Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 16/116/03. The contractual start date was in September 2018. The draft manuscript began editorial review in June 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Walsh et al. This work was produced by Walsh et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Walsh et al.
Chapter 1 Introduction
Musculoskeletal disorders (MSKDs) are the leading cause of disability in the UK with over 20 million people reportedly living with a MSKD;1,2 they account for approximately 30% of primary care consultations, with many patients repeatedly consulting due to non-resolution of their problem. 3,4 Lower-back pain is the most burdensome of these conditions1 and is the leading cause of years lived with disability in the UK. 5 The annual economic impact of MSKD more generally is vast, accounting for 23.3 million lost workdays in 2021,5 costing NHS England almost £5 billion6 and approximately £8.6 billion in personal independence payments in England, Scotland and Wales. 7
The volume of people with MSKD contributes to the significant financial and service delivery burden faced in primary care;8 2021–22 figures show that general practitioners (GPs) and other primary care staff delivered more appointments than in any other year on record9 and, given MSKD prevalence, a significant proportion will be attributed to these conditions. This is compounded by GP recruitment and retention difficulties10 which are likely to increase. Figures suggest that 13% of GPs under the age of 50 years, and 60% of those aged over 50 years expect to leave their position within the next 5 years. 11 The impact this is likely to have on patient care is substantial, and will inevitably affect waiting times, safety and levels of satisfaction, which are already causing concerns. 12 Given the exponentially increasing demand, coupled with the difficulties associated with GP recruitment and retention,8,10–12 alternative models of care that are implementable with relative ease, timeliness and affordability are essential. The pressing need for appropriate management is recognised by many integrated care boards, with primary care workforce initiatives representing an area of priority,13 and the area has been highlighted by the Primary Care Workforce Commission as requiring further evaluation and understanding. 10
By definition, GPs have an extensive knowledge of the initial and continuing management of multiple conditions. However, evidence suggests there is considerable variability in GP treatment of MSKDs, with care being offered that is inconsistent with national guidelines and under-use of cost-effective strategies, such as exercise and self-management. 14 Furthermore, data suggest that many referrals to secondary care orthopaedic and scanning services may be inappropriate, resulting in increased waiting times and the potential for delay in cases that do necessitate urgent attention. 14,15 There is a growing belief that GPs may not be the most appropriate healthcare professionals to manage the MSKD population, given their limited specialist musculoskeletal training. 16–18 By contrast, there is evidence that physiotherapists who are expert in MSKDs are effective in making diagnoses and achieving successful clinical outcomes, demonstrate good levels of patient satisfaction and save money on unnecessary referrals. 17,19–21 However, given the complexity of patients who may present with MSKD alongside multimorbidities, it is as yet unclear whether non-physician-led assessment and examination may lead to suboptimal management.
An emerging model and workforce development is first-contact physiotherapy, a rapidly developing approach to managing MSKD in primary care,22 whereby a specialist musculoskeletal first-contact physiotherapist (FCP) located within general practice undertakes the first patient assessment, diagnosis and management without the requirement for prior GP consultation. Furthermore, the expanding competency framework within physiotherapy means that in addition to the traditional skills of assessment, exercise provision, education and manual therapy, some first-contact physiotherapists can be accredited to prescribe medication, order scans, inject joints and list for surgery. 22 While FCP continues to expand across the UK, and is gaining significant commissioning momentum, there is limited evidence on the effectiveness of this approach and the context within which it is applied; local audits suggest that this model produces potential cost savings and service benefits. Pilot schemes throughout the UK indicate freeing-up of GP appointments, reduction in secondary care referrals, fewer scan requests, increased patient satisfaction and potential cost-savings within general practice. 23 Moreover, there is institutional support for the role evidenced by the investment in the Additional Roles Reimbursement Scheme (ARRS), which aims to introduce 26,000 new roles into multidisciplinary teams (MDTs), of which first-contact physiotherapists are an integral part. 24
There is a lack of robust research evidence investigating the FCP service initiative, so further investigation is required. Of particular importance is the choice of model in relation to contextual variations within and across sites in the UK. Current audits of the various service delivery models suggest variables such as competency levels (i.e. whether or not clinics employ first-contact physiotherapists with additional qualifications), the extent of treatment provision (i.e. diagnosis and immediate treatment in surgery or diagnosis only with onward referral for treatment) and employment status (i.e. employed via single general practice, deployed from NHS physiotherapy departments or federation/cluster roles) impact upon their functioning within sites, which, we argue, is essential to study with robust methodology. The complexity of this emergent service delivery initiative, including the likelihood of intended and unintended outcomes, produces a compelling argument supporting the use of realist evaluation methodology; an approach that can manage an analysis of the variation between sites employing different FCP models as well as the mechanisms within each model. We believe the evidence gained from this methodological approach will expedite the impact this has on clinical and commissioning practice and will facilitate the National Institute for Health and Care Research (NIHR) ‘Push-the-Pace’ initiative. 25
Aim
To evaluate FCP in general practice for patients with MSKDs and to provide evidence for the adoption of appropriate service delivery models with potential to:
-
provide optimal patient management
-
show meaningful patient benefit
-
relieve GP workload pressures
-
promote better use of healthcare resources
-
positively impact on whole-system musculoskeletal practice.
Using realist methodology, the primary research question was to establish how FCP works in practice, for whom and why? Each phase provided cumulative insight into the primary research question stated above.
Objectives
-
Determine key characteristics of FCP provision in primary care (survey).
-
Analyse current literature to determine key aspects of service architecture that may impact provision and create initial programme theories regarding ‘how’ FCP may work in practice (realist review and stakeholder consultation).
-
Establish the clinical and cost-effectiveness of the FCP model of care compared with GP-led approaches (case study evaluation – quantitative).
-
Explore the views and experiences of patients, healthcare professionals and practice staff regarding the FCP model of care (case study evaluation – qualitative).
-
Determine the impact of new ways of remote working post-COVID-19 on FCP staff (survey and interviews).
-
Integrate data to provide insight into how and why the FCP service works in practice (case study evaluation – qualitative and quantitative).
Report structure
The report is presented with each phase included as a separate chapter, including the related methods, analysis and brief overview of findings. Chapter 7 then brings the quantitative and qualitative findings together and includes implications for implementation and practice. Chapter 8 summarises key findings and Chapter 9 includes strengths and limitations and recommendations for future research.
Chapter 2 Patient and public involvement and engagement
Ethos
Patient and public involvement and engagement (PPIE) is a core principle of our research and essential to ensure public accountability and transparency. For this study, PPIE directly improved the quality of our research, making it relevant to people affected by MSKD and to those who give them support. Patients and public have endorsed our research as important and have helped us refine our original proposal in a preapplication focus group. Continuing to support the research throughout each phase of work, our patient partners, present on the study steering committee and project management group, helped us to conduct the research using methodologies acceptable and sensitive to our patient groups, and assisted us in presenting findings in ways that are accessible to a range of audiences.
From the outset, people with MSKDs have made a valuable contribution in shaping and developing our work, and we continued to embed PPIE throughout. We had patient representation on the study steering committee, a white woman in her 40s who experienced chronic widespread musculoskeletal pain. Co-applicant Foster, a white man in his 70s with osteoarthritis in multiple joints, was a patient representative and was an integral part of the project management group. All time was reimbursed according to NIHR recommended rates.
Our project management group patient research partner and study co-applicant attended realist methodology training to support his involvement in the study planning and interpretation of findings. He attended monthly project management group meetings where possible and provided regular written feedback on all study decision-making processes. DF has also co-authored study outputs.
The study steering committee patient research partner attended the majority of our 6-monthly meetings, providing impartial feedback of study progress and supporting the team with problem solving and decision-making. Meaningful inclusion throughout the project also helped us understand patients’ ongoing service needs and make sure that the perspectives of those affected by MSKDs were represented in future service delivery decision-making.
Specific work package input
Work package 1: survey
Contribution to content and interpretation of data. The co-applicant patient representative was a co-author of the study output.
Work package 2: realist review and stakeholder engagement
Attended realist methods training and contributed to the development of FCP service architecture and initial programme theories. We recruited four additional patient representatives through People in Health West of England to attend our stakeholder event to provide feedback on our emerging initial programme theories. The co-applicant patient representative was a co-author of the study output.
Work package 3: case study evaluation
Contribution to all patient facing literature, interview schedules and advised on time to complete outcome measures. One patient research partner participated in a ‘practice interview’ to allow researchers to refine their questioning and techniques in advance of actual patient interviews. The co-applicant patient representative was a co-author of the study output.
Limitations
Despite considerable efforts, we had limited diversity within our PPIE; this was also reflected in the research itself. While this may have been influenced by the impact of COVID-19 and the disproportionate way in which the pandemic impacted people from underserved communities, we recognise this as a significant limitation of both our PPIE and the research itself. We relied on traditional means of recruitment for our PPIE, including social media and existing PPIE networks, which may have had limited reach. We have since changed our practice and have now established partnerships with local community organisations and champions within the community to ensure that we recruit a more diverse sample. The equality, diversity and inclusion within the research sample are discussed in the relevant chapters.
Summary
We integrated PPIE throughout the study and relied on the valuable contributions to ensure our planning and conduct had the patient at the centre. Our patient partners provided us with considerable insight and guided us on decision-making and data interpretation in the project’s entirety. We are grateful to all the patients and members of the public who have contributed to FRONTIER from the outset.
Chapter 3 National survey and identification of key first-contact physiotherapy service models
Reproduced with permission from Halls et al. 26 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text..
Aim
To conduct a survey to scope existing provision and key aspects of models of FCP provision across the UK. This information was used to inform the selection of models for in-depth evaluation in work package (WP) 3.
Study design
A survey was co-designed, piloted and subsequently distributed to individuals involved in FCP service provision.
Ethical approval
Prior to initiation of the study, an application for ethical approval was submitted to the University of the West of England Faculty Research Ethics Committee. Ethical approval to proceed with the study was given on 20 July 2018 (REC reference number: HAS.18.07.204).
Survey development and pilot
The survey was developed by the research team (including researchers, clinical commissioners, patients, physiotherapists and GPs). Initially, a draft survey was designed by the immediate study team. Although it was intended that the survey would be distributed using an online survey platform, the early drafts were developed in Microsoft Word® (Microsoft Corporation, Redmond, WA, USA) for ease of editing. The draft survey included open and closed questions regarding but not limited to geographical location, patient demographics, current service providers, referral pathways, staffing (numbers, grades and competencies), access to services, service aims and financial arrangements.
The draft survey was piloted with three individuals, known to the research team, who work in the areas of FCP and/or MSKD commissioning. Each pilot involved the draft survey being reviewed by the external individual and subsequently comments and feedback were provided via e-mail, via telephone conversation and in person. The draft survey was then edited based on this feedback. The revised survey was then discussed with the wider research team at the first project management group meeting. Following this, the survey was again edited based on the feedback received. It was then formatted using Qualtrics® (Qualtrics, Provo, UT, USA), an online survey platform. Once finalised, the online link to the 42-question survey (see Appendix 1) was sent to five individuals known to the research team to check that there were no problems accessing the survey (e.g. NHS firewalls or differences across the devolved nations) prior to wider distribution.
Survey distribution
The survey was targeted at those providing FCP services as managers or physiotherapists. Two approaches to survey distribution were used: direct e-mail and online platforms. The direct e-mail approach involved sending a survey link to relevant individuals identified from the FCP development network e-mail list. This e-mail list contained predominantly those involved in England-based FCP services and the Chartered Society of Physiotherapy (CSP)-led English pilot, therefore contacts in Wales, Scotland and Northern Ireland assisted in distributing e-mails to their local contacts across the devolved nations. E-mails were addressed to individuals personally, provided a short description of the aim of the survey, invited them to participate by clicking the attached link, and provided study team contact details should they require further information.
The online platform approach used Twitter (now X; San Francisco, CA, USA) and the FRONTIER study website. The link to the survey was made available via these online platforms. Regular updates were posted and shared during the period that the survey was available. The aim of the survey was to achieve as large a sample as possible to determine the nature of service provision at that point in time.
Data management and analysis
Survey data were initially stored in Qualtrics. Following the closure of the survey, data were downloaded from Qualtrics into a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet for formatting and analysis.
Analysis involved basic descriptions (numbers and percentages) and graphical representation of survey data. Survey respondents also had the opportunity to provide free-text responses. These data were not analysed using formal qualitative methodology but, instead, were used to add context to responses provided to particular questions. Some survey respondents indicated potential interest in further case-study-based evaluation (WP3) and provided their names and contact details.
Results
Response
The survey received 102 responses; 81% (n = 83) provided fully complete data sets. Given the nature of distribution it was impossible to determine a response rate. Furthermore, NHS England primary care workforce returns were unable to explicitly or reliably identify FCP numbers at this stage.
Respondent demographics
Of the 102 respondents, 31% (n = 32) identified themselves as ‘service manager’ and 63% (n = 64) as ‘FCP physiotherapist’. Six respondents indicated ‘other’ as their professional role. These responses included four individuals reporting different physiotherapist titles including advanced practitioner physiotherapist, consultant therapist, telephone triage physiotherapist and consultant physiotherapy. One respondent reported that their role was ‘director of clinical integration’ and one respondent left their role unidentified. The largest proportion came from those based in England (59%, n = 60). There were 22% (n = 22) responses from Scotland, 14% (n = 14) responses from Wales and 2% (n = 2) responses from those based in Northern Ireland. Four responses (4%) were unidentified in relation to geographical location. A total of 93 respondents described the local area where their FCP service was based, which included inner city/urban (35%, n = 33), suburban (33%, n = 31) and rural (20%, n = 19). Ten respondents (11%) indicated that their first-contact physiotherapist was based in an ‘other’ local area, which they described as a mixture of above options. Finally, 48 respondents (47%) provided information regarding the patient population that their FCP service covered. Reports of patient populations ranged from 1200 to 600,000. Of these, 12 (25%) had a patient population ≤ 10,000, 24 (50%) had a patient population between 10,001 and 99,999 and 12 (25%) had a patient population ≥ 100,000.
First-contact physiotherapy service provision by individual physiotherapists
Reports of the number of hours worked per week ranged from 0 to 37.5 hours, with a median of 16 hours. Responses indicate that 58% of respondents worked in their FCP roles up to 0.5 full-time equivalent (FTE), while 17% were working in FCP roles at 1.0 FTE. Appointment times for both initial and follow-up patient appointments ranged from 15 to 30 minutes, with 20-minute appointments being reported by most (71%, n = 50).
Some respondents specifically indicated that their service was only available to new patients or that they had no follow-up patient appointments. One respondent stated that their service has ‘no follow-ups but patients can request a call back if they have seen us before’. Some respondents also reported that they provide telephone triage (prior to face-to-face appointments). These were reported as 5–10 minutes, or that appointment times were 30 minutes, which included time for telephone triage and administration time.
Banding
A total of 69 responses were received, most reported being Agenda for Change band 7 (43%, n = 30) or 8a (48%, n = 33). Only one respondent reported being band 6 (1%) and five reported being band 8b+ (7%).
Additional skills
Of the 66 responses received, 7 (10%) reported having no additional skills, while 55 (83%) reported having two or more of the extended scope capabilities listed. The most frequently selected extended scope capabilities were the ability to request imaging (86%, n = 57), request blood tests (68%, n = 45), and the ability to inject (67%, n = 44); 19 (29%) reported that they were able to interpret imaging and 11 (17%) reported that they were able to list for surgery.
Of the 27 (41%) who indicated that they were independent non-medical prescribers, 20 (74%) reported that they were able to prescribe directly, 4 (15%) could prescribe through the GP via patient-specific or group direction pathways, 2 (7%) were not permitted to prescribe in their FCP despite being qualified independent prescribers, and 1 (4%) did not know.
First-contact physiotherapy service delivery models
Service duration
Responses were provided by 93 (91%) respondents. FCP service durations ranged from 0 months to 9 years. Of the 93 responses, 9 reported that their services were currently still in development or not yet up and running (10%). Approximately one third of FCP services were reported to have been running for < 1 year (n = 30, 32%); just under half of all FCP services were reported to have been running between 1 and 3 years (n = 43, 46%). Only seven (8%) FCP services were reported to have been running for longer than 3 years.
First-contact physiotherapist allocation
Respondents were asked about the number of first-contact physiotherapists working within their service. A total of 89 responses (87%) were provided, of which 5 (6%) indicated that they did not know; 13 (15%) reported that their FCP service was provided by 1 practitioner, 14 (16%) by 2, 7 (8%) by 3, 19 (21%) by 4 and 31 (35%) by 5 or more practitioners.
In relation to the total number of hours of FCP provision available per week, through current FCP services (note, not individuals), 88 (86%) responses were provided. Of these, 12 (14%) indicated that they did not know or the provided response was unclear or zero. The remaining responses ranged from 4 to 763.5 hours, with just under half of those between 30 and 187.5 hours (49%).
Key service drivers
For this question, 86 responses (84%) were given; multiple responses were permitted. Most respondents (90%) stated the main driver was to relieve GP pressure; 76% suggested it was to provide better care for patients and to provide earlier access to specialist services (59%). Other responses included better use of the available workforce, to save money and because they were part of an earlier national pilot in England.
Access
In relation to how patients access FCP services, respondents could select ‘triage at reception’, ‘self-booking (e.g. online appointments)’ or ‘other’ or could select multiple responses if that was more relevant. Some 85 responses (83%) were provided; of these, approximately half selected a combination of responses (n = 45, 53%). The majority were triaged at reception (40%) or triage at reception and other strategies such as self-booking.
Service funding
The following three questions asked about how FCP services are commissioned, funded and provided. In relation to how FCP services were reported to be commissioned, 86 (84%) responses were provided. Of these, eight respondents (10%) did not know, but a range of other responses across the provided response options were given including commissioned by the Clinical Commissioning Group (17%) or funded by a practice group (15%).
Within ‘other’, respondents added detail about commissioning of their FCP services. Some respondents used other terms for group of GP practices to describe how FCP services were commissioned including ‘super GP partnership’ or ‘GP federation’. Others described that FCP services were commissioned by systems and funding relevant to different devolved nations, including health and social care partnerships (Scotland), health boards (Wales) and integrated joint boards (Northern Ireland).
In relation to how FCP services were reported to be provided, 82 (80%) responses were given. The response ‘NHS provider’ accounted for over 80% of responses. Few additional free-text responses were provided here to elaborate on ‘other’; those provided described that FCP services were funded by health and social care partnerships, physiotherapy services and a GP stakeholder company.
Additional information
A total of 27 respondents (26%) provided additional information about their FCP service or role. Some of these respondents commented about how their services were further expanding.
Appointment length and content was mentioned by three respondents:
15 mins session does not work, especially if you have an interpreter patient and you have to use language line.
I feel moving forward 20 min appointments would be better, allowing more time with patients, better Assessment and able to do all admin for patient within the slot. Would negate need for admin slot at end of session.
FCP banding and advanced practice capabilities were mentioned by two respondents, who both questioned the necessity and cost-effectiveness of advanced practice capabilities:
Banding currently at 7 but trying to re band as 8a given the service provided. In my view physiotherapy is making the same mistakes as ANP [advanced nurse practitioners] first did when starting the advanced role.
More than 95% of patients do not require any advance practice intervention.
Challenges with FCP services were also discussed, including recruitment and information technology (IT) systems:
The XX [IT system named] does not work well at all within a cluster setting. It is the single biggest problem we have with the role.
Study implications
This WP used a survey approach to identify FCP service provision across the UK. This section considers results specifically in relation to the objectives of this WP, which included understanding the models of FCP service provision available across the UK, understanding the key aspects of ‘standard’ and additional capabilities models and scoping potential interest in WP3.
The 102 responses received within the 29-day window that the survey was available indicated that there was considerable interest in the topic of FCP. Although as expected, most responses (59%) came from those based in England, the largest of the devolved nations, responses were received from all devolved nations, in particular in Scotland and Wales. Interest from outside England may have resulted from their lack of involvement in the CSP-led English pilot and evaluation. The interest and engagement in this work at the early stage from the devolved nations provided positive indicators for the next phases of the FRONTIER study considering the wider project aim to engage with and involve UK-wide FCP services. It also met the WP objective of identifying potential interest in WP3.
In relation to responses regarding geographical location, within each devolved nation apart from Northern Ireland, over half of the sustainability and transformation partnerships/health board regions that make up each nation were represented in survey responses. Limited response from Northern Ireland may have been due to the lack of availability of FCP services when the survey was conducted, but this service has subsequently developed.
The survey responses also provided the opportunity to identify key aspects of ‘standard’ [non-pharmacological (medication and/or injection) and ‘additional competency’ (prescription and/or injection) models of FCP provision for WP3].
In our survey sample, 91% (n = 66) of FCPs reported that they were either band 7 or 8a. Only seven (10%) reported having no additional capabilities, while 86% (n = 57) reported that they could request imaging, 67% (n = 44) reported that they could inject and 41% (n = 27) reported that they could prescribe.
The survey also allowed enhanced understanding of FCP models and service provision available across the UK. In relation to how long FCP services have been running, the survey sample revealed that 9% (n = 9) of FCP services were currently still in development, nearly one quarter (23%, n = 22) were < 5 months old and only seven (8%) were reported to have been running for longer than 3 years. These figures, together with additional free-text comments provided, indicate the future development and expansion of services and demonstrate the new and evolving nature of FCP.
With regard to the key drivers for FCP service initiation, nearly all those who responded to this question (90%, n = 77) selected ‘To relieve pressure on local GPs’. Although a common justification for FCP service initiation, this response was surprisingly high, given that the majority of respondents were not GPs. Other highly selected responses included ‘to provide better care for patients’ and ‘to provide earlier access to specialist services’. Interestingly, ‘To save money’, a commonly cited justification for FCP service initiation, was only selected by one third of respondents (30%, n = 26). These responses are likely a reflection of the majority of respondents being FCP service physiotherapists or managers rather than commissioners. The qualitative work within the WP3 case studies was able to draw out more detail regarding the perspectives on this from a range of staff. It also provided an opportunity to explore reasons for initial FCP service initiation and service development and continuation.
A commonly reported benefit of FCP is appointments are typically longer than GP appointments (typically 10 minutes or less). This was confirmed in the survey responses, with 71% (n = 50) reporting that their FCP services offered 20-minute appointments, with all ranging from 15 to 30 minutes. Some additional free-text comments indicated that FCP service appointment times may change, which was a consideration for WP3 in terms of understanding the context at individual sites, but also potentially in terms of site recruitment to ensure inclusion of services running a range of appointment durations.
With regard to how patients access FCP services, there were a few aspects of note. First, it was very common that patients were triaged into FCP services. However, this role was not only performed by reception staff, but also by clinical GP practice staff. Second, very few respondents selected ‘self-booking’ either as an individual response or in combination with another response option. Both these aspects may be a result of the relatively ‘new’ nature of many of the services represented in this survey. It may be the case that clinical staff identify appropriate patients during routine consultations until services become established and patients become aware of its availability and purpose. Additionally, despite suggestions that standardised scripts can be used for musculoskeletal triage, this was only mentioned by one respondent. When thinking about WP3, survey responses indicated that it may be that multiple approaches to patient access are in operation in GP practices. It was therefore important for the study team to be able to record ‘footfall’ from all patient access routes.
Finally, in terms of FCP service commissioning, funding and providers, there were a number of points of note. First, the providers of FCP services were clear with over three quarters (83%, n = 68) of respondents describing that their FCP service was provided by the NHS. Service commissioning and funding questions were less clear. Respondents reported across all the response options provided for the commissioning question and, in addition, nearly one quarter (n = 24) reported ‘other’ commissioning approaches. However, many comments related to how services were paid for or financed, rather than how they were planned and monitored. The subsequent question about how FCP services were funded had a poor response rate, potentially due to respondents feeling that they had answered this in the previous question. Despite the effort that went into designing the questionnaire, and these three questions in particular, question wording may have been a limitation.
Limitations
We were unable to identify how many individuals saw the questionnaire and chose not to respond. Equally, it was not possible to determine the potential number of participants and therefore report our sample size as a percentage of the potential sample. Given the relatively small numbers of respondents to this survey, this is recognised as a limitation of this work.
Conclusions and summary
In summary, an online survey was used to identify and understand models of FCP service provision across the UK. A total of 102 responses were received from physiotherapists, managers and others involved in the provision of FCP based across the devolved nations. A number of considerations and implications for the FRONTIER project were identified. First, the interest and engagement with WP1 was promising, particularly with the identification of 62 respondents who indicated potential interest in participation in WP3. Second, recruitment of sites for WP3 needed to consider inclusion of services with a range of appointment durations and representation of FCP services commissioned in different ways. Third, consideration needed to be given to how best understand the educational, resource and cost implications of different models of FCP. Fourth, areas for further contextual understanding were identified including perceptions of the FCP role from a range of stakeholders and reasons for initial service initiation and continued service development. These areas were therefore included in the development of preliminary programme theory and realist synthesis as part of WP2 and explored in depth in WP3. Finally, practical considerations for WP3 included ensuring that all patient access routes into FCP services could be captured in data collection, and that processes were in place to manage practices using no or multiple clinical data systems.
Chapter 4 Rapid realist scoping synthesis regarding provision of first-contact physiotherapy in primary care
Reproduced with permission from Jagosh et al. 27 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Aim
To develop initial programme theories to inform in-depth case-study evaluation.
Objectives
-
Conduct a rapid realist review to produce a set of realist initial programme theories regarding what works, for whom, in what context and with what resources.
-
Engage with key stakeholders to validate the programme theories and gather further evidence about how FCP models are currently working.
Research questions
-
Does FCP improve patient management over usual GP care? And if so, how?
-
Does FCP show meaningful patient benefit? And if so, how and for whom?
-
Does FCP relieve GP workload pressure?
-
Are there unintended consequences to GP workload that need to be understood?
-
Does FCP promote better use of healthcare resources? If so, how?
-
Does FCP positively affect whole systems musculoskeletal practice? If so, how?
-
Are there risks associated with FCP models? If so, what are they and how do they accrue?
Study design
Realist synthesis and stakeholder consensus.
Ethical approval
Prior to initiation of the study, an application for ethical approval was submitted to the University of the West of England Faculty Research Ethics Committee. Ethical approval to proceed with the study was given on the 20 July 2018 (reference number: HAS.18.07.204).
Methods
Methodological approach
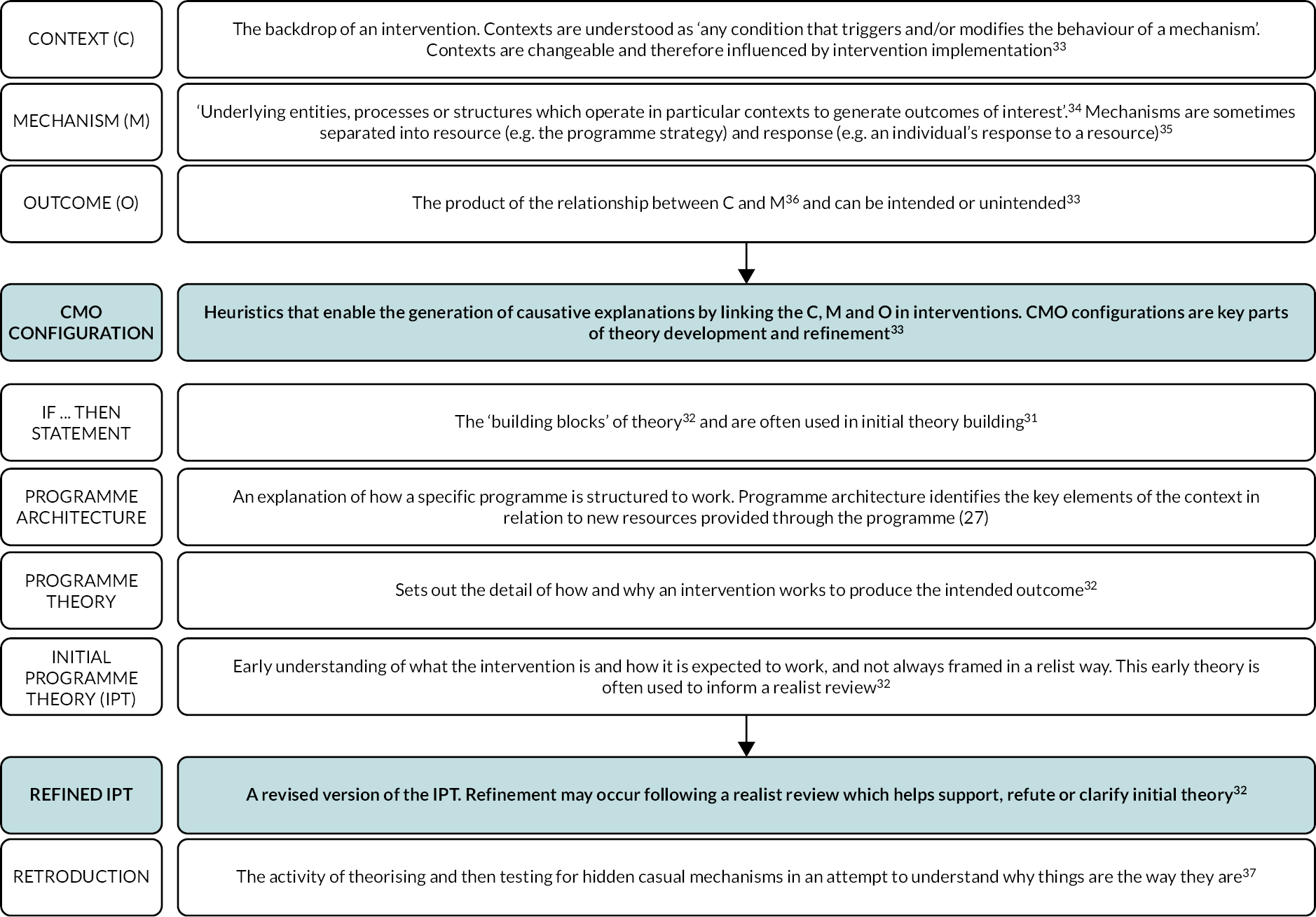
A realist-informed scoping synthesis was performed. Realist synthesis is a theory-driven approach designed to investigate complex social interventions. 28–30 It is described as being focused on understanding ‘what works (or does not work), for whom under what circumstances, how and why’. 28–30 Rather than assuming that interventions are the direct and linear cause of outcomes, the realist approach posits that ‘mechanisms’ are the causal explanations that result in outcomes. 28–30 As such, realist approaches look to identify relationships between contexts, mechanisms and outcomes (CMO) to allow explanation of how and why interventions are effective or not. 28–30 The key definitions relating to the realist approach used in this synthesis are shown in Figure 1.
FIGURE 1.
Realist definitions. C, contexts; IPT, initial programme theory; M, mechanisms; O, outcomes.
The realist approach was chosen for this synthesis for its value in investigating complexity, and the recognition that FCP is in itself a complex intervention, being implemented in a complex system (NHS). 31 Prior to commencement, the realist methodological expert on the team (JJ) completed a 2-day in-person training event with the co-applicant team to develop realist skills. NW had previously attended realist methodological training in advance of study application.
Finally, and importantly, the use of a realist informed approach was also necessary to develop initial programme theory to take forward as the theoretical foundation of the FRONTIER realist evaluation (WP3).
Search process
We adhered to the steps outlined in RAMESES (Realist And MEta-narrative Evidence Syntheses: Evolving Standards) guidelines32 in performing realist reviews or syntheses: (1) identifying potential theories; (2) searching for evidence; (3) appraising primary studies; (4) extracting data; (5) analysing and synthesising evidence; (6) consultation with key stakeholders and (7) theory refinement. Stages 6 and 7 were included to provide further validation of the emerging theories from key external stakeholders, naïve to the proposed theories38 (see Appendix 2 outlines theory development processes).
Step 1: identifying potential theories
To facilitate initial theorising, an exploratory scoping review of the FCP literature was undertaken in October 2018. Initial theories were developed through a series of iterative discussions with the full academic and MDT and conceptualised from the perspective of key stakeholders involved in the FCP model, at all levels of service provision (i.e. patients, physiotherapists, commissioners).
Although this and subsequent steps are described as a linear process, the theorising that occurred at each step was iterative and thus overlapped with other steps; considerable numbers of iterations of theory were generated, revised and refined throughout the synthesis process.
Step 2: searching for evidence
Following initial theorising, and in consultation with library services, an iterative literature search was performed in January 2019 to identify primary and grey literature. The search was deliberately broad to ensure the identification of a range of sources which could contribute information on this emerging topic area.
All study designs were eligible and no exclusion criteria were imposed other than English language sources only. Databases searched included the Allied and Complementary Medicine Database, Cumulative Index to Nursing and Allied Health Literature, MEDLINE, SPORTDiscus, PsycInfo® (American Psychological Association, Washington DC, USA, via EBSCO), EMBASE (via OVID), Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials.
The core synthesis team filtered the identified literature for inclusion in full-text review informed by consideration of the scope and breadth of the synthesis and for pragmatic reasons. The process involved duplicate removal, title screening and then rigorous, iterative rounds of abstract screening performed in synthesis team pairs who discussed abstracts with an independent synthesis team member in the event of disagreement. In addition to empirical literature, grey literature sources were also searched using basic search terms (e.g. first contact physiotherapy). Sources included the CSP and Royal College of General Practitioners websites and YouTube (Google Inc., Mountain View, CA, USA). A CSP FCP discussion forum and e-mail list and a discussion forum from Twitter (now X) focused on FCP (#PhysioTalk) were also included.
Step 3: appraising primary studies
Appraisal of identified sources was informed by consideration of their richness, relevance and rigour. Sources that contained detail to elucidate initial theories were considered conceptually rich and relevance pertained to the insight into the topic of investigation. 39 The core synthesis team was mindful of the relevance of non-UK derived literature given the unique context of the NHS, the timeliness of publication given the emerging nature of the FCP model and the recognised definition of FCP as co-located in primary care. Rigour was addressed through methodological appraisal of source credibility. No sources were excluded but considerations were documented which informed source influence on the developing theory.
Step 4: extracting data
All records were managed in an Excel database. Initially, information about each source including title, authors, date, type and abstract were extracted before assigning to members of the team. For consistency, a data extraction process was designed and piloted.
For data extraction, team members were asked to follow six steps for each assigned source: (1) source familiarisation and note taking; (2) consider the contribution of the source (e.g. the insight it generates, whether it illuminates initial theory) and its overall value; (3) write a summary capturing thoughts from step 2; (4) reread each source to identify causal links and CMO configurations; (5) extract specific data related to CMO if only partial information is available directly from the source (e.g. no mechanism stated), fill gaps with ‘hunches’ to propose logical causal hypotheses to complete the CMO configuration; and (6) add any additional comments about the source not captured elsewhere. Approximately 10% of sources were cross-checked by synthesis team pairs, who discussed sources in relation to relevance, reviewed source data extracted in the above six steps and resolved any differences in opinion through discussion.
Step 5: analysing and synthesising evidence
Following data extraction, a 2-day meeting was held with the core synthesis team where all data extracted during step 4 were discussed and reconfigured for clarity. Here, the extracted data refined the initial programme theory and were grouped into overarching research priority areas – person, place and time.
Step 6: consultation with key stakeholders
To consolidate and validate understanding and further refine theory development, an event with key stakeholders was held. The event was attended by stakeholders (n = 10) representing commissioners (n = 1), practice managers (n = 2), physiotherapists (n = 3), professional body (n = 1) and members of the public (n = 3). The event was facilitated by the research team (n = 6) who presented the candidate CMOs within each of the three priority areas (person, place and time) and facilitated small group discussions based on a modified nominal group technique approach.
The group was divided into two smaller subgroups for ease of discussion before reconvening into a larger whole group meeting. Each group was provided with the candidate CMOs and asked to discuss for their relevance, indicate their levels of agreement and to prioritise. The two groups then reconvened in a single group to present their individual findings, discuss any amendments and reprioritise as a whole group.
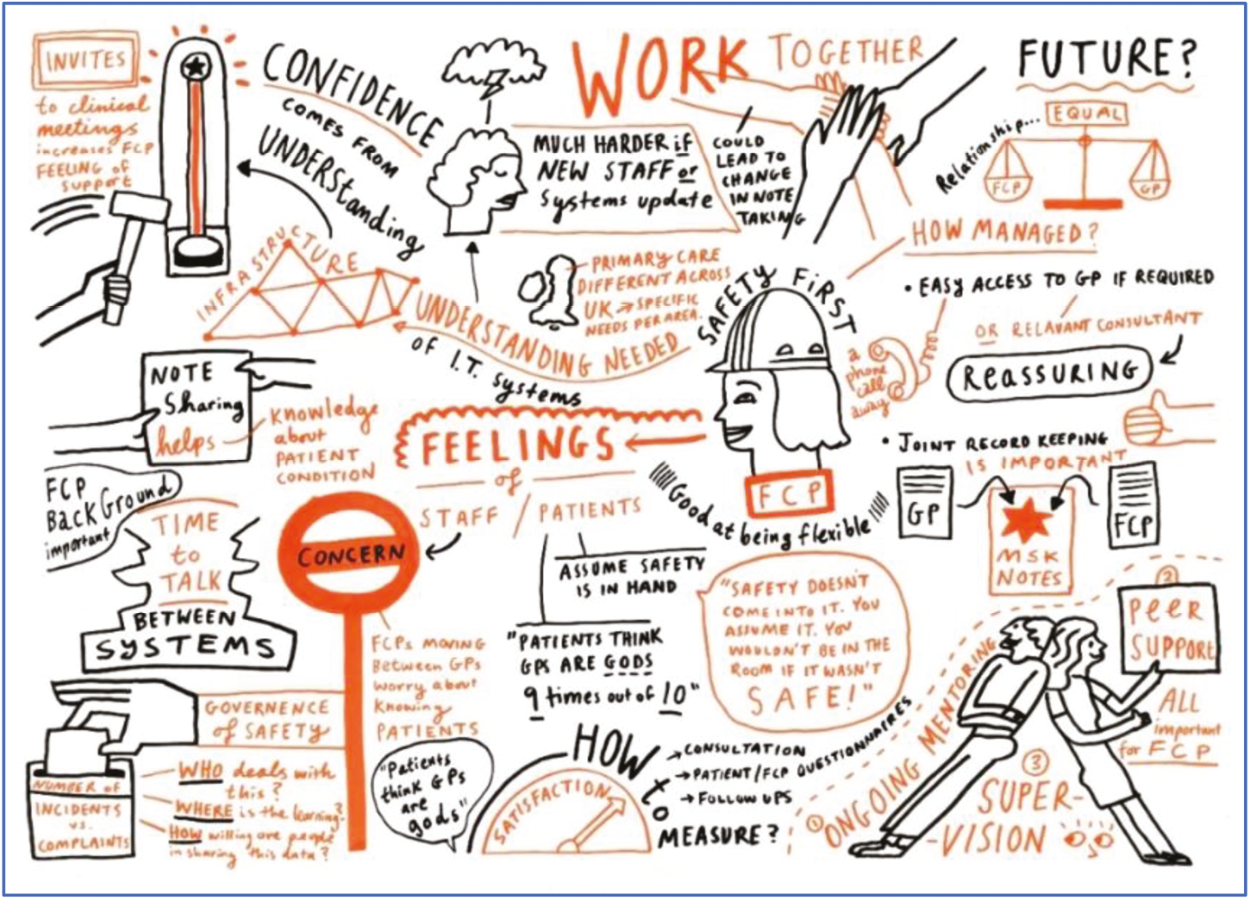
Discussions were audio recorded and field notes collected. In addition, discussions were professionally illustrated in real time to provide an accessible representation to the whole group and permit further discussion and group validation.
Step 7: theory refinement
Following the stakeholder event, three team meetings were held to consolidate theory refinement and reflect on stakeholder prioritisation to inform later project work.
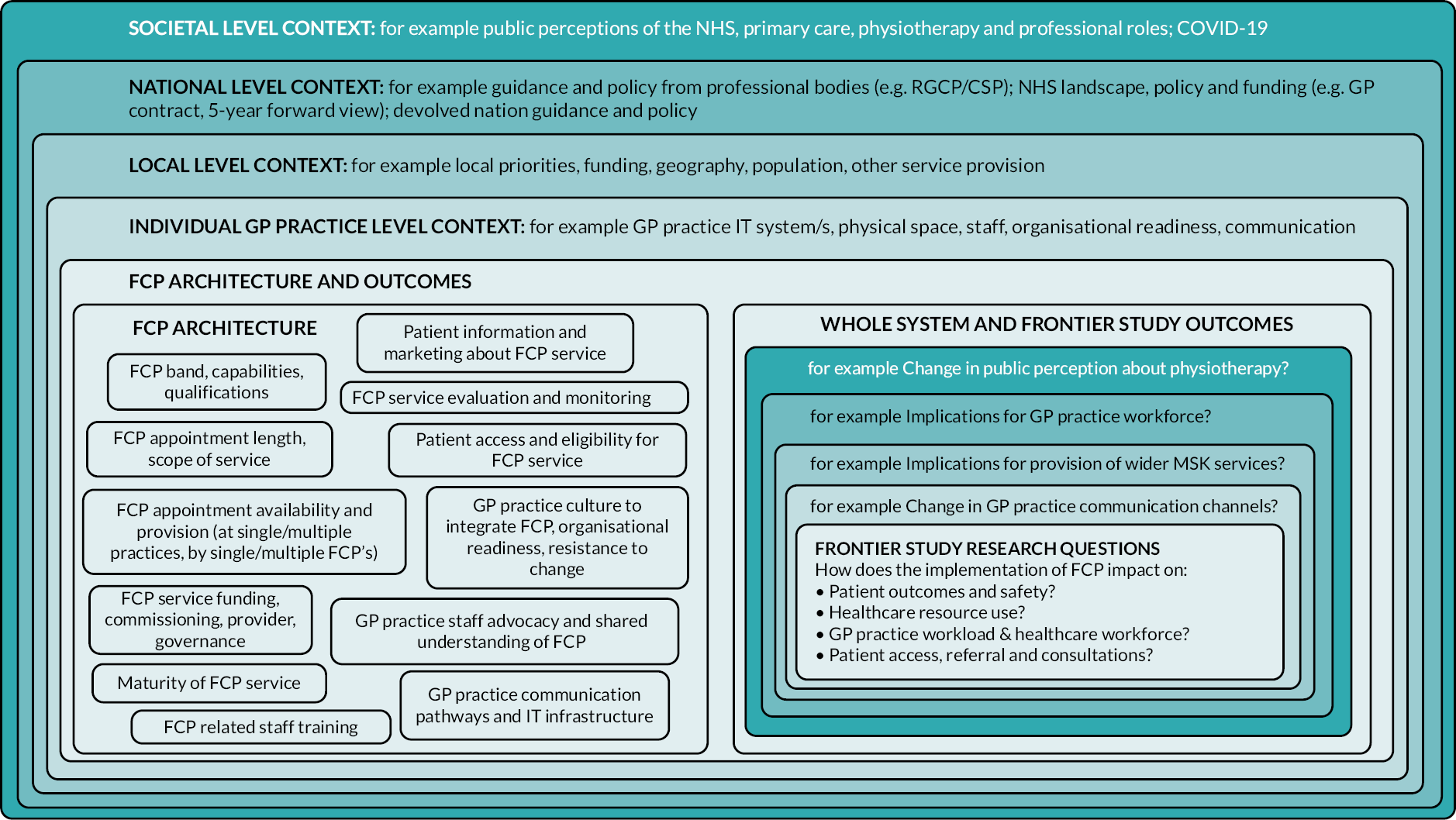
Results
Initial programme theory and first-contact physiotherapy architecture
Initial theorising through iterative team discussions identified key components of the ‘architecture’ of the FCP intervention, creating initial programme theories of how FCP may ‘work’. This was conceptualised at multiple levels of service provision, including broad ‘societal’ level contexts through to ‘individual GP practice’ level contexts (Figure 2). This provided understanding and appreciation of the wider context in which the FCP model was operating and how this may influence its functioning, for example by considering how funding streams, local models of delivery or public perceptions of primary care impact FCP delivery. It also developed an awareness of how outcomes resulting from the FCP model may impact on systems at a wider level; for example, if FCP reduces referrals to secondary care, then there may be implications on funding and provision in secondary care MSK services.
FIGURE 2.
Early conceptualisation of first-contact physiotherapy architecture. CSP, Chartered Society of Physiotherapy; RCGP, Royal College of General Practitioners.
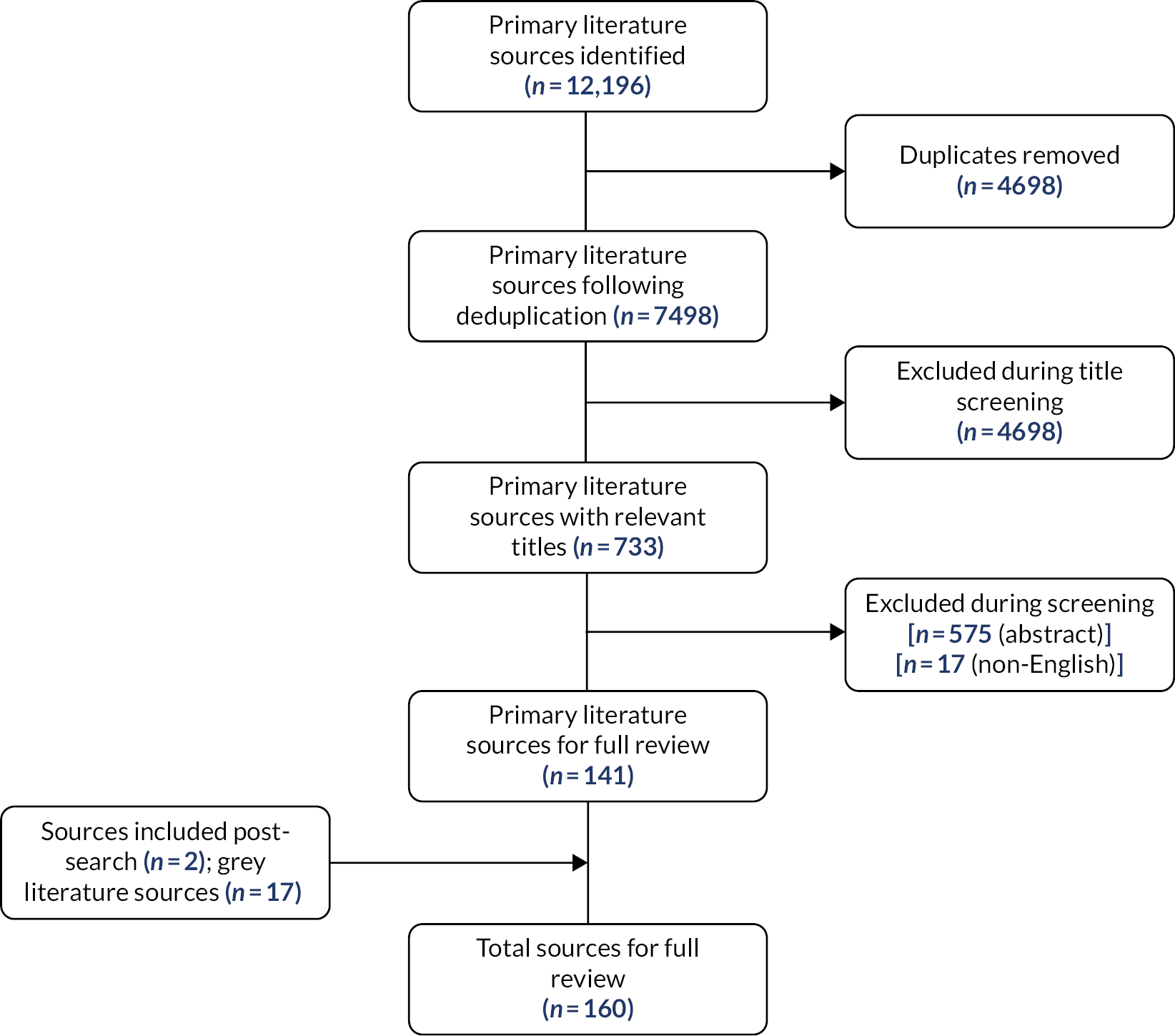
Summary of sources for synthesis
The sources identified and excluded during searching are detailed in Figure 3. The primary literature search identified 12,196 sources, which were reduced to 143 sources, including journal articles (n = 46), abstracts (n = 29), magazine articles (n = 63), letters (n = 4) and theses (n = 1). Grey literature searching identified 17 sources, CSP discussion fora and e-mail list (n = 3), Royal College of General Practitioners website (n = 1), YouTube videos (n = 12), Twitter (now X) #physiotalk discussion (n = 1). Searching totalled 160 sources for full-text review.
FIGURE 3.
Flow diagram of search process and source identification.
Preliminary programme theory synthesis and refinement
During the team meeting to reconfigure the extracted data, the initial programme theories (developed before the synthesis) were considered alongside 300 preliminary CMO configurations resulting from data extraction. CMO configurations were grouped by theme, refined to remove duplication and prioritised to meet the research objectives. This led to the development of CMO configurations which were grouped under three overarching research priority areas:
-
Awareness of and access to FCP: covering the approaches to sharing information about FCP (e.g. marketing, advocacy), accessing FCP services and how these considerations influence staff and patient feelings and perceptions about FCP.
-
FCP skills and knowledge: covering the unique value of the FCP role, skills and knowledge (and the distinction from GP role, skills and knowledge) and how these considerations influence staff and patient feelings and perceptions about FCP.
-
Safety and FCP: covering how patient safety are managed and performed in the FCP role and how this influences staff and patient feelings and perceptions about FCP.
Development of programme theory through the stakeholder event
At the stakeholder event, participants were presented with a refined and accessible version of the theory, presented using the overarching research priority areas described above.
Illustrations were produced that captured small group discussion and whole-group feedback of each of the three priority areas. Following the stakeholder event, the synthesis team met to deliberate the discussion points using field notes and illustrations as reminders. The event discussion points highlighted and prioritised three main areas (awareness and access to FCP; FCP skills and knowledge; patient safety and FCP), enhanced understanding of some of the issues surrounding the FCP model and clarified areas of uncertainty. This fed into the refined initial programme theory described below. Throughout the stakeholder event, an illustrator was employed to visually document discussions. This provided an accessible means of relaying information to participants and other groups thereafter. Summary illustrations are presented in Figures 4–6.
FIGURE 4.
Awareness of and access to the first-contact physiotherapist (person and place).

FIGURE 5.
Skills and knowledge of the first-contact physiotherapist (person and time).
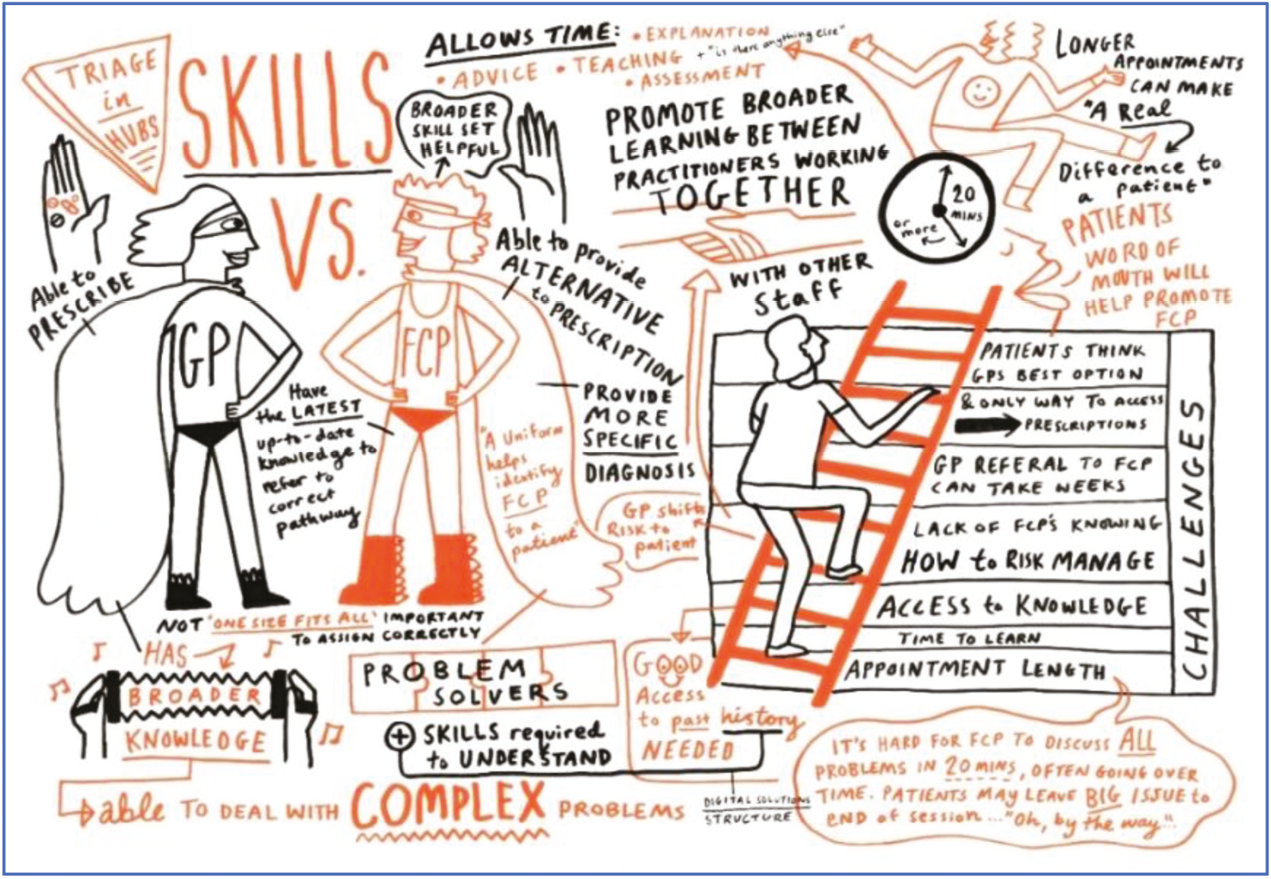
FIGURE 6.
Patient safety (person).
Refined initial programme theory
The stages of initial theorising, source synthesis and stakeholder event all systematically fed into the refined preliminary programme theory. This process was also influenced by the continually evolving wider context of FCP, which saw the model become more prominent during the study period and undergo its own refinement and adjustments to implementation. FCP was identified within NHS strategy as a high-impact intervention, the underpinning principle of which are that ‘patients should be seen by the right person, in the right place, first time’. 40 This underpinning principle was felt to summarise how the FCP programme was intended to work, while demonstrating the inextricable link between the FCP programme and the wider NHS and was therefore used to conceptualise the refined programme theory, considering all of the previous aspects of the work, including consultation. This conceptualisation proposed that FCP provides the opportunity for patients presenting with MSKDs to consult with a FCP rather than a GP (‘right person’), at their local GP practice (‘right place’), without the need for a prior GP consultation (‘first time’; Figures 7 and 8). See Appendix 2 for early theorising.
FIGURE 7.
Right person, right place, first time.
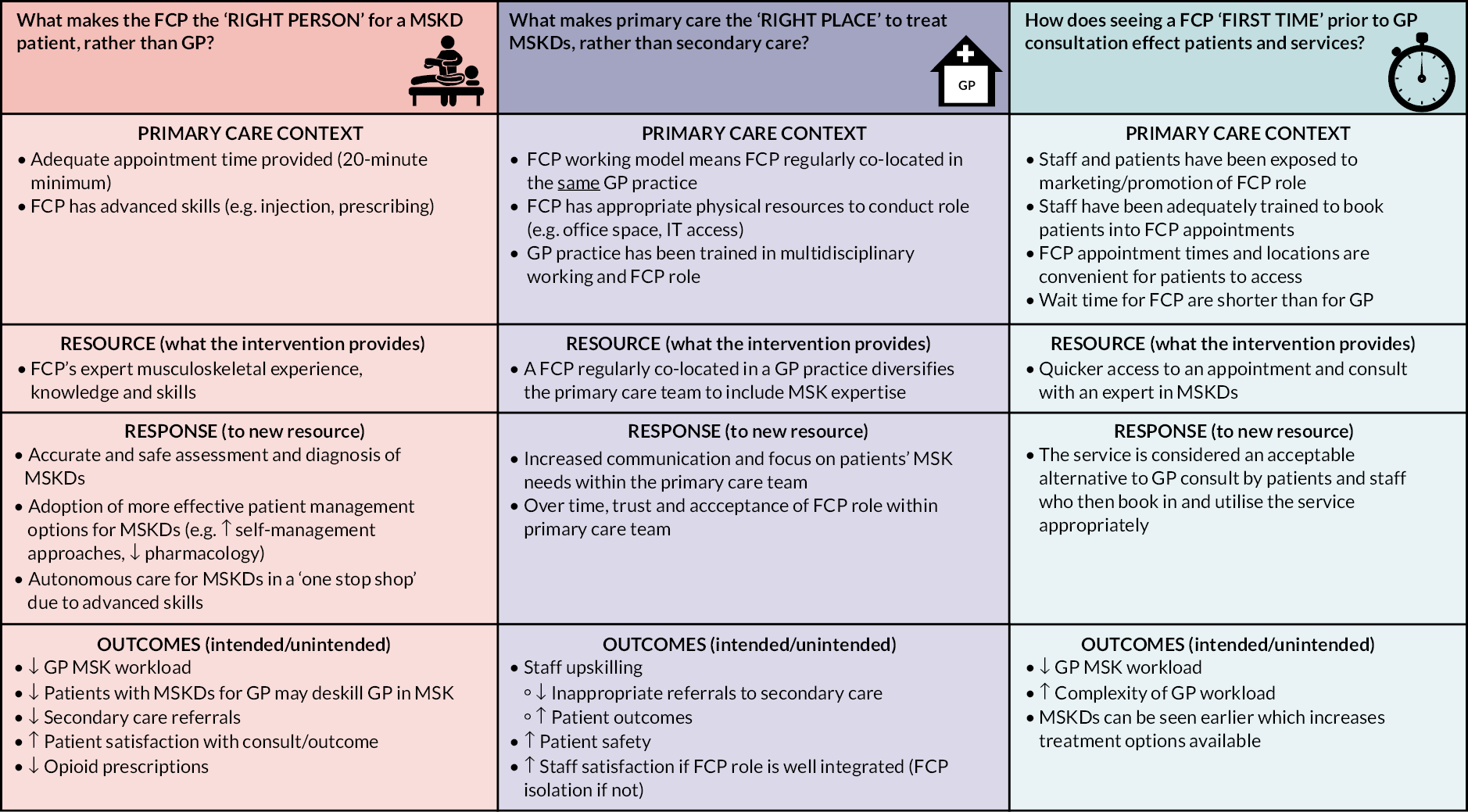
FIGURE 8.
Refined initial programme theories with hypothesised contexts, mechanisms and outcomes.
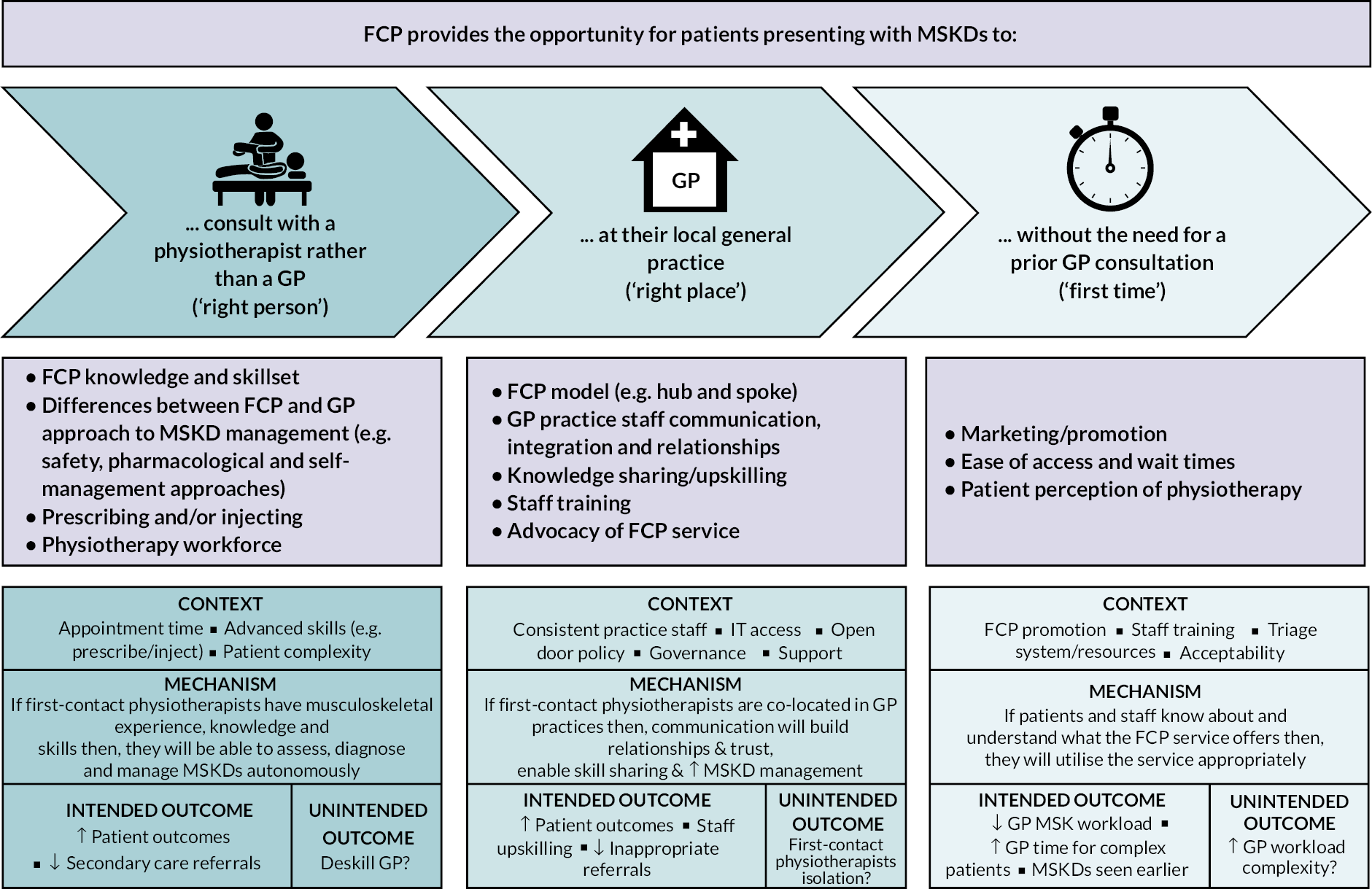
The key theory aspects relating to each of the three headings have been summarised under the main heading represented by (either ‘right person’, ‘right place’, or ‘right time’). However, there is a natural overlap across headings and key theory aspects; therefore, although visually represented by a single heading, the key theory aspects are in reality more interlinked.
