Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR135079. The contractual start date was in July 2021. The final report began editorial review in January 2022 and was accepted for publication in September 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Cantrell et al. This work was produced by Cantrell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 et al.
Chapter 1 Background and introduction
Rationale
Suicide prevention is a key priority of the NHS Long Term Plan (NHS, 2019). 1 In the most recently available figures (from 2020) a total of 5224 deaths by suicide were registered in England and Wales (ONS, 2020). 2 The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) annual report indicates that over a quarter of people who die by suicide have been in contact with mental health services within the last year (NCISH, 2021). 3 Suicide and self-harm represent the most acute forms of crises for children and young people.
Predicting and managing risk is an important element of mental healthcare planning in the UK. In mental health, risk is constructed as a potential negative outcome or behaviour arising from the unwanted actions of people using services. 4 This results in two main concerns: the risk the person presents to themselves in the form of suicide or vulnerability and the risk the person presents to others. 4 As mentioned above, the first of these risks is common. The risk of harm to others is rarer but adds substantial concerns for health staff and for the mental health system.
Throughout this report a distinction is made between the risk-assessment process and the tools that are used within the process. The risk-assessment process is used in response to many drivers and to meet many demands; these vary from offering a person-centred care approach through to seeking to predict the risk of future harm to self or others through risk screening. Some of these responses are considered to be appropriate and others are not. As a consequence, two broad types of tools can be identified; those that are designed with the intent of predicting risk, that is risk screening, specifically self-harm and suicide, and those that are intended for broader use in facilitating the risk-assessment process. Both of these approaches are explored in this report.
Approaches to risk assessment
Within the wider context of risk assessment, three main approaches have been identified: unstructured clinical judgement (based on professional gut feeling), actuarial (using validated tools to measure risk) and structured clinical judgement (a combination of the former two). 5 The current risk-averse climate, common to many areas of protection and safeguarding, has seen increased use of actuarial approaches to risk management. 6 Actuarial approaches utilise statistical techniques to generate risk predictors along with checklist approaches. Actuarial approaches seek to make it easier to demonstrate adherence with procedures and may simplify completion making the process little more than a tick-box exercise. Organisationally, checklists and scales facilitate standardisation of procedures and of documentation, particularly when included within integrated electronic records.
‘… Those advocating for their use suggest that they enrich assessment by providing “an anchor against the force of bias”,7 greater inter-rater reliability and scientific validity, greater transparency around decisions taken as well as providing documentation for review, audit and analysis should a negative event occur’. 5,8
Conversely, clinical approaches involve an assessment derived in part from the medical and mental health disciplines. Clinical approaches include the structured clinical approach, which uses prompts or checklists to guide and subsequently interpret the risk assessment. 9 Outside of a clinical context, this expertise-based approach may alternatively be labelled structured professional judgement. 10 Aside from these three reference points, additional terms are used to describe certain features or characteristics of approaches, either individually or collectively. Assessments that employ a theory-informed approach assume that, because the subsequent assessment is based on theory, it can prove superior to approaches that are simply determined by institutional requirements and the procedural structure of assessment guidelines. 11 Practitioners refer to a formulation process;12 in such circumstances they employ a systematic approach that identifies all factors critical to a specific risk assessment and considers the purpose of the assessment, scope and depth of the necessary analysis, analytical approach, available resources and outcomes, and overall risk-management goal. Others contrast a problem-orientated approach with a medical model approach. 13 Other descriptions may focus more on the intended aim of the assessment, as, for example, with the collaborative approach or therapeutic approaches. Approaches may reference the content, as in multifaceted approach or the overarching philosophy of care as in the interpersonal approach. Finally, increasing attention is being directed at a whole-system approach, recognising the complexity of the included interventions and of the context in which they are delivered. These diverse approaches can similarly be observed within the specific context of risk assessment for self-harm and suicide.
Although risk assessment remains contested within mental health care, efforts continue to focus on developing actuarial mechanisms for identifying and predicting future risk behaviours. The predictive accuracy of risk screening in mental health care falls short of the performance of commonly accepted tools from other branches of health care. 4 In the light of reviews that repeatedly document significant limitations of such scales, with consistent recommendations that scales are not used for routine clinical practice, there is a need to consider whether such scales truly meet the best interests of the individual child or adolescent mental health patient. 4
NICE guidance
NICE guidance describes risk assessment as:
a detailed clinical assessment that includes the evaluation of a wide range of biological, social and psychological factors that are relevant to the individual and, in the judgement of the healthcare professional conducting the assessment, relevant to future risks, including suicide and self-harm. 14
Risk assessments may be used as part of a broader assessment to inform treatment planning but have been frequently misused to guide clinician predictions of future behaviour. 15,16
Following submission of this review an update to the 2011 NICE guidance entitled Self harm: assessment, management and preventing recurrence [NG225] was published. This guidance is intended to fully update both: Self-harm in over 8s: short-term management and prevention of recurrence (CG16) and Self-harm in over 8s: long-term management (CG133), previously referenced within this report.
Risk-assessment tools and scales can form part of the risk-assessment process and are generally checklists to be completed by patient or health professional to give a quick and rough estimate of patient risk, for example high or low risk of suicide. However, concerns have been expressed about how risk assessments are undertaken across the UK. NICE guidance on long-term management of self-harm in the over-eights recommend the following ‘Do not use risk assessment tools and scales to predict future suicide or repetition of self-harm’ and ‘Do not use risk assessment tools and scales to determine who should and should not be offered treatment or who should be discharged’. 14 Risk screening may have unintended consequences in drawing the clinical encounter towards a focus on self-harm, which may itself have harmful effects. However, contrary to staff fears, there is little evidence to suggest that simply discussing the possibility of self-harm or suicide increases the chance that children or young people will contemplate such actions.
Suicides in children are very rare, and predicting them is difficult. The NICE Quality Standard on Depression in children and young people (NICE, 2019; NG 134) states that children and young people with suspected severe depression should be seen by a Child and Adolescent Mental Health Service (CAMHS) professional within 2 weeks of referral, or within a maximum of 24 hours if at a high risk of suicide. Prompt access to services is essential if children and young people are to receive the right treatment at the right time. 17 Arrangements should be in place so that children and young people referred to CAMHS with suspected severe depression and a high risk of suicide are kept in a safe place and seen as an emergency, within a maximum of 24 hours, to help prevent injury or worsening of symptoms. However, CAMHS service are currently experiencing extreme pressure.
A mental health professional called to assess a child or adolescent during a crisis situation, either in Accident and Emergency, in a CAMHS outpatient service or at young person’s home, needs to assess her/his suicide risk quickly. Assessment is typically conducted via an interview. Checklists and assessment instruments have been developed to facilitate the clinical encounter. They also offer a structure within which to obtain the necessary information on which to base a comprehensive assessment. NICE (2011) guidance recommends that risk assessment is used as part of a broader assessment to inform treatment planning. 18 However, they have been frequently misused to guide clinicians’ predictions of future behaviour.
Concern has been expressed that risk assessments frequently fail to capitalise on their clinical value, being translated into a perfunctory exercise that occurs in isolation from an overall assessment of a young person’s biopsychosocial need. This is particularly the case given that a primary motivation for completion of risk-assessment processes is likely to be seeking to avert recriminations relating to likely risk to others. A relatively rare, and yet high-profile, risk (harm to others) has therefore come to dominate risk-management considerations ahead of the more frequent occurrences of child or adolescent self-harm or suicide. A UK Royal College of Psychiatrists report titled ‘Rethinking risk to others’19 raised concerns about a culture of blame and the proliferation of invalidated tick-box assessment forms that are produced as a means of ‘back covering’ and that represent ‘a lazy and authoritarian approach to delivering health care .…’. 20
Aims and objectives
Our initial research question is as follows:
‘Which risk-assessment tools for self-harm and suicide are currently in use in CAMHS services in the UK and other English-speaking high-income countries?’
The review then addresses the main research question:
‘For whom and in what circumstances do risk assessments for self-harm and suicide change the clinical encounter for children and adolescents and what effect does this have on their mental health outcomes?’
Our aim is to address the initial research question by mapping the literature and then to explore the main research questions by a resource-constrained realist-informed review of published and ‘grey’ literature.
The review objectives were as follows:
To review the factors within the clinical encounter that impact upon risk assessments for self-harm and suicide within CAMHS, specifically,
-
to conduct a realist synthesis to understand underlying mechanisms for risk assessment, why they occur and how they vary by context
-
to conduct a mapping review of primary studies and reviews to identify and describe the available tools of potential applicability to the UK for undertaking risk assessments for self-harm and suicide within CAMHS.
The timescale for this review was 3 months; its purpose is to provide an overview, description and summary of the available evidence, particularly in terms of identifying when particular approaches to conducting a clinical encounter for risk assessment for self-harm and suicide are most or least suitable.
Our approach involved the following:
-
Conducting systematic searches across the major medical, psychology and health-related bibliographic databases and additional ‘grey’ literature searches.
-
Descriptively mapping retrieved items meeting broad inclusion criteria plus any additional included items identified from the reference lists of review articles.
-
Coding the items according to the following elements: risk-assessment tools used (their features, validity), training, the clinical setting where the risk-assessment tools for self-harm and suicide are used, characteristics of the health professional and young people use of the tools within the clinical encounter, the short-medium term impact of the risk assessment and long-term impacts.
-
Coding the data for explanations of how the risk-assessment process is perceived to work (context–mechanism–outcome configurations or CMOCs) to inform the realist analysis.
-
Summarising the findings in a final literature review report.
Chapter 2 Methods
The review comprised two stages. The first involved an analytic realist logic within a realist review. A realist review is specifically designed to answer questions such as ‘how?’, ‘why?’, ‘for whom?’, ‘in what circumstances?’ and ‘to what extent?’ complex interventions, such as risk assessment for self-harm and suicide within a clinical encounter, actually ‘work’. 21 Through a review of the literature, the review team develops an overarching programme theory, which they gradually refine using data from documents identified as the review progresses. 22,23 The second review involved a mapping review to identify the quantity and quality of the literature on risk assessment in CAMHS.
Rationale for a resource-constrained realist review
Conventional systematic reviews assume that outcomes result from a linear progress of cause leading to effect. 24 However, clinical encounters do not take place within a controlled experimental setting but occur within a complex, continually-shifting context. 25 In seeking to explain the processes that are taking place it becomes necessary to use a theory-driven approach; focusing on explanations of how interventions ‘work’ (programme theories). 26 Within this programme theory, the team uses a realist logic of analysis to explore outcome patterns. 27 Realist synthesis represents a tried and tested methodology, frequently used within the NIHR Health Services & Delivery Research Programme to generate, explore and test such explanations by synthesising complex evidence from diverse sources and thus offering an understanding of why and how complex interventions work. 28
In brief, mechanisms cause outcomes to occur, but the relevant mechanisms are only activated within conducive contexts. 29 By examining the ‘mechanisms’, exploring the ‘contexts’ where the intervention occurred, and then linking these contexts and mechanisms to the ‘outcome’ of the intervention a review team is able to examine the relationships between these three components. 30 Each combination of context (C), mechanism (M), and outcome (O) is labelled a ‘C–M–O configuration’. 31 Where patterns of C–M–O configurations recur they offer semi-predictable patterns/paths of how a program functions – broad ‘rules’ for how and when certain outcomes most typically occur. 32
A realist review typically requires as much as 12 months of research endeavour; time spent in exploring the literature and in generating subsequent analysis. In recognition that policy windows may not always accommodate extensive analysis some have coined the term ‘rapid realist review’ for circumstances intended to support an accelerated transition from research to policy/practice. 33 The review team resists this terminology, not least because, in contrast to other rapid forms of synthesis, rapid realist synthesis variants offer no concessions to an abbreviated methodology. Instead, the report privileges ‘resource-constrained realist review’, recognising that constraints do not impact upon the methodology, as such, but may restrict the number of programme theories to be explored or, in the case of this review, constrain the quantities of evidence assembled to sustain or negate each theory. By exploring all the candidate theories the review team hopes to facilitate overall conclusions while acknowledging the potential for further nuance and explanation of the hypothesis underpinning each programme theory.
Prior to this resource-constrained realist review, a prespecified protocol was produced, which is available via the website of the funder, the National Institute for Health Research Health Service & Delivery Research Programme. This protocol incorporates both realist review and mapping review elements and includes the research question, search strategy, synthesis methodology, inclusion criteria for relevance screening, data-extraction form, quality-assessment tool, and plans for dissemination. This overview of methods offered a framework within which the specific realist review methods could be reviewed, revised and enhanced as relevant evidence became apparent. This section of the report follows the RAMESES (Realist and Meta-narrative Evidence Syntheses: Evolving Standards) guidelines34 for reporting, modified to accommodate a resource-constrained realist review.
In addition to the data extraction to facilitate the review of tools, data were coded to inform the subsequent realist analysis. The codes were piloted with codes being refined based on emerging concepts throughout the analysis period. Coded text was selected according to its facility to address the following questions:
-
Does this section of text refer to context, mechanism or outcome?
-
How might this specific CMOC be described (whether partial or complete)?
-
(a) How does this (full or partial) CMOC relate to the clinical encounter? (b) Are there data that support how the CMOC relates to the clinical encounter? (c) In light of this CMOC and any supporting data, does the clinical encounter need to be changed?
-
(a) Is the evidence sufficiently trustworthy and rigorous to change the CMOC? (b) Is the evidence sufficiently trustworthy and rigorous to justify changing the clinical encounter?
Eligibility criteria
To be included in the mapping review a publication was required to meet the criteria provided in Table 1 and to not be excluded by the criteria given in Table 2.
| Primary list | ||
|---|---|---|
| Date | Evidence published between 1 January 2011 (year of NICE guideline) and 31 December 2021 | |
| Setting | Any setting in which structured formal child and adolescent mental health risk assessment for self-harm and suicide is conducted, which meets the above criteria (e.g. health or social care settings and child’s own home) | |
| Population | Child and adolescent mental health population (8 years and older to correspond with NICE guideline) and their family members and clinicians | |
| Study type | Systematic reviews OR Primary studies not restricted by study design (to include relevant audits or service evaluations in addition to formal research studies) but these must include quantitative or qualitative research or evaluation data |
|
| Model of care | Child and adolescent mental health and crisis care contexts | |
| Outcomes | Include any reported outcomes. Primary outcomes to include the following: health outcomes (suicide and self-harm, depression symptoms etc.), health service outcomes (admission, resource utilisation etc.) and individual outcomes (mood, anxiety etc.) | |
| Other | Individual studies from UK (for realist synthesis and review of tools). Discursive accounts, guidance and qualitative studies (realist synthesis) |
Systematic reviews that include studies from Australia, New Zealand, Canada, USA, UK and Ireland (review of tools) |
| Date | Evidence published before 1 January 2011 |
|---|---|
| Setting | Interventions/services that do not typically include structured formal risk assessment. Needs assessment as a form of psychological assessment. Studies only about self-harm were excluded as a single approach to self-harm/suicide is required |
| Population | Adults (18 years or older) and child under 8 years |
| Study type | Papers that describe interventions/services without providing any quantitative or qualitative data. Conceptual papers and projections of possible future developments |
| Model of care | Other first contact that does not involve risk assessment. Unstructured or informal approaches to risk assessment |
| Outcome | Studies that include no process (e.g. qualitative) or outcome (e.g. quantitative) data |
| Other | Studies conducted in low- or middle-income countries. Studies from non-Anglophone high-income countries. Papers not published in English |
Information sources
A broad search to identify published and peer-reviewed literature focused on how child and adolescent mental health risk assessment is delivered in the UK was conducted, including a search for relevant grey literature. The team sought to identify examples of current practice, pilots and other child and adolescent mental health initiatives carried out in the UK and review their robustness, applicability and scalability.
The search strategy combined thesaurus and free-text terms and relevant synonyms for the population (child and adolescent mental health population) and intervention [risk assessment (broad terms to retrieve research on the use of risk assessment, and risk-screening scales/tools; including terms for psychosocial assessment as the broad term for assessments including risk-assessment components)], using proximity operators where appropriate. Search terms were then combined using Boolean operators appropriately. Outcome terms were not included in the search as outcome information is not always included in the title or abstract, meaning that their use could impact negatively on the identification and retrieval of relevant studies. Similarly, the search strategy was not limited to self-harm and suicide with these inclusion criteria being assessed at the subsequent study selection stage (see Appendix 1, MEDLINE search strategy).
Once agreed with NIHR HS&DR and DHSC, the search strategy on MEDLINE was translated for other major medical and health-related bibliographic databases. The search was limited to research published in English from 2011–current to reflect developments since the NICE guidance (2011). Methodological search filters were not utilised to keep searching broad and ensure all relevant study types were retrieved. Geographical (i.e. UK)35 and review filters were used; first to restrict to the UK and subsequently, to retrieve systematic reviews.
MEDLINE (including Epub Ahead of Print & In-Process), PsycINFO, EMBASE, CINAHL, HMIC, Science and Social Sciences Citation Index and the Cochrane Library were all searched in September 2021. Targeted ‘grey’ literature searches were carried out in October 2021 to identify reports/case studies in websites including the following: Mental Health Foundation www.mentalhealth.org.uk, MindEd for Families www.mindedforfamilies.org.uk/young-people, Royal College of Paediatrics and Child Health www.rcpch.ac.uk/, Royal College of Psychiatrists www.rcpsych.ac.uk and Young Minds www.youngminds.org.uk. Additional evidence was identified from the reference lists and/or citation searching of included studies.
We also utilised expertise of colleagues working in mental health including Scott Weich and Elizabeth Taylor Buck and input from Dr Bernadka Dubicka, consultant and research lead in Pennine Care Foundation Trust, Greater Manchester and Chair of the Royal College of Psychiatrists (RCPsych) Child and Adolescent Faculty to identify additional documents and initiatives being carried out within a UK context to ensure that the review is as inclusive as possible.
Data management/data selection
Search results were downloaded to Endnote bibliographic management software.
Selection process
A pilot-study selection exercise involved members of the review team independently coding a small sample of records (200 each). Verdicts were compared and inter-rater reliability was rated as acceptable. The remaining records were distributed between the review team (AC, KS, ABo and DC) and then subject to independent single review. A sample of excluded records was reviewed to minimise the likelihood of exclusion in error. Where a verdict of unsure was recorded by one reviewer these records were passed to a second reviewer for agreement to be resolved by consensus. In the event of continued disagreement a third reviewer (ABo) arbitrated on eventual inclusion.
Data-collection process
Following piloting of a data-extraction form, a user-friendly Google form interface was used to input data into a Google Sheets/Excel spreadsheet. Summary tables were inserted within the final report and summarised data were produced for the summary report. In accordance with most rapid reviews, duplicate data extraction was not considered possible. However, data were iteratively checked and rechecked during writing of the final report.
Data items
Data to be extracted included the following:
-
year and place of study
-
the tool and risk-assessment method
-
the population included (age group, clinical characteristics and setting)
-
study design and outcomes measured [any outcomes measured by studies relevant to patient mental health (e.g. status of condition, risks and care planning as a result of the risk assessment) were included]
-
main findings
-
key messages including limitations.
Quality assessment
In line with realist-informed approaches, that privilege richness of data and relevance over rigour, preliminary quality assessment of each study focuses on generic limitations of study design, although specific design limitations were documented where identified. Given the diverse evidence to be included, the review team made the decision to only apply quality assessment to studies evaluating an actual tool. This allowed for the use of insights from qualitative data and process evaluations as well as implementation studies.
For the mapping review the team compiled published assessments relating to the different aspects of validity for the individual tools and documented these according to systematic methods (Table 8). Quality appraisal was then conducted independently using the appropriate sections (quantitative or qualitative or both) of the MMAT tool, and disagreements were resolved through discussion.
Data synthesis
Synthesis takes the form of descriptive, narrative approaches – such as textual, tabular and graphical presentation. However, following a mapping process, the team utilised a realist-based approach. A realist review seeks to explore the underlying causes for observed outcomes and when these might occur by reviewing published and grey literature.
Using the analytic building blocks known as CMOCs [i.e. propositions that describe what works (or happens), for whom and in what contexts and why] the team explored these contexts. 36 Contexts are conditions that activate or modify the behaviour of mechanisms. 22 This realist review seeks to identify and understand the contexts that impact on factors that determine the outcome of the risk-assessment process, whether that clinical encounter is successful or suboptimal. Realist methods offer an optimal vehicle for exploring the complex and dynamic nature of the clinical encounter.
The resource-constrained realist review sought to explore the contexts that influence risk assessment for mental health for children and adolescents by seeking to answer the following questions:
-
Which factors within the clinical encounter impact positively or negatively on risk assessment for self-harm and suicide in children and adolescents within CAMHS?
-
What are the underlying mechanisms, why do they occur and how do they vary in different contexts?
This resource-constrained realist review supports exploration of risk-screening tools and risk-assessment processes in child and adolescent mental health, including a descriptive analysis of tools most commonly used within the UK. As a result, this review focuses on the processes of risk assessment while acknowledging known limitations to the design and utilisation of specific risk-screening tools. The question on underlying mechanisms involved exploring key components and processes within risk assessment for self-harm and suicide and constructing programme theory statements for each stage or component – for assessment against the identified evidence. Individual team members extracted data from each allocated study and coded the context, mechanisms and outcomes within the studies.
Synthesis followed a pathway approach, as used in previous realist-based reviews for primary care and social care. 22,37 Resultant CMOCs were discussed within the research team. Comments from patient representatives and clinical experts were fed into the iterative, cyclical process of searching, data extraction, analysis and programme theory development.
The scope of the resource-constrained realist review was clarified through regular team meetings to discuss the protocol, review process and synthesis outputs. The agreed review question was ‘For whom and in what circumstances do risk assessments for self-harm and suicide change the clinical encounter for children and adolescents and what effect does this have on their mental health outcomes?’.
Although findings for CAMHS in general are privileged, the review team sought to identify specific age differences between children and adolescents where these may exert an influence on the conduct or outcome of the clinical encounter. Where contextual differences relate to the setting of the risk assessment these were also highlighted in the review findings.
Searching for relevant evidence: search strategy and eligibility criteria
To test the programme theory, a qualified information professional developed and implemented a search strategy to retrieve relevant primary studies and discursive contributions from both academic and grey literature. This complemented the overall search strategy as implemented for the mapping review and executed across multiple bibliographic databases (see Information sources). Items informing the programme theories were identified from the full bibliographic searches. Supplementary subject searches and forward citation were then executed on Google Scholar using the Publish or Perish desktop search engine. These electronic searches were complemented by innovative use of the scite tool to view ‘within publication citations’ in context and to establish whether the citation provides supporting or contrasting evidence for cited claims.
Relevance confirmation, data extraction and quality assessment
A single reviewer assessed each study to determine its relevance to the review question and to extract pertinent detail. Given the nature of the question and the available evidence (non-research designs) no attempt was made to appraise the quality of included studies. Assessment of relevance involved studies being assigned one of three categories based on conceptual relevance:
*** Directly relevant – evidence derived from a child and adolescent risk-management context.
** Partially relevant – evidence derived from a wider mental health risk-management context, which may or may not include child and adolescent populations.
* Indirectly relevant – evidence on risk assessment more generally (e.g. risk assessment for violence).
Patient and public involvement (PPI)
Patients and members of the public have been involved in this review through the Sheffield Evidence Synthesis Centre PPI group. This PPI group advises on the plain language summary and other relevant outputs and provides perspectives on relevant contextual factors and key messages for NHS staff.
Chapter 3 Results
This section begins by characterising the main approaches that feature in risk assessment. Both generically and specifically. Thereafter, the Results section falls into two subsections. First, programme theory components are examined and explored within a resource-constrained realist review. Second, the report presents a review of approaches to assessment and tools used specifically in the UK context.
The pathway to intervention
The risk-assessment process is clearly defined in NICE documentation and other guidance (Table 3; Box 1). Within this overarching structure latitude exists with regard to the purpose of risk assessment, how exactly it is performed, what scales or tools are used, if any, and how the outputs and outcomes from risk assessment are used.
| Stage | Detail |
|---|---|
| 1. Child presents to service | Presentations to accident and emergency departments, primary care, acute paediatric care etc. |
| 2. Initial triage and care | Initial assessment for risk (e.g. by paediatrician or registered children’s nurse) and assignment of immediate (e.g. physical) care |
| 3. Risk formulation | Brings together an understanding of personality, history, mental state, environment, potential causes and protective factors, or changes in any of these to provide a narrative of individual risk |
| 4. Development of care plan and risk-management plan | A risk-management plan should be included in the overall care plan |
| 5. Regular review of care plan | Plans should be updated, to include monitoring changes in risk and specific associated factors for the service user, and evaluation of impact of treatment strategies over time |
See Appendix 2 for an expansion of the stages of the risk-assessment pathway offering further detail on each of these processes.
-
Methods and frequency of current and past self-harm.
-
Current and past suicidal intent.
-
Depressive symptoms and their relationship to self-harm.
-
Any psychiatric illness and its relationship to self-harm.
-
The personal and social context and any other specific factors preceding self-harm, such as specific unpleasant affective states or emotions and changes in relationships.
-
Specific risk factors and protective factors (social, psychological, pharmacological and motivational) that may increase or decrease the risks associated with self-harm.
-
Coping strategies that the person has used to either successfully limit or avert self-harm or to contain the impact of personal, social or other factors preceding episodes of self-harm.
-
Significant relationships that may either be supportive or represent a threat (such as abuse or neglect) and may lead to changes in the level of risk.
-
Immediate and longer-term risks.
Results 1: Programme theories for risk assessment
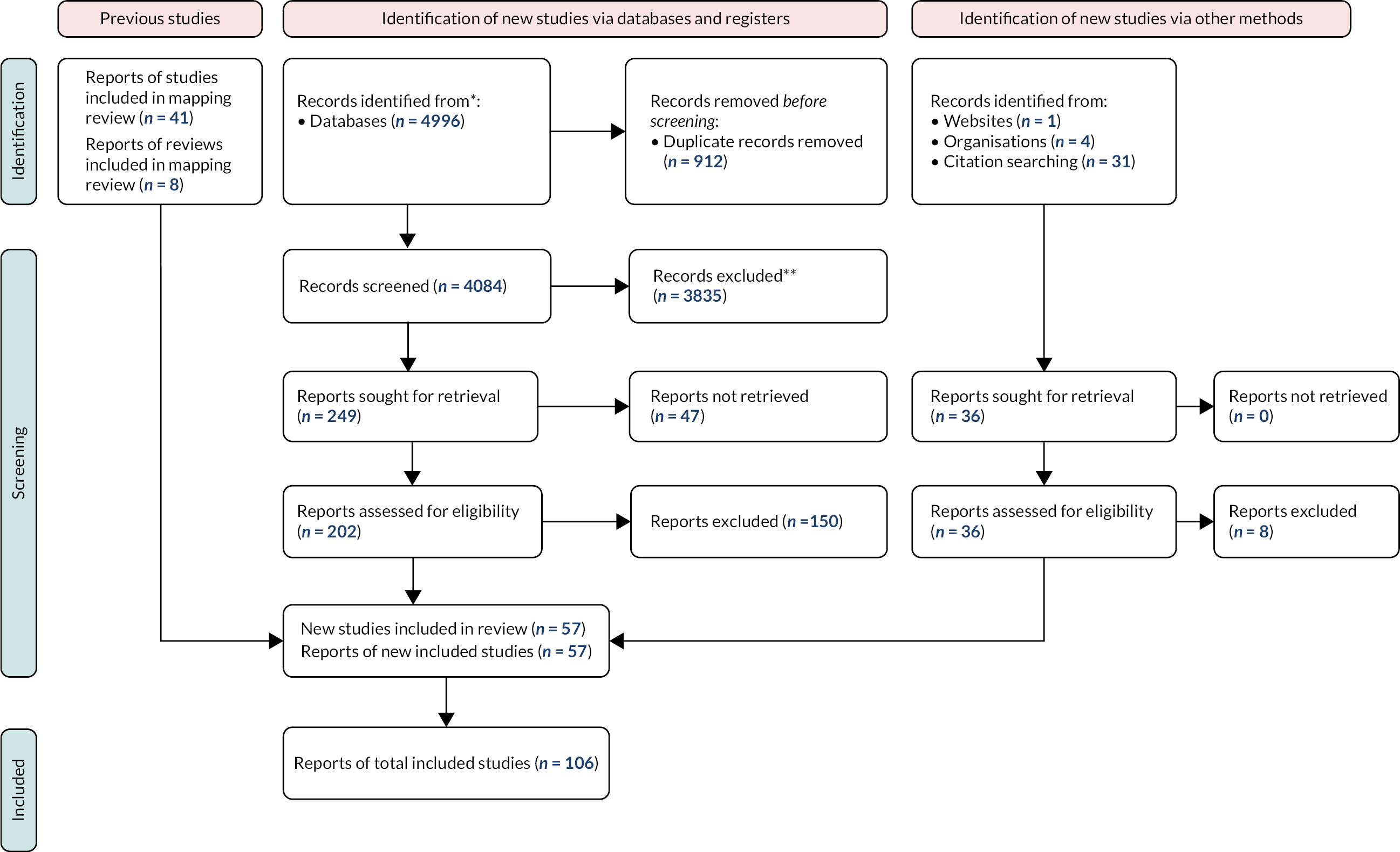
This section reports a resource-limited realist review of risk-assessment tools and processes in child and adolescent mental health. 57 papers were identified for inclusion in the realist review. These comprised 7 systematic reviews, 1 randomised controlled trial (RCT), 6 quantitative studies, 18 qualitative studies and 9 surveys with 7 discussion papers, 3 conventional literature reviews, and 1 opinion piece. There were two case studies and a further two case studies that combined case studies with qualitative research. Finally, there was a single case note review. The flow of information through the resource constrained realist review process is shown in Figure 1.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis flow chart for the realist review. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. DOI: 10.1136/bmj.n71
Initial theory
Initial theory for how, when and why risk assessment is intended to work within the clinical encounter in child and adolescent mental health was identified by undertaking a detailed examination of The assessment of clinical risk in mental health services. National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH). 38 This report asked 85 mental health trusts and health boards in the UK for details of the main risk-assessment tools and approaches that they currently used. Information on the nominated tools was documented, including structure, content and symptom profile. The Inquiry contacted clinicians, patients and carers asking them to share their experiences of tools via an online survey targeted across mental health services in general. 38 Importantly, it sought to represent clinician, patient and carer viewpoints as required when exploring a complex adaptive system. While this confidential inquiry was not specific to a child and adolescent population, the team considered it a suitable starting point because
-
the focus of the review question is not on the population but on the context of assessment within a mental health service (in its broadest sense) and
-
evidence would be privileged according to its relevance to the review question, meaning that the team would particularly seek and highlight nuances from a specific child and adolescent mental health context.
However, critical differences combine to make the application of an assessment of child or adolescent suicide and self-harm unique. 39 Power differentials, which will exist for both populations, are particularly amplified for younger children. Furthermore, a child at risk exists in a complex care system that includes both protective and risk factors. Assessment of young people in many contexts is conducted by non-mental health experts who lack specialist knowledge and experience to inform clinical decisions. 40 Further differences may relate to the focus of assessments, for example in acute paediatric care assessment typically takes place within an immediate (i.e. hours or days) window for potential self-harm or suicide. 39 In such contexts, assessments are performed in time-limited circumstances with children and adolescents with potentially dynamic and fluctuating mental health. In the UK, NICE (2004) guidelines advocate that children and adolescents who self-harm should be assessed for risk. 41 This assessment is intended to identify psychiatric illness and its relationship to self-harm, assess personal and social context together with any specific factors predicting self-harm. It is further required to recognise any significant relationships, either supportive or representing a threat. Such an assessment needs to consider the relatively immediate risk of self-harm or suicide in order to make time-critical risk-management decisions.
We formulated 14 programme theory components derived from the clinical implications of the NCISH report. In each case, the intention was to represent context (signified by IF), mechanisms (represented by THEN) and outcomes (designated by LEADING TO). When programme theory components were either underspecified or incomplete other sources of evidence are used to complete the CMOCs. A single reviewer extracted the following information from the source documents:
-
The activities associated with the risk-assessment process.
-
The setting in which the risk-assessment process took place, including physical environment, social setting, and wider social and economic climate (if specified).
-
The outcomes of each intervention, including both clinical outcomes and responses by adolescent or carer.
Through this preliminary review, successful interventions are considered to require the following:
-
IF risk-assessment approaches are simple, accessible and part of a wider assessment process THEN staff are able to generate standardised, informative and clinically useful assessments LEADING TO appropriate use of support and services.
-
IF clinical staff focus clinical risk-assessment processes on building relationships THEN clinicians and adolescents trust each other LEADING TO frank and open communication within the clinical encounter.
-
IF the emphasis of clinical risk-assessment processes is on gathering good-quality information on (i) the current situation, (ii) past history and (iii) social factors THEN staff use information to inform a collaborative approach to management LEADING TO coordinated and integrated care.
-
IF staff are comfortable asking young patients about suicidal thoughts THEN young service users share relevant information concerning their circumstances LEADING TO an appropriate service response.
-
IF risk-assessment processes are conducted consistently across mental health services THEN the quality of response to young service users does not depend upon each individual contact LEADING TO the availability of consistent information across services.
-
IF staff are trained in how to assess, formulate and manage risk, including appropriate referral THEN staff feel equipped to manage the risks for children and adolescents who present to health services LEADING TO an emphasis on positive risk taking.
-
IF staff are supported by on-going supervision THEN staff feel able to deliver a consistent approach to risk assessment LEADING TO a reduction in adverse events.
-
IF families and carers are involved in the assessment process THEN families and carers are given an opportunity to express their views on potential risk LEADING TO a collaboratively developed risk-management plan.
-
IF mental health staff communicate risk assessments with primary care THEN young people are directed to appropriate care LEADING TO successful health outcomes.
-
IF the management of risk is personal and individualised THEN young people don’t see their care as ‘protocol driven’ and won’t feel alienated LEADING TO their engagement with care.
-
IF organisations involved in risk assessment utilise a whole-system approach THEN this strengthens the standards of care for everyone, LEADING TO the safe management of supervision, delegation and onward referral.
As a complementary activity, the review team identified three ‘counter programme theories’, which relate to how the risk-assessment process might result in unintended consequences:
-
IF staff view risk-assessment tools as a way of predicting future suicidal behaviour THEN they incorrectly interpret individual levels of need for care LEADING TO inappropriate use of restrictive practices such as involuntary hospitalisation, restraint, sedation and seclusion (for the service user).
-
IF clinicians use risk-screening tools and scales in isolation within the risk-assessment process THEN treatment decisions are determined by a score LEADING TO incorrect interpretation of individual need for care and inappropriate utilisation of CAMHS (for the service).
-
IF staff develop tools for risk assessment locally THEN checklists and scales lack formal psychometric evaluation LEADING TO limited clinical utility of tools for risk assessment and unnecessarily restrictive treatment options.
