Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 16/53/17. The contractual start date was in January 2018. The final report began editorial review in July 2019 and was accepted for publication in April 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Baker et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Background
This chapter sets out the background and study context, explaining why it is important to enhance knowledge about restrictive practices in adult mental health inpatient settings and how the behaviour change technique (BCT) taxonomy can contribute to the development and understanding of interventions.
Restrictive practices in adult mental health inpatient settings
Incidents that threaten service user and staff safety, such as violence, aggression and self-harm, are not uncommon in mental health inpatient settings. 1 The Royal College of Psychiatrists’ (RCP) survey of violence in inpatient mental health settings in 20072 found violence and aggression to be commonplace, experienced by approximately three-quarters of all staff and one-third of service users. They are often managed using restrictive practices, which are defined by the Department of Health and Social Care as:
‘[. . .] deliberate acts on the part of other person(s) that restrict an individual’s movement, liberty and/or freedom to act independently in order to: take immediate control of a dangerous situation where there is a real possibility of harm to the person or others if no action is undertaken . . .’
Examples of restrictive practices include restraint (manual or mechanical holding of the service user), seclusion (isolating the service user in a locked room), coerced intramuscular injection of sedating drugs and constant observation (service user within eyesight or arm’s reach of one or more supervising nurses at all times).
Restrictive practices are widely used internationally4 although reliable prevalence data can be hard to find, and are influenced by discrepancies in definition and recording methods. 5 Cultural differences mean that across countries some forms of restrictive practice are more acceptable than others. For example, mechanical restraint is seen as an acceptable treatment in acute settings in the USA but unacceptable in UK acute settings. 6 Despite such differences, there is an emerging international consensus that restrictive practices are used too frequently. 7 Restrictive practices can cause serious physical and even lethal harm as well as psychological injury to service users and staff. 8 Face-down restraint has been associated with positional asphyxia. 8 Restrictive practices can also have a profoundly detrimental effect on therapeutic relationships between staff and service users. 9 Substantial costs arise from staff sickness10 and resource-intensive observation of service users. 11
Interventions to reduce restrictive practices
Restrictive practices began to attract wider attention following the occurrence of deaths attributed to their use. 12 In England and Wales, the Mental Health Units (Use of Force) Act 2018 has mandated that Mental Health Trusts must reduce the use of restrictive practices. 13 Despite a plethora of policies and initiatives in the UK and internationally to reduce the use of restrictive practices, there is no robust evidence to support the use of one intervention in preference to another. Furthermore, it has been noted that where one restrictive practice is reduced another might increase. 8,14 Safewards, an initiative to reduce conflict (violence, absconding, self-harm, rule breaking and medication refusal) and containment (restraint, seclusion and sedation),15 showed a reduction in incidences of both in the intervention arm. 16 It demonstrated that innovative, evidence-based interventions can reduce violence and containment usage in settings that are contending with the resource limitations characteristic of UK acute mental health services. A trial of Six Core Strategies17 demonstrated a reduction in ‘seclusion–restraint’ and observation days, although no differences in terms of violence.
Observation studies have reported the reduction of restrictive practices and violent behaviours after the delivery of interventions,18–20 although they are generally considered low quality, and other studies have reported no effect. 21 One study showed some evidence in favour of restraint training over de-escalation training. 22
In the UK, Safewards,16 Six Core Strategies23 and No Force First24 are examples of initiatives that have been promoted and adopted by some NHS Mental Health Trusts, while the National Coordinating Centre for Mental Health is promoting a quality improvement programme. However, the specific content of such initiatives and programmes has not been examined in detail; hence, the mechanisms through which they might change behaviour are not fully understood and, furthermore, it is not known whether or not interventions leading to reductions in the use of restrictive practices share common features.
Previous reviews14,18,25–31 have highlighted the paucity of research in this area and poor quality of the evidence. One study concluded that there is a lack of evidence from controlled studies to support the use of current non-pharmacological approaches to violent behaviour. 32 Although there is a clear imperative to identify the best-quality studies to reliably understand how effective an intervention is, this has little applicability in practice if the choice of interventions is extensive while awareness of their effectiveness is limited. Service providers thus require some way of knowing what interventions are available and how comparable they are.
There are repeated calls for restrictive practices reduction guidance to be based on robust transparent studies,33,34 and for interventions to be better described and better evaluated. A further challenge for reviewers of behavioural (non-pharmacological) interventions is how to synthesise content, especially when there are vast differences between procedures. Livingston et al. 18 reviewed training-based interventions to reduce restrictive practices. They highlighted the difficulty of reaching conclusions because of ‘different types of aggression management programs, which contain a variety of approaches’ [and that the] ‘focus, curriculum, and duration of the training vary substantially from one program to another’. 18 Another review found that only 39% of interventions were adequately described when published. 35 This does not necessarily mean that interventions are not described, but does suggest the absence of a common language with which to describe intervention components. 36,37
The behaviour change technique taxonomy
To address this issue, a taxonomy of BCTs was developed. 38 The taxonomy provides a reliable method of precisely specifying components of programmes in a transparent manner, using an established language. It is intended for application across theory-based programmes aimed at both patients and professionals.
The BCT taxonomy built on a previous taxonomy devised from content analysis of reports of interventions,39 and followed a series of context-specific taxonomies focusing on physical activity and healthy eating,40 and prevention of risky sexual behaviour,41 professional behaviour change,42 safe drinking43 and smoking cessation support. 44,45 It differed from these in that it was designed to be comprehensive and to encompass a wide range of behaviour change techniques. This taxonomy is widely used internationally to report on programmes and synthesise evidence. 46,47
The development of the BCT taxonomy involved an empirical approach aiming to achieve international consensus around content. Three distinct methodologies were employed: (1) Delphi methods were used to develop labels and definitions of the individual BCTs, (2) the reliability of coding these BCTs was tested and used to highlight BCTs requiring refinement by the study team, and (3) an open-sort grouping task was delivered via an online computer program, with statistical techniques, including hierarchical cluster analysis, applied to generate a hierarchical structure of technique clusters designed to increase the speed and accuracy of recall during use of the taxonomy.
The BCT taxonomy enables the robust synthesis of evidence that has previously been problematic to unpick and compare. A BCT is defined as ‘an observable, replicable, and irreducible component of a programme designed to alter or redirect causal processes that regulate behaviour’. 38 The taxonomy comprises 93 BCTs (e.g. ‘problem-solving’, ‘instruction on how to perform the behaviour’, ‘social comparison’) in 16 thematic clusters, such as ‘goals and planning’ (solving problems by identifying actions required, and setting and reviewing goals) ‘shaping knowledge’ (including instructions on performing the behaviour and information about antecedents), ‘antecedents’ (including factors that could influence whether or not restrictive practices can be avoided) and ‘feedback and monitoring’ (including the monitoring of ward data, and whether or not and how feedback was given).
All interventions to reduce restrictive practices use BCTs. For example, role-playing verbal de-escalation strategies could be coded as ‘rehearsal of relevant skills’ involving ‘social comparison’, ‘monitoring of emotional consequences’ and ‘feedback on behaviour’. An expert delivering information about the risks of restraint could involve ‘information about health consequences’ delivered by a ‘credible source’. The BCT taxonomy therefore provides a reliable method of precisely specifying intervention components and the mechanisms by which behaviour is changed. 36,37 Use of this standardised language promotes transparency through more accurate reporting and replication,45 as well as more successful implementation with proven effectiveness. 38
The taxonomy can be used prospectively in intervention design48,49 by assisting with the identification of BCTs potentially associated with effectiveness. 38 It can also be used retrospectively to describe completed interventions and has been used internationally to report interventions43 and synthesise evidence,41,50 including reanalysing existing interventions to explore their components. 40
Chapter 2 Methods
This chapter sets out the study aim and objectives and describes the methods used in a three-stage study design including literature search, data extraction and analysis.
Aim and objectives
The aim of this study was to identify, standardise and report the effectiveness of components of interventions that seek to reduce restrictive practices in adult mental health inpatient settings using the BCT taxonomy. 39
The study objectives were to:
-
provide an overview of interventions aimed at reducing restrictive practices in adult mental health inpatient settings
-
classify components of those interventions implemented in terms of behaviour change techniques, and determine their frequency of use
-
explore evidence of clinical effectiveness and cost-effectiveness by examining behaviour change techniques and intervention outcomes
-
identify behaviour change techniques showing the most promise of clinical effectiveness and cost-effectiveness, and that require testing in future high-quality evaluations.
Design
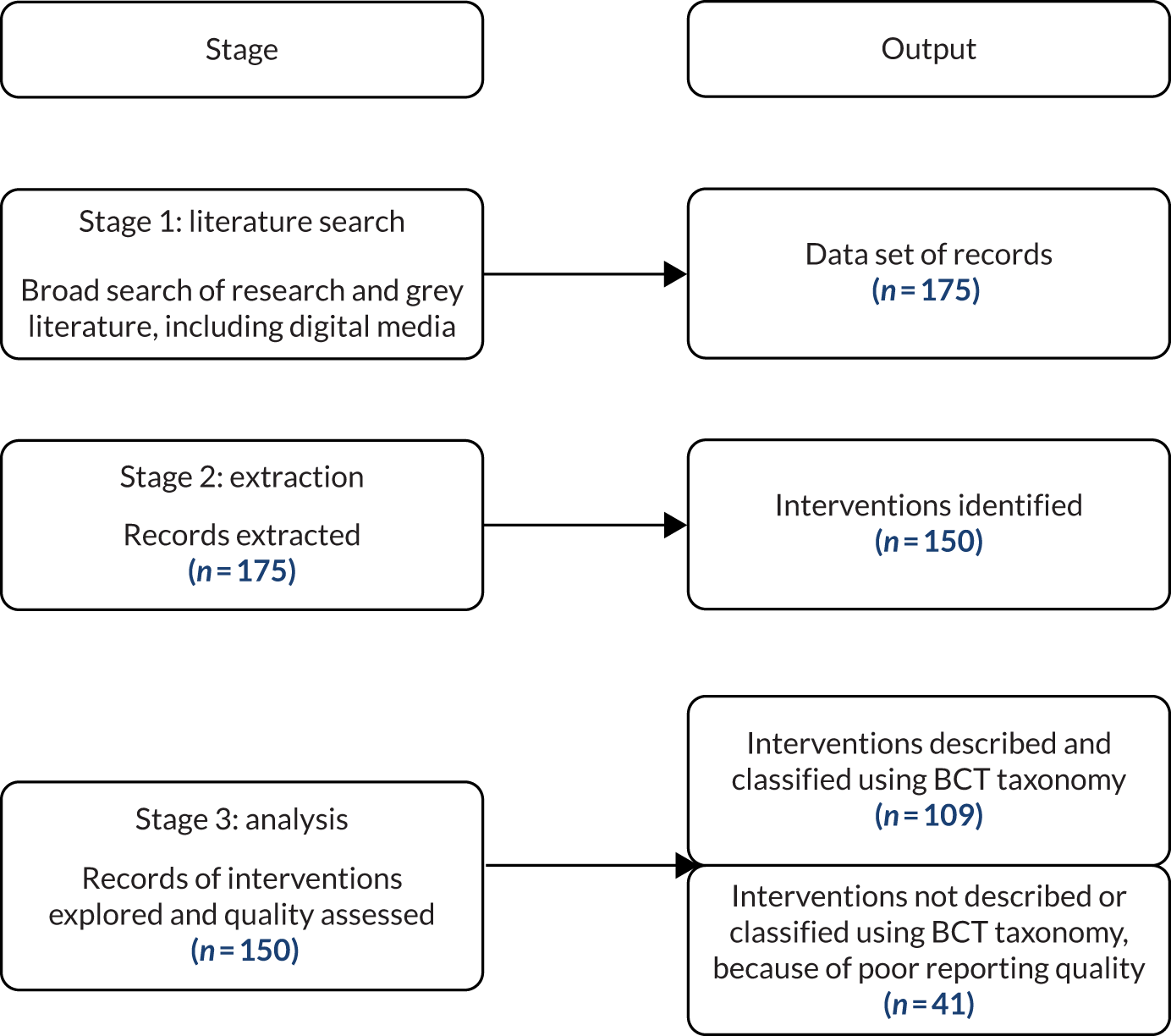
The study design comprised three stages. The purpose of stage 1 was to systematically search all English-language reports of interventions to reduce restrictive practices in inpatient mental health settings (objective 1). The aim of stage 2 was to extract data for analysis using the validated, structured BCT taxonomy to identify the content of the interventions (objective 2). The aim of stage 3 was to analyse the content of interventions using the BCT taxonomy, alongside a critical appraisal of all retrieved records using the Mixed Methods Appraisal Tool (MMAT), an appraisal tool specifically designed for mixed-methods reviews. 51 The application of the MMAT is described in Assessment of study quality using the Mixed Methods Appraisal Tool. The study design is illustrated in Figure 1 (see Chapter 3).
Stage 1: literature search
Introduction
Stage 1 focused on ascertaining the range and characteristics of interventions, irrespective of evidence of effectiveness, which involved systematically searching and reviewing all reports of interventions seeking to reduce the use of restrictive practices.
The search strategy approach drew on the increasingly utilised method of mapping52–56 to inform the purpose and output of the review. It differed from the method described in Bradbury-Jones et al. 52 because of the broad scope of the search and the inclusion of interventions in the current study. It was known that in addition to a small number of well-known interventions reported in the academic literature, there were numerous small-scale, standalone initiatives available for implementation in services. Not all of these would appear in a search restricted to the published research literature as they may be reported in unpublished literature or ‘non-research’ publications.
The search for relevant interventions records was informed by an ‘environmental scanning’57 approach suggested by Judy Wright, the project Information Specialist. Environmental scanning is a search methodology familiar in business contexts but relatively little used in health research. It permits the identification of more diverse information about an area than could be retrieved solely from published literature. In health-care settings, environmental scans have been used to inform future planning, to document evidence of current practice and to raise awareness. 57 It was therefore an appropriate choice for expanding the scope of the search strategy. Environmental scanning may involve a ‘passive’ approach that focuses on published and unpublished existing data or an ‘active’ approach where additional knowledge is generated through primary data collection. 57 In this study, a passive approach was used.
In keeping with objective 1 (to provide an overview of interventions aimed at reducing restrictive practices in adult mental health inpatient settings), the search criteria targeted diverse reports of non-pharmacological interventions aimed at changing the behaviour of inpatient adult mental health service staff to reduce restrictive practices. The scope of the searches was necessarily broad to include all records of an intervention, whether it was an evaluation or a descriptive report. 55 In order to include as many interventions as possible within the scope of the search, no quality threshold was imposed either indirectly (by restricting the search to high-impact journals)52 or directly via the search criteria or by screening. 54,56 Inclusion was not restricted by study design. 42 Interventions that solely involved policy change and those that aimed to reduce the use of one type of restrictive practice by replacing it with another were not eligible for inclusion.
In addition to interventions intended to reduce or eliminate restrictive practices, reports of interventions designed to improve quality or reduce or manage violence were included if their procedures and/or outcome measures addressed restrictive practices. Eligibility criteria are shown in Table 1.
| Criterion | Include | Exclude |
|---|---|---|
| Population | Adult (including older people) mental health inpatient settings (including acute, forensic and PICU services) | Children and Child and Adolescent Mental Health Services, learning disability and organic conditions |
| Date | 1999–2019 | |
| Interventions | Aimed at changing the behaviour of inpatient adult mental health service staff to reduce restrictive practices. Interventions may or may not have been implemented | Pharmacological only |
| Outcomes | Reduce restrictive practices | |
| Language | English language | Non-English language |
The starting date of 1999 was decided by the date of introduction of the UK National Service Framework for Mental Health,58 which precipitated new quality standards and a significant shift in the orientation of services. Because of the research team’s prior knowledge of the paucity of the evidence base, there were no restrictions on study design and no quality threshold was imposed. Searches were conducted from February until June 2018, and repeated in April 2019.
Two main searches were developed to identify interventions to reduce the use of restrictive practice in adults with mental health disorders. The first search aimed to identify reports from the academic bibliographic databases. The second search aimed to identify unpublished reports, including those occurring in the grey literature, social media and other digital resources.
Academic bibliographic databases search
The first search was conducted in February 2018. A wide range of academic bibliographic databases were searched for published studies, including:
-
British Nursing Index (BNI)
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL)
-
Cochrane Central Register of Controlled Trials (CCTR)
-
Cochrane Database of Systematic Reviews (CDSR)
-
Database of Abstracts of Reviews of Effects (DARE)
-
EMBASE
-
Health Technology Assessment (HTA) Database
-
HTA Canadian and International
-
Ovid MEDLINE®
-
NHS Economic Evaluation Database (NHS EED)
-
PsycInfo®
-
PubMed.
For full details of the databases, see Appendix 1.
The rationale for the academic databases was to select databases with good coverage of mental health studies and those covering studies of the nursing workforce, because the restraint reduction interventions are particularly important to this group that are dealing with aggressive and difficult situations on a ward. Two nursing databases (CINAHL and BNI), two of the largest medical databases (EMBASE and MEDLINE), the largest mental health database (PsycInfo), an evidence-based health database with good coverage of randomised controlled trials (RCTs) (Cochrane Library) and PubMed were searched to supplement the Ovid MEDLINE as they can contain some articles more recent than those included in Ovid MEDLINE. The team discussed and consented to this database selection, as proposed by the Information Specialist.
Search strategies were developed for the concepts: coercive interventions, mental health conditions and inpatients. Searches included subject headings and free-text words, identified by text analysis tools (PubReMiner), the Information Specialist (JW) and project team members. Further terms were identified and tested from known relevant papers. Searches were peer reviewed by a second Information Specialist. For full details of the search strategies, see Appendix 2 and Report Supplementary Material 1.
The search was updated and re-run in April 2019 in the same databases except for DARE and NHS EED, which were not searched as they had not received further content since the 2018 search. Owing to a change in database providers, BNI and HTA databases were searched via a different database host in 2018 rather than 2019. After checking index terms, two additional terms were added to the PsycInfo search: involuntary treatment/and psychiatric hospitalisation. All other searches remained the same.
Grey literature search
The second search was run from June 2018 to August 2018 to identify unpublished (grey) literature reports in databases, websites and social media sources. For full details, see Appendix 1.
The list of information resources to search was created collaboratively by the project team and information specialists. Websites for charities, government health departments, health-care organisations, health-care quality agencies, mental health organisations, professional societies/colleges and training providers were selected following an exercise to gather all potentially useful websites known by the project team, and those found by an information specialist scoping search. This large list was then organised into ‘types’ of organisations, such as health-care quality agencies, charities and government departments, and the team refined the list to include a set of 5–10 websites to search for each group that represented different countries/regions.
The team prioritised resources that were likely to provide relevant reports from North America, Australasia and Europe. Google (Google Inc., Mountain View, CA, USA) was used to search for interventions in 30 countries specifically identified in the 2016 Legatum Prosperity Index™ (a between-nations ranking system) as having the best health systems. A structured social media search incorporated YouTube (URL: www.youtube.com; YouTube, LLC, San Bruno, CA, USA), Facebook (URL: www.facebook.com; Facebook, Inc., Menlo Park, CA, USA) and Twitter (URL: www.twitter.com; Twitter, Inc., San Francisco, CA, USA).
The search strategies used in academic databases were adapted for use in grey literature databases, websites and social media sources. Website and social media searches used search terms similar to those used in the academic database searches, but fewer of them, and multiple short searches were run per resource, rather than one complex search. This ensured that the searches were consistent with the academic databases despite the limited ability of web and social media resources to process long strings of search terms or combine multiple searches. For further detail, see Appendix 2 and Report Supplementary Material 1.
In addition, an information request for unpublished interventions was sent to mailing lists for the health and medical community, clinical librarians and mental health librarians. No suggestions of restrictive practice reduction interventions were received from the mailing list information request. Project team members forwarded relevant reports they saw on their own social media accounts and through personal contacts with experts. When contact details were available, authors of identified interventions aimed at reducing the use of restrictive practices were contacted for further data. A request for information was circulated around Restraint Reduction Network members.
Backward citation searching of cited references and forward citation searching using Google and PubMed were used in order to access fuller descriptions of interventions, including development, procedures and implementation to supplement records with minimal detail, such as conference and poster abstracts, Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides and some non-research reports. This procedure was also used to identify journal publications associated with a dissertation/thesis and published reports associated with unpublished records and non-research reports. These strategies were also supported with a Google search for authors. Individual journals were hand-searched; however, because of the disparate nature of journals reporting the study topic, no key journals were identified.
The results of the published and grey literature database and website searches were stored and de-duplicated in EndNote (Clarivate Analytics, Philadelphia, PA, USA) referencing software libraries. The results of the social media searches were stored in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) file.
Screening
Free online citation screening software (Abstrackr beta version, Center for Evidence Synthesis in Health, Brown University, Providence, RI, USA) was used to assist with screening. Abstrackr uses artificial intelligence to help reduce screening time by determining the relevance of papers, based on inclusion and exclusion terms entered by reviewers, and subsequently displays references in order of predicted relevance. 59
Retrieved references were imported into Abstrackr and the following settings were selected: a pilot phase of 100, double-screening, display-all (i.e. title, authors, abstract, keywords) and order by relevance. Two researchers (KC and KB) independently screened the first 100 references, documenting their decision-making. Terms were discussed and shared to ensure maximum efficiency and coherence after screening the first 100 references, again after screening 600 and again after screening 1000. In total, 55 terms indicating relevance were entered, including restrain, intervention, psychiatry, inpatient, and the names of specific interventions of interest. In addition, 78 terms indicating irrelevance were entered, including child, community, dementia and learning disability. The full list is provided in Appendix 3. Once 1500 references had been screened, no further references appeared to be relevant. Following the recommendation of Rathbone et al. ,60 references without an abstract were screened separately (n = 998) to avoid compromising Abstrackr’s predictions. Screening conflicts were discussed and resolved between KC and KB. This process generated a subset of full texts to retrieve for further screening.
Stage 2: data extraction
Records were scrutinised to develop a sense of scope and content, and then extracted using a data extraction sheet informed by relevant data extraction tools.
A full list of extraction terms can be found in Appendix 4. Extraction was conducted using a standardised extraction tool supplemented with additional terms. The Workgroup for Intervention Development and Evaluation Research (WIDER) tool was used. WIDER was designed specifically to facilitate the identification and extraction of essential details of behaviour change interventions. 61 It comprises 20 recommendations under four broad headings for reporting behaviour change interventions: characteristics of those delivering the intervention, characteristics of the recipient, setting and mode of delivery. In order to capture the breadth of interventions identified in the retrieved records, the tool was adapted to include additional subheadings; for example, city, state/province, country, setting (type) and setting size (beds/wards) were added to subheadings under ‘setting’. These subheadings were developed inductively to reflect content, while retaining the validated structure of the WIDER recommendations. The subheadings under ‘setting’ are relatively descriptive, reflecting the different ways in which setting was reported.
Subheadings under ‘mode of delivery’ were developed in a more interpretive fashion, using the constant comparison technique62 to make judgements about whether one form of delivery was the same as or different from another. When a key detail of delivery mode was identified that did not fit under an existing subheading, another subheading was created for it.
Other headings for data extraction, for example publication type, year of publication and peer review, were drawn from modifiable Cochrane extraction templates63 and developed with reference to the study objectives. Extraction in stage 2 applied the first two screening questions in the MMAT to identify evaluation studies. Additional information using terms from the Cochrane template included, for example, funder (if any), design and outcome measures. The application of the MMAT is described in more detail in Assessment of study quality using the Mixed Methods Appraisal Tool.
Two researchers (KC and KB) extracted all data into a shared Microsoft Excel spreadsheet, where the data were stored and organised. Notes and clarifications were recorded directly on the spreadsheet. Decision-making during the process of extraction was documented for transparency.
Modification
Reports of modifications to the intervention protocol were recorded, including what was modified and how. 64 In this context, modification meant any planned deviation from the original intervention protocol.
Fidelity
When fidelity was recorded, it described reports of implementation as specified by the intervention protocol. 65
Theory
For the purposes of data extraction, theory was defined as a way of understanding, explaining and predicting behaviour, events and situations. Different scales of theory have been proposed:66 grand, mid and small.
Small theory or programme theory is how and why an intervention is proposed to work. It sets out the components of the intervention, the outcomes and how outcomes will be measured, often in the form of a logic model or driver diagram. 67 Although a 19-item measure for the assessment of the use of theory in interventions is available,48 it was apparent from screening and data extraction that few interventions made any use of theory, and most of the items in the measure would be recorded as ‘no’. Therefore, an adaptation was developed in which any interventions that explicitly referred to theory were examined for (1) whether or not they used theory to inform intervention design and implementation and (2) whether or not they related their findings back to the theory (this criterion was adapted from the theory coding scheme). 48 For example, a judgement would be made about whether or not a training intervention that was described as being informed by social learning theory had linked its training content and delivery back to the same theory, and subsequently whether or not the findings were discussed in relation to the theory.
Not reported
The term ‘not reported’ (NR) was used to indicate missing information, unless there was an explicit explanation of why the information was not provided, such as that costs were not recorded or a procedure was not followed. For example, if fidelity is not reported it can be assumed neither that fidelity was unmeasured nor that it was measured and unreported. The analysis and findings presented below therefore can reflect only what was reported.
Stage 3: analysis
The aim of stage 3 was to analyse the data by describing and classifying interventions using the BCT taxonomy, alongside quality assessment of those records which reported evaluations. The application of the BCT coding manual in this study is illustrated in Appendix 5.
A single record could contain multiple interventions (e.g. NHS documents describing examples of good practice) and multiple records could refer to the same intervention (e.g. initial study, longitudinal study and replication study of an intervention). Records were used to complete the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (see Figure 2) and to report sources and formats. These are presented by type (e.g. research, tool), format (e.g. journal article, thesis) and year of publication to provide a general overview of the range of records captured by the search (see Chapter 3, Characteristics of records identified).
A distinction was made between interventions that had been reported/implemented only once (as far as could be ascertained) and others that had been reported/implemented multiple times, so that multiple records of the same intervention would not skew the analyses. Multiple reports of a single intervention were grouped together and termed an ‘intervention family’. Chapter 4 provides detailed descriptions of the interventions identified under headings corresponding to recommendations in WIDER,61 where that information was reported. As some records contained multiple interventions and the focus here was on the content of each report, the unit of analysis was instances where an intervention was mentioned.
Records were screened using the MMAT,68 as its first level of screening establishes whether or not a report can be categorised as an evaluation. In order to capture different evaluation designs, outcomes and findings, the unit of analysis was the evaluation. They are presented under headings corresponding to Cochrane guidance63 (see Chapter 4).
Describing intervention content using the behaviour change technique taxonomy
Interventions to reduce restrictive practices use a variety of behaviour change techniques to change staff behaviour. The BCT taxonomy was used to describe and compare the content of the interventions identified. As described above, the BCT taxonomy can be retrospectively applied to completed interventions41,46 and to synthesise evidence. 41,50
Behaviour change technique coding
Two researchers (KB and KC) acted as coders and independently coded the documents using the BCTv139 as the basis for a coding manual for the data. Both researchers were trained in application of the BCT taxonomy and are experienced qualitative mental health services researchers. The analysis was also supported by NVivo 12 software (QSR International, Warrington, UK) for qualitative data analysis. NVivo provided an efficient means of storing, coding, checking and reviewing throughout the analysis. The software enables the generation of audit trails including spreadsheets with clear links to original data sets.
Twenty interventions of varying types were coded independently by both researchers before discussion about how BCTs had been identified and coded. The coding manual was developed as the two researchers (KB and KC) discussed and recorded details about how they had coded BCTs and for what reasons. Once the researchers were satisfied with the coding of this set of 20, the remainder were independently coded by one coder and then reviewed by the second. The researchers conferred when there was uncertainty and sought advice from author Ian Kellar, an expert in BCT, as required. Changes were made to the coding manual and coding to ensure consistency. Formal measures of agreement were not used because of the novelty of applying the taxonomy in this area. Appendix 4 provides further details.
Development of the coding manual
The starting point for the coding manual was the BCTv1 taxonomy and its definition and examples of each BCT. 39 However, most of the examples in the taxonomy referred to behaviour of health-care service users rather than health-care staff. In response to this discrepancy the current study applied the approach reported in Presseau et al. 47 For example, regarding ‘reframing’ in the context of staff–patient interactions, staff are supported to think of aggression as a response to trauma, that is the communication of distress. Further examples specific to the literature were developed to consider the content of the interventions to be described. As the coding progressed, additional examples and clarification based on areas of both discrepancy and consensus were added.
There were no intervention components that did not fit into the taxonomy. Some BCTs detected were aimed at health-care staff, for example instructions on how to perform a behaviour via training. Others were aimed at mental health service users, for example using distraction to reduce feelings of aggression and some were aimed at both groups, for example generating emotional and social support by encouraging socialising on mental health wards. Again, taking the approach of Presseau et al. ,47 these were treated separately. In line with the study aims, the focus was BCTs targeting staff behaviour.
The taxonomy deals with BCTs concerning both behaviour and outcomes of behaviour. Outcomes can be the stopping of a behaviour (e.g. stopping smoking and improving health) or the commencement of a behaviour (e.g. exercising and reducing weight). These were distinguished by treating incidents of restrictive practices as ‘outcomes’ and ‘behaviour’ as the efforts made to reduce these (e.g. de-escalation). The interventions contained more focus on outcomes than on behaviour as these are easier to record and report; however, some interventions did encourage the examination of near-misses and successes (i.e. where restrictive practices had been avoided), perhaps through team meetings, and these were seen as examples of monitoring of behaviour rather than outcomes.
One problematic aspect of the taxonomy is its use of ‘self’ in terms of ‘self-monitoring’, ‘self-reward’, ‘self as role model’, ‘valued self-identity’ and ‘self-talk’. The initial screening of the literature had revealed that there was very little reference to individual health-care staff at all and no self-monitoring from individuals. Therefore ‘self’ was interpreted in a collective sense and was applied in instances in which the ward team were, for example, self-monitoring rather than being monitored at arm’s length via management. This interpretation was validated during coding, since no examples of individuals (rather than ward teams) were detected, and, in addition, many ward-based initiatives had been generated from the ward staff, rather than from management or at a broader policy level. Therefore, when it was reported that a ward recorded its own incident data, this was classified as ‘self-monitoring of outcomes’. When data were recorded centrally, this was recorded as ‘monitoring of outcomes’. The other opportunity for self-monitoring was in interventions that used debriefing after an incident. If it was specified that staff were encouraged to reflect on their role in the incident, this was coded as ‘self-monitoring of behaviour and/or outcomes’.
One coding decision made in relation to staff training was that, if this was mentioned at all, it was coded as BCT 4.1 ‘instruction on how to perform the behaviour’, regardless of the level of detail (following Presseau et al. 47). Sometimes, interventions referred only to staff training in de-escalation, with no further detail; it was agreed that, in this circumstance, an assumption could be made that, at the minimum, there would be instruction involved. This is not in keeping with the specified instructions for coding BCTs, but had the rationale that, if only those interventions that had gone on to describe the actual content of this training had been coded, the presence of training within the interventions would have been severely under-reported.
Several of the BCTs refer to prompts or cues. It was agreed that, where a checklist or tool had been implemented on a ward (e.g. during a risk assessment on admission), this would be coded as a ‘prompt’, as it prompted staff to carry out behaviour that had the intention of avoiding restrictive practices. Care planning or risk assessment were treated within the context of ‘goals and planning’. This was because, although they were focused on the service user, ‘goals and planning’ can also refer to agreement on how staff will respond to service users’ needs. ‘Problem-solving, goals and planning’ could also be identified in post-incident debriefing, depending on how the debriefing was described.
The difference between ward and service level in monitoring of outcomes was also seen in a number of other BCTs that could be applied at the individual staff/service user level, ward level, organisation level and policy level. For example, ‘goal-setting (outcome)’ was detected at all of these levels (see Appendix 6 for further details).
Descriptive statistics were used to count which BCTs featured in each intervention to provide an overall frequency of the most commonly occurring BCTs across the data set, and what clusters they were from. It was further established which BCTs were used in interventions with particular components, for example training, or audit and review, or service user involvement.
Describing intervention outcomes and relating back to behaviour change technique content
The outcomes of evaluations were extracted and described. These outcomes were then related back to the BCTs contained in the intervention subject to evaluation. The BCTs in evaluations with both positive and negative findings were identified and described.
Assessment of study quality using the Mixed Methods Appraisal Tool
In stage 1, the primary objective was to identify and document all interventions in records that met the eligibility criteria. The quality of the records was of interest; however, although it was anticipated that the records would be diverse in quality, it was also expected that the data set would contain valuable information about the range of interventions being considered for use in practice. Therefore, no records were excluded on the basis of quality.
In the current study the MMAT51 was used at two levels: to identify records of interventions that had been evaluated and to assess the quality of the evaluation reports. To get a sense of the quality of the evidence, the screening questions of the MMAT51 were used during data extraction to establish whether or not the intervention had been subject to an evaluation. The MMAT was again used for further examination of evaluations during data analysis.
The MMAT was designed for use in complex systematic literature reviews that include quantitative, qualitative and mixed-methods studies. The MMAT was developed from theory and a literature review, and has been found to have good validity. 51,68 Quantitative and qualitative studies are judged against four criteria and mixed-methods studies are judged against three. Scores are between 0% and 100%, although caution is advised against relying solely on the score, and reviewers are encouraged to provide a narrative description of the study features that lead to that score. The quantitative domain is split into three subdomains: randomised controlled, non-randomised and descriptive. The characteristics of the MMAT meant that it was selected as the most suitable tool with which to judge study quality in the context of wide-ranging research methods.
Chapter 3 Results of the literature search and a detailed description of records
This following sections present the results of each of the three stages of the review. Figure 1 illustrates the study design with outputs.
FIGURE 1.
Study design with outputs.
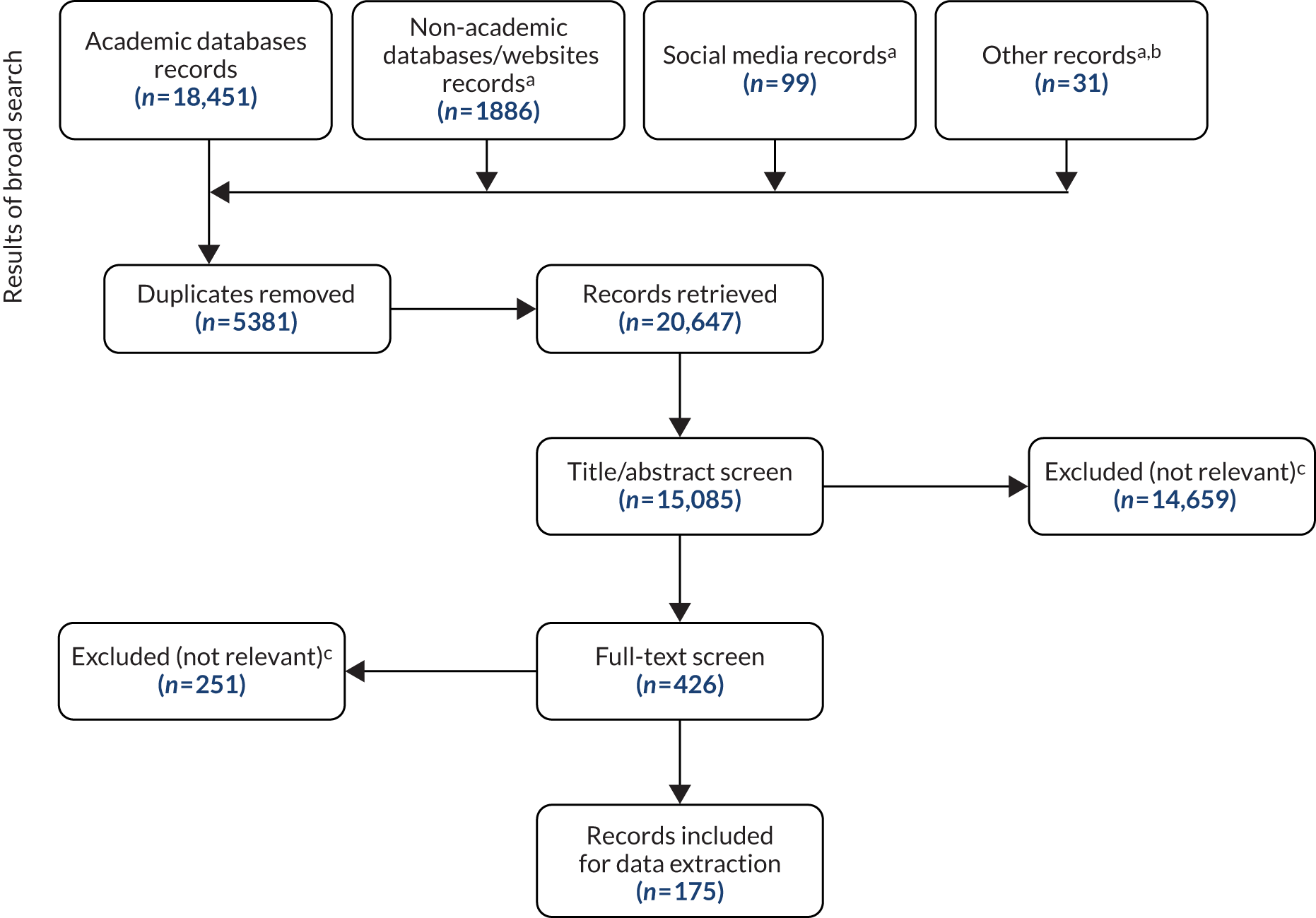
This chapter provides an overview of the literature search results, including a PRISMA flow diagram to indicate the extraction process. It describes in detail the records identified and highlights key characteristics of the data set.
Overview of the literature search results
As illustrated in the PRISMA flow diagram in Figure 2, the search of academic databases identified 18,451 records, and a further 1985 records were found in the grey literature (1886 in databases and websites, 99 in social media). Backward and forward citation searches, and contact with authors generated an additional 31 records. After removal of duplicates, 15,085 records were subject to title and abstract screening, which excluded 14,659. A total of 426 records were retrieved, of which 251 were excluded following full-text screening. The final data set consisted of 175 records for extraction. Further details are available in Appendices 1 and 2.
FIGURE 2.
The PRISMA flow diagram. a, Grey literature: non-academic databases and websites, social media and ‘other’ records; b, ‘other’ records: forward citation searches, contact with authors; c, excluded because not relevant (e.g. record does not describe an intervention, generic policy change, replacement of one restrictive practice with another).
The data set of 175 records was diverse in terms of how interventions were reported. Some interventions occurred in more than one record, some records reported more than one intervention and some reports were mentioned in more than one record. Overall, within the data set were 221 separate records of interventions, referring to 150 interventions in total. Of these, 109 had been evaluated and 41 had not been evaluated. This detail is illustrated in Figure 1.
The approach to analysis was designed to address study objectives 3 and 4, that is to explore evidence of effectiveness by examining behaviour change techniques and intervention outcomes, and to identify behaviour change techniques showing most promise of effectiveness and that require testing in future high-quality evaluations. Therefore, following extraction, the reports were organised into groups according to the intervention or interventions they described. This allowed for a primary focus on the evidence for each intervention, rather than the evidence per se.
Characteristics of records identified
Records were organised by type, the most common of which was research reports (Table 2 and see Appendix 8). The remaining records included brief descriptions of interventions presented in reports by organisations such as the Agency for Healthcare Research and Quality (AHRQ), the Care Quality Commission (CQC), NHS, Mind, the RCP (practice examples), and NHS trusts and hospitals (service reports); these non-research reports focused on interventions rather than a service setting (intervention reports), instructions for the performance of an intervention (instructions), links to training organisation websites (training links) and tools used as part of an intervention (tools). The majority of these were journal articles but they also included websites, leaflets, theses,69–75 abstracts,76–81 booklets,82–87 slides,84,88–92 videos,93–96 a podcast97 and a course syllabus. 98
| Record characteristic | Number of records (n = 175) | % |
|---|---|---|
| Record type | ||
| Research reports | 121 | 69 |
| Service reports | 15 | 9 |
| Tools | 14 | 8 |
| Training links | 9 | 5 |
| Intervention reports | 7 | 4 |
| Practice examples | 6 | 3 |
| Instructions | 3 | 2 |
| Format | ||
| Journal article | 116 | 66 |
| Website | 16 | 9 |
| Leaflet/handout | 10 | 6 |
| Booklet | 8 | 5 |
| Thesis/dissertation | 7 | 4 |
| Slides | 6 | 3 |
| Abstract | 6 | 3 |
| Video | 4 | 2 |
| Podcast | 1 | 1 |
| Syllabus | 1 | 1 |
| Year of publication | ||
| 1999–2004 | 21 | 12 |
| 2004–9 | 24 | 14 |
| 2009–14 | 49 | 28 |
| 2015–19 | 61 | 35 |
| No date | 20 | 11 |
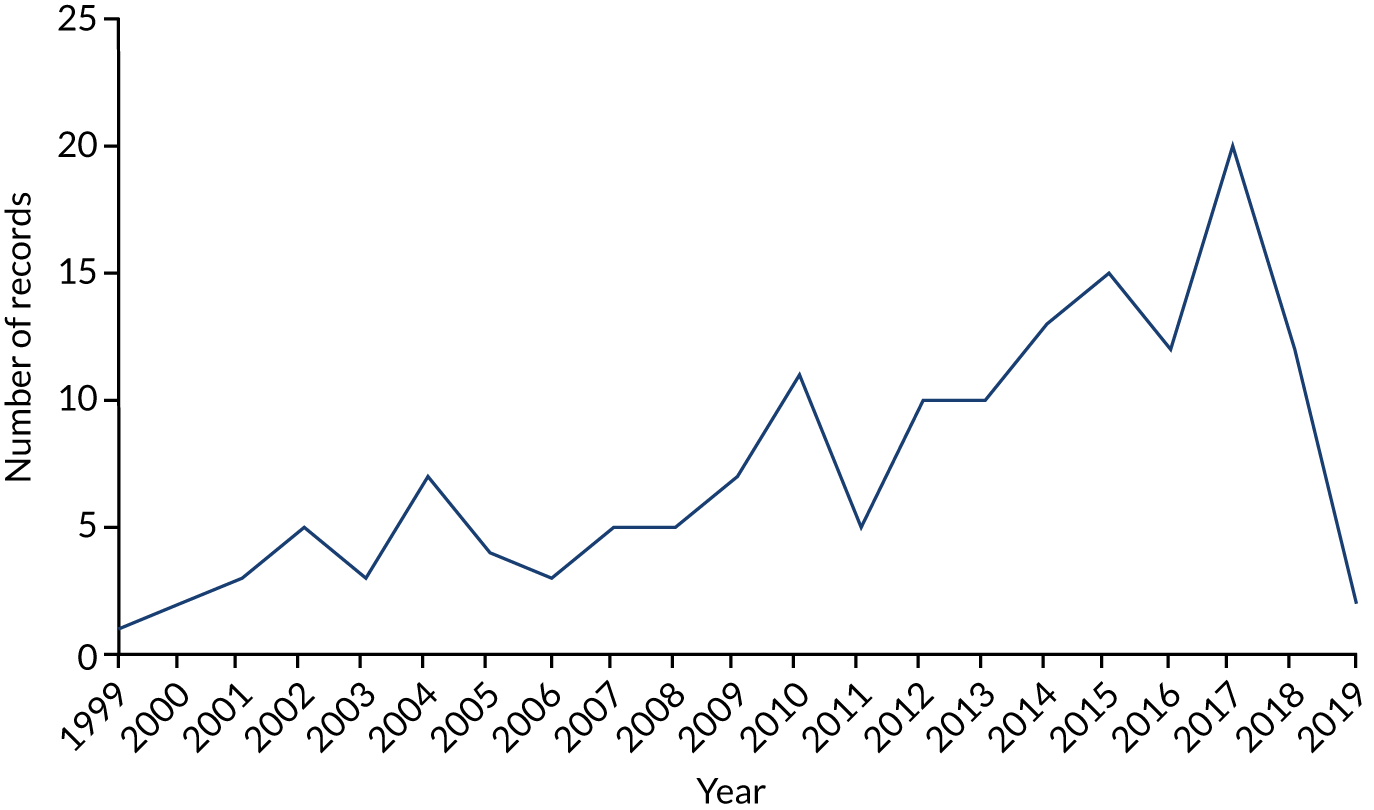
The number of records available steadily increased over the search period (i.e. 1999–2019), peaking at 20 in 2017, as illustrated in Figure 3. More than double the number of records in the period 2009–19 (n = 111) were identified compared with the previous 10-year period (n = 45). Twenty records were undated. These comprised all instructions, an intervention report and a service report (both in slide format), six tools (three of which were websites), the case examples on the AHRQ and RCP websites, and seven training links (three of which were videos). The context and content of these records indicated that they fell within the inclusion criteria.
FIGURE 3.
Records by year.
The distinction between records, standalone interventions and intervention families
The 175 records that were identified reported a total of 150 unique interventions (see Figure 1). Of these, 121 records reported standalone interventions. The remaining 54 records contained 100 references to 29 intervention families. Intervention families consisted of interventions with multiple records, sometimes in different formats and some of which have been implemented (and evaluated) multiple times (see Appendix 7). The intervention for which the most records were identified was Six Core Strategies (n = 18), including research reports, intervention reports, service reports and tools. With the exception of four records that pertained to two studies respectively,23,99 all other records were unrelated to each other – there were no follow-up or replication studies. Similarly, 10 records were identified for Safewards, which were unrelated research reports except for two that reported the same study in different formats. 88,100 Just three interventions had replication studies: City Nurse,101,102 Patient Focused Nursing103,104 and Review. 105,106 Two interventions had follow-up studies: Initiatives to Reduce Seclusion and Restraint107,108 and Open Door Policy. 109–111 One intervention (Brøset Violence Checklist112–114) had been evaluated in a pilot and a subsequent study. In the case of six interventions (Beacon Project,115,116 Recovery Based Principles,6,117 Early Recognition Method,118,119 REsTRAIN Yourself,22,85,87,120,121 Scottish Patient Safety Programme for Mental Health91,122–124 and Talk First83,86,125,126), the multiple records related to the same application or study of that intervention, often in different formats.
Chapter 4 Description of the interventions and evaluations
As per objective 1, and in keeping with the mapping approach, this chapter documents the overarching characteristics of the 150 interventions identified, including their scope and common features.
Comprehensiveness and consistency of reporting
A great deal of information was missing from the records about key aspects of the interventions. Recipient, setting, mode of delivery and aims were well reported but often lacked detail, whereas development, dose, who it was delivered by, and modification and fidelity were poorly reported (Table 3). Only 12% did not report setting. Remarkably few details were provided about who delivered the intervention, to whom, how, for how long or how often. These were usually ambiguous, describing implementation in a ward/unit, hospital or trust/administrative area without providing details of whether the sample consisted of staff and/or service users, front-line and/or managerial/administrative staff or how many of each were exposed to the intervention. Few specified whether the intervention was aimed at one or multiple professions. Most records did not include information regarding modification of or fidelity to the intervention protocol or the assumed change process that informed the intervention development (see Table 3).
| Reported (N = 221) | WIDER recommendation | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Detailed description of interventions | Assumed change process and design principles | Access to manuals/protocols | |||||||
| By whom delivered | Recipient | Setting | Mode of delivery in implementation | Dose: intensity and duration | Modification and fidelity | Aims/targets | Development | Materials | |
| Not applicable, n (%) | 17 (8) | 21 (9) | 32 (15) | 42 (19) | 29 (13) | 16 (7) | – | 18 (8) | 85 (39) |
| Not reported, n (%) | 99 (45) | 19 (9) | 27 (12) | 49 (22) | 130 (59) | 173 (78) | 46 (21) | 138 (63) | 84 (38) |
| Reported (including partial reporting), n (%) | 105 (47) | 181 (82) | 162 (73) | 130 (59) | 62 (28) | 32 (15) | 175 (79) | 65 (29) | 52 (23) |
Intervention setting
Clinical setting
Sixty-seven interventions (45%) did not provide any detail about the clinical setting other than it being adult inpatient (see Appendix 9). A further 27 interventions (18%) did not report clinical setting as they were not reporting implementation, for example training links. The intervention that has been applied in the widest clinical settings is Six Core Strategies. Six standalone interventions127–132 had been implemented in multiple settings within the same intervention/study, as had four intervention families (i.e. interventions with multiple records): Six Core Strategies (in acute and secure wards); Brøset Violence Checklist [in acute wards and psychiatric intensive care units (PICUs)]; Tower Hamlets Violence Reduction Collaborative (in multiple acute settings); and Initiatives to Reduce Seclusion and Restraint (in multiple, unreported settings). A further five interventions had been applied across various clinical settings: the Scottish Patient Safety Programme for Mental Health had been implemented in acute, PICU and forensic settings, the Dynamic Appraisal of Situation Aggression – Inpatient Version (DASA-IV) had been implemented in acute and high-dependency wards, the Novel Seclusion Reduction Program in acute and forensic wards, and Sensory Modulation and Sensory Rooms had both been implemented in acute wards and PICUs.
The most common setting for implementing interventions to reduce restraint and seclusion was acute wards (n = 40/150; 27%). Nevertheless, interventions had also been implemented on PICUs (n = 11), and on forensic (n = 10), secure (n = 8) and specialist geriatric (n = 6) wards. The least common settings were admission wards (n = 1) and high-dependency units (HDUs) (n = 1).
Geographical setting
Just five interventions (3%) had been implemented in different countries, with Six Core Strategies23,75,133 having the widest geographical spread covering six countries (i.e. Canada, England, Finland, New Zealand, Spain and the USA). No Force First24,134 had been applied in three countries (i.e. Australia, England and the USA), as had Sensory Modulation135–137 (Australia, Denmark and New Zealand) and Sensory Rooms138 (Australia, England and the USA). The Brøset Violence Checklist114 (Canada and Switzerland) and Patient Focused Nursing104,139 (Australia and the USA) had each been applied in two countries. Safewards16 was applied in three countries (Australia, Denmark and England). Overall, the countries applying the widest range of interventions were the USA (n = 60) and the UK (n = 59). The origins of two interventions were not reported (see Appendix 10).
Assumed change process and design principles
Intervention aims and targets
Three intervention aims were identified to (1) reduce, eliminate or prevent, (2) improve and (3) manage or monitor.
One hundred and five of the 150 interventions (60%) had a single aim, 35 (23%) had two aims and five (3%) had three aims88,131,133,140–142 (Table 4). The remaining 14% did not report an aim or target. 77
| Target | Standalone intervention | Intervention family | Total, n (%) |
|---|---|---|---|
| Multiple restrictive practices | |||
| Seclusion and restraint | 31 | 22 | 53 (24) |
| PRN and security involved in restraint | 1 | – | 1 (0.25) |
| PRN and restraint | – | 1 | 1 (0.25) |
| PRN, seclusion and restraint | – | 3 | 3 (1) |
| Single restrictive practices | |||
| Restraint only | 15 | 10 | 25 (11) |
| Seclusion/long-term segregation only | 7 | 14 | 21 (9.5) |
| Chemical only | 4 | 2 | 6 (2) |
| Generic | 8 | 21 | 29 (13) |
| Patient focused | |||
| Aggression/violence/assault | 14 | 12 | 26 (11) |
| Patient care/outcomes | 4 | 4 | 8 (3) |
| Early identification | 1 | 2 | 3 (1) |
| Patient experience | 3 | 3 | 6 (2) |
| Ward focused | |||
| Safety | 3 | 15 | 18 (8) |
| Quality | 6 | 5 | 11 (5) |
| Collaboration/communication | – | 4 | 4 (2) |
| Staff focused | |||
| Knowledge and skills | 12 | 2 | 14 (6) |
| Staff outcomes | 3 | – | 3 (1) |
As seen in Table 4, 81 interventions reported a single target, 29 had multiple targets and the remainder did not report a target. The most common target was seclusion and restraint (n = 53 interventions), followed by restraint only (mechanical, physical or prone restraint) (n = 25 interventions), seclusion [including long-term segregation (n = 21 interventions)] and generic terms [e.g. ‘restrictive practice’, ‘conflict and containment’, ‘coercive measure’ (n = 29 interventions)]. Another common target was service user behaviour [e.g. aggression, violence, ‘problem behaviour’ (n = 26)]. Just 11 interventions included pro re nata (PRN) medication or chemical restraint as a target: in six it was the sole target. One of these interventions specified eliminating unsupervised PRN medication (and reducing PRN medication overall),143 another aimed to replace PRN medication with ‘other clinical strategies’ (no further explanation provided),131 and another to reduce restraint associated with PRN medication and security involvement. 69 None of the interventions explicitly reported targeting the use of rapid tranquillisation, although Beckett et al. 130 referred to reviewing its use (in their procedures) and Sarkar78 examined the impact of their intervention on their use of rapid tranquillisation (reported in their outcome measures). Some interventions specified the type of restrictive practice they wanted to address, whereas others specified frequency115,131,144 or duration. 115,145,146
The most common aim for improvement was quality (e.g. environment, ward functioning, staff presence, service user to staff ratios, quality of care, ‘communication’) (n = 11). Other common targets for improvement included safety (n = 18), service user behaviour (‘dangerous’, ‘disruptive’, ‘risk’, ‘challenging’, ‘problem’, ‘aggression’) (n = 26),20,78,112–114,118,129,136,137,141,147–156 and staff skills and attitudes (n = 14). Three interventions targeted staff injury,129,157 anxiety141 and burnout,70 whereas 14 targeted service user outcomes and experiences, including service user harm,114 the service user experience (e.g. feeling of safety158), experience of care79,159 and service user outcomes. 160 Others targeting harm or safety did not specify service user or staff (e.g. Bell and Gallagher161) or included both (e.g. Lo74). In addition to those targeting quality of care (and implicitly targeting staff behaviour), five specifically targeted staff behaviour in terms of staff attitudes and perceptions,162 knowledge and efficacy,21,141,163 and culture. 132
Reference to theory
Mention of theory was absent from many interventions. Three interventions referred to having a ‘theory of change’85,153 but provided no further detail about what this was, how it had been developed and how it was tested and refined. Many of the ‘quality improvement’ interventions used a plan, do, study, act (PDSA) cycle: a mechanism to repeat and adjust interventions until they achieve the desired effect. 12,16,17
Some interventions130,137 made explicit cited reference to programme-level theories that had informed their intervention procedures, such as Sensory Modulation or Trauma-Informed Care. Other programme-level theories cited sought to explain staff behaviour, service user behaviour, therapeutic relationships and organisational change. These studies often sought to test or modify not the actual theory but rather the impact of using interventions based on them in relation to the reduction of restrictive practices.
The most frequently cited theory related to staff behaviour was social learning theory,71–73,152,164 which was used to support training interventions that sought to improve the self-efficacy of individual staff and staff teams.
Bonner’s theoretical model for debriefing and post-incident review165 informed one intervention166 and the general aggression model167 informed another that sought to reduce aggression via Sensory Modulation. 152 Kernberg’s theory of personality organisations and transference-focused psychotherapy168,169 informed clinical guidelines that aimed to reduce restraint. 170 Other theories mentioned included those seeking to explain care giving processes: Peplau’s interpersonal relations171 and Watson’s caring theory. 172 Both Safewards173 and City Nurse102 were based on the theoretical work of Bowers et al. 101 regarding conflict and containment, and the interaction between service users and staff.
Five interventions were informed by broad organisational change theories. Kanter’s structural empowerment theory sees organisational empowerment and potential for change as being influenced by the individuals within the organisation having access to information, resources and opportunities to learn. 174 The transtheoretical model of change175 is generally applied to individuals, explaining how people prepare for and enact change, although Colton176 applies it to organisations to structure a tool kit to prepare to reduce restrictive practices. Schein’s model of organisational culture177 informed the development of the Six Core Strategies. 178 This focuses on publicly espoused values and assumptions. Senge179 focuses on the capacity of organisations and, by extension, the individuals within them to learn and focuses on a common goal. 133 The Iowa Model of Evidence Based Practice was used to guide the implementation of a rapid response team. 74 The full analysis of behaviour change techniques used in the interventions can be found in Chapter 5.
Mode of delivery: intervention procedures
The extraction process highlighted the procedures used by each intervention to address restrictive practices. A total of 15 unique procedures were identified from the analyses and these were organised into six themes (Figure 4).
FIGURE 4.
Intervention procedures by theme. PPI, patient and public involvement.
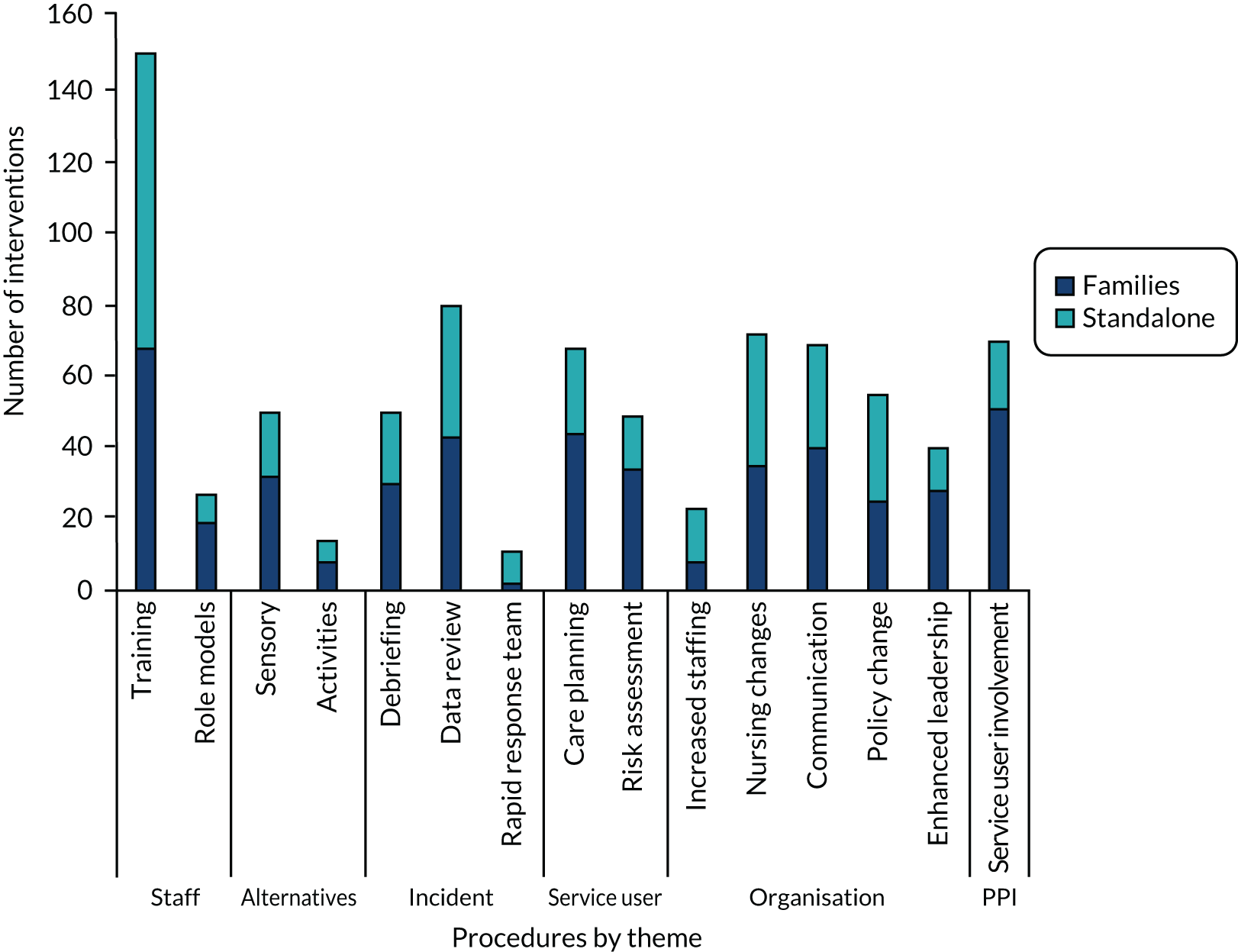
Staff-focused procedures
Staff-focused procedures were those that were aimed at and undertaken solely by staff with a view to influencing staff use of restrictive practices. One procedure was training, which could cover, among other topics, de-escalation (e.g. Laker et al.,21 Sullivan et al. ,104 Lee et al. 127 and Jonikas et al. 180) or crisis management (e.g. Steinert et al. 20 and Melin69). Another staff-focused procedure was role modelling, which could involve supervision or mentoring (e.g. Fletcher et al. 181 and Noorthoorn et al. 182) and identifying champions, experts or specialists (e.g. Bowers et al. ,102 Tully et al. 90 and Lombardo et al. 159) to set an example to ward staff.