Right person
The ‘right person’ component conceptualises that the FCP model provides patients presenting with MSKDs to consult with a first-contact physiotherapist rather than a GP. Key aspects relating to ‘right person’ include expert musculoskeletal skills and knowledge of the first-contact physiotherapist, how the FCP model compares with the traditional model of GP-led care, safety of the FCP model, additional training and qualifications relevant to FCP roles, and the impact of FCP on the wider physiotherapy workforce.
Right place
The ‘right place’ component conceptualises that the FCP model provides patients presenting with MSKDs the opportunity to consult with a first-contact physiotherapist at their local general practice. Key theory aspects relating to ‘right place’ include model of primary care provision, communication, staff integration and knowledge sharing. Although overlapping, aspects relating to patient awareness of and access to FCP services are captured within ‘first time’.
Right/first time
The ‘first time’ component conceptualises that the FCP model provides patients presenting with MSKDs the opportunity to consult with a first-contact physiotherapist without the need for prior GP consultation. Key theory aspects relating to ‘first time’ include service awareness, promotion and training, and acceptability.
A summary of the areas for further investigation is provided below. These are categorised into overarching areas rather than specific ‘if–then’ statements.
-
practice understanding of the role
-
integrating the first-contact physiotherapist into general practice
-
knowledge and skills of the physiotherapist
-
appointment structure
-
practice endorsement of FCP
-
patient acceptability of the first-contact physiotherapist role
-
employment and management of the first-contact physiotherapist role
-
impact of FCP on practice workload and wider resource use.
Implications for the FRONTIER project
The purpose of WP2 was to identify initial programme theories for further investigation in the qualitative aspect of WP3 (mixed-method realist evaluation). However, this phase of the work coincided with a rapidly evolving initiative to implement FCP, with service configurations changing constantly, including implementation toolkits and educational frameworks, all of which impacted on the architecture of FCP. Therefore, theories developed in this phase were useful for sensitising the team to the issues of interest, but possibly elucidated fewer established theories due to the changing contexts of FCP provision. Indeed, this was further impacted during the evaluation resulting from the COVID-19 pandemic that had significant impact on delivery of FCP models, namely to remote consultation from in-person contact.
The benefits of the realist methodology however allowed fluidity between the synthesis and consensus exercise (WP2), with the qualitative aspect of the evaluation (WP3), this is discussed further in Jagosh et al. 27
Limitations
The stakeholder consultation exercise was limited in numbers and did not include GP representatives or practice nurses who may have provider greater insight into the theorising and validation. Further challenges were the rapidly moving landscape of FCP which meant service initiatives were changing constantly. We addressed this issue in part by retaining some fluidity between our synthesis and consensus approach, and later stage qualitative evaluation, to ensure the theorising reflected on contemporary thought and practice. Furthermore, the literature base was developing at a rapid pace and some publications may have been missed; we also acknowledge there was very little literature at the time (and indeed at present) on the wider impact of FCP implementation on different levels of population deprivation.
Given the novelty of the service and the involvement of multiple stakeholders, we needed to provide some focus to our work to retain manageability and ensure it was completed within the project time and budget. We therefore adopted the ‘right person, place and time’ approach. This could be considered reductive and not representative of the full landscape and architecture of FCP. We recognise this as a limitation of our work but believe it does provide a useful insight to support implementation, and further research can explore the wider issues influencing and influenced by FCP implementation.
Conclusions and summary
The rapid realist synthesis identified multiple candidate initial programme theories and early CMO configurations. Theories that were related to service implementation were carried forward for further investigation in WP3. Hypothesised initial programme theories were used to inform interview schedules and iterative thinking in the case study evaluations.
Chapter 5 Surveying the impact of remote consultations on the first-contact physiotherapist’s mental health
Reproduced with permission from Anchors et al. 41 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In response to a NIHR call for an additional WP for current studies that could investigate mental health issues, we undertook a study investigating the impact of remote consultations, imposed by COVID-19, but integral to the NHS Long Term Plan drive for digital first. 42
Aim
To explore the health and well-being issues experienced by first-contact physiotherapists as a result of remote consultations.
Study design
A mixed-method sequential explanatory study was undertaken consisting of: (1) a nationwide e-survey with FCPs and (2) qualitative interviews with FCPs.
Ethical approval
Ethical approval to proceed with the study was given by the University of the West of England Faculty Research Ethics Committee HAS.19.06.204 on 15 December 2021.
Methods
Survey development
The draft survey was developed within the MDT. The attitude statements were derived from reanalysing transcripts described in Chapter 6 in relation to remote consultations. Nvivo (Lumivero, Denver CO, USA) was used to undertake a keyword search related to remote consultations, then attitude statements derived from the coded transcripts. Existing literature was also searched to identify any novel areas not represented in the transcripts.
The identified areas and related challenge statements were within the following domains:
-
isolation
-
increased workload
-
professional anxiety
-
frustration and job satisfaction
-
IT issues
-
mental strain
-
physical impacts.
The benefits statements were within the following domains:
-
improved access for patients
-
flexibility
-
expedited access
-
improved management of acute presentations
-
patient acceptability and satisfaction
-
increased productivity.
The draft was piloted once on a FCP and a research fellow at the University of West England to check the content, logic, routing and timing of the survey. Only minor changes were made to wording as a result.
Survey content
Instructions at the beginning of the survey included a link to the participant information sheets; participants were explicitly informed that responding to the survey constituted consent. Respondents were asked to provide a contact e-mail if they wished to be interviewed in phase 2 of the study.
Demographics
Work location (nation), deprivation level of work location, professional banding, professional experience, details regarding FCP employment model and number of practices worked at, and any training to undertake remote consultations.
Remote consultation usage
Types of remote consultation used and estimated time allocation for each.
Challenges and benefits of remote consultations
Participants rated their agreement with 19 attitude statements that related to either to a challenge (e.g. ‘Digital ways of working have made me feel quite isolated from the other practice staff’) or a benefit (e.g. ‘Digital ways of working have been useful for me, at least with patients with acute presentations’) of remote consultations on a five-point rating scale (1 = strongly disagree, 5 = strongly agree). The attitude statements were created from re-analysing transcripts described in Chapter 6 and from existing literature. Open-ended questions about benefits and challenges of remote consultations were also included.
Stress appraisal
Rated on a six-point Likert scale anchored between 1 (not at all) and 6 (extremely), two self-report items from the cognitive appraisal ratio were adapted to assess evaluations of task demands and personal coping resources towards remote consultations. 43 Specifically, demand evaluations were assessed by the item ‘In general, how demanding do you find digital consultations?’, while resource evaluations were assessed by the item ‘In general, how well do you cope with the demands of digital consultations?’. A stress appraisal score was calculated by subtracting demands from resources (range: −5 to 5), with zero and a positive score suggested to be reflective of a challenge state (i.e. coping resources match or exceed task demands) and a negative score representative of a threat state (i.e. task demands exceed coping resources). 44
The survey was open from 27 June to 1 August 2022. A copy of the survey can be found in Appendix 3.
Distribution
The e-survey targeted UK based first-contact physiotherapists and was distributed electronically via Qualtrics to FCP networks, the CSP FCP special interest group and personal contacts. E-mails were also sent to training hub contacts to share with local FCPs. E-mails provided a short description of the aim of the survey, invited them to participate by clicking the attached link, and provided study team contact details. The online platform approach used Twitter (now X) and the FRONTIER study website (frontierstudy.co.uk). Here, the link to the survey was made available via these online platforms. The link was redistributed on two occasions to promote further returns.
Eligibility
First-contact physiotherapists currently practicing in the UK and able to read and respond in English language. No other eligibility criteria were required.
Semistructured interviews
Survey respondents who expressed an interest in being interviewed, were contacted via e-mail and provided with an information sheet and consent form in advance of arranging. Interviews were conducted online via Microsoft Teams® (Microsoft Corporation, Redmond, WA, USA), digitally recorded and transcribed verbatim. The transcripts were double-checked for accuracy against the audio recording and anonymised before being imported into NVivo version 1.6.1.
Discussion guide
The interviews explored FCP experiences of remote consultations including implementation and usage, benefits and demands associated with remote consultations, impacts of remote consultations (on performance, health and well-being and burnout), coping responses, and training (past, current and level of interest).
Data analysis
Quantitative data were analysed descriptively in SPSS version 28 (IBM Corporation, Armonk, NY, USA). The qualitative data were analysed in NVivo by three team members using Braun and Clarke’s45 six-phase reflexive thematic analysis.
Results
Quantitative component
Participants
The survey was completed by 109 FCPs and included complete data sets (Table 1). Eleven others opened the survey and completed the first question, but provided no further data; they were therefore not included in the analysis. Almost half (46.8%) were based in England, with 39.4% in Scotland and smaller numbers based in Northern Ireland (8.3%) and Wales (5.5%). The areas of deprivation in which FCPs were working were evenly split, with 27.5% working in areas of high deprivation, 27.5% in low deprivation, 24.8% in mixed deprivation and 20.2% in areas of middle deprivation. The majority of participants had either 2–5 years (41.3%) or 1–2 years of experience (33.0%), with a smaller number having > 5 years (12.8%) or < 1 year of experience (12.9%) as a first-contact physiotherapist. Participants tended to be employed by an NHS community service provider (44.0%) or an NHS acute service provided (29.4%). Fewer were directly employed by the primary care network (PCN) (13.8%) and only 1 (0.8%) was employed by a single GP practice. Nearly 40% (39.4%) were working at two practices, one-fifth (20.2%) at one practice, one-fifth (20.2%) at three practices and one-fifth (20.2%) at four or more practices.
| Characteristic | Respondents (N = 109), n (%) |
|---|---|
| Work location | |
| England | 51 (46.3) |
| Northern Ireland | 9 (8.3) |
| Scotland | 43 (39.4) |
| Wales | 6 (5.5) |
| Description of deprivation area | |
| High | 30 (27.5) |
| Middle | 22 (20.2) |
| Low | 30 (27.5) |
| Mixed | 27 (24.8) |
| Band level | |
| 7 | 75 (65.1) |
| 8a | 36 (33.0) |
| 8b | 2 (1.8) |
| Length of time as a first-contact physiotherapist (years) | |
| < 0.5 | 3 (2.8) |
| 0.5–1 | 11 (10.1) |
| 1–2 | 36 (33.0) |
| 2–5 | 45 (41.3) |
| 5–10 | 14 (12.8) |
| Employment model | |
| Single GP practice | 1 (0.9) |
| Primary care network | 15 (13.8) |
| NHS community service provider | 48 (44.0) |
| NHS acute service provider | 32 (29.4) |
| Other | 11 (10.1) |
| Don’t know | 2 (1.8) |
| Practices employed (n) | |
| 1 | 22 (20.2) |
| 2 | 43 (39.4) |
| 3 | 22 (20.2) |
| ≤ 4 | 22 (20.2) |
Remote consultation usage
Of the 109 respondents who had used remote consultations in the past 2 years, 62.4% (n = 68) were using them for < 25% of their patient consultations. The majority of respondents (98.2%, n = 107) used telephone consultations, with 55.5% (n = 60) using a combination of other formats including video and 28.4% (n = 31) using text based remote consultations.
Benefits of remote consultations
Most agreed with the key benefits of the ease and flexibility of access of remote consultations for patients who found it difficult to come into the practice (64.2%, n = 70) and for those who preferred not to come into the practice (67.0%, n = 73). Half (50.5%, n = 55) agreed in the value of remote consultations allowing them to see certain patients quicker and 55.1% (n = 60) found them useful for patients with acute presentations. However, 44% (n = 48) did not agree that remote consultations allowed them to be more productive at work and 37.6% (n = 41) did not agree that remote consultations were popular with patients. Level of agreement responses are included in Table 2.
| Statement | Respondents, n (%) | ||||
|---|---|---|---|---|---|
| Strongly disagree | Somewhat disagree | Neither agree nor disagree | Somewhat agree | Strongly agree | |
| Been rewarding as they allow me to provide ease of access to patients who previously found it difficult to come into the practice | 4 (3.7) | 10 (9.2) | 25 (22.9) | 65 (59.6) | 5 (4.6) |
| Been satisfying as they enable me to provide a more flexible service as some people prefer not to come into the practice | 3 (2.8) | 9 (8.3) | 24 (22.0) | 61 (56.0) | 12 (11.0) |
| Been valuable to me as they have allowed me to see certain patients quicker as they would have to wait longer to see me face-to-face | 13 (11.9) | 19 (17.4) | 22 (20.2) | 44 (40.4) | 11 (10.1) |
| Been useful for me, at least with patients with acute presentations | 8 (7.3) | 20 (18.3) | 21 (19.3) | 51 (46.8) | 9 (8.3) |
| Been gratifying as they are very popular with patients as many of them are pleased with the digital consultation | 11 (10.1) | 30 (27.5) | 41 (37.6) | 24 (22.0) | 3 (2.8) |
| Allowed me to be more productive than ever at work | 20 (18.3) | 28 (25.7) | 36 (33.0) | 22 (20.2) | 3 (2.8) |
Challenges of remote consultations
Seven challenge themes were measured: isolation, increased workload, anxiety, frustrations and job satisfaction, IT issues, mental strain and physical impacts. The key challenge of remote consultations with the most agreement (81.6%, n = 89) was stress caused by technology not working correctly. This was followed by the challenges linked to frustrations and job satisfaction, where over 60% of respondents agreed that patients are frustrated with remote working and want to be seen face to face (65.2%, n = 47); remote consultations are not as effective as face to face (61.5%, n = 67); and that these types of consultations have removed the enjoyable face-to-face contact (61.4%, n = 67). Results are presented in Table 3.
| Statement | Mean (SD) | Strongly disagree, n (%) | Somewhat disagree, n (%) | Neither agree nor disagree, n (%) | Somewhat agree, n (%) | Strongly agree, n (%) |
|---|---|---|---|---|---|---|
| Isolation | ||||||
| Made me feel quite isolated from the other practice staff | 3.31 (1.18) | 8 (7.3) | 21 (19.3) | 27 (24.8) | 35 (32.1) | 18 (16.5) |
| Caused me to be more disconnected from my patients | 3.39 (1.05) | 4 (3.7) | 22 (20.2) | 23 (21.1) | 47 (43.1) | 13 (11.9) |
| Increased workload | ||||||
| Added to my workload as I have to spend additional time sending out resources to the patient | 3.00 (1.19) | 12 (11.0) | 31 (28.4) | 21 (19.3) | 35 (32.1) | 10 (9.2) |
| Added to my workload because appointments take longer because I have to ask more questions or patients take longer to explain the problem | 3.36 (1.14) | 5 (4.6) | 24 (22.0) | 25 (22.9) | 37 (33.9) | 18 (16.5) |
| Anxiety | ||||||
| Caused me to feel anxiety over missing an important detail about the patient | 3.41 (1.21) | 8 (7.3) | 20 (18.3) | 21 (19.3) | 39 (35.8) | 21 (19.3) |
| Caused me concern over patient privacy | 2.33 (0.92) | 20 (18.3) | 46 (42.2) | 31 (28.4) | 11 (10.1) | 1 (0.9) |
| Frustrations and job satisfaction | ||||||
| Been stressful because patients are frustrated with remote working and want to be seen face to face | 3.68 (1.09) | 3 (2.8) | 17 (15.6) | 18 (16.5) | 45 (41.3) | 26 (23.9) |
| Have removed the enjoyable face-to-face contact that I expected to have with patients as part of my role | 3.74 (1.06) | 2 (1.8) | 13 (11.9) | 27 (24.8) | 36 (33.0) | 31 (28.4) |
| Been frustrating as they are not as effective as face to face | 3.72 (1.05) | 3 (2.8) | 11 (10.1) | 28 (25.7) | 39 (35.8) | 28 (25.7) |
| IT issues | ||||||
| Been stressful when the technology does not work | 4.17 (0.94) | 2 (1.8) | 5 (4.6) | 13 (11.9) | 41 (37.6) | 48 (44.0) |
| Caused extra time pressures contacting patients (e.g. availability or IT issues) | 3.37 (1.08) | 3 (2.8) | 29 (26.6) | 14 (12.8) | 51 (46.8) | 12 (11.0) |
| Mental strain | ||||||
| Increased my mental fatigue as you are either on the phone or on a screen | 3.52 (1.18) | 7 (6.4) | 16 (14.7) | 24 (22.0) | 37 (33.9) | 25 (22.9) |
| Physical impacts | ||||||
| Have caused me to have physical aches and pains from being so desk bound | 3.42 (1.25) | 11 (10.1) | 18 (16.5) | 14 (12.8) | 46 (42.2) | 20 (18.3) |
Stress appraisal of digital consultations
Although respondents did rate the demands of digital consultations to be fairly high [mean 3.45, standard deviation (SD) 1.21], they rated their coping resources to be higher (mean 4.33, SD 0.82), therefore revealing a positive stress appraisal score (mean 0.88, SD 1.63). This positive score suggests that first-contact physiotherapists view digital consultations as a challenge type stress (i.e. their coping resources exceed the required demands) rather than a threat type stress (i.e. the task demands exceeded their coping resources).
Training
Nearly two-thirds (64.2%, n = 70) had not received training and over half (55%, n = 60) were interested in further development, particularly associated with IT and software training and remote assessment guidance. Participants also requested training on how to complete digital consultations in ‘general’ to ensure they can be more effective. Likewise, several references were made to improved communication techniques to ensure effectiveness.
Qualitative component
Participants
A total of 39 (35.8%) FCPs expressed an interest in taking part in an interview; 16 responded to follow-up e-mails and consented to take part in the qualitative component of this study. Interviews lasted for an average of 47.37 minutes (SD 9.29). Table 4 displays their characteristics. The sample was reviewed throughout data collection and considered sufficient when coding resulted in no further development.
| Participant pseudonym | Work location | Description of deprivation area | Consultations that are remote (%) | Remote consultation usage |
|---|---|---|---|---|
| Matt | England | Low | < 25 | Telephone, video and text |
| Justine | England | Low | < 25 | Telephone, video and text |
| Simon | England | High | 25–50 | Telephone, video and text |
| Lorraine | England | Low | < 25 | Telephone, video |
| Grace | England | Middle | > 50 | Telephone, text |
| Anna | Northern Ireland | High | 25–50 | Telephone only |
| Joanne | England | Mixed | < 25 | Telephone only |
| Sally | Scotland | Mixed | < 25 | Telephone, video and text |
| Damian | Scotland | High | < 25 | Telephone, video and text |
| Diane | Wales | Mixed | < 25 | Telephone, video |
| Vanessa | Scotland | Middle | < 25 | Telephone only |
| Lucy | Scotland | Mixed | < 25 | Telephone only |
| Abbie | Scotland | Middle | 25–50 | Telephone only |
| Paul | Northern Ireland | High | 25–50 | Missing data |
| Harriet | England | High | > 50 | Telephone only |
| Maxine | England | High | > 50 | Missing data |
Themes
Five overarching themes were identified through analysis of the interview data.
Theme 1: remote consultations provide logistical benefits to the patient
FCP participants perceived remote consultations as beneficial for the patient rather than for themselves and predominantly for logistical reasons. They were deemed useful for meeting the needs of patients who required flexibility with appointments because of employment, mobility issues, COVID-19 restrictions, holiday or preference for remote consultations:
To me it’s about them, not about me, it’s what suits them, but lots of patients are really happy with a phone consultation because they don’t have to take time off work. They can fit it in, it makes life a lot easier for them in lots of ways.
Grace
Likewise, remote consultations were considered useful for ‘simple’ presentations and for certain stages of the patient pathway, such as follow-up, providing results, sending information on exercises through e-mail and in certain circumstances, screening. However, there was no consistency where in the patient pathway remote consultations should be used, with some FCPs arguing that the first appointment should be face to face and others using the telephone to screen patients first.
Fewer references were made with regard to the benefit of remote consultations for the first-contact physiotherapist. However, some participants did agree that these types of appointments could offer them efficiency when dealing with participants:
They can be timesaving … if I run over, it is not the end of the world for the telephone. I just feel there’s not as much pressure on you with a telephone call, because you don’t have somebody sitting there in the waiting room for their appointment time. It is more efficient, generally.
Joanne
Other participants appreciated the control they experience when conducting remote compared with face-to-face appointments with regard to the ‘flow’ of the conversation and questioning:
I think as a clinician there is some ease in being remote in that you have time … If you have a problem you don’t know the answer to, you can say to somebody I need to go and ring and speak to somebody … It gives me time to go and do those things and come back. So, it’s quite flexible to my needs as a developing FCP.
Harriet
Theme 2: compromised efficacy is the key challenge of remote consultations
Perceived poor efficacy
Poor efficacy was seen as the key challenge of remote consultations. Reasons included: (1) problematic for certain patients; (2) inability to perform tests; (3) likelihood of missing red flags and (4) inability to build rapport.
-
Problematic for certain patients
Remote consultations were considered to be unsuitable for the elderly, people hard of hearing, patients with ‘complex’ presentations, male patients who some considered to be less open on the telephone and patients who were unable to access the phone or video.
-
Inability to perform tests
Participants readily discussed the inability to perform certain diagnostic tests in remote consultations that they used to aid their decision-making, consequently, gaps in clinical reasoning reduced effectiveness in some cases, with the potential for safety issues:
You can’t do any special tests, you can’t test for ligament integrity or you can’t fully assess muscle power remotely, it’s just not possible, it was an educated stab in the dark sometimes and that didn’t feel comfortable at all.
Lucy
-
Likelihood of missing red flags
Nearly all participants cited concerns about missing an important diagnosis or a ‘red flag’ when using remote consultations.
I suppose there’s always that wondering if you’ve missed something sinister and important, when you are taking your patient’s word for it, rather than being able to see anything.
Joanne
Face-to-face consultations were perceived as ‘safer’ and generally leading to more effective outcomes for the patient.
-
Inability to build rapport
Many expressed difficulties in building rapport with the patient with limited non-verbal cues, and therefore gaining patient trust could be compromised. The benefit of ‘therapeutic touch’ was also missed:
They like you to just have a look at things, this therapeutic effect of actually just touching the site of their pain … A patient comes in, they tell you the site of the pain … you put your finger on the exact site of the pain … and they think you’re wonderful because you’ve got the site of the pain.
Damian
Inefficiency
Duplication of appointments was the key reason for inefficiency with many first-contact physiotherapists choosing to bring in their patient for a face-to-face appointment following a telephone or video first appointment due to diagnostic uncertainty. It was also noted that many telephone and video appointments could take more time than a face-to-face appointment, with physiotherapists feeling ‘slowed down’ by IT.
Privacy concerns Patients often attended the consultations in inappropriate locations (e.g. public places such as supermarkets, on public transport, in their workplace):
I have had patients answer the phone and they have had a relative beside them and they are on speaker in the car, and I have tried to explain as part of this consultation I am going to have to ask some potentially sensitive medical questions.
Paul
Patients lack value for remote consultations Some first-contact physiotherapists believed that patients simply did not value the remote consultation to the same extent as a face-to-face appointment. Participants argued that for most patients, face-to-face still seemed to be the preference, with a sense of feeling ‘unseen’ by other health professionals as a result of the COVID-19 pandemic.
Theme 3: unique challenges exist for first-contact physiotherapists working in areas of high deprivation
Participants described a range of additional challenges when working in areas of high socioeconomic deprivation including lack of access to technology, poor digital literacy, language and communication barriers and poor health literacy. Specific coping strategies to deal with these challenges were also identified.
-
Lack of access to technology
Many of these patients did not have an appropriate device or the contact number could frequently change because of families sharing a mobile phone, or did not have an e-mail address, making it impossible to send follow-up information:
There are definitely some of your more deprived patients as well that maybe don’t have wi-fi at home, they’re maybe just picking it up on their mobile data, so again the call quality can be very, very poor. So yes, absolutely, you feel like you’re working at a disadvantage with these patients, it’s an extra level of barriers for them I suppose.
Lucy
-
Poor digital literacy
First-contact physiotherapists explained that ‘digitally literate’ patients in high deprivation areas were ‘very few and far between’. For those patients who did have a smartphone, they were often unsure how to access the camera on the handset and maybe unable to open attachments sent via e-mail.
-
Language and communication barriers
Many participants described the difficulties in remote consultations citing problems with longer appointments and information becoming ‘lost in translation’:
It’s very, very difficult … I think on a phone to interject … it’s going on and on and on and on and forwards and backwards and forwards and backwards between the patient and interpreter, and I think it is it’s much harder on the phone to say stop.
Lucy
-
Poor health literacy
The language barriers described above formed part of the challenge, but reduced engagement also created challenges. There was a belief that lack of engagement contributed to the challenge of low health literacy for patients in areas of high deprivation:
I would say a higher percentage of them [patients in high deprived areas] would probably be easier just to manage in a face-to-face, but I think that there are more complexities to some of those patients and some of those are around expectation of what NHS services can deliver and … I speak to a memorable number of patients through translation services where I’ve had the same conversation week in, week out and referrals have already been made, but those patients’ concerns have just not been answered.
Harriet
Physiotherapists discussed specific strategies that they employed when conducting remote consultations with patients in areas of high deprivation, although their own expectations were different:
You’ve got to have different expectations, I can’t expect the same outcomes, as if I was working in a PCN [primary care network] that has got very good health literacy, it’s not going to be the same.
Simon
Theme 4: digital consultations impact the health and well-being and work satisfaction of first-contact physiotherapists
Participants revealed that remote consultations have impacted their health and well-being and their work satisfaction.
-
Mental health impacts
Mental health impacts included stress and anxiety, and mental strain. As detailed earlier, many first-contact physiotherapists thought that missing red flags was a real likelihood, and in particular for less experienced physiotherapists:
I think that’s where my worry, sometimes, is that there are a lot of people within the role that don’t have enough clinical experience to recognise that. And, probably why a lot of other first-contact physiotherapists get worried about missing red flags, and I think that can play on people from a stress point of view.
Grace
Difficulties with IT, such as poor technology, added to the stress and anxiety:
There probably would be an anxiety kind of thing of are things going to work today, and I guess anxiety in how the patients were going to react to it if it wasn’t working well. Were they going to be upset, were they going to start getting angry, what was their level of expectation and just not having the confidence of being able to potentially manage and de-escalate situations virtually and remotely.
Lucy
Mental strain was also readily experienced as a result of both telephone and video consultations. Descriptions of these types of consultations included ‘mentally demanding’, ‘exhausting’, ‘mental fatigue’ and ‘brain fog’.
Many coping strategies were employed by participants to face these mental health impacts including safety netting, seeking support and using self-reflective techniques.
In addition, different forms of support were sought out by the participants which included from colleagues, peers, GPs, more senior physiotherapists or the practice staff in general. Finally, some participants relied upon self-reflective techniques to address some of their anxiety and stress. This meant acknowledging the level of risk involved in their role and accepting the level of risk:
I guess just trying to be practical about it, trying to absolutely acknowledge how I felt about it which I think is really important and acknowledging to myself you know what, this is how you feel and absolutely it’s completely valid to feel upset about these things, to feel anxious.
Lucy
-
Physical impacts
FCPs noted physical consequences of remote consultations included headaches, eye deterioration, fatigue, hip pain and tension and stiffness in the neck and back. Participants commented that it was not in their nature to be sedentary for long periods of time so particularly struggle with this requirement for these types of consultations.
-
Work dissatisfaction
Participants revealed frustration, isolation, lack of enjoyment and increased workload resulting from remote working. Frustration was raised as a result of patient difficulty describing symptoms or being asking to do inappropriate testing, as this physiotherapist explained:
I remember saying to someone over the telephone with a sprained ankle, can you stand on one foot. It belittles our profession; it totally belittles our profession.
Matt
Participants explained that ‘sitting in front of a screen all day’ was ‘very isolating’ and several physiotherapists experienced this as being separated from both their colleagues and their patients:
There are things that I love about my job, which are the patient contact and seeing that you’re making somebody, even think about changing their behaviour is as much as you can get sometimes. I wouldn’t be satisfied with my job if it was all digital.
Anna
Theme 5: strategies and facilitators improve the efficacy of remote consultations
Strategies directly employed by the first-contact physiotherapist and certain facilitators were both revealed to improve the process of remote consultations.
-
Strategies
Strategies to enhance the efficacy of virtual consultations involved practical, verbal and adaptive techniques. Practical strategies included time scheduling to allow for IT issues. Some practices also offered detailed information to the patient in advance of a consultation to ensure that the patient was familiar with the technology. Some physiotherapists also provided customised videos to patients for their prescribed exercises to assist the patient with their treatment.
Several verbal techniques designed to facilitate a virtual appointment were described by participants. These included ‘mirroring’ of patient’s language and providing and extracting precision descriptions of symptoms and location of pain from patients. Participants also explained that being honest about the limitations with the patient could facilitate remote consultations:
I tend to be up front with them and say, look, I don’t think we’re going to get as much information on the phone but we’ll do our best.
Matt
Likewise, reassurance was also a readily used technique with patients who questioned the virtual appointment and its efficacy:
The key thing I often get is patients will say, well, I don’t know how you can tell me what’s wrong without seeing me. And, I reassure them that over 90% of diagnosis are made by what you say to me, not what I see.
Grace
Finally, some techniques involved more adaptive clinical techniques in response to remote consultations. Several participants described their greater reliance on subjective reasoning believing they could not trust objective reasoning due to the lack of effective hands-on testing.
Generally, some participants explained they needed to learn to trust the patient more with their descriptions and others felt they would seek out more clinical support from either GPs in their practice or more senior physiotherapists.
-
Facilitators
The greater the physiotherapist’s experience, the more confidence they expressed with using remote consultations:
It’s a really, really scary role, I think, clinically, but maybe I’m just a little happier about running through red flags with patients over the phone and having a … I have a low threshold to bringing them in, either with me or a GP if I have any concerns … I can also read through red, herring, red flags, relatively well.
Grace
Previous experience and comfort with IT were also both determinants of a more successful remote consultation. Finally, in contrast to some physiotherapists who had little control over their appointment diaries, those who did have this autonomy observed its positive consequences for remote consultations:
I’m really lucky ... the slots are there but I can squeeze people in for an extra quick check, I can double up somebody if I think that’s what they need. I have a fair amount of autonomy over my diary once it’s opened to me and that doesn’t happen in lots of places.
Anna
Discussion
Findings from this supplementary study, together with the outcomes of the case-study evaluation, enabled a greater insight into FCP provision and how challenges associated with new ways of remote working may be addressed in the future. A strength of this study was the integration of qualitative and quantitative data, which provided further understanding of the challenges and benefits to remote consultation. A full discussion of the implications is integrated into the evaluation findings in Chapter 7; key issues are highlighted below.
From the perspective of the physiotherapist, remote consultations were largely perceived as being beneficial for the patient rather than the physiotherapists themselves in terms of providing them with convenience and flexibility, although there was recognition that some people were frustrated with remote consultations, with a preference for in-person appointments. Both the quantitative and qualitative components reported few benefits of remote consultations to the physiotherapist directly.
Challenges
The survey data revealed IT issues, perceived poor efficacy, anxiety over missing diagnostic details, isolation and increased workload to be key challenges associated with digital consultations. This was certainly supported in the qualitative data, where perceived poor efficacy was revealed as the key challenge, being explained by the likelihood of missing red flags, lacking for certain patients (e.g. the elderly, people with disabilities), inability to perform physical tests and lack of rapport with the patient.
One other notable challenge with the usage of remote consultations revealed in the qualitative data was their inefficiency, supported further in the survey data with the finding of increased workload. Despite one of the aims of the ‘digital first’ approach being to speed up patient traffic, our data revealed that remote consultations resulted in a ‘false efficiency’ through the duplication of appointments and increased appointment times from IT issues.
Impact
The qualitative data revealed impacts on physiotherapists’ mental health (stress and anxiety over missing red flags and dealing with IT issues and mental strain), physical health (e.g. headaches, eye deterioration and back and neck pain) and their work satisfaction (frustration, isolation, lack of enjoyment and increased workload). The survey data, however, revealed that they were viewing remote consultations as a ‘challenge’ (i.e. their coping resources exceed the required demands) rather than as a ‘threat’ (i.e. demands exceed coping resources). Despite the negative impacts to mental and physical health being detailed, physiotherapists were employing ‘problem-focused’ coping strategies (e.g. safety netting, seeking clinical support, regular movement breaks) to manage the challenges.
Strategies, facilitators and training
In addition to coping strategies, other strategies and facilitators were revealed to improve the quality of remote consultations. Techniques included practical, verbal and adaptive techniques (e.g. increasing appointment time, patient reassurance and subjective reasoning) and facilitators included previous experience (as a physiotherapist and with digital methods) and role autonomy. Many of the techniques were self-learnt during the increased use of remote consultations during COVID-19 rather than being taught by the practice or the PCN. The survey data revealed that nearly two-thirds of the physiotherapists had not received training in remote consultations, yet over half were interested in receiving relevant training. However, when prompted in interviews, many first-contact physiotherapists considered the training window for remote consultations to be ‘over’. Regardless, there is a necessity for better training to support physiotherapists to deliver remote consultations, particularly for inexperienced physiotherapists to better prepare them for a hybrid consultation role in primary care.
High socioeconomic deprivation
This study revealed additional challenges for FCPs working with patients living in high socioeconomic deprivation areas including lack of access, poor digital literacy, language and communication barriers, and poor health literacy. A few physiotherapists did attempt to increase their knowledge of patients in high deprivation areas and reached out to charities or community groups; however, most booked a face-to-face appointment to avoid the additional problems.
Limitations
The survey was piloted on only one FCP, and with more extensive piloting may have highlighted further formatting issues that may have increased the response rate and/or quality of the data. Additionally, the response rate was relatively low, so may not have presented a true picture of the communities’ views on remote consultations. It was not the purpose of this study to investigate the patient view of remote consultations, but further work investigating this viewpoint would be beneficial. While the interview numbers were limited, the sample size was monitored throughout to ensure no further development of coding.
Conclusion
Remote consultations posed challenges to first-contact physiotherapists, but their coping strategies and resilience meant that the demands were, on the whole, well managed. Coping levels need to be monitored to ensure that first-contact physiotherapists continue to cope with the demands of the role.
Chapter 6 Case study realist evaluation: a mixed-method study
Reproduced with permission from Walsh et al. 46 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Quantitative
Aim
To conduct a multiple case study site evaluation to determine effectiveness and costs of the FCP model in primary care.
Objectives
-
Empirically test the validated ‘initial programme theories’ arising from WP2 using a series of nationwide case studies at general practice sites.
-
Collect longitudinal cohort data for 6 months from patients attending GP surgeries with MSKDs to determine the impact of FCP (vs. no FCP) clinical outcomes, satisfaction and service use.
-
Analyse implications of models of FCP for healthcare resource use and costs, from the NHS perspective, compared with usual (no FCP) care and assess cost-effectiveness.
-
Present findings regarding effectiveness and contextual factors to help NHS decision makers to commission services that are safe, effective and cost-effective for their areas.
Research questions
-
Does FCP improve patient management over usual GP care? And if so, how?
-
Does FCP show meaningful patient benefit? And if so, how and for whom?
-
Does FCP relieve GP workload pressure?
-
Are there unintended consequences to GP workload that need to be understood?
-
Does FCP promote better use of healthcare resources? If so, how?
-
Does FCP positively affect whole systems MSK practice, If so, how?
-
Are there risks associated with FCP models? If so, what are they and how do they accrue?
Study design
Mixed-method case study realist evaluation. To assess the clinical and cost-effectiveness of FCP service delivery models and non-FCP physiotherapy provision, general practices were recruited from across the UK. We recruited patients within those practices who were actively undergoing physiotherapy management for a current MSKD and collected longitudinal data over a 6-month period. Qualitative interviews were also undertaken with key stakeholders to test initial programme theories.
Ethical approval
Research ethics approval was granted on the 18 June 2019 (IRAS ID: 261530; REC reference number: 19/NI/0108). Health Research Authority (HRA) approval was granted on 25 June 2019.
Methods
Case study sampling and recruitment
Sampling
We required 39 case study sites across the UK, representing key sampling criteria (e.g. geographical location) that were likely to impact on service delivery. Case study sites were categorised into three strands:
-
No FCP service. MSKD management continues with GP consultation, termed GP led
-
Standard FCP with no additional competencies for prescribing and/or injecting, termed FCP standard provision (ST)
-
Service offering a first-contact physiotherapist with additional competencies to prescribe and/or inject, termed FCP additional qualifications (AQ).
To achieve a wide geographical sample, case study sites were selected from England, Wales, Scotland and Northern Ireland with a range of urban and rural environments and deprivation based on GP population postcode deprivation index.
Recruitment
In WP1, we compiled a database of FCP practices who have expressed an interest in participating in this stage of the research and categorised these respondents according to the sampling criteria presented above. We also approached the NIHR local clinical research network to recruit the remaining sites.
All patients who attended a FCP appointment were provided with study recruitment materials by the clinician. Potential participants were encouraged to read the recruitment materials and contact the study team for further information or to express their willingness to participate.
Inclusion criteria
-
Patients consulting with a suspected MSKD episode, defined as any acute or chronic disorder related to the spinal or peripheral musculoskeletal system.
-
Not consulted for the same problem in preceding 3 months.
-
18 years and over.
Exclusion criteria
-
Under 18 years of age.
-
Receiving palliative care for a terminal illness.
-
If non-English speaking and unwilling to provide informed consent and communicate through an interpreter.
For general practices that did not have a FCP model, we provided study information packs to surgeries and requested GPs or reception staff to distribute to individuals consulting with a MSKD based on the preference of the individual practice. Some practices requested a recruitment method using the practice database each week to identify attendees who were then distributed the same study materials.
On receipt of the consent form, the baseline health economics questionnaire [Client Services Receipt Inventory (CSRI); see Appendix 4] was completed over the telephone. Information collected included the nature and duration of the musculoskeletal condition and associated service use in the previous 3 months, employment status and days off work or ability to perform usual activities. An outcome measure pack was then posted to participants for immediate completion.
Sample size
The aim of this research was to determine that FCP is not substantially worse (non-inferiority analysis) than GP-based practice. For the purpose of assay sensitivity, the study was designed as a three-arm design, which includes usual GP care, FCP(ST) and FCP(AQ). This sample size computation also accounted for the similarities of patients within each GP centre and treated each GP centre as a cluster within which patients are nested.
Based on Bishop et al. ,21 a non-inferiority margin of two units in Short Form questionnaire-36 items (SF-36) scale, that is the standard practice is either superior or worse no more than by two unit is assumed. Previous research in MSKD, such as Angst et al. ,47 has estimated a minimal clinically important difference from 4 points for the SF-36 PCS subscale. The SD of the difference between the SF-36 score between models was 6.5 based on Salisbury et al. 48 In a one-sided 0.05 significance non-inferior hypothesis test, to achieve 80% power, 132 subjects were required. To account for the hierarchical nature of the design, that is patients are nested within GP centres, this number was inflated by the design effect.
The design effect for a cluster size of 14 and an intracluster correlation coefficient of 0.007515 was 1.09, requiring a total sample size to 145 per arm. After allowing for attrition of 20%, the total subjects required per arm is increased up to 181, making the total of at least 13 GP centres per arm, and a per practice sample size of approximately 14.
Recruitment to the study was impacted by COVID-19, so recruitment figures were revisited in relation to attrition rates (running at 5%) and eventual number of recruited sites, extended due to recruitment challenges (n = 46). Targets were thus reviewed indicating that the total subjects required per arm was reduced to 154, requiring a total sample size of 462.
In the analysis, GP centres were intended to be included as a random effect in a general linear mixed model to account for similarity of patients within each GP centre. The sample size computation was performed using a combination of nQuery 8 (Statistical Solutions, Saugus, MA, USA) and SAS® version 9.4 software (SAS Institute Inc., Cary, NC, USA).
Assessment points
Data were collected from participants at the time points indicated in Table 5. Respondents who returned incomplete questionnaires were sent telephone/e-mail reminders. On completion of the 6-month outcome data, patients were sent a £10 voucher to thank them for their participation in the study.
| Patient-reported outcome measure | Measurement domain | Assessment points (months) | Direction of improvement |
|---|---|---|---|
| Primary outcome measure | |||
| SF-36 physical component summary49 | Physical function | 0, 3, 6 | Higher |
| Secondary outcome measures | |||
| SF-36 mental component summary49 | Mental health | 0, 3, 6 | Higher |
| EQ-5D-5L profile measure and visual analogue scale50 | Health-related quality of life | 0, 3, 6 | Higher |
| Roland–Morris disability questionnaire51 | Health status for low back pain | 0, 3, 6 (patients with lower-back pain only) | Lower |
| Musculoskeletal health questionnaire52 | Musculoskeletal symptoms | 0, 3, 6 | Higher |
| General practice assessment questionnaire53 | Satisfaction with receptionists, appointments, opening times, communication with healthcare staff, continuity of care and enablement | 0 | Higher |
| Client services receipt inventory54 | Healthcare utilisation | 0, 3, 6 | Not applicable |
| Return to work (self-report of absenteeism/change of work practices due to MSKD) | Function | 0, 3, 6 | Not applicable |
| Patient-Reported Experiences and Outcomes of Safety in Primary Care55 | Patient-reported safety in primary care | 0, 3, 6 | Higher |
Patient-reported outcome measures
Quantitative analysis
Primary outcome analysis
The change in SF-36 PCS from baseline to 3 months and from baseline to 6 months was compared between the three service models using a one-way analysis of variance. If a significant difference was seen, post hoc unpaired t-tests comparing each pair of service models was performed to determine the superior service model(s). Further comparisons of the three service models were undertaken in the context of stepwise linear regression modelling, incorporating the demographic and clinical features of the patients, including their baseline SF-36 PCS. Dummy variables were constructed to represent individual sites as required. Regression analyses considered multilevel modelling in the form of a general linear mixed model with site as a random effect.
Secondary outcomes analysis
The change in SF-36 mental health score, musculoskeletal health questionnaire and in EuroQol-5 Dimensions, five-level version (EQ-5D-5L) health-related quality of life from baseline to 3 months and from baseline to 6 months was compared between the three service models using a one-way analysis of variance. If a significant difference was seen, post hoc unpaired t-tests comparing each pair of service models was performed to determine the superior service model(s). A similar analysis was performed for the Roland–Morris disability questionnaire score, for patients with lower-back pain only, owing to the high prevalence and consultation rates for this disorder. For each of the three service models, the proportion of off work patients at baseline who reported having returned to work at 6 months was compared using a chi-square test.
Costs analysis
Comparisons of costs between the three service models was performed using appropriate statistical tests (according to the distributions of the relevant cost variables).
Health economics analysis
A patient-level analysis of outcomes and costs for the sample of patients with musculoskeletal conditions recruited to the study was undertaken. A customised version of the CSRI (see Appendix 4)48 was used to gather data retrospectively from participants on service use related to the musculoskeletal condition in the previous 3 months covering primary, community and hospital use, voluntary and informal care received, medications by prescription and devices purchased over the counter, access to private providers or the complementary medicine sector and out-of-pocket expenditures. The CSRI data were gathered by telephone interview at baseline (0 months), 3 and 6 months. Participants were also asked about time off work or inability to undertake usual activities during these telephone interviews.
The analysis of the individual patient-level data was undertaken through the application of a cost-effectiveness framework, with reference to the primary outcome, SF-36 PCS and to health-related quality of life measures (EQ-5D-5L). Adjustments were made for any baseline variations in patient characteristics. Differences identified between service models with regard to costs and/or health outcomes were explored, where possible, by an appropriate regression analysis. The base-case economic analysis adopted a direct NHS resource use cost perspective. The societal perspective was incorporated through the consideration of self-reported time off work. Participant reported out-of-pocket expenditures were also included to provide a private perspective. The full range of outcomes were also considered in a broader cost consequences framework.
Results
Recruitment
A total of 426 participants were recruited to the study. There were 110 (25.8%) from service model GP, 124 (29.1%) from service FCP(ST) and 192 (45.1%) from service model FCP(AQ). A total of 46 general practices were involved: 13 GP (with 1, 2, 2, 5, 6, 6, 7, 10, 11, 14, 14, 15 and 17 participants), 15 FCP(ST) (with 1, 3, 3, 3, 4, 4, 5, 7, 7, 9, 9, 14, 15, 17 and 23 participants) and 18 FCP(AQ) (with 1, 1, 4, 4, 6, 8, 8, 9, 11, 12, 14, 15, 15, 16, 16, 16, 17 and 19 participants).
Participating practice overview
Practices provided data regarding their patient population (including gender and predominant age ranges, and ethnic mix) and deprivation deciles. Deprivation data from Northern Ireland were provided as a geographical national ranking rather than based on deciles reported in England, Scotland and Wales.
A broad range of participating practices were recruited, representing different patient population size, ethnicity, deprivation and geographical location (Table 6). Descriptive summaries of each arm have been provided to prevent potential identification at individual practice level.
| Arm | Location | Deprivation decile | Population | Ethnicity |
|---|---|---|---|---|
| GP (n = 13) | Urban: 9/13 (69.2%) | Median: 7 | Mean: 12,600 | Mean percentage: 3.8% Asian, 1.6% mixed, 1.2% black, 0.5% other non-white (remaining 93.1% white groups) |
| Range: 1–10 | Range: 2800–31,000 | |||
| FCP(ST) (n = 15) | Urban: 12/15 (80.0%) | Median: 8 | Mean: 19,500 | Mean percentage: 2.4% Asian, 1.1% mixed, 0.8% black, 0.9% other non-white (remaining 94.8% white groups) |
| Range: 1–10 | Range: 4600–55,000 | |||
| FCP(AQ) (n = 18) | Urban: 13/18 (72.2%) | Median: 6.5 | Mean: 11,700 | Mean percentage: 1.7% Asian, 0.6% mixed, 0.1% black, 0.8% other non-white (remaining 96.8% white groups) |
| Range: 1–10 | Range: 5000–35,000 |
Participant demographics
All participants completed a baseline patient-reported outcome measure (PROM), which contained demographic data: gender, date of birth (giving age at baseline), ethnicity and highest level of education. The first baseline PROM was completed on 11 December 2019 and the last on 26 April 2022 (recruitment to the study was temporarily paused in 2020 due to the COVID-19 pandemic and recommenced according to national guidelines). Baseline features are summarised in Table 7, including employment at baseline CSRI. No statistically significant differences were found between the three service models for age, gender, highest level of education or employment status.
| Demographic feature | Total participants (N = 426) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Test | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | Minimum | Maximum | n | Mean | SD | Minimum | Maximum | n | Mean | SD | Minimum | Maximum | n | Mean | SD | Minimum | Maximum | ANOVA | |
| Age (years) | 425a | 63.0 | 13.2 | 21.1 | 94.1 | 109a | 63.2 | 13.3 | 21.5 | 89.9 | 124 | 63.1 | 12.8 | 21.1 | 83.6 | 192 | 62.8 | 13.4 | 24.5 | 94.1 | p = 0.962 |
| N | n | % | N | n | % | N | n | % | N | n | % | Chi-square | |||||||||
| Gender | |||||||||||||||||||||
| Male | 425 | 145 | 34.1 | 110 | 37 | 33.6 | 123 | 41 | 33.3 | 192 | 67 | 34.9 | p = 0.953 | ||||||||
| Ethnic group | |||||||||||||||||||||
| White | 417 | 408 | 97.8 | 107 | 106 | 99.1 | 122 | 116 | 95.1 | 188 | 186 | 98.9 | n/ab | ||||||||
| Education | 410 | 108 | 119 | 183 | Kruskal–Wallis | ||||||||||||||||
| Primary/secondary | 101 | 24.6 | 26 | 24.1 | 29 | 24.4 | 46 | 25.1 | p = 0.512 | ||||||||||||
| Further education | 179 | 43.7 | 51 | 47.2 | 57 | 47.9 | 71 | 38.8 | |||||||||||||
| Associate degree | 12 | 2.9 | 4 | 3.7 | 4 | 3.4 | 4 | 2.2 | |||||||||||||
| Bachelor’s degree | 70 | 17.1 | 18 | 16.7 | 16 | 13.4 | 36 | 19.7 | |||||||||||||
| Master’s degree | 24 | 5.9 | 6 | 5.6 | 6 | 5.0 | 12 | 6 | |||||||||||||
| Professional degree | 20 | 4.9 | 3 | 2.8 | 5 | 4.2 | 12 | 6.6 | |||||||||||||
| Doctorate | 4 | 1.0 | 0 | 0.0 | 2 | 1.7 | 2 | 1.1 | |||||||||||||
| Employment status | 418 | 108 | 121 | 189 | Chi-square | ||||||||||||||||
| Employed full-time | 109 | 26.1 | 26 | 24.1 | 31 | 25.6 | 52 | 27.5 | p = 0.749 | ||||||||||||
| Employed part-time | 68 | 16.3 | 19 | 17.6 | 24 | 19.8 | 25 | 13.2 | |||||||||||||
| Voluntary worker/unemployed and seeking work/Homemaker/carer | 40 | 9.6 | 9 | 8.3 | 13 | 10.7 | 18 | 9.5 | |||||||||||||
| Retired | 201 | 48.1 | 54 | 50.0 | 53 | 43.8 | 94 | 49.7 | |||||||||||||
Participant clinical features
In addition, up to two key MSKD areas were identified in relation to the current presentation at the GP surgery. In particular, it was noted whether or not lower-back pain was involved, given the previously reported high incidence of consultations for lower-back pain within primary care. 3 Further clinical data were collected in the PROM baseline questionnaire in the form of: the SF-36 health survey version 1.0, the EQ-5D-5L health questionnaire, the Musculoskeletal Health Questionnaire (MSK-HQ), the Roland–Morris Disability Questionnaire (collected only from those with back pain), the Patient Reported Experiences and Outcomes of Safety in Primary Care (PREOS-PC) Short Form on healthcare safety, the General Practice Assessment Questionnaire (GPAQ) and the Keele STarT MSK Stratification Tool® (Keele University, Keele, UK; baseline only).
Summary statistics of these clinical features for the 426 participants are presented in Table 8. Along each row, N indicates the total number of participants for whom information on the relevant clinical feature was available within each service model. For the key item of lower back pain (‘MSKD area included BACK’), n indicates the number of participants identified as having this condition within each service model; and, similarly, in the lower portion of the table for the PREOS-PC negative impact on health question (had a health problem that was caused, or made worse, by the health care received in GP surgery in past 12 months). For the STarT-MSK Risk question and the other PREOS-PC questions (all of which have ordinal response scales), response numbers for each category on the scale are indicated by n. For the remaining clinical features, all scored on a linear scale, summary statistics are given as mean with SD, minimum and maximum, with the exception of the PREOS-PC safety score, which is expressed as a median with interquartile range (IQR), owing to being heavily skewed towards the maximum score of 10 (‘completely safe’).
| Clinical feature | ALL participants (N = 426) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Comparison test | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | N | n | % | N | n | % | Chi-square | |||||||||
| MSKD area included BACK | 426 | 106 | 24.9 | 110 | 20 | 18.2 | 124 | 33 | 26.6 | 192 | 53 | 27.6 | p = 0.165 | ||||||||
| N | Mean | SD | Minimum | Maximum | N | Mean | SD | Minimum | Maximum | N | Mean | SD | Minimum | Maximum | N | Mean | SD | Minimum | Maximum | ANOVA | |
| SF-36: PCS | 403 | 35.6 | 10.5 | 10.2 | 62.3 | 103 | 35.3 | 9.3 | 15.7 | 55.7 | 118 | 36.8 | 10.2 | 12.6 | 57.0 | 182 | 35.0 | 11.3 | 10.2 | 62.3 | p = 0.338 |
| SF-36: MCS | 403 | 49.1 | 10.9 | 13.7 | 69.4 | 103 | 47.0 | 12.4 | 13.7 | 64.7 | 118 | 50.5 | 10.1 | 21.0 | 69.3 | 182 | 49.4 | 10.4 | 20.4 | 69.4 | p = 0.051 |
| EQ-5D-5L Score (England)a | 423 | 0.709 | 0.230 | −0.281 | 1.000 | 109 | 0.683 | 0.262 | −0.281 | 1.000 | 123 | 0.749 | 0.183 | 0.210 | 1.000 | 191 | 0.698 | 0.235 | −0.241 | 1.000 | p = 0.062 |
| EQ-5D-5L VAS | 422 | 68.8 | 19.3 | 0 | 100 | 109 | 66.7 | 20.0 | 15 | 95 | 122 | 72.6 | 17.3 | 10 | 100 | 191 | 67.6 | 19.9 | 0 | 100 | p = 0.036 |
| MSK-HQ Total | 414 | 33.8 | 10.4 | 5 | 54 | 106 | 32.1 | 10.2 | 8 | 53 | 123 | 35.5 | 9.2 | 9 | 54 | 185 | 33.5 | 11.1 | 5 | 54 | p = 0.044 |
| MSK-HQ Physical activity | 421 | 2.7 | 2.4 | 0 | 7 | 109 | 2.39 | 2.31 | 0 | 7 | 123 | 3.01 | 2.46 | 0 | 7 | 189 | 2.71 | 2.42 | 0 | 7 | p = 0.145 |
| Roland–Morrisb | 98 | 9.4 | 6.1 | 0 | 24 | 18 | 11.2 | 5.8 | 1 | 20 | 32 | 8.2 | 5.9 | 1 | 21 | 48 | 9.5 | 6.4 | 0 | 24 | p = 0.253 |
| STarT MSK pain intensity [0–10 (worst)] | 401 | 6.3 | 2.3 | 0 | 10 | 105 | 6.4 | 2.3 | 1 | 10 | 117 | 6.1 | 2.2 | 0 | 10 | 179 | 6.4 | 2.3 | 0 | 10 | p = 0.441 |
| STarT MSK risk | 105 | 116 | 180 | p = 0.129 | |||||||||||||||||
| Low | 15 | 14.3 | 33 | 28.4 | 38 | 21.1 | |||||||||||||||
| Medium | 63 | 60.0 | 58 | 50.0 | 96 | 53.3 | |||||||||||||||
| High | 27 | 25.7 | 25 | 21.6 | 46 | 24.4 | |||||||||||||||
| Baseline characteristics continue below | |||||||||||||||||||||
| PREOS-PC: question 1 | 360 | 98 | 101 | 161 | p = 0.498 | ||||||||||||||||
| Always | 110 | 25.8 | 30 | 30.6 | 30 | 29.7 | 50 | 31.1 | |||||||||||||
| Often | 69 | 16.2 | 23 | 23.5 | 20 | 19.8 | 26 | 16.1 | |||||||||||||
| Sometimes | 69 | 16.2 | 20 | 20.4 | 20 | 19.8 | 29 | 18.0 | |||||||||||||
| Rarely | 64 | 15.0 | 17 | 17.3 | 18 | 17.8 | 29 | 18.0 | |||||||||||||
| Never | 48 | 11.3 | 8 | 8.2 | 13 | 12.9 | 27 | 16.8 | |||||||||||||
| PREOS-PC: question 2 | 327 | 85 | 92 | 150 | p = 0.738 | ||||||||||||||||
| Always | 57 | 13.4 | 14 | 16.5 | 17 | 18.5 | 26 | 17.3 | |||||||||||||
| Often | 28 | 6.6 | 6 | 7.1 | 10 | 10.9 | 12 | 8.0 | |||||||||||||
| Sometimes | 51 | 12.0 | 11 | 12.9 | 14 | 15.2 | 26 | 17.3 | |||||||||||||
| Rarely | 48 | 11.3 | 16 | 18.8 | 13 | 14.1 | 19 | 12.7 | |||||||||||||
| Never | 143 | 33.6 | 38 | 44.7 | 38 | 41.3 | 67 | 44.7 | |||||||||||||
| PREOS-PC: question 3 | 353 | 95 | 96 | 162 | p = 0.589 | ||||||||||||||||
| Always | 16 | 3.8 | 0 | 0.0 | 5 | 5.2 | 11 | 6.8 | |||||||||||||
| Often | 35 | 8.2 | 5 | 5.3 | 7 | 7.3 | 23 | 14.2 | |||||||||||||
| Sometimes | 68 | 16.0 | 24 | 25.3 | 20 | 20.8 | 24 | 14.8 | |||||||||||||
| Rarely | 50 | 11.7 | 18 | 18.9 | 12 | 12.5 | 20 | 12.3 | |||||||||||||
| Never | 184 | 43.2 | 48 | 50.5 | 52 | 54.2 | 84 | 51.9 | |||||||||||||
| PREOS-PC: question 4 yes | 411 | 42 | 9.9 | 105 | 8 | 7.6 | 119 | 13 | 10.9 | 187 | 21 | 11.2 | p = 0.593 | ||||||||
| N | Median | IQR | N | Median | IQR | N | Median | IQR | N | Median | IQR | Kruskal–Wallis | |||||||||
| PREOS-PC: safety (scale 0–10 best) | 408 | 9 | 8–10 | 106 | 9 | 8–10 | 115 | 9 | 8–10 | 187 | 9 | 7–10 | p = 0.821 | ||||||||
With regard to these clinical assessments, no statistically significant differences were found between the three service models at baseline, with the exception of for EQ-5D-5L visual analogue scale (VAS) (where a significantly better state of health was reported in service model FCP) and for MSK-HQ total (where a more desirable musculoskeletal status was indicated in service model FCP).
Baseline experience of primary care consultations
At baseline only, the GPAQ-R2 was administered. This contains three questions relating to preferences in the way appointments are booked, which can be deemed to be demographic/personal features, together with 21 other questions encompassing three domains: ‘Healthcare professional aspects at the visit’, ‘Reception staff and appointments’ and ‘Overall performance’, which can be deemed to be outcomes from the baseline attendance at the GP surgery. Consequently, these are separated out in the top and bottom of Table 9.
| GPAQ-R2 appointment aspect | All GP practices (N = 426 participants) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Comparison test | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Booking time | N | n | % | N | n | % | N | n | % | N | n | % | Chi-square |
| CSRI baseline | N | Median | IQR | N | Median | IQR | N | Median | IQR | N | Median | IQR | Kruskal–Wallis |
| GPAQ-R2 domain | N | Median | IQR | N | Median | IQR | N | Median | IQR | N | Median | IQR | Kruskal–Wallis |
| Important to be able to book appointments ahead of time: Yes | 402 | 336 | 83.6 | 104 | 85 | 81.7 | 118 | 104 | 88.1 | 180 | 147 | 81.7 | p = 0.283 |
| Practice booking format | |||||||||||||
| Normally book in person | 411 | 54 | 13.1 | 106 | 14 | 13.2 | 122 | 20 | 16.4 | 183 | 20 | 10.9 | p = 0.384 |
| Normally book by telephone | 411 | 387 | 94.2 | 106 | 100 | 94.3 | 122 | 116 | 95.1 | 183 | 171 | 93.4 | p = 0.833 |
| Normally book online | 411 | 69 | 16.8 | 106 | 17 | 16.0 | 122 | 26 | 21.3 | 183 | 26 | 14.2 | p = 0.259 |
| Preferred booking format | |||||||||||||
| Prefer to book in person | 412 | 107 | 26.0 | 107 | 20 | 18.7 | 122 | 33 | 27.0 | 183 | 54 | 29.5 | p = 0.122 |
| Prefer to book by telephone | 412 | 321 | 77.9 | 107 | 88 | 82.2 | 122 | 96 | 78.7 | 183 | 137 | 74.9 | p = 0.333 |
| Prefer to book online | 412 | 184 | 44.7 | 107 | 43 | 40.2 | 122 | 58 | 47.5 | 183 | 83 | 45.4 | p = 0.519 |
| Days to get an appointment | 379 | 6.0 | 2.0–14.0 | 91 | 7.0 | 2.0–20.0 | 107 | 5.0 | 2.0–10.0 | 181 | 7.0 | 2.0–14.0 | p = 0.142 |
| The visita | 411 | 93.2 | 79.5–100.0 | 107 | 88.6 | 70.5–100.0 | 121 | 95.5 | 84.1–100.0 | 183 | 93.2 | 79.5–100.0 | p = 0.014 |
| Reception staff and appointmentsb | 400 | 62.5 | 41.7–81.7 | 105 | 70.0 | 47.5–83.3 | 117 | 58.3 | 39.6–83.3 | 178 | 61.1 | 37.5–78.1 | p = 0.052 |
| Overall performancec | 407 | 80.0 | 55.0–95.0 | 107 | 85.0 | 60.0–100.0 | 117 | 85.0 | 60.0–95.0 | 183 | 80.0 | 50.0–95.0 | p = 0.247 |
In Table 9, N indicates the number of participants for whom information on the relevant appointment aspect was available in each service model category. At the top of the table, n indicates the corresponding number of participants eliciting an affirmative response, while at the bottom, summary statistics in the form of median with IQR are shown for the continuous main assessment outcome domain scores in each service model category.
