Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR131238. The contractual start date was in November 2020. The final report began editorial review in January 2022 and was accepted for publication in May 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 O’Cathain et al. This work was produced by O’Cathain et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 O’Cathain et al.
Chapter 1 Background
Demand for primary and emergency care in the UK
There is considerable pressure on general practices, emergency departments (EDs) and emergency ambulances in the UK. In 2019, the Royal College of General Practitioners highlighted intense resource and workforce pressure on general practice out-of-hours services and expressed concerns about decreases in the number of general practitioners (GPs) per head of population, despite rising demand for general practice. In 2021, the Royal College of General Practitioners highlighted the lack of GPs to meet demand. 1 In 2019, policy-makers reported on the NHS England website that there were 110 million urgent patient contacts in England each year, with around 85 million being same-day GP appointments, and the rest attendances at EDs and minor injury units. NHS England estimated that between 1.5 million and 3 million attendances at EDs could be managed by other parts of the urgent care system. Emergency ambulance services deal with around 11 million calls annually, and around one in eight are dealt with through advice from a clinician by telephone. 2 Patients having these ‘hear-and-treat’ calls, that is calls that do not result in an ambulance being despatched, are offered self-care advice or are recommended to contact lower-acuity services. NHS England is currently encouraging people to use NHS 111 to help them make decisions about which service, if any, to use, including self-care and pharmacy. Demand for NHS 111 also outstrips supply, and policy-makers have attempted to ease demand for this service by encouraging people to use NHS 111 Online to help them make decisions about where in the NHS to seek care. 3
There is a need to consider ways of reducing pressure on emergency and primary care services. Although primary care is a setting that provides a first point of contact in the NHS for patients, and includes general practices, community pharmacies and dentists, a focus on general practice is important because of the current pressure on this service.
Minor health problems
Some people need to use emergency and urgent care, and it is important to maintain access to services to meet their needs. However, some people do not need the clinical resources or acuity level of primary or emergency care services. Some patients could contact their GP instead of calling for an emergency ambulance or attending an ED. Other patients could self-care or seek advice from a pharmacist instead of contacting general practice, the ED or the ambulance service. A variety of terms are used to describe this type of service use, such as ‘clinically unnecessary’,4 ‘primary care sensitive problems’ in emergency care,5 non-urgent or low acuity. The prevalence of this type of use varies depending on the definition used, but it is likely to be high. For example, 15% of attendances were classed as non-urgent in an analysis of routine data from EDs in the UK. 6
Some of these contacts in primary and emergency care are for minor health problems, injuries or ailments that could be managed through self-care or contact with a pharmacist. Examples of minor health problems include raised temperature in a child, musculoskeletal pain, eye discomfort, gastrointestinal disturbance and upper respiratory tract-related symptoms. 7 Research has shown that people attend EDs, general practice or a pharmacy with these minor health problems. When contacts with different services for similar minor health problems are compared, they have similar resolution rates, but the cost per consultation is higher for EDs and GPs than for pharmacy: £147 and £82, compared with £29, respectively. 7 People may also attend general practice out-of-hours services, as well as daytime general practice, for minor health problems. 8
Reasons why people attend primary and emergency care with minor health problems
There are a wide range of reasons why people contact services for minor health problems. A recent study of ‘clinically unnecessary’ use of ambulance services, EDs and GPs in the UK explored this issue using a realist review, qualitative interviews with patients and a national population survey. 4 Ten reasons were identified in the realist review9 and qualitative interviews:10
-
uncertainty about symptoms, causing anxiety
-
heightened awareness of risk as a result of experience or knowledge of traumatic health events, leading to anxiety
-
fear of consequences when responsible for others such as children or elderly people
-
inability to get on with daily life, such as going to work or looking after children
-
need for immediate pain relief
-
waited long enough for things to improve
-
stressful lives so cannot cope with any health problem
-
following advice of trusted others from NHS staff, family, friends, colleagues
-
perceptions or prior experiences of services, for example positive experiences of EDs lead to further use of EDs
-
perceived poor access to a GP in the time frame wanted.
These issues were measured in a national population survey of the tendency to contact primary and emergency care for minor health problems. Other issues that were less commonly identified in the literature were also measured, including awareness of alternative services, beliefs about how busy emergency and primary care services are and health literacy levels. The effect of people’s health literacy levels on their decision-making was measured because researchers in the USA found that people who attended EDs with non-urgent problems had lower levels of health literacy. 11 It was also possible that poor health literacy might underlie some of the reasons for using primary and emergency care for minor health problems. For example, people with low levels of health literacy might be more anxious about minor health problems because they do not understand what symptoms are associated with serious problems, they may be less likely to know how to manage pain, they may be more likely to look to others for advice, they may not know how long it takes for some minor problems to resolve and they may be unaware of alternative services. When a range of variables were tested in a population survey to explain tendency to contact primary and emergency care for minor health problems, lower health literacy levels were associated with this use of emergency ambulances and general practice, even when all other variables were controlled for. 9,12
The importance of health literacy
Given the role of health literacy in explaining the tendency to use emergency ambulances and general practice, and its relationship with the use of EDs for non-urgent problems, it is important to understand what it is, how it is measured, its relationship with use of primary and emergency care, and how it can be addressed to reduce the use of primary and emergency care for minor health problems.
What is health literacy?
Health literacy is defined by the World Health Organization as the resources needed for people to access, understand and use information and services to make decisions about their health. 13 There are different types of health literacy: functional or basic health literacy (reading and writing skills); communicative health literacy (cognitive and social skills to extract information and apply it); and critical health literacy, which requires more advanced cognitive and social skills to analyse information. 14
People with limited health literacy struggle with:
-
finding information
-
reading and understanding information
-
knowing how to act on information
-
knowing how to communicate with health professionals
-
knowing which services to use and when. 15
Aligned with health literacy is digital or e-health literacy, which has been defined as ‘the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem’. 16
Health literacy may be viewed as an individual skill, but an individual’s social support system (e.g. partner, family, community) and the context in which they live (e.g. the health-care system available) are also likely to be relevant. 17
How is health literacy measured?
There are a number of validated measures of health literacy that either test health literacy (one might call these ‘objective measures’) or measure people’s perceptions of their health literacy (one might call these ‘subjective measures’). Examples include the objective measure Newest Vital Sign, used in a study of health literacy among parents attending a paediatric ED for non-urgent problems;11 the subjective measure the Health Literacy Questionnaire, which measures multiple domains of health literacy;15 and the subjective measure the European Health Literacy Survey Questionnaire, which is available in multiple European languages. 18
Policy initiatives on health literacy in the UK
Improving health literacy is important to policy-makers in the UK. National policy in England currently focuses on improving health literacy in the management of chronic conditions and health improvement, and on improving health literacy awareness among the health-care, social care and third-sector workforces. NHS England has a health literacy lead and multiagency initiatives to improve health literacy. 13 NHS Scotland has a long-term plan to improve health literacy. 19 Health Education England generates tools and leads initiatives to improve health literacy. 20
The relationship between health literacy and demand for primary care and emergency services for minor health problems
Primary care
There is evidence that a lower level of health literacy is related to greater use of primary care, including contacting a GP,21 frequency of doctor visits22 and use of out-of-hours primary care services. 23 There is also evidence that it is related to greater demand for general practice for minor health problems. A recent British population survey of the demand for same-day general practice for minor health problems identified that people with a lower level of health literacy had a greater tendency to contact their GP in a multivariable analysis testing a wide range of variables. 12
Emergency care
There is systematic review evidence from 2011 that a lower level of health literacy is associated with greater use of emergency services. 24 More recent studies support this conclusion. Examples include unnecessary use of the ambulance service in Japan,25 ED use for minor or non-urgent problems in the USA,26 ED return rates27 and use of EDs by first-generation Chinese immigrants in Australia. 28 A 2020 British population survey of demand for emergency ambulances and EDs for minor health problems identified that people with a lower level of health literacy had a greater tendency to contact emergency ambulances. 4
Reasons for the relationship
The relationship between health literacy and the use of primary and emergency care for minor health problems could be explained simply by the educational status of patients. There is a correlation between health literacy and educational attainment, but educational attainment does not explain all of the variation in health literacy levels. For example, 29% of people attending EDs for non-urgent issues were found to have a college education and a low level of health literacy. 11
There is evidence that people with a lower level of health literacy may overestimate the severity of an illness and seek care sooner than people with a higher level of health literacy. 29 They may also be harder to reassure when a symptom is not serious. A study30 of factors determining parental reassurance for a child with fever in rural general practice showed that parents who lacked knowledge about complications of fever had higher levels of concern before consulting a doctor and were less likely to be reassured after consultation with a doctor, leading to a recommendation that further education of parents is required.
Research that does not support this relationship
Not all studies have found a relationship between use of health services for minor health problems and health literacy. For example, health literacy was found not to be associated with GP consultations, only with home consultations. 31 A survey of the British population found no relationship between health literacy and tendency to use EDs for minor health problems when other variables were adjusted for. 4
Need for interventions to address health literacy in this context
Research exploring help-seeking behaviour for minor health problems sometimes concludes that patient education is needed. Physicians and nurses cite lack of education and self-care when exploring the related area of frequent attendance,32,33 and a lack of awareness of the availability and capability of alternative services to EDs. 10 When GPs in the UK were interviewed about strategies for coping with increasing workload, they identified the need to educate patients about self-care, stating that they preferred that the government rather than GPs to be responsible for this education. 34
Improving health literacy is one of many solutions needed
This review focuses on health literacy because it is an important factor affecting demand for primary and emergency care for minor health problems. However, it is one of many factors; as a 2020 study concluded, ‘There is unlikely to be a single solution to these multiple, inter-related reasons for “clinically unnecessary” use of services. Rather, a series of solutions, undertaken concurrently, may be necessary’. 4 It is important to keep in mind that service-related issues are important, as well as health literacy; for example, some people may have tried to get an appointment with their GP before going to an ED, but have been unable to get one in the time frame they wanted. Addressing health literacy is a potential solution to consider, complementary to other initiatives.
NHS initiatives to address demand for primary and emergency care
Given that there is a need for multiple interventions to address demand for primary and emergency care for minor health problems, it is useful to consider the range of interventions that policy-makers, commissioners and service providers have introduced. They tend to focus largely on service and workforce reconfigurations that offer alternatives to the three pressurised services of general practice, EDs and emergency ambulances, or on initiatives to manage minor problems efficiently within each of these three services. Examples of these initiatives include provision of a Community Pharmacy Minor Ailment Service, the provision of walk-in centres, the extension of the role of pharmacists, GPs working in EDs, paramedics working in general practices and redirection of people attending EDs. Initiatives also include the national telephone helpline NHS 111 for urgent care whereby non-clinical call-takers direct people to the most appropriate service for their need, or pass callers to clinicians who assess more difficult cases and offer self-care advice or referral to services.
Intervention further back in the pathway of help-seeking behaviour may offer a complementary approach to these initiatives. That is, it may be possible to reduce population need to seek advice from health professionals in pharmacy or NHS 111 for minor health problems and thereby reduce demand for pressurised services. This will be useful at any time, and especially during pandemics, when some people stop attending primary care and emergency services for minor health problems and need to self-care or be able to distinguish between minor and serious problems.
Reviews in related areas
Prior to applying for funding for this systematic review, we undertook a scoping exercise and found no similar systematic reviews. We continued to search for other reviews during the study. We found a number of reviews in related areas, but no review of the same territory.
Reviews of interventions to improve health literacy
There are numerous systematic reviews of interventions to improve health literacy,24,35,36 including for enhancing digital health literacy. 37,38 These reviews tended to focus on interventions with the intention of improving health literacy as their primary outcome, and often did not go beyond this point in the pathway to consider the impact of this improved health literacy on service use. When the reviews did go beyond this point, they considered improvement in health and changes in service use for self-management of chronic conditions, rather than for minor health problems.
Reviews of behaviour change
A review focusing on health behaviours39 looked relevant to our work because health literacy interventions can aim to change behaviour regarding service use. This review did not include the types of interventions of interest in our review. It concluded that interventions could improve health literacy and result in lifestyle changes.
Reviews of self-management of chronic conditions
Some reviews focused on self-management interventions for chronic conditions, with the aim of reducing ED attendances and hospital admissions. 35 These interventions aimed to educate patients on how to prevent serious exacerbations that necessitate an emergency response. That is, they aimed to reduce ED attendance for serious problems, rather than minor problems. It is possible that they also reduced ED attendance for minor problems, but this was not the primary purpose of the intervention and so these reviews did not include interventions relevant to our review. The term ‘self-management’ rather than ‘self-care’ is usually used in the context of chronic conditions such as asthma and diabetes, whereby the aim is to prevent exacerbations using self-management.
Reviews of patient-focused interventions
A review of patient-focused interventions included one type aiming to improve health literacy. 40 Again, the focus was on health literacy rather than changing service use.
Reviews of health literacy interventions to reduce use of primary or emergency care
Prior to seeking funding for this study, we found a review that focused on parental health literacy and paediatric ED attendance, in which seven out of eight studies showed that interventions reduced ED use. 26 This review considered one specific patient group (parents of young children), so we still believed that it was important to undertake our review. We intended to include the papers from this review in our review, but found that most of them focused on the chronic condition of asthma and the prevention of serious problems, rather than the management of minor health problems.
Andrews et al. 41 reviewed the specific area of respiratory illness among children. Part of the focus was on primary care consultations, for which they found nine papers about eight interventions aiming to increase health literacy. Six studies measured reductions in the number of consultations, with these reducing by 13–40% in three studies, although some studies relied on self-report of service use. They authors concluded that interventions were best if they occurred prior to an illness episode, highlighting the importance of the timing of an intervention. Again, this review focused on a specific illness in a specific age group, so there was still a need to undertake our review, and to ensure that we included relevant papers from this review.
Paudyal et al. 42 undertook a systematic review of pharmacy-based minor illness schemes aiming to reduce use of other services. Although pharmacy use can be viewed as ‘supported self-care’, this review was not relevant because interventions did not focus on improving health literacy, but instead on offering an alternative health professional for advice.
Reviews of digital health literacy interventions
Some of the interventions in our systematic review are likely to be delivered digitally. Of interest was a 2011 systematic review that concluded that there were not enough studies to identify effective interventions for enhancing digital health literacy. 38 A more recent (2020) systematic review of digital interventions for the specific area of parents of acutely ill children in primary care found three studies. 43 Interventions were applications (hereafter referred to as ‘apps’) or a website offering self-triage or advice. Parents did not find two of the interventions easy to use. None of these interventions demonstrated reduced use of services for minor health problems. One study showed no difference in non-urgent ED attendances; one did not measure this outcome; and one measured intended, rather than actual, service use. Donovan et al. 43 proposed that the way in which interventions were developed could affect their usability and their effectiveness, and that co-design with patients was important.
Reviews of self-care for minor health problems
Richardson et al. 44 undertook three systematic reviews of qualitative and quantitative research on self-care for minor ailments. One review focused on evaluation of services/interventions and their impact on reduction of use of GPs and EDs. The focus of this review was much wider than that of our review, looking beyond health literacy and including interventions such as the use of NHS 111, pharmacies and walk-in centres. In addition, it focused only on the UK, rather than international literature. Richardson et al. 44 found that interventions using education only did not work and proposed that this was because a range of issues affected patient decision-making. They highlighted that people can be overwhelmed by anxiety. We included their education-based interventions in our review where relevant.
Reviews of self-triage/symptom checkers
An audit of self-triage interventions showed that most were risk averse and encouraged people to contact services when, in fact, self-care was reasonable. 45 This audit did not measure impact on service use.
The need for this review
Although a number of reviews have been undertaken in related areas, and some reviews addressed parts of the territory covered in this review, there was a research gap for a review of health literacy interventions aiming to reduce the use of primary and emergency care for minor health problems.
Chapter 2 Research aim, design, and patient and public involvement
Aim and objectives
The aim was to identify interventions that reduce the use of primary and emergency care for minor health problems by improving health literacy.
The objectives were to:
-
identify the effectiveness, cost-effectiveness and safety of interventions
-
identify the contexts in which different types of interventions are effective
-
describe interventions
-
identify the mechanisms of action of interventions
-
construct a typology of interventions relevant to service use reduction
-
describe the development process and its impact on effectiveness
-
describe the literacy levels of information-based interventions and their impact on effectiveness
-
identify patient, carer and staff views on the feasibility and acceptability of interventions
-
consider how UK stakeholders could operationalise the evidence in terms of identifying a set of interventions that they would find feasible, appropriate, meaningful and effective within their localities.
These objectives are slightly different from those in the proposal. For example, we originally intended to consider the literacy levels of effective interventions only, but we subsequently decided to do this for all the interventions we could find because we were interested in whether or not the readability or ease of use of an intervention had an impact on its effectiveness.
Design
We undertook a systematic review with stakeholder involvement. First we held a stakeholder event to inform the systematic review, then we conducted a systematic review to identify and synthesise the evidence and, finally, we held another stakeholder event to consider how to implement the evidence. We attended to guidance on good practice when involving stakeholders in systematic reviews. We drew on the Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2) framework to reflect on our patient and public involvement (PPI). 46 See Report Supplementary Material 1 for the GRIPP2 reporting guidance checklist.
Ethics approval
Some researchers may use research methods for stakeholder involvement, such as Delphi exercises,47 and this requires research ethics approval. Our stakeholder involvement was akin to PPI in that we held workshops to encourage research users to shape and interpret the systematic review. We did not require ethics approval for the stakeholder involvement or for the systematic review.
Patient and public involvement
Aim
We aimed to have patients and members of the public providing input to the development, conduct and dissemination of the review to ensure that the findings would be relevant and useful in supporting people making decisions about self-care or accessing health care.
What we proposed in the funding application
Margaret Ogden (a member of the Sheffield Evidence Synthesis Centre PPI group when we applied for funding) supported development of the funding application and was a co-applicant. We planned that Margaret would be part of the project management team, attending team meetings every couple of months and inputting into decision-making throughout the study.
We proposed that four members of the School of Health and Related Research (ScHARR) Evidence Synthesis Centre PPI group would be involved in different parts of the review process, including attending the two stakeholder events and supporting the development of the protocol (e.g. ensuring the salience of the search strategy, supporting the development of a dissemination strategy and providing feedback on the plain English summary included in the final report). We promised that we would keep the group informed throughout the project.
We proposed that we would also take our early findings to the Yorkshire and Humber Deep End Patient Panel. This is a panel of 10–15 people living in the most socioeconomically deprived areas in Sheffield, established by a local GP. We would also invite them to the second stakeholder event, expecting a maximum of five to attend.
What we did
Although our activities were in keeping with what we proposed, we had to respond to COVID-19 restrictions by quickly amending our plans to meet virtually, rather than face to face. This provided an opportunity to involve people from a wider geographical area while keeping within allocated costs. We also involved members of the Deep End Patient Panel from the start of the systematic review, rather than only at the findings stage. We involved PPI members in all stages of the review, including developing the funding application, deciding the scope of the review, designing the user-friendliness assessment and considering the implications of the findings.
Who was involved
We aimed to work with people representing the general public, rather than seeking out people with lower levels of health literacy or a history of using primary or emergency care for minor health problems.
Margaret Ogden was actively involved in the review. She supported the development of the funding application and was a co-applicant. She was a member of the project team, attending team meetings and supporting the development of the stakeholder events. She co-led the PPI group with Alexis Foster, seeking out new members to ensure diversity. She helped with developing the User-Friendliness Assessment Tool (UFAT) and undertaking assessments of the user-friendliness of included interventions (see Chapter 3). She commented on and edited the plain English summary in the final report. Using Pollock et al. ’s48 involvement framework, Margret Ogden’s involvement was categorised as both ‘controlling and influencing’: she was part of the research team, contributed to decision-making and undertook review activities by assessing the user-friendliness of interventions.
In the application for funding, we said that we would work with the Sheffield Evidence Synthesis Centre PPI group, but this ceased to exist by the start of the review. Instead we developed a new PPI group for the review, with membership expanding over time. We invited some members of the disbanded Sheffield Evidence Synthesis Centre PPI group to be involved; in addition to Margaret Ogden, one person agreed to be involved. As some of the potential interventions included in the review were aimed at parents of young children, we wanted to have representation from this demographic. Through our networks, we identified two people to be involved who had young children, one of whom had not undertaken PPI work before. We also invited members of the Deep End Patient Panel to join our PPI group. We did this because the Deep End Patient Panel was not meeting at the time because of COVID-19. A member of our team (AF) had links with several of the members, and so was able to support them to become involved in our group. As the review progressed, Margaret Ogden recruited three more experienced PPI members who were based in different parts of country, two of whom were carers. We took an open, flexible approach to PPI,48 recruiting people throughout the review and involving them in the review in different ways.
Although not all PPI members attended all the events, throughout the review 14 different people were involved and 10 people attended (or provided input into) each of the four PPI meetings. The PPI members were relatively diverse. Although the majority of people were based in Sheffield, we also had people based in the north-east of England, London and Gloucestershire. People were at different stages of their lives: some were retired whereas others had young children. We had a mix of males and females. People had different life experiences including being carers, being a refugee, being community activists and living in socioeconomically deprived areas. The involvement was categorised as ‘contributing’: PPI members influenced the review, for example by contributing to the scope of the review and interpretation of the findings. 48
Patient and public involvement meetings
We held four events attended by PPI members. Ten PPI members contributed to each of the two stakeholder events either by attending or offering insights after the event. In between the two stakeholder events, there was a PPI meeting to develop the UFAT and a meeting to discuss the preliminary findings of the review. After each meeting, we wrote up notes that documented points made and the actions the team would take based on these points.
Owing to COVID-19, all meetings were held virtually. The advantage was that it enabled people to participate from across the country. Furthermore, it meant that we were able to involve a larger number of PPI members because the budget could be used for remuneration rather than for travel and refreshment costs. The disadvantage was that some people found the technological aspect of virtual meetings difficult. For these people, a team member (AF) held discussions with some PPI members outside the meetings to enable them to share their views and/or supported them with using the technology such as having trial sessions on the technology. Over time, members became more confident at participating virtually. For example, one person went from having to speak outside the meeting by telephone to actively engaging in later PPI events virtually. Having ‘break-out rooms’ in the first stakeholder event helped to give an opportunity for everyone to participate. We did not do this in the second stakeholder event, which may have reduced participation from less confident members.
Keeping people informed between meetings
The team wanted to ensure that PPI members (and other stakeholders) were kept informed of the progress of the review between meetings. We did this through producing newsletters periodically throughout the project. These were written in plain English by a team member (AF) and Margaret Ogden reviewed them to ensure that they were easy to understand. Margaret Ogden also wrote part of one of the newsletters. We received positive feedback about the newsletter and intend to do this in future studies.
Remuneration and skills development
Patient and public involvement members were remunerated by direct transfer to their bank accounts. We generally paid £50 per attendance at a 2-hour meeting. People were also remunerated for supporting the UFAT work (explained in Chapter 4). To support skills development, we delivered training on using social media at the request of some PPI members. They wanted to learn how to use Twitter (Twitter, Inc., San Francisco, CA, USA) to support their PPI work and promote the findings from the review. We delivered this training to five people. The technological support and trial sessions for using technology for virtual meetings are likely to increase people’s skills and confidence in participating in future virtual meetings.
Chapter 3 First stakeholder event
Background
In the first month of the study (November 2020), we held a virtual stakeholder event. It had to be virtual because of COVID-19. We aimed to involve representatives from the following groups: patients, carers and members of the public; Clinical Commissioning Groups (CCGs); NHS England Emergency and Urgent Care directorate; the NHS England Health Literacy Lead; general practice; EDs; and emergency ambulance services. The aim was to elicit stakeholders’ perceptions of key issues that might further shape the review, such as suggestions about the key types of interventions to include. The virtual format facilitated people from different parts of the UK to attend the event.
Stakeholders attending the event
Fourteen stakeholders attended the event, along with research team members:
-
seven PPI representatives (three others provided input outside the event)
-
one urgent care commissioner from a CCG
-
one representative from NHS England
-
one ED consultant
-
one GP
-
one academic pharmacist
-
one representative from NHS Digital
-
one representative from the third sector.
We designed the event with our PPI co-applicant Margaret Ogden to ensure that PPI representatives were supported to engage in the event. Our stakeholder lead on the team (AF) contacted all of the PPI representatives by telephone or e-mail before the stakeholder event to discuss the review and to support people to attend by explaining how the virtual platform worked. Alexis Foster also facilitated input from three PPI representatives who could not attend the event. Two did not feel confident with the technology and one person could not make the date. Alexis Foster sent them the notes from the event and then had a telephone call with each of them to discuss the event and get their input. We ensured that we included their viewpoints in the write-up of the event. This additional involvement was important because we did not want to exclude people from the event because of lack of technical skills.
The event
The event was held on 10 November 2020 and lasted 2 hours. It was a mixture of presentations and discussions. Alicia O’Cathain delivered two short presentations (each < 10 minutes) to explain the review, to justify why the research was needed and to discuss how the research fits within research on help-seeking behaviour in emergency and primary care. Jonathan Berry, the health literacy lead from NHS England, also presented on initiatives being delivered within the NHS to increase health literacy.
The group was split into two smaller groups to facilitate discussion, with each small group facilitated by a member of the research team and including a mix of stakeholders. In the discussion we focused on potential factors we needed to consider in the review. We also discussed potentially relevant interventions. Attendees gave us potential sources of grey literature such as work undertaken by the World Health Organization Healthy Cities initiatives, and by specific CCGs in England.
The issues raised and actions taken
After the event we recorded the points made by stakeholders and our comments on how we would address each point in the review (Table 1). We circulated our write-up to the stakeholders so they could add to the document. Comments from people who had been unable to attend the meeting were added at this stage (this is indicated by ‘post meeting’ in Table 1).
| Issue | Detail | Action |
|---|---|---|
| Making connections with others doing similar work | People are doing a lot of work related to this area | We need to talk to people who may be doing work on this issue such as the Scottish Government and NHS Sheffield CCG |
| Type of literature | Initiatives will be happening in the real world so search websites (e.g. World Health Organization reports) and speak to people rather than just searching research published in academic journals | We are already planning to do this but we have made it more central to our search now and intend to start this early in our study, for example search websites of NHS Scotland and the World Health Organization Healthy Cities initiative |
| Focus of our review | Are we including in our review:
|
We are focusing on interventions that improve health literacy for minor problems and, by doing this, reduce the need for people to use urgent general practice services, A&E and ambulance for minor problems |
| A lot of this list is relevant to our work. Some of the list is not relevant to our specific study, but is important to the wider topic of health literacy | ||
| It is useful to have this list so that when we identify interventions we can think about what we have not found information on, as well as what we have found | ||
| International literature | Focus beyond high-income countries | We are already planning to look at all countries. We did not make this clear in our meeting. We agree that some health literacy interventions will be used in low- and middle-income countries, so will make sure we search for and value those |
| Framework of types of interventions | Level of interventions: focus on individuals or systems? (e.g. school curriculum would be a systems approach) | This helped us to think about our framework for interpreting findings. We are going to be focusing on both individual- and system-level interventions |
| Timing of intervention and relevance to people’s lives: makes more of an impact if given at the right time so people are receptive and interested? | We will include ‘timing/relevance’ in our framework now | |
| Language used in interventions | Simple ‘living-room speak’ is needed in any intervention | We are planning to assess the literacy levels of information-based interventions in our review. Some may not have been effective because they required people to have high levels of literacy or knowledge |
| When are people receptive to interventions | We spoke about when people are most receptive to interventions. For example, we wondered whether or not it is when someone is feeling ill and accessing services, rather than when they are well | We will check when the studies provide the intervention to people. For example, is the intervention provided to people when they access health-care service or to children at school? |
| People felt that school children and people moving into an area (e.g. students) need to be taught health literacy and also taught about local services as each area is different (systems approach) | ||
| Level of trust in who is giving the information | The success of interventions may depend on how much people trust the source/person delivering the intervention. For example, people may trust community workers they have an established relationship with more than doctors | We will explore whether or not any of the studies we find consider the influence of trust on the results of their research |
| People have a lot of trust in urgent care services (e.g. A&E). They are consistent throughout the country and people know a doctor will see them, even if they have to wait | ||
| People are increasingly getting information from social media and may get lots of opinions on, for example, ‘what is this rash?’. They may choose to believe those with similar health beliefs | ||
| Who people are making the decision for | People may be more likely to access urgent care for minor problems because they are worried about their child or someone they care for more than if it had been for themselves | We will consider who the interventions are aimed at, for example patients directly, parents, informal carers. We will reflect on how this may influence a study’s findings |
| COVID-19 | How and when people access services may not return to normal after the COVID-19 pandemic | We will need to reflect on the UK context when we meet in the second stakeholder event to consider which interventions are relevant |
| It is about more than health literacy | People struggle to get GP appointments and other types of services, and so may access urgent care services because they cannot get help from other sources | We totally agree that other things are important. Health literacy is only one piece of a bigger picture. We will make sure that this is explained when reporting our findings and also reflect on whether or not studies have considered these issues within their research |
| There are logistical challenges to accessing some services, such as public transport | ||
| People are becoming increasingly used to 24/7 access to things (e.g. online shopping), and so may expect this in terms of accessing support for their health | ||
| Some people are more pessimistic/worriers by nature and may worry that a symptom is serious, which influences how they access services | ||
| It was suggested that people may access urgent care services because of previous experiences. For example, someone may have tried to access a pharmacist before about a condition but been directed to urgent care, so they feel they might as well go straight to urgent care. Likewise, if someone has a positive experience of accessing other services, this may give them the confidence to do this again | ||
| Training and knowledge of health professionals | It is not just about individual patients/carers, but also the role of health professionals to support people to have conversations, signposting to services, etc. | We are looking at interventions aimed at patients, not health professionals. (Originally our response to this issue was to say we would include these interventions. We changed this response after reflecting that we needed to stay focused on our plan) |
| Post meeting: studies not written up in the English language | There may be research on the topic that has been published in languages other than English | Unfortunately, for this study we do not have the resources to translate articles not written in English. However, we will be recording how many studies we have not included because of this and if there are some, then we will recommend that further research is needed that does consider these studies |
| We will also feed back to reviewers more generally about the need to have the resources to translate studies in future reviews | ||
| Post meeting: how was the intervention designed? | It will be important to consider how the intervention was designed, especially in terms of whether or not people who may receive the intervention were involved in the design process. For example, who are the authors of the paper? | We will consider within the review how the interventions are designed, especially in terms of involving people who may receive the support |
Ongoing communication
Following the event, we circulated newsletters to keep stakeholders informed about the progress of the review and to give people the opportunity to provide further feedback.
Chapter 4 Systematic review methods and results
Design
We undertook a multicomponent review49 of quantitative and qualitative research. We registered the review on PROSPERO (registration number CRD42020214206). The funders played no role in the review.
Methods
Searches
We searched the following databases from inception to 11 January 2021: Ovid MEDLINE, The Cochrane Library (via Wiley Interscience), EMBASE (via Ovid), Cumulative Index to Nursing and Allied Health Literature (via EBSCO), PsycINFO (via Ovid), Web of Science and Sociological Abstracts. We also searched for evidence in other sources including Google (Google Inc., Mountain View, CA, USA) and web-based review databases, such as Epistemonikos, PROSPERO and the Joanna Briggs Institute database.
We undertook a structured grey literature search by searching websites including Social Care Online, Health Literacy UK (https://healthliteracy.org.uk/), Public Health England, NHS England, NHS Scotland, The Kings’ Fund and the Royal College of Nursing. We also undertook targeted Google searches of domains including ‘.gov.uk’ and ‘.org.uk’ (and their international counterparts). In addition, we searched the websites of specific organisations known to have run local initiatives (e.g. Sheffield CCG, Stoke CCG) and the websites of international projects, including Optimising Health Literacy and Access (OPHELIA) (Australia) and the World Health Organization Healthy Cities initiative. Finally, we compiled a list of known authors on the topic of health literacy and searched for their conference papers, reports and papers, as well as researchers citing their work on Google Scholar (Google Inc.).
Given that this review was multicomponent, we had proposed, if needed, to undertake supplementary searches after our initial search to ensure that we met the aims and objectives of the review. As the initial search progressed and synthesis began, we did not need to undertake further searches for different components. We did however undertake one further search in August 2021 to identify additional studies reporting evaluations of navigation tools because we had identified tools only from the USA in our original search.
Search terms
A professional information specialist within the information resources team in the ScHARR (MC) developed the search strategy using the standard search strategy of population, intervention, comparator, outcomes and setting/context.
-
Population. No search terms in relation to population were used because we wanted to include all populations.
-
Intervention. Interventions with the primary purpose of reducing primary or emergency service use for minor health problems by improving health literacy. ‘Minor health problems’ was not used to limit the initial search because researchers may not use this term (or similar terms), or explicitly articulate a focus on minor health problems. Instead we searched widely and then screened for interventions to reduce service use for minor health problems. We were not interested in interventions to improve health literacy for chronic conditions, where the aim is to reduce use of emergency care and hospitalisation through prevention of health problems. These chronic condition interventions tend to focus on self-management to prevent serious exacerbations, hence the interest in hospitalisation. We removed these at the screening stage. Nor were we interested in interventions in which health professionals made decisions about whether or not, or where, to seek health care and gave self-care advice as part of this (e.g. NHS 111).
-
Comparator. A range of study designs. When a design was a randomised controlled trial (RCT), the comparator could be usual care or a control assumed not to have the active intervention being tested.
-
Outcomes. (1) Changes in use of general practice, GP out-of-hours services, emergency ambulance, EDs, paediatric EDs (using a range of international terms for these services). (2) Changes in use of services overall or specifically for minor health problems. (3) Rate of adverse events, that is missed serious health problems for which people would otherwise have sought care. (4) Patient acceptability and health-care feasibility. (5) Changes in other outcomes, for example knowledge, health literacy, confidence.
-
Setting/context. We were interested in interventions that might work in the UK context. We searched for evidence without limiting the country/setting.
See Appendix 1 for search terms used on 11 January 2021.
Further inclusion/exclusion criteria
We limited the search to English-language literature. We limited the search to articles published between 1990 and 2020 to ensure relevance to the current health-care system.
Screening
We downloaded references into EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA]. We piloted the screening process by having three reviewers (AOC, AF and CC) independently screen the titles and abstracts (when available) of the same 100 records retrieved from the searches to determine whether or not a study met the predefined inclusion criteria and whether or not the criteria were being interpreted by all reviewers in the same way. We discussed and clarified any differences of interpretation and then one reviewer (CC) screened all the titles and abstracts, tagging each as ‘include,’ ‘exclude’ or ‘unclear’. We retrieved the full texts of all ‘include’ or ‘unclear’ articles and classified them as ‘include’, ‘exclude’ or ‘unclear’ (CC and AOC), with differences resolved through discussion. When this discussion did not lead to resolution, we consulted a fourth reviewer (LP). One reviewer (LP) screened the reference lists of relevant systematic reviews for further primary research studies. One reviewer (CC) checked the references of included studies to identify additional relevant studies.
Data extraction
Louise Preston developed a data extraction form to meet the study objectives. Four reviewers (CC, AOC, AF and LP) independently extracted data from three studies and discussed the process to ensure that we were clear about what we needed to extract and the level of detail required. Then one reviewer (CC) independently extracted data from each included study. The data extracted included the following.
-
General description (author, year of publication).
-
Study design.
-
Context. Although this was not a realist review, we were interested in characteristics of context that might contribute to reductions in use of primary care and emergency services. Contexts included the country where the research was conducted and the target population.
-
Delivery setting (emergency care, primary care, community, workplace, other).
-
Headline message.
-
Description of the intervention using the Template for Intervention Description and Replication (TIDieR) framework. 50
-
How the intervention was developed. Given that patient involvement in the development of interventions is noted as good practice to create usable and helpful interventions,51 we documented how authors of papers described the intervention development process. We did not search beyond the included papers.
-
Mechanisms of action of the intervention (see the next section about how we identified these).
-
Changes in service use: ED, general practice and emergency ambulance overall or for minor health problems. We also extracted how they were measured (actual use from patient records or patient-reported use) and time period of measurement (e.g. 6 months).
-
Costs and cost-effectiveness (see Costs and cost-effectiveness for explanation).
-
Safety or adverse events.
-
Displacement. We documented whether or not studies of interventions to reduce the use of primary care also measured any effect on EDs to ensure that we considered displacement of service contacts to higher-acuity services.
-
Any other outcomes measured, for example change in health literacy levels or knowledge of minor illness management.
-
Patient/carer and staff views on the feasibility or acceptability of the intervention.
-
Copy of written components of the intervention.
A second reviewer (LP) independently extracted data from 10% of the included studies and resolved differences by discussion with Christopher Carroll and Alicia O’Cathain. Discrepancies were related to the level of detail of extraction, rather than the accuracy of extraction.
Mechanisms of action
We began the review with three potential mechanisms in mind (information, education and empowerment), identified from reading background literature and some of the included intervention studies. An information mechanism might include ‘take your temperature’, education might include ‘this is how you take your temperature’ and empowerment might include ‘engendering confidence in making decisions based on a temperature reading’. One reviewer (CC) extracted authors’ stated mechanisms or assigned mechanisms based on this list of three mechanisms and the description of the interventions.
As we read existing reviews on self-care and health literacy, and read more of the included studies, we reconsidered the list of mechanisms. Richardson et al. 44 was particularly helpful in this endeavour. In their systematic review of self-care for minor ailments, they explored mechanisms using the theoretical domains framework. 52 They described the need to affect people’s willingness to self-care, which might be compromised by a lack of knowledge and skills to manage self-care. They identified the need to address people’s capability (knowledge, skills, beliefs about capabilities, decision-making processes) and motivation (beliefs about consequences, e.g. persuasion that EDs are overcrowded or that pharmacists are competent). Some authors of the included studies explicitly discussed the need for an intervention to address people’s anxiety about a specific symptom as a barrier to self-care. 53 Some interventions in the included studies also tailored the intervention to individuals’ symptoms and situations, rather than offering the same advice to all. We constructed an extended set of mechanisms and one reviewer (AOC) extracted these when the basic data extraction had been completed by Christopher Carroll. Authors of papers were rarely explicit about mechanisms; we identified them by interpreting text from the description of the intervention, or the background or discussion sections of a paper in which authors discussed the intervention aims, rationale or development. The six mechanisms are listed and described in Results.
