Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR133884. The contractual start date was in November 2021. The final report began editorial review in November 2022 and was accepted for publication in March 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Chambers et al. This work was produced by Chambers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Chambers et al.
Chapter 1 Background
Residents in care homes for older people include a high proportion of people with complex health and care needs, including frailty and dementia. 1 Consequently, they are at high risk of experiencing unplanned hospital admissions. While they are often necessary, such admissions can be distressing for the residents, their families and friends, and care home staff, and can also be costly. A report by the Health Foundation concluded that around 40% of unplanned admissions from care homes may be avoidable (conditions potentially manageable outside hospital). 2
Action to reduce unnecessary and/or unhelpful/potentially harmful unplanned admissions among people in care homes and the wider community is an important priority for health and social care both in the UK and internationally. The recent UK government White Paper Integration and Innovation set out plans to promote greater cooperation between health and social care. 3 The COVID-19 pandemic further demonstrates the need for health and social care systems to work together. An additional concern in the UK is ‘delayed discharge’ when patients admitted to hospital are unable to be discharged because of lack of social care support, which in turn affects patients requiring admission from emergency departments (EDs). 4 Reduction of unplanned admissions from care homes can help to alleviate this pressure on the wider health-care system and enable more holistic person-centred place-based care to be provided in the person’s home setting.
Interventions to reduce unplanned admissions from care homes or the community can potentially be implemented at various points in the health and social care system. 5 The University of York Centre for Reviews and Dissemination (CRD) conducted a scoping review on the topic for Northumberland Clinical Commissioning Group in 2014. 6 This review focused on interventions that were categorised as community geriatrician services, case management, discharge planning, integrated working between primary care and care homes, medicines management, the prevention of delirium and end-of-life care. The key finding of the CRD report was that ‘there is little good quality comparative evidence to inform strategies for reducing unplanned admissions from care homes’. The authors noted, however, that closer working between health-care and care home staff, training for care home staff and advanced care planning at end of life all appeared promising.
A systematic review of interventions to reduce admissions from care homes was published by Graverholt et al. around the same time as the CRD report. 7 This review included 4 systematic reviews and 5 primary studies, covering 11 different interventions. These were categorised as interventions to structure or standardise clinical practice, geriatric specialist services, and influenza vaccination. Both the CRD report and Graverholt et al. concluded that the quality of evidence was low but some interventions [e.g. advance care planning (ACP), palliative care, care pathways and ‘geriatric specialist services’] represent promising approaches that require further research. The need for an update is justified by the substantial volume of new research. An initial scoping search of Medline, the Cochrane Library and Cumulative Index to Nursing and Allied Health Literature (January 2014 to January 2021) identified 647 unique references.
We were not aware of any subsequent broad reviews of this topic at the outset of our review, which was commissioned in 2020. However, initial literature searching identified a more recent review by Buck et al. published in 2021. 8 We compare our findings with those of Buck et al. in the Discussion section of this review but our systematic treatment of issues related to implementation and applicability gives our work a broader focus.
The aim of this systematic review was to update the literature on health and/or social care interventions that might support home-based care for people living in care homes with or without nursing. Relevant interventions could be delivered in care homes, hospitals, or a mixture of the two, and could involve many different health and social care professionals. This means that the research evidence identified and synthesised in this review is of key importance in enabling further development of integrated working between health and social care.
Chapter 2 Methods
Patient and public involvement
The project was planned to incorporate public involvement led by a public co-applicant (Lynne Wright, who replaced Cynthia Atkin) supported by regular meetings of a public advisory group. The strategic public advisory group of the Sheffield Health and Social Care Delivery Research Programme (HS and DR) Evidence Synthesis Centre also discussed the review at an early stage and advised on recruitment of the public advisory group.
The topic-specific public advisory group and review team had four one-hour meetings, covering:
-
introductions and discussion of the project context, the methods used (including the public involvement plan and offer of optional training on evidence synthesis methods) and the objectives
-
discussion of ‘emerging’ findings
-
further discussion of review findings
-
focus on dissemination of the review findings and production of the final report (including plain language summary and reporting public involvement).
Members of the group contributed to the review by
-
highlighting issues from their own experience, primarily related to how services work in practice, for example inadequate needs assessment of people with complex problems leading to placement in a care home that is unable to meet their needs and hence increasing risk of unplanned hospital admission. Members also discussed examples of paramedic assessment and decision-making about taking people to hospital, and raised awareness of pressures on some care home managers to adopt a ‘risk averse’ approach to managing residents’ health
-
providing details of potentially relevant research based on involvement in other research projects, specifically a tool for identifying people at risk of deterioration
-
suggesting channels for disseminating review findings outside academia, for example charities such as Age UK, local carers’ groups (with links to both the NHS and local authorities), the Care Quality Commission and possibly Parliament (Health and Care Select Committee or All-Party Parliamentary Groups)
-
suggesting that many carers were unlikely to access material on academic websites even when this was labelled as being in plain language. Short printed summaries were seen as being more suitable for decision-makers than for carers, care home residents and the general public.
We also made contact with an existing group based in Leicester with an interest in older people’s health and care and we hope to work with them on the dissemination of the research findings.
We encountered a number of challenges:
-
The public co-applicant was unable to participate as planned for personal reasons. A member of the patient and public involvement (PPI) group, Lynne Wright, took on the role and attended meetings with the research team and clinical experts as well as contributing to the report.
-
Despite our best efforts, we were only able to recruit three active members for the topic-specific PPI group. This was obviously not ideal, although the members were knowledgeable and enthusiastic, represented different geographical areas and had diverse experiences of the care home sector.
-
We were unable to attend a meeting until late in the project with the existing PPI group based in Leicester but the group was interested in the project and we hope to work with them on dissemination of the review findings.
Statement by Lynne Wright
I joined this research project because I am very concerned about the present state of social care and the availability of care homes in the UK that are able to offer care to frail elderly people with complex needs. I am also concerned about the increasing number of care home residents being sent to accident and emergency (A&E) or ‘shipped off to hospital’ because their care needs are not being fully met. I feel that this research is extremely worthwhile and will hopefully be a valuable source of information.
The meetings have been productive and well run, and I feel that myself and my fellow PPI members have been listened to and given the opportunity to put across our own thoughts and perspective on the research.
I was the carer for my husband, who sadly died earlier this year; he had Parkinson’s with Lewy body dementia and other comorbidities. Three and a half years ago, as I was no longer able to meet my husband’s care needs at home, we made the sad joint decision that he should move into residential care. As a family, we put much thought and effort into finding a suitable care home that was close to our home, where he would be happy and that was able to meet his needs at that time. As my husband had a degenerative condition, we did realise that, as his condition progressed, he would probably need to move to a home that could offer more specialised care.
From my experience it is very important to find the right type of residential care to meet the resident’s specific care needs. This has been made more difficult of late due to the COVID-19 crisis.
Sending residents to A&E following minor injuries – where a paramedic or GP is called out – is something that should, if at all possible, be avoided. Residents are often taken alone by ambulance. The home may try to contact a relative, but it is not always possible for someone to get to A&E to be with their relative. This can be extremely upsetting and confusing for the resident. In the south-west, we now have two paramedics who are able to carry out minor interventions in situ. On two occasions one of these paramedics attended my husband and was able to treat minor cuts (by stitching or glueing) thus avoiding a visit to A&E. Hopefully, more paramedics will be trained and available to carry out these procedures.
More and more elderly people are being admitted to acute hospitals because a suitable care home cannot be found or their care package fails at the residential home they are living in. They are not ‘ill’ as such – they need care. This is not an ideal situation. There is a lack of elderly care wards and people find themselves on a busy acute ward where staff have little training in the needs of someone with multi-morbidity and also sometimes mild or severe dementia. Often, they do not understand why they are in hospital and for many due to lack of stimulation and help with mobilising their condition can quickly deteriorate. It is a similar scenario for many elderly people who after completing inpatient treatment are fit to be discharged but are no longer able to be safely discharged back to their home.
There is a shortage of homes, particularly nursing/dementia homes that are able meet the needs of someone with multimorbidities and dementia. My husband’s care package failed three times and he was admitted to an acute hospital twice. The second time he spent six months on an acute hospital ward (where his condition drastically deteriorated) before we were offered a placement that could meet his complex care needs and give him the care and support he needed and also give me ‘peace of mind’ knowing that he was in a safe and caring environment.
Equity, diversity and inclusion
As a systematic literature review, this project did not involve care home residents, family carers or members of the public as research participants. The research team included a public co-applicant (Lynne Wright, who replaced Cynthia Atkin) with extensive experience of the care home sector as carer for her late husband (see Patient and public involvement). The strategic and topic-specific public advisory groups included people from a diverse range of backgrounds (age, ethnicity and place of residence), although those involved in the topic-specific group tended to be older. We also discussed the project with a Leicester-based PPI group with a specific focus on health of older people (see Patient and public involvement).
Direct involvement of care home residents with appropriate capacity and interest would have made the project more inclusive but would have required considerable time and resources. The project was a systematic review, which meant that most of the research team had backgrounds in this field and lacked informal links with the care home sector. This probably acted as a barrier to including funding for this type of work in the research proposal.
The academic members of the research team were all highly experienced in their respective fields, reflecting the knowledge and experience required to gain funding and deliver the research. The overall team was balanced in terms of gender. The project was a development opportunity for the principal investigator (a late entrant to academic research) who undertook this role on a separately commissioned project for the first time.
Reflections on equity, diversity and inclusion arising from the review findings are presented below (see Chapter 5).
Review questions
The overall research questions were:
-
What interventions are used in the UK health and social care system to minimise unplanned hospital admissions of care home residents?
-
What candidate interventions used in other applicable settings could potentially be used in the UK?
-
What can we learn from research studies and ‘real-world’ evaluations about the effects of such interventions on admissions?
-
What is known about the feasibility of implementing such interventions in routine practice and their acceptability to care home residents, their families and staff?
-
What is known about the costs and value for money associated with these interventions?
Identification of evidence
A broad search was conducted to identify published and peer-reviewed literature on interventions to reduce unplanned admissions from care homes in the UK and other high-income countries. Additionally, a search was undertaken to retrieve relevant grey literature.
The search strategy was developed on MEDLINE and then agreed with the research team (see Appendix 1). The search includes thesaurus and free-text terms and relevant synonyms for the population (residents in care homes for older people) and intervention (interventions to reduce unplanned admissions and named interventions) and makes use of proximity operators where appropriate and the different terms for each concept were combined using the Boolean operator OR. Population and intervention search terms were then combined using the Boolean operator AND. Outcome terms were not included in the search as information on outcomes is not always included in title or abstracts, so including these terms could mean that relevant studies would potentially not be retrieved. The search was limited to research published in English from 2014 to December 2021 to reflect developments since the previous review. Methodological search filters were not applied to keep the search broad and to ensure that all relevant study types were retrieved. However, an attempt was made to remove non-empirical research using the Boolean operator NOT for letters, editorials, news, historical articles, comments and case reports. Additionally, to ensure that studies retrieved were on humans not animals, the Boolean operator NOT was used to remove terms likely to be in studies on animals not humans. The National Institute for Health and Care Excellence filter for Organisation for Economic Co-operation and Development countries was used to aid retrieval of studies from UK and other high-income countries. 9
Once the MEDLINE search had been agreed it was translated to the other major medical and health-related bibliographic databases in December 2021.
The following databases were searched:
-
Cumulative Index to Nursing and Allied Health Literature
-
EMBASE
-
PsycINFO® (American Psychological Association, Washington, DC, USA)
-
Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews
-
Science and Social Sciences Citation Indexes
-
Health Management Information Consortium
-
Social Care Online
-
Social Service Abstracts.
Following the main search, an extra focused search was conducted to identify studies investigating interventions to reduce falls in care homes in January 2022. The search used the MeSH term Accidental Falls/pc (Prevention and Control) and free-text terms, and was then combined with the main search population terms; the MEDLINE search is provided in Appendix 1.
Targeted grey literature searches were carried out to identify reports, guidelines and policy in January 2022. The websites of the following organisations were searched:
-
Department of Health and Social Care (https://www.gov.uk/government/organisations/department-of-health-and-social-care)
-
Health Foundation (www.health.org.uk)
-
National Institute for Health and Care Excellence (www.nice.org.uk)
-
Nuffield Trust (www.nuffieldtrust.org.uk)
-
The database OpenGrey (https://easy.dans.knaw.nl/ui/advancedsearch) was searched, although it is now an archive and no new items are being added.
Citation searching of the 49 initially included studies, from the screen of the main and extra falls searches, was undertaken on Web of Science on 9 March 2022.
Reference checking of included studies and relevant existing reviews was completed. Search results were downloaded to a bibliographic management database (EndNote X9, Clarivate, Philadelphia, PA, USA) and deduplicated. Records were exported to EPPI-Reviewer (EPPI Centre, University College London, London, UK) systematic review software for coding and analysis.
Inclusion and exclusion criteria
Population and participants
The population of interest is residents of care homes for older people, including both those with and without nursing. Studies in which the main participants belong to other groups (e.g. families and social networks of residents; care home staff, other health and social care professionals providing services for care home residents, and health and social care policy makers/service commissioners) were included if they met the other criteria with a focus on reducing residents’ unplanned hospital admissions. We also included residents in assisted living or extra-care housing (with a wide range of services available on-site).
Studies involving residential care for children/young people and vulnerable working age adults (e.g. people with learning disabilities) were excluded, as were studies of older adults living in the community, including sheltered housing and those receiving care at home. Studies of mixed samples with a separate subgroup analysis of care home residents were eligible for inclusion.
Interventions
Interventions delivered in care homes or hospitals to reduce unplanned admissions were included. The taxonomy used to classify interventions is presented in Table 1. The final version was modified from the provisional version presented in the protocol based on discussion among the review team during the study selection process.
| Type of intervention | Setting | Definition | Comments |
|---|---|---|---|
| QI programme | Care home | Complex intervention centred on improving staff skills and processes of care | |
| Integrated working | Care home | Complex intervention centred on improving links between external health care providers and care homes | |
| Training and workforce development | Care home | General training courses; vocational/educational qualifications | Simpler than QI programmes |
| Dealing with specific problems | Care home | Management of common causes of unplanned admissions (e.g. delirium, inappropriate prescribing, hydration and nutrition) | Includes specific training courses |
| Paramedic assessment/non-conveyance | Pre-hospital | Paramedic assessment and possible treatment at the scene | Includes qualitative studies of decision-making |
| ED interventions | ED | Specialist treatment during and shortly after admission | |
| ACP | Care home | Interventions to encourage ACP by residents and/or family carers | |
| Palliative/end-of-life care | Care home | Access to specialist palliative care services | |
| Other | Any | Relevant interventions not included elsewhere (e.g. protective flooring) |
Comparator/control
Optimally, included studies compared an intervention with an alternative (such as continuing current practice) using an experimental (e.g. a cluster randomised trial comparing two groups of care homes)10 or quasi-experimental design such as interrupted time series. We also included before/after studies with or without a control setting and noncomparative qualitative or mixed-methods studies.
Outcomes
The primary outcomes were measures of impact on unplanned admissions among care home residents (e.g. absolute numbers or statistical effect measures from comparative studies), perceived feasibility of implementing the intervention in UK settings (barriers/facilitators), and acceptability to care home residents, their families and staff involved in delivering the intervention. Secondary outcomes included other measures of admissions, costs/resource use and any measure of ‘cost-effectiveness’ (value for money). Patient-reported outcome measures (i.e. those reported directly by the patient or carer without interpretation by clinicians or others) were included where available.
Study types
We included studies of any design providing data on the outcomes of interest. This includes:
-
quantitative research studies of any design
-
qualitative research involving interviews, focus groups, etc.
-
mixed-methods studies
-
service evaluations from the UK only
-
UK-relevant guidelines, policy documents and grey literature.
We also included systematic literature reviews but in view of the volume of primary literature retrieved these were used for reference checking only.
Settings
The setting of interest is the UK social care and health system. Studies from other high-income countries (as defined by the World Bank) were included but synthesised separately and assessed for relevance to the UK context using the Framework for Intervention Transferability Applicability Reporting (FITAR) tool. 11
Additional exclusion criteria
Editorials, commentaries, opinion surveys, news and discussion articles, books, book chapters, theses and conference abstracts were excluded, as well as articles in languages other than English.
Study selection
Selection of studies for the review was carried out in stages. In view of the large number of records retrieved, keyword searching of EPPI-Reviewer for relevant terms in titles and abstracts was used as a preliminary filter. Search terms included ‘care home(s)’, ‘nursing home(s) (NHs)’, ‘assisted living’, ‘extra-care’, ‘ambulance’, ‘paramedic’, ‘skilled nursing facility’ and ‘residential aged care facility (RACF)’. Records that contained relevant terms but were obviously not relevant based on their title were excluded by a single reviewer. Titles and abstracts of remaining records were screened by two reviewers independently using the inclusion criteria above. Discrepancies were resolved by discussion and, if necessary, by reference to a third reviewer. Full-text items that appeared potentially to meet the inclusion criteria were obtained and evaluated by two reviewers independently, with disagreements resolved as above. Records of the process were maintained in EPPI-Reviewer.
Data extraction and quality (risk of bias) assessment
Data were extracted from included studies in EPPI-Reviewer Web (EPPI Centre, University College London, UK) using a customised set of codes covering the study characteristics, key findings/conclusions and strengths/limitations. Effect measures were extracted as reported by study authors. Data on intervention components and delivery were extracted using the Template for Intervention Description and Replication (TIDiER-Lite) checklist. We used the Promoting Action on Research Implementation in Health Services (PARIHS) framework to support extraction of relevant data on implementation of interventions from included UK studies and the FITAR tool to assess applicability of international evidence to the UK context. PARIHS incorporates domains covering evidence, context and facilitation. 12 FITAR covers elements of the intervention/initiative, features of workforce, features of services, systems leadership, financial and commissioning processes and patients/populations. 11
We assessed risk of bias for studies using recognised research designs using the following tools:
-
Joanna Briggs Institute checklists for randomised controlled trials (RCTs) and quasi-experimental studies. 13
-
National Heart, Lung and Blood Institute checklist for cohort and cross-sectional studies. 14
-
Mixed Methods Appraisal Tool for mixed methods and qualitative studies. 15
Assessments were performed by two reviewers independently, with discrepancies resolved by consensus or referral to a third reviewer.
In addition to risk of bias assessment, we extracted data on the strengths and limitations of each included study. Strengths and limitations were those reported by study authors and/or identified by members of the review team. Evidence sources with major limitations, namely absence of a control group and/or a small sample size (judged qualitatively) were described as low quality to reflect the need to treat such studies with caution as evidence of intervention effectiveness. This does not mean that the research was poorly conducted or not of value in its own setting.
Synthesis of evidence
The synthesis of evidence adopted a narrative synthesis approach as specified in the review protocol. Narrative synthesis has been described as ‘an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis’. 16 Narrative synthesis typically involves four stages: developing a theoretical model of how the intervention(s) of interest might work; developing a preliminary synthesis; exploring relationships in the data; and assessing robustness of the synthesis (strength of evidence). 16
Interventions to reduce unplanned hospital admissions of care home residents are diverse and involve different health and care professionals intervening at different stages of residents’ care pathways. Our taxonomy of interventions (see Table 1) identified these and formed the theoretical model for the narrative synthesis.
We grouped studies by type of intervention and setting (UK or international) and the preliminary synthesis was performed within these groups. We summarised study characteristics, findings and study quality (risk of bias assessment where applicable plus strengths and limitations) for each group, together with any general issues about implementation or applicability to the UK setting using the PARIHS and FITAR tools, respectively. For studies that reported sufficient detail, we extracted information on intervention characteristics and delivery using the TIDiER-Lite checklist. Studies were assigned to one intervention group, but the synthesis took account of links between intervention types; for example, ACP can be a stand-alone intervention, part of a quality improvement (QI) programme or linked to an approaching need for palliative/end-of-life care. We used the totality of extracted data for each type of intervention to seek to identify factors that might make the interventions more or less effective and/or influence their implementation in routine practice (described as ‘exploring relationships in the data’ by Popay et al. ). 16
We classified the overall strength of evidence for intervention effectiveness as ‘stronger’, ‘weaker’, ‘very limited’ or ‘inconsistent’ based on the following criteria:17
-
‘stronger evidence’ represents generally consistent findings in multiple studies with a comparator group design
-
‘weaker evidence’ represents generally consistent findings in one study with a comparator group design and several noncomparator studies or multiple noncomparator studies
-
‘very limited evidence’ represents an outcome reported by a single study
-
‘inconsistent evidence’ represents an outcome for which less than 75% of the studies agree on the direction of effect.
Evidence on effectiveness was considered alongside that on feasibility, acceptability and ‘cost-effectiveness’ to assist decision-makers in forming an overall assessment of the value of the intervention. We specifically aimed to identify which interventions are best supported by UK evidence and which interventions in use elsewhere may be suitable for adaptation and evaluation in the UK context. All studies included in the review were included in the analysis of the overall strength of evidence, with no exclusions based on study design or risk of bias.
Evidence summary tables are presented in the main text. Detailed tables on intervention characteristics, implementation and applicability are presented in (see Appendices 2 and 3, Tables 33–41). Risk of bias tables for different study designs are presented in Appendix 4, Tables 42–45.
Variations from protocol
As noted above, keyword searches were undertaken to prioritise records for screening in EPPI-Reviewer because of the large number of records retrieved by the search. A random 10% sample of remaining records was checked and no further references were selected for abstract or full-text screening. One relevant reference that would have been overlooked was subsequently discovered by chance as part of a separate EPPI-Reviewer search.
Chapter 3 Results
Results of literature search
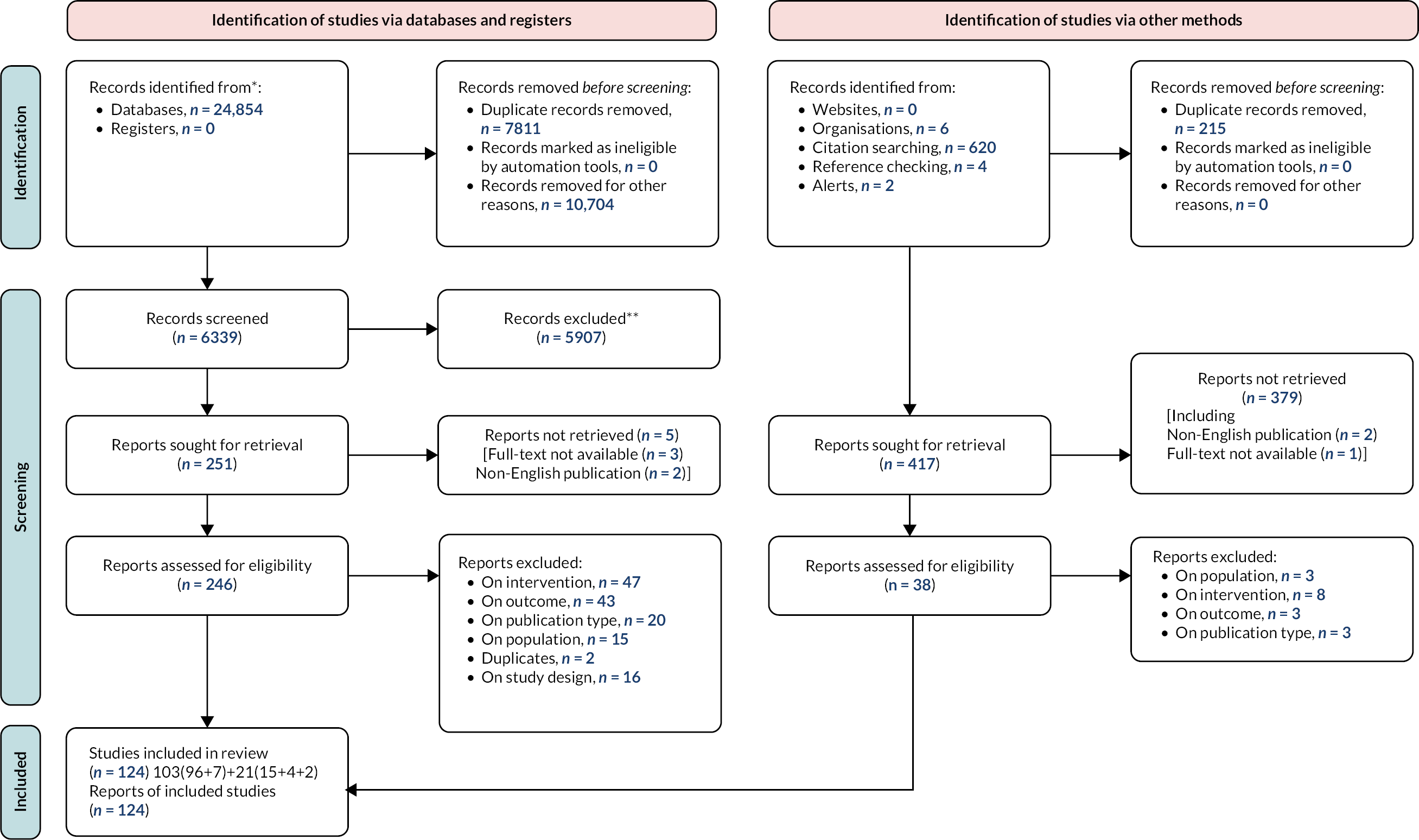
The database searches retrieved 24,656 references which were imported into Endnote X9. After the removal of 7691 duplicates there were 16,965 unique references. The unique references were then imported in EPPI-Reviewer systematic reviews software and a check for duplicates found a further 120 duplicates leaving 16,845 unique references. The large number of references would have taken up too much time and resources to screen; thus keyword searches were undertaken on EPPI-Reviewer to prioritise references for screening (see Variations from protocol). Single-reviewer title screening was then undertaken on 6141 references and 576 were then screened on abstract by two reviewers with 234 included for full-text screening. A total of 96 references were included in the full review from the original database search.
The extra focused database search for falls prevention retrieved 198 references after duplicates within the falls and from the original search were removed. All 198 references were screened on title and 22 were included for abstract screening; 17 references were included for full-text screening and 7 were included in the review.
Citation searches retrieved 620 references. After deduplication within the citation search results and the Endnote library, 406 references were imported into Endnote for screening. Title screening included 84 of these references for abstract screening and 32 were included for full-text screening with 15 included in the final review.
Reference checking of included studies found four further studies for inclusion in the review. A further two included studies were found from alerts. Search of websites of relevant organisations retrieved six potential additional publications, none of which were included.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram18 (see Figure 1) illustrates the study selection process. In summary, 124 publications were included in the review. Given that some interventions/programmes were represented by multiple publications, and that we included qualitative and implementation research as well as trials and service evaluations, the term ‘study’ is used to refer to any type of publication (primarily peer-reviewed journal articles) or report (primarily grey literature).
Summary of included studies
Of the 124 studies from which we extracted data, 30 were from the UK, 44 from the USA, 24 from Australia, 4 from New Zealand, 20 from other countries and 2 from multiple countries (see Table 2). The most common types of intervention were integrated working (particularly in the UK and Australia) and QI programmes (particularly in the USA).
| UK (n) | Australia (n) | USA (n) | New Zealand (n) | Other (n) | |
|---|---|---|---|---|---|
| QI programme | 3 | 1 | 19 | 4 | 1 |
| Integrated working | 13 | 15 | 4 | 0 | 5 |
| Training/workforce development | 4 | 0 | 1 | 0 | 2 |
| Management of specific problems | 4 | 1 | 5 | 0 | 4 |
| Paramedic assessment/non-conveyance | 0 | 0 | 0 | 0 | 1 |
| ED interventions | 0 | 1 | 0 | 0 | 1 |
| Advance care planning | 4 | 1 | 6 | 0 | 5 |
| Palliative/end-of-life care | 4 | 5 | 6 | 0 | 3 |
| Other | 0 | 0 | 3 | 0 | 1 |
In terms of study design, the largest single group was cluster RCTs (17 studies), followed by uncontrolled before–after (15), controlled before–after (13), non-RCTs (11), qualitative studies (11) and mixed-methods studies (10). Four studies used a step-wedge design, involving randomisation to introduce the intervention at different times during the study. Thirty-two studies used other designs, including cohorts and secondary data analyses. The studies reported a wide range of quantitative and qualitative outcomes but no patient-reported outcome measures were recorded.
Quality improvement programmes
UK evidence
We included three studies of interventions in UK settings that were classified as QI programmes. 19–21 The key feature of QI programmes is an emphasis on developing skills and expertise within the care home. Studies in which the intervention included elements of QI but the main emphasis was on integrating health and social care using expertise from outside the care home are discussed under Integrated working.
Two of the studies were regionally based and involved around 30 care homes each,19,20 while the third was smaller, with just three care homes involved. 21 Care homes in the study by Damery et al. 19 were predominantly care homes with nursing, while the study by Giebel et al. 20 included a mixture of care homes with and without nursing. All three studies used a before–after type of design with no separate control group. Formal risk of bias assessments were not performed because all the studies were potentially at high risk of bias. Study characteristics are summarised in Table 3; Appendix 2, Table 33 gives more details of the interventions. Two studies reported a significant improvement in at least one outcome following implementation of the QI intervention, while one reported a small increase in admissions. 1 These mixed results, together with the weak design of the included studies, suggest that evidence for the effectiveness of QI programmes in the UK is both weak and inconsistent.
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Damery et al.19 | Mixed methods | Nursing home: 28/29 provided nursing care | Care homes: 29 care homes from two localities in the West Midlands. Individuals: over 1000 care home staff received QI training | Standard care (before/after) | All admissions; transport to ED; feasibility of intervention | No effect: non-significant increase in admissions (p = 0.052); no effect on ED attendance |
| Giebel et al.20 | Interrupted time series | Nursing home: 15; residential home: 17 | Care homes: 32 care homes with 1314 beds. Individuals: unclear (no individual patient data were collected) | Standard care (before/after): 1 year pre and 4 years post implementation | Unplanned/preventable admissions: conveyance to hospital appears to be considered as a ‘potentially avoidable admission’; transport to ED; other (specify); emergency calls | Significant positive effect: 19% reduction in conveyance to hospital |
| Steel et al.21 | Uncontrolled before–after | Residential home | Care homes: 3 residential homes. Individuals: 34 care home residents | Standard care (before/after) | All admissions; costs/cost-effectiveness; other (specify); advance care planning; polypharmacy | Significant positive effect: 75% reduction in admissions at one care home |
Implementation
The two larger studies reported in some detail on implementation of the programmes while information was more limited for the smaller study by Steel et al. 21 (see Appendix 2, Table 34). Barriers to implementation centred around high staff turnover and resistance from some care home managers. Factors that acted as facilitators included active facilitation by programme staff, an emphasis on opportunities for career progression in one study20 and a policy environment in which reducing unplanned admissions is a high priority.
International evidence
The international evidence on QI programmes comes mainly from the USA (18 studies), with additional evidence from New Zealand (4 studies), Australia and Switzerland (1 study each).
The 18 US studies mainly reported on three QI programmes: Interventions to Reduce Acute Care Transfers (INTERACT); Missouri Quality Initiative (MOQI); and Optimising Patient Transfers, Impacting Medical Quality and Improving Symptoms: Transforming Institutional Care (OPTIMISTIC). Two studies summarised the results of an initiative launched by the US Centers for Medicare and Medicaid Services (CMS) in 2012. 26,36 This initiative covered QI programmes in seven US states, including MOQI and OPTIMISTIC (Indiana).