Service user-focused procedures
Service user-focused procedures were those that focused on and sometimes involved service users but always involved staff. One of these procedures was risk assessment – whereby service users’ triggers would be recorded – which was often undertaken using a tool designed for this purpose (e.g. Brøset Violence Checklist114 or the Early Detection Plan118). Another related procedure was care planning, in which service users and/or staff planned appropriate and preferred strategies to prevent or respond to distress and/or incidents. These sometimes involved service users in identifying their own triggers and forming their own plans, for example a ‘personal safety plan’132 and also included PDSA. 161
Alternative approaches
Two further procedures were classified as alternative approaches because they proposed alternative ways of either preventing or responding to service users’ distress. Sensory approaches included Sensory Modulation via the installation of sensory or Comfort Rooms (e.g. Novak et al. ,183 Barton et al. 184) and/or the availability of sensory equipment (e.g. Lee et al. 127) and/or use of Sensory Modulation techniques (e.g. Yakov et al. 185).
Incident-focused procedures
Other procedures were incident focused, that is, they were responses to incidents of restrictive practices. These included incident review procedures, in which organisations (staff and managers) conducted retrospective chart audits (e.g. Qurashi et al. 186) or collected and monitored their incident data (e.g. Donat106 and Friedman et al. 131) to establish baseline and progress rates, or to identify patterns for targeted intervention. In contrast to this whole-system review, debriefing was conducted immediately or soon after an incident, and included the staff and service users involved and possibly others who witnessed the incident (e.g. Duxbury et al. 120). The final procedure was rapid response, where specially trained rapid response teams were formed to respond to and provide support to incidents when they happened [e.g. psychiatric emergency response teams (PERTs); see Smith et al. 142 and Prescott et al. 128].
Organisation-focused procedures
We also identified several organisation-focused procedures. These were system-wide structural and cultural changes including making changes to staffing levels (e.g. Parasurum et al. 77), increased one-to-one nursing (e.g. Jungfer et al. 109) and/or staff availability to/contact with service users (e.g. Beezhold et al. 79 and Lewis et al. 132). Another procedure involved changing nursing approaches [e.g. such as implementing the City Nurse model,101 the Bergen model,129 a recovery approach (e.g. Repique et al. 187) or a trauma-informed approach (e.g. Madan et al. 108)]. This theme also included improvements to communication (e.g. Stead et al. 188), community meetings (e.g. Mistral et al. 189), de-escalation (e.g. Cowin et al. 163) and safety huddles (e.g. Taylor-Watt et al. 153 and Stead et al. 188). Another procedure involved policy change (e.g. Short et al. 157 and Sullivan et al. 190). Finally, leadership-related procedures involved senior management being involved in meetings, making statements of commitment.
Service user involvement in interventions
Forty-eight interventions involved service users in some way, but the type and extent of involvement varied greatly. In some cases, service users were involved in multiple ways, whereas in others they had limited roles. A number of interventions involved service users in a consultation or advisory role, for example as committee representatives,133 participants of project teams158 (e.g. working group on medicines and rapid tranquilisation130), service user panels,160 or advisory committees. 88,115,140,163 Service users were consulted for their views16 and feedback on rules,116 sensory rooms116,140 and research. 17,140 Others described involving service users in the design or co-production of parts of the intervention, such as safety plans,116 information leaflets,130 comfort rooms,23,191 training16,115,163 and the selection of intervention components. 16,116 Service users were involved in intervention delivery, for example in ward/community meetings,17,23,186,191 delivering activities,116 and training,88,116,137,163,182,192,193 displaying their positive messages for current service users,181,192,194,195 and as peer advocates,142 counsellors196 and support workers. 99,193 Only two interventions specified that service users were paid for their involvement. 24,197 The remainder that reported service user involvement provided no further detail.
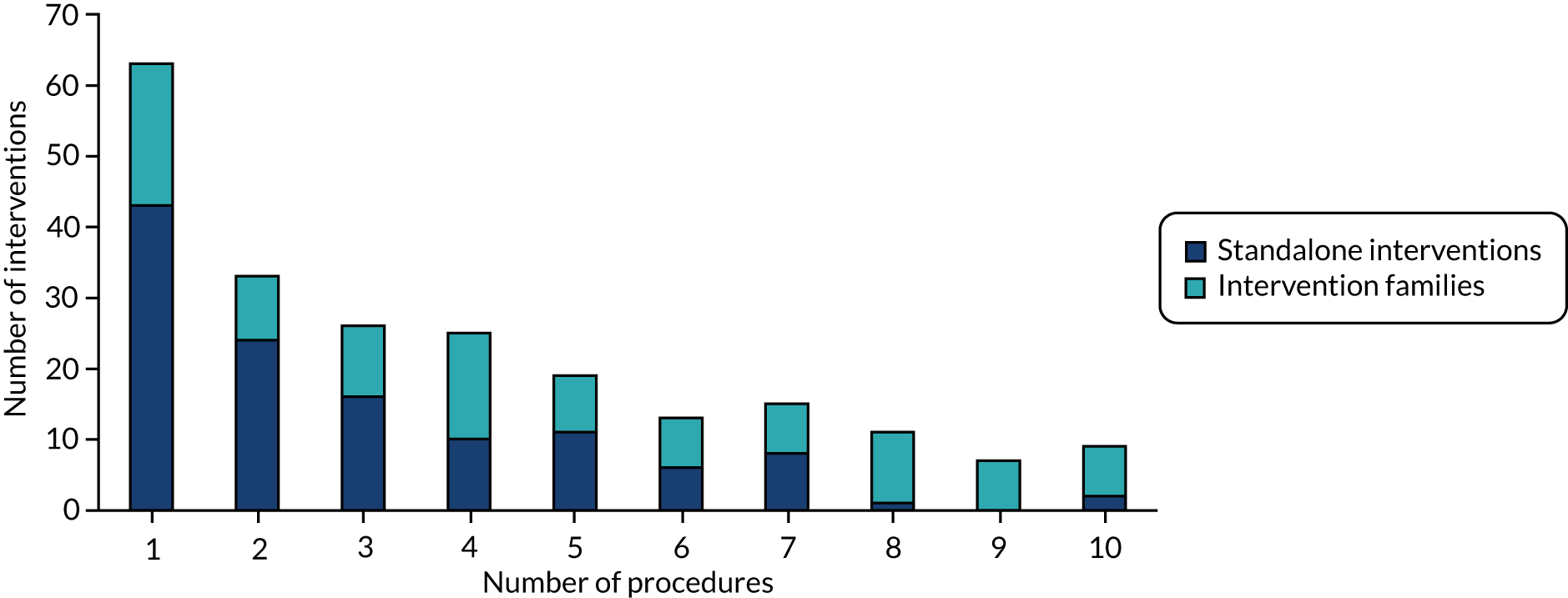
Seventy-one per cent (n = 158) of interventions involved multiple procedures, which ranged from 2 to 10 procedures (Figure 5).
FIGURE 5.
Number of procedures per intervention.
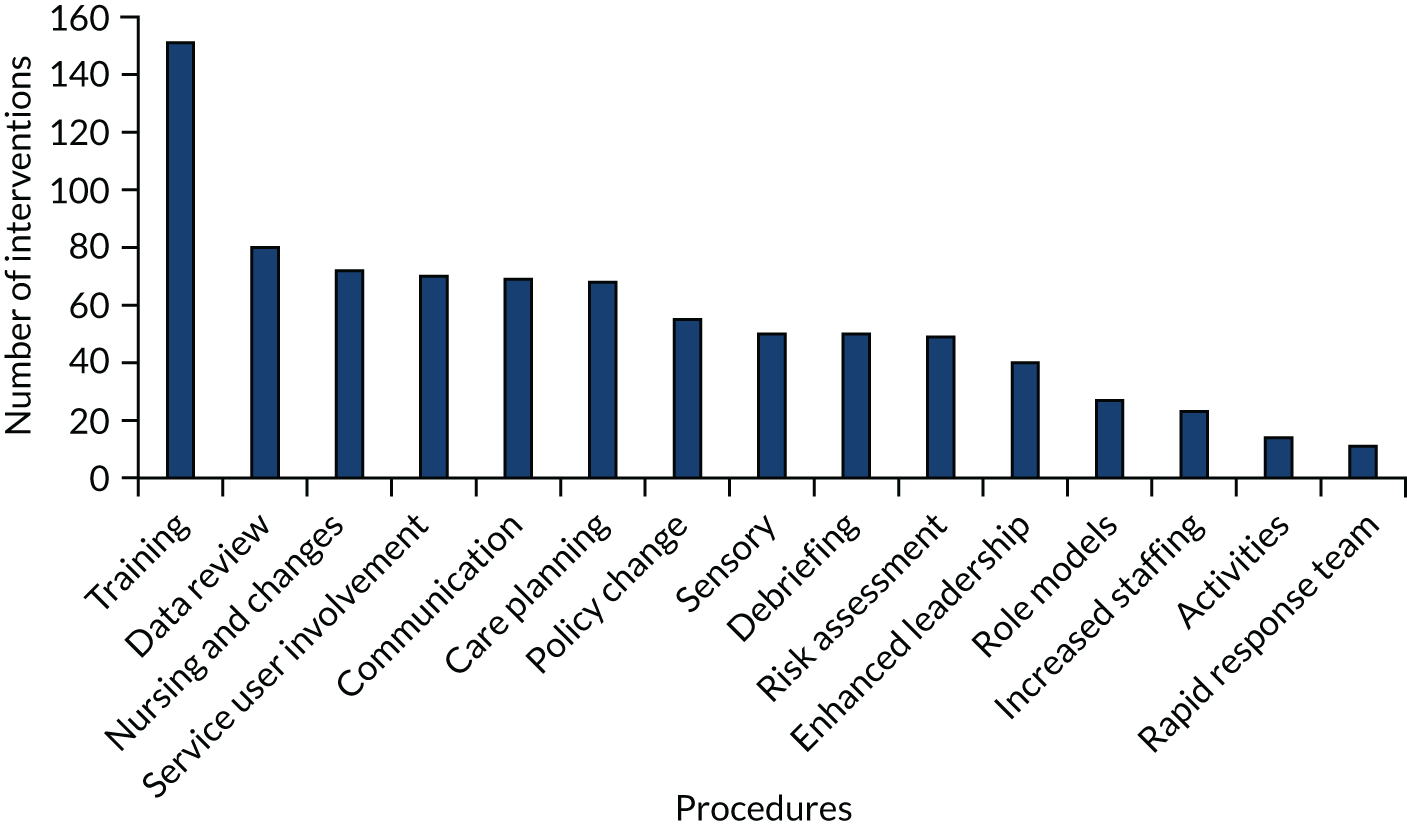
The most common procedures were training/education (n = 151), changes to nursing approaches (n = 72) (e.g. implementing Trauma-Informed Care or the Recovery Approach) and reviewing incident data (n = 80). Least mentioned were rapid response teams (n = 11) and activities (n = 14) (see Appendix 11).
As illustrated in Figure 6, although most interventions involved staff training, few reported the content, mode of delivery or training provider in any detail. The documentation reporting 89 interventions did not report any detail at all. The most common mode of delivery was group training or workshops (n = 37). Six reported using e-learning or online training and a further five reported multimedia components (e.g. video, PowerPoint) to their training. Four interventions reported using a train-the-trainer model. Others described training as one to one (n = 2), face to face (n = 3) or on the job (n = 1). Two interventions mentioned using champions and exchange visits respectively. Training was specified as provided in-house in 64 interventions and, of these, only seven specified the provider (these included quality improvement team, occupational therapists, unit manager or researcher). Training was delivered by external providers in 24 interventions, and 20 of these specified the provider. Providers mentioned included Bergen Model Representatives, Centre for Creative Leadership, City Nurse, Crisis Prevention Institute (CPI), ePsychNurse, Omega, Safewards, Substance Abuse and Mental Health Services Administration (SAMSHA), National Enforcement Training Institute, JKM Training, AQUA and Recovery Innovations. The remaining interventions did not report any information about the training provider.
FIGURE 6.
Distribution of procedures.
Intervention dose: duration and intensity
Many evaluations did not report details about the duration and intensity of the intervention. Partial details, such as overall duration of the intervention or of an individual component (usually training), were sometimes, but not always, provided. Often, the evaluation period and the duration of intervention implementation were not distinguishable. Similarly, the duration of individual intervention components was often not reported. With this proviso, interventions ranged in length from 10 months to 5 years. Some interventions described providing standalone training sessions, whereas others were conducted over a short period of time (e.g. 1 week) or longer (e.g. several months). One evaluation described offering refresher sessions. 152
Intervention materials
Interventions reported using various materials in the implementation of the intervention, including training materials, guidelines, multimedia resources, tools, posters, slides and policies. Some referred to materials that are publicly available on the internet (i.e. the Six Core Strategies, Safewards, Brøset Violence Checklist).
Costs and funding
Eighteen interventions referred to the cost of implementing the intervention or its financial impact. Costs were reported in the currency relevant to the study setting. Several studies provided details of the costs of one or more elements of the intervention, for example: US$10,000 for a Snoezelen room,198 US$11,456.98 for two Sensory Rooms,191 US$4000–5000 for sensory equipment,136,198 £70,000189 and £2000154 for environmental improvements, US$600 for PERT including office supplies and digital pagers,74 £69,285.25 for staff de-escalation and restraint training including replacement costs and overheads21 and US$20,000 for consulting fees. 198 Others referred to costs incurred but did not specify the amount, for example sensory equipment;127,196 camera, television monitor, three two-way radios;149 or staff training. 23,196 Putkonen et al. 17 reported the costs of their intervention as the equivalent to two person-years per year. Bell and Gallacher161 stated that their interventions incurred no costs.
Seven interventions reported who funded the intervention. Three reported receiving funding from the hospital where the intervention was implemented,23,74,127 whereas Mistral et al. 189 received funding from the mental health care trust. Putkonen et al. 17 specified that funding came via the hospital performance improvement project from research funding from the National Institutes of Health and Welfare. McEvedy et al. 137 reported receiving funding from the Victorian state government-funded programme. Lloyd et al. 136 reported that they received funding but did not specify the funder.
Nine interventions reported some cost–benefit analysis. Mistral et al. 189 reported a 62% reduction in time lost to staff short-term illness. Laker et al. 21 recommended further analysis, having been unable to draw conclusions from insufficient data regarding the costs of incidents, specifically damage to property, staff or service users and injury-related absence. Brown et al. 154 reported savings of 49% associated with reduced staff absence and injury (from £119,988 prior to implementation to £61,376 post implementation). Short et al. 157 reported a decrease of 77% in lost work days due to staff injury (90% of which were attributable to physical interventions). Lo74 argued that because the PERT intervention did not require any additional staffing resources it was likely to bring economic benefits. Finally, Putkonen et al. 17 reported 75% reduction in the number of sick days in the information period and 65% reduction in the intervention period, compared with the previous year; and in addition, reported 80–82% shorter duration of sick days.
Evaluations of interventions
Evaluations were identified using the screening questions of the MMAT: the presence of a research question and the collection of data required to answer that question. Those reports that passed the screening were then appraised using the MMAT to be given a score in the form of a percentage.
Of the 109 evaluations that we identified, 106 were research reports and there was one intervention report,92 one service report156 and one practice example. 159 Six theses and five abstracts were included. Most evaluations (n = 95) were published in 42 peer-reviewed journals spanning mental health, nursing, psychiatry and quality. The most common publication titles were Psychiatric Services (n = 12), Journal of Psychiatric and Mental Health Nursing (n = 7), Journal of Psychosocial Nursing and Mental Health Services (n = 5), International Journal of Mental Health Nursing (n = 6) and Psychiatric Quarterly (n = 7). The remaining journals featured between one and four records.
Evaluation design
Evaluation design was often not described and, when it was reported, a variety of terms were used. Accordingly, design had to be inferred from other study details in some cases. Most evaluations were non-randomised studies (n = 103) (see Appendix 12). Based on the MMAT screening questions, all of these evaluations were considered to have recruited participants who were representative of the target population and used suitable outcome measures. Several were not considered to have reported complete outcome data and only two-thirds adequately accounted for confounders. There was very little reporting of modifications and fidelity to the intervention protocol, with only 11% of evaluations reporting this. There were six RCTs, four of which were cluster RCTs (Table 5). The MMAT scores of these six RCTs varied from 0% to 80%. Five out of the six RCTs reported complete outcome data and four did not describe any deviation from the protocol. Only three had comparable groups at baseline and described rigorous randomisation processes. Two reported that outcome assessors were blinded.
| Study authors and year of publication | Design | Sample | Intervention | Control | Outcome measuresa | Findingsa |
|---|---|---|---|---|---|---|
| Bowers et al. 201516 | Cluster RCT | 16 intervention wards, 15 control (mean number of beds per ward was 19) | Safewards | Physical health intervention | Rates of (1) total conflict and (2) total containment (Patient–staff Conflict Checklist) | Rate of conflict reduced by 15% (95% CI 5.7% to 23.7%); rate of containment reduced by 23.2% (95% CI 9.9% to 35.5%; not significant) |
| Kontio et al. 2014199 | Cluster randomised trial | 5 intervention wards, 5 control wards | E-learning course | Treatment as usual | Rates and duration of seclusion and restraint | Duration of mechanical restraint decreased (p < 0.001) |
| Putkonen et al. 201317 | RCT | 2 intervention wards, 2 control wards | Six Core Strategies | Treatment as usual | Rates of seclusion, restraints, or room observation, duration of seclusion or restraint | Rates of seclusion, restraints and room observation decreased from 30% to 15% (IRR 0.88, 95% CI 0.86 to 0.90; p < 0.001). Duration of seclusion/restraint decreased from 110 to 56 hours per 100 patient-days (IRR 0.85, 95% CI 0.78 to 0.92; p < 0.001) |
| van de Sande et al. 2011200 | Cluster RCT | Two intervention wards, two control wards | Structured short-term risk assessment (Brøset Violence Checklist, Crisis Monitor, Kennedy–Axis V scale, Brief Psychiatric Rating Scale, Dangerousness Scale, Social Dysfunction and Aggression Scale) | Treatment as usual | Rates and duration of seclusion, number of secluded patients | Duration of seclusion decreased (p < 0.05) |
| Parasurum et al. 201177 (abstract) | RCT | Four intervention wards, four control wards | Nursing staffing level and care | Not reported | Physical restraints | No restrictive practice outcomes reported |
| Abderhalden et al. 2008113 | Cluster RCT | Four wards randomised to intervention, five wards randomised to control, five wards introduced intervention without randomisation | Structured short-term risk assessment (Brøset Violence Checklist) for every patient admission | Treatment as usual | Incidence rates of (1) severe aggressive events (SOAS–R) and (2) coercive measures (yes/no) | Coercive measures decreased by 27% (p < 0.001) |
Four qualitative studies were identified72,137,152,201 (Table 6), as were a further six that used mixed methods15,140,166,187,189,203 (Table 7). Goulet et al. 166 and Chandler201 reported using case study methodology. These evaluations used the following data collection and analytical methods: interviews,72,137,140,152,201 focus groups,15,152,166,187 document (policy) review,201 observation,201 thematic analysis15,72,140,152,187 and qualitative content analysis. 137,166,201 All of these studies evaluated different types of interventions, except McEvedy et al. 137 and Sutton et al. ,152 which both evaluated Sensory Modulation.
| Study authors and year of publication | Design and methods | Research question(s) | Setting and sample | Intervention | Findings |
|---|---|---|---|---|---|
| Sutton et al. 2013152 | Qualitative: narrative analysis | To examine the potential of using sensory-based approaches to develop the theory and practice of preventing, minimizing, and managing aggression in mental health settings | 4 units: 40 staff, 20 patients | Sensory Modulation (Six Core Strategies) | Identified three factors that contributed to the management of distress and agitation:
|
| Chandler 2012201 | Qualitative: case study appreciative inquiry approach,202 inductive content analysis | How has the unit decreased use of restraints and seclusion? | 20-bed unit: 11 staff | Six Core Strategies; TIC | Rates of seclusion and restraint decreased from 27 to 6; identified three factors that played a key role:
|
| Huckshorn 201272 | Qualitative: phenomenology | To explore and describe the experiences of leaders and staff who directed or participated in successfully reducing the use of seclusion and restraint | 2 units: 21 staff | Six Core Strategies | Identified key factors for change:
|
| McEvedy et al. 2012137 | Qualitative: descriptive | To report descriptions of the effectiveness of the train-the-trainer intervention | 19 mental health services: 22 staff interviews; 10 focus group participants | Sensory Modulation; TIC | Knowledge of Sensory Modulation and TIC was transferred to ‘a substantial number’ of mental health service staff – but the impact on practice is not evidenced |
| Study authors and year of publication | Design and methods | Research question(s) | Setting and sample | Intervention | Findings |
|---|---|---|---|---|---|
| Mistral et al. 2002189 | Mixed methods | To evaluate the effectiveness of the Interventions | One unit: 36 staff | Therapeutic community | Use of seclusion decreased; identified improvement in staff attitudes and ward atmosphere |
| Newman et al. 2018203 | Mixed methods | To evaluate the effects of a 90-minute TIC-based staff training | 18-bed unit: 88 staff | Staff training: TIC | Rates of seclusion decreased; identified four types of facilitators/barriers:
|
| Cabral and Carthy 201715 | Mixed methods | To provide a service evaluation of the Safewards implementation | Six wards: 102 staff; 89 patients | Safewards | Increase in EssenCES score; identified three main themes:
|
| Goulet et al. 2017166 | Mixed methods | To develop and evaluate a ‘post-seclusion and/or restraint review (PSRR) intervention | One unit: 12 staff, three patients | Post-incident review | Statistically significant reduction in rate (χ2 = 4.473; p = 0.046) and duration (U = 4.181, z = –2.175; p = 0.030) of seclusion but not restraint |
| Repique et al. 2016187 | Mixed methods | To reduce the use of restraints; assess staff knowledge, beliefs, perceptions and values; and evaluate the implementation process | One hospital: 42 pre intervention, 32 post intervention, two focus groups of four staff | Recovery-oriented nursing practice | Slight reduction in restraint rates; identified that staff thought training could be improved; would like feedback from patients and leadership involvement |
| Smith and Jones 2014140 | Mixed methods | To explore the impact of the introduction of a sensory room | 15-bed unit: 10 staff, seven patients | Sensory Rooms | No significant reduction in seclusion rates, despite staff perception of reduction |
The MMAT prompts an appraisal of whether or not qualitative methods are appropriate, whether or not the data collection methods are adequate and the findings and their subsequent interpretation are sufficiently reported, and whether or not the study has overall coherence. The qualitative studies all scored the highest score of 100% when appraised using the MMAT.
The six mixed-method studies all used the same combination of qualitative data and non-randomised quantitative data (see Table 7). The qualitative arms of these mixed-method studies scored better than the quantitative arms, but they generally scored lower than the qualitative-only studies. All were considered appropriate subjects for qualitative inquiry with adequate data collection methods to address the research question. Four of the studies appeared to report findings and interpretations both derived from and supported by the data, as well as having a coherence across the study. Two were unclear on this aspect. The quantitative data collection in each was considered representative of the target population and to be using an appropriate outcome measurement. It was unclear whether or not two of the six studies reported all outcomes, and three did not account for confounding variables in the analysis. Only one study reported fidelity in terms of intervention delivery. The integration of the mixed methods was generally weak. Although there was adequate rationale for using the approach in all but one study, only one study integrated outputs and only one (other) study addressed divergences between the qualitative and quantitative findings. The different arms were considered to adhere to quality criteria in only half of the six studies.
Just two evaluations had a participatory element (c.f. involvement in the intervention); Goulet et al. 166 involved a service user/partner researcher and Bowers et al. 102 described their study as incorporating elements of action research.
Outcome measures in evaluations
Seventy evaluations reported multiple outcome measures (range 2–7 outcome measures) and 37 reported a single measure (Figure 7 and see Appendix 13). The most common measures were the incidence of seclusion (n = 56) and restraint (n = 48), followed by, less often, the use of PRN medication and forced medication (n = 16). Others included the incidence of violence or other ‘challenging’ behaviour (n = 20), self-harm and suicidal gestures (n = 4), staff or service user injury (n = 6) and staff sickness or absence (n = 4). Twenty-three reported measuring the incidence of a generic term for restrictive practices. In 11 cases, they reported the number or percentage of service users. Evaluations also reported measuring the duration of seclusion (n = 22) and restraint (n = 16), with one reporting duration per service user. Thirty-three evaluations reported the time elapsed between incidents, number of incidents averted, staff and service user experiences, and staff knowledge.
FIGURE 7.
Number of outcome measures.
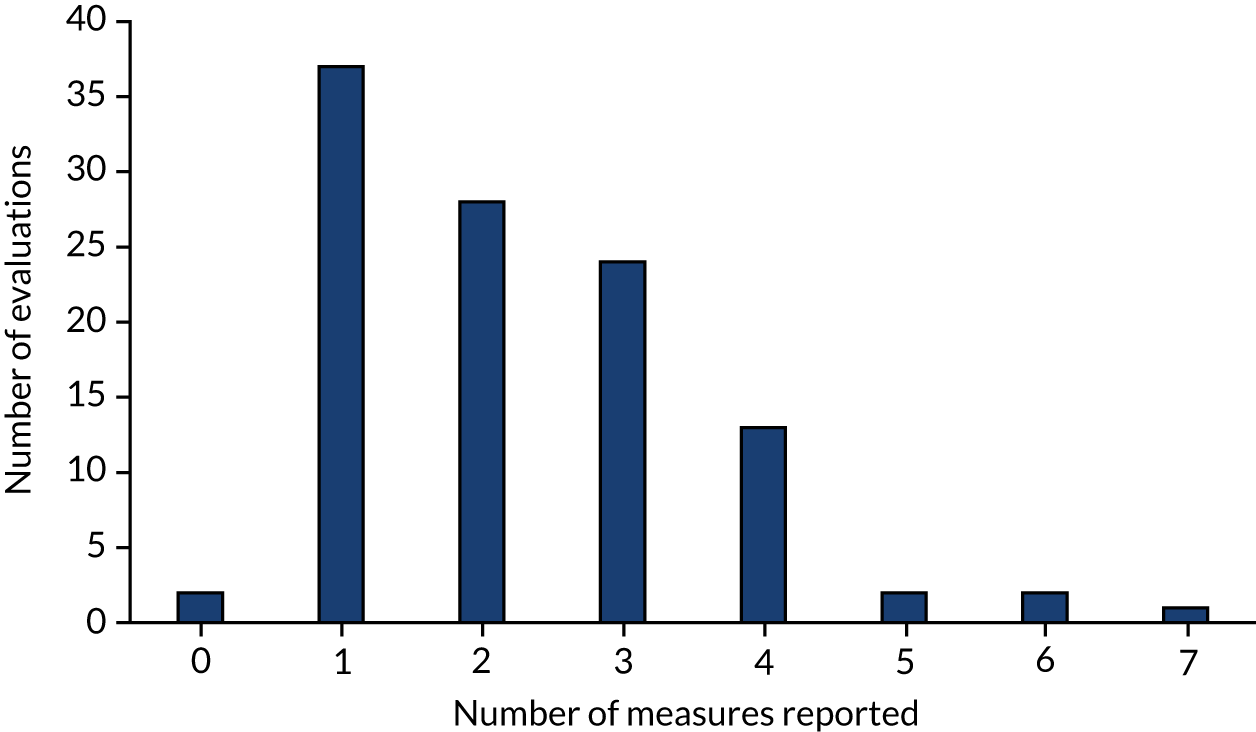
Several interventions used existing, routinely collected data for their evaluations, such as archived data, incident reports, nursing log-books, charts, institutional databases and electronic records. Five evaluations developed measures for the purposes of their evaluation: Alfred Psychiatry Safety Tool;127 Crisis Monitor;200 Patient Safety Climate Tool;161 Staff Observation Aggression Scale (SOAS);112 and Staff Observation Aggression Scale – Revised (SOAS-R). 118 Others developed or adapted surveys, created log-books or databases, or designed qualitative tools or visual analogue scales to collect data. We identified 40 standardised measures used 54 times in total. Thirty of these had been used just once and five had been used twice. The Heyman Staff Attitudes towards Seclusion Survey204 and the Patient–Staff Conflict Checklist Shift Report (PCC-SR)205 had both been used three times each, and the Brøset Violence Checklist206 and the Essen Climate Evaluation Schema (EssenCES)207 had both been used four times each.
Evaluation findings
The very wide variation in the 109 interventions described above presented considerable challenges for assessment of intervention effectiveness. The finding that most of the studies reported some positive outcomes in relation to reducing restrictive practices may be related to publication bias, especially in the grey literature. Many of the studies that reported evaluations contained anecdotal findings (i.e. did not present full figures), and these were excluded from this assessment. One hundred and seven evaluations were published in journals or via academic conferences, and these were examined in more detail. Twenty-six reported no positive findings related to the reduction of restrictive practices, and the majority of these evaluations used more than one procedure (e.g. training, audit, policy changes). As these procedure categories are broad, there is little to be learned from relating positive or negative outcomes back to their use. Interventions using a single procedure may be more useful in determining what type of procedures might reduce the use of restrictive practices. There were 13 of these: five used staff training (four reporting positive findings and one negative) and two used sensory methods (one positive finding and the other negative), but the remainder used a variety of strategies and all reported positive findings.
At least one positive finding in relation to reducing restrictive practices was reported in 51 of the evaluations; however, 32 did not report statistical significance. One evaluation77 (reported in a conference abstract) did not report findings.
Controlled trials
There were 18 evaluation studies that used a control for comparison purposes (see Appendix 12) and six RCTs (see Table 5). Fifteen reported significant findings in relation to the decrease in use of a restrictive practice. However, they did not all use the same definition for the restrictive practices, with two studies combining all restrictive practices. 16,113 Only one study reported an increase in restrictive practices but this was confounded by major service changes during the intervention. Of those studies that reported decreased use of restrictive practices, eight reported restraint, eight measured seclusion, two measured PRN medication and two measured observation.
Qualitative studies
Cabral and Carthy15 examined the staff experience of implementation of Safewards, including its perceived benefits and challenges. They reported that staff perceived benefits, but there was some resistance, and they also identified a knowledge and skills deficit of the model. McEvedy et al. 137 explored services’ feedback on the effectiveness of a train-the-trainer intervention on knowledge transfer and translation of this knowledge into practice. They reported that knowledge transfer to staff was achieved, with most services subsequently training further staff (in some cases adapting the train-the-trainer materials). However, they found little evidence of translation of Sensory Modulation or Trauma-Informed Care into practice. Goulet et al. 166 examined the staff and service users’ perspectives of the impact of the intervention, including barriers to and facilitators of its implementation. Staff reported that the post-incident review gave them the opportunity to discuss the service users’ feelings and restore the therapeutic relationship, while staff were able to learn from the experience. Smith and Jones140 explored staff and service users’ experiences of using the sensory room, reporting that they considered it to be a positive contribution to the unit, that it had been incorporated into care plans and improved communication. Staff perceived that there had been a reduction in the use of seclusion but it is unclear whether or not service users were asked. Repique et al. 187 explored nurses’ views of Recovery-Based Principles training and reported that they perceived the training materials to be good but lacking specific detail and examples, and stated a preference for a live presenter with the opportunity to ask questions. Nurses also expressed a desire for more direction from leadership and service user feedback.
Chandler201 reported that seclusion and restraint were reduced ‘dramatically’ (although this is not quantified) and explored how the unit achieved this reduction and promoted safety. The author described how opportunities, information, support, resources and relationships were the factors that gave staff the leadership to feel empowered and, in turn, they empowered service users. These factors were key to reducing restrictive practices and promoting safety. For example, staff were able to learn about the impact of trauma, service users’ sensorimotor needs and stress responses, and the establishment of respectful and trusting relationships. Staff were also able to reflect on their responses to service user stress.
Interventions subject to multiple evaluations
Two follow-up studies (n = 2), one pilot plus main study (n = 1) and two replication studies (n = 2) were identified.
Modification of and fidelity to intervention protocols
Eleven evaluations (n = 11) reported whether they tailored or modified the intervention protocol. Two described using some but not all of the Six Core Strategies90,144 and three reported modifying a tool. 113,188,208 Others reported tailoring the intervention to meet service users’ needs,140 making modifications as the intervention proceeded106 and allowing wards to choose the intervention. 209 One evaluation reported that modification was not planned but may have occurred unintentionally. 102
Twelve evaluations reported fidelity. The earliest of these was published in 2010 and the subsequent period saw fidelity reported with an increasing degree of precision. Two publications from 2010 made brief reference to fidelity; Lee et al. 127 reported that their Alfred Psychiatry Safety Tool had been completed by 50% of staff and that 81% of staff had read a completed tool, and Fluttert et al. 118 reported that their protocol achieved ‘uniform application’ and attributed this to it being structured and implemented during existing weekly meetings. Godfrey et al. 210 reported consideration of how to maintain fidelity (they implemented a team with advanced training to respond to incidents) but did not report or estimate fidelity rates.
Two interventions were identified that included the development of a tool to record and measure fidelity: one developed in the USA to assess fidelity to the Six Core Strategies [the 38-item Inventory of Seclusion and Restraint Reduction Interventions (ISRRI)],211 and the other developed in the UK to assess fidelity to Safewards (Safewards Researcher Visit Fidelity Checklist). 16 Wieman et al. 211 reported that fidelity to the Six Core Strategies (measured using a prototype of the ISRRI) fluctuated over time and across 43 settings, and recommended further research to understand the relationship between setting characteristics, fidelity patterns and outcomes.
In addition to the original Safewards study,16 four further interventions reporting fidelity utilised the Safewards protocol and Researcher Visit Fidelity Checklist. 15,181,194 Using this checklist, Bowers et al. 16 reported a mean fidelity rate of 38% [standard deviation (SD) 8%, range 27–54%, n = 271] during the outcome period. Bowers et al. 16 also assessed fidelity using a questionnaire, which identified a mean fidelity rate of 89% (SD 11%, range 62–100%, n = 79). Price et al. 194 reported a mean fidelity rate of 27.28% across the six wards in which the intervention was implemented. Cabral and Carthy15 were less precise, stating simply that ‘most of the 10 interventions had either been implemented or initiated across all six participating wards’. Fletcher et al. 181 modified the Researcher Visit Fidelity Checklist and measured fidelity over a 12-month period to assess ‘dose effects’ and reported ‘consistent improvement’, with services delivering an average of four interventions at the first time point and nine by the last. Maguire et al. 197 used Fletcher et al. ’s181 adapted checklist and reported a mean fidelity rate of 94.75%.
Bell and Gallacher161 reported an increased use of debriefing from 22% in the 6 months prior to the intervention to 60% in the final 6 months. Mann-Poll et al. 209 attributed ‘high levels of engagement’ to giving wards choices about participation in their intervention, but conceded that ‘We cannot be certain if the individual respondents working on participating wards were also actively participating in the [Seclusion Reduction Program]’.
Chapter 5 Results of the behaviour change technique synthesis
This chapter addresses objective 2 in describing the presence and frequency of BCTs in interventions.
Individual behaviour change techniques identified in interventions
As discussed, and illustrated in Figures 1 and 2, the result of the search strategy was a data set of 175 records, which, on analysis, was found to report a total of 150 different interventions. The 150 interventions were coded for BCT content. Description of intervention content was frequently found in the methods sections of studies, but additional detail was occasionally provided in the results or discussion sections. The heterogeneity of documents meant that the studies identified in the grey literature often did not report the intervention in a structured way, meaning that full texts had to be searched for content related to BCTs.
When interventions were examined by target, type of study or reported findings, it was apparent that there was a small group of BCTs that were most frequently found across all the interventions, that is ‘instruction on how to perform the behaviour’, ‘restructuring social environment’, ‘problem-solving’ and ‘action-planning’. Overall, 43 of the possible 93 BCTs within the BCT taxonomy were identified in the interventions (46%). The range of BCTs identified per intervention was 1–33 (mean 8 BCTs). BCTs found at least once across the interventions are shown in Figure 8 in terms of the percentage of interventions in which they were identified. For example, BCT 4.1, ‘instruction on how to perform the behaviour’, was detected in 91% of interventions, whereas BCT 10.10, ‘reward (outcome) of the behaviour, was detected in only 1% of interventions.
FIGURE 8.
Behaviour change techniques identified across all interventions.
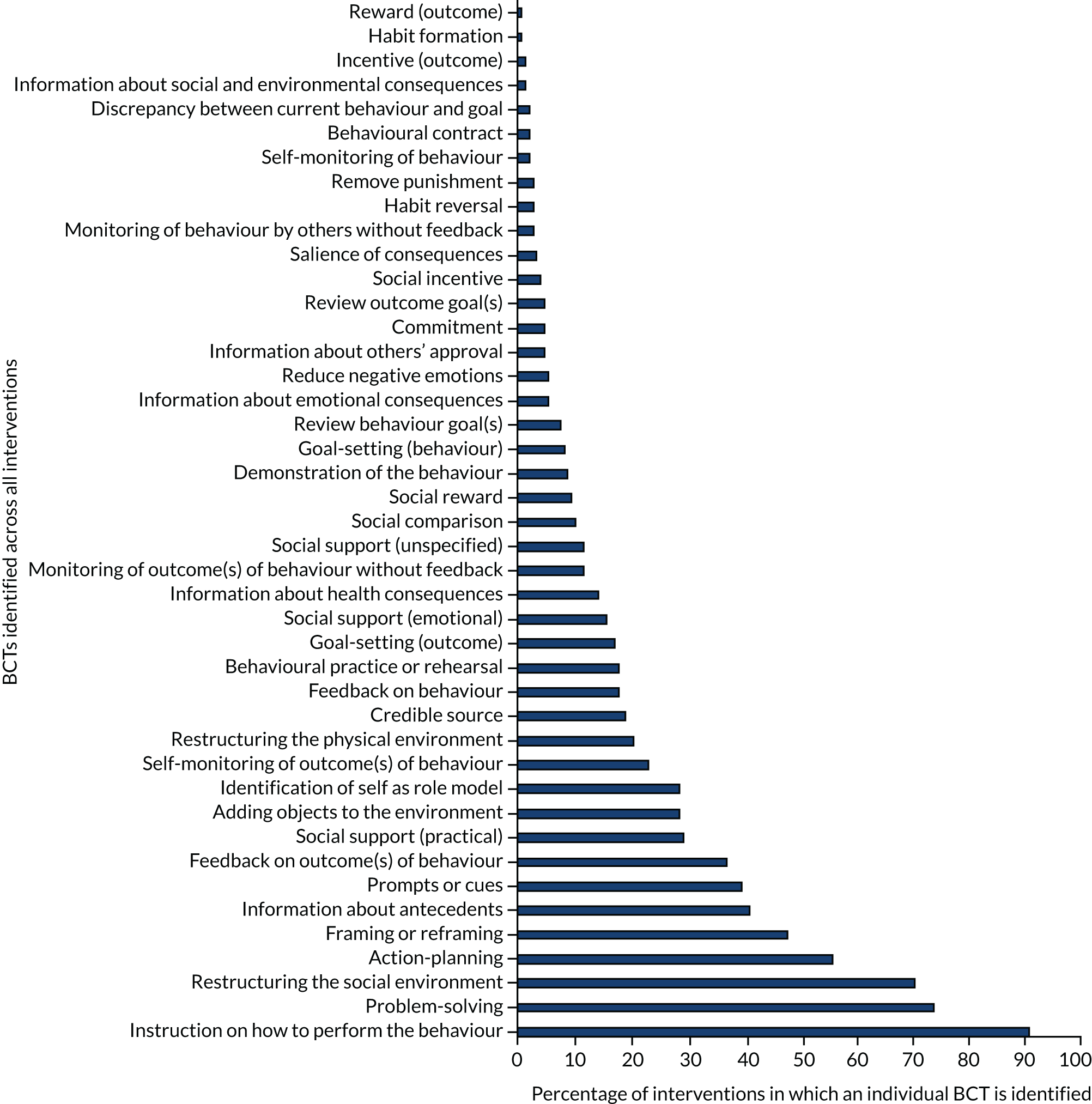
Further description of BCTs that featured in > 20% of interventions is provided in Table 8. This shows the most frequently identified BCTs, that is, those featuring in > 20% of interventions, together with an example of how the BCT was applied. For reference, the full BCT taxonomy as used in this study can be found in Appendix 6.
| BCT | Example | % | n |
|---|---|---|---|
| 4.1 Instruction on how to perform the behaviour | Receive tuition about how to perform effective de-escalation (e.g. as part of a staff training course) | 91 | 136 |
| 1.2 Problem-solving | Person/team is prompted to analyse factors influencing the behaviour (unsuccessful de-escalation resulting in increased restrictive practice) and find solutions or strategies to overcome the problems or increase facilitators (e.g. people become frustrated because of boredom, funding sought to provide ward activities) | 73 | 110 |
| 12.2 Restructuring the social environment | Making changes to the social environment that increase the potential for de-escalation (e.g. promote social contact between service users and staff by organising communal meals) | 70 | 105 |
| 1.4 Action-planning | Planning of how de-escalation will be carried out at either an individual level based on people’s preferences or on a more general level (e.g. when a service user is distressed, they inform staff in advance that they would prefer to be allowed time off the ward) | 55 | 82 |
| 13.2 Framing/reframing perspective on performing the behaviour | Suggesting the deliberate adoption of a (new) perspective on behaviour in order to change cognitions or emotions about performing the behaviour (e.g. seeing aggression as a manifestation of trauma and distress) | 47 | 70 |
| 4.2 Information about antecedents | Provide information about antecedents that reliably predict requirement of the behaviour (e.g. discussions about what often happens prior to an incident where restrictive practices are used) | 40 | 60 |
| 7.1 Prompts or cues | Introduce a stimulus with the purpose of prompting the behaviour (e.g. introducing a new risk assessment on admission) | 39 | 58 |
| 2.7 Feedback on outcome(s) of behaviour | Monitor and provide feedback on the outcome of performance of the behaviour (e.g. the number of restraints that have occurred on a ward) | 36 | 54 |
| 3.2 Social support (practical) | Advise on, arrange, or provide practical help (e.g. de-escalation rapid response team can be called to provide practical help to prevent an incident escalating) | 29 | 43 |
| 12.5 Adding objects to the environment | Add objects to the environment in order to facilitate performance of the behaviour (e.g. introducing a sensory box with equipment that could help staff to assist service users to manage distress) | 28 | 42 |
| 13.1 Identification of self as role model | Be aware that one’s own behaviour may be an example to others (e.g. staff attending training encouraged to promote de-escalation in their everyday practice) | 28 | 42 |
| 2.4 Self-monitoring of outcome(s) of behaviour | Establish a method for the person/team to monitor and record the outcome(s) of their behaviour (e.g. ward decides to monitor when restrictive practices are used with additional detail than is currently centrally requested) | 23 | 34 |
| 12.1 Restructuring the physical environment | Make changes to the physical environment that facilitate successful de-escalation (e.g. converting a seclusion room into a sensory room) | 20 | 30 |
Behaviour change technique clusters identified in interventions
The 43 different BCTs identified in the interventions were contained by 14 out of a possible 19 clusters within the BCT taxonomy. These are shown in Figure 9. The first four clusters contained over two-thirds of the BCTs; these were cluster 1 ‘goals and planning’, cluster 4 ‘shaping knowledge’, cluster 12 ‘antecedents’ and cluster 2 ‘feedback and monitoring’. The 14 clusters, the content that was coded to BCTs within them and those BCTs that were not identified are described below.
FIGURE 9.
Cluster of BCTs (%).
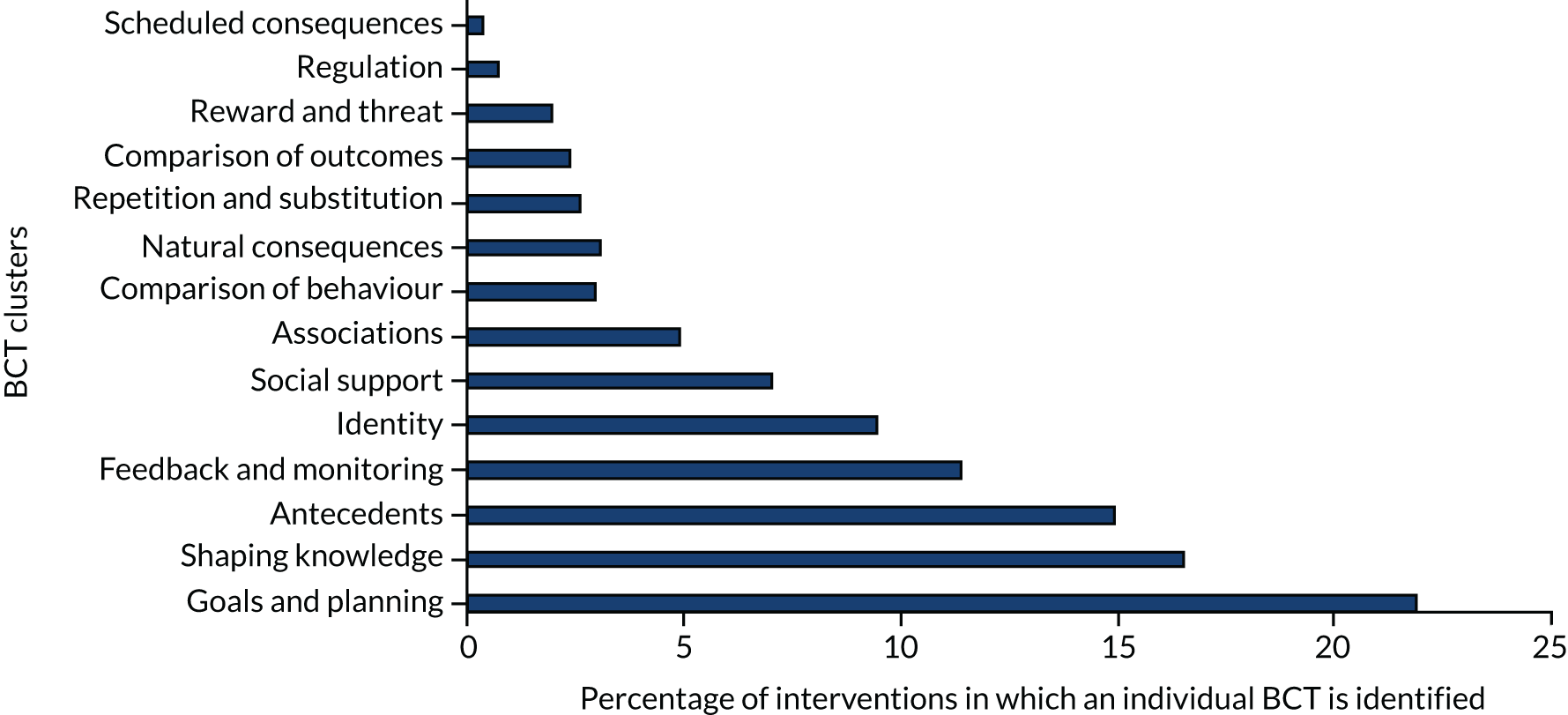
Goals and planning
Behaviour change techniques in the cluster ‘goals and planning’ were those identified most commonly in the interventions, with just over one-fifth (22%) of identified BCTs contained within this cluster (Figure 10). All the BCTs in this cluster were identified: ‘discrepancy between current behaviour and goal’ (BCT 1.6), ‘behavioural contract’ (BCT 1.8), ‘review for behaviour’ (BCT 1.5), ‘commitment’ (BCT 1.9), ‘review for outcomes’ (BCT 1.5), ‘goal-setting (behaviour)’ (BCT 1.1), ‘goal-setting (outcome)’ (BCT 1.3), ‘action-planning’ (BCT 1.4) and ‘problem-solving’ (BCT 1.2).
FIGURE 10.
Behaviour change technique cluster 1: goals and planning.
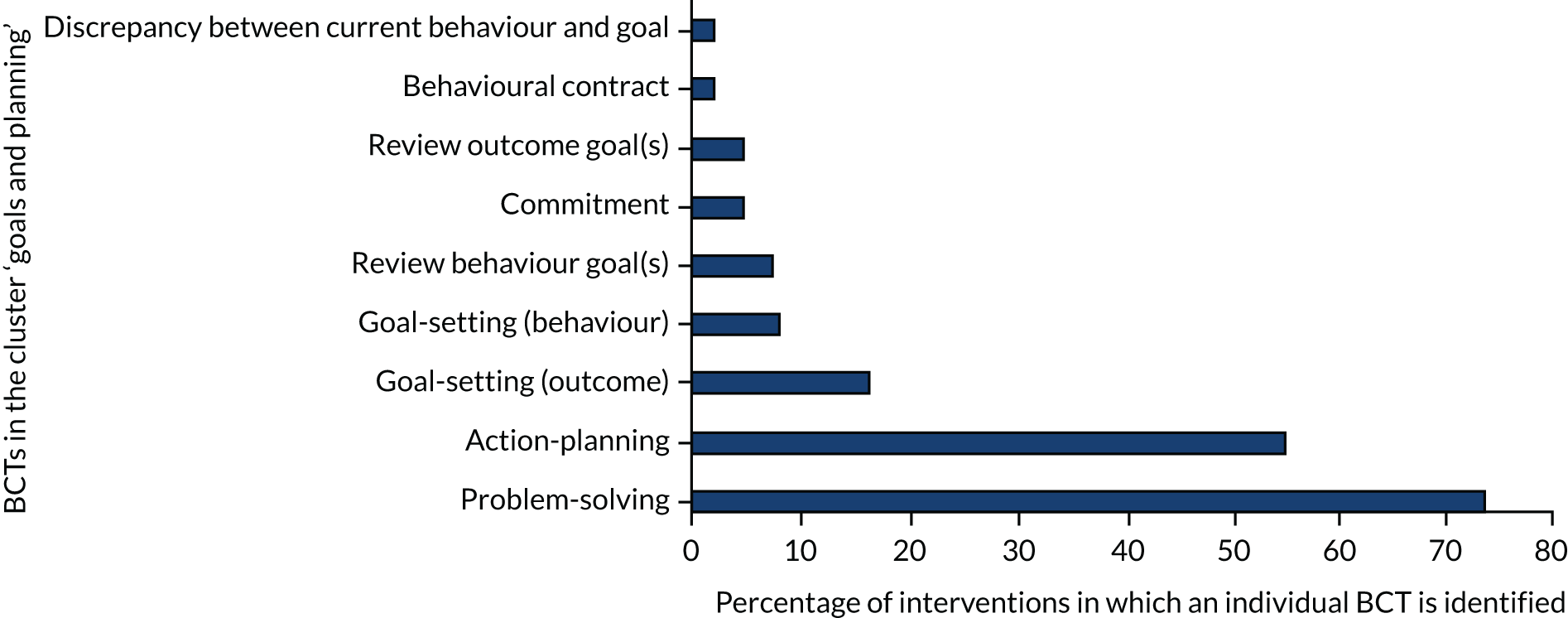
Problem-solving refers to when the individual or team is prompted to analyse what is influencing behaviour (unsuccessful de-escalation resulting in increased restrictive practice) and find solutions that attempt to overcome the problems or increase the likelihood of it happening. The ‘problem-solving’ described by interventions occurred in response to a problem of high rates of restrictive practices, or the resulting staff or service user injury. These problems could be identified at different levels: regional level, leading to a change in policy, within a service or in the review of individual service users. These reviews might involve the service user in the problem-solving process by taking place during individual care-planning meetings, debriefing after incidents or communal service user meetings. Problem-solving not involving service users took place during nursing handovers (e.g. McEwan et al. 123), staff clinical supervision (e.g. Prescott et al. 128) and in response to routine data review:
In weekly clinical supervision sessions, relevant data on seclusions and the circumstances leading up to its use were systematically discussed, in order to find ways to prevent future occurrence.
Mann-Poll et al. 212
Sometimes tools were used to support problem-solving, risk assessments and care plans:
A five-item recovery rounds checklist was developed by professional practice to prompt reflection and problem solving.
Hernandez et al. 99
A daily nursing assessment was also initiated by nursing staff. This included a brief mental state component . . . and assessment of risk of violence or harm to self or others, [resulting in an] individual service plan for the following 24 hours. This tool was important as its aided communication between nurses.
Sullivan et al. 104
‘Action-planning’ and ‘goal-setting’ followed a similar pattern, often as a result of problem-solving: planning with individual service users to try to prevent incidents that could result in restrictive practices, for example McEwan et al. ,123 or with staff teams when a ward had a target to reduce the number of episodes of restrictive practices, for example Lo. 74 There was also an indication of strategic action-planning and goal-setting, often through the formation of project steering groups to formulate institution-wide action plans to meet and review goals, for example Huckshorn. 133 Mention of reviewing goals was usually with reference to an individual service user and the goals documented in their care plan, for example Riemer. 156
Fewer interventions described ‘goal-setting’ than ‘action-planning’. Those that did consistently specified the reduction or elimination of restrictive practices, most commonly restraint and seclusion. 89 Other goals included improving staff cohesion and service culture:
The goals of the initiative included further reductions in S/R [seclusion and restraint] use and continued culture change to make the psychiatric inpatient and emergency services more patient centered and trauma informed.
Wale et al. 196
There were no examples of goal-setting with individual staff to reduce their use of restrictive practices.
Eight interventions24,176,190,201,213–216 described the use of a public ‘commitment’ (BCT 1.9) at strategic level to reduce restrictive practices:
Management has articulated (verbally and in writing) its intention of reducing the use of seclusion and restraint and/or to eliminate their use entirely.
Colton176
One of the more profound policy transformations was initiated by a declaration from the president and chief executive officer of RI [Recovery Interventions, Inc.], Gene Johnson, who mandated that seclusion and restraint practices would no longer be used and that the NFF [‘no force first’] policy would be implemented companywide, including in its crisis centers.
Ashcraft et al. 24
Three interventions described behavioural contracts to support individual staff commitment to reducing restrictive practices:16,137,217
[Trainees confirmed] that they would deliver the training when they returned to their service. The intention was that trainees should train end-users in all modules using the training materials they themselves had been trained with, in order to provide consistent training and maintain the integrity of the material.
McEvedy et al. 137
One other intervention made reference to a behaviour contract but it was unclear whether it referred to service user or staff behaviour. 103
Very few interventions discussed any discrepancy between the goal of the intervention and staff behaviour. Safewards has ‘clear mutual expectations’ that acknowledge this possibility, for instance to ‘. . . encourage the patients to refer to these expectations with staff, when they fail to uphold them’213 whereas Clark et al. 217 describe the commitment that staff make to refraining from using restrictive practices, via care plans with individual service users. Clark et al. 217 also report that patients are supported to challenge staff:
For example, if a tertiary intervention is used without any attempt at secondary intervention strategies, the patient is well within their rights to state that staff have not fulfilled their side of the contract and that the restrictive practices used may not have been justifiable.
Clark et al. 217
In only two instances was a discrepancy between current behaviour and intervention goal detected. 213,217
Shaping knowledge
The cluster ‘shaping knowledge’ contained 16% of the overall BCTs and included those that capture the imparted information about ‘antecedents’ (BCT 4.2) (40%; n = 60) and ‘instruction on performing the behaviour’ (BCT 4.1) (90%; n = 136), half of the four BCTs within this cluster (Figure 11). ‘Re-attribution’ (BCT 4.3) and ‘behavioural experiments’ (BCT 4.4) were not detected. Information about antecedents was detected as being provided at the theoretical, service, ward and individual service user levels.
FIGURE 11.
Behaviour change technique cluster 4: shaping knowledge.
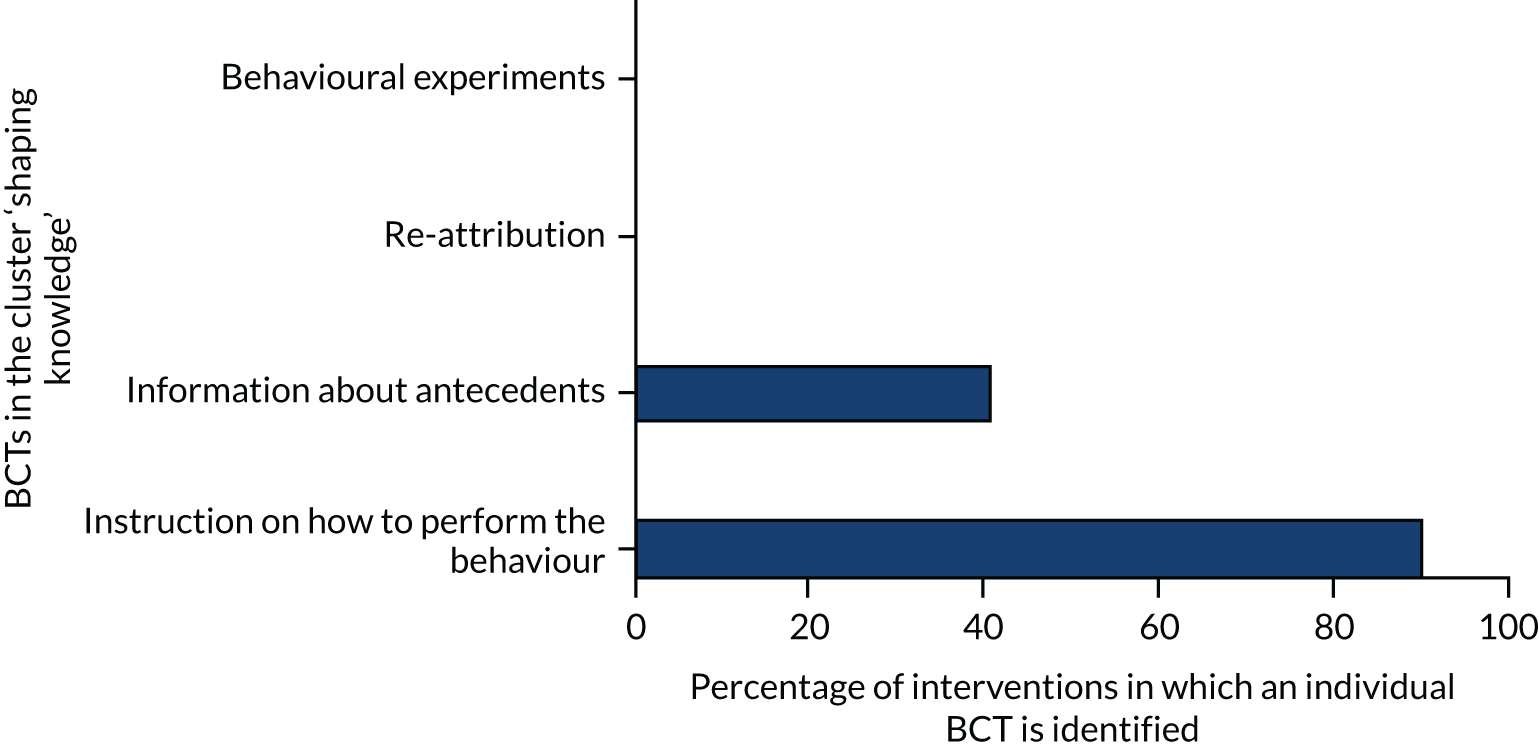
Information about antecedents for individual service users was sought either proactively on admission145,212 or on a regular basis (daily153 or weekly200) and either more broadly in a care plan or as part of a specific safety plan or risk assessment. Very few interventions reported the involvement of family in this process:145,182,212
Implementation of Safety Plans, a collaborative document completed by the patient with the staff that recorded stressors and triggers.
