Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR129209. The contractual start date was in March 2020. The final report began editorial review in January 2022 and was accepted for publication in August 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Duddy et al. This work was produced by Duddy et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Duddy et al.
Chapter 1 Background
This chapter introduces the National Health Service (NHS) Health Check (NHSHC), the existing evidence base that underpins the programme, recent developments that have affected its delivery, and the focus of this review project. The text below reproduces in part, and updates, the background information provided in our published protocol paper. 1
The NHS Health Check programme
Cardiovascular disease (CVD) causes one-quarter of all deaths in the United Kingdom (UK) and is the largest cause of premature mortality in deprived areas. Early detection and prevention of CVD are a priority for the NHS and the NHS Long Term Plan (2019) makes a clear commitment to early detection of risk factors and rapid initiation of treatment, with the ambitious aim of preventing over 150,000 heart attacks, strokes and dementia cases over 10 years. 2
The NHSHC programme is one pillar of England’s CVD prevention effort. Launched in 2009, the NHSHC aims to offer a five-yearly assessment of CVD risk factors to all adults in England aged between 40 and 74 years. The check involves the measurement of key CVD risk factors and calculation of an overall 10-year CVD risk (using QRisk®3), followed by advice, discussion and agreement on lifestyle and pharmacological approaches to manage and reduce risk. The latter steps may include the delivery of advice and ‘brief’ or ‘very brief’ interventions, signposting or formal referral to ‘lifestyle support’ services, such as stop-smoking and weight-management services, and clinical risk management (including prescribing) per relevant National Institute for Health and Care Excellence (NICE) guidelines. 3
The total eligible population for the NHSHC programme has been estimated at 15.5 million. 4 The largest and most recently published analysis of national data relating to the programme found that 10 million eligible people were offered a check between 2012 and 2017. 5 Of these, 52.6% (just over 5 million) received an NHSHC. Although national uptake rates have generally increased over time, there is significant regional variation, with uptake rates calculated for upper-tier local authority (LA) areas ranging from 25.1% to 84.7%. 5 These findings are in line with previous analyses that have identified significant regional variation in the invitation and uptake rates for the programme,6 as well as variation in other aspects of delivery and follow-up, including variation in the delivery of advice and onward referrals to lifestyle services. 7,8
History of the NHSHC programme
Originally commissioned by Primary Care Trusts (PCTs) across England, the NHSHC programme was developed to address high rates of death, disability and inequality in health outcomes associated with vascular disease. The programme was designed to build on success in secondary prevention, shifting the focus to early intervention and primary prevention,9 and supported by evidence compiled in a handbook produced by the UK National Screening Committee. 10 From the outset, the programme was intended not only to address individuals’ modifiable risk factors but also to address population-level health inequalities,9 and to do so via provision of pharmacological (e.g. statins and anti-hypertensives) and non-pharmacological (‘lifestyle’) interventions, focused on exercise, weight and smoking. 11
The original modelling for the programme estimated that it had the potential to deliver significant benefits, including the prevention of 1600 heart attacks and strokes, and 4000 new cases of diabetes each year. However, these modelled outcomes rested on key assumptions about the uptake of checks themselves, and of the uptake and compliance with interventions offered after the check. 11
The NHSHC programme was relaunched in 2013, when responsibility for commissioning many public health services was transferred from the NHS to LAs, and a new executive agency, Public Health England (PHE), was formed. 12 Minimum standards for the NHSHC delivery model became statutory requirements,13,14 and recommendations and guidance for programme delivery were produced and have since been regularly updated by PHE. 3 On 1 October 2021, following the disbandment of PHE, responsibility for oversight of the programme was formally transferred to the Office for Health Improvement and Disparities (OHID), a newly formed unit within the Department of Health and Social Care (DHSC).
Although minimum standards for NHSHC delivery are in place, LAs have flexibility in how and whom they commission to provide NHSHCs. As commissioning and delivery decisions are taken locally, with the aim of meeting the needs of local populations, there is inevitable variation in programme delivery, uptake and outcomes. In practice, most NHSHCs are delivered in general-practice settings but even so, there is significant variation in NHSHC delivery. 15,16
A summary of key programme milestones and documents is provided as part of Appendix 1 in this report.
Covid-19 and the NHS Health Check
The Covid-19 pandemic had a major impact on delivery of the NHSHC. In April 2020, NHS England and Improvement (NHSE&I) issued guidance for the prioritisation of community health services as part of the pandemic response, which included guidance to stop delivery of NHSHCs altogether. 17 PHE’s April 2020 Health Check e-Bulletin confirmed this plan, and outlined a delayed schedule for routine data collection relating to the programme. 18 To support the resumption of programme delivery after this pause, PHE issued ‘restart preparation’ guidance for commissioners and providers in April 2021. This guidance made it clear that decisions to restart delivery of the programme should be taken by LAs, in light of local assessments of safety and capacity (especially taking into account the need for general practices to prioritise Covid-19 vaccination work). 19
In recognition of the potential ‘limiting factor’ of workforce capacity in general practice, this guidance explicitly recommends that LA commissioners consider ‘alternative’ delivery models for future provision. It is clear that the pause and restart of the programme provoked a range of responses at local levels, including the introduction of new delivery models in some areas. 20 In recognition of this fact, we designed the survey component of this project to gather information from LAs on the extent and nature of changes in programme delivery in response to Covid-19.
In addition to these operational changes, official communications from PHE have placed a new emphasis on the potential benefits of the NHSHC in relation to Covid-19 outcomes, recognising that many of the risk factors that the NHSHC is designed to assess are also associated with increased risk of severe illness and death from Covid-19. 21,22 The potential for the NHSHC programme to help address risk factors associated with severe Covid-19 is acknowledged in the UK government’s Covid-19 recovery plan. 23
The NHS Health Check Review (2021)
Plans for a major review of the NHSHC programme were announced by the DHSC in August 2019, with an emphasis on personalisation and consideration of potential digital delivery methods. 24 In August 2020, the NHSHC e-Bulletin confirmed that this review was being undertaken by PHE21 and formal terms of reference were published in November 2020. The scope of the review included an assessment of the existing programme’s effectiveness, cost-effectiveness and limitations, as well as consideration of evidence relating to potential changes that might be made to both the content and delivery methods for the check. 25
The review’s findings were published in December 2021 by the new OHID unit. 26 The report sets out a new ‘vision’ for the NHSHC and makes six recommendations to government to guide delivery of the programme over the next decade. We have taken these recommendations into account in developing our own set of recommendations based on the findings of this project, aiming to complement and add to the recommendations published by OHID (see Chapter 4, Discussion).
Overview of existing evidence
The NHSHC programme has been controversial since its inception, and the value of the evidence underpinning its design and demonstrating its effectiveness has been subject to dispute. 27 Opponents of the programme cite an absence of data from randomised controlled trials (RCTs) demonstrating the effectiveness of mass CVD screening and prevention programmes. 28,29 PHE have responded by commissioning and producing a range of evidence that aims to demonstrate the effectiveness of the programme, and by setting up the NHSHC Expert Scientific and Clinical Advisory Panel (ESCAP) to regularly review and support delivery of the programme. 30
Observational studies collated in two PHE-commissioned rapid reviews suggest that the NHSHC is associated with increased rates of the detection of CVD risk factors and disease, statin prescribing, and referrals to lifestyle support services (including smoking cessation, weight management, exercise and alcohol support services). However, regional studies demonstrate wide variation both in these outcomes and in service delivery across England. Evidence on behaviour change and improvements in CVD risk factors and outcomes post-HC is sparse. The rapid reviews identified only six primary studies examining behaviour change, assessing only smoking. A limited number of studies have assessed improvements in body mass index (BMI), diastolic blood pressure, total cholesterol and overall CVD risk, but results are inconsistent and some studies found no evidence of an effect. 7,8
A more detailed overview of the existing evidence underpinning the NHSHC is available in our published protocol paper. 1
Project focus: what happens after the risk assessment in an NHS Health Check?
Our scoping searches and review of the existing research evidence identified a clear focus in the existing literature on the reach of the NHSHC programme, including on how to improve invitation, uptake and coverage. Less attention has been paid to what happens after the measurements and risk assessment have been undertaken, especially in relation to the delivery of advice, onward signposting or referral and ongoing support for lifestyle and behaviour change. In consultation with our key stakeholder, PHE (now OHID), we confirmed the value of a focus on these steps in this review. Our wider public and professional stakeholder groups (see Chapter 2) were also consulted on this proposed focus and confirmed the need for research in this area, reflecting their interest in the NHSHC as a programme with the potential to prompt and support behaviour and lifestyle change in attendees. The ability of the NHSHC to promote such behaviour change is a crucial underpinning assumption for the programme in relation to its aim to help attendees reduce their risk of experiencing a heart attack or stroke or developing some forms of dementia. 3 The rationale for choosing this project focus is further elaborated in Chapter 2 below (see Step 1: Locate existing theories).
What should happen after the risk assessment is completed in a Health Check?
PHE’s Best Practice Guidance3 and programme standards31 for the NHSHC make a number of clear recommendations in relation to what should happen after the measurements and risk assessments have been completed during a check. The documents are aimed at both commissioners and providers, and describe a range of advice and referral options, as well as clinical interventions that can be offered to attendees, with two objectives:
-
To promote and improve the early identification and management of the individual behavioural and physiological risk factors for vascular disease and the other conditions associated with those risk factors.
-
To support individuals to effectively manage and reduce behavioural risks and associated conditions through information, behavioural and evidence-based clinical interventions. 3
For commissioners, the Best Practice Guidance document makes some limited recommendations in relation to providing and ensuring clear referral pathways to other services that may be commissioned to support lifestyle and behaviour change. For example, in relation to smoking cessation, it suggests that LAs ‘may wish to’ put in place pathways to refer smokers to local stop-smoking services. However, it is also made clear that clinical follow-up remains the responsibility of primary care, and there is an emphasis placed on LAs’ legal responsibilities in relation to NHSHC delivery and data reporting – both focused on invitation and uptake. There is no legal requirement to ensure that NHSHCs include the provision of advice or referrals beyond the requirement to ‘ensure the individual having their NHS Health Check is told their cardiovascular risk score, and other results are communicated to them’, and that relevant data are recorded and sent to general practices to ensure appropriate clinical follow-up as required. 13,14
Despite this, PHE’s guidance documents aim to provide a level of standardisation in setting out recommendations for the steps following the mandatory measurements and risk assessments. The recommendations are not new or specific to the NHSHC programme; instead, the guidance invokes relevant NICE guidelines and so reflects what should be ‘usual care’, at least for those providers based in general practice. Both the Best Practice Guidance and the programme standards explicitly echo the ‘Making Every Contact Count’ competencies, intended to promote the opportunistic delivery of ‘brief’ and ‘very brief’ lifestyle interventions during routine interactions with health and care staff. 32 The NHSHC encounter is positioned as a means of extending the opportunity to deliver these interventions to an otherwise healthy population who may not otherwise have contact with healthcare services. 3
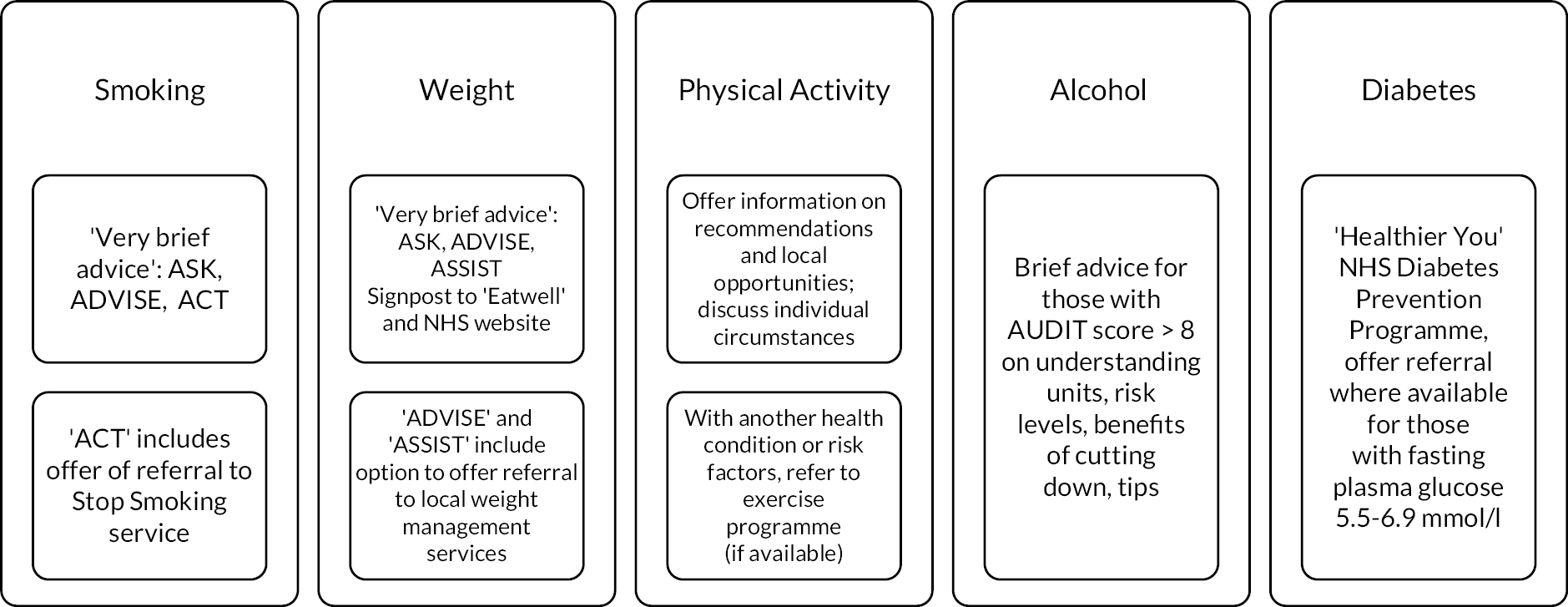
A summary of the recommendations in relation to advice, brief interventions and referrals in relation to each risk factor assessed during an NHSHC is provided in Figure 1.
FIGURE 1.
Recommendations for advice, brief intervention and referral.
Data on these potential activity outcomes for attendees of the NHSHC are not routinely collected or reported to PHE. A recent cross-sectional observational study of the NHSHC extracted data from primary care records in 90% of English general practitioner (GP) practices for the 5-year period 2012–2017. 5 The findings included data on the percentage of NHSHC attendees recorded as receiving advice, information or a referral after a check, in relation to each risk factor assessed. Table 1 reproduces Table 3 from this study, showing the percentage of all NHSHC attendees who received advice, information or referrals, as well as the percentage of all NHSHC attendees meeting the threshold for these interventions who received them.
| Intervention type | All attendees n (%) | Attendees with the CVD risk factor above threshold for intervention: n (%) |
|---|---|---|
| Alcohol consumption | 792,761 (15.5) | 46,611 (38.4) |
| Diet | 1,189,986 (23.3) | 766,521 (25.1) |
| Physical activity | 1,501,103 (29.4) | 434,326 (39.3) |
| General lifestyle/behaviours | 814,611 (16.0) | 211,571 (20.1) |
| Smoking cessation | 865,913 (17) | 467,119 (57.3) |
| Weight loss and obesity | 821,414 (16.1) | 599,380 (19.6) |
| Diabetes prevention programme | 4551 (0.1) | 3348 (0.9) |
| Total | 2,501,565 (49.0) | 565,047 (53.7) |
Although it is likely that data recording (coding into primary care records) for these activities is incomplete, the available data indicate that the rates at which they are delivered vary widely for different risk factors and appear to fall well below what the recommended thresholds for intervention suggest would be appropriate. These data also provide no detail on the nature of the advice, information and referrals offered, and the extent to which the specific recommendations made in the guidance are followed. These findings echo those from existing systematic reviews, which have also identified regional variation in ‘post-delivery management’ following an NHSHC. 7,8 In addition, this study and another recent observational study make it clear that most NHSHC attendees do not receive any treatment or referral after a check, and that statin prescribing in particular is much lower than guidelines recommend. 5,33 The rates recorded also fall short of those estimated in the initial economic modelling for the NHSHC programme. 34
Aims and objectives
Aim
The aim of this project was to understand how the NHSHC programme works in different settings for different groups, in order to recommend improvements to maximise intended outcomes. Following scoping searches and consultation with our stakeholders, we focused on the steps that follow the measurements and risk assessment undertaken during the check.
Objectives
-
To map how the programme is currently delivered across England, using findings from a PHE survey (October 2020) and data we collect using our own online survey of LAs (with a specific focus on what happens after the measurements and risk assessment and on Covid-19 related changes to delivery models).
-
To conduct a realist review to enable understanding of how the NHSHC programme works in different settings, for different groups, to achieve its outcomes (with a specific focus on what happens after the measurements and risk assessment).
-
To provide recommendations on tailoring, implementation and design strategies to improve the current delivery and outcomes of the NHSHC programme in different settings, for different groups.
Chapter 2 Methods
The project had two main strands – a survey of LAs and realist review – both supported by strong stakeholder engagement. This chapter begins with a section describing the role of our stakeholder groups throughout the project, before describing the methods used in our survey and realist review.
We conducted a survey of LAs with the aim of providing a comprehensive overview of how different localities across England implement the NHSHC programme. In addition, the survey aimed to gather additional material (including local knowledge, unpublished evaluations and examples of best practice and Covid-19-related innovation in delivery) for the review.
Our survey asked questions about current NHSHC delivery models (in 2021/2022, following the Covid-19-related pause to the service) and questions related to options for onward referral and follow-up of attendees after the Health Check encounter. It sought to identify the extent to which commissioners and providers had changed the way they commission and deliver the NHSHC programme in light of the Covid-19 pandemic. It also identified the extent to which services are available to support those identified as having modifiable risk factors, which has helped us to address our review focus on what happens after a Health Check, especially in relation to follow-up, onward referral and ongoing support for lifestyle and behaviour change. Our survey findings were considered alongside those from the previous PHE survey of LA commissioners, conducted in October 2020 as part of the wider review of the NHSHCs programme. 16
In addition, we conducted a realist review to enable us to better understand the important contexts that influence NHSHC delivery, and the mechanisms which produce both intended and unintended outcomes. Realist review is an interpretive, theory-driven approach to evidence synthesis that aims to develop an in-depth understanding of how, why, when and for whom complex interventions (such as the NHSHC) ‘work’. We chose this approach because existing research clearly demonstrates that the NHSHC programme is a complex intervention with context-sensitive outcomes, that is, the programme’s outcomes are highly dependent on the circumstances in which the NHSHC is delivered and received by attendees. There is significant heterogeneity in commissioning and delivery of the programme across England and wide variation in key outcomes, including rates of attendance, follow-up, and the provision of advice, onward referral and prescribing post-NHSHC. 7,8 Our review sought to improve understanding of this variation, via developing a programme theory that identifies the important contexts and mechanisms that produce NHSHC outcomes, with a specific focus on what happens after the measurements and risk assessment are complete.
The full project plan is presented in Figure 2. The project was registered with PROSPERO (CRD42020163822) in January 2020. The start date of the project was delayed to October 2020 due to Covid-19, and the project was conducted over 15 months, completed in December 2021.
FIGURE 2.
Project flow diagram.
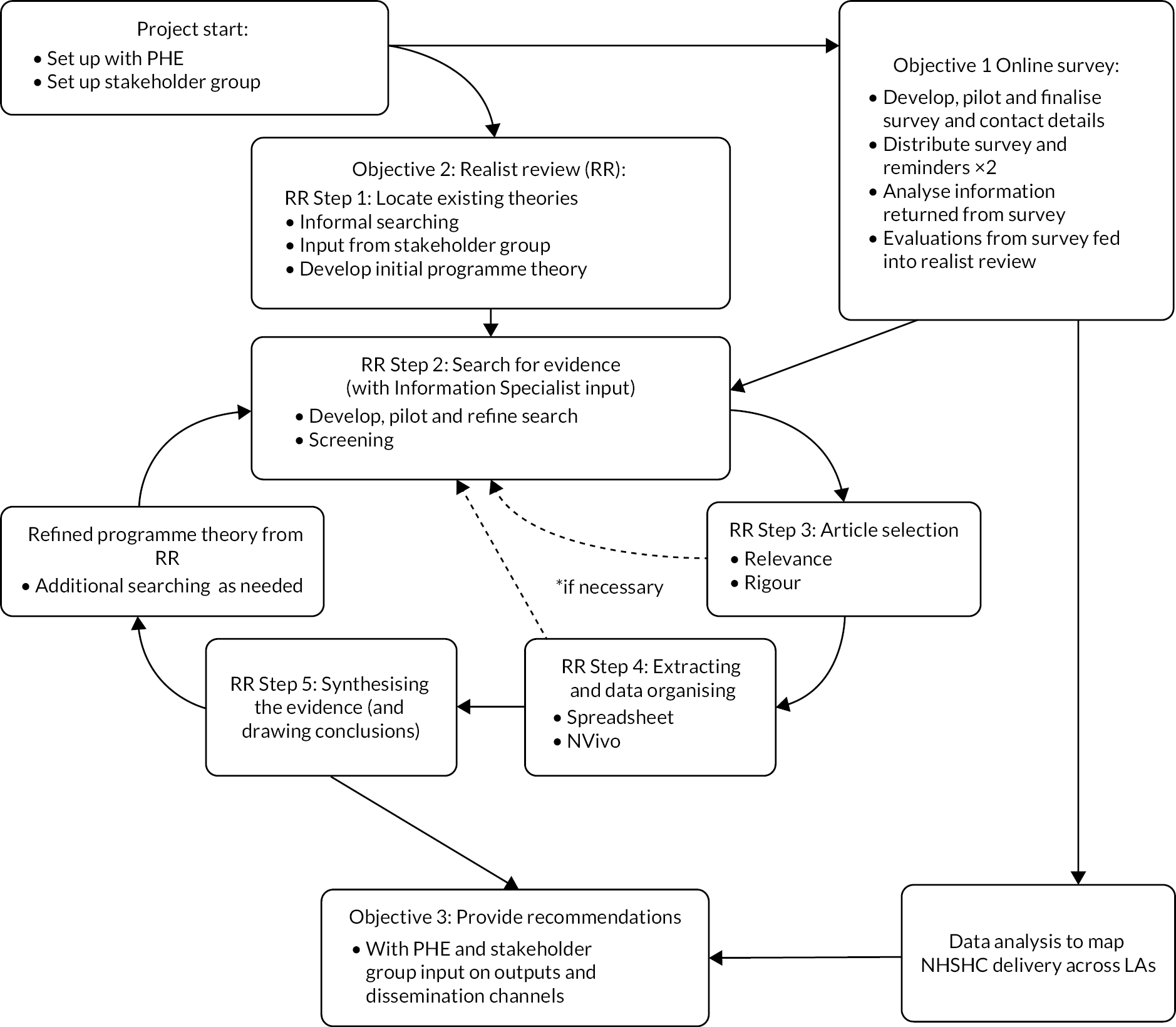
Our protocol was published in BMJ Open in April 2021. 1 The conduct and reporting of the review were informed by the Realist and Meta-narrative Evidence Synthesis: Evolving Standards (RAMESES) quality35 and publication36 standards. Ethical approval for the survey component of the project was granted by the University of Kent’s SRC Research Ethics Committee (SRCEA ID 0367) in February 2021.
Stakeholder groups
We recruited two stakeholder groups to provide us with content expertise and a range of perspectives throughout the project.
Throughout the project, our strategy for patient and public involvement (PPI) was informed by our PPI lead (VH). VH is an experienced PPI contributor (via the Public Involvement in Pharmacy Studies at Medway School of Pharmacy Group) and brought her valuable perspective as a member of the public and skills in group facilitation. In particular she supported us in developing lay summaries, advertising for further PPI contributors and supporting our PPI group throughout the project.
Our PPI group involved 10 members of the public from six different English regions, all of whom are eligible to receive the NHSHC. 37 This group was recruited by advertising via the Oxford Biomedical Research Centre website and the University of Kent’s Centre for Health Services Studies’ Opening Doors to Research group. We offered PPI contributors a shopping voucher as a token of our appreciation for their involvement, and covered any expenses they incurred in taking part. From those members of the public who came forward, we purposely selected a group who were as diverse as possible in relation to gender, age, ethnicity and geographical location, with the aim of capturing a range of different perspectives from individual members of the public.
Our ‘professional’ stakeholder group were recruited via our project team’s existing networks and snowballing from these, and included LA commissioners, NHSHC providers, an NHSHC trainer and representatives from relevant health charities. In addition, we maintained close contact with PHE’s (latterly OHID’s) CVD Prevention Programme lead throughout the project.
Both groups were consulted via regular online meetings throughout the project, using Microsoft Teams (Version 1.0, Microsoft Corporation) and Zoom (Version 5, Zoom Video Communications, Inc.) video conferencing software. Our approach to facilitating our meetings was driven by the need to work to ensure that these online discussions – necessary due to the Covid-19 pandemic – were as open and inclusive as possible. Based on the recommendation of our PPI lead (VH) we met with our PPI and professional stakeholder groups separately, to help ensure that members felt able to speak openly about their experience of receiving and/or commissioning/providing the NHSHC and to reduce the number of people in each meeting, giving individuals more opportunity to contribute. However, CD attended all meetings of both groups and, where relevant, reported discussions from the PPI group to the professional group and vice versa. Our PPI stakeholder group meetings were chaired by VH and our professional stakeholder group meetings by GW. To facilitate more in-depth discussion and give each participant more time to contribute, our PPI group was split into two smaller groups for the last two meetings.
Our final professional stakeholder group meeting was augmented with additional contributions from 36 individuals. They came from a range of professional backgrounds (LAs, Public Health, OHID and providers) and from geographically diverse parts of England. Individuals were recruited via OHID’s existing networks. These additional contributions were sought to ensure that we would get broader feedback and advice on our findings and recommendations.
We consulted the stakeholder groups in relation to the focus of the project and asked them to provide feedback on our emerging findings as they developed. To help facilitate discussion on our findings, we circulated summary material before each meeting and provided an overview slide presentation at the beginning of each meeting. We initiated discussions with sets of simple questions to help guide the participants; for example, we asked stakeholders how our findings related to their own knowledge and/or experience of commissioning, providing or attending the NHSHC, and we asked them about important influences on NHSHC delivery or the response to the NHSHC that seemed to be missing from our findings. Our aim was both to identify those findings with particular resonance for stakeholders, but also to highlight any important aspects of NHSHC delivery that are not well represented in the literature. We consulted the professional stakeholder group on the development of our survey questions, to ensure their relevance and importance, and on our survey design, with the aim of maximising clarity, validity and the likelihood of achieving a good response with full completion of questions.
The discussions held during these meetings helped to shape our analysis as the project progressed. Input from both the professional and PPI groups influenced the analysis of our survey responses and our interpretation of the data included in the review. For example, input from the professional stakeholder group informed the development of a typology of NHSHC delivery models and the identification of relevant factors to consider in our analyses. In discussions of the review’s emerging findings, our PPI group members emphasised the need for NHSHC attendees to have more control over what happens during and after a check, especially in relation to the discussion of ‘lifestyle’ advice and opportunities for referral to other services. As a result, we reconsidered our data on attendee responses to what providers offer or discuss at the end of an NHSHC encounter, to consider whether it could tell us more about potential mechanisms producing these important outcomes for attendees. (see e.g. CMOCs A16–A17, A30–32 in Chapter 3). Similarly, PPI members’ repeated observations on the ‘mismatch’ of the focus of the NHSHC with their own health needs and priorities helped us to shape our findings (see e.g. CMOCs A9–A11) and recommendations in this area. Overall, our PPI group felt strongly that they needed more clarity on the purpose of the NHSHC programme and the group’s in-depth discussions on this point are represented strongly throughout our findings and in our subsequent recommendations for policy and practice (see Chapter 3 and Chapter 4).
In the last meetings with each group, we asked the participants for their input to help us to develop and refine practical recommendations for NHSHC delivery based on our findings and to inform our dissemination strategies, to help us to develop tailored outputs and identify the key ‘players’ for dissemination amongst different audiences. We refined our recommendations and developed plans for dissemination activities and project outputs on the basis of feedback from both groups.
A summary of the stakeholder group meetings and important input from these groups is provided in Table 2.
| Date | Stakeholder members | Key discussion topics |
|---|---|---|
| 29/01/2021 | Professional group: seven attendees (one GP, one pharmacist, one trainer, two LA commissioners, two charity representatives) | Introduction to the project. Discussion focused on the potential gap between commissioning and delivery and the reality of NHSHCs delivery and on the project focus. On the survey, discussion focused on timing to ensure good response rates, clarity on the time periods referred to in survey questions, knowledge of the intended respondents (in LAs) and the balance between capturing detail while minimising burden for respondents. |
| 23/04/2021 | PPI group: 10 contributors | Introduction to the project. Discussion focused on contributors’ personal experiences of NHSHCs and included reflection on their awareness of the programme, negative and positive experiences of NHSHCs. |
| 21/05/2021 | PPI group: 10 contributors | Presentation of an initial set of emerging review findings focused on contexts influencing referral to other services as an outcome of an NHSHC. Discussion focused on the appropriateness of referrals, availability of services and the limitations of the NHSHC CVD focus. |
| 11/06/2021 | Professional group: six contributors (two GPs, one trainer, two LA commissioners, one charity representative) | Presentation of an initial set of emerging review findings focused on commissioner and provider perspective. Discussion focused on local variation in delivery, enthusiasm and engagement, leadership, workforce competencies and skills and the impact of Covid-19. |
| 10/09/2021 | PPI group: 10 contributors (split into meetings with five in each) | Presentation of review findings focused on attendee experience and response to the NHSHC. Discussion focused on medical versus ‘lifestyle’ interventions, the importance of follow-up, the need for personalised advice and support, and on the potential value and risks of digital checks. |
| 17/09/2021 | Professional group: four contributors (one GPs, one trainer, one LA commissioner, one charity representative) | Presentation of review findings focused on attendee experience and survey results. Discussion focused on the purpose of the HC, what ‘good’ looks like and what training is needed to achieve this, plus data and monitoring issues. Feedback was provided on emerging findings and the survey’s findings, typology and how it might be meaningfully described and analysed. |
| 05/11/2021 | PPI group: eight contributors (split into meetings with four in each group, follow up with two other members by email and separate online meeting) | Presentation of recommendations based on findings. Discussion focused on the need to recognise the impact of Covid-19 on individuals, variation in delivery between local areas and the need to clarify and communicate the purpose of the programme to the public. Contributors suggested outputs should include illustrative examples of good practice and a range of formats that could be appealing or accessible to different audiences (e.g. magazine articles, animations, social media posts). |
| 12/11/2021 | (Augmented) Professional group: 36 contributors (range of professional backgrounds – LAs, Public Health, OHID and providers and from geographically diverse parts of England) | Presentation of recommendations based on findings. Discussion focused on whether the recommendations resonated with them and on: tensions between case-finding and behavioural change; services to refer attendees onto after the NHSHC; challenges for providers; and wider issues impacting on NHSHC delivery. |
Survey methods
Survey aims and objectives
The aim of the survey was to enable us to gather additional material (local knowledge, unpublished evaluations and examples of good practice and Covid-19-related innovation) for the project, and to provide a comprehensive overview of how different localities across England implement the NHSHC programme. The objectives were:
-
To describe how NHSHCs are delivered across England, particularly in relation to what happens after the measurements and risk assessment.
-
To determine how the Covid-19 pandemic has changed the way NHSHCs are delivered in some areas.
-
To categorise, as far as possible, different models of NHSHC delivery employed across England.
-
To determine any associations between NHSHC delivery models and other variables, based on relevant publicly available data.
Survey development and piloting
An online survey (available in full on our project website www.journalslibrary.nihr.ac.uk/programmes/hsdr/NIHR129209/#/) was developed using Jisc Online Surveys, chosen as it is designed to generate professional academic survey formats. The survey was to cover all LAs in England with responsibility for commissioning the NHSHC programme (i.e. upper-tier and unitary). Given the timing of the survey – during the second year of the Covid-19 pandemic, and less than a year since PHE’s own survey on NHSHC programme delivery – we were concerned that our survey would add an unwanted and unwarranted burden, unless it asked new questions and was able to provide new information. The survey was therefore designed to capture (1) changes in delivery in response to the pandemic and (2) detail about the delivery of the programme with a focus on what happens after the measurements and risk assessment are complete.
We also used the survey to find out whether LAs had commissioned, conducted or been part of any assessments of the NHSHC programme in the previous five years (including evaluations, collection of attendee feedback, health equity audits, or any other type of study), and to request copies of these to be included in our review.
The survey questions were designed in collaboration with our stakeholders, who helped us to ensure that the content of the questionnaire addressed the objectives of the research, the instructions and questions were clear and concise, and the survey was straightforward and quick to complete (i.e. in less than 15 minutes).
The survey included a mix of simple closed- and open-ended questions. The latter were included to enable respondents to both explain their responses to closed questions and add any further information about commissioning and delivery. Four-point rating scales were used to obtain level of confidence in capacity, accessibility and usage of support services (where 1 means ‘not confident at all’, and 4 means ‘very confident’).
The resulting online survey was sent to seven LAs (NHSHC/Cardiovascular Health leads) on 30 April 2021 to ‘test’ the system in advance of full roll-out. The survey was completed in full by three respondents, and feedback on the survey itself was positive. One subsequent change was made to the survey prior to the main launch. This was to include a single additional question at the start (Q3: Has the delivery of NHSHCs in your area resumed since the Covid-19 pause? Yes/No).
Administering the survey
To ensure a maximal response, and to ensure the survey was correctly targeted to those best placed to answer it, we worked closely with PHE to distribute the survey and make use of their tried-and-tested processes for dissemination. PHE sent the survey on our behalf to two of their governance groups: the PHE regional NHSHC Leads, and their Local Implementor National Forum, which includes LA NHSHC implementers representing all of the PHE regions. These groups were then asked to disseminate the email to their networks (e.g. the regional leads were asked to cascade the message to contacts for the LAs in their area). PHE also publicised the survey through their established NHSHC programme webinar series. Following the launch on 17 May 2021, a first reminder was sent on 4 June, and another on 18 June (announcing an extension to the deadline). On 2 July, targeted reminders were sent to leads in regions with a response rate of less than 35% (West Midlands, North East, East of England and London), for further cascading to all LAs in their regions. The survey closed on 18 July 2021.
Data handling
Survey responses were recorded online then downloaded into Microsoft Excel and a statistical software package (IMB SPSS Statistics 27) to aid analysis. Respondents were allocated unique identifying codes (R01–R68). Respondents were asked to name the LA(s) on behalf of which they were responding. Where one respondent was responding on behalf of multiple LAs, responses to all remaining questions were copied for the relevant LAs. Each LA was then allocated a unique identifying code (LA01–LA74). Qualitative responses given in free-text boxes were used to clarify or amend responses where relevant. For a few responses that appeared confusing or limited, we conducted a search of that council’s website in order to double-check information given (e.g. with regard to where NHSHCs are made available).
Data analysis
Simple descriptive statistics were used to analyse quantitative responses to the questionnaire. Where relevant, qualitative responses were categorised to enable descriptive analysis; for example, the venues where the NHSHC was offered. Qualitative responses were also used to illustrate the quantitative data throughout, for example by contributing to case examples of delivery types.
In order to develop a typology of LAs based on delivery of the NHSHC, data from responses to several questions were combined. This enabled categories to be devised, based on how LAs were delivering NHSHCs before the Covid-19 pause and their use of remote methods after the pause. The following responses were used to categorise delivery models:
-
number and type of venues pre-Covid-19 pause
-
number and type of providers delivering face-to-face and/or remote health checks
-
number of remote methods used post-Covid-19 pause.
Based on their responses to these questions, LAs were grouped into three categories as outlined in Table 3.
| Category | Number of venues | Number of providers | Number of remote methods used post-Covid |
|---|---|---|---|
| General-practice delivery | Delivery in general practice only | All general-practice staff | No remote delivery |
| Blended delivery | Delivery in general practices plus/minus pharmacies. No other community provision. | General-practice staff plus/minus pharmacy staff | No or limited remote delivery post-Covid |
| Blended with outreach delivery | Delivery in multiple venues, including community settings | Mix of providers, including general-practice and non-general-practice staff | No or limited remote delivery post-Covid |
Associations between category of delivery and other factors
Associations with the following other survey responses were assessed:
-
total number of commissioned services reported
-
total number of referral processes reported
-
total number of methods used to prioritise invitations pre- and post-COVID pause
-
average reporter confidence in capacity and accessibility of support services, confidence in their usage (rating scale)
-
total number of monitoring aspects plus evaluation reported (categorised as none, minimal, above average).
In addition, key statistics related to the public health function, populations, and performance measures for NHSHC programme delivery at LA level were obtained from publicly available data. For each responding LA we recorded:
-
geographic region: PHE centres38
-
size: estimated population, 201939
-
budget: Public Health budget per head, 2019/2039
-
deprivation: Indices of Multiple Deprivation (IMD) 201940
-
NHSHC programme delivery performance: proportion of eligible people receiving an NHSHC between 2015/16 and 2019/20. 41
On the request of our stakeholder group, we also explored the possibility of including the rurality index in our analysis, as an external factor that is likely to influence NHSHC delivery. However, this was found to be problematic since rurality is classified at district level, meaning no classifications are available for the large county (upper tier) councils (of which there are 19 in our dataset). In addition, due to the number of classifications (six), and the exclusion of the county councils, there were very few responding LAs within any of the more rural classifications.
