Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA Programme on behalf of NICE as project number 07/53/01. The protocol was agreed in May 2007. The assessment report began editorial review in October 2007 and was accepted for publication in July 2008. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
RS Taylor is an author on two of the HTA reports included in this review, is a member of PenTAG, which prepares technology assessment reports for NCCHTA on behalf of the National Institute for Health and Clinical Excellence (NICE), and is a NICE Appraisal Committee member. J Elston is an Academic Speciality Registrar in Public Health on placement at PenTAG.
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NCCHTA, Alpha House, Enterprise Road, Southampton Science Park, Chilworth, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Aims and objectives
Aim
To explore the use of surrogate outcomes in Health Technology Assessment (HTA) and by doing so provide a basis for guidance for their future use, validation and reporting.
This report focuses on the role of surrogate outcomes in cost-effectiveness models (CEMs) within UK HTA Programme reports.
Objectives
Specifically, the objectives of the report are to:
-
summarise current guidelines for the use of surrogate outcomes in HTA and CEMs
-
survey the use of surrogate outcomes in CEMs in UK HTA Programme reports published in 2005 and 2006
-
review current practice around the use (i.e. validation, quantification and reporting) of surrogate outcomes in CEMs in UK HTA Programme reports
-
assess the validity of identified surrogates using existing frameworks
-
provide recommendations on the use of surrogate outcomes in CEMs within future HTA reports.
Before addressing these objectives, Chapter 2 provides an overview of the use of surrogates in clinical trials, economic analysis and HTA based on a non-systematic literature review.
Chapter 2 Background
Rationale for the use of surrogate outcomes
One of the most important factors in determining the duration, size and cost of a clinical trial of a new or existing treatment is the choice of outcome. Ideally, decisions on the use of treatment should be based on well-conducted randomised controlled trials (RCTs) that assess clinically important ‘final’ patient-relevant outcomes, that is, outcomes of which the patient is aware and wants to avoid, for example death or morbid end points (e.g. myocardial infarction, stroke or impaired quality of life). 1,2
However, conducting trials with final patient-relevant outcomes can require a very large sample size and/or periods of long follow-up for sufficient differences in outcome to be obtained to achieve statistical significance, particularly in the case of chronic diseases. Other end points can be used to substitute for, or act as a ‘surrogate’ for, the final outcome, the principal rationale being a more rapid accrual of data. Therefore, the use of surrogate outcomes may lead to shorter studies and faster times to licensing and dissemination of new treatments. In particular, when a patient’s risk of serious morbidity or mortality is high and/or his or her illness is rare, use of surrogate outcomes may provide an attractive option when it comes to approval of new treatments for market access. Some common surrogate outcomes that have been used to gain regulatory approval are listed in Table 1.
| Disease | Surrogate outcome | Final patient-relevant outcome |
|---|---|---|
| HIV infection | CD4 count | AIDS or death |
| Cancer | Tumour size reduction | Mortality |
| Colon cancer | Carcinoembryonic antigen | Disease progression |
| Prostate cancer | Prostate-specific antigen | Disease progression |
| Cardiovascular disease | Blood pressure, cholesterol level | Haemorrhagic stroke, myocardial infarction |
| Glaucoma | Intraocular pressure | Vision loss |
| Osteoporosis | Bone density | Bone fracture |
Surrogate outcome – definition
Terms such as ‘surrogate outcome or end point’, ‘biomarker’ or ‘biological marker’ are often used interchangeably. This heterogeneity in terminology has led to some confusion over the identification of what may be considered a surrogate outcome and the role of surrogate outcomes.
There are important differences between these terms, particularly in terms of what constitutes a surrogate outcome. The distinctions made by the Biomarkers Definitions Working Group of the United States National Institutes of Health (US NIH)4 are helpful in this respect and are summarised in Table 2.
| Term | Definition |
|---|---|
| Biological marker (biomarker) | A characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes or pharmacological response to a therapeutic intervention |
| Clinical (final) outcome | A characteristic or variable that reflects how a patient feels, functions or survives |
| Surrogate outcome | A biomarker that is intended to substitute for a clinical (final) outcome. A surrogate end point is expected to predict clinical benefit |
Two key tenets of a surrogate outcome are that it represents an end point that is intended to substitute for and be predictive of a final patient-relevant clinical outcome.
Risks of surrogate outcomes
The early use of surrogate outcomes has led to some dramatic breakthroughs in treatments. This is perhaps best illustrated by the dramatic surge of the AIDS epidemic and the impressive therapeutic results obtained with highly active antiretroviral therapy based on the use of CD4 cell counts and viral load, which substituted for time to clinical events and overall survival. 5
However, despite their potential appeal, and success in some areas, the use of surrogate outcomes in trials has been controversial. Their use, at least in some applications, has led to erroneous or even harmful conclusions. 6,7 One of the most well-known cases involved the approval of three cardiovascular drugs, encainide, flecainide and moricizine, by the United States Food and Drug Administration (FDA). The drugs were approved as they were shown to effectively suppress arrhythmias. It was believed that, because ventricular arrhythmia is associated with an almost fourfold increase in the rate of cardiac complication-related death, the drugs would reduce mortality. After the drugs had been approved and introduced into clinical practice the Cardiac Arrhythmia Suppression Trials (CAST I and II) were conducted to evaluate how the three drugs would affect the survival of patients who had a myocardial infarction and ventricular arrhythmia. Both trials showed that, although the drugs did suppress the rate of arrhythmia, the number of deaths among patients treated with the drugs was more than twice that observed in patients receiving placebo. 8
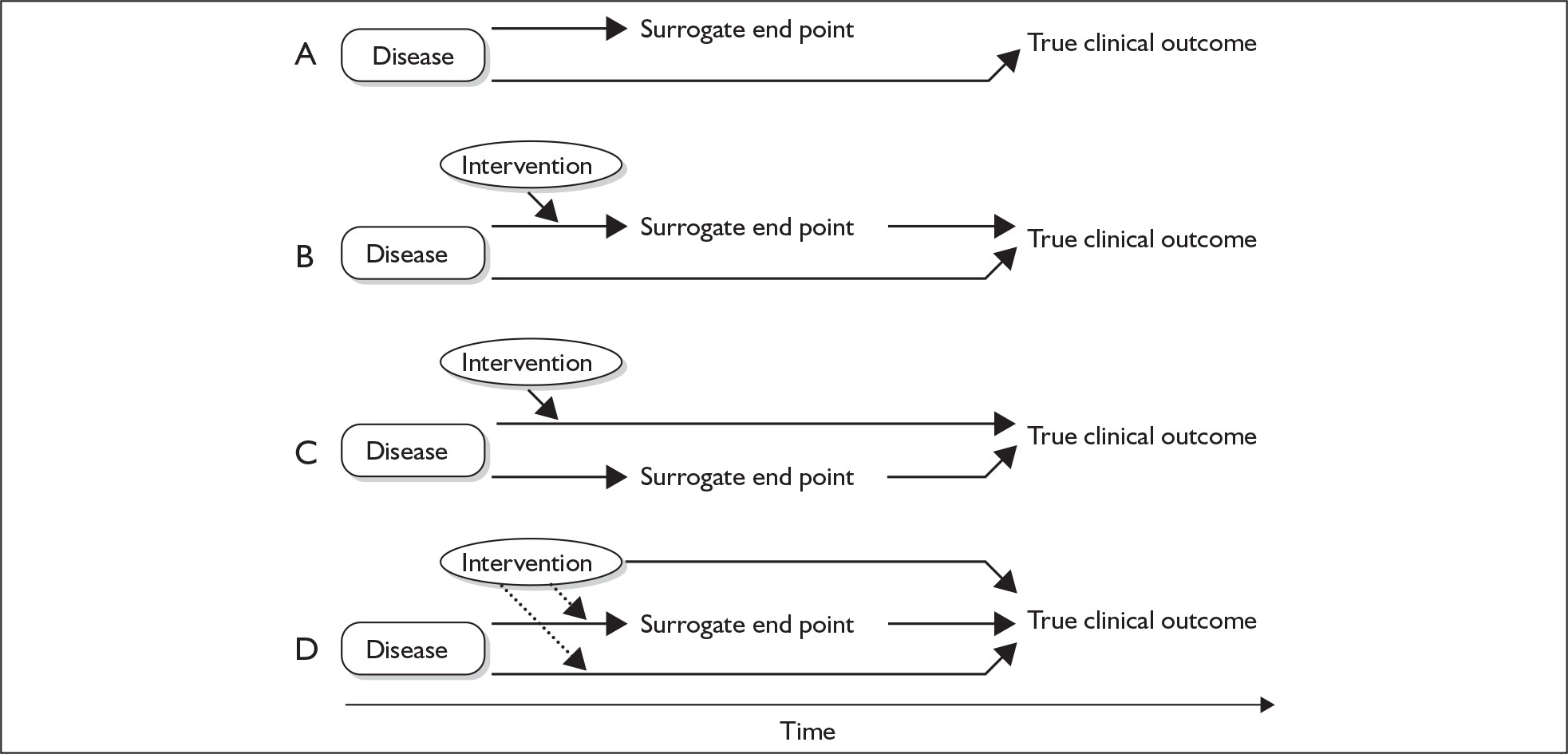
In addition to arrhythmia suppression, Fleming and DeMets6 catalogue several other examples of so-called ‘false-positive’ conclusions as the result of the early approval of drugs on the basis of surrogate outcomes. They also provide a number of potential explanations for these failures (as illustrated in Figure 1).
FIGURE 1.
Examples of the reasons for failure of surrogate outcomes. A. The surrogate is not on the causal pathway of the disease process. B. There are several causal pathways leading to the disease but the intervention affects only the pathway mediated through the surrogate. C. There are several causal pathways leading to the disease but the surrogate is not on the pathway that the intervention affects or is insensitive to its effects. D. The intervention may also have a mechanism of action that is independent of the disease process (dotted lines), affecting the final outcome directly. Adapted from Fleming and DeMets. 6
More recently, Ridker and Torres9 reviewed the various characteristics of 324 consecutive cardiovascular trials published in three major general medical journals [Journal of the American Medical Association (JAMA), the Lancet and the New England Journal of Medicine] between January 2000 and July 2005. The authors found that trials reporting a surrogate outcome as a primary outcome were more likely to report a positive treatment effect [77 out of 115 trials (67%)] than those trials that reported a final patient-related primary outcome [113 out of 209 trials (54%), p = 0.02].
The reviews of Fleming and DeMets6 and Ridker and Torres9 suggest that the use of surrogate outcomes in HTA may lead to two levels of error: (1) a conclusion that a new treatment has a greater health benefit than risk when the opposite is true (false positive); (2) an overestimate of the true level of benefit of a new treatment (bias). Furthermore, at least theoretically, the use of a surrogate outcome could lead to a false negative or underestimate of treatment effect. When possible, policy-makers and HTA analysts would seek to avoid such errors.
Validation of surrogate outcomes
The balance of potential advantages and risks in using surrogate outcomes within clinical trials highlights the need for criteria by which the validity of surrogate measures can be judged. The following broad hierarchy has been proposed as part of the International Conference on Harmonisation guidelines for the conduct of clinical trials for the registration of drugs (ICH-9). 10
In practice, the strength of the evidence for surrogacy depends upon (i) the biological plausibility of the relationship, (ii) the demonstration in epidemiological studies of the prognostic value of the surrogate for the clinical outcome and (iii) evidence from clinical trials that treatment effects on the surrogate correspond to effects on the clinical outcome.
ICH-9,10 p. 9
In passing, it is interesting to note the overlap between this hierarchy and Bradford Hill’s criteria for inferring causation versus association, as first stated in 1965. 11
The sources of evidence necessary to attain each of the three levels are summarised in Table 3.
| Hierarchical level | Evidence requirementa | Source of evidence |
|---|---|---|
| Level 3 | Biological plausibility of relationship between surrogate outcome and final patient-related outcome | Pathophysiological studies and understanding of disease process |
| Level 2 | Consistent association between surrogate outcome and final patient-related outcome | Epidemiological (observational) studies demonstrating an association between the surrogate outcome and final patient-related outcome |
| Level 1 | Treatment effects on the surrogate correspond to effects on the patient-related outcome | Clinical trial(s) showing that change in surrogate outcome with treatment is associated with a commensurate change in final patient-related outcome |
At the lowest level (level 3), understanding of the biology and pathophysiological studies makes it plausible that changes in the surrogate will lead to changes in the final patient-related outcome. Level 2 requires evidence of the association between the surrogate outcome and the final patient-related outcome. Typically, this evidence would come from cross-sectional observational studies in which both surrogate and final patient-related outcomes are available. The strength of association is reflected in statistics such as a correlation coefficient or relative risk. The larger the correlation, the more likely the causal link between the surrogate and final outcomes. In addition to the strength of association, the validity of the association depends on whether it is consistent across studies and, given the observational basis of the evidence, following adjustment for known confounders. Level 1 validation requires controlled trial evidence showing that the treatment-related change in the surrogate outcome is associated with a concomitant change in the final outcome.