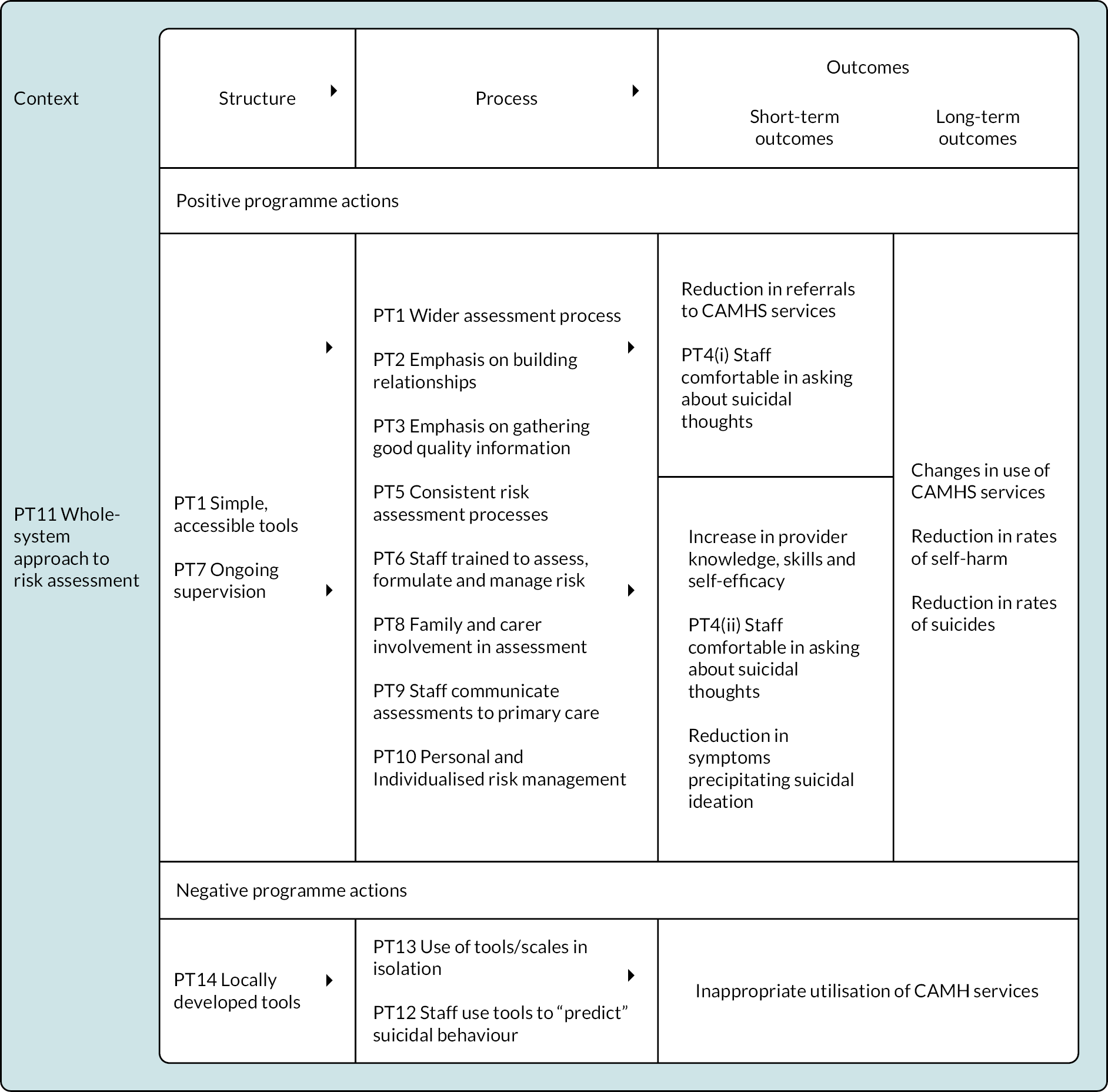
Following identification of programme theory components the team decided to construct an overall logic model as a ‘conceptual map’ within which to locate the diverse programme theories. An initial version was identified from a Screening and Referral Logic Model derived from a relevant publication from the RAND Corporation (Figure 2). 42 The team then overlaid the 14 programme theories on the initial logic model to create a logic model for the realist review (Figure 3).
FIGURE 3.
Logic model developed for the realist review.
Results
1. Usability
-
Programme Theory 1. IF risk assessment approaches are simple, accessible and part of a wider assessment process THEN staff are able to generate standardised, informative and clinically useful assessments LEADING TO appropriate use of support and services.
Supporting evidence
This programme theory component is based on the NCISH report, which promotes an assessment process that goes beyond strict actuarial approaches. 38
Evidence base: three systematic reviews, one NICE guidance document, one feasibility study, one qualitative study, one narrative review, one survey, five commentaries, and one textbook.
Risk-assessment scales are commonly used in clinical practice to quantify the risk of suicide, with 85% of NHS mental health trusts using checklist-style approaches. 38 Currently, no standardised risk-screening tool is available for use within clinical practice in the UK. 39 Furthermore, risk-screening tools that exist possess questionable validity, reliability and acceptability (see Validity and Table 8).
In contrast, NICE guidance (CG133) recommends that risk assessment should take place within a comprehensive assessment of the patient’s needs. 14 A recent systematic review43 concludes that current evidence is not yet sufficient to recommend that structured diagnostic assessments should be universally adopted as an adjunct to clinical practice. However, the reviewers suggest that structured diagnostic assessments could be applied cautiously and mindfully pending further evaluation. A minority of users of the Davies’ structured interview for assessing adolescents in crisis expressed concern that ‘having a form to fill in’ hampers the development of rapport and a relationship between the young person and the professional.
Critics of actuarial approaches comment on the paucity of empirical evidence to support the ability of tools to predict accurately. 16,44–46 See Programme Theory 12. Many argue that tools are based on information about groups, which is of limited value in predicting the behaviours of an individual. 5,44,47 Within adult mental health care the literature consistently affirms that the focus of mental health organisations is now on risk management,48,49 quality assurance and patient safety. 49 Recent studies suggest that this may also be true for CAMHS. 50,51 Risk assessment in isolation from the development and implementation of clinical judgment frameworks becomes potentially ineffectual. Clinicians should not shelter behind the ‘fallacy’ of risk assessment, instead of acknowledging that assessment tools are likely to serve the organisation more than the patient. 52
A possible corollary to Programme Theory 1 is that development of simple assessment tools within a complete assessment process could result in higher rates of referral for risk of self-harm and suicide, thereby increasing utilisation of CAMHS services.
2. Trust
-
Programme Theory 2. IF clinical staff focus clinical risk-assessment processes on building relationships THEN clinicians and adolescents trust each other LEADING TO frank and open communication within the clinical encounter.
Supporting evidence
This programme theory component on building relationships is based on the NCISH report, which found that clinicians believed that an important focus of risk assessment involved building a rapport such that the assessment flowed smoothly. 38
Evidence base: one NICE guidance document, five qualitative studies, two surveys, one case study, and one commentary.
NICE guidance 133 states that ‘health and social care professionals working with people who self-harm should: aim to develop a trusting, supportive and engaging relationship with them’. Such a recommendation is further informed by qualitative research using interviews with nurses on wards of four psychiatric hospitals. 53 Professionals are concerned about how risk assessment may influence their relationship with service users. Often mental health nurses tend to emphasise risk avoidance to maintain safety. 5,54,55 Literature describing nurses’ perceptions of safety in acute mental health reports that nurses perceive their role as mainly risk management. 5 Most packages focus on assessment skills, risk screens and risk-factor tools but do not address tensions between divergent views of people in distress and professionals involved and how to build empathic partnerships5 in time- and resource-poor environments.
A further tension relates to working environments that privilege ‘task-based nursing over therapeutic care’ and those that create ‘conditions for open and genuine communication’. Task-based working environments, exemplified by a preoccupation with tick-box risk assessment, often prove detrimental to person-centred care. Furthermore, within a mental health service context, a focus on risk management ‘inherently erodes the formation of a therapeutic relationship, as patients who are viewed as risky are not trusted’. 56
In contrast, where ‘conditions for open and genuine communication’ exist staff members seek to focus on ‘developing an accurate and meaningful picture of patients’. 53 As a consequence staff members can enhance their capacity for compassionate and considerate contact and communication with patients experiencing suicidal ideation.
Compassionate care is particularly important – unlike their feelings for the self-harm population in general, staff typically hold positive attitudes towards self-harm specifically in adolescents and young children. 40,57 If done well in an unhurried, empathetic and non-judgmental manner, the interview can be therapeutic and encourage the patient to seek future help. By contrast, negative attitudes and a focus on the patient’s physical needs might result in the patient avoiding emergency services in the future. A healthcare professional should not give false reassurance, because patients may doubt that they are taking their situation seriously. 58 If possible, they should seek to obtain a corroborative history of the event from a third party. 58
Assessing young people requires engagement, empathy and a genuine curiosity about what has happened to bring the young person to a point of acute risk. Such an approach seeks to increase the chances of openness and honesty and a collaborative risk assessment. Otherwise, young people will keep risky thoughts and plans hidden, particularly if they think they will be judged or punished.
When presenting to their GP, young people feel that it is important that their GPs initiate the conversation about mental health, suicide and self-harm. 59 If a GP asks directly about such topics this may overcome some of the barriers to disclosure of suicidal thoughts, depressive symptoms or mental health problems more generally.
In the context of risk assessments for suicidal behaviour and/or self-harm, young people dislike labels such as ‘risk’ and ‘risk assessment’. 59 They perceive such labels to be potentially stigmatising and problematic. Young people may be especially vulnerable to labels that could increase stigma; language and terms related to suicidality or self-harm may be perceived as ‘pathologising’. Awareness of these attitudes may help in a shift away from professional-focused terms such as ‘at-risk’ and ‘risk assessment’, to patient-focused language such as ‘coping assessment’. 60 However, participants in one qualitative study disliked the term ‘assessment’, suggesting the inclusion of language relating to ‘well-being’. 59
Young people endorse the need for ‘comprehensive psychosocial-based assessments that prioritise collaboration and the therapeutic alliance, are holistic, acknowledge that risk is dynamic over time, and are needs-driven’. 59 Individualised, needs-based approaches to assessment are key for young people. 59
A collaborative dialogue facilitates empowerment and creates opportunities for young people to be involved in decision-making and to meet their growing needs for autonomy, agency and control. 59 Such a dialogue is concordant with principles of patient-centred care, shared decision-making and patient engagement. Furthermore, patient-centred care is fundamental to a biopsychosocial approach and recognises the pivotal role of the family. Young people may be particularly sensitive to power disparities and condescension. A friendly, non-judgemental attitude is critical; poor attitudes and body language and impersonal, overmedicalised approaches impede the therapeutic alliance and the disclosure of suicidal behaviour/self-harm. 59
Young people’s views of self-harm services have not been extensively studied. 61 A recent study has explored the views of young people in relation to the role of GPs. 59 GPs have been found, in one study, to be the most frequent healthcare practitioner source for urgent referrals of children and young people for self-harm, suicidal thoughts or following overdose. Families may prefer to access their GPs when worried about these issues. GPs can feel dependent on specialist support and feel the need for increased training in supporting children and young people with mental health issues. 62 Young people expect GPs to be skilled and knowledgeable in providing practical resources and support for presentations of suicidal behaviour and self-harm, including crisis support. 59 Assistance from the GP with accessing crisis resources or using a safety plan is viewed as highly beneficial. 59 GPs taking the time to demonstrate resources to the young person was another expression of care and connection to assist a positive relationship. 59 Young people may have little previous experience of how the healthcare system is structured, and therefore might require more ‘scaffolding’ than adults. 63
Young people are typically ambivalent when seeking help. They may isolate themselves, feeling that it is not safe, or that they are not ready to disclose their suicidal thoughts and feelings (e.g. as a consequence of feeling shame). In response, nurses describe how they try to enable patients to communicate in an open and genuine way. 53 By presenting themselves as accessible and approachable, reaching out to patients, and encouraging patients to approach them and talk to them nurses are able to work on creating an open and communicative environment. 53 Nurses highlight the need to develop a trusting relationship, respect the emotions of patients and reassure patients that they can disclose suicidal ideation. 53
All the above suggests that ‘… policy makers and hospital leaders should aim to create environments where [staff] can be involved in multifaceted and interpersonal approaches to suicide risk assessment’. 64 In such environments organisations could create relationships between children and young people and professionals that release preventive and therapeutic potential, rather than encouraging impersonal observations and ineffective checklist approaches. See Programme Theory 1.
3. Credible information
-
Programme Theory 3. IF the emphasis of clinical risk-assessment processes is on gathering good-quality information on (i) the current situation, (ii) past history and (iii) social factors THEN staff use information to inform a collaborative approach to management LEADING TO coordinated and integrated care.
Supporting evidence
This programme theory component is based on the NCISH report,38 which found that clinicians believed that an important element of risk assessment is the quality of the information gathered. The clinicians interviewed noted the importance of gathering a thorough history of previous incidents, and having an awareness of triggers for distress, for example significant anniversaries. They reported that a good risk history should include details of the incident and its consequences as well as the likelihood of the incident being repeated. However, some highlighted the difficulty of predicting suicide. 38
Evidence base: two quantitative studies, one multicentre study, three qualitative studies, three surveys and three commentaries.
Critics argue that tools tend to focus on historical (static) risk factors thus ignoring the dynamic or situational variables, which impact on the person. 5,8 The Functional Analysis of Care Environments–Child and Adolescent Risk-Assessment Suite (FACE–CARAS) suite of tools promotes use of schedules that enquire about both historical (static) and current (dynamic) risk factors. 65
Key to risk assessment is a collaborative dialogue, which encompasses the provision of adequate, detailed information across all aspects of a young person’s care, including treatment options and confidentiality. 59 Assessment tends to focus on risks people with mental health diagnoses pose, which marginalises consideration of other risks like living in inadequate accommodation. 66 It constructs individuals as risks who need interventions rather than identifying issues within particular communities, such as those with higher levels of poverty, substance abuse and unemployment. 48 It may also obscure risks that come from accessing mental health services, which potentially include loss of liberty, forced treatment or negative experiences. 67,68
Young people value the protection of their privacy, particularly for sensitive issues. 59 However, this should not be interpreted as a reason not to ask them about their thoughts of self-harm or suicide. Health professionals should also be aware that different types of self-harm may be viewed differently by children and young persons (CYP). For example, stigma associated with cutting may make a child or young person more secretive whereas attempted suicide frequently signals that the young person has reached a point where they are no longer able to cope at all. 61 Young people also express concerns regarding the privacy and confidentiality of their medical information relating to mental health and suicidal behaviour/self-harm. 59
Challenges exist in relation to incompleteness of information. A survey of outpatient and inpatient adolescents in the UK showed that 20% reported at least one episode of self-harm on the questionnaire that was not recorded in the clinical record. 69 The authors concluded that ‘using a combination of clinical interviews (with multiple informants), paper-and-pencil tools and comprehensive clinical records’ keeping afford the best chance of identifying adolescents who self-harm’. 69 A multicentre study of self-harm in England70 reported that psychosocial assessment occurred in only 57% of presentations in the study, even though the three centres (six hospitals) involved had well-established specialised self-harm services. The authors concluded that this ‘low rate of completion demonstrates the extent to which hospitals fall short of implementing the national guideline recommendation that all self-harm patients should receive a specialist assessment’. 70 They suggest that this low completion requires further investigation, particularly as ‘non-assessment may have several causes (e.g. self-discharge, patient refusal, unavailability of staff, emergency department policy). 70 They argue that this is particularly critical given what they claim as ‘accumulating evidence that psychosocial assessment is associated with reduction in risk of repetition of self-harm’ and the fact that ‘provision of appropriate psychiatric and social care is unlikely in the absence of an assessment’. 70
The FACE–CARAS tools are predicated on a stepped approach to completion – such that subsequent tools are only completed when indicated by the overall risk profile – but even within the context of research and evaluation completion of subscales was found to be unacceptably incomplete. 65
While advances in computerisation and clinical records have shifted the exact nature of this challenge the need for multiple and complementary approaches remains as pressing as ever. Specific challenges relate to conducting suicide risk assessment. Self-report measures of suicidality are limited by reporting biases (e.g. young people may conceal suicidality to avoid anticipated negative consequences) and high temporal variability (i.e. self-reported suicidal ideation may fluctuate from moment to moment). 71
When patients feel able to communicate in an open and genuine way, nurses are able to get to know patients, can assess suicidal ideation and also identify risk and protective factors. Strategies used to characterise the presence and severity of suicidal ideation, include listening to and observing patients, asking patients about the presence of suicidal thoughts and plans, and checking with colleagues. 53 Nurses must be alert to expressions that might be indicative of suicidal ideation (e.g. self-harm and social isolation). Nurses describe how they depend upon their intuitive senses, and that their own emotional responses, including ‘feeling anxious about the potential of a suicidal attempt’, provide cues to emerging suicidal ideation. Conversely, such emotional responses may also make nurses more likely to assess suicide risk as higher than it actually is. 53
4. Communicative environment
-
Programme Theory 4. IF staff are comfortable asking young patients about suicidal thoughts THEN young service users share relevant information concerning their circumstances LEADING TO an appropriate service response.
Supporting evidence
This programme theory component is based on the NCISH report38 in which patients recommended that risk-assessment tools should incorporate a focus on suicidal thoughts, i.e. ‘to encourage staff to confidently tackle difficult questions’.
Evidence base: one meta-analysis, one quantitative study, one service improvement project, five qualitative studies, five surveys and one editorial comment.
Mental health nurses who are confident can make responsible decisions related to risk management. 5 Some nurses seem to have the interpersonal qualities and skills to move beyond checking and controlling suicide risk and instead make efforts to acknowledge and connect (with) the patient as a person, even during standardised assessments and observations. 53 These nurses adopt a focus that transcends a reductionist focus on static risk and protective factors and seems to open doors to a holistic picture of patients by being attentive to their needs and hopes and trying to understand the nature of their suicidal expressions. 20,72
One possible source of discomfort for staff members, particularly those who do not specialise in mental health, is the fear that asking patients about suicide might induce suicidal ideation. In general, nurses favour ‘daring to discuss’ suicidal ideation to support the patient’s communication. However, they also felt that they must not ‘force the conversation’. 53 Thirteen studies (2001–13) have examined whether asking about suicide induces suicidal ideation. 73 With samples including both adolescents and adults and both general and at-risk populations, none of the identified studies found a statistically significant increase in suicidal ideation in participants as a result of being asked about their suicidal thoughts. Findings suggest that acknowledging and talking about suicide with adolescent populations may in fact reduce, rather than increase suicidal ideation, with a suggestion that repeat questioning may benefit long-term mental health. 73 Studies in treatment-seeking populations suggest that asking people who are or have been suicidal about suicidality can lead to improvements in mental health. 73 Review findings suggest that recurring ethical concerns about enquiring about suicidality could be relaxed.
The fear that asking about suicide itself precipitates action (so-called iatrogenic risk) persists, especially among clinicians with a non-psychiatric background. A meta-analysis quantitatively synthesised 13 studies that explicitly evaluated the iatrogenic effects of assessing suicidality via prospective research designs. When pooled the overall effect of assessing suicidality did not demonstrate significant iatrogenic effects in terms of negative outcomes. A key strength of this study is that the review authors stratified studies according to the timing of their follow-up assessments, concluding that assessing suicidality did not result in any significant negative effects on immediate, short-term, or long-term follow-up assessments. The authors conclude that their findings support the appropriateness of universal screening for suicidality, and state that this should allay the fears of clinicians that assessing suicidality is harmful. 74
Clinicians’ anxieties may increase the reliance on undertaking an assessment based upon a checklist of phenomenological or epidemiologically valid items that provide few opportunities to account for individual differences that may provide a more accurate and richer suicide risk assessment. 75 Use of risk-assessment tools may provide false reassurance, assuaging the clinician burden and sense of dyscontrol, while giving the impression of effective working and so mediating corporate risk.
Losing a patient by suicide can impact on professional practices, including issues around objective clinical decision-making. It may lead to behaviours likened to learned helplessness, such as increased vigilance when dealing with future suicidal patients and avoidance of treating suicidal patients. 76,77 These in turn may lead to an ongoing reliance on the same systems for assessment and treatment. 75
One feature that might influence staff’s comfort and willingness to ask young people about suicidal ideation relates to whether young people themselves feel comfortable with such questioning. Increasing numbers of qualitative studies have found that, contrary to the beliefs of many, young people do not mind being asked about the presence or absence of suicidal thoughts. 78–81 Several tools utilise self-report approaches. For example, the developers of the Risk-Taking (RT) and Self-Harm (SH) Inventory for Adolescents (RTSHIA) point out how the quality of data produced by self-report measures is comparable to those obtained through clinical interviews. 82 They state that people may feel more comfortable admitting to sensitive thoughts and acts when they are asked to circle a response or write a brief explanation instead of providing a verbal report, which may be influenced by interpersonal reactions to interviewers. Reassurance of the confidentiality and anonymity of self-reports is also important for young people. Pragmatically, few alternatives to self-report data exist when requesting personal and sensitive information from young people.
5. Consistency of approach
-
Programme Theory 5. IF risk-assessment processes are conducted consistently across mental health services THEN the quality of response to young service users does not depend upon each individual contact LEADING TO the availability of consistent information across services.
Supporting evidence
Programme Theory 5 is based on the NCISH report,38 which found ‘little consistency in the length, content or use of risk tools, although there was greater consistency in some places than others’. Risk assessment also needs to be consistent across mental health services. 38
Evidence base: one systematic review, one mixed-methods study, one interrupted time series, one case series, one service improvement project and two surveys.
As articulated the programme theory relates to inconsistencies in the role and personal characteristics of the staff member making the contact and to inconsistencies resulting from contact with multiple, uncoordinated individuals. Patients who were critical of the assessment process felt that there was inconsistency between teams. 38 It is noteworthy that one of the strengths of the Wales Applied Risk Research Network (WARRN) initiative, as identified by clinicians, is the development of a consistent approach, within and between organisations. 83 Clinicians acknowledged that different agencies had created a common language and understanding that improved communication both across and between agencies. 83 These benefits have been similarly realised by a consistent two-step risk assessment and management process (Comp RA) within Northern Ireland. 38 Benefits can also extend to the development of standardised training and supervision procedures and processes, seen in the WARRN83 and the Collaborative Assessment and Management of Suicidality (CAMS) training programmes. 75
Programme Theory 5 is further supported by a mixed-methods study,84 which examined which risk-assessment tools were currently in use in the UK, and collected views from clinicians, service users and carers on the use of these tools. Findings showed little consistency in the use of these instruments. 84 Clinicians, patients and carers expressed both positive and negative views of the featured instruments. Findings attest to the need for assessment processes to be consistent across mental health services. Many professionals using the Davies’ structured assessment for adolescents in a crisis thought that it was good for a professional to have some structure and framework within which to operate so that ‘nothing would be missed’. Significantly, this view was not shared universally. Ongoing supervision is another provision to support consistency of approach. Care for self-harm within emergency departments appears to be particularly variable, with research showing it to be ineffective and delayed. 85
Areas where compliance needs to be improved include appropriate completion of the risk assessment. 86 A recent study extracted anonymised data from CAMHS at two time points. Data were compared with prevalence and population data and then a subsample was evaluated against NICE guidelines. Between time points there was a significant decrease in the number of cases that had a risk assessment completed appropriately and the number that had a full risk screen completed. 86 It is unlikely that this result was due to either a genuine reduction in the level of risk seen in CAMHS87 or that it represents a change in reporting practices. Even where a risk screen is completed somewhere in their notes, consistency needs to be improved to standardise risk monitoring and communication between services. For example, if a young person transitions to adult services having readily accessible information on risk is crucial.
Further variation relates to the experience of the clinician; experienced clinicians tend to use a positive risk-taking approach, whereas recently qualified clinicians do not feel as confident with suicidality cases unless they are routinely confronted with such cases (such as those working in a crisis team). 75
6. Self-efficacy
-
Programme Theory 6. IF staff are trained in how to assess, formulate and manage risk, including appropriate referral THEN staff feel equipped to manage the risks for children and adolescent who present to health services LEADING TO an emphasis on positive risk taking.
Supporting evidence
This programme theory component is based on the NCISH report,38 which found that healthcare professionals do not feel confident in being able to implement care plans, within which immediate risks can be mitigated, if they lack appropriate support and guidance to inform their assessment. 39
Evidence base: one systematic review, one RCT, three quantitative studies, one mixed-methods study, one qualitative study, one pre–post study, one service-improvement project, three surveys and one commentary.
Nurses with good confidence can make responsible decisions related to risk management. 5 Continuing education about the use of risk-assessment tools is needed to demonstrate that their use is compatible with therapy. 5 Staff need training if they are to use risk assessments in such a way that ensures their reliability. 88 A mixed-methods study in the UK reported little consistency in the use of instruments and highlighted a need for adequate training. 84 Nearly a third of clinicians surveyed in UK mental health services reported poor levels of training, highlighting practical issues in the use of tools and the poor quality of documented information. 84 Noticeably, training is a substantive component of both the Davies’ structured assessment for adolescents in a crisis and for the WARRN formulation-based approach83 – both indicating that familiarity with a structured process and how it integrates within clinical judgement should be considered more important than technical mastery of a tool or checklist. Over 2 days, the WARRN training modules cover basic clinical skills, such as how to conduct a clinical interview and what should be covered, techniques for asking difficult questions, how to formulate, and how to produce risk-management plans. The essential need for documentation and communication of presenting risks and the reasons underpinning these risks are highlighted. The value of co-production with the service user and family/carer is also covered. Standardised paperwork and forms to record the WARRN assessment and formulation are provided for use by clinicians following training. 83
Typically, healthcare professionals within emergency department environments have limited mental health training, and as such, feel ill equipped to assess and manage the associated risks apparent for children or adolescents presenting following an episode of self-harm or attempted suicide. 89 The limitations of these prediction methodologies likely impact on clinicians’ confidence when assessing suicide risk. Dealing with patients who self-harm and/or are suicidal is perhaps one of the most difficult challenges faced by clinicians. 75 One study estimated that 88% of mental health professionals have at least some level of fear relating to a patient dying by suicide, as well as discomfort around working with suicidal patients. 90 More than two-thirds of doctors practising emergency medicine believe that they are insufficiently trained at assessing those attempting self-harm. The limited training that health professionals receive relating to the assessment and management of suicidality may contribute to the burden felt by clinicians working in healthcare settings. Learned helplessness may result as suicide rates remain unaffected and predictive data have little impact on reversing this rate. The checklist-style structure of risk assessment within many NHS mental health services forms an ‘aide memoire’ of items characteristic of many suicide risk prediction tools.
Evidence highlights that training focusing specifically on the management of the suicidal drivers, or factors mediating the cognitions, emotions and behaviours augmenting suicidal risk, resulting in suicidal behaviours, can have a positive effect on clinicians’ confidence, clinical skills and implementation of evidence-based practices. 91,92 Greater awareness and accurate knowledge can de-stigmatise self-harm behaviour by staff enabling them to develop a greater understanding of contextual issues. 93 Additionally, education and attitude awareness may equip professionals with alternative explanations for self-harm behaviour that can help them to become more empathic and, subsequently, to alter their behaviours. 89,94
Training was a major component of a service-improvement initiative aimed at improving suicide prevention in North East Lincolnshire. 75 Three phases of training were delivered across the organisation: ‘suicide risk triage’ training, CAMS training, and CAMS concordance. All qualified staff were required to attend a mandatory 1-day training course entitled ‘risk triage training’ in groups of approximately 12 staff. Besides providing an overview of how the ‘suicide risk triage’ model was to be implemented within services, training collected data on factors that clinicians felt impacted on their confidence during the suicide risk assessment. The mandatory training also ensured all clinicians met a baseline level of ability and knowledge and was delivered to all new and newly qualified clinicians. Anecdotal feedback from the training highlighted the positive impact of a clear, structured approach to clinical risk decision-making to help clarify the most appropriate pathways to care for suicide risk presentations and the benefit of having support available for decision-making around challenging risk cases. The authors highlight evidence that CAMS training can significantly decrease clinician’s anxiety about working with suicidal risk and increase confidence, with results sustained at 3-month follow-up. 95 However, they acknowledge that the CAMS approach has yet to be evaluated in the UK.
Evidence from another study suggests that while training may help in ensuring staff can engage with the theoretical aspects of the situation they need additional provision for practical implementation. 96 Reflective peer review is suggested as one mechanism by which to help staff to reflect on their risk assessments, consider the knowledge and information that has informed their risk-management plans and discuss this with their peers in a supportive environment. 96 The authors claim that such a programme improved staff skills, confidence and documentation. 96
Similar findings are reported from a joint Australia–Switzerland initiative to investigate whether a training intervention increases GPs’ detection sensitivity for probable mental disorders in young people. 97 While improvements in detection were demonstrated these related only to more clearly detected cases and not to a more pragmatic clinical definition. The authors concluded that improving recognition of mental disorder among young people attending primary care is likely to require a multifaceted approach targeting young people and GPs. 97 Training is a necessary, but not sufficient condition for improved detection.
7. A role for supervision
-
Programme Theory 7. IF staff are supported by ongoing supervision THEN staff feel able to deliver a consistent approach to risk assessment LEADING TO a reduction in adverse events.
Supporting evidence
NICE guidelines specify that ‘Child and adolescent mental health service practitioners involved in the assessment and treatment of children and young people who have self-harmed should… have regular supervision’. 14
Evidence base: one clinical guideline, one service improvement project and one survey.
Successful suicide prevention requires that clinicians are confident when faced with suicide risk is a pertinent issue for suicide prevention. 75 There is conflicting evidence on whether clinicians focus on predicting the probability of suicide, despite little evidence supporting the utility of this approach. 75 A recent survey suggests that attitudes and behaviours towards the predictive ability of tools may differ between doctors and other health professionals. 38 However, the survey did not specify whether doctors were specialists or non-specialists or whether their experience was based on specialist training in mental health or rotations.
One NHS mental health provider implemented a service-wide, systems-level approach to suicidal risk (known as ‘suicide risk triage’),75 with supervision as a key component. This sought to address issues around clinicians’ confidence when assessing suicide risk, identified through training sessions, which highlighted the value of shared responsibility with senior supervising colleagues when considering more challenging suicide risk assessments. By addressing the concerns of all clinical staff, through a formal supervision hierarchy this system-level approach sought to ‘minimise confounders of objective, person-specific clinical risk decision’. 75 The supervision hierarchy was provided to support clinicians if they were unsure about the level of suicidal risk a service user presented with, the treatment plan they would develop for them, or if they felt that the risk was potentially life-threatening and therefore needed escalation for assessment and intervention. 75 Supervision arrangements included additional training for nominated clinicians within each team who were available to support/advise their colleagues when making difficult decisions around assessment and management of suicide risk. This support could be extended further up the hierarchy to trained clinicians and senior staff with extensive experience of managing clinical risk. 75 Clinicians affirmed the benefits of having a supervision structure in place, together with an organisation-wide approach for handling suicide risk cases.
8. Service user involvement
-
Programme Theory 8. IF families and carers are involved in the assessment process THEN families and carers are given an opportunity to express their views on potential risk LEADING TO a collaboratively developed risk-management plan.
Supporting evidence
This programme theory component is based on the NCISH report,38 which found that clinicians considered that closer contact with a patient’s family is the second most important risk-reduction factor in preventing suicide, after closer supervision of the patient. NICE guidance [NG 225] states that the professional should ‘discuss with the person and their families or carers (as appropriate), their current support network, any safety plan or coping strategies’. 14
Evidence base: one clinical guideline, one mixed-methods study, two qualitative studies, two service improvement projects and one survey.
One mixed-methods study from the UK reviewed risk-assessment tools currently in use and concluded that personalised management plans should be collaboratively developed with patients and their families and carers. 84 Engaging carers in discussions on risk has been shown to improve carer satisfaction. 98 Davies’ structured interview for assessing adolescents in crisis17 is one tool that includes structured interview/checklist assessment with ‘parenters’. The rationale cited is the need to guard against any omissions, for whatever reason, from the young person. Specifically, its developers point to how mood troughs are more critical than averages when conducting the risk assessment and that talking to significant others (e.g. parents) can serve to elicit such information.
More broadly, involvement of service users and their carers in mental healthcare planning is largely welcomed by mental health professionals. 99 However, tensions between user and carer involvement and professional accountability remain to be resolved. Conventional staff training programmes are commonly viewed as deficient, requiring that user involvement depends for its success on individual, relational skills. 99 Notwithstanding a generally favourable professional view of user involvement, challenges remain in relation to a lack of effective implementation support. 99
9. Interagency communication
-
Programme Theory 9. IF mental health staff communicate risk assessments to primary care THEN young people are directed to appropriate care LEADING TO successful health outcomes.
Supporting evidence
This programme theory component is based on the NCISH report,38 which identified a pressing need to improve access to and collaboration between primary care and mental healthcare services.
Evidence base: Three qualitative studies and one commentary.
Many UK studies describe issues that GPs have with mental healthcare services. Mental healthcare professionals are thought to tend to minimise GPs’ assessments of patients’ suicidal state. Adolescent contact with primary care presents an opportunity to conduct suicide screening and intervention. However, most primary care providers do not screen adolescents for suicide risk, perhaps because of suicide being a low base rate event. 100 Providers may feel that they lack formal psychiatric training or they may experience a general discomfort about screening adolescent patients for suicide risk. 100 Cumulatively, as many as 83% of adolescent suicide attempters are not identified as such by their primary care providers. 100
GPs report feeling stuck with patients, because they rarely meet the criteria for review and, therefore, remain in primary care. 101,102 A recent British study described how GPs feel professional isolation; being ‘lost in a referral maze’. 103 British GPs have also expressed the need for mental health staff based in GP practices. 103
10. Personalisation and individualisation
-
Programme Theory 10. IF the management of risk is personal and individualised THEN young people do not see their care as ‘protocol driven’ and don’t feel alienated LEADING TO their engagement with care.
Supporting evidence
This programme theory component is based on the NCISH report,38 which found that patients expressed a wish for ‘a personalised approach, not based on the completion of a checklist’. The team highlighted their previous research to suggest that risk is often individual and risk management should be personalised. 104,105
Evidence base: two qualitative studies, one mixed-method study, one pilot study, one service improvement project, one confidential inquiry, one survey and one commentary.
Young people dislike assessment approaches that are inflexible or binary; perceiving them as failing to capture nuance in their mental states and potentially impacting negatively on access to health care. 59 Instead, young people want to be treated in a holistic and individualised manner. 59 This finding reinforces recommendations that methods that categorise patients into ‘risk-level’ groups should not be used to determine treatment outcomes, as they can miss key opportunities for intervention. 18 In particular, methods that feel impersonal to young people, such as ‘tick-box’ or checklist-style approaches, are unwelcome. 59
A UK-based mixed-methods study, which examined risk-assessment tools in current use, highlighted the need for management plans that are personalised and collaboratively developed with patients and their families and carers. 84 These findings are substantiated by contemporary qualitative research exploring conversations of self-harm in the emergency department. 106 Patients identified two main types of approach:
-
A therapeutic interaction made people feel their life mattered and instilled hope for the future.