The 18 included studies are listed in Tables 4 and 5, which summarise the key reports (those providing original data on intervention effectiveness). Table 6 summarises details of the INTERACT, OPTIMISTIC and MOQI interventions as extracted from the key study reports.
| Reference | Programme name | Effect? | Comments |
|---|---|---|---|
| Blackburn et al. 22 | OPTIMISTIC | Yes | Before/after; highlights variation across facilities |
| Ersek et al.23 | OPTIMISTIC | Qualitative study | |
| Galambos et al.24 | MOQI | Stakeholder surveys | |
| Huckfeldt et al.25 | INTERACT | Yes | Varies by degree of implementation |
| Ingber et al. 26 | Summary of 7 initiatives | Yes | Relative to comparison groups |
| Kane et al. 27 | INTERACT | No | RCT of implementation support |
| Ouslander et al.28 | INTERACT | Secondary data analysis | |
| Ouslander et al.29 | INTERACT | Secondary data analysis | |
| Popejoy et al.30 | MOQI | Evaluates use of INTERACT tools | |
| Rantz et al.31 | MOQI | Yes? | Single-facility before–after |
| Rantz et al. 32 | MOQI | Yes | Before–after; main results paper |
| Rantz et al.33 | MOQI | Implementation, role of advanced practice registered nurse | |
| Rantz et al.34 | MOQI | Estimated cost savings | |
| Tappen et al.35 | INTERACT | No negative effect on safety | |
| Vadnais et al. 36 | Summary of 7 initiatives | Yes | Follow-up to Ingber et al.25 |
| Vogelsmeier et al.37 | MOQI | Analysis of avoidable transfers | |
| Vogelsmeier et al.38 | MOQI | Implementation: role of support team | |
| Vogelsmeier et al.39 | MOQI | Yes | 6-year follow-up before/after |
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Blackburn et al.22 | Uncontrolled before/after | Nursing home | Care homes: 19 facilities in Indiana enrolled in OPTIMISTIC programme October 2012 | Standard care (before/after) | All admissions: Kaplan–Meier curves estimating the probability of a resident being hospitalisation-free from time of eligibility were calculated overall and separately for each facility | Significant positive effect: probability of having no hospitalisations within 1 year, increasing from 0.51 to 0.57, which was statistically significant (p < 0.001) |
| Ingber et al.26 | Controlled before–after, mixed methods | Nursing home | Care homes: 7 ECCP organisations, 143 ECCP facilities, 262 comparison facilities. Individuals: 61,636 facility residents, 22,442 from 143 ECCP facilities, 38,194 from 262 comparison facilities | Standard care (before–after) | Unplanned/preventable admissions: all admissions; feasibility of intervention; processes, successes, challenges, lessons learned, and unintended consequences; acceptability to residents/families; costs/cost-effectiveness; Medicare expenditure | Significant positive effect |
| Kane et al.27 | Cluster RCT | Nursing home | Care homes: 85 (33 intervention, 52 control). Individuals: 23,478 (9050 intervention, 14,428 control) | Standard care (parallel control group) | Unplanned/preventable admissions: based on Medicare/Medicaid criteria; all admissions; transport to ED; ED visits without admission; other (specify); 30-day readmissions | No effect: effect for avoidable admissions not robust after correction for multiple comparisons |
| Rantz et al.32 | Uncontrolled before–after | Nursing home | Care homes: 16 within 80 miles of a major city in Missouri. Individuals: 5186 enrolled; average 1750 each day |
Standard care (before–after) | Unplanned/preventable admissions; all admissions | Significant positive effect: for all-cause admissions in some quarters |
| Vadnais et al.36 | Controlled before–after: pooled evaluation of 7 separate QI programmes in different US states under the CMS initiative to reduce avoidable hospitalisations among nursing facility residents | Nursing home | Care homes: not reported but target of 15–30 intervention homes per state. Individuals: baseline period intervention 24,978, comparison 41,986. Intervention period: intervention 67,315, comparison 117,383 | Standard care (before–after) | Unplanned/preventable admissions; all admissions | Significant positive effect: reduction in all-cause and potentially preventable hospital transfers compared with controls |
| Study ID | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| Blackburn et al.22 | Full-time registered nurses working with care home staff | Working together to assess changes in resident condition and implement QI measures. Additionally, OPTIMISTIC nurse practitioners provide in-person evaluations, and management of residents with acute condition changes. Evidence-based processes implemented under OPTIMISTIC include coordination of care through collaborative care reviews, advance care-planning facilitation, and the use of tools from INTERACT | Nursing home | Nurses employed full time | Not applicable |
| Kane et al.27 | INTERACT study team; INTERACT champion and co-champion in each NH | Training and support (primarily telephone/online) for implementing INTERACT, including tools to help nursing home staff identify and evaluate acute changes in nursing home resident condition and document communication between physicians; care paths to avoid hospitalisation when safe and feasible; and ACP and QI tools | Participating nursing homes | 1-year intervention period (March 2013 to February 2014) | Not reported |
| Rantz et al.32 | APRN (nurse practitioner or clinical nurse specialist) at each nursing home; project medical director; other MOQI team members, including QI coach, care transitions coach (coordinating ACP and end-of-life care) and health information technology coordinator; other stakeholders, including social services, primary care and nursing staff (see also Vogelsmeier et al.)38 | Early recognition, assessment and management of residents’ condition (APRNs); education of APRNs, advice to MOQI team, liaison with participating physicians (medical director); use of INTERACT tools, including root cause analysis for all hospital transfers; regular feedback to nursing home leadership; proactive discussions about end-of-life care and ACP | Participating nursing homes and other treatment settings | Full-time APRN in each nursing home supported by MOQI team | Not reported |
Initial evaluations of OPTIMISTIC22 and MOQI32 used a before–after design with no control group, placing them at high risk of bias. Subsequently, Ingber et al. 26 and Vadnais et al. 36 strengthened the evidence base by using administrative data to create comparison groups (matched by propensity scoring) for both intervention groups, together with five other initiatives funded by the CMS (see Table 5). INTERACT was the only programme to undergo a randomised trial, as well as a number of secondary data analyses (see Table 4). The trial was subject to unclear risk of bias as key details including method of randomisation were not reported in the paper. 27
The main component of INTERACT is a series of tools for care home staff to recognise acute changes in residents’ condition, document communication with physicians and use care pathways to avoid hospital admission when safe to do so. The trial performed by Kane et al. 27 compared implementation support for INTERACT with standard care in nursing homes that could be using INTERACT tools without support. By contrast, OPTIMISTIC and MOQI both involved study nurses working in nursing homes to improve staff skills and promote best practice. The MOQI programme also involved use of some of the QI tools developed by INTERACT (see Table 6).
In terms of effectiveness, the trial of implementation support for INTERACT27 reported a reduction in avoidable admissions that was not robust after correction for multiple comparisons. Subsequent analyses revealed that nursing homes in the intervention or control group reporting high usage of INTERACT achieved reductions in potentially avoidable admissions of 0.221 per 1000 resident‐days, representing an 18.9% relative reduction. 25 The MOQI and OPTIMISTIC studies reported reductions in unplanned admissions, but both were at high risk of bias, as noted above.
The initial analysis of the seven CMS-funded initiatives with a controlled before–after design reported mixed results for reductions in potentially avoidable admissions. 26 Three of the seven programmes reported statistically significant reductions against matched controls in 2014 and four did so in 2015. Only two programmes (MOQI and OPTIMISTIC) reported significant reductions in both years. These findings suggest the existence of ‘publication bias’ in the reporting of this initiative, with only the more successful programmes publishing their results in full. In a subsequent analysis, Vadnais et al. combined data from 2014–16 for all intervention and control groups to produce a single effect estimate. 36 The combined analysis reported an annual decrease in potentially avoidable admissions of 2.01 percentage points [95% confidence interval (CI) 2.86 to 1.15], representing an 18% relative reduction. Reductions in potentially avoidable acute care transfers and ED visits were also reported.
In summary, the studies of QI programmes implemented in US nursing homes broadly meet the criteria for ‘stronger’ evidence but the findings should be interpreted with caution because of possible confounding factors in uncontrolled studies and unclear risk of bias. The inclusion of MOQI and OPTIMISTIC as separate publications and as part of the combined analysis should also be taken into account.
Other studies
Three studies (four publications) described QI programmes evaluated in New Zealand care homes (see Table 7). The studies were performed by the same group of authors, were relatively large and performed in a diverse range of settings. Two studies were cluster RCTs and one was a repeated measures before/after study. The study by Boyd et al. 40 was at unclear risk of bias because of limited reporting and lack of blinding. The Aged Residential Care Healthcare Utilisation Study (ARCHUS) trial41 was better reported and appeared to be at lower risk of bias, although as usual with this type of intervention, only limited blinding was possible. The third study was at high risk of bias because there was no control group. 42
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Boyd et al.40 | Cluster RCT | Nursing home, residential home | Care homes: intervention facilities 29, comparison facilities 25. Individuals: intervention facilities 1425 residents, comparison facilities 1128 residents. | Standard care (parallel control group) | Unplanned/preventable admissions. Medical admissions considered as potentially preventable. All admissions. All resident hospitalisations | No effect. Acute hospitalisation rates increased for both groups, although less for intervention group |
| Connolly et al.41 | Cluster RCT | Nursing home; mixture of ‘private hospital care’ for those requiring assistance with activities of daily living and 24-hour nurse availability; dementia care (secure rest homes); and psychogeriatric care (for those with dementia and additional needs). Residential home: ‘rest homes’ not providing 24-hour nursing care | Care homes: 36 (18 in each group). Individuals: 1998 (1123 intervention; 875 control) | Standard care (parallel control group) | Unplanned/preventable admissions (defined as ambulatory-sensitive hospitalisations; i.e. admission for specific conditions); all admissions (all acute admissions); length of hospital stay; other (specify); mortality | No effect. No difference in avoidable admissions (RR 1.07, 95% CI 0.85 to 1.36) or mortality |
| Connolly et al.42 | Uncontrolled before–after | Nursing home; residential home; similar to Connolly 201541 | Care homes: 21 facilities with higher than expected ED presentation/admission rates. Individuals: 1296 beds | None: repeated measures before–after | Unplanned/preventable admissions; emergency admissions for specific conditions; paper appears to use presentation and admission interchangeably (authors note ED presentation more directly under control of care home staff); transport to ED | Significant positive effect: 25% reduction in ED admissions after intervention |
The interventions used in the three studies are summarised in Table 8. The first study involved a relatively simple intervention with gerontology nurse specialists providing on-site support to care home staff. 40 The ARCHUS study added a wider multidisciplinary team (MDT)41 and this intervention was also evaluated in the third study with some minor changes. 42
| Study ID | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| Boyd et al.40 | GNS working with care home staff and primary and secondary health care services | Clinical support; education and clinical coaching; and care coordination for high-risk residents | Care home | The GNS was on site at each facility for a mean of 1.9 hours per month. GNSs provided care coordination and comprehensive geriatric assessments for residents of concern as needed (mean 2.6 assessments per facility in 12 months). The GNS also provided care coordination for residents transitioning across healthcare settings, although much of this work was not well captured in GNS records | On-site visits every other month and delivery of standardized gerontology education sessions for nurses and care assistants (mean 5.5 sessions per facility in 12 months). Ad hoc on-site clinical coaching to discuss residents of concern (mean 2.3 sessions per facility in 12 months) occurred at the request of facility staff |
| Connolly et al.41 | GNS and study MDT | Facility baseline assessment and care plan; monitoring and benchmarking of indicators linked to care quality; MDT meetings to review individual residents’ needs; gerontology education and clinical coaching for care home nurses | Care home/facility | GNS support/education began with weekly visits and gradually reduced in intensity over the 9-month intervention period | Benchmarking: 3 times during the intervention period; MDT meetings monthly for the first 3 months at each site |
| Connolly et al.42 | GNSs and study MDT | Facility baseline assessment; clinical coaching for nurses and care givers; MDT meetings, including medication review | Care home/facility | Increased clinical coaching time at each facility (relative to ARCHUS) | Three 1-hour MDT meetings at each facility |
Neither of the randomised trials found that the intervention reduced potentially preventable admissions compared with standard care. A subsequent ‘post hoc’ analysis of the ARCHUS data reported a reduction in admissions for a group of five conditions (cardiac failure, ischaemic heart disease, chronic obstructive pulmonary disease, stroke and pneumonia) responsible for many admissions among care home residents43 but as an unplanned analysis this should be treated with caution. Connolly et al. 42 reported a reduction in admissions post intervention but causality is uncertain in the absence of a control group. This suggests that the evidence for QI programmes involving gerontology nurse specialists with or without MDT support in New Zealand is at best inconsistent.
Turning to single studies in other countries, the Early Detection of Deterioration in Elderly residents (EDDIE) programme was evaluated in a before/after study in Queensland, Australia. 44 The intervention involved advanced clinical skills training, decision support and access to additional diagnostic equipment, plus targeted collaboration with a wide range of external stakeholders. Implementation was supported by an on-site clinical lead and ‘clinical champions’. The EDDIE programme was associated with a 19% reduction in annual hospital admissions and a 31% reduction in the average length of stay from baseline, comparable to effects reported in other studies but with a relatively high risk of bias. One additional study evaluated a QI programme in Switzerland using a stepped-wedge design. 45 The intervention, designated INTERCARE, was similar to the US programmes described above, with a nurse appointed to each participating care home as a link between care home staff and physicians. INTERCARE also used tools from the INTERACT programme. As this was a non-randomised study, the risk of bias was higher than for similar stepped-wedge studies with randomisation. The study reported a significant reduction in unplanned hospital transfers compared with the pre-implementation period, thus strengthening the international evidence base for QI programmes of the INTERACT type.
Applicability
Three of the US studies of QI programmes (four publications) provided data relevant to assessing applicability to UK settings: a summary of the 2012 CMS initiative,26 one of its component studies (MOQI32,33) and the trial of implementation support for INTERACT. 27
The major differences between the US and UK health systems (insurance-funded vs. publicly funded) are less acute for care home research because many US care home residents are covered by the publicly funded Medicare (for older people) and/or Medicaid (for people on low incomes) programmes. Both the CMS initiative and the INTERACT trial stated that included participants were Medicare/Medicaid recipients, although MOQI included some privately paying residents in state-licensed beds.
A further difference from the UK is that many US care homes include a mixture of long-term residents and those admitted for short-term rehabilitation following hospital treatment – although this difference is becoming less marked over time with the widespread commission of short-term ‘discharge to assess’ beds in the care home sector. The CMS initiative included only long-stay residents, increasing applicability to the UK, but this was unclear for the INTERACT study.
Other relevant factors captured by the FITAR framework for assessing intervention transferability/applicability were:
-
Population (residents seemed to be comparable to UK populations in terms of age and sex or gender and representative of the general US population)
-
Organisation/finance (Medicare financial penalties for readmissions; not currently relevant to UK setting)
-
Leadership:
-
supportive and stable nursing home leadership was associated with success in reducing admissions
-
a high level of facilitation in the INTERACT study (which was a trial of implementation support)27 and MOQI (intervention support team)
-
-
Services/workforce/initiative:
-
care homes participating in MOQI had high standards of care and high admission rates (comparable to some UK care homes)
-
INTERACT largely provided support to existing workforce
-
MOQI was heavily dependent on advanced practice registered nurses and other specialist nurses working full-time in care homes (difficult to apply in UK with current workforce shortages)
-
legal restrictions affected services provided by advanced practice nurses in some states26
-
NH staff turnover limited buy-in to QI initiatives26
-
the CMS initiative lasted four years but researchers reported that attitudes and practices were only beginning to shift at the end of the study period.
-
Applicability data were extracted from three publications from New Zealand. 40–42 The setting was urban (Auckland) and participating care homes had a higher than expected level of potentially preventable admissions. Most participating facilities were equivalent to residential care homes, although the ARCHUS study also included some ‘private hospitals’ providing higher levels of long-term care. 41 The health and care system appeared to be more closely integrated than in the UK, with a district health board responsible for supporting and certifying care homes and also providing acute hospital services. Few details of leadership and facilitation were provided, although the ARCHUS study achieved good ‘buy-in’ from participating facilities. 41
Workforce is a key factor in evaluating the applicability of this New Zealand research to the UK. The interventions were led by gerontology nurse specialists with at least 10 years of gerontology experience who were employed by the district health board. 40 The ARCHUS study authors noted that nurse practitioners, most of whom can prescribe medications, might be able to provide a faster response for some conditions, but the study was unable to employ nurse practitioners. Boyd et al. 40 pointed out that employment of nurse practitioners in the care sector in New Zealand was low. Nurse practitioners are not currently employed in UK care homes, but they are increasingly employed by NHS providers, mainly as advanced clinical practitioners, to support care homes as part of the Enhanced Health in Care Homes (EHCH) model. However, Boyd et al. 40 noted that their intervention was relatively low in intensity compared with other interventions involving nurse specialists.
The one QI programme study from Australia44 shared some features with the English EHCH model and other initiatives, being initially developed by care home nursing staff with input from community healthcare providers. The presence of active implementation support in this study should be taken into account in assessing its applicability to the UK. Finally, the Swiss INTERCARE study45 involved an urban care home population with a median age and sex or gender distribution similar to the UK. Participating care homes were highly motivated and committed to implementing the complex study intervention, based on the use of registered nurses in extended roles.
Integrated working
UK evidence
We used ‘integrated working’ to cover interventions in which the central feature was enhanced health service support for care homes, albeit often as part of a complex intervention with several elements, for example staff training and patient advocacy. We included 13 UK studies in this group, most of which were part of the Care Home Vanguard Initiatives, which developed the model of care now delivered nationally through EHCH. 2,46–53 Data from these studies were analysed by the Health Foundation, Nuffield Trust and other independent organisations. The remaining publications described or evaluated local initiatives and were mainly published as grey literature. 54–56
Five of the Care Home Vanguard studies (six publications) reported on initiatives in specific English cities or districts (Nottingham, Sutton, Rushcliffe, outer East London and Wakefield) with support from local commissioners and health and social care organisations. Details of the interventions varied (see Appendix 2, Table 35) and all had multiple elements but strengthening links between care homes and local general practices was a key feature. One intervention differed from the others by including availability of support from a geriatrician. 51
Characteristics of these studies are summarised in Table 9. The studies used linked care home and hospital data to compare outcomes of residents in participating care homes with those of a matched control group in homes with similar characteristics but not receiving enhanced support. This means that the comparison was not randomised and limited data on resident characteristics were available. A further study used administrative data to estimate the effect of new integrated care models (including the Care Home Vanguards) on hospital admissions at the national level. 50
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Brine et al.46 | Controlled before–after | Nursing home, residential home | Care homes: 15 nursing and 23 residential care homes. Individuals: 782 residents | Standard care (before–after) | Unplanned/preventable admissions; all admissions; transport to ED; length of hospital stay; other (specify); proportion of deaths that took place outside hospital (as a proxy for dying in preferred place of death) | Significant positive effect: emergency admissions were 18% lower for the intervention group and potentially avoidable emergency admissions 27% lower. Differences were only significant for residential homes. There was no difference between groups in ED attendance |
| Conti et al.47 | Controlled before–after | Nursing home, residential home | Care homes: intervention group – 17 nursing homes and 11 residential care homes; matched control group – 97 care homes. Individuals: intervention group – 297 residents; matched control group – 243 individuals, 296 records |
Standard care (before–after) | Unplanned/preventable admissions: subset of ‘potentially avoidable’ emergency admissions, based on a list of conditions considered to be manageable in community settings or preventable through good quality care; emergency admissions; transport to ED; ED attendances; length of hospital stay; hospital bed days; other (specify); outpatient appointments; admissions with urinary tract infection as principal diagnosis; proportion of death occurring outside hospitals (taken indicator of successful end-of-life planning) | No effect |
| Lloyd et al.49 | Controlled before–after | Unclear or not available ‘care homes’ | Care homes: 23 Principia care homes; comparison group was from 64 care homes. Individuals: 588 residents from Principia care homes, 588 residents in comparison group |
Standard care (before–after) | Unplanned/preventable admissions; emergency admissions; all admissions; transport to ED; length of hospital stay; other (specify); outpatient attendances; death | No effect: significant reduction in emergency admissions only |
| Lloyd et al.48 | Controlled before–after | Nursing home, residential home | Care homes: nursing homes 10 intervention, 27 control; residential homes 13 intervention, 47 control. Individuals: 68 in each group |
Standard care (before–after) | Unplanned/preventable admissions; potentially preventable emergency admissions; all admissions; emergency admissions; transport to ED; length of hospital stay; other (specify); proportion of deaths outside hospital | Significant positive effect: residential care homes only |
| Morciano et al.50 | Controlled before–after | Nursing home, residential home | Care homes: not reported (care homes participating in 6 care home Vanguards were included). Individuals: not reported (residents in care homes participating in 6 care home Vanguard pilot projects were included) | Standard care (parallel control group); compares data from care home Vanguard sites with non-Vanguard sites; appears to be total hospital admissions and bed days | All admissions; emergency admissions; length of hospital stay; hospital bed days | Significant positive effect: significant reduction in rate of emergency admissions for care home Vanguard vs. non-Vanguard areas |
| Sherlaw-Johnson et al.51 | Mixed methods | Nursing home | Care homes: 4 [intervention (Health 1000) group]; 19 (comparator group). Individuals: 431 (intervention group); 1495 (comparator group) | Standard care (before–after) | All admissions; emergency admissions; transport to ED; length of hospital stay; acceptability to care home staff; costs/cost-effectiveness | Significant positive effect: 35% marginal reduction in emergency admissions (95% CI 6% to 55%) |
| SQW Ltd 201752 | Mixed methods | Nursing home, residential home | Care homes: all Sutton (CCG and local authority) care homes invited to participate. Individuals: not reported | None | Unplanned/preventable admissions; non-elective admissions; emergency admissions; transport to ED; length of hospital stay; acceptability to residents/families; costs/cost-effectiveness; other (specify); preferred place of death | No effect |
| Vestesson 201953 | Controlled before–after | Nursing home; residential home; assisted living/extra care housing; 2 supported living schemes received some parts of the support given to care homes | Care homes: 15 in intervention (Vanguard) and 30 in matched control group. Individuals: 526 residents in each group | Standard care (parallel control group); matched controls in similar care homes | Unplanned/preventable admissions; emergency admissions for specific conditions; emergency admissions; transport to ED; length of hospital stay; emergency and elective hospital bed days; other (specify); deaths in hospital | Significant positive effect: significant but not conclusive evidence for potentially avoidable admissions |
| Wolters 20192 | Other (specify): summary of learning from Health Foundation evaluations of initiatives in Sutton, Rushcliffe, Nottingham and Wakefield | Nursing home, residential home | Care homes: not reported (see reports on individual initiatives). Individuals: not reported (see reports on individual initiatives) | Standard care (before–after) | Unplanned/preventable admissions; emergency admissions; transport to ED; feasibility of intervention | Significant positive effect: varied across sites/outcomes |
Four of the five local interventions reported a decrease in emergency admissions, potentially preventable emergency admissions or both compared with matched control groups. The exception was the initiative in Sutton, which the authors suggested may have been evaluated too early for any effect to be detected. 5 Relative reductions of between 18% and 39% were reported but CIs suggested a range of effects from less than 5% to over 50%. A subgroup analysis of the Rushcliffe study indicated that the reduction in admissions was present for residential homes but not for nursing homes,48 possibly because the lower baseline level of support in these homes gave more scope for improving outcomes. Overall, this group of studies constitutes ‘stronger’ evidence for the effectiveness of integrated working initiatives but with uncertainty about the size and clinical significance of any effect.
Implementation
Studies with data extracted on implementation are summarised in Table 10. In terms of the PARIHS framework, none of the studies reported evidence as a barrier to implementation. By contrast, numerous barriers associated with the background context in the UK were identified. Some general practitioners (GPs) were opposed to alignment of specific GP practices with care homes,46 and in another study alignment proved difficult for reasons connected to organisational boundaries. 51 In Bradford and Airedale, some GPs preferred direct referral rather than referral via a telehealth hub and some care homes continued to turn to GPs first rather than contacting the telehealth service. 57 Several studies reported barriers arising from within the care home, including resistance from managers and staff,57 difficulties in ensuring that staff had time to attend training,52 low levels of information technology literacy, internal processes that conflicted with study protocols51 and high staff turnover. 57
| Study setting | Evidence as barrier | Context as barrier | Evidence as facilitator | Context as facilitator | Role of facilitation |
|---|---|---|---|---|---|
| Nottingham City46 | Not reported | Inconsistent implementation across area; GP and resident resistance | Not reported | CCG supported initiatives to improve health in care homes from 2007 | Evaluation covered a range of existing services |
| Sutton47,52 | Not reported | Difficulties arranging staff time for training; lack of information technology literacy; e-learning underused; some staff unfamiliar with link nurse role | Intervention components based on evidence of what works elsewhere | Some intervention components already existed in some form; small group of committed senior staff did initial groundwork | Facilitation by steering group and programme staff; funding from NHS England to support spread of Vanguard |
| East and North Hertfordshire57 | Not reported | Lack of baseline data; time and resource demands of information governance | Not reported | Single trade association providing training across area; pre-existing collaboration between local authority and CCG | ‘Complex care champions’ appointed; homes received funding to backfill posts |
| Bradford and Airedale57 | Not reported | Some reluctance to use remote service; care homes continued to contact familiar GPs or community teams | Use of highly trained staff as first point of contact rather than relying on pathways or algorithms | Involvement of all staff, including those not directly using the service; telehealth hub as single first point of contact | Not reported |
| Rushcliffe46,49 | Not reported | Varying standard of ‘usual care’ within and between homes | Residential home residents identified as potentially more likely to benefit from additional support | Area with relatively low levels of admissions and socioeconomic deprivation | Residential home staff received additional training compared with nursing home staff |
| Outer east London51 | Not reported | Nursing homes in ‘geographically difficult’ locations, difficult to align with general practice; homes privately owned, potential conflict between existing practice and intervention procedures | Model of care based on Wagner’s chronic care model | Mutual trust between care homes and GPs; high staff turnover not seen as a problem locally | Initiative driven forward by a group of committed individuals providing ‘strong leadership and clear vision’; support from prime minister’s Challenge Fund |
| Wakefield53 | Not reported | One GP practice per care home model was not implemented | Not reported | Care home Vanguard formed in March 2015 | Not reported |
At the organisational level, implementation of the intervention across the Nottingham city area was inconsistent. 46 The East and North Hertfordshire care home vanguard encountered barriers associated with recruitment and time/resources required to obtain information governance approval. 57 Evaluation was also hampered by a lack of baseline data for comparison.
Implementation of support for integrated working was supported by cited evidence of similar interventions proving effective in other settings51,52 and evidence of variation in use of hospital services between care homes, suggesting potential for improvement. 2
Contextual factors that favoured implementation were generally based on pre-existing services or partnerships (see Table 10). Rushcliffe and outer East London benefited from low baseline levels of socioeconomic deprivation and relatively low levels of staff turnover which reduced care home sector instability, respectively.
Some details of facilitation of implementation were reported from Sutton, Hertfordshire, Rushcliffe and outer east London (see Table 10). Two studies highlighted the role of committed individuals in key positions47,51,52 and these sites also received funding to support implementation of their interventions.
International evidence
The largest body of international evidence on integrated working interventions comes from Australia (15 studies), followed by the USA (4) and other countries (4).