Maguire et al. 116
This information could also be sought via debriefing after an episode of restrictive practice:
(d) identify triggers and antecedent behaviors that may have resulted in the use of restraint; (e) discuss alternative behavior and healthy coping strategies that may effectively minimize the future use of restraint should similar situations reoccur.
Riahi et al. , 201623
Information about antecedents could be informed by review of aggregate service data:153
Change ideas were developed through sharing theories about why violence was occurring and what would help to mitigate this. A range of stakeholders contributed to this theory-building in a facilitated workshop, including staff of all levels of seniority and different professional backgrounds, service users and the police liaison officer.
Taylor-Watt et al. 153
Staff training often included more general information about antecedents:
. . . staff were trained in early recognition of warning signs, thereby improving their risk-assessment skills, and their ability to prevent and manage aggression in early stages.
Georgieva et al. 150
‘Instruction on how to perform the behaviour’ (BCT 4.1) was one of the most frequently coded BCTs, present in 91% (n = 136) of interventions. Interventions varied as to how much detail they provided. Some merely reported that staff were trained in de-escalation, whereas others provided more detail. Specific instructions were provided, for example regarding how to resolve conflict and de-escalate situations or use Sensory Modulation strategies. Training often included Trauma-Informed Care (see BCT 13.2: ‘framing/reframing’) as well as avoiding restrictive practices through use of risk assessment, care planning and respectful communication. Many interventions also provided instruction for when de-escalation had failed with elements about managing violence, restraint skills and post-incident care, as well as legal and ethics issues.
Some training involved service users116 and when this was the case this had influenced the content of the training:
PMVA [Prevention Management of Violence and Aggression] training was revamped with much greater focus on communication, de-escalation and building therapeutic alliance.
Lombardo et al. 159
Very little mention was made of training supporting staff to regulate their own emotional responses; where it was mentioned it included raising awareness of and control of feelings, especially fear and anger. 15,129
Antecedents
The BCT cluster ‘antecedents’, involving factors that might influence whether or not restrictive practices can be avoided, was a theme throughout many interventions, typically in terms of preventing situations where service users might become distressed and conflict occur. ‘Antecedents’ was the third most populated cluster, containing 15% of BCTs (Figure 12). Half of the six BCTs constituting the antecedents cluster were identified: ‘restructuring the physical environment’ (BCT 12.1), ‘adding objects to the environment’ (BCT 12.5) and ‘restructuring the social environment’ (BCT 12.2). ‘Avoidance/reducing exposure to cues’ (BCT 12.3), ‘distraction’ (BCT 12.4) and ‘body changes’ (BCT 12.6) were not detected. Broader ward- and organisation-level changes to the physical and social environment described here as BCTs that aim to reduce antecedents by addressing individual service user needs are described elsewhere under ‘prompts’.
FIGURE 12.
Behaviour change technique cluster 12: antecedents.
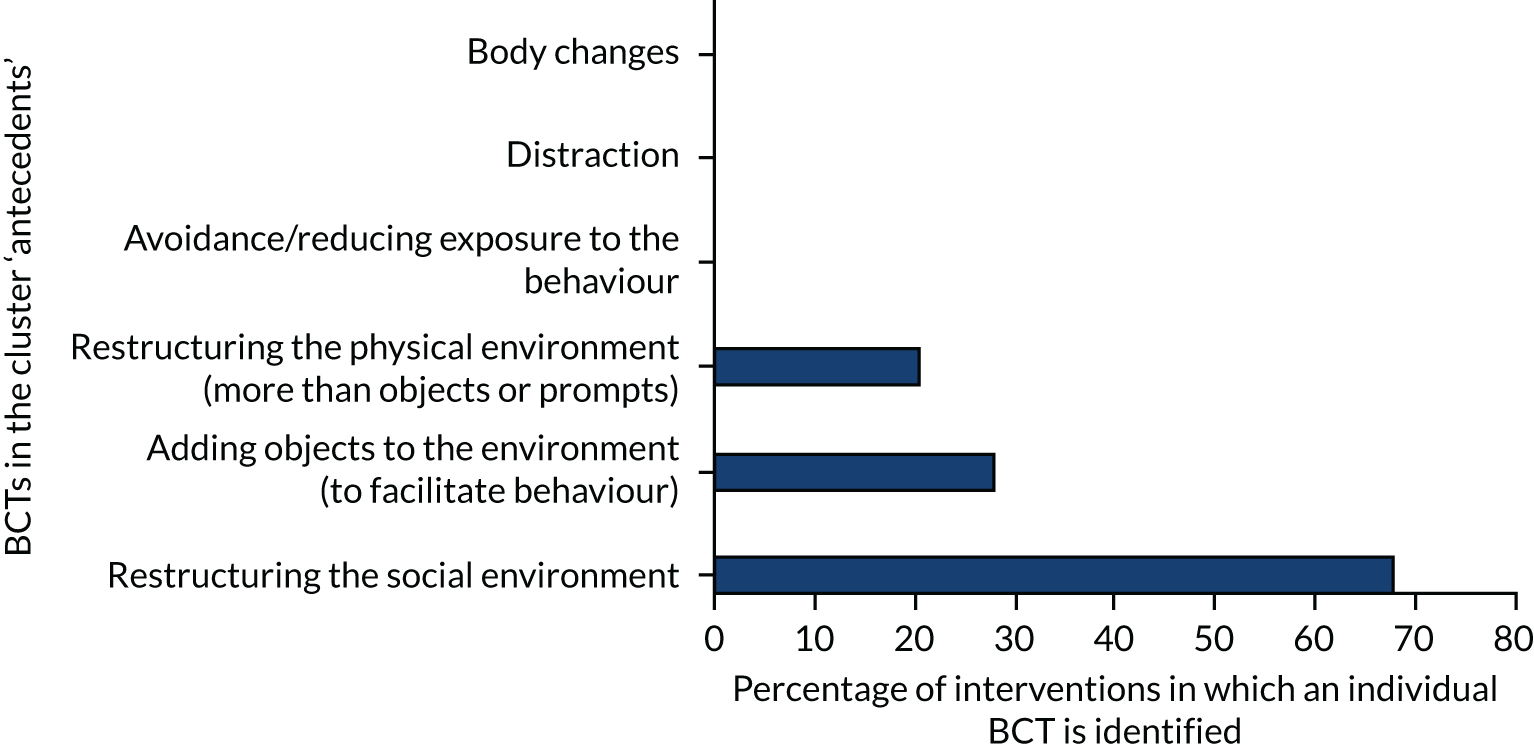
Restructuring the physical environment
‘Restructuring the physical environment’ was a feature of 20% (n = 30) of coded interventions and considered any changes made to the ward itself, including the introduction or removal of specific rooms and changes made to the fabric of the building. Nineteen (13%) interventions included the creation of private rooms (e.g. Lombardo et al. 159) with a low-stimulus environment, often created out of a seclusion room, called comfort, sensory, quiet or ‘Snoezelen’ rooms. Although these rooms were aimed at changing service user behaviour, they gave staff an alternative resource to help support their aim of de-escalation. Sivak191 reports that the walls were painted in a pale-green colour; one had a mural and another included an area of chalkboard paint at a convenient height for clients to use if they chose to do so. The noise level was reduced by the installation of drop ceilings, and light panels with sky scenes were used to create a sense of being outside. 191
Service users were often involved in deciding how they should be decorated:
[S]uggestion boxes were also placed in both ward sitting rooms [. . .]. Suggestions for the design and decor were made by patients, carers and staff. These included; colours of paint, design of curtains, style of pictures for the walls, types of furniture, brightness/levels of lighting and layout of furniture.
Smith and Millar158
Other changes to the general physical environment included upgrading of wards to make them feel more homely or comfortable:
. . . inexpensive physical changes, including repainting walls with warm colors, placement of decorative throw rugs and plants, and rearrangement of furniture.
Borckardt et al. 107
Two interventions included physical restructuring of outside areas with the creation of a ward garden and allotment. 83 Some interventions did not create Sensory Rooms but created separate space for service users to watch television or designated quiet areas. 158
Adding objects to the environment
Many interventions also added objects to the environment (BCT 12.5). The most frequently mentioned was Sensory Modulation equipment, which was used in 16 interventions; it could be a portable box of equipment or could be equipment kept within a sensory room:
This range of objects included a massage chair, rocking chair, beanbag, faux-fur blankets, weighted blankets, weighted soft toys, ‘stress’ balls, portable audio and DVD [digital versatile disc] players with relaxing sounds and visual scenes, aromatic oils and diffusers, scented hand creams, and adjustable coloured ambient lighting.
Sutton et al. 152
Objects such as rugs and plants provided a more homely feel, whereas others were there to provide activities for service users, and included games consoles, reading material, games and puzzles, DVDs and exercise equipment:
. . . exercise machines were added as options to help the service users burn energy and safely manage stress.
Riemer and Corwith192
Another category of object added to the environment were noticeboards displaying information for staff, service users or both. Safewards encouraged staff to have posters of de-escalation tips in their office:
To change the Soft Words poster every day or so. To remind other members of the team as to what the Soft Words are. To draw attention to the Message of the Day poster in the nurses office.
Safewards213
Another category of things added to the environment is items to alert staff of incidents; this includes personal alarms,150 two-way radios,218 pagers74 and closed-circuit television (CCTV),83 all of which were used in at least one intervention.
Restructuring the social environment
This BCT (12.2) is intended to record changes made to the social environment in order to facilitate the performance of a desired behaviour or create barriers to an unwanted behaviour. Many of the interventions made changes to the social environment of the setting including changing the way that people interact with each other, from the strategic through to the individual level. As such, this BCT was divided into four themes: stakeholder involvement, increased access to staff, improved communication and promoting social contact.
Stakeholder involvement
Stakeholders could be service users, relatives or ward staff. The main aspect of interventions coded under this category was that of service user involvement (referred to by 25% of interventions; see Service user involvement in interventions). When detail was provided, it was most often referred to in terms of involvement in individual care, either in care planning or debriefing after an incident of restrictive practice had occurred. Service user involvement that was not related to individual care was mostly consultation on aspects of an intervention, for example the design of a sensory room. Some interventions employed service users as consultants, sometimes in a paid capacity:
Two patients from the ward were recruited and paid for their time and input on the local working party.
Maguire et al. 197
A small number of these interventions employed service users to deliver training:
Consumer advocates provided staff education on such topics as respect, therapeutic approaches to providing care, trauma-informed care, and reducing the risk for violence.
Riemer and Corwith192
Other interventions had service user representation on committees, at either ward level or at a more strategic level:
We established a multidisciplinary seclusion/restraint minimisation committee, chaired by a peer specialist.
Ash et al. 6
Others consulted existing committees consisting only of service users:
The Consumer Advisory Group, whose membership comprised patient representatives and Consumer Consultants, was regularly consulted.
Ching et al. 115
There was very little involvement of relatives and informal carers. Two interventions provided support for families, one by providing education and support and the other by opening a resource centre:
To enhance the role of families in treatment and the organization, the Family Resource Centre opened in 2013 to provide a space for families to share experiences, access resources, attend family-specific groups, and connect with other families for support and encouragement.
Riahi et al. 23
The rest of the interventions that made references to families and informal carers did so with reference to either their involvement in care planning or post-incident debriefing.
Some interventions made specific reference to the involvement of ward staff in the development of some interventions. According to Cambridgeshire and Peterborough NHS Foundation Trust,85 all staff were engaged in considering new approaches for initiating proactive care and eliminating the use of force, which helped to promote positive conversations and avoid defensiveness. Ideas about small changes were encouraged and the appreciative inquiry model was used to develop questions, such as:
What are we doing well that we should continue and build on? What should we stop doing? What should we start doing or do differently?
Cambridgeshire and Peterborough NHS Foundation Trust85
The importance of ward staff in the implementation of interventions was acknowledged:
A combined top-down and bottom-up approach was used: leadership and support from the top was seen as essential while acknowledging that changes could not be implemented without the active involvement, participation and fiat of the professionals working on the wards.
Mann-Poll et al. 212
Explicit managerial support formed part of many interventions,23,106,116,133,192,212,219 either institutionally or at ward level. 106 Six Core Strategies implementation guidance emphasised that staff should be made aware of the involvement and commitment of senior staff in reducing seclusion and restraint, including the chief executive officer (CEO)/administrator, the medical director and other senior staff. 133
Many interventions had a specific steering group17,115,116 including senior managers who provided monitoring and strategic direction for the interventions. 83 In some interventions (n = 10), the multidisciplinary nature of these groups was emphasised:
Establishment of a project management structure that included consumer consultants, managers, clinicians and academics of all disciplines.
McEwan et al. 123
Improved interaction between staff and service users
Improving interaction between service users and staff was attempted in several ways, including increasing the number of staff available and promoting access to existing staff. Increased staffing was a feature of 12 interventions; some interventions simply increased staffing ratios,150,220 either all the time or in crisis situations. 109 Several interventions introduced a rapid response team with the aim of providing expertise in a crisis situation, for example Hernandez et al. ,99 whereas others added expert practitioners to ward teams:
Two City Nurses were appointed for the project and were recognized clinical experts in acute inpatient care with long experience of practice development work. They worked with the wards’ staff, 3 days per week, using the working model mentioned earlier, to bring about change towards low-conflict, low-containment, high-therapy nursing.
Bowers et al. 102
Other interventions sought to improve service user access to staff. One intervention used a direct booking facility for an appointment to see a doctor, whereby doctors’ availability was displayed in the communal area, enabling patients to book a mutually convenient slot. 83
However, others encouraged nursing staff to proactively approach service users209 and prioritise service user need over administrative duties or increased observations:113
. . . he asked can we go a walk and I said yes, let’s just go, and he said that he thought he had no chance as you were there on the computer.
McEwan et al. 123
Improved communication was a frequent part of the social restructuring of the service setting to reduce conflict. This aimed to improve communication between staff, between service users or between staff and service users. When the aim was to improve communication between staff and service users, it could take place with individual service users, prompting staff to support service users in expressing their feelings and wishes. 103,123 It could also be a collective endeavour with supportive ward community meetings to involve both service users and staff. 83 Putkonen et al. 17 also report the following:
They also suggested new ways and practices to decrease fear, violence, and coercion and brainstormed with staff and doctors about the ward rules and practices during weekly community meetings (45 minutes).
Putkonen et al. 17
Communication between staff about individuals and ward issues were enhanced in some interventions via ward meetings,17,212,221 case reviews,23,106 safety huddles or supervision:
. . . the IPCU [intensive psychiatric care unit] safety huddle was subsequently born. This was a 10-minute ‘huddle’ to focus on potential or actual safety issues. The focus was on anticipation and prevention; nursing assistant staff were involved and contributed to its facilitation.
McEwan et al. 123
Clinical supervision is an invaluable and objective way of communicating the plan across three shifts. One successful approach uses a single-person contact to meet with each of the employees across shifts.
Visalli and McNasser103
Few interventions mentioned communication with relatives and carers, for example Mann-Poll et al. ,212 with the exception of communicating service rules and behavioural expectations:
Clear boundaries and limitations with respect to acting out behavior were communicated at admission.
Mann-Poll et al. 212
There was some evidence of communication of behavioural expectations to staff; Safewards used ‘mutual expectations’ and ward rules and expectations of behaviour were publicly displayed:
Step 4, get your mutual expectations printed as a laminated poster to the ward, to your specified design with your specified content. Please hang this in a prominent and public space where it can be read by patients and staff.
Safewards213
One other intervention107 saw the introduction of a strategy to promote respectful communication with service users:
. . . all clinical staff to engage in the following communication behaviors with inpatients: ‘Acknowledge’ patients, ‘Introduce’ themselves, articulate the anticipated ‘Duration’ of the clinical contact, ‘Explain’ the reason for the contact, and ‘Thank’ patients for their cooperation.
Borckardt et al. 107
Several interventions included aspects surrounding rules or policy changes. Some rules aimed to change how restrictive practices were governed or recorded. 146 Maguire et al. 116 report that this involved documentation of care plans to identify conditions and interventions for ending seclusion, allowing ‘transparency for the patient and consistency for the clinical team’. In addition, a project officer was appointed and the changes to practice were captured in a rewritten Seclusion Policy and Procedure. 116
Several interventions reviewed existing rules with the intention of ascertaining whether or not they were necessary:107,116,139 For example, guidance for implementation of the 6 Cs draws attention to the need for staff to look critically at a facility’s regulations, identifying that they may be neither logical nor necessary:
Most inpatient facilities have historical rules that are habits or patterns of behavior that are not congruent with a non-coercive, recovery facilitating environment, for instance rules such as putting people who self-abuse in non-lethal ways in restraint, or putting people who are intrusive only in restraint.
Huckshorn133
. . . a team for each unit that was tasked with reviewing and modifying unit rules and policies to be less restrictive to patients or eliminating unit rules that were too restrictive.
Borckardt et al. 107
Promoting more flexible responses from staff to service users was an aspect of several reviews of rules:
. . . further flexible approach to supporting patients, e.g. to have several spells of time off the ward to defuse agitation.
McEwan et al. 123
Sometimes, increasing flexibility of rules was instigated by ward staff:
From a bottom-up perspective, teams could choose their own package of interventions tailored to their ward. They could for example choose to make their ward rules more flexible.
Mann-Poll et al. 212
Service users were occasionally involved in this process:17
Staff and patients collaborated to review the unwritten and arbitrary ‘unit rules’ that often are sources of conflict.
Maguire et al. 116
Promoting social contact
One aspect of restructuring the social environment to reduce conflict was promoting socialising, either between staff and service users139 or between service users. 83 Although interventions that provided greater opportunities for service users to socialise with each other are not specifically targeting staff behaviour, similar to Sensory Rooms, they give staff a broader repertoire of resources to use in de-escalation. 123 The ‘know each other’ aspect of Safewards was the most comprehensively described initiative promoting social interaction between service users and staff:
. . . with consent, capacity and confidentiality considered, staff and patients provide non-controversial information about each other, this could include hobbies, music, TV programmes. This information is then placed in a file and made available in communal areas.
Safewards213
Shared meals featured in some interventions:
Shared lunches with staff and patients on male High Dependency Unit, promoting engagement and establishment of relationships.
Northumberland, Tyne and Wear NHS Foundation Trust83
Other shared tasks promoted closer interaction; one intervention17 focused on restrictive practice. In accordance with patient requests:
. . . some patients and staff volunteered to work together 1 hour per week on building projects . . . Because many patients and staff found it difficult to discuss their experiences of coercion and violence, they wrote, photographed, and illustrated a book together, titled ‘Behind Locked Doors’.
Putkonen et al. 17
Only one intervention described creating opportunities for families and carers to socialise:
To enhance the role of families in treatment and the organization, the Family Resource Centre opened in 2013 to provide a space for families to share experiences, access resources, attend family-specific groups, and connect with other families for support and encouragement.
Riahi et al. 23
Activities on wards for service users were seen as a way of reducing restrictive practices. Activities might be individual or group-based activities groups were more frequently described. Staff were sometimes trained to deliver group activities or a specific staff member might be responsible; in one example, data analysis showed when incidents were more likely to occur on a female admission unit, and, in response, an activity coordinator was introduced on the unit throughout the week. 83
Some groups were explicitly treatment orientated, whereas others were recreational:
. . . treatment-based groups/classes are matched with a person’s assessed needs . . . As an educational endeavour, staff are trained to offer individual groups inside and outside the facility. Treatment groups or classes include communication, managing mental health, anger management, assertiveness training, problem solving, and community housing skills.
Visalli and McNasser139
One intervention recognised the importance of activities being available to all service users, even those in the PICU:133
Has leadership reviewed the facility’s plan for clinical treatment activities in an effort to assure that active, daily, person centered, effective treatment activities are offered to all persons receiving services; that these services are offered off living units preferably; and that persons attending have some personal choice in what activities they attend. The minimal criteria to meet under this objective is to assure that service recipients are not spending their days in enclosed areas with no active effective psycho-social or psychiatric rehabilitation occurring that is effective in teaching living, learning, recreational and working skills.
Huckshorn133
Only one initiative promoting activities – Star Wards – was described as having been developed by service users. Star Wards include 75 ideas for meaningful activities that service users can consider, especially in the evenings or at weekends when there are fewer planned activities. They range from simple changes, such as making magazines and newspapers available, to themed social events and activities. 125
Feedback and monitoring
Behaviour change technique cluster 2, ‘feedback and monitoring’, accounted for the monitoring of ward data and, if they were fed back to the ward, in what ways this feedback took place. Eleven per cent of BCTs were in this cluster (BCTs 2.1–2.7) (Figure 13). Both feedback and monitoring related primarily to outcomes (reduced restrictive practices) of the behaviour (de-escalation) although there was some evidence of monitoring of behaviour. Monitoring was either self-monitoring (including ward-level monitoring) or by others, for example at system level through incident reports. ‘Biofeedback’ (BCT 2.6) was not detected.
FIGURE 13.
Behaviour change technique cluster 2: feedback and monitoring.
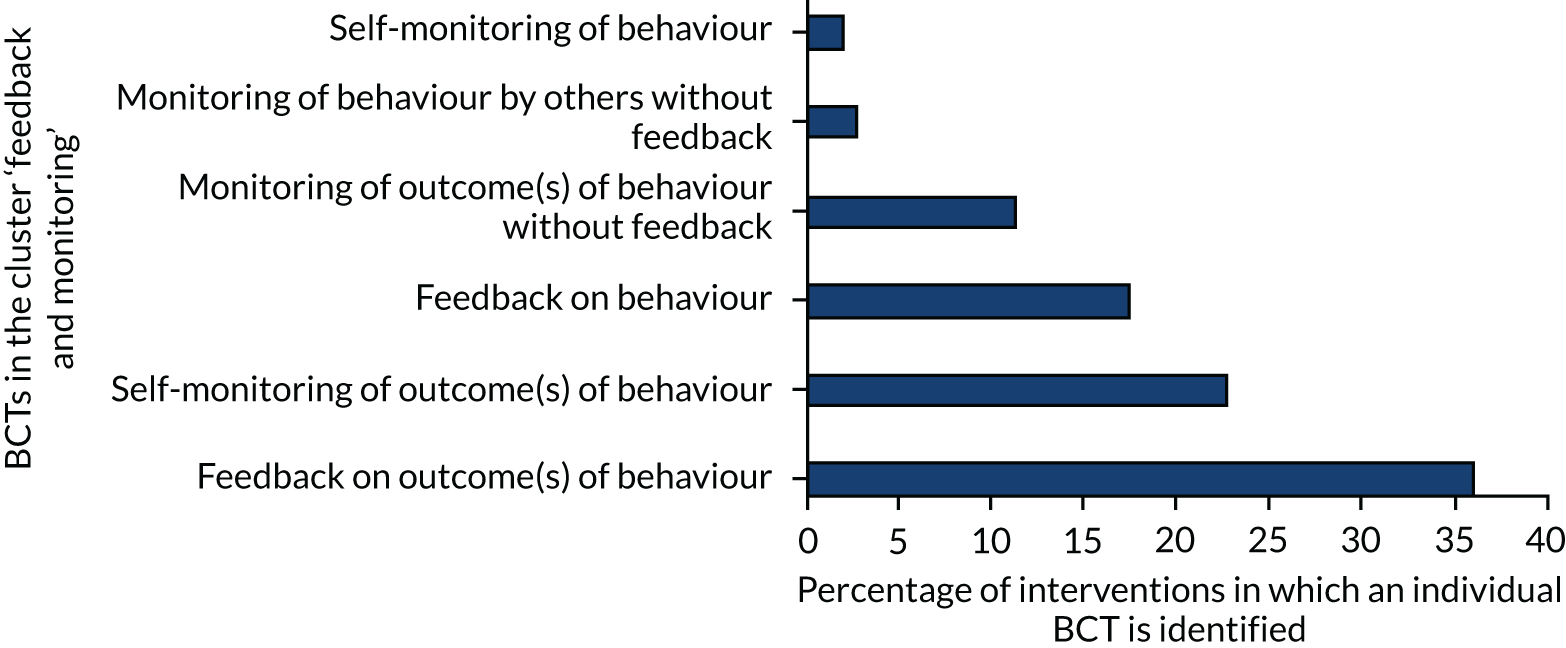
Feedback on behaviour
‘Feedback on behaviour’ (BCT 2.2) occurred through post-incident debriefing, team meetings or clinical supervision when near-misses were discussed. This feedback was supported by intervention structures such as the introduction of tools such as safety crosses:
Displaying safety crosses . . . a simple wall calendar that staff can mark in colour to show red days (when there was an incident of physical violence) or green days (incident-free). This evolved to include orange incidents, reflecting a near miss or build-up of hostility – which are not usually recorded in any form.
Self-monitoring of behaviour
‘Self-monitoring of behaviour’ (BCT 2.3) was coded when interventions encouraged ward staff to take the lead on reflecting on not just incidents but near-misses and times when de-escalation had been successfully used:
The nursing team started collecting and recording improvement data on safety crosses regarding safety huddle frequency, daily goal-setting frequency, and restraint incidence. Weekly improvement data were . . . collected on the quality of patient risk assessments and safety plans, as well as the extent of service user involvement in safety planning.
McEwan et al. 123
One intervention involved the service user in this process:
If a crisis was averted, staff members and the patient reviewed the crisis management plan and determined which strategies were most effective.
Jonikas et al. 180
Only one intervention described staff reflection on the way in which they individually related to service users:
. . . participants practised self-awareness techniques to gain a more profound understanding of their personal habits, ways of behaving on the ward in relation to patients and teams.
Kontio et al. 199
Monitoring of behaviour by others without feedback
Only three interventions described monitoring (as distinct from self-monitoring) staff behaviour (BCT 2.1). D’Orio et al. 149 used CCTV to monitor the behaviour of staff. Short et al. 157 monitored broader staff safety performance data and Hochstrasser et al. 110 described monitoring processes to prevent incidents.
Feedback on outcomes of behaviour
Many interventions monitored outcomes of behaviour in terms of the number of restrictive practices that occurred in the setting, for example the number of restraints or duration of seclusion. Most interventions fed back the outcomes of behaviour (i.e. the number of restraints) via institutional recording systems that was fed back at either ward186 or institutional level:132
Each morning the project senior nurse and cultural anthropologist – psychotherapist-counselor discussed with staff the violent incidents that occurred and reported on the practices, restrictions, and alternative methods used, according to the postevent analysis sheet. These meetings identified and praised successful interventions and otherwise helped the staff to improve their practices.
Putkonen et al. 17
It needed to capture the essential data relating to ‘how many’ incidents and qualitative information regarding the antecedents through meaningful postincident debriefs with patients and staff. This information enabled the ward team to make real-time changes to patients’ individual care plans. Good reporting practices translated data into usable information.
Lombardo et al. 159
Some interventions used debriefing including both service users and staff involved in an incident of restrictive practice. 222 This was seen as feedback on the outcomes of the behaviour (and could also include self-monitoring of the outcomes of behaviour), depending on the format of the debrief and whether or not staff were asked to reflect on their practice.
Self-monitoring of behaviour outcomes
Thirty-four interventions described using self-monitoring of outcomes of behaviour (BCT 2.4). This was where wards monitored their own incidents rather than monitoring being a centralised system-level process. Self-monitoring could also be a part of post-incident debriefing depending on how it was described as being carried out.
Monitoring behaviour outcomes without feedback
Feedback as a result of monitoring was not always provided, for example Short et al. 157 In a number of cases it was not reported whether or not these data were fed back to ward staff; for example, two studies79,223 were clear that data were being collected without staff knowledge, which led to the assumption these data were not being fed back during the intervention.
Identity
The cluster ‘identity’ referred to the identity of the individual staff members and 9% of the BCTs identified were in this cluster. Two of the five potential BCTs in this cluster were detected: ‘framing or reframing’ (BCT 13.2) and the ‘identification of the self as a role model’ (BCT 13.1). The BCTs ‘incompatible beliefs’ (BCT 13.3), ‘valued self-identity’ (BCT 13.4) and ‘identity associated with changed behaviour’ (BCT 13.5) were not detected (Figure 14).
FIGURE 14.
Behaviour change technique cluster 13: identity.
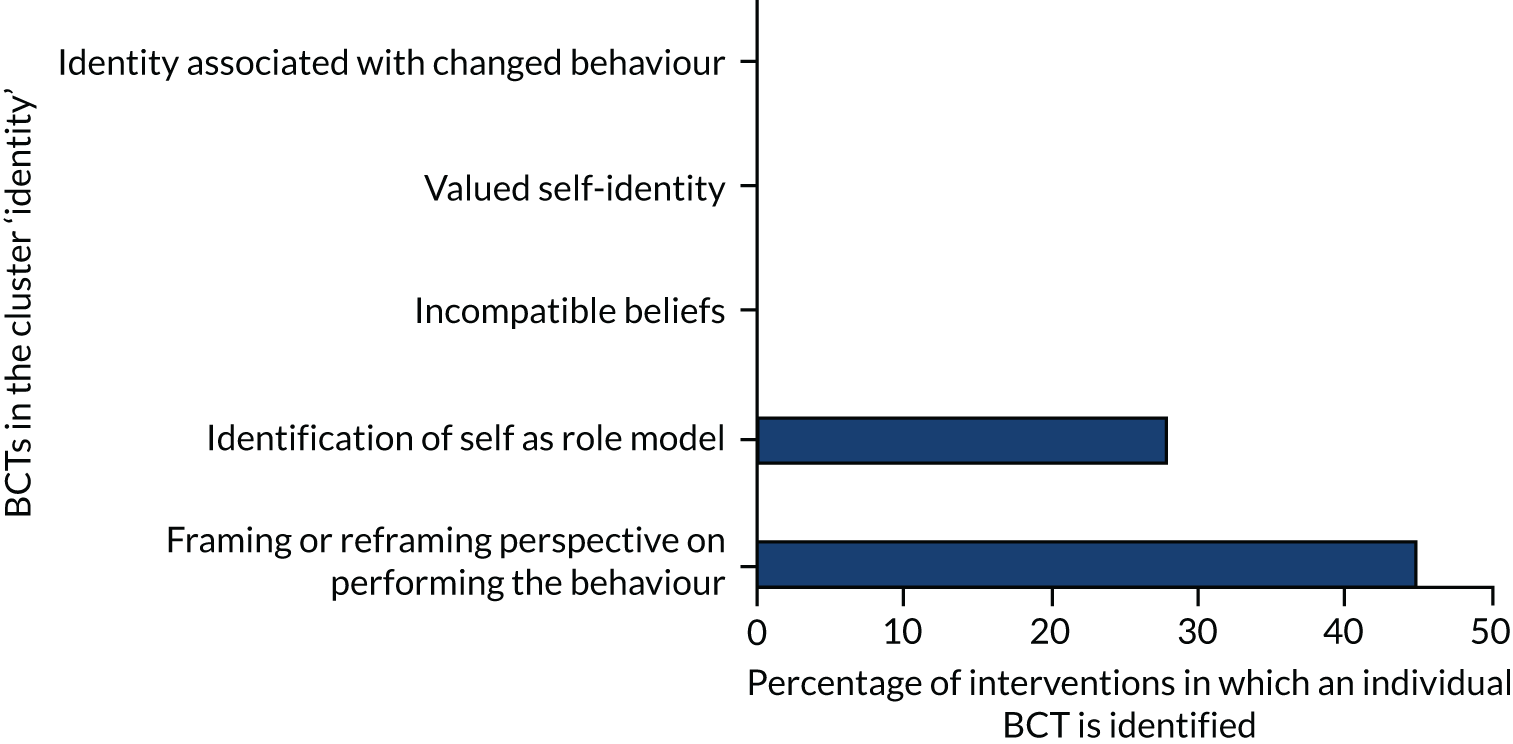
Framing/reframing
Framing is the conscious adoption of a different perspective on behaviour in order to change emotions about performing a behaviour. In terms of the interventions, this was dominated by those that introduced changes in nursing philosophy to service user-centred approaches. This is illustrated by the Safewards approach of having positive regard for service users:
Positive words: Aims to create a positive view of the patient at ‘handover’, even when a troublesome behaviour is being reported, by also saying something positive about the patient.
Cabral and Carthy15
Training sought to reframe restraint as avoidable and a true last resort:
Training is provided which gives staff the key competencies and supports the view that restraint is used as a last resort to manage risk behaviour associated with aggression, violence and acute behavioural disturbance.
Restraint Reduction Network214
Different ways of understanding service user distress were a common feature of interventions. Approaches described how behaviour might be affected by environmental/individual interaction. Maybo Conflict Management Training224 follows the principles of Positive Behaviour Support, emphasising how behaviour is used as a form of communication and heavily influenced by both internal and external factors. Participants have a greater empathy for individuals once these factors are understood and a greater appreciation of the depth to which quality of life is compromised. This involved training sessions about sensory processing models, and Trauma-Informed Care in particular:
For trauma-informed care, all unit staff attended a half-day standardized training seminar on the nature of trauma and its effects on patients’ experiences, physiology, and psychological processes, along with instructions on how to minimize engaging in behaviors that could exacerbate trauma related reactions from patients.
Borckhart et al. 107
. . . training explains how a client’s history can influence their experience and reaction to seclusion and restraint.
Colton176
Role modelling
Promoting ‘self-identification as a role model’ (BCT 13.1) was achieved in a number of ways. The most common was using a ‘train the trainers’ model, which was used in 16 interventions, for example Visalli and McNasser,139 when select staff members became trainers of their colleagues and often retained a mentoring expert role afterwards. Intervention champions were another commonly used method of role modelling, for example Yakov et al:185
There are Safewards champions for each ward, who provide practical support and help with implementation, training and coaching.
Twelve interventions85,88,90,97,100–103,129,132,135,159,181,185,187,197,225 used expert practitioners on wards to disseminate good practice:
Two City Nurses were appointed for the project, and were recognized clinical experts in acute inpatient care with long experience of practice development work.
Bowers et al. 101
Ambassadors from within the teams were appointed to discuss the use of coercive measures with their colleagues and to help stimulate changes in attitudes and practices.
Boumans et al. 225
Four interventions made use of information sharing and exchanges between organisations that was coded as role modelling in a broader manner:85,209,221,226
GGZ Nederland, the Dutch mental health umbrella organization, has supported exchange programs that organize quarterly meetings, allowing hospitals to learn from each other.
Noorthoorn et al. 221
Social support
The cluster ‘social support’ (Figure 15) accounted for 7% of the BCTs in the interventions and all three possible BCTs were identified as taking place within staff teams at ward level, more broadly within the organisation, or being shared with external agencies. Social support was either ‘unspecified’ (BCT 3.1), or further defined as either ‘emotional social support’ (BCT 3.3) or ‘practical social support’ (BCT 3.2).
FIGURE 15.
Behaviour change technique cluster 3: social support.
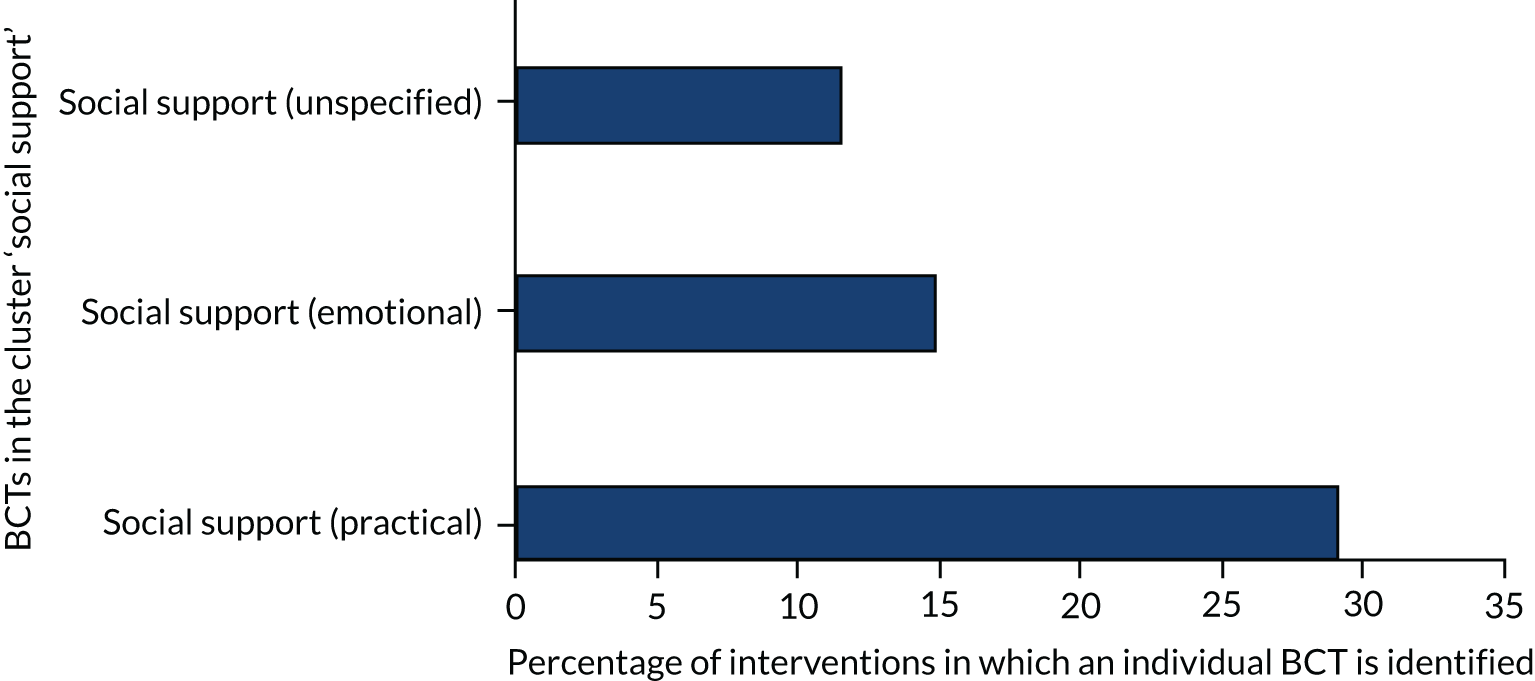
Practical support included ‘hands-on’ support in terms of sharing ideas for good practice in reducing restrictive practices. Taxis227 reported that at the outset a ‘weekly RN [registered nurse] discussion group’ was formed, with the goal of addressing practice issues, by raising awareness of the restraint and seclusion incidents, and to ‘build a consensus’ for increased use of less restrictive alternatives. Rather than providing ready-made answers for all situations, the goal was to ‘form a collegial environment in which these matters could be discussed’. This collegiality would serve as an important element as the programme progressed.
Melin69 reported that the meeting was intended to be a forum in which staff involved in treatment could have a positive and constructive dialogue about the interventions and the behaviour of colleagues. Guidelines included making sure that treatment staff were back in control before the meeting started, clarifying what happened, reviewing how staff responded and looking for ways to improve and strengthen responses in the future. Treatment staff were to be supported and encouraged, and trust in colleagues was to be expressed.
Safety huddles were coded as involving practical social support. The Northumberland, Tyne and Wear NHS Foundation Trust83 reported that the Positive Safe Team provide ongoing support including training, consultancy and opportunities for sharing good practice.
Some training providers offered ongoing practical social support for participants228 and, depending on the nature of training, it can offer practical social support in terms of feedback on role play.
The use of rapid response de-escalation teams, which featured in 12 interventions, was classed as providing practical social support.
Associations
As illustrated in Figure 16, associations were detected in 5% of BCTs in 57 interventions, although only one BCT ‘prompts or cues’ (BCT 7.1). None of the other BCTs in this cluster were detected: ‘cue signalling reward’ (BCT 7.2), ‘reduce prompts or cues’ (BCT 7.3), ‘remove access to the reward’ (BCT 7.4), ‘remove aversive stimulus’ (BCT 7.5), ‘satiation’ (BCT 7.6), ‘exposure’ (BCT 7.7) or ‘associative learning’ (BCT 7.8). Associations were predominantly prompts or cues (BCT 7.1) in the form of standardised assessments for service users on wards relating to risk of violence. 127 Mersey Care NHS Foundation Trust229 reported training staff in the PICU in the use of a structured risk assessment tool: the DASA-IV. DASA-IV scores were incorporated into daily care-planning. DASA-IV is a seven-item scale used for daily assessment of inpatients. Higher scores indicate a possible need for increased attention over the following 24 hours to reduce the risk of a serious violent incident.
FIGURE 16.
Behaviour change technique cluster 7: associations.
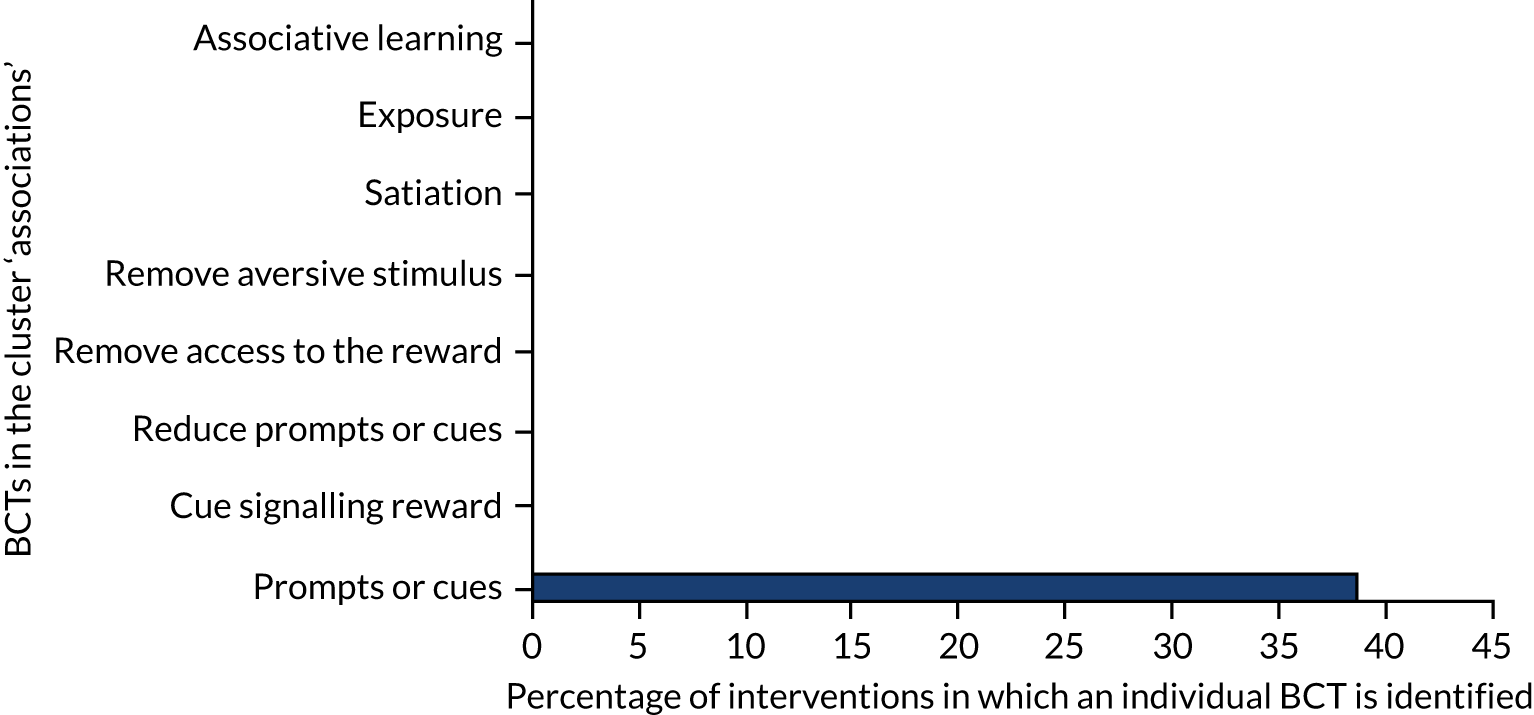
Other prompts included posters181,213 displayed in offices or wards and flow charts reminding staff of less restrictive practices (e.g. Alberta Health Services). 230
Comparison of behaviour
As illustrated in Figure 17, cluster 6, ‘comparison of behaviour’, comprises three BCTs: ‘demonstration of behaviour’ (BCT 6.1), ‘social comparison’ (BCT 6.2) and ‘information about others’ approval’ (BCT 6.3). Three per cent of detected BCTs were in this cluster and all three BCTs in this cluster were identified. Comparison of behaviour consists of experiencing demonstrations of the behaviour (BCT 6.1), usually as part of training sessions demonstrating successful de-escalation. ‘Social comparison’ (BCT 6.2) was found in everyday practice, through being compared with other wards or wards publicly acknowledging restraint rates, and receiving information about other people’s approval (BCT 6.3).
FIGURE 17.
Behaviour change technique cluster 6: comparison of behaviour.
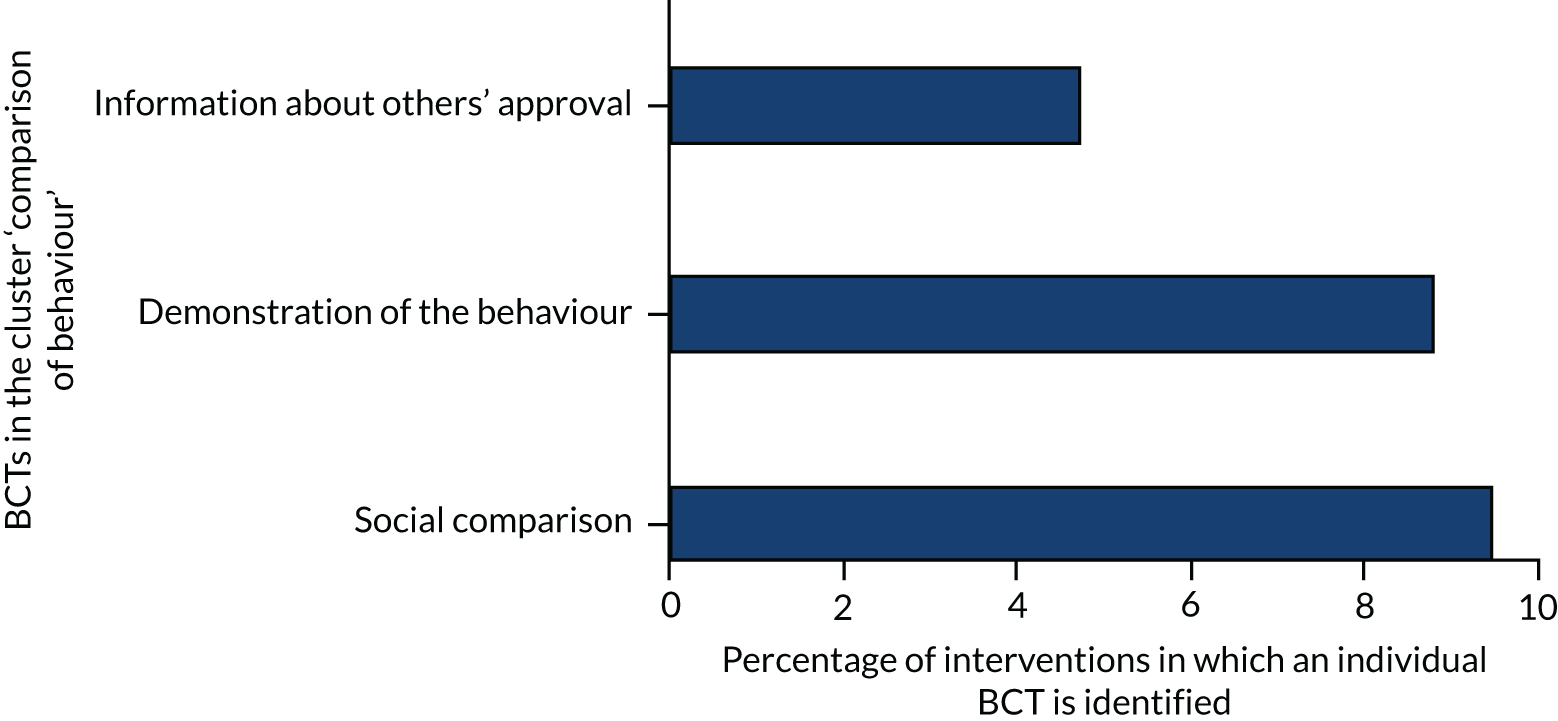
Thirteen references,16,93,95,96,141,144,162,176,184,198,208,231,232 described de-escalation behaviour being demonstrated (BCT 6.1) as part of their training intervention, either by trainers or through role-play scenarios. ‘The Six Core Strategies intervention used Social comparison’ (BCT 6.2) at ward level, encouraging linked facilities to engage in healthy competition (e.g. by displaying data in open areas).
The Restraint Reduction Network promoted similar social comparison as ‘peer assessment’, in which one team or unit would be responsible for assessing the performance of another. This was felt to be effective in increasing motivation and engagement, and also in enhancing deeper understanding of assessment, and sharing good practice. 233
It became a feature at individual staff level within two interventions, one using Safewards. A well-publicised ‘star of the week’ initiative at Northumberland, Tyne and Wear NHS Foundation Trust was enthusiastically supported by staff and patients, and allowed a mild sense of competition between peers. 83
‘Information about others’ approval’ (BCT 6.3) was identified when there were descriptions of communication of support and approval from others. At ward level, one study described growing support from a consultant psychiatrist for intervention activities that had been instigated by nursing staff. It was also a feature of the social comparison activities when peers or service users nominated the best de-escalator or ‘star of the week’. Safety crosses were displayed publicly to show when the last incident of restraint had occurred:
Displaying safety crosses in the public area of the ward. This is a simple wall calendar that staff can mark in colour to show red days (when there was an incident of physical violence) or green days (incident-free). This evolved to include orange incidents, reflecting a near miss or build-up of hostility – which are not usually recorded in any form. This was an accessible way to share incident data and provided a focal point on the ward for staff, people using the service and visitors.
Natural consequences
As illustrated in Figure 18, in the BCT cluster ‘natural consequences’ a distinction is made between natural consequences and scheduled consequences such as a predetermined reward for performing a behaviour. A total of 3% of BCTs identified were in this cluster and included four BCTs: ‘information about health’ (BCT 5.1), ‘information about emotional consequences’ (BCT5.6), ‘salience of consequences (BCT5.2)’, ‘information about social and environmental consequences’ (BCT 5.3). ‘Monitoring of emotional consequences’ (BCT 5.4) and ‘anticipated regret’ (BCT 5.5) were not detected in any interventions.
FIGURE 18.
Behaviour change technique cluster 5: natural consequences.
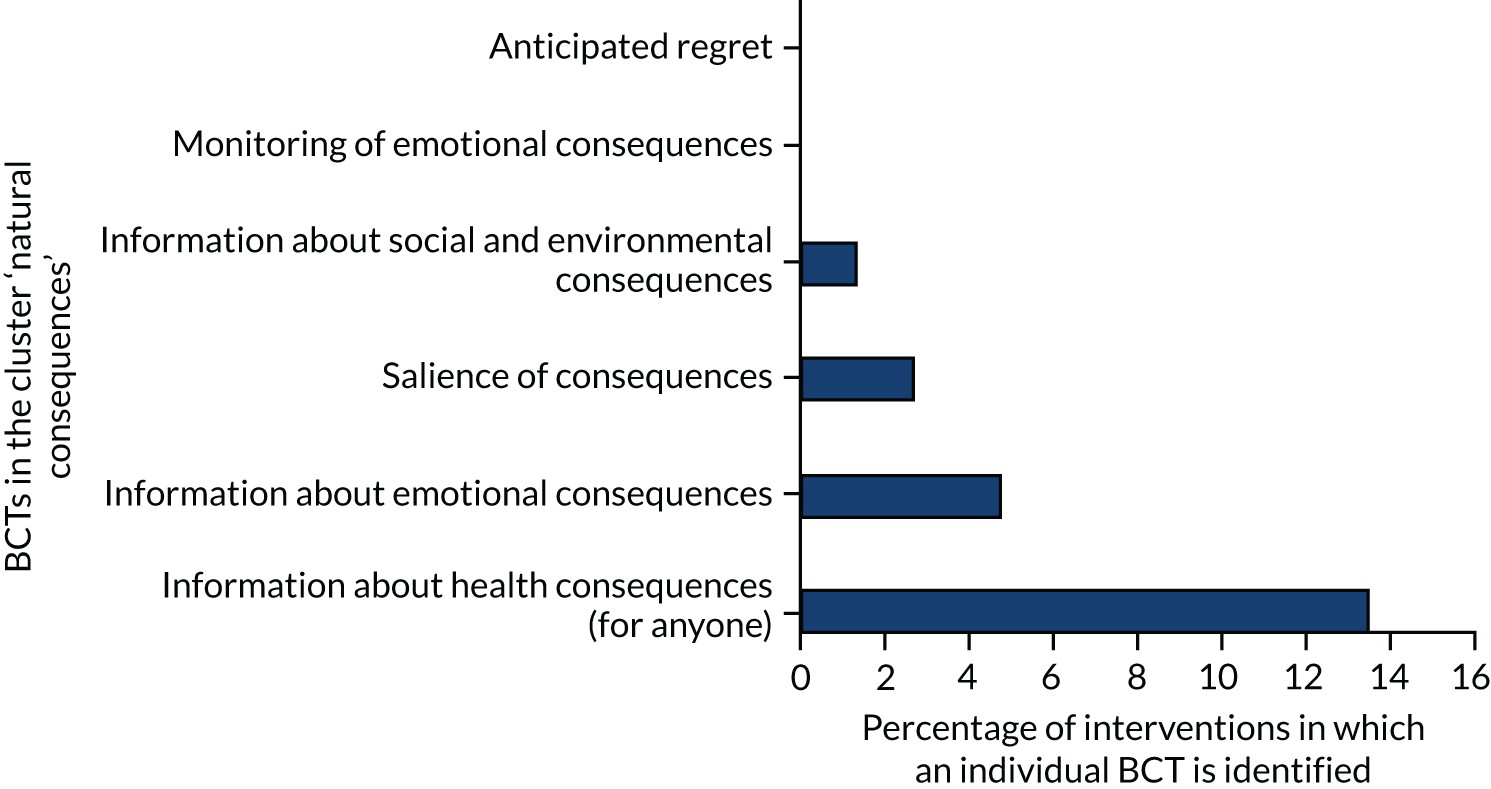
The consequence of the desired behaviour (defined as successful de-escalation) was the elimination of the harmful effects of restrictive practices. Interventions described consequences of de-escalation failure predominantly on service users, although some interventions also referred to consequences for staff (e.g. Forster et al. ). 234 Some interventions merely talked about ‘negative’ consequences without specifying what these were, and so these were coded as health consequences. Health consequences (BCT 5.1) were specifically described in 23 interventions, primarily about physical risks to the service user. For example, Space Training235 included emphasis on understanding inherent risks of physical interventions, with a specific focus on ‘positional asphyxia’.
Some interventions (n = 7) emphasised physical and/or emotional health consequences, including interventions with a noticeable focus on the impact of restraint on the service user,123,143,195 and others that focused on health consequences for staff:70,141,236
. . . the goal of the program was both to reduce episodes of seclusion and restraint and reduce staff injuries. This intervention was designed to counteract the frequently encountered attitude that the real outcome of such programs is to place staff members at higher risk.
Forster et al. 234
. . . a series of mandated workshops on trauma-informed care, were created that included education on the neurobiological and psychosocial effects of trauma, the relationship of dissociative symptoms and self-harm to posttraumatic stress disorder (PTSD), and the retraumatization that occurs from being restrained or witnessing use of restraints and seclusion.
Chandler201
The broader social and environmental consequences of restrictive practices were referred to by only one study:
Has leadership evaluated the impact of reducing S/R [seclusion and restraint] on the whole environment? (This includes issues such as increased destruction of property; extended time involved in de-escalation attempt, additional admission assessment questions, debriefing activities and processes to document event, etc.)
Huckshorn133
‘Salience of consequences’ (BCT 5.2) was coded when interventions used particular methods to emphasise the consequences of not performing successful de-escalation and restrictive practices being used:
Each staff member experienced 5-point restraints first-hand, and many cited that experience as pivotal in their decision whether or not to restrain a patient in a state of agitation when queried 1 year after the course.
Forster et al. 234
The service users educated the project workers in consumer specialist meetings (1 hour per week) about their own experiences with violence and coercion, individual triggers of violence, and effective calming activities.
Putkonen et al17
This often included service user testimony about the consequences of their traumatic experiences of restrictive practices, for example Riley et al. 134
Repetition and substitution
As illustrated in Figure 19, 3% of the BCTs detected were in the cluster ‘repetition and substitution’ and consisted of three of the seven possible BCTs: ‘behavioural practice/rehearsal’ (BCT 8.1), ‘habit formation’ (BCT 8.3) and ‘reversal’ (BCT 8.4). ‘Behaviour substitution’ (BCT 8.2), ‘overcorrection’ (BCT 8.5), ‘generalisation of target behaviour’ (BCT 8.6) and ‘graded tasks’ (BCT 8.7) were not detected in any interventions.
FIGURE 19.
Behaviour change technique cluster 8: repetition and substitution.
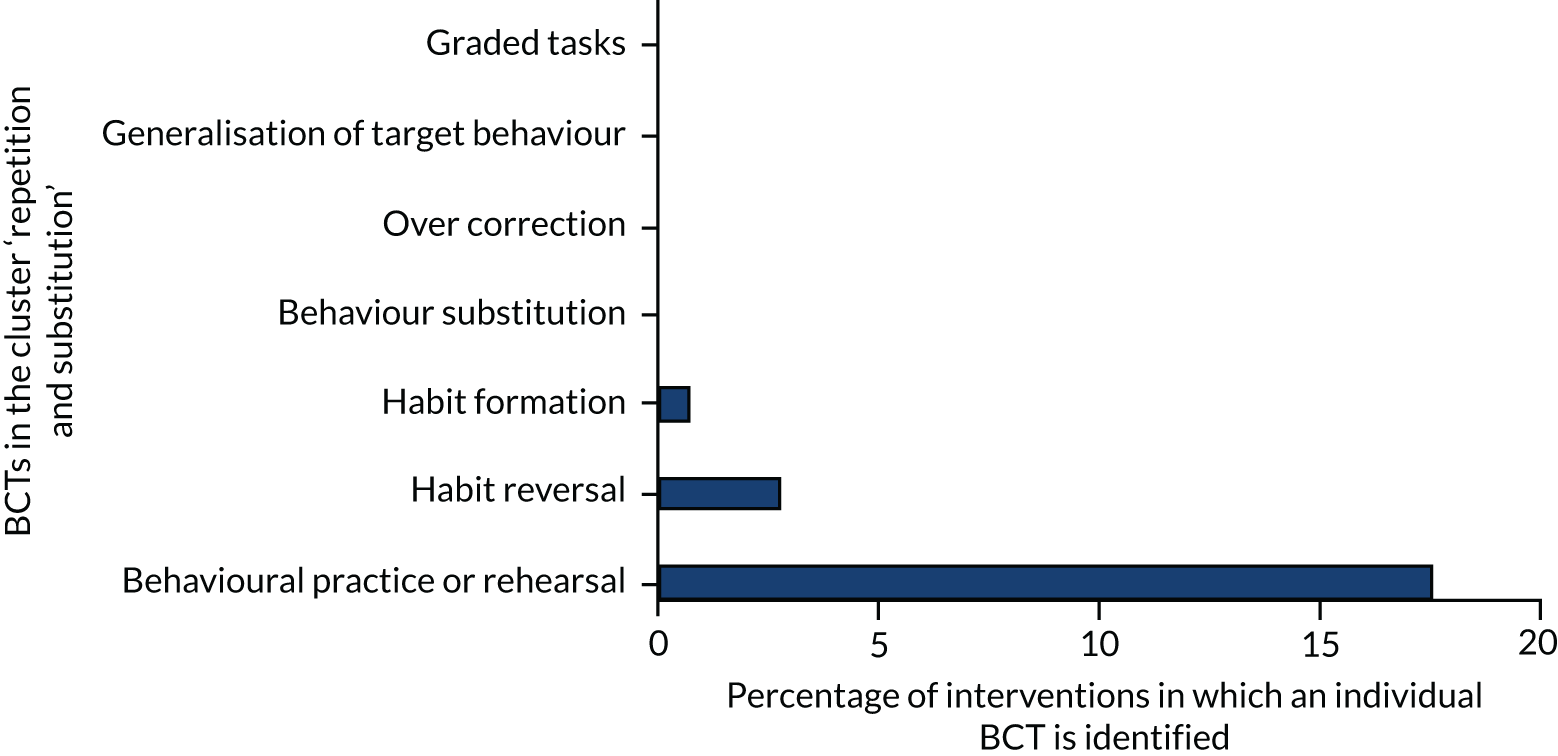
Twenty-eight interventions described staff taking part in activities to practise and rehearse de-escalation skills. This was most typically in the form of role-play activities:
These team-building exercises, it was hoped, would highlight the different roles staff members play in the restraint process, crisis intervention, and de-escalation techniques. It was expected that these exercises would help to clarify the roles staff members play in a crisis and allow them to practice crisis management techniques.
