Notes
Article history
The contractual start date for this research was in October 2020. This synopsis began editorial review in January 2023 and was accepted for publication in April 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Rattray et al. This work was produced by Rattray et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Rattray et al.
Introduction
Background
Nurses who worked in critical care areas of the NHS were at the forefront of the coronavirus disease caused by the SARS-CoV-2 virus (COVID-19) pandemic. Critical care was a highly charged environment that placed significant and sometimes unique demands on critical care nurses (CCNs) and nurses redeployed to critical care from other areas (RDNs). What has emerged in the literature over the last 2–3 years is the emotionally challenging experience of working in critical care with concerns about becoming personally infected and taking this to vulnerable family members, dealing with a significantly increased workload, and concerns around providing quality care. 1 Additionally, the mortality rate of COVID-19 patients was exceptionally high; care had to be delivered using full personal protective equipment (PPE); in the early stages of the pandemic, how to manage patients effectively was unclear, relatives had to be supported at a distance often via screens on mobile devices, staff worked while understanding the potential risks to personal (higher risks because of aerosol-generating procedures) and family health, and CCNs also had to supervise redeployed staff with limited or no critical care experience.
Participants described feelings of hopelessness; they reported a lack of managerial support2 and physical and emotional exhaustion. Several studies have highlighted nurses’ increased risk of psychological distress and burnout. 3–5 The pandemic also highlighted a general unpreparedness of healthcare systems at all levels. Staffing models changed,6 with non-CCNs redeployed to support this stretched workforce. Critical care nursing skills were crucial.
Most studies assessing the impact of COVID-19 on this occupational group are cross-sectional, with limited comparisons from before the pandemic. Furthermore, these studies tend not to be underpinned by any theoretical model or framework to guide the analyses and interpretation of findings. This makes identification of individual and organisational outcomes difficult.
How an organisation supports its workforce, especially at times of increased demand, is key to staff well-being, the ability to retain staff and achievement of its aims. We need also to recognise the enduring nature of psychological distress and post-traumatic stress symptoms, which can be difficult to treat, and increased staff sickness and turnover. Taken together, this emphasises the importance of supporting staff both during and as we emerge from the pandemic for the benefit of individual staff members, quality of critical care services, and ultimately outcomes for patients and their relatives.
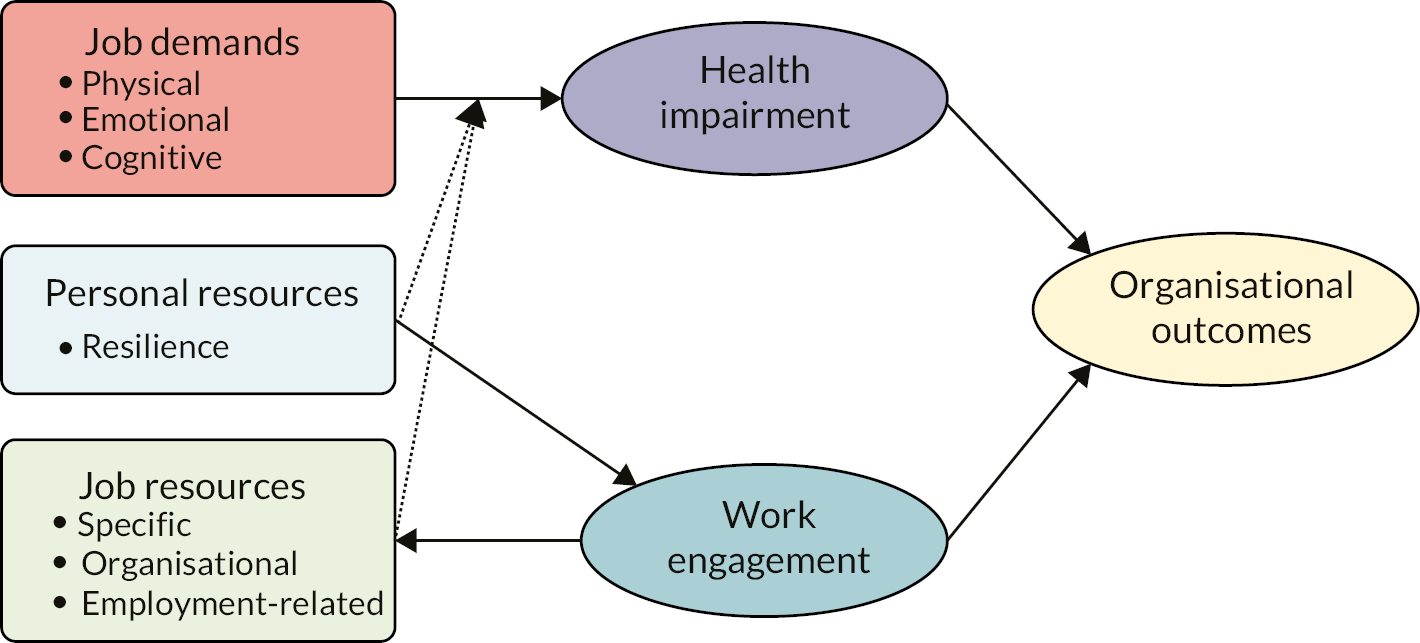
The aim of this study was to understand the impact of COVID-19 on CCNs and RDNs and NHS organisations. Our understanding of the impact of working in critical care during the pandemic was underpinned by a theoretical model of occupational stress, the Job demands−resources (JD-R) model7,8 (Figure 1). The JD-R model is a dual-process model that describes three outcomes, two of which can be thought of as outcomes for individual nurses, namely, health impairments and work engagement. It is a flexible model that allows application of a range of measures, and importantly facilitates flexible testing of relationships across antecedents and outcomes. 9 In this study, health impairments were conceptualised as indicators of stress, that is, psychological distress, burnout and symptoms of post-traumatic stress disorder (PTSD). Work engagement was operationalised as vigour (energy brought to work), dedication (pride and commitment) and absorption (concentration and immersion within work). The third group of outcomes are more appropriately considered as outcomes of importance for the organisation, such as nurses’ perceptions of patient safety, quality of care, job satisfaction, intention to change jobs etc.
The JD-R model also identifies job demands as sources of health impairment and resources (personal and job resources) as support for work engagement. Demands predict worse health, in this case, poorer mental health, higher burnout and increased symptoms of PTSD. Resources strengthen work engagement. Health impairments and work engagement are the proximal predictors of organisational outcomes. A healthier and more engaged workforce predicts more positive organisational outcomes, for example, better staff retention, higher job satisfaction and better quality of patient care. Various forms of the JD-R model are available that allow personal and job resources to predict health impairment directly and also to moderate the relationship between demands and health impairment. In this moderation version of the JD-R model, the negative impact of increased demands on health impairment is offset by the provision of job resources and personal resources, such as individual staff resilience. The current study examined the JD-R model as shown in Figure 1. We also examined the ability of resources to predict health impairment directly.
Summary of study methods
The current study adopted a concurrent mixed-methods approach (full details are described in the study protocol10). In phase 1, a quantitative survey assessed all components of the JD-R model [full details of the measures of the JD-R model can be found in Appendix 1 (Table 6)], and collected information about the support services offered and their perceived usefulness. Free-text responses also enabled nurses to describe their best and their worst shifts and any other aspect of their experience they wished to report. Baseline data were available for comparison from a very similar survey conducted with CCNs in Scotland in 2018. 11 In phase 2, nurses took part in in-depth interviews about their experience.
Participants
The study participants were critical care and redeployed nurses with substantive contracts who worked in critical care during the pandemic in any of 11 NHS Boards in Scotland (16 critical care units), 2 NHS Trusts in England (2 units) and 1 NHS Board in Wales (1 unit). In total, 661 nurses completed the survey (CCNs = 461, RDNs = 200). Survey data were collected between January 2021 and March 2022. Forty-four nurses were interviewed (CCNs = 28, RDNs = 16). Interview data were collected between April 2021 and June 2022. Full demographic details of survey and interview participants can be found in Appendix 1, Tables 7 and 8 respectively. 2018 participants: the baseline survey recruited CCNs only (n = 557) and from units in Scotland only (n = 19 units). Recruitment spanned 4–6 weeks on each unit, from 16 April to 16 October 2018. Demographic details for 2018 participants are shown in Appendix 1, Table 7.
Recruitment
A study champion was recruited in each unit. The study champion promoted the study with staff and placed paper copies of the survey study packs on the unit. Participants could complete the survey on paper or online; 75% of participants chose paper. Participants interested in taking part in an interview provided their contact details separately to the survey. When the survey collection period was complete, the surveys and interview contact slips were returned to the research team by courier. The pandemic precluded any member of the study team from travelling for purposes of participant recruitment. 2018 recruitment: a study champion was also used in the 2018 study. However, the researcher (McCallum) on the 2018 survey also visited each unit in person to aid recruitment and to collect the completed surveys. Survey completion was on paper only.
Outcome measures
Health impairment
Health impairment was measured as psychological distress (General Health Questionnaire, GHQ-12), burnout (three subscales from the Maslach Burnout Inventory Human Services Survey (MBI-HSS) namely, emotional exhaustion, depersonalisation and personal accomplishment) and PTSD symptoms (Post-traumatic Stress Disorder Checklist, PCL-5). None of the measures are diagnostic, but each has a threshold score for probable caseness, that is, an individual meeting or exceeding that score would probably meet the required diagnostic criteria for the relevant mental health condition. For example, for the PCL-5 caseness means that if a formal diagnostic interview were done it is likely that a diagnosis of PTSD would be made. These threshold values are for MBI emotional exhaustion ≥ 27, MBI depersonalisation ≥ 14, MBI personal accomplishment ≤ 30, PCL ≥ 31 and for GHQ ≥ 4.
Work engagement
This was measured using the three subscales of the Utrecht Work Engagement Scale (UWES-9), namely vigour, dedication and absorption.
Organisational outcomes
Six organisational outcomes were assessed: certainty about future, changing jobs, job satisfaction, commitment [Questionnaire on the Experience of Work (QEEW 2.0)], quality of care (Agency for Healthcare Research and Quality Hospital Survey) and patient safety (Perceptions of Care Undone).
Job demands
Nine job demands were measured: pace and amount of work, emotional load, mental load, physical effort, complexity of work, work organisation, role conflict (all subscales from the QEEW 2.0), and disproportionate relative/visitor expectations and verbal aggression from relatives/visitors (both subscales from the Customer Related Social Stressors Scale). In addition, four items assessed the demands from communication with relatives that were particular to the pandemic.
Job and personal resources
Ten job resources were measured using subscales from the QEEW 2.0, namely, learning opportunities, effectiveness in achieving goals, autonomy, task clarity, feedback, relationship with supervisor, relationship with colleagues, quality, well-being focus, and staffing. Personal resources (personal resilience) were measured using the Connor Davidson Resilience Scale.
Analyses summary
Survey data
Analysis of variance (ANOVA) was used to test differences in outcome means between CCNs before and during the pandemic. ANOVA was also used to test for differences between CCNs and RDNs during the pandemic. Logistic regression was used to obtain odds ratios (ORs) for stress outcomes dichotomised as probable caseness/not according to recommended cut-off scores. We estimate that having a sample size of 500 would have adequate power (> 0.8) to allow for a small effect to be detected in GHQ-12 outcomes between the 2108 and the current study samples with α = 0.05. Standard linear regression was used to explore outcome predictors. In the first step nursing experience and demographic variables that were significantly correlated with the dependent variable were entered. In the second/third step the relevant JD-R model subscales were entered.
Interviews
A semistructured topic guide was used flexibly throughout the interviews (the topic guide is provided in Appendix 1, Table 9). This was formulated in line with components of the JD-R model and was structured in five main sections to explore (1) the principal job demands, (2) job resources, (3) the impact of working during the pandemic on staff well-being, (4) the wider impact on the organisation and lastly (5) the availability and effectiveness of well-being provisions. Data were analysed using the five-stage Framework Method12 using the six constructs of the JD-R model as the analytic framework.
Rationale for research
Evidence emerging early in the pandemic suggested that the impact on CCNs was likely to be significant, particularly in relation to work-related stress. This workforce was and still is at the forefront of the response to COVID-19 and was and is crucial to the delivery of effective and safe critical care services. Without a pre-pandemic comparator it was difficult to quantify this impact; the 2018 data set was essential as a comparator. While the use of a historical comparator has methodological limitations, it was based on a PhD study that had included a systematic review, applied a theoretical framework and provided robust evidence. 11 Previous work exploring work-related stress in this occupational group had been largely atheoretical. A key finding of the systematic review for the PhD was that burnout and work stress were often stated as being synonymous with CCN work; however, this was not supported empirically. The literature was fraught with methodological and measurement issues. A national survey in 2018 was essential to overcome the issues in the existing literature and provided us with an understanding of the extent of the problem in the UK. No other published UK data could be found at that time. Our pre-pandemic data allowed these comparisons and, importantly, the use of a model of occupational stress contextualised staff well-being where predictors and potential interventions could be identified. The JD-R model has both negative and positive arms, thus recognising the complexity of a work environment and potential interactions between demands and resources. The NHS had staffing issues prior to COVID-19, and these are likely to be worsened post pandemic. Staff recruitment and retention require a healthy workplace and not just a healthy workforce; the JD-R model allows for the study of the workforce and their working environment.
Most NHS Boards and Trusts provided differing types of support which, unsurprisingly, had to be implemented quickly, and without any evaluation. This study provides evidence as to how CCNs and RDNs viewed these interventions mainly in terms of accessibility and utility, and these data are available to inform future supportive services.
We used a survey to assess the impact in terms of measurable outcomes and the magnitude of that impact, and one-to-one interviews to understand more fully experiences and identify aspects not captured by the applied model. This mixed-methods approach is a strength of this study.
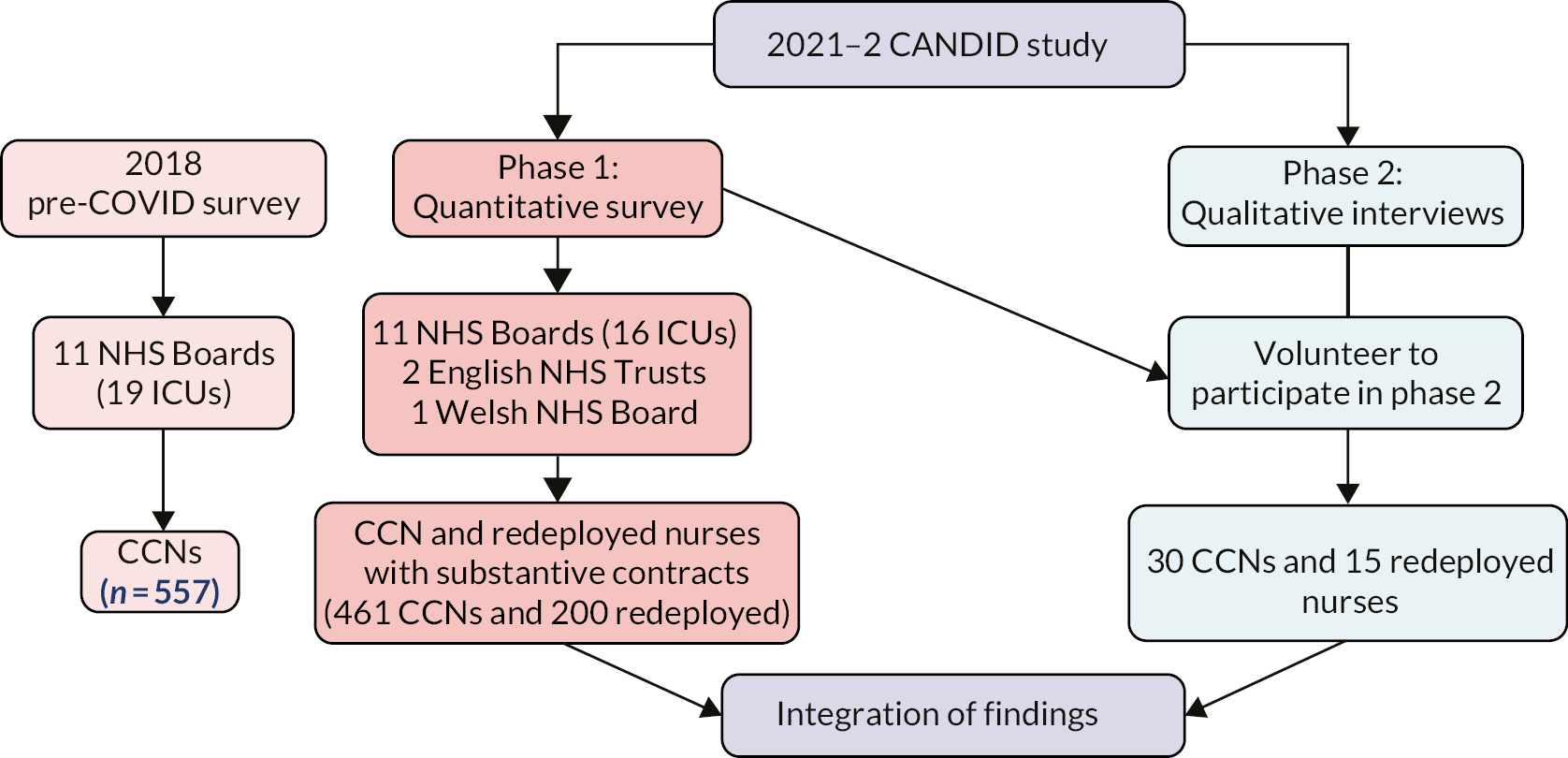
Research pathway diagram
This was a two-phase mixed-methods study: a survey and a series of in-depth interviews (Figure 2). Participants in the survey could then volunteer to take part in the interview phase of the study.