One-way analysis of variance was used to compare service provision, referral processes and delivery performance across delivery categories. Chi-squared tests were used to assess associations between delivery category and other variables. Spearman’s correlation was used to assess relationship between variables.
Review methods
Review questions
-
What are the mechanisms by which the current NHSHC programme produces its intended outcomes after the measurements and risk assessment?
-
What are the important contexts which determine whether the different mechanisms produce intended outcomes?
-
In what circumstances are such interventions likely to be effective?
Our realist review followed Pawson’s five iterative stages42 as outlined in our protocol. 1 The steps we followed are summarised below.
Step 1: Locate existing theories
The goal of this step was to identify existing theories that explain when, how and for whom the NHSHC programme is supposed to ‘work’, to achieve its desired outcome of reducing CVD risk and mortality. The rationale for this step is that interventions and programmes like the NHSHC are underpinned by implicit and explicit assumptions and theories about how they should work in practice. 43 To locate existing theories that might offer explanations for NHSHC processes and outcomes, we undertook two iterative processes:
-
We drew on the knowledge and experience of our own project team (including in general practice, pharmacy, public health and lived experience), and consulted with our stakeholders.
-
We informally searched the literature to identify:
-
existing theories, consulting both grey literature in the form of NHSHC programme documentation, and published research studies that employed formal or substantive theories to understand the NHSHC
-
existing reviews and evidence syntheses focused on the NHSHC programme to develop our understanding of the existing research landscape and identify gaps in knowledge.
-
For step (b), we identified NHSHC programme documentation via searching and browsing the NHSHC website (www.healthcheck.nhs.uk) and the UK DHSC website (http://dh.gov.uk), and archived versions of these websites (via the UK Government Web Archive (http://nationalarchives.gov.uk) and the Internet Archive WayBack Machine (http://archive.org/web/)). We identified existing theoretical literature by running searches in PubMed and Web of Science (Core Indexes – SCI-EXPANDED, SSCI, ESCI, AHCI), using a slightly modified version of Booth and Carroll’s BeHEMoTh approach for searching for theory. 44 We searched for the health context (the NHSHC) and terms relating to ‘theory’ and used citation tracking to identify additional studies. To identify published reviews, we consulted bibliographies produced by PHE, who have undertaken regular literature searches for evidence relevant to the NHSHC programme since 2015 (www.healthcheck.nhs.uk/commissioners-and-providers/evidence/literature-review/). The full details of the searches employed are available in Appendix 2.
Overall, we consulted 60 programme documents (policy papers and guidance) and identified 19 existing studies of the NHSHC that employed six formal theories or theoretical frameworks, and 10 existing reviews and evidence syntheses. Details of these documents are provided in Appendix 1.
In reviewing the existing research evidence relating to the NHSHC programme by consulting existing reviews and evidence syntheses, we identified an existing focus on the early steps of the initial programme theory (IPT) as outlined above, and especially on the processes involved in invitation and uptake of the NHSHC. Conversely, less research attention has been paid to later stages, and especially to what happens after measurements and risk assessment at the end of a check, in relation to advice, onward signposting and/or referral and ongoing support for lifestyle and behaviour change. As described above in Chapter 1 (see Project focus: what happens after the risk assessment in a Health Check?) we determined (in consultation with our stakeholder groups) to focus our own review on these later steps.
We combined our understanding of the programme from the literature reviewed with our own knowledge to develop and refine a coherent IPT for our realist review and to inform the subsequent stages of searching, data extraction and analysis. The IPT is presented in Figure 3; it maps out the steps involved in the delivery of an NHSHC and highlights our particular areas of focus and questions we considered in the course of the project.
FIGURE 3.
Initial programme theory for the realist review with project focus highlighted.

In recognition of the complex nature of the NHSHC programme, and the possibility (captured in our IPT) that important interactions and feedback loops may exist with earlier steps in the delivery of the check, we determined that we should not exclude evidence relating to other programme steps. Instead, we decided to focus initially on identifying those documents that could provide data relating to the later steps, and subsequently draw on data that may shed important light on relationships with other steps in the programme as necessary.
Step 2: Search for evidence
The aim of this step was to identify a relevant body of literature containing data that could be used to develop and refine the IPT developed in Step 1.
At the outset of this project, we were aware that PHE regularly undertakes literature searching for new evidence relating to the NHSHC. These regular searches employ a comprehensive search strategy across 13 relevant sources (PubMed, MEDLINE, Embase, Health Management Information Consortium (HMIC), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Global Health, PsycINFO, Cochrane Library, NHS Evidence, Google Scholar, Google, Clinicaltrials.gov and the ISRCTN registry). These searches have been used in previous review projects commissioned by PHE to identify and synthesise evidence relating to the NHSHC. 7,8 These published reviews have included additional searches in OpenGrey and/or Web of Science (Science Citation Index, SCI-EXPANDED); the most recent of these PHE-commissioned reviews captured studies published until the end of December 2019.
As described in our protocol, we did not duplicate this existing work, but aimed to re-use and extend it. As such, we identified documents to consider for inclusion in three main categories:
-
Documents included in two existing rapid reviews commissioned by PHE, as well as additional studies identified using the same search strategies and included in PHE’s published quarterly literature reviews. These were empirical (quantitative and qualitative) studies of the NHSHC. The eligibility criteria that were employed in the rapid reviews (and so determined our inclusion of documents from these sources) are summarised in Table 4.
-
Documents retrieved via additional focused searches that we ran to identify additional material that may have been excluded from the existing reviews and bibliographies. This included, for example, relevant commentary or opinion, which may still be included in a realist review where data from these documents may contribute to theory-building. 45 Our more specific search strategies focused on identifying documents focused on the NHSHC in England. We ran these more targeted searches in MEDLINE, Embase, CINAHL, HMIC and Web of Science (SCI-EXPANDED, SSCI indexes). These searches used specific free-text terms describing the NHSHC alongside relevant subject heading terms as appropriate. The full search strategies used are reproduced in Appendix 2.
-
Documents retrieved via a trawl of the NHSHCs website (www.healthcheck.nhs.uk/), including case studies, local evaluations and abstracts and posters presented at the Health Checks/Cardiovascular Disease Prevention annual conferences from 2014 to 2020. These sources represent an important source of data on local implementations of NHSHC and additional research studies that have been excluded from previous reviews. Our realist approach provides the opportunity to supplement and structure the informal collaborative knowledge-sharing that has been facilitated by these spaces. 46
| Inclusion criteria | Exclusion criteria |
|---|---|
| Intervention: NHSHC | Editorials, commentaries and opinion pieces |
| Study design: guidelines; RCT, cluster RCT, quasi RCT, cluster quasi RCT; controlled and uncontrolled pre–post studies with appropriate comparator groups; interrupted time series; cohort studies (prospective and retrospective); case-control studies; qualitative studies from any discipline or theoretical tradition with recognised qualitative methods of data collection and analysis; economic and health outcome modelling |
This main phase of searching and gathering documents was undertaken in October 2020. At the same time, a regular email alert for (NHS (‘health check’ or ‘health checks’)) was set up using Google Scholar, to help capture research studies and grey literature published over the course of the review. Some additional documents were provided by our professional stakeholder group members and by respondents to our survey, in response to our request for local evaluations or similar documents, as described above.
All documents identified via these processes were stored and deduplicated using Endnote X9 (Clarivate Analytics, Philadelphia, PA, USA) reference management software.
Additional searching
Additional searches for data may be undertaken in a realist review, for example, to help to develop and test particular aspects of the programme theory. Although we had anticipated that additional searches for documents containing empirical data may have been required for this review, the project team agreed that the material had been identified via the searching processes described above were sufficient to meet the needs of this project.
We conducted a small number of focused searches (in Google Scholar) to identify material related to one substantive theory, ‘street-level bureaucracy’,47 which has been used to help to frame and illuminate our final programme theory and discussion, and is described in more detail below (see Chapters 3 and 4). These searches are also reproduced in Appendix 2.
Step 3: Article selection
Documents were exported from Endnote X9 and imported into Rayyan QCRI (Qatar Computing Research Institute (Data Analytics), Doha, Qatar), a web-based tool designed to support screening for systematic reviews. Initially, CD and GW screened a small sample of documents (n = 25) in a pilot process to check for consistency in the application of our initial inclusion and exclusion criteria.
We then screened the full set of documents retrieved in Step 2 using a three-step process. CD screened the titles and abstracts (where available) of the documents retrieved via our searches and the NHSHC website following the eligibility criteria specified in our review protocol and outlined in Table 5. GW screened 10% of each of these sets of documents in duplicate (n = 67 documents retrieved via searching; n = 25 documents retrieved from the NHSHC website), and CD and GW discussed discrepancies in decision-making as a means of ensuring consistency in how the inclusion criteria were applied.
| Inclusion criteria | Exclusion |
|---|---|
| Intervention: NHSHC programme (all delivery models) Focus criteria: later steps in NHSHC delivery, including the provision of advice, signposting, referral, prescriptions |
Cardiovascular screening programmes run in countries other than England |
| Study design: all study designs | Other NHS screening programmes |
| Setting: any setting providing NHSHCs in England | Routine health checks offered to specific target populations by the NHS which are not part of the NHSHC programme |
| Participants: commissioners and providers of NHSHCs; all adults eligible for NHSHCs | |
| Outcome measures: all outcome measures related to NHSHCs Focus criteria: all outcomes relating to later steps in NHSHC delivery, including rates of provision of advice, signposting, referral, prescriptions, and behaviour and lifestyle change |
When this initial screening process was complete, CD re-screened all remaining documents in light of the review’s chosen focus, seeking to identify documents that were likely to include data on what happens after the measurements and risk assessments are complete in an NHSHC. This additional inclusion criterion was applied to identify documents that described, for example, the offer or delivery of advice, signposting or referral, ongoing support or prescriptions following an NHSHC. Where the coverage of any particular document was unclear from the title or abstract, it was included for full text screening. The application of this additional inclusion criterion permitted us to efficiently prioritise documents that were likely to contribute relevant data on our chosen focus.
For the documents included in the existing PHE-commissioned rapid reviews, we relied on the screening processes undertaken by these review teams. We therefore included for consideration in full text all of the documents included in these reviews that related to review questions which focused on the appropriate stage of the NHSHC, as follows:
-
How is primary care managing people identified as being at risk of CVD or with abnormal risk factor results? (Objective 4 in the rapid reviews)
-
What are patients’ experiences of having an NHSHC? (Objective 5 in the rapid reviews)
-
What is the effect of the NHSHC on disease detection, changing behaviours, referrals to local risk management services, reductions in individual risk factor prevalence, reducing CVD risk and on statin and anti-hypertensive prescribing? (Objective 6 in the rapid reviews).
In the final stage of screening, CD read all documents in full text, to assess whether or not they contained relevant data that could contribute to the development and refinement of the programme theory. This process continued and was repeated during Steps 4 and 5 (see below), as the documents were read and re-read closely multiple times and the analysis evolved over the course of the review.
All excluded documents were stored in an Endnote reference library so that they could be consulted later in the review as required.
At all stages, wherever we identified documents that included relevant data, we also considered the rigour or trustworthiness of those data at the point of inclusion. We did not apply a standard checklist to assess each study. Instead, each piece of extracted relevant data was first assessed in relation to the methods that were used to produce it (where applicable). We did not automatically exclude data that were judged to be of limited rigour, or data that were not produced directly by a specific research method, as we also made an overall assessment of rigour at the level of the programme theory developed over the course of the review. 45 Our overall assessment of rigour took into account the role that each piece of data played in the developing programme theory and focused on our judgement of the explanatory value of the theory produced. To make this assessment, we considered both the volume and the nature of the data that underpinned each part of our developing programme theory. We also assessed the plausibility and coherence of each aspect of the programme theory (each context-mechanism-outcome configuration (CMOC)), as well as the relationships between these and the programme theory as a whole. To do so, we applied three interrelated criteria to each of these levels45 (see Step 5 below for more detail):
-
Consilience: We considered the extent to which the theories explained the included data, and considered theories that explained more of the data to be more plausible than those that could only account for some data (while bearing in mind that the aim in realist research is to identify and explain ‘demi-regular’ patterns of outcomes, i.e. we anticipated some data may point to ‘exceptions to the rule’).
-
Simplicity: We considered the extent to which the theories were simple and did not require special assumptions to be added to ‘help’ them explain the data.
-
Analogy: We considered the extent to which the theories fit with what is already known from existing research and substantive (formal) theory and the extent to which the component parts of our theories fit with each other.
All of the review findings presented below were judged by our project team to meet these criteria and so represent our assessment of plausible and coherent theories that explain important outcomes related to what happens after the measurements and risk assessment are completed in an NHSHC. Some aspects of the programme theory are stronger and more plausible than others, being based on a greater volume of more trustworthy data. To ensure transparency, the findings are accompanied by a full account of the data underpinning them: see Table 21, Table 22 and Table 23. A separate data appendix with full details of all extracted data is available on request from the authors.
Step 4: Extracting and organising data
We extracted the main characteristics (bibliographic details and information relating to study design, participants, settings and main findings) of each included document into an Excel spreadsheet. These details are presented in Table 20 in Chapter 3.
The full text of included documents was uploaded into the qualitative data analysis software, NVivo (Version 12, QSR International, Warrington, UK). CD coded relevant sections of text in these documents where they were interpreted as being relevant to what happens after the measurements and risk assessment are completed in an NHSHC. Some coding was deductive (some codes were anticipated in advance of data extraction and analysis, based on the IPT and background reading) but most coding was inductive (codes were created to categorise data in the included studies during the data extraction process) and some was retroductive (codes were created based on an interpretation of the data extracted, where we inferred what the causal force was that generated observed outcomes, i.e. mechanisms). Each new element of data was incorporated into our analysis (as described below in Step 5) and as the analysis progressed and the programme theory was refined over the course of the review, documents were re-scrutinised to ensure that all relevant data were captured. The final version of the coding frame is reproduced in Appendix 3.
As with screening, a 10% set of documents were coded in duplicate. CD and EG coded 10% of documents (n = 22) independently and GW provided an additional check for this coding by reviewing a merged NVivo file. The coding decisions and coding frame were discussed by the wider project team to resolve discrepancies and ensure consistency in how codes were understood and applied. Following this, CD coded the remaining documents following the processes described above. This process is a slight deviation from the process planned in our protocol, which indicated that 10% checks would be conducted by GW alone. This change permitted an additional member of the research team (EG) to provide an additional independent check on data coding, while increasing her familiarity with the data included in the review.
Step 5: Synthesising the evidence and drawing conclusions
We used a realist logic of analysis to make sense of the data included in the review. This process began and moved in parallel with the decisions taken in Step 4, as data were included wherever they were considered sufficiently rigorous and were understood to have relevance to our focus in the NHSHC. When coding of the included documents was complete, the data contained within individual or across closely related categories were read and considered together. We interpreted the extracted data as relating to important contexts, mechanisms or outcomes (or the relationships between these) and used them to build CMOCs, describing why (by which mechanisms) particular outcomes were generated in particular contexts.
To do this, we compiled and interpreted data both within and across included documents. We used cross-case comparison to draw parallels wherever the data demonstrated that similar contexts and mechanisms were in operation to produce patterns of outcomes, and to understand when and how different outcomes were produced. Based on our interpretations, we constructed theoretical explanations in the form of CMOCs for the range of outcomes we observed in the data, where these were relevant to our focus on what happens after the measurements and risk assessment are completed in an NHSHC. We aimed to develop the CMOCs at an appropriate level of abstraction, such that they embodied potentially transferable explanations that encompassed a range of specific circumstances and outcomes. In practice, this meant that our interpretation focused on identifying the salient features of the circumstances described in the data that could be understood as functioning as context, and identifying the specific, proximal outcomes that were produced in those contexts, rather than focusing solely on the intended overall outcomes of the NHSHC. As our theories were refined, more specific CMOCs were merged, whenever they were understood to articulate specific cases of a more abstract phenomenon, while others were separated, when it became clear that more than one active context, mechanism or resulting outcome was in operation. Where mechanisms were not explicitly articulated in the included data, we used retroductive reasoning to infer likely causal forces, with a focus on the reasoning and responses of different participants involved in the NHSHC programme (commissioners, providers and attendees).
Our application of this process to an example CMOC is set out below, to help to illustrate what we did in more detail.
CMOC C1: When commissioners view the NHSHC programme as a means to improve people’s lives through behaviour change (C) they will try to exert their influence over providers to ensure that the programme is delivered with this in mind (O) because they believe this will maximise the potential benefits of the programme (M).
This CMOC is underpinned by data extracted from 12 documents: two research articles (one cohort study and one qualitative interview study), four local evaluations of the NHSHC, three conference abstracts or presentations, one unpublished working document provided by a LA who responded to our survey and two other reports focused on LA roles in programme delivery. The specific data underpinning this CMOC included:
-
Statements from the commissioners’ perspective (from local evaluations and reports focused on LA roles, which include local case studies) that illustrate the role of engagement and close working relationships with providers to ensure that NHSHCs are delivered as envisioned. For example:
There should be a dedicated programme team … to address, for example, day-to-day running, timely monitoring, provider quality control (especially training and audit), marketing and programme evaluation. 48
Data presented in this report reflect a high-performing [local] authority that works closely with general practices, stakeholders and patient representatives within it. 49
The commissioning body … has enthusiastically taken up the findings from their evaluation and created an information package for the participating GP Practices and has also held an information day…50
[The] importance of communications and relationship building should not be underestimated … it is important to build effective, collaborative working relationships between Commissioners and Providers. 51
-
Further statements from the same and additional sources draw attention to the potential for LA commissioners to use their influence and relationships to work to ensure providers retain a focus on the behaviour change purpose of the NHSHC. For example: (All our emphasis.)
Liaise with NHS England [Local Area Team] to ensure the information gained from an NHS Health Check is used by … General Practitioners to improve the health of the patient by ensuring there is appropriate: incorporation of the NHS Health Check results into patient records; follow up with their GP; referral to lifestyle interventions as required. 48
The results we are most proud of relate to bringing all our primary care practices together to deliver consistency of approach, re-invigorating staff to enable them to feel they can assist people to make the changes. 52
‘Softer’ measures of success are seen as: ensuring there is provision of appropriate follow-up lifestyle services to help those with health issues identified during the NHS Health Check. Many commissioners believe this is imperative to the spirit of the programme, even though there are no targets around this. 51
Taken together, our data represent multiple local examples where there was recognition of the importance of a route for LA commissioners to exert influence over NHSHC providers in relation to programme delivery, and that this influence may be used in particular to try to ensure that advice and referrals relating to the programme’s aim to support behaviour change are delivered. By including these observations in local evaluation reports, conference presentations and case studies, commissioners and evaluators have drawn attention to the importance of this role for LAs, and, by implication, a potential disconnection in commissioner and provider priorities that could affect programme delivery. This latter implication is borne out in other CMOCs developed from the commissioner (e.g. CMOCs C2–C10) and the provider perspective (e.g. CMOCs P1–P8), lending further support to CMOC C1 as part of our overall understanding of how the programme operates, as captured in our final programme theory.
Only six of the documents reported research or evaluation work that was undertaken using specific methods, and therefore an overall judgement of the quality and strength of the evidence collated here was required. Our judgement centred on the criteria outlined above in Step 4. We considered that, taken together, our data were consilient, in that CMOC C1 captures a causal explanation for the observed outcome that LA commissioners may work to exert influence over NHSHC programme delivery; simple, in that we did not feel there was need to specify any additional assumptions to support our explanation; and supported by analogy. 45 In this case, we did not draw on substantive theory during the development of this CMOC, but we draw attention to our observation that this CMOC makes sense when considered in relation to other CMOCs developed over the course of the review, as summarised in our final programme theory (see Chapter 4).
CD undertook this step and developed and shared sets of developing CMOCs, accompanied by explanatory narratives and their underpinning data, with the wider project team. Following discussion within the team, the CMOCs were refined and re-organised to help develop their explanatory value. This included re-ordering and grouping similar CMOCs together – considering the relationship of each CMOC to a developing overall programme theory – as well as consideration of the level of abstraction at which CMOCs were presented and discussion of potential mechanisms where these were unclear. Emerging findings were also shared with our PPI and professional stakeholder groups (see section Stakeholder groups and Table 2 above) and feedback from these discussions also informed the project team’s discussions and refinement of the CMOCs.
In the later stages of the review, we also considered whether substantive theory could play a role in supporting or developing our analysis. A small number of documents included in the review included theoretical perspectives, reflecting what we found during IPT development (see Appendix 1), but most of the literature that contributed data to our review was atheoretical. We considered whether substantive theory from various disciplines could help to support or illuminate aspects of our findings during project team discussions.
Overall, analysis and synthesis of the data was an interpretive and iterative process, involving returning to the documents and data and interpreting and re-interpreting their meaning, seeking additional data as needed and ongoing discussion within the project team throughout.
Chapter 3 Findings
This section describes the findings of both the survey and realist review components of this project. The findings of the survey are presented first, including descriptive information about our respondents, before quantitative and qualitative analysis of responses and a typology of NHSHCs delivery models are presented. For the review, a description of the included documents is followed by an overview of the CMOCs developed, accompanied by a narrative detailing the findings of the synthesis of the data extracted from those documents. The overall final programme theory is outlined and illustrated in Figure 18 in the final part of this section. The findings of the survey and review together underpin the conclusions and recommendations presented in Chapter 4.
Survey findings
Respondent details
In addition to the three pilot responses, we received 69 from the main survey launch, giving a total of 72. Four responses were duplicates from the same LA, one from the pilot and three within the main survey. The pilot respondents asked us to ignore their first response, which was therefore removed, while the second responses from the remaining three duplicates were removed, leaving 68 responses for analysis.
Five of these respondents were reporting on behalf of multiple LAs. Therefore, the total number of LAs represented by these 68 respondents was 74. These varied proportionally by region (Table 6).
| Geographic region | Number of LAs | Number of responding LAs | % of responding LAs |
|---|---|---|---|
| East Midlands | 9 | 5 | 56 |
| East of England | 12 | 8 | 67 |
| London | 33 | 18 | 55 |
| North East | 12 | 4 | 33 |
| North West | 23 | 9 | 39 |
| South East | 18 | 13 | 72 |
| South West | 15 | 6 | 40 |
| West Midlands | 14 | 4 | 29 |
| Yorks & Humber | 15 | 7 | 47 |
| Total | 151 | 74 | 49 |
Delivery of the NHS Health Check
Responses representing 64 councils reported that delivery of NHSHCs in their area had resumed since the Covid-19 pause. The remaining respondents, representing 10 councils, said the programme hadn’t yet been resumed in their area.
Face-to-face delivery of NHS Health Checks before and after Covid pause
Face-to-face delivery in most venues reduced following the Covid-19 pause, but particularly in community settings and pharmacies. One respondent indicated a Covid-19 vaccination centre was used after the pause (Table 7).
| Venue | Before | After |
|---|---|---|
| GP practice | 73 (99%) | 65 (87%) |
| Pharmacy | 16 (26%) | 9 (12%) |
| Mobile unit | 6 (8%) | 6 (8%) |
| Community setting: | 30 (41%) | 15 (20%) |
| Workplaces | 11 | |
| Community centres | 9 | |
| Places of worship | 4 | |
| Leisure centres/sports halls | 3 | |
| Libraries | 4 | |
| Wellbeing centre/hub | 3 | |
| Council offices | 2 | |
Alternative methods of delivery
The use of alternative (remote) methods of delivery increased significantly following the Covid-19 pause, with the telephone being the most frequently used means of communication (Table 8).
| Method | Before | After |
|---|---|---|
| Telephone | 2 | 26 |
| Video | 1 | 11 |
| Self-completion online | 2 | 5 |
All 11 LAs that use video consultations for elements of the NHSHC also use telephone; two of these also indicated using self-completion online. Two LAs were trying out online self-completion tools before the Covid-19 pause. One was carrying out a ‘Pilot of a remote digital check, bloods were not taken but the question was asked if they know their values. Digital check just used to garner a risk score to encourage attendance at F2F [face-to-face] for higher-risk patients’ (R61). This LA did not continue with this method after resuming following the Covid-19 pause, while the second did:
[the online self-completion tool] wasn’t available to all practices ‘before’. However, the offer is available to all practices now, but some have not engaged or decided not to take up the offer. (R32)
Eleven of the LAs offering partially remote NHSHCs (in a two-part service) require that the NHSHC attendee attends the practice for blood tests. However, six use data on file, as long as it is within three or sometimes six months. One respondent representing two LAs described a drive-through blood-testing service in the community, set up by the hospital (R08).
Fifty-four respondents (75%) said they would consider using remote methods in future, mostly in combination with face-to-face testing. Digital options that allowed a lifestyle questionnaire to be completed online were seen as a potential way of reducing the length of a subsequent physical appointment within the practice (which would include risk assessment and advice/referral) (R01), or as a way of helping providers to prioritise or target those most in need (R17, R31), or to focus the face-to-face appointment on risk communication, personal support and advice (R50, R66):
Online assessments prior to appointment, or some digital intervention to capture some basic information, but having the main consultation face-to-face – communicating the risk. (R66)
Alternatively, some saw the value of a two-part model in which an initial brief face-to-face appointment for physical measurements was then followed up by phone to discuss results and interventions (e.g. R04, R07, R20).
Looking at doing physical measures face to face and follow up appointment including risk management part of the check remotely. (R07)
This is in contrast with at least one LA which allows their providers to use their own judgement about how to use remote delivery, but ‘insist they [patients] need to come in to take their measurements and collect their results’ (R11). One respondent (on behalf of two LAs) suggested that their preference for face-to-face delivery was ‘to achieve best behaviour change results’ (R15).
There were some other novel proposals, and a high degree of uncertainty about what will work best in the future:
We are testing the feasibility and acceptability of remote blood testing using a kiosk in community setting and then linking back to an online questionnaire tool. This system would be for lower-risk patients predominantly. (R61)
The provider of our lifestyle service is developing an online health check model that we may pilot. (R25)
[We are] concentrating on community options to ease pressure on primary care and consider[ing] any remote options that are presented to us. (R47)
Many indicated they were wanting to learn how other areas got on with this hybrid model of providing NHSHCs, or were hoping to take part in a PHE-led pilot. One respondent expressed a concern about the ‘need to stick to the contents of the NHS Health Checks in order for interventions to be counted as a Health Check’ (R09). This respondent was therefore dissuaded from looking at digital alternatives. Comments from other LAs also suggested that they would be waiting for the lead to come from PHE/national guidance.
Which health professionals are commissioned to deliver the Health Checks?
None of the respondents told us they didn’t know which health professionals are commissioned to deliver the NHSHC. However, in later comments, respondents said that:
We commission GP practices to deliver it through suitably qualified, trained (and overseen) staff. It is then up to them who that actually is. (R30)
It’s often difficult to monitor Health Check activity from start to finish. Lack of contract monitoring meetings and data wrapped up in other service provision. (R03)
Healthcare assistants (HCAs) and/or nurses deliver the NHSHC in most (61) of the responding LAs. These same staff have also been used to deliver NHSHCs remotely. Respondents said that GPs deliver the NHSHC in 48 of the LAs, and also deliver remotely in 12 (Table 9).
| Provider | Face to face | Remotely |
|---|---|---|
| HCA | 61 | 19 |
| Nurse | 61 | 18 |
| GP | 48 | 12 |
| Pharmacist | 17 | 1 |
| Pharmacy assistant | 14 | 1 |
| Health trainer | 14 | 5 |
| Other | 9 | 3 |
Other providers included wellbeing advisers, health improvement practitioners, lifestyle coaches and paramedics. No respondents reported delivery via a ‘drive-through’ service.
Delivery has been affected by Covid-19 in some areas, with seven respondents reporting a change in who delivers the NHSHC following the Covid-19 pause. Delivery in leisure centres and by primary care staff was more problematic following Covid-19. In general, more HCAs were involved and fewer nurses or GPs:
Less involvement from Nursing team as they are being utilised for vaccine. (R05)
Other areas mentioned that there were fewer health trainers involved, and that some council staff and paramedics were taking over delivery.
Prioritisation of eligible candidates
Respondents were asked whether NHSHC candidates were prioritised by ethnicity, Covid-19 risk, indicators of deprivation, or by other risk factors, before and after the Covid-19 pause. The prioritising of eligible candidates appeared to increase following the pause (Table 10).
| Factor | Before | After |
|---|---|---|
| Ethnicity | 22 | 35 |
| Covid-19 risk | 21 | |
| Deprivation | 31 | 34 |
| Other | 28 | 33 |
Examples cited in the ‘other’ category included: diagnosed mental illness, homeless, from a traveller community, inactivity, routine and manual workers, and gender/age (e.g. men over 65). Covid-19 appeared to have prompted some areas to start targeting via risk where they hadn’t done so before.
There was evidence of increased targeting by ethnicity post-Covid-19:
As we have a high BAME population, we introduced a South Asian health check which is offered to residents of BAME origin aged between 30 and 39. (R56)
Risk factors which were specifically targeted in relation to both CVD and Covid-19 were high BMI and smokers. One area specified targeting those eligible for flu vaccines, but most described processes designed to identify those at high overall CVD risk, since the risk factors were similar for both CVD and Covid-19.
Have just been able to add Covid Risk to our list of priority people, they would’ve probably already been included in the priority list anyway. (R66)
Such targeting was not universally feasible, as indicated by the following comments:
Smoking status, BMI above 30, family history, ethnicity other than white, deprivation quintile 1. Practices tell us that this data is not always up to date and so it’s not easy to identify those at higher risk. (R13)
Our focus is on getting more practices to engage before we focus on any kind of prioritisation. For about 5 years we have struggled for various local reasons to get about a third of our practices to engage. Another third are only engaging in a limited way. (R30)
We have 48 providers (GPs) and each prioritise their invites according to their preference. We recommended they prioritised by ethnicity and predicted risk during lockdown. (R05)
Services to support risk reduction/management
As shown in Table 11 below, the majority of responding authorities had at least one service to support smoking cessation, alcohol and drug misuse, weight management, diabetes prevention, psychological support and social prescribing. In many LAs, there were two or sometimes three service providers for some of these services. Five respondents indicated in the open comments that their LAs also commission physical activity/exercise on referral services; one mentioned a generic lifestyle service.
| Service | Number of LAs in survey sample commissioning: | |||||
|---|---|---|---|---|---|---|
| Don’t know who commissions | No response / no service provider | 1 service provider | 2 service providers | 3 service providers | 4 service providers | |
| Smoking cessation | 1 | 2 | 45 | 18 | 8 | |
| Alcohol and drug misuse | 3 | 0 | 52 | 15 | 3 | 1 |
| Weight management | 5 | 6 | 45 | 16 | 2 | |
| Diabetes prevention | 7 | 2 | 60 | 4 | 1 | |
| Psychological support | 20 | 6 | 39 | 7 | 1 | 1 |
| Social prescribing | 10 | 2 | 46 | 13 | 3 | |
| Other services | 7 | |||||
As shown in Table 12, the majority of lifestyle and other relevant support services were provided through public, private or third-sector commissioning, with fewer provided by GP or LA staff.
| Service | Number of LAs responding that services are delivered in their area by: | ||||||
|---|---|---|---|---|---|---|---|
| GP staff | LA staff | Public sector | Private sector | Third sector | Other | Total services | |
| Smoking cessation | 26 | 20 | 22 | 28 | 9 | 0 | 105 |
| Alcohol | 8 | 3 | 27 | 30 | 26 | 1 | 95 |
| Weight management | 10 | 10 | 16 | 38 | 9 | 0 | 83 |
| Diabetes prevention programme | 10 | 0 | 16 | 38 | 5 | CCG: 2 | 71 |
| Psychological support | 5 | 0 | 33 | 6 | 13 | CCG: 2 NHS Trust: 1 |
60 |
| Social prescribing | 30 | 12 | 11 | 3 | 23 | CCG: 2 | 81 |
| Other | 0 | 0 | 4 | 2 | 1 | 0 | 7 |
| Total services | 89 | 45 | 129 | 145 | 86 | 8 | 502 |
Respondents were asked how confident they were that:
-
each set of services has sufficient capacity to meet the demand arising from NHSHCs. They were asked to think about, for example, waiting times, eligibility criteria, etc.
-
each set of services is accessible to NHSHC attendees requiring support. They were asked to think about, for example, days/times of services, location of services, cost to service users, etc.
Most of the 68 respondents gave their views on their level of confidence in the support services available in the LAs for which they were responding. Confidence in the capacity of these services was mostly positive (see Figure 4).
FIGURE 4.
Commissioners’ confidence in the capacity of services to support NHSHC attendees.

However, this level of confidence varied across the different services. Respondents told us:
We had increased our smoking cessation service just prior to Covid so they have the capacity, the rest have seen so many people coming through over the last year that there is a bit of a wait for some. (R66)
We have capacity within weight management, EoR and diabetes prevention. Concern is around IAPT [Improving Access to Psychological Therapies programme] capacity as there was a waiting list prior to COVID and I understand that there is now more pressure on this service. (R61)
Others expressed doubts about the capacity of services to meet potential demand:
If all who are eligible and ready to be referred were so, there would not be enough capacity in the system, specifically weight management and mental health alone. (R08)
[The LA] had capacity issues with its commissioned smoking cessation service following a huge increase in demand throughout COVID-19. There are known long waiting times for psychological support services and not all professionals are aware of social prescribing practices. (R28)
Three respondents cited financial difficulties in association with the availability of appropriate support services:
With austerity measures, the capacity in the system has become so limited that there is very little capacity available. (R13)
The local authority is unable to properly financially support referral services. (R34)
Both alcohol and psychological support services (mental health services) are far less well established and resourced. (R23)
One respondent suggested that ‘In general, capacity isn’t the issue. It’s the motivation and interest from the public that is the issue’, citing that group weight management sessions are offered, but not welcomed by the majority of the population (R18).
Responses to the question about confidence in capacity (shown in Figure 1) suggest that there are some LAs with significant gaps in commissioned support services. Indeed, one respondent commented:
There are no weight management and stop smoking services available locally. (R16)
However, several respondents felt unable to give a view about the capacity or accessibility of services, especially for services that were not commissioned by the LA. This is reflected in the variable amount of missing data and in several comments from respondents. This response highlights the difficulty of pulling together information across such a fragmented system:
NDPP [National Diabetes Prevention Programme] is funded by NHSE [NHS England] through CCG [Clinical Commissioning Group] who rarely provides information to LAs unless forced to do so; all others are LA funded except for tier 3 weight management – another CCG funded service which is non-existent in the last 4 years. (R54)
Confidence in the accessibility of the services (see Figure 5) was similar and directly correlated to confidence in the capacity (Spearman’s r = 0.752; p < 0.001). Respondents were least certain about whether psychological support services had sufficient capacity and accessibility, which may be because these services are generally commissioned by NHS organisations.
FIGURE 5.
Commissioners’ confidence in the accessibility of services to support NHSHC patients.
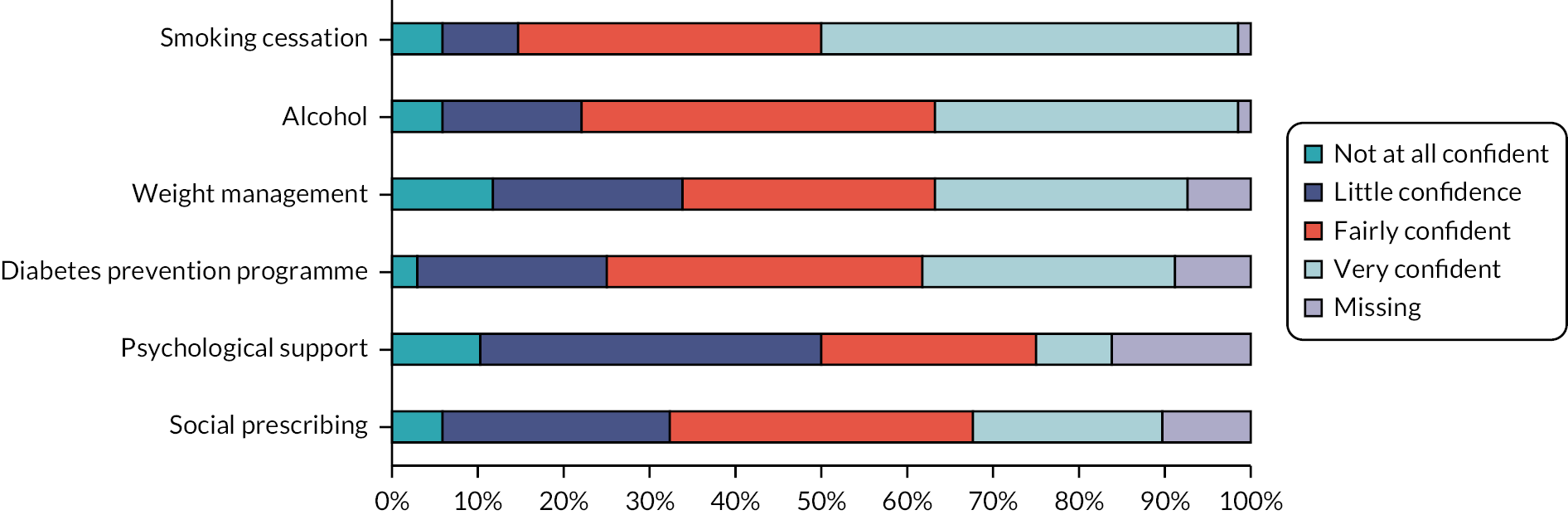
All respondents provided an opinion regarding the appropriate use made by NHSHC providers of the support services that are available. This was much lower, with over half of the respondents (n = 50; 68%) having relatively little confidence (Figure 6).