The waiting time for an appointment (collected at the baseline CSRI) is presented (also as median with IQR) in the middle of the GPAQ-R2 summary statistics as it pertains to the appointment.
No statistically significant differences were found between the three service models in relation to aspects of appointment preferences, nor for waiting time to obtain an appointment. Note that, although the FCP(ST) exhibited a lower median number of days, this was still not statistically significant when compared with the waiting time in either the GP or the FCP(AQ) models.
In terms of the three main assessment outcome domains, no statistically significant differences were found between the three service models except for ‘the visit’ domain, where a significantly higher (i.e. better) overall outcome score was reported in service models FCP(ST) and FCP(AQ). However, although the null hypothesis of no difference between the three service models was (marginally; p = 0.052) upheld for the ‘reception staff and appointments’ domain, there was found to be a statistically significant difference between GP and FCP(AQ), with GPs exhibiting higher (better) overall outcome scores.
See Appendix 5 for the breakdown of each GPAQ-R2 question responses by service model, and in total.
Participant retention
Of the 426 participants, 27 (6.3%) were lost to follow-up before 3 months. A further 8 (1.9%) were lost to follow-up after 3 months and before 6 months. There were four (0.9%) participants who only contributed PROM data at 6 months in addition to PROM and CSRI baseline data. The remaining 377 (88.5%) returned data at all three time points (baseline, 3 and 6 months), including 320 (75.1%) who completed both PROM and CSRI data at each time point. A full breakdown is shown in Appendix 6, indicating the number of participants who elicited each of the many possible combinations of data for the two data sources across the three time points.
Inspecting the service models associated with the 35 participants in the first five rows who delivered no data at 6 months and who were deemed to have dropped out, there were 9 among the 110 service model GP participants (8.2%), 7 among the 124 service model FCP(ST) participants (5.6%) and 19 among the 192 service model FCP(AQ) participants (9.9%). There was no statistically significant difference between these three drop-out rate percentages (chi-square test: p = 0.405).
For information, summary statistics on times from baseline to 3 months and from baseline to 6 months are shown at the foot of the table in Appendix 6.
Benefits and status change
Data relating to benefits were collected via the CSRI at baseline, 3 and 6 months, although there was very little reported provision of benefits. Appendix 7, Table 20 shows the prevalence of different benefits being received at baseline. In addition, the incidence rate is shown for when absence from work was covered by certification at baseline. Appendix 7, Tables 21 and 22 show very little change in circumstances over the observation period of 6 months and, consequently, no statistically significant differences between the three service models.
Primary outcome and secondary outcomes (excluding healthcare service use) comparisons
The primary outcome variable was the change in SF-36 PCS from baseline to 3 months and from baseline to 6 months. The results of the comparison of the three service models for this variable and the PROM-derived secondary outcome variables are shown in the ‘Change: comparison test’ column in Table 10.
| Primary outcome | Time point | Total participants (N = 426) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Change: comparison test | Improved: comparison test | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Months | N | Improved n (%) | Change mean | Change SD | Change range | N | Improved n (%) | Change mean | Change SD | Change range | N | Improved n (%) | Change mean | Change SD | Change range | N | Improved n (%) | Change mean | Change SD | Change range | ANOVA | Chi-square | |
| SF-36: PCS | 3 | 336 | 219 (65.2) | 2.72 | 8.42 | −32.27 to 36.28 | 86 | 47 (54.7) | 1.87 | 8.18 | −17.82 to 27.73 | 98 | 71 (72.4) | 3.69 | 8.05 | −15.19 to 23.70 | 152 | 101 (66.4) | 2.58 | 8.78 | −32.27 to 36.28 | p = 0.332 | p = 0.037a |
| 6 | 348 | 234 (67.2) | 4.15 | 9.78 | −38.86 to 35.54 | 89 | 57 (64.0) | 4.12 | 9.70 | −28.67 to 29.06 | 107 | 75 (70.1) | 4.18 | 8.98 | −20.90 to 27.00 | 152 | 102 (67.1) | 4.15 | 10.42 | −38.36 to 35.54 | p = 0.999 | p = 0.667 | |
| Secondary outcome | |||||||||||||||||||||||
| SF-36: MCS | 3 | 336 | 160 (47.6) | −0.14 | 8.25 | −24.14 to 27.52 | 86 | 46 (53.5) | 0.68 | 8.50 | −23.07 to 26.30 | 98 | 43 (43.9) | −0.23 | 8.07 | −24.14 to 27.52 | 152 | 71 (46.7) | −0.54 | 8.23 | −23.84 to 17.52 | p = 0.542 | p = 0.409 |
| 6 | 348 | 170 (48.9) | −0.43 | 8.78 | −32.12 to 32.59 | 89 | 46 (51.7) | 0.66 | 10.31 | −32.12 to 32.59 | 107 | 50 (46.7) | −1.05 | 7.93 | −24.15 to 16.66 | 152 | 74 (48.7) | −0.64 | 8.37 | −28.94 to 23.54 | p = 0.370 | p = 0.786 | |
| EQ-5D-5L score (England)b | 3 | 362 | 185 (51.1) | 0.0347 | 0.1662 | −0.656 to 0.897 | 96 | 44 (45.8) | 0.0370 | 0.1712 | −0.400 to 0.897 | 102 | 56 (54.9) | 0.0350 | 0.1549 | −0.350 to 0.519 | 164 | 85 (51.8) | 0.0331 | 0.1710 | −0.656 to 0.732 | p = 0.984 | p = 0.429 |
| 6 | 376 | 229 (60.9) | 0.0483 | 0.1639 | −0.525 to 0.897 | 95 | 56 (58.9) | 0.0480 | 0.1793 | −0.508 to 0.897 | 113 | 70 (61.9) | 0.0370 | 0.1463 | −0.525 to 0.519 | 168 | 103 (61.3) | 0.0561 | 0.1665 | −0.398 to 0.790 | p = 0.630 | p = 0.898 | |
| EQ-5D-5L VAS | 3 | 361 | 170 (47.1) | 0.96 | 14.01 | −55 to 70 | 96 | 42 (43.8) | 0.58 | 16.75 | −55 to 70 | 99 | 48 (48.5) | 1.49 | 11.99 | −35 to 45 | 166 | 80 (48.2) | 0.85 | 13.46 | −50 to 40 | p = 0.895 | p = 0.745 |
| 6 | 371 | 169 (45.6) | 0.50 | 16.94 | −67 to 76 | 94 | 40 (42.6) | 0.82 | 19.19 | −55 to 76 | 111 | 46 (41.4) | −1.05 | 15.70 | −67 to 55 | 166 | 83 (50.0) | 1.36 | 16.42 | −65 to 55 | p = 0.501 | p = 0.298 | |
| PREOS-PC Q5 [0 to 10 (best)] | 3 | 337 | 87 (25.8) | −0.09 | 1.74 | −9 to 6 | 90 | 21 (23.3) | −0.06 | 1.59 | −6 to 4 | 91 | 24 (26.4) | −0.26 | 2.17 | −9 to 6 | 156 | 42 (26.9) | −0.01 | 1.52 | −7 to 5 | p = 0.535 | p = 0.817 |
| 6 | 348 | 84 (24.1) | −0.22 | 1.89 | −8 to 5 | 90 | 22 (24.4) | −0.14 | 1.52 | −5 to 4 | 101 | 32 (31.7) | −0.18 | 2.22 | −8 to 5 | 157 | 30 (19.1) | −0.29 | 1.97 | −7 to 5 | p = 0.825 | p = 0.070 | |
| MSK-HQ total | 3 | 356 | 232 (65.2) | 3.29 | 8.05 | −25 to 32 | 93 | 58 (62.4) | 2.66 | 7.89 | −24 to 32 | 102 | 67 (65.7) | 3.61 | 7.98 | −14 to 30 | 161 | 107 (66.5) | 3.47 | 8.22 | −25 to 26 | p = 0.667 | p = 0.798 |
| 6 | 367 | 256 (69.8) | 4.78 | 8.67 | −23 to 34 | 92 | 68 (73.9) | 5.22 | 8.29 | −23 to 34 | 113 | 74 (65.5) | 4.78 | 8.86 | −18 to 32 | 162 | 114 (70.4) | 4.52 | 8.80 | −21 to 26 | p = 0.830 | p = 0.415 | |
| MSK-HQ physical | 3 | 362 | 118 (32.6) | 0.03 | 2.13 | −7 to 7 | 96 | 25 (26.0) | −0.10 | 2.11 | −7 to 7 | 102 | 34 (33.3) | −0.07 | 2.05 | −7 to 5 | 164 | 59 (36.0) | 0.17 | 2.20 | −7 to 7 | p = 0.520 | p = 0.252 |
| 6 | 371 | 125 (33.7) | 0.13 | 2.19 | −7 to 7 | 94 | 21 (22.3) | −0.09 | 1.99 | −5 to 7 | 112 | 46 (41.1) | 0.29 | 2.03 | −5 to 7 | 165 | 58 (35.2) | 0.15 | 2.40 | −7 to 7 | p = 0.462 | p = 0.016a | |
| Roland–Morrisc | 3 | 72 | 38 (52.8) | −1.36 | 3.42 | −10 to 6 | 11 | 5 (45.5) | −1.09 | 3.18 | −7 to 3 | 23 | 11 (47.8) | −1.17 | 3.96 | −10 to 6 | 38 | 22 (57.9) | −1.55 | 3.20 | −7 to 4 | p = 0.882 | p = 0.650 |
| 6 | 73 | 44 (60.3) | −1.95 | 3.72 | −10 to 8 | 13 | 10 (76.9) | −2.62 | 2.72 | −9 to 1 | 25 | 12 (48.0) | −1.20 | 4.31 | −10 to 8 | 35 | 22 (62.9) | −2.23 | 3.59 | −10 to 4 | p = 0.449 | p = 0.204 | |
In an unadjusted analysis, no statistically significant difference was found between the three service models and the nominated primary outcome variable, notably at 6 months where p = 0.999.
For information, the number and percentage of participants who improved (as opposed to delivering the same or a worse outcome score at 3 or 6 months as compared to baseline) is also displayed. Note that certain secondary outcomes have restricted scoring scales, so the number staying the same was considerable, for example, PREOS PC-Q5 (11-point scale: 0–10) and MSK-HQ physical (8-point scale: 0–7 days).
No statistically significant differences were detected using this two-way simplification of change in score, except for change in SF-36 PCS at 3 months (where a higher proportion of improved participants was seen in the FCP(ST) service model in comparison with the GP and FCP(AQ) service models) and for change in MSK-HQ physical activity level at 6 months [where once again a higher proportion of improved participants was seen in the FCP(ST) service model in comparison with the GP and FCP(AQ) service models; see ‘Improved: comparison test’ column in Table 10].
In an adjusted analysis, the three service models were compared in greater depth for the primary outcome change in SF-36 PCS (3 months – baseline) and for the primary outcome change in SF-36 PCS (6 months – baseline) using stepwise linear regression modelling. The following were nominated as predictors:
-
GP practice status: service model, in the form of a dummy variable for FCP and a dummy variable for FCP(AQ).
-
Demographic participant features: gender (male: yes/no), age in years at baseline, ethnic origin (white: yes/no), education (none beyond secondary school: yes/no and university educated: yes/no), employment status at baseline (full-time: yes/no and full-time or part-time: yes/no).
-
Clinical participant features: baseline SF-36 PCS, MSKD area at baseline included back (yes/no), MSKD area at baseline included knee or leg or hip or foot or ankle (yes/no), and whether the presented MSK condition had affected employment or ability to perform usual activities (yes/no) as reported at baseline.
Note that with the eventual inclusion of 46 general practices (including 4 with only 1 participant) instead of the intended 14 practices across the three service models, it was not feasible to include individual sites into the regression modelling process. Similarly, the possibility of multilevel modelling was also eliminated.
Backwards stepwise linear regression, with rerunning of the final model to include additional participants for whom data were missing only for non-significant predictors, led to the following model (with R2 = 0.112 and n = 321; see Appendix 8, Tables 1 and 2 for full details) for change in SF-36 PCS at 3 months:
Backwards stepwise linear regression, with rerunning of the final model to include additional participants for whom data were missing only for non-significant predictors, led to the following model (with R2 = 0.138 and n = 332; see Appendix 8, Tables 1 and 2 for full details) for change in SF-36 PCS at 6 + 2.129 (if participant months:
There were also no statistically significant differences between the three service models for the (PROM-derived) nominated secondary outcomes listed in Table 10, although the much smaller sample sizes for the change in Roland–Morris disability total score, owing to this measure being restricted to participants presenting with lower-back pain, should be noted.
However, when each of these change outcomes is simplified from the change in continuous score to an Improved or worsened/stayed the same scenario, a statistically significant difference between the three service models was seen in two instances. At 3 months, the FCP(ST) and FCP(AQ) service models delivered a statistically significant greater improvement rate for the primary outcome variable SF-36 PCS compared with the GP service model. Also at 6 months, the FCP(ST) and FCP(AQ) service models delivered a statistically significant greater improvement rate for the secondary outcome MSK-HQ physical compared with the GP service model.
Secondary outcome healthcare utilisation summary statistics
The secondary outcome variable measuring healthcare service use was only available from the CSRI data. These services spanned NHS services, private health care, outpatient referrals, planned/unplanned hospital admissions, investigations (tests), medications, exercise and wellness classes, help with home/garden and help with personal care.
Prescription medications are reported as total prescriptions and broken down into drug categories (Tables 11 and 13). Appendix 9 includes further detail on drug classification.
| Health services | Total (N = 370) | GP (N = 94) | FCP(ST) (N = 114) | FCP(AQ) (N = 162) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Users: n | F2F home | F2F practice | Pho- ne | Other | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Other | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Other | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Other | Total contacts | |
| Outpatient referralsa | Number of contacts | Number of contacts | Number of contacts | Number of contacts | ||||||||||||||||||||
| Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | |
| Hospital admissions | Users: n | 0 | 1 | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total |
| Tests | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts |
| Prescibed medications | Users: n | 0 | 1 | 2–3 | 4–8 | Total | Users: n | 0 | 1 | 2–3 | 4–8 | Total | Users: n | 0 | 1 | 2–3 | 4–8 | Total | Users: n | 0 | 1 | 2–3 | 4–8 | Total |
| Exercise and wellnessd | Number of sessions | Number of sessions | Number of sessions | Number of sessions | ||||||||||||||||||||
| Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | |
| GP | 52 | 1 | 13 | 37 | 1 | 74 | 29 | 1 | 3 | 24 | 1 | 47 | 10 | 0 | 5 | 5 | 0 | 11 | 13 | 0 | 5 | 8 | 0 | 16 |
| Practice nurse | 4 | l | 2 | l | 0 | 4 | 2 | 1 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 2 |
| District nurse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Physiotherapist | 90 | 4 | 58 | 26 | 2 | 135 | 9 | 2 | 0 | 6 | 1 | 18 | 27 | 1 | 20 | 6 | 0 | 43 | 54 | 1 | 38 | 14 | 1 | 74 |
| Occupational therapist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Social worker | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Orthotist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Physiotherapy | 38 | 331 | 18 | 18 | 2 | 80 | 16 | 77 | 5 | 10 | 1 | 42 | 11 | 103 | 6 | 4 | 1 | 20 | 11 | 151 | 7 | 4 | 0 | 18 |
| Rheumatology | 2 | 367 | 1 | 1 | 0 | 3 | 2 | 91 | 1 | 1 | 0 | 3 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| Orthopaedics | 16 | 353 | 13 | 3 | 0 | 20 | 9 | 84 | 7 | 2 | 0 | 12 | 3 | 111 | 2 | 1 | 0 | 4 | 4 | 158 | 4 | 0 | 0 | 4 |
| Other | 13 | 356 | 9 | 3 | 1 | 33 | 5 | 88 | 5 | 0 | 0 | 5 | 4 | 110 | 2 | 2 | 0 | 12 | 4 | 158 | 2 | 1 | 1 | 16 |
| Planned inpatient | 1 | 369 | 0 | 0 | 1 | 3 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 1 | 161 | 0 | 0 | 1 | 3 |
| Unplanned inpatient | 0 | 370 | 0 | 0 | 0 | 0 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 161 | 0 | 0 | 0 | 0 |
| Planned day case | 0 | 370 | 0 | 0 | 0 | 0 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| MRI | 12 | 358 | I | 12 | 0 | 0 | 12 | 5 | 89 | 5 | 0 | 0 | 5 | 3 | 111 | 3 | 0 | 0 | 3 | 4 | 158 | 4 | 0 | 0 |
| X-ray | 65 | 305 | bO | 4 | 1 | 72 | 22 | 72 | 19 | 2 | 1 | 27 | 15 | 99 | 14 | 1 | 0 | 16 | 28 | 134 | 27 | 1 | 0 | 29 |
| CT | 0 | 370 | 0 | 0 | 0 | 0 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| Ultrasound | 5 | 365 | 5 | 0 | 0 | 5 | 2 | 92 | 2 | 0 | 0 | 2 | 0 | 114 | 0 | 0 | 0 | 0 | 3 | 159 | 3 | 0 | 0 | 3 |
| Other scan | 7 | 363 | 7 | 0 | 0 | 7 | 2 | 92 | 2 | 0 | 0 | 2 | 1 | 113 | 1 | 0 | 0 | 1 | 4 | 158 | 4 | 0 | 0 | 4 |
| Blood test | 13 | 357 | 13 | 0 | 0 | 13 | 7 | 87 | 7 | 0 | 0 | 7 | 2 | 112 | 2 | 0 | 0 | 2 | 4 | 158 | 4 | 0 | 0 | 4 |
| Injections | 28 | 342 | 25 | 3 | 0 | 31 | 9 | 85 | 9 | 0 | 0 | 9 | 5 | 109 | 5 | 0 | 0 | 5 | 14 | 148 | 11 | 3 | 0 | 17 |
| Allb | 103 | 268 | 54 | 40 | 8 | 179 | 42 | 52 | 20 | 17 | 5 | 84 | 21 | 93 | 14 | 6 | 1 | 30 | 40 | 123 | 20 | 17 | 2 | 65 |
| Analgesics | 15 | 355 | 15 | 0 | 0 | 15 | 7 | 87 | 7 | 0 | 0 | 7 | 2 | 112 | 2 | 0 | 0 | 2 | 6 | 156 | 6 | 0 | 0 | 6 |
| NSAIDs | 43 | 327 | 39 | 4 | 0 | 47 | 16 | 78 | 14 | 2 | 0 | 18 | 7 | 107 | 7 | 0 | 0 | 7 | 20 | 142 | 18 | 2 | 0 | 22 |
| Steroids | 1 | 369 | 1 | 0 | 0 | 1 | 1 | 93 | 1 | 0 | 0 | 1 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| Tricyclic | 10 | 360 | 10 | 0 | 0 | 10 | 2 | 92 | 2 | 0 | 0 | 2 | 6 | 108 | 6 | 0 | 0 | 6 | 2 | 160 | 2 | 0 | 0 | 2 |
| Muscle relaxant | 7 | 363 | 5 | 2 | 0 | 9 | 5 | 89 | 4 | 1 | 0 | 6 | 1 | 113 | 0 | 1 | 0 | 2 | 1 | 161 | 1 | 0 | 0 | 1 |
| Anti-epileptic | 8 | 362 | 8 | 0 | 0 | 8 | 3 | 91 | 3 | 0 | 0 | 3 | 2 | 112 | 2 | 0 | 0 | 2 | 3 | 159 | 3 | 0 | 0 | 3 |
| Vitamins and minerals | s | 365 | 2 | 3 | 0 | 8 | 3 | 91 | 2 | 1 | 0 | 4 | 1 | 113 | 0 | 1 | 0 | 2 | 1 | 161 | 0 | 1 | 0 | 2 |
| Proton pump | 9 | 361 | 9 | 0 | 0 | 9 | 4 | 90 | 4 | 0 | 0 | 4 | 1 | 113 | 1 | 0 | 0 | 1 | 4 | 158 | 4 | 0 | 0 | 4 |
| Opioids | 53 | 317 | 46c | 6 | 1 | 63 | 27 | 67 | 22 | 4 | 1 | 35 | 6 | 108 | 6 | 0 | 0 | 6 | 20 | 142 | 18c | 2 | 0 | 22 |
| Other anti-depressant | 3 | 367 | 3 | 0 | 0 | 3 | 2 | 92 | 2 | 0 | 0 | 2 | 1 | 113 | 1 | 0 | 0 | 1 | 0 | 162 | 0 | 0 | 0 | 0 |
| Bisphosphonates | 1 | 369 | 1 | 0 | 0 | 1 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 1 | 161 | 1 | 0 | 0 | 1 |
| Gout | 1 | 369 | 0 | 1 | 0 | 2 | 1 | 93 | 0 | 1 | 0 | 2 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| New NHS classes | 3 | 366 | 1 | 2 | 0 | 19 | 0 | 94 | 0 | 0 | 0 | 0 | 1 | 113 | 0 | 1 | 0 | 4 | 2 | 159 | 1 | 1 | 0 | 15 |
| Private | Total (N = 370) | GP (N = 94) | FCP(ST) (N = 114) | FCP(AQ) (N = 162) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Users: n | Number of contacts | Users: n | Number of contacts | Users: n | Number of contacts | 0 | Number of contacts | |||||||||||||||||
| 0 | 1 | 2–5 | > 5 | Total contacts | 0 | 1 | 2–5 | > 5 | Total contacts | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 1 | 2–5 | > 5 | Total contacts | |||||
| OTC medications | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days |
| Exercise and wellnessc | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions |
| Physiotherapist | 26 | 344 | 8 | 9 | 9 | 105 | 11 | 83 | 4 | 4 | 3 | 41 | 5 | 109 | 1 | 3 | 1 | 16 | 10 | 152 | 3 | 2 | 5 | 48 |
| Osteopath or chiropractor | 13 | 357 | 3 | 6 | 4 | 60 | 7 | 87 | 2 | 3 | 2 | 35 | 2 | 112 | 1 | 1 | 0 | 3 | 4 | 158 | 0 | 2 | 2 | 22 |
| Complementary therapist | 11 | 361 | 1 | 9 | 1 | 33 | 3 | 91 | 0 | 3 | 0 | 8 | 3 | 111 | 0 | 3 | 0 | 8 | 5 | 157 | 1 | 3 | 1 | 17 |
| Sports therapist | 2 | 368 | 0 | 2 | 0 | 5 | 1 | 93 | 0 | 1 | 0 | 2 | 0 | 114 | 114 | 0 | 0 | 0 | 1 | 161 | 0 | 1 | 0 | 3 |
| Consultant | 8 | 362 | 7 | 1 | 0 | 9 | 5 | 89 | 4 | 1 | 0 | 6 | 2 | 112 | 2 | 0 | 0 | 2 | 1 | 161 | 1 | 0 | 0 | 1 |
| Surgery | 0 | 370 | 0 | 0 | 0 | 0 | 0 | 94 | 0 | 0 | 0 | 0 | 0 | 114 | 0 | 0 | 0 | 0 | 0 | 162 | 0 | 0 | 0 | 0 |
| Others | 7 | 363 | 5 | 1 | 1 | 13 | 4 | 90 | 2 | 1 | 1 | 10 | 0 | 114 | 0 | 0 | 0 | 0 | 3 | 159 | 3 | 0 | 0 | 3 |
| Oral analgesics | 100 (27.0) | 270 | 97 | 3 | 45.14 | 9.29 | 29 (30.9) | 65 | 29 | 0 | 41.70 | 10.90 | 33 (28.9) | 81 | 31 | 2 | 36.09 | 7.98 | 38 (23.5) | 124 | 37 | 1 | 57.13 | 9.26 |
| Paracetamola | 91 (24.6) | 279 | 91 | n/a | 42.41 | 7.81 | 25 (26.6) | 69 | 25 | n/a | 38.15 | 8.57 | 30 (26.3) | 84 | 30 | n/a | 32.10 | 6.17 | 36 (22.2) | 126 | 36 | n/a | 55.09 | 8.50 |
| Oral NSAIDs | 74 (20.0) | 296 | 73 | 1 | 31.43 | 3.74 | 16 (17.0) | 78 | 16 | 0 | 10.25 | 0.95 | 22 (19.3) | 92 | 22 | 0 | 28.89 | 2.57 | 36 (22.2) | 126 | 35 | 1 | 39.78 | 6.14 |
| Ibuprofenb | 70 (18.9) | 300 | 36 | n/a | 33.47 | 3.59 | 15 (16.0) | 79 | 15 | n/a | 10.29 | 0.84 | 20 (17.5) | 94 | 20 | n/a | 36.57 | 2.53 | 35 (21.6) | 127 | 35 | n/a | 39.86 | 5.89 |
| Topical analgesics | 7 (1.9) | 363 | 7 | 0 | Unknown | 0 | 2 (2.1) | 92 | 2 | 0 | Unknown | 0.00 | 2 (1.8) | 112 | 2 | 0 | Unknown | 0.00 | 3 (1.9) | 159 | 3 | 0 | Unknown | 0.00 |
| Topical NSAIDs | 25 (6.8) | 345 | 25 | 0 | 90.00 | 0.26 | 8 (8.5) | 86 | 8 | 0 | Unknown | 0.00 | 6 (5.3) | 108 | 6 | 0 | Unknown | 0.00 | 11 (6.8) | 151 | 11 | 0 | 90.00 | 0.59 |
| CAM and dietary supplements | 6 (1.6) | 364 | 5 | 1 | 90.00 | 0.25 | 1 (1.1) | 93 | 1 | 0 | Unknown | 0.00 | 2 (1.8) | 112 | 1 | 1 | Unknown | 0.00 | 3 (1.9) | 159 | 3 | 0 | 90.00 | 0.56 |
| Number of sessions | Number of sessions | Number of sessions | Number of sessions | |||||||||||||||||||||
| New private classes | 11 | 358 | 5 | 5 | 1 | 103 | 3 | 91 | 2 | 1 | 0 | 18 | 4 | 110 | 2 | 2 | 0 | 26 | 4 | 157 | 1 | 2 | 1 | 59 |
| Health services | Total (N = 348) | GP (N = 90) | FCP(ST) (N = 107) | FCP(AQ) (N = 151) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Users: n | F2F home | F2F practice | Pho- ne | Other | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Oth- er | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Oth- er | Total contacts | Users: n | F2F home | F2F practice | Pho- ne | Oth- er | Total contacts | |
| Number of contacts | a | Number of contacts | a | Number of contacts | a | Number of contacts | ||||||||||||||||||
| Outpatient referralsa | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts | Users: n | 0 | 1 | 2–5 | > 5 | Total contacts |
| Hospital admissions | Users: n | 0 | l | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total | Users: n | 0 | 1 | 2 | 3 | Total |
| Tests | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts | Users: n | 0 | 1 | 2 | 4 | Total contacts |
| Prescribed medications | Users: n | 0 | l | 2–5 | 4–8 | Total | Users: n | 0 | 1 | 2–5 | 4–8 | Total | Users: n | 0 | l | 2–3 | 4–8 | Total | Users: n | 0 | 1 | 2–3 | 4–8 | Total |
| Exercise and wellnessb | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total sessions |
| GP | 30 | 0 | 11 | 19 | 0 | 39 | 14 | 0 | 6 | 8 | 0 | 21 | 8 | 0 | 2 | 6 | 0 | 9 | 8 | 0 | 3 | 5 | 0 | 9 |
| Practice nurse | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 |
| District nurse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Physiotherapist | 38 | 1 | 21 | 14 | 2 | 69 | 5 | 0 | 1 | 3 | 1 | 14 | 11 | 1 | 1 | 3 | 0 | 26 | 22 | 0 | 13 | 8 | 1 | 29 |
| Occupational therapist | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Social worker | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Orthotist | 1 | 0 | 1 | 0 | 0 | 2 | 1 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Physiotherapy | 26 | 321 | 9 | 16 | 1 | 60 | 8 | 81 | 3 | 5 | 0 | 17 | 8 | 99 | 2 | 6 | 0 | 19 | 10 | 141 | 4 | 5 | 1 | 24 |
| Rheumatology | 4 | 343 | 2 | 1 | 1 | 12 | 1 | 88 | 0 | 1 | 0 | 2 | 2 | 105 | 1 | 0 | 1 | 9 | 1 | 150 | 1 | 0 | 0 | 1 |
| Orthopaedics | 13 | 334 | 11 | 2 | 0 | 18 | 4 | 85 | 4 | 0 | 0 | 4 | 4 | 103 | 3 | 1 | 0 | 6 | 5 | 146 | 4 | 1 | 0 | 8 |
| Other | 8 | 339 | 6 | 2 | 0 | 11 | 1 | 88 | 0 | 1 | 0 | 2 | 3 | 104 | 2 | 1 | 0 | 5 | 4 | 147 | 4 | 0 | 0 | 4 |
| Planned inpatient | 3 | 34S | l | 2 | 0 | 5 | 2 | 88 | 1 | 1 | 0 | 3 | 1 | 106 | 0 | 1 | 0 | 2 | 0 | 151 | 0 | 0 | 0 | 0 |
| Unplanned inpatient | 0 | 348 | 0 | 0 | 0 | 0 | 0 | 90 | 0 | 0 | 0 | 0 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | lSl | 0 | 0 | 0 | 0 |
| Planned day case | 0 | 348 | 0 | 0 | 0 | 0 | 0 | 90 | 0 | 0 | 0 | 0 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| MRI | 5 | 343 | 5 | 0 | 0 | 5 | 1 | 89 | 1 | 0 | 0 | 1 | 1 | 106 | 1 | 0 | 0 | 1 | 3 | 148 | 3 | 0 | 0 | 3 |
| X-ray | 9 | 339 | 9 | 0 | 0 | 6 | 0 | 90 | 0 | 0 | 0 | 0 | 3 | 104 | 3 | 0 | 0 | 3 | 6 | 145 | 6 | 0 | 0 | 3 |
| CT | l | 347 | l | 0 | 0 | 1 | l | 89 | l | 0 | 0 | 1 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Ultrasound | l | 347 | l | 0 | 0 | 1 | 1 | 89 | 1 | 0 | 0 | 1 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Other scan | 0 | 348 | 0 | 0 | 0 | 0 | 0 | 90 | 0 | 0 | 0 | 0 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Blood test | 3 | 345 | 3 | 0 | 0 | 3 | 0 | 90 | 0 | 0 | 0 | 0 | 2 | 105 | 2 | 0 | 0 | 2 | 1 | 150 | 1 | 0 | 0 | 1 |
| Injections | 12 | 336 | 11 | l | 0 | 13 | 4 | 86 | 4 | 0 | 0 | 4 | 3 | 104 | 3 | 0 | 0 | 3 | 5 | 146 | 4 | 1 | 0 | 6 |
| All | 66 | 282 | 37 | 23 | 6 | 113 | 27 | 63 | 15 | 8 | 4 | 51 | 16 | 91 | 8 | 7 | 1 | 26 | 23 | 128 | 14 | 8 | 1 | 36 |
| Analgesics | 13 | 335 | 13 | 0 | 0 | 13 | 7 | 83 | 7 | 0 | 0 | 7 | 2 | 105 | 2 | 0 | 0 | 2 | 4 | 147 | 4 | 0 | 0 | 4 |
| NSAIDs | 23 | 325 | 22 | l | 0 | 24 | 8 | 82 | 8 | 0 | 0 | 8 | 7 | 100 | 6 | 1 | 0 | 8 | 8 | 143 | 8 | 0 | 0 | 8 |
| Steroids | 1 | 347 | 1 | 0 | 0 | 1 | l | 89 | l | 0 | 0 | 1 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Tricyclic | 7 | 341 | 7 | 0 | 0 | 7 | 1 | 89 | 1 | 0 | 0 | 1 | 4 | 103 | 4 | 0 | 0 | 4 | 2 | 149 | 2 | 0 | 0 | 2 |
| Muscle relaxant | 2 | 346 | 2 | 0 | 0 | 2 | 1 | 89 | 1 | 0 | 0 | 1 | 0 | 107 | 0 | 0 | 0 | 0 | 1 | lSO | 1 | 0 | 0 | 1 |
| Anti-epileptic | 6 | 342 | 5 | 1 | 0 | 7 | 2 | 88 | 1 | 1 | 0 | 3 | 1 | 106 | 1 | 0 | 0 | 1 | 3 | 148 | 3 | 0 | 0 | 3 |
| Vitamins and Minerals | 4 | 344 | 1 | 3 | 0 | 7 | 2 | 88 | 1 | 1 | 0 | 3 | 1 | 106 | 0 | 1 | 0 | 2 | 1 | 150 | 0 | 1 | 0 | 2 |
| Proton pump | 4 | 344 | 4 | 0 | 0 | 4 | 1 | 89 | 2 | 0 | 0 | 1 | 2 | 105 | 2 | 0 | 0 | 2 | 1 | 150 | 1 | 0 | 0 | 1 |
| Opioids | 36 | 312 | 33 | 2 | 1 | 42 | 15 | 75 | 12 | 2 | 1 | 21 | 7 | 100 | 7 | 0 | 0 | 7 | 14 | 137 | 14 | 0 | 0 | 14 |
| Other anti-depressant | 2 | 346 | 2 | 0 | 0 | 2 | 2 | 88 | 2 | 0 | 0 | 2 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Bisphosphonates | 2 | 346 | 2 | 0 | 0 | 2 | 1 | 89 | 1 | 0 | 0 | 1 | 0 | 107 | 0 | 0 | 0 | 0 | 1 | 150 | 1 | 0 | 0 | 1 |
| Gout | 1 | 347 | 0 | 1 | 0 | 2 | 1 | 89 | 0 | l | 0 | 2 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| New NHS classes | 4 | 344 | 2 | 2 | 0 | 21 | 0 | 90 | 0 | 0 | 0 | 0 | 2 | 105 | 1 | 1 | 0 | 8 | 2 | 149 | 1 | 1 | 0 | 13 |
The over-the-counter (OTC) medications data are also reported in some detail (Tables 12 and 14), being classified into five categories: ‘oral analgesics’, ‘oral non-steroidal anti-inflammatory drugs’ (NSAIDs), ‘topical analgesics’, ‘topical NSAIDs’ and ‘complementary and alternative medicine, and dietary supplements’. OTC medications are fully itemised by category in Appendix 9.
| Private | Total (N = 348) | GP (N = 90) | FCP(ST) (N = 107) | FCP(AQ) (N = 151) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Users: n | Number of contacts | Users: n | Number of contacts | Users: n | Number of contacts | Users: n | Number of contacts | |||||||||||||||||
| 0 | 1 | 2–5 | > 5 | Total contacts | 0 | 1 | 2–5 | > 5 | Total contacts | 0 | 1 | 2–5 | > 5 | Total contacts | 0 | 1 | 2–5 | > 5 | Total contacts | |||||
| OTC medications | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days | Users: n (%) | Non- users: n | 1 type | 2 types | Users: mean days | All: mean days |
| Number of sessions | Number of sessions | Number of sessions | Number of sessions | |||||||||||||||||||||
| Exercise and wellnessc | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total Sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total Sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total Sessions | Users: n | 0 | 1–3 | 4–12 | 13–36 | Total Sessions |
| Physiotherapist | 8 | 340 | 3 | 4 | 1 | 20 | 3 | 87 | 2 | 1 | 0 | 5 | 3 | 104 | 0 | 2 | 1 | 11 | 2 | 149 | 1 | 1 | 0 | 4 |
| Osteopath or chiropractor | 12 | 336 | 5 | 5 | 2 | 38 | 7 | 83 | 3 | 3 | 1 | 20 | 2 | 105 | 1 | 0 | 1 | 11 | 3 | 148 | 1 | 2 | 0 | 7 |
| Complementary therapist | 8 | 340 | 1 | 5 | 2 | 28 | 3 | 87 | 1 | 2 | 0 | 6 | 2 | 105 | 0 | 2 | 0 | 6 | 3 | 148 | 0 | 1 | 2 | 16 |
| Sports therapist | 0 | 348 | 0 | 0 | 0 | 0 | 0 | 90 | 0 | 0 | 0 | 0 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Consultant | 5 | 343 | 3 | 2 | 0 | 7 | 3 | 87 | 2 | 1 | 0 | 4 | 0 | 107 | 0 | 0 | 0 | 0 | 2 | 149 | 1 | 1 | 0 | 3 |
| Surgery | 2 | 346 | 2 | 0 | 0 | 2 | 2 | 88 | 2 | 0 | 0 | 2 | 0 | 107 | 0 | 0 | 0 | 0 | 0 | 151 | 0 | 0 | 0 | 0 |
| Others | 2 | 346 | 1 | 1 | 0 | 3 | 1 | 89 | 0 | 1 | 0 | 2 | 1 | 106 | 1 | 0 | 0 | 1 | 0 | 151 | 0 | 0 | 0 | 0 |
| Oral analgesics | 66 (19.0) | 282 | 65 | 1 | 51.90 | 6.73 | 22 (24.4) | 68 | 21 | 1 | 55.83 | 8.38 | 18 (16.8) | 89 | 18 | 0 | 41.17 | 4.88 | 26 (17.2) | 125 | 26 | 0 | 56.44 | 7.10 |
| Paracetamola | 60 (17.2) | 288 | 60 | n/a | 51.24 | 5.83 | 19 (21.1) | 71 | 19 | n/a | 56.8 | 7.01 | 16 (15.0) | 91 | 16 | n/a | 40.20 | 3.98 | 25 (16.6) | 126 | 25 | n/a | 54.47 | 6.48 |
| Oral NSAIDs | 38 (10.9) | 310 | 37 | 1 | 30.86 | 2.05 | 10 (11.1) | 80 | 10 | 0 | 34.67 | 1.25 | 14 (13.1) | 93 | 14 | 0 | 19.50 | 1.80 | 14 (9.3) | 137 | 13 | 1 | 43.33 | 2.67 |
| Ibuprofenb | 36 (10.3) | 312 | 36 | n/a | 33.75 | 2.03 | 10 (11.1) | 80 | 10 | n/a | 34.67 | 1.25 | 12 (11.2) | 95 | 12 | n/a | 22.63 | 1.76 | 14 (9.3) | 137 | 14 | n/a | 43.33 | 2.67 |
| Topical analgesics | 3 (0.9) | 345 | 3 | 0 | Unknown | 0.00 | 2 (2.2) | 88 | 2 | 0 | Unknown | 0.00 | 0 (0.0) | 107 | 0 | 0 | n/a | n/a | 1 (0.7) | 150 | 1 | 0 | Unknown | 0.00 |
| Topical NSAIDs | 8 (2.3) | 340 | 8 | 0 | 90.00 | 0.00 | 3 (3.3) | 87 | 3 | 0 | Unknown | 0.00 | 0 (0.0) | 107 | 0 | 0 | n/a | n/a | 5 (3.3) | 146 | 5 | 0 | 90.00 | 0.61 |
| CAM and dietary supplements | 4 (1.1) | 344 | 4 | 0 | Unknown | 0.00 | 1 (1.1) | 89 | 1 | 0 | Unknown | 0.00 | 1 (0.9) | 106 | 1 | 0 | Unknown | 0.00 | 2 (1.3) | 149 | 2 | 0 | Unknown | 0.00 |
| New private classes | 12 | 336 | 7 | 4 | 1 | 91 | 2 | 88 | 1 | 1 | 0 | 9 | 4 | 103 | 3 | 1 | 0 | 15 | 6 | 145 | 3 | 2 | 1 | 67 |
Of the 426 participants in the study, CSRI information was obtained for 370 (86.9%) at 3 months; NHS and private service use totals are shown in Tables 11 and 12, respectively.
Two respondents reported receipt of help with home or garden at both 3 and 6 months, reporting 24 hours (self-paid) and 84 hours (free from family or friend) per week. One respondent reported receipt of help with personal care at 3 and 6 months (free from family or friend).
Comparing the three service models for usage of each of the seven OTC medication categories, the chi-square test produces p = 0.376, p = 0.645, p = 0.590, p = 0.487, p = 0.980, p = 0.650 and p = 0.883; that is, no statistically significant difference between the three service models for the usage of any of the seven OTC-type medications.
Of the 426 participants in the study, CSRI information was obtained for 348 (81.7%) at 6 months; NHS and private service use totals are shown in Tables 13 and 14, respectively.
Comparing the GP service model against the FCP models for the usage of opioids, a statistically significant higher prevalence was found at both time points – 3 months and 6 months. At 3 months, 27/94 (28.7%) GP patients had received opioids compared to 26/276 (9.4%) FCP patients; chi-square test: p < 0.001. At 6 months, 15/90 (16.7%) GP patients had received opioids compared to 21/258 (8.1%) FCP patients; chi-square test: p = 0.022.
Total costs
Unit costs were applied to the use of NHS services to compute the total cost for each participant (i.e. primary and community services, outpatient referrals, investigations and tests, including injections). An additional total cost was calculated, which also included inpatient events (planned surgery due to MSK condition). The costs of medications and private treatment were excluded, as were the cost of wellness and exercise classes, and additional expenses such as home help, personal care, home adaptations, mobility equipment and transport for treatment costs because reporting of these items was patchy and considered potentially unreliable.
The cost calculations were performed using the Unit Costs shown in Appendix 10.
The cost of the initial presentation (included in the Total Cost) for participants in the three service models was calculated as follows, excluding prior triage (typically performed by a receptionist or ‘care navigator’):
-
GP: £39
-
FCP(ST) band 7: £22
-
FCP(AQ) band 7: £22
Summary statistics, and comparisons between the three service models, are shown in Table 15, where N indicates the number of participants for whom the cost information was available across the relevant time period. Included at the end is a sensitivity exercise to examine the implication of an alternative costing for the FCP(AQ) physiotherapist, using the band 8a cost of £25 (£75 for each working hour of contact).
| Cost (£) | Time period (months) | Total participants (N = 425) | GP participants (N = 109) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Test | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Median | Minimum | Maximum | N | Mean | Median | Minimum | Maximum | N | Mean | Median | Minimum | Maximum | N | Mean | Median | Minimum | Maximum | Kruskal–Wallis | ||
| Total excluding inpatient | 0–3 | 370 | 112.42 | 44.00 | 22 | 1738 | 94 | 203.08 | 83.50 | 39 | 1738 | 114 | 89.73 | 22.00 | 22 | 922 | 162 | 72.30 | 41.00 | 22 | 679 | p < 0.001 |
| Total including inpatient | 0–3 | 370 | 193.66 | 44.00 | 22 | 15,906 | 94 | 238.65 | 83.50 | 39 | 3775 | 114 | 89.73 | 22.00 | 22 | 922 | 162 | 240.70 | 41.00 | 22 | 15,906 | p < 0.001 |
| Total excluding inpatient | 3–6 | 348 | 27.21 | 0 | 0 | 1838 | 90 | 22.38 | 0 | 0 | 752 | 107 | 19.97 | 0 | 0 | 561 | 151 | 35.21 | 0 | 0 | 1838 | p = 0.918 |
| Total including inpatient | 3–6 | 348 | 180.52 | 0 | 0 | 15,862 | 90 | 263.38 | 0 | 0 | 15,832 | 107 | 167.93 | 0 | 0 | 15,862 | 151 | 140.06 | 0 | 0 | 15,862 | p = 0.694 |
| Total excluding inpatient | 0–6 | 348 | 142.77 | 52.00 | 22 | 1964 | 90 | 235.56 | 105.50 | 39 | 1738 | 107 | 112.95 | 41.00 | 22 | 952 | 151 | 108.59 | 44.00 | 22 | 1964 | p < 0.001 |
| Total including inpatient | 0–6 | 348 | 382.47 | 52.00 | 22 | 16,784 | 90 | 507.44 | 105.50 | 39 | 16,334 | 107 | 260.92 | 41.00 | 22 | 16,784 | 151 | 394.11 | 44.00 | 22 | 15,922 | p < 0.001 |
| Total excluding inpatient, assuming band 8a (not band 7) for FCP(AQ) | 0–6 | 348 | 144.97 | 52.00 | 22 | 1967 | 90 | 235.56 | 105.50 | 39 | 1738 | 107 | 112.95 | 41.00 | 22 | 952 | 151 | 113.66 | 50.00 | 25 | 1967 | p < 0.001 |
| Total including inpatient, assuming band 8a (not band 7) for FCP(AQ) | 0–6 | 348 | 384.66 | 52.00 | 22 | 16,784 | 90 | 507.44 | 105.50 | 39 | 16,334 | 107 | 260.92 | 41.00 | 22 | 16,784 | 151 | 399.16 | 50.00 | 25 | 15,925 | p < 0.001 |
There were 370 participants who elicited CSRI data at 3 months. Of these, 22 did not elicit CSRI data at 6 months. No participants elicited CSRI at 6 but not at 3 months (see Appendix 6). The total cost for 0–6 months was thus only able to be calculated for 348 participants – those who elicited CSRI data at both 3 and 6 months.
Inspecting the entire 6 months of the study, and assuming a consistent band 7 unit cost for the FCPs, a statistically significant difference in total cost is seen between the three service models, irrespective of whether inpatient costs are included or excluded from the total cost calculation.
In both instances, the GP service model is found to be significantly more costly, with a median total cost of £105.50 per patient versus £41.00 for FCP(ST) and £44.00 for FCP(AQ). There was no statistically significant difference between the FCP(ST) and FCP(AQ) total cost.
A sensitivity analysis relating to a potential higher salary band for the FCP(AQ) physiotherapists did not contradict these findings, other than to detect a statistically significant higher total cost in the FCP(AQ) when compared with the FCP(ST) service model (Mann–Whitney U test: p < 0.001, when excluding and when including inpatient costs).
The total cost (£) excluding inpatient costs over the 0- to 6-month period was considered for modelling using stepwise linear regression. However, inspection of its histogram revealed a very large spike at £22 corresponding with FCP(ST) plus FCP(AQ) participants, and a further spike at £39 corresponding with GP participants, rendering linear regression statistically inappropriate. Given the impossibility of applying any standard transformation to dampen these spikes and, given that the same problem would have occurred (with an extremely large spike at £0) if initial presentation cost was excluded from this total, it was decided instead to model the presence or absence of any additional cost over the initial presentation cost using stepwise logistic regression. The following variables were entered as predictors:
-
General practice status: service model, in the form of a dummy variable for GP.
-
Demographic participant features: gender (male: yes/no), age in years at baseline, ethnic origin (white: yes/no), education (none beyond secondary school: yes/no and university educated: yes/no), employment status at baseline (full-time: yes/no and full-time or part-time: yes/no).
-
Clinical participant features: baseline SF-36 PCS, baseline SF-36 MCS, baseline EQ-5D-5L score (England), EQ-5D-5L general health VAS score, MSKD area at baseline included back (yes/no), MSKD area at baseline included knee or leg or hip or foot or ankle (yes/no), and whether the presented musculoskeletal condition had affected employment or ability to perform usual activities (yes/no).
Backwards stepwise logistic regression, with rerunning of the final model to include additional participants for whom data were missing only for non-significant predictors, led to the model in Table 16 (with Nagelkerke R2 = 0.089 and n = 334) for incurring additional cost (excluding inpatient costs) during 0–6 months.
| B | SE | Wald | df | Sig. | Adjusted odds ratio | 95% CI for adjusted odds ratio) | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Step 1a | Service model: GP | 0.780 | 0.279 | 7.839 | 1 | 0.005 | 2.181 | 1.264 | 3.764 |
| Baseline SF-36 PCS | −0.034 | 0.011 | 9.617 | 1 | 0.002 | 0.966 | 0.945 | 0.987 | |
| Constant | 1.468 | 0.418 | 12.307 | 1 | < 0.001 | ||||
The model demonstrates a significantly higher likelihood of incurring additional cost if under a GP service model, with such participants being 2.181 times more likely to incur additional cost compared to a participant under a FCP(ST) or FCP(AQ) service model.
Additionally, a statistically significant effect of baseline SF-36 PCS is seen, with higher scores being associated with a lower likelihood of incurring additional cost. The adjusted odds ratio of 0.966 implies that a participant with a baseline SF-36 PCS which is 10 points higher than another participant is 0.96610 = 0.708 times less likely to incur additional cost.
None of the other predictors were statistically significant, although the GP service model predictor could have been replaced with dummy variables for FCP(ST) and FCP(AQ), and these would have been statistically significant in the opposite direction, with each having a similar adjusted odds ratio [FCP: adjusted odds ratio (aOR) 0.401, 95% confidence interval (CI) from 0.216 to 0.746; FCP(AQ): aOR 0.507, 95% CI from 0.281 to 0.914].
In summary, the analysis demonstrated neither model was inferior in relation to clinical outcome at 6 months post consultation. The GP-led model of care was approximately two and a half times more costly than both the FCP(ST) and FCP(AQ) models.
Cost-effectiveness: National Health Service perspective
In summary, in relation to the primary outcome (SF-36 PCS), the analysis demonstrated that neither FCP(ST) or FCP(AQ) model was inferior to GP at 6 months post consultation. The GP-led model of care was more than twice as costly compared with both the FCP(ST) and FCP(AQ) models (based on NHS service use).
There were no significant differences in quality-of-life changes (based on EQ-5D-5L) seen between the models at 3 or 6 months, so, given the cost differentials and the lack of significant differences seen in quality of life changes, no further analysis was undertaken. This was also the case for other secondary outcomes.
Days of work and inability to perform usual activities
The CSRI returns at baseline, 3 and 6 months elicited (as a single item) days taken off work or (for those individuals who were not in paid employment), inability to perform usual activities. Baseline CSRI data also included employment status. Where data recorded a code of 999 for days off at any time point, the number of days was always assumed to be missing (i.e. the participant had not revealed this information); when a code of 888 (indicating not applicable) was present, the number of days reset was zero.
Table 17 shows summary statistics for days taken off work/unable to perform usual activities broken down by employment status. Note that the total sample size is 425; one participant did not elicit any CSRI information at any time point and is omitted from the analysis.
| Employment at baseline | Time point (months) | Total participants (N = 425) | GP participants (N = 109) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192)s | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Days lost known, n | Losing 0 days (%) | Days lost, mean | Days lost: IQR | Days lost, max. | N | Days lost known, n | Losing 0 days (%) | Days lost, mean | Days lost: IQR | Days lost, max. | N | Days lost known, n | Losing 0 days (%) | Days lost, mean | Days lost, IQR | Days lost, max. | N | Days lost known, n | Losing 0 days (%) | Days lost, mean | Days lost, IQR | Days lost, max. | ||
| Full-time | Base | 109 | 99 | 73.7 | 10.6 | 0–2 | 365 | 26 | 24 | 75.0 | 28.9 | 0–7.5 | 365 | 31 | 27 | 77.8 | 3.6 | 0–0 | 60 | 52 | 48 | 70.8 | 5.5 | 0–2 | 76 |
| 3 | 92 | 76 | 85.3 | 8.8 | 0–0 | 90 | 23 | 18 | 83.3 | 10.1 | 0–0 | 90 | 28 | 23 | 91.3 | 4.5 | 0–0 | 90 | 41 | 34 | 82.4 | 11.1 | 0–0 | 90 | |
| 6 | 80 | 64 | 85.9 | 7.6 | 0–0 | 90 | 21 | 15 | 86.7 | 6.1 | 0–0 | 90 | 25 | 20 | 90.0 | 5.9 | 0–0 | 90 | 34 | 29 | 82.8 | 9.5 | 0–0 | 90 | |
| Part-time | Baseline | 68 | 57 | 73.7 | 6.0 | 0–2 | 150 | 19 | 16 | 75.0 | 5.1 | 0–5.3 | 31 | 24 | 19 | 84.2 | 8.8 | 0–0 | 150 | 25 | 22 | 63.6 | 4.1 | 0–3.3 | 50 |
| 3 | 55 | 42 | 90.5 | 4.5 | 0–0 | 90 | 13 | 9 | 88.9 | 10.0 | 0–0 | 90 | 21 | 15 | 100.0 | 0.0 | 0–0 | 0 | 21 | 18 | 83.3 | 5.4 | 0–0 | 90 | |
| 6 | 51 | 39 | 89.7 | 8.5 | 0–0 | 90 | 12 | 9 | 88.9 | 10.0 | 0–0 | 90 | 19 | 13 | 84.6 | 11.5 | 0–0 | 90 | 20 | 17 | 94.1 | 5.3 | 0–0 | 90 | |
| All employed | Base | 177 | 156 | 73.7 | 8.9 | 0–2 | 365 | 45 | 40 | 75.0 | 19.4 | 0–5.3 | 365 | 55 | 46 | 80.4 | 5.7 | 0–0 | 150 | 77 | 70 | 68.6 | 5.1 | 0–2 | 76 |
| 3 | 147 | 118 | 88.1 | 7.2 | 0–0 | 90 | 36 | 27 | 88.9 | 10.0 | 0–0 | 90 | 49 | 38 | 94.7 | 2.7 | 0–0 | 90 | 62 | 53 | 83.0 | 8.9 | 0–0 | 90 | |
| 6 | 131 | 103 | 88.3 | 7.9 | 0–0 | 90 | 33 | 24 | 91.7 | 7.5 | 0–0 | 90 | 44 | 33 | 87.9 | 8.1 | 0–0 | 90 | 54 | 46 | 87.0 | 7.9 | 0–0 | 90 | |
| Voluntary worker/unemployed and seeking work/homemaker/carer | Base | 40 | 30 | 43.3 | 119.0 | 0–43.5 | 1576 | 9 | 7 | 42.9 | 27.9 | 0–84 | 90 | 13 | 9 | 44.4 | 62.7 | 0–95 | 365 | 18 | 14 | 42.9 | 200.9 | 0–127.5 | 1576 |
| 3 | 31 | 24 | 54.2 | 26.5 | 0–60 | 90 | 7 | 5 | 40.0 | 22.0 | 0–48 | 60 | 13 | 9 | 66.7 | 11.9 | 0–8.5 | 90 | 11 | 10 | 50.0 | 42.0 | 0–90 | 90 | |
| 6 | 31 | 22 | 68.2 | 27.3 | 0–90 | 90 | 7 | 5 | 80.0 | 12.0 | 0–30 | 60 | 13 | 9 | 88.9 | 10.0 | 0–0 | 90 | 11 | 8 | 37.5 | 56.3 | 0–90 | 90 | |
| Retired | Base | 201 | 169 | 66.9 | 21.2 | 0–14 | 365 | 54 | 50 | 72.0 | 8.8 | 0–7.8 | 90 | 53 | 40 | 67.5 | 35.1 | 0–22.3 | 365 | 94 | 79 | 63.3 | 22.1 | 0–14 | 365 |
| 3 | 188 | 138 | 71.7 | 17.5 | 0–7.8 | 90 | 51 | 42 | 64.3 | 24.6 | 0–67.5 | 90 | 49 | 31 | 77.4 | 18.4 | 0–0 | 90 | 88 | 65 | 73.8 | 12.4 | 0–4 | 90 | |
| 6 | 182 | 135 | 85.2 | 11.3 | 0–0 | 90 | 50 | 39 | 76.9 | 15.4 | 0–0 | 90 | 47 | 32 | 90.6 | 8.4 | 0–0 | 90 | 85 | 64 | 87.5 | 10.2 | 0–0 | 90 | |
| Unknown | Base | 7 | 3 | 33.3 | 72.3 | 0–210 | 210 | 1 | 0 | – | – | – | – | 3 | 1 | 0.0 | 210.0 | n/a | 210.0 | 3 | 2 | 50.0 | 3.5 | 0–7 | 7 |
| 3 | 4 | 4 | 0.0 | 71.0 | 33–90 | 90 | 0 | 0 | – | – | – | – | 3 | 3 | 0.0 | 90.0 | 90–90 | 90.0 | 1 | 1 | 0.0 | 14.0 | n/a | 14 | |
| 6 | 4 | 4 | 0.0 | 90.0 | 90–90 | 90 | 0 | 0 | – | – | – | – | 3 | 3 | 0.0 | 90.0 | 90–90 | 90.0 | 1 | 1 | 0.0 | 90.0 | n/a | 90 | |
| All | Base | 425 | 356 | 67.6 | 24.5 | 0–7 | 1576 | 109 | 97 | 71.1 | 14.5 | 0–8.5 | 365 | 124 | 96 | 70.8 | 25.4 | 0–4.8 | 365 | 192 | 165 | 63.6 | 29.8 | 0–7.5 | 1576 |
| 3 | 370 | 284 | 76.1 | 14.7 | 0–0 | 90 | 94 | 74 | 71.6 | 19.1 | 0–14.9 | 90 | 114 | 81 | 81.5 | 13.0 | 0–0 | 90 | 162 | 129 | 75.2 | 13.3 | 0–1 | 90 | |
| 6 | 348 | 264 | 83.7 | 12.5 | 0–0 | 90 | 90 | 68 | 82.4 | 12.4 | 0–0 | 90 | 107 | 77 | 85.7 | 11.7 | 0–0 | 90 | 151 | 119 | 83.2 | 13.1 | 0–0 | 90 | |
To facilitate realistic comparisons with the days lost in relation to employment/usual activities at 3 and 6 months, whenever the number of days lost at baseline was reported as > 90, it was capped at 90 days. This occurred 17 times: on 2 occasions in the GP-led service model (210 and 365 days), on 8 occasions in FCP(ST) [120, 150 (twice), 180, 210 and 365 days (3 times)] and on 7 occasions in FCP(AQ) [120, 180 (twice), 365, 420, 730 and 1576 days]. Note that, in Table 17, all summary statistics at baseline are calculated using the raw data prior to the days lost being capped at 90 days.
In Table 17, in each segment [All, GP arm, FCP(ST) arm and FCP(AQ) arm], N indicates the total number of participants belonging to the specified employment status at the specified time point and n indicates the number of participants among them N for whom information on days off work/ability to perform usual activities was available. The percentage who lost 0 days among these n participants is shown in the next column, and summary statistics (mean, IQR and maximum) for the days lost, incorporating those who lost 0 days, are shown in the next three columns.
The CSRI reported changes from baseline in days lost, after capping baseline days lost at 90, for all participants (irrespective of employment status) are summarised in Table 18; a negative number indicates that less days were lost than prior to baseline. In addition, changes at 3 and 6 months from baseline are shown and compared for when absence from work was covered by a certification.
| Employment/usual activities | Time point | Total participants (N = 426) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Comparison test | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Months | N | n | % | Mean, median (IQR) | N | n | % | Mean, median (IQR) | N | n | % | Mean, median (IQR) | N | n | % | Mean, median (IQR) | Kruskal–Wallis | |
| Change from baseline | Time point | TOTAL (334, 319 respondents), n (%) | GP (90, 87 respondents), n (%) | FCP(ST) (99, 93 respondents), n (%) | FCP(AQ) (145, 139 respondents), n (%) | Kruskal–Wallisa | ||||||||||||
| Months | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | ||
| Days lost | 3 | 284 | −5.0, 0 (−2 to 0) | 74 | 5.7, 0 (0–0) | 81 | −16.5, 0 (−10.5 to 0) | 129 | −3.9, 0 (−2 to 0) | p = 0.019 | ||||||||
| More | 37 | 13.0 | 14 | 18.9 | 5 | 6.2 | 18 | 14.0 | p = 0.049 | |||||||||
| Same | 173 | 60.9 | 46 | 62.2 | 51 | 63.0 | 76 | 58.9 | ||||||||||
| Fewer | 74 | 26.1 | 14 | 18.9 | 25 | 30.9 | 35 | 27.1 | ||||||||||
| Days lost | 6 | 264 | −8.7, 0 (−7 to 0) | 68 | −3.9, 0 (−7 to 0) | 77 | −20.5, 0 (−75 to 0) | 119 | −3.8, 0 (−3 to 0) | p = 0.063 | ||||||||
| More | 26 | 9.8 | 7 | 10.3 | 5 | 6.5 | 14 | 11.8 | p = 0.200 | |||||||||
| Same | 154 | 58.3 | 42 | 61.8 | 42 | 54.5 | 70 | 58.8 | ||||||||||
| Fewer | 84 | 31.8 | 19 | 27.9 | 30 | 39.0 | 35 | 29.4 | ||||||||||
| Was any absence from work covered by a doctor’s certificate? | 3 | 0 (0) | 4 (1.2) | 326 (97.6) | 4 (1.2) | 0 (0) | 2 (2.2) | 86 (95.6) | 2 (2.2) | 0 (0) | 2 (2.0) | 96 (97.0) | 1 (1.0) | 0 (0) | 0 (0) | 144 (99.3) | 1 (0.7) | p = 0.565 |
| 6 | 2 (0.6) | 1 (0.3) | 310 (97.2) | 6 (1.9) | 1 (1.1) | 1 (1.1) | 83 (95.4) | 2 (2.3) | 1 (1.1) | 0 (0) | 89 (95.7) | 3 (3.2) | 0 (0) | 0 (0) | 138 (99.3) | 1 (0.7) | p = 0.789 | |
A statistically significant difference was found at 3 months between the three service models, with FCP(ST) shown to have a greater improvement in days lost compared with the GP and FCP(AQ) arms. This effect was also exhibited at 6 months but did not reach statistical significance.
