants that specialist care was the gold standard of treatment. For instance, one respondent said:
I was thrombolysed and spent the night here, but I was told that I was very lucky that this particular consultant was here that day, because he’s usually at [trust name redacted] and I could have ended up coming here and then being blue lighted across to [trust name redacted], so it was good that he was here and I was able to stay here . . .
This sense was reinforced in the same focus group when a respondent said it would be better to stay at the local trust ‘for common conditions like stroke and things like that’ but that specialist input would be necessary for ‘more obscure, difficult things’.
Related to the issue of viewing specialist care as gold standard, participants were sometimes reluctant to support the notion of generalist roles as a preferred option in secondary care. For instance, when asked whether they would prefer a generalist clinician that can ‘take a step back and see you as a whole patient’, one respondent said ‘no, I don’t think that’s a good idea at all’. Only when pressed was the respondent able to accept that there could be a benefit in seeing a generalist, for instance when a patient had five or six things wrong under different specialties.
Where respondents were able to acknowledge a role for care co-ordination by a generalist, more than one appeared to view this co-ordinating role as one that should be performed by a general practitioner. One person saw generalist input in the community (i.e. from a general practitioner) as removing the need for generalist input in an acute setting. Another said:
. . . it comes down to the GP [general practitioner] who knows you and knows you as a person – she should be able to discern whether it needs just solely a cardiologist or a general physician that would take it on a broader level.
However, geriatric care was the one area where multiple respondents saw a potential benefit in a generalist role in secondary care, particularly where patients had dementia. As one respondent put it:
. . . if they’re presented with half a dozen different doctors, they usually don’t understand what it’s all about and it’s confusing. They get conflicting messages and it’s not good care. Particularly for the elderly I think you need one person . . .
Another respondent said:
At this stage in my life, I want to see a specialist. I might think differently if I start developing more complex conditions which have interactions on medicine, but I haven’t come across it.
This respondent saw a value in having generalist input in medicines management in particular, having an overview of all medicines being used to prevent interactions.
Another respondent suggested that having care overseen by a generalist might reduce emergency re-admissions by cutting the amount of time patients had to wait for specialist appointments. However, these views were not universal, with one participant expressing a preference for specialist care even when presented with the hypothetical situation of being an older patient with multiple complex conditions.
The success with which information about patients flowed within and between NHS organisations was seen by several FGPs as a significant factor in the potential success of both specialist and generalist models. One described how having generalist input could help in situations where patients had incomplete knowledge about their own care, such as not knowing all of the medications that they took on a regular basis. But the same respondent felt that benefits provided by a generalist in a hospital setting, such as being able to understand the patient’s medical history, would be covered via access to an electronic patient record.
However, other patients expressed dissatisfaction with having to repeatedly explain symptoms to health-care professionals. One participant, who had experienced care under one doctor on a generalist ward as well as care in a specialist unit and had found the flow of information broken at the specialist site, said the specialist unit had been ‘a nightmare because you’ve got to start again’, in that they had to explain their medical history and symptoms to each new clinician.
A further factor was the experience of respondents who had initially been treated by a specialist at a more distant trust and then transferred to the local hospital. One respondent mentioned their notes had taken a long time to arrive at the local trust, following specialist treatment at a more distant hospital, which had caused problems.
Several respondents were able to articulate the fact that demand was limited for certain very specialist roles at smaller hospitals, and that providing a full service might not be the best use of NHS resources. For instance, one respondent said ‘. . . but of course there’s only about 40 or 50 people a year thrombolysed at this hospital, so you can’t have a full 24 hour service – it’s just not practical’.
The same patient suggested that remote access to specialists via telemedicine was a solution to this problem, and when asked to choose between travelling to see a specialist and receiving treatment at the local hospital, even acknowledging the risks posed by delayed start to treatment, the patient said: ‘I think if it was better top-notch treatment, yes, you would want to go’.
Discussion
Although some FGPs saw the choice between specialist and generalist clinician as a personal preference, others initially viewed specialist care as a preferred option. This appeared to be on the basis that a specialist clinician would have greater expertise to be able to treat the presenting issue. In making this distinction, participants appear to place less weight on the value of effectively co-ordinated care within a secondary care setting.
When the potential benefit of the generalist role in care co-ordination was explained, particularly in relation to patients with multiple complex conditions, some participants were better able to appreciate the value of generalist care. However, some still maintained that they personally would prefer to see a specialist and others felt that care co-ordination should be a component of the general practitioner role, carried out in the community. This suggests that it may be necessary to place more focus on explaining to patients the significance of effective care co-ordination for good outcomes in a secondary care environment, and how this role differs from co-ordination in primary care.
Some participants understood that the costs of employing a full range of specialist clinicians could be prohibitive for a small hospital, and were able to outline potential solutions such as greater use of telemedicine, co-ordination of care by a generalist with visiting specialists, or provision of care at multiple locations. However, these patients still sometimes expressed a preference for specialist care for themselves when asked, revealing a certain level of cognitive dissonance. Patients were not asked to make trade-offs between different options for care in the focus group research and it will be important to see whether or not this cognitive dissonance is resolved when they are asked these questions in the DCE experiment component of the research programme.
List of abbreviations
- A&E
- accident and emergency
- AMU
- acute medical unit
- APD
- acute physician dominant
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CFIR
- Consolidated Framework for Implementation Research
- CHAIN
- Contact, Help, Advice and Information Network
- CI
- confidence interval
- CLAHRC
- Collaboration for Leadership in Health Research and Care
- CMG
- case-mix group
- COPD
- chronic obstructive pulmonary disorder
- CQC
- Care Quality Commission
- DCE
- discrete choice experiment
- DCS
- Day of Care Survey
- df
- degrees of freedom
- DGH
- district general hospital
- DToC
- delayed transfer of care
- ED
- emergency department
- FGP
- focus group participant
- FTE
- full-time equivalent
- GIM
- general internal medicine
- GP
- general practice
- HES
- Hospital Episode Statistics
- HRG
- Healthcare Resource Group
- HSCIC
- Health and Social Care Information Centre
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- IQR
- interquartile range
- LOS
- length of stay
- MRS
- marginal rates of substitution
- NCEPOD
- National Confidential Enquiry into Patient Outcome and Death
- NHSE
- NHS England
- NHSI
- NHS Improvement
- NIHR
- National Institute for Health Research
- PPI
- patient and public involvement
- RCP
- Royal College of Physicians
- SD
- standard deviation
- SpD
- specialist dominant
- STP
- sustainability and transformation plan
- WP
- work package
Notes
-
Framework analysis of telephone surveys and case study interviews
-
Investigating the economic costs associated with models of medical generalism in smaller hospitals
-
Additional material for the exploratory analysis of patient-related outcomes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09040).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