Although we are unaware of a single internationally agreed checklist for the validation of surrogate outcomes, our literature searches identified two groups that have independently published criteria for judging the adequacy of surrogate outcomes.
JAMA User’s Guide (XIX) to the use of surrogate end points
Bucher and colleagues,12 as part of the JAMA Users’ Guides to the Medical Literature series, produced advice on using journal articles reporting intervention effects based on a surrogate outcome. They propose that the validity of a surrogate depends on two issues. First, to be consistently reliable the surrogate must be on the causal pathway from the intervention to the final outcome. Second, in considering a particular intervention there must be confidence that there are no important effects of that intervention on the final outcome that are not mediated through, or captured by, the surrogate. The guide provides three questions to determine the validity of a surrogate outcome (Table 4).
| Guide | Requirement questions |
|---|---|
| 1 | Is there a strong, independent, consistent association between the surrogate outcome and the final outcome? |
| 2 | Is there evidence from randomised controlled trials in other drug classes that improvement in the surrogate outcome has consistently led to improvement in the final outcome? |
| 3 | Is there evidence from randomised controlled trials within the same drug class that improvement in the surrogate outcome has consistently led to improvement in the final outcome? |
Although they do not mention the requirement for biological plausibility, the JAMA User’s Guide questions are otherwise directly related to the levels of surrogate validation presented in Table 3, i.e. guide 1 is equivalent to level 2 evidence and guides 2 and 3 are equivalent to level 1 evidence. According to Bucher et al. ,12 for a surrogate to be considered valid there needs to be a positive response to guide 1 and one of guide 2 or guide 3.
By splitting level 1 evidence into two components, the JAMA User’s Guide provides an extension to the validation of surrogates, as RCT evidence may be available for the surrogate and final outcome from another drug (or other medical technology) class but not for the actual drug or another drug within the same class. However, this further level of validation may well be contrary to the desire of analysts and policy-makers for a more generic use of a surrogate outcome across treatments within a disease area.
OMERACT biomarker and surrogate end point evidence schema
The OMERACT (Outcomes Measures in Rheumatology Clinical Trials) Working Group recently published a quantitative scoring system that evaluates and ranks the surrogacy status of biomarkers. 13 Scoring was developed through literature review and therefore is again broadly based on the validation hierarchy in Table 4. The OMERACT scoring schema is based on four domains (Table 5).
| Domain | Definition | Scoring |
|---|---|---|
| A. Target | The final outcome that the surrogate substitutes fora | 0–5 |
| B. Study design | The level of evidence for the relationship between the surrogate outcome and the final outcome | 0–5 |
| C. Statistical strength | The strength of the association between the surrogate outcome and the final outcome and its statistical significance | 0–5 |
| D. Penalties | Lack of, opposing or inconsistent evidence from biology, clinical epidemiology or therapeutic trials | –1 to –3 |
| Total –3 to –15 |
In this schema the authors propose that a biomarker be recognised as a surrogate outcome only if it achieves a total score of 10 or more.
No rationale for the weighting of domains in the scoring system is provided. Furthermore, the authors emphasise the current very limited application of the schema and the need for its further development. Until such application takes place, the validity and acceptability of the OMERACT tool remains uncertain.
Finally, the last decade has seen considerable efforts made in the development of statistical methods for the validation of surrogate outcomes. Detailed discussion of these statistical methods is beyond the scope of this report but can be found elsewhere. 14,15 These statistical methods include concepts such as the proportion of treatment effect explained (PTE), which is intended to indicate the proportion of the treatment effect mediated by the surrogate outcome, and the relative effect (RE), which is the ratio of the effects of treatment upon the surrogate and final outcomes. The application of these methods in single trials has often faced the problem of low statistical power, which in turn has been overcome by further developments in approaches that allow multicentre patient-level data analysis and meta-analysis.
Regulatory consideration of surrogate outcomes
With growing pressure to reduce the time to regulatory approval for new medical technologies, surrogate outcomes are frequently used as the basis for marketing licence applications for drugs and medical devices, particularly when they affect patients with life-threatening diseases for which no effective therapy exists. This has particularly been the case for the regulatory authority in the US, the FDA, although less so for the European regulatory authority, the European Medicines Agency (EMEA). 15,16 A summary of the current policies of both agencies is given below.
US Food and Drug Administration
In 1992 the FDA formulated a new regulatory process – the accelerated approval process – for diseases that are serious or life threatening and for which no effective therapies exist. Part of the accelerated approval process (‘subpart H’) allows marketing approval for a new drug product to be granted on the basis of:
adequate and well-controlled clinical trials establishing that the drug product has an effect on a surrogate end point that is reasonably likely, based on epidemiological, therapeutic, pathophysiologic and other evidence, to predict clinical benefit or on the basis of an effect on a clinical end point other than survival or irreversible morbidity. Approval under this section will be subject to the requirement that the applicant study the drug further, verify and describe its clinical benefit, where there is uncertainty as to the relation of the surrogate end point to clinical benefit, or of the observed clinical benefit to ultimate benefit outcome. Post-marketing studies would usually already be under way. When required to be conducted such studies must also be adequate and well controlled. The applicant shall carry out such studies with due diligence.
Johnson et al. ,15 p. 1404
European Medicines Agency
In the European Union there is a different ‘accelerated approval’ process. Current European legislation allows for granting of marketing authorisation under ‘exceptional circumstances’ when comprehensive data cannot be provided at the time of the submission (e.g. orphan conditions when the disease is rare) and provided that the applicant agrees to a further programme of studies which will be the basis of a post-authorisation review of the benefit–risk profile of the drug. Although this primarily refers to situations in which RCTs are lacking or difficult to undertake, it equally applies to absence of data on an appropriate clinical end point. Although less formalised than the FDA accelerated approval process, in such circumstances the European accelerated approval of drugs may also accept evidence that uses surrogate outcomes to support applications. 16
In other international jurisdictions the regulatory acceptance of surrogates may differ. For example, in Japan proof of surrogacy through at least two RCTs collecting the final outcome is required as part of the post-marketing process. 16
Use of surrogate outcomes in Health Technology Assessment
The Centre for Reviews and Dissemination (CRD) at the University of York17 defines HTA as follows:
HTA considers the effectiveness, appropriateness, cost and broader implications of technologies using both primary research and systematic review. It seeks to meet the information needs of those who manage and provide care.
This definition emphasises two key aspects of HTA. First, its scope is to systematically review the clinical effectiveness and the cost (effectiveness) of a drug (or other form of health technology). Second, HTA aims to inform policy and has been increasingly used by governments and health-care payers as a means of supporting their reimbursement and funding decisions. Since 1999 the National Institute for Health and Clinical Excellence (NICE) has been responsible for providing guidance to the NHS in England and Wales on the use of health technologies, principally based on their clinical effectiveness and cost-effectiveness. These decisions have drawn on HTA reports commissioned by the Department of Health and undertaken by independent, university-based academic teams. These reports are based on a systematic review of the clinical effectiveness literature and determine cost-effectiveness typically using the common currency of cost per quality-adjusted life-year (QALY) gained. QALYs are a way of measuring both the quality and the quantity of life lived, as a means of quantifying the benefit of a treatment in terms of a universal/comparable health currency. In many instances the nature of clinical evidence is such that these cost-effectiveness analyses are based on a decision-analytic model.
A number of NICE decisions have been based on an estimate of cost-effectiveness predicated from surrogate outcomes, e.g. the use of orlistat and sibutramine in the treatment of obesity (short-term changes in body mass index predicting long-term changes in cardiovascular events and mortality) and the use of ezetimibe/statins in the treatment of primary hypercholesterolaemia (short-term changes in total cholesterol and cholesterol subfraction levels predicting cardiovascular events and mortality).
Laupacis18 recently commented that it was the experience of the Canadian Common Drug Review (which makes national reimbursement decisions on drugs based on technology assessment submissions from manufacturers) that ‘the use of unvalidated surrogates is increasing’ and that this presented ‘one of the difficult issues that [CDR] has struggled with’. Tappenden and colleagues19 summed up the importance of the appropriate use of surrogate outcomes in model-based cost-effectiveness analyses for cancer treatments:
it is imperative that the link between tumour response [surrogate outcome] and final outcome is explicitly quantified and preferably validated alongside the exploration of the uncertainty surrounding this relationship.
Tappenden et al. ,19 p. 870
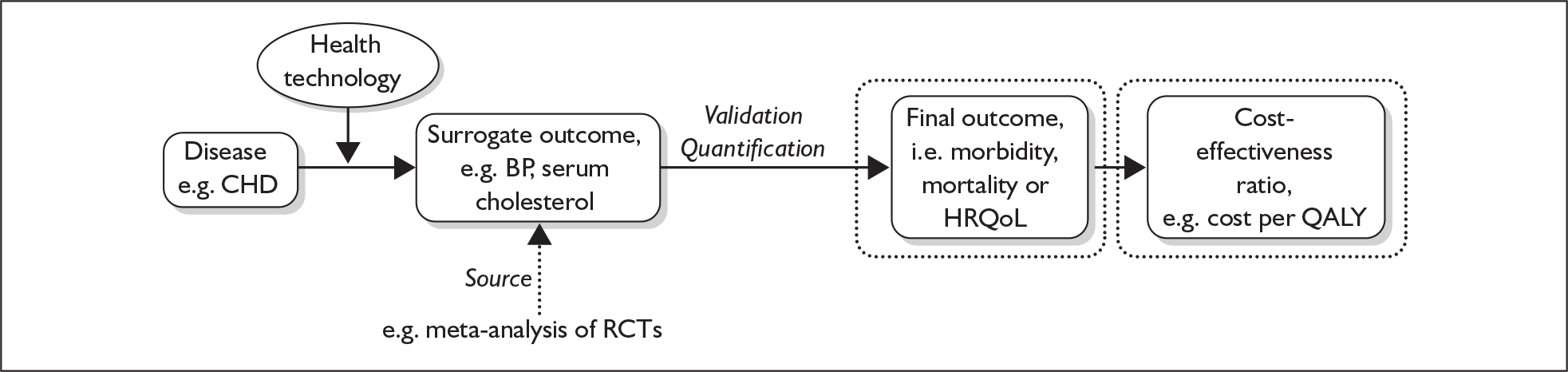
Surrogate outcomes, therefore, have the potential to play an important role in HTA model-based cost-effectiveness analyses and the reimbursement decisions based on these data. A schematic representation of the use of surrogate outcomes in an HTA CEM is illustrated in Figure 2.
FIGURE 2.
Schematic representation of the use of a surrogate outcome in a Health Technology Assessment cost-effectiveness model. ‘Source’ refers to the source of the surrogate outcome data (usually a systematic review/meta-analysis of clinical effectiveness literature in an HTA); ‘validation’ refers to the evidence supporting the relationship between the surrogate outcome and the final outcome; and ‘quantification’ refers to how this relationship has been quantified. The two dotted boxes show that quantification of the surrogate outcome to final outcome may take place either within or outside the cost-effectiveness model per se. BP, blood pressure; CHD, coronary heart disease; HRQoL, health-related quality of life; QALY, quality-adjusted life-year; RCT, randomised controlled trial.