Melin69
Detail was rarely provided about whether or not staff played the role of the service user. Some interventions did give details, with one using a fully immersive role-play scenario using actors in other roles.
There was little content in the interventions relating to habit, although one habit formation (BCT 8.3) technique was identified in Safewards, the requirement that staff:
. . . say something good about each patient at nursing shift handover . . .
Bowers et al. 16
There was one example of ‘habit reversal’ (BCT 8.4), used within four interventions,16,159,213,222 that encouraged staff to break the habit of saying ‘no’ to service user requests:
This has led to a culture of ‘say yes first’ at the trust, which helps patients to understand what needs to happen for a member of staff to say ‘yes’. The ‘reflect’ acronym helps staff to remember what they need to consider when answering a patient’s request: R – Reframe: What would it have taken to say yes? E – Easy: Was ‘no’ the easy option? F – Feeling: What would it have felt like? L – Listen: Did we listen? E – Explain: Did we explain? C – Creative: Were we creative enough? T – Time: Did we take the time?
East London NHS Foundation Trust, 2017. 85 Contains public sector information licensed under the Open Government Licence v3.0
First reflex should be saying ‘yes’, not ‘no’. Do you really need to say ‘no’? Can you justify saying ‘no’? Is this something that with a bit of effort or work or checking, you could say ‘yes’ or at least a partial ‘yes’ to?
Safewards213
Comparison of outcomes
As seen in Figure 20, cluster 9, ‘comparison of outcomes’, contained 2% of the BCTs with only one detected from the three within this cluster. ‘Pros and cons’ (BCT 9.2) and ‘comparative imagining of future outcomes’ (BCT 9.3) were not identified. The only BCT in this cluster was that of using a ‘credible source’ (BCT 9.1), usually as a way of imparting information. A variety of these credible sources were described within the interventions. Service users were used in 13 interventions:
When staff began to accept peers as co-workers and began to rely on them as a crucial part of the workforce, attitudes toward recovery changed significantly, and the tendency to use seclusion and restraint became more and more remote.
Ashcraft and Anthony193
FIGURE 20.
Behaviour change technique cluster 9: comparison of outcomes.
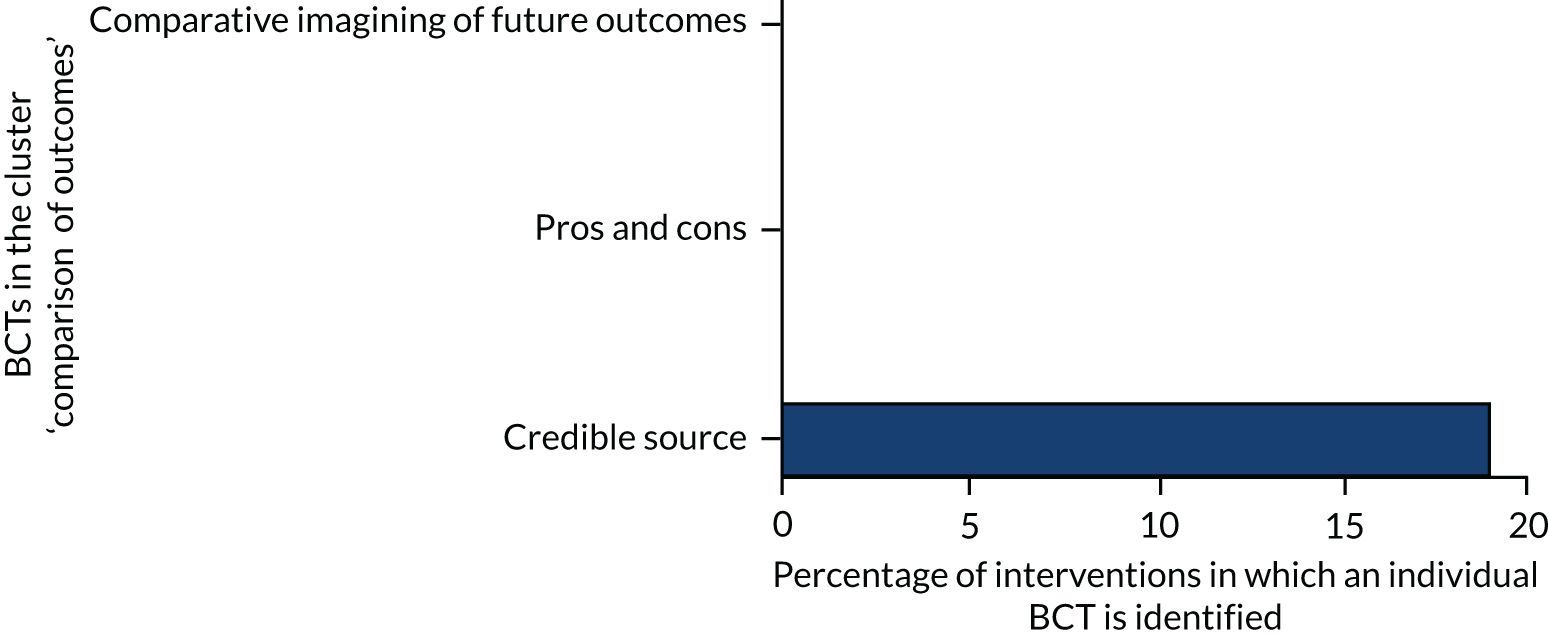
The psychological impact of restrictive practices was described by service users as part of training or other awareness-raising activities, this was also coded as ‘salience of consequences’ (BCT 5.2):
At the engagement sessions, delivered in partnership with service users, teams are introduced to No Force First and hear accounts of people’s experience of physical intervention.
Riley et al. 134
Clinical specialists were also described as credible sources in other interventions, either delivering training or describing the physical impact of restraint on the service user (e.g. a medical director in Madan et al. 108). One other type of credible source was academic researchers feeding back intervention data to ward staff (e.g. Mann-Poll et al. 212).
Reward and threat
As illustrated in Figure 21, cluster 10 (‘reward and threat’) contained 4 of the 11 possible BCTs. Future punishment, self-reward/incentive, non-specific reward/incentive and material reward/incentive (behaviour) were not detected. Two per cent of BCTs were in this cluster. Incentives and rewards could be ‘non-specific’ (BCT 10.6, BCT 10.3), ‘material’ (BCT 10.1, BCT 10.2) or ‘social’ (BCT 10.5, BCT 10.4). There could also be ‘self-incentive’ (BCT 10.7) and ‘self-reward’ (BCT 10.9), and could also be associated with ‘behaviour or outcome’ (BCT 10.8, BCT 10.10).
FIGURE 21.
Behaviour change technique cluster 10: reward and threat.
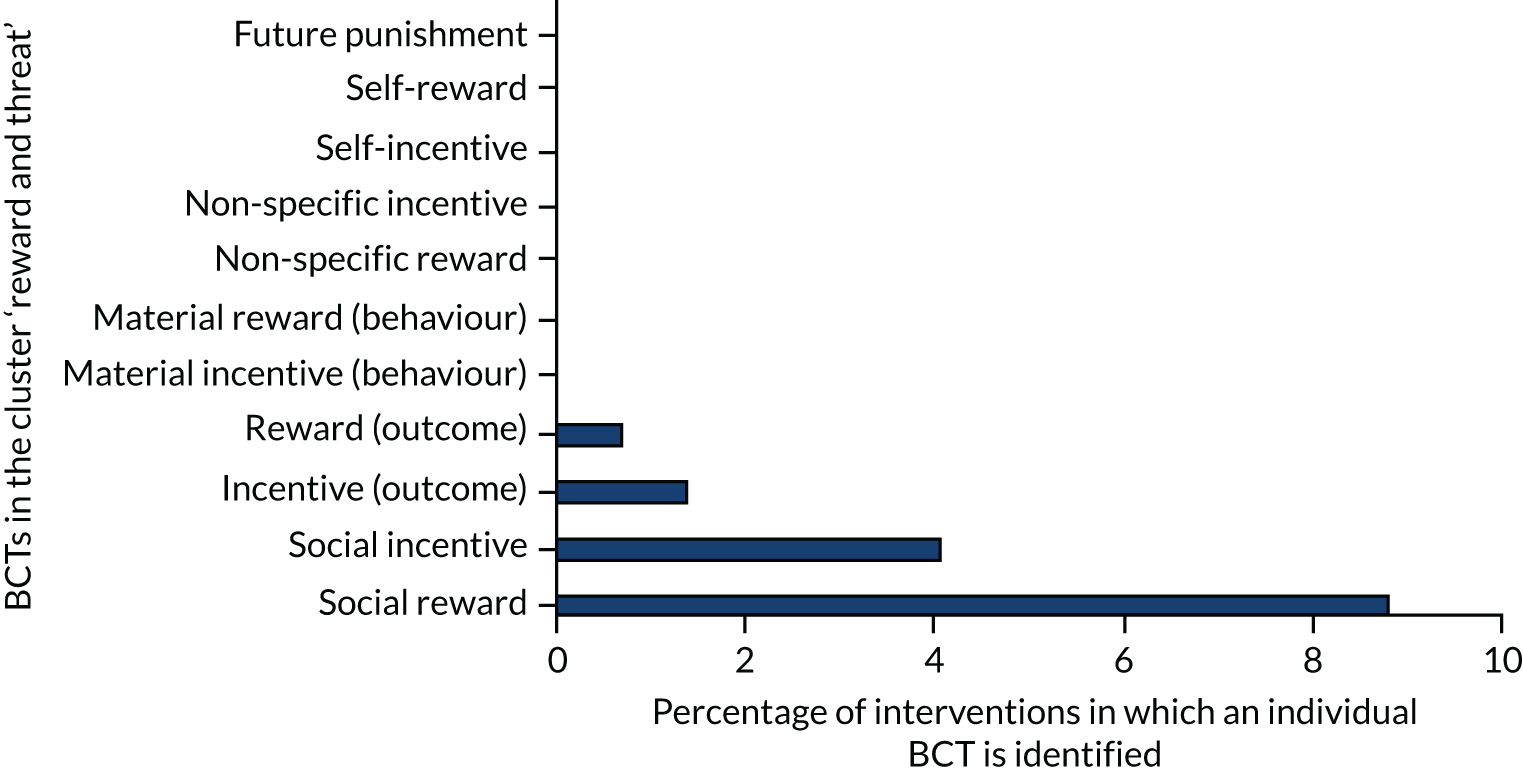
Most of the incentive and reward described within the interventions was of the social variety (BCT 10.4, BCT 10.5). In some interventions, wards or individuals were praised for reducing restrictive practices (e.g. Szypula and Martin89) through awarding certificates, celebrations of success, favourable publicity in service newsletters, and notice boards where positive messages can be left. For instance, a board in a staff office was used for staff to write supportive messages and compliments about the good work they were doing; this proved popular and eventually transferred into the patient area so that both patients and staff could write on it. 83
Blair and Moulton-Adelman222 reported the following:
Ongoing recognition of unit successes and individual staff initiatives related to improved patient care is encouraged. Such steps reinforce positive movement toward a therapeutic culture of care and improve overall morale and cohesiveness.
Blair and Moulton-Adelman222
Blair and Moulton-Adelman222 describe that success is acknowledged in many ways, including recognition of individuals in staff meetings, department-wide e-mails, and get-togethers organised across the unit for the purpose of celebrating the achievement of specific milestones. The celebrations help to reinforce awareness of the goals yet to be reached. 222
‘Material incentives and rewards’ (BCT 10.1, BCT 10.2) were few, although one intervention had a competition with a prize for the best performing ward, and cinema tickets were raffled among ward staff. 237 Continuing professional development (CPD) credits were used in one intervention as an incentive for attending training. 115
Regulation
Very few of the interventions used BCTs from the cluster ‘regulation’ (0.6%) and only one of the four possible BCTs was identified. As illustrated in Figure 22, ‘pharmacological support’ (BCT 11.1), ‘conserving mental resources’ (BCT 11.3) and ‘paradoxical instructions’ (BCT 11.4) were not identified. The only BCT detected in this cluster was ‘reduce negative emotions’ (BCT 11.2), which was targeted at reducing staff stress in order to promote the reduction of restrictive practices. Several interventions (n = 8) described a focus on reducing staff stress in general terms, although some addressed specific aspects of staff stress including anxiety,141 frustration236 or burnout:70
The strategy of allowing people to vent about possible negative outcomes was needed to create space for possibilities.
Ashcraft et al. 24
FIGURE 22.
Behaviour change technique cluster 11: regulation.
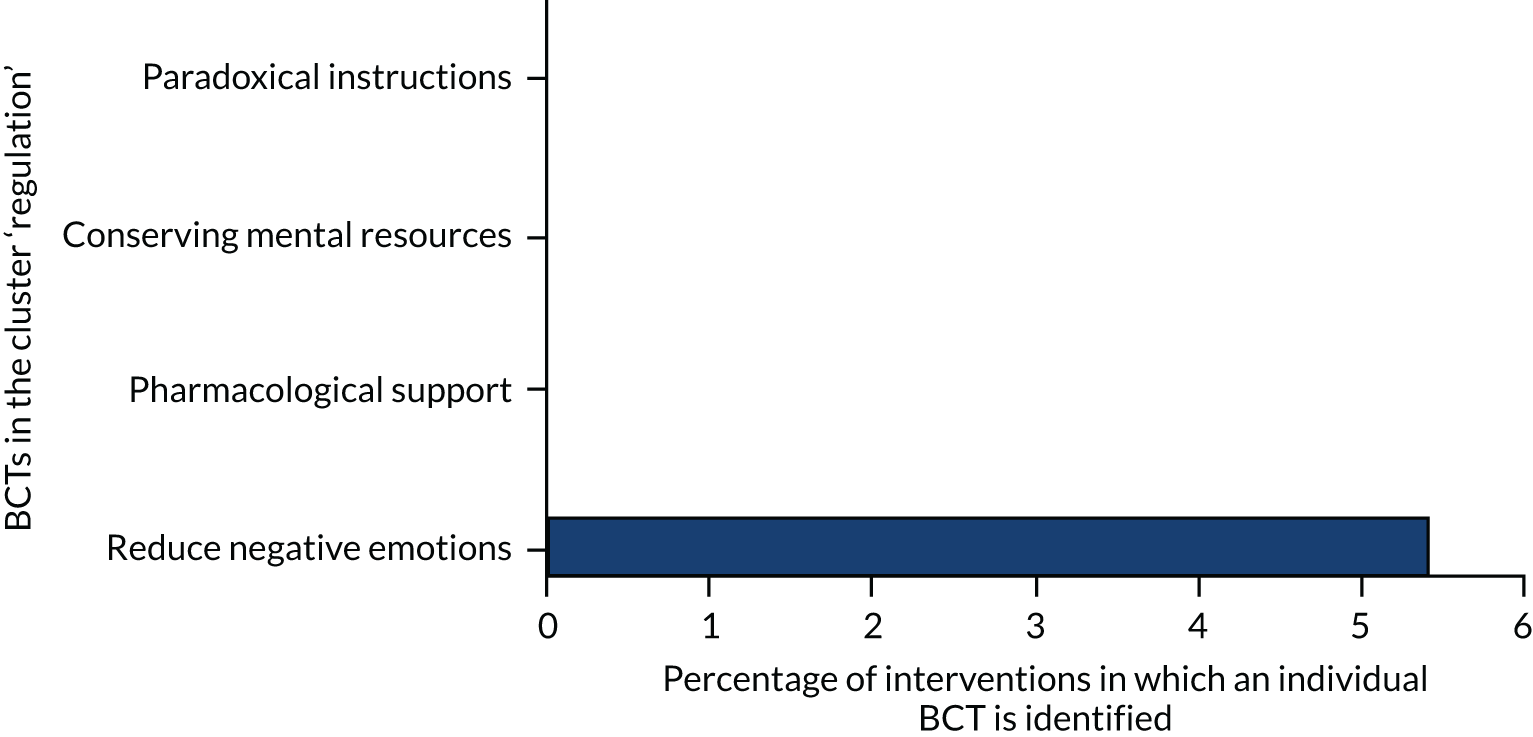
Other studies focused on reducing staff negative emotions during the post-incident debrief:
Opportunities are provided/scheduled to process the event with staff about their feelings, reactions, and safety.
Colton176
Scheduled consequences
Few aspects of cluster 14, ‘scheduled consequences’ (reward and punishment), were used in the interventions, with only 0.3% of BCTs being in this cluster and only one BCT identified: ‘remove punishment’ (BCT 14.10). ‘Behaviour cost’ (BCT 14.1), ‘punishment’ (BCT 14.2), ‘remove reward’ (BCT 14.3), ‘reward approximation’ (BCT 14.4), ‘rewarding completion’ (BCT 14.5), ‘situation-specific reward’ (BCT 14.6), ‘reward incompatible behaviour’ (BCT 14.7), ‘reward alternative behaviour’ (BCT 14.8) and ‘reduce reward frequency’ (BCT 14.9) were not identified (Figure 23).
FIGURE 23.
Behaviour change technique cluster 14: scheduled consequences.
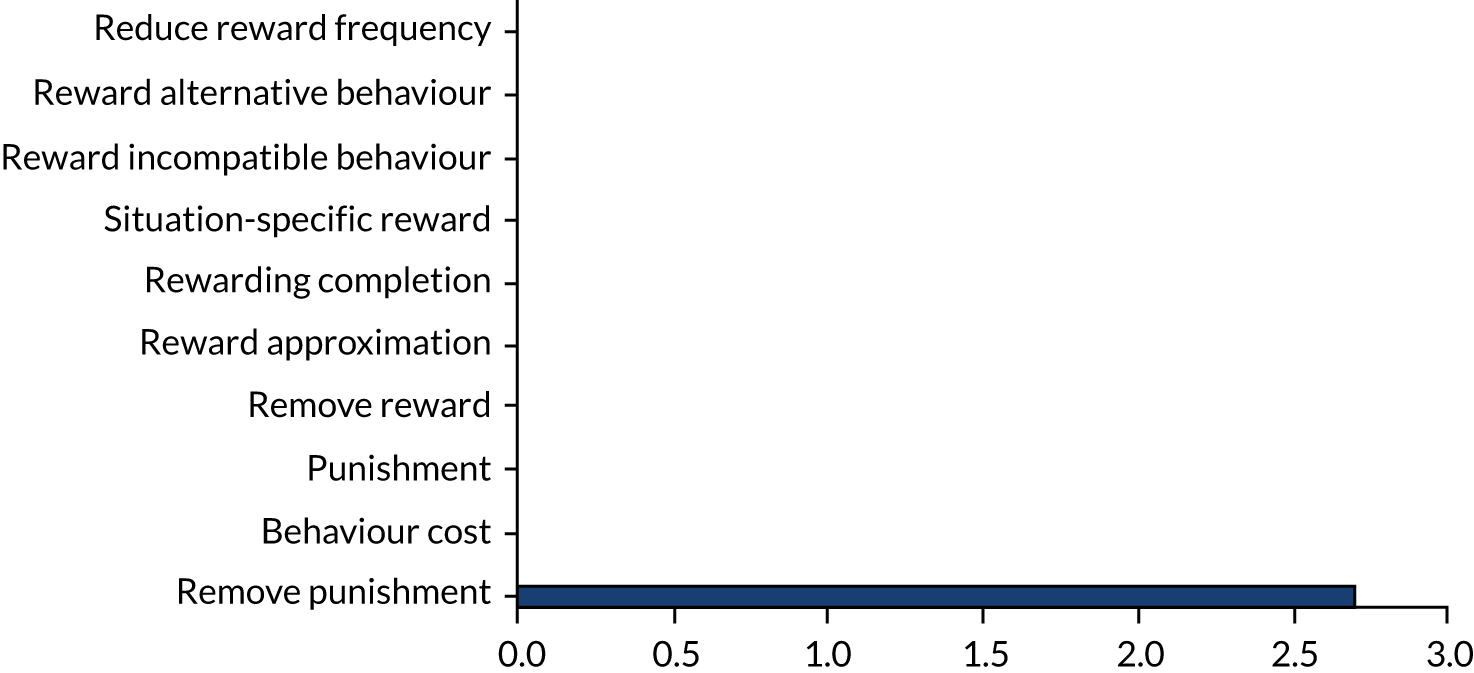
The removal of punishment referred to the removal of an unpleasant consequence if the desired behaviour is performed. In five interventions,132,133,159,238,239 this was described as ensuring that debriefing sessions were supportive and not blaming to promote reflection on attempted de-escalation from the staff members involved, even if the episode had resulted in the use of a restrictive practice:
There was a focus on performance, but the approach was one of curiosity and help rather than summative judgement.
Lombardo et al. 159
Administrators have carefully fostered a welcoming, nonthreatening atmosphere that helps direct care staff overcome their initial trepidation about attending the meetings in the medical director’s office. Leaders have purposefully avoided any appearance of assigning blame or ‘second guessing’ decisions that have been made by direct care staff.
Allen et al. 238
Unused or little used behaviour change technique clusters in interventions
Two clusters of BCTs, ‘self-belief’ and ‘covert learning’, were not detected in any of the interventions (Box 1). The ‘self-belief’ category contains techniques that aim to promote self-efficacy, a determinant that has a key role in reducing lapses and coping with behavioural barriers. 240
15.1. Verbal persuasion about capability.
15.2. Mental rehearsal of successful performance.
15.3. Focus on past success.
15.4. Self-talk.
16. Covert learning16.1. Imaginary punishment.
16.2. Imaginary reward.
16.3. Vicarious consequences.
Some clusters featured only by virtue of one BCT being coded (coded BCT in bold) (Box 2).
11.1. Pharmacological support.
11.2. Reduce negative emotions.
11.3. Conserving mental resources.
11.4. Paradoxical instructions.
14. Scheduled consequences14.1. Behaviour cost.
14.2. Punishment.
14.3. Remove reward.
14.4. Reward approximation.
14.5. Rewarding completion.
14.6. Situation-specific reward.
14.7. Reward incompatible behaviour.
14.8. Reward alternative behaviour.
14.9. Reduce reward frequency.
14.10. Remove punishment.
As illustrated in Box 2, there were two little-used BCT clusters: ‘regulation’ and ‘scheduled consequences’. Within these, ‘reduce negative emotions’ (highlighted in italics in Box 2) was coded in relation to stress reduction elements of an intervention, and ‘remove punishment’ (highlighted in italics in Box 2) referred to ensuring that, when de-escalation had failed and restrictive practices had been used, the staff member could debrief reflexively on what could have been done differently, rather than in anticipation of punishment.
It should be noted that, for a BCT to be identified in an intervention, there had to be evidence of its presence within the intervention materials. Therefore, there may be instances where a BCT remained unidentified owing to lack of evidence. See Appendix 14 for a full list of the BCTs that were not identified in the interventions.
Mechanisms of action
In behavioural science, mechanisms of action are posited as the theoretical constructs through which BCTs affect behaviour. Recent work has specified 26 mechanisms of action, drawn from the Theoretical Domains Framework241 and a systematic review of 83 behaviour change theories. 242 Understanding how specific BCTs have their effects on behaviour will help us to explain intervention effects and to evaluate interventions and, as evidence accumulates, potentially help us to develop more effective and/or efficient interventions. The Theory and Techniques Tool243 was used to identify the mechanisms of action for which there were identified links with the BCTs identified in studies reporting positive findings.
The BCTs that were used in studies reporting positive findings are shown in relation to their established links with mechanisms of action (Table 9). This shows that the most common mechanisms of action linked to BCTs in studies reporting successful findings were ‘environmental context and resources’ and ‘behavioural cueing’. ‘Environmental context and resources’ is defined as changes to aspects of a person’s situation or environment that discourage or encourage the behaviour (in this case de-escalation). BCTs linked with this were ‘restructuring the social environment’ (BCT 12.2), for example introducing social contact with service users; ‘prompts or cues’ (BCT 7.1), such as completing a daily risk assessment’; ‘restructuring the physical environment’ (BCT 12.1), perhaps by removing a seclusion room; and ‘adding objects to the environment’ (BCT 12.5), for example adding a sensory cart to a ward. ‘Behavioural cueing’ indicates processes by which behaviour is triggered from the external environment, from the performance of another behaviour or from ideas appearing in consciousness. The BCTs that used ‘behavioural cueing’ included ‘adding objects’ such as posters, ‘prompts’ such as risk assessment or flow charts, ‘action-planning’ through care-planning or team meetings, and ‘changes to the physical environment’, for example the introduction of a sensory room.
| BCT | Mechanisms of action | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Skill | Belief about capabilities | Behavioural regulation | Behavioural cueing | Feedback processes | Environmental context and resources | Social influences | Memory attention and decision processes | Attitude towards the behaviour | |
| 4.1 Instruction on how to perform the behaviour | ✗ | ✗ | ✗ | |||||||
| 12.2 Restructuring the social environment | ✗ | |||||||||
| 1.2 Problem-solving | ✗ | ✗ | ||||||||
| 1.4 Action-planning | ✗ | |||||||||
| 7.1 Prompts or cues | ✗ | ✗ | ✗ | |||||||
| 13.2 Framing/reframing | ✗ | |||||||||
| 2.7 Feedback on outcome(s) of behaviour | ✗ | |||||||||
| 4.2 Information about antecedents | ✗ | ✗ | ||||||||
| 12.5 Adding objects to the environment | ✗ | ✗ | ||||||||
| 12.1 Restructuring the physical environment | ✗ | ✗ | ||||||||
The second most common was that of ‘behavioural cueing’: processes by which behaviour is triggered from the external environment, the performance of another behaviour, or from ideas appearing in consciousness. The BCTs that used ‘behavioural cueing’ included ‘adding objects to the environment’, such as posters, ‘prompts or cues’ such as risk assessment or flow charts, and ‘action-planning’ through care-planning or team meetings as well as ‘changes to the physical environment’, such as the introduction of a sensory room.
The ‘knowledge’ mechanism of action was targeted by two BCTs. The first was ‘instruction of how to perform the behaviour’ (BCT 4.1), which was coded whenever training in effective de-escalation was present. ‘Information about antecedents’ (BCT 4.2) included education about what kind of factors often lead to incidents, at either an individual or a ward level.
Behavioural regulation was also targeted by the BCTs ‘information about antecedents’ (BCT 4.2) and ‘problem-solving’ (BCT 1.2), which could include discussion with an individual service user about how staff could behave towards them to ensure that incidents involving restrictive practice were avoided. This could also include discussion within staff teams, sometimes in the form of a safety huddle, where the overall needs of the ward were discussed and resources reallocated to avoid incidents developing.
Skill was targeted by ‘instruction on how to perform behaviour’ (BCT 4.1), in which staff were taught specific skills related to de-escalation, for example non-confrontational verbal approaches. Feedback processes were targeted by ‘feedback on outcomes of behaviour’ (BCT 2.7); this commonly involved wards receiving a weekly summary of how many incidents of restrictive practices had occurred. Attitude towards the behaviour was targeted by ‘framing/reframing’ (BCT 13.2). An example of this was when Trauma-Informed Care approaches were introduced to a service and staff were encouraged to view the use of restrictive practices as retraumatising, rather than as a necessary part of clinical work. Memory, attention and decision processes were targeted by ‘prompts or cues’ (BCT 7.1), such as carrying out a risk assessment as part of each admission.
It is worth noting that none of the BCTs in studies that reported significant positive findings targeted optimism, social/professional role and identity, needs, values or emotion. Of these, only emotion has any evidence of links with BCTs and there is only one (BCT 11.2: ‘reduce negative emotion’). As such, it may be that there are methods for targeting these mechanisms of action but no connections have so far been made between them and individual BCTs. Appendix 15 provides further detail regarding the identification of BCTs in evaluations of interventions that reduced restrictive practices.
Conclusion
The results of the application of the BCT taxonomy to 150 interventions that sought to reduce restrictive practices identified 43 out of a possible 93 BCTs within the intervention materials. The most frequently identified BCT was ‘instruction on how to perform the behaviour’ (BCT 4.1), reflecting the high use of training within interventions. The other most frequently identified BCTs were within the ‘goals and planning’ cluster, followed by ‘shaping knowledge’, ‘antecedents’ and ‘feedback and monitoring’. These four clusters contained over two-thirds of the BCTs.
Chapter 6 Results of the behaviour change technique synthesis: behaviour change techniques in intervention procedures
This chapter presents the results of the BCT synthesis. The BCTs found in the interventions are grouped and described here. The full list of records included in the review is provided in Appendix 16.
Behaviour change techniques by intervention procedure
Twelve per cent of interventions used only one procedure, with the rest containing multiple procedures, for example staff training and audit and feedback or nursing changes and service user involvement. The BCTs detected in individual procedures were extracted and are detailed below.
Training
As illustrated in Figure 24, staff training was the procedure most frequently reported in interventions. The most frequent BCT detected was that of instruction, although that was coded for every training intervention even if no detail was provided. Following instruction, there were numerous other BCTs detected; Figure 24 shows those featuring in > 10% of interventions. Reframing the beliefs of participants often involved education about Trauma-Informed Care or, less frequently, the recovery model. ‘Problem-solving’ featured within training when participants were asked to consider their own settings and examine what antecedents led to incidents, and ‘action-planning’ featured where it was decided to make changes to avoid them. ‘Restructuring of the social environment’ via training might include aspects such as encouraging staff to try to have more contact with service users.
FIGURE 24.
Procedures: training: 135 interventions coded.

Training often involved staff practising or rehearsing de-escalation by taking part in role play, with each other, with the trainers or even with actors. Feedback on performance could involve social support from peers and trainers. Training was delivered by professional trainers from specific companies, sometimes using a ‘train the trainer’ model. Other interventions used senior clinical staff to deliver training and external trainers often came from clinical backgrounds. Service users were included in training, delivering information about the consequences of experiencing restrictive practices and increasing the salience of those consequences through telling of their personal experience.
Some interventions encouraged trainees to see themselves as a role model by taking their learning back to the workplace and sharing it with other staff, as well as leading by example.
Audit and feedback
Audit and feedback are when clinical performance-related data are collected and fed back to health-care staff, and are often available in electronic format. As illustrated in Figure 25, the audit and feedback procedures in the interventions typically consisted of data being collected from ward staff about any restrictive practices that occurred on the ward. These data might be the number of restraints or seclusion, the duration of seclusion or the use of PRN medication. Data are often entered by ward staff onto a centralised system. A number of different variables affected how the data were fed back to staff teams. The frequency of feedback was variable and could be daily, weekly, monthly or quarterly. The level of detail varied in terms of whether it was ward- or service-level data. The means of feedback could be in person or electronically, to an individual or a team. Data could be made public or retained within the staff team. No data were fed back at individual staff level. The resulting discussion about the data could involve problem-solving and action-planning, particularly if the rates of restrictive practice had not decreased in line with goals. Practical social support was evident here with staff making suggestions and supporting each other, and celebrating successes, a type of social reward. Some wards self-monitored their rates of restrictive practices, perhaps collecting more detail than would be collected by central incident reporting systems, for example about antecedents. Comparison to others might feature if wards were comparing their rates with other wards. Some interventions also monitored outcomes without feeding them back to staff.
FIGURE 25.
Procedures: audit and feedback: 53 interventions coded.
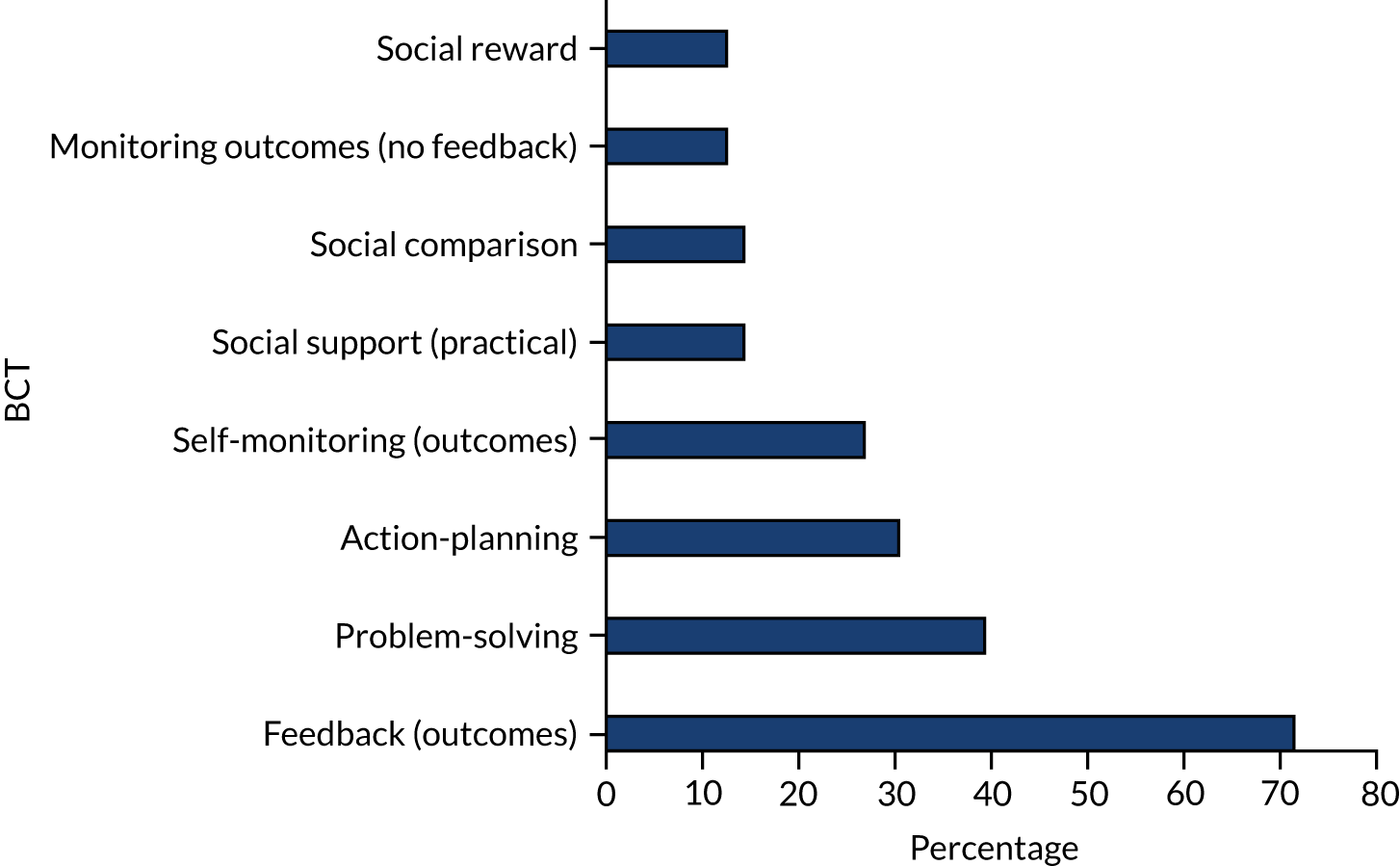
Nursing changes
As illustrated in Figure 26, the BCT detected most frequently in these interventions was ‘restructuring the social environment’. This often occurred through making staff more accessible and proactive to service user need as well as introducing new meetings to discuss ward safety (e.g. safety huddles), maybe with a regular prompt, often involving the ward staff monitoring their behaviour and providing each other with social support both practical and emotional. ‘Problem-solving and action-planning’ was carried out at individual and ward level with the overall milieu of the ward being the focus or individuals who might be experiencing distress. The underlying philosophy of care might be changed by adopting an approach such as Trauma-Informed Care or the recovery model. In these cases, ‘reframing’ would be used to change the beliefs of staff to view distress in a different way. Such approaches might encourage staff to see themselves as role models practising the new approach with service users and supporting other staff. Sometimes physical changes were made to service settings to make them more comfortable, or to include quiet areas: objects could be added such as exercise equipment or books and multimedia devices.
FIGURE 26.
Procedures: nursing changes: 48 interventions coded.
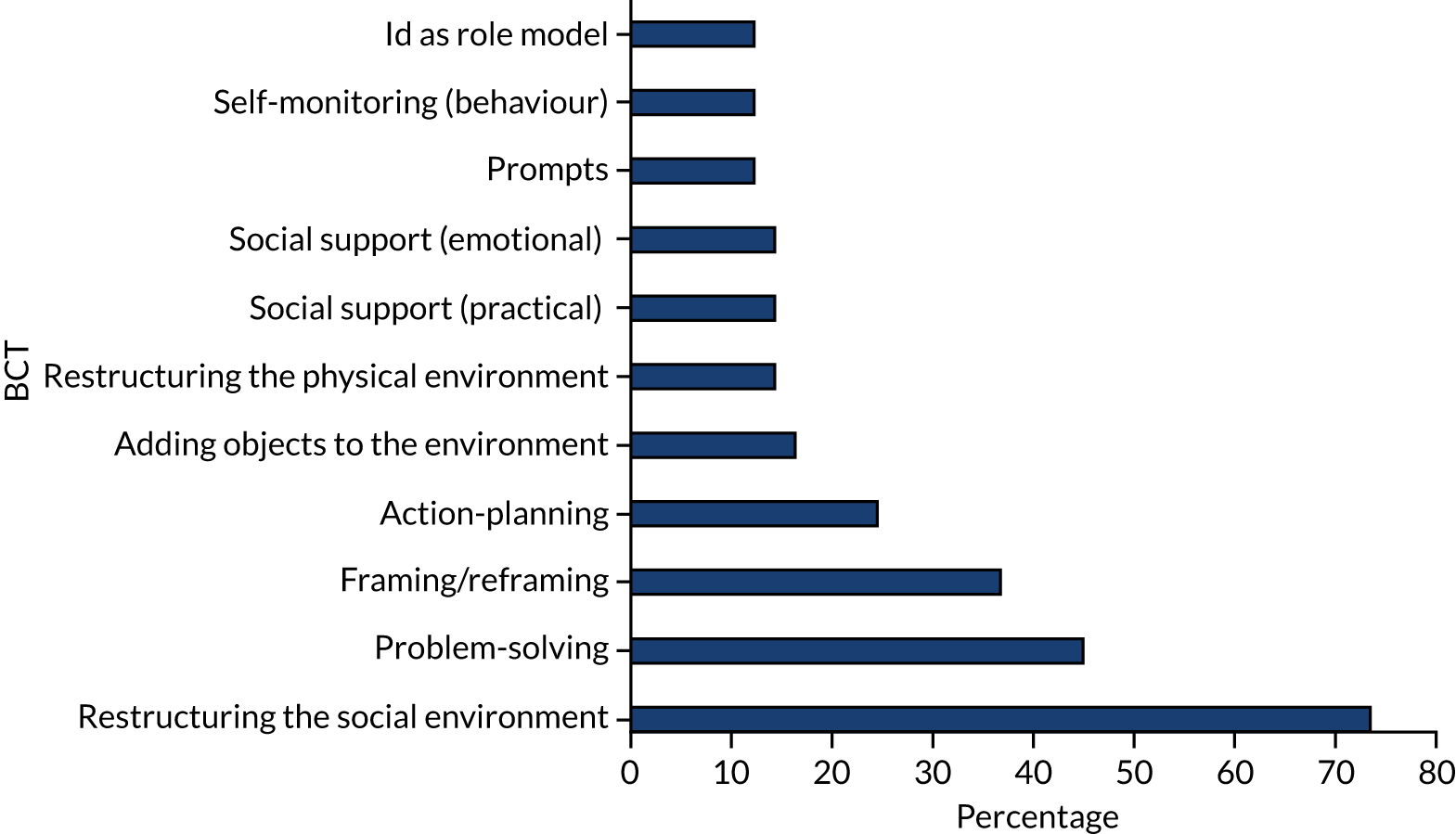
Service user involvement
As illustrated in Figure 27, the BCTs that were present with service user involvement were predominantly ‘restructuring the social environment’, ensuring that service users informed the development of interventions or parts of interventions. Service user committees were used for a variety of reasons including the ongoing monitoring of the behaviour of ward staff, reviewing the rates of restrictive practices and contributing towards problem-solving. Service users were part of delivering training, as a credible source testifying about the harms of restrictive practices, and were sometimes employed to provide staff with mentoring.
FIGURE 27.
Procedures: service user involvement: 37 interventions coded.
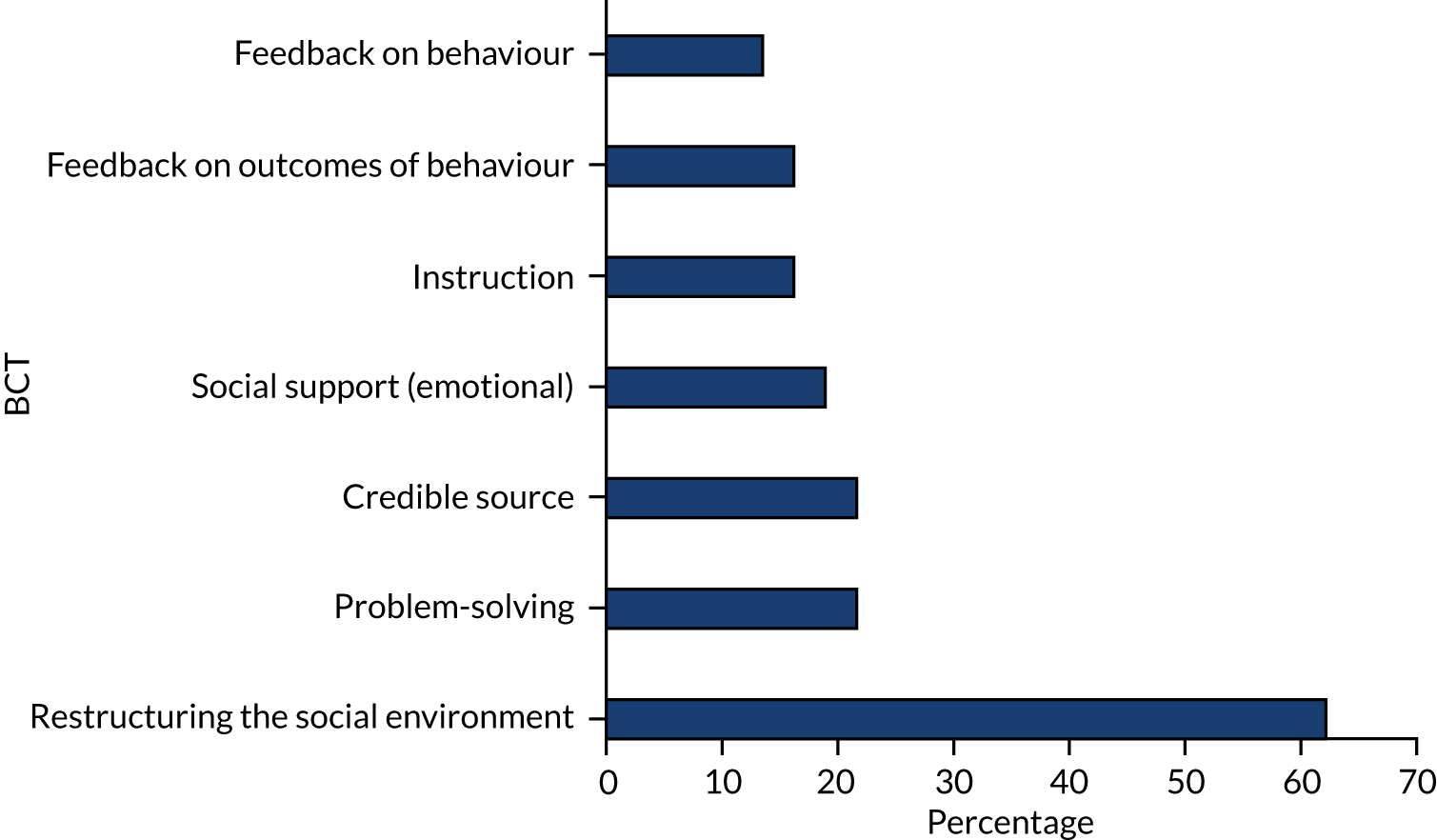
Care planning
As seen in Figure 28, care planning was one procedure used to reduce restrictive practices, primarily by attempting to problem-solve, by relating to service users’ needs while they were resident in a setting. The planning was frequently prompted by an admission, or might be carried out weekly with staff having a discussion with the service user about their current situation and/or previous experiences. It often included soliciting information about what ‘antecedents’ could cause distress and how they can be avoided. If a new method of care planning was introduced as part of the intervention, perhaps by placing greater value on service user perspectives, this might also be ‘restructuring the social environment’.
FIGURE 28.
Procedures: care planning: 37 interventions coded.
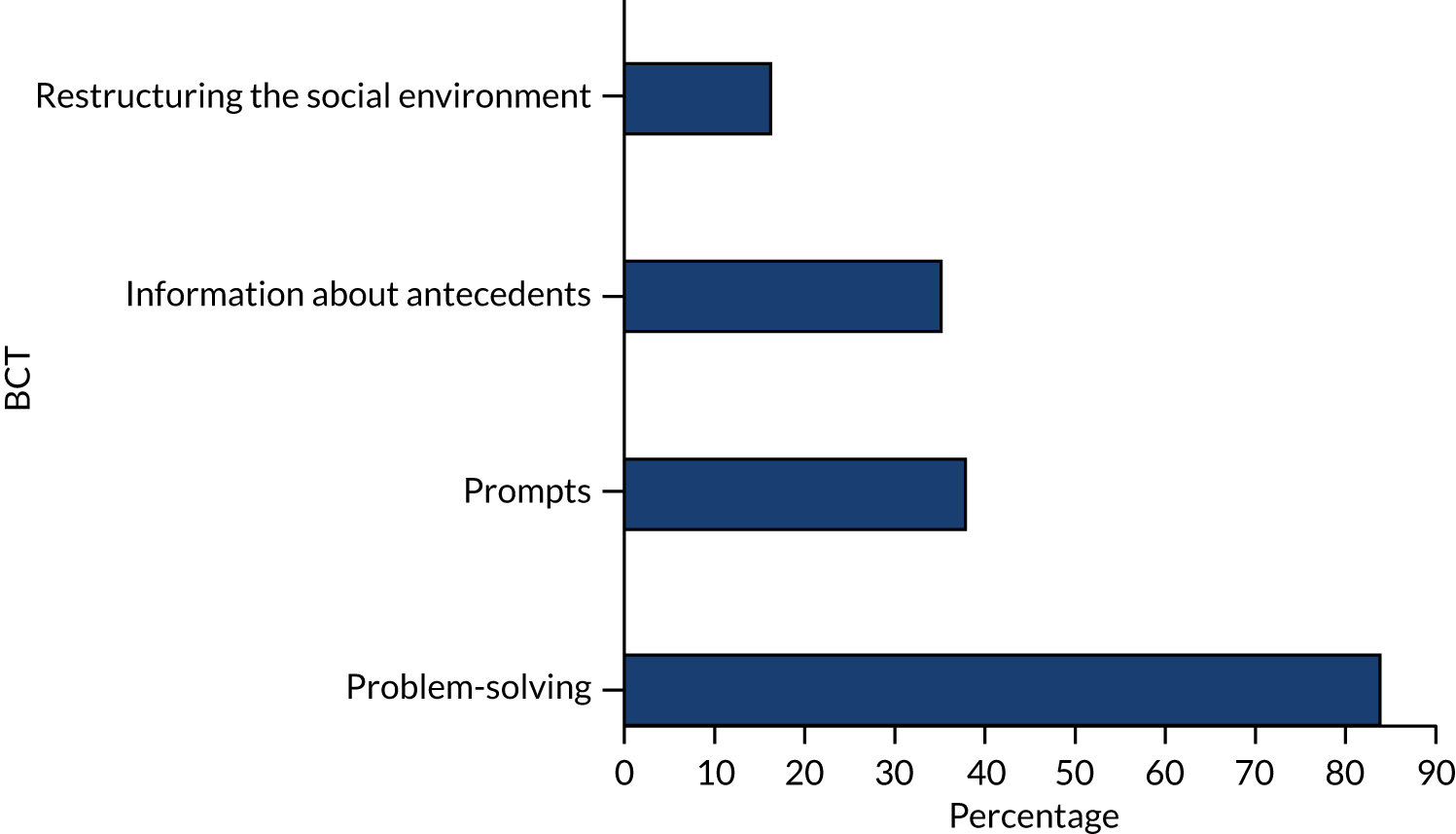
Communication strategies
As illustrated in Figure 29, procedures to improve communication focused on restructuring the social environment, often by introducing new fora for examining current behaviour and then problem-solving and action-planning with the provision of social support, sometimes involving service users.
FIGURE 29.
Procedures: communication: 32 interventions coded.
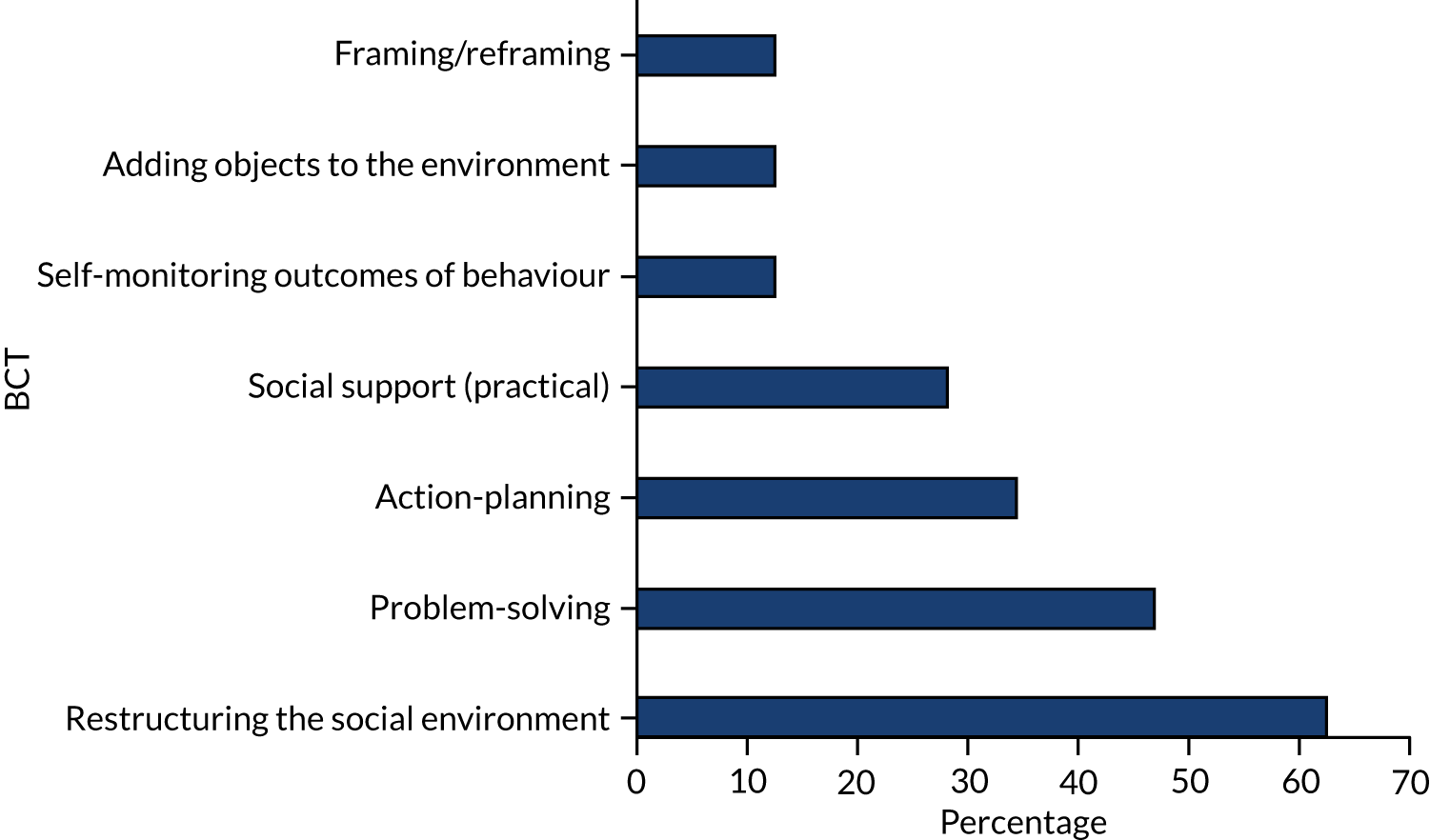
Procedures could add objects to support communication, for example a wall calendar allowing service users to book appointments with a doctor if they wished. These procedures were often informed by framing/reframing approaches such as Trauma-Informed Care and promoting service user involvement.
Debriefing
As illustrated in Figure 30, debriefing typically took place within a few hours of an incident of restraint. Debriefing after an incident when restrictive practices were used was an opportunity for both staff and service users to reflect on what happened (What antecedents had led up to the incident? What specific problems had arisen? Why had they not been solved? What could have been done differently? What would reduce the chances of the same thing happening again?) and its introduction was coded as a restructuring of the social environment. This involved problem-solving, action-planning and examining antecedents as well as receiving feedback on outcomes of the incident. The debrief was usually framed in positive terms so that staff did not feel that it was a form of punishment, rather an opportunity to reflect on what had happened and examine their behaviour. Debriefs involved a range of different people; they sometimes included only the staff member(s) involved but at other times included the service user, members of the broader staff team and senior managerial staff. One feature was the provision of social support, both practical and emotional.
FIGURE 30.
Procedures: debriefing: 30 interventions coded.
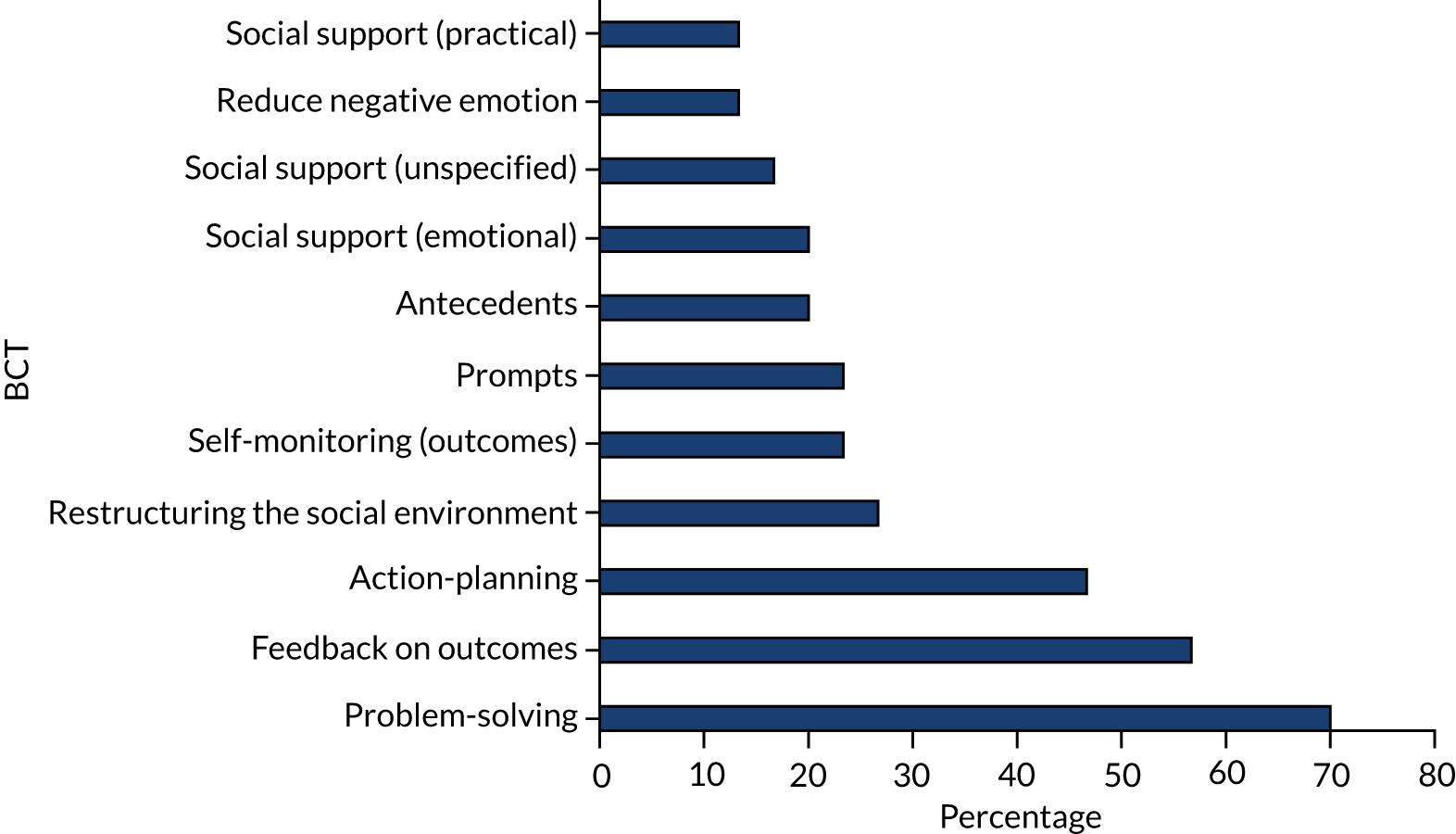
Sensory approaches
As illustrated in Figure 31, sensory procedures almost always included the addition of objects to the environment, usually sensory modulating equipment, available for service users to use on a ward. Some interventions restructured the physical environment by adding dedicated Sensory Rooms, quiet areas or even gardens. Assessments on admission for sensory preferences might become prompts to ensure that these facilities were tailored to the individual service user and involved problem-solving and action-planning.
FIGURE 31.
Procedures: sensory: 27 interventions coded.