Constructing a typology of interventions
We expected to see different types of interventions for improving health literacy with the aim of reducing the use of primary and emergency care. We planned to synthesise the evidence by type. We could find no existing framework of types of interventions, so we read a selection of included papers and papers in the wider health literacy literature. We inductively constructed a typology. We have used this inductive approach to developing taxonomies and frameworks successfully in other reviews. 54,55 We drew on Coulter and Ellins,40 who identified different types of health literacy interventions as written health information, alternative format resources, low literacy initiatives and targeted mass media campaigns. When we read a selection of included papers, we identified the following types: written information to navigate the health-care system, written information on managing illness, educational workshops, one-to-one health coaching and digital self-triage. These interventions came in different formats (paper; digital, including mobile phones; human; or mixed). They were also delivered at different times [to people who had used emergency or primary care for a minor health problem (‘specific’) or made available to the people at any time (‘general’)]. Although we had a number of other intervention characteristics to choose from, and we discussed the potential to use these (e.g. setting of delivery, target population aimed at, group vs. one-to-one delivery, tailored vs. not), we wanted to keep the typology simple. We constructed a typology of interventions based on the aim of the intervention (navigation, education or self-triage), how the intervention was delivered (e.g. written, person, digital) and when it was delivered (when a patient had used a service for a minor health problem, or it was offered to everyone). We selected timing of the intervention because a related review drew attention to its importance,41 and this was also raised in our first stakeholder event. We discussed the typology as a team and tested it on a range of included studies. When we were happy with the typology, one reviewer (AOC) coded each included study to it. A second reviewer (CC) checked the application of this typology and highlighted a few discrepancies. Alicia O’Cathain returned to the highlighted papers to double-check the coding of each study (see Results for the typology).
Quality assessment: risk of bias and risk to rigour
Given the wide variety of study types included in this review, we used a hybrid approach to risk-of-bias assessments. For RCTs, we used the Cochrane Risk of Bias tool. 56 For non-randomised studies, we used the Newcastle–Ottawa Scale (case–control and cohort studies). 57 For qualitative studies, we assessed risk to rigour using the Critical Appraisal Skills Programme (CASP) tool,58 and for mixed-methods studies we used the Mixed Methods Appraisal Tool (MMAT). 59 We did not use our assessment of risk of bias or of risk to rigour to exclude evidence from the review, but to assess the overall evidence base and the confidence with which we could use the evidence. One reviewer (CC) undertook the quality assessment. Another reviewer (LP) undertook an independent assessment of 10% of studies and identified minor differences, which were resolved via discussion with Christopher Carroll.
Assessment of readability and user-friendliness of written components of interventions
An important concern arising from the first stakeholder event was that interventions aimed at improving health literacy needed to be written in plain English and designed in a way that made it easy for the reader to comprehend what was written. For example, interventions using medicalised language or with long chunks of condensed text would be difficult for people to understand and act on. At least 43% of written materials containing health information are too complex for most adults to understand. 60 We decided to assess both the readability and the user-friendliness of the written components of included interventions.
Readability
The Flesch Reading Ease (FRE) and Flesch–Kincaid Grade Level (FKGL) are established approaches to readability assessment. 61 Readability is about the complexity of language being used, and thus the level of literacy someone may need to have to understand a document. 62 We used the FRE and the FKGL because they have been used in previous studies that consider health literacy and are the most commonly used assessments because they can be measured using Microsoft Word (Microsoft Corporation, Redmond, WA, USA). 63 Both the FRE and the FKGL consider the number of syllables in words and the average number of words per sentence. They differ in terms of the weightings they give to different parts of the formula. Therefore, there may be some differences in how an intervention is scored on the two assessments. 63
The readability assessments are automatically calculated using Microsoft Word. We needed to type the interventions into Microsoft Word. Rather than typing in the whole document, we followed an established procedure of choosing a selection of text from each intervention. 62 The selection was drawn from the first 100 words (excluding title/headings), 100 words from the middle and the last 100 words of a written component of an intervention. It is possible that an intervention may have been scored differently had the full text been assessed.
The FRE score ranges between 100 and 0, where 90–100 = very easy, 80–89 = easy, 70–79 = fairly easy, 60–69 = standard, 50–59 = fairly difficult, 30–49 = difficult and 0–29 = very confusing. A document scoring ≥ 70 is considered suitable for most adult readers. A score of 30–69 is considered somewhat difficult and suitable for only some adults. Anything scoring < 30 is considered difficult and inappropriate because it is written at a university graduate level. 64 More generally, documents are considered to be written in plain English if they have scores of at least 60. 65
The FKGL relates to the USA education grade a document is suitable for. The score ideally needs to be grade 8 or lower, as this reflects the reading level of most adults. Scores are categorised as follows: ≤ 8 (suitable for most adults), 9–12 (fairly difficult because it is written at a level suitable for high school students aged 14–18 years) and > 12 (difficult because it is written at a level suitable for university students).
Development of a User-Friendliness Assessment Tool
At the first stakeholder event, people raised the issue that interventions need to be user-friendly so that people feel able to understand and act on the information they contain. Stakeholders gave examples of text-heavy leaflets full of jargon, which would be barriers to people understanding and acting on the information provided. This would then have implications on the effectiveness of those leaflets. Consequently, as a research team, we wanted to assess the ‘user-friendliness’ of interventions, focusing on medicalised language/jargon, font and text style; whether or not content was broken down into short paragraphs/bullet points; and whether or not the intervention was written by someone patients trusted. We had to develop our own UFAT because we could not identify an existing tool. We found guidance from credible sources that recommended good practice for health literacy interventions. These were from the NHS in the UK66 and the Centers for Disease Control and Prevention in the USA. 67 We drafted a tool and shared this with our PPI members for feedback. Some PPI members also tested the UFAT on two interventions. We held a meeting in June 2021 with PPI members to discuss their feedback, and revised the tool substantially based on their feedback. Key changes included ensuring that at least two people assessed an intervention because of the divergence in views about the interventions, having four response options per item so that the tool was more sensitive, and adding additional questions on trustworthiness and confidence in the information provided. We also agreed that PPI members would be involved in assessing the user-friendliness of interventions. The UFAT is in Appendix 2. The tool consists of 14 items, each of which produces a score of 0–3. The scores from each question are combined to produce a maximum overall score of 42. Interestingly, Rughani et al. 63 published a paper assessing GP websites during our review and included a similar ‘design factors’ assessment tool in their work.
Process of assessment
Health literacy interventions can come in a range of formats including person-delivered, leaflets, websites and posters. The readability and user-friendliness assessments could be undertaken only on interventions that included a written component. Furthermore, we could only assess interventions that were in English and publicly available. For example, some of the websites were subscription only or in Dutch. Some papers showed an extract from the intervention rather than a link to, or copy of, the whole intervention; therefore, we used this extract. We were able to locate 13 interventions related to 20 articles included in the review; some interventions were reported in a number of papers. Some of the interventions were impossible to find because they were more than 20 years old, for example leaflets developed in 1991.
In addition to assessing the interventions in the review, we also assessed an intervention identified by PPI members and stakeholders that is currently in use in the NHS: The Little Orange Book. 68 This is an information resource aimed at parents of young children in the north-east of England to support them with understanding common childhood illnesses.
We calculated the FRE and the FKGL for each intervention. At least two people applied the UFAT to each intervention, typically two PPI members and one researcher (LP). The scores of the different assessors were combined and a mean calculated. We compared scores on readability and user-friendliness to assess their relationship. Very high levels of correlation would suggest that only the readability scores were necessary for use in our synthesis.
Synthesis
Presentation of the studies
One reviewer (CC) reported the included studies in alphabetical order in four tables: (1) context/characteristics, (2) description of the intervention (including mechanisms and typology), (3) service use outcomes and (4) other outcomes. A second reviewer (AOC) read the papers independently and checked the presentation of each study.
Synthesis of outcomes
We used the typology of interventions to identify common types and then we presented a narrative synthesis of service use outcomes for each common type, with data summarised in tables. We ordered studies in these tables in alphabetical order, or, if there was a subset of the type, we ordered by this subset and then alphabetically.
We could not use meta-analysis because of the heterogeneity in how service use outcomes were measured. We did not measure heterogeneity in reported effects because it was clear from the data extraction that there was considerable variation in the way the outcomes were measured and the time periods over which they were measured. We planned to use the typology to synthesise other outcomes and processes, but numbers were too small. Instead we undertook a narrative synthesis of all the studies for each outcome or process. We followed the synthesis without meta-analysis (SWiM) reporting guidelines. 69 The SWiM checklist can be found in Report Supplementary Material 2. When drawing conclusions from the synthesis, we gave weight to studies that used RCTs in preference to other designs, measured the impact on service use using routine data/records rather than self-reported service use, were assessed as being of higher quality, and had greater relevance to the UK because the research was undertaken in the UK or a country with a similar health-care system to that of the UK.
Costs and cost-effectiveness
We knew from scoping the evidence base that there would be few economic evaluations for synthesis. We intended to follow the ‘brief economic commentary’ for synthesis, rather than the ‘integrated full systematic review of economic evidence’ as set out in the Cochrane Handbook. 70 We planned to follow methods used by Angus et al. 71 to summarise any directly reported costs associated with interventions as reported in the literature and convert them to Great British pounds for a specific year. We planned to aggregate these data across intervention types to report costs for comparison and narratively synthesise cost-effectiveness and report the relationship between cost-effectiveness and context. Unfortunately, the cost data and cost-effectiveness analyses were often poorly undertaken or reported. Instead we undertook a simple narrative synthesis.
Qualitative research
We intended to analyse qualitative research using qualitative synthesis methods. 72 There were only four articles reporting qualitative research, focused mainly on digital interventions, so synthesis was limited.
Explaining variation in impact on service use
Ideally we would have identified size of effect of each intervention within a meta-analysis, but, as explained previously, this was not possible because of heterogeneity in outcome measurement. We might also have considered a meta-regression to explain size of effect. 73 Instead, we identified whether or not studies that measured service use in a full evaluation (as opposed to pilot studies, which are underpowered statistically) had statistically significant reductions for impact on use of different services. Then we used IBM SPSS Statistics 27 (IBM Corporation, Armonk, NY, USA) to test whether or not different characteristics of the study, context and intervention explained reductions in service use.
An alternative way of explaining variation in an outcome is to consider the relationship between context, mechanisms and outcomes by identifying context–mechanism–outcome chains associated with understanding messy complex interventions. 74 We did this by considering mechanisms within the narrative synthesis by type of intervention.
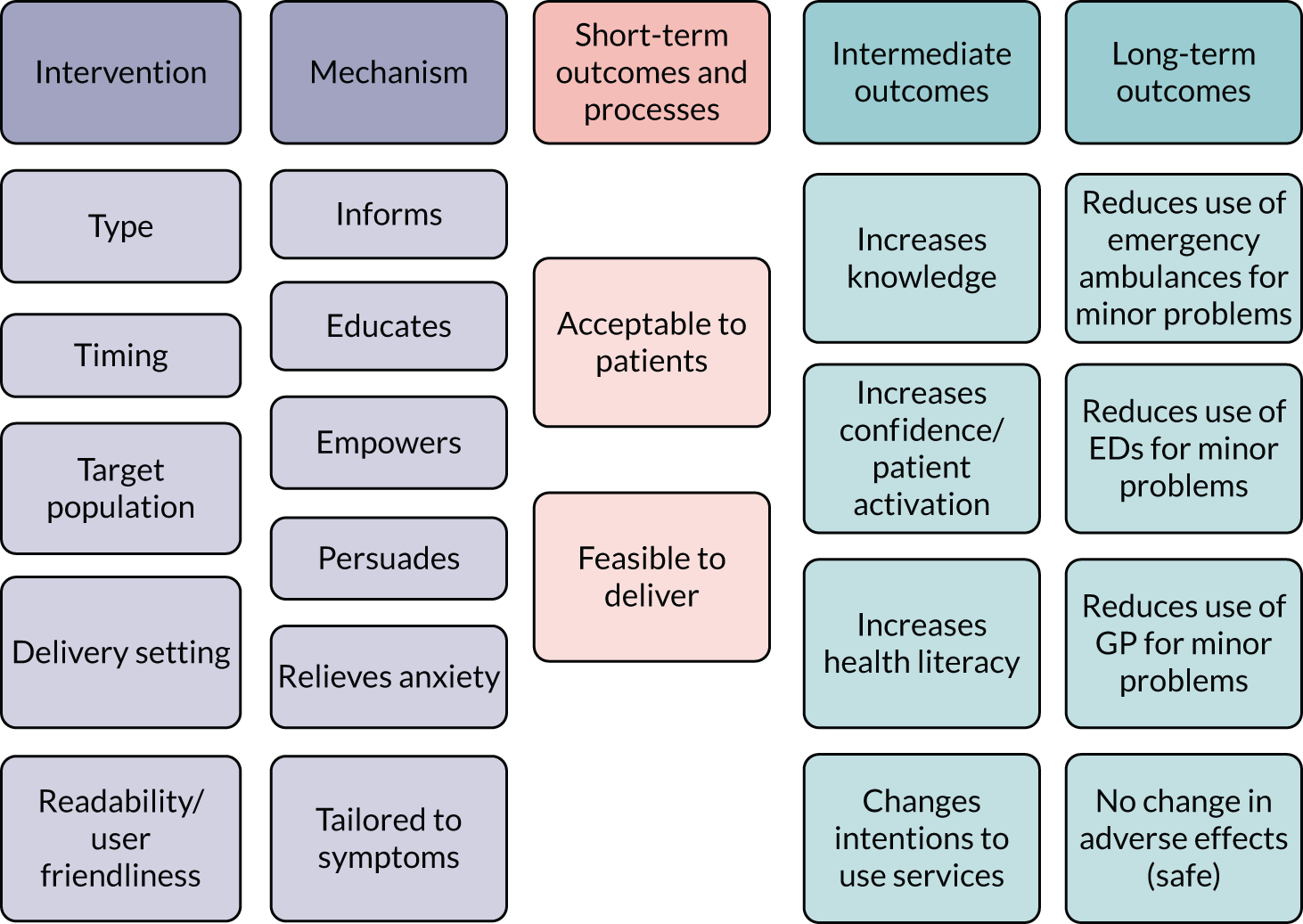
Articulating a programme theory
We constructed a logic model to present a programme theory of how characteristics and mechanisms of interventions might produce short- and intermediate-term outcomes that lead to long-term outcomes. We did this to facilitate interpretation of the synthesis (Figure 1).
FIGURE 1.
Logic model of health literacy interventions to reduce use of primary and emergency care.
Results
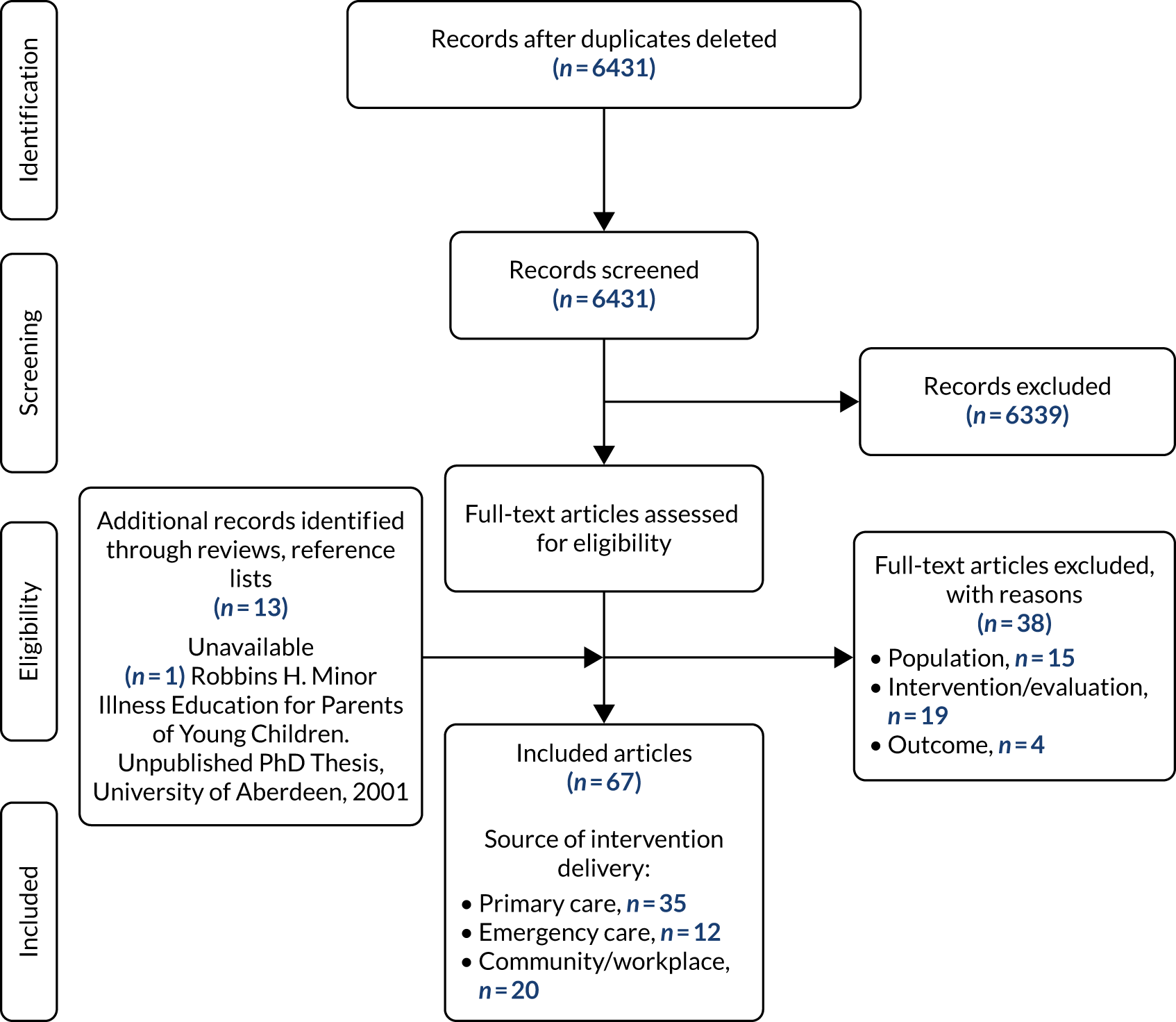
Included articles
We identified 67 articles that met our inclusion criteria (Figure 2). The decision about inclusion was challenging when studies met some, but not all, of the inclusion criteria. We excluded 38 articles at the full-text stage (see Appendix 3). Articles about frequent users of EDs tended to be excluded at the full-text stage because these studies focused on a population of people identified as having serious problems such as homelessness and substance abuse, rather than minor health problems. Articles about self-management of chronic conditions such as asthma were excluded when they were about prevention of acute severe problems, rather than management of minor health problems. Case management interventions tended to be excluded because they did not focus on minor health problems, but on serious problems that resulted in hospitalisations.
FIGURE 2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Characteristics or context of articles
The characteristics of each study are presented in Appendix 4. We describe each characteristic in the following sections.
Time of publication
The 67 articles were published over the three decades between 1990 and 2020, with half of articles published in 2010 or later (n = 32). In particular, interventions delivered in emergency care and community/other settings were undertaken more recently (e.g. 8/12 emergency care articles were published after 2010). This indicates the ongoing interest in this issue over time, and the more recent interest in interventions delivered in emergency care or community/other settings.
Country
The articles reported studies undertaken largely in North America (n = 37), the UK (n = 16) and the rest of Europe (n = 12). The Netherlands featured highly in the European group, specifically for interventions delivered in primary care. Only two articles were from the rest of the world (Taiwan and Australia). Most of the interventions delivered in emergency care were from North America (11/12), as were most of the community/other setting articles (15/20). This raises a potential concern about transferability of parts of the evidence base to the UK because of the role of payment and insurance for services in North American health-care systems, particularly in the USA.
Place of delivery of the intervention
The articles reported interventions delivered to users of primary care (n = 35), users of EDs (n = 12) and within community/other settings (n = 20). No intervention was delivered to ambulance service users.
Target population
Around half the articles were aimed at parents of young children (n = 32), some of which were aimed at parents of children aged < 5 years (14/32). Most articles about interventions delivered in EDs were aimed at parents of young children (9/12), demonstrating a paucity of evidence about interventions aimed at adults attending EDs. Some articles specified that the population aimed at, or the sample included in the study, was (1) socially deprived and/or (2) mainly from an ethnic minority group associated with poverty in that country and/or (3) had low health literacy levels (21/67).
Articles reporting the same study
Some articles reported different aspects of the same study or data set: Plass et al. ,75,76 Rutten et al. ,77,78 and Hibberd et al. 79 and Wagner et al. 80 There were 64 studies in total. Other articles were written by the same author, testing the same intervention in different ways on different populations,81–83 with Herman and Mayer82 undertaken as a pilot for Herman and Jackson. 81 Yardley et al. 53 was an exploratory RCT for Little et al. ’s84 full RCT.
Study design
The authors used a range of designs in the articles, mainly RCTs (n = 30), and single-arm or controlled cohort studies (n = 33). A few articles reported qualitative or mixed-methods research (n = 4). The cohort studies included controlled before-and-after studies (n = 11), before-and-after studies (n = 8) and non-RCTs (n = 4).
Description of interventions
The interventions reported in the 67 articles were described using TIDieR guidelines (see Appendix 5). This description included the rationale for the intervention; what was delivered and by whom, how, where, when and how much; and any tailoring/personalisation. The items of ‘modifications’ and ‘fidelity’ were also extracted, but were rarely reported and so are not presented in Appendix 5. Instead, these items are described in narrative form in the following sections Modifications and Fidelity. Appendix 5 also includes a summary of how the interventions were developed, their proposed mechanisms of action (subjective assessment by our team) and their type according to our typology.
Rationale for the intervention
The reported rationale for many interventions, whether delivered in primary or emergency care, was to reduce emergency care use for non-urgent complaints, including directing patients to primary care,83,85–95 and to reduce any and all health service use. 96–98 Some interventions were specifically designed to reduce reconsultation for a similar minor health problem, especially in primary care,99–101 and, in some cases, the interventions sought to modify patients’ and carers’ consultation behaviour related to specific minor problems, such as childhood fever,102,103 respiratory tract infections84 and cough. 77,78
Other primary and emergency care-delivered interventions were explicitly designed to improve patients’ and carers’ knowledge and confidence sufficiently to enable minor problems to be self-managed96,102,104–109 and/or to enable the selection of the appropriate service, for example primary instead of emergency care. 108–112 Many such interventions reported the corollary rationale of reducing unnecessary primary or emergency care use as a result of improved knowledge. 53,75,76,103,113,114
Unlike the primary and emergency care interventions, the majority of community and workplace-based interventions had the specific aim of improving self-care and participants’ knowledge, both of illnesses (including some specific minor problems such as childhood fever or cough)79–82,115–121 and when to access what service. 122,123 A smaller number of such studies explicitly reported that the aim of an intervention was to reduce use of primary care,124 emergency care125,126 or health services generally. 127–129
What was delivered and by whom, how, where, when and how much
The interventions were delivered either by a specific individual or designated team of health-care staff, (e.g. a GP, paediatric ED physician or nurse),75–78,88,99–102,107,109,112,130,131 a service generally (e.g. the primary care practice)84,86,92,106,132,133 or, in the case of some workplace or community interventions, an employer or an external organisation. 79,80,120,121,127,128 In some cases, the interventions were delivered by the researchers only. 83,85,89,94,110,134
Some interventions were delivered face to face to target groups of patients or carers at pre-set time points, in particular regular monitoring visits for babies and infants (e.g. Well Child Visits). 90,111,119,134,135 However, the majority of interventions directed at specific groups of patients or carers were delivered in direct response to a potentially unnecessary primary care or emergency care consultation and with the explicit purpose of preventing future, similar consultations. Such interventions were delivered principally at the time of the index consultation,75–78,83,85,94,95,99–103,109,130,131,136 but could also be delivered a little time later. 88,89,92,108,112,137
Another large group of interventions, principally in the community group, were delivered to people for consideration in the home setting. This might consist of written materials or information resources (e.g. websites) for specific patient groups,81,82,98,115,116,118,123,126,132,133 for all patients in a particular primary care practice96,104,105,138 or for all patients in a particular area or region. 53,79,80,117,122,124,125,129,139,140
Tailoring/personalisation
Many interventions do not appear to have involved any element of personalisation for the intended audience, carer or patient. When personalisation was undertaken, it most often involved one of the following approaches: most frequently, an interactive discussion between staff and the patient or carer concerning the content of the intervention (a leaflet, video, written material or workshop);85,99,102,103,108,112,115,120,128,130,136 individual case management or patient navigation services;87,91,93 the use of personalised data in automated systems;89,98,111,123 directing patients specifically to their own local services;94 and the use of the most appropriate language to communicate with patients and carers, for example English or Spanish. 95,125,126
Modifications
Reported modifications to an intervention during its implementation or delivery were rare. Only one study reported modifying a primary care-delivered intervention, by adding a social worker-delivered intervention to the original nurse-delivered intervention to see if this improved access to primary care among patients who had an unnecessary ED attendance (it did not). 137
Fidelity
Implementation fidelity was also considered infrequently. This consideration took two forms: (1) strategies to facilitate fidelity of implementation and (2) actual evaluations of implementation fidelity. The former included prompts built into systems to remind staff to do things with the intervention or to remind patients that the intervention existed and was available for them,102,107,117 staff training to facilitate implementation and regular monitoring to check that the intervention was being delivered properly. 79–81,94,139 The latter included quantitative evaluations of whether or not patients had received all of the intervention that they should have received90,92,108,121,126,139 and qualitative evaluations of what worked well and what did not work well. 104,112
How the interventions were developed
Eight approaches to intervention development were previously identified in a taxonomy: partnership, target population centred, evidence and theory based, implementation based, efficiency based, stepped or phased, intervention specific, and combination. 54 In the 67 articles in our review, there was often little description of the intervention development process in the article or its references (see Table 3 and Appendix 5). Twenty-two articles provided no details, and the description, if any, was brief. Sometimes authors reported using two approaches in combination, for example ‘target population centred’ and ‘evidence based’. The most common approach used was target population-based, where the intervention development involved surveys, interviews or focus groups with patients (n = 15). Authors were often vague about the focus of this work, and in some cases reported that it involved understanding the needs or problems of the patients, or assessing the acceptability of a developed intervention. Authors also reported using evidence-based (n = 8) or theory-based (n = 4) approaches. The theories used included the information, motivation, behavioural skills model;111 the common-sense model of self-regulation of illness and social cognitive theory to build self-confidence53,84 as part of the same programme of research; and Green and Kreuter’s predisposing, reinforcing and enabling constructs in educational diagnosis and evaluation–policy, regulatory and organisational constructs in educational and environmental development (PRECEDE–PROCEED) model. 130 Only one article reported a partnership approach whereby a primary care-based intervention for parents of young children was developed in collaboration with a Latino family advisory board. 111 One article reported using a stepped approach, but did not name it. 99 The authors of 19 articles described other ways of developing interventions, usually working with health professionals or their governance bodies.
Owing to the paucity of information about intervention development, we did not synthesise the outcomes of studies by the approach to intervention development.
Mechanisms of action
We identified mechanisms of action based on the text in the articles because authors were not always explicit about the intervention mechanisms or they used different language to describe similar mechanisms. The range of mechanisms we looked for are described in Table 2. Each intervention could have multiple mechanisms. When the different mechanisms were counted, educating people to understand symptoms and self-care techniques was the most common mechanism, present in most of the interventions (see Table 2). Where education was not present, awareness of services to help people navigate health care was present. The least common mechanism was explicitly addressing people’s anxiety about the seriousness of a symptom to allow them to self-care if appropriate.
| Mechanism (shorthand) | Description | Frequency in 67 articlesa |
|---|---|---|
| 1. Service awareness and knowledge to help navigate a complex system (service awareness and knowledge) | Informing people about services available, opening times, how to access them, types of treatments offered, when/in what circumstances to access pharmacy, GP, ED or ambulance | 23 |
| 2. Education in understanding symptoms and self-care techniques (education) | Informing and educating people about how to identify and diagnose symptoms, how to distinguish between minor and more severe symptoms, and how to self-manage and alleviate symptoms | 53 |
| 3. Empowerment by increasing confidence and self-efficacy (empowerment) | Empowering people to communicate with health professionals or have confidence in their decision-making abilities by increasing patient activation, resulting in reduced anxiety | 15 |
| 4. Addresses barrier of anxiety to help self-care (anxiety) | Explicitly help people to address anxiety levels so this, in turn, reduces the perceived need for contacting a health service or the perceived urgency of the problem | 8 |
| 5. Persuasion, towards or away from a service (persuasion) | Towards supported self-management at pharmacy or against inappropriate use/misuse of GP, ED or ambulance, including informing people about pressure services are under. May show advantages or disadvantages of going to a particular service | 12 |
| 6. Tailored, personalised to individual’s symptoms (tailored) | Speaks specifically to an individual and their situation, rather than offer the same information to everyone | 21 |
Typology of interventions
The final typology of interventions developed by the team is shown in Table 3. We assigned each study to a type. Members of the team disagreed over the categorisation of some papers. For example, Platts et al. 107 was considered typology A.II by one reviewer and as A.II and B.II by another. Although the doctor issued the booklets and encouraged their use, there was no discussion with the patient beyond this, so we finally categorised it as A.II.
| Mode and aim/timing | Given at the time of contacting a service for a minor illness (specific) | Available at any time (general) |
|---|---|---|
| A. Paper or video information | ||
| I. Navigation tool | ||
| II. Educational self-care tool | ||
| III. Self-triage tool | ||
| B. Person delivered | ||
| I. Navigation tool | ||
| II. Educational self-care tool | O’Neill-Murphy et al.103 | |
| C. Digital | ||
| I. Navigation tool | Anhang Price et al.123 | |
| II. Educational self-care tool on a website, an app or mobile phone text | Lepley et al.136 | |
| III. Self-triage software including app (includes self-care education C.II) | Not possible | |
| D. Mass media public education | ||
| Posters/television/radio/newspapers/website | Not possible | Hou et al.122 |
| E. Multicomponent | ||
| A.I and B.I | Davis et al.86 | |
| A.II and B.II | ||
| B.I and B.II | ||
| A.I, A.II, B.I and B.II | Sturm et al.94 | Robbins et al.108 |
| A.I and C.II | DeCamp et al.111 | |
| A.I and A.II | Rector et al.125 | |
| A.I and A.II and C.I | Beal et al.116 | |
| A.II and B.II and D | ||
Selecting types for evidence synthesis
There were too few examples in some types to make synthesis meaningful. Because of this, we decided to synthesise interventions given at a specific or general time together, and combine similar types. We created six common types in the evidence base and an ‘other’ type, making seven types for synthesis.
-
Navigation types (A.I, B.I, C.I and multicomponent A.I and B.I) in seven articles.
-
Written education about managing minor health problems (A.II and C.II) in 17 articles.
-
Person-delivered education (B.II and multicomponent B.I and B.II) in five articles.
-
Written education with person-delivered education (multicomponent A.II and B.II) in 17 articles.
-
Multicomponent education (e.g. multicomponent A.II and B.II and D) in five articles.
-
Self-triage (C.III and A.III) in nine articles.
-
Other in seven articles: a few studies did not fit these types and are described separately as ‘other’. Ohns118 is also included here so that all of the 67 articles are described by type in the synthesis in later sections.
Readability and user-friendliness of written information components
The interventions varied considerably in their readability (Table 4). Eight of the 13 interventions were assessed as being written in plain English (interventions scoring ≥ 60 on the FRE). In contrast, the NHS Choices and Triple Zero websites were assessed as difficult to comprehend and suitable only for people with higher levels of education, for example university students. It was interesting that the two lowest-scoring interventions were both websites. This reflects a concern, raised by Rughani et al. ,63 that the required reading age of health-related websites is often too high for the general population.
| Intervention | Type of intervention | Paper | FRE | FKGL | Mean user-friendliness scorea | ||
|---|---|---|---|---|---|---|---|
| Score | Categorisation | Score | Categorisation | ||||
| Plass et al.75 | Self-care booklet | Plass et al.75,76 | 93.4 | Very easy | 1.4 | Suitable for most adults | 17.3 |
| Purple Crying | Leaflet | Barr et al.115 | 90.2 | Very easy | 3.2 | Suitable for most adults | 37.6 |
| What to do if your child gets sick | Leaflet | 81.5 | Easy | 3.7 | Suitable for most adults | 36.7 | |
| bHolden89 | Booklet | Holden89 | 73.9 | Fairly easy | 5.0 | Suitable for most adults | 32 |
| Internet Doctor | Screenshots from website | 73.1 | Fairly easy | 7 | Suitable for most adults | 27 | |
| Macfarlane et al.101 | Letter | Macfarlane et al.101 | 68.1 | Standard | 9.1 | Fairly difficult: high school students | 10 |
| Take care of yourself | Booklet | Steinweg et al.120 | 62.6 | Standard | 8.4 | Suitable for most adults | 21 |
| Macfarlane et al.100 | Leaflet | Macfarlane et al.100 | 61.3 | Standard | 8.6 | Suitable for most adults | 17 |
| Sustersic et al.131 | Leaflet | Sustersic et al.131 | 60.9 | Standard | 7.7 | Suitable for most adults | 26.7 |
| Choosing Wisely | Leaflet | Huyer et al.112 | 59.5 | Fairly difficult | 7.9 | Suitable for most adults | 29.3 |
| Healthwise Handbook | Leaflet | 55.2 | Fairly difficult | 9 | Fairly difficult: high school students | 28 | |
| Family Medical Centre | Poster | Adesara et al.110 | 52.5 | Fairly difficult | 7.7 | Suitable for most adults | 22.2 |
| NHS Choices | Website | Murray et al.124 | 49.8 | Difficult | 9.9 | Fairly difficult: high school students | 27 |
| Triple Zero | Website | Hou et al.122 | 23.6 | Very confusing | 14.6 | Difficult: writing at university level | 27.5 |
The 13 interventions ranged considerably in their mean user-friendliness scores, from 10 to 37.6 out of 42 (see Table 4). Two of the interventions scored > 35, indicating that they had a high level of user-friendliness (i.e. ‘what to do if your child gets sick’ and Purple Crying). Both of these interventions were aimed at parents of young children. The Purple Crying leaflet was scored highly in terms of the trustworthiness of the source, layout of the intervention and clarity of language. Three of the interventions had a score < 21. 75,100,101 In Plass et al. ,75 the content was considered to be well ordered and the font appropriate, but it could have been better written and formatted using pictures to help explain the content. Interestingly, all three of these interventions scored well on the readability assessment. Interventions with a mean score in the middle of the range did not score ‘2’ across all the items: they scored high on some items, but low on others. For example, assessors scored the Internet Doctor resource as appropriate in tone (scored 3), but there was no reference to the resource being available in alternative formats (scored 0). Interventions often included excessive use of medicalised terms or jargon without having accompanying explanations in plain English.
Readability and user-friendliness scores did not always correlate. Three interventions were assessed as being ‘very easy’ or ‘easy’ to read, but only two of these were assessed as being user-friendly. Similarly, the interventions with poor readability scores did not necessarily have the worst user-friendliness scores. This indicates that readability scores and user-friendliness scores were assessing different issues.
We hypothesised that more recent interventions would have better levels of readability, given an increasing awareness of this issue over time. However, we found that there was no correlation between the date of the paper and the readability scores or the user-friendliness scores.
We were interested in how interventions currently being used in the NHS might fare under a similar assessment. So we assessed The Little Orange Book,141 which stakeholders identified early in our review. This is a web-based and paper-based booklet to educate people in how to self-care for minor health problems and look out for serious ones. It was developed and is used in the North-east of England. This intervention had a standard level of readability on the FRE score (66.6) and was suitable for most adults (FKGL score = 8.1). It was classed as being written in plain English. It was assessed as having a higher user-friendliness score than all the interventions in our review, with a mean score of 40 out of 42. Our assessors felt that it was well laid out, it used pictures to communicate messages, and the use of terminology and numbers was appropriate for readers.
Quality assessment
We identified an appropriate quality assessment tool for each study design and applied it to the 67 articles (see Appendix 6). The Cochrane Risk of Bias tool was used for RCTs, and it identified 20 out of 30 RCTs as having high risks of bias; only one RCT was deemed to be at low risk of bias. 90 The Newcastle–Ottawa Scale was used for cohort studies, identifying 17 out of 33 as weak. Only one study was identified as ‘strong’ (i.e. as having a low risk of bias). 87 Three of the remaining four studies were qualitative (for which the CASP tool was used), one of which was assessed as being a ‘strong’ study;112 and the final study was mixed methods, assessed using the MMAT, and judged to be weak. 104 The lack of RCTs deemed to be at low risk of bias, and the paucity of strong studies, was disappointing because it suggests that the evidence base is generally of low quality. However, it is worth noting that these tools can lead to harsh judgements (a high risk of bias assigned to any one domain can result in an overall assessment of a high risk of bias). 56 Researchers had to undertake evaluations of health literacy interventions in complex real-world environments where, for example, attrition rates are often high. Because of this, we also assessed quality in a more subjective way, identifying only worrying flaws that might reduce the credibility of findings. This informal assessment is reported in the text in later sections of the findings.
Synthesis of all studies
Service use
Of the 67 articles, 54 measured change in service use. Authors measured impact on ED attendances (n = 31) and GP consultations (n = 27) rather than impact on ambulance services or other primary care consultations. Even though Hou et al. 122 was about a campaign to reduce the use of ambulances, the indicator measured the percentage of ED attendances arriving by ambulance. The 54 articles and impact on service use are presented in alphabetical order in Appendix 7. Five of these were pilot studies that were never intended to have statistical power to show change in service use. 53,82,88,103,136 These are displayed in the type-specific tables (see Tables 5–17), but are not included in the narrative synthesis when considering the proportion of studies in each type showing a reduction in service use. Eight interventions aimed to increase the use of primary care because they persuaded patients to shift their focus from emergency to primary care. 91,93,94,116,125,130 Again we display these in our type-specific tables below, but exclude them when considering the proportion of studies in each type showing a reduction in GP use.
The way in which impact was measured varied across studies, and was measured over different time periods, so it was not possible to undertake a meta-analysis. Reporting of findings was so varied that it was not even possible to present similar indicators, such as percentage reduction in service use, and undertake a test of heterogeneity to check if these could be synthesised in a meta-analysis. As an alternative to a meta-analysis, we undertook a narrative synthesis. We also identified the proportion of studies that showed a statistically significant difference in each type of intervention, recognising that a lack of statistical power may have contributed to any null findings.
When we removed the five pilot studies and eight articles reporting interventions aiming to increase the use of primary care, around two-thirds of articles (31/50, 62%) measuring impact showed a statistically significant reduction in their selected measure of emergency or primary care use. Nineteen out of 30 (63%) showed a statistically significant reduction in ED attendances and 16 out of 27 (59%) showed a statistically significant reduction in GP consultations.
