Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/05/110. The contractual start date was in September 2018. The final report began editorial review in July 2021 and was accepted for publication in March 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Zoccatelli et al. This work was produced by Zoccatelli et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Zoccatelli et al.
Chapter 1 Context and research objectives
Some text in this chapter has been reproduced from Zoccatelli et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Enabling residents’ voices to be heard is vital for planning the provision of publicly funded health and social care services and ensuring that the wider systems – of which such services are a part – are accountable to the public, the communities and the patients they serve. National and international policies encourage the involvement of residents in health planning and provision. 2–4
In some countries, including England, there is a legal duty to consider public involvement in commissioning and providing health care, and at all stages in major health-care planning decisions,5,6 and this is a cornerstone of patient-centred health and care systems. There is increasing evidence of a positive association between public involvement and more ‘innovative, effective and efficient ways of designing, delivering and joining up services’ (contains public sector information licensed under the Open Government Licence v3.0). 7 For instance, it has been argued that NHS managers and staff are more informed as to the needs of the community they serve and will make better decisions about how to use limited resources when they listen to what matters to residents. 7 Other rationales for incorporating public and patient voice into decision-making and care improvement are more broadly about enhancing legitimacy and building consensus around often contentious health-care reorganisations. 8–13
In England, state-sponsored patient and public involvement (PPI) dates to 1974, when community health councils were established as a new model through which to represent the views of the public and advocate for local patients in each area health authority. Subsequently, arm’s-length bodies fulfilling the function of representing the public in the sphere of health care have been a persistent feature of the English policy landscape. 14 Nevertheless, since 2000, there have been three major reorganisations of the statutory system for PPI in England. 15
Community health councils were replaced by PPI forums in 2002, which were themselves abolished and replaced by local involvement networks (LINks) in 2008. LINks operated for only 4 years before they were superseded by Healthwatch, which was established as part of the coalition government’s 2012 reform of health and social care. Each iteration of the formal PPI system in England has involved different duties, powers, funding, composition and mechanisms for accountability (Table 1). 16
| 1976–2002: CHCs | 2003–7: PPI forums | 2008–13: LINks | 2013 to present day: Healthwatch | |
|---|---|---|---|---|
| Number | 185 | 572 | 151 | 150 |
| Funding | Regional NHS office | CPPIH | Local authority with funding from DHSC | Local authority with funding from DHSC |
| Cover | Locality | NHS and primary care trusts in England | Local authority | Local authority |
| Remit | NHS and public health | NHS and public health | Health and social care | Health and social care |
| Accountability | Unclear, but could be removed by nominating organisation | CPPIH | To be determined locally | Local authority |
| Staff | Selected by CHC members employed by the NHS | Employed through voluntary organisations who are contracted to support PPI forums | Employed by host organisations | Employed by Healthwatch independently or through its host organisations |
| Statutory powers | Request information, visit NHS premises, sit as observers on health authority boards, be consulted on major changes in health care, appeal to the Secretary of State | Request information and visit NHS premises | Request information, visit NHS premises, refer health and social care matters to local council’s overview and scrutiny committee | Request information, visit NHS premises, sit on local statutory health and well-being boards, signpost health and social care services, escalate issues to Healthwatch England or the CQC |
What is Healthwatch?
Originally conceived as a ‘consumer champion in health and care’, local Healthwatch is now ostensibly a major partner through which local government monitors the quality – and supports the design – of health and social care. 7,17 Healthwatch does this by providing NHS England, Clinical Commissioning Groups (CCGs), provider organisations and local authorities themselves with information and advice based on the views of residents and service users.
As we write, there are 150 local Healthwatch bodies across England. This number does not quite correspond with the number of local authorities in England because Healthwatch Dorset, Healthwatch West Central London and Healthwatch Northamptonshire each cover more than one local authority area.
Local Healthwatch work is supported at the national level by Healthwatch England, an independent statutory subcommittee of the Care Quality Commission (CQC), which provides local organisations with guidance and advice and draws on evidence collected locally to highlight national trends and issues. Local Healthwatch organisations have statutory powers to advise local authorities and NHS commissioners about their communities’ needs and concerns relating to the provision of health and social care, and these are embodied in Healthwatch’s six statutory functions (Box 1).
-
Obtain the views of people about their needs and experience of local health and social care services. Make these views known to those involved in the commissioning and scrutiny of care services e.g. CCGs, local authorities, hospital trusts.
-
Write reports and make recommendations about how those services could or should be improved.
-
Promote and support the involvement of people in the monitoring, commissioning and provision of local health and social care services.
-
Provide information and advice to the public about accessing health and social care services and the options available to them.
-
Make the views and experiences of people known to Healthwatch England, supporting its role as national champion.
-
Make recommendations to Healthwatch England to advise the CQC to carry out special reviews or investigations into areas of concern.
Adapted from the Healthwatch England website (URL: www.healthwatch.co.uk/our-history-and-functions) and reproduced from Zoccatelli et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The box includes minor additions and formatting changes to the original text.
Healthwatch organisations are commissioned by each local authority in England with funding from the Department of Health and Social Care (DHSC). The money is provided by the DHSC through two separate funding streams: (1) the central government grant to local government (distributed through the Ministry of Housing, Communities and Local Government) and (2) a supposedly smaller amount of funding provided directly to local authorities through the Local Reform and Community Voices (LRCV) grant. This funding is not ring-fenced. In addition to providing funding for Healthwatch, the LRCV grant is also used to fund deprivation of liberty safeguards in hospitals and the independent NHS complaints advocacy services. Although the bulk of Healthwatch funding is supposed to come from the Department for Levelling Up, Housing and Communities grant, Healthwatch England has recently highlighted that ‘a total of 71 local Healthwatch, almost half the network, now get most of their funding via the LRCV grant . . . and six local Healthwatch [ . . . rely exclusively on the] money provided through the LRCV grant to fund their statutory activities’. 16 Funding for Healthwatch has also substantially decreased since its launch in 2013. Originally set at £40.3M in 2013/14, funding has fallen to an estimated £25.5M in 2019/20, which is in line with wider reductions in funding to local government. 18 In general, there is a well-recognised lack of transparency in the way that local authorities allocate funding to their local Healthwatch, leading to significant variability in Healthwatch budgets across England. 18
Although all Healthwatch organisations are required to be social enterprises and are expected to involve volunteers in their activities and governance structures, there is no nationally mandated model for Healthwatch. Such flexibility in terms of organisational arrangements contributes to the range of organisational models on which Healthwatch can draw. For instance, Healthwatch organisations can be registered as charities, community interest companies or private limited companies. Some organisations may function as standalone or so-called ‘independent’ organisations that do only Healthwatch work, whereas other organisations may be part of larger organisations that also do work unrelated to Healthwatch. This situation raises hitherto underexplored questions about the relationship between local Healthwatch and non-statutory Voluntary, Community and Social Enterprise (VCSE) organisations, as well as how – and with what effects – their respective roles in the local health and social landscape are formed.
In terms of their institutional role, Healthwatch bodies are differentiated from earlier state-backed PPI systems – principally by their legally mandated functions and a statutory seat on local health and well-being boards. A cornerstone of the 2012 reforms, health and well-being boards were established to integrate health and social care and ensure the inclusion of a wide range of local stakeholders in the strategic planning of health care, social care and public health; they vary greatly in their role and operation. 19,20 Healthwatch’s membership of health and well-being boards was intended to provide Healthwatch organisations (and, therefore, patient and public voice) with a more extensive role in the local decision-making mechanisms through which health and social care services are commissioned and provided locally. However, the move to integrated commissioning and provision of care beyond local authority footprints and the role of health and well-being boards is increasingly unclear. 21 Nevertheless, as Gansu22 has stated, Healthwatch’s involvement in health and well-being boards points to an important, broader feature of its relationship to the local health and social care landscape:
. . . local Healthwatch are unique – they are the only organisation that has a helicopter view of an entire local Health and Wellbeing system. In the world of localism and integrated health and care this is key. 22
This ‘helicopter view’ is becoming more salient, given the transformation in NHS organisational structures towards integrated care at the regional, local and neighbourhood level in the years since 2013.
The organisation of health and care has changed dramatically since Healthwatch was conceived. Although the Health and Social Care Act 20125 prioritised the principles of competition and marketisation, the trend over the past 5 years has been towards greater collaboration and integration among NHS bodies and their partners. Of the many new structures that have emerged that affect the environment in which local Healthwatch work, integrated care systems (ICSs) are perhaps the most significant. ICSs are partnerships between NHS CCGs, providers and local authorities, together with VCSE organisations, across a given area (e.g. South East London or West Yorkshire and Harrogate). The NHS Long Term Plan23 envisaged that all areas in England would be covered by ICSs from 2021. Building on this, the government published a health and care white paper in February 2021. 24 The paper proposed that such ICSs be made statutory organisations with commensurate powers. However, although Healthwatch was mentioned in the 2021 White Paper as a way in which public and patient voice could be represented at the ICS level, its involvement was not formally mandated in the subsequent Health and Care Act 2022. 24
Studying Healthwatch
Although there have been several studies of Healthwatch’s predecessors,15,25–27 there has been little research into how local Healthwatch organisations are organised, how they build and maintain relationships with different stakeholders and, ultimately, whether or not they make a meaningful contribution as a key pillar of resident and patient involvement in the English NHS. In the period before Healthwatch became operational, a National Institute for Health and Care Research (NIHR)-funded study looked at how CCGs conduct PPI in relation to long-term conditions. 26 The study recommended that ‘further research is urgently required to examine how [PPI] is being developed within the reformed . . . NHS’. 26 However, since this report in 2014, there has been little research on the work of Healthwatch.
Related work has looked at public participation in large-scale health changes and has studied Healthwatch as one of many actors in that process. Although this work valuably explores how various iterations of PPI coalesce in situations of contest or controversy, Healthwatch itself is not its immediate focus. 28 Mixed-methods research commissioned by the DHSC examined the initial operations of local Healthwatch organisations in the first 18–21 months of their existence and noted the early variability of Healthwatch work, as well as its general reliance on positive relationships with local stakeholders to ‘build legitimacy, influence and create impact’ (contains information licensed under the Open Government Licence v3.0). 27 The research also highlighted activities that made Healthwatch effective in its early days and proposed recommendations for change. 27 More recent qualitative research on local Healthwatch organisations in one English region has pointed to a lack of clarity as to Healthwatch’s role in the landscape of health and social care planning and provision. 15,29,30 Here, the authors identify what they term as the ‘jurisdictional misalignment’ between local Healthwatch organisations, local authorities, health and well-being boards and the NHS organisations with which they must work as a key challenge. 20,30,31 Other tensions include competition with other third-sector and PPI organisations and processes and constrained local authority budgets from which local Healthwatch contracts are awarded, typically for 2 or 3 years at a time. 15,29,30 Reflecting on the design of ‘local Healthwatch quality statements’ launched in 2016 to encourage local Healthwatch organisations to collect information about and assess the quality of their work, Gansu22 similarly highlighted the importance of local context and of good-quality relationships between service managers, local authority leaders, CCG members and local Healthwatch organisations.
Although these studies point to the challenges and tensions faced by local Healthwatch organisations, they do not explore the various institutional landscapes in which Healthwatch operates, the daily practices through which its influence is created and maintained, and the reasons for, and implications of, different approaches to collecting and communicating evidence about residents’ needs and experiences. It is essential to consider the interconnection of these various practices and concepts. To address this gap, our study uses the theoretical framework of actor network theory (ANT).
Actor network theory
Originating in science and technology studies, ANT focuses on the role of mutually influencing relations between various human and institutional actors, as well as the sociomaterial contexts (e.g. objects, documents, buildings, meetings, technologies, data, policies, strategies, contracts, ideas) in which they operate (Box 2). 32,33
-
ANT is a theory developed by Bruno Latour, Michel Callon and John Law as part of science and technology studies during the 1980s.
-
Although ANT carries ‘theory’ in its name, it is better understood as a range of methods for doing social science research.
-
ANT sets out to describe the connections that link together humans and non-humans (e.g. objects, documents, buildings, meetings, technologies, data, policies, strategies, contracts, ideas). Both humans and non-humans are understood as ‘actors’ that can have an influence on phenomena of interest.
-
In particular, ANT describes how these connections come to be formed, what holds them together and what they produce in particular contexts. This system of mutual influence between and among humans and non-humans is called an ‘actor network’.
-
To study an actor network, ANT researchers employ some key qualitative research methods as part of their data collection:
-
non-participant observation (i.e. spending time in the places where the interactions between actors, both human and non-human, happen and decisions about them are taken) and recording them as field notes
-
interviews with relevant human actors to discuss their opinions, frustrations, emotions, hopes and beliefs, as well as the reasons underlying their practices
-
collection and analysis of relevant documents, particularly if they play a part in interactions.
-
In studies of health-care service and delivery, ANT has typically been advanced as a framework for investigating health-care organisations and technologies,34–36 and it has been applied successfully in other NIHR-funded studies. 37–40 For instance, three of the authors of this report – Amit Desai, Giulia Zoccatelli and Glenn Robert – were recently involved in a NIHR-funded project that used ANT to investigate and optimise the use of patient experience data in acute NHS trusts. 40 This work explored the mutually influencing relationship between different forms of patient experience data and technologies and the people and institutions that use (or fail to use) them to improve the quality of patient care. 40–42 Thinking with ANT meant that we built ethnographic descriptions of how patient experience data came to be formed in any given hospital and how these data were entangled in relationships that enabled them to act to affect improvement.
Our study of Healthwatch similarly pays attention to these ‘mutually influencing relations’ between various human and non-human actors in shaping the practices and strategies through which Healthwatch promotes patient and public voice. 43 Using ANT adds to our understanding of Healthwatch in two main ways. First, we are able to expand the range of actors beyond merely human or institutional actors, which had been the focus of previous studies,15 and this allows us to give due consideration to the ways in which relationships between Healthwatch and its local stakeholders are shaped and mediated on a daily basis by artefacts, such as organisational and governance structures, funding arrangements, institutional landscapes, data, technologies and evidence-gathering mechanisms (i.e. non-human actors) (Box 3).
-
Healthwatch staff and volunteers.
-
Patients.
-
Carers.
-
Local residents.
-
Charities staff and volunteers.
-
CCG members.
-
Local authority officers.
-
Local councillors.
-
Local GPs and others in general practices.
-
Trust staff (e.g. patient experience managers, engagement managers, nurses, clinicians).
-
Documents (e.g. ‘enter and view’ reports, strategy documents, ICS plans, Healthwatch quality statements).
-
Technologies (e.g. computers, software, patient experience data, surveys, internet, e-mail, telephones).
-
Funding and funding applications.
-
Policies.
-
Buildings.
-
Contracts.
GP, general practitioner.
As we explore in the mode of analysis (see Chapter 3), findings (see Chapters 4–7) and discussion (see Chapter 8) chapters that follow, thinking with ANT allows us to see and analyse the entanglements of which Healthwatch is a part and which shape the possibilities of its work. Therefore, for example, we trace the ways in which the health and social care institutional landscape in any given Healthwatch area of operation intersects with funding arrangements or Healthwatch organisational structure, and how these need to be considered together to understand the nature of key Healthwatch activities, such as engagement or evidence-gathering and communication.
Second, existing studies rely primarily on interviews and surveys that can provide only post hoc accounts of events. 15,27,30 Our study, although incorporating a survey and interviews, also prioritised a broadly ethnographic approach (endorsed by ANT) to capture the processual nature of relations, therefore uncovering the emergent and unexpected ways in which local Healthwatch organisations enhance patient and public voice.
By examining the nature and quality of interaction between local Healthwatch organisations and key stakeholders, as well as the non-human elements that enable such interaction, our study provides, to the best of our knowledge, the first comprehensive exploration of these hitherto largely neglected organisations.
Research aims and objectives
The aim of our study was to explore and enhance the operation and impact of local Healthwatch organisations in ensuring effective patient and public voice in the commissioning and provision of NHS services. We have achieved this aim by pursuing the following four objectives:
-
to establish current priorities, activities (e.g. advocacy, signposting, surveys, inspections) and organisational arrangements (e.g. staffing, funding, nature of contract, jurisdictions) of local Healthwatch organisations in England [method: survey (phase 1)]
-
to explore the processes and interactions that link local Healthwatch organisations to a range of individual and institutional actors [e.g. commissioners, general practitioners (GPs), CCGs, trusts, patients, local authority staff, care homes, third-sector organisations and Healthwatch England] and to the wider contexts through which they operate (e.g. funding, contracts, reports) to assess their impact on local health-care commissioning and provision [method: ethnographic fieldwork at five local Healthwatch organisations and engagement with members from 15 other Healthwatch organisations (phases 2 and 3)]
-
to build consensus about what might constitute ‘good practice’ in terms of the operation of local Healthwatch organisations [method: joint interpretive forums (JIFs) (phase 4)]
-
to distil and then disseminate generalisable principles around what facilitates and/or limits the influence of local Healthwatch as a key element of patient and public voice in the NHS [method: small-group discussions and online interviews with the Healthwatch Involvement Panel (HIP) and JIF (phase 3)].
Pursuing these objectives helped us answer our two key research questions:
-
What are the strategies, practices and sociomaterial structures that enable Healthwatch to enhance patient and public voice in the NHS?
-
How is PPI made impactful for residents themselves, as well as commissioners, providers and other NHS actors, as they are brought together through the daily work of Healthwatch?
Structure of the report
In this chapter, we have set out the context and relevant literature for our study, including the theoretical lenses we chose to adopt, as well as the aims and objectives of the study. In Chapter 2, we discuss the methodology we used and the changes we made to the original protocol.
In Chapter 3, we detail our data sources and our modes of analysis across the four phases of the study.
Chapter 4 presents the findings of our national survey of local Healthwatch mapping organisational structures, relationships and impact across the network.
Chapter 5 presents the findings from 16 months of ethnographic fieldwork at five local Healthwatch study sites and explores key axes of variability in Healthwatch’s arrangements, strategies and practices. The chapter is organised into four sections: (1) organisational structures, (2) funding arrangements, (3) institutional landscapes and (4) strategies and practices of engagement.
Chapter 6 combines insights from phases 2–4 of the study to produce statements of good practice relating to the collection, analysis and communication of patient and public voice. The bulk of the data presented here were collected at local JIFs held remotely at four of the study sites, and focused on what constitutes good and useful evidence for Healthwatch organisations and key partners, such as the NHS and local authorities, and what most effectively presents the voice of residents.
Chapter 7 draws on our research in phases 2 and 3 and explores how local Healthwatch organisations responded to the COVID-19 pandemic in England.
In Chapter 8, we demonstrate how our findings provide significant new knowledge about the everyday practices and strategies of local Healthwatch organisations. Before concluding the report, we draw out the implications of our study for policy, practice and research.
The appendices contain additional information that the reader may find useful, including profiles summarising key features of each of the five local Healthwatch study sites (see Appendix 1) and resource documents we produced for the JIFs (see Appendix 4).
Note on naming practices and pseudonyms
We have anonymised each of the study sites by giving them the following pseudonyms: Healthwatch Ashton, Healthwatch Beecham, Healthwatch Cherryburgh, Healthwatch Dogwood and Healthwatch Elmbridge. Similarly, the organisations that hosted three of our study sites are given the following pseudonyms: Achieve (Healthwatch Ashton), Community Together (Healthwatch Cherryburgh) and Direction Health (Healthwatch Dogwood).
Other Healthwatch organisations referred to in the report (e.g. those of HIP members) are also given pseudonyms. Where individual HIP members are quoted, they are not referred to by name but are, instead, given a number (e.g. HIP member 3).
Chapter 2 Methodology and changes to the protocol
Some text in this chapter has been reproduced from Zoccatelli et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
The study was organised in four phases.
-
Phase 1 (September 2018 to April 2019) comprised the design, development, distribution and analysis of our national survey of all local Healthwatch in England (objective 1).
-
Phase 2 (April 2019 to January 2021) included:
-
the recruitment of five case study sites and the recruitment of 15 members of the HIP
-
ethnographic data collection visits to gather documentary evidence, carry out observations and conduct interviews
-
a switch to virtual fieldwork in March 2020
-
data-gathering and iterative data analysis with the HIP (objective 2).
-
-
Phase 3 (March 2020 to April 2021) included online interviews and small-group discussions with HIP members to explore Healthwatch experiences during the COVID-19 pandemic and to generate statements of good practice (objective 4).
-
Phase 4 (January to June 2021) consisted of participatory sense-making workshops modelled on JIFs. 44 The first workshop was held virtually in January 2021 (with representatives from all five Healthwatch study sites) and it was followed by virtual workshops at four of the individual local Healthwatch study sites (May to June 2021) (objectives 3 and 4).
Phases 1–3 deepen our understanding of how Healthwatch organisations are structured and operate, whereas phase 4 is concerned with the related but separate issue of enhancing evidence-gathering strategies.
Phase 1: nationwide online survey
We conducted a national online survey between December 2018 and January 2019. The survey had the following three aims:
-
to explore the current organisational arrangements, relationships and impact of local Healthwatch organisations in England
-
to explore the extent to which these vary across local Healthwatch organisations
-
to use the data to help select our five study sites and members of the HIP in line with our broad sampling framework.
All local Healthwatch organisations in England were invited to take part in the survey. We obtained a list of 150 publicly available ‘info@’ e-mail addresses of local Healthwatch organisations from Healthwatch England and sent unique links to these addresses. We asked the local Healthwatch organisation chief executive, director or manager to complete it. The survey was conducted using the Jisc online survey platform (URL: www.onlinesurveys.ac.uk). We sent weekly reminders to potential respondents. We also reminded potential respondents through Facebook (URL: www.facebook.com, Meta Platforms, Inc., Menlo Park, CA, USA) and Twitter (URL: www.twitter.com, Twitter, Inc., San Francisco, CA, USA) and asked Healthwatch England to publicise the survey through its communication channels.
The survey was designed in consultation with:
-
participants (mainly Healthwatch chief executives, chairpersons and managers) at the Healthwatch Annual Conference in October 2018, where we ran a workshop to identify areas the survey should explore
-
Healthwatch England, in relation to the surveys and data returns they already conduct and collate from local Healthwatch organisations (so as avoid duplication in our survey)
-
our independent Project Advisory Group
-
five former local Healthwatch chief executive officers (CEOs) or directors.
The final version of the survey had 47 questions and examined three facets of local Healthwatch work (see Report Supplementary Material 1). The first section focused on Healthwatch organisational structure, particularly funding arrangements and staffing. The second focused on local Healthwatch engagement with key partners, location of relevant stakeholders and level of co-operation. The third explored the types and qualities of the impact achieved (or intended) by local Healthwatch organisations. Based on suggestions made by the former local Healthwatch chief executives and directors who piloted our survey, in this third section we opted for descriptive questions about the types of impact achieved and about practical examples of successful or failed impact experienced by local Healthwatch organisations in the past 3 years. This approach allowed us to account for a broad range of factors involved in successful/failed projects (e.g. project topics, their length, stakeholders involved and systemic challenges encountered). We avoided more general questions about the overall impact of each organisation because we regard ‘impact’ as the outcome of a complex array of inter-related factors, which are better suited to the in-depth qualitative investigation we carried out in the second phase of this research project.
The survey used a combination of open- and closed-response questions. The questionnaire mainly comprised questions requiring ‘yes/no’ responses [e.g. ‘Does your Healthwatch award funding (e.g. grant, contract) to other organisations?’] or the selection of possible answers from a drop-down menu (e.g. ‘How would you describe the overall quality of co-operation among key health and social care stakeholders in your local area?’, with respondents asked to indicate their views on a five-point scale from ‘excellent’ to ‘poor’). Most closed questions in the survey included an ‘other’ option and allowed for free-text responses in the form of a brief description.
Open questions were limited to the last two sections of the survey. In these sections, we asked respondents to briefly outline two specific pieces of work they had carried out in the past 3 years that they regarded as (1) successful and (2) unsuccessful. In these final sections, we used a combination of closed and open questions, requiring text responses in the form of a brief description. Open-ended questions asked, for example, ‘What was the piece of work about?’, ‘How was the impact delivered?’ and, in the case of unsuccessful projects, ‘What barriers did your Healthwatch experience in its work?’. We coded answers based on topic, duration of the project (i.e. ≤ 1 year, between 1 and 2 years or ≥ 2 years) and barriers to impact. Closed questions in these final two sections included ‘type of impact achieved or intended to be achieved’ (covering 13 options, e.g. ‘improved access to care and treatment for members of our community’, and participants could select more than one option) and, in the case of successful projects, ‘most important stakeholders involved’ (covering 19 options, including an ‘other’ option, and participants could select up to three options).
For data about numbers of [total and full-time equivalent (FTE)] staff and volunteers and Healthwatch grant/contract values, we relied on data compiled by Healthwatch England in the period 2013–18. These data were shared with the research team in February 2019.
Based on the findings of phase 1 survey, the team wrote a report for circulation to the network and presented it at the Healthwatch conference (2019).
Phase 2: ethnographic study
Below we present a description of our sampling and data collection methods for the two main research elements of the research work in phase 2; that is, (1) the fieldwork at our five case study sites before and during the COVID-19 pandemic and (2) the work of the HIP.
Fieldwork at five local Healthwatch study sites
We carried out interviews, observations and documentary analyses at five purposively sampled local Healthwatch organisations over a 17-month period (August 2019 to January 2021) (see Appendix 1 for a summary of characteristics for each study site). Although the project proposal and first version of the protocol envisaged only four local Healthwatch study sites, as phase 2 developed through the involvement of the HIP, it became clear that we needed to recruit a fifth local Healthwatch site to have a sample that better reflected the variability of Healthwatch, as perceived by staff and volunteers of Healthwatch themselves.
Sampling
To identify potential Healthwatch study sites, we constructed and adapted our sampling frame through an iterative process that included the following stages:
Survey results analysis
We built our sampling strategy for the selection of five case study sites from the results of the phase 1 survey, focusing particularly on the findings associated with the intersection of organisational structure, funding arrangements and type of local authority. In doing this, we slightly modified the sampling strategy outlined in the protocol, where we had said that we would focus particularly on the findings associated with the ‘jurisdictional contexts’ variable. This choice was justified by the fact that in designing the phase 1 survey we were advised by the people we consulted (see the list above) not to include many questions about Healthwatch jurisdictional context, as these would have duplicated information already collected by Healthwatch England or otherwise publicly available. Following discussion with our Advisory Group, we, instead, decided to build our sampling strategy using the following formula:
We selected a study site with typical organisational arrangements for each of the three main local authority types (i.e. county, unitary and London/Metropolitan). We grouped London and Metropolitan local authority types together, as their answers in the surveys were largely consistent.
The typical arrangements we found (based on the survey return), which are explained in greater detail in Chapter 4, were as follows:
-
unitary + small number of relationships + contract + hosted (represented by Healthwatch Dogwood)
-
London or Metropolitan + average number of relationships + contract + either hosted or standalone (represented by Healthwatch Cherryburgh)
-
county + large number of relationships + grant + standalone (represented by Healthwatch Beecham).
Advisory group
We presented our sampling strategy to our Advisory Group. The Advisory Group approved the three Healthwatch sites, listed above. The study team discussed with the Advisory Group the criteria for recruiting the fourth study site and these included:
-
a Healthwatch in an urban area outside London
-
a Healthwatch with a host with more than one Healthwatch contract.
These characteristics were deemed to complement those of the three Healthwatch sites mentioned above and allowed for a rounded sample of study sites taken as a whole. In May 2019, we recruited a Healthwatch study site that, hosted by an organisation with four Healthwatch contracts and based in an urban area outside London, met these inclusion criteria. However, in August 2019, the host lost the contract for this Healthwatch. We then approached two other Healthwatch sites with similar characteristics. In discussion with the Advisory Group, we agreed on the recruitment of Healthwatch Ashton, that, hosted by an organisation with two Healthwatch contracts and based in a mixed urban/rural area outside London loosely met the above criteria. The selection of Healthwatch Ashton was regarded by the Advisory Group as particularly valuable by virtue of the small size of its core local authority contract (< £100,000 per annum) as this characteristic was not present in any of the other three Healthwatch sites we had already recruited.
Healthwatch Involvement Panel
We held our first HIP meeting on 17 July 2019, where we discussed our sampling strategy and presented the anonymised core features of the four Healthwatch sites we planned to recruit. The panel members suggested that our sampling still did not fully reflect the range of local Healthwatch organisations in England. The panel members noted that the only standalone Healthwatch study site recruited was operating at county level and had an unusually large budget compared with the median Healthwatch core local authority funding (i.e. > £500,000 per annum). Therefore, the HIP suggested the recruitment of an additional standalone Healthwatch study site with the following characteristics:
-
a Healthwatch site operating in a smaller area than a county
-
a Healthwatch site with a smaller local authority core funding than Healthwatch Beecham.
The study team agreed that this gap was important to fill and at the end of July 2019 recruited Healthwatch Elmbridge, which met these inclusion criteria.
Ethnographic data collection
We carried out 75 days of face-to-face ethnographic fieldwork at the five local Healthwatch study sites during the period preceding the COVID-19 pandemic (August 2019 to March 2020). The two researchers Giulia Zoccatelli and Amit Desai carried out fieldwork at two study sites each (GZ: Healthwatch Beecham and Healthwatch Cherryburgh; AD: Healthwatch Dogwood and Healthwatch Elmbridge) and shared fieldwork at the fifth site (Healthwatch Ashton). Fieldwork at this latter site started in January 2020 because of recruitment issues. The researchers visited each Healthwatch site for meetings, informal conversations and formal individual interviews. The researchers also observed the daily work in Healthwatch offices and accompanied Healthwatch staff and volunteers to relevant daily activities and meetings. Although we observed interactions between Healthwatch staff and members of the public, and had interviewed and spoke informally to local residents and volunteers at all of our study sites, the principal aim of the study was to explore and enhance the practices and strategies of local Healthwatch itself. Furthermore, although communicating the voice of residents is a key aspect of Healthwatch work, data collection did not focus on residents themselves (other than volunteers), as they were not involved (with a few exceptions) in Healthwatch’s everyday work.
In line with the study’s ANT-informed theoretical approach, we collected the following three forms of data:
-
Ethnographic field notes, which included notes made when attending meetings (e.g. health and well-being board meetings, ICS meetings, overview and scrutiny committee meetings), accompanying staff and volunteers on data-gathering, outreach and inspection activities (e.g. enter and view visits, stalls at community events, hospital trusts, local libraries, engagement activities with local residents and specific patient cohorts), observing the daily work in Healthwatch offices and having informal chats with Healthwatch staff, volunteers and local stakeholders.
-
Eight-four individual semistructured interviews were carried out face to face and online both before and after the pandemic with employed staff of all levels, volunteers and local stakeholders, including local authority staff, ICS staff, councillors, representatives of local third-sector organisations and relevant provider representatives. Fifty-six interviews were audio- or video-recorded and transcribed for analysis. For a breakdown of the interviewees’ characteristics, see Table 8. Potential participants for one-to-one semistructured interviews were selected based on our observations and their involvement with Healthwatch work. External stakeholders were identified and introduced by Healthwatch staff at each study site. No-one refused to participate or withdrew from the study once they had agreed to participate. Interview transcripts were anonymised at the point of transcription and assigned a composite numeric identifier. A template of the interview schedules is included on the NIHR Journals Library website [URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/1705110/#/ (accessed 27 May 2022)].
-
Documentary evidence, such as internal documents, reports, health and well-being board minutes, and local Healthwatch and Healthwatch England strategy documents.
At each local Healthwatch site, we paid particular attention to the interaction between human and non-human actors (e.g. strategy documents, funding applications, data, reports) and observed the practices in which these interactions are embedded. The researchers took detailed hand-written notes during observations and interviews, which were then typed or written up into detailed field notes soon after. Observations included office work, meetings, the production and circulation of reports, the collection of data and everyday interactions between Healthwatch members and external actors, such as the CCG and local authority staff, NHS provider trusts, ICS staff and third-sector organisations.
Ethnographic data collection during the COVID-19 pandemic
On 23 March 2020, the government issued a broad range of regulations intended to curb the spread of COVID-19 in England, including ‘stay at home’ instructions. When this happened, we moved our ethnographic data collection online. Between March 2020 and January 2021, we carried out a total of 114 virtual contacts (i.e. observations, catch-up chats, interviews) with the five Healthwatch study sites. The researchers were able to start virtual fieldwork almost immediately after the issuing of the ‘stay at home’ regulations at four (Healthwatch Ashton, Cherryburgh, Dogwood, Elmbridge) out of five study sites. On request of the then chairperson of Healthwatch Beecham, fieldwork was suspended at this site between March 2020 and July 2020, as the organisation was appointing a new CEO and recruiting new trustees and members of the staff. Fieldwork at Healthwatch Beecham resumed in June 2020 and continued until January 2021, when fieldwork formally concluded in all sites.
During our virtual ethnography (March 2020 to January 2021) we collected the following four types of data:
-
Observational data about both internal and external Healthwatch meetings, including virtual team meetings, board meetings, health and well-being board meetings, overview and scrutiny committee meetings, ICS-level meetings and Healthwatch and external stakeholders annual general meetings. As almost all Healthwatch engagement activities moved online, researchers also observed virtual engagement events carried out by Healthwatch staff and volunteers at all five study sites, including engagement with specific patient cohorts, volunteers’ meetings and roundtables to discuss residents’ experiences and needs during the pandemic.
-
Catch-up conversations and interviews with Healthwatch staff, board members and other volunteers.
-
One-off interviews with external stakeholders, including CCG chief operating officers (COOs), directors of public health, local authority Healthwatch commissioners and contract managers, hospital staff, ICS officers and members of the public involved in Healthwatch engagement activities.
-
Documentary evidence, such as internal documents, reports, health and well-being board minutes and local Healthwatch and Healthwatch England strategy documents.
Ethnographic data collection at the five Healthwatch study sites was complemented by an expanded role and involvement of the HIP. Below we outline the work we conducted with the HIP and describe its changing role during the COVID-19 crisis.
Healthwatch Involvement Panel
The HIP was a panel of 15 local Healthwatch staff and volunteers recruited from 15 local Healthwatch organisations that were not case study sites. The HIP was conceived as a group that would help us analyse the ethnographic data from the five study-sites.
The purpose of the HIP was therefore to ensure:
-
the ongoing generalisability of our findings by ensuring that local Healthwatch staff and volunteers have the chance to jointly reflect on the data presented and provide ongoing interpretation and explanation based on their own experience
-
that our study outputs are meaningful to local Healthwatch staff and volunteers, therefore, improving the likelihood of beneficial change in the way in which Healthwatch currently operates
-
appropriate PPI in this phase through engagement with Healthwatch volunteers.
The operation of the HIP changed substantially after the start of the COVID-19 pandemic. We adapted our approach so that the HIP functioned as a data source about local Healthwatch work during the pandemic (as opposed to a data analysis partner). This way of working deepened our engagement with individual HIP members and we were able to ensure that the three purposes listed above were achieved.
Healthwatch Involvement Panel member selection
We recruited 15 HIP members over the course of spring 2019. The members comprised a mix of Healthwatch staff and volunteers.
The first HIP by role included nine senior staff [CEO/COO/director/manager], two other staff and three volunteers (including one board member); one member could not attend. Over the course of the HIP, there were several minor changes in composition by role (but not by organisation). One member in the ‘other staff’ category became a manager, one CEO began attending instead of a member of his staff, one manager left his organisation and was replaced on the HIP by his successor and one CEO left her organisation (at which point a board member attended instead).
The principal inclusion criterion for sampling for the HIP was a ‘yes’ response to question 46 in the survey (‘Would someone in your Healthwatch like to participate in the Healthwatch Involvement Panel?’). We also included those who approached us by e-mail to ask to be further involved in the study. In addition to wanting representation from each English geographical region, we also took account of the varieties of organisational structure (i.e. standalone or hosted, hosted by a large or small host, contract or grant) and institutional landscapes. For instance, we wanted to include a Healthwatch organisation from Greater Manchester, given the unique nature of the region’s devolved health budget. These considerations (except geographical region) reflected the same criteria as those used to select our five study sites. All HIP members’ Healthwatch organisations received funding from the local authority through a contract and none received a grant. In Tables 2–4 we present the composition of the HIP by organisation type, English region and type of local authority.
| Organisational type | Number of people in HIP |
|---|---|
| Standalone | 9 |
| Hosted | 6 (of which 2 were hosted by an organisation and 4 or more Healthwatch contracts) |
| English region | Number of people in HIP |
|---|---|
| London | 4 |
| South East | 2 |
| South West | 1 |
| East | 2 |
| West Midlands | 1 |
| East Midlands | 2 |
| North West | 1 |
| Yorkshire and the Humber | 1 |
| North East | 1 |
| Local authority type | Number of people in HIP |
|---|---|
| County | 5 |
| Unitary | 6 |
| London borough | 4 |
| Metropolitan borough | 3 |
We prepared a shortlist of possible Healthwatch candidates for the HIP and presented this to our Advisory Group. The Advisory Group endorsed our suggestions and noted that the Healthwatch candidates proposed would together form a panel of sufficient range and diversity.
We organised five HIP meetings in total between July 2019 and February 2021. Two of these meetings were held in London. Details of the meetings are presented in Appendix 2. The final three meetings were held online. The final meetings discussed a combination of findings from the ethnographic work conducted at the five case study sites (phase 2) and from the semistructured interviews and small-group discussion (phase 3).