Guidelines for the use of surrogate outcomes in Health Technology Assessment and cost-effectiveness analyses
In spite of their potential role, current guidance on the use (and validation) of surrogates in HTA reports, systematic reviews and cost-effectiveness analyses is variable. The recommendations from selected guidelines are summarised in Table 6.
| Guidelines document | Recommendation |
|---|---|
| Health Technology Assessment | |
| The International Network of Agencies for Health Technology Assessment (INAHTA) checklist for HTA reports, 200020 | No guidance on the use of surrogate outcomes |
| European Collaboration for Assessment of Health Interventions (ECHTA) Working Group 4 report, 200221 | ‘when assessing efficacy and effectiveness of therapeutic interventions, health-related outcomes (e.g. mortality) should be used. Using physiological or biochemical outcomes (i.e. “surrogate” outcomes) should be avoided as far as possible as they may not correlate with the health-related outcomes. Thus, if surrogate outcomes are used, the underlying assumptions have to be clearly stated, and results should be regarded carefully. Reliance on surrogate outcomes may be harmful and even lethal’ |
| Systematic reviews | |
| Centre for Reviews and Dissemination (CRD) systematic review guidelines, 200117 | ‘Use of intermediate, surrogate or proxy outcomes (e.g. intraocular pressure as a surrogate for visual field damage in ocular glaucoma or loss of bone mineral content as a surrogate for fractures in hormone replacement therapy) can lead to misleading conclusions from reviews’ (section 1.2.2.1) |
| Cochrane Handbook for Systematic Reviews of Interventions, 200622 | ‘One type of evidence that can be helpful in considering the likelihood of a cause–effect relationship between an intervention and an important outcome is indirect evidence of a relationship. This includes evidence relating to intermediate outcomes (such as physiological or biochemical measures that are markers for risk of the outcome of interest), evidence from studies of different populations (including animal studies) and evidence from analogous relations (i.e. similar interventions). Because conclusions regarding the strength of inferences about the effectiveness of an intervention are essentially causal inferences, reviewers might want to consider guidelines for assessing the strength of a causal inference, such as those put forward by Hill (Hill, 1971)’ (section 9.1) |
| ‘In addition to identifying limitations of the applicability of the results of their review, reviewers should discuss and draw conclusions about important variation in results within the circumstances to which the results are applicable. Is there predictable variation in the relative effects of the intervention, and are there identifiable factors that may cause the response or effects to vary? These might include . . . biochemical markers’ (section 9.2.4) | |
| Cost-effectiveness analyses and modelling | |
| Drummond 200523 | ‘The success of this approach depends on the extent to which the link between intermediate [surrogate] and final outcomes has been established. In some cases, where the size of the relative risk (for example, of death) comparing individuals with and without the risk factor is large, it may be possible to establish the link through observational or case–control studies . . .. However, in many situations it might be necessary to establish the link through studies of stronger methodology, such as intervention studies with random assignment of subjects to treatment groups . . . |
| When undertaking a CEA using effectiveness data relating to an intermediate end point the economic analyst should either (1) make a case for the intermediate end point having value of clinical relevance in its own right, (2) be confident that the link between intermediate and final outcomes has been adequately established by previous research, or (3) ensure that any uncertainty surrounding the link is adequately characterized in the economic study’ (Chapter 5, pp. 108–9) | |
| International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force on Modelling Good Practice, 200324 | ‘If evidence regarding structural assumptions is incomplete, and there is no universally accepted theory of disease process, then the limitations of the evidence supporting the chosen model structure should be acknowledged. If possible, sensitivity analyses using alternative model structures – for example, using alternative surrogate markers or intermediate variables – should be performed’ |
| Philips 200425 | ‘The methods and assumptions that are used to extrapolate short-term results to final outcomes (e.g. trial-based intermediate outcomes to survival) should be documented and evidence should be provided that the methodology is valid’ |
| NICE 200426 | ‘4.4.1 Evidence submitted to NICE |
| 4.4.1.2 The written submissions provide a unique contribution outlining the professional view of the place of the technology in current clinical practice. This includes evidence that relates to some or all of the following: | |
| – the identification of appropriate outcome measures and the appropriate use of surrogate outcome measures’ | |
| Use of surrogate outcomes to estimate final outcomes | |
| PBAC 200764 | ‘The claim that an incremental treatment effect on a surrogate outcome measured with the proposed drug quantitatively predicts a subsequent incremental treatment effect on a final outcome is more persuasively shown if attention is given to the following issues. |
| Step 1 Present a systematic review of the literature to examine whether epidemiological evidence and biological reasoning has established that there is a relationship between the surrogate outcome and the final outcome independent of any intervention. In a few instances, relationships have been established, or have been proposed, between surrogate outcomes and final outcomes. Examples include blood, left ventricular ejection fraction and survival after myocardial infarction, or viral load and cure of viral hepatitis. | |
| Step 2 Present a systematic review of the literature to examine whether randomised trial evidence using other drugs has shown that there is a basis to conclude that a treatment effect on the surrogate outcome has satisfactorily predicted a treatment effect on the final outcome. (If there is evidence of this type for the proposed drug, this might help support a biological argument for the treatment.) Based on this evidence, quantify the relationship between these treatment effects with an assessment of the uncertainty of the relationship. Discuss the reproducibility of these findings (e.g. whether they have been consistently shown across more than one trial and for more than one alternative drug and mechanism of action). | |
| Step 3 Explain why this relationship between the treatment effects on these outcomes with these other drugs is likely to apply to the proposed drug. Refer in this explanation to the mechanism of action of the proposed drug compared with the mechanism(s) of action of the drugs contributing evidence to Step 2 (a so-called “class effects” argument). At present, it is difficult to give categorical advice. | |
| Consider which outcomes are most appropriate and most feasible, given the data available. The clinical importance and patient relevance of the outcomes should be established and, where possible, supported with data. | |
| Having addressed the three steps above in transforming a treatment effect on a surrogate outcome to a treatment effect on a final outcome, explain in response to Subsection D.4 how this is included in the economic evaluation, including by specifying and referencing the sources of the longer term natural history (e.g. longitudinal population studies) as well as the transformed treatment effects’ (extracted from Section C2) | |
The International Network of Agencies for Health Technology Assessment (INAHTA) guidance for the reporting of HTA makes no mention of the methodological issues associated with the use of surrogate outcomes. 20 The European Collaboration for Assessment of Health Interventions (ECHTA) Working Group 4 report on good practice in HTA recommends that surrogate outcomes should be avoided or at least used with extreme care. 21 The CRD17 and the Cochrane Handbook for Systematic Reviews of Interventions22 both comment on the issue of surrogacy (‘intermediate outcome’ or ‘marker’) and the need for caution in interpreting the validity and reporting of outcomes.,
Cost-effectiveness methods guidelines, on the other hand, are generally more accepting of the need for surrogate outcomes in CEMs. Drummond and colleagues,23 in the third edition of Methods for the Economic Evaluation of Health Care Programmes, stress the importance of evidence of the linkage between the intermediate (surrogate) and final outcomes. The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force on Good Modelling Practice guidelines24 additionally highlight the need to undertake sensitivity analyses to assess the robustness of cost-effectiveness to structural assumptions around the relationship between the surrogate and final patient-related outcomes. Philips and colleagues25 (based on their systematic review of modelling good practice guidelines) stress the importance of transparency in describing the rationale for extrapolation between the surrogate (‘intermediate’) outcome and final outcome. Finally, the current NICE Guide to Methods of Technology Appraisal26 mentions the inclusion of evidence based on surrogate outcomes but provides no guidance on methods for the validation or reporting of such outcomes. The Pharmaceutical Benefits Advisory Committee (PBAC) guidelines for manufacturers’ submissions (updated 2007) provide detailed consideration of the use of surrogates.
Our literature searches found no empirical studies examining the use of surrogate outcomes in HTA and CEMs therein.
Chapter 3 Methods
Sampling frame
Reports published in the UK HTA Programme monograph series in 2005 and 2006 formed the sampling frame for this study. This period was chosen to reflect recent HTA practice and was limited to 2 years because of time and resources available for this project.
Selection of reports
Reports were selected on the following basis:
-
Inclusion criteria – the report addressed a treatment effectiveness/efficacy question and included a CEM and the CEM was primarily based on a surrogate outcome.
-
Exclusion criteria – the report addressed a diagnostic, screening, aetiology or prognostic question or the report was a methodological study.
A structured proforma was developed to ensure the consistent application of the selection criteria and piloted on five HTA reports (see Appendix 1). Piloting identified that it was not always possible to judge whether the CEM in an HTA report was based on a surrogate outcome. We initially used the US NIH Biomarkers Definitions Working Group definition of a surrogate end point (see Table 2), that is, ‘a biomarker that is intended to substitute for a clinical (final) outcome, and that a surrogate end point is expected to predict clinical benefit.’ However, this definition was difficult to operationalise in practice as the outcomes used in HTA reports were not what could be described as ‘biomarkers’ but were instead patient-related end points. A pragmatic approach was therefore taken that permitted such reports to be included if they otherwise fulfilled the definition of a surrogate outcome (i.e. substitution for and prediction of a final outcome). The inclusion and exclusion criteria were applied independently to all reports by the two authors (RST and JE).
Data extraction
The following categories of information were extracted from included CEM surrogate outcome reports:
-
characteristics of report (i.e. type of technology, disease area and whether report was on behalf of NICE)
-
summary of CEM [i.e. type of model and base-case incremental cost-effectiveness ratio(s) (ICER)]
-
characterisation of surrogate outcome used in CEM and identification of derived final outcome
-
source of surrogate outcome evidence used in CEM (e.g. systematic review of clinical trials)
-
evidence of validation of surrogate outcome
-
methods used in report to quantify link between surrogate outcome and final outcome (e.g. regression-based approach)
-
consideration of the uncertainty associated with using surrogate outcomes in the results or conclusions or elsewhere in the report.
Information was extracted by one of the authors using a standardised proforma (see Appendix 1) and checked by the second author.
Surrogate outcome scoring
In those reports identified as using surrogate outcomes, the evidence linking the surrogate and final outcomes was assessed according to the JAMA criteria12 and the OMERACT scoring schema. 13 Full copies of these scoring systems are provided in Appendix 2.
Data analysis and reporting
Information on all included and excluded reports was entered into a Microsoft Excel spreadsheet and summarised using counts and percentages. A narrative synthesis of the included reports was undertaken, presented in the form of tabular summaries and illustrative qualitative quotations from the text of the reports. Exploratory chi-squared analyses were planned to identify potential predictors of the use of surrogate outcomes across the included HTA reports.
Chapter 4 Results
Selection of reports
A total of 100 HTA monograph reports were published between 2005 and 2006. The characteristics of these reports are summarised in Table 7.
| Category | Number of reports |
|---|---|
| Technology type | |
| Drug | 30 |
| Medical device | 11 |
| Surgical procedure | 8 |
| Education or counselling | 9 |
| Diagnostic or screening | 22 |
| Methodological | 11 |
| Othera | 9 |
| Disease type | |
| Cancer | 12 |
| Cardiovascular | 14 |
| Mental health | 11 |
| Skeletomuscular | 9 |
| Dermatological | 6 |
| Renal urinary | 6 |
| Gastrointestinal | 5 |
| Infectious disease | 5 |
| Other diseases | 21 |
| Not applicable | 11 |
| Type of report | |
| Primary research | 33 |
| Secondary research | 66 |
| Both primary and secondary | 1 |
| Contains a cost-effectiveness decision model (CEM) | 50 |
| Report undertaken on behalf of NICE | 31 |
The majority of the HTA reports (52%) assessed either drugs or diagnostic/screening tests. The disease areas that were most frequently addressed were cancer, cardiovascular disease and mental health. About two-thirds (67%) of the reports addressed a secondary (or systematic review) research question and 50% of all the reports contained a CEM.
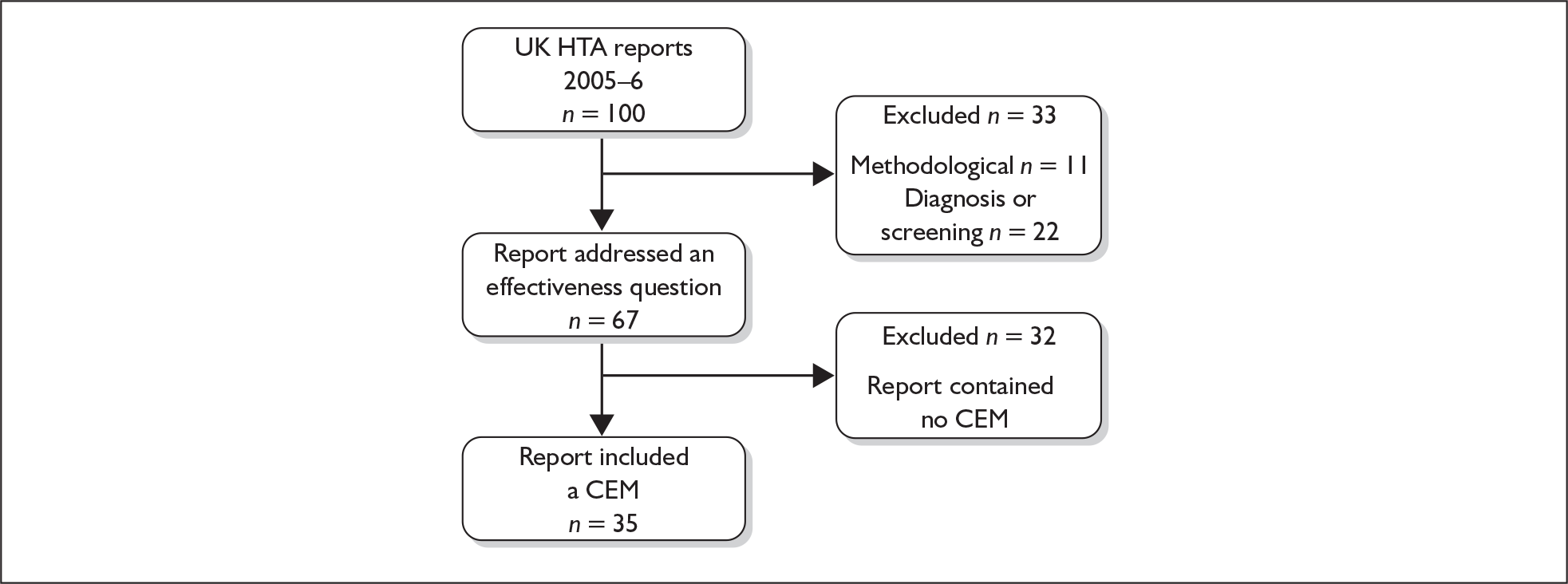
The process of report selection is summarised in Figure 3. A number of reports were initially excluded on the grounds that they addressed either a methodological or a diagnostic/screening question. Of the remaining 67 HTA reports, a further 32 reports were excluded as they did not contain a CEM. Appendix 3 contains the list of excluded reports and reasons for exclusion.