FIGURE 6.
Commissioners’ confidence in appropriate use made of support services by NHSHC providers.

Several respondents commented that the number of onward referrals from the NHSHCs remain low, for example:
There is a wealth of support available from [this council]. The issue is not all providers access the support available. (R18)
However, others mentioned that they ‘have no real data on referral to other services’ (R03), so they generally lack knowledge about uptake of referrals following NHSHCs:
I have been generous giving this a three [fairly confident]. We do highlight support services as part of our NHS Health check training but have no way of following patients through to know how many access support successfully. (R64)
The level of awareness of NHSHC providers was a major factor in low confidence in the use of these services:
A recent survey of our GP providers indicates lack of awareness and skills in initiating lifestyle conversations, communicating the NHS HC results or about the offer from the Lifestyle provider. Subsequently we suspect not all GP practices refer into the community offers that are available following a NHS HC. (R13)
However, where there was less fragmentation, this was seen to be improved:
Onward referrals from Health Checks into our own services are higher from our own team of Health Trainers, which suggests that we aren’t getting all the referrals we should be getting from other providers. (R23)
Several respondents noted that they are working (or were working, prior to Covid-19) on addressing low rates of referrals through training and through working closely with providers.
Forty respondents reported that there had been a change in either capacity or accessibility of support services since the Covid-19-related pause, 13 said there had been no change, and 15 said they didn’t know. In some cases, the move of some support services to online provision was perceived to affect both accessibility and capacity in both positive and negative ways.
Many of these services have had to move online for part of the time at least, possibly making them more accessible for some but less accessible for others. (R50)
Services moved onto telephone support where possible and this increased accessibility for people as in they did not have to travel to attend appointments. (R66)
For some services capacity has increased due to remote delivery. (R04)
F2F [face-to-face] services have moved online only which are more popular and more efficient, permitting advisers to see more clients. (R40)
In some cases, Covid-19 has prompted greater investment in support services:
Tier 2 weight management service has had increased funding and the service has expanded and lowered its referral threshold. There is more social prescribing as an increase in PCN [Primary Care Network] link workers funded by national scheme. More funding for substance misuse services as well. (R41)
Increase in funding for drug/alcohol services, plus increase in funding for weight management programmes have increased capacity and accessibility. (R10)
Referral processes
Most respondents provided information about referral processes for support services. The most commonly cited referral processes for accessing support services were the client making an appointment themselves or a provider making an appointment on their behalf (Table 13). However, some respondents did not know the referral processes in place in their area. As with awareness of service providers, the referral processes were least well known for psychological support services.
| Service | Number of LAs responding that the following referral routes are available in their area: | |||||
|---|---|---|---|---|---|---|
| Client makes own appointment | Provider makes appointment | Referral via link worker | Other | Don’t know | Missing response | |
| Smoking cessation | 59 | 41 | 22 | 2 Pharmacy/direct; London stop-smoking service | 4 | 3 |
| Alcohol | 42 | 38 | 24 | 1 drop-in | 16 | 1 |
| Weight management | 37 | 34 | 24 | 1 online | 10 | 5 |
| Diabetes prevention programme | 28 | 35 | 18 | 1 GP | 14 | 2 |
| Psychological support | 24 | 26 | 12 | 0 | 28 | 5 |
| Social prescribing | 22 | 28 | 25 | 0 | 23 | 4 |
| Other service | 6 | 7 | 3 | 0 | 7 | |
| Total referral processes | 218 | 209 | 128 | 5 | ||
Multiple processes for ensuring that patients can obtain appointments with follow-on services are apparent in many areas (see Table 14). For example, for smoking cessation services, in 36 areas, clients can either make an appointment themselves or a provider can make an appointment on their behalf, while in 13 of these areas referral via a link worker is a third option. The number of referral processes reported was strongly related to the number of services commissioned across the LAs (Spearman’s r = 0.423; p < 0.001).
| Service | Number of LAs | ||
|---|---|---|---|
| One process only | Two processes | Three or more processes | |
| Smoking cessation | 24 | 29 | 14 |
| Alcohol | 20 | 26 | 11 |
| Weight management | 29 | 23 | 7 |
| Diabetes prevention programme | 36 | 20 | 2 |
| Psychological support | 20 | 21 | 0 |
| Social prescribing | 26 | 17 | 5 |
Respondents representing 12 LAs indicated that referral processes had changed following the Covid-19 pause. For 45 LAs, respondents indicated no change. For the remaining 17, respondents gave no information. Changes were mainly positive:
Self-referrals are now possible to our social prescribing service which is a gateway to all other support services. (R41)
Weight management and stop smoking services transitioned to a new provider in January 2021. Referral routes are now more accessible. People can now self-refer on the website, through a freephone number, local number and email. Professionals/link workers can refer as above and through integrated SystmOne referral form. (R27)
Monitoring and evaluation
Monitoring of the outcomes of NHSHC programmes by LAs was relatively poor, with only 22 (31%) respondents indicating they gathered data on referrals to the GP, and 30 (42%) on the outcomes from such referrals, for example, new diagnoses. A similar proportion indicated they gathered data on referrals to lifestyle support services (24; 34%) and the outcomes from these, such as weight loss (19; 26%). Very few indicated they had data on whether prescriptions were taken up (8; 11%) or whether prescribing had resulted in changes in biomarkers (4; 6%). Respondents representing 33 LAs (46%) stated that they had undertaken some evaluation of their local programme (see Figure 7).
FIGURE 7.
Monitoring data routinely requested by commissioners.

Typology of local authorities
The number of LAs (N = 74) which fell into the three categories of delivery, are shown in Table 15.
| Delivery category | Number of LAs |
|---|---|
| General practice | 24 (32%) |
| Blended | 21 (28%) |
| Blended with outreach | 29 (39%) |
General-practice delivery
All LAs in this category delivered the NHSHC in the general practice setting only, by one or more of the following staff: GP, nurse, HCA, health trainer and pharmacist. None of the LAs in this category described using remote methods for delivering any aspect of the NHSHC post-Covid-19, although several were considering doing so.
Case examples:
In one LA (LA68), NHSHCs pre-Covid-19 were delivered face-to-face only in GP practices, by GPs and nurses. No remote methods have been used and they are not interested in developing such methods because of ‘limitations due to budget reductions’.
In another LA (LA32), NHSHCs pre-Covid-19 were delivered face-to-face only in GP practices, by nurses and HCAs. No remote methods were used, but the respondent was interested to ‘Explore options in light of Covid-19 impact on the acceptability of different models of health provision e.g. online consultations’.
Blended delivery
In this category, seven LAs delivered the NHSHC in GP practices and pharmacies, with or without some use of remote methods post-Covid-19. All others delivered in GP practices only, but also used remote methods to deliver part of the NHSHC. They were delivered by one or more of the following staff: GP, nurse, HCA, pharmacist, pharmacy assistant and paramedic.
Case examples:
In one LA (LA66), NHSHCs pre-Covid-19 were offered in general practices, by HCAs and nurses. Post-Covid-19, telephone consultations have been used to deliver part of the NHSHC, with patients attending the practice only for bloods and physical measurements. Interest in pursuing this method is positive, since ‘feedback from local medical committee is that patients like this form of e-consult’.
Another LA (LA36) offered NHSHCs pre-Covid-19 in general practices and pharmacies, but post-Covid they are no longer available in pharmacies. Post-Covid-19, telephone consultations have been used to deliver part of the NHSHC and the LA is also ‘looking at developing digital plus targeted face to face’.
Blended with outreach
All LAs except one in this category delivered the NHSHC in GP practices. In addition, they all delivered the NHSHC in at least one other venue, one of which was a community venue other than a pharmacy. Eighteen LAs in this category used no remote methods. Eleven used some form of remote methods.
Case examples:
In one LA (LA06), NHSHCs were provided pre-Covid-19 in GP practices and workplaces by practice nurses (PNs), HCAs and a community health improvement nurse. Post-Covid-19, they are delivered in practices only, but using a brief 5-minute face-to-face consultation followed by a telephone call. The intention is to continue with this: ‘2 part model: initial brief face to face appointment for physical measures with follow up by phone to deliver results and intervention’.
In another LA (LA22), NHSHCs were provided pre- and post-Covid-19 in GP practices, pharmacies, and in workplaces, faith halls, and ‘anywhere there are eligible populations’ using a mobile unit. Staff involved in face-to-face delivery include GPs, HCAs, nurses, pharmacists, pharmacy technicians and health trainers, while HCAs and nurses offer remote delivery via both telephone and video post-Covid-19. The LA are keen for this to continue. ‘We would welcome all opportunities to enable the population to access an NHS Health Check in a variety of ways that’s suits them.’ Methods for increasing reach were described: ‘1. Currently piloting a partnership approach with one practice and our community check provider. The GP practice invites males under 50 to attend their check at the community provider who is based in the same building as the practice. 2. Provided grants to NHS Healthcare Trusts to provide NHS Health Checks to their staff. 3. Community checks … delivered as part of an integrated Health and Well-being service.’
Associations between delivery category and other survey data
The number of commissioned services reported by each respondent to support smoking cessation, weight management, alcohol use, the diabetes prevention programme, psychological support, social prescribing and any other relevant services was totalled. Overall, there were 502 services reported for the 74 LAs (mean 6.78; median 6.0). The LAs were grouped into three categories, dependent on the number of services reported (see Table 16). Just over a third of the LAs (25; 34%) reported having a higher than average number of providers, over half of which (n = 14) were in the blended with outreach category of delivery.
| Number of commissioned support services | Number of LAs (n = 74) |
|---|---|
| Below average (5 or fewer) | 20 (27%) |
| Average (6/7) | 29 (39%) |
| Above average (more than 7) | 25 (34%) |
The mean number of commissioned services was significantly higher in the LAs which fell into the blended with outreach category (7.6) compared to the general practice (6.6) or blended categories (5.9) (F = 3.85; p = 0.026) (see Figure 8).
FIGURE 8.
Association between commissioned support services and NHSHC delivery category.
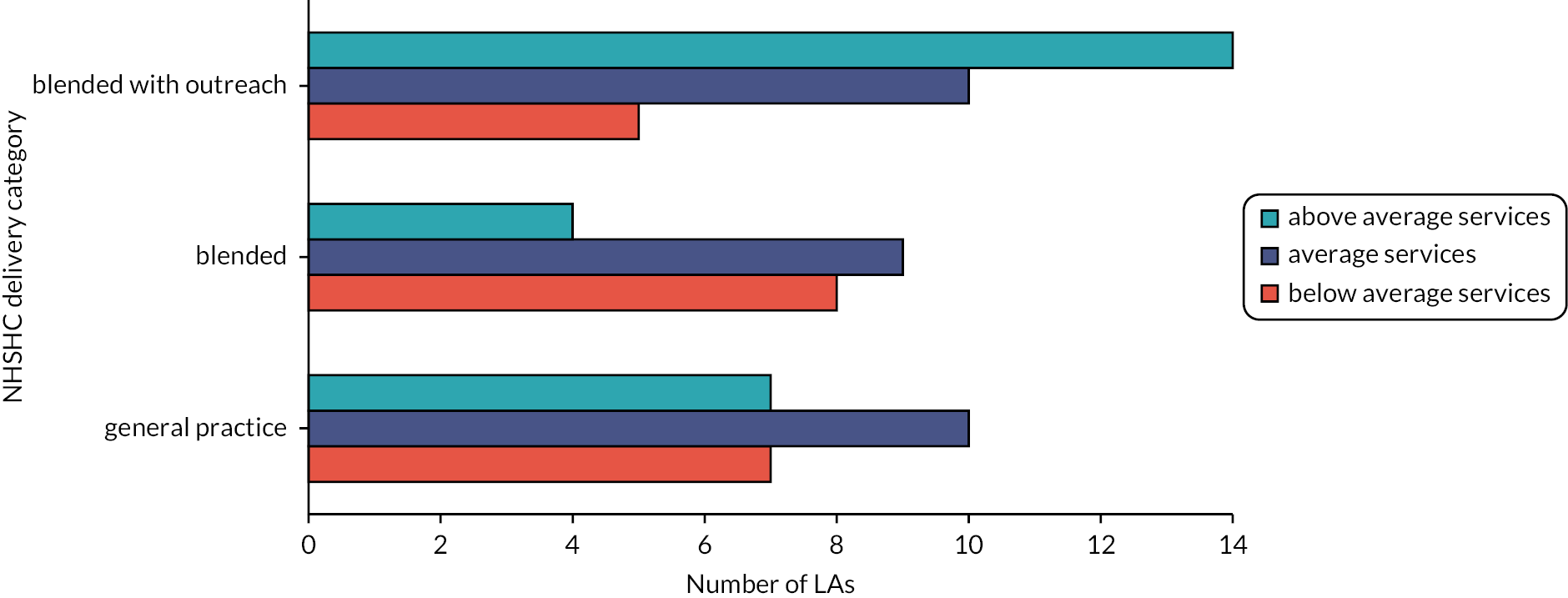
The total number of different referral processes into all support services reported by each respondent was 560. As three LAs reported no information about referral processes for any service, the overall mean number was 7.57, median 8.0, range 1 to 16. A third of the remaining 71 LAs (24; 34%) reported a below average number of referral processes, equivalent to one or fewer referral processes per major service (see Table 17).
| Number of referral methods for support services | Number of LAs (n = 71) |
|---|---|
| Below average (6 or fewer) | 24 (34%) |
| Average (7/8) | 16 (23%) |
| Above average (more than 8) | 31 (44%) |
The LAs which were categorised as offering blended with outreach delivery had the highest mean number of referral processes (8.0), compared to those categorised as general practice (7.5) and blended delivery (7.0), although the difference was not statistically significant (F = 0.311, p = 0.764) (see Figure 9).
FIGURE 9.
Association between referral processes and NHSHC delivery category.

The respondents’ average rating of confidence in both capacity and accessibility for each of the six main services was calculated, excluding missing responses. Their confidence in usage was rated as a single score for all support services. Confidence in the capacity, accessibility and usage of the support services varied little across the categories of delivery, although trends were visible in the confidence in accessibility and usage with the increasing use of non-general-practice-based NHSHC delivery (Table 18).
| Delivery category | Overall confidence ratings for all services | ||
|---|---|---|---|
| Capacity average (n = 72) | Accessibility average (n = 73) | Usage (single rating) (n = 74) | |
| General practice | 2.80 | 2.69 | 2.00 |
| Blended | 2.63 | 2.73 | 2.14 |
| Blended with outreach | 2.68 | 2.82 | 2.41 |
The total number of methods used to prioritise invitations was calculated for each LA both pre- and post-Covid-19. The number of methods was not related to the category of delivery, either pre- or post-Covid-19. In general, the number of prioritisation factors increased in all categories post-Covid-19. However, the increase in the mean number of prioritisation factors used was higher in the blended and blended with outreach categories, compared to the general-practice category (see Table 19 and Figure 10).
| Delivery category | Mean number of factors used to prioritise invitations | |
|---|---|---|
| Pre-Covid-19 | Post-Covid-19 | |
| General practice | 1.08 | 1.37 |
| Blended | 1.10 | 2.10 |
| Blended with outreach | 1.10 | 1.59 |
FIGURE 10.
Change in prioritisation pre- and post-Covid-19 by category of delivery.

The degree of monitoring and evaluation reported as being undertaken was generally low: mean number of aspects reported = 1.92; median 1.5. There were 19 LAs reporting doing none, 30 reporting monitoring/evaluating one or two aspects (minimal), and the remaining 25 reporting monitoring/evaluating more than two aspects (above average). The degree of monitoring and evaluation was not related to the category of delivery (see Figure 11).
FIGURE 11.
Monitoring and evaluation of NHSHCs by delivery category.
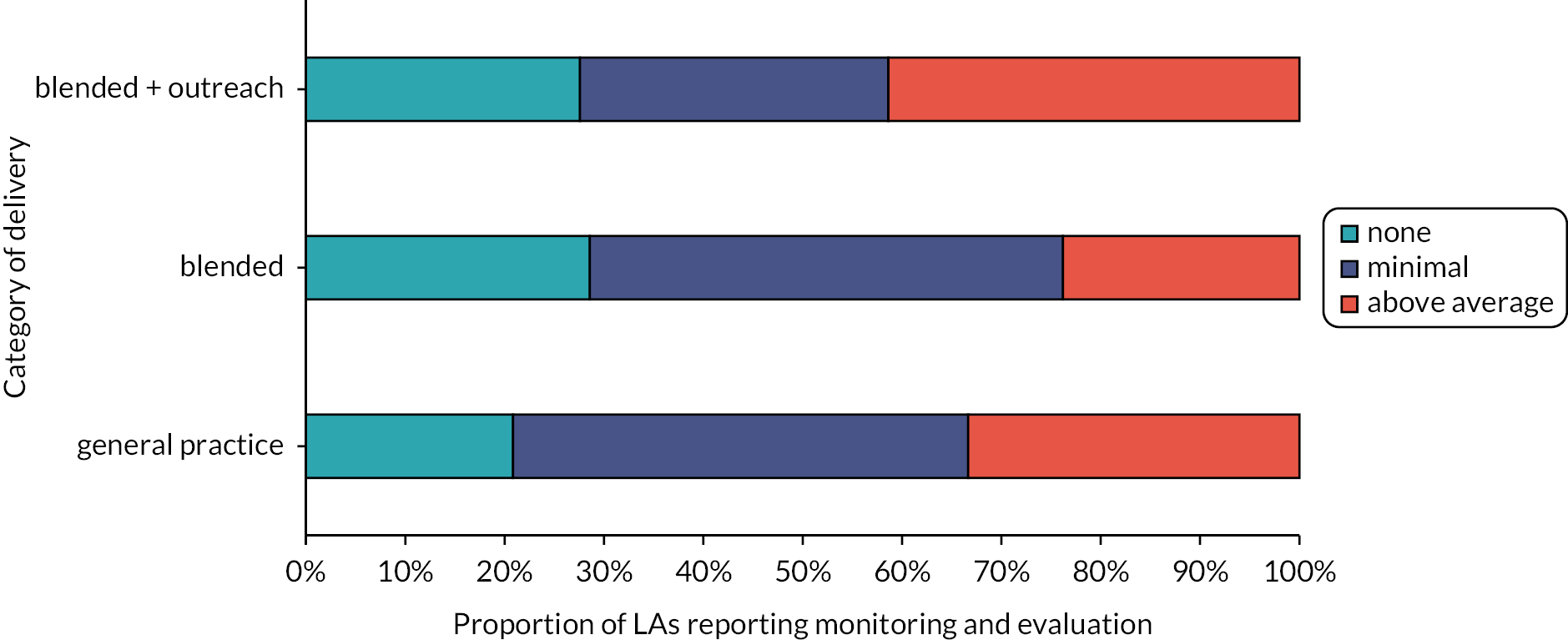
Associations between delivery category and data at local authority level
With regard to geographic region, there were notable differences in the proportions of LAs in the three NHSHC delivery categories in each PHE centre. Whilst five out of the seven responding LAs in Yorkshire and Humber fell in the ‘blended with outreach’ category, seven out of the nine responding LAs in the North West fell in the ‘general-practice delivery’ category (see Figure 12).
FIGURE 12.
Proportion of LAs in NHSHC delivery categories by geographic region.

With regard to LA size, there were no significant differences in the relative size of the LAs falling in each NHSHC delivery category, although there does appear to be a trend that those LAs delivering via community outreach tend to be larger (see Figure 13).
FIGURE 13.
Size of LAs in each NHSHC delivery category.

With regard to budget, there were no significant differences in the relative size of the public health budgets of LAs falling in each NHSHC delivery category (see Figure 14).
FIGURE 14.
Public health budgets of LAs in each NHSHC delivery category.
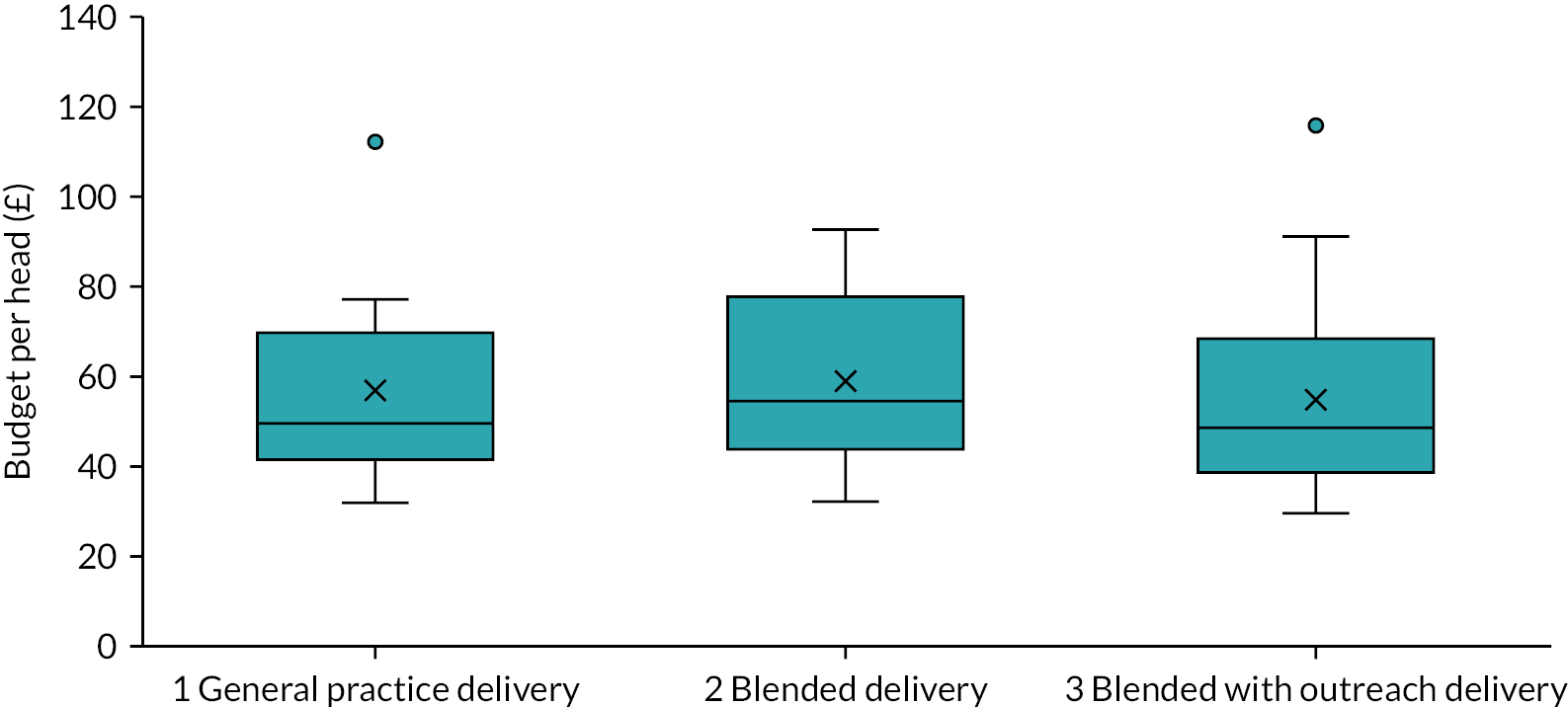
With regard to deprivation, there were no significant differences in the relative deprivation of LAs falling in each NHSHC delivery category. Below (see Figure 15) we have reported on the indicator ‘Rank of proportion of LSOAs in most deprived 10% nationally’, but other indicators (e.g. rank of local concentration) paint a similar picture.
FIGURE 15.
Deprivation within LAs in each NHSHC delivery category. LSOA, lower-layer super output area.

Finally, with regard to NHSHC programme delivery performance, according to the measures captured by PHE and published in Appendix 1 of their programme review41 (proportion of eligible people receiving an NHSHC between 2015/16 and 2019/20) LAs delivering NHSHCs using a ‘blended with outreach’ model achieved, on average, a lower coverage (37.8%) than those delivering using a general practice (46.7%) or blended (45.4%) delivery model (F = 3.217; p = 0.046) (see Figure 16).
FIGURE 16.
NHSHC performance measures (2015/16 to 2019/20) for LAs in each NHSHC delivery category.

Summary of survey findings
Our survey, covering 74 LAs across England, clearly demonstrates the variation in delivery of the NHSHC in terms of where and how it is provided and by whom. Whilst HCAs and/or nurses deliver the NHSHC in most (85%) responding LAs, GPs deliver at least some of the checks in two-thirds of the LAs. There is a wide range of other professionals responsible for delivering the checks, to a greater or lesser extent in different LAs. Some commissioners do not specify and are not aware of the type/grade of professional that delivers the check.
Our information on the delivery of the NHSHC before and after the Covid-19 pause has enabled us to create a typology of NHSHC delivery for the first time. We identify three main models in use prior to the Covid-19 pause: delivery in general practice only (used by 32% of responding LAs), delivery in general practice but also offering remote delivery (such as by phone or video consultation) and/or delivery in pharmacy (28%), and delivery in a range of settings that include community venues, with or without remote delivery (39%).
Our survey also provides new insight into what happens to attendees after their risk assessment. Whilst our survey found that most LAs commission at least one service to support key aspects of behavioural change (in relation to smoking, alcohol consumption and weight management), there are some LAs in which significant service gaps exist. Our survey shows that even though commissioners overall might feel reasonably confident about the capacity and accessibility of support services, they are much less confident that appropriate use is being made of the support services by NHSHC providers.
Our analyses show that LAs using a blended with outreach model tend to have a higher number of support services to support behaviour change following the check. The blended with outreach model is also associated with more post-Covid-19 prioritisation of NHSHC candidates, and greater confidence in the accessibility and usage of follow-on support services. There does appear to be a pattern with regard to LAs in the different regions commissioning different delivery models. For example, seven out of nine LAs in the North West employ a general-practice delivery model, whilst only one out of 13 LAs in the South East, one out of seven in Yorkshire and Humber and one out of six in the South West do so. Whilst there is no significant association, there appears to be a trend that those LAs delivering via community outreach tend to be larger in population size. However, our data show no apparent association between delivery model and the size of the public health per head, or level of deprivation. Finally, when looking at the programme performance indicators captured by PHE, programme coverage might be slightly less overall for LAs delivering via a blended with outreach model.
Review findings
Documents included in the review
The identification, screening and inclusion of documents in the review are summarised in Figure 17 (an adapted version of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram). 53 A total of 124 included documents contributed data to the review.
FIGURE 17.
Summary of searching and screening.
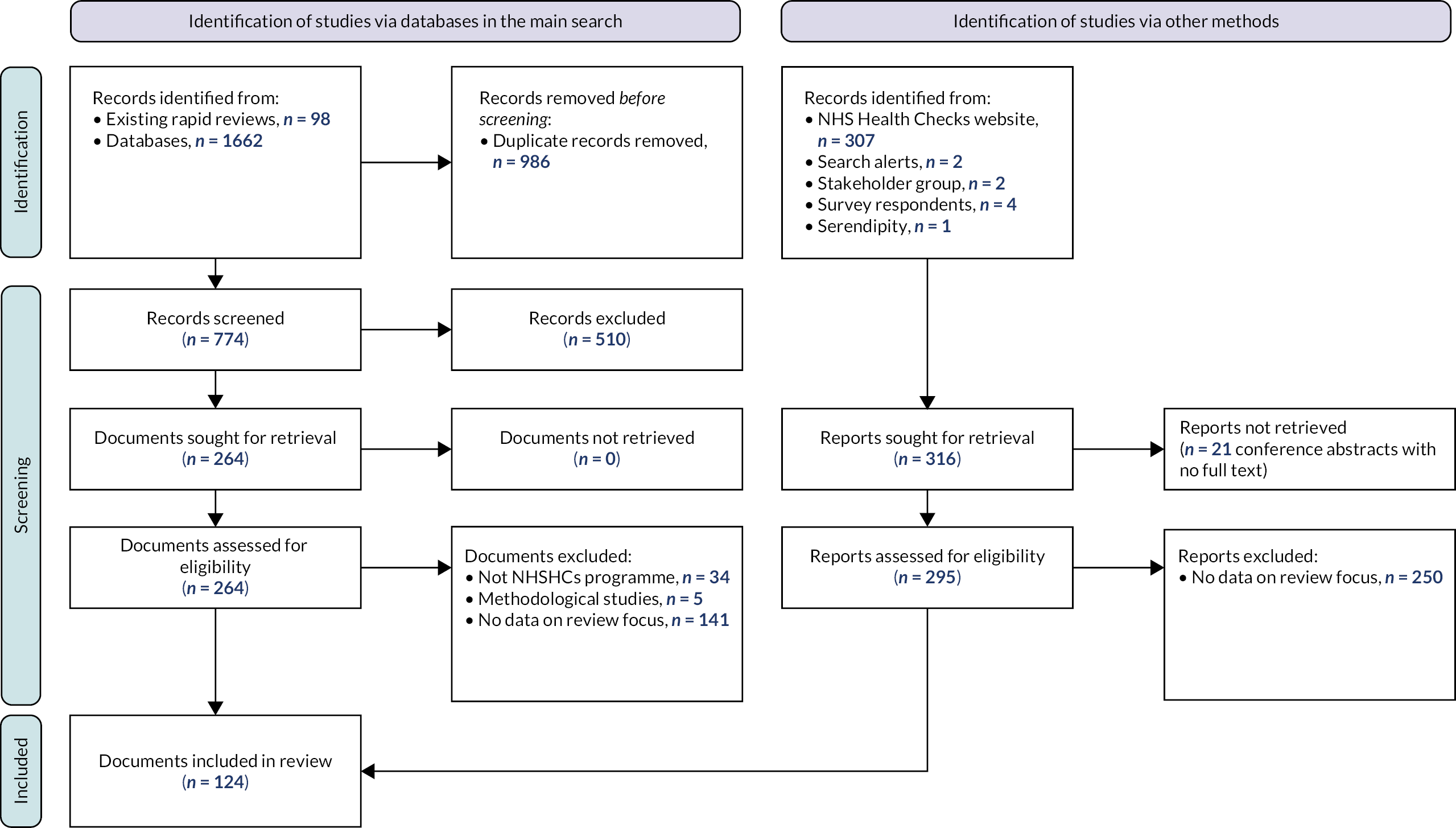
Of the 124 documents included, 59 were published research papers or reports, 20 were documents reporting local evaluations of services, 34 were conference materials (including presentations, abstracts and posters) and 11 were other types of documents, including policy reports, guidance, news articles and theses. Seventeen per cent (n = 21) of included documents contributed data describing the NHSHCs programme in relation to all of England; the rest focused on a single local area or small group of areas. The geographical distribution of included documents that represent individual local areas in England is illustrated in Figure 18. Details of the full set of included documents are provided in Table 20.
FIGURE 18.
Map of England showing geographical focus of included documents.