Phase 3: online interviews and small-group discussions with Healthwatch Involvement Panel members
Lessons emerging from COVID-19 pandemic
National restrictions to tackle the COVID-19 pandemic were imposed in England from mid-March 2020 onwards. As we described above, face-to-face fieldwork at our study sites was no longer possible. Similarly, we could no longer convene the HIP in person or hold long meetings with them as we had pre-pandemic. With the approval of our Advisory Group, we decided to modify the protocol to adapt the operation of the HIP to these new circumstances. Our fieldwork data showed that the pandemic was highlighting and catalysing existing Healthwatch practices and relationships. Understanding Healthwatch’s role in the pandemic response, therefore, represented a new and important part of achieving our study’s aims and objectives.
Alongside our ongoing data collection from the five study sites, we used the HIP as a key source of data about the work of local Healthwatch organisations during this time. This significantly expanded the role of the HIP in our study beyond its original scope as a partner in analysing data from the study sites. In addition, using the HIP in this way allowed us to access a broader range of insights from different organisations, as well as different roles, within Healthwatch. This change in HIP structure and role helped mitigate some of the challenges of conducting online fieldwork with our existing study sites. Data collection at these sites – although ongoing and valuable – had become less time intensive, and the benefits of the ethnographic method in conducting observations and informal conversations with study participants were attenuated in an online format. Moreover, as work had moved online, HIP members were accessible regardless of geographical location.
Over three panel meetings (in April 2020, October 2020 and February 2021), we developed a model for working with the HIP (see Table 10). We carried out semistructured individual or small-group online interviews with panel members 2 or three 3 in advance of a panel meeting. These interviews were recorded and transcribed. Amit Desai and Giulia Zoccatelli analysed the transcripts together and highlighted key findings and themes. At the online HIP meeting, the study team presented key themes emerging from both these interviews and small-group discussions and from fieldwork at the five study sites. We organised a plenary discussion around prepared questions based on the initial data analysis. The online HIP meeting was video- and audio-recorded and transcribed, the chat box saved and the transcript and chat box further analysed.
Production of emerging statements of ‘good practice’
We used data from the fieldwork at the five study sites (in phase 2), from the online interviews and small-group discussions (in phase 3) and from the JIFs (in phase 4) to draft a series of statements of ‘good practice’ about the practices and strategies used by local Healthwatch organisations to collect, organise and communicate patient and public needs to key stakeholders and the contexts where they might apply and work best. The emerging list of these statements of good practice was discussed and refined through an interactive process with HIP members and the participants at the local JIFs (see Phase 4: joint interpretive forums). In the last part of this interactive process (in July 2021) we circulated via e-mail a draft list of these statements to all HIP members and asked for their insights on their generalisability and usefulness. We obtained comments from five HIP members, which were incorporated to generate the final set of statements of good practice (see Chapter 6).
Phase 4: joint interpretive forums
In phase 4, we carried out a series of multistakeholder workshops in the format of JIFs (i.e. a type of group discussion aimed at encouraging ‘perspective taking’ and joint decision-making). 44 We organised five JIFs in total: one cross-site JIF (January 2021), which brought together representatives from each Healthwatch study site, and four local JIFs, one at each study site (May 2021–June 2021). The JIFs were attended by members of the Healthwatch team, Healthwatch board and key local stakeholders identified by each Healthwatch study site. Despite repeated attempts, we were unable to organise a local JIF with Healthwatch Ashton because of significant staff changes and work pressures at the organisation in May and June of 2021. All JIFs were held virtually over Microsoft Teams (Microsoft Corporation, Redmond, WA, USA).
Cross-site joint interpretive forum
Our first workshop was held in January 2021 and was attended by up to three representatives from all five Healthwatch study sites, as well as the study team (Table 5 shows a breakdown of JIF participants by roles in their respective local Healthwatch organisation).
| Healthwatch organisation | |||||
|---|---|---|---|---|---|
| Ashton | Beecham | Cherryburgh | Dogwood | Elmbridge | |
| Role | Manager | CEO | CEO | Manager | CEO |
| Volunteer co-ordinator | Office manager | Chairperson | Chairperson | Chairperson (volunteer) | |
| Healthwatch volunteer | Engagement manager | Board member | Research analyst | ||
The 2-hour workshop concluded the data collection at the five case study sites. The workshop aimed to allow participants to share information about key features of their Healthwatch organisation to enable discussion of early analytical themes (discussion was elicited with the aid of four deliberately provocative statements prepared by the research team based on our emerging findings) and provide a space for the presentation and discussion of preliminary findings from the study. Ahead of the workshop, we circulated a document outlining emerging themes from our analysis (see Appendix 4).
The cross-site JIF comprised three inter-related activities that were organised around a structure carefully planned to maximise participation and dialogue. These three activities were:
-
a discussion of pre-circulated Healthwatch profiles
-
a presentation of emerging themes from our fieldwork
-
a provocations activity.
We detail these activities in Appendix 3.
Local joint interpretive forums held at each Healthwatch study site
The local JIFs aimed to provide a platform for the sharing of perspectives between three broad groups of people (i.e. the study researchers, staff and officers of local Healthwatch study sites and key institutional stakeholders of these study site Healthwatch organisations). In May 2021, we held four local JIFs in total, each involving one of our study sites and their principal stakeholders, such as CCG, local authority, provider trust and VCSE representative (Table 6).
| Healthwatch | Participants by professional role |
|---|---|
| Beecham |
|
| Cherryburgh |
|
| Dogwood |
|
| Elmbridge |
|
We used local JIFs as part of the iterative process through which we generated statements of ‘good practice’ about the daily work of local Healthwatch organisations. To tailor the discussion to the needs and interests of our local Healthwatch study sites, in the planning phase (April 2021), we discussed with the Healthwatch CEO or manager at each study site the structure and content of the local JIFs. In dialogue with the Healthwatch CEO or manager, we developed three key questions that we used to guide the discussion during the meeting:
-
What evidence from Healthwatch about public and patient needs and experiences of local services do health and social care partners find most useful?
-
How can the collection and communication of such needs and experience be improved?
-
How can Healthwatch and its local health and care partners work better together to effect positive change for local people?
The CEOs or managers at all Healthwatch study sites were involved in planning the JIFs at their respective organisations and in the recruitment of participants among their health and social care partners. Participants for the JIF workshops were purposively selected by each local Healthwatch organisation based on their role in the organisation, relevance in Healthwatch daily work, participation in earlier phases of the study and their willingness and availability to participate. All four local JIFs were held remotely via Microsoft Teams and lasted between 90 and 120 minutes. Three local JIFs (i.e. Beecham, Dogwood and Elmbridge) were video- and audio-recorded and transcribed for analysis. Technical difficulties meant that the Cherryburgh local JIF was not recorded. Amit Desai and Giulia Zoccatelli took detailed notes.
Local JIFs were organised around two inter-related activities:
-
a presentation about Healthwatch history and statutory functions and about the aims, objectives, methods and outputs of the study
-
a plenary discussion of the current and potential practices used by Healthwatch to gather and communicate evidence about residents’ needs and experiences.
We describe these activities in Appendix 3.
Patient and public involvement
Patient and public involvement was an integral element throughout the study. The involvement of patients and members of the public in the study aimed to ensure that they could share their experiences about local Healthwatch organisations and contribute to the discussion about how Healthwatch might work better to serve their needs and interests.
In the planning phase, PPI shaped the formulation of the research questions, the study design and the plans for dissemination. During the study, patients and the public (including volunteers at local Healthwatch organisations) were involved in various ways across the four phases in an ongoing and embedded fashion:
-
In pre-study phase meetings, we involved 17 patients and members of the public to refine the research questions and the study design.
-
In phases 2 and 3, we involved local Healthwatch volunteers in the HIP. These Healthwatch volunteers helped us with the analysis of ethnographic data from the case study site during the first two HIP meetings and provided valuable insights about volunteers’ involvement in Healthwatch activities during the COVID-19 pandemic.
-
In phase 4, two Healthwatch volunteers attended the cross-site JIF and several Healthwatch volunteers (mainly board members) attended the local JIFs.
-
Our Advisory Group included two members of the public (recruited from the attendees to our pre-study phase focus groups).
-
In addition to this face-to-face PPI engagement, the study team established Twitter and Facebook accounts for the project through which we shared research activities and emerging findings.
Patients and members of the public who took part in the study were offered full support to contribute effectively to the study. This support included reimbursement of travel costs to face-to-face meetings, accommodation and subsistence (where appropriate) for HIP members, and training in qualitative methods during phase 2. In addition, we provided payments to PPI participants in accordance with INVOLVE guidelines.
In the sections that follow, we detail the four principal ways in which patients and the public were involved in our research.
Patient and public involvement meetings (pre-study phase, completed April 2017)
People involved
-
Meeting A: Research Expert Group at the Centre for Public Engagement, Kingston University (London, UK) and at St George’s University of London (London, UK):
-
Ten members of a standing ‘Research Expert Group’, including former and current NHS patients, carers, and former and current local Healthwatch volunteers.
-
-
Meeting B: local Healthwatch organisations and Healthwatch England, held at King’s College London (London, UK):
-
Nine people, including staff and volunteers from several London local Healthwatch organisations and Jacob Lant (Head of Policy and Partnerships at Healthwatch England).
-
Aims
-
To refine research questions, study design, objectives and pathways to impact and dissemination.
-
To identify the need for the research.
Methods
A presentation of the proposed study followed by general discussion.
Outcomes
The PPI meetings emphasised the need for this research, but rejected our initial proposal to focus exclusively on local Healthwatch organisation’s dementia-related work, which the group said would not be representative of the work of all local Healthwatch organisations in England. The group suggested that we adopt a broader focus by means of the phase 1 survey to account for the variability of each local Healthwatch organisation’s annually agreed priorities and identified variables. The group approved and refined our recruitment strategy for the HIP (see below) and suggested a Delphi phase (see Changes to protocol) to build consensus around ethnographic data analysis.
Healthwatch Involvement Panel (phase 2)
People involved
-
Four volunteers with local Healthwatch organisations that were not case study sites.
-
The HIP was chaired by Sally Brearley, who is an experienced patient and public representative and facilitator.
Aims
-
To involve Healthwatch volunteers, as well as staff, given that volunteers play a significant role in local Healthwatch organisations.
-
To ensure that volunteers, as well as staff, assist the analytical work of the study team based on their own experience and knowledge of local Healthwatch.
-
To look for points of similarity and difference with their own organisational practices to help build a broader picture of local Healthwatch activity across England.
-
To guide the research team with detailed suggestions on how to develop the ethnographic work in accordance with short- and medium-term fieldwork objectives.
-
To share with the research team their experiences of, and insights about, Healthwatch volunteering in the first year of the COVID-19 crisis.
Methods
All HIP members (including volunteers) took part in a qualitative research methods training delivered by the study team at King’s College London on 17 July 2019. At the first two HIP meetings, HIP members were presented with data from phase 1, the sampling strategy for the five case study sites and some emerging findings from the phase 2 ethnography. HIP members were asked to participate in activities and joint discussions in line with the aims articulated above. During the COVID-19 pandemic, HIP members (including volunteers) were invited to take part in two one-to-one interviews and one focus group to discuss their personal experience of the work of Healthwatch in this time. We conducted and recorded a total of six interviews with our volunteer HIP members and one focus group. The latter explored the experience of volunteering at Healthwatch during the pandemic. HIP member volunteers also took part in the activities and discussion during plenary HIP meetings.
Outcomes
The involvement of volunteers in the HIP helped us broaden our focus to include the experiences of non-staff members of local Healthwatch organisations. In addition, the involvement of volunteers provided an inclusive forum for engagement and joint reflection between staff and volunteers on the everyday practices and strategies of local Healthwatch work.
Joint interpretative forums (phase 4)
People involved
-
Of the 15 total participants at the cross-site JIF, two were volunteers.
Aims
-
To engage patients and the public as key stakeholders in joint reflection and interpretation of the findings from phases 1–3.
-
To discuss what forms of evidence and what dissemination strategies by local Healthwatch organisations would be more useful in affecting positive change for residents.
Method
The cross-site JIF involved one 2-hour virtual meeting involving three representatives from each study site (including volunteers). The meeting involved a mix of interactive activities, presentation of emerging research findings and joint discussion among participants.
Outcomes
The JIFs ensured that the patient and public voice was considered in the interpretation of study results, building the basis for collaboration to guarantee that patient and public voice was involved in the creation of resulting action at the local level.
Advisory Group (all phases)
People involved
-
Members of our Advisory Group included two patients and members of the public who were recruited among the participants of the PPI focus groups held in the pre-study phase.
Aims
-
To ensure that patient and public views are considered throughout the research process, along with those of academics, policy-makers and practitioners.
-
To ensure that patient and public perspectives contribute to the dissemination of research findings and recommendations.
Method
We held five 2-hour meetings over the course of the study, during which the study team consulted the Advisory Group about the sampling and recruitment of participants and research plans during the following months.
Outcomes
Patient and public involvement in the Advisory Group enabled us to consider the perspective of lay people on emerging research findings from the study and to tailor the planning of research outputs to various intended audiences.
Ethics approval
Following advice from our sponsor and the Research & Development Office at Guy’s and St Thomas’ NHS Foundation Trust on behalf of King’s College London – and with the agreement of the NIHR – we initiated two separate ethics approval processes with separate protocols. Phase 1 was split from the later phases. This was to ensure that phase 1 (i.e. the survey) could proceed on schedule without being unduly delayed by the more complicated ethics approval processes required for ethnographic fieldwork at specific study sites.
The survey phase was judged to pose a minimal ethics risk by King’s College London and received Research Ethics Minimal Risk Registration (MRA-18/19-8494) on 14 September 2018.
Ethics approval for the rest of the study was organised through Integrated Research Application System and Health Research Authority processes (Integrated Research Application System number 252993). As the study was largely non-NHS based and did not require the recruitment of NHS patients, it was judged to fall outside the purview of NHS Research Ethics Committee review. Therefore, we proceeded to apply for King’s College London ethics review and this was granted by PNM Research Ethics Panel on 12 July 2019 (reference LRS-18/19-12587). The Health Research Authority granted approval on 5 August 2019.
Changes to protocol
The following three substantive changes to our original protocol were made and agreed with the NIHR Health and Social Care Delivery Research programme.
First, the addition of a fifth case study site was a result of discussions with our HIP in July 2019 and following the successful completion of our national survey in phase 1. We presented a sampling frame to the HIP together with anonymised details of the four Healthwatch case study sites we proposed would become the focus of our ethnographic fieldwork in phase 2. The HIP felt that limiting ourselves to four sites would inevitably mean not being able to explore an important additional type of Healthwatch organisation and asked us to carefully consider whether or not we could add a fifth site that would enable us to include this additional type of Healthwatch organisation. Following discussions among the research team and with the chairperson of our Advisory Group, we added a fifth site. This was acknowledged by NIHR in its response to our second progress report (August 2019):
Thank you for explaining the two separate ethical approvals and both KCL [King’s College London] and HRA [Health Research Authority] approvals are now uploaded to the MIS [Management Information System]. This is good news as you can now commence your fieldwork. Your Healthwatch Improvement Panel is providing value, includes volunteers and have recommended that you recruit a fifth case study site, which you have added.
Communication from the funder's monitoring department, 2019, personal communication
Second, we replaced our proposed Delphi study with the greater involvement of our HIP (in combination with the end of study JIFs). The purpose of a Delphi is to reach consensus. Through the early phases of our empirical fieldwork, however, we discovered that the huge (and unexpected) variability of the 150 Healthwatch organisations in England and their activities would make consensus around uniform principles of good practice difficult to achieve and, arguably, inappropriate (this is also reflected in the important addition of the fifth case study site as outlined above). ‘Good practice’ principles achieved via a Delphi process would also be difficult for local Healthwatch organisations to implement, given their diversity. Instead, we used the JIFs together with the enhanced involvement of the redefined HIP (with a membership of 15 Healthwatch organisations) to formulate, test and refine more nuanced, tailored and targeted principles of good practice, which would be better able to take account of the diversity of Healthwatch organisations:
The Research Team proposed that the Delphi process (phase 3) be replaced with regional workshops based on emerging research findings, which would involve the HIP and possibly existing regional networks. The Advisory Group agreed that a Delphi would not be suitable at that point in the project because it would truncate the emerging complexity. They felt that the research team’s proposal would increase the value of the research.
Advisory Group meeting minutes, 6 November 2019
Third, the decision to explore the impact of COVID-19 on Healthwatch practices was discussed and agreed with the Advisory Group at a subsequent meeting. In addition to the 13 one-to-one interviews already carried out with HIP members, the study team proposed continuing direct engagement with panel members through virtual small-groups discussions and/or semistructured interviews with panel members. The two remaining HIP meetings, originally scheduled for phase 2, were eventually carried out alongside these new forms of engagement in the months following the end of fieldwork in January 2021. At the meeting on 21 May 2020, the study team remarked that the expanded role of the HIP throughout the study would enable a more nuanced understanding of the variability of Healthwatch work, particularly in the context of the COVID-19 pandemic.
Chapter 3 Data sources and modes of analysis
Some text in this chapter has been reproduced from Donetto et al. 40 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In addition, some text in this chapter has been reproduced from Zoccatelli et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Phase 1
Data sources
We received responses to our survey from 96 local Healthwatch organisations, achieving a response rate of 68% (note that eight Healthwatch organisations responded on behalf of two or more Healthwatch organisations that they operated as a combined organisation). Nineteen (19.8%) of our respondents were commissioned by county councils, 16 (16.6%) by London boroughs, 23 (24%) by metropolitan districts and 38 (39.6%) by unitary authorities. Table 7 presents a breakdown of the responses we obtained based on the geographical region.
| Region (na) | Total number of Healthwatch organisations | Number of survey respondents |
|---|---|---|
| East (1) | 11 | 9 |
| East Midlands (2) | 10 | 6 |
| London | 32 | 16 |
| North East | 12 | 6 |
| North West (2) | 23 | 12 |
| South East (1) | 18 | 15 |
| South West (1) | 15 | 11 |
| West Midlands | 14 | 13 |
| Yorkshire and the Humber | 15 | 8 |
| Total | 150 | 96 |
Modes of analysis
The survey data and analysis comprised descriptive statistics consisting of single variables and included frequency and percentage response distributions, measures of central tendency and dispersion measures, such as the range and standard deviation. All open comment responses were analysed using open coding and constant comparison. The survey was conducted using the Jisc online survey platform.
Phase 2
Data sources
Data sources include documents collected at the Healthwatch study sites [e.g. agendas and minutes from board meetings, committees and panel discussions, strategy documents, PowerPoint® presentations (Microsoft Corporation, Redmond, WA, USA), leaflets, feedback forms], transcripts of video- and audio-recorded interviews, ethnographic field notes from informal conversations and observations at each study site and written ethnographic notes and transcripts of HIP meetings. In Table 8, we present a breakdown of fieldwork data sources (observations and interviews) at each of the five study sites. Table 9 outlines the number and roles of attendees at the five HIP plenary meetings.
| Healthwatch | Days of fieldwork pre pandemic (n) | Contacts (e.g. online observations, catch-up chats, interviews) (n) | One-to-one interviews (total): (n) | Formal interviews recorded and transcribed (n) | Interview participants (n) (recorded and transcribed) |
|---|---|---|---|---|---|
| Ashton | 8 | 15 | 15 | 8 |
2 Healthwatch staff 2 Healthwatch board members 2 Healthwatch volunteers 2 VCSE representatives |
| Beecham | 17 | 26 | 28 | 18 |
8 Healthwatch staff 4 Healthwatch board members 2 Healthwatch volunteers 2 council staff (Healthwatch commissioner and council senior commissioning officer) 1 ICS programme director 1 CEO of neighbouring Healthwatch |
| Cherryburgh | 20 | 31 | 24 | 16 |
7 staff members (2 staff members were interviewed three times over the course of fieldwork) 2 Healthwatch board members 1 Healthwatch volunteer 1 council staff (director of public health) 1 elected councillor |
| Dogwood | 16 | 23 | 10 | 2 |
1 CCG chairperson and COO 1 Direction Health CEO |
| Elmbridge | 14 | 19 | 7 | 6 |
1 Healthwatch chairperson 1 Healthwatch board member 1 Healthwatch CEO 1 CCG staff member 1 local hospital trust engagement lead 1 local authority contract manager |
| Total | 75 | 114 | 84 | 50 |
| HIP meeting date | Number of participants | Participants by role |
|---|---|---|
| 17 July 2019 | 14 |
7 CEOs/COOs/directors 2 managers 3 other staff roles 1 volunteer 1 board member volunteer |
| 26 November 2019 | 15 |
6 CEOs/COOs/directors 2 managers 3 other staff roles 2 volunteers 2 board member volunteers |
| 23 April 2020 | 14 |
6 CEOs/COOs/directors 3 managers 2 other staff roles 1 volunteer 2 board member volunteers |
| 20 October 2020 | 15 |
6 CEOs/COOs/directors 3 managers 2 other staff roles 2 volunteers 2 board member volunteers |
| 23 February 2021 | 13 |
6 CEOs/COOs/directors 2 managers 2 other staff roles 1 volunteers 2 board member volunteers |
Modes of analysis
Our principal mode of analysis in phase 2 was informed by ANT, which was developed by Bruno Latour, Michel Callon and John Law as part of science and technology studies during the 1980s32,33 and which has been taken in several directions since its application to the study of health care and health organisations. 37,39,41,42 As discussed in more detail in Chapters 2 and 3, although it carries ‘theory’ in its name, ANT is better understood as a range of methods for conducting research. ANT aims to describe the connections that link together humans and non-humans (e.g. objects, technologies, policies and ideas) and seeks to describe how these connections come to be formed, what holds them together, and what they produce. Amit Desai, Giulia Zoccatelli and Glenn Robert had used this mode of analysis successfully in another study. 40
Our analysis was based on a combination of re-examination of our textual data (i.e. re-reading notes and transcripts, producing memos and reflective notes, and open coding, mostly manual) and discussion, in groups of different sizes, of observations and reflections on field visits. By this we mean that the analysis proceeded through discussion of emerging themes and ideas as much as through individual work. Two researchers on the team, Amit Desai and Giulia Zoccatelli, carried out fieldwork at two study sites each and shared another study site. Amit Desai and Giulia Zoccatelli were jointly responsible for preparing, convening and planning activities for the HIP. In addition, Amit Desai and Giulia Zoccatelli shared an office and met almost daily on Microsoft Teams during the COVID-19 pandemic and therefore had the opportunity to share views and nascent analytical threads as these emerged. These regular meetings allowed for discussion of the practices observed and the conversations had at the study sites. In our analysis, we relied on a mix of documents from Healthwatch and other sources, such as interview transcripts and field notes. Amit Desai and Giulia Zoccatelli met with Glenn Robert (principal investigator) every 2–4 weeks to discuss progress and ideas. Whole research team meetings were held every 2 months throughout the study to discuss emerging themes and potentially useful analytical and reporting approaches.
Individual analysis and group discussions were used to examine our descriptions for each Healthwatch organisation and compared practices and patterns both within each Healthwatch organisation and across Healthwatch (including data from the study sites and, in the later part of phase 2, from the HIP). Emerging data analysis was also sense-checked by the HIP to ensure validity. The findings emerging from these comparisons were used to structure and feed into the following study phases.
By observing practices and having several conversations with Healthwatch staff, board members, volunteers and key partners, we built rich descriptions of the ways in which different elements of Healthwatch work came together and showed identifiable patterns. Through the individual analysis and group discussions outlined above, we examined our descriptions for each Healthwatch study site and compared practices and structures of Healthwatch work [e.g. how Healthwatch staff (humans) interacted with a patient feedback database (non-human)]. Although we relied on the analysis of three types of data, in the presentation of our research findings in Chapters 5–7 we construct descriptions that combine different sources of data in an integrated way for the sake of clarity. This means that we refer to specific data sources (e.g. an interview quotation or an excerpt from a document) only when this adds to the narrative.
Phases 3 and 4
Data sources
Text data in phase 3 include documents shared by HIP members (e.g. strategy documents, PowerPoint presentations, leaflets, feedback forms), transcripts of video- and audio-recorded interviews and ethnographic field notes taken by the researchers during the interviews (Table 10 shows a breakdown of data sources from interviews and small-group discussions with HIP members from April 2020 to February 2021).
| Date | Method |
|---|---|
| April 2020 |
|
| October 2020 |
|
| February 2021 |
|
Data sources in phase 4 include transcripts of video-recorded JIF meetings (both cross-site and local JIFs at each study site) and written notes taken by the researchers during the meeting. The plenary discussion and the three small-group discussions at the cross-site JIF were audio- and video-recorded on Microsoft Teams and transcribed for analysis. Team members also took written notes about general themes emerging from the discussion. The discussions at the local JIFs were audio- and video-recorded on Microsoft Teams and transcribed for analysis. Owing to technical issues arising during the meeting, no recording was made of the Healthwatch Cherryburgh JIF. Instead, hand-written notes were taken by the researchers Giulia Zoccatelli and Amit Desai and used for the analysis.
Modes of analysis
Amit Desai and Giulia Zoccatelli carried out the interviews jointly. Amit Desai and Giulia Zoccatelli read and analysed each transcript separately – together with their notes from the interview – and then met to discuss common emerging themes. Analysis proceeded through this discussion of emerging themes and ideas as much as through individual work. Emerging themes and ideas were then presented by Amit Desai and Giulia Zoccatelli to the whole study team for further discussion and refinement. Initial analysis of findings from individual and small-group interviews with HIP members was presented for sense-checking and further refinement at HIP plenary meetings in April 2020, October 2020 and February 2021.
Chapter 4 Findings part 1: mapping local Healthwatch’s organisational structures, relationships and impact
Some text in this chapter has been reproduced from Zoccatelli et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
In this chapter, we report the findings from the first phase of our study; that is, the online survey of all 150 local Healthwatch organisations in England carried out between December 2018 and January 2019. The survey (1) mapped the current organisational arrangements, relationships and impact of local Healthwatch organisations in England and (2) illuminated the extent to which these vary across local Healthwatch organisations. We obtained responses from 96 local Healthwatch organisations (i.e. a response rate of 68%).
Organisational structure
Standalone or ‘hosted’?
We categorised local Healthwatch organisations as to whether they are (1) independent standalone organisations that only conduct Healthwatch work in one locality or (2) are part of other organisations that also carry out other work. Standalone Healthwatch organisations are sometimes referred to as ‘independent’ by people involved in the Healthwatch world, indicating that the Healthwatch in question is not part of another organisation. We use standalone throughout the report to mean these Healthwatch organisations. The other kind of Healthwatch organisations referred to are called ‘hosted’ organisations. Host types vary greatly across the Healthwatch network and include:
-
local community and voluntary sector support organisations that may hold several Healthwatch contracts
-
a local social enterprise (e.g. disability charity) that holds the local Healthwatch contract or grant alongside other activities
-
a local Healthwatch that holds the contract for additional Healthwatch organisations and does no other non-Healthwatch work.
Most Healthwatch organisations reported that they were ‘standalone’ (n = 56, 58.3%) and 40 (41.7%) Healthwatch organisations said that they were ‘hosted’.
To investigate if geographical size or complexity of local authority structures were associated with whether or not a local Healthwatch organisation is standalone or hosted, we cross-tabulated the above categorisations by size and type of local authority in which each Healthwatch organisation principally operated. There are four types of local authority in England that fund the work of local Healthwatch organisations: (1) county, (2) unitary, (3) metropolitan district and (4) London borough. Of these local authority types, counties are generally larger and more complex than the other three types. This is mainly because counties have two tiers of local government, which means that powers and responsibilities are split between county-level government and district-level local government, and Healthwatch could potentially operate at both these tiers. The other three types of local authority have a single tier. We found that a larger proportion of Healthwatch organisations in counties describe themselves as ‘standalone’ (78.9%) than Healthwatch organisations in unitary authorities (47.4%), metropolitan districts (56.5%) or London boroughs (62.5%). Conversely, Healthwatch organisations in unitary local authorities tend to report a higher proportion of hosted organisations (52.6%) than those in counties (21.1%), London boroughs (37.5%) or metropolitan districts (43.5%).
Contracts or grants?
We explored the different mechanisms by which Healthwatch organisations are funded by their local authority (i.e. contracts or grants). The main difference between contracts and grants is that the former must be tendered in accordance with government (UK and formerly European Union) procurement regulation and this process requires providers of local Healthwatch services to devote considerable time and resources to the management and renewal of their contract. Grants are not subject to these formalities. Applying for a continuation of funding may not be as onerous for grant-funded Healthwatch organisations, in that terms of a grant may be less prescriptive or exacting than a contract. However, grants are normally provided for shorter periods of time (usually 1 year), and shorter funding periods could have an affect on the long-term planning ability of a local Healthwatch organisation.
We found that the majority of local Healthwatch organisations are currently funded through a contract, whereas one-fifth (n = 19, 19.8%) are funded by a grant. One respondent chose the ‘other’ option and explained in the free-text section that their funding mechanism was currently under review (and probably moving from grant to contract). Geographical and local authority-based variations appeared to play a role in determining the funding mechanisms for Healthwatch. For example, although contracts are the main funding mechanism across Healthwatch organisations in England generally, the east of England is the only region in which the number of Healthwatch organisations with grants outnumber those with contracts. Grants make up a larger proportion of funding mechanisms than the England average in counties (n = 5, 26.3%) and unitary local authorities (n = 9, 23.7%), whereas Healthwatch organisations in London boroughs (n = 2, 12.5%) and metropolitan local authorities (n = 3, 13.0%) reported lower proportions of grants than the national picture. We found that a much smaller proportion of hosted Healthwatch organisations hold grants (n = 2, 5.0%) compared with Healthwatch organisations that describe themselves as ‘standalone’ (n = 17, 30.4%).
External funding
Since their launch in 2013, local Healthwatch organisations have undergone significant budget cuts. Publicly available data compiled by Healthwatch England show that the value of contracts or grants was reduced in four-fifths (n = 121, 79.3%) of all 150 Healthwatch organisations in England between 2013 and 2018, with nine Healthwatch organisations experiencing cuts in excess of 50% of their original budget. It is interesting to note that, in parallel, the number of Healthwatch organisations seeking and receiving funding beyond that provided by their local authority for their Healthwatch functions is thought to have increased since 2013. 16 In our survey, we found that 71 (74.0%) Healthwatch organisations were receiving such funding. The two most common services provided in exchange were ‘research on patient or service user experience’ (n = 56, 77.8%) and ‘development of patient/public engagement activities’ (n = 44, 61.1%). The sources of this external funding also varied. Forty-four (62.0%) of the 71 Healthwatch respondents who reported receiving this funding said that they received it from CCGs, 42 (59.2%) reported receiving this funding from local authorities, 25 (35.2%) reported receiving this funding from NHS providers and 24 (33.8%) reported receiving this funding from sustainability and transformation partnerships (STPs) (the precursor to ICSs). Funding sources varied based on local authority types and the geographical location of local Healthwatch organisations. For example, we found that all Healthwatch respondents from London boroughs that reported receiving external funding did so from the health sector. Conversely, outside London, the main source of funding for local Healthwatch organisations was reported to be their local authority.
Healthwatch as award funders
Twenty-seven (28.1%) Healthwatch organisations awarded funding to other organisations. Examples included contracting voluntary and community organisations to gather feedback from groups of people whom Healthwatch found hard to reach or setting up small community funding schemes that were used to engage local organisations to carry out research or engagement with specific patient groups.
Staffing
Publicly available data compiled by Healthwatch England for the period between April 2017 and March 2018 show that, for those Healthwatch organisations responding to the survey, the median number of total employed staff was 6 (range 2–15), the median number of FTE staff was 3 (range 1–13.5) and the median number of volunteers was 23 (range 3–743).
Overall, volunteers were reported to contribute significantly to ‘enter and view’ visits. These ‘enter and view’ visits are statutory powers used by Healthwatch organisations to observe and gather information from staff and users of health and social care services at sites of care (e.g. a general practice or a care home) to assess the quality and standard of care. Forty-two (43.8%) Healthwatch organisations said that ‘enter and view’ visits were carried out ‘mostly by volunteers with some employed staff contribution’, whereas 29 (30.2%) Healthwatch organisations said that they were ‘equally carried out by employed staff and volunteers’. Conversely, administrative and clerical work (n = 95, 99.0%), research and report writing (n = 87, 90.7%) and communications and social media (n = 92, 95.8%) were either ‘wholly carried out by employed staff’ or ‘mostly by employed staff with some volunteer contribution’.
Relationships
To build a picture of the network of Healthwatch relationships, we asked how many CCGs, hospital trusts, mental health trusts, community health trusts, general practice surgeries and care homes Healthwatch respondents engaged with (Figure 1) and we found that:
-
54 (56.3%) Healthwatch respondents engage with only one CCG and a small number (n = 9, 9.4%) of Healthwatch respondents engage with five or more CCGs
-
39 (40.6%) Healthwatch respondents engage with only one hospital trust and six (6.2%) Healthwatch respondents engage with five or more hospital trusts
-
79 (82.3%) Healthwatch respondents engage with only one mental health trust
-
60 (62.5%) Healthwatch respondents engage with only one community health trust and 23 (24.0%) Healthwatch respondents do not engage with any community health trusts
-
40 (41.7%) Healthwatch respondents engage with more than 40 general practice surgeries
-
one-third (n = 32, 33.3%) of all Healthwatch respondents engage with more than 50 care homes and five (5.2%) Healthwatch respondents engage with none.
FIGURE 1.
Percentage of Healthwatch organisations with numbers with zero to five or more stakeholders in each category.
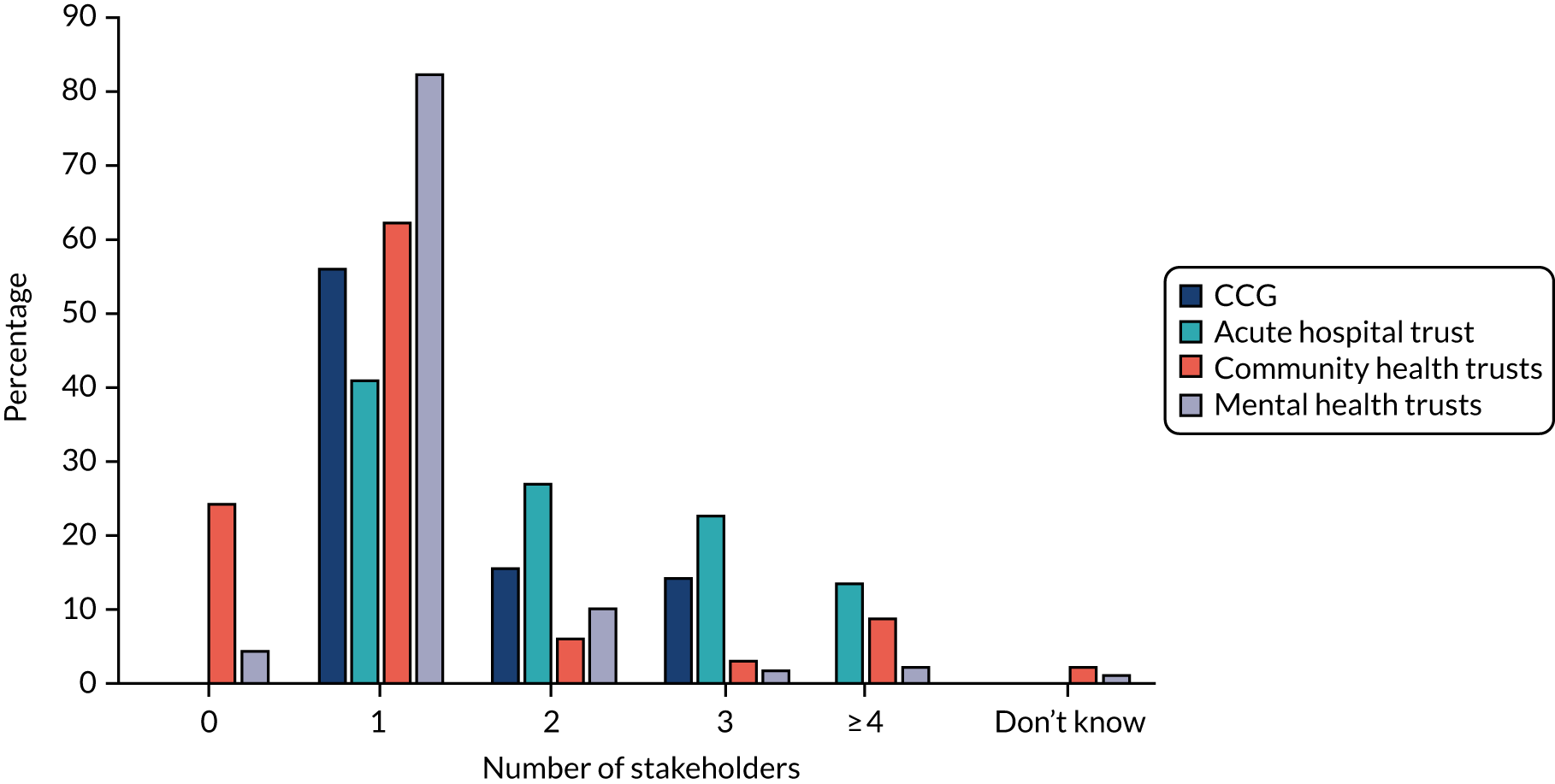
To provide further insight into the institutional and relational complexity of Healthwatch networks, we also asked whether or not local Healthwatch organisations engage only with stakeholders within the boundaries of their local authority, and two-fifths (n = 40, 41.7%) of all Healthwatch respondents said that this was the case. However, there was variation by (1) local authority type and (2) type of health or social care organisation. Healthwatch organisations in unitary local authorities are more likely than others to engage with organisations outside the boundaries of their local authority. For example, more than two-fifths (42.1%) of Healthwatch organisations located in unitary local authorities engage with CCGs outside their local authority area, compared with only three (15.8%) Healthwatch organisations in counties, four (17.4%) Healthwatch organisations in metropolitan districts and three (18.8%) Healthwatch organisations in London boroughs. Healthwatch organisations in unitary authorities (47.4%) are also more likely than Healthwatch organisations in other local authority types to engage hospital trusts outside their local authority area [seven (30.4%) Healthwatch organisations in metropolitan districts and five (26.3%) Healthwatch organisations in counties reported this].