For summary statistics of the number of days lost at each time point by service model, broken down by ‘in full-time employment’, ‘in part-time employment’, ‘voluntary worker/unemployed and seeking work/homemaker/carer’, ‘retired’ and ‘unknown’, see Table 17.
Out-of-pocket expenditures and use of private sector
At 3 months (see Table 12), of the 26 participants obtaining private physiotherapy at 3 months, 23 (88.4%) were not covered by private medical insurance. These 23 users incurred a median total cost (excluding additional costs, e.g. personal transport) of £200 (range £0–£600).
None of the 13 participants using a private osteopath or chiropractor at 3 months was covered by private medical insurance; the 13 users incurred a median total cost (excluding additional costs, e.g. personal transport) of £180 (range £0, stated by participant as a free initial consultation, to £559).
None of the 11 participants using private complementary therapists were covered by private medical insurance; the 11 users incurred a median total cost (excluding additional costs, e.g. personal transport) of £100 (range £30–£210).
At 6 months (see Table 14), of the 9 participants obtaining private physiotherapy at 6 months, seven (77.8%) were not covered by private medical insurance; these seven users incurred a median total cost (excluding additional costs, e.g. personal transport) of £150 (range £0, stated by participant as a free initial consultation, to £300).
None of the 12 participants using a private osteopath or chiropractor was covered by private medical insurance; the 12 users incurred a median total cost (excluding additional costs, e.g. personal transport) of £120 (range £35–£350).
None of the 8 participants using private complementary therapists was covered by private medical insurance; the eight users incurred a median total cost (excluding additional costs, e.g. personal transport) of £110 (range £40–£400).
Neither of the 2 participants who had surgery were covered by private medication insurance; one had a hip replacement (at a self-reported cost of £10,900) and one had a knee operation (at a self-reported cost of £11,400, including two consultations).
Limitations of the economic analysis
Two elements of the original health economics analysis plan were not undertaken.
First, the practice level analysis to compare workforce configurations and costs was impractical due to the expanded number of practices in the study, many of which recruited relatively small numbers of participants. Moreover, interviews with members of practice teams to explore the integration of physiotherapy had been completed and reported in other WPs.
Second, the collection of participants’ service use data from GP records was found to be problematic and had to be abandoned due to poor coding and difficulties ascertaining from searches what interventions had been received. Hence, the calculation of musculoskeletal-related costs was based on responses to the CSRI. These data were collected meticulously by interview, but some variation occurred in the timing of the 3- and 6-month follow-up data and there was some missing information. It is also possible that recall errors arose, in particular in OTC medications, when there was no prescription for the patient to reference. We do note, however, that the self-report process was identical across all arms.
Qualitative
Aim
Gather evidence to inform and supplement the quantitative data from case study sites implementing FCP in primary care.
Objective
-
Gather qualitative evidence from key stakeholders at case study sites to better understand the barriers and facilitators to FCP and the impact that FCP has on pathways and equitable access to care.
-
Provide information to inform implementation of the FCP model in primary care.
Methods
Sample
The qualitative arm of the study involved in-depth investigation at study sites involved in the quantitative data collection. Prior to qualitative investigation all sites had been recruited to the quantitative evaluation and were actively involved in patient recruitment.
On study initiation, we intended to interview sites that were GP-led in addition to the FCP arms, but early interviews with five sites suggested that this approach was not yielding particularly useful data, as sites were simply asked to speculate on having a FCP in place rather than reporting experiences. The subsequent interviews were therefore undertaken with sites with a FCP.
Sample size
Our indicative sample size was based on obtaining a variety of team members’ views within practice sites. Important team members were considered to be FCPs, GPs, other practice healthcare staff, reception staff and practice managers, in addition to patients who had experienced the service. A maximum variation approach to sampling was used to ensure that sites represented an array of types of FCP employment and demographic attributes. Practices were categorised according to their FCP provision model. Practices also reflected important demographic variables that would probably impact service provision, including geographical factors (urban or rural location) and level of deprivation (high, moderate or low). As such, we assumed a sample size of approximately 80–100 participants. This was not based on the concept of data saturation, but instead was aligned to the realist principles of understanding how individual site contexts impacted outcomes of interest.
Recruitment
Multiple stakeholders were approached at each site for interview, including staff and patients. Staff were approached via a gatekeeper at the site tasked with managing the study, who sent an e-mail to staff members enquiring as to whether they would like to take part in an interview.
Patients indicated whether they would like to take part in an interview when completing quantitative outcome measures as part of the wider realist evaluation.
Consent
Staff and patients who assented to contact from the FRONTIER study team were e-mailed or posted a participant information sheet, consent form and interview guide, and were then booked for a one-to-one interview. Interviews were conducted remotely, via Skype video or telephone call, depending on the preference of the participant, by members of the study team. All participants were informed of the purpose of the study, the role of the interviewer and, where appropriate, their profession.
Interviews
Interviews were guided by a realist expert (JJ). The interview schedules were developed in relation to the initial programme theories identified in the realist review (see Chapter 4).
-
practice understanding of the role
-
integrating the first-contact physiotherapist into general practice
-
first-contact physiotherapist’s knowledge and skills
-
appointment structure
-
practice endorsement of FCP
-
patient acceptability of the first-contact physiotherapist role
-
employment and management of the first-contact physiotherapist role
-
FCP impact on practice workload and wider resource use.
As detailed in the realist synthesis chapter, FCP was a rapidly shifting landscape as practices employed an increasing number of first-contact physiotherapists. Alongside this, the advent of COVID-19 created a sudden shift in the way all clinical work was delivered in primary care. To allow for these unknown variables, interviewers adopted an inductive approach to questions, as opposed to the more traditional ‘teacher–learner cycle’ of realist interview questioning. 57 In brief, the traditional realist approach to interviewing would be theory driven, investigating respondents' views and experiences on pre-established theorising. Given the rapidly changing nature of the FCP role and the impact of the COVID-19 pandemic, more exploratory questioning was employed to support novel theorising in addition to more traditional theory-driven approaches.
Interview schedules were designed for each stakeholder and used semistructured questions, which focused on the initial programme theory areas identified, if relevant to the stakeholder being interviewed, and also open general questions, to allow interviewees to address new areas of theorising. A realist approach to following up points of interest was used. This allowed the interviewer to pinpoint and summarise certain issues raised by the participant to ensure common understanding and to clarify any causal assertions they may have made. Where appropriate, the interviewer informally introduced theory ‘ideas’ to participants to gain their insights and requested they give examples of their experience to ground their claims in real-world examples.
All one-off interviews with practice staff and patients were undertaken by HS and SH, neither of whom were healthcare professionals but who were post-doctoral health services researchers, well informed of realist principles, who had conducted the realist synthesis. Both had led qualitative studies in the past.
Three additional interviews were undertaken by NW with an interface clinician, interface lead and university training lead for the physiotherapist/practitioner. It was deemed more appropriate for these interviews to be led by a physiotherapist (NW) who had a better understanding of the professional landscape and terminology used by these participants. NW has extensive post-doctoral experience of mixed-method research. All interviewers identified as female.
Interviewers were encouraged to make reflective notes on completion of interviews and use these alongside the analysis.
Analysis
All data were anonymised and transcribed by a university-approved transcriber. No transcripts were returned to participants for comment but study summary findings were provided. Transcripts were analysed in Microsoft Word and data extracted to an Excel spreadsheet. All transcripts were coded by one of two team members (SH, HS) with second coding provided by other team members (FC, MC, JJ, CL, RT, NW).
Data were extracted using a coding matrix cross matching extracted data to initial programme theories identified above and aspects related to context, mechanism and outcome. Initial programme theories were subsequently refined and presented as CMOs. Once all data were extracted, the team (SH, JJ, CL, HS, RT, NW), guided by realist methodological expert JJ, met multiple times to create and refine CMO statements. Patient research partner DF was also consulted on patient related CMO formation.
Findings
In total, representatives from 24 practices took part in the realist qualitative study, reflecting a variety of models of FCP provision in general practice and demographic attributes (Table 19). In total, 77 interviews were conducted between June 2020 and May 2021 with an array of stakeholders at each site (Table 11; 17 FCPs, 16 GPs, 8 practice managers, 6 receptionists, 2 advanced practitioners and 28 patients). Three additional interviews were conducted with an interface clinician, interface lead and university training lead for FCP/practitioner to gain wider contextual information. All interviews were conducted on a one-to-one basis. A total of n = 80 interviews were included in the analysis. Interviews lasted an average of 29 minutes.
| ID | Country | FCP category | Urban/rural | Deprivation | Interviews conducted with stakeholders | Total (n) |
|---|---|---|---|---|---|---|
| 01 | Wales | FCP(AQ) | Rural | High | FCP(AQ), GP, practice manager, receptionist, 2 patients | 6 |
| 02 | Scotland | FCP(AQ) | Urban | Low | FCP(AQ), practice manager, patient | 3 |
| 03 | Scotland | FCP(AQ) | Urban | Low | Patient | 1 |
| 05 | Wales | FCP(AQ) | Rural | Moderate | FCP(AQ), practice manager, GP, receptionist, 4 patients | 8 |
| 06 | Wales | FCP(AQ) | Urban | Moderate | FCP(AQ), GP | 2 |
| 10 | Scotland | FCP(AQ) | Urban | Moderate | FCP(AQ), GP, 2 patients | 4 |
| 11 | England | FCP(AQ) | Urban | Low | Four patients | 4 |
| 17 | England | FCP(AQ) | Rural | Moderate | GP, practice manager, FCP, 2 patients | 5 |
| 21 | England | GP led | Urban | Moderate | GP, Patient | 2 |
| 22 | England | FCP(ST) | Urban | High | FCP, 2 GPs, practice manager, receptionist | 5 |
| 23 | England | GP led | Rural | Moderate | GP, practice manager, receptionist | 3 |
| 26 | England | GP | Urban | Low | GP, 2 advanced practitioner nurse | 3 |
| 32 | Wales | FCP(ST) | Urban | High | FCP | 1 |
| 35 | England | GP | Urban | Low | Physiotherapist (non-FCP), GP, practice manager, receptionist | 4 |
| 37 | England | FCP(AQ) | Urban | High | FCP(AQ), receptionist, patient | 3 |
| 40 | England | GP | Rural | Low | GP, practice manager | 2 |
| 41 | England | FCP(AQ) | Rural | Moderate | FCP, GP, 2 patients | 4 |
| 42 | England | FCP(AQ) | Urban | High | Patient | 1 |
| 43 | England | FCP(ST) | Urban | High | FCP(AQ), 2 patients | 3 |
| 45 | England | FCP(ST) | Rural | Moderate | FCP, GP, 2 patients | 4 |
| 47 | England | FCP(AQ) | Urban | High | FCP(AQ), GP, patient | 3 |
| 48 | England | FCP(ST) | Urban | Moderate | Two FCP, GP, patient | 4 |
| 50 | England | FCP(AQ) | Rural | Moderate | Patient | 1 |
| 52 | England | FCP(ST) | Rural | Low | FCP | 1 |
Following the interviews, theories were refined and were encapsulated under three areas and are presented with related CMOs below.
These were titled:
-
understanding the first-contact physiotherapist role and integration into healthcare teams
-
the FCP approach in practice; impact on workload and resource use
-
employment of the first-contact physiotherapist role.
Understanding the first-contact physiotherapist role and integration into healthcare teams
Promoting the first-contact physiotherapist role to patients
Practices emphasised how effective promotion of the FCP role was key to making the service an acceptable alternative to GP appointment for patients. For some practices, effective promotion was adopted after experiencing pushback or uncertainty from patients about seeing a FCP. Promotion included both verbal explanations from reception staff and print media, such as posters, leaflets, newsletters, newspapers, websites and social media.
I think from the initial outset patients were a bit wary because I think we weren’t selling it very well, if I’m honest because you’d say ‘Oh the physio will see you’, ‘I don’t need a physio’ that’s what we’d get, you know? Now we do have a bit of a spiel. ‘The advanced physio will see you, who can assess, diagnose, can prescribe …’ We have to do all that really and then they’re very reassured at the outset that they’re going to get the one-stop shop ... and they will use her again as well.
Practice manager, 05W
However, despite promotion of the role, some patients refused referral to a physiotherapist appointment by a receptionist and opted to see a GP instead. In these cases, it was possible for the receptionist and GP to work together to build patient confidence in the FCP skillset if the GP endorsed the role.
[A] couple of times they’ve not been booked in with the physio because they’ve said they didn’t want to, they wanted to speak to a GP, but actually when the doctor says ‘Oh no, no, the physio can deal with this’ then they go ‘Oh ok, ok’ and they quite happily go for it. So, perhaps that bit of validation that it’s a service that we’re encouraging and supporting and is working well.
GP, 45E
There were challenges when describing the FCP role to patients and variation in the terms used; for example, ‘musculoskeletal specialist’, ‘first-contact physio’, ‘senior physiotherapist’ or ‘physiotherapist’. This impacted patient understanding and expectations of what the service would provide. Using terms like ‘senior’ or ‘advanced’ were used to highlight the specialism of the role and encourage patient confidence to try out FCP. However, some clinicians also expressed concerns that the phrase ‘first contact’ implied that patients were not allowed to go back to the physiotherapist (GP2, 22E) or that the physiotherapist should provide ‘physical contact’ to assess the problem (practice manager, 22E).
I wasn’t sure what to expect. I just knew that I was going for an assessment, just to see the physio … I didn’t know whether he would just give me some exercises to do or exactly what. Having had private physio, to be honest I thought ‘Oh, maybe he’ll just do some sort of manipulation, massage on it once he’s assessed what it was’. It was more like seeing a GP because it was more him assessing what the problem was rather than doing hands-on work on it. It was a shorter session than I was expecting … you expect you’re going to go in and you’re going to come out completely cured.
Patient 1, 43E
Developing staff understanding of the first-contact physiotherapist role
It was important to provide consistent understanding of the FCP role scope across practice staff to ensure appropriate patients were referred to the FCP and the role scope was well communicated to patients. However, there were challenges to implementing this in practice because of FCPs working within large and dispersed staff teams, often across multiple practices, in some cases a lack of physical colocation of the role and the use of trainee or locum staff. The onus was on the physiotherapist to communicate their role to staff in these complex settings; however, this could be challenging due to the need to balance clinical workload with these administrative duties. When they had the time, first-contact physiotherapists used a variety of techniques to improve practice staff understanding of their role and referral including, regular training for front office and clinical staff about the role using targeted group or one-to-one meetings and daily reminders, staff feedback, information sheets and videos. They were able to target their feedback to staff through monitoring the first contact rate and checking whether patients with musculoskeletal conditions were wrongly referred to the GP. Through being proactive in their communication, FCP staff could build relationships that encouraged practice staff to approach them when they were uncertain about patient referral.
I work at three GP practices, one of them, they haven’t put me in the same building as the admin people and that was the hardest one to get sorted, because I wasn’t having small chats with them every day about things and feeding back as easily … I do keep an eye out to see what’s been referred to GPs, so I will let them know whether they’re appropriate for me. I go on the App where people send their referrals in and link them over to me … If anyone’s inappropriate, I let them know
First-contact physiotherapist 41E
C: FCP role scope and referral processes are new to primary care. This takes time for staff and practices to develop familiarity, particularly if first-contact physiotherapists have limited face-to-face contact with staff, either due to remote working or covering multiple practices.
M: Providing the first-contact physiotherapist with time and materials to educate staff and patients about their role (resource) helps develop other staff and patient knowledge about the scope of the role, trust in the role, staff confidence to promote and endorse the role to patients, and familiarity regarding which patients the first-contact physiotherapist sees (response).
O: Over time, FCP caseload improves (relevance, scope of practice), which shortens patient pathway leading to reduced GP appointment use and improved patient and staff acceptability of the role.
When first-contact physiotherapists experienced challenges communicating the role to practice staff then they found that GPs may unnecessarily refer patients to them leading to duplicated workload and increased patient pathways, perhaps indicating the workload pressures that GPs are currently facing.
I tried to indicate that that needs to go onto MSK physio, not to an FCP if he’s [GP] already made the diagnosis and he’s more or less using me as a more expert physio in-house, as opposed to an FCP and I don’t think he’ll change his mind on that easily ... It even gets to the point he puts his referrals under my door ... I think a few of the GPs are trying to struggle with things and they think ‘I know, bump to the FCP’.
First-contact physiotherapist, 45E
The respondent, who worked in a dual FCP and physiotherapy role, also highlighted the need to avoid conveying this complexity to GPs to avoid issues around referral; ‘the GPs know me only as a FCP, they don’t know me as a physio. Otherwise, that’s too complicated’ (first-contact physiotherapist, 45E).
C: Patients are reluctant to consult with a first-contact physiotherapist as ‘traditional’ models of care require an initial GP consultation to determine the problem and most appropriate course of management. Additionally, understanding of the first-contact physiotherapist skillset and role within the patient pathway is limited resulting in further patient uncertainty and reticence.
M: Providing promotional materials; reception staff addressing patient reluctance and refusal to consult with first-contact physiotherapists through explanation and differentiation from standard GP, supported by further endorsement from GPs regarding the nature of the consultation (resource) enhances patient understanding, reassures them of the role and benefit of the first-contact physiotherapist (response).
O: Over time the patient defaults to FCP consultation for MSKDs, making better use of FCP and GP appointment allocation and skillset.
Secondary care and dual-role physiotherapists
FCPs who worked dual roles or had moved into their role from local secondary care provision, were often well integrated into musculoskeletal pathways outside of general practice. This knowledge of clinicians and pathways allowed them to make more targeted and appropriate onward referrals for general practice patients, which first-contact physiotherapists felt accelerated the patient journey and provided reassurance for patients about their management plan. In some instances, secondary care had put a limitation on accepting referrals from first-contact physiotherapists due to problems with workload and wait lists, and requested these referrals were sent by the GP or by local musculoskeletal assessment teams. This added workload to these teams and increased the patient pathway.
Not all secondary care places will take referrals from us and that’s variable, depending on where you work, and so that’s a little bit of a barrier … I think they think they’ll be inundated … I’ll write the letter, e-mail it to the GP, who then just cuts and pastes it, so it’s essentially my referral.
First-contact physiotherapist, 10S
C: FCP provision to practices through a provider model delivers a more consistent service for both practitioners and GP practice.
M: First-contact physiotherapists continue to be employed on their substantive contracted terms and conditions via a central provider, have access to peer support networks and professional development opportunities and may work within a rotational model that still exposes them to traditional physiotherapy department placements (resources). For the practice, this provides a more stable service as the FCP employment, professional development and performance is managed centrally (resource).
O: This enables a more secure employment opportunity for first-contact physiotherapists, professional support and improves job satisfaction (response). For the practice, it improves service effectiveness, and knowledge of the system (response).
Integrating the first-contact physiotherapist into the practice
At some practices, physically co-locating the FCPt was problematic and they had to manage changes in room space (22E), inaccessibly located rooms (26E) and rooms that were too small or lacked the necessary equipment (37E). However, co-locating first-contact physiotherapists in general practice provided advantages to patients, particularly in rural areas, who no longer had to travel long distances to access physiotherapy at the hospital (05W).
Initially, room space was an issue and it may well be in the future. When I first was doing the pilot for three months I never knew which room I was going to be in when I came in … I now have a regular room, which makes a big difference. Doesn’t seem much, does it? But it does, just knowing where you’re going when you come in … starts the day off a bit more calmly.
First-contact physiotherapist, 22E
It is likely that where the FCP is physically located in the practice will affect how accessible they are to practice staff which has implications for clinical discussions and developing understanding of the role, and, in turn, the first-contact physiotherapist’s sense of integration with the practice.
Practices varied in how successfully they were able to integrate first-contact physiotherapists and practices which had established methods of staff communication were able to foster better relationships among staff and improve clinical communication likely leading to improved patient outcomes.
[FCP is] most efficient when the multi-disciplinary primary care team work together. So, every day between half ten, quarter to eleven … the clinical team, I guess really, all down tools where possible … the triage nurse who’s been speaking with patients in the morning can hand over any patients to MSK or to GP. MSK can escalate anything to the GP, not only at that time but it does happen primarily then. But we very much have an open-door policy and a duty GP, so there’s always someone available for escalated discussions.
Practice manager, 02S
FCPs highlighted the need for formal and informal, virtual and face-to-face opportunities for communication with staff teams, and the need to know who they could approach each day for clinical discussions. These issues became more pertinent for physiotherapy staff who were not employed directly by practices, as some described not being automatically invited to meetings or missing meetings if they did not coincide with their session times. This led to a perception of less integration and multidisciplinary working.
I don’t feel fully integrated into the practice … the GP practices that we cover are all part of one larger group ... I was only at the practice … each one of them one day a week … one of them that I worked at was just really friendly and, like I say, I knew who the GPs were and I felt comfortable to, you know, send them a message and just sort of go ‘Oh, I’ve got this person, can I just chat it through with you?’ Or knock on a door or something. Whereas, at the other practice, I don’t feel like I knew who any of them were and, although I would still send those messages, I would just kind of feel a bit more like ‘Oh they don’t know me and I don’t know who they are’ and ‘I don’t even know who’s working today so I don’t even know who’s available for me to contact’ … at the other practice it was just taken as the norm that everyone just piles into the staff room at lunchtime.
First-contact physiotherapist, 52E
C: Practices who work in a multidisciplinary way, with established methods of communication are able to better support the embedding of first-contact physiotherapists.
M: First-contact physiotherapists spend more sessions within fewer practices, have allocated time for networking and open communication avenues. They can access and share clinical expertise to facilitate more informed clinical decisions. Integration allows continuous feedback to staff regarding referral management (resource), making them feel part of the team, and leading to better integration (response).
O: Shortened patient pathway and improved patient outcomes, reduced GP appointment use/workload over time, Staff satisfaction, improved service efficiency.
Being able to work in a multidisciplinary way was key to successful implementation of the FCP role. This was because, although first-contact physiotherapists are expert practitioners, they have limits to how quickly they see patients, their role scope and knowledge of patient history compared with GPs, and require regular communication with other clinical experts to practice safely.
in the other GP practice that she works in there’s a patient that has … spoken with the GP but then had been referred to her, but there had been a lengthy wait to see her and then COVID happened … that the patient, I think, had something, I’m afraid to say, sinister and … it wasn’t missed, it just wasn’t possibly managed and I think she [FCP] felt that, at that practice there wasn’t a great … ability to speak with everyone … there’s times when people can bypass and not see each other for a long period of time and I think definitely communication is king.
Practice manager, 02S
Despite this one instance, FCPs were reported by other clinicians to work safely with patients and escalate red flags appropriately. Clinical conversations about the boundaries of the role scope were important way for GPs to develop confidence in FCP expertise, which in turn provided a sense of relief that they could safely refer patients with musculoskeletal conditions to another staff member.
Impact of the first-contact physiotherapy approach in general practice on workload and resource use
The first-contact physiotherapy approach
There was agreement between the majority of staff and patients that FCP musculoskeletal expertise was at a higher level than the GP, which provided them with a wider knowledge base to draw from for diagnosis and management options.
He’s very good diagnostically – we value that. We’re all taught in that, we all know our musculoskeletal stuff to an extent but I always feel like physios … they know a lot more than us GPs! They’re much more thorough. They can get to the bottom of things very quickly … he’s a level up from us isn’t he?
GP, 41E
First-contact physiotherapists experienced a range of appointment times with most falling between 15 and 30 minutes. It was acknowledged by GPs and first-contact physiotherapists that, to conduct the depth of FCP assessment and associated improved patient management, it was key to provide FCPs with longer appointments slots than the GP. This is turn led to reduced prescribing and appointment use over time.
We [FCPs] get longer than the GP don’t we? … we can allow patients to explain themselves rather than directing sessions with closed questions … they see them multiple times, whereas I would see some of these people once, they see them four or five times for the same thing … so, say if you get a back pain, because they only have 10 minutes, they’ll be safety-netting them, checking for red flags and then it’s usually pain relief and they’re not usually sign-posted to information, it’s ‘Here’s your pain relief, see you later’ and they will check them up periodically and people are phoning in more to have painkiller reviews and things rather than addressing what’s actually going on
First-contact physiotherapist, 41E
The additional appointment time was well received by patients who described feeling listened to and understood by the FCP, and more confident in their approach.
I felt it was very thorough and, as I say, the exercises she suggested I do, seemed to be very relevant … I think just it was nice to not feel rushed … sometimes with the GP appointments, you can feel that you’ve only got a short amount of time there to rattle through things … she explained what she suspected the problem was … she obviously took the time to show me the exercises she wanted me to do and then she got me to sort of try doing them
Patient 127, 10S
In general, the first-contact physiotherapists were perceived positively by patients. However, a minority described finding the FCP approach, which prioritises self-management and only uses onward referral for scans and X-rays where clinically indicated, challenged the acceptability of the role.
I thought ‘No, I want an X-ray’ and I didn’t want to wrangle with him over my shoulder because I was in agony with my shoulder and the experience I’d before that it was exercises, exercises
Patient 1, 01W
This issue was acknowledged by FCPs too, who had to challenge patient expectations around scans, while not increasing the likelihood of patients using additional GP appointments if the first-contact physiotherapist had not met their expectations.
I’ve got one or two patients with niggly back pain that desperately want a scan and they didn’t get one and I’m quite sure they were upset with me with that, but I think, hopefully, a GP wouldn’t have sent them for a scan either. But, of course, sometimes that does happen
First-contact physiotherapist, 45E
Similarly, theFCPs recommendations that patients use exercises and self-management for musculoskeletal conditions had mixed responses from patients. If patients were able to understand and engage with self-management advice and had confidence that it might help, then they were more likely to engage in recommendations and experience an improvement in symptoms. However, those who found it hard to engage with this type of advice may experience less improvement in their condition and therefore may opt to see a GP in future.
At the time I thought ‘Oh, this’ll never do any good’ because it was so painful but, in fact, it probably did, because it does feel a lot better now … I think the exercises have done me good
Patient 2, 05W
A key aspect of the FCP intervention was the offer of follow-up or review after a set time frame for patients after their initial consultation. The majority of first-contact physiotherapists did offer patients a follow-up call if needed, which enabled patients to monitor their condition and feel reassured that they would receive ongoing care, if necessary. However, if this was missed then it created uncertainty for the patient as to what would happen next which might lead to GP appointment use.
H] said he would call four weeks after I had my injection and I’ve not heard from him … you don’t get the follow-up call or the follow up after that, then that kind of disheartens you to thinking … ‘I might as well just go back to my GP then’ … only because if I have to do all the chasing and all the following up, whereas normally, with a GP, they would put an appointment in … it would be mad I think to go on a different route, after going down that one … you can’t get closure if you’ve not got any [follow up] … if it does not get better or it doesn’t get fixed you can’t get closure on that injury,
Patient 1?, 03S
C: FCPs have specialist musculoskeletal knowledge compared with most GPs and are allocated longer appointment times (20 + minutes) by the practice.
M: This enables the first-contact physiotherapist to conduct a more thorough assessment, diagnose more complicated musculoskeletal disorders, determine the necessity for further investigation and provide instant access to specific non-pharmacological interventions, such as tailored exercise regimens (resource) and condition-related advice (resource). This reassures and empowers patients to take self-directed action (response) and reduces the need for them to wait for GP onward referral for physiotherapy input (response).
O: Improved patient outcomes and satisfaction; staff satisfaction; fewer appointments required (in onward referral); fewer prescriptions.
First-contact physiotherapist with additional qualifications and workload
Additional qualifications of the FCP were another key factor that impacted the way in which the role could alleviate practice workload. First-contact physiotherapists with prescribing and injection qualifications were able to take on a higher proportion of patients with musculoskeletal conditions and manage them in a more autonomous way than those without these qualifications. This led to a reduction in GP workload, as GPs no longer needed to manage these patients’ conditions or provide as much clinical supervision of FCP management. Physiotherapists with qualifications to give injections provided a perceived bigger reduction to the GP’s workload than prescribing, due to the additional time it takes for the clinician to administer injections.
I think he [first-contact physiotherapist] undertakes other things as well, for example, joint injections and things so quite hands-on. I used to do that sort of thing before in previous surgery and I’m more than happy to do that now. But the need isn’t there because the FCP does that … I suppose it allows me to deal with other things. I’m not bogged down with just musculoskeletal.
GP, 01W
C: Some first-contact physiotherapists have additional qualifications (e.g. injections/prescribing) meaning they can independently manage a higher proportion of patients with musculoskeletal conditions and deal with patients largely autonomously.
M: This frees up GP musculoskeletal workload (resource) to deal with other patients (response). First-contact physiotherapists with additional pharmacological qualifications (resource) may also reduce GP workload through decreased appointments (response); number of prescriptions/injections may also reduce due to the physiotherapist’s ability to use other skillsets, for example tailored exercise and self-management approaches.
O: Improved patient outcomes for patients with and without musculoskeletal conditions, GP satisfaction, shorter patient pathway, patient satisfaction, reduced healthcare resource use, reduced burden on secondary care appointments.
Given the governance requirement to enable FCPs to prescribe and/or inject, clinical supervision from the GP is required to support competency sign-off, which does place additional pressure on GPs while these competencies are met.
C: For first-contact physiotherapists to gain their clinical competence in prescribing and/or injecting, GPs are required to provide mentoring and supervision time, as there are insufficient other practice staff to fulfil these supervisory roles at present.
M: More time is initially required from GPs (resource) to provide supervision and mentorship, placing additional burden on their time (response).
O: While in the short term this may lead to frustration and uncertainty as to the value of these supportive mechanisms, overtime the benefits are actualised as the first-contact physiotherapist can manage more patients independently and therefore can enable the GP to use appointments for managing other patient consultations.
FCPs without additional qualifications and first-contact physiotherapists who experienced IT or governance barriers to being able to administer prescriptions, had to task GPs or other clinicians to provide patients with prescriptions, yet this was still perceived by GPs as a reduction in workload because they did not have to conduct the whole patient consultation themselves. Some first-contact physiotherapists were frustrated that they were not legislated to provide patients with fit notes, which they felt would be a useful addition to their role that would save the patient time a reduce the burden on GP workload.
It’s a lot easier to talk to you guys [FCPs] than have a whole conversation with the patient. I’d rather you have done all the leg work and come to me and say ‘This is what I’ve chosen because of this, this and this’. It’s a lot less time-consuming than having that conversation with the patient. So, it does decrease load in that respect
GP, 06W
Interestingly, some FCPs (with and without the injecting qualification) reported taking an alternative perspective to using injections than traditionally adopted in general practice. This conservative approach reduced the number of injections used and, instead, used other treatments leading to improved condition management for patients in the long term. One first-contact physiotherapist noted that this approach was in conflict with some practices that are financially rewarded for providing injections.
[I]t doesn’t take much just to inject a patient but I think the education and the information about what the injection is and how that’s going to help them going forward … obviously, we’re trying to move away from just the current injection, injection, injecting tendon pains and things like that so it’s … it’s making sure you’ve exhausted all the conservative treatments and everything else first before we start … I think we had something like 60 people waiting for an injection at one point, and I cleared that list, really. I went through that list and I probably only injected about a third of those patients in the end.
First-contact physiotherapist 61, 48E
C: First-contact physiotherapists without additional qualifications (either because they are not working towards them or the practice does not want them) cannot entirely manage patients independently and autonomously if a need for prescription and/or injection is identified.
M: First-contact physiotherapists may task the GP or pharmacist to prescribe medication, which requires sign off according to local governance procedures (resource); this generates additional workload for the tasked clinician, could delay patient treatment and may add to appointment use (resource).
O: Increased practice workload, inefficient appointment use, possible patient dissatisfaction. A reduction in GP workload, as they are not doing full consultation.
Managing referral of complex musculoskeletal conditions and staff training in these conditions
There was variation among practices in how to best manage patients presenting with complex or multiple conditions alongside a musculoskeletal problem. In some practices, these patients’ conditions were managed solely by the GP to provide a more streamlined interaction for the patient and reduce appointment use (05W, 01W). In another practice, one problem was dealt with by the GP and the musculoskeletal problem was then referred to the FCP to free up GP time (45E). Another practice made a pragmatic decision to share musculoskeletal workload among both first-contact physiotherapists and GPs because there was too little first-contact physiotherapist time to manage all the musculoskeletal patients and GPs liked this type of work (10S). One site reported an advantage to bringing together the expertise of the first-contact physiotherapists and GP to managing complexity (47E).
[M]y colleague GP and myself, we both very closely work and review at the same time pain medication also, especially chronic conditions because we tend to see in this practice, repeat patients. They keep coming back again and again and again. So, we wonder what’s going on you know? Whether we diagnosed properly and then, if needed, we do further investigations and find the problem and right medication and right exercise advice
First-contact physiotherapist, 47E
Similarly, it was not always clear whether patients who had a chronic musculoskeletal problem and were under GP care could be referred to the first-contact physiotherapist, as they fell outside the CSP eligibility criteria for an ‘acute musculoskeletal problem’. However, some practices referred these patients to FCP to ensure that these lists were full or to use the physiotherapist’s expertise to improve patient care.
[W]e were a bit like ‘Well, how’s that [FCP as first point of contact only] going to work? What if we have a day when there’s hardly anyone with musculoskeletal problems?’ … strictly speaking we can’t book in with him. If a patient comes to us first, strictly speaking we’re not supposed to send them onto [name] because that sort of defeats the object. But there is a bit of flexibility with it. We have discussed patients with him that we’re concerned about and he’s arranged to see them. I don’t know whether that’s actually allowed, strictly speaking, but it definitely helps … our problem is, NHS physios, the waiting list for that at the hospital for here is just, I don’t know, I dread to think how many months or weeks it is … he’s picking stuff off the list so that’s reducing our workload, which we really need at the moment because we’re drowning a bit.
GP, 41E
C: The practice adopts a flexible approach to FCP referral and refers patients who have previously seen a GP for their musculoskeletal problem without resolution or diagnostic uncertainty.
M: GP–first-contact physiotherapist review/discussion of patients with complex musculoskeletal conditions in conjunction with a referral for a thorough assessment by the first-contact physiotherapist (resource) provides new ideas for management of the condition that may rely less on medication (response).
O: Improved patient care and outcomes, reduced prescriptions, GP upskilling and fewer referrals to onward physiotherapy or unnecessary investigations.
While FCPs undoubtedly provided advantages to patients care and GP workload, it was also important to ensure that other staff could access some of these patients to retain their musculoskeletal skillsets and develop experience in this area.
[M]y concern is for our GP trainees … I am trying to make sure that they get some musculoskeletal stuff booked in, or if they get stuff booked in that they don’t just kind of push it on to the first-contact physiotherapist … I remember my training, we did an awful lot of joint examination and that sort of thing at university but, certainly, the trainees we’ve got now I think they’re quite lacking confidence in terms of musculoskeletal problems.
GP, 45E
FCPs were considered an important musculoskeletal training resource in general practice. Practice staff used first-contact physiotherapists for clinical discussions to develop their musculoskeletal diagnostic and management skills (43E, 47E, 48E), for shadowing (35E), for joint appointments (47E) and to provide training in weekly clinical meetings (10S, 40E).
[Y]esterday I said ‘Look, if you have somebody that you’ve seen, why don’t you book a double appointment – one for yourself, one for the FCP and watch how they would assess that patient?’ Then that way you will learn for yourself what a professional assessment from a physiotherapist would be like and you can use that to assess your own skillset.
GP, 35E
Remote consultation and e-consult
During the COVID-19 pandemic, there was a rapid increase in the use of remote consultations by first-contact physiotherapists. This new context required FCPs to offer patients telephone or video triage first to determine their problem and, if appropriate, to manage this condition remotely, and only to allocate face-to-face appointments to patients presenting with complexity or risk, to patients unable to access remote communication or to certain presentations (e.g. back pain) less suited to telephone assessment. Patients and staff across practices reported that remote consultation was convenient, quick and effective for patients whose presenting problem and access requirements were suited to this approach.
[H]e said ‘Right, I’m going to set up this on-line consultation’, this video thing, took us 20 minutes to get it right [laughs] and, anyway, I was able to … he did a very thorough consultation, I showed him my heel on the phone, he asked me all the symptoms … and he gave me the exercises to do and within two weeks I was walking again.
Patient 1, 01W
Video consultations provided helpful visual information for FCP assessment; however, first-contact physiotherapists and patients frequently experienced challenges with the technology, which prohibited its use. Conducting triage or consultations via telephone removed visual cues about the patient that were helpful when determining diagnosis and treatment plans, which led to uncertainty that the physiotherapist might miss things.
I certainly worry more over the phone than seeing them face to face, because when you see someone it’s quite reassuring … It creates anxiety doesn’t it? You feel a bit more vulnerable to missing things and litigation and things I suppose … Yeah, I suppose [it does affect satisfaction in the role] … I’ve not enjoyed it since COVID as much at all.
First-contact physiotherapist, 41E
To account for this new risk to patient safety, FCPs made sure that they understood patient histories, safety-netted patients and encouraged them to come back for reviews if their symptoms did not resolve.
[since remote working] we do get a few more [reviews] now than we used to … Some of the challenges of remote working in that, you know, did we get things right at that first appointment or not and has the patient fully understood what we were asking them to do, because you can’t demonstrate the exercises.
First-contact physiotherapist, 52E
First-contact physiotherapy staff reported that conducting remote consultation over long periods impacted their satisfaction in the role. They missed the patient rapport of face-to-face appointments, and found the role became more sedentary and isolating. To alleviate this pressure, one practice (06W) limited the number of remote consult patients per day by recruiting additional staff from other physiotherapy teams.
[T]he enjoyment level’s definitely gone down because … well, I can spend five or six hours on the phone and it’s dire … It’s just the fact that when a patient comes in at least you walk up to the door, and you assess them and you’re moving around. You can be stuck at your desk for hours … so physically having aches and pains, yes. And well-being.
First-contact physiotherapist, 41E
Remote consultations also led some patients, who had an expectation that face-to-face assessment was necessary or who lacked confidence in their ability to describe their problem, to feel uncertain that the FCP understood their condition.
I think I’d feel … as if I was getting better treatment if I was going face to face rather than just on the telephone. I’d prefer somebody to touch … the painful area … then they would see exactly where the pain was, rather than me trying to tell them on the telephone.
Patient, 02S
Other patients trusted the FCPt enough to allow them to determine what was the best form of assessment for their problem. One patient highlighted that this trust was dependent on the patient’s confidence in their ability to articulate their problem over the telephone. This issue was also highlighted by first-contact physiotherapists, who found variability in patients’ ability to verbally describe their problem impacted their certainty in diagnosis.
[W]hen you talk to someone over the phone, they feel that they have to tell you 10 times that their shoulder is hurting … They go on and on and on. It’s tiring … they’ve done my head in by their terrible description of what’s going on and I’ve got no idea which bit of the body they’re even talking about!
First-contact physiotherapist, 05W
Both staff and patients had concerns that, for some patients, remote consultation may ultimately lead to duplication of work and increase appointment use over time. Duplication occurred if patients were triaged remotely and then required face-to-face assessment thereby using two appointments, or if problems were not adequately assessed and managed at the first consult due to the limitations of telephone working.
[T]hey sort of tried to save time with the appointments by talking to you over the phone and not offering you a follow-up appointment … actually you’ve ended up having to use so many appointments to get to the bottom of what’s going on … It cost me five months of complete and utter distress and it cost them far more money in the end … some things, they [GP and first-contact physiotherapist] do need to see you for.
Patient, 47E
C: Remote consultation imposed through circumstances (i.e. COVID-19) or as a result of practice approaches to consultation, mean that diagnoses and decisions regarding management are made without seeing the patient in person, resulting in anxiety and frustration for patient and the first-contact physiotherapist.
M: Creating systems that allow time for patients to explain symptoms and follow-up appointments to manage uncertainty (resource) allays first-contact physiotherapist concerns regarding missed diagnoses (response) and provides patients with confidence that their condition is fully understood and managed appropriately (response).
O: Impact on resource use through double appointments but longer-term more effective use of resource as less likelihood of misdiagnosis or patients presenting to GPs.
Practices imagined that going forward beyond the COVID-19 pandemic that they would offer patients a ‘hybrid approach’ of face-to-face and remote consultations. This would provide increased access and convenience for those happy with remote consultations but ensure that patients could retain the choice of having a face-to-face appointment. This was important to ensure equitable access to provision for those unable to interact with remote ways of working. This reasoning also applied to the use of e-consult to book appointments. Practice staff highlighted barriers to remote access for those with poor internet connection, limited availability of mobile data or wi-fi, little confidence in using technology or limited health literacy or ability to describe their condition. To overcome these issues, one practice offered patients the opportunity to complete shortened e-consult forms over the telephone.
[T]he other thing worth mentioning is that when you have only open access that, for the health illiterate and the people that GP will always be the first point of contact, which is your less well-educated, so you fuel health inequality in some respects, because those who are health literate will have instant access to advanced physio, whereas those that aren’t have this delayed GP presentation referral route.
GP, 10S
C: Some patients with musculoskeletal conditions cannot access e-consult forms or engage in remote consultation due to low health literacy, data poverty or difficulty accessing technology. These patients may experience delays in seeing the first-contact physiotherapist and may wait longer for an appointment.
M: Patients register their need for an appointment and the receptionist conducts a shortened e-consult in person or calls them from the practice (resource). The first-contact physiotherapist provides face-to-face appointments for patients who need them (resource). Patients with access requirements gain equitable access to musculoskeletal advice (response).
O: Equitable access to FCP appointments.
Employment of first-contact physiotherapists
Recruiting experienced physiotherapists to the role
Practices highlighted the importance of recruiting FCPs who had a specific level of training and experience to embed the role successfully and safely within a general practice population. Witnessing first-contact physiotherapists managing musculoskeletal conditions successfully enabled GP and other practice staff to build trust in the role and safely delegate patients to them, thereby relieving GP workload.
Our experience with the fully funded roles, the ARSS [Additional Roles Reimbursement Scheme] roles … is that it’s very, very much dependent on the person who’s in role … they are taking risks, they’re taking a responsibility and that ability to manage that risk and responsibility is all down to experience and their skills … the GMC rules are quite clear on that, is that when you’re delegating responsibilities you have a responsibility to make sure that they’ve got the ability to do that work for you, because you’re still held responsible for their mistakes … there is a risk involved in that and protocol and clinical governance, document and contract only go so far. So, it’s important that we get the right person.
GP, 35E
However, practices noted that there were not enough advanced or experienced physiotherapists available for them to recruit into general practice. Practices were concerned that they were pulling physiotherapy staff out of secondary care posts and that staff coming into general practice would require additional training and mentoring to develop their competencies. Despite guidance that explicitly states this role should be provided by band 7 or 8 physiotherapists, there was evidence that this was not being adhered to in practice.
If FCPs [are] employed without past experience then they will find the role more challenging – mentoring maybe more important for these FCPs … we have an FCP, she’s like a band 6 or something, when I had a one-to-one with her she was saying she was not that confident seeing all the ankles and foot injuries
First-contact physiotherapist, 37E
Training, supervision and support of first-contact physiotherapists
The impact on general practice of recruiting less experienced FCPs was that they needed to provide additional time for the physiotherapist to engage in training and development and allow other staff time to provide supervision, daily debriefs or to sign off training competencies. Practices also needed to fund the advanced practice courses. Less experienced physiotherapists described how important clinical discussions were to maintaining patient safety (43E, 45E) but also mentioned how the time it took to have these conversations impacted on their caseloads, which could increase stress levels, and it was felt that the pressure put on first-contact physiotherapists more generally was impacting their health, burnout and willingness to remain in the role. Similarly, first-contact physiotherapists reported a lack of time to complete the advanced practice training requirements.
[A]t the moment, as an FCP you really do ‘do’ the clinical part well but it’s finding time to do the other things, and I certainly think we probably … we have training time as part of our role and I think that needs to increase a bit more … you can’t just do clinical – I think you would burn out … I think there should be perhaps 70/30 or even 60/40.
First-contact physiotherapist, 10S
I just think these guys have had their accreditation coursework to do, a lot of them are doing their injection courses because that’s become a must, they’re trying to do their roles, they’re trying to see their patients, they’re trying to keep up to date with their admin, and they’re exhausted.
Interface clinician
Supervision of the role was fundamental to FCP development and ensuring safe practice. While this was recognised at some practices, at others first-contact physiotherapists reported that supervision input was inadequate, or supervisors were not clearly identified or accessible.
I’m new into post and sometimes I think just having a little bit more support from GPs, but also from the nurses … just to be able to tap into that a little bit more easily … I think that’s very important … I’ve not had any supervision from any of the GPs at all. I’m not aware that anyone has gone through any of the patients I’ve seen to check that they’re happy with my handling of the patients … the other FCP, who is more experienced, we only work on a Monday together … we don’t actually physically ever see each other … a couple of times when I’ve had a very complex patient I would have valued somebody just to sit and chat through. When I very first started, the first week, I said ‘Who do I have time with to chat over patients?’ and one of the GPs said ‘Why would you be needing to do that?’… they’re expecting [name], the other FCP to be a supervisor for each other.
First-contact physiotherapist, 45E
FCPs valued their connections with colleagues in general practice, yet they highlighted that the nature of the role could be clinically isolating at times, particularly for physiotherapists employed in areas without other first-contact physiotherapists nearby. To alleviate this problem, many first-contact physiotherapists accessed other avenues of support beyond general practice, such as FCP or physiotherapy colleagues in primary or secondary care using face to face meetings, or remote groups, such as WhatsApp (Meta, Mountain View, CA, USA), NHS Futures or Zoom.
C: First-contact physiotherapists are new to primary care and feel isolated compared to working in busy outpatient departments. Rural locations, part time and remote working, and PCN employment models (which may inhibit integration into one practice team) make it difficult for first-contact physiotherapists to gain face-to-face support from their peers. Having clinical discussions with other experts in musculoskeletal conditions is important for confidence and development in the role.
M: First-contact physiotherapists use clinical networks and peer support within and outside general practice using face-to-face and virtual communication (resource). This improves clinical decision-making and a feeling of clinical support which reduces feelings of isolation (response) and enhances safety-netting (response).
O: Improved patient outcomes and safety, development of staff skillset and staff satisfaction.
Employment models for first-contact physiotherapists
FCPs described variation in their employment experience based on how they were employed. For example, some were employed under a PCN structure to meet the needs of patients with musculoskeletal conditions across several practices, whereas other were employed directly by a single practice or practice group. Being employed directly by a single practice or group provided first-contact physiotherapists with some clarity about who held responsibility for supporting their role.
I’m employed by the practice … main thing is that, um … they are now my employer, and so there’s a responsibility there. Um, and, you know, I’m part of the team and I’m integrated into the team and my training is done in-house … just being there full-time, as well, that probably makes a big difference … from an integration point of view
First-contact physiotherapist 61, 48E
Some FCPs employed under a more centralised structure (e.g. PCN, trust or health board) experienced more barriers in tailoring aspects of their employment to meet individual needs, for example, accessing laptops for home working or negotiating leave.
I actually self-isolated with my daughter and that created quite a bit of a rift in one sense, and it’s more ... about the differences in ‘Well, we pay for these sessions, this is what you should be providing’ you know, etc. … that’s coming through the PCN and the practice manager’s side of things … So I actually ended up working from home, but it was ‘who is responsible for setting that up and developing it between the trust and the hand who’s paid for what and that’s the business end of it’? That I just don’t want to be involved with!. at one point it felt like, I was pretty much stuck in the middle of it all and you’re trying the best for both areas … we are in the process of really doing is learning from that experience and saying ‘OK, who does what and who’s responsible for what?’
First-contact physiotherapist, 17E
In certain instances, this higher-level employment model could be advantageous for both practice and FCPs, as it provided opportunities for larger groups of physiotherapists to connect and be part of a team rather than working in silos at individual practices. This led to more training opportunities and autonomy to develop the role among themselves.
[W]e’re managed centrally, if you like, so we’re not employed by the GPs, we’re managed by the health and care social partnership … we all work very differently depending on where we work, but our clinical governance, if you like, and our CPD, all those sort of things, are run more centrally … essentially we’re kind of in charge of everything else, which works well because we’re not … we can sort out the CPD and all the sort of training issues amongst ourselves rather than have to rely on an individual practice. So, we’ve got that support network
First-contact physiotherapist, 10S
Similarly, there could be advantages to practice of not having to negotiate individual contracts and benefiting from the FCP skillset without the burden of managing the role.
[W]e’ve got our physio through the CMAC team, and I’ll try and remember what the CMAC team is when I get a minute! So, all that was sorted out between those really, the SLA and what their salary would be or how much would we be prepared to … there was probably a bit of negotiation went on. You know, how many hours he could work for us.
Practice manager, 01W
C: FCP provision to practices through a provider model delivers a more consistent service for both practitioners and GP practice.
M: First-contact physiotherapists continue to be employed on their substantive contracted terms and conditions via a central provider, have access to peer support networks and professional development opportunities and may work within a rotational model that still exposes them to traditional physiotherapy department placements (resources). For the practice, this provides a more stable service as the employment, professional development and performance are managed centrally (resource).
O: This enables a more secure employment opportunity for first-contact physiotherapists, professional support and improves job satisfaction (response). For the practice, it improves service effectiveness and knowledge of the system (response).
The biggest issue highlighted by FCPs of working under a centralised employer to cover multiple practices was the difficulty in getting to know the teams, processes and IT systems across a variety of workplaces quickly. While they reported that they were able to understand these differences over time, it meant that they experienced a steep learning curve on entry to the role; learning new processes was time consuming and there was a risk of mistakes during this period impacting patient care. One practice highlighted the importance of moving towards using more standardised systems between practices.
[O]ver time, when you’re having staff that work over multiple practices and that number of staff increase, then there’ll have to become, by the back door, some more uniformity. So, we’re really lucky because we got some funding from NHS England through something called Quick Start and so, all the practices have been working together to change all of their templates so that we all use exactly the same template … Because we do occasionally get, like … we’re getting them now, significant errors where the pharmacists have put a recall on for somebody to come and have a blood test for safety, but they’ve used the wrong code for that particular practice because there were options. And, so, it’s the same for the physio, you know, if they’ve not actually booked the patient in for a follow-up and they’ve just put a code on thinking that somebody in an office some where’s going to call back and it’s not a code that that particular practice search on you have a problem. And the same for adding drugs, you know, like injections and things.
GP, 40E
C: First-contact physiotherapists are required to work across multiple sites with different IT systems or processes in place, which may restrict access for staff and can be confusing and time consuming. This can lead to mistakes being made that impact patient care/safety and is inefficient for staff.
M: Governance and practice systems can be managed centrally to develop standardised systems (resource), which will be quicker and easier for staff to use across different locations (response) and ensure that first-contact physiotherapists have access to all patient information.
O: Improved consistency of service, staff satisfaction, improved patient safety and better clinical decision-making.
Service design and implementation
Safe, effective and efficient FCP service delivery requires appropriate planning and support, and the right skill/experience level. Data highlighted that, because of demand, staff have moved into roles without the necessary patient mileage and skill level which has placed them in a potentially precarious and unsafe position.
I think it was rushed … I felt it was implemented very incorrectly. I think a lot of the FCP staff have been hung out to dry a little bit. I think a lot of the FCP staff aren’t qualified enough to do that role.
Interface clinician
I don’t know whether we’re training physios and we’re getting enough band 5s to come in. We need that flow of staff that are coming through that we’re training up and I know a few years ago we didn’t have that. I don’t know what that training position is now, but we certainly need to increase that in order to supply staff to a completely new sector.
Interface lead
The data emphasised the potential for FCP to bring about additional benefits if practices moved away from the traditional throughput model in primary care. Spending time doing joint consults, upskilling other professionals (and themselves) could enhance the patient and the system, but the system is not set up for this. First-contact physiotherapists are not in the role to simply manage workload, they need to add value to patient management, and their ways of working need to be respected if they are to maximise their system potential.
My understanding is that it’s all about numbers and getting through patients and I suppose that comes back to the culture of primary care and is that culture around that throughput or is it around the quality and the learning and the development of staff? FCPs could be brilliant if we have the right FCP in and they were doing a lot more of those joint consultations and that learning and case discussions. I think they could really improve care for patients ... it was an opportunity to put physios in and to change some of that culture and to take some of that pressure and just to slow things down to improve on the quality of things rather than being on that treadmill where they’re just trying to get through numbers.
Interface lead
Provision of FCPs should not be at the expense of other physiotherapy roles; it should be in addition to them if the system is to work effectively. The ongoing issue of moving staff around is having a system wide impact. Taking experienced staff from physiotherapy departments is resulting in reduced skill and capability to provide effective rehabilitation and supervise more junior staff.
We’ve taken all of the good Band 6 and Band 7 more experienced physios out of department and into FCP, so now the Band 5s are struggling, which is putting more pressure on the 8s that are around in departments and that are in the hospital, like myself. It’s upped my e-mail and telephone workload massively.
Interface clinician
You needed 20 or 30 new physios to do the FCP and keep all those physios in department, because all you’re doing is robbing Peter to pay Paul and that, for me, is where the waiting lists are going up
Interface clinician
C: The demand for staff to fill first-contact physiotherapist roles means that either senior staff are migrating from department-based physiotherapy services into FCP; or more junior, less experienced staff are taking up first-contact physiotherapist roles. This reduces the senior, experienced skill set in physiotherapy departments and/or places staff with less experience in frontline roles.
M: Creating a system whereby junior staff are supported to develop FCP skills within their departmental roles and exposed to FCP alongside more senior staff (resource) would provide opportunity for role development and preparation (response).
O: This would create a more structured pathway for career progression allowing staff to gain FCP-specific skills earlier within their careers enabling better preparation into FCP roles and develop a workforce ready to move into FCP roles without detriment to department-based services.
Discussion
Quantitative results of the evaluation investigating the clinical effectiveness and costs of FCP models of care and the continued GP-led model showed that clinical outcomes at the primary end point of 6 months do not differ significantly between models. However, it was found that patients who saw the FCP(ST) and FCP(AQ) recovered sooner compared with those who saw the GP; patients who saw the FCP(ST) had a greater improvement in days lost compared with those who saw the GP and FCP(AQ). Patient satisfaction with their ‘visit’ was significantly better when comparing the GP with the FCP(AQ) but not significantly different compared with the FCP(ST). When considering total costs, the GP model was significantly higher than both the FCP(ST) and FCP(AQ) models of care.
The associated qualitative findings highlighted the barriers and facilitators affecting how the FCP role is currently impacting the wider musculoskeletal system and referral pathways, and the ways in which the role is supporting primary care capacity by introducing an advanced level of clinical practice. Findings emphasised factors influencing degrees of embeddedness into primary care teams, as well as highlighting the importance of satisfaction of the role from the point of view of the first-contact physiotherapist.
The following chapter discusses the findings in greater detail, integrating the mixed-method findings in relation to service implementation.
Chapter 7 Discussion
The realist evaluation of effectiveness and costs of FCP-led models [throughout this discussion, FCP relates to both models of FCP(ST) and FCP(AQ)], supported by the other WPs including a survey, realist synthesis and mixed-method study investigation of remote consultation and staff well-being resulted in programme theories described in terms of CMO. Data were triangulated and are presented below in relation to the original project aims of how the FCP model of care could:
-
provide optimal patient management
-
show meaningful patient benefit
-
relieve GP workload pressure
-
promote better use of healthcare resources
-
positively impact on whole-systems musculoskeletal practice.
Within the following discussion, particular emphasis is placed on implementation considerations, as since this study commenced there has been significant investment in expanding the FCP role with ubiquitous provision across all UK nations. In England, all adults consulting with MSKDs in primary care will have access to FCP in 2023–24, as such provision of implementation considerations is helpful to assist in service planning.
Provide optimal patient management
The primary research question for FRONTIER was to determine the effectiveness and costs of the FCP-led programme compared with GP management. Quantitative analysis showed that both GP- and FCP-led models were equally effective at managing MSKD, evidenced by the SF-36 outcomes at the 6-month primary end point. However, a greater proportion of patients who saw either the FCP(ST) or FCP(AQ) recovered more quickly at 3 months compared with those who consulted with the GP. While the recovery trajectory for MSKDs can vary widely depending on the diagnosis, symptom severity and individual psychosocial factors, this may be explained by the likelihood that FCP-led approaches allowed more consultation time, which may have enabled more refined diagnosis and targeted plan for treatment provision (e.g. specific exercises). While it should be noted that patients in the FCP(ST) arm of the study presented with significantly better MSK-HQ and EQ-5D-5L VAS scores, indicating a better state of MSKD health, this was not reflected in the FCP(AQ) arm, so is unlikely to account for the differences in recovery time. Indeed, previous work has highlighted GP propensity for pharmacological management, rather than guideline-based rehabilitation strategies for MSKDs,14,58 so this may feasibly account for differences in recovery. Whether the deviation from evidence-based guidelines results from awareness and competency levels is unclear; potentially reduced GP consultation time may account for diagnostic uncertainty, a reduced opportunity to understand the psychosocial impact of MSKDs and to address self-management strategies, all of which are critical for MSKD management. 59 It should be noted however that recent GP consultation duration data demonstrated that, in England, almost one third of GP consultations lasted more than 15 minutes, with around 19% lasting more than 20 minutes. 60 This is probably a representation of the complexity of many GP patient consultations, but may not be reflective of the time afforded to MSKD consultations, which GPs considered a simpler problem. Interview data from this study demonstrated that GPs perceived MSKD presentations as a quick consultation, and almost a relief from the complex nature of other conditions. While this may be the case for some acute injuries, for example, this does not reflect the majority of MSKD presentations, and could account for the less than optimal disease management. 61
Patient interviewees in this study valued the time spent with first-contact physiotherapists, the time taken to assess, explain and address the problem, and the provision of empowering self-management advice which may have impacted satisfaction. This was reflected in GPAQ scores related to the visit, where satisfaction was higher for physiotherapy-led appointments compared with GPs, although reported satisfaction with the reception appointment process was better for the GP compared with FCP(AQ). This may be related to patient expectations regarding which healthcare professional they expected or wanted to see for their condition and relates to appropriate advocacy and signposting discussed later. It should be acknowledged however that some patients were not satisfied with FCP approaches, particularly when they did not align with their own expectation and preferences. This was noted when first-contact physiotherapists did not support radiographical investigations, choosing instead to use their clinical reasoning to determine that scans were not required to manage the condition effectively; there was a concern that this may mean that GPs would be consulted instead, and would offer these investigations, thus undermining the first-contact physiotherapist’s decision-making.
Findings from the realist synthesis and interviews highlighted the importance of the extended FCP appointment time both from a professional and patient perspective, and in line with CSP guidance62 the majority of FCP appointments within the FRONTIER study were of 20 minutes’ duration, and resource use costs were based on this premise, although several did acknowledge that their contact time had either been reduced or was under threat from practice managers, seeking to align provision to GP consultations. As discussed, the additional time permitted thorough assessment of biopsychosocial issues, diagnosis, provision of immediate tailored advice, prescription where appropriate and onward referral where necessary. Whether reduction in FCP-led appointment times would elicit the same outcomes is unknown but, given the levels of satisfaction and outcome success (clinical and cost), it would seem prudent to retain the extended nature of the appointment.
A further proposed outcome derived from the earlier realist phases suggested fewer prescriptions would be administered by FCP-led models, either through independent prescription [FCP(AQ)] or via locally agreed processes for those without prescribing licenses. This was supported by the case-study evaluation, which identified higher proportions of patients managed pharmacologically by GPs compared with those who saw the physiotherapists. Of note was the higher number of opioid derivatives in the GP-led group. While there has been a significant drive to reduce opioid use, with significant progress having been made,63 GP use is still notable and considerably more prevalent than controlled drug prescription by physiotherapists. Indeed, the qualitative work highlighted that prescribing licenced FCP(AQ)s used their qualification to deprescribe in many instances, a phenomenon described elsewhere among UK-based first-contact physiotherapists. 64
From an onward resource use perspective, data showed relatively small reliance on other services within each model. For services that were used there was a greater number of referrals to outpatient physiotherapy by GPs, as would be expected, and an indication of a greater proportion of patients referred for X-rays in the first 3 months post consultation; other work has suggested GP overuse of magnetic resonance imaging but this was not reflected in this study. 65
The self-reported low engagement/referral to exercise classes was surprisingly low across all groups. Recommendations and guidelines for all MSKD management highlight the benefit of exercise as a core intervention. It is possible that referral to exercise programmes, such as ESCAPE-pain,66 for example for those presenting with osteoarthritis or low back pain, was hampered by COVID-19, and it is also likely that FCP consultations resulted in targeted exercise prescription, but this cannot be verified from the resource data.
From a within practice staff perspective, the qualitative work suggested an overall level of satisfaction with FCP-led models. Reception/care navigation staff valued the opportunity to offer patients appointments with FCP staff; GPs recognised the benefits of additional, alternative skill sets to their own, and other trainee and qualified clinical practice staff noted opportunities for shared learning assist them with their management of MSKDs. Interestingly, there was a perception that one of the benefits of the FCP models was expedited access to care, but CSRI data showed that the median wait for a GP appointment was 7 days, identical to the FCP(AQ), while the FCP(ST) median wait for an appointment was only 2 days sooner, with a 5-day wait.