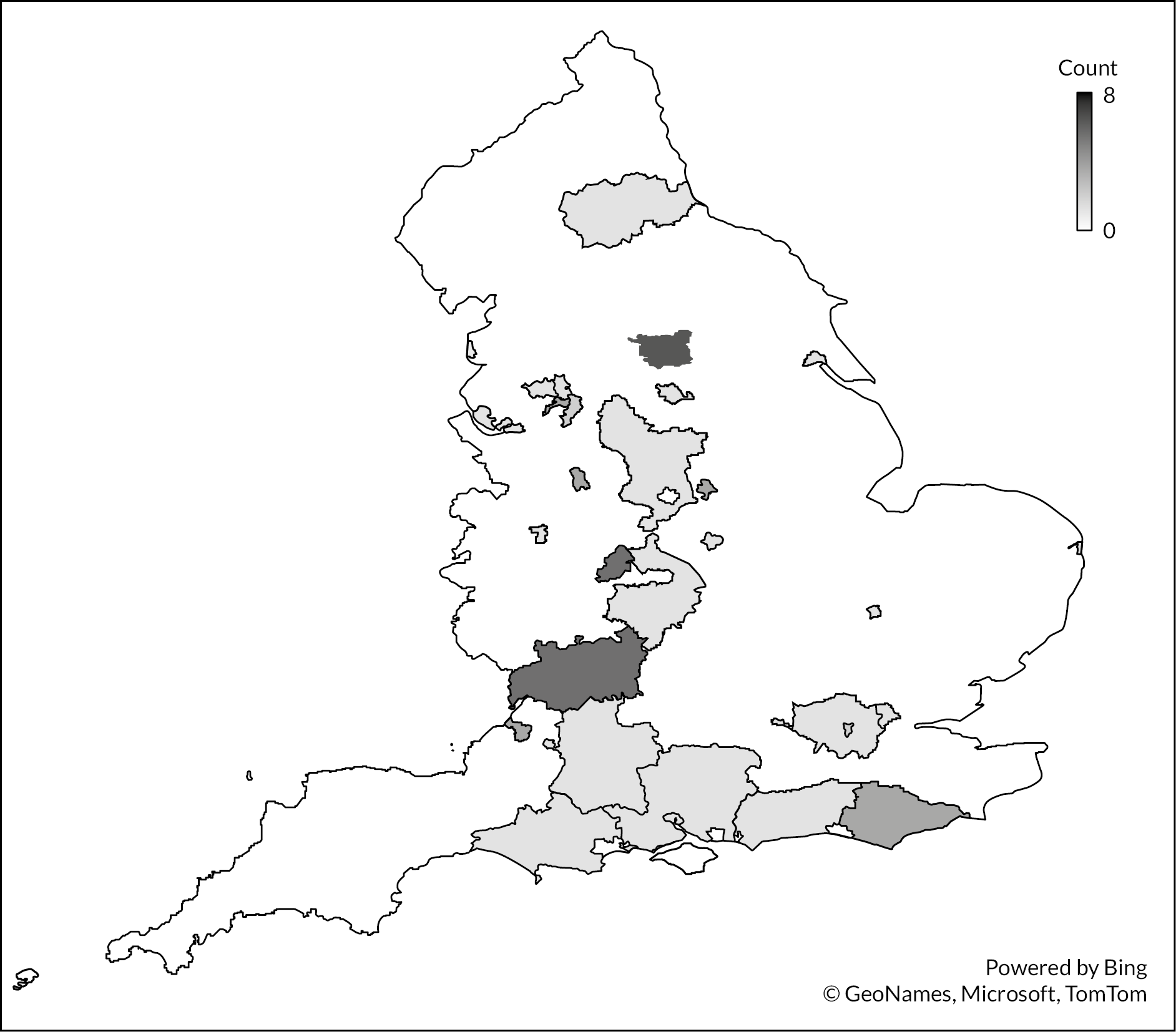
| First author | Year | Document type | Aim or purpose of document | Study design (if applicable) | Perspective(s) | Local area(s) | Commissioning perioda | Contributed data to CMOCs | Total contributions to CMOCs | Source | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C-CMOCs | P-CMOCs | A-CMOCs | ||||||||||
| Alageel54 | 2018 (1) | Conference presentation | Summary of results of qualitative interview study (Alageel 2018) | Qualitative interview study | Providers | Lambeth and Lewisham | LA | P7 | 1 | NHSHC website | ||
| Alageel55 | 2018 (2) | Journal article | To identify barriers and facilitators to implementing multiple health behaviour change interventions for CVD risk reduction in primary care | Qualitative interview study | Providers | Lambeth and Lewisham | LA | C14 | P1, P2, P6, P7, P8, P10, P11, P13, P15, P20, P22, P24, P27 | A1, A2, A27, A30, A32, A35, A38, A39 | 22 | Existing review |
| Alageel56 | 2020 | Journal article | To examine factors that might influence engagement and adherence to lifestyle change interventions and medication amongst people recently assessed at medium or high risk of CVD | Qualitative interview study | Attendees | Lambeth and Lewisham | LA | C14 | P23 | A2, A6, A10, A12, A15, A25, A28, A30, A31, A32, A35, A36, A38, A43, A44 | 17 | Existing review |
| Alford57 | 2010 | Evaluation report | To explore behaviour changes made following community-based NHSHC and experience of NHSHCs | Qualitative interview study | Attendees | Knowsley | PCT | A40, A44 | 2 | Existing review | ||
| Al-Osaimi58 | 2020 | Conference abstract | To describe the implementation of software to manage the NHSHC | n/a | Commissioners | Sandwell | LA | C2, C7 | 2 | NHSHC website | ||
| Artac59 | 2013 | Journal article | To assess whether the NHSHC was associated with a reduction in CVD risk after one year | Pre/post | Attendees | Hammersmith and Fulham | PCT | P12 | 1 | Existing review | ||
| Atkins60 | 2020 | Journal article | To identify behaviours and actors relevant to uptake, delivery and follow-up of NHSHCs and influences on those behaviours | Systematic review | n/a | n/a | n/a | C14 | A35 | 2 | Searches – MEDLINE | |
| Baker61 | 2014 (1) | Evaluation report | To assess the impact of the NHSHC programme and inform future commissioning (summary) | Cross-sectional | Attendees | Gloucestershire | PCT | C9 | P12, P17 | 3 | NHSHC website | |
| Baker62 | 2014 (2) | Journal article | To investigate the perceptions and opinions of patients who attended an NHSHC | Survey | Attendees | Gloucestershire | PCT | C14 | P1, P8, P20, P25 | A1, A15, A18, A22, A23, A26, A34 | 12 | Existing review |
| Baker63 | 2015 (1) | Journal article | To investigate health professionals’ experiences and perspectives of implementation of the NHSHC | Survey including qualitative analysis of free-text responses | Providers | Gloucestershire | PCT | C2 | P10, P11, P18 | 4 | Existing review | |
| Baker64 | 2015 (2) | Journal article | To investigate how the local NHSHC pathway was followed and interpreted | Cross-sectional | n/a | Gloucestershire | PCT | P2, P12 | 2 | Existing review | ||
| Bell65 | 2019 | Conference abstract | To describe the outcomes of NHSHCs delivered in an integrated model with lifestyle services | Cross-sectional | Commissioners | Medway | LA | C3 | P19 | 2 | NHSHC website | |
| Boase66 | 2012 | Journal article | To explore the perspectives of PNs in their role of communicating CVD risk to patients | Qualitative interview study | Providers | Cambridge | PCT | P4, P22, P27 | A8, A19 | 5 | Searches – MEDLINE | |
| Boseley67 | 2020 | Conference presentation | To describe a local model of NHSHC delivery with integrated lifestyle services | Mixed methods | Commissioners | East Sussex | LA | C3, C6, C7 | P14, P15, P19 | A4 | 7 | NHSHC website |
| Brutus48 | 2013 | Evaluation report | To review the design of the local NHSHC programme and analyse delivery options available | Cross-sectional | Various | Croydon | PCT | C1, C2, C7 | P1, P13, P15, P19 | A6, A40 | 9 | NHSHC website |
| Burgess68 | 2016 | Conference presentation | Summary results of a qualitative interview study (Alageel 2020) | Qualitative interview study | Attendees | Lambeth and Lewisham | LA | P1, P23 | A2, A5, A10, A20, A23, A28, A33, A42 | 10 | NHSHC website | |
| Burke69 | 2015 | Conference presentation | To describe local delivery of NHSHCs with a focus on vulnerable groups | n/a | Commissioners | Leeds | LA | A5, A38 | 2 | NHSHC website | ||
| Carter49 | 2016 | Journal article | To evaluate local outcomes of NHSHCs with a focus on diagnosis and management after checks | Retrospective cohort | Attendees | Leicester | PCT, Transition | C1 | 1 | Existing review | ||
| Centre for Public Scrutiny70 | 2014 | Other report | A report on the role of Council Scrutiny in local reviews of NHSHC programmes | n/a | n/a | Various | LA | C1, C11 | P1 | 3 | Searches – HMIC | |
| Chatterjee71 | 2017 | Journal article | To assess the knowledge, use, and confidence in national physical activity and Chief Medical Officer guidelines and tools among GPs in England | Survey | Providers | England | LA | P21 | 1 | Searches – MEDLINE | ||
| Chipchase72 | 2011 | Evaluation report | To explore people’s views and experiences of the NHSHC | Qualitative interview study | Various | Birmingham | PCT | P1, P14 | A1, A2, A11, A12, A19, A20, A40 | 9 | Existing review | |
| Clarke73 | 2020 | Conference presentation | To describe the of data to inform local CVD prevention work | n/a | Commissioners | Barnsley | LA | C8 | A33 | 2 | NHSHC website | |
| Cochrane74 | 2012 (1) | Journal article | To compare changes in population CVD risk factors between those who receive an NHSHC and those who receive an NHSHC with additional lifestyle support | RCT | n/a | Stoke on Trent | PCT | P26 | A9 | 2 | Existing review | |
| Cochrane75 | 2013 | Journal article | To review response, attendance and treatment uptake following NHSHCs | Cross-sectional | n/a | Stoke on Trent | PCT | A9 | 1 | Existing review | ||
| Coffey76 | 2014 | Evaluation report | To assess the level of uptake of NHSHCs | Cross-sectional | n/a | Salford | PCT | P12, P20 | 2 | Existing review | ||
| Coghill77 | 2018 | Journal article | To assess uptake and outcomes of NHSHCs in general practice | Cross-sectional | n/a | Bristol | PCT, Transition, LA | P12, P16 | 2 | Existing review | ||
| Collins78 | 2011 | Evaluation report | To evaluate the effectiveness of an ‘outreach’ delivery model for NHSHCs | Mixed methods | n/a | Medway | PCT | P17 | A4 | 2 | NHSHC website | |
| Corlett79 | 2016 | Journal article | To assess the findings of NHSHCs delivered in pharmacy settings, referrals to GPs and client views | Mixed methods | n/a | Lewisham | Transition, LA | A2, A13, A15, A25, A35, A38 | 6 | Existing review | ||
| Coward80 | 2020 | Conference presentation | To describe processes linking NHSHCs with local services that aim to promote physical activity | n/a | n/a | Dorset | LA | C2, C7, C8 | P17, P19, P26, P27, P28 | 8 | NHSHC website | |
| Cupit81 | 2018 | PhD thesis | To explore how patients’ and healthcare professionals’ knowledge and practices about CVD prevention are socially organised | Ethnography | n/a | Unknown | LA | C8, C13, C14 | P2, P4, P9, P10, P20, P24 | A11, A23, A25, A27, A31, A35, A38, A44 | 17 | NHSHC website |
| Dalton82 | 2011 | Journal article | To examine the uptake of NHSHCs and statin prescribing | Cross-sectional | n/a | Ealing | PCT | P2, P3 | 2 | Existing review | ||
| Derbyshire County Council83 | 2015 | Evaluation report (Health Equity Audit) | To identify health inequalities in relation to the NHSHC programme | Cross-sectional | Commissioner | Derbyshire | LA | C9, C10 | P2, P12, P15, P16, P17, P20, P22, P25 | A35 | 11 | NHSHC website |
| Edmans84 | 2013 | Other report | To describe local training provision in relation to the dementia component of NHSHCs | n/a | Providers | Southwark | LA | P20 | 1 | NHSHC website | ||
| Fenton85 | 2018 | Conference presentation | To describe local CVD prevention work and NHSHCs | Cross-sectional | n/a | Southwark | LA | P1, P3 | 2 | NHSHC website | ||
| Forster86 | 2015 | Journal article | To evaluate the ‘yield’ of NHSHCs (in relation to identification of risk factors, diagnoses and prescribing) | Retrospective cohort | n/a | England | PCT, Transition, LA | P2, P6, P12, P16 | 4 | Existing review | ||
| Forsyth87 | 2012 | Conference abstract | To test a delivery model using pharmacists to deliver health checks to the South Asian community (NB describes checks delivered in Scotland) | Mixed methods | n/a | Glasgow | PCT | A17 | 1 | Searches – Embase | ||
| Frazer88 | 2020 | Conference presentation | To describe the delivery of NHSHCs with integrated lifestyle services | n/a | Commissioners | West Sussex | LA | C3 | 1 | NHSHC website | ||
| Gidlow89 | 2020 | Journal article | To examine the content of NHSHC, patient-practitioner communication balance and differences when using QRISK2 versus JBS3 CVD risk calculators | Observation (video recorded NHSHCs) | n/a | West Midlands | LA | P10, P20 | A6, A13, A39 | 5 | Searches – MEDLINE | |
| Gidlow90 | 2021 (1) | Research report | To explore the extent of physical activity and alcohol measurement in the NHSHC | Observation (video recorded NHSHCs) | n/a | West Midlands | LA | P20 | 1 | NHSHC website | ||
| Gidlow91 | 2021 (2) | Research report | To explore practitioner and patient understanding of CVD risk, associated advice or treatment and the response of patients to the NHSHC supported by the QRISK2 or JBS3 risk calculators | Mixed methods | n/a | West Midlands | LA | P10 | A9, A10, A13, A29 | 4 | Search alerts | |
| Graley92 | 2011 | Journal article | To describe a ‘postcode lottery’ effect in relation to NHSHCs | Cross-sectional | Commissioner | North-west London | PCT | C9, C10, C13, C14 | P12, P13 | 6 | Existing review | |
| Greaves93 | 2015 | Journal article | To assess the feasibility of delivering an intervention to promote healthy eating and physical activity and of conducting a full-scale RCT | Pilot RCT | n/a | Bath | PCT | P28 | A30, A37, A40 | 4 | Searches – MEDLINE | |
| Green94 | 2018 | Evaluation report | To understand the NHSHC patient journey from invitation through to behaviour change or clinical intervention | Mixed methods | Attendees | East Sussex | LA | C7 | P10, P24 | A1, A8, A12, A24, A29, A35 | 9 | Stakeholder group |
| Gregory95 | 2018 | Conference presentation | To describe the role of healthcare professionals in treatment of tobacco dependency | n/a | n/a | England | LA | P25 | 1 | NHSHC website | ||
| Gulliford96 | 2018 | Journal article | To compare CVD risk scores for ‘invited’ and ‘opportunistic’ NHSHCs | Retrospective cohort | n/a | Lambeth and Lewisham | Transition, LA | P11 | 1 | Existing review | ||
| Hardman97 | 2014 | Evaluation report | To describe local delivery of an NHSHC programme with Health Trainers | n/a | Various | Bolton | PCT | C3 | P7, P14, P19 | A13, A30 | 6 | NHSHC website |
| Haringay Council98 | 2012 | Evaluation report | Scrutiny review focused on men’s health needs and life expectancy gap | Mixed methods | n/a | Haringay | PCT | C7 | A10, A13, A14, A16, A30, A37 | 7 | NHSHC website | |
| Hawking99 | 2018 | Conference poster | To describe a visual risk communication tool designed for use in NHSHCs | n/a | Providers, attendees | Newham | LA | A44 | 1 | NHSHC website | ||
| Hawking100 | 2019 | Journal article | To explore patient perspectives and experiences of a personalised risk report during an NHSHC | Qualitative interview study | Attendees | Newham | LA | P28 | A1, A9, A10, A18, A19, A20, A40, A44 | 9 | Existing review | |
| Hinde101 | 2017 | Journal article | To assess the cost-effectiveness of NHSHCs | Economic evaluation | n/a | England | LA | C12, C13 | 2 | Existing review | ||
| Homer102 | 2015 | Journal article | To determine the characteristics of patients prescribed statins for primary prevention according to their CVD risk | Cross-sectional | n/a | Newham, City & Hackney, Tower Hamlets (London) | LA | P3 | 1 | Serendipity | ||
| Honey103 | 2013 | Journal article | To identify the attitudes of primary healthcare professionals towards the delivery of lifestyle advice in NHSHCs | Q methodology | Providers | Leeds | PCT | P2, P6, P7, P18, P22, P24, P27 | 7 | Searches – MEDLINE | ||
| Honey104 | 2015 | Journal article | To examine the perspectives of patients identified as being at ‘high risk’ of CVD events | Qualitative interview study | Attendees | Leeds | PCT | P27 | A2, A3, A4, A5, A7, A9, A10, A13, A19, A20, A22, A27, A29 | 14 | Searches – MEDLINE | |
| Hooper105 | 2014 | Journal article | To estimate the case detection of five health conditions by NHSHCs | Cross-sectional | Attendees | Warwickshire | PCT | C10 | 1 | Existing review | ||
| Hyseni106 | 2020 | Journal article | To report the results of a workshop that aimed to facilitate engagement with stakeholders who will be involved in co-production of an NHSHC modelling tool for commissioners | Qualitative interview study | Commissioners, providers, policy-makers | Various | LA | C5, C7, C11, C12, C13, C14 | P12 | 7 | Searches – MEDLINE | |
| Ismail50 | 2015 | Journal article | To explore the challenges and barriers faced by staff involved in the delivery of the NHSHC | Qualitative interview study | Providers | Leeds | LA | C1, C7, C9, C14 | P6, P10, P12 | A35, A36, A44 | 10 | Existing review |
| Ismail107 | 2016 | Journal article | To provide an insight into the process of patients receiving NHSHCs and determine the extent to which they were supported to reduce CVD risk through behaviour change | Qualitative interview study | Attendees | Leeds | PCT | P2, P27 | A2, A6, A8, A11, A12, A30, A31, A38 | 10 | Existing review | |
| Ismail108 | 2019 | Research report (NIHR) | To test the clinical and cost effectiveness of an ‘enhanced lifestyle motivational interviewing’ intervention for patients at high risk of CVD in group and individual settings, compared with usual care | RCT | n/a | South London | LA | P6, P7 | A6, A16, A17, A26, A27, A30, A31, A32, A34, A40, A44 | 13 | Searches – WoS | |
| Jones52 | 2020 | Conference poster | To describe local CVD prevention work and NHSHCs | n/a | n/a | Telford | LA/CCG | C1 | P6, P17 | A14 | 4 | NHSHC website |
| Kearney109 | 2015 | Conference presentation | To describe factors that influence GP engagement with NHSHCs and potential solutions | n/a | n/a | n/a | LA | C4 | P1 | 2 | NHSHC website | |
| Kennedy110 | 2019 | Journal article | To evaluate uptake, risk factor detection and management from the NHSHC | Quasi-RCT | n/a | Hampshire | PCT, Transition, LA | P13 | 1 | Existing review | ||
| Kirkpatrick111 | 2016 | Conference presentation | To describe staff development and training for NHSHC providers | n/a | Providers | Salford | LA | P8 | 1 | NHSHC website | ||
| Krska112 | 2010 | Evaluation report | To evaluate a CVD screening service offered in pharmacy settings and obtain views of prospective users about the acceptability of the service | Mixed methods | n/a | Sefton | PCT | P25 | A2 | 2 | NHSHC website | |
| Krska113 | 2013 | Conference abstract | To compare the views of the general public, pharmacists and patients invited to the NHSHC and to compare experiences of NHSHCs delivered by pharmacies and general practices | Survey and qualitative interviews | Providers, attendees | Sefton | PCT | A14 | 1 | Searches – Embase | ||
| Krska114 | 2014 | Journal article | To explore the views and experiences of patients with potentially high CVD risk | Survey | Attendees | Sefton | PCT | P7, P10 | A15 | 3 | Existing review | |
| Krska115 | 2016 (1) | Journal article | To seek the views of GPs and practice managers on NHSHC implementation | Survey | Providers | Sefton | PCT | C9 | P10, P13 | 3 | Existing review | |
| Krska116 | 2016 (2) | Journal article | To evaluate NHSHC implementation in relation to data recording, advice provided, referrals, prescribing and new diagnoses | Cross-sectional | Providers | Sefton | PCT | C10 | 1 | Existing review | ||
| Kumar117 | 2015 | Conference presentation | To describe work to improve GP engagement with NHSHCs | n/a | n/a | Stoke on Trent, Havering (London) | LA | C1 | 1 | NHSHC website | ||
| Lake118 | 2010 | Conference presentation | To describe a community-based NHSHC service | n/a | n/a | Camden | PCT | C11 | P19, P28 | A5, A14 | 4 | NHSHC website |
| Lambert119 | 2016 | Journal article | To assess indicators of programme reach available to local service commissioners | Assessment of indicators | n/a | NE England | PCT, Transition | P12 | 1 | Existing review | ||
| Lennon120 | 2020 | Conference presentation | To describe local responses to Covid-19 in relation to NHSHCs and social prescribing | n/a | n/a | Redbridge | LA | C6 | 1 | Stakeholder group | ||
| Liverpool City Council121 | 2020 | Conference poster | To describe the local Health Trainer service available to NHSHC attendees | n/a | n/a | Liverpool | LA | P6, P8, P19, P26, P27, P28 | A6, A14, A16, A30, A36, A40 | 12 | NHSHC website | |
| Local Government Association122 | 2015 | Other report | Report on the transfer of public health responsibilities to LAs | n/a | Commissioners | Various | LA | C1, C5, C8, C11, C12, C13 | 6 | Existing review | ||
| LA A123, b | 2019 | Evaluation report | Evaluation of local NHSHC programme | Mixed methods | Commissioners | [Redacted] | LA | C1, C2, C11 | P16, P17 | A15 | 6 | Survey respondent |
| LA B124, b | 2019 | Evaluation report | Evaluation of local NHSHC programme | Mixed methods | Commissioners | [Redacted] | LA | C7, C11, C12 | 3 | Survey respondent | ||
| LA C125, b | nd | Working document | Report describing quality assurance considerations in relation to NHSHCs | n/a | Commissioners | [Redacted] | LA | C1, C2, C4, C7 | P9 | 5 | Survey respondent | |
| LA C126, b | 2019 | Evaluation report | To measure, monitor and report on performance and quality of NHSHCs against a quality framework | Mixed methods | Commissioners | [Redacted] | LA | C2, C7, C10, C12 | 4 | Survey respondent | ||
| London Borough of Bromley127 | 2018 | Conference presentation | To assess the prevention of diabetes through NHSHCs | Cross-sectional | n/a | Bromley | LA | C14 | P8, P25 | 3 | NHSHC website | |
| Loo128 | 2011 | Conference abstract | To derive information on community pharmacists’ activities and attitudes in relation to NHSHCs | Survey | Providers | Various | PCT | P13 | 1 | Existing review | ||
| Lumley129 | 2015 | Conference presentation | To describe the role of the NHSHC in addressing high blood pressure | n/a | Commissioners, providers | Blackpool | LA | C1, C7 | 2 | NHSHC website | ||
| Maddern130 | 2020 | Conference abstract | To describe the role of local political scrutiny in developing and improving NHSHCs | n/a | Commissioners | Wiltshire | LA | C11 | 1 | NHSHC website | ||
| Martin131 | 2011 | Practitioner article | To describe challenges in delivery of NHSHCs | n/a | Provider | East Sussex | PCT | C13 | P14 | 2 | Searches – CINAHL | |
| McDermott132 | 2015 | Conference presentation | Summary of research exploring the implementation of NHSHCs in primary care settings | Qualitative interview study | Providers | Lambeth and Lewisham | PCT, Transition | C9 | P1, P10, P13 | 4 | NHSHC website | |
| McMillan133 | 2018 | Journal article | Report on a workshop with members of the public to inform design of a ‘digital adjunct’ intervention for the NHSHC | Co-production | Attendees | Manchester | LA | A6, A44 | 2 | Searches – MEDLINE | ||
| McNaughton134 | 2011 | Journal article | To evaluate delivery of the NHSHC in community pharmacies | Qualitative interview study | Providers | Tees Valley | PCT | C13 | P20, P27 | A14, A15 | 5 | Existing review |
| McNaughton135 | 2014 | Journal article | To understand factors that influenced adherence to medication and advice in ‘high risk’ patients identified by the NHSHC | Qualitative interview study | Attendees | North East England | PCT | A3, A9, A10, A25, A27, A28, A35, A38, A40, A42 | 10 | Existing review | ||
| Mills136 | 2017 | Journal article | To synthesise data concerning the views of commissioners, managers and healthcare professionals towards the NHSHC | Systematic review | Commissioners, providers | n/a | n/a | P10, P13 | 2 | Searches – MEDLINE | ||
| Nahar137 | 2020 | Journal article | Protocol for a mixed-methods implementation study of a community-based CVD risk assessment and coaching intervention | Mixed methods (protocol) | n/a | Sussex, Nottingham | LA | A14 | 1 | Searches – MEDLINE | ||
| Nasir138 | 2018 | Conference abstract | To describe a local project that aimed to increase NHSHC uptake and referrals to local lifestyle services | Cross-sectional | n/a | Kingston (London) | LA | A35, A37 | 2 | NHSHC website | ||
| Newman139 | 2018 | Conference presentation | To describe Health Coaching techniques | n/a | n/a | n/a | LA | P27 | 1 | NHSHC website | ||
| NHS Greenwich140 | 2011 | Evaluation report | To assess the outcomes of a community-based NHSHC delivery model | Mixed methods | n/a | Greenwich | PCT | P14 | A4, A13, A17 | 4 | Existing review | |
| NHS Midlands and East141 | 2011 | Evaluation report | To evaluate a pilot programme aiming to deliver lifestyle interventions through the NHSHC | Mixed methods | n/a | Bedfordshire; Great Yarmouth and Waveney | PCT | C2, C7 | P1, P7, P10, P17, P19 | A40 | 8 | NHSHC website |
| NICE142 | 2014 | Guidance | Guidance for LAs on commissioning and delivery of the NHSHC | n/a | Commissioners | England | LA | C11 | 1 | Searches – HMIC | ||
| Nicholas143 | 2012 | Journal article | To evaluate the organisation of the NHSHC in general practices | Survey | Providers | Lambeth and Lewisham | PCT | P2 | 1 | Existing review | ||
| O’Flaherty144 | 2021 | Research report | To develop a model for commissioners to quantify cost-effectiveness and potential for equitable population health gain of the NHSHC | Mixed methods | Commissioners | Various | LA | C7 | 1 | Search alerts | ||
| Onyia145 | 2016 | Conference presentation | To describe the impact of Health Trainers on uptake of lifestyle services after NHSHCs | Cross-sectional | n/a | Halton | LA | P6, P8, P25, P26 | 4 | NHSHC website | ||
| Oswald146 | 2010 | Evaluation report | To evaluate the implementation and outcomes of the ‘Tees Vascular Assessment Programme’ (precursor to NHSHC) | Mixed methods | n/a | Tees Valley | PCT | C8, C9, C13, C14 | P1, P2, P7, P11, P14, P28 | A1, A2, A4, A9, A13, A10, A18, A28, A29, A31, A32, A33, A40, A41, A42, A43 | 26 | Existing review |
| Palladino147 | 2020 | Journal article | To assess associations between coverage of the NHSHC and detection and management of incident cases of non-diabetic hyperglycaemia and type 2 diabetes | Retrospective cohort | n/a | England | PCT | P5 | 1 | Searches – MEDLINE | ||
| Patel5 | 2020 | Journal article | To describe the uptake and outputs of the NHSHC programme | Cross-sectional | n/a | England | Transition, LA | P3, P12 | 2 | Searches – MEDLINE | ||
| Paxton148 | 2020 | Journal article | To assess the fidelity of delivery of NHSHCs in general practice | Fidelity assessment | n/a | East of England | PCT | P20, P21 | 2 | Searches – MEDLINE | ||
| Perkins149 | 2020 | Conference presentation | Presentation describing CVD prevention initiatives | n/a | n/a | England | LA | A2, A38 | 2 | NHSHC website | ||
| Perry150 | 2014 | Journal article | To explore experiences of engaging with a community-based NHSHC | Qualitative interview study | Attendees | Knowsley | PCT | P14, P28 | A2, A4, A7, A13, A18, A25, A35, A38, A40, A44 | 12 | Existing review | |
| PHE3 | 2020 | Guidance | Best Practice Guidance for commissioners and providers | n/a | n/a | England | LA | P12 | A12 | 2 | NHSHC website | |
| Rawlinson151 | 2019 | Journal article | To evaluate an ‘enhanced health promotion service’ in a physiotherapy-led musculoskeletal service providing NHSHCs and diabetes checks | Mixed methods | n/a | Salford | LA | C6 | P6, P7, P8, P14, P17, P19, P26 | 8 | Searches – CINAHL | |
| Research Works51 | 2013 | Evaluation report | To assess commissioners’ and providers’ experiences of the NHSHC and gain an understanding of the engagement of public health professionals with NHSHCs | Qualitative interview study | Commissioners, providers | Various | PCT, Transition | C1, C4, C7, C11, C13 | P7, P9, P10, P13, P14, P19 | A13 | 12 | Existing review |
| Richardson152 | 2016 | News article | Article responding to research demonstrating lower coverage of NHSHCs and limited evidence of effectiveness of NHSHCs | n/a | n/a | n/a | LA | P18 | A16 | 2 | Searches – CINAHL | |
| Riley153 | 2015 | Journal article | To examine the feasibility and acceptability of community outreach NHSHCs targeted at the Afro-Caribbean community | Ethnography | Providers, attendees | Bristol | LA | P10 | A2, A3, A13, A14, A16, A17, A21, A23, A25, A26, A40, A44 | 13 | Existing review | |
| Riley154 | 2016 | Journal article | To examine the experiences of patients attending and healthcare professionals conducting NHSHCs | Qualitative interview study | Providers, attendees | Bristol | LA | P4, P8, P10, P27 | A1, A3, A11, A19, A20, A21, A22, A25, A33, A35, A38, A44 | 16 | Existing review | |
| Robson155 | 2015 | Journal article | To describe implementation and results of the NHSHCs | Cross-sectional | n/a | City & Hackney, Newham, Tower Hamlets | PCT | P9 | 1 | Existing review | ||
| Robson156 | 2017 | Journal article | To describe the coverage and impact of NHSHCs on cardiovascular risk management and identification of new comorbidities | Retrospective cohort | n/a | City & Hackney, Newham, Tower Hamlets | PCT, Transition, LA | P9 | 1 | Existing review | ||
| Saramunee157 | 2015 | Journal article | To explore the experience of and willingness to use seven pharmacy public health services related to cardiovascular risk among the general public in England (including the NHSHC) | Mixed methods | Attendees | Sefton | A15, A29 | 2 | Searches – MEDLINE | |||
| Shaw158 | 2015 | Journal article | To explore healthcare professionals’ and patients’ experiences of delivering and receiving the NHSHC | Qualitative interview study | Providers, attendees | Birmingham | PCT | C14 | P8, P12, P23, P24, P27 | A2, A3, A4, A6, A9, A24, A26, A32, A35, A36, A38, A40 | 18 | Existing review |
| Shaw159 | 2016 | Journal article | To evaluate the implementation of the NHSHC from the perspective of GPs | Qualitative interview study | Providers | Birmingham | PCT | P1, P5, P6, P9, P10, P11, P13, P17, P20, P21, P26, P27 | A1, A6, A10, A12, A20, A30, A39 | 19 | Existing review | |
| Simon160 | 2020 | Conference presentation | Presentation describing physical activity interventions for prevention and management of health conditions | n/a | n/a | England | LA | P26 | 1 | NHSHC website | ||
| Solutions Strategy161 | 2017 | Evaluation report | To evaluate the pilot and assess the feasibility of extending the NHSHC to include a dementia risk reduction component | Mixed methods | n/a | Birmingham, Bury, Manchester, Southampton | P26 | A13, A15, A26 | 4 | Searches – HMIC | ||
| Strutt162 | 2011 | PhD thesis | To investigate patients’ experiences of and responses to NHSHCs | Qualitative interview study / ethnography | Attendees | n/a | PCT | P1, P16 | A2, A5, A6, A7, A11, A13, A15, A20, A21, A22, A25, A26, A29, A30, A34, A35, A44 | 19 | Existing review | |
| Tanner8 | 2020 | Research report | To update PHE-commissioned rapid evidence synthesis and summarise evidence to address several research questions relating to the implementation of NHSHCs | Systematic review | Various | n/a | n/a | P2 | 1 | NHSHC website | ||
| Thompson163 | 2016 | Conference presentation | Presentation describing PHE’s ‘StARS’ framework for assessment of NHSHCs | n/a | Commissioners | England | LA | C11 | 1 | NHSHC website | ||
| Thompson164 | 2019 | Conference abstract | Summary of implementation and outcomes of an integrated cardiovascular service | Cross-sectional | Commissioner | Slough | LA | C3 | P19 | 2 | NHSHC website | |
| Trueland165 | 2013 | News article | Article based around an interview with NHSHC supporter Professor Michael Kirby | n/a | Commissioners | n/a | LA | C8 | 1 | Searches – HMIC | ||
| Turner166 | 2013 | Journal article | To evaluate variation in statin take-up following risk assessment in the NHSHC | Qualitative interview study | Attendees | Nottingham | PCT | A15, A28, A41, A42, A43 | 5 | Searches – HMIC | ||
| Usher-Smith7 | 2017 | Research report | To provide a rapid synthesis of published research evidence on NHSHCs | Systematic review | n/a | n/a | n/a | P8 | 1 | NHSHC website | ||
| Visram167 | 2012 | Evaluation report | To investigate the implementation and accessibility of the ‘health trainer community check’ service | Mixed methods | Various | Durham | PCT, Transition | C1, C5, C9 | P6, P12, P19, P27 | A2, A3, A4, A5, A31, A32, A33 | 14 | NHSHC website |
| Williams168 | 2018 | Conference presentation | Presentation describing physical activity training and use of the GPPAQ tool to assess physical activity levels | n/a | n/a | England | LA | P21, P26 | 2 | NHSHC website | ||
The findings from our realist review describe what our included data tell us about what happens after the measurements and risk assessment are completed in an NHSHC. Our explanations of what happens (and what does not happen) in practice during and after a check centre on the reasoning and responses of three groups of actors:
-
Commissioners, who make decisions about who will provide the NHSHC in local areas, how the programme should be delivered, how providers will be remunerated and how delivery will be monitored, and may also be responsible for commissioning other local lifestyle services that may be available to NHSHC attendees.
-
Providers, who make decisions about the advice, brief interventions, referrals and clinical interventions that it is appropriate to offer to each attendee, and who deliver and record the delivery of these activities during the NHSHC.
-
Attendees, who respond to the NHSHC and the offer or provision of advice, brief interventions, referral or prescriptions, and may ultimately choose to make lifestyle changes or take medicine to lower their CVD risk, or not.
Overview of CMOCs
In total 86 CMOCs were developed based on the data included in the review. Each CMOC describes the relationship between an important context (for a group of actors) and certain outcomes, and the underlying mechanisms in operation when these outcomes occur. The CMOCs are not mutually exclusive and may interact; instead, our findings illustrate how the delivery and outcomes of individual NHSHC encounters are shaped by a wide range of influences. Multiple important contexts influence commissioners, providers and NHSHC attendees and provoke many different responses from these groups.
The full set of CMOCs are summarised in Table 21, Table 22 and Table 23 with an overview of the data that underpinned each one. A detailed narrative that draws on these individual CMOCs follows each.