The 15 publications from Australia reported on 10 different interventions. Of these, seven were delivered by hospital-based teams. The studies used a wide range of designs (see Table 11). Sample size for quantitative studies ranged from 1 to 81 care homes. The number of participants involved also varied widely but was less clearly reported, for example as the number of beds rather than the number of individuals recruited or analysed. Many of the studies were at high risk of bias because of weak study designs or small sample sizes. Of the RCTs included, one was small (45 participants)58 and the other used a step wedge rather than a parallel control group design. 59 Details of risk of bias for individual studies can be found in Appendix 4.
| Reference | Intervention | Delivered from | Study design and sample size | Effect measure |
|---|---|---|---|---|
| Amadoru et al.64 | Residential in-reach | Hospital | Qualitative; 8 care homes, 40 staff | N/A |
| Chan et al.65 | Acute geriatric outreach | Hospital | Before–after; 12 nursing homes | Rate ratio 10% reductiona |
| Cordato et al.58 | Post-discharge visits (REAP) | Hospital | RCT; 21 care homes, 45 residents | Readmissions, ⅔ reductiona |
| Craswell et al.60 | Nurse practitioner candidate: enhanced primary care | Primary care | NRCT 1 intervention site |
ED admissions 44.6 vs. 59%a |
| Dai et al.62 | Acute geriatric outreach | Hospital | ITS; 12 care homes | Admissions 42.8 to 27.1/montha |
| Dwyer et al.61 | Nurse practitioner: community-based residential acute care service | Community | Qualitative; 10 care homes, 15 interviewees | N/A |
| Fan et al.63 | HiNH | Hospital | CBA; 1 hospital catchment area, > 2000 beds | Admissions rate ratio 0.62a |
| Fan et al.67 | HiNH | Hospital | Economic evaluation of Fan et al.63 | Reduction in net costs to health servicea |
| Haines et al.59 | In-house GPs | Primary care | Step wedge RCT; 15 care homes | Unplanned hospital transfers rate ratio 0.53; admissions 0.52a |
| Hullick et al.68 | ACE; nurse-led telephone triage+ | Hospital (ED) | CBA; 4 intervention, 8 control homes | 40% reduction in ED admissionsa |
| Hullick et al.69 | ACE | Hospital | Stepped wedge; 81 facilities, 9 EDs | ED admissions rate ratio 0.79a |
| Hullick et al.70 | ACE + video-telehealth | Hospital | CBA; 5 intervetion, 8 control homes | No difference in ED visits and admissions |
| Hutchinson et al.71 | Geriatrician-led outreach service (RECIPE) | Hospital | Cohort/ITS; 73 facilities in hospital catchment area | Reduction in admissions from 3.03 to 2.4/resident/quartera |
| Kwa et al.72 | Residential in-reach (linked to Amadoru et al.63) | Hospital | Uncontrolled before–after; 52 care homes | Unplanned ED presentations 2.4 vs. 0.8%a |
| O’Neill et al.65 | Hospital avoidance | Care home collaborating with specialist in-reach team and other specialists | Qualitative; 1 care home, 21 interviewees | N/A |
Table 12 summarises the interventions evaluated in the Australian studies. Interventions delivered by hospital-based teams were described as ‘residential in-reach’, ‘acute geriatric outreach’, ‘regular early assessment post-discharge’ (REAP), ‘hospital in the nursing home’ (HiNH), ‘aged care emergency service’ (ACE; with or without telehealth) and ‘geriatrician-led outreach service’ (Residential Care Intervention Program in the Elderly). Services described as ‘in-reach’ and ‘outreach’ overlapped in terms of intervention content and the distinction between them was unclear. The REAP programme differed from the others by being delivered after discharge with a view to reducing unplanned readmissions.
| Study ID | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| Amadoru et al.64 | RACF staff, GPs and residential in-reach RNs | A residential in-reach service operating in Melbourne. It is geriatrician-led and operates seven days a week, from 9 a.m. to 5 p.m.. This service offered telephone advice, geriatrician or nursing reviews, acute interventions such as intravenous antibiotics and hydration, palliative care, changing or reinsertion of urinary catheters and percutaneous endoscopic gastrostomy tubes, management of elective hospital day admissions for blood transfusions and acute medical admissions, discharge follow-up and coordination of specialist consultations | Care homes in an urban setting | Operates seven days a week, from 9 a.m. to 5 p.m. | Occurred per referral from GP or care home staff |
| Chan et al.66 | Acute geriatric outreach service: 2 part-time geriatricians initially, subsequently joined by 1 nurse; advanced trainee in geriatric medicine available both pre and post intervention but not consistently | Geriatric outreach service targeting acute conditions such as pneumonia, cellulitis and urinary tract infections. Members could cannulate, order blood tests on the same day and order imaging investigations. They sometimes also provided staff education and training | Participating nursing homes | Geriatricians each work 0.5 FTE; service operates 9 a.m. to 5 p.m. Monday to Friday | Not applicable |
| Cordato et al.58 | 7 geriatricians and 1 nurse practitioner | Usual post-discharge care (as for the control group) plus regular joint geriatrician and nurse practitioner evaluations. Additional investigations and/or treatments recommended/arranged in concert with the resident’s GP/primary care physician, who retained ultimate responsibility | Nursing home | Visits involved both geriatrician and nurse practitioner; length of sessions not reported | First visit within 1 week after discharge from hospital admission, then monthly visits for 6 months |
| Craswell et al.60 | NPC working with GPs and care home staff | NPC provided triage, assessment, preliminary diagnosis and primary care for acutely unwell or deteriorating residents to reduce potentially preventable transfer to hospital. Identification was achieved by regularly visiting all resident areas, discussing resident conditions with all levels of clinical staff of the facility and visiting residents with a history of known comorbid conditions. NPC also collaborated with the GP in the care of residents, promoted ACP, and provided opportunistic education to care staff | Care home | During the 12-month study period, NPC completed 1790 consultations with 266 residents, the median number of consultations per resident 4 | Not applicable |
| Dai et al.62 | Geriatricians and nurse triage referrals and visit care homes to assess and manage patients there with ‘hospital in the home’ interventions | ‘Hospital at home interventions’ including cannulation, intravenous drugs (antibiotics, furosemide), and subcutaneous fluids. Other interventions provided include symptom management, difficult urinary catheterisations, ACP, and medication reviews. The service relies on private pathology and radiology providers for investigations. It works collaboratively with private wound nurse practitioners and community nursing services. Hyperacute problems such as stroke and acute coronary syndromes are excluded | Care homes in catchment area | Available during weekdays, staffed by 1 FTE geriatrician, 1 FTE aged care nurse, and 1 FTE geriatric trainee | Not applicable |
| Dwyer et al.61 | 2 nurse practitioners (1 gerontology and 1 chronic disease endorsed), care home nurse managers, RNs, allied health professionals and residents’ GPs | Community-based ‘in-reach’, service called RACS. RACS team respond to calls from care facilities and provide a responsive, mobile triage service | Care home | Two FTE NPs working office hours Monday to Friday | Not applicable |
| Fan et al.63/Fan et al.67 | ED-based nurses working in partnership and coordinating with RACF staff and other health providers (further details not reported) | Four main components: (1) HiNH staff manage acute symptoms in nursing home residents who might otherwise require transfer to ED; (2) support and education for nursing home staff and GPs; (3) HiNH team seeks senior medical decision-making at an early stage after presentation to ED and coordinates subsequent care; (4) HiNH team coordinates discharge of residents from ED and inpatient care | Care home and ED | Programme involved ‘2 or 3’ ED-based nurses as main programme staff; Fan et al.67 | Not applicable |
| Haines et al.59 | In-house GP; clinical manager; RN in charge; community RNs/EENs; care staff | Clinical manager supports the GP in managing medical practice, RN in overall charge; other RNs/EENs act as team leader for a small group of personal care attendants responsible for a ‘community’ of residents. Personal care attendants assist residents with their medications | Nursing home | 1 full-time GP was employed for each 150 residents | Not applicable |
| Hullick et al.68 | ED advanced practice nurse led and coordinated the service, working with care home and ambulance staff, GPs, ED staff and the primary care organisation | Clinical care manual to support care in the facility; nurse led telephone triage line; education of care home staff; establishing goals of care prior to ED transfer; case management when in the ED; and development of collaborative relationships between stakeholders | Care home and ED | Over 20 evidence-based algorithms; 2-hour educational presentation with extra education as required; telephone advice 12 hours/day, 7 days/week | Not applicable |
| Hullick et al.69 | See Hullick et al.68 | 24-hour nurse-led telephone consultation service for care facilities; evidence-based algorithms for common problems; establishing goals of care before transfer to ED; case management by specialist aged care nurses in the ED; empowerment and education of care facility staff; community of practice involving all stakeholders; ongoing change management and coordination among stakeholders. See also Hullick et al.68 | Participating care facilities and EDs | Telephone advice 24 hours/day; education used a ‘train the trainer’ approach with a 2-day workshop at each ‘step’ | Quarterly meetings of community of practice |
| Hullick et al.70 | Care home staff, ED/aged care RN/advanced practice RN supported the programme 1 day per week including trouble shooting | The video telehealth pathway was available 7 days a week for calls between 8 a.m. to 4 p.m. This involved two-way, real-time interactive communication between the resident with support from care home staff and nursing staff in the ED. Care home staff member activated the call, managed the patient, managed the camera and equipment and undertook tasks to support the telehealth call. They also considered the recommendations from the ED regarding management including whether transfer to the ED was needed. Out of hours, telephone support continued to be provided by the primary health organization as part of the Aged Care Emergency programme, with no video enhancement. The video telehealth technology was also used to provide follow-up of patients discharged from hospital up to 1 week following their discharge to ensure clinical handover was complete | ED and care homes | 7 days a week 8 a.m. to 4 p.m. | As needed |
| Hutchinson et al.71 | Referral by hospital staff (ED, ambulance or other), care home staff or primary care; triage and care home visit by aged care specialist (nurse specialist, registrar or geriatrician); additional services as required | Triage (same day or same week response); care home visit: assessment, care planning, arrange interventions/pathology, referral to hospital in the home if required, development of long-term care plan (including ACP with advance directive if appropriate) with primary care and care home staff | ED and care home | Same day or same week response depending on needs | Additional visits if required once enrolled in the programme |
| Kwa et al.72 | Hospital RIR team serving care homes within the catchment area | Change of medical staff from rotating ED physician support to a consistent consultant geriatrician; co-location of an existing ward-based RAC liaison nurse role to work with the RIR team; stakeholder engagement to encourage referral for review and continued care after hospital discharge | Care homes and tertiary referral hospital | Before implementation, the RIR team consisted of a nurse (1.0 FTE) and consultant physician (0.5 FTE), Monday–Friday, 9 a.m. to 5 p.m. In 2014, the service was redesigned without incurring any increase in operating cost or FTE allocation | Not applicable |
| O’Neill et al.65 | Primarily nursing staff at nursing homes, but also community clinical staff including geriatricians and wound care nurses | Decision-support tools; advanced clinical skills training; specialist clinical support and collaboration; medical equipment | Nursing home and hospital (to support early discharge) | Not clear but package of training and referral pathways which appear to be continuously implemented | Continuous |
Core components of the interventions included geriatrician and/or nurse practitioner leadership; telephone advice and case review; visits to care homes as required; tests and investigations; and hospital-level treatments such as cannulation. However, most services were only available during set hours and mainly on weekdays.
Primary care or community-based studies evaluated nurse practitioner-led services60,61 and a model of care supervised by in-house GPs supported by a clinical manager. 59 This latter model was unusual and the study was affected by difficulties in recruiting GPs to work in and across care homes.
With one exception, all the quantitative studies reported a significant reduction in one or more outcomes related to admissions, ED visits or health service costs. The size of effect and the effect measure used varied but controlled studies typically reported relative reductions of a third or more compared with standard care for both hospital-based62,63 and primary care/community-based60 interventions (see Table 11).
Qualitative studies reported that the rate of referral to in-reach services was influenced by the perceived responsiveness of the service and outcomes of care. 61,64 In a further study, care home staff welcomed the introduction of a hospital avoidance programme involving collaboration with community-based specialists alongside use of QI tools. 65 The qualitative studies were all from the perspective of care home staff, mainly nurses.
Of the four US studies (see Table 13), two evaluated the use of telemedicine for remote consultation72,73 and the others evaluated specific models of care. 75,76 Further details of the interventions are presented in Appendix 3, Table 39.
| Reference | Intervention | Delivered from | Study design and sample size | Effect measure |
|---|---|---|---|---|
| Brickman et al.75 | MDT | Hospital ED | Non-randomised trial; 1 intervention, 101 control sites | Annual unplanned admissions: 55% reduction |
| Grabowski et al.73 | Out-of-hours telemedicine | Medical call centre | Step-wedge RCT; 11 care homes | Hospitalisation rate: significant reduction for higher users |
| Hofmeyer et al.74 | Telemedicine consultations | Telemedicine ‘hub’ with on-call specialists | Uncontrolled pilot study | Transfer rate decreased from 54% in 2013 to 17% in 2015 |
| Stadler et al.76 | MDT | Hospital (tertiary geriatric centre) | Uncontrolled before/after; 3 rural facilities | 35% reduction in monthly ED transfers and 30.5% reduction in monthly hospitalisations |
Other studies
Of the four remaining studies, three examined measures to strengthen medical support for care home residents (see Table 14) and one (two publications) evaluated early geriatrician follow-up after discharge. Same-day access to a physician, assignment of a dedicated GP to nursing homes and changes in reimbursement policy were all associated with reductions in admissions in single studies. While all the studies had some kind of control group, study designs were observational and/or non-randomised, suggesting that the findings should be interpreted cautiously. These studies add to the UK and international body of evidence for the effectiveness of improving access to primary care physicians in reducing unplanned admissions.
| Reference and country | Intervention | Delivered from | Study design and sample size | Effect measure |
|---|---|---|---|---|
| Kobewka et al.79 Canada |
Same-day physician access | Not applicable (association study) | Retrospective cohort; 161 care homes | Hospitalisations 21% reduction (rate ratio 0.79) |
| Kumpel et al.80 Germany |
Additional reimbursement for physicians | Policy change | Controlled before–after; 22,000 nursing home residents | 8% (absolute) reduction in ambulatory care-sensitive admissions |
| Pedersen et al.77,78 Denmark |
Follow-up visit by geriatric team after discharge | Hospital geriatric team | Quasi-randomised trial; 648 (330 intervention, 318 control) in 2018 study | Readmissions 37% reduction (adjusted hazard ratio 0.63; 95% CI 0.42 to 0.95) |
| Weatherall et al.81 Denmark |
Dedicated GPs attached to nursing homes | Primary care | Non-randomised trial; 16 nursing homes | Preventable admissions, 27% relative reduction |
Two studies by Pedersen et al. 77,78 evaluated early follow-up visits by a nurse and doctor from a geriatric team following hospital discharge as a way of reducing early readmissions. The first study recruited a general population of older people with frailty admitted to hospital (with care home residents as a subgroup)77 while a later paper reported specifically on care home residents. 78 In the 2018 study,78 readmissions were reduced by 37% in the intervention group relative to standard care. The study was at risk of bias from non-random assignment to treatment groups and possible differences between groups at baseline. A similar intervention evaluated in Australia by Cordato et al. 58 reported a two-thirds reduction in readmissions (see Table 11). Taken together, the two studies represent ‘weaker’, albeit promising, evidence for this type of intervention.
Applicability
Applicability data were extracted from 12 of the 15 Australian studies (see Table 15). Key points relevant to applicability/transferability were as follows:
| Reference | Population | Organisations/finance | Leadership | Services/workforce/initiative |
|---|---|---|---|---|
| Amadoru et al.64 | Not reported; limited details reported above under ‘limitations’ | Not reported | Not reported | Not reported |
| Chan et al.66 | Mean age of treated patients was 85.7 years and 52% were females; 69.4% were acute patients (deemed to require ED transfer if not seen the same day) | Service established by geriatric and ED specialists to serve NHs in hospital catchment area. Additional funding was obtained to establish the acute geriatric outreach service | Not reported | Referrals from nursing home staff and patients/carers increased from 29% in 2013 to 76% |
| Cordato et al.58 | Catchment area of study generally middle-income and culturally diverse. Patients unable to complete study questionnaires (e.g. with severe dementia) were excluded | Care homes were within the catchment area of St George’s Hospital (specific local government areas of Sydney). Authors note findings relevant to most developed nations as they face similar challenges to Australia and there is overlap in delivery of health and social care. About 2/3 of hospital beds in Australia publicly funded through Medicare. Care homes provided by private and not-for-profit organisations, subsidised by federal government, with ongoing medical care through Medicare | Not reported | Support of residents’ GPs pivotal to success of the intervention. Key elements include targeting the post-hospitalisation period and regularity and frequency of follow-up |
| Craswell et al.60 | Residents referred to the NPC were on average 86 years of age and 67% were female | Intervention facility described as ‘multisite’; ED described as ‘local’ so relatively close to intervention and other facilities. Study was funded via a competitive grant from the Department of Social Services (now Commonwealth Department of Health) | Not reported | Intervention delivered by nurse practitioner candidate undertaking advanced training so could potentially mitigate a shortage of qualified nurse practitioners. Intervention of relatively low complexity and limited spread; part of larger research project: Care coordination through ED, residential aged care and primary health collaboration |
| Dai et al.62 | Care home residents from 17 residential aged care facilities in the Bankstown catchment area. Not clear if nursing or non-nursing care. | Bankstown-Lidcombe Hospital introduced the acute geriatric outreach service. The service was provided by the hospital but not clear how it was funded/commissioned. Service also involves private providers | Not reported | Service was designed to improve on previous sub-acute model. During the study period, Australia funded more home care support, which may have meant people entering residential care had more complex health needs than previously. Service delivered by 1 full time geriatrician, 1 full time aged care nurse, and 1 full time geriatric trainee. Service was hospital-based; no other details reported. Service successfully delivered since January 2015, suggesting good longevity |
| Fan et al.63 | Residents presenting to ED were mainly aged 75–94 and about 63% were female | All nursing homes in the catchment areas of the intervention and control hospitals were federal funded, and their performance was assessed against a set of legislated accreditation standards. The composition of nursing homes in the 2 areas was also similar, with comparable percentage of high- and low-care beds. HiNH programme funded by Queensland State Government | Not reported. Lack of reporting may reflect HiNH programme operating since 2006 | See above; elements of intervention delivered in care home and ED. ED nurses key to intervention but grade and hours worked not reported. HiNH programme implemented at intervention hospital since 2006, hence long-lasting initiative |
| Haines et al.59 | Not reported | Intervention initiated by Bupa Aged Care. GPs and other staff employed directly by Bupa Aged care | Not reported | Trial sites in different cities/states; common ownership implies similar standards of care. Intervention aimed to improve access to GPs and expand role of RNs; four facilities were unable to recruit GPs during the study. Complex initiative requiring significant reorganisation of roles; 30-month trial plus pre- and post-intervention periods supports longevity |
| Hullick et al.68 | Mean resident age approximately 86 years in both groups | Setting was a local health district in New South Wales, Australia with a range of tertiary and primary services. The tertiary referral hospital, in which the intervention ED is located, is surrounded by a number of RACFs that refer patients to the ED. Three of the intervention RACFs were not-for-profit organisations and one for-profit, with a total of 413 residents. Three of the intervention facilities had RNs onsite 24 hours a day. One facility had RNs on call overnight. Care in RACFs is subsidised by the Australian federal government with the majority of services provided by not- for profit organisations. State governments fund acute care services. The context for the study was that there was no additional funding for RNs in RACFs | Development of collaborative relationships among stakeholders a key part of the intervention | High rate of ED attendance in intervention facilities; intervention and control sites matched on number of total beds, dementia specific beds, and ratio of high to low care beds. RNs in RACFs account for 15 % of the direct care workforce with the majority of staff being AINs or PCAs. RNs in provide oversight of entire facilities with supervision of AINs and PCAs. Nurse practitioners are advanced practice nurses whose numbers are limited and closely controlled by state and federal funding (0.2% of staff). Intervention operates before and during transfer to the ED; advice and coordination provided by ED staff |
| Hullick et al.69 | Study covered the Hunter New England Health Local Health District in northern and western New South Wales, Australia, including the metropolitan region of Greater Newcastle along with regional and rural communities | Participating EDs ranged from a small rural ED that saw 11,106 patients in total to a large tertiary referral trauma hospital ED that saw 79,952 patients in 2018. For financial information, see Hullick et al.67 | Two advanced practice nurses provided leadership for the programme. Community of practice brought together key stakeholders | Participating facilities varied in baseline rate of ED transfer. For workforce details, see Hullick et al.67 Intervention operates before and during transfer to the ED; advice and coordination provided by ED staff and staff from the local primary care/general practice organisation |
| Hullick et al.70 | Nursing home population in Australia, homes varied in provision of dementia care and respite care | The 5 intervention RACS all belonged to 1 not-for-profit aged care organisation. Intervention and control homes referred patients to the same community hospital ED | Initiative for the study came from the care home organisation running the intervention sites | ACE hospital avoidance programme operating for at least 9 months before study data collection started. Local health district telehealth personnel were available by telephone when required; they recommended equipment and assisted with training both hospital and care home staff. An APRN supported the programme 1 day per week including trouble shooting, change management and training as well as monthly project meetings with stakeholders. The RN trained the care home and hospital administrative and nursing staff. Stakeholders included a nurse educator and nurse practitioner from the care home organisation, the ACE program advanced practice RN, local health district telehealth support as well as ED and older persons’ ward representatives from the hospital. Video consultation to help evaluate unwell residents and provide follow-up of residents recently discharged from hospital. The ACE program has engaged 81 RACS that primarily transfer residents to nine EDs across a large regional local health district of Northern and Western New South Wales, Australia, including regional and rural communities |
| Hutchinson et al.71 | Median age of 84 years, 61% female | Not reported | Not reported | Service based on assessment by aged care specialists; authors note shortage of trained staff a barrier to providing palliative care services in residential care settings. RECIPE service introduced in 2002, so high longevity |
| Kwa et al.72 | Patients seen by RIR were marginally older in the second period (median age pre: 86 years, IQR: 80‒91, vs. post: 87 years, IQR: 81‒91). The 5 most common conditions that were treated during RIR visits were skin conditions; respiratory; ‘other geriatric assessment’; end-of-life care; and catheter care | Service provided by tertiary referral hospital to 52 care homes in its catchment area, covering three local government areas. Authors state that service redesign did not incur any additional costs | Not reported but this was redesign of an established service rather than introduction of a completely new service | Service redesign required a consultant geriatrician with experience in acute care of the older patients including in care home settings and a ward-based liaison nurse integrated with the RIR team. RIR service began in 2009 and was restructured in 2014 |
| O’Neill et al.65 | Nursing home staff in general population nursing home Queensland | Not reported | Intervention included ‘clinical champions’ | Partial integration; early evaluation in one setting |
-
Population:
-
Most studies reported some details of the patient population (e.g. age, gender or sex distribution) and setting. There were no specific issues affecting applicability (e.g. highly selected or indigenous populations) but the type of setting could influence applicability.
-
-
Organisation/finance:
-
Cordato et al. 58 noted that their findings were ‘relevant to most developed nations’ because different countries face similar challenges and have overlapping health and social care systems. In Australia, Their summary provides further details relevant to the applicability of study findings from Australia to the UK setting. In Australia, about two-thirds of hospital beds are publicly funded through Medicare. Care homes are provided by private and not-for-profit organisations, subsidised by federal government, with continuing medical care through Medicare. 58 State governments fund acute care. 68
-
The Australian studies involved a wide range of organisations. Although EHCH in England is based upon a national specification across England, it is coordinated at a regional level through integrated care systems. This mirrors, in many ways, the regional organisation of approaches described in Australian literature. Services were designed to cover care homes within the catchment area of particular hospitals66 or at the level of the local health district. 68 In another study, the care home provider, Bupa Aged Care, implemented and evaluated an intervention involving employment of GPs to work within care homes. 59 This latter intervention could have limited application to the UK, where GPs are generally external to care homes and serve patients in the community as well as care home residents.
-
Most studies involved all care homes in the study area that wished to participate, generally a mixture of privately owned and not-for-profit homes. 63,66,68 Others involved working with homes belonging to a single care organisation. 70
-
Some studies reported limited details of the organisations involved. 71
-
Across the range of studies, financial support was reported from an unspecified source of ‘additional funding’;66 the Department of Social Services;60 and the Queensland State Government. 63 One study reported that service redesign incurred no extra costs. 72
-
-
Leadership:
-
Details of systems leadership were not reported for most studies. Hullick et al. 69 reported that advanced practice nurses provided leadership and a community of practice brought together key stakeholders. In another study by the same group,70 the initiative was originated by the owners of the care homes where the intervention was implemented. The hospital avoidance programme reported by O’Neill et al. 65 included ‘clinical champions’.
-
-
Services/workforce/initiative:
-
One study reported that the research took place at a time of increased public funding for care homes, which may not be applicable to the UK. 62
-
The role of government accreditation of care homes, highlighted in one study,63 is similar to that seen across all four UK nations.
-
In terms of workforce, the included studies identified issues that appear applicable to the UK, including the importance of support from residents’ GPs58 and the need to take into account shortages of healthcare professionals, including GPs,59 specialist nurses68 and geriatricians. 72
-
Specific features of workforce and organisations were of uncertain applicability to UK practice but should be taken into account. These include key roles for particular staff such as nurse practitioners in advanced training;60 the overall balance of the workforce, about 15% of care staff in Australia being registered nurses and just 0.2% nurse practitioners;68 and the role of staff based in different settings,68 staff from EDs working more closely with care homes in Australia than the UK.
-
Other studies
Applicability data were extracted from three of the four integrated working studies conducted in the USA. 73–76 Key findings related to applicability were:
-
Population:
-
Organisations/finance:
-
Leadership:
-
In a study of telemedicine, some care homes made little use of the service, likely a generalisable outcome of lack of leadership at that level. 73
-
Prior to implementation of the reducing avoidable facility transfers intervention, members of the provider’s geriatric team served as medical directors of participating facilities76 (not readily applicable to the UK).
-
-
Services/workforce/initiative:
-
Of the two MDT-type interventions, one identified issues applicable to UK settings (complexity of intervention, requirement for training of care home staff). 75
-
The other study reported that internal medicine physicians with little experience of working in care homes were assigned to provide out-of-hours medical coverage, an issue unlikely to be applicable to UK care home settings. 76
-
Looking at studies conducted in other countries, applicability data were extracted from the Danish studies by Pedersen et al. 78 (early geriatric follow-up) and Weatherall et al. 81 (dedicated GPs). A major difference from the UK is that nursing homes in Denmark are publicly owned, with relatively uniform staffing and resources; this facilitates integration with the health-care system. 78 Pedersen et al. 78 also noted that hospital admissions in Denmark tend to be short (hence the potential value of early geriatric follow-up), suggesting that the problem of delayed transfer of care is less acute than in the UK. The study of dedicated GPs81 found recruitment challenging (despite GPs being able to continue their own practice alongside work in nursing homes) and this would likely be applicable to a similar intervention in the UK.
Training/workforce development
Interventions classified as training/workforce development were more specific than QI programmes. These interventions focused on training within a specific speciality, for example dementia, or to manage a specific problem such as delirium or recognising acute physiological deterioration.
UK evidence
We included four studies of interventions in UK settings that were classified as training/workforce development. 52,82–84 All of the studies were regionally based. 52,82–84 The vanguard study included all care homes in the London Borough of Sutton: 81 in 2018, although numbers varied during the study period. 52 The other studies were smaller, with 23 care homes,84 14 care homes83 and, in the smallest study, 4 care homes. 82 Care homes in three of the studies were a mix of nursing and residential homes,52,82,83 the type of care homes was unclear in the other study. 84 Two of the studies designs were mixed methods,52,84 one was a feasibility cluster RCT83 and the other an uncontrolled before–after study. 82 Formal risk of bias assessment was conducted for the RCT,83 identifying possible concerns over differences between treatment groups at baseline and lack of blinding. The other studies were at high risk of bias because of weak design and small sample size. 82,84
The studies investigated a variety of different training and workforce interventions; a dementia learning community,84 the PiTSTOP study of ‘STOP Delirium!’ a delirium educational package,83 a self-contained training intervention on recognising deterioration and other topics82 and training/workforce development within the Vanguard programme,52 which is discussed in greater detail within the integrated working section. Study characteristics are summarised in Table 16; Appendix 2, Table 37 gives more details of the interventions. The STOP Delirium! educational package outcomes measured were feasible and a larger trial following further modification to the intervention is feasible and needed to assess the impact of the education package, for which this trial was not designed. 83 Establishing a dementia community was also found to be feasible with ‘plan, do, study, act’ cycles the more active ‘active ingredient’ of the community. 84 No significant differences were found for intervention homes compared with control care homes in changes in rate of ambulance call-outs and across all sites change in rate of all admissions was not associated with changes in Quality of Life in Dementia Scale scores or more specifically the rates of emergency admissions. This was a small trial of just 23 care homes and further larger studies over a longer period could be needed to determine the impact of the learning community on unplanned hospital admissions. The self-contained training intervention on recognising deterioration and similar topics82 found that the training programme was well-received by carers but attendance rates for staff were low from 5% to 28%, indicating that the programme was not reaching all care home staff. The study did observe reductions in hospital admissions and specifically avoidable admissions, but these reductions were not analysed statistically and it was hard to demonstrate causality for this small QI project. Another promising intervention that could be investigated in a larger trial. The UK training/workforce development intervention evidence is weak. The included studies demonstrate potentially promising interventions for care homes but would all require further larger trials to properly demonstrate their potential impact.
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Armstrong et al.82 | Uncontrolled before/after | Nursing home, residential home | Care homes: 4 care homes in Enfield, UK. Individuals: about 190 residents and 206 staff (varying over the course of the project) | Standard care (before–after) | Unplanned/preventable admissions; all admissions; other (specify); percentage of staff completing training | No effect: reductions observed but not analysed statistically |
| Sheaff et al.83 | Mixed methods realist evaluation | Unclear | Care homes: 23 (13 intervention, 10 control). Individuals: control 330 residents, 245 staff; intervention 288 residents, 298 staff | Standard care (parallel control group) | Emergency admissions; Feasibility of intervention; evaluated presence/absence of elements of intervention programme theory; other (specify); ambulance call-outs end-of-life planning | No effect: emergency admissions did not change |
| Siddiqi et al.82 | Feasibility cluster RCT | Nursing home, residential home | Care homes: 14 care homes. Individuals: 215 care home residents | Standard care (parallel control group) | All admissions; costs/cost-effectiveness; other (specify); delirium; delirium severity; medications; falls; deaths | No effect |
| SQW 201752 | Mixed methods | Nursing home, residential home | Care homes All Sutton (CCG and local authority) care homes invited participated in intervention. January 2017, Sutton CCG had: 81 care homes. Care home population not static, residents moved in and died and care homes, opened and closed. 2015–16 focused on nursing homes from Autumn 2016 residential homes more involved. Individuals: not reported |
None | Unplanned/preventable admissions; non-elective admissions; emergency admissions; transport to ED; length of hospital stay; acceptability to residents/families; costs/cost-effectiveness; other (specify); preferred place of death | No effect |
All of the UK training/workforce development studies reported on implementation of the programme as this is an important part of investigating the feasibility of a new intervention, this information is provided in Appendix 2, Table 38. Barriers to implementation included, competing pressures on staff time making it hard for them to have time to attend training,52,82 information technology facilities and support,52,82 high staff turnover,82 low attendance rates at training,82 shift work. 82 Facilitators to implementation of these interventions were having champions from within the care homes,83,84 a flexible delivery approach including evening sessions, webinars, podcasts to enable more care home staff to participate,82 information technology systems to enable virtual meetings82 and stable management. 82 Recently set government targets for dementia training acted as a facilitator for care home management in establishing a dementia learning community. 84 Armstrong et al. 82 also discussed the training material highlighting the importance of an activity-based curriculum, embedding of key messages with each session and aligning topics with admissions data.
International evidence
We included three studies, from countries other than the UK, of intervention classified as training and workforce development, one study from Canada,85 Norway86 and USA,87 respectively (see Table 17). The Canadian study had the largest sample, 135 nursing homes in the province of Saskatchewan, the US study investigated 85 assisted living facilities across three states and the study from Norway investigated 30 nursing homes from one county. The studies from Norway and USA were both RCTs; one was a cluster RCT87 and the other a step-wedge RCT;86 risk of bias for these studies is provided in Appendix 4, Table 42. Randomisation and a reasonably sized sample were strengths of the cluster RCT and limitations were missing data due to COVID-19, a relatively homogenous white sample and timing for data collection varied meaning that percentages could not be compared between periods. The step-wedge RCTs’ strengths were the reasonably sized sample and design and limitations were problems collecting data, the two groups for comparison were not identical and the original power calculation was for a standard RCT not a step wedge. 86 The study from Canada had a retrospective observational study design; formal risk of bias was not undertaken due to the high risk of bias inherent in this study design. Characteristics of these studies are summarised in Table 17; Appendix 3, Table 40 gives more details of the interventions. The study investigating training in function-focused care for care home staff in assisted living facilities in USA found no effect on emergency room or hospital transfers although there was a decrease in falls in the intervention group at 12 months. 87 A structured educational programme in intravenous treatment of dehydration and infections had a positive effect on the number of nursing home residents treated in the nursing home instead of the hospital. 86 The study investigating the legislation that long-term care facilities need to have a registered nurse on duty 24 hours a day, 7 days a week found that lower nurse availability was associated with an increased risk of hospital admission. 85
| Study ID and country | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| McGregor et al.85 (Canada) | Retrospective observational study | Nursing home | Care homes: 135 care homes in Saskatchewan. Individuals: 15,214 residents in included facilities | Standard care (parallel control group) | All admission; transport to ED | Significant positive effect: lower nurse availability associated with increased risk of admission |
| Resnick et al.87 (USA) | Cluster RCT | Assisted living/extra care housing | Care homes: 85 assisted living facilities; facilities across 3 states: 32 in Maryland, 33 in Pennsylvania and 19 in Massachusetts. Individuals: 781; treatment group 440, control group 341 | Standard care (parallel control group) | All admissions; transport to ED; other (specify); falls; cognition function; transfer to nursing homes | No effect |
| Romoren et al.86 (Norway) | Step wedge RCT | Nursing home | Care homes: 30 nursing homes. Individuals: 330 cases in 296 nursing home residents | Standard care (parallel control group) | Unplanned/preventable admissions; number treated in nursing home instead of hospital; length of hospital stay; harms of intervention; mortality at 30 days; other (specify); number of days treated; type of antibiotics used | Significant positive effect |
The applicability of the international evidence to the UK is limited due to the specific regions investigated,85 the type of facilities included in the study which were all public/not-for-profit facilities which is different to the UK where the majority are facilities are run for profit85 and where there are differences in health care systems. 87
There is limited evidence from the international studies of the impact of training/workforce development interventions due to potential biases in all of the included studies.