While FCP job satisfaction remained positive, there was an impact on appointment format with the increased use of remote consultation, initially imposed by the COVID-19 pandemic, but also encouraged within the NHS Long Term Plan’s ‘digital first’ aspirations. 43 Most first-contact physiotherapists reported remote working to be more convenient for many patients but not as effective from the clinician perspective, and impactful on their own health and well-being; in fact, many had reverted to in-person appointments as restrictions lifted, recognising the diagnostic restrictions of this format and the limitation in some patient groups, such as those who had limited English language use, had hearing difficulties, or when IT use was restricted. Interestingly, the patients’ view of remote appointments was mixed, with many suggesting they ‘hadn’t had an appointment’ if it was a telephone consultation, with others recognising the convenience.
Of utmost importance when considering role substitution and supplementation is that safety levels are retained, and this was indeed identified with the realist synthesis as an important outcome. Analysis of the PREOS-PC outcome measure, which measures patient perceptions of ‘safe care’, identified no significant differences across models.
From an implementation recommendation perspective, key issues to consider are:
-
Extended appointment times (20 minutes) should be maintained so that first-contact physiotherapists can deliver patient-centred, personalised care while remaining clinically and cost-effective.
-
Employing either FCP(ST)s or FCP(AQ)s results in the same clinical outcomes with no obvious benefit of additional competency qualifications.
-
Retain extended appointment times of at least 20-minute duration.
-
It is not necessary to employ first-contact physiotherapists with additional pharmacological qualifications to achieve an effective service.
Show meaningful patient benefit
In addition to the impact on clinical outcomes detailed above, in particular, the expedited recovery in FCP-led models of care, the data suggest that patients in FCP-led models of care demonstrated considerably fewer days off work than those within the GP arm. Previous work has demonstrated the significant impact on days lost, with an average of 15.2 days per year in 2021/22 for those impacted by MSKDs. 67 Interestingly, provision of fit-note certificated absence was particularly low in the FCP(AQ) led-model (3.8%), while the GP-led and FCP(ST) models recorded 14.7% and 16%, respectively.
FRONTIER recruitment was completed by the end of April 2022, and it was not until July 2022 that the legislation for fit-note provision changed, permitting physiotherapists (along with other non-medical professionals) to issue fit-notes. 68 As such, patients within the non-GP-led arms would have required GPs to issue fit-notes either at the request of the consulting first-contact physiotherapist or through a subsequent appointment with the GP, both of which require additional resource use. Changes to legislation therefore have a positive impact on GP demands, but from the current data, it is not possible to determine whether the change has resulted in altered behaviour regarding fit-note provision.
The findings of fewer workdays lost following FCP consultation is a positive one. An earlier national evaluation found that 54% of patients who consulted a first-contact physiotherapist reported reduced impact on their ability to work over a 3-month period following consultation, yet only 29% reported receiving work-related advice. 23 The current study did not record whether work-related conversations were undertaken; nevertheless impact on ability to work showed positive outcomes.
Meaningful patient benefit of healthcare interventions is often perceived in terms of condition improvement or recovery and better quality of life. At the primary end point of 6 months, a similar proportion of patients improved in relation to their physical function (primary outcome SF-36 PCS) irrespective of their consultation model. This equated to 67% in the GP-led arm; 70% in FCP(ST) and 67% among the FCP(AQ) consultees. This, however, suggests that approximately 30% of all consultees did not improve. This is reflected in UK-wide data, which suggest that approximately one third of the population live with a MSKD, an issue which creates significant burden on individuals and the healthcare system as a whole. 69 Of note is the change in quality of life scores, which, while similar and not significantly different across arms, only demonstrated around 50% of patients’ quality of life improved after 6 months. While this may be reflective of previous criticisms of the EQ-5D-5L as an outcome measure,70 or indeed the likelihood that, when reporting outcomes, patients conflate the impact of other conditions in their appraisal, it remains a concern that quality of life remains significantly impacted by a large proportion of patients.
-
There is a clear, meaningful benefit on days lost when individuals consult with a FCP(ST) for a MSKD. First-contact physiotherapists could be provided with additional training and support to improve work-related conversations and advice further to build on current provision.
-
Provide training in work-related conversations and management to maximise consultation outcomes.
Relieve general practitioner workload pressure
When considering human resource use, an original driver for extending primary care skill mix both in the NHS Long Term Plan36 and subsequently with the ARRS, was to reduce the burden on GPs,24,40 with continued rhetoric in this area. Yet reports consistently show that GP demand continues to increase and will continue to do so as the overall population grows, and in particular the increase in the over-65 years population, who are higher users of primary care services. 9,71,72
First-contact physiotherapy-led models of care do not reduce GP burden per se as inevitably demand is taken up by other conditions, which may in fact be more complex, but it does potentially free up appointments for other conditions that necessitate GP consultation. To date, there are few data to support this suggestion, however, with patient satisfaction continuing to fall; only 56% of patients considered their experience of making an appointment as good or better in 2022, a reduction from 70% the previous year. Furthermore, more than 1 in 4 people reported difficulties in making appointments and therefore gave up, an increase from just under 1 in 10 the previous year. 73 An early case study evaluation of a site introducing FCP into their service reported a 9-day decrease (from 19 days) in non-urgent GP appointment times, which they attributed to FCP introduction. 74 Data from FRONTIER, however, suggest that the median wait for a GP appointment was 7 days (IQR 2–20 days); FCP(ST) 5 days (IQR 2–10 days); and FCP(AQ) 7 days (2–14 days). Recently reported figures suggest that non-urgent patients receive a GP appointment within 2 weeks (in England),75 so there is a possibility that our sample (across the UK) is not entirely reflective of current wait times.
There are no robust data that demonstrate how wait times for FCP are changing over time, but certainly in our qualitative work there was a perception from practice staff and patients that access to FCP was easier compared to seeing a GP, but this is largely unsubstantiated in the current study. Perceptions of decreased wait may be due to practice staff reflecting on the early stages of FCP implementation, as interviewees frequently stated it took time for both patients and reception staff to be aware of and use the new model, so diaries were remaining relatively free and therefore accessible as the service became established.
A previous evaluation of FCP services in England reported that GP workload was positively impacted, as the majority of patients did not consult their GP with the same problem within 3 months of seeing the first-contact physiotherapist. 23 This was supported within FRONTIER, with very few patients consulting with the GP for the same problem having seen the first-contact physiotherapist, whereas many more patients who initially consulted their GP, reconsulted for the same problem within the study period.
If the success of FCP-led models of care are considered in terms of reduced GP burden, this may be a challenging argument to evidence76,77 given the continued pressure placed on GP staff. Within the realist synthesis, some GPs noted additional burden placed on them as a result of ARRS implementation (including FCP) due to increased supervision time, more complex team management and changes in caseload complexity. One of the supervisory burdens relates to FCP staff seeking to gain prescribing and injecting competencies, either as part of a progression to advanced practice or to extend their clinical capabilities; furthermore, some first-contact physiotherapists also reported the excessive burden placed upon them to achieve additional qualifications or work towards advanced practice. There was very little representation of advanced practice within FRONTIER, so difficult to determine any benefits or otherwise to the service of this level of practice. However, there were no significantly apparent service benefits of employing a FCP(AQ) compared with a FCP(ST) within practice, so given the necessity for GP involvement to support development of FCP(AQ)s, it may be more efficient to employ a FCP(ST) assuming that there are pathways to manage prescription of drugs that adhere to all governance and legal requirements. It should be noted, however, that in Northern Ireland all are employed at advanced practice level, with additional prescribing qualifications [FCP(AQ)]. Only one practice with a physiotherapy-led model of care was recruited in Northern Ireland, so meaningful analysis of this approach is not possible.
Research on the impact of prescribing is mixed. A national evaluation of independent prescribing among physiotherapists and podiatrists demonstrated that while there were high levels of patient satisfaction and acceptability, alongside clinical effectiveness, this was no different from that provided by non-prescribing staff supported by medical prescription. 78 Another study investigating independent prescribing activity of physiotherapists (not necessarily FCP) in musculoskeletal clinics noted that most activity was for medicines optimisation (dose adjustments) (18.1%) followed by recommendations for OTC medication (15.5%); only 4.1% of reported activity was for prescription of a new medicine. 79
While there may not be excessive benefits to patient management resulting from independent physiotherapy prescribing, it should be noted that there is a current shortage of GPs in practice, with no obvious improvement envisaged. Extending the competencies of other staff to fulfil at least in part some of the roles traditionally undertaken by GPs will help to address some of the workforce challenges and maintain quality care at the first point of access. Prescribing also supports the progression of individuals in advanced practitioner roles.
-
FCP(ST) and FCP(AQ) models deliver equal service outcomes so there is no clear benefit to employing a first-contact physiotherapist with additional qualifications, particularly given the additional burden placed on staff in association with this.
-
Benefits of FCP-led models need to be carefully conveyed to GPs and practice management staff to manage expectations; basing service success on reduction in GP workload is unlikely to achieve the desired aims.
-
Provide clear guidance regarding the scope of FCP practice for patients and practice staff members.
-
Convey the wider benefits of FCP to the practice team regarding impact on medication use, other healthcare resources and recovery time.
-
Do not suggest that FCP ‘frees up’ GP time per se; make it clear that it will reduce the musculoskeletal caseload, allowing patients with other more complex needs to access GP appointments.
-
As first-contact physiotherapists with additional qualifications grow in number, support these staff to become mentors with capability to supervise and sign-off competencies to reduce the requirements of GPs.
Promote better use of healthcare resources
The previous text has detailed some of the resource use benefits associated with consultations, prescriptions and investigations. FRONTIER adopted a non-inferiority analysis of GP, FCP(ST) and FCP(AQ) models, assuming that each would be effective and safe. This assumption was supported at the 6-month primary end point, with analysis of the SF-36 PCS primary outcome measure demonstrating no significant differences across service delivery models. Furthermore, in relation to the EQ-5D-5L, there were also no significant differences in outcome analysis at 6 months. Given the similar clinical outcomes, implementation decisions can be driven by the costs associated with the delivery models and cost minimisation considered. Based on consultations and subsequent resource use, the median cost per patient on the GP-led model of care equated to £105.50; costs for FCP(ST) and FCP(AQ) were £41.00 and £44.00, respectively. There was therefore a clear benefit to implementing FCP-led models of care at a ratio of approximately 2.5 : 1 compared with GP care, which would incur significant cost savings given the extent of MSKD consultations in primary care. 1,3,15
The main analysis was based on band 7 physiotherapists filling both the FCP(ST) and FCP(AQ) roles, as this was the banding of most of the participating FCP staff and fulfils CSP recommendations for non-advanced practitioners. 80 However, given the drive towards advanced practice,80 and the Northern Irish requirement for advanced practitioners fulfilling these roles,81 a sensitivity analysis based on band 8a staff fulfilling the FCP(AQ) roles still retained the significant cost reduction compared with GP-led models, but did detect a statistically significant higher total cost when compared with the FCP(ST) band 7 costed model.
FRONTIER recruitment and data collection occurred throughout the COVID-19 pandemic, so consultation format was impacted by social distancing restrictions, although cost analysis did take this into account. Going forward, however, and in relation to the NHS Long Term Plan drive for ‘digital first’,43 it will be important to monitor resource use associated with this approach. Qualitative work in the study focusing on remote consultations suggested that first-contact physiotherapists were inclined to review patients on the telephone, but frequently bring them in for a face-to-face reconsultation due to diagnostic uncertainty, given their responsibility as the first consulting clinician. Indeed, the nationwide survey of staff demonstrated that most first-contact physiotherapists had largely reverted to in-person appointments, noting this to be more effective and satisfying to them as clinicians, and more inclusive for those who, for a variety of reasons, found remote consultations challenging. As the digital agenda progresses, this has the potential to significantly impact resource use if further appointments are required to confirm diagnoses. It may be, however, that as staff get more experience and confidence in their more autonomous role, willingness to make decisions remotely may become more likely.
Findings here, supported by earlier work by Moffatt et al. ,76 also highlighted best use of resource relied on a clear understanding of the FCP role to ensure appropriate referrals were made, and therefore reduced appointment wastage. In some cases, the role of the FCP was unclear to practice staff, leading to unnecessary referrals and duplication of workload. Typically, the responsibility to communicate the scope of the role fell to the first-contact physiotherapists themselves, which was particularly difficult if they were covering multiple practices, and when they were challenged with balancing workload with such additional tasks of practice staff training. Those practices with self-reported established methods of communication (including team meetings; time for first-contact physiotherapists to discuss their role with other staff; supporting literature (for patients and staff); electronic communication channels) described stronger relationships between staff, improved understanding of the role, and therefore more appropriate appointment booking.
-
Both FCP(ST) and FCP(AQ) band 7 models provide a better investment compared with GP-led models of care; band 8a employment is significantly more expensive than the band 7 model but still better value than the GP-led model of care.
-
Remote consultation may result in additional resource use as first-contact physiotherapists are inclined to conduct an additional in-person assessment to confirm diagnosis so retention of face-to-face or hybrid models may prove more effective than ‘digital first’ approaches.
-
Appropriate appointment allocation requires staff education of the FCP remit; this is facilitated by FCP staff spending more time within the practice and becoming integrated into the team and practice meetings.
-
Consider both band 7 and band 8a FCP employment.
-
More experienced physiotherapists who move into FCP roles may manage the demands on new remote ways of working more effectively.
-
Embedding staff within the practice, supporting team bonding and trust is likely to create a more effective working environment.
Positive impact on whole systems musculoskeletal practice
While the other FRONTIER aims each demonstrated a positive impact of FCP-led models, the impact on whole systems MSKD management is more ambiguous. While there were no quantitative data to support these issues, they were addressed in the realist synthesis and qualitative work. Positive impacts included GP upskilling in MSKD management through reviewing shared record systems, team discussions and, in some cases, in-service training sessions on musculoskeletal assessment. This has been recognised in other work where both GPs and practice nurses suggested skill development through interaction with FCP practice staff. 76 It should be noted; however, that in both studies, there was also a suggestion that introducing first-contact physiotherapists may have a detrimental effect on GPs as ‘siphoning off’ MSKD cases would reduce the opportunity for GPs to develop skills in this area. 76 This is likely to be an unfounded concern as FCP provision is still considerably outstripped by GP numbers, making it very unlikely that all MSKD cases could be managed non-medically.
A further benefit arose from employing physiotherapists into FCP roles who were employed within other parts of the system (e.g. within main provider physiotherapy departments), as this created a sound understanding of local pathways and referral processes, which could sometimes be less obvious to GP colleagues and could potentially impact on efficient patient management. We were unable to identify any other studies that reported this finding.
Of concern, however, was the potential that FCP-led models had a negative impact on the system as a whole. These concerns were mainly derived from shifting the workforce from other parts of the system (notably community or secondary care physiotherapy departments) to meet the employment resource requirements of primary care, leaving a departmental void of senior staff and the supporting role they provided to more junior colleagues. There were also suggestions that the exponential increase in FCP opportunities, mainly fuelled by the ARRS,24,40 meant that less-experienced staff were being appointed to roles resulting in concerns regarding their suitability to perform the role safely and effectively, a finding also reported by Moffatt et al. 76 who noted GPs and FCP staff expressed concerns regarding care quality among less-experienced staff. Within FRONTIER, particular concern was expressed when PCNs or individual practices were independently employing their own first-contact physiotherapist without the supporting professional governance network in place to monitor and support performance and development.
Employment via a provider model, whereby the main provider of physiotherapy services also provides primary care FCP services, may address some of the issues of concern raised, but also provide a more positive employment experience for FCP staff and the practices themselves as contracting and governance are managed by the provider; continuing training and personal development is supported centrally, and cover for absence remains the responsibility of the provider institution. Respondents within FRONTIER recognised the benefits of employment and provision through a provider model, and this is also reflected in a paper by Ingram et al. ,82 describing service benefits using this approach in South West England. A further benefit of this model is the supportive network this provides through access to other colleagues. Participants in FRONTIER, and elsewhere,82 recognised the potential loneliness of the FCP role (compounded by remote consultations), and lack of related professional support for decision-making, but valued the opportunity to contact colleagues when uncertainties arose. Individuals employed outside of the provider model did not have such supportive mechanisms.
Of note however, some first-contact physiotherapist respondents did suggest benefits associated with single practice or small PCN employment, as more sessions could be spent in fewer locations, rather than the wider range of practices frequently covered within provider models. The additional embedded time was thought to facilitate better team working, knowledge of the service and individuals involved, which led to a greater understanding of the service offered. Indeed, we note throughout the importance of the MDT in supporting successful implementation. This is through service advocacy, understanding of the role, skillset and benefits of a first-contact physiotherapist to both patients and other practice staff. Our data suggest there that is no established understanding on initial implementation but, with time and experience, understanding and trust develops, which facilitates more effective team working, more appropriate patient targeting and mutual support among practice staff.
Misunderstandings of the concept of the FCP offer was frequently repeated by these staff within the FRONTIER study and also in a recent paper evaluating the FCP role in Wales. 83 The original concept was based on a triage and assess model for genuine new presentations. It has been noted, however, that services frequently accept some referral from GPs for patients who have consulted the GP but who were referred on immediately, or those that are not resolving and GPs are seeking a second opinion. While this may not align with first-contact principles, it may provide better patient management without the necessity of onward referral outside of primary care, and therefore reduce waiting times in these locations, and was reported in case study sites within FRONTIER, although these patient participants did not meet inclusion criteria for inclusion on the study. It does, however, impact on timely provision in primary care if genuine first-contact appointments are delayed due to such referrals, coupled with session demand outstripping availability. Indeed, Lewis and Gill83 report that wait times increased to 3–4 weeks when limited appointment slots were filled with onward referrals from GPs. When provision comes via a provider model, service level agreements can influence these issues and provide less opportunity for service flexibility or misuse, whereas direct employment through practices or PCNs results in greater potential for service fluidity to meet practice demands.
-
Service provision models require careful consideration. While there are pros and cons to both the provider and local employed approaches, the provider model is likely to provide greater service provision stability and create a more supportive network development structure and governance than the practice employed approaches.
-
The impact of moving staff around the system requires careful monitoring. Shifting more experienced, senior staff from department-based services into FCP roles may impact junior staff supervision and development opportunities which over time may impact the quality of physiotherapy services and staff satisfaction. Providing structured development opportunities and split roles may improve workforce development over time and maintain physiotherapy service stability across the pathway.
-
Flexibility in FCP provision may be required to better meet the needs of primary care. Service level agreements must ensure that priority is given to genuine first contact consultations, but determining criteria and number of referrals may, in the longer term, create more efficiencies and quality of care across the whole system.
-
Supportive networks need to be in place to support FCP staff with decision-making and to create opportunities for professional development. For practice-employed staff, the GP may need to provide mentorship if access to physiotherapy professional support is not obtainable.
-
Staff employed through the practice or PCN may feel more embedded within the team. For these employees finding suitable ways to ensure professional support and continued development is essential, alongside ensuring terms and conditions are commensurate with the role.
-
For staff who are centrally employed, reducing the number of practices they cover, and providing more time within fewer practices will help with embedding the first-contact physiotherapist and building a team culture.
-
Early discussion regarding referral pathways (i.e. first or second contact) will ensure appointments are used appropriately and team satisfaction is retained.
-
Where possible, provide roles that include more than one clinical approach. For example, coupling FCP with interface services will help with job satisfaction and reduce likelihood of burnout.
-
Monitor impact of FCP provision on physiotherapy department waiting lists to ensure shifting personnel does not adversely impact on other parts of the musculoskeletal pathway.
Wider implementation considerations
The FRONTIER study was conducted with physiotherapists but ARRS, of which FCP is part, includes multiple other new roles or new remits for established healthcare professional within primary care. 24 The findings from the current study are likely to resonate with other professionals and supporting roles as they are introduced into established MDTs. A paper by Jones et al. 84 interviewed ARRS staff and those involved with the implementation of the multiple roles noting implementation challenges associated with sustainability of the workforce and opportunities for career progressions, managing scope and expectations, navigating supervision and development, successful integration into the team, tensions among other staff when role blurring occurs, and their impact on wider systems function. Much of these resonated with FRONTIER findings, although it should be noted that physiotherapy is an established profession, whereas other ARRS staff, nursing associates for example, are a new ‘profession’ and therefore may experience additional challenges in establishing their role and value. Interestingly, a recent realist synthesis investigating the role of paramedics in general practice reported almost identical findings to FRONTIER, identifying that the key criteria influencing success were staff understanding and acceptance of the role, induction processes that supported training, supervision and development, patient understanding and acceptance, and different employment models to suit practice needs. 85 Given the similarities across different roles already reported in the literature, it is important that, as further staff are integrated into general practice, lessons are learned from other professions that are more established in novel working locations and in emerging roles.
Patient and public involvement and engagement
Throughout the study, we worked with people who had experience of consulting GPs and physiotherapists for MSKDs, in addition to NHS commissioners, physiotherapy managers and first-contact physiotherapists themselves who were not part of the project team but were consulted in engagement events. This helped to shape the study processes, interview questions and interpretation of findings.
Regarding patient involvement, the most impactful and insightful input was in relation to creating early theories and prioritisation of areas for investigation. For many theories, the views of patients and professional staff and academics aligned, but whereas issues of safety were prioritised by professionals, patients suggested this was a given if somebody was working in the role within the NHS and was not therefore a priority for them for further investigation; this was confirmed in PREOS-PC data, where no safety issues were identified.
Consultation and engagement with healthcare professionals and NHS managers facilitated understanding of the emerging issues around FCP implementation as it underwent expedited rollout, and particularly during the pandemic, which posed additional challenges. This helped to shape our interview questions, which needed to be flexible, given the significant contextual changes throughout the study.
Summary
First-contact physiotherapy provides a clinically effective model of care that is equal to GP provision; it is also safe and cost-effective and, from a cost-minimisation perspective, is superior to GP-led models of care. Patients who consult with first-contact physiotherapists recover sooner and experience fewer days off work or from their normal activities.
The next chapter summarises the findings in relation to each of the stated aims.
Chapter 8 Summary of findings
The aims of FRONTIER were to:
-
provide optimal patient management
-
show meaningful patient benefit
-
relieve GP workload pressure
-
promote better use of healthcare resources
-
positively impact on whole systems musculoskeletal practice.
Provide optimal patient management
First-contact physiotherapy-led models produce the same clinical outcomes 6 months post consultation as GP-led models of care. Patients who consult the first-contact physiotherapist are likely to recover sooner, with a higher proportion of patients reporting improvements in their condition 3 months post consultation compared with GP consultation.
First-contact physiotherapy consultation times are longer than time spent consulting a GP, which is valued by patients. This extended time is likely to contribute to the expedited recovery period, as it permits additional time to advise patients on condition management including simple exercise and self-management techniques.
Patients who see the first-contact physiotherapist are less likely to be managed pharmacologically, in particular with fewer opioid-derivative prescriptions.
Optimal management includes timely access to appointments for patients. There was very little difference in access times between the FCP- and GP-led models, but patients who saw the first-contact physiotherapist were provided with more specialised musculoskeletal assessment, diagnosis and management sooner in the management pathway.
Appointment format continues to evolve, and while COVID-19 restrictions saw a move to remote working, this has now largely reverted to in-person consultations. Whether remote consultation provides optimal management is questionable, with many physiotherapists stating that they provided convenience but not effective management.
Ultimately, optimal management is determined by safe and effective practice; outcome measures on safety showed no differences between models of care.
Show meaningful patient benefit
Patients who consulted with the first-contact physiotherapist demonstrated a quicker recovery rate compared with GP consultees, and this was coupled with fewer days of loss productivity (time off work or away from usual activities).
While similar numbers of patients reported an improvement in their symptoms at the 6-month primary end point, approximately 30% of patients in each arm did not improve. This is indicative of the nature of MSKDs with about one third of the population living with chronic musculoskeletal pain, impacting on personal quality of life and placing significant demands on healthcare and societal resources. Furthermore, approximately 50% showed improvement in their quality of life 6 months post consultation. This may be a criticism of the outcome measure but also other factors impacting well-being.
The propensity for GPs to use pharmacological interventions, particularly opioid derivatives, may be detrimental to patients in the longer term, so FCP management is likely to provide more optimal management without inducing iatrogenic complications.
Relieve general practitioner workload pressure
While one of the initial drivers of the FCP programme was to ease the pressure on GPs, there is no strong evidence from FRONTIER or other FCP-related studies to suggest this is the case. It could be argued that if patients consult a first-contact physiotherapist and do not then subsequently consult a GP (as evidenced in FRONTIER), the need for GP appointments is reduced. Indeed, in the qualitative study, some GPs did report a perceived positive impact of first-contact physiotherapists on their workload. It is likely that for the burden of MSKD workload on GPs to be adequately relieved, considerably more first-contact physiotherapist need to be recruited and embedded into practices.
However, given the recognised growing demand on GP time, the need for appointments remains high. There is also a recognition that GP caseload is changing, in part due to the presence of first-contact physiotherapists but also other roles within primary care, which may be relieving GPs of the need to see patients with less complex conditions. This is potentially leading to greater demands on GP time, as consultees present with more complex conditions, which require longer consultation time. While this may present a better use of the GP skillset, it does come with additional pressure. The impact that this additional demand has over time needs careful monitoring to ensure that the schemes introduced to reduce pressure on GPs do not in themselves result in unanticipated consequences or create further stress through shifts in caseload.
Furthermore, the growing size and complexity of primary care teams may also place further demands on GPs to manage staff and to provide support for development and mentorship to advanced practice. Arguably, this may reduce over time as more intraprofessional mentorship is provided when further FCP staff have achieved qualifications themselves that permit them to sign off others’ competencies. Further consideration on team formation and leadership and management structures may also address some of the additional pressure placed on GPs. Currently GPs lead multiprofessional clinical teams including nurses, allied health professionals and other support staff (e.g. social prescribing link workers) but this could be reconsidered and reconfigured to allow other professions at advanced practitioner level to adopt more extensive team management roles.
Promote better use of healthcare resources
Given the non-significant differences in clinical outcomes, FCP models present may present a better use staff resource compared to the GP-led model of care for patients with MSKDs. Based on consultation costs and subsequent healthcare resource use, first-contact physiotherapists are approximately 2.5 times cheaper than GPs, achieving the same clinical outcomes after 6 months. This also enables GPs to direct their attention to more complex presentations beyond MSKDs.
Interestingly, there appears to be no significant difference in patient outcomes irrespective of whether the first-contact physiotherapist has additional qualifications to prescribe or inject. Most at present are band 7, but even when analysing the impact of band 8a staff in the FCP role, it still represents a significant cost saving compared with the GP, although would be significantly more expensive if band 8a staff fulfilled the FCP(AQ) role compared with the FCP(ST). Consideration must therefore be given to whether there is any benefit employing staff with additional prescribing and/or injecting capabilities given the lack of clinical benefit compared with those without these competencies. In Northern Ireland, this remains a requirement for FCP appointment but, given the challenges in healthcare budgets, this may prove prohibitive in the future in the absence of evidence supporting the associated benefits. However, consideration of the wider benefits of first-contact physiotherapists achieving these competencies is necessary. First, achieving the prescribing capability facilitates decisions about deprescribing and, given the acknowledgment in this study that patients who saw a first-contact physiotherapist achieved similar outcomes to GPs with fewer medications, this is something that could significantly impact on patient management and resource use. Second, career progression and roadmap pathways to advanced practice may include additional qualifications to inject and/or prescribe, so they remain an important aspect of career development. Given the volume of work in general practice and the challenges of staff retention, maintaining staff satisfaction and providing career development opportunities are likely to have a positive impact on recruitment and retention.
Positive impact on whole-system musculoskeletal practice
The impact of the FCP model on whole systems MSKD practice remains uncertain. While there are benefits to introducing expert care earlier in the pathway and the upskilling of other primary care staff when extending the team, there are suggestions that GP staff, in particular, may become deskilled in MSKD management. While this seems unlikely, given the extent of the problem, it is something that needs monitoring.
A further challenge is the impact of shifting the workforce from secondary care or community-based roles into primary care has on the system. There are concerns that gaps are appearing in these services, with more senior, skilled staff taking FCP roles, leaving more junior staff without the professional and clinical support required. Furthermore, given the vast increase in first-contact physiotherapist numbers over a short period, there is also concern regarding the suitability of some less experienced staff in FCP roles.
Finally, the employment model may also impact on system stability. Provision of FCP services via the main provider supports benefits for both the FCP staff and the GP practices as governance, contracting and professional development remain the responsibility of the provider. This is also likely to lead to better workforce planning in the longer-term.
Chapter 9 Strengths, limitations and future research
This study was conceived and funded in advance of the implementation of the ARRS, which was initiated in 2019. While the study commenced in advance of the COVID-19 pandemic, work continued throughout and afterwards, but was significantly hampered by lockdown restrictions and additional pressures placed on primary care. As such, limitations should be considered in light of these significant occurrences.
Strengths
This is the first study to investigate the different models of FCP provision compared with GP-led models of care. It provides extensive and robust evidence regarding clinical and cost outcomes; safety; satisfaction; and resource use. It also included sites from across all four nations of the UK, the first study of FCP to provide such extensive geographical coverage.
The methodological approach, which used mixed-method realist evaluation, provides evidence of whether the programme (FCP) works, but in addition and importantly how it works, for whom and in what circumstances. This therefore provides invaluable contextual information regarding service implementation and development.
Since this study commenced, there has been a national pilot in England of FCP, with associated qualitative work which provided evidence of programme benefits and limitations. FRONTIER, however, has provided significant additional understanding of FCP and provides novel information not reported in current literature.
Limitations
The design of the evaluation WP of the FRONTIER study relied heavily on recruiting general practices, and patients and staff within those practices. The circumstances imposed by COVID-19 severely hampered all aspects of recruitment and data collection, which impacted on study success. These included:
-
Challenges recruiting practice sites early on in the study, particularly across all four nations. While the required number of sites was reached, and indeed exceeded, the numbers of individual patient recruits within each site varied greatly, with some sites recruiting just one participant. Sites tried multiple approaches to recruitment, but this was clearly not a priority given the pressures that services were under at the time. Furthermore, for much of the recruitment period, patients and the public were living under lockdown rules, social distancing and many were self-isolating. All these issues created uncertainty and anxiety and inevitably impacted people’s willingness to engage in research activities. As a result, we fell short of the required sample size, although we still provide the largest data set with longest follow-up available for FCP. Given the range of site recruitment numbers and the underpowered sample, caution must be exerted when interpreting findings.
-
In the early stages of recruitment, the ARRS was implemented in England. This provided financial incentives for practices to employ FCP staff, which resulted in challenges to practice recruitment. In some cases, practice sites would agree to participate in the study within the GP-led arm, but would then employ a first-contact physiotherapist, making them ineligible for further recruitment. Additionally, recruiting sites to the GP-led arm was challenging, as sites in England reported their intention to employ a first-contact physiotherapist in the future, so were unwilling to take part in the study.
-
As reported within the health economics analysis previously, two elements of the original health economics analysis plan were not undertaken. First, the practice level analysis to compare workforce configurations and costs was impractical due to the expanded number of practices in the study, many of which recruited relatively small numbers of participants. Moreover, interviews with members of practice teams to explore the integration of physiotherapy had been completed and reported in other WPs. Second, the collection of participants’ service use data from GP records was found to be problematic and had to be abandoned due to poor coding and difficulties ascertaining from searches what interventions had been received. Hence, the calculation of MSKD-related costs was based on responses to the CSRI. These data were collected meticulously by interview, but some variation occurred in the timing of the 3- and 6-month follow-up data and there was some missing information. It is also possible that recall errors arose. This may be of particular relevance to OTC medications when no prescription detail was available for the patient to consider – this was, however, an identical process across each arm.
-
At the funding stage, we were asked to include a WP investigating the impact of the outputs from FRONTIER. We had intended to integrate this work throughout the study but the climate and changes to our timeline prevented this happening. However, we have now integrated this into the planned dissemination and implementation work.
-
The research was led by a physiotherapist and included several physiotherapy co-applicants, which may be considered to bring a biased view of the FCP role. None were first-contact physiotherapists or involved in the implementation or promotion of the FCP service, but it could be argued they were inherently aligned to the professional value of the FCP role. To mitigate, we included other professionals within the team including a GP, psychologist and health services researchers with no affiliation to the profession alongside methodologists who all contributed to analysis and interpretation of results.
Equality, diversity and inclusion limitations
Given the number of sites, across all four nations and the impact of primary care workload, it proved challenging to get sites to return their patient approach data, which would have allowed us to determine how representative the research sample was, compared with the cohort who sought FCP consultation. We therefore used practice-level data to compare demographics of research participants to practice populations. It was very apparent that the recruited FRONTIER cohort was not representative of the practice population. Our sample was overwhelmingly white, and not representative of the diverse nature of many of the recruited practices. It is difficult to determine the reason for this discrepancy. At the time, people from Black and Asian communities were disproportionately impacted by the COVID-19 pandemic, which may have created reluctance to participate in research. However, even after lockdown restrictions eased, recruitment in diverse populations failed. This may be a result of the cohort who access first-contact physiotherapists, due to awareness of the offer and perceived acceptability – this is an area that requires further investigation. As a result of the skewed sample, we cannot claim with any certainty the benefits or otherwise of FCP in under-represented communities.
We also recognise that our recruitment methods may have limited including people from non-English speaking populations (other than Welsh, where all legal requirements were met). We relied on GP practice staff inviting all patients who attended appointments but the study information was provided in English, and we were not asked by recruiting sites to provide information in any other languages or approached by representatives of potential recruits to provide interpreter services. We do not know whether our lack of diversity is through potential participant choice or because our recruitment methods were prohibitive.
Further research
Findings from the FRONTIER study highlight areas for further research detailed below:
-
Gaining further insight into the reasons related to expedited recovery demonstrated by patients who consult with first-contact physiotherapists may lead to improved services for all patients. Gaining a better understanding through qualitative appraisal of why and how patients who consult with a first-contact physiotherapist rather than a GP achieve a quicker recovery may highlight key issues related to the consultation or advice given. Identifying these important aspects and sharing with other healthcare professionals may enhance the outcome for all patients consulting with MSKDs, with positive impact on direct and indirect costs.
-
Greater understanding of how FCP is advertised to all practice cohorts is important given the skewed access of patients reported in FRONTIER and elsewhere. Qualitative research that explores how FCP, along with other emerging roles within general practice are advertised, understood and accepted among patient cohorts is important to ensure there is equitable access for all, in addition to making the best use of available resources. The recruited cohort in the study was highly skewed towards those of white ethnicity, which may be indicative of recruitment processes, but conversations with clinical collaborators suggest that the cohort consulting with first-contact physiotherapists is not representative of the overall practice ethic mix, suggesting that this anomaly does warrant further investigation.
-
Understanding the whole systems impact of introducing FCP into the MSKD pathway is imperative to ensure the viability of physiotherapy provision in the future. This study focussed on the impact of introducing first-contact physiotherapists into general practice but this change in service provision impacts on other aspects of the MSK pathway including orthopaedic interface services and department-based physiotherapy provision. Understanding how shifting services impacts on waiting lists in addition to the impact of FCP roles on stress, anxiety and burnout is important to ensure that this part of the workforce is not subject to the same pressures experienced by GPs; this will ensure a sustainable future workforce.
-
Investigating the natural course of MSKDs may assist with decision-making on when to intervene. Data from this study show that a similar proportion of patients improved irrespective of the type of intervention they received (i.e. GP or FCP directed). Equally almost one third of patients did not improve and were therefore considered to be living with a chronic MSKD. Gaining a better understanding of the profile of individuals who do not improve with first-line interventions, including the time to consultation following symptom presentation may assist with decision-making on how and when to intervene.
-
Determining how FCP staff work effectively alongside other new and emerging roles in general practice. Given the extent of new roles being introduced into general practice, it will be important to investigate how first-contact physiotherapists work alongside other staff to maximise the potential of the entire team. For example, MSKDs are prolific, and often have physical and psychological triggers and impact. Embedding staff with responsibility for mental health alongside first-contact physiotherapists may provide a more effective, holistic management pathway for many patients living with MSKDs and, in particular, those who experience chronic pain. Investigating team composition and outcomes may be beneficial.
Additional information
CRediT contribution statement
Nicola E Walsh (https://orcid.org/0000-0002-0499-4829): Conceptualisation (lead), Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Alice Berry (https://orcid.org/0000-0002-3863-6835): Formal analysis, Investigation, Project administration, Validation, Visualisation, Writing – draft, Writing – reviewing and editing.
Serena Halls (https://orcid.org/0000-0002-0737-8255): Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Validation, Visualisation, Writing – reviewing and editing.
Rachel Thomas (https://orcid.org/0000-0003-3726-5179): Analysis, Investigation, Methodology, Project administration, Supervision, Visualisation, Writing – reviewing and editing.
Hannah Stott (https://orcid.org/0000-0002-2177-3577): Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Visualisation, Writing – reviewing and editing.
Cathy Liddiard (https://orcid.org/0000-0002-9384-1866): Data curation, Analysis, Investigation, Project administration, Software, Writing – reviewing and editing.
Zoe Anchors (https://orcid.org/0000-0002-3090-2334): Data curation, Formal analysis, Investigation, Methodology, Validation, Visualisation, Writing – draft, Writing – reviewing and editing.
Fiona Cramp (https://orcid.org/0000-0001-8035-9758): Formal analysis, Investigation, Writing – reviewing and editing.
Margaret Cupples (https://orcid.org/0000-0002-4248-9700): Data curation, Formal analysis, Investigation, Writing – draft, Writing – reviewing and editing.
Peter Williams (https://orcid.org/0000-0001-7885-0564): Conceptualisation, Data curation, Analysis (statistics lead), Investigation, Methodology, Project administration, Resources, Validation, Visualisation, Writing – draft, Writing – reviewing and editing.
Heather Gage (https://orcid.org/0000-0002-2049-9406): Conceptualisation, Data curation, Analysis (health economics lead), Investigation, Methodology, Project administration, Resources, Validation, Visualisation, Writing – draft, Writing – reviewing and editing.
Dan Jackson (https://orcid.org/0000-0003-2253-7880): Analysis, Methodology, Writing – draft, Writing – reviewing and editing.
Paula Kersten (https://orcid.org/0000-0003-4038-0442): Formal analysis, Investigation, Writing – reviewing and editing.
Dave Foster: Patient research partner (lead), Analysis, Writing – reviewing and editing.
Justin Jagosh (https://orcid.org/0000-0001-6807-2957): Conceptualisation, Data curation, Analysis (realist methodological lead), Investigation, Methodology, Validation, Visualisation, Writing – reviewing and editing.
Acknowledgements
The authors would like to thank our funder, NIHR, for their support with this study.
We would also like to acknowledge:
-
All participants that took part in each aspect of this study. In particular, we would like to thank everyone at each participating practice site. This study was conducted before, during and after the pandemic and required considerable commitment at some very challenging times. Thank you for your support and enthusiasm.
-
All PPIE members who contributed to the study design and conduct, both in preparing the study and throughout; in particular, Dave Foster, our PPIE lead representative, co-applicant and co-author.
-
Study steering committee members: Professor Katrina Turner (Chair); Professor Jeremy Horwood; Dr Eric Lenguerrand; Dr Elsa Marques; Dr Emma Gibbard; Dr Rob Stenner; Ruth Ten Hove; Abi Henderson; Dr Claire Lowe. Thank you for your support and guidance throughout.
-
Dr Alison Llewellyn; Dr Jen Pearson; Dr Pete Young for your input into the original application and Gemma Artz for providing insight into NHS commissioning.
-
Thanks to Dr Jude Hancock for your input into dissemination plans and strategy.
-
Our NIHR project managers Ellie Fairbank and Harry Gibbs for your continued support and patience.
-
Our grant hosts at Bristol, North Somerset, South Gloucestershire Integrated Care Board. Thank you, Paul Roy, Katalin Bagi and Dr Alison Diaper for your expertise throughout.
Data-sharing statement
All data requests should be submitted to the corresponding author. Access will be granted where possible in line with Open Access principles, providing all anonymity is preserved.
Ethics statement
All governance and ethical approvals were in place before studies commenced. Chapter 3 FCP Survey and Chapter 4 Realist review and consensus exercise: ethical approval to proceed with the study was given on the 20 July 2018 (UWE FREC reference number: HAS.18.07.204). Chapter 5 Remote consultations survey: ethical approval to proceed with the study was given by the UWE FREC HAS.19.06.204 on 15.12.21. Chapter 6 Case study evaluation: research ethics approval was granted on the 18 June 2019 by the Northern Ireland REC (IRAS ID: 261530; REC reference number: 19/NI/0108). HRA approval was granted on 25 June 2019.
Information governance statement
The University of the West of England (UWE) Bristol is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, UWE Bristol is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (www.uwe.ac.uk/about/structure-and-governance/data-protection).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/RTKY7521.
Primary conflicts of interest: All team members were financially supported via this grant to undertake this work. Nicola E Walsh is a member of the NIHR Health and Social Care Delivery Research (Seacole) Panel and receives funding through NIHR Applied Research Collaborative West to lead a research theme. Paula Kersten provides tuition for advanced practice courses and receives reimbursement. Fiona Cramp is a member of NIHR Doctoral Clinical Academic Fellowship Committee. We have no other declarations or conflicts to report.
Publications
Halls S, Thomas R, Stott H, Cupples ME, Kersten P, Cramp F, et al. Provision of first contact physiotherapy in primary care across the UK: a survey of the service. Physiotherapy 2020;108:2–9. https://doi.org/10.1016/j.physio.2020.04.005
Jagosh J, Stott H, Halls S, Thomas R, Liddiard C, Cupples M, et al. Benefits of realist evaluation for rapidly changing health service delivery. BMJ Open 2022;12:e060347. https://doi.org/10.1136/bmjopen-2021-060347
Anchors Z, Jones B, Thomas R, Berry A, Walsh N. The impact of remote consultations on the health and wellbeing of first contact physiotherapists in primary care: a mixed methods study. Musculoskeletal Care 2023;21:1–12. https://doi.org/10.1002/msc.1737
Walsh N, Halls S, Thomas R, Berry A, Liddiard C, Cupples ME, et al. First contact physiotherapy: an evaluation of clinical effectiveness and costs. Br J Gen Pract 2024;74:e717–26. https://doi.org/10.3399/BJGP.2023.0560
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Murray C, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2197-223.
- Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2163-96.
- Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord 2010;11.
- Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain 2004;110:361-8.
- Versus Arthritis . The State of Musculoskeletal Health 2023.
- Right Care . The NHS Atlas of Variation in Healthcare: Reducing Unwarranted Variation to Increase and Improve Quality 2011.
- HM Treasury . Autumn Statement 2016 n.d. www.gov.uk/government/publications/autumn-statement-2016-documents/autumn-statement-2016 (accessed August 2017).
- Quality First . Managing Workload to Deliver Safe Patient Care 2015 2015.
- Institute for Government . Performance Tracker 2022 23: Spring Update 2023. www.instituteforgovernment.org.uk/performance-tracker-2022-23 (accessed 30 May 2024).
- Roland M (Chair). Primary Care Workforce Commission . The Future of Primary Care: Creating Teams for Tomorrow 2015.
- ICM Unlimited . British Medical Association National Survey of GPs. The Future of General Practice 2015 Full Report 2015.
- British Medical Association. Pressure in General Practice Data Analysis. British Medical Association; 2024. n.d. URL: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed 26 July 2024)">https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis">n.d. URL: https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/pressures/pressures-in-general-practice-data-analysis (accessed 26 July 2024).
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed April 2023).
- Margham T. Musculoskeletal disorders: time for joint action in primary care. Br J Gen Pract 2011;61:657-8. https://doi.org/10.3399/bjgp11X601541.
- Mallen CD, Thomas E, Belcher J, Rathod T, Croft P, Peat G. Point-of-care prognosis for common musculoskeletal pain in older adults. JAMA Intern Med 2013;173:1119-25.
- Malhotra A, Maughan D, Ansell J, Lehman R, Henderson A, Gray M, et al. Choosing wisely in the UK: the Academy of Medical Royal Colleges’ initiative to reduce the harms of too much medicine. BMJ 2015;350.
- Goodwin RW, Hendrick P. Physiotherapy as a first point of contact in general practice: a solution to a growing problem?. Prim Health Care Res Dev 2016;6:489-502.
- Oakley C, Shacklady C. The clinical effectiveness of the extended‐scope physiotherapist role in musculoskeletal triage: a systematic review. Musculoskeletal Care 2015;13:204-21.
- Chartered Society of Physiotherapists . First Contact Physiotherapy Case Studies n.d. www.csp.org.uk/professional-clinical/improvement-innovation/first-contact-physiotherapy/case-studies (accessed January 2017).
- Chartered Society of Physiotherapists . GPs Support Physios As a First Point of Contact in Surgeries 2016. www.csp.org.uk/news/2016/04/26/gps-support-physios-first-point-contact-surgeries (accessed February 2024).
- Bishop A, Ogollah RO, Jowett S, Kigoz1 J, Tooth S, Protheroe J, et al. STEMS pilot trial: a pilot cluster randomised controlled trial to investigate the addition of patient direct access to physiotherapy to usual GP-led primary care for adults with musculoskeletal pain. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-012987.
- Physiopedia . First Contact Physiotherapy n.d. www.physio-pedia.com/First_Contact_Physiotherapy (accessed March 2024).
- Stynes S, Jordan KP, Hill JC, Wynne-Jones G, Cottrell E, Foster NE, et al. Evaluation of the first contact physiotherapy (FCP) model of primary care: patient characteristics and outcomes. Physiotherapy 2021;113:199-208. https://doi.org/10.1016/j.physio.2021.08.002.
- Primary Care Strategy and NHS Contracts Group and Systems Transformation Group . Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance 2019. www.england.nhs.uk/publication/network-contract-directed-enhanced-service-additional-roles-reimbursement-scheme-guidance (accessed January 2024).
- Moran R, Butt J, Heller S, Hinks J, Kerridge L, Samuels M, et al. Health research systems in change: the case of ‘Push the Pace’ in the National Institute for Health Research. Health Res Policy Syst 2019;17. https://doi.org/10.1186/s12961-019-0433-2.
- Halls S, Thomas R, Stott N, Cupples ME, Kersten P, Cramp F, et al. Provision of first contact physiotherapy in primary care across the UK: a survey of the service. Physiotherapy 2020;108:2-9. https://doi.org/10.1016/j.physio.2020.04.005.
- Jagosh J, Stott H, Halls S, Thomas R, Liddiard C, Cupples M, et al. Benefits of realist evaluation for rapidly changing health service delivery. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-060347.
- Pawson R, Tilley N. Realist Evaluation. London: Cabinet Office; 2004.
- Jagosh J. Introduction to Realist Evaluation and Synthesis [video 57 Minutes] n.d. https://realistmethodology-cares.org (accessed April 2023).
- Pawson R, Tilley N. Realistic Evaluation. Thousand Oaks, CA: SAGE Publications Ltd; 1997.
- Rycroft-Malone J, Seers K, Eldh AC, Cox K, Crichton N, Harvey G, et al. A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0811-0.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46.
- Astbury B, Leeuw F. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. https://doi.org/10.1177/1098214010371972.
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0237-x.
- Sims S, Leamy M, Davies N, Schnitzler K, Levenson R, Mayer F, et al. Realist synthesis of intentional rounding in hospital wards: exploring the evidence of what works, for whom, in what circumstances and why. BMJ Qual Saf 2018;27:743-57. https://doi.org/10.1136/bmjqs-2017-006757.
- Jagosh J. Retroductive theorizing in Pawson and Tilley’s applied scientific realism. J Crit Realism 2020;19:121-30. https://doi.org/10.1080/14767430.2020.1723301.
- Gilmore B, McAuliffe E, Power J, Vallières F. Data analysis and synthesis within a realist evaluation: toward more transparent methodological approaches. Int J Qual Methods 2019;18. https://doi.org/10.1177/1609406919859754.
- Pearson M, Brand SL, Quinn C, Shaw J, Maguire M, Michie S, et al. Using realist review to inform intervention development: methodological illustration and conceptual platform for collaborative care in offender mental health. Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0321-2.
- NHS England and NHS Improvement . Right Person, Right Place, First Time. Elective Care High Impact Interventions: First Contact Practitioner for MSK Services 2019.
- Anchors Z, Jones B, Thomas R, Berry A, Walsh N. The impact of remote consultations on the health and wellbeing of first contact physiotherapists in primary care: a mixed methods study. Musculoskeletal Care 2023;21:655-66. https://doi.org/10.1002/msc.1737.
- NHS England . The NHS Long Term Plan 2019.
- Tomaka J, Palacios R, Champion C, Monks S. Development and validation of an instrument that assesses individual differences in threat and challenge appraisal. J Depress Anxiety 2018;7:1-10. https://doi.org/10.4172/2167-1044.1000313.
- Moore LJ, Young T, Freeman P, Sarkar M. Adverse life events, cardiovascular responses, and sports performance under pressure. Scand J Med Sci Sports 2018;28:340-7. https://doi.org/10.1111/sms.12928.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Walsh N, Halls S, Thomas R, Berry A, Liddiard C, Cupples ME, et al. First contact physiotherapy: an evaluation of clinical effectiveness and costs [published online ahead of print 1 March 2024]. Br J Gen Pract 2024. https://doi.org/10.3399/BJGP.2023.0560.
- Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum 2001;45:384-91.
- Salisbury C, Montgomery A, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ 2013;346.
- Ware JE, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36v2 Health Survey. Lincoln, RI: QualityMetric; 2007.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36.
- Roland M, Morris R. A study of the natural-history of back pain: development of a reliable and sensitive measure of disability in low back-pain. Spine 1983;8:141-4.
- Musculoskeletal Health Questionnaire (MSKHQ). Chesterfield: Versus Arthritis; 2014.
- Mead N, Bower P, Roland M. The general practice assessment questionnaire (GPAQ): development and psychometric characteristics. BMC Fam Pract 2008;9.
- Knapp M. The Economic Evaluation of Mental Health Care. Aldershot: Arena; 1995.
- Ricci-Cabello I, Avery AJ, Reeves D, Kadam UT, Valderas JM. Measuring patient safety in primary care: the development and validation of the ‘patient reported experiences and outcomes of safety in primary care’ (PREOS-PC). Ann Fam Med 2016;14:253-61. https://doi.org/10.1370/afm.1935.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60. https://doi.org/10.1177/1356389016638615.
- Wallis JA, Ackerman IN, Brusco NK, Kemp JL, Sherwood J, Young K, et al. Barriers and enablers to uptake of a contemporary guideline-based management program for hip and knee osteoarthritis: a qualitative study. Osteoarthr Cartil Open 2020;2. https://doi.org/10.1016/j.ocarto.2020.100095.
- Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev 2018;4. https://doi.org/10.1002/14651858.CD010842.pub2.
- Bostock N. One in Five GP Appointments Last More Than 20 Minutes n.d. www.gponline.com/one-five-gp-appointments-last-20-minutes/article/1794470 (accessed June 2023).
- NHS England . Musculoskeletal Health n.d. www.england.nhs.uk/elective-care-transformation/best-practice-solutions/musculoskeletal (accessed April 2023).
- Chartered Society of Physiotherapy . FCP Services 2021. www.csp.org.uk/professional-clinical/improvement-innovation/first-contact-physiotherapy/first-contact-physio-2 (accessed March 2023).
- NHS England . Opioid Prescriptions Cut by Almost Half a Million in Four Years As NHS Continues Crackdown 2023. www.england.nhs.uk/2023/03/opioid-prescriptions-cut-by-almost-half-a-million-in-four-years-as-nhs-continues-crackdown (accessed March 2023).
- Mullan J, Smithson J, Walsh N. The experiences of physiotherapy independent prescribing in primary care: implications for practice. Prim Health Care Res Dev 2023;24. https://doi.org/10.1017/S1463423623000142.
- Sajid IM, Parkunan A, Frost K. Unintended consequences: quantifying the benefits, iatrogenic harms and downstream cascade costs of musculoskeletal MRI in UK primary care. BMJ Open Quality 2021;10. https://doi.org/10.1136/bmjoq-2020-001287.
- Hurley MV. Enabling Self-management and Coping with Arthritic Pain Using Exercise. London: ESCAPE-pain; n.d.
- Department for Work and Pensions . Getting the Most Out of the Fit Note: Guidance for Healthcare Professionals 2023. www.gov.uk/government/publications/fit-note-guidance-for-healthcare-professionals/getting-the-most-out-of-the-fit-note-guidance-for-healthcare-professionals (accessed March 2024).
- Health and Safety Executive . Working Days Lost in Great Britain 2022. www.hse.gov.uk/statistics/dayslost.htm (accessed March 2023).
- Versus Arthritis . The State of Musculoskeletal Health 2021: Arthritis and Other Musculoskeletal Conditions in Numbers 2021. www.versusarthritis.org/media/24653/state-of-msk-health2-2021.pdf (accessed December 2022).
- Caplan N, Robson H, Robson A, Kelly M, Wilkes G. Changes in health-related quality of life (EQ-5D) dimensions associated with community-based musculoskeletal physiotherapy: a multi-centre analysis. Qual Life Res 2018;27:2373-82. https://doi.org/10.1007/s11136-018-1883-7.
- Office for National Statistics . Estimates of the Population for the UK, England and Wales, Scotland and Northern Ireland 2022. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed March 2023).
- Department of Health . Resource Allocation: Weighted Capitation Formula 2011. www.gov.uk/government/publications/resource-allocation-weighted-capitation-formula (accessed April 2023).
- NHS England . GP Patient Survey 2022 n.d. www.england.nhs.uk/statistics/2022/ 07/14/gp-patient-survey-2022 (accessed April 2023).
- NHS England . Pickering Medical Practice, North 2020. www.england.nhs.uk/gp/case-studies/routine-gp-appointment-waiting-times-reduced-by-47-pickering-medical-practice-north/#:~:text=The%20average%20waiting%20time%20for,routine%20appointment%20to%20come%20round (accessed March 2024).
- NHS Digital . Appointments in General Practice, October 2022 2022. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/october-2022#:~:text=38.9%25%20of%20appointments%20in%20October,day%20that%20they%20were%20booked.&text=89.4%25%20of%20all%20appointments%20were%20attended%20in%20October%202022.&text=43.5%25%20of%20all%20appointments%20in,were%20carried%20out%20by%20nurses (accessed March 2023).
- Moffatt F, Goodwin R, Hendrick P. Physiotherapy-as-first-point-of-contact-service for patients with musculoskeletal complaints: understanding the challenges of implementation. Prim Health Care Res Dev 2018;19:121-30.
- Goodwin R, Moffatt F, Hendrick P, Stynes S, Bishop A, Logan P. Evaluation of the First Contact Physiotherapy (FCP) model of primary care: a qualitative insight. Physiotherapy 2021;113:209-16. https://doi.org/10.1016/j.physio.2021.08.003.
- Carey N, Edwards J, Otter S, Gage H, Williams P, Courtenay M, et al. A comparative case study of prescribing and non-prescribing physiotherapists and podiatrists. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05918-8.
- Noblet T, Jadhakhan F, Bennett A, McCrum C, O’Shea S, Hensman-Crook A, et al. A multi-site prospective, observational study of physiotherapist independent prescribing activity across musculoskeletal clinics in the United Kingdom. Musculoskelet Sci Pract 2022;61.
- Health Education England . Multi-Professional Framework for Advanced Clinical Practice in England 2017. https://advanced-practice.hee.nhs.uk/multi-professional-framework-for-advanced-clinical-practice-in-england (accessed March 2024).
- Chartered Society of Physiotherapy . First Contact Physiotherapy Career Development in Northern Ireland 2021. www.csp.org.uk/professional-clinical/improvement-innovation/first-contact-physiotherapy/career-guide/local-guidance/northern-ireland (accessed February 2024).
- Ingram S, Stenner S, Acton T, Armitage K. Implementation of a provider based musculoskeletal first contact physiotherapy service model: key points to consider. Musculoskeletal Care 2020;19:232-5. https://doi.org/10.1002/msc.1527.
- Lewis MW, Gill P. Facilitators and barriers regarding the implementation and interprofessional collaboration of a first contact physiotherapy service in primary care in Wales: a qualitative study. Int J Ther Rehabil 2023;30:1-12.
- Jones B, Anchors Z, Voss S, Walsh N. A qualitative investigation of the Additional Roles Reimbursement Scheme in primary care. Br J Gen Pract 2023;74:e315-22. https://doi.org/10.3399/BJGP.2023.0433.
- Stott H, Goodenough T, Jagosh J, Gibson A, Harris N, Liddiard C, et al. Understanding paramedic work in general practice in the UK: a rapid realist synthesis. BMC Prim Care 2024;25. https://doi.org/10.1186/s12875-024-02271-1.
- Jones K, Burns A. Unit Costs of Health and Social Care 2021. Canterbury: Personal Social Services Research Unit, University of Kent; 2021.
- NHS England . 2020/21/National/Cost/Collection/Data/Publication n.d. www.england.nhs.uk/publication/2020-21-national-cost-collection-data-publication (accessed 14 April 2023).