| CMOC | Summary of data | |
|---|---|---|
| Understanding and engagement with the NHSHC programme: case-finding or enabling behaviour change? | ||
| CMOC C1 | When commissioners view the NHSHC as a means to improve people’s lives through behaviour change (C) they will try to exert their influence over providers to ensure the programme is delivered with this in mind (O) because they believe this will maximise the potential benefits of the programme (M) | Data extracted from 12 documents: 2 research articles (1 cohort study, 1 qualitative interview study); 4 local evaluation reports; 3 conference materials; 1 unpublished LA working document; 2 other reports focused on LA roles in NHSHCs |
| CMOC C2 | When commissioners view the NHSHC as a means to improve people’s lives through behaviour change (C) they will try to establish closer working relationships between different parts of the wider system (the NHSHC, lifestyle services and primary care) to improve referral pathways (O) because they believe this will maximise the potential benefits of the programme (M) | Data extracted from 8 documents: 1 research article (survey); 4 local evaluation reports; 2 conference materials; 1 unpublished LA working document |
| CMOC C3 | When commissioners view the NHSHC as a means to improve people’s lives through behaviour change (C) they may develop ‘integrated’ models of service delivery with the NHSHC delivered alongside lifestyle services (O) because they believe this will maximise the potential benefits of the programme (M) | Data extracted from 5 documents: 1 local evaluation report; 4 conference materials |
| CMOC C4 | When providers are sceptical and less engaged with the NHSHC programme (C) commissioners may be unable to exert their influence over them (O1) or establish close working relationships between different parts of the system (O2) because providers are resistant and unwilling to engage (M) | Data extracted from 3 documents: 1 local evaluation report; 1 conference presentation; 1 unpublished LA working document |
| CMOC C5 | When commissioners have a focus on the wider social determinants of health (C) they are more likely to commission ‘alternative’ NHSHC providers (i.e. to move away from a medical model based on primary care) (O) because they believe this will maximise the benefits of the programme (M) | Data extracted from 3 documents: 1 research article (qualitative interviews/workshop); 1 local evaluation report; 1 report focused on LA roles in NHSHCs |
| CMOC C6 | When commissioners have a focus on the wider social determinants of health (C) they may integrate NHSHC delivery with other services that address other problems (O) because they believe this will maximise the potential benefits of the programme (M) | Data extracted from 3 documents: 1 research article (mixed-methods evaluation); 2 conference materials |
| CMOC C7 | When commissioners view the NHSHC as a means to improve people’s lives through behaviour change (C) they are more likely to collect data related to what happens after the measurements and risk assessment are completed in a check (O) because they believe these are important data to monitor and evaluate programme performance (M) | Data extracted from 15 documents: 2 research articles (1 qualitative interviews/workshop, 1 qualitative interview study); 1 research report (mixed-methods study); 7 local evaluation reports; 4 conference materials; 1 unpublished LA working document |
| CMOC C8 | When commissioners view the NHSHC as a means to improve people’s lives through behaviour change (C) they are more likely to collect data related to the needs of the local population to inform the commissioning of lifestyle support services (O) because they believe this will maximise the benefits of the programme (M) | Data extracted from 6 documents: 1 PhD thesis (ethnography); 1 local evaluation report; 2 conference materials; 1 report focused on LA roles in NHSHCs; 1 news article |
| CMOC C9 | In some circumstances, commissioners may cede more control over delivery to primary-care-based providers (e.g. GP practices) (O) but the contexts in which this happens and the mechanisms underpinning this outcome are not clear (C, M not defined) | Data extracted from 8 documents: 3 research articles (1 qualitative interview study, 1 survey, 1 cross-sectional study); 4 local evaluation reports; 1 conference materials |
| CMOC C10 | In some circumstances, commissioners may focus only on mandatory data collection (monitoring invitation, uptake and coverage) (O) but the contexts in which this happens and the mechanisms underpinning this outcome are not clear (C, M not defined) | Data extracted from 5 documents: 3 research articles (3 cross-sectional studies); 2 local evaluation reports |
| Practical constraints: politics and funding | ||
| CMOC C11 | Where there is local political support and engagement with the NHSHC programme (C), local delivery is more likely to be evaluated (O1) and developed or improved (O2) because commissioners and public health teams are empowered to focus on the programme (M) | Data extracted from 10 documents: 1 research article (qualitative interview study); 3 local evaluation reports; 3 conference materials; 2 other reports focused on LA roles in NHSHCs; 1 guidance document |
| CMOC C12 | When funding for public health programmes is constrained (C1) and commissioners or public health teams are convinced of the NHSHCs long-term effectiveness and value (C2) local delivery is more likely to be evaluated (O1) and developed or improved (O2) because these activities are considered worthwhile (M) | Data extracted from 5 documents: 2 research articles (1 qualitative interview study, 1 economic evaluation); 2 local evaluation reports; 1 other report focused on LA roles in NHSHCs |
| CMOC C13 | When funding for public health programmes is constrained (C) commissioners may select providers who offer the best value for money / lowest cost per NHSHC delivered (O) because they must prioritise mandatory public health programme delivery (‘prescribed functions’) before funding additional services (M) | Data extracted from 9 documents: 4 research articles (2 qualitative interview studies, 1 cross-sectional, 1 economic evaluation); 2 local evaluation reports; 1 PhD thesis (ethnography); 1 other report focused on LA roles in NHSHCs; 1 practitioner-facing article |
| CMOC C14 | When funding for public health programmes is constrained (C) commissioners must prioritise funding mandatory services (‘prescribed functions’) (M) leading to cuts and reduced capacity in non-mandatory services (e.g. local lifestyle support services) (O) | Data extracted from 11 documents: 8 research articles (5 qualitative interview studies, 1 survey, 1 cross-sectional study, 1 systematic review); 1 local evaluation report; 1 PhD thesis (ethnography); 1 conference presentation |
| CMOC | Summary of data | |
|---|---|---|
| Understanding and engagement with the NHSHC programme: scepticism versus ‘buy in’ | ||
| CMOC P1 | When providers are sceptical about the NHSHC programme as a behaviour change intervention (C) they may prioritise completing the mandatory elements of the check and fail to engage with the delivery of advice, brief interventions or referrals (O) because they do not believe these will help attendees (M) | Data extracted from 14 documents: 3 research articles (2 qualitative interview studies, 1 survey); 1 research report (mixed-methods study); 4 local evaluation reports; 4 conference materials; 1 other report focused on LA roles in NHSHCs; 1 PhD thesis (ethnography) |
| CMOC P2 | When providers are sceptical about the NHSHC programme as a behaviour change intervention (C1) or sceptical about the effectiveness of behaviour change to reduce the risk of CVD (C2) they are more likely to consider medication (e.g. statins or anti-hypertensives) as an appropriate intervention for those assessed at higher risk (O) because they believe these will help attendees (M) | Data extracted from 11 documents: 7 research articles (2 qualitative interview studies, 1 survey, 2 cross-sectional studies, 1 cohort study, 1 Q-methodology study); 2 local evaluation reports; 1 research report (systematic review); 1 PhD thesis (ethnography) |
| CMOC P3 | When providers (who are able to prescribe) are sceptical about the recommended thresholds for prescription (C) they are less likely to prescribe (O) because they do not believe it will help attendees (M) This CMOC may apply to other interventions but we lack data to confirm or refute this. |
Data extracted from 4 documents: 3 research articles (3 cross-sectional studies); 1 conference presentation |
| CMOC P4 | When providers are worried about labelling healthy people as sick (C) they may avoid offering advice, referrals or prescriptions (O) because they are concerned about the potential harms of overdiagnosis (M) | Data extracted from 3 documents: 2 research articles (2 qualitative interview studies); 1 PhD thesis (ethnography) |
| CMOC P5 | When providers are highly engaged with preventive healthcare (C) they are more likely to be highly engaged with the NHSHC programme (O) as they understand it to be a useful means of reaching more patients with this agenda (M) | Data extracted from 2 documents: 2 research articles (1 qualitative interview study, 1 cohort) |
| CMOC P6 | When providers believe that lifestyle modification is an effective means of reducing CVD risk (C) they are more likely to offer attendees advice, brief interventions or referrals to lifestyle support services (especially as a first line of action) (O) because they believe these may help attendees (M) | Data extracted from 11 documents: 6 research articles (2 qualitative interview studies, 1 cohort study,1 mixed-methods study, 1 Q-methodology study); 1 research report (RCT); 1 local evaluation report; 3 conference materials |
| CMOC P7 | When providers buy in to the NHSHC as an opportunity to support behaviour change (C) they are more likely to offer attendees advice, brief interventions or referrals to lifestyle support services (O) because they believe these will help attendees (M) | Data extracted from 11 documents: 5 research articles (1 qualitative interview study, 1 survey, 1 mixed-methods study, 1 Q-methodology study); 1 research report (RCT); 4 local evaluation reports; 1 conference presentation |
| CMOC P8 | When providers have the specific skills they need to support the delivery of advice, brief interventions and referrals (C) they are more likely to engage with and prioritise these activities (O) because they feel confident to deliver them during the NHSHC encounter (M) | Data extracted from 10 documents: 5 research articles (3 qualitative interview studies, 1 survey, 1 mixed-methods study); 1 local evaluation report; 3 conference materials; 1 research report (systematic review) |
| Practical constraints: time and money | ||
| CMOC P9 | When funding arrangements for delivery of checks incentivise volume of delivery (C) providers may prioritise completing mandatory elements of the check and minimise time spent delivering advice, brief interventions or offering referrals (O) because they are aware they do not have to complete these (M) | Data extracted from 6 documents: 3 research articles (1 qualitative interview study, 1 retrospective cohort, 1 cross-sectional); 1 local evaluation report; 1 PhD thesis (ethnography); 1 LA internal working document |
| CMOC P10 | When providers have many competing priorities (C) they may prioritise completing mandatory elements of the check and minimise time spent delivering advice, brief interventions or offering referrals (O) because of expediency (M) | Data extracted from 16 documents: 10 research articles (4 qualitative interview studies, 1 systematic review, 3 surveys, 1 ethnography, 1 observational study based on video recordings); 3 local evaluation reports; 1 research report (mixed methods); 1 PhD thesis (ethnography), 1 conference presentation |
| CMOC P11 | When there is a focus on increasing the volume of checks delivered (C) providers may offer more checks ‘opportunistically’ (i.e. not in a standalone appointment) (O) as they feel this is more efficient (M) | Data extracted from 5 documents: 4 research articles (2 qualitative interview studies, 1 retrospective cohort, 1 survey, 1 mixed methods); 1 local evaluation report |
| CMOC P12 | It is clear that data about non-mandatory elements of a check are often under-recorded or recorded inconsistently (O) but the contexts in which this happens and the mechanisms underpinning this outcome are not clear (C, M not defined). Potentially important contexts here include competing priorities, a focus on delivery of mandatory elements of checks, lack of monitoring and/or incentivisation to collect particular data items, or difficulty in recording certain activities within existing data collection systems | Data extracted from 15 documents: 10 research articles (3 qualitative interview studies, 4 cross-sectional studies, 1 pre/post study, 1 retrospective cohort, 1 study assessing the validity of indicators); 3 local evaluation reports; 1 guidance document; 1 conference abstract |
| CMOC P13 | When providers do not feel they are adequately compensated for delivering checks (C) they may prioritise completing mandatory elements of the check and minimise time spent delivering advice, brief interventions, or offering referrals (O) because they do not feel it is worth the cost (M) | Data extracted from 10 documents: 6 research articles (2 qualitative interview studies, 1 cross-sectional study, 1 quasi-RCT, 1 survey, 1 systematic review); 2 local evaluation reports; 2 conference materials |
| CMOC P14 | When providers ‘buy in’ to the NHSHC programme (see CMOC P7 above) (C1) and have adequate time and/or flexibility to deliver each check (C2) they may offer more personalised and in-depth advice and support (O) because they believe these may help attendees (M) | Data extracted from 9 documents: 2 research articles (1 qualitative interview study, 1 mixed methods); 5 local evaluation reports; 1 conference presentation; 1 practitioner-facing article |
| Practical constraints: referrals and follow-up | ||
| CMOC P15 | When multiple modifiable risk factors are identified during a check (C1) and separate lifestyle services exist for each (C2) providers (and attendees) may agree to prioritise addressing one risk factor first (M) so the delivery of advice, brief interventions and referrals reflect this priority (O) | Data extracted from 4 documents: 1 research article (qualitative interview study); 2 local evaluation reports; 1 conference presentation |
| CMOC P16 | When providers don’t perceive available lifestyle services to be a good ‘fit’ for individuals (C) they may avoid making referrals to these services (O) because they do not believe it will help attendees (M) | Data extracted from 4 documents: 2 research articles (1 retrospective cohort, 1 cross-sectional study); 2 local evaluation reports; 1 PhD thesis (interviews/ethnography) |
| CMOC P17 | When information about local lifestyle services and referral routes is disparate and difficult to access (C) it is harder for providers to make referrals (O) because providers are unaware of available services and how to refer (M) | Data extracted from 9 documents: 2 research articles (1 qualitative interview study, 1 mixed methods); 4 local evaluation reports; 3 conference materials |
| CMOC P18 | When providers have concerns about the quality of lifestyle support services (C) they may avoid making referrals (O) because they doubt they will help attendees (M) | Data extracted from 3 documents: 2 research articles (1 survey, 1 Q-methodology study); 1 news article |
| CMOC P19 | When providers have established relationships and referral pathways to trusted lifestyle services (C) they are more likely to offer referrals (O) because this becomes a delivery norm (M) | Data extracted from 12 documents: 1 research article (mixed methods); 5 local evaluation reports; 6 conference materials |
| Practical constraints: relationships and confidence in the delivery of advice | ||
| CMOC P20 | When providers are concerned that discussion of a particular risk factor may cause offence or upset an attendee (C) they may avoid bringing it up or discussing it in-depth (O) because they lack confidence and want to avoid confrontation (M) | Data extracted from 11 documents: 6 research articles (3 qualitative interview studies, 1 survey, 1 observational study based on video recordings, 1 fidelity assessment); 2 local evaluation reports; 1 research report (observational study); 1 PhD thesis (ethnography); 1 other report |
| CMOC P21 | When providers lack knowledge about recommendations in relation to a particular risk factor (C) they may avoid bringing it up or discussing it in-depth during a check (O) because they lack confidence in their advice (M) | Data extracted from 4 documents: 3 research articles (1 qualitative interview study; 1 survey; 1 fidelity assessment); one conference presentation |
| CMOC P22 | When providers perceive that an attendee is unlikely to want to, or be able to change their lifestyle (C) they may avoid giving them advice or offering referrals to support this (O) because they do not think it will help (M1) or because they are worried it could damage their relationship (M2) | Data extracted from 4 documents: 3 research articles (2 qualitative interview studies; 1 Q-methodology study); 1 local evaluation report |
| CMOC P23 | When providers feel they themselves are not good role models for healthy lifestyles (C) they may be reluctant to deliver advice or brief interventions, or make referrals (O) because they are worried about appearing hypocritical and lacking credibility (M) | Data extracted from 2 documents: 1 research article (qualitative interview study) and 1 conference presentation |
| CMOC P24 | When providers have lived experience of (trying to) make lifestyle changes (C) they may share this and empathise with attendees (O) because they want to build rapport and a therapeutic alliance during checks (M) | Data extracted from 5 documents: 3 research articles (2 qualitative interview studies, 1 Q-methodology study); 1 local evaluation report; 1 PhD thesis (ethnography) |
| CMOC P25 | When discussing a risk factor is normalised and routine (C) providers may be more likely to deliver advice, brief interventions and offer referrals related to that risk factor (O) because they feel comfortable and practiced in doing so (M) | Data extracted from 6 documents: 1 research article (survey); 2 evaluation reports; 3 conference materials |
| CMOC P26 | When providers receive training (C1) or have regular practice (C2) in delivering lifestyle advice, they are more likely to deliver it regularly during checks (O) because they feel more confident (M) | Data extracted from 9 documents: 3 research articles (1 qualitative interview study, 1 mixed methods, 1 RCT); 1 local evaluation report; 5 conference materials |
| CMOC P27 | When providers take into account attendees’ own priorities, constraints and wishes during a check (C) they may adapt the advice, brief interventions or referrals offered to take these into account (e.g. make fewer but more appropriate referrals) (O) because they share the decision with attendees (M) | Data extracted from 12 documents: 8 research articles (7 qualitative interview studies, 1 Q-methodology study); 1 local evaluation report; 3 conference materials |
| CMOC P28 | When providers are aware of attendees’ own priorities, constraints and wishes (C) they may identify and emphasise the benefits of simple changes that are more acceptable and achievable for attendees (O) because they believe this will help attendees (M) | Data extracted 7 from documents: 3 research articles (2 qualitative interview studies, 1 pilot RCT); 1 local evaluation report; 3 conference materials |
| CMOC | Summary of data | |
|---|---|---|
| Understanding and engagement with the NHSHC programme: expectations and priorities | ||
| CMOC A1 | When attendees understand the NHSHC as a screening opportunity aimed at identifying individuals with disease (C) they may be less likely to engage with advice, brief interventions or offers of referrals (O) because what is offered does not meet their expectations (M) | Data extracted from 9 documents: 6 research articles (5 qualitative interview studies, 1 survey); 3 local evaluation reports |
| CMOC A2 | When attendees are already aware of risk factors and/or potential improvements they could make to their lifestyle (C) they may be more receptive to receiving advice, brief interventions or referrals (O) because they are mentally prepared for it (M) | Data extracted from 15 documents: 8 research articles (6 qualitative interview studies, 1 ethnography, 1 mixed methods); 4 local evaluation reports; 1 PhD (ethnography); 2 conference materials |
| CMOC A3 | When attendees are unaware that they have risk factors for CVD and receive results that indicate that they are at high risk (C) they may need extra support and information from providers (O) because they are shocked and upset (M) | Data extracted from 6 documents: 5 research articles (4 qualitative interview studies, 1 ethnography); 1 local evaluation report |
| CMOC A4 | In some circumstances attendees who receive results that indicate that they are at high risk may be prompted to make immediate lifestyle changes (O) because they are shocked and upset (M), but the contexts in which this happens (and for whom) are not clear (C undefined) | Data extracted from 8 documents: 3 research articles (3 qualitative interview studies); 4 local evaluation reports; 1 conference presentation |
| CMOC A5 | When providers are able to explain the implications of risk factors to attendees in a way they can understand (C) attendees may be more receptive to advice, brief interventions or referrals (O) because they appreciate its importance for their own lives (M) | Data extracted from 6 documents: 1 research article (qualitative interview study); 1 local evaluation report; 1 PhD thesis (interviews/ethnography); 3 conference materials |
| CMOC A6 | When providers are able to link advice, brief interventions and offers of referrals to attendees’ own priorities for their health and lifestyle (C) attendees may be more likely to engage with these (O) because they want to achieve these (M) | Data extracted from 10 documents: 6 research articles (4 qualitative interview studies, 1 co-production study, 1 observational study using video-recordings); 1 research report (RCT); 1 local evaluation report; 1 PhD thesis (interviews/ethnography); 1 conference poster |
| CMOC A7 | When attendees have multiple risk factors (C) they may choose to focus on the advice, brief interventions or referrals offered in relation to those lifestyle changes that are easier to change (O) because they feel it is better than nothing (M) | Data extracted from 3 documents: 2 research articles (qualitative interview studies); 1 PhD thesis (interviews/ethnography) |
| CMOC A8 | When attendees feel a personal responsibility for their own health and lifestyle (C) they may be unlikely to take up offers of referrals or ongoing support or follow-up (O) because they feel obliged to try to make changes on their own (M) | Data extracted from 3 documents: 2 research articles (2 qualitative interview studies); 1 local evaluation report |
| CMOC A9 | When attendees are not motivated to change their lifestyle or behaviour (C) they are unlikely to engage with advice, brief interventions or take up offers of referrals to lifestyle services (O) because they do not believe they need to, and have other priorities (M) | Data extracted from 8 documents: 6 research articles (4 qualitative interview studies, 1 RCT, 1 cross-sectional study); 1 research report (mixed methods); 1 local evaluation report |
| CMOC A10 | When attendees are fatalistic about their health (C) they are unlikely to engage with advice, brief interventions or take up offers of referrals to lifestyle services (O) because they think they are pointless (M) | Data extracted from 8 documents: 4 research articles (4 qualitative interview studies); 1 research report (mixed methods); 1 local evaluation report; 1 conference presentation |
| CMOC A11 | When attendees have health concerns and priorities that fall outside the remit of the NHSHC programme (C) they may be disappointed with the check (O1) and unlikely to engage with advice, brief interventions or take up offers of referrals to lifestyle services (O2) because these do not feel important to them, and they have other priorities (M) | Data extracted from 5 documents: 2 research articles (2 qualitative interview studies); 1 local evaluation report; 2 PhD theses (ethnography, interviews/ethnography) |
| CMOC A12 | When attendees receive an ‘opportunistic’ check (C) they are less likely to (receive and) engage with advice, brief interventions or offers of referrals (O) because they do not understand that this is the purpose of the check (M) | Data extracted from 6 documents: 3 research articles (3 qualitative interview studies); 2 local evaluation reports; 1 guidance document |
| CMOC A13 | When attendees have the opportunity and time to discuss and ask questions during a check (C) they may be more likely to receive and engage with advice, brief interventions and offers of referrals (O) because they understand that this is the purpose of the check (M) | Data extracted from 13 documents: 5 research articles (2 qualitative interview studies, 1 ethnography, 1 mixed-methods study, 1 observational study using video-recordings); 6 local evaluation reports; 1 research report (mixed methods); 1 PhD thesis (interviews/ethnography) |
| CMOC A14 | When checks are delivered in a non-medical setting (i.e. not in general practice) (C) attendees may be more likely to engage in discussions about risk factors and lifestyle change (O) because they feel relaxed and comfortable (M) | Data extracted from 8 documents: 3 research articles (1 qualitative interview study, 1 ethnography, 1 protocol for a mixed-methods study); 1 local evaluation report; 4 conference materials |
| Understanding and engagement with the NHSHC programme: credibility and trust | ||
| CMOC A15 | When attendees receive advice, brief interventions, offers of referral or prescriptions from a professional they consider to be suitably qualified (C) they may be more likely to engage with or accept these interventions (O) because they consider them to be credible (M) | Data extracted from 10 documents: 7 research articles (3 qualitative interview studies, 2 surveys, 2 mixed-methods studies); 2 local evaluation reports; 1 PhD thesis (interviews/ethnography) |
| CMOC A16 | When attendees receive advice, brief interventions or offers of referral from a provider who seems to understand their circumstances (C) they may be more likely to engage with these interventions (O) because they consider them to be credible (M) | Data extracted from 5 documents: 1 research article (ethnography); 1 research report (RCT); 1 local evaluation report; 1 conference poster; 1 news article |
| CMOC A17 | When providers can deliver culturally appropriate lifestyle advice (C) attendees may be more likely to engage with it (O) because they consider it to be more credible and relevant (M) | Data extracted from 4 documents: 1 research article (ethnography); 1 research report (RCT); 1 local evaluation report; 1 conference abstract |
| CMOC A18 | When the measurements and risk assessment completed during a check identify attendees as ‘low risk’ (C) attendees may be less receptive to any advice, brief interventions or referrals offered (O) because they are reassured and do not think they need to take action (O) | Data extracted from 4 documents: 3 research articles (1 qualitative interview study, 1 survey, 1 mixed-methods study); 1 local evaluation report |
| CMOC A19 | When providers downplay risks or temper advice about lifestyle (C) attendees may feel there is no need to make any changes (O) because they are reassured (M) | Data extracted from 5 documents: 4 research articles (4 qualitative interview studies); 1 local evaluation report |
| CMOC A20 | When providers are able to convey the importance and urgency of NHSHC risk assessments to attendees (C) attendees may be more receptive to advice, brief interventions or referrals (O) because they feel important (M) | Data extracted from 6 documents: 3 research articles (3 qualitative interview studies); 1 local evaluation report; 1 PhD thesis (interviews/ethnography); 1 conference presentation |
| CMOC A21 | When the measurements and risk assessment completed during a check identify attendees as ‘low risk’ (C) attendees’ healthy lifestyle habits may be reinforced (O) because they understand these have tangible benefits, reflected in their results (M) | Data extracted from 3 documents: 2 research articles (1 qualitative interview study, 1 ethnography); 1 PhD thesis (interviews/ethnography) |
| CMOC A22 | When attendees receive measurements and risk assessment results from non-professionals (C1) or do not receive results at all (C2) they may be less likely to consider the results to be important (O) because they trust that providers will alert them to significant results that require action (M) | Data extracted from 4 documents: 3 research articles (2 qualitative interview studies, 1 survey); 1 PhD thesis (interviews/ethnography) |
| CMOC A23 | When attendees perceive providers to be disengaged with the check (C) they may be less likely to engage with advice, brief interventions or offers of referral (O) because they do not believe these are important (M) | Data extracted from 4 documents: 2 research articles (1 ethnography, 1 survey); 1 PhD thesis (ethnography); 1 conference presentation |
| CMOC A24 | When attendees receive advice, brief interventions or offers of referral from a provider who does not seem to ‘practice what they preach’ (C) they may be less likely to engage with these interventions (O) because they consider these to lack credibility (M) | Data extracted from 2 documents: 1 research article (qualitative interview study); 1 local evaluation report |
| CMOC A25 | When attendees receive advice or information relating to healthy lifestyles that they are already familiar with during a check (C) they may perceive the advice to be useless (O) because they have heard it before (M) | Data extracted from 8 documents: 6 research articles (4 qualitative interview studies, 1 ethnography, 1 mixed-methods study); 2 PhD theses (ethnography, interviews/ethnography) |
| CMOC A26 | When attendees learn something new and important to them during a check (C) they may attempt to make changes to their lifestyle in light of this (O) because they have an improved understanding of risk factors or lifestyle advice (M) | Data extracted from 6 documents: 3 research articles (1 qualitative interview study, 1 ethnography, 1 survey); 1 research report (RCT); 1 local evaluation report; 1 PhD thesis (interviews/ethnography) |
| CMOC A27 | When attendees are aware of conflicting or inconsistent guidance about healthy lifestyles (C) they may reject or ignore advice delivered during a check (O) because they doubt its credibility (M1) or are confused (M2) | Data extracted from 4 documents: 2 research articles (2 qualitative interview studies); 1 research report (RCT); 1 PhD thesis (ethnography) |
| CMOC A28 | When attendees are aware of controversy in relation to recommended medication (statins) (C) they may be ambivalent about accepting or adhering to a prescription (O) because they are uncertain of the benefits (M) | Data extracted from 5 documents: 3 research articles (3 qualitative interview studies); 1 local evaluation report; 1 conference presentation |
| CMOC A29 | When attendees have doubts about the accuracy of the tests and tools used to measure and assess risk during a check (C) they may be less receptive to advice, brief interventions, referrals or prescriptions offered to address identified risks (O) because they are unsure that the assessments are credible (M) | Data extracted from 6 documents: 2 research articles (1 qualitative interview study, 1 mixed-methods study); 1 research report (mixed-methods study); 2 local evaluation reports; 1 PhD thesis (interviews/ethnography) |
| Practical constraints: referrals and follow-up | ||
| CMOC A30 | When attendees receive continuity of care and follow-up after a check (C) they may be more likely to engage with advice, take up referrals or attempt to make lifestyle changes (O) because they are reminded of what they are meant to be doing and why (M) | Data extracted from 10 documents: 5 research articles (4 qualitative interview studies, 1 pilot RCT); 1 research report (RCT); 2 local evaluation reports; 1 PhD thesis (interviews/ethnography); 1 conference poster |
| CMOC A31 | When attendees receive continuity of care and follow-up after a check (C) they may be more likely to engage with advice, take up referrals or attempt to make lifestyle changes (O) because they feel supported and valued (M) | Data extracted from 5 documents: 2 research articles (2 qualitative interview studies); 1 research report (RCT); 1 local evaluation report; 1 PhD thesis (ethnography) |
| CMOC A32 | When attendees are repeatedly offered follow-up and feedback on progress after a check (C) they may be motivated to attempt and maintain lifestyle changes (O) because they can monitor their progress (M) | Data extracted from 6 documents: 3 research articles (3 qualitative interview studies); 1 research report (RCT); 2 local evaluation reports |
| CMOC A33 | When attendees can see tangible benefits of making lifestyle changes after a check (C) they are more likely to maintain these (O) because they are motivated to continue (M) | Data extracted from 5 documents: 1 research article (qualitative interview study); 2 local evaluation reports; 2 conference materials |
| CMOC A34 | When attendees are not offered any follow-up (beyond the five-year NHSHC programme cycle) (C) they may lack motivation to attempt any lifestyle changes (O) because they interpret the absence of follow-up to mean there is no urgent need to make changes (M) | Data extracted from 3 documents: 1 research article (survey); 1 research report (RCT); 1 PhD thesis (interviews/ethnography) |
| CMOC A35 | When attendees don’t consider local lifestyle services to be convenient, appropriate or likely to meet their needs (C) they are less likely to take up referrals or attend these services (O) because they feel it is pointless (M) | Data extracted from 14 documents: 9 research articles (7 qualitative interviews studies, 1 systematic review, 1 mixed-methods study); 2 local evaluation reports; 2 PhD theses (ethnography, interviews/ethnography); 1 conference abstract |
| CMOC A36 | When local lifestyle support services are designed to be more accessible (e.g. in terms of timing, location, cost) (C) attendees may be more likely to start and continue to attend (O) because they feel they are more convenient, affordable or relevant (M) | Data extracted from 4 documents: 3 research articles (3 qualitative interview studies); 1 conference poster |
| CMOC A37 | When attendees have the option to try out a lifestyle service or are supported to try one by a provider (C) they may be more likely to take up an offer of a referral (O) because they feel more confident to do so (M) | Data extracted from 3 documents: 1 research article (pilot RCT); 1 local evaluation report; 1 conference abstract |
| Practical constraints for attendees: person-centredness | ||
| CMOC A38 | When attendees receive advice about healthy lifestyles that does not take account of their personal circumstances (C) they are less likely to engage with it (O) because they believe it is unworkable for them (M) | Data extracted from 10 documents: 8 research articles (7 qualitative interview studies, 1 mixed-methods study); 1 PhD thesis (ethnography); 1 conference presentation |
| CMOC A39 | When attendees receive advice about healthy lifestyles that they believe they cannot achieve (e.g. because it seems to require big changes) (C) they are less likely to engage with it (O) because they feel overwhelmed and hopeless (M) | Data extracted from 3 documents: 3 research articles (2 qualitative interview studies, 1 observational study using video recordings) |
| CMOC A40 | When attendees receive advice about healthy lifestyles that attendees feel they can fit into their lives (e.g. around other commitments) (C) they may be more likely to engage with it (O) because they perceive the changes to be less disruptive (M) | Data extracted from 13 documents: 6 research articles (4 qualitative interview studies, 1 ethnography, 1 pilot RCT); 1 research report (RCT); 5 local evaluation reports; 1 conference poster |
| CMOC A41 | When attendees feel that significant lifestyle change is unworkable for them (C) they may be more likely to accept prescriptions (e.g. for statins) (O) because they still want to do something to reduce their CVD risk (M) | Data extracted from 2 documents: 1 research article (qualitative interview study); 1 local evaluation report |
| CMOC A42 | When attendees anticipate or experience medication side effects or burdens (C) they may be more ambivalent about accepting or adhering to prescriptions (O) because they are uncertain of the benefits and concerned about harms (M) | Data extracted from 4 documents: 2 research articles (2 qualitative interview studies); 1 local evaluation report; 1 conference presentation |
| CMOC A43 | When attendees anticipate or experience medication side effects or burdens (C) they attempt lifestyle change (O) because they prefer this option (M) | Data extracted from 3 documents: 2 research articles (2 qualitative interview studies); 1 local evaluation report |
| CMOC A44 | When attendees are encouraged and supported by friends, family or peers to make and sustain lifestyle changes (C) they may be more likely to attempt and maintain changes (O) but the mechanism for this is unclear (M not defined) | Data extracted from 11 documents: 7 research articles (5 qualitative interview studies, 1 ethnography, 1 co-production study); 1 research report (RCT); 1 local evaluation report; 2 PhD theses (ethnography, interviews/ethnography) |
Local authority commissioners
Some variation in NHSHC delivery is intended and built into the programme at this level: LAs are encouraged to commission services and set service specifications to meet local needs and priorities. 3,31 Our data suggest that commissioners’ decisions are partly based on their understanding of the purpose and utility of the NHSHC programme, but are constrained by practicalities, primarily centred on the availability of resources and funding. Both the overall approach and capacity of local public health teams play an important role in setting local plans and expectations for delivery of the NHSHC.
Understanding and engagement with the NHSHC: case-finding or enabling behaviour change?
The data suggest that a dual understanding of the purpose of the NHSHC programme exists. At one end of the spectrum, the programme is understood primarily in a pathogenic model, as a ‘case-finding’ intervention, designed to screen the population to identify those individuals who meet disease thresholds or are at high risk of doing so. At the other end, the NHSHC is understood as an opportunity to prompt or support ‘healthy lifestyles’, in a more salutogenic model that may encompass a more holistic understanding of the causes of, and potential responses to, CVD and CVD risk.
When public health teams and commissioners understand the NHSHC programme as a behaviour change intervention – that is, as a viable means of improving individuals’ health by provoking or encouraging them to make certain lifestyle changes – this can colour their overall approach to commissioning and monitoring the programme. There may be increased engagement with the whole NHSHC ‘pathway’ and longer-term outcomes, reflected in work to build closer working relationships across the local systems in which the NHSHC operates.
These commissioners may work to avoid a ‘medical model’ of the NHSHC where the emphasis is on recording relevant test results and necessary follow-up in primary care. They may attempt to exert their influence over providers by, for example, building relationships, maintaining regular contact, and offering training that emphasises behaviour change (CMOC C1). Local teams who adopt this stance may also work to establish and maintain relationships and referral pathways between different parts of the wider system that exists around the NHSHC itself, that is, between providers of the NHSHC, primary care and lifestyle support services (CMOC C2). This work may result in these referral pathways becoming smoother and more familiar, facilitating referrals between services and so potentially increasing access to lifestyle support. In some local areas, this approach reaches a logical conclusion in the development of ‘integrated’ models of NHSHC delivery, where the check itself and subsequent support are delivered in a single setting, by one provider, or a group of providers working closely together (CMOC C3). These collaborative and integrative efforts on the part of LAs aim to increase standardisation and improve quality in programme delivery, but also to ensure that the programme reflects its intended purpose in encouraging and supporting lifestyle change.
Local authorities may face difficulties in establishing close working relationships with providers who understand the purpose of the NHSHC differently or are less engaged with it. In particular, when providers are sceptical about the programme’s aims and efficacy, providers may be uninterested or even resistant to the close working and integration of services that exists in other areas (CMOC C4; and see CMOCs P1, P2, P3, P4 below in relation to NHSHC Providers).
As suggested above, this focus on the NHSHC as a potentially salutogenic intervention, capable of prompting behaviour and lifestyle change in attendees, may lead commissioners to move away from traditional programme delivery models that are centred on delivery in general-practice settings. Commissioning a range of alternative providers – including those who may specialise in supporting lifestyle change, such as provider models led by Health Trainers, coaches or ‘community champions’ – may also enable LAs to exert more control over programme delivery and reflect their concern with delivering ongoing support for behaviour and lifestyle change, as well as the wider, ‘social determinants’ of health and wellbeing (CMOC C5). Although it is not the focus of this review, other data in the literature emphasise that a further key motivation here is in extending the reach or coverage of the NHSHC, and especially as a potential means of addressing disparities of access and use of primary healthcare services such as GPs. In some areas, this may be the primary motivation for adopting non-traditional delivery models, but the shift away from a medical model towards a focus on supporting lifestyle change is a natural fit for these providers.
In some areas, integrated delivery models combine delivery of the NHSHC not only with relevant lifestyle support services, but with local services that address other important determinants of health and wellbeing, including mental health, housing and work (CMOC C6). This approach might include, for example, providing access to link workers or social prescribing services that can offer NHSHC recipients ongoing support, signposting or referral into a wide range of local services. In these delivery models, LAs have found a way to leverage the NHSHC to support local priorities and fit into a worldview that recognises that individual health and wellbeing depend on a holistic assessment of medical and social factors.
A focus on the whole NHSHC ‘pathway’ and longer-term outcomes for attendees may also be reflected in LAs’ activities and priorities in relation to monitoring and evaluation of the programme. LAs who understand the check as a behaviour change intervention and who focus on the need for ongoing support post-check may be more likely to exceed the minimum data returns required by PHE. Data collection may reflect their priorities and understanding of the programme, including data on activities and outcomes post-check to support monitoring and evaluation of programme delivery and impact (CMOC C7). These efforts may extend into investment in specialist software designed to guide NHSHC delivery and automatically collect such data (and simultaneously supporting standardisation of delivery, as described in CMOC C1 above). This focus is also likely to extend into the collection and use of meaningful data on local populations to inform the commissioning of appropriate local lifestyle services that may be offered to NHSHC attendees, potentially leading to the provision of services that are a better ‘fit’ for local populations (CMOC C8).
The data included in our review and reported by LAs in recent surveys (conducted by PHE and ourselves, as part of this project – see Survey findings above) suggest that not all LAs are keen or able to adopt a model of delivery as described above (and reflected in CMOCs C1–C8). In some local areas, it may make sense for commissioners to cede more control of programme delivery to long-standing NHSHC providers (usually general practices, although this may include community pharmacies in some areas) (CMOC C9). Less engaged LAs may also focus on mandated data collection and collect minimal or no data on later steps in NHSHC delivery and post-NHSHC outcomes. The most important (and legally required) outcomes to measure are those related to invitation, uptake and overall coverage of the programme, reflecting a priority to maximise the proportion of eligible individuals who receive a check (CMOC C10). However, we are not able to define with our current data the contexts in which this commissioning model is more likely, or the mechanisms that may underpin it.
Drawing on the data underpinning CMOCs C1–C8 above, we suggest that different approaches may reflect different understandings of the purpose of the programme. For example, where commissioners understand the NHSHC as primarily a clinical intervention, they may feel that it should be delivered by, and remain wholly or primarily the responsibility of, primary care services (especially general practices). However, other more pragmatic constraints may play a greater role in limiting what LAs can deliver and the extent of their influence on programme delivery and some of these are outlined in more detail in the next section below.
Practical constraints for commissioners: politics and funding
Although our data give a clear indication that the overall approach and understanding of the NHSHC adopted by LAs is an important factor that influences commissioning and implementation of the programme in different areas, it is also important to recognise that commissioners are constrained by more practical concerns. Our data suggest that political ‘buy in’ and scrutiny of the programme (and of public health and prevention initiatives more generally) are crucial factors in determining levels of support and attention devoted to the NHSHC in local areas (CMOC C11). Local political support and awareness of the programme can drive evaluation and improvement efforts. Such engagement may be driven by individual counsellors or local decision-making bodies (e.g. Health and Wellbeing Boards) and may therefore rest in turn on the composition of such bodies.
Engagement with the programme may also rest on how its outcomes and ‘effectiveness’ are measured and understood. In a broader context of financial restraint,169 engagement with the NHSHC may rest on the perception that it represents value for money or a ‘return on investment’ (CMOC C12). However, severe financial constraints and pressure to reduce spending in the present may still prevent LAs from attempting to realise health benefits and cost savings that are measured in the longer term, or on others’ balance sheets. 6,101
Funding constraints create pressure for LAs to commission NHSHC providers with a focus on maximising invitation, uptake and coverage, that is, the measurable outcomes that are prioritised in legislation and reporting requirements, and delivering the mandatory elements of the NHSHC for the least cost (CMOC C13). Spending on the programme as a whole decreased by 23.8% in the period between 2016/17 and 2020/21. 169 The extent of funding constraints may constrict commissioners’ choices of delivery models and service specifications. Some data included in our review suggest that community-based or ‘outreach’ models of delivery, as well as those that integrate additional support for attendees post-check, are more expensive than the most common general-practice-led delivery model.
Funding constraints and budget cuts in recent years have also limited the availability and capacity of commissioned (and wider) lifestyle support services. Although there are exceptions (such as the National Diabetes Prevention Programme, launched in 2016 and commissioned nationally by NHS England,170 and the new NHS Digital Weight Management Programme),171 local services are generally commissioned by LAs, who have been forced to divert funds and prioritise funding for statutory (i.e. mandatory) services (CMOC 14). Within the ring-fenced funding available to LAs to support public health, delivery of the NHSHC programme itself is a ‘prescribed function’,172 which must be delivered and reported on. Lifestyle services that could support individuals after an NHSHC are non-prescribed and so subject to increased pressure on budgets. The ring-fenced public health grant has itself been shrinking since LAs took on responsibility for these functions in 2013, resulting in significant cuts in spending on a wide range of public health services. 169,173
Our data point to wide variation in the availability of lifestyle services between local areas and over time. Limited availability and limited access to these services are commonly cited in reports that collate the reviews of HC providers and commissioners, attributed to funding cuts during years of austerity in the UK. The impact of these cuts on NHSHC providers is discussed further below (see CMOCs P16, P17, P18).
Providers
Our data suggest that a further layer of variation in delivery of the NHSHC is generated at the level of individual providers. As for LA commissioners, variation in what happens after the measurements and risk assessments are completed during a check can result from differences in attitudes towards the programme and understanding of its purpose and effectiveness. However, as above, our data also point to important practical constraints on providers’ activity, including the need to deliver each check within a limited timeframe, the ease with which referral pathways can be accessed, and important social and relational elements of the interaction between providers and NHSHC attendees. Some of these constraints are directly influenced by LA commissioning decisions and demonstrate the ways and extent to which LAs can influence programme delivery ‘on the ground’.
Understanding and engagement with the NHSHC: scepticism versus ‘buy in’
The NHSHC programme has been controversial since its inception and has been the subject of significant debate about its effectiveness, cost-effectiveness and evidence base. 27–29,174–176 Our data point to a split in NHSHC providers in relation to their belief in the programme’s potential to help those who attend, and suggests that provider ‘buy in’ to the programme’s objectives and approach is a fundamental context that affects delivery. In particular, providers’ belief in the ability of the NHSHC to provoke and support behaviour and lifestyle change for attendees (or not) and their perception of the relative importance of lifestyle modification over clinical intervention to reduce CVD risk influence what providers offer attendees at their check. The data included in our review suggest that providers who have not ‘bought in’ to the programme and are sceptical about its ability to promote lifestyle change or reduce CVD risk may fail to engage with guideline recommendations in relation to the delivery of advice, brief interventions and referrals to lifestyle services (CMOC P1). In this context, there may instead be an emphasis on efficiency in delivery, minimising workload, and collecting sufficient data about attendees to record an NHSHC as complete from the commissioners’ perspective (to ensure the provider is compensated for supplying the check). Attendees may perceive such providers as offering a ‘tick-box’ approach to the NHSHC and failing to offer adequate explanation, discussion or personalised advice (see also CMOC A12 below).
Scepticism about the NHSHC programme as an effective behaviour change intervention, or about the effectiveness of behaviour and lifestyle change to significantly reduce CVD risk, may mean that providers are more likely to consider medication to be an appropriate intervention for those at higher risk levels. Providers may be more likely to offer prescriptions for statins or anti-hypertensives – or refer attendees on to their GP with this in mind, if they are not able to prescribe themselves (CMOC P2).
Data from existing systematic reviews7,8 and from Patel et al.’s (2020) large observational study5 indicate that NHSHC attendance is associated with increased rates of statin prescribing (c. 3–4% higher than for those who do not attend a check) for those at high CVD risk, and similar increased rates of anti-hypertensive prescriptions. 5 However, rates of prescribing vary, and there are some data to suggest that prescribers (usually GPs or nurse practitioners) exercise discretion and do not always follow best practice or NICE guidance. Our data suggest that this discretion may be related to providers’ beliefs about the efficacy of medication versus ‘behaviour change’ in general, or for certain groups, especially those believed to be at higher CVD risk, such as those from particular ethnic groups. Overall, rates of prescribing fall below those that were modelled at the outset of the NHSHC programme,34 or that might be expected if all NHSHC providers followed existing guidance for all attendees. 5 In 2014, guidance from NICE was updated to recommend statins for all those deemed to have a CVD risk in excess of 10% over 10 years. 177 Lower rates of statin prescribing in particular may reflect scepticism on the part of GPs about the recommended thresholds at which intervention should be offered or recommended (CMOC P3). Similar reasoning may apply to other interventions that may be offered during an NHSHC, including referrals to lifestyle services, although there are few data available to confirm or refute this.
For some providers, there appears to be a more general concern associated with the potential for the NHSHC to label healthy people (who may have some risk factors) as sick. Providers who are concerned about overdiagnosis may feel that the tests and measurements conducted on otherwise healthy people during a check are of low benefit, or even potentially harmful, especially in relation to causing anxiety or shame, or provoking attendees to adopt a ‘sick role’. These providers may still deliver the check, but they may communicate results differently and potentially temper or avoid giving too much advice, offers of prescriptions or referrals (CMOC P4).
In contrast to those who are sceptical, some providers are highly engaged with the NHSHC programme and view it as an opportunity to reach more people and assess their CVD risk. These providers may be highly committed to preventive healthcare in general and so are highly engaged with the programme as the dominant screening programme for prevention of CVD in England (CMOC P5). Other providers perceive the NHSHC programme as an opportunity to support behaviour and lifestyle change and are therefore more likely to offer more in-depth advice and onward referrals to relevant lifestyle support services. The data suggest providers must have confidence both in the effectiveness of lifestyle changes to reduce CVD risk (CMOC P6) and in the NHSHC programme itself to prompt attendees to make lifestyle changes, or as a means of offering patients relevant advice, support or referrals (CMOC P7). There is a sense in the data that such providers understand behaviour and lifestyle change to be the primary purpose of the NHSHC and have a preference for lifestyle modification over medication (at least as a first recourse).