FIGURE 2.
Schematic of the phase 1 and phase 2 CANDID studies and the 2018 baseline study. ICUs, intensive care units.
Principal findings and analyses
The response rate for the 2018 study was 47%. In the pandemic study, the response rate in Scotland was 32%; the response rates in England and Wales could not be determined because denominators for these sites could not be identified accurately; however, they were substantially lower. There were no differences between the 2018 and the pandemic samples in terms of age, gender or years of critical care experience.
The pandemic and job demands
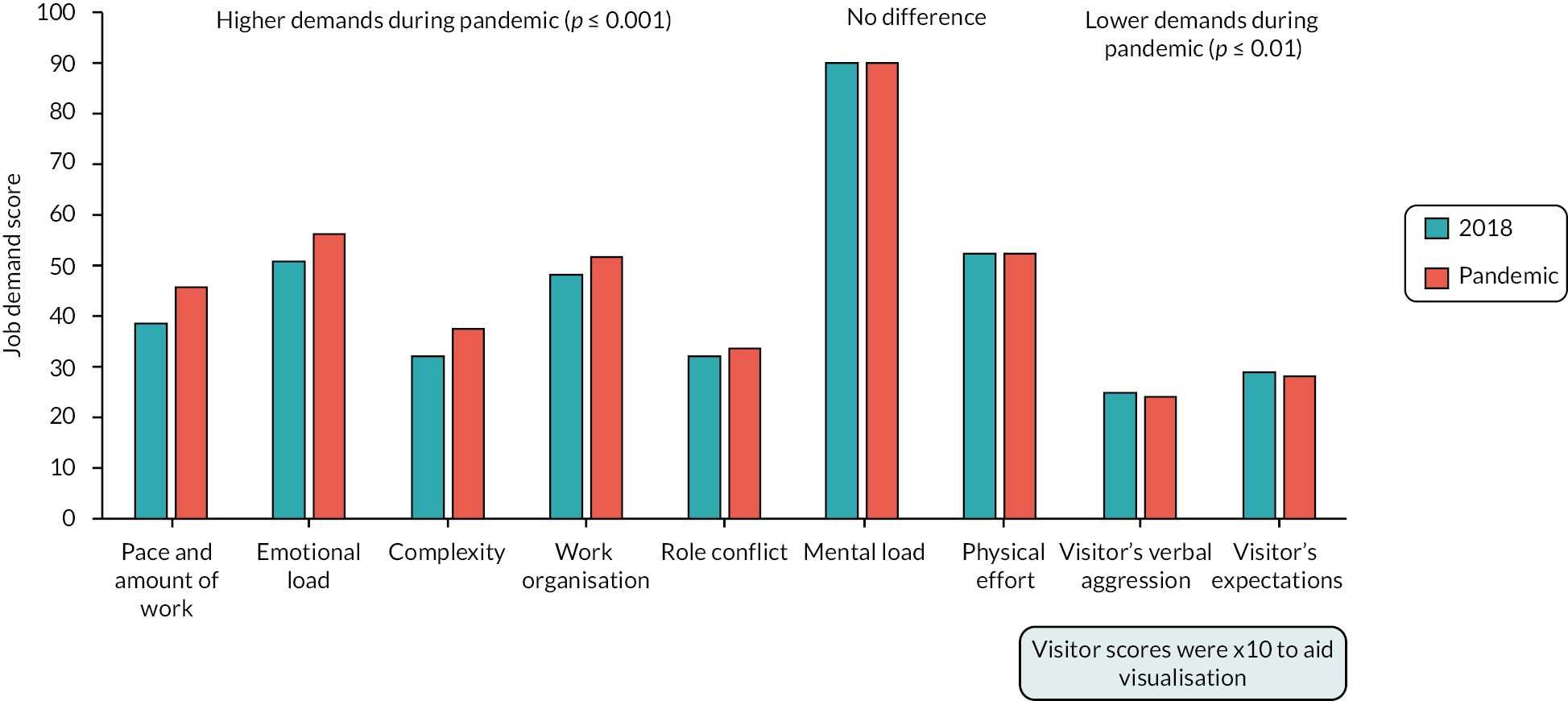
Survey: demands
For CCNs, five demands were higher during the pandemic (pace and amount of work, emotional load, complexity, work organisation, role conflict), two demands stayed the same (mental load, physical effort) and two demands were lower (visitor verbal aggression and visitor expectation) (Figure 3). The reduced demand from visitors is perhaps explained by their exclusion from visiting their relatives/friends. The rank order of demands for CCNs was unchanged. A job demand that was perceived as high by CCNs before the pandemic remained so and, in some cases, increased.
FIGURE 3.
Levels of job demands for CCNs in 2018 and during the pandemic.
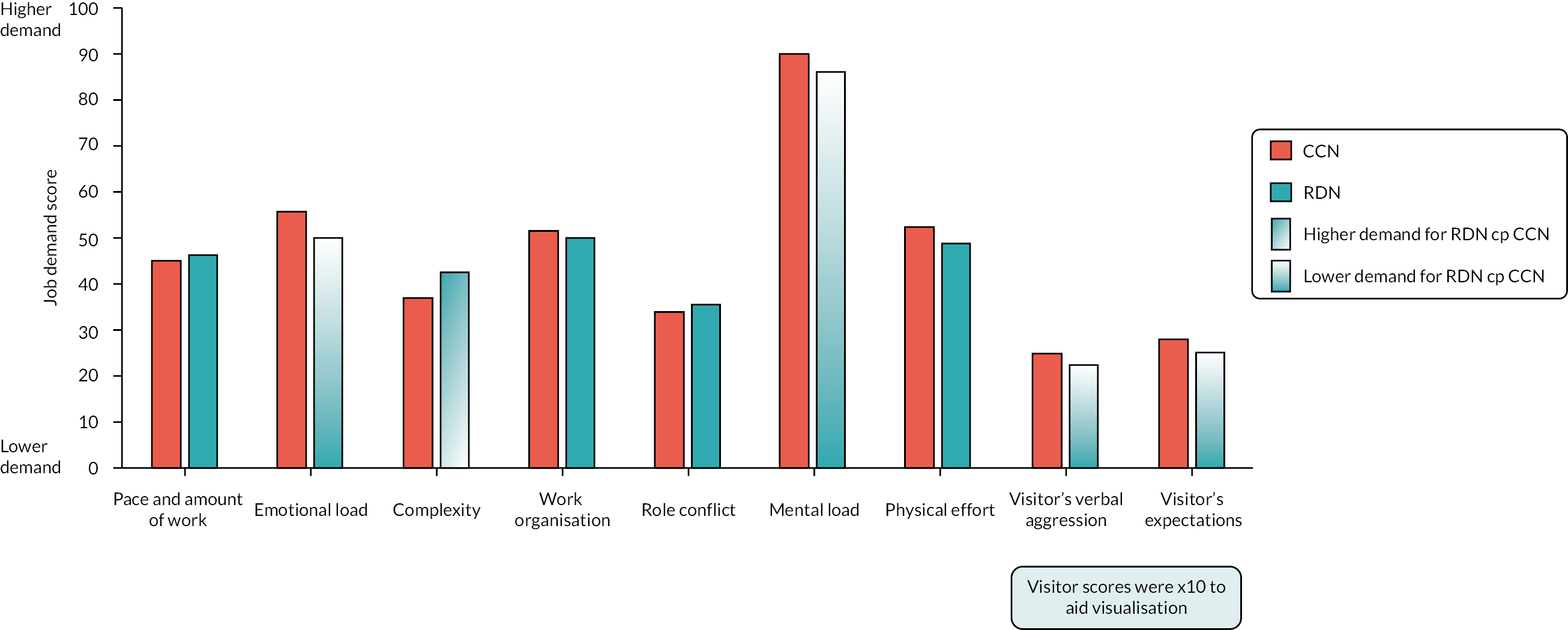
Compared to CCNs, RDNs reported four demands to be lower (emotional load, mental load, visitor’s verbal aggression and expectations) and one demand to be higher (complexity of their work) compared with CCNs (Figure 4). There were no differences between CCNs and RDNs in the level of demand experienced during the pandemic from the pace and amount of work, physical effort and role conflict.
FIGURE 4.
Levels of job demands for CCNs and RDNs during the pandemic.
Interviews: demands
Interview data were coded to each of the seven job demands measured in the survey, and the quotes shown in Table 1 illustrate nurses’ experiences of these. One job demand, namely, pace and amount of work, was divided into two subcomponents: staff–patient ratios and supporting redeployed staff. Staff experienced prolonged heightened job demands throughout the course of the pandemic. This primarily concerned intensified pace and amount, complexity, and the physical and emotional effort expended during their work in intensive care unit (ICU). For redeployed staff, role conflict represented a uniquely challenging demand.
| Job demand subcomponents | Job demand illustrative quotes |
|---|---|
| Pace and amount of work: Revised staff–patient ratios |
I had four patients and they were really sick, and I just felt like the whole shift I was chasing my tail and fighting fires, just making sure that everybody’s infusions didn’t run out. CCN 8, Band 5, 2 years of ICU experience |
| Pace and amount of work: Supporting redeployed staff |
They redeployed people from other healthcare backgrounds, I was working with people from physiotherapy, who are able to help you to roll a patient, things like that, but they weren’t familiar with the documentation. They … of course not, I’m not blaming them. But to have to deal with that as well, I’d rather I was on my own than having so called helpers. I found them a chain and ball. CCN 22, Band 5, 29 years of ICU experience |
| Emotional load | The emotional involvement was … I found more than … you never used to get involved with your patients, but … it just seemed so much more intense ’cos you were, kind of, fighting with them and that only contact with their family as well. It’s … it was just horrible. Horrible for the family, horrible for the staff. RDN 14, Band 5, 9 years of experience |
| Mental load | You get pulled in so many different directions because you get so many people come to your bedside and … you feel a bit like a headless chicken sometimes … if you’re not physically fatigued, you’re mentally fatigued because there’s always something, you’re constantly thinking of something, there’s always something needs to be done. CCN 23, Band 5, 18 months of ICU experience |
| Physical effort: Working in PPE |
You only had three breaks in a shift and you’re there for 13 hours. So, I remember taking off my mask and it’s the greatest feeling in the world when you took this mask off, but it was only for half an hour break and then you’d have to put it back on. But you had so many layers on you were sweating and … oh it was really hard work. And my poor face was all, you know, misshapen and lined. RDN 16, Band 7+, 28 years of experience |
| Work complexity: Patient acuity |
Basically, you had a shift shadowing, and then it was, good luck, off you go. Which you just can’t underestimate the absolute fear and terror you have the whole time, because you have somebody who’s critically unwell, and you know what you don’t know. RDN 8, Band 7+, 18 years of experience |
| Work complexity: Working in PPE |
When we had the big visor … the big, like, helmet visors on, it sounds hilarious, but we all hit our heads a lot on different pieces of equipment because you just couldn’t … it’s really hard to explain, but you just couldn’t really figure out how close you were to something. And then all of a sudden, you’ve hit your … the top of your head on your bedside screen or something. CCN 17, Band 5, 3.5 years of ICU experience |
| Role conflict | Because we were in Recovery, we didn’t have the usual ventilators that we use on ITU, we were stuck with the anaesthetic machines, which are what they normally use in theatre, so none of us knew how to use those or anything like that. So, it was just a bit, I don’t know, it kind of just got left a bit, sort of very much out of my depth. CCN 11, Band 5, 15 months of ICU experience |
| Work organisation Working in satellite ICU units |
The challenge was that the unit we were in wasn’t designed as a ward unit, so it was the theatre admissions suite, so the physical area wasn’t appropriate. So there was bed … the spaces … so it was designed to take trolleys, like theatre trolleys and ICU beds are really wide and really long, and then they’ve got a ventilator and all your pumps and all your equipment, and the unit that we were actually in had screens, curtains round the bed space, but the bed space was designed for a small trolley, so when you tried … when you were doing personal care on your patient, the curtains kind of cut the bed in half, and you couldn’t walk around the bed. RDN 2, Band 6, 18 years of experience |
The pandemic and job and personal resources
Survey: resources
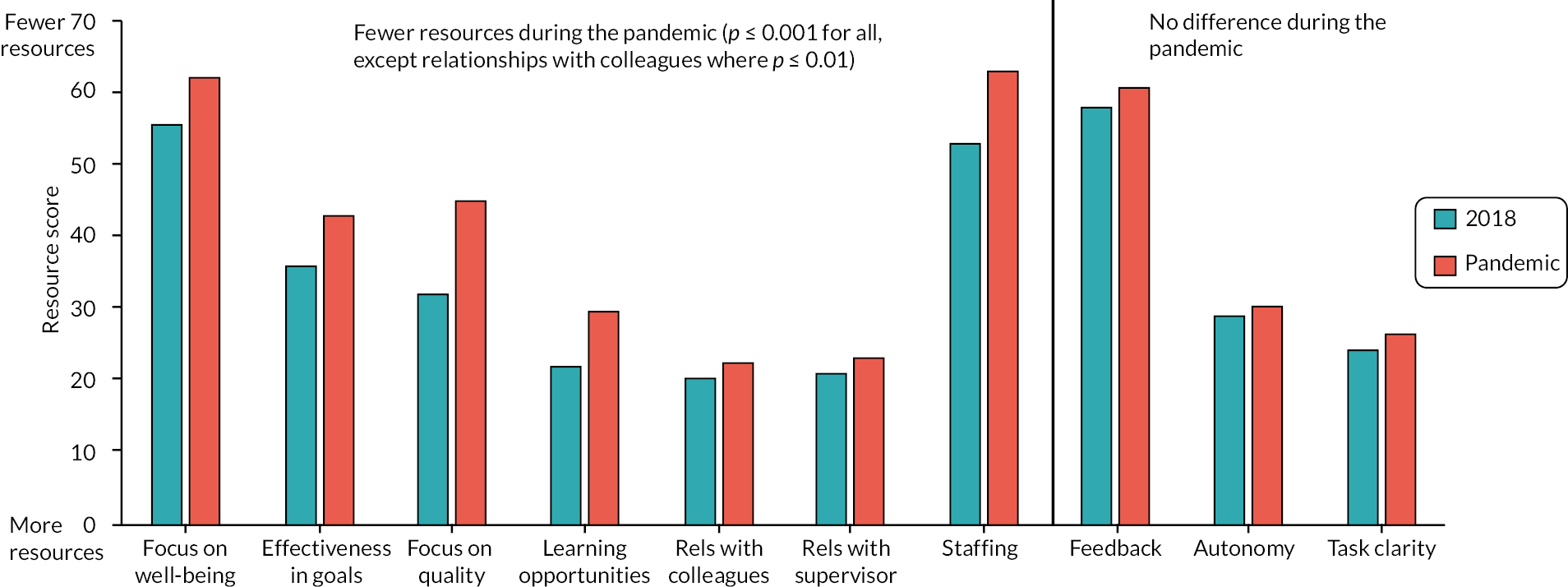
Seven job resources were worse for CCNs during the pandemic compared with 2018 (Figure 5; please note a higher resource score = fewer resources). The rank order of resources for CCNs was relatively unchanged during the pandemic. If a resource was perceived as poor before the pandemic, it remained so. Of note is the importance the organisation places on quality, its focus on staff well-being, feedback and staffing levels, all of which are job resources. These are areas of potential intervention. The personal resource of resilience was also reduced during the pandemic [F(1,1013) = 31.55; p ≤ 0.001, ω2 0.03].