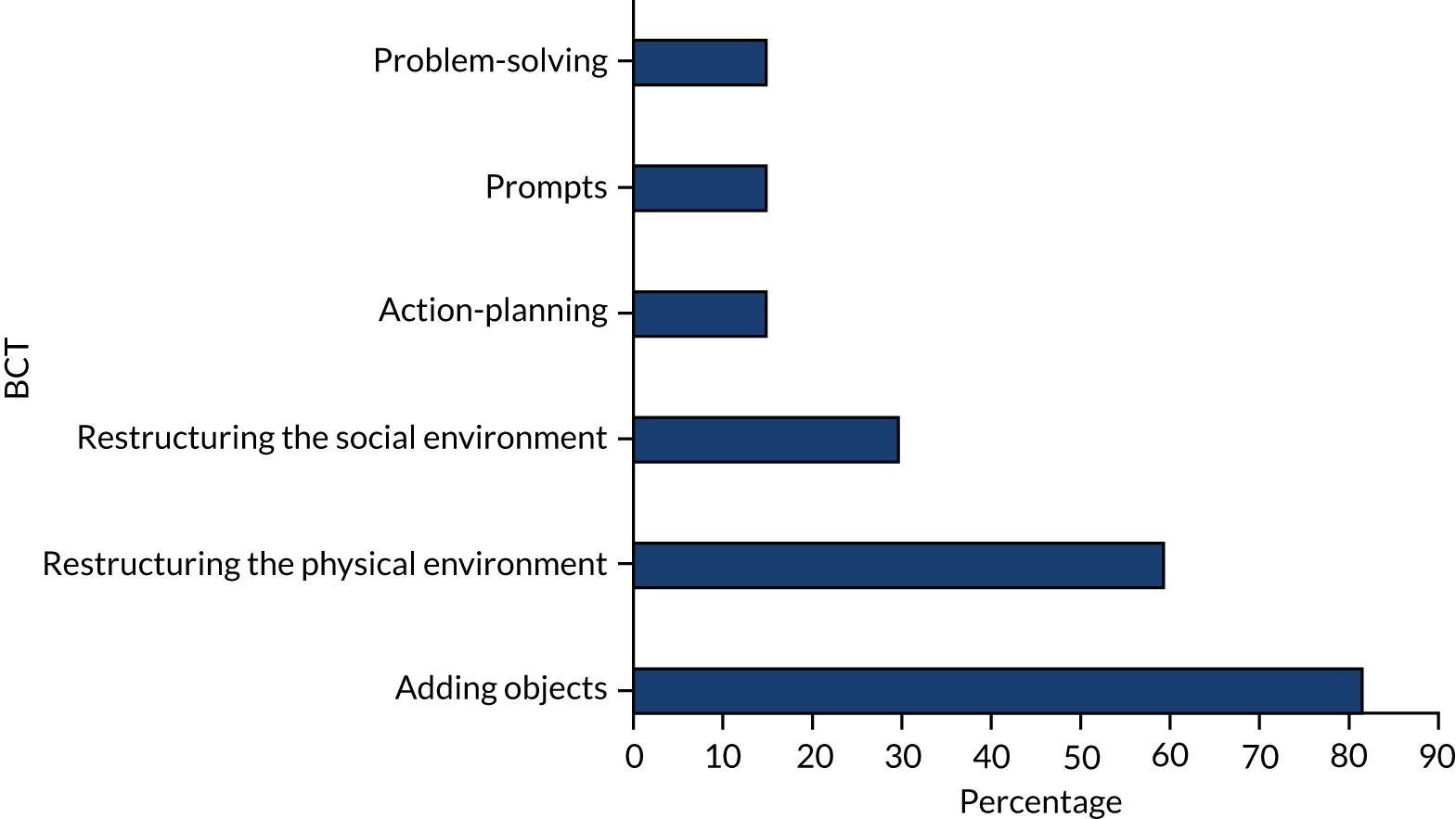
Policy change
Procedures that involved a change of policy or rules restructured the social environment (Figure 32). Some also involved framing/reframing such as adopting a recovery approach, social support through restructuring meetings, prompts to carry out regular risk assessments, and problem-solving and goal-setting often through meetings. Objects added to the environment included posters displaying information about service rules.
FIGURE 32.
Procedures: policy: 26 interventions coded.
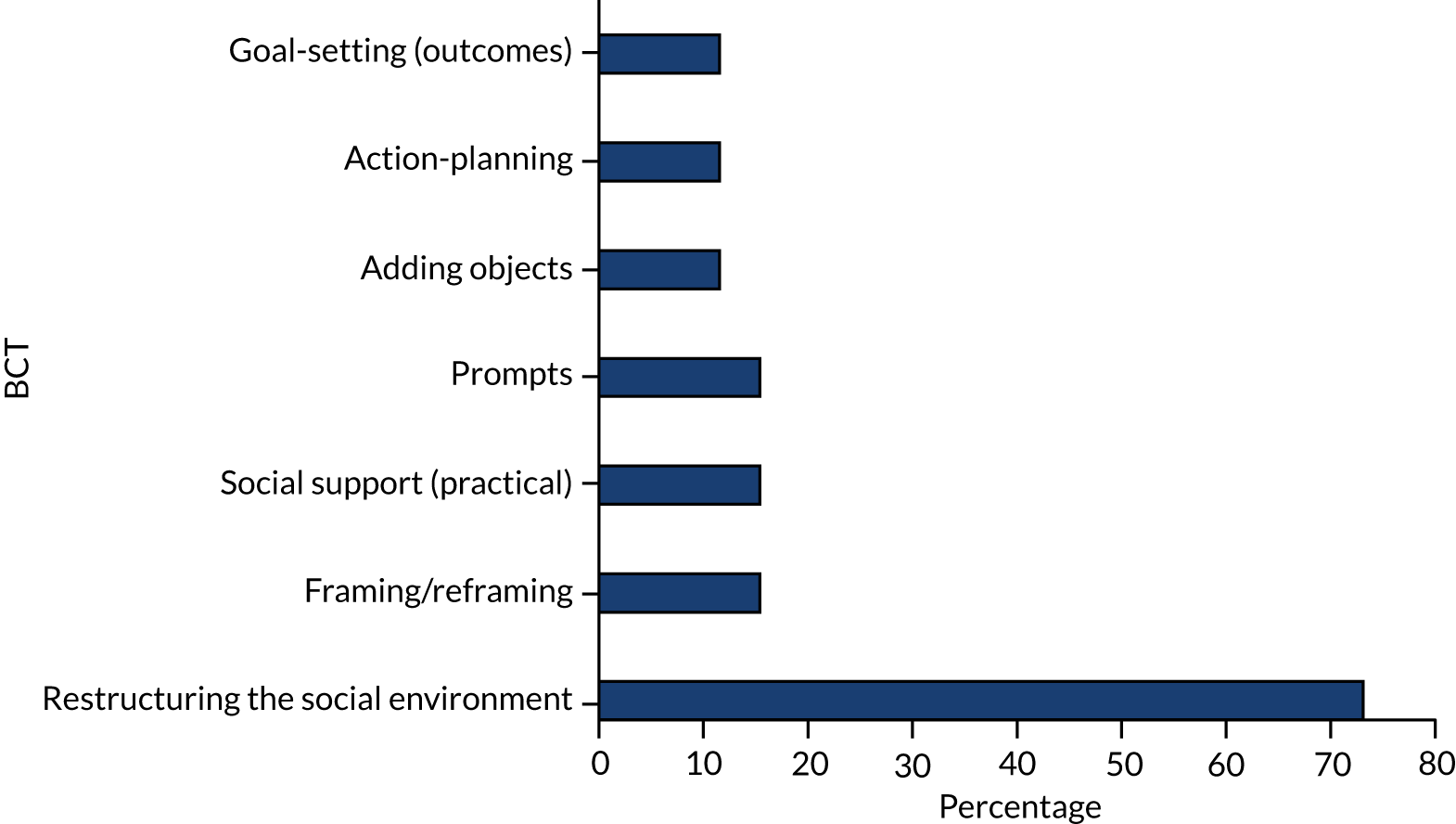
Risk assessment
As illustrated in Figure 33, the procedures for risk assessment were similar to care planning but focused on risk and safety. The most common BCT was the staff member identifying antecedents, problem-solving and action-planning with or about the service user. As with more general care planning, risk assessment was often prompted on admission to services or was carried out on a regular basis. This change in practice could sometimes be part of a broader change in the social environment.
FIGURE 33.
Procedures: risk assessment: 29 interventions coded.
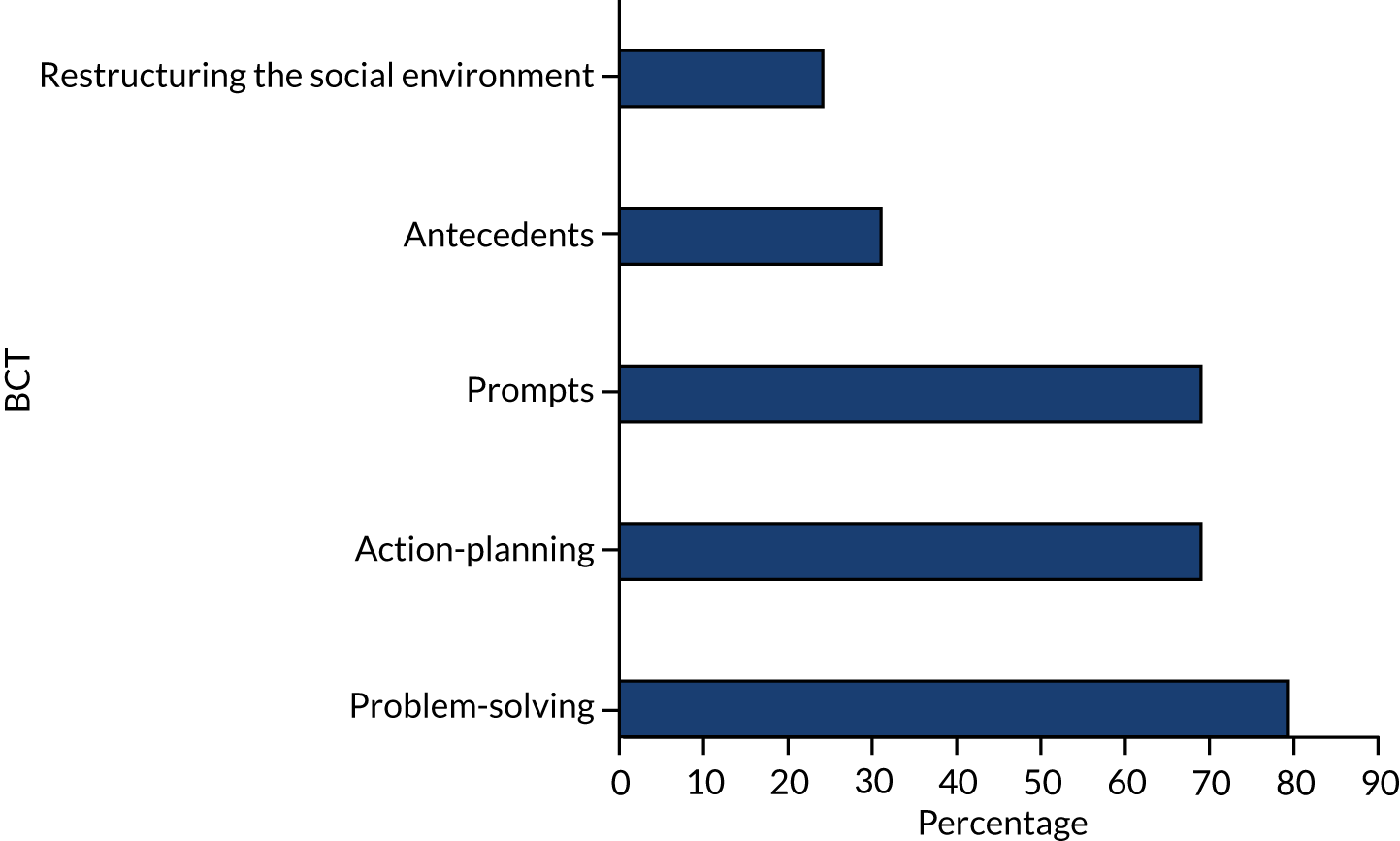
Enhanced leadership
Procedures to enhance leadership were dominated by changes in the social environment (Figure 34), sometimes involving a wholesale adoption of an approach such as Trauma-Informed Care. These procedures included more contact with ward staff, the formation of project steering groups reviewing both behaviour and outcomes, and managers working on wards and being seen as role models in the attempts to reduce restrictive practices. Other aspects often informed through these mechanisms were problem-solving, action-planning and goal-setting for both behaviour and outcomes.
FIGURE 34.
Procedures: enhanced leadership: 29 interventions coded.
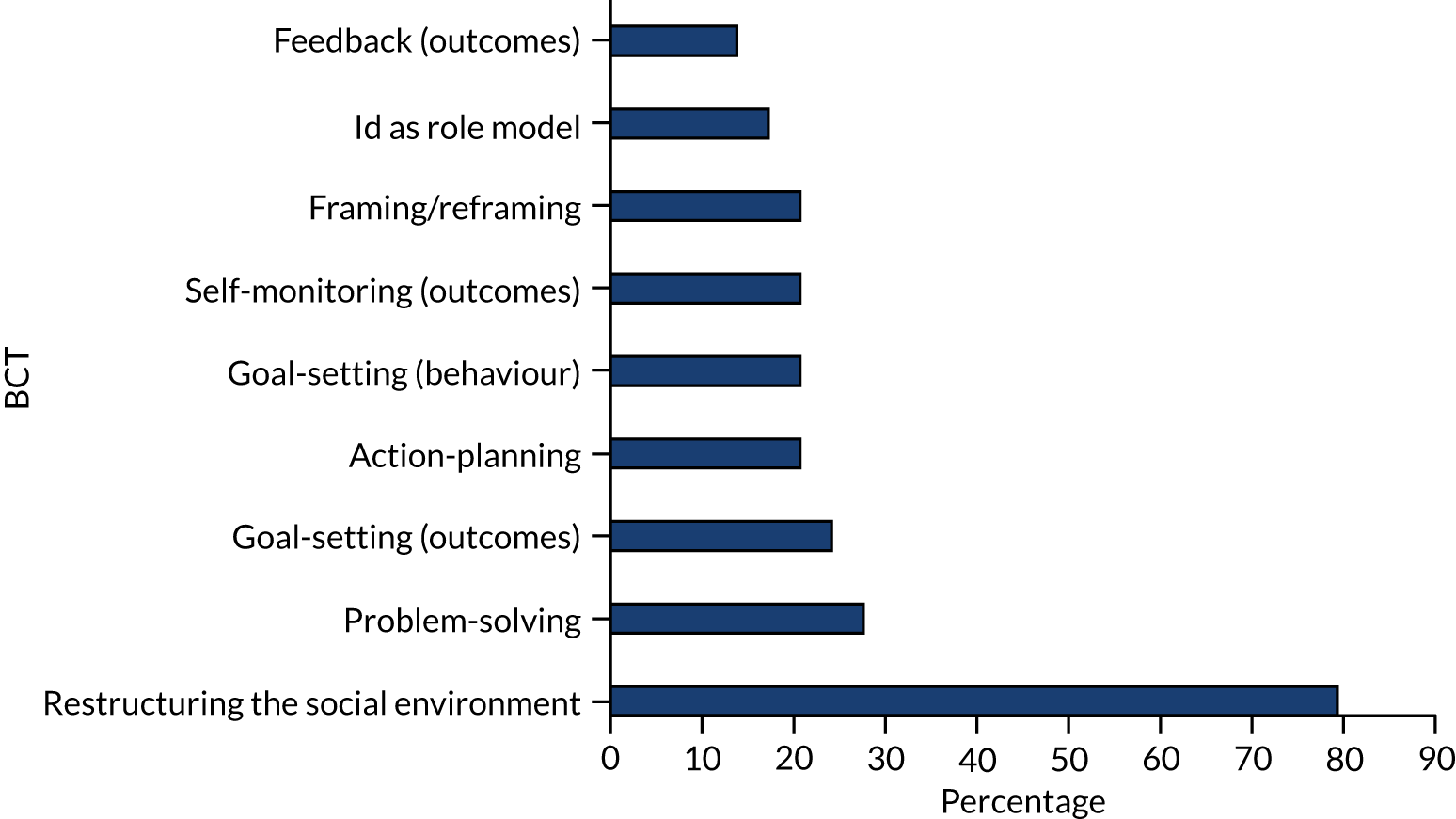
Role modelling
As illustrated in Figure 35, the development of staff as role models involved them self-identifying as a role model, operating as such within the staff team, predominantly by providing social support to their colleagues. The use of role models often involved restructuring the social environment in terms of introducing new staff who were the role models, or training existing staff to fulfil this position.
FIGURE 35.
Procedures: role models: 11 interventions coded.
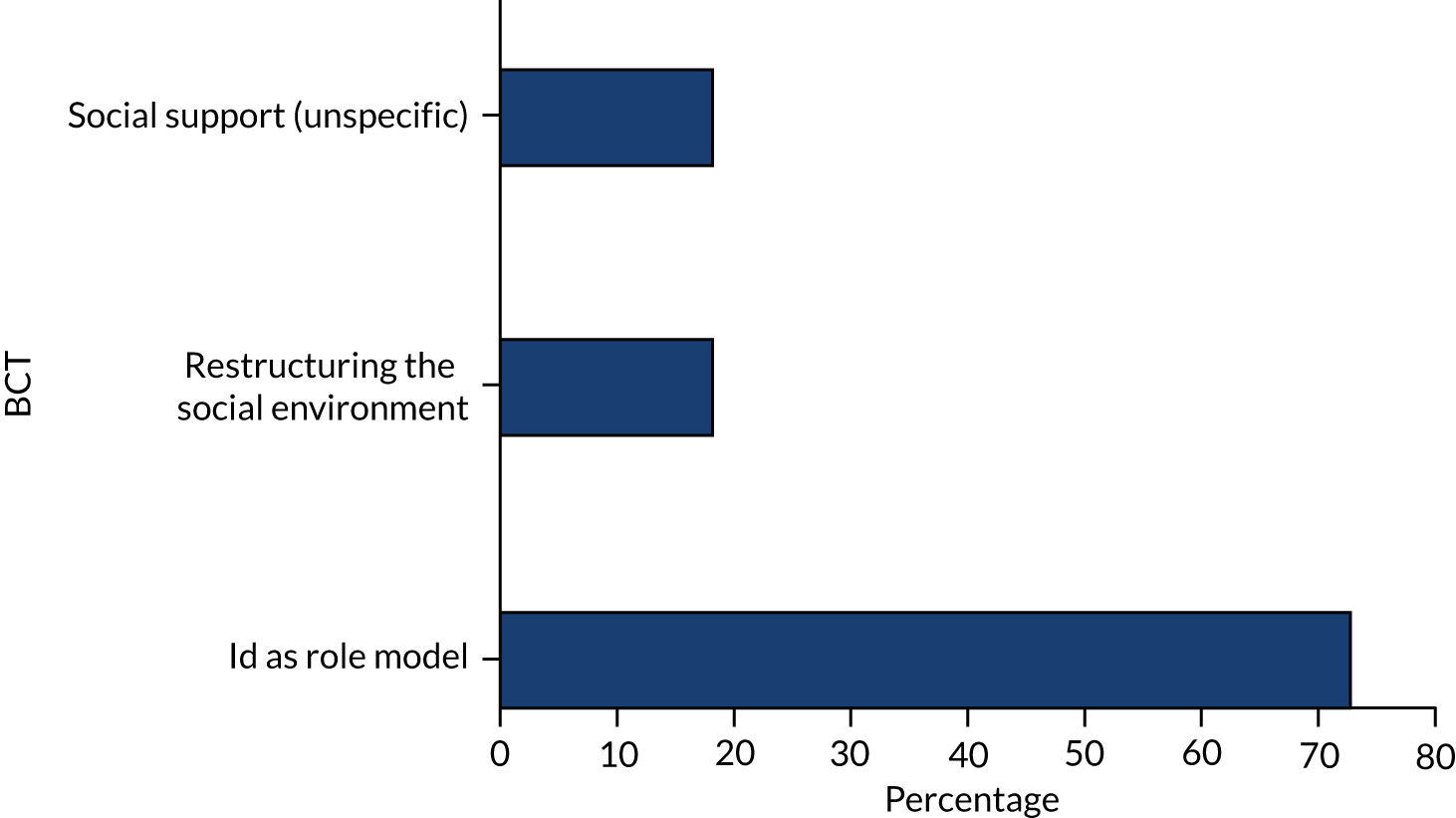
Increased staffing
Increased staffing was rarely associated with any other BCT other than restructuring the social environment, coded in 91% (n = 11/12) of the interventions.
Activities for service users
As illustrated in Figure 36, few BCTs were detected in relation to the introduction of activities for service users. These changed the social environment to reduce the use of restrictive practices by improving the options open for staff when working with service users. They could include adding objects to the environment, such as sports equipment or games consoles.
FIGURE 36.
Procedures: activities: seven interventions coded.
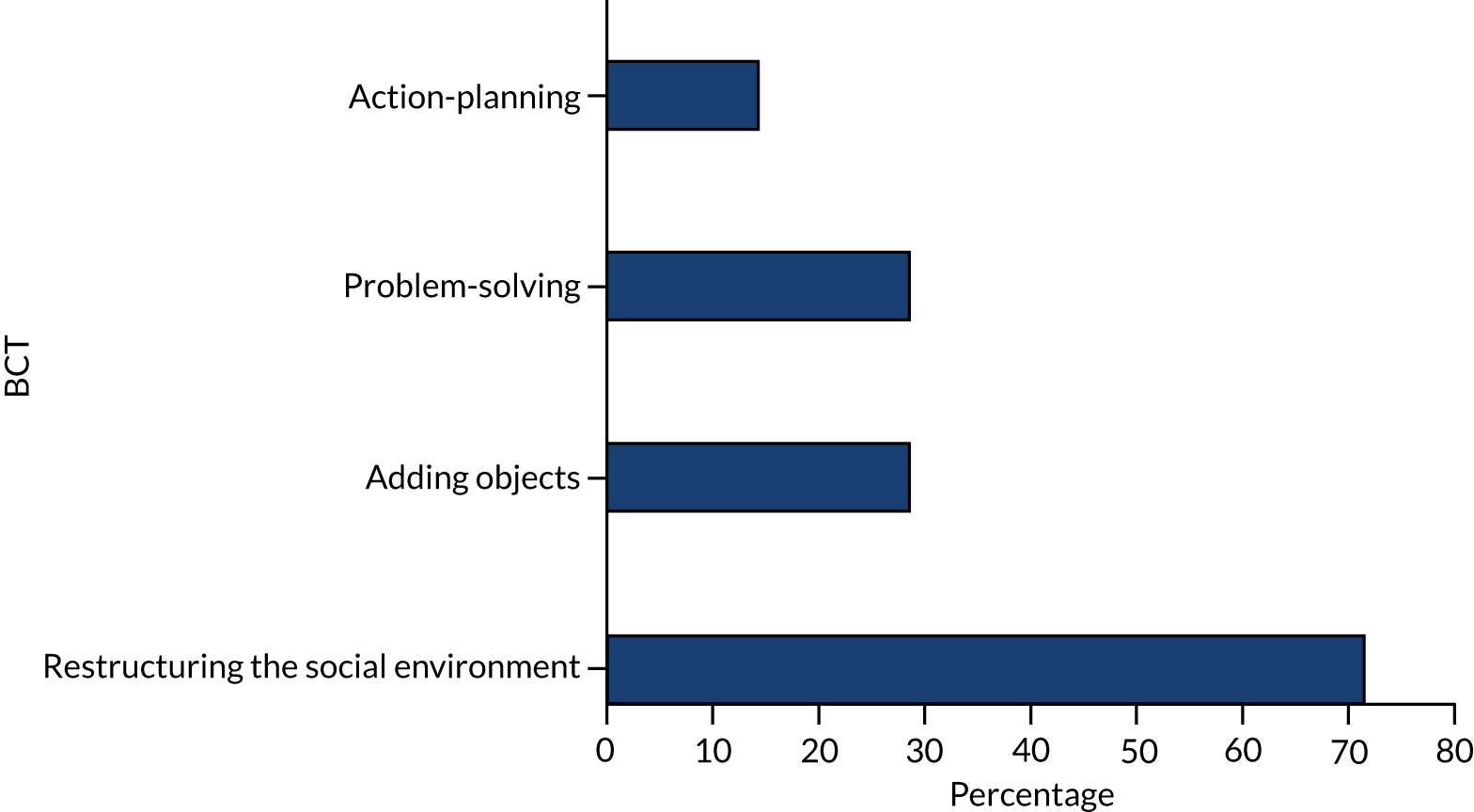
Rapid response teams
Several interventions (n = 8) made use of rapid response teams although few BCTs were detected within these descriptions. The availability of teams restructured the social environment of the ward and included staff of varying professional backgrounds, including nursing and security staff who had received instruction in de-escalation. On arrival they provided practical, social support to ward staff; there were also elements of problem-solving and action-planning detected in two of them.
Chapter 7 Behaviour change techniques and evaluation outcomes
Objective 3 of the study was to identify and prioritise BCTs showing most promise of effectiveness and that require testing in future high-quality evaluations. Ninety-six of the interventions coded for BCTs had been evaluated on 109 occasions using a range of outcome measures namely, restraint (duration and incidence), seclusion (duration and incidence), PRN medication use, observation, or multiple measures reported in combination so that it was not possible to disaggregate them (see Appendix 13). Ninety per cent of evaluations reported at least one positive finding, although not all of the evaluations reported statistics to indicate whether or not their findings had statistical significance, with only 58 studies reporting tests of significance. Only one study reported a statistically significant increase in restrictive practices,129 six reported no effect69,101,102,145,192,231 and the remainder reported at least one significant positive outcome. Figure 37 illustrates the BCTs used in studies that reported statistically significant positive outcomes. These were:
FIGURE 37.
Behaviour change techniques identified in studies reporting statistically significant positive findings.
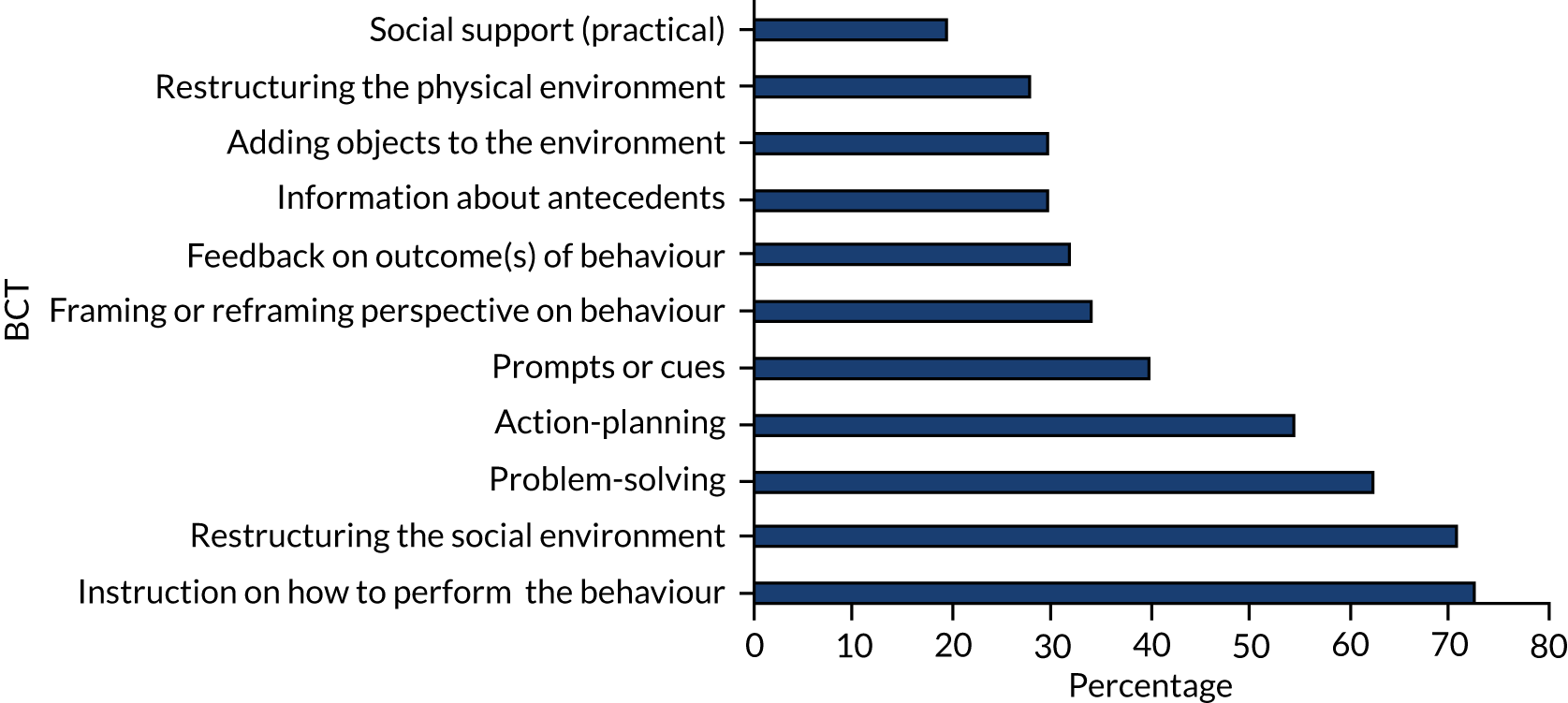
-
social support (practical)
-
restructuring the physical environment
-
adding objects to the environment
-
information about antecedents
-
feedback on outcome(s) of behaviour
-
framing/reframing perspective on behaviour
-
prompts or cues
-
action-planning
-
problem-solving
-
restructuring the social environment
-
instruction on how to perform the behaviour.
This order is different from the frequency with which BCTs are found across all the interventions, as can be seen in Table 10.
| Number | All interventions | Evaluations of interventions with statistically significant positive findings |
|---|---|---|
| 1 | Instruction on how to perform the behaviour | Instruction on how to perform the behaviour |
| 2 | Problem-solving | Restructuring the social environment |
| 3 | Restructuring the social environment | Problem-solving |
| 4 | Action-planning | Action-planning |
| 5 | Framing/reframing | Prompts |
| 6 | Antecedents | Framing |
| 7 | Prompts | Feedback on outcomes |
| 8 | Feedback on outcomes of behaviour | Antecedents |
| 9 | Social support (practical) | Adding objects to the environment |
| 10 | Adding objects to the environment | Restructuring the physical environment |
Behaviour change techniques reporting significant findings in reductions in restraint, seclusion and pro re nata medication
Interventions reported outcomes related to restrictive practices, namely seclusion, restraint, PRN medication, observation and a combination of these that could not be disaggregated (see Chapter 3). Figures 38–40 show the different BCTs identified in interventions that reported significant findings in reductions in PRN medication, restraint and seclusion.
FIGURE 38.
All BCTs found in evaluations that reduced PRN medication.
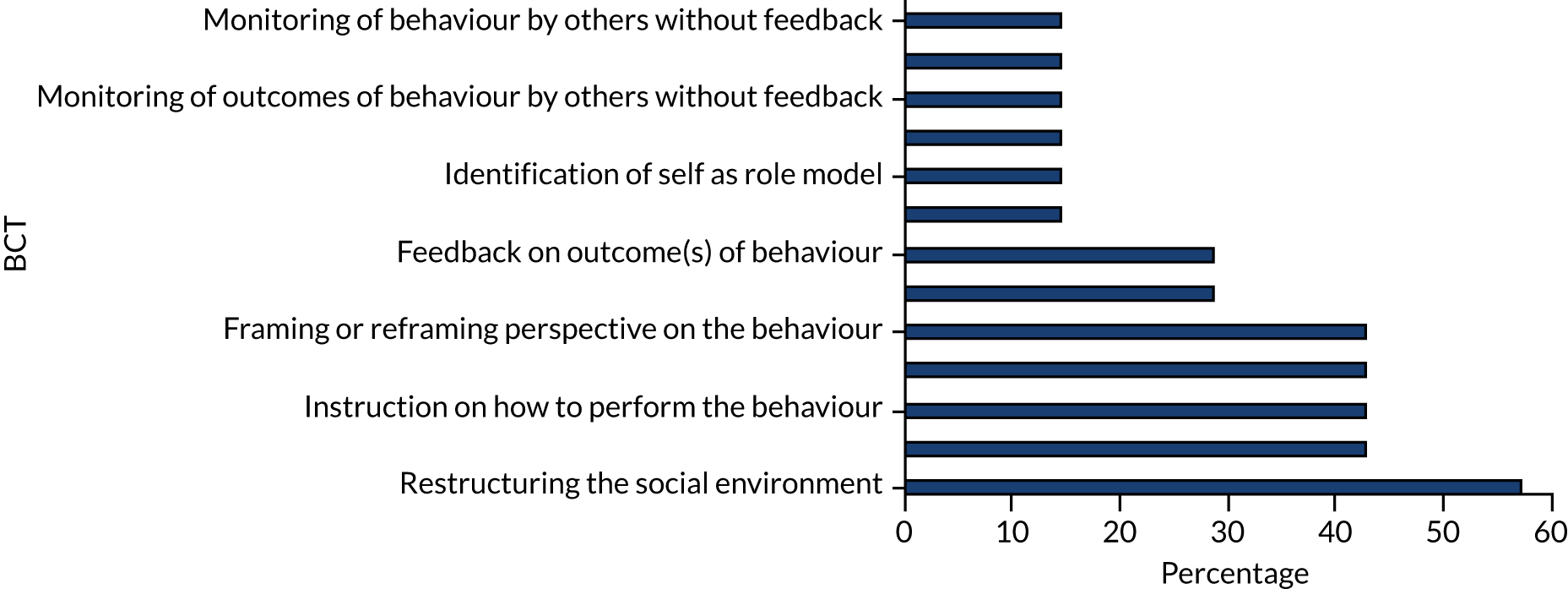
FIGURE 39.
Behaviour change techniques found in > 20% of evaluations that reduced restraint.
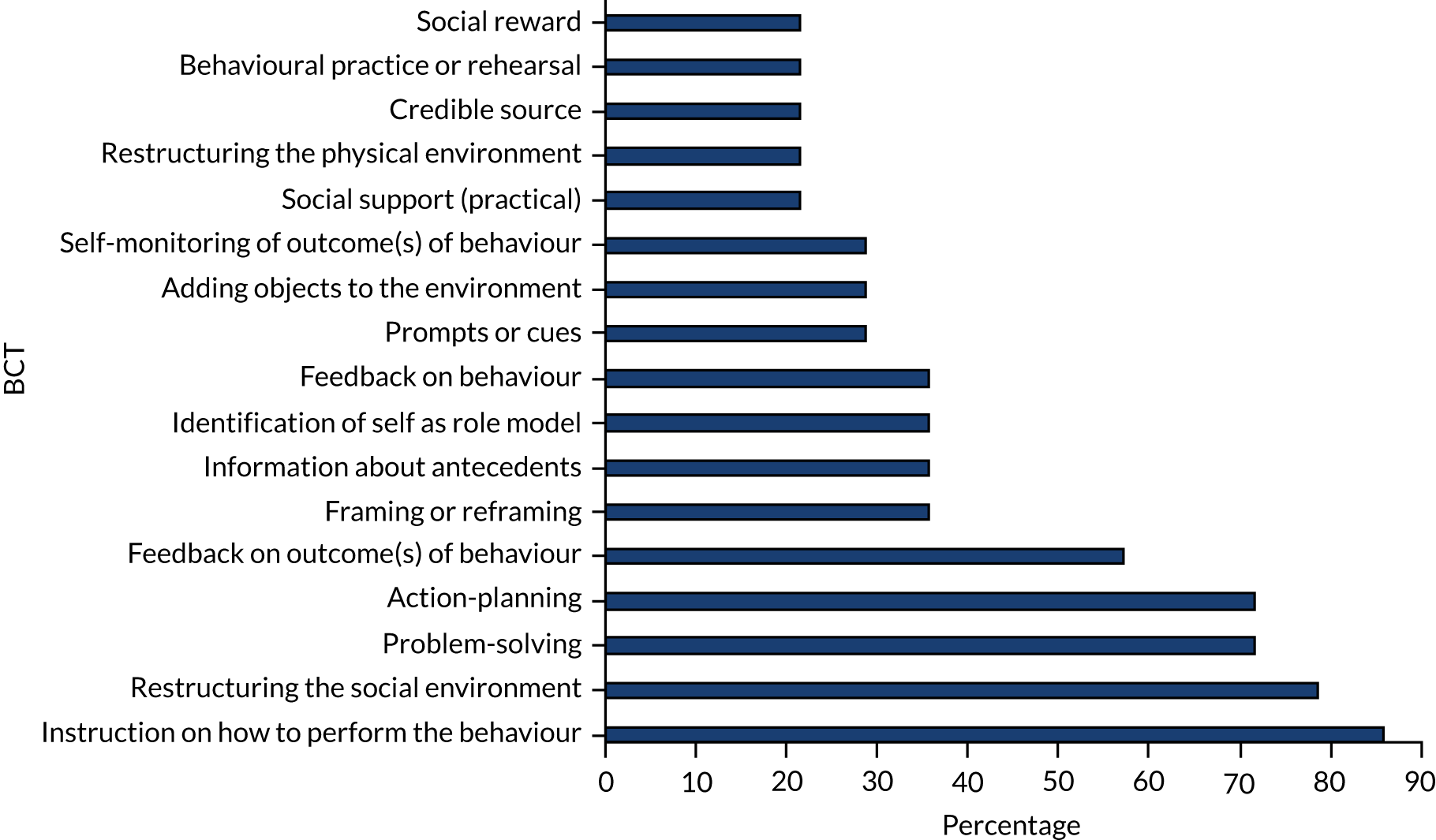
FIGURE 40.
Behaviour change techniques found in > 20% of evaluations that reduced seclusion.
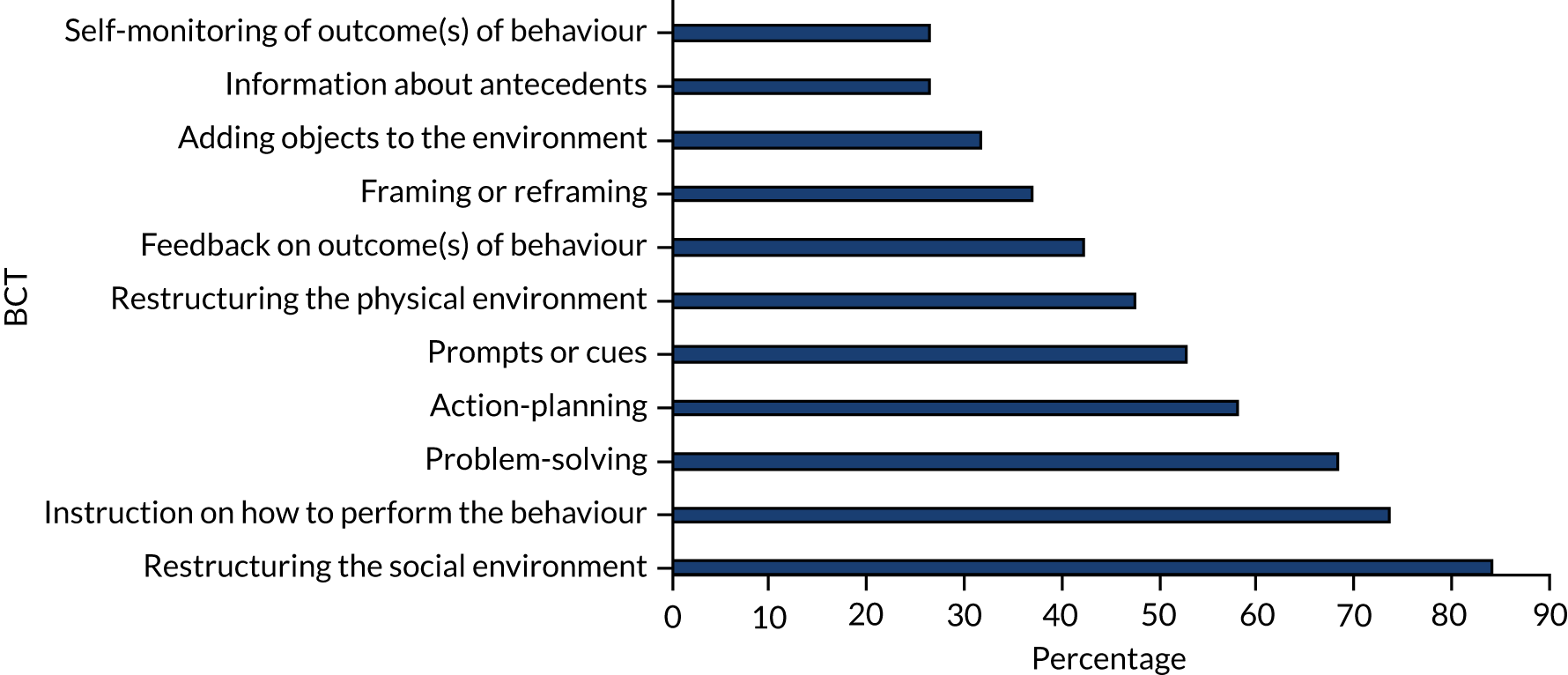
The majority of all interventions looking at the reduction of seclusion and restraint used ‘instruction’, ‘problem-solving’, ‘action-planning’ and ‘restructuring of the social environment’. ‘Prompts’ were used more often in reducing seclusion, and ‘restructuring the physical environment,’ and ‘feedback on outcomes of behaviour’ were used more in reducing restraint. A higher percentage of the interventions that reduced PRN use used ‘reframing’.
Outcomes of randomised controlled trials
As the evaluations were of varied quality it was of interest to look only at the evidence from the five RCTs that reported outcomes, as illustrated in Figure 41. All reported at least one significantly positive outcome.
FIGURE 41.
Behaviour change techniques used in RCTs.
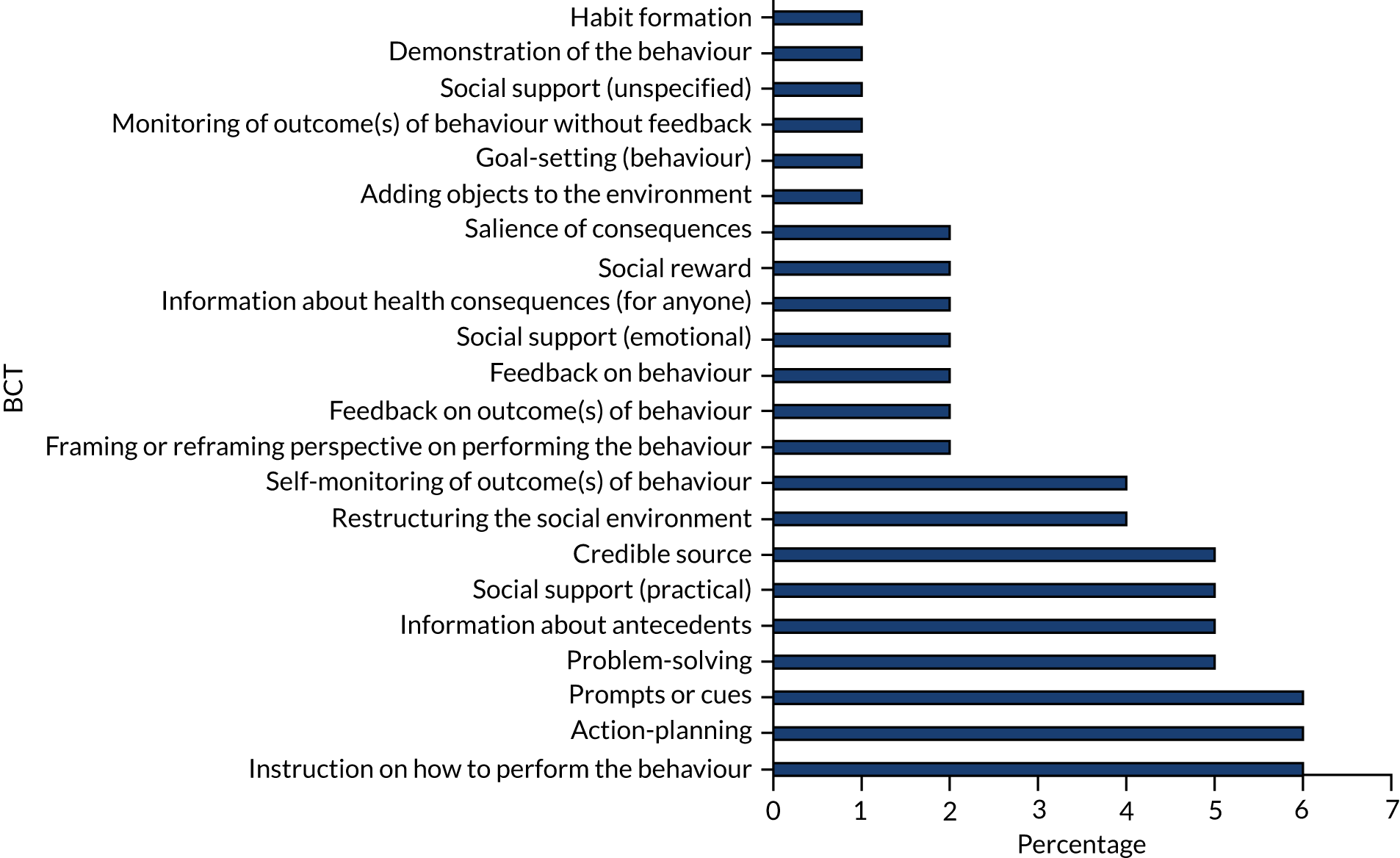
Twelve studies reported no positive findings. The BCTs identified as having been used in these 12 studies are shown in Figure 42. ‘Instruction’, ‘action-planning’ and ‘problem-solving’ remain the most popular BCTs in common with all the studies taken as a whole, whereas ‘restructuring the social environment’ is less common and the use of prompts becomes more frequent, albeit still in only a small number of studies.
FIGURE 42.
Behaviour change techniques of studies showing no positive outcomes.
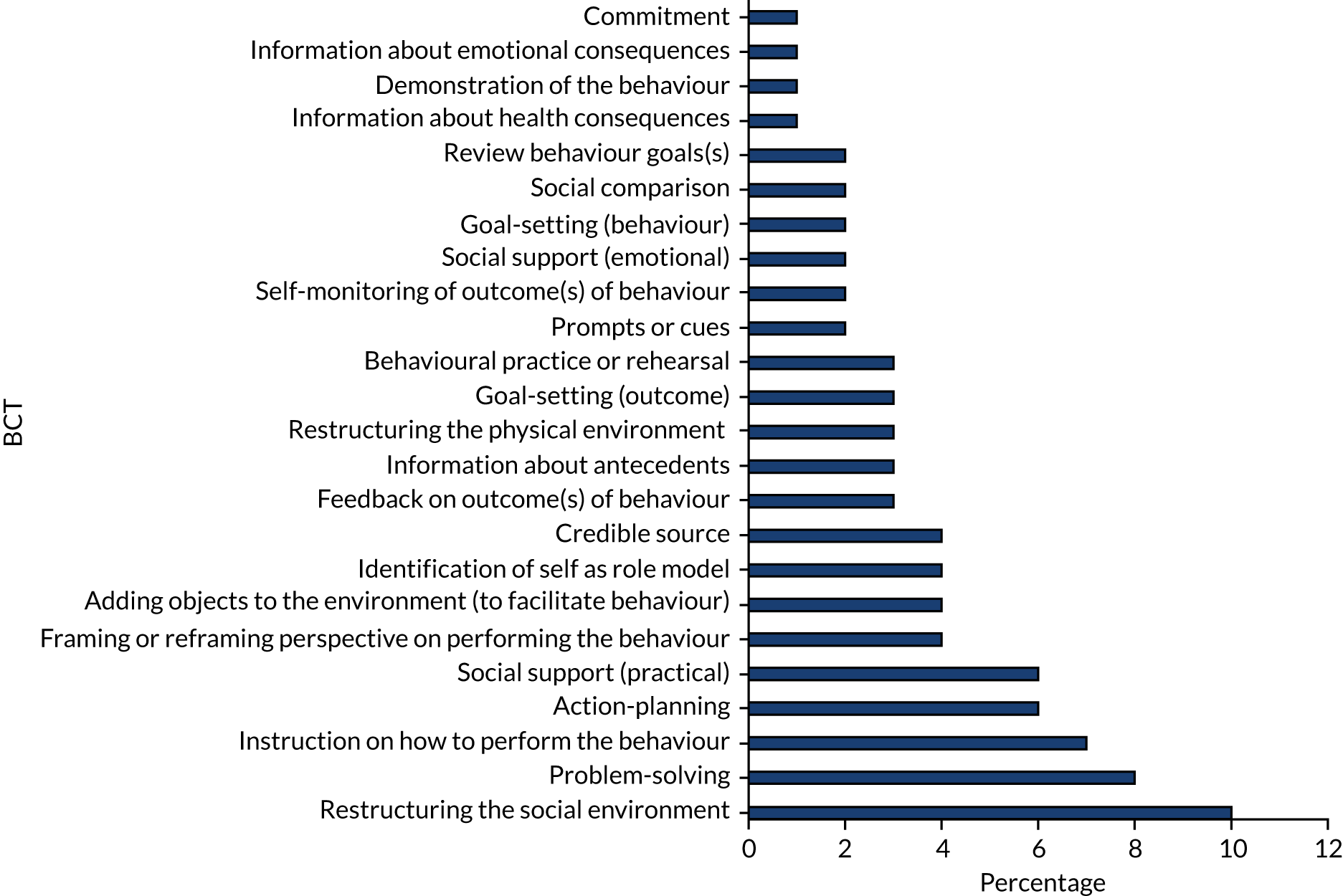
‘Instruction’ remains the most commonly identified BCT. Similarly, ‘action-planning’ and ‘problem-solving’ are ranked second and fourth. ‘Prompts’ are more frequently used, ranking third, compared with seventh across all interventions.
The BCTs used in the RCTs contained some differences to those used in studies with no effects. Although both frequently contained ‘instruction on how to perform the behaviour’, ‘action-planning’ and ‘problem-solving’, these were detected in different frequencies with instruction featuring in 88% of RCTs compared with 58% of studies detecting no effects. The use of ‘prompts or cues’ and ‘information about antecedents’ featured more in RCTs; all but one reported at least one positive finding. The most frequently identified BCT in studies that found no effects was ‘restructuring the social environment’, the least specific BCT applied in this study.
Chapter 8 Summary and discussion of mapping results
This chapter summarises the results of the analysis of our broad and extensive searching of databases and the grey literature that identified 175 records containing 150 unique interventions.
Summary of the literature search results
Overview
The overall purpose of the study was to document the range of interventions developed to reduce restrictive practices, describe their characteristics and identify any overarching patterns. The search identified a disparate and complex collection of interventions in many sources and formats, steadily increasing over the 20-year search period since the introduction of the UK National Service Framework for Mental Health in 1999, and peaking in 2017. Most interventions can be found in research reports published in nursing journals. Various mental health-related and other non-governmental organisations provide resources for service providers in the form of links to training providers and examples of good practice in the reduction of restrictive practices.
Characteristics of interventions
The search found a total of 150 unique interventions to reduce restrictive practices. This included 29 intervention families (interventions with multiple records) and 121 standalone interventions (with only single records). Six Core Strategies was the largest intervention family and had been implemented in the broadest range of countries (n = 6) and clinical settings (n = 6). Safewards had also been implemented in multiple countries (n = 3) and clinical settings (n = 2). The highest numbers of interventions (and widest range) were found in the UK and the USA; others were identified in Canada, Australia, New Zealand, Singapore and several European countries. Most interventions were implemented in unspecified adult mental health inpatient settings, but, where more detail was provided, the most common setting in which to undertake an intervention to reduce restrictive practices was an acute ward.
Variation in intervention reporting
Unsurprisingly, given the broad inclusion criteria and the number of interventions subsequently identified, there was enormous variation in intervention reporting. The interventions were often intended to address multiple restrictive practices and related issues (e.g. service user behaviour, staff skills, quality, safety and adverse consequences) in varying combinations. The most common intervention target was seclusion or restraint; however, 11 interventions targeted PRN medication. Similarly, most interventions used multiple procedures, in some cases as many as 10, and, again, in varying combinations. The most common procedure was Training, although Changes to Nursing Approaches and Review of Incident Data were also often used. Despite the popularity of training as a key procedure, detailed descriptions of the training content and providers were often lacking. The least common procedures were Rapid Response Teams and Activities for Service Users. Forty-eight interventions reported involving service users in some way, but the type and extent of their involvement varied greatly. In some cases, service users were involved in multiple ways, whereas in others they had limited roles.
One hundred and three out of the 109 evaluations used a non-randomised design and there were just six RCTs; the remainder were qualitative or mixed-methods studies. Just two evaluations reported service user involvement in the evaluation. Seventy of the evaluations reported multiple outcome measures, and these most frequently focused on the incidence of seclusion or restraint; however, there was limited consistency as some noted the timing of incidents and others the severity. Only 18 made any reference to the cost of implementing the intervention or its financial impact.
Discussion of analysis
The study clearly shows that there has been an upturn in publications and research endeavour in this field in recent years. In the UK, at least, this is possibly a response to the publication of the Department of Health and Social Care’s response to events at Winterbourne View. Restrictive practices began to attract attention following deaths that occurred during their use, and this increased further when the abuse of patients at Winterbourne View Hospital was documented in 2011. 244
Nevertheless, regardless of an increase in the volume of the literature, the analysis highlighted gaps and huge inconsistency in study design and units of analysis across both sample size and settings. Reporting was generally poor and inconsistent, despite guidelines such as WIDER,61 which recognises the need to standardise reporting of complex social interventions aimed at changing behaviour and provides tools to address the issue. One explanation for this is that it is difficult to capture or measure who is exposed to the intervention, for what duration and at what intensity. To some extent, the level and clarity of detail provided were determined by the format of the retrieved record, and the nature of the intervention and its procedures. Although training might be conducive to measurement, many other procedures, including changes to policy, nursing approach or the physical environment, could be described as standalone events or as ongoing. Therefore, notwithstanding the advent of tools such as WIDER, the analysis showed that limitations remain when it comes to measuring fidelity, and dose, of interventions designed to reduce restrictive practices.
Discussion of quality assessment
The evidence base for interventions to reduce restrictive practices appears to be small; only six RCTs were identified, and variations in their targets and outcome measures precluded any meta-analysis. Most evaluations were published in nursing journals of low impact. The evaluation methods themselves were often poorly described and, in particular, lacked detail about the interventions or methodology that had been applied or the theoretical basis for the intervention. Forty-one potentially eligible evaluations of interventions were excluded from the analysis as they did not pass the MMAT screening questions.
Issues of quality and reporting are particularly problematic when trying to provide precise descriptions of interventions subject to evaluation because of the implications for replication and meta-analysis: ‘to facilitate replication, further development, and scale-up of the interventions’. 61 This clearly had an impact on the ability to apply the taxonomy, make meaningful comparisons of interventions or undertake a meta-analysis of the results. For those studies identified outside the academic literature, experience suggests that other types of reports/formats cannot be relied on to provide comprehensive details of an intervention.
On balance, the evidence suggests that interventions place greater emphasis on service users’ contribution to circumstances that lead to the use of restrictive practices than on the impact that restrictive practices (or their reduction) have on them. Many interventions reported that they sought to improve service user experience by, for example, promoting recovery or providing Trauma-Informed Care and included specific aims to improve quality of care, service user experience, a feeling of safety and recovery. Nevertheless, few reported examining service user outcomes such as injury or perception of safety. Although they measured the incidence, and sometimes duration, of restraint or seclusion, they did not report these incidents in terms of their impact on service users. Although service users were sometimes involved in intervention delivery, they were rarely involved in intervention design or evaluation. A good proportion of the interventions that were reported included procedures aimed at changing service user behaviour and engaging service users in identifying their own triggers, strategies and preferences. In contrast, interventions inviting managers and frontline professionals to reflect on their practice required a focus not on their triggers, for example, but instead on understanding service users’ histories.
Chapter 9 Summary and discussion of the behaviour change technique results
In this chapter, we summarise and discuss the BCT results, reflecting on the application of the BCT taxonomy and drawing out key issues identified from the synthesis.
Summary of the behaviour change technique synthesis results
The application of the BCT taxonomy to provide descriptions of interventions to reduce restrictive practices in a systematic way is, to our knowledge, the first time such an approach has been taken. This review has identified that over two-thirds of all interventions identified employ strategies to shape knowledge, use goals and planning, provide feedback and monitoring, and address antecedents in order to reduce restrictive practices.
Records relating to the 150 identified interventions were coded for BCTs and contained 43 of the possible 93 BCTs (47%). The number of BCTs identified per intervention ranged from 1 to 33 (mean 8 BCTs). The BCT taxonomy39 places BCTs into 16 thematic clusters. The 43 BCTs identified in the interventions were contained in 14 of these clusters; BCTs from ‘self-belief’ and ‘covert learning’ were not detected. The first four clusters were ‘goals and planning’, ‘shaping knowledge’, ‘antecedents’ and ‘feedback and monitoring’ and contained over two-thirds of the BCTs.
The BCTs related to ‘goals and planning’ appeared most frequently, with just over one-fifth (22%) of BCTs identified contained within this category, of which ‘problem-solving’ (BCT 1.2) and ‘action-planning’ (BCT 1.4) appeared most frequently. The cluster ‘shaping knowledge’ contained 16% of the overall BCTs and included those capturing imparting information about ‘antecedents’ (BCT 4.2) (40%) and ‘instruction on performing the behaviour’ (BCT 4.1) (90%). The BCT cluster ‘antecedents’, related to factors that might influence whether or not restrictive practices could be avoided, contained 15% of BCTs. Three BCTs were identified: ‘restructuring the physical environment’ (BCT 12.1), ‘adding objects to the environment’ (BCT 12.5) and ‘restructuring the social environment’ (BCT 12.2). BCT cluster 2, ‘feedback and monitoring’, accounted for the use of data, accounting for 11% of BCTs. ‘Data monitoring and feedback’ related primarily to outcomes (reduced restrictive practices) rather than behaviour (de-escalation).
Behaviour change techniques were examined with regard to procedures used in interventions, such as staff training, audit and feedback, or nursing changes. This demonstrated which BCTs were associated with the individual procedures of multiprocedural interventions. The most commonly used procedure was staff training (135 interventions), which was dominated by the use of ‘instruction on how to perform the behaviour’ (BCT 4.1) (77%) and ‘framing/reframing’ (BCT 13.2) (33%). ‘Audit and feedback’ (53 interventions) most frequently contained ‘feedback on outcomes of behaviour’ (BCT 2.7) (71%) and ‘problem-solving’ (BCT 1.2) (39%). Nursing changes (48 interventions) used ‘restructuring the social environment’ (BCT 12.2) (73%) and ‘problem-solving’ (BCT 1.2) (45%).
The BCTs that were identified most frequently in interventions reporting statistically significant reductions of restrictive practices were ‘instruction on how to perform the behaviour’ (BCT 4.1), ‘restructuring the social environment’ (BCT 12.2 ) and ‘problem-solving’ (BCT 1.2), within the three clusters of ‘antecedents’, ‘shaping knowledge’ and ‘goals and planning’.
Shaping knowledge
The majority of interventions used staff training as a mechanism to reduce restrictive practices. The training was usually a procedure of the intervention, for example to improve de-escalation skills, but could also form part of another procedure of the intervention such as training to use a risk assessment tool. Training was most likely to be part of a single-procedure intervention but, as the content was poorly described in many instances, it was not possible to determine the delivery, content, duration and frequency of the training. Training can contain a variety of different BCTs, for example social support, shaping knowledge, information about consequences, demonstration of the behaviour, rehearsal, identity, comparison of outcomes and self-belief. It may be that some of these BCTs are more effective in changing behaviour than others and some might have no discernible effect. Theorising how training might be expected to change behaviour would allow for the selection of some of these BCTs and their subsequent testing.