-
A formulaic assessment focusing on risk made people feel their life did not matter and hopeless about the future (see Table 4).
| Therapeutic interaction | Formulaic assessment |
|---|---|
| Unscripted conversation, really listening and acknowledging distress | Checklist questions that are a barrier to trust, disclosure and listening |
| Warmth, positive non-verbal communication that fosters trust and disclosure | Feeling judged and unworthy of help |
| Difficult yet direct conversations helping people understand their feelings | Trivial treatment suggestions |
| A co-produced treatment plan | Feeling unsafe to go home |
Even though patients interviewed were 18 years and older (eligibility was 16+ years) the data explores staff approaches rather than patient-specific factors so is likely to be transferable conceptually to the experience of children and adolescents presenting to the emergency department.
In the wider context of safeguarding it has been observed that health and social care professionals are in constant tension, accountable for promoting individual autonomy while seeking to predict accurately the level of risk resulting from subsequent action. 107 This tension is equally present within risk assessment for children and adolescents and reflects a wider literature, which contends that the focus of mental health organisations is now on risk management and quality assurance and patient safety. 108 Even where this imperative is not explicit it is revealed in how the purpose of tools is explained. For example, Davies’ structured assessment for adolescents in a crisis concludes by stating that ‘a structured interview or checklist of questions offers a fail-safe for clinicians to make sure that all important factors are considered when making an assessment’. 17
11. Integration within a whole-system approach
Programme Theory 11. IF organisations involved in risk assessment utilise a whole-system approach THEN this strengthens the standards of care for everyone, LEADING TO the safe management of supervision, delegation and onward referral.
Supporting evidence
This programme theory component is based on the NCISH report, which stated that risk assessment should form ‘one part of a whole-system approach that should aim to strengthen the standards of care for everyone, ensuring that supervision, delegation and onward referral are all managed safely’. 38
Evidence base: one systematic review, one qualitative study, one survey and two commentaries.
The need for a whole-system approach is noted by the most recent systematic review considered within this realist synthesis. 109 It noted the policy direction of numerous best practice and policy guidelines for the assessment of risk from the UK, USA and Australia among others, all of which identified the need for ‘a whole system, multiagency, and collaborative approach’. 109 The same systematic review drew attention to ‘a clear lack of specificity as to how to implement the recommendations in practice’. 109 Furthermore, the review pointed out how ‘no single model of risk assessment was discussed in more than one document’,109 substantiating the conclusions of variability and fragmentation. Research suggests that paternalistic professional attitudes, homogenisation of service users, and organisational structures prevent the cultural change required to shift to a strengths-based approach to risk. 5,49,107,110
As a complementary activity the review team identified three ‘counter programme theories’, which relate to how the risk-assessment process might result in unintended consequences.
12. Trying to predict
Programme Theory 12. IF staff view risk-assessment tools as a way of predicting future suicidal behaviour THEN staff incorrectly interpret individual levels of need for care LEADING TO inappropriate use of restrictive practices such as involuntary hospitalisation, restraint, sedation and seclusion (for the service user).
Supporting evidence
This programme theory component is based on the NCISH report,38 which reported that risk assessment has traditionally focused on prediction; patients being categorised into low, medium or high risk of a particular outcome.
Evidence base: two clinical guidelines, three systematic reviews – one with meta-analysis, one narrative review, two cohort studies, one observational study, one mixed-methods study, two surveys and four commentaries.
NICE guidelines state that risk-assessment tools and scales should not be used to predict future suicide or repetition of self-harm (risk screening), or to determine who should or should not be offered treatment. 14 The NCISH report38 found that scores on checklists also determined management decisions; contrary to national guidelines for self-harm assessment.
The NCISH report38 highlights research that suggests that categorising risk in such a way is unhelpful in guiding the treatment and management of a patient,111,112 and has poor predictive value. 16,113–116 It is supported by a mixed-methods study in the UK, which collected views from clinicians, service-users and carers on the use of risk-assessment tools. 84 Graney et al. highlight how most patients who died by suicide in the UK had been assessed as low risk in their last contact with mental health services. 84 They concluded that, in line with national guidance, risk assessment should not be seen as a way to predict future behaviour and risk screening should not be used as a means of allocating treatment. 84 The NICE guidelines suggest risk assessments might be used as prompts or measures of change. 18 Evidence suggests that risk-screening tools are no more accurate at predicting risk than expert specialist mental health professional clinical judgement in non-acute psychiatric outpatients. 114 A later review suggested the pooled positive predictive value for suicide was 5%: for every 100 people rated at high risk, five would go on to die by suicide. 117 More importantly, risk scales would miss suicide deaths in the large ‘low-risk’ group. 117
Most tools identified in the NCISH survey38 encouraged staff to make predictions of future behaviours and stratify risk, for example, into high, medium, and low or numeric risk categories. Overall, 80 (94%) tools used risk categorisation to inform care. In mental health services risk assessment has traditionally focused on prediction (risk screening). Around a third of nurses (n = 15, 32%) and managers (n = 11, 38%), but none of the doctors, thought tools had predictive value, compared to around two-thirds of psychologists (n = 20, 70%). 38
Notwithstanding acknowledged risk factors for such harmful acts as suicide and violence, no evidence has substantiated that identifying and responding to risk factors is useful in predicting, preventing or reducing risk of harm. 20 Even where risk assessment is believed to be useful, incorrect interpretation of individual need for care118 can lead to restrictive mental health practices, such as involuntary hospitalisation, restraint, sedation and seclusion. 20,119 Unintended consequences of such practices themselves present competing risks, placing both patients and staff at risk of harm. 20,120
In summary, then, no widely accepted tools exist for clinically assessing a patient’s risk of subsequent self-harm or suicide. 121 Specifically, within a child and adolescent population context, many promising measures for use in child and adolescent populations have insufficient psychometric data, and require further research. 121
13. Trying to score
Programme Theory 13.IF clinicians use risk-screening tools and scales in isolation within the risk-assessment process THEN treatment decisions are determined by a score LEADING TO incorrect interpretation of individual need for care and inappropriate utilisation of CAMHS (for the service).
Supporting evidence
This programme theory component is based on the NCISH report,38 which found that, contrary to national guidance, scores on locally used tools determined management decisions. Indeed, one of the clinical messages of the report is that ‘Risk is not a number, and risk assessment is not a checklist. (Risk screening) Tools if they are used …should be considered part of a wider assessment process. Treatment decisions should not be determined by a score’. 38
Evidence base: one systematic review, three qualitative studies, one service improvement project, two surveys and six commentaries.
A recent systematic review surveyed the available tools and concluded that limitations in the use of risk-screening tools in isolation as a predictor needs to be recognised. 109 The review concluded that no one risk-screening scale was supported by sufficient evidence to sustain its use in clinical practice. The review authors argued that this lack of empirical evidence should be used to engineer a radical shift in the contemporary discourse in the patient safety literature on risk assessment. Furthermore, they claim that the focus on risk-screening tools may deter the development of sound clinical judgement frameworks. Clinical judgement is considered essential for the use of Davies’ structured interview for assessing adolescents in crisis. 17 Its originators reason that sometimes a person only ticks a few boxes when they are at significant risk of harming themselves. Weighting within the items of a tool may mean that these important indicators in isolation may fail to trigger a clinical threshold. Furthermore, the development team reason that ‘mood troughs’, not averages, are more critical within the risk assessment. 17
Numerous writers have discussed the advantages and disadvantages of using risk assessment tools to assess risk. 8,48 Survey research suggests that nurses favour ‘interpretative’ approaches to assessment, relying on their own ‘instinct’ to guide assessment. In contrast, other studies suggest that most respondents believe that risk-assessment tools facilitate professional decision-making. 5 Critics point out that despite claims that risk-assessment tools help to manage risk, there is little evidence to support such assertions. 48 For instance, 87% of respondents in a survey of 1937 psychiatrists endorsed the view that ‘tools provide a false sense of security, as there is little direct evidence that tools help to reduce adverse events’. 19
The literature available suggests that intuition or the unstructured approach continues to form a key part of how nurses determine decisions about risk,122,123 with some studies suggesting that nurses see risk assessment as the doctor’s responsibility,122 and try to offset clinical responsibility when practising risk assessment and management by referring decisions to a psychiatrist or the team. 124 In relation to risk-assessment tools, only one study was located that reported nurses using validated tools or derivatives to guide their practice;66 while some of the community mental health nurses (CMHNs) in this study reported using tools they still favoured clinical judgement and ‘interpretative’ approaches. Nurses in other studies also report some ambivalence towards using tools, viewing them as a technology of psychiatry designed to erode clinical expertise or as bureaucratic instruments without value or purpose. 122,125 Conversely, others propose that they facilitate discussion between practitioners about risk and enhance care documentation. 122 They are also viewed as providing a measure of legal protection from liability and an important way of documenting and justifying decisions. 123 However, nurses also view risk-assessment approaches as little more than strategies to protect organisations, should an adverse event occur,124 contributing to defensive antitherapeutic practices. 126
14. Trying to do things differently
Programme Theory 14. IF staff develop their own tools for risk assessment THEN checklists and scales lack formal psychometric evaluation LEADING TO limited clinical utility of tools for risk assessment and unnecessarily restrictive treatment options.
Supporting evidence
This programme theory component is based on the NCISH report,38 which concluded that ‘there is little place for locally developed tools’. Approximately two-thirds of NHS mental health organisations use locally devised adaptations that lack formal psychometric validation. 115
Evidence base: one systematic review, three qualitative studies, two quantitative studies, one mixed-methods study, one observational study, one cohort study, one service-improvement project, two surveys and two commentaries.
Recent research confirms the limited clinical utility for predicting suicide and self-harm using risk-screening scales. 113,114,116 Furthermore, the use of such scales may result in unnecessarily restrictive treatment options for those categorised as ‘high-risk’. 127 Evidence reviewing the predictive value of widely used risk-screening scales in the UK has highlighted the low specificity of such scales for suicide and self-harm, which may result in individuals remaining within mental health services for longer than necessary. 113 In such cases, where staff inappropriately identify suicide risk, targeted treatment to assist suicidality may be superseded by restrictive care planning, such as compulsory detainment and hospitalisation. 127
Individuals with suicidality present with needs that are not exclusively mental-health-based, including societal, community, relationship and individual risk factors. 128 Assuming that suicidality is the result of a mental health diagnosis may place an unnecessary burden on mental health professionals to prevent suicide, as well as increased blame if an individual who does not seek help completes suicide. 129 Previous research estimates that, for those individuals who do have contact with healthcare services, only between 3% and 22% of individuals had reported suicidal intent at their final appointment with a health-care professional before their suicide,130–132 suggesting suicide risk identification is more complex than a simple dyadic relationship between suicide expression and psychiatric disorder. Unsurprisingly, UK suicide rates remain high, given the limited utility of suicide risk prediction methodologies that remain routine practice across mental health providers.
Almost without exception, the above programme theories focus on conducting a risk assessment that extends beyond a mere tick-box exercise to embrace all elements of a thorough biopsychosocial assessment. An overarching line of argument encapsulating all 14 programme theories might read as follows:
If risk assessment to support the mental health of children and adolescents takes place within a wider assessment process (PT1) using simple accessible, standardised tools (PT1) that are not developed locally (PT14) and not used in isolation (PT13) THEN staff are able to focus on building relationships (PT2) and to feel comfortable when asking about suicidal thoughts (PT4). Consistent risk-assessment processes (PT5) that gather good-quality information (PT3), offer personalised and individualised risk management and do not seek to ‘predict’ suicidal behaviour (PT12) are facilitated by family and carer involvement in assessment (PT8) and good communication with primary care. Staff are supported to deliver risk assessment within a context where they receive good-quality on-going supervision (PT7) and where they have been appropriately trained to assess, formulate, manage and refer risk (PT6). As a consequence, staff gain increased knowledge, skills and self-efficacy, CAMHS services achieve a reduction in inappropriate referrals and more effective use of CAMHS services, ultimately leading to a reduction in rates of self-harm, symptoms precipitating suicidal ideation, and rates of suicide.
While success (‘what works’) can be conceived in terms of producing a treatment plan to manage the current and future needs of the child or adolescent patient it necessarily extends to the effectiveness of interventions to reduce self-harm, suicidal ideation and suicide attempts. Such a link proves challenging to demonstrate.
The next section examines the tools and approaches that exist and the extent to which these demonstrate both the rigour and relevance required to use these tools in UK clinical practice.
Results 2: Approaches to risk assessment for self-harm and suicide
We used two approaches for identifying tools and approaches to identify self-harm and suicide in children and adolescents. We looked for (i) primary studies that evaluated individual tools or approaches and we also sought to identify (ii) reviews of multiple tools and approaches. We identified 49 tools or approaches and eight reviews and mapped their contents within a mapping review.
Risk assessment tools and approaches for self-harm and suicidality
We identified 49 papers reporting tools or approaches to assess the risk of self-harm and suicidality among children and adolescents (see Figures 4 and 5). Tools were all used in UK-based studies (development of the tool may have occurred elsewhere) or reported from surveys conducted in a UK context (see Table 5). Nine of the tools and approaches are used for generic risk assessment within UK services according to recent UK or regional surveys. 38,115 Five instruments have been developed specifically for use within a UK paediatrics setting. Fourteen scales were developed outside the UK for specific use with a child or adolescent target group. The remaining 21 were generic tools for suicide or aspects of harm that have been adapted, tested and/or used in a child and adolescent patient group.
FIGURE 4.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram for mapping review: primary studies.
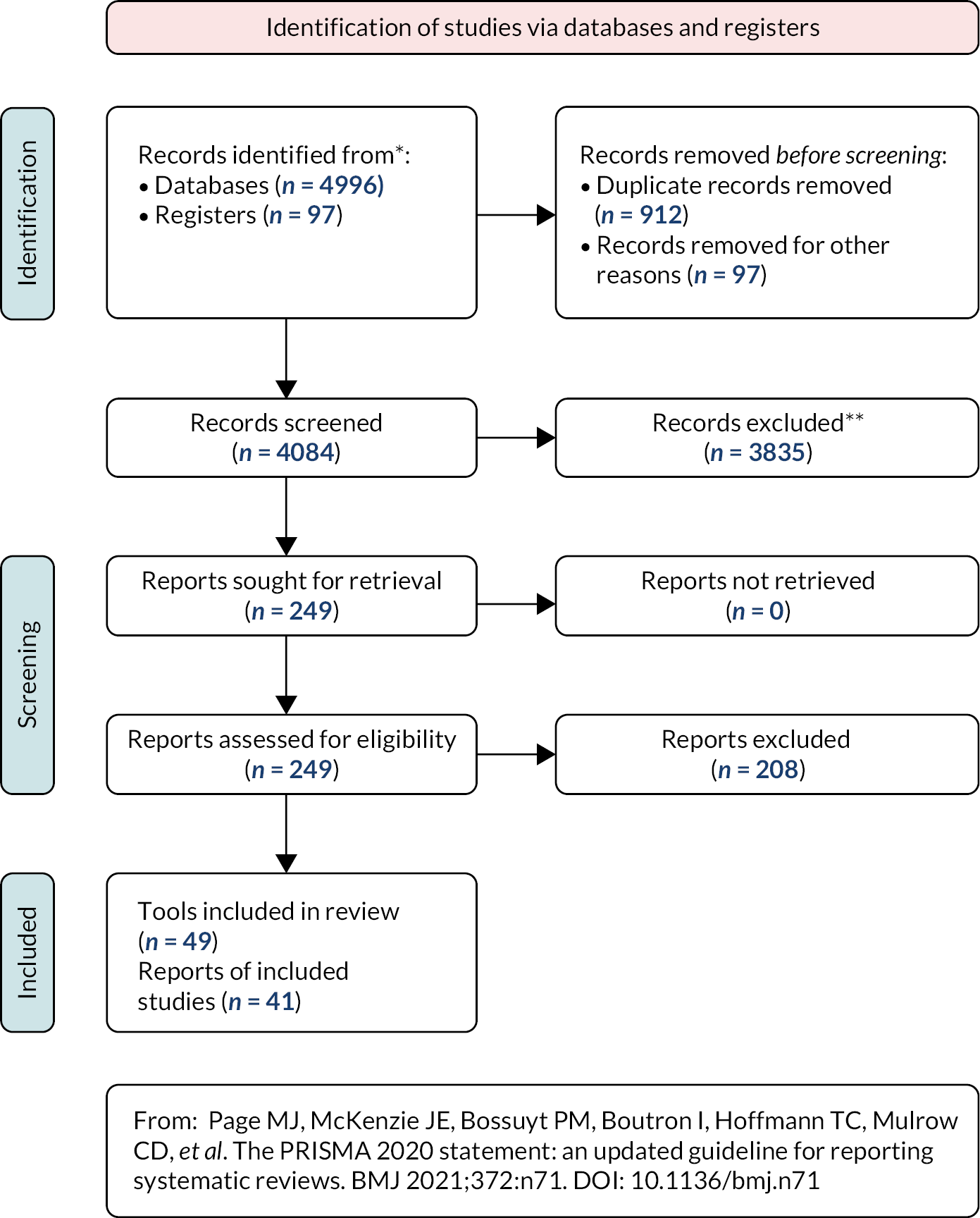
FIGURE 5.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis diagram for mapping review: systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. DOI: 10.1136/bmj.n71
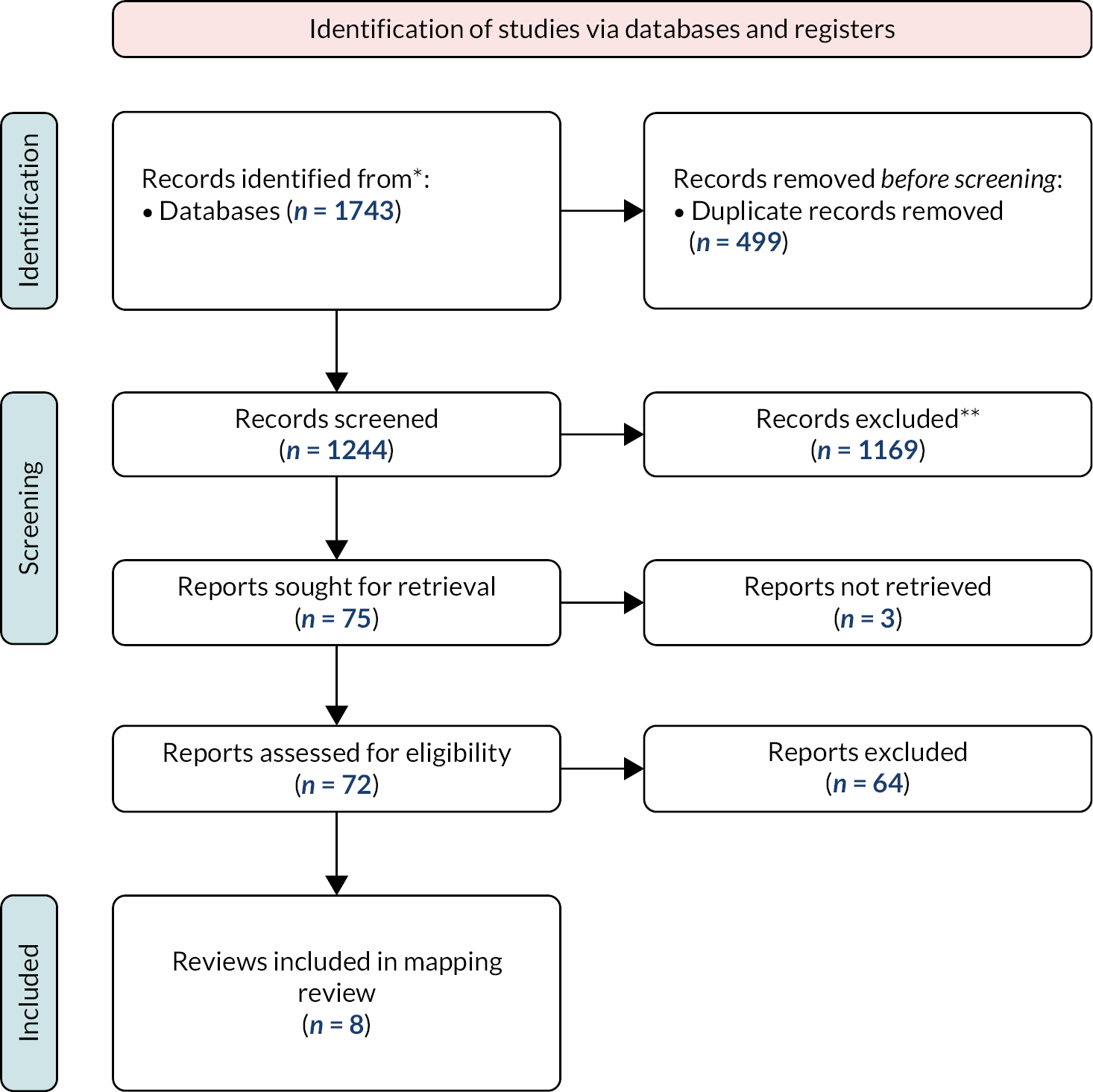
| Term given to assessment focus (associated studies) | Biological approach | Psychological approach | Social approach | Biopsychosocial approach |
|---|---|---|---|---|
| Context CAMHS-child assessments | ||||
| Psychosocial assessment (of mental state, risks, and needs)70,133,135,138,142 | ○ | ● | ● | ○ |
| Clinical assessment139,141,143 | ○ | ● | ● | ○ |
| Context CAMHS-family assessments | ||||
| Extended family assessment134,137 | ○ | ● | ● | ○ |
| Context – primary care | ||||
| Clinical management – primary care140 | ○ | ● | ● | ○ |
| Context – other professionals | ||||
| Screening for suicide and self-harm (Youth Justice System)136 | ○ | ● | ○ | ○ |
| Guidelines and associated studies | ||||
| Clinical assessment145 | ○ | ● | ● | ○ |
| Self-harm: assessment, management and preventing recurrence14,144 Royal College of Psychiatrists Managing Self-Harm in Young People15 |
● | ● | ● | ● |
| Special Educational Needs (Special Educational Needs code of practice, 2014)145 | ||||
Mapping assessment literature
The next section aims to map the included studies and guidelines on clinical risk assessments more generally (as opposed to the following section, which focuses on the utility of scales or tools).
Eleven studies discussed an assessment process for risk assessment70,133–143 in contrast to studies that focus on specific risk-assessment tools or scales. Four guidelines and associated papers on risk assessment were also identified. 14,15,144,145
Table 5 maps biological, psychological and social elements of assessment approaches to assessment approaches (including studies that also include a tool) for self-harm and suicidality focused assessments only. Quality assessment was undertaken on the empirical studies. One tool was excluded because it did not carry a suicide/self-harm focus. 142
This section begins by looking at elements of the guidelines identified in Table 8. All elements are identified in the NICE (2011) guidance,14 which states that:
A risk assessment is a detailed clinical assessment that includes the evaluation of a wide range of biological, social and psychological factors that are relevant to the individual and, in the judgement of the healthcare professional conducting the assessment, relevant to future risks, including suicide and self-harm (p. 20).
This is reinforced by the Royal College of Psychiatrists guidelines for Managing Self-Harm in Young People,15 which present with acute self-harm in the emergency department, stating:
Admission should be to a paediatric, adolescent or medical ward or to a designated unit. This is indicated regardless of the individual’s toxicological state so that comprehensive physical and psychosocial assessments can occur and management/crisis intervention can be planned and initiated.
The emphasis is, therefore, consistent with a psychosocial approach with physical assessment.
The 2021 National Confidential Inquiry into Suicide and Safety in Mental Health: Annual Report145 emphasises psychological elements and so-called co-morbidities, but biological assessment is less clear. The guidance states:
Suicide in people aged under 25 Clinical services should ensure that services for children, young people, and young adults have the skills to respond to the clinical complexity of many younger patients, including combinations of personality disorder diagnosis, eating disorder, self-harm and alcohol or drug misuse. These co-morbidities add to suicide risk but can act as a reason for non-acceptance by services designed for single conditions (p. 8).
The Department of Education code of practice145 specifies the role of schools in mental health responsibilities towards children. The guidance provides statutory guidance for education and health services in the early identification and support of children and young people with mental health problems. ‘Where there are concerns [about a child’s mental health needs], there should be an assessment to determine whether there are any causal factors such as undiagnosed learning difficulties, difficulties with communication or mental health issues’ (p. 96). 145 Schools should work closely with the local authority and other providers to agree the range of local services and clear arrangements for making appropriate requests (this includes CAMHS) (p. 103). However, the guidance is not framed as a risk assessment. 145
In the context of CAMHS the psychosocial assessment term was used in five studies. 70,133,135,138,142 The psychosocial assessment was viewed as an integrated assessment of needs and risk that informs clinical management in line with clinical guidelines. A specific study about internet use and self-harm reports that clinicians found it acceptable to ask about internet use during psychosocial assessments to inform perceptions of risk and decision-making. 142 The term ‘clinical management’135 was used, which included reference to psychosocial assessment in the study of episodes of self-harm and repetition presenting to three UK centres over a 10-year period (2000–9) to examine the relationship between four aspects of management and repetition of self-harm within 12 months. Provision of a psychosocial assessment by mental health staff was associated with a 40% lower risk of repetition following self-harm in two of the three study centres (p. 3). A separate analysis found no association with a lower risk of repetition than psychosocial assessment alone than (1) psychosocial assessment and specialist community mental health follow-up, (2) psychosocial assessment, medical admission and specialist community mental health follow-up, (3) psychosocial assessment and psychiatric admission.
Studies using the term clinical assessments139,141,143 only referred to psychological and social elements, although not within an explicit psychosocial approach. Patton et al. discuss how self-harm in adolescents is associated with continued behavioural, emotional, and social problems well into adulthood. 141 Horowitz et al. 139 imply that physical or biological concerns are missed in the case of youth suicides, finding ‘Over one-third of the youth who killed themselves had a medical illness, most often a young person-specific condition such as asthma or acne. Without comorbid psychiatric diagnoses, these young patients … may easily pass through the healthcare system undetected’ (p. e12).
Two studies specifically involved family members in the assessment process. 134,136 Participants in a psychoanalytic qualitative study to understand suicidal behaviour in young people referred to specialist CAMHS were offered an extended individual and family assessment. 134 The fractured reality potentially identified leads to incongruence in the young person’s presentation, which may be misleading when assessing risk.
One cohort study of primary care clinical management assessments following episodes of self-harm stratified variables by sex, age group, and practice level deprivation. 140 Mental illness comorbidity was examined across a broad range of diagnoses. 140 This study focused on outcomes (self-harm episodes, clinical management and mortality) (discussed in Impact on mental health assessment processes and outcomes). However, it does convey the elements included in clinical management through assessment according to the likelihood of referral to mental health services and psychotropic drug prescribing. The importance of gaining ‘the social picture’ are reiterated in papers without a specific self-harm or suicide focus. 146 One study of screening for self-harm derived from the context of youth offending. 136 The role of youth justice staff is principally seen in signposting the young person to mental health services and then supporting them during their engagement with those services. 136
Table 6 shows how tools from Davies, FACE, SDQ and WARRN tools map to outcomes from NICE (2011) recommendations.
| Study (CAMHS context featuring real-world practice) | Features of assessment (including RA tools) – and associated textual evidence | Previous incidences of self-harm | Identification of depressive symptoms | Diagnosis of other psychiatric illnesses | Social relationships and contexts (history) | Identification of risk factors and protective factors | Identification of relationships (un)supportive | Identification of longer-term risks | Integrated care and risk-management plan | Outcomes and role of RA tool (including changes reported in clinical encounter) |
| Therapeutic assessment148 Uses Therapeutic Assessment Quality Assurance Tool (TAQAT, primary outcome measure)149 |
Followed by 30-min intervention covering:
Family members involved in all stages of TA whenever possible. |
? | ? | ? | ● | ? | ? | ? | ○ | Only those with non-suicidal self-harm showed improvement on Children’s Global Assessment Scale score following brief therapeutic intervention. No interaction between treatment and suicidality. Columbia Classification Algorithm of Suicide Assessment used in sampling of RCT for suicidal and non-suicidal self-harm categories |
| Davies’ structured interview for assessing adolescents in crisis17 Structured assessment Three structured interviews as checklist of key questions to be asked by health professionals assessing suicide risk of children and adolescents in crisis situations. Questions allow for quick and comprehensive assessment, reminding clinicians of factors to consider when deciding if a risk is significant or not, and ensuring that factors are not neglected or overlooked |
Proposed structured interview/checklist assessment in three parts:
Questions address both fixed factors (e.g. age, gender etc.) and fluid factors (e.g. level of hopelessness). Includes questionnaire for parent/carer, to guard against omissions from young person. Questions for clinician are to help analyse information obtained during other structured interviews and face-to-face contact. Information can then be shared with colleagues, and informed clinical judgement can be made on the risk. If any significant risks are identified then a risk-management plan is put into place |
○ | ● | ○ | ○ | ● | ? | ? | ● | From checklist: informed clinical judgement can be made on risk. From study: learning points and observations made by professionals in acceptability of checklist |
| WARRN-A formulation-based risk-assessment procedure for CAMHS83 Staff asked their opinion of WARRN training and the risk-evaluation process |
Formulation-based RA: Personalised evidence-based explanation of ‘to who’, ‘when’, ‘where’ and ‘why’ there may be a risk. Examination of individual’s previous problem behaviours is analysed to identify themes, contexts and motivations for the target behaviours. Hypothesising what behaviours may be risky (based on case history, interviews, discussion with family and carers, and other professionals, etc.), identifying situational factors that may increase or decrease risk, along with positive protective factors that might mitigate against risk. Risk formulation feeds directly into safety planning and risk management | ? | ? | ? | ● | ● | ? | ? | ? | Service evaluation of WARRN-A tool Clinicians reported increased clinical skills, increased confidence in their assessment and management of risk and in safety planning, the increased safety of service users and the general public, and a belief that WARRN had saved lives. Qualitative data showed that clinicians thought a common risk evaluation instrument across Wales and different agencies had created a common language and understanding that improved communication |
| Psychosocial assessment and Suicide intent scale Problem drug use, drug misuse and self-harm. Psychosocial assessment by member of the general hospital psychiatric service. Mental health professionals carrying out psychosocial assessment complete 18-item checklist indicating whether or not, in their opinion, specific problems are present |
Psychosocial assessment by a member of the general hospital psychiatric service. Following this assessment, the member of staff records detailed information about the patient and the episode of self-harm on a standard data entry form. Presence/absence of psychiatric and personality disorder is recorded, usually according to ICD-10 clinical criteria. The Suicidal Intent Scale part of psychosocial assessment Any number of 18 problem areas (e.g. legal problems, alcohol consumption) may be recorded as present |
● | ? | ● | ● | ? | ● | ? | ? | 18 risk factors rather than outcomes Repetition within 12 months of the index episode of self-harm More severe disorders being recorded. Clinical staff conducting psychosocial assessments tend to use a problem-orientated rather than a medical model approach |
| Examines characteristics of 64 young men, consecutively admitted to Bluebird House, an NHS mixed gender, adolescent forensic, medium secure hospital | Focused on young men’s clinical presentations, as informed by the Millon Adolescent Clinical Inventory, and their ICD10 diagnoses. - aids clinician in understanding the difficulties, Young men’s responses clustered in three main groups (Personality Patterns, Expressed Concerns and Clinical Syndromes. p. 24) Also examines their risk profiles, especially with regards to others, as informed by Structured Assessment of Violence Risk in Youth findings and staff recorded incidents. (Assessment is completed using information from multiple sources, including interviews with the adolescent, as well as their primary caregivers and from observations and incidents as recorded by staff during admission). Risk information was additionally derived from ‘Incident forms’ completed by nursing staff |
● | ? | ? | ○ | ○ | ○ | ? | ? | Study outcomes: Trajectory for some young men into adult personality disorders, their presentation and prognosis compared to female counterparts, and how their presentation contrasts with adult male forensic populations |
| FACE-CARAS150 - to record and analyse clinicians’ views of the proposed FACE-CARAS | Proposed FACE-CARAS assessment system: Screening questions (the ‘FACE Risk Profile’) guide clinician to complete further specific schedules from choice of nine, given previous risk factors flagged and clinical experience of the rater. Both historical (static) and current (dynamic) risk factors. Provides anchor point descriptions so items can be coded as absent or representing a perceived low, moderate or high level of risk in that domain. Information used to develop a risk formulation and management plan, as well as assign global scores to a number of risk domains |
? | ? | ? | ● | ○ | ○ | ? | ● | Qualitative study - Emerging themes highlighted need to add items such as criminality and fire-setting to the violence RA schedule; a structured approach for risk of sexual harm be utilised; and an eating disorder RA be included |
| SDQ151 investigated associations between family reports of child mental (using self and parent SDQ) and clinician-reported levels of functioning (CGAS). Also used SDQ AVS, which attempts to adjust the estimated change for regression to the mean and other non-treatment-related factors | Emphasises importance of taking account of multiple viewpoints when making appraisals of functioning and symptom severity. CGAS: clinician-rated scale of general functioning rated from 1 to 100, with 100 signifying superior functioning and 1 indicating extreme impairment152 SDQ: standardised emotional and behavioural screening questionnaire comprising 25 items on five scales: emotional symptoms, hyperactivity, conduct, pro-social behaviour and peer relationships153 SDQ AVS. The SDQ AVS estimates impact of treatment over and above what might be expected without intervention. Presenting problems checklist. Clinician-rated checklist developed by CORC. Includes hyperkinetic disorder, emotional disorder, conduct disorder, eating disorder, psychotic disorder, self-harm, autistic spectrum disorder, learning disability, developmental disability, habit disorder, substance disorder and other presenting problems154 |
● | ● | ● | ○ | ○ | ● | ? | ○ | Data set of 161,979 episodes of care collected by the CORC - self-harm represented 6.2% of sample. Outcomes in study associations between family reports of child mental (using self and parent SDQ) and clinician-reported levels of functioning (CGAS). Small-to-medium correlations found between family and clinician ratings. Ratings diverged for the lowest-function CGAS bands. Regression analyses showed that prosocial ratings from both child and parent contributed to clinician ratings. Knowing child-reported emotional problem severity made parent ratings of emotions irrelevant to clinician judgements. Positive association between SDQ AVS and CGAS; as hypothesised, CGAS showed more change than SDQ AVS, suggesting that clinicians overestimate change. Of measures included in study, parent SDQ was most prevalent in CORC data set |
This consideration commences by briefly reviewing the approaches specifically developed in the UK for children and adolescents (Table 7).
Tools and approaches developed in the UK for children and adolescents
Tools and approaches developed in the UK for children and adolescents are outlined in Tables 8–10.
| Developed in the UK for generic (i.e. child, adolescent and adult) use | Developed in the UK for children and adolescents | Developed non-UK for children and adolescents | Developed non-UK |
|---|---|---|---|
|
|||
|
|||
|
|||
Children and Young People - Mental Health Safety Assessment Tool
Contemporaneously (2018) with a scoping review of assessment tools of immediate risk of self-harm and suicide in children and young people by Carter et al.,39 the authors published a protocol for the development and psychometric evaluation of such an assessment tool; the Children and Young People - Mental Health Safety Assessment Tool (CYP-MH SAT). 147 The authors claimed this as the first UK-based study to develop an assessment tool to ascertain immediate risk of suicide and self-harm in children and young people presenting to acute paediatric hospital settings in mental health crisis. As a strength for the UK context, the protocol was tailored towards an English-speaking population, while recognising that further national and international testing and adaptations are required for generalisability. A corresponding weakness is its untried status with regard to ethnic minority populations within the UK population. The protocol used an opportunistic sample of self-selected experts to inform development of the assessment tool, recognising that such experts might be more motivated to take part and/or exhibit allegiances that might lead them to respond in a particular way.