FIGURE 5.
Levels of job resources for CCNs in 2018 and during the pandemic.
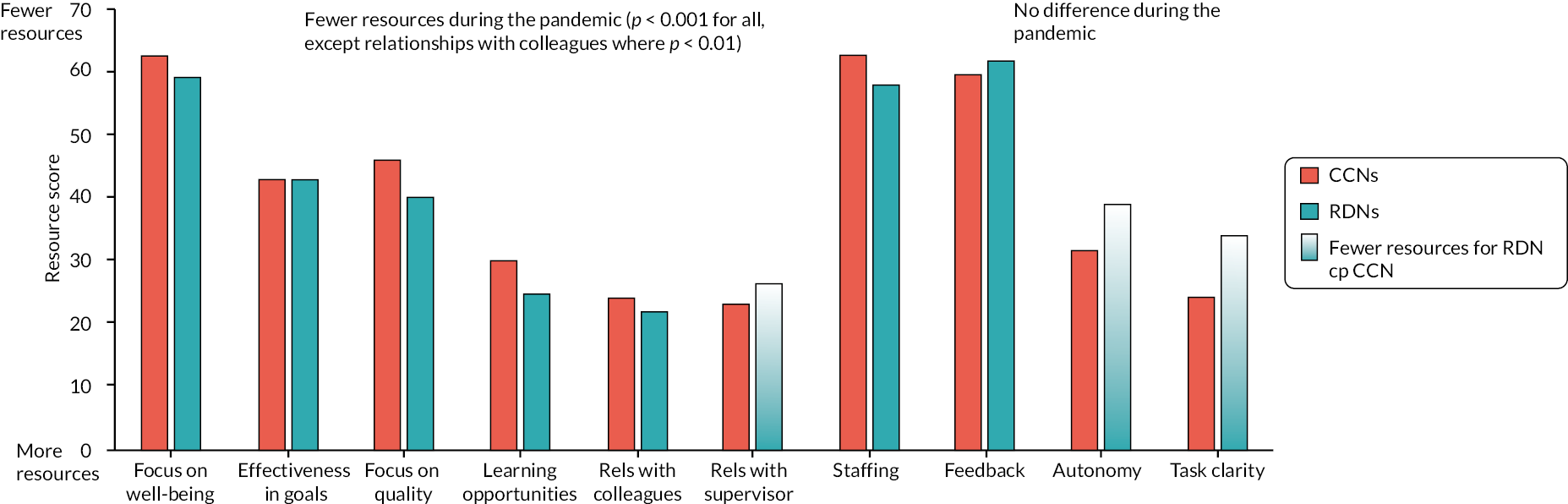
Most job resources were of an equivalent level for both RDNs and for CCNs except for three job resources (Figure 6). Specifically, RDNs reported less task clarity, less autonomy and poorer relationships with their supervisor compared with CCNs.
FIGURE 6.
Levels of job resources for CCNs and RDNs during the pandemic.
For CCNs, the combination of clearly increased demands together with reduced resources would be expected to result in an increase in stress, that is, worse health impairment, and reduced work engagement and a consequent negative impact on organisational outcomes.
Interviews: resources
Interview data could also be coded to each of the ten job resources and to the personal resource of resilience (Table 2 for illustrative quotes). Positive relationships with colleagues and supervisors were heralded as a core job resource during the pandemic. For redeployed staff, maintaining positive relationships with staff and supervisors from within their own unit was important to reduce isolation during their redeployment.
| Job resource subcomponents | Job resource illustrative quotes |
|---|---|
| Job autonomy | It’s such a huge amount of trust, and it’s nice. It’s nice to know that you’re trusted enough, and actually that you have to be educated enough to make these decisions. I think it’s one of the really wonderful things about Critical Care nursing, because you can make decisions and just get on with it, you can help your patients. CCN 8, Band 5, 2 years of ICU experience |
| Task clarity: Low task clarity |
I didn’t know what people, you know, the people who were next to me, what they were able to do. There was one person next to me, and I said, can you help me with that, and she said, oh I don’t know what to do either. And I thought, my God. There was theatre staff who had been redeployed to help as well, nobody really knew what they were doing. RDN 5, Band 7+, 27 years of experience |
| Quality | So it was kind of yeah, just running about and making sure that they all had their drugs ready and everything. It was just about making sure that they were safe and everything else. It was like...if they’ve not been repositioned, that’s not the end of the world, it’s not a priority. We just have to make sure that x, y and z’s done, and it became very task focused and not person centred any more. CCN 13, Band 5, 2 years of ICU experience |
| Feedback: Positive feedback staff and patients’ families |
But one of the good things in all of this was, they sent an email to thank me for being so compassionate, and allowing them the time to have seen him, you know. And I’ve kept that, you know, and it was the one thing that I thought, well I have made a difference to someone, and me doing that has impacted that. RDN 5, Band 7+, 27 years of experience |
| Relationship with superior: High resource |
The senior management team were very patronising and condescending. It was even so frustrating that I had to tell them that ‘what are you guys doing? I know that you are managing the staffing but why can’t you be on the bed space?’. Which was really frustrating, that they just come to you and ask, like, oh how are you, how are you getting on, how are the numbers of staff. It was so condescending. There was even a point that I was with the bed space nurse, trying to do a CPR. We were in the middle of a CPR and one of the matrons tried to call me and ask me for three more staff. CCN 9, Band 6, 10 years of ICU experience |
| Relationship with colleagues High resource |
And it was a real, sort of … teamwork and a real sense of we’re in this together. You know, that first time is … I’m sure everybody would tell you that, the first time round it really was that, we’re absolutely in this together. CCN 19, Band 6, 9 years of ICU experience |
| Learning opportunities | The feeling that you’re doing something worthwhile was amazing, and you know, it makes you think a lot more about the bodily systems and how things work. You know, you could see how altering, you know, a blood pressure medication would have an effect on the heart rate and then have an effect on how they breathe, or vice versa, you change the setting on the ventilator, and you could see the problems that you might give the heart and ultimately the person’s blood pressure, which then affects their kidneys and the urine output. So you can actually see how the whole bodily system works, and that was really interesting. RDN 3, Band 7+, 5 years of experience |
| Effectiveness in achieving goals | To give you an idea, I think the ITU nurses have about 12 weeks, being shadowed … they have 12 weeks being shadowed before they can kind of go solo. So we were supposed to have a day, and it was a kind of tick list – ventilator, pumps, suctioning – that’s you. And then by lunchtime they said, actually we’re too busy, we’re going to have to cut it. So that was our introduction to ITU, pretty much. RDN 8, Band 7+, 18 years of experience |
| Staffing: Low staffing resources |
It’s so hard to be the nurse in charge and look after all other ten patients, basically. Because you have three ICU nurses. But these three ICU nurses are very junior. They’re, like, three months only in intensive care and sometimes you don’t get to go for a break or for a toilet break even, because these COVID patients are very unpredictable and they deteriorate very quickly. And you can’t just leave them with someone who doesn’t have enough experience. CCN 9, Band 6, 10 years of ICU experience |
| Well-being focus | There was no such thing. What break out rooms? What are you talking about? What rooms? Where could any of us walk away from our patient group or our patients or whatever and just say to our colleagues, well actually I’m having a wee hard time today so I’m going to go and sit in another room for 45 minutes and cry into my coffee. It was absolutely … to be honest, we were slightly outraged. CCN 5, Band 5, 20 years of ICU experience |
The pandemic and health impairment
Survey: health impairment outcomes
Compared to 2018, during the pandemic health impairment scores for CCNs were worse across all subscales. There were no differences between CCNs and RDNs on the measures of health impairment during the pandemic, suggesting the conclusions about the impact of the pandemic on mental health will equally apply to RDNs.
Critical care nurses experienced substantial elevation in risk of clinically significant health impairment during the pandemic compared to 2018 (Figure 7). Seventy-six per cent of CCNs reached threshold score for probable psychological distress. This represents a sixfold elevation in risk compared with 2018 {GHQ-12, OR 6.03 [95% confidence interval (CI) 4.75 to 7.95]}. Similarly, 55%, 14% and 43% of CCNs reached threshold score for burnout on the emotional exhaustion, depersonalisation and personal accomplishment subscales of the MBI, respectively. There was significant elevation of risk on all three subscales of burnout [emotional exhaustion, OR 4.02 (3.07 to 5.26); depersonalisation, OR 3.18 (1.99 to 5.07); personal accomplishment, OR 1.53 (1.18 to 1.97)]. A measure of PTSD symptoms was not included in the 2018 survey, precluding calculation of the change in risk. However, a third of CCNs reported clinically concerning PTSD symptoms.
FIGURE 7.
Percentage of CCNs in 2018 vs. during the pandemic reaching threshold score for probable caseness on measures of health impairment.
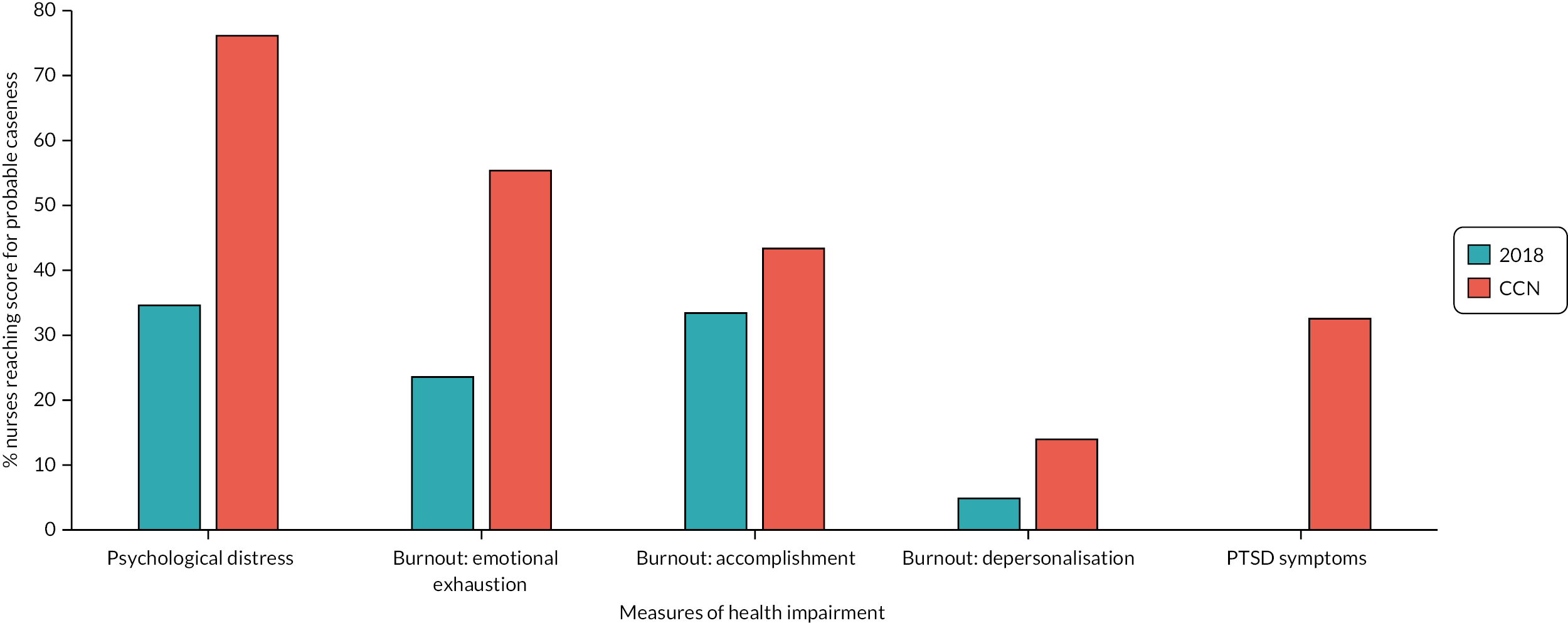
These findings are consistent with rates reported in critical care healthcare workers in the UK3,13 and internationally14 during the pandemic. 15 The PTSD risk data for CCNs are three times higher than comparator occupations that are likely to experience traumatic events, namely, rescue workers and ambulance workers,16,17 with risk factors relating to the trauma, the person and the environment.
Interviews: health impairment outcomes
Nurses described in vivid detail how working in critical care had impacted on their mental health and their physical heath (Table 3 for illustrative quotes). It was clear from the interviews that heightened job demands, notably the negative emotional load arising from increased exposure to death and navigating end-of life care in the absence of relatives, had a damaging impact on staff physical and psychological well-being. Most described emotional and physical exhaustion, burnout, symptoms of PTSD and impaired sleep.
| Health impairment components | Health impairment illustrative quotes |
|---|---|
| Burnout: Emotional exhaustion |
So, whilst I was in ITU I literally just hated going to work, I hated it. It’s the only way I can describe it, I just hated it. And I cried a lot. It was the whole experience – I just hated it. I hated doing the shift, I hated how I felt when I was at work, unsafe and just exhausted. And like you were just saying about patients, just feeling like I wasn’t even being a nurse, not a proper nurse in the way that I’d known it. RDN 11, Band 6, 15 years of experience |
| Distress: Anxiety and depression |
I think to summarise, the fact that I have had three months absence from work with anxiety, is probably a representation of how bad that has been. It was just so stressful …. I think at one point I was unable to leave the house, I felt so anxious that I couldn’t even leave the house, as I briefly mentioned about the staff support mental health nurse who … literally talking me through going to the hairdressers. CCN 7, Band 6, 16 years of ICU experience |
| PTSD symptoms | Things I really struggled with is memories afterwards, like one of our patients was listening to music, so there’s certain music, if I hear it, it takes me straight back, I can’t listen to it as much, and it’s all the kind of phone calls with family and that that kind of haunt you afterwards. In the second wave, out of all the ventilators I looked after, only one survived, so it’s just a lot to think about. RDN 7, Band 6, 8 years of experience |
| Detaching from work | When I get home, I get home, I leave everything at work. When I go to work, I’m at work; whatever I have at home I will leave it at home. But during those times it was quite hard. Like, it makes you rethink about your choices in life. It makes you think about life. Should I shift jobs? Would I, like …? What did I do today? Was it correct? Did I make the proper thing? Like, there’s a lot of things going on in your mind each and every day. CCN 9, Band 6, 10 years of ICU experience |
| Recovery after work | I was just so exhausted, I don’t remember doing anything other than … I tell you something that was odd was that I couldn’t concentrate on TV, which is unusual for me. ’Cos I remember distinctly that the new series of Killing Eve was on and I just couldn’t concentrate at all. In fact, I couldn’t really concentrate on anything, I just kept flitting between TV, phone, whatever, anything. But I couldn’t really concentrate on stuff. RDN 11, Band 6, 15 years of experience |
| Sleep impairment | My sleep I’ve just struggled with so much. So, I’m trying everything. And it just does not work. I’ll lie in bed for an hour and a half, wide awake. I can’t get to sleep, and then once I am asleep, I’ll wake up several times throughout the night. So, my sleeping is awful. And then once I come into work I’m shattered. So, I’m always moaning at work that I’m so tired. RDN 9, Band 5, 2 years of experience |
The ability of job demands and resources to explain health impairment outcomes was assessed (details provided below). Job demands predicted health impairment and resources were associated with a reduction in the negative impact of job demands on health impairment, but this moderating role of resources was not observed at higher levels of demand. Lack of resources, especially reduced learning opportunities, and two organisational resources, that is, lack of focus on staff well-being, and reduced focus on quality predicted worse organisational outcomes.