Appendix 1 First-contact physiotherapy service provision across the United Kingdom
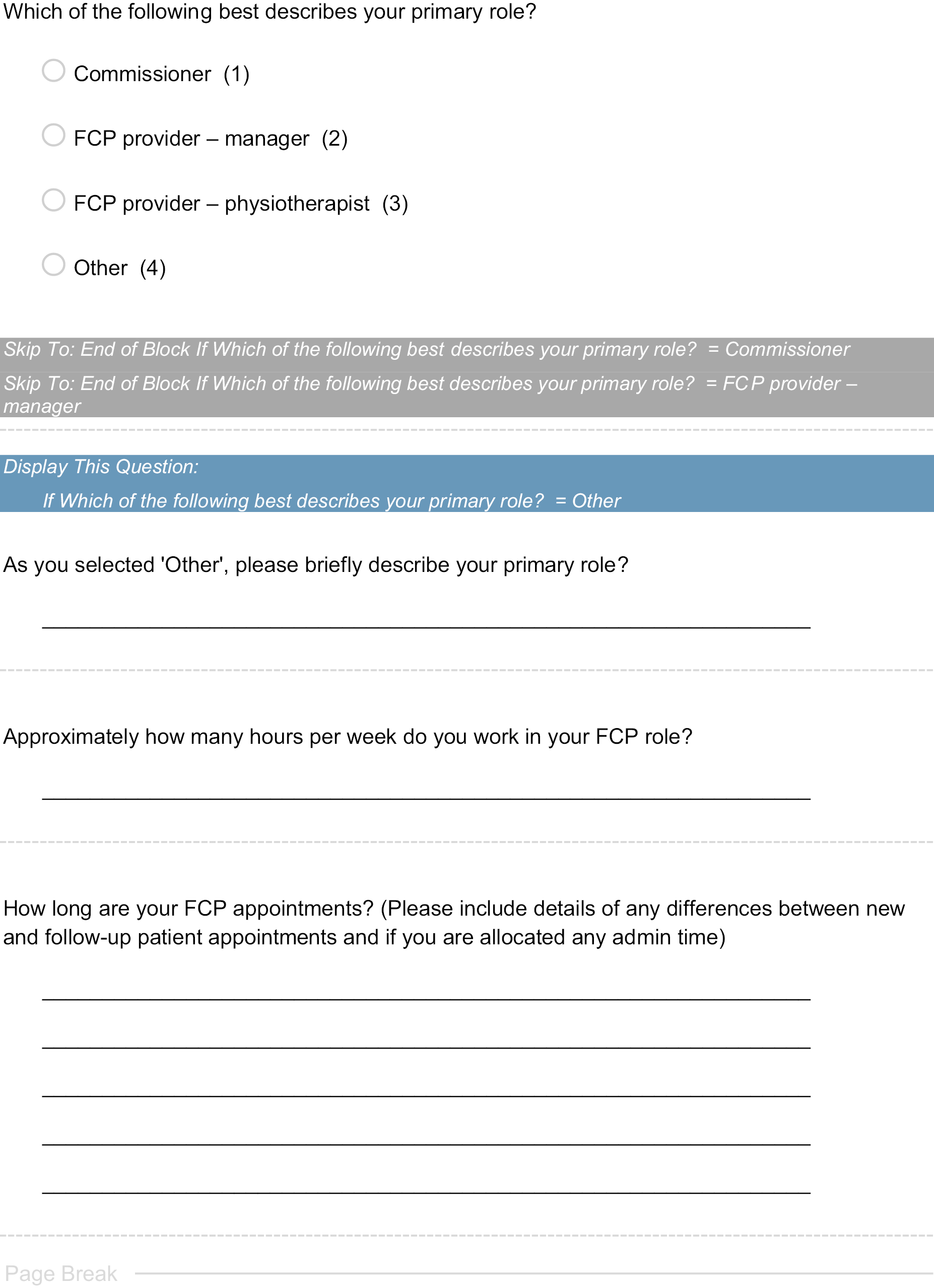
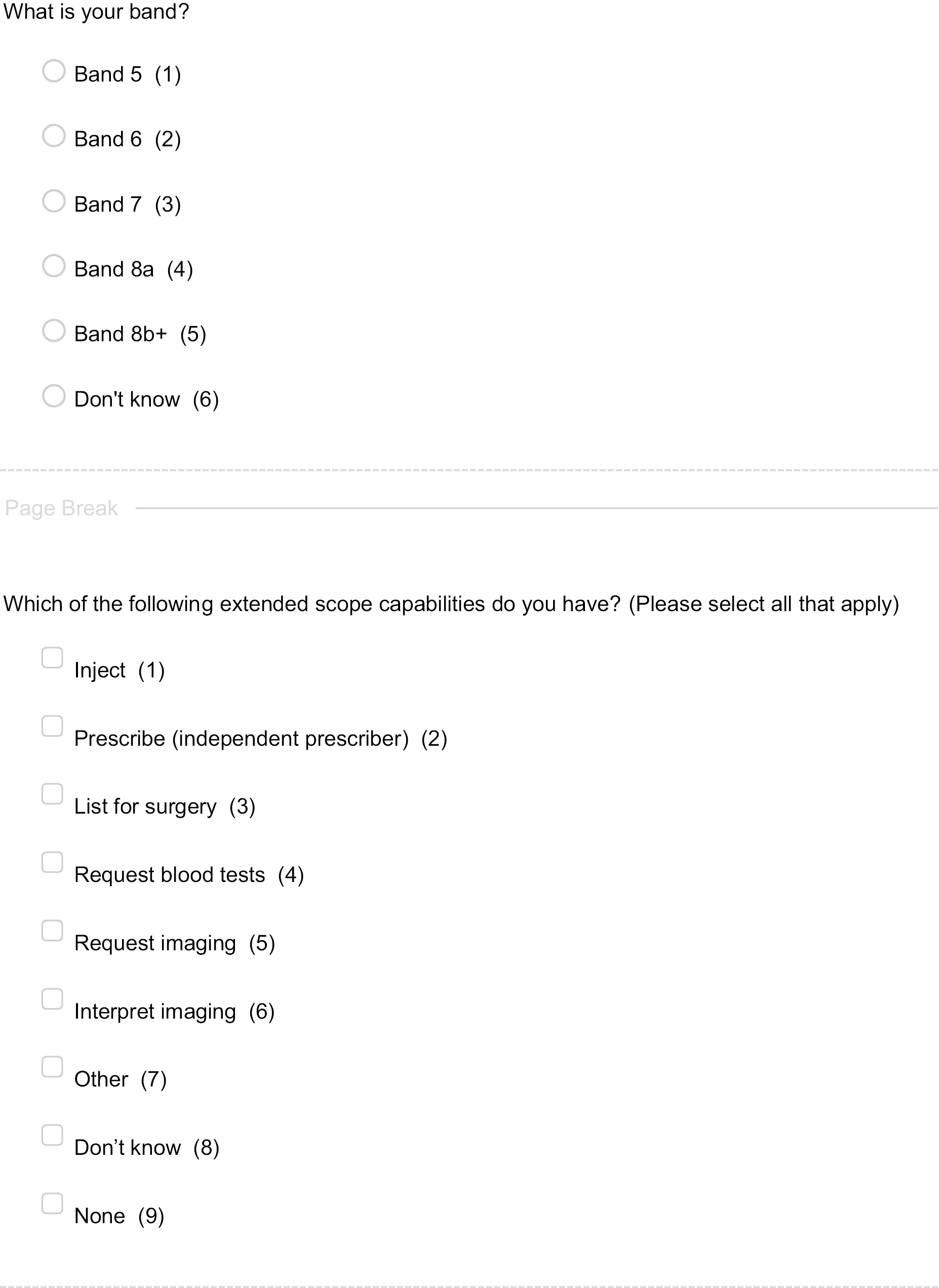
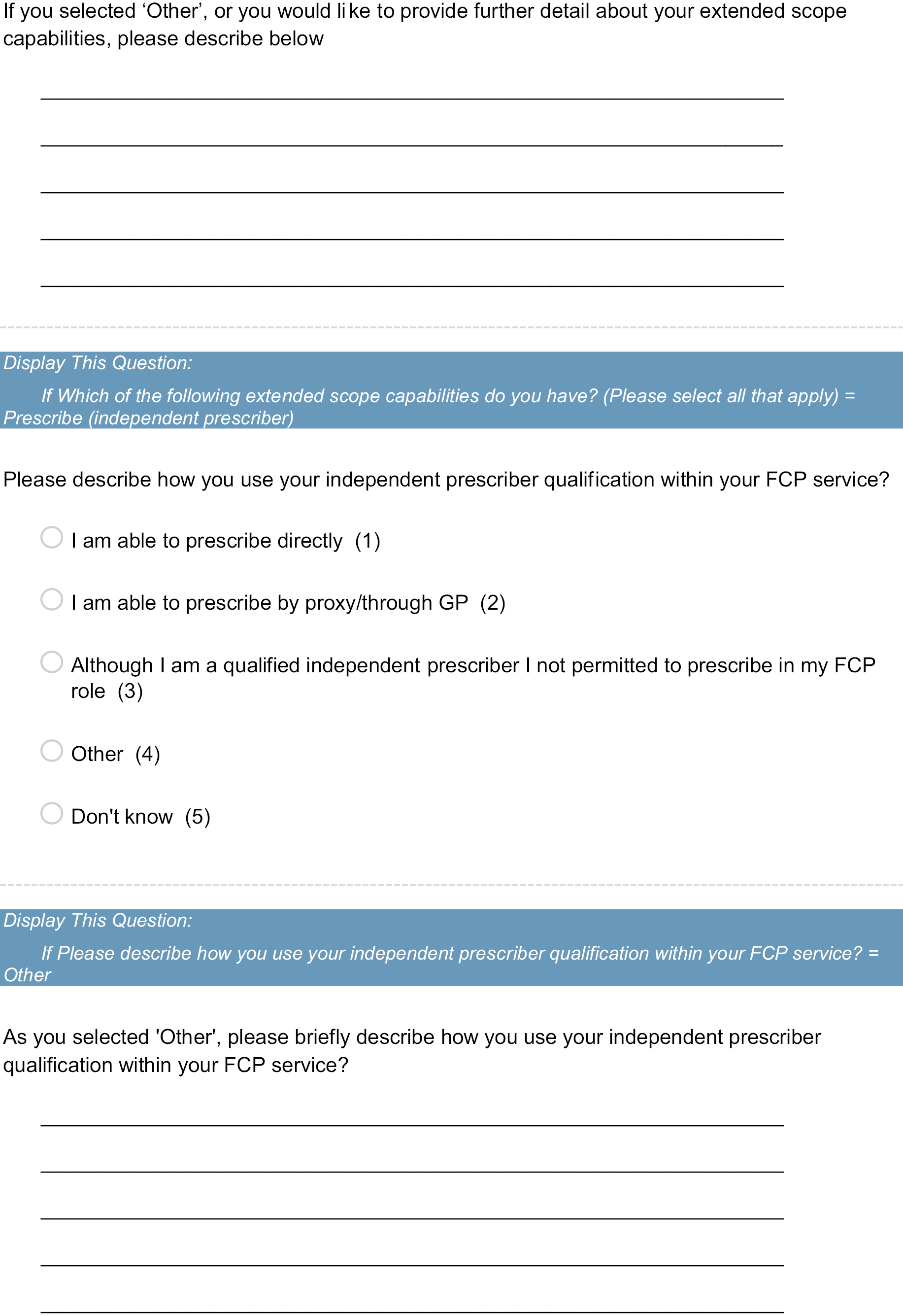
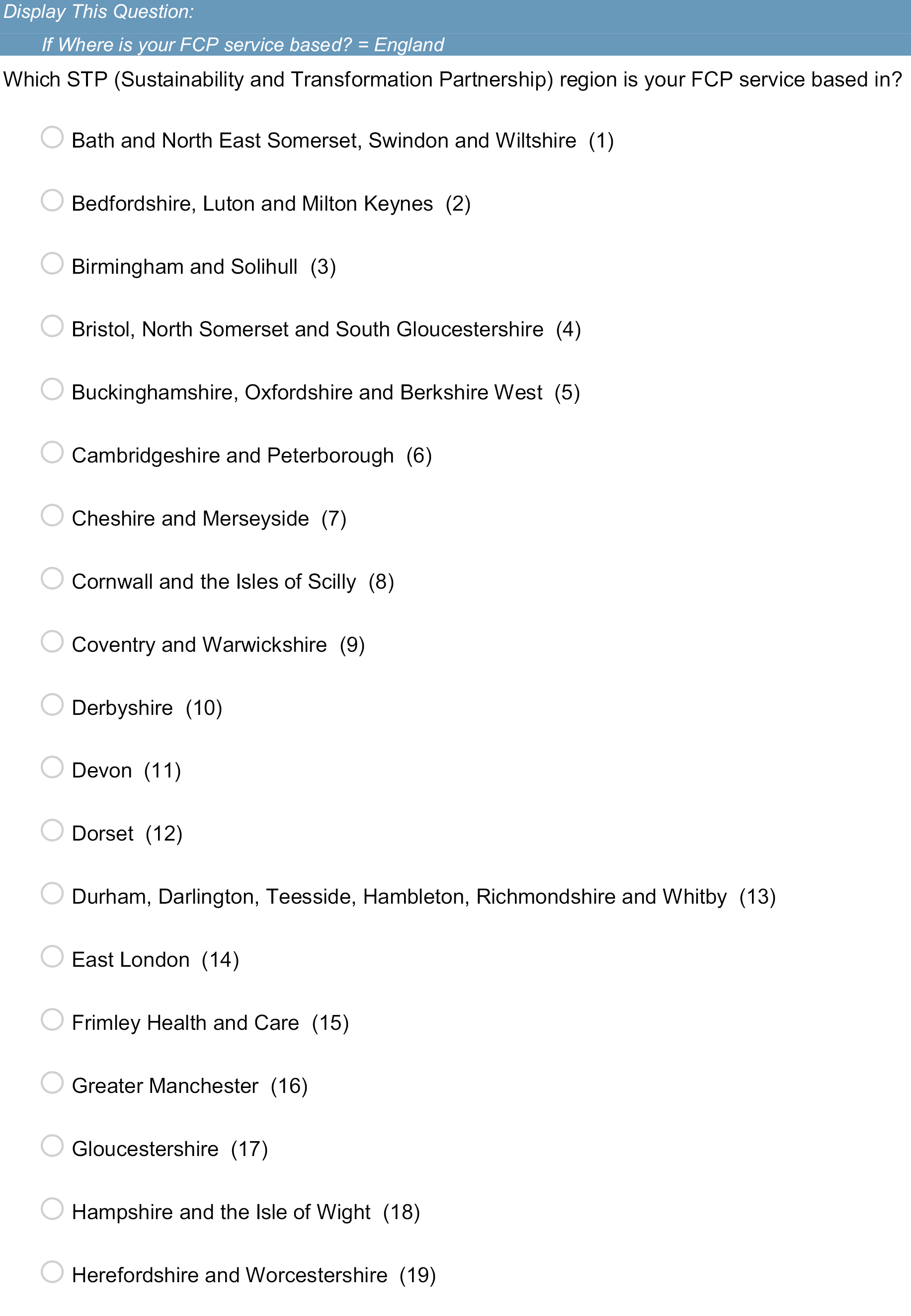
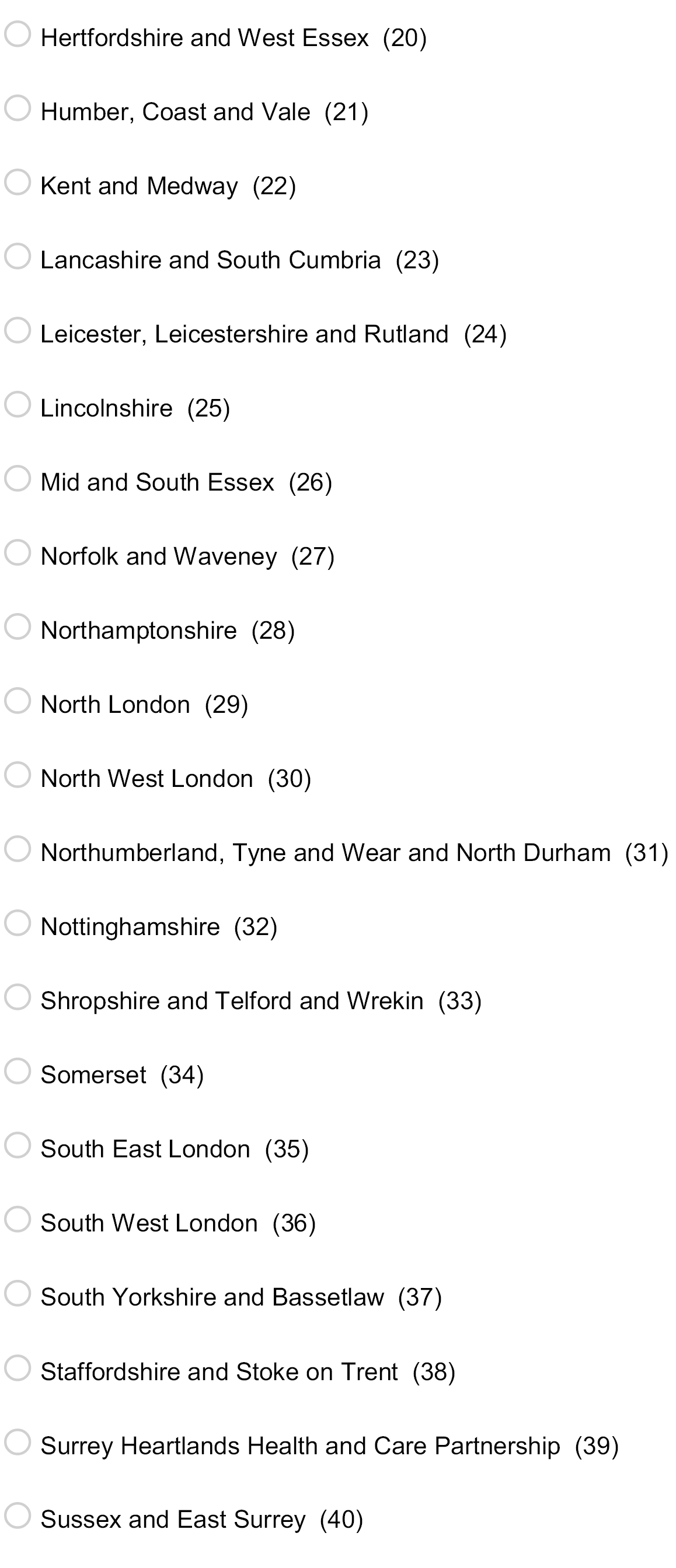
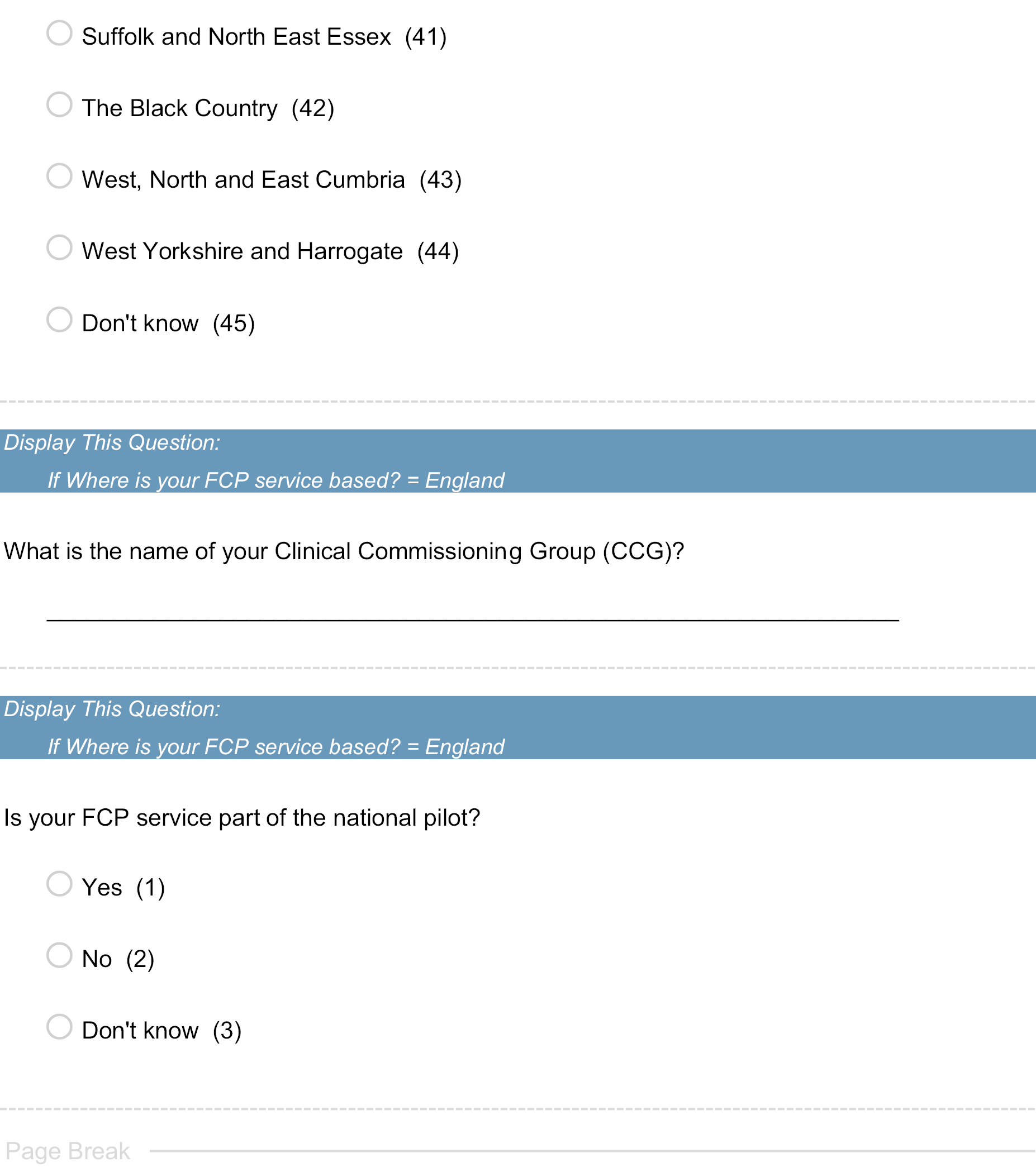
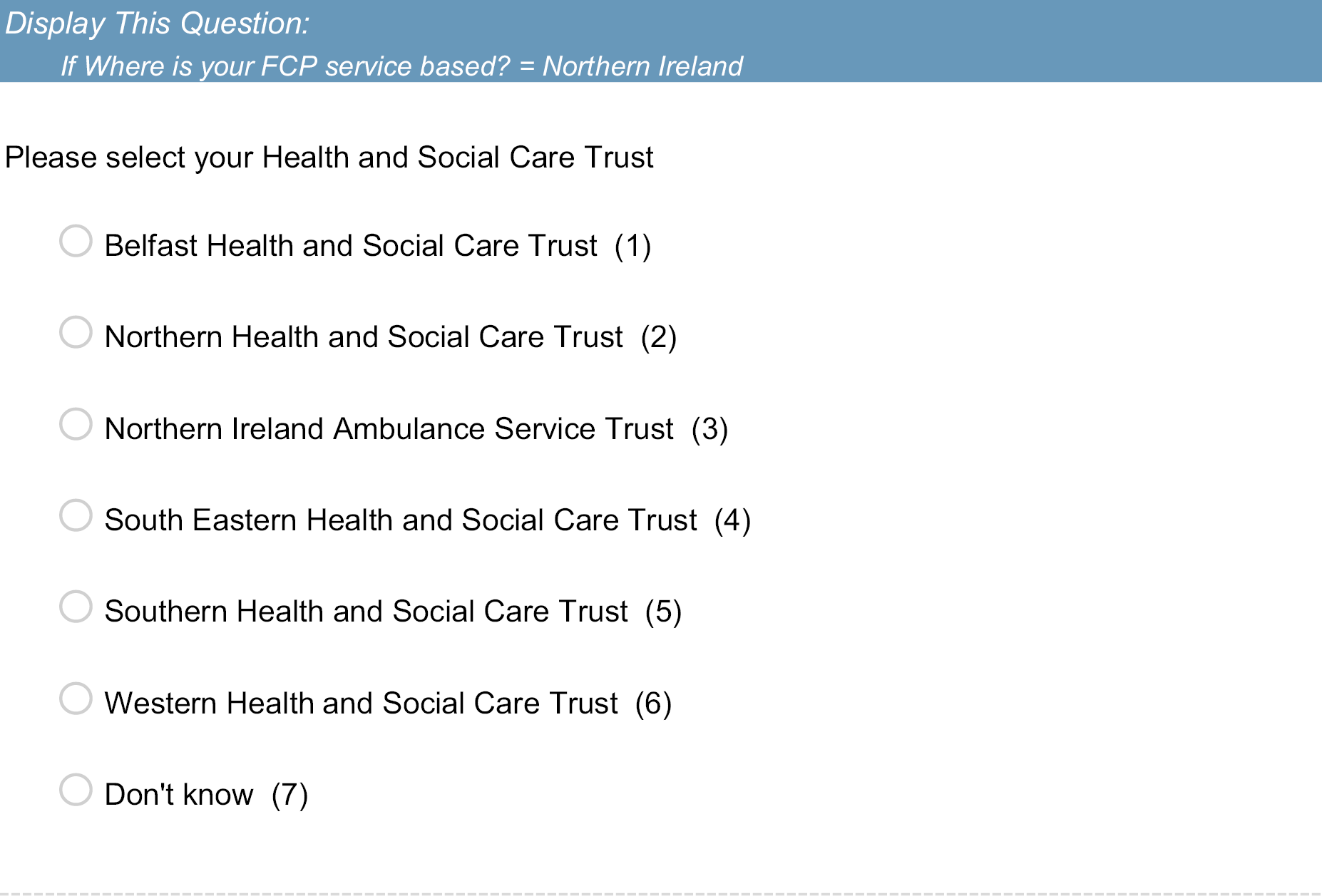
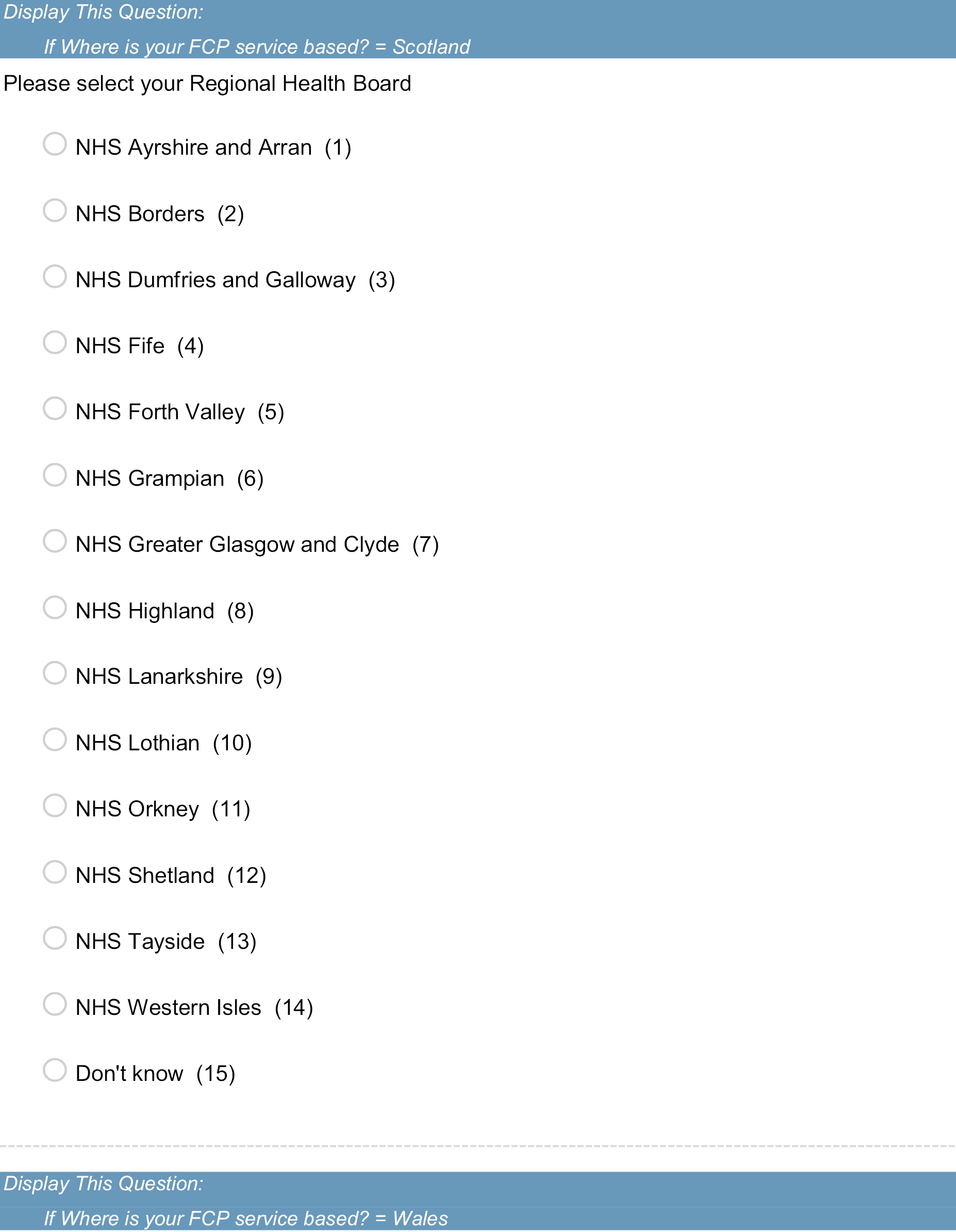
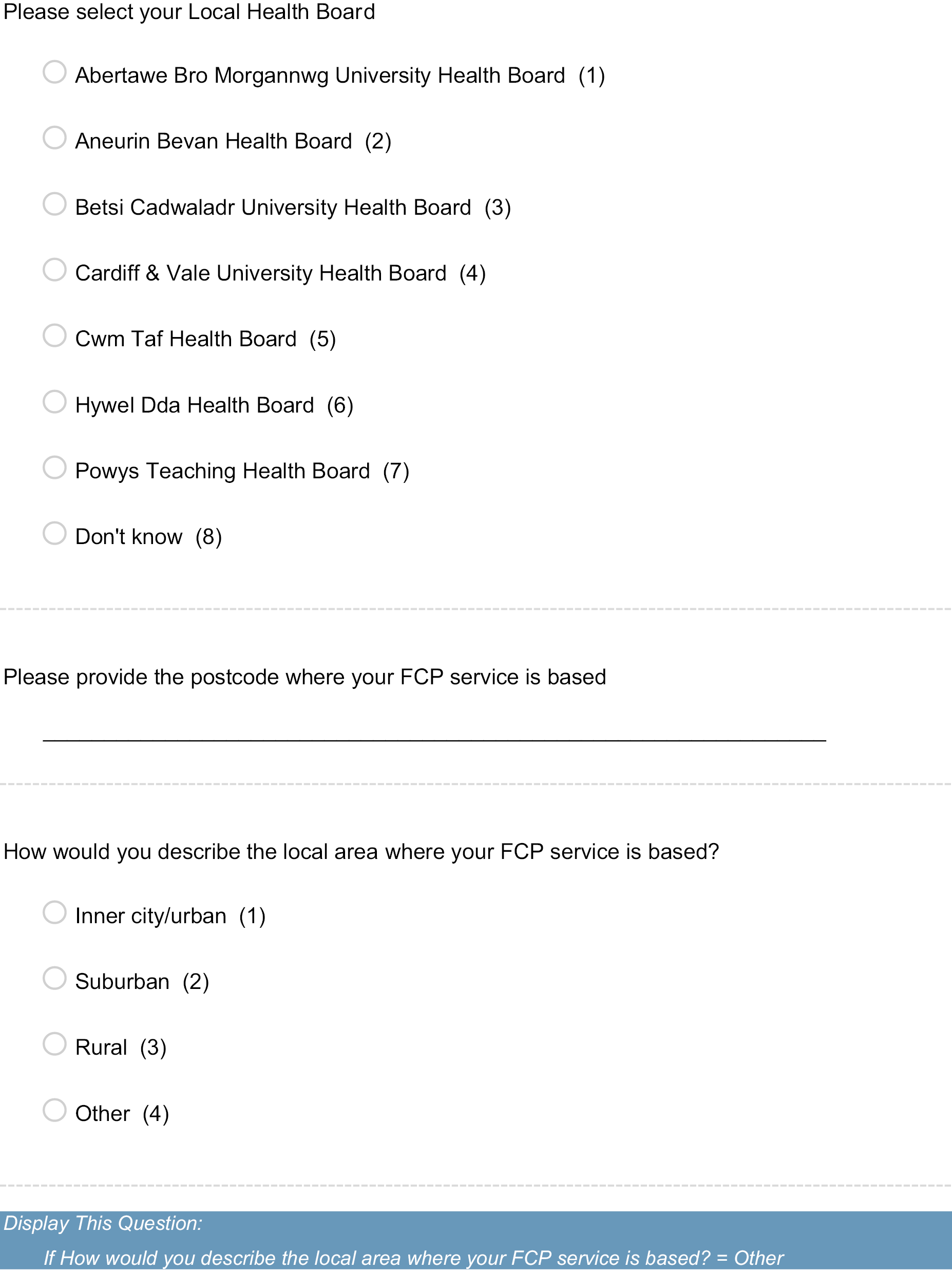
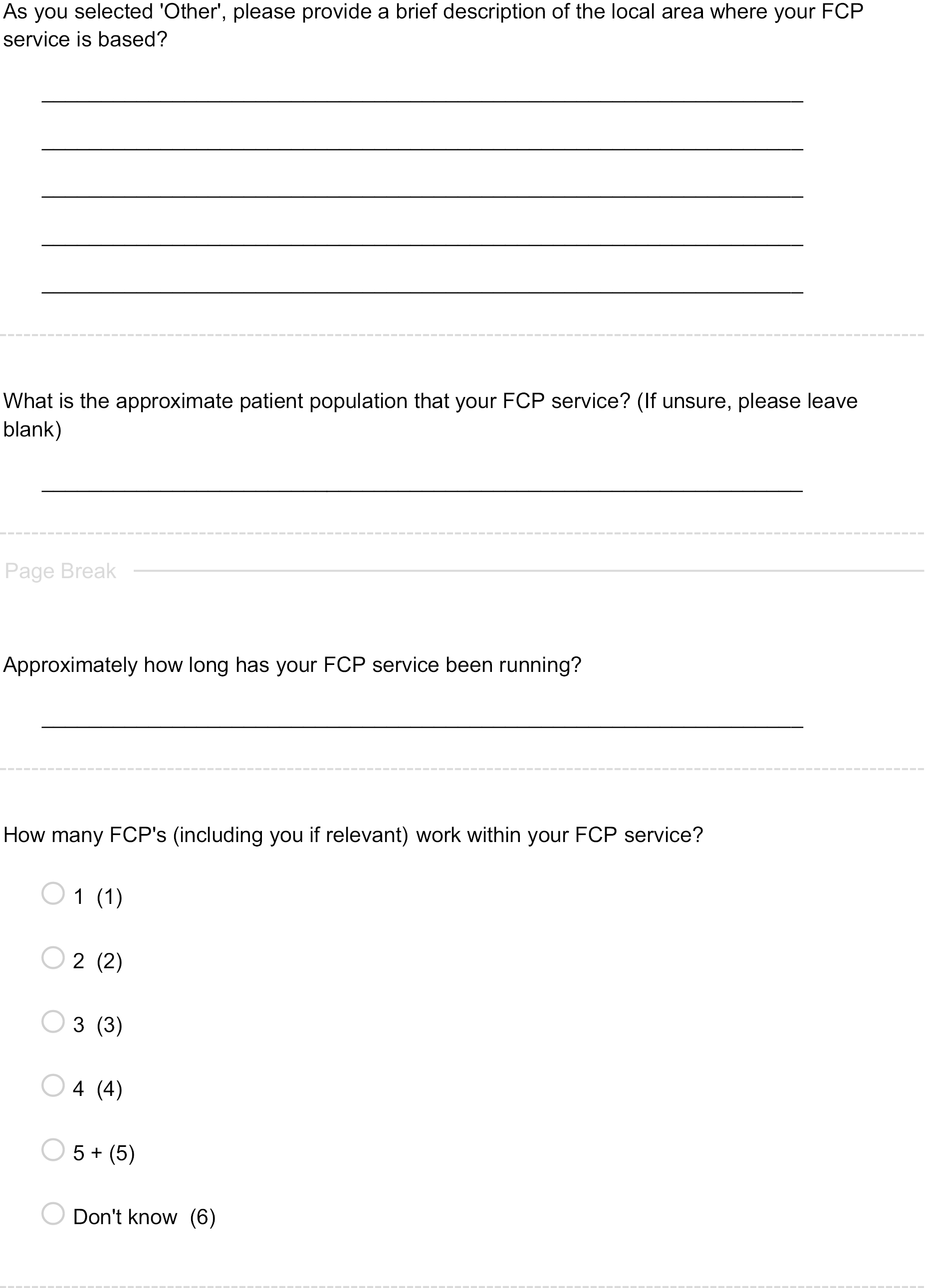
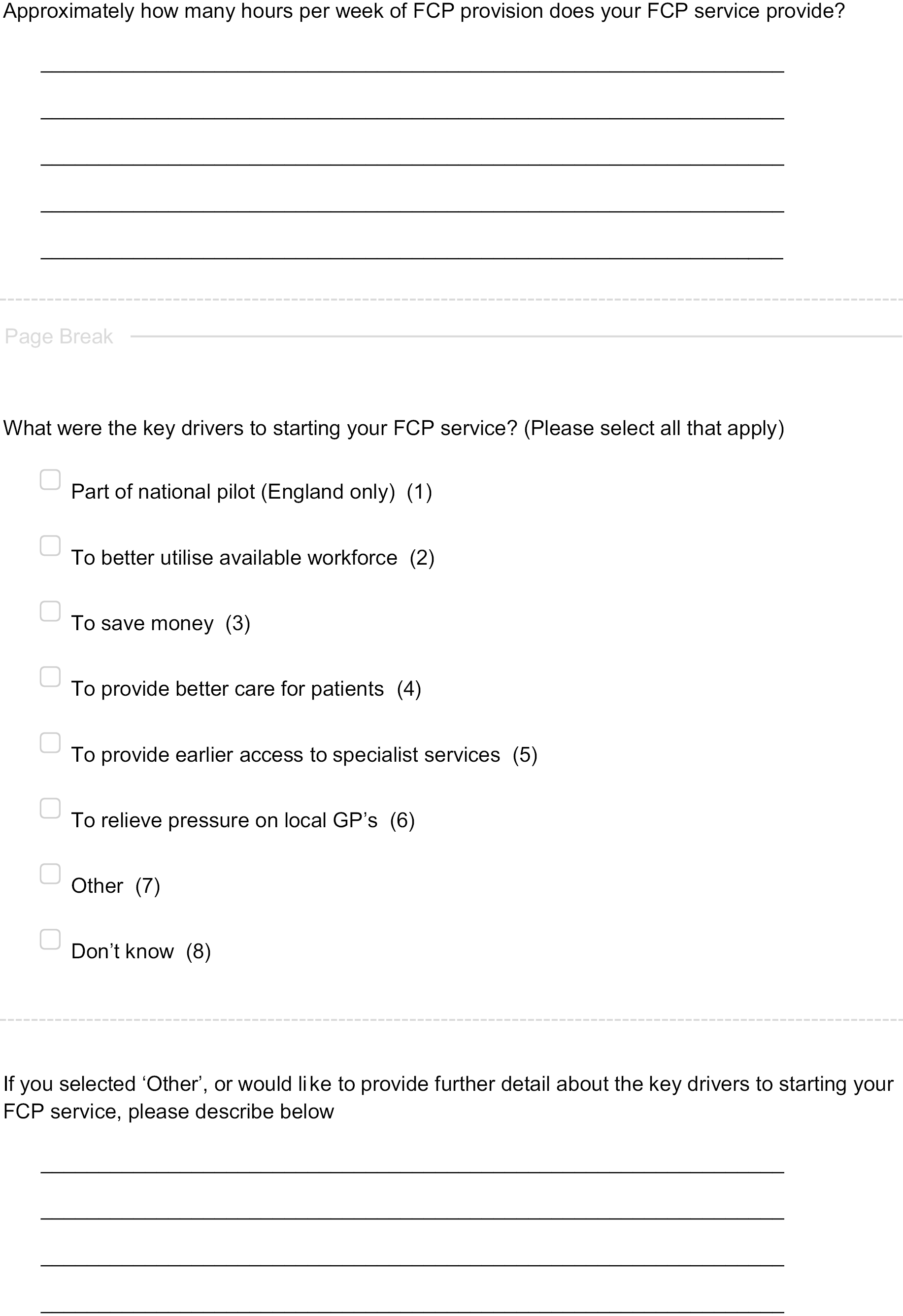
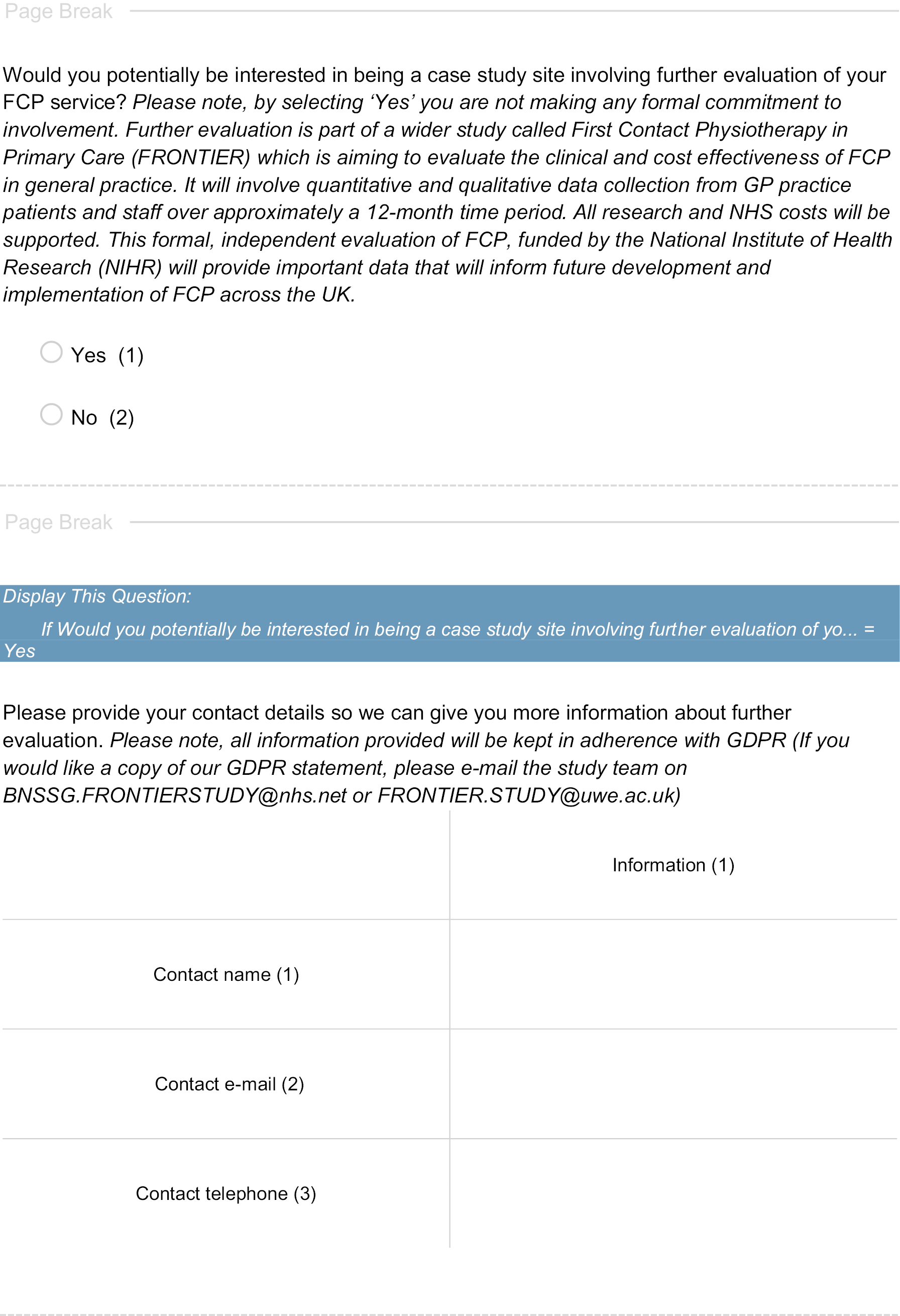
Appendix 2 Realist theory development and flow chart
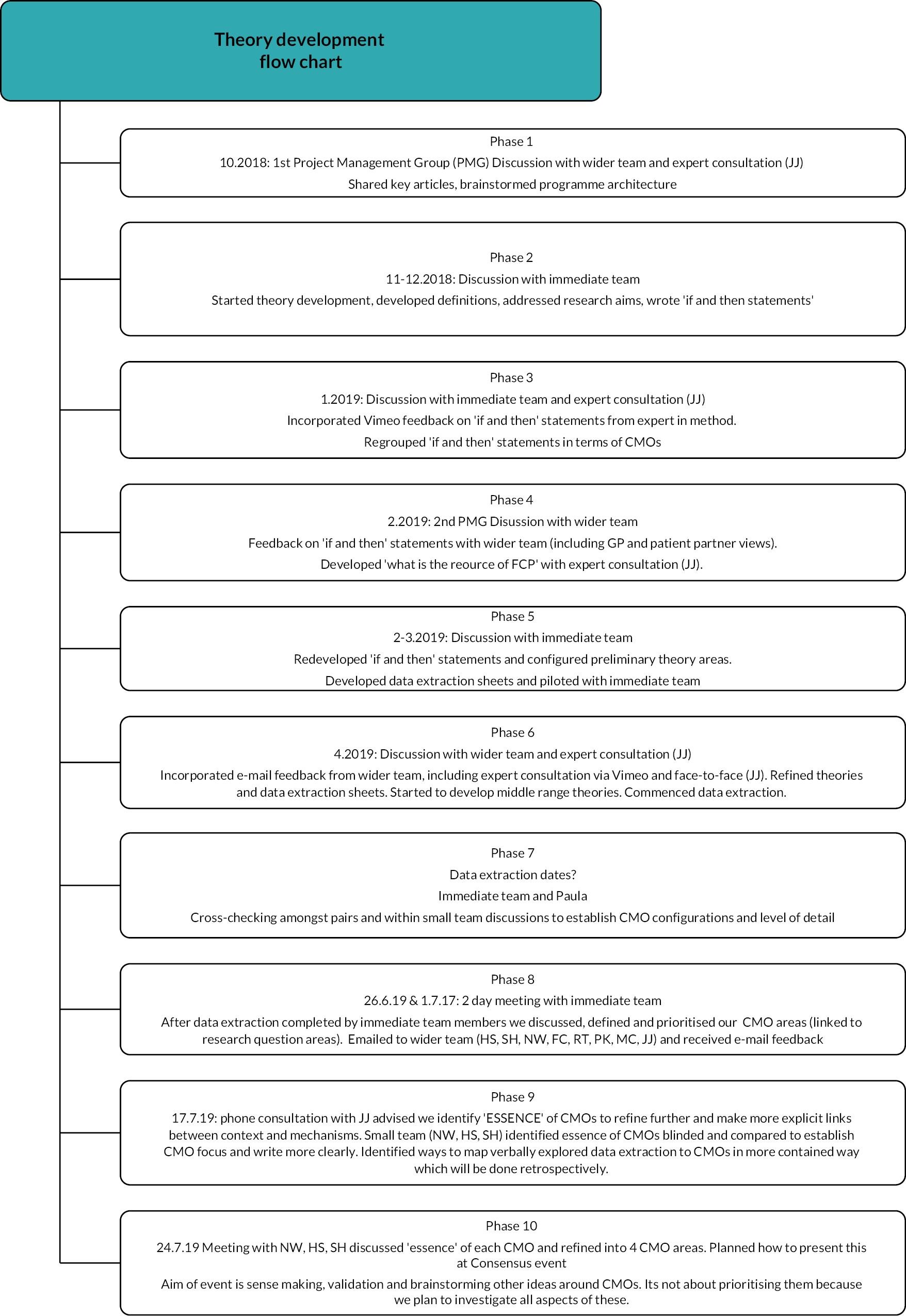
Initial programme theory development areas
Theory areas
Right time
How changes to referral processes and which practitioner is the first point of patient contact affect access and take up of FCP services. How does take up of FCP appointments create intended and unintended outcomes?
In the old system, the patient went direct to GP appointment, which was booked by a receptionist. There was a cultural belief that doctors know best. Physios were generally located outside of primary care.
Since FCP has been introduced, physios have been moved into primary care which has changed the first point of patient contact and eliminated the need for GPs to fill this role in all cases. It has also increased the staffing and therefore the appointment capacity for patients with musculoskeletal conditions. Patients have the option to self-refer to this service or be booked in via a receptionist. This is intended to make it quicker and easier for patients with musculoskeletal conditions to get a primary care appointment.
This has changed referral processes in primary care for both patients and staff and challenged the cultural belief about who should offer first point of contact appointments in primary care.
To change their previous referral behaviours, staff and patients need to have adequate knowledge of the new service and new referral processes. This will help them be more able to trust that this service will meet the needs of patients and primary care, and they will then try it out and access these appointments. Over time, as more patients and staff refer to the service and experience acceptable outcomes, this process will become embedded (normalisation process theory) and the old referral processes and beliefs that ‘doctor knows best’ will change.
If patients take up these new musculoskeletal appointments:
-
GPs should experience reduced MSK workload.
-
Admin should experience reduced appointment booking pressure.
-
Patients should experience shorter wait times for appointments.
-
Patients should experience increased satisfaction due to shorter wait times and having more choice about which professional to access.
-
Patients should experience earlier detection of musculoskeletal conditions.
Ripple – If patients experience earlier detection of musculoskeletal conditions due to changes to access then (links to ‘right person’ theory area):
-
Patients should experience an increased motivation to engage in self-management.
-
Increased patient satisfaction due to symptom resolution.
-
Early detection reduces chronicity, so more patients can be managed in primary care.
-
Reduced need for appointments in both primary and secondary care.
Contextual factors will affect how much patients and staff know about the new FCP service and the new referral processes. Contextual factors include:
-
Training of admin staff to develop knowledge of the new FCP service and confidence to use new referral or screening tools.
-
If IT systems make it easy to adopt new referral processes and book FCP appointments.
-
Promotion of the service to patients (marketing/welcome message).
-
Admin staff perceptions of whether the FCP service can meet a patients’ needs (complex/older patients to GP).
-
GP or other staff endorsement of the FCP service.
-
.Patient openness to new services and ability to access new referral routes (younger/more educated patients more likely to self-refer).
Certain contextual factors may undermine the need to change old referral behaviours:
-
If waiting lists for FCP are higher than GP then the incentive to try the new service is removed.
Right place
How does moving physiotherapists into the FCP role in primary care influence musculoskeletal communication among this PCN and how does this effect patient management? How does this change in physical location of physio services and team structure create intended and unintended outcomes?
In the old system, physio services were usually located as outpatient services in various secondary, community or primary care settings. They conducted assessment, diagnosis and treatment. Services were accessed by referral from primary care (e.g. GP) or in some areas via self-referral. Waiting times varied but in many settings were likely to be weeks. Physios worked within a team and received specialist supervision/management.
Since the top-down introduction of FCP, physios have been moved quite quickly into primary care services, creating changes in staffing structures and skill sets in both primary and secondary care. It has changed the physical location in which a physio works and, due to complex staffing models within primary care, first-contact physiotherapists may not sit within one practice but often perform roles covering multiple primary care locations. The physio role has been adapted into the FCP model to fit the needs of primary care (shorter appointments offering only assessment and simple advice – the effects of shorter appointments are discussed in the next theory area: 3 ‘right person’). There have also been changes to the MDT network within which a physio works. The novelty of the FCP role in primary care teams may mean physios feel insecure moving to this new setting as they establish their role and feel that they have to prove their worth to retain their new employment. This is also influenced by the medical hierarchy within primary care, which suggests that ‘doctors know best’, alongside uncertainty around whether a practice or multiple practices ‘employ’ the first-contact physiotherapist, which might link to a sense of support, belonging or professional development.
The intention is that through locating musculoskeletal skills in primary care, at the front end of the patient pathway, that primary care musculoskeletal management will improve through introducing musculoskeletal skills into primary care which can be communicated between this new MDT. This will reduce the burden on secondary care physio provision and, in conjunction with the previous theory area (2: ‘right time’), shorten the patient pathway. Over time this new MDT will be embedded (NPT) and this will normalise the involvement of first-contact physiotherapists in primary care and the role will be seen as more valuable/trustworthy. If there is a lack of communication this may create uncertainty that FCP is an acceptable service (relates to previous theory area 1: right time).
If these new primary care teams are able to communicate and build relationships, they will see the value of the other practitioners’ scope of practice. If the first-contact physiotherapist is embraced as part of the MDT, this has the potential to achieve beneficial outcomes including:
-
Education of primary care staff in musculoskeletal conditions and patient management through shadowing roles, discussion and reading patient notes leading to improved management of patients with musculoskeletal conditions (this links to knowledge in theory area 1: access).
-
Enhance patient safety as complex cases can be easily discussed in the MDT.
-
FCP staff satisfaction as they feel valued/supported within the team (links to staff retention – hunch).
-
GP staff satisfaction as they feel better supported in their musculoskeletal practice (hunch) (links to reduced GP workload – hunch).
Ripple – As a result of a better skilled musculoskeletal primary care team then:
-
This will reduce improve communication with secondary care teams about musculoskeletal referrals and increase the appropriateness of onward referrals/requests for tests or imaging.
-
This will reduce appointment use in primary care as GPs are upskilled in musculoskeletal management and provide more appropriate interventions and referrals.
-
This will create a more consistent approach to musculoskeletal management between staff in primary care which will reduce the need for patients to request second opinions.
However, there may be unintended consequences of locating a first-contact physiotherapist within a primary care team.
-
The first-contact physiotherapist is no longer part of wider physio team and feels isolated in this new MDT primary care role.
-
First-contact physiotherapists work in an isolated way within primary care which impacts patient safety.
-
First-contact physiotherapists feel unsupported by primary care and have reduced opportunities for continuing professional development.
-
Secondary care experience shortages in physio staffing.
-
GPs feel deskilled as they no longer see as many patients with musculoskeletal conditions.
Contextual factors may affect the ability to build these communication and relationships between staff:
-
Staff consistency – frequency of rotation or temporary FCP and GP staff, are PCNs small enough to allow clinicians to get to know one another?
-
Employment/ownership of the FCP role – who provides funding and support for skills development.
-
Practical infrastructure – surgery space and IT set up (referrals, tasking, patient notes).
-
Availability of networks between first-contact physiotherapists and other physios within or outside primary care team.
-
Practitioner time, skills (personal or IT) and infrastructure/policy to engage in MDT communication.
-
Primary care staff openness to MDT working – do they value physio input or are they suspicious?
(If there is a low need for FCP services in the area then the primary care team may be resistant to beginning MDT working, if so the value of FCP will not be recognised.)
Right person
How does the skillset of the first-contact physiotherapists influence outcomes in primary care?
Prior to the introduction of FCP, musculoskeletal expertise was usually accessed as an outpatient following GP referral from primary care or referral from a secondary care service, or in some areas via direct access/self-referral to physio services. These services often had a waiting list of several weeks which might in some cases increase the chronicity of musculoskeletal conditions. These appointments are usually 45 minutes and involve an in depth, biopsychosocial assessment, diagnosis and recommendations for treatment which might involve returning to the same service for multiple treatment sessions. This provides increased opportunity for the practitioner to build up an understanding of a patients’ condition and ensure their recommendations are of benefit.
There has been an evolving understanding of the musculoskeletal skills required in primary care. Originally it was thought that Band 6 physios could conduct the role with supervision, yet more recently the CSP has recommended that band 7–8a physios perform the role who likely have the additional clinical qualifications which may benefit the role and reduce patient contacts in primary care for example NMP or injection. This might mean that the FCP role is perceived as an attractive route for career progression. The high demand for physios to fill FCP roles in primary care and a lack of band 7–8a physios to meet this need may have led to lower-skilled practitioners being employed with supervision or mentoring. There has also been discussion about the effects on patient safety for a musculoskeletal specialist to provide first point of contact over a generalist practitioner.
The appointment structure and role specifications for FCP in primary care is very different from other physio roles. Appointments are usually between 15 and 30 minutes in length, although in some practices may be as short as 10 minutes. The role is primarily about assessment, diagnosis and brief advice or onward referral, as opposed to treatment. Owing to time constraints, it is likely that the assessment that can be provided may not be as in depth as other physio services.
The intention of locating this musculoskeletal skillset in primary care is that it will provide a higher level (although a smaller dose) of musculoskeletal expertise at the front end of the primary care pathway. This musculoskeletal skillset provides enhanced assessment, diagnosis and musculoskeletal condition management (compared with usual GP care) which enables the first-contact physiotherapist to have the confidence to work autonomously and removes the pressure on GPs to perform this role which might feel out of their scope of expertise.
If the first-contact physiotherapist is able to provide patients with the benefits of their musculoskeletal expertise, then the likely outcomes are:
-
Improved musculoskeletal assessment and management first time.
-
Wider variety/more effective musculoskeletal management options used – reduced prescriptions, increased self-management, reduced diagnosis/pathologising conditions.
-
Patient more reassured (first time), educated about musculoskeletal conditions, increased confidence to independently manage their condition/reduced negative strategies.
-
Improved patient outcomes/reduced chronicity.
-
Reduced repeat appointments in primary care for the same condition (quick ‘discharge’).
-
More appropriate onward referrals to secondary care.
-
Safe practice – as first-contact physiotherapists identify/refer non-musculoskeletal conditions that are out of their scope.
-
More satisfied patients – with appointment, practitioner, advice and outcome.
Secondary outcomes
-
Reduced GP musculoskeletal workload – patients not needing to see GP for ongoing musculoskeletal conditions.
-
Reduced pressure on GP to practice out of their scope.
-
More appropriate secondary care referrals will reduce ‘whole-system’ musculoskeletal resource use.
Ripple – as a result of musculoskeletal expertise at the front end of the care pathway there will be:
-
More effective musculoskeletal management and more musculoskeletal educated patients earlier in their condition trajectory, which will reduce musculoskeletal symptom severity/chronicity and therefore primary care appointment use over time.
-
More management of conditions in primary care (and reduced chronicity) alongside appropriate use of secondary care resources will reduce the pressure/burden on secondary care and reduce waiting lists over time.
Contextual factors will affect the ability of the first-contact physiotherapist to perform their role:
-
Skills/staffing
-
First-contact physiotherapist banding, additional clinical qualifications and experience will create a balance that will affect the ability of a practitioner to practice autonomously, which in turn will impact the use of ‘repeat’ appointments in primary care and both staff and patient perceptions of value/satisfaction with the role.
-
Primary care expectations and infrastructure to support the use of or development of additional clinical qualifications by first-contact physiotherapists varies. Some surgeries may expect GPs to perform injections/prescribing or IT systems may not be set up to allow first-contact physiotherapists to use these skills. This may lead to the use of additional primary care appointments as first-contact physiotherapists task GPs to perform these skills. Physiotherapists may feel undervalued if their skills are underused or if they are not offered professional development to acquire these skills. Surgeries/PCNs may feel exploited/frustrated if they are unnecessarily paying for higher banded physios but not benefiting from the pay-off of reducing appointment use which the FCP role is intended to provide.
-
Difficulties identifying higher banded physiotherapists to staff the role may mean lower banded/experienced physiotherapists are recruited to perform the role. If these first-contact physiotherapists are not supervised sufficiently then there may be an impact on patient outcomes and patient safety.
-
-
Appointment length
-
Surgery expectations of FCP appointment length will affect depth of assessment and management options that the physiotherapist can deliver, which might affect patient outcomes. If the appointment length is much shorter than in standard physio and the patient is only seen for one session, it may be difficult to provide physio services that provide outcomes which negate the need for referral to standard physio care (however, this is likely to be no worse than standard GP care – is this a hunch?). It is not clear whether seeing a physio for a short time at an early point is sufficient to achieve patient behaviour change/self-management and improved outcomes or if over time there likely to be ‘repeat’ appointment use.
-
Shorter appointments affect pressure experienced by the first-contact physiotherapist in the role to complete tasks within a certain timeframe. This may lead to the physiotherapist working longer/unpaid hours, which might reduce satisfaction in the role. This may be exacerbated by difficulty/lack of clarity of how to adapt the physio role in secondary care and training for the role to a primary care setting and the needs of a primary care population. The first-contact physiotherapist may find that shorter appointments, the changed nature of the role and loss of treatment skills and patient relationship affects their satisfaction within the role.