FIGURE 3.
Selection of reports. CEM, cost-effectiveness model.
| Study | Report volume (issue) | Primary/secondary research | NICE TAR | Population | Intervention | ‘Outcome(s)’ used in CEM | Source of outcome | ‘Final outcome’ classification | Commentary on the approach to the use of outcome in the CEM | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Death | Clinical event | Disease severity | Function | HRQoL | |||||||||
| Greenhalgh 200527 | 9 (9) | Secondary | Yes | Depressive illness, schizophrenia | Electroconvulsive therapy | Treatment response as assessed by depression | Meta-analysis of RCTs | ✓ | Utility values a pplied to health states based on treatment response | ||||
| Treatment response as assessed by psychotic symptoms | Single RCT | ✓ | |||||||||||
| Green 200528 | 9 (11) | Secondary | Yes | Severe sepsis | Drotrecogin alpha | Overall mortality | Single RCT | ✓ | Utility values applied to survivor health state | ||||
| McCormack 200529 | 9 (14) | Secondary | Yes | Inguinal hernia | Laparoscopic surgery | Hernia recurrence, pain and return to usual activities | Meta-analysis of RCTs and non-RCTs | ✓ | Utility values applied to health states based on recurrence and pain | ||||
| Wilby 200530 | 9 (15) | Secondary | Yes | Epilepsy in adults | Antiepileptic drugs | Treatment response as assessed by reduction in seizures | Meta-analysis of RCTs | ✓ | Utility values applied to health states based on seizure response | ||||
| Hartwell 200531 | 9 (17) | Secondary | Yes | Acute myocardial infarction | Immediate angioplasty | Overall mortality and cardiovascular events | Meta-analysis of RCTs | ✓ | ✓ | Fixed utility value applied to health states associated with cardiovascular events | |||
| Woodroffe 200532 | 9 (21) | Secondary | Yes | Adults undergoing renal transplantation | Immunosuppressive drugs | Biopsy-confirmed acute rejection | Meta-analysis of RCTs | a | a | a | a | a | Biopsy-confirmed acute rejection used to predict graft survival. QALYs were then driven by graft survival rates |
| Stevenson 200533 | 9 (22) | Secondary | Yes | Postmenopausal osteoporosis | New drugs | Fractures (hip, vertebral, wrist and proximal humerus) | Meta-analysis of RCTs | ✓ | Mortality and utility applied according to site of fracture | ||||
| Wilson 200534 | 9 (25) | Secondary | Yes | Gastrointestinal stromal tumours | Imatinib | Overall mortality and functional status as assessed by Eastern Cooperative Oncology Group (ECOG) performance status | Single uncontrolled trial | ✓ | ✓ | ECOG used to map to HRQoL utility | |||
| Robinson 200535 | 9 (27) | Secondary | Yes | Acute coronary syndrome | Glycoprotein antagonists | Overall mortality, MI, vascularisation and GI bleeding | Meta-analysis of RCTs | ✓ | ✓ | Fixed utility value applied to health states associated with cardiovascular events | |||
| Tillin 200536 | 9 (28) | Primary | No | Bowel incontinence | Electrically stimulated neosphincter surgery | HRQoL as assessed by EQ-5D | Non-RCT study | ✓ | Trial EQ-5D used directly | ||||
| Garside 200537 | 9 (29) | Secondary | Yes | Atopic eczema | Pimecrolimus and tacrolimus | Severity scale – Investigator Global Assessment (IGA) and assessment of treatment response with Physician Global Evaluation (PGE) | Meta-analysis of RCTs | ✓ | Utility values applied to health states based on severity | ||||
| Cochrane 200538 | 9 (31) | Primary | No | Lower limb osteoarthritis | Water-based therapy | Pain and functional status assessed on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scale and HRQoL assessed by SF-36 and EQ-5D | Single RCT | ✓ | ✓ | Trial EQ-5D used directly | |||
| Castelnuovo 200539 | 9 (43) | Secondary | Yes | Atrioventricular block and sick sinus syndrome | Dual chamber pacemakers | Overall mortality, atrial fibrillation, pacemaker syndrome and complications | Meta-analysis of RCTs | ✓ | ✓ | Utility applied to health states based on cardiovascular outcomes | |||
| Clegg 200540 | 9 (45) | Secondary | Yes | End-stage heart failure | Left ventricular assist devices | Overall mortality and HRQoL as assessed by Minnesota Living with Heart Failure (MLWHF) score | Single RCT, controlled and uncontrolled data | ✓ | ✓ | MLWHF mapped to utility scores | |||
| Clar 200541 | 9 (47) | Secondary | Yes | Cartilage defects in knee joints | Autologous chronocyte implantation | HRQoL (SF-36) | RCTs and uncontrolled data | ✓ | Illustrative threshold analysis to assess change in utility necessary to achieve cost-effectiveness | ||||
| Dretzke 200542 | 9 (50) | Secondary | Yes | Conduct disorder in children | Parent training | Child behaviour as assessed by the Child Behaviour Checklist (CBCL) and the Eyberg Child Behaviour Inventory (ECBI) | Meta-analysis of RCTs | ✓ | Examined what the QALY gains would have to be for unit change in behavioural outcomes needed to achieve cost-effectiveness | ||||
| Loveman 200643 | 10 (1) | Secondary | Yes | Alzheimer’s disease | Donepezil, rivastigmine, galantamine and memantine | Cognitive function as assessed by the Alzheimer’s Disease Assessment Scale, cognitive subscale (ADAS-cog) score | Meta-analysis of RCTs | a | a | a | a | a | ADAS-cog used to predict outcome of need for full-time care |
| Connock 200644 | 10 (7) | Secondary | Yes | Epilepsy in children | Antiepileptic drugs | Treatment response as assessed by freedom from seizures and side effects | RCTs | ✓ | Utility values applied to health states based on treatment response and side effects | ||||
| Main 200645 | 10 (9) | Secondary | Yes | Advanced ovarian cancer | Topotecan, doxorubicin and paclitaxel | Overall mortality and progression-free survival | RCTs | ✓ | ✓ | Utility values applied to health states based on disease state | |||
| Connock 200646 | 10 (20) | Secondary | Yes | Fabry’s disease and mucopolysaccharidosis | Enzyme replacement therapy | None | Not applicable | a | a | a | a | a | Assumed that on treatment patients regain full health |
| Wright 200647 | 10 (21) | Primary | No | Mild chronic hepatitis C | Alpha-interferon and ribavirin | HRQoL assessed by EQ-5D | Single RCT | ✓ | Trial EQ-5D values used directly | ||||
| King 200648 | 10 (23) | Secondary | Yes | Attention deficit disorder in children and adolescents | Methylphenidate, dexamphetamine and atomoxetine | Treatment responses as assessed on global symptom improvement (GSI-I) and severity (GSI-S) scales | Meta-analysis of RCTs | ✓ | Utility values applied to health states based on treatment response | ||||
| Connock 200649 | 10 (24) | Secondary | Yes | Gaucher’s disease | Enzyme replacement therapy | Disease severity as assessed by the Severity Score Index (SSI) | Non-RCTs | ✓ | Utility values mapped from severity scores | ||||
| Thomas 200650 | 10 (25) | Secondary | No | Cutaneous warts | Salicylic acid and cryotherapy | Cure rate | Meta-analysis of RCTs | ✓ | ICER is cost per 1% cure | ||||
| Buxton 200651 | 10 (27) | Secondary | No | Risk of sudden cardiac death due to arrhythmias | ICD | Overall mortality, arrhythmia, hospitalisation | RCTs and survey | ✓ | ✓ | No utility gain with ICD assumed in base case | |||
| Shepherd 200652 | 10 (28) | Secondary | Yes | Chronic hepatitis B | Adefovir dipivoxil and pegylated interferon alpha-2a | Response to treatment as assessed by alanine aminotransferase (ALT) and hepatitis B virus (HBV) levels and seroconversion rates | RCTs | a | a | a | a | a | Cirrhosis, liver cancer, liver transplant and death predicted from seroconversion rates based on natural history model. Utility values applied to health states based on disease state |
| Woolacott 200653 | 10 (31) | Secondary | Yes | Psoriatic arthritis | Etanercept and infliximab | Function/disability assessed by Health Assessment Questionnaire (HAQ) | RCTs | ✓ | Utility values predicted from HAQ | ||||
| Pandor 200654 | 10 (41) | Secondary | Yes | Colon cancer | Oxaliplatin and capecitabine | Progression-free survival and overall mortality | RCTs | ✓ | ✓ | Utility values applied to health states based on disease state | |||
| Kaltenthaler 200655 | 10 (33) | Secondary | Yes | Depression and anxiety; obsessive–compulsive disorder | Computerised cognitive behaviour therapy | Depression severity as assessed by the Beck Depression Inventory (BDI) | RCTs | ✓ | Utility values mapped to severity categories via BDI | ||||
| Treatment response as assessed by the Yale–Brown Obsessive Compulsive Scale (YBOCS) | ✓ | Utility values mapped from YBOCS | |||||||||||
| Chen 200656 | 10 (42) | Secondary | Yes | Rheumatoid arthritis in adults | Adalimumab, etanercept and infliximab | Function/disability assessed by HAQ | Meta-analysis of RCTs | ✓ | Utilities predicted from HAQ | ||||
| Davies 200657 | 10 (44) | Secondary | No | Individuals undergoing non-urgent surgery | Cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion | Need for transfusion, overall mortality, morbidity and adverse events | Meta-analysis of RCTs | ✓ | ✓ | External source of utility values applied to morbidity and adverse events | |||
| Murray 200658 | 10 (45) | Secondary | Yes | Colorectal cancer | Laparoscopic surgery | Mortality, cancer recurrence, complications | ✓ | ✓ | Fixed utility values applied to health states associated with disease states | ||||
| Woolacott 200659 | 10 (46) | Secondary | Yes | Psoriasis | Etanercept and efalizumab | Disease severity assessed by Psoriasis Area and Severity Index (PASI) | RCTs | ✓ | HRQoL utilities predicted from PASI | ||||
| Sharples 200660 | 10 (48) | Primary/secondary | No | Severe heart failure | Ventricular assist devices | Mortality and HRQoL as assessed by EQ-5D | Non-RCT study | ✓ | ✓ | EQ-5D used directly | |||
| Yao 200661 | 10 (49) | Secondary | Yes | Children undergoing renal transplantation | Immunosuppressive drugs | Biopsy-confirmed acute rejection | Meta-analysis of RCTs | a | a | a | a | a | Biopsy-confirmed acute rejection used to predict graft survival |
Four32,43,52,61 of the 35 reports (11%) were identified as using an outcome in the CEM based on prediction of a different end point reported in the clinical effectiveness review. These reports were therefore judged to be examples of the use of surrogate outcomes (highlighted in grey in Table 8) and are discussed in further detail below.
The remaining 31 HTA reports used a range of ‘final outcomes’ in their CEMs, including mortality or definitive clinical events (e.g. myocardial infarction, fracture) (n = 17), patient-related measures of disease severity (e.g. eczema severity scale) (n = 7) and functional status [e.g. Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)] (n = 4). Six reports directly used a health-related quality of life (HRQoL) outcome in their CEM. Of these, four primary research reports used the EQ-5D generic utility measure and two secondary research reports used either a disease-specific [i.e. Minnesota Living with Heart Failure (MLWHF) scale] or a generic [i.e. Short Form 36 questionnaire (SF-36)] HRQoL measure, mapped to EQ-5D.
In those reports that did not use a direct measure of mortality or HRQoL in their CEM, changes in clinical outcome (i.e. disease severity, functional status) had to be converted into utility scores. Reports broadly used two conversion approaches: (1) a judgement on health states based on the clinical outcome (e.g. treatment response) to which specific utility values were then applied and (2) direct mathematical mapping of the clinical outcome to utility values. A more detailed analysis of the conversion of clinical outcome into utility in these reports was deemed to be outside the scope of this report; however, this issue will be discussed again in Chapter 5 of this report. The remainder of this section focuses on the four HTA reports that used surrogate outcomes.
Reports with a CEM based on a surrogate outcome
Characteristics of reports
All four HTA reports32,43,52,61 based on surrogates were commissioned on behalf of NICE. They covered a range of diseases: two reports (from the same academic team) were on renal transplants; one was on Alzheimer’s disease; and one was on chronic hepatitis B infection.