Taken together, these findings have substantive implications for the mental well-being, recruitment and retention of nurses who worked in critical care during the pandemic. Both PTSD symptoms and burnout can have enduring trajectories with the risk of the individual developing PTSD, and burnout is contagious,18 such that prevalence may increase through horizontal transfer. 8 This raises concerns about the ability of staff to recover without appropriate psychological treatment, support and/or reductions in workplace demands and improved resourcing. Further, burnout has a negative impact on quality of care and career engagement19 and PTSD symptoms carry significant additional functional impairment,5 with implications for patient safety and quality of care. Collectively, these findings have implications for a workforce that is still experiencing high levels of clinical activity and staff attrition within a challenging work environment.
The pandemic and work engagement
Survey: work engagement outcomes
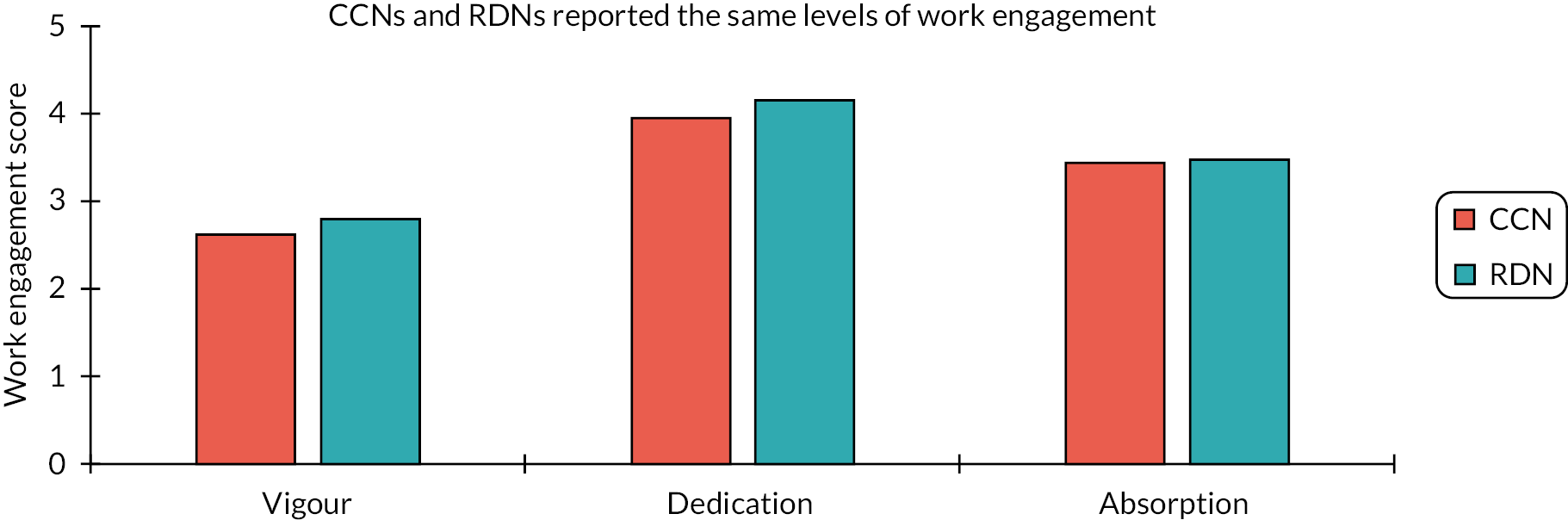
CCNs were significantly less engaged by their work during the pandemic (Figure 8). The three components of work engagement, namely vigour, dedication and absorption, were all reduced (ω2 0.04, 0.02 and 0.007 for vigour, dedication and adsorption, respectively). There were no differences between CCNs and RDNs on any of the three components of work engagement (Figure 9).
FIGURE 8.
Levels of work engagement by CCNs in 2018 and during the pandemic.
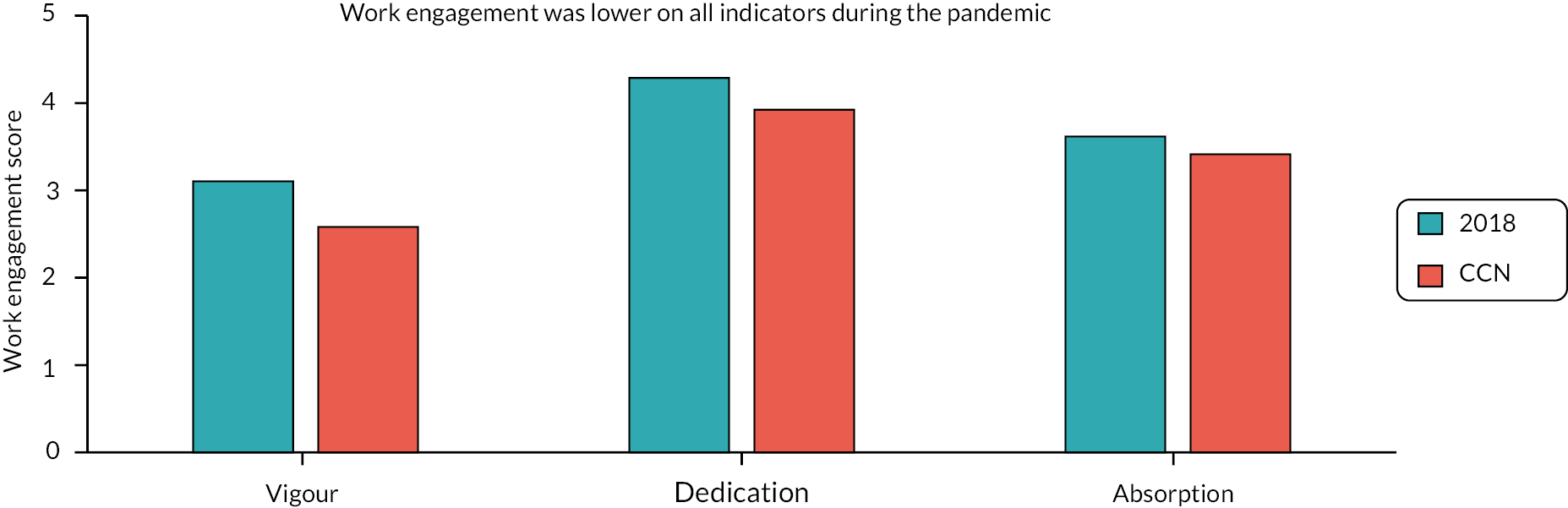
FIGURE 9.
Levels of work engagement by CCNs and RDNs during the pandemic.
Interviews: work engagement outcomes
The impact of the pandemic had complex effects on nurses’ relationship with their work (Table 4 for illustrative quotes). Many described feeling less engaged with their work. However, others spoke of feeling especially committed to their role and to their colleagues.
| Work engagement subcomponents | Work engagement illustrative quotes |
|---|---|
| Depleted engagement | I just feel as well, I’m … I’ve never been someone before that, kind of, just went to work, if you know what I mean. Whereas now I tend to just feel like I’m … I’ll just go to work, look after my patient and go home. Whereas I was never that kind of person before. CCN 17, Band 5, 3.5 years of ICU experience |
| High commitment | I just felt it was my job to work during the pandemic, I had to do what I had to do … I mean, I’m saying it has been horrific but in actual fact I wouldn’t have changed it. I would have gone in and done exactly the same as what I’ve done if I have to do it again. [When asked to describe why this was] Because I love being a nurse. CCN 15, Band 7+, 23 years of ICU experience |
The pandemic and organisational outcomes
Organisational outcomes
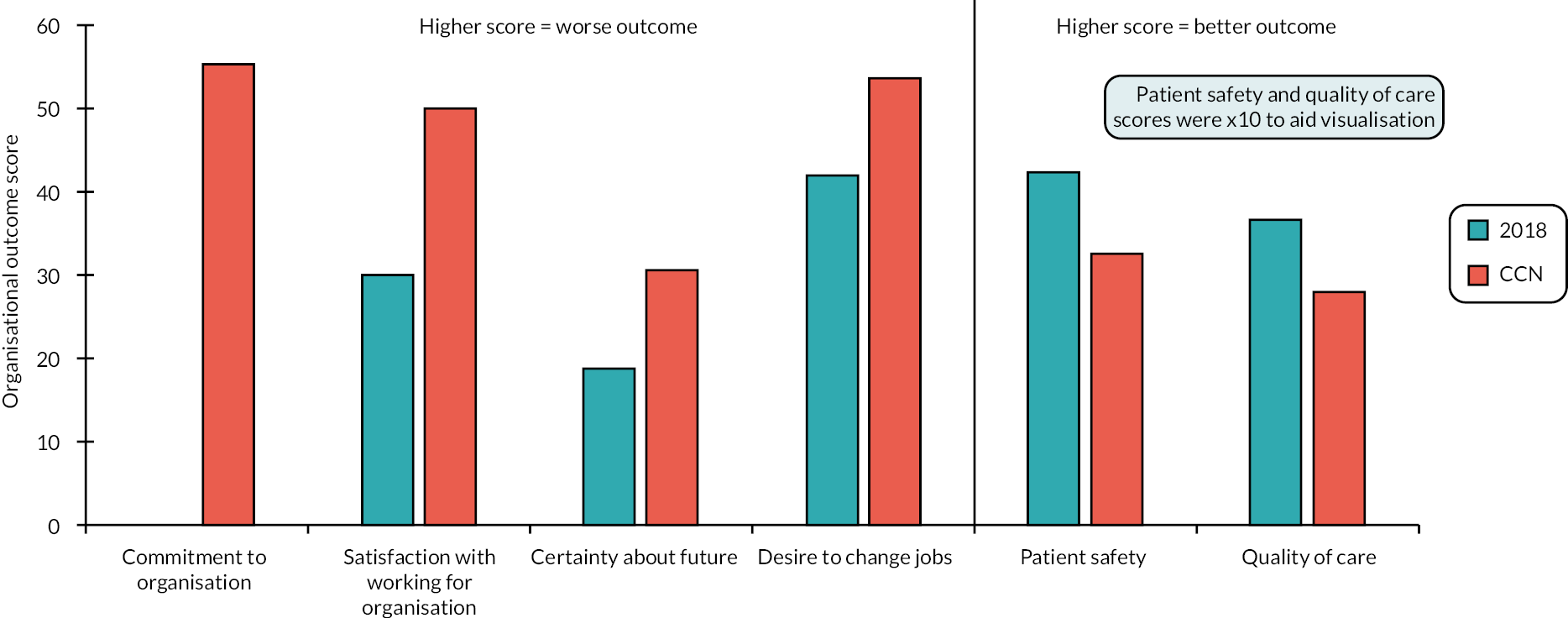
Five organisational outcomes were measured in 2018 and during the pandemic; all five outcomes worsened for CCNs (Figure 10). The pandemic had a large negative effect on job satisfaction (ω2 0.18), perceived quality of care (ω2 0.23) and patient safety (ω2 0.23). Medium-sized effects were seen on CCNs’ certainty about their future at work (ω2 0.06) and their desire to change jobs (ω2 0.05). Seventy per cent of CCNs were thinking of changing their job, and 28% were already planning to change their job within the next year. These figures are higher than a recent Belgian study conducted during the fourth and fifth waves, assessing intention to leave ICU and the profession, where 43% of CCNs indicated they were going to leave critical care and 24% the profession. 20 A key element from the Belgian study was the variation across units. Where the work environment was more positively rated, nurses were less likely to indicate a desire to leave the profession. This aligns with key findings from CANDID, where job resources and nurses’ perceptions of how they and their work were valued predicted work engagement and organisational outcomes.
FIGURE 10.
Organisational outcomes for CCNs in 2018 and during the pandemic.
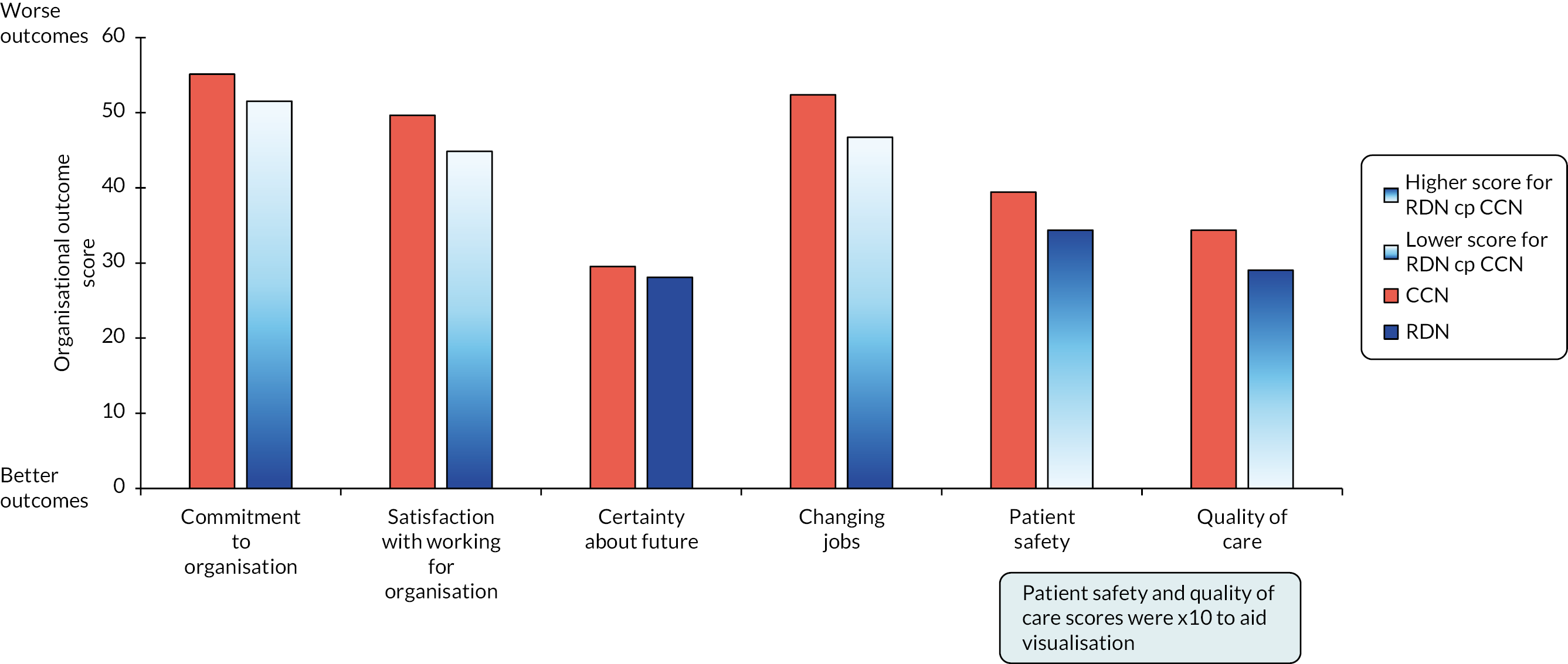
Redeployed nurses reported greater job satisfaction, lower desire to change jobs, and higher patient safety and quality of care compared to CCNs (Figure 11). However, these differences were not substantial enough to impact on RDNs’ decision-making in relation to job retention; 60% of RDNs were thinking of changing their job, and 21% were planning to change their job within the next year.
FIGURE 11.
Organisational outcomes for CCNs and RDNs during pandemic.