Quality of relationships
We asked how local Healthwatch organisations rated (1) the overall quality of the co-operation among key health and social care stakeholders in their local area and (2) their level of engagement in the development of planning frameworks for health and social care services (e.g. ICSs). Most Healthwatch organisations reported both positive relationships among local stakeholders and a good level of involvement in ICSs (Table 11). However, the survey highlighted significant regional variation across the network. For instance, we found that five out of six Healthwatch respondents in the north-east of England reported having no or limited involvement in ICSs’ development.
| Quality of co-operation in local area | Involvement in development of STPs/ICSs | ||
|---|---|---|---|
| Response | n (%) | Response | n (%) |
| Excellent | 7 (7.3) | A high level of involvement | 14 (14.6) |
| Good | 54 (56.3) | A good level of involvement | 38 (39.6) |
| Neither good nor bad | 20 (20.8) | Some involvement | 31 (32.3) |
| Limited | 15 (15.6) | Not much involvement | 8 (8.3) |
| Poor | 0 | No involvement | 5 (5.2) |
More than half (n = 31, 57.4%) of the Healthwatch organisations that reported a ‘good’ overall quality of co-operation among stakeholders in their area reported either a ‘high’ or ‘good’ involvement in ICSs. In contrast, three-fifths (n = 9, 60.0%) of Healthwatch organisations in areas of ‘limited’ co-operation reported only ‘some’ or ‘not much’ involvement in ICSs.
Impact
Healthwatch organisations overwhelmingly reported impacts that were local in nature. The most common response among the 13 options provided was ‘Improved access to care and treatment for members of our community’, selected by 73 (76.0%) Healthwatch respondents, followed by ‘Increased levels of participation in co-production of people who use a service’ (n = 65, 67.7%). National-level impacts were selected by far fewer respondents. Ten (10.4%) local Healthwatch respondents reported that they had influenced changes in national policy or specialist commissioning and eight (8.3%) Healthwatch respondents had escalated an issue to Healthwatch England that was later actioned.
We explored the relationship between the number of FTE staff and (1) the number of types of local impact reported by respondents and (2) whether or not they reported national impact. We found that the greater the number of FTE staff, the larger the number of types of local impact, as well as the greater the likelihood of reporting a national impact.
Examples of successful impact
We asked respondents to identify a successful piece of work they had completed in the past 3 years. The responses represent a broad range of cases of perceived impact achieved by local Healthwatch organisations, along with an indication of the type of impact, the time needed to achieve that impact, the ways in which impact was delivered and three key stakeholders involved in each piece of work. In Box 4, we present two examples of the returns we obtained in this section of the survey.
Activities in care homes: study looking at the level of activities in care homes and the impact on the well-being of residents.
What was the key impact you achieved?
Other: influenced care home providers to develop their activity programmes to offer a more varied and stimulating programme of activities for residents.
How long did it take to achieve this impact?
12 months.
How was the impact delivered (e.g. research presenting evidence, publicity activity)?
Research, followed by a conference, social media attention.
Which of the following local stakeholders did you involve to achieve this impact? Please select the three most important
Social care providers.
Media.
Local CQC inspectors.
Example 2
What was the piece of work about?
Access to eyecare: to give people a strong voice and ensure their experiences and views are considered and influence how eye care services are provided.
What was the key impact you achieved?
Improved access to care and treatment for members of our local community.
How long did it take to achieve this impact?
While the project took 2 years from proposal through to our final evidence-based research report, action was quickly taken based on our recommendations.
How was the impact delivered (e.g. research presenting evidence, publicity activity)?
Evidence/findings presented in a research report following focus groups, site visits and interviews with members of the public.
Which of the following local stakeholders did you involve to achieve this impact? Please select the three most important
Other: local eye health network.
Local patient or condition-specific groups.
Community voluntary sector organisations.
The topics covered in the examples chosen by Healthwatch respondents varied, with hospital care (n = 14, 16.5%), primary care (n = 11, 12.9%), social care (n = 10, 11.8%) and disability (n = 10, 11.8%) being the most common (Table 12).
| Topic | Project duration | Total number (%) | ||
|---|---|---|---|---|
| ≤ 1 year | > 1 and < 2 years | ≥ 2 years | ||
| Hospital care | 10 | 1 | 3 | 14 (16.5) |
| Disability (excluding mental health) | 7 | 3 | 0 | 10 (11.8) |
| Primary care: GPs, eyecare, NHS 111 (no dentistry) | 6 | 4 | 1 | 11 (12.9) |
| Social care | 8 | 2 | 0 | 10 (11.8) |
| General engagement activities with patients and the public | 5 | 2 | 1 | 8 (9.4) |
| Mental health | 4 | 3 | 1 | 8 (9.4) |
| Children and young adults: general | 4 | 3 | 0 | 7 (8.2) |
| Seldom-heard groups: other (e.g. homelessness, drug and alcohol abuse, prisoners) | 4 | 1 | 0 | 5 (5.9) |
| Dentistry | 5 | 0 | 0 | 5 (5.9) |
| Palliative care and end-of-life care | 3 | 0 | 0 | 3 (3.5) |
| Seldom-heard groups: black, minority ethic and refugees | 0 | 0 | 1 | 1 (1.2) |
| Service users transport | 1 | 1 | 0 | 2 (2.4) |
| Carers | 0 | 1 | 0 | 1 (1.2) |
| Intermediate care | 1 | 0 | 0 | 1 (1.2) |
| Phlebotomy | 1 | 0 | 0 | 1 (1.2) |
| Other | 1 | 0 | 0 | 1 (1.2) |
| Total | 60 (68.2) | 21 (23.5) | 7 (8.2) | 88 (100) |
Regarding the type of impact achieved, almost one-third (n = 29, 30.2%) of respondents selected a project that led to an ‘improvement in the access to care and treatment for the members of their community’. Sixteen (16.7%) Healthwatch respondents selected an initiative through which they ‘influenced new commissioning or commissioning intentions’, 12 (12.5%) chose a project that ‘produced changes to local contract specifications’ and the same number chose a project that ‘improved the quality of care’.
The most commonly reported stakeholders involved in successful projects were ‘CCG board and staff’ (n = 40, 41.7%), ‘service users or service users groups’ (n = 33, 34.4%), ‘health and well-being board members’ (n = 26, 27.1%), ‘community voluntary sector organisations’ (n = 25, 26.0%) and ‘local authority overview and scrutiny committee’ (n = 21, 21.9%). Conversely, ‘governors of trusts’ (n = 0), ‘local MPs [Members of Parliament]’ (n = 1, 1%), ‘NHS England’ (n = 2, 2.1%), ‘staff at neighbouring Healthwatch’ (n = 3, 3.1%) and ‘local STP/ICS boards’ (n = 3, 3.1%) were only selected by a limited number of respondents.
Examples of failed impact
We asked respondents to briefly outline a piece of work that they had completed in the past 3 years that they regarded as being unsuccessful. We also asked respondents to select the type of impact that they wanted to achieve and to describe the main barriers to impact they faced on its delivery (Box 5).
Need for residents with autism.
What was the impact you wanted to achieve?
Promote issues which were adopted into a strategy (locally, regionally or nationally).
Please briefly describe the barriers to impact you experienced.
The commissioner writing the strategy was really engaged and also put us in contact with a variety of relevant departments and NHS commissioners (who actually ended up acting on our feedback and making a change on their side). However, the commissioner left, and the post’s responsibilities were left vacant for some time. We are still waiting for an opportunity to discuss the findings again. A board set up to look at the strategy did discuss the report and told us it was insightful but we have not been able to look at a longer term influence.
Example 2
What was the piece of work about?
Community dental services – access to procedures carried out under general anaesthesia.
What was the impact you wanted to achieve?
Improve access to care and treatment for members of our local community.
Please briefly describe the barriers to impact you experienced.
We ended up in a morass of different organisations with different responsibilities. Not everything they were each telling us could be true, as they were contradictory. The commissioner (NHS England) has been helpful in some ways but defensive in others. But we haven’t given up. We continue to press for answers. It is over 2 years since we began work on this.
Local Healthwatch respondents chose examples of unsuccessful projects that covered a broad range of topics. The most common topics were primary care (n = 17, 17.7%), hospital care (n = 14, 14.6%), disability (n = 10, 10.4%) and mental health (n = 9, 9.4%). Regarding the type of impact intended to be achieved, the majority (n = 45, 46.9%) of our Healthwatch respondents selected projects intended to ‘improve access to care and treatment’ for members of their local community.
The two most common barriers to impact identified by local Healthwatch respondents were the ‘lack of co-operation among or by key institutional stakeholders’ (n = 36, 37.5%) and the ‘systemic complexity or lack of clarity among stakeholders about respective organisational roles, responsibilities’ (n = 27, 28.1%), which, when combined, were selected by almost two-thirds of our survey respondents. Despite widespread concern about decreasing Healthwatch budgets, only 10 (10.4%) local Healthwatch respondents identified a ‘lack of resources’ as the main barrier to impact.
Summary
The findings of our phase 1 survey bring to the fore the variability in Healthwatch arrangements and highlight some interesting trends. In terms of organisational structure, although a majority of Healthwatch organisations do, indeed, operate as standalone social enterprises, the number of ‘hosted organisations’ is still significant, with more than two-fifths of Healthwatch organisations reporting being run by a host. Types of hosts also vary greatly, ranging from small social enterprises to large organisations that hold the contracts of several Healthwatch organisations in geographically dispersed areas. Healthwatch organisations within unitary local authorities are more likely to be hosted – rather than independent – organisations. Healthwatch organisations in counties, conversely, report the smallest proportion of hosted organisations, and one reason for this may be that Healthwatch organisations that are hosted by another organisation may struggle to operate at the larger geographical scale of a county. Although economies of scale, in terms of back-office functions, are likely to make large host organisations more competitive in the tender for a Healthwatch contract, they may be easier to realise in smaller geographical areas (i.e. unitary local authorities) rather than in larger areas (i.e. counties). Alternatively, it might be a function of the relative population density of the different local authority types. Based on data from the Office for National Statistics,45 none of the county councils fall into the top 50% of local authority areas by population density and it is, therefore, plausible that the third sector in such comparatively sparsely populated locales is less developed than in London boroughs, unitary authorities and metropolitan districts. Consequently, this may mean that there are fewer potential host organisations that might bid for Healthwatch contracts in county council areas.
Survey responses also mirror the challenging financial landscape in which most local Healthwatch organisations currently operate. As data from Healthwatch England reveal, and as we discuss in Chapter 1, four out of the five local Healthwatch organisations in this study have seen their funding reduced since 2013, and cutting operational costs as well as finding alternative sources of funding have become important for securing Healthwatch’s organisational sustainability. We found that over 70% of Healthwatch organisations are now receiving external funds in addition to their core local authority contract or grant and these funds cover a broad range of activities, ranging from research on patients’ and service users’ experiences to the provision of the NHS Complaints Advocacy Service. Sources of funding also vary greatly across the network. Most common are funds from health organisations and local authorities, but with geographical variation. In the face of shrinking core funding, such ancillary funding may well be a vital supplement to ensure the viability of some local Healthwatch organisations. However, given the importance attached to their role as the principal conduit for the views of patients and service users on health and social care, dependence on these extra sources of funding may bring with it challenges around autonomy.
The variety of organisational and funding arrangements mirrors the diversity in the type and complexity of relationships with key stakeholders in health and social care, like CCGs, acute, community and mental health hospitals, GPs and care homes. Although many Healthwatch organisations engage in relatively simple institutional landscapes featuring only a limited number of stakeholders located within the boundaries of their local authorities, other Healthwatch organisations are embedded in complex institutional landscapes involving large numbers of commissioners and providers of health and social care services (e.g. five or more CCGs, five or more hospital trusts) located both within and outside the boundaries of their local authority. For example, our survey findings show that Healthwatch organisations in more complex institutional landscapes report more varied forms of impact (see Chapter 5, Institutional landscapes).
Looking more broadly at the quality of the relationship between local stakeholders and the level of involvement reported by Healthwatch in the development of key planning frameworks for health and social care services, like ICSs, our findings highlighted further variation. For instance, we found that although most Healthwatch respondents reported a high or good level of involvement in ICSs, five out of six Healthwatch respondents in the north-east of England reported having no or limited involvement in their development.
The quality of collaborative relationships with a range of partners also appeared to crucially influence the impacts described by participating Healthwatch organisations, including where impact had not been achieved. Local impacts predominated over national-level impact, reflecting the remit of local Healthwatch organisations. However, only 1 of the 10 participating Healthwatch organisations perceived that it had influenced a national-level policy change and this suggests that there is scope for further co-ordination of such activity, with a key role for Healthwatch England in securing wider impact.
Chapter 5 Findings part 2: exploring key axes of Healthwatch variability
In Chapter 4, we drew on the findings of our national online survey of local Healthwatch organisations to map the variability of Healthwatch’s organisational structures, relationships and impact across England.
In this chapter, we use (1) findings of our phase 2 ethnographic study of five Healthwatch study sites (see Figure 2 for the basic characteristics of each of the five study sites) and (2) insights from the discussion held among Healthwatch representatives at each study site during the cross-site JIF in phase 4. Drawing on these data, we explore in greater detail the following four key axes of Healthwatch variability that shape Healthwatch’s everyday strategies and practices:
-
organisational structures: ‘hosted’ or ‘standalone’
-
funding arrangements
-
institutional landscape
-
strategies and practices of engagement.
FIGURE 2.
Study sites’ basic characteristics. All details correct as of January 2021. FTE, full-time equivalent; LA, local authority.
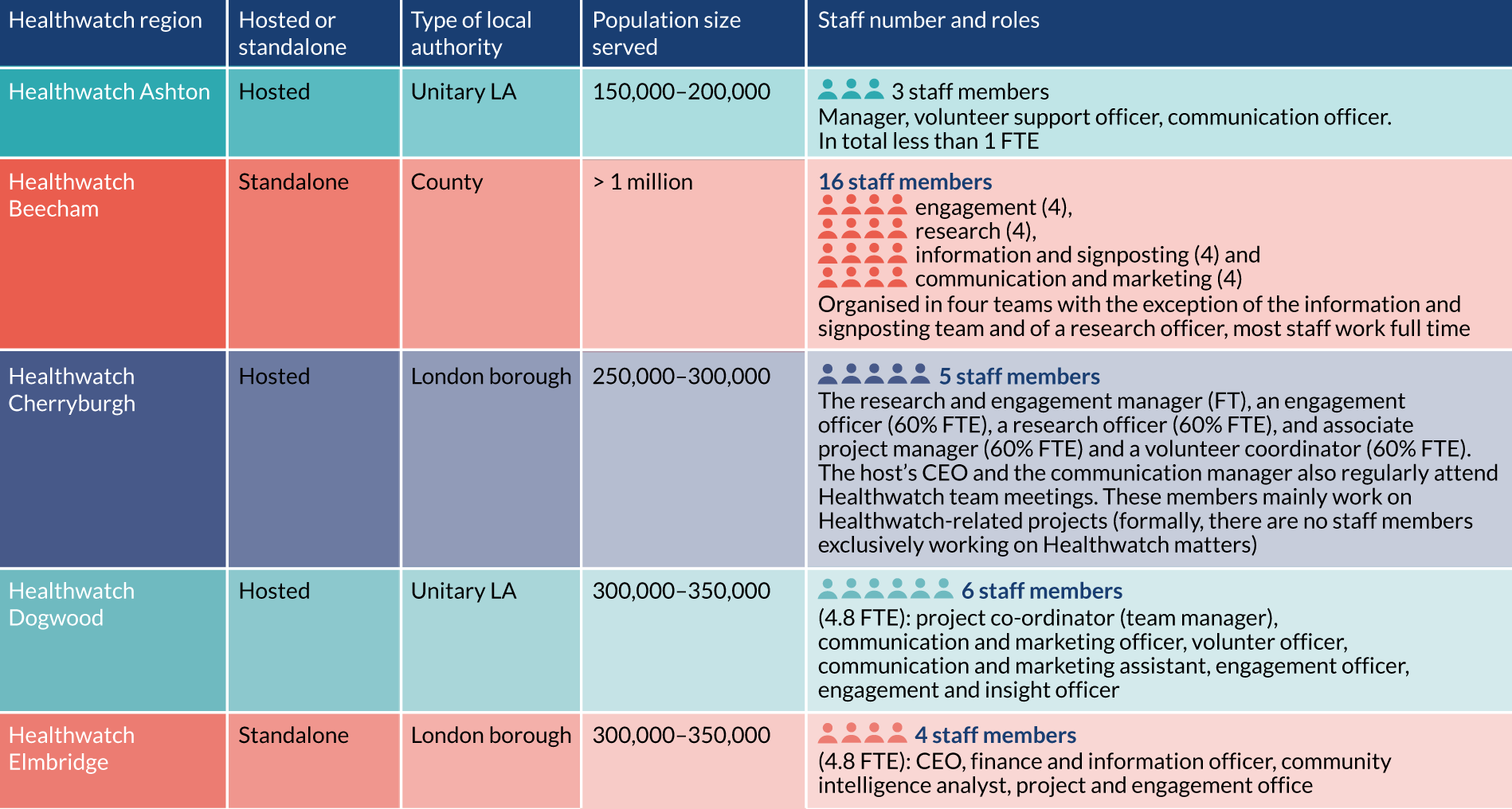
To approach the analysis of these areas, we use the theoretical framework of ANT. As we have outlined in greater detail in Chapter 1, ANT focuses on the analysis of the connections that link humans and non-humans (e.g. objects, documents, buildings, meetings, technologies, data, policies, strategies, contracts, ideas). ANT describes how these connections come to be formed, what holds them together and what they produce in particular contexts. From the ANT point of view, organisations (e.g. Healthwatch), as well as the immaterial concepts they actualise through their work (e.g. patients and public voice), are always the product of a system of mutual influence between humans and the material structures with which they come in contact every day. From this perspective we argue that, despite the fixed nature of Healthwatch’s statutory functions, what Healthwatch actually is, and what it does in its daily operation, is far from fixed.
Drawing on this approach, we organise our discussion in four short sections, with each exploring a specific axis of Healthwatch variability. The axes, we argue, are the direct product of Healthwatch’s entanglement with the key sociomaterial structures that shape their work.
Drawing on the extended ethnographic description of everyday practices and arrangements at our five Healthwatch study sites, we ultimately show how what is univocally called ‘Healthwatch’ is the multifaceted outcome of these entanglements, which shape Healthwatch’s everyday strategies and practices, and its potential and influence in representing the voice and needs of patients and public in health and care decisions. Each of these entanglements are mutually influencing and, therefore, closely related to each other.
Organisational structures: ‘hosted’ or ‘standalone’
As we discussed in Chapter 4, one of the main ways in which Healthwatch organisations are categorised is whether they are (1) standalone organisations that conduct only Healthwatch work and do so in one locality or (2) part of other organisations that also carry out other work. These latter Healthwatch organisations are referred to as ‘hosted’. According to our survey findings, most Healthwatch organisations reported being standalone (n = 56, 58.3%), with 40 (41.7%) Healthwatch organisations reporting that they are ‘hosted’.
The dualism between hosted and standalone organisations is commonly referred to by Healthwatch as a crucial way to discuss intrinsic differences between various Healthwatch organisations. The centrality of this dualism, for instance, emerged during our first HIP meeting when we presented the key characteristics of the four Healthwatch organisations we sampled to become our study sites. On that occasion, HIP members felt strongly that our selection was skewed towards hosted organisations and suggested that we recruit an additional site to reflect the specificity of a ‘small, standalone Healthwatch’ organisation. HIP members’ stress that the distinction between standalone and hosted Healthwatch organisations mirrors the general concern for this specific aspect of Healthwatch’s organisational set-up across the Healthwatch network. In 2018, for instance, Glenn Robert and Amit Desai attended the Healthwatch National Conference (Stratford-upon-Avon, UK), where a lively debate broke out about the risks posed by ‘predatory’ host organisations that bid for many Healthwatch contracts. The impression among many of those from standalone Healthwatch organisations was that Healthwatch organisations run by hosts would prioritise the needs of said hosts, become less responsive to the needs of local people and, therefore, not be ‘truly independent’ (a key Healthwatch value). This was reiterated during the course of our study and through our engagement with the HIP.
Our ethnographic findings, however, suggest that this easy dualism between standalone and hosted Healthwatch organisations conceals important aspects of Healthwatch’s organisational structures. In fact, we found that there is a great variability even within these two categories and such variability is determined by a far more complex array of factors (e.g. local histories, institutional landscapes, funding arrangements and staffing issues).
Drawing on this background, we address the following questions:
-
How does the variability of organisational arrangements affect the everyday work of local Healthwatch organisations?
-
Are hosted Healthwatch organisations so like each other that they form a distinct category from standalone Healthwatch organisations?
-
Are the labels of ‘standalone’ or ‘hosted’ meaningful in understanding how local Healthwatch organisations work? In other words, is the distinction between the two labels consequential?
We address these questions by outlining the key aspects in the organisational arrangements at all our five study sites.
Healthwatch Ashton (hosted by a charity that also runs another Healthwatch organisation)
Healthwatch Ashton’s contract had been held by Achieve since the launch of Healthwatch in 2013. Achieve is a charitable company that was established in the late 1990s and works to promote health and well-being and address health inequalities in the broader region in which it is based. At the time of our fieldwork, Achieve also held the contract for Healthwatch Oakleigh (which was not a study site). In addition, until recently, Achieve held the contracts for a number of other Healthwatch in areas that adjoin that of Healthwatch Ashton.
Achieve delivered a range of other services in the area, which were funded variously by local authorities, the CCG and the National Lottery Community Fund. These services included leading a project to promote the involvement of seldom-heard groups in council decision-making, advocacy services, networking and research services for the local voluntary sector, and social prescribing projects.
Most of this other work took place outside the local authority covered by Healthwatch Ashton. Healthwatch Ashton’s manager explained that this was why Healthwatch Ashton appeared to operate on its own, separately from Achieve:
One thing I would add is I think Healthwatch Ashton as a contract is fairly self-contained. I mean I know it’s really small but I think it operates, I mean as I said, that doesn’t sort of – I guess what I’m trying to say is we wouldn’t necessarily [work with other parts of Achieve], because it’s in a different geographical area to I suppose [to] the other contracts’ work.
Healthwatch Ashton manager, interview, 6 January 2021
Two members of staff, including the manager, were shared across Healthwatch Ashton and Healthwatch Oakleigh; however, the Healthwatch organisations remained separate operations and were not in geographically contiguous areas. The small size of Healthwatch Ashton’s budget meant that Healthwatch Ashton relied on an active cohort of volunteers to set priorities and to carry out most of its activities (see Box 7).
Although formal governance responsibility for Healthwatch Ashton lies with Achieve’s board, Healthwatch Ashton had also formed its own executive board, which set its strategic and organisational priorities. This board was comprised staff members and volunteers.
Healthwatch Beecham (standalone Healthwatch organisation with a consultancy arm)
At the time of our fieldwork, Healthwatch Beecham was a standalone Healthwatch organisation that was funded through annual grants and run by a charitable company that conducted only Healthwatch work.
In 2016, Healthwatch Beecham established ‘Beecham Voice’, which was a separate company specialised in bidding for and delivering separate engagement and research projects. At the start of our fieldwork in August 2019, Beecham Voice was delivering three projects external to the Healthwatch contract, all of which were commissioned by the local council. These projects included a large 5-year contract awarded in 2019 to develop and facilitate engagement activities with disabled adults, the value of which exceeded that of Healthwatch Beecham’s core grant. Even although all of Beecham Voice’s projects were delivered by Healthwatch Beecham’s staff, during the time of our fieldwork, Beecham Voice was in the process of setting up an independent board, wholly separate from that of Healthwatch Beecham.
In the spring of 2020, Healthwatch Beecham appointed a new CEO and board chairperson and, following these changes, a decision was made to move Beecham Voice to dormant status. Beecham Voice’s independent board was dissolved and it ceased activity in March 2021. The contracts delivered by Beecham Voice were transferred to Healthwatch Beecham, which is now delivering those as Healthwatch projects. Healthwatch Beecham has not reached a final decision about the fate of Beecham Voice. When asked about Beecham Voice by other Healthwatch representatives during the cross-site JIF, the Healthwatch Beecham CEO explained:
I don’t think [Beecham Voice] did fail. We set it up for a specific purpose at a specific time. It delivered that purpose, and it no longer is. So, we were having two sets of accounts, two sets of boards, two sets of board papers, because we had the trading arm [Beecham Voice]. We needed the trading arm at the time when it was set up. It was useful, it’s no longer fit for the need that we have at the moment in the current climate we’re in. A lot of the external funding that we’re getting outside of the core grant is from applying for funds, applying for grants, and they need to be done through a charity. Most of them need you to be a charity in order to be able to apply for the funds, which means that [Beecham Voice] isn’t a vehicle to apply for that work through, so that’s why we’ve moved it to a dormant status so we can reignite it at a point in time if we need to. At this point in time we don’t see the need to invest in it.
Healthwatch Beecham CEO, cross-site JIF, 28 January 2021
Healthwatch Beecham’s board was still undergoing renewal at the end of our fieldwork in December 2020. At that time, it was composed of members mainly selected for their professional expertise (finance, research, charity work, etc.).
Healthwatch Cherryburgh (Healthwatch as a ‘project’ of its host organisation)
Healthwatch Cherryburgh’s contract was delivered by Community Together (Tamworth, UK), which is a community interest company specialised in service improvement through user engagement. Community Together was set up in April 2015 and took over the Healthwatch team and the novated contract from Healthwatch’s previous host, which was a local charity that had previously delivered the LINks contract and whose chairperson, at the time of our fieldwork, was also Community Together’s chairperson.
Since its launch, Community Together has expanded its range of activities and in 2020 was delivering several other contracts alongside Healthwatch Cherryburgh. These contracts included local social prescribers and community navigators, the delivery of support services to local residents who are aged ≥ 50 years, a CCG project to help develop Patient Participation Groups (PPGs) at the level of primary care networks (PCNs), and adviser services to tenants and leaseholders of social housing estates. Healthwatch Cherryburgh was the only Healthwatch contract delivered by Community Together.
The embeddedness of Healthwatch Cherryburgh within its host was reflected in Community Together’s organisational set up. Although five members of Community Together’s staff worked mainly on Healthwatch-related projects, Community Together did not have any formally dedicated Healthwatch staff members exclusively working on Healthwatch matters. Healthwatch Cherryburgh also did not have a dedicated board. Strategic direction for all projects, including those of Healthwatch Cherryburgh, was provided by Community Together’s board, which comprised local residents who were current and retired professionals working in organisation management, research and health and social care. No board member led on Healthwatch’s activities. Community Together’s independent chairperson received an annual salary for their work and represented Healthwatch at the health and well-being board and in several other council and NHS meetings.
In our chats and interviews with them, Community Together’s staff and board members consistently described how Healthwatch Cherryburgh could not be conceived of as separate from its host. Rather, Community Together’s staff and board members talked about Healthwatch as one among the many ‘projects’ in Community Together’s portfolio. For instance, as Community Together’s director told us:
Healthwatch Cherryburgh doesn’t exist. It is just a project [ . . . ] At Community Together, we badge things [projects] differently depending on the situation. If it’s useful for us, if it makes the project more recognizable, then I’d badge something – a stall, an event – as Healthwatch, but the next time I could badge it differently. It depends. Usually, when it’s about health, I’d use the Healthwatch logo, because it’s easier for people to understand what we are about. You know, Healthwatch brings a lot of kudos and a lot of clout.
Healthwatch Cherryburgh’s CEO, interview, 14 September 2020
Healthwatch Dogwood (hosted by a local charity that holds no other Healthwatch contract)
Healthwatch Dogwood was a ‘hosted’ Healthwatch organisation. The contract had been held since 2013 by local charity Direction Health, which provided services to people with disabilities. Direction Health was also the host employer for the local PCN’s social prescribers and held the contract for the local authority’s independent advocacy service. Healthwatch Dogwood had its offices at a complex owned by Direction Health where the host organisation itself was also based. In addition, Direction Health also let office space to other local VCSE organisations. Direction Health charged the Healthwatch contract a management fee, which comprised roughly one-tenth of the value of the contract.
Although formal governance responsibility for Healthwatch Dogwood lay with Direction Health’s board, Healthwatch Dogwood had its own active board that provided it with strategic direction. The board included two types of member; that is, (1) local residents with a background in the health and social care or the VCSE sector (referred to as ‘independent members’) and (2) representatives from local VCSE organisations (including the CEO of Direction Health) and a local authority officer (referred to as ‘co-opted’ members). Given the size of the area Healthwatch Dogwood covers, the board aimed for geographical representativeness among its independent members. Like Healthwatch Cherryburgh, the chairperson of the Healthwatch board was remunerated for their time commitment of 3 days per month. Unlike Healthwatch Cherryburgh’s chairperson, the chairperson of the Healthwatch Dogwood board was not independent and was a full board member.
The existence of a separate Healthwatch Dogwood board, which made decisions about Healthwatch Dogwood’s organisational priorities, allocation of resources and strategic vision, headed by a paid chairperson, meant that in many respects Healthwatch Dogwood looked like a separate organisation from Direction Health. Although staff were formally employees of Direction Health, most staff carried out Healthwatch work exclusively. Only one member of staff had a split role and divided their time between Healthwatch and the host. However, Direction Health maintained involvement in operational decisions and the Healthwatch manager often consulted its CEO in this regard.
According to Healthwatch Dogwood’s chairperson and manager, being hosted suited Healthwatch Dogwood well, as it allowed the Healthwatch board to focus on the Healthwatch work of best conveying public voice into the health and social care system without being distracted by legal, human resources or financial sustainability concerns (these were the domain of Direction Health). Therefore, Healthwatch Dogwood staff said that they felt freer than if they were a ‘standalone’ Healthwatch organisation. Staff found it to be beneficial that, rather than being compelled to recruit board members for their expertise in human resources, legal, finance or fundraising, the board itself included members who could access, and indeed be the voice of the public. Related to this was that Healthwatch Dogwood’s board did not necessarily regard its work as commercially sensitive or private. For instance, in pre-pandemic times, members of the public and VCSE organisations were invited to a coffee morning and asked to stay and observe the board meeting that followed.
Healthwatch Elmbridge (small standalone Healthwatch organisation)
Healthwatch Elmbridge described itself as a standalone Healthwatch organisation. Healthwatch Elmbridge was a charitable company that carried out only Healthwatch work and did not hold the contract of any other Healthwatch organisation. The charitable company was set up in 2013 specifically to hold the local Healthwatch contract and had held it continuously since.
As a charitable company, Healthwatch Elmbridge had a board of trustees with formal governance responsibilities. The board had seven members who were a mix of people working or formerly working in health care, local government or qualitative research, and residents and healthcare users with an interest in public involvement in health. Healthwatch Elmbridge had two co-chairpersons who represented different styles of Healthwatch. One co-chairperson was a senior commissioner in a neighbouring local authority and brought an institutional and strategic perspective, whereas the other co-chairperson had a long history in local health activism and represented a more ‘grassroots’ understanding of Healthwatch. Like Healthwatch Dogwood, where a representative from the council sat on the board, at Healthwatch Elmbridge, the local authority contract manager attended board meetings but was not a trustee. However, there was ongoing discussion within Healthwatch Elmbridge as to whether or not the presence of the contract manager – who was responsible for monitoring performance – at board meetings was appropriate. The board met in private. A suggestion from the local authority contract manager that Healthwatch Elmbridge might consider meeting in public was rejected by trustees, as they felt that this was based on a misunderstanding of the role of Healthwatch Elmbridge’s board, which, for them, was centrally about organisational governance rather than public participation.
Healthwatch Elmbridge used the services of external consultants to conduct some of its activities and these services complemented the skills of employed staff. For instance, one of the main features of Healthwatch Elmbridge’s work was the development of a database of patient and public feedback (see Chapter 6), which was managed by an external information manager who also carried out work for several other Healthwatch in the region. Healthwatch Elmbridge also used an ethnographic research consultancy to plan and carry out projects on specific communities.
Summary
This section presented the variability of Healthwatch’s organisational arrangements at our five study sites. Such variability complicates the straightforward dualism between ‘hosted’ and ‘standalone’ organisations and shows how Healthwatch’s organisational structures are actually the product of a broader range of factors, including organisational histories and board composition (e.g. Healthwatch Ashton, Healthwatch Cherryburgh, Healthwatch Dogwood), strategic planning to better exploit financial opportunities (as in the case of Healthwatch Beecham’s creation of a consultancy arm or Healthwatch Cherryburgh’s ambiguity in terms of the boundaries between Healthwatch and its host’s respective remits) and the lack of geographical overlap between the work of the host organisation and hosted Healthwatch, leading to a degree of separateness (e.g. Healthwatch Ashton).
Looking specifically at the three study sites ‘hosted’ by other organisations (i.e. Healthwatch Ashton, Healthwatch Cherryburgh and Healthwatch Dogwood), our findings show a great variability in their organisational arrangements. Although both Healthwatch Cherryburgh and Healthwatch Dogwood were hosted by a small local charitable company that held only one Healthwatch contract, their respective ways of organising and conceiving Healthwatch work were different.
Healthwatch Cherryburgh did not appear and work as an organisation in the way that, for example, Healthwatch Dogwood seemed to, despite their common hosted status. Staff and outputs were deployed strategically across Community Together, and who or what was labelled ‘Healthwatch’ shifted and bore little relation to the funding purpose for that work. For instance, Community Together had been commissioned by the local authority to gather the experiences of local adult social care users. The outputs of this work were routinely presented to the outside world as being produced by Healthwatch Cherryburgh, even though it was not funded or carried out as a ‘Healthwatch’ piece of work. However, branded as a Healthwatch piece of work, it could be presented at the local health and well-being board at which Healthwatch Cherryburgh has a statutory seat. Such ‘rebranding’, therefore, had the effect of boosting the visibility of that work locally.
Conversely, Healthwatch Dogwood appeared as a quasi-organisation separate to that of its host; that is, Direction Health had an arms-length relationship with Healthwatch Dogwood. The latter had its own board, dedicated staff and projects. At local voluntary sector engagement events, for instance, Direction Health and Healthwatch Dogwood had separate stalls with different staff at each. Healthwatch Dogwood had features which resembled those of standalone Healthwatch such as Healthwatch Elmbridge. Both Healthwatch Dogwood and Healthwatch Elmbridge set their own priorities, deployed their staff and carried out their projects in an autonomous Healthwatch-named way. In terms of backgrounds and professional interests, Healthwatch Dogwood and Healthwatch Elmbridge also looked very similar in composition, although one point of difference is that Healthwatch Dogwood’s board had members who represented other VCSE organisations. Interestingly, although Healthwatch Dogwood’s board was happy to meet in public, Healthwatch Elmbridge’s board was not. Nevertheless, the similarities between the two blur the presumed distinctiveness of hosted Healthwatch organisations compared with standalone Healthwatch organisations. This was very different from Healthwatch Cherryburgh, where, as its CEO described, ‘Healthwatch Cherryburgh doesn’t exist. It is just a project’ (Healthwatch Cherryburgh’s CEO, interview, 14 September 2020).
Similar to Healthwatch Dogwood, Healthwatch Ashton – also a hosted Healthwatch – behaved autonomously, despite being part of a much larger charity (Achieve), which had supralocal activities and one other Healthwatch contract. Healthwatch Ashton had its own board and staff, as well as an active cohort of Healthwatch volunteers separate from those of Achieve. As Healthwatch Ashton’s manager discussed above [see Healthwatch Ashton (hosted by a charity that also runs another Healthwatch organisation)], part of the reason for this autonomy was that Achieve’s other contracts were for activities in other local authorities, CCGs and ICS to that in which Healthwatch Ashton operates. Therefore, Healthwatch Ashton, even although it was hosted, looked organisationally much more like Healthwatch Elmbridge than Healthwatch Cherryburgh (one of the other hosted Healthwatch organisations among our study sites). This complicates the categories of ‘hosted’ and ‘standalone’ Healthwatch organisations. Although these terms have a basic descriptive function and are also used rhetorically to make claims, they cannot in themselves explain how Healthwatch organisations function. We have shown how this applies to ‘hosted’ organisations; however, it also applies to standalone Healthwatch organisations such as Healthwatch Beecham [see Healthwatch Beecham (standalone Healthwatch organisation with a consultancy arm)], the structures of which produced a different manifestation of a standalone Healthwatch compared with Healthwatch Elmbridge. Healthwatch Beecham and Beecham Voice ran alongside each other as separate organisations, each with its own board and projects, but delivered by the same staff. One effect of this was to complicate the chains of accountability of Healthwatch Beecham, as it was linked via its staff to the operations and priorities of Beecham Voice.
Funding arrangements
As we detailed in Chapter 1, Healthwatch organisations across England receive different levels of funding from their local authority contracts. The range of funding is large, ranging from £42,000 per year for Healthwatch City of London to over £500,000 per year for several Healthwatch organisations that cover whole counties. Healthwatch funding is not ring-fenced, nor do local authorities across England follow a uniform formula for calculating Healthwatch funding. In general, Healthwatch organisations serving large populous counties or cities receive more money in absolute terms than Healthwatch organisations working in small unitary authorities. Such variability alongside the fluctuation of Healthwatch funding decisively shapes not only Healthwatch’s organisational structures but also, and more importantly, its ability to fulfil its mission.