Woodroffe et al. 200532
This report examined the clinical effectiveness and cost-effectiveness of a number of new immunosuppressive therapies (tacrolimus, basiliximab, daclizimab, mycophenolate mofetil and sirolimus) compared with existing therapy (ciclosporin and azathioprine) in adults undergoing kidney replacement. A systematic review identified a total of 33 RCTs across the various drugs comparisons. Most trials were short term (≤ 12 months) and were therefore of insufficient sample size and duration to detect differences between drugs in terms of relevant patient-related final outcomes, i.e. survival of the kidney graft and mortality. However, virtually all trials reported biopsy-confirmed acute rejection (BPAR). The authors of the report describe BPAR as ‘acute episodes heralded by a reduction in graft function (seen on biochemistry), and clinical features such as fluid retention and occasionally graft tenderness and fever and confirmed through a histological sample taken of the effected graft.’ Furthermore, ‘the importance of acute rejection is not only the risk of acute graft loss, but also that it may be more likely that a patient will subsequently lose the [kidney] graft.’ BPAR was used as a surrogate outcome to predict graft survival.
Shepherd et al. 200652
The aim of this study was to assess the clinical effectiveness and cost-effectiveness of two antiviral agents [adefovir dipivoxil (ADV) and pegylated interferon alpha-2a (PEG)] for the treatment of adults with chronic hepatitis B infection. The report’s systematic review identified seven RCTs that assessed the effectiveness of ADV and three trials evaluating the effectiveness of PEG. These trials reported treatment effects as the short-term biochemical response [e.g. levels of alanine aminotransferase (ALT) for liver function], virological response [e.g. presence of hepatitis B virus (HBV) DNA as evidence of viral replication] and seroconversion [e.g. hepatitis B virus e antigen (HBeAg) loss/anti-HBe; hepatitis B virus surface antigen (HBsAg) loss/anti-HBs]. The authors used seroconversion rates as a surrogate outcome in a transition natural history model to predict liver cirrhosis, liver cancer, liver transplant and death.
Loveman et al. 200643
This study assessed the clinical effectiveness and cost-effectiveness of new drugs (donepezil, rivastigmine, galantamine and memantine) for Alzheimer’s disease. A total of 12 RCTs were included. The four drugs were shown to be effective when assessed by a cognitive function outcome measure, i.e. the Alzheimer’s Disease Assessment Scale, cognitive subscale (ADAS-cog) score. The ADAS-cog score was used as a surrogate by the authors to predict the outcome of needing full-time care.
Yao et al. 200661
This sister report to that of Woodroffe et al. 32 examined the clinical effectiveness and cost-effectiveness of a number of new immunosuppressive therapies in children. The analysis was undertaken by the same academic group and an adaptation of the CEM developed in the previous report was used. The same group of drugs were compared and the systematic review identified 14 RCTs and non-RCTs. As in the Woodroffe report,32 BPAR was used as a surrogate outcome to predict graft survival.
Surrogate validation
The evidence supporting the use of surrogate outcomes (Table 9) was assessed according to the evidence framework presented earlier in this report (see Table 3).
| Report | Evidence of validation? | Evidence | Level of evidence |
|---|---|---|---|
| Woodroffe 200532 | Yes | Systematic review of observational evidence of relationship between surrogate outcome and final outcome | 2 |
| Loveman 200643 | Yes | Observational study of individual patient data comparing cognitive function and need for full-time care | 2 |
| Shepherd 200652 | Yes | Systematic review of disease natural history | 3 |
| Yao 200661 | Yes | Systematic review of observational evidence of relationship between surrogate outcome and final outcome | 2 |
| Comparison of change in surrogate outcome in one RCT | 1 |
Woodroffe et al. 32 provided evidence from a systematic review and meta-analysis of observational studies to demonstrate the relationship between BPAR (surrogate outcome) and graft survival, i.e. level 2 evidence:
A key assumption in the cost-effectiveness modelling framework of this review is the linkage between BPAR, graft and patient survival, quality of life and costs. The selection of acute rejection is supported by a systematic review of potential prognostic predictors for graft survival (Novartis submission, Addendum 7).
Woodroffe et al. ,32 p. 68
Yao et al. 61 updated this systematic review to include evidence in children. To limit bias and confounding, the authors limited the systematic review to observational studies with multivariate analyses with 5-year or longer follow-up times. The authors identified one of two studies in children that confirmed the relationship between the surrogate outcome (BPAR) and the final outcome (graft survival) – level 2 evidence:
In summary, this updated review of surrogate outcome predictors in children appears to support the findings that acute rejection is a strong predictor of future graft loss.
Yao et al. ,61 p. 7
In addition, Yao et al. 61 examined whether the relationship between the surrogate outcome and the final outcome held up in a trial setting:
To investigate the level of extrapolation between observational data and RCTs for this review, we compared the change in surrogate levels to the change in graft survival seen in the paediatric RCT by Filler and colleagues.
Yao et al. ,61 p. 7
They found that:
In this trial, an improvement in 2-year graft survival with tacrolimus (p = 0.04) was associated with improvements in both GFR and the incidence of acute rejection at 6 months to 1 year in the tacrolimus group.
Yao et al. ,61 p. 7
that is, level 1 evidence.
The report of Shepherd et al. 52 recognises the limitations of the outcomes assessed in the trials and the need to predict a more final outcome of chronic hepatitis B:
Clinical trial data relating to the effectiveness of interventions included in this appraisal are limited to measurements of short-term serological, virological and histological changes. In order to estimate the impact of these intermediate effects on final outcomes for patients, a natural history model for CHB was required.
Shepherd et al. ,52 p. 81
Following a literature search on the natural history and epidemiology of chronic hepatitis B the authors developed a Markov disease state transition model. These epidemiological data were judged to represent level 3 evidence:
the principal effect of antiviral treatment is to change patients’ serological, biochemical, histological or virological status to place them in health states where they are less likely to develop progressive liver disease.
Shepherd et al. ,52 p. 82
Loveman et al. 43 based their decision to use cognitive function as a predictor for full-time care on a previously developed CEM for Alzheimer’s disease (AHEAD model). The authors state that the relationship between cognitive function and full-time care is based on individual patient data analysis undertaken by the developers of the AHEAD model. 62 On checking this source reference, the study concerned was identified to be a cohort comparison of cognitive function outcome and full-time care in Alzheimer’s disease, i.e. level 2 evidence.
Surrogate quantification
A range of approaches was used across the four reports to quantify the relationship between the surrogate outcome and the final outcome. The CEM in both the Woodroffe et al. 32 and the Yao et al. 61 reports used a hazard ratio [derived from a systematic review of observational studies examining the patient-level relationship between the surrogate outcome (BPAR) and the final outcome (graft survival)] to numerically represent this relationship.
The authors reported that the pooled hazard ratio (HR) for allograft survival based on an acute rejection episode was 1.95 (95% confidence interval (CI):1.42 to 2.67).
The adult BSA model was adapted for paediatrics . . . [and] . . . use made of a paediatric-specific HR of 1.41, 95% CI: 1.15 to 1.74.
Yao et al. ,61 p. 43
Shepherd et al. 52 assessed the relationship between seroconversion rate (surrogate outcome) and final outcome (e.g. chronic hepatitis, liver cancer) within a natural history CEM. The link between the surrogate outcome and the final outcome was quantified as a transition probability within this model, as shown in Table 10.
| Health state | Transition probability | |
|---|---|---|
| From | To | |
| HBeAg | HBsAg | 0.02 |
| HBeAg | R | |
| CHB | 0.03 | |
| CC | 0.01 | |
| HCC | 0.001 | |
Loveman et al. 43 quantified the impact of cognitive function (surrogate outcome) on full-time care (final outcome) using a predictive risk equation developed by the AHEAD model authors. 59 This equation was developed using a Cox proportional hazards model and contains coefficients for cognitive function, age at disease onset and the presence of psychotic symptoms (PSY) and extrapyramidal syndrome (EPS) and treatment duration (Table 11).
| Variable | EPS | PSY | < 65 years at disease onset | Cognitive function | Duration | |
|---|---|---|---|---|---|---|
| Risk equation index | Coefficient | –0.9419 | –0.4027 | –0.4848 | –0.0724 | 0.0617 |
Handling uncertainty
In their discussion, Woodroffe et al. 32 identified the link between surrogate outcome (BAPR) and final outcome (graft survival) in their model as a potential limitation:
In contrast, certain limitations were placed on the review . . . to estimate long-term effectiveness (and cost-effectiveness), extrapolation from trial 1-year BAPR to graft survival was undertaken.
Woodroffe et al. ,32 p. 68
In addition, in the executive summary of their report they state that:
The absence of both long-term outcome and quality of life from trial data makes assessment of the clinical and cost-effectiveness of the newer immunosuppressants contingent on modelling based on extrapolations from short-term trial outcomes.
Woodroffe et al. ,32 p. xi
Yao et al. 61 took a quantitative approach to handling the uncertainty associated with the use of a surrogate outcome in their CEM. Using sensitivity analysis, they explored how the ICER would alter when varying the hazard ratio for the relationship between the surrogate outcome and the final outcome. Two hazard ratio values were chosen: (1) 1.41, based on a single paediatric observational study (base-case value); and (2) 1.69, taken from a meta-analysis of adult observational studies. Sensitivity analysis shows that the ICER for each of the pairwise comparisons remains relatively consistent (i.e. either dominant or > £50,000/QALY), providing evidence that the CEM results are relatively insensitive to the quantification of the relationship between the surrogate outcome and the final outcome (Table 12).
| Drug comparison | Hazard ratio | ICER |
|---|---|---|
| CAS vs TAS | 1.41 | £145,540/QALY |
| 1.69 | £58,801/QALY | |
| CAS vs CMS | 1.41 | £194,559/QALY |
| 1.69 | £76,958/QALY | |
| CAS vs BCAS | 1.41 | Dominant |
| 1.69 | Dominant | |
| CAS vs DCAS | 1.41 | Dominant |
| 1.69 | Dominant | |
| TAS vs BTAS | 1.41 | Dominant |
| 1.69 | Dominant |
Furthermore, in the report’s discussion the authors raise the dependence on surrogate outcome as a specific limitation of the CEM:
Surrogate outcomes – The short duration of follow-up of RCTs necessitated the prediction of long-term graft loss [final outcome] and all-cause mortality from 1-year BPAR [surrogate outcome]. The authors of this report updated a previous systematic review of the literature in order to source the predictive value of BPAR associated with children [see section ‘Surrogate outcomes and prediction of long-term graft survival’ (p. 6)].
Yao et al. ,61 p. 55
In addition, they note that there was inadequate validatory evidence to use two other possible markers as surrogate outcomes in the CEM:
We found insufficient evidence to support the predictive use of graft function outcomes (i.e. serum creatinine and [glomerular filtration rate] GFR [surrogate outcomes].
Yao et al. ,61 p. 55
Shepherd et al. 52 quantified the impact of uncertainty associated with the use of surrogates through sensitivity analysis, varying the assumptions of the structure of the CEM, as shown in Table 13.
| Cost per QALY | ||||
|---|---|---|---|---|
| IFN | PEG | LAM | ADV | |
| Baseline analysis | £5994 | £6119 | £3685 | £16,569 |
| Structural assumption: | ||||
| Zero transition probability from compensated cirrhosis to HBeAg seroconverted state | £5275 | £5696 | £3513 | £30,494 |
| Zero transition probability from HBeAg seroconverted state to HCC | £5864 | £6047 | £3615 | £16,220 |
Also through sensitivity analysis, Loveman et al. 43 assessed the impact of a 1-point shift (in both directions) for the surrogate outcome (ADAS-cog) (Table 14).
| Cost per QALY | |||
|---|---|---|---|
| Donepezil 10 mg | Rivastigmine 6–12 mg | Galantamine 24 mg | |
| Base case | £96,797 | £70,438 | £81,910 |
| +1 point on base-case ADAS-cog | £66,505 | £49,065 | £57,119 |
| –1 point on base-case ADAS cog | £150,214 | £120,915 | £122,571 |
Furthermore, in the discussion section the authors highlight the limitation of the use of surrogate outcomes:
It is difficult to know what the changes [in cognitive function] demonstrated on each measure really mean.