Both sustained workplace demands and the negative impact of these demands on staff well-being incurred negative organisational consequences (Table 5 for illustrative quotes). Nurses reported problems with staffing in terms of increased staff turnover and staff sickness. They perceived their employing organisation to have reduced commitment to quality of care and reduced patient safety. While some staff experienced positive job satisfaction, it was more often the case that nurses discussed how they are considering leaving their specialty or nursing altogether.
| Organisational subcomponents | Organisational outcomes illustrative quotes |
|---|---|
| High staff turnover | There’s been more staff left our unit than we could ever replace. Like, currently in our unit there’s 40 vacancies for just staff nurses. CCN 19, Band 6, 9 years of ICU experience |
| High staff sickness | I just burst out crying and I just said, I can’t do this anymore, so I went to my … well, it was one of the other charge nurses who was in charge that day, my senior charge nurse was off, and they just said, look, you shouldn’t go back, and I was like, I can’t go back, I just … and then I’ve been off ever since. RDN 7, Band 6, 8 years of experience |
| Reduced patient safety | I felt that I was forced to become very unsafe and, you know, there were even times that I had to fight with the senior management team. I didn’t even care any more that if, like, if they are matron or head of nursing or whatever they are. CCN 9, Band 6, 10 years of ICU experience |
| Reduced quality of care | In terms of patient care, I think I left most shifts feeling quite almost morally traumatised because I hadn’t done the bits of TLC that you … that you are responding to that person like they are a human. You are brushing their hair or you are making sure their mouth is really well moisturised. None of these things are going to kill anybody but that was really difficult, that you just didn’t feel like you were actually looking after people as well as you should have. RDN 12, Band 6, 9 years of experience |
| Certainty about future | I have actually agreed to cut my hours back. I was actually going to leave. I got an interview for a new job which I never thought I would do because I love my job. But I knew it was affecting me out of work. But I think what I have done so far so good. I cut my hours and work part time over winter and see if that gets me through. CCN 14, Band 7, 9 years of ICU experience |
| High job satisfaction | I remember his family made a point of saying how well they felt I was treating them. But as I pointed out that’s why I’m there and by caring for his family I’m helping to care for him. But the best bit was again talking to the family and I always speak to the patients, he wasn’t really conscious and his wife smiled and she touched my hand and said, if he had been well, he’d have loved you, you’re just the sort of nurse that he would want to be looked after by …. I went home that night feeling that I have done my job well, I have made a difference to these people in what is the most horrendous of situations. RDN 1, Band 5, 17 years of experience |
| Low job satisfaction | There was no satisfaction, you know, in anything, because the moment you achieved something, it just felt like you took one step forward and three steps back, and I mean, three steps back’s not even just one step back, they just got sicker and sicker, no matter how much of your skills and your knowledge and experience that you put into looking after them, what would have made somebody better before didn’t work. RDN 2, Band 6, 18 years of experience |
These results indicate a serious threat to staffing critical care adequately, now and in the future. The quotations illustrate clearly the emotional and demanding nature of working in critical care during the pandemic and the potential impact on this crucial workforce and, significantly, organisations. Understaffing is a serious risk, which will have an additional negative impact on staff well-being and development. Of particular concern would be the loss of experienced staff, which has adverse implications for the support, supervision and retention of staff new to critical care, who in the post-pandemic era are increasingly required to fill gaps in staffing. Staff expressed perceptions of reduced quality of care and patient safety, which is concerning and has implications for patients, their families and staff. Any further reductions in staffing are likely to exacerbate these negative findings, which also have applicability to nursing outside critical care.
Predicting health impairment, work engagement and organisational outcomes
Predictors of health impairment
Demographic factors, job demands, job resources and personal resources combined to account for over 40% of the variability in mental health and PTSD symptoms and over 50% of the variability in burnout (emotional exhaustion) for CCNs (Figure 12), with very similar findings for RDNs.
FIGURE 12.
Predictors of health impairment for CCNs (only significant predictors are included in the table). Data are standardised beta coefficients. Darker colours indicate stronger associations. Higher scores on all outcomes indicate worse outcomes, i.e. poorer mental health, greater emotional exhaustion and worse PTSD symptoms. R2 = % variance accounted for in each outcome. *p < 0.05, **p < 0.01, ***p < 0.001.
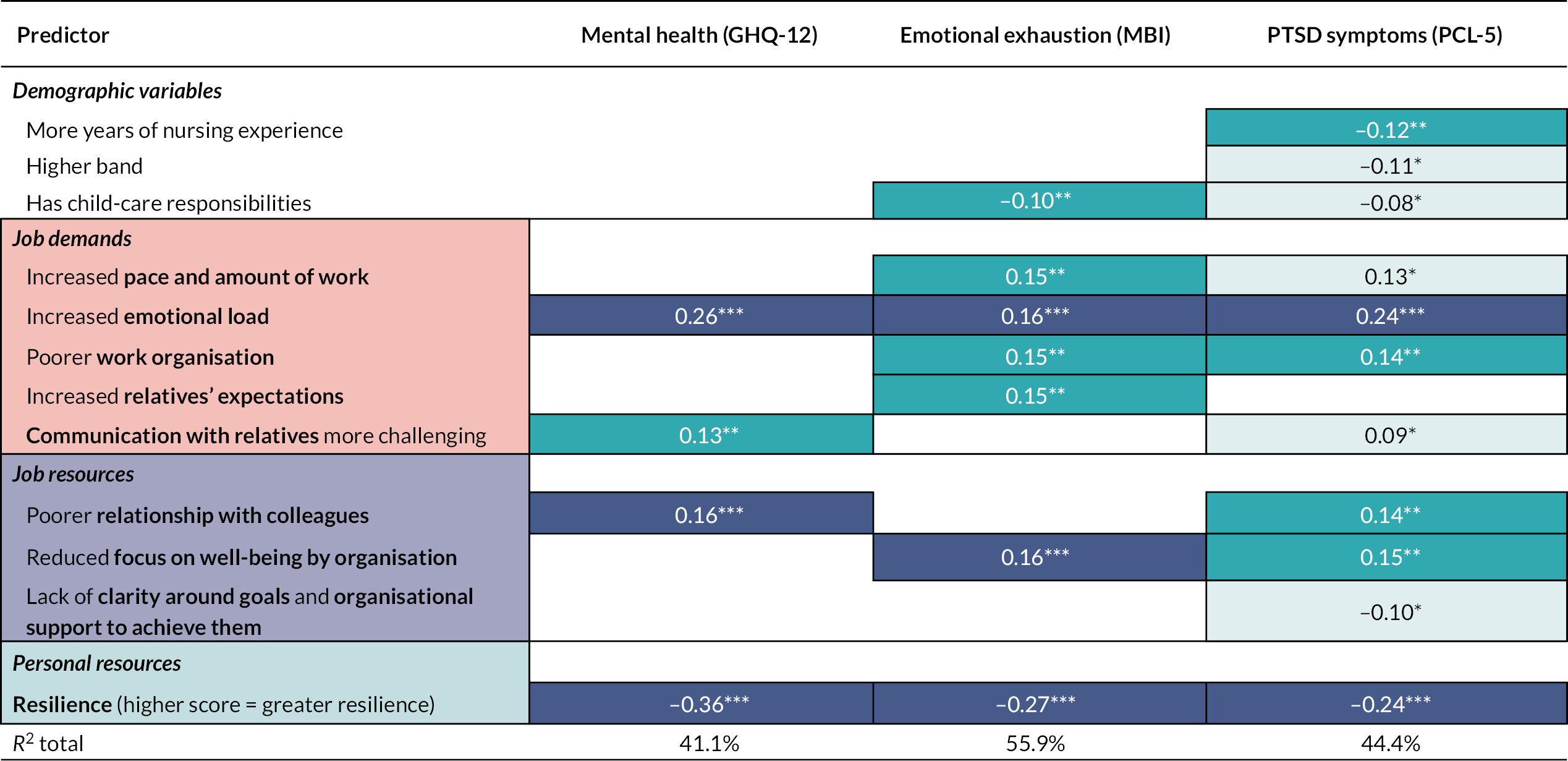
Health impairment outcomes were predicted by demographic factors, job demands and resources. Some demographic factors were protective; for example, having more nursing experience, being at a higher employment band and having child-care responsibilities were associated with fewer PTSD symptoms. Increased demands predicted worse outcomes for all three measures of health impairment. The demands from an increased emotional load were particularly burdensome, being strongly predictive of poorer mental health, increased burnout and worse PTSD symptoms. Similarly, poor work organisation, increased pace and amount of work and challenging communications with relatives were associated with greater burnout and worse PTSD symptoms. Depleted resources were also predictive of worse outcomes. Depleted resilience was particularly problematic, being strongly associated with worse mental health, greater burnout and worse PTSD symptoms. In addition, poorer relationships with colleagues and reduced focus on well-being by the organisation were each associated with worse outcomes on two of the three health impairment measures.
The association between demands and resources and all three health impairment outcomes identifies potential intervention targets to support staff well-being. However, moderation analyses examined the ability of resources to mitigate the negative effect of demands on health impairment outcomes. Moderators were identified for mental health (GHQ-12), burnout emotional exhaustion (MBI-EE) and PTSD symptoms (PCL-5). Simple slopes analyses indicated that resources reduced the negative effect of demands on mental health and burnout emotional exhaustion. However, this moderation effect was stronger at lower levels of demand; as demands increased, the moderation effect reduced. At lower levels of demand, learning opportunities mitigated the negative impact of demands on PTSD symptoms, whereas this moderation effect was not apparent at high levels of demand. These moderation analyses suggest that at high levels of demands the provision of extra resources alone does not reduce the negative effects of demands on health impairment; rather, what is required are interventions to reduce the level of demand or to prevent excessive increases in demand.
Predictors of work engagement
Three resources accounted for ~28–35% of the variability in measures of engagement. CCNs were more engaged when the organisation valued quality and they had access to learning opportunities. When resilience was depleted CCNs were less engaged.
Predictors of organisational outcomes
Organisational outcomes were predicted by job demands, job resources, health impairment and work engagement outcomes (Figure 13). Increased demands, fewer resources, worse health impairment and lower work engagement were each associated with worse organisational outcomes. However, job resources and health impairment outcomes were the more robust predictors. Seven of the ten job resources measured were predictive. For example, fewer learning opportunities were associated with reduced job commitment, increased intention to change jobs, reduced certainty about the future, lower job satisfaction, reduced perceived patient safety and reduced perceived quality of care. Similarly, poorer mental health (GHQ-12) was associated with worse outcomes on four of the six organisational outcomes. The JD-R model was able to account for between 26% and 54% of the variability in organisational outcomes.
FIGURE 13.
Predictors of organisational outcomes for CCNs. Data are standardised beta coefficients. Darker colours indicate stronger associations. Higher scores on all outcomes indicate worse outcomes, e.g. less commitment, increased intention to change jobs, less certainty about the future, lower job satisfaction, reduced patient safety and quality of care. R2 variance accounted for in each outcome. *p < 0.05, **p < 0.01, ***p < 0.001.
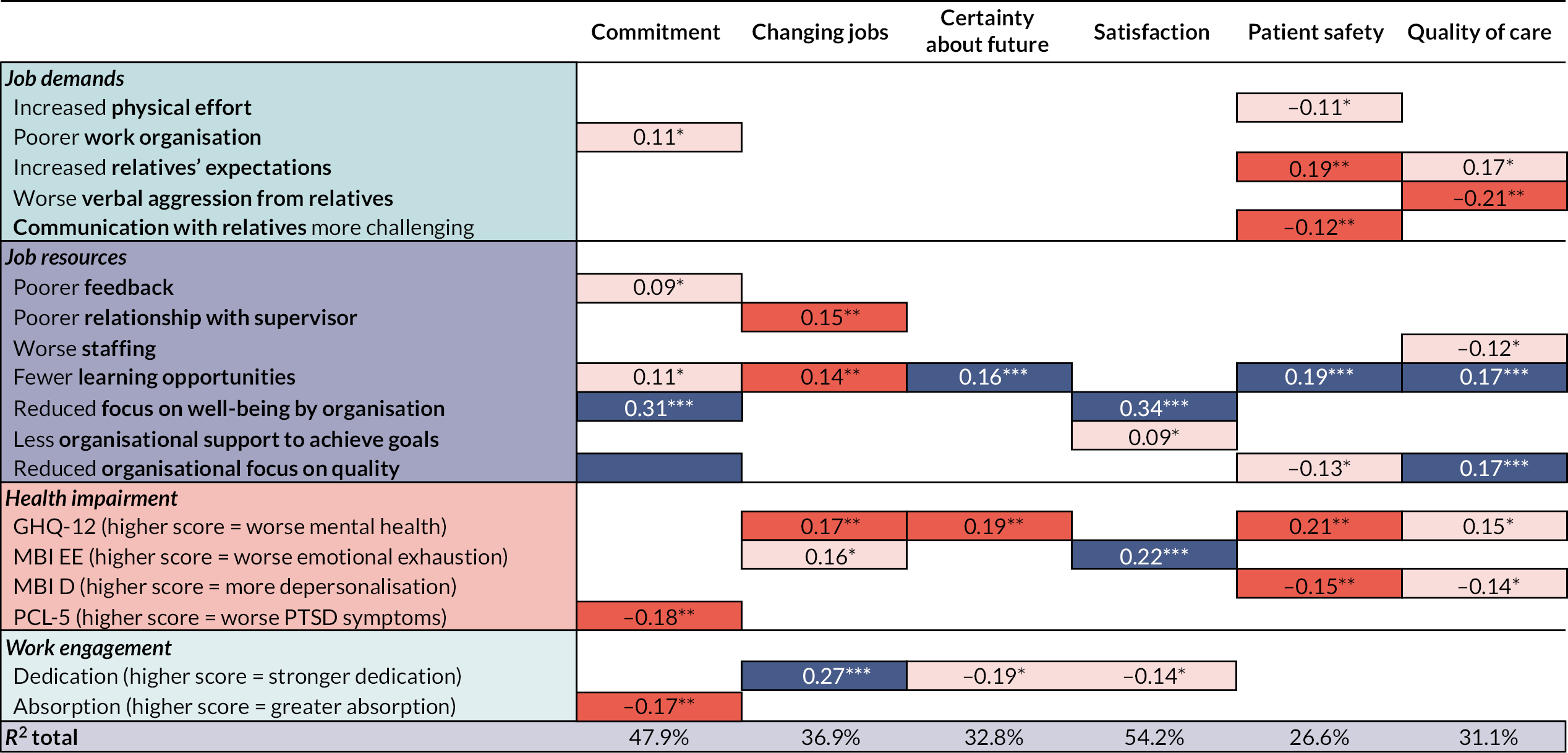
These results demonstrate the important role job resources and psychological/mental health have in relation to organisational outcomes. When staff are working in an environment that provides learning opportunities within an organisation that supports their well-being and focuses on quality, they are less likely to be thinking about or planning to change jobs, are more certain about their future, are more satisfied with their job and more committed to it. They are also more likely to rate patient safety and quality of care more positively.
Survey: supportive measures
Participants were invited to list the supportive measures they were offered and then to rate each measure as to its ease of access and usefulness. A range of supportive measures were provided. The most common (317 responses) of these were ‘Environment/Spaces’ that included ‘quiet rooms’, ‘well-being/resilience hubs’ and in essence were places where nurses could relax away from units for refreshments or, on some occasions, access specific therapeutic interventions. Around 37% of staff were unable to access these and this was reflected in reported utility, with 39% indicating the spaces were not useful. The next most common measure (298 responses) was ‘Therapeutic Contact’ with a clinical psychologist/counsellor, chaplain or equivalent. Again, 30% of those responding could not easily access these people and 28% did not find the service useful. The other measures included practical support and support from colleagues. Interestingly, ‘Signposting’ to online sites or telephone support was easy to access (around 90% indicated this) but was no more useful than these other measures.