In this section, we explore the effects of these differential levels of absolute funding. We consider the following questions:
-
How does the value of a local Healthwatch’s funding affect its ability to attract funding external to the Healthwatch contract to build a range of relationships with key stakeholders, recruit and retain specialist staff and disseminate its work appropriate audiences?
-
Ultimately, how does this affect its ability to convey the voice of patients and the public to its local systems?
To address these questions, we examine two of our case study sites which provide an instructive contrast; one site (Healthwatch Beecham) holds one of the largest contracts in England and the other (Healthwatch Ashton) holds one of the smallest contracts in England. We then examine the effects of external funding on Healthwatch’s daily operations. In Figure 3, we summarise the funding arrangements of our five local Healthwatch study sites.
FIGURE 3.
Study sites’ funding arrangements.
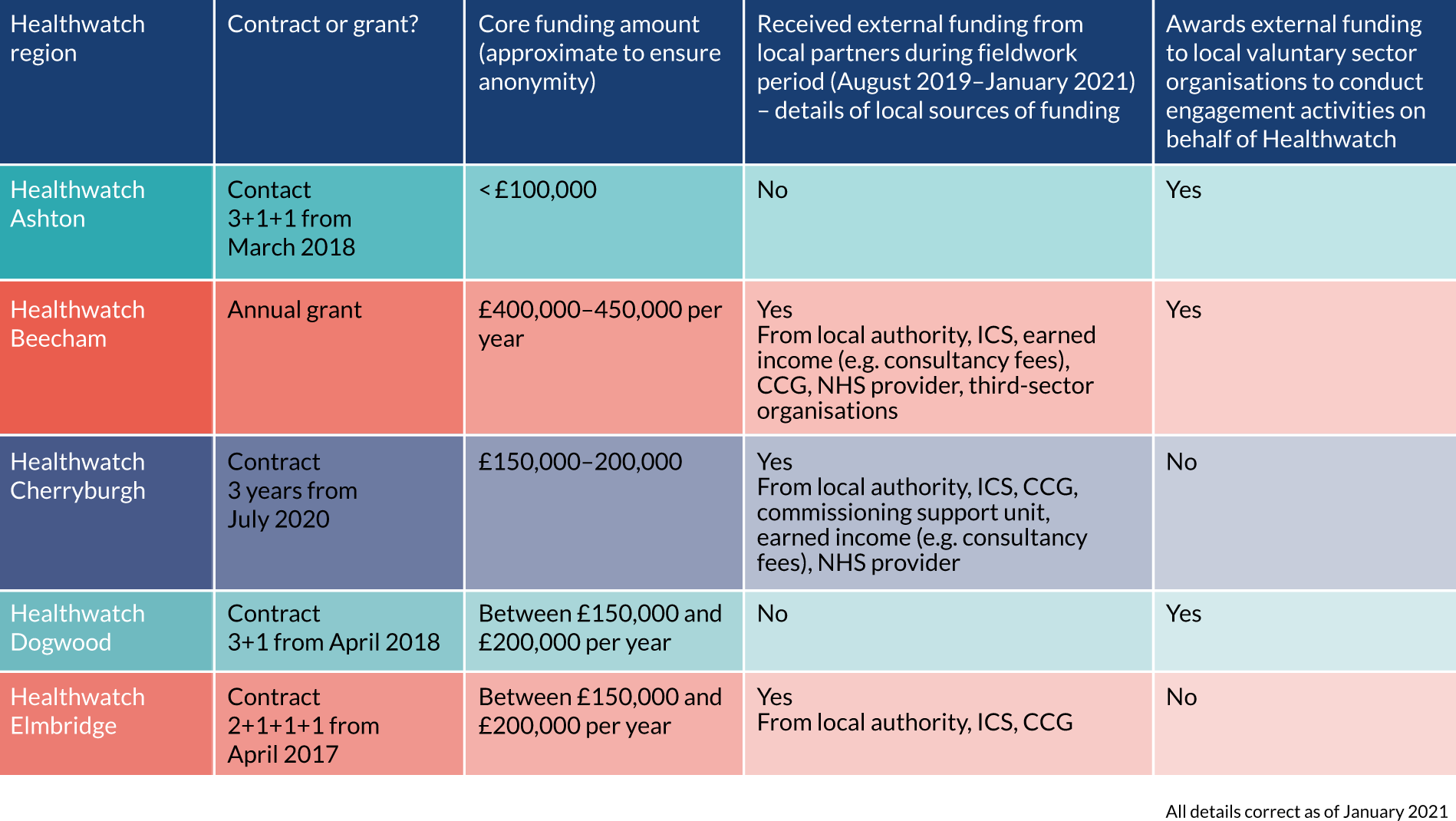
Healthwatch Beecham: large funding and larger opportunities
Healthwatch Beecham had the largest core funding among our five study sites. Funded through a local authority grant that was renegotiated yearly, Healthwatch Beecham had a core budget of £540,000 at the beginning of our fieldwork in 2019. Of this, £120,000 was specifically awarded for the delivery of signposting services for health and social care in the area, but this additional money was cut from the 2020–21 grant. However, even without this amount, in 2020–21 Healthwatch Beecham was still one of the best-funded Healthwatch organisations (in absolute terms) in the entire national network.
Although Healthwatch Beecham’s large budget was justified by its officers based on the size of its local population, its funding was not used to ensure a greater presence of Healthwatch across the large county where it is based (e.g. through the establishment of local Healthwatch Beecham branches in different districts). Rather, funds were principally used to employ highly specialised members of staff. In addition to the CEO and office manager, Healthwatch Beecham employed 13 other staff members split into four teams (i.e. engagement, research, information and signposting, and communication and marketing). Apart from those in the information and signposting team and one research officer, most staff members worked full-time.
Healthwatch Beecham’s staff included people trained at PhD (Doctor of Philosophy) level (e.g. research manager), as well as people who have had high-profile and successful careers in their respective fields (e.g. communication lead). Staff members played a key role in shaping the activities and profile of Healthwatch Beecham locally; for example, they regularly designed and followed sophisticated strategies for platforms such as radio, television, local newspapers, podcasts, guest lectures at local universities and community workshops (as well as attending policy stakeholders’ meetings, such as those with the local authority and CCG) to disseminate Healthwatch Beecham’s work. In addition, work by these members of staff is occasionally published in peer-reviewed journals and academic-edited volumes.
These specialised members of staff were also instrumental in creating new opportunities for the organisation, helping it to attract additional funding, as well as skilled staff members. For example, during the time of our fieldwork, Healthwatch Beecham’s research manager was involved in the design of two successful seed fund applications for projects funded through UK Research and Innovation and the NIHR Applied Research Collaboration in partnership with two local universities. One of these projects drew on Healthwatch Beecham’s previous connections with a network of charities and community groups looking to support people living with neurological disorders. The project aimed to involve the charities and community groups in the design of further research projects proposed by the VCSE, which would be delivered collaboratively by the local university, VCSE and Healthwatch Beecham.
The involvement of Healthwatch Beecham in formal partnerships with local universities allowed the organisation to access the often substantial additional funding derived from successful grant applications. An indirect consequence of these academic partnerships was that Healthwatch Beecham then became aware of, and was able to access more effectively, additional skilled staff at subsidised cost through university and government training schemes. For example, in January 2021, two members of Healthwatch Beecham’s communication and marketing team were apprentices on a 4-year programme in collaboration with a local university. One member of the research team was a secondee from the CASE (Collaborative Awards in Science and Engineering) PhD Studentship programme and was on a 12-week placement as part of her PhD at another local university.
Like Healthwatch Beecham, other Healthwatch organisations were also aware of the potential of collaborating with universities to access academic research funding. We found, however, that different levels of funding have an important impact on the ability of local Healthwatch to exploit the possibilities offered by a closer collaboration with local universities. In Box 6 we present the experience of a member of the HIP; that is, the CEO of a Healthwatch organisation with a core budget of less than £100,000, in collaborating with universities.
Although her Healthwatch had been involved in co-ordinating patient engagement for research projects in the past, Healthwatch Mapleton’s CEO was aware that their Healthwatch organisation lacked the specialist skills required to conduct more extensive research of an academic level and that it did not have the budget to employ specialist staff with those skills. In turn, this meant that opportunities for collaboration were more limited:
If we had more money then yes, we’d be able to employ somebody with research skills. As it is, we just try our best. We can learn a lot from universities, an awful lot, and perhaps we could access training as well. It’s just, it’s finding that time to do it while we’re still – we’re only tiny. [ . . . ] So, I know especially one of my team would love to have more research skills but it’s just finding the time to do that training on top of everything else, otherwise she might have to do it on her own, in her own time. So, if we had more money we’d employ somebody. And I think that to be a valued member, a valued partner of organisations that we need to step up a bit more with the research, because there are organisations that will say actually yeah, but how did you do that and how did you come to those outcomes and blah, blah. And we can say it to a certain degree, but not in the way that a university would, like a proper research fellow or whatever. We’d just be like ‘Well this is as good as you’re going to get I’m afraid’. Do you see what I mean? It’s frustrating. It really is frustrating, but it is what it is.
HIP member 3, interview, 3 February 2021
As this illustrates, limited funding and the consequent impossibility of most local Healthwatch organisations to employ specialised staff mean that smaller Healthwatch organisations are precluded from pursuing opportunities for meaningful collaboration with relevant partners like local universities. As the case of Healthwatch Beecham shows, these collaborations are important ways through which Healthwatch enhances its profile and therefore its ability to credibly represent patient and public voice locally. Furthermore, collaborating with academic partners offers important financial opportunities and the possibility to attract specialised staff.
Healthwatch Ashton: the effects of a small contract
In contrast with Healthwatch Beecham, Healthwatch Ashton had one of the smallest annual contracts of any Healthwatch in England (a total of £80,000 between local authority funding and LRCV funding). Healthwatch Ashton’s core funding from the local authority was approximately £40,000 per year and was paid in four instalments. Healthwatch Ashton also received £40,000 per year that must be used to fund local VCSE to carry out engagement work on its behalf. This latter funding came from the LRCV grant and was paid to Healthwatch Ashton at different times every year and specifically when grant payments did not coincide with the payment of its core funding. This was an unusual arrangement for Healthwatch funding, as most Healthwatch organisations received the LRCV grant bundled with their core local authority contract and could use it at their discretion. These funding arrangements had several interlinked consequences.
First, the core funding from the local authority contract was not enough to cover Healthwatch Ashton’s operating expenses as they arose through the year and, therefore, the shortfall was covered by Healthwatch Ashton’s host Achieve. The shortfall was then repaid when the LRCV grant was released by the local authority. The uncertainty associated with the LRCV grant in terms of its timing and amount meant that Healthwatch Ashton found it difficult to plan its work.
Second, the small size of the core contract funding meant that Healthwatch Ashton had a staff team of < 1 FTE in total, which greatly limited its capacity to carry out conventional Healthwatch activities. Consequently, the team had to develop a way of working that relied heavily on the contribution of volunteers (Box 7). At the time of our fieldwork, Healthwatch Ashton’s staff was composed of a manager, volunteer support officer and a communications officer, all of whom were part time and whose total FTE was < 1. A significant proportion of staff time was spent supporting volunteers in their activities; in fact, this was the main responsibility of one of its three dedicated officers. The small budget also meant that Healthwatch Ashton needed to make difficult choices about what to prioritise. At the start of its most recent contract, Healthwatch Ashton had to decide whether to focus its work either on engagement or volunteer support, and, given its need to involve volunteers, they chose the latter; however, this meant that it had no capacity itself to carry out engagement work with the public and patients. This put pressure on staff and led to the volunteer support officer also doing engagement work when she could.
The funding constraints meant that Healthwatch Ashton had to rely on the involvement of volunteers to an unusual extent among Healthwatch organisations. Healthwatch Ashton volunteers often carried out activities that would in other Healthwatch organisations be performed by paid staff. For instance, Healthwatch Ashton had a system of granting responsibility to individual volunteers to serve as the link between Healthwatch and each of the main care providers in the area. At the time of our fieldwork, the link volunteers attended relevant internal meetings at these providers (e.g. patient experience groups, quality committees) at which they presented any feedback Healthwatch Ashton had received from the public about services and conveyed back to Healthwatch Ashton any updates from the providers. This link function was a key way in which Healthwatch Ashton could keep abreast of any developments in its local health and social care system. Healthwatch volunteers were also active in reviewing quality accounts generated annually by each provider. This involved receiving a draft of the account from the provider and discussing it among themselves. The volunteer support officer then drew together their comments and drafted a response to the provider, suggesting areas of further inquiry. The volunteer support officer also organised a meeting (which she also attended) between the link volunteer, other volunteers who have commented on the accounts, and the appropriate person in charge of quality at the provider, such as the director of nursing.
Healthwatch Ashton’s volunteers were heavily involved in the projects funded through the LRCV grant in two ways. First, the volunteers selected the projects to be funded and, second, each funded project was assigned a link volunteer who liaised with the project lead and checked on progress. In one such project, for instance, the link volunteer, a former director of nursing, learnt that the grant-holder was struggling to complete their proposed work because of staffing issues. Together with a staff member from Healthwatch Ashton, the link volunteer helped design a survey to be used in the engagement project. Although not all link workers were called on in this way, this example and the others above show how Healthwatch Ashton’s funding structure led to a greater involvement of volunteers in operational matters than those in most other Healthwatch organisations.
Third, as Healthwatch Ashton could not use the money from the LRCV in an unrestricted way (e.g. to carry out targeted and planned engagement activities itself), but had to – in effect – outsource engagement work to local VCSE organisations (e.g. conducting surveys of particular groups), Healthwatch Ashton had no opportunity to develop its own engagement capacity. The manager of Healthwatch Ashton explained that, this led to some confusion about how Healthwatch works on the part of the volunteers, who were so central to its the running:
[Healthwatch Ashton’s volunteers] say ‘why do we have to give that money away to other organisations?’.
Fieldnotes, 18 February 2020
External funding
The example above shows the effect of a small core budget in absolute terms. There is another aspect related to the fluctuation of funding and well-established trend towards falling Healthwatch budgets: as we discussed in Chapter 4, publicly available data show that, since their launch in 2013, local Healthwatch organisations have undergone significant budget cuts. The value of contracts or grants was reduced in four-fifths (n = 121, 79.3%) of all 150 Healthwatch organisations in England between 2013 and 2018.
Such a funding squeeze has led to increased discussions within and among Healthwatch organisations about the desirability of generating income in addition to their core contracts. Our survey showed that a majority of Healthwatch organisations now bid for external funding [and 71 (74.0%) Healthwatch organisations among our survey respondents were receiving such funding]. Some Healthwatch representatives argued that soliciting and accepting external funding was problematic because it fundamentally encroaches on Healthwatch’s key principle of independence. Healthwatch Cherryburgh’s chairperson, for instance, described this situation in the following terms during the cross-site JIF:
I mean Healthwatch is one of a number of, oh, it’s the last of a number of attempts to establish an independent voice for patients and the public and I think we had high hopes at the outset that it would be able to be the independent voice, and certainly when we started in Cherryburgh we had lots of dosh to do it! We had lots of ambitions as to how we could sustain that independence – but slowly but surely the money has become less and less and we were obliged really to enter into a whole range of contracts with different parts of the NHS and social care, and I think relationships are reasonably friendly but there’s a lot more that we would be able to do if we had the resources to really inject a thorough, independent voice into the systems [ . . . ] There’s a continuum between independence and slavery, I suppose, and I think we’ve very much slid back towards the slavery over the period. That’s not to undermine what we’ve done but it’s very far from the independent free-speaking outfit that I would have liked to have seen.
Healthwatch Cherryburgh chairperson, cross-site JIF, 28 January 2021
Healthwatch Dogwood’s chairperson offered a slightly different perspective, which was less absolute. Healthwatch Dogwood’s chairperson recognised that different Healthwatch organisations would make different decisions based on their level of funding. In addition, Healthwatch Dogwood’s chairperson felt that Healthwatch Dogwood was relatively comfortable financially and, therefore, did not need to charge for additional work:
I think they should seek commissioned work and work in partnership when there’s a particular need, but I don’t think it should be funded because that may – it may – colour the independence. [ . . . ] But I would say within that it depends on the financial state of the Healthwatch because I think Healthwatch Dogwood has not had its funding reduced in the last 2 or 3 years – he says, touching wood – but I’m sure that other Healthwatch whose financial state is much less secure than ours, then I would understand they may have a different perspective.
Healthwatch Dogwood chairperson, cross-site JIF, 28 January 2021
This was borne out by fieldwork at Healthwatch Dogwood. For instance, staff at Healthwatch Dogwood had carried out an engagement project with PPGs at a PCN for which they did not charge. The Healthwatch manager explained that, although the PCN offered to pay for this work, Healthwatch Dogwood refused because it did not need the additional income and it was more important to develop good relations and obtain experience of this kind of activity.
Among our study sites, a minority of Healthwatch respondents and HIP members expressed an opposing view to those of Healthwatch Cherryburgh and Healthwatch Dogwood’s chairpersons. Rather than viewing external funding as a problem, some Healthwatch respondents and HIP members regarded it as a way to ensure that their work achieves better impact, as Healthwatch Beecham’s business manager explained:
I think that it’s [external funding] allowed us to be able to be independent but also to hold the stakeholders to account because they’re obviously paying for a service so they need to listen to what these people are saying.
Healthwatch Beecham business manager, cross-site JIF, 28 January 2021
Healthwatch Elmbridge’s chairperson echoed this sentiment. Although Healthwatch Elmbridge’s chairperson recognised that the search for external funding was a result of issues of financial sustainability, not being solely reliant on local authority core contract funding also allowed Healthwatch to be more independent:
I want to say that we actively seek commissioned work because, you know, with a new commissioning round coming up, we don’t believe that we’re going to be able to keep the same level of commissioning from the local authority and we need to diversify our revenue streams in order to be sustainable. And also in order to be independent.
Healthwatch Elmbridge chairperson, cross-site JIF, 28 January 2021
In Box 8, we present an example of the complex entanglement of ethics and financial considerations surrounding a Healthwatch organisation’s decision to explore external funding opportunities.
At the beginning of 2020, Healthwatch Elmbridge was trying to encourage more key partners to use an insights database of patient and public feedback on health and social care services that it had developed and that it uses as the main vehicle through which it channels ‘the voice of the people’ to the local system (see Chapter 6 for more details about this).
Although the local hospital trust was keen to pay for access and to support it, the CEO also wanted the local ICS to start using and developing the database across the footprint. The CEO, therefore, asked the hospital trust to approach the ICS and ask whether or not the latter would match-fund the local trust’s offer. After several months, this happened, and the insights database began to be used across the ICS footprint and by all the Healthwatch organisations in the area. Moreover, each local Healthwatch organisation was paid by the ICS to support its use of the database. Therefore, Healthwatch Elmbridge, not only succeeded in generating income for itself, but also for other neighbouring Healthwatch organisations, and the match-funding by the ICS ensured that Healthwatch was in a better position to co-ordinate providing patient and public voice across the footprint.
Highlighting the importance of the institutional landscape in which Healthwatch operate and which shape the possibilities of its work, the discussion at the finance subcommittee also considered how Healthwatch Elmbridge could talk about itself as an innovator within an innovative local system. The CEO commented that Elmbridge is a system leader, as evidenced, for instance, by the advanced development of its PCNs. The CEO asked, ‘Are we, as a Healthwatch, an innovator and leader because of this general innovation?’, and suggested that Healthwatch Elmbridge ‘talk about this more’, as it would help them attract additional income.
The subcommittee also discussed the possibility of research partnerships with universities of a kind already pursued by Healthwatch Beecham (discussed above) and this was uncontroversial among board members. However, a proposal by the co-chairperson that Healthwatch Elmbridge seek corporate funding for its young persons’ panel was met with some disquiet. Healthwatch Elmbridge’s CEO felt uncomfortable with this idea and remarked that the corporate sponsor ‘would only be doing it for a photo op’. The issue remained unresolved.
Summary
Money is a major axis of variability between Healthwatch organisations. Different amounts of funding in different areas enable the creation and maintenance of radically different sorts of organisations, which, nevertheless, ostensibly share the same mission. Healthwatch contract value is partly justified based on population. Therefore, larger local authority areas tend to have larger absolute amounts of funding than smaller areas. However, these larger absolute amounts of funding are not used to help these Healthwatch organisations replicate the services of smaller Healthwatch organisations on a larger scale, rather the larger contract value enables such Healthwatch organisations to hire larger numbers of more varied staff and, therefore, offer different services. In so doing, larger Healthwatch organisations become very different from smaller Healthwatch organisations, despite the name they share. This point has been reinforced by interviews with managers of large Healthwatch organisations in our study sites and our HIP. Towards the end of the fieldwork period, for instance, managers reported that five of the larger Healthwatch organisations by contract value had created an informal network to discuss issues that are specific to them and not catered for by the official Healthwatch network infrastructure, which tends to be geographically organised.
The value of its contract influences the ability of a Healthwatch organisation to engage local people and promote their involvement in the monitoring and planning of services. Consider the specialisation of staff and engagement of the two Healthwatch study sites we considered above, Healthwatch Beecham, for instance, could link up with academics and involve specialist and expert VCSE organisations, as well as condition-specific patients in longer-term projects. Moreover, Healthwatch staff, there had the skills to facilitate co-design processes. Compare this with Healthwatch Ashton, which was unable to conduct its own engagement activities within the funding awarded by the local authority, as the then Healthwatch Ashton manager explained when reflecting on the effect of their funding structure:
. . . our size does affect our ability to have a voice.
Fieldnotes, 12 November 2019
We have also seen how a fall in the value of local Healthwatch contracts over the past 8 years meant that many Healthwatch organisations chose to solicit additional funding from the NHS and local authorities themselves. This has raised questions for some Healthwatch organisations about whether this lessens their independence or enhances it. It may also be the case that those larger Healthwatch organisations are in a better position than smaller ones to obtain substantial external funding for research or engagement activities, therefore widening the gap between Healthwatch organisations even further and raising questions of equity for people in different areas of England. Perhaps the most striking consequence of the differential levels of funding is the effect on the capacity of Healthwatch as an organisation to grow and diversify and, in doing so, expand not only the notion of Healthwatch, but also the notion of voice itself.
Institutional landscapes
Healthwatch organisations operate in varied institutional landscapes and this variation is found in both the type and number of health and social care actors, as well as the jurisdictional context of the local authority (Figure 4, see also Figure 2). On the latter point, there are Healthwatch organisations in different types of local authority (e.g. counties, London boroughs, metropolitan and unitary), which are organised at considerably different scales and have different features. Healthwatch in counties, for instance, have a broader geographical area to cover and they may find it challenging to maintain contacts with lower-tier local authorities, such as district councils, and with hyperlocal health and social care providers. These organisations contrast, for instance, with Healthwatch organisations in smaller local authorities (e.g. London or metropolitan boroughs), which may be part of relatively simple networks featuring a limited number of local stakeholders only.
FIGURE 4.
Number of stakeholders in study site areas. Data from survey phase December 2018–January 2019. All details correct as of January 2021. LA, local authority.
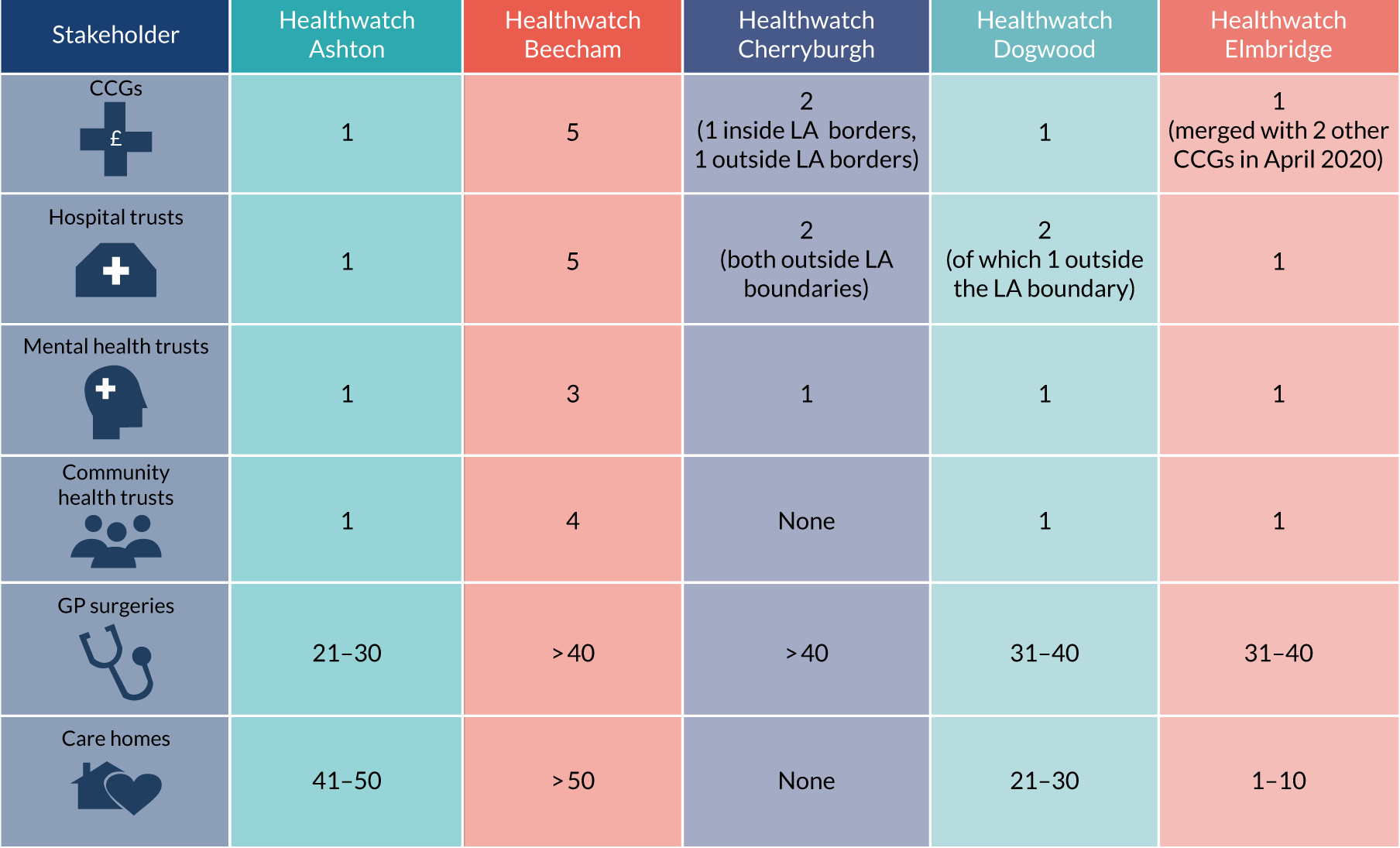
The range of health and social care actors that populate these landscapes are also varied and affect the kinds of environment and possible relationships within which Healthwatch organisations work. Significant actors shaping Healthwatch strategies and practices include:
-
local authorities and their boards and committees (e.g. health and well-being board)
-
CCGs
-
ICSs
-
integrated care partnerships (ICPs)
-
NHS provider trusts
-
GPs and PCNs
-
VCSE organisations and networks.
Below, we consider three contrasting institutional landscape types to address the following questions:
-
What effect does the scale, range and quality of local relationships have on the organisation of Healthwatch’s daily work?
-
How do these relationships affect the potential impact of local Healthwatch organisations?
A fragmented institutional landscape and its effects on Healthwatch’s practices and strategies: the example of Healthwatch Beecham
The local authority area in which Healthwatch Beecham is located is a large county (Beecham) characterised by a large number of health and social care actors. For instance, there are five CCGs, three ICSs (all of which also cover other local authority areas) and 293 general practices. Beecham’s health and well-being board provides strategic oversight of all these actors.
The size and fragmentation of the institutional landscape of the county make it difficult for Healthwatch Beecham to scrutinise services and to participate in meetings and events held in each lower-tier local authority in the county. For instance, during our research, Healthwatch Beecham was attending only the county-level health and wellbeing boards and not the 12 district-level health and well-being boards, despite invitations to attend them. The new CEO (since August 2020) discussed with us how she was planning to expand Healthwatch volunteering programmes so as to have ‘volunteers sitting on those and feeding information back up to us’ (Healthwatch Beecham CEO, cross-site JIF, 28 January 2021). This volunteering project had not yet been launched at the end of our fieldwork in Healthwatch Beecham.
The challenges posed by the size and fragmentation of its local system significantly influenced the practices and strategies adopted by Healthwatch Beecham in its daily work. The large number of local providers was, for instance, cited as one of the key reasons why Healthwatch Beecham had decided not to conduct any enter and view visits. Instead of trying to build relationship with a large number of providers, Healthwatch Beecham chose to adopt a more in-depth and broad-scale focus on specific themes, which it explored through the lived experiences of local people (see Healthwatch Beecham: long-term in-depth engagement shaped by the interests of staff members for details), as Healthwatch Beecham’s CEO (until March 2020) explained to us:
At Healthwatch Beecham we can’t do the same things that other Healthwatch do. We don’t go to the council and say ‘we visited all the GP surgeries in the county and we gathered feedbacks in each one of them’. Honestly, so what? What we do is identifying gaps in the market. There is still no work done on this topic, we do it.
Fieldnotes 28 August 2019
This more focused and theme-led way of working had limitations that were sometimes highlighted in our conversations with local partners. Limitations included the fact that Healthwatch Beecham staff did not necessarily know how the system worked as a whole, and did not have the range of contacts that other Healthwatch organisations might have maintained. This can be seen in an interview with Healthwatch Beecham’s commissioner (5 November 2020):
Is there anything you would improve in how Healthwatch operates and –
I think I’m seeing improvements now, you know, in terms of leadership and, you know, sometimes their connections and their kind of knowledge of the health and social care system [ . . . ] hasn’t always been as good as it could be. One of the projects I had to explain the difference between personal health budgets and personal budgets in a social care context – that sort of thing I would kind of expect them to skill themselves up over – so the context of how health and social care works should, for me, be stuff that they are aware of. Obviously, they won’t know all the detail but, broadly speaking, they should be aware of [the context].
A dominant and successful provider: the example of Healthwatch Dogwood
From Healthwatch Dogwood’s perspective, one of the most important features of Dogwood’s health and social care institutional landscape was the presence of a large and successful provider trust. At the time of our research, the trust ran acute and community health services in the area, along with adult social care. The trust also had a subsidiary primary care arm that ran several general practices in both Dogwood and in a neighbouring CCG patch. The trust was one of the few English trusts to have consistently received an ‘outstanding’ rating from the CQC. Moreover, many of the area’s key stakeholders also had formal roles at the trust or had held positions with it in the past. For instance, the CEO of the local authority was also an executive director of the trust. In addition, Healthwatch Dogwood’s own chairperson was for several years a non-executive director of the trust.
One of the area’s health and social care leaders described this dominance:
. . . we have brilliant healthcare, we have brilliant providers, but they are very difficult to control and to influence because at the end of the day, some of their departments – their financial department just says ‘shut up, we’re rich and successful. Go away, you’re little and trivial’ . . . the trust are very dominant . . . and they like to be dominant and they like to use that and they are incredibly successful.
Dogwood CCG chairperson, interview, 1 October 2020
The trust had an active and well-resourced engagement and communications department, which, in Healthwatch Dogwood’s view, was very protective of the trust’s operations. Therefore, Healthwatch Dogwood found it difficult to make its voice heard with regard to the services the trust provides. For instance, Healthwatch Dogwood’s reports on the trust’s hospital services were often responded to in a minimal way or ignored completely, partly because of a history of tension between Healthwatch Dogwood and the trust (the cause of which was a hospital closure consultation conducted several years ago). Although relations had improved greatly since then, Healthwatch Dogwood occasionally received mild informal complaints from the trust about the way in which conducted its work. For instance, a misunderstanding arose between this Healthwatch organisation and the trust about the characterisation of a patient story that had been published in a Healthwatch England document. Although the story was not identified with the trust and was presented as a generic issue, the trust nevertheless felt that Healthwatch Dogwood ought to have given them advance notice.
One way in which Healthwatch Dogwood had begun to make space for itself in this particular institutional landscape was to engage more actively with other providers in the area, such as the mental health trust and PCNs, as well as with the VCSE sector, and to improve relations with the CCG. For instance, it had recently been formally involved in the mental health trust’s planning and commissioning of a new recovery college to be delivered by VCSE partnerships. Healthwatch Dogwood’s contribution was sought because of its knowledge and connections with smaller VCSE organisations in the county.
A joined-up health and care landscape: Healthwatch Cherryburgh and Healthwatch Elmbridge
Healthwatch Cherryburgh and Healthwatch Elmbridge are both located in areas where there is a strong history of integration of key health and social care actors.
In Healthwatch Cherryburgh, the integration of the local health-care system was being formalised during the time of our research through the establishment of a borough partnership board. Healthwatch Cherryburgh was actively involved in the development of the board and was a member of a working group that regularly met to develop and define both the strategic (i.e. health and well-being strategy) and operational (i.e. delivery plan) aspects of the future working of the board. According to Healthwatch Cherryburgh’s CEO, the operations of the working group were going smoothly. After attending a successful working group meeting with one of the fieldworkers, Healthwatch Cherryburgh’s CEO explained that the main reason for this was the local health and care system’s history of working in partnership, even before the formal establishment of the partnership board:
Frank [pseudonym] said that members of the working group were able to collaborate very well because they are used to working together. They worked together even before the formal work they are now doing to establish the partnership board. In Cherryburgh people don’t change, they are always the same people you keep on meeting at various boards and committees. They have learned how to communicate; they know which personalities are there around the table and they generally listen to each other.
Fieldnotes, 7 January 2020
The cohesiveness of the local system and Community Together’s active involvement in the integrated work of local stakeholders meant that Healthwatch was able to establish itself as a recognisable partner in the system. As part of the development work for the borough partnership, Healthwatch Cherryburgh’s director was, for instance, made responsible, alongside the CCG’s head of communication and engagement, for producing the ‘partnership’s engagement and co-production strategy’.
Compared with the relative novelty of Cherryburgh’s formal integration, Elmbridge had formally established an ICP involving commissioners, providers, the local authority and the VCSE for almost a decade at the time of our fieldwork. Healthwatch Elmbridge is not a board member of the partnership. Healthwatch Elmbridge was offered a place, but decided that, as it already sits on the health and well-being board, which oversees the work of the partnership, such a dual role might have proved complicated. Instead, Healthwatch Elmbridge sat on each of the three workstreams of the partnership that look, respectively, at the health and social care of young people, healthy adults and older people. The existence of an advanced partnership in Elmbridge affected the ways in which Healthwatch Elmbridge conducted its work into patient and service user experience and also the ways in which such work was received by various stakeholders. For instance, Healthwatch Elmbridge organised some of its engagement projects and report-writing around ‘localities’ (the borough is divided into four localities), which was one of the key ways in which the partnership organised and targeted its work. Similarly, Healthwatch Elmbridge was increasingly using ‘I statements’ (e.g. ‘I am supported to make healthy lifestyle choices’) sourced from the partnership’s own outcomes framework to track how local people understood their health and social care support. Healthwatch Elmbridge also attempted to triangulate its data from engagement work with public health, local authority, GP and CCG data to create a richer picture of patient and public experiences and needs. In Box 9, we present an example of Healthwatch Elmbridge’s work in its ICP.
A new UTC was opened by the area’s GPs on the site of the main acute hospital. The intention was to relieve A&E pressures at the hospital and provide a better service for local people. However, the UTC providers were finding that take-up of the service was low among patients and asked Healthwatch Elmbridge to investigate why this might be the case. Healthwatch Elmbridge’s approach was to track the entire patient pathway into A&E and/or UTC and to gather insights from patients. This way of doing the research, that is, looking at pathways across different health providers, reflected the integrated way in which the landscape is organised more broadly.
A&E, accident and emergency; UTC, urgent treatment centre.
Summary
Healthwatch is embedded in an ecosystem of relationships with people in the health and social care system, as well as in the material and institutional infrastructures of the areas where they operate (e.g. a successful provider trust, a long-standing partnership board, a larger number of district-level health and well-being boards). In the ethnographic examples provided above, we have described how these various ecosystems shape individual Healthwatch strategies and practices.
One example of this is Healthwatch Beecham’s focus on the in-depth, lived experience of local people about specific health and social care topics, which was influenced by the challenges posed by the sheer complexity and size of the health and social care system. In its daily work, Healthwatch Beecham was confronted with a large number of possible institutional partners and associated meetings (both formal and informal) at which projects might be discussed and at which decisions about commissioning and provision might be taken. In this context, at the time of our research, Healthwatch Beecham embraced a more thematic way of working that did not rely on continuously maintaining a large number of relationships, something which would have consumed huge resources. However, this more focused approach made Healthwatch Beecham’s staff less familiar with the day-to-day working and priorities of individual institutional actors.
This point is further illuminated by the contrast with other study sites. Healthwatch Cherryburgh and Healthwatch Elmbridge were part of well-integrated systems even before the formal development of their ICPs. In these areas, the relationships forged by Healthwatch were more predictable because of the smaller identifiable number of people and institutions with whom Healthwatch can have regular and consistent contact. As the CEO of Healthwatch Cherryburgh reported, in these systems people are used to collaborating and know each other’s work and capacities, and this meant that these Healthwatch’s practices and strategies were more easily embedded in local institutional conversations around health and social care.