Such providers may have experienced positive outcomes from encouraging and supporting NHSHC attendees (or other patients) to engage with behaviour change efforts. This level of engagement with the programme may be more common amongst dedicated NHSHC providers (e.g. Health Trainers), especially those who understand supporting lifestyle change to be part of their professional role and who may have undertaken extensive training in this area (see also CMOC P26 below). Some of our data appear to suggest that the existence of the NHSHC programme itself has helped to foster engagement with preventive healthcare, raising awareness and shifting clinical practice norms to incorporate more early detection and intervention.
Our data suggest that training for NHSHC providers can help to generate the ‘buy in’ context described above, giving providers a sense of the programme as a behaviour change intervention that can make a real difference to people’s lives, and emphasising a focus on follow-up, advice and referrals. Providers who are knowledgeable about the potential benefits of these activities may be more likely to deliver them, and training may also increase providers’ confidence in these areas (CMOC P8). Such training must therefore include more than just the practical elements focused on testing and measurement in the check and shift the emphasis to the NHSHC encounter as an opportunity to offer attendees advice, brief interventions or referrals. It may include specific skills cited in PHE’s Best Practice Guidance, including motivational interviewing or health coaching, where the focus is on developing the skills providers need to help people to set personal goals and make plans to achieve lifestyle change. 3 As above, those in dedicated roles are more likely to have received more extensive training of this kind, which can serve to reinforce professional norms and expectations in these roles. Other data indicate that many providers have themselves identified a need for training that focuses on the ‘next steps’ following testing and measurement during a check, describing deficient training as a barrier to delivery.
Practical constraints for providers: time and money
As for commissioners, it is clear from our data that providers’ delivery of the NHSHC programme is influenced not only by their understanding of and engagement with it, but also by practical constraints, often focused on the requirement to deliver checks with limited resources, and alongside numerous competing priorities. The extent of what can be delivered within an NHSHC is most obviously limited by the time available to deliver it. PHE’s guidance for commissioners and providers does not make any specific recommendation about the duration of a check, and there is clear evidence of wide variation in both the time allotted to and the time actually spent delivering each check. Within an NHSHC encounter, providers must manage the time they have available to conduct multiple tests and measurements, as well as having a conversation with the attendee, explaining test results and risk factors, delivering personalised advice and appropriate brief intervention(s) and potentially making appropriate referrals to other services.
Different funding models exist: in PHE’s 2020 survey of LAs, 71.4% reported that providers were paid based on activity (i.e. per NHSHC delivered) while 15.6% were paid a fixed amount. In a small number of areas, compensation is tied to performance and designed to incentivise reaching particular population groups or increasing invitation or offer rates. 16 However, no matter which of these funding models is adopted, providers may be affected by time pressure on appointments. Most funding arrangements ensure that there is clear incentive for providers to increase the number of checks delivered, leading to a focus on delivery of the mandated or monitored aspects of the NHSHC, and so potentially reducing the time available for in-depth discussion, personalised advice or shared decision-making about what to do next (CMOC P9; and see CMOC C13 above).
In addition, those providers – such as general practices and community pharmacies – who deliver the NHSHC alongside many other services may consider that the programme adds to workload, adversely affecting other activities and so producing a clear incentive to deliver checks as efficiently as possible. For example, GPs may consider that limited staff time may be better spent in caring for those who are already unwell, rather than engaged in preventive care, or focusing on activities they judge to be more clinically important for a particular patient (CMOC P10).
Time constraints in the delivery of checks and a subsequent focus on meeting targets to deliver large numbers of checks within existing resources can lead to more checks being delivered ‘opportunistically’, that is, NHSHC tests and measurements are completed during an existing encounter with a healthcare professional, whenever it becomes apparent that the person is eligible to receive a check (CMOC P11). This approach may be efficient for providers, increasing the volume of NHSHCs they deliver, but it is unlikely to ensure sufficient time for in-depth discussion and personalisation of advice and referrals.
A focus on efficiency in delivery may also be reflected in data recording during checks. Data collection is focused on those aspects of NHSHC delivery that are monitored (primarily: coverage and uptake) and there are serious inconsistencies and potential under-recording of data relating to other NHSHC activities, which are frequently highlighted in local evaluation documents and research studies. For example, a large volume of data from both types of document makes it clear that data on referrals are not necessarily prioritised and are therefore inconsistently captured, if at all. Recorded levels of these activities may underestimate the actual activity that takes place during NHSHC encounters (CMOC P12). The reasons for this are not clear. It may be that when the emphasis in a check is placed on the ‘mandatory’ elements, data on activities such as delivering advice or offering referrals are less well recorded. However, some data suggest that this effect may be ameliorated wherever LAs specifically prioritise capturing data on certain activities and outcomes, and take action to improve data collection. For example, some LAs have invested in software that aims to improve data capture and can be used to monitor delivery of the checks, and they may mandate certain data collection requirements in service specifications (see CMOC C7 above). It is also worth noting that incentives from elsewhere may play a role in incentivising providers to collect certain types of data. For example, advice and referrals relating to smoking cessation appear to be consistently better recorded and more frequent than advice and referrals relating to other risk factors. This may reflect the inclusion of these activities in the Quality and Outcomes Framework, such that recording data in these areas is directly incentivised for GP practices. 178
Our data suggest that for some providers (and especially general practices) this aim of efficiency in delivery of NHSHCs may also be provoked by a sense that they are inadequately compensated for delivery of the NHSHC (CMOC P13). In particular, it is notable that current funding arrangements usually mean that any follow-up required after an NHSHC appointment is uncompensated, and such follow-up and ongoing care may be significant, especially when the programme identifies large numbers of people at higher CVD risk. Follow-up and continuity of care within general-practice settings may also take on a new importance where access to other support services is limited by difficult referral pathways or funding cuts (see CMOC C12 above, and CMOCs P16, P17, P18, P19 below). These outcomes associated with the contexts of time pressure and competing priorities may be especially marked where there is a prevailing context of provider scepticism about the NHSHC (see CMOCs P1, P2, P3, P4).
Conversely, delivery models that are based on service specifications or practice that provide dedicated appointments of adequate duration, or flexibility in delivery that allows providers to extend the length of appointments when needed, can provide space for more in-depth and personalised advice and support to be offered (CMOC P14). Providers who have ‘bought in’ to the NHSHC and are working within delivery models like this are able to prioritise these activities for those attendees who they feel will benefit (see also CMOCs C1, C2, C3).
Practical constraints for providers: referrals and follow up
Providers’ actions during the NHSHC are also influenced by the availability and accessibility of additional lifestyle services in the local area.
Some variability in recorded rates of advice and referrals in relation to different risk factors may reflect a process of prioritisation undertaken by NHSHC providers and attendees. When a check identifies multiple risk factors, behaviour change efforts may be focused on just one risk factor at a time, in line with an emphasis seen in some of the literature on making small changes and harm reduction (CMOC P15). This outcome also reflects evidence that suggests that separate services may be more effective than more holistic models of support that might focus on lifestyle change in general. Some data seem to suggest that providers may make judgements about the appropriateness of lifestyle services for individual NHSHC attendees, based on various characteristics, such as gender or age (CMOC P16). For example, some data seem to suggest that older people may be referred to exercise classes or smoking cessation services less frequently than younger people. These decisions are likely to be influenced by specific local service provision (see CMOCs C8 and C14 above) and it is important to note that the observed patterns also may also reflect the preferences and priorities of NHSHC attendees (see CMOCs A35, A36, A37) or joint decisions reached in discussion between providers and attendees.
In order to offer them to attendees, providers need to be aware of the availability and extent of local services that may be available, and the appropriate pathways for referral or signposting into them (CMOC P17). Several pieces of data included in the review indicate that this is a potential blockage that must be addressed before providers can be relied upon to take advantage of available local services; in particular, local evaluation reports describe this problem directly, or highlight it indirectly by identifying a need to improve or collate information on local services and programmes. Providers who are aware of local services may still hesitate to refer NHSHC attendees on, especially if they have concerns about the quality of local services, or where they compare them unfavourably with support they feel they could deliver themselves in the form of advice, brief interventions or ongoing follow-up and support (CMOC P18). Both of these factors should be understood in the prevailing context of funding cuts, which have affected the availability and continuity of many locally provided services (see CMOC C14 above).
Supporting these findings are data that suggest that onward referrals to lifestyle support services are facilitated by the existence of well-established relationships and pathways to trusted local services. Services may be trusted because they have been in place for some time, have demonstrated past success, or where there are good working relationships between services and NHSHC providers (CMOC P19). As noted above, LAs may have worked to help develop and embed these relationships and some areas have introduced integrated provision of NHSHCs and onward support services (see CMOCs C2 and C3 above). Provision of the NHSHC and lifestyle support services in a single setting or by a single organisation makes onward referral simple, allowing it to become a normal and expected part of NHSHC delivery.
Practical constraints for providers: relationships and confidence in the delivery of advice
Despite the clear variation in its recorded delivery, large numbers of NHSHC attendees are recorded in research studies and local evaluations as having received advice or education relating to healthy lifestyle. This advice may be general, or focused on a specific risk factor, especially where these are identified as affecting individual attendees during the check. This step of the check is the least defined and remains unmonitored at a national level, although PHE’s Best Practice Guidance points NHSHC providers to numerous sources of existing guidance and recommendations relating to the delivery of advice and ‘brief’ or ‘very brief’ interventions that could be delivered as part of the check. Our data suggest that when it is delivered, the content and nature of the advice provided is highly variable. This component of the check is not only constrained by the time available to deliver the check (see CMOCs P9, P10, P11) but also influenced by a wide range of other factors, including social and professional factors that play a role in how advice is delivered.
The confidence and comfort of providers in communicating risk and delivering lifestyle advice plays an important part in what happens after testing and measurements are completed. Several sources of data point to a reluctance on the part of some providers to discuss certain lifestyle risk factors, especially where these are considered to have the potential to cause distress or upset for attendees (CMOC P20). Our data suggest that this may apply to various risk factors, including weight, levels of physical activity and especially alcohol consumption. Some data also suggest that providers may experience discomfort in discussing the risk of dementia during a check. To save attendees and themselves from discomfort, providers may simply avoid in-depth discussion of certain topics during the check, or limit themselves to providing brief, generic advice, without asking attendees for many details or attempting to personalise the discussion. Providers may also lack confidence in delivering advice when they are aware that they lack knowledge about current evidence and recommendations about a particular lifestyle risk factor (CMOC P21). This may be a particular problem when guidance is recent or is regularly updated.
Providers may also lack confidence in delivering advice whenever they anticipate that it will not be well received by attendees. When a provider suspects that someone will be reluctant to discuss lifestyle change, or may struggle to make or sustain meaningful changes, they may avoid discussing risk factors or offering advice. There is a concern that giving advice or offering referrals in these circumstances could damage the relationship between the provider and attendee, which may be a particular concern where the provider-attendee relationships are ongoing outside of the NHSHC encounter, such as in general practice or community pharmacy settings (CMOC P22). Providers may also be concerned that advice will not be well received when they have concerns that they themselves are not good role models for ‘healthy’ lifestyles, and may therefore lack credibility for attendees (CMOC P23, and see also CMOC A24 below). However, in some cases, it appears that providers are able to turn this to their advantage – those with lived experience of risk factors or making lifestyle changes may be better able to empathise with NHSHC attendees in a similar position and can share their own experiences to help build rapport and establish a therapeutic alliance (CMOC P24).
For some providers, the delivery of advice and offer of referrals in relation to lifestyle factors appear to be easier and more routine. This is especially the case when discussing and advising on a lifestyle factor become more normalised and well-established as a key part of delivering the NHSHC (CMOC P25). For example, the delivery of advice and interventions in relation to smoking cessation is now well-established in healthcare settings, as smoking cessation messages have become more embedded in cultural norms. Whenever providers are more practised in discussing and providing advice on any particular topic, and when they might reasonably anticipate that attendees will be unsurprised to discuss it, providers are more likely to feel more comfortable in dispensing it.
As noted above in relation to generating ‘buy in’ to the NHSHC’s goals, training can potentially play an important role in addressing providers’ knowledge gaps and potentially equipping them with new skills to support more in-depth discussion of lifestyle and personalised advice and support (CMOC 26). Some data suggest that when NHSHCs are delivered by dedicated providers who have undertaken more extensive training (and have more practice in delivering NHSHCs) rates of advice delivered on potentially ‘sensitive’ topics are higher.
Similarly, when NHSHC providers have a professional norm of shared decision-making and in-depth discussion with attendees, they may be more likely to vary the delivery of an NHSHC in response to attendees’ individual circumstances and preferences (CMOC P27). This may be an overlooked but important driver of the apparent variability in what happens after measurements and risk assessment are completed during a check. When providers have adopted this approach, we might expect, for example, that providers offer fewer, but potentially more appropriate and welcome, referrals to lifestyle services, and offer more workable lifestyle advice that takes into account attendees’ individual constraints and preferences. Some of our data suggest that when providers take wider factors about attendees’ lives and preferences into account, they can emphasise the benefit of making smaller changes, which may be more likely to be acceptable, achievable and sustainable over the longer term (CMOC P28).
Attendees
The findings presented above offer explanations that describe how important contextual influences and commissioners’ and providers’ responses to those conditions can influence the delivery of the NHSHC programme. This section presents our findings relating to what might be the most important step in the NHSHC programme theory: what shapes the response and subsequent actions of those who attend and receive a check. As above, our data point to yet further sources of variation, this time in how attendees receive, understand and respond to the advice, brief interventions, referrals and prescriptions that they may be offered at the end of a check. Attendees’ responses are influenced by a wide range of factors, including their own understanding of the NHSHC, features of local delivery models and other important external contexts in attendees’ own lives.
Understanding and engagement with the NHSHC: expectations and priorities
Our data suggest that attendees, like commissioners and providers, have different understandings of the purpose of the NHSHC programme and different expectations about what it will provide. Some of these understandings and expectations are pre-existing attitudes that attendees bring to the check. Others are formed in response to the delivery model adopted by commissioners and providers, which has the potential to send important signals to attendees about the purpose of the check and how they should respond to what they are offered. The experience of a check for an individual attendee is produced at the intersection of these expectations of what will be offered, and attendees’ own priorities for their health and lifestyle.
For some attendees, the NHSHC is interpreted as a screening opportunity: the focus is placed on the measurements and risk assessment conducted during the check and on the potential to identify hitherto undetected ill health (or high risk factors that could themselves be construed as ill health), and then on initiating any necessary medical treatment. For these attendees, any advice, brief interventions or referrals relating to lifestyle or behaviour change may seem misplaced, and something they are not interested in considering (CMOC A1). Attendees may arrive with this perception of the check – this may be related to the programme’s name (‘NHSHC’), how the programme is advertised and how potential attendees are informed about its purpose, although this is out of the scope of this review project; see, for example, references 72, 107 and 179.
The extent to which attendees are willing to engage with the NHSHC programme as a behaviour change intervention can also rest on their existing attitudes and priorities in relation to health and lifestyle. Data on behaviour changes after the check are sparse: the literature includes a volume of anecdotal evidence demonstrating that, for some individuals, the check may trigger significant lifestyle changes, and a significant volume of self-reported change or intention to change. Large observational studies have identified an association between HC attendance and improvements in some clinical markers and measurements (e.g. overall CVD risk, blood pressure, cholesterol, BMI), either over time (pre/post check) or in comparisons of attendees versus matched non-attendees. 7,8 However, the observational nature of most of these studies means that the direction of causation is unclear, and it is not possible to directly attribute improvements to the NHSHC itself; it may be the case that those who choose to attend are more likely to have wanted to or changed their lifestyle and improved these outcomes anyway.
Some data included in our review may lend weight to this argument: some attendees appear to be more receptive to the delivery of advice or offer of referrals designed to support behaviour change than others. This includes attendees who arrive at the check with an awareness or understanding of health risks, or of areas where they feel their lifestyle could be improved (CMOC A2). This includes those attendees who are aware of increasing risks associated with age, prompting them to take more care of their health, and those who have personal experience of the consequences of poor cardiovascular health. The data underpinning this CMOC are dominated by the influence of family history, but people may also be exposed to the consequences of poor cardiovascular health in their local area, peer group or at work, if they are healthcare professionals themselves. For these attendees, the HC encounter may provide a crucial prompt to make lifestyle changes. Data relating to earlier steps in the NHSHC programme pathway suggest that this group may be more likely to accept an invitation and attend a check in the first place (although this is out of the scope of this review). 8
Some attendees receive unexpected results during a check. When attendees are unprepared, they may be shocked and upset to learn about serious risk factors, and require more time, explanation and sensitive support from providers to help them to understand and reduce the risk, so that they do not disengage with the whole process (CMOC A3). For some attendees, this shock alone appears to be enough to prompt sometimes significant lifestyle changes, but it is difficult within our data to ascertain the contexts in which and for whom this happens, or whether these changes are sustained over the longer term (CMOC A4).
Overall, there is a sense that for some attendees, the NHSHC aligns with their own personal priorities. There are also some data to suggest that providers can also play an important role in communicating the relevance of the NHSHC for individual attendees. For example, where providers are able to make the risk factors identified at a check or potential benefits of lifestyle change more tangible and understandable for attendees, they may be more receptive to the advice they receive and more inclined to consider making lifestyle changes (CMOC A5). Similarly, a shared process of priority-setting may enable a greater focus on attendees’ preferences, priorities and plans for the future. Some data included in our review suggest that (as well as motivating people to attend) a focus on what attendees are improving their health for may be motivating and support lifestyle changes (CMOC A6). Some recommended approaches to the delivery of advice and brief interventions within the NHSHC are based on these principles. For example, motivational interviewing and health coaching (informed by behavioural change techniques) require providers to move away from simply providing information, towards a more collaborative approach that focuses on motivating change and setting goals. Such approaches may help to ensure that the NHSHC encounter feels more relevant for individual attendees, as well as potentially helping to ensure that any advice or referrals offered are acceptable and achievable (see also CMOCs A38, A39, A40, A41).
It is worth noting that some of our data suggest that routes to attempted behaviour change are not necessarily straightforward for attendees. Some of our data point to a complicated process of negotiation and customisation that can take place during a check and afterwards, as attendees contemplate making lifestyle changes. To some extent, attendees may pick and choose which pieces of advice to follow, adopting some, rejecting others, and making adaptations to render advice about lifestyle changes acceptable and ensure they fit with their own preferences and priorities (CMOC A7). For other attendees, a strong sense of personal responsibility for lifestyle behaviours may mean that offers of support or referrals are rejected in favour of trying to make changes alone (CMOC A8).
For other attendees, there appears to be a significant mismatch between the focus and design of the NHSHC programme and those of its attendees. It is clear from our data that there is a group of attendees who are not motivated to make changes to their lifestyle and behaviour, and are therefore very unlikely to engage with any advice offered, or to accept any referrals to lifestyle services (CMOC A9). Attendees in this group simply have other priorities and reject the idea that making and sustaining lifestyle changes is necessary or desirable for them. They may only have attended their check because they felt compelled by the invitation. Some attendees have fatalistic attitudes about their health; this group may feel the NHSHC as a whole is a pointless exercise for them (CMOC A10). For other attendees, the content and focus of the NHSHC programme may not reflect their own health priorities. This group may have more pressing concerns and find the focus on CVD risk factors to be irrelevant and potentially frustrating (CMOC A11). Many in this group express their disappointment that the HC does not cover, or is not flexible enough to accommodate, a more wide-ranging set of health issues that are important to them.
Important aspects of how checks are delivered can also play a role in signalling the purpose and importance of the check to attendees. It is clear from a range of data included in the review that not all checks are delivered in a dedicated encounter with a provider. In particular, when checks are delivered in general-practice settings, they may be delivered ‘opportunistically’; that is, relevant test results and measurements may be recorded during an appointment focused on another problem or problems (NB this mode of delivery should not be confused with ‘opportunistic’ checks delivered in community-based settings without appointments; the same term is used to describe both delivery models in the literature). This approach to delivery is actively encouraged by some commissioners and providers, and PHE’s Best Practice Guidance is clear that checks that are delivered in this way should count towards the figures for checks ‘offered’ as well as delivered. When a check is delivered opportunistically, attendees may not even be aware that they have received a check, let alone had time for any in-depth discussion of risk factors or advice (CMOC A12). As noted above (see CMOC P11) this delivery model is likely to reduce the time available for each check and so makes it more likely that the emphasis is placed on recording mandatory test results and measurements, with less focus on the delivery of advice, brief interventions or onward referrals. Although this model of delivery may save time and increase the coverage of the programme, it may also be an important signal for attendees that the NHSHC is composed of a series of measurements and risk assessment alone.
Conversely, our data suggest that where more time is available for a check, attendees can take advantage of this opportunity to ask questions and engage with the discussion about risk factors and lifestyle (CMOC A13, and see CMOC P14 above). Some of the data underpinning this CMOC emphasise the value that attendees may place on face-to-face interactions with providers, as a means of facilitating extended discussions and the provision of advice, brief interventions and offers of referrals.
Other data included in the review suggest that the setting in which NHSHCs are delivered matters. PHE surveys indicate that most NHSHCs are still delivered in general-practice setting; in 2019/20, 70% of LAs commissioned checks delivered in GP practices. 16,180 Our own survey confirms this finding (see above in Survey findings). Most research and evaluative work to date on ‘outreach’ settings for the HC has focused on the adoption of alternative delivery settings as a means of increasing the reach of the programme, facilitating access and coverage. However, there are some data to suggest that checks delivered in a non-medical setting, and especially in a more informal, familiar setting, may also facilitate more in-depth discussion, because attendees are more relaxed and may be more willing to speak openly about risk factors and lifestyles, away from the formality (and potential time pressures – see CMOCs P9, P10, P11) that may be associated with general-practice-based appointments (CMOC A14). Delivery in alternative settings may work to counter an impression of the check as a series of measurements and risk assessment (as described above in CMOC A1).
Understanding and engagement with the NHSHC: credibility and trust
Closely related to the question of where NHSHCs are delivered is the question of who delivers them. As noted above, our survey results suggest that when checks are provided in general-practice settings, they are most likely to be delivered by a HCA or PN. When checks are provided in other settings, such as community pharmacies, or other community venues, they may be delivered by other professionals, including pharmacists, pharmacy technicians, Health Trainers and coaches, or others. No matter who provides a check, providers have the potential to wield significant influence over attendees, and the credibility of the provider matters to them.
For some people, this credibility may be enhanced by the involvement of a familiar professional whom they trust. They may be more likely to engage with offers of advice, referrals and prescriptions when these are delivered by a professional that attendees associate with healthcare, or who has provided them with healthcare before (CMOC A15). There may be some overlap here with the perception of the NHSHC as a medical or clinical intervention (see CMOC A1 above). In this case, credibility may be attributed to the trust that attendees place in certain healthcare professions. Some of the data underpinning this CMOC are more negative and present the converse view: some attendees express doubts about the credibility of advice provided by, for example, HCAs or Health Trainers.
For other attendees, the credibility of any lifestyle advice provided during a check may be enhanced where it is provided by someone who seems to understand their life circumstances and experiences. For example, when the NHSHC is delivered via an outreach or community-based model, commissioners or providers may have made a conscious effort to ensure that staff reflect the local communities that they serve. These efforts (though often primarily intended to increase uptake of checks) also affect what happens after the risk assessments and measurements are completed. Documents describing these delivery models emphasise the value of good rapport between providers and attendees in the delivery of advice and offers of onward referrals. Attendees may be more inclined to engage with pragmatic advice delivered by someone like them or who they feel understands their lived experience (CMOC A16). For attendees from ethnic minority groups, the ability of providers to deliver advice that is culturally appropriate is an important factor in ensuring advice is both credible and workable for attendees (CMOC A17) (and see also CMOCs A38, A39, A40, A41).
Attendees’ response to the NHSHC is also affected by the manner in which providers communicate with them during a check and our data are clear that providers wield significant influence in how the check and the results of the check are understood. In particular, some data suggest that providers can (possibly inadvertently) leave attendees with a sense that there is nothing to worry about and no recommendation to make any lifestyle changes. This is most obvious when the NHSHC measurements and risk assessment indicate that attendees have a low or average CVD risk score (CMOC A18) but our data suggest that providers may downplay risks and dilute advice even when attendees are calculated to be at high CVD risk, leading to a sense of reassurance and an understanding that no lifestyle change is strongly recommended or required (CMOC A19). Our data do not illuminate the contexts and mechanisms underpinning this behaviour in providers, but it may be related to feelings of scepticism or concerns about the check, or reluctance to discuss certain lifestyle issues in depth (see CMOCs P1, P2, P20 above).
Conversely, some data suggest that certain features of delivery models can underline the importance of NHSHC risk assessments and help to convey a sense of urgency about taking action to attendees – including, for example, when results are provided in writing (CMOC A20). Other data included in the review suggest that receiving a ‘low’ risk score may help to reinforce and encourage attendees to maintain healthy lifestyle behaviours (CMOC A21).
The credibility and significance of the check and the results of the risk assessment can also be signalled to attendees by the professional role of the provider. For some attendees, there is a strong sense that receiving results, or related follow-up, from a recognised clinician (such as their GP or a PN) is an important part of this. In some cases, there are data to suggest that results and risk scores that are low to average may not even be communicated to attendees at all (CMOC A22). Our data also suggest that attendees recognise disengaged providers, and that this disengagement may be passed on: attendees can take a cue from some providers that the check is unimportant (a ‘tick-box exercise’) and are therefore less likely to engage with any interventions offered (CMOC A23). Finally, a smaller set of data points to another factor that may influence the credibility of some providers. Mirroring data about providers’ concerns about appearing hypocritical in giving healthy lifestyle advice (see CMOC P23), some attendees also describe their scepticism or discomfort in receiving advice from providers who they perceive not to follow it (CMOC A24).
The credibility of NHSHC providers is particularly important in light of the fact that attendees may come to the check with some awareness of current (and past) recommendations in relation to ‘healthy lifestyles’ and of the advice and interventions that may be offered after a check. Attendees who are already familiar with common recommendations are more likely to feel dissatisfied with ‘generic’ information and advice being delivered as part of the check (CMOC A25). Some data point to a more positive impact when attendees can learn something new or have a misconception about CVD risk factors corrected. In these circumstances, attendees are enabled to think about making lifestyle changes with an improved understanding of the potential benefits (CMOC A26). However, when attendees’ existing knowledge extends to knowledge of controversies and changes in guidance and recommendations relating to behavioural risk factors (especially diet) (CMOC A27) and medicines (especially statins) (CMOC A28) they are likely to feel ambivalence about any interventions they are offered at a check.
Further to this, for some attendees, there is doubt about the accuracy of some of the tools used to assess behaviour and measure risk during the check, which providers may need to address. When attendees harbour doubts about how their lifestyle is being assessed, this can undermine the check and leave them unreceptive to any interventions that are offered (CMOC A29). Some of the data collected here seem to suggest that ‘harder’ results (such as the results of blood tests or blood pressure measurements) may be considered to be more trustworthy than those based wholly or in part on self-reported behaviours.
Practical constraints for attendees: referrals and follow-up
Mirroring the findings from the provider perspective, attendees’ responses to the NHSHC programme are also significantly influenced by local arrangements and infrastructure in relation to onward referral and follow-up. The extent of ongoing support for attendees is an important aspect of overall delivery of the programme. It may take the form of onward referrals to other services, or follow-up from the original provider of the check. Attendees frequently cite the need for ongoing support after a check, and there is a clear sense in the data that some kind of ongoing support and input – regularly reminding attendees about advice or goals set during the check – may be necessary to support sustained attempts at lifestyle change (CMOC A30). Sustained involvement and support from a healthcare professional may also help to give attendees a sense that someone else cares about their health. Ongoing contact and follow-up is a means for providers to demonstrate care, and this kind of support can help to ensure that attendees feel valued and encouraged in any attempts to make lifestyle changes (CMOC A31).
Some of our included data indicate that the opportunity for follow-up (especially where this might involve repeat tests or measurements) may help make the benefits of adhering to prescribed drugs or instigating lifestyle changes more tangible for those who attempt them, potentially reinforcing these and helping attendees maintain them over the longer term (CMOC A32). Some data do indicate that attendees who make lifestyle changes and then see or feel tangible benefits from doing so may be more likely to maintain these changes (CMOC A33). In both cases, attendees are aware that lifestyle changes have had a positive impact and this may be an important factor in determining whether further lifestyle changes are attempted, or if they can be maintained over the longer term.
Where attendees are aware that they will not receive follow up beyond the standard ‘5 year’ invitation cycle, there is a sense of frustration in the data that the check is rendered pointless. There is a lack of motivation to make changes, because the absence of follow-up implies that there is no urgent need to make any lifestyle changes (CMOC A34).
Attendees vary in their response to ongoing support in the form of referrals or signposting on to ‘lifestyle support’ services. Data on uptake of these services are sparse (as are data on whether they are offered, especially when they are informal ‘signposts’ rather than more formal ‘referrals’) but the data that are available suggest that uptake and sustained engagement with these services are highly variable. Reflecting data for providers’ willingness to offer referrals to attendees (see CMOC P16 above), some data suggest that attendees themselves also make decisions about these services on the basis of their perceived appropriateness. Attendees may reject offers of referrals to onward services that they cannot fit into their current responsibilities (work, childcare etc.) or cost too much. Sometimes attendees who are signposted or offered onward referral may not feel that the services available are a good fit for them in ‘softer’ ways, including whether other people of a similar age, gender and background attend, or whether services can accommodate other health needs and comorbidities – and they may be unfamiliar with what the services will be like (CMOC A35).
The data included in our review indicate the value of lifestyle support services that are provided in convenient locations, at convenient times, and are subsidised or available free of charge – reducing the barriers to uptake may at the very least encourage eligible attendees to try a service out, because important barriers are removed (CMOC A36). In addressing the ‘softer’ issues, some data included in our review suggest that small interventions like offering ‘taster’ sessions or having someone (e.g. a Health Trainer) accompany people to their first session may help them to access such services for the first time by demystifying them and helping attendees feel more confident about attending (CMOC A37).
Practical constraints for attendees: person-centredness
Other data included in our review demonstrate that the specific content of the advice and further support offered to attendees, as well as the way in which this support is offered, also have an impact on how they are received. There is a need for providers to ensure that the lifestyle advice and/or referrals that they offer attendees are appropriate and workable, and that advice is tailored to suit the person in front of them. Recommending lifestyle changes that are unworkable in the face of attendees’ work or caring responsibilities, financial situation or wider health is unlikely to provoke successful behaviour change attempts (CMOC A38; and see also CMOC A35 above in relation to the appropriateness of referrals to lifestyle services). Similarly, advice about lifestyle changes that is perceived to have far-reaching implications may be seen as being too overwhelming and cause attendees to feel hopeless before they have even begun to make changes (CMOC A39). When providers take an approach that emphasises the value of making small changes, one at a time, attendees may be more receptive and find that they are able to try to make changes with less effort (CMOC A40).
Attendees have to balance their health priorities with their lifestyle preferences, and make these decisions within the constraints that exist in their lives. For some attendees at higher risk levels, this may present as an opportunity to balance recommended lifestyle changes against the need to take prescribed medicine as a means of reducing their risk of CVD. When attendees perceive recommended behavioural changes to be unworkable – either because they cannot or because they prefer not to make these changes – they may accept a prescription for a drug like a statin as an acceptable means of reducing their risks (CMOC A41). As noted above, providers’ attitudes towards the NHSHC programme and towards behaviour and lifestyle change more generally may also have an important influence on decision-making here (see CMOC P2). On the other hand (like those attendees who are aware of controversy surrounding statins) other attendees are ambivalent or reluctant to take medication – they may anticipate or experience side effects or burden and inconvenience, including about the cost burden of lifelong prescriptions. These attendees may prefer to at least attempt lifestyle changes as a strategy to reduce their risk (CMOC A42, CMOC A43).
Finally, a further set of data included in the review highlights the importance of broader social networks in enabling and supporting behaviour change, which may carry implications for the individualised approach that is embedded in the NHSHC programme delivery model. The data included here suggest that the support of attendees’ social networks, including family members, friends and other peers, can be a crucial factor in enabling sustained change (CMOC A44). The mechanisms underpinning these outcomes are less clear: individuals may be motivated by the support of others, a sense of solidarity or even a feeling of peer pressure from the wider social group. A small section of the data underpinning this CMOC hints that lifestyle changes made in this context could have a broader ripple effect, helping to motivate and support others across family and social networks to make and sustain changes that could improve their health, too.
Final programme theory
Our final programme theory is presented in Figure 19, which summarises our findings and the CMOCs on which they are based. This figure is intended to illustrate the important contexts that affect the delivery of the NHSHC after the measurements and risk assessments are completed. In particular, it aims to highlight that both variation in understanding and engagement with the programme can affect the way in which it is commissioned and delivered. The figure also includes the important practical constraints that limit what can be delivered within the programme’s remit and affect the delivery of advice and referrals after a check. Finally, the diagram identifies connections between delivery models and processes and the experiences of NHSHC attendees; these experiences are equally various, and may or may not meet their expectations and needs.
FIGURE 19.
Final programme theory.

Chapter 4 Discussion
This project has explored what happens in the NHSHC programme after the measurements and risk assessments are completed. The success of the programme as a prevention initiative rests on this stage, when attendees may (or may not) be offered advice, referrals or prescriptions to help them to manage and potentially to reduce their risk of developing CVD. Our focus on this area reflected not only its importance, underlined and confirmed by our stakeholder groups, but also our aim to address the relatively sparse body of existing research with this focus. Research on the implementation of the NHSHC programme has focused largely on processes related to invitation, uptake and coverage,7,8 although we note that recent NIHR-funded projects have also focused on supporting commissioning144 and on risk communication. 91 Our project sought to shed light on the final steps in the NHSHC pathway, to improve our understanding of what influences the delivery of these aspects of the NHSHC and how they are received by those who attend.
Both our survey of LAs and our realist review have gathered evidence of variation in the delivery of checks in relation to the advice, prescriptions and referrals that are offered to NHSHC attendees. Our review synthesised data from a diverse range of sources, including published research and material documenting and evaluating local NHSHC programme implementation. Based on our review findings, we offer evidence-based theoretical causal explanations for the varied outcomes that are observed. These include factors that influence commissioning decisions in relation to the programme, providers’ behaviour and approach to delivery, and attendees’ responses to what they are offered during and after an NHSHC. Below, we summarise out findings and draw on substantive theory to offer a framework to understand how the worldview and constraints faced by commissioners and providers ultimately determine the NHSHC experience for attendees, and the multiple routes which produce variation in programme delivery and affect programme outcomes. We also situate our findings in the wider literature and finally set out our recommendations for policy-makers, commissioners and providers.
Variation in NHSHC delivery: street-level bureaucracy
Our findings draw attention to wide variation in delivery of what happens after the measurements and risk assessment are completed during an NHSHC. Large-scale observational studies indicate that the Best Practice Guidance relating to the delivery of advice, ‘brief interventions’, referral and prescriptions is not always followed, with rates of delivery falling well below guideline thresholds. 5,33 Regional and local studies indicate wide variation in the delivery and uptake of these activities. 7,8 Inconsistencies in the recording and collation of data relating to the delivery and uptake of advice, referrals and prescribing post-check mean that it is not currently possible to produce a comprehensive picture of this variation across England. 5,119 However, the data that we gathered in our survey and synthesised in our review provide a starting point to understand delivery in this area and highlight the roles that LA commissioners and providers play.
Our survey identified variation between LAs in commissioned NHSHC providers and both variation and gaps in the commissioning and use of services to support risk management and reduction for attendees post-check. Our review underlines these findings and identifies other factors at work, centred on commissioners’ and providers’ understanding of the purpose of the NHSHC, local levels of engagement with the programme and a range of practical constraints that limit what can be achieved within the programme’s remit.
Our review goes a step further and considers how these differences in commissioned and actual delivery models for the NHSHC influence how individual NHSHC encounters are experienced by attendees, as well as the additional, external influences that affect their response to what they are offered by NHSHC providers. Data from research focused on attendee experience of the NHSHC suggest that responses to the programme are as varied as its delivery but that understanding and engagement and practical constraints also play a major role in how much attendees are willing and able to do to address any risks identified during their check.
Our understanding of the processes at work in driving this variation draws on Lipsky’s concept of ‘street-level bureaucracy’, borrowed from the international relations literature. 47,181 We are not the first to make use of this concept to aid understanding of how the NHSHC programme182 and wider health policies in the UK setting have been implemented in practice. 183,184 Lipksy’s framework emphasises the discretion of those charged with implementing policies and the resulting significant influence of their decisions on outcomes, as well as street-level bureaucrats’ responses to limited resources.