-
Appendix 3 The impact of digital consultations on first-contact physiotherapists
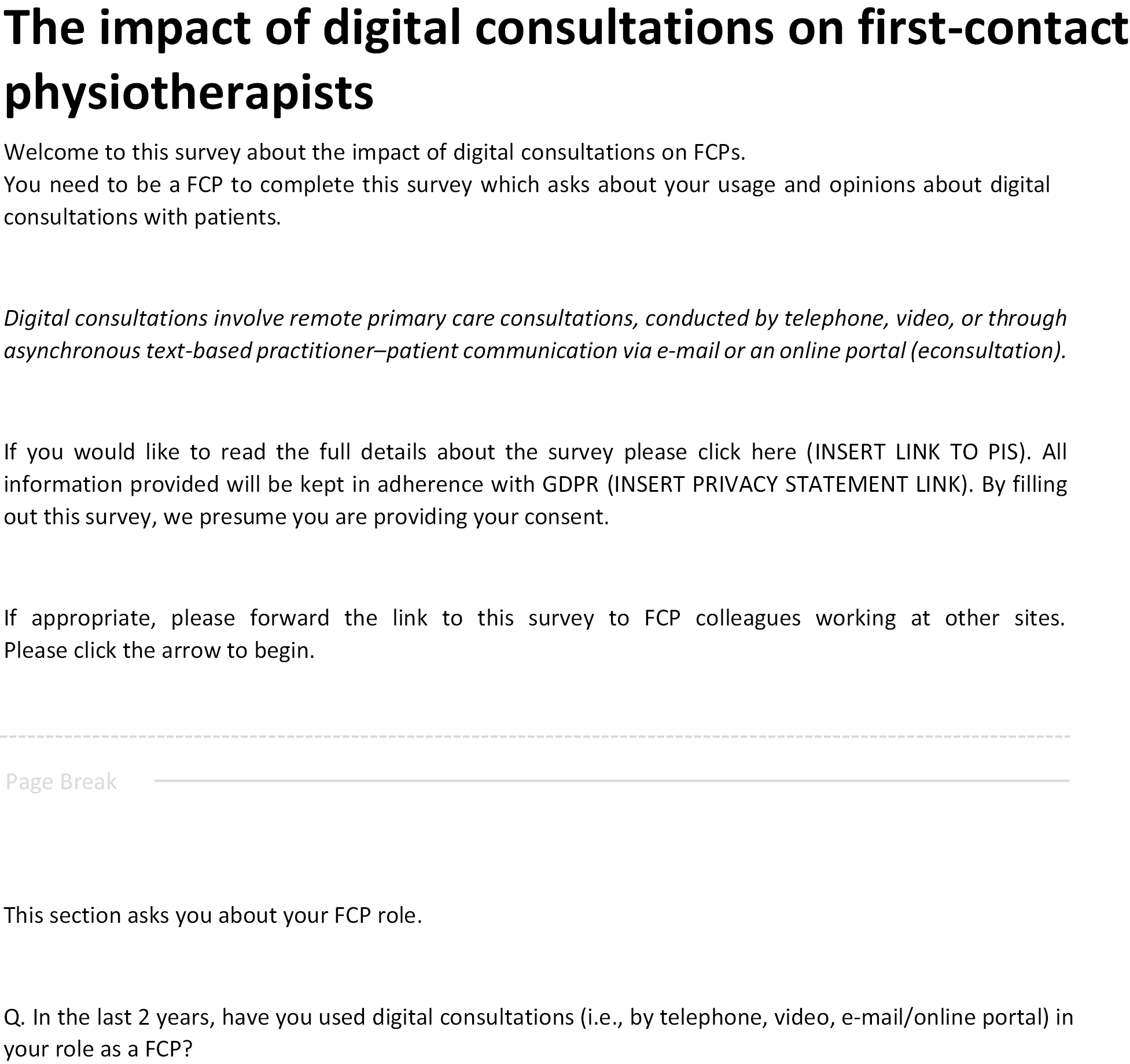
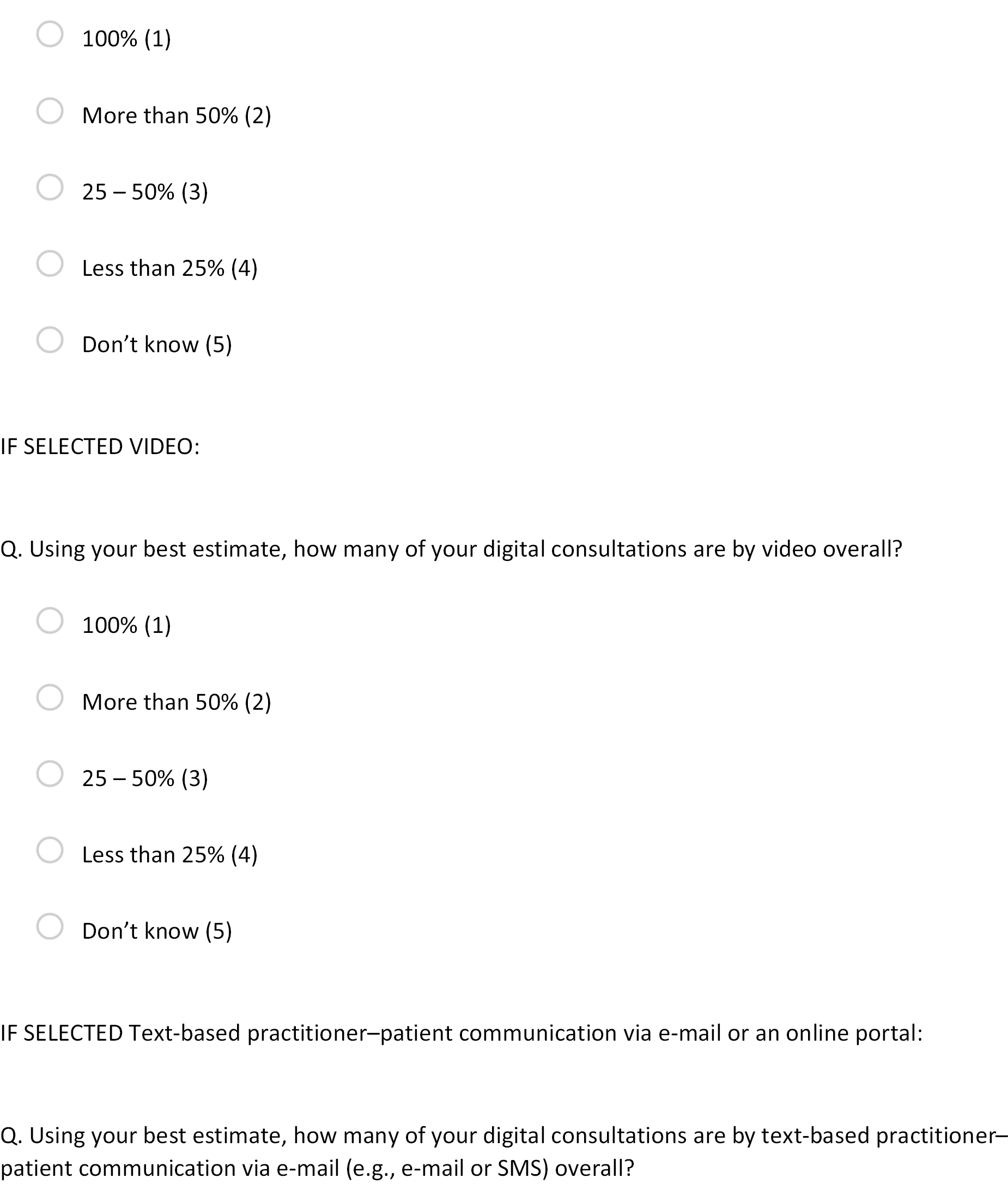
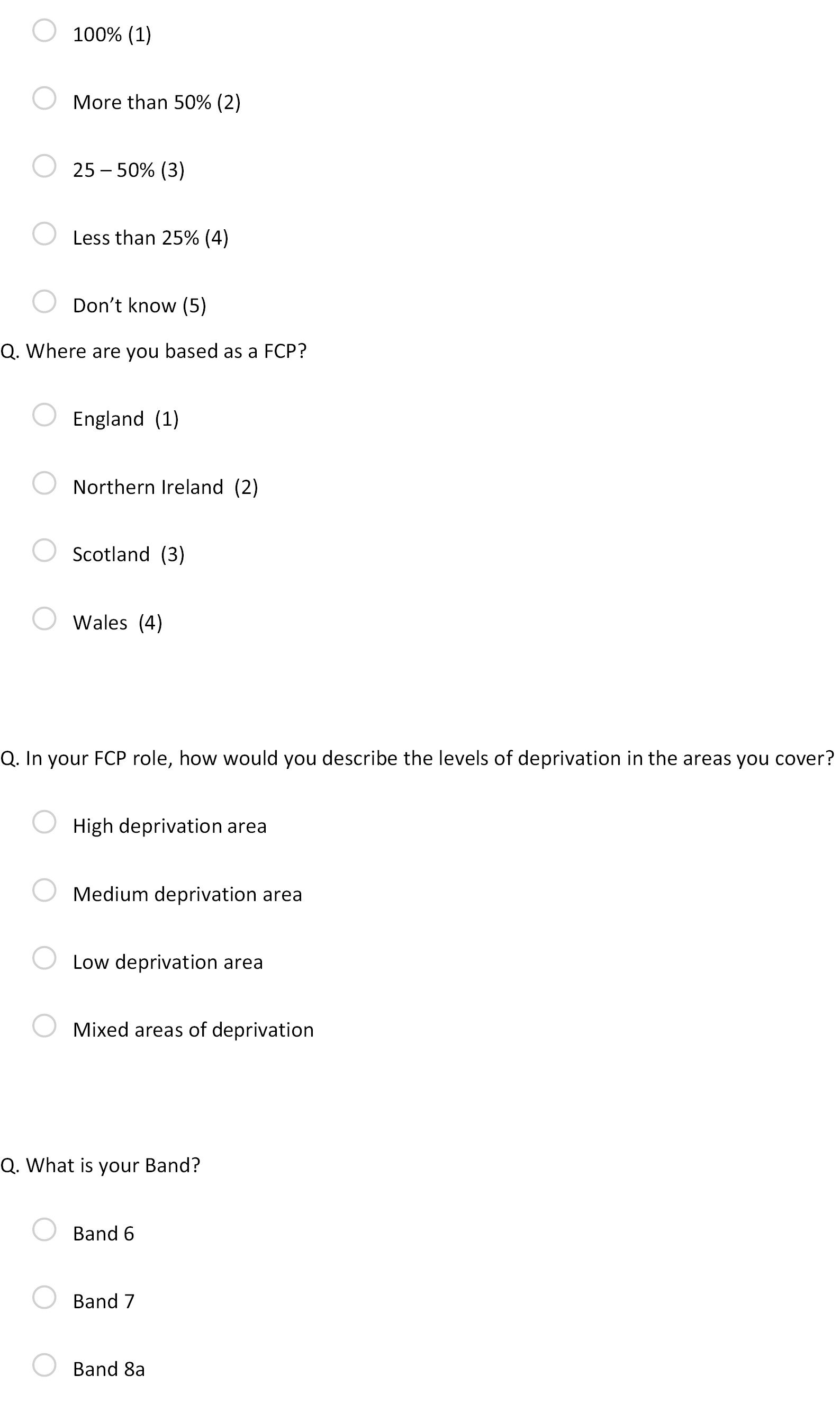

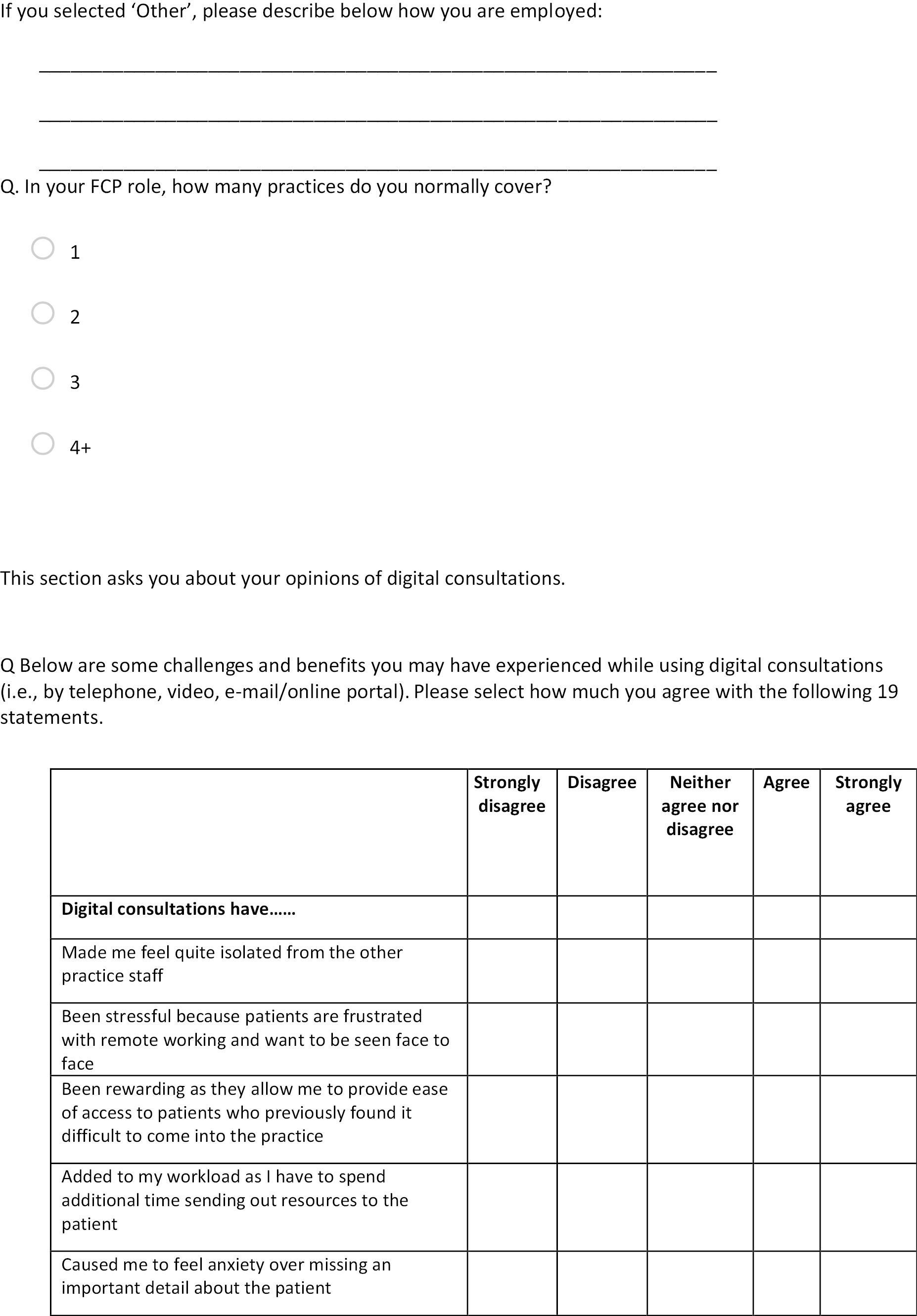
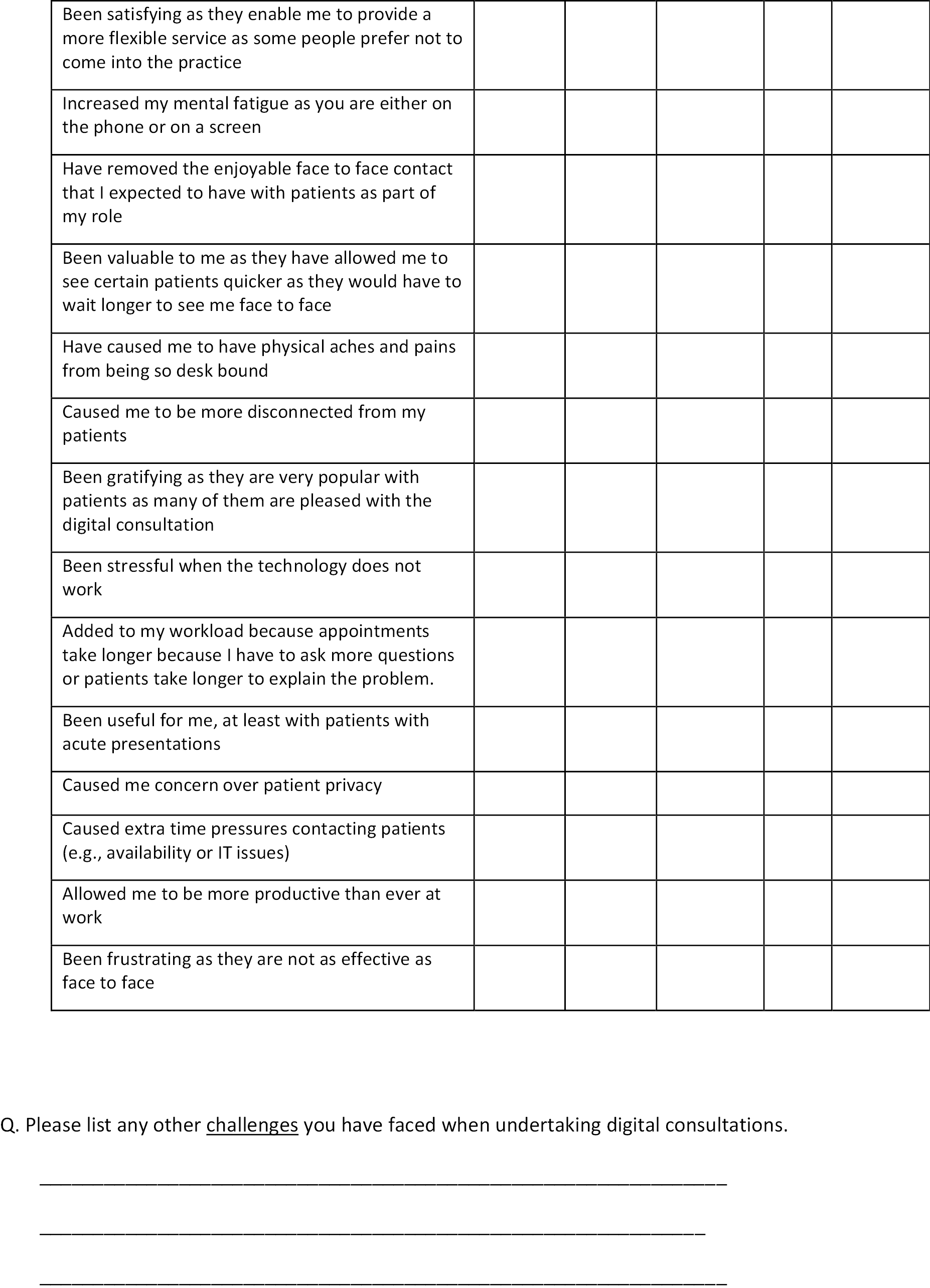
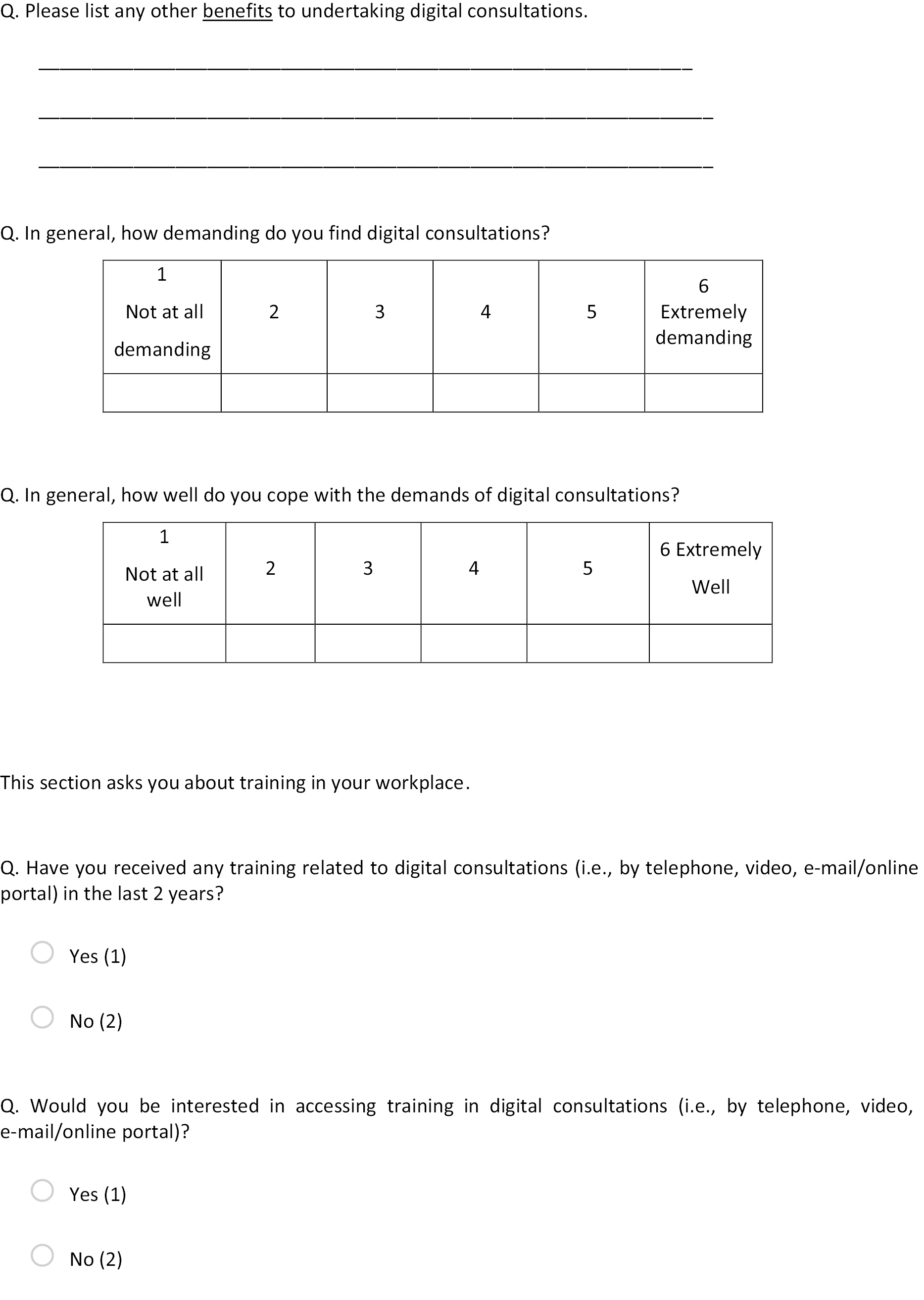
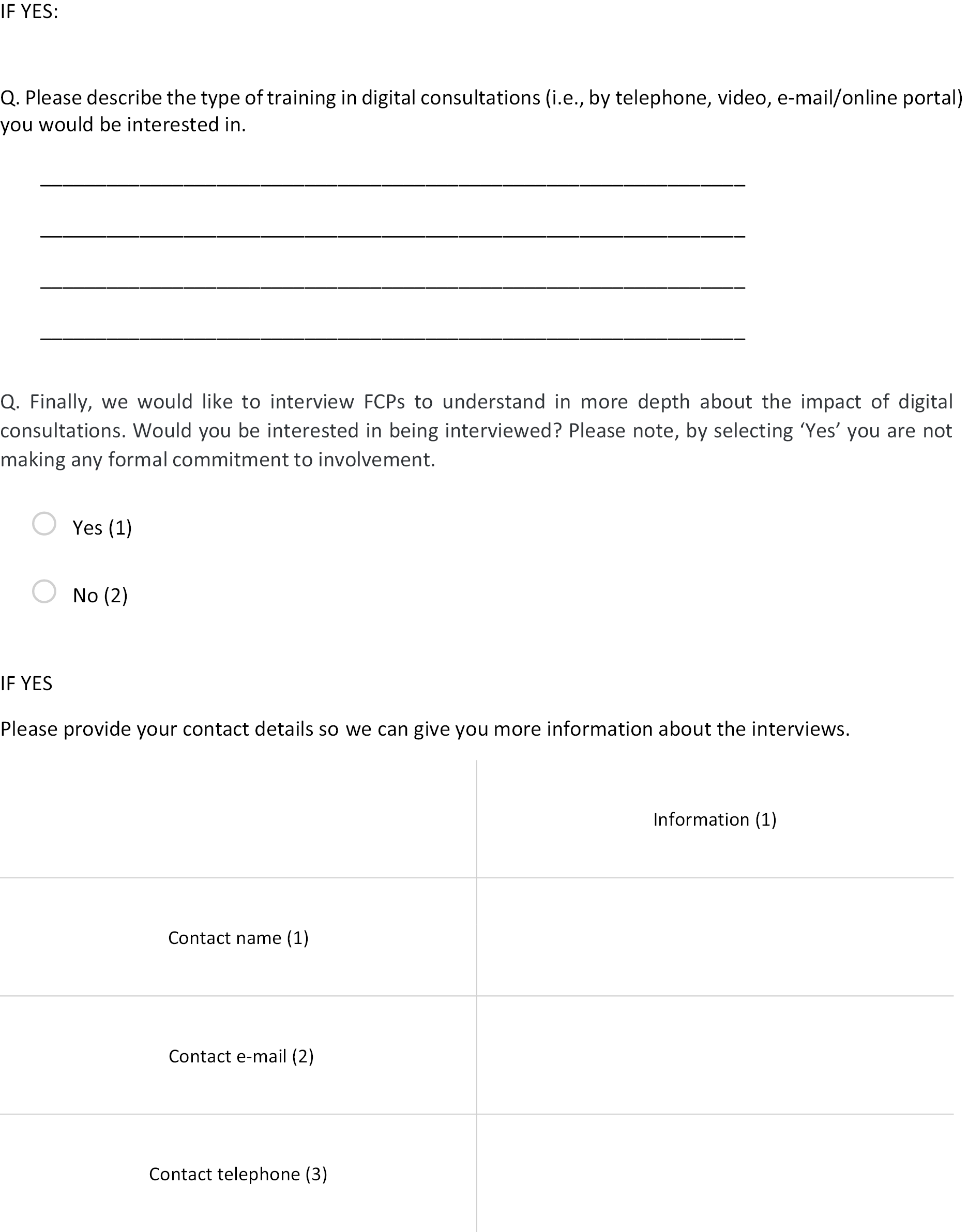
Appendix 4 Client Service Receipt Inventory
Client services receipt inventory version 3
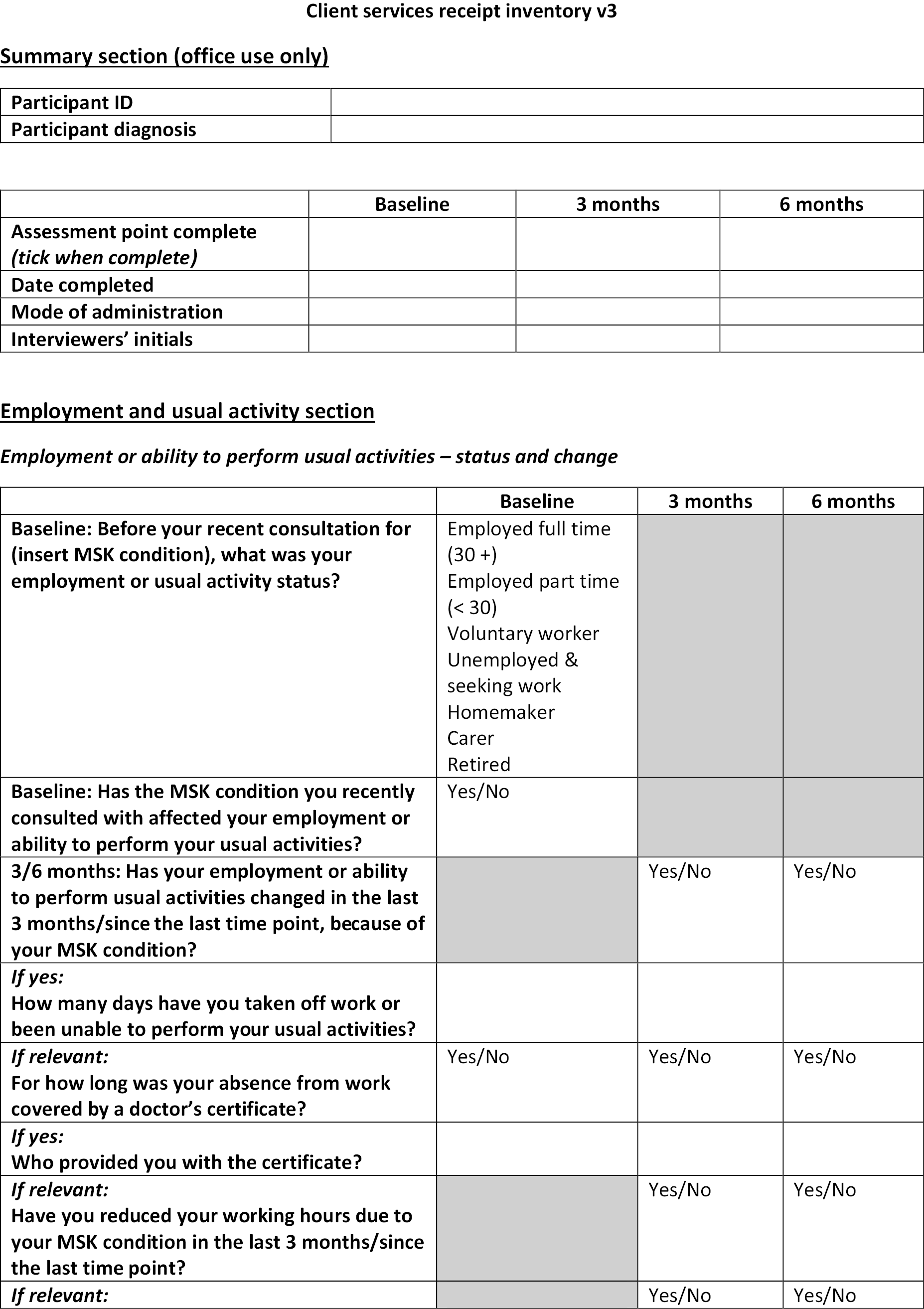
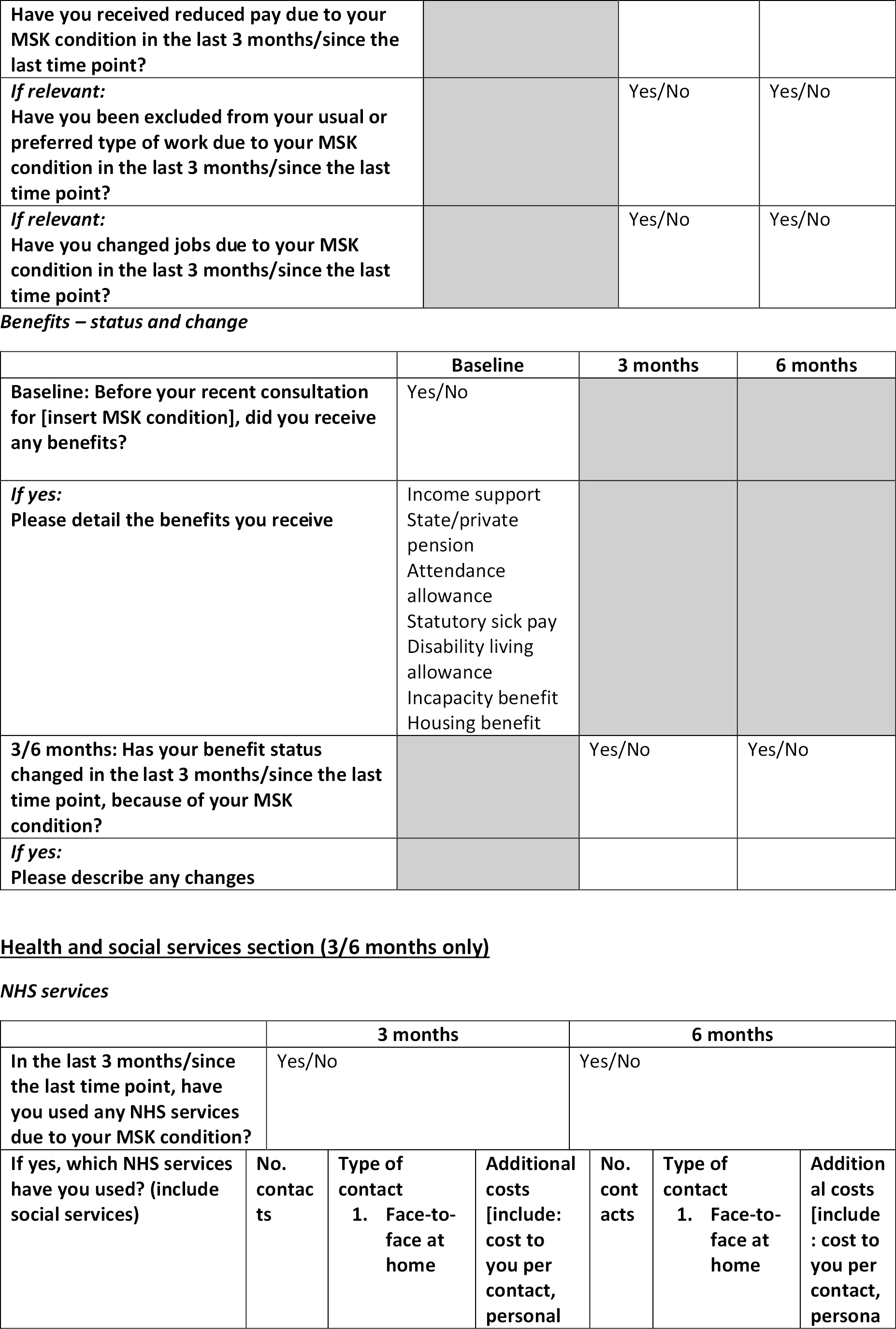
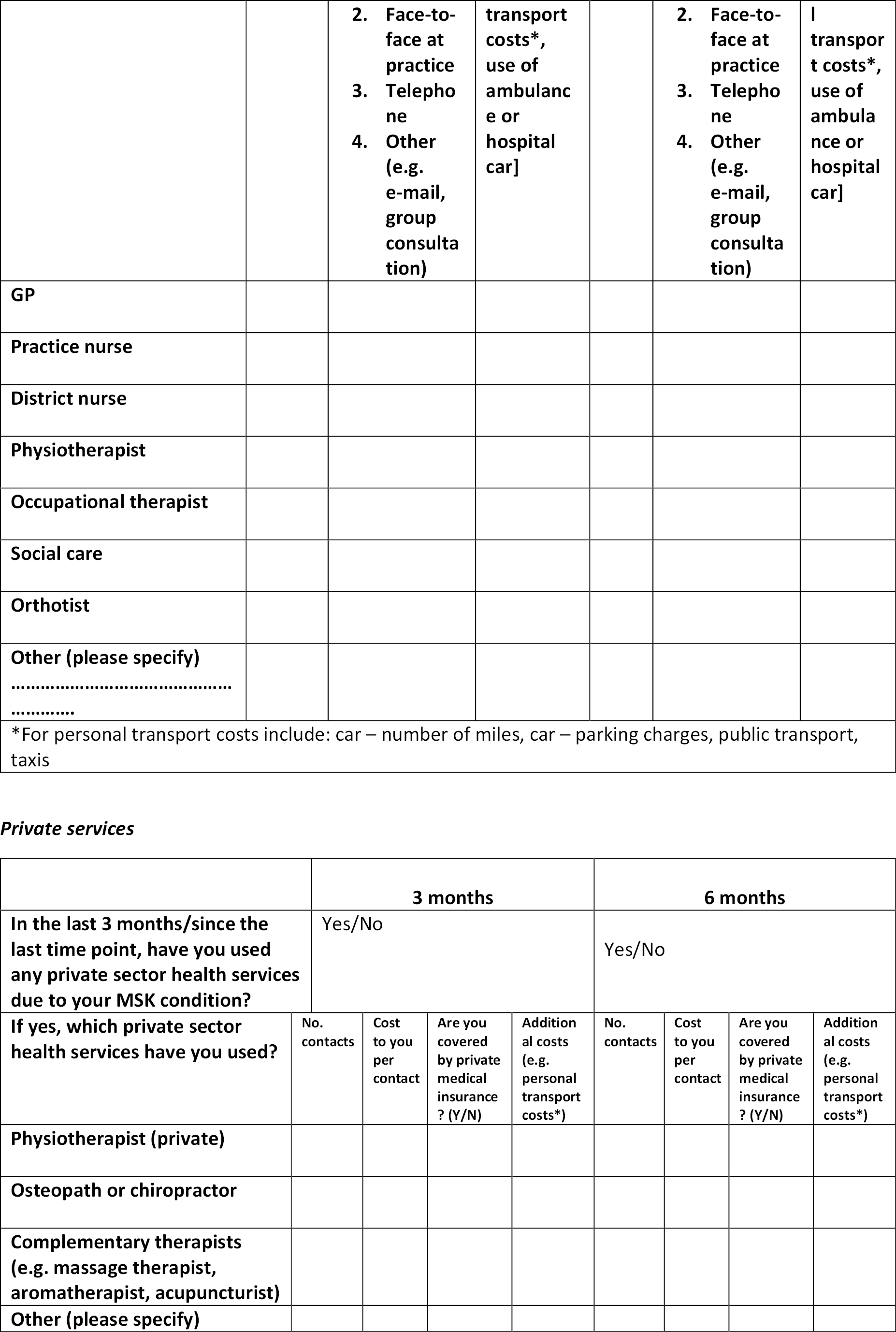
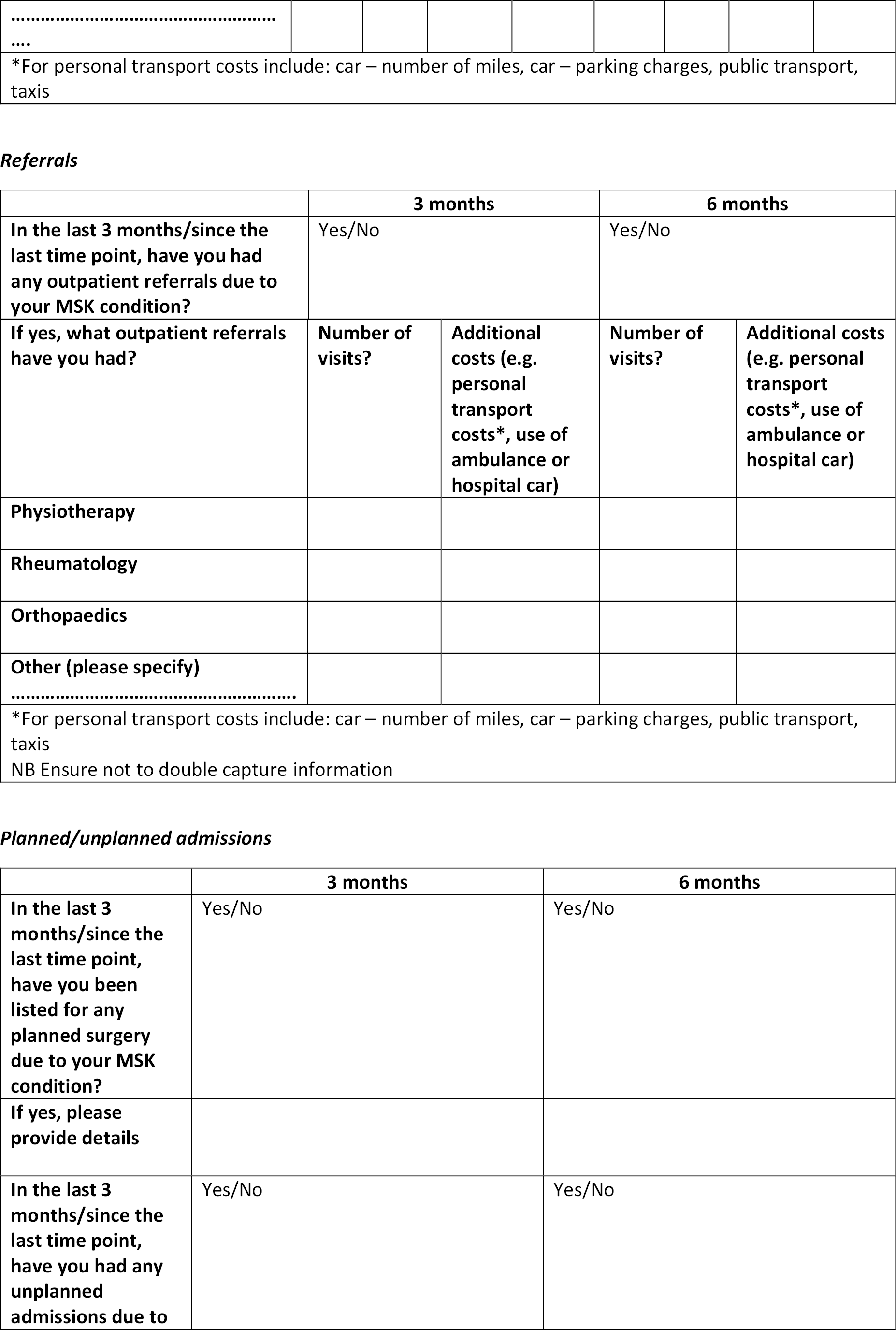
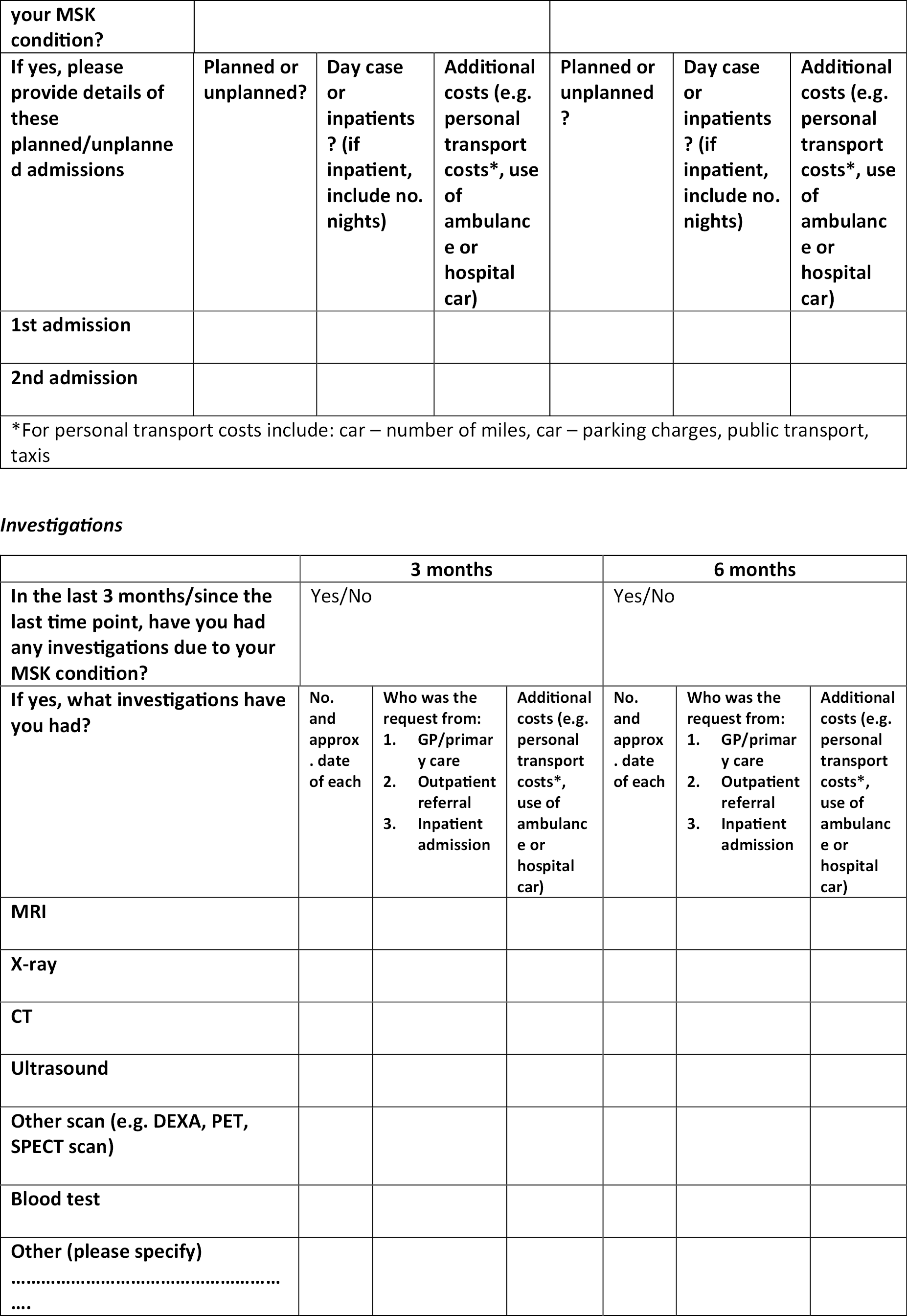
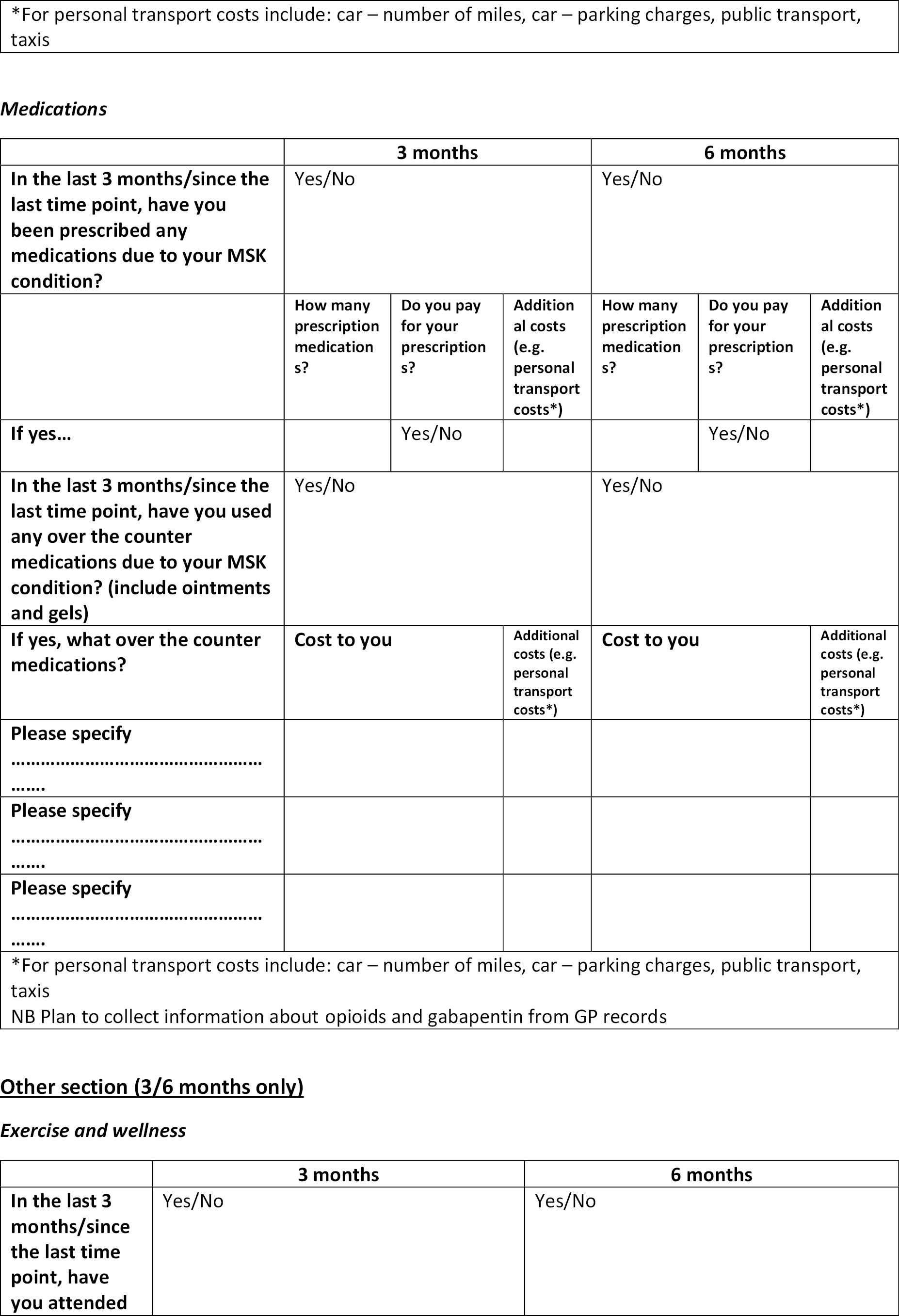
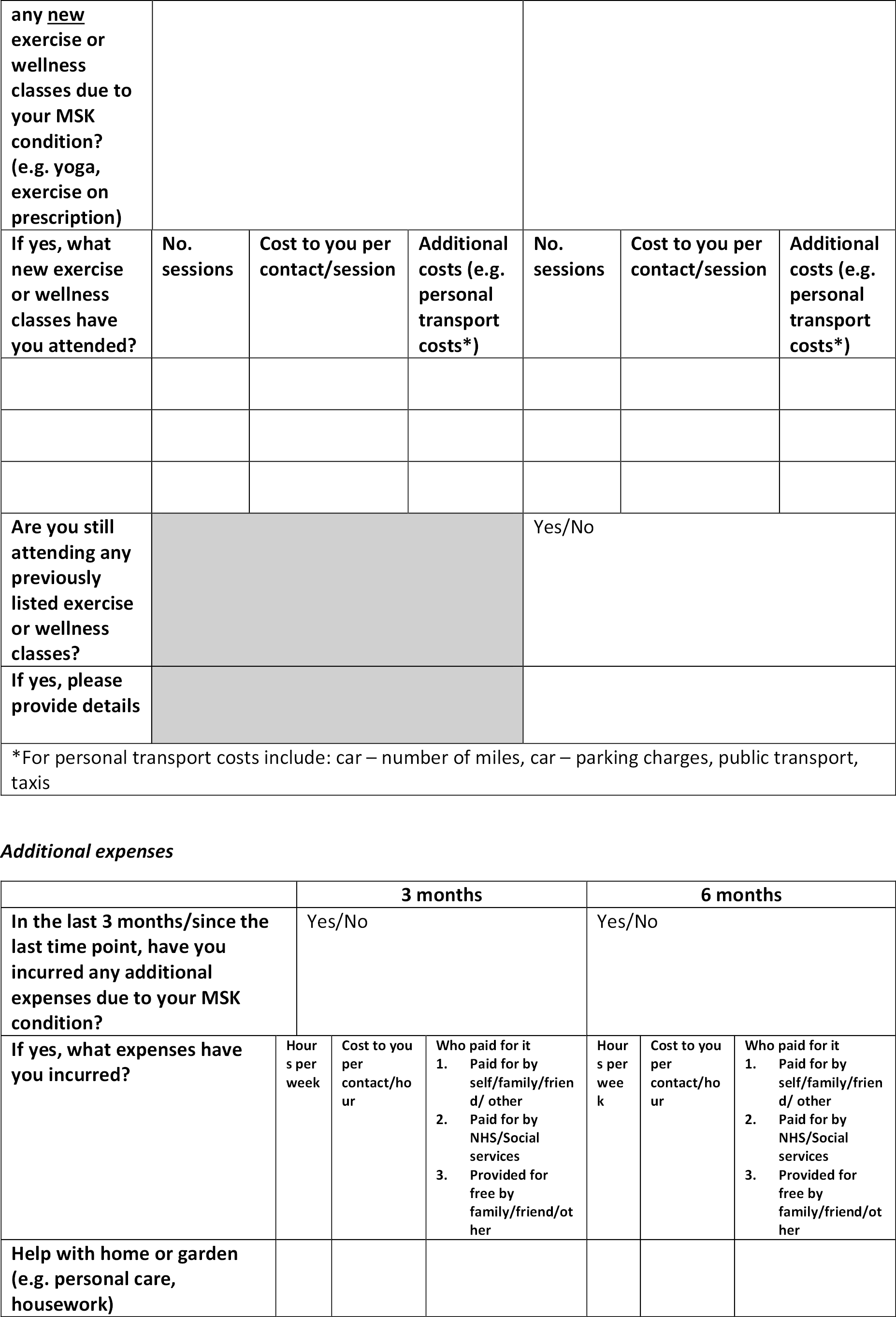
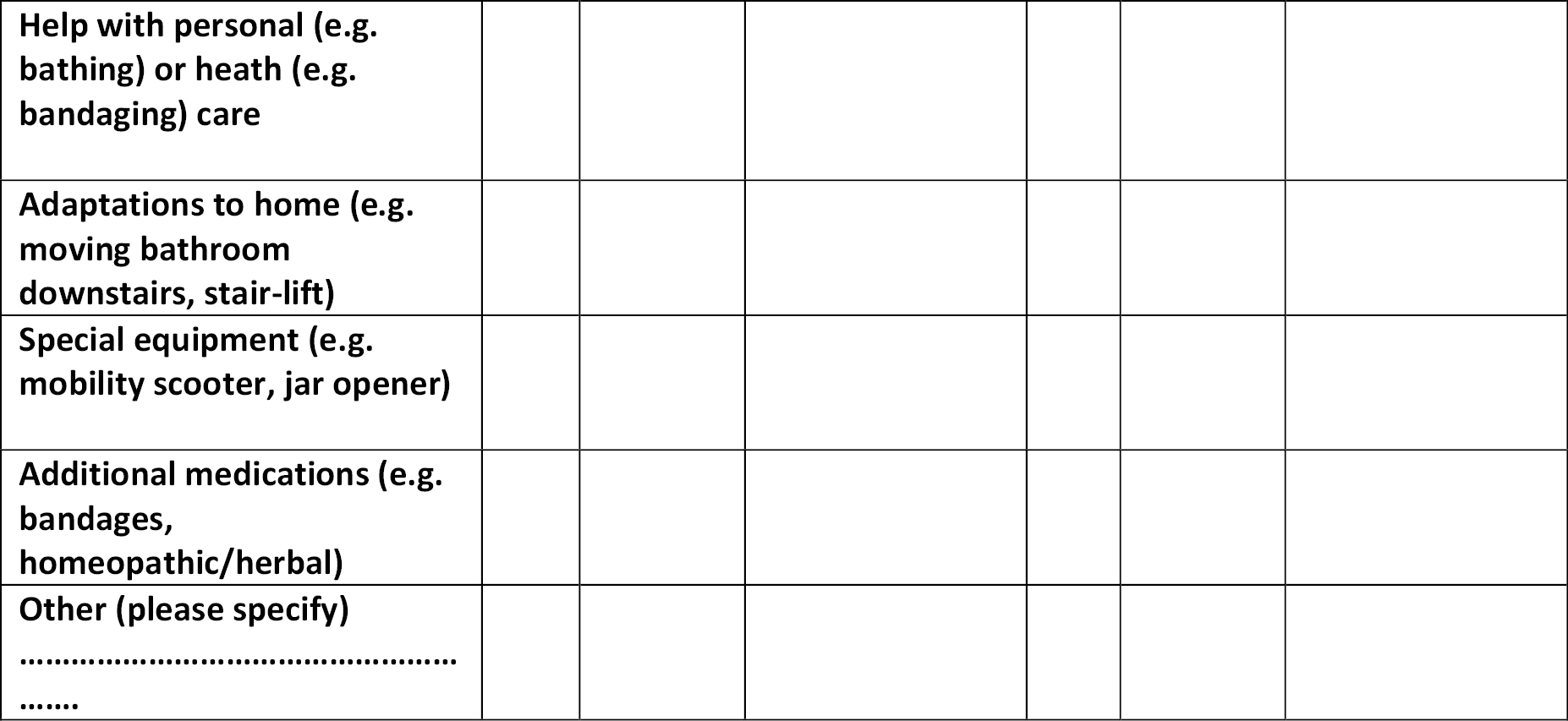
Appendix 5 General Practice Assessment Questionnaire-R2 responses within each domain, by service model
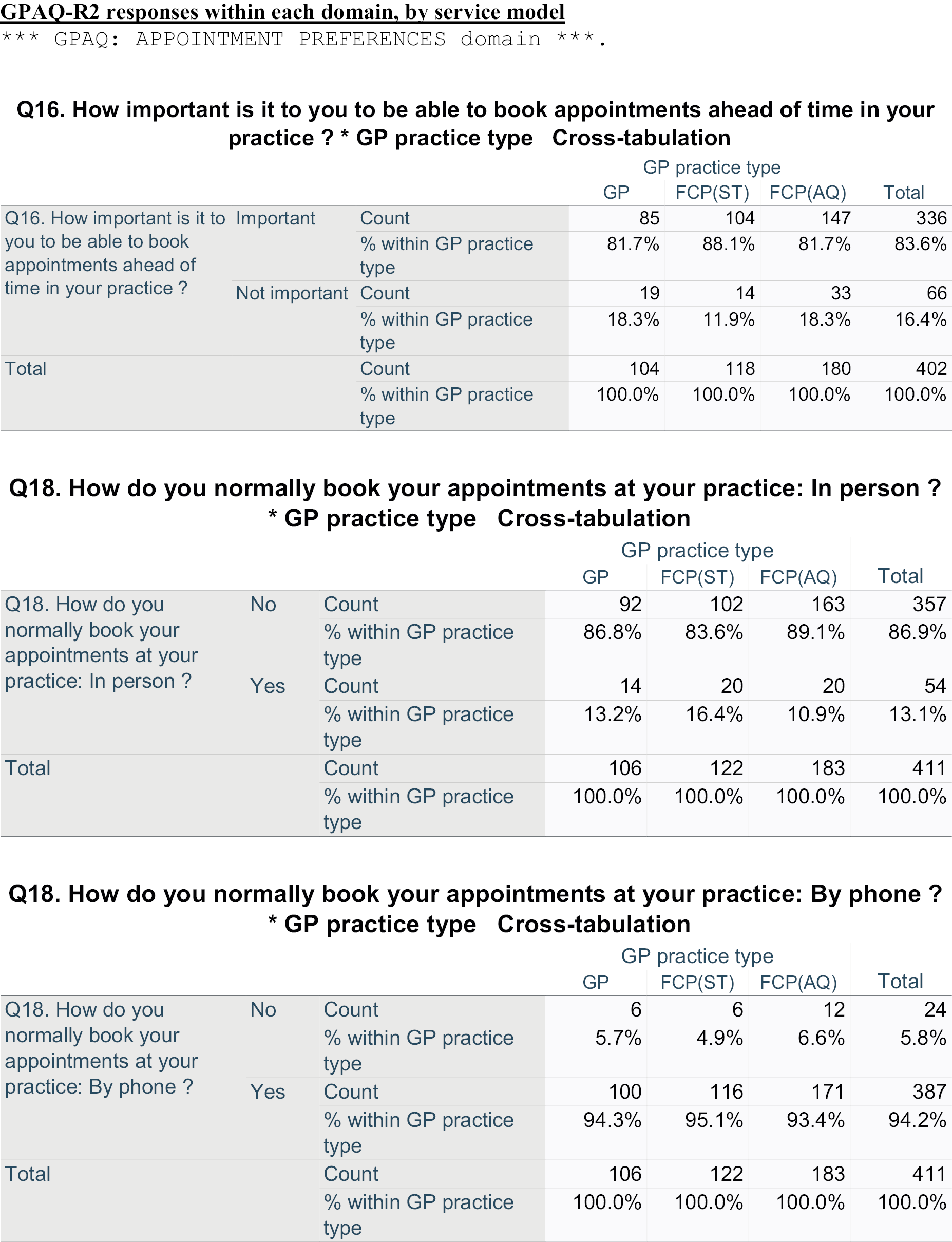
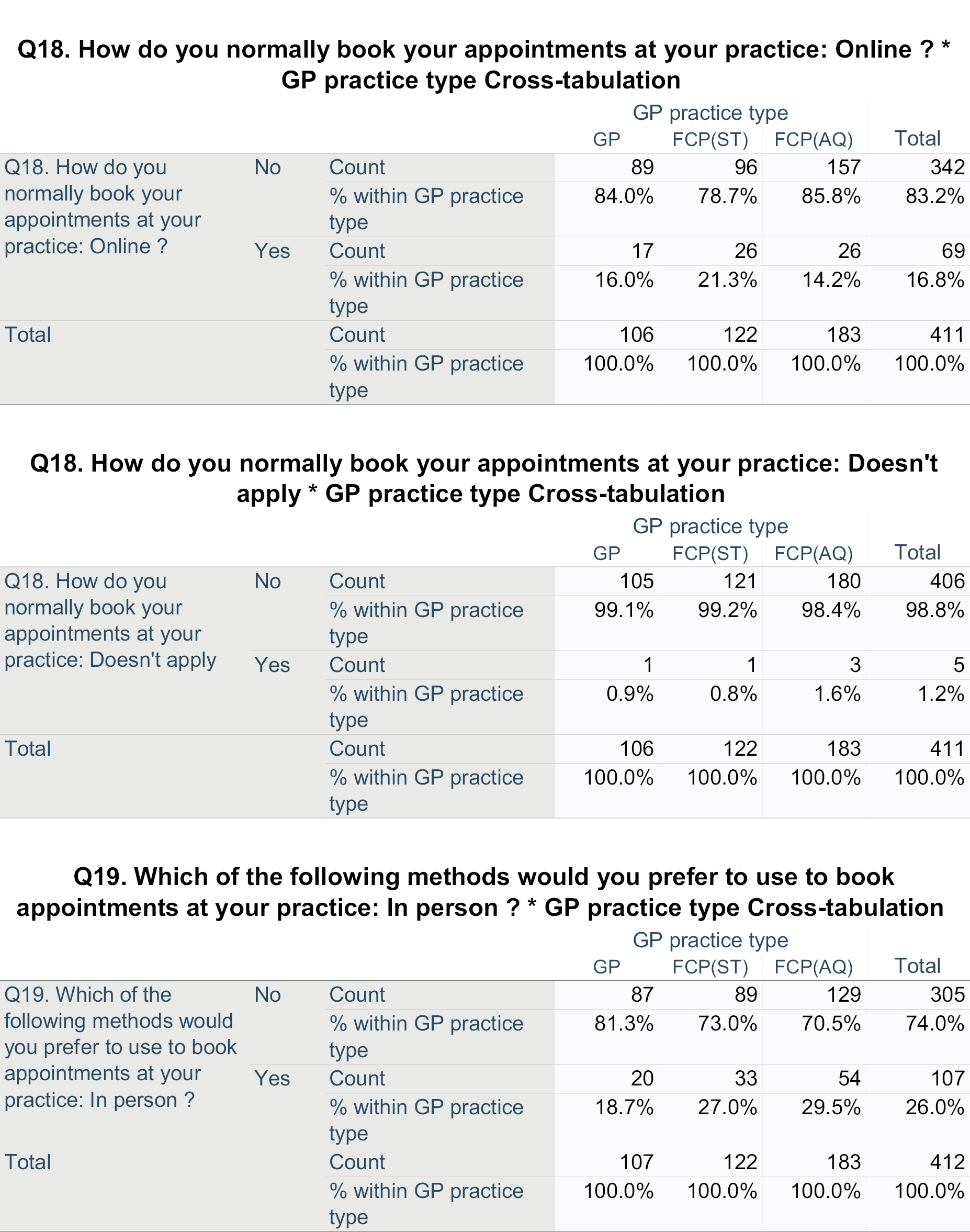
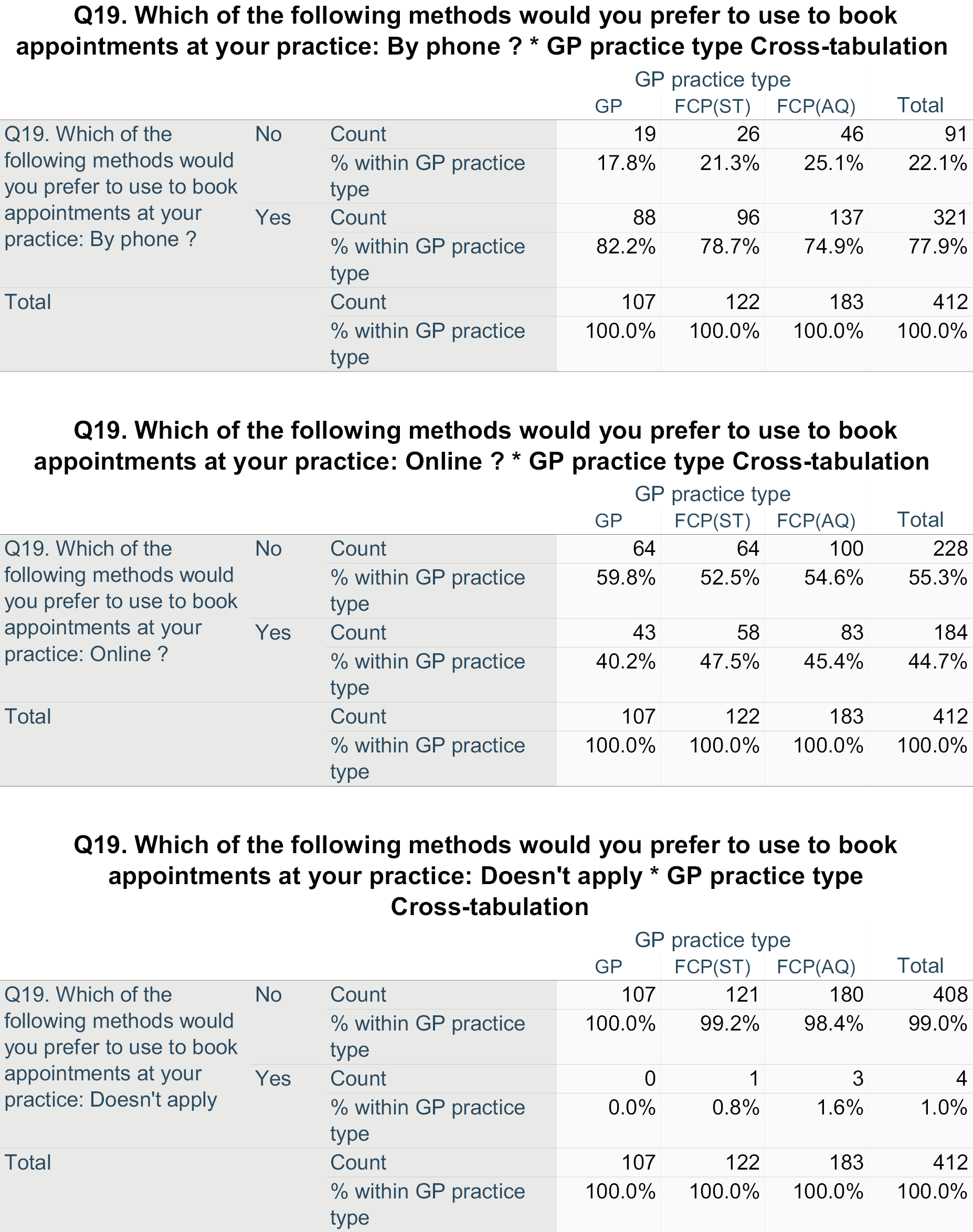
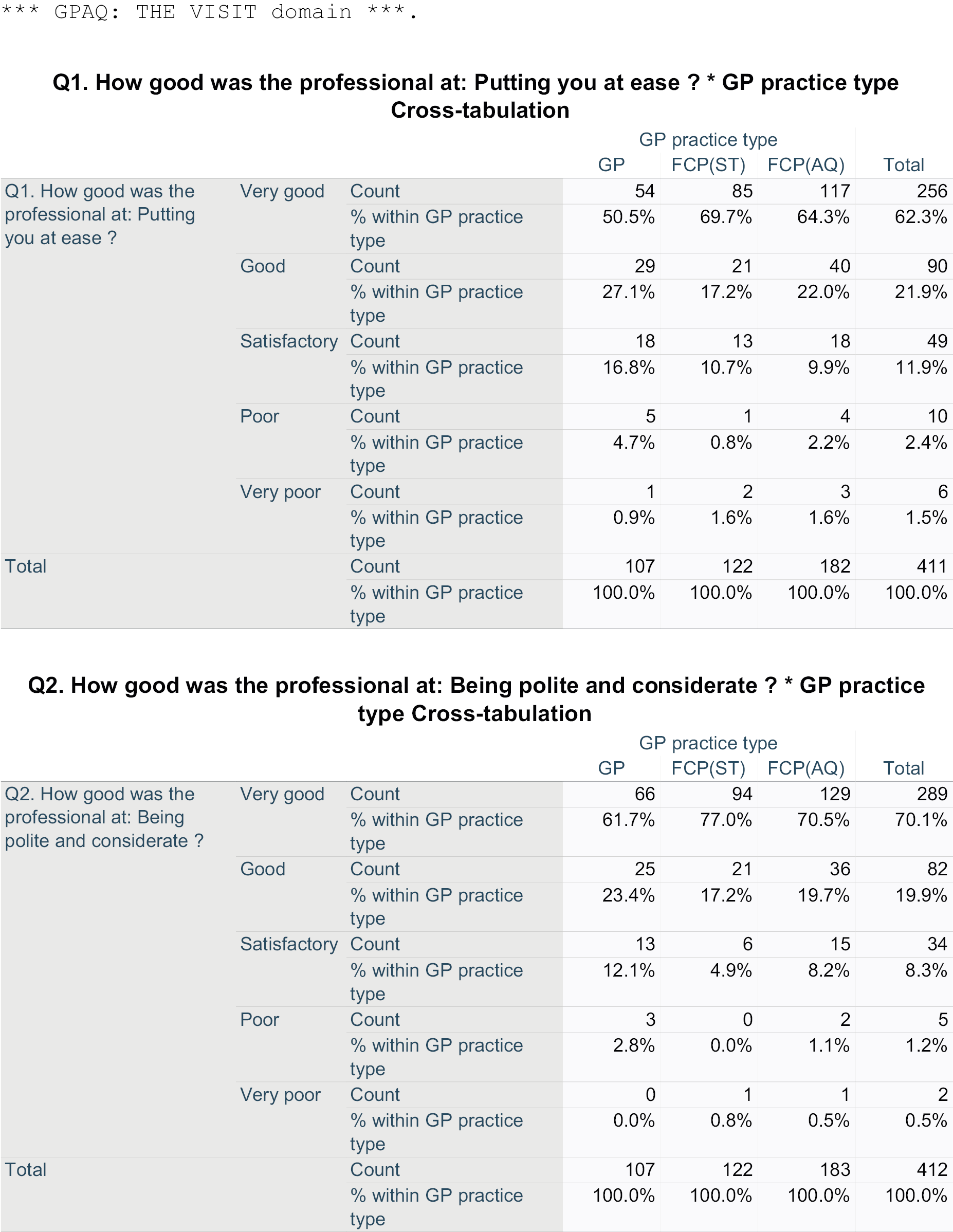
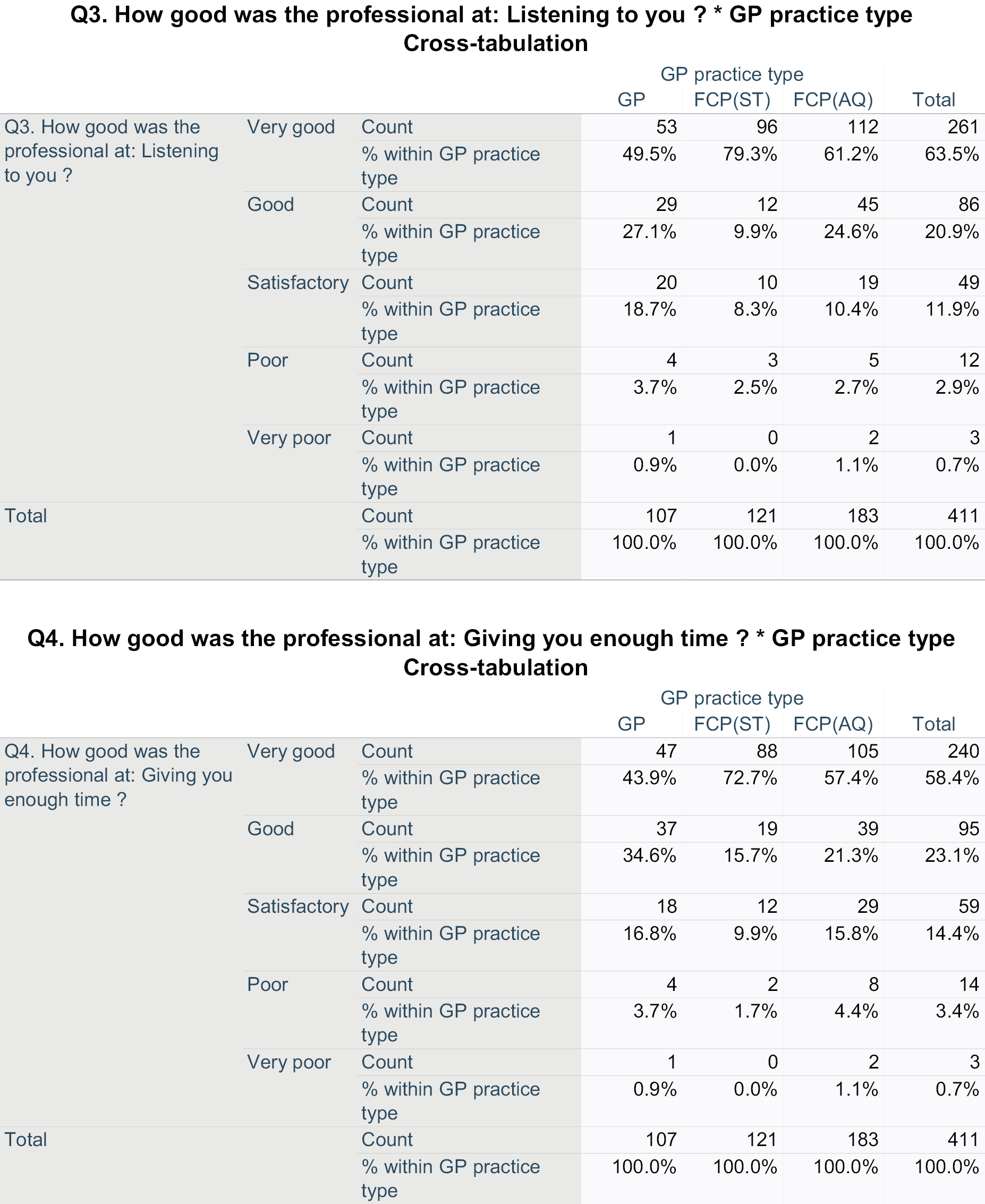
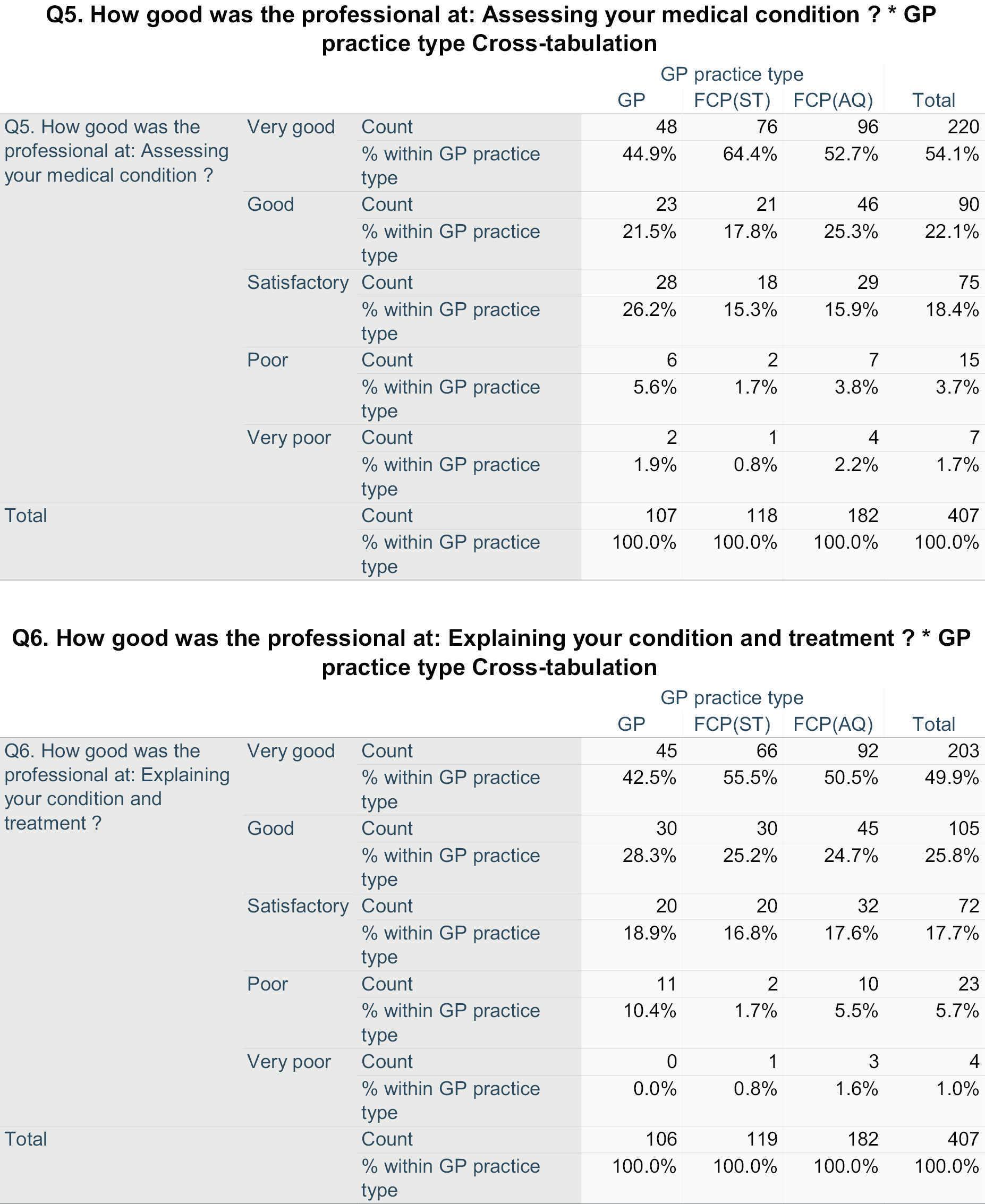
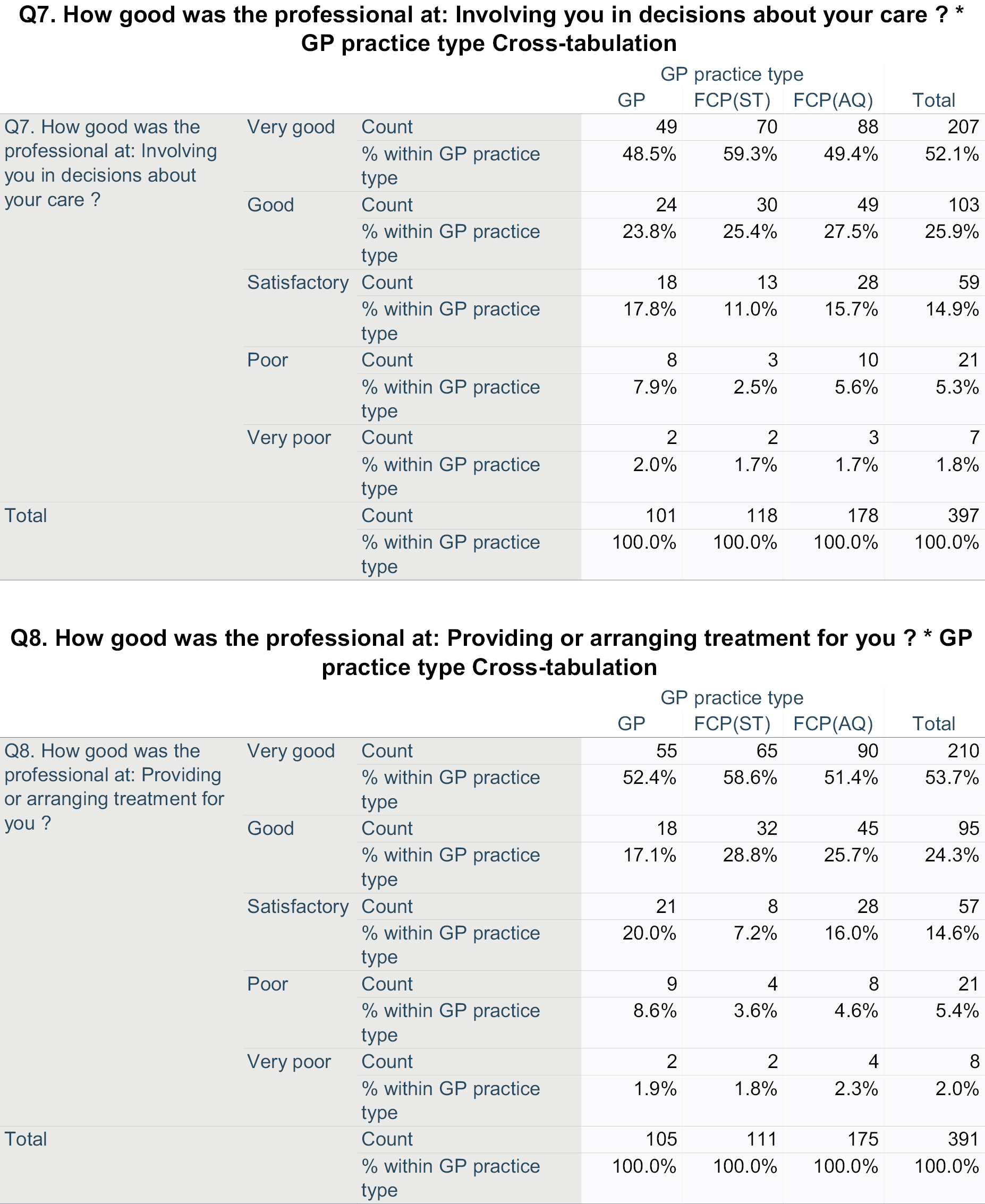
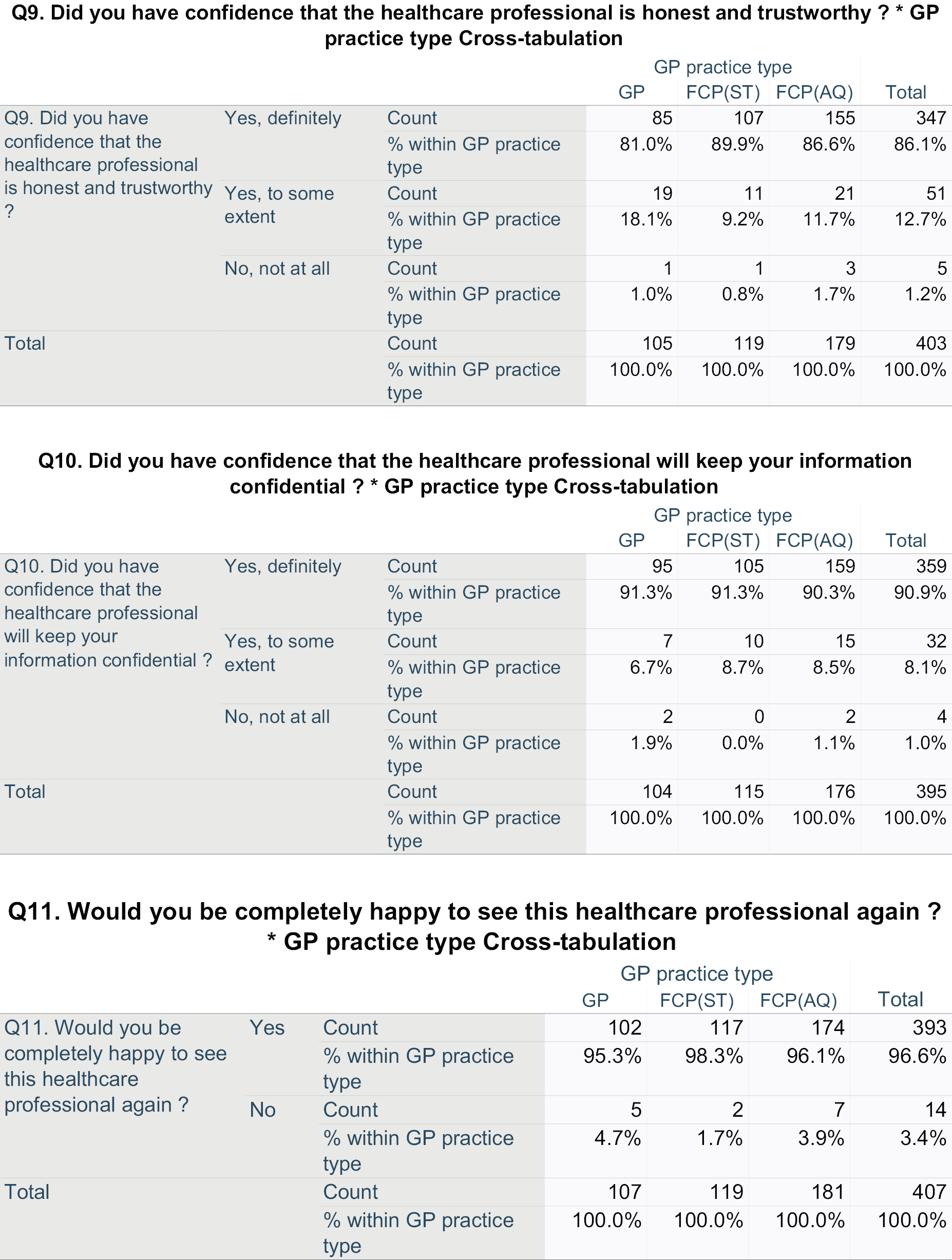

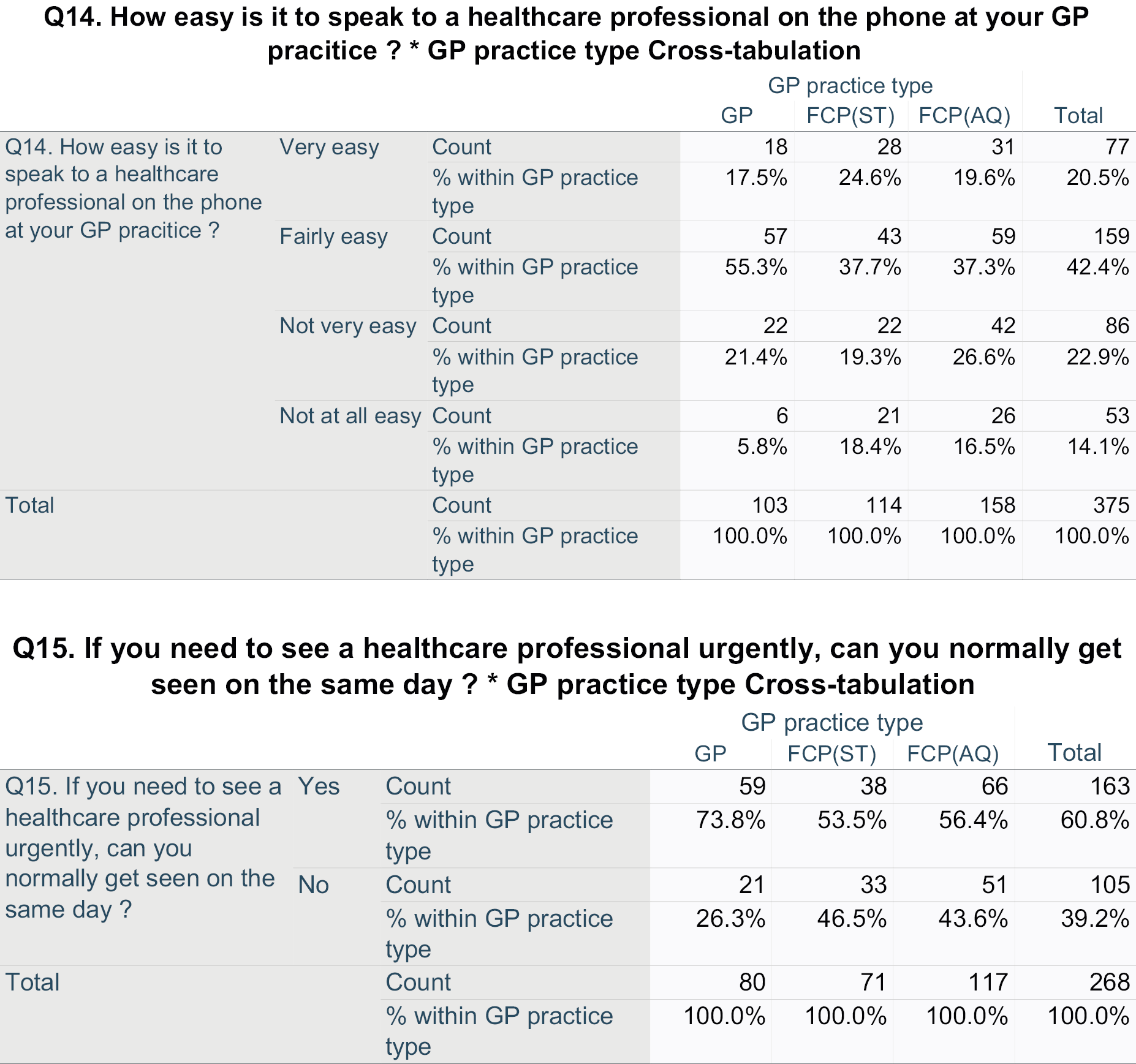
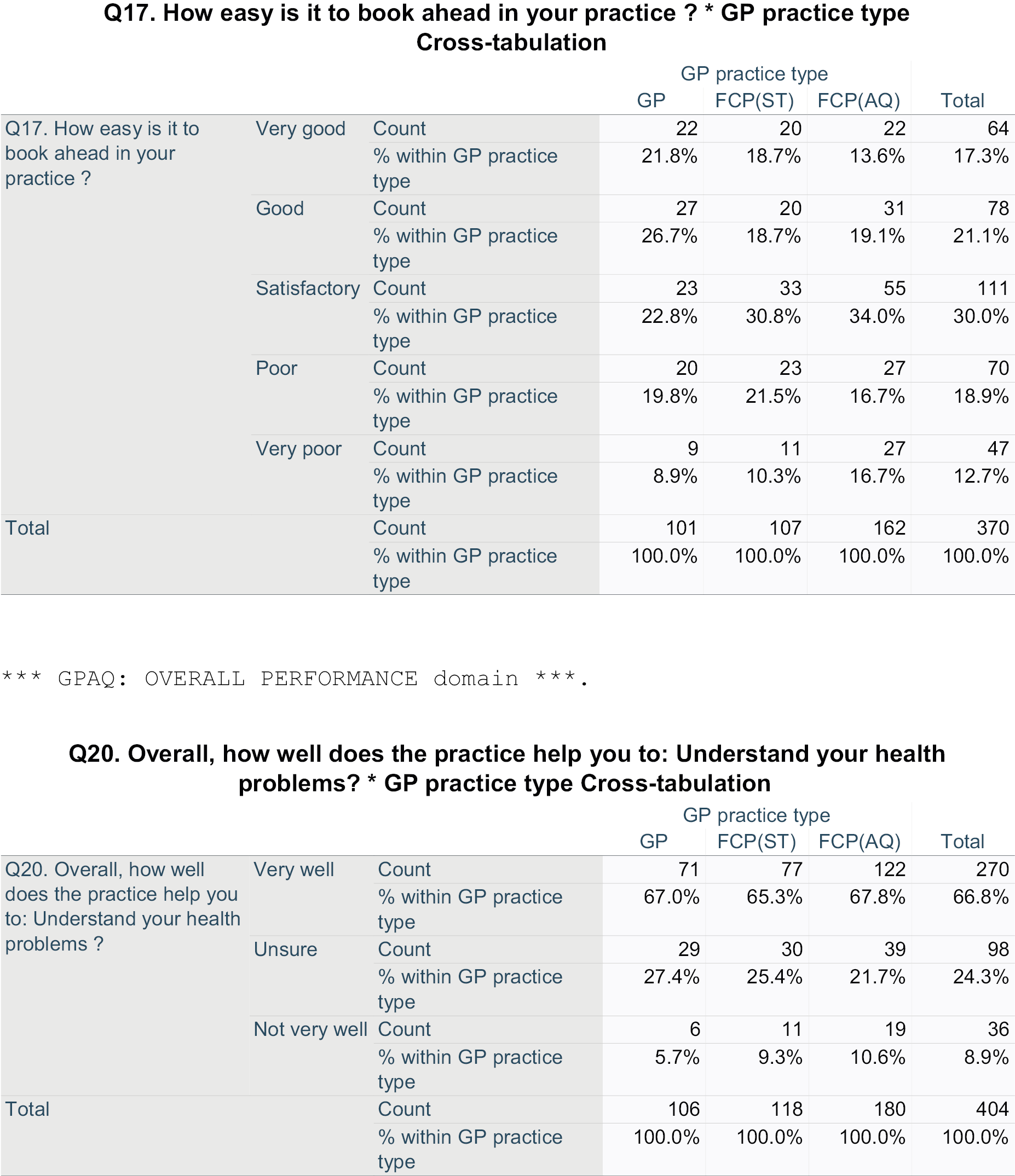
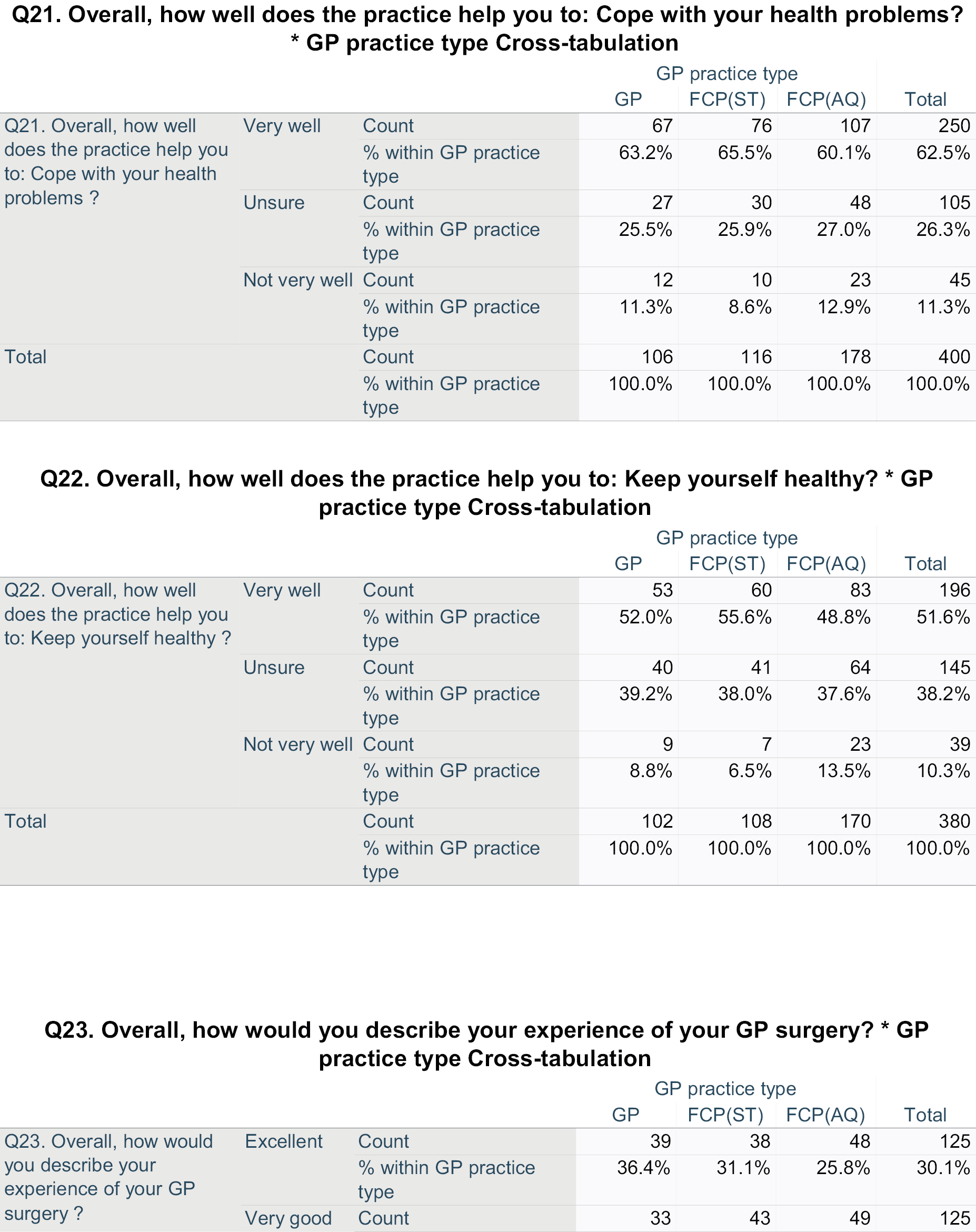
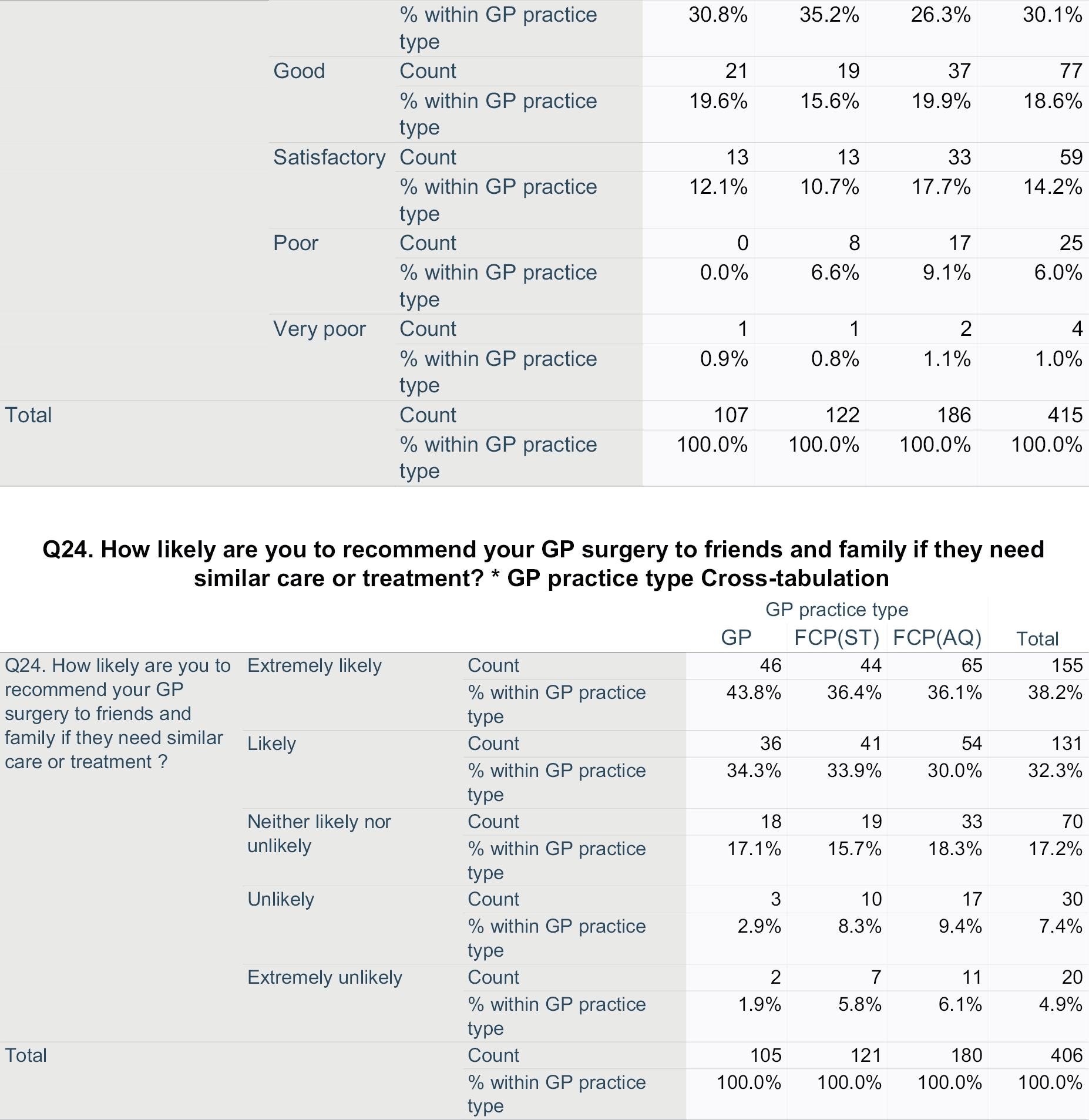
Appendix 6 Breakdown of patient-reported outcome measures and Client Service Receipt Inventory data availability
| Data source: overall data profile | PROM: baseline | CSRI: baseline | PROM: 3 months | CSRI: 3 months | PROM: 6 months | CSRI: 6 months | Participants | |
|---|---|---|---|---|---|---|---|---|
| (n) | (%) | |||||||
| Baseline only | Yes | No | No | No | No | No | 1 | 0.2 |
| Yes | Yes | No | No | No | No | 26 | 6.1 | |
| Baseline and 3 months only | Yes | Yes | Yes | No | No | No | 4 | 0.9 |
| Yes | Yes | No | Yes | No | No | 1 | 0.2 | |
| Yes | Yes | Yes | Yes | No | No | 3 | 0.7 | |
| Baseline and 6 months only | Yes | Yes | No | No | Yes | No | 4 | 0.9 |
| Baseline, 3 and 6 months | Yes | Yes | No | Yes | No | Yes | 5 | 1.2 |
| Yes | Yes | No | Yes | Yes | Yes | 20 | 4.7 | |
| Yes | Yes | Yes | No | Yes | No | 21 | 4.9 | |
| Yes | Yes | Yes | Yes | No | Yes | 3 | 0.7 | |
| Yes | Yes | Yes | Yes | Yes | No | 18 | 4.2 | |
| Yes | Yes | Yes | Yes | Yes | Yes | 320 | 75.1 | |
| Number with corresponding baseline(n) | – | – | N = 369 | N = 370 | N = 383 | N = 348 | Total: 426 | |
| Number of days from corresponding baseline: Mean (SD) | – | – | 85.3 (17.0) | 121.3 (56.1) | 180.3 (26.0) | 196.0 (28.5) | – | |
Appendix 7 Benefits/social support summary statistics
| Benefit received | TOTAL participants (N = 426) | GP participants (N = 110) | FCP(ST) participants (N = 124) | FCP(AQ) participants (N = 192) | Comparison test | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | N | n | % | N | n | % | Chi-square | |
| Income support | 419 | 16 | 3.8 | 107 | 3 | 2.8 | 121 | 4 | 3.3 | 191 | 9 | 4.7 | p = 0.670 |
| State/private pension | 415 | 208 | 50.1 | 106 | 52 | 49.1 | 121 | 66 | 54.5 | 188 | 90 | 47.9 | p = 0.503 |
| Attendance allowance | 419 | 7 | 1.7 | 107 | 4 | 3.7 | 121 | 0 | 0.0 | 191 | 3 | 1.6 | p = 0.088a |
| Statutory sick pay | 419 | 3 | 0.7 | 107 | 0 | 0.0 | 121 | 1 | 0.8 | 191 | 2 | 1.0 | p = 0.581a |
| Disability living allowance | 419 | 18 | 4.3 | 107 | 5 | 4.7 | 121 | 4 | 3.3 | 191 | 9 | 4.7 | p = 0.816 |
| Incapacity benefit | 419 | 4 | 1.0 | 107 | 1 | 0.9 | 121 | 1 | 0.8 | 191 | 2 | 1.0 | p = 0.981 |
| Housing benefit | 419 | 10 | 2.4 | 107 | 2 | 1.9 | 121 | 2 | 1.7 | 191 | 6 | 3.1 | p = 0.647a |
| Absence certificate | 111 | 11 | 9.9 | 34 | 5 | 14.7 | 25 | 4 | 16.0 | 52 | 2 | 3.8 | p = 0.132 |
| Benefit received | TOTAL (N = 370) | GP (N = 94) | FCP(ST) (N = 114) | FCP(AQ) (N = 162) | Comparison test | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Benefit status: baseline → 3 months | Benefit status: baseline → 3 months | Benefit status: baseline → 3 months | Benefit status: baseline → 3 months | ||||||||||||||
| No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | Kruskal–Wallisa | |
| Income support | 0 (0) | 14 (3.8) | 350 (96.2) | 0 (0) | 0 (0) | 2 (2.2) | 91 (97.8) | 0 (0) | 0 (0) | 4 (3.6) | 107 (96.4) | 0 (0) | 0 (0) | 8 (5.0) | 152 (95.0) | 0 (0) | p = 1.000 |
| State/private pension | 0 (0) | 186 (51.2) | 177 (48.8) | 0 (0) | 0 (0) | 47 (51.1) | 45 (48.9) | 0 (0) | 0 (0) | 61 (55.0) | 50 (45.0) | 0 (0) | 0 (0) | 78 (48.8) | 82 (51.2) | 0 (0) | p = 1.000 |
| Attendance allowance | 1 (0.3) | 6 (1.6) | 357 (98.1) | 0 (0) | 1 (1.1) | 3 (3.2) | 89 (95.7) | 0 (0) | 0 (0) | 0 (0) | 111 (100) | 0 (0) | 0 (0) | 3 (1.9) | 157 (98.1) | 0 (0) | p = 0.233 |
| Statutory sick pay | 0 (0) | 3 (0.8) | 361 (99.2) | 0 (0) | 0 (0) | 0 (0) | 93 (100) | 0 (0) | 0 (0) | 1 (0.9) | 110 (99.1) | 0 (0) | 0 (0) | 2 (1.3) | 158 (98.8) | 0 (0) | p = 1.000 |
| Disability living allowance | 0 (0) | 15 (4.1) | 349 (95.9) | 0 (0) | 0 (0) | 3 (3.2) | 90 (96.8) | 0 (0) | 0 (0) | 4 (3.6) | 107 (96.4) | 0 (0) | 0 (0) | 8 (5.0) | 152 (95.0) | 0 (0) | p = 1.000 |
| Incapacity benefit | 0 (0) | 2 (0.5) | 362 (99.5) | 0 (0) | 0 (0) | 1 (1.1) | 92 (98.9) | 0 (0) | 0 (0) | 0 (0) | 111 (100) | 0 (0) | 0 (0) | 1 (0.6) | 159 (99.4) | 0 (0) | p = 1.000 |
| Housing benefit | 0 (0) | 7 (1.9) | 357 (98.1) | 0 (0) | 0 (0) | 1 (1.1) | 92 (98.9) | 0 (0) | 0 (0) | 2 (1.8) | 109 (98.2) | 0 (0) | 0 (0) | 4 (2.5) | 156 (97.5) | 0 (0) | p = 1.000 |
| Benefit received | TOTAL (n = 348) | GP (n = 90) | FCP(ST) (n = 107) | FCP(AQ) (n = 151) | Comparison test | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Benefit status: baseline → 6 months | Benefit status: baseline → 6 months | Benefit status: baseline → 6 months | Benefit status: baseline → 6 months | ||||||||||||||
| No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | No → Yes | Yes → Yes | No → No | Yes → No | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | Kruskal–Wallisa | |
| Income support | 1 (0.3) | 14 (4.1) | 330 (95.7) | 0 (0) | 0 (0) | 2 (2.2) | 88 (97.8) | 0 (0) | 0 (0) | 4 (3.8) | 100 (96.2) | 0 (0) | 1 (0.7) | 8 (5.3) | 142 (94.0) | 0 (0) | p = 0.526 |
| State/private pension | 0 (0) | 182 (52.8) | 163 (47.2) | 0 (0) | 0 (0) | 46 (51.1) | 44 (48.9) | 0 (0) | 0 (0) | 59 (56.7) | 45 (43.3) | 0 (0) | 0 (0) | 77 (51.0) | 74 (49.0) | 0 (0) | p = 1.000 |
| Attendance allowance | 0 (0) | 7 (2.0) | 338 (98.0) | 0 (0) | 0 (0) | 4 (4.4) | 86 (95.6) | 0 (0) | 0 (0) | 0 (0) | 104 (100) | 0 (0) | 0 (0) | 3 (2.0) | 148 (98.0) | 0 (0) | p = 1.000 |
| Statutory sick pay | 0 (0) | 2 (0.6) | 342 (99.1) | 0 (0) | 0 (0) | 0 (0) | 90 (100) | 0 (0) | 0 (0) | 1 (1.0) | 103 (99.0) | 0 (0) | 0 (0) | 1 (0.7) | 149 (98.7) | 0 (0) | p = 0.526 |
| Disability living allowance | 0 (0) | 15 (4.3) | 330 (95.7) | 0 (0) | 0 (0) | 3 (3.3) | 87 (96.7) | 0 (0) | 0 (0) | 4 (3.8) | 100 (96.2) | 0 (0) | 0 (0) | 8 (5.3) | 143 (94.7) | 0 (0) | p = 1.000 |
| Incapacity benefit | 1 (0.3) | 2 (0.6) | 342 (99.1) | 0 (0) | 1 (1.1) | 1 (1.1) | 88 (97.8) | 0 (0) | 0 (0) | 0 (0) | 104 (100) | 0 (0) | 0 (0) | 1 (0.7) | 150 (99.3) | 0 (0) | p = 0.243 |
| Housing benefit | 0 (0) | 7 (2.0) | 338 (98.0) | 0 (0) | 0 (0) | 1 (1.1) | 89 (98.9) | 0 (0 | 0 (0) | 2 (1.9) | 102 (98.1) | 0 (0) | 0 (0) | 4 (2.6) | 147 (97.4) | 0 (0%) | p = 1.000 |
Appendix 8 Regression models for 36-Item Short-Form survey physical component summary
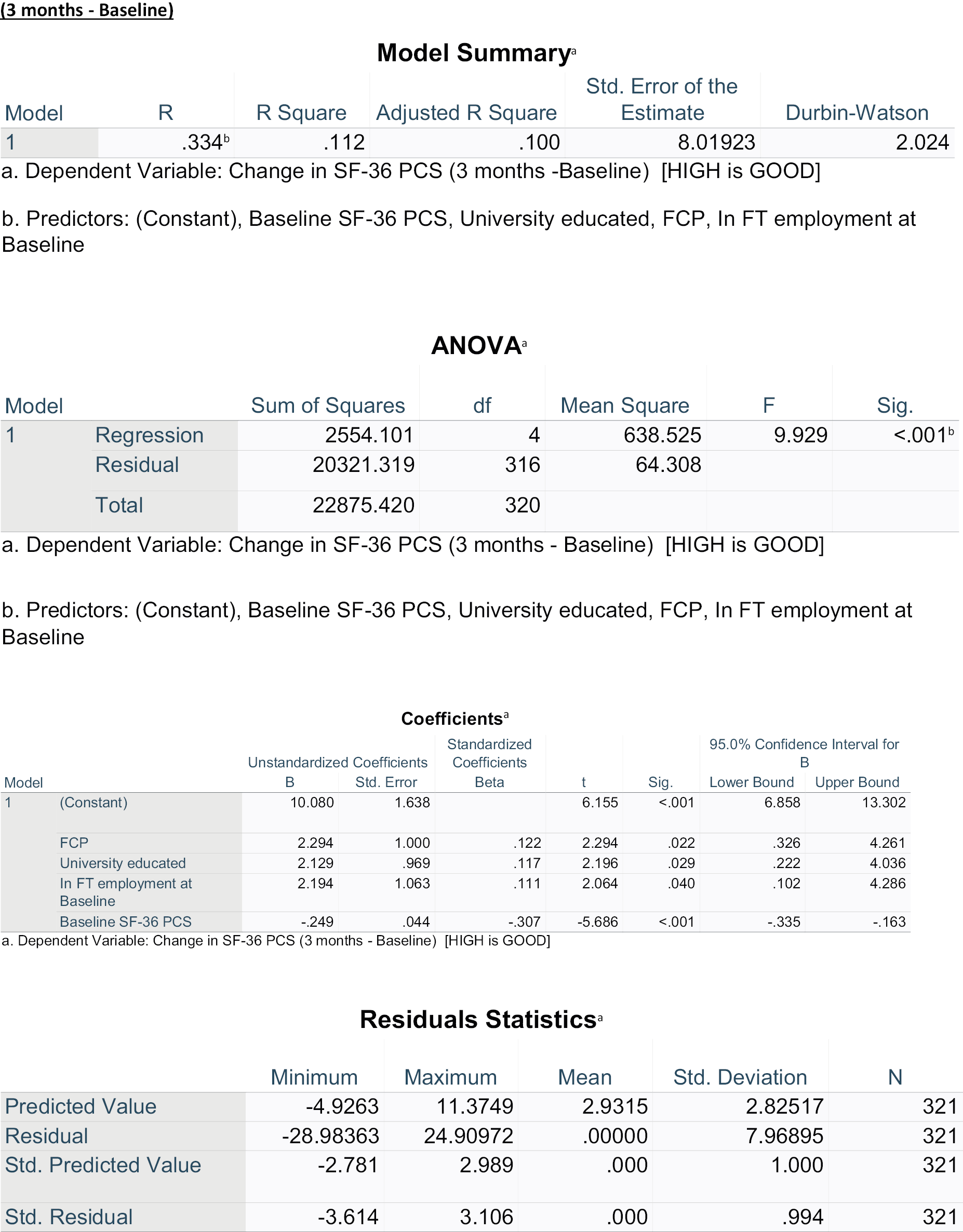
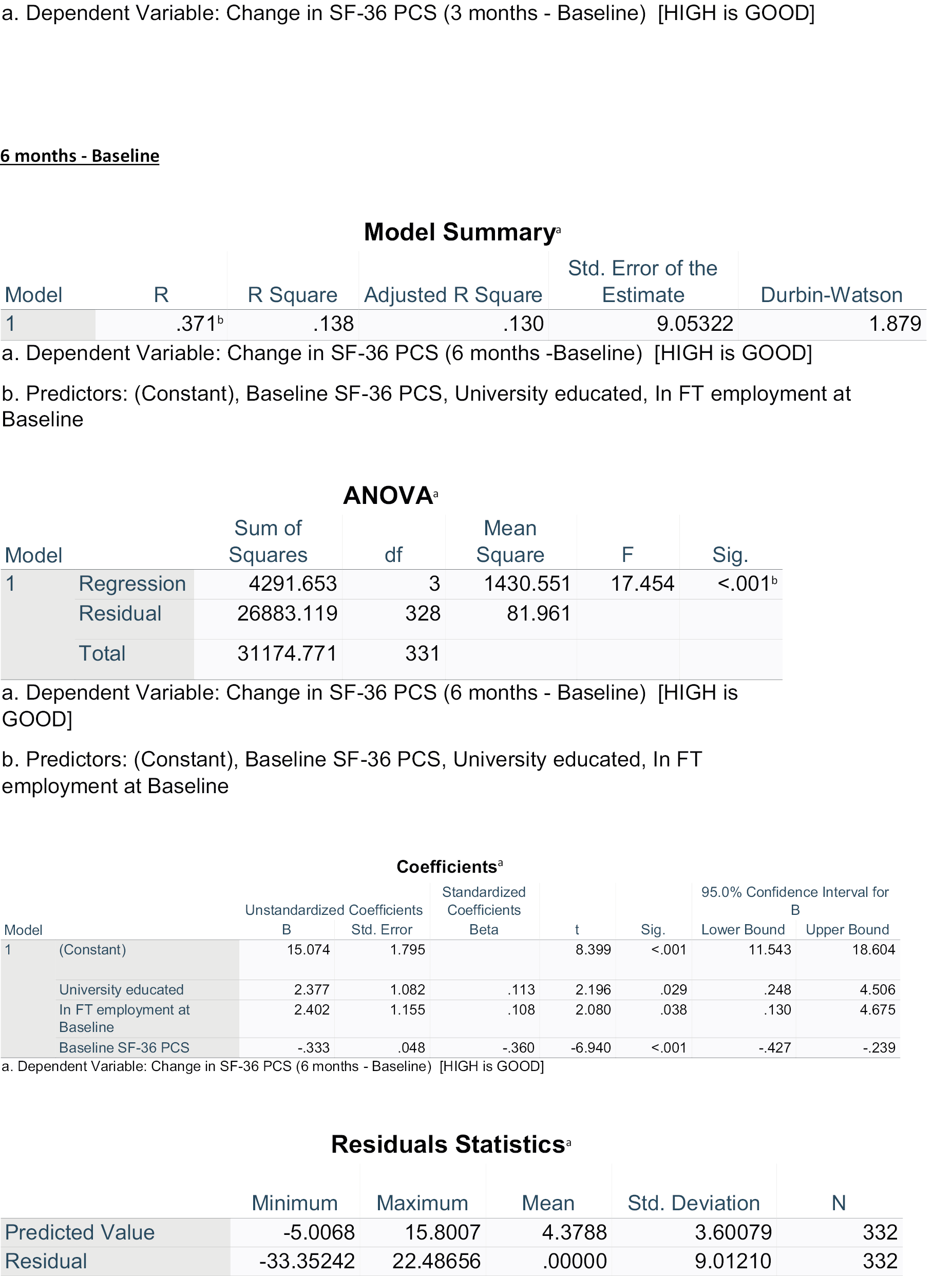