The partnerships involving Healthwatch Cherryburgh and Elmbridge contain some actors who were more powerful than others. However, no single actor emerged as totally dominant. This was not the case in Healthwatch Dogwood’s area of operation. For Healthwatch Dogwood, the local provider trust presided over the health and social sector by virtue of its size, financial status and success, and this had an impact on the everyday work of Healthwatch Dogwood. In its daily work, Healthwatch Dogwood was constantly reflecting on its positioning within the system and whether or not any given course of action would have resulted in conflict with the trust and others. For instance, some of those involved in Healthwatch Dogwood were more willing to take a less cautious approach than others within the organisation. One response that sidestepped this ever-present tension was that Healthwatch Dogwood had begun to cultivate relationships with other institutional actors in configurations that do not involve the dominant provider trust. As we outlined above, these new relationships include relationships with the mental health trust and the VCSE sector.
Strategies and practices of engagement
Healthwatch engagement is commonly understood as Healthwatch staff or volunteers soliciting the views of patients and residents through a range of activities with the aim of shaping health and care service provision.
The sociomaterial structures (e.g. funding, staffing, relationships) that shape the varied ways in which Healthwatch organisations work have a direct effect on the ways in which engagement is carried out by each different Healthwatch organisation. Below, we explore these entanglements by describing common engagement practices and strategies at each of the five study sites. In doing so, we address the following questions:
-
What different strategies and practices of engagement do local Healthwatch organisations pursue?
-
How do the organisational and funding arrangements affect the type of engagement in each study site?
In the summary, we highlight cross-cutting themes and issues raised by these different ways of ‘doing engagement’.
Healthwatch Ashton: engagement projects carried out by local Voluntary, Community and Social Enterprises
Most Healthwatch organisations carry out their own engagement projects. However, Healthwatch Ashton’s small contract value and peculiar funding model (see A fragmented institutional landscape and its effects on Healthwatch’s practices and strategies: the example of Healthwatch Beecham) means that, at the time of our research, it was unable to conduct substantial engagement projects itself, except for small projects supported by Healthwatch England or NHS England. Instead, Healthwatch Ashton used the LRCV funding (which it received separately from its core contract) to fund local VCSE organisations, which then conducted engagement with the public and patients.
Healthwatch Ashton runs a competitive process for these grants every year. Healthwatch Ashton’s executive board, which was composed largely of volunteers who are local residents, reviewed the applications, scored them and decided which projects to fund and at what level. Healthwatch Ashton stipulated that the projects had to be consistent with the mission of Healthwatch. In addition, the board often set other criteria (e.g., encouraging applications that proposed hearing from seldom-heard groups and rural communities). Projects that received funding committed to completing the work within a certain time and to producing a final report that would feature Healthwatch Ashton’s logo, as well as granting Healthwatch Ashton (and its host Achieve) the right to use any data gathered as a result of the engagement project.
Completed projects were presented to Healthwatch staff and volunteers, and staff discussed with recipients of grants ways in which the findings from their reports might be developed. For instance, at a meeting in late 2019, a local young persons’ charity CEO presented their work on collecting young people’s experiences of non-statutory mental health care and support. One finding of the CEO’s work was that young people with minor mental health issues in the area did not relate well to adult support workers and, therefore, young people found it difficult to talk to adult support workers. This finding – together with others – pointed to an increased role for peer mentoring of young people with mental health issues. The charity CEO said that there were no organisations offering this service and they were looking for ways in which they could plug the gap. Healthwatch Ashton responded in two ways in the meeting. First, Healthwatch Ashton said that it would take these findings to the local health overview and scrutiny committee and ask for them to be given an agenda item, therefore bringing it to the attention of the commissioner and providers attending the meeting. Second, Healthwatch Ashton could support the charity with applications to obtain funding for a peer support programme.
This example demonstrates several aspects of this way of conducting engagement. The intention of Healthwatch Ashton was to access the voices of people whom it otherwise finds difficult to access. This particular meeting featured presentations from two Healthwatch-funded engagement projects on young people on mental health services. These are voices that Healthwatch Ashton did not hear through other channels, as one of its executive board members said at the meeting:
. . . in the last hour, we’ve heard more about children’s mental health services than in the last 2 years.
Ideally, these projects were intended to give Healthwatch Ashton data that it could take to key statutory stakeholders and suggest changes with. Conversely, the VCSE grantees of engagement funding wanted the access to mental health commissioners, which they believed Healthwatch could offer.
However, there were significant limitations for Healthwatch Ashton in conducting engagement in this way. Although Healthwatch Ashton decided which proposals to fund, it had little control over the applications it received. Taken together with the requirement that the LRCV funding had to be spent within a certain period of time, this meant that Healthwatch Ashton funded projects that do not necessarily fall within conventional definitions of ‘engagement’ (e.g. increasing telephone support capacity at a charity providing services for unpaid carers). As has happened in the past, there is also a risk that projects are not completed. Given Healthwatch Ashton’s staffing constraints, Healthwatch Ashton had limited ability to mitigate these risks in a practical way (e.g. by seconding a skilled member of staff to support the organisation in its work).
Healthwatch Beecham: long-term in-depth engagement shaped by the interests of staff members
Most of Healthwatch Beecham’s engagement projects involved long-term in-depth collection of people’s ‘lived experience’. Projects were mainly identified based on the personal interests of Healthwatch Beecham’s staff, and then selected based on importance and potential impact. Topics and dissemination strategies were identified in line with Healthwatch Beecham’s priority areas, externally commissioned work or knowledge gaps identified by the staff. As the office manager explained to us at the beginning of our research, the choice to carry out a specific engagement project was ultimately always made by individual team members:
. . . as a rule of thumb, we always let people decide whether they want to do something, so they are interested. We want passionate people, we don’t want people to do projects they are not passionate about.
Fieldnotes, 7 October 2019
Once they identified a project they wanted to carry out, staff members drafted a proposal. In the proposal staff identified the need for the project being conducted, the evidence to be collected, the intended impact and possible sources of funding external to Healthwatch’s core grant. This information alongside the project’s budget were then presented to Healthwatch Beecham’s board. If the board agreed, then the project was then signed off and could start.
At the time of our study, each member of Healthwatch Beecham’s engagement and research team was busy conducting at least one long-term engagement project that aligned with their personal interest. For instance, Paul (pseudonym), an engagement officer who joined Healthwatch in 2018 after a career in the police had been carrying out a project looking at perceptions of, and support for, poor mental health among emergency service staff. Paul’s work had involved interviews, focus groups and observations carried out over a period of 7 months with police officers, British Transport Police staff, paramedics and acute hospital staff. Staff in the communication and marketing team helped Paul with the design of his 42-page report.
The dissemination strategy of Paul’s project also reflected his particular strengths, personal concerns and previous experience. As in the case of many other Healthwatch Beecham staff reports, Paul’s report was promoted on Healthwatch Beecham’s website and social media channel. The report was sent to several relevant stakeholders with whom Paul had been in contact during the engagement phase of this work, including staff in the local police, transport police, ambulance services, one local hospital, CCG and ICS. Paul had also been invited to give guest lectures and seminars at the nursing and occupational health departments of two local universities, and planned to produce a podcast episode featuring interviews with the project’s participants.
Given the sensitivity of the project’s topic, Healthwatch Beecham decided to avoid using more mainstream channels (e.g. local radio, newspapers and TV channels) to disseminate report findings, as they would normally do otherwise.
Healthwatch Cherryburgh: blurring the distinction between Healthwatch and its host’s engagement work
As with other aspects of Healthwatch Cherryburgh’s work, there was little distinction between the engagement work conducted as Healthwatch Cherryburgh and that conducted as Community Together. Some projects were branded as Healthwatch projects, even when they were engagement activities commissioned from Community Together.
For instance, since 2017, Community Together had been commissioned by the local authority to organise and oversee the activities of nine reference groups of local residents who used adult social care services. The chairpersons of each reference group were also members of a joint partnership board (JPB) that meets every 2 months and is co-chaired by Community Together’s chairperson. Both the JPB and the individual reference groups were regularly attended by council, CCG and ICS representatives, depending on the topic. During the five meetings of the reference groups and of the JPB that we attended, service users, carers and general residents actively participated in the discussion about strategic priorities (e.g. the council’s new carers strategy) and the planning of services they used (e.g. the redevelopment of a day centre for people with learning disabilities).
To carry out this engagement work, Community Together had appointed a ‘partnership manager’ whose job was entirely dedicated to the organisation and management of the project. Despite being a Community Together employee paid with funding external to the Healthwatch contract, the partnership manager was considered by Community Together’s staff to be a member of the Healthwatch team. The partnership manager was one of the five people who regularly attended the monthly Healthwatch Cherryburgh team meetings alongside Community Together’s CEO and the communication manager. The reports that the partnership manager produced through engagement work with the reference groups and the JPB were usually presented at formal council and CCG meetings as Healthwatch reports. When we asked Healthwatch Cherryburgh’s CEO if the council also considered this to be a ‘Healthwatch project’, rather than a ‘Community Together project’, the CEO explained to us:
For this work, the council probably approached us as Healthwatch. As I told you, for us Healthwatch is like a hat we put on when it is more useful, when it makes things clearer for our partners. So, normally, if it [a project] has to do with health and social care, we’d do it with our Healthwatch hat on.
Healthwatch Cherryburgh’s CEO, interview 7 January 2020
Healthwatch Dogwood: engagement project prompted by feedback from local people
Healthwatch Dogwood considers itself a ‘listening organisation’ and, therefore, found it valuable to launch engagement projects prompted by unsolicited feedback from members of the public or patient groups.
For instance, in spring and summer 2019, Healthwatch Dogwood began receiving feedback from local residents, informing them that a hearing aid repair ‘drop-in’ service that they relied on was being withdrawn. This ‘drop-in’ service was provided by a local hearing loss charity and it ran sessions in accessible settings, such as libraries and general practices, around the county. The ‘drop-in’ service also offered information about living with hearing loss at these sessions. The charity could no longer run the service because of a loss of funding. Users would, therefore, have to travel to NHS audiology clinics at a limited number of hospital locations. As hearing aids need regular maintenance and repair, users contacted Healthwatch Dogwood because they were concerned that the ‘clinic-only’ service would be inaccessible to people who relied on public transport or lived in remote parts of this large rural county. There was fear, therefore, that people would be compelled to use defective equipment, severely affecting the quality of their lives.
On the basis of this unsolicited feedback, Healthwatch Dogwood decided to examine the impact of the closure of the ‘drop-in’ service by collecting the experience of users of audiology services. Healthwatch Dogwood had, at that time, two members of staff who carried out engagement work: Lorna and Vicky. Vicky also worked on ‘insight’ and analysed evidence and drafted reports. Lorna and Vicky discussed the project with the hearing loss charity and the trust that provided audiology services in the county, and both the charity and the trust were enthusiastic about the work.
Over the course of 2 months in autumn 2019, Lorna and Vicky held a number of feedback sessions at both community settings (general practices and libraries) that had formerly hosted the hearing aid repair services, and at the hospital-based clinics. Lorna and Vicky distributed a survey at these sessions and listened to user experience as told to them. Lorna and Vicky also invited people with hearing loss to attend a focus group. Vicky analysed the data and wrote the report over the course of 4 months.
A draft of the report was shared with the trust and the CCG, and both sent responses that were ultimately included in the published version. Although Healthwatch Dogwood’s manager noted that these responses were ‘a bit bland’, in that they offered very little specific action, Healthwatch Dogwood’s manager was nevertheless excited that the team had produced a detailed and investigative report that had its origin in unsolicited feedback and highlighted an issue that had hitherto gone unreported. This way of working provided a model for the future and the Healthwatch Dogwood’s manager told us that she wants to ‘do more targeted, specific work like the Audiology project . . . it comes from the bottom-up . . . [and] it’s about building the evidence base ourselves’ (fieldnotes, 28 October 2020).
Healthwatch Elmbridge: engaging residents on the social determinants of health in co-ordination with the local system
Healthwatch Elmbridge had, in recent years, expanded the sphere of its engagement work beyond the more usual Healthwatch focus of collecting local people’s experiences of health and social care services. Healthwatch Elmbridge had conducted several projects gathering views and experiences of what are commonly called the social determinants of health, for example income and job security, housing (overcrowding, etc.), access to green space and shops selling fresh vegetables (versus proximity to unhealthy takeaway shops) and air pollution. As outlined in the examples below, the holistic understanding of health influencing this engagement emerged as a result of Healthwatch’s collaboration with the local NHS, public health and local authority, and the well-developed local ICP (all of whom were invested in this ‘social’ approach to questions of health and well-being). The impetus also came from Healthwatch Elmbridge’s board members, who regularly discussed Healthwatch work in ‘social’ terms (e.g. wanting to explore the health and life experiences of people living in poor housing or who are subject to crime or air pollution).
For instance, from 2019 to 2020, Healthwatch Elmbridge was involved in planning and carrying out engagement work on the area’s new health and well-being strategy. Working in collaboration with the public health department, other local authority officials and the CCG, Healthwatch Elmbridge organised several day-long events at different libraries in the borough. The engagement activities consisted of Healthwatch staff talking at length to local residents (for 30–60 minutes) one on one about their lives, family and experiences of health, well-being, poverty, precarity, diet and environment. Healthwatch staff used a 20-page booklet to guide their questioning and in which they noted respondent answers. We attended planning meetings for this work and one of the engagement events in December 2019.
The health and well-being strategy engagement work built on an earlier project carried out by Healthwatch Elmbridge as part of the local consultation around the NHS Long Term Plan23 in May 2019. The engagement work was planned around talking to residents about their health at street markets in all four ‘localities’ of the borough. The locality focus emphasised Healthwatch Elmbridge’s desire to understand its area in more granular terms and draw out any differences that housing, wealth and environment had on people’s experiences and expectations around their health and well-being. Importantly, the data from this engagement work were linked in their report to ‘I statements’ (e.g. ‘I am supported to make healthy lifestyle choices’) developed by the local ICP to structure its outcomes framework.
As a way of concluding this section, in Box 10, we outline how our five study sites organised their engagement with Healthwatch volunteers.
All of our Healthwatch study sites had volunteer involvement (Figure 5). We found that local arrangements (e.g. funding and staffing, geographical size of the Healthwatch organisation’s patch) shape how volunteers contribute to Healthwatch activities. There are different types of volunteering associated with Healthwatch. First, there are those who are identified as ‘Healthwatch volunteers’. ‘Healthwatch volunteers’ are referred to as volunteers because of the official volunteer infrastructure that a local Healthwatch organisation creates, which often involves a volunteer co-ordinator who trains them, sends them updates and offers them opportunities to get involved. Second, some Healthwatch organisations also convene regular engagement panels or groups and these often have a fairly stable membership. The members of these panels are not often referred to as ‘Healthwatch volunteers’, although they do make time to be involved in Healthwatch activities. Finally, some Healthwatch organisations have boards of differing types, which are mainly composed of people who contribute their labour for free. Figure 5 outlines volunteer engagement and structures at each of the five study sites.
FIGURE 5.
Healthwatch volunteers at the five Healthwatch study sites. All details correct as of January 2021. c., circa.
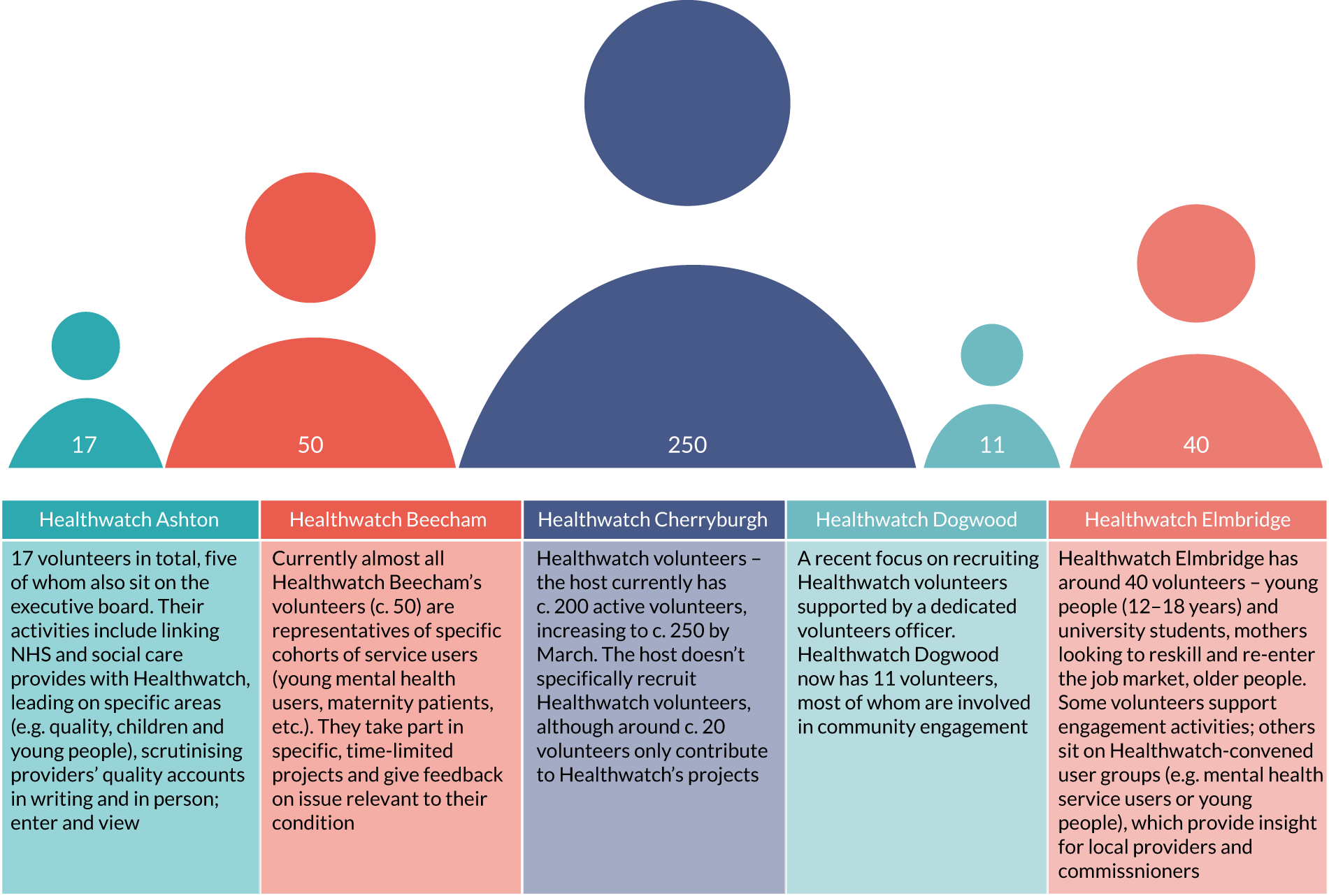
Summary
One of the key statutory functions of Healthwatch is to ‘obtain the views of people about their needs and experience of local health and social care services’. 46 Many Healthwatch organisations receive unsolicited feedback, conduct surveys of local residents and patients (both by type of service or type of user), carry out enter and view visits, and organise Healthwatch stalls in public places and events. However, as the examples above show, the strategies and practices of engagement are varied and are substantially determined by individual Healthwatch organisation’s organisational structure, funding and local landscape.
Healthwatch Ashton and Healthwatch Beecham provide an instructive comparison about how engagement is shaped by different levels of funding. The funding arrangements of Healthwatch Ashton meant that it could not initiate or substantially direct engagement activities itself. Rather, the main source of its engagement was work carried out by other organisations, such as local VCSE, that are granted money from the LRCV. This means that Healthwatch Ashton had little control over the design, execution and end results of the engagement that was carried out in its name. Conversely, Healthwatch Beecham – the best-funded Healthwatch among our study-sites – had a great deal of autonomy over the type of engagement projects it undertook. This autonomy extended to individual members of Healthwatch staff who were largely free to pursue projects based on their personal or professional interests (as long as the projects were regarded as within Healthwatch’s remit by senior managers, the board or the local authority commissioner).
Differential structures of funding also had an impact on how engagement work can be effectively managed. Therefore, although Healthwatch Cherryburgh was funded to employ a partnership manager to direct the work of JPB, Healthwatch Ashton had no additional resource to manage the LRCV money that it must distribute to VCSE organisations to conduct engagement on their behalf. Healthwatch Ashton recognised that this limits the potential of the engagement work in the ways described above. In fact, Healthwatch Ashton asked the local authority to allow it to use some of the LRCV money to employ someone to properly manage the engagement projects it funded, but the council refused.
The local health and social care landscape also influenced how engagement was initiated and performed. For instance, Healthwatch Dogwood’s manager emphasised that she preferred doing ‘bottom-up work’, such as the audiology project described in Healthwatch Dogwood: engagement project prompted by feedback from local people, as this work allowed them to carve out their own space for engagement. Healthwatch Dogwood’s engagement was rarely carried out in partnership with its major local stakeholders, which were dominated by a large and successful provider trust. The trust had a large engagement team and historically does not engage with Healthwatch. The trust have had diverging views about engagement and Healthwatch’s role locally. Healthwatch Elmbridge, on the other hand, had successfully managed to conduct engagement in ways that remain independent from the system, but still closely co-ordinated with it. This was largely because the key health and care actors had long become used to working in an integrated way and regarded Healthwatch Elmbridge as an equal and valuable partner.
Chapter 6 Findings part 3: the current and potential impact of Healthwatch in gathering and using patient and public voice – principles of good practice and insights from local joint interpretative forums
Enabling residents’ voices to be heard is a vital part of a patient-centred, publicly funded health and social care system, as it ensures that it is accountable to members of the public, communities and service users. Healthwatch was set up in 2013 to understand the needs and experiences of patients and residents, and to ensure residents’ views are heard and acted on. The policy document that launched the idea of Healthwatch during the passage of the Health and Social Care Act 20125 described Healthwatch as ‘a strong voice for people’ (contains public sector information licensed under the Open Government Licence v3.0). 17 Although the Act5 made provision for the fora at which such a voice would be conveyed by Healthwatch (e.g. health and well-being boards), it left open what constituted such a voice and how it should be communicated. What evidence should be produced to represent public voice into the local health and social care system? Should it be qualitative or quantitative or a mixture of the two? How are people’s personal experiences of care collected by local Healthwatch organisations translated (if at all) into evidence that is useful for local systems?
In this chapter, we explore these questions by presenting the findings and activities from the four local JIFs that we held in phase 4 of our study. At these JIFs, we presented different examples of gathering and communicating evidence, which largely emerged from the fieldwork with the five study sites. We asked Healthwatch staff, board members and their key partners to consider ways in which these methods might or might not be useful in their work to better evidence public and patient voice.
The analysis of phase 4 findings combined with the ethnographic data from phases 2 and 3 was used by the team to draft a series of ‘principles of good practice’ relating to how Healthwatch collects, organises and communicates evidence about people’s experiences of health and care to their local system. These ‘principles’ were later circulated to HIP members to test their relevance and usefulness to the broader Healthwatch network beyond the specificities of the five Healthwatch study sites. The production of the principles of good practice meets objective 3 of our study (i.e. to build consensus about what might constitute good practice in terms of the operation of local Healthwatch organisations) and objective 4 of our study (i.e. to distil and disseminate generalisable principles around what facilitates and/or limits the influence of local Healthwatch organisations as a key element of patient and public voice in the NHS).
We chose to focus on ‘evidence’ because Healthwatch’s practices and strategies for the gathering and use of patient and public voice constitute the very core of its mission and are crucial to better inform health and social care commissioning and provision. This focus was substantiated by insights from all five case study sites during the planning of phase 4. Reflecting on Healthwatch’s statutory functions and seat on local authority health and well-being boards, Healthwatch Elmbridge’s chairperson explained the distinctive way in which ‘voice’ is transformed into ‘evidence’:
So all the Healthwatches will have that and what comes with that is we are, you know, not just representing voices, we’re actually taking a strategic overview of the evidence that we have and feeding into the development and monitoring and implementation of strategy and that’s happening at the health and well-being board and I think that’s quite important.
Healthwatch Elmbridge chairperson, JIF Elmbridge, 21 May 2021
Evidence is a key way in which relationships between Healthwatch and its partners are built. As we show below, both ‘sides’ are intensely interested in the ways in which Healthwatch can act most effectively on behalf of the residents it serves. The quality of evidence is important because, as the chairperson of Healthwatch Elmbridge indicated above, it has the potential to be relied on to develop important local health and care strategies, such as joint strategic needs assessments. If there is conflict between Healthwatch and key partners about the quality or status of evidence, then this can affect relationships. Reflecting on a past period of tension between the CCG and the local Healthwatch organisation, a CCG COO we interviewed at another study site drew a distinction between ‘views of the community’ and ‘evidence’:
[I]f Healthwatch come along and say ‘look, here’s the evidence to prove you’re wrong’, we would look at it very carefully and we would change our minds if they were right. You can only make sensible decisions on evidence-based practice. What you then do with the evidence, and how you think you can best answer it, is much more imaginative but you’ve got to start off with evidence and I think we just went through that period when the views of the community were mistaken for evidence.
CCG COO, interview, 1 October 2020
In this chapter, we first introduce five examples about evidence-gathering, organisation and communications, which we used as the basis for the discussion at the local JIFs. Three of these examples are based on material already discussed in Chapter 5 and, in these cases, we simply signpost the reader to the parts of this report where they feature. In the following sections, we focus on describing the two evidence-gathering techniques not presented in other parts of this report. Later, we present key elements from the discussion at the four local JIFs organised by themes. At the end of the chapter, we draw our findings from these phases to propose five statements of Healthwatch good practice regarding the collection and communication of evidence that represent potentially fruitful ways of better representing the voice of residents. Here, we also highlight the contribution of the HIP in refining the original draft.
Ways of producing evidence
At local JIFs, a combination of the following types of evidence-gathering techniques were presented:
-
The community insights repository of patient and public experiences [see Healthwatch Elmbridge: the community insights repository of patient and public experiences (quantitative and qualitative)].
-
Investigating social determinants of health in economically diverse neighbourhoods (see Chapter 5, Healthwatch Elmbridge: engaging residents on the social determinants of health in co-ordination with the local system).
-
Gathering evidence about the experiences of specific ethnic minority groups (see Box 12).
-
Acting on unsolicited feedback from patients and the public (see Chapter 5, Healthwatch Dogwood: engagement project prompted by feedback from local people).
-
Qualitative reports (see Chapter 5, Healthwatch Beecham: long-term in-depth engagement shaped by the interests of staff members).
-
Evidence collected by other VCSE organisations (see Chapter 5, Healthwatch Ashton: engagement projects carried out by local Voluntary, Community and Social Enterprises)
-
Evidence from residents’ panel (see Healthwatch Beecham: an expansive use of residents’ panels).
These techniques were largely based on the ethnographic data coming from our five Healthwatch study sites. In Table 13, we outline the ‘ways of collecting evidence’ templates that were discussed at each local JIF.
| Healthwatch | ‘Ways of collecting evidence’ discussed |
|---|---|
| Beecham |
|
| Cherryburgh |
|
| Dogwood |
|
| Elmbridge |
|
Below, we present, in detail, two examples of translating local people’s experiences into evidence. The examples are from two of our Healthwatch study sites: Healthwatch Elmbridge and Healthwatch Beecham. We focus on these examples because they have not been discussed elsewhere in the report.
A full list of the summaries circulated to JIF participants is available in Appendix 6.
Healthwatch Elmbridge: the community insights repository of patient and public experiences (quantitative and qualitative)
Healthwatch Elmbridge developed a comprehensive database of patient and public feedback on health and social care services. The database has become the central vehicle through which Healthwatch Elmbridge attempts to channel ‘the voice of the people’ to the local system.
The database contains coded qualitative feedback (e.g. free-text comments from surveys, patient stories) that is used to produce reports on patient or public views and experience on particular themes or services over a defined period of time. The coding is organised by different elements of a patient’s pathway and also includes additional codes that relate to the social determinants of health (poverty, clean air, housing, etc.). A single piece of feedback can generate several coded items, and each item is also given a positive, negative or neutral value. Healthwatch Elmbridge’s CEO explained the database further:
We have an [insights database] which is based on a Microsoft Access [Microsoft Corporation, Redmond, WA, USA] database and we have a coding frame that’s nationally recognised so any kind of data that comes to us, whether it is through surveys or through people who just contact us at the office, outreach focus groups, all those types of data that would normally be in very different formats . . . [A]s long as they express a value judgement of any kind of service, we can put them in the same place, code them in the same way and have some . . . automatically-generated Excel [Microsoft Corporation, Redmond, WA, USA] reports which we then use to do some more in-depth analysis.
Healthwatch Elmbridge CEO, cross-site JIF, 28 January 2021
Importantly, the Healthwatch Elmbridge team also includes feedback received by health and social care providers and commissioners. For instance, Healthwatch Elmbridge regularly asks for, and receives, patient experience data collected by the main hospital trust in the area, which is then added to the database. Healthwatch Elmbridge would like local partners to input the data themselves, run analyses and produce reports according to their own needs without the direct involvement of Healthwatch staff. To this end, Healthwatch Elmbridge’s research analyst runs regular database training sessions for local authority, public health, CCG and trust staff. The people who attend the training are attracted by the qualitative sources of such data, which they hope will complement their own largely quantitative data sets. As the research analyst explained to those attending one such training session we observed, the database’s ‘biggest strength is its very diverse range’. The research analyst emphasised that the multitude of data gathered together in this accessible database ‘creates richer and more relevant data sets’. However, the direct use by local health and social care system partners – unmediated by Healthwatch Elmbridge – is limited, despite two key partners (i.e. the CCG and the local authority’s public health directorate) paying to access it.
Nevertheless, the database is deployed in many arenas by Healthwatch Elmbridge’s staff themselves, and the data they extract and disseminate are used by their partners. For instance, Healthwatch Elmbridge sends out regular reports to providers and commissioners on themes specific to its service area and the data from these reports, produced by the database, are used by service providers. One such service provider is the local GP federation, which triangulates its own data with those produced by Healthwatch Elmbridge, and includes the data in its own analyses and reports. As Healthwatch Elmbridge’s CEO commented, ‘they think we’re reliable enough to be used for QI [quality improvement]’ (fieldnotes, 22 January 2020). Healthwatch Elmbridge’s CEO went on to emphasise that the GP federation was using Healthwatch’s data in an integrated way, which indicated for her the weight given to their data.
The database, therefore, fulfils two key functions in establishing Healthwatch Elmbridge’s authority to communicate ‘voice’. First (as in the example of the GP federation above), it translates individual qualitative comments into aggregated numbers that are more easily communicated to partners and more readily used in partners’ own projects and reports. The Healthwatch Elmbridge chairperson explained:
[The insights database] does reduce a lot of the stories that we capture to percentages and when we’re talking to the science-based people on the health and well-being board, they respond to ‘79%’ much more than ‘the lived experience of the people they tell us is this’.
Healthwatch Elmbridge chairperson, cross-site JIF, 28 January 2021
Second, the prominence of the database in Healthwatch Elmbridge’s work – and their reference to it in almost all the meetings we observed – means that the database contributes to establishing the basis from which Healthwatch Elmbridge speaks more generally:
[Our health and social care partners] recognise that we have a great evidence base and so therefore when I speak at the health and well-being board, I’m able to cite it and people know that I’m citing evidence.
Healthwatch Elmbridge chairperson, cross-site JIF, 28 January 2021
Healthwatch Beecham: an expansive use of residents’ panels
In contrast to Healthwatch Elmbridge, Healthwatch Beecham’s approach to evidence is almost entirely qualitative, based on the collection of the ‘lived experiences’ of local people, which are gathered through long-term in-depth engagement with specific subgroups of the local population. Healthwatch Beecham collects lived experiences through both staff-initiated projects, which usually involve interviews, and observations of people and services [e.g. among emergency service staff (see Chapter 5, Healthwatch Beecham: long-term in-depth engagement shaped by the interests of staff members) or among patients in a secure mental health unit], as well as through externally funded engagement activities (e.g. a panel to discuss the health-care needs of people with various forms of disability in the county). This latter case is particularly useful to illuminate how local people’s experiences are translated into evidence in Healthwatch Beecham, as well as what experiences count as evidence.
The panel is composed of members chosen by Healthwatch Beecham. The members are chosen not only because they have a particular form of disability or are the carers of someone living with a disability, but also because of the network of people they can involve in the work of the forum. For this reason, most panel members are representatives of communities and local charities addressing the needs of people living with specific disabilities (e.g. visually impaired, veterans). Panel meetings are only ‘the beginning of our engagement’, as Healthwatch Beecham’s engagement officer, who was in charge of the project, explained to us. General meetings are used to raise issues and themes that are then explored in more detail in specially organised focus groups attended by a larger number of people affected by that specific form of disability. Action points and solutions are also usually discussed and planned outside panel meetings and in collaboration with the communities and organisations with which panel members are associated.
The integration between the work of the panel and the more granular engagement carried out through specific focus groups makes it possible for Healthwatch Beecham to translate individual lived experiences of panel members into forms of evidence about the collective experience of a broader network of local people affected by a specific condition. This was considered to be important by both Healthwatch staff and members of the panel who, in several instances, discussed with us how a single individual’s lived experience could not be considered a good enough form of evidence in itself. Discussing the first meeting of the forum, when panel members were recruited simply based on their conditions rather than based on their ability to link with a broader network of relevant people and organisations, a panel member told us:
You had other people in that room that day who just wanted to speak about their specific – not people who have got the same injury as them or disability as them, but their specifics, so there was one guy who said ‘I have an issue with my local bus service’, you know, that doesn’t apply to anyone else in that room, or the thousands of people that they’re representing – that is one specific issue and that could take up 10 minutes talking about that. I sat there thinking if you were to do this for everybody’s specific issue you’ll never achieve anything, not possible, you know, and I fed that back at the time, I said, you know, ‘you have to have a fixed agenda, you have to have people submit what they want to talk about in advance, because if you just have it as an open forum you ain’t ever getting anywhere’.
Healthwatch Beecham’s forum participant, interview, 29 October 2020
In Box 11, we provide an example of the work of the panel to address the concerns of visually impaired residents during the early phases of the COVID-19 crisis.
During a general panel discussion about the impact of COVID-19 on the lives of local people living with a form of disability, a visually impaired panel member shared his frustrations with the fact that most social distancing indications in supermarkets were in written form and were impossible for people with sight loss to be aware of. The panel member reported having been sometimes verbally abused because of his lack of compliance with social distancing regulations. Healthwatch decided to take action about this panel member’s experience. Together with other visually impaired members of the panel and their contacts among local organisations of blind people, Healthwatch organised a series of focus groups to explore whether or not this was a shared experience among people with sensory impairment. The experiences gathered through the focus groups were noted as concerns in the ‘co-production plan’, which was a live document shared between Healthwatch and the local council that commissions the work of the panel. After having become aware of the concerns raised in the focus groups, the council decided to fund the production of two short films about the experiences of people with sensory impairment during the pandemic. The films have been planned in discussion with the groups and charities involved in the focus groups.
In the next section, we present some of the themes discussed in the JIFs.
The local joint interpretive forums: discussing different types of evidence collected by Healthwatch
The nature of Healthwatch evidence
Most Healthwatch participants at the local JIFs were clear that using a diversity of qualitative approaches to collecting and communicating patient and public voice was desirable and that no one approach should necessarily dominate. Healthwatch Cherryburgh’s engagement manager, for instance, stated that her Healthwatch produced evidence through a combination of all the ways described in the document presented, except for the insights database. Most Healthwatch and external stakeholders alike emphasised the value of the qualitative nature of the evidence Healthwatch could provide to the system. For instance, the local authority commissioner of Healthwatch Dogwood discussed how qualitative data about the aspirations of local people relating to their long-term care requirements as they age might help the local authority better plan its market position statement for providers:
I quite like the idea of the qualitative reports based on . . . long-term research, particularly with some of the issues that are going on in Dogwood and some of the impact of COVID around care homes and the longer-term ramifications for care homes . . . we have to start planning the services that we’re going to be delivering in the future, that we’re going to be commissioning in the future.
Local authority commissioner, Dogwood local JIF, 26 May 2021
These qualitative data were also welcomed by Healthwatch Dogwood’s manager who foresaw new avenues for improving the impact of Healthwatch through working in this way:
I think that qualitative[ly] asking people about their aspirations about services is really, really positive and I think because . . . that could lead directly into an impact which is helping to shape a market positioning statement, so effectively a commissioning position . . . I think that’s a really interesting approach to Healthwatch work.
Healthwatch Dogwood manager, Dogwood local JIF, 26 May 2021
The crucial importance of integrating the qualitative ‘lived experience’ of local residents and service users for planning changes to the way health and care is delivered was echoed (perhaps more forcefully) by an ICS programme director who attended Healthwatch Beecham’s JIF:
[W]e need to kind of be really, really clear that the transformation process includes lived experience, that lived experience should be independent and actually should have that diversity as well. If we’re not investing in that lived experience then we’re not really properly going about the way we’re doing transformation.
ICS programme director, Beecham local JIF, 25 May 2021
This commitment to ‘lived experience’ expressed by the ICS programme director aligned well with Healthwatch Beecham’s long-standing focus on this particular way of conducting engagement and communicating evidence.
This type of mutual agreement between Healthwatch Beecham and its key external stakeholders was also evident at Healthwatch Elmbridge’s JIF. However, although the participants at Healthwatch Elmbridge’s JIF agreed about the importance of rich and qualitative ‘lived experience’, Healthwatch Elmbridge and its stakeholders alike expressed the need for qualitative and quantitative data to work together. Discussing Healthwatch Elmbridge’s insights database, the area’s GP quality lead lauded the blend of insights it made possible:
[F]or me the balance of the narrative with the quant[itative] stuff is really powerful and it’s something that I think it would be a massive loss for us as an organisation to not have that stuff at our fingertips and it’s really interesting when we’re working in other [areas] that don’t have that data to work with, you’re kind of scrabbling around for stuff . . .