Health literacy
Only 9 out of 67 articles measured health literacy among participants either at baseline or as an outcome. 88,90,108,111,118,119,121,126,136 Seven of the nine articles were conducted in the USA, and two were conducted in the UK. 108,121 The most commonly used tool was the Newest Vital Sign,142 which was used in five studies. 90,111,118,126,136 One of these studies also used the Short Test of Functional Health Literacy in Adults. 126,143 The remaining four studies developed their own health literacy questionnaires based on a variety of illness scenarios,88,108 a single scenario (e.g. fever)119 or specifically around service use. 121
Six articles used the health literacy tool to assess baseline health literacy only (Ohns118), of which five used the tool to determine comparability between intervention and control groups. 90,111,119,126,136 Three studies tested participants before and after the intervention (including comparisons with controls), sometimes at multiple time points, and found improvements in participants’ health literacy, knowledge or confidence regarding certain scenarios, although this improvement might not have been long term. 88,108,121
Satisfaction or helpfulness
Twenty out of 67 articles measured satisfaction with the intervention, or views of how helpful users had found the intervention. Eighteen out of 20 articles found high levels of satisfaction, or higher levels than a control group. A qualitative study of a digital intervention, eConsult, showed that patients valued the flexibility gained from using the intervention because it allowed them to fit seeking health-care advice around their lives and lifestyle. 104 A quotation documented in this paper illustrates these views: ‘As someone who works 9–5 it is very convenient service. It is trustworthy and reliable which makes it even better’. Patients also valued help with deciding how serious a symptom might be so they did not waste the time of pressurised services: ‘It is a good service to have especially if you feel you don’t want to waste time taking a valuable appointment when it may not be necessary to see someone face to face’. Another qualitative study asked people to select their preferred type of intervention. 118 People preferred the mobile app version rather than paper versions, and younger people were more likely to hold this preference. However, there was very little detail about why they held this preference. There was brief discussion about people liking the freedom of being able to check the mobile app no matter where they were.
Knowledge about minor health problems
Eight out of 67 articles measured a change in knowledge or understanding of minor health problems, or a change in knowledge compared with a control group. Seven out of eight articles showed positive results.
Enablement
Seven out of 67 articles measured enablement, confidence or locus of control in terms of people feeling able to take actions after being given the intervention. Six out of seven articles showed positive results.
Change in behaviour or intentions
Sixteen out of 67 articles measured whether or not users had changed their intentions around service use after using the intervention; 16/16 articles showed positive results.
Facilitators of and barriers to the interventions
The few articles with qualitative components described facilitators and barriers. These were often specific to the type of intervention. The interventions explored using qualitative research tended to be at the more complex end of interventions, with digital components and health professional engagement required. 112,114 Therefore, this section lacks transferability to the whole evidence base.
Literacy, digital literacy and equity
Nijland et al. 114 considered the feasibility of their digital intervention and the barriers affecting it. They identified that patients underused or misused their digital application because of a lack of education. Health professionals also had concerns about patient equity of access and the exclusion of those without access to new technology.
The fit with existing services
Interventions requiring interaction with health professionals could meet barriers related to this factor. When an intervention also included an e-mail consultation if required, health professionals were unclear about regulations and felt that there was insufficient reimbursement for it, and applications could not be integrated with existing patient information systems or medical records. 114 The wider organisation had to be behind any initiative, for example the hospitals in which the ED was situated, otherwise there might be conflicting systems for health professionals to follow. 112
User-friendliness
Patients faced technical problems and unattractive web page layouts. 114 Health professionals also faced technical problems in terms of identifying software bugs and unclear features. 114
Not meeting needs
Patients had problems with a digital intervention. 114 They found that the information offered was not always relevant; the information provided by the digital medical encyclopaedia was too general to be useful; information in other parts of the system was too limited to be useful; self-care advice was insufficiently tailored to their personal needs; they could not always understand the information; and they struggled to understand medical terms used or to describe their problem to enter into the system. Health professionals using this intervention felt that patients still required contact with them rather than the intervention facilitating self-care. 114 If health professionals had to respond to a patient and offer e-mail advice, they found this time-consuming because responses had to be worded with care to prevent legal problems.
Sign-up from health professionals
If health professionals had to hand out information or follow a script, they might have their own views about the appropriateness of this for some types of patients or more generally. 112 This could be overcome if health professionals were very concerned about overcrowding in their ED. Furthermore, health professionals could sympathise with the anxiety of patients even though the symptoms they came with were not serious, so they were concerned about judging people too harshly.
Cost and cost-effectiveness
Fifteen of the 67 articles reported cost data in the results sections of the papers. 79–82,86,87,95,104,120,124,127,128,135,138 Thirteen of these studies were conducted in the USA, and two in the UK. 104,124
Eleven of these studies reported the results of formal analyses of the intervention: 10 studies reported findings in terms of cost savings81,86,95,104,120,124,127,128,135 and one study reported on return on investment. 138 Nine of the 11 studies were from the USA, and two were from the UK;104,124 five of the studies were conducted in primary care populations,95,104,124,135,138 four in community/other settings81,120,127,128 and two in emergency care. 86
All 10 studies reporting economic data found that their interventions generated substantial cost savings. 81,86,95,104,120,124,127,128,135 In terms of intervention types, different types were found to be cost-effective: person-delivered navigation;87 written and person-delivered navigation;86 written education alone;95 written and person-delivered education,81,120,127,135 including with the support of mass media;128 digital education alone;124 and digital self-triage. 104 One study of a type of written education alone also reported that return on investment was estimated to be twice as much as the savings from avoided visits. 138
Given the heterogeneity of settings, interventions and locations, it was not possible to perform any formal analysis of the cost data. It was also concerning that all the analyses showed cost savings. We were concerned about the desire of authors to promote their intervention as cost-saving. We were also concerned that these analyses did not always use credible effectiveness data, and we had rated many studies as having problems.
Another nine studies mentioned cost data in the papers’ discussion or conclusion sections:83,101,107,117,119,129,134,137,139 four studies were conducted in the USA;83,119,134,137 two in the UK,101,107 and one each in Canada,117 the Netherlands129 and Taiwan. 139 These calculations were not accompanied by methods and therefore are not considered in our synthesis.
Safety
Our PPI colleagues were concerned that promotion of patient decision-making about which symptoms were serious or not could lead to patients delaying help-seeking for serious health problems. Only eight of the included studies assessed safety as an explicit outcome or compared surrogate outcomes such as hospitalisation across study arms. The explicit safety assessments included instances when patients should have accessed a service, but did not do so on account of the intervention. For example, people may have believed incorrectly that their, or their child’s, complaint was non-urgent and should be managed using self-care, thus resulting in higher numbers of urgent admissions or severe illness in an intervention group. When assessed, no safety problems were identified. Hospitalisation rates tended to be similar: 2.7% for the intervention group versus 2.6% for controls (p = 0.96);92 3.5% for the intervention group versus 6.2% for the usual care group (p = 0.11). 98 In a RCT of digital self-triage for respiratory problems, there was no difference in hospitalisation rates between the arms in the trial at 12 months; indeed, the intervention group had a lower level (not statistically significant). 84 Sometimes articles reported the numbers of hospitalisations or adverse events, rather than rates. Again these tended not to show problems: three participants in the intervention group and four in the control group were subsequently admitted to hospital or observed in a paediatric assessment unit. 99 No adverse events were associated with the intervention in a RCT of an educational booklet in EDs. 89 Sometimes the intervention group was followed up, and again no problems were identified: a 3-year medical record review of children in the intervention group showed no evidence of serious problems that might be associated with delaying seeking treatment;135 there was no delay in seeking help for a cough that lasted more than3 weeks78 and a reduction in GP consultations for non-serious coughs was accompanied by an increase in consultations for coughs with alarming symptoms. 77 Other measures of safety included premature death (there was no sign of a link between premature death at 6 months and the interventions91) and breaking the rules of engaging with the intervention (there was some violation of rules, but not enough for the authors to be worried about139).
On the whole, any reduction in service use was perceived to be a success; there was usually no subanalysis to determine if some of that reduction was not appropriate.
Displacement
When we planned the systematic review, we were mindful of what we called ‘displacement’. This is when patients seek care at an alternative ED instead of self-caring. If use of that alternative service is not measured, it may look as if the intervention works when, in fact, it has merely replaced use of one ED with use of another. This is most relevant to interventions aiming to reduce the use of primary care, during which patients may attend the ED instead of the GP. It is also relevant to EDs when patients have access to a number of EDs but the intervention is used, and service use measured, in only one ED. This issue was rarely attended to in the 67 papers. The only attention paid to it was when researchers identified a limitation of their studies as measurement of ED use in a single hospital only.
Synthesis by type
Service use
We have summarised the proportions of articles showing a reduction in ED (Figure 3) or GP use (Figure 4) by type of intervention. The numbers in each intervention type are small, so it is not possible to say whether or not some types were more likely to show a reduction in service use. Although navigation tools look like they may be more likely to show reductions, there were a number of poor-quality studies in this type.
FIGURE 3.
Numbers of studies showing a reduction or no change in ED attendances, by type.
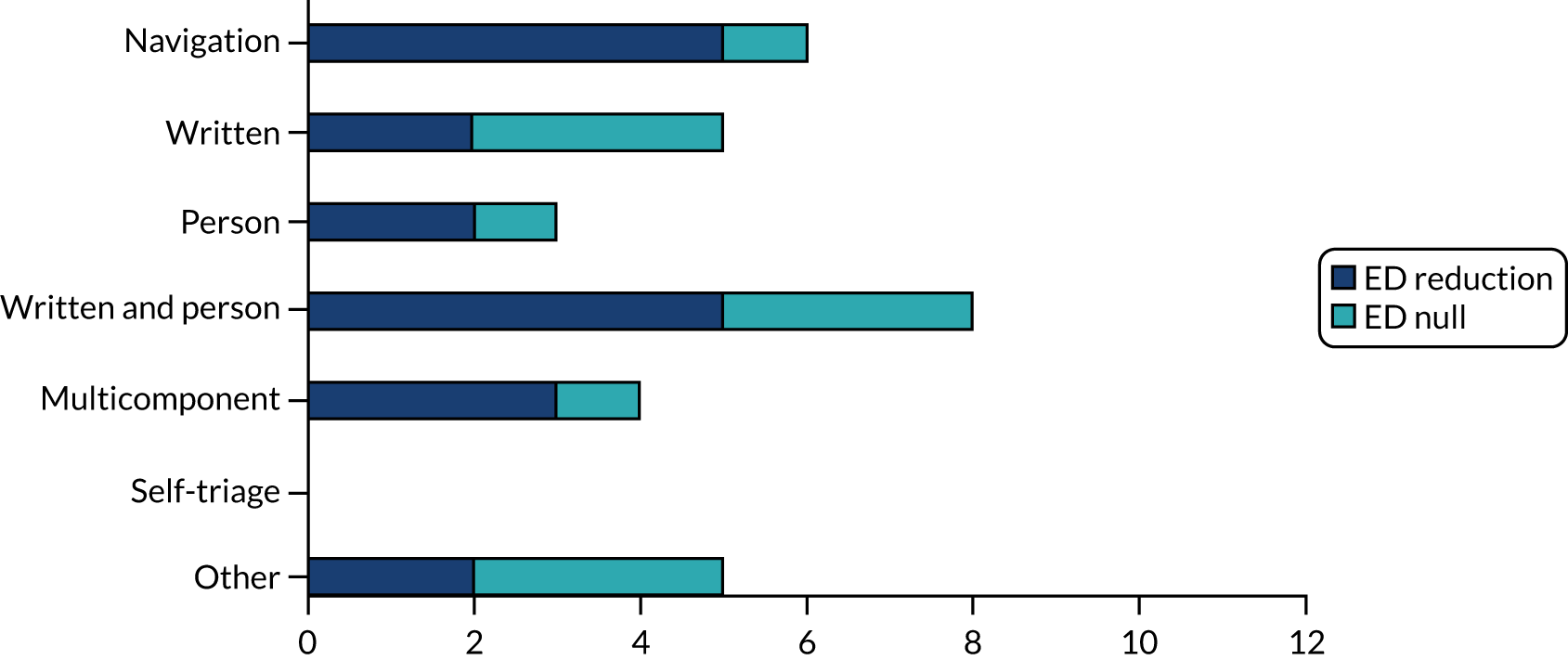
FIGURE 4.
Numbers of studies showing a reduction or no change in GP consultations, by type.
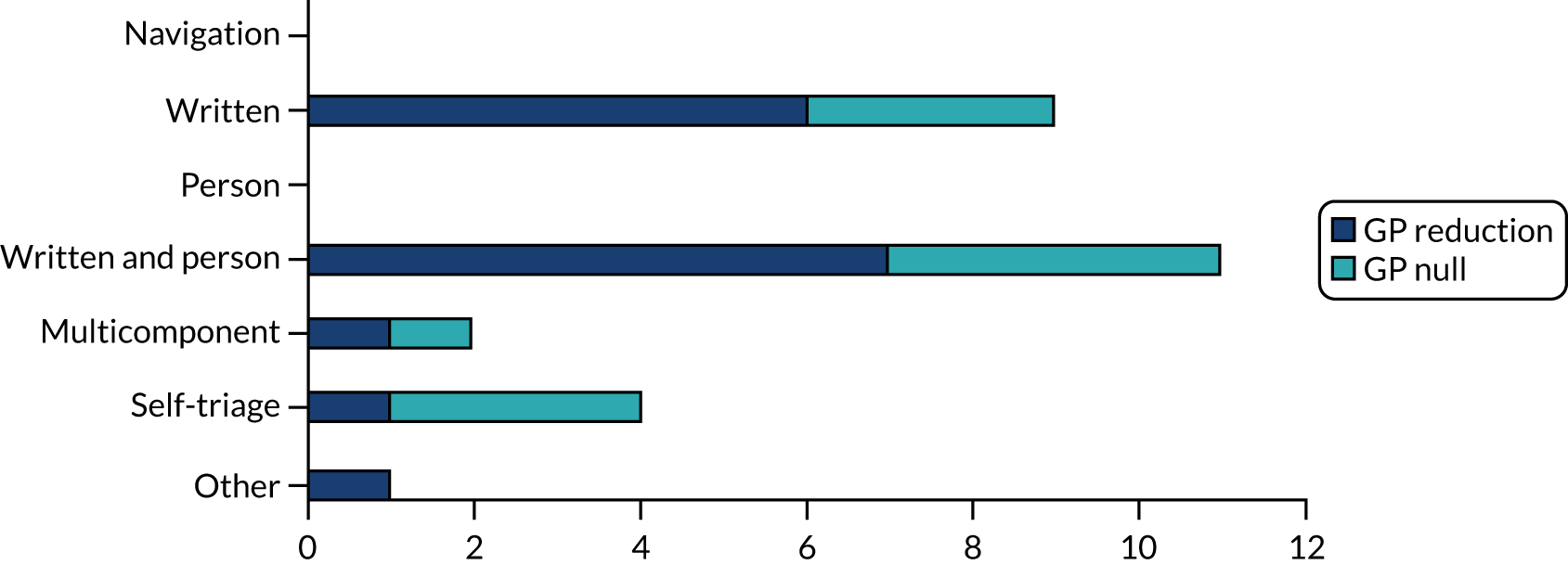
1. Navigation types (A.I, B.I and C.I)
Size and quality of the evidence base
Seven studies testing eight interventions aimed to guide people to the most appropriate service (including self-care) for their minor health problem. They included written navigation tools (A.1),91,110 person-delivered navigation tools (B.I),87,91,92,130 digital navigation tools (C.I)123 and a multicomponent written and person-delivered navigation tool (A.I and B.I). 86
The studies focused on interventions that persuaded patients to use primary care rather than EDs. All the studies were undertaken in the USA, where funding systems for health care (e.g. an insurance system) can save money directly if their patients use primary care rather than EDs. The studies mainly used strong designs for testing impact: either RCTs or controlled before-and-after studies. Only one study87 was rated as being of high quality using a formal assessment tool. We also had concerns about the quality of some studies in terms of the analyses undertaken,92,130 clerical errors potentially affecting the data collection,91 lack of intention-to-treat analyses91 and the potential that patients attended a different ED from the one being measured. 87 On a positive note, the studies measured service use using routine records, although they used different time periods for measurement.
Intervention description and mechanisms
These interventions tended to use the mechanisms of ‘raising awareness’ and ‘persuasion’. The person-delivered interventions took an active and targeted approach by communicating the message via ‘patient navigators’87 or health professionals91,92,130 to people who had used an ED for a minor health problem.
Impact on service use
In Table 5, ‘+’ indicates a statistically significant reduction in service use, ‘–’ indicates a null result and ‘±’ indicates that results were mixed. Five of the six articles measuring impact on EDs showed a reduction, although, in two studies,91,92 this was not a simple overall reduction. Racine et al. 92 showed no reduction overall in ED attendances, but then tested the data for types of service use, which showed a statistically significant reduction. Patel et al. 91 showed a reduction when they looked at subgroups, rather than for the sample overall. So strictly, a statistically significant reduction in ED attendances was found in three out of six studies. The studies that measured primary care use had an intention to increase use of this service because the aim of the intervention was to shift users from EDs to primary care. Given that increasing use of primary care was not a relevant aim of our study, we have not indicated that results were + or – in Table 5. There was some indication that different age groups might be persuaded using different delivery approaches: a postal approach for younger patients and a telephone approach for older patients. 91
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| A.I Written | |||||||
| Adesara et al.,110 USA | CBA study | Weak | Awareness, persuasion | 6 months | Records | All: (+) ED visits attributable to intervention patients – pre = 6.83%; during = 6.22%; post = 6.15%. Approximately 40 ED visits saved per month. Internal medicine clinic: pre = 1.34%; during = 1.69% (difference pre–during vs. intervention p < 0.001); post = 1.43% (difference pre–post vs. intervention p < 0.001) | |
| Patel et al.,91 USA | RCT with three arms | High risk of bias | Awareness, tailoring | 6 months | Records | All: (±) no change in the whole sample, but change in ED use differed by age group and intervention type, with reductions for older people getting a telephone call and younger people being mailed information. Telephone intervention vs. matched control outcome (model): 0.92 (0.77–1.10); p = 0.36 [≥ 65 years: 0.78 (0.62–0.99); p = 0.04]. Mail intervention vs. matched control outcome: 1.07 (0.92–1.23); p = 0.40 [< 65 years: 0.73 (0.55–0.98); p = 0.03] | All:
|
| B.I Person-delivered | |||||||
| Chande and Kimes,130 USA | RCT | High bias | Awareness, education, persuasion and tailoring | 12 months | Records, self-report | All: (–) ED – at study entry, 94 out of 102 in the intervention group and 87 out of 93 in the control group had made at least one visit to the ED (p = 0.79). At the 1-year follow-up, 84 out of 102 in the intervention group and 73 out of 93 in the control group had made at least one visit to the ED (p = 0.59). There was no significant difference in rates of use of the ED | All: at study entry, 95 out of 102 in the intervention group and 75 out of 93 in the control group had seen their PCP at least once (p = 0.59). At the 1-year follow-up, 81 out of 102 in the intervention group and 77 out of 93 in the control group made at least one visit to their PCP (p = 0.59); however, the total number of PCP visits by both groups increased by almost 50%. Although there was no difference between the control and intervention groups at the 1-year follow-up, the total increase in visits for both groups is significant (p < 0.001) |
| Minor: (–) at study entry, 55 out of 102 (54%) in the intervention group and 55 out of 93 (59%) in the control group had made two or more ED visits for minor illness in the preceding year. At the 1-year follow-up, 61 out of 102 (60%) in the intervention group and 57 out of 93 (61%) in the control group had made two or more ED visits for minor illness (p = 0.95) | |||||||
| Enard and Ganelin,87 USA | CBA study | Strong | Awareness, persuasion, tailoring | 12 months and 24 months | Records | All: (+) for people who did not use the ED frequently in the previous year, the mean number of primary care-related ED visits declined significantly in the corresponding post-observation period, compared with controls. The OR was 0.83 (95% CI 0.71 to 0.98) for people who had a baseline attendance of one or more visits at 12 months. At 24 months, this was 0.55 (95% CI 0.47 to 0.63) | |
| Racine et al.,92 USA | RCT | Some concerns | Awareness, persuasion | 12 months | Records | All: (±) both intervention and control groups were as likely to return to the PED after their initial PED visit (intervention, 38%; control, 39%; p = 0.26). But, looking at visits, the adjusted odds of returning to a PED rather than another service was 0.88 (95% CI 0.82 to 0.94). PED, n (%): 2145 (17.7) vs. 2329 (20.4); p < 0.001. Hospitalisation, n (%): 325 (2.7) vs. 302 (2.6); p = 0.96. Subspecialty, n (%): 2744 (22.6) vs. 2220 (19.5); p < 0.001 |
|
| A.I and B.I | |||||||
| Davis et al.,86 USA | BA study | Moderate/weak | Awareness, persuasion | 3 and 12 months | Records | All: (+) 62 fewer PED visits than the same 3 months the previous year. The numbers continued to decrease at 12 months: a decrease of 284 in the total number of PED visits (29.8%). In 2015, the clinic was at 71.5 visits per 100 persons per year. Following interventions, in 2017, the rate changed to 41.9 visits per 100 persons per year | All: the proportions of paediatric patients using the (GP) clinic instead of the ED also shifted from 2015 to 2017: 47.5% (64 patients) used the clinic for upper respiratory infections in 2015; in 2017, that number increased to 78.2% (97 patients) who were seen in the clinic as opposed to the ED (p < 0.0001) |
| Minor: (±) 41.1% decrease (from n = 82 to n = 48) in level-3 (urgent) visits to the ED and a 16.7% decrease (from n = 120 to n = 100) in level-4 (less urgent) visits in the initial 3 months. These changes were maintained when examining the data 1 year later. The number of level-5 (not acute) visits remained unchanged | Minor: Walk-in clinic visits during this time continued to increase. Similar shifts were seen in fever and otitis media; however, the sample size was not great enough to draw significant conclusions | ||||||
Other outcomes
Only one weak prospective cohort study of a navigation tool reported any findings on users’ satisfaction with the intervention: 90% of the respondents reported that they were satisfied with the triage website Strategy for Off-site Rapid Triage (SORT) for Kids. 123 The other six studies of this type reported no relevant outcome data on satisfaction. 86,87,91,92,110,130
Current examples in the NHS
The NHS in England makes use of navigation tools routinely to make the general public aware of the range of services they can use, and in what circumstances, so that they use EDs only when they need to. An example of this is the Choose Well page on the Sheffield Children’s NHS Foundation Trust website: www.sheffieldchildrens.nhs.uk/patients-and-parents/choose-well/ (accessed 7 September 2021). This type of information is also disseminated by social media. For example, Sheffield Teaching Hospitals NHS Foundation Trust tweeted a navigation tool in July 2021 under the title of ‘Injured or unwell?’ (Figure 5). These navigation tools present different service options and when to use them. They can use the mechanism of ‘positive persuasion’ in terms of the promise of quicker advice if people use alternatives to EDs. We also found an example of a person-delivered navigation process (with a leaflet) to persuade users of an urgent care centre with minor problems to look for alternative sources of care in their future health-seeking. 144 There are also videos available through YouTube (YouTube, LLC, San Bruno, CA, USA) that make people aware of new services in primary care that might reduce demand for face-to-face care. An example is produced by West Yorkshire Health and Care Partnership,145 which includes the use of British Sign Language and animation to facilitate accessibility.
FIGURE 5.
Sheffield Teaching Hospitals NHS Foundation Trust ‘navigation tool’ tweet.

Conclusion and relevance to English NHS
The evidence base identified that there was potential that people could be persuaded to use their primary care provider, rather than an ED. However, the quality of the studies was not high and the evidence base was likely to be context specific because it was generated in the USA where there are incentives to make cost savings within a health insurance agency context. In terms of relevance to England, the navigation tools in use in England are different from those used in the evidence base. Tools in England mainly attempt to disseminate information to potential service users, rather than actively communicate a message to a targeted group of recent ED users. The NHS tools use a light-touch persuasion technique, compared with the persuasive techniques used in the evidence base. So the evidence base is not relevant to the NHS tools in routine use. We would recommend that consideration is given to identifying how these NHS tools could be used in a more proactive and targeted way in England, and that this approach is evaluated.
Box 1 provides a plain English summary of this section.
Some tools tried to persuade people to use their GP rather than go to A&E. Some of them worked. But the quality of the studies was not high. And the studies were done in the USA, where they have health insurance. This is different from the UK. The tools were different from ones used in the UK in other ways. They used nurses to persuade people who had gone to A&E with a small problem to go to their GP next time. In the UK we tend to have information on hospital websites and this is aimed at everyone. So the studies we found were not relevant to the NHS at the moment. We wonder what would happen if the NHS tried to target the information on their websites to the people who need it the most. Then we could test if this works.
A&E, accident and emergency.
2. Written information about how to care for minor ailments in leaflets, booklets, books and websites (A.II and C.II)
Size and quality of the evidence base
Seventeen articles focused on written education in paper format given at a specific time when patients sought care for a minor health problem,89,100,101,107,109,119 paper format given at a general time95–97,105,106,117,138 and a website given at a specific136 or general time. 90,124,129 Fourteen of these measured impact on service use. These are presented in Table 6 in the three groups of articles ‘at a specific time’, ‘at a general time’ and ‘digital’. There was one pilot study so this was not powered to detect a difference. Of the articles measuring impact, seven were undertaken in the UK, five in the USA, one in Denmark and one in the Netherlands. The study designs were strong, mainly RCTs; in fact, all the studies used controls. All the studies used records rather than self-report. The formal quality assessment identified only one high-quality study. Our more informal assessment identified some concerns with papers: limited results available because yet to be formally published,89 low statistical power,119 or poor analysis or presentation of the findings. 95,97,105,107,138 We felt that, given the difficulties of undertaking research in this area, and the harshness of the formal quality assessment, we identified some good-quality studies with strong designs undertaken in the UK. 84,89,96,100,101 We also considered the controlled before-and-after study undertaken in the Netherlands, which made use of a national database on GP consultations to measure outcomes, to be highly relevant to the UK and of good quality. 129
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| Paper based, specific time | |||||||
| Holden,89 UK | RCT | Some concerns | Education | 11 months | Records | Minor: (–) average number of non-urgent attendances (including reattendances):– intervention, mean 1.3 (SD 0.8); control, 1.3 (SD 0.7). Reattendance rate: intervention, 23.2%; control, 24.6% | |
| Macfarlane et al.,101 UK | RCT | High risk of bias | Education | 1 month | GP-recorded reconsultations | All: (+) for the whole group, patients who received the leaflet had significantly fewer reconsultations for the same symptoms over the following month (14.9%) than those who did not receive a leaflet (21.4%); (OR 1.56, 95% CI 1.11 to 2.19; p = 0.007). For the 723 patients who were treated with antibiotics, significantly fewer patients receiving a leaflet reconsulted (60/369, 16%), than those who did not receive the leaflet (81/354, 23%) (OR 1.53, 95% CI 1.03 to 2.26; p = 0.02) | |
| Macfarlane et al.,100 UK | RCT | High risk of bias | Education | 1 month | Records | All: (–) the reconsultation rates were similar for all patients: leaflet, 11/104; no leaflet, 14/105 | |
| Platts et al.,107 UK | RCT | High risk of bias | Education | 12 months | Records | All: (–) the differences between the groups in the number of visits to EDs and in the numbers of telephone calls, home visits and nurse clinic visits were small and not statistically significant | All: (–) mean annual consultation rates, including routine GP consultations and emergency consultations with a GP or nurse practitioner, for the 12-month period of the study, classified by age group, sex and book group, did not, in general, differ between the three arms of the study. Use of NHS Direct telephone service: a total of 160 participants made an average of 1.19 calls to the NHS Direct telephone service. In a multivariable logistic regression model, the odds of calling NHS Direct were nearly doubled for being allocated to the NHS Direct group rather than to control or to the self-care book group (p < 0.01) |
| Steelman et al.,119 USA | Non-RCT | Weak | Education | 4 months | Records | Minor: (–) intervention vs. control: appropriate ED and clinic visits: 5 vs. 9; inappropriate visits: 6 vs. 8; p > 0.99 | |
| Paper based, general time | |||||||
| Elsenhans et al.,138 USA | Non-RCT | Moderate/weak | Education | 4 months | Records |
|
|
| Hansen,105 Denmark | RCT | High risk of bias | Education | 6 months | Records | All: (+) families that received the booklet reported significantly more self-teatments, had significantly fewer consultations and had significantly fewer consultations in which worry was the main reason. Mean number of patient-initiated consultations: intervention 0.288 (2SD 0.3–0.2) vs. control 0.426 (2SD 0.5–0.4). For home visits: intervention 0.098 (2SD 0.1–0.7) vs. control 0.195 (2SD 0.2–0.2) (no p-values given). Worry was a reason for consultation: intervention 19% vs. control 31% (p = 0.0075). GP assessed appropriateness of consultation: intervention 88% vs. control 81% | |
| Heaney et al.,96 UK | RCT | High risk of bias | Education | 1 year pre intervention, 1 year post intervention | Records |
|
|
| Little et al.,106 UK | RCT | High risk of bias | Education | 12 months | Records | Minor: (+) compared with the control group, fewer patients in the booklet and summary card groups attended frequently with minor illnesses – booklet: OR 0.81 (95% CI 0.67 to 0.99; p = 0.043); summary card: OR 0.83 (95% CI 0. 27 to 0.96; p = 0.011) | |
| Usherwood,97 UK | RCT | High risk of bias | Education | 12 months | Contact record completed by practice staff | Minor: (±) although there was no significant difference between booklet and control groups for daytime health centre contacts, there were differences for daytime home visits and for contacts out of hours. For daytime home visits, the mean frequency of initial contacts was substantially lower in the booklet group than in the control group for households with one or two children. For out-of-hours contacts for booklet symptoms, the mean frequencies of initial contacts were higher in the booklet group than in the control group for all sizes of household | |
| Yoffe et al.,95 USA | CBA study | Weak/moderate |
|
18 months | Records | Minor: (+) there was a dramatic drop in ED use rates by children seen in the clinic in which the booklet was distributed. The reductions ranged from 55% to 81%, compared with the same month of the previous year and compared with other geographies. Compared with the control groups, the decline in use rates by intervention patients was statistically significant (p < 0.001) | |
| Digital | |||||||
| Ladley et al.,90 USA | RCT | Low risk of bias | Education | 12 months | Records |
|
|
| Lepley et al.,136 USA | RCT (pilot) | High risk of bias | Education | 6 months | Records, self-report | All: (–) record review – no significant difference in rate of ED visits between the application group and the control group (14% more visits in the application group; IRR 1.14, 95% CI 0.56 to 2.34), between the book group and the control group (22% fewer visits in the application group; IRR 0.78, 95% CI 0.34 to 1.74) or between the book and application group and the control group (40% fewer visits in the application group; IRR 0.60, 95% CI 0.25 to 1.42) | |
| Spoelman et al.,129 the Netherlands | CBA study | Moderate | Education | 3 years | Records |
|
|
Intervention description and mechanisms
Leaflets or booklets varied in size and in the range of minor conditions addressed. They were sometimes endorsed by health professionals within a slide presentation,119 a covering letter if a booklet was sent by post105,106,138 or by personally handing the leaflet/booklet to the patient. 95,101,107 The role of the health professionals was different from the role taken for person-delivered education interventions (B.II, discussed in later section) in that there was no discussion with patients of the content of the booklet/leaflet. In one study, patients had the option of calling a doctor with questions, but we did not consider this to be person-delivered because it was optional. 119 In another study, the intervention was a leaflet and verbal advice from the doctor, compared with verbal advice as the control, so the intervention being tested was a leaflet. 100 The common mechanism was ‘education’.
Impact on service use
In Table 6, (+) indicates a statistically significant reduction in service use, (–) indicates a null result and (±) indicates that results were mixed. Pilot studies are indicated by italics. Five articles of paper-based interventions measured the impact on Eds, and two of these identified a reduction. 90,95 We had concerns about the quality of one of these positive studies, and the formal quality assessment rated the other as having a low risk of bias, so results were not determined by the quality of the research. Of the null studies, one was very small119 and one was a good-quality UK study (according to our informal assessment), involving posting a leaflet to ED non-urgent users and measuring further attendances. 89 Again, research quality did not explain null results.
Of the nine studies measuring impact of written interventions on GP consultation rates, six showed a reduction. The two good-quality UK RCTs (based on our informal assessment) had conflicting results. 96,106 One study’s positive result relied on a subgroup analysis. 97 The single website intervention measuring GP consultations129 identified a reduction in GP consultations in the population for symptoms that were frequently accessed on the website, compared with consultations for conditions not frequently accessed on the website.
Other outcomes
Six articles reported no relevant outcome data on satisfaction. 89,95,96,100,101,129 Eleven of the 17 articles reported one or more relevant outcomes (Table 7). Seven of the 17 articles reported findings on users’ satisfaction with the intervention. In all seven articles, users reported being satisfied or very satisfied with the intervention, regardless of whether the intervention was aimed at general populations,97,106,138 aimed at a specific group109 or was web based. 90,124,136 However, in some cases, participants might have been satisfied with the intervention, but also satisfied with the control intervention,109 or expressed preferences for one format of the intervention over another. 136 Six of these seven articles were assessed either as being weak (two non-RCTs) or at high risk of bias (four RCTs); only one RCT was judged to be at low risk of bias. 90
| Study | Design | Quality | Mechanisms | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Paper based, specific | ||||||
| Platts et al.,107 UK | RCT | High risk of bias | Education | 3 and 12 months | Questionnaire |
|
| Steelman et al.,119 USA | Non-RCT | Weak | Education | Baseline and 2 and 4 months | Self-report instrument | (+) Knowledge: evaluation of knowledge on fever – average number of incorrect responses:
|
| Wood et al.,109 USA | CBA study | Weak | Education | 2 months | 5-question survey |
|
| Paper based, general | ||||||
| Elsenhans et al.,138 USA | Non-RCT | Moderate/weak | Education | 6 months | Telephone survey | (+) Satisfaction: there was general enthusiasm among members and staff and the majority recommended the continued use of self-care manual; no dissatisfaction was expressed |
| Hansen,105 Denmark | RCT | High risk of bias | Education | 6 months | Self-report instrument (survey and interview) | (+) Enablement: self-management of episodes of illness – 51% in the intervention group and 36% in the control group reported some kind of self-treatment. This difference was statistically significant |
| Little et al.,106 UK | RCT | High risk of bias | Education | 12 months | Survey | (+) Satisfaction: most respondents could remember receiving a leaflet or booklet (booklet 85%, card 70%, control 52%; p < 0.001) and found them useful (booklet 81%, card 78%, control 62%; p < 0.001) |
| Mullett and Hills,117 Canada | Prospective cohort study | Weak | Education | 12 months | Diary | Helpfulness: examples from patient diaries describing how the handbook helped them make decisions and self-care, and also what was missing from the handbook |
| Usherwood,97 UK | RCT | High risk of bias | Education | 12 months | Questionnaire | (+) Satisfaction: perceived usefulness of the booklet – frequency of response:
|
| Digital | ||||||
| Ladley et al.,90 USA | RCT | Low risk of bias | Education | 12 months | Survey | (+) Enablement: high levels of satisfaction and engagement at 12-month survey in intervention group: 91% (75/79 who completed the survey) felt more comfortable making decisions about when to take their baby to the ED |
| Lepley et al.,136 USA | RCT (pilot) | High risk of bias | Education | 6 months | Telephone survey | (+) Satisfaction: modified intention to treat – combined app (n = 37) vs. combined book (n = 37) vs. control (n = 23): |
(–) Satisfaction: per-protocol analysis – combined app (n = 20), combined book (n = 37), combined control (n = 23):
|
||||||
| Authors note in the discussion that the mHealth app used a lot of medical jargon and was not good for people with lower health literacy levels | ||||||
| Murray et al.,124 UK | Survey | Weak | Education | At the time of using the website or visiting the GP | Survey | (+) Satisfaction:
|
(+) Knowledge: online sample (n = 1559) – patients who agree/strongly agree that use of NHS Choices for their GP appointments means:
|
||||||
Three studies of paper-based formats reported improved knowledge and understanding among patients. 107,109,119 The same finding was reported in a study of an NHS website,124 and improved confidence was found among users of a general paper-based intervention. 105
People changed their minds about the actions they would take after using one of the interventions. 107
Current examples in the NHS
The NHS in the UK has a number of sources of web-based educational materials about how to care for minor ailments and when to seek health care. The NHS website [www.nhs.uk (accessed 31 August 2022)] has a section titled ‘Health A to Z’ where a minor symptom such as ‘sore throat’ can be searched for and self-care advice is offered in writing and a short video, along with the role a pharmacist could play. Figure 6 shows a screenshot of a page (accessed 7 September 2021). It is aimed at everyone. People find it by searching the internet.
FIGURE 6.
NHS website screenshot. Contains public sector information licensed under the Open Government Licence v3.0.
There are also regional versions of web-based education to help parents of young children to self-care for minor ailments, advertised under the banner of ‘Healthier Together’. For example, a version of Healthier Together146 is available for people in the South Yorkshire and Bassetlaw area (Figure 7). The website link is emailed directly to parents and addresses common illnesses and conditions that affect children and young people aged 0–18 including rashes, fever, coughs, asthma, sickness, earache, conjunctivitis, head injuries, and limps. It offers a traffic light system of seriousness from ‘minor’ to ‘urgent’. A Consultant Paediatrician from local highly regarded children’s hospital signs the letter.
FIGURE 7.
Healthier Together screenshot.
Another example of a regional resource for parents is The Little Orange Book68 produced by Newcastle and Gateshead CCG for parents with young children (Figure 8).
FIGURE 8.
The Little Orange Book screenshot.