The resulting instrument underwent rebranding as the CYP-MH SAPhE instrument when it appeared in 2021. 50 The published study sought to psychometrically assess the CYP-MH SAPhE instrument for identification of immediate risk of self-harm in children and adolescents, aged 10–19 years, in acute paediatric wards or emergency departments. Through the scoping review and subsequent collaboration with expert academics and clinicians, an instrument was developed to assess immediate risk of suicide and/or self-harm in children and adolescents in mental health crisis to acute paediatric hospital settings and emergency departments. Testing of the instrument across three acute hospital sites (Paediatric Emergency Departments and Acute Paediatric Wards) within the UK resulted in an eight-item instrument, weighted within two constructs (self-harm and suicidality). The authors justify development of separate self-harm and suicide facets based on extant literature that defines them as separate constructs. The authors claim that the strength of CYP-MH SAPhE lies in ‘its co-development by those in clinical practice’ for use within a clinical practice setting. 50
Despite recognised limitations (see Validity), the authors claim that the CYP-MH SAPhE instrument is a rapid and sensitive instrument to identify immediate risk of self-harm and suicidality in children and adolescents aged 10–19 years presenting to acute paediatric care. The authors conclude that the CYP-MH SAPhE tool has ‘potential utility as a screener by the paediatric health professional in the inpatient ward or emergency department as part of a holistic assessment’. Key to the authors’ claim is the phrase ‘as part of a holistic assessment’ – the role of stand-alone risk screening tools for risk prediction is no longer championed. They recommend that the CYP-MH SAPhE instrument requires further evaluation ‘to confirm its suitability and effectiveness in clinical practice’. 50
Davies’ structured interview for assessing adolescents in crisis
Having previously produced the Describe the risk; identify the options; choose your preferred option(s); explain your choice; share your thinking (DICES) System for Risk Assessment in Mental Health and Risk Management in Mental Health, the team at the Association of Psychological Therapies decided to extend their work with a tool for children. The team devised a structured interview/checklist assessment in three parts for parenters [‘parenter’ is the term used for the person(s) doing the parenting], the young person themselves and the clinician. The questions address both fixed factors (e.g. age, gender etc.) and fluid factors (e.g. current level of hopelessness at any specific point in time). Clinicians can then share information with colleagues and make an informed clinical judgement, recognising that a young person may only tick a few boxes even when they are at significant risk of harming themselves. Once significant risks are identified then a risk-management plan is put into place.
At the time of information (July 2013) only about 30 people had received the structured interviews. Much of the claim for its utility is indirectly attributed from the DICES Series of checklists to which more than 6000 people had subscribed to use. Although most professionals welcomed a tool to ensure they ‘covered all the bases’, a minority thought that ‘having a form to fill in’ hampered the development of rapport and a relationship between the young person and the professional. Many (though not all) agreed that ‘it was good that the professional had some framework and structure to operate within’, and that ‘nothing would be missed’.
Clinical judgement is vital when assessing suicide risk. Fluid factors, such as hopelessness, are not easily weighted in statistical models. Mood troughs, not averages, are more critical to an assessment; such information is only elicited by talking to the person and their ‘significant others’ (usually parents) and taking into account fluid factors, such as hopelessness and how they say they feel. The team claim that a structured interview or checklist of questions offers a fail-safe for clinicians to make sure that all important factors are considered when making an assessment.
Functional Analysis of Care Environments (FACE-CARAS) suite of tools
The FACE-CARAS toolkit has been developed to support practitioners in CAMHS in performing a structured risk assessment. 150 It covers multiple risk domains including violence, suicide, self-harm, experienced abuse and exploitation. The FACE-CARAS involves comprehensive risk assessment, including a risk scale – to produce a FACE Risk Profile and a clinical management plan (paper/electronic). Schedules enquire about both historical (static) and current (dynamic) risk factors.
Functional Analysis of Care Environments–Child and Adolescent Risk-Assessment Suite comprises a suite of tools – the practitioner completes an overall risk profile before selecting other tools for a more in-depth assessment where indicated. The three-step process comprises completing a Young Person’s Risk Profile as a ‘screening’ step, then one or more Focused Schedules as indicated at the screening stage, and then the ‘Formulation and Management Plan’ section of the Young Person’s Risk Profile as appropriate to the Focused Schedule(s). Items are either coded as absent or as representing a perceived low, moderate or high level of risk in that domain. The resulting information is then used to develop a risk formulation and management plan, as well as to assign global scores to each of a number of risk domains.
The tool was designed for a youth mental health setting; the mean age of original sample was 15.94 (range 12.23–18.71) with 36 males/69 participants. 157 Predictive ability was tested with a sample of 123 young people with clinician-completed FACE-CARAS ratings. These were examined in a retrospective file review to extract data on a relevant list of adverse outcomes at 3 and at 6 months following the assessment. 65 Although this was not a prospective longitudinal study, researchers were blind to the clinicians’ ratings, allowing valid testing of predictive power. The FACE-CARAS profile score was considered a good potential predictor of risks of self-harm, suicidal behaviours, serious self-neglect, abuse or exploitation by others, and violence to others at both 3 and 6 months. It was weakly ‘predictive’ of accidental self-harm and no better than chance at signalling physical ill health.
Evaluation indicated the usefulness of the ‘profile summary’ section of the tool as likely to generate clinically useful risk predictions, notwithstanding that guidance recommends that tools for risk assessment should not be used for risk screening in a predictive way. 14 In practice, clinicians often did not complete the subscales – the authors therefore recommend further work. 157
Risk-Taking (RT) and Self-Harm (SH) Inventory for Adolescents82
Its originators claim that the RTSHIA, a self-report measure designed to assess adolescent RT and SH in community and clinical settings, offers an improvement over existing measures by providing information about the full spectrum of potentially self-destructive behaviours alongside other significant information. As a self-report measure, they claim the benefits of standardised administration, wording and scoring and faster, more economical administration and scoring. Furthermore, they state that the quality of data produced by self-report measures compares to that from clinical interviews. People may be more comfortable admitting to sensitive thoughts and acts when asked to circle a response or write a brief explanation instead of providing a verbal report. Moreover, assuring participants of the confidentiality and anonymity of self-reports seems to be easier. In any case, few alternatives to self-report data exist when requesting personal and sensitive information from young people.
Furthermore, the RTSHIA was developed for, and validated in a clinical population of, adolescents because ‘behaviours defined by adults as risky or self-destructive do not have the same function in adolescents’. The study included a large and highly diverse sample of participants drawn from a wide range of age groups.
Another claimed advantage is that the RTSHIA assesses the frequency of self-harm behaviour, as opposed to simply recoding its presence/absence.
Several limitations must be acknowledged. First, the RTSHIA is primarily a self-report measure, and therefore dependent upon respondents’ comprehension of items, concentration ability and openness. Despite reassurance with regard to anonymity and confidentiality, participants may hesitate to give personal information to authority figures. In addition, younger adolescents, may feel that certain items are not applicable to them. Second, the wording of the questions does not discriminate between current and past history behaviours. Finally, concern has been expressed over whether the two scales are sufficiently comprehensive. Although both scales have been shown to work, have good psychometric properties and appear reliable and valid, results are preliminary and need replication with different samples.
In summary, the RTSHIA responds to a need to supplement in-depth interview-based instruments and captures wider presentations of self-harm. It supports the need to rely on multiple assessment methods. The authors acknowledge the likely added value of obtaining interview data beyond self-report questionnaires. They suggest that the RTSHIA can be used as a primary screening measure to be supplemented by interviews or focused measures, especially in clinical settings, where in-depth information is required. For the present, the RTSHIA appears to offer potential for use as a multifocused screening tool for identifying diverse problem behaviours/thoughts in adolescence and as a tool for assessing young people who self-harm. Although it is premature to draw conclusions about the utility of the scale, the RTSHIA currently represents a psychometrically sound, comprehensive tool with the potential for further empirical investigation.
The Self-Harm Questionnaire (SHQ)69 was designed to improve identification of self-harm in adolescents. The complete questionnaire consists of three screening questions enquiring about past incidents of self-harming behaviour or thinking, followed by 12 additional questions that are only presented to adolescents reporting previous self-harm.
Wales Applied Risk Research Network
WARRN is a formulation-based technique for the assessment and management of serious risk for users of mental health services, adopted across Wales. The developers of WARRN recognised that structured professional judgments were impractical to use in many NHS settings due to time constraints, the need for training on each instrument, and the multiplicity of possible risks faced by any service user. The development team, therefore, aimed to develop a ‘formulation-based’ approach to risk assessment to equip clinical staff with skills for implementation.
WARRN was previously in use in adult mental health services across Wales. The ‘youth’ version was modified in consultation with senior CAMHS staff from across Wales; the only changes required were to take a developmental framework to the assessment and to use age appropriate training vignettes. Training was implemented via a training the trainer cascade programme.
A service evaluation was conducted to evaluate WARRN and its impact across CAMHS in Wales. An online survey was disseminated to 88 NHS clinicians in CAMHS to evaluate their perceptions of the use and effectiveness of WARRN. Clinicians reported increased clinical skills, increased confidence in their assessment and management of risk and in safety planning, the increased safety of service users and the general public, and a belief that WARRN had saved lives. Qualitative data showed that clinicians thought a common risk-evaluation instrument across Wales and different agencies had created a common language and understanding that improved communication both across and between agencies. WARRN appears well accepted in CAMHS services, exerting positive effects on service-user well-being and safeguarding with potential implementation in other services. However, this favourable view of the WARRN tool is based mainly on internal evaluations and remains to be replicated by independent evaluation teams.
| Scale/tool/approach | Focus of assessment | No. of items/ subscales | Population tested | Completion format | Response format |
|---|---|---|---|---|---|
| Children and Young People-Mental Health Self-harm Assessment in Paediatric healthcare Environments (CYP-MH SAPhE)50 (formerly CYP-MH SAT)147 | Self-harm in acute paediatric wards or emergency departments | 8 items | 163 CYP presenting at acute hospital settings with primary mental health (cases) or physical health (non-cases) conditions50 | Self-report | Likert scale and dichotomous items |
| Davies’ structured interview for assessing adolescents in crisis17 | Depression in children and young people | Proposed structured interview/ checklist assessment in three parts:
Questions allow for quick and comprehensive assessment, reminding clinicians of factors to consider when deciding if risk is significant, and ensuring that factors are not neglected or overlooked |
Limited details of use (details from 2013) | Clinician completed | Three structured interviews with checklist of key questions for health professionals to ask when assessing suicide risk of children and adolescents in crisis situations |
| FACE-CARAS of tools157 | Self-harm of various forms | Suite of tools:
|
Youth mental health setting65,150; mean age of 15.94 (range 12.23–18.71) with 36 males/69 participants157 Retrospective file review of records from 123 young people with FACE-CARAS ratings examined for outcomes at 3 and 6 months.65 FACE-CARAS profile score good potential predictor of self-harm and suicidal behaviours at 3 and 6 months. Weakly ‘predictive’ of accidental self-harm and no better than chance for physical ill health |
Clinician report | Comprehensive risk assessment including risk scale – to produce FACE Risk Profile and clinical management plan. Schedules enquire about historical and current risk factors. Items coded as absent or as low, moderate or high risk. Information used to develop a risk formulation and management plan, and to assign global scores to risk domains |
| RTSHIA82 | Adolescent RT and SH in community and clinical settings | Questionnaire includes two subscales assessing separately risk-taking behaviours and self-injurious behaviours | 651 young people from secondary schools in England (11.6–18.7 years) and 71 young people referred to mental health services for SH behaviour in London (11.9–17.5 years) completed RTSHIA along with standardised measures of adolescent psychopathology. | Self-report | Questionnaire that assesses simultaneously risk-taking and self-harm behaviours. Items are rated on a 4-point scale (0 = never; 3 = many times), referring to lifelong history |
| WARRN83 | Serious risk (e.g. violence to others, suicide) | Not applicable (formulation-based approach; standardised paperwork and forms provided) | Not applicable (study evaluated clinician opinions)83 | Clinician report; coproduction with service user and family carers encouraged | Documented risk assessment and ‘formulation’ |
Table 5 presents summary information on the risk-assessment scales and tools included in the review. Data for these tables were extracted from included primary studies and from the seminal scoping review (2019). 39 This scoping review from Carter et al. (2019) originally reviewed 22 different tools. Our review team has not referred to the original papers reporting on the development of these tools, some of which date to the 1960s, or to the extensive literature on validation in different populations and settings. Our approach reflects a focus on use of the tools in clinical practice together with the resource constraints of this review. References to other studies are cited in the papers included in the tables.
The scoping review published in 2019 identified 26 risk-assessment tools reported in 22 full-text articles. 39 However, a high percentage (59%) of included studies were developed over 20 years ago. Concerns about psychometric properties are typically raised in connection with older tools and instruments.
Our analysis extended the comprehensive list of assessment tools included in the scoping review;39 adding two recent tools82,147 and expanding beyond formal tools to include overall approaches. The original scoping review39 started with 22 tools. This review added ten tools to those tools used for self-harm and suicide in a general population. We excluded tools previously included in the scoping review39 to reflect only tools used in a UK context and to capture the primary focus on suicide. As reported in the scoping review, tools varied in length, response and scoring format, age ranges and degree of psychometric testing. 39 Most assessments were tested across broad age ranges, and so lack sensitivity to the age groups of particular interest to this review. The relative lack of tools for children, as opposed to adolescents, is noticeable although this imbalance does seem to follow the self-harm and suicide age trajectory. Some tools, such as the SIQ and the SIQ-JR have undergone age-based revisions/adaptations. 39
The scoping review concluded that many tools were subject to limited psychometric testing, and no single tool was valid or reliable for use with children presenting in mental health crisis to non-mental health settings. 39 It recommended development of a ‘clinically appropriate, valid and reliable tool that assesses immediate risk of self-harm and suicide in paediatric settings’. 39
Tool development continues to see different rationales in terms of whether to focus only on suicide risk or whether to incorporate risk items relating to self-harm. No measure assessed risk of self-harm in isolation. 39 As with much psychological tool development most assessment tools were tested only in the USA and primarily with inpatients. Where studies report psychometric testing in UK populations this is indicated in the accompanying tables. 39 UK guidelines remain unable to promote the use of any one assessment tool to safely manage immediate risk of self-harm or suicide to inform clinical decisions in acute paediatric settings. 192 The accompanying analysis indicates that the ongoing preoccupation to identify or develop such a tool has proved something of a distraction when attention should focus on a holistic biopsychosocial assessment conducted within a whole-system approach to assessment.
| Scale/tool | Focus of assessment | No. of items/subscales | Population tested | Completion format | Response format |
|---|---|---|---|---|---|
| Children’s Global Assessment Scale152 [Added] |
Overall functioning | 10 deciles | Samples from CAMHS services in England151 | Clinician-rated | Scored within each decile to produce overall score (1–100) |
| C-CASA148 [Added] |
Suicide and self-harm | 8 items (categories) | 12–18 years. 71% female; self-harm; UK148 | Adverse event reports from trial sponsors | Categories ranging from ‘completed suicide’ to ‘not enough information’ |
| START:AV [Added] | Aggression and self-harm | 22 items in pilot version used for study | 90 adolescents (55 male) with and without developmental disabilities; medium secure adolescent service in UK166,167 | Completed by multidisciplinary care team | 3-point scale for each item as strength and vulnerability |
| SIQ-JR (Reynolds, 1987a)* |
Frequency and severity of suicidal ideation | 15 items | 11–18 years. Males/females; mixed ethnicity; students, psychiatric, suicide ideators, parentally bereaved; inpatients, school, outpatients, community | Self-report | 7-point Likert scale continuum Scores: 0-6 Total score: 0-90. Cut off: 31 |
| SIQ (Reynolds, 1987b)* |
Frequency and severity of suicidal ideation | 30 items | 13–19 years; males/females; mixed ethnicity; students, suicide attempters, suicide ideators, nonsuicidal controls. medical/surgical, psychiatric; Inpatient, emergency department, school, community | Self-report | 7-point Likert scale continuum Scores of 0-6 Total score 0-180. Cut-off: 41 |
| SIS188* | Suicide intent | 20 items 2 subscales |
Ages not defined. Males/females; mixed ethnicity; psychiatric, non-suicide attempters, suicide attempters; inpatient | Clinician-rated | Three-item Likert scale Scores: 1–3 Total score: 1–60 |
| The Child Maltreatment Interview Schedule173 [Added] |
Maltreatment | 5 categories (reduced to 4 for study) | 11–17 years presenting to Emergency Assessment Service in Princess Alexandra Hospital, Essex (UK) Population includes overdose in addition to self-harm189 | Clinician-rated? (Semistructured interview) | Appears to be yes/no |
| STOP-SAS*170 | Suicide risk | 14 items- children 19 items adolescent, parents, clinician |
8–18 year olds; males/females; mixed ethnicity; psychiatric,170 medicated;170 outpatients;170 Spain,170 UK,170 Italy,170 France,170 Germany,170 Netherlands170 | Self-report; parent- report; clinician report | 6-point Likert scale Adolescents, Parents, Clinicians: 0–5 scores Total score: 0–95; 4-point Likert scale Children: 0–3 scores; Total score: 0–42 |
| Adolescent Dissociative Experiences Scale (A-DES; version 1.0)172 [Added] |
Developed as screening tool of serious dissociative and post-traumatic disorders among adolescents |
30 self-administered items; four subscales capture (1) amnesia, (2) absorption and imaginative overinvolvement, (3) passive influence and (4) depersonalisation | 11–17 years. Presenting to Emergency Assessment Service in Harlow, Essex (UK) Population includes overdose in addition to self-harm189 | Self-administered | Likert-type Scale from 0 to 10 (‘0’ = ‘never’ and ‘10’ = ‘always’). Mean score of 4 + indicates pathologically significant dissociation |
| SAVRY182 [Added] |
Used in assessment of male/female adolescents. For use by professionals in diverse disciplines who conduct assessments and/or make intervention/plans concerning violence risk in youth | 24 items in three risk domains (historical risk factors, social/contextual risk factors, and individual/clinical factors). Collected details of young men’s clinical presentations Adolescent Clinical Inventory, and ICD10 diagnoses | 12–18 years. 64 young men, consecutively admitted to Bluebird House, an NHS mixed gender, adolescent forensic, medium secure hospital190 | Information from multiple sources, including patient and carer interviews and institutional records | Each risk item has three-level rating structure with specific rating guidelines (low, moderate, or high). In addition to 24 risk factors, includes six protective factor items rated as present/ absent |
| Family perceptions scale [Added] |
Questionnaire to allow family members to report perceived functioning across; nurture, problem-solving, behavioural boundaries, Responsibility and expressed emotion |
29-item questionnaire | Compares self-reported family functioning of 21 adolescents presenting at four UK medical wards with self-harming behaviour with those obtained from a sample of adolescents drawn from the local community.191 | Self-report questionnaire | Produces scores for five subscales, Likert-type scale: not true, somewhat true, certainly true |
| HAM-D175 [Added] |
Severity of depression | 21 items | 12–18 years. Admitted following an episode of self-harm191 | Clinical interview | Score 0–4 for each item (higher score represents more severe depression); total score based on first 17 items |
| SHQ69 [Added] |
Identification of self-harm | 3 screening questions and 12 questions for those endorsing self-harm | 12–17 years. 100 young people (71 female); UK Hospital Trust69 | Self-report | Binary yes/no |
| Strengths & Difficulties Questionnaire - SDQ [Added] | Emotions and behaviour | 25 items on 5 scales | 4–18 years; samples from 45 CAMHS services in the UK151 | Parent/teacher and self-report versions | Produces score of 0–10 on each subscale |
| Therapeutic Assessment (TA)149,a [Added] |
Self-harm | Not reported | Clinicians (n = 24) involved in self-harm assessment149 | Clinician assessment | Not reported |
Validity
A review team member extracted data from overviews of reliability and validity testing of the tools as presented in included studies (Tables 11–14). Internal consistency and test–retest reliability across the identified tools was generally moderate to good. As Carter et al. observes,39 this suggests consistency across the same construct (i.e. risk of suicide) meaning that the tools are able to produce similar scores when tested over a number of time points, respectively. Limitations in test–retest reliability continue to persist and this has been illustrated by studies that have shown that suicide/self-harm risk may be sensitive to change even within a matter of a few hours.
| Scale/tool | Reliability | Validity |
|---|---|---|
| Adolescent Dissociative Experiences Scale (A-DES; version 1.0)172,189 | Psychometric properties validated | Not reported |
| Child Maltreatment Interview Schedule173,189 | Not reported | Not reported |
| Children and Young People-Mental Health Self-harm Assessment in Paediatric healthcare Environments (CYP-MH SAPhE)50 | Good inter-rater agreement (kappa = 0.65) but sometimes conducted up to 4 hours apart50 allowing changes in clinical presentation | Potentially reliable and valid instrument. Non-cases did not complete Columbia-Suicide Severity Rating Scale. Unable to establish convergent validity in those with a non-mental health-related primary presentation |
| Children’s Global Assessment Scale151 | Test–retest and inter-rater undertaken | Not reported |
| C-CASA148 | Inter-rater undertaken | Not reported |
| FACE-CARAS of tools157 | Component schedules could be reliably rated, with near perfect to moderate agreement. Internal reliability consistency values (Cronbach’s alpha) moderate to high in all cases | Not reported |
| FPS191 | Not reported | Validated for use in adolescent populations191 |
| HAM-D175,191 | Not reported | Well-validated checklist, widely used in adolescent populations |
| SHQ69 | Inter-rater agreement (kappa) 0.78 (95% CI 0.60 to 0.96) | Concurrent validity tested by comparing SHQ results with young person’s clinical record; no significant difference in predicting future self-harm over 3 months |
| START:AV166,167 | Inter-rater reliability undertaken | Not reported |
| Strengths and difficulties questionnaire – SDQ151 | Extensively investigated | Extensively investigated |
| SAVRY182,190 | Not reported | Validated risk-assessment tool |
| SIQ-JR39,183 | Internal consistency and test-retest undertaken | See Carter et al.39 for details |
| SIQ39 | Excellent internal consistency | See Carter et al.39 for details |
| STOP-SAS39,170 | Excellent internal consistency; inter-rater undertaken (medium-large effect size) | See Carter et al.39 for details |
| SIS39,188 | Good internal consistency | See Carter et al.39 for details |
| Therapeutic Assessment (TA)149 | Not reported | Not reported |
| WARRN83 | Not reported | Not reported |
As Carter et al. observes,39 few assessment tools have investigated inter-rater reliability, thus little evidence exists to demonstrate that current assessment tools provide consistent results across different raters. There is little evidence of real-world testing with most being ‘tested with raters (i.e. clinician, self and parent) with limited scientific or clinical justification’. 39
Face validity is typically considered prerequisite to other validity/reliability tests. However this is not exemplified by the patterns of development and testing demonstrated by the tools in this review and even where this has been attempted it has not generally been performed satisfactorily. 39 Little consideration has focused on developmental issues associated with the child and adolescent populations targeted by this review. Substantial differences in cognitive ability, perception and understanding between younger children and those closer to 18 years of age continue to throw doubt on the ability of current tools ‘to provide accurate representation of potential risk for children and adolescents across the age range’. 39 The authors of the CYP-MH SAPhE instrument claim face validity given that it was acceptable and understandable to children and adolescents as evident from minimal missing data. 50
The CYP-MH SAPhE instrument possesses high internal consistency across two constructs (self-harm and suicidality) and high inter-rater reliability. CYP-MH SAPhE also demonstrated high congruent validity with a previously developed in-depth instrument designed to assess suicide risk, and high levels of discriminant validity suggesting it can adequately discriminate between children and adolescents with a primary mental health crisis and those with a primary physical medical illness or injury. 50 Future exploration of ‘suicidality’ is required to determine the robustness of this factor given its poor reliability. In a psychometric evaluation of the RTSHIA, risk-taking and self-harm were validated as related, but different constructs, rather than elements of a single continuum. Inter-item and test–retest reliability were high for both components. The authors claim that robust psychometric data emerged in support of the measure’s convergent, concurrent and divergent validity and its reliability with participants from the whole range of secondary education. Among a sample of psychiatric service inpatients and outpatients, the SHQ has demonstrated good concurrent and predictive validity. 69
Generalisability of the CYP-MH SAPhE instrument may be limited by use of a homogeneous sample of predominantly female children and adolescents, with white British ethnicity. 50 The RTSHIA is similarly limited in connection with its external validity and the generalisability of the findings. The samples, although diverse, were not all selected to be representative of the broader adolescent population.
The FACE-CARAS profile score was a good potential predictor of risks of self-harm, suicidal behaviours, serious self-neglect, abuse or exploitation by others, and violence to others at both 3 and 6 months. 65 It was weakly ‘predictive’ of accidental self-harm and no better than chance at signalling physical ill health. Clinical use of the scale did not conform to research standards and often left subscales incompletely rated. Collectively, these limitations need to be comprehended and mitigated in future evaluations.
Tools have also been identified for use in mental health crises beyond self-harm and suicide assessments. Those specific to particular populations with certain conditions or characteristics are listed. Since these do not apply to the entire child population they are not included within the tools on self-harm and suicidality.
Specific populations
Among specific populations (Table 12) several mental health conditions were assessed. These included the following: individuals with intellectual disabilities – behaviour problems;193 adolescents with possible paranoia;194 self-harm, children in care;195 self-harm and autism risk factors; autistic individuals;196 individuals with personality disorder in adolescents who self-harm;197 child well-being – used with children with a parent in the military;198 scale – depression;199 those who need a comprehensive needs assessment; adolescents with intellectual disabilities;200 general mental health, transgender and gender diverse youth;201 patients with persistent major depressive disorder (PMDD)-depression screening;202 adult offenders and forensic psychiatric patients – future violent behavior;203 autistic individuals – self-harm;196 inpatient CAMHS patients – well-being (risk factors);204 adolescents in secure unit violence (risk factors);205 individuals with autism, severe intellectual disabilities – self-harm;196,206 detection of individuals with psychosis207 and adolescents at risk of psychosis. 208,209
| Name of tool Associated articles |
Population | Other features of study |
|---|---|---|
| Assessment of Concerning Behavior199 | Children and Young People with ASD | Assess Mental Health and Concerning Behaviors in Children and Young People with ASD199 |
| Behavior Problems Inventory – Short Form193 | Individuals with Intellectual Disabilities – behaviour problems | Includes UK children Comparison of scales to assess validity |
| Behaviour problems Bird Checklist of Adolescent Paranoia194 [added to Carter et al. (2019)]39 |
Adolescents with possible paranoia | Evaluates psychometric properties of new measure, tests for measurement invariance, and assesses its potential for computerised adaptive testing. Participants from clinical sample recruited from community outpatient CAMHS (n = 271) and adolescent inpatient unit (n = 30) in Oxfordshire (Bird et al., in review). Patients 11–17 years |
| Brief Assessment Checklist*195 | Self-harm, children in care | Tool used with Strength and Difficulties Questionnaire to assess mental health of children in care |
| CBQ*196 | Self-harm and autism risk factors in autistic individuals | Identifies ‘novel, robust and stable profile of behavioural characteristics associated with persistent self-injury’ using multiple measures.
|
| Comprehensive Assessment of At-Risk Mental States208,209 | Adolescents at risk of psychosis. | Evaluated knowledge and attitudes of clinicians in a CAMHS in relation to ‘At-Risk Mental State’ concept in psychosis through survey208 |
| Developmental Behaviour Checklist (DBC – primary carer and teacher versions)200 | Adolescents with Intellectual Disabilities | UK sample. Identification of those at risk and undertaking of a comprehensive needs assessment |
| Expanded ACEs Scale201,210 | General mental health, Transgender and gender diverse youth | Transgender and Gender Diverse Youth’s Experiences of Gender-Related Adversity. Sample seeking services at a paediatric gender centre |
| Gender Minority Stress and Resilience measure201,211,212 | General mental health, Transgender and gender diverse youth | Transgender and Gender Diverse Youth’s Experiences of Gender-Related Adversity. Sample seeking services at a paediatric gender centre |
| General Health Questionnaire 12198,213 | Child well-being – used with children with parents in the military Scale – general mental health, well-being |
Investigates impact of father’s military deployment on child well-being in primary schoolchildren and compares measures of adjustment with matched group of children with fathers deployed on military training (non-combat) deployment |
| Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA)*197 | Individuals with personality disorder in adolescents who self-harm | Evaluates personality disorder in repeated self-harm in adolescence and its impact on self-harm psychopathology and adaptation outcomes over 1 year. (n = 366) of adolescents presenting with repeated self-harm aged 12–17 years. Trial took place in eight CAMHS settings within North West England (2002–6) |
| Parenting stress. The Parenting Stress Index/Short Form (SF)198 | Children with a parent in the military – child well-being | Investigates impact of parent’s military deployment on child well-being in primary schoolchildren and compares measures of adjustment with a matched group of children with parents deployed on military training (non-combat) deployment |
| PHQ-9202 | Patients with PMDD – depression screening | 187 secondary care patients with PMDD recruited to a RCT and allocated to either a specialist depression team arm or a general mental health arm; their PHQ-9 score was measured at baseline, 3, 6, 9 and 12 months |
| RBQ198 | Child well-being – used with children with a parent in the military Scale – child behaviour |
Investigates impact of parent’s military deployment on child well-being in primary schoolchildren. Class teachers and parents (non-deployed) completed a measure of child behaviour and parents completed a measure of parenting stress and general health |
| Self-esteem. The Self-Concept Inventory (one of five self-report scales in The Beck Youth Inventories (BYI) for Children and Adolescents (second edition; BYI-II)198,214 | Children with a parent in the military – Child Well-Being Scale – Anxiety |
Investigates impact of parent’s military deployment on child well-being in primary schoolchildren. For details see above |
| The Children’s Revised Impact of Event Scale198,215 | Children with a parent in the military – Child Well-Being – Scale – general mental health, well-being, behaviour |
Investigates impact of parent’s military deployment on child well-being in primary schoolchildren. For details see above |
| The Depression Self-Rating Scale198,216 | Child well-being – used with children with a parent in the military Scale – Depression |
Investigates impact of parent’s military deployment on child well-being in primary schoolchildren and compares measures of adjustment with a matched group of children with parents deployed on military training (non-combat) deployment. Class teachers/parents (non-deployed) completed measure of child behaviour. Parents completed measure of parenting stress and general health |
| The Structured Assessment of Protective Factors for Violence Risk, Historical, Clinical, Risk Management–20 and Psychopathy Checklist–Screening Version203 | Adult offenders and forensic psychiatric patients – future violent behaviour | Supplement to Historical Clinical Risk Management–20 to assess protective factors and their relationship to future violent behaviour in adult offenders and forensic psychiatric patients. Administered in a sample of 261 patients in UK forensic, general inpatient, and community mental health settings |
| The Screen for Child Anxiety-Related Disorders;217 child version, 41 items)198 | Children with a parent in the military – Child Well-Being Scale – self-esteem |
Investigates impact of parent’s military deployment on child well-being in primary schoolchildren and compares measures of adjustment with a matched group of children with parents deployed on military training (non-combat) deployment. Class teachers and parents (non-deployed) completed measure of child behaviour and parents completed measure of parenting stress and general health |
| The Self-Restraint Questionnaire*196 | Autistic individuals – self-harm | Identified novel, robust and stable profile of behavioural characteristics associated with persistent self-injury through use of several measures. Measures as detailed above |
| SCQ196 | Autistic individuals – self-harm | Identified novel, robust and stable profile of behavioural characteristics associated with persistent self-injury through use of several measures. Measures as detailed above |
| The Social Connectedness Scale204 | Inpatient CAMHS patients –well-being (risk factors) | Sought to evaluate utility and acceptability of a measure of social connectedness in inpatient CAMHS |
| SAVRY182,205 | Adolescents in secure unit violence (risk factors) | UK study – characteristics of female patients admitted to an adolescent secure forensic psychiatric hospital |
| The Wessex Behaviour Rating System (used to assess self-help adaptive functioning)196,206 | Individuals with autism, Severe intellectual disabilities – self-harm | Identified profile of behavioural characteristics associated with persistent self-injury through use of several measures.196 Measures as detailed above |
| Transdiagnostic risk calculator for automatic detection of psychosis218 | Detection of individuals with psychosis | Paranoia assessment protocol |
Summary
Pile et al. (2020) contextualise risk assessments among NICE guideline recommendations for depression. 86 (Risk assessment appropriately completed; cases requiring a full risk screen; consideration of parental mental health; parental mental health issues identified; self-report questionnaire administered; evidence-based psychological intervention offered; currently or previously prescribed antidepressant medication.) This conceptualisation of risk-assessment tools and those used to meet the broader requirements of the guidelines, has informed the parameters of this review. This was an important step as the studies identified in this review (either as research on the efficacy of risk-related tools or research about application of tools), do not tend to differentiate between tools applied within risk assessments, screening and self-report questionnaires. 86 Therefore, this review includes tools that help clinicians to build a picture of risk, as opposed to only tools that are referred to as risk-assessment checklist tools. NICE guidelines for self-harm in the over-eights consider risks that include the following: previous incidences of self-harm, identification of depressive symptoms, diagnosis of other psychiatric illnesses, social relationships and contexts history, identification of risk factors and protective factors, identification of relationships (un)supportive, and identification of longer-term risks. Risk-assessment tools may be considered to help structure risk assessments as long as they include the areas identified in NICE recommendation 1.3.6 (1.3.13).
Another recommendation is to develop an integrated care and risk-management plan, which could be viewed as an outcome (see Impact on mental health assessment processes and outcomes).
Use to assess self-harm or suicide
Several individual tools assess the risk of suicidal thoughts or self-harm within a broader set of tools to assess general mental health issues (Children’s Global Assessment*; Columbia Suicide Severity Rating Scale*, obsessive compulsive inventory for children, Revised Children’s Anxiety and Depression Scale), or as tools for a particular population [Brief Assessment Checklist*195 (children in care) Challenging Behaviour Questionnaire (CBQ), The Self-Restraint Questionnaire – Laverty; HoNOSCA – individuals with personality disorder (See Table 15]. 197
Combinations of tools
Four studies describe application of a combination of tools. 196,198,230,239 Laverty et al. used a combination of The Revised Children’s Anxiety and Depression Scale, the Obsessive Compulsive Inventory for Children, the Children’s Revised Impact of Events Scale, the Columbia Suicide Severity Rating Scale, the KIDSCREEN-10 Index, the Children’s Global Assessment Scale, and the Child Anxiety Life Interference Scale to create a behaviour profile assessment to enable clinicians to identify characteristics associated with persistent self-injury through the use of several measures. 196 Laverty et al. reported on self-harm but specifically for individuals with autism. The authors identified a novel, robust and stable profile of behavioural characteristics associated with persistent self-injury through the use of several measures (a demographic questionnaire detailing the following: CBQ; The Activity Questionnaire; impulsivity; Social Communication Questionnaire; Repetitive Behaviour Questionnaire and the Self-Restraint Questionnaire).