Within the broad constraints of the legal framework13,14 and Best Practice Guidance3 underpinning the NHSHC programme, our analysis clearly demonstrates that the ways in which NHSHC providers actually deliver checks in everyday practice affect how attendees’ experience the programme, and effectively determine the actual remit and purpose of the programme on the ground. As Lipsky describes it
the decisions of street-level bureaucrats, the routines they establish, and the devices they invent to cope with uncertainties and work pressures, effectively become the public policies they carry out. 181
For NHSHCs, the extent to which discretion can be exercised may be greater towards the end of the programme pathway. Processes relating to the identification of eligible attendees, invitation and the measurements and risk assessment that should be administered during each check are restricted by the legal framework underpinning the programme13,14 and supported by clearer guidance offering less room for local adaptation. 3 The subsequent steps are less prescribed, more dependent on local delivery models (and the availability of other local services) and activity is less well recorded and monitored, leaving commissioners and providers with more discretion to determine what local delivery will look like.
Although much of the existing work that uses this framework to understand how health policies have been enacted on the ground focuses on those engaged in delivery of policies, and on those who interact directly with the recipients of those policies – in our case, NHSHC providers – our analysis is novel in that it also highlights the discretion exercised by LA commissioners in decision-making about local programme specifications and support. Although not directly public-facing, LA commissioners interpret the requirements of the NHSHC programme, exercising discretion of their own to adapt the programme to meet local needs and fit within local constraints. Their decisions and overall approach directly influence NHSHC providers, forming important local contexts in which local versions of the programme are delivered.
Our analysis points to commissioners’ and providers’ understanding and engagement with the NHSHC programme, as well as a range of practical constraints in driving decision-making about programme delivery. These two aspects mirror Lipsky’s focus on street-level bureaucrats’ discretion in the enactment of public policies, and their response to and attempts to implement policies within the confines of limited resources. Finally, our analysis also draws out outcomes relating to attendees’ experience of the NHSHCs programme that are related to the contexts created by commissioners’ and providers’ decision-making. Commissioner and provider decisions and resulting delivery models and practice inform attendees’ own understanding and engagement with NHSHCs, but their experience and response to what the programme offers are also affected by other external factors relating to their individual attitudes and circumstances.
Understanding and engagement with the NHSHC
Our review findings identify variation in how the primary purpose of the NHSHC programme is understood as a crucial factor driving variation in commissioning and delivery. The NHSHC programme was designed to fulfil two purposes, seeking both to identify cases of diagnosable illness or individuals at ‘high risk’ and to support individuals to manage and reduce CVD risk, via prescribing or by prompting behaviour change in relation to ‘lifestyle factors’ associated with CVD. Both purposes focus on the individual attendee, but while the former reflects a purely biomedical approach, the latter requires an extension to consider wider psychosocial factors that influence CVD risk, albeit with a focus on ‘lifestyle’ and individual behaviour.
Our data suggest that both commissioners and providers may tend to prioritise one purpose over the other, and that this prioritisation is then reflected in commissioning decisions and delivery models. In particular, differences in understanding or prioritisation of one aim of the programme at the expense of the other can affect delivery of what happens after the measurements and risk assessments have been completed during a check (see Figure 19). For example, favouring a particular purpose can drive variation in who delivers the check and the training they have received, where checks are delivered, the time allocated to each check, the availability, accessibility and referral pathways to local lifestyle services and important differences in data collection and monitoring, as well as funding models. As commissioners and providers set about implementing the programme at ‘street-level’, their values and intentions for the programme can be understood as informing their exercise of discretion in commissioning and delivery of these aspects. However, it is important to be aware that the NHSHC has been in existence for 13 years and that commissioning and delivery in individual local areas are not static, but rather may have undergone multiple changes over this period – a fact that was emphasised by our professional stakeholder group.
The double layer of discretion (at commissioner and provider levels) in how the NHSHC programme is enacted in each locality in England means that the relationship between LA commissioners and providers is crucial. Commissioners determine service specifications and funding models and engage in monitoring of NHSHC delivery. But, unless they are also acting as providers themselves (as is the case for some provision in some local areas), there is a limit to the extent that they can influence the day-to-day practice of all providers. Shared understanding and levels of engagement with programme delivery have the potential to underpin a coherent local delivery model and work at both levels to achieve the programme’s aims. However, there is also a potential here for commissioners or providers to undermine and contradict each other. In particular, the data included in our review point to problems where LA commissioners or public health teams may struggle to engage local general practices. Different levels of engagement with the programme may reflect differences in understanding of its purpose, scepticism about its ability to deliver positive outcomes for attendees, but also more practical concerns, especially around competing priorities, workload and delivering NHSHCs within limited resources – these constraints can create tension between potentially competing models in commissioning and delivery (see below, Practical constraints).
The delivery models commissioned and implemented locally send important signals to NHSHC attendees that inform their understanding and engagement with the programme in turn. Delivery of checks in general-practice settings and a focus on completing measurements and risk assessment may suggest to attendees that the check should be understood as a screening tool or clinical intervention. Delivery elsewhere, in community settings, or with a greater focus on the delivery of advice, space for discussion and offers of referral to lifestyle support services, sends a very different message. In some local areas, NHSHCs are delivered alongside integrated lifestyle services, and the programme facilitates links to link workers or social prescribing functions, enabling providers to offer more holistic support to attendees that may better reflect individual needs. As our data suggest that attendees’ engagement with offers of advice and referral may depend on what they expect to receive during a check, it is important to ensure that local advertising and communication about the programme accurately depict its purpose. Providers themselves can also (un)intentionally transmit ‘softer’ signals to attendees. In particular, the extent of provider engagement with the programme is often apparent during a check, and providers have the potential to convey urgency, but also the potential to imply that the check is not much more than a ‘box-ticking’ exercise. This finding underlines the importance of work to engage providers and generate a shared understanding and ‘buy in’ for its intended aims.
Overall, just as providers can exercise discretion in how they deliver advice, offer referrals or recommend prescriptions, attendees themselves can exercise discretion in their response. The focus of the check on individuals and their behaviour also carries the important implication of the ‘responsibilisation’ of attendees – there is an expectation that attendees will engage in individual work to address identified ‘lifestyle risk factors’. 185 However, just as commissioners and providers face practical constraints that affect what they are able to deliver within the programme’s remit, attendees must also contend with constraints in their own lives – individual limited resources that affect the extent to which they are able to consider taking on board advice, taking up referrals, and, ultimately, making changes to their behaviour to help manage or reduce their CVD risk. Others have drawn attention to the risks inherent in this strategy, including the potential for any positive health impacts to be unfairly distributed amongst attendees. 186
Practical influences on the NHSHC
Commissioners’ and providers’ approach to organising and delivering NHSHCs is influenced by much more than their understanding and engagement with the programme. Practical factors influence decision-making about the programme and limit what it is realistic to deliver locally, within each NHSHC encounter. LA commissioners have the discretion to set important boundaries for providers in setting service specifications and determining funding models for the programme. The extent to which commissioners’ focus on ensuring delivery of the mandatory measurements and risk assessment during checks versus the delivery of aspects of the check that might prompt and support behaviour change affects what providers are able to offer. This includes, for example, how local funding models incentivise different delivery methods, the relationship between funding and the time allocated for each check, the availability of local lifestyle services and the ease with which referrals can be made to these services.
Providers contracted to deliver the NHSHC are also influenced by the need to ensure that staff involved in delivering checks have confidence in every aspect of delivery. Our data suggest that not all providers feel they have the knowledge and skills required to deliver those elements of the check that are more focused on prompting behaviour change, including delivering advice or offering referrals. These findings raise questions about when and how providers receive training to deliver the check, and whether this training focuses on the completion of measurements and risk assessment, or whether it includes training focused on the delivery of advice and supporting discussions about lifestyle with attendees. In addition, when checks are delivered in settings where providers may face competing demands on their time (in general-practice or pharmacy settings, for example) these workload and time pressures may translate into ‘leaner’ delivery of checks, with a focus on the essential mandatory parts of the NHSHC that are more closely monitored. There is a risk that personalised advice, discussion and offers of referral become secondary concerns and may not be delivered consistently in these settings.
Delivery is affected by the availability of resources across primary and community healthcare and public health, and in particular for disease prevention and health improvement activities. These resources include funding envelopes for public health programmes, workforce capacity and structural, cultural and status differentials that present challenges to collaborative working across the many different organisations involved in these activities. Community health services are diverse, with complex patterns of commissioning and provision; the dynamic relationship between these services and the other parts of the system is often overlooked. The identification of practical constraints that influence NHSHC commissioners and providers has implications for national and local policy. In particular, it is clear that the delivery of personalised, individual advice and discussion at the end of a check is a more intensive and costly proposition than the delivery of a simpler programme focused on case-finding. In addition, increasing referrals from the NHSHC to local and national lifestyle support services requires an assessment of their capacity.
Our data suggest that there is a relationship between the practical influences facing commissioners and providers and their understanding and engagement with NHSHCs. Both groups of actors may to some extent exercise discretion and adapt their understanding of the purpose of the programme based on their knowledge and experience of the potentially limited resources available to deliver it. Despite the common mantra of ‘doing more with less’, the realities of the funding envelopes available send clear signals to commissioners and providers to prioritise efficient and lean delivery models, and, as our data make clear, these models tend to favour the ‘case-finding’ function of the NHSHC programme. Local scepticism about the likely impact of the programme on the part of providers is likely to be compounded by the perception that both the NHSHC programme itself and the lifestyle support services on which it depends are difficult to access.
We have shown that these influences also affect attendees’ experience of the programme and place significant limitations on what they can be offered post-check. The extent to which attendees can be offered meaningful, personalised advice and support for behaviour or lifestyle change within the current programme is open for debate. Attendees’ own lives and needs are more complicated and are unlikely to be improved using generic advice about ‘healthy lifestyles’. Ethnographic work that has explored NHSHC delivery has identified the ways in which the highly structured nature of the measurements and risk assessment are conducted within checks and limited time available to providers to complete these can ultimately impede meaningful discussion and exploration of attendees’ priorities and personal circumstances. 81,162 Similarly, limited availability of lifestyle services in some localities and difficulties in accessing services that will fit into individual attendees’ lives mean that these options are unrealistic or very limited for many. There is an ethical component to the effects of these limitations – attendees faced with results that indicate that their risk of CVD is elevated may be left without support to help them to attempt or sustain lifestyle changes, leaving them with limited options (e.g. inaction, medication and/or attempting to make changes alone). This ethical dilemma and the potential harms for attendees are absent from the literature that we have reviewed and are an area that would benefit from future exploration and research (see Chapter 5). If local implementation of the NHSHC cannot accommodate and respond to the constraints and priorities of individual attendees, its potential role in prompting and supporting behaviour change is weakened.
Covid-19 and the NHSHC
Our survey gathered data from 74 LAs on their local responses to the Covid-19 pandemic in relation to NHSHC programme delivery. Findings suggest that the pandemic has prompted further changes in programme delivery, perhaps leading to even greater variation across the country. Our results suggest that commissioners may be placing a greater emphasis on prioritising candidates amongst those eligible, following the pandemic (i.e. targeting potentially higher-risk groups and individuals). Many commissioners have commissioned or are considering different delivery models, particularly to shift the focus from currently overburdened general-practice settings. These changes could result in wider uptake of community-based or outreach delivery models, using a range of settings and a range of provider organisations and staff. Within this there is some novelty, for instance, in using paramedics to deliver the NHSHC, or in delivering the NHSHC within a flu or Covid-19 vaccination clinic. The changes might also see increased use of remote methods of delivery, with some LAs already using or actively considering a digital self-directed completion, or the use of phone or video consultations for a part of the check. This is one area of innovation where several survey respondents told us they were waiting for evidence-based guidance and direction.
In addition to prompting some innovation in NHSHCs delivery, the effects of the Covid-19 pandemic and the associated pause in delivery of checks have the potential to exacerbate existing contexts, and to create new contexts that put pressure on the delivery of checks. In particular, calls for a ‘catch up’ following the pause and concerns about delayed or missed diagnoses may result in a shift in emphasis towards the programme’s case-finding function. 187 In addition, the spiralling workload crisis in primary care and significant competing priorities for general practice (not least in relation to the continuing Covid-19 vaccination programme) may increase disengagement amongst general-practice-based providers of the check. At the time of writing this report, NHSE&I had issued new guidance to divert resources to ‘increase capacity’ to deliver Covid-19 vaccinations and boosters,188 which is likely to result in reduced or paused delivery of NHSHCs in settings involved in delivering the vaccination programme.
LA commissioners may need to respond to these ongoing problems by considering whether alternative delivery models based elsewhere could help to ensure continued delivery of NHSHCs, and potentially free general practices from one burden too many.
Comparison with existing literature
Most previous research on the NHSHC undertaken using survey methods has focused on providers, especially general-practice staff and managers,63,115,128,143,189,190 or on actual or potential NHSHC attendees. 79,113,114,191,192 One previous study included a survey of eight LAs. 92 A systematic review (based on a PHE-commissioned rapid review project) collating studies on the views of commissioners, managers and healthcare professionals identified only two existing studies including the perspectives of commissioners: one qualitative interview study, and one including commissioner interviews as part of a wider mixed methods evaluation. 136 More recently, an NIHR-funded study to develop a cost-effectiveness modelling tool for local commissioners involved a survey of the 16 ‘best-performing’ LAs, that is, those that achieved the highest rates of uptake in the 2013–2017 delivery cycle. 144 Our survey therefore extends the current survey literature, capturing detailed delivery information and the views of LA commissioners in relation to the programme.
Our survey of LAs complements and extends previous survey work undertaken by PHE. 15,16 Collectively, these surveys have all highlighted the considerable variation in delivery practice across England. With regard to whom the NHSHC is delivered by, the PHE surveys have asked which provider organisations deliver the NHSHC. However, they have never asked which health professionals are commissioned to conduct the check. Our review highlights the importance of the discretion and capacity of the delivering professional, and their relationship with the attendee, for influencing the attendee’s experience and subsequent action following a check. However, there is limited knowledge, even amongst some commissioners, about who, exactly, is delivering the checks.
Our survey is the first to create a typology of delivery models. The previous PHE surveys found that the majority of LAs commission general practice to deliver the NHSHC. Our survey also found that general practice remains by far the most typical setting of the NHSHC, both before and after the Covid-19 pause, with almost a third of responding LAs providing NHSHCs only in this setting. Looking across the PHE surveys and our data, the use of community outreach in NHSHC delivery reduced from 2014 to 2020, but may be seeing a subsequent increase again following the Covid-19 pause. Unfortunately, there are currently no data that would enable a comparison of different delivery models and programme outcomes, such as reach (particularly in relation to potentially higher-risk groups), referrals to support or subsequent changes in behaviours and/or risk scores.
Whilst PHE’s 2014 survey found that ‘lifestyle interventions’ were provided in (and usually commissioned by) most LAs, these data were not collected in their 2020 survey. Our survey therefore was an important first attempt to systematically collect data focused on services and referrals for attendees post-assessment, and to find out whether data related to this part of the programme are routinely collected by commissioners. It revealed the complexity and fragmented nature of this follow-on support, with multiple services being provided by different providers in different areas. Whilst this might help to ensure a range of different services to suit a range of different people, it is also likely to be difficult for the providers of the NHSHC programme to navigate. Unfortunately, commissioners are not generally in a position to assess the use being made of support services, since only a minority of respondents told us they routinely requested data on whether referrals were taken up, or indeed what the outcomes are of any subsequent support offered.
Our review is the first realist review to focus on the NHSHC programme, but the programme has been the subject of several previous evidence syntheses (see Appendix 1 for details of review projects that we identified at the outset of this project). Previous reviews have focused on a wide range of areas and steps in the NHSHC programme pathway and have identified significant variation in delivery models. 8,193 Our review is the first to focus solely on what happens after the measurements and risk assessments are complete, although four existing reviews have synthesised evidence that relates to this step and the findings correspond well with those of our review. The evidence included in two PHE-commissioned rapid reviews is discussed in more detail in Chapter 1. Briefly, these reviews include evidence of geographical variation in referral to ‘lifestyle services’ and capture some data relating to healthcare professionals’ doubts about the NHSHC’s long-term effectiveness and training needs. These reviews also identified broad themes describing NHSHC attendee experience, including attendees’ perspectives on the quality of the information provided during checks, perceptions of ‘genetic determinism’ (fatalism) and the important ‘environmental’, ‘resource’ and ‘cost and time’ factors that constrain individual attendees’ ability to respond to advice and offers of referral.
In addition to these, Shaw et al.’s 2016 international review of qualitative evidence focused on patient experience of CVD and diabetes prevention programmes and mapped this evidence using the Theoretical Domains Framework (TDF). 194 As in our project, the authors found evidence relating to attendees’ perception of the purpose of such programmes, their attitudes and understanding of their own ability to make lifestyle changes, the resources and infrastructure that existed to support programmes. Atkins et al.’s 2020 review coded evidence relating to the behaviours of commissioners, providers and attendees using the capability-opportunity-motivation-behaviour and TDF models. 60 Reflecting our own review, most included studies related to the behaviour of NHSHC attendees (called patients in this review). This review identified evidence relating to several behaviours that are relevant to our project’s focus. In particular, their findings relating to providers’ knowledge, skills and attitudes towards the delivery of advice or behavioural interventions, providers’ belief in those interventions, the resources available to deliver checks, the need to take account of attendees’ wider ‘social context’ in the delivery of advice and the availability of funded services that can accept referrals from the programme all echo aspects of our findings. Our review complements and extends the work undertaken in these reviews, by developing causal explanations for the variation in how NHSHCs are delivered, and how attendees experience the programme. The broad inclusion criteria in our review have allowed us to include much more data related to commissioners and providers, and to relate this directly to data focused on attendees. This has helped us to demonstrate how commissioner and provider discretion can affect attendees’ experience of the NHSHC, as well as how variation in delivery can influence how attendees respond to what they are offered during their check.
During this project, PHE were commissioned by the DHSC to undertake their own review of the NHSHC programme. This review was published by OHID in December 2021,26 accompanied by a summary of the evidence and analyses that were used to inform the recommendations made in the report. 41 Several aspects of the evidence gathered here echo our own findings, including the evidence presented on follow-up (section 2.7 of the main report) which highlights the crucial influence that providers have over attendees in relation to supporting behaviour change, the ‘structural factors’ that can impede the delivery of advice and onward referrals, and the potential need for ongoing follow-up. The evidence annex also includes the observation that data recording and collection during checks may be incomplete and presents new data in relation to what NHSHC attendees are offered during their check (termed ‘Outputs’ in the review report annex). These data indicate that the type of intervention offered to attendees (which could be advice, referral, prescriptions or further tests) varies according to age, ethnicity and deprivation. Although this is presented positively in the report, as evidence that providers are tailoring offers to meet differing needs, there is no evidence that this apparent tailoring is appropriate or beneficial for attendees. Our own findings demonstrate clearly that what providers offer attendees during checks is subject to a wide range of influences and it is unclear from the data if these patterns reflect the needs of attendees’, or even represent the outcomes of rational decision-making processes for providers. More research is needed to build on our review findings and develop a better understanding of how providers’ make decisions in relation to what to offer NHSHC attendees (see Chapter 5).
The OHID review presents three goals for a ‘transformed’ NHSHC programme, as follows:26
-
engage people in maintaining good health and preventing non-communicable disease by empowering and supporting them to understand their risks and to take early, sustained action to reduce those risks
-
reduce the health inequality that results largely from different levels of major non-communicable diseases and their underlying risk factors
-
act as a gateway to the wider wellness ecosystem by integrating the service with other non-communicable disease prevention programmes and by promoting joint-working and cost-sharing.
These goals appear to put the programme’s focus on supporting behaviour change and the development and maintenance of ‘healthy lifestyles’ front and centre, and we have reflected this emphasis in how we have framed our own recommendations below. We also note that the third goal for the NHSHC to become a ‘gateway’ programme through which attendees could access other services is echoed in our own recommendations and was well-supported by our professional and PPI stakeholder groups. However, we note that the findings of both our survey and our review raise a note of caution for the second goal, to reduce health inequalities. Our project has demonstrated the extent of local variation in commissioning and delivery of the NHSHC, especially in those aspects of the check that might most directly support the reduction of CVD risks. Our review shows that the causes of this variation are multifaceted, and achieving this aim will require solutions that address the complexity that affects delivery at this step of the NHSHC pathway.
The OHID review was also accompanied by an annex describing the governance arrangements for their project, including the role of its steering group and expert panel. 195 A letter from the panel chair raises important questions about the programme’s effectiveness and implementation, and notes the limitations of what can be achieved by the NHSHC alone. The panel have made a strong recommendation for a ‘thorough evaluation’ of the programme, ‘to assess the effectiveness of the end to end pathway (from identification through to outcomes (or good proxies thereof))’. Our own findings have provided a starting point and highlighted the need for more thorough examination of what happens at one particular step of the pathway – what happens after the measurements and risk assessments are complete – and would support the case for such an evaluation, to include a focus on this under-researched step (see Chapter 5 for more detail).
Recommendations for policy and practice
Based on our survey and review findings, we have drawn out the implications for the NHSHC programme, with the overall aim of increasing the focus on, and improving delivery of, what happens after the measurements and risk assessments are completed. Our recommendations below sought to respond to a series of questions that were raised by our survey and review findings:
-
What is the NHSHC for?
-
Do people think the NHSHC ‘works’?
-
Is there a mismatch between NHSHC priorities and those of attendees?
-
Is the NHSHC adequately resourced?
-
What other services does the NHSHC depend on?
-
Can the NHSHC take attendees’ real lives into account?
Our recommendations suggest potential changes in programme design, guidance, and commissioning and delivery on the ground, hence are differentially aimed at NHSHC policy-makers (in OHID), LA commissioners and NHSHC providers. These were developed in consultation with our stakeholder groups, composed of members of the public eligible to receive NHSHCs and a range of professionals involved in NHSHC policy, commissioning and delivery (see Chapter 2, Stakeholder groups). The recommendations are derived from four important implications that arise from our findings. These are the need for: clarifying the purpose of the NHSHC, working to create ‘buy in’ and engagement with the programme, focusing NHSHCs on attendee needs, and improving the links between the NHSHC and other parts of the system.
OHID have also made recommendations for the programme: (1) build sustained engagement; (2) launch a digital service; (3) start younger; (4) improve participation; (5) address more conditions; and (6) create a learning system. Within these headline recommendations, there are many specific recommendations that echo our own; wherever this is the case, we have highlighted this.
Our nine recommendations for policy and practice, the major implications from our findings and the evidence on which they were based are set out in Table 24.
| What we recommend (intended target audience in brackets) | Why we recommend it (implications and evidence) | Related recommendations from OHID review | |
|---|---|---|---|
| Guidance and documentation | R1 (OHID) Review national guidance, documentation and engagement materials (for commissioners, providers and attendees):
|
Clarify the purpose of the NHSHC Different interpretations of the primary purpose of the NHSHC drive variation in commissioning and delivery of the programme, and subsequently in how attendees understand and experience their check. There is a need for greater clarity to reduce unintended variation in what |
Recommendation 1: Build sustained engagement. This recommendation aims to ensure there is a ‘clear focus on promoting lasting health and wellbeing’ in NHSHCs. |
| R2 (LAs) Review local guidance, documentation and engagement materials (for providers and attendees, as above). | attendees are offered during and after their check. | ||
| Funding | R3 (OHID) Assess programme funding in relation to delivery of the programme’s aims:
|
Work to create ‘buy in’ to NHSHCs Commissioners, providers and attendees have varying levels of engagement with the programme. Scepticism about NHSHCs, limited resources and competing priorities for providers can undermine the quality of delivery. Focus NHSHCs on attendee needs NHSHC attendees are diverse and arrive at their check with different levels of knowledge, priorities for their health and constraints within their own lives. NHSHCs that can deliver more personalised advice and/or offers of referrals to appropriate services may be more successful at engaging them. It is unclear if current funding arrangements for the programme are always sufficient to ensure delivery of this part of the check. |
No specific recommendations are made in relation to funding for the programme or supporting services, although the OHID review notes that recommendations could be implemented within five years ‘subject to investment’. Recommendations that relate to extending the programme’s scope and coverage of younger people, as well as a recommendation for ICS and health and care partnerships to ensure ‘sufficient provision’ of NHS and LA interventions for attendees post-check, carry obvious funding implications. |
R4 (LAs) Assess the impact of, and consider changes to local funding models to support delivery of the programme’s aims:
|
|||
| Data and monitoring | R5 (OHID/ LAs) Review national and local data monitoring (and evaluation work) in relation to the programme’s intended purpose(s):
|
Clarify the purpose of the NHSHC The current emphasis in national (and often local) data collection is on invitation, uptake and coverage, encouraging a high-volume, case-finding model of delivery. Focus NHSHCs on attendee needs; Improve links between the NHSHC and other services Currently, data collection in relation to the advice and/or referrals that attendees are offered (and take up) post check is inconsistent, so it is not possible to assess whether attendees are offered appropriate, personalised support. |
No specific recommendations are made in relation to data and monitoring for the NHSHC that relate to our own, although the potential for a digital solution to provide NHSHCs to simultaneously capture and enable sharing and reporting of data is noted. Our recommendation would be for such data to include a focus on the delivery and uptake of advice and referrals. |
| Provider training and skills | R6 (OHID/ LAs/ Providers) Consider whether existing training provision and provider skills support the delivery of the programme’s aims:
|
Focus NHSHCs on attendee needs Checks that can deliver more personalised advice and offers of appropriate referrals may be more successful in engaging attendees. There is a need to review exactly who delivers the check and ensure they have received adequate training to either deliver personalised support themselves or signpost/refer attendees on. |
Recommendation 1: Build sustained engagement. This recommendation includes specific recommendations to develop a national training offer that emphasises long-term behaviour change, and for LAs to ensure that contracts require staff to undertake training that includes behaviour change techniques. |
| Buy in and engagement | R7 (OHID) Continue to produce/commission and publicise evidence for NHSHC effectiveness and evidence that demonstrates how positive outcomes for attendees can be achieved:
|
Work to create ‘buy in’ to NHSHCs Commissioners, providers and attendees have varying levels of engagement with the programme. Some scepticism about NHSHCs is related to the limitations of the existing evidence base supporting the programme. |
Recommendation 6: Create a learning system. This recommendation for a ‘rigorous, ongoing independent scientific evaluation’ of the NHSHC is welcome and we note that our own recommendations could be taken into account in the development of evaluation projects. |
| Referrals and follow up | R8 (OHID) Review the extent to which the NHSHC is a ‘one off’ encounter with a provider and the potential for a check to be the beginning of a longer-term engagement:
|
Focus NHSHCs on attendee needs Personalised support for some attendees is likely to require ongoing follow-up, multiple opportunities to engage with advice or referrals and support and feedback on progress. Improve links between the NHSHC and other services The success of the NHSHC programme and its ability to help attendees to reduce their CVD risks rests on what happens after the measurements and risk assessment are complete. Links between the NHSHC and primary care and other support services are essential, and NHSHC providers must be able to navigate and use these to their full potential. |
Recommendation 1: Build sustained engagement includes a recommendation for ICS and health and care partnerships to ‘ensure there is sufficient provision’ of services for NHSHC attendees to access post-check. We endorse this recommendation but would extend it as work should also focus on ensuring that referral criteria and pathways are known and clear to NHSHC providers and attendees, such that services can be accessed easily. |
R9 (LAs/ Providers) Review the extent to which local provision of the NHSHC can support longer-term engagement with the programme’s aims for attendees:
|
We note that while some recommendations in the OHID review fall outside the scope of our own work, our findings raise concerns about the implementation of others. In particular, two of the recommendations – to ‘start younger’ and ‘address more conditions’ – propose to significantly expand the scope and coverage of the NHSHC. Our review findings relating to the experience of attendees suggest that the latter recommendation to make the NHSHC more ‘holistic’ by including other health concerns may be welcomed by some, but overall, our findings suggest that policy-makers should be cautious about any expansion of the programme. Assessment of the feasibility of these recommendations must take into account current conditions in the wider health system, including the limited capacity of primary care and community and public health services. Without appropriate follow-up services, these extensions of the programme risk leaving attendees with few or no options for ongoing support to help them to manage any risks or conditions identified. In the absence of additional investment, the availability of accessible follow-on services and of convincing evidence of clinical and cost-effectiveness, expansion could risk increasing provider scepticism and disengagement from the programme. There is also a risk that expanding the programme’s scope and coverage could increase confusion about its purpose, and so drive increasing variation in commissioning and delivery.
The OHID review’s second recommendation to launch a digital offer for the NHSHC should take into account the findings of our review. In particular, any digital offer should not neglect the final steps in the NHSHC pathway and the need to ensure that attendees are offered personalised advice and referral as appropriate. There are risks inherent in any digital offer that some attendee groups could be excluded, but also a need to evaluate the effectiveness of digital versus face-to-face delivery of checks, to identify what works and for whom.
OHID’s fourth recommendation to ‘improve participation’ continues the existing emphasis on invitation and uptake, although we note that there is also a focus here on targeting those groups at highest risk of CVD. Nonetheless, policy-makers should be cognisant that measures that encourage high-volume delivery may inadvertently detract attention and focus away from more intensive delivery of personalised advice and support for behaviour change.
Chapter 5 Conclusions
Summary of key findings
This project set out to understand how the NHSHC programme works in different settings for different groups, in order to recommend improvements to maximise intended outcomes. Within this broad remit, we focused on the end of the NHSHC pathway: what happens after the measurements and risk assessment have been undertaken, especially in relation to the delivery of advice, onward signposting or referral and ongoing support for lifestyle and behaviour change?
Our survey of LAs has collected novel data describing local delivery models of both the NHSHC itself and the support services essential for enabling behaviour change. It has revealed significant variation areas across the country in how NHSHCs are provided and the extent to which relevant support services are available. In particular, it is clear that some areas offer greater accessibility of both the NHSHC and support services than others, regardless of public health budget, although this is not matched by greater uptake. Our survey has also gathered novel data detailing local responses to the Covid-19 pandemic, including innovations in NHSHC delivery that deserve further consideration, development and evaluation in their own right.
Our realist review of the literature has generated evidence-based theoretical causal explanations for this variation, building an understanding of when (in which contexts) and how (by which mechanisms) a range of outcomes occur. The outcomes of interest in this review are those that relate to the commissioning, delivery and response to NHSHCs, with a focus on what happens after the measurements and risk assessments have been completed. Our analysis suggests that the variation reported in the literature and by our survey respondents is the result of the exercise of discretion by commissioners and providers in the delivery of checks. Commissioners’ decisions in relation to local programme implementation, funding and monitoring, and providers’ decisions about how checks are delivered on the ground and their behaviour during those checks are influenced by multiple factors. These factors include their understanding of the purpose of the NHSHC and their engagement with the programme and its aims – but this understanding, and their actual behaviour in relation to delivery, is constrained by important practical factors.
Prevailing conditions, including existing funding envelopes, current funding and monitoring arrangements and workforce pressures for providers, tend to push commissioners and providers towards a delivery model that focuses on the ‘case-finding’ purpose of the NHSHC, to the detriment of work that could prompt or support behaviour change. However, in some local areas, commissioners and providers have been able to work against this tide and attempt to deliver NHSHCs that focus on its purpose as a means of supporting attendees to make changes to help reduce their CVD risk. Whether or not these efforts can be sustained in the aftermath of Covid-19 is uncertain at present, especially given ongoing and increasing workload pressures in primary care.
Recommendations for future research
In addition to the recommendations for policy and practice set out above (in Chapter 4) we make several specific recommendations for future research in relation to the NHSHC programme. We first make a general recommendation that more research efforts should be directed to consider the final steps in the NHSHC pathway (i.e. on what is delivered after the measurements and risk assessments are complete) and on the role and place of the NHSHC programme within the wider prevention and inequalities agenda. In addition, we support the call from the NHSHC Expert Panel for a thorough ‘end to end’ evaluation of the programme and would urge those undertaking such an evaluation to ensure detailed consideration of what is delivered and offered to attendees, and the links between the NHSHC, primary care/general practice and national and local ‘lifestyle services’.
Other more specific recommendations for future research that have arisen from this project are as follows:
-
Our survey findings could be complemented and extended by:
-
Survey and qualitative research with NHSHC providers and attendees about the delivery and experience of the NHSHC, with a focus on the final steps in the pathway and delivery of advice and offers of referral and/or prescriptions, including work to explore the routes between the NHSHC and support services;
-
Work to build on the typology of NHSHC delivery models that we have developed in this review, for example, to consider whether this typology could be refined with additional data, to map all English LAs against these categories and to compare outcomes across these different delivery models;
-
Additional research (via survey, freedom of information request or document analysis using information from LA and provider websites) to address the gaps in our survey response and build a more complete picture of delivery across all areas in England;
-
Follow-up surveys to assess delivery, timed to capture the results of commissioning decisions made post-Covid, which may reflect the outcomes of innovations employed during the pandemic, pressures affecting general-practice providers and/or commissioners’ actions in relation to the recommendations made in the OHID review;
-
Additional research into innovations including digital delivery methods and new methods for prioritising NHSHC invitations (to assess their feasibility and acceptability to different groups, potential equality impacts and impact on NHSHC uptake and outcomes).
-
-
Our review findings raise a number of areas for further development and exploration:
-
Future research with a focus on the final steps in the NHSHC pathway should include a range of perspectives and use a variety of methods to help to improve our understanding of the delivery of offers of advice and referrals.
-
Qualitative research with providers could provide further insight into their decisions about which interventions are offered to which NHSHC attendees.
-
Qualitative research with providers and attendees should use an ethical framework to consider problems posed where NHSHCs are delivered but options for attendees post-check are limited (e.g. because access to local lifestyle services is limited).
-
Quantitative and qualitative research is needed to address the relative scarcity of data that could be used to assess equality and diversity in relation to what is offered to attendees during and after their check. OHID have published evidence indicating that offers of prescription and referral vary by age and ethnicity. Additional work to collect and analyse data on these activities and variables is needed to assess potential disparities in delivery; new qualitative work could compare the experience of different groups of attendees, or provider attitudes and approach to different groups.
-
Anecdotal data suggest that some NHSHC attendees make and maintain significant lifestyle changes. In-depth qualitative work with NHSHC attendees could help to identify important contexts that may help to explain why a small number of people are motivated to do this and the role of the NHSHC itself.
-
-
Survey and/or qualitative research to address the relative scarcity of literature focused on LA commissioners and public health teams in relation to the NHSHC. Such research should focus on answering questions related to the important contexts identified in our review: what informs commissioner understanding and engagement with the NHSHC programme? How do they respond to the local practical constraints they face and make decisions about local delivery models? How do LA-provider relationships vary across England, and what informs these? Our professional stakeholder group informed us that LA ‘ethos’ and political stances may play an important role and could be explored.
-
Survey and observational research to assess and model local capacity for NHSHC delivery, to help inform local decisions about delivery models and workforce planning (e.g. which and how many providers can be commissioned).
-
Strengths and limitations
Our project has a number of key strengths. The two components (survey and realist review) complement each other, providing both new primary data and new interpretations of existing secondary data relating to what happens at the end of the NHSHC pathway. Our project focus on what happens in NHSHCs after the measurements and risk assessments have been completed helps to address the relative lack of research on this particular aspect of NHSHC delivery.
The project as a whole was strengthened by close working with our PPI lead, Vivienne Hibberd, and our committed PPI and professional stakeholder groups. Both groups were diverse: our PPI contributors represented a range of ages, gender, ethnicities and local areas in England; our professional stakeholders comprised members from a variety of professional roles and representing different localities. Our stakeholders helped us to focus the project, provided detailed feedback on our emerging findings and helped to shape our interpretations of our data and the recommendations that we developed as a result. We are continuing to involve these groups in the development of additional outputs from this project, which we plan to produce to communicate our findings and recommendations to non-academic audiences, including policy-makers (OHID), LA commissioners and providers of NHSHCs. At the time of writing, our plans for these additional outputs centre on providing brief and accessible information about our main findings, and are likely to include briefing documents for these audiences, and a short video.
Our survey of LAs complements previous surveys undertaken by PHE, gathering new data relating to our project’s focus on what happens after the measurements and risk assessments are completed in an NHSHC. To our knowledge, it is the first survey of LAs to gather data on local availability of lifestyle support services, referral processes and routine monitoring of the programme, and it has allowed us to develop a novel typology of NHSHC delivery models. Our typology of LAs clearly demonstrates wide variation in delivery. In addition, our survey is the first attempt to systematically gather data in relation to LAs’ responses to Covid-19 in relation to the NHSHC programme. However, it was limited by the low response rate, covering just under half of all LAs in England. This is lower than previous surveys undertaken by PHE, but was anticipated in view of extensive work being undertaken by LAs during the ongoing pandemic. Given the large proportion of non-responding LAs, we considered it was not feasible to search their websites for additional data. Unfortunately therefore, our findings, the typology we have developed and the analysis of external factors associated with different delivery models inevitably fail to take account of any delivery models or approaches being used by non-responding LAs. We were unable to access data from the most recent PHE survey as planned, but the relevant findings were available for comparison, hence this did not detract from our analysis.
As noted above, the qualitative survey data and discussions with our stakeholders have made it clear that the picture of delivery generated by our survey data is a snapshot in time, and that delivery models are likely to undergo significant change.
Our realist review followed the RAMESES quality standards for realist synthesis. By adopting a realist approach to our analysis, we have been able to develop explanations for the causes of variation in commissioning, delivery and response to the NHSHC programme, and to draw on substantive theory (street-level bureaucracy) to help further elucidate our findings.
Our review drew on a diverse range of material and in particular on data extracted from a wide range of grey literature. Our approach allowed us to synthesise data from conference materials and local documentation and evaluation work (including some unpublished internal documents) with data extracted from published research studies and helped to enrich our findings with local contextual detail. We had hoped that more of the material shared by our survey respondents could have been included for this reason, but (as with the literature more widely) most of the material shared with us focused on the common issues of invitation, uptake and coverage of NHSHCs.