GP quality lead, Elmbridge local JIF, 21 May 2021
Moreover, Healthwatch Elmbridge discussed the ways in which its quantitative evidence from the insights database could be used alongside more qualitative ‘direct experience’ evidence of resident or user experience provided by specialist voluntary sector organisations. This had the effect of lending more weight to such experience in the eyes of key audiences, such as the area’s health and well-being board:
I think it’s worked quite well when the actual qualitative voice or the user voice has actually come from the voluntary sector from within particular specialist groups . . . because they are specialist groups who represent that voice, but what we’ve been able to do is basically provide a broader picture to that voice to say ‘well let’s reflect the voice of the wider group’ and using the community insights to underpin the personal story . . . and using ours to give it a bit of clout.
Healthwatch Elmbridge CEO, Elmbridge local JIF, 21 May 2021
Healthwatch Elmbridge’s insight database attracted some interest at the other study site JIFs. The research manager at Healthwatch Beecham, for instance, said that, although such a database ‘would be the dream’ for him, he foresaw significant problems in its practice, particularly regarding the uniform and consistent coding of qualitative comments if more than one person was involved in it. Healthwatch Cherryburgh’s engagement manager suggested that the resources needed to manage such a database would mean that her Healthwatch would be unable to do much else. The area’s director of public health added that he valued Healthwatch Cherryburgh’s flexibility in its approach and found the idea of a database too ‘cumbersome’.
Broader issues relating to Healthwatch research processes were also discussed at some of the JIFs. Healthwatch participants at Healthwatch Beecham’s JIF called for a more professional scientific approach to the collection of data – such as proper sampling of participants or informants for surveys, focus groups or interviews. Healthwatch Beecham’s CEO argued that such ‘professionalisation’ of evidence would make it more effective:
I know I’m in the privileged position of having two research doctorates on my team and two teachers on my team – but that’s something we could definitely support the wider Healthwatch in, because they have access to such a wide group of stakeholders, they have the time to listen to those stories, so actually being able to professionalise that experience gives it a lot more rigour and makes it a lot more robust, so I think that’s definitely something we should explore moving forward.
Healthwatch Beecham CEO, Beecham local JIF, 25 May 2021
A Healthwatch Elmbridge board member – who is a social science researcher and in the past has pushed for such scientific techniques to apply to the work that Healthwatch Elmbridge conducts – also observed that any method, qualitative or quantitative, must be tailored to the particular question being asked:
. . . a question comes on why you’re doing what you’re doing, what’s the question, people asking the question, people asking will then dictate what methodology you use, so it’s not a case [of] do we want a story or do we want numbers, it’s what’s the question and then depending on the focus of the question we’ll say ‘actually a quantitative methodology will be more effective than a qualitative one or vice versa’.
Healthwatch Elmbridge board member, Elmbridge local JIF, 21 May 2021
Panels as a source of insight
The idea of user panels as outlined in the resource document (see Appendix 6), proved popular among Healthwatch staff and external stakeholders at most JIFs. Healthwatch staff and external stakeholders liked the concept of the panel as a partnership between local authority, VCSE and Healthwatch, and agreed that it would mitigate some of their past problems with this form of gathering service user and resident insight. Healthwatch Elmbridge’s CEO remarked:
My initial thought about the first idea, the one with the panels, was that we do run for example a mental health task group, we have [a young persons group], so we kind of already are doing a little bit of that but I quite like the aspect of the council people being involved and attending the meetings for these types of panels, actually having transparency about what happens to their insights and their visions after the people from the council hear about them.
Healthwatch Elmbridge CEO, Elmbridge local JIF, 21 May 2021
The chairperson of the health and well-being board in Elmbridge agreed that panels structured in this way could be an effective way to access experiences:
I think some of that qualitative experience and the panel approach makes some of those stories really compelling which forces that change.
Councillor in Elmbridge, Elmbridge local JIF, 21 May 2021
At Healthwatch Dogwood’s JIF, the chairperson of Healthwatch Dogwood also suggested that panels, along the lines of that described in the resource document (see Appendix 6), might be a means of reinvigorating PPGs in the newly formed PCNs:
. . . there’s huge potential in terms of Patient Participation Groups which might morph into sort of mini residents’ panels and so on. So I think there’s a huge amount of work potentially with the primary care networks, the residents’ panels potentially in those areas, PPGs.
Chairperson Healthwatch Dogwood, Dogwood local JIF, 26 May 2021
He also pointed out that Healthwatch and its partners in the health and care landscape should co-ordinate to ensure that there would not be an unnecessary duplication of panels across different institutions. The council commissioner who worked with Healthwatch Beecham on setting up the programme of panels (described in Appendix 6) summarised the approach as enabling bottom-up, user-identified issues while allowing the local authority to ask about needs and experiences on topics that are strategically important for it:
. . . because that forum was always – in our design of it – meant to create the space for both, so that the forum members could table themes that were absolutely coming from that unsolicited end and the independence side in terms of the things that people say are most important to them to raise, versus us creating the space for the things that strategically are important for us to work with people on in relation to people with lived experience, so I think it is about both.
Local authority Healthwatch commissioner, Beecham local JIF, 25 May 2021
Different sorts of evidence: locality and the social determinants of health
The resource document (see Appendix 6) outlined Healthwatch Elmbridge’s work, which involved examining the varying health needs and experiences of populations based on where they live and other social determinants of health (see Chapter 5 for a fuller exposition). This was the topic of much discussion at the Healthwatch Beecham and Healthwatch Dogwood JIFs in particular, as this sort of approach is not generally adopted by Healthwatch Beecham and Healthwatch Dogwood. Nevertheless, the approach was endorsed by external stakeholders. Therefore, at Healthwatch Beecham’s JIF, an ICS programme director said that a localised approach to collecting and communicating lived experience would be valued by the system:
[W]e need that range, there’s no one type of data or information to tell the story, we need quantitative information, qualitative information, but as we’re starting to look at for example data from population health management approaches and those sorts of things, it’s the story that’s so important and to help to add that interpretation because there is a risk there, isn’t it, that we don’t really properly understand the story and make assumptions about that, so I just absolutely endorse the fact that if we’re thinking as a system much more locally and place based and neighbourhood based then we need to understand stories at place and neighbourhood base as well.
ICS programme director, Beecham local JIF, 25 May 2021
An approach that took account of both locality and the wider determinants of health was achievable and desirable for this ICS manager, who had experience of (1) the communities’ health and care needs during the COVID-19 pandemic and (2) Healthwatch Beecham’s emphasis on collecting and communicating people’s lived experiences:
I think the story over the last year and a half in particular has been a big reminder about just how we need to move away from dividing people up and putting them into different categories and boxes. Certainly the recent experience about the sheer intersectionality of a lot of the issues that our communities are facing needs to be the thing moving forward. So I’d just make a plea for kind of not trying to divide things up, but almost embrace that complexity of people and their lived experience because that, at the end of the day, is what we’ve got to deal with and respond to as a health and care system.
ICS programme director, Beecham local JIF, 25 May 2021
Likewise, a CCG manager at JIF Dogwood encouraged Healthwatch to consider the wider determinants of health, echoing what other CCG officials had told us in interviews during fieldwork:
I think it is more around, there needs to be more focus on the wider determinants, it’s not all about health services because obviously all of the wider determinants have an impact on how and why people need the services.
CCG manager, Dogwood local JIF, 26 May 2021
Representatives from Healthwatch Dogwood seemed open to the possibility of exploring this, but indicated that this additional work would need to be resourced. Healthwatch Dogwood’s local authority commissioner commented on how this would be examined holistically in the context of the next specification for the Healthwatch contract in her area:
. . . but as the commissioner of Healthwatch, it is something that we’re going to be looking at going forward because obviously we have to look at the service specification, what Healthwatch does and this is probably very timely in taking forward that piece of work as well. So I mean I alluded to it before around the longer-term pieces of work but obviously what we need to look at as well is the resources that would be required for that and I’ve listened to what other partners have said about being involved in work around the wider determinants and I do actually think that is something that potentially could inform quite a lot of the work that we do within health and social care.
Local authority commissioner, Dogwood local JIF, 26 May 2021
Therefore, although stakeholders recognised the potential value of Healthwatch collecting more experiences beyond those directly of care services they had received (or would like to receive), stakeholders also recognised that Healthwatch, as currently commissioned in that area, would not be able to fulfil this desire.
How to provide evidence at the integrated care system level?
At each JIF, we also discussed the involvement of Healthwatch in the ICS and asked whether or not the nature and level of insight Healthwatch conventionally provide would have to change to meet the demands of working at a larger scale. At all JIFs, both Healthwatch representatives and key partners (sometimes including ICS staff) emphasised that they valued Healthwatch’s local focus and ability to provide independent public and patient voice:
I’ve been to meetings with other systems and I can’t understand why or how it is that local Healthwatch are not part of their system arrangements because they have a statutory role, so for the public, you know, this is the route through which you can actually have your voice listened to, so surely we need to respect the statutory role of Healthwatch as much as the statutory role of a local NHS trust or commissioners or the county council, whatever, I just think it’s time that that needs to be written down properly and followed.
ICS programme director, Beecham local JIF, 25 May 2021
Healthwatch Beecham and Healthwatch Elmbridge were involved in their respective ICSs to a much greater degree than our other study sites, largely because of the more advanced nature of their development. The insights database used by Healthwatch Elmbridge was now being used at an ICS level by all the Healthwatch organisations in that particular ‘footprint’. From Healthwatch Elmbridge’s perspective, this and other ways of collaborating on collecting and producing evidence has led to an increase in Healthwatch influence:
I was just going to say I think that Healthwatch’s influence has actually increased since the ICS and the fact that we’re working more collaboratively almost gives us more clout and there isn’t the sort of divide and rule kind of thing, because we’re able to join up our evidence that evidence has more weight because there’s more of it. And so instead of having, you know, eight Healthwatch that are all doing their own thing, we’ve got eight Healthwatch that are doing the same thing. And we’ve got a quite powerful body of evidence to which we could be – I think what I’d like to see is feeding into what will be an unprecedented sort of level of service redesign post COVID and that our evidence can be used to support genuine community leadership and the designing of services across a whole range of health and social care providers.
Healthwatch Elmbridge CEO, Elmbridge local JIF, 21 May 2021
The ICS representative at the JIF agreed:
I think [it] has really been of value, the way that the Healthwatches have particularly come to work together on the community insight system and, as a result of that, the development of relationships across all the Healthwatches and a really quite strategic way of thinking about things.
ICS manager, Elmbridge local JIF, 21 May 2021
This way of working is challenging, however, and requires financial and other support, as Healthwatch Dogwood’s chairperson pointed out:
. . . it is not for one single Healthwatch to undertake that. Healthwatches have to work together and if Healthwatch is to pass on a consistent, coherent, collective view to these partners and these systems, then that takes a lot of time to get representatives from [all the] Healthwatches in the [footprint] to get them to work together for a collective evidence based voice. There’s a huge amount of work in that for somebody somewhere and I think that’s the key issue.
Healthwatch Dogwood chairperson, Dogwood local JIF, 26 May 2021
Who is your audience?
We also asked Healthwatch representatives at the local JIFs about their key audiences for the evidence they collect from local residents and how different audiences might require different engagement. Reflecting on their experience of presenting evidence to key committees during the COVID-19 pandemic, Healthwatch Elmbridge’s research officer described the ways in which their reports became shorter and more graphic-heavy so that their audience – public health, CCG, health providers and local authority staff working under pressure – could digest key points quickly:
. . . what happened with us was that our reports became a lot more infographic, like, you know, in terms of my own practice I found myself almost never using Word [Microsoft Corporation, Redmond, WA, USA] again. Nowadays I just do the report directly in infographic format in Canva [Canva, Sydney, NSW, Australia]. Having this very infographic approach that’s very tailored for meetings and presentations and very fast skimming actually made us better and more effective.
Healthwatch Elmbridge staff, Elmbridge local JIF, 21 May 2021
Reflecting on Healthwatch’s dissemination strategies, the chairperson of the health and well-being board at Healthwatch Elmbridge’s JIF suggested that, in her area, ‘some of these stories can be told more and louder’. When we asked Healthwatch Elmbridge’s CEO about this comment, she interpreted it as follows:
. . . the sense that I get from her [is] that she sees Healthwatch as a really important partner to her role and that she sees that somehow we can work with councillors and almost giving an independent voice so that they can basically perform their role better because obviously we’re external to the council staff and therefore give them a slightly different perspective, but also it’s a really quick way of them of understanding a little bit about what constituents are saying, you know, because for them it’s their voters really isn’t it.
Healthwatch Elmbridge CEO, interview, 3 June 2021
By way of striking contrast, at Healthwatch Beecham’s JIF, a key local partner – the ICS – suggested that Healthwatch widen its audience to include the health and care sector to a greater extent:
And, you know, please don’t underestimate the importance of having really high-quality products that enable that story to travel and to be heard by a range of different audiences, because it’s as important to, kind of, you know, the health and care kind of community to hear those stories as for the public and MPs [Members of Parliament] and so on as well.
ICS programme director, Beecham local JIF, 25 May 2021
This contrast highlights the range of work that Healthwatch carries out to communicate evidence effectively to a wide array of audiences.
Statements of good practice for Healthwatch on evidencing patient and public voice
Practices and strategies relating to evidence is central to Healthwatch and helps local Healthwatch organisations fulfil their mission to effectively convey patient and public voice to health and care partners. The complexity of the discussions at the local JIFs demonstrates the importance of both good evidence-gathering practices and communication strategies so that Healthwatch organisations are in the best possible position to influence decision-making on behalf of local residents. Combining the findings of phase 4 with the ethnographic data we collected in phases 2 and 3, we drafted statements of good practice on which local Healthwatch organisations can practically draw on to enhance their impact. We circulated a draft of these statements to our HIP members (see Appendix 5) to test their relevance and usefulness to the broader Healthwatch network. Below, we summarise the key points made by HIP members who commented on the draft.
Insights from the Healthwatch Involvement Panel to refine statements of good practice
We received comments from five HIP members. One HIP member expressed concerns that the statement did not make reference to the impact of the financial challenges experienced by local Healthwatch organisations, which was discussed by many HIP members during the course of phases 2 and 3. We responded to this concern by clarifying that the issue of budgetary constraints was addressed and discussed in the main body of the report (see Chapter 5, Funding arrangements) and that these statements focused specifically on highlighting good practice that local Healthwatch organisations may themselves implement or seek additional funding for.
The other four HIP members were broadly supportive of the statements. However, we received comments on the following aspects.
Three members of the HIP warned about the expansion of Healthwatch activities to include investigations of the social determinants of health, which, although valuable, were not included as part of Healthwatch’s official remit (defined by statute). The HIP members interpreted Healthwatch’s official remit as being focused on engaging people about their experiences of care services, as one HIP member stated:
I would be reluctant to promote investigation of social determinants without some reflection that it’s a grey area in terms of the statutory functions.
HIP member 2, e-mail communication, 29 June 2021
The HIP members suggest, however, that they would be willing to conduct such work, as long as it the local authority funded it separately and in addition to their core contracts to fulfil their statutory functions. Responding to the e-mail thread, a fourth HIP member disagreed with this assessment, arguing that local authorities were entitled to commission Healthwatch in any way they chose:
Although we do have our statutory duties, I’ve rarely seen them enforced. The only paymaster is the council. Accordingly, we can to a large degree influence our own direction if we satisfy the commissioners. HWE [Healthwatch England] can suggest and guide, but the paymasters ultimately decide.
HIP member 1, e-mail communication, 30 June 2021
As a result of this discussion, we modified the wording of statement 2 as follows. In addition, the following amendments to statements were made:
-
One member of the HIP observed that engaging formally with VCSE organisations to gather evidence on Healthwatch’s behalf (either through panels or commissioned work) fell within the statutory function of ‘promoting, and supporting, the involvement of local people in the commissioning, provision and scrutiny of local care services’ (HIP member 2, e-mail communication, 30 June 2021). Therefore, we modified statement 5 to emphasise this aspect and reassure Healthwatch that it could legitimately proceed in this way.
-
The same HIP member asked that statement 3 more clearly explain that co-ordination between Healthwatch organisations would better help ICS leaders ‘get a fuller picture of the experiences, needs and wishes of the population they serve’ (HIP member 2, e-mail communication, 29 June 2021). Therefore, we changed the wording of statement 3 to emphasise this point.
-
Another HIP member proposed, in relation to statement 5, that processes of co-production would be preferable to panels and we now mention co-production as an important element of a panel process.
Statements of good practice for the gathering and use of patient and public voice
Healthwatch works best when it uses a broad range of techniques to collect patient and public voice and to communicate this to local partners
We found that stakeholders and Healthwatch alike value a varied and flexible approach that does not privilege one way of collecting and communicating evidence over another. This approach allows Healthwatch to tailor evidence-gathering and communication and to adopt a sensible approach to the specificity of the topics being investigated, as well as the needs of the people and organisations involved. Even those Healthwatch organisations that identified their ‘brand’ more closely with a particular technique (e.g. a database of local patient and public feedback) felt the need to maintain and develop other methods of collecting, analysing and communicating evidence.
Healthwatch can enhance its influence by adopting a more locality-based approach to patient and public voice
The needs and experiences of residents in relation to health and care vary according to neighbourhood or locality within a given local authority area, and this is due to varying levels of deprivation across the local authority, as reflected, for example, in population density, access to local services and green spaces. We found that it is not common for Healthwatch to organise its work to capture these local or neighbourhood specificities. When such work is carried out, however, it has been highly regarded by local stakeholders, such as public health directorates, NHS trusts, CCGs. In those areas where Healthwatch has not worked in this way, local partners indicated a strong interest in a more sustained focus on locality. This interest is directly linked to the move towards understanding and improving population health outlined in NHS strategies, such as the NHS Long Term Plan,23 and the greater importance attached to the social determinants of health and inequalities, partly prompted by the COVID-19 pandemic. Healthwatch may enhance its influence and, therefore, the voice of patients and the public by adopting this more granular approach. For larger Healthwatch organisations, this might involve rethinking organisational structures to enable them to cover a range of localities in depth. If Healthwatch was to investigate the social determinants of health (e.g. engaging residents about how they experience air pollution or crime, and the subsequent impact on their health), then this may need resource in addition to Healthwatch’s core contracts, as this area does not fall within Healthwatch’s statutory functions.
Healthwatch organisations benefit from co-ordinating evidence-gathering with other Healthwatch organisations in their integrated care system area
Providing evidence about patient and public voice to the ICS is an increasingly important area of work for many local Healthwatch organisations. Although ICSs are still forming, and Healthwatch involvement will become better defined through the passage of the Health and Care Act 2022,47 it is already clear that Healthwatch organisations provide a fuller picture of the needs and experiences of local people to ICS leaders when they co-ordinate their evidence-gathering and communicating work with other Healthwatch organisations in the ICS through formal mechanisms, such as memoranda of understanding or planning and conducting joint projects across the ICS footprint. Healthwatch organisations can do this while still maintaining a clear focus on the specific needs and experiences of patients and residents in their local area, which is valued by ICS leaders.
Healthwatch organisations can engage well with local democratic representatives when they adapt their communication strategies in innovative ways
Most of the evidence gathered by Healthwatch organisations about the needs and experiences of their residents is shared with local NHS and council staff. In addition to these audiences, Healthwatch organisations find it valuable to target a broader range of local stakeholders less commonly addressed in their work and some of these local stakeholders have explicitly indicated an interest to work more closely with local Healthwatch organisations. One such example are local councillors who, in some areas, have used the evidence produced by Healthwatch to better understand the health needs and experiences of their constituents. On these occasions Healthwatch’s independence has been considered a particularly valued asset, allowing councillors to hear constituent views that would otherwise be difficult for them to access. To engage councillors better, some Healthwatch organisations have modified their communication strategies and instead of long and detailed reports they have produced regular ‘quick-read’, graphic-heavy briefings, which are better suited for the specific needs of this audience.
Panels can be a rich and sustainable source of insight if organised as a partnership between Healthwatch and statutory and voluntary sector organisations
Healthwatch organisations often explore new ways to collect patient and public voice. Panels of service users organised by locality or health condition have been convened by many Healthwatch organisations in the past. We heard from Healthwatch organisations that such panels were often beset by problems of diversity, over-reliance on individual anecdote and increasing apathy among members as they see little change resulting from their discussions. In addition, some Healthwatch organisations experienced logistical difficulties in organising panels on a regular basis because of these issues. However, we found that panels could be a rich and effective source of insight where local Healthwatch organisations worked in partnership with (1) a network of VCSE organisations and (2) a statutory body, such as the local authority or NHS. This combination of partners contributing to the panel’s operation means that (1) panels can draw on a broader and fresh network of service users and (2) panel discussions become more directly embedded in health and care decision-making processes via formal mechanisms of mutual accountability between Healthwatch and local stakeholders, therefore, becoming a process of co-production. The involvement of a variety of VCSE organisations means that the panel will have access to informal networks of people, many of whom would otherwise find it difficult to share their experiences. The involvement of the VCSE in Healthwatch work in this way falls within the existing remit of Healthwatch as provided by statute. While local Healthwatch facilitates panels and allows said panels to operate independently, they are working in partnership with other actors and are therefore not solely responsible for ensuring the panels’ success or effectiveness. This modified way of organising panels addresses many of their previously experienced limitations.
Chapter 7 Findings part 4: Healthwatch and the COVID-19 pandemic
Some text in this chapter has been reproduced from Zoccatelli et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
On 23 March 2020, the UK government issued a broad range of advice and regulations intended to curb the spread of COVID-19 and prevent the NHS from being overwhelmed by people needing care. Consequently, health and social care in England were radically reorganised (e.g. cancelling all elective surgery, moving primary care consultations online, relaxing hospitals’ discharge obligations to patients). In this chapter, we explore the impact of the sweeping changes brought forward by the COVID-19 pandemic on the operation of local Healthwatch organisations. We draw on data collected in the five study sites in phase 2, as well as the data we collected through online interviews and small-group discussion with HIP members in phase 3, to discuss how Healthwatch adapted its work to continue representing the voice of local patients and public in decision-making processes about health and care.
Healthwatch in the first phase (spring 2020)
For Healthwatch organisations in England, the new ‘stay at home’ regulations had immediate effects. For Healthwatch staff, all face-to-face intelligence-gathering activities with the public were suspended and ‘enter and view’ visits to hospitals, care homes and general practices were cancelled. Local governance fora attended by Healthwatch staff were also largely suspended in the initial phases of the pandemic.
In adjusting the ways in which they worked, Healthwatch staff had to choose which of their statutory functions to prioritise. In the first few weeks of the COVID-19 crisis, the priority of the health and care system was for people to adhere to the new regulations to protect its ability to cope under the strain of an already large number of hospital admissions. Most local Healthwatch organisations were immediately enlisted by their local health and care systems to disseminate official information through different channels, including their websites, bulletins and newsletters. Some local Healthwatch organisations also reported compiling lists of NHS and government websites, creating directories of voluntary sector organisations and signposting members of the public to appropriate support agencies.
However, the lockdown posed practical challenges to Healthwatch’s ability to fulfil some of its functions. Healthwatch organisations were no longer able to access public and patient views as they had, nor could they contribute to health and social care scrutiny and decision-making at a formal level because boards and committees were either no longer meeting or were meeting in new configurations (e.g. virtual meetings arranged at short notice), which tended to exclude Healthwatch.
In this context, many Healthwatch organisations described a shift in the relative emphasis placed on their statutory functions. Before the pandemic most Healthwatch organisations regarded the provision of information and signposting of local services as a marginal part of their role; however, as the pandemic unfolded these functions moved to centre stage. In the initial phases of the crisis, ‘acting as a messenger’, as one Healthwatch CEO put it, led Healthwatch to primarily become a voice of the system to the people, but what spaces were then left for conveying the voice of the people to the system at this time?
This question provoked dilemmas for Healthwatch staff. Talking about her frustration for the lack of interest shown by overwhelmed local organisations to engage with feedback, a Healthwatch CEO in the north-east of England told us:
. . . I think at the moment [ . . . ] the explanation to come back, [ . . . ] is ‘look, we just can’t do anything at the moment, we have to deal with this’. But, for us, it would be ‘well let’s just see how long that [explanation] goes on for because life still goes on, there’s people still needing operations, there’s still people getting diagnosed with cancer and other different illnesses and things, they still need that help’.
HIP member 3, interview, 2 April 2020
To discuss how local Healthwatch organisations tried to tackle such dilemmas, we provide three examples of innovative strategies deployed by Healthwatch to ensure that the voice of local people was still heard by local systems in the early days of the pandemic.
Finding the voice of the people
Healthwatch Limefield: socially distanced public engagement
Soon after the beginning of the pandemic, Healthwatch Limefield moved its engagement activities online and set up two types of weekly ‘engagement and support’ Zoom (Zoom Video Communications, San Jose, CA, USA) meetings, which were open to residents to attend. The first type of meeting was aimed at gathering feedback from specific local communities, for example unpaid carers, people with learning disabilities, ethnic minority communities and young people. For this work, Healthwatch Limefield linked up with community organisations, working closely with them to collate the experiences of different demographics and different communities.
The second type of ‘engagement and support’ Zoom meeting was open to all residents to join. Participants were encouraged to share experiences and challenges in accessing services during the pandemic and to ask questions about COVID-19 and local health and social care planning and provision. In organising this work, Healthwatch Limefield’s manager described focusing most of his efforts on liaising with local stakeholders, including patient experience teams at local hospitals, commissioners, council staff and quality accreditation officials. Once the fora were set up, Healthwatch Limefield’s manager invited these officials to propose relevant topics for discussion. For example, Healthwatch Limefield’s manager told us that his local contacts in the CQC proposed dedicating a forum to discussing the drop in the number of people contacting GPs and community health-care providers. According to the CQC, there was a risk that some health conditions (such as diabetes or cancer) could go undetected if the trend continued. The discussion at Healthwatch Limefield’s Zoom meetings highlighted that people were, indeed, more reluctant to contact health-care providers in the first few weeks of the pandemic. Most forum attendees said that this was because they did not want to put extra pressure on local NHS services. As a consequence, the CQC was considering whether or not ‘the messaging needed to be changed slightly’ to help address this attitude.
Healthwatch Elmbridge: virtual intelligence gathering
At first, Healthwatch Elmbridge stopped gathering data about residents’ experience of the health and care system and feeding these data back to the NHS or local authorities, as Healthwatch Elmbridge’s CEO initially told us ‘they don’t want to hear anything right now’ (fieldnotes, 17 March 2020). Shortly after, however, Healthwatch Elmbridge’s CEO reported that her position was changing. Talking with senior managers at the local hospital, Healthwatch Elmbridge’s CEO learned that they were keen to hear how people were coping with the pandemic and gaps in care or services.
Healthwatch Elmbridge found two ways of gathering people’s experiences while complying with physical distancing. First, the team designed and circulated an ongoing online survey to residents. Second, the team asked to join the WhatsApp (Meta Platforms, Inc., Menlo Park, CA, USA) groups of the numerous mutual aid societies established by local residents to identify and support people who were self-isolating. After joining the WhatsApp groups, Healthwatch staff encouraged their members to feed back their views to Healthwatch. In addition, Healthwatch staff monitored members’ exchanges in the groups to identify trends or themes of concern.
By the end of April 2020, Healthwatch Elmbridge had already produced two reports presenting the analysis of data gathered and making recommendations as to how the local authority and NHS might address emerging issues. The reports covered a broad range of topics relating to residents’ health and well-being during the pandemic, including physical, mental and economic well-being, understanding of government advice and experiences of accessing health and social care services.
The reports received considerable attention from elected officials in local government and health-care providers. Healthwatch Elmbridge’s CEO was asked to present the findings regularly to the local authority’s pandemic committee (i.e. a central co-ordination body bringing together local health and social care leaders), as well as to the only health-related local authority committee meeting running at the time. The reports seemed to have real influence on the local provision of some services. For instance, Healthwatch Elmbridge found that pregnant women, classed as a vulnerable group, were reporting high levels of anxiety and would welcome a tailored programme of information provided through midwives and health visitors, as well as online consultations instead of telephone consultations. The local maternity service providers responded by committing to redesign their work to take account of these wishes.
Healthwatch Birchington: co-ordinating local administrators to address inconsistencies in system responses
At the beginning of the pandemic, Healthwatch Birchington received numerous telephone calls from members of the public who reported being unsure about the government’s advice on COVID-19. In particular, these people reported inconsistencies in who was categorised as ‘vulnerable’ and which regimes of isolation applied to different categories of vulnerability.
Through their contacts in the local system, Healthwatch Birchington’s staff began investigating the information local administrators were using to identify people especially vulnerable to COVID-19. Healthwatch Birchington discovered that the local authority (which is responsible for social care and public health) was using different sources of information than the local NHS (which is responsible for health-care services and for officially categorising people according to clinical risk). As the CEO of Healthwatch Birchington described, by taking up the role of the ‘go-between between the local authority and the CCG who were doing completely their own thing’, Healthwatch Birchington helped ensure better communication between key stakeholders in an area with a history of weak co-operation (interview, HIP member 5, 7 April 2020) and this eventually led to the public having clearer instructions about what to do, as well as more information on what support was available to them.
Healthwatch Birchington’s CEO also realised the need to similarly facilitate co-ordination between local officials and the voluntary sector. This was particularly important for small community groups, including condition-specific support groups (e.g. diabetes), faith-based associations and street-based neighbourhood groups, of which the council had been hitherto unaware. Healthwatch Birchington collated a database of voluntary sector activity during the pandemic, which included these smaller community groups, and made it available to the council and to the local organisation responsible for co-ordinating local voluntary sector activity. By facilitating communication between grassroots groups, the voluntary sector, the council and the NHS, Healthwatch Birchington addressed the need of local people to access support and information that was tailored to their needs.
Intensification of work (summer–autumn 2020)
Across most of England, cases of COVID-19 dropped to low levels from June 2020 until the autumn. Some Healthwatch staff returned to their offices with staggered shifts to maintain adequate social distancing. However, engagement activities and other meetings were all still conducted online. In certain parts of the country (e.g. Leicester, the North West and Yorkshire), the number of cases remained relatively large, prompting additional restrictions through the summer and early autumn. During this period we continued our research with the five study sites and carried out interviews with their staff, volunteers and local stakeholders, as well as observations of the engagement activities and meetings local Healthwatch organisations were organising and attending online. Alongside our work in the five study sites, we carried out four focus groups with HIP members, which we grouped thematically as follows: (1) those working in urban areas with local restrictions, (2) those in urban areas without local restrictions, (3) members of rural Healthwatch organisations and (4) Healthwatch volunteer members of our panel. We also convened a plenary HIP meeting where we presented emerging findings from the focus groups and engaged the panel in a general discussion about the work of Healthwatch in this period.
The research activities illuminated how the initial concerns some Healthwatch organisations had about the shifting nature of their role (i.e. becoming the voice of the system to the people, rather than the voice of the people to the system) had instead given way to a significant intensification of Healthwatch work on all fronts. This intensification was effectively described by one HIP member, a Healthwatch CEO:
My first worry was what are we going to do, because our bread and butter is being out there and that was a real concern, but within two weeks the amount of work that was coming through has continued to rise [ . . . ] and I know from our regional meetings – it’s across the board. The worry then was we’re going to have a burn out because everyone was just doing so much, no-one was flinching. Our board recently wrote a letter to every team member to thank them [ . . . ] For us, for me, it was burnout.
HIP member 3, small-group discussion, 14 October 2020
Although conventional in-person engagement activities were still suspended, many other elements of Healthwatch work intensified, as the Healthwatch CEO quoted above describes (HIP member 3, small-group discussion, 14 October 2020). This intensification of work was mainly linked to the increased number and range of meetings attended by Healthwatch staff. Committees and boards that local Healthwatch organisations regularly attended pre-pandemic had resumed meeting virtually after a brief hiatus in the spring. Many Healthwatch organisations were now ever more closely involved in aspects of local system pandemic response, as one Healthwatch staff member described:
I’ve never been so busy in all my life through lockdown, because I suddenly was in a lot more meetings, I talked myself in through existing relationships into some of the weekly resilience calls and things and was welcomed.
HIP member 4, small-group discussion, 14 October 2020
The increased use of virtual meetings rather than face-to-face interactions meant that people with whom Healthwatch had relationships were more accessible than before the pandemic because of the way diary time had come to be organised (e.g. several back-to-back virtual meetings, meetings being squeezed in between others). The project manager in charge of the organisation of Healthwatch Cherryburgh’s reference groups discussed this development:
So there is an opportunity there that we are [ . . . ] exploiting, which is the use of technology to bring people together [ . . . ] We [can] actually use this opportunity to get hold of people that we wouldn’t otherwise be able to. And that is working, not just for service users’ voices but also getting in touch with people from the council. Because on a normal everyday they’ll be like, ‘Oh I’m sorry, I’m busy in meetings. I have to be at this place and I have to be at that place’, whereas now most people are working from home, and they can always try and give five minutes of their time to you. So it’s been much better actually than before for me.
Project manager, Healthwatch Cherryburgh, interview, 18 May 2020
Moreover, as virtual meetings obviate the need to travel, Healthwatch staff could attend many more and different types of meetings on any given day and this was particularly important for Healthwatch staff covering large geographical areas:
I would say for being involved in a lot more of the regional meetings, it’s been really, really good, you know, Zoom and Teams has opened up a whole new world really and it’s worked really well for us, because we’re a small team the travel time, you know, to go all the way up to [place 2] or all the way down to [place 3] and that type of thing, so it’s proved really, really good for us in that sense . . .
HIP member 3, small-group discussion, 14 October 2020
Although the intensification of work created by the larger number of meetings in which Healthwatch was involved affected the workload of CEOs and managers most directly, it also affected other members of staff who carried out the new engagement activities discussed at those meetings. The participation of Healthwatch in pandemic response meetings meant their work became more responsive and staff needed to carry out work in shorter timescales. Pre-pandemic, local Healthwatch organisations may have carried out engagement work on an issue raised by patient feedback over a period of months, including producing a detailed report that would be shared with key stakeholders. During this second phase of the pandemic, however, this way of working largely ceased. Instead, at local system meetings, Healthwatch organisations often identified gaps in system information about particular seldom-heard groups (e.g. experiences and needs of particular ethnic minority communities, refugees or homeless people). The Healthwatch organisations then contacted relevant grassroots community organisations to gather feedback directly or indirectly and relayed this to local system leaders at their now regular meetings, which happened more frequently and were more accessible than before. In Box 12, we provide an example of Healthwatch Cherrybourgh’s engagement work with Pakistani-origin communities in their local area during this phase.
Healthwatch Cherryburgh is located in a highly diverse local authority. Thirty-eight per cent of local residents are from ethnic minority groups. When, in England, in the first phases of the COVID-19 crisis, it became clear that ethnic minority communities were being disproportionately affected by the pandemic, Healthwatch Cherryburgh launched a pilot project to explore how the local Pakistani-origin community was managing the challenges brought about by COVID-19. Healthwatch Cherryburgh’s aim was to use the case of the Pakistani-origin community as a starting point to explore broader issues affecting all ethnic minority communities in the areas. These issues included language barriers that could hamper the access to correct information, the role of comorbidities (e.g. diabetes and lung conditions) that are particularly prevalent among ethnic minority communities and cultural differences in the use of health-care services (e.g. greater reliance on emergency departments rather than GPs). Beside the large number of Pakistani-origin people in the area, another key factor that led Healthwatch Cherryburgh to choose these communities was because one of their engagement officers is ethnically Pakistani. The engagement officer spoke the language and had already established connections with local community groups, making it easier for Healthwatch Cherryburgh to access information quickly and present it to the council in a shorter time frame, as the engagement officer explained to us at the beginning of the project:
. . . because my ethnic background is Pakistani and I am able to speak the language, so – it was very, you know, it was the obvious choice kind of, you know, I speak it, I know the community very well, I know their challenges very well and then there’s a lot of, kind of, reasons why we should do it as well.
Healthwatch Cherryburgh engagement officer, interview, 19 May 2020
Healthwatch Cherryburgh’s engagement officer distributed a short survey to community organisations in their own local authority area and a neighbouring borough. All the community organisations involved had developed initiatives supporting local Pakistani-origin residents directly. Healthwatch Cherryburgh learnt that community organisations were operating as emergency help centres and food banks, offering befriending services, information and advice. Healthwatch Cherryburgh’s research officer also conducted online and telephone interviews with the staff and volunteers within these organisations and with local councillors and NHS staff from Turkish and Kurdish backgrounds.
In June 2020, Healthwatch Cherryburgh produced a report about the engagement work carried out with the Pakistani community, which was circulated and presented to the council, CCG and the main VCSE organisation working with other ethnic minority groups in the area. In addition, the report was sent to Healthwatch England.
The impact the report produced was immediate. In direct response to the report, in September 2020, the council launched a £150,000 programme of work aimed at creating and maintaining community engagement networks for COVID-19 prevention and health and care messages to improve the health and well-being of local people in the long term. In their call for expressions of interest in the programme, the director of public health and the assistant director of commissioning referenced Healthwatch Cherryburgh as the source of the research that highlighted the need for such a targeted programme. Healthwatch Cherryburgh, a local mental health charity and the local VSCO infrastructure organisation were chosen to lead this programme of work.