Pexton et al.’s study investigates the impact of a parent’s military deployment to Afghanistan on child well-being in primary schoolchildren and compares measures of adjustment with a matched group of children with parents deployed on military training (non-combat) deployment. 198 Class teachers and parents (non-deployed) completed a measure of child behaviour and parents completed a measure of parenting stress and general health. Oliver et al. (2012) explored early risk markers for self-injury and aggression through high-frequency repetitive or ritualistic behaviours. 206 Finally, Hurrell et al., used responses from psychosocial questionnaires, including the Paediatric Quality of Life Inventory (PedsQL 4.0 Generic Core and Family Impact Module), the Strengths and Difficulties Questionnaire (SDQ), the Paediatric Index of Emotional Distress (PI-ED), and the Hospital Anxiety and Depression Scale (HADS) in conjunction with clinical psychology consultations to evaluate a range of psychosocial aspects in Bladder Exstrophy and Epispadias Complex (BEEC) paediatric patients. 239 Certain individual scores did fall within clinical ranges, highlighting a potential need for further assessment. 207
Making the connection: Effect of risk assessment on mental health outcomes
Prospective studies examining the association between high risk, as identified by risk-assessment tools, and death by suicide are notably lacking. 240 Empirical studies have been unable to demonstrate that categorising patients at low risk or high risk of future fatal or non-fatal self-harm can contribute to a reduction in overall rates of these adverse events. 48 A systematic review of 11 studies aimed to evaluate the ability of 10 separate risk tools to predict the future episodes of suicide/self-harm in adolescents. The majority of the studies were rated with an unclear risk of bias. Meta-analysis was not possible due to high heterogeneity between studies and tools. The ability of the tools to correctly identify adolescents going on to attempt self-harm/suicide ranged from 27% (95% CI 10.7% to 50.2%) to 95.8% (95% CI 78.9% to 99.9%). 16 The authors conclude that the predictive ability of these tools varies greatly. As a practical consequence, no single tool is considered suitable for predicting a higher risk of suicide or self-harm in adolescent populations.
| Study ID | Country | Setting | Tool | Design |
|---|---|---|---|---|
| Ballard et al. (2017)219 | USA | Emergency department | Ask Suicide Screening Questions | Retrospective |
| Cha et al. (2016)220 | USA | Inpatient unit | Self-Injurious Thoughts and Behaviours Interview Self-Injury Implicit Association Test |
Prospective |
| Chitsabesan et al. (2003)221 | UK | Home | SIQ | Prospective |
| Czyz et al. (2016)222 | USA | Emergency department | C-SSRS Self-Assessed Expectation of Suicide Risk Scale |
Retrospective |
| Gipson et al. (2015)223 | USA | Emergency department | C-SSRS | Prospective |
| Horwitz et al. (2015)224 | USA | Emergency department | C-SSRS | Retrospective |
| King et al. (2014)225 | USA | Inpatient unit | SIQ-JR | Prospective |
| King et al. (2010)226 | USA | Inpatient unit | Beck Hopelessness Scale SIQ-JR |
Prospective |
| Ougrin and Boege (2013)69 | UK | Mixed inpatient/ outpatient clinics | SHQ | Prospective |
| Posner et al. (2013)174 | USA | Open treatment trial | C-SSRS | Prospective |
| Yen et al. (2013)227 | USA | Inpatient unit | SIQ | Prospective |
| Study ID | Outcomes | Measures | Measurement period |
|---|---|---|---|
| Ballard et al. (2017)219 (ASQ) |
Predictive ability for suicide | Sensitivity 95.8%, specificity 5.8%, positive predictive value 16.8% and negative predictive value 87.5% |
6 months |
| Cha et al. (2016)220 (SI-IAT and SITBI) |
Repeat self-harm Repeat self-harm |
SI-IAT – (unadjusted OR 3.10, 95% CI 0.39 to 9.94; p ≥ 0.05) SITBI – (adjusted OR 1.82, 95% CI 1.25 to 2.65; p = 0.002) |
3 months 3 months |
| Chitsabesan et al. (2003)221 (SIQ) |
Accuracy to classify patient as high/low risk for self-harm repetition | Sensitivity 27.3%, specificity 99.2%, positive predictive value 85.7% and negative predictive value 85.6% |
6 months follow-up |
| Czyz et al. (2016)222 (C-SSRS) |
Future suicide attempt | Unadjusted OR ranged from 1.09 (95% CI 1.01 to 1.17) to 3.85 (95% CI 1.07 to 13.86) for every 1-point increase in score. Adjusted OR ranged from 1.15 (95% CI 1.03 to 1.29) to 1.51 (95% CI 1.24 to 1.84) for every 1-point increase in score | - |
| Gipson et al. (2015)223 (C-SSRS) |
Future suicide attempt | Unadjusted OR from 1.09 (95% CI 1.01 to 1.17) to 3.85 (95% CI 1.07 to 13.86) for every 1-point increase in score. Adjusted OR from 1.15 (95% CI 1.03 to 1.29) to 1.51 (95% CI 1.24 to 1.84) for every 1-point increase in score | - |
| Horwitz et al. (2015)224 (C-SSRS) |
Future suicide attempt | Unadjusted OR from 1.09 (95% CI 1.01 to 1.17) to 3.85 (95% CI 1.07 to 13.86) for every 1-point increase in score. Adjusted OR from 1.15 (95% CI 1.03 to 1.29) to 1.51 (95% CI 1.24 to 1.84) for every 1-point increase in score | - |
| King et al. (2014)225 (SIQ-JR) | Future suicide attempt | For every 1-point increase in score, RR of no future attempt was 0.93 | - |
| King et al. (2010)226 (SIQ-JR) | Future suicide attempt | For every 10-point increase in score, unadjusted HR of future suicide attempt was 1.30 (95% CI 1.14 to 1.48; p ≤ 0.001). Subsequent multivariate regression model reported adjusted HR of 1.23 (95% CI 1.08 to 1.40; p = 0.003) | - |
| Ougrin and Boege (2013)69 (SHQ) | Predictive validity for self-harm | Sensitivity 94.7%, specificity 34.6%, positive predictive value 25.4% and negative predictive value 96.6% |
3 months |
| Posner et al. (2013)174 (C-SSRS) |
Future suicide attempt | Unadjusted OR from 1.09 (95% CI 1.01 to 1.17) to 3.85 (95% CI 1.07 to 13.86) for every 1-point increase in score. Adjusted OR from 1.15 (95% CI 1.03 to 1.29) to 1.51 (95% CI 1.24 to 1.84) for every 1-point increase in score | |
| Yen et al. (2013)227 (SIQ) |
Future suicide attempt | In univariate regression, statistically significant HR of 1.01 (95% CI 1.00 to 1.02; p ≤ 0.05) for high/low suicidal intent score. After multivariate analysis, despite HR being same at 1.01 (95% CI 1.00 to 1.02; p ≥ 0.05), no longer statistically significant |
| Name of tool (associated articles) | Crisis/MH condition | Other features of study |
|---|---|---|
| The Anhedonia Scale228 | Loss of interest or pleasure (depression) | For adolescents Self-report scale Development and validation of tool |
| Children’s Global Assessment*151,229 | Anxiety, depression, obsessive-compulsive disorder, post-traumatic stress disorder | Child Anxiety Life Interference Scale, Children’s Revised Impact of Events Scale and Children’s Global Assessment230 Predictors of change in global psychiatric functioning at an inpatient adolescent psychiatric unit229 Compares clinician rating on CGAS and family ratings on SDQ151 |
| Depression Anxiety Stress Scale (DASS-21)87 | Depression, anxiety, stress | Administered to caregivers, study applied three scales |
| Juvenile Victimisation Questionnaire231,232 | Emotional well-being, maltreatment | UK study uses using self-report measures to assess the emotional well-being of maltreated children, young people and young adults |
| NICE guidelines86 | Depression | Assessment and treatment of depression in children and young people in the UK. Study investigates whether guidelines around risk, parental mental health, questionnaire use and psychological and pharmacological intervention are implemented in CAMHS |
| Me and My School Questionnaire233 | General mental health, school | Self-report mental health measure for children and adolescents – aims to assess its clinical sensitivity to justify its utility as a screening tool in schools |
| Moods and Feelings Questionnaire – C/P*87,234,235 | Anxiety, self-harm and depression in young adulthood (including in sexual minorities) | Used in combination with two other scales – Used 11-item Version of Revised Children’s Anxiety and Depression Scale to Identify Anxiety and Depressive Disorders in Adolescents234 Analysed association of self-harm and depression in young adulthood in sexual minorities235 |
| PSCY236 | General mental health, school | Mental health screening in school setting |
| Revised Children’s Anxiety and Depression Scale*87,230,234 | Suicide, Anxiety, depression, obsessive-compulsive disorder, and post-traumatic stress disorder (risk factors) | To identify Anxiety and Depressive Disorders in adolescents. In addition, they examined whether adding items assessing suicidal ideation (Moods and Feelings Questionnaire – C/P) and symptom impact and duration (items adapted from the Strengths and Difficulties Questionnaire – SDQ)234 |
| Trauma Symptom Checklist for Young Children237 - shortened 26-item version232 | Emotional wellbeing, childhood adversity (maltreatment and other types of victimisation) | UK study using standardised scores from self-report measures, to assess emotional wellbeing of maltreated children, young people and young adults taking into account other types of childhood victimisation, different perpetrators, non-victimisation adversities and variables known to influence mental health |
| Unusual Experiences Questionnaire238 | Risk factors for mental health problems Screened for unusual, or ‘psychotic-like’, experiences are perceptions or beliefs |
Used with Strength and Difficulties Questionnaire. Reports on feasibility of a routine screening methodology, and screening outcomes, in CAMHS in South East London, UK |
Growing evidence suggests that combinations of risk factors do not accurately identify those at greatest risk of further self-harm and suicide. 241 A five-hospital multicentre prospective cohort study of adults referred to psychiatric liaison services following self-harm tested predictive utility of items from five risk scales. 241 Even though some individual items outperformed the scale from which they were derived, no items were superior to clinician or patient risk estimations. This finding in adult populations adds confirmation to the fact that risk-assessment scales should play little role in the management of people who have self-harmed. 241 There is every reason to believe that these methodological limitations translate equally to a paediatric context, potentially even more so given developmental variability within the child and adolescent age groups.
Impact on mental health assessment processes and outcomes
Other studies seek to make a connection between tools and scales and other health or health service outcomes, beyond self-harm and suicide. Generally, these links are supported by isolated studies and are not based on strong and consistent evidence. Pile et al. (2020) investigated whether NICE guidelines impact upon the implementation of risk assessment in CAMHS for children with depression. 86 Findings showed adherence to NICE guidance was mostly good at around 1 year. 86 Subsequently, a decrease was observed in correct completion of risk assessments. 86 The study also reported a significant decrease in the number of cases where a full risk screen (for those at higher risk) was completed. The authors note that compliance and consistency to the guidelines needs to increase to standardise risk monitoring and communication between services. 86
Terrelong and Fugard (2017) demonstrated the importance of multi-informant data gathering and integrating multiple clinician perspectives when monitoring outcomes. 151 Welsh et al. (2011) identified a need for further training for CAMHS clinicians in relation to the psychosis risk syndrome. 208 One study assessed symptoms and tracked progress197 using the HoNOSCA to assess global functioning. 197 The study evaluated personality disorder in repeated self-harm in adolescents and its impact on self-harm psychopathology and adaptation outcomes over 1 year. Another study of symptom-based outcomes assessed the clinical sensitivity of the Me and My School questionnaire (a self-report measure for children aged 8 years) to justify its utility as a screening tool in schools. 233 Sinclair et al. used the Paediatric Symptom Checklist for Youths to assess the mental health surveillance of adolescents, within a school setting. 236
Phillips et al. (2019) analysed the utility and acceptability of a tool on social connectedness – a concept linked with well-being and risk in young people in relation to subjective well-being and recovery outcomes. 204 The Developmental Behaviour Checklist (primary carer and teacher versions) was applied to adolescents with intellectual disabilities200 to identify those at risk. The study also used a clinical interview to assess service utilisation and medication prescribing.
Kennedy et al. 229 aimed to identify personal and environmental factors that influence outcome in an adolescent unit that accepts both emergency and planned admissions. This study explores risk-assessment tools indirectly as one of several predictors of outcomes. Similarly, Laverty et al. used risk-assessment tools to create a profile of behavioural characteristics associated with persistent self-injury. Findings support an early intervention strategy targeted towards individuals identified at higher risk of developing self-injurious behaviour. 196
Fusar-Poli et al. (2019) proposed a protocol for real-world detection of Individuals at Risk of Psychosis. 218 Tarren-Sweeny et al. linked the use of checklist tools to improved mental health screening for children in care using the Strengths and Difficulties Questionnaire and the Brief Assessment Checklists. 195 Tarver et al. 199 and Bird et al. (2020) similarly focus on instruments of potential use in clinical practice. 194
Rojan et al. (2012) assess the accuracy of a tool for evaluation and research purposes. Gin et al. (2018) applied a checklist to screen for distressing ‘psychotic-like’ or unusual experiences (UEDs) in under 18s. 238
Chapter 4 Discussion
This review has revealed, through two complementary evidence syntheses, that considerable diversity exists in connection with risk assessment in children and adolescents. Diversity exists at every level; from why professionals view risk assessment as important, how it should be done, how it could be used and what tool(s) should be used and indeed whether formal tools should be used at all. Some clear principles have emerged and these have been confirmed by the clinical informants to the review.
For whom and in what circumstances do risk assessments change the clinical encounter?
Risk assessment is an important, indeed essential, stage of the clinical encounter and results in useful deliverables, such as the formulation, the care plan and definite plans for follow-up. Several meta-analyses of quantitative studies, together with qualitative studies, reveal that young people who present in relation to self-harm or attempted suicide do not generally respond poorly to being asked about their intent. However, certain types of self-harm carry particular stigma, such as cutting, and need to be handled with sensitivity. Evidence further suggests that young people prefer not to be thought of as being a ‘risk’. The use of the term in the context of a clinical encounter evokes other words like danger and safety and elicits fear and anxiety.
What impact does risk assessment have?
The review of the predictive ability of tools for assessing risk of self-harm reveals that their predictive ability is consistently poor. Factors that are thought to have an association with future self-harm or suicide ideation are diffuse, the evidence on their influence is inconsistent and, therefore, tools have included different permutations of these factors. Conversely, consistently reported factors such as previous suicide history might be expected to be explored through any thorough risk-assessment process and are not dependent upon use of any specific tool. Nevertheless, attempts continue in the pursuit of a tool that will meet the diverse needs of emergency departments, general paediatric settings and specialist CAMHS services. However, many contemporary approaches are shifting instead to a focus on a holistic risk-assessment process with a view to making the process consistent and complete.
The realist review strongly supports the need for risk assessment for self-harm and suicide to take place within a wider assessment process (PT1). Consistent risk-assessment processes (PT5) should gather good-quality information (PT3), offer personalised and individualised risk management and not seek to ‘predict’ suicidal behaviour. Tools that are used to inform and structure the overall process should be simple, accessible and standardised (PT1). These tools should be locally applicable but not developed locally (PT14) and, rather than being used in isolation these tools should support the wider biopsychosocial assessment that includes, but does not focus on, risk (PT13).
NICE recommendations offer a structure for reviewing the risk-assessment process and deciding whether it is complete and fit for purpose. Recommendations for content include the following: previous incidences of self-harm, identification of depressive symptoms, diagnosis of other psychiatric illnesses, social relationships and contexts (history), identification of risk factors and protective factors, identification of (un)supportive relationships, identification of longer-term risks and an integrated care and risk-management plan. Many, but not all, of these features are present within existing risk-assessment approaches.
The realist synthesis confirms that the quality of the clinical encounter is an important contributor to the risk-assessment process; a health professional can make a difference through a successful interaction with a young person. Staff should be enabled so that they can focus on building relationships (PT2) and are able to feel comfortable when asking about suicidal thoughts (PT4). Risk-assessment processes are facilitated by family and carer involvement in assessment (PT8) and good communication with primary care. Staff should therefore be supported to deliver risk assessment within a context where they receive good-quality on-going supervision (PT7) and where they have been appropriately trained to assess, formulate, manage and refer risk (PT6). As a consequence, staff are able to gain increased knowledge, skills and self-efficacy, CAMHS services are likely to achieve a reduction in inappropriate referrals and more impactful use, ultimately leading to a reduction in rates of self-harm, symptoms precipitating suicidal ideation, and rates of suicide.
Strengths of the evidence
A large number of tools and approaches have been identified by this review. Subsequent to the previous scoping review,39 additional tools have been produced and validated. 82,147 As seen from the foregoing analysis there is emerging consensus (i) that no single tool meets current clinical needs, (ii) that tools are not to be used for prediction and (iii) in agreeing the components of a wide-ranging and comprehensive biopsychosocial assessment.
Limitations of the evidence
Individually, some of the tools for risk screening demonstrate strong psychometric properties. However, in the context of risk assessment they lack the very psychometric property that is critical to their successful use; their predictive ability, both individually and collectively, is poor. As a consequence, the identification of wider approaches to risk assessment is likely to prove more valuable to the reader.
This review confirms previous findings from earlier reviews, namely identification of key gaps and deficits in the evidence base. Principal among these is the limited availability of psychometrically tested assessment tools in specific contexts and regions. However, recent publication of a tool developed specifically for assessing risk of self-harm in acute paediatric settings seeks to address one identified gap. 50 However, this development in some ways counters widespread recognition that no single tool is likely to meet clinical needs.
Many risk instruments for child and adolescent self-harm and suicide have been developed in other countries and thus may not be valid or culturally suitable for a UK-based CAMHS population. Even tools developed for and in the UK may not meet the specific requirements of ethnic minority populations. Additionally, many were developed in paper format and cannot always be meaningfully entered into electronic patient records, as increasingly adopted within the UK NHS.
Strengths of the review
Findings from this mapping review and realist synthesis are based on comprehensive and extensive searches of seven databases, supported by reference checking and forward citation chaining. The review has built upon existing reviews to provide and extend a summary of the characteristics, and ratings of reliability and validity of assessments tools of immediate self and suicide risk in children and adolescents. Use of a systematic review methodology, albeit within time and resource constraints, has served to mitigate the acknowledged deficiencies of previous scoping reviews. This increases the confidence that significant additional risk-assessment tools, that have been developed and psychometrically tested, have not been overlooked. Moreover, by extending beyond the terms ‘self-harm’ and ‘deliberate self-harm’ in the search strategy we have been able to identify additional studies that might otherwise have been missed through use of alternative terminology. Fourteen empirical studies that evaluated a tool were quality assessed to ensure consistency of approach.
Limitations of the review
The focus of the review was on mapping the topic and then analysing what contributes to effective risk-assessment processes. The heterogeneous studies exploring specific risk-assessment tools prevented the use of meta-analysis. However, the review team did harness existing systematic reviews where these could contribute to an understanding of the limitations of the evidence base. Furthermore, the realist synthesis was conducted within a resource-constrained context. As a consequence the evidence base was limited to a small number of indicative studies mobilised around each of the fourteen programme theories. Generation of the candidate programme theories was undertaken using one main source38 and several subordinate sources (See Appendix 3 and Table 17) and interpretation was undertaken by one experienced reviewer, although corroborated by other team members.
Time constraints, combined with ethical challenges, meant that it was not possible to access either CYP or families of CYP who have accessed mental health services in the standing PPI group. The absence of meaningful involvement of users of mental health services for children and young people in the design and implementation of this review is a recognised challenge in rapid synthesis activities. Further user involvement could help in specifying the language and concepts used and in assisting with applicability and relevance of the study. The review questions were generated using Department of Health and Social Care prioritisation processes and were not amenable to further specification by a PPI group.
Lessons learned
Experience when conducting this review confirms the review context as one of many where tensions between the risk-averse operational culture of the NHS and drivers towards patient-centred care are currently playing out. The checklists have become apparatus that is associated in the minds of patients, family members and professionals with a tick-box mentality that shows little interest in the individualised needs of the patient. An initial focus on tools and checklists has, through literature review and consultation with clinical experts, become an imperative for a holistic exploration of the risk-assessment process. The thorough biopsychosocial assessment offers a professionally acceptable alternative to checklist-based approaches but is increasingly ‘squeezed out’ by time and resource constraints. However, these options do not represent genuine alternatives because of the absence of evidence that risk assessment bears any relation to the eventual prognosis of child and adolescent service users. Structured professional judgement remains an important component of the decision-making process and so the precise choice of a tool by which to structure this process may be less critical than the overall process itself. Having recognised that choice of process may be informed by training and personal preference it should be acknowledged that consistency of approach both within and across organisations may also prove an important consideration with potential benefits highlighted by the standardised WARRN approach across Wales.
Implications for service delivery/policy and practice
Much of the literature highlights the absence of a universally accepted suicide/self-harm risk-assessment tool validated for use in inpatient paediatric settings where there may be an immediate risk of self-harm or suicidal behaviour (i.e. within hours of the triage assessment). Despite attempts to develop additional tools for risk assessment, recent additions share many of the limitations of their precursors in relation to different types of reliability and validity, of which predictive validity is foremost. Equally importantly, none of these additional tools overcome persistent challenges, namely that (i) no single tool can carry the onerous requirements for biopsychosocial assessment, including a specific requirement to assess young people at risk for self-harm and suicide, and (ii) multiagency whole-system approaches to risk assessment may be facilitated by the availability of suitable tools but are not ensured by them.
Healthcare professionals working within paediatric inpatient settings find themselves reliant on their own clinical judgement. In contrast to staff working in CAMHS who have received training in difficult aspects of handling the child or adolescent at risk for self-harm or suicide, many front-line staff may lack experience and training in this sensitive and critical area of service delivery. Risk-assessment tools offered as the default choice within their setting may not have been developed for the specific needs of this population/setting. Staff perceptions need to be changed through further training regarding what constitutes a risk assessment. Overestimation of risk may lead to inappropriate utilisation of resources at the possible expense of more immediate priorities. Conversely, underestimation of risk may lead to non-intervention, potentially leading to self-harm consequences and distress for families and to affected care staff, themselves.
Future research
Mental health problems among young people continue to increase and this is likely to continue as the long-term impacts of the pandemic are felt within CAMHS. At present, those making mental health risk assessments on the frontline do not have a first-choice suicide/self-harm risk-assessment tool. As a consequence, healthcare professionals working across diverse paediatric settings employ diverse approaches and typically have to depend heavily upon their own clinical judgement. Staff may also find themselves using a risk-assessment framework/tool that has not been developed for the specific needs of this population/setting or using the tool for purposes that are not intended. An inaccurate assessment of risk may result in either over or underestimation of risk rating, inappropriate safety-management strategies and inefficient utilisation of CAMHS and resources. It remains to be seen whether recent development of the CYP-MH SAPhE instrument147 fulfils its promise and, indeed whether its utility extends beyond the immediate acute paediatric care context for which it has been designed. More importantly, any preferred instrument must be used within an overall psychosocial assessment, not simply as a tick-box exercise.
Before further research is commissioned, consultation needs to take place with children, young people and their families to establish the next steps for future research. With a focus on an overall risk-assessment process for self-harm and suicide, not on further development of checklist-based approaches, it remains to be established how the 14 propositions can best be implemented in practice to enhance the clinical encounter and ameliorate mental health outcomes.
Further research is also required to evaluate the value to young persons, health professionals and health services of a complete and holistic assessment, not simply provision of an alternative tool. An evaluated approach to overall assessment could then be used to support safety-management decisions across acute paediatric care settings.
Chapter 5 Conclusions
Overall, the evidence in this review suggests that risk-assessment procedures that are sensitive to the values and preferences of young persons are likely to elicit more complete information and to contribute to a more positive relationship between health professionals and the young patients themselves. However, it is not possible to link the outcomes from the risk-assessment process directly to clinical outcomes, particularly given the variability of the available tools and the considerable range in technical performance that these tools deliver. Features that are likely to enhance the value of the risk-assessment process itself include involvement of the family, where appropriate, and the incorporation of an approach to risk assessment within a thorough biopsychosocial assessment. In addition, benefits seem to accrue within and across organisations when standardisation of processes, but not necessarily tools, is secured.
While the UK research base is not as broadly populated as that for the USA, in terms of development and validation of tools, it remains to be seen whether these should function primarily within a context of research and service evaluation, rather than possessing clinical utility. Little evidence was available to evaluate the interaction between clinician and child or adolescent. This is perhaps not surprising given the vulnerability of young people, which may impede or even thwart some forms of qualitative research, and also the critical context of the interaction in terms of non-specialist health staff in emergency settings under time-critical and resource pressures. Nevertheless, training, possibly to include role play, and supervision by experienced staff may help to improve the quality and consistency of the clinical encounter. Lessons remain to be learnt from training initiatives and potentially from the Lincolnshire whole system approach to management of self-harm and suicide.
We believe that further studies evaluating the utility of specific tools and instruments are not warranted, although additional evaluations of risk-assessment processes more widely would benefit from further qualitative insights. In particular, health systems and organisational leadership initiatives could benefit from close examination of risk management more broadly, in particular how the theoretical tensions between risk minimisation and patient-centred care are enacted at a practical and operational level.
What this study adds
This study confirms that the technical development of tools generally, and of tools and instruments for risk assessment in particular, should not be allowed to deflect the research agenda away from holistic (individually) and whole-system (organisationally) imperatives. In particular, it provides research-based corroboration for insights gained from national surveys and articulated individually and collectively by clinical experts. It also validates recommendations in clinical guidelines in relation to the need to avoid using risk-assessment tools for prediction or for determining clinical management decisions.
Key learning points
The value of realist synthesis is evidenced in being able to explore how insights generated from a national survey play out in the published literature. In particular, realist synthesis was able to engage with diverse types of evidence to fill in knowledge gaps not addressed by documentation of validation studies as performed by earlier scoping and systematic reviews. Nevertheless, realist synthesis accrues most value when it addresses what works questions in conjunction with a focus on contexts and mechanisms and not simply as a supplement to existing effectiveness data.
Acknowledgements
We gratefully acknowledge input from Dr Bernadka Dubicka, consultant and research lead in Pennine Care Foundation Trust, Greater Manchester and Chair of the Royal College of Psychiatrists (RCPsych) Child and Adolescent Faculty.
Contributions of authors
Anna Cantrell (https://orcid.org/0000-0003-0040-9853) was the lead reviewer, lead author and managed the project.
Katie Sworn (https://orcid.org/0000-0001-6247-4007) was the second reviewer.
Duncan Chambers (https://orcid.org/0000-0002-0154-0469) provided additional reviewer input as required.
Andrew Booth (https://orcid.org/0000-0003-4808-3880) is the Co-Director of the Evidence Synthesis Centre and chief methodologist for the project. He is also the guarantor for the data and compiled the final report.
Elizabeth Taylor Buck (https://orcid.org/0000-0003-2596-2655) provided subject expertise.
Scott Weich (https://orcid.org/0000-0002-7552-7697) provided subject expertise.
Information governance
This review was conducted under School of Health and Related Research (ScHARR) Information Governance procedures. All staff members are compliant with University of Sheffield policies and procedures and have submitted to regular training in relevant aspects of governance.
Data-sharing statement
All available data can be obtained on request from the corresponding author.
Funding
Support/Sources: NIHR Health Services & Delivery Research Funding Programme
Sponsor: NIHR Health Services & Delivery Research
Role of sponsor or funder
The sponsor identified the original topic through prioritisation processes and commissioned the Evidence Synthesis Centre to conduct the review. Following input into the protocol, the funder had no further input into the process or findings of the review.
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- NHS . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/.
- Office for National Statistics . Suicides in England and Wales: 2020 Registrations 2021.
- NCISS . National Confidential Inquiry into Suicide and Safety in Mental Health: Annual Report: England, Northern Ireland, Scotland and Wales 2021 2021.
- Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect 2017;20:471-83. https://doi.org/10.1111/hex.12474.
- Downes C, Gill A, Doyle L, Morrissey J, Higgins A. Survey of mental health nurses’ attitudes towards risk assessment, risk assessment tools and positive risk. J Psychiatr Ment Health Nurs 2016;23:188-97.
- Stewart A, MacIntyre G. Safeguarding Adults: Key Themes and Issues. London: Palgrave; 2017.
- Jones J, Plowman C. Multidisciplinary Working in Forensic Mental Health Care. London: Elsevier; 2005.
- Doyle M, Dolan M. Violence risk assessment: combining actuarial and clinical information to structure clinical judgements for the formulation and management of risk. J Psychiatr Ment Health Nurs 2002;9:649-57.
- Homaifar B, Matarazzo B, Wortzel HS. Therapeutic risk management of the suicidal patient: augmenting clinical suicide risk assessment with structured instruments. J Psychiatr Pract 2013;19:406-9.
- Bouch J, Marshall JJ. Suicide risk: structured professional judgement. Adv Psychiatr Treat 2005;11:84-91.
- Cramer RJ, Kapusta ND. A social-ecological framework of theory, assessment, and prevention of suicide. Front Psychol 2017;8. https://doi.org/10.3389/fpsyg.2017.01756.
- Pisani AR, Murrie DC, Silverman MM. Reformulating suicide risk formulation: from prediction to prevention. Acad Psych 2016;40:623-9.
- Boyce P, Carter G, Penrose-Wall J, Wilhelm K, Goldney R. Summary Australian and New Zealand clinical practice guideline for the management of adult deliberate self-harm (2003). Austr Psych 2003;11:150-5.
- NICE . Self-Harm: Assessment, Management and Preventing Recurrence NICE Guideline [NG225] 2022.
- Royal College of Psychiatrists . Managing Self-Harm in Young People (Guideline Number CR192) 2014.
- Harris IM, Beese S, Moore D. Predicting future self-harm or suicide in adolescents: a systematic review of risk assessment scales/tools. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029311.
- NICE . Davies’s Structured Interview for Assessing Adolescents in Crisis 2013.
- National Collaborating Centre for Mental Health . NCCfM. Self-Harm. The NICE Guideline on Longer-Term Management 2011.
- Royal College of Psychiatrists . Rethinking Risk to Others in Mental Health Services 2008.
- Wand T, Isobel S, Derrick K. Surveying clinician perceptions of risk assessment and management practices in mental health service provision. Austr Psych 2015;23:147-53.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
- Ford JA, Wong G, Jones AP, . Access to primary care for socioeconomically disadvantaged older people in rural areas: a realist review. BMJ Open 2016;6.
- Booth A, Wright J, Briscoe S. Doing Realist Research. London: Sage; 2018.
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons; 2019.
- Shuttleworth J, Britton J, Keenan A, Thomaidis-Zades K. Psychoanalysis, the NHS, and Mental Health Work Today. London: Routledge; 2018.
- Aromatario O, Van Hoye A, Vuillemin A, Foucaut A-M, Pommier J, Cambon L. Using theory of change to develop an intervention theory for designing and evaluating behavior change SDApps for healthy eating and physical exercise: the OCAPREV theory. BMC Public Health 2019;19:1-12.
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91.
- Fletcher A, Jamal F, Moore G, Evans RE, Murphy S, Bonell C. Realist complex intervention science: applying realist principles across all phases of the Medical Research Council framework for developing and evaluating complex interventions. Evaluation 2016;22:286-303.
- Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7:1-10.
- Minian N, Corrin T, Lingam M, deRuiter WK, Rodak T, Taylor VH, et al. Identifying contexts and mechanisms in multiple behavior change interventions affecting smoking cessation success: a rapid realist review. BMC Public Health 2020;20:1-26.
- Greenhalgh J, Manzano A. Understanding ‘context’in realist evaluation and synthesis. Int J Soc Res Methodol 2021;25:1-13. https://doi.org/10.1080/13645579.2021.1918484.
- Saul JE, Willis CD, Bitz J, Best A. A time-responsive tool for informing policy making: rapid realist review. Implement Sci 2013;8:1-15.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11:1-14.
- Ayiku L, Levay P, Hudson T, Craven J, Finnegan A, Adams R, et al. The medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID medline. Health Info Libr J 2017;34:200-16. https://doi.org/10.1111/hir.12187.
- De Brún A, McAuliffe E. Identifying the context, mechanisms and outcomes underlying collective leadership in teams: building a realist programme theory. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05129-1.
- Booth A, Hock E, Preston L, Uttley L. Social Care Access for Adult BAME and LGBT+ Populations: A Rapid Realist Review. Southampton: National Institute for Health Research; 2021.
- The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) . The Assessment of Clinical Risk in Mental Health Services 2018.
- Carter T, Walker GM, Aubeeluck A, Manning JC. Assessment tools of immediate risk of self-harm and suicide in children and young people: a scoping review. J Child Health Care 2019;23:178-99. https://doi.org/10.1177/1367493518787925.
- Crawford MJ, Aldridge T, Bhui K, Rutter D. User involvement in the planning and delivery of mental health services: a cross-sectional survey of service users and providers. Acta Psychiatr Scand 2003;107:410-4. https://doi.org/10.1034/j.1600-0447.2003.00049.x.
- NICE . The Short-Term Physical and Psychological Management and Secondary Prevention of Selfharm in Primary and Secondary Care, CG16 2004.
- Eberhart NK, Cerully JL, Shearer AL, . Evaluation Approaches for Mental Health Prevention and Early Intervention Programs. Santa Monica: RAND; 2017.
- Reeves K, Charter E, Ford T. Measurement issues: is standardised diagnostic assessment feasible as an adjunct to clinical practice? A systematic review. Child Adolesc Ment Health 2015;21:51-63. https://doi.org/10.1111/camh.12089.
- Wand T. Positioning mental health nursing practice within a positive health paradigm. Int J Ment Health Nurs 2012;22:116-24. https://doi.org/10.1111/j.1447-0349.2012.00848.x.
- Boland B, Bremner S. Squaring the circle: developing clinical risk management strategies in mental healthcare organisations. Adv Psychiat Treat 2013;19:153-9. https://doi.org/10.1192/apt.bp.111.010009.
- McCallum J, Eagle K. Risk assessment: a reflection on the principles of tools to help manage risk of violence in mental health. Psychiat Psychol Law 2014;22:378-87. https://doi.org/10.1080/13218719.2014.959155.
- Kumar S, Simpson AIF. Application of risk assessment for violence methods to general adult psychiatry: a selective literature review. Austr N Z J Psychiat 2005;39:328-35. https://doi.org/10.1080/j.1440-1614.2005.01579.x.
- Wand T. Investigating the evidence for the effectiveness of risk assessment in mental healthcare. Issues in Mental Health Nursing 2012;33:2-7. https://doi.org/10.3109/01612840.2011.616984.
- Clancy L, Happell B, Moxham L. The language of risk: common understanding or diverse perspectives?. Issues Ment Health Nurs 2014;35:551-7. https://doi.org/10.3109/01612840.2014.880139.
- Manning JC, Carter T, Walker G, Coad J, Aubeeluck A. CYP-MH-SAT Study Group . Assessing risk of self-harm in acute paediatric settings: a multicentre exploratory evaluation of the CYP-MH SAPhE instrument. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2020-043762.
- MacDonald S, Sampson C, Biddle L, Kwak SY, Scourfield J, Evans R. Theorising health professionals’ prevention and management practices with children and young people experiencing self-harm: a qualitative hospital-based case study. Sociol Health Illn 2021;43:201-9. https://doi.org/10.1111/1467-9566.13211.