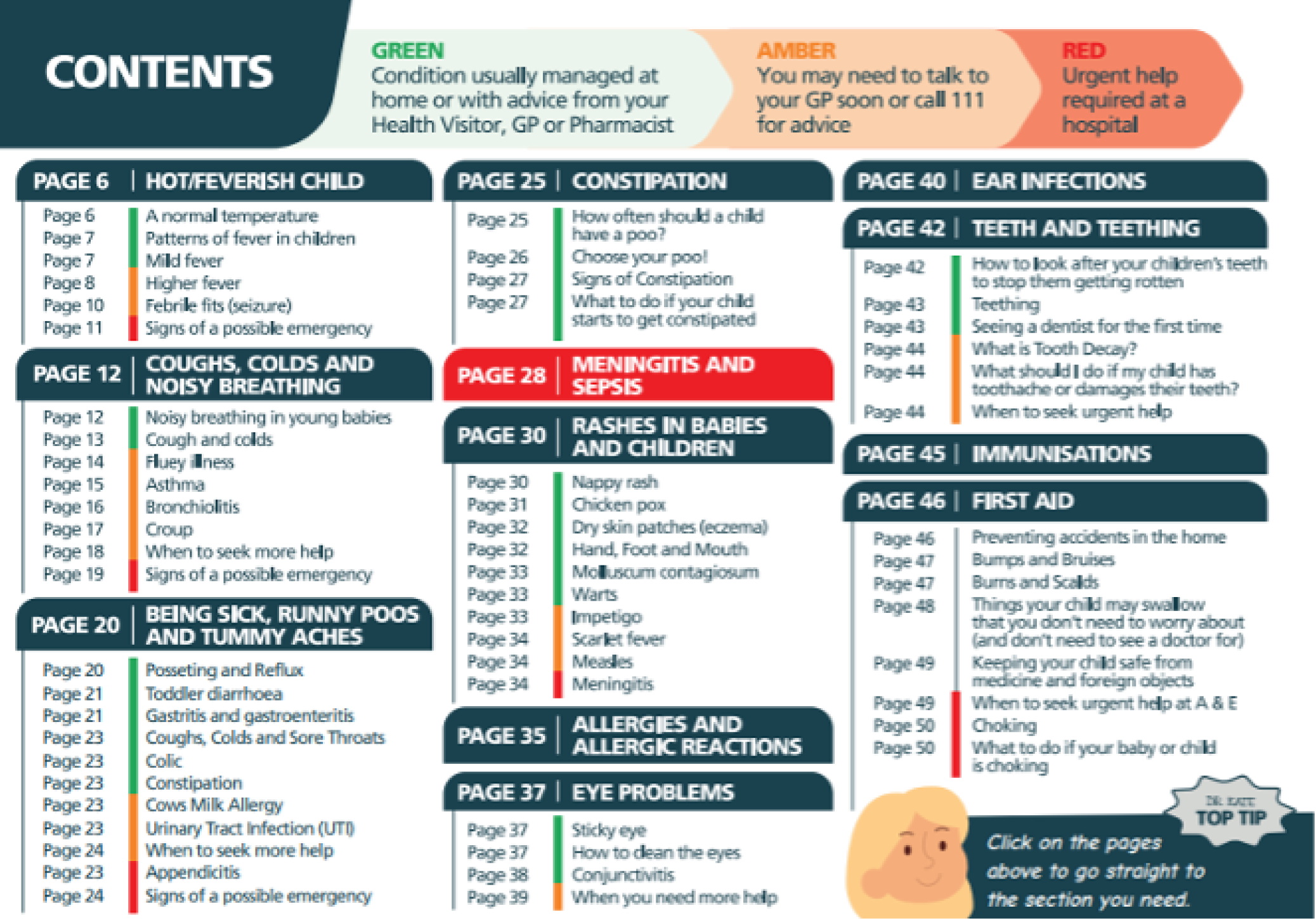
Conclusions and relevance to the NHS
There is a reasonable size of evidence base about sending booklets or leaflets to patients, but limited evidence about digitally available written information. There is a reasonable amount of evidence from the UK and the rest of Europe. The outcome of interest measured was more likely to be impact on GP consultations than ED attendances. Unfortunately, the results of different studies were not consistent. There was no apparent reason why some good-quality studies showed reductions in service use and others not. However, there were enough positive studies to consider this type of intervention as having potential. Given the availability of digital educational information in the NHS currently, it may be beneficial to undertake a high-quality evaluation of such information, specifically considering how any information is disseminated to relevant people. Our PPI colleagues were keen that ways of educating people other than through digital means should also be used because of a lack of digital health literacy in the UK population and the lack of access to technology. Some regional educational information is also available in paper format, for example The Little Orange Book. 68
Box 2 provides a plain English summary of this section.
Booklets, leaflets and websites that tell people how to look after minor problems have been tested. People find them helpful and think that they know more about what to do when they are ill. But some research says they reduce the use of a GP or A&E and some research says they do not. They have potential, but need to be tested more.
A&E, accident and emergency.
3. Person-delivered education (B.II, and multicomponent B.I and B.II)
Size and quality of the evidence base
Three interventions focused on a person delivering education about managing minor health problems,88,103,126 and two had an additional component of a navigation tool. 93,137 They are presented in Table 8 in that order, alphabetically for each group. All the studies were undertaken in the USA. Only one study was a full RCT. Two studies were pilots, and so did not have statistical power to detect changes in service use. 88,103 None of the studies was assessed as being of good quality in the formal assessment. In addition, we were concerned about the analysis or presentation of results for one study,137 and two studies relied on self-report. 103,126 So the evidence base was small and poor for this type of intervention.
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| B.II only | |||||||
| Fieldston et al.,88 USA | BA pilot | Moderate/weak | Education, empowerment | 6 months | Records | All: (–) the mean number of ED visits for the index child reduced following the intervention, although the difference was not significant: 0.67 mean ED visits before, and 0.58 after (p = NS) | All: (–) the mean number of ambulatory visits for the index child reduced following the intervention, although the difference was not significant: 2.7 before vs. 2.3 after (NS). After-hours telephone calls to the PCP rose significantly from 0.33 per patient to 1.46 per patient ( p = 0.047) |
| O’Neill-Murphy et al.,103 USA | RCT pilot | High risk of bias | Education, empowerment | 2 weeks and 8 weeks | Self-report | All: (–) only one child, in the control group, had visited the ED in the time period, even though 30% (n = 11) of the control and 43% (n = 10) of the intervention had a fever in the previous 2 weeks | |
| Stockwell et al.,126 USA | RCT | High risk of bias | Awareness, education, empowerment | 5 months | Self-report | All: (+) children < 4 years of age in intervention families had fewer PED visits per illness episode than the standard curriculum group [18/205 (8.8%) vs. 29/191 (15.2%), respectively; p = 0.049]. The majority of this difference was for children aged 6–48 months [intervention families 16/194 (8.2%) vs. standard curriculum group 29/185 (15.7%) PED visits per illness episode; p = 0.025]. The relationship between intervention status and fewer PED visits was also significant on the family level (p = 0.03). For intervention families attending all three classes, 6.2% of illness episodes resulted in a PED visit for a child aged 6–48 months (5/80); for those attending two classes, this was 7.8% (8/102), and for those attending zero or one class, it was 25% (3/12) (p = 0.087) | |
| B.I and B.II | |||||||
| DeSalvo et al.,137 USA | Non-RCT | Weak | Awareness, education, persuasion, tailoring | 3 and 6 months | Records, self-report | All: (–) these patients had an average of 0.16 emergency room visits per patient in the 3 months subsequent to the index visit. In contrast, there were 0.29 subsequent visits per patient in the control group (p < 0.01). By the end of the first 3 months, the difference had disappeared (intervention 0.32 vs. control 0.28; p = 0.14). The addition of a social worker to the team in the second phase did not result in a change in emergency room use (0.3 visits per patient in both the intervention and control groups; p = 0.5) | |
| Shnowske et al.,93 USA | Retrospective cohort study | Moderate/weak | Awareness, education, tailoring | 3 months | Records |
|
All: mean number of PCP visits per month before was 0.31 ± 0.64, and after assignment was 0.28 ± 0.68 (p = 0.30). Had expected to see an increase |
Intervention description and mechanisms
The interventions were delivered by nurses88,137 or community health workers126 and varied in terms of length of time spent on training patients and the number of minor illnesses addressed. For example, a paediatric ED nurse delivered a 90-minute training session to parents,88 and community health workers gave three 90-minute training sessions on minor illness. 126 The mechanisms included both education and empowerment, as patients were trained in self-management.
Impact on service use
In Table 8, (+) indicates a statistically significant reduction in service use, (–) indicates a null result, and (±) indicates that results were mixed. Pilot studies are indicated by italics. Removing the pilot studies, three studies measured impact on EDs and two of these showed a reduction in use. Only one full study measured impact on GP consultations; they expected an increase because they aimed to shift care from EDs.
Other outcomes
One RCT that was judged to be at high risk of bias, evaluating person-delivered education, reported high levels of satisfaction with the upper respiratory infection intervention. 126 Two studies judged to be weak or at high risk of bias reported improved knowledge scores following the intervention,88,126 but a third trial, also at high risk of bias, found that the intervention did not improve participants’ confidence when faced with fever in a child: anxiety was reduced more in the control group. 103 One study of this type reported no relevant outcome data on satisfaction or intentions at all (Table 9). 137
| Study | Design | Quality | Mechanisms | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Fieldston et al.,88 USA | BA pilot | Moderate/weak | Education, empowerment | 6 months | Knowledge tests | (+) Knowledge: the intervention increased knowledge as measured by performance on the 19-item evaluation questionnaire, with mean scores increasing from 55% in the pre-intervention assessment to 77% (p < 0.001) immediately following the intervention. All three content areas (colds, fever and trauma) saw increase in knowledge, comparing the pre-intervention and post-intervention test results. Among the 20 participants, the mean score on the follow-up test declined from the value immediately after intervention (79% for those 20 participants to 71%; p = 0.031), but remained higher than before the intervention (61%; p = 0.015). For the same group, at follow-up, the mean scores for specific content areas were not significantly different from post-intervention scores, except for trauma, in a negative direction (74–62%; p = 0.044) |
| O’Neill-Murphy et al.,103 USA | RCT pilot | High risk of bias | Education, empowerment | 2 weeks and 8 weeks | Telephone interview | (–) Anxiety levels: > 40% of parents in each group reported that they had moderate to high levels of anxiety related to their child’s fever on arrival to the ED. After either fever education programme, parents in both groups reported reduced levels of fever anxiety: control group, 82%; intervention group, 85%. At the 2-week follow-up, parents in both groups reported that they felt less anxious when their child has a fever (86% of the control group and 50% of the intervention group) |
| Stockwell et al.,126 USA | RCT | High risk of bias | Awareness, education, empowerment | 5 months | Knowledge–Attitudes instrument |
|
Current examples in the NHS
We are aware that multiple types of health professional in the NHS educate patients informally about managing minor ailments when patients attend for care for that ailment, for example GPs, health visitors and pharmacists. We could find no examples of health professionals or trainers routinely offering formal education in managing minor health problems in the UK. The NHS has ‘care navigators’ who work in general practice and guide patients to the right clinician within a practice, and offer support for long-term conditions and social support. There are also social prescribers in primary care or volunteers who may offer some education and navigation.
Conclusions and relevance to the NHS
The evidence base for person-delivered education was small, context specific (USA only) and had some underpowered pilot studies, so few conclusions can be drawn. Although the NHS may have services similar to this type of intervention, we feel that there are no routinely available interventions currently in the NHS. The NHS would have to introduce this type of intervention and evaluate it. The feasibility of such an initiative delivered by health professionals is doubtful in times of staff shortage, and costs are likely to be prohibitive. Our PPI panel wondered about the use of volunteers to offer training, but also pointed out that patients need to trust the expertise of any trainers.
Box 3 provides a plain English summary of this section.
There was not much research on doctors or nurses educating patients about minor problems. The research was done in the USA. It may not be possible to use it in the UK because there is a shortage of doctors and nurses.
4. Combination of written education and person-delivered education (A.II and B.II)
Size and quality of the evidence base
Seventeen articles (15 studies) assessed leaflets/booklets and an interactive session with a person to educate people about minor health problems (Table 10). Ten were offered at a specific time in a patient’s care75–78,83,85,99,102,112,131 and seven at a general time. 81,82,120,121,127,134,135 They are presented in Table 10 in alphabetical order within these two groups. The evidence base for interventions given at a specific time was largely generated in Europe, whereas interventions offered at a general time were largely undertaken in the USA. There were seven RCTs and four controlled before-and-after studies that measured impact on service use. The formal quality assessment showed a mix of medium- to poor-quality studies. Seven articles relied on self-report and/or we had concerns about quality in terms of large loss to follow-up,83,127 the control group being very different from the intervention group,75 poor analysis with reliance on subgroup analysis78 or very short follow-up. 131
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| Specific | |||||||
| Chande et al.,85 USA | RCT | High risk of bias |
|
6 months | Records |
|
|
| de Bont et al.,102 the Netherlands | Cluster RCT | Some concerns |
|
|
Records | Minor: (–) reconsultation with OOH service within 2 weeks: usual care group (N = 13,410): n = 861 (5.5%); access to booklet group (N = 11,945): n = 741 (5.4%); access to booklet, OR 0.95 (95% CI 0.83 to 1.09). Reconsultation with OOH service in 6 months: OR 0.99 (95% CI 0.84 to 1.18) | |
| Francis et al.,99 UK | RCT | Some concerns |
|
2 weeks | Self-report | Minor: (–) there was no significant difference between the intervention and control groups in the odds of reconsulting in primary care during the 2 weeks after registration. Primary care reconsultation for same illness episode within the first 2 weeks: intervention 33/256 (12.9%) vs. control 44/272 (16.2%); OR 0.75 (95% CI 0.41 to 1.38). There was no significant intervention effect when telephone consultations were counted as reconsultations along with face-to-face primary care consultations (OR 0.81, 95% CI 0.47 to 1.42), or when consultations at EDs were included along with primary care consultations (OR 0.85, 95% CI 0.48 to 1.51) | |
| Herman et al.,83 USA | BA study | Weak | Education | 6 months | Self-report | All: (+) visited the ED – 73% pre vs. 43% post, p < 0.0001; visited the ED more than once: 36% pre vs. 26% post, p = 0.19 | |
| Plass et al.,75 the Netherlands | CBA study | Moderate |
|
24 months | Records | Minor: (+) intervention group – a significant decrease in self-reported care-seeking behaviour concerning minor ailments and self-limiting health problems (p < 0.001). At baseline, the participants reported that, during the previous 6 months, they had consulted their GP 3.0 (SD 2.2) times because of 4.9 (SD 2.1) different minor illnesses. Six months later, they reported that they had consulted their GP 2.1 (SD 2.0) times for 5.1 (SD 3.2) different minor illnesses. One year after the intervention, they reported 1.7 (SD 1.8) consultations for 5.3 (SD 2.7) different minor illnesses. Control group: the number of consultations for minor illnesses was, on average, 2.4 (SD 2.3) for 5.4 (SD 3.7) different minor illnesses | |
| Rutten et al.,77 the Netherlands | RCT | High risk of bias | Education | 12 months | Not clear | All: (+) in both groups, the consulting behaviour changed. In the experimental practices, the GP was confronted less often with everyday cough (16 before vs. 11 after, compared with 28 before vs. 34 after in control practices) and more often with alarming symptoms (31 before vs. 47 after, compared with 16 before vs.19 after in control practices; p < 0.05) | |
| Sustersic et al.,131 France | RCT | Some concerns | Education | 2 weeks | Self-report | Minor: (+) 23.4% consulted for the same symptoms in the households of the intervention group, compared with 56.2% in the control group (p < 0.01) | |
| General | |||||||
| Bertakis,134 USA | RCT | High risk of bias |
|
12 months | Records | Minor: (–) appropriate visits: 0.2 ± 1.1 vs. 0.03 ± 0.9; p = 0.095. Appropriate visits: 75.3% ± 40.7% control vs. 84% ± 35.2% intervention; p = 0.072 | Minor: (+) appropriate visits: 97.6% ± 11.2% control vs. 99.5% ± 4.8% intervention; p = 0.016 |
| Herman and Mayer,82 USA | CBA pilot | Weak |
|
6 months | Self-report | All: (+) 32 fewer visits to the ED (p < 0.01) | All: (+) visits to doctor or clinic – post intervention, there were 161 fewer visits to the doctor or clinic (p < 0.01) and 67 fewer calls to the doctor (p < 0.03) |
| Herman and Jackson,81 USA | BA | Weak |
|
6 months | Self-report | All: (+) number of visits decreased from 0.79 per year to 0.33 i.e. by 58% (95% CI¼51%–66%) | All: (+) the pre-training mean number of clinic visits per child was 3.69 per year (0.3072 per child per month). The post-training mean was 2.1922 per year (0.1851 per child per month), showing a reduction of 1.47 visits per child per year (p < 0.001). Tracking survey data showed that doctor or clinic visits decreased by 42% (95% CI 33% to 46%) |
| McWilliams et al.,135 USA | CBA study | Moderate |
|
12 months | Records |
|
Minor: (–) 28% decrease in primary care visits for ear pain in the intervention sites [from 762 (1249) to 550 (1064) visits], compared with no change in control sites [from 667 (1491) to 639 (1269), 4% decrease], but after regression models, no change (p = 0.14) |
| Powell,127 USA | Prospective cohort study | Weak | Education | 5 months | Self-report | All: (+) reduced ED visits by 52 | All: (+) reduced GP visits by 126 |
| Steinweg et al.,120 USA | Survey | Weak |
|
6 months | Self-report | Minor: (+) a total of 181 ED visits avoided, with 39.8% of the respondents indicating that they avoided at least one visit | Minor: (+) 72% of the respondents avoided at least one clinic visit. A total of 423 clinic visits were avoided during the 6-month study period |
| White et al.,121 UK | CBA study | Moderate |
|
6 months | Records | All: (–) no statistically significant changes were seen in ED use when comparing the intervention group with the comparison (OR 1.64, 95% CI 0.84 to 3.32; p = 0.157), or in use of NHS Direct (OR 1.36, 95% CI 0.88 to 2.11; p = 0.169) | All: (–) the intervention did not make a detectable difference to the number of consultations with GPs or other PHCPs in the follow-up period. Expected number of PHCP consultations for a person in the intervention group was 1.17 times that of their counterpart in the comparison group (95% CI 0.93 to 1.46; p = 0.182). The proportion of people using services in the follow-up period was statistically significantly increased in the intervention group than in the comparison group for OOH services (OR 2.26, 95% CI 1.10 to 4.92; p = 0.031) |
Intervention description and mechanisms
The interactive part of the intervention was provided by a researcher,85,134 a doctor in a consultation,75,78,99,102,112,131 a nurse135 or trainers/employers. 81,82,120,121,127 Because of the interactive component, there were additional mechanisms to the education mechanism in purely written educational interventions: tailoring, anxiety reduction and empowerment were common.
Impact on service use
In Table 10, (+) indicates a statistically significant reduction in service use, (–) indicates a null result and (±) indicates that results were mixed. Pilot studies are indicated by italics. Three articles did not report impact on service use. 76,78,112 Nine studies measured impact on ED attendances, but one was a pilot study (see Table 10). Five out of the eight full studies showed a reduction in any indicator of service use. Twelve measured impact on GP consultations, but one was a pilot study. Seven of the 11 full studies showed a reduction in the number of GP consultations.
In Table 10, one article showed an unexpected increase in the use of GP out-of-hours services and a non-statistically significant increase in the use of primary care generally,121 raising the issue of unintended consequences of trying to increase health literacy. The authors raise the concern that a lot of data were missing in their routine data set and their results should be treated with caution. Furthermore, they measured service use overall, rather than for minor conditions, so it is possible that any increase in service use was for major problems. Nonetheless, it is important to recognise the possibility that service use might be increased by these interventions.
Other outcomes
Eleven of the 17 articles reported relevant outcomes (Table 11). Four articles reported no relevant outcome data on these outcomes. 75,85,102,112,134
| Study | Design | Quality | Mechanisms | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Specific | ||||||
| Francis et al.,99 UK | RCT | Some concerns |
|
2 weeks | Telephone questionnaire | (–) Satisfaction: there were no significant differences in terms of satisfaction, level of reassurance, parental enablement, or the parent’s rating of the ‘usefulness of any information received in the consultation’ |
| Herman et al.,83 USA | BA study | Weak | Education | 6 months | Telephone survey | (+) Intention: hypothetical responses to low-acuity child medical problem scenarios:
|
| Rutten et al.,78 the Netherlands | RCT | High risk of bias | Education | Unclear | Not clear | (+) Behaviour: changes in consulting behaviour –
|
| Sustersic et al.,131 France | RCT | Some concerns | Education | 2 weeks | Telephone interview/survey | (+) Behaviour: for the whole population (adults and adults accompanying children), those in the PIL group significantly showed behaviour that was closer to that recommended by the PIL than those in the group that had not received a PIL (mean behaviour score 4.9 vs. 4.2; p < 0.01). This was confirmed by the alternative analytical approach, whereby the behaviour scores were dichotomised and used in univariate analysis (recommended behaviour 71.8% vs. 43.0%; p < 0.01) |
| (+) Knowledge: likewise, those in the PIL group had a mean knowledge score that was significantly higher than that of those in the control group (mean knowledge score 4.2 vs. 3.6; p < 0.01).The adult patient subgroup showed behaviour that was closer to that recommended by the PIL than adult patients in the control group (mean behaviour score 4.9 vs. 4.0; p < 0.01). The adult and child group showed the same tendency, but did not reach significance (mean behaviour score 4.9 vs. 4.5; p = 0.11) For the adult patient subgroup, knowledge was significantly better in the group that received a PIL (mean knowledge score 4.2 vs. 3.5; p < 0.01), irrespective of the condition studied or of sociodemographic parameters (with the exception of the level of education, for which the difference was not significant) | ||||||
| General | ||||||
| Herman and Mayer,82 USA | CBA pilot study | Weak |
|
6 months | Self-report instrument |
|
| (+) Behaviour: accessing health information – according to the survey, exposure to the self-care book or to the book with additional training affected the way many parents accessed their health information. Before the intervention, about half of the parents (52%) claimed to derive health information ‘from the doctor or clinic’. Following the intervention, however, only 18% claimed to access health information this way, a decrease of 34%. The effects of the training were evident in parents’ responses to the question ‘When your child is sick, where do you first go for help?’. In the control group (those who received the book without the additional training), 69% responded that they would ‘call [their] child’s regular doctor or health phone line’. In the intervention group, however, which received both the book and training in how to use it efficiently, 58% responded that they would ‘look in a book’, with only 28% reporting that they would ‘call [their] child’s regular doctor or health phone line’. (Only 1% of those in the control group responded that they would ‘look in a book’ first.) Eight per cent of those in the control group had noted that they would ‘take [their] child to the emergency room’, whereas only 3% of those in the intervention group claimed that they would take that route when a child was sick (17% in the control group would ‘call family or friends’, whereas only 7% in the intervention group chose that option). Overall, then, 6 months following the intervention, more parents claimed that they would turn to a book and fewer claimed that they would take a child to the clinic or ED in response to a perceived illness | ||||||
|
||||||
|
(+) Intention: parent responses to mild conditions, including what they would do if their child had a fever of 99.5 °F, had an earache, was vomiting and had diarrhoea, or had a runny nose and a cough. In each case, more parents would look in a book and fewer would call 911, go to the ED or go to the doctor or a clinic Change in parent responses regarding method of treatment, from pre to post intervention: |
||||||
| Herman and Jackson,81 USA | BA study | Weak |
|
6 months | Self-report instrument |
|
| (+) Anxiety: after participating in the intervention and receiving training in the use of a health book, the percentage of parents who reported being ‘very worried’ when their child is sick decreased by one-third | ||||||
| (+) Missed workdays: workdays missed by the primary caretaker per year decreased by 42% (95% CI 35% to 50%), and school days missed per year decreased by 29% (95% CI 23% to 35%). Changes in school days missed were confirmed through examination of school records | ||||||
| McWilliams et al.,135 USA | CBA study | Moderate |
|
12 months | Questionnaire | (+) Satisfaction: using a scoring system from −10 to 10, parents at the 15-month WCV strongly endorsed this intervention, showing support for both aspects of the intervention (nurse teaching and access to prescription). Support for this intervention remained high for those seen at the 24-month WCV, even for families who had not experienced an episode of ear pain after the nursing intervention |
| (+) Intentions: when surveyed at the 24-month WCV, 42.0% of parents indicated that their children had in fact experienced ear pain since the 15-month WCV. More than 80% of this subgroup believed that the nursing education helped them avoid an ED or after-hours visit: 54.3% ‘strongly agreed’, 31.4% ‘somewhat agreed’, 8.6% ‘were unsure’, 5.7% ‘somewhat disagreed’ and 0% ‘strongly disagreed’. Likewise, > 80% of these same parents indicated that access to antipyrine–benzocaine otic drops helped avoid an ED or after-hours visit: 62.9% ‘strongly agreed’, 25.7% ‘somewhat agreed’, 11.4% ‘were unsure’, 0% ‘somewhat disagreed’ and 0% ‘strongly disagreed’ | ||||||
| Powell,127 USA | Prospective cohort study | Weak | Education | 5 months | Questionnaire | (+) Intentions: (usefulness, understanding, etc.) > 90% for 607 employees who returned questionnaire; 70% felt that using the guide would help them visit the doctor less frequently |
| Steinweg et al.,120 USA | Survey | Weak |
|
6 months | Survey | (+) Enablement: programme outcome – confidence to treat minor illness: increased, 77%; no change, 23%; decreased, 0% |
| White et al.,121 UK | CBA study | Moderate |
|
6 months | Questionnaire | (+) Enablement (locus of control) – change in scores from baseline:
|
| (–) Knowledge: there was no statistically significant effect of being in the intervention group on perceived health status, levels of social support or knowledge about children’s cough, back pain or crying in babies at 6 and 12 months’ follow-up, controlling for baseline, gender and setting | ||||||
| (+) Intentions: statistically significant positive effects of being in the intervention group were seen at 6 months in intention to use GP services less for minor ailments and, at 12 months in knowledge about back pain. Intention to use services: at baseline, > 90% of all participants stated an intention to use the family doctor, and > 80% stated an intention to use the pharmacist or family for support. At the 12-month follow-up, intention to use support from friends, hospital, the library, occupational health workers and social workers had increased in the intervention group, but not the comparison group. Intention to use support from health visitors and midwives had decreased in the comparison group, but not in the intervention group | ||||||
Only two of these articles reported on participants’ satisfaction with the interventions. 99,135 Both were of moderate quality (or were assessed as having some concerns); both were also for interventions targeted at parents: one found no significant differences in terms of satisfaction, level of reassurance, parental enablement or the parent’s rating of the ‘usefulness of any information received in the consultation’,99 whereas the other reported high levels of satisfaction with the education provided at well-child visits for infants. 135
Eight articles evaluated patients’ reported changes in behaviours and intentions to consult following an intervention, and each of these studies found a positive direction of change, regardless of whether the intervention was aimed at a specific group78,83,131 or populations more generally. 81,82,121,127,135 Five of the eight articles were judged to be weak or at high risk of bias; two non-RCTs were assessed as being of moderate quality121,135 and one RCT was judged to have some concerns. 131
Two studies also reported increased confidence among participants to deal with minor illness120 or improved locus of control following the intervention. 121
Two studies compared knowledge between intervention and control groups: a moderate-quality trial of a targeted intervention reported a significant improvement in knowledge in the intervention group,131 whereas a moderate-quality controlled before-and-after study of a more general intervention found no such difference, despite improvements across other measures such as intentions and locus of control. 121
Current examples in the NHS
We could find no examples of this type of intervention in routine use in the NHS.
Conclusion and relevance to the NHS
Even though this type of intervention had additional mechanisms to written material only, the conclusions from the evidence base were similar to those drawn about written information only. There is potential for this type of intervention to affect service use, but there is no strong evidence base to say that it does.
Box 4 provides a plain English summary of this section.
A lot of research looked at a person training patients in how to look after minor problems and giving them leaflets or booklets too. The findings were the same as for leaflets and booklets by themselves.
5. Multicomponent interventions (A.II and B.II with mass media campaigns D)
Size and quality of the evidence base
Five articles (four studies) used additional components to the written information combined with a person-delivered approach described in the previous section, adding mass media advertisements79,80,115,128,139 (Table 12). They were based in North America, with one based in Taiwan. 139 None of the studies was a RCT. They were of moderate quality in our formal quality assessment, but in our informal assessment of quality, we identified concerns about a downwards trend in service use in the control group,79 and service use based on self-report. 80
Description of interventions and mechanisms
The mass media components included public education campaigns in a specific geographical area, or the use of posters to promote training workshops. The mechanisms tended to include empowerment as well as education.
Impact on service use
In Table 12, (+) indicates a statistically significant reduction in service use, (–) indicates a null result and (±) indicates that results were mixed. One study did not measure service use. 139 Three articles measured impact on ED attendances and three of these showed a reduction in use. Two measured impact on GP consultations, with one showing a reduction. Note that Hibbard et al. 79 and Wagner et al. 80 are different components of the same study, with the former using routine data to measure impact and the latter using a controlled before-and-after survey of self-reported use.
| Study | Design | Quality | Mechanism | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| Barr et al.,115 Canada | BA study | Moderate |
|
6 months | Records | Minor: (+) visits for non-disease-related crying: pre intervention: 724/20,394 (3.5%) of visits. The relative risk of a visit for crying or colic in the post-implementation period compared with the pre-implementation period was 0.705 (95% CI 0.59 to 0.85; p < 0.001), representing an overall 29.5% reduction in visits | |
| Hibbard et al.,79 USA | Non-RCT | Moderate |
|
12 and 24 months | Records | All: (+) emergency rooms visits began to decline in the intervention group following the intervention | |
| Minor: (±) TLAS visits showed a steady decline in the comparison communities. In the intervention communities, however, TLAS visits increased during the first follow-up year, but decreased during the second period. They remained higher during that period than at baseline and were higher in the intervention communities than in the other two comparison communities by a factor of nearly two. But they were lower in the second follow-up period than the first follow-up period. ED visits began to decline the intervention communities, whereas they increased in one comparison community | |||||||
| Powell et al.,128 USA | BA study | Moderate |
|
12 months | Records | All: (+) the frequency of ED visits decreased by 100 visits or 19.8% | All: (+) the frequency of health-care provider office visits decreased by 932 visits (18.4%). All categories of health-care provider office visits showed declines (freestanding laboratory, accidents, consultations, regular, all other). The frequency of all outpatient visits declined by 1032, or 18.5%. This averaged a little over 1 fewer visit per employee. All 938 subscribers (371 employees and 567 dependents): frequency of health-care provider office visits decreased by 522 visits, or 12.2%. The frequency of subscriber total outpatient visits declined by 495 visits, or 10.8% |
| Wagner et al.,80 USA | CBA study | Moderate/weak |
|
12 months | Self-report | All: (–) seeing a doctor (0 vs. ≥ 1 visits) – at baseline, 84.5% of the intervention group had visited a doctor in the past year, and 86.1% of the control group had done so. At 1 year: 88.9% intervention vs. 86.8% control; difference in differences = 3.7%, or = 1.38 (95% CI 0.97 to 1.95); p = NS. Number of visits: baseline – 3.69 intervention vs. 3.84 control; 1 year: 3.73 intervention vs. 3.67 control; p = NS. After adjusting for observable characteristics, both seeing a doctor and number of visits were not statistically associated with the Healthwise Communities Project intervention |
Other outcomes
Three of the five articles of the multicomponent type reported other outcomes (Table 13). Two studies of this type reported no relevant outcome data on satisfaction or intentions. 80,115
| Study | Design | Quality | Mechanism | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Chiu et al.,139 Taiwan | Survey | Weak |
|
9 months | Survey | (+) Satisfaction: 80% (n = 80) of the respondents were aware of the existence of the ESCMSs, and the MMI service was known to most residents and was used by most of them. Compared with respondents who had not used the MMI service (n = 30), those who had used the service (n = 50) considered the ESCMSs more helpful (90% vs. 77%; p < 0.05) |
| (+) Intentions: compared with respondents who had not used the MMI service (n = 30), those who had used the service (n = 50) had greater willingness to seek help from the ESCMS in the future (88% vs. 57%; p < 0.01) | ||||||
| Hibbard et al.,79 USA | Non-RCT | Moderate |
|
12 and 24 months | Survey | (+) Behaviour: the effects observed for manual use appeared to be greater in the intervention community than in the comparison communities. The intervention respondents were more likely to indicate that using a self-care manual helped them self-treat a symptom and saved them a visit to the doctor. The magnified effect observed in the intervention community for manual use does not occur for users of a nurse advice line or computer program. Thus, it appears that the intervention increased the use of manuals as well as the effects of using a manual |
| Powell et al.,128 USA | BA study | Moderate |
|
12 months | Survey | (+) Satisfaction: workshop evaluation – the results show a high level of satisfaction with the guide and the workshop:
|
| (+) Understanding: 89% of employees reported having a better understanding of when to see the health-care provider; 92% of employees feel that they are wiser health-care consumers | ||||||
| (+) Intentions: 73% of employees think that they will need to visit their health-care provider less frequently; 66% of employees think that they will be absent from work less often |
Examples in the NHS
We could find no examples of this type of intervention in routine use in the NHS.
Conclusion and relevance to the NHS
The findings for this type of intervention were essentially the same as for the combination of written information with person-delivered education, and for written information by itself.
Box 5 provides a plain English summary of this section.
Not a lot of research has been done on using leaflets, people giving training in looking after minor health problems, and advertising in newspapers, etc. at the same time. Some of the research showed a reduction in use of A&E and GPs, but some did not.
A&E, accident and emergency.
6. Self-triage (C.III and A.III)
Size and quality of evidence base
Nine studies reported self-triage interventions: most of them were digital self-triage interventions,53,84,98,104,113,114,140 and two older studies report a paper-based symptom-scoring system akin to self-triage. 132,133 They are presented in Table 14 in alphabetical order within these digital and paper groups. The digital self-triage evidence base was highly relevant to the UK because three articles were undertaken in the UK and four in the Netherlands. Some did not measure outcomes. 104,114 Of the ones that did, some were RCTs,84,98 with another RCT acting as an exploratory study for one of these full RCTs. 53 The formal quality assessment did not identify these RCTs as being of high quality. Our own informal assessments identified concerns that only very educated people were included98 and that there was reliance on self-report for some outcomes on service use. 84 Yardley et al. 53 was an exploratory study/pilot, and so did not have the necessary statistical power to detect a change in GP consultations. The paper-based self-triage evidence base was small and limited to a scoring system for very young children.
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | GP use |
|---|---|---|---|---|---|---|
| Digital | ||||||
| Little et al.,84 UK | RCT | High risk of bias |
|
5 and 12 months | Records | All: (±) based on self-report, a modest increase in contacts for NHS Direct among those who had a RTI in the intervention group [37/1574 (2.4%) vs. 20/1661 (1.2%), multivariate RR 2.25, 95% CI 1.00 to 5.07; p = 0.048], but reduced contact with doctors [239/1574 (15.2%) vs. 304/1664 (18.3%), RR 0.71, 95% CI 0.52 to 0.98; p = 0.037]. There was no evidence that self-management advice resulted in delayed consultations for serious illnesses (e.g. lobar pneumonia, meningitis, septicaemia) and, hence, an increased number of hospitalisations; in fact, the number of hospitalisations reduced, albeit not statistically significantly, both in the shorter term (20 weeks) and longer term (1 year). Use of primary care records at 12 months showed no difference in consultations at the GP (RR 0.85, 95% CI 0.65 to 1.12; p = 0.259) and the hospitalisation rate was lower in intervention group, but this was not statistically significant (RR 0.35, 95% CI 0.11 to 1.10; p = 0.073) |
| Yardley et al.,53 UK | Exploratory RCT | High risk of bias |
|
4 weeks | Self-report | All: of the people in the internet doctor group, 11 (11.6%) had consulted their doctor or used other health-care services (mainly NHS Direct) for their symptoms, compared with a substantially greater proportion ( n = 21, 17.6%) in the control group, although this difference did not approach significance in this small sample ( p = 0.22) |
| van der Gugten et al.98 the Netherlands | RCT | Some concerns |
|
12 months | Records | All: (–) intervention (N = 314) vs. control (N = 305):
|
| Paper | ||||||
| Thomson et al.,132 UK | RCT | Some concerns |
|
6 months | Records | All: (–) no differences were detected between groups in the use of primary care services, excluding number of child health surveillance and immunisation attendances: intervention, median 2; control, median 2 (p = 0.26). Use of OOH service did not differ either (86 vs. 85 consultations; p = 0.93) |
| Thornton et al.,133 UK | Prospective cohort study | Weak |
|
6 months | Self-report | All: only reports numbers of mothers reporting contact with health-care professionals. Contacts with their health visitor, midwife and doctor were mostly for minor complaints |
Description of interventions and mechanisms
The digital interventions included eConsult104 and an especially developed digital triage intervention. 53,84 Three interventions focused on respiratory problems, either in the general population in the UK53,84 or among children in the Netherlands. 98 The paper-based system was the same in both studies, asking parents to score symptoms. The common mechanisms were education and tailoring, with some interventions also offering attention to anxiety reduction. One of the interventions adopted reinforcement techniques by sending e-mail reminders to users on an ongoing basis to maintain awareness of the intervention. 84
Impact on service use
In Table 14, (+) indicates a statistically significant reduction in service use, (–) indicates a null result and (±) indicates that results were mixed. Pilot studies are indicated by italics. Five studies measured impact on service use (see Table 14), focusing on GP use. One study was a pilot and one study offered such limited information about impact on service use that we could not interpret the findings. Two studies were of key interest because they were relatively recent digital tools. 84,98 Little et al. 84 offered a positive picture of digital self-triage, showing fewer GP consultations when this intervention was used. In Little et al. ,84 the proportions of GP consultations were 15% in the self-triage group vs. 18% in the control group, based on self-report of those who had a respiratory illness; a similar difference was evident when routine records were used, although this was not statistically significant because all consultations were included, not simply those for respiratory illness. In contrast, there was no difference in GP consultations for the European study. 98 Authors of this study point out that they tested the intervention on a highly educated sample and that their results may not be generalisable to those in lower socioeconomic groups.
Other outcomes
Seven of the nine included articles of the self-triage type reported relevant outcomes (Table 15). Of these seven articles, all but two were assessed as being weak or at high risk of bias; the exceptions being a moderate-quality qualitative study114 and a RCT with only some concerns. 98 Two studies of this type reported no relevant outcome data on satisfaction or intentions at all. 84,132
| Study | Design | Quality | Mechanisms | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Digital | ||||||
| Nijland et al.,114 the Netherlands | Qualitative | Moderate | Education | 6 months | Survey | (–) Satisfaction: user-friendliness – 106 (40.8%) out of the 260 times the 14 patients used the apps, they faced usability problems; quality of care – 146 (56%) times, they faced quality-of-care problems, such as comprehensiveness of information |
| Nijland et al.,113 the Netherlands | Survey | Weak | Education | 54 weeks | Survey | (–) Enablement (self-care advice): 15% of patients were given self-care advice, so authors considered it to be a very cautious intervention |
| (±) Intentions: patients used the triage system to gather information about their complaint (n = 72, 49%), more than for deciding whether or not a doctor has to be contacted (n = 38, 26%) | ||||||
| Preceding the triage consultation, nearly half of patients (n = 73, 49%) had the intention to visit a GP for their complaint. Of the patients with an intention to visit (n = 72), most expected self-care advice (n = 30) and fewer expected to be advised to visit a GP (n = 22), or had no expectations at all (n = 20). All the patients who expected to be advised to visit a GP (n = 22) received such advice, whereas, of the patients who expected tailored self-care advice (n = 30), the majority (63%) received advice to visit a GP. In most cases, contact with a doctor (GP advice) was given (n = 54, 76%) | ||||||
| A positive attitude towards advice was strongly related to the perceived usefulness of the advice, as reflected in understandability, reliability of information, applicability in daily life and effectiveness. It appeared that 57% actually had complied with the advice. Patients who complied with the advice were more highly educated (55%) and frequent users of medication (40%); furthermore, the received advice corresponded, in most cases (84%), with expected advice. Reasons for non-compliance were lack of confidence in the advice and fear to follow-up the provided advice | ||||||
| Yardley et al.,53 UK | Exploratory RCT | High risk of bias |
|
4 weeks | Patient enablement instrument | (+) Enablement: the median patient enablement score was significantly greater in the internet doctor group than in the control group [median score of 3 vs. 2, respectively (IQR 0–5), for the whole sample; p = 0.03] |
(+) Satisfaction with web-delivered advice in the internet doctor vs. control groups (n = 332) (scale/item mean for each group) –
|
||||||
| (+) Intentions to consult the doctor declined between baseline and the intermediate (48-hour) follow-up; although the decline was greater in the internet doctor group, this difference did not reach significance. Consultation necessity beliefs and emotional reactions to illness declined at follow-up to a similar extent in both groups. Poor understanding of illness declined in the internet doctor group, but slightly increased in the control group, resulting in a just significant interaction between time and group effects. Self-confidence to self-care remained stable, similar and high in both groups at both time points | ||||||
| van der Gugten et al.,98 the Netherlands | RCT | Some concerns |
|
12 months | Questionnaire | (+) Satisfaction:
|
| (+) Behaviour: changed (when applicable) – yes, because of the information I went to the doctor, 3.8%; yes, because of the information I did not go to the doctor, 5.8%; no, I wanted to go and I did, 65.4%; no, I did not want to go and I did not go, 25.0% | ||||||
| Verzantvoort et al.,140 the Netherlands | Prospective cohort study | Weak |
|
Within 24 hours of app use | Survey, telephone interview |
|
|
||||||
| Paper | ||||||
| Thornton et al.,133 UK | Prospective cohort study | Weak |
|
6 months | Questionnaire | (+) Satisfaction: they all found Baby Check easy to use; between 68% and 81% found it useful, and 96% would recommend it to others |
Six of the nine articles of the self-triage type reported on participants’ satisfaction. Four articles reported clear satisfaction with the intervention,53,98,133 one reported that only slightly more than 50% of respondents were satisfied or very satisfied with the intervention app,140 and one study reported barriers to the acceptability of the website for self-triage. 114
The mixed findings on satisfaction for the app and website were also reflected in respondents’ intentions: satisfaction with the app or website was highest for those respondents who received advice commensurate with their prespecified intentions. 113,140 Two studies that reported a positive change in behaviour and intentions to consult also reported positive effects on either satisfaction53 or satisfaction and confidence. 98
Current examples in the NHS
The NHS in England has recently introduced NHS 111 Online, a digital self-triage service. Anyone can check a symptom, either to get advice about where and when to seek help, or to get general information about the symptom and how to manage it. Symptoms are checked only for patients aged > 5 years; people using the self-triage for young children are asked to contact NHS 111 by telephone. The service is available at https://111.nhs.uk (accessed 7 September 2022), and a page is shown in Figure 9.