Management of specific problems
UK evidence
We included three UK studies (four publications) of interventions to reduce unplanned admissions by tackling specific problems that were not primarily training interventions (see Table 18). The Better Health in Residents of Care Homes with Nursing (BHiRCH-NH) study88,89 evaluated a complex intervention to improve early detection and treatment of urinary tract and respiratory infections, chronic heart failure and dehydration. The other studies in this group evaluated pharmacist-led medication review90 and delirium prevention. 83 Two of the studies were cluster randomised trials at low risk of bias83,88,89 but the study of medication review was at high risk of bias as there was no control group. 90
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Downs et al.88 | Cluster RCT | Nursing home | Care homes: 14 NHs recruited but 2 withdrew before the intervention began. Individuals: 148 nursing home staff; 95 family carers; 245 residents | Standard care (parallel control group) | All admissions; feasibility of intervention; costs/cost-effectiveness | No effect: intervention not implemented as planned |
| McKee et al.90 | Service evaluation | Nursing home | Care homes: 16 nursing homes. Individuals: 727 patients had medication reviews | Standard care (before–after) | Emergency admissions; monthly presentations; all admissions; costs/cost-effectiveness; estimated drug cost savings; other (specify); to enable comparisons between clinics where the consultant pharmacist worked alone and where they worked with a consultant geriatrician extra data were collected for 100 patients on type of clinical intervention by pharmacist and medication appropriateness. | Significant positive effect |
| Sampson et al.89 | Cluster RCT | Nursing home | Care homes: 14 nursing homes (7 intervention, 7 control) in London and West Yorkshire. Individuals: 245 residents, 95 family carers, 148 staff | Standard care (parallel control group) | Unplanned/preventable admissions; all admissions; transport to ED; feasibility of intervention; acceptability to care home staff; acceptability to residents/families; costs/cost-effectiveness; harms of intervention; no evidence of harm | No effect |
| Siddiqi et al.83 | Feasibility cluster RCT | Nursing home, residential home | Care homes: 14 care homes. Individuals: 215 care home residents | Standard care (parallel control group) | All admissions; costs/cost-effectiveness; other (specify); delirium (delirium severity; medications; falls; deaths) | No effect |
Details of the interventions are presented in Table 19. The BHiRCH-NH and ‘Stop Delirium!’ interventions were relatively complex while the remaining study reported a relatively simple intervention (medication review) that could be delivered by a single health professional. The medication review study was the only one that reported a positive effect, constituting ‘very limited’ evidence, with ‘inconsistent’ evidence for this heterogeneous group of interventions as a whole.
| Study ID | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| McKee et al.90 | Consultant pharmacist working alone or with geriatrician; nursing home staff | Comprehensive medication review; meeting with nursing home staff 6 weeks later to assess uptake of recommendations and identify educational needs | Nursing home | Comprehensive review of medication prescribed | One clinic per participating nursing home |
| Sampson et al.89 | Care home nursing staff and assistants | 3 key components, adapted from the INTERACT programme and paper based as UK nursing homes have variable use of electronic records: (1) Stop and Watch early warning tool: care assistants or nurses used this when they noted a change in a resident’s condition. They circled observed changes, notified the nurse and placed the tool in the resident’s nursing home records. (2) Care pathway: this was a two-step clinical guidance and decision-support system, focusing on symptoms and signs of four key ACSC conditions (acute exacerbation of congestive heart failure, respiratory and urinary tract infections, dehydration). The initial ‘primary’ assessment comprised screening questions with the potential to trigger a more detailed ‘secondary’ assessment. If the primary or secondary assessment result was ambiguous, the care pathway was administered at 6-hour intervals, until concerns had resolved and/or appropriate intervention was instigated. The nurse recorded the outcome of the primary and secondary assessment and their care plan in the resident’s records and decided on the next course of action. This may have included further monitoring using the Stop and Watch early warning tool, treatment initiated in the nursing home, or communication with primary care using the SBAR tool. Copies of the completed care pathway were kept with the resident’s record. (3) The SBAR method: a structured method for communicating critical information to primary care used by nurses to seek primary care intervention for the resident after the care pathway indicated a risk of decline | In the nursing home | For deteriorating residents | As required |
| Siddiqi et al.83 | Specialist delirium practitioner (mental health nurse with expertise in delirium) Delirium champion from each home | Stop Delirium! intervention – a multifaceted enhanced educational package incorporating multiple strategies to change practice delivered to each care home over 16 months. Specialist delirium practitioner delivered education sessions. Facilitated working groups of care home staff, groups identified targets around delirium prevention and developed solutions for their care home. Delirium champion from care home staff was training by practitioner. Each home had delirium box of resources to support learning | Care homes | 3 education sessions | Not provided |
Implementation
Implementation data were collected for the two complex interventions (see Table 20). Despite active implementation support in both studies, various contextual factors within the participating care homes produced substantial barriers to implementation of the study interventions.
| Reference | Barriers | Facilitators | Active facilitation |
|---|---|---|---|
| Downs et al.88 | Barriers to implementation at the level of the care home included insufficient support from management with respect to staff workload allocation. Nursing home managers were not sufficiently visible in their endorsement of this new way of working. The education strategy for the intervention may not have been sufficient to lead practice change and only included a 1-day training workshop and telephone support that was not acted on | Intervention development included a rapid research review, interviews and consensus workshops | Implementation support included identifying two practice development champions (PDCs) in each intervention home, and supporting them with a training workshop, practice development support group, monthly coaching calls, handbooks and web-based resources. PDCs from five of six intervention homes attended the training workshop, following which they had variable engagement with implementation support |
| Siddiqi et al.83 | Summary home-level data for hospital admissions (obtained from care homes) were missing for two homes, and rates were lower than estimated from other sources. Recording of falls differed markedly with some homes recording any instances where a resident was found on the floor as a fall, and others limiting recording to observed falls only; falls data were not, therefore, analysed further. However, only two-thirds of hearing tests were conducted due to lack of appropriate space in the care home. Resident-level data collection diaries were found not to be feasible for completion by residents and too burdensome for staff. Care-home-level diaries were also only partially completed by staff due to time pressures. It was uncommon for friends and family members to be either present to complete proxy forms or to have spent sufficient time observing the resident to be able to comment | A delirium champion was identified in four, and there was evidence of outputs from working groups being used in 5 of the 7 homes | Specialist delirium practitioner delivered training and facilitated working groups. Working groups consisted of care home staff and they set targets and decide on solutions that suited their home. Delirium champions in each home. Overall, 84.4% of staff completed at least one education session; in four homes, over 90% of staff completed all three sessions. Working groups were established in all homes. Delivery of the intervention was compromised in the later part of the study due to first sickness absence and then maternity leave of the delirium practitioner (9 of 22 months) |
International evidence
The international evidence for interventions to manage specific problems comprised 10 studies, of which 5 evaluated medication review/deprescribing, 4 evaluated vaccination of residents and/or care workers and 1 evaluated pharmacological prophylaxis of influenza (see Table 21). Four of the studies reported no significant effect on hospital admissions, which may reflect the fact that these studies were not primarily focused on admissions. Niznik et al. 91 reported that deprescribing acetylcholinesterase inhibitors was associated with reduced risk of hospitalisation from falls and fractures in residents with dementia, with no increase in the overall risk of adverse events. Risk of bias assessment did not identify any major issues with this study other than lack of blinded outcome assessment.
| Reference (country) | Intervention | Study type | Type of care home | Sample size | Comparator | Intervention effect |
|---|---|---|---|---|---|---|
| Frankenthal et al.98 (Israel) | Medication review | Individual RCT | Nursing home | Individuals: 359 | Standard care (parallel control group) | No effect: there was no significant group difference in the average number of hospitalisations (p = 0.10), and the trend toward a reduction in the average number of hospitalisations in the intervention group was not significant (p = 0.40) |
| Gorisek et al.96 (Slovenia) | Pharmacological influenza prophylaxis | Observational | Nursing home | Care homes: 3 nursing homes in Slovenia. Individuals: 208, 167 and 164 residents in the participating homes | Standard care (parallel control group); prophylaxis for all residents was compared with prophylaxis for directly exposed residents only and no pharmacological prophylaxis. Non-pharmacological measures were the same in all nursing homes | No statistical analysis of differences between nursing homes |
| Gravenstein et al. 92 (USA) | Influenza vaccination | Cluster RCT | Nursing home | Care homes: 823 facilities were recruited to the study between March and August, 2013 | Standard care (parallel control group) | Significant positive effect: incidence of respiratory-related hospital admissions was significantly lower in facilities where residents received high-dose influenza vaccines than in those that received standard-dose influenza vaccines (0–185 per 1000 resident-days or 3.4% over 6 months vs. 0.211 per 1000 resident-days or 3·9% over 6 months; unadjusted RR 0.888, 95% CI 0.785 to 1.005; p = 0.061, and adjusted RR 0.873, 95% CI 0.776 to 0.982; p = 0.023). For all-cause admissions: 3509 (1.021%) high dose group vs. 3788 (1.113%) standard group. Unadjusted RR 0.920 (95% CI 0.859 to 0.985) 0.017 |
| Junius-Walker et al.99 (Germany) | Medication review | Cluster RCT | Nursing home | Care homes: 44 nursing homes with 862 residents were randomised, 23 of them (with 452 residents) to the intervention group and 21 (with 410 residents) to the control group | Standard care (parallel control group) | No effect; there were no significant differences in terms of the number of hospitalisations or the proportion of nursing-home residents requiring emergency or rescue services on at least one occasion in the preceding 6 months |
| McConeghy et al.93 (USA) | Influenza vaccination | Cluster RCT | Nursing homes | Care homes: 823 nursing homes, housing 50, 012 eligible residents, to adjuvant or standard vaccine | Standard care (parallel control group) | Significant positive effect |
| Nymberg et al.94 (Sweden) | Medication review | Controlled trial (non-randomised); follow-up of RCT with control group members able to receive intervention | 75% of participants were nursing home residents | Care homes: not reported. Individuals: 369 (182 intervention, 187 control; 139 and 140, respectively, were nursing home residents) | Standard care (parallel control group); compared randomised intervention and control groups | No effect: significant at 12 months if control patients who received MRI were excluded |
| Mor et al.95 (USA) | SARS-CoV-2 vaccination | Controlled trial (non-randomised) | Nursing home | Care homes; 280 nursing homes in 21 states | Standard care (parallel control group) | Significant positive effect |
| Niznik et al.91 (USA) | Deprescribing | Cohort study | Nursing home | Not reported | Standard care (parallel control group); compares residents with and without evidence of deprescribing | Significant positive effect: reduced likelihood of hospitalisation due to falls or fractures |
| Pop-Vicas et al.94 (USA) | Influenza vaccination | Retrospective cohort | Nursing home | Care homes: across 122 cities under influenza surveillance. Individuals: not applicable | Compares seasons with high and low match between circulating strains and vaccines | Significant positive effect |
| Sluggett et al.100 (Australia) | Medication review | Cluster RCT | Nursing home | Care homes: 8 South Australian residential homes: 99 residents participated in the intervention arm and 143 in the comparison arm | Standard care (parallel control group) | No effect: no significant differences in the rate of falls, hospitalisations, or mortality were observed between the 2 study arms at follow-up in both the unadjusted and adjusted analyses |
Turning to prevention of common infections, large RCTs in the USA reported that high-dose influenza vaccine is more effective than low-dose92 and adjuvanted vaccine more effective than non-adjuvanted93 for preventing hospital admission of care home residents. A further retrospective cohort study of influenza vaccination reported that a 50-percentage-point increase in the A/H3N2 match rate (from < 25% to > 75%) reduced long-stay nursing home resident deaths by 2.0% and pneumonia/influenza hospitalisations by 4.2%. 94 For SARS-CoV-2 vaccination, a trial of earlier compared with later vaccination found that facilities with earlier vaccination had fewer hospitalisations and deaths over the short-term (five to eight weeks) than those vaccinated later. 95 These trials support the effectiveness of vaccination policies but as would be expected none had a control group without vaccination. A study of oseltamivir prophylaxis of influenza compared hospitalisation rates in homes with prophylaxis for all residents (3.6%), directly exposed residents (7.8%) and no prophylaxis (16.1%). 96 The study involved only three care homes, numbers of residents were small and there was no statistical analysis, making the findings difficult to interpret.
Applicability
Applicability data were extracted from seven of the studies (not tabulated). Issues that could potentially affect applicability of individual study findings to UK settings were possible differences in influenza strains and vaccination rates of care home staff (USA vs. UK);92 Medicare coverage (USA vs. UK);93 mixed population and well established and funded programme of medication review (Sweden vs. UK);97 and reliance on a single vaccine provider (USA vs. UK). 95
Paramedic assessment/non-conveyance
Only one included study dealt with paramedic assessment and decision-making when there is uncertainty about taking a care home resident to hospital or treating them in situ. 101 This qualitative focus group study involved 18 German paramedics. Participants perceived that hospital transfers were potentially avoidable in some cases of urinary catheter complications, infections and falls. Uncertainties about legal liability were seen as a key factor favouring transfer of residents to hospital. Although not a UK study, the findings may be applicable to UK paramedics and could inform implementation of specialist paramedic services and training for paramedics attending care homes. See also the qualitative study of decision-making at the end of life by Murphy-Jones et al. 102 described below (see Palliative/end-of-life care).
Emergency department interventions
ED interventions were defined as interventions which were initiated in the ED or conducted by ED staff. Two studies met this definition (see Table 22) and were both conducted in Australia. 70,103 Both studies are before and after studies conducted at single regional EDs which receive admissions from multiple care homes within their catchment area. One study included 5991 and the other study included 1271 ED attendances in analysis. Marsden et al. 103 included no control group and was rated as higher risk of bias than Hullick et al. ,70 which included control care homes which did not receive the intervention; however, allocation was not randomised.
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Hullick et al.70 | Controlled before–after | Nursing home | 13 (5 intervention, 8 control) care homes; 1271 ED attendances | Standard care | Hospital admissions and ED visits | No significant difference in hospital admission or ED visits after the introduction of telehealth |
| Marsden et al.103 | Uncontrolled before–after study | Unclear | 5991 ED presentations from care homes over the study period (pre-GEDI 1209; interim GEDI 3324; and post-GEDI 1458) | Standard care | Hospital admissions | When controlling for all other variables, the hazard ratio for discharge for those patients presenting in the post intervention period was 1.15 (95% CI 1.05 to 1.26), indicating a significant reduction in hospital admission in the post-intervention period |
Marsden et al. 103 present a nurse-led multidisciplinary intervention delivered in the ED who receive referrals from care homes and expedite geriatric assessment and other clinical management in the ED. When controlling for all other variables, the hazard ratio for discharge for those patients presenting in the post intervention period was 1.15 (95% CI 1.05 to 1.26), indicating a significant reduction in hospital admission in the post-intervention period. When controlling for all other variables the hazard ratio for reduced length of hospital stay for those patients presenting in the intervention period was 1.49 (95% CI 1.24 to 1.78) and 1.44 (95% CI 1.30 to 1.60) for the interim intervention period. Hullick et al. 70 evaluated a video telehealth consultation with hospital ED staff in addition to an existing QI programme aimed at reducing ED attendances from care homes. Fourteen months’ pre- and post-intervention data were analysed. There was no significant difference in hospital admission or ED visits after the introduction of telehealth.
The evidence is low quality from single centres outside the UK setting. Therefore, we are unable to recommend use of either intervention. That said, models of geriatric assessment in the ED like that described by Marsden et al. are used in some centres in the UK as part of a frailty service104,105 and both the clinical and cost effectiveness require evaluation.
Advance care planning
Promoting ACP was part of most QI interventions included in the review. This section includes studies of ‘stand-alone’ interventions to encourage ACP.
UK evidence
We included four UK studies of ACP interventions (see Table 23). A mixed-methods study106 and a service evaluation107 evaluated effects on outcomes. A further mixed-methods study108 and a qualitative study109 explored feasibility and acceptability to care home staff.
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Alcorn et al.108 | Mixed methods; case review of notes of care home residents who died in hospital plus interviews | Care homes with either on site nurses or district nurses – medical care provided by GPs | Care homes: 2 teaching hospitals serving 89 care homes were eligible and residents identified were from 61 of these care homes. Individuals: 109 residents who died over a 6-month period. Interviews with 26 staff from 14 care homes discussing 26 of the 109 patients | None | Advanced care planning preferences for patients who eventually died in hospital. | Not applicable |
| Amador et al.106 | Mixed methods: costed health and social care services used by residents, including medication and accommodation in phase one. In phase two worked with care homes in which some of these residents lived and undertook an intervention. Compared total cost and cost components for residents whose care homes had participated in the intervention | Residential home | Care homes: 6 care homes for older people, offering personal care and specialist support in dementia care without onsite nursing care and representing a range of demographic characteristics | Standard care (before/after); Wilcoxon matched pairs sign-rank tests were conducted to compare total cost and cost components during phases 1 and 2 for those residents who participated in both | Emergency admissions; length of hospital stay; feasibility of intervention; qualitative evidence; costs/cost-effectiveness; cost reduction related to reduced health service use, both community and hospital | No effect |
| Garden et al.107 | Service evaluation | Residential home | Care homes: 7 care homes in Boston. Individuals: 283 places registered for care of people with dementia | Standard care (before–after); data were collected from the local hospital information department for the calendar years before and after introduction of the service | All admissions; feasibility of intervention; costs/cost-effectiveness; other (specify); place of death; staff confidence following training; carer satisfaction with how care planning was conducted | Significant positive effect: first-year admissions fell by 37% from baseline and in second and third years they fell by 55%. 102 care plans in place by April 2013. Of the residents who died during follow-up 67/68 died in their preferred place. Significant improvements in staff confidence following training. 64 carers completed a questionnaire on their satisfaction with ACP; 92% of the 64 carers rated the service > 9/10 |
| Harrad-Hyde et al.109 | Qualitative | Nursing homes; residential homes | Care homes: 6 care homes (3 nursing, 2 residential and 1 dual registered). Individuals: 30 (7 managers, 3 deputy managers, 7 registered nurses, 7 senior carers and 6 carers) | Not applicable | Acceptability to care home staff | Not applicable |
The interventions comprised an ‘appreciative enquiry’ intervention designed to improve end-of-life care for residents with dementia106 and a service combining training for staff with ACP for residents with dementia107 (details not shown). Both studies were at high risk of bias because of weak study designs. Both studies included residents with dementia, so their relevance to general care home populations is uncertain. The study by Amador et al. 106 focused on residential care homes without on-site nursing.
Amador et al. 106 reported cost reductions related to reduced health service use following the intervention but the effect on admissions was unclear. 106 By contrast, the service evaluation found that admissions fell by 37% from baseline in the first year and 55% in the second and third years. 107 This limited body of evidence meets our criteria for ‘inconsistent’ evidence. Overall, the evidence for promotion of ACP suggests that it is best undertaken as part of a clearly specified QI programme.
Alcorn et al. 108 examined 109 cases of care home residents who died in hospital and reported that ACP regarding hospital admission was recorded in 44% of cases. Barriers to care home staff looking after dying residents were uncertain trajectories of decline, acute events, challenges of ACP, relationship with family and lack of external support. 108 The qualitative interview study by Harrad-Hyde et al. 109 identified some similar issues. Care home staff favoured ACP in principle but were concerned about possible repercussions, especially when residents’ families wanted them to be taken to hospital. A key finding was that hospital transfers are more likely to occur if plans are not specific enough for care home staff to interpret them confidently. 109
Implementation
Implementation data were extracted for the two intervention studies (see Table 24). These studies reported relatively few barriers to implementation, possibly reflecting their early publication dates.
| Reference | Barriers | Facilitators | Active facilitation |
|---|---|---|---|
| Amador et al.106 | 2 homes from phase 1 of the study declined to take part in phase 2 | Availability of standard cost data and data on service use and characteristics of residents; participating care homes had favourable Care Quality Commission inspection reports | Co-design approach to intervention development facilitated by research team |
| Garden et al.107 | Not reported | Initial funding, leadership and implementation; empowerment of care home staff, families and doctors by affirming knowledge and using care planning to manage the uncertain end-of-life trajectories of people with dementia. This service was implemented in an urban setting where proximity between care homes and acute hospital may favour high admission rates | Nurse seconded to implement service, support of consultant liaison psychiatrist |
International evidence
International evidence around ACP comprised 12 studies (see Table 25): 6 from the USA, 1 from Australia and the remainder from other countries (including 1 multinational study). 115
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Adekpedjou et al.110 (Canada) | Retrospective cohort | Unclear or NA; described as ‘long-term care homes’ | Care homes: not reported. Individuals: 123,003 | Standard care (parallel control group); compares people with and without ‘do not resuscitate’ or ‘do not hospitalise’ orders | All admissions | Significant positive effect; both types of order were associated with decreased odds of hospitalisation but ‘do not hospitalise’orders were often ignored |
| Cohen et al.111 (USA) | Qualitative; semistructured interviews of nursing home staff | Nursing home | Care homes: 8 facilities, 4 with high hospitalisation rates, 4 with low hospitalisation rates. Individuals: 31 interviews | Standard care (parallel control group); this was not an intervention study but 2 groups were compared: those with high hospitalisation rates and those with low hospitalisation rates | All admissions; acceptability to care home staff; acceptability to residents/families | Not applicable |
| Galambos et al.112 (USA) | Service evaluation | Nursing home | Care homes: 16 nursing homes. Individuals: (2013) 1876 records reviewed acted as comparator, (2014) 1711 records reviewed, (2015) 1730 records reviewed, (2016) 1544 records reviewed | Standard care (before–after); baseline data from 2013 used for comparison | Unplanned/preventable admissions; all admissions; transport to ED; other (specify); number of advance directives in medical records of MOQI participants – through annual AD record/chart inventory | Significant positive effect: residents who did not have an AD were 29% more likely to be transferred. Using a logistic mixed model, results indicated statistical significance (p < 0.001) for increased AD documentation |
| Hendriks et al.113 (the Netherlands) | Prospective cohort | Nursing home | Care homes: 28 facilities in the Netherlands. Individuals: 372 newly admitted nursing home residents with dementia | None | All admissions; other (specify); treatment goals, do-not-treat (resuscitate/hospitalise) orders | No effect: study could not determine causation |
| Hickman et al.114 (USA) | Observational cohort study (part of larger OPTIMISTIC programme) | Nursing home | Care homes: 19 urban and suburban nursing facilities in Indiana. Individuals: 1482 residents | Standard care (parallel control group); outcomes compared for residents with (1) physician orders for scope of treatment comfort measures or do not hospitalise orders; (2) ACP orders with no hospitalisation limit (e.g. code status only); and (3) no ACP | Unplanned/preventable admissions; all admissions | No effect: no significant difference after adjusting for age, functional status and cognitive functioning |
| Honinx et al.115 (multinational) | Cross-sectional survey | Nursing home | Care homes: 322 nursing homes. Individuals: 1707 deceased residents | None | All admissions; other (specify); place of death | Not applicable |
| Houttekier et al.116 (Belgium) | Cross-sectional survey | Nursing homer | Care homes: 69 nursing homes in Flanders. Individuals: 198 deceased residents | None | All admissions | Not applicable |
| Martin et al.117 (Australia) | Cluster RCT | Nursing home; RACF is the term used to refer to permanent nursing care homes providing care to those no longer able to live independently in Australia | Care homes: 45 homes approached, 8 agreed to participate; 6 were placed into 3 clusters of 2 homes per cluster. Individuals: total potential study population was 445 residents, with 418 fitting inclusion criteria and 326 continuing to randomisation. In the 6 RACFs involved, the mean study participation rate was 78%. In total, at study commencement, there were 145 residents in the control group and 181 in the intervention group | Standard care (parallel control group) | Emergency admissions; transport to ED; length of hospital stay | Significant positive effect: intervention did not result in a statistically significant change at 6 months; however, at 12 months, it reached statistical significance with 40% reduction in ED visits and hospitalisations compared with controls, with an incident rate ratio 0.63 (95% CI 0.41 to 0.99; p = 0.044). Mortality rates show increased likelihood of dying in the RACF, with statistical significance at 6 months at a relative risk ratio of 2.19 (95% CI 1.16 to 4.14; p = 0.016) |
| Moyo et al.118 (USA) | Cluster RCT | Nursing home | Care homes: 119 intervention and 241 control. Individuals: 923 intervention and 1925 control | Standard care (parallel control group) | All admissions; (1) hospital transfers in the last 90 days of life (admissions, ED visits without admission and observation stays); (2) 3 or more hospital transfers in the last 90 days of life; (3) late transition (defined as hospital transfer in the last 3 days of life or hospice admission in the last day before death); other (specify): outcome of ‘burdensome treatment use’ which defined as experiencing any of tube feeding, parenteral therapy (for medication delivery or hydration), admission to an intensive care unit, and invasive mechanical ventilation | Significant positive effect: receipt of 1 or more potentially burdensome treatments was less common in the intervention compared with the control arm (21.7% vs. 25.7%; p = ¼0.02); statistically significant reduction in the prevalence of 90-day hospital transfers among decedents with advanced illness (marginal proportion differences: 1.7%, 95% CI 3.2% to 0.1%) |
| Mullaney et al.119 (USA) | Mixed methods; a convergent mixed-method design. Quantitative data collected on the MRA scores as undertaken by nurse practitioners and patient outcomes. Qualitative approach to explore nurse practitioner perceptions of the impact of MRA on advanced care planning discussions and patient outcomes | Nursing home | Individuals: 187 individuals newly enrolled in Medicare; advantage across 3 states; 14 nurse practitioners from 80 invited across a sample from 2 of the 3 states in which the Medicare individuals were enrolled | None | All admissions | Significant positive effect: significant difference was found in relationship between the number of ACP discussions and the number of hospitalisations. The more ACP discussions that occurred the less likely a patient was to be admitted to hospital (p = 0.0025) |
| Nakashima et al.120 (USA) | Cross-sectional | Nursing home | Standard care (parallel control group); residents who did not have an advance directive (36%) | All admissions; hospital stays; transport to ED; ED visits | Significant positive effect: residents with DNH orders had significantly fewer hospital stays in the past 90 days than those without DNH orders (3.0% vs. 6.8%, p < 0.0001) and residents with DNH orders also had significantly fewer ED visits (2.8% vs. 3.6%, p = 0.03). Dementia residents with DNH orders had significantly fewer hospital stays than those without DNH orders (2.7% vs. 6.3%, p < 0.0001) but no difference in ED visits (2.8% vs. 3.5%, p = 0.11) | |
| Overbeek et al.121 (the Netherlands) | Cluster RCT | Nursing home; residential care homes including adults receiving home care; assisted living/extra care housing; residential care homes including adults receiving home care | Care homes: 16 residential homes and people receiving home care who lived near to the homes. Individuals: at study initiation, 97 in intervention group and 100 in control group; at follow-up, 77 in intervention group and 83 in control group | Standard care (parallel control group) | Other (specify); primary measure – patient activation measure (measures individual knowledge, skills and confidence to manage health and healthcare). Secondary outcome measures were quality of life, satisfaction with healthcare, documentation of care preferences in an AD, appointment of a surrogate decision-maker and use of medical care | No effect: no effect of ACP on use of hospital care, diagnostic procedures or a selection of medical interventions |
On closer examination, two of the US studies, although focused on ACP, were reporting results from named QI programmes (MOQI112 and OPTIMISTIC114) and are not discussed further in this section. Two studies involved ‘do not hospitalise’ (DNH) orders (see next paragraph). The remaining studies evaluated a video-assisted ACP intervention using a cluster RCT design118 and nurse practitioner-led ACP discussions using a mixed-methods design with no control group. 119 Both studies found a significant positive effect in terms of reduced hospitalisations and together constitute ‘weaker’ evidence of effect in the US setting.
Two further US-based studies dealt specifically with DNH orders. A quantitative cross-sectional study reported that residents with DNH orders were significantly less likely than those without to be transferred to hospital, although those with DNH orders only comprised 6% of the study sample. 120 However, a qualitative study of nursing home staff found that they do not tend to interpret DNH orders literally. Rather, DNH orders were seen as ‘a signal that hospitalisation should be questioned and discussed with the family when an acute event occurred’. 111
Settings outside the USA provided ‘inconsistent’ evidence for the effect of interventions to promote ACP on residents’ hospital admissions at the end of life. A cluster RCT of the ‘goals of patient care’ process in Australia reported a 40% reduction in hospitalisations compared with control after 12 months. 117 In Europe, cross-sectional data from six countries indicated that residents without an advance directive were more likely to be hospitalised in the last month of life. Absence of conversation about ACP increased the risk of dying in hospital. 115
Three further studies of DNH orders from Canada,110 the Netherlands113 and Belgium116 complemented evidence from the United Statea that these orders reduce but by no means eliminate hospitalisations. The study from Belgium (a cross-sectional survey) reported that residents with dementia without a DNH ‘general physician order’ were more likely to be hospitalised. 116
Considering the international evidence as a whole, there appears to be ‘stronger’ evidence that DNH orders are not fully effective for reducing hospital admissions at the end of life. Evidence for interventions promoting discussion of ACP is ‘inconsistent’.
Applicability
Applicability of findings about ACP from international settings to UK practice needs to take into account legal and cultural differences with regard to end-of-life care. The relevance of DNH (as distinct from ‘do not resuscitate’) orders to UK practice is uncertain.
Palliative/end-of-life care
UK evidence
Three UK studies evaluated palliative care interventions (see Table 26). Authors reported that the palliative care programmes described resulted in avoided admissions at the end of life and/or a reduction in deaths in hospital. However, statistical significance was unclear for two of the studies. All the studies had methodological weaknesses and constitute borderline ‘very limited’ or ‘weaker’ evidence.
| Reference | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Kinley et al.122 | Service evaluation | Residential home | Care homes: 2011–12, 4 homes (baseline?); 2012–13, 16 homes; 2013–14, 28 homes; 2014–15, 23 homes. Individuals: number of deaths 2011–12, 18; 2012–13, 68; 2013–14 136; 2014–15, 115 | Standard care (before–after); audit data were collected from the records of all deceased residents 1 year prior to start of programme and then continuing every month | Feasibility of intervention; other (specify); number of deaths in care home; number of residents with a document ACP; numbers of residents with a DNACPR form | Significant positive effect: audit of 4 years of programme, showed an increase of the number of deaths in the care homes from 44% (8/18) in 2011–12 in 4 care homes to 64% (74/115) in 2014–15 in 23 residential care homes |
| Smith et al.123 | Uncontrolled before/after; 1-year pilot study | Nursing home | Care homes: 3 nursing homes in North Brent. Individuals: not reported | Standard care (before–after) | Other (specify); deaths in hospital (admissions not explicitly reported) | Not reported; 25% reduction in hospital deaths for 2015–16 vs. 2014–15 |
| Springett et al.124 | Service evaluation | Nursing home; residential home | Care homes: 11 (6 nursing, 5 residential). Individuals: not reported | None | Unplanned/preventable admissions; prticipating care homes reported 95 admissions and 30 avoided admissions over 1 year | Not reported; magnitude/significance of effect unclear |
An additional qualitative study102 analysed data from semistructured interviews with six paramedics relating to decision-making about taking residents nearing the end of life to hospital. Tensions between the perceived best interests of residents and those of others resulted in contrasting approaches by paramedics.