- Kapur N, Goldney RD. Suicide Prevention. Oxford: Oxford University Press; 2019.
- Vandewalle J, Beeckman D, Van Hecke A, Debyser B, Deproost E, Verhaeghe S. Contact and communication with patients experiencing suicidal ideation: a qualitative study of nurses’ perspectives. J Adv Nurs 2019;75:2867-7. https://doi.org/10.1111/jan.14113.
- Clancy L, Happell B, Moxham L. Perception of risk for older people living with a mental illness: balancing uncertainty. Int J Ment Health Nurs 2015;24:577-86. https://doi.org/10.1111/inm.12175.
- Felton A, Repper J, Avis M. The construction of people with mental health problems as risk objects: findings of a case study inquiry. J Psychiatr Ment Health Nurs 2018;25:558-68. https://doi.org/10.1111/jpm.12501.
- White MR, Stein-Parbury J, Orr F, Dawson A. Working with consumers who hear voices: The experience of early career nurses in mental health services in Australia. Int J Ment Health Nurs 2019;28:605-15. https://doi.org/10.1111/inm.12566.
- Anderson M, Standen PJ. Attitudes towards suicide among nurses and doctors working with children and young people who self-harm. J Psychiatr Ment Health Nurs 2007;14:470-7. https://doi.org/10.1111/j.1365-2850.2007.01106.x.
- Suarez N, Saunders K. Assessment and management of self harm. BMJ 2012;344.
- Bellairs-Walsh I, Perry Y, Krysinska K, Byrne SJ, Boland A, Michail M, et al. Best practice when working with suicidal behaviour and self-harm in primary care: a qualitative exploration of young people’s perspectives. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-038855.
- Stallman HM. Coping planning: a patient-centred and strengths-focused approach to suicide prevention training. Australas Psychiat 2018;26:141-4. https://doi.org/10.1177/1039856217732471.
- McAndrew S, Warne T. Hearing the voices of young people who self-harm: implications for service providers. Int J Ment Health Nurs 2014;23:570-9. https://doi.org/10.1111/inm.12093.
- Neufeld SA, Jones PB, Goodyer IM. Child and adolescent mental health services: longitudinal data sheds light on current policy for psychological interventions in the community. J Public Ment Health 2017;16:96-9.
- Roisman GI, Masten AS, Coatsworth JD, Tellegen A, . Salient and emerging developmental tasks in the transition to adulthood. Child Dev 2004;75:123-33. https://doi.org/10.1111/j.1467-8624.2004.00658.x.
- Cutcliffe JR, Barker P. Considering the care of the suicidal client and the case for ‘engagement and inspiring hope’ or ‘observations’. J Psychiatr Ment Health Nurs 2002;9:611-1. https://doi.org/10.1046/j.1365-2850.2002.00515.x.
- Evans SA, Young D, Tiffin PA. Predictive validity and interrater reliability of the FACE-CARAS toolkit in a CAMHS setting. Crim 2019;29:47-56. https://doi.org/10.1002/cbm.2104.
- Godin P. ‘You don’t tick boxes on a form’: a study of how community mental health nurses assess and manage risk. Health Risk Soc 2004;6.
- Vassilev I, Pilgrim D. Risk, trust and the myth of mental health services. J Ment Health 2007;16:347-57.
- Flintoff A, Speed E, McPherson S. Risk assessment practice within primary mental health care: a logics perspective. Health (London) 2019;23:656-74. https://doi.org/10.1177/1363459318769471.
- Ougrin D, Boege I. Brief report: the self harm questionnaire: a new tool designed to improve identification of self harm in adolescents. J Adolesc 2013;36:221-5.
- Hawton K, Bergen H, Waters K, Ness J, Cooper J, Steeg S, et al. Epidemiology and nature of self-harm in children and adolescents: findings from the multicentre study of self-harm in England. Eur Child Adolesc Psychiatry 2012;21:369-77. https://doi.org/10.1007/s00787-012-0269-6.
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J Abnorm Psychol 2017;126:726-38. https://doi.org/10.1037/abn0000273.
- Higgins A, Doyle L, Downes C, Morrissey J, Costello P, Brennan M, et al. There is more to risk and safety planning than dramatic risks: mental health nurses’ risk assessment and safety-management practice. Int J Ment Health Nurs 2016;25. https://doi.org/10.1111/inm.12180.
- Dazzi T, Gribble R, Wessely S, Fear NT. Does asking about suicide and related behaviours induce suicidal ideation? What is the evidence?. Psychol Med 2014;44:3361-3. https://doi.org/10.1017/S0033291714001299.
- DeCou CR, Schumann ME. On the iatrogenic risk of assessing suicidality: a meta-analysis. Suicide Life Threat Behav 2018;48:531-43. https://doi.org/10.1111/sltb.12368.
- Brown S, Iqbal Z, Burbidge F, Sajjad A, Reeve M, Ayres V, et al. Embedding an evidence-based model for suicide prevention in the national health service: a service improvement initiative. Int J Environ Res Public Health 2020;17.
- Rothes IA, Henriques MR. Health professionals’ explanations of suicidal behaviour: effects of professional group, theoretical intervention model, and patient suicide experience. OMEGA-J Death Dying 2017;76:141-8.
- Rothes I, Henriques M. Health professionals facing suicidal patients: what are their clinical practices?. Int. J. Environ Res Public Health 2018;15. https://doi.org/10.3390/ijerph15061210.
- Horowitz L, Ballard E, Teach SJ, Bosk A, Rosenstein DL, Joshi P, et al. Feasibility of screening patients with nonpsychiatric complaints for suicide risk in a pediatric emergency department: a good time to talk?. Pediatr Emerg Care 2010;26:787-92. https://doi.org/10.1097/PEC.0b013e3181fa8568.
- Ballard ED, Bosk A, Snyder D, Pao M, Bridge JA, Wharff EA, et al. Patients’ opinions about suicide screening in a pediatric emergency department. Pediatr Emerg Care 2012;28:34-8. https://doi.org/10.1097/PEC.0b013e31823f2315.
- Ross AM, White E, Powell D, Nelson S, Horowitz L, Wharff E, et al. To ask or not to ask? Opinions of pediatric medical inpatients about suicide risk screening in the hospital. J Pediatr 2016;170:295-300. https://doi.org/10.1016/j.jpeds.2015.11.052.
- Mathias CW, Michael Furr R, Sheftall AH, Hill-Kapturczak N, Crum P, Dougherty DM. What’s the harm in asking about suicidal ideation?. Suicide Life Threat Behav 2012;42:341-1. https://doi.org/10.1111/j.1943-278X.2012.0095.x.
- Vrouva I, Fonagy P, Fearon PR, Roussow T. The risk-taking and self-harm inventory for adolescents: development and psychometric evaluation. Psychol Assess 2010;22:852-65. https://doi.org/10.1037/a0020583.
- Gray NS, Tiller J, Snowden RJ. WARRN-A formulation-based risk assessment procedure for Child and Adolescent Mental Health Services (CAMHS): The view of clinicians. J Forensic Pract 2019;21:228-39. http://doi.org/10.1108/JFP-06-2019-0025.
- Graney J, Hunt IM, Quinlivan L, Rodway C, Turnbull P, Gianatsi M, et al. Suicide risk assessment in UK mental health services: a national mixed-methods study. Lancet Psychiat 2020;7:1046-53. https://doi.org/10.1016/s2215-0366(20)30381-3.
- Burns J, Dudley M, Hazell P, Patton G. Clinical management of deliberate self-harm in young people: the need for evidence-based approaches to reduce repetition. Aust N Z J Psychiatry 2005;39:121-8.
- Pile V, Shammas D, Smith P. Assessment and treatment of depression in children and young people in the United Kingdom: comparison of access to services and provision at two time points. Clin 2020;25:119-32. https://doi.org/10.1177/1359104519858112.
- Orchard F, Pass L, Marshall T, Reynolds S. Clinical characteristics of adolescents referred for treatment of depressive disorders. Child Adolesc Psychiatry Ment Health 2017;22:61-8. https://doi.org/10.1111/camh.12178.
- Michail M, Tait L. Exploring general practitioners’ views and experiences on suicide risk assessment and management of young people in primary care: a qualitative study in the UK. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009654.
- Crawford T, Geraghty W, Street K, Simonoff E. Staff knowledge and attitudes towards deliberate self-harm in adolescents. J Adolesc 2003;26:619-29.
- Jahn DR, Quinnett P, Ries R. The influence of training and experience on mental health practitioners’ comfort working with suicidal individuals. Prof Psychol Res Pr 2016;47.
- LoParo D, Florez IA, Valentine N, Lamis DA. Associations of suicide prevention trainings with practices and confidence among clinicians at community mental health centers. Suicide Life Threat Behav 2019;49:1148-56. https://doi.org/10.1111/sltb.12498.
- Oordt MS, Jobes DA, Fonseca VP, Schmidt SM. Training mental health professionals to assess and manage suicidal behavior: can provider confidence and practice behaviors be altered?. Suicide Life Threat Behav 2009;39:21-32.
- Timson D, Priest H, Clark-Carter D. Adolescents who self-harm: professional staff knowledge, attitudes and training needs. J Adolesc 2012;35:1307-14. https://doi.org/10.1016/j.adolescence.2012.05.001.
- Anderson M, Standen PJ, Noon JP. A social semiotic interpretation of suicidal behaviour in young people. J Health Psychol 2005;10:317-31. https://doi.org/10.1177/1359105305051418.
- Schuberg K, Jobes D, Ballard E. Pre/Post/Post/Evaluations/of/CAMS-Trained/VA/Clinicians 2009.
- McLaughlin S, Bailey D, Bonner G, Canning C. Improving confidence in suicide risk assessment. Nurs Times 2014;110:16-8.
- Ambresin AE, Otjes CP, Patton GC, Sawyer SM, Thuraisingam S, English DR, et al. Training general practitioners to detect probable mental disorders in young people during health risk screening. J Adolesc Health 2017;61:302-9. https://doi.org/10.1016/j.jadohealth.2017.03.015.
- Jackson H, Wray J, Gardiner E, Flanagan T. Involving carers in risk assessment: a study of a structured dialogue between mental health nurses and carers. J Res Nurs 2019;24:330-41. https://doi.org/10.1177/1744987119851533.
- Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud 2015;52:1834-45. https://doi.org/10.1016/j.ijnurstu.2015.07.008.
- Horowitz LM, Ballard ED, Pao M. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr 2009;21:620-7. https://doi.org/10.1097/MOP.0b013e3283307a89.
- Leavey G, Mallon S, Rondon-Sulbaran J, Galway K, Rosato M, Hughes L. The failure of suicide prevention in primary care: family and GP perspectives – a qualitative study. BMC Psychiatry 2017;17. https://doi.org/10.1186/s12888-017-1508-7.
- Saini P, Windfuhr K, Pearson A, Da Cruz D, Miles C, Cordingley L, et al. Suicide prevention in primary care: general practitioners’ views on service availability. BMC Res Notes 2010;3. https://doi.org/10.1186/1756-0500-3-246.
- Saini P, Chantler K, Kapur N. General practitioners’ perspectives on primary care consultations for suicidal patients. Health Soc Care Community 2016;24:260-9. https://doi.org/10.1111/hsc.12198.
- Suicide NCIi, Illness HbPw M. Making Mental Health Care Safer: Annual Report and 20-Year Review 2016.
- Rahman MS, Kapur N. Quality of risk assessment prior to suicide and homicide. Psychiatr Bull 2014;38:46-7. https://doi.org/10.1192/pb.38.1.46b.
- Xanthopoulou P, Ryan M, Lomas M, McCabe R, . Psychosocial assessment in the emergency department. Crisis 2021;20210527. https://doi.org/10.1027/0227-5910/a000786.
- King E, Davies K, Abendstern M. Positive risk taking: debating the research agenda in the context of adult protection and COVID. J Adult Prot 2021;23:317-24.
- Clancy L, Happell B. Tensions of difference: reconciling organisational imperatives for risk management with consumer-focused care from the perspectives of clinicians and managers. J Clin Nurs 2014;23:3177-87. https://doi.org/10.1111/jocn.12564.
- Saab MM, Murphy M, Meehan E, Dillon CB, O’Connel S, Hegarty J, et al. Suicide and self-harm risk assessment: a systematic review of prospective research. Arch Suicide Res 2021:1-. https://doi.org/10.1080/13811118.2021.1938321.
- Wilson SC, Carryer J, Brannelly T. New risks: the intended and unintended effects of mental health reform. Nurs Inq 2016;23:200-10. https://doi.org/10.1111/nin.12130.
- Large MM, Ryan CJ, Carter G, Kapur N. Can we usefully stratify patients according to suicide risk?. BMJ 2017;359. https://doi.org/10.1136/bmj.j4627.
- NHS Resolution . Learning from Suicide Related Claims: A Thematic Review of NHS Resolution Data 2018.
- Chan MK, Bhatti H, Meader N, Stockton S, Evans J, O’Connor RC, et al. Predicting suicide following self-harm: systematic review of risk factors and risk scales. Br J Psychiatry 2016;209:277-3.
- Quinlivan L, Cooper J, Meehan D, Longson D, Potokar J, Hulme T, et al. Predictive accuracy of risk scales following self-harm: multicentre, prospective cohort study. Br J Psychiatry 2017;210:429-36. https://doi.org/10.1192/bjp.bp.116.189993.
- Quinlivan L, Cooper J, Steeg S, Davies L, Hawton K, Gunnel D, et al. Scales for predicting risk following self-harm: an observational study in 32 hospitals in England. BMJ Open 2014;4.
- Steeg S, Quinlivan L, Nowland R, Carrol R, Casey D, Clements C, et al. Accuracy of risk scales for predicting repeat self-harm and suicide: a multicentre, population-level cohort study using routine clinical data. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1693-z.
- Carter G, Milner A, McGill K, Pirkis J, Kapur N, Spittal MJ. Predicting suicidal behaviours using clinical instruments: systematic review and meta-analysis of positive predictive values for risk scales. Br J Psychiatry 2017;210:387-95. https://doi.org/10.1192/bjp.bp.116.182717.
- Granello DH. The process of suicide risk assessment: twelve core principles. J Couns Dev 2010;88:363-70.
- Gerson R, Malas N, Mroczkowski MM. Crisis in the emergency department: the evaluation and management of acute agitation in children and adolescents. Child Adolesc Psychiatr Clin N Am 2018;27:367-86.
- Darby C, Cardwell P. Restraint in the care of children. Emergency Nurse 2011;19.
- Haney EM, O’Neil ME, Carson S, Low A, Peterson K, Denneson LM, et al. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. Washington, DC: Department of Veterans Affairs (US); 2012.
- Muir-Cochrane E, Gerace A, Mosel K, O’Kane D, Barkway P, Curren D, et al. Managing risk: clinical decision-making in mental health services. Issues Ment Health Nurs 2011;32:726-34. https://doi.org/10.3109/01612840.2011.603880.
- Woods P. Risk assessment and management approaches on mental health units. J Psychiatr Ment Health Nurs 2013;20:807-13. https://doi.org/10.1111/jpm.12022.
- Manuel J, Crowe M. Clinical responsibility, accountability, and risk aversion in mental health nursing: a descriptive, qualitative study. Int J Ment Health Nurs 2014;23:336-43. https://doi.org/10.1111/inm.12063.
- Gerace A, Curren D, Muir-Cochrane E. Multidisciplinary health professionals’ assessments of risk: how are tools used to reach consensus about risk assessment and management?. J Psychiatr Ment Health Nurs 2013;20:557-3. https://doi.org/10.1111/jpm.12026.
- Stickley T, Felton A. Promoting recovery through therapeutic risk taking. Ment Health Pract 2006;9.
- Mulder R, Newton-Howes G, Coid JW. The futility of risk prediction in psychiatry. Br J Psychiatry 2016;209:271-2. https://doi.org/10.1192/bjp.bp.116.184960.
- Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet 2016;387:1227-39. https://doi.org/10.1016/S0140-6736(15)00234-2.
- Pridmore S, Ahmadi J, Reddy A. Suicide in the absence of mental disorder. Working Paper of Public Health 2012;1. https://doi.org/10.4081/wpph.2012.6772.
- Isometsa ET, Heikkinen ME, Marttunen MJ, Henriksson MM, Aro HM, Lonnqvist JK. The last appointment before suicide: is suicide intent communicated?. Am J Psychiatry 1995;152:919-22. https://doi.org/10.1176/ajp.152.6.919.
- Matthews K, Milne S, Ashcroft GW. Role of doctors in the prevention of suicide: the final consultation. Br J Gen Pract 1994;44:345-8.
- Pearson A, Saini P, Da Cruz D, Miles C, While D, Swinson N, et al. Primary care contact prior to suicide in individuals with mental illness. Br J Gen Pract 2009;59:825-32. https://doi.org/10.3399/bjgp09X472881.
- Murphy E, Kapur N, Webb R, Cooper J. Risk assessment following self-harm: comparison of mental health nurses and psychiatrists. J Adv Nurs 2011;67:127-39. https://doi.org/10.1111/j.1365-2648.2010.05484.x.
- Anderson J, Hurst M, Marques A, Millar D, Moya S, Pover L, et al. Understanding suicidal behaviour in young people referred to specialist CAMHS: a qualitative psychoanalytic clinical research project. J Child Psychother 2012;38:130-53. http://doi.org/10.1080/0075417X.2012.684484.
- Kapur N, Steeg S, Webb R, Haigh M, Bergen H, Hawton K, et al. Does clinical management improve outcomes following self-harm? Results from the multicentre study of self-harm in England. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0070434.
- Knowles SE, Townsend E, Anderson MP. Youth Justice staff attitudes towards screening for self-harm. Health Soc Care Community 2012;20:506-15. https://doi.org/10.1111/j.1365-2524.2012.01061.x.
- Taylor PJ, Wood AM. Discrepancies in parental and self-appraisals of prosocial characteristics predict emotional problems in adolescents. Br J Clin Psychol 2013;52:269-84. https://doi.org/10.1111/bjc.12013.
- Hiles S, Bergen H, Hawton K, Lewin T, Whyte I, Carter G. General hospital-treated self-poisoning in England and Australia: comparison of presentation rates, clinical characteristics and aftercare based on sentinel unit data. J Psychosom Res 2015;78:356-62. http://dx.doi.org/10.1016/j.jpsychores.2015.01.006.
- Horowitz L, Bridge JA. Analysis of multisource data establishes wide-ranging antecedents of youth suicide in England. Evid Based Ment Health 2017;20. https://doi.org/10.1136/eb-2016-102565.
- Morgan C, Webb RT, Carr MJ, Kontopantelis E. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ 2017;359. https://doi.org/10.1136/bmj.j4351.
- Patton G, Borschmann R. Responding to the adolescent in distress. Lancet 2017;390:536-8. http://doi.org/10.1016/S0140-6736%2817%2931331-4.
- Padmanathan P, Biddle L, Carroll R, Derges J, Potokar J, Gunnell D. Suicide and self-harm related internet use. Crisis 2018;39:469-78. https://doi.org/10.1027/0227-5910/a000522.
- O’Reilly M. Social media and adolescent mental health: the good, the bad and the ugly. J Ment Health 2020;29:200-6. http://doi.org/10.1080/09638237.2020.1714007.
- O’Reilly M, Kiyimba N, Karim K. ‘This is a question we have to ask everyone’: asking young people about self-harm and suicide. J Psychiatr Nurs 2016;23:479-8. https://doi.org/10.1111/jpm.12323.
- Department of Education . Special Educational Needs and Disability Code of Practice: 0 to 25 Years 2014.
- Jobanputra S, Singh S. What Are General Practitioners’ Views on the Management of Adolescents With Mental Health Disorders? A Qualitative Study 2020.
- Manning JC, Walker GM, Carter T, Aubeeluck A, Witchell M, Coad J. The CYP-MH SAT study group . Children and Young People-Mental Health Safety Assessment Tool (CYP-MH SAT) study: protocol for the development and psychometric evaluation of an assessment tool to identify immediate risk of self-harm and suicide in children and young people (10-19 years) in acute paediatric hospital settings. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-020964.
- Ougrin D, Zundel T, Kyriakopoulos M, Banarsee R, Stahl D, Taylor E. Adolescents with suicidal and nonsuicidal self-harm: clinical characteristics and response to therapeutic assessment. Psychol Assess 2012;24:11-20. http://dx.doi.org/10.1037/a0025043.
- Ougrin D, Zundel T, Ng AV, Habel B. Teaching therapeutic assessment for self-harm in adolescents: training outcomes. Psychol Psychother 2013;86:70-85. https://doi.org/10.1111/j.2044-8341.2011.02047.x.
- Daniel MR, Weir S, Tiffin PA. A novel CAMHS risk assessment system: Clinicians’ views. J Forensic Pract 2013;15:182-1. http://doi.org/10.1108/JFP-09-2012-0011.
- Terrelonge DN, Fugard AJ. Associations between family and clinician ratings of child mental health: a study of UK CAMHS assessments and outcomes. Clin 2017;22:664-74. https://doi.org/10.1177/1359104517713240.
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children’s global assessment scale (CGAS). Arch Gen Psychiatry 1983;40:1228-1. https://doi.org/10.1001/archpsyc.1983.01790100074010.
- Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Wolpert M, Ford T, Trustam E, Law D, Deighton J, Flannery H, et al. Patient-reported outcomes in child and adolescent mental health services (CAMHS): use of idiographic and standardized measures. Int J Ment Health 2012;21:165-73. https://doi.org/10.3109/09638237.2012.664304.
- Mackway-Jones K. Pain Assessment as Part of the Triage Process. London: BMJ Publishing Group; 1997.
- Pierce DW. Suicidal intent in self-injury. Br J Psychiatry 1977;130:377-85.
- Tiffin PA, Kitchen CEW, Weir S. Innovations in practice: piloting a new child and adolescent risk assessment suite in the UK. Child Adolesc Ment Health 2015;20:225-9. https://doi.org/10.1111/camh.12110.
- Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, et al. Ask Suicide-Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med 2012;166:1170-6. https://doi.org/10.1001/archpediatrics.2012.1276.
- Pfeffer CR, Jiang H, Kakuma T. Child–Adolescent Suicidal Potential Index (CASPI): a screen for risk for early onset suicidal behavior. Psychol Assess 2000;12.
- Larzelere RE, Andersen JJ, Ringle JL, Jorgensen DD. The child suicide risk assessment: a screening measure of suicide risk in pre-adolescents. Death Studies 2004;28:809-27.
- Shaffer D, Scott M, Wilcox H, Maslow C, Hicks R, Lucas CP, et al. The Columbia suicidescreen: validity and reliability of a screen for youth suicide and depression. J Am Acad Child Adolesc Psychiatry 2004;43:71-9. https://doi.org/10.1097/00004583-200401000-00016.
- Orbach I, Feshbach S, Carlson GA, Ellenberg L. Attitudes toward life and death in suicidal, normal, and chronically ill children: an extended replication. J Consult Clin Psychol 1984;52:1020-7. https://doi.org/10.1037/0022-006x.52.6.1020.
- Osman A, Downs WR, Kopper BA, Barrios FX, Baker MT, Osman JR, et al. The reasons for living inventory for adolescents (RFL-A): development and psychometric properties. J Clin Psychol 1998;54:1063-78. https://doi.org/10.1002/(sici)1097-4679(199812)54:8<1063::aid-jclp6>3.0.co;2-z.
- Angelkovska A. The Development and Validation of an Instrument to Identify Risk of Self-Harm in Children. University of Western Australia; 2007.
- Angelkovska A, Houghton S, Hopkins S. Differential profiles of risk of self-harm among clinically referred primary school aged children. Sch Psychol Int 2012;33:646-60.
- Sher MA, Gralton E. Implementation of the START:AV in a secure adolescent service. J Forensic Pract 2014;16:184-93. https://doi.org/10.1108/JFP-04-2013-0021.
- Sher MA, Warner L, McLean A, Rowe K. A prospective validation study of the START:AV. J Forensic Pract 2017;19:115-29. http://doi.org/10.1108/JFP-10-2015-0049.
- Cotton CR, Range LM. Suicidality, hopelessness, and attitudes toward life and death in clinical and nonclinical adolescents. Death Stud 1996;20:601-10. https://doi.org/10.1080/07481189608252765.
- Reynolds WM, Mazza JJ. Assessment of suicidal ideation in inner-city children and young adolescents: reliability and validity of the suicidal ideation Questionnaire-JR. Sch Psychol Rev 1999;28:17-30. https://doi.org/10.1080/02796015.1999.12085945.
- Flamarique I, Santosh P, Zuddas A, Arango C, Purper-Quakil D, Hoekstra PJ, et al. Development and psychometric properties of the Suicidality: Treatment Occurring in Paediatrics (STOP) Suicidality Assessment Scale (STOP-SAS) in children and adolescents. BMC Pediatr 2016;16.
- Reynolds WM. Development of a semistructured clinical interview for suicidal behaviors in adolescents. J Consult Clin Psychol 1990;2:382-90. https://doi.org/10.1037/1040-3590.2.4.382.
- Armstrong JG, Putnam FW, Carlson EB, Libero DZ, Smith SR, . Development and validation of a measure of adolescent dissociation: the adolescent dissociative experiences scale. J Nerv Ment Dis 1997;185:491-7.
- Vizzard E. Clinical Approaches to Sex Offenders and Their Victims. New York: Wiley; 1991.
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011;168:1266-77.
- Hamilton M. The Hamilton Depression Scale—accelerator or break on antidepressant drug discovery. Psychiatry 1960;23:56-62.
- Range LM, Lewis LS. Life orientation inventory: a method of assessing suicide risk. J Psychoeduc Assess 1992;10:296-7.
- Miller IW, Norman WH, Bishop SB, Dow MG. The modified scale for suicidal ideation: reliability and validity. J Consult Clin Psychol 1986;54:724-5. https://doi.org/10.1037/0022-006x.54.5.724.
- Horowitz LM, Wang PS, Koocher GP, Burr BH, Smith MF, Klavon S, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics 2001;107:1133-7. https://doi.org/10.1542/peds.107.5.1133.
- Patterson WM, Dohn HH, Bird J, Patterson GA. Evaluation of suicidal patients: the SAD PERSONS scale. Psychosomatics 1983;24:343-5. https://doi.org/10.1016/s0033-3182(83)73213-5.
- Bolton JM. Suicide risk assessment in the emergency department: out of the darkness. Depress Anxiety 2015;32:73-5. https://doi.org/10.1002/da.22320.
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol 1979;47:343-52. https://doi.org/10.1037//0022-006x.47.2.343.
- Borum R, Bartel P, Forth A. Manual for the Structured Assessment of Violence Risk in Youth (SAVRY©): version 1.1. University of South Florida; 2003.
- Reynolds WM. Suicidal ideation questionnaire (SIQ). Odessa, FL: Psychological Assessment Resources; 1987.
- Harriss L, Hawton K. Suicidal intent in deliberate self-harm and the risk of suicide: the predictive power of the Suicide Intent Scale. J Affect Disord 2005;86:225-33. https://doi.org/10.1016/j.jad.2005.02.009.
- Cull JG, Gill WS. PsycTESTS Dataset. American Psychological Association (APA); 1982.
- Plutchik R, van Praag HM, Conte HR, Picard S. Correlates of suicide and violence risk 1: the suicide risk measure. Compr Psychiatry 1989;30:296-302. https://doi.org/10.1016/0010-440x(89)90053-9.
- Conrad AK, Jacoby AM, Jobes DA, Lineberry TW, Shea CE, Arnold Ewing TD, et al. A psychometric investigation of the suicide status form II with a psychiatric inpatient sample. Suicide Life Threat Behav 2009;39:307-20. https://doi.org/10.1521/suli.2009.39.3.307.
- Beck AT, Resnik AT, Lettieri DJ. PsycTESTS Dataset. American Psychological Association (APA); 1974.
- Hoyos C, Mancini V, Furlong Y, Medford N, Critchley H, Chen W. The role of dissociation and abuse among adolescents who self-harm. Aust N Z J Psychiatry 2019;53:989-99. https://doi.org/10.1177/0004867419851869.
- Hill SA, Argent SE, Lolley J, Freya W. Characteristics of male patients admitted to an adolescent secure forensic psychiatric hospital. J Forensic Psychiatry Psychol 2016;27:21-37. https://doi.org/10.1080/14789949.2015.1094117.
- Palmer E, Welsh P, Tiffin PA. Perceptions of family functioning in adolescents who self-harm. J Fam Ther 2016;38:257-73. https://doi.org/10.1111/1467-6427.12069.
- Horowitz LM, Bridge JA, Pao M, Boudreaux ED. Screening youth for suicide risk in medical settings: time to ask questions. Am J Prev Med 2014;47:S170-5. https://doi.org/10.1016/j.amepre.2014.06.002.
- Rojahn J, Rowe EW, Sharber AC, Hastings R, Matson JL, Didden R, et al. The behavior problems inventory-short form for individuals with intellectual disabilities: Part II: reliability and validity. J Intellect Disabil Res 2012;56:546-65. https://doi.org/10.1111/j.1365-2788.2011.01506.x.
- Bird JC, Loe BS, Kirkham M, Fergusson EC, Shearn C, Stratford H, et al. The assessment of paranoia in young people: item and test properties of the Bird Checklist of Adolescent Paranoia. Schizophr Res 2020;220:116-22. https://doi.org/10.1016/j.schres.2020.03.046.
- Tarren-Sweeney M, Goemans A, Hahne AS, Gieve M. Mental health screening for children in care using the strengths and difficulties questionnaire and the brief assessment checklists: guidance from three national studies. Dev Child Welfare 2019;1:177-96. http://dx.doi.org/10.1177/2516103219829756.
- Laverty C, Oliver C, Moss J, Nelson L, Richards C. Persistence and predictors of self-injurious behaviour in autism: a ten-year prospective cohort study. Mol Autism 2020;11. https://doi.org/10.1186/s13229-019-0307-z.
- Ayodeji E, Green J, Roberts C, Trainor G, Rothwell J, Woodham A, et al. The influence of personality disorder on outcome in adolescent self-harm. Br J Psychiatry 2015;207:313-9. https://doi.org/10.1192/bjp.bp.113.138941.
- Pexton S, Farrants J, Yule W. The impact of fathers’ military deployment on child adjustment. The support needs of primary school children and their families separated during active military service: a pilot study. Clin 2018;23:110-4. https://doi.org/10.1177/1359104517724494.
- Tarver J, Vitoratou S, Mastroianni M, Heaney N, Bennett E, Gibbon F, et al. Development and psychometric properties of a new questionnaire to assess mental health and concerning behaviors in children and young people with Autism Spectrum Disorder (ASD): the Assessment of Concerning Behavior (ACB) Scale. J Autism Dev Disord 2021;51:2812-28. https://doi.org/10.1007/s10803-020-04748-1.
- Hassiotis A, Turk J. Mental health needs in adolescents with intellectual disabilities: cross-sectional survey of a service sample. Appl Res Intellect Disabil 2012;25:252-61. https://doi.org/10.1111/j.1468-3148.2011.00662.x.
- Price MA, Hollinsaid NL, Bokhour EJ, Johnston C, Skov HE, Kaufman GW, et al. Transgender and gender diverse youth’s experiences of gender-related adversity. Child Adolesc Social Work J n.d. https://doi.org/10.1007/s10560-021-00785-6.
- Guo B, Kaylor-Hughes C, Garland A, Nixon N, Sweeney E, Simpson S, et al. Factor structure and longitudinal measurement invariance of PHQ-9 for specialist mental health care patients with persistent major depressive disorder: exploratory structural equation modelling. J Affect Disord 2017;219:1-8. https://doi.org/10.1016/j.jad.2017.05.020.
- Haines A, Brown A, Javaid SF, Khan F, Noblett S, Omodunbi O, et al. Assessing protective factors for violence risk in U.K. general mental health services using the structured assessment of protective factors. Int J Offender Ther Comp Criminol 2018;62:3965-83. https://doi.org/10.1177/0306624X17749449.
- Phillips K, Whatson BL, Wells E, Milson G, Hartley S. Capturing the impact of adolescent inpatient admissions: the social connectedness scale. Clin Child Psychol Psychiatry 2019;24:631-41. https://doi.org/10.1177/1359104518807745.
- Hill SA, Brodrick P, Doherty A, Lolley J, Wallington F, White O. Characteristics of female patients admitted to an adolescent secure forensic psychiatric hospital. J Forensic Psychiatry Psychol 2014;25:503-19. http://doi.org/10.1080/14789949.2014.933863.
- Oliver C, Petty J, Ruddick L, Bacarese-Hamilton M. The association between repetitive, self-injurious and aggressive behavior in children with severe intellectual disability. J Autism Dev Disord 2012;42:910-9. https://doi.org/10.1007/s10803-011-1320-z.
- Fusar-Poli P, Werbeloff N, Rutigliano G, Oliver D, Davies C, Stahl D, et al. Transdiagnostic risk calculator for the automatic detection of individuals at risk and the prediction of psychosis: second replication in an independent national health service trust. Schizophr Bull 2019;45:562-70. http://doi.org/10.1093/schbul/sby070.
- Welsh P, Mediavilla JL, Tiffin PA. Attitudes and knowledge of child and adolescent mental health clinicians in relation to the psychosis risk syndrome. Early Interv Psychiatry 2011;5:355-9. https://doi.org/10.1111/j.1751-7893.2011.00285.x.
- Welsh P, Brown S. ‘I’m not insane, my mother had me tested’: the risk and benefits of being labelled ‘at-risk’ for psychosis. Health Risk Soc 2013;15:648-2. http://dx.doi.org/10.1080/13698575.2013.848846.
- Karatekin C, Hill M. Expanding the original definition of Adverse Childhood Experiences (ACEs). J Child Adolesc Trauma 2019;12:289-306. https://doi.org/10.1007/s40653-018-0237-5.
- Hidalgo MA, Petras H, Chen D, Chodzen G. The gender minority stress and resilience measure: psychometric validity of an adolescent extension. Clin Pract Pediatr Psychol 2019;7:278-90. https://doi.org/10.1037/cpp0000297.
- Testa RJ, Habarth J, Peta J, . Development of the gender minority stress and resilience measure. Psychol Sex Orientat Gend Divers 2015;2.
- Goldberg DP. User’s Guide to the General Health Questionnaire. Windsor: NFER-NELSON; 1988.
- Beck J. Manual for the Beck Youth Inventories. San Antonio, TX: Harcourt Assessment; 2005.
- Dyregrov A, Kuterovac G, Barath A. Factor analysis of the impact of event scale with children in war. Scand J Psychol 1996;37:339-50. https://doi.org/10.1111/j.1467-9450.1996.tb00667.x.
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. J Child Psychol Psychiatry 1981;22:73-88. https://doi.org/10.1111/j.1469-7610.1981.tb00533.x.
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 1997;36:545-53. https://doi.org/10.1097/00004583-199704000-00018.
- Fusar-Poli P, Oliver D, Spada G, Patel R, Stewart R, Dobson R, et al. Real world implementation of a transdiagnostic risk calculator for the automatic detection of individuals at risk of psychosis in clinical routine: study protocol. Front Psychiat 2019;10. http://dx.doi.org/10.3389/fpsyt.2019.00109.