FIGURE 9.
NHS 111 Online screenshot. Contains public sector information licensed under the Open Government Licence v3.0.
We found that Buckinghamshire CCG had a similar service called ‘AskFirst’, that is a symptom checker that offers self-care advice and helps people find local services [www.buckinghamshireccg.nhs.uk/public/your-services/feeling-unwell/askfirst/ (accessed 18 November 2021)]. It can be downloaded onto a mobile phone.
A large number of general practices in the UK have signed up to eConsult where patients can get advice about self-managing symptoms and direction to services such as pharmacy [https://econsult.net/nhs-patients/how-to-use-econsult (accessed 23 September 2021)]. It appears that a patient makes a query online, and a GP triages that query, rather than self-triage by the patient. We included the Cowie et al. 104 study in our review, which used eConsult. In Cowie et al. ,104 eConsult was described as offering self-care advice, so we included it in our review. However, descriptions of its use routinely in the NHS imply that a GP makes decisions, not the patient.
Conclusion and relevance to the NHS
This type of intervention has potential, but the evidence base needs strengthening for impact on primary care, and does not exist for the impact on emergency care. NHS 111 Online is a relatively new service in England that offers digital self-triage. A RCT of the active use of NHS 111 Online (potentially with reminders to use it), with measurement of its impact on EDs as well as GP consultations, would add considerably to the evidence base.
Box 6 provides a plain English summary of this section.
There is not a lot of research on computer sites that check patients’ symptoms. This type of service is available in the NHS, so it is important to test if it helps to reduce the use of A&E or a GP for minor problems.
A&E, accident and emergency.
7. Other types of interventions
Size and quality of the evidence base
Seven articles did not fit the six common types of interventions. Six of these were a rare type of intervention94,108,111,116,122,125 and one was a qualitative study focusing on five interventions, and therefore could not be included in the typology. 118
Description of intervention and mechanisms
All six interventions included in the typology had awareness as a mechanism, and four also had education as a mechanism.
Impact in service use
In Table 16, (+) indicates a statistically significant reduction in service use, (–) indicates a null result and (±) indicates that results were mixed. Six of the studies measured the impact on either emergency or primary care. Two of the five articles showed a reduction in ED use and the single study that measured GP use, expecting to see a reduction, showed a reduction. Hou et al. 122 is an interesting study because the intervention was a community campaign to reduce the use of ambulances for minor problems. The indicator measured was ED use, specifically arriving at an ED by ambulance, so it is described in the ‘impact on ED’ column in Table 16. In the UK, minor problems are dealt with by ambulance personnel at a person’s home/location of the call and are not taken to an ED, so Hou et al. ’s 122 indicator is not a good indicator of ambulance use in the UK.
| Study | Design | Quality | Mechanisms | Time period of measurement | Data source | Impact on ED | Impact on GP consultations |
|---|---|---|---|---|---|---|---|
| Beal et al.,116 USA | CBA study | Moderate |
|
12 months | Records, self-report | All: (–) no significant changes in emergency care visits after accounting for covariates | All: non-urgent health-care use significantly decreased for both enrolled and comparison youth in the year after study launch (t[150] = 5.65; p < .01; and t[150] = 5.13; p < .01, respectively), but the decrease for the intervention group was smaller for than hoped for |
| DeCamp et al.,111 USA | RCT | Some concerns |
|
15 months | Records | All: (+) reduced use of EDs. Salud al Día (n = 79) vs. usual care (n = 78): ED visits, mean 1.23 (SD 1.66) vs. 1.82 (SD 1.64); p = 0.03; IRR 1.48 (95% CI 1.04 to 2.12) for control vs. intervention. Frequency of ED use differed (p = 0.03):
|
|
| Hou et al.,122 Australia | BA study | Weak |
|
3 months | Records |
All: (+) fewer patients arrived at the ED by road ambulance or other means, as opposed to own transport (OR 0.90, 95% CI 0.80 to 1.00; p = 0.055) Minor: other results were counterintuitive. Patients arriving at the ED had significantly lower clinical urgency after the campaign than before the campaign. The changes were mainly driven by the decrease of ATS 3 from 46.5% to 44.0% and the increase of ATS 4 from 26.7% to 29.5%. Patients attending the ED were significantly less likely to have higher clinical urgency after the campaign than before the campaign (Wald χ2 test; p = 0.0007) |
|
| Rector et al.,125 USA | RCT | Some concerns |
|
6 months | Records |
|
All: the hypothesis was that GP-type visits would increase. Neither health plan differed significantly in the percentage of intervention households or household members who visited an office-based physician. There were also no differences when subgrouping by age (< 19 years and ≥ 19 years) |
| Robbins et al.,108 UK | RCT | High risk of bias |
|
7 months | Records |
|
|
| Sturm et al.,94 USA | RCT | High risk of bias |
|
6 and 12 months | Records | All: (–) PED follow-up at 6 and 12 months. Control (N = 168) vs. intervention (N = 164): high acuity follow-up –
|
All: the intervention group had 203 well-child visits (1.23 per patient), compared with 195 (1.16 per patient) in the control group (rate difference 0.02 per person-year (95% CI –0.2 to 0.3; p = 0.87). The intervention group had 139 sick visits during the follow-up period (0.85 visits per patient), compared with 109 in the control group (0.65 per patient) (rate difference 0.19 per person-year (95% CI 0.013 to 0.39; p = 0.036). That is, the treatment group used the PCP more, as planned |
Minor: (±) PED follow-up at 6 and 12 months. Control (N = 168) vs. intervention (N = 164): low acuity follow-up –
|
Other outcomes
Only two of the seven articles of this miscellaneous type reported relevant outcomes (Table 17). One was a controlled before-and-after study of moderate quality. 116 This study of adolescents leaving the care system reported that the majority found the intervention, the I Care Guide, helpful. 116 The second was a qualitative study using focus groups to rank caregivers’ preferences regarding different types of educational interventions for childhood illness: the most preferred was the mobile app, and the least preferred were printouts for specific illnesses; this was the same regardless of a participant’s baseline level of health literacy. 112 There was little qualitative information available about why people preferred an intervention, although there were some comments about the accessibility of the mobile app and the comprehensiveness of the information.
| Study | Design | Quality | Mechanisms | Data collection time points | Data source | Impact on other outcomes |
|---|---|---|---|---|---|---|
| Beal et al.,116 USA | CBA study | Moderate |
|
12 months | Records, self-report | (±) Satisfaction: the majority of adolescents reported that the I Care Guide was somewhat (46%) or very helpful (42%), and 78% of participants who responded to surveys at the 12-month follow-up reported that they still had the guide (42% of all participants who received a guide at enrolment). The majority of youth (80%) reported using the I Care Guide at least once during the study, with sections discussing emergency care, reproductive health and symptoms most commonly endorsed |
| Ohns,118 USA | Qualitative | Strong | Education | Cross-sectional | Focus groups |
|
Current examples in the NHS
Not relevant.
Conclusion and relevance to the NHS
It is difficult to draw conclusions about this miscellaneous type.
Impact on service use: multivariable regression
Using a logistic regression of reduction in ED use versus null, we tested whether or not characteristics of the study, context or intervention were more likely to result in reductions. We repeated this for reduction in GP consultations versus null. We tested the decade in which the study was published, the country, the place of delivery, whether or not the intervention was targeted at people in poverty/with low health literacy, whether it was targeted at a parent of a young child or all people, whether it was given at a specific or a general time, the type of intervention, the study design, the quality of research, the time period measured, whether or not records were used for measurement, the presence of mechanisms of impact, the Flesch score and usability. The Flesch score and usability were available for some papers only. We could not measure approach to intervention development because this was so poorly described in most papers. Numbers were small for this analysis (low statistical power) and a large number of variables were tested, so it is a problematic analysis. There were no statistically significant findings, with the exception of the decade in which articles were published: the 2000s had a greater proportion of studies showing a reduction in ED attendance and GP consultations. There is no explanation for this.
Chapter 5 Second stakeholder event
Background
Towards the end of the study, we held a virtual PPI event (in September 2021) followed by a virtual stakeholder event that included PPI members (in October 2021). The aim was to elicit stakeholders’ perceptions of the findings and actions that could be taken. We held the PPI event first so we could hear PPI views alone before hearing the views of all stakeholders together. Both meetings were virtual because of COVID-19. In the stakeholder event, we aimed to involve representatives from the following groups: patients, carers and members of the public, CCGs, NHS England urgent and emergency care, general practice, EDs and emergency ambulance services; we also aimed to involve the NHS England health literacy lead. We report the two meetings together because they discussed similar issues.
Stakeholders attending the events
Ten PPI members attended the PPI event. Nineteen stakeholders attended the stakeholder event along with research team members:
-
eight PPI representatives (two provided input outside the meeting)
-
five NHS England and CCG commissioners
-
one representative from NHS England Health Literacy
-
one ED consultant
-
one GP
-
one NHS trust manager
-
two ambulance service representatives (a medical director and a paramedic).
We invited the same stakeholders from the first stakeholder event and some additional stakeholders who had learnt about our review. As the meeting was held virtually, people were able to attend from different parts of England, including the north-east, south-west, London and Yorkshire.
The events
At the PPI event, the team presented study findings in a series of short presentations, leaving most of the time for discussion. We heard useful feedback on how the findings may be relevant to the NHS, the role of family and friends when accessing services, and factors that influence people’s use of urgent care. The second stakeholder event was held on 13 October 2021 and lasted 2 hours. The team presented the findings of the review, including the following:
-
the types of interventions identified
-
the effectiveness of different types of interventions
-
the readability and user-friendliness of interventions
-
implications of the review for the NHS, considering how feasible, appropriate, meaningful and effective the interventions were.
We also discussed potential ways of disseminating the findings to influence practice. Margaret Ogden (PPI co-applicant) helped to organise the events, gave a presentation to stakeholders about the user-friendliness of the interventions, and supported the facilitation of the events.
The issues raised and actions taken
After the events, we recorded the points made by attendees at the PPI event and the second stakeholder event and how we would address each point in the report (Table 18). We circulated our write-up to the stakeholders so they could add to the document; none responded.
| Issue | Detail | Action |
|---|---|---|
| Number of studies found | Attendees were surprised that so few studies were found, and how few were based in the UK. People discussed how they knew of interventions that were being used in parts of the UK, but have not necessarily been evaluated, and thus would not have been included in the review | We will include this reaction in the report when we reflect on the evidence base. We will also discuss how interventions are delivered in the NHS that have not undergone evaluation resulting in publication |
| Health literacy is not the only issue | Attendees described how sometimes people need to see their GP (and other health professionals) for some issues and struggle to get an appointment. Consequently, people end up accessing more urgent care. Improving health literacy is not going to help this. People expressed frustration about access to GPs | We will be clear in the report that people face difficulties accessing care and that health literacy is one of many issues that need to be addressed. We will be clear that we are not saying health literacy is the only issue, or the most important one |
| Wider system capacity | Attendees discussed that, although the interventions may be valuable, the current health-care system has a lot of problems, such as delays getting through to 111 or seeing a GP. So, it is not just the effectiveness of interventions within a research context, but whether or not they work within the wider health-care system, and the accessibility of alternative services to GPs and A&E | We will reflect on how the health-care system affects whether or not interventions can be used in practice (feasibility) |
| Local infrastructure | Attendees discussed how access to services was partly shaped by local infrastructure, for example was the A&E nearer to the patient than the minor injuries unit? They felt that this issue may influence behaviour and, again, is not about health literacy | We will ensure that, in our report, we discuss how there are many factors beyond health literacy that influence people’s use of health-care services |
| People need to have increased health literacy, not just awareness of other services | Attendees discussed how the decision not to attend an A&E department was about more than simply having awareness of alternative services. It was also about having the confidence in the moment of a health crisis to access services. For example, an attendee described how the majority of people surveyed in one A&E felt that they would make the same decision to use A&E again, despite now knowing an alternative service might be more suitable | It will be important to consider that interventions need to take account of the fact that people make decisions when they or someone they support are experiencing a health crisis. We will reflect on the fact that people are being asked to change their behaviour and make decisions when experiencing stress |
| Knowing about interventions being used in the NHS | Attendees had not seen some of the interventions that are available in the NHS (e.g. NHS 111 Online). The group discussed how to promote them, for example put on television screen in general practice waiting rooms, use of schools and local newsletters. Attendees felt that it needed to be easy to access where anyone can check out symptoms and find out what to do | We will have a recommendation in the report that any interventions need to be known about by the intended recipients |
| Lack of studies focused on ambulance services | The review did not identify any studies delivered by ambulance services or measuring the impact of use of ambulance services. We discussed whether or not people were surprised about this and the initiatives that may be happening in the NHS currently | We will include in our report the reflection that no studies had been identified in this setting and the potential for interventions to be developed to be used with people using ambulance services for minor problems |
| Settings for the interventions | Attendees discussed how the interventions found in the review were generally delivered in health-care contexts such as leaflets handed out by GPs, but there could be scope to use places like food banks to reach other people | We will reflect in our findings about the scope for delivering interventions in alternative settings |
| Targeted vs. universal interventions | Attendees discussed that there could be a need for both more universal interventions, such as leaflets delivered to everyone in a town, and more targeted interventions, for example coaching support with people who need more support to improve their health literacy | We will reflect in the report about the different intensities and purposes of different interventions and whether or not a ‘stepped’ approach is feasible |
| Care navigators | We showed that some of the studies in the review evaluated people being provided with support from care navigators, but said that these interventions are not in use in the UK. Attendees pointed out that there are care navigator-type projects being conducted in the UK. For example, some general practices use volunteer community health champions to advise people on potential services. Social prescribing is being rolled out throughout general practices and one of its functions could be supporting people to feel more confident accessing alternative forms of support | We will discuss the findings of the review with our social prescribing networks. We will relate these NHS initiatives to the evidence base in our report |
| Role of community pharmacists and trust | Attendees discussed that, in the UK, we do not have as much of a culture of using pharmacists as a form of advice as other countries such as France. Some general practices are starting to employ pharmacists to provide advice to patients, for example those on multiple medications | This raised the issue of trust in different services and interventions. We are assessing the trustworthiness of interventions in our review using our user-friendliness tool. We will also reflect, in the discussion section of our report, about the importance of addressing people’s trust in alternative sources of support |
| People felt that there needed to be greater promotion of the training, qualifications and skills pharmacists have, to help increase the public’s trust of getting support from different types of health-care professionals | ||
| Needing to have people we trust to promote interventions (e.g. family members) | Attendees discussed the importance of having people you trust recommending the interventions, such as people supporting a relative to use the NHS website or a health visitor recommending support | In the discussion section of the report, we will reflect on how engagement with interventions may rely on people learning about them through family members, friends and health professionals |
| Volunteers | Attendees proposed that volunteers could support the delivery of interventions such as care navigators to help make interventions more cost-effective. Person-delivered interventions do not have to be delivered by health-care professionals | In the discussion section of the report, we will reflect on the potential role of volunteers to deliver interventions |
| Online triage tools | Although some attendees had used online triage tools, such as eConsult, through their GPs, a challenge is that having underlying health conditions often excludes people from using these | We will reflect on whether or not, in any of the included studies, patients with underlying health conditions were included |
| User-friendliness of interventions | Attendees discussed how developing the UFAT was an important part of the review. They felt that it was something that could be used beyond the review, including by people designing patient-facing information. People gave the example that general practice websites are often not well designed | In the report, we will include information on how the user-friendliness tool could be used to assess other patient-facing materials such as general practice websites |
| Having resources available in different languages and accessible in different formats | Attendees spoke about the need to have resources available in different languages and different formats. But they appreciated that funders did not always have the budget for this and that a considerable range of languages would be needed. One attendee discussed the Recite Me software (Recite Me, Gateshead, UK), which can change websites into more accessible formats | Within the user-friendliness tool, we are assessing whether or not interventions include information about how to access the tool in different formats or languages. In our report, we will also reflect on the importance of ensuring that this is taken account of when designing health literacy interventions |
| Having well-designed, user-friendly resources | Attendees spoke about the importance of having well-designed interventions, such as a clear layout and reasonable font size. They felt that the user-friendliness of interventions may affect the chance to improve health literacy | We are assessing the user-friendliness of interventions in the review. We will explore whether or not the user-friendliness scores are associated with the effectiveness of interventions. Doing this will help us understand the potential impact of having a well-designed intervention |
| Tone of interventions | Attendees said that it is important that any interventions are appropriate in their tone and not patronising | We have assessed the tone of interventions through the user-friendliness tool and this will be included in the results section of the report |
| Reaching everyone | Attendees discussed that there are some people who are not engaged in mainstream media/digital platforms, etc. It is important to consider how these people can be reached through interventions | We will reflect in our report about whether or not any of the studies in the review considered how to reach less engaged people |
| COVID-19 brings opportunities | Attendees discussed that, although COVID-19 has been disruptive, it may also provide opportunities. People have got used to accessing services differently and have realised how important it is to look after our health | We will reflect in our report about the impact of the COVID-19 pandemic and how it may be an opportune time to try and improve health literacy to change service use for minor health problems |
| Finding interventions at the right time | Attendees discussed the need for interventions to be on hand when they need them. Attendees described how sometimes leaflets get put in a drawer and people cannot find them when they need them. Booklets can be stored on a bookshelf. The PPI members liked The Little Orange Book, feeling that they could have it to hand in paper format | We will have a section in the report about finding interventions when they are needed |
| Changing ingrained behaviours | Attendees discussed how people may have grown up accessing specific services, for example A&E in countries where primary care may not be available. Other people said they had grown up not accessing A&E because it was far from their home, so they would not think about accessing it. We discussed how ingrained experiences of accessing services may be and education needs to be from a young age or aimed at people new to the country/area (e.g. students and refugees) | We will highlight that there appears to be a gap in interventions that are aimed at children (as opposed to parents) or people new to a country |
| Educating people about alternative methods of support | Attendees spoke about the need to provide education to people to increase health literacy, such as courses or education in schools | We will reflect on whether or not there is a gap in the types of interventions that have been evaluated and whether or not further research is needed on education sessions in schools |
| Being risk averse when making decisions for other people | Attendees discussed how people were often more risk averse when making decisions for children or people they care for than when making decisions for themselves, such as teachers having to decide whether to take a schoolchild to A&E | We have included a number of interventions aimed at parents of young children in our review. We have not found interventions aimed at people in other caring relationships and will explain that this is a gap in the research |
| Positive experiences shape people’s future use | Attendees discussed that a positive experience of an alternative source of support, such as using an internet website, will increase people’s willingness to use it again instead of attending urgent care services | In the report, we will reflect on people building on their experiences of new interventions |
| Keeping interventions updated | Attendees pointed out that leaflets can get out of date. They were keen that interventions are kept up to date, for example websites are updated and health services have strategies for ensuring that leaflets are replaced | We will reflect on whether or not any of the included studies considered the long-term use of interventions, such as how to keep them up to date |
| Safety: what if it’s something serious? | PPI members felt that there will always be cases when people do not know if their indigestion is a heart attack or a cyst is breast cancer. Attendees wondered how interventions strike that balance of helping people to assess whether something is non-urgent or serious | The safety of interventions is important and one of the adverse effects of the interventions could be people not accessing urgent care when they need to. There will be a section in the findings of the report about the safety of interventions |
| Which interventions work for whom? | Attendees discussed how the interventions had been tested in different populations, in different settings and given at different times. People felt that it might be worthwhile including in the report a matrix based on all of the intervention formats and looking at what could work for whom | We are doing a multiple regression analysis to see if there are any characteristics of interventions or people that result in reduced use of primary or emergency care |
| Interventions can be relatively low cost, so even a little impact makes it worth it | Attendees discussed how interventions such as a leaflet can be relatively cheap. So even if they only have some impact on a small number of people, it could be worthwhile doing them | We will reflect on the level of impact interventions need to have given their cost (although the cost data we have are very poor) |
| Finding out why some interventions work and others do not | Attendees were really intrigued by why some interventions were effective and others were not. They thought that it was an important area of learning to help with designing future interventions | We are doing a multiple regression analysis to see if there are any characteristics of interventions or people that result in reduced use of primary or emergency care |
| Reducing use of A&E may increase use of services such as general practice | Attendees were concerned that reducing the use of A&E may increase use of services such as general practice | Some of the interventions in the review aimed to reduce use of A&E by increasing use of the GP. Indeed this may be a consequence of reducing use of A&E |
| It can be difficult to monitor the impact of interventions in practice | Attendees pointed out that it can be difficult to measure the impact of NHS initiatives on A&E because of issues of data quality. Therefore, it can be difficult to understand the impact of initiatives | In our report, we will reflect on the challenges of understanding the impact of health literacy interventions, especially when trying to use routine data in evaluations rather than data specifically collected for a research study |
| Interest in interventions currently being used in the NHS | Attendees discussed that there are many interventions that are being used in routine practice, such as The Little Orange Book or the Sheffield ‘Plan B’ social media campaign. However, because they are not being formally evaluated as part of an academic study, people may not know about their existence or benefit from their learning | In our report, we will discuss that a future area of research could be undertaking an exploratory study to learn what interventions are being used in the UK and learn from their experiences |
Chapter 6 Discussion and conclusions
Summary of findings
A total of 67 articles (64 studies) were included: 37 from the USA, 16 from the UK, 12 from the rest of Europe and two from the rest of the world. There were seven intervention types: navigation tools directing people to the range of services available (n = 7); written education about managing minor health problems in booklet or website format (n = 17); person-delivered education (n = 5); written education with person-delivered education (n = 17); multicomponent of written education, person-delivered education and mass media campaign (n = 5); self-triage (n = 9); and other (n = 7). Most articles reporting satisfaction with the intervention, enablement and perceived changes to behaviour showed positive results. Nineteen out of 30 (63%) articles measuring impact on ED attendances showed a reduction. Sixteen out of 27 (59%) articles measuring impact on GP consultations showed a reduction. Returning to the logic model specified earlier in the report (see Figure 1), the interventions appeared to improve short-term and intermediate-term outcomes (when measured), but there was variation in whether or not they affected the longer-term outcomes of reduced use of EDs or GPs. There was no indication that variation in the evidence base was explained by any of a range of population, research design or intervention characteristics, including complexity of the intervention. Interventions ranged in reading age and user-friendliness. The few articles reporting safety (n = 8) showed that interventions were safe.
Strengths and limitations of the evidence base
The evidence base had six strengths. First, the evidence base was generally very recent (almost half of the included articles had been published since 2010: 32/67), which increases its applicability to current contexts. Second, it derives from the multiple settings of primary care, secondary care and the community, rather than interventions delivered in a single setting only. Third, around one in four articles were conducted in the UK (16/67), and so a sizeable part of the evidence base is highly applicable to the context of interest. Fourth, it was extensive, covering a range of intervention types. Fifth, multiple study designs were used, including a high number of RCTs and quasi-experimental studies. Sixth, there were a considerable number of studies aimed at parents of young children, a group that has been identified as high users of emergency and primary care for minor health problems. 4
The evidence base had seven limitations. First, members of the PPI panel reflected that the evidence base was much smaller than they had expected. Second, the quality of the evidence base was often assessed as being poor, with many RCTs assessed as being at high risk of bias, and all but one non-randomised study being assessed as being of only moderate or weak quality. Third, the evidence base was highly heterogeneous in terms of the study designs, intended populations, the details of the interventions themselves, outcome measurements, and lengths of follow-up. This was especially the case for the measurement of service use outcomes, both in terms of the indicator used and the time period of measurement. This prevented the statistical pooling of interventions and outcomes, so the size of any positive effects for any particular intervention type could not be precisely quantified. Fourth, a large proportion of the studies were conducted in the USA (37/67), which has a financially distinct health and social care system, compared with the UK, which is likely to moderate patient decisions around accessing care. Fifth, cost data or analyses were rarely reported; if they were reported, it was sometimes as a discussion point, rather than details of methods used to calculate costs. So it could not be determined whether or not even a small statistically significant effect might be cost-effective, especially for relatively basic, low-resource intervention types. Sixth, there was almost no explicit assessment of safety. Seventh, there were surprisingly few interventions delivered in emergency care, and none delivered by ambulance services. The emergency care-delivered interventions were dominated by recently published North American studies of interventions aimed at parents of young children, rather than aimed at adults seeking help for their own health.
Relevance of the evidence base
Approximately one-quarter of articles were conducted in the UK (16/67), and so a sizeable part of the evidence base was highly applicable to the UK context. The interventions in the evidence base were similar to interventions in current use in the NHS, for example booklets about minor health problems, NHS website symptom checker, NHS 111 Online.
Fit with other evidence
Do educational leaflets/booklets work in other areas?
We found that there was evidence that leaflets/booklets could help to reduce the use of emergency and primary care for minor health problems, but the evidence base was too mixed and not of high enough quality to draw firm conclusions about this. The best we could say was that they have the potential to work. Educational leaflets/booklets are used in other areas. For example, a leaflet-based intervention was used for people calling out an emergency ambulance when they had a hypoglycaemic event, resulting in a reduction in repeat calls to the ambulance service for hypoglycaemia. 147 The evidence base in other areas can be limited. A 2021 systematic review of health literacy interventions in cancer identified 87 intervention studies, but found that most of them focused on the early stage of developing interventions, rather than evaluating outcomes of developed interventions. 148
Ease of reading and reading age
We found a range of readability scores for interventions in our review. This is reflected in other research. Other studies have made judgements about patient-facing written materials, identifying FRE scores of 54, compared with our range of 23–93, where 100 is very easy. 149 These authors highlighted the importance of assessing readability so that improvements can be made to materials. A lack of attention to literacy levels for patient information leaflets in general practice has been found. Only 24% of patient information leaflets met recommended reading criteria. 62 A recent study of the readability of general practice websites using FRE and the FKGL found that less than one in four were at or below the recommended reading age for online content of 9–14 years in an assessment of approximately 1000 general practices in Scotland. 63 Our assessment of an existing intervention in the NHS, (The Little Orange Book,68 judged to be suitable for most adults, having a FRE score of 67 and scoring almost perfectly in our user-friendliness assessment) shows that the NHS can produce excellent educational materials.
Has COVID-19 changed things?
A question that emerged in the PPI meetings was whether things were different since the pandemic and might this affect the transferability of evidence across time. We believe that the need for self-care increased during the lockdown periods of the global COVID-19 pandemic, as ED attendances dropped and face-to-face GP consultations were partly replaced with online ones because of fear of catching COVID-19. A survey and qualitative interview study of people who contacted primary care during the lockdown in New Zealand identified that health-care-seeking decisions were influenced by their ability to self-care and self-triage. 150 The conclusions of that study were that more support for people to self-care and self-triage would help pressurised services in emergency situations, such as a pandemic, as well as in usual times. They may also help patients attend to minor health problems when they are fearful of attending services.
Developing interventions
We found very little information about how interventions were developed. There is a lot of interest in co-design approaches to intervention development currently, that is the people who will use an intervention help to design it. There is also interest currently in the use of psychological theories when developing interventions for behaviour change. We did find some examples of co-design and use of psychological theories in our review, but we did not have enough examples or enough information about the development processes to determine if taking these approaches was more likely to result in effective interventions. Co-design of educational leaflets for minor health problems in combination with attention to psychological theory is occurring in recently produced interventions. 151
Trusting the source of information
Our team expected to see trust in the source of information as a possible mechanism of action. PPI members identified it as an important issue. It did not make a significant appearance in our review, even though it has been identified as affecting behaviour. 152,153
Strengths and limitations of the review
The systematic review had eight strengths. First, all processes (study selection, data extraction and quality assessment) were carried out by experienced reviewers. Second, the literature search was undertaken by a qualified senior information specialist and was comprehensive, involving the interrogation of multiple databases, supplemented by further techniques, such as reference-checking of included studies and reviews, searching of many grey literature sources (e.g. websites of relevant organisations) and focused searching for the publications of known relevant authors. This was an important issue because of the nebulous nature of the intervention we were interested in. Third, the data were not appropriate for statistical analysis, but the synthesis involved the application of a novel typology, going beyond standard narrative synthesis techniques to deliver practical findings. Fourth, focusing specifically on health literacy interventions, rather than considering them as a subgroup in a wider set of interventions, allowed for a more nuanced understanding of this type of intervention. Fifth, the focus on both emergency and primary care allowed the bringing together of similar interventions used for the same purpose of reducing the use of services. Sixth, assessing the readability and user-friendliness of interventions, as well as effectiveness, drew attention to a strength or weakness of an intervention that might affect its ability to have an impact on service use. Seventh, the extensive involvement of PPI, including having a PPI co-applicant, four events for PPI, and inclusion of members of the Deep End Patient Panel from one of the most socially deprived areas in the UK, grounded the review and findings in the reality of people’s lives. Eighth, the engagement of a wide range of stakeholders helped to ensure that the findings were useful to them. For example, it led to us identifying an intervention produced and used within the NHS currently that we included in our user-friendliness assessment and could recommend for wider use in terms of being a high-quality resource.
The systematic review had seven limitations. First, we found studies mainly from the USA, the UK and the rest of Europe. We may have missed research from the rest of the world, but it is also plausible that interest in improving health literacy to reduce the use of emergency and primary care is limited to those countries. There is some support for this: there has been an exponential growth in publications about health literacy more generally, with a dominance of the USA, Australia and the UK,154 which makes it unlikely that we missed global health literature. Second, we are likely to have missed grey literature and literature that did not measure primary and emergency care use. Towards the end of the review, one of our stakeholders identified a small-scale evaluation of The Little Orange Book undertaken by a patient group. 141 The findings were very similar to those in our review in that users of the intervention found the intervention very helpful. An additional finding was that staff regarded it highly. From discussions with our stakeholders, there are likely to be more of these types of studies that are not published in peer-reviewed journals or easily found using grey literature searches. It is also possible that we missed relevant studies published in databases because we required a focus on reduction of service use. When finalising the report, we found an article reporting the development and evaluation of a component of a mass media campaign to reduce the use of emergency ambulance services for non-emergencies. 155 The campaign was successful in terms of reaching people and changing their attitudes towards ambulance use. That is, it was similar to the findings of our review in that it was successful for short-term outcomes. The next step for the research group was to measure the effect on ambulance use. Third, the majority of each systematic review process (study selection, data extraction and quality assessment) was performed by a single reviewer (CC). However, as an initial step, and to ensure complete clarity and consistency in the application of inclusion criteria and data extraction, four project team members (CC, LP, AOC and AF) all screened 100 titles and abstracts, and extracted three studies, to identify, discuss and resolve any ambiguities. There was also independent checking by a second reviewer (LP) of a minimum of 10% of the article data extractions and critical appraisals (n = 7), and disagreements were found to be rare and easily resolved. All decisions were also checked with reference to a third member of the project team (AOC or AF). Fourth, it was sometimes difficult to stay clear about the boundaries of the research when health professionals such as pharmacists and health visitors offer advice to patients about managing future minor health problems. We have ensured that we are clear that the review was about interventions to help patients make decisions themselves without input from health professionals. Fifth, we could not access all the interventions to do readability testing and user-accessibility assessments. Sixth, we had intended to use context–mechanism–outcome chains in our synthesis, but this did not feel like a helpful process, so we did not do it. Seventh, the ‘feasible, appropriate, meaningful and effective’ framework was not helpful during our second stakeholder event. It may have been more useful if we had identified one intervention or intervention type that stood out as effective and warranted further detailed discussion about its use in the NHS.
Strengths and limitations of the patient and public involvement activity
The GRIPP2 checklist46 and Pollock et al. ’s48 framework were used to help us reflect on our PPI. The PPI activity had seven strengths. First, we involved 14 different people, each with different characteristics and life experiences. Second, we had a PPI member (MO) as an active member of the project team. This ensured that, when conducting the review, there was always a PPI voice who provided valuable advice, feedback and support throughout the project. Third, one of our co-applicants was the stakeholder lead (AF), ensuring that there was researcher and administrator time dedicated to supporting people. Fourth, we involved PPI members throughout the review, including at protocol development stage, developing the UFAT and when considering the implications of the results. Fifth, we kept people informed throughout the study by having a project newsletter, and our stakeholder lead (AF) encouraged telephone and e-mail exchanges if people wanted to contribute outside meetings. Sixth, we remunerated people for their involvement. Seventh, we provided additional support to facilitate involvement, including training on engaging in virtual meetings and on using Twitter.
The PPI activity had three limitations. First, because of COVID-19, we held all our events virtually. We feel that we mitigated against problems with technology, but could have made more use of small breakout rooms during meetings to allow quieter members to contribute. Virtual meetings also reduced any opportunity for informal rapport-building, such as chatting over coffee. Second, there was a long gap of no PPI meetings between the November 2020 and June 2021 meetings. Although we kept the PPI group updated about the review through newsletters, an interim meeting in the spring may have been valuable. We did not undertake any meetings in that period because we were at the search/extraction stage of the review and we wanted to work with PPI members when we had emerging findings to discuss. Third, the university’s financial systems made remuneration complex for some members. This caused stress and resulted in delays in payments for some people. Our department is working with the university to simplify PPI payments so that it does not become a barrier to engagement.
Reflections on doing this type of research
We have five recommendations for researchers doing this work in the future. First, measure actual use of services using records, rather than relying on self-report. Second, be consistent as a research community about the measurement time period. The most common measurement time periods were 6 months and 1 year. Third, we noted that some studies used records from a single hospital only; intervention users may have actively sought care outside this hospital if they felt that their local ED was trying to persuade them not to attend. If possible, we recommend also measuring impact on surrounding EDs. Fourth, not many studies measured safety, and this is a really important issue to patients and the public. It is heartening that those that measured safety found these interventions to be safe. Fifth, we felt that the low scoring in the formal quality assessment of these studies was harsh given the difficulty of undertaking research in such complex environments. This was particularly the case for the RCTs in our review. Researchers could review these assessment tools for application to pragmatic RCTs.
Implications for decision-makers
A number of health literacy interventions are used in the NHS currently. Commissioners and service providers have developed booklets and websites to help parents of young children and the general population to manage minor health problems and decide where best to go for care. Policy-makers have developed NHS 111 Online for self-triage. Rather than develop further new interventions, commissioners and service providers could contact their counterparts in different regions and make use of existing good-quality interventions. It might also be helpful to have a space where local evaluations can be shared. Once commissioners and service providers locate a relevant intervention, they could assess the reading age and user-friendliness, and improve these if necessary. This is important for websites as well as information in booklet format. Our PPI members were keen that commissioners and service providers look for ways to make existing interventions available to more people (e.g. through school) and available in different languages or formats, such as online videos. We know that NHS 111 Online is advertised on bus stops and some navigation tools are posted on social media, yet the PPI members often had not seen them. The PPI members were concerned about a lack of digital literacy in some parts of the population and a lack of access to technology; they described initiatives they had come across such a health champion in general practice who could help people to look things up on a tablet. They also described a system that, when added to a website, reads the website content aloud and translates it into different languages. Finding ways of making existing good-quality interventions more accessible and used by the general population might benefit people’s ability to care for minor health problems and seek health care from the most appropriate place. It is also important to continue to evaluate existing interventions in terms of measuring impact on service use and cost-effectiveness, because this cannot be taken for granted.
Recommendations for further research
-
Focus on understanding how to improve access to existing good-quality interventions (particularly those currently used in the NHS), rather than develop new interventions.
-
Continue to evaluate the effectiveness and cost-effectiveness of these types of interventions, given that these types of interventions have potential to reduce the use of emergency and urgent care, and that self-care for minor health problems may be necessary during pandemics and to facilitate the sustainability of emergency and urgent care provision.
-
Measure the safety of these interventions.
-
Focus on understanding why an intervention did or did not work, rather than only measuring impact on service use, that is use mixed-methods evaluations of RCTs/quasi-experimental designs and process evaluation/qualitative research.
-
Undertake more rigorous economic evaluation of these interventions.
-
Evaluate interventions aimed at adults using EDs for minor health problems because few studies did this.
-
Pay more attention to ‘displacement’, whereby people use different services from the ones being measured.
-
As a research community, measure changes in service use in a consistent way and at a consistent time post intervention. This will facilitate a future meta-analysis. Consider measuring change in attendances at a service for minor health problems/non-urgent reasons at 1 year post intervention.
-
Consider ways of making it easier to monitor change in service use over time using routine data.
Conclusions
Health literacy interventions have potential to reduce emergency and primary care use. They need further rigorous evaluation to determine which work best and for whom.
Acknowledgements
Acknowledgement for individuals
Thanks to Vera Fibisan for her administrative skills, support for the PPI endeavour and organisation of the stakeholder events.
Thanks to PPI members and stakeholders for their time and insights (some people did not want their names included):
-
Aidan Barry
-
Kristin Bash
-
Jude Beng
-
Jonathan Berry
-
Mary Bramhall
-
Jo Chalmers
-
Colleen Ewart
-
Debbie Floyd
-
Kate Grudzinska
-
Carrie Hedderwick
-
Carole Hobson
-
Sarah Illingworth
-
Linda Jones
-
Kenye Karemo
-
Kerry Knox
-
Rashmi Kumar
-
Liz Lingard
-
Margaret Mellor
-
Mike Oliver
-
Sam Pilkington
-
Vickie Riley
-
Niro Siriwardena
-
Alan Smith
-
Debs Smith
-
Jill Smith
-
Irene Soulsby
-
Josie Soutar
-
Helen Twohig
-
Frances Verey.