International evidence
We included five palliative care studies from Australia, of which four publications evaluated nurse-led palliative care needs rounds (including one focused on feasibility127). The fifth study evaluated a similar nurse-led palliative care consultative service. 128 The studies that reported on effectiveness produced ‘inconsistent’ evidence overall (see Table 27).
| Reference | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Chapman et al.125 | Controlled trial (non-randomised) | Nursing home; nursing home care mentioned in abstract | Care homes: 4 care homes. Individuals: 104 intervention, 173 historical controls | Standard care (parallel control group) | All admissions; length of hospital stay; costs/cost-effectiveness | No effect; significant reduction in length of stay |
| Forbat et al.126 | Step-wedge RCT | Nursing home; nursing aides are most of the staff in care homes in Australia with a small number of registered nurses | Care homes: 12 care homes. Individuals: 1700 residents | Standard care (parallel control group); stepped-wedge RCT: intervention commenced with 2 sites with other sites crossing over from control bimonthly in clusters of 2–3 sites. Trial finished 6 months after final site started receiving intervention. Control condition involved usual care, which consisted of the specialist palliative care clinicians providing ad hoc reactive clinical consultations when referred by facility staff | All admissions; overall number of admissions; length of hospital stay; length of staff calculated for those residents who were hospitalised for longer than 24 hours; costs/cost-effectiveness; cost of admissions | Significant positive effect: significantly reduced length of stay in hospital; clinically significant reduction in the number of hospitalisations; reduced admissions led to annual net cost-saving |
| Koerner et al.127 | Qualitative; interviews embedded in a larger RCT | Residential home; care home | Care homes: 11 care homes. Individuals: 21 staff members | Not applicable | Feasibility of intervention Acceptability to care home staff |
Not applicable |
| Mitchell et al.128 | Mixed methods | Unclear or not available; level of nursing care not explicitly stated | Care homes: 3 facilities in Queensland, Australia. Individuals: facilities cared for 277 residents, with 24 deaths in the pre-intervention period and 44 during the intervention | Standard care (before–after); 12 months before and after intervention for quantitative outcomes | All admissions; acceptability to care home staff; acceptability to residents/families; other (specify); qualitative data on improvements in palliative care | Significant positive effect: hospital transfers decreased between pre-and post-intervention periods |
| Rainsford et al.129 | Controlled trial (non-randomised) | Residential home; RACF | Care homes: 2 RACFs with a total of 112 beds. Individuals: all residents who died between April 2018 and March 2019 were included in the intervention group (43). There was a subgroup of decedents who were discussed in needs rounds (17/43). Control cohort consisted of all residents who died during the 3-year period prior to the introduction of needs rounds (113) | Standard care (before–after) | Unplanned/preventable admissions; emergency admissions; transport to ED | No effect; no statistical differences in overall number of ED presentations, hospital admissions or length of hospital stay |
Six publications from the USA, of which three came from the same group, evaluated palliative care teams, hospice enrolment and integration of palliative care with infection management (see Table 28). The majority of studies reported a positive effect for palliative care consultations (borderline ‘stronger’/‘weaker’ evidence) while evidence for the other interventions was ‘very limited’ (one study each).
| Study ID | Study type | Type of care home | Sample size | Comparator | Outcomes | Intervention effect |
|---|---|---|---|---|---|---|
| Harrison et al.130 | Other (specify); cross-sectional observational study | Nursing home | Care homes: 838 nursing homes providing complete data. Individuals: 143,223, including 42,761 with advanced dementia, CHF or COPD | None | All admissions; also admissions due to infection | Significant positive effect: significant association between integration and all-cause or infection-related admission for some groups |
| Miller et al.131 | Other (specify): observational cohort | Nursing home | Care homes: 286 nursing homes in 24 counties. Individuals: not reported | Standard care (parallel control group); compared nursing homes with and without palliative care consultations over 10 years (2000–10) | All admissions; admissions in the last 30 days of life; other (specify); hospital death rates | Significant positive effect: reduction in end-of-life hospitalisations |
| Miller et al.132 | Retrospective cohort study | Nursing home | Care homes: 46 nursing homes in 2 US states. Individuals: 1651 (477 consultation recipients, 1174 controls) | Standard care (parallel control group); residents without consultation matched by propensity scoring | All admissions; admissions in last 7, 30 and 60 days of life; transport to ED; ED visits in last 30 and 60 days of life; other (specify); other ‘potentially burdensome care transitions’ | Significant positive effect; residents with consultations had lower hospitalisation rates |
| Miller et al.133 | Cohort with matched controls | Nursing home | Care homes: 31 NHs in 2 US states; Individuals: unclear | Standard care (parallel control group); matched control group without consultation | All admissions; hospitalisation and acute care use 7 and 30 days before death; other (specify): potentially burdensome transitions of care | Significant positive effect: rduction in hospitalisations and burdensome transitions |
| Temkin-Greener et al.134 | Multi-armed RCT; 2-armed controlled trial with a third nonrandomised group to assess placebo effect of the RCT | Nursing home | Care homes; treatment nursing homes 14; control nursing homes 11; nonrandomised ‘facilities’ 609 | Standard care (parallel control group) plus a nonrandomised control group | All admissions; number of hospitalisations | No effect; overall, no statistically significant effect of the intervention |
| Zheng et al.135 | Controlled before–after | Nursing home | Care homes: 14,030 nursing homes. Individuals: 747,641 individuals included in modelling – 505,851 in nonhospice group and 241,790 in hospice group | Standard care (parallel control group) | All admissions; other (specify): staff competencies | Significant positive effect |
Finally, studies on an integrated palliative care programme involving telemedicine (Singapore);136 a multicomponent palliative care programme comprising staff education and organisational support (seven European countries);137 and a palliative care training programme for care home staff (Finland)138 all reported no significant effect of the intervention.
Other interventions
A single study from the USA evaluated a decision aid in a mixed-methods RCT. 139 Residents and families rated the decision aid as very helpful but it did not decrease hospital transfers compared with the control group. Installation of ‘compliant flooring’ to reduce fall-related injuries and hospitalisations also had no effect in a randomised trial conducted in Canada. 140
The Veterans’ Administration Medical Foster Home Programme is discussed below.
Interventions applied in assisted living and similar settings
Only one study reported on an intervention to reduce unplanned admissions in residents in assisted living settings. In a US cluster RCT, ‘function-focused care’ was shown to be safe but there was no treatment effect on ED or hospital transfers. 87
The Veterans’ Administration Medical Foster Home programme involves people receiving nursing-home-level care in small units owned by the primary care provider with medical support from Veterans’ Administration staff. Two publications from the same group reported reductions in potentially preventable admissions following enrolment in the programme. 141,142
Chapter 4 Economic evidence
A total of 28 included studies reported costs or ‘cost-effectiveness’ (broadly defined) as an outcome measure: 5 for QI programmes, 11 for integrated working, 2 for training/workforce development, 4 for management of specific problems, 2 for ACP, 3 for palliative care and 1 for other interventions. Most of these studies were not designed as full economic evaluations, meaning that not all relevant costs and benefits may have been taken into account.
UK economic evidence
Table 29 summarises UK studies reporting economic outcomes. The majority of studies reported cost savings but weak study designs and limited reporting mean that the findings should be treated with great caution. One report extrapolated findings from one area across the whole of England to estimate possible cost savings. 56 Some reports were produced by manufacturers56 or professional bodies55 with a potential conflict of interest. One report indicated that the intervention increased costs in the first two years,52 probably reflecting the introduction of new ways of working. The programme would require reductions in costs (preferably from reduced hospital admissions) to be sustainable without additional funding.
| Reference | Type of intervention | Main findings | Comments |
|---|---|---|---|
| Steel et al.21 | QI programme | Admission costs fell from £55,678 pre intervention to £49,653 post intervention | Data for 1 care home; no comparator |
| Holder et al.57 | Integrated working (telemedicine) | Incremental difference in costs found in evaluation between telemedicine and control group were £1.2 million with a return on investment of £6.74 per £1 spent by the clinical commissioning group | Airedale NHS Foundation Trust |
| Royal Pharmaceutical Society55 | Integrated working (MDT) | Net annualised savings of £184 per person could be achieved by medication review and, for every £1 invested in intervention, £2.38 could be released from medicines budget | Comparison unclear |
| Sherlaw-Johnson et al.51 | Integrated working (dedicated primary care service) | Marginal reduction in commissioners’ costs associated with emergency admissions was £1032 (95 % CI £30 to £1673) | |
| SQW Ltd52 | Integrated working (Sutton Homes of Care) | Vanguard saved £466,282 in 2016/17 but spent £1.05 million in same period. Report notes that achievement of net savings will depend on maintaining or continuing to reduce activity levels such as nonelective admissions without such high levels of programme funding | |
| Tunstall56 | Integrated working (telehealth and telecare) | Based on case studies, the report estimates that, if clinically led technology-enabled models in care homes were scaled up across NHS England, it would save approximately £1billion per annum and avoid over 226,000 emergency admissions and 2.5 million bed days | Extrapolated findings from local area initiatives with no comparator |
| Siddiqi et al.83 | Training in delirium prevention | Using data obtained directly from hospitals overall cost for intervention home residents was estimated at £3281 and in the control homes £7210 | Feasibility trial |
| Downs et al.88 Sampson et al.89 | Complex intervention to tackle specific problems | The incremental cost per quality-adjusted life year gained of BHiRCH-NH vs. TAU was £12, 633. Residents receiving the intervention accrued a nonsignificantly higher cost and a very small increase in quality-adjusted life years; the intervention has a 65% probability of being cost-effective at a WTP of £20, 000 | Pilot trial, full trial not recommended |
| McKee et al.90 | Medication review clinics | Total estimated drug cost savings for the project over 2-years were £213,000 | |
| Amador et al.106 | ACP for residents with dementia | Following intervention, total service costs fell by 43% and hospital care costs by 88% | |
| Garden et al.107 | ACP for residents with dementia | Estimated cumulative net savings over 3 years between £150,000 and £300,000 | No details of methodology reported |
The two most rigorous studies83,89 collected promising economic data but they were both feasibility trials and in one case the intervention proved impossible to implement, making a full trial unviable. 89
International economic evidence
Table 30 summarises the international evidence base. Economic evaluations are sensitive to differences in context between countries and changes in costs and currency fluctuations over time also need to be taken into account.
| Reference | Country | Type of intervention | Main findings | Comments |
|---|---|---|---|---|
| Carter et al.44 | Australia | QI programme | Intervention more effective and less costly than usual care | Cost-effectiveness data from cohort study |
| Ingber et al.26 | USA | QI programme (data from 7 different states) | In 2015, average per resident Medicare expenditures were reduced by $60–2248 for all-cause hospitalisations and by $98–577 for potentially avoidable hospitalisations | |
| Rantz et al.33 | USA | QI programme (MOQI) | Programme improved outcomes while reducing costs | Uncontrolled before–after study |
| Rantz et al.34 | USA | QI programme (MOQI) | Savings to payers in participating nursing homes between 2015 and 19 were over $30 million | As above |
| Chan et al.66 | Australia | Integrated working | For every $1 spent, a saving of $5.50 was realised | Uncontrolled beforeafter study |
| Cordato et al.58 | Australia | Integrated working | Total costs were 50% lower in the intervention group, with lower total hospital inpatient and total ED costs | Data from small RCT |
| Craswell et al.60 | Australia | Integrated working (REAP) | Lower costs for residents transferred to hospital | Data from controlled trial |
| Fan et al.67 | Australia | Integrated working (HiNH) | 95% certainty that the values of net costs would fall within the range from −AU$15,018,055 to −AU$3,358,820. | Cost study suggesting substantial savings |
| Grabowski et al.73 | USA | Integrated working (telemedicine) | Average savings to Medicare for a nursing home that was more engaged with telemedicine was estimated at $151,000 per nursing home per year, relative to the less-engaged facilities. Annual cost of telemedicine service was $30,000 per nursing home, implying net savings of roughly $120,000 per nursing home per year in the more-engaged facilities | Covers selected nursing homes rather than whole sample |
| Kwa et al.72 | Australia | Integrated working (residential in-reach) | ED cost and inpatient admission costs were each lower in the period following changes to care model | Uncontrolled before–after study |
| Chapman et al.125 | Australia | Palliative care (needs rounds) | Cost savings associated with shorter admissions | Controlled (quasi-experimental) study |
| Forbat et al.126 | Australia | Palliative care (needs rounds) | Across 12 care homes, a conservative estimate of annual net cost-saving from reduced admissions was AU$1,759,011 (US$1.3 m; UK£0.98 m). | Stepped wedge RCT |
| Lamppu et al.138 | Finland | Palliative care (training) | Total hospital costs were similar in the intervention and control groups. | Data from cluster RCT |
| Pracht et al.142 | USA | VA Medical Foster Home Programme | Costs associated with avoidable admissions fell by 39% over 180 days following enrolment in the programme | Uncontrolled before–after study |
As with the UK studies, most of the international studies reported cost savings associated with the study intervention, including QI programmes, various types of integrated working, palliative care and the Veterans’ Administration Medical Foster Home Programme. Most of the studies were primarily designed to evaluate effectiveness and many had methodological flaws such as absence of a control group. For this reason, risk of bias assessment using a tool designed for economic evaluations was not attempted. It should be noted, however, that the more rigorously designed studies, such as the cost analysis of the Queensland HiNH programme,67 produced estimates of large cost savings similar to those derived from smaller or uncontrolled studies.
Chapter 5 Discussion and conclusions
This review had broad inclusion criteria and covered interventions ranging from improved access to primary care through to palliative care for residents nearing the end of life. We discuss the findings in relation to the specified review questions. Overall strength of evidence for UK and international studies is summarised in Tables 31 and 32.
| Type of intervention | Relevant studies | Strength of evidence | Comments |
|---|---|---|---|
| QI programmes | Damery et al.,19 Giebel et al.,20,a Steel et al.21,a | Inconsistent | Evidence strengthened by significant QI elements in most integrated working interventions (next row) |
| Integrated working | Brine et al.,46,a Conti et al.,47/SQW Ltd,52 Lloyd et al.,49,a Lloyd et al.,48,a Morciano et al.,50,a Sherlaw-Johnson et al.,51,a Vestesson et al.53,a | Stronger | |
| Training/workforce development | Armstrong,82 Sheaff et al.,84 Siddiqi et al.,83 SQW52 | No evidence of effect | |
| Management of specific problems | Downs et al.88/Sampson et al.,89 McKee et al.90,a | Inconsistent | Inclusion of Siddiqi et al. here rather than row above makes no difference |
| ACP | Amador et al.,106 Garden et al.107,a | Inconsistent | |
| Palliative/end-of-life care | Kinley et al.,122,a Smith et al.,123 Springett et al.124 | Very limited | Significance of effect unclear for Smith et al. and Springett et al. |
| Type of intervention | Relevant studies | Strength of evidence | Comments |
|---|---|---|---|
| QI programmes | United States: Blackburn et al.,22,a Ingber et al.,26,a Kane et al.,27 Rantz et al.,32,a Vadnais et al.36,a | Stronger, inconsistent Stronger, borderline stronger, inconsistent |
Evidence weakened by duplication of data between reports Statistical significance unclear for some studies |
| New Zealand: Boyd et al.,40 Connolly et al.,41 Connolly et al.42,a | |||
| Integrated working | Australia: Chan et al.,66,a Cordato et al.,58,a Craswell et al.,60,a Dai et al.,62,a Fan et al.,63,a Haines et al.,59,a Hullick et al.,68,a Hullick et al.,69,a Hullick et al.,70 Hutchinson et al.,71,a Kwa et al.72,a | ||
| USA: Brickman et al.,75,a Grabowski et al.,73,a Hofmeyer et al.,74 Stadler et al.76,a | |||
| Other countries: Kobewka et al.79 (Canada); Kumpel et al.80 (Germany); Pedersen et al.,77,78,a Weatherall et al.81 (Denmark) | |||
| Training/workforce development | McGregor et al.85,a (Canada); Resnick et al.87 (USA), Romoren et al.86,a (Norway) | Inconsistent | |
| Management of specific problems | Medicine review: Frankenthal et al.98 (Israel); Junius-Walker et al.99 (Germany); Nymberg et al.97 (Sweden); Niznik et al.91,a (USA); Sluggett et al.100 (Australia) | Inconsistent, stronger | |
| Infection prevention: Gorisek et al.96 (Slovenia); Gravenstein et al.92,a McConeghy et al.,93,a Mor et al.,95,a Pop-Vicas et al.94,a (USA) | |||
| ED interventions | Hullick et al.70 (Australia); Marsden et al.103,a (New Zealand) | Inconsistent | |
| ACP | Martin et al.117,a (Australia); Houttekier et al.116 (Belgium); Adekpedjou et al.110,a (Canada); Honinx et al.115 (multinational); Hendriks et al.,113 Overbeek et al.,121 (the Netherlands); Cohen et al.,111 Galambos et al.,112,a Hickman et al.,114 Moyo et al.118,a Mullaney et al.119,a Nakashima et al.120,a (USA) | Inconsistent | |
| Palliative/end-of-life care | Australia: Chapman et al.,125 Forbat et al.,126,a Koerner et al.,127 Mitchell et al.,128,a Rainsford et al.129 | Inconsistent, stronger | |
| United States: Harrison et al.,130,a Miller et al.,131–133,a Temkin-Greener et al.,134 Zheng et al.135,a |
Interventions in use in the UK
That the quantity of the evidence was lower for the UK compared with other countries combined is to be expected, given that the UK is only one country, but it covered almost all the intervention categories in our taxonomy.
A particular focus in the UK literature has been on links with primary care and community services through the care home vanguards programme, which has subsequently provided the basis for EHCH. The vanguards, and subsequently EHCH, combined elements of integrated working with QI and locally important elements. The vanguards programme involved substantial support being given to the localities selected as pilot sites, something that has not been continued at the same level for national roll-out of EHCH, raising questions about how easy it might be to embed and sustain such programmes longer term. Early research has outlined the considerations during implementation that enable care home interventions to embed and sustain, but this has been based upon a small number of studies, largely focussed around QI. 143 There is much potential for researchers and practitioners to both test these processes and learn from successes and failures during national roll-out of EHCH.
Other interventions used in the UK included local QI and training programmes, initiatives to tackle specific problems such as delirium and inappropriate prescribing, or to introduce components of ACP and palliative/end-of-life care. Quantitative studies of paramedic-led interventions were lacking, although qualitative research highlighted the complexities and tensions involved in decision-making. These findings reinforce long-standing findings about the difficulty of negotiating care during acute crises in care homes due to uncertain organisational boundaries, roles and responsibilities when residents’ health deteriorates. 144,145 A decade after these findings first appeared, work is needed to better standardise operating procedures between care homes and ambulance providers during medical crises.
UK care home research is in its infancy,144,145 but research considering those receiving social care in other settings, for example assisted living (with more limited services available on site), is even less well developed. It was to a certain extent unsurprising that we found a paucity of publications around such settings.
International interventions
The range of interventions used in other high-income countries was broadly similar to that seen in the UK. The US Medicare system has evaluated a range of QI programmes with memorable acronyms such as INTERACT and OPTIMISTIC. New Zealand is also a source of important studies of QI interventions.
An important group of studies from Australia evaluated responsive services provided to groups of care homes by hospital-based MDTs, often with an emergency medicine background. Details of the service models varied (e.g. in-reach, outreach, HiNH) but studies suggested substantial reductions in unplanned admissions and other outcomes, albeit sometimes with weak study designs. Such models are not standard in the UK. Hospital at Home in the UK mirrors some of the approaches undertaken in Australia. Care homes were excluded from the largest RCT of Hospital at Home in the UK,146 but are supported by some local Hospital at Home services. 147 Urgent Community Response, which describes short-duration intensive healthcare support in the community for older people who have experienced acute deterioration and which is part of the NHS England Ageing Well programme, also excludes care home residents from its core specification. 148 The national roll-out in England of Hospital at Home as part of the Frailty Virtual Wards initiative, alongside Urgent Community Response, provides an opportunity to evaluate the applicability of approaches evidenced to work in Australia in the UK setting. This would, though, require care home residents to be included and for focused evaluation around these questions.
Telehealth interventions have been evaluated in the USA and other settings (including to a small extent in the UK) with mixed results. There is a fairly substantial international evidence base evaluating ACP and palliative care interventions, although results have been inconsistent (see Table 32). The considerations when implementing telehealth in care home settings have been well described, although there remain specific challenges around implementing video consultations for residents with cognitive or sensory impairment and further research is required to better understand the role of telehealth in such groups. 149
We found only one study based in an assisted living setting (in the USA). The Veterans’ Administration Medical Foster Home model is another evaluated intervention with no apparent equivalent in the UK.
Effectiveness of interventions
We graded evidence for effectiveness according to a relatively simple scheme. Much of the evidence was graded as ‘weaker’ because of a shortage of controlled studies or ‘inconsistent’. Interventions with ‘stronger’ evidence included improved links with primary/community care and QI programmes with staff attached to care homes. Diversity of outcome measures and heterogeneity of interventions precluded meta-analysis but claimed reductions (against control or baseline) were often of the order of 30–50%, which would imply significant reductions in resource use. Groupings presented in our tables are not the only ones and readers can form their own assessment (but note that single studies always constitute ‘very limited’ evidence).
Implementation in UK
The barriers to implementation of healthcare interventions in care homes are well described. and include staff shortages, high staff turnover and care homes changing ownership or going out of business. Problems affecting service delivery in care homes affect the wider urgent/emergency care system and vice versa. A recurrent theme, throughout the literature, both prior to and during the pandemic, is insufficient recognition or engagement with expertise held in and by the care home sector. Serial studies have shown a willingness and enthusiasm among care home staff to make healthcare better for their residents, but a tendency among NHS providers to engage with them late in service design, if at all, with services designed to give care home staff little latitude in how they are implemented at an individual care home level. 89,150–153
Facilitators to implementation were identified, including building on existing services/relationships and the role of committed leaders in both the care home and health sectors. Key within this will be empowerment of care home providers and staff to shape the design and implementation of care home healthcare interventions. Integrated care boards bring together local authorities and NHS commissioners and providers. Care home providers, though, are predominantly corporate or third sector and remain largely ‘outside the room’. There is promise that this may change with the appointment of a chief nurse for social care, who might better facilitate consultation with national care home provider organisations, but specific work is required to build relationships with care home providers and staff at a local and regional level. 154 The situation will not improve without investment in such relationships.
Applicability of international evidence
Much is made in the literature of the differences in service delivery between care home sectors internationally. This is important in the way that it influences: the core competencies of staff employed in care homes (for example through mandatory minimum training in the USA and Australia): the availability of in situ resident medical staff (e.g. elderly care physicians in the Netherlands); the role of medical staff in determining care home policies (for example through the medical director initiative in the USA) and the sense of care homes as being ‘inside’ the system (more common where care homes are publicly funded, as in Denmark or the Netherlands).
An important overarching consideration, however, is that the cohorts of residents living in care homes are very similar around the globe. 155 This was evidenced in the markedly similar way that COVID-19 affected care home residents internationally. 156 Long-term care systems are no more similar or different than healthcare systems. UK and US long-term care arguably have more in common than do acute hospital systems in the respective countries. It is therefore possible to transfer approaches between countries, so long as attention is paid to the differences and similarities between systems, and so long as new models from overseas are evaluated in parallel with implementation when introduced for the first time.
The FITAR tool proved useful for identifying a wide range of issues that could affect applicability of international evidence. Examples included mixtures of long-stay and short-stay residents in some nursing homes (USA), cultural attitudes to ACP/palliative care (USA/Europe), workforce regulations and roles of different grades (especially nurses; USA/Australia) and public ownership of care homes (Denmark). Extraction of data at the level of the country rather than the individual study would have saved time in the overall review process.
Economic evidence
We identified a relatively large amount of economic evidence for the UK but this was mostly of low quality. International evidence was included for completeness but there is a a need for particular caution in extrapolating from other countries or time periods. Costing social care interventions has long provided difficulties in the UK, as NHS and social care costs are collated differently and separately. 157 Additional challenges come from understanding how costs are transferred between health and social care commissioners and providers. 158 An intervention that saves the NHS money may ultimately generate cost, opportunity cost, or both for care home providers. Finally, quality of life measures have limited applicability in care home residents because of the prevalence of dementia in this setting, and this limits some types of health economic evaluation. 159 Substantial work is required to develop frameworks to better evaluate costs, and cost-effectiveness of interventions that straddle the interface between health and social care, and in care home research more generally.
Strengths and limitations
Strengths of the review include its broad coverage of UK and international evidence, a thorough search including grey literature and citation searching into 2022 and reference list checking and use of two independent reviewers for most standard review processes.
We extracted data on details of interventions, which is important for understanding complex interventions; the relevant tables may be a useful resource for designing new care models.
Coverage of the international literature was sufficient to answer our research question about possible candidate interventions that could be relevant to UK practice. We evaluated risk of bias for most included studies using design-specific tools. Statements about overall strength of evidence were informed by risk of bias assessment even where the key considerations are not explicitly stated.
Our findings were broadly similar to a review of specialist health-care services in care homes by Buck et al. published in 2021. 8 This review used a slightly different framework of interventions to ours but with many common elements. The study reported that interventions addressing residents’ general health needs, assessment and management services and non-training initiatives involving medical staff can reduce hospital admissions, while there was also promising evidence for services targeting residents at imminent risk of hospital admission or post-hospital discharge and training-only initiatives. There was evidence that end-of-life care services may enable residents to remain in the home at the end of life, but the high number of poor-quality studies (authors’ terminology) undermined confidence in this result. Buck et al. 8 used a ‘vote counting’ approach to evidence synthesis with binomial testing to assess statistical significance of the findings. This contrasts with our more qualitative approach to assessing strength of evidence by intervention and setting. Our assessment of implementation and applicability issues and our specific focus on unplanned admissions differentiates our approach from that of Buck et al. 8 Both reviews have relevance for supporting evidence-informed decision-making by service commissioners and providers.
The large number of records identified by our searches led us to prioritise items for screening by searching for relevant keywords. This is not uncommon and is allowed for in the latest version of the PRISMA flow diagram. We checked a random sample of unscreened records which confirmed that the risk of missing relevant items through this approach was likely to be low. We did not attempt any meta-analyses because of the heterogeneity of included studies for most types of intervention together with lack of availability of the required data and/or diversity of effect measures in some cases.
A further possible limitation was the framing of our analysis around a predefined taxonomy of interventions. This worked well in most cases but inevitably, there was an element of subjectivity in placement of a few studies. Our approach was to assign each study to one group but it would be possible to conduct a sensitivity analysis by adding or removing ‘marginal’ studies to identify any effects on the overall assessment of strength of evidence.
Our overall assessment was less comprehensive than that provided by Grading of Recommendations, Assessment, Development and Evaluation (GRADE) and similar systems. This reflects our decision to produce a broadly focused review and the recognition that much of the evidence either fell outside the domains of GRADE or would be heavily downgraded because of the use of nonrandomised study designs. It is also worth noting that qualitative evidence, while relevant to some aspects of the review, is not adequately assessed by either our system or GRADE.
Equity, diversity and inclusion
This section complements the discussion of review processes above (see Chapter 2). Diversity in care home populations is likely to be increasing in many countries in line with that of society as a whole, although research on this topic was outside the scope of our review. We cannot be certain how far the care homes, residents and staff in our included studies were representative of the wider care home population. However, there is evidence that care home residents worldwide are relatively similar at the population level (see Chapter 5). Equity and diversity issues affecting care homes may thus reflect those present in society as a whole and specifically in the health and care system.
Decision-making about admission of care home residents to hospital can raise issues of equity, although given our focus on implementing and evaluating interventions these were only touched on in our review. Family advocacy may influence the decision-making process (see Chapter 3). Residents with dementia represent a particularly vulnerable group whose needs require attention to support equitable treatment.
The health and social care workforce is disproportionately female and highly diverse in terms of characteristics such as ethnicity and socioeconomic status. Research involving care home staff should seek to ensure that all groups are appropriately represented, for example in qualitative studies and surveys. Our review included too small a sample of such studies to draw meaningful conclusions, but this could be an interesting topic for further research.
Implications for service delivery
We have identified the following implications for service delivery:
-
Opportunities to reduce unplanned admissions exist at all stages of residents’ care journeys from routine care to palliative care at end-of-life.
-
Types of intervention such as QI programmes or integrated working between care homes and primary care/community services differ in aspects such as workforce requirements, technology, intensity of the intervention etc. Services can consider adapting described interventions to their own context, including possibilities for simplification where evidence supports this.
-
Evidence suggests that care home managers and staff support proposed interventions that will help them to deliver better care for their residents. Early and genuine consultation to assess feasibility and acceptability of interventions could be a major factor in successfully implementing new service models.
-
Specific work is required to build relationships between NHS and care home providers and staff at a local and regional level.
-
There is some evidence to guide where changes to services are more likely to improve outcomes; for example, care homes without nursing may benefit more than those with nursing from some forms of support because of their lower baseline level of staffing and because of differences in case mix.
-
In attempting to transfer approaches between countries, attention should be paid to the differences and similarities between systems, and new models from overseas should be evaluated in parallel with implementation in the UK setting. Changes to how care is delivered to older people in the community, including Hospital at Home and Urgent Community Response, mirror some initiatives targeted at care homes overseas and could provide an opportunity to test and evaluate imported models of working if care homes are adopted within remit.
-
Work is needed to better understand and standardise operating procedures between care homes and ambulance providers seeking to negotiate care for residents during medical crises, particularly with regard to lines of responsibility and shared liability for decision making.
Implications for research
We have identified the following priorities for research:
-
Researchers should carefully consider what is realistic in terms of study design and data collection given the current UK context of extreme pressure on care homes. As with changes to service delivery, genuine involvement of care home residents, family members and staff is required to design and deliver high-quality research. Development and reporting of appropriate patient-reported outcome measures is recommended.
-
Research is needed to better understand the factors that enable effective interventions to become embedded and sustained in practice over the long term.
-
There is a need for rigorous economic evaluations, ideally using measures that can be used to compare different interventions and taking into account costs associated with implementation, particularly how costs are transferred between health and social care commissioners and providers.
-
The national roll-out in England of Hospital at Home as part of the Frailty Virtual Wards initiative, alongside Urgent Community Response, provides an opportunity to evaluate the applicability of approaches evidenced to work in Australia in the UK setting.
-
Further research is required to evaluate approaches based on paramedic assessment and potential non-conveyance, including assessment of safety and qualitative studies of resident, family carer and care home staff/management perspectives.
-
Further research is required to better understand the role of telehealth in reducing unplanned admissions of residents with cognitive or sensory impairments.
-
We found only one study based in an assisted living setting (in the USA). Research to evaluate interventions to reduce unplanned admissions from such settings in the UK is required, bearing in mind the lower levels of both resident need and on-site services.
Conclusions
This updated and extended systematic review has identified a substantial body of relevant research (124 publications) published between 2014 and early 2022. Much of the evidence is of low quality because of flaws such as uncontrolled study designs and small sample size. Despite this, it is clear that interventions at various stages of residents’ care pathways can reduce unplanned admissions if implemented effectively. Most interventions are complex and require co-operation between health and social care staff. This suggests that intervention effectiveness in routine practice is likely to be influenced by local contextual factors.
In the UK and internationally, integrated working and QI programmes have the strongest evidence of effectiveness. Integrated working takes a variety of forms, with primary and community care links being emphasised in UK practice and the role of hospital-based MDTs being more prominent in Australia. Simpler training and staff development initiatives have shown mixed results. ACP is key to ensuring that residents’ and families’ wishes are respected at the end of life but ‘do not hospitalise’ orders cannot be recommended. Qualitative research has identified key themes around decision-making involving paramedics, care home staff and residents/family carers but further work is required to optimise ways of working together and minimise unplanned admissions. Access to high-quality palliative care for care home residents is an ethical requirement but the best way to deliver this is unclear in the face of inconsistent and generally low-quality evidence.
The relevance of international evidence to UK practice is often debated. We were able to identify key factors that decision-makers may want to take into account in evaluating the suitability of international care models for testing in UK settings. Fundamental similarity of the characteristics of care home residents included in research studies tends to support transferability of evidence between different health and care systems.
The UK care home sector, like the health and care system generally, is under great pressure as a result of well-known problems including staff shortages, financial instability and the COVID-19 pandemic. The PARIHS framework identified these and other barriers to implementing interventions to reduce unplanned admissions. Facilitators were also identified, and the Care Home Vanguard studies included in this review led to the roll-out of the EHCH care model in England. Even when interventions have been successfully implemented, the pressures on the system mean that longer-term sustainability cannot be taken for granted and should be considered from an early stage.
Finally, we identified priorities for research, including better economic evaluations; evaluation of ‘HiNH’ and similar approaches; and appropriate interventions to reduce unplanned admissions from assisted living settings. Research studies should have realistic design and objectives and involve care home staff, managers and residents/families from the outset.
Acknowledgements
We are grateful to all the members of public involvement advisory groups based in Sheffield and Leicester for their contributions and insight.