Although the work of Healthwatch staff intensified, the lack of face-to-face engagement and the suspension of enter and view visits in health and care settings inversely affected the involvement of volunteers in Healthwatch activities. Healthwatch volunteers are largely involved in public-facing activities and, with the shift of Healthwatch work online, many volunteers were unable to contribute because the Healthwatch activities in which they ordinarily took part prepandemic were suspended. This inability to contribute sometimes stemmed from the volunteers themselves being at high risk of COVID-19 (owing to their age or medical conditions). The need to retain volunteers despite the lack of volunteering opportunities was creating concerns for many research participants in our study sites and the HIP, and these concerns were reported to us as a further factor that contributed to the intensification of Healthwatch work in this period. One HIP member, a Healthwatch CEO, described it as follows:
I am starting to come up with issues on our volunteers, we did a lot of social interactions with them throughout the pandemic and they were really receptive to that, but actually with their age group and the cohort that they are, they can’t actually do very much with or for us at the moment – and that is starting to become a problem – so there is starting to become this, you know, we want to see every survey that you send out and we’ll help you input and that’s coming from the chair all the way down to what we call champions, so it’s really difficult to manage that at the moment, which I wasn’t expecting.
HIP member 5, small-group discussion, 5 October 2020
Some Healthwatch organisations found a solution to the problem posed by potentially disengaged volunteers and this was to use volunteers as a source of feedback about local people’s experiences of the pandemic (Box 13).
In England, when the pandemic began, Healthwatch Dogwood had 11 volunteers on its books. Most of these volunteers had been recently recruited as part of a new focus on volunteering to support Healthwatch activities to promote the creation of links to different communities across the large and diverse geographical area in which they worked. During the successive periods of national restrictions, the kinds of activities such volunteers might carry out were restricted. Concerned at the risk that these newly recruited volunteers – many of whom had yet to begin Healthwatch work – might lose interest and, therefore, imperil this new strategy, the volunteer support officer proposed new ways of engaging them.
Healthwatch Dogwood had recently launched an initiative to solicit online feedback from local people about their experiences of health and care during the pandemic. This consisted of a free-text box on its website and residents were encouraged to write it as a ‘story’. The volunteer support officer asked the new volunteers to submit their stories. As the volunteer support office told us, this was an example of ‘micro-volunteering’, which, in the Healthwatch context, meant the use of volunteers’ own experiences as feedback about local health and social care services.
Implications for Healthwatch of intensification of work
This intensification of work had several implications. One generally positive implication of increased Healthwatch activity was that its profile had been raised with its stakeholders and with members of the public. This raise in profile was a result of the accessibility of virtual forms of engagement and the new responsive ways of working with local pandemic management partners, as one HIP member, a Healthwatch CEO, described:
I would say there’s definitely been a shift. We’ve definitely got our feet underneath the table. Before, we were always forever knocking on doors until we were let in, but now we’re actually being invited in, you know, rather than bulldozing our way through!
HIP member 3, interview, 3 February 2021
Several Healthwatch managers and CEOs reported that they were able to reach larger numbers of local residents through varied forms of digital engagement. As larger numbers of local people now attended virtual events, health professionals and managers increasingly found Healthwatch events more useful than in the past. For instance, the same Healthwatch CEO quoted above described how her team’s use of the Facebook Live platform not only attracted a large local audience but raised their profile with clinicians:
. . . we have been so busy and we’ve adapted so well and we’ve been doing live Facebook sessions and we’ve been attracting more and more people to talk to us and then clinicians because of the live Facebook have been coming along saying ‘oh, that’ll be great for the flu vaccinations, we can do question and answers and things like that’.
HIP member 3, interview, 3 February 2021
Another Healthwatch CEO said that although he had struggled in the past to get residents to attend in-person engagement events, he was astonished at the numbers now attending virtually:
. . . by moving business online, I mean [ . . . ] the numbers that we can reach out to digitally just surpass the numbers that we would see conventionally. So, for example we did a talk to the University of the Third Age; we had 87 people on the call. We’ve never had 87 people turn up to a village hall to talk about Healthwatch. Now I appreciate that a lot of those people have just probably got nothing else to do on a Wednesday afternoon than to join a Zoom call, but the numbers attending our public board meetings have gone up.
HIP member 6, interview, 8 February 2021
Similarly, Healthwatch Elmbridge held a public lecture given by a renowned specialist in health inequalities that attracted over 400 attendees, something Healthwatch Elmbridge’s chairperson said would have proved impossible were it to have been held face to face:
Now, I think we’re braced with the pandemic on this one because we would not have gone out and hired a hall for 500 people, you know, we wouldn’t have been able to afford it. Zoom has its upsides too.
Healthwatch Elmbridge chairperson, interview, 5 October 2020
Moreover, the newer, more responsive way of working, with quicker turnaround times, has also had the effect of generating more awareness of Healthwatch’s work and usefulness to local health and social care systems, as one Healthwatch CEO said:
I’m really aware that during the pandemic I have tried to take every opportunity to increase awareness of us as an organisation because there’s been an appetite to understand things in perhaps a much more live way than we would normally get, and a much less sort of overly constructed way as well. So people want things a bit faster, a bit more raw, kind of like ‘help us right at this moment’ and I think that’s produced some really interesting opportunities for us and I think that’s been great in terms of our awareness in our local places.
HIP member 7, interview, 15 February 2021
One consequence of the increased awareness of Healthwatch in various locales in England was that Healthwatch’s staff had to learn to navigate new areas of activity and new relationships and this meant that, in some instances, local Healthwatch organisations found themselves in uncomfortable territory (e.g. being solicited by regional or national media about elements of the local pandemic response while having to avoid appearing overly critical or political). On a more technical level, Healthwatch staff had to spend time learning new ways of organising events online, as in the case of Healthwatch Elmbridge’s public lecture, which involved training facilitators of Zoom breakout rooms, for instance.
Healthwatch staff not only had to experiment with digital engagement, they also had to learn how to represent Healthwatch in digital meetings without some of the benefits of ‘corridor chat’, etc., as one Healthwatch member of staff put it:
I feel almost slightly you have to be a bit more shouty – I don’t mean shouty in an aggressive way – but a bit more kind of ‘hello it’s Healthwatch’ and say something Healthwatch-ey, rather than it being as easy to join the meeting, get the feel of the meeting, use a bit of body language and join the group a bit, I mean, we all have different styles, but I don’t think I would join a group and then start rocking the boat.
HIP member 4, interview, 10 February 2021
The combination of the greater awareness of Healthwatch’s potential, the accessibility provided by digital forms of engagement and the new ways of working that this continuously entailed led to a cycle of intensification of work for Healthwatch during this period. Compounding this was that many Healthwatch staff found it difficult to refuse invitations to meetings during this time. There was a sense that Healthwatch had an important role to play in local responses during such an unprecedented health emergency and there was, therefore, a strongly articulated ethics dimension to Healthwatch work, as a Healthwatch CEO and HIP member described:
. . . it’s not necessarily that there has been an external sort of ‘you have to do more’, it’s more kind of, like, ‘at this time if we’re going to be helpful and we’re going to get it right, we need to do more’ – and so I am thrilled to work with people who have that in their DNA but at the same time I worry all the time about people ending up off on long-term sick because they have taken on so much and they’re under so much strain that actually they’re not going to be able to manage when something does happen that’s challenging.
HIP member 7, small-group discussion, 5 October 2020
As the quotation above highlights, this intensification of Healthwatch work raised significant issues of staff exhaustion that worried many Healthwatch managers and CEOs and, in autumn 2020, led them to question the sustainability of this pace of work. This commitment to being involved meant that Healthwatch staff felt ‘guilty’ if they rejected offers of participation in health and social care:
[There is] this feeling of guilt about taking time off . . . when there’s such a thing happening as there is and everybody else is out there risking their lives you’re thinking it would be wrong to take time off.
HIP member 8, small-group discussion, 14 October 2020
The increased accessibility of those with whom Healthwatch maintained relationships and its higher profile, as well as the ethics commitments to the Healthwatch work and mission in a time of crisis, all contributed to the intensification of activities in summer and autumn 2020.
A return to normal? (The view from February 2021)
By February 2021, the pandemic situation in England had deteriorated. A few weeks after our HIP meeting in October 2020, national restrictions were imposed once again because infections and hospitalisations were rising, particularly in the north of England. The restrictions were lifted in early December, during which time the more transmissible ‘Alpha variant’ (B.1.1.7) of COVID-19 gained a foothold in London and the south-east of England and spread to other parts of England. Greater restrictions were imposed progressively on various parts of the country from mid to late December until England went into a third national ‘lockdown’ on 4 January 2021.
From December 2020, the UK’s COVID-19 vaccination programme also began in earnest. Information campaigns were launched that targeted groups in society (e.g. ethnic minorities) who were seen as ‘vaccine hesitant’ and at risk of lower uptake.
We wanted to track the development of Healthwatch work since October 2020, including whether or not the intensification of activity we had found for the earlier period had continued into the winter as the pandemic entered a new phase. We also wanted to explore Healthwatch’s involvement, if any, in the vaccination programme. To this end, we held one-to-one interviews with 12 HIP members over 2 weeks in February 2021 and organised a final plenary HIP meeting where members also offered reflections on how their Healthwatch organisation had changed over the course of the pandemic since March 2020.
Our interviews showed that the intensification of work of the preceding 10 months had largely abated and this was for two reasons. First, many interviewees mentioned that, as they had already intimated during the second phase, the pace of work – especially in ‘responsive’ mode – had been unsustainable and they were concerned about ‘burnout’, and this issue of burnout had become more pressing because primary and secondary schools were closed during much of the third period of national restrictions and many Healthwatch staff were, therefore, educating their children at home.
Second, and associated with the issue of ‘burnout’, some Healthwatch CEOs and managers felt a loss of control over their schedule of work and priorities. The CEOs and managers had decided to reinstate more ‘normal’ ways of working and planning their projects; however, they were still conscious of being buffeted by events outside their control, as one of our HIP members, a Healthwatch CEO, described:
It seems to me like in the last year that’s been transformed into a very reactive role again, which is something that I’ve spent 5 years trying to move us away from. And that’s where I’m struggling at the moment. I’m trying to create this work plan for this year and I’m very, very tentative about what can I focus on and be reactive to, because there is still so much up in the air.
HIP member 5, 3 February 2021
Moreover, some Healthwatch boards were keen for Healthwatch – and their local health and social care systems – to re-orient their activities to non-COVID-19 work. In this period Healthwatch Dogwood’s chairperson, for instance, wrote repeatedly to the chairperson of his area’s health and well-being board and to the director of public health, asking them to begin including more non-COVID-19-related items to their meeting agenda. One Healthwatch CEO told us how the mood had shifted in her organisation’s board and she was now being asked to focus less directly on COVID-19:
There is increasing pressure on us from the trustee board, and a little bit from our contract manager about offering something that fits in with the historic view of what Healthwatch has been. So that kind of we need to get back to doing what we’ve always done . . . we need to pick up some of the pieces of work that we might have picked up before the pandemic started, to evidence that we still have a more diverse range than just being a COVID public voice . . .
HIP member 7, interview, 15 February 2021
Partly, this return to more ‘normal’ ways of working was also born of a desire to keep Healthwatch staff engaged, as staff also expressed the importance of an ethic of ‘listening to the voice of the people’, which had been modified by working in responsive mode to the system. Therefore, the same CEO described how she aimed to enable voice in a more targeted way, arising from concerns they themselves were hearing. Healthwatch hoped to achieve a more balanced approach in this latter period:
. . . there’s a lot of different things trying to pull us in all sorts of different directions, which is a bit exhausting and a bit difficult to manage, as well as trying to make sure that the staff stay onside and that we’re responding to what people tell us. Because we did a big piece of COVID engagement in the summer and that had loads and loads of insight in it. So what we’ve tried to do this time is pick out the things that perhaps wouldn’t have been the big key themes, when we did that first piece, but the stuff that sat underneath it that perhaps would impact a particular group. And the staff are really passionate about that because that’s responding to the voice of the public . . .
HIP member 7, interview, 15 February 2021
Some local Healthwatch organisations were also able to step back from the active co-ordination work between the local authority, NHS and community groups that they had previously taken up and this was partly because the relationships between these other partners had now been well established and Healthwatch’s initial facilitating role was no longer needed as the pandemic went on, as one Healthwatch CEO told us:
I think the one thing that’s transformed locally for me is how the local authorities and the ICS/CCGs have interacted with people. The sort of real powerful sort of push that we put [in spring 2020] on them not talking to people or informing people, but actually getting people round the table. That was quite transformational last year. They used to come to us a lot for ‘can you speak to these people for us and gather this information for us?’ but because of the pandemic they have got those links, they’ve got the COVID champions up, they’ve got massive links with a lot of the communities now, so I find our role is not so much talking to the seldom heard and gathering those voices, but actually ensuring that those voices are sat around the right tables at the right times at a more sort of strategic level rather than going out doing a survey with black and ethnic minorities.
HIP member 5, HIP 5, 23 February 2021
We described above how the ethics commitment of many Healthwatch staff to contribute to the pandemic response alongside colleagues from the health and social care sector led to feelings of being unable to refuse to be involved, even at the cost of exhaustion. Another corollary of this ethics commitment was that many local Healthwatch organisations undertook considerable extra work outside the remit of their contracts and for free, and this continued in the third phase. One CEO told us about how her Healthwatch organisation became involved in the vaccination programme to such an extent that it overshadowed other aspects of her work for several weeks. The CEO found herself working in ‘responsive’ mode again, despite her efforts at resuming ‘ordinary service’; and her work was not compensated:
I am invited ad hoc to the primary care network meetings where they talk about how they’re delivering vaccination, so literally since the start of January my whole job has become about trying to bring in public voice into some of the vaccination work. And of course there’s no additional funding for doing something like that and for trying to get the system to work together on something. And there was no sign that that was going to be the ask of us until the start of January, so none of that was planned in.
HIP member 7, interview, 15 February 2021
Now that their attention was turning to matters beyond the immediate pandemic response, some Healthwatch managers and CEOs felt the loss of their usual face-to-face ways of working more acutely, particularly in relation to their powers of ‘enter and view’. Much like their criticism of the ‘responsive’ way of working, this was characterised as a lack of control. Therefore, although Healthwatch would work with health and social care providers to organise visits in the past, some Healthwatch organisations were reporting that providers were now less inclined to facilitate such visits or even to discuss possible alternatives:
But we’ve also lost a lot of control . . . [W]hen we start to raise the idea of doing [enter and view] in a different way, we sort of get backed backwards and I think hospitals, particularly health and social care, are quite comfortable with the fact that we’re not going in and not viewing and observing and talking to patients in that way at the moment.
HIP member 9, HIP 5, 23 February 2021
For these Healthwatch organisations, the inability to be physically present on care premises meant they were not able to deploy their professionally honed senses of observation, as one Healthwatch CEO added:
. . . [I]f you go into a care home, your whole sense – all your senses – are being used, you’re not just talking to someone on a screen. So for me it would be about, ‘what does it smell like when I go in? What am I hearing in the background?’
HIP member 9, HIP 5, 23 February 2021
Another Healthwatch CEO echoed this sentiment:
. . . we need to get back to be able to doing some hands-on work. It’s exactly the same as walking into an A&E [accident and emergency] department and getting a sense for whether or not it feels organised or not.
HIP member 6, HIP 5, 23 February 2021
In February 2021, there was still a great deal of uncertainty among Healthwatch staff about their ability to return to previous ways of working. What was clear was the desire to reduce the intensity of work and, although some staff tried to facilitate this by, for example, attempting to set their own workplans, they often found themselves at the mercy of their local systems’ needs and felt compelled to contribute in this most severe phase of the pandemic so far.
Lessons for Healthwatch and others from the COVID-19 pandemic
Below, we outline three lessons for Healthwatch from our findings relating to its activities and experiences during part of the COVID-19 pandemic (from March 2020 to February 2021):
-
Crucial to Healthwatch’s ability to act effectively in conveying patient and public voice throughout the course of the pandemic was its formally mandated position in England’s health and social care system. For instance, as in Healthwatch Elmbridge’s example, involvement in mutual aid groups’ WhatsApp chats allowed access to the views and experiences of people (e.g. those who were self-isolating), which might otherwise be difficult to access. However, it was Healthwatch’s status as a formal statutory organisation (as well as the expertise, reputation and relationships built up over time because of that status) that provided it with a direct channel through which to communicate these views back to people with decision-making power in the health and social care system.
-
Healthwatch Birchington’s expanded co-ordinating role similarly demonstrates the uniqueness of Healthwatch in the English health and social care governance landscape. Combined with its broad and deep knowledge of the local voluntary sector, Healthwatch Birchington was able to gather feedback from residents and seek answers from and co-ordinate information between health and council agencies. A statutory organisation like Healthwatch is well positioned to mobilise relationships with different stakeholders because of the status provided by Healthwatch’s legal mandate.
-
Local Healthwatch organisations reported the tension between being responsive to the needs of the system during an emergency and managing their own sense of autonomy to set their own work agenda not only was this tension bound up for some in a cherished notion of Healthwatch independence but it also had practical effects, such as the increased risk of staff burnout, which, respondents feared, would in the long run lead to a less effective local Healthwatch organisation. Therefore, local Healthwatch organisations learned that they needed to pay attention to the ways in which they balance their own mission as providing the voice of local people, their responsibilities in that role to the wider health and care landscape and the existential needs of their own organisations and working lives.
Chapter 8 Discussion, implications for decision-makers and conclusions of the study
Discussion
There is a legal duty for the NHS to consider public involvement in commissioning and providing health care, including at all stages in major health-care planning decisions,34 and this is a cornerstone of a patient-centred, publicly funded NHS. 35 There is increasing evidence of a positive association between public involvement and more ‘innovative, effective and efficient ways of designing, delivering and joining up services’ (reproduced with permission from the World Health Organization; URL: www.euro.who.int/:data/assets/pdf_file/0014/303026/Compendium-of-initiatives-in-the-WHO-European-Region-rev1.pdf). 2 It is argued that NHS managers and staff are better equipped to understand the needs of the community they serve and to make better decisions about how to use limited resources when they listen to what matters to residents. 2
Although in theory Healthwatch may be well placed to provide this, there has been little research into how local Healthwatch organisations are organised, how they build and maintain relationships with different stakeholders and, ultimately, whether or not they are making a meaningful contribution as a key pillar of residents and patient involvement in the English NHS. Existing studies15,27,30 about Healthwatch have discussed some of the challenges and tensions faced by local Healthwatch organisations. However, because of the aims and design of the studies,15,27,30 which relied primarily on interviews and surveys, these studies could provide only post hoc reflections of events. Therefore, they could not capture the processual nature of relations and provided little evidence about the contexts in which Healthwatch operates, the daily practices through which its influence is created and maintained, and how this enables or hampers the improvement of services for patients. 15,27,30 This evidence gap is particularly problematic given Healthwatch’s role as a key partner in monitoring the quality – and supporting the design – of health and social care locally by providing the NHS and local authorities with information and advice based on the views of residents and patients. 5
In this study, we drew on ANT to explore how the variability of Healthwatch organisations emerged through the sociomaterial environments in which they work. These environments include mutually influencing connections among human actors (e.g. Healthwatch staff, volunteers and board members) and non-humans (e.g. funding, local authority and NHS meetings, governance arrangements, feedback forms and databases). For instance, we have shown that the official characterisation of different Healthwatch organisational structures as ‘standalone’ or ‘hosted’ tells us very little about how such organisations actually work and orient their practices of engagement. Rather, contingent interactions between human and non-human actors create a reality that does not necessarily accord with the fixed binary of Healthwatch types (i.e. ‘standalone’ or ‘hosted’). Nevertheless, this binary is regarded by Healthwatch as a crucial way of discussing intrinsic differences between its various organisations, and also as a factor in Healthwatch's ability to effectively present patient and public voice. However, our findings complicate this straightforward dualism (i.e. ‘hosted’ vs. ‘standalone’) and show that Healthwatch’s organisational structures are actually the product of a broader range of factors, including organisational histories, board composition, and strategic planning to better exploit financial opportunities. This complexity also emerges from the other sociomaterial structures, which we present in Chapter 5. Consider the effect of different funding arrangements in shaping the possibilities of Healthwatch and its ability to represent patient and public voice in its local systems. As we showed, different absolute amounts of local authority funding, the ways in which the funds are allocated and the different abilities and possibilities for Healthwatch organisations to attract funding external to the local authority contracts give rise to organisations across Healthwatch that not only look different (e.g. large Healthwatch organisations vs. small Healthwatch organisations), but deliver very different services to their respective local populations and systems. These findings show how Healthwatch actively emerges from these structures and creates its well-documented variability. Therefore, despite the fixed nature of local Healthwatch organisations’ statutory functions, and their supposedly uniform mission and identity, local Healthwatch organisations cannot be approached as intrinsically coherent organisations (i.e. there is no such a thing as an ideal Healthwatch organisation against which others are measured).
Local Healthwatch organisations’ variability in terms of organisational structures has far-reaching implications for their potential and influence in representing the voice and needs of patients and public in their local health and care systems. Such variability has potentially serious consequences, as it leads to unequal opportunities for people in different parts of England to participate meaningfully in health and care decision-making. Consider here the contrasting examples presented in Chapter 5, Institutional landscapes. Healthwatch Ashton was constrained in its ability to plan and conduct its own engagement activities with local people not only by the small amount of money it received but also by the particular mechanism by which its funding was allocated. Subsequently, this meant that Healthwatch Ashton largely relied on third parties to collect the views and experiences on its behalf, and also on its small cohort of volunteers to relay issues in an ad hoc way. These arrangements limited Healthwatch Ashton’s ability to hear and address the needs and views of the local community and to effectively prioritise some issues over others. Healthwatch Beecham, however, with its large and stable local authority and external funding, was able to recruit a range of staff with different specialist skills who could lead on specific streams of work and create and maintain partnerships with valuable local stakeholders, such as universities. These partnerships not only further enabled Healthwatch Beecham to bring in additional money and staff, but also enabled Healthwatch Beecham to carry out PPI in more rigorous ways. It is undeniable that the residents of Ashton had far fewer opportunities for their voices to be heard through Healthwatch than those of Beecham. This is an effect of the fact that Healthwatch’s involvement strategies and practices are a product of the sociomaterial structures in which, and through which, their work is performed. These practices cannot be analysed without taking account of the specific environments and organisational arrangements of the Healthwatch organisation through which it is delivered.
The aim of the study was to explore and enhance the local operation and impact of Healthwatch. Our discussion above has shown how Healthwatch works and produces effects, and has highlighted Healthwatch’s variability. The second aspect of our aim was to ‘enhance’ Healthwatch’s operation and impact and we did so through JIFs, which we detail in Chapter 6. During the JIFs, we discussed different examples of gathering and communicating evidence with Healthwatch staff, board members and their key partners, and jointly reflected with them on ways in which these methods might or might not be useful in their work to better evidence public and patient voice. We chose to focus on ‘evidence’ because Healthwatch’s practices and strategies for the gathering and use of patient and public voice constitute the very core of its mission and are crucial to better inform health and social care commissioning and provision. Like any other aspect of Healthwatch’s work, Healthwatch’s practices of gathering and creating evidence are shaped by the contingent entanglements of sociomaterial structures (e.g. funding arrangements, institutional landscapes) and these are largely defined as ‘local’ structures, demonstrated (and evidenced) by the variability among different Healthwatch organisations. The JIFs held at four of the five study sites were, therefore, ‘local’ in nature, gathering actors that contribute to defining the possibilities of that local Healthwatch organisation. However, the discussion at the JIFs indicated areas of similarity and agreement around the issue of evidence, which emphasised practices of collecting and deploying evidence valued by both Healthwatch and its key partners beyond the specificities of their local area. The JIFs led us to create a series of statements of good practice that related to how Healthwatch organisations collect, organise and communicate evidence about people’s experiences of health and care to their local system. By putting Healthwatch people and their partners in dialogue in an analytical evidence-influenced space in which dilemmas, aspirations and experiences could be discussed, the study provides an actionable output that all Healthwatch organisations can use to maximise the impact of the patient and public voice they represent in their local systems.
It remains to be seen what (if any) long-term transformative impact the COVID-19 pandemic will have on the relationships, practices and strategies we describe. The pandemic has raised new questions about Healthwatch’s role in local health and care systems. Our findings, relating to the period from March 2020 to February 2021, indicate that Healthwatch’s status derived from its statutory functions allowed it to be seen as a relevant and valued partner in local pandemic responses. Some local Healthwatch organisations, for instance, co-ordinated various local partners, especially among the VCSE sector, and, therefore, took up a role that is not formally included as a statutory function. This ability emerged from Healthwatch’s pre-existing institutional relationships and engagement with various sectors of the local health and care systems and was, therefore, an effect of the sociomaterial entanglements we describe above. Some local Healthwatch organisations were better able to mobilise resources, engagement strategies and relationships, whereas other Healthwatch organisations, which had struggled to find a meaningful place in their systems, found themselves (happily or not) marginal to the pandemic response effort. Therefore, the pandemic catalysed existing differences among Healthwatch organisations, possibly exacerbating the existing unequal opportunities for people to be meaningfully involved in local health and care decision-making processes.
Patient and public involvement was an integral element of this research project. In the planning phase, PPI successfully shaped the formulation of research questions, study design and plans for dissemination. During the study, members of the public (including volunteers at local Healthwatch organisations) were involved in various ways across the four phases, with varying degrees of success. As we discuss in Limitations, the fact that Healthwatch is not widely known among members of the public means that our public involvement was restricted to local volunteers of our Healthwatch study sites and HIP members. Although we hoped that patients and members of the public would be able to contribute effectively to the sense-making phases of the study and have their say in how Healthwatch might work better to serve their interest, the national COVID-19 restrictions, and the pressures faced by local Healthwatch organisations and their local partners who were our gatekeepers, made recruitment of these categories of local patients and public challenging.
Limitations
Self-reported impact in the survey
There are limitations to the usefulness of this kind of self-reported information on impact. For instance, we were unable to draw conclusions from the survey data as to whether or not particular organisational arrangements and relationship types lead to better impact among our local Healthwatch respondents.
Study site characteristics
There were two limitations relating to our study sites.
First, we did not ultimately succeed in recruiting a Healthwatch site with a host that held several Healthwatch contracts. Although we initially secured a local Healthwatch site with this characteristic, the host lost many of its contracts in the period between recruitment and the start of fieldwork. We approached other Healthwatch sites that matched this profile, but we were not successful in recruiting them. However, we decided that working with a Healthwatch site whose host had recently lost Healthwatch contracts would be of value to the broader aims of the study and we, therefore, aimed to recruit one of the remaining local Healthwatch sites of the host organisation we had initially approached. Importantly, this local Healthwatch site has one of the smallest value contracts in England and staff were enthusiastic about participating. Nevertheless, we ensured that the HIP contained two local Healthwatch sites that were hosted by organisations that hold more than four contracts and this mitigated the limitation to a certain extent.
Second, we would have liked to recruit a local Healthwatch site operating in a large urban area outside London. The Healthwatch site we initially recruited (referred to above) fulfilled this criterion. However, when we lost the study site because of the provider changing, we had already recruited our other study sites and, therefore, had very little flexibility to re-organise the selection. Having such a Healthwatch site would have given us a view of the challenges faced in urban areas outside London. We mitigated this limitation by including several Healthwatch sites from large urban areas in the HIP.
Involvement of local residents in the study
Although we observed interactions between Healthwatch staff and members of the public, and had interviewed and spoke informally to local residents and volunteers at all of our study sites, the direct voice of local residents is not prominent in this report. This is for two main reasons. First, the principal aim of the study was to explore and enhance the practices and strategies of local Healthwatch organisations. Second, although communicating the voice of local residents is a key aspect of Healthwatch work, residents themselves (other than volunteers) are not involved (with a few exceptions) in Healthwatch’s everyday work.
Effect of the COVID-19 pandemic in England
The COVID-19 pandemic made access to people and meetings more challenging during this time, as key people in the NHS, local authorities and Healthwatch were busier than before the emergency. Moving our phase 2 research online in 2020 resulted in less textured data from our study sites. Although we attended and observed meetings online and talked to staff before and after the events, we were less able to take advantage of the serendipitous and unplanned encounters, conversations and meetings that are possible in real life. This also reflected the new ways of working that our participants (including Healthwatch staff) were experiencing in their own working lives. Consequently, this may have resulted in us obtaining less rich data in that latter period of phase 2 than we might otherwise have obtained.
Recommendations for future research
-
Future research should explore the consequences for local Healthwatch organisations of the development of ICSs, as this is pertinent, given the passage of the Health and Care Act 2022,47 which has abolished CCGs and replaced them with Integrated Care Boards, which establishes ICSs on a statutory basis.
-
Future research should explore Healthwatch in an international comparative perspective. Healthwatch is the latest iteration of a long-standing practice in England of formal PPI in health service decision-making. Therefore, it may prove instructive to conduct a comprehensive comparison of such provision across the nations of the UK, and between England and other health systems around the world.
-
Future work should examine how the response to the COVID-19 pandemic has reconfigured the voluntary sector locally. The response to COVID-19 created new ways of working between the statutory and voluntary sector locally and nationally (including Healthwatch) and it may be important to track these changes and their effects so as to optimise the ways in which health and care planning and provision is organised post-pandemic.
-
Future research should investigate how Healthwatch responds formally and informally to newly emerging focus on public health and health inequalities. This further research may look not only at how health inequalities affect the work of Healthwatch (e.g. recruitment of staff in areas of deprivation), but also at how Healthwatch addresses demands by its system partner to reorient its focus to better understand local health inequalities.
Implications for policy, practice and research
Our findings have the following implications for policy, practice and research.
Review basis for national funding allocations to local Healthwatch organisations
There is significant variability in the work of Healthwatch that raises questions about whether or not there is equitable treatment of people across England in their ability to participate effectively in local health and social care planning and provision. A key element of this variability is the funding of local Healthwatch organisations. Our study shows that funding arrangements significantly shape everyday strategies and practices of collecting and transmitting patient and public voice. Healthwatch organisations with larger-value contracts can provide a more varied and specialised service to local people and the health and social care system. In addition, these larger Healthwatch organisations are better able to attract additional external funding, therefore further entrenching their differential abilities. Policy-makers and Healthwatch commissioners may want to consider the effect of different funding arrangements on exacerbating the variability of local Healthwatch organisations across England, therefore determining differential outcomes in Healthwatch’s ability to represent patient and public voice in each area and across England as a whole.
Clarify the role of Healthwatch in the changing commissioning landscape
Local Healthwatch organisations’ operations are determined by the different institutional landscapes in which they work. Changes in health and social care commissioning and provision – particularly the development of ICSs – raise questions about Healthwatch’s institutional location and role, which has remained formally unchanged since 2012. For instance, Healthwatch is granted a seat by statute on health and well-being boards. However, given not only the development of ICSs but also of other local forms of partnership, health and well-being boards may not be the optimal forum through which to provide formal contributions. Although Healthwatch was mentioned in the 2021 White Paper24 as a way in which public and patient voice could be represented at the ICS level, its involvement was not formally mandated in the subsequent Health and Care Act 2022. Certainly, Healthwatch’s involvement in integrated care to date has been variable. By reviewing and clarifying Healthwatch’s role in these new local and regional partnerships, policy-makers and commissioners may ensure that Healthwatch can more effectively influence the decision-making process on behalf of the patients and residents it serves.
Retain the statutory role of Healthwatch
The statutory nature of Healthwatch’s function is key to its ability to represent local voice to its health and social care partners. The fact that Healthwatch is legally mandated and that local Healthwatch organisations have statutory powers means that it has an official status that distinguishes it from other VCSE organisations, and this was highlighted during the COVID-19 pandemic when the health and social care system came under extreme stress; in most places during this period, Healthwatch was treated as a partner in the system’s pandemic response. This is important to note for various Healthwatch stakeholders, given the changes to the health and care system authorised by the Health and Care Act 2022. Likewise, local Healthwatch organisations may wish to reflect on how they made use of their formal status during the pandemic and how they can learn from this in the future, as this would enhance their participation in existing and new spaces so that the voice of the public is not neglected in local decision-making processes.
Recognise the important local co-ordinating role of Healthwatch
Many local Healthwatch organisations have successfully embraced a co-ordinating role between key stakeholders (both statutory and from the voluntary sector) in local health and care systems. However, although this role is not formally included in Healthwatch’s statutory functions, it nonetheless proved key in ensuring the involvement of local communities and addressing the needs of vulnerable populations, particularly in the COVID-19 pandemic response. Healthwatch may enhance its ability to represent local voices by actively cultivating this function to facilitate the participation of community groups, especially those that might otherwise go unnoticed. Local stakeholders, including Healthwatch commissioners, may be able to better support local Healthwatch organisations and their missions by acknowledging the importance of this function and the resources it requires.
Producing deep and broad findings is possible in varied organisations, such as Healthwatch, if researchers regularly involve many non-study site participants to sense-check data and to offer their own experiences and analysis as data. The combination of research methods and our innovative and sustained engagement with relevant stakeholders, such as the HIP and JIFs, ensured that our findings were locally and nationally relevant, contextually sensitive and generalisable. These engagements strengthened collaborations between the study team and the study participants as well as among participants themselves (as in the case of our HIP members). These engagements also contributed to participants’ ownership of the research process, making study outputs more clearly useful for them.
Conclusion
In this study, we have explored the local operation and impact of Healthwatch in England. We have pointed to ways in which its role in ensuring effective patient and public voice in the commissioning and provision of health and care services can be enhanced. We pursued a mixed-methods approach, incorporating surveys, ethnographic fieldwork (i.e. interviews and observations) and collaborative sense-making. We mapped the diversity of organisational structures, activities, relationships and impact across the Healthwatch network in England. We explored the strategies, practices and sociomaterial infrastructures that shape the possibilities of Healthwatch organisations in any given local environment, and traced how actors come together to form the work of local Healthwatch organisations. We found that the diversity of the Healthwatch network belies its otherwise unitary appearance. This diversity – especially in differential funding arrangements – has considerable implications for equity of access to influencing health and care planning and provision for residents across England. Nevertheless, the study produced generalisable principles of good practice regarding the collection and communication of evidence. We suggest that the adoption of these practices will enhance the operation and impact of Healthwatch.
Acknowledgements
We thank the large number of people who made this study possible. Foremost, we thank the staff, board members and volunteers of the five local Healthwatch study sites for their enthusiasm and commitment to the project. These participants kindly allowed us to shadow them at meetings and events and pester them for chats and interviews, and introduced us to their partners in their local areas. We also thank all those NHS, local authority staff and representatives of voluntary sector organisations who agreed to be interviewed by us, as well as those who took part in the JIFs.
The 15 members of the HIP generously gave their time and their thoughts and adapted marvellously to the challenges and opportunities of moving our discussions online during the COVID-19 pandemic, and this study would be infinitely poorer without their participation.
The production of our phase 1 national survey was made possible by the advice of six former Healthwatch CEOs and managers who offered invaluable comments on survey questions. Thanks too to Trevor Murrells for bringing his statistical skills to bear on the survey data analysis.
We thank Healthwatch England for giving us an opportunity to publicise the study and to discuss some of its early findings at two consecutive Healthwatch conferences. We would like to thank Jacob Lant at Healthwatch England for his unflagging support of the study and for his stimulating discussions about the work and direction of Healthwatch more broadly.
Finally, we are grateful to the following members of our Advisory Group for their advice and support throughout the project:
-
Dr Jonathan Boote, independent researcher
-
Councillor Rebecca Charlwood, Leeds City Council
-
Professor Michael Dent (chairperson), Staffordshire University
-
Pete Flavell, Healthwatch Sutton
-
Dr Andy Gibson, University of West of England Bristol
-
Tim Gilling, formerly of the Centre for Governance and Scrutiny
-
Jacob Lant, Healthwatch England
-
Dr Helen Lloyd, University of Plymouth
-
Shani Shamah, PPI advisor
-
Monica Stannard, PPI advisor.
We thank the NIHR reviewers and editors for their insightful comments and suggestions for improvement.
Contributions of authors
Giulia Zoccatelli (https://orcid.org/0000-0001-9292-5155) (Research Fellow, King’s College London) is a joint first author, contributed substantially to the study design, led and conducted data collection in all four phases, led and contributed to overall data analysis, and led and contributed substantially to report writing.
Amit Desai (https://orcid.org/0000-0003-2234-2872) (Research Fellow, King’s College London) is a joint first author, contributed substantially to the study design, led and conducted data collection in all four phases, led and contributed to overall data analysis, and led and contributed substantially to report writing.
Glenn Robert (https://orcid.org/0000-0001-8781-6675) (Professor of Healthcare Quality and Innovation, King’s College London) was the principal investigator, managed the project, led the overall study design, co-ordinated the study team, conducted data collection and analysis with the HIP, contributed to overall data analysis, contributed to report writing and gave final approval of the manuscript.
Graham Martin (https://orcid.org/0000-0003-1979-7577) (Professor, and Director of Research, The Healthcare Improvement Studies Institute, University of Cambridge) contributed to overall study design, conducted data collection and analysis with the HIP, contributed to overall data analysis and report writing, and gave final approval of the manuscript.
Sally Brearley (https://orcid.org/0000-0001-7918-7485) (Visiting Senior Research Fellow, King’s College London) contributed to overall study design, conducted data collection and analysis with the HIP, contributed to overall data analysis and report writing, and gave final approval of the manuscript.
Data-sharing statement
All qualitative data generated that can be shared are contained within the report. All data queries and requests should be submitted to the corresponding author for consideration.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Zoccatelli G, Desai A, Martin G, Brearley S, Murrels T, Robert G. Enabling ‘citizen voice’ in the English health and social care system: a national survey of the organizational structures, relationships and impacts of local Healthwatch in England. Health Expect 2020;23:1108-17. https://doi.org/10.1111/hex.13086.
- World Health Organization . Lessons from Transforming Health Services Delivery: Compendium of Initiatives in the WHO European Region 2016.