Contributions of authors
Alicia O’Cathain (https://orcid.org/0000-0003-4033-506X) (Professor of Health Services Research) led the study.
Alexis Foster (https://orcid.org/0000-0002-7978-2791) (Research Fellow) led the stakeholder engagement and the user-friendliness of interventions component, and co-led the PPI.
Christopher Carroll (https://orcid.org/0000-0002-6361-6182) (Reader) conducted the systematic review.
Louise Preston (https://orcid.org/0000-0001-7477-4517) (Senior Research Fellow) contributed to design and conduct of the systematic review.
Margaret Ogden (https://orcid.org/0000-0002-4611-5095) (PPI member) co-led PPI input.
Mark Clowes (https://orcid.org/0000-0002-5582-9946) (Research Associate) conducted the searches.
Joanne Protheroe (https://orcid.org/0000-0002-9608-1487) (Director of General Practice Education, Director of Clinical Academic Training, Past Chair of Health Literacy UK, and NHS Clinical Adviser for Health Literacy) advised on health literacy aspects of the review.
Ethics statement
This study is a systematic review with stakeholder involvement and did not need ethics approval.
Data-sharing statement
This report generated no new data; therefore, there are no further data to be shared other than those included in the report. Any further queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Royal College of General Practitioners . Simply Not Enough GPs to Meet Demand n.d. www.rcgp.org.uk/about-us/news/2021/june/simply-not-enough-gps-to-meet-demand.aspx (accessed 26 October 2021).
- NHS England . Ambulance Quality Indicators Data 2021–22 n.d. www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2021-22/ (accessed 26 October 2021).
- NHS England . New Campaign to Help Public Get NHS Advice Quickly Ahead of ‘Winter Like No Other’ n.d. www.england.nhs.uk/2021/11/new-campaign-to-help-public-get-nhs-advice-quickly-ahead-of-winter-like-no-other/ (accessed 2 November 2021).
- O’Cathain A, Knowles E, Long J, Connell J, Bishop-Edwards L, Simpson R, et al. Drivers of ‘clinically unnecessary’ use of emergency and urgent care: the DEUCE mixed-methods study. Health Soc Care Deliv Res 2020;8. https://doi.org/10.3310/hsdr08150.
- Booker MJ, Shaw ARG, Purdy S. Why do patients with ‘primary care sensitive’ problems access ambulance services? A systematic mapping review of the literature. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-007726.
- O’Keeffe C, Mason S, Jacques R, Nicholl J. Characterising non-urgent users of the emergency department (ED): a retrospective analysis of routine ED data. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0192855.
- Watson MC, Ferguson J, Barton GR, Maskrey V, Blyth A, Paudyal V, et al. A cohort study of influences, health outcomes and costs of patients’ health-seeking behaviour for minor ailments from primary and emergency care settings. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006261.
- Welle-Nilsen LK, Morken T, Hunskaar S, Granas AG. Minor ailments in out-of-hours primary care: an observational study. Scand J Prim Health Care 2011;29:39-44. https://doi.org/10.3109/02813432.2010.545209.
- O’Cathain A, Connell J, Long J, Coster J. ‘Clinically unnecessary’ use of emergency and urgent care: a realist review of patients’ decision making. Health Expect 2020;23:19-40. https://doi.org/10.1111/hex.12995.
- Long J, Knowles E, Bishop-Edwards L, O’Cathain A. Understanding young adults’ reasons for seeking ‘clinically unnecessary’ urgent and emergency care: a qualitative interview study. Health Expect 2021;24:1535-44. https://doi.org/10.1111/hex.13301.
- Morrison AK, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad Pediatr 2014;14:309-14. https://doi.org/10.1016/j.acap.2014.01.004.
- O’Cathain A, Simpson R, Phillips M, Dickson JM. Tendency to contact general practice instead of self-care: a population vignette study. BJGP Open 2020;4. https://doi.org/10.3399/bjgpopen20X101024.
- NHS England . Enabling People to Make Informed Health Decisions n.d. www.england.nhs.uk/ourwork/patient-participation/health-decisions/ (accessed 26 October 2021).
- Nutbeam D. Defining and measuring health literacy: what can we learn from literacy studies?. Int J Public Health 2009;54:303-5. https://doi.org/10.1007/s00038-009-0050-x.
- Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-658.
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006;8. https://doi.org/10.2196/jmir.8.2.e9.
- Heijmans M, Uiters E, Rose T, Hofstede J, Devillé W, van der Heide I, et al. Study On Sound Evidence For a Better Understanding of Health Literacy in the European Union. Brussels: Consumers, Health, Agriculture and Food Agency, European Commision; 2015.
- Sørensen K, Van den Broucke S, Pelikan J, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-948.
- Scottish Government . Making It Easier: A Health Literacy Action Plan 2017–2025 n.d. www.gov.scot/publications/making-easier-health-literacy-action-plan-scotland-2017-2025/ (accessed 26 October 2021).
- NHS Health Education England . Improving Health Literacy n.d. www.hee.nhs.uk/our-work/knowledge-library-services/improving-health-literacy (accessed 26 October 2021).
- van der Heide I, Heijmans M, Schuit AJ, Uiters E, Rademakers J. Functional, interactive and critical health literacy: varying relationships with control over care and number of GP visits. Patient Educ Couns 2015;98:998-1004. https://doi.org/10.1016/j.pec.2015.04.006.
- Berens EM, Vogt D, Ganahl K, Weishaar H, Pelikan J, Schaeffer D. Health literacy and health service use in germany. Health Lit Res Pract 2018;2:e115-e122. https://doi.org/10.3928/24748307-20180503-01.
- Jansen T, Rademakers J, Waverijn G, Verheij R, Osborne R, Heijmans M. The role of health literacy in explaining the association between educational attainment and the use of out-of-hours primary care services in chronically ill people: a survey study. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3197-4.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97-107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005.
- Ueki S, Komai K, Ohashi K, Fujita Y, Kitao M, Fujiwara C. Parental factors predicting unnecessary ambulance use for their child with acute illness: a cross-sectional study. J Adv Nurs 2019;75:2811-19. https://doi.org/10.1111/jan.14161.
- Morrison AK, Myrvik MP, Brousseau DC, Hoffmann RG, Stanley RM. The relationship between parent health literacy and pediatric emergency department utilization: a systematic review. Acad Pediatr 2013;13:421-9. https://doi.org/10.1016/j.acap.2013.03.001.
- Griffey RT, Kennedy SK, D’Agostino McGowan L, Goodman M, Kaphingst KA. Is low health literacy associated with increased emergency department utilization and recidivism?. Acad Emerg Med 2014;21:1109-15. https://doi.org/10.1111/acem.12476.
- Zhang L, Ding D, Neubeck L, Gallagher R. Health literacy as a predictor of emergency department visits and self-rated health among Chinese immigrants: findings from an Australian survey. Patient Educ Couns 2020;103:2353-60. https://doi.org/10.1016/j.pec.2020.04.017.
- May M, Brousseau DC, Nelson DA, Flynn KE, Wolf MS, Lepley B, et al. Why parents seek care for acute illness in the clinic or the ED: the role of health literacy. Acad Pediatr 2018;18:289-96. https://doi.org/10.1016/j.acap.2017.06.010.
- Chapron A, Brochard M, Rousseau C, Rousseau AC, Brujean M, Fiquet L, et al. Parental reassurance concerning a feverish child: determinant factors in rural general practice. BMC Fam Pract 2018;19. https://doi.org/10.1186/s12875-017-0686-1.
- Vandenbosch J, Van den Broucke S, Vancorenland S, Avalosse H, Verniest R, Callens M. Health literacy and the use of healthcare services in Belgium. J Epidemiol Community Health 2016;70:1032-8. https://doi.org/10.1136/jech-2015-206910.
- Oslislo S, Heintze C, Schmiedhofer M, Möckel M, Schenk L, Holzinger F. How to decide adequately? Qualitative study of GPs’ view on decision-making in self-referred and physician-referred emergency department consultations in Berlin, Germany. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-026786.
- Sandín-Vázquez M, Conde-Espejo P. Primaria Grupo de Investigación sobre Utilización de Servicios en Atención Primaria . Frequent attendance: the primary care professional’s perceptions on the influence of social factors and health care system organisation. Rev Calid Asist 2011;26:256-63. https://doi.org/10.1016/j.cali.2011.03.006.
- Fisher RF, Croxson CH, Ashdown HF, Hobbs FR. GP views on strategies to cope with increasing workload: a qualitative interview study. Br J Gen Pract 2017;67:e148-e156. https://doi.org/10.3399/bjgp17X688861.
- Sheridan SL, Halpern DJ, Viera AJ, Berkman ND, Donahue KE, Crotty K. Interventions for individuals with low health literacy: a systematic review. J Health Commun 2011;16:30-54. https://doi.org/10.1080/10810730.2011.604391.
- Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-6331-7.
- Jacobs RJ, Lou JQ, Ownby RL, Caballero J. A systematic review of eHealth interventions to improve health literacy. Health Informatics J 2016;22:81-98. https://doi.org/10.1177/1460458214534092.
- Car J, Lang B, Colledge A, Ung C, Majeed A. Interventions for enhancing consumers’ online health literacy. Cochrane Database Syst Rev 2011;6. https://doi.org/10.1002/14651858.CD007092.pub2.
- Walters R, Leslie SJ, Polson R, Cusack T, Gorely T. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health 2020;20. https://doi.org/10.1186/s12889-020-08991-0.
- Coulter A, Ellins J. Patient-Focused Interventions: A Review of the Evidence. London: The Health Foundation; 2006.
- Andrews T, Thompson M, Buckley DI, Heneghan C, Deyo R, Redmond N, et al. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: a systematic review and meta-analysis. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0030334.
- Paudyal V, Watson MC, Sach T, Porteous T, Bond CM, Wright DJ, et al. Are pharmacy-based minor ailment schemes a substitute for other service providers? A systematic review. Br J Gen Pract 2013;63:e472-81. https://doi.org/10.3399/bjgp13X669194.
- Donovan E, Wilcox CR, Patel S, Hay AD, Little P, Willcox ML. Digital interventions for parents of acutely ill children and their treatment-seeking behaviour: a systematic review. Br J Gen Pract 2020;70:e172-e178. https://doi.org/10.3399/bjgp20X708209.
- Richardson M, Khouja C, Sutcliffe K, Hinds K, Brunton G, Stansfield C, et al. Self-Care for Minor Ailments: Systematic Reviews of Qualitative and Quantitative Research. London: EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London; 2018.
- Semigran HL, Linder JA, Gidengil C, Mehrotra A. Evaluation of symptom checkers for self diagnosis and triage: audit study. BMJ 2015;351. https://doi.org/10.1136/bmj.h3480.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a scoping review. Syst Rev 2018;7. https://doi.org/10.1186/s13643-018-0852-0.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Development of the ACTIVE framework to describe stakeholder involvement in systematic reviews. J Health Serv Res Policy 2019;24:245-55. https://doi.org/10.1177/1355819619841647.
- Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev 2012;1. https://doi.org/10.1186/2046-4053-1-28.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Howard Wilsher S, Brainard J, Loke Y, Salter C. Patient and public involvement in health literacy interventions: a mapping review. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0081-z.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. https://doi.org/10.1186/1748-5908-7-37.
- Yardley L, Joseph J, Michie S, Weal M, Wills G, Little P. Evaluation of a web-based intervention providing tailored advice for self-management of minor respiratory symptoms: exploratory randomized controlled trial. J Med Internet Res 2010;12. https://doi.org/10.2196/jmir.1599.
- O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud 2019;5. https://doi.org/10.1186/s40814-019-0425-6.
- O’Cathain A, Thomas KJ, Drabble SJ, Rudolph A, Hewison J. What can qualitative research do for randomised controlled trials? A systematic mapping review. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002889.
- The Cochrane Collaboration . RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials n.d. https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed 30 September 2022).
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses n.d. www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 28 November 2021).
- Critical Appraisal Skills Programme . CASP Checklist n.d. https://casp-uk.net/wp-content/uploads/2018/03/CASP-Qualitative-Checklist-2018_fillable_form.pdf (accessed 28 November 2021).
- Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT): Version 2018 – User Guide n.d. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf (accessed 28 November 2021).
- Rowlands G, Protheroe J, Winkley J, Richardson M, Seed PT, Rudd R. A mismatch between population health literacy and the complexity of health information: an observational study. Br J Gen Pract 2015;65:e379-86. https://doi.org/10.3399/bjgp15X685285.
- Jindal P, MacDermid JC. Assessing reading levels of health information: uses and limitations of flesch formula. Educ Health 2017;30:84-8. https://doi.org/10.4103/1357-6283.210517.
- Protheroe J, Estacio EV, Saidy-Khan S. Patient information materials in general practices and promotion of health literacy: an observational study of their effectiveness. Br J Gen Pract 2015;65:e192-7. https://doi.org/10.3399/bjgp15X684013.
- Rughani G, Hanlon P, Corcoran N, Mair FS. The readability of general practice websites: a cross-sectional analysis of all general practice websites in Scotland. Br J Gen Pract 2021;71:e391-e398. https://doi.org/10.3399/BJGP.2020.0820.
- Kher A, Johnson S, Griffith R. Readability assessment of online patient education material on congestive heart failure. Adv Prev Med 2017;2017. https://doi.org/10.1155/2017/9780317.
- NHS England . The Information Standard Principles: The Information Standard for Health and Care Information Production Quality Statements n.d. www.england.nhs.uk/tis/the-info-standard/#end-product (accessed 18 September 2022).
- NHS Digital . Design Principles n.d. https://service-manual.nhs.uk/design-system/design-principles (accessed 4 November 2021).
- Centers for Disease Control and Prevention . Research Summaries &Amp; Science Bites n.d. www.cdc.gov/healthliteracy/researchevaluate/evidence-research.html (accessed 4 November 2021).
- NHS Newcastle Gateshead Clinical Commissioning Group . The Little Orange Book: Expert Advice on Helping Babies and Young Children When They’re Poorly 2021. newcastlegatesheadccg.nhs.uk/wp-content/uploads/sites/12/2020/08/Little-Orange-Book.pdf (accessed 7 September 2021).
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368. https://doi.org/10.1136/bmj.l6890.
- Aluko P, Graybill E, Craig D, Henderson C, Drummond M, Wilson ECF, et al. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2. London: Cochrane; 2021.
- Angus C, Latimer N, Preston L, Li J, Purshouse R. What are the implications for policy makers? a systematic review of the cost-effectiveness of screening and brief interventions for alcohol misuse in primary care. Front Psychiatry 2014;5. https://doi.org/10.3389/fpsyt.2014.00114.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. https://doi.org/10.1186/1471-2288-8-45.
- Deeks JJ, Higgins JPT, Altman DG. 9.6.4 Meta-Regression n.d. https://handbook-5-1.cochrane.org/chapter_9/9_6_4_meta_regression.htm (accessed 28 November 2021).
- Shaw J, Gray CS, Baker GR, Denis JL, Breton M, Gutberg J, et al. Mechanisms, contexts and points of contention: operationalizing realist-informed research for complex health interventions. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0641-4.
- Plass AMC, Timmermans DRM, van der Wal G. Decreasing the number of consultations for minor illnesses of Turkish and Dutch inhabitants of a deprived area in The Netherlands: an intervention study. Fam Pract 2005;22:51-7. https://doi.org/10.1093/fampra/cmh703.
- Plass AMC, Timmermans DRM, van der Wal G. Does stimulating self-care increase self-care behaviour for minor illnesses of Dutch and Turkish inhabitants of a deprived area in The Netherlands?. Patient Educ Couns 2006;63:97-103. https://doi.org/10.1016/j.pec.2005.09.005.
- Rutten GE, Beek MM, van Eijk JT. Effects of systematic patient education about cough on the consulting behaviour of a general practice population. Patient Educ Couns 1993;22:127-32. https://doi.org/10.1016/0738-3991(93)90092-B.
- Rutten G, Van Eijk J, Beek M, Van der Velden H. Patient education about cough: effect on the consulting behaviour of general practice patients. Br J Gen Pract 1991;41:289-92.
- Hibbard JH, Greenlick M, Jimison H, Capizzi J, Kunkel L. The impact of a community-wide self-care information project on self-care and medical care utilization. Eval Health Prof 2001;24:404-23. https://doi.org/10.1177/01632780122034984.
- Wagner TH, Hibbard JH, Greenlick MR, Kunkel L. Does providing consumer health information affect self-reported medical utilization? Evidence from the Healthwise Communities Project. Med Care 2001;39:836-47. https://doi.org/10.1097/00005650-200108000-00009.
- Herman A, Jackson P. Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention. J Health Commun 2010;15:895-910. https://doi.org/10.1080/10810730.2010.522228.
- Herman AD, Mayer GG. Reducing the use of emergency medical resources among Head Start families: a pilot study. J Community Health 2004;29:197-208. https://doi.org/10.1023/b:johe.0000022026.20770.f4.
- Herman A, Young KD, Espitia D, Fu N, Farshidi A. Impact of a health literacy intervention on pediatric emergency department use. Pediatr Emerg Care 2009;25:434-8. https://doi.org/10.1097/PEC.0b013e3181ab78c7.
- Little P, Stuart B, Andreou P, McDermott L, Joseph J, Mullee M, et al. Primary care randomised controlled trial of a tailored interactive website for the self-management of respiratory infections (Internet Doctor). BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009769.
- Chande VT, Wyss N, Exum V. Educational interventions to alter pediatric emergency department utilization patterns. Arch Pediatr Adolesc Med 1996;150:525-8. https://doi.org/10.1001/archpedi.1996.02170300079015.
- Davis T, Meyer A, Beste J, Batish S. Decreasing low acuity pediatric emergency room visits with increased clinic access and improved parent education. J Am Board Fam Med 2018;31:550-7. https://doi.org/10.3122/jabfm.2018.04.170474.
- Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag 2013;58:412-27. https://doi.org/10.1097/00115514-201311000-00007.
- Fieldston ES, Nadel FM, Alpern ER, Fiks AG, Shea JA, Alessandrini EA. Effects of an education and training intervention on caregiver knowledge of nonurgent pediatric complaints and on child health services utilization. Pediatr Emerg Care 2013;29:331-6. https://doi.org/10.1097/PEC.0b013e31828512c7.
- Holden B. Distribution of Targeted Educational Materials to Families After They Attend Emergency or Urgent Care Services With a Child Under 5 Years-Old in a Non-Urgent Situation, in Order to Reduce Future Repeat Non-Urgent Attendances. Report No. ISRCTN74381956 2020.
- Ladley A, Hieger AW, Arthur J, Broom M. Educational text messages decreased emergency department utilization among infant caregivers: a randomized trial. Acad Pediatr 2018;18:636-41. https://doi.org/10.1016/j.acap.2018.02.003.
- Patel PB, Vinson DR, Gardner MN, Wulf DA, Kipnis P, Liu V, et al. Impact of emergency physician-provided patient education about alternative care venues. Am J Manag Care 2018;24:225-31.
- Racine AD, Alderman EM, Avner JR. Effect of telephone calls from primary care practices on follow-up visits after pediatric emergency department visits: evidence from the Pediatric Emergency Department Links to Primary Care (PEDLPC) randomized controlled trial. Arch Pediatr Adolesc Med 2009;163:505-11. https://doi.org/10.1001/archpediatrics.2009.45.
- Shnowske K, Berg DD, Guntern P, Hop D. Care guide use for repeated non-emergent complaints and its effect on emergency department visit frequency. Am J Emerg Med 2018;36:1697-8. https://doi.org/10.1016/j.ajem.2018.01.036.
- Sturm JJ, Hirsh D, Weselman B, Simon HK. Reconnecting patients with their primary care provider: an intervention for reducing nonurgent pediatric emergency department visits. Clin Pediatr 2014;53:988-94. https://doi.org/10.1177/0009922814540987.
- Yoffe SJ, Moore RW, Gibson JO, Dadfar NM, McKay RL, McClellan DA, et al. A reduction in emergency department use by children from a parent educational intervention. Fam Med 2011;43:106-11.
- Heaney D, Wyke S, Wilson P, Elton R, Rutledge P. Assessment of impact of information booklets on use of healthcare services: randomised controlled trial. BMJ 2001;322:1218-21. https://doi.org/10.1136/bmj.322.7296.1218.
- Usherwood TP. Development and randomized controlled trial of a booklet of advice for parents. Br J Gen Pract 1991;41:58-62.
- van der Gugten AC, Uiterwaal CS, Verheij TJ, van der Ent CK. E-health and consultation rates for respiratory illnesses in infants: a randomised clinical trial in primary care. Br J Gen Pract 2015;65:e61-8. https://doi.org/10.3399/bjgp15X683485.
- Francis NA, Butler CC, Hood K, Simpson S, Wood F, Nuttall J. Effect of using an interactive booklet about childhood respiratory tract infections in primary care consultations on reconsulting and antibiotic prescribing: a cluster randomised controlled trial. BMJ 2009;339. https://doi.org/10.1136/bmj.b2885.
- Macfarlane J, Holmes W, Gard P, Thornhill D, Macfarlane R, Hubbard R. Reducing antibiotic use for acute bronchitis in primary care: blinded, randomised controlled trial of patient information leaflet. BMJ 2002;324:91-4. https://doi.org/10.1136/bmj.324.7329.91.
- Macfarlane JT, Holmes WF, Macfarlane RM. Reducing reconsultations for acute lower respiratory tract illness with an information leaflet: a randomized controlled study of patients in primary care. Br J Gen Pract 1997;47:719-22.
- de Bont EGPM, Dinant GJ, Elshout G, van Well G, Francis NA, Winkens B, et al. Booklet for childhood fever in out-of-hours primary care: a cluster-randomized controlled trial. Ann Fam Med 2018;16:314-21. https://doi.org/10.1370/afm.2265.
- O’Neill-Murphy K, Liebman M, Barnsteiner J. Fever education: does it reduce parent fever anxiety?. Padiatr Emerg Care 2001;17:47-51. https://doi.org/10.1097/00006565-200102000-00014.
- Cowie J, Calveley E, Bowers G, Bowers J. Evaluation of a digital consultation and self-care advice tool in primary care: a multi-methods study. Int J Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15050896.
- Hansen BW. A randomized controlled trial on the effect of an information booklet for young families in Denmark. Patient Educ Couns 1990;16:147-50. https://doi.org/10.1016/0738-3991(90)90089-4.
- Little P, Somerville J, Williamson I, Warner G, Moore M, Wiles R, et al. Randomised controlled trial of self management leaflets and booklets for minor illness provided by post. BMJ 2001;322:1214-16. https://doi.org/10.1136/bmj.322.7296.1214.
- Platts A, Mitton R, Boniface D, Friedli K. Can self-care health books affect amount of contact with the primary health care team? A randomized controlled trial in general practice. Scand J Prim Health Care 2005;23:142-8. https://doi.org/10.1080/02813430510031289.
- Robbins H, Hundley V, Osman LM. Minor illness education for parents of young children. J Adv Nurs 2003;44:238-47. https://doi.org/10.1046/j.1365-2648.2003.02798.x.
- Wood EB, Harrison G, Trickey A, Friesen MA, Stinson S, Rovelli E, et al. Evidence-based practice: video-discharge instructions in the pediatric emergency department. J Emerg Nurs 2017;43:316-21. https://doi.org/10.1016/j.jen.2016.11.003.
- Adesara R, Spencer JP, Bost JE. Office-based patient education decreases non-emergent emergency department visits. J Med Pract Manage 2011;27:131-5.
- DeCamp LR, Godage SK, Valenzuela Araujo D, Dominguez Cortez J, Wu L, Psoter KJ, et al. A texting intervention in Latino families to reduce ED use: a randomized trial. Pediatrics 2020;145. https://doi.org/10.1542/peds.2019-1405.
- Huyer G, Chreim S, Michalowski W, Farion KJ. Barriers and enablers to a physician-delivered educational initiative to reduce low-acuity visits to the pediatric emergency department. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0198181.
- Nijland N, Cranen K, Verlinden S, Kelders SM, Boer H, van Gemert-Pijnen JEWC. Computer Generated Self-Care Advice via Web-Based Triage of Complaints in Primary Care n.d. https://doi.org/10.1109/eTELEMED.2009.17.
- Nijland N, van Gemert-Pijnen J, Boer H, Steehouder MF, Seydel ER. Evaluation of internet-based technology for supporting self-care: problems encountered by patients and caregivers when using self-care applications. J Med Internet Res 2008;10. https://doi.org/10.2196/jmir.957.
- Barr RG, Rajabali F, Aragon M, Colbourne M, Brant R. Education about crying in normal infants is associated with a reduction in pediatric emergency room visits for crying complaints. J Dev Behav Pediatr 2015;36:252-7. https://doi.org/10.1097/DBP.0000000000000156.
- Beal SJ, Nause K, Lutz N, Greiner MV. The impact of health care education on utilization among adolescents preparing for emancipation from foster care. J Adolesc Health 2020;66:740-6. https://doi.org/10.1016/j.jadohealth.2019.12.009.
- Mullett J, Hills M. What information and support do people seek to help them make decisions about self-care?. Int J Health Promot Educ 2002;40:111-9. https://doi.org/10.1080/14635240.2002.10806209.
- Ohns MJ. Identifying the preferred method to educate low income caregivers about common childhood illnesses: a step toward health literacy through a focus group study. J Pediatr Nurs 2019;47:131-5. https://doi.org/10.1016/j.pedn.2019.05.003.
- Steelman J, Kotchmar GS, Brehm W, Greenwall K. Childhood fever education in a military population: is education enough?. J Miss State Med Assoc 1999;40:407-9.
- Steinweg KK, Killingsworth RE, Nannini RJ, Spayde J. The impact on a health care system of a program to facilitate self-care. Mil Med 1998;163:139-44. https://doi.org/10.1093/milmed/163.3.139.
- White A, South J, Bagnall AM, Forshaw M, Spoor C, Marchant P, et al. The self-care for people initiative: the outcome evaluation. Prim Health Care Res Dev 2012;13:382-94. https://doi.org/10.1017/S146342361200014X.
- Hou XY, Zhao J, Chu K. Impact of a government Triple Zero awareness campaign on emergency department patient characteristics. Emerg Med Australas 2012;24:393-400. https://doi.org/10.1111/j.1742-6723.2012.01560.x.
- Anhang Price R, Fagbuyi D, Harris R, Hanfling D, Place F, Taylor TB, et al. Feasibility of web-based self-triage by parents of children with influenza-like illness: a cautionary tale. JAMA Pediatr 2013;167:112-18. https://doi.org/10.1001/jamapediatrics.2013.1573.
- Murray J, Majeed A, Khan MS, Lee JT, Nelson P. Use of the NHS Choices website for primary care consultations: results from online and general practice surveys. JRSM Short Rep 2011;2. https://doi.org/10.1258/shorts.2011.011078.
- Rector TS, Venus PJ, Laine AJ. Impact of mailing information about nonurgent care on emergency department visits by Medicaid beneficiaries enrolled in managed care. Am J Manag Care 1999;5:1505-12.
- Stockwell MS, Catallozzi M, Larson E, Rodriguez C, Subramony A, Andres Martinez R, et al. Effect of a URI-related educational intervention in early head start on ED visits. Pediatrics 2014;133:e1233-40. https://doi.org/10.1542/peds.2013-2350.
- Powell D. Control health care costs by controlling demand. Hum Resour Prof 1995;8:19-22.
- Powell DR, Sharp SL, Farnell SD, Smith PT. Implementing a self care program. Effect on employee health care utilization. AAOHN J 1997;45:247-53. https://doi.org/10.1177/216507999704500506.
- Spoelman WA, Bonten TN, de Waal MWM, Drenthen T, Smeele IJM, Nielen MMJ, et al. Effect of an evidence-based website on healthcare usage: an interrupted time-series study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-013166.
- Chande VT, Kimes D. A health promotion intervention for families in a Medicaid managed care plan. Acad Emerg Med 1999;6:823-7. https://doi.org/10.1111/j.1553-2712.1999.tb01215.x.
- Sustersic M, Jeannet E, Cozon-Rein L, Maréchaux F, Genty C, Foote A, et al. Impact of information leaflets on behavior of patients with gastroenteritis or tonsillitis: a cluster randomized trial in French primary care. J Gen Intern Med 2013;28:25-31. https://doi.org/10.1007/s11606-012-2164-8.
- Thomson H, Ross S, Wilson P, McConnachie A, Watson R. Randomised controlled trial of effect of Baby Check on use of health services in first 6 months of life. BMJ 1999;318:1740-4. https://doi.org/10.1136/bmj.318.7200.1740.
- Thornton AJ, Morley CJ, Green SJ, Cole TJ, Walker KA, Bonnett JM. Field trials of the Baby Check score card: mothers scoring their babies at home. Arch Dis Child 1991;66:106-10. https://doi.org/10.1136/adc.66.1.106.
- Bertakis KD. Impact of a patient education intervention on appropriate utilization of clinic services. J Am Board Fam Pract 1991;4:411-18.
- McWilliams DB, Jacobson RM, Van Houten HK, Naessens JM, Ytterberg KL. A program of anticipatory guidance for the prevention of emergency department visits for ear pain. Arch Pediatr Adolesc Med 2008;162:151-6. https://doi.org/10.1001/archpediatrics.2007.30.
- Lepley BE, Brousseau DC, May MF, Morrison AK. Randomized controlled trial of acute illness educational intervention in the pediatric emergency department: written versus application-based education. Pediatr Emerg Care 2020;36:e192-e198. https://doi.org/10.1097/PEC.0000000000001719.
- DeSalvo A, Rest SB, Nettleman M, Freer S, Knight T. Patient education and emergency room visits. Clin Perform Qual Health Care 2000;8:35-7. https://doi.org/10.1108/14664100010333017.
- Elsenhans VD, Marquardt C, Bledsoe T. Use of self-care manual shifts utilization pattern. HMO Pract 1995;9:88-90.
- Chiu YK, Sun YC, Wang YW, Yeh JI. Establishing a community-run GP-supervised self-care program for minor illnesses in remote areas in Taiwan: an observational study. Fam Pract 2012;29:338-44. https://doi.org/10.1093/fampra/cmr090.
- Verzantvoort NCM, Teunis T, Verheij TJM, van der Velden AW. Self-triage for acute primary care via a smartphone application: practical, safe and efficient?. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0199284.
- Involve North East . The Little Orange Book Six Month Review: The Views of Health Care Professionals and Parents Carers 2018.
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the Newest Vital Sign. Ann Fam Med 2005;3:514-22. https://doi.org/10.1370/afm.405.
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33-42. https://doi.org/10.1016/S0738-3991(98)00116-5.
- Groom N, Kidd T, Carey N. Urgent care centre redirection: evaluation of a nurse-led intervention. Emerg Nurse 2018;25:25-30. https://doi.org/10.7748/en.2018.e1768.
- West Yorkshire Health and Care Partnership . GP Online Consultation Animation – British Sign Language (BSL) Version n.d. www.youtube.com/watch?v=S0Y7922MTSY (accessed 30 August 2022).
- Healthier Together, Royal College of Paediatrics and Child Health, NHS . Healthier Together – a South Yorkshire and Bassetlaw Initiative n.d. https://sybhealthiertogether.nhs.uk/ (accessed 7 September 2021).
- Botan V, Law GR, Laparidou D, Rowan E, Smith MD, Ridyard C, et al. The effects of a leaflet-based intervention, ‘Hypos can strike twice’, on recurrent hypoglycaemic attendances by ambulance services: a non-randomised stepped wedge study. Diabet Med 2021;38. https://doi.org/10.1111/dme.14612.
- Housten AJ, Gunn CM, Paasche-Orlow MK, Basen-Engquist KM. Health literacy interventions in cancer: a systematic review. J Cancer Educ 2021;36:240-52. https://doi.org/10.1007/s13187-020-01915-x.
- Moore JE, Millar BC. Improving COVID-19 vaccine-related health literacy and vaccine uptake in patients: Comparison on the readability of patient information leaflets of approved COVID-19 vaccines. J Clin Pharm Ther 2021;46:1498-500. https://doi.org/10.1111/jcpt.13453.
- Imlach F, McKinlay E, Kennedy J, Pledger M, Middleton L, Cumming J, et al. Seeking Healthcare During Lockdown: Challenges, Opportunities and Lessons for the Future [published online ahead of print April 13 2021]. Int J Health Policy Manag 2021. https://doi.org/10.34172/ijhpm.2021.26.
- Hayes CV, Mahon B, Sides E, Allison R, Lecky DM, McNulty CAM. Empowering patients to self-manage common infections: qualitative study informing the development of an evidence-based patient information leaflet. Antibiotics 2021;10. https://doi.org/10.3390/antibiotics10091113.
- Figueiras M, Ghorayeb J, Coutinho M, Marôco J, Thomas J. Levels of trust in information sources as a predictor of protective health behaviors during COVID-19 pandemic: a UAE cross-sectional study. Front Psychol 2021;12. https://doi.org/10.3389/fpsyg.2021.633550.
- Maykrantz SA, Gong T, Petrolino AV, Nobiling BD, Houghton JD. How trust in information sources influences preventative measures compliance during the COVID-19 pandemic. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18115867.
- Qi S, Hua F, Xu S, Zhou Z, Liu F. Trends of global health literacy research (1995-2020): analysis of mapping knowledge domains based on citation data mining. PLOS ONE 2021;16. https://doi.org/10.1371/journal.pone.0254988.
- Borg K, Wright B, Sannen L, Dumas D, Walker T, Bragge P. Ambulances are for emergencies: shifting attitudes through a research-informed behaviour change campaign. Health Res Policy Syst 2019;17. https://doi.org/10.1186/s12961-019-0430-5.
- NHS Digital . Content Style Guide: How We Write n.d. https://service-manual.nhs.uk/content/how-we-write (accessed January 2021).
- Powell DR. HealthyLife® Self-Care Guide. Farmington Hills, MI: American Institute for Preventive Medicine; 1994.
Appendix 1 Final search strategy
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R).
Date range searched: 1946 to 11 January 2021.
-
Health Literacy/or (health literacy or educational intervention* or self triage).mp.
-
*health education/or *health promotion/or *patient education as topic/or *prenatal education/or *“Caregivers”/ed [Education]
-
(pamphlet* or booklet* or information leaflet* or patient leaflet*).ti,ab. or (digital intervention* or internet or web-based or text* or SMS or mobile app*).ti,hw,kw.141287
-
exp *Primary Health Care/
-
*community pharmacy services/or *call centres/or *hotlines/or *triage/
-
*Family Practice/or *General Practice/or *Practice Management, Medical/or *“Telemedicine”/
-
(((urgent or emergency) adj2 (treatment or department or care or services)) or minor injur* or minor illness* or general practi* or GP or (consult* adj2 doctor) or primary care or primary health* or community health cent* or “out of hours”).ti,ab,kw.
-
exp *Health Services Accessibility/or *“Health Services Needs and Demand”/
-
(empower* or ((manag* or reduc* or decreas* or cope* or mitigat* or influenc* or effect or affect*) adj3 (preventable or unnecessar* or non-urgent or non-urgent or avoidable or low acuity or frequent) adj3 (demand* or pressure* or “use” or usage or utili* or admission* or visit* or crowding or surge))).ti,ab.
-
Self-care/or (self-manag* or self-care or treatment seeking or help seeking or care seeking or self-limiting).ti,ab,kw.
-
1 or 2 or 3
-
4 or 5 or 6 or 7
-
8 or 9 or 10
-
12 and 13
-
14 or *“General Practice”/sn or *Emergency Service, Hospital/sn
-
11 and 15
-
limit 16 to English language.
Appendix 2 User-Friendliness Assessment Tool
The following criteria assess the user-friendliness of interventions. By user-friendliness, we mean how easy it is to understand the information being communicated. It has been developed based on health literacy guidance from NHS Digital156 in the UK and the Centers for Disease Control and Prevention67 in the USA. Furthermore, we have consulted patients and members of the public about the tool.
Assess the intervention for each of the items below and total it up to provide a total score (maximum score of 42).
Appendix 3 Articles excluded at full-text stage
Wrong population (not patients accessing services for minor illness, non-urgent care, e.g. chronic illness)
-
Agarwal G, Pirrie M, McLeod B, Angeles R, Tavares W, Marzanek F, et al. Rationale and methods of an evaluation of the effectiveness of the community paramedicine at home (CP@home) program for frequent users of emergency medical services in multiple Ontario regions: a study protocol for a randomized controlled trial. Trials 2019;20:75.
-
AHC M. Better patient education can lead to lower medical costs: focus on health literacy. Case Manage Advis 2020;31:1–3.
-
Blancafort Alias S, Monteserin Nadal R, Moral I, Roque Figols M, Rojano I Luque X, Coll-Planas L. Promoting social capital, self-management and health literacy in older adults through a group-based intervention delivered in low-income urban areas: results of the randomized trial AEQUALIS. BMC Public Health 2021;21:84.
-
Botelho A, Dias IC, Fernandes T, Pinto LMC, Teixeira J, Valente M, et al. Overestimation of health urgency as a cause for emergency services inappropriate use: insights from an exploratory economics experiment in Portugal. Health Soc Care Community 2019;27:1031–41.
-
Bronsky ES, McGraw C, Johnson R, Giordano K, Orlando A, Bar-Or D. CARES: a community-wide collaboration identifies super-utilizers and reduces their 9-1-1 call, emergency department, and hospital visit rates. Prehosp Emerg Care 2017;21:693–9.
-
Cambon J, Cordier T, Munnich EL, Renda A, Kapur B, Hoxhaj S, et al. Effects of educational messaging on urgent and emergent care-seeking behaviors among publicly insured populations. Am Health Drug Benefits 2018;11:86–93.
-
Greene JC, Haun JN, French DD, Chambers SL, Roswell RH. Reduced hospitalizations, emergency room visits, and costs associated with a web-based health literacy, aligned-incentive intervention: mixed methods study. J Med Internet Res 2019;21:e14772.
-
Hibbard JH, Greene J. The impact of an incentive on the use of an online self-directed wellness and self-management program. J Med Internet Res 2014;16:e217.
-
Judson TJ, Odisho AY, Neinstein AB, Chao J, Williams A, Miller C, et al. Rapid design and implementation of an integrated patient self-triage and self-scheduling tool for COVID-19. J Am Med Inform Assoc 2020;27:860–6.
-
Kelley L, Capp R, Carmona JF, D’Onofrio G, Mei H, Cobbs-Lomax D, et al. Patient navigation to reduce emergency department (ED) utilization among Medicaid insured, frequent ED users: a randomized controlled trial. J Emerg Med 2020;58:967–77.
-
Michelen W, Martinez J, Lee A, Wheeler DP. Reducing frequent flyer emergency department visits. J Health Care Poor Underserved 2006;17(1 Suppl.):59–69.
-
Nejtek VA, Aryal S, Talari D, Wang H, O’Neill L. A pilot mobile integrated healthcare program for frequent utilizers of emergency department services. Am J Emerg Med 2017;35:1702–5.