- Ballard ED, Cwik M, Van Eck K, Goldstein M, Alfes C, Wilson ME, et al. Identification of at-risk youth by suicide screening in a pediatric emergency department. Preven Sci 2017;18:174-82.
- Cha CB, Augenstein TM, Frost KH, Gallagher K, D’Angelo EJ, Nock MK. Using implicit and explicit measures to predict nonsuicidal self-injury among adolescent inpatients. J Am Acad Child Adolesc Psychiatry 2016;55:62-8. https://doi.org/10.1016/j.jaac.2015.10.008.
- Chitsabesan P, Harrington R, Harrington V, Tomenson B. Predicting repeat self-harm in children. How accurate can we expect to be?. Eur Child Adolesc Psychiatry 2003;12:23-9. https://doi.org/10.1007/s00787-003-0302-x.
- Czyz EK, Horwitz AG, King CA. Self-rated expectations of suicidal behavior predict future suicide attempts among adolescent and young adult psychiatric emergency patients. Depress Anxiety 2016;33:512-9. https://doi.org/10.1002/da.22514.
- Gipson PY, Agarwala P, Opperman KJ, Horwitz A, King CA. Columbia-suicide severity rating scale: predictive validity with adolescent psychiatric emergency patients. Pediatr Emer Care 2015;31:88-94. http://doi.org/10.1097/PEC.0000000000000225.
- Horwitz AG, Czyz EK, King CA. Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. J Clin Child Adolesc Psychol 2015;44:751-61. https://doi.org/10.1080/15374416.2014.910789.
- King CA, Jiang Q, Czyz EK, Kerr DCR. Suicidal ideation of psychiatrically hospitalized adolescents has one-year predictive validity for suicide attempts in girls only. J Abnorm Child Psychol 2014;42:467-77. https://doi.org/10.1007/s10802-013-9794-0.
- King CA, Kerr DC, Passarelli MN, Foster CE, Merchant CR. One-year follow-up of suicidal adolescents: parental history of mental health problems and time to post-hospitalization attempt. J Youth Adolesc 2010;39:219-32. https://doi.org/10.1007/s10964-009-9480-2.
- Yen S, Weinstock LM, Andover MS, Sheets ES, Selby EA, Spirito A. Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychol Med 2013;43:983-93. https://doi.org/10.1017/s0033291712001912.
- Watson R, McCabe C, Harvey K, Reynolds S. Development and validation of a new adolescent self-report scale to measure loss of interest and pleasure: the Anhedonia Scale for Adolescents. Psychol Assess 2021;33:201-17. http://dx.doi.org/10.1037/pas0000977.
- Kennedy J, Hembry P, Green D, Skuse D, Lewis S. Predictors of change in global psychiatric functioning at an inpatient adolescent psychiatric unit: a decade of experience. Clin 2020;25:471-82. https://doi.org/10.1177/1359104519898215.
- Krause KR, Chung S, Adewuya AO, Albano AM, Babins-Wagner R, Birkinshaw L. International consensus on a standard set of outcome measures for child and youth anxiety, depression, obsessive-compulsive disorder, and post-traumatic stress disorder. Lancet Psychiatry 2021;8:76-8. https://doi.org/10.1016/S2215-0366(20)30356-4.
- Hamby S, Finkelhor D, Ormrod R, . The Juvenile Victimization Questionnaire (Jvq): Child Self-Report Version. Durham, NH: Crimes against Children Research Center; 2004.
- Radford L, Corral S, Bradley C, Fisher HL. The prevalence and impact of child maltreatment and other types of victimization in the UK: findings from a population survey of caregivers, children and young people and young adults. Child Abuse Negl 2013;37:801-13. https://doi.org/10.1016/j.chiabu.2013.02.004.
- Patalay P, Deighton J, Fonagy P, Vostanis P, Wolpert M. Clinical validity of the Me and My School questionnaire: a self-report mental health measure for children and adolescents. Child Adolesc Psychiatry Ment Health 2014;8. https://doi.org/10.1186/1753-2000-8-17.
- Radez J, Waite P, Chorpita B, Creswell C, Orchard F, Percy R. Using the 11-item version of the RCADS to identify anxiety and depressive disorders in adolescents. Res Child Adolesc Psychopathol 2021;49:1241-57. https://doi.org/10.1007/s10802-021-00817-w.
- Irish M, Solmi F, Mars B, King MB. Depression and self-harm from adolescence to young adulthood in sexual minorities compared with heterosexuals in the UK: a population-based cohort study. Lancet Child Adolesc Health 2019;3:91-8. http://dx.doi.org/10.1016/S2352-4642%2818%2930343-2.
- Sinclair J, Holden S. The mental health surveillance of adolescents, within a school setting. Ment Health Rev J 2013;18:83-92. https://doi.org/10.1108/MHRJ-10-2012-0028.
- Briere J, Johnson K, Bissada A, Damon L, Crouch J, Gil E, et al. The Trauma Symptom Checklist for Young Children (TSCYC): reliability and association with abuse exposure in a multi-site study. Child Abuse Negl 2001;25:1001-14.
- Gin K, Banerjea P, Abbott C, Browning S, Bracegirdle K, Corrigall R, et al. Childhood unusual experiences in community Child and Adolescent Mental Health Services in South East London: prevalence and impact. Schizophr Res 2018;195:93-6. https://doi.org/10.1016/j.schres.2017.08.046.
- Hurrell RA, Fullwood C, Keys J, Dickson AP, Fishwick J, Whitnall B, et al. Psychosocial screening at paediatric BEEC clinics: a pilot evaluation study. J Pediatr Urol 2015;11:79.e71-6. https://doi.org/10.1016/j.jpurol.2014.10.013.
- Goldston DB. Assessment of Suicidal Behaviors and Risk Among Children and Adolescents. Bethesda, MD: National Institute of Mental Health; 2000.
- Taylor AK, Steeg S, Quinlivan L, Gunnell D, Hawton K, Kapur N. Accuracy of individual and combined risk-scale items in the prediction of repetition of self-harm: multicentre prospective cohort study. BJPsych Open 2020;7. https://doi.org/10.1192/bjo.2020.123.
- Self-Harm, Suicide and Risk: Helping People Who Self-Harm. London: Royal College of Psychiatrists; 2010.
- Rees N, Rapport F, Snooks H. Perceptions of paramedics and emergency staff about the care they provide to people who self-harm: constructivist metasynthesis of the qualitative literature. J Psychosom Res 2015;78:529-35. https://doi.org/10.1016/j.jpsychores.2015.03.007.
- Erps KH, Ochs S, Myers CL. School psychologists and suicide risk assessment: role perception and competency. Psychol Sch 2020;57:884-900.
- National Collaborating Centre for Mental Health (UK) . Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care 2004.
- Gipson P, King C. Health behavior theories and research: implications for suicidal individuals’ treatment linkage and adherence. Cogn Behav Pract 2012;19:209-7.
- Olfson M, Gameroff MJ, Marcus SC, Bridge JA. Emergency treatment of young people following deliberate self-harm. Arch Gen Psychiatry 2005;62:1122-8. https://doi.org/10.1001/archpsyc.62.10.1122.
- Sisler SM, Schapiro NA, Nakaishi M, Steinbuchel P. Suicide assessment and treatment in pediatric primary care settings. J Child Adolesc Psychiatr Nurs 2020;33:187-200. https://doi.org/10.1111/jcap.12282.
- Goodyer IM. Suicide in Children and Adolescents. Cambridge: Cambridge University Press; 2003.
- American Academy of Child and Adolescent Psychiatry . Practice parameter for the assessment and treatment of children and adolescents with suicidal behavior. American Academy of Child and Adolescent Psychiatry. J Am Acad Child Adolesc Psychiatry 2001;40:24s-51s. https://doi.org/10.1097/00004583-200107001-00003.
- O’Reilly M, Karim K, Stafford V, Hutchby I. Identifying the interactional processes in the first assessments in child mental health. Child Adolesc Ment Health 2015;20:195-01. https://doi.org/10.1111/camh.12077.
- Barbot B, Eff H, Weiss SR, McCarthy JB. The role of psychopathology in the relationship between history of maltreatment and suicide attempts among children and adolescent inpatients. Child Adolesc Ment Health 2021;26:114-21. https://doi.org/10.1111/camh.12393.
- Vatne TM, Finset A, Ørnes K, Ruland CM. Application of the verona coding definitions of emotional sequences (VR-CoDES) on a pediatric data set. Patient Educ Couns 2010;80:399-404. https://doi.org/10.1016/j.pec.2010.06.026.
- Bennardi M, McMahon E, Corcoran P, Griffin E. Risk of repeated self-harm and associated factors in children, adolescents and young adults. BMC Psychiatr 2016;16. https://doi.org/10.1186/s12888-016-1120-2.
- Bridge JA, Olfson M, Fontanella CA, Marcus SC. Emergency department recognition of mental disorders and short-term risk of repeat self-harm among young people enrolled in Medicaid. Suicide Life Threat Behav 2018;48:652-60. https://doi.org/10.1111/sltb.12377.
- Sayal K, Roe J, Ball H, Atha C, Kaylor-Hughes C, Guo B, et al. Feasibility of a randomised controlled trial of remotely delivered problem-solving cognitive behaviour therapy versus usual care for young people with depression and repeat self-harm: lessons learnt (e-DASH). BMC Psychiatr 2019;19. https://doi.org/10.1186/s12888-018-2005-3.
- Troya MI, Cully G, Leahy D, Cassidy E, Sadath A, Nicholson S, et al. Investigating the relationship between childhood sexual abuse, self-harm repetition and suicidal intent: mixed-methods study. Bjpsych Open 2021;7. https://doi.org/10.1192/bjo.2021.962.
- Smith GL, McGuinness TM. Adolescent psychosocial assessment: the HEEADSSS. J Psychosoc Nurs Ment Health Serv 2017;55:24-7. https://doi.org/10.3928/02793695-20170420-03.
- Armstrong M. Nursing Skills for Children and Young People’ Mental Health. Cham, Switzerland: Springer; 2020.
- NICE . Depression (Amended): Management of Depression in Primary and Secondary Care. CG23 2007.
- NICE . Depression: The NICE Guidelines on the Treatment and Management of Depression in Adults Clinical Guideline CG90 (Updated ed.) 2010.
- Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics 2010;126:1117-23. https://doi.org/10.1542/peds.2010-0852.
- Fiedorowicz JG, Weldon K, Bergus G. Determining suicide risk (hint: a screen is not enough). J Fam Pract 2010;59:256-60.
- Gibbons R. Seminars in the Psychotherapies. Cambridge, UK: Cambridge University Press; 2021.
- Weerasekera P. Multiperspective Case Formulation: A Step towards Treatment Integration. Krieger Publishing Company; 1996.
- House A, Owens D. General hospital services in the UK for adults presenting after self-harm: little evidence of progress in the past 25 years. Br J Psychiatr 2020;217:661-2. https://doi.org/10.1192/bjp.2020.85.
- Kapur N. Services for self-harm: progress and promise?. Br J Psychiatr 2020;217:663-4. https://doi.org/10.1192/bjp.2020.104.
- Kendall T, Taylor C, Bhatti H, Chan M, Kapur N. Guideline Development Group of the National Institute for Health and Clinical Excellence. Longer term management of self harm: summary of NICE guidance. BMJ 2011;343. https://doi.org/10.1136/bmj.d7073.
- Harris IM, Beese S, Moore D. Predicting repeated self-harm or suicide in adolescents and young adults using risk assessment scales/tools: a systematic review protocol. Syst Rev 2019;8. https://doi.org/10.1186/s13643-019-1007-7.
- Last A, Henley W, Norman S, Goodman R, Ford T. Innovations in Practice: Feasibility of the development and well-being assessment as an adjunct to clinical assessment in child and adolescent mental health services. Child Adolesc Ment Health 2013;19:142-6. https://doi.org/10.1111/camh.12017.
Appendix 1 MEDLINE search strategy
Database: Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations and Daily <1946 to September 02, 2021>
Search strategy
-
exp adolescent/ (2119054)
-
Child/ (1772715)
-
(adolescen* or boy? or boyfriend or boyhood or girlfriend or girlhood or child* or girl? or juvenil* or kid? or minors or minors* or paediatric* or peadiatric* or pediatric* or puber* or pubescen* or school* or teen* or underage? or under-age? or youth*).ti,ab,kf. (2241109)
-
or/1-3 (3895754)
-
suicide/ or suicidal ideation/ or suicide, attempted/ (61686)
-
Self-Injurious Behavior/ or Self Mutilation/ (11693)
-
(suicid* or parasuicid* or auto mutilat* or automutilat* or self destruct* or selfdestruct* or self harm* or selfharm* or self immolat* or selfimmolat* or self inflict* or selfinflict* or self injur* or selfinjur* or selfmutilat* or self mutilat* or self poison* or selfpoison* or (self adj2 (cut or cuts or cutting or cutter? or burn or burns or burning or bite or bites or biting or hit or hits or hitting)) or head bang* or headbang*).ti,ab,kf,kw. (97846)
-
Crisis Intervention/ (5851)
-
cris?s.ab,ti. (73370)
-
Mental Health/ (46480)
-
Mental Disorders/ (169157)
-
mental health.ti,ab. (165684)
-
exp Mental Health Services/ (100187)
-
or/5-13 (534832)
-
4 and 14 (154687)
-
Risk Assessment/ (287241)
-
((risk* or psychosocial) adj3 assessment*).ab,ti. (93939)
-
(((assess* or predict* or risk*) adj2 (form*1 or checklist* or check list* or index* or indices or interview* or instrument* or inventor* or item*1 or measure* or psychometric* or question* or scale* or score* or scoring or self report* or subscale* or test* or tool*)) or (comprehensive adj (assessment* or evaluation*))).ti,ab. (382459)
-
or/16-18 (691499)
-
15 and 19 (10340)
-
exp United Kingdom/ (378288)
-
(national health service$ or nhs$).ab,in,ti. (226818)
-
(english not ((published or publication$ or translat$ or written or language$ or speak$ or literature or citation$) adj5 english)).ti,ab. (41605)
-
(gb or ‘g.b.’ or britain$ or (british$ not ‘british columbia’) or uk or ‘u.k.’ or united kingdom$ or (england$ not ‘new england’) or northern ireland$ or northern irish$ or scotland$ or scottish$ or ((wales or ‘south wales’) not ‘new south wales’) or welsh$).ab,in,jw,ti. (2218033)
-
(bath or ‘bath’s’ or ((birmingham not alabama*) or (‘birmingham’s’ not alabama*) or bradford or ‘bradford’s’ or brighton or ‘brighton’s’ or bristol or ‘bristol’s’ or carlisle* or ‘carlisle’s’ or (cambridge not (massachusetts* or boston* or harvard*)) or (‘cambridge’s’ not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (‘canterbury’s’ not zealand*) or chelmsford or ‘chelmsford’s’ or chester or ‘chester’s’ or chichester or ‘chichester’s’ or coventry or ‘coventry’s’ or derby or ‘derby’s’ or (durham not (carolina* or nc)) or (‘durham’s’ not (carolina* or nc)) or ely or ‘ely’s’ or exeter or ‘exeter’s’ or gloucester or ‘gloucester’s’ or hereford or ‘hereford’s’ or hull or ‘hull’s’ or lancaster or ‘lancaster’s’ or leeds* or leicester or ‘leicester’s’ or (lincoln not nebraska*) or (‘lincoln’s’ not nebraska*) or (liverpool not (new south wales* or nsw)) or (‘liverpool’s’ not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (‘london’s’ not (ontario* or ont or toronto*)) or manchester or ‘manchester’s’ or (newcastle not (new south wales* or nsw)) or (‘newcastle’s’ not (new south wales* or nsw)) or norwich or ‘norwich’s’ or nottingham or ‘nottingham’s’ or oxford or ‘oxford’s’ or peterborough or ‘peterborough’s’ or plymouth or ‘plymouth’s’ or portsmouth or ‘portsmouth’s’ or preston or ‘preston’s’ or ripon or ‘ripon’s’ or salford or ‘salford’s’ or salisbury or ‘salisbury’s’ or sheffield or ‘sheffield’s’ or southampton or ‘southampton’s’ or st albans or stoke or ‘stoke’s’ or sunderland or ‘sunderland’s’ or truro or ‘truro’s’ or wakefield or ‘wakefield’s’ or wells or westminster or ‘westminster’s’ or winchester or ‘winchester’s’ or wolverhampton or ‘wolverhampton’s’ or (worcester not (massachusetts* or boston* or harvard*)) or (‘worcester’s’ not (massachusetts* or boston* or harvard*)) or (york not (‘new york*’ or ny or ontario* or ont or toronto*)) or (‘york’s’ not (‘new york*’ or ny or ontario* or ont or toronto*))))).ti,ab,in. (1540924)
-
(bangor or ‘bangor’s’ or cardiff or ‘cardiff’s’ or newport or ‘newport’s’ or st asaph or ‘st asaph’s’ or st davids or swansea or ‘swansea’s’).ti,ab,in. (61304)
-
(aberdeen or ‘aberdeen’s’ or dundee or ‘dundee’s’ or edinburgh or ‘edinburgh’s’ or glasgow or ‘glasgow’s’ or inverness or (perth not australia*) or (‘perth’s’ not australia*) or stirling or ‘stirling’s’).ti,ab,in. (227664)
-
(armagh or ‘armagh’s’ or belfast or ‘belfast’s’ or lisburn or ‘lisburn’s’ or londonderry or ‘londonderry’s’ or derry or ‘derry’s’ or newry or ‘newry’s’).ti,ab,in. (29131)
-
or/21-28 (2786627)
-
(exp africa/ or exp americas/ or exp antarctic regions/ or exp arctic regions/ or exp asia/ or exp oceania/) not (exp great britain/ or europe/) (3072494)
-
29 not 30 (2647369)
-
20 and 31 (1310)
-
limit 32 to yr=‘2011 -Current’ (892)
-
limit 33 to english language (889)
***************************
Appendix 2 Risk-assessment pathway
This risk-assessment pathway is based largely upon NICE guidance and descriptive papers that outline the steps of the risk-assessment process. This work underpinned the realist synthesis allowing identification of critical points that lead to variation in outcomes. Table 16 within this Appendix provides a condensed version of this process.
| Study conducted to compare risk assessments by psychiatrists and mental health nurses following an episode of self-harm133 | Aim – to examine RA in relation to clinical management in practice. Psychiatric form included sociodemographic data, clinical information, precipitating factors, method of harm, circumstances of the act, a current mental state assessment, an RA and clinical follow-up arrangements. Patients classified as low-, moderate- or high-risk (study focused on high-risk patients) |
● | ? | ● | ● | ● | ● | ? | ? | Study – Standard RA form including detailed demographic and clinical data completed by the assessing psychiatrist or nurse. Outcomes compared: Positive predictive value of RAs for subsequent self-harm.
|
| Positive predictive value of RAs for self-harm repetition 25% (95% CI 20 to 31) among nurses and 23% (95% CI 13 to 37) among psychiatrists. Strong agreement on factors associated with RA of high-risk by both professions. Following RA of high-risk, psychiatrists much more likely than nurses to admit people for inpatient treatment (RR = 5Æ6, 95% CI 3Æ2 to 9Æ7) |
||||||||||
| General hospital-treated self-poisoning in England and Australia: Comparison of presentation rates, clinical characteristics and aftercare based on sentinel unit data138 |
In Oxford, majority of patients received a psychosocial assessment by psychiatric clinicians. Patients not receiving assessment identified through emergency department and medical records. Comparison of presentation rates, clinical characteristics and aftercare based on sentinel unit data Demographic, clinical and hospital management data on each episode collected by clinicians using standardised forms. Data from assessments entered into an electronic database by trained blinded data entry staff |
● | ? | ? | ? | ? | ? | ? | ? | Compared presentation rates, patient characteristics, psychosocial assessment and aftercare in the UK and Australia |
| To examine how the management that patients receive in hospital relates to subsequent outcome. Identified episodes of self-harm presenting to three UK centres (Derby, Manchester, Oxford) between 2000–9. Examined relationship between four aspects of management (including psychosocial assessment) and repetition of self-harm within 12 months | Four aspects of Management:
Examined repetition of self-harm within 12 months |
● | ? | ● | ? | ? | ? | ? | ○ | Main outcome was repeat self-harm within 12 months of an individual’s index episode during study period |
| Psychosocial assessment investigated population-based rates of self-harm in children and adolescents by gender and age groups, trends in rates over time, methods used for self-harm, diurnal and annual temporal patterns, clinical characteristics, aftercare and repetition of self-harm. Also examined adherence to national guidance on psychosocial assessment and admission of under-16-year olds | Psychosocial assessment and admission Admission to a hospital bed for self-harm presentations, diurnal and annual temporal patterns, clinical characteristics, aftercare and repetition of self-harm. Relationship problems examined |
● | ? | ? | ? | ? | ● | ? | ? | Psychosocial assessment and admission During 2005–7 specialist psychosocial assessment occurred in 57.0 % (N = 1500) of episodes (four not known). Admission to a hospital bed for self-harm presentations occurred in 70.7 % (N = 1063) in Oxford and Manchester. The majority of individuals aged under 16 years admitted (84.1 %), significantly more than those aged 16–18 years. Frequent repetition of self-harm (53.3 % had history of prior self-harm and 17.7 % repeated within a year). Relationship problems were predominant difficulties associated with self-harm |
| Mental health assessment.144 Specifically evaluating self-harm and suicide risk. Purposeful sample of all consenting first assessment appointments within UK CAMHS. Initial multidisciplinary assessments followed institutional requirement and assessment guidelines. Children assessed by minimum of two practitioners including consultant, staff grade and trainee child and adolescent psychiatrists, clinical psychologists, assistant psychologists, community psychiatric nurses (CPNs), occupational therapists and psychotherapists) |
Evaluating self-harm and suicide risk (including through direct questioning) Format of assessments not informed by any specific theoretical approach |
● | ? | ? | ? | ? | ? | ? | ? |
Explores 15 cases where practitioners did not ask specifically about self-harm or suicidal ideation.
|
| Qualitative psychoanalytic clinical research project Each clinician planned to offer an extended assessment to five cases fulfilling the inclusion criteria, that is a young person who had been referred to specialist CAMHS with self-harm or suicidal behaviour and who attended mainstream schooling, did not have a statement of special educational needs and was not suffering with anorexia nervosa |
Extended assessments – included history taking, assessment of risk (including suicidality), familial relationships Risk assessments drew information from the following sources: Physical presentation
|
? | ● | ? | ● | ● | ? | ? | ○ | Detailed case history is needed. P. 141 The use of the Truth Danger Theory and assessing risk- Estimating risk: Acknowledges that risk tools are only a ‘useful adjunct’ to clinical experience in assessing risk Findings revealed obstacles to accurate assessment of current and enduring risk: Lack of Congruence between components of a young person’s presentation may lead to inaccurate assessment of their current and enduring risk |
The overall pathway
Non-mental health professionals, such as paediatricians and registered children’s nurses, are increasingly involved in conducting an initial assessment of these children. 39 Not only must they identify the immediate physical and emotional health needs of these children but they also need to assess any immediate risk of suicide and self-harm. In contrast with specialist mental health care delivered by professionals (including psychiatrists, nurses, social workers and psychologists) with specialist training, skills and knowledge2 these health professionals receive little specialist mental health training. 89
Risk assessment is a critical step towards a formulation, treatment plan, and successful intervention. Not only does it seek to respond appropriately to children and adolescents at risk of self-harm, suicidal ideation and suicide attempt, it is also important in managing those children who might not currently require the most urgent level of response, potentially diverting staff resources from where they are needed at that particular point in time.
As this report makes clear, evidence suggests that risk-assessment tools are no more accurate at predicting risk than expert specialist mental health professional clinical judgement. Assessments focus on immediate (i.e. hours or days) risks of self-harm or suicide while in receipt of acute paediatric care. Additionally, assessments are performed in time-limited circumstances in children and adolescents with potentially dynamic and fluctuating mental health. 39 Therefore, when implementing a plan of care where immediate risks can be mitigated, healthcare professionals require appropriate support and guidance. NICE guidelines feature numerous risk-assessment components. 14 Previous incidents of self-harm is the most common characteristic incorporated into risk assessments.
Setting
Children or adolescents at risk are most likely to present to primary care, and accident and emergency departments. Acute paediatric care settings place unique demands upon assessment of risk for suicide or self-harm. 39 Paediatricians and registered children’s nurses lead initial triage and care of children and adolescents in acute paediatric settings, including emergency departments and paediatric inpatient wards. 147
Self-harm is one of the top five causes of acute medical admission to hospitals,242 yet only a minority (10–20%) present to hospital. 243 Prevalence is probably between 1% and 5% of the general population. In addition, significant concerns may be raised within a school context or when the family or individual engages with social services. Teachers and other school personnel who interact with students daily have a unique opportunity and responsibility to be aware of, and recognise, signs of suicide. 244 Typically, their response is to try to ensure that the young person seeks to access health or mental health services.
Initial triage and care
NICE (2004) guidelines on self-harm advocate that children and adolescents who self-harm should be assessed for risk. 89,245 This initial stage seeks to ensure that children and adolescents are appropriately assessed such that they are safe until definitive and expert mental health assessment is undertaken. Nursing professionals identify providing care for children and adolescents experiencing mental health crisis as one of the most complex and stressful duties undertaken in practice. 96 Poor experience and outcome at this acute phase may trigger a knock-on negative impact on adherence with follow-up and future mental health. Non-adherence to follow-up is, in turn, a predictor of poor outcomes, seen not only in repeated self-harm and suicide but also in numerous diverse psychosocial outcomes. 246
Assessment
Where immediate physical care is not required, children or adolescents may spend over 5 hours in emergency departments before receipt of specialised health care or assessment. 50 A health professional assessing children and adolescents who are experiencing a mental health crisis should (i) identify the main clinical and demographic features known to be associated with their mental health crisis, and (ii) identify the key psychological characteristics associated with risk, in particular depression, hopelessness and continuing suicidal intent. 245 In addition, they should address any immediate physical health needs. 247 The health professional should ensure the safety of the child or adolescent until expert assessment is undertaken by specialist mental health professionals. 147
Risk assessment requires identification of any positive risk factors as well as any relevant protective factors. A structured assessment comprises multiple steps:58
-
Take a chronological history of the event. 248
-
Identify mental or physical illness by history and examine the patient’s mental state.
-
Conduct a risk assessment and, finally, based on the risk assessment
-
Identify management options.
Invariably health professionals have to conduct assessments in time limited circumstances and with children and adolescents with potentially changing mental health status. Therefore, they focus the assessment on identifying the most pertinent risks (i.e. immediate risk of self-harm or suicide). They also take into account risk factors, coping abilities and assessment of lethality of previous suicidal and self-harm behaviour. 249 Such factors can help staff to differentiate between high-risk and low-risk suicidal and self-harm behaviours. 250 For each young person staff will also consider their emotional regulation ability, communication style, readiness to engage and to accept help, and where they are positioned in their illness/recovery trajectory. Key components include introductions, reasons for attendance, problem presentation, decision-making and session closure. 251 Health professionals try to identify relevant stress factors that might have influenced the patient, which could be targeted for future management. 58 Risk factors can include a heightened vulnerability for stigma, guilt and acute distress. 252 Furthermore, they consider the seriousness of the patient’s intent. 248 Assessment explores the person’s family, social situation and child protection issues.
Risk assessment should also consider the developmental age of the children and adolescents as children can often find verbal expression difficult, especially when in emotional distress. 253 Where young persons find it difficult to disclose feelings or emotions (e.g. adolescent males), risk-assessment tools may offer a mechanism by which they can express and describe their feelings and distress. Otherwise a young person may simply choose not to engage at all. Furthermore, the risk assessment should include assessment of previous A&E presentations39 as this represents one of the strongest predictors of future A&E reattendance. 254
Biopsychosocial assessment
Most sources endorse a thorough biopsychosocial assessment. 165,255–257 This may be challenging given time pressures. A holistic biopsychosocial assessment, that includes but does not focus upon risk assessment, may not be viewed as important within a culture that focuses on risk aversion. Mental health professionals need to be vigilant for a broad range of biopsychosocial factors when conducting a risk assessment. 252 If health professionals outside of CAMHS (such as paediatricians and children’s nurses) are to implement a plan of care that seeks to mitigate immediate risks, they need to be supported in making an informed assessment.
The Home, Education/Employment, Eating, Activities, Drugs, Sexuality, Suicidal ideation and Safety (HEEADSSS) assessment is considered by some as a practical, youth-relevant strategy for adolescent patients who attend A&E with self-harm/mental health concerns. 258 The HEEADSSS assessment provides a systematic approach to developing rapport with the young person and performing a holistic, biopsychosocial resilience and risk assessment across the domains of home, education, eating (and/or employment), activities, drugs and alcohol, sexuality, suicide, and mental health and safety.
Perspectives of health professionals
NICE clinical guidelines (CG 16) state that children and young people should be assessed by professionals experienced in the assessment of children and young people who self-harm. 14 Mental health nurses may be concerned about the influence of risk assessment on their relationship with service users and may feel that they have to emphasise risk avoidance in order to maintain safety. 5,54
General practitioners
General practitioners (GPs) should respect the young person’s desire for privacy. They should ensure that young people are aware of how their information is collected, stored and used, and doing so is likely to result in improved disclosure of suicidal behaviours and/or self-harm. 59 Time constraints pose a significant barrier to empathetic listening and sensitive discussion. The challenge for GPs and other time-pressured individuals is how to ensure that young people experience a positive therapeutic interaction during their engagement with services. Youth-friendly care, including being non-judgemental, genuine, respectful, empathetic, and listening, may help to promote a sense of connection and being cared for, and inspire hope. Positive interactions may also address barriers to disclosure and identification of suicidal behaviour and/or self-harm, laying a foundation for open and honest communication.
GPs may feel that they lack the confidence and skills to enquire about and discuss suicidality and self-harm with young people. 59 They may also worry about possible negative outcomes associated with asking about these issues. Negative reactions from GPs to a disclosure could serve to escalate or exacerbate the young person’s symptoms. Young people, and GP themselves, have expressed how they would welcome training for GPs in communication skills to overcome this obstacle to providing patient-centred care. 59 Indeed, some anxiety over negative outcomes seems to stem from recognition that GPs could conduct these assessments and then refer to CAMHS services.
CAMHS staff
Different CAMHS across the UK have different structures and teams. Often CAMHS services may include self-harm teams or crisis/liaison teams whose role is to undertake urgent hospital/community assessments. 259 The majority of staff in these teams are mental health nurses. 259 Staff working within CAMHS report feeling more effective than A&E staff and teachers in responding to adolescent self-harm behaviour. 93 In feeling more effective they also felt less negative. It has been suggested that CAMHS staff may have invested more in the therapeutic relationship with young people and thereby have a better understanding than staff assigned to treat those who self-harm medically. 93
Intervention
Risk-assessment tools and scales are usually checklists to be completed and scored by a health professional or, sometimes, by the service user. They are designed to give a crude indication of the level of risk (e.g., high or low) of a particular outcome, most often suicide. The use of risk scales for suicidal ideation or behaviour is controversial. 115 Some clinical guidance advises the use of risk scales over locally developed proformas, but others argue that scales should only be used to structure assessments and not to predict future risk of suicidal behaviour or decide upon aftercare. 16,241 Quinlivan et al. investigated the use of risk scales following self-harm within National Health Service (NHS) emergency departments and specialist mental health treatment settings. The most frequently used suicide risk-assessment instruments were unvalidated, locally developed scales. 115 Indeed, 22 of 32 (68.8%) English hospitals included in the study used an unvalidated instrument. The authors concluded that there is presently little consensus among clinicians and hospital systems regarding the best instrument to use to assess suicide risk. 115 In the remaining third of English hospitals included in the study, the SAD PERSONS scale (SPS) emerged as the most frequently used standardised approach to suicide risk assessment. The SPS has been implemented despite evidence suggesting it is no better than chance at predicting future suicide attempts among ED psychiatric patients. 180 There is growing evidence that risk scales do not accurately predict repeat self-harm and suicide. 16,241 and this has been demonstrated specifically in scales for children and adolescents. 16
Currently, GPs may use the Patient Health Questionnaire-9 (PHQ-9) for assessing and monitoring depression260 and ‘biopsychosocial assessments’ to assess patients’ risk. 261 Biopsychosocial assessments are designed to offer a holistic assessment about diverse factors, not exclusively risk of self-harm and suicide. A study of the usability of the PHQ-9 in an adolescent population (13–17 year olds) concluded that it is an excellent tool for screening depression with this age range in primary care settings. 262 Psychosocial assessment instruments have been developed to provide healthcare professionals in multidisciplinary contexts with a framework with which to discuss young people’s psychological, social, behavioral and environmental concerns. NICE guideline (CG 133) suggests areas to be included in a structured risk assessment. 14
The NICE guideline (CG 133) cautions that a health professional14
-
should not use risk-assessment tools and scales to predict future suicide or repetition of self-harm
-
should not use risk-assessment tools and scales to determine who should and should not be offered treatment or who should be discharged
-
may use risk-assessment tools to help structure risk assessments as long as they include the areas identified in Box 2.
Evidence confirms that health professionals should not be afraid of discussing suicide with the patient; doing so does not make a suicide attempt more likely to happen again. 263 When discussing the outcome of the incident, a health professional should ask whether the patient regrets either their attempt or the failure of their attempt, and how they are likely to act in the future if the same stress factor presents itself. 58 This approach is a useful marker of risk, although determined patients may be able to hide their emotions and future intent.
Follow-up
Young people emphasise the importance of follow-up after a presentation involving risk of suicidal behaviour or self-harm. Active follow-up by GPs can ‘provide an opportunity for further assistance, strengthen the therapeutic relationship and potentially mitigate isolation, hopelessness and increased vulnerability that can occur with disengagement’. 59 Health professionals should use information gained to plan follow-up in the form of
-
a care plan, and
-
a risk-management plan in conjunction with the person who self-harms and their family, carers or significant others if agreed with the person.
They should provide copies for the service user and share them with their GP. If there is disagreement between health and social care professionals and the person who self-harms about their needs or risks, the young person could be given the opportunity to write this in their notes.
Risk formulation
Health professionals should begin by summarising key areas of needs and identifying the risks and triggers, and how these interact. The information gained is then used to develop a risk formulation and management plan. 150 The risk formulation is a brief summarising statement of an estimate of the nature and level of perceived risks, the target of these risks and the timescale of the risk prediction. 150 Typically, the risk formulation (i) identifies ‘why’ someone engages in problematic behaviour not just ‘if’ they will engage in it, and (ii) goes beyond simply identifying risk factors to thinking about how key variables interact and connect in the expression of risk. 38 Twenty-nine (34%) of 85 services surveyed used the ‘five Ps model’ (facilitating the understanding of a case, its context and the way in which factors interact)264 to underpin risk formulation. 265
Longer-term treatment and management of self-harm
Mental health services (including community mental health teams and liaison psychiatry teams) are generally responsible for the routine assessment and the longer-term treatment and management of self-harm. 266,267 In children and young people this should be the responsibility of the CAMHS. The following section is largely based upon the NICE guideline (CG 133)14 and an associated commentary. 268
Care plans
Care plans should be multidisciplinary and developed collaboratively with the person who self-harms and, provided the person agrees, with their family, carers or significant others. 268 Members of the team should discuss, agree and document the aims of longer-term treatment in the care plan. 14 They should review the person’s care plan with them, including the aims of treatment, and revise it at agreed intervals of not more than one year.