Loveman et al. ,43 p. 14
OMERACT scoring schema and JAMA criteria
The scoring on the OMERACT surrogate schema domains for the four reports is summarised in Table 15. The low OMERACT schema score of 4 for the Shepherd et al. 52 report reflects the fact that, although the authors ‘embedded’ the relationship between seroconversion (surrogate outcome) and chronic hepatitis/liver cancer (final outcome) in the disease history CEM, they did not present specific biological or epidemiological evidence to support this link. The reports of Woodroffe et al. ,32 Loveman et al. 43 and Yao et al. 61 each scored 9 out of the potential maximum OMERACT score of 15; however, they all just failed to meet the threshold cut-off score of ≥ 10 that the authors of the schema deemed to represent the minimum level of evidence that an end point should reach to support its use as a surrogate outcome.
| Domain | Woodroffe 200532 | Shepherd 200652 | Loveman 200643 | Yao 200661 |
|---|---|---|---|---|
| A. Targeta | 4 (renal graft survival) | 4 (chronic hepatitis, liver cancer) | 4 (need for full-time care) | 4 (renal graft survival) |
| B. Study design | 2 (at least one prespecified population-based study) | 0 (review of disease natural history) | 2 (at least one prespecified population-based study) | 2 (at least one prespecified population-based study) |
| C. Statistical strength | 3 (at least good association between marker change and target change in all individual studies) | 0 (no relevant data) | 3 (at least good association between marker change and target change in all individual studies) | 3 (at least good association between marker change and target change in all individual studies) |
| D. Penalties | 0 | 0 | 0 | 0 |
| Overall score | 9 | 4 | 9 | 9 |
The studies of Woodroffe et al. ,32 Loveman et al. 43 and Yao et al. 61 were judged to broadly meet the JAMA level of guide 1, i.e. strong, independent, consistent association between the surrogate outcome and the final outcome. With RCT evidence showing the relationship between surrogate and final outcomes, the report of Yao et al. 61 also fulfilled the level of guide 2 and thus met the JAMA requirement of a valid surrogate.
Predictors of the use of surrogate outcomes
Given the small number of HTA reports with CEMs based on surrogate outcomes, an analysis of predictive factors was not possible.
Chapter 5 Discussion
This study aimed to examine the use of surrogate outcomes in CEMs in HTA by undertaking both a non-systematic review of the literature on the use of surrogate outcomes in HTA and a survey of the use of surrogate outcomes in CEMs in UK HTA reports published in 2005 and 2006.
The terms ‘surrogate outcome or end point’, ‘biomarker’ and ‘biological marker’ are often used interchangeably, which has led to confusion over the identification of what may be considered a surrogate outcome and the role of surrogate outcomes. For the purposes of this report we applied the following definition of a surrogate outcome: an end point that substitutes for and predicts a patient-relevant final outcome (i.e. mortality, important clinical events or health-related quality life).
Findings
Review of the literature
There is a long tradition of the use of surrogate outcomes (e.g. blood pressure, tumour size reduction) in clinical trials and drug regulation. However, the use of surrogate outcomes is controversial and a number of cases have been documented in which use of a surrogate outcome has led to the adoption of a health technology that has later been found to be harmful. 6,7 UK and international guidelines on HTA methods currently provide little or no specific advice on the appropriate selection and use of surrogate outcomes. 20,21,26
Through a synthesis of ICH-9 guidelines10 and the work of the US NIH Biomarker’s Definitions Working Group4 an evidence hierarchy for surrogate validation can be derived: level 1 – controlled trial evidence showing that the treatment-related change in surrogate outcome is associated with a concomitant change in the final outcome; level 2 – evidence from observational studies of an association between the surrogate outcome and the final patient-related outcome; and level 3 – understanding of the biology and pathophysiological studies make it plausible that the changes in the surrogate outcome will lead to changes in the final patient-related outcome.
Survey of UK HTA reports
Out of a total of 100 HTA UK reports published between 2005 and 2006, 35 addressed an effectiveness/efficacy question and contained a CEM. Of these, four (11%) reports were found to have based their cost-effectiveness analysis on a surrogate outcome: two reports32,61 of patients undergoing kidney transplantation used an outcome of biopsy-confirmed acute rejection (BPAR) (final outcome – graft survival); one report43 of Alzheimer’s disease used the cognitive function score (final outcome – need for full-time care); and one report52 of chronic hepatitis used seroconversion (final outcome – chronic hepatitis/liver cancer).
All four reports sourced treatment-related changes in surrogate outcomes through a systematic review of the literature, in some cases also undertaking meta-analysis. However, there was some variability in the consistency and transparency by which these reports provided evidence of the validation for the surrogate–final outcome relationship. Most usefully, some reports used sensitivity analyses to explore the impact of the potential uncertainty of the surrogate–final outcome relationship on cost-effectiveness. Only one of the reports61 undertook a systematic review to specifically seek the evidence base for the surrogate–final outcome link. Furthermore, this was the only report to provide level 1 surrogate–final outcome validation evidence, i.e. RCT data showing a strong association between the change in surrogate outcome (BPAR) and the change in final outcome (graft survival) at an individual patient level. Two of the other three reports reported level 2 evidence, i.e. observational study data showing the relationship between the surrogate outcome and the final outcome. 32,43 However, none of the reports achieved a sufficient score on the OMERACT schema to be judged to have acceptable evidence of a surrogate outcome by its authors. Having been only recently developed, the OMERACT schema requires further testing against a range of surrogate outcomes to fully assess its suitability as a practical tool.
It is interesting to note that the four reports based on the use of surrogate outcomes were all undertaken on behalf of NICE, whose reference case seeks a cost per QALY analysis. 26 There may therefore be a particular pressure on HTA analysts when undertaking work directly for policy-makers to extrapolate from surrogate outcomes to QALYs to formally quantify the cost-effectiveness of a health technology.
The 31 remaining reports used a wide range of patient-relevant final outcomes in their CEMs. In total, 17 reports used what might be regarded as a ‘definitive’ final outcome, i.e. death or important clinical events (e.g. myocardial infarction, fracture). Six reports used a HRQoL outcome as assessed by the EQ-5D or a non-preference HRQoL measure (e.g. SF-36). Seven reports used outcomes that, although potentially important to patients, were not what might be regarded as a ‘final outcome’ in that disease area, e.g. improvement in osteoarthritis function assessed on the Health Assessment Questionnaire (HAQ) or reduction in severity assessed on the Psoriasis Area and Severity Index (PASI). 53,59 A number of authors called these near final outcomes ‘intermediate’ outcomes. In CEMs these outcomes require some process of further translation to quantify the health benefit and determine the cost-effectiveness. For example, one HTA report used a previously published algorithm to compute the utility gain from the observed change in functional outcome score (HAQ) in arthritis patients. Other reports derived utility by linking the outcome to a particular disease state (e.g. pain). This process of extrapolating clinical outcomes from intermediate outcomes to utility is known as ‘mapping’. 63 Although outside the direct scope of this study, it is noteworthy that the process of utility mapping shares the same issues of outcome translation as surrogate outcomes. For example, it cannot be assumed that outcome measures that can be partially or fully perceived by patients at a point in time linearly map on to HRQoL outcomes at a later stage. This raises the question as to whether the evidence requirements for utility mapping should be similar to those applied to the surrogates.
In summary, in spite of the importance and risks of the use of surrogate outcomes in CEMs, the four HTA reports identified in this survey varied considerably in their approaches to handling and reporting surrogates. The strength of evidence for the surrogate–final outcome relationship, transparency of quantification and exploration of uncertainty of this relationship were found to vary considerably. Recommendations for handling and reporting of surrogate outcomes in CEMs in future HTA reports are made below.
Report strengths and limitations
We believe this to be the first empirical study of the use of surrogate outcomes in HTA. Previous surrogate outcome surveys have focused on their use in clinical trials and often used a purposive sampling strategy to identify examples that have led to surrogate failure. 6,7,9 This report provides an overview of the various issues relating to the use of surrogate outcomes in HTA, including definitional uncertainty, a framework for surrogate validation and a summary of current methodological guidelines for the use of surrogates.
However, because of limited resources and time, the sample of HTA reports surveyed was relatively small and limited to the UK. The small sample size and the limited number of HTA reports with a CEM based on a surrogate outcome potentially limits the generalisability of the findings of this study. The report focused on inclusion of HTA reports in which there was clear evidence of the dependence of the CEM on a surrogate outcome. We may have therefore excluded reports that used surrogate outcomes but which were unclear about this in their CEM description or reports in which the CEM depended on a mix of final and surrogate outcomes (in terms of the operational definition of this review). Documentary analysis was used to assess the content of included reports. It is therefore important to acknowledge that the absence of mention of an issue in the text should not necessarily imply the absence of consideration of that issue by the report’s authors. Finally, for the purposes of this report we have focused on identifying HTA reports with CEM models that have used definitive examples of surrogate outcomes. However, we recognise that rather than a dichotomy there is effectively a continuum between what might be regarded as ‘true surrogate outcomes’ and what might be regarded as ‘true final outcomes’. Nevertheless, we would contend that the recommendations remain applicable.
Proposed recommendations for studies selecting and/or using surrogate outcomes in HTA reports
Recommendations are proposed for the use of surrogate outcomes (any end point that substitutes for and predicts a final patient-related outcome, i.e. mortality, important clinical events or HRQoL) in future HTA reports. These recommendations are based on the findings of the review of the literature on the use of surrogate outcomes, the experience of the survey of the use of surrogates in UK HTA reports and feedback and discussion on the draft recommendations from InterTasc [UK HTA groups who undertake technology assessment reports commissioned by the National Institute for Health Research (NIHR) HTA Programme] and the technology assessment team at NICE. The rationale and source of each recommendation are shown in parentheses. These recommendations are intended to act as a list of considerations that policy-makers and HTA analysts should take into account when faced with the use of surrogate outcomes in CEMs in HTA reports. It is acknowledged that the practicalities and resource implications of implementing these recommendations have not been formally tested within this project.
-
Ideally, the assessment of clinical effectiveness and cost-effectiveness of a health technology should be based on final patient-related outcomes (i.e. mortality, important clinical events and HRQoL) (for rationale see Chapter 2, Risks of surrogate outcomes). To minimise the risk of bias this evidence should be identified from a systematic review (and meta-analysis) of well-conducted RCTs.
-
When this is not possible and there is a requirement to use a surrogate outcome2 the following should be undertaken:
-
A review of the evidence for the validation of the surrogate–final outcome relationship (for rationale see Chapter 2, Validation of surrogate outcomes). To minimise the risk of bias such a review should be systematic.
-
The evidence on surrogate validation should be presented according to an explicit hierarchy such as the following: level 1: evidence demonstrating treatment effects on the surrogate correspond to effects on the patient-related outcome (from clinical trials); level 2: evidence demonstrating a consistent association between surrogate outcome and final patient-related outcome (from epidemiological/observational studies); level 3: evidence of biological plausibility of relationship between surrogate outcome and final patient-related outcome (from pathophysiological studies and/or understanding of the disease process) (for rationale see Chapter 2, Validation of surrogate outcomes). To achieve level 1 classification a surrogate must fulfil the level 1 and level 2 and level 3 criteria. To achieve level 2 classification a surrogate must fulfil the level 2 and level 3 criteria.
-
Consideration should be given to carrying out a CEM analysis based on a surrogate outcome when there is level 1 or 2 validation evidence (for rationale see Chapter 2, Risks of surrogate outcomes).
-
-
When a CEM analysis based on a surrogate outcome is undertaken:
-
Provide a transparent explanation as to how the relationship between the surrogate and final outcomes is quantified within the CEM (for rationale see Chapter 4, Reports with CEMs based on a surrogate outcome).
-
Explicitly explore and discuss the uncertainty associated with use of the surrogate outcome in the CEM, especially through sensitivity analysis (for rationale see Chapter 4, Reports with CEMs based on a surrogate outcome). In accordance with recent HTA methodological developments, such uncertainty may be quantified using probabilistic sensitivity analysis.
-
Make specific research recommendations regarding the need for future research on the surrogate–final outcome relationship (for rationale see Chapter 4, Reports with CEMs based on a surrogate outcome). In accordance with recent HTA methodological developments, the impact of the surrogate outcome on decision uncertainty may be quantified by value of information analysis.
-
Include the term ‘surrogate outcome’ in the report executive summary/abstract to assist bibliographic identification (for rationale see Chapter 4, Reports with CEMs based on a surrogate outcome).
-
Areas for future research
The following areas are suggested for further research:
-
Given both the UK focus and relatively small number of HTA reports with a CEM explicitly based on surrogate outcomes identified, the generalisability of the findings may be limited. This supports a more extensive survey of the use of surrogate outcomes in HTA across international jurisdictions. Consideration should be given to the role of surrogate outcomes in both the clinical effectiveness and the cost-effectiveness components of these reports. Furthermore, future empirical studies need to address those situations in which HTA reports may combine both surrogate and final outcomes and the validity of using surrogates across technology classes.
-
The review of the literature in this report identified only two previous empirical studies designed to quantify the potential bias associated with the use of surrogate outcomes. Further empirical studies are needed to assess the potential biases of the use of surrogate outcomes in HTA and cost-effectiveness analyses, for example a comparison of the findings of cost-effectiveness analyses based on surrogate outcomes versus cost-effectiveness analyses based on final outcomes.