-
Pascual FT, Hoang K, Hollen C, Swearingen R, Hakimi AS, King JA, et al. Outpatient education reduces emergency room use by patients with epilepsy. Epilepsy Behav 2015;42:3–6.
-
Pillow MT, Doctor S, Brown S, Carter K, Mulliken R. An Emergency department-initiated, web-based, multidisciplinary approach to decreasing emergency department visits by the top frequent visitors using patient care plans. J Emerg Med 2013;44:853–60.
-
Yu J, Zhang HW, Shao YK, Lei Y, Chen H, Pu ZH, et al. A smartphone-based online tool for prehospital self-triage of COVID-19. Chin J Acad Radiol 2020;3:175–80.
Wrong intervention/not a primary research evaluation
-
Anonymous. Distribution of health handbook leads to reduction in ER visits. Healthc Demand Dis Manag 1999;5:31–2.
-
Anonymous. CMs educate members on appropriate ED use: program targets frequent flyers. Case Manag Advis 2007;18:125–6.
-
Anonymous. Program helps beneficiaries avoid unnecessary ED visits: care coordination steers members toward primary care. Case Manag Advis 2008;19:65–7.
-
Anonymous. Reducing ‘frequent fliers’ in the emergency room: Medicaid members connect with primary care. Case Manag Advis 2008;19:51–2.
-
Anonymous. Patient education program slashes ED readmissions. ED Manag 2009;21:42–3.
-
Anonymous. In review of ED utilization reduction strategies, data regarding impact on safety, outcomes in short supply. ED Manag 2014;26:8–10.
-
Botelho A, Dias IC, Fernandes T, Pinto LMC, Teixeira J, Valente M, et al. Overestimation of health urgency as a cause for emergency services inappropriate use: insights from an exploratory economics experiment in Portugal. Health Soc Care Community 2019;27:1031–41.
-
Chastonay OJ, Lemoine M, Grazioli VS, Canepa Allen M, Kasztura M, Moullin JC, et al. Health care providers’ perception of the frequent emergency department user issue and of targeted case management interventions: a cross-sectional national survey in Switzerland. BMC Emerg Med 2021;21:1–10.
-
DeVries A, Li C-H, Oza M. Strategies to reduce non-urgent emergency department use: experience of a Northern Virginia Employer Group. Medical Care 2013;51:224–30.
-
Eminovic N, Wyatt JC, Tarpey AM, Murray G, Ingrams GJ. First evaluation of the NHS Direct Online clinical enquiry service: a nurse-led web chat triage service for the public. J Med Internet Res 2004;6(2).
-
Grossman LK, Rich LN, Johnson C. Decreasing non-urgent emergency department utilization by Medicaid children. Paediatrics 1998;102(1 Pt 1):20–4.
-
Gustafsson S, Martinsson J, Wälivaara BM, Vikman I, Sävenstedt S. Influence of self-care advice on patient satisfaction and healthcare utilization. J Adv Nurs 2016;72:1789–99.
-
Gustafsson S, Savenstedt S, Martinsson J, Walivaara B-M. Need for reassurance in self-care of minor illnesses. J Clin Nurs 2018;27:1183–91.
-
Houghton J. Minor illness management: empowering parents through shared knowledge. Paediatr Nurs 2005;17:24–5.
-
Kantonen J, Lloyd R, Mattila J, Kauppila T, Menezes R. Impact of an ABCDE team triage process combined with public guidance on the division of work in an emergency department. Scand J Prim Health Care 2015;33:74–81.
-
Nguyen CA, Shih JA, Lin KV, Aladesanmi OA. Targeting national emergency department overuse: a case for primary care, financial incentives, and community awareness. Harvard Health Policy Rev 2014;14:23–6.
-
Peetoom KKB, Smits JJM, Ploum LJL, Verbakel JY, Dinant G-J, Cals JWL. Does well-child care education improve consultations and medication management for childhood fever and common infections? A systematic review. Arch Dis Child 2017;102:261–7.
-
Trevett AJ, Martin JR, Ross WA, Macfarlane E. The introduction of a daily telephone advice service: how is it used and is it worth the effort? Scott Med J 1998;43:57–8.
-
Williams K, White L, Plorde M, Eisenberg M. Empowering the patient: after-care instructions reduce calls and improve quality of life. J Emerg Med Serv 2008;33:42–9.
Wrong outcome
-
Baker MD, Monroe KW, King WD, Sorrentino A, Glaeser PW. Effectiveness of fever education in a paediatric emergency department. Paediatr Emerg Care 2009;25:565–8.
-
Lass M, Tatari CR, Camilla Hoffmann M, Huibers L, Maindal HT. Contact to the out-of-hours service among Danish parents of small children – a qualitative interview study. Scand J Prim Health Care 2018;36(2).
-
Olsen JR, Gallacher J, Piguet V, Francis NA. Development and validation of the Molluscum Contagiosum Diagnostic Tool for parents: diagnostic accuracy study in primary care. Br J Gen Pract 2014;64:e471–6.
-
South J, Darby F, Bagnall A-M, White A. Implementing a community-based self-care training initiative: a process evaluation. Health Soc Care Community 2010;18:662–70.
Appendix 4 Characteristics of included studies (studies in alphabetical order)
| Study | Country | Study design | Brief intervention description (na) | Control (n) | Population | Parent or all | Delivery setting | Headline finding |
|---|---|---|---|---|---|---|---|---|
| Adesara 2011110 | USA | CBA study | Educational posters in family medical centre; family medical centre letter sent to non-admitted non-emergency ED attendees after ED discharge in clinic hours only (1114 patient records reviewed; 316 non-emergency, and 281 sent a letter) | NR | People aged 18–70 years who had used ED service for a non-emergency problem (general) | All | ED | Brief office-based intervention resulted in a reduction in the number of ED visits of 40 per month |
| Anhang Price 2013123 | USA | Prospective cohort study (pilot) | SORT for Kids: triage website for adults and carers to determine if PED is appropriate (294) | N/A | Individuals seeking care for a child aged < 18 years with influenza-like illness attending a PED with a temperature, cough or sore throat | Parent | Community/workplace/other | This pilot study suggests that web-based decision support to help parents and adult caregivers self-triage children with influenza-like illness is feasible. However, prospective refinement of the clinical algorithm is needed to improve its specificity without compromising patient safety because it classified a lot of children as high risk |
| Barr 2015115 | Canada | BA study | Period of PURPLE Crying prevention programme (NR) | Pre intervention (20,394) | Parents of newborns (0–5 months of age) in metropolitan area | Parent | Community/workplace/other | The findings imply that improved parental knowledge of normal crying, secondary to a public health programme, may reduce medical ED use for crying complaints in the early months of life |
| Beal 2020116 | USA | CBA study | I Care Guide and companion website (www.icare2check.org) (151) | Usual care (151) | Adolescents (aged ≥ 16 years) expecting to leave child protective services custody for at least 12 months. Mainly African American | All | Community/workplace/other | As expected, ICare2Check was associated with increased engagement in health care generally and non-urgent ambulatory care specifically, but no change in emergency care use |
| Bertakis 1991134 | USA | RCT | FPC patient advisor booklet with an educational intervention (108) | FPC patient advisor booklet without educational intervention (106) | New patients attending the FPC | All | ED | The educational intervention did not change the total number of patient visits or telephone calls, but did affect the appropriateness of patient use of health-care services |
| Chande 199685 | USA | RCT | Specialised educational materials, including 10-minute videotape on paediatric health care issues to be watched in the PED and an informational booklet to take away on common paediatric ailments (69 families) | No intervention: standard discharge instructions (61 families) | People who have used a PED for a minor problem (general); parents; family carers. Mainly African American | All | ED | A one-time educational intervention in the PED does not alter long-term ED use habits for minor illness |
| Chande 1999130 | USA | RCT | Health promotion intervention (102) | No intervention (93) | Children < 13 months of age, enrolled in a Medicaid managed care plan, who used the PCP for primary care and presented to the PED with minor illness | All | ED | There was no difference in health-care use between the intervention and control groups at the 12-month follow-up. The health promotion intervention did not alter use habits |
| Chiu 2012139 | Taiwan | Survey | CGPSC programme implemented through easy-access self-care medical spots | N/A | Population of remote mountainous area in Tai-Tung County located in Eastern Taiwan | All | Community/workplace/other | The CGPSC programme was a viable option to help residents in remote areas to manage minor illnesses |
| Cowie 2018104 | UK (Scotland) | MM study | eConsult web-based triage: provides individuals with self-care assessment and advice for the most common conditions seen in general practice, and also a consultation system | N/A | Primary care patients from general practices (a mix of urban/rural areas) | All | ED | Expectations that eConsult would offer an additional and alternative method of accessing GP services were largely met, but less certain that it has fulfilled expectations of promoting self-help |
| Davis 201886 | USA | BA study | Family medicine clinic opening hours increased and standardised and patient education provided (unclear) | Pre intervention (NR) | Individuals seeking care for others (parents), individuals seeking care for others aged 0–18 years, Medicaid users | Parent | Primary care | Increasing access to primary care clinic and improving patient education decreased low-acuity PED visits |
| de Bont 2018102 | Netherlands | Cluster RCT | Illness-focused interactive booklet (10 GP OOH co-operatives and 11,945 consultations) | Usual care (10 GP OOH co-operatives and 13,410 consultations) | Children aged 3 months to 12 years with fever from 20 large, rural and urban GP OOH centres | Parent | Primary care | Mainly focused on antibiotic prescribing as primary outcome. Benefit of intervention was largely restricted to the cases in which family physicians actually used the booklet. Secondary outcome showed reduced intention to consult for similar illnesses |
| DeSalvo 2000137 | USA | Non-RCT | Individualised patient education (first phase: 288; second phase: NR) | Usual care (NR) | Primary care clinic patients who had visited the ED, serving financially disadvantaged patients | All | ED | The attempt to change patients’ behaviour and move patients from emergency rooms to primary care settings had minimal success |
| DeCamp 2020111 | USA | RCT | Salud al Día (Health Up-to-Date) interactive text message service, including appointment reminders, support for obtaining medicines, support for completing referrals, illness care monitoring and education (79) | Usual care (78) | Individuals seeking care for others (parents): singleton infant < 2 months of age, self-identification as Latino or Latina, preferred health-care language of Spanish, and one household mobile phone in urban primary care centre; 87% had limited or marginal health literacy | Parent | Primary care | This Spanish-language text messaging intervention reduced ED use and increased influenza vaccine receipt among a population at high risk of health-care disparities. Tailored text message interventions are a promising method for addressing disparities |
| Elsenhans 1995138 | USA | Non-RCT | Self-care manual mailed to 2144 people aged 22–40 years; all people presenting with targeted complaints given a booklet (NR) | No intervention (NR) | Those aged 22–40 years with heaviest use of internal medicine unit with selected visit type, (e.g. upper respiratory infections, aches and pains), and everyone who attended with targeted complaints | All | ED | Identifying high users of discretionary visit types and targeting them for self-care interventions is associated with a measurable shift in the pattern of visit use |
| Enard 201387 | USA | CBA study | Patient navigation programme (1905) | No intervention (11,737) | Primary care-related patients attending ED. Culturally and linguistically diverse Medicaid and uninsured patients aged 18 months to 65 years, mainly black and Hispanic, who frequently use the ED for primary care | All | ED | Intervention was associated with decreased odds of returning to the ED among less frequent primary care-related ED users within 12 months and all users within 24 months. The savings associated with reduced primary care-related ED visits were greater than the cost to implement the programme |
| Fieldston 201388 | USA | BA pilot study | Health education and training intervention by PED nurses to 32 caregivers in primary care | Pre intervention (NR) | Caregivers (mothers, fathers and grandmothers) of children (aged 7 months to 5 years) from four urban primary care centres, largely ethnic minority communities | Parent | Primary care | Intervention led to increased caregiver knowledge regarding management of common minor childhood illnesses, increased after-hours telephone use, but no significant decrease in ED use |
| Francis 200999 | UK | Cluster RCT | Interactive booklet on childhood respiratory tract infections in 30 practices with patients (274 patients) | Usual care (31 practices, 284 patients) | Children (aged 6 months to 14 years) consulting with a respiratory tract infection (cough, cold, sore throat, earache for ≤ 7 days) and their parents | Parent | Primary care | No change in primary outcome of reconsultation for same illness episode in 2 weeks. Intervention led to important reductions in antibiotic prescribing and reduced intention to consult (self-reported) without reducing satisfaction with care |
| Hansen 1990105 | Denmark | RCT | Health booklet on minor illnesses: stuffy or runny nose, sore throat, cough, vomiting, diarrhoea, fever and minor trauma (50 families) | No intervention (48 families) | Individuals seeking care for others (parents of children aged 0–8 years), individuals seeking care for others (family carers) | Parent | Primary care | Families that received the booklet reported significantly more self-treatments, demanded significantly fewer consultations and had significantly fewer consultations in which worry was the main reason |
| Heaney 200196 | UK | RCT | What Should I Do? booklet: 40 common health problems and information on when to self-care or consult a doctor (1702 participants at end of study). Health-care manual: 50 common health problems and information about keeping healthy (1688) | No intervention (1563) | General population (no history of service use for minor problems) and OOH users in previous 12 months | All | ED | Widespread distribution of information booklets about the management of minor illness is unlikely to reduce demand for health services |
| Herman 200482 | USA | CBA study (pilot) | Training class plus book What to Do When Your Child Gets Sick, which offers easy-to-understand information on > 50 common childhood medical problems. Aim was to evaluate the training aspect (236) | Received book only (170) | Head Start parents (low-income parents of children aged 0–5 years), many of whom lack basic health literacy skills | Parent | Community/workplace/other | During the 6-month follow-up, parents who received the book reported a 48% reduction in ED visits and a 37.5% reduction in clinic visits |
| Herman 200983 | USA | BA study | Health literacy intervention (self-help book on child health problems) (61) | Pre-intervention period (113) | Parents bringing children to ED for non-urgent complaints. Mainly Latina mothers on Medicaid or Medicare | Parent | ED | Health literacy interventions may reduce non-urgent ED visits and help mitigate ED overcrowding and rising costs of care |
| Herman 201081 | USA | BA study | Health literacy intervention: training class plus book What to Do When Your Child Gets Sick, plus subsequent reinforcement, based on booklet (9240 at baseline; 7281 at 6-month follow-up) | N/A | Head Start parents (low-income parents of children aged 0–5 years), a vulnerable population, ethnically diverse | Parent | Community/workplace/other | The average number of ED and doctor visits among parents decreased by 58% and 41%, respectively (p < 0.001). Workdays missed by the primary caretaker per year decreased by 42%, and school days missed per year decreased by 29% (p < 0.001) |
| Hibbard 200179 | USA | Non-RCT | Community-wide self-care information project (Healthwise Communities Project) (959, with 718 at the 36-month follow-up) | Two comparison communities. Unclear but probably no action taken at all (1954, with 1617 at the 36-month follow-up) | A regional community of 250,000 people in 112,000 households | All | Community/workplace/other | The intervention increased the use of self-care resources. Users believe that these products help them make better decisions regarding when to seek care and how to self-treat problems. The utilisation data findings provide some evidence to support this conclusion |
| Holden 202089 | UK | RCT (not published yet, ISRCTN record used) | Targeted education (1963 families) | Usual care (1969 families) | Parents and carers of children (aged < 5 years) who attend PED or urgent care centre with a non-urgent health problem | Parent | ED | There was no difference in service use between treatment and control arms |
| Hou 2012122 | Australia | BA study | Triple Zero community awareness campaign for appropriate ambulance usage (17,793 ED attenders post intervention; 17,920 pre intervention) | N/A | Patients attending the ED for 3 months pre/post campaign | All | Community/workplace/other | The campaign had no significant impact on the arrival mode of the patients, but the illness acuity of the patients decreased, whereas the illness severity of the patients increased |
| Huyer 2018112 | Canada | Qualitative | PED physician-delivered education using two-page pamphlet entitled ‘Choosing Wisely’ (42) | N/A | Individuals seeking care for others (other care relationship) | All | ED | Barriers to and enablers of pamphlet use were identified. Sustaining doctor participation was a challenge owing to many factors, including unclear communication by the organisation and the fact that the intervention was aimed at all attenders, including high acuity |
| Ladley 201890 | USA | RCT | Enhanced standard of care + text messages (108) | Enhanced standard of care (99) | Caregivers of newborns (0–10 weeks of age) receiving primary care at a single urban high-volume academic primary care clinic who were offered the intervention for the first 6 months of a child’s life. Largely ethnic minority communities, 70% with low health literacy | Parent | Primary care | Educational text messages reduced ED use |
| Lepley 2020136 | USA | RCT (pilot) | Acute illness educational intervention:
|
Instructional handout on car seat safety (25) | English-speaking parents or guardians of children (aged < 12 years) presenting to PED with non-urgent complaints. Half had low household incomes | Parent | ED | Giving understandable, written health information with short introductory videos to vulnerable populations in a PED has the capacity to empower parents with knowledge to care for a sick or injured child |
| Little 2001106 | UK | RCT |
|
One-page leaflet with surgery times and how to contact the doctor in an emergency | Random sample of patients from practice registers recruited by post | All | ED | Fewer patients attended with minor illnesses in the booklet and leaflet groups. Data suggest that posting detailed information booklets about minor illness to the general population would have a limited effect |
| Little 201684 | UK | RCT | Internet-delivered intervention providing advice to manage respiratory tract infections (852 reported at least one illness) | No access to intervention (920 reported at least one illness) | Adults (aged ≥ 18 years) registered with GPs (43,769 people invited; 3044 consented) | All | ED | There was reduced contact with GPs and a slight increase in contact with NHS Direct for symptoms that did not warrant immediate medical attention, without increasing hospitalisations |
| Macfarlane 1997101 | UK | RCT | Information leaflet on lower respiratory tract infection handed out by GP at consultation (501) | No leaflet (505) | Consecutive, previously well adults (aged > 16 years) who consulted with a lower respiratory tract infection | All | ED | Informing previously well patients about the natural history of lower respiratory tract infection symptoms is an effective strategy for reducing reconsultations |
| Macfarlane 2002100 | UK | RCT | GP verbal advice on the need for antibiotics and information leaflet (106) | GP verbal advice on need for antibiotics, but no leaflet (153) | Previously well adults presenting with acute bronchitis | All | ED | Rates of antibiotic use were lower in the leaflet group, but reconsultation rates were the same in both groups, and no patients required referral to hospital for respiratory illness during follow-up |
| McWilliams 2008135 | USA | CBA study | Anticipatory guidance at well-child visit (nurse teaching and prescription access) (191) | Usual care (133) | Children who attended a 15-month well-child visit | All | Primary care | Nurse-administered anticipatory guidance reduced ED visits for ear pain in toddlers and was well appreciated by parents |
| Mullett 2002117 | Canada | Prospective cohort study | Partnerships for Better Health (self-care intervention) (153) | N/A | Delivered to 27,000 people in a region | All | Community/workplace/other | We were provided with concrete examples of how the resources provided the information the public needed to gain the confidence to be fully informed partners in looking after their health |
| Murray 2011124 | UK | Two surveys of NHS Choices users | NHS Choices website (1559 completed an online survey); 125 GP waiting-room survey participants. Framed as a primary care service, but not offered in general practice, so included here | N/A | User of online NHS Choices (aged > 18 years) and general practice participants recruited from the waiting room | All | Community/workplace/other | NHS Choices has been shown to alter health-care-seeking behaviour, attitudes and knowledge among its users, and results in reduced demand for primary care consultations among young, healthy users for whom reduced health service use is likely to be appropriate |
| Nijland 2008114 | Netherlands | Qualitative research: scenarios and interviews | Web-based primary care apps for supporting self-care (28) | N/A | 14 health staff (included GPs, physicians specialising in communicable diseases, and a psychologist); 14 patients | All | ED | Patients’ and caregivers’ expectations did not correspond with their experiences of the use of the internet-based apps. User-friendliness and quality of care were important aspects of the intervention |
| Nijland 2009113 (in this group because the software is described in Nijland 2008114 as for use in primary care) | Netherlands | Retrospective cohort study of routine data and survey | Web-based triage (6538 in cohort, 192 in online survey) | N/A | Public | All | ED | Web-based triage can promote self-management for minor ailments, especially for patients who have a positive attitude towards computer-generated advice |
| Ohns 2019118 | USA | Qualitative study | Paper summary of five interventions to reduce non-urgent ED use: a commonly used diagnosis-specific handout, a booklet of the most common childhood illnesses and symptoms, a comprehensive book of common childhood illnesses and symptoms, a 24-hour nurse call line, and a mobile app, KidsDoc, developed by the American Academy of Pediatrics (30) | N/A | Parents of children aged < 10 years, low income | Parent | Community/workplace/other | KidsDoc was the preferred method. Materials should be redesigned using best practices to reduce health literacy demands and match consumer preferences. This focus group provides valuable information and a step towards future research to address health literacy using materials identified by low-income consumers |
| O’Neill-Murphy 2001103 | USA | RCT (pilot) | Interactive fever education (pamphlet + discussion and training) (44) | Standard fever education (pamphlet alone) (43) | Parents/primary caretakers with children aged 3 months to 5 years who presented to the ED with a chief complaint of fever. Mainly African American and lower socioeconomic group | Parent | ED | The control group had as much reduction of their level of anxiety after receiving written information, in the form of a pamphlet, as the interactive intervention group |
| Patel 201891 | USA | RCT (three arms) | Education and information about alternative venues of care: emergency physician telephone call to discuss services; mailed information on services (609); mailed information only (771) | Matched controls (1827 and 1542) | Aged > 18 years, low acuity. Low-risk adults with a recent treat-and-release ED visit. Younger and older patients (aged < 65 and ≥ 65 years) analysed separately | All | ED | Patients aged ≥ 65 years (telephone follow-up by an emergency physician) had a 22% reduction in ED use; patients aged < 65 years (mailed educational information) had a 27% reduction in ED use |
| Plass 200575 | Netherlands | CBA study | Self-care booklet for minor illness handed out by GP (162), and 132 who were in a group that was not interviewed | No intervention (85) | Patients (Turkish, Dutch and other nationalities) who frequently visit their GP (five times a year), living in deprived areas of The Hague | All | ED | The results indicate that distribution by the GP of booklets with tailored information when a patient is ill leads to a reduction in consultations for minor illnesses |
| Plass 200676 | Netherlands | BA study structured interview | Self-care booklet for minor illness (117 at 1 year) | N/A | Patients (Turkish and Dutch) who frequently visit their GP (five times a year), living in deprived areas of The Hague | All | ED | Despite the reduction in consultations up to 2 years post intervention, there was no change in self-reported self-care behaviours |
| Platts 2005107 | UK | RCT | Self-care health book (660); NHS Direct (659) of those completing the questionnaire at 12 months | No intervention (648) | Primary care adult patients in South East England, an affluent area | All | ED | Handing out of self-care health books provided qualitative benefits for patients, but did not reduce attendance at the general practice |
| Powell 1995127 | USA | Prospective cohort study | Reports two studies:
|
N/A | Employees | All | Community/workplace/other | By managing their employees’ demands with comprehensive self-care materials, employers can have a significant impact on health-care use and, potentially, health-care costs |
| Powell 1997128 | USA | BA study | Self-care workshop and booklet (328) | N/A | Employees at Berk-Tek, Inc. (New Holland, PA, USA), a manufacturer of copper and fibre optic data communication wire and cable | All | Community/workplace/other | Reduction in demand for health-care services can be accomplished by teaching employees to make better decisions about when they should see their health-care provider or go to the ED vs. when they should self-care |
| Racine 200992 | USA | RCT | Follow-up telephone call by the primary care practice within 72 hours of the initial PED visit to counsel about the availability of after-hours advice and when to access the PED (2166) | Usual discharge instructions (2080) | Families of paediatric patients (aged 0–21 years) from four participating primary care practices with an index PED visit (April–December 2005). Large proportions of African American and Hispanic populations | Parent | Primary care | Follow-up telephone calls from primary care practices after PED visits counselling patients on the use of services can modulate subsequent care-seeking behaviour and decrease future PED use |
| Rector 1999125 | USA | RCT | Mailing booklet about non-urgent care to Medicaid beneficiaries (3579) | No booklet (3344) | Urban Medicaid populations with a history of ED use (mostly families with children, so a mix of adults and children) | All | Community/workplace/other | Intervention did not have a significant effect on use of EDs |
| Robbins 2003108 | UK | RCT | Home visit and booklet (54) | No intervention (49) | Parents of 6-week-old babies | Parent | Primary care | The trial showed a reduction in the use of a child health clinic, but no effect on use of other services. It demonstrated reduction in parents’ intentions to consult a doctor |
| Rutten 199178 | Netherlands | RCT (practices randomised) | Rational practice policy/patient education about cough (224) | No intervention (324) | Patients aged 1–60 years consulting with an ‘everyday’ cough at least twice in the pre-intervention period (and having at least one cough consultation in the post-intervention period also) | All | ED | A rational practice policy and the provision of patient education stimulated patients to modify their consulting behaviour by reducing their subsequent consultations for cough. This could result in a reduction in the costs of health care |
| Rutten 199377 | Netherlands | RCT (practices randomised) | Systematic patient education about cough (224) | No intervention (324) | Patients consulting with an ‘everyday’ cough at least twice in the pre-intervention period (and having at least one cough consultation in the post-intervention period also) | All | ED | The consulting pattern was changed in the desired direction (reducing consultations for everyday cough and increasing them for coughs with alarming symptoms) by means of a relatively simple modification of the usual policy |
| Shnowske 201893 | USA | Retrospective cohort study | Care guide use for repeated non-emergent complaints (287) | N/A | Patients aged > 18 years who repeatedly present to the ED for non-emergency complaints | All | ED | Although there was a statistically significant decrease in ED visits after care guide initiation, this may be due, in part, to the diminished prescription of opioids in the ED |
| Spoelman 2016129 | Netherlands | CBA study | Nationwide evidence-based health website (912,000 patients who visited their GP) | Reference group of topics not viewed on the website | General population, although framed as a community primary care population | All | Community/workplace/other | This study showed that, 2 years after the launch of an evidence-based health website, nationwide primary care usage decreased by 12%. This effect was most prominent for telephone consultations |
| Steelman 1999119 | USA | Non-RCT | Fever education: slide presentation on well-infant care topics + additional presentation on fever and mailed reminders (50, but only 17 completed the study) | Slide presentation on well-infant care topics (43, but only 14 completed the study) | Military paediatric well-infant clinic population | Parent | Community/workplace/other | Intervention improved parental knowledge, but did not translate into anticipated improvement in clinic and emergency room use patterns |
| Steinweg 1998120 | USA | Survey | Self-care intervention programme coupled with a health promotion pharmacy (276 eligible; 191 responded) | N/A | Military setting | All | Community/workplace/other | Increased knowledge of personal health issues; confidence to treat minor illnesses; 72% of respondents reported avoiding at least one clinic visit; 39.8% reported avoiding at least one ED visit |
| Stockwell 2014126 | USA | RCT | URI-related educational intervention + standard curriculum (76 families; 99 children) | Standard curriculum (78 families; 98 children) | Predominantly Latino Early Head Start families with children aged < 4 years | Parent | Community/workplace/other | An URI health literacy-related educational intervention embedded into Early Head Start decreased PED visits and adverse care practices |
| Sturm 201494 | USA | RCT | PCP-specific teaching + standard discharge instructions(164) | Standard discharge instructions (168) | Children (aged 3 months to 16 years) seen in the PED for non-urgent concerns. Mainly African American | All | ED | A simple low-cost intervention was able to decrease non-urgent PED use and redirect these patients to their PCP for future sick visits over a 12-month period |
| Sustersic 2013131 | France | Cluster RCT (doctor) | Four patient information leaflets (181 patients, 15 physicians) | No leaflet (207 patients, 15 physicians) | All consecutive adults and children (aged < 18 years and accompanied by an adult) diagnosed with acute gastroenteritis or tonsillitis | All | ED | Patient information leaflets given by the physician during the consultation significantly modified the patient’s behaviour and knowledge of the disease, compared with patients not receiving the leaflets. There were fewer visits for the same symptoms for people in the same household |
| Thomson 1999132 | UK | RCT | Baby Check + Play It Safe (accident prevention leaflet) (497) | Play It Safe (accident prevention leaflet) only (500) | Mothers of newborns: mothers of babies born in the participating practices over 14 months. English-speaking mothers only | Parent | Primary care | Distributing illness assessment guidelines to an unselected group of mothers may be well received, but tangible benefits to the parents, babies or health-care providers are difficult to detect. No difference in primary care use |
| Thornton 1991133 | UK | Prospective cohort study × 2 | Baby Check scorecard (70); Baby Check scorecard + nurse validation visit (104) | None | Mothers of term babies | Parent | Primary care | Mothers found it useful. There was no comparison of service use, so no relevant conclusions could be drawn |
| Usherwood 199197 | UK | RCT | Booklet and covering letter (210 households) | No intervention (209 households) | Parents registered with primary care with children aged 2–12 years | Parent | Primary care | The overall effect of the booklet was a statistically non-significant reduction in consultations for the symptoms that it addressed (‘booklet symptoms’) |
| van der Gugten 201598 | Netherlands | RCT | WHISTLER-online intervention: internet programme to inform on respiratory symptoms and support decisions about contacting primary care physicians (323) | Usual care (i.e. no specific programme to support decision-making) (322) | Parents of children who participated in the ongoing WHISTLER prospective cohort study of determinants of respiratory illnesses. Recruited at age 2–3 weeks from primary health-care centres and followed for 1 year. Needed to have access to a computer | Parent | Primary care | Although parents greatly appreciated the provided facilities, a personalised e-support programme on respiratory illnesses in infants did not substantially reduce health-care use for respiratory symptoms |
| Verzantvoort 2018140 | Netherlands | Prospective cohort study | Self-triage for acute primary care via a smartphone application (group 1: survey – 4456; group 2: telephone group to check if the right triage occurred – 126) | N/A | Primary care users | All | ED | The app ‘Should I see a doctor?’ could be a valuable tool to guide patients in contacting the OOH primary care clinic for acute care |
| Wagner 200180 | USA | CBA study | Community-wide self-care information project (Healthwise Communities Project): handbook, website, advice line, media campaign (5909 questionnaires returned for all groups) | No intervention likely (5909 questionnaires returned for all groups) | A regional community | All | Community/workplace/other | The Healthwise Communities Project had a small (non-statistically significant) effect on overall self-reported use |
| White 2012121 | UK | CBA study | Self-care skills training course (868 undertaking the intervention and 544 completing data collection) | No intervention (700 joining the control group and 414 completing data collection) | People voluntarily attending self-care skills training courses, which were held in parent and child groups and in workplaces in intervention areas | All | Community/workplace/other | The training programme had a small but positive effect, which was still evident at 12 months, on individuals’ knowledge and confidence levels with regard to managing their own health, but did not lead to reductions in health service use |
| Wood 2017109 | USA | CBA study | Brief video discharge instructions added to standard written/verbal discharge instructions (41) | Standard discharge instructions (42) | PED attendees: caregivers of children (aged up to 21 years) presenting with one of three common paediatric diagnoses: gastroenteritis, bronchiolitis or fever | Parent | ED | Analysis found that the video group achieved significantly higher knowledge scores on the post-test survey (p < 0.001) than the control group, particularly regarding treatment and when to seek further medical care |
| Yardley 201053 | UK | Exploratory RCT | Tailored theory-based, web-based intervention providing tailored advice for self-management of minor respiratory symptoms (368) | Static web page with advice on reducing consultations and undertaking self-care, used in Little 2001106 (346) | Online volunteers with unknown characteristics, but advertised to university students | All | ED | Our findings provide initial evidence that tailored web-based advice could help patients self-manage minor symptoms to a greater extent |
| Yoffe 201195 | USA | CBA study in realistic evaluation | Parent-focused educational intervention booklet given in a primary care setting (NR, but 6000 booklets distributed) | Pre intervention and clinics in other areas (NR) | Children aged ≤ 10 years from clinic serving low-income population | Parent | Primary care | There was a substantial and statistically significant reduction in ED use for non-urgent care of children in the intervention group, and a proportional reduction in ED charges for this group |
Appendix 5 Description of interventions (studies in alphabetical order)
| Study | Brief intervention description | Why | Who, where/when | How, how much, materials and procedures | Tailoring/modifications | How developed | Mechanism of action | Type |
|---|---|---|---|---|---|---|---|---|
| Adesara 2011110 | Educational posters in FMC; FMC letter sent to non-admitted ED attendees after ED discharge | To teach/encourage patients to be seen in primary care rather than ED |
|
Individual and general: written letters sent to individuals who had ED record of non-urgent visit; poster in the waiting area, examination rooms and triage room of the FMC | No | No details |
|
A.I, specific |
| Anhang Price 2013123 | SORT for Kids: triage website for adults and carers of children with influenza-like illness | To determine if PED is appropriate |
|
Individual; website; written: based on the child’s age and usual health status, the algorithm assigns a child with influenza-like illness to one of three risk groups: (1) high-risk cases who should receive immediate care in an ED; (2) intermediate-risk cases who warrant expedited evaluation by the child’s paediatrician or another PCP; and (3) low-risk children who should be able to safely recover at home, provided their condition does not worsen. Website based on guidance from the CDC/AAP clinical algorithm produced during the 2009 novel influenza A (H1N1) pandemic to help health-care professionals and call centre personnel efficiently triage children | By question response | Evidence-based: algorithm based on clinical guidance developed by the CDC to help parents and adult caregivers determine if a child with influenza-like illness requires ED care. Converted into plain English to help health literacy |
|
C.I general |
| Barr 2015115 | Period of PURPLE Crying prevention programme | To support caregivers in their understanding of early infant crying and to prevent shaken baby syndrome |
|
|
Interaction with nurses | No details |
|
A.II and B.II and D general |
| Beal 2020116 | I Care Guide and companion website, (www.icare2check.org) (n = 151) | To assist foster youth in navigating the health-care system and maintaining connections to primary care |
|
|
None | Target population based: designed by experts from the Live Well Collaborative engaged with foster youth and stakeholders; the format, organisation and styling of information was informed by youth focus groups |
|
A.I and A.II and C.I general |
| Bertakis 1991134 | FPC patient advisor booklet with an educational intervention | To support patients to use services more appropriately | Researcher delivered it to new patients at their first appointment at a FPC |
|
During the session, patients were encouraged to ask questions about the book and its use | No details |
|
A.II and B.II general |
| Chande 199685 | Specialised educational materials: video and booklet | To reduce the number of PED visits by educating parents about use of their PCP and providing information about common paediatric illnesses |
|
|
Researcher doctor read the booklet with the parents and answered their questions while they were waiting to be discharged | With the assistance of a professional with expertise in urban community health education to make it understandable to the patient population |
|
A.II and B.II specific |
| Chande 1999130 | Health promotion intervention | To encourage patients to seek care from their PCP and reduce the number of visits to the PED for minor illness |
|
|
Parents were encouraged to ask any questions they had about accessing their PCP | Theory-based: designed to affect the factors identified by Green and Kreuter’s PRECEDE–PROCEED model |
|
B.I specific |
| Chiu 2012139 | Community-run and GP-supervised self-care for minor illnesses programme implemented through ESCMSs | To provide a service for minor illnesses |
|
|
No | Target population based: authors conducted a survey (pre test) to gather the information on residents’ personal experiences of, and their needs for, the self-care of minor illnesses and minor injuries |
|
A.II and B.II and D general |
| Cowie 2018104 | eConsult website: provides individuals with self-care assessment and advice for the most common conditions seen in general practice | To provide patients with a means of self-care |
|
|
Self-triage and facility to request a response from health professionals to a questionnaire | Developed by the Hurley Group, an NHS partnership led by practising GPs |
|
C.III general |
| DeSalvo 2000137 | Individualised patient education | To improve access to the primary care clinics |
|
|
Personalised information offered by nurse | Target population based: based on a survey of people who had frequently used the local ED |
|
B.I and B.II specific |
| Elsenhans 1995138 | Self-care manual: the Healthwise Handbook | To reduce the demand for primary care services for selected visit types |
|
|
Unclear | Healthwise Handbook was developed in the USA | Education | A.II general |
| Enard 201387 | Patient navigation programme | To decrease ED use by effectively connecting uninsured and Medicaid patients with medical homes and other support resources |
|
|
PNs document and tailor the intervention on the basis of the clients’ responses | By the Memorial Hermann Community Benefit Corporation (Houston, TX, USA) in November 2008 as a performance improvement initiative in its largest hospital |
|
B.I specific |
| Heaney 200196 | What Should I Do? booklet, and a health-care manual | To reduce unnecessary consultations and to enhance self-care |
|
|
No | What Should I Do? booklet developed in the Netherlands; health-care manual, developed by a GP and practice nurse in Dunkeld, Scotland | Education | A.II general |
| Herman 200482 | Training class plus book | To enhance knowledge and self-care |
|
|
No | Selected self-care tool is part of a series of easy-to-read self-help books published by the Institute for Healthcare Advancement |
|
A.II and B.II general |
| Herman 200983 | Health literacy intervention (self-help book on child health problems) | To reduce future ED and outpatient clinic resource use |
|
|
None | No details | Education | A.II and B.II specific |
| Herman 201081 | Training class plus book, plus subsequent reinforcement, based on booklet | To enhance knowledge and self-care (skill development and literacy) |
|
|
No | Selected self-care tool is part of a series of easy-to-read self-help books published by the Institute for Healthcare Advancement |
|
A.II and B.II general |
| Hibbard 200179 | Community-wide self-care information project (Healthwise Communities Project) | To enhance self-care and, in turn, decrease unnecessary use of health care and reduce costs |
|
|
No | No details |
|
A.II and B.II and D general |
| Holden 202089 | Targeted educational materials for families who attend emergency or urgent care services with a child aged < 5 years in a non-urgent situation | To reduce future repeat non-urgent attendances |
|
|
Personalised letter | No details | Education | A.II specific (and small A.I) |
| Hou 2012122 | Triple Zero community awareness campaign | To raise public awareness of appropriate ambulance use |
|
|
No | No details |
|
D general |
| Huyer 2018112 | ED physician-delivered education using two-page pamphlet | To educate caregivers and influence future PED use by equipping them to better distinguish emergency from non-emergency conditions and offer alternative sources for care |
|
|