Goals and planning
The use of goals and planning to reduce restrictive practices included strategic goals and planning at several levels (i.e. individual planning with service users, ward team goals, and at the wider organisational or health system level). It is of interest whether or not health system level goals and planning have as much impact as those generated at ward level and whether or not goals and planning with individual service users is more effective at reducing restrictive practices. Some interventions claimed that those initiatives generated at ward level had greater ‘buy-in’ from staff, whereas others claimed similar importance of top-down initiation and support. These often occurred simultaneously in the same intervention so were difficult to distinguish. Coding of BCTs found at individual, team and system levels would go some way to address this difficulty, although that was beyond the scope of this study as it sought to describe content overall and via individual procedures. Theorising why using ‘goals and planning’ employed at these different levels might effect change would allow these effects to be tested in isolation.
Antecedents
The social environment of mental health services was thought to contribute to the use of restrictive practices, and many interventions sought to improve it through the promotion of interaction between service users and staff. This became a broad category, somewhat reducing its sensitivity. The physical environment was frequently involved, although generally limited to changes made to wards to make them more therapeutic, something recently highlighted by the CQC in the UK. There was less attention paid to the overall architecture and design of wards, which was unsurprising when few services have resources for a full redesign. There may be aspects of overall structure, such as visibility of staff and service users, natural light, opportunities for private space or fresh air, that reduce restrictive practices. Again, these modifications were often made in conjunction with other intervention procedures, meaning that the effect on behaviour of physical restructuring alone is unknown.
Feedback and monitoring
This was a frequently identified component of many of the interventions and has a range of BCTs associated with it. As described above, it is difficult to identify feedback on behaviour within these interventions as successful de-escalation may not be recorded, whereas outcomes of the (failed) behaviour are routinely recorded. As well as the feedback and monitoring BCTs, other BCTs relating to social support, information about antecedents, social comparison and reward within these procedures were also detected; it is of interest what role these play in these procedures. There was little description of how the data were fed back to staff, whether delivered verbally, in writing, electronically or during a meeting. It was often unclear what level of detail was provided in the data, whether it was at ward level or service level, over what time period and how identifiable incidents would be to those involved. These might be important factors to test to better determine whether or not feedback and monitoring changes behaviour, and again the use of theory would allow these factors to be tested.
Discussion of behaviour change technique synthesis
The BCT taxonomy has been used more frequently to systematically describe interventions that are targeted at service users rather than at health-care professionals, and although this is not the first study to apply the taxonomy to interventions targeting staff behaviour it is a relatively new area. 47 Previous work in this area has made modifications to the taxonomy definitions to enable a better fit, and this was required here. 47 Most of the BCTs could be applied directly to the interventions, but some were more complicated because of the different contexts in which they could occur. For example, the BCT ‘problem-solving’ could feature in a number of settings such as with individual service users on admission or after an episode of restrictive practice, between staff during a ward safety huddle, or via meetings involving managers, staff and service users. These difficulties were addressed by further coding these BCTs using and identifying and reporting subthemes that capture this variety of use.
Targeting behaviour of staff versus behaviour of service users
One of the challenges of this approach was associated with the target that the intervention was focused on, that is staff or service user behaviour, and subsequently how to code this. Many instances were detected in interventions when a BCT was being used that was targeting the service user but that could also change staff behaviour, for example the introduction of a sensory room aiming to change the behaviour of service users and facilitate self-care to reduce distress. In that respect it was targeting service user behaviour; however, it also changed staff behaviour because the introduction of a sensory room provides an additional resource that they can use to support people experiencing distress. This has come about through either restructuring the physical environment or adding objects to the environment to either reduce antecedents to conflict or promote de-escalatory behaviour if conflict arises. As such, this was included and coded as a BCT. The interpersonal relationships between service users and health-care staff are extremely important and it cannot be assumed that the escalation of conflict behaviour is always generated by the service user: the staff member may contribute equally, whether intentionally or not. An intervention such as a sensory room can therefore facilitate de-escalatory behaviour from the staff member as it might promote calmer behaviour from the service user.
A further example was apparent in ‘action-planning’, and this often included care planning with an individual service user. It could be seen that this was an attempt to change the service user’s behaviour in the event of them becoming distressed and, on one level, this may prove the case; however, the activity of action-planning with the service user may also cause the staff to action-plan. They may discover that when this service user becomes distressed, they are made more distressed by a noisy environment. They can then plan to help the service user to find a quieter space in the event of distress, which in turn successfully avoids the use of restrictive practices. As interventions can affect the behaviour of staff, service users and visitors in the therapeutic milieu to different degrees, it is important that this is acknowledged while retaining the focus on staff behaviour and how it might be changed.
The one BCT that lacked sensitivity in this study was also one of the most frequently used, namely ‘restructuring the social environment’. This was used to capture a broad range of changes implemented by interventions from a strategic management level through to everyday interactions between service users. The decision to create subcategories (e.g. access to staff, management support, promote socialisation) for this BCT to retain this detail addresses this difficulty to a certain degree but it might be considered a limitation when viewing the overall summaries of the BCTs coded in this study.
Future development of BCT coding could consider the use of subcategories. Some of this information could be seen as contextual rather than relating to a specific BCT. For example, it is unclear whether a new type of staff meeting is a BCT in itself or the BCT is only what happens during the meeting, for example problem-solving and practical social support. This may be a grey area that was specific to these data and not easily addressed through the use of subcategories. Presseau et al. 47 also found that this code required more specificity when coding system-level interventions, and recommended the addition of what is ‘restructured’, preferably within an explicit programme theory.
‘Behaviour’ versus ‘outcomes of behaviour’
For this study, the target ‘outcome of the behaviour’ was an absence of something happening, such as reduced seclusion episodes or fewer restraints. The target ‘behaviour’ was successful de-escalation, which is itself not an absence of carrying out restrictive practice but a proactive attempt to avoid it by using other strategies. Although it was clear for this study that the desired ‘behaviour’ was that which sought to reduce the use of restrictive practice, often described as de-escalatory behaviour, this was almost never measured or even accounted for among the interventions. The focus was always on the ‘outcomes’ of the behaviour, such as the number of restraints or seclusions. This meant that feedback about the ‘behaviour’ could rarely be identified as the focus was on feedback on ‘outcomes of behaviour’. This somewhat fails to acknowledge successful de-escalation.
Behaviour change technique dosage
The frequency of use of BCTs whether they were present or not within an intervention was summarised, not how many times evidence of their use was detected. Therefore, this does not reflect the ‘dose’ of each BCT. It is possible to report this cumulatively using NVivo software, but is not meaningful across a large number of interventions.
The use of theory was not explicit in many of the interventions, which is not unusual in health services research. 66 This is a significant weakness of this evidence as the explicit use of theory would allow better comparison between interventions in terms of what assumptions the intervention is based on, how the techniques that have been employed are expected to have an effect, and how effective this ultimately was. It is recommended that developers of future interventions make more explicit use of theory.
Comparison with previous research
There is little previous research with which to compare the results of the current study. The only other study to apply the BCT taxonomy to interventions seeking to change professional behaviour, Presseau et al. ,47 reported some similar findings, albeit in a different area of health care (diabetes care).
Pressau et al. 47 identified 21 BCTs in 11 clusters, compared with 43 in 14 clusters identified in the current study. The BCTs identified most frequently in Pressau et al. 47 differed from those reported here, which is not unexpected as the two studies concerned interventions targeting different issues. Pressau et al. 47 did not find covert learning, self-belief (similar to the current study findings) or use of regulation and scheduled consequences (in contrast with the current study findings) evident in intervention materials. The current study detected small numbers of one of the BCTs in each of these categories. In addition, Pressau et al. 47 detected no BCTs targeting identity, whereas role modelling and ‘reframing’ occurred within many of the interventions reported in the current study. This latter point may be related to the reality that moving to a Trauma-Informed Care system involves reframing perspectives on restrictive practices as a key element.
Therefore, the current study contributes further insights into the potential of the BCT taxonomy to understand mechanisms for change in the behaviour of staff in health settings. Potentially, further research into the use of BCTs may facilitate the emergence of a recognisable set of BCTs likely to be effective across diverse health settings, and others which are particularly helpful in specific contexts.
Chapter 10 Conclusions
This chapter addresses the strengths and limitations of the study, reflecting on how the scope and quality of the evidence base has had an impact on the study outcomes. The chapter highlights implications for practice and makes recommendations for future research.
Strengths and limitations
The study objectives were to:
-
provide an overview of interventions aimed at reducing restrictive practices in adult mental health inpatient settings
-
classify components of those interventions implemented in terms of BCTs and determine their frequency of use
-
explore evidence of effectiveness by examining BCTs and intervention outcomes
-
identify BCTs showing the most promise of effectiveness and that may require testing in future high-quality evaluations.
Strengths
As demonstrated in Chapters 4–6, the study was successful in meeting objectives 1 and 2. The current report provides a high level of detail concerning the range, components and application of interventions using BCTs.
A rigorous approach to coding documents was employed, supported by qualitative analysis software (NVivo). All intervention information was stored in one project and the initial coding frame took the form of the BCT taxonomy. Adopting a deductive qualitative analysis for the BCT coding enabled within-BCT-category coding, which allowed the identification of subthemes within the more populated BCTs. It also supported the use of memos to allow communication between the two coders about areas of divergence. This approach was, on reflection, considered to have been a success and will be repeated with a similar study.
Limitations
The broad search strategy that included a wide range of grey literature in diverse formats, together with no criteria for exclusion on the basis of quality, was developed in response to the research team’s familiarity with the research field and prior awareness that, although the research evidence was likely to be sparse, there were a large number of interventions being used in practice, with potential to be mapped onto the BCT taxonomy. Our novel approach to searching was comprehensive, and effective in its results, yet records of interventions were disparate in terms of focus and quality. The strategy was thus useful for identifying the number and range of available interventions; however, it does raise questions about how such diverse evidence can be assimilated and appraised in a meaningful way.
Quality of description
With some exceptions, the quality of the description of the content of interventions was very poor. This meant that it is not possible to detect precisely what is happening without information from individual staff. Given that the reporting of the content of interventions is poor, this is a weakness of all reviews of this sort. Contact details for obtaining further information for 140 records were extracted but there were only 14 replies to 100 requests for further information. Four interventions devised by commercial training companies charged a fee for access to their materials. Those resources that had been developed often lacked sufficient detail for coding or had been poorly stored, for example citing outdated URL links. Standards for reporting the development of health research [e.g. via the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) network]245 do not often appear to have been applied. The use of appropriate guidelines would greatly enhance the quality of research in this area. The reporting of outcomes is a particular difficulty owing to the diverse nature of outcomes used and metrics applied.
Our approach to BCT coding, for example the overcoding of certain BCTs, predominantly ‘instruction on how to perform the behaviour’ (BCT 4.1), may be considered a risk because this may have enabled the recognition of specifics of training that may not have occurred. Given that this BCT has been used in nearly all of the interventions, it was unfortunate that it was frequently very poorly described and, as aspects of training can vary dramatically, an understanding as to the exact content of much of the training was not gained. However, if this code had not been used whenever training was involved then it would have been under-reported. On balance, it was concluded to be preferable to over-report, with an accompanying call for clarity, rather than disregard. ‘Restructuring the social environment’ (BCT 12.2) was also used in a wide variety of circumstances and consequently there is some overlap with contextual factors such as service user involvement. It was thought better to have some duplication in this important area than not to code it. The impact of joint working between service users and health-care staff might deter the use of restrictive practices, potentially caused by staff knowing the service user through this different relationship.
Setting
As this was an exploratory piece of work it was limited to adult mental health services. Although a range of adult inpatient settings were included (including acute, forensic and PICU services) this review excluded a range of services and settings where restrictive practices are commonplace. This included Child and Adolescent Mental Health Services, and interventions targeting people with learning disabilities and organic conditions. It may be worthwhile conducting similar research to explore the techniques used to reduce restrictive practices across other settings.
English language as an inclusion criterion
It was beyond the study remit to include material that was not reported in English. It is likely that, by limiting the review to records in English, it was predisposed to identifying interventions from the USA, Canada, Europe and Australia. It is difficult to assess how many additional records might have been included in this review had this limit not been imposed. There are international efforts to reduce restrictive practices across adult psychiatric institutions. For example, there are widespread efforts across Europe that are published in non-English-language journals. Further afield, the use of Pasung (physical restraint and confinement) in Indonesia has been under considerable scrutiny. It is likely that some interventions in some countries that aim to reduce restrictive practices may not have been included.
Implications for policy and practice
There continues to be an urgent need to reduce restrictive practices in inpatient mental health settings. This has been recommended by a range of stakeholders in the UK [including, for example, the National Institute for Health and Care Excellence (NICE) and CQC] and internationally. Service providers urgently require high-quality evidence regarding the effectiveness of interventions to reduce restrictive practices.
The evaluations of interventions frequently report positive results in terms of reductions in restrictive practices. Publication bias aside, the majority of evaluations report positive findings. This implies that, in general, the approaches being used can and do work. However, the evidence base is limited by poor reporting and disregard for theory, and leads to a tendency for individual organisations to develop ad hoc untested interventions or to implement known interventions inconsistently (for example, Safewards, Six Core Strategies, No Force First). Their implementation is often poorly evaluated and studies frequently fail to measure the fidelity to the interventions used,246 which is crucial to understand how interventions might have been modified during implementation. When they are successful at a local level, there is often a poor understanding of the active components that resulted in the reduction of restrictive practices, hampering the ability to implement them more broadly.
This study describes the extent of the current evidence base and, despite its complexity, indicates where the focus of interventions to date has been with regard to BCTs, and suggests that this is leading to reductions in restrictive practices.
Research recommendations
Multiple procedures
The multiple components and multiple aims of the interventions causes further obscurity. Although a single target might on the face of it be ‘reducing restrictive practices’, this is a target made up of a range of different practices. Many of the interventions had multiple components; however, without individual testing of the components of interventions, resources might be wasted on elements that are simply not effective, or are perhaps effective only when coterminous with another intervention. This study shows that complex interventions have been developed and implemented, potentially ahead of the rigorous testing required to develop a robust evidence base. For example, the current review did not find evidence to answer questions such as Is repeated staff training necessary? How important is action-planning? Is overall care planning better than specific safety planning or risk assessment?
Outcomes
Restrictive practices include a variety of outcomes and they are often reported in diverse ways using a range of units of analysis, for example restraints per service user, or restraints per day. Studying the reduction in the use of PRN medication might require a quite different approach to outcomes evaluation, compared with reducing restraint. For example, where one restrictive practice is reduced, another might increase.
The potential for so much variety here makes it difficult to compare studies and meta-analyse outcome data. There is little consideration of service user-reported outcome measures, and the development of such measures would be a helpful addition to the increasing body of research in this area.
Behaviour change techniques showing the most promise
When interventions were examined by target, type of study or reported findings, it was apparent that there was a small group of BCTs that were most frequently found across all the interventions, such as ‘instruction on how to perform the behaviour’, ‘restructuring the social environment’, ‘problem-solving’ and ‘action-planning’.
A complication of this finding was that the BCT ‘restructuring the social environment’ was a broad category that, for the purposes of this study, encompassed several subcategories. There were some variations that might tentatively indicate that some BCTs were more effective in reducing restrictive practices than others. The RCTs appeared to make more use of ‘prompts or cues’ and ‘information about antecedents’ than those studies that reported no positive findings. Caution in interpreting this finding is required owing to the small number of RCTs and, indeed, the small number of studies reporting no effects.
Because of the generally weak evidence base around interventions evaluation, including the small number of RCTs, this review cannot confidently recommend the testing of specific BCTs that show promise. Instead, there appears to be a strong argument for intervention developers to consider the specific components of interventions, and why and how these individual components might be tested.
Undetectable behaviour change techniques
Fifty BCTs were either not found at all, or found only rarely. Of these, some will not be applicable, some might have been presented in practice but were undetectable from available reports, and others might never have been considered and yet could be effective. Videos of training sessions and observational work would help elaborate on this and could be considered in future studies.
As BCTs using reward and threat were rarely detected, it may be valuable to explore the potential of this area to have an impact on the reduction of restrictive practices.
Pro re nata medication
That so few studies have focused on chemical restraint/rapid tranquillisation is concerning. There is widespread and frequent use of chemical restraint (rapid tranquillisation) in acute mental health wards. Given that most medicines given at this time are either benzodiazepines or antipsychotics, further research in this area is warranted. It is also clear that the process of offering and/or refusing PRN medication can lead to an escalation in the use of restrictive practices, and additional understanding of this process may lead to a subsequent reduction in restrictive practices.
Concluding comments
Despite numerous policy initiatives and recommendations from bodies such as NICE, the CQC and the Royal College of Psychiatry, there seems to be ongoing concern about the use of restrictive practices in adult inpatient mental health settings. The care of individuals detained in hospitals will remain suboptimal unless there is a sustained focus on reducing these practices. The impact of restrictive practices on the psychological and physical welfare of both service users and staff should not be underestimated. Without sustained effort these practices will continue to occur in institutional settings worldwide.
This study identified a large number of interventions that have been implemented over the past two decades. The findings suggest that there is potential to rationalise complex interventions. More often than not, they have targeted multiple restrictive practices, using multiple procedures and – where they have been measured – applied multiple outcomes. The content of these procedures appears to share common ground in terms of the clusters of behaviour change techniques used. Evaluated interventions tend to report positive findings. This suggests an understated set of assumptions about how interventions are intended to work, and through which mechanisms. Making these assumptions explicit through the use of theory would enable the testing, measurement and refinement of interventions to maximise their effect.
It is proposed that the learning from this study should be applied to the development and testing of future interventions to reduce restrictive practices through targeting health-care staff behaviour. This study has identified commonly used BCTs and they do appear to result in the reduction of restrictive practices. However, future interventions should be theoretically informed, test procedures in isolation, be rigorously described and measure their outcomes using a common language.
Acknowledgements
We are grateful to the National Institute for Health Research (NIHR) and colleagues who have supported this study.
Contributions of authors
John Baker (https://orcid.org/0000-0001-9985-9875) was responsible for leading the study, protocol development, contributed to literature searches, data extraction and analysis, and writing and editing the report.
Kathryn Berzins (https://orcid.org/0000-0001-5002-5212) was responsible for co-ordinating the study, contributed to literature searches, data extraction and analysis, BCT mapping and writing and editing the report.
Krysia Canvin (https://orcid.org/0000-0001-6571-6411) contributed to literature searches, data extraction and analysis, BCT mapping and writing and editing the report.
Iris Benson (https://orcid.org/0000-0001-5710-4706) (MBE) our patient and public involvement (PPI) representative throughout the project, contributed to the Steering Group, the plain English summary and the dissemination strategy.
Ian Kellar (https://orcid.org/0000-0003-1608-5216) provided expertise in BCT mapping, and contributed to writing and editing the report.
Judy Wright (https://orcid.org/0000-0002-5239-0173) developed and advised on the search strategies and contributed to the final report.
Rocio Rodriguez Lopez (https://orcid.org/0000-0003-2460-8128) developed and advised on the search strategies and contributed to the final report.
Joy Duxbury (https://orcid.org/0000-0002-1772-6874) provided expertise in restrictive interventions.
Tim Kendall (https://orcid.org/0000-0003-3825-3022) provided policy expertise.
Duncan Stewart (https://orcid.org/0000-0001-7355-4280) provided expertise in restrictive interventions and contributed to writing and editing the final report.
Data-sharing statement
No new data have been created in the preparation of this report and, therefore, there is nothing available for access and further sharing. All queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Bowers L, Stewart D, Papadopoulos C, Dack C, Ross J, Khanom H, et al. Inpatient Violence and Aggression: A Literature Review. Report from the Conflict and Containment Reduction Research Programme 2011.
- Royal College of Psychiatrists (RCP) . Healthcare Commission National Audit of Violence 2006–7 2007.
- Social Care, Local Government and Care Partnership Directorate . Positive and Proactive Care: Reducing the Need for Restrictive Interventions 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/300293/JRA_DoH_Guidance_on_RP_web_accessible.pdf (accessed 23 July 2020).
- Noorthoorn E, Lepping P, Janssen W, Hoogendoorn A, Nijman H, Widdershoven G, et al. One-year incidence and prevalence of seclusion: Dutch findings in an international perspective. Soc Psychiatry Psychiatr Epidemiol 2015;50:1857-69. https://doi.org/10.1007/s00127-015-1094-2.
- Steinert T, Lepping P, Bernhardsgrütter R, Conca A, Hatling T, Janssen W, et al. Incidence of seclusion and restraint in psychiatric hospitals: a literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol 2010;45:889-97. https://doi.org/10.1007/s00127-009-0132-3.
- Ash D, Suetani S, Nair J, Halpin M. Recovery-based services in a psychiatric intensive care unit – the consumer perspective. Australas Psychiatry 2015;23:524-7. https://doi.org/10.1177/1039856215593397.
- Department of Health and Social Care (DHSC) . Positive and Proactive Care: Reducing the Need for Restrictive Interventions 2014.
- Stewart D, Bowers L, Simpson A, Ryan C, Tziggili M. Manual restraint of adult psychiatric inpatients: a literature review. J Psychiatr Ment Health Nurs 2009;16:749-57. https://doi.org/10.1111/j.1365-2850.2009.01475.x.
- Mind . Mental Health Crisis Care: Physical Restraint in Crisis 2013.
- NHS Security Management Service (NHS SMS) . Cost of Violence Against NHS Staff: A Report Summarising the Economic Cost to the NHS of Violence Against Staff 2007 2008 2010.
- Flood C, Bowers L, Parkin D. Estimating the costs of conflict and containment on adult acute inpatient psychiatric wards. Nurs Econ 2008;26:325-30.
- Norfolk, Suffolk and Cambridgeshire Strategic Health Authority . Independent Inquiry into the Death of David Bennett: An Independent Inquiry Set Up Under HSG(94)27 2003.
- Great Britain . Mental Health Units (Use of Force) Act 2018 2018.
- Stewart D, Van der Merwe M, Bowers L, Simpson A, Jones J. A review of interventions to reduce mechanical restraint and seclusion among adult psychiatric inpatients. Issues Ment Health Nurs 2010;31:413-24. https://doi.org/10.3109/01612840903484113.
- Cabral A, Carthy J. Can Safewards improve patient care and safety in forensic wards? A pilot study. Br J Ment Health Nurs 2017;6:165-71. https://doi.org/10.12968/bjmh.2017.6.4.165.
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J. SUGAR . Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud 2015;52:1412-22. https://doi.org/10.1016/j.ijnurstu.2015.05.001.
- Putkonen A, Kuivalainen S, Louheranta O, Repo-Tiihonen E, Ryynänen OP, Kautiainen H, et al. Cluster-randomized controlled trial of reducing seclusion and restraint in secured care of men with schizophrenia. Psychiatr Serv 2013;64:850-5. https://doi.org/10.1176/appi.ps.201200393.
- Livingston JD, Verdun-Jones S, Brink J, Lussier P, Nicholls T. A narrative review of the effectiveness of aggression management training programs for psychiatric hospital staff. J Forensic Nurs 2010;6:15-28. https://doi.org/10.1111/j.1939-3938.2009.01061.x.
- Ashcraft L, Anthony WA, Jaccard S. Rein in seclusion and restraints: they are not compatible with recovery-oriented services. Behav Healthc 2008;28:6-7.
- Steinert T, Eisele F, Goeser U, Tschoeke S, Uhlmann C, Schmid P. Successful interventions on an organisational level to reduce violence and coercive interventions in in-patients with adjustment disorders and personality disorders. Clin Pract Epidemiol Ment Health 2008;4. https://doi.org/10.1186/1745-0179-4-27.
- Laker C, Gray R, Flach C. Case study evaluating the impact of de-escalation and physical intervention training. J Psychiatr Ment Health Nurs 2010;17:222-8. https://doi.org/10.1111/j.1365-2850.2009.01496.x.
- Duxbury J, Baker J, Downe S, Jones F, Greenwood P, Thygesen H, et al. Minimising the use of physical restraint in acute mental health services: the outcome of a restraint reduction programme (‘REsTRAIN YOURSELF’). Int J Nurs Stud 2019;95:40-8. https://doi.org/10.1016/j.ijnurstu.2019.03.016.
- Riahi S, Dawe IC, Stuckey MI, Klassen PE. Implementation of the Six Core Strategies for restraint minimization in a specialized mental health organization. J Psychosoc Nurs Ment Health Serv 2016;54:32-9. https://doi.org/10.3928/02793695-20160920-06.
- Ashcraft L, Bloss M, Anthony WA. Best practices: the development and implementation of ‘no force first’ as a best practice. Psychiatr Serv 2012;63:415-17. https://doi.org/10.1176/appi.ps.20120p415.
- Scanlan JN, Novak T. Sensory approaches in mental health: a scoping review. Aust Occup Ther J 2015;62:277-85. https://doi.org/10.1111/1440-1630.12224.
- Dahm KT, Leiknes KA, Husum TL, Kirkehei I, Hofmann B, Myhrhaug HT, et al. Interventions for Reducing Seclusion and Restraint in Mental Health for Adults. Oslo: Knowledge Centre for the Health Services at the Norwegian Institute of Public Health (NIPH); 2012.
- Sailas E, Fenton M. Seclusion and restraint for people with serious mental illnesses. Cochrane Database Syst Rev 2000;2. https://doi.org/10.1002/14651858.CD001163.
- Gaskin CJ, Elsom SJ, Happell B. Interventions for reducing the use of seclusion in psychiatric facilities: review of the literature. Br J Psychiatry 2007;191:298-303. https://doi.org/10.1192/bjp.bp.106.034538.
- Bak J, Brandt-Christensen M, Sestoft DM, Zoffmann V. Mechanical restraint – Which interventions prevent episodes of mechanical restraint? – A systematic review. Perspect Psychiatr Care 2012;48:83-94. https://doi.org/10.1111/j.1744-6163.2011.00307.x.
- Mugoya GCT, Kampfe CM. Reducing the use of PRN medication in in-patient psychiatric hospitals. J Life Care Plan 2010;19:37-46.
- Scanlan JN. Interventions to reduce the use of seclusion and restraint in inpatient psychiatric settings: what we know so far a review of the literature. Int J Soc Psychiatry 2010;56:412-23. https://doi.org/10.1177/0020764009106630.
- Muralidharan S, Fenton M. Containment strategies for people with serious mental illness. Cochrane Database Syst Rev 2006;3. https://doi.org/10.1002/14651858.CD002084.pub2.
- Wynn R. The use of physical restraint in Norwegian adult psychiatric hospitals. Psychiatry J 2015;2015. https://doi.org/10.1155/2015/347246.
- Möhler R, Meyer G. Development methods of guidelines and documents with recommendations on physical restraint reduction in nursing homes: a systematic review. BMC Geriatr 2015;15. https://doi.org/10.1186/s12877-015-0150-9.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-40.
- Davidson KW, Goldstein M, Kaplan RM, Kaufmann PG, Knatterud GL, Orleans CT, et al. Evidence-based behavioral medicine: what is it and how do we achieve it?. Ann Behav Med 2003;26:161-71. https://doi.org/10.1207/S15324796ABM2603_01.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. https://doi.org/10.1007/s12160-013-9486-6.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. https://doi.org/10.1037/0278-6133.27.3.379.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. https://doi.org/10.1037/a0016136.
- Abraham C, Good A, Warren MR, Huedo-Medina T, Johnson B. Developing and testing a SHARP taxonomy of behavior change techniques included in condom promotion interventions. Psychol Health 2011;26.
- Brett J, Staniszewska S, Newburn M, Jones N, Taylor L. A systematic mapping review of effective interventions for communicating with, supporting and providing information to parents of preterm infants. BMJ Open 2011;1. https://doi.org/10.1136/bmjopen-2010-000023.
- Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 2012;107:1431-40. https://doi.org/10.1111/j.1360-0443.2012.03845.x.
- West R, Walia A, Hyder N, Shahab L, Michie S. Behavior change techniques used by the English Stop Smoking Services and their associations with short-term quit outcomes. Nicotine Tob Res 2010;12:742-7. https://doi.org/10.1093/ntr/ntq074.
- Michie S, Hyder N, Walia A, West R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict Behav 2011;36:315-19. https://doi.org/10.1016/j.addbeh.2010.11.016.
- Berzins KM, Gray TA, Waterman H, Francis JJ. Specifying active components of educational interventions to promote adherence to treatment in glaucoma patients: application of a taxonomy of behavior change techniques. Psychol Res Behav Manag 2015;8:201-9. https://doi.org/10.2147/PRBM.S74664.
- Presseau J, Ivers NM, Newham JJ, Knittle K, Danko KJ, Grimshaw JM. Using a behaviour change techniques taxonomy to identify active ingredients within trials of implementation interventions for diabetes care. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0248-7.
- Michie S, Prestwich A. Are interventions theory-based? Development of a theory coding scheme. Health Psychol 2010;29:1-8. https://doi.org/10.1037/a0016939.
- Michie S, Churchill S, West R. Identifying evidence-based competences required to deliver behavioural support for smoking cessation. Ann Behav Med 2011;41:59-70. https://doi.org/10.1007/s12160-010-9235-z.
- NHS Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness: CRD'S Guidance for Those Carrying Out or Commissioning Reviews. CRD Report 4 (2nd Edition) 2001.
- Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49:47-53. https://doi.org/10.1016/j.ijnurstu.2011.07.002.
- Bradbury-Jones C, Breckenridge JP, Clark MT, Herber OR, Jones C, Taylor J. Advancing the science of literature reviewing in social research: the focused mapping review and synthesis. Int J Soc Res Methodol 2019;22:451-62. https://doi.org/10.1080/13645579.2019.1576328.
- Carter EW, Lane KL, Crnobori M, Bruhn AL, Oakes WP. Self-determination interventions for students with and at risk for emotional and behavioral disorders: mapping the knowledge base. Behav Disord 2011;36:100-16. https://doi.org/10.1177/019874291103600202.
- Clapton J, Rutter D, Sharif N. SCIE Systematic Mapping Guidance. London: Social Care Institute for Excellence; 2009.
- Cooper DI. What is a ‘mapping study’?. J Med Lib Assoc 2016;104:76-8. https://doi.org/10.3163/1536-5050.104.1.013.
- Perryman CL. Mapping studies. J Med Lib Assoc 2016;104:79-82. https://doi.org/10.3163/1536-5050.104.1.014.
- Graham P, Evitts T, Thomas-MacLean R. Environmental scans: how useful are they for primary care research?. Can Fam Physician 2008;54:1022-3.
- Department of Health and Social Care (DHSC) . The National Service Framework for Mental Health: Modern Standards and Service Models 1999.
- Wallace B, Small K, Brodley C, Lau J, Trikalinos T. Deploying an Interactive Machine Learning System in an Evidence-Based Practice Center: Abstrackr n.d. https://doi.org/10.1145/2110363.2110464.
- Rathbone J, Hoffmann T, Glasziou P. Faster title and abstract screening? Evaluating Abstrackr, a semi-automated online screening program for systematic reviewers. Syst Rev 2015;4. https://doi.org/10.1186/s13643-015-0067-6.
- Albrecht L, Archibald M, Arseneau D, Scott SD. Development of a checklist to assess the quality of reporting of knowledge translation interventions using the Workgroup for Intervention Development and Evaluation Research (WIDER) recommendations. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-52.
- Dye JF, Schatz IM, Rosenberg BA, Coleman ST. Constant comparison method: a kaleidoscope of data. Qual Rep 2000;4:1-10.
- Cochrane Collaboration . Data Collection Form for Intervention Reviews for RCTs and Non-RCTs – Template 2014. https://dplp.cochrane.org/sites/dplp.cochrane.org/files/public/uploads/CDPLPG%20data%20collection%20form%20for%20intervention%20reviews%20for%20RCTs%20and%20non-RCTs.doc (accessed 23 October 2020).
- Cotterill S, Knowles S, Martindale AM, Elvey R, Howard S, Coupe N, et al. Getting messier with TIDieR: embracing context and complexity in intervention reporting. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-017-0461-y.
- O’Shea O, McCormick R, Bradley JM, O’Neill B. Fidelity review: a scoping review of the methods used to evaluate treatment fidelity in behavioural change interventions. Phys Ther Rev 2016;21:207-14. https://doi.org/10.1080/10833196.2016.1261237.
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Kelly B, Perkins DF. Handbook of Implementation Science for Psychology in Education. New York, NY: Cambridge University Press; 2012.
- Pluye P, Gagnon MP, Griffiths F, Johnson-Lafleur J. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int J Nurs Stud 2009;46:529-46. https://doi.org/10.1016/j.ijnurstu.2009.01.009.
- Melin RD. Team responses to inpatient aggression: the effects of institutional training on restraint utilization patterns. Diss Abstr Int B 2002;63.
- Gonzalez TD. Impact of active listening training at a California state hospital: a quantitative study. Diss Abstr Int B 2009;70.
- Bybel B. Does Education of Alternative Measures Decrease the Use of Physical Restraints and Seclusion?. Phoenix, AZ: University of Phoenix; 2011.
- Huckshorn KA. Reducing Seclusion and Restraint Use in Mental Health Settings: A Phenomenological Study of Hospital Leader and Staff Experiences 2012.
- Omolewa P. The Impact of Instructive Educational Program on Physical Restraint Reduction in Acute Mental Health Hospitals 2012.
- Lo CT. Implementation of a Psychiatric Emergency Response Team on Adult Psychiatric Inpatient Units 2015.
- Wolfaardt T. An Evaluation of the Efficacy of the Six Core Strategies Intervention to Reduce Seclusion and Restraint Episodes in an Acute Mental Health Unit 2013.
- Hayashi F, Harsany A, Varvara M, Wong PY, Lantz MS. The elimination of seclusion in a geriatric inpatient unit: using environmental modification to effect a cultural change. Am J of Geriat Psychiat 2015;23:S122-3. https://doi.org/10.1016/j.jagp.2014.12.122.
- Parasurum R, Chua PS, Kannusamy P. A randomised controlled study examining the impact of a staffing model and nursing care delivery system on patient, nurse and organisational outcomes. Ann Acad Med Singapore 2011;1.
- Sarkar J. Reducing violence through the use of structured therapies. Ann Acad Med Singapore 2013;1.
- Beezhold J, Williams P, Taylor J, Harris A, Kandasamy S. A quasi-experimental controlled intervention to reduce violence on an acute psychiatric ward. Eur Psychiatry 2010;25. https://doi.org/10.1016/S0924-9338(10)70864-6.
- Burhan A, Black E, Ross T, Toogood P, O’Regan T. The impact of a primary nursing care delivery approach upon the frequency and effectiveness of PRN medication. Am J of Geriat Psychiat 2010;1:S82-S3.
- Wishnowsky G. Lessons in reducing seclusion and restraint in aged person’s mental health. HNE Hand Nurses Midwives 2013;6. www.semanticscholar.org/paper/Lessons-in-reducing-seclusion-and-restraint-in-aged-Wishnowsky/bf838f5087943072ac2b826026a7c4d79c1a9c6c (accessed 20 November 2020).
- Trevarrow R. Chill Out Room Project. Newcastle upon Tyne: Northumberland Tyne and Wear NHS Foundation Trust; 2019.
- Northumberland Tyne and Wear NHS Foundation Trust . Positive and Safe Care Annual Report 2018 2018.
- Substance Abuse and Mental Health Services Administration (SAMSHA) . Alternatives to Seclusion and Restraint SAMHSA State Infrastructure Grant: Evaluation Overview 2006.
- Care Quality Commission (CQC) . Mental Health Act: A Focus on Restrictive Intervention Reduction Programmes in Inpatient Mental Health Services 2017.
- NHS Improvement . Valued Care in Mental Health: Improving for Excellence – A National Mental Health Improvement Model 2018.
- Mind . Restraint in Mental Health Services 2015.
- Higgins N, Dart N, Meehan T, Fulbrook P, Kilshaw M, Anderson D. Implementation of Safewards Across Three Inpatient Mental Health Units 2017. https://insight-prod.s3.ap-southeast-2.amazonaws.com/public/uploads/20170426.2.pdf (accessed 4 August 2020).
- Szypula F, Martin M. Balancing Risk & Safety When Reducing Restraint &Amp; Seclusion n.d.
- Tully J, McSweeney L, Harfield KL, Castle C, Das M. Innovation and pragmatism required to reduce seclusion practices. CNS Spectr 2016;21:424-9. https://doi.org/10.1017/S1092852916000481.
- Scottish Patient Safety Programme . Restraint and Seclusion Driver Diagram n.d. http://ihub.scot/media/1967/seclusion-restraint-v18.pdf (accessed 20 November 2020).
- Huckshorn KA. Preventing Violence, Trauma, and the Use of Seclusion and Restraint in Mental Health Settings: Preventing Conflict, Violence and the Use of Seclusion Restraint 2010. https://iacc.hhs.gov/meetings/iacc-meetings/2010/services-workshop/november8/slides_kevin_ann_huckshorn_110810.pdf (accessed 8 January 2021).
- Hart C. Using De-Escalation Skills in a Mental Health Setting: Twenty First Century Media 2015. www.youtube.com/watch?v=Q4T-x1za6lg (accessed 4 August 2020).
- Taylor A, Brown S. Minimising Seclusion and Restraint: Sensory Approaches in the Adult Inpatient Psychiatric Setting 2013. https://webcast.gigtv.com.au/Mediasite/Play/9fa51cf1682e41aba3408700cccf8bfb1d?catalog=78ae969f64c24b8787fd5d40d5fd4b8b21 (accessed 23 October 2020).
- Crisis Prevention Institute (CPI) . De-Escalation Techniques 2010. www.youtube.com/watch?v=pBe4A32fpyI (accessed 22 October 2020).
- Meeks T. Non-Violent De-escalation for Therapists. Seattle, WA: Harborview Medical Center; 2016.
- Crisis Prevention Institute (CPI) . How CentraCare Health Reduced Worker’s Comp Costs. Unrestrained Episode 26, Guest: James Gulbranson and Paul Ruegemer [Internet]. Part 1: Non-Violent Crisis Intervention; Part 2: Behavioral Escalation Response Team 2016. www.crisisprevention.com/en-CA/Blog/March-2016/Unrestrained-Episode-26-Guests-James-Gulbranson-Pa (accessed 19 November 2020).
- Royal College of Psychiatrists (RCP) . Prevention and Management of Violence and Aggression Training Plan (TEWV): Reducing Restrictive Practice Programme 2020.
- Hernandez A, Riahi S, Stuckey MI, Mildon BA, Klassen PE. Multidimensional approach to restraint minimization: the journey of a specialized mental health organization. Int J Ment Health Nurs 2017;26:482-90. https://doi.org/10.1111/inm.12379.
- Higgins N, Dart N, Meehan T, Fulbrook P, Kilshaw M, Anderson D, et al. The Safewards Program in Queensland public hospital acute mental health settings. Aust Nurs Midwifery J 2016;23.
- Bowers L, Brennan G, Flood C, Lipang M, Oladapo P. Preliminary outcomes of a trial to reduce conflict and containment on acute psychiatric wards: City Nurses. J Psychiatr Ment Health Nurs 2006;13:165-72. https://doi.org/10.1111/j.1365-2850.2006.00931.x.
- Bowers L, Flood C, Brennan G, Allan T. A replication study of the city Nurse intervention: reducing conflict and containment on three acute psychiatric wards. J Psychiatr Ment Health Nurs 2008;15:737-42. https://doi.org/10.1111/j.1365-2850.2008.01294.x.
- Visalli H, McNasser G. An effective model of practice without contention. Soins Psychiatr 2000;210:30-2.
- Sullivan D, Wallis M, Lloyd C. Effects of patient-focused care on seclusion in a psychiatric intensive care unit. Int J Ther Rehabil 2004;11:503-8. https://doi.org/10.12968/ijtr.2004.11.11.17202.
- Donat DC. An analysis of successful efforts to reduce the use of seclusion and restraint at a public psychiatric hospital. Psychiatr Serv 2003;54:1119-23. https://doi.org/10.1176/appi.ps.54.8.1119.
- Donat DC. Employing behavioral methods to improve the context of care in a public psychiatric hospital: reducing hospital reliance on seclusion/restraint and psychotropic PRN medication. Cogn Behav Pract 2002;9:28-37. https://doi.org/10.1016/S1077-7229%2802%2980036-0.
- Borckardt JJ, Madan A, Grubaugh AL, Danielson CK, Pelic CG, Hardesty SJ, et al. Systematic investigation of initiatives to reduce seclusion and restraint in a state psychiatric hospital. Psychiatr Serv 2011;62:477-83. https://doi.org/10.1176/ps.62.5.pss6205_0477.
- Madan A, Borckardt JJ, Grubaugh AL, Danielson CK, McLeod-Bryant S, Cooney H, et al. Efforts to reduce seclusion and restraint use in a state psychiatric hospital: a ten-year perspective. Psychiatr Serv 2014;65:1273-6. https://doi.org/10.1176/appi.ps.201300383.
- Jungfer HA, Schneeberger AR, Borgwardt S, Walter M, Vogel M, Gairing SK, et al. Reduction of seclusion on a hospital-wide level: successful implementation of a less restrictive policy. J Psychiatr Res 2014;54:94-9. https://doi.org/10.1016/j.jpsychires.2014.03.020.
- Hochstrasser L, Fröhlich D, Schneeberger AR, Borgwardt S, Lang UE, Stieglitz RD, et al. Long-term reduction of seclusion and forced medication on a hospital-wide level: implementation of an open-door policy over 6 years. Eur Psychiatry 2018;48:51-7. https://doi.org/10.1016/j.eurpsy.2017.09.008.
- Hochstrasser L, Voulgaris A, Möller J, Zimmermann T, Steinauer R, Borgwardt S, et al. Reduced frequency of cases with seclusion is associated with ‘opening the doors’ of a psychiatric intensive care unit. Front Psychiatry 2018;9. https://doi.org/10.3389/fpsyt.2018.00057.
- Needham I, Abderhalden C, Meer R, Dassen T, Haug HJ, Halfens RJ, et al. The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study. J Psychiatr Ment Health Nurs 2004;11:595-601. https://doi.org/10.1111/j.1365-2850.2004.00767.x.
- Abderhalden C, Needham I, Dassen T, Halfens R, Haug HJ, Fischer JE. Structured risk assessment and violence in acute psychiatric wards: randomised controlled trial. Br J Psychiatry 2008;193:44-50. https://doi.org/10.1192/bjp.bp.107.045534.
- Clarke DE, Brown AM, Griffith P. The Brøset Violence Checklist: clinical utility in a secure psychiatric intensive care setting. J Psychiatr Ment Health Nurs 2010;17:614-20. https://doi.org/10.1111/j.1365-2850.2010.01558.x.
- Ching H, Daffern M, Martina T, Thomasa S. Reducing the use of seclusion in a forensic psychiatric hospital: assessing the impact on aggression, therapeutic climate and staff confidence. J Forens Psychiatry Psychol 2010;21:737-60. https://doi.org/10.1080/14789941003681361.
- Maguire T, Young R, Martin T. Seclusion reduction in a forensic mental health setting. J Psychiatr Ment Health Nurs 2012;19:97-106. https://doi.org/10.1111/j.1365-2850.2011.01753.x.
- Ash D, Metcalfe P, Burton C. Reduction in the use of seclusion with the introduction of recovery principles in an acute psychiatric unit. Schizophr Res 2014;1:S292-S3. https://doi.org/10.1016/S0920-9964(14)70828-X.
- Fluttert FA, Van Meijel B, Nijman H, Bjørkly S, Grypdonck M. Preventing aggressive incidents and seclusions in forensic care by means of the ‘Early Recognition Method’. J Clin Nurs 2010;19:1529-37. https://doi.org/10.1111/j.1365-2702.2009.02986.x.
- Fluttert FA, Van Meijel B, Bjørkly S, Van Leeuwen M, Grypdonck M. The investigation of early warning signs of aggression in forensic patients by means of the ‘Forensic Early Signs of Aggression Inventory’. J Clin Nurs 2013;22:1550-8. https://doi.org/10.1111/j.1365-2702.2012.04318.x.
- Duxbury J, Thomson G, Scholes A, Jones F, Baker J, Downe S, et al. Staff experiences and understandings of the REsTRAIN Yourself initiative to minimize the use of physical restraint on mental health wards. Int J Ment Health Nurs 2019;28:845-56. https://doi.org/10.1111/inm.12577.
- Advancing Quality Alliance (AQUA) . REsTRAIN Yourself Toolkit 2014. www.aquanw.nhs.uk/resources/restrain-yourself-toolkit/20917 (accessed 22 October 2020).
- NHS Scotland. Scottish Patient Safety Programme . Patient Safety Including Trauma Informed Care and Usage of Seclusion and Restraint 2014. https://ihub.scot/media/1863/iimhl-spsp-v03.pdf (accessed 24 November 2020).
- McEwan S, McClarty D, Porter L. Achieving violence and restraint reduction in an IPCU. Br J Ment Health Nurs 2016;5:38-42. https://doi.org/10.12968/bjmh.2016.5.1.38.
- Cheema F, McKechnie L, Riley P, Carlyle A, Ross J, Renwick C, et al. Improving patient safety in mental health through quality risk management. Euro Psychiat Conf 2013;28. https://doi.org/10.1016/S0924-9338(13)76792-0.
- Northumberland Tyne and Wear NHS Foundation Trust . Positive and Safe Care Annual Report 2017 2017.
- Royal College of Psychiatrists (RCP) . Reducing Restrictive Practice Programme: Tools – Talk First 2019. www.rcpsych.ac.uk/improving-care/nccmh/reducing-restrictive-practice (accessed 28 February 2019).
- Lee S, Cox A, Whitecross F, Williams P, Hollander Y. Sensory assessment and therapy to help reduce seclusion use with service users needing psychiatric intensive care. J Psychiatric Int Care 2010;6:83-90. https://doi.org/10.1017/S1742646410000014.
- Prescott DL, Madden LM, Dennis M, Tisher P, Wingate C. Reducing mechanical restraints in acute psychiatric care settings using rapid response teams. J Behav Health Serv Res 2007;34:96-105. https://doi.org/10.1007/s11414-006-9036-0.
- Björkdahl A, Hansebo G, Palmstierna T. The influence of staff training on the violence prevention and management climate in psychiatric inpatient units. J Psychiatr Ment Health Nurs 2013;20:396-404. https://doi.org/10.1111/j.1365-2850.2012.01930.x.
- Beckett P, Holmes D, Phipps M, Patton D, Molloy L. Trauma-informed care and practice: practice improvement strategies in an inpatient mental health ward. J Psychosoc Nurs Ment Health Serv 2017;55:34-8. https://doi.org/10.3928/02793695-20170818-03.
- Friedman R, Nurenberg JR, Birnbaum S, Schleifer SJ. Using structured clinical feedback to encourage alternatives to use of ‘P.R.N.’ medication in a state psychiatric hospital. J Psychiatr Pract 2012;18:381-7. https://doi.org/10.1097/01.pra.0000419823.69914.c7.
- Lewis M, Taylor K, Parks J. Crisis prevention management: a program to reduce the use of seclusion and restraint in an inpatient mental health setting. Issues Ment Health Nurs 2009;30:159-64. https://doi.org/10.1080/01612840802694171.
- Huckshorn KA. Six Core Strategies for Reducing Seclusion and Restraint Use. Alexandria, VA: National Association of State Mental Health Program Directors; 2006.
- Riley D, Benson I, Kilcoyne J, Angus D. No Force First: eliminating restraint in a mental health trust. Nurs Times 2018;114:38-9.
- Andersen C, Kolmos A, Andersen K, Sippel V, Stenager E. Applying sensory modulation to mental health inpatient care to reduce seclusion and restraint: a case control study. Nord J Psychiatry 2017;71:525-8. https://doi.org/10.1080/08039488.2017.1346142.
- Lloyd C, King R, Machingura T. An investigation into the effectiveness of sensory modulation in reducing seclusion within an acute mental health unit. Adv Men Health 2014;12:93-100. https://doi.org/10.1080/18374905.2014.11081887.
- McEvedy S, Maguire T, Furness T, McKenna B. Sensory modulation and trauma-informed-care knowledge transfer and translation in mental health services in Victoria: evaluation of a statewide train-the-trainer intervention. Nurse Educ Pract 2017;25:36-42. https://doi.org/10.1016/j.nepr.2017.04.012.
- Department of Mental Health and Addiction Services (DMHAS) . DMHAS Guidelines for Development of Comfort Rooms 2019.
- Visalli H, McNasser G. Reducing seclusion and restraint: meeting the organizational challenge. J Nurs Care Qual 2000;14:35-44. https://doi.org/10.1097/00001786-200007000-00007.
- Smith S, Jones J. Use of a sensory room on an intensive care unit. J Psychosoc Nurs Ment Health Serv 2014;52:22-30. https://doi.org/10.3928/02793695-20131126-06.
- Calabro K, Mackey TA, Williams S. Evaluation of training designed to prevent and manage patient violence. Issues Ment Health Nurs 2002;23:3-15. https://doi.org/10.1080/01612840252825446.
- Smith GM, Davis RH, Bixler EO, Lin HM, Altenor A, Altenor RJ, et al. Pennsylvania State Hospital system’s seclusion and restraint reduction program. Psychiatr Serv 2005;56:1115-22. https://doi.org/10.1176/appi.ps.56.9.1115.
- Hayes A, Russ MJ. Discontinuing the use of PRN intramuscular medication for agitation in an acute psychiatric hospital. Psychiatr Q 2016;87:25-9. https://doi.org/10.1007/s11126-015-9359-1.
- Guzman-Parra J, Aguilera Serrano C, García-Sánchez JA, Pino-Benítez I, Alba-Vallejo M, Moreno-Küstner B, et al. Effectiveness of a multimodal intervention program for restraint prevention in an acute Spanish psychiatric ward. J Am Psychiatr Nurses Assoc 2016;22:233-41. https://doi.org/10.1177/1078390316644767.
- Hellerstein DJ, Staub AB, Lequesne E. Decreasing the use of restraint and seclusion among psychiatric inpatients. J Psychiatr Pract 2007;13:308-17. https://doi.org/10.1097/01.pra.0000290669.10107.ba.
- Guzman-Parra J, Garcia-Sanchez JA, Pino-Benitez I, Alba-Vallejo M, Mayoral-Cleries F. Effects of a regulatory protocol for mechanical restraint and coercion in a Spanish psychiatric ward. Perspect Psychiatr Care 2015;51:260-7. https://doi.org/10.1111/ppc.12090.
- Long CG, West R, Afford M, Collins L, Dolley O. Reducing the use of seclusion in a secure service for women. J Psychiat Int Care 2015;11:84-9. https://doi.org/10.1017/S174264641400017X.
- Geoffrion S, Goncalves J, Giguère CÉ, Guay S. Impact of a program for the management of aggressive behaviors on seclusion and restraint use in two high-risk units of a mental health institute. Psychiatr Q 2018;89:95-102. https://doi.org/10.1007/s11126-017-9519-6.
- D’Orio BM, Purselle D, Stevens D, Garlow SJ. Reduction of episodes of seclusion and restraint in a psychiatric emergency service. Psychiatr Serv 2004;55:581-3. https://doi.org/10.1176/appi.ps.55.5.581.
- Georgieva I, de Haan G, Smith W, Mulder CL. Successful reduction of seclusion in a newly developed psychiatric intensive care unit. J Psychiat Int Care 2010;6:31-8. https://doi.org/10.1017/S1742646409990082.
- Aremu B, Hill PD, McNeal JM, Petersen MA, Swanberg D, Delaney KR. Implementation of trauma-informed care and brief solution-focused therapy. J Psychosoc Nurs Ment Health Serv 2019;56:16-22. https://doi.org/10.3928/02793695-20180305-02.
- Sutton D, Wilson M, Van Kessel K, Vanderpyl J. Optimizing arousal to manage aggression: a pilot study of sensory modulation. Int J Ment Health Nurs 2013;22:500-11. https://doi.org/10.1111/inm.12010.
- Taylor-Watt J, Cruickshank A, Innes J, Brome B, Shah A. Reducing physical violence and developing a safety culture across wards in East London. Br J Ment Health Nurs 2017;6:35-43. https://doi.org/10.12968/bjmh.2017.6.1.35.
- Brown J, Fawzi W, McCarthy C, Stevenson C, Kwesi S, Joyce M, et al. Safer wards: reducing violence on older people’s mental health wards. BMJ Open Quality 2015;4. https://doi.org/10.1136/bmjquality.u207447.w2977.
- Van der Schaaf PS, Dusseldorp E, Keuning FM, Janssen WA, Noorthoorn EO. Impact of the physical environment of psychiatric wards on the use of seclusion. Br J Psychiatry 2013;202:142-9. https://doi.org/10.1192/bjp.bp.112.118422.
- Riemer D. Creating sanctuary: reducing violence in a maximum security forensic psychiatric hospital unit. On the Edge 2009;15.
- Short R, Sherman ME, Raia J, Bumgardner C, Chambers A, Lofton V. Safety guidelines for injury-free management of psychiatric inpatients in precrisis and crisis situations. Psychiatr Serv 2008;59:1376-8. https://doi.org/10.1176/appi.ps.59.12.1376.
- Smith P, Millar M. The quiet room: improving the acute care psychiatric environment. FoNS Improv Insights 2014;9:1-20.
- Lombardo C, Van Bortel T, Wagner AP, Kaminskiy E, Wilson C, Krishnamoorthy T, et al. PROGRESS: the PROMISE governance framework to decrease coercion in mental healthcare. BMJ Open Qual 2018;7. https://doi.org/10.1136/bmjoq-2018-000332.
- Zuehlke JB, Kotecki RM, Kern S, Sholty G, Hauser P. Transformation to a recovery-oriented model of care on a veterans administration inpatient unit. Psychiatr Rehabil J 2016;39:361-3. https://doi.org/10.1037/prj0000198.
- Bell A, Gallacher N. Succeeding in sustained reduction in the use of restraint using the Improvement Model. BMJ Qual Improv Rep 2016;5. https://doi.org/10.1136/bmjquality.u211050.w4430.
- Chang NA, Grant PM, Luther L, Beck AT. Effects of a recovery-oriented cognitive therapy training program on inpatient staff attitudes and incidents of seclusion and restraint. Community Ment Health J 2014;50:415-21. https://doi.org/10.1007/s10597-013-9675-6.
- Cowin L, Davies R, Estall G, Berlin T, Fitzgerald M, Hoot S. De-escalating aggression and violence in the mental health setting. Int J Ment Health Nurs 2003;12:64-73. https://doi.org/10.1046/j.1440-0979.2003.00270.x.
- Bandura A, Walters RH. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977.
- Bonner G, Lynch JE, Trenoweth S. Contemporary Issues in Mental Health Nursing. London: Wiley-Blackwell; 2008.
- Goulet MH, Larue C, Lemieux AJ. A pilot study of ‘post-seclusion and/or restraint review’ intervention with patients and staff in a mental health setting. Perspect Psychiatr Care 2017:1-9. https://doi.org/10.1111/ppc.12225.
- Anderson CA, Bushman BJ. Human aggression. Ann Rev Psychol 2002;53:27-51. https://doi.org/10.1146/annurev.psych.53.100901.135231.
- Kernberg OF, Magnavita JJ. Handbook of Personality Disorders: Theory and Practice. New York, NY: Wiley; 2004.
- Foelsch PA, Kernberg OF. Transference-focused psychotherapy for borderline personality disorders. Session: Psychothera Pract 1998;4:67-90. https://doi.org/10.1002/(SICI)1520-6572(199822)4:2<67::AID-SESS5>3.0.CO;2-5.
- Gonzalez-Torres MA, Fernandez-Rivas A, Bustamante S, Rico-Vilademoros F, Vivanco E, Martinez K, et al. Impact of the creation and implementation of a clinical management guideline for personality disorders in reducing use of mechanical restraints in a psychiatric inpatient unit. Prim Care Companion CNS Disord 2014;16. https://doi.org/10.4088/PCC.14m01675.
- Peplau HE. Peplau’s theory of interpersonal relations. Nurs Sci Q 1997;10:162-7. https://doi.org/10.1177/089431849701000407.
- Watson J. Human Caring Science. Burlington, MA: Jones & Bartlett Publishers; 2011.
- Bowers L. Safewards: a new model of conflict and containment on psychiatric wards. J Psychiatr Ment Health Nurs 2014;21:499-508. https://doi.org/10.1111/jpm.12129.
- Kanter RM. Men and Women of the Corporation. New York, NY: Basic Books; 1993.
- Prochaska JO, Johnson S, Lee P, Shumaker SA, Ockene JK, Riekert KA. The Handbook of Health Behavior Change. New York, NY: Springer Publishing Company; 2009.
- Colton D. Checklist for Assessing your Organization’s Readiness for Reducing Seclusion and Restraint. Staunton, VA: Commonwealth Center for Children and Adolescents; 2004.
- Schein EH. Organizational Culture and Leadership. Hoboken, NJ: John Wiley & Sons Inc.; 2004.
- Huckshorn KA. Re-designing state mental health policy to prevent the use of seclusion and restraint. Adm Policy Ment Health 2006;33:482-91. https://doi.org/10.1007/s10488-005-0011-5.
- Senge PM. The Fifth Discipline: The Art and Practice of the Learning Organization. New York, NY: Doubleday; 1990.
- Jonikas JA, Cook JA, Rosen C, Laris A, Kim JB. A program to reduce use of physical restraint in psychiatric inpatient facilities. Psychiatr Serv 2004;55:818-20. https://doi.org/10.1176/appi.ps.55.7.818.
- Fletcher J, Spittal M, Brophy L, Tibble H, Kinner S, Elsom S, et al. Outcomes of the Victorian Safewards trial in 13 wards: impact on seclusion rates and fidelity measurement. Int J Ment Health Nurs 2017;26:461-71. https://doi.org/10.1111/inm.12380.
- Noorthoorn E, Janssen W, Theunissen J, Hesta H, de Vries W, Hutschemaekers G, et al. The power of day-to-day motivational techniques and family participation in reducing seclusion. Int J Ment Health 2008;37:81-98. https://doi.org/10.2753/IMH0020-7411370304.
- Novak T, Scanlan J, McCaul D, MacDonald N, Clarke T. Pilot study of a sensory room in an acute inpatient psychiatric unit. Australas Psychiatry 2012;20:401-6. https://doi.org/10.1177/1039856212459585.
- Barton SA, Johnson MR, Price LV. Achieving restraint-free on an inpatient behavioral health unit. J Psychosoc Nurs Ment Health Serv 2009;47:34-40. https://doi.org/10.3928/02793695-20090101-01.
- Yakov S, Birur B, Bearden MF, Aguilar B, Ghelani KJ, Fargason RE. Sensory reduction on the general milieu of a high-acuity inpatient psychiatric unit to prevent use of physical restraints: a successful open quality improvement trial. J Am Psychiatr Nurses Assoc 2017. https://doi.org/10.1177/1078390317736136.
- Qurashi I, Johnson D, Shaw J, Johnson B. Reduction in the use of seclusion in a high secure hospital: a retrospective analysis. J Psychiatric Intensive Care 2010;6:109-15. https://doi.org/10.1017/S174264640999015X.
- Repique RJ, Vernig PM, Lowe J, Thompson JA, Yap TL. Implementation of a recovery-oriented training program for psychiatric nurses in the inpatient setting: a mixed-methods hospital quality improvement study. Arch Psychiatr Nurs 2016;30:722-8. https://doi.org/10.1016/j.apnu.2016.06.003.
- Stead K, Kumar S, Schultz TJ, Tiver S, Pirone CJ, Adams RJ, et al. Teams communicating through STEPPS. Med J Aust 2009;190:S128-32. https://doi.org/10.5694/j.1326-5377.2009.tb02619.x.