As with any review project, our findings were limited by the availability and quality of the available literature. We must acknowledge that the material identified for the review covers a wide date range and some older material describes NHSHCs delivery when the programme was commissioned by PCTs. This may limit its applicability to the present day, although we considered each piece of data on its own merits before inclusion in our analysis and aimed to select data that it was reasonable to consider still relevant in terms of identifying contexts that still apply, or mechanisms likely still to be in operation. Our stakeholder groups also helped us to ensure that our findings resonated with contemporary experience of commissioning, delivering or attending NHSHCs.
Our chosen project focus did limit the availability of material that could be included in the review and we note that some of our findings touch on areas that are well-researched in their own right, including shared decision-making about medication, risk communication and behaviour and lifestyle change. Deeper consideration of these aspects of the NHSHC was beyond the scope of this project, but we acknowledge that links to these wider literatures are important and could help to deepen understanding of some aspects of programme delivery and responses to it. The documents included in this review were diverse in type but also in rigour. The CMOCs developed in the course of the project vary in terms of the volume, type and robustness of the data that underpin them. We have provided a full transparent account of those data, so that the strength of each CMOC is made apparent to those reading this report, including those CMOCs that are underdeveloped and could benefit from additional data. Where relevant, we have identified particular areas where new research would be welcome and help to develop the evidence base further.
Acknowledgements
We would like to express our thanks for the help, feedback and advice provided by all of our wonderful stakeholders and PPI contributors. We would especially like to thank PHE and OHID for continuing to be engaged and involved throughout the project and for their help with: the recruitment of stakeholders; distribution and reminders for the survey and; for providing opportunities for dissemination of our findings and outputs.
Contributions of authors
Ms Claire Duddy (https://orcid.org/0000-0002-7083-6589) (Realist Reviewer) developed the research project and led the review work, devised, piloted and carried out the scoping and main literature searches for the review, screened the resulting references, carried out data coding, applied a realist logic of analysis to the data, developed and refined the CMOCs and final programme theory, presented emerging findings to the PPI and professional stakeholder groups, and drafted and revised the final report.
Dr Erica Gadsby (https://orcid.org/0000-0002-4151-5911) (Senior Research Fellow, Public Health) developed the research project and led the survey work, devised, piloted and administered the survey, analysed the survey data, carried out consistency checks on data coding for the review, contributed to the development and refinement of the CMOCs and final programme theory, and contributed to the final report.
Ms Vivienne Hibberd (https://orcid.org/0000-0001-6863-9562) (PPI lead) developed the research project, provided PPI input, facilitated PPI group meetings, contributed to the development and refinement of the CMOCs and final programme theory and contributed to our final report.
Professor Janet Krska (https://orcid.org/0000-0002-4148-5652) (Professor of Clinical and Professional Pharmacy) conceived and developed the research project, analysed the survey data, provided relevant methodological and content support and input, contributed to the development and refinement of the CMOCs and final programme theory, and contributed to the final report.
Associate Professor Geoff Wong (https://orcid.org/0000-0002-5384-4157) (Associate Professor of Primary Care) conceived and developed the research project, led and facilitated the professional stakeholder group meetings, carried out consistency checks on the screening and data coding for the review, provided relevant methodological and content support and input, contributed to the development and refinement of the CMOCs and final programme theory, and contributed to the final report.
Publications
Duddy C, Wong G, Gadsby EW, et al. NHS Health Check programme: a protocol for a realist review. BMJ Open 2021;11:e048937. doi: 10.1136/bmjopen-2021-048937
Gadsby EW, Krska J, Duddy C et al. The NHS Health Check programme: a survey of programme delivery in England before and after the Covid-19 pandemic response [version 1; peer review: awaiting peer review]. NIHR Open Res 2023;3:32. https://doi.org/10.3310/nihropenres.13436.1
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised survey data may be granted following review. The full set of extracted data used to inform our realist review is available on request.
Ethics statement
Ethics approval was granted by the University of Kent SRC Ethical Review Panel (for the Division of Law, Society and Social Justice) in February 2021 (SRCEA id 0367). NHS Research Ethics Committee approval was not required for this study. Individual participants were able to respond to the survey anonymously, only choosing to enter their name and email address if they wished to receive further information on the outputs of the research. Informed consent was given by participants based on the information we provided about the purpose of the survey, how the data were to be handled, our plans for analysing the data, and how their confidentiality would be ensured in the reporting of any data.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
Appendix 1 Documents informing initial programme theory
Existing studies using substantive theories to understand the NHSHC
| First author | Year | Study method(s) and aim(s) | Summary of findings | Application of theory | Area(s) of focus from IPT | |
|---|---|---|---|---|---|---|
|
Theoretical Domains Framework (TDF), Behaviour Change Wheel (BCW), COM-B
Integrated frameworks of theories of behaviour change organised into several ‘domains’ (TDF), related to interventions via the BCW based on the ‘COM-B’ system of behaviour (capability, opportunity, motivation) |
Atkins | 2020 | Systematic review; To apply behavioural science frameworks to identify behaviours and actors relevant to uptake, delivery and follow up of HCs. |
Thirty seven studies reported nine behaviours and influences for eight behaviours. Included physical opportunity for HCs (for both HCPs and patients); motivational (e.g. beliefs about consequences, social influences). | COM-B and TDF were used to code direct quotes from participants and primary study authors’ interpretations of barriers and facilitators in the included studies. | All steps in IPT |
| Alageel | 2020 | Framework analysis of interview data; To examine factors that may influence engagement and adherence to lifestyle change/medication amongst those assessed as ‘high risk’. |
Identified themes relating to meaning of ‘risk’, past experience with medication and lifestyle change attempts. Participants were positive about the HC and being motivated to try to change. Lifestyle services and social support were facilitators. | TDF and the ‘necessity concerns framework’ (see below) informed the interview schedule | Behaviour change post-HC Medication adherence post-HC |
|
| Alageel | 2018 | Thematic analysis of interview data; To identify barriers/facilitators of implementing multiple health behaviour change interventions for CVD risk reduction in primary care. |
Identified themes relating to HCP conceptualisation of health behaviour change, delivering multiple health behaviour change interventions and delivering HCs. | TDF informed the interview topic guide and data from the interviews was coded in relation to TDF. | Behaviour change post-HC (from perspective of HCPs). | |
| Shaw | 2016 | Systematic review; To examine patients’ preferences for prevention programmes for cardiovascular disease and diabetes. |
Identified themes relating to knowledge, beliefs, cues to action/inaction, social influences, role and identity, and context. | TDF structured the framework synthesis. | All steps in IPT (from perspective of patient). | |
| Trivedy | 2016 | Mixed methods evaluation; To describe the process and results of opportunistic health checks at cricket matches (‘Boundaries for Life’). |
Uptake was reported to be high (compared with HCs at other sporting venues) and positive feedback was received from participants. Participants especially cited convenience and the authors concluded that the intervention provides both capability and opportunity for uptake. | COM-B used to classify reasons for attendance and non-attendance. | Uptake/attendance. | |
| Burgess | 2015 | Framework analysis of interview data; To explore influences on people’s decisions to take up the offer of a HC. |
Identified themes relating to lack of awareness, beliefs about susceptibility to CVD, beliefs about civic responsibility, issues with access/appointments, beliefs about consequences of having a HC. | TDF informed the interview schedule and the analytic framework for analysis of data. | Uptake/attendance. | |
| Elwell | 2012 | Thematic analysis of focus group data; To examine patients’ and health professionals’ perspectives on lifestyle behaviour change and inform intervention development. |
Identified themes relating to lack of time/resources, starting interventions too late, personal circumstances, need for continuous effort. | As participants identified a wide range of influences on behaviour, the authors concluded an “integrative behaviour change model” like TDF should inform intervention development. | Behaviour change post-HC. | |
|
Normalization Process Theory
Conceptual framework for understanding implementation, embedding and integration of innovations; normalisation needs coherence, cognitive participation, collective action and reflexive monitoring |
Stone | 2020 | Thematic analysis of interview data; To examine the experience of staff delivering telephone outreach to improve equity of HC uptake in deprived and BAME communities. |
Identified themes relating to coherence (outreach workers more convinced about HCs than primary care staff, recruitment of workers with community knowledge/connections, provision of training, involvement of commissioners and outreach workers and primary care staff working together. | NPT used to analyse and understand interview data. | Uptake/attendance. |
| McNaughton | 2018 (2020, 2011) | Secondary analysis of interview data; To understand the factors that influence individuals’ engagement with the HC programme (2020, 2011 are related papers describing the methods employed). |
The wider social system was found to be ‘integral to engagement’ with the HC programme at all stages. | NPT informed interview schedules, was used to make sense of emerging themes and NPT constructs were considered in relation to the findings to make sense of these. | Uptake/attendance; Behaviour change post-HC. |
|
| McNaughton | 2015 | Thematic analysis of interview data; To understand factors that influenced adherence to medication and advice in ‘high risk’ patients. |
Advice and discussion offered, and subsequent initiation of, and adherence to medication and lifestyle changes highly variable. The HC is the start of a process of adaptation and may require personalised/tailored ongoing support. | NPT informed interview schedules (but was not used to frame the results in this publication). | Behaviour change post-HC Medication adherence post-HC |
|
|
Andersen’s Behavioural Model of Health Service Use
Identifies three explanatory domains: predisposing characteristics (demographics, social structure, health beliefs), enabling resources (personal/family, community relations) and need (perceived). |
Wilson | 2019 | Cross sectional study assessing HC attendance at age 68; To assess associations between factors associated with health care utilisation and HC attendance in later life. |
Factors found to be associated with attendance included not smoking, worse health in adulthood. Some factors differed between men and women. Health-related factors were more important than socio-economic factors. | Andersen’s model was used to identify predisposing, enabling and need factors to include in the analysis. | Uptake/attendance |
| Mason | 2018 | Regression analysis using national HCs data and LA annual expenditure returns; To evaluate the effects of LA expenditure on programme invitation, coverage and uptake rates. |
Higher per capita spend was associated with increases in invitation rate and coverage rate but did not affect uptake. | Andersen’s model was used to categorise the control variables used in the regression analysis (identified via literature review). | Uptake/attendance | |
|
Necessity-Concerns Framework
Developed to understand medication adherence whereby perceptions of the necessity of medication are balanced with concerns about medication |
Alageel | 2020 | As above | As above | As above | Behaviour change post-HC Medication adherence post-HC |
|
Protection Motivation Theory
The intention to undertake health-protective behaviour is understood as resulting from assessment of threat (e.g. risk of CVD) and coping (e.g. consequences of behaviour change). Responses to threat can be adaptive or maladaptive. |
Gidlow | 2019 | Protocol: qualitative analysis of 240 video recorded health checks plus interviews; quantitative process evaluation to compare HC content with outcomes; 10 in-depth case studies; To explore practitioner and patient CVD risk perceptions when using QRISK2/JBS3 tools, associated advice/treatment and patients’ responses. |
N/a, protocol paper | PMT will be used as the coding framework for qualitative data. | Delivery of HC; Behaviour change post-HC |
| Sallis | 2019 | Randomised controlled trial (three arms); To assess whether ‘behaviourally informed’ invitation letters containing ‘sunk costs’ or ‘counterargument’ messages improve uptake of HCs. |
Intervention letters increased uptake versus the national template letter (control). | PMT informed intervention design: the authors hypothesised that the letters’ effects were the result of increased perceptions of ‘threat’ and response efficacy via ‘counterarguments’. The ‘sunk costs’ letter was hypothesised to work via the ‘sunk costs fallacy’. |
Uptake/attendance | |
| Usher-Smith | 2017 | Secondary analysis of trial data: thematic analysis of interview data and quantitative usage data; To explore individual-level factors associated with usage of a web-based lifestyle intervention. |
Low engagement found to be associated with having a negative emotional reaction to receiving risk score, perception that the intervention did not provide new lifestyle information and being less likely to have reported feeling obliged to complete the intervention as part of the study. Also maybe with negative past experience of attempted behaviour change (but not stat sig). | PMT used to frame and understand results. | Behaviour change post-HC | |
|
‘Candidacy’
Theoretical construct describing how individuals’ perceive their ‘candidacy’ for certain health conditions/access to health services, and this is influenced by social circumstances, cultural norms and previous interactions with health systems. |
Ellis | 2015 | Thematic analysis of interviews; To explore how HC non-attenders perceive the programme, identify reasons for non-attendance and inform strategies to improve uptake. |
Identified themes relating to the positive perception of the HC concept, perceived lack of personal relevance, ineffective invitation method and appointment inconvenience. | Concept of candidacy used to summarise and explain main findings. | Uptake/attendance |
NHSHC programme documentation

Major National Health Service Health Check (NHSHC) programme documents were identified via browsing and searching current and archived versions of United Kingdom (UK) government and NHS websites. Major programme milestones and publications are outlined on the timeline below.
Existing reviews focused on the NHSHC
We identified existing reviews and evidence syntheses relating to the NHSHC by consulting PHE’s regularly updated bibliographies, available on the NHSHC website (https://www.healthcheck.nhs.uk/commissioners-and-providers/evidence/literature-review/). We identified 10 published reviews; 4 of these present findings from the PHE-commissioned rapid review by Usher-Smith et al. (2017).
| Review | Summary of review aim(s) | Included study designs | Setting(s) | Approach to synthesis | No. included studies | Main finding(s) | Areas of focus from IPT |
|---|---|---|---|---|---|---|---|
| Cooper 2014 | Identify from existing reviews the key factors that influence uptake of health screening; to review the international evidence to assess factors that influence uptake of HCs and increase/inhibit uptake. | No restrictions listed; Quantitative study designs/findings included (Authors recommend qualitative research is needed). | Primary care, community, occupational No geographical limits but focus on transferability to England and NHS (all included studies are from England). |
Rapid review; narrative synthesis | 7 papers reporting 5 studies | Limited evidence of demographic/health factors associated with HC uptake. Older age, higher risk, non-smokers and females seem to be key predictors. Ethnic minority uptake seems better where there is “sufficient GPs of ethnic concordance”. Smaller GP practices seem better at attracting uptake. |
Uptake (socioeconomic and demographic differences; who offers the check and where?) Describes patterns but no causal explanations (how, why, for whom, in what circumstances…). |
| Shaw 2016 | To review patients’ experiences of prevention programmes for CVD and diabetes. | Qualitative studies | Primary care or community No geographical limits |
Framework and thematic synthesis using TDF domains to organise findings; conceptual model summarising findings | 14 | Conceptual model illustrates ‘complex interactions’, including: Social influences feeding into knowledge/beliefs about for example, health and citizenship, autonomy Context incl conceptualising HCPs as educators; community contexts altering HCP roles and facilitating access “the evidence suggests that the significance of each factor is not fixed and that different combinations … will play out differently on different occasions”. |
Covers the whole IPT, from invitation and uptake to behaviour change. Focus on patient experience and perceptions at each stage. Recommendations therefore focus on how to address patients’ knowledge, beliefs, social influences (with careful framing that emphasises increasing uptake/compliance). |
| Mills 2017 | To synthesise data concerning the views of commissioners, managers and HCPs towards the NHSHC (including challenges of implementation) NB the findings of this review are also included in Usher-Smith et al. (2017a). |
Quantitative surveys and qualitative studies. | NHSHC delivery settings. | Descriptive synthesis of quantitative data Thematic synthesis of qualitative data |
15 | Evidence that these groups could see the benefit of the HC, but the largest survey of GPs found only half viewed HC as important and beneficial. Range of reviews in qualitative studies; pharmacists are notably all positive, citing professional/business opportunities. |
Covers the whole IPT to some extent, but focus is on overall perception of programme, especially benefits to patients, and implementation with a focus on delivery of the assessment and advice. |
| Usher-Smith 2017a | To provide a rapid synthesis of the published research evidence on NHSHCs, addressing six questions: Who is and who is not having a HC? What are the factors that increase take-up? Why do people not take up the offer of a HC? How is primary care managing people identified as being at risk of CVD or with abnormal risk factor results? What is the effect of the HC on disease detection, changing behaviours, referrals to local risk management services, reductions in individual risk factor prevalence, reducing CVD risk and on statin and antihypertensive prescribing? |
Qualitative and quantitative studies. | NHSHC delivery settings. | Rapid; Descriptive synthesis of quantitative results; Thematic synthesis of qualitative data. |
68 | Substantial variation in HC coverage across regions/settings, but consistently higher in older people/Females/More deprived. Lack of national studies Uptake may be improved by changes to invitation methods/text messages Range of reasons people do not take up HC, incl lack of awareness, competing priorities, misunderstanding purpose, aversion to preventive medicine, difficulty getting appt, concerns about privacy (in pharmacy). Wide variation in process/delivery/content. Common challenges are workloads, IT, funding, training. HCs associated w/small increases in disease detection and 3–4% increase in prescription of statins; lack of data on behaviour change or referral to lifestyle services. |
Review covers the whole IPT to some extent but speaks mainly to first steps (invitation, uptake) and delivery (content, process). This review identifies a lack of data relating to post-HC steps including referrals and behaviour change. |
| Usher-Smith 2017b | To review the experiences of patients attending HCs in England NB the findings of this review are also included in Usher-Smith et al. 2017a |
Qualitative and quantitative studies. | NHSHC delivery settings. | Thematic synthesis of qualitative data; Descriptive synthesis of quantitative data. |
20 | Patient satisfaction surveys consistently show high levels of satisfaction. Interview data shows some patients left with unmet expectations, confusion about purpose of HC, confusion about CVD risk scores. Lifestyle advice was regarded as too simple/not personalised. However interview data also indicated many felt the HC was a ‘wake up call’. |
Focus on the delivery (assessment and advice) elements of the IPT (who, how and where; accessibility and acceptability). |
| de Waard 2018 | To identify characteristics, barriers and facilitators to participation in HCs for cardiometabolic diseases in primary care. | Qualitative and quantitative studies. | Primary care settings No geographical limits. |
Narrative synthesis organised around 4 themes (personal characteristics, attitude towards outcome/preventive care, practical issues, related to HCP). | 39 | Barriers: lower age, lower education, smoking and living alone (but results not consistent); also not wanting to know, worry about the outcome, feeling healthy and low perceived severity/susceptibility to disease. Facilitators: wanting to know/reassurance, feeling responsible for one’s health, concerns about health. Also important are invitation, sufficient information, requested time investment, ease of getting appt. |
Uptake (socioeconomic and demographic differences; who offers the check and where?) Describes patterns with some inconsistencies. No causal explanations (how, why, for whom, in what circumstances…). |
| Harte 2018 | To review why people do not attend NHSHCs NB the findings of this review are also included in Usher-Smith et al . 2017a |
Qualitative studies. | NHSHC delivery settings. | Thematic synthesis. | 9 | Review identifies three groups of non-attenders: those unaware of HC programme; aware of programme but do not appreciate preventive nature; those who recognise preventive nature of HC but actively choose not to engage bc they do not want to be ‘told off’ or refer not to know. Also evidence of practical barriers: time constraints, competing priorities, perceived/actual difficulties in making appts, concerns about privacy in pharmacy. |
Uptake (who offers the check and where; patient attitudes and preferences). Describes various explanations for lack of attendance at HCs. |
| Martin 2018 | To review quantitative evidence on coverage, uptake and impact of NHSHC
NB the findings of this review are also included in Usher-Smith et al . 2017a |
Quantitative | NHSHC delivery settings | Narrative synthesis | 26 | In the 5 year cycle 2013-2018 evidence suggests 45.6% of eligible adults have attended; % varies significantly by region (from 18.9% – >100%). Higher coverage (% of eligible population): older, family history of CHD, deprived areas, some ethnic groups. Uptake (% of invitees) also varies. 48.2% of those invited attend. Uptake also higher if older, female but results are lower for those living in most deprived areas. Impact studies w/comparator groups show attendance associated with small increase in disease detection, increased likelihood of statin and antihypertensive prescription, small decreases in modelled CVD risk. V few studies have reported impact on behaviours. |
Focus on coverage, invitation and uptake (socioeconomic and demographic differences), and on certain patient outcomes: disease detection, prescribing and health related behaviour. In the latter category, data is only available relating to smoking. |
| Atkins 2020 | To identify behaviours and actors relevant to uptake, delivery and follow up of NHSHCs and influences on these behaviours, and to signpost to example intervention content | Qualitative and quantitative studies; systematic reviews | NHSHC delivery settings | Framework and thematic analysis using COM-B and TDF domains to organise findings; classification of themes as barriers/facilitators | 37 | Identified 9 behaviours and barriers/facilitators for 8 of these: HCPs inviting – time consuming to identify eligible ptx; Patients attending – family history, desire for reassurance; need to see HC as relevant to them; HCPs delivering – perceived need for training and more time/space; some disagreement about benefits and behavioural vs pharmacological intervention; need to take account of ptx social context and appropriate message framing; lack of confidence in delivering behavioural support; HCPs referring – lack of availability of services; Patients attending referral – belief in importance; Patients changing behaviour – ‘wake up call’, but varied understanding of CVD risk, lack of awareness of behaviours that influence risk; influence of friends and family; HCP role; fatalistic beliefs; small incremental changes welcomed. Patients re-attending – intentions to re-attend; HCPs recording data – hindered if multiple invitation methods used; Managers/commissioners synthesising/disseminating data – no barriers/facilitators identified. |
Covers the whole IPT, from invitation and uptake to behaviour change. Focus on behaviour of relevant actors and specific barriers/facilitators at each step. Sequencing of steps is clear but the mechanisms underpinning these findings are not, nor are the contexts in which different behaviours are more or less likely to occur and affect outcomes. |
| Bunten 2020 | To highlight interventions and invitation methods that increase the uptake of NHSHCs, and to identify whether the effectiveness of these interact with broader patient and contextual factors. | Quantitative studies (RCT, observational cohort, cross-sectional). | NHSHC delivery settings. | Systematic review following PRISMA and CASP; narrative synthesis following ESRC. | 9 | Letters are most widely used invitation method but least effective versus telephone / opportunistic f2f invitation. Behavioural insights-inspired changes to letters improve attendance. One study found effectiveness of invitation method varied by patient ethnicity |
Uptake (socioeconomic and demographic differences; who offers the check and where?) Describes patterns with some inconsistencies. No causal explanations (how, why, for whom, in what circumstances…). |
| Dubois (Ongoing?) | Protocol To identify and compare local and regional studies that have undertaken an evaluation of the NHSHC programme in England. |
Qualitative and quantitative (but notes expecting to include cohort and cross-sectional case studies – evaluations). | NHSHC delivery settings. | Quantitative data to be ‘pooled’ and meta-analysis conducted ‘if relevant’ Qualitative data to be pooled via thematic analysis. |
- | - | Outcomes of interest include coverage, identifying new interventions, increased risk of CHD, new diagnoses. Whole IPT may be covered depending on availability of data in evaluations. |
Appendix 2 Search strategies
This appendix provides details of the search strategies employed to identify documents relevant to the realist review. As described in the methods section (see Chapter 2).
Searches to locate existing theories (Step 1)
We searched PubMed and Web of Science (Core Collection) using a combination of terms relating to HCs, and terms relating to theory, adopting a slightly modified version of Booth and Carroll’s (2015) ‘BeHEMoTh’ approach. As the HC programme is a specific health context (H) and we were interested in theorisation of all steps in the programme, no individual behaviours (Be) were specified.
PubMed (11 October 2020)
-
“Health Check” OR “Health Checks” (3847).
-
UK OR United Kingdom OR England OR Britain OR British (1790010).
-
model OR models OR modelling OR theor* OR concept* OR framework* (4625627).
-
1 AND 2 AND 3 (130 hits).
Web of science (SCI-EXPANDED, SSCI, AHCI, ESCI) (11 October 2020)
-
“Health Check” OR “Health Checks” (topic) (3474).
-
UK OR “United Kingdom” OR England OR Britain OR British (topic) (623802).
-
Model OR models OR modelling OR theor* OR concept* OR framework* (topic) (11284654).
-
1 AND 2 AND 3 (70 hits).
These searches identified 11 studies utilising 6 theoretical models or frameworks. An additional search for each of these named theories, plus terms relating to the NHSHC, was conducted in Google Scholar. In addition, we also searched Google Scholar for papers relating to the NHSHC that also cited the key citations related to each identified theory. These two steps were conducted in October 2020 and identified a further 8 (5 + 3) papers.
Searches for evidence on NHSHC (Step 2)
MEDLINE (via Ovid, 11 November 2020)
-
health check*.ti,ab,kw (6084);
-
(NHS or National Health Service or United Kingdom or UK or England or English).ti,ab,kw (370078);
-
exp England/ (107308);
-
2 or 3 (440075);
-
1 and 4 (468);
-
limit 5 to (english language and yr = “2008-Current”) (325).
Embase (via Ovid, 11 November 2020)
-
health check*.ti,ab,kw (8572);
-
(NHS or National Health Service or United Kingdom or UK or England or English).ti,ab,kw (487112);
-
England/ (24573);
-
2 or 3 (494513);
-
1 and 4 (521);
-
limit 5 to (english language and yr = “2008-Current”) (459).
CINAHL (via EbscoHost, 11 November 2020)
-
TX “health check* (2391);
-
TI (NHS OR “National Health Service” OR “United Kingdom” OR UK OR England OR English) OR AB (NHS OR “National Health Service” OR “United Kingdom” OR UK or England OR English) (178298);
-
MH “England” (62863);
-
S2 OR S3;
-
S1 AND S4;
-
Limiters: published date: 20080101–20201231; English language; Expanders: Apply equivalent subjects (378).
HMIC (via Ovid, 11 November 2020)
-
health check*.mp (598)
-
(NHS or National Health Service or United Kingdom or UK or England or English).mp (118285);
-
exp England/ (26501);
-
exp health authorities in England/ (6680);
-
or/2-4 (135421);
-
1 and 5 (321);
-
limit 6 to (English language and yr = “2008-Current”) (191).
Web of science (SCI-EXPANDED, SSCI; 11 November 2020)
-
TOPIC: (“health check*”) (5144);
-
TOPIC: (NHS OR “National Health Service” OR “United Kingdom” OR UK OR England OR English) (522053);
-
#1 AND #2 (358);
-
Refined by: PUBLICATION YEARS: (2020 OR 2012 OR 2019 OR 2011 OR 2018 OR 2010 OR 2017 OR 2009 OR 2016 OR 2008 OR 2015 OR 2014 OR 2013) AND LANGUAGES: (ENGLISH) (309).
Additional searches for theory
A short series of highly focused searches for documents describing street-level bureaucrats or street-level bureaucracy were run in Google Scholar in October and November 2021. The details of these searches and results screened (on screen) are provided below.
Google Scholar, 6 October 2021
-
(“street level bureaucracy” OR “street level bureaucrats”) AND (“public health”) (8,160);
-
(“street level bureaucracy” OR “street level bureaucrats”) AND (“primary care”) (2090);
-
(“street level bureaucracy” OR “street level bureaucrats”) AND (“general practice” OR “general practices”) (889);
-
(“street level bureaucracy” OR “street level bureaucrats”) AND (“local authority” OR “local authorities”) (6320).
Appendix 3 Coding frame
| Name | Description |
|---|---|
| Organisational factors | Mother node for child nodes relating to organisational or system features that may influence commissioning/implementation/delivery/outcomes of HCs |
| Availability of appropriate lifestyle services | Data relating to the availability (or otherwise) of lifestyle or other support services for onward referral for HCs participants who meet referral thresholds. Includes data where services are nominally available but inappropriate for needs, for example, only available in work hours, or unappealing to some groups. |
| Commissioner priorities | Data relating to commissioners' targets or priorities in relation to the HC programme or wider related goals (e.g. CVD prevention, health inequalities) that may influence commissioning decisions, and wider messages, initiatives and policies that may influence these priorities. |
| Data collection – monitoring | Data relating to providers or commissioners collection and use of data to monitor or evaluate HCs and post-HCs services. |
| Competing – complementary programmes | Describing other interventions, programmes or pathways (usually but not exclusively focused on CVD) that are available and exist in parallel and alongside the HC and may complement/compete with HCs. |
| Financial incentives | Data relating to remuneration arrangements that may incentivise different approaches to HCs delivery, for example, flat fee vs payment that incentivises activity, prescriptions, targeting, or anything else. Data relating to costs of delivery may also live here (none identified at time of node creation). |
| LA-provider relationships | Data describing relationships, communication and support and engagement between the LA commissioners and HC providers. |
| Provider organisation buy-in | Data relating to provider organisations (usually GP practices) ‘buy in' and engagement with the HCs programme (or otherwise). Closely related to Financial Incentives, and LA-provider relationships codes. A potential driver of variation. See also data under HCP engagement relating to individual provider attitudes and engagement. |
| Provider time and workload | Data relating to time and workload pressures that may constrain prioritisation and delivery of the HC, as well as post-HC follow up, ongoing support and so on. |
| Provider training and skills | Describing (variation in) training provided to or received by HC providers or their skill levels in relation to different apsects of HCs delivery. |
| Referral pathways, thresholds and follow up routes | Data relating to the patient pathway through the HC, especially to important decision points, including decisions to provide advice or refer onwards (and if so, to where). Closely related to (but not duplicating) data on referral outcomes. |
| Integration of services | Data relating to the integration of services that provide different aspects of the Health Checks pathway, especially integrated check and referral/lifestyle services. This code has been moved to become a child of Referral pathways/thresholds as data here may represent extreme cases of very short pathways/easy referrals. |
| Outcomes and patterns | Mother node for child notes relating to broad categories of observed outcomes post-HC. |
| Advice and brief interventions | Data relating to the provision of advice within the HC, including the delivery of ‘brief interventions’ that aim to provoke lifestyle/behaviour change. Closely related to codes on Communicating Risk, Reassurance, Difficult Conversations, and especially Personalised, Tailored Advice (and nested children). |
| Behaviour or lifestyle change | Data relating to actual or intended outcomes related to lifestyle or behaviour changes post-HC. |
| Clinical outcomes | Data relating to actual clinical or health related outcomes, for example, reductions in BMI, blood pressure, cholesterol levels; morbidity, mortality. |
| Disease detection or case finding | Outcomes related to the detection and diagnosis of disease or risk factors for disease, that is, where it’s reported that the HC led to X new diagnoses of Y or similar. |
| Prescribing drugs | Data relating to prescribing decisions post-HC (usually for statins and/or antihypertensives). |
| Declining drugs or non-adherence | Data related to HC attendees/patients who decline prescriptions (especially for statins) or reasons for declining, or data suggesting people may not adhere to medication. |
| Referral outcomes | Data relating to referrals to lifestyle services post-HC, including smoking cessation, weight management, healthy eating, physical activity and other services. |
| Uptake and adherence to lifestyle services | Specifically relating to uptake of, or attendance/adherence to lifestyle services where people have been referred post-HC. |
| Variation in delivery | Describes variation in delivery or implementation of the Health Check (O) |
| Social, behavioural, relational | Mother node for child nodes relating to social, behavioural or relational factors that affect HCs commissioning/implementation/delivery/outcomes (previously ‘Social and behavioural factors’). Nothing is coded here directly. |
| Communicating and understanding risk | Data relating to patients’ and providers’ understanding of CVD risk and risk management, and/or on communicating about these risks (some previously coded in ‘health attitudes and literacy’ and ‘difficult conversations’). |
| Fatalism and family history | Understandings of CVD risk that are coloured by a sense of fatalism (or disconfirming cases), especially related to family history of CVD. Closely related to Health Literacy child codes (this data previously coded as Health Attitudes and Literacy) |
| Reassurance | Data relating to HC attendees’ seeking reassurance or being reassured by the HC; the question of whether the perception of the HC as a ‘check' and for reassurance means it is not perceived as a vehicle for behaviour change. Close links with data in the “getting older” and “family history” codes, and ‘HC expectations’. |
| Continuity of care | Data relating to ongoing support and continuity of care and follow up post-HC, including data on attendee preferences for (usually relational) continuity and the actual delivery of such continuity. |
| Difficult conversations, sensitive subjects | Data relating to the difficulties of discussing behavioural and lifestyle change with HC attendees and how this might affect relationships. Previously included data re: CVD risk communication and giving advice, now in separate buckets. |
| HC expectations | Data relating to HC attendees understanding of the purpose of the HC and often their disappointment or unmet expectations in relation to the HC, e.g. related to it’s breadth of coverage, delivery methods, interactions or the advice received. A focus on ‘checking’ (an ‘MOT’) may have implications for behaviour change? See also ‘Reassurance’ (Previously: ‘Unmet expectations’). |
| HCP attitudes and engagement | Data relating to HC provider attitudes and engagement with the programme, including scepticism of its clinical and cost effectiveness. Formerly also coded data relating to practices/organisations now coded at Provider Organisation Buy In. |
| Health attitudes and literacy | Mother node for codes relating to various health attitudes that may affect uptake of the HC and subsequent behaviour change. Nothing is coded here. |
| Friends and family influences | Data relating to how individuals’ social networks can affect their health attitudes and behaviours, for example, by acting as a trigger to change or supporting ongoing change; and vice versa – data about how lifestyle changes may be shared more widely than the original HC attendee. |
| Getting older | Data relating to how getting older, or reaching particular age milestones, may be a trigger for worrying about health and (intentions about?) behaviour or lifestyle changes. May overlap with Fatalism code. |
| Good patients, citizens | Data relating to HC attendees’ desire to be ‘good’ patients or citizens, e.g. feeling social pressure to attend HCs. Focus is on uptake of the HC but does this translate forward into post-HC services/behaviour? If this is a powerful mechanism, could it be leveraged? |
| Health literacy | Data relating to HC attendees’ understanding of (especially CVD-related) health and healthy behaviours, including data on attendees’ beliefs about their own health, what constitutes a ‘healthy’ lifestyle and confusion over changing guidance (big overlaps with communicating and understanding risk). |
| Seeking help or preventive care, attitudes to | Data relating to eligible HC attendees’ attitudes re: accessing health care services, especially GP practices, and on attitudes towards ‘prevention’. Includes data on the extent to which attendees consider prevention to be within the GP’s remit, or what is a legitimate reason to use an appointment(s). |
| Worried well, low risk | Data relating to the ‘worried well’, suggesting or refuting the idea that HCs are used primarily by those who are already at low risk and/or motivated to sustain or improve their ‘healthy’ lifestyles. Much focuses more on uptake of the check – but may translate forward into post-HC steps? |
| Personalised, tailored advice and support | Data relating to the personalisation or tailoring of post-HC advice and/or support. Includes data relating to attendees’ preferences for personalisation as well as actual personalisation; data that describes the HC as more than a generic, ‘tick box’ exercise (or vice versa). Previously included data on shared decision making and especially on declining referrals/prescriptions, now coded in separate buckets. Close links with small changes/setting goals buckets. |
| Community-based, peer support | Data relating to the involvement of ‘peers’ in providing the HC or subsequent lifestyle support services, for example, via recruitment of people from local communities (or data relating to providers having features like this, e.g. Health Trainers, Lay Health Workers etc). |
| Competing priorities and comorbidities | Data relating to other life-related factors that may affect engagement with the HC and subsequent follow up for attendees (‘life getting in the way’). Includes data on comorbidities and busy lives, and also data describing patients' preferences for ‘bad’ lifestyles taking priority over ‘healthy’ behaviours. |
| Setting goals | Describing the use of a tactic of advising (from providers) or adopting (for attendees) setting goals in order to support or facilitate changes to lifestyle, or prioritising some changes over others as a way of making changes more likely/manageable and/or sustainable. Closely related to ‘Setting goals’. |
| Small changes, harm reduction | Describing the use of a tactic of advising (from providers) or adopting (for attendees) making small changes to lifestyle, or prioritising some changes over others as a way of making changes more likely/manageable and/or sustainable. Closely related to ‘Setting goals’. |
Glossary
- Context
- In realist research, the conditions or circumstances in which mechanisms that generate observed outcomes are ‘triggered’ or activated.
- Context-mechanism-outcome configuration
- A heuristic used to present a realist causal explanation for an outcome, presented as a relationship between some particular context(s) and mechanism(s).
- Demi-regularity
- A semi-predictable pattern of outcomes that occur in the same context(s).
- Mechanism
- In realist research, the underlying context-sensitive causal force that generates an outcome, often conceptualised as the response of an individual actor to important context(s).
- Programme theory
- A set of theoretical explanations about how a programme, intervention or process is understood to work. Realist programme theories explain the process by which outcomes of interest are thought to be generated, using causal explanations captured in the form of context-mechanism-outcome configurations.
- Substantive theory
- An established, formal theory drawn from any discipline that can be used to help understand the programme, intervention or process under examination.
List of abbreviations
- BMI
- body mass index
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMOC
- context-mechanism-outcome configuration (see glossary for a definition)
- CVD
- cardiovascular disease
- DHSC
- Department of Health and Social Care
- GP
- general practitioner
- HCA
- healthcare assistant
- HMIC
- Health Management Information Consortium
- IPT
- initial programme theory
- LA
- local authority
- NHS
- National Health Service
- NHSE
- NHS England
- NHSE&I
- NHS England and Improvement
- NHSHC
- NHS Health Check
- NICE
- National Institute for Health and Care Excellence
- OHID
- Office for Health Improvement and Disparities
- PCT
- Primary Care Trust
- PHE
- Public Health England
- PN
- practice nurse
- PPI
- patient and public involvement
- RAMESES
- Realist and Meta-narrative Evidence Synthesis: Evolving Standards
- RCT
- randomised controlled trial
- TDF
- Theoretical Domains Framework