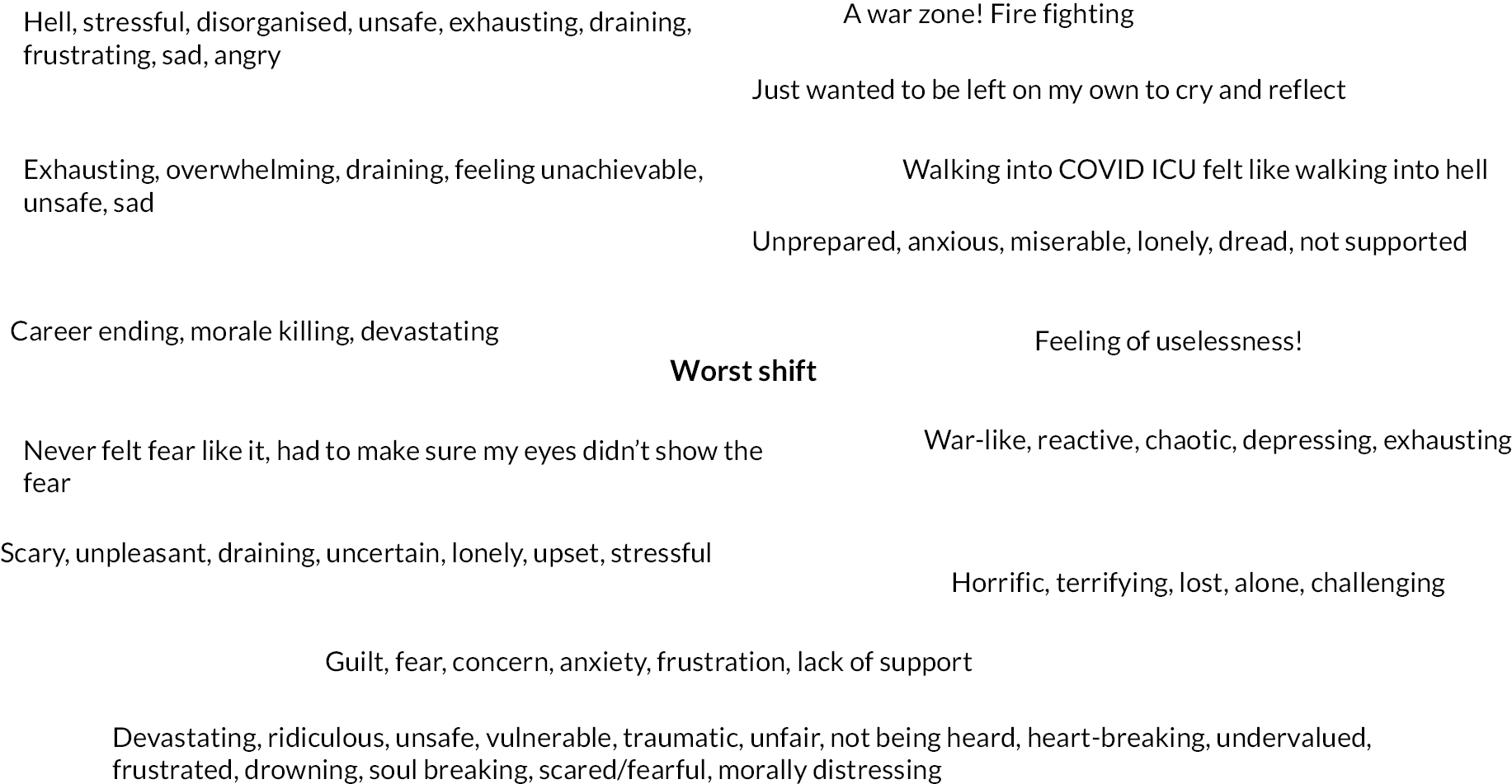
Survey: free-text responses
At the end of the survey, nurses were asked to identify which words they would use to describe their worst (n = 592 nurses) and best shifts (n = 561) and if there was anything else they would like to tell us (n = 465). These represented a range of emotions and were related to a number of aspects of working during the pandemic, and many likened this to being ‘at war’. Stress and distress were clearly demonstrated in the descriptions of their worst shift (Figure 14). They described also how it made them feel, including how prepared and supported they were to meet the challenges.
FIGURE 14.
Free-text responses to describe the worst shift.
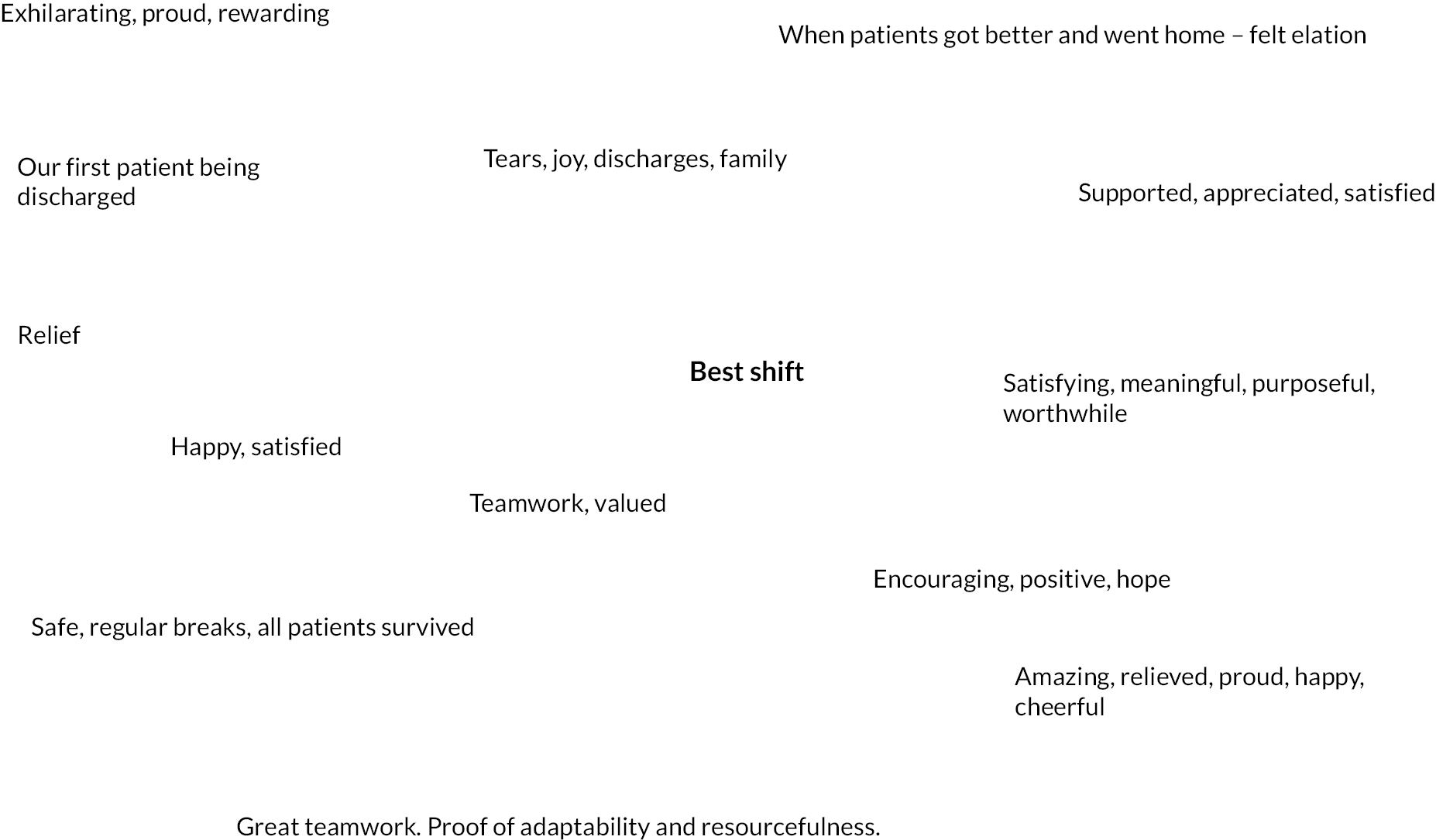
However, there were also positive aspects; typical descriptions of the best shift are shown in Figure 15. There was a sense of achievement when patients survived, and this made nurses feel good about their shift. Teamwork was another positive aspect.
FIGURE 15.
Free-text responses to describe the best shift.
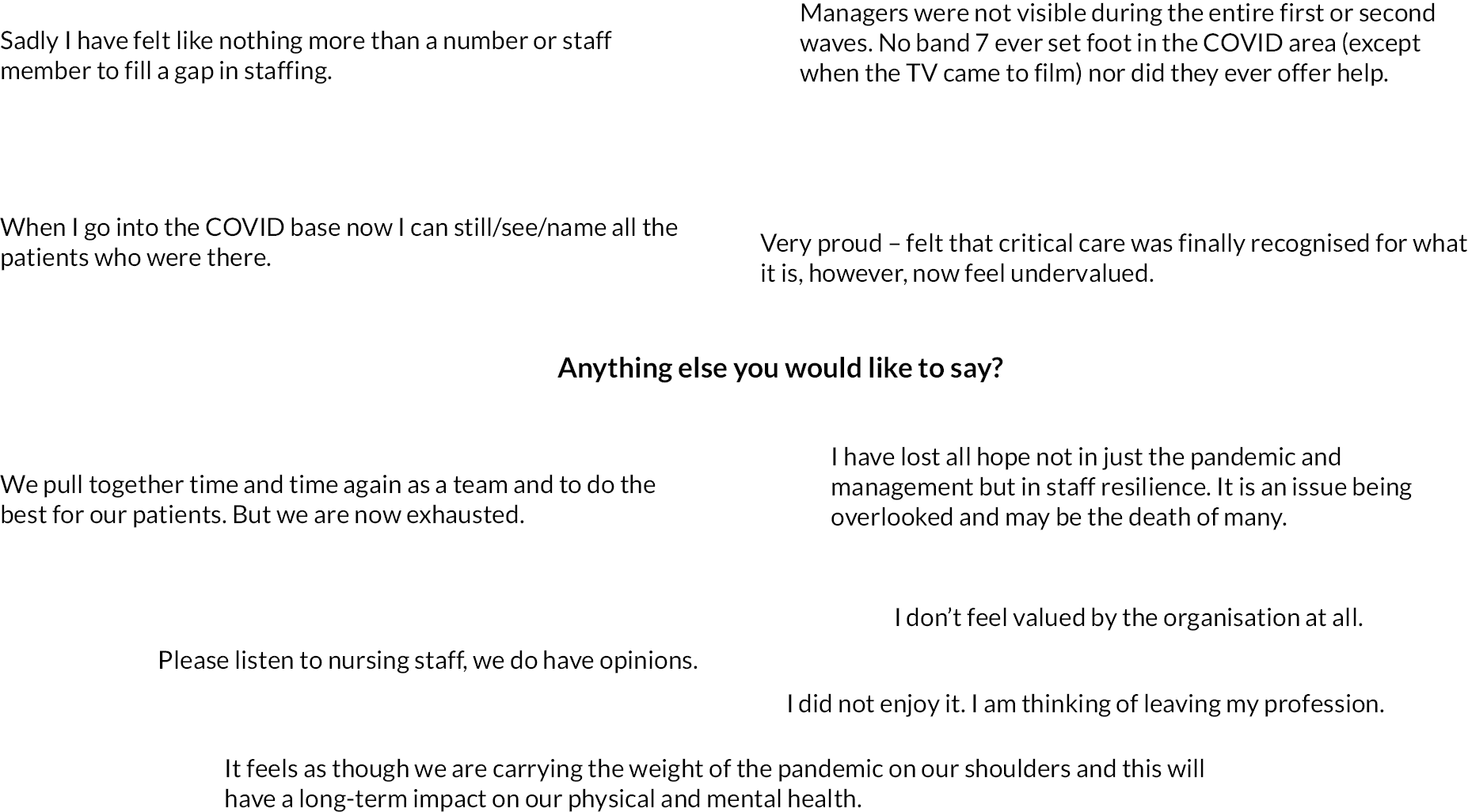
Responses that represent the content of the free-text box that enabled nurses to tell us anything else related to their experience of working during the pandemic are shown in Figure 16. These tended to represent both negative and positive views, with the former relating mainly to how valued staff were feeling when completing the survey, and how they view the consequences for critical care services. These quotes serve to illustrate the quantitative results and are very much in line with the results of the in-depth qualitative interviews.
FIGURE 16.
Free-text responses to the invitation to add anything else about their experiences.
Integration of mixed-methods approach
We applied and integrated our concurrent mixed-methods design in several ways. Firstly, our research questions required to be answered using both quantitative and qualitative approaches. Secondly, our applied theoretical framework both informed the survey content by representing all elements of the model and provided the focus for the interview schedule. Thirdly, the model also was applied to both types of analyses. Statistical analyses explored the levels of and relationship across and between the key variables, to allow us to identify presence and magnitude of the consequences of working in critical care through the pandemic. An a priori application of the model to the qualitative data allowed us to further understand and explain nurses’ experience in relation to our quantitative findings, while also identifying areas not addressed by the JD-R model. By using this design, our results will be of value to key healthcare stakeholders, managers and policy-makers.
Strengths of the study in relation to other studies
The study has several major strengths in relation to other studies that have reported the impact of the pandemic on healthcare workers. First, baseline data were available from a previous study, conducted by members of the research team in 2018. This pre-pandemic comparator data set enabled the CANDID study to report changes in health impairment, work engagement and organisational outcomes resulting from the pandemic. Other studies were limited to reporting point prevalence rates primarily for mental health outcomes only.
Second, the application of a model of occupational stress enabled CANDID to move beyond a description of the impact of the pandemic to an explanation of those impacts. The JD-R model identifies the demands that predict health impairments and the resources that protect health and foster positive work engagement. In addition, the model also provides insight into how staff health impairment and engagement factors affect outcomes of importance to their employing organisation. Hence, the model moves the evidence base forward from being purely outcome-focused. The use of a model of occupational stress, therefore, can be used to design interventions that support staff and organisational outcomes by targeting the structure of the workplace as well as individual staff, and that target prevention of harm in addition to treatment of illness.
Limitations
Response rates in Scotland (32%) were below those of the 2018 study (47%); however, this is unsurprising given recruitment took place during a pandemic when staff were extremely over stretched. It is of note that some units had very high levels of participation, others much lower, and this may reflect several issues which we have no solid evidence of and, hence, which we have not speculated upon in the report. This lower response may or may not be related to not seeing the value of research, being burnt out by the sheer volume and difficulty of the work they have been – or still were – doing, being involved in other research studies etc.
We were unable to calculate the response rate for units outside Scotland. The response rate here was certainly much lower than that obtained in Scotland. This means the results, especially of the survey data, will be more representative of nurses working in Scotland and their local working conditions and the national policies of the government at Holyrood than nurses and their local environments in England and Wales. The dominance of Scotland in the sample also has equality, diversity and inclusion (EDI) implications; in the 2011 census, 96.02% of the population of Scotland reported that they were ‘white’. Consequently, nurses from other ethnic backgrounds are under-represented in the survey data in particular. We discuss EDI limitations of the study in more detail in the Equality, diversity and inclusion.
Survey data were collected between January 2021 and March 2022 and interview data were collected between April 2021 and June 2022. Large variations in the time taken to obtain research and development (R&D) approvals from each Health Board/Trust account for the prolonged period of data collection. We did not plan for the analysis of a longitudinal data set and hence have not undertaken such analyses. We recognise that both critical care unit staffing and the volume of work within critical care will have varied across this period and that our analyses do not take account of this variability.
While mental health can only be measured by self-report, other measures in the study, such as quality of care, patient safety and staffing, are amenable to more objective measures. The study was not resourced to obtain more objective measures. Any interpretation of the data should be made alongside the understanding that our measures assessed perceptions of factors such as quality of care, patient safety and staffing. That said, experiential factors such as perceptions are important drivers of behaviour; for example, NHS employees who responded to the Nursing and Midwifery council’s 202021 survey of staff who were leaving the register reported ‘too much pressure, workplace culture, staffing and disillusionment with the quality of care’ (p. 2) as reasons for leaving.
Summary and implications for decision-makers
This study revealed the considerable adverse impact of the pandemic on the well-being of nurses working in critical care, particularly in relation to risk of work-related stress and the impact on NHS organisations. Up to three-quarters of CCNs are at risk of significant psychological distress, up to half at risk of burnout and a third reported PTSD symptoms at a level that would require formal clinical assessment. Crucially, having pre-COVID-19 comparative data strengthens the importance of these results. These levels of probable mental health impairment are consistent with rates reported in critical care healthcare workers in the UK3,4 and internationally14 during the pandemic. CCN risk is three times higher than comparator occupations that are likely to experience traumatic events, namely, rescue workers and ambulance workers,16,17 with risk factors relating to the trauma, the person and the environment.
This study has significant implications for strategic government and NHS Health Board/Trust decision-makers. We have clearly demonstrated the negative impact for nurses of working in critical care during COVID-19 and it is likely that our results will apply to other staff groups both within and outwith critical care. Of great concern is the ongoing and enduring nature of the sources of stress, symptoms of distress and post-traumatic stress. The levels demonstrated in this study may worsen without appropriate support and action. Importantly, burnout is also contagious, which may mean that these levels may increase and affect staff new to the specialty. 18 Given current staff recruitment and retention challenges, this has serious implications for critical care services which are dealing still with COVID cases and the clinical backlog of cases resulting from the pandemic.