Contributions of authors
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) (Research Fellow in Public Health) managed the project and contributed to all review processes and report writing.
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) (Research Fellow in Health Economics and Decision Science) performed the literature searches and contributed to all review processes and report writing.
Louise Preston (https://orcid.org/0000-0001-7477-4517) (Senior Research Fellow in Health Economics and Decision Science) contributed to all review processes and report writing.
Carl Marincowitz (https://orcid.org/0000-0003-3043-7564) (NIHR Academic Clinical Lecturer in Emergency Medicine) acted as a topic expert advisor and contributed to all review processes and report writing.
Lynne Wright (https://orcid.org/0009-0008-6637-2911) (public co-applicant) acted as a topic expert advisor and contributed to writing the plain English summary and PPI sections of the report.
Simon Conroy (https://orcid.org/0000-0002-4306-6064) (Professor of Geriatric Medicine) acted as a topic expert advisor and contributed to writing the report.
Adam Lee Gordon (https://orcid.org/0000-0003-1676-9853) (Professor of the Care of Older People) acted as a topic expert advisor and contributed to writing the report.
Ethical review
Not required.
Information governance statement
As a literature review, this study did not handle any personal data.
Data-sharing statement
Any additional data not included in this report and its appendices are available on request. All queries should be submitted to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing 2014;43:97-103. https://doi.org/10.1093/ageing/aft077.
- Wolters A, Santos F, LLoyd T, Lilburne C, Steventon A. Emergency Admissions to Hospital From Care Homes: How Often and What For?. London: Health Foundation; 2019.
- Department of Health and Social Care . Integration and Innovation: Working Together to Improve Health and Social Care for All 2021.
- Limb M. Delayed discharge: how are services and patients being affected?. BMJ 2022;376. https://doi.org/10.1136/bmj.o118.
- Huntley AL, Chalder M, Shaw ARG, Hollingworth W, Metcalfe C, Benger JR, et al. A systematic review to identify and assess the effectiveness of alternatives for people over the age of 65 who are at risk of potentially avoidable hospital admission. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016236.
- Centre for Reviews and Dissemination . Interventions to Reduce Unplanned Admissions From Care Home Settings 2014.
- Graverholt B, Forsetlund L, Jamtvedt G. Reducing hospital admissions from nursing homes: a systematic review. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-36.
- Buck D, Tucker S, Roe B, Hughes J, Challis D. Hospital admissions and place of death of residents of care homes receiving specialist healthcare services: a systematic review without meta-analysis. J Adv Nurs 2021;17. https://doi.org/10.1111/jan.15043.
- Ayiku L, Levay P, Hudson T. The NICE OECD countries’ geographic search filters: part 1: methodology for developing the draft MEDLINE and EMBASE (Ovid) filters. J Med Lib Assoc 2021;109:258-66.
- Gordon AL, Logan PA, Jones RG, Forrester-Paton C, Mamo JP, Gladman JRF, et al. Medical Crises in Older People Study Group . A systematic mapping review of randomized controlled trials (RCTs) in care homes. BMC Geriatr 2012;12. https://doi.org/10.1186/1471-2318-12-31.
- Baxter S, Johnson M, Chambers D, Sutton A, Goyder E, Booth A. Towards greater understanding of implementation during systematic reviews of complex healthcare interventions: the framework for implementation transferability applicability reporting (FITAR). BMC Med Res Methodol 2019;19. https://doi.org/10.1186/s12874-019-0723-y.
- Rycroft-Malone J. The PARIHS framework—a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual 2004;18:297-304.
- Joanna Briggs Institute n.d. https://jbi.global/critical-appraisal-tools (accessed 22 February 2023).
- National Heart, Lung and Blood Institute n.d. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed 22 February 2023).
- Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 2018;34:285-91. https://doi.org/10.3233/EFI-180221.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. London: ESRC Methods Programme; 2006.
- Chambers D, Cantrell A, Johnson M, Preston L, Baxter SK, Booth A, et al. Digital and online symptom checkers and health assessment/triage services for urgent care to inform a new digital platform: a systematic review. Health Serv Deliv Res 2019;7:1-87. https://doi.org/10.3310/hsdr07290.
- Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 2021;372. https://doi.org/10.1136/bmj.n71.
- Damery S, Flanagan S, Jones J, Jolly K. The effect of providing staff training and enhanced support to care homes on care processes, safety climate and avoidable harms: evaluation of a care home quality improvement programme in England. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18147581.
- Giebel C, Harvey D, Akpan A, Chamberlain P. Reducing hospital admissions in older care home residents: a 4-year evaluation of the care home innovation Programme (CHIP). BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-4945-9.
- Steel A, Hopwood H, Goodwin E, Sampson EL. Multidisciplinary residential home intervention to improve outcomes for frail residents. BMC Health Serv Res 2022;22. https://doi.org/10.1186/s12913-021-07407-y.
- Blackburn J, Stump TE, Carnahan JL, Hickman SE, Tu W, Fowler NR, et al. Reducing the risk of hospitalization for nursing home residents: effects and facility variation from OPTIMISTIC. J Am Med Dir Assoc 2020;21:545-549.e1. https://doi.org/10.1016/j.jamda.2020.02.002.
- Ersek M, Hickman SE, Thomas AC, Bernard B, Unroe KT. Stakeholder perspectives on the optimizing patient transfers, impacting medical quality, and improving symptoms: transforming institutional care (OPTIMISTIC) project. Gerontologist 2018;58:1177-87. https://doi.org/10.1093/geront/gnx155.
- Galambos C, Vogelsmeier A, Popejoy L, Crecelius C, Canada K, Alexander GL, et al. Enhancing physician relationships, communication, and engagement to reduce nursing home residents hospitalizations. J Nurs Care Qual 2021;36:99-104. https://doi.org/10.1097/ncq.0000000000000542.
- Huckfeldt PJ, Kane RL, Yang Z, Engstrom G, Tappen R, Rojido C, et al. Degree of implementation of the interventions to reduce acute care transfers (INTERACT) quality improvement program associated with number of hospitalizations. J Am Geriatr Soc 2018;66:1830-7. https://doi.org/10.1111/jgs.15476.
- Ingber MJ, Feng Z, Khatutsky G, Wang JM, Bercaw LE, Zheng NT, et al. Initiative to reduce avoidable hospitalizations among nursing facility residents shows promising results. Health Aff (Millwood) 2017;36:441-50. https://doi.org/10.1377/hlthaff.2016.1310.
- Kane RL, Huckfeldt P, Tappen R, Engstrom G, Rojido C, Newman D, et al. Effects of an intervention to reduce hospitalizations from nursing homes: a randomized implementation trial of the INTERACT program. JAMA Intern Med 2017;177:1257-64. https://doi.org/10.1001/jamainternmed.2017.2657.
- Ouslander JG, Engstrom G, Reyes B, Tappen R, Rojido C, Gray-Miceli D. Management of acute changes in condition in skilled nursing facilities. J Am Geriatr Soc 2018;66:2259-66. https://doi.org/10.1111/jgs.15632.
- Ouslander JG, Reyes B, Yang Z, Engstrom G, Tappen R, Newman D, et al. Nursing home performance in a trial to reduce hospitalizations: implications for future trials. J Am Geriatr Soc 2021;69:2316-26. https://doi.org/10.1111/jgs.17231.
- Popejoy LL, Vogelsmeier AA, Alexander GL, Galambos CM, Crecelius CA, Ge B, et al. Analyzing hospital transfers using INTERACT acute care transfer tools: lessons from MOQI. J Am Geriatr Soc 2019;67:1953-9. https://doi.org/10.1111/jgs.15996.
- Rantz MJ, Flesner MK, Franklin J, Galambos C, Pudlowski J, Pritchett A, et al. Better care, better quality: reducing avoidable hospitalizations of nursing home residents. J Nurs Care Qual 2015;30:290-7. https://doi.org/10.1097/NCQ.0000000000000145.
- Rantz MJ, Popejoy L, Vogelsmeier A, Galambos C, Alexander G, Flesner M, et al. Successfully reducing hospitalizations of nursing home residents: results of the Missouri quality initiative. J Am Med Dir Assoc 2017;18:960-6. https://doi.org/10.1016/j.jamda.2017.05.027.
- Rantz MJ, Popejoy L, Vogelsmeier A, Galambos C, Alexander G, Flesner M, et al. Reducing avoidable hospitalizations and improving quality in nursing homes with APRNs and interdisciplinary support: lessons learned. J Nurs Care Qual 2018;33:5-9. https://doi.org/10.1097/NCQ.0000000000000302.
- Rantz M, Vogelsmeier A, Popejoy L, Canada K, Galambos C, Crecelius C, et al. Financial and work-flow benefits of reducing avoidable hospitalizations of nursing home residents. J Nutr Health Aging 2021;25:971-8. https://doi.org/10.1007/s12603-021-1650-2.
- Tappen RM, Newman D, Huckfeldt P, Yang Z, Engstrom G, Wolf DG, et al. Evaluation of nursing facility resident safety during implementation of the INTERACT quality improvement program. J Am Med Dir Assoc 2018;19:907-913.e1. https://doi.org/10.1016/j.jamda.2018.06.017.
- Vadnais AJ, Vreeland E, Coomer NM, Feng Z, Ingber MJ. Reducing transfers among long-stay nursing facility residents to acute care settings: effect of the 2013-2016 Centers for Medicare and Medicaid Services Initiative. J Am Med Dir Assoc 2020;21:1341-5. https://doi.org/10.1016/j.jamda.2020.01.002.
- Vogelsmeier A, Popejoy L, Kist S, Harrell R, Alexander G, Rantz M. Avoiding nursing home to hospital transfers rethinking avoidability. J Nurs Care Qual 2019;34:189-93. https://doi.org/10.1097/ncq.0000000000000409.
- Vogelsmeier A, Popejoy L, Kist S, Shumate S, Pritchett A, Mueller J, et al. Reducing avoidable hospitalizations for nursing home residents: role of the Missouri quality initiative intervention support team. J Nurs Care Qual 2020;35:1-5. https://doi.org/10.1097/NCQ.0000000000000444.
- Vogelsmeier A, Popejoy L, Canada K, Galambos C, Petroski G, Crecelius C, et al. Results of the Missouri quality initiative in sustaining changes in nursing home care: six-year trends of reducing hospitalizations of nursing home residents. J Nutr Health Aging 2021;25:5-12. https://doi.org/10.1007/s12603-020-1552-8.
- Boyd M, Armstrong D, Parker J, Pilcher C, Zhou L, McKenzie-Green B, et al. Do gerontology nurse specialists make a difference in hospitalization of long-term care residents? Results of a randomized comparison trial. J Am Geriatr Soc 2014;62:1962-7. https://doi.org/10.1111/jgs.13022.
- Connolly MJ, Boyd M, Broad JB, Kerse N, Lumley T, Whitehead N, et al. The Aged Residential Care Healthcare Utilization Study (ARCHUS): a multidisciplinary, cluster randomized controlled trial designed to reduce acute avoidable hospitalizations from long-term care facilities. J Am Med Dir Assoc 2015;16:49-55. https://doi.org/10.1016/j.jamda.2014.07.008.
- Connolly MJ, Broad JB, Bish T, Zhang X, Bramley D, Kerse N, et al. Reducing emergency presentations from long-term care: a before-and-after study of a multidisciplinary team intervention. Maturitas 2018;117:45-50. https://doi.org/10.1016/j.maturitas.2018.08.014.
- Connolly MJ, Broad JB, Boyd M, Zhang TX, Kerse N, Foster S, et al. The ‘Big Five’. Hypothesis generation: a multidisciplinary intervention package reduces disease-specific hospitalisations from long-term care: a post hoc analysis of the ARCHUS cluster-randomised controlled trial. Age Ageing 2016;45:415-20. https://doi.org/10.1093/ageing/afw037.
- Carter HE, Lee XJ, Dwyer T, O’Neill B, Jeffrey D, Doran CM, et al. The effectiveness and cost effectiveness of a hospital avoidance program in a residential aged care facility: a prospective cohort study and modelled decision analysis. BMC Geriatr 2020;20. https://doi.org/10.1186/s12877-020-01904-1.
- Zuniga F, Guerbaai RA, de Geest S, Popejoy LL, Bartakova J, Denhaerynck K, et al. Positive effect of the INTERCARE nurse-led model on reducing nursing home transfers: a nonrandomized stepped-wedge design. J Am Geriatr Soc 2021;70:1546-57. https://doi.org/10.1111/jgs.17677.
- Brine R, Conti S, Wolters A. The Impact of Providing an Enhanced Package of Care for Care Home Residents in Nottingham City: Briefing. London: Health Foundation; 2019.
- Conti S, Gori C, Caunt M, Steventon A. Briefing: The Impact of Providing Enhanced Support for Sutton Homes of Care Residents. London: Health Foundation; 2018.
- Lloyd T, Conti S, Santos F, Steventon A. Effect on secondary care of providing enhanced support to residential and nursing home residents: a subgroup analysis of a retrospective matched cohort study. BMJ Qual Saf 2019;28:534-46. https://doi.org/10.1136/bmjqs-2018-009130.
- Lloyd T, Wolters A, Steventon A. Briefing: The Impact of Providing Enhanced Support for Care Home Residents in Rushcliffe. London: Health Foundation; 2017.
- Morciano M, Checkland K, Billings J, Coleman A, Stokes J, Tallack C, et al. New integrated care models in England associated with small reduction in hospital admissions in longer-term: a difference-in-differences analysis. Health Policy 2020;124:826-33. https://doi.org/10.1016/j.healthpol.2020.06.004.
- Sherlaw-Johnson C, Crump H, Curry N, Paddison C, Meaker R. Transforming Health Care in Nursing Homes: An Evaluation of a Dedicated Primary Care Service in Outer East. London: Nuffield Trust; 2018.
- SQW Ltd, Social Care Institute for Excellence . Evaluation of Sutton Homes of Care Vanguard: End of Year Report 2017.
- Vestesson E, LLoyd T. The Impact of Providing Enhanced Support for Care Home Residents in Wakefield: Briefing. London: Health Foundation; 2019.
- Healthwatch I. Experiences of Integrated Care and the Integrated Care Ageing Team. London: Healthwatch Islington; 2015.
- Society RP. Sustainability and Transformation Partnerships. London: Royal Pharmaceutical Society; 2018.
- Tunstall . NHS Demand Management from Care Homes: A £1bn Opportunity for NHS England 2018.
- Holder H, Kumpunen S, Castle-Clarke S, Lombardo S. Managing the Hospital and Social Care Interface: Interventions Targeting Older Adults. London: Nuffield Trust; 2018.
- Cordato NJ, Kearns M, Smerdely P, Seeher KM, Gardiner MD, Brodaty H. Management of nursing home residents following acute hospitalization: efficacy of the ‘regular early assessment post-discharge (REAP)’ intervention. J Am Med Dir Assoc 2018;19:276.e11276e11-276.e19. https://doi.org/10.1016/j.jamda.2017.12.008.
- Haines TP, Palmer AJ, Tierney P, Si L, Robinson AL. A new model of care and in-house general practitioners for residential aged care facilities: a stepped wedge, cluster randomised trial. Med J Aust 2020;212:409-15. https://doi.org/10.5694/mja2.50565.
- Craswell A, Wallis M, Coates K, Marsden E, Taylor A, Broadbent M, et al. Enhanced primary care provided by a nurse practitioner candidate to aged care facility residents: a mixed methods study. Collegian 2020;27:281-7. https://doi.org/10.1016/j.colegn.2019.08.009.
- Dwyer T, Craswell A, Rossi D, Holzberger D. Evaluation of an aged care nurse practitioner service: quality of care within a residential aged care facility hospital avoidance service. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-1977-x.
- Dai J, Liu F, Irwanto D, Kumar M, Tiwari N, Chen J, et al. Impact of an acute geriatric outreach service to residential aged care facilities on hospital admissions. Aging Med (Milton) 2021;4:169-74. https://doi.org/10.1002/agm2.12176.
- Fan L, Hou XY, Zhao J, Sun J, Dingle K, Purtill R, et al. Hospital in the Nursing Home program reduces emergency department presentations and hospital admissions from residential aged care facilities in Queensland, Australia: a quasi-experimental study. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1275-z.
- Amadoru S, Rayner J-A, Joseph R, Yates P. Factors influencing decision-making processes for unwell residents in residential aged care: Hospital transfer or Residential InReach referral?. Australas J Ageing 2018;37:E61-7. https://doi.org/10.1111/ajag.12512.
- O’Neill BJ, Dwyer T, Reid-Searl K, Parkinson L. Managing the deteriorating nursing home resident after the introduction of a hospital avoidance programme: a nursing perspective. Scand J Caring Sci 2017;31:312-22. https://doi.org/10.1111/scs.12349.
- Chan DKY, Liu FX, Irwanto D, Prasetyo D, Ozorio G, Li F, et al. Experience of establishing an acute geriatric outreach service versus subacute service to nursing homes. Intern Med J 2018;48:1396-9. https://doi.org/10.1111/imj.14104.
- Fan L, Lukin B, Zhao J, Sun J, Dingle K, Purtill R, et al. Cost analysis of improving emergency care for aged care residents under a Hospital in the Nursing Home program in Australia. PLOS ONE 2018;13. https://doi.org/10.1371/journal.pone.0199879.
- Hullick C, Conway J, Higgins I, Hewitt J, Dilworth S, Holliday E, et al. Emergency department transfers and hospital admissions from residential aged care facilities: a controlled pre-post design study. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0279-1.
- Hullick CJ, Hall AE, Conway JF, Hewitt JM, Darcy LF, Barker RT, et al. Reducing hospital transfers from aged care facilities: a large-scale stepped Wedge evaluation. J Am Geriatr Soc 2021;69:201-9. https://doi.org/10.1111/jgs.16890.
- Hullick C, Conway J, Hall A, Murdoch W, Cole J, Hewitt J, et al. Video-telehealth to support clinical assessment and management of acutely unwell older people in Residential Aged Care: a pre-post intervention study. BMC Geriatr 2022;22. https://doi.org/10.1186/s12877-021-02703-y.
- Hutchinson AF, Parikh S, Tacey M, Harvey PA, Lim WK. A longitudinal cohort study evaluating the impact of a geriatrician-led residential care outreach service on acute healthcare utilisation. Age Ageing 2015;44:365-70.
- Kwa J-M, Storer M, Ma R, Yates P. Integration of inpatient and residential care in-reach service model and hospital resource utilization: a retrospective audit. J Am Med Dir Assoc 2021;22:670-5. https://doi.org/10.1016/j.jamda.2020.07.015.
- Grabowski DC, O’Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for medicare. Health Aff (Millwood) 2014;33:244-50.
- Hofmeyer J, Leider JP, Satorius J, Tanenbaum E, Basel D, Knudson A. Implementation of telemedicine consultation to assess unplanned transfers in rural long-term care facilities, 2012-2015: a pilot study. J Am Med Dir Assoc 2016;17:1006-10. https://doi.org/10.1016/j.jamda.2016.06.014.
- Brickman KR, Silvestri JA. The emergency care model: a new paradigm for skilled nursing facilities. Geriatr Nurs 2020;41:242-7. https://doi.org/10.1016/j.gerinurse.2019.10.004.
- Stadler DS, Oliver BJ, Raymond JG, Routzhan GE, Flaherty EA, Stahl JE, et al. Reducing avoidable facility transfers (RAFT): outcomes of a team model to minimize unwarranted emergency care at skilled nursing facilities. J Am Med Dir Assoc 2019;20:929-34. https://doi.org/10.1016/j.jamda.2019.03.010.
- Pedersen LH, Gregersen M, Barat I, Damsgaard EM. Early geriatric follow-up after discharge reduces readmissions – a quasi-randomised controlled trial. Eur Geriatr Med 2016;7:443-8. https://doi.org/10.1016/j.eurger.2016.03.009.
- Pedersen LH, Gregersen M, Barat I, Damsgaard EM. Early geriatric follow-up visits to nursing home residents reduce the number of readmissions: a quasi-randomised controlled trial. Eur Geriatr Med 2018;9:329-37. https://doi.org/10.1007/s41999-018-0045-3.
- Kobewka DM, Kunkel E, Hsu A, Talarico R, Tanuseputro P. Physician availability in long-term care and resident hospital transfer: a retrospective cohort study. J Am Med Dir Assoc 2020;21:469-475.e1. https://doi.org/10.1016/j.jamda.2019.06.004.
- Kumpel C, Schneider U. Additional reimbursement for outpatient physicians treating nursing home residents reduces avoidable hospital admissions: results of a reimbursement change in Germany. Health Policy 2020;124:470-7. https://doi.org/10.1016/j.healthpol.2020.02.009.
- Weatherall CD, Hansen AT, Nicholson S. The effect of assigning dedicated general practitioners to nursing homes. Health Serv Res 2019;54:547-54. https://doi.org/10.1111/1475-6773.13112.
- Armstrong SF, Gluck T, Gorringe A, Stork A, Jowett S, Nadicksbernd JJ, et al. Care homes education: what can we learn?. BMJ Open Qual 2021;10. https://doi.org/10.1136/bmjoq-2020-001153.
- Siddiqi N, Cheater F, Collinson M, Farrin A, Forster A, George D, et al. The PiTSTOP study: a feasibility cluster randomized trial of delirium prevention in care homes for older people. Age Ageing 2016;45:652-61. https://doi.org/10.1093/ageing/afw091.
- Sheaff R, Sherriff I, Hennessy CH. Evaluating a dementia learning community: exploratory study and research implications. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-2894-3.
- McGregor MJ, Murphy JM, Poss JW, McGrail KM, Kuramoto L, Huang HC, et al. 24/7 registered nurse staffing coverage in Saskatchewan nursing homes and acute hospital use. Can J Aging-Revue Canadienne Du Vieillissement 2015;34:492-505. https://doi.org/10.1017/s0714980815000434.
- Romoren M, Gjelstad S, Lindbaek M. A structured training program for health workers in intravenous treatment with fluids and antibiotics in nursing homes: a modified stepped-wedge cluster-randomised trial to reduce hospital admissions. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0182619.
- Resnick B, Boltz M, Galik E, Zhu S. the impact of a randomized controlled trial testing the implementation of function-focused care in assisted living on resident falls, hospitalizations, and nursing home transfers. J Aging Phys Act 2021;29:922-30. https://doi.org/10.1123/japa.2020-0426.
- Downs M, Blighe A, Carpenter R, Feast A, Froggatt K, Gordon S, et al. A complex intervention to reduce avoidable hospital admissions in nursing homes: a research programme including the BHiRCH-NH pilot cluster RCT. Programme Grants Appl Res 2021;9:1-200. https://doi.org/10.3310/pgfar09020.
- Sampson EL, Feast A, Blighe A, Froggatt K, Hunter R, Marston L, et al. Pilot cluster randomised trial of an evidence-based intervention to reduce avoidable hospital admissions in nursing home residents (Better Health in Residents of Care Homes with Nursing-BHiRCH-NH Study). BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-040732.
- McKee H, Miller R, Cuthbertson J, Scullin C, Scott MG. Nursing Home Outreach Clinics show an improvement in patient safety and reduction in hospital admissions in residents with chronic conditions. Eur J Pers Cent Healthc 2016;4:650-5.
- Niznik Joshua D, Zhao X, He M, Aspinall Sherrie L, Hanlon Joseph T, Hanson Laura C, et al. Risk for health events after deprescribing Acetylcholinesterase inhibitors in nursing home residents with severe dementia. J Am Geriatr Soc 2020;68:699-707. https://doi.org/10.1111/jgs.16241.
- Gravenstein S, Davidson HE, Taljaard M, Ogarek J, Gozalo P, Han L, et al. Comparative effectiveness of high-dose versus standard-dose influenza vaccination on numbers of US nursing home residents admitted to hospital: a cluster-randomised trial. Lancet Respir Med 2017;5:738-46. https://doi.org/10.1016/S2213-2600(17)30235-7.
- McConeghy KW, Davidson HE, Canaday DH, Han L, Saade E, Mor V, et al. Cluster-randomized trial of adjuvanted versus nonadjuvanted trivalent influenza vaccine in 823 US nursing homes. Clin Infect Dis 2021;73:e4237-43. https://doi.org/10.1093/cid/ciaa1233.
- Pop-Vicas A, Rahman M, Gozalo PL, Gravenstein S, Mor V. Estimating the effect of influenza vaccination on nursing home residents’ morbidity and mortality. J Am Geriatr Soc 2015;63:1798-804. https://doi.org/10.1111/jgs.13617.
- Mor V, Gutman R, Yang X, White EM, McConeghy KW, Feifer RA, et al. Short-term impact of nursing home SARS-CoV-2 vaccinations on new infections, hospitalizations, and deaths. J Am Geriatr Soc 2021;69:2063-9. https://doi.org/10.1111/jgs.17176.
- Gorisek Miksic N, Ursic T, Simonovic Z, Lusa L, Lobnik Rojko P, Petrovec M, et al. Oseltamivir prophylaxis in controlling influenza outbreak in nursing homes: a comparison between three different approaches. Infection 2015;43:73-81. https://doi.org/10.1007/s15010-014-0703-4.
- Milos Nymberg V, Lenander C, Borgstrom Bolmsjo B. The impact of medication reviews conducted in primary care on hospital admissions and mortality: an observational follow-up of a randomized controlled trial. Drug Healthc 2021;13:1-9. https://doi.org/10.2147/DHPS.S283708.
- Frankenthal D, Lerman Y, Kalendaryev E, Lerman Y. Intervention with the screening tool of older persons potentially inappropriate prescriptions/screening tool to alert doctors to right treatment criteria in elderly residents of a chronic geriatric facility: a randomized clinical trial. J Am Geriatr Soc 2014;62:1658-65. https://doi.org/10.1111/jgs.12993.
- Junius-Walker U, Krause O, Thurmann P, Bernhard S, Fuchs A, Sparenberg L, et al. Drug safety for nursing-home residents – findings of a pragmatic, cluster-randomized, controlled intervention trial in 44 nursing homes. Dtsch Arztebl Int 2021;118:705-12. https://doi.org/10.3238/arztebl.m2021.0297.
- Sluggett JK, Hopkins RE, Chen EYH, Ilomaki J, Corlis M, Van Emden J, et al. Impact of medication regimen simplification on medication administration times and health outcomes in residential aged care: 12 Month follow up of the SIMPLER randomized controlled trial. J Clin Med 2020;9. https://doi.org/10.3390/jcm9041053.
- Pulst A, Fassmer AM, Hoffmann F, Schmiemann G. Paramedics’ perspectives on the hospital transfers of nursing home residents-a qualitative focus group study. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17113778.
- Murphy-Jones G, Timmons S. Paramedics’ experiences of end-of-life care decision making with regard to nursing home residents: an exploration of influential issues and factors. Emerg Med J 2016;33:722-6. https://doi.org/10.1136/emermed-2015-205405.
- Marsden E, Taylor A, Wallis M, Craswell A, Broadbent M, Barnett A, et al. Effect of the geriatric emergency department intervention on outcomes of care for residents of aged care facilities: a non-randomised trial. Emerg Med Australas 2020;32:422-9. https://doi.org/10.1111/1742-6723.13415.
- Preston L, van Oppen JD, Conroy SP, Ablard S, Buckley Woods H, Mason SM. Improving outcomes for older people in the emergency department: a review of reviews. Emerg Med J 2021;38:882-8. https://doi.org/10.1136/emermed-2020-209514.
- van Oppen JD, Thompson D, Tite M, Griffiths S, Martin FC, Conroy S. The Acute Frailty Network: experiences from a whole-systems quality improvement collaborative for acutely ill older patients in the English NHS. Eur Geriatr Med 2019;10:559-65. https://doi.org/10.1007/s41999-019-00177-1.
- Amador S, Goodman C, King D, Ng YT, Elmore N, Mathie E, et al. Exploring resource use and associated costs in end-of-life care for older people with dementia in residential care homes. Int J Geriatr Psychiatry 2014;29:758-66. https://doi.org/10.1002/gps.4061.
- Garden G, Green S, Pieniak S, Gladman J. The Bromhead Care Home Service: the impact of a service for care home residents with dementia on hospital admission and dying in preferred place of care. Clin Med 2016;16:114-8. https://doi.org/10.7861/clinmedicine.16-2-114.
- Alcorn G, Murray SA, Hockley J. Care home residents who die in hospital: exploring factors, processes and experiences. Age Ageing 2020;49:468-80. https://doi.org/10.1093/ageing/afz174.
- Harrad-Hyde F, Armstrong N, Williams C. Using advance and emergency care plans during transfer decisions: a grounded theory interview study with care home staff. Palliat Med 2021;36:200-7. https://doi.org/10.1177/02692163211059343.
- Adekpedjou R, Heckman GA, Hebert PC, Costa AP, Hirdes J. Outcomes of advance care directives after admission to a long-term care home: DNR the DNH?. BMC Geriatr 2022;22. https://doi.org/10.1186/s12877-021-02699-5.
- Cohen AB, Knobf MT, Fried TR. Do-not-hospitalize orders in nursing homes: ‘call the family instead of calling the ambulance’. J Am Geriatr Soc 2017;65:1573-7. https://doi.org/10.1111/jgs.14879.
- Galambos C, Rantz M, Popejoy L, Ge B, Petroski G. Advance directives in the nursing home setting: an initiative to increase completion and reduce potentially avoidable hospitalizations. J Soc Work End Life Palliat Care 2021;17:19-34. https://doi.org/10.1080/15524256.2020.1863895.
- Hendriks SA, Smalbrugge M, Hertogh C, van der Steen JT. Changes in care goals and treatment orders around the occurrence of health problems and hospital transfers in dementia: a prospective study. J Am Geriatr Soc 2017;65:769-76. https://doi.org/10.1111/jgs.14667.
- Hickman SE, Unroe KT, Ersek M, Stump TE, Tu W, Ott M, et al. Systematic advance care planning and potentially avoidable hospitalizations of nursing facility residents. J Am Geriatr Soc 2019;67:1649-55. https://doi.org/10.1111/jgs.15927.
- Honinx E, Piers RD, Onwuteaka-Philipsen BD, Payne S, Szczerbinska K, Gambassi G, et al. PACE collaborators . Hospitalisation in the last month of life and in-hospital death of nursing home residents: a cross-sectional analysis of six European countries. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-047086.
- Houttekier D, Vandervoort A, Van den Block L, van der Steen JT, Vander Stichele R, Deliens L. Hospitalizations of nursing home residents with dementia in the last month of life: results from a nationwide survey. Palliat Med 2014;28:1110-17. https://doi.org/10.1177/0269216314535962.
- Martin RS, Hayes BJ, Hutchinson A, Tacey M, Yates P, Lim WK. Introducing goals of patient care in residential aged care facilities to decrease hospitalization: a cluster randomized controlled trial. J Am Med Dir Assoc 2019;20:1318-1324.e2. https://doi.org/10.1016/j.jamda.2019.06.017.
- Moyo P, Loomer L, Teno JM, Gutman R, McCreedy EM, Belanger E, et al. Effect of a video-assisted advance care planning intervention on end-of-life health care transitions among long-stay nursing home residents. J Am Med Dir Assoc 2021;23:394-8. https://doi.org/10.1016/j.jamda.2021.09.014.
- Mullaney SE, Devereaux Melillo K, Lee AJ, MacArthur R. The association of nurse practitioners’ mortality risk assessments and advance care planning discussions on nursing home patients’ clinical outcomes. J Am Assoc Nurse Pract 2016;28:304-10. https://doi.org/10.1002/2327-6924.12317.