- Mistral W, Hall A, McKee P. Using therapeutic community principles to improve the functioning of a high care psychiatric ward in the UK. Int J Ment Health Nurs 2002;11:10-7. https://doi.org/10.1046/j.1440-0979.2002.00220.x.
- Sullivan AM, Bezmen J, Barron CT, Rivera J, Curley-Casey L, Marino D. Reducing restraints: alternatives to restraints on an inpatient psychiatric service – utilizing safe and effective methods to evaluate and treat the violent patient. Psychiatr Q 2005;76:51-65. https://doi.org/10.1007/s11089-005-5581-3.
- Sivak K. Implementation of comfort rooms to reduce seclusion, restraint use, and acting-out behaviors. J Psychosoc Nurs Ment Health Serv 2012;50:24-3. https://doi.org/10.3928/02793695-20110112-01.
- Riemer D, Corwith C. Application of core strategies: reducing seclusion and restraint use. On the Edge 2007;13:7-10.
- Ashcraft L, Anthony W. Eliminating seclusion and restraint in recovery-oriented crisis services. Psychiatr Serv 2008;59:1198-202. https://doi.org/10.1176/appi.ps.59.10.1198.
- Price O, Burbery P, Leonard S, Doyle M. Evaluation of Safewards in forensic mental health. Ment Health Pract 2016;19:14-21. https://doi.org/10.7748/mhp.19.8.14.s17.
- Cockerton R, O’Brien A, Oates J. Implementing positive and proactive care. Mental Health Practice 2015;19:36-9. https://doi.org/10.7748/mhp.19.4.36.s21.
- Wale JB, Belkin GS, Moon R. Reducing the use of seclusion and restraint in psychiatric emergency and adult inpatient services – improving patient-centered care. Perm J 2011;15:57-62. https://doi.org/10.7812/TPP/10-159.
- Maguire T, Daffern M, Bowe SJ, McKenna B. Risk assessment and subsequent nursing interventions in a forensic mental health inpatient setting: associations and impact on aggressive behaviour. J Clin Nurs 2018;27:e971-83. https://doi.org/10.1111/jocn.14107.
- Agency for Healthcare Research and Quality . Multipronged Strategy Reduces Use of Seclusion and Restraints to Manage Aggression at Inpatient Behavioral Health Facility 2009. https://innovations.ahrq.gov/profiles/multipronged-strategy-reduces-use-seclusion-and-restraints-manage-aggression-inpatient (accessed 22 October 2020).
- Kontio R, Pitkänen A, Joffe G, Katajisto J, Välimäki M. eLearning course may shorten the duration of mechanical restraint among psychiatric inpatients: a cluster-randomized trial. Nord J Psychiatry 2014;68:443-9. https://doi.org/10.3109/08039488.2013.855254.
- van de Sande R, Nijman HL, Noorthoorn EO, Wierdsma AI, Hellendoorn E, Van der Staak C, et al. Aggression and seclusion on acute psychiatric wards: effect of short-term risk assessment. Br J Psychiatry 2011;199:473-8. https://doi.org/10.1192/bjp.bp.111.095141.
- Chandler GE. Reducing use of restraints and seclusion to create a culture of safety. J Psychosoc Nurs Ment Health Serv 2012;50:29-36. https://doi.org/10.3928/02793695-20120906-97.
- Whitney D, Cooperrider D. Appreciative Inquiry: A Positive Revolution in Change 2011.
- Newman J, Paun O, Fogg L. Effects of a staff training intervention on seclusion rates on an adult inpatient psychiatric unit. J Psychosoc Nurs Ment Health Serv 2018;56:23-30. https://doi.org/10.3928/02793695-20180212-02.
- Heyman E. Seclusion. J Psychosoc Nurs Ment Health Serv 1987;25:8-9. https://doi.org/10.3928/0279-3695-19871101-04.
- Bowers L, Douzenis A, Galeazzi G, Forghieri M, Tsopelas C, Simpson A, et al. Disruptive and dangerous behaviour by patients on acute psychiatric wards in three European centres. Soc Psychiatry Psychiatr Epidemiol 2005;40:822-28. https://doi.org/10.1007/s00127-005-0967-1.
- Woods P, Almvik R. The Brøset Violence Checklist (BVC). Acta Psychiatr Scand 2002;106:103-5. https://doi.org/10.1034/j.1600-0447.106.s412.22.x.
- Schalast N, Redies M, Collins M, Stacey J, Howells K. EssenCES, a short questionnaire for assessing the social climate of forensic psychiatric wards. Crim Behav Ment Health 2007;18:49-58. https://doi.org/10.1002/cbm.677.
- Chabora N, Judge-Gorny M, Grogan K. The Four S Model in action for de-escalation: an innovative state hospital-university collaborative endeavor. J Psychosoc Nurs Ment Health Serv 2003;41:22-8.
- Mann-Poll PS, Smit A, van Doeselaar M, Hutschemaekers GJ. Professionals’ attitudes after a seclusion reduction program: anything changed?. Psychiatr Q 2013;84:1-10. https://doi.org/10.1007/s11126-012-9222-6.
- Godfrey JL, McGill AC, Jones NT, Oxley SL, Carr RM. Anatomy of a transformation: a systematic effort to reduce mechanical restraints at a state psychiatric hospital. Psychiatr Serv 2014;65:1277-80. https://doi.org/10.1176/appi.ps.201300247.
- Wieman DA, Camacho-Gonsalves T, Huckshorn KA, Leff S. Multisite study of an evidence-based practice to reduce seclusion and restraint in psychiatric inpatient facilities. Psychiatr Serv 2014;65:345-51. https://doi.org/10.1176/appi.ps.201300210.
- Mann-Poll PS, Smit A, Noorthoorn EO, Janssen WA, Koekkoek B, Hutschemaekers GJM. Long-term impact of a tailored seclusion reduction program: evidence for change?. Psychiatr Q 2018;89:733-46. https://doi.org/10.1007/s11126-018-9571-x.
- Safewards . Resources for Safewards Implementation n.d. www.safewards.net/ (accessed 22 October 2020).
- Restraint Reduction Network . Six Key Restraint Reduction Strategies 2019. https://restraintreductionnetwork.org/wp-content/uploads/2016/11/Six-Key-Restraint-Reduction-Strategies.pdf (accessed 5 October 2020).
- Cummings KS, Grandfield SA, Coldwell CM. Caring with comfort rooms: reducing seclusion and restraint use in psychiatric facilities. J Psychosoc Nurs Ment Health Serv 2010;48:26-30. https://doi.org/10.3928/02793695-20100303-02.
- Allen D, Lowe K, Brophy S. Predictors of restrictive reactive strategy use in people with challenging behaviour. J Appl Res Intellect Disabil 2009;22:159-68. https://doi.org/10.1111/j.1468-3148.2008.00484.x.
- Clark LL, Shurmer DL, Kowara D, Nnatu I. Reducing restrictive practice: developing and implementing behavioural support plans. Br J Ment Health Nursing 2017;6:23-8. https://doi.org/10.12968/bjmh.2017.6.1.23.
- D’Orio B, Wimby G, Haggard PJ. Reducing risk associated with seclusion and restraint. Psychiatric Times 2007;24:48-52.
- Guez R, Skolnick J, Scott B. The Six Core Intervention. Boston, MA: Massachusetts Department of Mental Health SAMHSA State Infrastructure Grant ‘Alternatives to Restraint and Seclusion’; 2006.
- Donat DC. Impact of improved staffing on seclusion/restraint reliance in a public psychiatric hospital. Psychiatr Rehabil J 2002;25:413-16. https://doi.org/10.1037/h0094994.
- Noorthoorn EO, Voskes Y, Janssen WA, Mulder CL, van de Sande R, Nijman HL, et al. Seclusion reduction in Dutch mental health care: did hospitals meet goals?. Psychiatr Serv 2016;67:1321-7. https://doi.org/10.1176/appi.ps.201500414.
- Blair M, Moulton-Adelman F. The Engagement Model for reducing seclusion and restraint: 13 years later. J Psychosoc Nurs Ment Health Serv 2015;53:39-45. https://doi.org/10.3928/02793695-20150211-01.
- Beaglehole B, Beveridge J, Campbell-Trotter W, Frampton C. Unlocking an acute psychiatric ward: the impact on unauthorised absences, assaults and seclusions. BJPsych Bull 2017;41:92-6. https://doi.org/10.1192/pb.bp.115.052944.
- Maybo . Positive and Safer Outcomes. RRN Approved Training for Learning Disability and Autism Services 2020. www.maybo.com/sector/social-care/learning-disabilities/ (accessed 20 November 2020).
- Boumans CE, Egger JI, Bouts RA, Hutschemaekers GJ. Seclusion and the importance of contextual factors: an innovation project revisited. Int J Law Psychiatry 2015;41:1-11. https://doi.org/10.1016/j.ijlp.2015.03.001.
- Alegent Health Mental Health Services, Omaha NE and Council Bluffs IA . Trauma Informed Care 2008.
- Taxis JC. Ethics and praxis: alternative strategies to physical restraint and seclusion in a psychiatric setting. Issues Ment Health Nurs 2002;23:157-70. https://doi.org/10.1080/016128402753542785.
- Positive Response Training and Consultancy . Positive Response Training and Consultancy n.d. https://positive-response.co.uk/ (accessed 22 October 2020).
- NHS Improvement . Mersey Care NHS Foundation Trust – Using the DASA Tool to Assess the Risk of Violence Among Psychiatric Inpatients 2018.
- Alberta Health Services . Restraint As a Last Resort Flowchart 2017. https://extranet.ahsnet.ca/teams/policydocuments/1/clp-prov-restraint-r-restraint-use-procedure-flowchart.pdf (accessed 15 September 2020).
- Martin BA, Suane SN. Effect of training on sensory room and cart usage. Occup Ther Ment Health 2012;28:118-28. https://doi.org/10.1080/0164212X.2012.679526.
- American Psychiatric Nurses Association (APNA) . 2017 – Seclusion and Restraint: Assessment and Risk Mitigation 2017. https://e-learning.apna.org/products/2017-seclusion-and-restraint-assessment-and-risk-mitigation#tab-product_tab_overview (accessed 1 March 2019).
- Stirling C, Aiken F, Dale C, Duxbury J. Reducing Restrictive Practices Checklist. Manchester: Crisis Prevention Institute; 2015.
- Forster PL, Cavness C, Phelps MA. Staff training decreases use of seclusion and restraint in an acute psychiatric hospital. Arch Psychiatr Nurs 1999;13:269-71. https://doi.org/10.1016/S0883-9417(99)80037-5.
- Space Training Consultants Ltd . Space Training n.d. www.spacetraining.co.uk/ (accessed 22 October 2020).
- Royal College of Psychiatrists . Reducing Restrictive Practice Programme 2018. www.rcpsych.ac.uk/improving-care/nccmh/reducing-restrictive-practice (accessed 1 March 2019).
- McCue RE, Urcuyo L, Lilu Y, Tobias T, Chambers MJ. Reducing restraint use in a public psychiatric inpatient service. J Behav Health Serv Res 2004;31:217-24. https://doi.org/10.1007/BF02287384.
- Allen DE, de Nesnera A, Souther JW. Executive-level reviews of seclusion and restraint promote interdisciplinary collaboration and innovation. J Am Psychiatr Nurses Assoc 2009;15:260-4. https://doi.org/10.1177/1078390309342749.
- National Association of State Mental Health Program Directors . Environments for the Reduction of Restraint &Amp; Seclusion 2007. www.nasmhpd.org/sites/default/files/VIII_SuccessStoryMadden.ppt (accessed 22 October 2020).
- Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev 2016;10:277-96. https://doi.org/10.1080/17437199.2016.1151372.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. ‘Psychological Theory’ Group. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. https://doi.org/10.1136/qshc.2004.011155.
- Carey RN, Connell LE, Johnston M, Rothman AJ, de Bruin M, Kelly MP, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med 2019;53:693-707. https://doi.org/10.31234/osf.io/x5372.
- Human Behaviour Change Project . The Theory and Techniques Tool 2020. https://theoryandtechniquetool.humanbehaviourchange.org (accessed 14 September 2020).
- Bubb SJ. Winterbourne View – Time for Change: Transforming the Commissioning of Services for People with Learning Disabilities and/or Autism. London: NHS England; 2014.
- EQUATOR Network . The Enhancing the QUAlity and Transparency Of Health Research (EQUATOR) Network n.d. www.equator-network.org (accessed 22 October 2020).
- James K, Quirk A, Patterson S, Brennan G, Stewart D. Quality of intervention delivery in a cluster randomised controlled trial: a qualitative observational study with lessons for fidelity. Trials 2017;18. https://doi.org/10.1186/s13063-017-2189-8.
- Health Prince Edward Island . Self Directed Resource Guide: Least Restraint 1 – Introduction n.d. www.gov.pe.ca/photos/original/src_least_restr.pdf (accessed March 2019).
- Morrow J, Huckshorn K, Leff H.S, Wieman D, Camacho-Gonsalves T, Anderson T. Alternatives to Seclusion and Restraint SAMHSA State Infrastructure Grant Evaluation Overview n.d.
- Substance Abuse and Mental Health Services Administration (SAMSHA) . Coordinating Center: Alternatives to Restraint &Amp; Seclusion (ARS) State Infrastructure Grant (SIG) Program – First Round of ARS SIG Grantees 2009.
- British Institute of Learning Disabilities . Accreditation Provider List 2019. www.bild.org.uk/our-services/pitrainingaccreditation/accreditation-provider-list/ (accessed 1 March 2019).
- Ascot Team Broadmoor Hospital . A Pilot Evaluation of Strategies to Reduce Long Term Segregation on Ascot Ward, Broadmoor Hospital 2015.
- Tees Esk and Wear Valleys NHS Foundation Trust . 2017–18 Annual Report 2018.
- Tees Esk and Wear Valleys NHS Foundation Trust . Positive Approaches Team 4 Day Course 2017.
- Respect Training . Respect Training From NAVIGO n.d. www.navigocare.co.uk/our-services/training-and-opportunities/respect-training-solutions/ (accessed 1 March 2019).
- Stensgaard L, Andersen MK, Nordentoft M, Hjorthøj C. Implementation of the Safewards model to reduce the use of coercive measures in adult psychiatric inpatient units: an interrupted time-series analysis. J Psychiatr Res 2018;105:147-52. https://doi.org/10.1016/j.jpsychires.2018.08.026.
- John J. Reducing Restrictive Practices Bradley Brook n.d. www.slideserve.com/Audrey/environments-for-the-reduction-of-restraint-seclusion (accessed 22 October 2020).
- Kayes D, Humphris E. Introduction of restraint and seclusion reduction program in Margaret Tobin Centre. Aust Nurs Midwifery J 2015;3.
- Natale G, Fitzgerald A, Landry M, Harmon K. Applying Jean Watson’s caring theory to reduce restraint use in the acute psychiatric area. Pelican News 2017.
- American Hospital Association . Learning From Each Other: Success Stories and Ideas for Reducing Restraint Seclusion in Behavioral Health n.d. www.aha.org/content/00-10/learningfromeachother.pdf (accessed 1 March 2019).
- D.ESCAL8 . PBS and De-Escalation: Developing Positive Relationships, Supporting Those in Distress n.d. http://de-escalate.com (accessed 22 October 2020).
- JKM Training, Inc . Reducing Restraints. n.d. www.safecrisismanagement.com/reducing-restraints.aspx (accessed 1 March 2019).
- VSA . Behavioural Support Strategies n.d. www.vsa.org.uk/other-services/behavioural-support-strategies/ (accessed 1 March 2019).
- CALM Training . Calm Training. n.d. https://calmtraining.co.uk/ (accessed 1 March 2019).
- PRICE Training . PRICE Training n.d. www.pricetraining.co.uk/ (accessed 1 March 2019).
- Safe Crisis Management Europe . Safe Crisis Management Europe n.d. www.safecrisismanagement.org/ (accessed 1 March 2019).
- Specialist Service Training Solutions Ltd . Specialist Services Training Solutions Ltd n.d. https://sstsuk.com/ (accessed 1 March 2019).
- St Anne’s Community Service (St-ACS) Team . ST-ACS Positive Behaviour Support (PBS) Training. n.d. www.st-annes.org.uk/our-services/st-acs-positive-behaviour-support-pbs-training/ (accessed 1 March 2019).
- Loddon Foundation Ltd . PROACT-SCIPr-UK® n.d. www.proact-scipr-uk.com/proact-scipr-uk/ (accessed 1 March 2019).
- Northumberland Tyne and Wear NHS Foundation Trust . Talk 1st Ward Assessment 2019.
- Northumberland Tyne and Wear NHS Foundation Trust . Positive and Safe Debrief Policy and Tool 2019.
- Northumberland Tyne and Wear NHS Foundation Trust . Positive and Safe Positive Practice Process Outline 2018.
- South Australia Health . Mental Health Restraint and Seclusion Toolkit Fact Sheet 7 2019. www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+topics/mental+health/restraint+and+seclusion+in+mental+health (accessed 1 March 2019).
- West London NHS Trust . Positive and Safe: Violence Reduction and Management Programme – Instructors Manual 2015. https://westlondon.nhs.uk/pmva-manual/ (accessed 24 November 2020).
- Pollard R, Yanasak EV, Rogers SA, Tapp A. Organizational and unit factors contributing to reduction in the use of seclusion and restraint procedures on an acute psychiatric inpatient unit. Psychiatr Q 2007;78:73-81. https://doi.org/10.1007/s11126-006-9028-5.
- Khadivi AN, Patel RC, Atkinson AR, Levine JM. Association between seclusion and restraint and patient-related violence. Psychiatr Serv 2004;55:1311-12. https://doi.org/10.1176/appi.ps.55.11.1311.
- Fletcher E, Stevenson C. Launching the Tidal Model in an adult mental health programme. Nurs Stand 2001;15:33-6. https://doi.org/10.7748/ns2001.08.15.49.33.c3074.
- Yang CP, Hargreaves WA, Bostrom A. Association of empathy of nursing staff with reduction of seclusion and restraint in psychiatric inpatient care. Psychiatr Serv 2014;65:251-4. https://doi.org/10.1176/appi.ps.201200531.
- Donat DC. Impact of a clinical-administrative review procedure on reducing reliance on psychotropic PRN medication. Psychiatr Rehabil J 2006;29:215-18. https://doi.org/10.2975/29.2006.215.218.
- Björkdahl A, Heilig M, Palmstierna T, Hansebo G. Changes in the occurrences of coercive interventions and staff injuries on a psychiatric intensive care unit. Arch Psychiatr Nurs 2007;21:270-7. https://doi.org/10.1016/j.apnu.2007.06.007.
- Mahmoud KF, Terhorst L, Lindsay D, Brager J, Rodney T, Sanchez M, et al. Psychometric properties of the person-centered version of the alcohol and alcohol problems perceptions questionnaire (PCAAPPQ). Alcohol Alcohol 2020;55:652-9. https://doi.org/10.1093/alcalc/agaa061.
- Brown C, Dunn W. Adolescent/Adult Sensory Profile. San Antonio, TX: Psychological Corporation; 2002.
- McLeod H, Deane F, Hogbin B. Changing staff attitudes and empathy for working with people with psychosis. Behav Cogn Psychother 2002;30:459-70. https://doi.org/10.1017/S1352465802004071.
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep 1962;10:799-812. https://doi.org/10.2466/pr0.1962.10.3.799.
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyenet TD, . Assessment of client/patient satisfaction: development of a general scale. Eval Progr Plann 1979;2:197-20. https://doi.org/10.1016/0149-7189(79)90094-6.
- Martin T, Daffern M. Clinician perceptions of personal safety and confidence to manage inpatient aggression in a forensic psychiatric setting. J Psychiatr Ment Health Nurs 2006;13:90-9. https://doi.org/10.1111/j.1365-2850.2006.00920.x.
- Baars van A, De Schaal voor Gevaar, Mulder CL, Snijdewind A. De Epidemie van Dwangtoepassingen in de Psychiatrie. Mension; 2006.
- Vaughan B, Carter A, Macfarlane C, Morrison T. The DREEM, part 1: measurement of the educational environment in an osteopathy teaching program. BMC Med Educ 2014;14. https://doi.org/10.1186/1472-6920-14-99.
- Ogloff JR, Daffern M. The dynamic appraisal of situational aggression: an instrument to assess risk for imminent aggression in psychiatric inpatients. Behav Sci Law 2006;24:799-813. https://doi.org/10.1002/bsl.741.
- Champagne T, Stromberg N. Sensory approaches in inpatient psychiatric settings: innovative alternatives to seclusion and restraint. J Psychosoc Ment Health Serv 2004;42:34-4.
- Allen JJ, Anderson CA, Bushman BJ. The General Aggression Model. Curr Opin Psychol 2018;19:75-80. https://doi.org/10.1016/j.copsyc.2017.03.034.
- Harris MG, Sparti C, Scheurer R, . Measurement properties of the Health of the Nation Outcome Scales (HoNOS) family of measures: protocol for a systematic review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021177.
- Long C, West R, Afford M, Collins L, Dolley O. Dolan and Fulham (2001) (unpublished) . Reducing the use of seclusion in a secure service for women. J Psychiatric Intens Care 2015;11:84-9. https://doi.org/10.1017/S174264641400017X.
- Kennedy JA. Fundamentals of Psychiatric Treatment Planning. Washington, DC: American Psychiatric Press; 1992.
- Huang HT, Chuang YH, Chiang KF. Nurses’ physical restraint knowledge, attitudes, and practices: the effectiveness of an in-service education program. JNR 2009;17:241-8. https://doi.org/10.1097/JNR.0b013e3181c1215d.
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. Menlo Park, CA: Mind Garden, Inc.; 2016.
- Martin DC, Walker HK, Hall WD, Hurst JW. Clinical Methods: The History, Physical, and Laboratory Examinations. Boston: Butterworths; 1990.
- Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. The Overt Aggression Scale for the objective rating of verbal and physical aggression. Am J Psychiatry 1986;143:35-9. https://doi.org/10.1176/ajp.143.1.35.
- Bowers L. Association between staff factors and levels of conflict and containment on acute psychiatric wards in England. Psychiatr Serv 2009;60:231-9. https://doi.org/10.1176/ps.2009.60.2.231.
- Rush AJ, South CC, Jha MK, Grannemann BD, Trivedi MH. Toward a very brief quality of life enjoyment and satisfaction questionnaire. J Affec Disord 2019;242:87-95. https://doi.org/10.1016/j.jad.2018.08.052.
- Donabedian A. Evaluating the quality of medical care. Milbank Q 2005;83:691-729. https://doi.org/10.1111/j.1468-0009.2005.00397.x.
- Bech P. The Bech, Hamilton and Zung Scales for Mood Disorders: Screening and Listening. Berlin, Heidelberg: Springer; 1996.
- Morken T, Valborg B, Johnsen GE, Rypdal K, Palmstierna T, Johansen I. The Staff Observation Aggression Scale – Revised (SOAS-R) – adjustment and validation for emergency primary health care. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3157-z.
- Stevenson C, Barker P, Fletcher E. Judgement days: developing an evaluation for an innovative nursing model. J Psychiatr Ment Health Nurs 2002;9:271-6. https://doi.org/10.1046/j.1365-2850.2002.00472.x.
- Laker C, Rose D, Flach C, Csipke E, McCrone P, Craig T, et al. Views of the Therapeutic Environment (VOTE): stakeholder involvement in measuring staff perceptions of acute in-patient care. Int J Nurs Stud 2012;49:1403-10. https://doi.org/10.1016/j.ijnurstu.2012.06.001.
- Hallett N, Huber J, Sixsmith J, Dickens G. Measuring the violence prevention climate: development and evaluation of the VPC-14. Int J Nurs Stud 2018;88:97-103. https://doi.org/10.1016/j.ijnurstu.2018.09.002.
- Rossberg J, Friis S. A suggested revision of the Ward Atmosphere Scale. Acta Psychiatr Scand 2003;108:374-80. https://doi.org/10.1034/j.1600-0447.2003.00191.x.
- Belanger S. The ‘S.R challenge’: reducing the use of seclusion and restraint in a state psychiatric hospital. J Healthc Qual 2001;23:19-24. https://doi.org/10.1111/j.1945-1474.2001.tb00319.x.
- Blair EW, Woolley S, Szarek BL, Mucha TF, Dutka O, Schwartz HI, et al. Reduction of seclusion and restraint in an inpatient psychiatric setting: a pilot study. Psychiatr Q 2017;88:1-7. https://doi.org/10.1007/s11126-016-9428-0.
- Dewey K, Brill C. Decrease in restraint use in a study of a geropsychiatric unit. J Psychosoc Nurs Ment Health Serv 2000;38:14-8.
- Fluttert FAJ, Van Meijel B, van Leeuwen M, Bjørkly S, Nijman H, Grypdonck M. The development of the forensic early warning signs of aggression inventory: preliminary findings. Toward a better management of inpatient aggression. Arch Psychiatr Nurs 2011;25:129-37. https://doi.org/10.1016/j.apnu.2010.07.001.
- Hyde S, Fulbrook P, Fenton K, Kilshaw M. A clinical improvement project to develop and implement a decision-making framework for the use of seclusion. Int J Ment Health Nurs 2009;18:398-40. https://doi.org/10.1111/j.1447-0349.2009.00631.x.
- Maudsley Simulation . Maudsley Simulation n.d. www.maudsleysimulation.com/ (accessed 1 March 2019).
Appendix 1 Databases and resources searched
Academic databases searched for published studies: February 2018 and April 2019
-
BNI (via ProQuest): 1992 to February 2018.
-
BNI (Healthcare Databases Advanced Search via ProQuest): 1992 to April 2019.
-
CINAHL (via EBSCOhost): 1981 to present.
-
CCTR (via Wiley Online Library): issue 1 of 12, January 2018.
-
CCTR (via Wiley Online Library): issue 4 of 12, April 2019.
-
CDSR (via Wiley Online Library): issue 2 of 12, February 2018.
-
CDSR (via Wiley Online Library): issue 4 of 12, April 2019.
-
DARE (via Wiley Online Library): issue 2 of 4, April 2015.
-
EMBASE Classic + EMBASE (via Ovid): 1947 to 2019 April 16.
-
HTA Database (via Wiley Online Library): issue 4 of 4, October 2016.
-
HTA Canadian and International (Centre for Reviews and Dissemination, University of York) (on 24 April 2019).
-
Ovid MEDLINE®: 1946 to April Week 1 2019.
-
Ovid MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily to 16 April 2019.
-
NHS EED (via Wiley Online Library): issue 2 of 4, April 2015.
-
PubMed (National Library of Medicine) 1946 to present.
Grey literature resources
Databases searched for unpublished studies
-
ClinicalTrials.gov (US National Institutes of Health).
-
Dissertations & Theses A&I (ProQuest): 1743 – present.
-
Evidence Search (NICE).
-
International Clinical Trials Registry Platform (World Health Organization).
-
OpenGrey (INIST-CNRS).
Websites searched
Websites and search engines were searched for research and non-research reports of interventions.
The search engine Google was used plus the following websites.
Mental health organisations
-
European Violence in Psychiatry Group (EViPRG) (http://eviprg.eu/).
-
Mental Welfare Commission for Scotland (www.mwcscot.org.uk/).
-
National Mental Health Consumer and Carer Forum (https://nmhccf.org.au/).
-
CPI (www.crisisprevention.com/).
-
Safe Crisis management (https://safecrisismanagement.com).
-
Healthcare Improvement Scotland (http://ihub.scot/).
Health-care organisations
National
-
NICE Evidence (UK) (see database section above).
-
SAMHSA (USA) (www.samhsa.gov/).
-
National Association of State Mental Health Program Directors (USA) (www.nasmhpd.org/).
-
Canadian Mental Health Commission (www.mentalhealthcommission.ca/English/).
-
Depression and Bipolar Support Alliance (DBSA) (https://dbsalliance.org).
Regional
-
Seclusion and Restraint Reduction Leadership Group (Texas, USA) (http://tnoys.org/srr-leadership-group/).
Societies/colleges
Psychiatrists
-
The World Association of Social Psychiatry (WASP) (www.waspsocialpsychiatry.com; https://coercioninpsychiatry.com/references/).
-
European Psychiatric Association (www.europsy.net/).
-
American Psychiatric Association (www.psychiatry.org/).
Nurses
-
International Society of Psychiatric Mental Health Nurses (www.ispn-psych.org/).
-
Mental Health Nurses Association (MHNA) (UK) (www.unitetheunion.org/how-we-help/list-of-sectors/healthsector/healthsectoryourprofession/mhna/).
-
American Psychiatric Nurses Association (APNA) (www.apna.org/i4a/pages/index.cfm?pageid=1).
-
Australian College of Mental Health Nurses (www.acmhn.org/).
Charities
-
Rethink (www.rethink.org/).
-
MIND (www.mind.org.uk/).
-
Mental Health Foundation (www.mentalhealth.org.uk/statistics).
-
National Alliance on Mental Illness (www.nami.org/).
-
Mental Health Australia (https://mhaustralia.org).
National government health departments
-
Department of Health and Social Care (UK) (www.gov.uk).
-
Australian Government. Department of Health (https://agedcare.health.gov.au).
-
US Department of Health and Human Services (HHS) (www.hhs.gov/).
-
Ministry of Health. New Zealand (www.health.govt.nz/).
Health-care quality agencies
-
NICE Quality Standards (www.nice.org.uk/standards-and-indicators).
-
CQC (UK) (www.cqc.org.uk/).
-
NHS Improvement (https://improvement.nhs.uk/).
-
AHRQ (www.ahrq.gov/).
-
Australian Commission on Safety and Quality in Health Care (www.safetyandquality.gov.au/).
-
Health Quality Ontario (www.hqontario.ca/).
-
Health Quality & Safety Commission New Zealand (www.hqsc.govt.nz/).
Training providers
-
Skills for Health (UK) (www.skillsforhealth.org.uk/).
-
CPI (www.crisisprevention.com/).
-
Restraint Reduction Network (http://restraintreductionnetwork.org/).
-
Dynamic intervention (https://dynamicinterventions.org).
-
Challenging Behaviour Foundation (UK) (www.challengingbehaviour.org.uk/).
-
Royal College of Nursing (www.rcn.org.uk/).
-
CALM (www.calmtraining.co.uk/).
-
BILD (www.bild.org.uk/).
-
Caring Solutions (www.caringsolutionsukltd.com/).
-
Centre for Mental Health (www.centreformentalhealth.org.uk/).
-
Scottish Association for Mental Health (SAMH) (www.samh.org.uk/).
-
Support in Mind Scotland (www.supportinmindscotland.org.uk/).
E-mail lists
E-mail lists contacted for research and non-research reports of interventions:
-
LIS-MEDICAL@jiscmail.ac.uk
-
CLIN-LIB@Jiscmail.ac.uk
-
MENTAL-HEALTH-LIBRARIES@jiscmail.ac.uk.
Social media
Social media resources searched for research and non-research reports of interventions:
-
YouTube
-
Facebook
-
Twitter.
Appendix 2 Search strategies
Search strategies are summarised and tabulated below. For the detailed search strategy and strings, see Report Supplementary Material 1.
Summary of search strategies
| Academic databases |
|---|
| BNI (ProQuest): 1992 to February 2018 |
| BNI (Healthcare Databases Advanced Search via ProQuest): 1992 to April 2019 |
| CINAHL (EBSCOhost): 1981 to present |
| CCTR (Wiley Online Library): issue 1 of 12, January 2018 |
| CCTR (Wiley Online Library): issue 4 of 12, April 2019 |
| Cochrane Database of Systematic Reviews (Wiley Online Library): issue 2 of 12, February 2018 |
| Cochrane Database of Systematic Reviews (Wiley Online Library): issue 4 of 12, April 2019 |
| DARE (Wiley Online Library): issue 2 of 4, April 2015 |
| EMBASE Classic + EMBASE (Ovid): 1947 to 2019 April 16 |
| HTA Database (Wiley Online Library): issue 4 of 4, October 2016 |
| HTA Canadian and International (Centre for Reviews and Dissemination, University of York) |
| Ovid MEDLINE(R): 1946 to April week 1 2019 |
| Ovid MEDLINE(R) Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily to 16 April 2019 |
| NHS Economic Evaluation Database (Wiley Online Library): issue 2 of 4, April 2015 |
| PubMed (National Library of Medicine): 1946 to present |
| Databases and registers containing unpublished studies |
| ClinicalTrials.gov (US National Institutes of Health) |
| Dissertations & Theses A&I (ProQuest): 1743 to present (searched April 2018 and February 2019) |
| Evidence Search (NICE) |
| International Clinical Trials Registry Platform (World Health Organization) |
| OpenGrey (INIST-CNRS) |
| Websites |
| Mental health organisations |
| Health-care organisations |
| Societies/colleges of (i) psychiatrists and (ii) nurses |
| Charities |
| National government health departments |
| Health-care quality agencies |
| Training providers |
| Google (advanced search interface): national and international |
| E-mail requests for information |
| Social media |
| YouTube |
Appendix 3 Terms entered into Abstrackr
| Terms indicating relevance | ||
|---|---|---|
| 4 steps to safety | mental health | psychiatry |
| 4pi national involvement standards | mental health nursing simulation on workplace violence | psychogeriatric |
| 6 core strategies | methodical work approach | psycho-geriatric |
| adults | multimodal functional model | reduce |
| alternative to restraint flowsheet | no force first | reducing |
| calm | no restraint policy | respect |
| city nurse | non-pharmacological | restrain yourself |
| de-escalate | nonviolent crisis intervention | restrain yourself |
| de-escalation | omega program | restraint |
| exbelt | pasung | restraint reduction network |
| force | positive alternatives to restraint and seclusion | restrictive |
| forced medication | positive and safe champions network | restrictive practices |
| fours model | positive and safe initiative | Safewards |
| four steps to safety | positive behaviour support | Scottish patient safety programme |
| handle with care | program | seclusion |
| initiative | project beta | seclusion and restraint reduction initiative |
| inpatient | promise | six core strategies |
| intervention | psychiatric | staying safe |
| teamstepps | ||
| Terms indicating irrelevance | ||
| administration | factors associated | prevalence |
| adolescent | diabetes | perception |
| alcohol withdrawal | drinking | perspectives |
| alzheimer | early intervention service | pharmaceutical |
| alzheimer’s | earthquake | pharmacologic |
| antibiotic | falls | pharmacological |
| arthritis | general | pharmacy |
| assertive community treatment | hiv | philosophy |
| associated with | intellectual disability | physical |
| attitudes | intellectual disability | primary care |
| behavioural disabilities | intellectually disabled | prison |
| brain injury | learning disability | quadriplegia |
| cancer | mental disabilities | rats |
| cardiac | mental retardation | refugee |
| care home | military | relationship |
| child | minors | risk factors |
| children | neurocognitive disorders | risk profile |
| community | nonpsychiatric | sars |
| critical care | nursing home | school |
| delirium | outpatient | self-harm |
| dementia | outpatient commitment | stroke |
| determinants | pain | surgical |
| developmental disabilities | palliative | tinnitus |
| emergency department | paediatric | views |
| erratum | predict | youth |
| factors affecting | predictors | |
Appendix 4 Extraction items
| Recommendations | Extracted |
|---|---|
| COCHRANE 1. Record |
1.1 Author(s) 1.2 Title 1.3 Journal 1.4 Peer reviewed (y/n) 1.5 Year 1.6 Publication format |
| COCHRANE 2. Evaluations |
2.1 Evaluation (y/n)? 2.2 Design 2.2.1 Randomised? 2.2.2 Controlled? 2.3 Evaluation period (if not available: overall length of study) 2.4 Outcome measures used 2.4.1 Standardised outcome measure used 2.4.2 Data collection from existing records or developed/recorded for study 2.5 Findings reported (y/n) 2.5.1 Significant outcome reported (y/n)? 2.6 Study funder |
| WIDER 1. Detailed description of interventions in published papers | |
|---|---|
| 1.1 Characteristics of those delivering the intervention |
1.1.1 Provider: in-house/external 1.1.2 Provider: organisation name 1.1.3 Provider: detail |
| 1.2 Characteristics of the recipients |
1.2.1 Sample: size (n of people) 1.2.2 Sample: description |
| 1.3 The setting |
1.3.1 City 1.3.2 State/province 1.3.3 Country 1.3.4 Setting: size (n of beds/wards) |
| 1.4 The mode of delivery |
1.4.1 Training education 1.4.2 Sensory room 1.4.3 Role models 1.4.4 Care-planning 1.4.5 Debriefing 1.4.6 Assessing risk 1.4.7 Reviewing incident data 1.4.8 Increased staffing 1.4.9 Nursing changes TIC 1.4.10 Improved communication 1.4.11 Change in policy rules 1.4.12 Enhanced leadership 1.4.13 Activities 1.4.14 Rapid response team 1.4.15 Service user involvement 1.4.16 Miscellaneous |
| 1.5 The intensity | 1.5.1 How often |
| 1.6 The duration |
1.6.1 Intervention: date done 1.6.2 Intervention: start date 1.6.3 Intervention components: duration 1.6.4 Permanent (y/n) |
| 1.7 Adherence/fidelity to delivery protocols |
1.7.1 Voluntary/mandatory 1.7.2 Report tailoring or modification (y/n) 1.7.3 Report fidelity (y/n) |
| 1.8 Detailed description of the intervention content provided for each study group | 1.8.1 Delivery of control described |
| WIDER 2. Clarification of assumed change process and design principles | |
| 2.1 The intervention development |
2.1.1 Service user involvement in intervention development (y/n) 2.1.2 Service user involvement detail 2.1.3 Costs of intervention |
| 2.2 The change techniques used in the intervention | [See BCT coding] |
| 2.3 The causal processes targeted by these change techniques |
2.3.1 Aim of intervention [See BCT coding] |
| WIDER 3. Access to intervention manuals/protocols | |
| 3.1 Submit protocols or manuals for publication to make these supplementary materials easily accessible (i.e. online) |
3.1.1 Materials available? 3.1.2 Website 3.1.3 Contact available for information? (y/n) 3.1.4 Contact name 3.1.5 E-mail |
| WIDER 4. Detailed description of active control conditions | |
| THEORY coding |
Explicit mention of theory (name)? (y/n) Theory used in intervention design? (y/n) Theory used in interventions implementation? (y/n) Results related back to the theory? (y/n) |
Appendix 5 Coding manual
Behaviour change technique coding: issues and assumptions
Assumptions
-
We are applying the BCT taxonomy to interventions that aim to change staff behaviour in terms of how staff interact with patients.
-
The intervention target is interaction between staff and patients: ‘The final target of most interventions was to organically change interactions between patients and between staff and patients’. 16
-
Objects added to make environment more comfortable, etc., are for patients but aimed at increasing quality of interaction and reducing conflict and aggression (which leads to restrictive practices).
-
‘Self’ can include individual and groups of staff as opposed to management.
-
Knowing that data are being collected is not the same as receiving feedback.
Common interventions and potential behaviour change technique codes
| Intervention procedure | BCT code |
|---|---|
| Behavioural plans/contracts for patients/patient plan |
|
| Data review |
|
| Debrief/witnessing |
|
| Leadership or management changes |
|
| Meetings between frontline and management staff (no patients) |
|
| Meetings between frontline staff (no patients) (e.g. safety huddle) |
|
| Care-planning meetings between individual staff and patient |
|
| Meetings between staff and patients (group)/community meeting |
|
| Posters |
|
| Rapid response team |
|
| Risk assessment |
|
| Rule changes |
|
| Sensory equipment |
|
| Sensory Rooms |
|
| Sharing learning events |
|
| Staff visibility |
|
| Tools |
|
| Train the trainers |
|
| Training/education |
|
| Trauma-informed care, etc. (change of nursing model) |
|
Clarify difference between similar codes
| Code | Decisions |
|---|---|
| Problem-solving | Patient/staff identify triggers, influences, strategies |
| Information about antecedents | Information from external source, for example training, not from, for example, patient or staff |
| Re-attribution |
|
| Framing/reframing |
Patient response to trauma About how staff behaviour is framed (e.g. improve quality and safety) |
| Restructuring the physical environment |
More than just adding objects Creating a sensory room, making a ward more comfortable |
| Adding objects to the environment |
To facilitate the behaviour, not prompt or cue – so have removed from risk assessment. Have included poster and safety crosses More than information (so how do we code information leaflets?) |
| Prompts or cues | For example, a risk assessment on admission |
| Monitoring by self | Where ‘self’ is ‘staff’ (e.g. ward teams) |
| Monitoring by others | System-wide monitoring through Datix (Datix Limited, London) etc. |
| Habit reversal | For example, ‘no’ audit. Habit is to say ‘no’; change to trying to say ‘yes’ |
| Goals and planning |
Problem-solving includes activity discussing difficulties with patients, staff or management For action-planning to be coded it must mention planning Goal-setting – for both behaviour and outcomes and review of same Commitment and contracts – must be explicitly mentioned |
| Feedback and monitoring |
Self-monitoring of outcomes and behaviour (as almost always conflated) are treated as the same thing: records and discussion about successes and failures that take place at ward level, including debriefing with a patient (ward is treated as ‘the self’ as no individuals are ever mentioned) Monitoring of outcomes and behaviour by others without feedback (system-level monitoring, e.g. by a researcher) Feedback on outcomes and behaviour – data generated centrally and sent back to the ward; debriefing with a patient present or not |
| Social support | Practical if helping to de-escalate in a group – rapid response team. Emotional if reflecting and discussion |
| Removing punishment | Non-punitive environment (always debriefing related) |
| Consequences |
If no detail or detail of asphyxiation, etc. (e.g. ‘negative consequences of restraint’), code as health consequences Emotional – specific reference to psychological trauma Social and environmental – hardly anything but damage to property, time taken form-filling, impact on team Salience of consequences, only if talking specifically about personal stories of restrictive practices. Can be video or written, not just in person |
| Reward and threat | Celebrations, plaque, cinema ticket, prizes |
| Training |
Only coded demonstration if it specifically says that Instruction is the one to code all mention of training Behaviour practice if it includes role play or interactive element |
Definitions within COMPARE (present study)
| Term used in BCT | Definition in COMPARE |
|---|---|
|
Outcome Outcome goal (positive outcome of wanted behaviour) |
|
| Target (behaviour) |
|
|
Behaviour goal Wanted behaviour The behaviour to be achieved |
|
| The behavioural problem |
|
Appendix 6 Behaviour change technique coding levels applied in this review
| Group | BCT | Coding level | |||
|---|---|---|---|---|---|
| Individual | Unit (ward) | Service | Policy | ||
| 1. Goals and planning | 1.1. Goal-setting (behavior) | ✗ | ✗ | ||
| 1.2. Problem-solving | ✗ | ✗ | ✗ | ||
| 1.3. Goal-setting (outcome) | ✗ | ✗ | ✗ | ✗ | |
| 1.4. Action-planning | ✗ | ✗ | ✗ | ||
| 1.5. Review behavior goal(s) | ✗ | ✗ | |||
| 1.6. Discrepancy between current behavior and goal | ✗ | ✗ | |||
| 1.7. Review outcome goal(s) | ✗ | ✗ | ✗ | ||
| 1.8. Behavioral contract | ✗ | ✗ | ✗ | ||
| 1.9. Commitment | ✗ | ✗ | ✗ | ||
| 2. Feedback and monitoring | 2.1. Monitoring of behavior by others without feedback | ✗ | |||
| 2.2. Feedback on behavior | ✗ | ✗ | |||
| 2.3. Self-monitoring of behavior | ✗ | ✗ | |||
| 2.4. Self-monitoring of outcome(s) of behavior | ✗ | ✗ | |||
| 2.5. Monitoring of outcome(s) of behavior without feedback | ✗ | ||||
| 2.6. Biofeedback | ✗ | ||||
| 2.7. Feedback on outcome(s) of behavior | ✗ | ✗ | |||
| 3. Social support | 3.1. Social support (unspecified) | ✗ | ✗ | ✗ | |
| 3.2. Social support (practical) | ✗ | ✗ | ✗ | ||
| 3.3. Social support (emotional) | ✗ | ✗ | ✗ | ||
| 4. Shaping knowledge | 4.1. Instruction on how to perform the behavior | ✗ | ✗ | ✗ | |
| 4.2. Information about antecedents | ✗ | ✗ | ✗ | ||
| 4.3. Re-attribution | ✗ | ✗ | ✗ | ||
| 4.4. Behavioral experiments | ✗ | ✗ | |||
| 5. Natural consequences | 5.1. Information about health consequences | ✗ | ✗ | ✗ | |
| 5.2. Salience of consequences | ✗ | ✗ | ✗ | ||
| 5.3. Information about social and environmental consequences | ✗ | ✗ | ✗ | ||
| 5.4. Monitoring of emotional consequences | ✗ | ✗ | ✗ | ||
| 5.5. Anticipated regret | ✗ | ✗ | |||
| 5.6. Information about emotional consequences | ✗ | ✗ | ✗ | ||
| 6. Comparison of behavior | ✗ | ✗ | ✗ | ||
| 6.1. Demonstration of the behavior | ✗ | ✗ | ✗ | ||
| 6.2. Social comparison | ✗ | ✗ | ✗ | ||
| 6.3. Information about others’ approval | ✗ | ✗ | |||
| 7. Associations | 7.1. Prompts or cues | ✗ | ✗ | ||
| 7.2. Cue-signalling reward | ✗ | ✗ | |||
| 7.3. Reduce prompts or cues | ✗ | ✗ | |||
| 7.4. Remove access to the reward | ✗ | ✗ | |||
| 7.5. Remove aversive stimulus | ✗ | ✗ | |||
| 7.6. Satiation | ✗ | ||||
| 7.7. Exposure | ✗ | ||||
| 7.8. Associative learning | ✗ | ||||
| 8. Repetition and substitution | 8.1. Behavioral practice/rehearsal | ✗ | ✗ | ✗ | |
| 8.2. Behavior substitution | ✗ | ✗ | |||
| 8.3. Habit formation | ✗ | ✗ | |||
| 8.4. Habit reversal | ✗ | ✗ | |||
| 8.5. Overcorrection | ✗ | ||||
| 8.6. Generalisation of target behavior | ✗ | ✗ | |||
| 8.7. Graded tasks | ✗ | ||||
| 9. Comparison of outcomes | 9.1. Credible source | ✗ | ✗ | ✗ | |
| 9.2. Pros and cons | ✗ | ✗ | |||
| 9.3. Comparative imagining of future outcomes | ✗ | ✗ | |||
| 10. Reward and threat | 10.1. Material incentive (behavior) | ✗ | ✗ | ✗ | |
| 10.2. Material reward (behavior) | ✗ | ✗ | ✗ | ||
| 10.3. Non-specific reward | ✗ | ✗ | ✗ | ||
| 10.4. Social reward | ✗ | ✗ | ✗ | ||
| 10.5. Social incentive | ✗ | ✗ | ✗ | ||
| 10.6. Non-specific incentive | ✗ | ✗ | ✗ | ||
| 10.7. Self-incentive | ✗ | ✗ | |||
| 10.8. Incentive (outcome) | ✗ | ✗ | ✗ | ||
| 10.9. Self-reward | ✗ | ✗ | |||
| 10.10. Reward (outcome) | ✗ | ✗ | ✗ | ||
| 10.11. Future punishment | ✗ | ✗ | ✗ | ||
| 11. Regulation | 11.1. Pharmacological support | ✗ | |||
| 11.2. Reduce negative emotions | ✗ | ✗ | ✗ | ||
| 11.3. Conserving mental resources | ✗ | ||||
| 11.4. Paradoxical instructions | ✗ | ||||
| 12. Antecedents | 12.1. Restructuring the physical environment | ✗ | ✗ | ✗ | ✗ |
| 12.2. Restructuring the social environment | ✗ | ✗ | ✗ | ✗ | |
| 12.3. Avoidance/reducing exposure to cues for the behavior | ✗ | ✗ | |||
| 12.4. Distraction | ✗ | ||||
| 12.5. Adding objects to the environment | ✗ | ✗ | ✗ | ||
| 12.6. Body changes | ✗ | ||||
| 13. Identity | 13.1. Identification of self as role model | ✗ | ✗ | ||
| 13.2. Framing/reframing | ✗ | ✗ | ✗ | ||
| 13.3. Incompatible beliefs | ✗ | ||||
| 13.4. Valued self-identify | ✗ | ||||
| 13.5. Identity associated with changed behavior | ✗ | ||||
| 14. Scheduled consequences | 14.1. Behavior cost | ✗ | |||
| 14.2. Punishment | ✗ | ||||
| 14.3. Remove reward | ✗ | ||||
| 14.4. Reward approximation | ✗ | ||||
| 14.5. Rewarding completion | ✗ | ||||
| 14.6. Situation-specific reward | ✗ | ||||
| 14.7. Reward incompatible behavior | ✗ | ||||
| 14.8. Reward alternative behavior | ✗ | ||||
| 14.9. Reduce reward frequency | ✗ | ||||
| 14.10. Remove punishment | ✗ | ||||
| 15. Self-belief | 15.1. Verbal persuasion about capability | ✗ | |||
| 15.2. Mental rehearsal of successful performances | ✗ | ||||
| 15.3. Focus on past success | ✗ | ||||
| 15.4. Self-talk | ✗ | ||||
| 16. Covert learning | 16. Covert learning | ||||
| 16.1. Imaginary punishment | ✗ | ||||
| 16.2. Imaginary reward | ✗ | ||||
| 16.3. Vicarious consequences | ✗ | ||||
Appendix 7 Intervention families (interventions with multiple records)
| Intervention family | Records | Intervention report | Research report | Service report | Tool | Practice example | Training link | Study type | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Same study | Follow-up study | Replication study | Pilot study | ||||||||
| 1. Six Core Strategies | 18 | ✗92 | ✗17,72,74,75,144,203,211 | ✗89,192,219,247 | ✗133,214 | ||||||
| ✗248,249 | Y | ||||||||||
| ✗23,99 | Y | ||||||||||
| 2. Beacon Project | 2 | ✗115,116 | Y | ||||||||
| 3. Behavioural Support Planning | 2 | ✗217 | ✗217 | Y | |||||||
| 4. Brøset Violence Checklist | 3 | ✗112–114 | Y | ||||||||
| 5. City Nurse | 2 | ✗101,102 | Y | ||||||||
| 6. Comfort Rooms | 2 | ✗215 | ✗191 | ||||||||
| 7. CPI/MAPA | 2 | ✗95,250 | |||||||||
| 8. DASA-IV | 2 | ✗86,236 | |||||||||
| 9. Early Recognition Method | 3 | ✗118 | ✗118,119 | Y | |||||||
| 10. Initiatives to Reduce Seclusion and Restraint | 2 | ✗107,108 | Y | ||||||||
| 11. Mutual Help Meetings | 3 | ✗83,236 | |||||||||
| 12. No Force First | 3 | ✗24,134 | ✗85 | ||||||||
| 13. Novel Seclusion Reduction Program | 2 | ✗90 | ✗251 | ||||||||
| 14. Open-Door Policy | 3 | ✗109,111 | Y | ||||||||
| 15. Patient-Focused Nursing | 2 | ✗104,139 | Y | ||||||||
| 16. Positive and Safe | 2 | ✗252 | ✗253 | ||||||||
| 17. Positive Behaviour Support | 2 | ✗85,236 | |||||||||
| 18. PROMISE | 2 | ✗85,159 | |||||||||
| 19. Recovery-Based Principles | 2 | ✗6,117 | Y | ||||||||
| 20. Respect Training | 3 | ✗87,236 | ✗254 | ||||||||
| 21. REsTRAIN Yourself | 4 | ✗22 | ✗121 | ✗85,87 | Y | ||||||
| 22. Review | 2 | ✗106,220 | Y | ||||||||
| 23. Safewards | 10 | ✗15,16,181,194,195,197,255 | |||||||||
| ✗88,100 | Y | ||||||||||
| 24. Scottish Patient Safety Programme For Mental Health | 4 | ✗122,123 | ✗124 | ✗91 | Y | ||||||
| 25. Seclusion Reduction Program | 4 | ✗182,209,212,221 | |||||||||
| 26. Sensory Modulation | 4 | ✗135–137,152 | |||||||||
| 27. Sensory Rooms | 3 | ✗158,183,231 | |||||||||
| 28. Talk First | 5 | ✗83,125 | ✗126 | ✗86,236 | Y | ||||||
| 29. Tower Hamlets Violence Reduction Collaborative | 2 | ✗153 | ✗85 | ||||||||
| Total | 100 | – | – | – | – | – | – | 9 | 2 | 3 | 1 |
Appendix 8 Interventions by type and format
Practice examples
| Author(s) | Description | Intervention examples described |
|---|---|---|
| AHRQ198 |
Code Grey (crisis response team) SPARK |
|
| Lombardo et al.159 | PROMISE | |
| CQC85 | Effective approaches to reduce restrictive practice |
HOPES model No Force First Positive Behaviour Support PROMISE REsTRAIN Yourself Tower Hamlets Violence Reduction Collaborative |
| Mind87 | Good practice initiatives |
Respect REsTRAIN Yourself |
| NHS229 | Illustrative case studies |
DASA-IV NHS Improvement Talk First |
| RCP236 | Tools and resources for change ideas |
Accredited training courses, peer-support PMVA tutors, PMVA training tool Co-produced posters DASA-IV Expert by experience mentors to staff Mutual Help Meetings No audit: reflect to reframe Peer support Personal Behavioural Support plans PMVA training Positive Behaviour Support framework PMVA training plan Reducing restrictive practice RESPECT Training: ‘No pain, no panic’ Safety crosses Simulated training Talk First Values and attitudes training tool |
Service reports
| Author(s)/service | Intervention |
|---|---|
| Alegent Health | Trauma-Informed Care |
| Worcester State Hospital92 | Six Core Strategies |
| John J Madden Mental Health Centre256 | Environments for the reduction of restraint and seclusion |
| Barton et al.184 | Achieving Restraint-free |
| Blair and Moulton-Adelman222 | Engagement Model |
| Cockerton et al.195 | Safewards |
| Guez et al.219 (Massachusetts Department of Mental Health) | Six Core Strategies |
| Kayes and Humphris257 | Restraint and Seclusion Reduction Program |
| Natale et al.258 | Caring Theory |
| Northumberland Tyne and Wear NHS Foundation Trust125 | Talk First; Positive and Safe |
| Northumberland Tyne and Wear NHS Foundation Trust83 | Talk First; Positive and Safe |
| Riemer and Corwith192 | Six Core Strategies |
| SAMSHA249 | Six Core Strategies |
| Sivak191 | Comfort Rooms |
| Szypula and Martin89 | Six Core Strategies |
| Tees Esk and Wear Valleys NHS Foundation Trust252 | Positive and Safe |
| Trevarrow82 (Northumberland Tyne and Wear NHS Foundation Trust) | Positive and Safe |
| Tully251 | Novel Seclusion Reduction Program |
| Wishnowsky81 | Reducing Seclusion and Restraint |
Intervention reports
| Author(s) | Intervention |
|---|---|
| APA, APNA and NAPHS259 | Ideas for reducing restraint/seclusion |
| CPI97 | BERT |
| Higgins et al.100 | Safewards |
| Huckshorn92 | Six Core Strategies |
| McEwan et al.123 | Scottish Patient Safety Programme for Mental Health |
| Morrow248 | Six Core Strategies |
| Scottish Patient Safety Programme122 | Scottish Patient Safety Programme for Mental Health |
Trainer links
| Author(s)/provider | Title/intervention |
|---|---|
| CPI95 | CPI training extract |
| D.Escal8260 | http://de-escalate.com 260 |
| Harborview96 | Training course |
| Hart93 | Training video |
| JKM Training, Inc.261 | Reducing Restraints |
| Navigo254 | Respect Training |
| Tees Esk and Wear Valleys NHS Foundation Trust253 | Positive Approaches Team 4-day course (Positive and Safe) |
| APNA232 | APNA e-learning centre (2017): seclusion and restraint – assessment and risk mitigation |
| APNA e-learning centre (2014–17): shifting the culture – identifying essential elements to reduce workplace violence in health care | |
| BILD | |
| Behavioural Support Strategies262 | Behavioural Support Strategies programme |
| Calm Training263 | CALM |
| CPI95 | MAPA |
| Maybo224 | SAFER approach |
| NAPPI UK Ltd | NAPPI |
| Positive Response Training and Consultancy228 | Positive Response |
| PRICE264 | PRICE |
| Safe Crisis Management Europe265 | Safe Crisis Management Europe |
| Space Training Consultants Ltd235 | Space Training |
| Specialist Service Training Solutions Ltd266 | Specialist Service Training |
| St-ACS Team267 | Positive Behaviour Support training and development programme |
| Loddon Foundation Ltd268 | PROACT-SCIPr-UK® |
Tools
| Author(s) | Tool description/intervention |
|---|---|
| Alberta Health Services230 | Restraint as a last resort flow chart |
| Aqua121 | REsTRAIN Yourself toolkit |
| Clark et al.217 | Behavioural Support Planning chart |
| Colton176 | Checklist for assessing your organisation’s readiness for reducing seclusion and restraint |
| Fluttert et al.118 | FESAI tool (Early Recognition Method) |
| Fluttert et al.119 | Early Recognition Method protocol |
| Huckshorn et al.133 | Six Core Strategies planning tool |
| Northumberland Tyne and Wear NHS Foundation Trust269 | Talk First ward assessment |
| Northumberland Tyne and Wear NHS Foundation Trust270 | Positive and Safe debrief policy and tool |
| Northumberland Tyne and Wear NHS Foundation Trust271 | Positive and Safe positive practice process outline |
| Restraint Reduction Network214 | Six Key Restraint Reduction Strategies (Six Core Strategies) |
| Scottish Patient Safety Programme91 | Restraint and seclusion driver diagram phase two |
| South Australia Health272 | Mental health restraint and seclusion toolkit (COPING model) |
| Stirling et al.233 | Reducing restrictive practices checklist |
Instructions
| Author | Instructions description/intervention |
|---|---|
| Health Prince Edward Island247 | Self-directed resource guide: least restraint 1 – introduction |
| DMHAS138 | DMHAS guidelines for development of Comfort Rooms |
| West London NHS Trust273 | Positive and Safe: violence reduction and management programme – instructors manual |
Websites
-
https://e-learning.apna.org (accessed 20 November 2020)
-
https://www.bild.org.uk (accessed 20 November 2020)
-
https://respecttraining.org (accessed 20 November 2020)
-
https://safecrisismanagement.com/scm-specialty-workshops/ (accessed 20 November 2020)
-
https://de-escalate.com/courses (accessed 20 November 2020)
-
https://aqua.nhs.uk/resource_toolkit/toolkit/ (accessed 20 November 2020)
-
https://restraintreductionnetwork.org/wp-content/uploads/2016/11/Reducing-Restrictive-Practices-Checklist.pdf (accessed 20 November 2020)
-
https://ihub.scot/project-toolkits/safety-principles/safety-principles/least-restrictive-practice-principle/restraint-monitoring-and-training/ (accessed 20 November 2020)
-
https://restraintreductionnetwork.org (accessed 20 November 2020)
-
https://innovations.ahrq.gov/profiles/multipronged-strategy-reduces-use-seclusion-and-restraints-manage-aggression-inpatient (accessed 20 November 2020)
-
https://www.clahrc-eoe.nihr.ac.uk/2016/07/8095/ (accessed 20 November 2020)
-
http://www.gov.pe.ca/photos/original/src_least_restr.pdf (accessed 20 November 2020)
-
https://westlondon.nhs.uk/pmva-manual/ (accessed 20 November 2020)
-
https://www.rcpsych.ac.uk (accessed 20 November 2020)
-
https://www.nabh.org/wp-content/uploads/2018/06/LearningfromEachOtherFINAL.pdf (accessed 20 November 2020).