There are two elements to supporting staff. Firstly, some staff need support now and although there are a range of services currently that may provide this it is important to note that in our study, approximately one-third of staff could not or did not access such services. Secondly, the importance of resources indicates an area where leaders and managers could develop. The importance of valuing staff well-being and the quality of their work should not be underestimated, along with learning opportunities. These issues emerged very strongly in the study and were key topics in our stakeholder events. CCNs were concerned about the erosion of standards that occurred during the pandemic and were concerned that this was neither recognised nor would be addressed. The work environment needs to be a place where staff thrive, develop and learn to deal with and cope with challenge and not somewhere that will cause harm and damage. Consideration needs to be given to how to meaningfully improve the critical care workplace. Our results indicate a range of areas where this might occur. We offer specific recommendations for NHS organisations and governments. The list of recommendations is not given in priority order; it is likely that each Board and each unit would be able to identify a priority order most suitable to their local needs. However, that said, the need to provide support for staff who are currently experiencing psychological distress as a result of working during the pandemic is urgent.
Specific recommendations for NHS organisations and governments:
-
Monitor CCN and RDN levels of stress, distress and post-traumatic stress symptoms annually for the next 3 years. PTSS and burnout are often enduring and result in functional impairment, likely further exacerbating the current staffing challenges. For the health and well-being of staff and the quality of care of patients, it is imperative that we continue to monitor these consequences, to support this staff group and the critical care services.
-
Support existing staff recovery from the pandemic, through accessing appropriate current services whether that be well-being services, occupational health, general practice or psychological/mental health services. This study found many staff did not or could not access services. We need to understand the reasons more fully for this and develop solutions to optimise staff access.
-
Listen to nurses. Seek input from nurses about their working environment and how it can be structured to improve their working lives and outcomes for their patients.
-
Build upon those supportive measures that were introduced during the pandemic (i.e. access to clinical psychology/counselling, well-being spaces), but ensure all staff can access these. The importance of staff well-being and commitment by organisations/governments should not be underestimated and interestingly was not rated highly prior to the pandemic.
-
Recognise and reward staff contributions to organisations by valuing quality care. This was an important element from the stakeholder events. Staff are proud of the quality of care they deliver but felt this was under-appreciated.
-
Resource nurses to engage in continual professional development and provide learning opportunities. Learning opportunities emerged as an important predictor of work engagement and organisational outcomes.
-
Promote work environments that are conducive to building upon individual and team resilience. The lack of direct managerial support emerged as a concern across participating sites. There were examples of excellent support, but often the lack of managerial presence was concerning.
Research recommendations
This study has identified workplace factors that predict indicators of psychological health, work engagement and other outcomes of value to the NHS. It is possible that predictive factors and/or the strength of the associations between those factors and outcomes will differ between Boards and between units. Future research should:
-
Use theoretical models able to generate an explanation of the factors that affect occupational stress. The area would benefit from the use of models that account for additional factors, such as workplace culture, team working and broader workplace systems. The application of theories able to identify targets for intervention, other than treatment of individual staff who are ill, would promote a prevention rather than treatment approach to staff well-being.
-
Conduct longitudinal studies that would progress the area from a position of being able to identify predictors of psychological distress and workplace engagement to being able to identify the causes of psychological distress and workplace engagement. This understanding would improve our ability to design effective preventive interventions.
-
Consider that interventions likely to make a positive and sustained difference for staff are likely to be locally produced to meet local needs and will likely be multilevel. Intervention development may need to include CCNs, unit managers and NHS Board/Trust senior managers. Hence, participatory research/action Research methods may be best suited for intervention development relevant for specific units.
Challenges faced and lessons learnt for future research
Challenge 1: research and development approvals
CANDID faced challenges around obtaining permissions to recruit from each unit and then actual recruitment of nursing staff from critical care areas and beyond. Ethical approval was in place quickly, but the need to obtain R&D approval separately from each Board or Trust caused delays. The study information requested varied widely, with some Boards granting approvals within a week while others required Caldicott applications and took almost a year to provide approval. This caused delays to the original timetable and additional administration work that had to be undertaken by the study RA. Lesson learnt: recruitment from the NHS during the pandemic was challenging to all. It was especially challenging in ICU. In future studies, we would be inclined to allocate more time for recruitment and would request resource to support specialist administrator time for this work.
Challenge 2: unit access
We were prevented, by local unit managers, from accessing the largest two units in Scotland, despite the Executive Nurse Director and the Board’s R&D department not having any objections to the study (we were given access to the third unit in that Board). Senior Nurse Managers also were unable to facilitate our access. The reasons for this are unclear. We knew from various sources that nurses in those units wanted to take part in the study. The research team are unanimous in the belief that this is an unethical situation and that local managers should not have the ability or authority to prevent staff taking part voluntarily in research work of this kind. Feedback from the stakeholder events highlighted the importance this study has in giving CCNs a ‘voice’. CCNs from these units were denied this. Lesson learnt: we will alert the Chief Scientist, Chief Medical Officer and Chief Nurse in Scotland in an attempt to prevent a similar situation arising in the future.
Challenge 3: extending study beyond Scotland
The original application was exclusively located within Scotland. NIHR requested recruitment from units outside Scotland to enable representation of very large units and a more diverse sample of nurses. We fully appreciated the reasons for this request and added three sites in England. However, this caused additional delays to the project and significantly increased the administrative workload. We encountered serious delays to obtaining the required permissions to access each site. Eventually we took the decision to remove one unit in England from the study for this reason. We then added one unit in Wales. We had completed the survey recruitment in Scotland in November 2021 but did not complete recruitment in the rest of the UK until the end of March 2022. Further, the study response rates in the rest of the UK were substantially lower than in Scotland, which was disappointing and a challenge to the desire to broaden the diversity of the survey sample, although the recruitment beyond Scotland resulted in the interview data being drawn from a more diverse sample. These lower recruitment rates are probably due to the research team having a much closer working relationship with many of the units in Scotland compared to our being very remote from those in the rest of the UK. In addition, we are aware that the London units were already taking part in many locally based survey studies. We continue to believe that the strength of this study is the availability of pre-pandemic data with which to compare the COVID-19 data. Lesson learnt: when challenged by a funder to change the planned recruitment, carefully consider the implications for the administrative workload, the study timetable and the possible impact on response rates. If need be, engage in a dialogue with the funder before accepting the suggested changes.
Patient and public involvement
We have involved CCNs at different stages of this study. A current CCN (TS) who worked in critical care during the pandemic is a co-applicant and has been involved in the design and implementation of the study and the dissemination events. Prior to the start of data collection, six CCNs, who were working during the pandemic, were provided with a draft of the study questionnaire. The CCNs were interviewed to sense-check questionnaire content and provide feedback, especially in relation to its ease of self-completion and any gaps in questionnaire content, especially in relation to working conditions in ICU that were particular to the pandemic. The study steering group then provided feedback on the modified questionnaire. The study steering group included four CCNs: a retired CCN, the Chair of the British Association of Critical Care Nurses, the Chief Nurse for Research and Development at NHS Lothian, and the Chair of the UK Critical Care Research Group, who also sits on the Intensive Care Society Council and the UK Critical Care Nursing Alliance.
For the interview component of the study, the interview guide was developed iteratively in consultation with the research team [which included three former and one current CCN (TS)]. The interview guide was then assessed for appropriateness during two pilot interviews with a current CCN (TS) and a retired CCN and member of the study steering group.
Preliminary analyses of the study findings were presented to two stakeholder workshops, which included 15 CCNs, 1 redeployed nurse, 7 middle-level managers, 4 steering group members, 1 representative from the Scottish Intensive Care Society and 1 representative from NHS Education Scotland. Participants provided feedback on the results. We continue to present the study findings to staff from the Health Boards and Trusts that took part in the study and to receive feedback from them.
Additional information
Acknowledgements
The authors would like to extend their thanks and gratitude to all the nurses who took part in the study. We are especially grateful to all those nurses who acted as study champions in their local units. They worked hard to promote the study at a time when they were under high and sustained workload levels. We are also grateful for the guidance provided by the study steering group throughout the project. We thank Mr Barrie Tullet of Caseroom Press and the University of Lincoln for his design of the CANDID study logo.
Equality, diversity and inclusion
In acknowledgement of the comparatively low levels of diversity within the Scottish general population, the survey and interview recruitment were expanded on request from NIHR to include two NHS Trusts in England (two units) and one NHS Board in Wales (one unit). While 7 of the 44 (15%) interview participants identified as being of non-white ethnicity, survey participation rates in units outside Scotland were low, meaning the large majority of survey data are from white nurses. This is regrettable and probably due to two main issues. First, travel restrictions meant that we could not travel to provide in-person support for recruitment locally. Second, unlike in Scotland, we had no current working relationships with these units. We did not have the time or resources to replicate the recruitment strategy of the UK-REACH group (please see details below); we did liaise with the Chair of the British Association of Critical Care Nurses (who sat on our Expert Advisory Panel) and advertised the study via social media among professional groups, including the Caribbean Nurses and Midwives Association and the Filipino Nurses Association. However, we are very mindful that the quantitative evidence collected in the study is lacking in representation from nurses from a wider variety of ethnicities. This is an especially important omission given the increased mortality rate and risk of COVID-related complications for individuals of different ethnic groups.
Here we wish to note the work of the UK-REACH group (UK Research study into Ethnicity And COVID-19 outcomes in Healthcare workers: see website UK-REACH). There are likely lessons to be learnt from their exemplary, targeted recruitment strategy, which included letters of invitation and awareness-raising via professional bodies, awareness-raising via their communication channels and social media, and direct invitation and recruitment via UK healthcare providers. We also note that the UK-REACH study has reported that healthcare workers from ethnically diverse backgrounds, 20% of whom were nurses or midwives, experienced increased psychological burden as a result of working during the pandemic (Qureshi I, Gogoi M, Al-Oraibi A, Wobi F, Chaloner J, Gray L, et al.; UK-REACH Collaborative Group. Factors influencing the mental health of an ethnically diverse healthcare workforce during COVID-19: a qualitative study in the United Kingdom. Eur J Psychotraumatol 2022;13:2105577). The findings of Qureshi et al.’s qualitative study show overlap with the interview data from the CANDID study. Participants in the REACH study reported anxiety due to ongoing changes in protocols and policies, fears about infection risk, trauma because of the exposure to severe illness and death (of patients, colleagues and loved ones), guilt around the potential to expose loved ones to infection, and stress from increased workload and longer working hours. That said, it is likely that, for nurses whose own ethnicity and the ethnicity of their families placed them at greater risk of serious outcomes from COVID, their fears may have been greater than those of nurses who did not face those elevated risks.
Dissemination to participants and related patient and public communities
The research team has disseminated findings across a range of key stakeholders including study participants. Two of the research team (PR and LMcC) are members of the Intensive Care Society Workforce Development Group, whose remit (amongst others) is to support activities related to the group’s Peer Support, Staff Well-being and Conditions to Thrive groups.
Stakeholder dissemination events
Two stakeholder dissemination events were held in Glasgow and Stirling in 2022. These were publicised to all units in Scotland. All NHS Board Executive Nurse Directors in areas that provided critical care services were invited along with Scottish government representatives, the study steering group, key stakeholders from the Scottish Intensive Care Society, all unit managers, and all unit contacts. Across the 2 events, there were 29 attendees: 4 steering group members, 15 CCNs, 5 senior managers, 1 redeployed nurse, 2 research managers, 1 representative from the Scottish Intensive Care Society, and 1 representative from NHS Education (Scotland). Discussion centred on a number of key issues:
-
CCNs were not surprised by the findings and viewed the results as a validation of their experience.
-
Significant issues of staffing, skill mix, quality of care, management visibility and support, and learning and development opportunities were identified, with CCNs concerned about the future delivery of high-quality critical care services.
-
CCNs felt that quality of care had been eroded during the pandemic. There was an overwhelming sense that staff needed support now, and in the future.
-
Lessons need to be learnt at all levels in NHS organisations and government, with a sense that the culture needed to change to become a more open and caring environment.
-
Positive aspects were identified with examples of reduced bureaucratic systems, increased local autonomy and decision-making, recognition of the CCN skill set and an understanding of other disciplines’ roles.
-
There was an increasing sense of ‘pulling together’ and working as a team.
Presentations to Health Boards/Trusts
The team also presented the study findings with participating NHS Boards/Trusts:
-
Key findings were presented in a brief report to NHS Lothian.
-
Presentations given to NHS Highland and NHS Lanarkshire.
-
Key findings were presented and discussed with managers and psychologists in one English NHS Trust.
-
Key findings were presented and discussed with one Welsh NHS Board.
Presentation to government
The principal investigators met with the Chief Nursing Officer (Scotland) and presented and discussed findings.
Other dissemination work
-
Dixon D, Rattray J. Psychological Impacts of COVID 19 on Staff: Research Updates. Webinar hosted by the Intensive Care Society February 2023.
-
Salisbury L, on behalf of the CANDID Investigators. Poster presentation: ‘I just burst out crying and said I can’t do this any more’. Scottish Intensive Care Society Annual Meeting, March 2023.
-
McCallum L, on behalf of the CANDID Investigators. Oral presentation: ‘Like fighting a fire with a water pistol’: a theoretically informed study of the impact on critical care nurses of working through he pandemic. UK Critical Care Research Group Annual Meeting, February 2023
-
Scott T, Rattray J, Dixon D. NHS nurse on ‘heartbreak and hell’ of ICU amid staff burnout crisis. Scottish Television News, April 2023.
-
McCallum L, on behalf of the CANDID investigators. Poster presentation: International Council of Nurses Congress 2023 (Montreal).
-
Dixon D. Health professional wellbeing. British Psychological Society, Division of Health Psychology. CPD webinar, May 2023.
-
McCallum L, Scott T, on behalf of the CANDID investigators. Symposium Oral presentation. ‘Like fighting a fire with a water pistol’: a theoretically informed study of the impact on critical care nurses of working through he pandemic. British Association of Critical Care Nurses Annual Conference, September 2023.
-
Ramsay P, on behalf of the CANDID investigators. Symposium Oral presentation. ‘The terror and the pride’: a theoretically informed, mixed methods study of the impact on redeployed nurses of working in ICU during the pandemic. British Association of Critical Care Nurses Annual Conference, September 2023.
-
Scott T, on behalf of the CANDID investigators, presented the study findings to an NHS Grampian Senior Nurses meeting.
-
McCallum L, on behalf of the CANDID Investigators. Oral presentation. ‘Like fighting a fire with a water pistol’: a theoretically informed study of the impact on critical care nurses of working through the pandemic. University of Glasgow Postgraduate Research Conference, May 2023.
-
Royal College of Nursing International Nursing Research Conference, September 2023 N.B. Accepted symposium, but not presented due to illness.
-
Dixon D, on behalf of the CANDID Investigators. Health Psychology Research During COVID. Invited talk at the University of Stirling, September 2023.
CRediT contribution statement
Janice Rattray (https://orcid.org/0000-0002-0563-8498): Conceptualisation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Visualisation, Writing – original draft.
Jordan Miller (https://orcid.org/0000-0003-2068-5951): Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – editing and reviewing.
Beth Pollard (https://orcid.org/0009-0003-4881-4708): Data curation, Formal analysis, Methodology, Writing – editing and reviewing.
Louise McCallum (https://orcid.org/0000-0002-7334-9153): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – editing and reviewing.
Alastair Hull (https://orcid.org/0000-0003-0672-8804): Conceptualisation, Funding acquisition, Methodology, Writing – editing and reviewing.
Pam Ramsay (https://orcid.org/0000-0003-3545-4275): Conceptualisation, Formal analysis, Funding acquisition, Writing – editing and reviewing.
Lisa Salisbury (https://orcid.org/0000-0002-1400-3224): Conceptualisation, Formal analysis, Funding acquisition, Methodology, Writing – editing and reviewing.
Teresa Scott (https://orcid.org/0000-0003-1656-6255): Funding acquisition, Methodology, Resources, Writing – editing and reviewing.