Risk-management plans
A risk-management plan should be clearly identifiable within the overall care plan and should14
-
address each of the long-term and more immediate risks identified in the risk assessment
-
address specific factors (psychological, pharmacological, social and relational) identified as associated with increased risk, with the agreed aim of reducing the risk of repetition of self-harm and/or the risk of suicide
-
include a crisis plan outlining self-management strategies and how to access services during a crisis when self-management strategies fail
-
ensure consistency with the long-term treatment strategy.
The team should inform the person who self-harms of the limits of confidentiality and that information in the plan may be shared with other professionals. 14 Risk-management plans should be updated, to include monitoring changes in risk and specific associated factors for the service user, and evaluation of the impact of treatment strategies over time.
Appendix 3 Evidence included from realist synthesis
| Publication identifier | Relevance | Publication/ study type | Aim | Results | Implications |
|---|---|---|---|---|---|
| Ambresin et al. (2017)97 Australia and Switzerland |
*** | RCT | To investigate whether training intervention increases general practitioners’ (GPs’) detection sensitivity for probable mental disorders in young people | GPs’ detection sensitivity improved after intervention if having probable mental disorder was defined as high K10 score and self-perceived mental illness (odds ratio: 2.81; 95% CI 1.23 to 6.42). No significant difference in sensitivity of GPs’ detection for preferred definition, high K10 or self-perceived mental illness (.37 in both; odds ratio: 0.93; 95% CI 0.47 to 1.83). Detection accuracy comparable (specificity: 0.84 vs. 0.87, positive predictive values: 0.54 vs. 0.60, and negative predictive values: 0.72 vs. 0.72) | Improving recognition of mental disorder among young people attending primary care is likely to require a multifaceted approach targeting young people and GPs |
| Anderson and Standen (2007)57 | *** | Questionnaire study | To investigate the attitudes towards suicide in nurses and doctors who work with children and young people who self-harm | 179 nurses and doctors working in accident and emergency; paediatric medicine and adolescent inpatient mental health services. Nurses and doctors indicated agreement on Mental Illness, Cry for Help, Right to Die, Impulsivity, Normality and Aggression scales, and less agreement on the Religion and Moral Evil scale. Only scores for Mental Illness statistically different by professional group | Complex attitudes need to be taken into account in training for healthcare professionals and in the development of contemporary suicide prevention policy |
| Ballard et al. (2012)79 | *** | Qualitative study | To understand how children react to suicide screening in an emergency department (ED) to inform implementation strategies | 106/156 patients (68%) presented to ED with non-psychiatric complaints and 50 (32%) presented with psychiatric complaints. All patients answered the question of interest, and 149 (96%) of 156 patients supported the idea that nurses should ask youth about suicide in the ED. Most frequently endorsed themes: (1) identification of youth at risk (20%), (2) desire to feel known and understood by clinicians (20%), (3) connection of youth with help/resources (18%), (4) prevention of suicidal behaviour (16%), and (5) lack of other individuals to speak to about these issues (12%) | Paediatric patients in the ED support suicide screening after being asked a number of suicide-related questions. Further work should evaluate the impact of suicide screening on referral practices and link screening efforts with evidence-based interventions |
| Bee et al. (2015)99 | * | Qualitative interviews and focus groups with data combined and subjected to framework analysis | To explore professional perceptions of delivering collaborative mental healthcare planning and involving service users and carers in their care | Care planning reveals philosophical tensions between user involvement and professional accountability. Professionals emphasised individual, relational skills as the core facilitator of involvement, highlighting important deficiencies in conventional staff training programmes | User-involved care planning is poorly defined and lacks effective implementation support. It requires greater recognition of the historical and contemporary contexts in which statutory mental health care occurs |
| Boland and Bremner (2013)45 | * | Opinion piece | To explore challenges of developing clinical risk management practice and policy within large mental healthcare organisations | Explores how clinical risk relates to clinical quality. Benefits of standardisation explored. Highlights complexities and conflicts of implementing standardised procedures, given evidence base, and difficulties when applying to clinical practice | Using concepts from strategic planning and psychology, suggests an approach to respond to these factors at a local level to achieve better outcomes for service users and clinicians |
| Brown et al. (2020)75 | *** | Quality improvement initiative | To outline novel systems-level approach to objectively differentiate level of severity for each suicide risk presentation and provide fast-track pathways for all, including life-threatening cases | Organisation-wide bespoke ‘suicide risk triage’ system utilising CAMS was implemented across all services. Preliminary impacts on suicidality, suicide rates and service user outcomes were described | Implemented in English NHS secondary care mental health provider open-access 24/7 crisis and home treatment service |
| Burns et al. (2005)85 | ** | Systematic review | To examine the evidence for the effectiveness of clinical interventions designed to reduce the repetition of self-harm in adolescents and young adults | Three RCTs, four clinical control trials and three quasi-experimental studies were identified. Group therapy, trialled in a RCT, was the only programme that led to a significant reduction in rates of repetition of self-harm. Attendance at follow-up did not improve significantly regardless of the intervention. One clinically controlled trial of intensive intervention resulted in poorer attendance at follow-up. One quasi-experimental study of family therapy resulted in significant reduction in suicidal ideation | The evidence base for treatments designed to reduce the repetition of self-harm in adolescents and young adults is very limited. Expensive interventions such as intensive aftercare offer no clear benefit over routine aftercare. Given that self-harm among young people is a common clinical problem further good-quality treatment studies are warranted. Process evaluation required to determine which individual components of any given intervention are effective |
| Carter et al. (2017)117 | ** | Systematic review and meta-analysis | To identify studies of predictive instruments and to calculate positive predictive value estimates for suicidal behaviours | For all scales combined, pooled positive predictive values were as follows: suicide 5.5% (95% CI 3.9 to 7.9%), self-harm 26.3% (95% CI 21.8 to 31.3%) and self-harm plus suicide 35.9% (95% CI 25.8 to 47.4%). Subanalyses on self-harm found pooled positive predictive values of 16.1% (95% CI 11.3 to 22.3%) for high-quality studies, 32.5% (95% CI 26.1 to 39.6%) for hospital-treated self-harm and 26.8% (95% CI 19.5 to 35.6%) for psychiatric in-patients | No ‘high-risk’ classification was clinically useful. Prevalence imposes a ceiling on positive predictive value. Treatment should reduce exposure to modifiable risk factors and offer effective interventions for selected subpopulations and unselected clinical populations |
| Chan et al. (2016)113 | ** | Systematic review and meta-analysis | To undertake first systematic review and meta-analysis of prospective studies of risk factors and risk-assessment scales to predict suicide following self-harm | Twelve studies on risk factors and seven studies on risk scales included. Four risk factors emerged from meta-analysis, with robust effect sizes that showed little change when adjusted for confounders. These included the following: previous episodes of self-harm (hazard ratio (HR) = 1.68, 95% CI 1.38 to 2.05, K = 4), suicidal intent (HR = 2.7, 95% CI 1.91 to 3.81, K = 3), physical health problems (HR = 1.99, 95% CI 1.16 to 3.43, K = 3) and male gender (HR = 2.05, 95% CI 1.70 to 2.46, K = 5). Studies evaluated only three risk scales (BHS, SIS and Scale for Suicide Ideation). Meta-analyses where possible (BHS, SIS) were based on sparse data and high heterogeneity was observed. Positive predictive values ranged from 1.3 to 16.7% | The four risk factors that emerged, although of interest, are unlikely to be of practical use being comparatively common in clinical populations. No scales have sufficient evidence to support their use. Use of these scales, or an over-reliance on the identification of risk factors in clinical practice, may provide false reassurance and is, therefore, potentially dangerous. Comprehensive psychosocial assessments of the risks and needs that are specific to the individual should be central to management of people who have self-harmed |
| Clancy et al. (2014)49 | * | Qualitative, exploratory approach using individual interviews and focus groups | To enhance understanding of how risk is conceptualised within an older persons’ setting | Language of risk was a major theme. This language, familiar to providers of services, was not familiar to consumers and carers. A reframing of risk is necessary to reflect consumers’ and carers’ experiences and understandings | Approach will be essential in promoting consumer and carer participation within recovery-based services, reflecting significant goals of government policy |
| Clancy and Happell (2014)108 | * | Qualitative exploratory methods | To understand the impact of risk management and assessment on the delivery of mental health care from the perspectives of managers and clinicians | Identified tensions between accountability and attending to risk issues and consumer-centred care, with concerns being raised that procedural and bureaucratic accountability influence (often negatively) provision of care. Different perspectives of clinicians and managers have different perspectives in relation to how they see evidence-based practice contributing to risk | Prioritising risk management may interfere with capacity of clinicians and managers to provide quality and consumer-focused mental health care. Deeper examination and reconceptualisation of role and importance of risk in mental health care needed to ensure service delivery remains consumer-focused |
| Crawford et al. (2003)89 | *** | Questionnaire survey | To investigate knowledge, attitudes and training needs concerning self-harm in adolescents, among professionals involved in the assessment and management of adolescence who self-harm | Mean percentage of correctly answered knowledge questions, across all professional groups, was 60%. With regard to knowledge, over three-quarters of participants were unaware that homosexual young men and those who had been sexually abused are at greater risk of self-harm. One-third of staff were unaware that adolescents who self-harm are at increased risk of suicide. Staff who felt more effective felt less negative towards this group of patients | Forty-two per cent of the participants wanted further training in self-harm among adolescents |
| Cutcliffe and Barker (2002)64 | * | Discussion paper | To explore contested positions regarding appropriate care for the person who is at risk of suicide; summarised as the ‘engagement and hope inspiration’ position and the ‘observations’ position | Describes policy context of care for the suicidal client. Focuses on ‘observations’ and identifies well-established, empirically based drawbacks to approach. Then focuses on ‘engagement, inspiring hope’ and points out key processes of engagement: forming a relationship, a human–human connection, conveying acceptance and tolerance, and hearing and understanding. Considers criticisms of engagement-inspiring hope approach in detail | Reiterates need to replace ‘observations’ with ‘engagement-hope inspiration’ as principal approach to caring for suicidal mental health clients |
| Dazzi et al. (2014)73 | ** | Literature review | To conduct review of published literature examining whether enquiring about suicide induces suicidal ideation in adults and adolescents, and general and at-risk populations | No studies found statistically significant increase in suicidal ideation among participants asked about suicidal thoughts. Findings suggest acknowledging and talking about suicide may reduce, rather than increase suicidal ideation, and may lead to improvements in mental health in treatment-seeking populations | Recurring ethical concerns about asking about suicidality could be relaxed to encourage and improve research into suicidal ideation and related behaviours without negatively affecting the well-being of participants |
| DeCou and Schumann (2018)74 | ** | Systematic review and meta-analysis | To quantitatively synthesised research concerning iatrogenic risks of assessing suicidality | Thirteen articles met inclusion criteria. Evaluation of pooled effect of assessing suicidality for negative outcomes did not demonstrate significant iatrogenic effects | Findings support appropriateness of universal screening for suicidality, and should allay fears that assessing suicidality is harmful |
| Downes et al. (2016)5 | ** | Anonymous survey with 13 attitudinal statements, rated on 5-point Likert scale, completed by 381 mental health nurses working in adult services in Ireland | To explore mental health nurses’ attitudes towards completing RAs, use of tools as an aid, and therapeutic or positive risk | Indicates strong support for RA. Nurses believe that RA tools facilitate professional decision-making but express concern that use of tools may negatively impact upon therapeutic engagement with service users. Most participants have positive attitudes towards therapeutic risk, believing service users have the right to take informed risks within recovery-orientated care | Relevance limited by adult services and context of Ireland |
| Felton et al. (2018)55 | * | Case study inquiry, using interviews with mental health professionals and observations in acute ward and assertive outreach team | To explore how practitioners, experience potential tensions arising from delivering recovery-orientated care and enforcing containment | Hilgartner’s theory of risk explains how risk dominates identity of people with mental health problems at cost of recovery. This results in increased monitoring, surveillance and medication to enact control | To undermine dominance of risk, professionals should reconnect with the subjective experiences of people with mental health problems and challenge the acceptance of risk as central to their role |
| Flintoff et al. (2019)68 | * | Discourse theory | To present an analysis of audio recordings of risk assessments completed within a primary care mental health service | Assessments function according to social logics of well-oiled administration and preservation, whereby bureaucratic processes are prioritised, contingency ironed out or ignored, and a need to manage potential risks to the service are dominant operational frames | Observed processes obscure or background problems with risk assessment, by generating practices that favour and offer protection to assessors, at the expense of those being assessed, to challenge stated aims of risk-assessment practice |
| Godin (2004)66 | ** | Interviews with 20 community mental health nurses from various geographical and practice areas | To develop greater understanding of how community mental health nurses, who have become frontline operatives of new regime of community mental health care, reflect on and practise risk assessment and risk management | Some nurses considered standardised methods of risk assessment to be too reductive, stifling and unnecessary, while others found them useful and informative. ‘Professional intuition’ was valued by many as an alternative method of risk assessment, particularly when assessing their own safety. Though their risk assessments concentrated on assessment of patients’ potential to harm others or themselves, some thought about risk in terms of risks faced by their clients from iatrogenic consequences of treatment and psychiatric care, and of victimisation within a hostile community | Highly rational new regime of community mental health care (‘epidemiological clinic’) has not had a totalising effect on work of community mental health nurses |
| Granello (2010)118 | ** | Discussion paper | To articulate guiding principles of the process of suicide assessment | Contains 12 core process principles that highlight broader philosophical tenets to guide suicide risk assessment | Twelve principles serve as to complement the current focus on content in suicide assessment |
| Graney et al. (2020)84 | *** | Survey of views from clinicians, service-users and carers on use of risk-assessment tools | To examine which suicide RA tools are in use in the UK; establish views of clinicians, carers and service users on the use of these tools; and identify how risk-assessment tools have been used with mental health patients before suicide | Obtained 156 RA tools from all 85 UK NHS mental health organisations. In total, 85 tools were included in the analysis. There was little consistency in the use of instruments. Overall, 39% of organisations use locally developed tools. Most tools aimed to predict self-harm or suicidal behaviour and scores used to determine management decisions. Clinicians described positive (facilitating communication and enhancing therapeutic relationships) and negative views (inadequate training and time-consuming nature). Patients/carers reported positive views, but emphasised little involvement and lack of clarity on what to do in a crisis | Comprehensive coverage of UK mental health organisations |
| Harris et al. (2019)16,269 | *** | Systematic review of cohort studies, case–control studies and RCTs | To evaluate the ability of risk tools to predict the future episodes of suicide/self-harm in adolescents | Predictive ability of 10 tools (across eleven studies) varies greatly. No single tool is suitable for predicting higher risk of suicide or self-harm in adolescent populations | First systematic review to explore use of tools to predict future self-harm/future suicide attempts in an adolescent population. High heterogeneity means that meta-analysis was not possible. Results highlight the need for further risk prediction work |
| Higgins et al. (2016)72 | ** | Self-completed survey administered to 381 mental health nurses in Ireland. [See Downes et al.5 (above).] | To explore mental health nurses’ practices and confidence in RA and safety planning | Nurses focus on risk to self and risk to others. Risk from others and ‘iatrogenic’ risk were less frequently considered. Results demonstrate lack of engagement with respect to collaborative safety planning, identification and inclusion of protective factors, and inclusion of positive risk-taking opportunities. Respondents report lack of confidence working with positive risk taking and involving family/carers in RA and safety-planning | Relevance limited by adult services and context of Ireland |
| Horowitz et al. (2010)78 | *** | Suicide screening using SIQ | To determine the feasibility of screening children for suicide risk when they present to the emergency department (ED) with non-psychiatric complaints | For patients entering ED for non-psychiatric reasons (n = 106), 5.7% (n = 6) reported previous suicidal behaviour, and 5.7% (n = 6) reported clinically significant suicidal ideation. No significant differences for mean length of stay in ED for non-psychiatric patients with positive triggers and those who screened negative. In total, 96% of participants agreed that suicide screening should occur in the ED | Suicide screening of non-psychiatric patients in the ED is feasible in terms of acceptability to parents, prevalence of suicidal thoughts and behaviours, practicality to ED flow, and patient opinion. Future efforts should address brief screening tools validated on non-psychiatric populations |
| Horowitz et al. (2009)100 | ** | Case studies | To review suicide screening in three different settings: schools, primary care clinics and EDs | Valid, brief and easy-to-administer screening tools can be utilised to detect risk of suicide in children and adolescents. Targeted suicide screening in schools, and universal suicide screening in primary care clinics and EDs may be most effective way to recognise and prevent self-harm | Settings must be equipped to manage youth who screen positive with effective and timely interventions. Most importantly, impact of suicide screening in various settings needs to be further assessed |
| Jackson et al. (2019)98 | *** | Before-and-after study. Carer-nurse risk consensus scores measured pre- and postintroduction of a structured dialogue | To investigate the impact of an intervention on consensus between nurses and carers on perceptions of risk | Findings support increasing carer contribution to discussions regarding risk. Further work required to embed carer involvement | |
| Jahn et al. (2016)90 | * | Quantitative survey | To identify what may contribute to fear of patient death by suicide by examining relations between suicide-focused training, professional experience, fear of suicide-related outcomes, comfort with and skills in working with suicidal patients, and knowledge of suicide risk and protective factors | Practitioners who worked with suicidal patients reported more knowledge of suicide risk and protective factors but did not report significantly different fear of patient death by suicide or patient suicide attempt than practitioners who did not work with suicidal patients | Results suggest that suicide-focused training may be critical to reducing practitioner fear of negative suicide-related outcomes and increasing comfort working with suicidal individuals. Providing such training may improve practitioners’ knowledge and skills, enhancing clinical outcomes |
| Kleiman et al. (2017)71 | * | Ecological studies | To examine (a) how does suicidal ideation vary over short periods of time? and (b) to what degree do risk factors for suicidal ideation vary over short periods and are such changes associated with changes in suicidal ideation? | For nearly all participants, suicidal ideation varied dramatically over the course of most days: more than one-quarter of all ratings of suicidal ideation were a standard deviation above/below previous response from a few hours earlier. Nearly all participants had at least one instance of intensity of suicidal ideation changing from one response to the next. Across both studies, risk factors for suicidal ideation (e.g. hopelessness, burdensomeness, and loneliness) varied considerably over just a few hours and correlated with suicidal ideation, but limited in predicting short-term change in suicidal ideation | These studies represent the most fine-grained examination of suicidal ideation ever conducted. Results advance understanding of how suicidal ideation changes over short periods and provide a novel method of improving the short-term prediction of suicidal ideation |
| Last et al. (2013)270 | *** | Questionnaire(s) | To explore whether completion of structured diagnostic assessments as an adjunct to clinical assessment avoids placing too great a burden to parents and services, and if the resulting information is useful to practitioners | Most parents found interview easy to understand. Many reported that experience of completing the interview changed how they thought about their child’s difficulties in a positive manner. Practitioner reports were mainly positive. Mean helpfulness score (out of 1–5 for very unhelpful to very helpful) was 4.04. No association between practitioner access to DAWBA and parent reported satisfaction on Experiences of Services Questionnaire | With right supporting arrangements in place, the DAWBA would be a feasible assessment tool in community CAMHS |
| Leavey et al. (2017)101 | ** | Qualitative study of 72 relatives or close friends bereaved by suicide and 19 GPs who have experienced the suicide of patients | To examine systemic inadequacies in suicide prevention from the perspectives of bereaved family members and GPs | Relatives highlight failures in detecting symptoms and behavioural changes and the inability of GPs to understand the needs of patients and their social contexts. A perceived overreliance on antidepressants is a major source of criticism by family members. GPs lack confidence in recognition and management of suicidal patients, and report structural inadequacies in service provision | Mental health and primary care services must find innovative and ethical ways to involve families in the decision-making process for patients at risk of suicide |
| LoParo et al. (2019)91 | * | Zero Suicide Workforce Survey: measure to evaluate staff knowledge, practices, and confidence in caring for patients at risk of suicide | To examine whether (1) behavioural health providers were more likely to implement best practices when they were more confident in their abilities, (2) number of suicide prevention trainings was positively associated with perceived confidence in abilities and implementation of evidence-based practices, and (3) specific trainings were more impactful than others on increasing providers’ level of confidence and/or practices | Moderate association between provider’s practice and confidence. The number of attended trainings had a significant correlation with both practice and confidence. Particular trainings demonstrated differential effects on provider’s practice and confidence | Results suggest that behavioural health providers who are confident in their skills in assessing and treating suicide risk are more likely to incorporate best practices into their clinical work. Also, it appears there is a small but significant benefit to multiple trainings for increasing both practice and confidence among providers |
| Manuel and Crowe (2014)124 | * | Descriptive, qualitative design | To examine how mental health nurses understood clinical responsibility and its impact on their practice | Three major themes: being accountable involves weighing up patients’ therapeutic needs against potential for blame in organisational culture of risk management. Fostering patient responsibility describes deciding when patients could take responsibility for their behaviour. Shifting responsibility describes culture of defensive practice fostered by organisational risk aversion | Highlights the challenges mental health nurses experience in relation to clinical responsibility in practice, including the balancing required between the needs of patients, the needs of the organisation, and the perceived need for self-protection |
| Mathias et al. (2012)81 | * | Repeated testing of suicidal ideation at 6-month intervals for up to 2 years | To examine if asking about suicidal thoughts can result in iatrogenic increases of such thoughts, especially among at-risk samples | Change in suicidal ideation tested using several analytic techniques, each pointed to a significant decline in suicidal ideation in the context of repeated assessment | Suggests that asking an at-risk population about suicidal ideation is not associated with subsequent increases in suicidal ideation |
| McCallum et al. (2014)46 | * | Literature review | To explore why structured clinical judgement is not utilised more in front-line assessment of risk for violence in those with mental and personality disorders | Literature review on mental disorder and violence, risk assessment and risk management suggests that front-line mental health professionals can employ structured clinical judgement underpinned by principles of risk-assessment tools | Ongoing resource development, education and availability of expertise should aid development of uniform approaches to violence risk management and therapeutic amelioration of the likelihood for violence |
| Michail et al. (2016)88 UK |
*** | Qualitative focus group study using framework analysis | To explore GP views and experiences of assessing, communicating with and managing suicidal young people with the aim of co-producing an educational intervention on youth suicide prevention tailored to GPs’ perceived needs | Three themes emerged from data in relation to GPs’ attitudes and beliefs towards suicide; the challenges GPs experience when it comes to the assessment and management of suicide risk in young people; and optimal ways of addressing some of these challenges through the provision of specialist education and training targeting GPs’ knowledge and clinical skills | Reveals wide variations in understanding and operationalisation of risk among GPs, with subsequent implications to how GPs perceive risk should be assessed. GP education on suicide risk assessment and management in youth should promote holistic understanding and assessment of risk and its individual, social and contextual influences |
| Muir-Cochrane et al. (2011)122 | ** | Qualitative study | To investigate the risk-assessment practices of a multidisciplinary mental health service | Mental health professionals draw on both managerial and therapeutic approaches to risk management, integrating these approaches into their clinical practice | Rather than being dominated by managerial concerns regarding risk, participants demonstrate professional autonomy and concern for needs of their clients |
| Mulder et al. (2016)127 | * | Discussion paper | To explore the value of risk prediction in psychiatry | Significant efforts have been made to identify risk factors associated with suicide. Evidence suggests that risk categorisation may be of limited value, or worse, potentially harmful | Argues for a shift in focus towards real engagement with the individual patient, their specific problems and circumstances |
| Oordt et al. (2009)92 | * | Before-and-after 6-month study | To investigate whether training in an empirically based assessment and treatment approach administered through a continuing education workshop could meaningfully impact professional practices, clinic policy, clinician confidence, and beliefs post training and 6 months later | At 6-month follow-up 44% of practitioners reported increased confidence in assessing suicide risk, 54% reported increased confidence in managing suicidal patients, 83% reported changing suicide care practices, and 66% reported changing clinic policy | Suggests that brief and carefully developed workshop training can potentially change provider perceptions and behaviours with a subsequent impact on clinical care |
| Pearson et al. (2009)132 | ** | Retrospective case-note study and semistructured interviews | To investigate the frequency and nature of general practice consultations in the year before suicide for patients in current, or recent, contact with secondary mental health services | In total, 91% of individuals (n = 224) consulted their GP at least once in the year before death. The median number of consultations was 7. GPs reported patient safety concerns in 27% of cases. Only 16% of GPs thought suicide could have been prevented. Poor agreement between GPs and mental health teams on risk of suicide. Both sets of clinicians rated moderate to high levels of risk in only 3% of cases | Consultation prior to suicide is common but suicide prevention in primary care is challenging. Possible strategies might include examining the potential benefits of risk assessment and collaborative working between primary and secondary care |
| Reeves et al. (2015)43 | * | Systematic review | To review studies that assess the utility, feasibility and acceptability of SDAs in the assessment of psychopathology among children and young people in routine clinical practice | Overall, attitudes towards SDAs were positive, with lack of training in administration and interpretation of SDAs and concern for validity being key barriers. Two RCTs and case series suggest that SDAs might aid detection of emotional disorders | Current evidence is not yet sufficient to recommend that SDAs should be universally adopted as an adjunct to clinical practice, but findings suggest that they can be used if applied cautiously and mindfully pending further evaluation |
| Ross et al. (2016)80 | * | Qualitative survey | To describe opinions about suicide risk screening in a paediatric medical inpatient sample | Majority (62.3%) of adolescents who participated had not been previously asked about suicide and were supportive of suicide risk screening (81.0%). Five salient themes emerged from qualitative analysis: prevention, elevated risk, emotional benefits, provider responsibility and lack of harm in asking | Majority of youth screened for suicide risk on medical inpatient units were supportive of suicide risk screening. Opinion data can assure clinicians that suicide risk screening is acceptable to paediatric patients and parents. Medical setting is a unique opportunity to capture youth at risk for suicide |
| Saab et al. (2021)109 | *** | Systematic review | To examine the effect of RA strategies on predicting suicide and self-harm outcomes among adult healthcare service users | Insufficient evidence exists to support any one tool, inclusive of clinician assessment of risk, for self-harm and suicidality. Discourse on risk assessment needs to move towards broader discussion on safety of patients at risk for self-harm/suicide | |
| Saini et al. (2016)103 | ** | Semistructured interviews | To explore GPs’ interpretations of patient communication and treatment in primary care leading up to suicide and to investigate relationship between GPs and mental health services prior to a patient’s suicide | Three themes emerged from GP interviews: (i) GP interpretations of suicide attempts or self-harm; (ii) professional isolation; and (iii) GP responsibilities vs. patient autonomy. GPs in this study may have different views from GPs who have never experienced patient suicide or who have experienced the death of a patient by suicide who was not under specialist services. Findings may not be representative of rest of the UK, although many issues are likely to apply across services | Highlights recommendations for suicide prevention in general practice: increasing GP awareness of suicide-related issues and improving training and RA skills; removing barriers to accessing therapies/ treatments in primary care; improving liaison and collaboration between services; and increasing awareness in primary care about why patients may not want treatments offered by focusing on each individual’s situational context |
| Saini et al. (2010)102 | ** | Questionnaire and interview study in the North West of England | To describe services available in general practices for the management of suicidal patients and to examine GPs views on these services | Responses suggested greater availability of services and training for general mental health issues than for suicide prevention. Three key themes from GP interviews were as follows: barriers accessing primary or secondary mental health services; obstacles faced when referring a patient to mental health services; managing change within mental healthcare services | Health professionals have an important role to play in preventing suicide. However, GPs expressed concerns about the quality of primary care mental health service provision and difficulties with access to secondary mental health services. Addressing these issues could facilitate future suicide prevention in primary care |
| Stickley and Felton (2006)55 | * | Discussion paper | To explore whether nurses can manage to promote a service user’s liberty, while simultaneously endeavouring to protect the individual and society from danger | Mental health nurses have a responsibility to promote individual’s right to freedom while at the same time promote society’s right to be protected from danger | Considers tension in mental health policy and practice that promotes freedom and choice and yet appears to endorse control, and how this affects nurses |
| Turecki and Brent (2016)128 | * | Discussion paper | - | With no effective algorithm to predict suicide in clinical practice, improved recognition and understanding of clinical, psychological, sociological and biological factors might help to detect high-risk individuals and assist in treatment selection | Regular follow-up of people who attempt suicide by mental health services is key to prevent future suicidal behaviour |
| Vandewalle et al. (2019)53 | * | Qualitative study | To uncover and understand core elements of how nurses in psychiatric hospitals make contact with patients experiencing suicidal ideation | Nurses seek to ‘create conditions for open and genuine communication’ while maintaining focus on ‘developing an accurate and meaningful picture of patients’. These represent nurses’ attention to relational processes like building trust as well as focus on assessing suicide risk. Nurse contacts depend on whether they are guided more by checking and controlling suicide risk or by acknowledging and connecting (with) the person | Relevance limited – nurses in psychiatric hospitals in Belgium |
| Vassilev and Pilgrim (2007)67 | * | Discussion paper | To problematise the taken for granted notion of ‘mental health services’ by drawing upon general sociological work on ‘risk’ and ‘trust’ | Outlines the risks to and from patients in routine mental health work, and the betrayal of trust as both a normal part of care and its corruption in mental health work | Concludes that ‘mental health services’ are a myth being mostly concerned with mental disorder and control (at least to most patients who form the focus of activity) |
| Wand (2012)48 | ** | Conventional literature review | To establish research evidence for effectiveness of a risk-assessment approach in mental health. Searched professional literature on RA in mental health, specifically for research on the effectiveness of risk assessment in reducing risk of harm to self or others | Search found limited research on effectiveness of risk assessment. ‘Structured professional judgement’ possibly reduces aggression risk but no evidence that risk assessment is effective in relation to self-harm or suicide reduction | |
| Wand (2012)44 | * | Discussion paper | To outline the emerging field of positive health, which eschews a psychiatric disorder and illness focus, being oriented towards identification of strengths, abilities, hopes, and the individual’s preferred future | The shift in positive health, from illness towards wellness, aims to build health literacy and decision-making capacity and thereby make more effective use of healthcare services. Promotes a positioning of mental health nursing practice within a positive health paradigm | Tables solution-focused assessment questions to contrast to current format for mental health assessment, which rather than being ‘comprehensive’, is predominantly concerned with problem and risk identification, and the search for pathology in the individual |
| White et al. (2019)56 | * | Qualitative exploratory descriptive study | To explore early career registered nurses’ understanding of providing care to mental health consumers who hear voices, a qualitative exploratory descriptive study with nine nurses regarding their experiences of caring for people who hear voices | Relevance limited by experience of nurses from Australia | |
| Wilson et al. (2016)110 | * | Critical discourse analysis | To examine mental health policies and guidelines, and to interview service users, families, nurses and the police about experiences of accessing services | For those who attempt to access services early in crisis, as suggested to lead to a better outcome, provision of services and rights appear to be reversed by an attempt to exclude them through practices that screen them out, rather than prioritising a choice in access | The discursive practice of being labelled ‘risky’ results in divergence between law and policy, which creates for nurses the obligation to manage a tension between medicalisation and normalisation |
| Woods (2013)123 Canada | * | Exploratory and descriptive study | To (1) identify and describe current risk assessment and management approaches used in the adult inpatient mental health and forensic units; and (2) identify good practice and shortfalls in current approaches | Participants reported that they had not considered risk assessment and management as a proactive structured process. Education and training was limited and skills were developed over time through practice | Five key issues: reliance on clinical judgement alone is not the best choice; need to consider risk as a whole concept; risk management being more reactive than proactive; education and training; and client involvement in risk assessment |
| Xanthopoulou et al. (2021)106 |
** | Interviews and inductive thematic analysis | To explore patient experiences of psychosocial assessment after presenting with self-harm/suicidality | People described two different experiences; a therapeutic interaction that made people feel their life mattered and instilled hope for the future and a formulaic assessment about the ‘risk’, which made people feel their life did not matter and hopeless about the future | Psychosocial assessment impacts on hope for people in crisis. A focus on therapeutic communication that is about the person, as well as the risk, improves patient experience, decreases distress, and instils hope that life is worth living |
Glossary
- Deliberate self-harm
- term no longer favoured by the Royal College of Psychiatrists, prefer self-harm.
- Risk assessment
- a detailed clinical assessment to include evaluation of biological, social and psychological factors that are relevant to the child/adolescent and, in the judgement of the healthcare professional conducting the assessment, relevant to future risks, including suicide and self-harm.
- Risk formulation
- the process of summarising the assessment, identifying the risks and triggers, and how these interact together. Risk formulation (i) identifies ‘why’ someone engages in problematic behaviour not just ‘if’ they will engage in it, and (ii) encourages a shift away from simply identifying risk factors to thinking about how key variables interact and connect in the expression of risk.
- Risk-management plan
- a clearly identifiable part of the care plan that should address the long-term and more immediate risks identified in the risk assessment as well as addressing specific psychological, pharmacological, social and relational factors associated with increased risk, with the agreed aim of reducing risk of repetition of self-harm and/or the risk of suicide. It should include a crisis plan outlining self-management strategies and how to access services during a crisis and ensure consistency with the long-term treatment strategy.
- Risk screening
- the specific use of tools within the risk-assessment process to try to predict the likelihood of risk of self-harm and/or suicide.
- Self-harm
- any act of self-poisoning or self-injury carried out by an individual irrespective of motivation. This commonly involves self-poisoning with medication or self-injury by cutting. Important exclusions include harm to the self arising from excessive consumption of alcohol or recreational drugs, or from starvation arising from anorexia nervosa, or accidental harm to oneself.
- Suicidal ideation
- often called suicidal thoughts or ideas, a broad term used to describe a range of contemplations, wishes, and preoccupations with death and suicide.
List of abbreviations
- CAMHS
- child and adolescent mental health services
- CAMS
- Collaborative Assessment and Management of Suicidality
- CBQ
- Challenging Behaviour Questionnaire
- CMOC
- context–mechanism–outcome configuration
- CYP
- children and young persons
- CYP-MH SAT
- Children and Young People – Mental Health Safety Assessment Tool
- DICES
- Describe the risk; Identify the options; Choose your preferred option(s); Explain your choice; Share your thinking
- FACE–CARAS
- Functional Analysis of Care Environments–Child and Adolescent Risk-Assessment Suite
- HEEADSSS
- Home, Education/Employment, Eating, Activities, Drugs, Sexuality, Suicidal ideation and Safety
- NCISH
- National Confidential Inquiry into Suicide and Safety in Mental Health
- PHQ-9
- Patient Health Questionnaire-9
- PMDD
- persistent major depressive disorder
- RCT
- randomised controlled trial
- RTSHIA
- Risk-Taking (RT) and Self-Harm (SH) Inventory for Adolescents
- SHQ
- Self-Harm Questionnaire
- SI-IAT
- Self-Injury Implicit Association Test
- SIQ
- Suicide Ideation Questionnaire
- SPS
- SAD PERSONS Scale
- TAQAT
- Therapeutic Assessment Quality Assurance Tool
- WARRN
- Wales Applied Risk Research Network