- Government of Canada . The Health Canada Policy Toolkit for Public Involvement in Decision Making 2005. www.canada.ca/en/health-canada/corporate/about-health-canada/reports-publications/health-canada-policy-toolkit-public-involvement-decision-making.html (accessed 10 July 2021).
- NHS England . Engaging Local People – A Guide for Local Areas Developing Sustainability and Transformation Plans 2017. www.england.nhs.uk/wp-content/uploads/2017/06/engaging-local-people-stps.pdf (accessed 10 July 2021).
- Great Britain . Health and Social Care Act 2012 2012.
- Scottish Government Health and Social Care Directorate . CEL 4 (2010) - Informing, Engaging and Consulting People in Developing Health and Community Care Services 2010. www.sehd.scot.nhs.uk/mels/CEL2010_04.pdf (accessed 26 May 2022).
- NHS England . Patient and Public Participation in Commissioning Health and Care: Statutory Guidance for CCGs and NHS England 2017. www.england.nhs.uk/wp-content/uploads/2017/05/patient-and-public-participation-guidance.pdf (accessed 7 July 2021).
- Flood CM. Scoping the shape of an iceberg: the future of public involvement in heath policy: reflecting on ‘public involvement policies in health: exploring their conceptual basis’. Health Econ Policy Law 2015;10:381-5. https://doi.org/10.1017/S1744133115000092.
- Bruni RA, Laupacis A, Martin DK. University of Toronto Priority Setting in Health Care Research Group . Public engagement in setting priorities in health care. CMAJ 2008;179:15-8. https://doi.org/10.1503/cmaj.071656.
- Florin D, Dixon J. Public involvement in health care. BMJ 2004;328:159-61. https://doi.org/10.1136/bmj.328.7432.159.
- Tritter J, Koivusalo M, Ollila E, Dorfman P. Globalisation, Markets and Healthcare Policy: Redrawing the Patient as Consumer. Abingdon-on-Thames: Routledge; 2010.
- Wait S, Nolte E. Public involvement policies in health: exploring their conceptual basis. Health Econ Policy Law 2006;1:149-62. https://doi.org/10.1017/S174413310500112X.
- Duschinsky R, Paddison C. ‘The final arbiter of everything’: a genealogy of concern with patient experience in Britain. Soc Theory Health 2018;16:94-110. https://doi.org/10.1057/s41285-017-0045-2.
- Stewart E, Ercia A, Greer SL, Donnelly PD. Between a rock and a hard place: comparing arms’ length bodies for public involvement in healthcare across the UK. Health Policy 2020;124:454-61. https://doi.org/10.1016/j.healthpol.2020.02.004.
- Martin GP, Carter P, Bevir M, Waring J. Decentring Health Policy. Abingdon-on-Thames: Routledge; 2017.
- Hogg CNL. Patient and public involvement: what next for the NHS?. Health Expect 2007;10:129-38. https://doi.org/10.1111/j.1369-7625.2006.00427.x.
- Department of Health and Social Care (DHSC) . Local Healthwatch: A Strong Voice for People – the Policy Explained 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/215097/dh_133288.pdf (accessed 10 July 2021).
- Healthwatch England . State of Support: Funding for Local Healthwatch 2019 20 2020.
- Coleman A, Checkland K, Segar J, McDermott I, Harrison S, Peckham S. Joining it up? Health and wellbeing boards in English local governance: evidence from Clinical Commissioning Groups and Shadow Health and Wellbeing Boards. Local Gov Stud 2014;40:560-80. https://doi.org/10.1080/03003930.2013.841578.
- Humphries R. Health and wellbeing boards: policy and prospects. J Integr Care 2013;21:6-12. https://doi.org/10.1108/14769011311305521.
- Visram S, Hunter DJ, Perkins N, Adams L, Finn R, Gosling J, et al. Health and wellbeing boards as theatres of accountability: a dramaturgical analysis. Local Gov Stud 2021;47:931-50.
- Gansu M. What Do People Think About Local Healthwatch and Why? 2015. https://localdemocracyandhealth.com/2015/12/07/what-do-people-think-about-local-healthwatch-and-why/ (accessed 7 July 2021).
- NHS . NHS Long Term Plan 2019. www.longtermplan.nhs.uk/publication/nhs-long-term-plan (accessed 27 May 2022).
- Department of Health and Social Care (DHSC) . Integration and Innovation: Working Together to Improve Health and Social Care for All 2021. assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/960549/integration-and-innovation-working-together-to-improve-health-and-social-care-for-all-print-version.pdf (accessed 26 May 2022).
- Taylor J, Tritter J. Local Involvement Networks: Learning from the Early Adopter Programme. Coventry: National Centre for Involvement; 2007.
- Peckham S, Wilson P, Williams L, Smiddy J, Kendall S, Brooks F, et al. Commissioning for long-term conditions: hearing the voice of and engaging users – a qualitative multiple case study. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02440.
- Gilburt H, Dunn P, Foot C. Local Healthwatch – Progress and Promise. London: The King’s Fund; 2015.
- Djellouli N. Public Involvement in Decisions to Change Health Services at a Large-Scale 2020.
- Carter P, Martin G. Engagement of patients and the public in NHS sustainability and transformation: an ethnographic study. Crit Soc Policy 2018;38:707-27. https://doi.org/10.1177/0261018317749387.
- Carter P, Martin G. Challenges facing Healthwatch, a new consumer champion in England. Int J Health Policy Manag 2016;5:259-63. https://doi.org/10.15171/ijhpm.2016.07.
- Hunter DJ, Perkins N, Visram S, Adams L, Finn R, Forrest A, et al. Evaluating the Leadership Role of Health and Wellbeing Boards As Drivers of Health Improvement and Integrated Care Across England 2018. https://eprints.whiterose.ac.uk/151457/1/Evaluating%20HWBs%20FINAL%20REPORT%20-%20April%202018%20Final.pdf (accessed 26 May 2022).
- Law J, Hassard J. Actor Network Theory and After. Oxford: Blackwell Publishing; 1999.
- Latour B. Reassembling the Social: An Introduction to Actor-Network-Theory. New York, NY: Oxford University Press; 2007.
- Cresswell KM, Worth A, Sheikh A. Actor-Network Theory and its role in understanding the implementation of information technology developments in healthcare. BMC Med Inform Decis Mak 2010;10. https://doi.org/10.1186/1472-6947-10-67.
- Cresswell K, Worth A, Sheikh A. Implementing and adopting electronic health record systems: how actor-network theory can support evaluation. Clin Gov Int J 2011;16:320-36. https://doi.org/10.1108/14777271111175369.
- Nguyen L, Bakewell L, Wickramasinghe N, Haddad P, Muhammad I, Moghimi H, et al. Transition from paper to electronic nursing documentation in residential aged care: an actor network theory analysis. Electron J Health Inform 2015;9:1-12.
- Greenhalgh T, Swinglehurst D, Stones R. Rethinking resistance to ‘big IT’: a sociological study of why and when healthcare staff do not use nationally mandated information and communication technologies. Health Serv Deliv Res 2014;2. https://doi.org/10.3310/hsdr02390.
- Tomlin Z, Peirce S, Elwyn G, Faulkner A. The Adoption Space of Early-Emerging Technologies: Evaluation, Innovation, Gatekeeping (PATH). Final Report 2012.
- Williams I, Harlock J, Robert G, Mannion R, Brearley S, Hall K. Decommissioning health care: identifying best practice through primary and secondary research – a prospective mixed-methods study. Health Serv Deliv Res 2017;5. https://doi.org/10.3310/hsdr05220.
- Donetto S, Desai A, Zoccatelli G, Robert G, Allen D, Brearley S, et al. Organisational strategies and practices to improve care using patient experience data in acute NHS hospital trusts: an ethnographic study. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07340.
- Desai A, Zoccatelli G, Adams M, Allen D, Brearley S, Rafferty AM, et al. Taking data seriously: the value of actor-network theory in rethinking patient experience data. J Health Serv Res Policy 2017;22:134-6. https://doi.org/10.1177/1355819616685349.
- Donetto S, Desai A, Zoccatelli G, Allen D, Brearley S, Rafferty AM, et al. Patient experience data as enacted: sociomaterial perspectives and ‘singular-multiples’ in health care quality improvement research. Sociol Health Illn 2021;43:1032-50. https://doi.org/10.1111/1467-9566.13276.
- Akrich M, Callon M, Latour B, Monaghan A. The key to success in innovation part I: the art of interessement. Int J Innov Manag 2002;6:187-206. https://doi.org/10.1142/S1363919602000550.
- Mohrman SA, Gibson CB, Mohrman AM. Doing research that is useful to practice a model and empirical exploration. Acad Manage J 2001;44:357-75. https://doi.org/10.5465/3069461.
- Office for National Statistics . Population Density Tables n.d. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationdensitytables (accessed 26 May 2022).
- Healthwatch . Our History and Functions 2021. www.healthwatch.co.uk/our-history-and-functions (accessed 26 May 2022).
- Great Britain . Health and Care Act 2022 2022.
- Zoccatelli G, Desai A, Martin G, Brearley S, Robert G, Beresford P, et al. COVID-19 and Co-production in Health and Social Care Research, Policy and Practice. Volume 1: The Challenges and Necessity of Co-production. Bristol: Policy Press and Bristol University Press; 2021.
Appendix 1 Healthwatch study site profiles
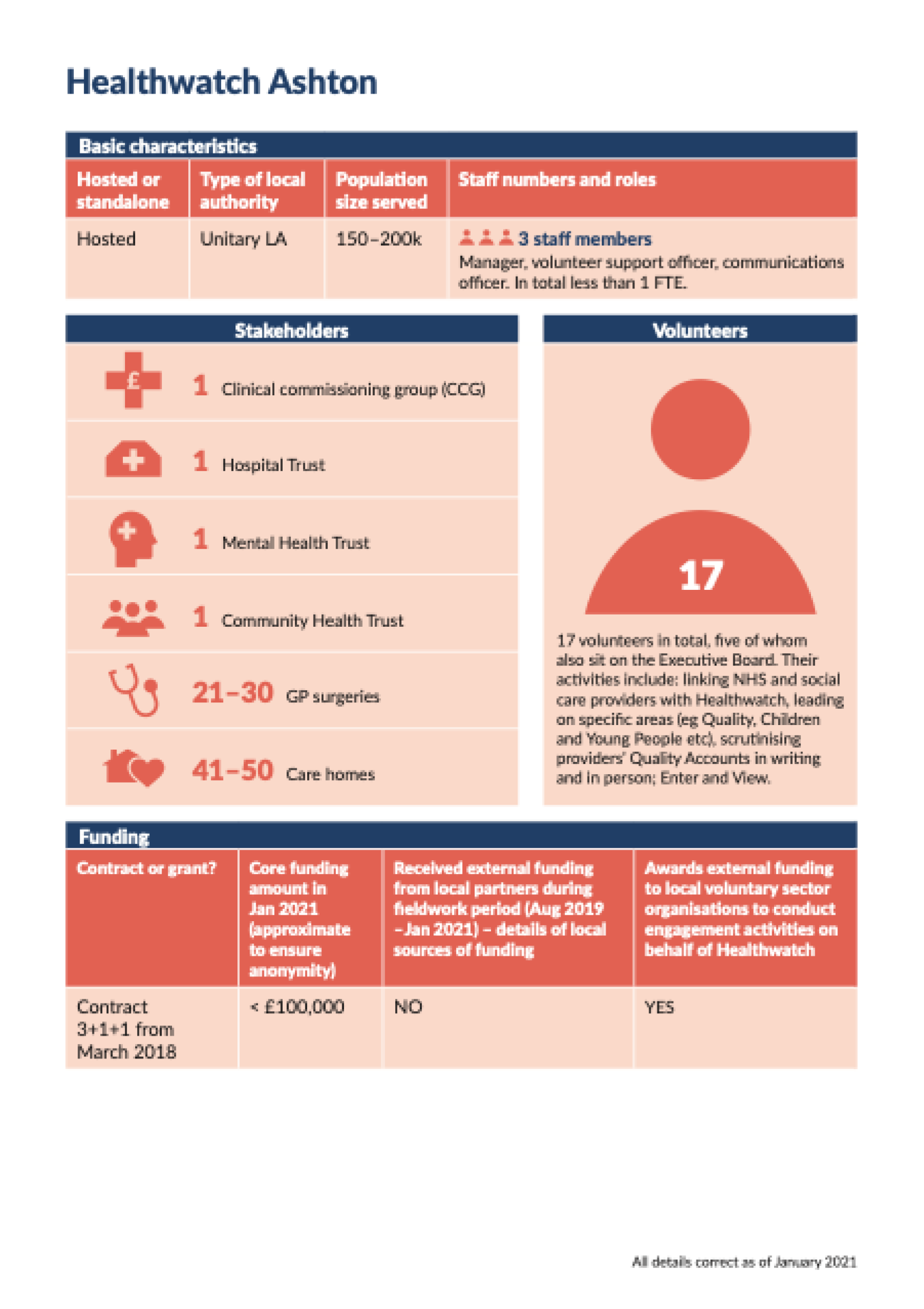
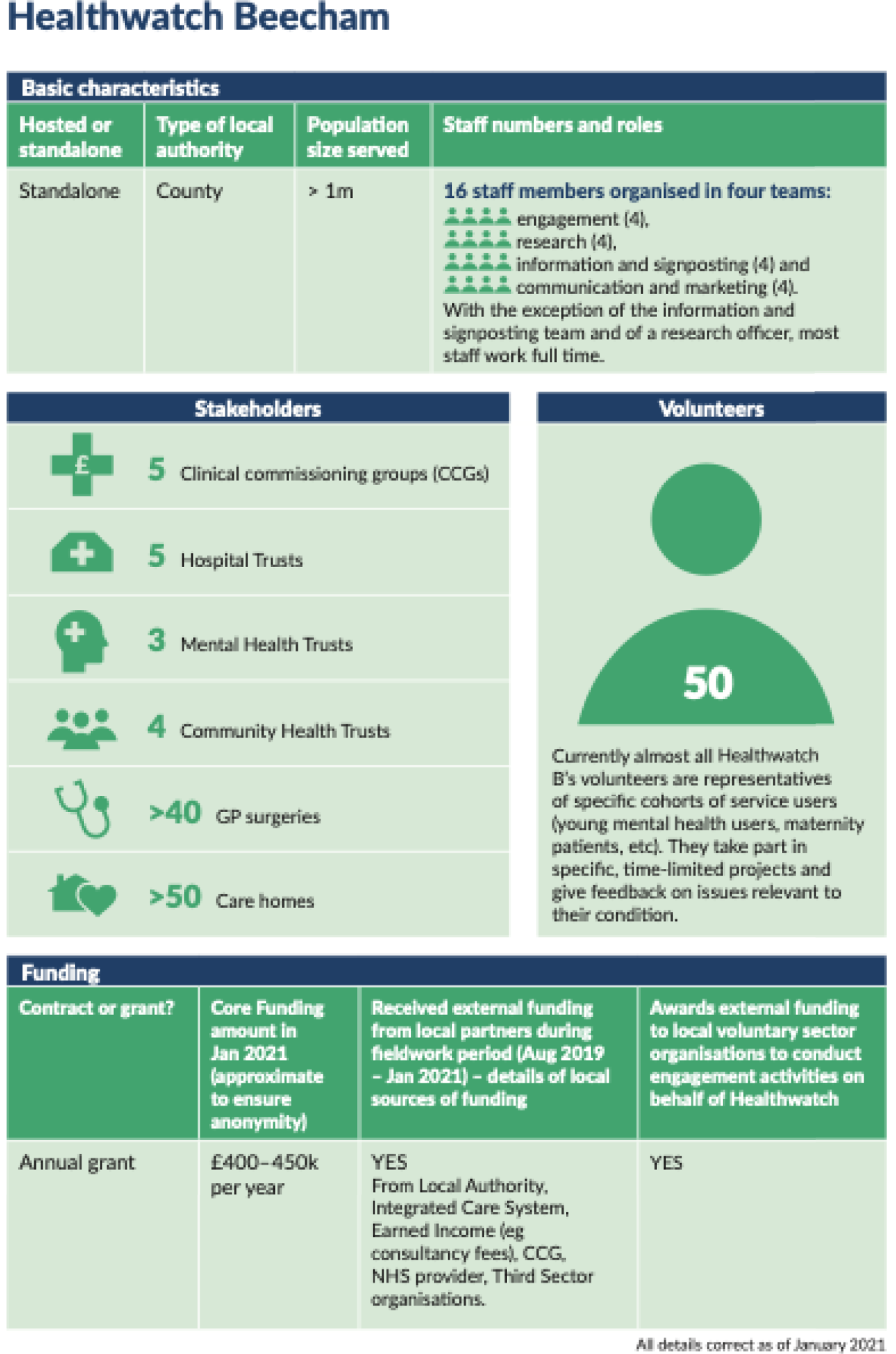
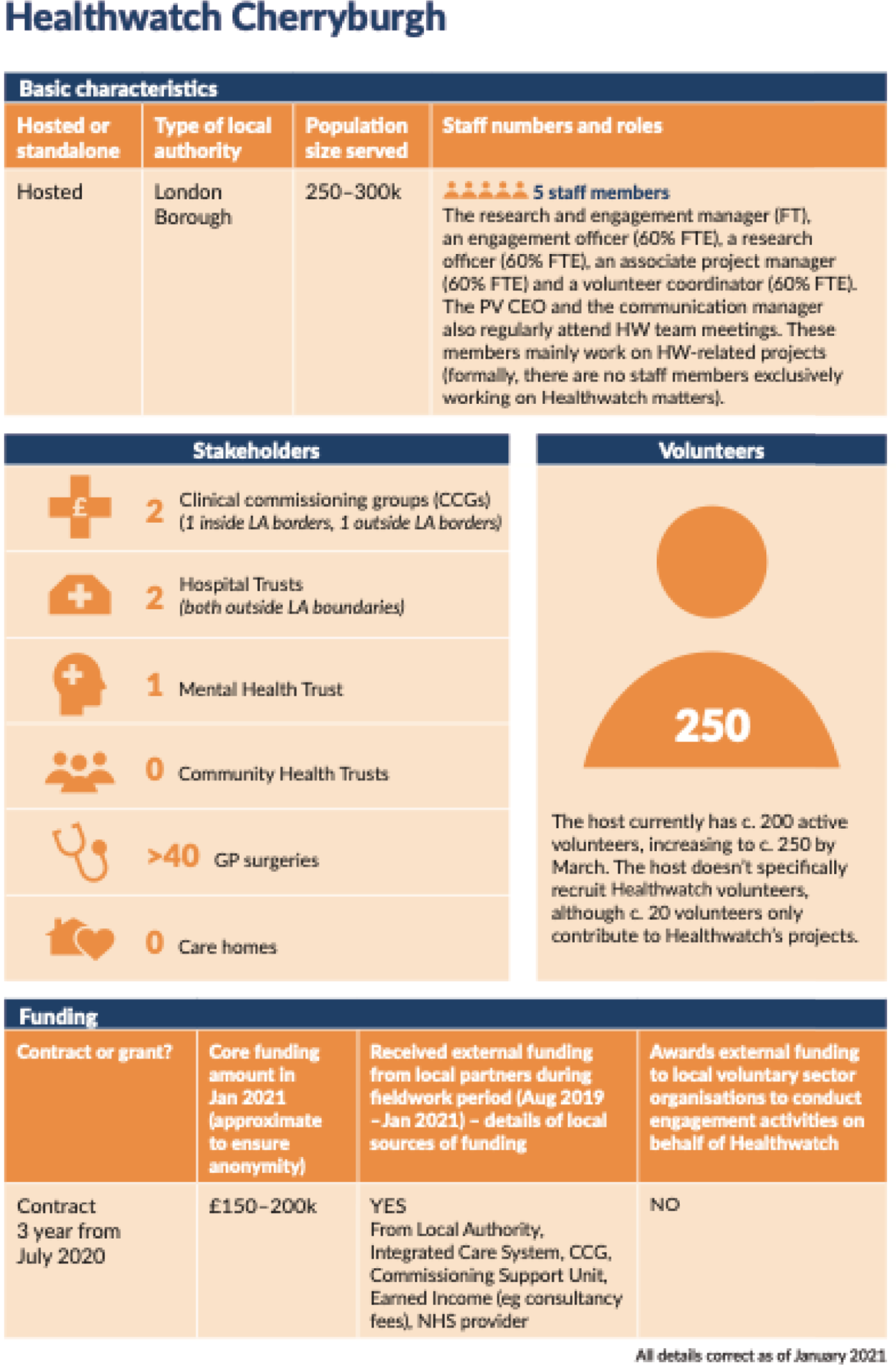
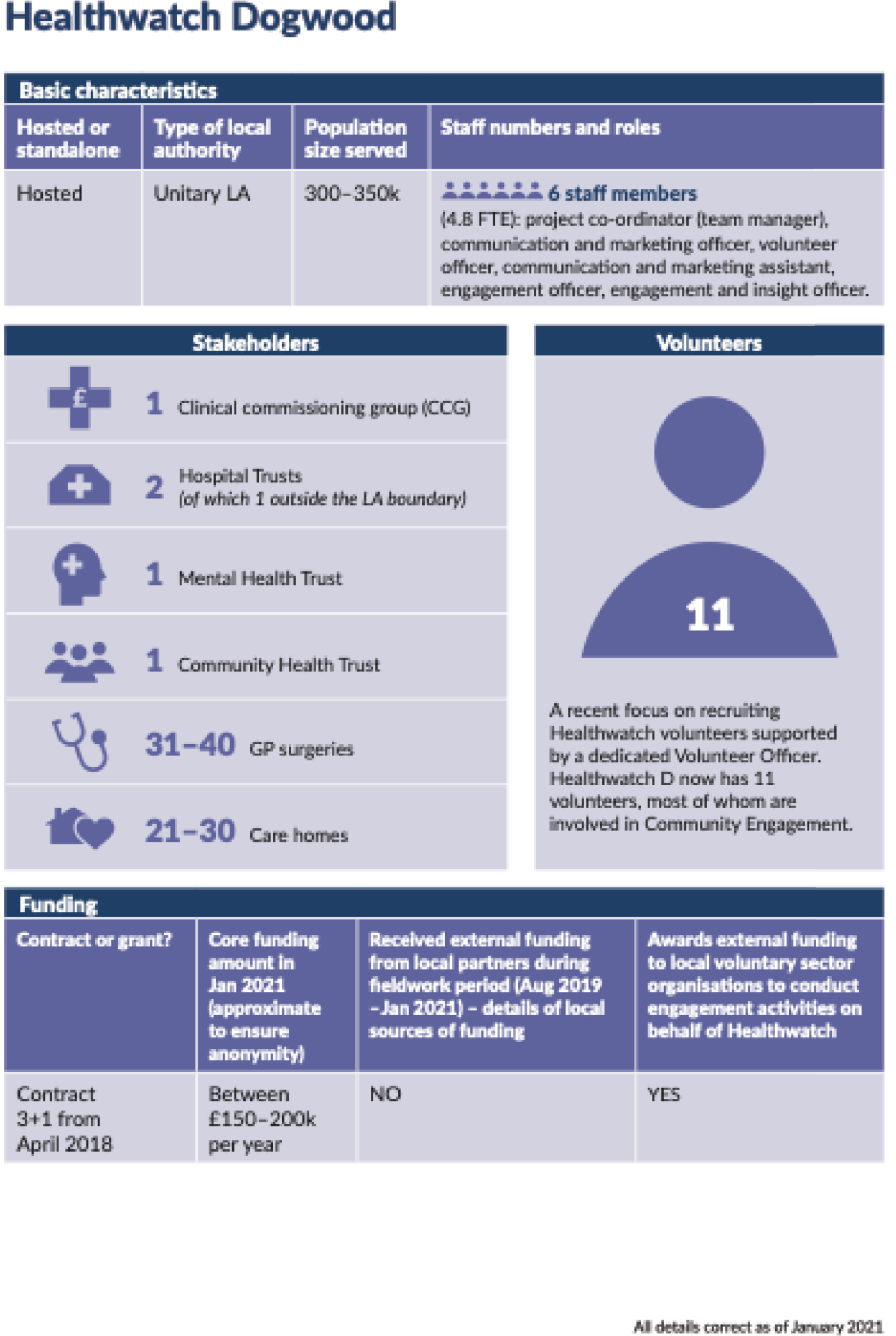
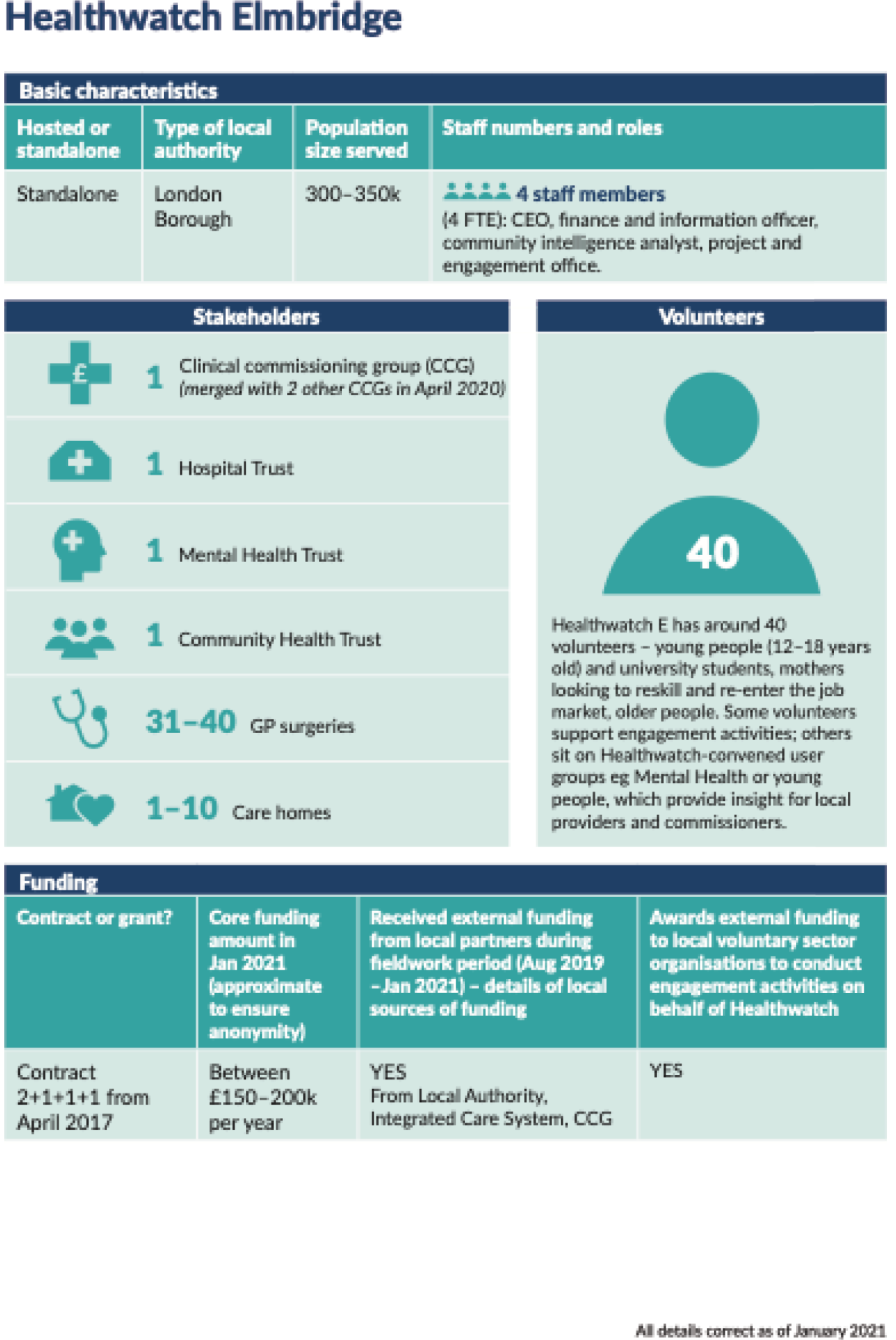
Appendix 2 Detailed description of pre-pandemic Healthwatch Involvement Panel meetings
Healthwatch Involvement Panel meeting 1 (July 2019)
The first meeting of the HIP took place over the course of a whole day. Fourteen members of the HIP attended. The HIP met in July 2019 and by this point we had recruited our phase 2 study sites but had not yet begun fieldwork.
The morning was devoted to establishing the ground rules for the HIP and introducing the study and its methods to them. In the afternoon, we held a ‘poster activity’ to introduce the study sites and to learn more about the HIP members’ Healthwatch organisation. We created a large format poster outlining the key features of each of the Healthwatch study sites. We asked each HIP member to browse the posters, discuss them with fellow HIP members and attach Post-it® (3M, Cynthiana, KY, USA) note comments or questions raised by the key features, which the study team would then answer or reflect on. We also asked each HIP member to select a study site that was most similar to their own and to give their reason for that choice. It was during this activity that HIP members first suggested that an additional Healthwatch study site that was both standalone and had a relatively low contract value be included (see Chapter 2, Fieldwork at five local Healthwatch study sites).
We also wanted to learn more about the range of views about Healthwatch present in the HIP. To this end, we organised a small-group and plenary discussion session centred around several statements or ‘provocations’ about aspects of Healthwatch work.
The provocations were as follows:
-
Healthwatch is unable to make real impact in areas where the local authority has a poor record of working with, and supporting, civil society.
-
Healthwatch cannot be a ‘critical friend’ to their local health and social care stakeholders. If they try, they fail.
-
The NHS is overwhelmed by patient feedback. Healthwatch should not be providing more patient feedback which the NHS lacks the resources to act on.
Towards the end of the first meeting, we facilitated a discussion of the HIP’s role in the study and reflections on the first meeting to ensure that members could air their views about their involvement and on the project more broadly.
Healthwatch Involvement Panel meeting 2 (November 2019)
The second HIP meeting took place in November 2019 when Amit Desai and Giulia Zoccatelli had been conducting fieldwork at four of the five study sites for 3 months. During our data collection at the study sites, we had become aware of the increasing importance of new integrated NHS structures (i.e. ICSs and PCNs) to the work of local Healthwatch organisations. We were also becoming aware of some differences among and within our Healthwatch study sites about how they conceptualised and practised Healthwatch ‘independence’. The HIP meeting lasted 3.5 hours and 15 HIP members attended.
The first activity probed the HIP’s views and experiences of the emerging NHS structures. We employed a 1–2–4 process to structure the discussion. Panel members were asked to reflect on Healthwatch’s role and relationships with the ICSs/PCNs individually, in pairs, in groups of four and then, finally, in plenary. At each stage, the study team posed questions to structure the discussion.
The second activity aimed to explore the question of Healthwatch’s role in the health and social care system. We facilitated a debate on the following motion:
This House believes that Healthwatch should focus on listening to the patient and public voice and transmitting it to others with the power to act; it is not Healthwatch’s role to collaborate in the design and implementation of changes to services.
The HIP members split into two teams to support and oppose the motion. Study team members facilitated the discussion and took notes during the debate.
Appendix 3 Description of activities at cross-site and local joint interpretive forums
Cross-site joint interpretive forum
Discussion of pre-circulated Healthwatch study site profiles
An objective of the cross-site JIF was to provide an opportunity for study sites to learn about each other’s organisational and funding arrangements, relationships, and daily strategies and practices. Until then, Healthwatch study sites had been kept anonymous from each other and participants were keen to learn the identities and activities of the other participating study sites. Based on some research and team members’ previous experience with holding JIFs40 we concluded that asking each Healthwatch team to present this information themselves at the workshop would be passive, time-consuming and subject to variation in quality and format, particularly given the constraints of holding the workshop virtually. To allow for participants to be actively engaged in the workshop, we decided to pre-circulate key information about each Healthwatch site’s structure and organisation by way of five ‘Healthwatch profiles’; that is, one for each study site. Participants were asked to read the profiles before the meeting and prepare three comments or questions to ask each other based on this information. The activity allowed the research team and JIF participants to gauge what participants found interesting about each study site’s structures, strategies and practices. Each Healthwatch profile consisted of the following seven elements:
-
general information about each Healthwatch (e.g. name of the local authority, whether that Healthwatch was hosted or standalone and a brief 50-word outline of the history and characteristics of each organisation/host organisation)
-
the composition and role of the Healthwatch/host organisation board
-
number of staff, FTE and roles
-
number and type of volunteers, as well as a brief 50-word description of their level of involvement in the organisation
-
financial arrangements (e.g. contract or grant, funding amount, length of the contract, amount, type and source of external funding if received)
-
outline of the key feature of each Healthwatch’s institutional landscape
-
‘talking points’ that mentioned a noteworthy aspect of each Healthwatch’s practices and strategies.
Presentation of emerging themes from fieldwork
During the workshop, the research team gave two presentations, discussing the following four inter-related emerging themes from the fieldwork:
-
relationships and ethics
-
scale and scope
-
engagement
-
volunteering.
The emerging themes were produced through discussions among members of the study team over several meetings in December 2020 and January 2020. A summary of the four themes was shared with all participants before the cross-site JIF and included research of some key questions that guided the study team’s analysis in relation to each topic. A copy of these summaries is included in Appendix 4. We wanted to check that our overall approach and emerging findings were accurate and relevant to Healthwatch study sites before drafting our report. The purpose of the presentation (and of the JIF as a whole) was to test if the kinds of analysis and ideas we were producing, and which we considered valuable, would be of interest to Healthwatch study sites or, alternatively, would need refining to make them more relevant to Healthwatch daily practice.
‘Provocations’ activity
After presenting the emerging themes from fieldwork, we held two small-group discussions of four ‘provocations’ directly relating to the topics presented. The ‘provocations’ were statements designed to spark debate among JIF participants. They were formulated by Amit Desai and Giulia Zoccatelli and were presented to the whole study team during a meeting held to plan for the workshop. Wording was subsequently refined by the other members of the study team to ensure maximum benefit from the ensuing discussions. The four provocations were as follows:
-
Healthwatch should refrain from seeking additional commissioned work from local stakeholders. This constraints Healthwatch’s independence and its ability to hold the system to account.
-
If decision-making processes move to the level of ICS or merged CCGs, the work of local Healthwatch will become irrelevant.
-
There is little point in gathering health and social care experiences from a large number of undifferentiated service users with the aim of improving the quality of care. Healthwatch must focus on specific marginalised groups in society to help the system address health inequalities.
-
Volunteering in Healthwatch is more trouble than it’s worth, both for the organisation and for the volunteers themselves. If Healthwatch engaged the public effectively and comprehensively, it would have no need of volunteers.
Participants were divided into three groups (‘breakout rooms’), each of which contained a representative from each different Healthwatch site, and were chaired by Glenn Robert, Graham Martin and Sally Brearley. The groups discussed each provocation for 10 minutes, with a short summary of the discussion presented to all JIF participants by group chairpersons after each round. The entire JIF, including the breakout rooms, were recorded and transcribed.
Local joint interpretive forums
Presentation on Healthwatch and the study
The study team gave a 15-minute presentation about:
-
aims of the meeting
-
historical overview of Healthwatch and its statutory functions
-
study aims and objectives
-
study methods and existing data sources
-
study outputs.
At the end of the presentation, the team asked for comments and took questions from the audience.
Discussion about different types of evidence collected by Healthwatch
The plenary discussion was based on the content of a document prepared by the study team, which detailed several ways in which Healthwatch study sites produce evidence to reflect the views and experiences of their residents. The material in this document was sourced from data from our phase 2 fieldwork. The document was adapted for each JIF to present and discuss ‘ways of producing evidence’ less commonly used at that Healthwatch study site. The team circulated the document via e-mail the day before the JIF. Participants were able to read the document ahead of the meeting, but time was also allocated during each meeting for participants to read the document, make notes and prepare questions.
Amit Desai and Giulia Zoccatelli chaired a plenary discussion that involved Healthwatch staff, board members and local stakeholders taking part in the meeting. The discussion took between 60 and 90 minutes (depending on the overall length of the meeting and as agreed at each Healthwatch) and was structured around the following questions:
-
How do these different approaches compare with current practices used by your local Healthwatch?
-
From your different perspectives, would any of these be desirable approaches for your local Healthwatch to pursue?
-
For external stakeholders: which type of evidence would be useful for your organisation to receive? Why? How would you envisage using it?
-
For Healthwatch staff and board members: would any of these practices of producing evidence help you be more effective in representing local people to your local health and care partners?
After addressing these questions, participants were asked to reflect on the impact on local Healthwatch practices and strategies of evidence production from the COVID-19 pandemic and from recent changes in health and care services commissioning and provision (e.g. ICSs, PCNs).
Appendix 4 Cross-site joint interpretive forum materials: emerging themes
Appendix 5 Draft statements of good practice relating to Healthwatch practices and strategies of producing evidence
Appendix 6 Seven ways of producing evidence (circulated to participants at local joint interpretive forums)
List of abbreviations
- ANT
- actor network theory
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- COO
- chief operating officer
- CQC
- Care Quality Commission
- DHSC
- Department of Health and Social Care
- FTE
- full-time equivalent
- GP
- general practitioner
- HIP
- Healthwatch Involvement Panel
- ICP
- integrated care partnership
- ICS
- integrated care system
- JIF
- joint interpretive forum
- JPB
- joint partnership board
- LINk
- local involvement network
- LRCV
- Local Reform and Community Voices
- NIHR
- National Institute for Health and Care Research
- PCN
- primary care network
- PhD
- Doctor of Philosophy
- PPG
- Patient Participation Group
- PPI
- patient and public involvement
- STP
- sustainability and transformation partnership
- VCSE
- Voluntary, Community and Social Enterprise
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/YUTI9128).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