Stephen Cole (https://orcid.org/0009-0008-5307-5248): Funding acquisition, Writing – editing and reviewing.
Diane Dixon (https://orcid.org/0000-0001-7099-204X): Conceptualisation, Data curation, Funding acquisition, Methodology, Project administration, Visualisation, Writing – original draft.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/PWRT8714.
Primary conflicts of interest: None of the authors have any competing interests.
Data-sharing statement
On completion of the study and publications arising from, it the anonymised transcripts will be available from corresponding authors on request.
Ethics statement
The study was approved by the Ethical Review Board for the School of Medicine, Medical Sciences and Health at the University of Aberdeen (CERB/2020/10/1993).
Information governance statement
The University of Aberdeen is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Aberdeen is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer, here https://www.abdn.ac.uk/staffnet/governance/data-protection-6958.php.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
Publications
Rattray J, McCallum L, Hull A, Ramsay P, Salisbury L, Scott T, et al. Work-related stress: the impact of COVID-19 on critical care and redeployed nurses: a mixed-methods study. BMJ Open 2021. https://doi.org/10.1136/bmjopen-2021-051326
McCallum L, Rattray J, Pollard P, Miller J, Hull A, Ramsay P, et al. The CANDID Study: impact of COVID-19 on critical care nurses and organisational outcomes: implications for the delivery of critical care services – a questionnaire study before and during the pandemic. medRxiv 2022. https://doi.org/10.1101/2022.11.16.22282346
Miller J, Young B, Mccallum L, Rattray J, Ramsay P, Salisbury L, et al. ‘Like fighting a fire with a water pistol’: a qualitative study of the work experiences of critical care nurses during the COVID-19 pandemic. J Adv Nurs 2024. https://doi.org/10.111/jan.15773
In preparation
McCallum L, Dixon D, Salisbury L, Pollard B, Hull A, Miller J, et al. The CANDID Study: the impact on and experiences of working in critical care during the COVID-19 pandemic on Redeployed Nurses: a mixed-methods study. In submission with Intensive and Critical Care Nursing.
Study registration details
This study is registered as researchregistry6126.
Funding
This synopsis presents independent research funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme as award number NIHR132068.
This synopsis reports on one component of the research award A model of occupational stress to assess impact of COVID-19 on critical care and redeployed nurses: a mixed-methods study. For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/NIHR132068).
About this synopsis
The contractual start date for this research was in October 2020. This synopsis began editorial review in January 2023 and was accepted for publication in April 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This synopsis was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Rattray et al. This work was produced by Rattray et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- CCNs
- critical care nurses
- COVID-19
- coronavirus disease caused by the SARS-CoV-2 virus
- GHQ-12
- General Health Questionnaire
- ICU
- intensive care unit
- JD-R model
- Job-Demands Resource model
- MBI-HSS
- Maslach Burnout Inventory Human Services Survey
- PCL-5
- Post-traumatic Stress Disorder Checklist for DSM-5
- PPE
- personal protective equipment
- PTSD
- post-traumatic stress disorder
- QEEW 2.0
- Questionnaire on the Experience of Work
- RDNs
- redeployed nurses
- UWES-9
- Utrecht Work Engagement Scale
References
- González-Gil MT, González-Blázquez C, Parro-Moreno AI, Pedraz-Marcos A, Palmar-Santos A, Otero-García L, et al. Nurses’ perceptions and demands regarding COVID-19 care delivery in critical care units and hospital emergency services. Intensive Crit Care Nurs 2021;62.
- Calkins K, Guttormson J, McAndrew NS, Losurdo H, Loonsfoot D, Schmitz S, et al. The early impact of COVID-19 on intensive care nurses’ personal and professional well-being: a qualitative study. Intensive Crit Care Nurs 2023;76.
- Hall CE, Milward J, Spoiala C, Bhogal JK, Weston D, Potts HWW, et al. The mental health of staff working on intensive care units over the COVID-19 winter surge of 2020 in England: a cross sectional survey. Br J Anaesth 2022;128:971-9.
- Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during COVID-19. Occup Med (Lond) 2021;71:62-7.
- Stocchetti N, Segre G, Zanier ER, Zanetti M, Campi R, Scarpellini F, et al. Burnout in intensive care unit workers during the second wave of the COVID-19 pandemic: a single center cross-sectional Italian study. Int J Environ Res Public Health 2021;18.
- Endacott R, Blot S. Fundamental drivers of nurses’ experiences of ICU surging during the coronavirus disease 2019 (COVID-19) pandemic. Curr Opin Crit Care 2022;28:645-51.
- Bakker AB, Demerouti E. Job demands–resources theory: taking stock and looking forward. J Occup Health Psychol 2017;22:273-85.
- Bakker AB, Demerouti E. The Job Demands-Resources model: state of the art. J Manag Psychol 2007;22:309-28.
- Bakker AB, Demerouti E, Sanz-Vergel A. Job Demands–Resources theory: ten years later. Annu Rev Organ Psychol Organ Behav 2023;10:25-53.
- Rattray J, McCallum L, Hull A, Ramsay P, Salisbury L, Scott T, et al. Work-related stress: the impact of COVID-19 on critical care and redeployed nurses: a mixed-methods study. BMJ Open 2021;11.
- McCallum CL. Work Related Stress and Wellbeing in Critical Care Nurses and Their Relationship with Patient Safety. Dundee: University of Dundee; 2022.
- Ritchie J, Spencer L. Analyzing Qualitative Data. London: Routledge; 1994.
- Greenberg N, Rafferty L. Post-traumatic stress disorder in the aftermath of COVID-19 pandemic. World Psychiatry 2021;20:53-4.
- Crowe S, Howard AF, Vanderspank-Wright B, Gillis P, McLeod F, Penner C, et al. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: a mixed method study. Intensive Crit Care Nurs 2021;63.
- Bruyneel A, Smith P, Tack J, Pirson M. Prevalence of burnout risk and factors associated with burnout risk among ICU nurses during the COVID-19 outbreak in French speaking Belgium. Intensive Crit Care Nurs 2021;65.
- Petrie K, Milligan-Saville J, Gayed A, Deady M, Phelps A, Dell L, et al. Prevalence of PTSD and common mental disorders amongst ambulance personnel: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol 2018;53:897-909.
- Berger W, Coutinho ES, Figueira I, Marques-Portella C, Luz MP, Neylan TC, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc Psychiat Psychiatr Epidemiol 2012;47:1001-11.
- Bakker AB, Le Blanc PM, Schaufeli WB. Burnout contagion among intensive care nurses. J Adv Nurs 2005;51:276-87.
- Hodkinson A, Zhou A, Johnson J, Geraghty K, Riley R, Zhou A, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ 2022;378.
- Bruyneel A, Bouckaert N, Maertens de Noordhout C, Detollenaere J, Kohn L, Pirson M, et al. Association of burnout and intention-to-leave the profession with work environment: a nationwide cross-sectional study among Belgian intensive care nurses after two years of pandemic. Int J Nurs Stud 2023;137.
- Leavers’ Survey 2020: Why Do People Leave the NMC Register?. London: Nursing and Midwifery Council; 2020.
Appendix 1
| Constructs and measures | Score range | Construct description |
|---|---|---|
| Outcome measures | ||
| Organisational outcomes | ||
| Quality of care [Agency for Healthcare Research and Quality Hospital Survey (1 item)] | 1–5a | Perceptions of quality of care |
| Patient safety (1 item) | 1–5a | Perceptions of patient safety |
| Certainty about futureb (3 items) | 0–100 | Certainty of remaining in job for next year |
| Changing jobsb (3 items) | 0–100 | Intention to remain in current job |
| Job satisfactionb (1 item) | 0–100 | Level of satisfaction with the job |
| Commitmentb,c (6 items) | 0–100 | Level of commitment to the organisation |
| Health impairment outcomes | ||
| Psychological health (GHQ-12; 12 items) | 0–36 | Mental health wellbeing/psychological distress |
| Burnout (MBI; 22 items in 3 subscales) | ||
| Emotional exhaustion | 0–54 | Feeling exhausted or overwhelmed |
| Depersonalisation | 0–30 | Impersonal responses towards recipients of care |
| Personal accomplishment | 0–48a | Feelings of competence and achievement |
| Post-traumatic stress disorder symptoms (PCL-5c; 20 items) | 0–80 | Intrusive thoughts, avoidant behaviours, negative changes in thinking and mood, and changes in physical and emotional reactions |
| Recovery from workb (6 items) | 0–100 | Immediate effects of work on home life |
| Detachment from workb (3 items) | 0–100 | Ability to psychologically disconnect from work |
| Work engagement outcomes | ||
| UWES (9 items in 3 subscales) | ||
| Vigour | 0–6a | High energy and resilience |
| Dedication | 0–6a | Sense of pride and commitment |
| Absorption | 0–6a | Concentration and immersion within work |
| Sources of stress | ||
| Job demands | ||
| Pace and amount of workb (6 items) | 0–100 | Speed and pressure of work |
| Emotional loadb (5 items) | 0–100 | How emotionally demanding is the job |
| Mental loadb (3 items) | 0–100 | Cognitive demands of work |
| Physical effortb (3 items) | 0–100 | Amount of physical effort required |
| Complexity of workb (3 items) | 0–100 | Complexity and difficulty of work |
| Work organisationb (6 items) | 0–100 | Interruptions and hindrances to work |
| Role conflictb (5 items) | 0–100 | Aspects of work that are disliked or unclear |
| Disproportionate relative/visitor expectations (8 items) | 1–5 | Unrealistic demands from relatives |
| Verbal aggression from relatives/visitors (5 items) | 1–5 | Verbal aggression from relatives/visitors |
| Communication with relatives/visitors (4 items)c | 1–10 | |
| Sources of work engagement | ||
| Job resources | ||
| Learning opportunitiesb (2 items) | 0–100 | Opportunities for growth and development |
| Effectiveness in achieving goalsb (4 items) | 0–100 | Clarity of what needs to be achieved and organisational support to meet these goals |
| Autonomyb (4 items) | 0–100 | Having freedom to decide or organise activities |
| Task clarityb (4 items) | 0–100 | Demarcation of responsibility for specific tasks |
| Feedbackb (4 items) | 0–100 | Feedback on purpose and results of work |
| Relationship with supervisorb (6 items) | 0–100 | Support from supervisor |
| Relationship with colleaguesb (6 items) | 0–100 | Collegial nature of relations within the team |
| Qualityb (4 items) | 0–100 | How quality is evaluated by the organisation |
| Well-being focusb (5 items) | 0–100 | Extent that the organisation prioritises and values staff well-being |
| Staffingb (4 items)d | 0–100 | Sufficient numbers of and use of agency/temporary staff |
| Personal resources | ||
| Resilience [Connor Davidson Resilience Scale (CDRS; 10 items)] | 0–4c | Extent to which an individual prospers in the face of hardship |
| 2018 | CCN | RDN | CCN vs. RDN | ||
|---|---|---|---|---|---|
| Number of participants | 557 | 461 | 200 | ||
| Age [mean (standard deviation)] | 40.37 (10.19) | 39.36 (10.86) | 42.00 (11.03) | F(1587) = 7.35** | |
| Gender: % women | 90.1 | 89.8 | 94.0 | χ2(1) = 2.93 ns | |
| Years of nursing experience [mean (standard deviation)] | 15.93 (10.09) | 15.10 (10.42) | 16.68 (11.54) | F(1654) = 3.00 ns | |
| Years of critical care experience [mean (standard deviation)] | 11.72 (9.00) | 11.49 (9.31) | – | ||
| Staff grade (%) | Band 5 | 72.1 | 65.2 | 62.8 | χ2(2) = 3.63 ns |
| Band 6 | 21.3 | 26.5 | 24.1 | ||
| Band 7 + | 6.6 | 8.3 | 13.1 | ||
| Int N | Age | Gender | Ethnicity | Role | Working experience (years) | Pay banda | Network/nationb | |
|---|---|---|---|---|---|---|---|---|
| Nursing | Critical care | |||||||
| Interviews conducted in wave 2 of the pandemic c | ||||||||
| 1 | 55 | Female | White British | RDN | 17 | N/A | 5 | North |
| 2 | 53 | Female | White British | CCN | 25 | 20 | 5 | East |
| 3 | 29 | Female | White British | CCN | 6 | 6 | 5 | North |
| 4 | 44 | Female | White British | CCN | 25 | 22 | 7 + | East |
| 5 | 25 | Female | White British | CCN | 4 | 1.5 | 5 | East |
| Interviews conducted in wave 3 of the pandemic c | ||||||||
| 6 | 54 | Male | White British | CCN | 20 | 20 | 5 | East |
| 7 | 45 | Female | White British | RDN | 18 | N/A | 6 | North |
| 8 | 29 | Male | White British | CCN | 9 | 7 | 5 | North |
| 9 | 51 | Male | White British | RDN | 5 | N/A | 7 + | East |
| 10 | 38 | Female | White British | CCN | 17 | 16 | 6 | West |
| 11 | 26 | Female | White British | CCN | 4 | 2 | 5 | England |
| 12 | 35 | Male | Asian/Asian British | CCN | 14 | 10 | 6 | England |
| 13 | 34 | Female | White British | RDN | 3 | N/A | 6 | West |
| 14 | 54 | Female | White British | CCN | 33 | 28 | 6 | West |
| 15 | 28 | Male | Black/African/Caribbean/Black British | CCN | 3 | 1.33 | 5 | England |
| 16 | 49 | Female | White British | RDN | 27 | N/A | 7 + | West |
| 17 | 47 | Female | White British | RDN | 26 | N/A | 5 | North |
| 18 | 53 | Female | White British | CCN | 30 | 29 | 6 | West |
| 19 | 33 | Female | White British | CCN | 6 | 2 | 5 | West |
| 20 | 31 | Female | White British | RDN | 8 | N/A | 6 | West |
| 21 | 37 | Female | White British | CCN | 15 | 9 | 7 + | North |
| 22 | 44 | Female | White British | CCN | 23 | 23 | 7 + | West |
| 23 | 36 | Female | White and Asian | CCN | 10 | 7 | 6 | North |
| 24 | 51 | Male | White British | RDN | 18 | N/A | 7 + | West |
| 25 | 26 | Female | White and Asian | RDN | 2 | N/A | 5 | England |
| 26 | 54 | Female | White British | RDN | 32 | N/A | 7 + | East |
| 27 | 26 | Female | White British | CCN | 5 | 3.5 | 5 | East |
| 28 | 52 | Female | White British | CCN | 30 | 24 | 6 | East |
| 29 | 42 | Female | White British | CCN | 19 | 9 | 6 | East |
| 30 | 61 | Female | White British | CCN | 24 | 17 | 7 + | East |
| 31 | 27 | Male | White British | CCN | 3 | 2 | 5 | England |
| 32 | 38 | Female | White British | RDN | 15 | N/A | 6 | England |
| 33 | 33 | Female | White British | RDN | 9 | N/A | 6 | England |
| 34 | 54 | Female | Other white background | CCN | 32 | 29 | 5 | England |
| 35 | 29 | Female | White British | CCN | 1.8 | 1.5 | 5 | Wales |
| 36 | 30 | Female | White British | CCN | 5 | 5 | 5 | Wales |
| 37 | 39 | Female | White British | CCN | 17 | 14 | 7 + | North |
| 38 | 49 | Female | White British | RDN | 27 | N/A | 7 + | North |
| 39 | 48 | Female | White British | RDN | 9 | N/A | 5 | West |
| 40 | 36 | Female | Other white background | CCN | 5 | 4 | 6 | West |
| 41 | 40 | Female | Other white background | CCN | 19 | 16 | 7 + | North |
| 42 | 56 | Female | White British | RDN | 33 | N/A | 5 | West |
| 43 | 49 | Male | White British | RDN | 28 | N/A | 7 + | North |
| 44 | 41 | Female | White British | CCN | 19 | 17 | 6 | West |
| Background questions |
|
| Experience of working in ICU during the pandemic |
|
| Job demands |
|
| Job resources |
|
| Exploring best and most challenging shifts |
|
| Impact on well-being |
|
| Identifying well-being initiatives |
|
| Effectiveness |
|
| Accessibility |
|
| Gaps in provision |
|
| Closing |
|