Appendix 9 Interventions by setting
| Interventions | Acute | Admission | Female PD | Geriatric | PICU, including secure | HDU, including secure | Medium/high security | Forensic, secure | Multiple settings | No details | Not applicable |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Standalone intervention | a | b | a | a | a | b | a | d | a | ||
| Intervention family | |||||||||||
| Six Core Strategies | e | e | e | d | f | ||||||
| Beacon Project | c | ||||||||||
| Behavioural Support Planning | c | f | |||||||||
| Brøset Violence Checklist | e | e | e | ||||||||
| City Nurse | c | ||||||||||
| Comfort Rooms | g | ||||||||||
| CPI/MAPA | f | ||||||||||
| DASA-IV | e | e | |||||||||
| Early Recognition Method | c | f | |||||||||
| Initiatives to Reduce Seclusion and Restraint | e | d | |||||||||
| Mutual Help Meetings | e | d | |||||||||
| No Force First | e | d | |||||||||
| Novel Seclusion Reduction Program | e | e | |||||||||
| Open-Door Policy | e | d | |||||||||
| Patient-Focused Nursing | e | d | |||||||||
| Positive and Safe | g | ||||||||||
| Positive Behaviour Support | g | ||||||||||
| PROMISE | e | d | |||||||||
| Recovery-Based Principles | c | ||||||||||
| Respect Training | f | ||||||||||
| REsTRAIN Yourself | g | f | |||||||||
| Review | g | ||||||||||
| Safewards | e | d | |||||||||
| Scottish Patient Safety Programme For Mental Health | e | e | e | f | |||||||
| Seclusion Reduction Programme | e | d | |||||||||
| Sensory Modulation | e | e | |||||||||
| Sensory Rooms | e | e | d | ||||||||
| Talk First | e | d | |||||||||
| Tower Hamlets Violence Reduction Collaborative | e | e | |||||||||
| Total number of interventions | 40 | 1 | 1 | 6 | 11 | 1 | 8 | 5 | 10 | 65 | 27 |
Appendix 10 Interventions by geographical location
Interventions by country
| Intervention | USA | Netherlands | Switzerland | Australia | Canada | Spain | Finland | New Zealand | Denmark | UK | Singapore | Germany | Sweden | Not known |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Standalone intervention | a | a | a | a | a | b | b | a | a | b | a | a | ||
| Intervention family | ||||||||||||||
| Six Core Strategies | c | c | c | c | c | c | ||||||||
| Beacon Project | d | |||||||||||||
| Behavioural Support Planning | d | |||||||||||||
| Brøset Violence Checklist | c | c | ||||||||||||
| City Nurse | d | |||||||||||||
| Comfort Rooms | d | |||||||||||||
| CPI/MAPA | c | c | ||||||||||||
| DASA-IV | d | |||||||||||||
| Early Recognition Method | d | |||||||||||||
| Initiatives to Reduce Seclusion And Restraint | d | |||||||||||||
| Mutual Help Meetings | d | |||||||||||||
| No Force First | c | c | c | |||||||||||
| Novel Seclusion Reduction Program | d | |||||||||||||
| Open-Door Policy | d | |||||||||||||
| Patient-Focused Nursing | c | c | ||||||||||||
| Positive and Safe | d | |||||||||||||
| Positive Behaviour Support | d | |||||||||||||
| Promise (Proactive Management of Integrated Services and Environments) | d | |||||||||||||
| Recovery-Based Principles | d | |||||||||||||
| Respect Training | d | |||||||||||||
| REsTRAIN Yourself | d | |||||||||||||
| Review | d | |||||||||||||
| Safewards | c | c | c | |||||||||||
| Scottish Patient Safety Programme for Mental Health | d | |||||||||||||
| Seclusion Reduction Programme | d | |||||||||||||
| Sensory Modulation | c | c | c | |||||||||||
| Sensory Rooms | c | c | c | |||||||||||
| Talk First | d | |||||||||||||
| Tower Hamlets Violence Reduction Collaborative | d | |||||||||||||
| Total number of interventions | 60 | 5 | 2 | 16 | 7 | 3 | 2 | 3 | 2 | 59 | 2 | 1 | 2 | 2 |
Appendix 11 Procedures
| Author(s) | Training | Nursing changes | Reviewing data | Communication | Care-planning | Sensory room | Change in policy | Assessing risk | Debriefing | Enhanced leadership | Role models | Increased staffing | Service user involvement | Rapid response | Miscellaneous | Activities | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Putkonen et al.17 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 10 | ||||||
| 2. Huckshorn92 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 11 | |||||
| 3. Riemer and Corwith192 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 10 | ||||||
| 4. Lewis et al.132 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 10 | ||||||
| 5. Lombardo et al.159 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 10 | ||||||
| 6. Riahi et al.23 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 9 | |||||||
| 7. Lo74 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 9 | |||||||
| 8. Duxbury et al.22 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 9 | |||||||
| 9. Wieman et al.211 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 8 | ||||||||
| 10. Noorthoorn et al.182 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 8 | ||||||||
| 11. Tully et al.90 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 8 | ||||||||
| 12. Wolfaardt75 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 13. Ash et al.117 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 14. Ash et al.6 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 15. Björkdahl et al.129 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 16. Bowers et al.16 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 17. Long et al.147 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 18. Mann-Poll et al.209 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 19. Taxis227 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 9 | |||||||
| 20. Short et al.157 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 21. Smith et al.142 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 22. Sullivan et al.190 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 23. Hochstrasser et al.111 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||||||
| 24. Zuehlke et al.160 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 25. Smith and Millar158 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 26. Georgieva et al.150 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 27. Madan et al.108 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 28. Ching et al.115 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 29. Blair et al.222 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 30. Borckardt et al.107 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 31. Aremu et al.151 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 32. Taylor and Brown94 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||||||
| 33. Qurashi et al.186 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 34. Maguire et al.116 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 35. Mistral et al.189 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 36. Fletcher et al.181 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 37. Price et al.194 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 38. Cabral and Carthy15 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 39. Maguire et al.197 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 40. Stead et al.188 | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | |||||||||||
| 41. D’Orio et al.149 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 42. Bell and Gallacher161 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 43. Yakov et al.185 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 44. Godfrey et al.210 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 45. Steinert et al.20 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 46. Jonikas et al.180 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 47. Sullivan et al.104 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 48. Mann-Poll et al.212 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 49. Forster et al.234 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 50. Noorthoorn e et al.221 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 51. Fluttert et al.118 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 52. Jungfer et al.109 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 53. Boumans et al.225 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 54. Guzman-Parra et al.146 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 55. Chandler201 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 56. Beezhold et al.79 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 57. Bowers et al.102 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 58. Pollard et al.274 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 59. Hernandez et al.99 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 60. Taylor-Watt et al.153 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 61. Clarke et al.114 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 62. Sarkar78 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 63. McEvedy et al.137 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 64. Andersen et al.135 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 65. Martin and Suane231 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 66. Goulet et al.166 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 67. Khadivi et al.275 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 68. Hellerstein et al.145 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 69. Calabro et al.141 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 70. Lee et al.127 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 71. Brown et al.154 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 72. Prescott et al 2007128 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 73. Donat106 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 74. Beaglehole et al.223 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 75. Hochstrasser et al.111 | ✗ | ✗ | ✗ | 3 | |||||||||||||
| 76. Melin69 | ✗ | ✗ | 2 | ||||||||||||||
| 77. Cowin et al.163 | ✗ | ✗ | 2 | ||||||||||||||
| 78. McCue et al.237 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||||||
| 79. Needham et al.112 | ✗ | ✗ | 2 | ||||||||||||||
| 80. Sutton et al.152 | ✗ | ✗ | 2 | ||||||||||||||
| 81. Repique et al.187 | ✗ | ✗ | 2 | ||||||||||||||
| 82. Fletcher and Stevenson276 | ✗ | ✗ | 2 | ||||||||||||||
| 83. Lloyd et al.136 | ✗ | ✗ | 2 | ||||||||||||||
| 84. Novak et al. 2012183 | ✗ | ✗ | 2 | ||||||||||||||
| 85. Björkdahl et al.129 | ✗ | ✗ | 2 | ||||||||||||||
| 86. Yang et al.277 | ✗ | ✗ | 2 | ||||||||||||||
| 87. Gonzalez70 | ✗ | ✗ | 2 | ||||||||||||||
| 88. Chang et al.162 | ✗ | ✗ | 2 | ||||||||||||||
| 89. Beckett et al.130 | ✗ | ✗ | 2 | ||||||||||||||
| 90. Bowers et al.101 | ✗ | ✗ | 2 | ||||||||||||||
| 91. van de Sande et al.200 | ✗ | ✗ | 2 | ||||||||||||||
| 92. Burhan et al.80 | ✗ | ✗ | 2 | ||||||||||||||
| 93. Guzman-Parra et al.144 | ✗ | ✗ | 2 | ||||||||||||||
| 94. Hayes and Russ143 | ✗ | ✗ | 2 | ||||||||||||||
| 95. Laker et al.21 | ✗ | 1 | |||||||||||||||
| 96. Omolewa73 | ✗ | 1 | |||||||||||||||
| 97. Geoffrion et al.148 | ✗ | 1 | |||||||||||||||
| 98. Bybel71 | ✗ | 1 | |||||||||||||||
| 99. Kontio et al.199 | ✗ | 1 | |||||||||||||||
| 100. Cummings et al.215 | ✗ | 1 | |||||||||||||||
| 101. Smith and Jones140 | ✗ | 1 | |||||||||||||||
| 102. Gonzalez-Torres et al.170 | ✗ | 1 | |||||||||||||||
| 103. Abderhalden et al.113 | ✗ | 1 | |||||||||||||||
| 104. Donat278 | ✗ | 1 | |||||||||||||||
| 105. Friedman et al.131 | ✗ | 1 | |||||||||||||||
| 106. Parasurum et al.77 | ✗ | 1 | |||||||||||||||
| 107. Donat220 | ✗ | 1 | |||||||||||||||
| 108. Stensgaard et al.255 | ✗ | 1 | |||||||||||||||
| 109. Newman et al.203 | ✗ | 1 | |||||||||||||||
| Total | 86 | 47 | 45 | 40 | 38 | 32 | 29 | 26 | 23 | 22 | 18 | 17 | 17 | 8 | 8 | 7 |
Appendix 12 Non-randomised evaluations (n = 85)
Non-controlled evaluations
| Author(s) | Wards | Significant outcomes |
|---|---|---|
| 1. Aremu151 | 1 ward | None |
| 2. Ash et al.6 | 10 beds/1 unit | Reduced seclusion episodes |
| 3. Ash et al.117 | 10 beds/1 unit | Reduced seclusion episodes |
| 4. Beaglehole et al.223 | 64 beds/1 service | Seclusion duration went down |
| 5. Beckett et al.130 | 27 beds (6/HDU and 21/acute) | Seclusion rates reduced, use of security staff decreased |
| 6. Bell and Gallacher161 | 30 beds/1 ward | Restraint use went down |
| 7. Björkdahl et al.129 | 41 wards/8 hospitals (12–18 beds each) | Significantly more positive attitudes from staff after training |
| 8. Björkdahl et al.279 | 28 beds/1 ward reducing to 12 mid-study | Increase in restrictive practices but likely to be confounded by bed reduction |
| 9. Blair222 | 120 beds/1 service | Decreased seclusion events but duration increased, duration of restraint increased |
| 10. Bowers et al.101 | 18 beds/2 wards | Reductions in conflict only |
| 11. Brown et al.154 | 50 beds/3 wards | Decreased incidents and staff injury |
| 12. Bybel71 | NR | Relationship between staff training and decrease s/r |
| 13. Cabral and Carthy15 | 6 wards | Improved ward atmosphere |
| 14. Calabro et al.141 | 12 wards/1 hospital | Improved attitudes, behavioural intention, self-efficacy |
| 15. Chandler201 | 1 ward | Decrease in s/r |
| 16. Chang et al.162 | 24 beds/1 unit | Decrease in s/r |
| 17. Ching et al.115 | 118 beds/5 units | Reduction in total number and duration of seclusion |
| 18. Clark et al.114 | 11 beds/PICU; 80 beds/centre; 2 units/centre of 92 beds | Reduced seclusion |
| 19. Cowin et al.163 | NR | None |
| 20. Donat106 | 1 hospital | Reduced seclusion restraint and PRN |
| 21. Donat 220 | 245 beds/1 hospital | As staff ration increased s/r decreased |
| 22. Donat278 | 310 bed/1 hospital | Reduced PRN use |
| 23. D’Orio et al.149 | 1 unit | Reduced seclusion and restraint 39% |
| 24. Fletcher and Stevenson276 | 2 wards | 67% decrease in restraint |
| 25. Fluttert et al.118 | 16 wards | Significant decrease in seclusions |
| 26. Forster et al.234 | 83 beds/1 facility | Significant decrease in restraint |
| 27. Friedman et al.131 | 500 beds/6 units plus cottages/1 hospital | Reduction in psychotropic PRN and seclusion and restraint |
| 28. Geoffrion et al.148 | 24 beds/2 ward (12 beds/PICU plus 12 beds/emergency) | Decrease in seclusion and restraints in PICU only not emergency department |
| 29. Georgieva et al.150 | 4 beds/1 unit | Reduced seclusion |
| 30. Godfrey et al.210 | 216/2 units (140/acute plus 76/transition) in 398-bed hospital | Mechanical restraint staff injuries all reduced |
| 31. Gonzalez-Torres et al.170 | 42 beds/1 ward | Restraint use went down |
| 32. Goulet et al.166 | 27 beds | Reduction in seclusion events and duration |
| 33. Guzman-Parra et al.144 | 42 beds/1 ward | Reduction in restraint |
| 34. Guzman-Parra et al.146 | 42 beds/1 ward | Reduced duration but not rate |
| 35. Hayes and Russ143 | 206 beds/9 units | Reduced PRN – did not increase restraint seclusion or assaults |
| 36. Hellerstein et al.145 | 58 beds/3 units | Reduced s/r |
| 37. Hernandez et al.99 | 326 beds/1 facility | Reduced s/r |
| 38. Hochstrasser et al.111 | 260 beds/15 wards | Seclusion and forced medications decreased |
| 39. Hochstresser et al.111 | 4 wards | Yes – decreased frequency of seclusions |
| 40. Huckshorn92 | 350 beds | NR |
| 41. Jonikas et al.180 | 3 units/1 hospital | Reduction of physical restraint |
| 42. Jungfer et al.109 | 277 beds/1 service | Reduced seclusion and forced medication on open wards |
| 43. Khadivi et al.275 | NR | Reduced seclusion and restraint and increased assaults |
| 44. Lee et al.127 | 30/1 unit | Reduction in seclusion |
| 45. Lewis132 | 88 beds/5 units/1 facility of 900 beds | 75% reduction in S/R |
| 46. Lo74 | 100 beds/5 units/1 hospital of 454 beds (each 20 beds) | No significant findings |
| 47. Lombardo et al.159 | 20 wards | Reduced restraint |
| 48. Long et al.147 | 40 beds/3 wards/1 facility | Less seclusion and less time in seclusion |
| 49. Maguire et al.116 | 116 beds/5 units | Reduction in frequency and duration of seclusion |
| 50. Maguire et al.197 | 20 beds/1 ward/1 hospital of 116 beds | None |
| 51. Mann-Poll et al.212 | 5 wards/1 hospital | Decreased rate and duration of seclusion immediately but not later |
| 52. Martin and Suane231 | NR | Increase in knowledge and use of Sensory Rooms |
| 53. McCue et al.237 | 135 beds/1 hospital | Reduced restraint |
| 54. McEvedy et al.137 | NR | Positive qualitative results |
| 55. Mistral et al.189 | 14 beds/3 wards/1 hospital | Reduction in seclusion |
| 56. Needham et al.112 | 24 beds/2 wards/1 hospital (12 plus 12) | On some analysis rates of coercion went down |
| 57. Newman et al.203 | 1 unit | None |
| 58. Noorthoorn et al.221 | 68 wards/8 hospitals in 2008 increasing to 1826 wards/66 hospitals in 2013 | Seclusion decreased; forced medications increased |
| 59. Novak et al.183 | 40 beds/1 unit | None |
| 60. Pollard et al.274 | 1 unit | Reduced s/r |
| 61. Prescott et al.128 | 36 beds (22/adult plus 14/observation) in 1 hospital | None |
| 62. Qurashi et al.186 | 1 hospital | Reduced seclusion |
| 63. Repique et al.187 | 192 beds | None |
| 64. Riahi et al.23 | 326 beds/1 facility | None |
| 65. Riemer and Corwith192 | 21 beds/1 unit | Reduced s/r incidents and duration |
| 66. Sarkar78 | NR | Not reported |
| 67. Short et al.157 | 200 beds/1 facility | Reduced seclusion restrain injury and fewer complaints |
| 68. Smith and Millar158 | 30 beds/1 ward | Not reported |
| 69. Smith et al.142 | 9 hospitals | Rate and duration of seclusion/r dropped |
| 70. Smith and Jones140 | 1 ward | None |
| 71. Stead et al.188 | NR | Seclusion reduced |
| 72. Steinert et al.20 | 18 beds/1 ward | Seclusion and restraint fell but not mechanical restraint for PD in one setting |
| 73. Stensgaard et al.255 | 26 wards | Decrease in coercive measure in general, and forced sedation |
| 74. Sullivan et al.104 | 8 beds/1 unit | Reduced duration rather than number of seclusions |
| 75. Sullivan et al.190 | 117 beds/5 units/1 hospital of 525 beds | Reduction in seclusion |
| 76. Sutton et al.152 | NR | Positive qualitative findings |
| 77. Taxis227 | 86 beds/1 facility | Reduction in s/r |
| 78. Taylor and Brown94 | 30 beds/1 unit | No detail |
| 79. Taylor-Watt et al.153 | 76 beds/6 wards | Reduction in violence restraint down 60% |
| 80. Tully et al.90 | NR | Reduced seclusion |
| 81. Wieman et al.211 | 50–200 beds/43 facilities | Yes |
| 82. Wolfaardt75 | 32 beds/1 unit | Not significant |
| 83. Yakov et al.185 | 20 beds/1 ward/1 facility | Reduction in restraints and assaults |
| 84. Yang et al.277 | 4 wards | None |
| 85. Zuehlke et al.160 | 15 beds/1 ward | Yes |
Non-randomised evaluations with a controlled design (n = 18)
| Author(s) | Design | Wards | Control | Significant findings |
|---|---|---|---|---|
| 1. Andersen et al.135 | Case control | 2 wards | NR | Restraint and PRN decreased (95% CI) |
| 2. Beezhold et al.79 | Quasi-experimental | NR | NR | Restraint and observation decreased (non-significant) |
| 3. aBorckardt et al.107 | Experimental design | 5 units | Pre-intervention wards as own control | Seclusion and restraint decreased (p = 0.008) |
| 4. aBoumans et al.225 | Experiment, explorative | 4 wards | Other wards with restrictive practice reduction initiatives taking place | Seclusion increased |
| 5. Bowers et al.102 | Non-randomised controlled trial, before/after including action research | 8 wards | NR | No significant findings |
| 6. Burhan et al.80 | Pre–post | 3 wards | NR | PRN use decreased (p = < 0.0001) |
| 7. Cummings et al.215 | Non-randomised controlled trial | NR | NR | No significant findings |
| 8. Duxbury et al.22 | Pre–post, controlled trial | 14 wards | Non-matched wards | Overall rate of restraint reduced by an average of 22% |
| 9. Fletcher et al.181 | Pre–post | 44 wards | NR | Seclusion decreased (p = 0.04) |
| 10. Gonzalez70 | Quasi-experimental, quantitative study | 2 units | NR | No restrictive practice outcomes reported |
| 11. Laker et al.21 | Pre–post, quasi-experimental | NR | NR | No restrictive practice outcomes reported |
| 12. Lloyd et al.136 | Pre–post | 40 beds/1 hospital (2 × 20 beds (14 acute and 6 PICU) | NR | Decreased seclusion (p < 0.001) |
| 13. aMadan et al.108 | Experimental naturalistic design, follow-up | 5 units | NR | Seclusion and restraint decreased (p < 0.001) |
| 14. Mann-Poll et al.209 | Pre–post | 4 wards | Other professionals | No restrictive practice outcomes reported |
| 15. Melin69 | Pre–post measures, quasi-experimental | 3 wards | NR | No restrictive practice outcomes reported |
| 16. Noorthoorn et al.182 | Prospective cohort | 2 wards | NR | Seclusion decreased |
| 17. Omolewa73 | Non-randomised controlled trial | 4 units | NR | No restrictive practice outcomes reported |
| 18. Price et al.194 | Non-randomised controlled trial | 6 units | Treatment as usual then Safewards | Seclusion (including duration) (95% CI 0.78 to 0.92; p < 0.001), restraint (including duration) and observation decreased (95% CI 0.86 to 0.90; p < 0.001) |
Appendix 13 Outcome measures
| Author(s) | Incidence | Duration | Other | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Seclusion | Restraint | Chemical | Generic | Violence | Self-harm | Injury | Staff sickness/absence | Seclusion | Restraint | Generic | |||
| 1. Abderhalden et al.113 | α | ✗ | ✗ | 3 | |||||||||
| 2. Andersen et al.135 | α | α | S | 2 | |||||||||
| 3. Aremu et al.151 | ED | S | 2 | ||||||||||
| 4. Ash et al.117 | αEP | 1 | |||||||||||
| 5. Ash et al.6 | αEP | 1 | |||||||||||
| 6. Beaglehole et al.223 | ✗ | ✗ | 2 | ||||||||||
| 7. Beckett et al.130 | ✗ | 1 | |||||||||||
| 8. Beezhold et al.79 | αE | E | E | 3 | |||||||||
| 9. Bell and Gallacher161 | ✗S | 1 | |||||||||||
| 10. Björkdahl et al.129 | ✗ | ✗ | 2 | ||||||||||
| 11. Björkdahl et al.279 | S | 1 | |||||||||||
| 12. Blair et al.222 | ✗ | ✗ | S | ✗ | ✗ | 4 | |||||||
| 13. Borckardt et al.107 | α | α | S | 2 | |||||||||
| 14. Boumans et al.225 | Sa | ✗ | 2 | ||||||||||
| 15. Bowers et al.102 | ✗ | 1 | |||||||||||
| 16. Bowers et al.16 | α | 1 | |||||||||||
| 17. Bowers et al.101 | ✗ | 1 | |||||||||||
| 18. Brown et al.154 | αE | αE | E | E | 4 | ||||||||
| 19. Burhan et al.80 | α | ✗ | 2 | ||||||||||
| 20. Bybel71 | α | α | 2 | ||||||||||
| 21. Cabral and Carthy15 | S | 1 | |||||||||||
| 22. Calabro et al.141 | ✗ | 1 | |||||||||||
| 23. Chandler201 | ✗ | ✗ | 2 | ||||||||||
| 24. Chang et al.162 | α | α | S | 3 | |||||||||
| 25. Ching et al.115 | ✗ | ✗ | S | 3 | |||||||||
| 26. Clarke et al.114 | ✗ | SP | 2 | ||||||||||
| 27. Cowin et al.163 | D | 1 | |||||||||||
| 28. Cummings et al.215 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||
| 29. Donat106 | ✗P | ✗P | ✗ | 3 | |||||||||
| 30. Donat220 | ✗ | ✗ | ✗ | 3 | |||||||||
| 31. Donat278 | ✗ | 1 | |||||||||||
| 32. D’Orio et al.218 | α | α | ✗ | 3 | |||||||||
| 33. Duxbury et al.22 | E | 1 | |||||||||||
| 34. Fletcher and Stevenson276 | ✗ | ✗ | ✗ | 3 | |||||||||
| 35. Fletcher et al.181 | α | 1 | |||||||||||
| 36. Fluttert et al.118 | α | D | 2 | ||||||||||
| 37. Forster et al.234 | ✗ | ✗ | 2 | ||||||||||
| 38. Friedman et al.131 | ✗ | ✗ | D | ✗ | 4 | ||||||||
| 39. Geoffrion et al.148 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||
| 40. Georgieva et al.150 | ✗ | ✗ | 2 | ||||||||||
| 41. Godfrey et al.210 | E | E | E | E | 4 | ||||||||
| 42. Gonzalez70 | E NR | 1 | |||||||||||
| 43. Gonzalez-Torres et al.170 | ✗ | 1 | |||||||||||
| 44. Goulet et al.166 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||
| 45. Guzman-Parra et al.146 | ✗ | α | 2 | ||||||||||
| 46. Guzman-Parra et al.144 | ✗ | ✗ | 2 | ||||||||||
| 47. Hayes and Russ143 | ✗ | ✗ | α | ✗ | 3 | ||||||||
| 48. Hellerstein et al.145 | ✗P | ✗P | ✗ | ✗ | ✗ | ✗ | 6 | ||||||
| 49. Hernandez et al.99 | E | E | E | 3 | |||||||||
| 50. Hochstrasser et al.111 | E | E | 2 | ||||||||||
| 51. Hochstrasser et al.111 | EP | EP | E | 3 | |||||||||
| 52. Huckshorn92 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 6 | ||||||
| 53. Jonikas et al.180 | E | 1 | |||||||||||
| 54. Jungfer et al.109 | αE | αE | 2 | ||||||||||
| 55. Khadivi et al.275 | E | E | E | 3 | |||||||||
| 56. Kontio et al.199 | E | αE | E | E | 4 | ||||||||
| 57. Laker et al.21 | E NR | E | 2 | ||||||||||
| 58. Lee et al.127 | αD | S | 1 | ||||||||||
| 59. Lewis et al.132 | αE | αE | E | E | E | S | 5 | ||||||
| 60. Lloyd et al.136 | α | ✗ | S | 3 | |||||||||
| 61. Lo74 | 0 | ||||||||||||
| 62. Lombardo et al.159 | D | D | 2 | ||||||||||
| 63. Long et al.147 | α | S | 1 | ||||||||||
| 64. Madan et al.108 | αE | αE | 2 | ||||||||||
| 65. Maguire et al.116 | XP | ✗ | S | 2 | |||||||||
| 66. Maguire et al.197 | ✗ | S | 2 | ||||||||||
| 67. Mann-Poll et al.209 | ✗ | ✗ | 2 | ||||||||||
| 68. Mann-Poll et al.212 | S | 1 | |||||||||||
| 69. Martin et al.231 | ✗ | ✗ | DS | 2 | |||||||||
| 70. McCue et al.237 | ✗ | ✗ | ✗ | 3 | |||||||||
| 71. McEvedy et al.137 | ✗ | 1 | |||||||||||
| 72. Melin69 | NR | 1 | |||||||||||
| 73. Mistral et al.189 | ✗ | S | S | 3 | |||||||||
| 74. Needham et al.112 | D | 1 | |||||||||||
| 75. Newman et al.203 | E | E | E | 3 | |||||||||
| 76. Noorthoorn et al.182 | α | ✗ | 1 | ||||||||||
| 77. Noorthoorn et al.221 | α | ✗ | 1 | ||||||||||
| 78. Novak et al.183 | ✗ | 1 | |||||||||||
| 79. Omolewa73 | S | 1 | |||||||||||
| 80. Parasurum et al.77 | NR | ✗ | S | 3 | |||||||||
| 81. Pollard et al.274 | ✗ | 1 | |||||||||||
| 82. Prescott et al.128 | ✗ | 1 | |||||||||||
| 83. Price et al.194 | α | S | S | 1 | |||||||||
| 84. Putkonen et al.17 | α | α | ✗ | ✗ | 2 | ||||||||
| 85. Qurashi et al.81 | ✗ | 1 | |||||||||||
| 86. Repique et al.187 | ✗ | 1 | |||||||||||
| 87. Riahi et al.23 | ESP | ESP | ES | ES | 4 | ||||||||
| 88. Riemer et al.192 | ✗ | ✗ | 2 | ||||||||||
| 89. Sarkar78 | ✗ | ✗ | ✗ | ✗ | 4 | ||||||||
| 90. Short et al.157 | α | α | ✗ | α | ✗ | 4 | |||||||
| 91. Smith and Millar140 | D | D | D | D | D | S | 5 | ||||||
| 92. Smith and Jones158 | 0 | ||||||||||||
| 93. Smith et al.142 | αP | ✗ | ✗ | 3 | |||||||||
| 94. Stead et al.188 | ✗ | 1 | |||||||||||
| 95. Steinert et al.20 | EP | EP | EP | EP | 4 | ||||||||
| 96. Stensgaard et al.255 | EP | E | E | 3 | |||||||||
| 97. Sullivan et al.190 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | 7 | |||||
| 98. Sullivan et al.104 | ✗ | 1 | |||||||||||
| 99. Sutton et al.152 | S | 1 | |||||||||||
| 100. Taxis227 | ✗ | 1 | |||||||||||
| 101. Taylor et al.94 | ✗ | 1 | |||||||||||
| 102. Taylor-Watt et al.153 | ✗ | ✗ | ✗ | S | 3 | ||||||||
| 103. Tully et al.90 | ✗ | DS | 2 | ||||||||||
| 104. van de Sande et al.200 | αSP | SD | S | 3 | |||||||||
| 105. Wieman et al.211 | ✗ | ✗ | ✗ | ✗ | S | 4 | |||||||
| 106. Wolfaardt75 | ✗ | ✗ | S | 3 | |||||||||
| 107. Yakov et al.185 | αE | αE | E | 2 | |||||||||
| 108. Yang et al.277 | ✗ | ✗ | ✗ | 3 | |||||||||
| 109. Zuehlke et al.160 | ✗ | ✗ | ✗ | 3 | |||||||||
| Total | 56 | 48 | 16 | 23 | 20 | 4 | 6 | 4 | 22 | 16 | 1 | 33 | |
| Standardised outcome measures | n |
|---|---|
| AAPPQ280 | 1 |
| Adult/Adolescent Sensory Profile (Brown and Dunn281) | 2 |
| Argus Scale200 | 2 |
| Attitudes towards working with people with psychosis (McLeod et al.282) | 1 |
| Behavioural Profile Tool | 1 |
| BPRS283 | 1 |
| Brøset Violence Checklist 206 | 4 |
| Client Satisfaction Questionnaire284 | 1 |
| Confidence in Managing Inpatient Aggression Survey (Martin and Daffern285) | 2 |
| CT-R Interview (Chang et al.162) | 1 |
| Dangerousness Scale286 | 1 |
| DREEM287 | 1 |
| Dynamic Appraisal of Situational Aggression Risk Assessment (Ogloff and Daffern288) | 1 |
| Emotions Activity Rating Scale (Champagne and Stromberg289) | 1 |
| EssenCES (Schalast et al.207) | 4 |
| General Aggression Model (Allen et al.290) | 1 |
| Heyman Staff Attitudes towards Seclusion Survey (Heyman204) | 3 |
| HoNOS291 | 1 |
| Inpatient behaviour rating scale (Dolan)292 | 1 |
| ISRRI: fidelity measure211 | 1 |
| Kennedy-Axis V293 | 1 |
| Knowledge of Physical Restraint Use, Attitudes of Physical Restraint Use, and Practice of Physical Restraint Use (Huang et al.294) | 1 |
| Maslach Burnout Inventory295 | 1 |
| Mental Status Assessment296 | 1 |
| Nursing staff questionnaire | 1 |
| Overt Aggression Scale (Yudofsky et al.297) | 1 |
| Patient Safety Climate Tool161 | 2 |
| PCC-SR298 | 3 |
| Presencia tool to measure risk of restraint (Guzman-Parra et al.144) | 1 |
| PATS-Q209 | 1 |
| Q-LES-Q-SF299 | 1 |
| Quality of Care measure300 | 1 |
| Safewards Implementation Audit Checklist, Safewards Researcher Visit Fidelity Checklist16 | 2 |
| Social Dysfunction and Aggression Scale301 | 1 |
| SOAS-R302 | 1 |
| Tidal Monitoring Assessment Tool303 | 1 |
| VOTE (Laker et al.304) | 1 |
| Violence prevention and management climate via ‘E13’ a 13-item questionnaire305 | 1 |
| Ward atmosphere scale306 | 1 |
Appendix 14 Individual behaviour change techniques not used
| Grouping | BCT |
|---|---|
| Feedback and monitoring | 2.6 Biofeedback |
| Shaping behaviour |
4.3 Re-attribution 4.4 Behavioural experiments |
| Natural consequences | 5.5 Anticipated regret |
| Associations |
7.2 Cue signalling reward 7.3 Reduce prompts or cues 7.4 Remove access to reward 7.5 Remove aversive stimulus 7.6 Satiation 7.7 Exposure 7.8 Associative learning |
| Repetition and substitution |
8.2 Behavioural substitution 8.5. Overcorrection 8.6. Generalisation of target behaviour 8.7. Graded tasks |
| Comparison of outcomes |
9.2. Pros and cons 9.3. Comparative imagining of future outcomes |
| Reward and threat |
10.1. Material incentive (behaviour) 10.2. Material reward (behaviour) 10.3. Non-specific reward 10.5. Social incentive 10.6. Non-specific incentive 10.7. Self-incentive 10.8. Incentive (outcome) 10.9. Self-reward 10.10. Reward (outcome) 10.11. Future punishment |
| Regulation |
11.1. Pharmacological support 11.3. Conserving mental resources 11.4. Paradoxical instructions |
| Antecedents |
12.3. Avoidance/reducing exposure to cues for the behaviour 12.4. Distraction 12.6. Body changes |
| Identity |
13.3. Incompatible beliefs 13.4. Valued self-identify 13.5. Identity associated with changed behaviour |
| Scheduled consequences |
14.1. Behaviour cost 14.2. Punishment 14.3. Remove reward 14.4. Reward approximation 14.5. Rewarding completion 14.6. Situation-specific reward 14.7. Reward incompatible behaviour 14.8. Reward alternative behaviour 14.9. Reduce reward frequency 14.10. Remove punishment |
| Self-belief |
15.1. Verbal persuasion about capability 15.2. Mental rehearsal of successful performance 15.3. Focus on past success 15.4. Self-talk |
| Covert learning |
16.1. Imaginary punishment 16.2. Imaginary reward 16.3. Vicarious consequences |
Appendix 15 Behaviour change techniques identified in evaluations of interventions that reduced restrictive practices
| Author(s) | Instruction on how to perform the behaviour | Restructuring the social environment | Problem-solving | Action-planning | Framing/reframing | Prompts or cues | Feedback: outcome(s) of behaviour | Information about antecedents | Adding objects to the environment | Social support (practical) | Restructuring the physical environment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Abderhalden et al.113 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 2. Andersen et al.135 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
| 3. Aremu et al.151 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 4. Ash et al.117 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| 5. Ash et al.6 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 6. Beaglehole et al.223 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| 7. Beckett et al.130 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
| 8. Beezhold et al.79 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9. Bell and Gallacher161 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 |
| 10. Blair et al.222 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 |
| 11. Borckardt et al.107 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 |
| 12. Bowers et al.16 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| 13. Burhan et al.80 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14. Bybel71 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15. Chandler201 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| 16. Chang et al.162 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 17. Ching et al.115 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 |
| 18. Clarke et al.114 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 19. D’Orio et al.149 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 0 |
| 20. Donat106,220 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 21. Donat278 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 22. Donat220 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 23. Duxbury et al.22 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 |
| 24. Fletcher and Stevenson276 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 25. Fletcher et al.181 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| 26. Fluttert et al.118 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| 27. Forster et al.234 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| 28. Friedman et al.131 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 29. Geoffrion et al.148 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 30. Georgieva et al.150 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 31. Godfrey et al.210 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 |
| 32. Gonzalez70 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 33. Goulet et al.166 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 |
| 34. Guzman Parra et al.146 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 35. Guzman-Parra et al.144 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| 36. Hayes and Russ143 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 37. Hernandez et al.99 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 38. Hochstrasser et al.111 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 39. Hochstrasser et al.111 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 40. Jonikas et al.180 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
| 41. Jungfer et al.109 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 42. Khadivi et al.275 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| 43. Kontio et al.199 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 0 |
| 44. Lee et al.127 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 |
| 45. Lewis et al.132 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| 46. Lloyd et al.136 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 |
| 47. Lombardo et al.159 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 |
| 48. Long et al.147 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| 49. Madan et al.108 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 1 |
| 50. Maguire et al.116 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| 51. Mann Poll et al.212 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 |
| 52. McCue et al.237 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 53. Mistral et al.189 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 |
| 54. Needham et al.112 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| 55. Newman et al.203 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 56. Noorthoorn et al.221 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| 57. Novak et al.183 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 58. Pollard et al.274 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 59. Price et al.194 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 |
| 60. Putkonen et al.17 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 |
| 61. Qurashi et al.186 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 |
| 62. Repique et al.187 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 63. Riahi et al.23 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| 64. Sarkar et al.78 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 65. Short et al.157 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| 66. Sivak191 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 |
| 67. Smith and Millar140 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 68. Smith and Millar158 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 |
| 69. Smith et al.142 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 |
| 70. Stead et al.188 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 0 |
| 71. Steinert et al.20 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| 72. Stensgaard et al.255 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 73. Sullivan et al.104 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| 74. Sullivan et al.104 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| 75. Taxis et al.227 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 76. Tully et al.90 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 77. van de Sande et al.200 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 |
| 78. Wieman et al.211 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 79. Wolfaardt75 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| 80. Yakov et al.185 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 |
| 81. Yang et al.277 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| 82. Zuehlke et al.160 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
Appendix 16 Full list of records included in the review
| Author(s) | Title |
|---|---|
| 1. Abderhalden et al.113 | Structured risk assessment and violence in acute psychiatric wards: randomised controlled trial |
| 2. AHRQ198 | Multipronged Strategy Reduces Use of Seclusion and Restraints to Manage Aggression at Inpatient Behavioral Health Facility |
| 3. Alberta Health Services230 | Restraint as a Last Resort Flowchart |
| 4. Allen et al.238 | Executive-level reviews of seclusion and restraint promote interdisciplinary collaboration and innovation |
| 5. Andersen et al.135 | Applying sensory modulation to mental health inpatient care to reduce seclusion and restraint: a case control study |
| 6. Health PEI | Alegent Health: Trauma Informed Care, Transforming Our Future |
| 7. American Hospital Association259 | Learning From Each Other: Success Stories and Ideas for Reducing Restraint/Seclusion in Behavioral Health |
| 8. American Psychiatric Nurses Association232 | 2017-Seclusion and Restraint: Assessment and Risk Mitigation |
| 9. AQUA121 | REsTRAIN Yourself toolkit |
| 10. Aremu et al.151 | Implementation of trauma-informed care and brief solution-focused therapy |
| 11. Tully251 | A pilot evaluation of strategies to reduce long term segregation on Ascot Ward, Broadmoor |
| 12. Ash et al.117 | Reduction in the use of seclusion with the introduction of recovery principles in an acute psychiatric unit |
| 13. Ash et al.6 | Recovery-based services in a psychiatric intensive care unit – the consumer perspective |
| 14. Ashcraft and Anthony193 | Eliminating seclusion and restraint in recovery-oriented crisis services |
| 15. Ashcraft et al.24 | Best practices: the development and implementation of ‘no force first’ as a best practice |
| 16. Barton et al.184 | Achieving restraint-free on an inpatient behavioral health unit |
| 17. Beaglehole et al.223 | Unlocking an acute psychiatric ward: the impact on unauthorised absences, assaults and seclusions |
| 18. Beckett et al.130 | Trauma-informed care and practice: practice improvement strategies in an inpatient mental health ward |
| 19. Beezhold et al.79 | A quasi-experimental controlled intervention to reduce violence on an acute psychiatric ward |
| 20. Belanger307 | The ‘S and R challenge’: reducing the use of seclusion and restraint in a state psychiatric hospital |
| 21. Bell and Gallacher161 | Succeeding in sustained reduction in the use of restraint using the Improvement Model |
| 22. ST-ACS Team267 | ST-ACS Positive Behaviour Support (PBS) Training |
| 23. Björkdahl et al.129 | The influence of staff training on the violence prevention and management climate in psychiatric inpatient units |
| 24. Björkdahl et al.279 | Changes in the occurrences of coercive interventions and staff injuries on a psychiatric intensive care unit |
| 25. Blair et al.308 | Reduction of seclusion and restraint in an inpatient psychiatric setting: a pilot study |
| 26. Blair and Moulton-Adelman222 | The Engagement Model for reducing seclusion and restraint: 13 years later |
| 27. Borckardt et al.107 | Systematic investigation of initiatives to reduce seclusion and restraint in a state psychiatric hospital |
| 28. Boumans et al.225 | Seclusion and the importance of contextual factors: an innovation project revisited |
| 29. Bowers et al.101 | Preliminary outcomes of a trial to reduce conflict and containment on acute psychiatric wards: City Nurses |
| 30. Bowers et al.102 | A replication study of the City Nurse intervention: reducing conflict and containment on three acute psychiatric wards |
| 31. Bowers et al.16 | Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial |
| 32. Brown et al.154 | Safer wards: reducing violence on older people’s mental health wards |
| 33. Burhan et al.80 | The impact of a primary nursing care delivery approach upon the frequency and effectiveness of PRN medication |
| 34. Bybel71 | Does Education of Alternative Measures Decrease the Use of Physical Restraints and Seclusion? |
| 35. Cabral and Carthy15 | Can Safewards improve patient care and safety in forensic wards? A pilot study |
| 36. Calabro et al.141 | Evaluation of training designed to prevent and manage patient violence |
| 37. CQC85 | ExampIe 1: improved leadership and governance [example 1 of 5] |
| 38. Chabora et al.208 | The Four S Model in action for de-escalation: an innovative state hospital–university collaborative endeavor |
| 39. Chandler201 | Reducing use of restraints and seclusion to create a culture of safety |
| 40. Chang et al.162 | Effects of a recovery-oriented cognitive therapy training program on inpatient staff attitudes and incidents of seclusion and restraint |
| 41. Cheema et al.124 | Improving patient safety in mental health through quality risk management |
| 42. Ching et al.115 | Reducing the use of seclusion in a forensic psychiatric hospital: assessing the impact on aggression, therapeutic climate and staff confidence |
| 43. Duxbury et al.22 | Minimising the use of physical restraint in acute mental health services: the outcome of a restraint reduction programme (‘REsTRAIN YOURSELF’) |
| 44. Hart93 | Using De-escalation Skills in a Mental Health Setting: Twenty First Century Media |
| 45. Clark et al.217 | Behavioural Support Chart |
| 46. Clark et al.217 | Reducing restrictive practice: developing and implementing behavioural support plans |
| 47. Clarke et al.114 | The Brøset Violence Checklist: clinical utility in a secure psychiatric intensive care setting |
| 48. Cockerton et al.195 | Implementing positive and proactive care |
| 49. Colton176 | Checklist for Assessing your Organization’s Readiness for Reducing Seclusion and Restraint |
| 50. Cowin et al.163 | De-escalating aggression and violence in the mental health setting |
| 51. CPI95 | De-escalation Techniques |
| 52. Cummings et al.215 | Caring with comfort rooms: reducing seclusion and restraint use in psychiatric facilities |
| 53. D.Escal8260 | PBS and De-escalation: Developing Positive Relationships, Supporting Those in Distress |
| 54. DMHAS138 | DMHAS Guidelines for Development of Comfort Rooms |
| 55. Dewey and Brill309 | Decrease in restraint use in a study of a geropsychiatric unit |
| 56. Donat106 | Employing behavioral methods to improve the context of care in a public psychiatric hospital: reducing hospital reliance on seclusion/restraint and psychotropic PRN medication |
| 57. Donat278 | Impact of a clinical-administrative review procedure on reducing reliance on psychotropic PRN medication |
| 58. Donat220 | Impact of improved staffing on seclusion/restraint reliance in a public psychiatric hospital |
| 59. D’Orio et al.149 | Reduction of episodes of seclusion and restraint in a psychiatric emergency service |
| 60. Fletcher and Stevenson276 | Launching the Tidal Model in an adult mental health programme |
| 61. Fletcher et al.181 | Outcomes of the Victorian Safewards trial in 13 wards: impact on seclusion rates and fidelity measurement |
| 62. Fluttert et al.310 | Forensic Early Signs of Aggression Inventory [FESAI] |
| 63. Fluttert et al.119 | Protocol Early Recognition Method |
| 64. Fluttert et al.118 | Preventing aggressive incidents and seclusions in forensic care by means of the ‘Early Recognition Method’ |
| 65. Forster et al.234 | Staff training decreases use of seclusion and restraint in an acute psychiatric hospital |
| 66. Friedman et al.131 | Using structured clinical feedback to encourage alternatives to use of ‘P.R.N.’ medication in a state psychiatric hospital |
| 67. Geoffrion et al.148 | Impact of a program for the management of aggressive behaviors on seclusion and restraint use in two high-risk units of a mental health institute |
| 68. Georgieva et al.150 | Successful reduction of seclusion in a newly developed psychiatric intensive care unit |
| 69. Godfrey et al.210 | Anatomy of a transformation: a systematic effort to reduce mechanical restraints at a state psychiatric hospital |
| 70. Gonzalez70 | Impact of active listening training at a California state hospital: a quantitative study |
| 71. Gonzalez-Torres et al.170 | Impact of the creation and implementation of a clinical management guideline for personality disorders in reducing use of mechanical restraints in a psychiatric inpatient unit |
| 72. Goulet et al.166 | A pilot study of ‘post-seclusion and/or restraint review’ intervention with patients and staff in a mental health setting |
| 73. CPI97 | Unrestrained – BERT Team Intervention Approach |
| 74. Guzman-Parra et al.144 | Effectiveness of a multimodal intervention program for restraint prevention in an acute Spanish psychiatric ward |
| 75. Guzman-Parra et al.146 | Effects of a regulatory protocol for mechanical restraint and coercion in a Spanish psychiatric ward |
| 76. Meeks96 | Non-Violent De-escalation for Therapists |
| 77. Hayashi et al.76 | The elimination of seclusion in a geriatric inpatient unit: using environmental modification to effect a cultural change |
| 78. Hayes and Russ143 | Discontinuing the use of PRN intramuscular medication for agitation in an acute psychiatric hospital |
| 79. Hellerstein et al.145 | Decreasing the use of restraint and seclusion among psychiatric inpatients |
| 80. Hernandez et al.99 | Multidimensional approach to restraint minimization: the journey of a specialized mental health organization |
| 81. Higgins et al.100 | The Safewards Program in Queensland public hospital acute mental health settings |
| 82. Higgins et al.88 | Implementation of Safewards Across Three Inpatient Mental Health Units |
| 83. Hochstrasser et al.110 | Long-term reduction of seclusion and forced medication on a hospital-wide level: implementation of an open-door policy over 6 years |
| 84. Huckshorn133 | Six Core Strategies© to Reduce the Use of Seclusion and Restraint Planning Tool |
| 85. Huckshorn92 | Preventing Violence, Trauma, and the Use of Seclusion and Restraint in Mental Health Settings: Real Reduction Experiences – What Worked? |
| 86. Huckshorn72 | Reducing Seclusion and Restraint Use in Mental Health Settings: A Phenomenological Study of Hospital Leader and Staff Experiences |
| 87. Hyde et al.311 | A clinical improvement project to develop and implement a decision-making framework for the use of seclusion |
| 88. JKM Training, Inc.261 | Reducing Restraints |
| 89. Jonikas et al.180 | A program to reduce use of physical restraint in psychiatric inpatient facilities |
| 90. Jungfer et al.109 | Reduction of seclusion on a hospital-wide level: successful implementation of a less restrictive policy |
| 91. Kayes and Humphris257 | Introduction of restraint and seclusion reduction program in Margaret Tobin centre |
| 92. Khadivi et al.275 | Association between seclusion and restraint and patient-related violence |
| 93. Kontio et al.199 | eLearning course may shorten the duration of mechanical restraint among psychiatric inpatients: a cluster-randomized trial |
| 94. Laker et al.21 | Case study evaluating the impact of de-escalation and physical intervention training |
| 95. Lee et al.127 | Sensory assessment and therapy to help reduce seclusion use with service users needing psychiatric intensive care |
| 96. Lewis et al.132 | Crisis prevention management: a program to reduce the use of seclusion and restraint in an inpatient mental health setting |
| 97. Lloyd et al.136 | An investigation into the effectiveness of sensory modulation in reducing seclusion within an acute mental health unit |
| 98. Lo74 | Implementation of a Psychiatric Emergency Response Team on Adult Psychiatric Inpatient Units |
| 99. Lombardo et al.159 | PROGRESS: the PROMISE governance framework to decrease coercion in mental healthcare |
| 100. Long et al.147 | Reducing the use of seclusion in a secure service for women |
| 101. Madan et al.108 | Efforts to reduce seclusion and restraint use in a state psychiatric hospital: a ten-year perspective |
| 102. Maguire et al.116 | Seclusion reduction in a forensic mental health setting |
| 103. Maguire et al.197 | Risk assessment and subsequent nursing interventions in a forensic mental health inpatient setting: associations and impact on aggressive behaviour |
| 104. Mann-Poll et al.212 | Long-term impact of a tailored seclusion reduction program: evidence for change? |
| 105. Mann-Poll et al.209 | Professionals’ attitudes after a seclusion reduction program: anything changed? |
| 106. Martin and Suane231 | Effect of training on sensory room and cart usage |
| 107. Maudsley Simulation312 | Maudsley Simulation |
| 108. McCue et al.237 | Reducing restraint use in a public psychiatric inpatient service |
| 109. McEvedy et al.137 | Sensory modulation and trauma-informed-care knowledge transfer and translation in mental health services in Victoria: evaluation of a statewide train-the-trainer intervention |
| 110. McEwan et al.123 | Achieving violence and restraint reduction in an IPCU |
| 111. Melin69 | Team Responses to Inpatient Aggression: The Effects of Institutional Training on Restraint Utilization Patterns |
| 112. Mind87 | Restraint in Mental Health Services |
| 113. Mistral et al.189 | Using therapeutic community principles to improve the functioning of a high care psychiatric ward in the UK |
| 114. Morrow et al.248 | Alternatives to Seclusion and Restraint SAMHSA State Infrastructure Grant Evaluation Overview |
| 115. Natale et al.258 | Applying Jean Watson’s caring theory to reduce restraint use in the acute psychiatric area |
| 116. Needham et al.112 | The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study |
| 117. Newman et al.203 | Effects of a staff training intervention on seclusion rates on an adult inpatient psychiatric unit |
| 118. NHS Improvement229 | Mersey Care NHS Foundation Trust – Using the DASA Tool to Assess the Risk of Violence Among Psychiatric Inpatients |
| 119. Noorthoorn et al.182 | The power of day-to-day motivational techniques and family participation in reducing seclusion |
| 120. Noorthoorn et al.221 | Seclusion reduction in Dutch mental health care: did hospitals meet goals? |
| 121. Novak et al.183 | Pilot study of a sensory room in an acute inpatient psychiatric unit |
| 122. Northumberland Tyne and Wear NHS Foundation Trust125 | Positive and Safe Care Annual Report 2017 |
| 123. Northumberland Tyne and Wear NHS Foundation Trust269 | Talk 1st Ward Assessment |
| 124. Northumberland Tyne and Wear NHS Foundation Trust270 | Positive and Safe Debrief Policy and Tool |
| 125. Northumberland Tyne and Wear NHS Foundation Trust271 | Positive and Safe Positive Practice Process Outline |
| 126. Northumberland Tyne and Wear NHS Foundation Trust83 | Positive and Safe Care Annual Report 2018 |
| 127. Omolewa73 | The Impact of Instructive Educational Program on Physical Restraint Reduction in Acute Mental Health Hospitals |
| 128. Parasurum et al.77 | A randomised controlled study examining the impact of a staffing model and nursing care delivery system on patient, nurse and organisational outcomes |
| 129. Pollard et al.274 | Organizational and unit factors contributing to reduction in the use of seclusion and restraint procedures on an acute psychiatric inpatient unit |
| 130. Prescott et al.128 | Reducing mechanical restraints in acute psychiatric care settings using rapid response teams |
| 131. Price et al.194 | Evaluation of Safewards in forensic mental health |
| 132. Putkonen et al.17 | Cluster-randomized controlled trial of reducing seclusion and restraint in secured care of men with schizophrenia |
| 133. Qurashi et al.186 | Reduction in the use of seclusion in a high secure hospital: a retrospective analysis |
| 134. RCP126 | Reducing Restrictive Practice Programme: Tools – Talk First |
| 135. Repique et al.187 | Implementation of a recovery-oriented training program for psychiatric nurses in the inpatient setting: a mixed-methods hospital quality improvement study |
| 136. Respect Training254 | Respect Training from NAVIGO |
| 137. Restraint Reduction Network214 | Six Key Restraint Reduction Strategies |
| 138. Riahi et al.23 | Implementation of the Six Core Strategies for restraint minimization in a specialized mental health organization |
| 139. Riemer and Corwith192 | Application of core strategies: reducing seclusion & restraint use |
| 140. SAMSHA249 | Coordinating Center: Alternatives to Restraint & Seclusion (ARS) State Infrastructure Grant (SIG) Program – First Round of ARS SIG Grantees |
| 141. Sarkar78 | Reducing violence through the use of structured therapies |
| 142. Scottish Patient Safety Programme122 | Patient Safety Including Trauma Informed Care and Usage of Seclusion and Restraint |
| 143. Scottish Patient Safety Programme91 | Restraint and Seclusion Driver Diagram |
| 144. Short et al.157 | Safety guidelines for injury-free management of psychiatric inpatients in precrisis and crisis situations |
| 145. Sivak191 | Implementation of comfort rooms to reduce seclusion, restraint use, and acting-out behaviors |
| 146. Smith et al.142 | Pennsylvania State Hospital system’s seclusion and restraint reduction program |
| 147. Smith and Millar158 | The quiet room: improving the acute care psychiatric environment |
| 148. Smith and Jones140 | Use of a sensory room on an intensive care unit |
| 149. South Australia Health272 | Mental Health Restraint and Seclusion Toolkit Fact Sheet 7 |
| 150. Stansgaard et al.255 | Implementation of the Safewards model to reduce the use of coercive measures in adult psychiatric inpatient units: an interrupted time-series analysis |
| 151. Stead et al.188 | Teams communicating through STEPPS |
| 152. Steinert et al.20 | Successful interventions on an organisational level to reduce violence and coercive interventions in in-patients with adjustment disorders and personality disorders |
| 153. Stirling et al.233 | Reducing Restrictive Practices Checklist |
| 154. Sullivan et al.190 | Reducing restraints: alternatives to restraints on an inpatient psychiatric service – utilizing safe and effective methods to evaluate and treat the violent patient |
| 155. Sullivan et al.104 | Effects of patient-focused care on seclusion in a psychiatric intensive care unit |
| 156. Sutton et al.152 | Optimizing arousal to manage aggression: a pilot study of sensory modulation |
| 157. Szypula and Martin89 | Balancing Risk & Safety When Reducing Restraint & Seclusion |
| 158. Taxis227 | Ethics and praxis: alternative strategies to physical restraint and seclusion in a psychiatric setting |
| 159. Taylor and Brown94 | Minimising Seclusion and Restraint: Sensory Approaches in the Adult Inpatient Psychiatric Setting |
| 160. Taylor-Watt et al.153 | Reducing physical violence and developing a safety culture across wards in East London |
| 161. Tees Esk and Wear Valleys NHS Foundation Trust252 | 2017–18 Annual Report |
| 162. Tees Esk and Wear Valleys NHS Foundation Trust253 | Positive Approaches Team 4 Day Course |
| 163. Trevarrow82 | Chill Out Room Project |
| 164. Tully et al.90 | Innovation and pragmatism required to reduce seclusion practices |
| 165. van De Sande et al.200 | Aggression and seclusion on acute psychiatric wards: effect of short-term risk assessment |
| 166. Visalli and Mcnasser139 | Reducing seclusion and restraint: meeting the organizational challenge |
| 167. Wale et al.196 | Reducing the use of seclusion and restraint in psychiatric emergency and adult inpatient services – improving patient-centered care |
| 168. West London NHS Trust273 | Positive and Safe: Violence Reduction and Management Programme – Instructors Manual |
| 169. Wieman et al.211 | Multisite study of an evidence-based practice to reduce seclusion and restraint in psychiatric inpatient facilities |
Glossary
- Behaviour change technique
- A specific, irreducible, active component of an intervention designed to change behaviour, for example providing ‘information about health consequences’.
- Behaviour change technique taxonomy
- A list of 93 behaviour change techniques organised into 16 clusters, for standardised reporting of behaviour change interventions. Note that the taxonomy was published in US English and, therefore, US spelling is used here when referring to behaviour change technique taxonomy terms.
- Chemical restraint
- The use of medication that is intended to prevent, restrict or subdue movement of any part of the service user’s body.
- Evaluations
- Evaluations of interventions are reported in research articles and anecdotal reports; replication studies and follow-up studies are counted as separate evaluations; reports of different analyses from the same study are counted as a single evaluation.
- Instructions
- Instructions for the performance of an intervention.
- Intervention
- Action or actions intended to address restrictive practices in adult mental health acute settings, for example a staff training initiative with or without organisational change. Some interventions are developed within and for an individual setting. Others may be well-known interventions that have been developed previously and are applied across several time periods or settings.
- Isolation
- Any seclusion or segregation that is imposed on a service user.
- Manual restraint
- A hands-on method of physical restraint.
- Mechanical restraint
- A method of physical intervention involving the use of equipment.
- Mixed Methods Appraisal Tool
- A tool suitable for appraising studies with diverse designs.
- Pro re nata medication
- Medication given when needed, rather than at a regular time.
- Procedures
- The actions taken as part of intervention, for example a training session.
- Restrictive practices
- Deliberate actions undertaken with the aim of restricting an individual’s movement, liberty and/or freedom to act independently. The intervention is intended to take rapid control of a dangerous situation where there is a real possibility of harm to the person or others.
- Seclusion
- The confinement of a service user in a room, which may be locked.
List of abbreviations
- AHRQ
- Agency for Healthcare Research and Quality
- BCT
- behaviour change technique
- BNI
- British Nursing Index
- CCTR
- Cochrane Central Register of Controlled Trials
- CCTV
- closed-circuit television
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPI
- Crisis Prevention Institute
- CQC
- Care Quality Commission
- DARE
- Database of Abstracts of Reviews of Effects
- DASA
- Dynamic Appraisal of Situation Aggression
- DASA-IV
- Dynamic Appraisal of Situation Aggression – Inpatient Version
- EQUATOR
- Enhancing the QUAlity and Transparency Of health Research
- EssenCES
- Essen Climate Evaluation Schema
- HDAS
- Healthcare Databases Advanced Search
- HDU
- high-dependency unit
- HTA
- Health Technology Assessment
- INIST-CNRS
- Institut de l'information scientifique et technique – Centre national de la recherche scientifique
- ISRRI
- Inventory of Seclusion and Restraint Reduction Interventions
- MMAT
- Mixed Methods Appraisal Tool
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIH
- National Institutes of Health
- NLM
- National Library of Medicine
- NR
- not reported
- PCC-SR
- Patient–Staff Conflict Checklist Shift Report
- PDSA
- plan, do, study, act
- PERT
- psychiatric emergency response team
- PICU
- psychiatric intensive care unit
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRN
- pro re nata
- RCP
- Royal College of Psychiatrists
- RCT
- randomised controlled trial
- SAMSHA
- Substance Abuse and Mental Health Services Administration
- SD
- standard deviation
- SOAS
- Staff Observation Aggression Scale
- SOAS-R
- Staff Observation Aggression Scale – Revised
- WHO
- World Health Organization
- WIDER
- Workgroup for Intervention Development and Evaluation Research
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hsdr09050).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