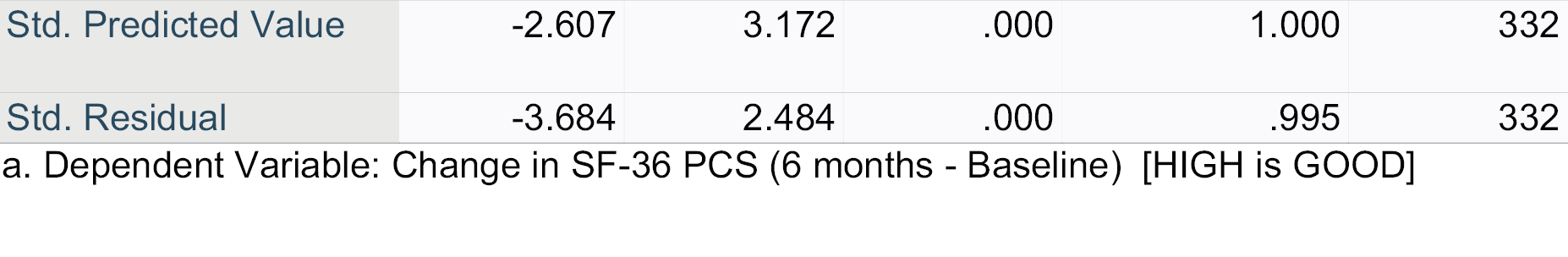
Appendix 9 Prescription medications
Classification of drug categories
| Analgesics (non- opioid) | NSAIDs | Steroids | Tricyclic antidepressant/pain | (Benzodiazipines) muscle relaxant | Anti-epileptic (neuromodulator) | Vitamins and minerals (bone health) | Proton pump inhibitors | Other antidepressants | Bisphosphonates | Xanthine oxidase inhibitors (gout) |
|---|---|---|---|---|---|---|---|---|---|---|
| Paracetamol | Voltarol® (Haleon, Weybridge, UK) | Prednisolone | Amitriptyline | Diazepam | Pregabalin | Vitamin D | Omeprazole | Citalopram | Alendronic acid | Allopurinol |
| Ibuprofen | Gabapentin | Calcium carbonate | Mirtazapine | Febuxostat | ||||||
| Naproxen | ||||||||||
| Diclofenac | ||||||||||
| Celebrex® (Upjohn, Hatfield, UK) |
Classification of over-the-counter medications
| Oral analgesia | Oral NSAIDs | Topical analgesia | Topical NSAIDs | Complementary and alternative medicine and dietary supplements |
|---|---|---|---|---|
| Paracetamol | Ibuprofen | Heat rubs and gels | Voltarol cream | Glucosamine/chondroitin |
| Co-codamol | Nurofen® (Reckitt Benckiser Healthcare, Slough, UK) | Deep Relief® gel (Mentholatum, East Kilbride, UK) | Voltarol gel | Turmeric tablets |
| Panadol | Anti-inflammatories (unnamed by patient) | Deep Heat® (Mentholatum, East Kilbride, UK) gel/heat gel | Anti-inflammatory gel (unnamed by patient) | Glucosamine gold gel |
| Solpadeine | Cuprofen® (Reckitt Benckiser Healthcare, Slough, UK) | Ibuprofen gel | Green lip mussel | |
| Zapain | Diclofenac | Movelat® cream (Thornton & Ross, Huddersfield, UK) | Iodex® (Haleon, Weybridge, UK) cream | |
| Ibuleve gel | Tiger Balm® (Haw Par Healthcare, Singapore) |
Appendix 10 Unit costs
The initial consultation for musculoskeletal condition will assumed to be face to face with either a GP or a FCP(ST) or a FCP(AQ) (depending on group).
We will assume Agenda for Change band 7 and 20 minutes face-to-face consultations with FCP(ST) and FCP(AQ) (based on CSP recommendations and the majority of sites within the study). We will also assume face-to-face consultations with the GP; the national unit costs will be used for this (i.e. 9.22 minutes, as below). A sensitivity analysis will use band 8a for FCP(AQ).
Service use related to the musculoskeletal condition beyond the initial consultation is drawn from self-reported data collected through the CSRI,54 customised for the project (see Appendix 3). It was originally intended to use GP records, but this proved problematic. In addition, there were doubts about coding these records and identifying the interventions that participants had received.
Participants reported use of a limited number of NHS health services; with the exception of GP and physiotherapists, the numbers of reported consultations were very low. Nationally validated unit costs primary and community care86 and hospital care87 were used to calculate total costs of health services used for the musculoskeletal condition at an individual level. The assumptions underlying this calculation are summarised in the table below.
| Service | Source: | Cost/contact £ | ||
|---|---|---|---|---|
| Healtha (primary and community) | GP surgery face-to-face | Jones and Burns, 2021, Section II, community-based healthcare staff | Chapter 10.3b surgery consultation 9.22 minutes | 39 |
| GP home visit | Assume 3 × a surgery consultation | 117 | ||
| GP telephone | Chapter 10.5 telephone triage £15.52 in 2013, uplifted using NHS cost inflation index (chapter 15.3), rounded | 19 | ||
| GP other | None (all reallocated to other categories) | |||
| Practice nurse | Chapter 10.2 £42/working hour, assumed 20-minute consultation | 14 | ||
| Practice nurse home visit | Assume 3 × a surgery consultation | 52 | ||
| Physiotherapist | Chapter 9, scientific and professional, band 7, £66/working hour, assumed 20-minute consultation (band 8a for sensitivity analysis: £75/working hour) | 22 [£25] | ||
| Physiotherapist home visit | Assume 3 × a surgery consultation | 66 | ||
| Orthotist (and podiatrist from ‘other’) | Chapter 9, scientific and professional, band 6 (as specialist podiatrist), £54/working hour, assumed 20-minute consultation | 18 | ||
| Outpatient | Physiotherapist | National Schedule of NHS Costs, FY 2020–21 | One to one adult currency code A08A1 | 104 |
| Podiatrist | Specialist care currency code A09D | 123 | ||
| Occupational therapist | One-to-one adult currency code A06A1 | 115 | ||
| Pain clinic/service/team | Consultant-led face-to-face first visit currency code 191 | 362 | ||
| Online pain group | Assume physiotherapist and 8 per group | 104/8 = 13 | ||
| Rheumatologist | Consultant-led face-to-face first visit currency code 410 | 316 | ||
| Orthopaedist | ||||
| Neurosurgeon | Consultant-led face-to-face first visit currency code 150 | 335 | ||
| Dr/consultant not specified | Consultant-led face-to-face first visit currency code 100 (general surgery) | 237 | ||
| Consultant for steroid injection | As orthopaedist | 316 | ||
| Musculoskeletal phone call | Assume orthopaedist × 0.25 | 39 | ||
| Accident and emergency department | AE index sheet | 297 | ||
| Inpatientb | Total hip replacement | Assume major non-trauma adult HRG elective procedure HN13D | 15,832 | |
| Total knee replacement | Assume major non-trauma adult HRG elective procedure HN23B | 11,450 | ||
| Drainage of fluid from knee | Assume minimal non-trauma knee procedure elective procedure HN26A | 1393 | ||
| Shoulder procedure | Assume intermediate non-trauma adult elective procedure HN54B | 5858 | ||
| Minor wrist surgery | Assume Minor non-trauma hand surgery elective procedure HN45B | 2779 | ||
| Tests | Magnetic resonance imaging | Outpatient IMAGOP | 311 | |
| X-ray | Diagnostic imaging 812 | 30 | ||
| computed tomography | ||||
| Ultrasound | ||||
| Other scan | ||||
| Blood test | Haematology, phlebotomy DAPS05 DAPS08 | 9 | ||
| Electromyography | Outpatient procedure neurology AA32Z | 530 | ||
| Colonoscopy (to confirm musculoskeletal cause) | Elective inpatient diagnostic colonoscopy FE32Z | 1527 | ||
Private costs: Costs of over-the-counter medications and private use of physiotherapy, osteopathy, chiropractic and complementary therapy will be based on expenditures reported by participants.
Ibuprofen and paracetamol – costs vary (3p to 20p) depending on type (e.g. capsule, tablet, liquid) and dosage (mgs). Assume 10p per dose.
Ibuprofen gel – £6 (40 gm max strength)
Deep Heat – 50 ml roll-on £5.
List of abbreviations
- ARRS
- Additional Roles Reimbursement Scheme
- CMO
- context, mechanism, outcome
- CSP
- Chartered Society of Physiotherapy
- CSRI
- Client Service Receipt Inventory
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- FCP(AQ)
- first-contact physiotherapist with additional qualifications
- FCP(ST)
- first-contact physiotherapy standard provision
- FTE
- full-time equivalent
- GP
- general practice/practitioner
- GPAQ
- General Practice Assessment Questionnaire
- HRA
- Health Research Authority
- IT
- information technology
- MDT
- multidisciplinary team
- MSKD
- musculoskeletal disorder
- NIHR
- National Institute for Health and Care Research
- NSAID
- non-steroidal anti-inflammatory drug
- OTC
- over the counter
- PCN
- primary care network
- PPIE
- patient and public involvement and engagement
- PREOS-PC
- Patient Reported Experiences and Outcomes of Safety in Primary Care
- PROM
- patient-reported outcome measure
- SF-36
- Short Form questionnaire-36 items
- VAS
- visual analogue scale
- WP
- work package