- Nakashima T, Young Y, Hsu WH. Are hospital/ED transfers less likely among nursing home residents with do-not-hospitalize orders?. J Am Med Dir Assoc 2017;18:438-41. https://doi.org/10.1016/j.jamda.2016.12.004.
- Overbeek A, Korfage IJ, Jabbarian LJ, Billekens P, Hammes BJ, Polinder S, et al. Advance care planning in frail older adults: a cluster randomized controlled trial. J Am Geriatr Soc 2018;66:1089-95. https://doi.org/10.1111/jgs.15333.
- Kinley J, Stone L, Butt A, Kenyon B, Lopes NS. Developing, implementing and sustaining an end-of-life care programme in residential care homes. Int J Palliat Nurs 2017;23:186-93. https://doi.org/10.12968/ijpn.2017.23.4.186.
- Smith D, Brown S. Integrating a palliative care approach into nursing care homes for older people. Int J Palliat Nurs 2017;23:511-5. https://doi.org/10.12968/ijpn.2017.23.10.511.
- Springett A. Practice improvement as a result of an end of life care programme for care homes. Nurs Older People 2017;29:23-7. https://doi.org/10.7748/nop.2017.e890.
- Chapman M, Johnston N, Lovell C, Forbat L, Liu WM. Avoiding costly hospitalisation at end of life: findings from a specialist palliative care pilot in residential care for older adults. BMJ Support 2018;8:102-9. https://doi.org/10.1136/bmjspcare-2015-001071.
- Forbat L, Liu W-M, Koerner J, Lam L, Samara J, Chapman M, et al. Reducing time in acute hospitals: a stepped-wedge randomised control trial of a specialist palliative care intervention in residential care homes. Palliat Med 2020;34:571-9. https://doi.org/10.1177/0269216319891077.
- Koerner J, Johnston N, Samara J, Liu WM, Chapman M, Forbat L. Context and mechanisms that enable implementation of specialist palliative care Needs Rounds in care homes: results from a qualitative interview study. BMC Palliat Care 2021;20. https://doi.org/10.1186/s12904-021-00812-4.
- Mitchell G, Melaku M, Moss A, Chaille G, Makoni B, Lewis L, et al. Evaluation of a commissioned end-of-life care service in Australian aged care facilities. Prog Palliat Care 2022;30:229-37. https://doi.org/10.1080/09699260.2021.1905146.
- Rainsford S, Liu WM, Johnston N, Glasgow N. The impact of introducing Palliative Care Needs Rounds into rural residential aged care: a quasi‐experimental study. Aust J Rural Health 2020;28:480-9. https://doi.org/10.1111/ajr.12654.
- Harrison JM, Agarwal M, Stone PW, Gracner T, Sorbero M, DI AW. Does integration of palliative care and infection management reduce hospital transfers among nursing home residents?. J Palliat Med 2021;24:1334-41. https://doi.org/10.1089/jpm.2020.0577.
- Miller SC, Dahal R, Lima JC, Intrator O, Martin E, Bull J, et al. Palliative care consultations in nursing homes and end-of-life hospitalizations. J Pain Symptom Manage 2016;52:878-83. https://doi.org/10.1016/j.jpainsymman.2016.05.017.
- Miller SC, Lima JC, Intrator O, Martin E, Bull J, Hanson LC. Palliative care consultations in nursing homes and reductions in acute care use and potentially burdensome end-of-life transitions. J Am Geriatr Soc 2016;64:2280-7. https://doi.org/10.1111/jgs.14469.
- Miller SC, Lima JC, Intrator O, Martin E, Bull J, Hanson LC. Specialty palliative care consultations for nursing home residents with dementia. J Pain Symptom Manage 2017;54:9-16.e5. https://doi.org/10.1016/j.jpainsymman.2017.03.005.
- Temkin-Greener H, Mukamel DB, Ladd H, Ladwig S, Caprio TV, Norton SA, et al. Impact of nursing home palliative care teams on end-of-life outcomes: a randomized controlled trial. Med Care 2018;56:11-8. https://doi.org/10.1097/MLR.0000000000000835.
- Zheng NT, Mukamel DB, Friedman B, Caprio TV, Temkin-Greener H. The effect of hospice on hospitalizations of nursing home residents. J Am Med Dir Assoc 2015;16:155-9. https://doi.org/10.1016/j.jamda.2014.08.010.
- Ho P, Lim Y, Tan LLC, Wang X, Magpantay G, Chia JWK, et al. Does an integrated palliative care program reduce emergency department transfers for nursing home palliative residents?. J Palliat Med 2001;25:361-7. https://doi.org/10.1089/jpm.2021.0241.
- Honinx E, Smets T, Piers R, Pasman HRW, Payne SA, Szczerbińska K, et al. Lack of effect of a multicomponent palliative care program for nursing home residents on hospital use in the last month of life and on place of death: a secondary analysis of a multicountry cluster randomized control trial. J Am Med Dir Assoc 2020;21:1973-1978.e2. https://doi.org/10.1016/j.jamda.2020.05.003.
- Lamppu PJ, Finne-Soveri H, Kautiainen H, Laakkonen ML, Laurila JV, Pitkala KH. Effects of staff training on nursing home residents’ end-of-life care: a randomized controlled trial. J Am Med Dir Assoc 2021;22:1699-1705.e1. https://doi.org/10.1016/j.jamda.2021.05.019.
- Tappen RM, Worch SM, Newman DO, Hain D. Evaluation of a novel decision guide ‘go to the hospital or stay here?’ for nursing home residents and families: a randomized trial. Res Gerontol Nurs 2020;13:309-19. https://doi.org/10.3928/19404921-20201002-01.
- Mackey DC, Lachance CC, Wang PT, Feldman F, Laing AC, Leung PM, et al. The Flooring for Injury Prevention (FLIP) Study of compliant flooring for the prevention of fall-related injuries in long-term care: a randomized trial. PLOS Med 2019;16. https://doi.org/10.1371/journal.pmed.1002843.
- Levy CR, Alemi F, Williams AE, Williams AR, Wojtusiak J, Sutton B, et al. Shared homes as an alternative to nursing home care: impact of VA’s Medical Foster Home program on hospitalization. Gerontologist 2016;56:62-71.
- Pracht EE, Levy CR, Williams A, Alemi F, Williams AE. The VA Medical Foster Home program, ambulatory care sensitive conditions, and avoidable hospitalizations. Am J Med Qual 2016;31:536-40.
- Devi R, Martin GP, Banerjee J, Gladman JR, Dening T, Barat A, et al. Sustaining interventions in care homes initiated by quality improvement projects: a qualitative study. BMJ Qual Saf 2022. https://doi.org/10.1136/bmjqs-2021-014345 (accessed 22 March 2022).
- Robbins I, Gordon A, Dyas J, Logan P, Gladman J. Explaining the barriers to and tensions in delivering effective healthcare in UK care homes: a qualitative study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003178.
- Gordon AL, Bennett C, Goodman C, Achterberg WP. Making progress: but a way to go-the age and ageing care-home collection. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afab213.
- Singh S, Gray A, Shepperd S, Stott DJ, Ellis G, Hemsley A, et al. Is comprehensive geriatric assessment hospital at home a cost-effective alternative to hospital admission for older people?. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afab220.
- Knight T, Lasserson D. Hospital at home for acute medical illness: the 21st century acute medical unit for a changing population. J Intern Med 2022;291:438-57. https://doi.org/10.1111/joim.13394.
- NHS England n.d. https://www.longtermplan.nhs.uk/areas-of-work/ageing-well (accessed 10 November 2022).
- Warmoth K, Lynch J, Darlington N, Bunn F, Goodman C. Using video consultation technology between care homes and health and social care professionals: a scoping review and interview study during COVID-19 pandemic. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afab279.
- Goodman C, Davies SL, Gordon AL, Dening T, Gage H, Meyer J, et al. Optimal NHS service delivery to care homes: a realist evaluation of the features and mechanisms that support effective working for the continuing care of older people in residential settings. Health Serv Deliv Res 2017;5:1-204. https://doi.org/10.3310/hsdr05290.
- Marshall F, Gordon A, Gladman JRF, Bishop S. Care homes, their communities, and resilience in the face of the COVID-19 pandemic: interim findings from a qualitative study. BMC Geriatr 2021;21. https://doi.org/10.1186/s12877-021-02053-9.
- Peryer G, Kelly S, Blake J, Burton JK, Irvine L, Cowan A, et al. Contextual factors influencing complex intervention research processes in care homes: a systematic review and framework synthesis. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afac014.
- Bunn F, Goodman C, Corazzini K, Sharpe R, Handley M, Lynch J, et al. Setting priorities to inform assessment of care homes’ readiness to participate in healthcare innovation: a systematic mapping review and consensus process. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17030987.
- Gordon AL, Spilsbury K, Achterberg WP, Adams R, Jones L, Goodman C. From Warkworth House to the 21st century care homes: progress marked by persistent challenges. Age Ageing 2022;51. https://doi.org/10.1093/ageing/afac169.
- Achterberg WP, Everink IH, van der Steen JT, Gordon AL. We’re all different and we’re the same: the story of the European nursing home resident. Age Ageing 2019;49:3-4. https://doi.org/10.1093/ageing/afz145.
- Aalto UL, Pitkala KH, Andersen-Ranberg K, Bonin-Guillaume S, Cruz-Jentoft AJ, Eriksdotter M, et al. COVID-19 pandemic and mortality in nursing homes across USA and Europe up to October 2021. Eur Geriatr Med 2022;13:705-9. https://doi.org/10.1007/s41999-022-00637-1.
- Curtis LA, Burns A. Unit Costs of Health and Social Care 2015. Unit Costs of Health and Social Care. Report Number: 3. Personal Social Services Research Unit 2015.
- Rocks S, Berntson D, Gil-Salmeron A, Kadu M, Ehrenberg N, Stein V, et al. Cost and effects of integrated care: a systematic literature review and meta-analysis. Eur J Health Econ 2020;21:1211-21. https://doi.org/10.1007/s10198-020-01217-5.
- Usman A, Lewis S, Hinsliff-Smith K, Long A, Housley G, Jordan J, et al. Measuring health-related quality of life of care home residents: comparison of self-report with staff proxy responses. Age Ageing 2019;48:407-13. https://doi.org/10.1093/ageing/afy191.
Appendix 1 MEDLINE search strategies
Main search strategy
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review and Other Non-Indexed Citations and Daily <1946 to 14 December 2021>
Search strategy:
-
residential facilities/or homes for the aged/or nursing homes/(47,896)
-
‘residential care’.ab,ti. (3754)
-
‘care home*’.ab,ti. (4721)
-
‘nursing home*’.ab,ti. (32,554)
-
Assisted Living Facilities/(1528)
-
‘assisted living’.ab,ti. (2410)
-
‘extra care housing’.ab,ti. (16)
-
or/1–7 (65,730)
-
exp *aged/or exp *geriatrics/or exp *geriatric nursing/or (centarian* or centenarian* or elder* or eldest or frail* or geriatri* or nonagenarian* or octagenarian* or octogenarian* or old age* or older adult* or older age* or older female* or older male* or older man or older men or older patient* or older people or older person* or older population or older subject* or older woman or older women or oldest old* or senior* or senium or septuagenarian* or supercentenarian* or very old*).ti,kf. (306,918)
-
8 or 9 (355,492)
-
Patient Admission/(25,826)
-
(unplanned adj3 (admission* or hospital*)).ab,ti. (2672)
-
(avoidable adj3 (admission* or hospital*)).ab,ti. (947)
-
‘community geriatric* service*’.ab,ti. (8)
-
Case Management/(10,401)
-
‘case management’.ab,ti. (11,442)
-
(discharg* adj3 plan*).ab,ti. (5382)
-
‘Delivery of Health Care, Integrated’/(13,761)
-
(integrated adj3 (working or care)).ab,ti. (12,152)
-
Delirium/pc (Prevention and Control) (1248)
-
(prevent* adj3 deliri*).ab,ti. (1173)
-
[(medicine* or medication*) adj3 (manag* or monitor* or review*)].ab,ti. (25,092)
-
Terminal Care/(30,296)
-
‘terminal care’.ab,ti. (1553)
-
‘end of life care*’.ab,ti. (10,925)
-
care, end-of-life.ab,ti. (128)
-
eol.ab,ti. (2217)
-
Advance Care Planning/(3619)
-
‘advance care planning’.ab,ti. (3566)
-
Fluid Therapy/(21,238)
-
(hydration adj3 nutrition).ab,ti. (1154)
-
(‘non convey*’ or nonconvey*).ab,kw,ti. (52)
-
‘specialist paramedic*’.ab,ti. (8)
-
(paramedic* adj3 assess*).ab,ti. (196)
-
‘training course* ’.ab,ti. (5569)
-
[(vocational or educational) adj qualification*].ab,ti. (804)
-
‘hydration and nutrition’.ab,ti. (232)
-
‘geriatric* specialist’.ab,ti. (40)
-
Vaccination/(90,966)
-
[(influenza* or flu*) adj3 vaccin*].ab,ti. (26,583)
-
covid-19 vaccines/or influenza vaccines/ (32,036)
-
[(covid* or corona* or ‘SARS CoV 2’) adj3 vaccin*].ab,ti. (11,950)
-
Pneumococcal Vaccines/(8162)
-
‘pneumo* vaccine*’.ab,ti. (4107)
-
Oxygen Inhalation Therapy/(15,411)
-
(oxygen adj1 therap*).ab,ti. (12,517)
-
or/11–46 (320,076)
-
10 and 47 (16,212)
-
letter/(1,162,749)
-
editorial/(589,748)
-
news/(210,552)
-
exp historical article/(406,561)
-
anecdotes as topic/(4746)
-
comment/(942,690)
-
case report/(2,232,728)
-
(letter or comment*).ti. (172,085)
-
or/49–56 (4,669,568)
-
randomized controlled trial/or random*.ti,ab. (1,404,034)
-
57 not 58 (4,640,014)
-
animals/not humans/(4,896,931)
-
exp animals, laboratory/(924,650)
-
exp animal experimentation/(9971)
-
exp models, animal/(613,504)
-
exp rodentia/(3,391,961)
-
(rat or rats or mouse or mice).ti. (1,384,553)
-
or/59–65 (10,383,418)
-
48 not 66 (14,900)
-
afghanistan/or africa/or africa, northern/or africa, central/or africa, eastern/or ‘africa south of the sahara’/or africa, southern/or africa, western/or albania/or algeria/or andorra/or angola/or ‘antigua and barbuda’/or argentina/or armenia/or azerbaijan/or bahamas/or bahrain/or bangladesh/or barbados/or belize/or benin/or bhutan/or bolivia/or borneo/or ‘bosnia and herzegovina’/or botswana/or brazil/or brunei/or bulgaria/or burkina faso/or burundi/or cabo verde/or cambodia/or cameroon/or central african republic/or chad/or exp china/or comoros/or congo/or cote d’ivoire/or croatia/or cuba/or ‘democratic republic of the congo’/or cyprus/or djibouti/or dominica/or dominican republic/or ecuador/or egypt/or el salvador/or equatorial guinea/or eritrea/or eswatini/or ethiopia/or fiji/or gabon/ or gambia/ or ‘georgia (republic)’/ or ghana/ or grenada/ or guatemala/ or guinea/ or guinea-bissau/ or guyana/ or haiti/ or honduras/ or independent state of samoa/ or exp india/ or indian ocean islands/ or indochina/ or indonesia/ or iran/ or iraq/ or jamaica/ or jordan/ or kazakhstan/ or kenya/ or kosovo/ or kuwait/ or kyrgyzstan/ or laos/ or lebanon/ or liechtenstein/ or lesotho/ or liberia/ or libya/ or madagascar/ or malaysia/ or malawi/ or mali/ or malta/ or mauritania/ or mauritius/ or mekong valley/ or melanesia/ or micronesia/ or monaco/ or mongolia/ or montenegro/ or morocco/ or mozambique/ or myanmar/ or namibia/ or nepal/ or nicaragua/ or niger/ or nigeria/ or oman/ or pakistan or palau/or exp panama/or papua new guinea/or paraguay/or peru/or philippines/or qatar/or ‘republic of belarus’/or ‘republic of north macedonia’/or romania/or exp russia/or rwanda/or ‘saint kitts and nevis’/or saint lucia/or ‘saint vincent and the grenadines’/or ‘sao tome and principe’/or saudi arabia/or serbia/or sierra leone/or senegal/or seychelles/or singapore/or somalia/or south africa/or south sudan/or sri lanka/or sudan/or suriname/or syria/or taiwan/or tajikistan/or tanzania/or thailand/or timor-leste/or togo/or tonga/or ‘trinidad and tobago’/or tunisia/or turkmenistan/or uganda/or ukraine/or united arab emirates/or uruguay/or uzbekistan/or vanuatu/or venezuela/or vietnam/or west indies/or yemen/or zambia/or zimbabwe/(1,186,145)
-
‘Organisation for Economic Co-Operation and Development’/(404)
-
australasia/or exp australia/or austria/or baltic states/or belgium/or exp canada/or chile/or colombia/or costa rica/or czech republic/or exp denmark/or estonia/or europe/or finland/or exp france/or exp germany/or greece/or hungary/or iceland/or ireland/or israel/or exp italy/or exp japan/or korea/or latvia/or lithuania/or luxembourg/or mexico/or netherlands/or new zealand/or north america/or exp norway/or poland/or portugal/or exp ‘republic of korea’/or ‘scandinavian and nordic countries’/or slovakia/or slovenia/or spain/or sweden/or switzerland/or turkey/or exp united kingdom/or exp united states/(3,363,943)
-
European Union/(17,009)
-
Developed Countries/(21,011)
-
69 or 70 or 71 or 72 (3,379,076)
-
68 not 73 (1,099,831)
-
67 not 74 (14,273)
-
limit 75 to english language (12,989)
-
limit 76 to year=‘2014–Current’ (6385)
MEDLINE extra falls search
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review and Other Non-Indexed Citations and Daily <1946 to 14 January 2022>
Search strategy:
-
residential facilities/or homes for the aged/or nursing homes/(48,006)
-
‘residential care’.ab,ti. (3775)
-
‘care home*’.ab,ti. (4774)
-
‘nursing home*’.ab,ti. (32,705)
-
Assisted Living Facilities/(1531)
-
‘assisted living’.ab,ti. (2433)
-
‘extra care housing’.ab,ti. (16)
-
or/1–7 (65,979)
-
exp *aged/or exp *geriatrics/or exp *geriatric nursing/or (centarian* or centenarian* or elder* or eldest or frail* or geriatri* or nonagenarian* or octagenarian* or octogenarian* or old age* or older adult* or older age* or older female* or older male* or older man or older men or older patient* or older people or older person* or older population or older subject* or older woman or older women or oldest old* or senior* or senium or septuagenarian* or supercentenarian* or very old*).ti,kf. (308,664)
-
8 or 9 (357,423)
-
Patient Admission/(25,879)
-
[unplanned adj3 (admission* or hospital*)].ab,ti. (2699)
-
[avoidable adj3 (admission* or hospital*)].ab,ti. (954)
-
‘community geriatric* service*’.ab,ti. (8)
-
Case Management/(10,408)
-
‘case management’.ab,ti. (11,481)
-
(discharg* adj3 plan*).ab,ti. (5413)
-
‘Delivery of Health Care, Integrated’/(13,793)
-
[integrated adj3 (working or care)].ab,ti. (12,255)
-
Delirium/pc (Prevention and Control) (1261)
-
(prevent* adj3 deliri*).ab,ti. (1192)
-
[(medicine* or medication*) adj3 (manag* or monitor* or review*)].ab,ti. (25,285)
-
Terminal Care/(30,376)
-
‘terminal care’.ab,ti. (1556)
-
‘end of life care*’.ab,ti. (10,999)
-
care, end-of-life.ab,ti. (129)
-
eol.ab,ti. (2238)
-
Advance Care Planning/(3646)
-
‘advance care planning’.ab,ti. (3612)
-
Fluid Therapy/(21,285)
-
(hydration adj3 nutrition).ab,ti. (1161)
-
(‘non convey*’ or nonconvey*).ab,kw,ti. (53)
-
‘specialist paramedic*’.ab,ti. (8)
-
(paramedic* adj3 assess*).ab,ti. (197)
-
‘training course* ’.ab,ti. (5611)
-
[(vocational or educational) adj qualification*].ab,ti. (810)
-
‘hydration and nutrition’.ab,ti. (235)
-
‘geriatric* specialist’.ab,ti. (39)
-
Vaccination/(91,649)
-
[(influenza* or flu*) adj3 vaccin*].ab,ti. (26,718)
-
covid-19 vaccines/or influenza vaccines/(32,861)
-
[(covid* or corona* or ‘SARS CoV 2’) adj3 vaccin*].ab,ti. (13,156)
-
Pneumococcal Vaccines/(8196)
-
‘pneumo* vaccine*’.ab,ti. (4126)
-
Oxygen Inhalation Therapy/(15,473)
-
(oxygen adj1 therap*).ab,ti. (12,610)
-
or/11–46 (322,683)
-
10 and 47 (16,328)
-
letter/(1,166,322)
-
editorial/(592,842)
-
news/(210,646)
-
exp historical article/(407,003)
-
anecdotes as topic/(4746)
-
comment/(947,871)
-
ase report/(2,239,554)
-
(letter or comment*).ti. (173,104)
-
or/49–56 (4,685,317)
-
randomized controlled trial/or random*.ti,ab. (1,411,760)
-
57 not 58 (4,655,618)
-
animals/not humans/(4,909,832)
-
exp animals, laboratory/(928,170)
-
exp animal experimentation/(10,021)
-
exp models, animal/(616,756)
-
exp rodentia/(3,403,886)
-
(rat or rats or mouse or mice).ti. (1,387,516)
-
or/59–65 (10,416,012)
-
48 not 66 (15,012)
-
afghanistan/or africa/or africa, northern/or africa, central/or africa, eastern/or ‘africa south of the sahara’/or africa, southern/or africa, western/or albania/or algeria/or andorra/or angola/or ‘antigua and barbuda’/or argentina/or armenia/or azerbaijan/or bahamas/or bahrain/or bangladesh/or barbados/or belize/or benin/or bhutan/or bolivia/or borneo/or ‘bosnia and herzegovina’/or botswana/or brazil/or brunei/or bulgaria/or burkina faso/or burundi/or cabo verde/or cambodia/or cameroon/or central african republic/or chad/or exp china/or comoros/or congo/or cote d’ivoire/or croatia/or cuba/or ‘democratic republic of the congo’/or cyprus/or djibouti/or dominica/or dominican republic/or ecuador/or egypt/or el salvador/or equatorial guinea/or eritrea/or eswatini/or ethiopia/or fiji/or gabon/or gambia/or ‘georgia (republic)’ /or ghana/or grenada/or guatemala/or guinea/or guinea-bissau/or guyana/or haiti/or honduras/or independent state of samoa/or exp india/or indian ocean islands/or indochina/or indonesia/or iran/or iraq/or jamaica/or jordan/or kazakhstan/or kenya/or kosovo/or kuwait/or kyrgyzstan/or laos/or lebanon/or liechtenstein/or lesotho/or liberia/or libya/or madagascar/or malaysia/or malawi/or mali/or malta/or mauritania/or mauritius/or mekong valley/or melanesia/or micronesia/or monaco/or mongolia/or montenegro/or morocco/or mozambique/or myanmar/or namibia/or nepal/or nicaragua/or niger/or nigeria/or oman/or pakistan/or palau/or exp panama/or papua new guinea/or paraguay/or peru/or philippines/or qatar/or ‘republic of belarus’/or ‘republic of north macedonia’/or romania/or exp russia/or rwanda/or ‘saint kitts and nevis’/or saint lucia/or ‘saint vincent and the grenadines’/or ‘sao tome and principe’/or saudi arabia/or serbia/or sierra leone/or senegal/or seychelles/or singapore/or somalia/or south africa/or south sudan/or sri lanka/or sudan/or suriname/or syria/or taiwan/or tajikistan/or tanzania/or thailand/or timor-leste/or togo/or tonga/or ‘trinidad and tobago’/or tunisia/or turkmenistan/or uganda/or ukraine/or united arab emirates/or uruguay/or uzbekistan/or vanuatu/or venezuela/or vietnam/or west indies/or yemen/or zambia/or zimbabwe/(1,192,175)
-
‘Organisation for Economic Co-Operation and Development’/(411)
-
australasia/or exp australia/or austria/or baltic states/or belgium/or exp canada/or chile/or colombia/or costa rica/or czech republic/or exp denmark/or estonia/or europe/or finland/or exp france/or exp germany/or greece/or hungary/or iceland/or ireland/or israel/or exp italy/or exp japan/or korea/or latvia/or lithuania/or luxembourg/or mexico/or netherlands/or new zealand/or north america/or exp norway/or poland/or portugal/or exp ‘republic of korea’/or ‘scandinavian and nordic countries’/or slovakia/or slovenia/or spain/or sweden/or switzerland/or turkey/or exp united kingdom/or exp united states/(3,372,732)
-
European Union/(17,054)
-
Developed Countries/(21,036)
-
69 or 70 or 71 or 72 (3,387,922)
-
68 not 73 (1,105,653)
-
67 not 74 (14,378)
-
limit 75 to english language (13,092)
-
limit 76 to year=‘2014–Current’ (6488)
-
Accidental Falls/pc (Prevention and Control) (10,120)
-
[fall* adj3 (prevent* or avoid* or manag* or intervention* or project* or program*)].ab,ti. (10,401)
-
78 or 79 (16,211)
-
8 and 80 (1071)
-
81 not 66 (1016)
-
82 not 74 (980)
-
limit 83 to english language (869)
-
limit 84 to year=‘2014–Current’ (333)
-
hospitalization/or patient admission/(147,809)
-
hospitali?ation.ab,ti. (160,421)
-
12 or 13 or 86 or 87 (267,445)
-
85 and 88 (33)
-
89 not 77 (21)
Appendix 2 Additional tables for Chapter 2 (UK evidence)
| Short title | Reference | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|---|
| Damery et al. | Damery et al.19 | Staff involved: 2 full-time facilitators working with care home staff | Safer Provision and Caring Excellence programme. QI intervention with 3 linked components: training in QI methods; use of QI tools to track trends in avoidable harms; and regular manager forums, ‘celebrating success’ events and newsletters | Care home | One-to-one coaching, small groups and larger training workshops | 24-month programme (December 2016 to December 2018); 8 half/full day shared learning events; monthly training on specific topics |
| Giebel et al. | Giebel et al.20 | Community matrons responsible for specific care homes; care home staff; MDT care team including district nurses, palliative care nurses, urgent care teams, community geriatricians and medicines management; televideo advanced nurse practitioner | Programme based on QI principles with the inclusion of ‘plan, do, study, act’ cycles. Community matron responsible for reactive care and ACP; televideo system providing access to clinical advice; 13 Care Home Innovation Programme protocols for initial management of common presentations; training of care home staff; monthly newsletter; bimonthly workstream meetings and quarterly collaborative meetings to update on progress and share good practice | Participating care homes | Community matron service 9 a.m. to 5 p.m. on weekdays; televideo service available 24 hours/7 days; regular meetings and newsletters (see above); one-off training for care home staff | One-off assessment by care manager and staff training session; regular meetings and newsletter (see above); other components as required over 4 years |
| Steel et al. | Steel et al.21 | MDT including senior and trainee GPs, trainees in geriatrics, psychiatry, pharmacist and residential home senior staff | MDT reviews for residents identified as needing attention: preparation; prereview MDT meeting; patient review, including comprehensive geriatric assessment; post-evaluation MDT discussion; educational session; follow-up by GP and psychiatry trainee (where required) | Participating residential homes | Not applicable | Monthly sessions conducted over 2 cycles |
| Reference | Barriers | Facilitators | Active facilitation |
|---|---|---|---|
| Damery et al.19 | Evidence: existing evidence of high workloads, high rates of staff turnover and difficulty recruiting and retaining competent staff. | Evidence: supports association between a positive safety culture and improved outcomes/reduced risk of harm. A previous study in south-east England found that QI training improved knowledge and awareness of resident safety and reduced harms in some homes | ‘Passionate facilitators with an in-depth understanding of issues within the care home sector, who tailored programme support accordingly’ were identified as key to success of the SPACE intervention. In addition to training events, facilitators visited each home to give ad hoc support and one-to-one QI coaching |
| Context: some managers and staff initially feared SPACE would increase bureaucracy and workloads. Programme depended on support of individual managers and ten homes changed manager at least once during the study. Annual staff turnover averaged 31% (range 9.6% to 78.3%). Engagement of individual homes also varied, with a small number showing minimal participation throughout. High staff turnover was also a potential barrier to sustaining the intervention. | Context: programme gave high priority to workforce development and highlighted opportunities for career progression | ||
| Giebel et al.20 | Evidence: not reported | Evidence: US study found QI intervention reduced ED attendance by 17%. Routine data on 999 calls, ED attendances and use of televideo system were available as part of contract with providers | Quarterly collaborative meetings for participating homes were considered vital for team building and promoting joined up working for a shared vision |
| Context: high turnover of care home managers and staff required new staff to be trained and training repeated. Other challenges included cultural differences between homes and lack of contractual levers | Context: NHS Long Term Plan (2019) prioritised measures to reduce hospital admissions in older people and to strengthen NHS support for care homes. The baseline standard (CQC rating) of participating homes was ‘good’ in 56%, ‘required improvement’ in 44%, and one home was graded ‘inadequate’ | ||
| Steel et al.21 | Evidence: not reported | Evidence as facilitator Details Project was underpinned by the EHCH implementation framework |
Limited details reported; a GP trainee took the lead role for the second cycle to encourage trainee leadership |
| Context: care home where cycle 2 took place was rated ‘inadequate’ by CQC (December 2018) | Context: integrated health care for older people identified as a key NHS priority in the Long Term Plan and 5-year Forward View |
| Reference | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| Brine et al.46 | Dementia outreach team; care home nursing team (community nurses, advanced nurse practitioners and support workers, working closely with geriatricians); Age UK Nottingham and Nottinghamshire Advocacy; GPs | Specialist input and training around dementia; case management of residents with dementia; nursing support to residential homes and nursing homes where required; advocacy support for residents and families; linking specific GP practices to care homes and providing an enhanced level of support | Participating care homes | Not reported | Not applicable |
| Conti et al.47 | Staff from partner organisations: Sutton CCG (GPs); community services; the local hospital trust; the London Ambulance Service and London Borough of Sutton (care home staff) | Pillar 1 (improving integrated care): weekly health and well-being rounds; multidisciplinary care home support team; and hospital transfer pathway; pillar 2 (supporting care home staff): tailored e-learning; resource package; and care home forum; pillar 3 (supporting quality assurance and safety): joint intelligence group with all partners represented; quality dashboard; and initiative to foster engagement with residents, carers and families | Participating care homes and local hospitals | Some interventions were available to all Sutton care homes (e.g. educational resources and the Care Home Forum). Overall, the focus of the vanguard from November 2015 to July 2016 was on NHs. Attention shifted to residential homes in November 2016 | Frequency and availability of different elements varied during the study period |
| Lloyd et al.49 | Community interest company (Principia) involving a partnership of general practices, community services and patients in Rushcliffe (Nottinghamshire) with support from the local CCG | Enhanced specification of GP care involving aligning care homes with specific practices. Includes review of new residents, comprehensive geriatric assessment within 2 weeks and regular GP visits to the home. Advocacy and independent support delivered by Age UK Notts and supported by volunteers Improved community nursing support, including peer-to-peer support and training for care home nurses Engagement with care home managers | Participating care homes | Not reported | Varied between elements, for example GP visits to care homes could be weekly or fortnightly |
| Sherlaw-Johnson et al.51 | MDT, including GPs, specialist doctors, nurses, physiotherapists, occupational therapists, pharmacists, key workers and social workers | Geriatrician available to support GPs and families; comprehensive medication reviews; named clinician and key workers for each nursing home; support for providing end-of-life care; ward rounds with advice and training for nursing home staff; assessment of acute problems by Health 1000 staff in the nursing home | Participating nursing homes | Advice available 8 a.m. to 8 p.m., 7 days per week | Frequency of particular elements not reported |
| Vestesson et al.53 | Representatives of voluntary organisations; MDT comprising professionals from areas including mental health, physiotherapy and nursing; GPs from 26 practices with patients living in Vanguard care homes | Voluntary sector: activities outside and inside care homes; signposting to services for residents identified as requiring extra help MDT: screening process to identify residents at risk of admission; falls risk assessments; training sessions for care home staff. Primary care: ‘1 GP practice, 1 care home’ model with associated key performance indicators | Participating care homes and local community services | MDT delivered 49 training sessions to 286 care home staff. MDT planned to screen all residents for unmet needs but from April 2016 this was limited to residents considered high risk by care home staff | MDT met weekly; frequency of GP visits varied between care homes and was largely based on the practice’s relationship with the care home and the Vanguard |
| Reference | Barriers | Facilitators | Active facilitation |
|---|---|---|---|
| Brine et al.46 | Evidence : not reported | Evidence: not reported | Not reported |
| Context: elements of the intervention were not implemented consistently across the CCG area, for example the nursing team did not cover the whole area until 2017. With regard to GP support, some GPs did not want to take on all residents in a care home and some residents were unwilling to change their GP | Context: Nottingham City CCG supported initiatives to enhance health of care home residents since 2007; EHCH vanguard formed in 2015 | ||
| Conti et al.47 | Evidence: not reported | Evidence: not reported | Not reported |
| Context: not reported | Context: homes of care vanguard built on initiatives developed by the partner organisations that were already in place | ||
| Lloyd et al.49 | Evidence: not reported | Evidence: not reported | Not reported |
| Context: not reported | Context: from April 2015, Principia was chosen as a vanguard site for the New Care Models programme that followed from the NHS 5-year Forward View area with relatively low baseline levels of admissions and socioeconomic deprivation | ||
| Sherlaw-Johnson et al.51 | Evidence: not reported | Evidence: model of care based on Wagner’s chronic care model | Authors state that ‘Health 1000 has been driven forward by a group of committed individuals’ in the organisations involved and emphasise the importance of ‘strong leadership and clear vision’ |
| Context: nursing homes were in ‘geographically difficult’ locations and unable to be aligned with a single general practice. Nursing homes were privately owned and had their own procedures which sometimes conflicted with the Health 1000 approach | Context: mutual trust between GPs and nursing home staff locally was cited as an important element in success. Communication between Health 1000 and nursing home managers was emphasised throughout. High staff turnover and instability among care home providers were not identified as issues locally. Development of Health 1000 was supported by the Prime Minister’s Challenge Fund | ||
| Vestesson et al.53 | Evidence: not reported | Evidence: not reported | Not reported |
| Context: ‘1 GP practice, 1 care home’ model was not implemented during the study period | Context: EHCH Vanguard formed in March 2015 to pilot new care model announced in the NHS 5-year Forward View |
| Short title | Reference | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|---|