Rating of the seriousness of the child’s presenting condition | Target population based: by a multidisciplinary team including PED physicians, hospital administrators, public relations and patient education experts, with input from and piloting by parent groups. The pamphlet’s design and content were based on published initiatives aimed at educating patients and caregivers about ED use |
|
A.II and B.II specific |
| Lepley 2020136 |
|
To determine if a brief educational intervention mHealth app is feasible (or used), and to determine its acceptability and usefulness with/without a written intervention |
|
|
Advice/instructions given to each parent |
|
Education | C.II specific |
| Little 2001106 |
|
To help patients’ confidence in managing minor illness, help in their decision to consult the doctor, and hence reduce rates of consultation for minor illness |
|
|
No |
|
Education | A.II general |
| Little 201684 (see Yardley 201053 using the same intervention) | Internet-delivered interactive intervention providing advice to manage respiratory tract infections | To reduce the number of contacts with GPs for individuals who experienced a respiratory tract infection |
|
|
On logging on to the website, users could select tailored advice based on their personal symptoms | Theory based: commonsense model of self-regulation of illness and social–cognitive theory to build self-confidence. Website was piloted and evaluated by researchers |
|
C.III general |
| Macfarlane 1997101 | Information leaflet on LRTI | To investigate if a simple leaflet affects reconsultation rates for previously well adults presenting to their GP with a LRTI |
|
|
No | Target population based: researchers designed the leaflet with the advice of the GP researchers and some patients | Education | A.II specific |
| Macfarlane 2002100 | Leaflet: verbal advice on antibiotics for bronchitis and information leaflet compared with verbal advice alone | To assess whether or not written advice affects the likelihood of patients’ reconsultating for original illness over and above verbal advice |
|
|
No | Researchers developed leaflet based on LRTI leaflet (Macfarlane 1997101) | Education | A.II specific |
| Mullett 2002117 | Partnerships for Better Health (self-care intervention) | To test if a self-care intervention affects self-care attitudes, knowledge and behaviour enough to influence participants’ use of medical services |
|
|
No | No details | Education | A.II general |
| Murray 2011124 | NHS Choices website | To determine if a website can reduce the frequency of primary care consultations among young, healthy users who may not require F2F consultation |
|
|
No | NHS Choices was developed and funded by the UK Department of Health and Social Care | Education | C.II general |
| Nijland 2008114 | Web-based primary care apps for supporting self-care | To determine user-centred criteria for successful application of internet-based technology for supporting self-care |
|
|
Includes potential individual responses | References for apps provided | Education | C.III general |
| Nijland 2009113 | Web-based triage | To evaluate the feasibility of such a system for self-care and triage |
|
|
Patient complaint generates specific advice | System was developed with 25 ‘entry’ complaints based on the criteria: high frequency, no physical contact required to assess the medical situation, and the possibility to rule out emergencies | Education | C.III general |
| Ohns 2019118 | Paper summary describing five patient educational options in a variety of formats and media | To help caregivers manage common childhood illnesses at home and determine when additional care is needed |
|
Individual, written, telephone, mobile app
|
No (other than specificity to illness for some interventions) | No details | Education | Not applicable |
| O’Neill-Murphy 2001103 | Interactive fever education (pamphlet + discussion and training) | To reduce parental fever anxiety, increase parent fever home management and reduce number of return ED visits |
|
|
Interactive discussion: parents were given the opportunity to share their current level of practice regarding fever management and to express any concerns that may be linked to anxiety | No details |
|
B.II specific |
| Patel 201891 | Education and information about alternative venues: EP telephone call to discuss services plus mailed information on services; another arm received mailed information only | To reduce future ED use for low-acuity problems |
|
|
Conversation closed with opportunity for feedback and questions | No details |
|
A.I specific and B.I specific |
| Self-care booklet for minor illnesses | To reduce care-seeking behaviour (GP consultations) by stimulating self-care behaviour for minor illnesses among Turkish and Dutch inhabitants of a deprived area |
|
|
The booklet was compiled and delivered by the local GP to make it as relevant to the local population as possible | Local GPs compiled this booklet based on an existing, more extensive booklet |
|
A.II and B.II specific | |
| Platts 2005107 | Self-care health book; NHS Direct book | To determine if provision of a self-care health book with implied GP endorsement (handed out in a consultation) could successfully encourage patients to self-care |
|
|
No |
|
Education | A.II specific |
| Powell 1995127 | Demand management programme | To reduce employees’ health service use, increase self-efficacy and satisfaction, and reduce costs |
|
|
No | No details | Education | A.II and B.II general |
| Powell 1997128 | Self-care workshop and booklet | To reduce employees’ health service use, increase self-care and reduce costs |
|
|
Workshops were interactive (included discussions) and were held at all times to accommodate shift work. Materials were personalised for the worksite | No details |
|
A.II and B.II and D general |
| Rector 1999125 | Mailing booklet about non-urgent care to Medicaid beneficiaries | To encourage use of alternatives to emergency care, including care by office-based physicians, telephone nursing assistance and self-care | Health provider (United HealthCare Services, Inc., Minnetonka, MN, USA) |
|
English; people could request Spanish version | Target population based: UnitedHealth Group and the Channing L. Bete Company (Deerfield, MA, USA), using a focus group, developed the First Look booklet |
|
A.I and A.II general |
| Rational practice policy and systematic patient education (leaflet) about cough | To modify consulting behaviour of patients with cough |
|
|
No | No details | Education | A.II and B.II specific | |
| Shnowske 201893 | Care guide use for repeated non-emergent complaints | To reduce ED visit frequency by directing patients to a more appropriate service for care |
|
|
Individualised case management | No details |
|
B.I and B.II specific |
| Spoelman 2016129 | Nationwide evidence-based health website | To determine whether or not the release of a nationwide evidence-based health website is associated with reduction in health-care resource use |
|
|
None | Evidence based: content of website is based on NHG guidelines | Education | C.II general |
| Steelman 1999119 | Fever education: slide presentation on well-infant care topics + additional presentation on fever and mailed reminders | To improve parental understanding and management of childhood fever |
|
|
Not reported | No details | Education | A.II specific (and very minor B.II) |
| Steinweg 1998120 | SCIP coupled with a HPP | To increase participant confidence, knowledge and self-efficacy, and decrease the number of participant clinic visits for self-limiting conditions |
|
|
Participants conclude the SCIP with a confidential consultation with a health-care provider | No details |
|
A.II and B.II general |
| Stockwell 2014126 | URI-related educational intervention + standard curriculum | To decrease the number of PED visits and adverse care practices for URIs |
|
|
English, Spanish | No details |
|
B.II general |
| Sturm 201494 | Information about services offered by a patient’s specific PCP and standard discharge instructions | To reduce non-urgent PED visits |
|
|
Information is specific to the parents’ own PCP; patients could ask questions |
|
|
A.I and B.I and A.II and B.II specific |
| Sustersic 2013131 | PILs | To assess if PILs have an impact on patient behaviour |
|
|
No | Evidence based: PILs written by first author with cited sources, for example relevant Cochrane reviews | Education | A.II and B.II specific |
| Verzantvoort 2018140 | Self-triage for acute primary care via a smartphone application ‘Should I see a doctor?’ | To assess the impact of the app on patients’ decisions to contact the OOH service for acute care, as well as to provide reassurance, information and self-care options |
|
|
Personalised to patient’s symptoms | Apeldoorn OOH GP clinic and Van Campen Consulting (Zaltbommel, the Netherlands), in collaboration with NHG |
|
C.III general |
| Wagner 200180 | Community-wide self-care information project (Healthwise Communities Project): handbook, website, advice line, media campaign | To give consumers skills and resources to make more informed self-care and health-care decisions, and reduce unnecessary health-care use |
|
|
None | No details |
|
A.II and B.II and D general |
| White 2012121 | Self-care skills training course | To determine if skills training leads to increased knowledge and skills, confidence to undertake self-care, intention to self-care and changes in patterns of service use |
|
|
None | No details |
|
A.II and B.II general |
| Wood 2017109 | Brief VDI added to standard written/verbal discharge instructions | To improve knowledge about the child’s diagnosis, treatment and illness duration, and when to seek further medical care |
|
|
None | The interprofessional EBP team developed VDI scripts for the three most common ED diagnoses. The scripts mirrored the content of the written discharge instructions plus images | Education | A.II specific |
| Yardley 201053 (further tested by Little 201684) | Tailored theory-based intervention: web-based intervention – internet doctor providing tailored advice for self-management of minor respiratory symptoms | To determine if intervention improves patient ‘enablement' (i.e. perceived ability to self-manage health and illness) and use of health services (i.e. contacting the doctor) |
|
|
Complex algorithm enabled patient to follow decision-making process depending on their symptoms | Evidence and theory based: by research team using latest relevant evidence and theory (common sense model, social cognitive theory) |
|
C.III general |
Appendix 6 Quality assessment (by study design)
Risk-of-bias assessments (cohort studies): modified Newcastle–Ottawa Scale (in alphabetical order)
| Study | Selection of intervention group | Selection of control group | Comparability of cohorts | Assessment of outcome | Adequacy of follow-up | Overall assessment |
|---|---|---|---|---|---|---|
| Adesara 2011110 | Adult patients from a single primary care site who had visited an ED for a non-emergency reason during clinic hours (n = NR) | Similar clinic for adult patients only on same site (n = NR) | Limited reporting (with clear differences in non-emergency ED visits pre intervention) | Records | Inadequate (6 months: 3 during intervention, 3 post intervention) | Weak |
| Anhang Price 2013123 | Convenience sample of caregivers attending PED with influenza-like illness (n = 294) | Not applicable | Same cohort (n = 165), but no details on differences | Structured interview (survey) | Inadequate (7 days for reconsultation rates); cross-sectional for usability | Weak |
| Barr 2015115 | Detailed and consistent identification of relevant attendances (infants aged 0–5 months) for one site (n = NR) | Historical (same criteria, same site) (n = 724) | Not reported | Records | Adequate (3 years) | Moderate |
| Beal 2020116 | Convenience sample of adolescents in child protective services (n = 151) | Matched controls (n = 151) | Differences between cohorts across a number of variables | Records, structured interview (survey) | Adequate (1 year) | Moderate |
| Chiu 2012139 | Convenience sample of residents with access to service (n = 100) | Not applicable | Not applicable | Survey | Cross-sectional | Weak |
| Davis 201886 | Detailed and consistent identification of relevant attendances (paediatric) for one primary care site (n ≥ 1000) | Historical (same criteria, same site) (n ≥ 1000) | NR (only numbers for each time period) | Records | Adequate (1 years) | Moderate/weak |
| DeSalvo 2000137 | Convenience sample of ED attendees from primary care clinics (odd-numbered patient records) (n = 288) | ED attendees from same primary care clinics with even-numbered patient records (n = NR) | NR | Records | Inadequate (6 months) | Weak |
| Elsenhans 1995138 | Purposive sample of internal medicine clinic-registered age group with heaviest ED use rates (n = 2144) | Same age group with heaviest ED use rates at comparable internal medicine clinic (n = NR) | Limited data, but generally comparable | Records for total ED use and ED use for specific complaints | Inadequate (4 months) | Moderate/weak |
| Enard 201387 | Convenience sample of frequent users of ED for primary care complaints, aged 18–65 years (n = 1907) | Sample with similar characteristics but who did not receive the intervention (n = 11,737) | Adequate | Records | Adequate (1 and 2 years) | Strong |
| Fieldston 201388 | Convenience sample of caregivers of children aged 6 months–5 years) attending four primary care sites (n = 32) | Historical (same sample) (n = 32) | Same cohort | Records | Inadequate (6 months) | Moderate/weak |
| Herman 200482 | Convenience sample of Head Start families at named sites (n = 236 families) | Head Start families at named sites that did not receive the full intervention (n = 170 families) | NR | Survey | Inadequate (6 months) (total number of families with 6-month data: 224) | Weak |
| Herman 200983 | Convenience sample of caregivers of children (aged 0–18 years) attending the PED for non-emergency complaints (n = 113) | Historical (same sample) (n = 61) | Same cohort (comparable to pre-intervention across variables) | Questionnaire | Inadequate (6 months) | Weak |
| Herman 201081 | Convenience sample of Head Start families at named sites (n = 7281 families) | Not applicable | Not applicable | Survey | Inadequate (6 months) | Weak |
| Hibbard 200179 | One intervention community (n = 959) | Two comparison communities (n = 1954) | Unclear | Records, survey | Adequate (3 years) | Moderate |
| Hou 2012122 | Patients attending ED post implementation (n = 17,920) | Historical (same criteria, same site): pre implementation (n = 17,793) | Some significant differences between cohorts | Records | Inadequate (3 months) | Weak |
| McWilliams 2008135 | All parents attending a 15-month WCV at one site (n = 191) | Historical (same criteria, same site) and alternative sites of same provider (n = 133) | Differences across some variables | Records | Adequate (1 year) | Moderate |
| Mullett 2002117 | Small convenience sample of volunteers who had received the intervention handbook (n = 153) | Not applicable | Not applicable | Diary | Adequate (1 year) | Weak |
| Murray 2011124 | Convenience sample of intervention users and primary care patients with access to intervention (n = 1559 and n = 125) | Not applicable | Not applicable | Survey | Cross-sectional | Weak |
| Nijland 2009113 | Convenience sample of intervention users (n = 192) | Not applicable | Not applicable | Survey | Cross-sectional | Weak |
| Plass 200575 | Purposive sample of adult patients who frequently consulted primary care for minor illness (n = 294) | Sample with same consultation criteria, except not only minor illness, from alternative sites in same area (n = 85), plus reference group | Differences across some variables | Records, interviews | Adequate (2 years) | Moderate |
| Plass 200676 | Purposive sample of adult patients who frequently consulted primary care for minor illness (n = 162) | Not applicable | Not applicable | Structured interview (survey) | Adequate (1 year) | Moderate (self-report of use) |
| Powell 1995127 | Employees at a single organisation (n = 1000) | Not applicable | Not applicable | Survey, records | Cross-sectional | Weak |
| Powell 1997128 | Employees at a single organisation (n = 371) | Historical (same criteria, same site) | Not applicable | Records, survey | Adequate (1 year) | Moderate |
| Shnowske 201893 | Convenience sample of patients who frequently attended ED with non-urgent complaints and who received the intervention (n = 287) | Historical (same sample) (n = 287) | Same cohort | Records | Inadequate (3 months) | Moderate/weak |
| Spoelman 2016129 | Purposive sample of general practices | Historical (same criteria), plus reference group | NR | Records | Adequate (3 years) | Moderate |
| Steelman 1999119 | Convenience sample of parents attending 2-, 4- and 6-month WCVs at one site (n = 50) | Convenience sample of parents attending 2-, 4- and 6-month WCVs at one site (n = 43) | NR | Records, survey | Inadequate (unclear, 4 months?) | Weak |
| Steinweg 1998120 | Participants in a military setting (n = 283) | Not applicable | Not applicable | Survey | Inadequate (6 months) | Weak |
| Thornton 1991133 | New mothers on a birth register (n = 104) | Not applicable | Not applicable | Questionnaire | Inadequate (6 months) (too few instances of illness to evaluate) | Weak |
| Verzantvoort 2018140 | Convenience sample of intervention users who volunteered to participate (n = 126) | Not applicable | Not applicable | Structured interview (survey) | Cross-sectional | Weak |
| Wagner 200180 | Random households in an intervention community (n = 1899) | Same criteria in two comparison communities (n = 4010) | NR | Questionnaire | Adequate (1 year) | Moderate/weak |
| White 2012121 | Convenience sample of patients from three primary care trusts (n = 868) | Convenience sample of patients from two primary care trusts (n = 700) | Differences across some variables | Records, survey | Adequate (1 year) | Moderate |
| Wood 2017109 | Convenience sample of caregivers of children (aged 0–21 years) attending the PED for non-emergent complaints (n = 83) | Historical (same sample) | Same cohort | Questionnaire | Inadequate (immediately before and after intervention) | Weak |
| Yoffe 201195 | All parents of children aged ≤ 10 years at a primary care site (n = NR) | Historical (same criteria, same site) and alternative sites in same area (n = NR) | Differences across some variables | Records | Adequate (18 months) | Weak/moderate |
Risk-of-bias assessments (randomised controlled trials): Cochrane Risk of Bias Tool v.2.0 (in alphabetical order)
| Study | Bias arising from the randomisation process (sequence generation, allocation concealment, balance between groups) | Bias due to deviations from intended intervention (blinding, deviations, likely effect on outcomes) | Bias due to missing data (attrition) | Bias due to measurement of outcome (blinding of assessors, potential for differences between groups) | Bias in selection of reported results (prespecified outcomes, potentially different measures) | Overall bias |
|---|---|---|---|---|---|---|
| Bertakis 1991134 | High | Some concerns | Low | Low | Some concerns | High |
| Chande 199685 | Some concerns | High | Low | Some concerns | Some concerns | High |
| Chande 1999130 | Low | High | Low | Some concerns | Some concerns | High |
| de Bont 2018102 | Low | Low | Low | Some concerns | Low | Some concerns |
| DeCamp 2020111 | Low | Low | Low | Low | Some concerns | Some concerns |
| Francis 200999 | Low | Some concerns | Low | Low | Some concerns | Some concerns |
| Hansen 1990105 | High | Some concerns | Low | Some concerns | Some concerns | High |
| Heaney 200196 | Low | Some concerns | Some concerns | Some concerns | Some concerns | High |
| Holden 202089 | Some concerns | Some concerns | Low | Some concerns | Low | Some concerns |
| Ladley 201890 | Low | Low | Low | Low | Low | Low |
| Lepley 2020136 | Some concerns | Some concerns | High | High | Some concerns | High |
| Little 2001106 | Some concerns | Some concerns | High | Low | Some concerns | High |
| Little 201684 | Low | Some concerns | High | Low | Some concerns | High |
| Macfarlane 1997101 | Some concerns | Low | Low | Some concerns | Some concerns | High |
| Macfarlane 2002100 | High | Some concerns | Low | Some concerns | Some concerns | High |
| O’Neill-Murphy 2001103 | High | Some concerns | High | High | Some concerns | High |
| Patel 201891 | Some concerns | High | Some concerns | Some concerns | Some concerns | High |
| Platts 2005107 | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | High |
| Racine 200992 | Low | Low | Low | Low | Some concerns | Some concerns |
| Rector 1999125 | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns |
| Robbins 2003108 | High | Some concerns | High | Some concerns | Some concerns | High |
| Rutten 199178 | Some concerns | High | High | Some concerns | Some concerns | High |
| Rutten 199377 | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | High |
| Stockwell 2014126 | Some concerns | Some concerns | Low | Some concerns | Some concerns | High |
| Sturm 201494 | High | Some concerns | Low | Low | Some concerns | High |
| Sustersic 2013131 | Low | Some concerns | Low | Some concerns | Some concerns | Some concerns |
| Thomson 1999132 | Low | Low | Low | Low | Some concerns | Some concerns |
| Usherwood 199197 | High | Some concerns | Some concerns | Some concerns | Some concerns | High |
| van der Gugten 201598 | Low | Low | Low | Low | Some concerns | Some concerns |
| Yardley 201053 | Low | Some concerns | High | Some concerns | Some concerns | High |
Risk-to-rigour assessments: modified Critical Appraisal Skills Programme (qualitative studies)
| Study | Clear statement of aims | Qualitative methodology appropriate | Recruitment strategy appropriate | Data collection appropriate | Researcher reflexivity | Ethics issues addressed | Data analysis sufficiently rigorous | Clear statement of findings | Overall assessment |
|---|---|---|---|---|---|---|---|---|---|
| Huyer 2018 § | Yes | Yes | Yes | Yes | Not reported | Yes | Yes | Yes | Strong |
| Nijland, 2008† | Yes | Yes | Unclear | Yes | Not reported | Not reported | Yes | Yes | Moderate |
| Ohns, 2019§ | Yes | Yes | Yes | Yes | Not reported | Yes | No | Limited | Moderate |
Risk-to-rigour assessments: Mixed Methods Appraisal Tool (mixed-methods studies)
| Study | Adequate rationale for using a mixed-methods design to address the research question? | Are the different components of the study effectively integrated to answer the research question? | Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | Overall assessment |
|---|---|---|---|---|---|---|
| Cowie 2018104 | Yes | No (very limited, principally only regarding costs) | No (very limited) | Unclear | Qualitative: yes; quantitative: limited | Weak |
Appendix 7 Impact on service use (studies in alphabetical order)
| Study | Brief intervention description (n) | Follow-up | Data source |
Service use: 1. ED all visits 2. ED minor/non-urgent/inappropriate visits 3. GP all visits 4. GP minor/non-urgent visits/inappropriate visits |
|---|---|---|---|---|
| Adesara 2011110 | FMC educational posters and letter sent to non-admitted ED attendees after discharge | Baseline, 6 months | Records |
|
| Beal 2020116 | I Care Guide and companion website | 12 months | Records, self-report |
|
| Bertakis 1991134 | Family practice clinic patient advisor booklet with/without an educational intervention | 12 months | Records | Control group vs. experimental group (note that this is the booklet vs. booklet + seminar):
|
| Chande 199685 | Specialised educational materials: video and booklet | 6 months | Records |
|
| Chande 1999130 | Health promotion intervention | 12 months | Records, self-report (data combined for outcomes) |
|
| Davis 201886 | Family medicine clinic opening hours increased and standardised and patient education provided | 3 and 12 months | Records |
|
| de Bont 2018102 | Illness-focused interactive booklet | Within 2 weeks for same illness episode and 6 months for OOH repeated consultation | Records, self-report used for service use intention |
|
| DeSalvo 2000137 | Individualised patient education | 3 months pre intervention, 3 and 6 months post intervention | Records, self-report |
|
| DeCamp 2020111 | Salud al Día (Health Up to Date) interactive text message service | 15 months | Records |
1. (+) Reduced use of EDs. Salud al Día, n = 79; usual care, n = 78. ED visits, mean (SD): 1.23 (1.66) vs. 1.82 (1.64); p = 0.03; IRR 1.48 (95% CI 1.04 to 2.12) for control vs. intervention. Frequency of ED use differed (p = 0.03) (intervention vs. control): |
| Elsenhans 1995138 | Self-care handbook | 4 months | Clinic records | Service use (intervention unit vs. control unit):
|
| Enard 201387 | Patient navigation programme | 12 and 24 months | Records |
|
| Fieldston 201388 | Health education and training by PED nurses | 6 months | Records |
|
| Francis 200999 | Interactive booklet on childhood respiratory tract infections | 2 weeks | Self-report | (–) There was no significant difference between the intervention and control groups in the odds of reconsulting in primary care during the 2 weeks after registration, but the intervention group was less likely to intend to consult for a similar illness in the future
|
| Hansen 1990105 | Booklet about common illnesses | 6 months | Self-report of illness and self-treatment; GP records for consultations |
|
| Heaney 200196 | What Should I Do? booklet and health-care manual | 1 year pre intervention, 1 year post intervention | Records | Change of use: mean rates of health service (primary care) use in year before and year after intervention (95% CI for estimated effect of booklet adjusted for baseline) –
|
| Herman 200482 | Training class plus book | 6 months | Self-report |
|
| Herman 200983 | Health literacy intervention (self-help book on child health problems) | 6 months | Self-report | Months pre intervention (n = 110) vs. post intervention (n = 61):
|
| Herman 201081 | Training class plus book, plus subsequent reinforcement, based on booklet | 6 months, and then 3 years for a subsample | Self-report on survey |
|
| Hibbard 200179 | Community-wide self-care information project (Healthwise Communities Project) | 12 and 24 months | Records |
|
| Holden 202089 | Targeted educational materials for families who attend emergency or urgent care services with a child aged < 5 years in a non-urgent situation | 11 months | Records |
|
| Hou 2012122 | Triple Zero community awareness campaign | 3 months | Records |
|
| Ladley 201890 | Anticipatory guidance at WCV + text messages | 12 months |
|
|
| Lepley 2020136 |
|
6 months | Records, self-report |
|
| Little 2001106 |
|
12 months | Records |
|
| Little 201684 | Internet-delivered intervention providing advice to manage respiratory tract infections | 5 and 12 months | Self-report, records for reconsultations in primary care |
|
| Macfarlane 1997101 | Information leaflet on lower respiratory tract infection | 1 month | GP recorded reconsultations | Reconsultation rates:
|
| Macfarlane 2002100 | Verbal advice on antibiotics and information leaflet, compared with verbal advice only | 1 month | Records |
|
| McWilliams 2008135 | Anticipatory guidance at WCV and prescription | 12 months for service use | Records for service use | Visit use for ear pain before and after the nurse-administered anticipatory guidance programme, compared with control sites; mean (SD) rates per 1000 before programme (n = 168) and after programme (n = 191):
|
| Murray 2011124 | NHS Choices website | At the time of visiting the website | Self-report |
|
| O’Neill-Murphy 2001103 | Interactive fever education (pamphlet + discussion and training) | 2 and 8 weeks | Self-report |
|
| Patel 201891 | Education and information: emergency physician telephone call to discuss services plus mailed information on services; mailed information only | 6 months | Records |
|
| Plass 200575 | Self-care booklet for minor illness | 12 months pre intervention and 24 months post intervention | Records for service use, self-report |
Control group: the number of consultations for minor illnesses that the participants in the reference group reported was an average of 2.4 (SD 2.3) for 5.4 (SD 3.7) different minor illnesses, and did not differ significantly from the number of consultations reported by the intervention group at time 2. However, there was a difference based on nationality. The medical records of both the intervention group [t(94) = 3.3; p = 0.001] and the control group [t(122) = 2.7; p = 0.007] showed a significant decrease in care-seeking behaviour concerning minor illnesses. This effect remained 2 years after the intervention, in particular among the Dutch participants in the intervention group [t(31) = 2.4; p = 0.02] The medical records of both the intervention group (p = 0.001) and the second intervention group that did not get lots of interviews as part of the research (p = 0.007] showed a significant decrease in care-seeking behaviour concerning minor illnesses. This effect remained 2 years after the intervention. The medical records of the controls did not show a change in the number of consultations for minor illnesses during the research period |
| Platts 2005107 | Self-care health book; NHS Direct | 12 months | Records | Consultation rates:
|
| Powell 1995127 | Health guide given as part of health screening | 5 months | Self-report |
|
| Powell 1997128 | Self-care workshop and booklet | 12 months | Records |
|
| Racine 200992 | Follow-up counselling telephone call by the primary care practice within 72 hours of the initial PED visit to counsel about appropriate services | 12 months | Records | All intervention vs. control follow-up visits by type of visit within 1 year of index visit (N = 23,516), type of visit:
|
| Rector 1999125 | Mailing booklet (First Look) about non-urgent care to Medicaid beneficiaries | 6 months | Records |
|
| Robbins 2003108 | Home visit and booklet | 7 months | Case note review for service use |
|
| Rutten 199377 | Systematic patient education about cough | 12 months | Not clear |
|
| Shnowske 201893 | Care guide use for repeated non-emergent complaints | 3 months (compared with 12 months previously) | Records |
|
| Spoelman 2016129 | Evidence-based health website | 3 years | Records (website and health records) | Trend in total number of consultations per 1000 patients per month before and after launch of the website:
|
| Steelman 1999119 | Fever education: slide presentation on well-infant care topics + additional presentation on fever and mailed reminders | 4 months | Records |
|
| Steinweg 1998120 | SCIP coupled with a HPP | 6 months | Self-report |
|
| Stockwell 2014126 | URI-related educational intervention + standard curriculum | 5 months | Self-report |
|
| Sturm 201494 | PCP-specific teaching and standard discharge instructions | 6 and 12 months | Records |
|
| Sustersic 2013131 | Patient information leaflets | 2 weeks | Self-report in telephone interview |
|
| Thomson 1999132 | Baby Check scorecard and accident prevention leaflet | 6 months | Records | Consultation rates
|
| Thornton 1991133 | Baby Check scorecard/booklet and nurse validation visit | 6 months | Self-report | Medical contacts
|
| Usherwood 199197 | Booklet and covering letter | 12 months | Contact record completed by practice staff | Initial contacts recorded for booklet symptoms per household:
|
| van der Gugten 201598 | WHISTLER-online intervention to inform on respiratory symptoms and support decisions on contacting appropriate services | 12 months | Records for service use, and self-report for preceding month on monthly questionnaire (data combined for some outcomes) | Number of visits for respiratory symptoms during the entire first year of life
|
| Wagner 200180 | Community-wide self-care information project (Healthwise Communities Project): handbook, website, advice line, media campaign | 12 months | Self-report |
|
| White 2012121 | Self-care skills training course | 6 months, with 12-month gap between baseline and after period | Records | Consultations:
1. None |
| Yardley 201053 | Web-based intervention providing tailored advice for self-management of minor respiratory symptoms | 4 weeks | Self-report |
|
| Yoffe 201195 | Parent-focused educational intervention booklet | 18 months | Records |
|
Appendix 8 Other outcomes (studies in alphabetical order)
| Study | Brief intervention description (n) | Follow-up | Data source | Views regarding interventions, intentions, behaviour, knowledge and confidence, effect of intervention (non-service use) |
|---|---|---|---|---|
| Anhang Price 2013123 | SORT for Kids: triage website for adults and carers of children with influenza-like illness | Cross-sectional |
|
|
| Beal 2020116 | I Care Guide and companion website | 12 months | Self-report |
|
| Chiu 2012139 | Community-run and GP-supervised self-care for minor illnesses programme implemented through ESCMSs | 9 months | Self-report | (+) Use: 80% (n = 80) of the respondents were aware of the existence of the ESCMSs, and the MMI service was known to most residents and was used by most of them. Compared to respondents who had not used the MMI service (n = 30), those who had used the service (n = 50) considered the ESCMSs more helpful (90.00% vs. 76.67%; p < 0.05) and had greater willingness to seek help from the ESCMSs in the future (88.00% vs. 56.67%; p < 0.01) |
| Cowie 2018104 | eConsult website: self-care assessment and advice for the conditions most commonly presented to GPs | 5 months | System log data and self-report patient surveys |
|
| Elsenhans 1995138 | Self-care manual | 12 months | Self-report | Satisfaction: there was general enthusiasm among members and staff, and the majority recommended the continued use of the self-care manual; no dissatisfaction was expressed |
| Fieldston 201388 | Health education and training by PED nurses in primary care | 6 months | Knowledge tests |
|
| Francis 200999 | Interactive booklet on childhood respiratory tract infections | 2 weeks | Self-report | (–) Satisfaction: there were no significant differences in terms of satisfaction, level of reassurance, parental enablement or the parent’s rating of the ‘usefulness of any information received in the consultation’ |
| Hansen 1990105 | Health booklet on minor illnesses | 6 months | Self-report | (+) Confidence: self-management of episodes of illness – 51% in the intervention group and 36% in the control group reported some kind of self-treatment. This difference was significant |
| Herman 200482 | Training class plus book | 6 months | Self-report |
|
| Herman 200983 | Health literacy (self-help book on child health problems) | 6 months | Self-report | (+) Intention: hypothetical responses to low-acuity child medical problem scenarios:
|
| Herman 201081 | Training class plus book, plus subsequent reinforcement, based on booklet | 6 months | Self-report |
|
| Hibbard 200179 | Community-wide self-care information project (Healthwise Communities Project) | 12 and 24 months | Self-report | (+) Use: the effects observed for manual use appeared to be greater in the intervention community than in the comparison communities – the intervention respondents were more likely to indicate that using a self-care manual helped them self-treat a symptom and saved them a visit to the doctor. The magnified effect observed in the intervention community for manual use does not occur for use of a nurse advice line or computer program. Thus, it appears that the intervention increased the use of manuals, as well as the effects of using a manual |
| Huyer 2018112 | ED physician-delivered education using two-page pamphlet | Cross-sectional | Self-report |
|
| Ladley 201890 | Text messages | 12 months | Self-report | High levels of satisfaction and engagement at the 12-month survey in the intervention group: 91% (75/79 who completed the survey) felt more comfortable making decisions about when to take their baby to the ED |
| Lepley 2020136 |
|
6 months | Self-report |
|
| Little 2001106 |
|
12 months | Self-report |
|
| McWilliams 2008135 | Anticipatory guidance at WCV and prescription for ear drops | Measured at 24-month clinic, so 9 months later | Self-report |
|
| Mullett 2002117 | Partnerships for Better Health (self-care intervention), including the Healthwise Handbook | 12 months | Diary | Examples from patient diaries describing how the handbook helped them make decisions and self-care, and also what was missing from the handbook |
| Murray 2011124 | NHS Choices website | At the time of using the website or visiting the GP | Self-report | Satisfaction:
|
| Nijland 2008114 | Web-based primary care apps for supporting self-care | 6 months | Self-report |
Patients – lack of education, underuse or misuse of applications because of lack of education, uncertainty about regulations for using internet for self-care Caregivers (health professionals) – unclear regulations about e-mail consultation: lack of a transparent protocol for e-mail consultation; unclear regulations about prerequisites for using e-mail consultation; lack of quality inspection of e-mail consultation applications; insufficient reimbursement for e-mail consultation. Lack of education and training: underuse or misuse of applications because of lack of education. Interoperability of systems: applications could not be integrated with the existing patient information system or medical records. Concerns about patient equity of access: concerns about the risk of widening of the gap between those who have access to new technology and those who have been excluded Patients – navigation problems: lack of a search engine; lack of an adequate search option; unclear navigation structure; hyperlinks were non-existent or useless; unclear or unattractive layout of web pages; no features for printing information; user-friendliness [40.8% (106/260) of the times the 14 patients used the apps, they faced usability problems]; quality of care [146 (56%) said they faced quality-of-care problems such as comprehensiveness of information]; technical problems: software bugs, drop-down menus or back buttons failed Caregivers (health professionals) – navigation problems: unclear navigation structure, hyperlinks lacking or useless; lack of feedback features; lack of documentation features; unclear answer procedures/formats; technical problems: software bugs Patients – problems with relevance of information: information provided by the digital medical encyclopaedia was too general to be useful; information provided by the virtual body was too limited to be useful; self-care advice insufficiently tailored to personal needs. Problems with comprehensibility of information: semantic mismatch between system and users because of unclear medical terms and lack of features to verbalise a problem in their own vocabulary; self-care advice hard to interpret; self-care advice frightening. Problems with responsiveness: caregiver used more than prescribed response time to answer patients’ questions Caregivers (health professionals) – non-profitability of e-mail consultation: requests from patients still required personal contact with a caregiver. Concerns about a higher chance of interpretation difficulties: carefulness with formulating answers to patient requests, such as being extremely careful when formulating the answer because of possible legal consequences. Concerns about a higher chance of misuse: requests from unknown patients through using the account of known patients |
| Nijland 2009113 | Web-based triage | 54 weeks | Self-report |
|
| Ohns 2019118 | Patient education information in a variety of formats and media | Cross-sectional | Focus groups |
|
| O’Neill-Murphy 2001103 | Interactive fever education (pamphlet + discussion and training) | 2 and 8 weeks | Self-report | (–) Confidence: > 40% of parents in each group reported that they had moderate to high levels of anxiety related to their child’s fever on arrival to the ED. After either fever education programme, parents in both groups reported reduced levels of fever anxiety: control group, 82%; intervention group, 85%. At the 2-week follow-up, parents in both groups reported that they felt less anxious when their child has a fever (86% of the control group and 50% of the intervention group) |
| Plass 200676 | Self-care booklet for minor illness | 12 months | Self-report | Behaviour: mean scores on determinants of self-care behaviour, All:
|
| Platts 2005107 | Self-care health book; NHS Direct | 12 months | Self-report |
Similarly, although both books were found to be easy to understand by most participants, the self-care book was seen as better for understanding (p < 0.001), and better for knowing what to do (p < 0.001); the advice from the self-care book was followed more often (p = 0.002), and using the self-care book was more often likely to lead to a change of mind on what to do (p = 0.003) Participants whose educational qualifications were below A Level were more likely to report that they found the information in the self-care book ‘harder to understand’ than those whose qualifications were at or above A Level, at both 3 months (p = 0.004) and 12 months (p = 0.006). Similarly, at 3 months, those whose educational qualifications were below A Level were more likely to report that they found the information in the NHS Direct book ‘useful for knowing what to do’ than those whose qualifications were at or above A Level (3 months, p = 0.012; 12 months, p = 0.009) |
| Powell 1995127 | Demand management programme | Cross-sectional | Self-report | (+) Satisfaction and understanding (usefulness, understanding, etc.): > 90% for 607 employees who returned the questionnaire; 70% felt that using the guide would help them visit the doctor less frequently |
| Powell 1997128 | Self-care workshop and booklet | Post intervention, 6 months | Self-report |
|
| Robbins 2003108 | Home visit and booklet | 7 months | Self-report |
|
| Rutten 199178 | Patient education about cough | Unclear | Unclear |
|
| Steelman 1999119 | Fever education: slide presentation on well-infant care topics + additional presentation on fever and mailed reminders | 4 months | Self-report | (+) Knowledge: evaluation of knowledge on fever – average incorrect response:
|
| Steinweg 1998120 | Self-care intervention programme coupled with a health promotion pharmacy | 6 months | Self-report | (+) Confidence: programme outcome – confidence to treat minor illness: increase, 77%; no change, 23%; decrease, 0% |
| Stockwell 2014126 | URI-related educational intervention + standard curriculum | 5 months | Self-report |
|
| Sustersic 2013131 | PILs | 10–15 days | Self-report in structured telephone interview |
|
| Thornton 1991133 | Booklet for one cohort, booklet and visit for second cohort | 6 months | Self-report | Satisfaction: they all found Baby Check easy to use, between 68% and 81% found it useful, and 96% would recommended it to others |
| Usherwood 199197 | Booklet and covering letter | 12 months | Self-report | (+) Satisfaction: perceived usefulness of the booklet – frequency of response:
|
| van der Gugten 201598 | WHISTLER-online intervention to inform on respiratory symptoms and support decisions on contacting appropriate services | 12 months | Self-report | (+) Satisfaction and behaviour: information needed and behaviour change –
|
| Verzantvoort 2018140 | Self-triage for acute primary care via a smartphone app | Within 24 hours of app use | Self-report |
|
| White 2012121 | Self-care skills training course | 6 and 12 months | Self-report, interviews |
|
| Wood 2017109 | Brief VDI added to standard written/verbal discharge instructions | 2 months | Five-question survey |
|
| Yardley 201053 | Web-based intervention providing tailored advice for self-management of minor respiratory symptoms | 48 hours | Self-report |
|
Glossary
- Digital health literacy or e-health literacy
- ‘the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem.’ (Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006;8:e9).
- Health literacy
- Health literacy is defined by the World Health Organization as the resources needed for people to access, understand and use information and services to make decisions about their health [www.england.nhs.uk/ourwork/patient-participation/health-decisions/ (accessed 26 October 2021)]. There are different types of health literacy: functional or basic health literacy (reading and writing skills); communicative health literacy (cognitive and social skills to extract information and apply it); and critical health literacy, which requires more advanced cognitive and social skills to analyse information (Nutbeam D. Defining and measuring health literacy: what can we learn from literacy studies? Int J Public Health 2009;54:303–5).
List of abbreviations
- CASP
- Critical Appraisal Skills Programme
- CCG
- Clinical Commissioning Group
- ED
- emergency department
- FKGL
- Flesch–Kincaid Grade Level
- FRE
- Flesch Reading Ease
- GP
- general practitioner
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public 2
- MMAT
- Mixed Methods Appraisal Tool
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- ScHARR
- School of Health and Related Research
- SORT
- Strategy for Off-site Rapid Triage
- SWiM
- synthesis without meta-analysis
- TIDieR
- Template for Intervention Description and Replication
- UFAT
- User-Friendliness Assessment Tool
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/IVQJ9044).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