-
Testing of the new OMERACT surrogate scoring schema and the development of similar tools.
-
Explore the transferability of the hierarchy of evidence framework for surrogate–final outcomes to the process of mapping disease-specific outcomes to HRQoL utility in CEM analyses.
Chapter 6 Conclusions
Policy decisions on the adoption of health technologies should be based on evidence of effectiveness and cost-effectiveness from well-conducted RCTs that report final patient-relevant outcomes, i.e. death, morbid end points (such as myocardial infarction, stroke) or impaired HRQoL. Contrary to this there is increasing pressure on health-care policy-makers to reduce the time to health technology regulatory approval and reimbursement by the use of surrogate outcomes (that substitute for and predict final patient-related outcomes). However, given that reliance on surrogate outcomes can ultimately lead to harmful patient outcomes, the use of such outcomes in HTA remains controversial.
In this survey of UK HTA reports about 10% of the CEMs therein were explicitly based on surrogate outcomes. The strength of evidence for the surrogate–final outcome relationship, transparency of quantification and exploration of uncertainty of this relationship were found to vary considerably. Recommendations are made for the use of surrogate outcomes in future HTA reports.
Acknowledgements
We would like to acknowledge Dr Colin Green (Senior Lecturer in Health Economics, Peninsula Medical School, Universities of Exeter and Plymouth), Mr Paul Tappenden (Senior Cost-effectiveness Modeller, Health Economics and Decision Science, School of Health and Related Research, University of Sheffield) and Professor Ken Stein (Professor in Public Health, Peninsula Medical School, Universities of Exeter and Plymouth) for their support and comments on an early draft of this report.
Thanks also go to Jo Perry, Sue Whiffin and Gabriel Rodgers for administrative project support and assistance with formatting of this report and to InterTasc, UK TAR groups and the technology assessment team at NICE for their comments on the draft recommendations of this report.
Contribution of authors
Rod Taylor devised and led the study, drafted the initial version of the protocol and report, assessed reports for inclusion and exclusion, extracted data and had overall responsibility for the project. Julian Elston contributed to the development of the protocol, contributed to the editing of the report, assessed reports for inclusion and exclusion and extracted data.
About PenTAG
PenTAG is part of the Institute of Health Services Research at the Peninsula Medical School. PenTAG was established in 2000 and carries out independent health technology assessments for the UK HTA Programme and other local and national decision-makers. The group is multidisciplinary and draws on individuals’ backgrounds in public health, health services research, computing and decision analysis, systematic reviewing, statistics and health economics. The Peninsula Medical School is a school within the Universities of Plymouth and Exeter. The Institute of Health and Social Care Research is made up of discrete but methodologically related research groups, among which health technology assessment is a strong and recurring theme. Projects to date include:
The effectiveness and cost-effectiveness of imatinib (STI 571) in chronic myeloid leukaemia: a systematic review. Health Technol Assess 2002;6(3).
Screening for hepatitis C among injecting drug users and in genitourinary medicine (GUM) clinics: systematic reviews of effectiveness, modelling study and national survey of current practice. Health Technol Assess 2002;6(31).
Systematic review of endoscopic sinus surgery for nasal polyps. Health Technol Assess 2003;7(17).
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling. Health Technol Assess 2004;8(3).
The effectiveness and cost-effectiveness of imatinib for first line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis. Health Technol Assess 2004;8(28).
Do the findings of case series studies vary significantly according to methodological characteristics? Health Technol Assess 2005;9(2).
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema – a systematic review and economic modelling. Health Technol Assess 2005;9(29).
The effectiveness and cost-effectiveness of dual chamber pacemakers compared to single chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome – systematic review and economic evaluation. Health Technol Assess 2005;9(43).
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling. Health Technol Assess 2006;10(8).
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end stage renal disease patients on dialysis: a systematic review and economic evaluation Health Technol Assess 2007;11(18).
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation. Health Technol Assess 2007;11(45).
The effectiveness and cost-effectiveness of cardiac resynchronisation therapy for heart failure: a systematic review and economic evaluation. Health Technol Assess 2007;11(47).
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA Programme or the Department of Health.
References
- Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess 1998;2.
- US Department of Health and Human Services FDA Center for Drug Evaluation and Research . Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 2006;4.
- Burzykowski T, Molenberghs G, Buyse M. The evaluation of surrogate endpoints. New York: Springer; 2005.
- Biomarkers Definitions Working Group . Biomarkers and surrogate endpoints: preferred and conceptual framework. Clin Pharmacol Ther 2001;22:485-502.
- Hughes MD, Daniels MJ, Fischl MA, Kim S, Schooley RT. CD4 cell count as a surrogate endpoint in HIV clinical trials: a meta-analysis of studies of the AIDS Clinical Trials Group. AIDS 1998;12:1823-32.
- Fleming TR, DeMets DL. Surrogate end points in clinical trials: are we being misled?. Ann Intern Med 1996;125:605-13.
- Gotzsche PC, Liberati A, Torri V, Rossetti L. Beware of surrogate outcome measures. Int J Technol Assess Health Care 1996;12:238-46.
- Cardiac Arrhythmia Suppression Trial (CAST) Investigators . Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med 1989;321:406-12.
- Ridker PM, Torres J. Reported outcomes in major cardiovascular clinical trials funded by for-profit and not-for-profit organizations: 2000–2005. JAMA 2006;295:2270-4.
- International Conference on Harmonisation guidelines for the conduct of clinical trials for the registration of drugs . E9: Statistical Principles for Clinical Trials n.d. www.ich.org/LOB/media/MEDIA485.pdf (accessed 1 October 2007).
- Hill AB. The environment and disease: association or causation?. Proc R Soc Med 1965;58:295-300.
- Bucher HC, Guyatt GH, Cook DJ, Holbrook A, McAlister FA. Users’ guides to the medical literature: XIX. Applying clinical trial results. A. How to use an article measuring the effect of an intervention on surrogate end points. Evidence-Based Medicine Working Group. JAMA 1999;282:771-8.
- Lassere MN, Johnson KR, Boers M, Tugwell P, Brooks P, Simon L, et al. Definitions and validation criteria for biomarkers and surrogate endpoints: development and testing of a quantitative hierarchical levels of evidence schema. J Rheumatol 2007;34:607-15.
- Weir CJ, Walley RJ. Statistical evaluation of biomarkers as surrogate endpoints: a literature review. Stat Med 2006;25:183-20.
- Johnson JR, Williams G, Pazdur R. End points and United States Food and Drug Administration approval of oncology drugs. J Clin Oncol 2003;21:1401-11.
- Chakaravarty A, Burzykowski T, Molenberghs G, Buyse M. The evaluation of surrogate endpoints. New York: Springer; 2005.
- NHS Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Those Carrying Out or Commissioning Reviews n.d. www.york.ac.uk/inst/crd/report4.htm (accessed 1 May 2007).
- Laupacis A. Economic evaluations in the Canadian Common Drug Review. Pharmacoeconomics 2006;24:1157-62.
- Tappenden P, Chilcott J, Ward S, Eggington S, Hind D, Hummel S. Methodological issues in the economic analysis of cancer treatments. Eur J Cancer 2006;42:2867-75.
- International Network of Agencies for Health Technology Assessment (INAHTA) . HTA Checklist 2000 n.d. www.inahta.org/HTA/Checklist/ (accessed 1 July 2007).
- Busse R, Orvain J, Velasco M, Perleth M, Drummond M, Gurtner F, et al. Best practice in undertaking and reporting health technology assessments. Working Group 4 Report. Int J Technol Assess Health Care 2002;18:361-422.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 n.d. www.cochrane.org/resources/handbook/hbook.htm (accessed 25 July 2007).
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart BL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
- Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices – Modeling Studies. Value Health 2003;6:9-17.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8.
- NICE . Guide to the Methods of Technology Appraisal 2004. www.nice.org.uk/download.aspx?o=201973 (accessed 1 July 2007).
- Greenhalgh J, Knight C, Hind D, Beverley C, Walters S. Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies. Health Technol Assess 2005;9.
- Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al. Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris) for the treatment of severe sepsis in adults: a systematic review and economic evaluation. Health Technol Assess 2005;9.
- McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al. Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 2005;9.
- Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al. Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation. Health Technol Assess 2005;9.
- Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al. Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation. Health Technol Assess 2005;9.
- Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al. Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study. Health Technol Assess 2005;9.
- Stevenson M, Jones ML, De Nigris E, Brewer N, Davis S, Oakley J. A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Assess 2005;9.
- Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al. Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation. Health Technol Assess 2005;9.
- Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al. Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling. Health Technol Assess 2005;9.
- Tillin T, Chambers M, Feldman R. Outcomes of electrically stimulated gracilis neosphincter surgery. Health Technol Assess 2005;9.
- Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al. The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation. Health Technol Assess 2005;9.
- Cochrane T, Davey RC, Matthes Edwards SM. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess 2005;9.
- Castelnuovo E, Stein K, Pitt M, Garside R, Payne E. The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation. Health Technol Assess 2005;9.
- Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al. The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation. Health Technol Assess 2005;9.
- Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al. Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation. Health Technol Assess 2005;9.
- Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al. The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children. Health Technol Assess 2005;9.
- Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al. The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease. Health Technol Assess 2006;10.
- Connock M, Frew E, Evans BW, Bryan S, Cummins C, Fry-Smith A, et al. The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review. Health Technol Assess 2006;10.
- Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al. Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation. Health Technol Assess 2006;10.
- Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al. A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1. Health Technol Assess 2006;10.
- Wright M, Grieve R, Roberts J, Main J, Thomas HC; UK. Mild Hepatitis C Trial Investigators. Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation. Health Technol Assess 2006;10.
- King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al. A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents. Health Technol Assess 2006;10.
- Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al. The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review. Health Technol Assess 2006;10.
- Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al. Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model. Health Technol Assess 2006;10.
- Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al. A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost-utility for these groups in a UK context. Health Technol Assess 2006;10.
- Shepherd J, Jones J, Takeda A, Davidson P, Price A. Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation. Health Technol Assess 2006;10.
- Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al. Health Technol Assess 2006;10.
- Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P. The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation. Health Technol Assess 2006;10.
- Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al. Health Technol Assess 2006;10.
- Chen YF, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al. A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness. Health Technol Assess 2006;10.
- Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C. Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model. Health Technol Assess 2006;10.
- Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al. Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation. Health Technol Assess 2006;10.
- Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Vergel YB, et al. Etanercept and efalizumab for the treatment of psoriasis: a systematic review. Health Technol Assess 2006;10.
- Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al. Evaluation of the ventricular assist device programme in the UK. Health Technol Assess 2006;10.
- Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al. A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children. Health Technol Assess 2006;10.
- Caro JJ, Getsios D, Migliaccio-Walle K, Raggio G, Ward A. AHEAD Study Group . Assessment of health economics in Alzheimer’s disease (AHEAD) based on need for full-time care. Neurology 2001;57:964-71.
- Brazier J, Ratcliffe J, Salomon J, Tsuchiya A. Measuring and valuing health benefits for economic evaluation. Oxford: Oxford University Press; 2007.
- Australian Government Department of Health and Ageing . Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (Version 4.2), December 2007 n.d. www.health.gov.au (accessed 1 September 2008).