| Armstrong et al. | Armstrong et al.82 | 1 trainer delivered all the sessions. Research team (UCL partners staff and Medicus Health partners clinicians) involved throughout, helped with data collection, analysis and generating change ideas | Education programme: topics covered deterioration recognition, care of the dying, falls, UTIs and strokes; programme delivery flexible – some care homes opted for frequent, short sessions and others requested periodic, all-day training | 4 care homes in Enfield London receiving clinical care from Medicus Health partner | Year-long programme. Programme delivery flexible (see above) | One-off programme over 1 year with evaluation at 3-, 6-, 9- and 12-month points, following evaluations change ideas were generated for the next cycle |
| Sheaff et al. | Sheaff et al.84 | NHS dementia nurse specialists, care home staff | Training programme on dementia. Introduction of dementia learning community – identification of dementia champion by dementia learning facilitators. Dementia champion and care home staff trained in dementia awareness and conducting ‘plan, do, study, act’ cycles. Dementia learning facilitators then worked with champions | Participating homes | 8-hour multimodule training programme; learning visitors regularly visit champion and also use teleconferences, awards, newsletters, etc. | ‘Plan, do, study, act’ cycles determine by champion; monthly awards; annual conference |
| Siddiqi et al. | Siddiqi et al.83 | Specialist delirium practitioner (mental health nurse with expertise in delirium); delirium champion from each home | Stop Delirium! intervention – a multifaceted enhanced educational package incorporating multiple strategies to change practice delivered to each care home over 16 months. Specialist delirium practitioner delivered education sessions. Facilitated working groups of care home staff, groups identified targets around delirium prevention and developed solutions for their care home. Delirium champion from care home staff was training by practitioner. Each home had delirium box of resources to support learning | Care homes | 3 education sessions | Not provided |
| Reference | Barriers | Facilitators | Active facilitation |
|---|---|---|---|
| Armstrong et al.82 | Evidence: barriers included competing priorities on time; shift work; low attendance rates. Evening sessions good way to offer flexible delivery but limited by professionals time. High staff turnover in social care sector made it difficult to train all staff. | Evidence: flexible delivery approach – evening sessions, webinars, podcasts; activity-based curriculum, alignment topics with admission data, embedding key messages in each tutorial | Nominating teaching monitor and developing individualised learning plans encouraged care homes to take ownership. Reminder phone calls and emails prior to teaching encouraged participation |
| Context: different perception of value of teaching; internal communication systems within care home; no IT facilities for virtual meetings; instability of management | Context : stability of management; communication systems IT facilities enabling virtual meetings | ||
| Sheaff et al.84 | Evidence: our results also expose the challenging case mix, low quality of care and organisational instability of some care homes in the locality studied | Evidence: government had recently set targets for dementia training | Dementia learning facilitators supported and worked with ‘dementia champions’ in each home. Dementia champions identified by care home managers, apart from 2 who took on role themselves |
| Context: not reported | Context: all study homes privately owned; homes volunteered to participate, DLC introduced at control homes after evaluation DLC homes with high well- and ill-being scores were generally bigger and had higher staffing ratio. | ||
| Siddiqi et al.83 | Evidence: summary home-level data for hospital admissions (obtained from care homes) were missing for 2 homes, and rates were lower than estimated from other sources. Recording of falls differed markedly with some homes recording any instances where a resident was found on the floor as a fall, and others limiting recording to observed falls only; falls data were not, therefore, analysed further | Evidence: not reported | Specialist delirium practitioner delivered training and facilitated working groups. Working groups consisted of care home staff who set targets and decided on solutions that suited their home. Delirium champions in each home. Overall, 84.4% of staff completed at least 1 education session; in 4 homes, over 90% of staff completed all 3 sessions. Working groups were established in all homes. Delivery of the intervention was compromised in the later part of the study due to first sickness absence and then maternity leave of the delirium practitioner (9 of 22 months) |
| Context: only two-thirds of hearing tests were conducted due to lack of appropriate space in the care home. Resident-level data collection diaries were found not to be feasible for completion by residents and too burdensome for staff. Care-home-level diaries were also only partially completed by staff due to time pressures. It was uncommon for friends and family members to be either present to complete proxy forms or to have spent sufficient time observing the resident to be able to comment | Context: delirium champion identified in 4 homes, and evidence of outputs from working groups being used in 5 of the 7 homes | ||
| SQW Ltd52 | Evidence: not reported | Evidence: intervention components (e.g. health and well being rounds) based on evidence of what works elsewhere | Sutton Homes of Care Vanguard had a steering group on which a wide range of NHS, social care and voluntary sector organisations were represented. Programme staff included a programme director and project manager, with funding for communications, administrative support and a GP clinical lead. NHS England awarded £250,000 later in the year (2016/17) to facilitate the spread of the Vanguard |
| Context: challenges included ensuring that care home staff had time for training and attending events, and communicating with care homes where staff lacked IT literacy. E-learning was less valued than expected (staff preferred face-to-face training). Some staff were unfamiliar with the link nurse role, suggesting resources may have been too thinly spread | Context: some intervention elements already existed in some form, including the Joint Intelligence Group, the Care Home Forums, the link and Supportive Care Home Team nurses, and the provision of educational resources. Initial groundwork that laid the foundations for subsequent developments was done by a small group of senior staff, with personal interest and a high level of commitment to improving the quality of care for Sutton’s care home residents |
Appendix 3 Additional tables for Chapter 3 (international evidence)
| Reference | By whom | What | Where | To what intensity | How often |
|---|---|---|---|---|---|
| Brickman et al.75 | MDT of physician specialists (emergency care, wound care, vascular, infectious disease, cardiology, physiatry, psychiatry, etc.), and APPs (e.g. nurse practitioners, physician assistants); trained nursing home staff | Protocols for managing common problems within the care home where appropriate; training of care home nursing staff; access to an ED physician and APP for advice; MDT evaluations of residents’ health; nursing coordinator to supervise the MDT and initial acute care management | Care home | Access to advice 24 hours/day | Resident evaluation weekly and on acute care visits |
| Grabowski et al.73 | Telemedicine call centre staffed by a medical secretary and three providers: a registered nurse, a nurse practitioner, and a physician. Calls were triaged by the medical secretary to the appropriate provider | Intervention homes had a cart with equipment for two- way videoconferencing and a high-resolution camera for use in wound care. When a nursing home resident had an off-hours medical problem, a staff member brought the cart into the resident’s room and contacted the telemedicine service | Nursing home | Telemedicine service operated evenings (5–11 p.m.) and weekends (10 a.m. to 7 p.m.) | Not applicable |
| Hofmeyer et al.74 | Advanced practice providers and registered nurses based at central hub, plus director of electronic long-term care and service line manager | Two-way video and peripherals allowing real-time consultation between care home staff and residents and on-call specialists. Specialist equipment included a two-way stethoscope and high-definition camera | Rural long-term care homes in USA (mainly South Dakota) | Service available 24/7 | As required; facilities involved in this pilot study had an average of 23 electronic long-term care consultations per site per year |
| Stadler et al.76 | Physicians, nurse practitioner, physician’s assistant, social worker, nurse | Reducing avoidable facility transfers comprises following elements: (1) longitudinal care and after-hours calls managed by small team of providers; (2) ACP became standard practice in SNFs; (3) increased engagement of provider during acute care events; (4) case review of hospital transfers | Participating SNFs | Small team providers managed all care, with at least 1 of team on site every business day, and after-hours calls. ACP became standard practice for SNFs. Nursing staff received education session on engaging provider early. Case review of most recent of most recent hospital transfers | Nursing staff received one education 1 on engaging provider early. Case review took place monthly for 1 hour and discussed approximately 15–20 cases |
| Reference | By whom | How often | To what intensity | Where | What |
|---|---|---|---|---|---|
| Resnick et al.87 | Research nurse facilitator; champion from staff in assisted living facilities; stakeholder team | Monthly visits from research nurse facilitator for 12 months; weekly emails | Research nurse facilitator visited each facility monthly for 2 hours. Weekly tidbits (function focused care webpage, 2014) were sent via e-mail to all stakeholder team members to provide new updates relevant to physical activity, innovative approaches to increase function and physical activity among residents, and opportunities to participate in contests either within the setting or between settings (e.g. best approach to engage residents in physical activity during Valentine’s day) | Assisted living facilities | Step I: environment and policy assessments; step II: education; step III: establishing resident function focused care service plans; step IV: mentoring and motivating |
| Romoren et al.86 | 2 skilled nurses trained all health workers in nursing homes | Once, after completing the training programme the nursing homes then had competencies to provide intravenous treatment locally | 1 day | Nursing homes | Educational programme included theory and practical training in intravenous treatment of dehydration and infection |
| Reference | Elements of intervention/initiative | Features of workforce | Features of services | Systems leadership | Financial and commissioning processes | Features of organisations | Patients and populations |
|---|---|---|---|---|---|---|---|
| Resnick et al.87 | Evidence of treatment fidelity based on delivery with a mean of 11.00 (SD 2.13) stakeholder meetings completed, education of 965 staff provided across all settings with a mean of 88% correct on the knowledge test, completion of policy and environment assessments in all settings, and mentoring and motivation activities were provided based on interventionist documentation (e.g. observations and positive feedback and verbal encouragement provided, contests provided) | Despite the many benefits associated with implementation of function-focused care, assisted living staff express concerns that engaging residents in function and physical activity will increase the risk of falling and subsequent transfers to the hospital setting | There may have been differences in regulatory issues or policies within settings that influenced transfers, such as caring for patients on hospice. Despite the high rate of falls in these settings, only about 50% of assisted living settings report having a plan for how falls are evaluated and/or prevented | FFC-AL-EIT used a four-step approach to implementation and included having a research nurse facilitator work with a champion identified by the setting and a stakeholder team (includes administrative and clinical staff that could affect or be affected by the intervention being implemented) | Patients on hospice. These could be considered in future work. At the time of this study, Maryland and Massachusetts were noted to have some Medicaid coverage for assisted living for eligible residents although Pennsylvania did not. Some Pennsylvania settings, however, allowed residents to pay for their stay in assisted living based on their full social security income (Eldercare Financial Assistance Locator, 2020). These differences may have influenced findings | Assisted living facilities similar in UK | Study was limited due to inclusion of a relatively homogenous sample of white residents from only 3 states and 85 settings |
| Romoren et al.86 | Over 90% of the health personnel (nurses and nursing assistants) in the 30 nursing homes received the intervention. Feedback during the training, follow-up meetings and evaluations. was positive. Among advantages described, patients were treated in surroundings and by personnel familiar to them, by personnel knowing them well; and the general phrase: ‘That hospitalization was avoided’. Among disadvantages described were practical difficulties with placing and keeping the PVC and confrontation with ethical dilemmas with end-of-life treatment. As a solution to the former, the ambulance service offered to assist in the practical problems with the PVC when necessary. All nursing homes were actively planning to continue providing intravenous treatment in the future | Mean man-years for nurses in the nursing homes was 14.1 (range 3.5–40.2), mean man-years for nursing assistants were 26.2 (range 5–105) | The local hospital and the Teaching nursing home in Vestfold County, Norway, decided to conduct and evaluate an intervention to increase the competence in administrating intravenous fluids and antibiotics in all nursing homes in the county. | In each of the nursing homes as well as in each hospital department, 1 or several nurses served as primary contact for the study team. These were responsible for including and registering information about the patients receiving intravenous treatment in standardised data collection forms. The nursing homes were followed closely by the study team, both regarding the local intravenous treatment and the patient inclusion and data collection. The primary contacts were contacted for a follow-up by telephone on a regular basis. In addition, the study team was available for support to the nursing homes and on e-mail and telephone on a daily basis. The nursing homes received a follow-up visit some months after the intervention, a few were visited several times | Not reported | 30 participating nursing homes had 12–124 beds (median 41), in total 1379 beds. They had one to eight departments, and either one type of beds or a combination of beds: for rehabilitation, short-term and long-term care, palliative care and special departments for patients with dementia | Study nursing homes were the vast majority of public and private nursing homes in 1 county, and probably without relevant differences from Norwegian nursing homes in general. |
Appendix 4 Risk of bias tables
| Reference | Questiona | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
| Boyd et al.41 | Unclear; method of randomisation not reported | Unclear | Unclear; residents similar for age but other characteristics not reported | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes; authors discuss design limitations of the study |
| Connolly et al.41 | Yes | Unclear | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Downs et al.87 | Yes | Yes | Yes | No | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes; cluster RCT justified |
| Forbat et al.126 | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes; cluster RCT justified |
| Frankenthal et al.98 | Yes | No | Yes | No | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Grabowski et al.73 | Unclear; states ‘we randomly assigned...’. but no information on how the process | Unclear; no information but would all get intervention eventually so less relevant? | Unclear; as a result, the two groups were relatively equal in terms of their overall five-star ratings. Compared with the control facilities, the treatment facilities were larger but they had fewer admissions per bed. Staffing levels of nurses and nurse aides in the two groups were relatively similar | Not applicable | Not applicable | Unclear | Yes | Yes | Yes | Yes | Unclear; nursing home billing data used to record hospitalisations did not provide time of resident’s transfer to hospital, nor did billing data include ED visits, which might also be influenced by use of telemedicine. Unfortunately, billing data also did not allow us to distinguish between hospitalisations for short-stay residents and those for long-stay residents | Yes | Yes |
| Gravenstein et al.92 | Yes | Yes | Yes | Unclear | No; open label vaccines supplied | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes; cluster randomisation and use of Medicare data justified |
| Haines et al.59 | Yes; random number | Yes | Unclear; limited resident data | No | No | No | Unclear | Unclear; lack of resident data | Yes; intention-to-treat | Yes | Yes | Yes | Yes; step-wedge cluster design and analysis justified |
| Honinx et al.137 | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Unclear |
| Junius-Walker et al.99 | Yes | Yes | Yes | No | No | No | Yes | Yes; small difference in loss to follow-up between groups | Yes; intention to treat analysis | Yes | Yes | Yes | Yes; cluster design justified |
| Kane et al.27 | Unclear; no details of randomisation reported | Unclear | Yes, applies to nursing home residents | Unclear | No | No | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes; analysis accounted for cluster randomisation |
| Lamppu et al.138 | Yes | Yes | Yes (see Table 1) | Unclear; defines residents as participants | No | Yes; nurses undertaking assessments were blinded | Yes | Yes | Unclear; 16 residents died before intervention complete and were excluded from the analysis | Yes | Yes | Yes | Yes; authors justified cluster randomisation and matching |
| Mackey et al.140 | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Martin et al.117 | Yes | No | Yes | No | No | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes |
| McConeghy et al.93 | Yes; independent statistician | Yes; likely as done independently | Yes; except more African Americans in the trivalent influenza vaccine group | Unclear | Unclear | Not applicable; used Medicare routine data | Yes | Yes | Yes; intention to treat analysis | Yes | Yes | Yes | Yes; authors justified cluster design, etc. |
| Moyo et al.118 | Yes | No | Yes | No | No | No | Unclear | Unclear | Yes | Yes | Yes | Yes | Yes |
| Overbeek et al.121 | Yes | No | Yes | No | No | Unclear | No; education level | Yes | Yes | Yes | Yes | Yes | Yes |
| Resnick et al.87 | Yes | Unclear | Yes | No | No | Yes | Yes | Yes; full flow diagram | Yes; ‘intent-to-treat philosophy’ | Yes | Yes | Yes | Yes; cluster design justified |
| Romoren et al.86 | Yes; randomisation at nursing home level. Randomisation was stratified based on nursing home size and followed 2 computer-based lists, 1 with the 7 large and 1 with the 21 small homes. To get a balanced randomisation, we randomised 3 small homes then 1 large home consecutively | Unclear; randomization list was open to the intervention team, and the 2 nurses who ran the training program cooperated so that each of them included every second nursing home consecutively according to the list | Unclear; patients in the control and intervention groups were similar in most characteristics except a higher proportion of women in the control group; a higher proportion of patients with cancer in the intervention group and a higher proportion of combined pneumonia and urinary tract infection in the control group | Unclear; nursing home staff knew if in intervention groups as had training. Don’t think residents would be aware if nursing home in intervention or control | No | Unclear; nurses assessing patient outcome in hospital could be blind to whether nursing home in intervention or control. Nurses assessing patient outcomes in nursing homes would know if their home was in intervention or control group | Yes | Unclear; not all patients treated locally were included in study and data collection forms were incomplete for a number of patients. We have no reason to believe that patients not included in the study differed from patients included or that the main results could have been altered, but it may have led to an underestimate of the need for intravenous treatment among nursing home patients | Yes | Yes | Yes | Yes | Unclear; original power calculation was for a standard RCT, allowance for the number of steps and allowance for any repeated measures on individuals was not included in this sample size estimate |
| Sampson et al.89 | Yes; independent, computer generated | Yes | Yes (see Table 2) | Unclear; unclear for residents | No | No; ‘not feasible for those collecting data’ | Yes | Yes; analysis included loss to follow-up | Yes | Yes | Yes | Yes; pilot trial so mainly descriptive | Yes; protocol/methods published |
| Siddiqi et al.83 | Yes; independent computer-generated list | Yes, as above | Unclear; ‘There were differences between allocation arms at baseline, with the Stop Delirium! group having a higher proportion of residents who were male, in nursing (as opposed to residential) care, lacking capacity to consent and with a dementia diagnosis’ | No | No | No | Yes | Yes | Unclear | Yes | Yes | Yes | Yes; full protocol available |
| Sluggett et al.100 | Unclear; no details reported | Unclear | Unclear: ‘Residents randomised to the intervention were more likely to be male, have shorter duration of stay in the RACF, and live in a regional area’ | No | No | No; trial was ‘non-blinded’ | Yes | Yes | Yes; ‘constrained longitudinal data analysis’ | Yes | Yes | Yes | Yes; cluster RCT of individual intervention |
| Tappen et al.139 | Yes; computer-generated random numbers | Yes, as question 1 | Yes (see Table 2) | No | No | Unclear | Yes | Yes; similar numbers lost to follow-up | Yes | Yes | Yes | Yes | Yes |
| Temkin-Greener et al.134 | Unclear; not reported | Unclear | Yes | No | No | Unclear | Yes | Unclear | Yes | Yes | Yes | Yes | Yes |
| Reference | Questiona | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| Brickman et al.75 | Yes | Yes; no individual data collected but homes owned by same company and historically similar | Yes; homes owned by same company and historically similar | Yes | No; post intervention only reported | Not applicable; no individual data collected | Yes | Yes | Yes |
| Brine et al.46 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Conti et al.47 | Yes | Unclear; statistical methods used in the evaluation mean that the control group was selected to be as similar to the Sutton residents in the study as possible on a range of demographic, socioeconomic, health and hospital use characteristics. Some of the differences at care home level were not expected to be substantially reduced through matching, since Sutton features a preponderance of small, independent care homes in a largely urban setting relative to the rest of England. These differences included the size, age category and rural classification of the care homes. We were also unable to measure differences relating to the quality of care delivered in care homes or other measures of the care home market, due to lack of data available to the improvement analytics unit. As such, these could not be addressed by the risk adjustment. We did however attempt to minimise the risk of introducing a significant bias by selecting care home residents from multiple areas | Unclear; notwithstanding similarities, it is possible that unmeasured differences may have existed between the Sutton residents in the study and the matched comparison group, for example in the availability of informal care support or local authority funding. It is also possible that there were greater similarities than anticipated in the care provided by some of the care homes included in the control group and those supported by the Sutton Homes of Care vanguard. For example, there may have been enhanced care initiatives being implemented in the comparison care homes. This would have made it harder to discern an effect of theSutton homes of Care vanguard compared with the control | Yes | Yes | Yes | Yes | Yes | Yes |
| Craswell et al.60 | Yes | Yes | Yes | Yes | Not applicable | Yes | Yes | Yes | Yes |
| Dai et al.62 | Yes | Not applicable | Not applicable | No; ITS analysis | Yes | Not applicable | Not applicable | Yes | Yes |
| Fan et al.63 | Yes | Unclear; only includes data for intervention site | Yes | Yes | Yes | Not applicable | Yes | Yes | Yes |
| Hullick et al.68 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Hullick et al.69 | Yes | Yes | Yes | Yes | No; only pre and post overall | Unclear | Yes | Yes; administrative data | Yes |
| Hullick et al.70 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Lloyd et al.49 | Yes | Yes; matched comparison group on care home characteristics and resident characteristics. However, some small differences remained even after matching, and the regression models adjusted for those | Yes | Yes; matched comparison group on care home characteristics and resident characteristics | Unclear | Yes | Yes | Yes | Yes |
| Marsden et al.103 | Yes | Yes | Unclear | No | Yes | Yes | Yes | Yes | Yes |
| Mor et al.95 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Pedersen et al.77 | Yes | Yes | Yes | Yes | No | Yes; drop-out similar between groups | Yes | Yes | Yes; electronic medical records |
| Pedersen et al.78 | Yes | Unclear | Yes | Yes | Not applicable | Yes | Yes | Yes | Yes |
| Sherlaw-Johnson et al.51 | Yes | Unclear; higher rate of dementia in comparator group | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Vestesson et al.53 | Yes | Yes | Yes | Yes; matched control group We ensured that the matched control group was as similar as possible to the vanguard residents in the study on observed characteristics (eg demographic mix, co-morbidities and past hospital activity). Vanguard and control residents may, however, have still differed in unobservable ways (for instance in degree of family support) | No | Yes | Yes | Yes | Yes |
| Furthermore, we did not identify as many care home residents as expected and we are unable to determine whether the missing residents (vanguard and non-vanguard) were different to the residents included the study. This could have affected the results | |||||||||
| Weatherall et al.81 | Yes | Yes; (see Table 1) | Yes | Yes | Yes; national routine data used | Not applicable; use of routinely collected data | Yes | Yes | Yes |
| Zheng et al.135 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Reference | Questiona | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Adekpedjou et al.110 | Yes | Yes | No; < 50% of long-term care home residents included | Yes | No | Not applicable | Yes; do not resuscitate or DNH order | Yes | NA; used administrative data | Yes |
| Carter et al.44 | Yes | Yes | Yes | Yes | No | Not applicable | Not applicable | Yes | No | No |
| Gorisek et al.96 | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Unclear | No |
| Harrison et al.130 | Yes, completed by DC | Yes | No; appears < 50% of NHs surveyed had complete data | Yes, within groups, e.g. advanced dementia | No | Yes; degree of integration | Yes | Yes | Not applicable; routine administrative data used | Yes |
| Hendriks et al.113 | Yes | Yes | Unclear | Yes | No | Not applicable | Not applicable | Yes | No; data from residents’ physicians | Unclear |
| Hickman et al.114 | Yes, completed by DC | Yes | Yes; < 1% opted out of participating | Yes | No | Yes; different levels of ACP | Yes | Yes | No; assessment by study nurses | Yes |
| Kobewka et al.79 | Yes | Yes | Not applicable; study used routine data | Yes; Ontario care home residents | No | Not applicable | Yes | Yes | No | Yes |
| Levy et al.141 | Yes | Yes | Not applicable; routine data used | Yes | No | Not applicable | Not applicable | Yes | Not applicable; routine administrative data used | Yes; matched groups used |
| Miller et al.131 | Yes; added by DC | Yes | Yes; nursing home-level data used | Yes | No | Yes; volume of consultations in different nursing homes | Yes | Yes | Not applicable; administrative data used | Yes |
| Miller et al.132 | Yes | Yes | Yes; administrative data used | Yes | No | No | Not applicable | Yes | Not applicable | Yes |
| Nymberg et al.97 | Yes | Yes | Yes | Yes | No | No | No | Yes | Unclear | No |
| Niznik et al.91 | Yes | Yes | Yes; routine data used | Yes | No | No | Yes | Yes | Not applicable; administrative data used | Yes |
| Pop-Vicas et al.94 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes |
| Reference | Questionsa | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening | Qualitative | Mixed methods | ||||||||||
| S1 | S2 | 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | 5.1 | 5.2 | 5.3 | 5.4 | 5.5 | |
| Alcorn et al.108 | – | – | – | – | – | – | – | Yes | Yes | Yes | Yes; e.g. discussion of how care home staff hoped residents may ‘bounce back’ after hospital treatment but most died after a short stay | Yes; appears well conducted and reported |
| Amador et al.106 | – | – | – | – | – | – | – | Yes | Yes | Yes | Unclear; limited overlap between qualitative and quantitative analyses | Unclear; limited details of qualitative methods |
| Amadoru et al.64 | Yes | Yes | Yes; checked by DC | Yes | Yes | Yes | Yes | – | – | – | – | – |
| Cohen et al.111 | Yes | Yes | Yes | Yes | Yes; supported by quotes | Yes | Yes | – | – | – | – | – |
| Dwyer et al.61 | Yes | Yes | Yes; question is about how to reduce admissions though high-quality care | Yes; interviews with service providers and users | Yes; data analysis theory-based and rigorous | Yes; substantial quotes included | Yes | – | – | – | – | – |
| Harrad-Hyde et al.109 | Yes | Yes | Yes; completed by DC | Yes | Yes | Yes; relevant quotations included | Yes | – | – | – | – | – |
| Ingber et al.26 | Yes | Yes | – | – | – | – | – | Yes; complex intervention being implemented in real-world settings | Yes; paper provides data on both effectiveness and the complexities of implementation | Yes; qualitative data help to explain quantitative results overall and at the state level | Unclear; no obvious inconsistencies but qualitative results reported in less detail | Unclear; qualitative methods not reported in detail |
| Koerner et al.127 | Yes | Yes | Yes; interviews with staff in homes using needs rounds | Yes | Yes; implementation science frameworks and thematic analysis used | Yes; relevant quotations included | Yes | – | – | – | – | – |
| Mitchell et al.128 | Yes | Yes | – | – | – | – | – | Yes; palliative care has both quantitative and qualitative benefits | Yes | Yes | Yes; e.g. discussion of why some residents were not referred | Yes |
| Mullaney et al.119 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes |
| Murphy-Jones et al.102 | Yes | Yes | Yes | Yes | Yes | Yes | Unclear; trustworthiness of study was influenced by the primary author holding the position of an ‘insider’, being an experienced prehospital clinician, employed as a paramedic in the same trust as participants and having specialist education in the subject area. This enabled participants to be relaxed and converse as colleagues using everyday language but impacted on confirmability. Researcher’s clinical knowledge may have led to misinterpretations of responses and data may have been missed by not exploring concepts. To counter this, participants were asked to explain colloquial terms and confirm the researcher’s interpretations. To reduce bias, the researcher adopted a reflexive approach, recording field notes and maintaining a research diary | – | – | – | – | – |
| O’Neill et al.65 | Yes | Yes | Yes | Yes; focus groups | Yes; thematic analysis | Yes; quotes included | Yes | – | – | – | – | – |
| Sheaff et al.84 | Yes | Yes | – | – | – | – | – | Yes; implementation and impact components | Yes | Yes | Yes; see Discussion section in main text | Unclear; limited qualitative methods/data |
| SQW Ltd52 | Yes | Yes | – | – | – | – | – | Yes | Yes | Yes | Unclear | Yes |
List of abbreviations
- A&E
- accident and emergency
- ACP
- advance care planning
- ARCHUS
- Aged Residential Care Healthcare Utilisation Study
- BHiRCH-NH
- Better Health in Residents of Care Homes with Nursing
- CI
- confidence interval
- CMS
- Centers for Medicare and Medicaid Services
- CRD
- Centre for Reviews and Dissemination
- DNH
- do not hospitalise
- ED
- emergency department
- EDDIE
- Early Detection of Deterioration in Elderly Residents
- EHCH
- Enhanced Health in Care Homes
- FITAR
- Framework for Intervention Transferability Applicability Reporting
- GP
- general practitioner
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluation
- HiNH
- Hospital in the Nursing Home
- INTERACT
- Interventions to Reduce Acute Care Transfers
- MDT
- multidisciplinary team
- MOQI
- Missouri Quality Initiative
- OPTIMISTIC
- Optimising Patient Transfers, Impacting Medical Quality and Improving Symptoms: Transforming Institutional Care
- PARIHS
- Promoting Action on Research Implementation in Health Services
- PPI
- patient and public involvement
- PRISMA
- Preferred reporting items for systematic reviews and meta-analyses
- QI
- quality improvement
- RACF
- residential aged care facility
- RCT
- randomised controlled trial
- REAP
- regular early assessment post-discharge
- TIDieR-Lite
- Template for Intervention Description and Replication (adapted)