Appendix 1 Inclusion/exclusion criteria and data extraction proforma
| No. | Question | |
|---|---|---|
| 1 | Identification number of HTA report | Volume: |
| Edition: | ||
| 2 | First author and year (2005/6) | |
| 3 | Reviewer: | RT |
| JE | ||
| 4 | Date extracted (format DD/MM/YY) |
| Key word search terms | Number of hits in report |
|---|---|
| surrog* | |
| biomarker | |
| intermediate outcome | |
| marker | |
| predictive factor |
Section A: General information – to be completed for all HTA reports
| No. | Question | Answer |
|---|---|---|
| 1 |
Type of health technology (exclude reports addressing non e.g. diagnosis, aetiology) Circle appropriate answer or answers |
Drug |
| Surgical procedure | ||
| Education or counselling | ||
| Diagnostic or screening | ||
| Health promotion | ||
| Medical device | ||
| Other (specify) | ||
| 2 |
Disease area Provide details |
|
| 4 |
Type of research report Circle appropriate answer |
Primary |
| Secondary | ||
| Not sure | ||
| 5 |
Undertook economic modelling? Circle appropriate answer |
Yes |
| No | ||
| Not sure | ||
| 6 |
NICE TAR? Circle appropriate answer |
Yes |
| No | ||
| Not sure | ||
| 7a |
Was the economic model based on a surrogate outcome(s)? (NIH definition of surrogate end point: a biomarker intended to substitute for a clinical end point. A clinical investigator uses epidemiological, therapeutic, pathophysiological, or other scientific evidence to select a surrogate end point that is expected to predict clinical benefit, harm, or lack of benefit or harm) Circle appropriate answer |
Yes |
| No | ||
| Not sure | ||
| 7b | If no, name main outcome(s) used in model | |
| 8 |
Type of decision model Circle appropriate answer or answers |
Decision tree |
| Markov model | ||
| Both | ||
| Other | ||
| 9 |
Base case ICER (£/QALY or £/health outcome gain) List result or results |
If answers to Questions 5 and 7a are both yes then include
| Include □ Exclude □ Unsure □ |
Section B: Surrogate HTA report – to be completed only for HTA reports with surrogate outcomes used in the economic model
| No. | Question | Answer |
|---|---|---|
| 10 | Characteristics of surrogate | |
| 11a | Surrogate outcome used? Name: | |
| Final outcome sought? Name: | ||
| 12b |
Type of surrogate (specify) Circle appropriate answer |
Biochemical |
| Physiological | ||
| Radiological imaging | ||
| Immunological | ||
| Histological | ||
| Other | ||
| Not sure | ||
| 13c |
Source of surrogate data used in model Circle appropriate answer |
Meta-analyses of RCT |
| Single study – RCT | ||
| Single study – non-RCT | ||
| Other | ||
| Not sure | ||
| 14 | Evidence of validation of surrogate | |
| 14 | Did the authors provide evidence of validation for the use of surrogate outcome used in the report? | Yes |
| No | ||
| Not sure | ||
| If yes, which of the following criteria did they mention? | ||
| 14a | Biological plausibility/pathophysiology | Yes |
| No | ||
| 14b | Epidemiological (correlation) studies | Yes |
| No | ||
| 14c | Treatment effect studies (RCTs) | Yes |
| No | ||
| 15 | Did the authors refer to any validation framework? | Yes |
| No | ||
| Not sure | ||
| If yes, which framework did they refer to? | ||
| 15a | Bucher criteria | Yes |
| No | ||
| 15b | Prentice criteria | Yes |
| No | ||
| 15c | Other | Yes |
| No | ||
| 15d | Other comments | |
| 16 | Validation scoring | |
| To be completed by reviewer | ||
| 16a | Bucher framework | Attached |
| 16b | Lassere framework | Attached |
| 17 | Quantification of surrogate in the model | |
| What statistical methods did the authors use to quantify the surrogate outcome in their economic model? | ||
| Regression-based approach | Yes | |
| No | ||
| Not sure | ||
| Confidence profile (Eddy) method | Yes | |
| No | ||
| Not sure | ||
| Other methods (give details) | Yes | |
| No | ||
| Not sure | ||
| 18 | Discussion/interpretation of surrogates in report | |
| 18 | Did the authors consider uncertainty associated with using surrogate outcomes in the results? | Yes |
| No | ||
| Not sure | ||
| 18a | If yes, was this consideration: | Narrative |
| Quantitative | ||
| Both | ||
| Not sure | ||
| 18ai | If narrative, provide quote (or cite relevant page/paragraph numbers) (e.g. did the authors discuss the influence of use on surrogate on interpretation of results?) | |
| 18b | Did the authors consider uncertainty associated with using surrogate outcomes in the conclusions | Yes |
| No | ||
| Not sure | ||
| 19 | To be selected as a case study? (i.e. was the report a ‘good’ example of how to use and report use of surrogates in HTA)? | Suitable |
| Not suitable |
Appendix 2 Surrogate outcome scoring
JAMA criteria – scoring
| Criteria | Circle appropriate response | Comments |
|---|---|---|
| 1. Necessary but not sufficient: Is there a strong, independent, consistent association between the surrogate end point and the clinical end point? | Yes | |
| No | ||
| Unsure | ||
| 2. Is there evidence from randomised trials in other drug classes that improvement in the surrogate end point has consistently led to improvement in the target outcome? | Yes | |
| No | ||
| Unsure | ||
| 3. Is there evidence from randomised trials in the same drug class that improvement in the surrogate end point has consistently led to improvement in the target outcome? | Yes | |
| No | ||
| Unsure |
OMERACT criteria – scoring
Circle appropriate rank for domains A–D and provide total score.
| Domain | Rank | Criteria |
|---|---|---|
| A. Target (for all studies ranked in domain B) | 0 | All targets studied are disease centred and reversible |
| 1 | At least one target studied that is disease centred is irreversible | |
| 2 | At least one patient-centred target that is reversible | |
| 3 | At least one patient-centred target of irreversible minor organ morbidity or minor irreversible clinical burden of disease | |
| 4 | At least one patient-centred target of irreversible major organ morbidity or major irreversible clinical burden of disease | |
| 5 | Death | |
| B. Study design (requires as baseline appropriate study quality, study power and study duration) | 0 | Evidence from in vitro or animal studies or case reports or cross-sectional observational or retrospective observational cohorts studies evaluating the relationship between marker and target |
| 1 | At least one prespecified non-population-based prospective observational study with collection of all covariates needed to adjust for known confounding and effect modification evaluating the relationship between marker and target | |
| 2 | At least one prespecified non-population-based prospective observational study with collection of all covariates needed to adjust for known confounding and effect modification evaluating the relationship between marker and target or one randomised controlled trial of the same drug class of an intervention evaluating the relationship between marker and target | |
| 3 | At least two randomised controlled trials of the same drug class of an intervention evaluating the relationship between marker and target | |
| 4 | At least two randomised controlled trials in each of two drug classes of an intervention evaluating the relationship between marker and target | |
| 5 | At least three randomised controlled trials in each of three known drug classes of an intervention evaluating the relationship between marker and target or at least three randomised surrogate objective trials | |
| C. Statistical strength | 0 | No association/prediction or no relevant data |
| 1 | At least fair association or better between marker change and target change in most single-study analyses | |
| 2 | At least fair association or better between marker change and target change in all single-study analyses or fair prediction in an across-study analysis evaluating the effect of treatment on marker change and target change | |
| 3 | At least good association or better between marker change and target change in all single-study analyses or good prediction in an across-study analysis evaluating the effect of treatment on marker change and target change | |
| 4 | At least very good association or better between marker change and target change in all single-study analyses and very good prediction in an across-study analysis evaluating the effect of treatment on marker change and target change | |
| 5 | Excellent association or better between marker change and target change in all single-study analyses and excellent prediction in an across-study analysis evaluating the effect of treatment on marker change and target change | |
| D. Penalties due to lack of evidence or evidence to the contrary | –1 | No in vitro or animal study evidence to support surrogacy validity or no epidemiological evidence to support surrogacy validity |
| –1 | At least one randomised controlled trial that does not demonstrate statistically significant surrogacy validity (i.e. evidence of no effect in at least one adequately powered randomised controlled trial) | |
| –1 | At least one epidemiological study that supports opposite assertion | |
| –1 | At least one epidemiological study that does not demonstrate surrogacy validity (i.e. evidence of no effect in at least one adequately powered epidemiological study) | |
| –1 | At least one randomised controlled trial that demonstrated evidence of significant clinical heterogeneity | |
| –2 | At least one randomised controlled trial that supports opposite assertion | |
| –3 | At least one randomised controlled trial that demonstrates use of marker confers patient harm | |
| –3 | Does not meet the threshold criterion of a rank of 3 in at least one domain if score is 7 or more | |
| Total score |
Appendix 3 Excluded HTA reports
| Study | Vol. no. | Issue no. | Primary reason for exclusion |
|---|---|---|---|
| Ozolins 2005 | 9 | 1 | No cost-effectiveness model |
| Dalziel 2005 | 9 | 2 | Methodological report |
| Wilson 2005 | 9 | 3 | No cost-effectiveness model |
| Fowler 2005 | 9 | 4 | No cost-effectiveness model |
| Shenfine 2005 | 9 | 5 | No cost-effectiveness model |
| Taylor 2005 | 9 | 6 | Diagnostic and screening question |
| Grant 2005 | 9 | 7 | Methodological report |
| Robinson 2005 | 9 | 8 | Methodological report |
| Smith 2005 | 9 | 10 | Methodological report |
| Dinnes 2005 | 9 | 12 | Methodological report |
| Willis 2005 | 9 | 13 | Diagnostic and screening question |
| Peveler 2005 | 9 | 16 | No cost-effectiveness model |
| Kalra 2005 | 9 | 18 | No cost-effectiveness model |
| Woloshynnowych 2005 | 9 | 19 | No cost-effectiveness model |
| Raftery 2005 | 9 | 20 | No cost-effectiveness model |
| Smith 2005 | 9 | 23 | No cost-effectiveness model |
| Roderick 2005 | 9 | 24 | No cost-effectiveness model |
| Glenny 2005 | 9 | 26 | Methodological report |
| Newman 2005 | 9 | 30 | Diagnostic and screening |
| Price 2005 | 9 | 33 | No cost-effectiveness model |
| Symmons 2005 | 9 | 34 | No cost-effectiveness model |
| King 2005 | 9 | 35 | Methodological report |
| Bryant 2005 | 9 | 36 | No cost-effectiveness model |
| Bartlett 2005 | 9 | 38 | Methodological report |
| Epps 2005 | 9 | 39 | No cost-effectiveness model |
| Hobbs 2005 | 9 | 40 | Diagnostic and screening question |
| Durham 2005 | 9 | 42 | No cost-effectiveness model |
| Knowles 2005 | 9 | 44 | Diagnostic and screening question |
| Kwartz 2005 | 9 | 46 | Diagnostic and screening question |
| McDaid 2005 | 9 | 48 | No cost-effectiveness model |
| Roderick 2005 | 9 | 49 | No cost-effectiveness model |
| Dennis 2006 | 10 | 2 | No cost-effectiveness model |
| Black 2006 | 10 | 3 | Diagnostic and screening question |
| Whiting 2006 | 10 | 4 | Diagnostic and screening |
| Dundar 2006 | 10 | 5 | Methodological report |
| Martin 2006 | 10 | 6 | Diagnostic and screening question |
| Garside 2006 | 10 | 8 | Diagnostic and screening question |
| Szczepura 2007 | 10 | 10 | Diagnostic and screening question |
| Wu 2006 | 10 | 11 | Diagnostic and screening question |
| Nelson 2006 | 10 | 12 | Diagnostic and screening question |
| Michaels 2006 | 10 | 13 | No cost-effectiveness model |
| Speight 2006 | 10 | 14 | Diagnostic and screening question |
| Goodacre 2006 | 10 | 15 | Diagnostic and screening question |
| Brazzelli 2006 | 10 | 16 | No cost-effectiveness model |
| Lewis 2006 | 10 | 17 | No cost-effectiveness model |
| Rodgers 2006 | 10 | 18 | Diagnostic and screening question |
| Kennedy 2006 | 10 | 19 | No cost-effectiveness model |
| Nixon 2006 | 10 | 22 | No cost-effectiveness model |
| Harvey 2006 | 10 | 29 | No cost-effectiveness model |
| Wardlan 2006 | 10 | 30 | Diagnostic and screening question |
| Castelnuovo 2006 | 10 | 32 | Diagnostic and screening question |
| Williams 2006 | 10 | 34 | Prognostic question |
| Brazier 2006 | 10 | 35 | No cost-effectiveness model |
| Whiting 2006 | 10 | 36 | Diagnostic and screening question |
| O’Dowd 2006 | 10 | 37 | No cost-effectiveness model |
| Brown 2006 | 10 | 38 | No cost-effectiveness model |
| Waugh 2006 | 10 | 39 | Diagnostic and screening question |
| Williams 2006 | 10 | 40 | Diagnostic and screening question |
| Brown 2006 | 10 | 43 | No cost-effectiveness model |
| Liu 2006 | 10 | 47 | No cost-effectiveness model |
| Henison 2006 | 10 | 50 | Diagnostic and screening question |
List of abbreviations
- ADAS-cog
- Alzheimer’s Disease Assessment Scale, cognitive subscale
- ADV
- adefovir dipivoxil
- ALT
- alanine aminotranferase
- BPAR
- biopsy-confirmed acute rejection
- CEA
- cost-effectiveness analysis
- CEM
- cost-effectiveness model
- CRD
- Centre for Reviews and Dissemination, University of York
- FDA
- Food and Drug Administration
- GFR
- glomerular filtration rate
- HAQ
- Health Assessment Questionnaire
- HR
- hazard ratio
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ICH
- International Conference on Harmonisation
- JAMA
- Journal of the American Medical Association
- NICE
- National Institute for Health and Clinical Excellence
- OMERACT
- Outcomes Measures in Rheumatology Clinical Trials
- PEG
- pegylated interferon alpha-2a
- PTE
- proportion of treatment effect explained
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SF-36
- Short Form 36 questionnaire
- TAR
- technology assessment report
- US NIH
- United States National Institutes of Health
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
Health Technology Assessment Programme
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NCCHTA
-
Dr Andrew Cook, Consultant Advisor, NCCHTA
-
Dr Peter Davidson, Director of Science Support, NCCHTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NCCHTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NCCHTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NCCHTA
HTA Commissioning Board
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programmes, Research and Development Directorate, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington