Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA Programme as project number 05/09/07. The contractual start date was in January 2006. The draft report began editorial review in May 2007 and was accepted for publication in June 2008. As the funder, by devising a commissioning brief, the HTA Programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
If funding bodies commission research in line with our recommendations, some of the report’s authors may apply.
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NCCHTA, Alpha House, Enterprise Road, Southampton Science Park, Chilworth, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Aims of the review
This review has two aims:
-
to identify, appraise and synthesise research across a range of study designs that are relevant to selected UK National Screening Committee (NSC) criteria for a screening programme in relation to domestic (partner) violence
-
to make a judgment on whether current evidence is sufficient for fulfilment of selected NSC criteria for the implementation of screening for domestic (partner) violence in health-care settings.
Previous systematic reviews of partner violence studies
Screening
Our previous systematic review,1,2 based on an evaluation of quantitative studies that addressed the NSC criteria, concluded that these criteria were not fulfilled and that implementation of a screening programme was not justified. Contemporaneous reviews by North American colleagues have come to similar conclusions. 3 The Canadian Task Force on Preventive Health Care used a broad analytic framework but only critically appraised intervention studies; its conclusion, that no recommendation could be made for or against screening, was based largely on those studies. 4 The US Preventive Task Force included and critically appraised assessment as well as intervention studies and concluded that there was insufficient evidence for a screening programme. 5 The main findings from these reviews are detailed in Appendix 1. The most recent systematic reviews evaluating the effectiveness of screening included studies published up until December 2002. No previous reviews have included qualitative studies to address any of the review questions.
The effectiveness of screening may vary between different health-care settings because of variation in prevalence of partner violence in different groups of patients, across the life course, and because of differences in acceptability within different health-care settings and between groups of health-care practitioners. Previous reviews of screening have not addressed this potential heterogeneity. Therefore it is possible that criteria for screening may be fulfilled in some settings with specific groups of patients but not in others. Our previous review evaluating the effectiveness of screening1 included three studies from primary care – community health centres, an internal medicine practice, and HMO (health management organisation) primary care clinics – two studies from antenatal settings and four from accident and emergency (A&E) departments.
Interventions after screening
A key element in the justification for a screening programme is an effective intervention or interventions following a positive screening test. In addition to reviews specifically designed to inform policy about screening, since 1998 there have been six systematic reviews of partner violence intervention studies relevant to health-care settings: Chalk and King,6 Abel,7 Hender,8 Cohn and colleagues,9 Klevens and Sadowski,10 and Ramsay and colleagues. 2 The most recent review of intervention studies, commissioned by the Department of Health’s policy research programme,11 included studies cited on the source bibliographic databases before October 2004.
This is a growing research field, and new studies may change the overall negative conclusion about the appropriateness of screening based on previous reviews.
Use of the term ‘partner violence’
A variety of terms are in current use to denote domestic violence perpetrated against an intimate partner, such as ‘partner violence’, ‘intimate partner violence’ (IPV), ‘spouse abuse’, ‘partner abuse’ and ‘battering’. There is still no international, or even national, consensus about the most appropriate term to use for this form of domestic violence. However, many experts in the field believe that ‘domestic violence’ is a misleading term because ‘domestic’ implies that the violence always happens within the home. Similarly, many see ‘IPV’ as inappropriate, as there is nothing ‘intimate’ about an abusive relationship. In this review we use the term ‘partner violence’ as this better reflects the nature of the problem. However, although this is our preferred term, when citing other sources we have retained their terminology where appropriate. We define partner violence against women as physical, sexual or emotional abuse with coercive control of a woman by a man or woman partner who is, or was, in an intimate relationship with the woman. In the US research literature ‘battered women’ is a common term; in this review we have consistently replaced this term with ‘survivors of partner violence’.
What about male survivors of partner violence?
Our overall review question is restricted to screening for partner violence perpetrated against women. Partner violence against men in heterosexual or same sex relationships is a social problem with potential long-term health consequences for male survivors,12 but is not the focus of this review. Although some population studies suggest that the lifetime prevalence of physical assaults against a partner is comparable between genders, even those studies report that violence against women is more frequent and more severe, and that women are three times more likely than men to sustain serious injury and five times more likely to fear for their lives. 13
Definitions of screening and routine enquiry
Screening, as defined by the NSC, is a public health service in which members of a defined population, who do not necessarily perceive they are at risk of, or are already affected by a disease or its complications, are asked a question or offered a test, to identify those individuals who are more likely to be helped than harmed by further tests or treatment to reduce the risk of a disease or its complications. 14
Routine enquiry, as it pertains to partner violence, refers to ‘asking all people within certain parameters about the experience of domestic violence, regardless of whether or not there are signs of abuse, or whether domestic violence is suspected.’15
The use of the term ‘screening’ as defined by the NSC refers to the application of a standardised question or test according to a procedure that does not vary from place to place, and that is how we use the term in this report. We acknowledge that many understand the term in a more general sense than this definition. To avoid confusion it is preferable to use the term routine enquiry where procedures are not necessarily standardised, but where question(s) are asked routinely, for example at every visit within time-specific or other parameters. Although there is not always a clear distinction between routine enquiry and screening, there is a flexibility of application in the former that is absent in the latter; a policy of routine enquiry does not necessarily have to fulfil the criteria for a screening programme. 16 Our review focuses on the criteria for screening, but in our final chapter we discuss the limitations of the screening model in relation to partner violence.
Extending the scope of previous reviews
We extended the scope of previous reviews in three ways. First, earlier reviews did not include a full assessment of the test characteristics of screening tools. We therefore aimed to evaluate the predictive properties of screening tools that could be used in clinical practice. Second, previous reviews have generated a vigorous correspondence,17 including an oft-repeated criticism that restriction to quantitative studies omits important evidence about the acceptability and value of screening or routine enquiry about partner violence in health-care settings. We therefore have included qualitative evidence in this review when it helped to answer a specific review question. Third, no previous review has addressed the economic costs related to the provision of services for abused women. We therefore searched for studies that evaluated the cost or cost-effectiveness of interventions for partner violence relevant to health-care settings and have also reported the economic modelling of a primary care partner violence intervention.
Chapter 2 Objectives and the review questions
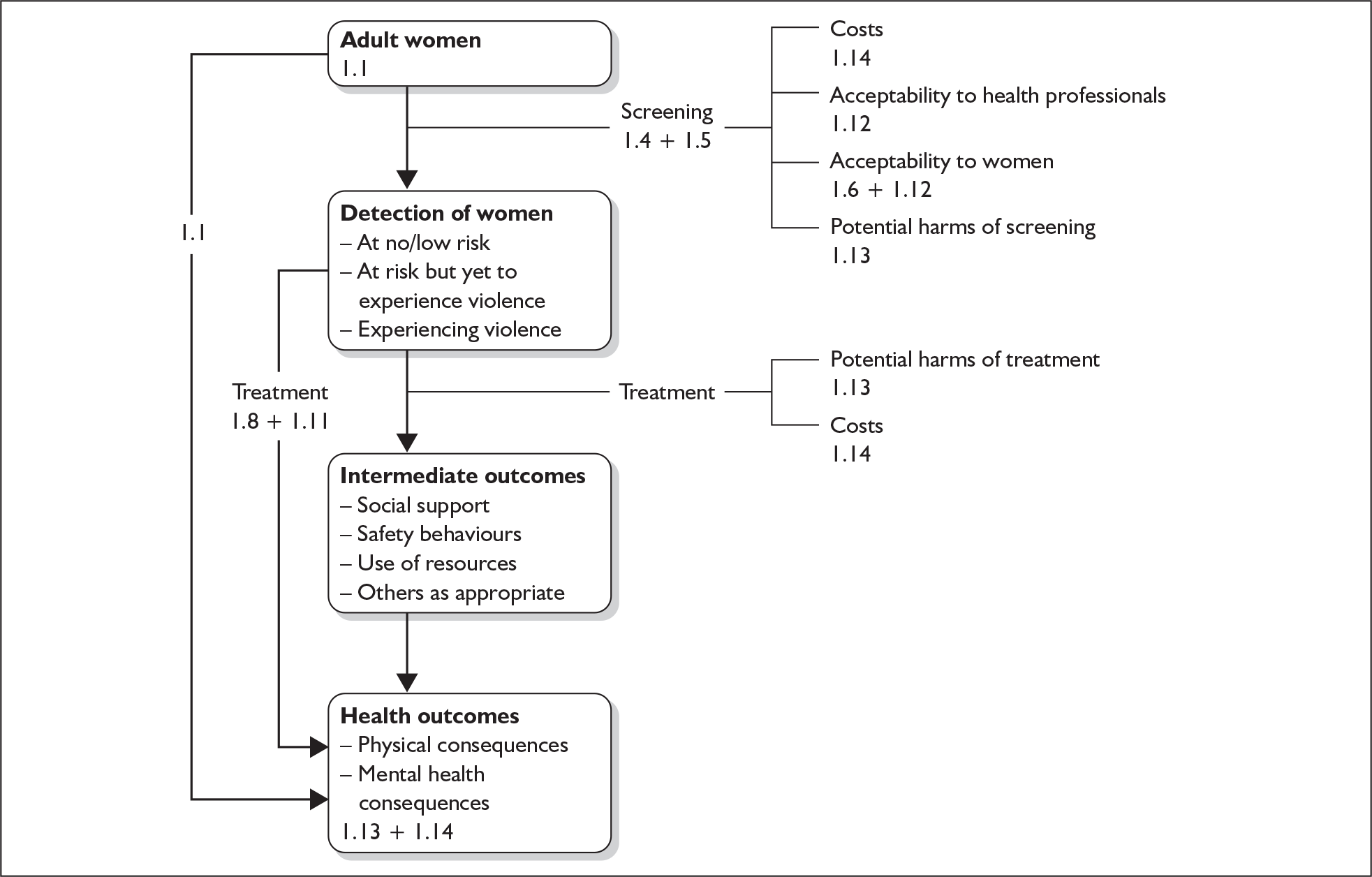
There are seven review questions. We have linked each of these to key NSC criteria for a screening programme. The figure in Appendix 2 places the criteria we are reviewing in an analytic framework for research on partner violence and health, and is adapted from a framework used by the Canadian Preventive Task Force. 18
Question I: What is the prevalence of partner violence against women and its health consequences?
There is no longer any debate about the public-health impact of partner violence, although prevalence rates and the magnitude of health sequelae vary depending on population and study design. But even the lower estimates for prevalence, morbidity and mortality make partner violence a potentially appropriate condition for screening and intervention. To answer this question we systematically searched for reviews from 1990 onwards on the health impact of partner violence, and summarised these along with prevalence data from individual studies from the UK published from 1995 onwards.
Question II: Are screening tools valid and reliable?
We reviewed the predictive properties and validity of current partner violence screening questions where they are evaluated against a standard criterion, such as the Conflict Tactics Scale. 19,20 We also summarised more general information about the screening tools, such as the number of items asked and the length of time required to administer the tool.
Specific questions:
-
Can screening efficiently and accurately identify women at risk of or experiencing partner violence?
-
Does accurate identification differ as a function of the number of items asked or the setting in which the tool is administered?
The distribution of test values in women experiencing partner violence was extracted and analysed.
Question III: Is screening for partner violence acceptable to women?
We reviewed acceptability of screening for partner violence by searching for quantitative surveys and qualitative studies eliciting the views of women. Findings from the different study designs were triangulated.
Specific review questions:
-
Is screening generally acceptable to women?
-
Do women’s views about screening differ as a function of previous exposure to screening?
-
Do women’s views about screening differ as a function of abuse status?
-
Are there any other factors associated with acceptability/non-acceptability?
-
age and ethnicity
-
health-care setting
-
mode of screening.
-
-
What harms do women report associated with screening for partner violence (qualitative studies only)?
Question IV: Are interventions effective once partner violence is disclosed in a health-care setting?
We reviewed quantitative studies of interventions that are relevant to women identified through screening procedures. This included studies of interventions initiated as a direct result of screening by health professionals, or interventions conducted outside of screening that nevertheless show what could be achieved if a woman’s abuse status was ascertained. We endeavoured to identify any evidence for a differential effect of early treatment on outcomes. We extended our previous systematic review,11 which included studies cited on the source bibliographic databases before October 2004.
Specific review questions:
-
Is there an improvement in abused women’s experience of abuse, perceived social support, quality of life and psychological outcome measures as a result of interventions accessed or potentially accessible as a result of screening (quantitative studies only)?
-
Is there an improvement for abused women’s children in terms of quality of life, behaviour and educational attainment following their mothers’ participation in programmes accessed or potentially accessed as a result of screening (quantitative studies only)?
-
What are the positive outcomes that abused women want for themselves and their children from programmes that include screening or other health-care-based interventions (qualitative studies only)?
We considered direct and indirect harms of whole screening programmes, where reported, by reviewing evidence from the intervention studies and qualitative studies.
Question V: Can mortality or morbidity be reduced following screening?
We searched for evidence from randomised controlled trials (RCTs) and reviewed these if available. We also included other controlled studies of interventions that implemented screening programmes or included partner violence screening as an aim in educational interventions for health-care professionals.
Specific review questions:
-
What are the changes in identification, information giving and referrals (made and attended) from screening and other system-based interventions in health-care and community/voluntary sector settings?
-
Is there evidence from RCTs and other controlled studies that there is a cessation or reduction in abuse following abused women’s participation in programmes including screening (quantitative studies only)?
-
Are there any measured harms from screening interventions (quantitative studies only)?
Question VI: Is a partner violence screening programme acceptable to health professionals and the public?
We reviewed quantitative and qualitative studies of acceptability to health professionals.
The issue of whether the test is acceptable to the public is addressed in question III, albeit only from the perspective of women. We did not address the issue of whether the programme is acceptable to male members of the general public.
Specific review questions:
-
Is screening for partner violence generally acceptable to health professionals?
-
Do health professionals’ views about screening differ as a function of previous experience of screening?
-
Do health professionals’ views about screening differ as a function of their role (e.g. physician, nurse, psychiatrist) or the setting in which they work (e.g. family practice, A&E, antenatal, dental practice)?
-
Are there any other factors associated with acceptability/non-acceptability?
-
age and ethnicity
-
training on partner violence.
-
Question VII: Is screening for partner violence cost-effective?
-
We reviewed studies evaluating the cost-effectiveness of screening. We complemented this with a cost-effectiveness model based on a pilot study of a primary care-based intervention that aimed to improve the identification of women patients experiencing partner violence.
NSC criteria not addressed by this review
We did not address this criterion because of its problematic application to the issue of partner violence: partner violence is not a condition in the disease model sense, and screening is not limited to detection of early stages of abuse.
In terms of partner violence, primary prevention interventions are largely in educational and media settings and we did not review these. This criterion is not relevant to a decision to implement a screening programme in health-care settings.
Review of evidence for criteria 8, 9 and 12 were part of our original proposal. Below we explain why we did not include them in the final review.
Further ‘diagnostic investigation’ is not relevant to the care of women who are identified in partner violence screening programmes.
Although some primary studies in our review discussed choices available to women disclosing abuse, there are no ‘evidenced-based policies’ for these treatment choices and, in the context of our resources for the reviews, we judged this criterion of secondary importance compared with those we did review.
The following criteria need to based on audit and policy research. They only need to be considered once the evidence-based criteria are met:
NSC criterion 12: Clinical management of the condition and patient outcomes should be optimised by all health-care providers prior to participation in a screening programme.
NSC criterion 17: There should be a plan for managing and monitoring the screening programme and an agreed set of quality assurance standards.
NSC criterion 18: Adequate staffing and facilities for testing, diagnosis, treatment and programme management should be available prior to the commencement of the screening programme.
NSC criterion 19: All other options for managing the condition should have been considered (e.g. improving treatment, providing other services), to ensure that no more cost effective intervention could be introduced or current interventions increased within the resources available.
NSC criterion 20: Evidence-based information, explaining the consequences of testing, investigation and treatment, should be made available to potential participants to assist them in making an informed choice.
NSC criterion 21: Public pressure for widening the eligibility criteria for reducing the screening interval, and for increasing the sensitivity of the testing process, should be anticipated. Decisions about these parameters should be scientifically justifiable to the public.
Chapter 3 Review methods
Inclusion and exclusion criteria
The generic criteria that applied to all seven questions are listed in Tables 1 and 2.
| Inclusion criteria | Review questionsb | ||||||
|---|---|---|---|---|---|---|---|
| QI | QII | QIII | QIV | QV | QVI | QVII | |
| Participants | |||||||
| Women aged over 15 years | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ |
| Women that report a lifetime experience of partner violence | ✓ | × | ✓ | ✓ | ✓ | × | ✓ |
| Settings | |||||||
| Health-care settings – no restrictions on geographical/national setting | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Primary studies conducted in services outside health-care systems to which referral can be made from a health-care setting | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ |
| Study designs | |||||||
| Randomised controlled studies, non-randomised parallel group studies, interrupted time series studies, before-and-after studiesa | ✓ | × | ✓ | ✓ | ✓ | ✓ | × |
| Cohort studies | ✓ | × | ✓ | ✓ | × | ✓ | × |
| Case–control studies | ✓ | × | ✓ | ✓ | ✓ | × | × |
| Cross-sectional studies | ✓ | × | ✓ | × | × | ✓ | × |
| Clusters of case studies | × | × | ✓ | × | × | ✓ | × |
| Prevalence studies | ✓ | × | ✓ | × | × | × | × |
| Qualitative designs | × | × | ✓ | × | × | ✓ | × |
| Questionnaire surveys | × | × | ✓ | × | × | ✓ | × |
| Studies where verbal interaction (researcher–participant) aids results’ formulation | × | × | ✓ | × | × | ✓ | × |
| Studies where abused women’s views discussed separately | × | × | ✓ | × | × | × | × |
| Studies evaluating a screening tool against a standard criterion | × | ✓ | ✓ | × | × | × | × |
| Economic evaluations of screening interventions | × | × | ✓ | × | × | × | ✓ |
| Aims of studies included | |||||||
| Interventions aimed at reducing abuse or improving the health of the women | ✓ | × | × | ✓ | ✓ | × | × |
| Interventions aimed at training staff | × | × | × | × | × | × | × |
| Interventions aimed at providing more organisation/system resources | × | × | × | × | × | × | × |
| Studies determining effectiveness of screening interventions | × | × | × | ✓ | × | × | × |
| Studies determining prevalence of partner violence | ✓ | × | × | × | × | × | × |
| Studies determining validity and reliability of screening | × | ✓ | × | × | × | × | × |
| Studies determining cost-effectiveness of screening | × | × | × | × | × | × | ✓ |
| Studies determining acceptability of screening to women | × | × | ✓ | × | ✓ | ✓ | × |
| Studies determining harms associated with screening | × | × | × | × | ✓ | × | × |
| Studies determining acceptability of screening to health professionals and public | × | × | × | × | × | ✓ | × |
| Included outcomes | |||||||
| Incidence of abuse (physical, sexual, psychological, emotional, financial) | ✓ | × | × | ✓ | ✓ | × | ✓ |
| Physicalc and psychosociald health | ✓ | × | × | ✓ | ✓ | × | ✓ |
| Proxy measurese | × | × | × | ✓ | ✓ | × | ✓ |
| Measures of validity and reliability of screening tools | × | ✓ | × | × | × | × | × |
| Degree of acceptability of screening amongst women | × | × | ✓ | × | × | × | × |
| Degree of acceptability of screening to health professionals | × | × | × | × | × | ✓ | × |
| Cost of providing screening | × | × | × | × | × | × | ✓ |
| Changes in identification, information giving and referrals from screening | × | × | × | × | ✓ | × | × |
| Included reporting formats | |||||||
| Studies published in peer-reviewed journals and in books by academic publishers | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Funder-published research reports | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Studies reported in European languagesf | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Reviews, from 1990, on the health impact of partner violence | ✓ | × | × | × | × | × | × |
| Studies, from 1995, reporting prevalence data for partner violence from the UK | ✓ | × | × | × | × | × | × |
| Exclusion criteria | Review questionsa | ||||||
|---|---|---|---|---|---|---|---|
| QI | QII | QIII | QIV | QV | QVI | QVII | |
| Participants | |||||||
| Female survivors of partner violence aged under 15 years | ✓ | × | ✓ | ✓ | ✓ | × | × |
| Female survivors of other (non-partner) abuse (e.g. stranger rape, adult survivors of child abuse, elder abuse) | ✓ | × | ✓ | ✓ | ✓ | × | × |
| Male survivors of partner abuse of any age | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Children of abused women, abused children, and the perpetrators of abuse | ✓ | × | ✓ | ✓ | ✓ | × | ✓ |
| Participants with no previous history of partner violence | ✓ | × | × | ✓ | ✓ | × | × |
| Settings | |||||||
| Studies conducted in non-health-care settings that are not considered relevant to health-care policy | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Study designs | |||||||
| Single case studies | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Study aims excluded | |||||||
| Interventions targeted at perpetrators of partner violence | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Studies reporting joint treatments, such as couple and family therapy (even if the therapy was administered separately to women) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Interventions aimed at helping the survivors of child or elder abuse | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Intervention studies initiated to help the survivors of abuse committed by other family members (such as in-laws) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Interventions targeted directly at helping children of women being abused by intimate partners | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Interventions aimed at abused men | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Studies determining the acceptability of screening that have not distinguished the perspectives of male and female members of the public | × | × | ✓ | × | × | ✓ | × |
| Community and societal interventions conducted with the aim of increasing public awareness of the problem of partner abuse | ✓ | ✓ | × | ✓ | × | × | ✓ |
| Criminal justice interventions | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Excluded outcomes | |||||||
| Studies that do not report outcomes relating to abuse | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Studies that do not report outcomes relating to at least one of: physical and psychosocial health, socioeconomic indicators and other proxy measures | ✓ | × | × | ✓ | ✓ | × | ✓ |
| Primary studies that only measure change in knowledge or attitudes of professionals about partner abuse | ✓ | ✓ | ✓ | × | ✓ | × | ✓ |
| Studies that only measure identification of abused women or documentation or safety assessments | ✓ | × | ✓ | × | × | ✓ | ✓ |
| Excluded reporting formats | |||||||
| Self-published research reports | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| PhD theses, masters’ and undergraduate dissertations | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Papers published in non-European languages | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Conference abstracts | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Reviews, before 1990, on the health impact of partner violence | ✓ | × | × | × | × | × | × |
| Prevalence data for partner violence from the UK reported before 1995 | ✓ | × | × | × | × | × | × |
Further question-specific criteria are listed below. All criteria were applied independently by two reviewers and disagreements were adjudicated by a third reviewer.
-
Primary studies of prevalence restricted to UK populations from 1995 onwards.
-
Review of health consequences restricted to systematic reviews from 1990 onwards.
-
Included study designs had to be validation studies, i.e. they evaluated a screening tool against a standard criterion/comparator.
-
The comparator had to have high sensitivity and specificity.
-
The comparator could have any number of items, but the index screening tool had to comprise 12 items or fewer. The rationale behind this postprotocol decision was the requirement for screening tools to be used in a clinical, not research setting. Long screening tools would be unsuitable due to the time needed to complete them, and we chose 12 items as an arbitrary cut-off. This reduced the number of screening tools reviewed but improved the clinical applicability of our findings.
-
Studies were excluded if non-standardised clinical interviews were used as the comparator.
-
Studies only reporting women’s perceived barriers to disclosure but not their views about the acceptability of screening were excluded.
-
Intervention studies on co-morbid populations were included if all the participants had experienced partner violence or if the outcome data for those who had experienced partner violence were reported separately.
-
Studies of interventions with children were included if the mothers were also involved; either the mothers received their own interventions or they played a role in interventions targeted at their children.
-
Studies that measured mortality, morbidity or quality of life outcomes for women were included.
-
Studies of screening intervention studies that measured proxy measures that were potentially associated with decreased morbidity and mortality were included, particularly documentation of abuse or referral to expert partner violence services.
-
Studies where documentation was limited to recording the disclosure of abuse, without recording more detailed information (about, e.g., context, safety and, perhaps, the perpetrator), were excluded.
-
Studies reporting changes in identification rates with no other outcomes were excluded.
-
Studies that only reported one proxy outcome were excluded, unless this was referral to expert partner violence services.
-
In addition to survey studies, intervention studies reporting attitude change were included and the before and after data reported separately.
-
We did not include studies addressing the issue of whether screening is acceptable to male members of the public.
-
Papers that only reported on the perceived barriers to screening were excluded.
-
Studies were excluded if they only measured screening behaviour without reporting attitudes towards screening for partner violence.
-
Studies had to include an analysis of costs of a health-care-based partner violence intervention or screening programme.
Identification of primary studies
We systematically searched for relevant studies using strategies that combined content terms and study designs (search strings available from authors). Searches were made of the international literature for published peer-reviewed studies. The following sources were used to identify studies.
Electronic databases
-
Cochrane Collaboration Central Register (CENTRAL/CCTR)
-
Biomedical sciences databases:
-
MEDLINE
-
EMBASE
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature)
-
Database of Abstracts of Reviews for Effectiveness (DARE)
-
National Research Register (NRR)
-
Health Management Information Consortium (HMIC)
-
MIDIRS (Midwives Informatin and Resource Service)
-
British Nursing Index (BNID)
-
NHS Economic Evaluation.
-
-
Social sciences databases:
-
Social Science Citation Index (SSCI)
-
International Bibliography of the Social Sciences (IBSS)
-
PsycINFO
-
Applied Social Sciences Index and Abstracts (ASSIA).
-
Searches of these databases included all studies referenced from their respective start dates to 31 December 2006. In addition to original research papers, we also searched for any relevant review articles.
In the case of Question I, we only searched for review articles in six of the electronic databases: Medline, Embase, Cinahl, DARE, British Nursing Index and Social Science Citation Index. We also used backward and forward citation tracking to identify other studies and we scrutinised papers in the reference lists of included studies.
Other sources
-
Personal communication with the first or corresponding authors of all included articles.
-
Consultation with members of partner violence organisations/research networks in the UK, Western Europe, North America and Australasia.
We did not hand search any journals.
Selection of studies
Two reviewers independently selected studies for inclusion in the review. Where possible, disagreement between the two reviewers was resolved by discussion. If agreement could not be reached then a third reviewer adjudicated. Agreement rates across all databases ranged from 70% to 98%, the average inter-rater agreement being 88%. If additional information was needed to resolve a disagreement, then this was sought either from the first or corresponding author of the study in question.
Data extraction and methodological appraisal by reviewers
Data from included studies were extracted by one reviewer and entered onto electronic collection forms. All of the extractions were independently checked by a second reviewer. Again, where possible, any disagreements between the two reviewers were resolved by discussion. If this was not possible, then a third reviewer adjudicated and all such decisions were documented. Where necessary, the first authors of studies or the correspondence authors were contacted to assist in resolving the disagreement. One reviewer appraised study quality and strength of design in relation to the review questions.
Analysis of primary data extracted
The data extraction forms were used to compile summary tables of the data and quality classification. These formed the basis for our narrative synthesis of the primary studies. We grouped the findings of the primary studies and analysed differences between studies in relation to setting (country, type of health-care facility), populations (ethnicity, socioeconomic status, method of identification/disclosure) and, in the case of intervention studies, the nature of the intervention. We performed narrative sensitivity analysis for each question, testing whether the overall findings persisted when the poor-quality studies were excluded. When effect sizes were not reported, we calculated Cohen’s d if the mean changes and standard deviations were reported in the papers or were available from the authors. For the quantitative studies, after consideration of the heterogeneity of interventions and outcomes and the overall purpose of this review – assessing the extent to which criteria for a screening programme were fulfilled – we chose not to pool the data from different studies.
Application of the appraisal criteria to our reviews
We appraised our reviews of intervention studies (Questions 4 and 8) using the Quality of Reporting of Meta-analyses of Randomised Controlled Trials (QUORUM) criteria. 21 We appraised our review of prevalence studies using the Meta-analysis of Observational Studies in Epidemiology (MOOSE) criteria. 22
Synthesis of the qualitative data
There is no standard method for combining qualitative studies. We therefore used a type of qualitative meta-analysis. 23 We drew on Schutz’s framework of constructs24 and on the metaethnographic method articulated by Britten and colleagues,25,26 although we prefer the term ‘meta-analysis’ as the studies analysed were not ethnographies. The analysis started with two parallel strands: (1) identification and examination of first- and second-order constructs in the primary studies, and (2) methodological appraisal. These strands were brought together in the formulation of third-order constructs expressing the conclusions of the meta-analysis.
First-order constructs were based on results in the primary studies relevant to the review question. Second-order constructs were the interpretations or conclusions of the primary investigators that related to the review question. These constructs were identified and grouped from data on the extraction forms, referring back to the original papers when necessary. For identification of second-order constructs, where the investigators only presented recommendations, we interpreted these as the authors’ conclusions. We intended to examine three different types of relationship between the constructs extracted from the studies:
-
constructs that were similar across a number of studies (reciprocal constructs) and, through a process of repeated reading and discussion, would yield third-order constructs that would express our synthesis of findings that were directly supported across different studies
-
constructs that seemed in contradiction between studies; we planned to explain these contradictions by examining factors in the studies and, where there was a plausible explanation, to articulate these as third-order constructs
-
unfounded second-order constructs; i.e. conclusions by primary study authors that did not seem to be supported by first-order constructs.
This method allows generalisations to be made that are not possible from individual qualitative studies.
Further details of the analysis by review question are given below.
We summarised the prevalence data reported in primary studies and the evidence for health consequences in systematic reviews. We plotted incidence and prevalence with 95% confidence intervals and tested the effect on variation of type of population (clinical versus community) and types of violence with logistic regression models. For health consequences, when we cited primary studies this was for illustrative purposes only.
In our narrative analysis of the results of these studies we evaluated the effectiveness and accuracy of the screening tools in terms of: test sensitivity and specificity, test positive and negative predictive values, positive and negative likelihood ratios, and the diagnostic odds ratio. Where feasible, we had also planned to pool results from primary studies of the same screening tool that were graded good or fair and that had comparable effect measures (e.g. sensitivity/specificity, predictive values, risk estimates). 27 However, no meta-analyses of the screening tool evaluations were possible because of the heterogeneity of the index tools used in the primary studies. Some of the primary studies did not fully report diagnostic accuracy, but did report the numbers of true positives, false positives, true negatives and false negatives for both the index and comparator tools. In those cases we calculated the diagnostic accuracy of the index tool. If the raw data were not available, we requested it from the authors. Reliability was judged by Cronbach’s alpha, coefficient alpha or Cohen’s kappa.
In addition to summarising the data in terms of the acceptability of screening to women, we also examined if attitudes varied as a function of women-related variables (such as age, ethnicity, abuse status, educational status), demographic features (such as the country where the study was conducted, the setting in which the women were recruited) and features relating to the screening process (such as the questions asked and who asked them). In a synthesis of the interview- and focus group-based qualitative and questionnaire-based quantitative studies, we explored whether and how these factors are associated with women’s positive attitudes towards partner violence screening. We did not perform a meta-regression of the surveys because of the heterogeneity of the clinical settings, of the demographic data collected from the informants, and the measures of acceptability.
We calculated effect sizes where means and standard deviations were reported or were obtainable from the authors of studies. Meta-analyses of the studies were planned, but the data could not be pooled because of the heterogeneity of settings, demographics of the women participants, study designs (including the duration of follow-up) and the outcomes measured. It was not possible to construct funnel plots to investigate potential publication bias.
Where data were reported, we calculated confidence intervals for differences in identification and referrals between intervention and control groups. Pooling of data to calculate an overall effect size was not feasible because of the weak study designs: there was only one RCT.
These data were summarised in terms of the acceptability of screening to health professionals (women’s views are given above and we did not seek to include studies examining the views of male members of the public). We also analysed if attitudes varied as a function of individual health professional-related variables (such as age, ethnicity, previous training on partner violence, personal experience of caring for abused patients), demographic features (such as the country where the study was conducted, the occupation of the health professional) and features relating to the screening process (such as the questions asked, who should ask the questions, where the screening should occur, barriers to screening). By examining these factors we explored whether and how these factors interact to increase or decrease health professionals’ positive attitudes towards screening women for partner violence.
In anticipation of a paucity of cost-effectiveness (or any economic) studies of screening for partner violence in health-care settings, we modelled the impact of an intervention in general practice to increase identification and referral of women experiencing partner violence. We used real cost data from a pilot study (PreDoVe, Prevention of Domestic Violence) we completed in three east London practices. 28 This model allowed us to link intermediate outcomes such as referrals and levels of abuse, to medium- and longer-term outcomes and costs such as abuse measures, quality of life, employment, housing and civil justice. We combined our data with secondary sources to estimate the impact on outcomes and costs that could not be measured within the pilot study. The model estimated the cost-effectiveness of the intervention and gave special attention to the following aspects:
-
Micro-level data collection – PreDoVE collected detailed resource use by women data, and we have combined these with unit cost data available from the NHS and relevant studies. 29
-
Confidence intervals around the estimates – we estimated the distribution of costs and outcomes of partner violence. This allowed us to investigate the probability that the intervention is cost-effective and to establish a confidence interval around the cost-effectiveness estimate.
-
Sensitivity analyses – we varied all costs and outcomes by 25% in univariate analyses.
-
The time lag between cause and effect – the study captured the extent to which women access services over time, including periods of time when the women choose to delay seeking additional help.
Appraisal of methodological quality
The quality of the primary studies was assessed using appraisal tools in accord with the different review questions and the nature of the data collected.
The papers reporting the prevalence studies were appraised using the current version of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist. 30 In assessing the studies for inclusion, the following methodological issues were considered: selection, confounding and measurement bias. In this review, for each item in the checklist a score of zero or one was assigned. The maximum total score was 22. Although this tool focuses on reporting rather than the quality of the primary studies per se, it does discriminate between studies of better or worse quality. We appraised the methodological quality of reviews with the Critical Appraisal Skills Programme (CASP) systematic review appraisal tool31. The scores for individual items informed a judgment about whether the review was high, medium or low quality. This judgment was made independently by two reviewers who did not disagree.
The papers reporting the validation of screening tools were appraised using the 14-item Quality Assessment of Diagnostic Accuracy Studies (QUADAS). 32 The tool allows studies to be rated for bias (eight items), variability (one item) and reporting (five items); these include patient spectrum, selection criteria, reference standard, disease progress, partial verification, differential verification, incorporation, test execution, blind analysis, interpretation, indeterminate results and study withdrawals (see Appendix 3.1). The QUADAS does not have a scoring system and the outputs are narrative results relating to the various sources of bias rather than a single score. This is an advantage in assessing diagnostic accuracy studies, as total scores tend to ignore the importance of individual items and do not take account of the direction of bias under different contexts. We used the QUADAS to assess both within-study bias (the level of methodological quality of each primary study) and between-study bias (the proportion of studies that have not accounted for a particular bias) to give an overall picture of the quality of the validation studies in this field.
Question III: Is screening for partner violence acceptable to women? Quantitative studies that examined women’s attitudes towards screening for partner violence were appraised using the STROBE30 checklist (see Question I above). In addition to scoring the individual primary studies, we ranked all the studies and carried out a sensitivity analysis by comparing results for those studies in the top quartile with the results for all the studies.
We appraised the methodological quality of qualitative studies for this question with the CASP qualitative appraisal tool. 31 The tool has 10 questions that address three broad issues: rigour (has a thorough and appropriate approach been applied to key research methods in the study?); credibility (are the findings well presented and meaningful?); and relevance (how useful are the findings?). In this review, for each item in the checklist a score of zero or one was assigned and a maximum score of 41 was possible. As for the quantitative studies, the resulting scores of the primary studies were ranked and those in the upper quartile were used for a sensitivity analysis. We have shown in a previous study that ranking of CASP scores for qualitative studies is a relatively robust method for ranking them by quality. 33
The United States Preventative Services Task Force (USPSTF)34 quality appraisal framework was used to assess the primary intervention studies included in the review. This tool rates the internal validity of a study (in terms of good, fair or poor) and its external validity, as well as the quality of execution of the study and its study design. The overall strength of evidence for each type of intervention could then be determined on the basis of the following criteria: the suitability of study design (greatest, moderate and least); the quality of execution of the study (based on the internal validity of the primary studies); the number of studies that fulfilled minimum suitability and quality criteria; and the size and consistency of reported effects. The combination of these factors determined the final score for evidence of effectiveness for each category of interventions (strong, sufficient or insufficient). For studies that used an RCT design, we also applied the Jadad score35 to obtain a further assessment of quality. Trials with lower Jadad scores are associated with overestimates of treatment effect. For further details of the USPSTF and Jadad quality appraisal methods, see Appendices 3.2 and 3.3.
These studies were also appraised using the USPSTF quality appraisal framework34 and the Jadad score. 35
In accordance with our assessment of the methodological quality of studies included under Question III, we once again used the STROBE checklist30 to appraise the quality of the quantitative studies and the CASP tool31 to appraise the qualitative studies we included. Sensitivity analyses of those studies that ranked in the upper quartiles for methodological quality were also performed.
We did not find any studies that fulfilled our inclusion criteria.
Application of review evidence to National Screening Committee criteria
Once the review was completed, its findings were summarised in relation to NSC criteria. The research group systematically considered each of these criteria against the review evidence using informal consensus to judge the extent to which the criteria were fulfilled. As noted in our proposal, the timescale of the review did not allow engagement with an external reference group. We did present our initial findings to a meeting of the National Domestic Violence and Health Research Forum. These findings and the design of the reviews were discussed by the Forum. There were no specific suggestions for further searching or analysis; comments on the questionable applicability of the NSC criteria to domestic violence screening informs our discussion of this issue in Chapter 11. We approached Health Ending Violence and Abuse Now (HEVAN), the domestic violence practitioners’ forum (Loraine Bacchus was secretary of the group), but no meeting was possible within the timescale of the review.
Chapter 4 What is the prevalence of partner violence against women and its impact on health? (Question I)
Prevalence of partner violence against women in the UK
One of the prerequisites for an effective screening programme in clinical settings, and the first NSC criterion, is that the condition is an important health problem. Two dimensions of importance are prevalence and health impact. In this section we review prevalence studies in England, Wales, Scotland and Northern Ireland.
Methodological challenges
Measuring the prevalence of partner violence is problematic; studies employ different definitions, use different questions, and examine different populations and time frames. Additionally, there are various methods of administering questions, for example self-completed or researcher-completed, which may affect responses. 36
The most common definition of partner violence used in UK prevalence studies only includes physical violence. More recent studies have broadened the definition to include emotional, sexual, psychological and financial abuse, as well as stalking. Others, although making reference to emotional and sexual violence in the definition of partner violence, only report the prevalence of physical violence. Even with this restricted focus, there are disparities: some researchers include threats of physical violence, others include only severe physical violence. The number and content of questions used to measure prevalence vary between studies. An additional obstacle to comparing studies is the modification of instruments without detailing how, or if, the instrument in its adapted format has been validated. Prevalence rates are reported over differing time frames. Reporting lifetime prevalence rates may suffer from the problem of recall bias. However, reporting 1-year prevalence (abuse in the past year) may under-represent the problem as women may not yet have had sufficient time to acknowledge or identify their experiences as partner violence. These disparities go some way to accounting for the varying prevalence rates.
Prevalence studies are likely to under-represent the extent of the problem, as violence may not be disclosed to the researcher. Furthermore, it is likely that some women experiencing partner violence are beyond the reach of epidemiological studies as their abusive partners may not allow them to speak to a researcher alone, or may not even allow them to leave the house.
Results
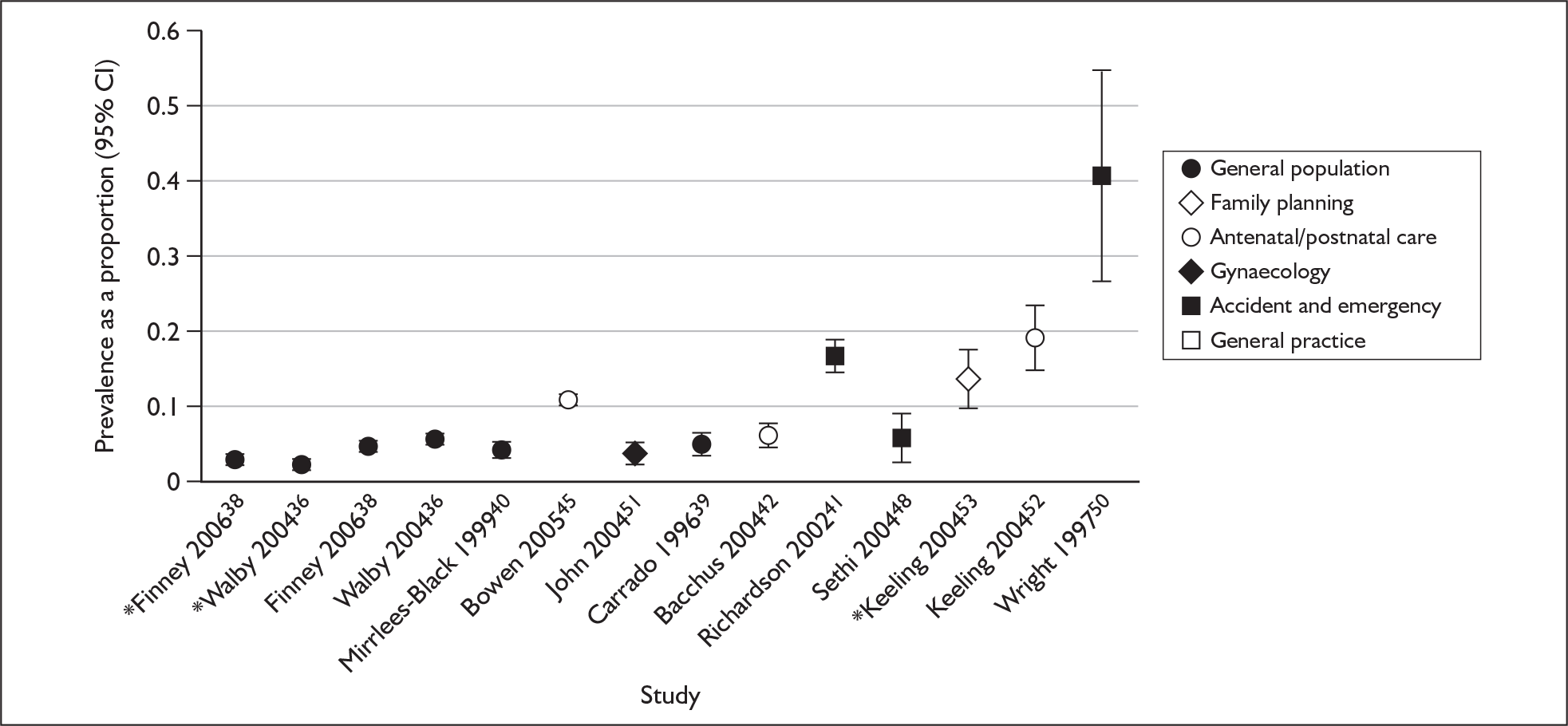
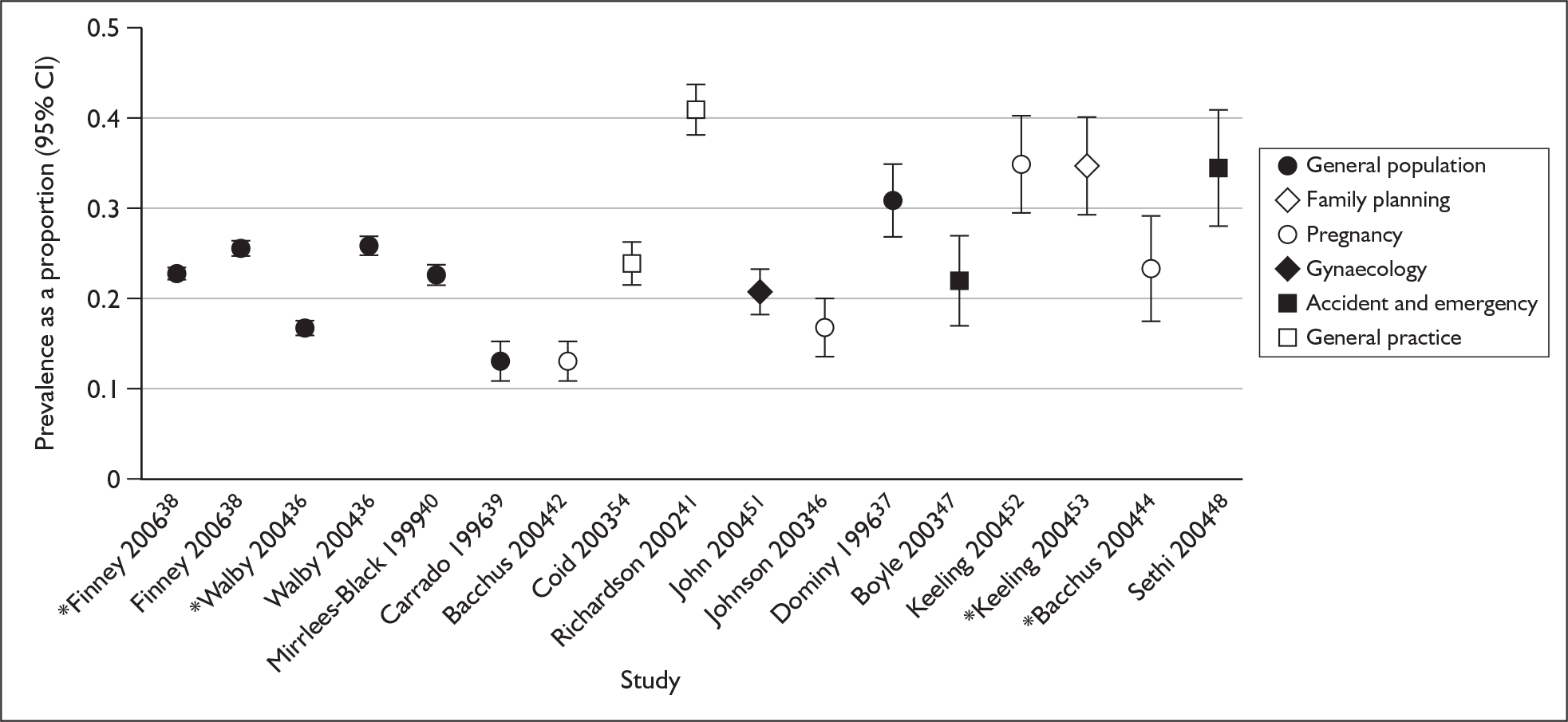
Sixteen studies (reported in 18 papers) met our inclusion criteria. Lifetime prevalence ranged from 13% to 31% in the five community-based samples (general population) and from 13% to 41% in the 11 studies of women recruited in health service settings (clinical populations). One-year prevalence ranged from 4.2% to 6% in the general population studies and from 4% to 19.5% in the clinical population studies. For details of study design, study results and quality appraisal, see Appendix 4.1.
General population
A study by Dominy and Radford37 reported a 31% lifetime prevalence of physical, emotional, sexual and psychological abuse in women living in Surrey. A random sample of 484 women in shopping malls and markets was administered a questionnaire. The sample was intended to be representative of the population of married women or those with long-term partners. However, the venues and timing of the sampling meant that women in full-time employment or education were likely to be under-represented. Women isolated by their partner or having their movements closely monitored by a partner were also likely to be under-represented. For these reasons, both the prevalence cited for partner isolation and the overall prevalence of partner violence may be an underestimate.
Walby and Allen36 measured the prevalence of physical and sexual violence in England and Wales. The study recruited a sample of 22,463 people, weighted to ensure that it was nationally representative. A lifetime prevalence of 25.9% and 1-year prevalence of 6%* were found for female respondents reporting physical, emotional and financial abuse, threats or force. Lifetime prevalence of sexual assault was estimated at 16.6% and 2.1%. These figures may be an underestimate as only people living in private households were included in the sampling frame, so women staying in refuges or with relatives were not included. The study found that younger women and those who were separated were at greater risk of violence.
An updated version of the above study38 used a computerised self-completion method to estimate the prevalence of physical, emotional and financial abuse, threats or force amongst a nationally representative sample of 24,498 men and women. Prevalence figures were adjusted to make them comparable with figures from the above study. The adjusted lifetime prevalence was 25.4% and the 1-year prevalence was 4.7%. The lifetime prevalence of sexual assault was 22.7% and the 1-year prevalence was 2.7%.
A study by Carrado39 used sampling quotas to ensure the sample of 971 women asked about partner violence was representative of the general population with regards to age, socioeconomic group, relationship status and geographical region. The questions relating to violence were administered as a self-completion questionnaire, part of a regular commercial bimonthly survey. The questions were derived from the Conflict Tactics Scale. 19 The study found a 13% lifetime prevalence of physical assault and 1-year prevalence of 5%. It also reported a higher prevalence in women who are young and single.
Mirrlees-Black and Byron40 used a representative sample of 6098 women to estimate the prevalence of partner violence (defined as physical assault) in 16–59-year-olds in England and Wales. They found a lifetime prevalence of 22.7% and 1-year prevalence of 4.2%. They also found that prevalence decreased with age.
Clinical populations
General practice
A study by Richardson et al. 41 measured the prevalence of partner violence in 1207 women attending a general practice, finding a 41% lifetime prevalence and a 17% 1-year prevalence of physical abuse by a partner. Prevalence was higher among women who were divorced or separated, and amongst women aged 16–24 years, and lower in women born outside the UK.
Antenatal/postnatal care
We found five papers (four studies) that estimated the prevalence of partner violence in women attending antenatal or postnatal clinics in the UK.
Bacchus and colleagues42 measured the lifetime prevalence and 1-year prevalence of physical, sexual and emotional abuse in a cohort of 892 women attending maternity services in south London; they asked about partner violence at booking, at 34 weeks of gestation and postpartum. The study reported a lifetime prevalence of 13% and prevalence (during the pregnancy) of 6.4%.
A second study conducted by Bacchus and colleagues43,44 measured a 23.5% lifetime prevalence of partner violence (physical, sexual and psychological) from a sample of 200 women receiving antenatal or postnatal care at a south London hospital.
In a study based on a cohort of 7591 women from 18 weeks’ gestation to 33 months postpartum, Bowen and colleagues45 found that the prevalence (during pregnancy and a 33-month postpartum period) of partner violence steadily increased through the second half of pregnancy and after delivery. At 18 weeks’ gestation, 5.1% of the women experienced some form of abuse (physical, sexual or emotional) and this increased to 11% at 33 months after the birth. However, this study had substantial limitations, including a high attrition rate (45%), which may result in an underestimated prevalence, because those experiencing partner violence were more likely to be lost to follow-up. Moreover, the questionnaires were posted to women, which may have discouraged some respondents from reporting abuse if they were still living with the abuser. A further complication of this study is that the women who completed the study differed from those lost to follow-up: they were more likely to have attended higher education, have fewer children, be married, be at least 25 years old when their first child was born, and be homeowners.
A questionnaire survey by Johnson and colleagues46 of 500 consecutive women in an antenatal booking clinic in a hospital in the north of England found a 17% lifetime prevalence of physical, sexual and emotional abuse in pregnant women. Abuse was most prevalent in women aged between 26 and 30 years.
Thus lifetime prevalence of partner abuse in women receiving antenatal or postnatal care in the UK ranges from 13% to 24%. One-year prevalence was estimated at 6.4% or 11% depending on the type of study and the stage of pregnancy at which women are asked about abuse.
Accident and emergency departments
We found three primary studies that measured the prevalence of partner violence in women attending accident and emergency departments in the UK.
In a study by Boyle and Todd,47 using randomly allocated time blocks, complete data were collected from 256 patients attending the emergency department of a Cambridge hospital. The study reported a 22.1% lifetime prevalence of physical, sexual and emotional abuse.
Sethi and colleagues48,49 purposefully sampled 22 nursing shifts, representative of day, night and weekend shifts. A questionnaire was administered to 198 women attending an inner city accident and emergency department. The study found a 34.8% lifetime prevalence of physical abuse. Prevalence was highest in women aged 30–39 and not in paid employment. A 6.1% 1-year prevalence of physical abuse in the past year was also reported. Neither this nor the Cambridge study reported which specific instrument was used to measure the rate of violence, so the difference in prevalence between the two studies might also be due to the use of different instruments in addition to population differences.
Wright and Kariya50 sought to ask consecutive assault victims attending a Scottish accident and emergency department over a 2-month period about partner violence. The paper reported that 41% of the 46 women asked had experienced partner violence in the past 2 months and that 63% of the women who were survivors of partner violence had experienced previous incidents. The paper did not define types of assault and probably only measured physical assault.
Among women attending accident and emergency departments in the UK, the prevalence of partner violence has been estimated between 22% and 35% depending on the definition adopted.
Gynaecology clinics
We found one study that examined the prevalence of partner violence in women attending gynaecology clinics in the UK. The study, by John and colleagues,51 reported a 21% lifetime prevalence of physical violence and a 1-year prevalence of 4%, with most abuse being perpetrated by ex-husbands or ex-boyfriends (32% and 29% respectively). Prevalence was highest in women aged 31–40 years.
Pregnancy counselling
A study by Keeling52 of women attending pregnancy counselling when seeking a termination reported a 35.1% lifetime prevalence for physical and emotional abuse, with 19.5% of the women having experienced abuse in the past year.
Family planning
A study by Keeling and Birch53 of women attending family planning clinics reported a 34.9% lifetime prevalence of physical, sexual, emotional and financial abuse, with a 1-year prevalence of 14%. Higher prevalence rates were observed in women aged 35–39 years and 45–49 years.
Figures 1 and 2 display the 1-year and lifetime prevalences (with 95% confidence intervals) of partner violence reported in the primary studies, in order of standard error. Table 3 lists the studies and the definitions of intimate partner violence (IPV) used.
FIGURE 2.
Plot of lifetime prevalence of partner violence with 95% confidence intervals. *See Table 3 for definitions of IPV used in these studies.
| Study | Definition of IPV | Study | Definition of IPV |
|---|---|---|---|
| Bacchus et al., 200442 | Physical, sexual, emotional | Johnson et al., 200346 | Physical, sexual, emotional |
| *Bacchus et al., 200444 | Physical, sexual, psychological | Keeling, 200452 | Physical, emotional |
| Bowen et al., 200545 | Physical, sexual, emotional | *Keeling and Birch, 200453 | Physical, sexual, emotional, financial |
| Boyle and Todd, 200347 | Physical, sexual, emotional | Mirrlees-Black and Byron, 199940 | Physical |
| Carrado, 199639 | Physical | Richardson et al., 200241 | Physical |
| Coid et al., 200354 | Sexual | Sethi et al., 200448 | Physical |
| Dominy and Radford, 199637 | Physical, emotional, sexual and psychological | Walby and Allen, 200436 | Physical, emotional, financial and threats |
| *Finney, 200638 | Physical, emotional, financial and threats | *Walby and Allen, 200436 | Sexual |
| *Finney, 200638 | Sexual | Wright and Kariya, 199750 | Physical |
| John et al., 200451 | Physical |
Table 4 shows the results of a logistic regression model testing whether the definition of IPV used in the studies or type of population (community versus clinical) is associated with variation in prevalence. We found that community populations have significantly lower prevalence, but there was no consistent relationship between the number of different types of IPV measured and the reported prevalence.
| Comparison | Incidence rate ratio | 95% Lower confidence limit | 95% Upper confidence limit | p-Value |
|---|---|---|---|---|
| Lifetime prevalence | ||||
| Setting: community vs clinical | 0.77 | 0.73 | 0.82 | < 0.001 |
| Count of 2 vs 1 | 1.22 | 1.18 | 1.25 | < 0.001 |
| Types of 3 vs 1 | 0.74 | 0.66 | 0.82 | < 0.001 |
| Violence 4 vs 1 | 1.27 | 1.04 | 1.56 | 0.02 |
| One-year prevalence | ||||
| Setting: community vs clinical | 0.24 | 0.22 | 0.27 | < 0.001 |
| Count of 2 vs 1 | 1.83 | 1.70 | 1.96 | < 0.001 |
| Types of 3 vs 1 | 0.93 | 0.83 | 1.05 | 0.24 |
| Violence 4 vs 1 | 1.19 | 0.86 | 1.65 | 0.30 |
Discussion
Estimates of prevalence based on community samples can underestimate the extent of partner violence,56 and estimates of prevalence in clinical samples will overestimate population prevalence, as survivors of partner violence are more likely to need health care than the general public (see below). Both types of studies are useful, however. Community samples will give a better estimate of population prevalence, and clinical samples are essential for understanding the impact of partner violence on health services. Several studies excluded non-English speakers, which may affect the generalisability of results, particularly in UK urban areas.
Those general population studies that scored most highly on the STROBE36,39 assessment tool (see Appendix 4.1) had estimates of prevalence that differed from the lower quality studies; however, there was similar variation in prevalence rates between high-quality studies, so this variation cannot be accounted for by study quality (see Appendix 4.2). It was difficult to compare the clinical population studies due to the heterogeneity of settings, age of the women and the definition of partner violence, but again study quality does not seem to predict prevalence. Within the clinical population studies, the prevalence seems to be highest in women attending accident and emergency departments. The lowest prevalence appears to be in antenatal populations; however, this may be due to women in these samples being younger than in other clinical populations.
Health impact
Results
We found 13 reviews reporting the health consequences of partner violence. Publication dates ranged from 1995 to 2006. Three reported mental health outcomes,57–59 five reported reproductive health effects 60–64 and five reported effects on children. 65–69 For details of review study design and quality appraisal see Appendix 4.3.
Mental health
A meta-analysis by Stith and colleagues70 synthesised results from primary studies published between 1980 and 2000 that measured the association of partner violence with depression and with alcohol abuse. Six studies, with a total of 899 participants, reported the association with depression. The pooled effect size was moderately large (r = 0.28, p < 0.001). The authors state that it is reasonable to assume that depression is a consequence of partner violence, although they did not substantiate this as a separate analysis of longitudinal studies. Eleven studies, with a total of 7084 participants, reported the association between alcohol abuse and partner violence, which was relatively small (r = 0.13, p < 0.001), with some evidence for a bidirectional effect.
Golding57 conducted a meta-analysis and reviewed results from published English language studies on physical abuse and threats of physical force as risk factors for mental health problems in women. Studies were excluded if no specific prevalence rates were given or if the study was limited to women experiencing abuse during pregnancy. Authors looked at the strength of association, consistency, temporality and biological gradient. Significant associations were found between partner violence and all outcome measures: depression, suicidality, post-traumatic stress disorder (PTSD), alcohol abuse or dependence, and drug abuse or dependence. When prevalence rates of mental health problems among survivors of partner violence were compared with those reported in general populations, the association with abuse was strong. A second indicator of strength of association was the odds ratio calculated from the subset of studies of survivors of partner violence in which comparison groups were used. The weighted mean odds ratio ranged from 3.6 to 3.8 in studies of depression, suicidality and PTSD, and was 5.6 in studies of alcohol and drug abuse or dependence. Although absolute prevalence rates varied across studies, the magnitude of association between partner violence and mental health problems was more consistent. The size of this association was statistically homogeneous in studies of PTSD, alcohol abuse and drug abuse. In studies of depression and suicidality, the variability among odds ratios was accounted for by sampling frames. The studies indicate that depression tends to lessen following the cessation of violence, and depression and PTSD seem to respond to the presence or absence of violence. Severity or duration of violence was associated with the prevalence or severity of both depression and PTSD, suggesting that dose–response relationships appear to exist for these disorders. Overall this review provides compelling evidence that adverse mental health outcomes can be a consequence of physical abuse or the threat of physical violence.
Jones and colleagues58 reviewed 43 studies of survivors of partner violence published between 1991 and 2001, to estimate the association of partner violence and PTSD. A consistent finding across varied samples (from clinical settings, refuges, hospitals and community agencies) was that a substantial proportion of survivors (31–84%) exhibit PTSD symptoms. The review also found that the partner violence refuge population is at a higher risk for PTSD than survivors who are not in refuge. The extent, severity and type of abuse were found to be associated with the intensity of PTSD.
Reproductive health
In a review of 14 published case–control and cohort studies, Murphy and colleagues64 determined whether there is evidence for an association between physical, sexual or emotional abuse during pregnancy and low birthweight. Studies had to have English language abstracts, focus on women abused during pregnancy or pregnant women with a past abusive relationship, and fulfil quality criteria. Only 8 out of 14 studies fulfilled all the inclusion criteria and were entered into a meta-analysis; this gave a pooled odds ratio of 1.4 (95% confidence interval 1.1–1.8) for a low birthweight baby in women who reported physical, sexual or emotional abuse during pregnancy, compared with non-abused women. Removing the two case–control studies from the analysis reduced the odds ratio to 1.3 (95% confidence interval 1.0–1.8). This meta-analysis provides tentative evidence of an association between partner violence during pregnancy and low birthweight babies.
Boy and Salihu62 reviewed 30 peer-reviewed studies on the impact of partner violence (physical, sexual and emotional) on pregnancy and birth outcomes. To be included in their review, studies must have been peer reviewed and research based, included a study population of at least five women, pertained to partner violence, included pregnant participants and included data on the outcomes searched. One study, which focused on partner violence and trauma during pregnancy, found that 88% of the pregnant women who had been physically injured had been attacked by their husband or boyfriend. In this population eight fetal deaths occurred, with one fetal death being the result of an assault, yielding a violence-related fetal mortality rate of 16.0 per 1000. Of the six studies focusing on maternal mortality, one case–control death review found that a woman abused during pregnancy was three times more likely to be killed by a partner as a woman who is not abused (odds ratio 3.08, 95% confidence interval 1.9–5.1). The remaining five studies on maternal mortality were based on death reviews and reported that more than half the deaths were the result of murder; the involvement of a husband or boyfriend was documented in multiple instances. Three death reviews focused on intentional trauma deaths; all noted that the majority of homicides were the result of partner violence. Twenty-three studies looked at partner violence and pregnancy outcomes. Three cohort studies found no significant differences between abused women and non-abused women, 7 studies reported mixed results, and the remaining 13 found significant differences between the outcomes of abused women and non-abused pregnant women. The three cohort studies that found no association between physical violence and negative outcomes did, however, note differences between abused and non-abused pregnant women: abused women were more likely to have uterine contractions and increased peripartum complications (p < 0.05)71 and were also significantly more likely to report substance use during the pregnancy (p < 0.001). 72 Out of the seven studies reporting mixed results, two addressed fetal death and found that mothers abused during pregnancy were 3.7 times more likely to have a fetal death (95% confidence interval 1.36–9.94); they also suffered higher rates of miscarriage (p < 0.05). None of the seven studies indicated a relationship with low birthweight or preterm delivery; however, two studies found the smallest babies were born to abused women. Six of the seven studies reported a variety of negative behaviours and complications in abused women. Abused women were found to have more kidney infections (odds ratio 2.7, 95% confidence interval 1.3–5.5) and were 1.5 times more likely to deliver by Caesarean section. Three studies reported significantly higher rates of substance abuse during pregnancy in abused compared with non-abused women. Ten of the 13 studies with significant differences found a significantly higher proportion of low birthweight babies in women abused during pregnancy. In the studies reporting a relationship between low birthweight and partner violence, the percentage of abused women delivering a low birthweight infant ranged from 9% to 22%. Preterm delivery was also reported as a negative outcome due to violence. Four studies reported an increased risk of preterm delivery among abused women compared with non-abused women. One study found a statistically significant difference only in a private hospital. The relative risk for delivering a preterm infant if the pregnant woman was abused ranged from 1.6 (95% confidence interval 1.14–2.28) to 2.7 (95% confidence interval 1.7–4.4). Victims of violence were more likely to have negative health behaviours during pregnancy: 10 studies reported greater use of alcohol and other substances when compared with non-abused women; and two studies also noted that abused women were at increased risk of low weight gain during pregnancy.
A review of nursing studies (including qualitative designs) published after 1995 on the relationship between partner violence and women’s reproductive health was conducted by Campbell and colleagues. 61 Two studies examined the effects of forced sex on women’s health. One study found that sexually assaulted women had significantly more gynaecological problems than those who were not sexually assaulted (p = 0.026). That study also found that women reporting more forced sex experiences reported significantly greater levels of depression (p = 0.018) and a less positive physical self-image than those not sexually assaulted. The second study found that women who were sexually and physically abused had more symptoms than those who were only sexually abused. One study investigated the association between abuse and risk of sexually transmitted infections, and found the rate among the abused, assaulted and raped groups (29%, 31% and 31.3% respectively) was significantly higher than in non-abused women (14.9%, p = 0.0001). One study examined records from 389 sexual assault victims, 71% of whom knew the perpetrator; it found that more than three-quarters (78.3%) of those resuming sexual activities reported sexual difficulties and 17.1% reported gynaecological pain, but almost all of them had normal general physical (98%) and gynaecological (95%) examinations.
A literature review by Jasinski60 reviewed findings on the relationship between partner violence and pregnancy, including the health consequences for the mother and child. Two studies were found that suggested partner violence was associated with late booking into antenatal care. Five studies found an association between partner violence and low birthweight, whereas two did not. The author raised the possibility that the finding of no relationship may be due to confounding variables, such as low socioeconomic status and gestation. Sample size differences and the lack of a standard cut-off for what constitutes low birthweight may also account for the conflicting findings. Evidence regarding the relationship between partner violence and premature labour was also found to be contradictory, with four studies finding an association and three finding none.
Nasir and Hyder63 reviewed findings from three English language studies on the impact of partner violence on adverse pregnancy outcomes in developing countries. A study in Nicaragua demonstrated that women with low birthweight babies were more likely to have experienced abuse during pregnancy (odds ratio 2.07 for threats, 3.27 for slaps, 5.04 for blows), and a multivariate analysis showed partner violence to be a strong risk factor. A study in India reported that women who had suffered beatings were significantly more likely to have experienced miscarriage or infant death (p < 0.05). Another study failed to demonstrate any significant difference in pregnancy outcomes between abused and non-abused women in China; however, it is not stated which outcomes were measured.
Impact on children’s health
In total, we identified five reviews reporting the impact that witnessing partner violence had on the health of child witnesses. Publication dates range from 1995 to 2006.
Buehler and colleagues65 conducted a meta-analysis of 68 studies (including dissertations), published in English, to explore whether interparental conflict is associated with internalising and externalising problems in children aged 5–18 years. The average effect size of the association between interparental conflict and youth problem behaviour was 0.32 (weak to moderate effect). Variability in these effects was explained by the characteristics of participants and methodological variables. The review provides some evidence that conflict between parents is one of several important familial correlates of internalising and externalising youth problem behaviours; however, the authors state this conclusion must be tempered given that 66% of the effects in this meta-analysis were non-significant.
A review by Bair-Merritt and colleagues,66 measuring the relationship between exposure to partner violence and postnatal physical health using contemporaneous control groups, contained 22 studies. Eight studies addressed general health and use of health services. Although children exposed to partner violence are at risk of under-immunisation, the evidence is inconclusive regarding overall health status and use of health services. Evidence was insufficient to draw a conclusion about whether abused women are less likely to breastfeed than non-abused women, as only one study was found which addressed this issue. Evidence was also insufficient to draw a conclusion about whether infants born to abused mothers were more likely to have poor weight gain than infants born to non-abused mothers, as only two studies addressed this issue. Based on seven studies, there was an association between witnessing partner violence and adolescent and adult risk-taking behaviours (including smoking, alcohol abuse, drug abuse, sexually transmitted infections, teenage pregnancy and unintended adult pregnancy).
Kitzmann and colleagues67 conducted a meta-analysis of 118 studies reported in English and published before 2000 (including dissertations) examining psychological, emotional, behavioural, social and academic outcomes of children exposed to physical aggression between parents or carers. Similar estimates of effect were obtained for a range of outcomes. Exposure to partner violence is associated with children internalizing and externalising problems to a similar degree. The effect sizes for social and academic outcomes were of similar magnitude as those found for internalising and externalising. The authors also synthesised effect sizes for measures of children’s specific cognitive, behavioural and emotional responses to simulated or hypothetical episodes of conflict between adults. As a group, effect sizes based on these specific measures did not differ from those based on measures of general adjustment. Relative to other children, children exposed to partner violence showed greater negative affect and more negative cognitions in response to stimulated or hypothetical conflict between adults, and were more likely to report that they would intervene or show aggression in response to conflict. There was less consistent evidence that witnesses were more likely to withdraw or show less positive coping, perhaps because these responses are more difficult to assess.
An ‘integrative’ review was conducted by Attala and colleagues. 68 The reviewers included 11 studies reported in peer-reviewed journals (with over 800 children and their parents); the studies investigated the effects on children, aged up to 18 years, of witnessing partner violence. Three of the studies were qualitative. Four studies examined partner violence and the impact on children’s emotional conditions or physical aggression. The first study found marital distress was positively associated with increased concern and social support-seeking by children. Children whose parents reported marital aggression and dissatisfaction were also found to demonstrate more preoccupation with physical aggression, concern and support-seeking responses than children with non-distressed parents. The second study found that preschoolers who had experienced familial violence had below-average self-concept scores. Preschool children were reported to have more difficulties in adjustment than children at school. The third study found that children who had recently witnessed violence between parents tended to have the lowest levels of social competence ratings, whereas their mothers reported the greatest health and emotional difficulties. The fourth study found that there was no significant difference in the amount of behavioural problems demonstrated by children who had witnessed partner violence, children who had been abused by their parents, and children who had experienced child abuse and witnessed partner violence.
Three studies examined partner violence and the impact on children’s externalising and internalising behaviours. The first study found that, compared with controls, survivors reported feeling more highly stressed as parents. The amount of stress was the most powerful predictor of children’s behaviour problems. Children from violent families had more internalising behaviour problems and were more aggressive than children from the comparison group. The second study found that witnessing physical and verbal interparental violence was related to the type and extent of behaviour problems displayed by young children. Residents of refuges showed significant levels of externalising and internalising behaviours with lower levels of functioning than the non-refuge group. The third study found that, compared with controls, children who witness abuse and are abused themselves showed the most distress, followed by those witnessing abuse. Preschool children were reported to have more difficulties in adjustment than children at school. Two studies examined the impact of partner violence on children’s conduct problems. The first found that parental marital abuse was associated with conduct problems in children who witnessed it. The second study found that two-thirds of the child residents of a partner violence refuge had experienced abuse or neglect. Of 21 schoolchildren, 46% had academic problems; of 28 preschoolers, 39% showed developmental delays; and of 48 children of all ages, 75% demonstrated behaviour problems. Two studies examined partner violence and the impact on parental aggression. The first found that parental aggression was highly associated with having witnessed partner violence as a child. This association did not vary by gender or by single or dual parent status of the family. The second study found a significant association between marital conflict and children’s behaviour problems. Boys exposed to marital conflict were at risk of being abusive in their adult relationships. One study examined the impact of partner violence on children’s depressive symptoms and found that children who were physically abused by their parents and who witnessed violence were more likely to report depressive symptoms. Mothers of all groups reported more problem behaviours than the children acknowledged. Fathers in the same study groups were no more likely to report behavioural problems than fathers from the control group.
Kolbo and colleagues69 reviewed 29 studies of the initial effects on children of witnessing partner violence, extending a previous review by another group. 73 Their findings indicated that children who witness partner violence are at risk for maladaptation in one or more of the following domains of functioning: (1) behavioural, (2) emotional, (3) social, (4) cognitive and (5) physical. The case studies examining behavioural functioning all shared a high degree of congruence in their findings of witnesses’ undesirable behaviour; however, 4 of the 16 correlational studies found no significantly higher instances of conduct problems, hyperactivity and aggression among witnesses of abuse than among comparison children. When only the findings from the recently conducted studies are compared, only one study does not find significant differences. This suggests that the evidence of the effects of witnessing partner violence on children’s behavioural functioning is less equivocal than in previous reviews. However, the reviewers do not state whether recently conducted studies are of a higher quality than those included in previous reviews.
Emotional functioning was assessed in 21 correlational studies and five case studies. Although the results of the case studies were relatively similar, 3 of the 13 correlational studies found no significant differences between witness and comparison groups. As a whole, these equivocal findings are consistent with previous reviews. However, when looking at only the most recently conducted studies, significant differences in emotional functioning and behavioural functioning are consistently found between witness and comparison groups. Thus the recent research is unequivocal in its finding that witnessing partner violence affects children’s emotional functioning, although the reviewers do not comment on whether the recent studies have a higher quality of design or execution.
Eleven studies examined social functioning as an outcome. Six studies documented a significant relationship between social functioning and witnessing partner violence; however, four of the five recently conducted studies did not find child witnesses to have significantly lower social competence scores than comparison groups. Although some children from violent homes appear to be at increased risk of developing problems in social functioning, the relationship between witnessing partner violence and the social functioning of these children remains unclear, with the majority of recent studies finding no significant relationship. Eight studies assessed cognitive functioning; three of these had been conducted since the previous review. Except for the findings of Christopoulos and colleagues,74 the recently conducted studies all found that children who witness abuse are at risk for problems in cognitive functioning. However, the limited number of recent studies makes it difficult to draw firm conclusions of a cause–effect relationship, and no mention is made of the quality of these studies.
Ten of the studies examined physical health. One of the only two studies using standardised measures suggested a causal relationship after finding clinical levels of somatic complaints among witnesses of abuse. The second study did not find any neurological deficit among such children, and evidence of a causal link between exposure to violence and health problems remains equivocal. The reviewers concluded that although there is still some uncertainty about the magnitude and consistency of detrimental effects on children’s social, cognitive and physical development, the evidence for effects on children’s emotional and behavioural development is far less equivocal.
Strengths and limitations
The strengths of this review of prevalence and health impact studies include the independent quality appraisal of primary studies by two reviewers (using the STROBE quality appraisal tool for prevalence studies and the CASP systematic review tool for health impact reviews) and the sensitivity analysis based on study quality. These reviews fulfil the QUORUM and most of the MOOSE reporting criteria lines (see Appendix 11.1 for MOOSE criteria and Appendix 11.2 for a flowchart of this review). Limitations of this review include the small number (six) of databases searched for studies, and the exclusion of reviews of health impact conducted prior to 1990 and prevalence studies conducted prior to 1995. Limitations of the primary prevalence studies include investigators’ modification of instruments to measure partner violence without reporting how, or if, the adapted version of the instrument was validated. Comparisons between the studies were problematic because of different definitions of partner violence, different questions to establish the presence of partner violence and different questionnaire administration methods. Limitations of the reviews of health impact studies include a lack of detailed reporting of search strategies, no quality appraisal of primary studies and no pooling of data. A major limitation in the field of domestic violence research is the absence of systematic reviews of physical consequences synthesising primary studies.
Discussion
The reviews provide strong evidence that partner violence can have a substantial detrimental effect on mental health. Evidence for the impact on pregnancy is more equivocal, but it is likely that low birthweight is a consequence of abuse during pregnancy. Recent studies on the impact on children show a greater prevalence of behavioural and mental health problems among children who witness partner violence, as well as diminished educational attainment. When the better-quality systematic reviews are considered, the findings on mental health, pregnancy and child health consequences are similar to the overall findings, although comparison between reviews is problematic because they report different outcomes.
Synthesis of prevalence and health impact studies
Differences in definition, methodology, sampling and assessment make it difficult to estimate precisely the prevalence of partner violence in the UK. Nonetheless, the studies reported here delineate the lower boundaries of partner violence prevalence, although possibly not the upper limit as under-reporting is likely. It is unarguable that partner violence against women is a common problem. To fulfil the NSC screening criterion for an important health problem, it also has to have a substantial impact on health. The reviews of health impact that we have considered, notwithstanding heterogeneity of morbidity estimates associated with partner violence, demonstrate that partner violence significantly increases the risk of mental illness and substance abuse and is likely to increase the risk of pregnancy complications.
We have not systematically reviewed individual studies of other health problems associated with partner violence, but they probably support the conclusion that partner violence has a substantial and persistent detrimental effect on the health of women. The most consistent and largest physical health difference between abused and non-abused women is in the prevalence of gynaecological problems. 75 Population-based studies from the USA show that the likelihood of abused women having gynaecological symptoms is three times greater than average. 76 Other conditions include chronic pain and neurological symptoms,75 gastrointestinal disorders77 and self-reported cardiovascular conditions. 78 The evidence for the substantial effect of partner violence on population health includes the results from the systematic reviews of outcomes on children that we have reported here.
Chapter 5 Are screening tools valid and reliable? (Question II)
Eighteen tools were assessed in 15 validation studies. The total number of participants was 10,289; studies reporting diagnostic accuracy comprised 8433 participants. The tools ranged from single questions to 30-item research inventories (see Appendix 5.1 for details of individual tools). Twelve tools were tested as index tools and eight as comparators; the Woman Abuse Screening Tool (WAST) and the Women’s Experience with Battering Scale (WEB) served in both capacities in different studies. Of the 15 studies, only 10 reported sufficient data to calculate diagnostic accuracy. The majority of studies were conducted in the USA (11), with two in Canada, and the remaining two in France and Brazil. Settings varied from general practice (six), accident and emergency departments (four), antenatal clinics (three), women’s health-care centres (two), women’s homes (two), domestic violence refuges (two) and an urgent care centre within a hospital (one). Publication dates ranged from 1992 to 2006. For details of primary studies see Appendix 5.3, and for detailed results by study see Appendix 5.4. Below we have presented the main findings in a narrative form.
The screening tools
Women’s Experience with Battering Scale (WEB)
Coker and colleagues79 tested the WEB against the Index of Spouse Abuse-Physical (ISA-P) in two university-associated family (general) practice clinics. The original ISA-P has 25 items assessing physical abuse; the investigators used a modified version consisting of 15 items. Prevalence was reported as 11% with the ISA-P. Reliability was good: Cohen’s kappa was 60% between the two measures, and a Pearson correlation of 0.67 between the two continuous measures supports the kappa statistic. Sensitivity was 86% and specificity 91%. The scores for each tool were compared with partner violence-associated injuries, adverse mental health outcomes, and perceived levels of health and health-care utilisation. Because the contents of each tool overlap and the authors wanted to identify which tool was more strongly associated with the health outcomes of interest, they performed a stratified analysis. Controlling for the ISA-P, WEB was found to be significantly associated with poor mental health, anxiety, depression, drug abuse, PTSD and low social support, whereas the ISA-P was only significantly associated with more physician visits when controlling for the WEB. In women currently experiencing physical partner violence only, the continuous ISA-P score (adjusting for continuous WEB score) was significantly associated with having a partner violence-related injury requiring medical care (relative risk 1.06); the WEB was not (relative risk 0.99). Amongst women reporting an event that could lead to PTSD (n = 356), the WEB score was associated with higher PTSD symptom scores (relative risk 2.02) and the ISA-P score was not (relative risk 0.93). The authors conclude that the WEB may identify more women experiencing both physical and psychological battering and thus increase its clinical value. The study has shown the positive scores on the WEB to be strongly associated with partner violence-related health outcomes.
Ongoing Violence Assessment Tool (OVAT)
In an accident and emergency department, Ernst and colleagues80 tested the OVAT against the Index of Spouse Abuse (ISA). The ISA detected a prevalence of 21% in women and 20% when both men and women were included. Reliability was reasonable, with a Cronbach’s alpha of 0.6 and a kappa of 0.58 (95% confidence interval 0.53–0.63). Similar to the WEB, the OVAT showed reasonable diagnostic accuracy: a sensitivity of 86% and specificity of 83%.
‘Hurts, Insults, Threatens and Screams at her’ (HITS) scale
The HITS scale has been compared with a number of tools in different cultural settings. Chen and colleagues81 trained medical students to administer the HITS alongside the ISA-P and WAST in an urban family (general) practice site. Approximately 70% of the practice population was of Hispanic origin; thus English and Spanish versions of the tools were used. Prevalence rates varied between the two comparators: ISA-P gave a prevalence of 5.4%, the WAST 9.9%; overall, 10.9% screened positive on the ISA-P or WAST. Diagnostic accuracy analyses were computed for both English and Spanish populations. To assess the nature and extent of misclassifications, receiver operating characteristic (ROC) analyses were used, which also help derive cut-off scores that highlight the greatest sum of sensitivity and specificity. Minor differences emerged when looking at the two comparisons.
Comparison of the English versions revealed good reliability (Cronbach’s alpha) for the HITS (0.76), ISA-P (0.80) and the WAST (0.78). English HITS total scores were also significantly correlated with ISA-P total scores (r = 0.76, p < 0.001) and WAST total scores (r = 0.75, p < 0.001).The area under the curve (AUC) for English HITS was 0.99, using ISA-P as the criterion. English HITS was effective as a screening tool for partner violence (p < 0.001). For those using the English language, HITS was compared with an English version of the ISA-P. A cut-off score of 10.5 created the greatest sum of sensitivity (86%) and specificity (99%).
For the Spanish versions, reliability was slightly lower (HITS = 0.61, ISA-P = 0.77 and WAST = 0.80); however, correlations between the Spanish tools were slightly higher than those found between the English tools (HITS and ISA-P r = 0.81, p < 0.001; HITS and WAST r = 0.78, p < 0.001). This pattern of high correlations was also repeated for the total sample. For those answering in Spanish, the HITS was compared with a translated Spanish version of WAST. The AUC for the Spanish HITS was 0.95, and HITS was found to be effective as a screening tool (p < 0.001). A cut-off of 5.5 maximised sensitivity (100%) and specificity (86%).
HITS has several advantages over WAST. It is an acronym (making it easier to remember the individual questions), its cut-off scores for identifying partner violence are easier to remember, and it has a simple scoring protocol compared with the WAST multiple scoring protocols. One limitation of HITS is that it is only validated for detection of current abuse. The different cut-off points for the HITS between English-speaking and Spanish-speaking populations may reflect different views about what constitutes abuse. Hispanic women may view certain types of abuse as less abusive than other cultural groups.
Sherin and colleagues82 used a modified version of the Conflict Tactics Scale (CTS) as a comparator against the HITS. In the first phase of the study, women were recruited from a family (general) practice setting in order to assess reliability and concurrent validity of the HITS. In the second phase the reliability and concurrent validity of the HITS were tested in self-identified survivors of partner violence from either a refuge or an accident and emergency department. The two groups were then compared to assess the construct validity of the HITS. In the first phase, HITS showed good reliability (Cronbach’s alpha = 80). The distribution of CTS and HITS scores suggests a low prevalence of partner violence in this population, although no prevalence figures were reported. Correlation between the two measures revealed a positive linear relationship (r = 0.85); the subscores for items measuring physical violence and verbal violence also showed a good positive association (0.82 and 0.81, respectively). No significant difference in scores was found due to presentation effects. In the second phase of the study, the scores from the practice population were compared with those of self-identified survivors and improvised diagnostic accuracy data were computed. With a cut-off score of 10.5 on the HITS, 96% of victims and 91% of non-victims were correctly identified (analogous to sensitivity and specificity analysis). This study provides good support for the use of HITS as a screening tool, although the accuracy analysis is contestable as a modified version of CTS (four reasoning items were removed) was employed.
Abuse Assessment Screen (AAS)
The Abuse Assessment Screen (AAS) has been tested against a number of tools, although only one study reported diagnostic accuracy data. Reichenheim and Moraes83 validated the AAS against the Revised Conflict Tactics Scale (CTS2) in postnatal maternity wards in Brazil. Three case levels of partner violence were specified in this study: minor, major and overall. Minor cases were those where the participant answered ‘yes’ to at least one of five items asking about less severe physical acts such as being grabbed, pushed or slapped; major cases were defined as when at least one of seven more severe acts were reported, such as being choked, beaten up or kicked; overall cases were those that featured at least one positive response from both subsets. Prevalence of partner violence found with the CTS2 varied depending on the definition of cases used. Prevalence of minor cases was 18%, for major cases it was 8%, and overall it was 19%. Diagnostic accuracy data for minor cases revealed a poor sensitivity at 32%, whereas specificity was very good (99%). Analysis of major cases showed an improved sensitivity of 61%, and specificity of 98%. Analysis of overall violence reduced sensitivity to 32%, with specificity at 99%. The AAS detects more major cases of abuse than either minor or overall violence. This observation is further supported by analysis of the false negatives; up to 50% of those who screened positive for ‘pushed or shoved’ or ‘grabbed’, and 60% of those who ‘had something thrown at them that could hurt’, were missed by the AAS.
Partner Violence Screen (PVS)
The Partner Violence Screen (PVS) has been tested against the ISA and CTS by Feldhaus and colleagues84 in an accident and emergency department setting. The ISA revealed a current prevalence of abuse of 24% (95% confidence interval 19–30%) and the CTS showed a prevalence of 27% (95% confidence interval 22–34%). The study found reasonable diagnostic accuracy for the PVS. When compared with the ISA, the sensitivity of the PVS was 65% and specificity 80%. The physical violence item and two safety items of the PVS also showed moderate linear sensitivity (53% and 48%, respectively) and reasonable specificity (89% and 88%, respectively) when individually compared with the ISA. Similarly, comparison with the CTS gave reasonable results. Overall, sensitivity was 71% and specificity 84%; the physical violence item had greater sensitivity and specificity (68% and 95%) compared with the ISA, whereas the safety item showed slightly lower diagnostic values than the ISA (sensitivity was 40%, specificity was 87%). The single physical abuse question of the PVS was more sensitive and specific than the questions regarding safety. The negative predictive value was also good, with sensitivity of 88% and specificity of 89%. The PVS is a three-question tool that takes only 20 seconds to administer. About one in every four women who entered the emergency department had a history of physical or non-physical partner abuse, and the PVS was able to detect between 65% and 71% of these women.
MacMillan and colleagues85 reported a validation of the PVS and WAST (see paragraph below) against the Composite Abuse Scale (CAS). Recruitment took place in two accident and emergency departments, two family practices and two women’s health clinics. The study’s original aim was to investigate the effects of presentation method of the two index tools; specifically computerised, face-to-face interview, or pencil and paper presentation. Prevalence of partner violence for the CAS was 10%. The PVS showed only moderate diagnostic accuracy, with a sensitivity of 49% and a specificity of 94%, although overall accuracy was stated as 89%, calculated as the number of true positives plus the number of true negatives divided by the total sample size.
Woman Abuse Screening Tool (WAST)
MacMillan and colleagues85 validated the WAST against the CAS. Like the PVS, they found only moderate diagnostic accuracy data, with a sensitivity of 47% and a specificity of 96%, although the overall accuracy was 91%.
Slapped, Threatened or Thrown (STaT) scale
Paranjape and colleagues86 validated the STaT against the ISA in an urgent care centre in an inner city hospital that provides primary care. For most recent relationships, the ISA revealed a lifetime prevalence of 33% and a current prevalence of 15%. Diagnostic accuracy data were computed for each STaT score. For scores ≥ 1, sensitivity was 95% (95% confidence interval 90–100%), specificity was 37% (95% confidence interval 29–44%); for scores ≥ 2, sensitivity was 85% (95% confidence interval 77–92%) and specificity was 54% (95% confidence interval 46–62%); and finally a score of 3 had a sensitivity of 62% (95% confidence interval 51–73%) and a specificity of 66% (95% confidence interval 59–73%). Although showing good sensitivity, the tool has only moderate specificity.
Behavioural Risk Factor Surveillance Survey (BRFSS)
Bonomi and colleagues87 compared the Behavioural Risk Factor Surveillance Survey (BRFSS) against the WEB using a telephone survey of randomly selected women enrolled for at least three years in a Group Health Cooperative. Prevalence was found to be 7% using the WEB. The authors computed diagnostic accuracy data for various elements of the BRFSS. For any kind of abuse, good sensitivity and specificity were found (72% and 90%, respectively). Sensitivity for sexual abuse was 21% and specificity 99%, whereas sensitivity for physical abuse was 42% and the specificity 95%. For detecting fear due to threats, sensitivity was 48% and specificity 97%. Detection of controlling behaviour was slightly better, with a sensitivity of 65% and specificity of 94%. The difference between these two tools is based on their conceptual framework; the BRFSS is based upon behavioural acts of abuse, whereas the WEB employs a more consequence-orientated approach.
Single question
The use of a single question was investigated by Peralta and Fleming,88 who asked women within a family (general) practice setting ‘Do you feel safe at home?’ and compared this with a modified version of the CTS (six items instead of 19, five of which related to psychological and one to physical violence). Period prevalence (90 days) of abuse was high at 44%, as measured by the modified CTS. The researchers examined diagnostic accuracy for the single question in three ways: (1) any violence, (2) physical violence with or without psychological violence, and (3) psychological violence with or without physical violence. For any violence, sensitivity was very poor at 9%, whereas specificity was high at 96%. For physical violence with or without psychological abuse, sensitivity was slightly improved at 15% and specificity was 95%. For psychological violence with or without physical violence, sensitivity was 9% and specificity was 96%. These results suggest that a single question about safety is a poor screening tool for partner violence.
Studies that did not assess the diagnostic accuracy data of index tools
Abuse Assessment Screen (AAS)
McFarlane and colleagues89 tested the AAS against the CTS, ISA and the Danger Assessment Scale (DAS) in antenatal clinics. The population was ethnically heterogeneous: African Americans 39%, Hispanics 34% and whites 27%. Prevalence measured with the AAS was 26% within the last year, 17% during pregnancy and 55% when these two were combined. When the physical abuse (ISA-P) and non-physical abuse (ISA-NP) scores were compared against AAS scores, those positively screened with the AAS were more likely to have a significantly higher score on the ISA. This study showed physical abuse during pregnancy to be more than twice as high as reported in previous literature. A possible explanation for the increased rates may be due to the primary care provider, rather than a researcher, asking the questions. Another explanation may be that a woman was assessed three times in pregnancy; abuse may not have occurred until the third trimester or women who at first did not want to disclose abuse did so when asked again. Although the prevalence of abuse in pregnancy was similar for the AAS and both parts of the ISA, the absence of reliability or diagnostic accuracy data makes it hard to draw any conclusions on the validity and reliability of the AAS from this study.
Perinatal Self-Administered Inventory (PSAI)
Sagrestano and colleagues90 administered the Perinatal Self-Administered Inventory (PSAI) and the CTS to women in antenatal clinics. Based on the CTS, the prevalence of verbal aggression was 84%, and 17% of women had experienced physical violence in the past year. During the current pregnancy, the prevalence of verbal aggression was 68% and that of physical violence was 13%. From the PSAI, the question ‘Are you experiencing severe conflicts with anyone at home?’ did not correlate with measures of verbal aggression, and there were no significant differences in scores of verbal or physical violence between those who endorsed the single question and those who did not. The other partner violence-related question of the PSAI, ‘Are you suffering from mental or physical violence abuse right now?’, was not correlated with either verbal or physical abuse as determined by the CTS, nor were there any significant differences in verbal aggression scores between those who did and did not respond in the affirmative to the suffering abuse question. For the violence subscale, paradoxically, those who responded in the affirmative to the single question (only 3% of the sample) scored significantly lower than those who did not. From these findings, the abuse questions of the PSAI are unlikely to be reliable screening tools for either verbal or physical violence within an antenatal setting; however, there are no diagnostic accuracy data to support this conclusion.
Woman Abuse Screening Tool (WAST)
Brown and colleagues91 conducted a validation study in a Canadian family (general) practice setting comparing the WAST with the Abuse Risk Inventory (ARI). Prevalence detected with the WAST was 9%. The WAST showed good internal consistency (coefficient alpha = 0.75) and was significantly correlated with the ARI (r = 0.69, p = 0.01). In 2001, Brown repeated the study in a French-speaking population in a domestic violence refuge and private homes setting, and reported good internal consistency. As neither study reported diagnostic accuracy no conclusion about construct validity can be drawn.
Single question
Connelly and colleagues92 used the CTS as a comparator to test a single question incorporated into a hospital admission protocol: ‘Are you in a relationship in which you have been threatened, scared or hurt by someone? If yes, whom? [sic]’ The specific clinical setting in which the protocol was administered is not clear. The CTS gave a prevalence of 18%. No diagnostic accuracy data were reported.
Diagnostic accuracy
The data for diagnostic accuracy are summarised in Table 5. The sensitivity of partner violence screening tools ranges from poor to good (9–100%). Tools that scored sensitivity greater than 85% include the HITS (both Spanish and English versions), STaT, WEB and OVAT. Specificity was good across all but one of the tools, ranging from 83% to 99%. The one outlier was the STaT scale, with a specificity of 37%. Index tools with a specificity greater than 85% included the AAS, HITS, single question ‘Are you safe at home?’, WAST, PVS, WEB and the BRFSS.
| Decreasing predictive power | Sensitivity | Specificity | Overall (Sen + spec) | |||
|---|---|---|---|---|---|---|
| ↓ | HITS (Spa) | 100 | AAS | 99.2 | HITS (imp) | 187 |
| HITS (imp) | 96 | HITS (Eng) | 99 | HITS (Spa) | 186 | |
| STaT | 94.9 | Single questiona | 95.8 | HITS (Eng) | 185 | |
| HITS (Eng) | 86 | WAST | 95.6 | WEB | 177 | |
| WEB | 85.9 | PVSb | 93.7 | OVAT | 168.8 | |
| OVAT | 85.7 | WEB | 91.1 | BRFSS | 162.1 | |
| BRFSS | 72.4 | HITS (imp) | 91 | PVS | 150.3 | |
| PVS | 68 | BRFSS | 89.7 | PVSb | 142.9 | |
| PVSb | 49.2 | HITS (Spa) | 86 | WAST | 142.6 | |
| WAST | 47 | PVS | 82.3 | STaT | 131.6 | |
| AAS | 31.7 | OVAT | 83.1 | AAS | 130.9 | |
| Single questiona | 8.8 | STaT | 36.6 | Single questiona | 104.6 | |
The relatively small number of studies for each index tool and the heterogeneity of settings, demography of participants and comparator tools precluded pooling of the diagnostic accuracy data.
Concurrent validity
Five studies reported concurrent validity (Table 6); generally this was high, the exception being the PSAI.
| Decreasing concurrent validity | Comparison (index vs comparator) | Correlation (r value) | p-Value |
|---|---|---|---|
| ↓ | HITS (imp) vs CTS (any) | 0.85 | Not stated |
| HITS (imp) vs CTS (physical) | 0.80 | ||
| HITS (imp) vs CTS (verbal) | 0.81 | ||
| HITS (Spa) vs ISA-P | 0.81 | < 0.001 | |
| HITS (Spa) vs WAST | 0.81 | < 0.001 | |
| HITS (Eng) vs ISA-P | 0.76 | < 0.001 | |
| HITS (Eng) vs WAST | 0.75 | < 0.001 | |
| WAST vs ARI | 0.69 | 0.01 | |
| WEB vs ISA-P | 0.67 | Not stated | |
| PSAI ‘Are you experiencing severe conflicts with anyone in your home?’ vs CTS | 0.16 | 0.035 | |
| PSAI ‘Are you experiencing severe conflicts with anyone in your home?’ vs CTS (verbal) | 0.10 | > 0.05 | |
| PSAI ‘Are you suffering mental or physical abuse now?’ vs CTS | 0.03 | > 0.05 | |
| PSAI ‘Are you suffering mental or physical abuse now?’ vs CTS (verbal) | – 0.05 | > 0.05 |
Reliability
Six primary studies reported two types of reliability data (Table 7): (1) internal consistency, a measure based on the correlations between different items on the same test (coefficient alpha and Cronbach’s alpha); and (2) inter-rater reliability, the degree of agreement among scorers (Cohen’s kappa). Most studies reported good reliability of the tools that were tested.
| Decreasing reliability | Index tool | Type | Value |
|---|---|---|---|
| ↓ | WASTa | Coefficient alpha | 0.95 |
| HITS (imp) | Cronbach’s alpha | 0.80 | |
| HITS (Eng) | Cronbach’s alpha | 0.76 | |
| WASTb | Coefficient alpha | 0.75 | |
| HITS (Spa and Eng combined) | Cronbach’s alpha | 0.71 | |
| HITS (Spa) | Cronbach’s alpha | 0.61 | |
| WEB | Cohen’s kappa | 0.60 | |
| OVAT | Cohen’s kappa | 0.58 |
Sensitivity analyses
If we exclude studies with three or more areas of bias as determined by the QUADAS appraisal tool, four studies remain, as shown in Table 8.
| Study | Tools assessed (index vs comparator) | Predictive power | Concurrent validity | Reliability |
|---|---|---|---|---|
| Feldhaus et al., 199784 | PVS vs ISA and CTS | 142.9 | Not stated | Not stated |
| Brown et al., 200091 | WAST vs ARI | 142.6 | r = 0.69, p = 0.01 | 0.75 |
| Chen et al., 200581 | HITS vs WAST: | |||
| HITS (Spa) | 186 | ISA-P r = 0.81, p < 0.001 WAST r = 0.81, p < 0.001 | 0.61 | |
| HITS (Eng) | 185 | ISA-P r = 0.76, p < 0.001 WAST r = 0.75, p < 0.001 | 0.76 | |
| HITS (Spa and Eng combined) | 0.71 | |||
| MacMillan et al., 200685 | PVS and WAST vs CAS | PVS 142.9 WAST 142.6 | Not stated | Not stated |
| Paranjape et al., 200686 | Single question ‘Do you feel safe at home?’ vs modified CTS | 104.6 | Not stated | Not stated |
The five higher-quality studies all report diagnostic accuracy data, although three84–86 do not report any psychometric properties of the index tools they validated, a shortcoming that is not captured by the QUADAS. The high-quality studies tested the PVS, WAST, HITS and the single question ‘Do you feel safe at home?’ as index tools and found that the WAST and HITS performed best overall.
The number of items in a tool was not associated with diagnostic accuracy. There were not enough studies testing tools in different health settings to judge whether they were more accurate with some groups of patients than others.
Which tools are valid and reliable?
When considering the rank of the diagnostic accuracy data (sensitivity, specificity and sensitivity plus specificity; see Table 5), the HITS scale consistently emerges as top ranked, followed by the WEB and the OVAT. HITS, an acronym derived from the four short questions, is quick to administer. Women answer each question using a five-point scale from 1 (never) to 5 (frequently); answers are then summed to give a potential total score ranging from 4 to 20. A cut-off score of 10 gives the highest combined sensitivity and specificity. It has good diagnostic accuracy in both English- and Spanish-speaking populations. A limitation of the HITS scale is that it fails to ask about sexual abuse or ongoing violence, thus it may need to be administered alongside another screening tool to detect these forms of abuse.
The WEB assesses abuse by characterising women’s perceptions of their vulnerability to physical and psychological danger or loss of control in relationships. The tool comprises 10 items and uses a six-point Likert-type scale giving a potential range of scores from 10 to 60. A score greater than 20 indicates battering. A disadvantage of the WEB is that women may not link abusive behaviours or tactics directly to the emotional impact the abuse is having on them. Although the WEB identifies abuse, it does not necessarily identify the acts of abuse, thus further enquiry from the clinician would be needed for adequate documentation in medical records. As shown in Tables 6 and 7, respectively, the WEB has good concurrent validity against the ISA-P and reasonable reliability although the study has more than two areas of bias.
The OVAT aims to detect current abuse asking about physical and non-physical violence within the past month. The four questions are quick to administer and score: three questions are true/false answers, the other is answered on a five-point Likert response: 1 (never) to 5 (very frequently). The OVAT takes 1 minute or less to administer and can be scored immediately. Table 5 shows the OVAT has good predictive power. Although no concurrent validity was reported in the primary study, the OVAT has reasonable reliability (see Table 7)
On current evidence, tools that scored a low combined sensitivity and specificity, such as the single question ‘Are you safe at home?’ or the AAS, are not good candidates for screening programmes in clinical settings.
Methodological considerations
Several areas of weakness have emerged from this review of screening tools. First, only Sherin and colleagues82 and Chen and colleagues81 report presentation effects, yet studies that account for data on presentation effects are more robust. Priming of responses due to type of wording or impact of questions may influence subsequent answers on later questions. Second, modified comparators (featured in four studies) may inflate or decrease the diagnostic accuracy, particularly if those tools have not been psychometrically tested. Furthermore, these studies are not truly comparable with other studies using the full version of the tool, thus comparisons within the field are more problematic. Third, discrete categories of violence should be analysed if possible. Peralta and Fleming88 analysed the diagnostic accuracy data in three ways: any violence, physical violence with or without psychological violence, and psychological violence with or without physical violence. The last two categories overlap, making it difficult to ascertain what the tool has identified and what the tool can accurately identify.
Study quality ranged from good to poor (see Appendix 5.5). When the number of positive responses was totalled for each study (a higher number denotes that fewer types of bias occurred in the study), 11 out of 15 primary studies scored 10 or more, i.e. had four or fewer different types of bias in the study; two scored nine, i.e. had five types of bias. There was ambiguous reporting in three of the studies: it is unclear whether Coker and colleagues79 used two separate tools or combined them into one, which may have increased multi-colinearity between the tools; Reichenheim and Moraes83 had unclear selection criteria, and Ernst and colleagues80 did not adequately report their selection criteria and their execution of the index test was uncertain.
None of the studies analysed the score of the index tool blinded to the score of the comparator. This may be a less important source of bias than others because there is little room for interpretation of the questionnaire data. Suitable comparators to use against an index tool include the CTS2, ISA or the CAS. But investigators also used the WAST, ARI, WEB, CTS, modified CTS and a modified CTS2 as comparators, although they are not adequately validated. Multi-colinearity may have featured in those studies that combined index and comparator tools into one instrument. This may be further influenced by using the index tool score to inform the final diagnosis. Unreported withdrawals from the studies may indicate a selection bias, particularly if such a feature is systematic across all the studies.
Strengths and limitations
The strengths of this review on screening tools include quality appraisal of primary studies using criteria from the QUADAS and the sensitivity analysis based on quality, the calculation of diagnostic accuracy (if this was not reported in the primary study and data were available) and a methodological critique of studies. Furthermore, this review question was quality appraised using the modified QUORUM checklist, which indicates that all the QUORUM criteria were met (see Appendix 11.3 for QUORUM checklist and flowchart).
Limitations of the review include the arbitrary choice of 12 items or less as a criterion for an index screening tool. A tally of 12 items was chosen by the authors because this was deemed to be a practical number of items to administer for screening purposes. Further limitations relate to the quality of the primary studies and heterogeneity of screening tools used by each study, making it impossible to pool the studies into a meta-analysis.
Discussion
There are valid and reliable screening tools for partner violence against women that can be used in health-care settings, fulfilling the NSC criterion, although the number of studies reporting validation and reliability for any one tool is small. The HITS scale shows most diagnostic accuracy, concurrent validity and reliability. Even if the study by Sherin and colleagues82 is disregarded due to its improvised diagnostic accuracy, the HITS still ranks above the other tools and has been validated in at least one good-quality study. 81 A total of 141 papers were initially selected, which covered a wide range of validation studies. We excluded many studies because of our upper limit of 12 items in a screening tool. It is possible that some of the excluded studies may have identified tools that had good diagnostic accuracy, but more than 12 questions would be impractical for use in clinical settings. The majority of studies came from North America, so their generalisability to UK clinical settings is uncertain. The choice of a tool for the NHS would need to take into account the use of different terms, such as ‘battering’, which is not used in the UK but is central to the WEB. The lack of UK studies in this review could reflect a lower priority given to validation of partner violence screening tools, as screening is not current policy within the NHS.
Finally, we need to heed the caution of Fogarty and colleagues94 about judging screening questions for partner violence as we would screening tools for medical conditions. A woman experiencing partner violence who discloses to a clinician has gone through ‘…a complex process. Factors involved in this process include the woman’s recognition of a problem, her willingness to trust her clinician with this information, and her perception of the clinician’s openness to hearing her story with compassion and without judgment.’
Chapter 6 Is screening for partner violence acceptable to women? (Question III)
Qualitative studies
Thirteen journal articles and one UK Home Office report (total of 13 studies) published between 2001 and 2006 fulfilled our inclusion criteria for this question. For details of the studies and quality appraisal scores see Appendix 6.1. Ten of the studies were conducted in the USA, two in the UK and one in Sweden. The total number of participants was 1393, ranging between 795 and 879. 96 The quality score of the primary studies, appraised with the CASP criteria, was between 2097 and 34,98,99 with most of the studies scoring more than 27 out of a possible 41.
First-order constructs
We identified 10 first-order constructs reflecting women’s attitudes towards screening in health-care settings.
Informants said that raising awareness in addition to eliciting disclosure of abuse should be an aim of screening. Women who did not want to disclose abuse still found screening beneficial as it helped to remove the stigma attached to partner violence, raised awareness of partner violence, gave them a sense of validation and conveyed to them that when they were ready they could talk to their health professional about abuse. Although women may not disclose abuse immediately, screening may facilitate disclosure later on when they feel more comfortable with the health-care professional or when their circumstances change and they feel the need to get help.
Some women thought that if they could have the opportunity to talk with someone about abuse, they would feel there is someone to support and encourage them. One woman said ‘What I really think helped me last pregnancy was people talking to me, not at me. Not having that better than [thou] attitude. I felt people really, genuinely cared’. 100
Some women found it more acceptable to be screened when they already knew and trusted the health-care professional.
Women emphasised the importance of professionals listening to them without judging or condemning them; not listening was viewed as inhibiting disclosure. Women felt more comfortable being screened and being asked sensitive questions by health-care professionals who they felt understood the complexity of partner violence.
Some women expressed concern that appointments were not long enough to make effective use of confidential time or that there was no time to listen.
Many of the women felt that screening gave them the opportunity to disclose abuse, either then or at a later stage, and that without this opportunity it would be harder for them to seek help.
Common concerns included the potential legal consequences of revealing abuse and fears that abusive partners might find out that the relationship had been discussed. Some women reported feeling ashamed and concerned that the health-care professional would judge them harshly for staying in an abusive relationship.
Some women stated that part of their fear and suspicion about screening and disclosing partner violence arose from not being sure of the health provider’s intentions when asking and the possible negative consequences of disclosure. Some women felt that they were being screened because health-care professionals did not think they were caring for their children properly and saw screening as part of an investigation of child neglect or abuse.
Opinions on whether screening should be conducted via a written questionnaire or face-to-face were mixed. Some women preferred to talk about their experience and others preferred writing it down and not having to disclose out loud.
Some women showed a preference for being screened by women; however, most women stated that a health-care professional’s interpersonal qualities were more important than their gender or profession. Others voiced a preference for being screened by older rather than younger health-care professionals and by doctors rather than nurses.
Second-order constructs
These constructs represent the conclusions of the authors of the primary studies.
-
Women believe the primary aim of screening should be education rather than eliciting disclosure.
-
Screening is generally acceptable to women.
-
Certain factors increase women’s acceptability of screening, such as the health-care professional’s manner, being asked in a safe and confidential environment, giving a reason for asking, not pressuring women to disclose, and the quality of the relationship the woman has with the professional.
-
Women have concerns about screening, such as lack of time, potential breach of confidentiality and fear of involvement of child protection services.
Contradictions within and between the studies
There were no major contradictions between constructs either within or between studies. With regard to first-order constructs 9 and 10, there was variability within and between studies on women’s preferences for being screened face-to-face or by written questionnaire, and their preferences about the gender and the profession of the person performing the screening. There were no contradictions between the second-order constructs.
These interview- and focus group-based studies found that women’s views on partner violence screening in health-care settings are complex. The emerging constructs were largely consistent across studies and did not vary by study quality. Generally, the informants find screening acceptable with certain caveats, such as the manner of asking and the nature of the initial response. One study found that women who suffered emotional abuse did not feel that they had been appropriately screened as the questions asked only covered physical violence. 100 This raises the possibility that women’s acceptance of screening may vary depending on the type of abuse they experienced. However, the majority of studies did not provide a breakdown of the type of abuse experienced by the women, and we were not able to explore this further. Given the number of qualitative studies, we were surprised there were not more contradictory findings. Without access to the data it is impossible to say whether contradictions were not present or were not reported by the authors, many of whom seemed to assume that screening for partner violence was an essential part of a health-care response.
Quantitative studies
Nineteen journal papers (18 cross-sectional studies and one case–control study) fulfilled our inclusion criteria. For details of the studies see Appendix 6.2. One study was a telephone survey,101 the others were based on face-to-face interviews or self-completed questionnaires. Twelve studies were conducted in the USA, two in the UK, one in Ireland, one in Canada, one in Australia, one in Italy and one in Germany. Response rates ranged between 49%102 and 100%,103 and the number of participants was between 95104 and 3455,105 with a total of 11,849 across all the studies. Twelve studies were conducted in a range of hospital settings, including one in a maternity unit and one in an ambulatory care clinic. Three studies recruited women patients from general practices, two from health maintenance organisations (HMOs), one recruited women attending a family planning clinic and one recruited women from a combination of general practice, partner violence programmes and refuges. There was variation in attitudes towards screening between countries and between settings within the same country (agreement with partner violence screening varied between 35% and 99%).The quality score assessed by STROBE30 was between 9106 and 20,107 with most of the studies scoring more than 14 out of a possible 22. For quality scores and results see Appendix 6.3.
Bair-Merritt and colleagues108 conducted a survey in an US paediatric emergency department, comparing responses of mothers and other female caregivers before (pre) and after (post) implementation of a screening programme that included displaying partner violence posters and cards in the waiting area. The two groups did not significantly differ with respect to age, race, education or personal partner violence history. The post group was less likely to find paediatric emergency department partner violence screening acceptable (pre, 76%; post, 63%; odds ratio 0.5; 95% confidence interval 0.3–0.9) and was less likely to say that they would disclose abuse (pre, 85%; post, 75%; odds ratio 0.6; 95% confidence interval 0.3–1.1). Notwithstanding this reduction, the majority of respondents found screening acceptable and said they would disclose if asked. There was no difference between previously abused and non-abused women with regard to the acceptability of displaying resources or routine screening.
Brzank and colleagues106 surveyed 18–60-year-old women attending an accident and emergency department in a German hospital. Overall, 32% of the 806 participants would have wanted to be asked about partner violence by their physicians. This number increased to 41% in the case of patients who had experienced sexual violence, and to 44% in the case of patients who experienced physical or emotional violence. Almost 65% of the participants generally thought that questions about partner violence experience should be part of routine history taking.
Caralis and Musialowski109 administered a questionnaire to 406 women in ambulatory clinics at a US Veterans Affairs Medical Center. They reported that 77% of non-abused and 70% of abused women agreed that doctors should routinely screen for abuse in their practices.
Friedman and colleagues110 administered a questionnaire to 164 women attending a primary care physician in the USA. Routine enquiry about physical and sexual abuse was favoured by 78% and 68% respectively. Older patients were more in favour of routine physical abuse enquiry, but responses about sexual abuse enquiry did not vary by age. Among patients who had not graduated from high school education, there was a higher proportion in favour of routine enquiry about physical abuse and sexual abuse.
The study by Gielen and colleagues111 included 202 abused women and 240 randomly selected non-abused women recruited from a US metropolitan health maintenance organisation. Forty-eight percent of the sample agreed that health-care providers should routinely screen all women. Women thought that screening would make it easier for abused women to get help (86%), although concerns were raised about increased risk of abuse with screening (43%).
Glass and colleagues105 conducted a study based in 11 mid-sized community-level hospital emergency departments in the USA, and recruited 3455 women patients. Those who were physically or sexually abused in the past year were less likely to agree with routine screening than women who reported a lifetime history of abuse or who reported no partner violence (80% versus 89%, p < 01), although the majority of both groups agreed with screening.
The participants in a study by Hurley and colleagues103 were 304 non-critically ill women, aged 16–95 years, who presented to emergency departments at two Canadian health centres. Eighty-six percent supported universal screening of women patients for partner violence, with no age differences.
McCaw and colleagues101 selected two random samples of women patients (total 397) – members of a non-profit, closed-panel, group-model US health maintenance organisation (Kaiser Permanente) – before and after an intervention that included a screening programme. The majority of women (80%) felt that clinicians should screen all their women patients for partner abuse. Responses to questions about the appropriateness of clinicians screening all women patients were similar pre- and post-intervention and did not differ by abuse status or by age.
McDonnell and colleagues112 recruited 481 patients attending their first antenatal appointment at an Irish hospital. Of the women who answered the questions regarding acceptability of partner violence screening, 468 (99%) found the questions acceptable and considered that all women should be asked these questions. There were no differences in acceptability by abuse status or by age.
A study by McNutt and colleagues113 recruited women from a health maintenance organisation (HMO), partner violence programmes and refuges. The survey incorporated questions on what women want nurses and physicians to ask, and what they want them to do and not do in order to help abused women. Forty percent of women in the HMO and community-based programmes and 64% in refuges agreed with screening.
Newman and colleagues114 conducted a survey of 451 women who were unaccompanied by a male partner in a paediatric emergency department in a US hospital. When asked if it was appropriate to screen them for partner violence when they sought care for their children, 75% of women stated it was. Forty-four percent preferred direct verbal questioning, 36% a written questionnaire, and 20% suggested other methods of screening.
Renker and Tonkin102 used anonymous computer interviews in two maternity units in the USA. Topics covered in the interview included screening and interventions, past disclosure to health-care providers, preferences or attitudes towards violence screening, pregnancy violence and violence severity screening. Feelings of anger, embarrassment or being offended were not experienced by the majority (97%) of women screened by their prenatal care providers for partner abuse.
Richardson and colleagues41 surveyed 1207 women in 13 randomly selected general practices in London. Eighty percent of women reported that they would not mind being asked by their general practitioner about abuse or violence in their relationship if they had come about something else.
Romito and colleagues107 conducted a survey in six family practice sites in Italy. Women were approached and asked if they would like to participate in a study to improve how health services respond to women’s health problems. Eighty-five percent of respondents believed the family doctor should ask all women about violence, 7% thought doctors should not ask, and 8% were uncertain. A higher percentage of women experiencing current abuse agreed that doctors should ask about abuse compared with women not currently experiencing abuse, although this association was not significant. Younger women were significantly less likely to agree that all doctors should ask about abuse.
Sethi and colleagues48 administered a modified World Health Organization (WHO) Multi-country Domestic Violence Study questionnaire in an inner-city accident and emergency department in a British hospital. The questions asked about the nature of violence and abuse experienced and women’s views on being asked about abuse in an accident and emergency department setting. Overall, 76% felt comfortable when asked about partner violence. Eighteen percent felt slightly uncomfortable, 5% felt uncomfortable and 1% felt very uncomfortable. Feelings of being uncomfortable were higher in those who had experienced abuse compared with those who had not (10% versus 3%, p = 0.02). In response to a question about the desirable frequency of being asked about partner violence, 35% felt it should be on all occasions, 26% felt they should usually be asked, 38% said seldom and 2% felt never. Many women commented on the need for privacy and safety and expressed concern about direct questions being asked of women presenting with injuries.
Zeitler and colleagues115 recruited women aged between 15 and 24 years who presented for family planning services to a US clinic. Almost 90% of those surveyed felt that universal screening by health-care providers is a ‘very good’ or ‘somewhat good’ idea. When respondents were categorised according to how much they minded being asked about violence, there were no differences according to ethnicity, school enrolment, parity, family violence or lifetime dating violence experience. However, compared with women aged 19–21 years, women aged 15–18 years were 2.9 times more likely to voice some concern regarding violence screening by a provider (36%, p < 0.01).
Webster and colleagues116 administered a self-report questionnaire to 1313 women from five Australian hospitals during the visit following the consultation at which they had been screened for partner violence. Ninety-eight percent of respondents believed it was a good idea to ask women about partner violence when visiting a hospital. There was no difference in the responses of women from rural, remote or inner city sites, nor were there differences between sites in terms of how women felt when asked partner violence questions. Ninety-six percent felt ‘OK’ about being asked, 1% felt relieved to be able to talk to someone about their problem, and 2% felt uncomfortable. Three-quarters of women who felt uncomfortable still agreed that it was a good idea to ask about partner violence.
Weinsheimer and colleagues104 recruited 95 consecutive women in a level 1 trauma centre to a questionnaire survey. Although 18% of women thought screening infringed their privacy, the overwhelming majority (> 90%) felt that it was appropriate to ask about partner violence and that women should be asked about it in a trauma setting. Nearly all (93%) of the 44 women who reported a history of partner violence thought a trauma centre health-care provider could assist them with a safety plan, but about one in four abused women thought reporting would increase their chances of further harm.
Witting and colleagues117 surveyed 146 patients attending an accident and emergency department, giving three hypothetical scenarios of varying partner violence risk. Patients’ support for ‘screening’ increased as the scenarios increased in severity: 86% expected it for the high-risk versus 17% for the low-risk scenario. The majority of patients felt that a physician, rather than a nurse, should have the primary responsibility for partner violence screening, but that the gender of the screener did not matter. A higher proportion of patients with lower educational status supported screening in the emergency department.
Synthesis
We have combined data from the interview- and focus group-based qualitative studies with the data from the questionnaire-based quantitative studies. The main focus of this review question was the acceptability to women patients of screening for partner violence. This included physical and sexual violence, emotional abuse and controlling behaviours by current partners or ex-partners. Although the proportion of survey respondents who found screening by health-care professionals acceptable varied between 35% and 99%, our main finding is that the majority of survey respondents and informants in the qualitative studies did find it acceptable even if it made them uncomfortable. There was variation in attitudes towards screening between countries and between health-care settings and by abuse and educational status. In the UK-based studies, 20% of respondents did not support screening in a general practice context, and 40% thought women should seldom or never be asked about partner violence in an accident and emergency department.
In the sensitivity analysis of the survey estimates of acceptability of screening, the variation in results could not be explained by the variation in STROBE quality scores. Higher-quality studies showed the same variation as in the total pool of studies.
Below we explore the role of the following factors in the acceptability of screening by health-care professionals:
-
the woman’s age, level of education, financial autonomy, and ethnicity
-
whether the woman has ever been abused and is currently abused by their partner or ex-partner
-
type of health-care setting
-
type of screening questions
-
type of health-care professional.
Age
Younger women, especially those aged 15–19 years, were less likely to agree with screening for partner violence. 102,107,115 Friedman and colleagues found that older patients were more in favor of routine physical abuse enquiry. 110 Age, however, did not influence the acceptability of routine enquiry for sexual abuse, although most surveys did not collect data on that issue.
Education
Witting and colleagues found that a higher proportion of respondents with lower education status supported partner violence screening. 117 Friedman and colleagues also found that, regardless of setting, patients who had not completed high-school education were more in favour of routine enquiry about physical abuse and sexual abuse. 110
Ethnicity
Although many of the surveys had ethnically diverse samples, most did not report acceptability by ethnic group. Zink and colleagues found that Latina mothers felt greater discomfort with partner violence questions than white American women. 118 The issue was not discussed in the qualitative studies.
Abuse status
Seven quantitative studies reported results by abuse status, and there was no consistent difference in acceptability by abuse status, although several found that a lower proportion of women with a history of partner violence were in favour of screening compared with women without that history. Caralis and Musialowski reported that 77% of non-abused women and 70% of abused women agreed with screening. 109 Glass et al. reported that 80% of women who were acutely abused or who were physically or sexually abused in the past year agreed with routine screening compared with 89% of women who reported a lifetime history of abuse or who reported no partner violence. 105 Zeitler and colleagues reported a similar result: women who had experienced physical violence in the last year were significantly less likely to report that they felt it was a good idea for health-care providers to ask all women about violence; but even so, 80% of this group were in favour of all women being asked. 115 However, Friedman and colleagues found that 80% of those who reported sexual abuse favoured routine physician enquiry about sexual abuse compared with 64% of those who reported never being sexually abused. 110 In the same study, patients who reported abuse were just as likely to favour routine enquiry as patients who reported never being abused. Gielen and colleagues found that 48% percent of their sample agreed that health-care providers should routinely screen all women, with abused women more likely than non-abused women to support this policy (54% versus 42%),111 which concurred with the findings of Sethi and colleagues that 43% of accident and emergency department patients with a history of abuse thought that women should always be asked about experience of partner violence, compared with 30% among those who had not been abused. 48
Screening settings
There were no consistent differences in acceptability of screening by health-care setting. Most of the studies were conducted in various hospital settings, with some in general practices, in refuges or where women attended their support groups; one was in a family planning clinic and some included different settings. In several of the qualitative studies, informants did say that they would prefer screening to be carried out by a clinician with whom they already had a relationship, which implies that primary care is a more acceptable context than an accident and emergency department. This finding also implies that it may be less appropriate to ask about abuse at the first antenatal appointment than at subsequent appointments.
Method of administering screening questions
Most quantitative studies did not test acceptability of screening in relation to screening modality. Those that did and the qualitative studies found a range of preferences; there was no single preferred modality.
Type of health-care professional
Acceptability of screening may vary according to the gender and the profession of the health-care provider asking the questions. Some women preferred being screened by female health-care professionals; however, the qualitative studies found that most women felt that a professional’s interpersonal skills were more important than their gender or profession. Others voiced a preference for being screened by older health-care providers and doctors. Richardson and colleagues41 found that 20% of women reported that they would mind being asked by their general practitioner about abuse or violence in their relationship if they had come about something else, with 23% objecting to a nurse asking; 42% reported that they would find it easier to discuss these issues with a woman doctor, and 3% expressed a preference for a male doctor.
Romito and colleagues found that women’s responses concerning who they would like to discuss violence issues with ranged from (more than one answer was possible) the family doctor (54%), a psychologist (28%), women who had similar experiences (22%), a social worker (9%) and the police (7%). 107 Webster and colleagues116 also reported a range of responses from women when asked about which health-care professionals should screen for partner violence: 1068 (65%) of the women nominated midwives, 1055 (64%) nominated general practitioners, 809 (49%) selected social workers, and 771 (47%) selected hospital doctors. Only 42 (2%) thought no one should ask. A number of women wrote comments such as ‘anyone who cares should ask’.
From the qualitative studies it seems that in general women gain a sense of support and relief from discussing their situation with a health-care professional. Some women found it more acceptable to be screened by a health-care professional where there was an already-established relationship and trust had been built up. Women also placed great emphasis on the capacity of health-care professionals to listen to them discuss their problems without judging or condemning them; not listening was viewed as inhibiting disclosure. Women felt more comfortable being screened and asked sensitive questions by health-care professionals who they felt understood the complexity of partner violence and who established a personal connection. 95,97,98,100,119,120 Some women also stated that part of their fear and suspicion associated with disclosing partner violence and being screened arose from not being sure of the health provider’s intentions in asking and what would happen if they told the provider. Some women felt that they were being screened because the health-care providers did not think they were caring for their children properly, and saw screening as a search for child neglect or abuse. 119 By giving a reason for screening, health-care providers may alleviate these fears and build up trust. Some women expressed concern that appointments were not long enough to make effective use of confidential time, or felt that health-care professionals did not have the time to listen. 119 Many of the women felt that screening gave them the opportunity to disclose abuse, either then or at a later stage, and that without this opportunity it would be harder for them to seek help. Women expressed concerns with possible negative repercussions of screening, such as breach of confidentiality, the involvement of children’s services, legal repercussions and being judged. 120 Common concerns highlighted included the legal repercussions of revealing abuse and fears that abusive partners might find out that the relationship had been discussed. Some women reported feeling ashamed and concerned that others would judge them poorly.
Strengths and limitations
The strengths of this review include the synthesising of qualitative and quantitative studies to answer this question, the quality appraisal of studies (using the STROBE checklist for quantitative studies and the CASP tool for the qualitative studies) and the performance of a sensitivity analysis. Respondent-related variables, such as demographic features and abuse status, and features relating to the screening process, such as setting, type of questions and the health-care professionals, were examined to assess how they interact to increase or decrease the acceptability of screening. This review meets the relevant QUORUM reporting criteria (see Appendix 11.4 for checklist and flowchart). A limitation is that we did not include studies, if they exist, of the views of men about health-care-based screening of women for domestic violence.
Discussion
Most of the surveys of women patients in health-care settings show that the majority agree with screening or routine questioning about partner violence, but there is variation, not explained by study quality, abuse status, setting or demographic factors. The quality of the surveys was generally good. A possible explanation for the variation of screening acceptability could be the variation in wording of the acceptability questions. Acceptability was measured by questionnaire statements to which women ‘agreed’ or ‘disagreed’. Most papers did not report the exact wording of the questions; however, these were not necessarily comparable. For example authors referred to statements like ‘women would have wanted to be asked’106 or ‘felt it was appropriate to screen them’. 101 The term ‘screening’ was not necessarily used and authors often did not clarify whether the question addressed violence when the women were attending with an apparently unrelated health problem. We excluded studies where the reported questionnaire item was vague and could be interpreted as acceptability of any question about partner violence.
In interviews and focus groups, women say they find screening beneficial, even if they are not yet ready to disclose abuse. Informants perceived screening as a method of raising awareness rather than eliciting disclosure of abuse. Women who were not yet ready to disclose abuse still found screening beneficial as it helped to remove the stigma attached to partner violence, raised awareness of partner violence, gave them a sense of validation and let them know there is somewhere they can go if they need help when they are ready to disclose. Although women may not disclose abuse immediately, screening may facilitate disclosure later when they feel more comfortable with the health-care professional, or when their circumstances change and they feel the need to get help.
Chapter 7 Are interventions effective once partner violence is disclosed in a health-care setting? (Question IV)
We found 33 studies measuring the effectiveness of interventions for women who have experienced partner violence and their children. Nineteen of these studies were examined in a previous systematic review,11 and have been summarised below with the new studies. Publication dates of the 14 studies not included in the previous review range from 2000 to 2006. The majority of these new studies were conducted in the USA, a few were conducted in Canada, two in Spain, one in Mexico and one in Hong Kong. The settings varied and included refuges, community settings, women’s homes, antenatal clinics, a methadone maintenance programme and primary care ‘public health’ clinics. Study designs included nine randomised controlled trials, two case–control studies and two before-and-after studies. For details of the included studies see Appendix 7.1. For results and quality scores of studies see Appendix 7.2. The assessments of individual studies using the USPSTF criteria and the Jadad tool are detailed in Appendices 7.3 and 7.4, respectively.
No qualitative studies were found that explored what outcomes abused women want for themselves and their children from programmes that include screening or other health-care based interventions.
Advocacy interventions with abused women
Eleven studies (four newly reviewed and seven from our previous review) evaluated the use of advocacy for women experiencing partner violence: one in Hong Kong, one in Canada and nine in the USA.
Studies published since our previous review
In an individually randomised controlled trial of an advocacy intervention in an urban public hospital antenatal ward, conducted by Tiwari et al.,121 advocacy benefited abused pregnant women who were still in a relationship with the abuser. Abused women at less than 30 weeks’ gestation and identified by screening were randomised to the intervention group, which received advice on safety, choice-making and problem-solving, or to the control group, which received a referral card listing community resources and sources of partner violence services. The intervention sessions lasted about 30 minutes, and afterwards women were given a brochure reinforcing the information provided. Follow-up was 6 weeks post-delivery, and hence ranged from 16 to 34 weeks from the intervention, depending on gestational age at recruitment. At follow-up, the intervention group reported significantly less psychological abuse and less minor physical abuse; however, the rate of severe abuse and sexual abuse did not differ between the groups. The intervention group had significantly greater physical functioning and significantly improved scores on role limitation measures for both physical and emotional problems. Although the women did not report any adverse effects as a result of participation in the study, the intervention group reported more bodily pain than the control group. There were no differences between groups on outcomes of general health, vitality, social functioning and mental health. Significantly fewer women in the intervention group had postnatal depression at follow-up than in the control group.
A pilot study by Constantino and colleagues of an advocacy intervention with a therapeutic component was conducted with first-time residents of an urban domestic violence refuge. 122 This individually randomised controlled trial compared a structured nurse-led social support intervention with unstructured discussion sessions. Both groups continued to receive standard refuge services. The intervention comprised eight weekly sessions (each lasting 90 minutes) and sought to empower abused women through the provision of four dimensions of social support: belonging, evaluation, self-esteem and tangible support (BEST). It provided resources to the women as well as information on further resources; it allowed them time to access resources when these were available; and provided an environment where they could talk with a counsellor and friends. Follow-up did not extend beyond the intervention period. At the end of the programme the experimental group had significant improvements on the ‘belonging’ function of social support, and had significant reductions in psychological distress and health-care utilisation. The authors reported non-significant improvements in ‘tangible’ social support and total social support, but no data were presented.
An individually randomised controlled trial conducted by McFarlane and colleagues in two urban primary care public health clinics and two women, infants and children clinics compared a nurse case management intervention with a referral card that listed a safety plan and sources of partner violence services. 123 Project nurses received a 40-hour training programme based on the March of Dimes protocol prior to study implementation. Advocacy sought to empower the women by increasing independence and control through encouraging the use of a 15-item safety-promoting behaviour checklist, supplemented with supportive care and anticipatory guidance by a nurse and guided referrals tailored to the women’s individual needs, such as job training. There were five 20-minute case management sessions. The control group received standard refuge services provided to all residents. No effect for the intervention was found at the 24-month follow-up: all outcomes (use of safety behaviours and community resources, threats, assault, homicide risk and work harassment) improved over time, regardless of group allocation. Study participants did not report any adverse effects. For findings relating to the children of the participants, see Interventions with children of abused women below.
Sullivan and colleagues tested the effect of an advocacy intervention aimed at abused women and their children (aged between 7 and 11 years) using an individually randomised controlled trial study design. 124 The intervention took place in women’s homes in an urban setting. Advocacy was based on the individual needs of the mother and child, but all sessions actively assisted mothers in accessing community resources. The majority (79%) of the women were recruited when leaving a domestic violence refuge and the remainder were recruited from community family service organisations or social services. Unspecified control group care was compared with a multicomponent intervention consisting of: (1) a highly trained paraprofessional who worked for 16 weeks and helped mothers to mobilise and access community resources; (2) the same paraprofessional who advocated similarly for the children for 16 weeks; (3) a 10-week support and education group attended by the children within the 16 weeks. Families saw their advocates for a mean of 10 hours a week, averaging 5 hours with the children and an additional 2.7 hours with the women. The basis of advocacy and the content of the sessions was similar to that of earlier intervention studies by Sullivan and her colleagues125–129 (reported under Studies included in our previous review below). An important part of the intervention was ensuring that the advocate was no longer needed after 16 weeks. At a 4-month follow-up, women in the intervention group had significantly reduced depression and improved self-esteem. Mothers who received advocacy also reported better quality of life than mothers in the control group, although this was not statistically significant. However, the intervention did not have an effect on the incidence of actual abuse or social support. For findings relating to the children, see Interventions with children of abused women below.
Studies included in our previous review
Here we summarise the findings of studies examined in our previous review. 11 In two separate randomised controlled studies (a pilot and a main study) by Sullivan and colleagues,125–129 undergraduate psychology students were trained to provide 10 weeks of community-based advocacy to severely abused women exiting from refuges. Advocacy was tailored to the individual women’s needs to help them to access community resources (such as housing, employment, legal assistance, transport and childcare), as well as empowering the women themselves. A number of beneficial outcomes were observed over time. In the main study, at the end of the advocacy period, there was a significant improvement in the women’s perceived effectiveness in obtaining resources, quality of life and perceived social support as compared with baseline and control group scores. At 10 weeks postintervention, the women who received advocacy reported improvement in their quality of life, and this was maintained at 6 months after the cessation of the programme. Initial improvements in perceived effectiveness in obtaining resources and perceived social support were no longer statistically significant at 6 months. However, when followed up 2 years after the cessation of advocacy, women in the advocacy group reported significantly less physical abuse and still had a significantly higher quality of life than women in the control arm. Subsequent to the review by Ramsay and colleagues, a 3-year follow-up130 has been conducted. This shows that advocacy continued to have a positive impact on the women’s quality of life and level of social support, although there was no continuing benefit in terms of revictimisation.
Advocacy and associated services also benefited pregnant abused women who were still in a relationship with the abuser, according to a parallel group intervention study conducted by McFarlane and colleagues. 131–133 The women, attending an antenatal clinic, were offered an intervention of three brief sessions of individual advocacy (not described in any detail) – education, referral and safety planning – spread over their pregnancies. Additionally, half of the intervention group was offered three further support group sessions at a local refuge, but outcomes for these were not considered separately. The investigators found that women receiving the intervention significantly increased their use of safety behaviours, including hiding keys, hiding clothes, asking neighbours to call the police, establishing a danger code with others, and hiding money. At a 12-month follow-up, women in the intervention group reported significantly improved resource use but not use of the police, and there were also significant reductions in violence, threats of violence and non-physical abuse against the women compared with women in the control group
Another advocacy study was also conducted in an antenatal setting by McFarlane and colleagues. 134 In this randomised controlled trial, abused Hispanic women were allocated to one of three intervention groups: (1) ‘brief’, where women were offered a wallet-sized card with information on community resources and a brochure; (2) ‘counselling’, where for the duration of the pregnancy women were offered unlimited access to a bilingual domestic violence advocate who was able to provide support, education, referral and assistance in accessing resources; and (3) ‘outreach’, which included all aspects of the ‘counselling’ intervention, plus the additional services of a bilingual trained non-professional mentor mother who offered support, education, referral and assistance in accessing resources. The investigators found that violence and threats of violence decreased significantly across time for all three intervention groups. At 2 months postdelivery, violence scores for the ‘outreach’ group were significantly lower compared with the ‘counselling’-only group; but there was no significant difference when compared with the ‘brief’ intervention group women who had received only a resource card and brochure. Subsequent follow-up evaluations at 6, 12 and 18 months found no significant differences between the three intervention groups. Use of resources was low for each of the groups and did not differ significantly by type of intervention at any of the follow-up evaluations.
A third advocacy study by the same research group was a randomised controlled trial,135,136 based in a family violence unit of a large urban district attorney’s office. All women received the usual services of the unit, which included processing of civil protection orders and optional advocacy referral, and the phone number of a caseworker for further assistance. They also received a 15-item safety-promoting behaviour checklist. In addition the intervention group received six follow-on phone calls over 8 weeks to reinforce the advice on adopting safety behaviours. The number of safety-promoting behaviours increased significantly in the intervention group, both compared with the control group and up to 18 months later.
An advocacy study by Feighny and Muelleman137 took place in a hospital’s accident and emergency department. The advocate saw the woman within 30 minutes of disclosure, discussed the incident with her, addressed safety issues, provided education about the cycle of violence, and informed her of community resources. A before-and-after design with historical controls was employed to evaluate outcomes, with data obtained from police/judicial, refuge and medical records. Women receiving advocacy significantly increased their use of refuges and refuge-based counselling services in comparison with preintervention controls. However, there was no effect on subsequent experience of abuse as measured by the number of repeat visits to the department over a mean follow-up period of 65 weeks, nor was there any significant difference in the number of police calls made by women after their initial visit, or in the number of women who went on to obtain full protection orders.
Tutty138 considered the effects of advocacy for women leaving refuges using a before-and-after study design. The intervention programme of support and advocacy, of longer duration than the model used by Sullivan, was provided by a graduate social worker and provided counselling and other help for the women. The main goals of the advocacy were to respond to the individual woman’s needs and to coordinate support services so that the woman could remain independent and safe. Tutty found that this programme of advocacy resulted in significant improvements over baseline scores for physical abuse and for ‘appraisal support’ (the availability of someone to talk to about one’s problems). However, there was no significant improvement for ‘belonging support’ (obtaining support from friends and family) or perceived stress levels.
In our previous review11 we found that evidence regarding the effectiveness of advocacy interventions is weakest for women who are still in an abusive relationship and there was little evidence that women identified through screening had improved outcomes from advocacy. In this update we found one well-executed study121 showing that an advocacy intervention may be effective for women who disclose current abuse as a result of screening in an antenatal clinic, and a fairly well-executed study in primary care public health clinics and women, infants and children clinics123 showing no difference between intervention and control arms. The strongest evidence for advocacy-based interventions, emerging from the relatively well-executed trials of Sullivan and colleagues, is for an intensive advocacy programme for women leaving a refuge. The evidence for the effectiveness of advocacy with a less intensive intervention or for women identified in health-care settings is less robust, either because study designs were more prone to bias or because the execution of the studies was flawed. Yet most studies show some benefit from advocacy for some outcomes and therefore this is a legitimate referral option for health-care professionals. Evidence from advocacy studies suggests that this form of intervention, particularly for women who have actively sought help from professional services, can reduce abuse, increase social support and quality of life, and lead to increased usage of safety behaviours and accessing of community resources. Five of the studies121–124,130 were well-executed studies of good or fair design. Considering only these high-quality studies did not alter the overall findings, although two of the less well conducted studies134,137 showed less effect of advocacy. Continued severe abuse or revictimisation was the outcome most resistant to advocacy, although this may partly be a function of short follow-up, as one of Sullivan’s trials showed no decrease in abuse at 4 months follow-up,124 but did find it at 2 years after the advocacy intervention. 125–129 Moreover, abuse is a factor over which the survivor has least direct control.
Support group interventions with abused women
Two studies (one from our previous review and one newly reviewed) evaluated support groups for abused women; both of these were based in Canada.
Study published since our previous review
The study reported by Fry and Barker139 after our previous review was published had a case–control design and compared the effectiveness of a story-telling intervention with minimal care where women attended information-giving support groups. The geographical setting was not reported. The intervention group participated in 30–90-minute sessions in which each woman was given an opportunity to narrate a story about six salient events that she had experienced in the previous 4–6 months and that she believed had had the strongest impact on her self-confidence, self-esteem and self-worth. A group facilitator attempted to put relevant structure on the reminiscence process by offering encouragement, directing questions and steering the contents. At the 4-month follow-up, women who had received the intervention demonstrated significant reductions in depression, and significant improvements in self-esteem, global self-efficacy scores, the ability to share feelings, feelings of personal adequacy and a sense of reality.
Study included in our previous review
The study included in our previous review11 had a before-and-after design and was reported in two papers by Tutty and colleagues. 140,141 They evaluated 12 feminist-informed support groups for survivors of partner violence, as part of a community family violence programme. The goals of the groups were to stop violence by educating participants about male/female socialisation, building self-esteem and helping group members to develop concrete plans. The groups were facilitated by professionals over a 10–12-week period. A number of statistically significant benefits were observed immediately after the end of the intervention, including improvements in all physical and non-physical abuse measures, perceived belonging support, locus of control, self-esteem, and perceived stress and coping. At 6 months’ follow-up, there were continued reductions in physical abuse and one measure of non-physical abuse, and increases in self-esteem and perceived stress and coping. Improvements in social support and locus of control were sustained. Using multivariable analysis, the investigators showed that groups with two facilitators, rather than one alone, may be more effective in reducing emotional abuse.
Both these studies were poorly executed with weak designs and therefore there is insufficient evidence on which to judge the effectiveness of support groups for women experiencing partner violence.
Psychological interventions with abused women
Seventeen studies (11 from our previous review and six newly reviewed) evaluated the use of psychological interventions. Most studies were conducted in the USA. Ten of the 17 studies reported on the effects of group interventions: one of these compared a group intervention with a slightly modified version, one included overall findings from 54 different partner violence programmes (which incorporated individual, group, or both individual and group counselling sessions), and one compared group and individual therapy. Seven studies considered the benefits of individual therapy, with two of these also each comparing two different interventions.
In the studies that compared two types of psychological intervention, both groups tended to have improved outcomes, but there were no differences between the interventions. It is unclear whether this means that (1) neither intervention is effective, as there is spontaneous improvement in these outcomes once a woman has left an abusive situation; or (2) one intervention is more effective than the other, but with insufficient power to detect the difference; or (3) both interventions are equally effective (i.e. superior to no intervention). Positive outcomes from studies comparing a psychological intervention with no intervention suggest that (1) is unlikely.
Individual psychological interventions
Studies published since our previous review
Koopman and colleagues142 conducted an individually randomised controlled trial in an urban setting comparing the effectiveness of an expressive writing intervention with a neutral writing control arm. Women were recruited through fliers, newspaper advertisements and electronic postings. Participants in the intervention group were asked to use expressive writing and to write about the most stressful events of their lives, exploring their deepest emotions and feelings. At the 4-month follow-up, women in the intervention group had significant reductions in depression compared with the control group. However, the reverse was true for bodily pain: women in greater pain at baseline benefited more if allocated to the control arm. The intervention had no effect on PTSD.
A ‘matched, yoked and randomised’ experimental and control group design was used by Reed and Enright,143 in an urban setting, to compare the effectiveness of forgiveness therapy against an alternative treatment consisting of discussions about the validity of anger regarding the injustice of past abuse, present strategies for healthy assertive choices, and interpersonal relationship skills. Women, all self-selected volunteers, in the intervention group engaged in weekly 1-hour sessions based on the Enright forgiveness process model. Participants determined the time spent on each forgiveness topic, and the intervention finished when each participant reported that she had completed the work of forgiving her former partner. The mean treatment time (one session per week) for the pairs was 8 months, with a minimum of 5 months and a maximum of 12 months. The intervention group demonstrated a significantly greater increase in forgiving their former abusive partner, self-esteem, environmental mastery (everyday decisions), finding meaning in suffering (moral decisions) and in ‘new stories’ (survivor identity). The intervention group also had significant reductions in trait anxiety, depression, post-traumatic stress symptoms and in old stories (victim identity). However, they did not have significant decreases in state anxiety scores.
Labrador and colleagues conducted a case–control study in an urban setting in Spain to assess the efficacy of an intervention for the treatment of chronic PTSD in women experiencing domestic violence. 144 The intervention consisted of four components: (1) self-evaluation and problem-solving; (2) breathing control; (3) exposure therapy (which involved recalling past events and confronting flashbacks); and (4) cognitive therapy. It was delivered in eight weekly sessions of 60 minutes. Women in the intervention group were split into two groups, with one group receiving the components of the intervention in the above order, and the second group receiving the cognitive therapy component before the exposure therapy to establish whether the efficacy of the intervention was affected by the order in which the cognitive and exposure therapy components were delivered. Women were referred from the ‘municipal centre for women’ and victim support centres, by judges of domestic violence cases and by housing advisors. Women in the intervention group showed significant decreases in depression and ‘maladaptation’ and significant increases in self-esteem 2 months from baseline. Although women in the intervention group had reductions in PTSD symptoms post-treatment, these were not significant when compared with the control group, apart from negative cognitions. No differences were found between the two intervention groups.
Studies included in our previous review
In our previous review11 we examined two randomised controlled trials of a psychological intervention conducted by Kubany and colleagues. 145,146 The intervention was based on cognitive behavioural therapy and was targeted at women survivors of partner violence who had PTSD. Specifically, the intervention included elements from existing treatments for PTSD, feminist modules that focused on self-advocacy and empowerment strategies, assertive communication skill building, the managing of unwanted contact with former partners, and identifying potential perpetrators to avoid revictimisation. The two evaluation studies, both randomised controlled trials, found a sustained improvement at 3 and 6 months, respectively, in a range of mental health measures including PTSD, depression and self-esteem.
In a randomised controlled study by Mancoske and colleagues, women who contacted a partner violence agency were provided with a rapid response crisis intervention. 147 They were then randomly assigned either to feminist-oriented counselling or to grief resolution-oriented counselling, both of which were provided over eight weekly sessions by trained social workers and included basic problem-solving and psychoeducation. At the end of counselling, both groups showed improvements over baseline in self-esteem and self-efficacy, although these were only significant for women who received grief resolution-oriented counselling.
In a parallel group study of women resident in a refuge or receiving refuge-associated services, conducted by McNamara and colleagues, two types of intervention were compared: individual counselling versus case management. 148,149 When assessed after three sessions, women in both groups showed significantly improved life satisfaction and coping ability compared with baseline values. Additionally, women who had received individual counselling showed a significantly greater increase in global improvement scores than women in the case management group.
Group psychological interventions
Studies published since our previous review
Gilbert and colleagues150 conducted a pilot study using a randomised controlled trial design to test the feasibility, safety and short-term preliminary effects of a relapse prevention and relationship safety (RPRS) intervention in reducing drug use and partner violence among women in methadone maintenance treatment programmes (MMTPs); the geographical region was not reported. The RPRS intervention consisted of eleven 2-hour group sessions and one individual session. The intervention was tailored to the realities of low-income, African American and Latina women and focused on the enhancement of self-worth, ethnic pride and risk avoidance in the future. Materials and exercises incorporated social cognitive skill building. At the end of each session, participants were asked to commit to specific skills practice exercises between sessions. The control group received an information session consisting of a 1-hour didactic presentation of a wide range of local community services that women in MMTPs can access, tips on help-seeking, and a comprehensive directory of local partner violence services. At the follow-up assessment women in the intervention group demonstrated reductions in minor physical, sexual and/or injurious partner violence in the past 90 days. They were also more likely than women in the information group to report a decrease in both minor and severe psychological partner violence. Other changes in abuse measures did not reach significance. Women in the intervention group also demonstrated decreases in depression at the 3-month follow-up. Compared with women in the control group, women in the intervention group were more likely to report a decrease in having sex while high on illicit drugs. Improvements regarding substance use and PTSD after receiving the intervention did not reach significance. No adverse events were detected.
A cognitive behavioral therapy programme for women referred from social services, counsellors and the judiciary who displayed post-traumatic stress symptoms but did not meet the diagnostic criteria for PTSD was evaluated in a case–control study by Arinero and Crespo conducted in an urban setting in Spain. 151 The intervention, administered in a health-care setting, included psychoeducation, breathing controlling techniques, self-esteem improvement procedures, cognitive therapy, problem-solving and communication skills training as well as specific strategies for relapse prevention. Eight 90-minute sessions were conducted with groups of 3–5 women. Women in the intervention group, compared with the waiting list control group, showed a decrease in post-traumatic and depressive symptoms and an improvement in adaptation levels up to 6 months’ follow-up. There were no significant changes in the levels of self-esteem, although there may have been a ceiling effect as self-esteem levels were already high at the outset compared with other studies. The authors point out that the effect sizes were not as large as those in previous studies, such as that of Kubany et al. ,145 and suggested that this might be because participants in their study had lower (i.e. better) symptom scores at baseline, producing a ceiling effect. There were significant decreases in depression for the intervention group post-treatment; the authors state this was still significant at 6 months but no data were presented. The effect size post-treatment was 0.95, and at the 1-month follow-up it was 0.66, but effect sizes for the 3- and 6-month follow-ups were not presented.
A before-and-after study, conducted in Mexico by Cruz and Sanchez,152 assessed the effectiveness of a group cognitive behavioural intervention on promoting self-esteem, coping strategies and assertiveness in abused spouses of problem drinkers. The intervention comprised three components: (1) identifying and correcting cognitive biases and defective information; (2) establishing emotional regulation strategies; and (3) acquiring assertiveness skills. Women received eighteen 150-minute weekly group sessions. Women’s self-esteem was found to have improved significantly from pre-test at the 3-, 6- and 18-month follow-ups, but not immediately after the intervention. There were also significant improvements in coping strategies at the 3-, 6- and 18-month follow-ups. Women’s assertiveness increased significantly from pre-test to the 3- and 6-month follow-up, but this was not sustained at the 18-month follow up.
Studies included in our previous review
Included in our previous review11 was a parallel group study by Cox and Stoltenberg153 in which new refuge residents were recruited to a personal and vocational group psychological programme that included cognitive therapy, skills building and problem-solving. The 16 Personality Factors instrument (16PF) was administered to half of the intervention group, which was then given full feedback, creating two intervention subgroups. The control group received normal refuge care, which included weekly non-structured counselling sessions. When assessed immediately after the cessation of the intervention, both intervention groups showed significant improvements over baseline levels of self-esteem. However, all other benefits over time, including anxiety, depression, hostility and assertiveness, were limited to those women who received the intervention without any feedback from the 16PF. Neither of the two intervention groups improved in terms of locus of control. None of the outcome measures improved over time for women in the control group.
Cognitive behavioural therapy was also the method used by Laverde in a randomised controlled trial in Columbia. 154 Abused women in the intervention arm were given cognitive behavioural therapy, with lectures and structured exercises. The women were shown models of appropriate and inappropriate behaviour in different situations, and this was then followed by role play. Twenty 3-hour group sessions were held over a period of 11 weeks. Abused women allocated to the control condition attended a support group; these sessions were unstructured and aimed to discuss issues around partner violence and to provide information about the women’s legal rights and the availability of services. It was found that the frequency and intensity of abuse decreased markedly in both groups at 15, 30 and 45 days postintervention, but the numbers were too small for any conclusions to be drawn. Other benefits over time for intervention group participants were also observed. In comparison with their baseline scores, women in this group significantly improved on several measures: communication skills, handling of aggression, assertiveness, and their feelings towards their partners and the relationship, such as feeling less sentimental. These improvements did not extend to the control group, and significant between-group differences were observed.
A psychoeducational group programme was evaluated in a parallel group study by Limandri and May. 155 The content of this programme included information about partner violence, safety planning, stress management, building self-esteem, coming to terms with loss and grief, and developing a number of life skills. Women were recruited primarily through the victim witness programmes of two district attorney offices. Follow-up did not extend beyond the 12-week intervention. At the end of the intervention, self-efficacy scores improved for the women receiving group counselling, but declined slightly for women in the control arm of the study. There was an improvement in women’s perception of abuse across time in both groups. There were no between-group comparisons, no scores for the outcome measures and no reporting of any statistical analysis.
Variable results were obtained by Melendez and colleagues156 in a randomised controlled trial of group counselling, in which abused and non-abused women recruited from a family planning clinic were offered four or eight group sessions of cognitive behavioural therapy to prevent human immunodeficiency virus (HIV)/sexually transmitted disease (STD) infection. (The data for the abused and non-abused women were reported separately and only those relating to the abused women are given here.) Two measures were used to test safe-sex practices: condom use in general and episodes of unprotected sex. At 1 month and 12 months of follow-up, abused women who received eight sessions of counselling were significantly more likely to say that they used condoms at least sometimes, compared with controls or with women receiving only four sessions of counselling. However, there was no difference between groups in the number of unprotected sex occasions. Short-term benefits were reported in the use of alternative safer-sex strategies in both intervention groups, and negotiation over safer sex after eight sessions of therapy, but these were not maintained at 12-months’ follow-up. There was no difference in abuse outcomes between the intervention and control groups at any postintervention assessment.
A parallel group study by Rinfret-Raynor and Cantin in Canada evaluated feminist-informed therapy for survivors referred to social services, either in individual or group sessions. 157 The intervention was compared with the normal non-structured therapy provided to clients by the agencies. The therapies were administered in a number of settings, including community health centres. When followed up after 12 months, women in all three arms of the study showed similar improvement over time in terms of abuse, self-esteem and assertiveness.
Another group intervention was reported by Kim and Kim158 in a parallel-group evaluation in Korea, conducted with women survivors of partner violence residing long-term in a refuge. The intervention group women were given eight weekly sessions of counselling based on an empowerment crisis-intervention model that was problem focused and goal directed. Follow-up was restricted to an immediate postintervention assessment. Women who received counselling had significantly reduced levels of trait anxiety compared with women in the control group. There were no differences between groups for state anxiety and depression scores, which decreased in both. Self-esteem did not change between or within groups.
A before-and-after evaluation conducted by Howard and colleagues159 considered counselling delivered by 54 partner violence providers in Illinois, USA. These providers varied in terms of theoretical framework and delivery. Generic counselling significantly improved the well-being and coping of physically abused women who approached support services for help, and was of particular benefit to women who had been both physically and sexually assaulted as compared with women who had suffered physical assault on its own.
In summary, there was a wide range of individual psychological interventions, which demonstrated improvements in psychological outcomes including depression, PTSD and self-esteem. Two fairly well-executed trials125–129,145,146 of individual cognitive therapy-based interventions for women with PTSD who were no longer experiencing violence provide reasonable evidence for this intervention, but this cannot be extrapolated to the women who were still in an abusive relationship. Consideration of only the high-quality studies142,143,145,146 for individual interventions did not alter the findings.
Although there are 10 studies of group psychological interventions, all showing improvement in one or more psychological or mental health outcome, all but one are poorly executed. Consequently, the effectiveness of this type of intervention remains uncertain, particularly for women who are still experiencing partner violence.
Interventions with children of abused women
Five studies (seven papers) evaluated the use of interventions with children where there was also a degree of involvement of the mothers. These are all newly reviewed studies; such interventions were not included in our previous review. Four of the studies were conducted in the USA and one was conducted in Canada.
An individually randomised controlled trial, conducted by Lieberman and colleagues,160,161 examined the effectiveness of child–parent psychotherapy compared with case management plus referrals for individual treatment in the community for abused mothers and their children. The geographical region was not reported. Child–mother dyads were recruited if the child was aged between 3 and 5 years, mothers had experienced marital violence and the perpetrator was not living at home. These dyads were referred from family courts, partner violence service providers, medical providers, preschools, self-referrals, other agencies, child protective services and former clients. Dyads were referred because of clinical concerns about the child’s behaviour or the mother’s parenting after the child had witnessed or overheard marital violence. The intervention (setting not specified) consisted of weekly joint child–parent sessions interspersed with individual sessions for the mothers, offered for 50 weeks (average attendance: 32 sessions). Children in the intervention group had significant reductions in symptoms of PTSD after the intervention. There was also a significant reduction in the children’s behaviour problems, which remained significant at the 6-month follow-up. Mothers in the intervention group reduced their number of avoidant PTSD symptoms and their number of current distress symptoms postintervention. The reductions in mothers’ number of current distress symptoms remained significant at the 6-month follow-up.
Jouriles and colleagues162 conducted an individually randomised controlled trial to assess the effectiveness of an intervention in reducing conduct problems among the children of survivors of partner violence and improving the mothers’ child management skills. The women were recruited from urban refuges. Recruited children were aged between 4 and 9 years, met the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders IV) criteria for oppositional defiant disorder or conduct disorder, and lived with their mother but not the perpetrator. The intervention had two components: (1) providing mothers and children with problem-solving skills; and (2) teaching mothers to use certain child management skills designed to help reduce their children’s conduct problems. The intervention consisted of weekly sessions of 1–1.5 hours, began after the subjects had left the refuge, and continued for up to 8 months, with the families attending 23 sessions on average. Mothers in the control group were contacted monthly, either in person or by telephone, and were encouraged to use existing community or refuge services. Both mothers and children benefited from participating in the intervention. At the 16-month follow-up, the intervention group’s mean level of child externalising problems did not differ from the mean of the normative population, whereas the mean level of externalising problems in the control group did. Children’s internalizing problems diminished over time, with similar rates of change in both groups. Mothers in the intervention group displayed a significantly higher mean level of child management skills at the 8-month follow-up. Psychological distress of the women diminished over time but there was no difference between the two groups. At 2 years after cessation of treatment163 there was no significant difference between the intervention and control groups with regard to recurrence of violence against the mothers. At baseline all the children met DSM-IV criteria for either oppositional defiant disorder or conduct disorder. By follow-up, 15% of the children in the intervention group and 53% in the control group were reported to have externalising problems at clinical levels. There was a similar differential reduction in conduct problems. Children in the intervention group significantly improved in terms of happiness/social relationships. Externalising and internalising behaviour scores for children in the intervention and control groups did not differ significantly from one another at the 24-month follow-up.
McFarlane and colleagues evaluated the effects on children’s behaviour of a nurse case management intervention for mothers. 164,165 For details of the intervention, see Advocacy interventions with abused women above. The level of children’s behavioural problems was assessed over a 24-month period, but there was no statistically significant beneficial effect of the intervention. The extent of behavioural problems for both young and older children improved over time regardless of the trial arm allocation of their mothers. The scores of children aged 5 years or below improved most, whereas scores of the teenagers improved the least.
Sullivan and colleagues considered the effect of a 16-week advocacy intervention for abused women and their children. 124 For details of the intervention, see Advocacy interventions with abused women above. Children’s scores for self-worth, physical appearance and athletic ability all increased, and the effect of the intervention on these variables was found to be significant over and above the effects of time. Children’s witnessing of abuse decreased in both groups, and again this effect was found to be significant over and above the effects of time. Assailant’s abuse of the child decreased in both the intervention and control group, but the within- and between-groups change decreases were not significant.
A before-and-after study by Ducharme and colleagues evaluated an intervention seeking to improve parent–child cooperation in women who were not living with the abuser. 166 The geographical region was not reported. Two groups received immediate intervention and two received delayed treatment. The intervention used ‘errorless compliance training’, a success-based, non-coercive intervention involving the hierarchical introduction of more demanding parental requests at a gradual pace, and lasted between 14 and 29 weeks. Mother–child dyads were self-referred or referred from child welfare agencies, school boards, women’s refuges and other social service agencies. Children were aged between 3 and 10 years and had severe behaviour problems. All of the children came from families where the mothers had experienced partner violence. Data for all four groups were pooled and showed that all children demonstrated increased compliance following the intervention. There was significant improvement in perception by mothers of their children’s externalising, internalising and total behaviour problems. Mothers rated their children as being significantly more cooperative after the intervention, and reductions in maternal stress and improvements on the parenting stress index were seen both on child and parent characteristics.
Four of the five studies examining the effectiveness of interventions with children of abused women were randomised controlled trials and well executed. These studies suggest that this type of intervention is promising and helps to reduce children’s behaviour problems and mother’s stress and PTSD symptoms. Such interventions may also increase a mother’s child management skills. The majority of these interventions were conducted with women who had left the abusive relationship, so these findings may not be generalisable to women who remain with an abusive partner.
Sensitivity analysis
As we did not meta-analyse the studies, we could not formally test the effect of study quality on pooled effect sizes with a subgroup analysis or metaregression. We examined variation for comparable outcomes (see Appendix 7.5) and made a qualitative judgment on whether study quality was related to effect size. Before-and after studies were not included in this sensitivity analysis due to the inherent risk of bias in this study design. Where studies did not report effect sizes, values for Cohen’s d between group effect sizes were calculated using means and standard deviations when such data were present. There were a sufficient number of studies measuring PTSD, depression, self-esteem and physical abuse to explore study quality on these outcomes. Five studies (four RCTs) measured PTSD as an outcome. 142–146,160,161 The better-quality studies had smaller effect sizes. 162–166 Five studies (four RCTs) measured the effects of the intervention on depression,126,142–146,150,157 with the better-quality studies showing smaller effect sizes. Four studies (two RCTs)138,140,143–146,152,153,157 measured the effects of the intervention on self-esteem. There was no clear relationship between effect size and study design and execution. Three studies (all RCTs)121,123,126,140 measured the effects of interventions on physical abuse. There was little variation in the effect sizes, which were all low. This sensitivity analysis highlights the importance of a high standard of design and execution of intervention studies.
Strengths of this review
We did not exclude studies on the basis of language, translating those that were not reported in English. We appraised the quality of all primary studies: the Jadad score was applied to randomised controlled trials, and all studies were appraised using the USPSTF quality criteria, which give a measure of internal and external validity, and also the strength of evidence of the studies as a whole, which can be used to assess the level of evidence for the particular type of intervention being assessed. Effect sizes were calculated where means and standard deviations were reported or obtainable from the authors. Our review meets all the relevant QUORUM reporting criteria (see Appendix 11.5 for QUORUM checklist and flowchart).
Limitations of this review
We did not pool outcomes for any of the interventions for several reasons: heterogeneity of outcome measures, variable follow-up between studies and, in the case of psychological treatments, the content of the interventions. Incomplete reporting of effect sizes would also have made meta-analysis difficult. It was not possible to test for publication bias with a funnel plot because the small number of studies reporting effect sizes would make the results misleading. 167 The largely positive findings of most of the studies suggest that publication bias may be operating in this field.
Limitations of our review originating in the primary studies include the absence of effect sizes or the data needed to calculate them, a lack of detailed reporting of the content of interventions, and poor study design or execution. These limitations weaken the strength of evidence for the various interventions.
Discussion
The level of evidence for effectiveness of advocacy interventions was assessed using the USPSTF criteria. We have already mentioned the incomplete reporting of effect sizes as a major limitation in the application of these criteria. Furthermore, whether or not overall effect sizes are ‘sufficient’ or not is a matter of judgment, as effect sizes may be sufficient for one outcome, but not for others. When analysed with the USPSTF criteria, the level of evidence for the effectiveness of advocacy interventions was borderline between insufficient and sufficient. We decided not to average the effect sizes for all the outcomes, but consider them individually, as it is arguable that one positive important outcome may be sufficient evidence to endorse an intervention. This is, however, a very conservative measure of the level of evidence as it is only based on four studies121–123,126 – the other studies included in our review either did not meet the quality criteria for inclusion in this analysis or did not provide the data required to calculate effect sizes.
The level of evidence for individual psychological interventions is sufficient, based on five studies,142–146 two of which were conducted by the same authors. Another reason for caution when interpreting this finding is that the interventions are quite different from each other, ranging from forgiveness therapy to expressive writing to cognitive trauma therapy designed for women with PTSD. The level of evidence for effectiveness of group psychological interventions is currently insufficient owing to a lack of studies meeting the quality criteria and having the necessary data from which to calculate effect sizes.
The level of evidence for effectiveness of support groups is currently insufficient owing to a lack of studies meeting the quality criteria and having the necessary data from which to calculate effect sizes. Although the evidence for psychological interventions and work with women and their children has grown more robust with recent trials, most did not recruit women identified in health-care settings. In those that did, it is not clear that the women were identified through screening. We have kept these studies in our review because our inclusion criteria covered interventions to which survivors of partner violence could have access through health services.
The strength of evidence for effectiveness of interventions with children of abused women is currently insufficient. Only three studies met the quality criteria and had the data required to calculate effect sizes;160–165 however, the effect sizes were not sufficient or consistent between these studies.
If one takes into account additional good-quality studies that could not be analysed with the USPSTF criteria124,125 there is enough evidence to justify access to advocacy services for survivors of partner violence in general, but the evidence is weakest for women who are identified through screening. Most of the studies measuring the effect of advocacy recruited women who have already disclosed abuse and have actively sought help. Many of the participants in these studies were recruited in refuges. We cannot confidently extrapolate the findings of these studies to women identified in health-care settings, whether by screening or case finding. Those advocacy studies that did identify and recruit women in health-care settings were based in antenatal clinics, therefore the evidence for the effectiveness of advocacy for women identified in health-care settings is strongest for antenatal services.
A big caveat in this judgment on advocacy services is the range of outcomes that were measured and the potential gap between women’s perception of benefit and these measures. Although part of this review question included a question about what outcomes women would want from advocacy and other interventions, we did not find any qualitative studies that addressed this.
Most studies did not specifically assess potential harm from the interventions, although worse outcomes in intervention groups compared with controls would have been an important indication of harm. The only examples of this from our review are two studies, one evaluating the effectiveness of advocacy,121 the other looking at individual psychological therapy,142 which found that women in the intervention arms experienced more bodily pain. The types of harm that would not have been detected unless the investigators specifically tried to measure them are more akin to adverse events in pharmacological trials. In the qualitative studies reviewed in Chapter 5, women cited breaches of confidentiality, stigmatisation and judgments by health-care providers as actual or potential harms of screening.
Chapter 8 Can mortality or morbidity be reduced following screening? (Question V)
We identified eight studies of interventions to implement screening with a total patient sample of 16,272 (one study did not report the number of participants). Publication dates ranged from 1998 to 2006, and the majority of studies were based in the USA. One study was conducted in Australia. Settings varied and included family practice sites and community clinics, health maintenance organisations (HMOs), women’s health clinics, and accident and emergency departments. One study trained nurses who visited vulnerable women in their homes. Experimental designs included seven before-and-after studies with varying follow-up periods (6 months to 2 years), and one randomised controlled trial. For further details of the design of included studies see Appendix 8.1. Results of included studies and quality scores are detailed in Appendix 8.2.
Morbidity and mortality are central to this NSC criterion, but we found no studies that measured these outcomes. Therefore we have included studies with proxy outcomes: identification of women experiencing partner violence after a system-based intervention to implement screening plus one other activity (such as referral to partner violence advocacy, or full documentation of the abuse). Studies that only reported one proxy outcome were excluded, unless this was referral to expert partner violence services. The justification for including identification plus another activity as relevant outcomes is that there is evidence that these additional activities may be associated with improved morbidity or mortality. As we discussed in Chapter 7, advocacy improves outcomes for survivors of partner violence and this may also be the case for psychological interventions.
The other specific outcome in our review protocol was harm associated with screening, but no studies reporting evidence of harms were found during this review.
The sections below are organised by health-care setting.
Health-care setting
Primary care, community clinics and health maintenance organisations
Harwell and colleagues168 used a before-and-after design with a 3-month follow-up at community health centres in the USA. The effects of the RADAR (Routine screening; Ask direct questions; Document your findings; Assess patient safety; Review patient options and referrals) training project was assessed via medical chart reviews, extracting data that allowed calculation of relative risk for screening being performed, suspicion and identification of partner violence, safety assessment, documentation of abuse, and referral to internal and external partner violence services. Training of all community health centre staff in the intervention group was 3–6 hours. Using trauma theory as a framework, it included a video on the emotional impact of partner violence, introduction to the use of and modelling of RADAR, and a survivor’s story. Follow-up support tailored to the needs of the centre staff continued for 2 years after training. Baseline measurements taken at pretraining for both phases were used as control data. During the intervention period women were more likely to have partner violence suspected (2% versus 6%, relative risk 1.49, 95% confidence interval 1.13–1.99), to have a safety assessment performed (5% versus 17%, relative risk 1.65, 95% confidence interval 1.39–1.97) and to be referred to an outside agency (0% versus 4%, relative risk 1.81, 95% confidence interval 1.45–2.28) compared with women in the baseline period. The authors state no differences were found for confirmation of partner violence; however, reported confidence intervals suggest a significant effect (2% versus 5%, relative risk 1.49, 95% confidence interval 1.08–1.97). This study showed improved proxy outcomes after implementation of RADAR.
Thompson and colleagues169 studied the impact of a system-based intervention to implement screening and effective responses to disclosure of partner violence in an HMO, recruiting five primary care clinics in a cluster randomised trial design. Utilising the Precede/Proceed model, the intervention focused on changing practitioner predisposing factors (such as knowledge and attitudes), enabling factors (environmental and infrastructure processes supporting the intervention) and reinforcing factors (i.e. the use of feedback). Staff attended two separate half-day training sessions, targeting skills building and empowering practice teams to ask about partner violence. Additionally, four educational sessions on skills improvement, community resources and early results were attended, with opinion leaders attending three extra training sessions. In intervention sites, posters about partner violence were displayed, cue cards given to clinicians, and screening questionnaires and newsletters periodically sent to participating health-care professionals. Identification of women experiencing partner violence at the intervention sites had increased at 9 months’ follow-up, although this was not significant (2% at baseline to 4% at follow-up, odds ratio 1.5, 95% confidence interval 0.73–3.17). At the intervention sites, the morbidity outcomes depression and physical injury did not improve and pelvic pain actually showed a significant increase (from 4% to 8%, odds ratio 3.8, 95% confidence interval 1.1–12.5).
McCaw and colleagues101 conducted a before-and-after study with historical controls within various departments of an HMO. Although the paper reporting the study was entitled ‘Beyond screening for domestic violence’, increased screening by clinicians was an aim of the intervention. The intervention was designed to take advantage of existing infrastructures and to avoid taking clinicians away from their clinical practice. Several brief training and information sessions were delivered to clinical staff and receptionists. Additionally, using a systems model approach, the HMO actively sought to improve its links with community services, inform patients about partner violence and appropriate services, provide clinicians with information and prompts, and employ an on-site domestic violence specialist. Nine months after training started, referrals had increased from 51 to 134. Unfortunately there was insufficient information to determine referral rates and no statistical analysis.
Coyer and colleagues170 conducted a before-and-after study in a rural, nurse-managed US health-care centre, testing whether the addition of a screening protocol into the clinic would increase the identification of violence against women. The system-centred intervention was relatively informal and involved discussions with nursing staff, which identified a need for improving their knowledge of local community resources. Due to staff interest, two local agencies that support women in violent situations visited the members of the clinic in order to provide background information, local statistics, information about the resources available and the processes of referrals, and a strategy on how to manage patients who gave a ‘yes’ response to the question ‘Is anyone hurting you?’. An audit of the medical notes 12 months prior to the intervention revealed no notation of abuse or use of partner violence services in any of the records. During the 12 months after the intervention, chart audit showed six women had notation of abuse in their medical records, and of these, four were referred to domestic violence refuges or the local drug treatment facility, and one was provided with the abuse hotline telephone number.
Women’s health services
In a parallel group study in an antenatal setting, Wiist and McFarlane171 provided clinic staff with a single session of 90 minutes of didactic training about screening for partner abuse and associated procedures, including making referrals to an on-site bilingual counsellor. This was supplemented with a protocol and with weekly visits by the trainer to provide support and for training any new staff. Referrals at follow-up showed an increase from 0% to 67% of women disclosing abuse at 3 months, and 53% at 12 months.
Ulbrich and Stockdale172 used a before-and-after design with historical controls to evaluate the implementation, in rural family-planning clinics, of ‘routine screening’ for partner violence. All staff were given didactic core training, pocket cue cards and a protocol to follow; key staff also received intensive follow-on training over 2 years. As part of the intervention, community-based domestic violence agencies provided advocates. At three of the clinics, the advocates worked mostly off-site but attended the clinics in emergency situations; at the fourth clinic, an on-site service was available for 1 day per week. Due to the low numbers in the study, only descriptive statistics were reported. For nurse-practitioners and registered nurses, a trend for discussing partner violence with patients on a weekly basis increased from 19% at pretraining to 57% at the 6-month follow-up (difference 38.3%, 95% confidence interval 37.0–39.6). Self-reported referrals over the past 3 months increased from 0% for four or more referrals to 21% at the 6-month follow-up (difference 21.4%, 95% confidence interval 20.0–22.8).
Accident and emergency department
In a before-and-after study with historical controls, Ramsden and Bonner173 evaluated the implementation of screening by nursing staff of all women aged over 15 years. The staff training focused on partner violence, screening protocols and a referral pathway. Information about resources, including local services and contact numbers, was also provided. Regardless of the patient’s response, all screened women were supposed to receive an information resource card. The duration and frequency of training was not stated. No data were presented on adherence to the protocol or on identification rates. It was found that the number of referrals to a social worker or to the police nearly doubled (8 compared with 14) as compared with preintervention numbers. However, the authors did not report enough information for referral rates to be calculated; neither did they report the findings of any statistical analyses.
Home visit
The before-and-after study with historical controls conducted by Shepard and colleagues174 differed from the others in that the health professionals who were instrumental in the intervention were nurses who routinely visited women in their own homes as part of a maternal and child health programme. For this project, the nurses received training in partner violence, and a partner violence response protocol was developed to increase referrals and information-giving. The protocol included a general question about the women’s history of abuse. Two years after the protocol was introduced, the authors reported that referral rates increased from 3% at preintervention to 17%. This positive trend was not statistically significant; however, the data on referral before and after the intervention were not fully comparable. Increases were found in both information-giving by nurses following the intervention (0.03% to 78%) and identification of partner violence (6% to 9%), although only the former was significant.
Sensitivity analyses
When considering outcomes by settings, system-level screening interventions in primary care and women’s health clinics are more effective than those within accident and emergency departments and home visits. Some of the studies did not adequately report data on referral outcomes, or combined several different outcomes under one category; thus it is hard to judge changes in these outcomes.
In terms of study quality, only one study169 had the ‘greatest’ strength of design and a ‘fair’ execution rating. The other seven studies rated ‘poor’ for execution and ‘moderate’ for strength of study design, most using a before-and-after method. Details of the assessment of execution of individual studies are in Appendix 8.3. Due to all but one of the studies having a poor execution rating, there is insufficient evidence for system-centred interventions increasing identification, referral and other activities aimed at reducing morbidity and mortality. The lack of variation in study quality precludes a detailed sensitivity analysis by quality. Yet it is striking that the highest quality study,169 and the only randomised controlled trial, did not find a significant increase in identification.
Strengths and limitations
By extending to proxy outcomes it was possible to explore the potential benefit of system-based screening interventions. For those studies where no statistical analysis was given, we calculated 95% confidence intervals for differences in the proportions if absolute numbers were reported, thus allowing some assessment of the precision of the comparisons reported by the authors. The USPSTF quality appraisal criteria were used to rate the primary studies. This not only gives us a measure of internal and external validity, but also the strength of evidence of the studies as a whole. This review fulfils the relevant QUORUM reporting criteria (see Appendix 11.6 for QUORUM checklist and flowchart).
Limitations are twofold, those arising from our review and those related to the primary studies. Excluded studies included those that only measured identification; it may well be that an intervention could have excellent efficacy in increasing detection rates, or improving the rapport and communication skills of staff, which improves patient disclosure. However, identification is a necessary but not sufficient condition of improved outcomes for women, and the additional activity inclusion criterion brings it further along a causal pathway towards patient benefit. Limitations of some of the primary studies include incomplete reporting of outcome data (as a result we could not construct a funnel plot to test for publication bias), no statistical analysis and poor reporting of the intervention. No reporting of adherence to screening protocols limits the interpretation of identification rates. These study limitations weaken overall findings and ultimately reduce the strength of evidence of these primary studies. The main limitations arising from the primary studies are failure to measure or lack of power to detect actual morbidity (in the case of the study by Thompson and colleagues169) and the generally weak study designs.
Discussion
Despite the finding that interventions in primary care settings produced overall a trend for increased identification and other activities aimed at reducing morbidity and mortality, there is insufficient evidence of effectiveness. The most methodologically robust study showed least effect on identification rates.
Chapter 9 Is screening for partner violence acceptable to health-care professionals? (Question VI)
Qualitative studies
We identified 10 journal articles and one UK Home Office report reporting the attitudes of health-care professionals towards screening for partner violence. For details of study design and quality scores see Appendix 9.1. Four studies were conducted in the USA, three in the UK, two in Sweden, one in Australia and one in New Zealand. There are six studies exploring midwives’ attitudes, one about nurses, two about physicians, one about nurses and mental health service providers, and one about a range of professionals. The total number of recruited health-care professionals was 446, ranging between 8 and 124 per study. The methodological quality score assessed by CASP was between 19 and 37, with most of the studies scoring more than 31.
First-order constructs
We identified 12 first-order constructs concerning health-care professionals’ views about partner violence screening. There were variations between studies regarding the first-order constructs but there were no systematic differences in relation to country or health-care setting.
Edin and Högberg found that the idea of asking all pregnant women questions about abuse, as is done with respect to smoking and alcohol, was acceptable to almost all the midwives they interviewed. 175 Stenson and colleagues also found that health-care professionals generally consider routine questioning about partner violence acceptable. A typical statement from their informants: ‘Regarding certain questions, routine is very important; to raise them at this point in time because then you know it will get done’. 176
It was felt that all health professionals need to be aware of the issues involved and share responsibility for detecting partner violence and supporting the women concerned. 177,178 Screening was seen as an expression of wanting to make a difference to the social issue of partner violence. 179
Edin and Högberg reported that one justification for screening expressed by their midwife informants was that asking every pregnant woman in their antenatal clinics questions about abuse ‘would play down the issue; no one would need to feel singled out when confronted with a sensitive question’. 175
Some accident and emergency staff thought that asking all women about abuse was an indication of good care. 180
Timing of screening was considered important by informants. Screening during routine medical intake, such as during the triage process, was considered inappropriate. 120 Concerns were raised about patients with a range of conditions: drug and alcohol intoxication, acute psychosis, active labour, stroke, heart attack or other acute conditions. These groups might be unable to respond appropriately to screening or their priority is immediate medical management. 181 The informants of Edin and Högberg suggested the issue could be brought up during the first antenatal visit of the women or at a later visit. 175 In the study by Stenson and colleagues, midwives did not perceive questions about violence as being more delicate than many other questions that are ordinarily asked in antenatal care. 176 Others said that ‘they did not feel it to be a problem to ask, although they reported different situations when they found questioning about abuse inappropriate’. Although different opinions were expressed regarding screening, some midwives suggested the use of routine questions; other informants preferred including asking as part of an ordinary conversation, because of the threat questions might pose to the integrity of the woman. 175
In general, informants felt there should be a dedicated health-care professional or paraprofessional assigned to do the screening120 or they believed the screening could be handled more appropriately by somebody else in a different department (‘Nurses asked why physicians do not screen, nurses suggested that the question be asked once a patient is transferred to the Women & Infants unit, and the emergency department staff questioned the practice of screening patients who are in a medical crisis.’). 175
Time constraints and poor infrastructure of the working environment were identified as major obstacles by most informants. A female physician stated: ‘It’s irresponsible for us to initiate screening if we don’t have the staff and resources. Can we appropriately direct them and meet their needs?’120 Staff requested greater feedback on whether screening provided any real benefit to patients (i.e. ‘Is there positive feedback on anyone we have helped or from referral sources?’). 181 When health-care professionals were not trained in responding to disclosure they were concerned about encouraging women to talk about abuse. Clinical staff in an accident and emergency department mentioned that the department did not provide patient follow-up and they did not want to initiate a process that they were neither able to complete nor felt certain would be completed elsewhere in the hospital. 180
Some informants noted that ‘there is no data on how effective asking is’,181 and this appeared to be a major reason for those informants who did not find screening by health-care professionals acceptable.
Fear of offending caregivers (when women attended with their children) and patients was also a recurrent theme from nurse and physician informants. 120,176 In a study by Hindin the importance of the relationship with women was reported by all midwives as one of the foundations of their professional practice. 182 The informants said that they did feel able to discuss a range of sensitive subjects with women because they gave time to listen to the women.
Midwives emphasised the importance of seeing the woman without her partner when screening for partner violence or if there was a known history of partner violence. 176,177,183
Some midwives expressed frustration about the perceived passivity of many women in the face of partner violence and their apparent inability to seek help or leave the abusive relationship. 177 Some informants also were sceptical about getting an ‘honest’ response to screening questions. 175
Second-order constructs
The second-order constructs representing authors’ interpretations are presented below.
-
Uncertainty about the appropriateness and value of screening for some patient presentations and in some clinical settings.
-
Range of opinion on which health-care professionals should screen for partner violence.
-
Inadequate health-care professional expertise resulting in feelings of frustration.
-
Concerns about time and increased workload associated with screening.
-
Concerns about screening increasing vulnerability to abuse and violence to the woman and potentially to the health-care professional.
-
Concerns about the effectiveness of screening in terms of improved outcomes for women.
-
Potential to stigmatise women as a result of screening for partner violence.
-
The importance of a good relationship between health-care professionals and women as a context for screening.
The second-order constructs were generally supported by the first-order constructs in all studies.
Contradictions between studies
Although most of the informants thought it was the responsibility of health-care professionals to screen for partner violence, some midwives remained anxious and sceptical about screening women for abuse. 177 In the study by Minsky-Kelly et al. ,181 informants expressed frustration over being required to screen all patients, feeling that ‘no one across the country ... is doing this’. They further questioned, ‘How much responsibility do I own to save the world?’. Many participants found screening for partner violence to be a disconcerting experience, arousing feelings of discomfort and embarrassment. 179 When they felt that screening was not having an impact, there was a sense of hopelessness in the face of what seemed like an insurmountable problem.
Informants in some studies expressed the view that screening for partner violence indicates openness of the health-care professional towards the problem, but Loughlin and colleagues found that clinical staff in an accident and emergency department were concerned that a screening protocol might have a negative impact on the public’s perception of the department. 180
Quantitative studies
Twenty papers reporting 20 studies fulfilled our inclusion criteria (see Appendix 9.2 for characteristics of included studies). Eleven studies were conducted in the USA, five in the UK, one in Pakistan, one in Kuwait, one in Northern Ireland and one in Belgium. Two studies were self-report postal questionnaires, one was an online self-report questionnaire, and the others were based on face-to-face interviews or self-completed questionnaires. There were seven studies of physician attitudes, four of midwives, one of nurses, one of medical students, one of midwife students, and six including different types of health-care professionals. Response rates were between 17% and 100%, and the number of recruited health-care professionals ranged between 27 and 976, with a total of 4553 respondents. The quality score assessed by STROBE was between 11 and 19, with most of the studies scoring more than 15. There was a wide range of acceptability of partner violence screening among health-care professionals, from 15% to 95%. Results and quality scores are detailed in Appendix 9.3.
Bair-Merritt and colleagues184 assessed residents’ views of partner violence screening in a postal questionnaire survey sent to all civilian paediatric residency programmes in the USA, with a 68% response rate. Ninety-three percent of chief residents felt that paediatricians should screen for partner violence. Seventy-one percent of respondents felt that their training was not sufficient to make them comfortable performing this screening.
Bair-Merritt and colleagues185 surveyed 151 clinicians in a US urban paediatric emergency department. Sixty-five percent agreed that they should screen for partner violence. Age, gender and role in the emergency department did not affect opinions about screening.
Baig and colleagues186 surveyed 167 residents across six primary care (internal medicine, obstetrics and gynaecology, paediatrics, family medicine, emergency medicine and combined medicine/paediatrics) residency programmes in a US hospital. Ninety-five percent of respondents thought partner violence screening was ‘important’. Resident characteristics, such as gender, year in residency and personal history of abuse, were not independently associated with importance placed on screening or on stated intention to screen for partner violence. Residents who managed a survivor of partner violence were more likely to report that screening was very important than those who had never taken care of a partner violence victim. In multivariate logistic regressions, emergency medicine residents were less likely than other residents to consider that partner violence screening was important. Some paediatric residents did not screen because of privacy concerns and thus may miss partner violence among their adolescent patients. Residents reported lack of time, personal discomfort and forgetting to ask as personal barriers to partner violence screening. Although residents cited lack of or poor training in partner violence as a barrier, training in residency was not independently associated with priority placed on screening or on stated intention to screen.
Baird187 surveyed 29 preregistration midwifery students about their views on routine enquiry about partner violence. Fifty-two percent of respondents felt it was the midwife’s role routinely to inquire about partner violence, 38% were unsure, whereas 10% felt there was no role for the midwife. Sixty-eight percent thought that women may be offended if asked about partner violence by a midwife.
Barnett188 surveyed midwives in Scotland about their attitudes towards routine enquiry. One hundred and thirty-two midwives responded. Sixty-six percent of midwives thought that they should ask women about partner violence, 27% were unconvinced and 7% believed that it was inappropriate. The majority said that it should be a multidisciplinary task with general practitioners and health visitors (who would know the whole family) asking routinely about partner violence. Ninety-two percent felt strongly that robust referral systems should be in place before they asked women about partner violence and feared that if this was not the case then questioning could in fact make a woman’s situation worse.
Ellis,189 in a survey of nurses in an emergency department in the USA, elicited 40 responses. Although 88% of the respondents had attended in-service training on partner violence, only 53% felt that nurses should screen all women for partner violence.
Fikree and colleagues190 surveyed a stratified random sample of 100 obstetricians in Pakistan. Almost half of the respondents were favourably inclined towards routinely screening patients. Among the three categories of obstetricians interviewed, junior obstetricians (59%) were more likely to be favourably inclined towards routine screening compared with either senior (42%) or trainee (43%) obstetricians. Reasons articulated by those obstetricians who did not consider routine screening important included no solution to the problem (30%), enquiry was an invasion of privacy (19%), and insufficient time to inquire (9%).
In a survey of 27 primary care attending physicians in two US hospitals, Friedman and colleagues110 found that one-third believed that physical abuse and sexual abuse questions should be asked routinely.
Goff and colleagues191 surveyed 541 physicians, general dentists and nurse practitioners in one town in Texas, with a 34% response rate. Twenty-nine percent of the health-care professionals believed that they did not see enough survivors of partner violence to do screening, 29% believed they should screen in the presence of non-specific complaints, 22% believed they should screen if patients present with a physical injury, 20% believed all women should be screened, and 2% believed a women should be asked once about abuse, during her first consultation.
Lazenbatt and colleagues192 surveyed all midwives in Northern Ireland, eliciting a response rate of 57%. Fifty-three percent of respondents thought that every pregnant woman should be screened for partner violence. When midwives were asked if they had ever raised the issue of partner violence with a client, only 28% had done so.
Nayak193 surveyed medical students at a Kuwait university. Of the 106 respondents, 93% felt that training in issues related to interpersonal violence is necessary, but only 25% agreed that patients should be routinely assessed for a history of victimisation.
Nicolaidis and colleagues194 surveyed 278 health-care professionals from 31 US family practices. Sixty-two percent had prior partner violence training. The majority agreed that it is the primary care provider’s responsibility to ask about partner violence when seeing patients for health maintenance visits (66%), chronic pain (56%) or injuries (62%). Fifteen percent agreed with screening for partner violence at every visit.
Price and Baird195 sent a questionnaire to all midwives in an acute trust in the UK. Fourteen percent of the respondents did not believe it was the role of health-care professionals to screen at all, with 39% stating that routine screening should not occur within professional practice. When asked who should screen, a wide range of responses was given, from ‘any one who is in contact with women to specialists’. A large majority of hospital-based midwives felt that it was the responsibility of the primary health-care team, specifically naming relevant individuals or by responses such as ‘any health professional that has an ongoing relationship with the woman, i.e. a community midwife’.
Richardson and colleagues196 surveyed general practitioners, practice nurses and health visitors in one London health authority. Among the 401 respondents, 32% thought that health visitors should routinely ask about partner violence, 15% thought this for practice nurses, and 14% for general practitioners. Practice nurses were significantly less likely than health visitors or general practitioners to think that routine enquiry about partner violence should take place (odds ratio 0.46, 95% confidence interval 0.27–0.77, p = 0.003). Other predictor variables were not significant in a multivariable regression model.
Roelens and colleagues197 surveyed 289 board-certified obstetrician-gynaecologists in Flanders, Belgium, with a 52% response rate. Seventy percent disagreed with universal screening of women patients and 81% disagreed with screening women once each trimester of pregnancy.
Salmon and colleagues,198 in an evaluation of an educational programme on midwives’ knowledge, skills, attitudes and implementation of routine antenatal enquiry for partner violence, surveyed 70 community midwives in one acute trust. At baseline 89% agreed with a statement that screening for partner violence was important, rising to 98% after the programme.
Shye and colleagues199 surveyed 203 primary care clinicians in a health maintenance organisation in north-western USA, finding that 75% would prefer routinely to ask patients at health maintenance visits, 8% would prefer to ask only women who are at high risk, 15% would let the clinician decide who to ask, and 2% percent would let the woman bring the subject up herself.
Synthesis
There was heterogeneity in the results of qualitative and survey studies about the acceptability to health-care professionals of partner violence screening. In the surveys, acceptability ranged between 15% and 95% of respondents.
Across the surveys, a higher proportion of physicians were in favour of screening compared with midwives, who raised different concerns and reported frustration regarding partner violence screening. Nevertheless, there was considerable heterogeneity within professions, including midwives. Acceptability of screening was generally lower outside the USA, although there was considerable variation among US health-care professionals in different surveys. There was no consistent association between type of health-care setting and acceptability, with the exception of paediatric emergency and ambulatory care, in which a large majority of clinicians were in favor of screening caregivers.
Findings from the qualitative studies showed that some informants thought screening was important but should be carried out by another health-care professional, and these findings were reinforced by the surveys. For example, midwives identified general practitioners and health visitors as being well placed to screen for partner violence. 188 Other health-care professionals felt there should be a dedicated professional or paraprofessional assigned to do the screening,120 or they believed the screening could be handled more appropriately by somebody else in a different department. 175
Those studies that measured respondents’ personal characteristics, such as gender, age and personal history of abuse, and tested their association with acceptability of screening generally found that they were not independently associated. 117,185,186 However, Baig and colleagues186 found that physicians who had managed survivors of partner violence were more likely to state that partner violence screening was very important.
In sensitivity analyses excluding the poorer quality studies, as assessed by STROBE for quantitative studies and the CASP criteria for qualitative studies, we did not find a relationship between study quality and the findings on the acceptability of screening. We also scrutinised the reported survey data to determine whether there was a relationship between survey response rates and the acceptability of screening, but found none even when studies were stratified by type of health professional (see Appendix 9.4).
Strengths and limitations
Strengths of this review include the synthesising of qualitative and quantitative studies to answer this question, the quality appraisal of studies (using the STROBE checklist for quantitative studies and the CASP tool for the qualitative studies) and the performance of a sensitivity analysis. This review fulfils the relevant QUORUM reporting criteria (see Appendix 11.7 for QUORUM checklist and flowchart). Health professional-related variables, demographic features and features relating to the screening process were examined to assess how they interact to increase or decrease the acceptability of screening by health-care professionals. A limitation is that the attitudes of male members of the public towards screening were not examined. Many of the response rates in the quantitative studies were generally less than 70% and often less than 50%. This is a limitation because it implies that the acceptability rates may well be inflated, as non-respondents are less likely to consider partner violence an important clinical issue and would be less likely to consider screening acceptable.
Discussion
There is a wider variation in the acceptability of partner violence screening among health-care professionals than among women (see Chapter 6), with many surveys showing that a majority of clinicians do not find it acceptable. Although we do not report the data here, those studies that also measured screening behaviour found an even smaller proportion of health-care professionals performing screening, even in the USA where this is policy in many health-care settings. There is scepticism about the benefit of screening and, again in contrast to the views of women, little mention of potential benefits beyond eliciting disclosure. From the qualitative studies we learn that, even when health-care professionals find screening acceptable, they are wary of implementation without training and possibly additional resources to deal with referrals after disclosure. The findings of surveys of clinicians internationally and in the UK and of the qualitative studies mean that the criterion of acceptability of partner violence screening in health-care settings is not fulfilled.
Chapter 10 Is screening for partner violence cost-effective? (Question VII)
In this chapter we investigate whether screening for partner violence in any health-care settings is cost-effective. First, we conducted a systematic review of the primary studies that reported the cost-effectiveness of partner violence screening. Second, a cost-effectiveness model was constructed based on a pilot trial of a system-based intervention to implement routine enquiry about partner violence in a primary care setting.
Systematic review of cost-consequence and cost-effectiveness studies
The search for economic analyses of screening interventions in health-care settings for partner violence retrieved nine potentially eligible papers detailing eight studies published between 1986 and 2005. All studies were sited in the USA. None of these studies fulfilled our inclusion criteria.
Six studies did not evaluate two alternative interventions; they simply measured costs of assault and homicide within families,200 hospital charges associated with partner violence,201 and costs of correct and false detection of partner violence. 202 The other three papers described the costs associated with resource utilisation by survivors of partner violence compared with women who have never experienced it. 203–205
Clark and colleagues206 performed a cost–benefit analysis on the implementation of the Violence against Women Act (VAWA) of 1994, suggesting that the benefit of the VAWA outweighs implementation costs from a societal viewpoint in the USA. However, the results of this analysis cannot inform the question whether screening programmes in health-care settings are cost-effective.
Two articles from Domino and colleagues reported the results from the Women, Co-occurring Disorders, and Violence Study (WCDVS), a multicentre, non-randomised trial comparing an integrated counselling and advocacy service with usual services as control. 207,208 The study recruited women with a mental health or substance abuse diagnosis and a co-occurring history of physical or sexual abuse. Follow-up of the women took place at 6 and 12 months. Screening for and detection of partner violence was not part of the study protocol, however, and the analyses therefore do not address the research question for this review. In spite of this, the study can serve as an indication of the effectiveness and costs of a partner violence intervention. For the population of 2026 women in the study, the intervention of integrated counselling and advocacy was likely to be cost-effective when compared with usual care.
The analysis was based on changes in four clinical outcome measures: the Addiction Severity Index drug and alcohol composite scores (ASI-D and ASI-A), the Global Severity Index (GSI) and the Post-traumatic Stress Disorder Symptom Scale (PSS). The analysis at the 6-month follow-up207 evaluated the cost from a Medicaid perspective, which included service delivery costs, as well as a societal perspective, which also comprised additional costs to service such as housing schemes and crime-related costs.
At the 12-month follow-up,208 costs were evaluated from a societal perspective, which included service delivery plus participants’ costs for time and transportation. Clinical outcomes were reported to be in favour of the intervention, and incremental cost-effectiveness ratios (ICERs) were presented per unit improvement on each of the four clinical outcome measures. Quality-adjusted life-years (QALYs) were not calculated. ICERs ranged from $123 to $12,227, and bootstrapped confidence intervals included 0, which was interpreted as uncertainty that incremental costs or savings are achieved. These results have to be viewed in the light of usual care containing a structured counselling intervention already, which partly explains similarities in treatment costs in both arms. Generalisations to other populations and countries would therefore strongly depend on existing usual care provisions, although it is likely that a similar intervention in an NHS context would also be cost-effective if the clinical outcomes were comparable. What Domino and colleagues have not demonstrated, however, is that screening in a health-care setting can be cost-effective.
Cost-effectiveness model of PreDoVe: a pilot trial of a primary care-based system-level intervention to improve identification and referral of women experiencing partner violence
The pilot study investigated a general practice-based intervention in the UK and tested the feasibility of this intervention in four general practices (three acting as an intervention and one as a control). The multifaceted, system-based intervention aimed to change the behaviour of clinicians towards women experiencing partner violence, and was designed to increase routine enquiry about partner violence and thereby disclosure of current partner violence. Following disclosure, clinicians were prompted to refer women to an advocate based in a domestic violence specialist agency or to a psychologist with specific training related to partner violence. The system-based intervention included initial educational sessions for all clinicians within the practice, which emphasised a pragmatic approach to enquiry and referral and also gave an overview of the wider community response. The referral component of the intervention was supported by a direct referral pathway to a domestic violence advocate and a psychologist, both of whom were involved in the initial training. In addition, prompts in the electronic medical record were used to probe for partner violence during routine consultations based on a four-item screening tool termed HARK (an acronym based on the dimensions of abuse, i.e. Humiliation, Afraid, Rape and Kick) linked to a range of coded diagnoses such as depression, insomnia, sexually transmitted infections and fatigue. 209 The HARK questions and a prompt to refer women to the advocate or psychologist were installed as a template onto the electronic medical record in the practices. Although the aim of the intervention was not a comprehensive screening programme for all women, it aimed to implement screening or routine enquiry for women presenting with other problems. We maintain that an economic analysis of this intervention is relevant to the question of whether screening for domestic violence could be cost-effective.
Model
A Markov model was developed to combine the intervention costs and benefits. It was fitted comparing the PreDoVe programme with usual care and used the differences between the two simulations to calculate the incremental net benefit. The model evaluated the impact of increased assessment and referral rates upon further violence and quality of life over a 10-year period. Partner violence affects several public services as women experiencing such violence come into contact with, for example, local authority housing departments and social services. Women experiencing violence who come into contact with the criminal justice system are now routinely recorded. Taking a societal perspective permitted a wide range of data from sources to be incorporated into the model. See Appendix 10.1 for summary of data sources for the model.
The model defines six health states in which women can find themselves (Figure 3). Following assessment, women experiencing partner violence can (1) remain unidentified, or are (2) identified and subsequently referred and treated, or (3) identified but decline referral to advocacy or psychology services. Women who receive treatment following disclosure during assessment can (4) drop out without improvement, or (5) enter a state of medium-term improvement where they can stay or move to the no-abuse or identified/untreated state. Women can also (6) die of non-related causes or specifically from partner violence. The transition probabilities for movement between these states were taken from the literature or in discussion with partner violence researchers. See Appendix 10.2 for details of transition probabilities. The average length of time a woman remains in contact with advocacy services is 6 months, and therefore the model cycle length was set to 6 months with a time horizon of 10 years. Following the approach suggested by the National Institute for Health and Clinical Excellence (NICE), we discounted both costs and outcomes at 3.5% per annum. The reason for this is that it is the approach most commonly taken in UK cost-effectiveness analyses, facilitating comparison of our results with other studies.
FIGURE 3.
Diagram of Markov model states of PreDoVe intervention.
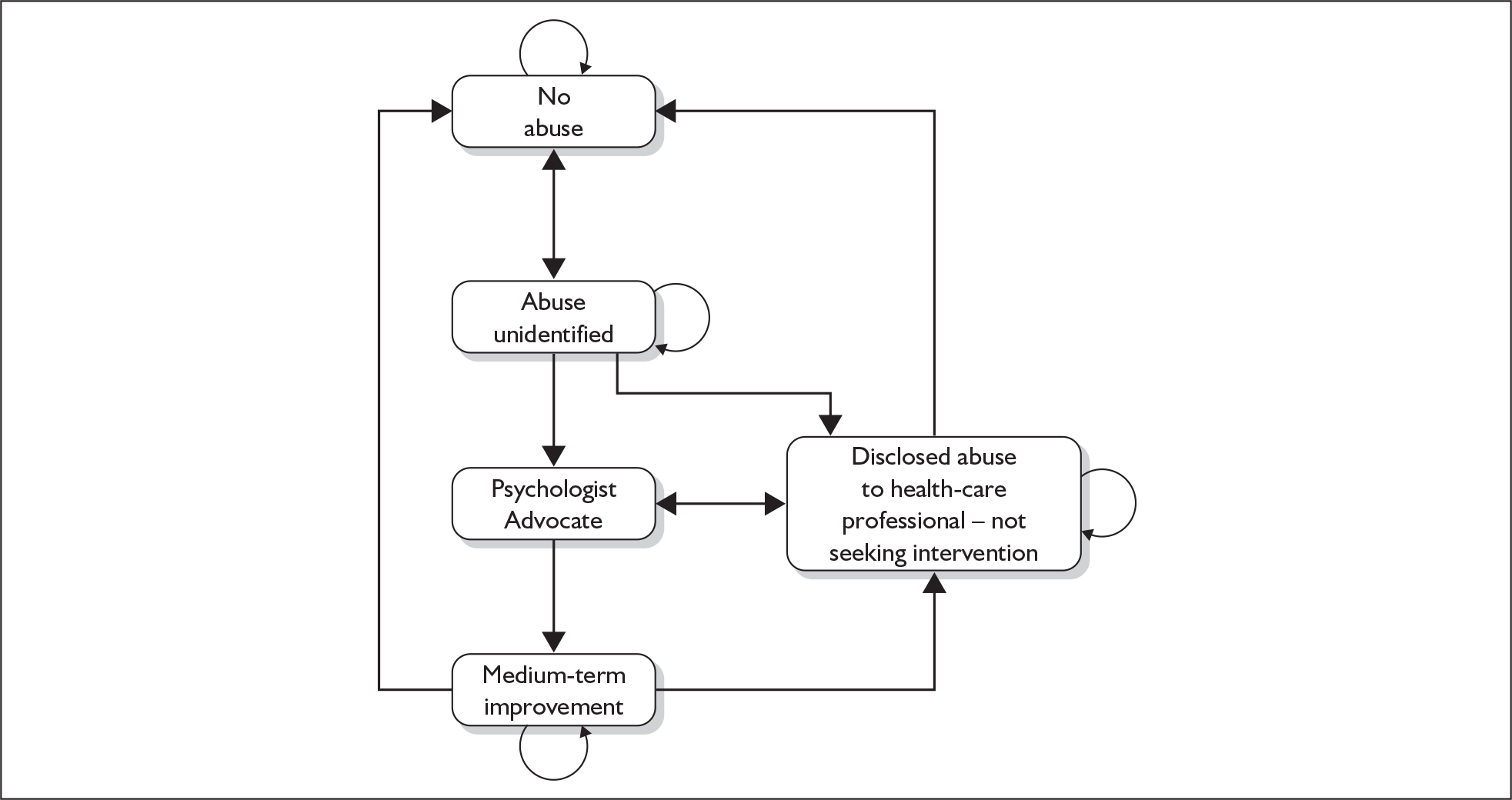
Costs associated with advocacy and/or psychological interventions were collated for each woman in the PreDoVe pilot trial, and averaged across all women in the arm. These directly recorded pilot data were used to populate the model with the number of women attending the practices, the number who were asked about partner violence by GPs or practice nurses, the number of women disclosing partner violence, the number of subsequent referrals to the advocate or psychologist, and the number of women who declined to take up the referral to these services.
Simplifying assumptions about current abuse incidence included: 16 years as a woman’s minimum age for first experiencing partner violence; a lifetime prevalence of 40%; and that moving to a state of abuse occurs at a constant rate over a woman’s lifetime. Assessment rates at intervention and control practices were assumed to be 10.7% of abused women and 7.1% of non-abused women, based on actual rates of asking and extrapolation from the prevalence of partner violence found in east London general practices.
Costs comprised health-care use in terms of assessment, mental health and treatment costs as well as other social costs. Social costs included criminal justice costs, civil justice costs and cost of divorce involving children, societal employment loss, temporary housing costs and costs of social services.
Quality of life was based on survey data using the Short Form 12 (SF-12) measurement tool. SF-12 data were converted into quality of life utilities between 0 (equivalent to death) and 1 (equivalent to optimal health) for those with less severe and more severe violence, based on the US study by Wittenberg and colleagues. 272 See Appendix 10.3 for a summary of treatment cost sources, and Appendix 10.4 for other costs and QALYs per woman per year for each state.
The majority of women in the model are likely to be in ‘No abuse’ (State 1) although a flow of women will become ‘Abuse unidentified’ (State 2). Following assessment, women experiencing partner violence can remain unidentified (State 2), or be referred to a psychologist and/or advocate (States 3 and 4), or disclose abuse to a health-care professional but not be seeking intervention (State 5). If the psychologist and/or advocate intervention is successful, the women can be termed as ‘Medium-term improvement’ (State 6) and, if this does not worsen, can return to the ‘No abuse’ category.
Results
Univariate sensitivity analysis was carried out, and model parameters were both increased and decreased by 25%, unless these figures were internally invalid (such as if probabilities were less than zero or greater than one). For transition probabilities for which the intervention was assumed to be preferable to the control, the sensitivity analysis was constrained to assume the transition probabilities were at worst equal. In addition, the sensitivity analysis used an upper and lower confidence interval for the impact of abuse on health.
Combining net benefits and net costs in the model resulted in an incremental cost-effectiveness ratio (ICER) of £2450 per QALY. This result would be considered cost-effective had a service use perspective been applied under the implicit willingness-to-pay threshold applied by NICE. Including costs from a societal perspective will result in lower costs per QALY. The estimated cost-effectiveness was most sensitive to women taking up an intervention and the success of these interventions ‘downstream’ from disclosure to a health-care professional (in PreDoVe this entailed partner violence advocacy and a psychological intervention), and to the likelihood that medium-term improvement will continue into living outside of an abusive relationship. Most ICERs did not increase above £5000 per QALY and only one was greater than the £30,000 notional threshold for cost-effectiveness in the UK. For details of the sensitivity analysis results, see Appendix 10.5.
We have made a number of simplifying assumptions in our model that could be addressed with more research. We considered the possibility that women may relapse into an abusive relationship, but we did not capture the fact that women with past histories of partner violence have a greater likelihood of entering into another abusive relationship. We also did not differentiate between women in a relatively new abusive relationship and those in longer-standing relationships or long-term harassment after they have left an abusive relationship. The latter group may take longer to change their situation. Our model draws upon the available evidence for the effect of partner violence programmes but these studies are based upon different populations and this may affect the accuracy of our findings. For instance, the main intervention effects were based on data from the PreDoVe pilot trial, based in inner city general practices with multiethnic, relatively deprived populations in the UK. The population targeted in PreDoVe were patients in primary care, and the majority of referrals were women who had not previously disclosed abuse. By contrast, our estimate of effect of advocacy came from a US study126 focused on a refuge population who had already self-identified and sought help, not necessarily in the context of health care. There is considerable uncertainty regarding both the modelling of partner violence, and the costs and quality of life for the women involved.
A limitation of the model for estimating the cost-effectiveness of screening is that the intervention was aimed at implementing routine enquiry of women presenting with a range of specific conditions, rather than a comprehensive screening programme within a health-care setting.
Discussion
In our review we were unable to identify any studies that tested the cost-effectiveness of screening women in health-care settings for partner violence. We did find a study that calculated the costs and service use for women with co-occurring mental health and substance abuse disorders who were survivors of partner violence and taking part in an intervention programme. Overall costs were the same for women within and without the programme and clinical outcomes were improved, which suggests that the intervention was cost-effective. Our cost-effectiveness model of a pilot trial of a primary care intervention that resulted in increased enquiry about partner violence by clinicians supports the hypothesis that this type of intervention could be cost-effective.
Chapter 11 Conclusions of the reviews and implications for health care
On the basis of our review findings, we believe that the NSC criteria are not fulfilled for a policy of screening women in health-care settings for partner violence. The main unmet criterion is evidence of improved morbidity and mortality from screening programmes (Question V). Notwithstanding the poor methodological quality of most studies of screening interventions, there is a trend for increased identification and referral to partner violence advocacy services. However, the strength of this evidence is insufficient as there is only one randomised controlled trial of a screening intervention showing a limited impact on the identification of partner violence. More importantly, there is no robust evidence that screening for partner violence has any direct benefits in terms of reducing levels of abuse or in improving the physical and psychological health of abused women. A further gap in the evidence base is that none of the screening studies has measured whether screening is associated with an increase in potential harm for abused women. Those that measured health outcomes for women, such as the cluster randomised controlled trial of Thompson and colleagues,169 would have been able to detect harm if the participants in the control group had better outcomes than those in the intervention group, but would not have been able to detect adverse events that were not outcome measures. We do know that two of the intervention studies (Question IV) found increases in bodily pain in treatment arms, although this may have been a temporary state, and arguably part of the therapeutic process. 210 The question of potential harm from a screening programme was also raised by survivors of partner violence in interview and focus group studies reported in Chapter 6, although the breaches in confidentiality they were particularly concerned about are not specific to screening. The risk of breaches of confidence should be negligible if health-care professionals have adequate training in appropriate and safe responses to disclosure of partner violence. 211 Health-care professionals also were concerned about adverse effects of screening, although the worry about offending patients raised in some of the studies reviewed in Chapter 9 was not confirmed by the survivors participating in the interviews and focus group studies or the surveys.
To what extent are the NSC criteria fulfilled?
NSC criterion 1, that the condition should be an important health problem, is met. Abuse of women by their partners or ex-partners is widespread internationally212 and there is no longer any debate about the large public health impact of partner violence, although prevalence rates and the magnitude of health sequelae vary depending on population and study design. However, even based on the lower estimates for prevalence, morbidity and mortality, it is clear that partner violence is a potentially appropriate condition for screening and intervention.
A variety of partner violence screening tools are available, ranging from single-question tools to 30-item research inventories. We limited our review to screening tools comprising 12 items or less, for ease of administration in busy health-care environments. NSC criterion 5 states that the screening test should be simple, safe, precise and validated, the distribution of test values in the target population should be known, and a suitable cut-off level defined and agreed. We reviewed the diagnostic accuracy of 12 screening tools, none of which had been evaluated in terms of the subsequent safety of women following their administration. Overall, the 4-item HITS (Hurts, Insults, Threatens and Screams) screening tool demonstrates the best predictive power, concurrent and construct validity and reliability, with a suitable cut-off score. It fulfils the NSC criterion and could be used to screen for partner violence in a variety of health-care settings. However, it does not ask about sexual abuse or ongoing violence, and so it may need to be administered alongside another screening tool to detect these forms of abuse. Alternative short screening tools, such as the WAST and the AAS, perform almost as well as the HITS in the health-care settings in which they were tested. The North American context of diagnostic accuracy studies of screening tools requires extrapolation of these findings to the NHS, but there is no a priori reason why the tools should perform substantially worse in a UK setting.
NSC criterion 7 is that the screening test should be acceptable to the population. We therefore evaluated both the quantitative and qualitative evidence eliciting the views of women. In general, the evidence from the survey studies of women patients in health-care settings shows that most agree with screening or being asked routinely about partner violence. However, from the qualitative studies, it is also clear that women perceive the purpose of screening as lying outside the public health screening framework and differently from health-care professionals. On the whole, health-care professionals see screening as a method for obtaining disclosure of abuse, which then leads to appropriate care being offered. By contrast, women tend to view screening as a method of raising awareness rather than eliciting disclosure of abuse. Thus, even though abused women may not disclose immediately, screening may facilitate later disclosure when the women feel more comfortable with the health-care professional, or when their circumstances change and they feel the need to get help. This has implications for health service policy in relation to screening and the training of health-care professionals in relation to partner violence, as we discuss further below. Although only 2 out of the 18 surveys were based in UK populations, their results are consistent with the range of opinion in the totality of studies.
NSC criterion 10 is that there should be an effective intervention for patients identified through early detection, with evidence of early treatment leading to better outcomes than late treatment. Further, the benefit from the screening programme should outweigh the physical and psychological harm caused by the test, diagnostic procedures and treatment. We reviewed studies that have evaluated the effectiveness of interventions for women who have disclosed abuse, including evidence from an increasing number of randomised controlled trials. Most were targeted at women who had already disclosed abuse, many from refuge populations, so extrapolation to women identified through screening is problematic. None of the studies tested whether early detection of partner violence leads to better outcomes. The evidence of effectiveness of advocacy interventions is growing, although using the USPSTF criteria for sufficiency of evidence for policy, it is on the borderline between insufficient and sufficient. As we discuss in Chapter 7, this is probably too conservative a judgment. On the whole, well-designed studies show improvements in outcomes for women receiving advocacy, but the evidence is strongest for women who have actively sought help or are already in a refuge. This evidence has informed UK central government funding of specialist independent domestic violence advocates (IDVAs) attached to both statutory and voluntary agencies. The only studies of advocacy interventions in women identified through screening in health-care services were based in antenatal clinics. 121,131–133 The evidence for individual psychological interventions is sufficient according to the USPSTF criteria, but this is based on only three studies and, more so than the advocacy studies, the interventions are very heterogeneous. The evidence for group psychological interventions and that for mother and child programmes is insufficient as a basis for policy. Overall, considering all types of interventions that women might be offered following disclosure, there is still uncertainty about their effectiveness. However, there is little evidence that they are ineffective. As none of the controlled studies of interventions was based in the UK, the uncertainty about their effectiveness within the NHS is even greater.
This question addresses NSC criterion 13, that there must be evidence from high-quality randomised controlled trials that the screening programme is effective in reducing mortality or morbidity. We extended the review to include proxy outcomes for improved morbidity and mortality, particularly referral to partner violence advocacy and other community support agencies following screening. We found no studies that directly measured morbidity and mortality. Although most of the studies measuring proxies showed improvements in these outcomes, study design and execution were generally poor. The most robust study methodologically showed the least effect on identification rates. There was no measurement of potential harms of screening, although these were raised by women and health-care professionals in the qualitative studies. Criterion 13 remains unfulfilled. As none of the studies was based in the UK, this is even more the case for NHS policy than it is for US health-care policy.
To fulfil the NSC criterion 14, there has to be evidence that the complete screening programme (test, diagnostic procedures, treatment/intervention) is clinically, socially and ethically acceptable to health professionals. We reviewed quantitative and qualitative studies of acceptability to clinicians. There was heterogeneity in the findings of qualitative and survey studies about the acceptability to health-care professionals of partner violence screening, but overall the evidence shows that this NSC criterion is not met. This contrasts with the surveys of women, which reported largely positive views of screening in health-care settings. The surveys of health-care professionals reported that a majority of clinicians do not find a screening programme to be acceptable, although the proportion of respondents who thought it acceptable ranged between 15% and 95%. The qualitative studies tended to report more positive views of screening from health-care professionals. However, even when clinicians think that there should be screening for partner violence, some held the view that it is other groups of health-care professionals who should be carrying out the screening. The qualitative studies also demonstrate that positive attitudes towards screening are tempered by a wariness of implementation without training and the possible need for additional resources to deal with referrals after disclosure. Although only 5 out of 20 surveys of health-care professionals were conducted among UK populations, the results of these were consistent with the range of opinion in the totality of surveys.
This question addressed NSC criterion 16, that the cost of the screening programme (including testing, diagnosis, treatment, administration, training and quality assurance) should be economically balanced in relation to expenditure on medical care as a whole (i.e. screening for partner violence should give value for money). We sought to review studies evaluating the cost-effectiveness of screening and we complemented this by modelling of costs and outcomes using data from a pilot study in primary care. We found no studies examining the cost-effectiveness of screening women for partner violence. Our cost-effectiveness model, based on pilot data, suggested that a system-level intervention in primary care that improves identification (well below the disclosure rate one might expect with a screening programme) and referral of women survivors of partner violence is likely to be cost-effective. Nevertheless, at present this NSC criterion is not fulfilled.
Strengths and limitations of this report
We have broken down a complex health-care policy issue with multiple criteria – should women be screened for partner violence in health-care settings? – into seven questions amenable to systematic review. We carried out these reviews to a high methodological standard and concluded that there was insufficient evidence to recommend screening as a policy. We have synthesised quantitative and qualitative studies for the two reviews on the views of health-care professionals and women patients respectively. Changes in our protocol included not reviewing three NSC criteria: (1) there should be an agreed policy on the further diagnostic investigation of individuals with a positive test result and on the choices available to those individuals; (2) there should be agreed evidence-based policies covering which individuals should be offered treatment; and (3) management of the condition and patient outcomes should be optimised. The criteria we reviewed are more central to a policy decision about screening, and reviews of these additional three criteria would not have changed our conclusions. We have highlighted limitations of the individual reviews in the relevant chapters. Generic limitations of all our reviews include: no hand searching for primary studies, no forward citation tracking, quality appraisal performed by one reviewer, and no funnel plots for publication bias. These additional components would not have changed the overall conclusion of our report. The main limitations of this report are the relatively small number and poor quality (or poor reporting) of primary studies and the absence of controlled studies of interventions in the UK.
Are the NSC criteria appropriate tests for a partner violence screening programme?
From our review of current research evidence, it is clear that key criteria for the effectiveness and appropriateness of a partner violence screening programme are not fulfilled, not even in antenatal clinics for which the Department of Health has a policy of ‘routine enquiry’. 213 This term is broader than ‘screening’, ranging from asking every woman patient about abuse to enquiry only in particular groups of patients. 16 Although reference to routine enquiry rather than screening seems to circumvent the NSC criteria, its implementation as policy still needs to be based on research evidence showing that it is safe and effective, which brings us back to the evidence we have reviewed here, with three notable differences.
First, the purposes of routine enquiry can include information about partner violence and signal to the patient that the clinician is a potential source of support if she discloses. Disclosure or identification is no longer the only outcome, as it is within a screening paradigm. One of the striking findings of our review is that survivors of partner violence value purposes other than identification for routine enquiry, although this view is not widely shared by the health-care professionals interviewed in the qualitative studies. Proponents of routine enquiry maintain that there are other benefits, such as reducing stigma214 about partner violence and changing prevailing social attitudes,211 although there is no compelling evidence that this is an outcome of routine enquiry. Second, routine enquiry does not require standardised screening tools, allowing a greater flexibility in how women are asked about abuse and, potentially, greater sensitivity to differences between women in how they might want to be asked. Third, there is less potential for the woman to feel pressurised to disclose abuse, as this is not the only purpose of routine enquiry. The Department of Health’s current policy of routine enquiry during pregnancy is not based on trial evidence of improved outcomes for women who are asked about abuse antenatally, although the trial by Tiwari and colleagues121 of advocacy suggests that women who do disclose abuse in pregnancy may benefit from an advocacy-based intervention, notwithstanding these differences.
Chamberlain, in her response215 to the lack of support for screening by the United States Preventive Service Task Force on intimate partner violence, concluded that the evidence criteria for a positive recommendation were too narrow and reflected a lack of understanding of the nature of partner violence by the task force. Specialists within domestic violence services highlight the dynamic nature of partner abuse and the legitimate reasons women may have for not wanting to disclose it to a particular health-care professional, with implications for any evaluation of its effectiveness. Nevertheless, if controlled evaluations of screening programmes are intrinsically problematic and the NSC criteria are flawed in relation to a problem like partner violence, we are left with the dilemma of how to judge whether a policy of screening or even routine enquiry is justified.
The debate about screening for partner violence and the shift in emphasis, at least in the UK, to routine enquiry has distracted attention from the uncontested importance of training for health-care professionals in being open to disclosure of partner violence and responding appropriately, whether they ask about abuse routinely or not. The remit of this review was the evidence for a policy of domestic violence screening, and we have not reviewed the evidence for other policy questions and recommendations.
Research questions
-
Do system-level interventions in health-care settings improve the response of health services to survivors of partner violence? Trials to answer this question may incorporate routine or selective enquiry and, potentially, could compare differences in outcomes between the two policies, although those outcomes would need to be broader than identification.
-
Do system-level interventions in health-care settings improve outcomes for women? Trials to answer this question are logistically more challenging in terms of recruitment and long-term follow-up of participants than those needed to answer research question 1.
-
Do psychological and advocacy interventions after disclosure of partner violence to health-care professionals in health-care settings – whether this is the result of screening, routine enquiry or selective enquiry – reduce violence and improve quality of life and mental health? These trials should have follow-up for years, not months, and include mental health and quality of life outcomes.
-
Study designs for research questions 2–4 need to incorporate the theoretical basis for different components of domestic violence interventions in order to enhance our understanding of how such interventions work (or do not work), for whom and in what contexts.
-
What do women want from health-care or health-care-related interventions after disclosure of partner violence? Qualitative studies would inform the design of these interventions and choice of outcome measures to evaluate them.
-
What is the ‘natural’ history of partner violence? This question includes exploring individual risk factors for survivors, factors supporting resilience of survivors and perpetrators, the trajectory of abuse across the life course, and predictors of severity and outcomes.
-
What is the long-term prognosis for survivors of partner violence after identification in health-care settings?
Research questions 6 and 7 are best addressed in cohort studies with long-term follow-up, studies that are almost absent in the field of domestic violence research.
Programmes addressing these seven research questions need to have the resources and expertise to include participants from majority and ethnic minority communities in the UK.
Listing important research questions is de rigeur for a systematic review. We believe it is almost as important to discuss research that does not need to be pursued. From this review, we conclude that the following types of study are not a priority in the UK.
-
Cross-sectional prevalence studies from antenatal clinics, accident and emergency clinics and, probably, general practice. Although there are only a few of these studies at present, more precise or generalisable estimates of prevalence will not materially inform health service policy.
-
Surveys of attitudes of health-care professionals towards partner violence, unless in the context of interventions to improve care, in which case measurement of attitudes may help to explain the results.
-
Surveys of women’s attitudes towards routine enquiry. Measuring the size of the minority of women who do not want routine enquiry about partner violence is not going to help develop policy.
We are not saying that this research should never be undertaken in the UK or funded in the future; but that in a competitive funding environment, where historically there has been little support of health-related domestic violence research, the priority should be given to the seven research questions listed above. We have found that the epidemiology of domestic violence in clinical populations in the UK is not particularly robust, but more precise measures of prevalence in different health-care settings and of health-care professional and patient attitudes towards screening is not the best use of resources while these questions remain unanswered.
Acknowledgements
We would like to thank all the investigators who responded to our queries about their studies, or to our request for additional studies, or provided us with copies of their papers: Arshiva Baig, Megan Bair-Meritt, Adrian Boyle, Petra Brzank, Cheryl Buehler, Jacqueline Campbell, M. Denise Dowd, Kerstin Edin, Prem Fry, Barbara Gerbert, Felicity Goodyear-Smith, Jeanne Hathaway, Katrina Hurley, Kim Jaffe, Ellen Jamieson, Jane Knapp, Cheryl Koopman, Alice Kramer, Harriet MacMillan, Randy Magen, Brigid McCaw, Renee McDonald, Judith McFarlane, Christina Nicolaidis, Chen Ping-Hsin, Stacey Plichta, Elizabeth Powell, Gail Robinson, Judy Rollins, Lynda Sagrestano, Debra Salmon, Daniel Saunders, Amer Shakil, Kevin Sherin, Vanja Stenius, Kristina Stenson and Robert Thompson.
We would also like to thank Marie Westwood for her guidance on the assessment of screening tools, the UK Domestic Violence and Health Research forum for their comments on our preliminary review findings, and Stephen Bremner for plotting prevalence rates and the logistic regression model in Chapter 4.
Contributions of authors
Gene Feder (professor of primary health care) designed the reviews, managed the project, supervised the analysis and edited the report. Camelia Arsene (reviewer) searched for primary studies, extracted and analysed data for Questions 3 and 6, and drafted the relevant chapters. Loraine Bacchus (research fellow, women’s health) designed the reviews and commented on results and drafts of the report. Danielle Dunne (reviewer) searched for the primary studies, extracted and analysed data for Questions 1, 3 and 4, and drafted the relevant chapters. Gill Hague (professorial research fellow, women’s health) designed the reviews and commented on results and drafts of the report. Stefanie Kuntze (health economics fellow) extracted and analysed data for the review part of Question 7 and drafted that section of the chapter. Richard Norman (health economics fellow) designed and performed the cost-effectiveness analysis in Chapter 10 and drafted that section of the chapter. Jean Ramsay (senior research fellow, primary care) designed the reviews, participated in the analysis, drafted Chapters 1, 2 and 11, and edited the report. Mark Rose (reviewer) searched for primary studies, extracted and analysed data for Questions 2 and 5, and drafted the relevant chapters. Anne Spencer (senior lecturer, health economist) designed and supervised the cost-effectiveness analysis in Chapter 10. Ann Taket (professor of primary care) designed the reviews and commented on results and on drafts of the report. Alison Warburton (senior research fellow, mental health) designed the reviews and commented on results and drafts of the report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA Programme or the Department of Health.
References
- Ramsay J, Richardson J, Carter YH, Feder G. Appraisal of evidence about screening for domestic violence n.d. www.library.nhs.uk/MENTALHEALTH.
- Ramsay J, Richardson J, Carter YH, Davidson LL, Feder G. Should health professionals screen women for domestic violence? Systematic review. BMJ 2002;325:314-18.
- Waalen J, Goodwin MM, Spitz AM, Petersen R, Saltzman LE. Screening for intimate partner violence by health care providers. Barriers and interventions. Am J Prev Med 2000;19:230-7.
- Wathen G, Macmillan H. Prevention of violence against women. Recommendation statement from the Canadian Task Force on Preventative Health Care. CMAJ 2003;69:582-4.
- Nelson HD, Nygren P, McInerney Y, Klein J. Screening women and elderly adults for family and intimate partner violence: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2004;140:387-96.
- Chalk R, King P. Violence in families: assessing prevention and treatment programs. Washington DC: National Academy Press; 1998.
- Abel EM. Psychosocial treatments for battered women: a review of empirical research. Res Social Work Prac 2000;10:55-77.
- Hender K. Is therapy/counselling/group work more effective than no treatment for women who are victims of domestic violence? Centre for Clinical Effectiveness, Evidence Report 19 2001.
- Cohn F, Salmon ME, Stobo JD. Confronting chronic neglect: the education and training of health professionals on family violence. Washington DC: National Academy Press; 2002.
- Klevens J, Sadowski L. Domestic violence towards women. Clin Evid 2005;13:2293-302.
- Ramsay J, Rivas C, Feder G. Interventions to reduce violence and promote the physical and psychosocial well-being of women who experience partner abuse: a systematic review. London: Department of Health; 2005.
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 2002;23:260-8.
- Canadian Centre for Justice Statistics . Family Violence in Canada: A Statistical Profile 2005 2005.
- UK National Screening Committee . What Is Screening? n.d. www nsc nhs uk/whatscreening/ (accessed January 2009).
- Department of Health . Domestic Violence: A Resource Manual for Health Care Professionals n.d. www.dh.gov.uk/ (accessed January 2009).
- Taket A, Nurse J, Smith K, Watson J, Shakespeare J, Lavis V, et al. Routinely asking women about domestic violence in health settings. BMJ 2003;327:673-6.
- Various . Rapid responses to: Should health professionals screen women for domestic violence? Systematic review. BMJ 2003. http://bmj.bmjjournals.com/cgi/eletters/325/7359/314 (accessed April 2007).
- MacMillan HL, Wathen CN. Prevention and treatment of violence against women: systematic review and recommendations. London, ON: Canadian Task Force on Preventative Health Care; n.d.
- Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. J Marriage Fam 1979;41:55-88.
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scale (CTS2). J Fam Issues 1996;17:283-316.
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet 1999;354:1896-900.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008-12.
- Schreiber R, Crooks D, Stern P, Morse J. Completing a qualitative project: details and dialogue. Thousand Oaks, California: Sage; 1997.
- Schutz A. Collected papers. The Hague: Martinus Nijhoff; 1962.
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Services Res Policy 2002;7:209-15.
- Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 2003;56:671-84.
- Walter SD, Jadad AR. Meta-analysis of screening data: a survey of the literature. Stat Med 1999;18:3409-24.
- Feder G. Prevention of Domestic Violence: A Pilot Study in Primary Care (PREDOVE). n.d. http://portal.nihr.ac.uk (accessed January 2008).
- Walby S. The Cost of Domestic Violence n.d. www.equalities.gov.uk.
- STROBE group . STROBE Statement (strengthening the Reporting of Observational Studies in Epidemiology) n.d. www.strobe-statement.org/PDF/STROBE-Checklist-Version3.pdf (accessed April 2005).
- NHS Learning and Development Public Health Resource Unit . CASP Appraisal Tools n.d. www.phru nhs.uk/casp/critical_appraisal_tools.htm (accessed April 2006).
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3.
- Feder G, Hutson M, Ramsay J, Taket A. Women exposed to intimate partner violence. Expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Int Med 2006;166:22-37.
- Harris R, Helfand M, Woolf S, Lohr K, Mulrow C, Teutsch S, et al. Curent methods of the US Preventive Services Task Force. Am J Prev Med 2001;20:21-35.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Control Clin Trials 1996;17:1-12.
- Walby S, Allen J. Domestic Violence, Sexual Assault and Stalking: Findings from the British Crime Survey 2004. www.crimereduction.gov.uk/domesticviolence42.htm.
- Dominy R, Radford L. Domestic violence in Surrey: developing an effective inter-agency response. London: Surrey County Council/Roehampton Institute; 1996.
- Finney A. Domestic violence, sexual assault and stalking: findings from the 2004/05 British Crime Survey. London: Home Office Online Report 12/06; 2006.
- Carrado M. Aggression in British heterosexual relationships: a descriptive analysis. Aggressive Behav 1996;22:401-15.
- Mirrlees-Black C, Byron C. Domestic violence: findings from the BCS self-completion questionnaire. London: Home Office; 2004.
- Richardson J, Coid J, Petruckevitch A, Chung WS, Moorey S, Feder G. Identifying domestic violence: cross sectional study in primary care. BMJ 2002;324.
- Bacchus L, Mezey G, Bewley S. Prevalence of domestic violence when midwives routinely enquire in pregnancy. BJOG 2004;111:441-5.
- Mezey G, Bacchus L, Bewley S, White S. Domestic violence, lifetime trauma and psychological health of childbearing women. BJOG 2005;112:197-204.
- Bacchus L, Mezey G, Bewley S. Domestic violence: prevalence in pregnant women and associations with physical and psychological health. Eur J Obstet Gynecol Reprod Biol 2004;113:6-11.
- Bowen E, Heron J, Waylen A, Wolke D. Domestic violence risk during and after pregnancy: findings from a British longitudinal study. BJOG 2005;112:1083-9.
- Johnson J, Haider F, Ellis K, Hay DM, Lindow SW. The prevalence of domestic violence in pregnant women. BJOG 2003;110:272-5.
- Boyle A, Todd C. Incidence and prevalence of domestic violence in a UK emergency department. Emerg Med J 2003;20:438-42.
- Sethi D, Watts S, Zwi A, Watson J, McCarthy C. Experience of domestic violence by women attending an inner city accident and emergency department. Emerg Med J 2004;21:180-4.
- Boyle A, Robinson S, Atkinson P. Domestic violence in emergency medicine patients. Emerg Med J 2004;21:9-13.
- Wright J, Kariya A. Characteristics of female victims of assault attending a Scottish accident and emergency department. J Accid Emerg Med 1997;14:375-8.
- John R, Johnson J, Kukreja S. Domestic violence: prevalence and association with gynaecological symptoms. BJOG 2004;111:1128-32.
- Keeling J. Pregnancy counselling clinic: a questionnaire survey of intimate partner abuse. J Fam Plan Reprod H 2004;30:165-8.
- Keeling J, Birch L. The prevalence rates of domestic abuse in women attending a family planning clinic. J Fam Plan Reprod H 2004;30:113-14.
- Coid J, Petruckevitch A, Chung WS, Richardson J, Moorey S, Cotter S, et al. Sexual violence against adult women primary care attenders in east London. Br J Gen Pract 2003;53:858-62.
- Finney A. Alcohol and intimate partner violence: key findings from the research. London: Home Office; 2004.
- Krahe B, Bieneck S, Moller I. Understanding gender and intimate partner violence from an international perspective. Sex Roles 2005;52:807-27.
- Golding JM. Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence 1999;14:99-132.
- Jones L, Hughes M, Unterstaller U. Post traumatic stress disorder (PTSD) in victims of domestic violence. A review of the research. Trauma Violence Abus 2001;2:99-119.
- Stith SM, Rosen KH, McCollum EE. Effectiveness of couples treatment for spouse abuse. J Marital Fam Ther 2003;29:407-26.
- Jasinski JL. Pregnancy and domestic violence. A review of the literature. Trauma Violence Abus 2004;5:47-64.
- Campbell JC, Woods AB, Chouaf KL, Parker B. Reproductive health consequences of intimate partner violence. A nursing research review. Clin Nurs Res 2000;9:217-37.
- Boy A, Salihu HM. Intimate partner violence and birth outcomes: a systematic review. Int J Fertil 2004;49:159-63.
- Nasir K, Hyder AA. Violence against pregnant women in developing countries: review of evidence. Eur J Public Health 2003;13:105-7.
- Murphy C, Schei B, Myhr T, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ 2001;164:1567-72.
- Buehler C, Anthony C, Krishnakumar A, Stone G, Gerard J, Pemberton S. Interparental conflict and youth problem behaviors: a meta-analysis. J Child Fam Studies 1997;6:233-47.
- Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: a systematic review. Pediatrics 2006;117:278-90.
- Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witness to domestic violence: a meta-analytic review. J Consult Clin Psychol 2003;71:339-52.
- Attala JM, Bauza K, Pratt H, Vieira D. Integrative review of effects on children of witnessing domestic violence. Issues Compr Pediatr Nurs 1995;18:163-72.
- Kolbo JR, Blakely EH, Engleman D. Children who witness domestic violence: a review of empirical literature. J Interpers Violence 1996;11:281-93.
- Stith SM, Smith DB, Penn CE, Ward DB, Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggress Violent Behav 2004;10:65-98.
- Pak L, Reece A, Chan L. Is adverse pregnancy outcome predictable after blunt abdominal trauma?. Am J Obstet Gynecol 1998;179:1140-4.
- Hilliard PJ. Physical abuse in pregnancy. Obstet Gynecol 1985;66:185-90.
- Fantuzzo JW, Lindquist CU. The effects of observing conjugal violence on children: a review and analysis of research methodology. J Fam Violence 1989;4:77-94.
- Christopoulos C, Cohn D, Shaw D, Joyce S, Sullivan-Hanson J, Kraft S, et al. Adjustment at time of shelter residence. J Marriage Fam 1987;49:611-19.
- Campbell JC. Health consequences of intimate partner violence. Lancet 2002;359:1331-6.
- McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, et al. The ‘battering syndrome’: prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Int Med 1995;123:737-46.
- Coker AL, Smith PH, Bethea L, King MR, McKeown RE. Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med 2000;9:451-7.
- Tollestrup K, Sklar D, Frost FJ, Olson L, Weybright J, Sandvig J, et al. Health indicators and intimate partner violence among women who are members of a managed care organization. Prev Med 1999;29:431-40.
- Coker AL, Pope BO, Smith PH, Sanderson M, Hussey JR. Assessment of clinical partner violence screening tools. J Am Med Womens Assoc 2001;56:19-23.
- Ernst AA, Weiss SJ, Cham E, Hall L, Nick T. Detecting ongoing intimate partner violence in the emergency department using a simple 4-question screen: the OVAT. Violence Vict 2004;19:375-84.
- Chen P, Rovi S, Vega M, Jacabs A, Johnson M. Screening for domestic violence in a prodominantly Hispanic clinical setting. Fam Pract 2005;22:617-23.
- Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: a short domestic violence screening tool for use in a family practice setting. Fam Med 1998;30:508-12.
- Reichenheim M, Moraes C. Comparison between the abuse assessment screen and the revised conflict tactics scales for measuring physical violence during pregnancy. J Epidemiol Commun Health 2003;58:523-7.
- Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA 1997;277:1357-61.
- MacMillan HL, Wathen CN, Jamieson E, Boyle M, McNutt LA, Worster A, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA 2006;296:530-6.
- Paranjape A, Rask K, Liebschutz J. Utility of STaT for the identification of recent intimate partner violence. J Natl Med Assoc 2006;98:1663-9.
- Bonomi AE, Thompson RS, Anderson M, Rivara FP, Holt VL, Carrell D, et al. Ascertainment of intimate partner violence using two abuse measurement frameworks. Inj Prev 2006;12:121-4.
- Peralta RL, Fleming MF. Screening for intimate partner violence in a primary care setting: the validity of ‘feeling safe at home’ and prevalence results. J Am Board Fam Pract 2003;16:525-32.
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. JAMA 1992;267:3176-8.
- Sagrestano LM, Rodriguez AC, Carroll D, Bieniarz A, Greenberg A, Castro L, et al. A comparison of standardized measures of psychosocial variables with single-item screening measures used in an urban obstetric clinic. J Obstet Gynecol Neonatal Nurs 2002;31:147-55.
- Brown JB, Lent B, Schmidt G, Sas G. Application of the Woman Abuse Screening Tool (WAST) and WAST-short in the family practice setting. J Fam Pract 2000;49:896-903.
- Connelly CD, Newton RR, Landsverk J, Aarons GA. Assessment of intimate partner violence among high-risk postpartum mothers: concordance of clinical measures. Women Health 2000;31:21-37.
- Brown JB, Schmidt G, Lent B, Sas G, Lemelin J. Screening for violence against women. Validation and feasibility studies of a French screening tool. Can Fam Physician 2001;47:988-95.
- Fogarty CT, Burge S, McCord EC. Communicating with patients about intimate partner violence: screening and interviewing approaches. Fam Med 2002;34:369-75.
- Belknap RA, Sayeed P. Te contaria mi vida: I would tell you my life, if only you would ask. Health Care Women Int 2003;24:723-37.
- Stenson K, Saarinen H, Heimer G, Sidenvall B. Women’s attitudes to being asked about exposure to violence. Midwifery 2001;17:2-10.
- Hathaway JE, Willis G, Zimmer B. Listening to survivors’ voices. Addressing partner abuse in the health care setting. Violence Against Women 2002;8:687-719.
- Chang JC, Decker MR, Moracco KE, Martin SL, Petersen R, Frasier P. Asking about intimate partner violence: advice from female survivors to health care providers. Patient Educ Couns 2005;59:141-7.
- Chang JC, Cluss PA, Ranieri L, Hawker L, Buranosky R, Dado D, et al. Health care interventions for intimate partner violence: what women want. Womens Health Issues 2005;15:21-30.
- Lutz K. Abused pregnant women’s interactions with health care providers during the childbearing year. J Obstet Gynecol Neonatal Nurs 2005;34:151-62.
- McCaw B, Berman WH, Syme SL, Hunkeler E. Beyond screening for domestic violence. A systems model approach in a managed care setting. Am J Prev Med 2001;21:170-6.
- Renker PR, Tonkin P. Women’s views of prenatal violence screening: acceptability and confidentiality issues. Obstet Gynecol 2006;107:348-54.
- Hurley KF, Brown M, Campbell SG, Wallace T, Venugopal R, Baggs D. Emergency department patients’ opinions of screening for intimate partner violence among women. Emerg Med J 2005;22:97-8.
- Weinsheimer RL, Schermer CR, Malcoe LH, Balduf LM, Bloomfield LA. Severe intimate partner violence and alcohol use among female trauma patients. J Trauma 2005;58:22-9.
- Glass N, Dearwater S, Campbell J. Intimate partner violence screening and intervention: data from eleven Pennsylvania and California community hospital emergency departments. J Emerg Nurs 2001;27:141-9.
- Brzank P, Hellbernd H, Maschewsky-Schneider U. Domestic violence against women: negative health consequences and need for care – results of a survey among first-aid-patients in the framework of the S.I.G.n.A.L. – accompanying research. Gesundheitswesen 2004;66:164-9.
- Romito P, De M, Turan J, Bottaretto R, Tavi M. Identifying violence among women patients attending family practices: the role of research in community change. J Community Appl Soc 2004;14:250-65.
- Bair-Merritt MH, Mollen CJ, Yau PL, Fein JA. Impact of domestic violence posters on female caregivers’ opinions about domestic violence screening and disclosure in a pediatric emergency department. Pediatr Emerg Care 2006;22:689-93.
- Caralis PV, Musialowski R. Women’s experiences with domestic violence and their attitudes and expectations regarding medical care of abuse victims. South Med J 1997;90:1075-80.
- Friedman LS, Samet JH, Roberts MS, Hudlin M, Hans P. Inquiry about victimization experiences – a survey of patient preferences and physician practices. Arch Intern Med 1992;152:1186-90.
- Gielen AC, O’Campo PJ, Campbell JC, Schollenberger J, Woods AB, Jones AS, et al. Women’s opinions about domestic violence screening and mandatory reporting. Am J Prev Med 2000;19:279-85.
- McDonnell E, Holohan M, Reilly MO, Warde L, Collins C, Geary M. Acceptability of routine inquiry regarding domestic violence in the antenatal clinic. Ir Med J 2006;99:123-4.
- McNutt LA, Carlson BE, Gagen D, Winterbauer N. Reproductive violence screening in primary care: perspectives and experiences of patients and battered women. J Am Med Womens Assoc 1999;54:85-90.
- Newman JD, Sheehan KM, Powell EC. Screening for intimate-partner violence in the pediatric emergency department. Pediatr Emerg Care 2005;21:79-83.
- Zeitler MS, Paine AD, Breitbart V, Rickert VI, Olson C, Stevens L, et al. Attitudes about intimate partner violence screening among an ethnically diverse sample of young women. J Adolesc Health 2006;39:119-8.
- Webster J, Stratigos S, Grimes K. Women’s responses to screening for domestic violence in a health-care setting. Midwifery 2001;17:289-94.
- Witting MD, Furuno JP, Hirshon JM, Krugman SD, Perisse AR, Limcangco R. Support for emergency department screening for intimate partner violence depends on perceived risk. J Interpers Violence 2006;21:585-96.
- Zink T, Levin L, Wollan P, Putnam F. Mothers’ comfort with screening questions about sensitive issues, including domestic violence. J Am Board Fam Med 2006;19:358-67.
- Bacchus L, Mezey GC, Bewley S. Women’s perceptions and experiences of routine enquiry for domestic violence in a maternity service. BJOG 2002;109:9-16.
- Dowd MD, Kennedy C, Knapp JF, Stallbaumer R. Mothers’ and health care providers’ perspectives on screening for intimate partner violence in a pediatric emergency department. Arch Pediatr Adolesc Med 2002;156:794-99.
- Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOG 2005;112:1249-56.
- Constantino R, Kim Y, Crane P. Effects of a social support intervention on health outcomes in residents of a domestic violence shelter: a pilot study. Issues Ment Health Nurs 2005;26:575-90.
- McFarlane J, Groff JY, O’Brien JA, Watson K. Secondary prevention of intimate partner violence. A randomized controlled trial. Nurs Res 2006;55:52-61.
- Sullivan C, Bybee D, Allen N. Findings from a community-based program for battered women and their children. J Interpers Violence 2002;17:915-36.
- Bybee DI, Sullivan CM. The process through which an advocacy intervention resulted in positive change for battered women over time. Am J Community Psychol 2002;30:103-32.
- Sullivan CM, Bybee DI. Reducing violence using community-based advocacy for women with abusive partners. J Consult Clin Psychol 1999;67:43-5.
- Sullivan CM, Campbell R, Angelique H, Eby KK, Davidson WS. An advocacy intervention program for women with abusive partners: six-month follow-up. Am J Community Psychol 1994;22:101-22.
- Sullivan CM, Tan C, Basta J, Rumptz M, Davidson WS. An advocacy intervention program for women with abusive partners: initial evaluation. Am J Community Psychol 1992;20:309-32.
- Sullivan CM, Davidson WS. The provision of advocacy services to women leaving abusive partners: an examination of short-term effects. Am J Community Psychol 1991;19:953-60.
- Bybee D, Sullivan C. Predicting re-victimization of battered women 3 years after exiting a shelter program. Am J Community Psychol 2005;36:85-96.
- Parker B, McFarlane J, Soeken K, Silva C, Reel S. Testing an intervention to prevent further abuse to pregnant women. Res Nurs Health 1999;22:59-66.
- McFarlane J, Parker B, Soeken K, Silva C, Reel S. Safety behaviors of abused women after an intervention during pregnancy. J Obstet Gynecol Neonatal Nurs 1998;27:64-9.
- McFarlane J, Soeken K, Reel S, Parker B, Silva C. Resource use by abused women following an intervention program: associated severity of abuse and reports of abuse ending. Public Health Nurs 1997;14:244-50.
- McFarlane J, Soeken K, Wiist W. An evaluation of interventions to decrease intimate partner violence to pregnant women. Public Health Nurs 2000;17:443-51.
- McFarlane J, Malecha A, Gist J, Watson K, Batten E, Hall I, et al. An intervention to increase safety behaviors of abused women: results of a randomized clinical trial. Nurs Res 2002;51:347-54.
- McFarlane J, Malecha A, Gist J, Watson K, Batten E, Hall I, et al. Protection orders and intimate partner violence: an 18-month study of 150 black, Hispanic, and white women. Am J Public Health 2004;94:613-18.
- Feighny KM, Muelleman RL. The effect of a community-based intimate partner violence advocacy program in the emergency department on identification rate of intimate partner violence. Mo Med 1999;96:242-4.
- Tutty LM. Post-shelter services: the efficacy of follow-up programs for abused women. Res Social Work Prac 1996;6:425-41.
- Fry P, Barker L. Female survivors of abuse and violence: the influence of storytelling reminiscence on perceptions of self-efficacy, ego strength, and self-esteem. New York: Springer Publishing; 2002.
- Tutty LM, Bidgood BA, Rothery MA. Support groups for battered women: research on their efficacy. J Fam Violence 1993;8:325-43.
- Tutty LM, Bidgood BA, Rothery MA. Evaluating the effect of group process and client variables in support groups for battered women. Res Social Work Prac 1996;6:308-24.
- Koopman C, Ismailji T, Holmes D, Classen CC, Palesh O, Wales T. The effects of expressive writing on pain, depression and posttraumatic stress disorder symptoms in survivors of intimate partner violence. J Health Psychol 2005;10:211-21.
- Reed GL, Enright RD. The effects of forgiveness therapy on depression, anxiety, and posttraumatic stress for women after spousal emotional abuse. J Consult Clin Psychol 2006;74:920-9.
- Labrador FJ, Fernandez-Velasco MD, Rincon PP. Efficacy of a brief and individual participation program by posttraumatic stress disorder in female victims of domestic violence. Int J Clin Health Psychol 2006;6:527-47.
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD: preliminary findings. J Trauma Stress 2003;16:81-9.
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, et al. Cognitive trauma therapy for battered women with PTSD (CTT-BW). J Consult Clin Psychol 2004;72:3-18.
- Mancoske RJ, Standifer D, Cauley C. The effectiveness of brief counseling services for battered women. Res Social Work Pract 1994;4:53-6.
- McNamara JR, Ertl M, Neufeld J. Problem-solving in relation to abuse by a partner. Psychol Rep 1998;83:943-6.
- McNamara JR, Ertl M, Marsh S, Walker S. Short-term response to counseling and case management intervention in a domestic violence shelter. Psychol Rep 1997;81:1243-51.
- Gilbert L, El-Bassel N, Manuel J, Wu E, Go H, Golder S, et al. An integrated relapse prevention and relationship safety intervention for women on methadone: testing short-term effects on intimate partner violence and substance use. Violence Vict 2006;21:657-72.
- Arinero M, Crespo M. A treatment-outcome study of cognitive-behavioural therapy for battered women: preliminary findings. Psicologia Conductual 2004;12:233-49.
- Cruz AGM, Sanchez S. Empowering women abused by their problem drinker spouses: effects of a cognitive-behavioral intervention. Salud Ment 2006;29:25-31.
- Cox JW, Stoltenberg CD. Evaluation of a treatment program for battered wives. J Fam Violence 1991;6:395-413.
- Laverde DI. Efectos del tratamiento cognoscitivo-conductual en el maltrato fisico en la pareja. Revista De Aalisis Del Comportamiento 1987;3:188-95.
- Limandri BJ, May BA. Psychoeducational Intervention to Enhance Self-Efficacy of Abused Women n.d.
- Melendez RM, Hoffman S, Exner T, Leu C, Ehrhardt AA. Intimate partner violence and safer sex negotiation: effects of a gender-specific intervention. Arch Sex Behav 2003;32:499-511.
- Rinfret-Raynor M, Cantin S, Kantor GK, Jasinski JL. Out of the darkness. Contemporary perspectives on family violence. Thousand Oaks, CA: Sage Publications; 1997.
- Kim S, Kim J. The effects of group intervention for battered women in Korea. Arch Psychiatr Nurs 2001;XV:257-64.
- Howard A, Riger S, Campbell R, Wasco S. Counseling services for battered women. A comparison of outcomes for physical and sexual assault survivors. J Interpers Violence 2003;18:717-34.
- Lieberman AF, Van Horn P, Ippen CG. Toward evidence-based treatment: child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry 2005;44:1241-8.
- Lieberman AF, Ippen CG, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2006;45:913-18.
- Jouriles EN, McDonald R, Spiller L, Norwood WD, Swank PR, Stephens N, et al. Reducing conduct problems among children of battered women. J Consult Clin Psychol 2001;69:774-85.
- McDonald R, Jouriles EN, Skopp NA. Reducing conduct problems among children brought to women’s shelters: intervention effects 24 months following termination of services. J Fam Psychol 2006;20:127-36.
- McFarlane JM, Groff J, O’Brien JA, Watson K. Behaviors of children following a randomized controlled treatment program for their abused mothers. Issues Compr Pediatr Nurs 2005;28:195-211.
- McFarlane JM, Groff JY, O’Brien JA, Watson K. Behaviors of children exposed to intimate partner violence before and 1 year after a treatment program for their mother. Appl Nurs Res 2005;18:7-12.
- Ducharme J, Atkinson L, Poulton L. Success-based, noncoercive treatment of oppositional behavior in children from violent homes. J Am Acad Child Adolesc Psychiatry 2000;39:995-1004.
- Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ 2006;333:597-600.
- Harwell TS, Casten RJ, Armstrong KA, Dempsey S, Coons HL, Davis M. Results of a domestic violence training program offered to the staff of urban community health centers. Evaluation Committee of the Philadelphia Family Violence Working Group. Am J Prev Med 1998;15:235-42.
- Thompson RS, Rivara FP, Thompson DC, Barlow WE, Sugg NK, Maiuro RD, et al. Identification and management of domestic violence: a randomized trial. Am J Prev Med 2000;19:253-63.
- Coyer S, Plonczynski D, Bladwin K, Fox P. Screening for violence against women in a rural health care clinic. Online J Rural Nurs Health Care 2006;6. www.rno.org/journal/.
- Wiist WH, McFarlane J. The effectiveness of an abuse assessment protocol in public health prenatal clinics. Am J Public Health 1999;89:1217-21.
- Ulbrich PM, Stockdale J. Making family planning clinics an empowerment zone for rural battered women. Women Health 2002;35:83-100.
- Ramsden C, Bonner M. An early identification and intervention model for domestic violence. Aust Emerg Nurs J 2002;5:15-20.
- Shepard M, Elliot BA, Falk DR, Regal RR. Public health nurses’ responses to domestic violence: a report from the enhanced domestic abuse intervention project. Public Health Nurs 1999;16:359-66.
- Edin KE, Högberg U. Violence against pregnant women will remain hidden as long as no direct questions are asked. Midwifery 2002;18:268-78.
- Stenson K, Sidenvall B, Heimer G. Midwives’ experiences of routine antenatal questioning relating to men’s violence against women. Midwifery 2005;21:311-21.
- Mezey GC, Bacchus L, Haworth A, Bewley S. Midwives’ perceptions and experiences of routine enquiry for domestic violence. BJOG 2003;110:744-52.
- Taylor P, Zaichkin J, Pilkey D, Leconte J, Johnson BK, Peterson AC. Prenatal screening for substance use and violence: findings from physician focus groups. Matern Child Health J 2006;11:241-7.
- McCosker H, Kain V, Anderson DJ, Webster J. The impact on midwives of undertaking screening for domestic violence: focus group findings. Birth Issues 2005;14:49-56.
- Loughlin S, Spinola C, Stewart L, Fanslow J, Norton R. Emergency department staff responses to a protocol of care for abused women. Health Educ Behav 2000;27:572-90.
- Minsky-Kelly D, Hamberger L, Pape D, Wolff M. We’ve had training, now what?: qualitative analysis of barriers to domestic violence screening and referral in a health care setting. J Interpers Violence 2005;20:1288-309.
- Hindin PK. Intimate partner violence screening practices of certified nurse-midwives. J Midwifery Womens Health 2006;51:216-21.
- Price S, Baird K, Salmon D. Asking the question: antenatal domestic violence. Pract Midwife 2005;8:21-5.
- Bair-Merritt MH, Giardino AP, Turner M, Ganetsky M, Christian CW. Pediatric residency training on domestic violence: a national survey. Ambulatory Pediatrics 2004;4:24-7.
- Bair-Merritt MH, Mollen CJ, Yau PL, Fein JA. Health care providers’ opinions on intimate partner violence resources and screening in a pediatric emergency department. Pediatr Emerg Care 2006;22:150-3.
- Baig A, Shadigian E, Heisler M. Hidden from plain sight: residents’ domestic violence screening attitudes and reported practices. J Gen Intern Med 2006;21:949-54.
- Baird K. Domestic violence: learning to ask the question. Pract Midwife 2005;8:18-22.
- Barnett C. Exploring midwives’ attitudes to domestic violence screening. Br J Midwifery 2005;13:702-5.
- Ellis JM. Barriers to effective screening for domestic violence by registered nurses in the emergency department. Crit Care Nurs Q 1999;22:27-41.
- Fikree FF, Jafarey SN, Korejo R, Khan A, Durocher JM. Pakistani obstetricians’ recognition of and attitude towards domestic violence screening. Int J Gynecol Obstet 2004;87:59-65.
- Goff H, Byrd T, Shelton A, Parcel G. Health care professionals’ skills, beliefs, and expectations about screening for domestic violence in a border community. Fam Commun Health 2001;24:39-54.
- Lazenbatt A, Thompson-Cree ME, McMurray F. The use of exploratory factor analysis in evaluating midwives’ attitudes and stereotypical myths related to the identification and management of domestic violence in practice. Midwifery 2005;21:322-34.
- Nayak MB. Factors influencing hesitancy in medical students to assess history of victimization in patients. J Interpers Violence 2000;15:123-33.
- Nicolaidis C, Curry M, Gerrity M. Health care workers’ expectations and empathy toward patients in abusive relationships. J Am Board Fam Pract 2005;18:159-65.
- Price S, Baird K. Tackling domestic violence: an audit of professional practice. Pract Midwife 2003;6:15-8.
- Richardson J, Feder G, Eldridge S, Chung WS, Coid J, Moorey S. Women who experience domestic violence and women survivors of childhood sexual abuse: a survey of health professionals’ attitudes and clinical practice. Br J Gen Pract 2001;51:468-70.
- Roelens K, Verstraelen H, Van EK, Temmerman M. A knowledge, attitudes, and practice survey among obstetrician-gynaecologists on intimate partner violence in Flanders, Belgium. BMC Public Health 2006;6.
- Salmon D, Murphy S, Baird K. An evaluation of the effectiveness of an educational programme promoting the introduction of routine antenatal enquiry for domestic violence. Midwifery 2006;22:6-14.
- Shye D, Feldman V, Hokanson CS, Mullooly JP. Secondary prevention of domestic violence in HMO primary care: evaluation of alternative implementation strategies. Am J Manag Care 2004;10:706-16.
- Straus MA. Medical care costs of intrafamily assault and homicide. Bull N Y Acad Med 1986;62:556-61.
- Finlayson T, Saltzman L, Sheridan D, Taylor W. Estimating hospital charges associated with intimate violence. Violence Against Women 1999;5:313-35.
- Varjavand N, Cohen DG, Novack DH. An assessment of residents’ abilities to detect and manage domestic violence. J Gen Intern Med 2002;17:465-8.
- Coker AL, Reeder CE, Fadden MK, Smith PH. Physical partner violence and medicaid utilization and expenditures. Public Health Rep 2004;119:557-67.
- Ulrich Y, Cain KC, Sugg NK, Rivara FP, Rubanowice DM, Thompson RS. Medical care utilization patterns in women with diagnosed domestic violence. Am J Prev Med 2003;24:9-15.
- Wisner CL, Gilmer TP, Saltzman LE, Zink TM. Intimate partner violence against women: do victims cost health plans more?. J Fam Pract 1999;48:439-43.
- Clark KA, Biddle AK, Martin SL. A cost-benefit analysis of the Violence Against Women Act of 1994. Violence Against Women 2002;8:417-28.
- Domino M, Morrissey JP, Nadlicki-Patterson T, Chung S. Service costs for women with co-occurring disorders and trauma. J Subst Abuse Treat 2005;28:135-43.
- Domino ME, Morrissey JP, Chung S, Huntington N, Larson MJ, Russell LA. Service use and costs for women with co-occurring mental and substance use disorders and a history of violence. Psychiat Serv 2005;56:1223-32.
- Sohal A, Eldridge S, Feder GS. The sensitivity and specificity of four questions (HARK) to identify intimate partner violence: a diagnostic accuracy study in general practice. BMC Fam Pract 2007;8.
- Barkham M, Stiles WB, Shapiro DA. The shape of change in psychotherapy: longitudinal assessment of personal problems. J Consult Clin Psychol 1993;61:667-77.
- Taket A. Tackling Domestic Violence: The Role of Health Professionals 2004. www.homeoffice.gov.uk/rds/pdfs04/dpr32.pdf (accessed December 2008).
- Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet 2006;368:1260-9.
- Department of Health . Responding to Domestic Violence: A Handbook for Health Professionals 2005.
- Bradley F, Smith M, Long J, O’Dowd T. Reported frequency of domestic violence: cross sectional survey of women attending general practice. BMJ 2002;324.
- Chamberlain L. The USPSTF recommendation on intimate partner violence: what we can learn from it and what we can do about it. Fam Violence Prevention Health Pract 2005;1:1-21.
- Briss PA, Brownson RC, Fielding JE, Zaza S. Developing and using the Guide to Community Preventive Services: lessons learned about evidence-based public health. Annu Rev Public Health 2004;25:281-302.
- Yegidis BL. Abuse risk inventory manual. Palo Alto, CA: Consulting Psychologist Press; 1989.
- Hegarty K, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: development and preliminary validation of the Composite Abuse Scale. J Fam Violence 1999;14:399-415.
- Hegarty K, Bush R, Sheehan M. The composite abuse scale: further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Vict 2005;20:529-47.
- Straus MA. Measuring intrafamily conflict and violence: the Conflict Tactics (CT) scales. J Marriage Fam 1979;41:75-88.
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): development and preliminary psychometric data. J Fam Issues 1996;17:283-316.
- Campbell JC. Nursing assessment for risk of homicide with battered women. ANS Adv Nurs Sci 1986;8:36-51.
- Berk RA, Berk SF, Loseke DR, Finkelhor D, Gelles RJ, Hotaling GT. The dark side of families. Beverly Hills, CA: Sage; 1983.
- Hudson WW, McIntosh SR. The assessment of spouse abuse: two quantifiable dimensions. J Marriage Fam 1981;43:873-88.
- Hudson WW. Partner abuse scale physical. Tempe, AZ: Walmyr Publishing; 1991.
- Parker B, McFarlane J. Nursing assessment of the battered pregnant woman. Maternal-Child Nursing J 1991;16:161-4.
- Soeken K, McFarlane J, Parker B, Lominack M. The Abuse Assessment Screen: a clinical instrument to measure frequency, severity, and perpetrator of abuse against women. Thousand Oaks, CA: Sage Publications; 1998.
- Prevalence of intimate partner violence and injuries – Washington, 1998. MMWR 2000;49:589-92.
- Brown JB, Sas G. Focus groups in family practice research: an example study of family physicians’ approach to wife abuse. Fam Pract Res J 1994;14:19-28.
- Weiss SJ, Ernst AA, Cham E, Nick TG. Development of a screen for ongoing intimate partner violence. Violence Vict 2003;18:131-41.
- Weiss S, Garza A, Casaletto J, Stratton M, Ernst A, Blanton D, et al. The out-of-hospital use of a domestic violence screen for assessing patient risk. Prehosp Emerg Care 2000;4:24-7.
- Ashur ML. Asking about domestic violence: SAFE questions. JAMA 1993;269.
- Neufeld B. Safe questions: overcoming barriers to the detection of domestic violence. Am Fam Physician 1996;53:2575-80.
- Paranjape A, Liebschutz J. STaT: a three question screen for intimate partner violence. J Womens Health 2003;12:233-39.
- Brown JB, Lent B, Brett PJ, Sas G, Pederson LL. Development of the Woman Abuse Screening Tool for use in family practice. Fam Med 1996;28:422-8.
- Smith PH, Earp JA, DeVellis R. Measuring battering: development of the Women’s Experience with Battering (WEB) scale. Womens Health 1995;1:273-88.
- Moonesinghe LN, Rajapaksa LC, Samarasinghe G. Development of a screening instrument to detect physical abuse and its use in a cohort of pregnant women in Sri Lanka. Asia Pac J Pub Health 2004;16:138-44.
- McFarlene J, Hughes RB, Nosek MA, Groff JY, Swedlend N, Dolan MP. Abuse assessment screen-disability (AAS-D): measuring frequency, type, and perpetrator of abuse toward women with physical disabilities. J Women Health Gen B 2001;10:861-6.
- Wasson JH, Jette AM, Anderson J, Johnson DJ, Nelson EC, Kilo CM. Routine, single-item screening to identify abusive relationships in women. J Fam Pract 2000;49:1017-22.
- Short LM, Rodriguez R. Testing an intimate partner violence assessment icon form with battered migrant and seasonal farmworker women. Women Health 2002;35:181-92.
- Yoshihama M, Clum K, Crampton A, Gillespie B. Measuring the lifetime experience of domestic violence: application of the life history calendar method. Violence Vict 2002;17:297-31.
- Attala JM, Hudson WW, McSweeney M. A partial validation of two short-form Partner Abuse Scales. Women Health 1994;21:125-39.
- Straus MA, Straus MA, Gelles RJ. Physical violence in American families: risk factors and adaptations to violence in 8,145 families. New Brunswick, NY: Transaction; 1990.
- Boris NW, Heller SS, Sheperd T, Zeanah CH. Partner violence among homeless young adults: measurement issues and associations. J Adolesc Health 2002;30:355-63.
- Tolman RM. The development of a measure of psychological maltreatment of women by their male partners. Violence Vict 1989;4:173-89.
- Tolman R. The validation of the Psychological Maltreatment of Women Inventory. Violence Vict 1999;14:25-37.
- Marshall L. Development of the Severity of Violence Against Women Scales. J Fam Violence 1992;7:103-19.
- McIntyre LM, Butterfield MI, Nanda K, Parsey K, Stechuchak KM, McChesney AW, et al. Validation of a trauma questionnaire in veteran women. J Gen Intern Med 1999;14:186-9.
- Hoff LA, Rosenbaum L. A victimization assessment tool: instrument development and clinical implications. J Adv Nurs 1994;20:627-34.
- Lewis B. The development and initial validation of the Wife Abuse Inventory. Tampa, FL: College of Education, University of South Florida; 1983.
- Lewis B. The Wife Abuse Inventory: a screening device for the identification of abused women. Soc Work 1985;30:32-5.
- Furbee PM, Sikora R, Williams JM, Derk SJ. Comparison of domestic violence screening methods: a pilot study. Ann Emerg Med 1998;31:495-501.
- Wetmore M, Fairbairn CD. A regional California program to screen adolescent patients for intimate partner violence. J Emerg Nurs 2003;29:373-6.
- Bateman W, Whitehead K. Health visitors’ domestic violence routine questioning tool: an exploration of women’s experience, effectiveness and acceptability. Int J Health Promotion Educ 2004;42:14-22.
- Fikree FF, Jafarey SN, Korejo R, Afshan A, Durocher JM. Intimate partner violence before and during pregnancy: experiences of postpartum women in Karachi, Pakistan. J Pak Med Assoc 2006;56:252-7.
- Anderst J, Hill TD, Siegel RM. A comparison of domestic violence screening methods in a pediatric office. Clin Pediatr (Phila.) 2004;43:103-5.
- Scholle SH, Buranosky R, Hanusa BH, Ranieri L, Dowd K, Valappil B. Routine screening for intimate partner violence in an obstetrics and gynecology clinic. Am J Public Health 2003;93:1070-2.
- Webster J, Holt V. Screening for partner violence: direct questioning or self-report?. Obstet Gynecol 2004;103:299-303.
- Bair-Merritt M, Feudtner C, Mollen CJ, Winters S, Blackstone M, Fein J. Screening for intimate partner violence using an audiotape questionnaire: a randomized clinical trial in a pediatric emergency department. Arch Pediatr Adolesc Med 2006;160:311-16.
- McFarlane J, Greenberg L, Weltge A, Watson M. Identification of abuse in emergency departments: effectiveness of a two-question screening tool. J Emerg Nurs 1995;21:391-4.
- Ramsden C, Bonner M. A realistic view of domestic violence screening in an emergency department. Accident Emerg Nurs 2002;10:31-9.
- Ross J, Walther V, Epstein I. Screening risks for intimate partner violence and primary care settings: implications for future abuse. Soc Work Health Care 2004;38:1-23.
- McFarlane J, Christoffel K, Bateman L, Miller V, Bullock L. Assessing for abuse: self-report versus nurse interview. Public Health Nurs 1991;8:245-50.
- Dutton MA, Mitchell B, Haywood Y. The emergency department as a violence prevention centre. J Am Med Womens Soc 1996;51:92-5.
- Chang JC, Decker M, Moracco KE, Martin SL, Petersen R, Frasier PY. What happens when health care providers ask about intimate partner violence? A description of consequences from the perspectives of female survivors. Journal of the American Medical Women’s Society 2003;58:76-81.
- Lutenbacher M, Cohen AJ, Mitzel J. Do we really help? Perspectives of abused women. Public Health Nurs 2003;20:56-64.
- Zink T, Jacobson J. Screening for intimate partner violence when children are present. The victim’s perspective. J Interpers Violence 2003;18:872-90.
- Zink T, Elder N, Jacobson J, Klostermann B. Medical management of intimate partner violence considering the stages of change: precontemplation and contemplation. Ann Fam Med 2004;2:231-9.
- Brzank P, Hellbernd H, Maschewsky-Schneider U. Domestic violence against women: health consequences and need for care – results of a survey among first-aid patients in the framework of the S.I.G.n.A.L. – accompanying research. Gesundheitswesen 2004;66:164-9.
- Renker PR, Tonkin P. Women’s views of prenatal violence screening: acceptability and confidentiality issues. Obstet Gynecol 2006;107:348-54.
- Knapp JF, Dowd MD, Kennedy CS, Stallbaumer-Rouyer J, Henderson DP. Evaluation of a curriculum for intimate partner violence screening in a pediatric emergency department. Pediatrics 2006;117:110-16.
- Wittenberg E, Lichter EL, Ganz ML, McCloskey LA. Community preferences for health states associated with intimate partner violence. Med Care 2006;44:738-44.
- Home Office . Criminal Statistics England and Wales 2001 2002.
- Netten A, Rees T, Harrison G. Unit costs of health and social care. Canterbury, Kent: University of Canterbury; 2001.
- Schiff M, Zeira A. Dating violence and sexual risk behaviors in a sample of at-risk Israeli youth. Child Abuse Neglect 2005;29:1249-63.
- Jain D, Sanon S, Sadowski L, Hunter W. Violence against women in India: evidence from rural Maharashtra, India. Rural Remote Health 2004;4.
- Mahony DL, Campbell JM. Children witnessing domestic violence: a developmental approach. Clin Excell Nurse Pract 1998;2:362-9.
- Wiebe ER, Janssen P. Universal screening for domestic violence in abortion. Women’s Health Issues 2001;11:436-41.
- Coid J, Yang M, Roberts A, Ullrich S, Moran P, Bebbington P, et al. Violence and psychiatric morbidity in a national household population – a report from the British Household Survey. Am J Epidemiol 2006;164:1199-208.
- Duxbury F. Recognising domestic violence in clinical practice using the diagnoses of posttraumatic stress disorder, depression and low self-esteem. Br J Gen Pract 2006;56:294-300.
- Duffy SJ, McGrath ME, Becker BM, Linakis JG. Mothers with histories of domestic violence in a pediatric emergency department. Pediatrics 1999;103:1007-13.
- Stark E, Flitcraft A. Killing the beast within: woman battering and female suicidality. Int J Health Serv 1995;25:43-64.
- Perrin S, Van Hasselt, V, Hersen M. Validation of the Keane MMPI-PTSD Scale against DSM-III-R criteria in a sample of battered women. Violence Vict 1997;12:99-104.
- Anetzberger G. Elder abuse identification and referral: the importance of screening tools and referral protocols. J Elder Abuse Neglect 2001;13:3-22.
- Champion J. Woman abuse, assimilation, and self-concept in a rural Mexican American community. Hispanic J Behav Sci 1996;18:508-21.
- Ejaz F, Bass D, Anetzberger G, Nagpaul K. Evaluating the Ohio elder abuse and domestic violence in late life screening tools and referral protocol. J Elder Abuse Neglect 2001;13:39-57.
- Punukollu M. Domestic violence: screening made practical. J Fam Pract 2003;52:537-43.
- Schofield M, Reynolds R, Mishra G, Powers J, Dobson A. Screening for vulnerability to abuse among older women: Women’s Health Australia Study. J Appl Gerontol 2002;21:24-39.
- Falk DR, Shepard M, Elliot BA. Evaluation of a domestic violence assessment protocol used by employee assistance counselors. Employee Assistance Q 2002;17:1-15.
- Pearce C, Hawkins J, Kearney M, Peyton C, Dwyer J, Haggerty L, et al. Translation of domestic violence instruments for use in research. Violence Against Women 2003;9:859-78.
- Waltermaurer E. Measuring intimate partner violence (IPV): you may only get what you ask for. J Interpers Violence 2005;20:501-6.
- Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict 2004;19:507-20.
- Prospero M. The role of perceptions in dating violence among young adolescents. J Interpers Violence 2006;21:470-84.
- Sisley A, Jacobs LM, Poole G, Campbell S, Esposito T. Violence in America: a public health crisis – domestic violence. J Trauma 1999;46:1105-12.
- Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. ‘Between me and the computer’: increased detection of intimate partner violence using a computer questionnaire [see comment]. Ann Emerg Med 2002;40:476-84.
- Canterino JC, VanHorn LG, Harrigan JT, Ananth CV, Vintzileos AM. Domestic abuse in pregnancy: a comparison of a self-completed domestic abuse questionnaire with a directed interview. Am J Obstet Gynecol 1999;181:1049-51.
- Moraes CL, Hasselmann MH, Reichenheim ME. Portuguese-language cross-cultural adaptation of the Revised Conflict Tactics Scales (CTS2), an instrument used to identify violence in couples. Cadernos De Saude Publica 2002;18:163-76.
- Meneghel SN, Camargo M, Fasolo LR, Mattiello DA, da Silva RC, Santos TC, et al. Women caring for women: a study at the ‘Viva Maria’ shelter, Porto Alegre, Rio Grande do Sul, Brazil. Cadernos De Saude Publica 2000;16:747-57.
- Saltzman L, Salmi L, Branche C, Bolen J. Public health screening for intimate violence. Violence Against Women 1997;3:319-31.
- Reichenheim ME, Moraes CL, Hasselmann MH. Semantic equivalence of the Portuguese version of the Abuse Assessment Screen tool used for the screening of violence against pregnant women. Revista De Saude Publica 2000;34:610-6.
- Ernst AA, Weiss SJ, Cham E, Marquez M. Comparison of three instruments for assessing ongoing intimate partner violence. Med Sci Monitor 2002;8:CR197-201.
- Houry D, Feldhaus K, Peery B, Abbott J, Lowenstein S, Al-Bataa-de-Montero S, et al. A positive domestic violence screen predicts future domestic violence. J Interpers Violence 2004;19:955-66.
- Bonomi A, Holt V, Thompson R, Martin D. Ascertainment of intimate partner violence in women seeking legal protection. Am J Prev Med 2005;28:52-8.
- Waller AE, Hohenhaus SM, Shah PJ, Stern EA. Development and validation of an emergency department screening and referral protocol for victims of domestic violence. Ann Emerg Med 1996;27:754-60.
- Hilton NZ, Harris GT, Rice ME, Lang C, Cormier CA, Lines KJ. A brief actuarial assessment for the prediction of wife assault recidivism: the Ontario domestic assault risk assessment. Psychol Assessment 2004;16:267-75.
- Heckert DA, Gondolf EW. Battered women’s perceptions of risk versus risk factors and instruments in predicting repeat reassault. J Interpers Violence 1919;19:778-800.
- Sprecher AG, Muelleman RL, Wadman MC. A neural network model analysis to identify victims of intimate partner violence. Am J Emerg Med 2004;22:87-9.
- Parker B, McFarlane J, Soeken K, Torres S, Campbell D. Physical and emotional abuse in pregnancy: a comparison of adult and teenage women [see comment]. Nursing Res 1993;42:173-8.
- Cecil H, Matson SC. Sexual victimization among African American adolescent females: examination of the reliability and validity of the Sexual Experiences Survey. J Interpers Violence 2006;21:89-104.
- Lazzaro MV, McFarlane J. Establishing a screening program for abused women. J Nurs Admin 1991;21:24-9.
- Norton LB, Peipert JF, Zierler S, Lima B, Hume L. Battering in pregnancy: an assessment of two screening methods. Obstet Gynecol 1995;85:321-5.
- Lavoie F, Vezina L. Female victimization in the context of dating violence in adolescence: development of an instrument (VIFFA). Can J Commun Ment Health 2001;20:153-71.
- Majdalani MP, Aleman M, Fayanas R, Guedes A, Mejia RM. Validation of a short questionnaire to use in clinical consultations to detect gender violence. Rev Panam Salud Publ 2005;17:79-83.
- Swahnberg IM, Wijma B. The NorVold Abuse Questionnaire (NorAQ): validation of new measures of emotional, physical, and sexual abuse, and abuse in the health care system among women. Eur J Public Health 2003;13:361-6.
- Wolfe DA, Scott K, Reitzel-Jaffe D, Wekerle C, Grasley C, Straatman AL. Development and validation of the Conflict in Adolescent Dating Relationships Inventory. Psychol Assessment 2001;13:277-93.
- Yost NP, Bloom SL, McIntire DD, Leveno KJ. A prospective observational study of domestic violence during pregnancy. Obstet Gynecol 2005;106:61-5.
- Higgins LP, Hawkins JW. Screening for abuse during pregnancy: implementing a multisite program. Am J Maternal Child Nurs 2005;30:109-14.
- Campbell JC, Sharps P, Glass N, Pinard GF, Pagani L. Clinical assessment of dangerousness: empirical contributions. Cambridge: Cambridge University Press; 2001.
- Moraes CL, Reichenheim ME. Cross-cultural measurement equivalence of the Revised Conflict Tactics Scales (CTS2) Portuguese version used to identify violence within couples. Cadernos De Saude Publica 2002;18:783-96.
- Mears M, Coonrod DV, Bay RC, Mills TE, Watkins MC. Routine history as compared to audio computer-assisted self-interview for prenatal care history taking. J Reprod Med 2005;50:701-6.
- McFarlane J, Parker B, Soeken K. Abuse during pregnancy: frequency, severity, perpetrator, and risk factors of homicide. Public Health Nurs 1995;12:284-9.
- Jory B. The Intimate Justice Scale: an instrument to screen for psychological abuse and physical violence in clinical practice. J Marital Fam Ther 2004;30:29-44.
- Heyman R, Feldbau K, Ehrensaft M, Langhinrichsen R, Leary K. Can questionnaire reports correctly classify relationship distress and partner physical abuse?. J Fam Psychol 2001;15:334-46.
- Flowers A, Lanclos N, Kelley M. Validation of a screening instrument for exposure to violence in African American children. J Pediatr Psychol 2002;27:351-61.
- Fals-Stewart W, Birchler G, Kelley ML. The timeline followback spousal violence interview to assess physical aggression between intimate partners: reliability and validity. J Fam Violence 2003;18:131-42.
- Janssen PA, Holt VL, Sugg NK. Introducing domestic violence assessment in a postpartum clinical setting. Maternal Child Health J 2002;6:195-203.
- Lo VF, Bhatia A, Sciallo D. Screening for domestic violence in the emergency department. Eur J Emerg Med 1998;5:441-4.
- Campbell DW, Campbell J, King C, Parker B, Ryan J. The reliability and factor structure of the index of spouse abuse with African-American women. Violence Vict 1994;9:259-74.
- Bass DM, Anetzberger GJ, Ejaz FK, Nagpaul K. Screening tools and referral protocol for stopping abuse against older Ohioans: a guide for service providers. J Elder Abuse Neglect 2001;13:23-38.
- Anderson B, Marshak H, Hebbeler D. Identifying intimate partner violence at entry to prenatal care: clustering routine clinical information. J Midwifery Womens Health 2002;47:353-9.
- Wahl RA, Sisk DJ, Ball TM. Clinic-based screening for domestic violence: use of a child safety questionnaire. BMC Med 2004;2.
- Benight CC, Harding-Taylor AS, Midboe AM, Durham RL. Development and psychometric validation of a Domestic Violence Coping Self-efficacy Measure (DV-CSE). J Trauma Stress 2004;17:505-8.
- Schofield M, Mishra G. Validity of self-report screening scale for elder abuse: Women’s Health Australia study. Gerontologist 2003;43:110-20.
- Mohr W, Tulman L. Children exposed to violence: measurement considerations within an ecological framework. Adv Nurs Sci 2000;23:59-68.
- Kubany E, Leisen M, Kaplan A, Watson S, Haynes S, Owens J, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assessment 2000;12:210-24.
- McNamara JR, Fields SA. The abuse disability questionnaire: internal consistency and validity considerations in two samples. J Fam Violence 2001;16:37-45.
- Varvaro F. Violence against women: the role of orthopaedic nurses in the identification, assessment, treatment, and care for the abused woman. Orthopaedic Nursing 1998;96:33-40.
- Gerard M. Domestic violence: how to screen and intervene. RN 2000;63:52-6.
- Fishwick NJ. Assessment of women for partner abuse. J Obstet Gynecol Neonat Nurs 1998;27:661-70.
- Ward S, Spence A. Training midwives to screen for domestic violence. MIDIRS Midwifery Digest 2002;12:S15-S17.
- Babcock J, Costa D, Green C, Eckhardt C. What situations induce intimate partner violence? A reliability and validity study of the Proximal Antecedents to Violence Episodes (PAVE) Scale. J Fam Psychol 2004;18:433-42.
- Shackelford TK, Goetz AT. Men’s sexual coercion in intimate relationships: development and initial validation of the Sexual Coercion in Intimate Relationships scale. Violence Vict 1919;19:541-56.
- Gregg GR, Parks ED. Selected Minnesota multiphasic personality inventory – 2 scales for identifying women with a history of sexual abuse. J Nerv Ment Dis 1995;183:53-6.
- Covington DL, Diehl SJ, Wright BD, Piner M. Assessing for violence during pregnancy using a systematic approach. Matern Child Health J 1997;1:129-33.
- Covington DL, Dalton VK, Diehl SJ, Wright BD, Piner MH. Improving detection of violence among pregnant adolescents. J Adolesc Health 1997;21:18-24.
- Cascardi M, Avery-Leaf S, O’Leary KD, Slep AMS. Factor structure and convergent validity of the Conflict Tactics Scale in high school students. Psychol Assessment 1999;11:546-55.
- Berlinger J. Helping abuse victims, part 1: taking an intimate look at domestic violence. Nursing (Lond) 2004;34:42-6.
- Datner EM, Shofer FS, Parmele K, Stahmer SA, Mechem CC. Utilization of the 911 system as an identifier of domestic violence. Am J Emerg Med 1999;17:560-5.
- Gagan MJ. Correlates of nurse practitioners’ diagnostic and intervention performance for domestic violence. West J Nurs Res 1998;20:536-53.
- Hilton NZ, Harris GT. Predicting wife assault: a critical review and implications for policy and practice. Trauma Violence Abuse 2005;6:3-23.
- Halpern LR, Susarla SM, Dodson TB. Injury location and screening questionnaires as markers for intimate partner violence. J Oral Maxillofac Surg 2005;63:1255-61.
- Williams GB, Dou M, Leal CC. Violence against pregnant women. These two screening tools may prove valuable in identifying women at risk [see comment]. Association of Women’s Health, Obstetric and Neonatal Nurses Lifelines 2003;7:348-54.
- Koziol M, Coates C, Lowenstein S. Predictive validity of a screen for partner violence against women. Am J Prev Med 2001;21:93-100.
- Gendron C. The development of a questionnaire for identification of women who are victims of violence in the conjugal milieu. Can J Nurs Res 1991;23:21-32.
- Dub M, Rinfret R, Drouin C. An exploratory study of the point of view of women and men on the services used concerning conjugal violence. Sante Ment Que 2005;30:301-20.
- Szafran W, Fossion P. Marital violence. Revue Medicale De Bruxelles 2005;26:S340-3.
- Rinfret R, Turgeon J, Dube M. A systematic screening protocol of domestic violence: measurement of efficiency. Can J Commun Ment Health 2002;21:85-99.
- Hasselmann MH, Reichenheim ME. Cross-cultural adaptation of the Portuguese version of the Conflict Tactics Scales Form R (CTS-1) used to assess marital violence: semantic and measurement equivalence. Cadernos De Saude Publica 2003;19:1083-93.
- Heron SL, Thompson MP, Jackson E, Kaslow NJ. Do responses to an intimate partner violence screen predict scores on a comprehensive measure of intimate partner violence in low-income black women?. Ann Emerg Med 2003;42:483-91.
- O’Leary KD. Psychological abuse: a variable deserving critical attention in domestic violence. Violence Vict 1999;14:3-23.
- Miscellaneous . Resources for clinicians: assessment for intimate partner violence in clinical practice. J Midwifery Womens Health 2002;47:386-90.
- Rodrigeuz R, Campbell JC. Empowering survivors of abuse: health care for battered women and their children. London: Sage; 1998.
- Barthauer L. Domestic violence in the psychiatric emergency service. San Francisco, CA: Jossey-Bass; 1999.
- Chuang CH, Liebschutz JM. Screening for intimate partner violence in the primary care setting: a critical review. J Clinical Outcomes Management 2002;9:565-71.
- Wyszynski ME. Screening women for family violence in the maternal child healthcare setting. Clin Excell Nurse Pract 2000;4:76-82.
- King MC, Ryan J. The role of nurse-midwives in assessment. J Nurse-Midwifery 1996;41:436-41.
- Coulthard P, Yong S, Adamson L, Warburton A, Worthington HV, Esposito M. Domestic violence screening and intervention programmes for adults with dental or facial injury. Cochrane Database of Systematic Reviews 2006.
- Pontecorvo C, Mejia R, Aleman M, Vidal A, Majdalani MP, Fayanas R, et al. Violencia domestica contra la mujer una encuesta en consultorios de atencion primaria. Medicina (Mex) 2004;64:492-6.
- Cook S, Goodman L. Beyond frequency and severity – development and validation of the Brief Coercion and Conflict Scales. Violence Against Women 2006;12:1050-72.
- Goetz AT, Shackelford TK, Schipper LD, Stewart-Williams S. Adding insult to injury: development and initial validation of the Partner-Directed Insults Scale. Violence Vict 2006;21:691-706.
- Williams KR, Grant SR. Empirically examining the risk of intimate partner violence: the revised Domestic Violence Screening Instrument (DVSI-R). Public Health Rep 2006;121:400-8.
- Parmar A, Sampson A, Diamond A. Tackling Domestic Violence: Providing Advocacy and Support to Survivors of Domestic Violence 2005:1-12.
- Fogarty CT, Brown JB. Screening for abuse in Spanish-speaking women. J Am Board Fam Pract 2002;15:101-11.
- Perry CM, Shams M, DeLeon CC. Voices from an Afghan community. J Cult Divers 1998;5:127-31.
- Freund KM, Bak S, Blackhall L. Identifying domestic violence in primary care practice. J Gen Intern Med 1996;11:44-7.
- McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, et al. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. J Behav Health Serv Res 2005;32:113-27.
- Kramer A. Domestic violence: how to ask and how to listen. Nurs Clin North Am 2002;37:189-210.
- Keeling J, Birch L. Asking pregnant women about domestic abuse. Br J Midwifery 2004;12:746-9.
- McCauley J, Yurk RA, Jenckes MW, Ford DE. Inside ‘Pandora’s Box’. Abused women’s experiences with clinicians and health services. J Gen Intern Med 1998;13:549-55.
- Thurston WE, Cory J, Scott CM. Building a feminist theoretical framework for screening of wife-battering: key issues to be addressed. Patient Educ Couns 1998;33:299-304.
- Kramer A, Lorenzon D, Muelle G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Women’s Health Issues 2004;14:19-2.
- Magen R, Conroy K, Del T. Domestic violence in child welfare preventative services: results from an intake screening questionnaire. Child Youth Serv Rev 2000;22:251-74.
- Sleutel MR. Women’s experiences of abuse: a review of qualitative research. Issues Ment Health Nurs 1998;19:525-39.
- Hamberger LK, Saunders DG, Hovey M. Prevalence of domestic violence in community practice and rate of physician inquiry. Fam Med 1992;24:283-7.
- Curnow SA. The Open Window Phase: helpseeking and reality behaviors by battered women. Appl Nurs Res 1997;10:128-35.
- Hamberger LK, Ambuel B, Marbella A, Donze J. Physician interaction with battered women: the women’s perspective. Arch Fam Med 1998;7:575-82.
- Moracco KE, Hilton A, Hodges KG, Frasier PY. Knowledge and attitudes about intimate partner violence among immigrant Latinos in rural North Carolina: baseline information and implications for outreach. Violence Against Women 2005;11:337-52.
- Panchanadeswaran S, Koverola C. The voices of battered women in India. Violence Against Women 2005;11:736-58.
- Lewis MJ, West B, Bautista L, Greenberg AM, Done-Perez I. Perceptions of service providers and community members on intimate partner violence within a Latino community. Health Educ Behav 2005;32:69-83.
- Sankar P, Jones NL. To tell or not to tell – primary care patients’ disclosure deliberations. Arch Intern Med 2005;165:2378-83.
- Weisz AN, Black BM. Evaluating a sexual assault and dating violence prevention program for urban youths. Soc Work Res 2001;25:89-100.
- Yoshioka MR, Gilbert L, El-Bassel N, Baig-Amin M. Social support and disclosure of abuse: comparing South Asian, African American, and Hispanic battered women. J Fam Violence 2003;18:171-80.
- O’Donnell SFMMP. Abuse in pregnancy – the experience of women. Ir Med J 2000;93:229-31.
- Jackson S. Abuse in dating relationships: young people’s accounts of disclosure, non-disclosure, help-seeking and prevention education. N Z J Psychol 2002;31:79-86.
- Zweig JM, Schlichter KA, Burt MR. Assisting women victims of violence who experience multiple barriers to services. Violence Against Women 2002;8:162-80.
- Cord-Duncan EC, Floyd M, Kemp EC, Bailey B, Lang F. Detecting potential intimate partner violence: which approach do women want?. Fam Med 2006;38:416-22.
- Boyle A, Jones PB. The acceptability of routine inquiry about domestic violence towards women: a survey in three healthcare settings. Br J Gen Pract 2006;56:258-61.
- Jones C, Bonner M. Screening for domestic violence in an antenatal clinic. Aust J Midwifery 2002;15:14-20.
- Hester M, Westmarland N. Tackling domestic violence: effective interventions and approaches. London: Home Office; 2005.
- Varcoe C. Abuse obscured: an ethnographic account of emergency nursing in relation to violence against women. Can J Nurs Res 2001;32:95-115.
- Bates L, Hancock L, Peterkin D. ‘A little encouragement’: health services and domestic violence. Int J Health Care Qual Assur 2001;14:49-56.
- Rodriguez MA, Quiroga SS, Bauer HM. Breaking the silence. Battered women’s perspectives on medical care. Arch Fam Med 1996;5:153-8.
- Dienemann J, Glass N, Hyman R. Survivor preferences for response to IPV disclosure. Clin Nurs Res 2005;14:215-33.
- Peterson R, Moracco KE, Goldstein KM, Clark KA. Women’s perspectives on intimate partner violence services: the hope in Pandora’s box. Women’s Health 2003;58:185-90.
- Curry M, Powers L, Oschwald M. Development of an abuse screening tool for women with disabilities. J Aggression 2003;8:123-41.
- Liang B, Goodman L, Tummala-Narra P, Weintraub S. A theoretical framework for understanding help-seeking processes among survivors of intimate partner violence. Am J Commun Psychol 2005;36:71-84.
- Taylor CA, Sorenson SB. Injunctive social norms of adults regarding teen dating violence. J Adolesc Health 2004;34:468-79.
- Crandall M, Senturia K, Sullivan M, Shiu-Thornton S. ‘No way out’: Russian-speaking women’s experiences with domestic violence. J Interpers Violence 2005;20:941-58.
- Sullivan M, Senturia K, Negash T, Shiu-Thornton S, Giday B. ‘For us it is like living in the dark’: Ethiopian women’s experiences with domestic violence. J Interpers Violence 2005;20:922-40.
- Mattson S, Shearer N, Long C. Exploring telehealth opportunities in domestic violence shelters. J Am Acad Nurse Prac 2002;14:465-70.
- Battaglia TA, Finley E, Liebschutz JM. Survivors of intimate partner violence speak out. Trust in the patient-provider relationship. J Gen Intern Med 2003;18:617-23.
- McNutt LA, van RM, Clark C, Fraiser I. Partner violence and medical encounters: African-American women’s perspectives. Am J Prev Med 2000;19:264-9.
- O’Connor M. Consequences and outcomes of disclosure for abused women. Int J Gynecol Obstet 2002;78:S83-9.
- Renker PR. Keeping safe: teenagers’ strategies for dealing with perinatal violence. J Obstet Gynecol Neonat Nurs 2002;32:58-66.
- Taylor JY. Moving from surviving to thriving: African American women recovering from intimate male partner abuse. Res Theory Nurs Pract 2004;18:35-50.
- Koziol-McLain J, Gardiner J, Batty P, Rameka M, Fyfe E, Giddings L. Prevalence of intimate partner violence among women presenting to an urban adult and paediatric emergency care department [see comment]. N Z Med J 2004;117.
- Davis K, Taylor B. Voices from the margins part 2: narrative accounts of the support needs of indigenous families experiencing violence. Contemp Nurse 2002;14:76-85.
- Washington PA. Disclosure patterns of black female sexual assault aurvivors. Violence Against Women 2001;7.
- McMurray A, Moore K. Domestic violence: are we listening? Do we see?. Aust J Adv Nurs 1994;12:23-8.
- Gerbert B, Johnston K, Caspers N, Bleecker T, Woods A, Rosenbaum A. Experiences of battered women in health care settings: a qualitative study. Women Health 1996;24:1-17.
- Kearsey K. Listening for silent screams: abused women hope to be ‘found’ by nurses and other health-care professionals. Registered Nurse J 2002;14:12-7.
- McCarraher DR, Bailey PE, Martin SL. Are reproductive health services a good place to screen for intimate partner violence? Evidence from Bolivia. Violence Against Women 2003;9:989-1002.
- Campbell JC, Soeken KL. Women’s responses to battering: a test of the model. Res Nurs Health 1999;22:49-58.
- Plichta SB, Duncan MM, Plichta L. Spouse abuse, patient-physician communication, and patient satisfaction. Am J Prev Med 1996;12:297-303.
- Weingourt R. Wife rape: barriers to identification and treatment. Am J Psychother 1985;39:187-92.
- Rodriguez MA, Bauer HM, Flores-Ortiz YG, Quiroga SS. Factors affecting patient-physician communication for abused Latina and Asian immigrant women. J Fam Pract 1998;47:309-11.
- Hayden SR, Barton ED, Hayden M. Domestic violence in the emergency department: how do women prefer to disclose and discuss the issues?. J Emerg Med 1997;15:447-51.
- Bacchus L, Mezey GC, Bewley S. Experiences of seeking help from health professionals in a sample of women who experienced domestic violence. Health Soc Care Community 2003;11:10-8.
- Hou W, Wang H, Chung H. Domestic violence against women in Taiwan: their life-threatening situations, post-traumatic responses, and psycho-physiological symptoms: an interview study. Int J Nurs Stud 2005;42:629-36.
- Peckover S. ‘I could have just done with a little more help’: an analysis of women’s help-seeking from health visitors in the context of domestic violence. Health Soc Care Community 2003;11:275-82.
- Scheiman L, Zeoli A. Adolescents experiences of dating and intimate partner violence: ‘Once is not enough’. J Midwifery Womens Health 2003;48:226-8.
- McCosker H, Madl R, Harris M, Anderson D, Mannion J. Evaluation of a self-paced education package on violence against women for rural community-based health workers. Aust J Rural Health 1999;7:5-12.
- Flinck A, Paavilainen E, Stedt-Kurki P. Survival of intimate partner violence as experienced by women. J Clin Nurs 2005;14:383-93.
- De Mendoza V. Culturally appropriate care for pregnant Latina women who are victims of domestic violence. J Obstet Gynecol Neonat Nurs 2001;30:579-88.
- Choi M, Harwood J. A hypothesized model of Korean women’s responses to abuse. J Transcult Nurs 2004;15:207-16.
- Brendtro M, Bowker L. Battered women: How can nurses help?. Issues Ment Health Nurs 1989;10:169-80.
- Petersen R, Moracco K, Goldstein K, Clark K. Moving beyond disclosure: women’s perspectives on barriers and motivators to seeking assistance for intimate partner violence. Women Health 2004;40:63-76.
- Grynbaum M, Biderman A, Levy A, Petasne W. Domestic violence: prevalence among women in a primary care center – a pilot study. Israel Med Assoc J 2001;3:907-10.
- Fugate ML, Ritch L, Navarro F, Engel B. Barriers to domestic violence help seeking: implications for intervention. Violence Against Women 2005;11:290-31.
- Bauer HM, Rodriguez MA, Szkupinski Quiroga S, Flores-Ortiz YG. Barriers to health care for abused Latina and Asian immigrant women. J Health Care Poor Undeserved 2000;11:33-44.
- Gerbert B, Bronstone A, Pantilat S, McPhee S, Allerton M, Moe J. When asked, patients tell: disclosure of sensitive health-risk behaviors. Med Care 1999;37:104-11.
- Chatzifotiou S. Violence against women and institutional responses: the case of Greece. Eur J Soc Work 2003;6:241-56.
- Edwards M. Raising the subject of domestic violence. Pract Nurse 2005;29:26-30.
- Fraser IM, McNutt LA, Clark C, Williams-Muhammed D, Lee R. Social support choices for help with abusive relationships: perceptions of African American women. J Fam Violence 2002;17:363-75.
- Richardson J, Feder G. Domestic violence: a hidden problem for general practice. Br J Gen Pract 1996;46:239-42.
- Campbell JC, Pliska MJ, Taylor W, Sheridan D. Battered women’s experiences in the emergency department. J Emerg Nurs 1994;20:280-8.
- Sethi D, Watts S, Watson J, McCarthy C, Zwi A. Experience of ‘screening’ for domestic violence in Women’s Services. J Public Health 2001;23:349-50.
- Milberger S, Israel N, LeRoy B, Martin A, Potter L, Patchak-Schuster P. Violence against women with physical disabilities. Violence Vict 2003;18:581-91.
- Dienemann J, Campbell J, Wiederhorn N, Laughon K, Jordan E. A critical pathway for intimate partner violence across the continuum of care. J Obstet Gynecol Neonat Nurs 2002;32:594-603.
- Yam M, Oradell NJ. Seen but not heard: battered women’s perceptions of the ED experience. J Emerg Nurs 2000;26:464-70.
- El-Khoury MY, Dutton MA, Goodman LA, Engel L, Belamaric RJ, Murphy M. Ethnic differences in battered women’s formal help-seeking strategies: a focus on health, mental health, and spirituality. Cultur Divers Ethnic Minor Psychol 2004;10:383-93.
- Goodyear-Smith F. National screening policies in general practice: a case study of routine screening for partner abuse. Appl Health Econ Health Policy 2002;1:197-209.
- McCloskey LA, Lichter E, Ganz ML, Williams CM, Gerber MR, Sege R, et al. Intimate partner violence and patient screening across medical specialties. Acad Emerg Med 2005;12:712-22.
- Busch NB, Wolfer TA. Battered women speak out: welfare reform and their decisions to disclose. Violence Against Women 2002;8:566-84.
- Gill A. Voicing the silent fear: South Asian women’s experiences of domestic violence. Howard J Criminal Justice 2004;43:465-83.
- Edwardsen EA, Pless NA, Fiscella KA, Horwitz SH, Meldrum SC. Pilot educational outreach project on partner violence. Prev Med 2004;39:536-42.
- Rodriguez MA, Sheldon WR, Bauer HM, Perez-Stable EJ. The factors associated with disclosure of intimate partner abuse to clinicians. J Fam Pract 2001;50:338-44.
- Gerbert B, Abercrombie P, Caspers N, Love C, Bronstone A. How health care providers help battered women: the survivor’s perspective. Women Health 1999;29:115-35.
- Burge S, Schneider F, Ivy L, Catala S. Patients’ advice to physicians about intervening in family conflict. Ann Fam Med 2005;3:248-54.
- Zink T, Jacobson J, Regan S, Pabst S. Hidden victims: the healthcare needs and experiences of older women in abusive relationships. J Women Health 2004;13:898-90.
- Hegarty K, Taft AJ. Overcoming the barriers to disclosure and inquiry of partner abuse for women attending general practice. Aust N Z J Public Health 2001;25:433-7.
- Romito P, Gerin D. Asking patients about violence: a survey of 510 women attending social and health services in Trieste, Italy. Soc Sci Med 2002;54:1813-24.
- Larsen T, Brodersen P, Larsen A, Bendtsen F. Violence to women in their partnership. IV. Contact pattern to public institutions. Ugeskr Laeger 1985;147:1801-4.
- Stenius VM, Veysey BM. ‘It’s the little things’: women, trauma, and strategies for healing. J Interpers Violence 2005;10:1155-74.
- Savage A, Russell LA. Tangled in a web of affiliation: social support networks of dually diagnosed women who are trauma survivors. J Behav Health Serv Res 2005;32:199-214.
- Reed B, Mazelis R. Scholarship, collaboration, struggle, and learning in the Women, Co-occurring Disorders, and Violence Study: introduction to the 6-month outcome papers. J Subst Abuse Treat 2005;28:87-9.
- Finkelstein N, Rechberger E, Russell LA, VanDeMark NR, Noether CD, O’Keefe M, et al. Building resilience in children of mothers who have co-occurring disorders and histories of violence: intervention model and implementation issues. J Behav Health Serv Res 2005;32:141-54.
- Jaffe P, Wilson S, Wolfe D. Promoting changes in attitudes and understanding of conflict resolution among child witnesses of family violence. Can J Behav Sci 1986;18:356-66.
- McCaw B, Bauer HM, Berman WH, Mooney L, Holmberg M, Hunkeler E. Women referred for on-site domestic violence services in a managed care organization. Women Health 2002;35:23-40.
- Foshee VA, Bauman KE, Ennett ST, Suchindran C, Benefield T, Linder GF. Assessing the effects of the dating violence prevention program ‘safe dates’ using random coefficient regression modeling. Prev Sci 2005;6:245-58.
- Riesen Y, Porath M. Perceived social support of maritally abused women and their children’s global self-worth. Can J Commun Ment Health 2004;23:109-15.
- Sullivan CM, Basta J, Tan C, Davidson WS. After the crisis: a needs assessment of women leaving a domestic violence shelter. Violence Vict 1992;7:267-75.
- Foshee VA, Bauman KE, Ennett ST, Linder GF, Benefield T, Suchindran C. Assessing the long-term effects of the Safe Dates Program and a booster in preventing and reducing adolescent dating violence victimization and perpetration. Am J Public Health 2004;94:619-24.
- Davies D. Intervention with male toddlers who have witnessed parental violence. Fam Soc 1991;72:515-24.
- Khemka I, Hickson L, Reynolds G. Evaluation of a decision-making curriculum designed to empower women with mental retardation to resist abuse. Am J Ment Retard 2005;110:193-204.
- Weisz AN. Reaching African American battered women: increasing the effectiveness of advocacy. J Fam Violence 2005;20:91-9.
- Cannon J, Sparks J. Shelters – an alternative to violence: a psychosocial case study. J Commun Psychol 1989;17:203-13.
- McBride D, Korell G. Wilderness therapy for abused women. Can J Counselling 2005;39:3-14.
- Rhodes R, Zelman A. An ongoing multifamily group in a women’s shelter. Am J Orthopsychiatry 1986;56:120-30.
- Angless T, Maconachie M, Van Z. Battered women seeking solutions: a South African study. Violence Against Women 1998;4:637-58.
- Attala J, Warmington M. Clients’ evaluation of health care services in a battered women’s shelter. Public Health Nurs 1996;13:269-75.
- Frick-Helms SB. ‘Boys cry better than girls’: play therapy behaviors of children residing in a shelter for battered women. Int J Play Ther 1997;6:73-91.
- Evans D, Shaw W. A social group work model for latency-aged children from violent homes. Soc Work Groups 1993;16:97-116.
- Grusznski R, Brink J, Edleson J. Support and education groups for children of battered women. Child Welfare 1988;67:431-44.
- Walker S. Domestic violence: analysis of a community safety alarm system. Child Abuse Rev 2001;10:170-82.
- Thomas CR, Miller G, Hartshorn JC, Speck NC, Walker G. Telepsychiatry program for rural victims of domestic violence. Telemed J E-Health 2005;11:567-73.
- Drotar D, Flannery D, Day E, Friedman S, Creeden R, Gartland H, et al. Identifying and responding to the mental health service needs of children who have experienced violence: a community-based approach. Clin Child Psychol Psychiatry 2003;8:187-203.
- Kozlowska K, Hanney L. An art therapy group for children traumatized by parental violence and separation. Clin Child Psychol Psychiatry 2001;6:49-78.
- Hillard PJA. Physical abuse in pregnancy. Obstet Gynecol 1985;66:185-90.
- Short LM, Hadley SM, Bates B. Assessing the success of the WomanKind program: an integrated model of 24-hour health care response to domestic violence. Women Health 2002;35:101-19.
- Bennett L, Dawe D, Power J. Children’s needs in shelters: mother’s perceptions. Can J Commun Ment Health 1999;18:57-76.
- Sullivan CM. Using the ESID model to reduce intimate male violence against women. Am J Commun Psychol 2003;32:295-303.
- Vives C, Gil G, Carrasco-Portiño M, Alvarez-Dardet C. Early screening of intimate partner violence. An evidence-based intervention?. Med Clin (Barc) 2006;126:101-4.
- Few A. The voices of black and white rural battered women in domestic violence shelters. Fam Relat 2005;54:488-500.
- Kerig PK, Fedorowicz AE, Brown CA, Warren M. Assessment and intervention for PTSD in children exposed to violence. J Aggression Maltreat Trauma 2000;3:161-84.
- Cook DR, Frantz-Cook A. A systemic treatment approach to wife battering. J Marital Fam Ther 1984;10:83-9.
- Gehart DR, Morales DL. Reclaiming one’s voice: a narrative intervention for women who have been battered. J Fam Psychother 2000;11:69-73.
- Yoshihama M. Policies and services addressing domestic violence in Japan: from non-interference to incremental changes. Women Stud Int Forum 2002;25:541-53.
- Webb W. Treatment issues and cognitive behaviour techniques with battered women. J Fam Violence 1992;7:205-17.
- Milner J. From ‘disappearing’ to ‘demonized’: the effects on men and women of professional interventions based on challenging men who are violent. Crit Soc Policy 2004;24:79-101.
- Martin G. Psychotherapy with abused women in a women’s agency. J Soc Work Pract 1993;7:153-61.
- Datner EM, O’Malley M, Schears RM, Shofer FS, Baren J, Hollander JE. Universal screening for interpersonal violence: inability to prove universal screening improves provision of services. Eur J Emerg Med 2004;11:35-8.
- Scott-Tilley D. Nursing interventions for domestic violence. Am J Nurs 1999;99.
- van Dalen A, Glasserman M. My father, Frankenstein: a child’s view of battering parents. J Am Acad Child Adolesc Psychiatry 1997;36:1005-7.
- Usdin S, Scheepers E, Goldstein S, Japhet G. Achieving social change on gender-based violence: a report on the impact evaluation of Soul City’s fourth series. Soc Sci Med 2005;61:2434-45.
- Coker AL, Watkins KW, Smith PH, Brandt HM. Social support reduces the impact of partner violence on health: application of structural equation models. Prev Med 2003;37:259-67.
- Frohmann L. The Framing Safety Project: photographs and narratives by battered women. Violence Against Women 2005;11:1396-419.
- Mueller D, Thomas H. The effectiveness of public health interventions to reduce or prevent spousal abuse toward women. London, ON: Effective Public Health Practice Project; 2001.
- Jones SM, Bogat GA, Davidson WS, von Eye A, Levendosky A. Family support and mental health in pregnant women experiencing interpersonal partner violence: an analysis of ethnic differences. Am J Commun Psychol 2005;36:97-108.
- Rosen KH, Stith SM. Intervention strategies for treating women in violent dating relationships. Fam Relat 1993;42:427-33.
- Kataoka SH, Fuentes S, O’Donoghue VP, Castillo-Campos P, Bonilla A, Halsey K, et al. A community participatory research partnership: the development of a faith-based intervention for children exposed to violence. Ethnic Dis 2006;16:89-97.
- Silvern L, Karyl J, Landis T. Individual psychotherapy for the traumatized children of abused women. Thousand Oaks, CA: Sage Publications; 1995.
- Rabenstein S, Lehmann P. Mothers and children together: a family group treatment approach. J Aggression 2000;3:185-20.
- Ahmed SM. Intimate partner violence against women: experiences from a woman-focused development programme in Matlab, Bangladesh. J Health Popul Nutr 2005;23:95-101.
- Becker MA, Gatz M. Introduction to the impact of co-occurring disorders and violence on women: findings from the SAMHSA Women, Co-occurring Disorders and Violence Study. J Behav Health Serv Res 2005;32:111-2.
- Kheder S, VandenBosch T. Intimate partner violence a health system’s response. Continuum 2001:15-22.
- Rhodes KV, Levinson W. Interventions for intimate partner violence against women: clinical applications. JAMA 2003;289:601-5.
- Ambuel B, Hamberger LK, Lahti J. Partner violence: a systematic approach to identification and intervention in outpatient health care. Wis Med J 1996;95:292-7.
- Campbell JC, Sharps P, Sachs C, Yam M. Medical lethality assessment and safety planning in domestic violence cases. Clin Fam Pract 2003;5:101-11.
- Berkowitz CD. Recognizing and responding to domestic violence. Pediatr Ann 2005;34:395-401.
- Duggan A, McFarlane E, Fuddy L, Burrell L, Higman SM, Windham A, et al. Randomized trial of a statewide home visiting program: impact in preventing child abuse and neglect. Child Abuse Neglect 2004;28:597-622.
- Mattson S, Ruiz E. Intimate partner violence in the Latino community and its effect on children. Health Care Women Int 2005;26:523-9.
- Webb E, Shankleman J, Evans MR, Brooks R. The health of children in refuges for women victims of domestic violence: cross sectional descriptive survey. BMJ 2001;323:210-13.
- Ham R, Gordon EE, Jarvis KL, Novaco RW. Life constraints and psychological well-being of domestic violence shelter graduates. J Fam Violence 2005;20:109-21.
- Goodkind JR, Sullivan CM, Bybee DI. A contextual analysis of battered women’s safety planning. Violence Against Women 2004;10:514-33.
- Vinton L. A model collaborative project toward making domestic violence centers elder ready. Violence Against Women 2003;9:1504-13.
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu WL, Elliott MN, et al. A mental health intervention for schoolchildren exposed to violence – a randomized controlled trial. JAMA 2003;290:603-11.
- Quinlivan JA, Evans SF. Impact of domestic violence and drug abuse in pregnancy on maternal attachment and infant temperament in teenage mothers in the setting of best clinical practice. Arch Women Ment Health 2005;8:191-9.
- McDermott MJGJ. When advocacy for domestic violence victims backfires: types and sources of victim disempowerment. Violence Against Women 2004;10:1245-66.
- Peled E. Intervention with children of battered women: a review of current literature. Child Youth Serv Rev 1997;19:277-99.
- Walton-Moss BJ, Campbell JC. Intimate partner violence: implications for nursing. Online J Issues Nurs 2002;7.
- Hotch D, Grunfeld A, Mackay K, Cowan L. An emergency department-based domestic violence intervention program: findings after one year. J Emerg Med 1996;14:111-17.
- Breton M, Nosko A. Group work with women who have experienced abuse. New York: Oxford University Press; 2005.
- Sudermann M, Marshall L, Loosely S. Evaluation of the London (Ontario) Community Group Treatment Programme for Children who have Witnessed Woman Abuse. J Aggression 2000;3:127-46.
- Pynoos R, Eth S. Special intervention programs for child witnesses to violence. Philadelphia, PA: Brunner/Mazel; 1986.
- Foshee VA, Bauman KE, Arriaga XB, Helms RW, Koch GG, Linder GF. An evaluation of Safe Dates, an adolescent dating violence prevention program. Am J Public Health 1998;88:45-50.
- Goodman L, Dutton MA, Vankos N, Weinfurt K. Women’s resources and use of strategies as risk and protective factors for reabuse over time. Violence Against Women 2005;11:311-36.
- Bybee DI, Sullivan CM. The process through which an advocacy intervention resulted in positive change for battered women over time. Am J Commun Psychol 2002;30:103-32.
- Allen NE, Bybee DI, Sullivan CM. Battered women’s multitude of needs. Evidence supporting the need for comprehensive advocacy. Violence Against Women 2004;10:1015-35.
- Statham J. Effective services to support children in special circumstances. Child Care Health Dev 2004;30:589-98.
- Groves B. Mental health services for children who witness domestic violence. Future Child 1999;9:122-32.
- Tutty L, Weaver G, Rothery M. Residents’ views of the efficacy of shelter services for assaulted women. Violence Against Women 1999;5:898-925.
- Graham-Bermann SA, Hughes HM. Intervention for children exposed to interparental violence (IPV): assessment of needs and research priorities. Clin Child Fam Psych 2003;6:189-204.
- Haggerty L, Goodman L. Stages of change-based nursing interventions for victims of interpersonal violence. J Obstet Gynecol Neonat Nurs 2003;32:68-75.
- Ogle RL, Baer JS. Addressing the service linkage problem – increasing substance abuse treatment engagement using personalized feedback interventions in heavy-using female domestic violence shelter residents. J Interpers Violence 2003;18:1311-24.
- Davis K, Taylor B, Furniss D. Narrative accounts of tracking the rural domestic violence survivors’ journey: a feminist approach. Health Care Women Int 2001;22:333-47.
- Gutman SA, Diamond H, Holness P, Brandofino DN, Pacheco DG, Jolly E, et al. Enhancing independence in women experiencing domestic violence and possible brain injury: an assessment of an occupational therapy intervention. Occup Ther Ment Health 2004;20:49-7.
- Norton IM, Schauer J. A hospital-based domestic violence group. Psychiatr Serv 1997;48:1186-90.
- Chalk R. Assessing family violence interventions: linking programs to research-based strategies. J Aggression Maltreat Trauma 2000;4:29-53.
- Wathen CN, MacMillan HL. Interventions for violence against women: scientific review. JAMA 2003;289:589-600.
- Noether CD, Finkelstein N, VanDeMark NR, Savage A, Reed BG, Moses DJ. Design strengths and issues of SAMHSA’s Women, Co-occurring Disorders, and Violence Study. Psychiatr Serv 2005;56:1233-6.
- Sullivan C, Allen N. Evaluating coordinated community responses for abused women and their children. Washington, DC: American Psychological Association; 2001.
- Peled E, Edleson JL. Predicting children’s domestic violence service participation and completion. Res Soc Work Pract 1998;8:698-712.
- Bullock L. Nursing interventions for abused women on obstetrical units. Thousand Oaks, CA: Sage Publications; 1998.
- Stone L. Shelters for battered women: a temporary escape from danger or the first step towards divorce. Victimology 1984;9:284-9.
- Chambers S. Group work with women from refuges. FSU Quarterly 1988;43:10-2.
- Barber M, Jenkins R, Jones C. A survivors’ group for women who have a learning disability. Br J Dev Disabil 2000;46:31-4.
- Gilson S. The YWCA Women’s Advocacy Program: a case study of DV and sexual assault services. J Commun Pract 1997;4:1-26.
- Gondolf EW. Characteristics of court-mandated batterers in four cities. Violence Against Women 1999;5:1277-93.
- Zust BL. Effect of cognitive therapy on depression in rural, battered women. Arch Psychiatr Nurs 2000;XIV:51-63.
- Veysey BM, Clark C. Responding to physical and sexual abuse in women with alcohol and other drug and mental disorders: program building. Introduction. Alcoholism Treatment Quarterly 2004;22:1-18.
- McHugo GJ, Kammerer N, Jackson EW, Markoff LS, Gatz M, Larson MJ, et al. Women, Co-occuring Disorders, and Violence Study: evaluation design and study population. J Subst Abuse Treat 2005;28:31-107.
- Preston SL. Claiming our place: women with serious mental health issues and support groups for abused women. Can J Commun Ment Health 2002;21:101-13.
- Mullender A, Debbonaire T, Hague G, Kelly L, Malos E. Working with children in women’s refuges. Child Fam Soc Work 1998;3:87-98.
- Brown J, Languedoc S. Components of an aboriginal-based family violence intervention program. Fam Soc-J Contemp H 2004;85:477-83.
- Ulrich YC. What helped most in leaving spouse abuse: implications for interventions. Association of Women’s Health Obstetric and Neonatal Nurses Clin Issues Perinat Womens Health Nurs 1993;4:385-90.
- Shavers CA, Levendosky AA, Dubay SM, Basu A, Jenei J. Domestic violence research: methodological issues related to a community-based intervention with a vulnerable population. J Appl Biobehav Res 2005;10:27-38.
- Seagull EA, Seagull AA. Healing the wound that must not heal: psychotherapy with survivors of domestic violence. Psychotherapy 1991;28:16-20.
- Clapp L. Ending domestic violence is everyone’s responsibility: an integrated approach to domestic violence treatment. Nurs Clin North Am 2000;35:481-8.
- Campbell J. A survivor group for battered women. Adv Nurs Sci 1986;8:13-20.
- Gorgen T, Nagele B. Domestic elder abuse and neglect – conclusions from the evaluation of a model project. Z Gerontol Geriat 2005;38:4-9.
- Morrissey JP, Ellis AR, Gatz M, Amaro H, Reed BG, Savage A, et al. Outcomes for women with co-occurring disorders and trauma: program and person-level effects. J Subst Abuse Treat 2005;28:121-33.
- Krishnan SP, Hilbert JC, McNeil K, Newman I. From respite to transition: women’s use of domestic violence shelters in rural New Mexico. J Fam Violence 2004;19:165-74.
- Dutton-Douglas MA, Dionne D, Steinman M. Woman battering: policy responses. Cincinnati, OH: Anderson Publishing; 1991.
- Anglin D, Sachs C. Preventive care in the emergency department: screening for domestic violence in the emergency department. Acad Emerg Med 2003;10:1118-27.
- Crockford M, Kent G, Stewart N. Play friendly and safe: a therapeutic group model for young children (5–8 years old) who have witnessed wife assault. J Child Youth Care 1993;8:77-86.
- Jaffe P, Wilson S, Wolfe D. Specific assessment and intervention strategies for children exposed to wife battering: preliminary empirical investigations. Can J Commun Ment Health 1988;7:157-63.
- Whipple J, Lindsey R. Music for the soul: a music therapy program for battered women. Music Therapy Perspectives 1999;17:61-8.
- Peled E, Edleson J. Multiple perspectives on groupwork with children of battered women. Violence Vict 1992;7:327-46.
- Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits LM. Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiat Serv 2005;56:1213-22.
- Curry MA, Durham L, Bullock L, Davis J. Nurse case management for pregnant women experiencing or at risk for abuse. J Obstet Gynecol Neonat Nurs 2006;35:181-92.
- Padala PR, Madison J, Monnahan M, Marcil W, Price P, Ramaswamy S, et al. Risperidone monotherapy for post-traumatic stress disorder related to sexual assault and domestic abuse in women. Int Clin Psychopharmacol 2006;21:275-80.
- Kane KE. The phenomenology of meditation for female survivors of intimate partner violence. Violence Against Women 2006;12:501-18.
- Shim WS, Haight WL. Supporting battered women and their children: perspectives of battered mothers and child welfare professionals. Child Youth Serv Rev 2006;28:620-37.
- Bullock L, Bloom T, Davis J, Kilburn E, Curry MA. Abuse disclosure in privately and medicaid-funded pregnant women. J Midwifery Womens Health 2006;51:361-9.
- Katz LF, Windecker-Nelson B. Domestic violence, emotion coaching, and child adjustment. J Fam Psychol 2006;20:56-67.
- Parker JS, Stewart GSGC. Research and intervention with adolescents exposed to domestic violence. Fam Ther 2006;33:45-52.
- Zust BL. Meaning of INSIGHT participation among women who have experienced intimate partner violence. Issues Ment Health Nurs 2006;27:775-93.
- Ford-Gilboe M, Wuest J, Varcoe C, Merritt-Gray M. Developing an evidence-based health advocacy intervention for women who have left an abusive partner. Can J Nurs Res 2006;38:147-67.
- Buschel BS, Madsen LH. Strengthening connections between mothers and children: art therapy in a domestic violence shelter. J Aggression Maltreat Trauma 2006;13:87-108.
- Bergeron M, Hebert M. Evaluation of a group intervention from a feminist approach with female victims of sexual assault. Child Abuse Neglect 2006;30:1143-59.
- Brienza RS, Whitman L, Ladouceur L, Green ML. Evaluation of a women’s safe shelter experience to teach internal medicine residents about intimate partner violence: a randomized controlled trial. J Gen Intern Med 2005;20:536-40.
- Coonrod DV, Bay RC, Rowley BD, Del Mar NB, Gabriele L, Tessman TD, et al. A randomized controlled study of brief interventions to teach residents about domestic violence. Acad Med 2000;75:55-7.
- Larkin G, Rolniak S, Hyman K, MacLeod B, Savage R. Effect of an administrative intervention on rates of screening for domestic violence in an urban emergency department. Am J Public Health 2000;90:1444-8.
- Holtrop TG, Fischer H, Gray SM, Barry K, Bryant T, Du W. Screening for domestic violence in a general pediatric clinic: be prepared. Pediatrics 2004;114:1253-7.
- Olson L, Anctil C, Fullerton L, Brillman J, Arbuckle J, Sklar D. Increasing emergency physician recognition of domestic violence. Ann Emerg Med 1996;27:741-6.
- Morrison LJ, Allan R, Grunfeld A. Improving the emergency department detection rate of domestic violence using direct questioning. J Emerg Med 2000;19:117-24.
- Wenzel JD, Monson CL, Johnson SM. Domestic violence: prevalence and detection in a family medicine residency clinic. J Am Osteopath Assoc 2004;104:233-9.
- McFarlane J, Wiist WW. Documentation of abuse to pregnant women: a medical chart audit in public health clinics. J Women Health 1996;5:137-42.
- Ernst A, Weiss S. Intimate partner violence from the emergency medicine perspective. Women Health 2002;35:71-8.
- Richter K, Surprenant Z, Schmelzie K, Mayo M. Detecting and documenting intimate partner violence: an intake form question is not enough. Violence Against Women 2003;9:458-65.
- DuMont MJ, Forte T, Cohen MM, Hyman I, Romans S. Changing help-seeking rates for intimate partner violence in Canada. Women Health 2005;41:1-19.
- Spinola C, Stewart L, Fanslow J, Norton R. Developing and implementing an intervention. Evaluation of an emergency department pilot on partner abuse. Eval Health Prof 1998;21:91-119.
- Campbell JC, Coben JH, McLoughlin E, Dearwater S, Nah G, Glass N, et al. An evaluation of a system-change training model to improve emergency department response to battered women. Acad Emerg Med 2001;8:131-8.
- Perrin KM, Boyett TP, McDermott RJ. Continuing education about physically abusive relationships: does education change the perceptions of health care practitioners?. J Contin Educ Nurs 2000;31:269-74.
- Siegel RM, Joseph EC, Routh SA, Mendel SG, Jones E, Ramesh RB, et al. Screening for domestic violence in the pediatric office: a multipractice experience. Clin Pediatr 2003;42:599-602.
- Stenson K, Heimer G, Lundh C, Nordstrom ML, Saarinen H, Wenker A. The prevalence of violence investigated in a pregnant population in Sweden. J Psychosom Obstet Gynaecol 2001;22:189-97.
- Dodge AC, McLoughlin E, Saltzman LE, Nah G, Skaj P, Campbell JC, et al. Improving intimate partner violence protocols for emergency departments: an assessment tool and findings. Violence Against Women 2002;8:320-38.
- Garcia FAR, Parsons ML. Effective screening for domestic violence in the inpatient obstetric setting. Primary Care Update Gyns 2002;9:94-7.
- Kothari CL, Rhodes KV. Missed opportunities: emergency department visits by police-identified victims of intimate partner violence. Ann Emerg Med 2006;47:190-9.
- Coker AL, Bethea L, Smith PH, Fadden MK, Brandt HM. Missed opportunities: intimate partner violence in family practice settings. Prev Med 2002;34:445-54.
- Sixsmith DM, Weissman L, Constant F. Telephone follow-up for case finding of domestic violence in an emergency department. Acad Emerg Med 1997;4:301-4.
- Korenstein D, Thomas DC, Foldes C, Ross J, Halm E, McGinn T. An evidence-based domestic violence education program for internal medicine residents. Teach Learn Med 2003;15:262-6.
- Hollander JE, Schears RM, Shofer FS, Baren JM, Moretti LM, Datner EM. The effect of written informed consent on detection of violence in the home. Acad Emerg Med 2001;8:974-9.
- Garcia-Moreno C. Dilemmas and opportunities for an appropriate health-service response to violence against women. Lancet 2002;359:1509-14.
- Agar K, Read J, Bush J. Identification of abuse histories in a community mental health centre: the need for policies and training. J Ment Health 2002;11:533-43.
- Paluzzi P, Gaffikin L, Nanda J. The American College of Nurse-Midwives’ Domestic Violence Education Project: evaluation and results. J Midwifery Womens Health 2000;45:384-91.
- Shields G, Baer J, Leininger K, Marlow J, DeKeyser P. Interdisciplinary health care and female victims of domestic violence. Soc Work Health Care 1998;27:27-48.
- Porcerelli JH, Cogan R, West PP, Rose EA, Lambrecht D, Wilson KE, et al. Violent victimization of women and men: physical and psychiatric symptoms. J Am Board Fam Pract 2003;16:32-9.
- Espinosa L, Osborne K. Domestic violence during pregnancy: implications for practice. J Midwifery Womens Health 2002;47:305-17.
- Berenson A. Perinatal morbidity associated with violence experienced by pregnant women. Am J Obstet Gynecol 1994;170:1760-9.
- Wallace A. Domestic violence: an education programme for hospital staff. J Fam Health Care 2002;12:65-7.
- Shattuck S. A domestic violence screening program in a public health department. J Commun Health Nurs 2002;19:121-32.
- Matevia M, Goldman W, McCulloch J, Randall P. Detection of intimate-partner violence among members of a managed behavioral health organization. Psychiatr Serv 2002;53:555-7.
- Tilden VP, Shepherd P. Increasing the rate of identification of battered women in an emergency department: use of a nursing protocol. Res Nurs Health 1987;10:209-15.
- Roberts GL, Lawrence JM, O’Toole BI, Raphael B. Domestic violence in the Emergency Department: 2. Detection by doctors and nurses. Gen Hosp Psychiatry 1997;19:12-5.
- Bergman B, Brismar B. A 5-year follow-up study of 117 battered women. Am J Public Health 1991;81:1486-9.
- Muelleman RL, Feighny KM. Effects of an emergency department-based advocacy program for battered women on community resource utilization. Ann Emerg Med 1999;33:62-6.
- Wessel L, Campbell JC. Providing sanctuary for battered women: Nicaragua’s casas de la mujer. Issues Ment Health Nurs 1997;18:455-76.
- Vives C, Caballero P, Alvarez-Dardet C. Temporal analysis of mortality due to intimate partner violence in Spain. Gaceta Sanitaria 2004;18:346-50.
- Allert CS, Chalkley C, Whitney JR, Librett A. Domestic violence: efficacy of health provider training in Utah. Prehosp Disaster Med 1996;12:52-6.
- Glowa PT, Frasier PY, Wang L, Eaker K, Osterling WL. What happens after we identify intimate partner violence? The family physician’s perspective. Fam Med 2003;35:730-6.
- Thompson RS, Meyer BA, Smith-DiJulio K, Caplow MP, Maiuro RD, Thompson DC, et al. A training program to improve domestic violence identification and management in primary care: preliminary results. Violence Vict 1998;13:395-410.
- Davis JW, Parks SN, Kaups KL, Bennink LD, Bilello JF. Victims of domestic violence on the trauma service: unrecognized and underreported. J Trauma 2003;54:352-5.
- Kohl PL, Barth RP, Hazen AL, Landsverk JA. Child welfare as a gateway to domestic violence services. Child Youth Serv Rev 2005;27:1203-21.
- Davila YR. Increasing nurses’ knowledge and skills for enhanced response to intimate partner violence. J Contin Educ Nurs 2006;37:171-7.
- McNulty A, Andrews P, Bonner M. Can screening for domestic violence be introduced successfully in a sexual health clinic?. Sex Health 2006;3:179-82.
- McCaw B, Kotz K. Family violence prevention program: another way to save a life. The Permanente Journal 2005;9:65-8.
- Duncan M, McIntosh PA, Stayton C, Hall CB. Individualized performance feedback to increase prenatal domestic violence screening. Matern Child Health J 2006;10:443-9.
- Short LM, Surprenant ZJ, Harris JM. A community-based trial of an online intimate partner violence CME program. Am J Prev Med 2006;30:181-5.
- Wong SL, Wester F, Mol SS, Lagro-Janssen TL. Increased awareness of intimate partner abuse after training: a randomised controlled trial. Br J Gen Pract 2006;56:249-57.
- Hsieh NK, Herzig K, Gansky S, Danley D, Gerbert B. Changing dentists’ knowledge, attitudes and behavior regarding domestic violence through an interactive multimedia tutorial. J Am Dental Assoc 2006;137:596-603.
- Jonassen J, Mazor K. Identification of physician and patient attributes that influence the likelihood of screening for intimate partner violence. Acad Med 2003;78:S20-3.
- Rodriguez MA, Bauer HM, McLoughlin E, Grumbach K. Screening and intervention for intimate partner abuse. Practices and attitudes of primary care physicians. JAMA 1999;282:468-74.
- Harris JM, Kutob RM, Surprenant ZJ, Maiuro RD, Delate TA. Can internet-based education improve physician confidence in dealing with domestic violence?. Fam Med 2002;34:287-92.
- Gerber MR, Leiter KS, Hermann RC, Bor DH. How and why community hospital clinicians document a positive screen for intimate partner violence: a cross-sectional study. BMC Fam Prac 2005;6:48-5.
- D’Avolio D, Hawkins JW, Haggerty LA, Kelly U, Barrett R, Durno Toscano SE, et al. Screening for abuse: barriers and opportunities. Health Care Women Int 2001;22:349-62.
- Kripke EN, Steele G, O’Brien MK, Novack DH. Domestic violence training program for residents. J Gen Intern Med 1998;13:839-41.
- Danis FS. Social work response to domestic violence: encouraging news from a new look. AFFILIA J Women Soc Work 2003;18:177-91.
- Gunn J, Hegarty K, Nagle C, Forster D, Brown S, Lumley J. Putting woman-centered care into practice: a new (ANEW) approach to psychosocial risk assessment during pregnancy. Birth 2006;33:46-55.
- Valdez S, Arenas M, Hernández T. The midwives’ experiences in the identification of battered women in pregnancy. Salud Publica Mex 2004;46:56-63.
- Krueger PM, Schafer S. Physician awareness of domestic violence: does continuing medical education have an impact?. J Am Osteopath Assoc 2000;100:145-8.
- Lavoie F, Martin G. Psychosocial assistance offered by physicians to abused women. Can J Public Health 1991;82:101-3.
- Leblanc L, Ouellet N. Screening for spousal abuse: the nurse’s role. Perspective infirmière: Revue Officielle De l’Ordre Des Infirmières Et Infirmiers Du Quebec 2004;1:39-43.
- Role of victims’ services in improving IPV screening by trained maternal and child health-care providers . Morbidity Mortality Weekly Report 2000;49:114-17.
- Zink T, Elder N, Jacobson J. How children affect the mother/victim’s process in intimate partner violence. Arch Pediatr Adolesc Med 2003;157:587-92.
- Saunders DG, Holter MC, Pahl LC, Tolman RM, Kenna CE. TANF workers’ responses to battered women and the impact of brief worker training: what survivors report. Violence Against Women 2005;11:227-54.
- Scobie J, McGuire M. The silent enemy: domestic violence in pregnancy. Br J Midwifery 1999;7:259-62.
- Zink T, Siegel R, Chen L, Levin L, Pabst S, Putnam F. Physician knowledge and management of children exposed to domestic violence in Ohio: a comparison of pediatricians and family physicians. Clin Pediatr (Phila) 2005;44:211-19.
- Borowsky IW, Ireland M. Parental screening for intimate partner violence by pediatricians and family physicians. Pediatrics 2002;110:509-16.
- Lapidus G, Beaulieu C, Gelven E, Sherman K, Duncan M, Banco L. A statewide survey of domestic violence screening behaviors among pediatricians and family physicians. Arch Pediatr Adolesc Med 2002;156:332-6.
- Glaister J, Kesling G. A survey of practicing nurses’ perspectives on interpersonal violence screening and intervention. Nurs Outlook 2002;50:137-43.
- Gerbert B, Gansky S, Tang J, McPhee S, Carlton R, Herzig K, et al. Domestic violence compared to other health risks: a survey of physicians’ beliefs and behaviors. Am J Prev Med 2002;23:82-90.
- Gadomski A, Wolff D, Tripp M, Lewis C, Short L. Changes in health care providers’ knowledge, attitudes, beliefs, and behaviors regarding domestic violence, following a multifaceted intervention. Acad Med 2001;76:1045-52.
- Chamberlain L, Perham H. The impact of perceived barriers on primary care physicians’ screening practices for female partner abuse. Women Health 2002;35:55-69.
- Goff H, Shelton AJ, Byrd T, Parcel G. Preparedness of health care practitioners to screen women for domestic violence in a border community. Health Care Women Int 2003;24:135-48.
- McGrath ME, Bettacchi A, Duffy SJ, Peipert JF, Becker BM, St A. Violence against women: provider barriers to intervention in emergency departments. Acad Emerg Med 1997;4:297-300.
- Zink T, Regan S, Goldenbar L, Pabst S, Rinto B. Intimate partner violence: what are physicians’ perceptions?. J Am Board Fam Pract 2004;17:332-40.
- Steen M, Bharj K. Midwives’ reflections: exploring attitudes, feelings and experiences when caring for women who are being abused. MIDIRS Midwifery Digest 2003;13:115-18.
- Price S, Baird K. Domestic violence in pregnancy: how can midwives make a difference?. Pract Midwife 2001;4:12-4.
- Moore ML, Zaccaro D, Parsons LH. Attitudes and practices of registered nurses toward women who have experienced abuse/domestic violence. J Obstet Gynecol Neonatal Nurs 1998;27:175-82.
- Brown JB, Lent B, Sas G. Identifying and treating wife abuse. J Fam Pract 1993;36:185-91.
- Dickson F, Tutty LM. The role of public health nurses in responding to abused women. Public Health Nurs 1996;13:263-8.
- Horan DL, Chapin J, Klein L, Schmidt LA, Schulkin J. Domestic violence screening practices of obstetrician-gynecologists. Obstet Gynecol 1998;92:785-9.
- Ortiz J, Ford L. Existence of staff barriers to partner violence screening and screening practices in military prenatal settings. J Obstet Gynecol Neonatal Nurs 2005;34:63-9.
- Ferris LE. Canadian family physicians’ and general practitioners’ perceptions of their effectiveness in identifying and treating wife abuse. Med Care 1994;32:1163-72.
- Janssen PA, Landolt MA, Grunfeld AF. Assessing for domestic violence exposure in primary care settings – the transition from classroom to clinical practice. J Interpers Violence 2003;18:623-33.
- Lanzilotti SS, Jones P, Dai J, Bentzien V. EMS & the domestic violence patient: a report card of existing policy, protocol & training. J Emerg Med Serv 1999;24:58-66.
- Williams JM, Chinnis AC, Gutman D. Health promotion practices of emergency physicians. Am J Emerg Med 2000;18:17-21.
- Tower L. Barriers in screening women for domestic violence: a survey of social workers, family practitioners, and obstetrician-gynecologists. J Fam Violence 2006;21:245-57.
- Chamberlain L, Perham-Hester KA. Physicians’ screening practices for female partner abuse during prenatal visits. Matern Child Health J 2000;4:141-8.
- Guedes A, Bott S, Cuca Y. Integrating systematic screening for gender-based violence into sexual and reproductive health services: results of a baseline study by the International Planned Parenthood Federation, Western Hemisphere Region. Int J Gynecol Obstet 2002;78:S57-63.
- Ahmed AM, Abdella ME, Yousif E, Elmardi AE. Response of Sudanese doctors to domestic violence. Saudi Med J 2003;24:1077-80.
- Smith PH, Danis M, Helmick L. Changing the health care response to battered women: a health education approach. Fam Commun Health 1998;20:1-18.
- Derk S. Rural health-care providers’ attitudes, practices, and training experiences regarding intimate partner violence – West Virginia 1997. Morbidity Mortality Weekly Report 1998;47:670-3.
- Borowsky IS, Ireland M. National survey of pediatrician’s violence prevention. Arch Pediatr Adolec Med 1999;153:1170-6.
- Garimella R, Plichta SB, Houseman C, Garzon L. How physicians feel about assisting female victims of intimate-partner violence. Acad Med 2002;77:1262-5.
- Pakieser RA, Lenaghan PA, Muelleman RL. Battered women: where they go for help. J Emerg Nurs 1998;24:16-9.
- Bacigalupe G. Family violence in Chile: exploring prevalence and clinical dimensions. J Fam Psychother 2000;11:39-57.
- Tilden VP. Response of the health care delivery system to battered women. Issues Ment Health Nurs 1989;10:309-20.
- Weiss SJ, Ernst AA, Blanton D, Sewell D, Nick TG. EMT domestic violence knowledge and the results of an educational intervention. Am J Emerg Med 2000;18:168-71.
- Sugg NK, Inui T. Primary care physicians’ response to domestic violence. Opening Pandora’s box. JAMA 1992;267:3157-60.
- Tudiver F, Permaul-Woods JA. Physicians’ perceptions of and approaches to woman abuse. Can Fam Physician 1996;42:1475-80.
- Melvin SY. Domestic violence: the physician’s role [see comment]. Hosp Pract (Minneap) 1995;30:45-52.
- Chescheir N. Violence against women: response from clinicians. Ann Emerg Med 1996;27:766-8.
- Limandri BJ, Tilden VP. Nurses’ reasoning in the assessment of family violence. Image J Nurs Sch 1996;28:247-52.
- Director TD, Linden JA. Domestic violence: an approach to identification and intervention. Emerg Med Clin North Am 2004;22:1117-32.
- Chez R. Woman battering. Am J Obstet Gynecol 1988;158:1-4.
- Jones RF. Domestic violence: let our voices be heard. Obstet Gynecol 1993;81:1-4.
- Forcier M, Patel R, Kahn JA. Pediatric residents’ attitudes and practices regarding adolescent dating violence. Ambulatory Pediatrics 2003;3:317-23.
- Groth B, Chelmowski MK, Batson TP. Domestic violence: level of training, knowledge base and practice among Milwaukee physicians. Wisconsin Med J 2001;100:24-8.
- Varjavand N, Cohen DG, Gracely EJ, Novack DH. A survey of residents’ attitudes and practices in screening for, managing, and documenting domestic violence. J Am Med Wom Assoc 2004;59:48-53.
- Currier GW, Barthauer LM, Begier E, Bruce ML. Training and experience of psychiatric residents in identifying domestic violence. Psychiatr Serv 1996;47:529-30.
- Gerbert B, Caspers N, Bronstone A, Moe J, Abercrombie P. A qualitative analysis of how physicians with expertise in domestic violence approach the identification of victims. Ann Intern Med 1999;131:578-84.
- Larkin GL, Hyman KB, Mathias SR, Amico F, MacLeod BA. Universal screening for intimate partner violence in the emergency department: importance of patient and provider factors. Ann Emerg Med 1999;33:669-75.
- Parsons LH, Zaccaro D, Wells B, Stovall TG. Methods of and attitudes toward screening obstetrics and gynecology patients for domestic violence. Am J Obstet Gynecol 1995;173:381-6.
- Erickson MJ, Hill TD, Siegel RM. Barriers to domestic violence screening in the pediatric setting. Pediatrics 2001;108:98-102.
- Haggblom AM, Hallberg LR, Moller AR. Nurses’ attitudes and practices towards abused women. Nurs Health Sci 2005;7:235-42.
- Davis RE, Harsh KE. Confronting barriers to universal screening for domestic violence. J Prof Nurs 2001;17:313-20.
- Ferris LE, Tudiver F. Family physicians’ approach to wife abuse: a study of Ontario, Canada, practices. Fam Med 1992;24:276-82.
- Heinzer MM, Krimm JR. Barriers to screening for domestic violence in an emergency department. Holistic Nurs Pract 2002;16:24-33.
- Varvaro FF, Gesmond S. ED physician house staff response to training on domestic violence. J Emerg Nurs 1997;23:17-22.
- de Wit K, Davis K. Nurses’ knowledge and learning experiences in relation to the effects of domestic abuse on the mental health of children and adolescents. Contemp Nurse 2004;16:214-27.
- Shearer HM, Forte ML, Dosanjh S, Mathews DJ, Bhandari M. Chiropractors’ perceptions about intimate partner violence: a cross-sectional survey. J Manipulative Physiol Ther 2006;29:386-92.
- Renker PR. Perinatal violence assessment: teenagers’ rationale for denying violence when asked. J Obstet Gynecol Neonatal Nurs 2006;35:56-67.
- Rodriguez-Bolanos RL, Marquez-Serrano M, Kageyama-Escobar ML. Gender-based violence: knowledge and attitudes of health care providers in Nicaragua. Salud Publica Mex 2005;47:134-44.
- Mendez H, Valdez S, Viniegra V, Rivera R, Salmerón C. Violence against women: knowledge and attitudes of healthcare providers at the Mexican Institute of Social Security in Morelos, Mexico. Salud Publica Mex 2003;45:472-82.
- Tower L. Domestic violence screening: education and institutional support correlates. J Soc Work Educ 2003;39:479-94.
- Bryant SA, Spencer GA. Domestic violence: what do nurse practitioners think?. J Am Acad Nurse Pract 2002;14:421-7.
- Cann K, Withnell S, Doll H. Domestic violence: a comparative study of levels of detection, knowledge, and attitudes in healthcare workers. Public Health 2001;115:89-95.
- Elliott L, Nerney M, Jones T, Friedmann P. Barriers to screening for domestic violence. J Gen Intern Med 2002;17:112-16.
- Hinderliter D, Doughty A, Delaney K. The effect of intimate partner violence education on nurse practitioners’ feelings of competence and ability to screen patients. J Nurs Educ 2003;42:449-54.
- Schoening A, Greenwood J, McNichols J. Effect of an intimate partner violence educational program on the attitudes of nurses. J Obstet Gynecol Neonatal Nurs 2004;33:572-9.
- Davies J, Harris MH, Roberts G, Mannion J, McCosker H, Anderson D. Community health workers’ response to violence against women. Aust N Z J Ment Health Nurs 1996;5:20-31.
- Glowa PT, Frasier PY, Newton WP. Increasing physician comfort level in screening and counseling patients for intimate partner violence: hands-on practice. Patient Educ Couns 2002;46:213-20.
- Kurz D. Emergency department responses to battered women: resistance to medicalisation. Soc Probl 1987;34:69-81.
- Kelso EJR. Selection from current literature: clinical detection of abuse. Fam Pract 1996;13:408-13.
- Krimm J, Heinzer M. Domestic violence screening in the emergency department of an urban hospital. J Natl Med Assoc 2002;94:484-91.
- Krantz G, Phuong TV, Larsson V, Thuan NTB, Ringsberg KC. Intimate partner violence: forms, consequences and preparedness to act as perceived by healthcare staff and district and community leaders in a rural district in northern Vietnam. Public Health 2005;119:1048-55.
- Cohen S, De V, Newberger E. Barriers to physician identification and treatment of family violence: lessons from five communities. Acad Med 1997;72:S19-S25.
- Johnson LE, Benight CC. Effects of trauma-focused research on recent domestic violence survivors. J Trauma Stress 2003;16:567-71.
- Gremillion DH, Kanof EP. Overcoming barriers to physician involvement in identifying and referring victims of domestic violence. Ann Emerg Med 1996;27:769-73.
- Coeling HV, Harman G. Learning to ask about domestic violence. Women Health Issues 1997;7:263-8.
- Shadigian E. Domestic violence: identification and management for the clinician. Compr Ther 1996;22:424-8.
- Stayton C, Duncan M. Mutable influences on intimate partner abuse screening in health care settings: a synthesis of the literature. Trauma 2005;6:271-85.
- Kim J, Motsei M. ‘Women enjoy punishment’: attitudes and experiences of gender-based violence among PHC nurses in rural South Africa. Soc Sci Med 2002;54:1243-54.
- Durant T, Colley GB, Saltzman LE, Johnson CH. Opportunities for intervention: discussing physical abuse during prenatal care visits. Am J Prev Med 2000;19:238-44.
- Ronnberg AK, Hammarstrom A. Barriers within the health care system to dealing with sexualized violence: a literature review. Scand J Public Health 2000;28:222-9.
- Protheroe L, Green J, Spiby H. An interview study of the impact of domestic violence training on midwives. Midwifery 2004;20:94-103.
- Krugman SD, Witting MD, Furuno JP, Hirshon JM, Limcangco R, Perisse AR, et al. Perceptions of help resources for victims of intimate partner violence. J Interpers Violence 2004;19:766-77.
- Loring MT, Smith RW. Health care barriers and interventions for battered women. Public Health Rep 1994;109:328-38.
- Reid SA, Glasser M. Primary care physicians’ recognition of and attitudes toward domestic violence. Acad Med 1997;72:51-3.
- Gerbert B, Caspers N, Milliken N, Berlin M, Bronstone A, Moe J. Interventions that help victims of domestic violence. A qualitative analysis of physicians’ experiences. J Fam Pract 2000;49:889-95.
- Larance LY, Porter ML. Observations from practice. Support group membership as a process of social capital formation among female survivors of domestic violence. J Interpers Violence 2004;19:676-90.
- Ferris LE. Detection and treatment of wife abuse in Aboriginal communities by primary care physicians. J Womens Health 1994;3:265-71.
- Shea C. Breaking through the barriers to domestic violence intervention. Am J Nurs 1997;97:26-33.
- Mortlock T. The battered woman in the Accident and Emergency department. Accident Emerg Nurs 1996;4:187-9.
- Chung M. Wife battering in Hong Kong: Accident and Emergency nurses’ attitudes and beliefs. Accident Emerg Nurs 1996;4:152-5.
- Peltzer K, Mashego TA, Mabeba M. Attitudes and practices of doctors toward domestic violence victims in South Africa. Health Care Women Int 2003;24:149-57.
- Peckover S. Focusing upon children and men in situations of domestic violence: an analysis of the gendered nature of British health visiting. Health Soc Care Comm 2002;10:254-61.
- Hamberger K. Evaluation of a health care provider training program to identify and help partner violence victims. J Fam Violence 2004;19:1-79.
- Zachary MJ, Schechter CB, Kaplan ML, Mulvihill MN. Provider evaluation of a multifaceted system of care to improve recognition and management of pregnant women experiencing domestic violence. Womens Health Issues 2002;12:5-15.
- Carbonell JL, Chez RA, Hassler RS. Florida physician and nurse education and practice related to domestic violence. Womens Health Issues 1995;5:203-7.
- Taft A, Broom DH, Legge D. General practitioner management of intimate partner abuse and the whole family: qualitative study. BMJ 2004;328:618-21.
- Steen M. Developing midwifery responses to women in their care who are living with violent men. MIDIRS Midwifery Digest 2000;10:313-17.
- McKie L, Fennell B, Mildorf J. Time to disclose, timing disclosure: GPs’ discourses on disclosing domestic abuse in primary care. Sociol Health Ill 2002;24:327-46.
- Trute B, Sarsfield P, Mackenzie D. Medical response to wife abuse: a survey of physicians’ attitudes and practices. Can J Commun Ment Health 1988;7:61-7.
- Davidson LL, Grisso JA, Garcia-Moreno C, Garcia J, King VJ, Marchant S. Training programs for healthcare professionals in domestic violence. J Women Health Gen-B 2001;10:953-69.
- Bessette H, Peterson S. Attitudes of adult nurse practitioner students toward women experiencing domestic violence. J Nurs Educ 2002;41:227-30.
- Wright L. Asking about domestic violence. Br J Midwifery 2003;11:199-202.
- Bates L, Brown W. Domestic violence: examining nurses’ and doctors’ management, attitudes and knowledge in an accident and emergency setting. Aust J Adv Nurs 1998;15:15-22.
- Marchant S, Davidson L, Garcia J. Addressing domestic violence through maternity services: policy and practice. Midwifery 2001;17:164-70.
- Corbally M. Factors affecting nurses’ attitudes towards the screening and care of battered women in Dublin A&E departments: a literature review. Accident Emerg Nurs 2001;9:27-3.
- Frost M. Health visitors’ perceptions of domestic violence: the private nature of the problem. J Adv Nurs 1999;30:589-96.
- Scales B. Domestic violence awareness in the perianesthesia setting. J Perianesth Nurs 2004;19:11-7.
- Sullivan M, Bhuyan R, Senturia K, Shiu T, Ciske S. Participatory action research in practice: a case study in addressing domestic violence in nine cultural communities. J Interpers Violence 2005;20:977-95.
- McAfee RE. Domestic violence as a women’s health issue. Womens Health Issues 2001;11:371-6.
- Dowd MD. The emerging role of the pediatric emergency department in intimate partner violence. Clin Pediatr Emerg Med 2004;5:276-83.
- Shadigian EM, Bauer ST. Screening for partner violence during pregnancy. Int J Gynecol Obstet 2004;84:273-80.
- Ely G. Domestic violence and immigrant communities in the United States: a review of women’s unique needs and recommendations for social work practice and research. Stress 2004;7:223-41.
- Daniels K. Intimate partner violence and depression: a deadly comorbidity. J Psychosoc Nurs Ment Health Serv 2005;43:44-51.
- Jaeger JR. Screening for domestic violence. Hosp Pract 2000;35:15-8.
- Lehrman FL, Berner LS. Physician as detective: discerning and recording domestic violence injuries. J Women Health 1997;6:267-70.
- Cox E. Synergy in practice: caring for victims of intimate partner violence. Crit Care Nurs Q 2003;26:323-30.
- Koziol-McLain J, Campbell JC. Universal screening and mandatory reporting: an update on two important issues for victims/survivors of intimate partner violence. J Emerg Nurs 2001;27:602-6.
- Klein SJ. Screening for risk of domestic violence within HIV partner notification: evolving practice and emerging issues. J Public Health Manag Pract 2001;7:46-9.
- Goodman L, Epstein D. Refocusing on women: a new direction for policy and research on intimate partner violence. J Interpers Violence 2005;20:479-87.
- Resick PA. A suggested research agenda on treatment-outcome research for female victims of violence. J Interpers Violence 2004;19:1290-5.
- Watts N. Screening for domestic violence. A team approach for maternal/newborn nurses. Association of Women’s Health and Neonatal Nurses Lifelines 2004;8:211-19.
- Biroscak BJ, Smith PK, Roznowski H, Tucker J, Carlson G. Intimate partner violence against women: findings from one state’s ED surveillance system. J Emerg Nurs 2006;32:12-6.
- Zlotnick C, Johnson DM, Kohn R. Intimate partner violence and long-term psychosocial functioning in a national sample of American women. J Interpers Violence 2006;21:262-75.
- Eisenstat SA, Bancroft L. Domestic violence. N Engl J Med 1999;341:886-92.
- Heath I. Domestic violence as a women’s health issue. Women Health Issues 2001;11:376-81.
- Physical violence during the 12 months preceding childbirth – Alaska, Maine, Oklahoma, and West Virginia, 1990–1991. Morbidity Mortality Weekly Report 1994;43:132-7.
- Carlson BE. The most important things learned about violence and trauma in the past 20 years. J Interpers Violence 2005;20:119-26.
- Ferris LE, McMain-Klein M, Silver E. Documenting wife abuse: a guide for physicians. Can Med Assoc J 1997;156:1015-22.
- Mayer L, Liebschutz J. Domestic violence in the pregnant patient: obstetric and behavioral interventions. Obstet Gynecol Surv 1998;53:627-35.
- Attala JM, McSweeney M, Mueller A, Bragg B, Hubertz E. An analysis of nurses’ communications in a shelter setting. J Community Health Nurs 1999;16:29-40.
- Nelms TP. An educational program to examine emergency nurses’ attitudes and enhance caring intervention with battered women. J Emerg Nurs 1999;25:290-3.
- Jezierski M. Family violence screening: opportunities in prehospital settings. J Emerg Nurs 1999;25:201-5.
- Campbell JC, Sheridan DJ. Emergency nursing interventions with battered women. J Emerg Nurs 1989;15:12-7.
- Williams-Evans SA, Sheridan DJ. Exploring barriers to leaving violent intimate partner relationships. Assoc Black Nurs Faculty 2004;15:38-40.
- Loraine K. Battered women: the ways you can help. RN 1981;44:22-8.
- Short S, Tiedemann JC, Rose DE. Family violence: an intervention model for dental professionals. Northwest Dent 1997;76:31-5.
- Goldner V. Morality and multiplicity: perspectives on the treatment of violence in intimate life. J Marital Fam Ther 1999;25:325-36.
- Davidhizar R, Giger JN. ‘Domestic violence’. J Pract Nurs 2002;52:18-22.
- Humphreys J, Parker B, Campbell JC. Intimate partner violence against women. Annu Rev Nurs Res 2001;19:275-306.
- Schiavone FM, Salber PR. Hitting close to home: domestic violence and the EMS responder. J Emerg Med Serv 1994;19:112-15.
- Stark E. Insults, injury, and injustice – rethinking state intervention in domestic violence cases. Violence Against Women 2004;10:1302-30.
- Thompson RS, Krugman R. Screening mothers for intimate partner abuse at well-baby care visits: the right thing to do. JAMA 2001;285:1628-30.
- Griffin MP, Koss MP. Clinical screening and intervention in cases of partner violence. Online J Issues Nurs 2002;7.
- Gantt L, Bickford A. Screening for domestic violence. How one hospital network started asking about abuse. Association of Women’s Health and Neonatal Nurses Lifelines 1999;3:36-42.
- El-Bayoumi G, Borum ML, Haywood Y. Domestic violence in women. Med Clin North Am 1998;82:391-40.
- Weiss GG. Domestic violence: shattering the silence. Med Econ 2005;82:62-6.
- Hannigan MA. Domestic violence: the response of healthcare. J Healthcare Protect Manag 1999;15:95-101.
- Cassidy K. How to assess and intervene in domestic violence situations. Home Healthcare Nurse 1999;17:664-72.
- Davidhizar R, Dowd S, Giger JN. Recognizing abuse in culturally diverse clients. Health Care Superv 1998;17:10-2.
- Chiodo GT, Tolle SW, Tilden VP. The dentist and family violence. Gen Dent 1998;46:20-5.
- Butler MJ. Domestic violence: a nursing imperative. J Holistic Nurs 1995;13:54-69.
- Cattaneo LB, Goodman LA. Risk factors for reabuse in intimate partner violence: a cross-disciplinary critical review. Trauma Violence Abuse 2005;6:141-75.
- Rickert VI, Vaughan RD, Wiemann CM. Adolescent dating violence and date rape. Curr Opin Obstet Gynecol 2002;14:495-500.
- King C. Changing women’s lives: the primary prevention of violence against women. AWHONN’s Clin Issues Perinat Womens Health Nurs 1993;4:449-57.
- Lundy M, Grossman S. Clinical research and practice with battered women: what we know, what we need to know. Trauma 2001;2:120-41.
- Ford-Gilboe M, Wuest J, Merritt-Gray M. Strengthening capacity to limit intrusion: theorizing family health promotion in the aftermath of woman abuse. Qual Health Res 2005;15:477-501.
- Coombes R. Making a fist of it. Health Serv J 2004;114.
- Helton A, McFarlane J, Anderson E. Prevention of battering during pregnancy: focus on behavioral change. Public Health Nurs 1987;4:166-74.
- Berlinger JS. Domestic violence: how you can make a difference, real ways to help a victim find safety. Nursing (Lond) 2001;31:58-64.
- Harris M, Anderson D, Madl R, Mannion J, McCosker H. The road to freedom: ending violence against women. Women Health Issues 1997;7:99-108.
- Taket A, Mann C. Clinical effectiveness information bulletin, 18. Information and resources on domestic violence. Community Practitioner 2005;78:1-4.
- Evans R. Children living with domestic violence. Emerg Nurse 2001;9:22-6.
- Garcia J, Davidson L. Researching domestic violence and health: National Perinatal Epidemiology Unit. MIDIRS Midwifery Digest 2002;12:S25-9.
- Henderson AD, Ericksen JR. Enhancing nurses’ effectiveness with abused women: awareness, reframing, support, education. J Psychosoc Nurs Ment Health Serv 1994;32:11-5.
- Hoff LA. Battered women: intervention and prevention. A psychosociocultural perspective, Part 2. J Am Acad Nurse Pract 1993;5:34-9.
- Wescott CS. Help for the hurting: when pregnant women are battered. Childbirth Instructor Magazine 1995;5:18-22.
- Germain CP. Sheltering abused women: a nursing perspective. J Psychosoc Nurs Ment Health Serv 1984;22:24-31.
- Baird K, Salmon D, Price S. Learning from the Bristol Pregnancy and Domestic Violence Programme. Br J Midwifery 2005;13:692-6.
- Hardacre S. Routine enquiry into domestic abuse: the All-Wales clinical pathway. Br J Midwifery 2005;13:697-701.
- Power C. Domestic violence: what can nurses do?. Aust Nurs J 2004;12:21-3.
- Kipps S. Sexual health needs of women in violent relationships. Primary Health Care 2005;15:27-32.
- Willis D, Porche D. Male battering of intimate partners: theoretical underpinnings, intervention approaches, and implications. Nurs Clin North Am 2004;39:271-82.
- Attala JM. Danger signs: detecting abuse against women in the home. Home Care Provid 1996;1:12-8.
- McFarlane J, Goodmark L. Preventing abuse during pregnancy. A clinical protocol. Am J Matern Child Nurs 1998;23:22-6.
- Harris M, Fallot RD, Berley RW. Qualitative interviews on substance abuse relapse and prevention among female trauma survivors. Psychiatr Serv 2005;56:1292-6.
- Hassouneh Phillips D. Understanding abuse of women with physical disabilities: an overview of the Abuse Pathways Model. Adv Nurs Sci 2005;28:70-8.
- Peled E, Edleson J. Advocacy for battered women: a national survey. J Fam Violence 1994;9:285-96.
- Mohr WK, Fantuzzo JW, Abdul-Kabir S. Safeguarding themselves and their children: mothers share their strategies. J Fam Violence 2001;16:75-92.
- Weitlauf JC, Smith RE, Cervone D. Generalization effects of coping-skills training: influence of self-defence training on women’s efficacy beliefs, assertiveness, and aggression. J Appl Psychol 2000;85:625-33.
- Turnbull L. Domestic violence. Pract Nurse 2001;21:25-30.
- Onyskiw JE. Research on violence and abuse in Canada: challenges and opportunities. Can J Nurs Res 2001;32:117-24.
- Ryan J, King MC. Scanning for violence. Association of Women’s Health and Neonatal Nurses Lifelines 1998;2:36-41.
- Belfiglio G. Should primary care providers screen for domestic violence?. Am J Manag Care 2001;2:147-50.
- Hague G, Malos E. Tackling domestic violence: a guide to developing multi-agency initiatives. Bristol: Policy Press-University of Bristol; 1996.
- Henrion R. Domestic violence during pregnancy: screening and management. J Gynecol Obstet Biol Reprod 2005;34:S62-7.
- Chez N. Helping the victims of domestic violence. Traces of blows. Krankenpflege – Soins Infirmiers 1995;88:17-22.
- Nicolaidis C, Touhouliotis V. Addressing intimate partner violence in primary care: lessons from chronic illness management. Violence Vict 2006;21:101-15.
- Roberts AR, Roberts B. Ending intimate abuse. Practical guidance and survival strategies. Oxford: Oxford University Press; 2005.
- Gazmararian JA, Lazorick S, Spitz AM, Ballard T, Saltzman LE, Marks JS. Prevalence of violence against pregnant women. JAMA 1996;275:1915-20.
- Brook A, Griffiths C. Trends in the mortality of young adults in England and Wales, 1961 to 2001. Health Stats Q 2003;19.
Appendix 1 Previous systematic reviews of partner violence screening
| Review authors and date | Number of databases searched (census date) | Types of studies reviewed | Number of papers | Findings |
|---|---|---|---|---|
| Waalen et al., 20003 | 3 (Jan 1999) | Studies reporting barriers to screening, and interventions to change provider behaviours related to screening | 24 | Barriers to screening are similar across health-care settings (e.g. lack of DV education/time/effective interventions, fear of offending patient). Studies evaluating interventions to increase screening found those limited to education had no significant effect on screening or identification rates. However, most interventions incorporating strategies in addition to education (e.g. providing specific screening questions) were associated with significant increases in identification |
| Ramsay et al., 20021,2 | 3 (Feb 2001) | Studies of interventions initiated in health-care settings, women’s and health professionals’ attitudes to screening | 20 | Screening increases the identification of abused women, and many women do not object to being asked. However, the majority of health professionals do not agree with screening women in health-care settings. Insufficient evidence to show if screening and subsequent interventions lead to improved outcomes for abused women, and no study investigated whether it may cause harm |
| Wathen and Macmillan, 20034 (Canadian Task Force) | 5 (Dec 2002) | Studies of interventions initiated in primary care; had to be applicable to Canadian clinical practice | 22 studies | Screening instruments exist to identify women experiencing partner violence. No comparative studies examining effectiveness of screening for improved women-outcomes (as opposed to abuse identification). No high-quality evidence evaluating effectiveness of shelters to reduce violence, but for women spending at least one night there is fair evidence that advocacy/counselling services decrease re-abuse and improve quality of life. Benefits of other interventions unclear, primarily because of a lack of suitably designed research measuring appropriate outcomes. In most cases, the potential harms of interventions are not assessed |
| Nelson et al., 20045 (US Preventive Services Task Force) | 6 (Dec 2002) | Studies of effectiveness of screening tools and interventions (for DV and elder abuse); had to be applicable to US clinical practice | 18 | No trials of effectiveness of screening in reducing harm have been published. Several screening instruments have been developed, some with fair to good reliability and validity, but none evaluated against measurable violence or health outcomes. Few intervention studies conducted; those existing focus on pregnant women; study limitations restrict their interpretation |
Appendix 2 Mapping of selected NSC criteria onto analytic framework for research on partner violence screening
Appendix 3 Quality appraisal
Appendix 3.1 Biases measured by quality assessment of diagnostic accuracy studies (QUADAS)
| Bias | Explanation |
|---|---|
| Spectrum bias | Are the results from the sample generalisable to the population? If not, then we cannot generalise to other populations |
| Selection criteria | Clear inclusion/exclusion criteria |
| Reference standard | What is the strength of the gold standard? If it cannot effectively distinguish cases and non-cases, this will influence diagnostic accuracy data |
| Disease progress | Whether index and comparator were collected at the same point in time. If not, then disease status may change between administrations of tools |
| Partial verification | Have all of the participants received confirmation of disease status with the gold standard? If not, a biased estimate of diagnostic accuracy may occur |
| Differential verification | Were the index tool results compared to different comparators? If so, they may only be suitable in certain contexts, thus impacting on diagnostic accuracy |
| Incorporation | Was the index tool used to inform the final diagnosis? If so, this may increase agreement between the index and comparator. Furthermore, if the index and comparator are administered as one tool, this may increase multi-colinearity |
| Test execution | To ensure both tools were given under the same conditions and for ease of replication. Different administration procedures may affect diagnostic accuracy |
| Blind analysis | If tools are subjective, knowledge of one tool may influence and bias the outcome of the other tool |
| Interpretation | The availability of clinical data may influence the interpretation of test outcomes, particularly if the tool requires a degree of subjectivity |
| Indeterminate results | Were these reported? If not, they may be correlated to the disease and can influence interpretation of results |
| Study withdrawals | If a systematic dropout has occurred, test performance may be biased |
Appendix 3.2 Quality appraisal of primary studies (US Preventative Task Force)
The United States Preventative Services Task Force (USPSTF) quality appraisal framework34,216 was used to assess the primary studies in this review. The USPSTF tool rates both internal and external validity. Quality of execution of the study is rated on a three-point scale (good, fair or poor), based on the following design-specific criteria:
-
for randomised controlled trials, there must be adequate randomisation and consideration of confounders
-
for other study designs, consideration of other potential confounders must be reported
-
all studies need to maintain comparable groups and no greater loss to follow-up than 20%
-
all measurements must be equal, reliable and valid
-
definition of interventions must be clear
-
all important outcomes should be considered or a good match of outcomes to goals
-
analysis is either intention to treat for RCTs, or statistical adjustments are made for confounders if other study designs are used.
Study design is also rated on a three-point scale (greatest, moderate and least). Prospective studies with parallel controls are rated greatest suitability; all retrospective studies or multiple assessment before-and-after studies without parallel controls are given a moderate rating; and single before-and-after measurements and no parallel control, or case studies and series designs are rated as least suitability.
The strength of evidence of each study is then considered with the following criteria:
-
quality of execution of the study
-
suitability of study design
-
number of studies that fulfilled minimum suitability and quality criteria
-
size and consistency of reported effects.
The combination of these factors determined the final score for evidence of effectiveness for each category of interventions: strong, sufficient or insufficient, in accordance with Table 10, adapted from the US Task Force on Community Preventive Services. 216
| Definition | Grade |
|---|---|
| Quality of execution | |
| A study (including meta-analyses or systematic reviews) that meets all design-specific criteriaa well | Good |
| A study (including meta-analyses or systematic reviews) that does not meet (or it is not clear that it meets) at least one design-specific criteriona but has no known ‘fatal flaw’, i.e. any or all of the following problems may occur, without the limitations noted in the ‘poor’ category below: generally comparable groups are assembled initially, but some question remains about whether some (although not major) differences occurred in follow-up; measurement instruments are acceptable (although not the best) and generally applied equally; some but not all important outcomes are considered; and researchers account for some but not all potential confounders | Fair |
| A study (including meta-analyses or systematic reviews) that has at least one design-specifica ‘fatal flaw’, or four lesser flaws. Fatal flaws are: groups assembled initially are not close to being comparable or are not maintained throughout the study; unreliable or invalid measurement instruments are used or are not applied at all equally among groups; and key confounders are given little or no attention or a number, i.e. criteria 2, 4 or 7.34 | Poor |
| Study design | |
| Prospective study with parallel controls | Greatest |
| All retrospective studies (e.g. historical controls), or multiple assessment before-and-after studies without parallel controls | Moderate |
| Single before-and-after measurements and no parallel control, or case studies and series | Least |
| Design suitability (D) (greatest, moderate, least) | Execution (E) (good, fair, poor) | Number of studies satisfying both D and E | Consistent direction of effect of these studies? | Effect sizea | Evidence of effectiveness |
|---|---|---|---|---|---|
| Greatest | Good | At least 2 | Yes | Sufficient | Strong |
| Greatest/moderate | Good | At least 5 | Yes | Sufficient | |
| Greatest | Good/fair | At least 5 | Yes | Sufficient | |
| Greatest | Good | 1 | Not applicable | Sufficient | Sufficient |
| Greatest | Good/fair | At least 3 | Yes | Sufficient | |
| Greatest/moderate | Good/fair | At least 5 | Yes | Sufficient | |
| Poor execution or least quality design | Too few studies | Inconsistent | Small | Insufficient | |
Appendix 3.3 Quality appraisal (Jadad score)
Randomised controlled trials were also given a Jadad score using a modified version of the Jadad criteria. 35 The Jadad score was calculated using the five items in Table 11. Four of the items are indications of good quality, and each counts as one point towards an overall quality score. The other item indicates poor quality, and a point is subtracted if its criteria are met. The range of possible scores is 0–4.
| Item | Score |
|---|---|
| Was the study described as randomised (this includes words such as randomly, random and randomisation)? | 0/1 |
| Was the method used to generate the sequence of randomisation described and appropriate (table of random numbers, computer-generated, etc.)? | 0/1 |
| Was there a description of withdrawals and dropouts? | 0/1 |
| Deduct one point if the method used to generate the sequence of randomisation was described and it was inappropriate (patients were allocated alternately, or according to date of birth, hospital number, etc.). | 0/–1 |
| Blinded assessment of outcomes | 0/1 |
| Total (out of 4) | 4 |
Appendix 4 Prevalence and health impact studies
Appendix 4.1 Characteristics, results and quality scores of studies of prevalence
| Study | Population | Geographical location | Sample size (women) | Type of sampling | Definition of IPV | Lifetime prevalence (%) | One-year prevalence (%) | Age group(s) (%) | Marital status (%) | Quality score (Strobe) total 22 |
|---|---|---|---|---|---|---|---|---|---|---|
| Carrado, 199639 | General population | Great Britain | 971 | Community | Physical | 13 | 5 | Not reported | Not reported | 19 |
| Dominy and Radford, 199637 | Women in Surrey | Southeast England | 484 | Community | Physical, emotional, sexual, psychological | 31 | Not reported | Not reported | Not reported | 12 |
| Finney, 200638 | General population | England and Wales | 24,498 men and women | Community |
Physical, emotional, financial, threats Sexual assault |
25.4a 22.7 |
4.7 2.7 |
Not reported | Not reported | 11 |
| Mirrlees-Black and Byron, 199940 | General population | England and Wales | 6098 | Community | Physical | 22.7 | 4.2 | Not reported | Not reported | 17 |
| Walby and Allen, 200436 | General population | England and Wales | 12,226 | Community |
Physical, emotional, financial, threats Sexual assault |
25.9b 16.6 |
6.0 2.1 |
Not reported |
Married: 2 Single: 6.9 Divorced/separated: 14.5 Stable relationship: 6.2 |
19 |
| Coid et al., 200354 | Women attending GP | London, urban, England | 1207 | Clinical | Sexual | 24 | Not reported | Not reported | Not reported | 17 |
| Richardson et al., 200241 | As above | As above | As above | As above | Physical, sexual | 41 | 17 | Not reported |
Married: 14 Single: 17 Divorced/separated: 28 Stable relationship: 16 |
21 |
| Bacchus et al., 200442 | Pregnant women | South London, England | 892 | Clinical | Physical, sexual, emotional | 13 | 6.4 | Not reported | Not reported | 19 |
| Bacchus et al., 200444 | Pregnant women | London, urban, England | 200 | Clinical | Physical, sexual, psychological | 23.5 | Not reported | Not reported | Not reported | 20 |
| Mezey et al., 200543 | As above | As above | As above | As above | As above | As above | As above | As above |
Married: 38.3 Single: 61.7 |
20 |
| Bowen et al., 200545 | Pregnant women and postpartum | Southwest England |
Start: 14,541 End: 7591 |
Clinical | Physical, sexual, emotional | Not reported | 11 | Not reported | Not reported | 20 |
| Johnson et al., 200346 | Pregnant women | North England | 475 | Clinical | Physical, sexual, emotional | 17 | Not reported |
< 16: 1 16–20: 11 21–25: 25 26–30: 40 > 30: 29 |
Married: 30 Single: 31 Divorced/separated: 11 Stable relationship: 28 |
15 |
| Boyle and Todd, 200347 | Women in emergency departments | Cambridge, England |
Not reported Men and women = 256 |
Clinical | Physical, sexual, emotional | 22.1 | Not reported | Not reported | Not reported | 20 |
| Sethi et al., 200448 | Women in emergency departments | Inner city, urban, England | 198 | Clinical | Physical | 34.8 | 6.1 |
18–29: 30.0 30–39: 44.7 40–49: 35.7 > 49: 35.1 |
Not reported | 20 |
| Wright and Kariya, 199750 | Women attending a Scottish A&E department | Scotland | 46 | Clinical | Physical | Not reported | 41 in 2 months | Not reported | Not reported | 16 |
| John et al., 200451 | Gynaecology patients | North England | 825 | Clinical | Physical | 21 | 4 |
< 20: 4 21–30: 26 31–40: 39 41–50: 23 51–60: 5 > 60: 3 |
Married: 37 Single: 16 Divorced/separated: 13 Stable relationship: 31 |
17 |
| Keeling, 200452 | Women attending pregnancy counselling | Northwest England | 312 | Clinical | Physical, emotional | 35.1 | 19.5 | Not reported | Not reported | 18 |
| Keeling and Birch, 200453 | Women attending family planning clinics | Not reported | 292 | Clinical | Physical, sexual, emotional, financial | 34.9 | 14 |
16–24: 32.4 25–29: 30.4 30–34: 38.3 35–39: 45.2 40–44: 24.0 45–49: 55.6 > 50: 18.2 |
Not reported | 19 |
Appendix 4.2 Sensitivity analysis of prevalence studies
| Setting | Studies ordered by quality score (figures in bold) and grouped by setting | Frequency of partner violence (%) | Definition |
|---|---|---|---|
| General population | Carrado, 199639 | Prevalence: 13 | Physical |
| 19 | One-year prevalence: 5 | ||
| Walby and Allen, 200436 | Prevalence: 25.9 | Physical, emotional, financial, threats | |
| 19 | One-year prevalence: 6 | ||
| Mirrlees-Black and Byron, 199940 | Prevalence: 22.7 | Physical | |
| 17 | One-year prevalence: 4.2 | ||
| Dominy and Radford, 199637 | Prevalence: 31 | Physical, emotional, sexual, psychological | |
| 12 | |||
| Finney, 2006 38 | Prevalence: 25.4 | Physical, emotional, financial, threats | |
| 11 | One-year prevalence: 4.7 | ||
| Clinical population | Richardson et al., 200241 | Prevalence: 41 | Physical, sexual |
| 21 | Incidence: 17 | ||
| Mezey et al., 200543 | Prevalence: 23.5 | Physical, sexual, psychological | |
| 20 | |||
| Bowen et al., 200545 | 18 weeks’ gestation to 33 months’ postnatal prevalence: 11 | Physical, emotional, sexual | |
| 20 | |||
| Boyle and Todd, 200347 | Prevalence: 22.1 | Physical, emotional, sexual | |
| 20 | |||
| Sethi et al., 200448 | Prevalence: 34.8 | Physical | |
| 20 | One-year prevalence: 6.1 | ||
| Bacchus et al., 200442 | Prevalence: 13 | Physical, emotional, sexual | |
| 19 | One-year prevalence: 6.4 | ||
| Keeling and Birch, 200453 | Prevalence: 34.9 | Physical, emotional, sexual, financial | |
| 19 | One-year prevalence: 14 | ||
| Keeling, 200452 | Prevalence: 35.1 | Physical, emotional | |
| 18 | One-year prevalence: 19.5 | ||
| Coid et al., 200354 | Prevalence: 24 | Sexual | |
| 17 | |||
| John et al., 200451 | Prevalence: 21 | Physical | |
| 17 | One-year prevalence: 4 | ||
| Wright and Kariya, 199750 | Two-month prevalence: 41 | Physical | |
| 16 | |||
| Johnson et al., 200346 | Prevalence: 17 | Physical, emotional, sexual | |
| 15 | |||
| Definition | Studies ordered by quality score (figures in bold) and grouped by definition | Frequency of partner violence (%) | Setting |
| Physical | Sethi et al., 200448 | Prevalence: 34.8 | A&E |
| 20 | One-year prevalence: 6.1 | ||
| Carrado, 199639 | Prevalence: 13 | General population | |
| 19 | |||
| Mirrlees-Black and Byron, 199940 | Prevalence: 22.7 | General population | |
| 17 | One-year prevalence: 4.2 | ||
| John et al., 200451 | Prevalence: 21 | Gynaecology patients | |
| 17 | One-year prevalence: 4 | ||
| Wright and Kariya, 199750 | Prevalence: 41 | Assault victims in a Scottish A&E department | |
| 16 | |||
| Physical, sexual | Richardson et al., 200241 | Prevalence: 41 | Women attending GPs |
| 21 | One-year prevalence: 17 | ||
| Walby and Allen, 200436 | Prevalence: 45 | General population | |
| 19 | One-year prevalence: 13 | ||
| Physical, sexual, emotional | Boyle and Todd, 200347 | Prevalence: 22.1 | A&E department |
| 20 | |||
| Bowen et al., 200545 | 18 weeks’ gestation to 33 months’ postnatal prevalence: 11 | Pregnant women | |
| 20 | |||
| Mezey et al., 200543 | Prevalence: 23.5 | Pregnant women | |
| 20 | |||
| Bacchus et al., 200444 | Prevalence: 13 | Pregnant women | |
| 19 | One-year prevalence: 6.4 | ||
| Johnson et al., 200346 | Prevalence: 17 | Pregnant women | |
| 15 | |||
| Sexual | Coid et al., 200354 | Prevalence: 24 | Women attending GPs |
| 17 | |||
| Physical, emotional | Keeling and Birch, 200453 | Prevalence: 35.1 | Women attending pregnancy counselling |
| 18 | One-year prevalence: 19.5 | ||
| Physical, sexual, emotional, financial | Keeling, 200452 | Prevalence: 34.9 | Women attending family planning clinics |
| 19 | One-year prevalence: 14 |
Appendix 4.3 Characteristics and quality scores of systematic reviews of health impact
| Review author(s)/date | Review question | Dates of search | Inclusion criteria | Exclusion criteria | No. of primary studies | Total number of participants | Meta-analysis conducted? | Quality score |
|---|---|---|---|---|---|---|---|---|
| Boy and Salihu, 200462 | To examine the evidence on the association between physical and emotional abuse and pregnancy outcomes | Not reported |
Peer-reviewed, research-based studies Population at least five women Pertained to IPV Included pregnant participants Included outcomes data on at least one of the following: birthweight, preterm birth, perinatal mortality, maternal mortality, stillbirth and adverse pregnancy outcomes Studies must be available to the reviewers |
30 | Not reported | No | Poor | |
| Campbell et al., 200061 | To examine nursing research related to IPV and women’s reproductive health | Focused on research published since 1995 |
Published, nursing research Focused on reproductive health |
17 (2 qualitative, 2 quantitative with qualitative element) | 8311 | No | Poor | |
| Golding, 199957 | To review literature on battering as a risk factor for mental health problems | Not reported | Studies that inferred mental health problems using clinical interviews, chart reviews, standardised survey interviews, and symptom checklists |
Non-English language papers Studies exclusively of abuse during pregnancy |
18 – Depression 13 – Suicidality 11 – PTSD 10 – Alcohol abuse 4 – Drug abuse |
1420 – Depression 2492 – Suicidality 817 – PTSD 1195 – Alcohol abuse 2057 – Drug abuse |
Yes | Good |
| Jasinski, 200460 | To synthesize the interdisciplinary empirical research on pregnancy-related violence | 1996–2004 | Focus of the review was primarily on research conducted with samples from the USA | Studies included in the review by Gazmararian et al., 1996847 | 17 on prevalence of pregnancy-related violence and 16 on consequences of pregnancy-related violence | Not reported | No | Poor |
| Jones et al., 200158 | To analyse data from literature based on studies of battered women to determine (1) the correlation of domestic violence and PTSD; (2) the best treatment strategies for PTSD; and (3) the evidence of PTSD treatment effectiveness with battered women | 1991–2000 |
Research-based articles published in the past 10 years Reports on domestic violence, PTSD, domestic violence/treatment/intervention, domestic violence and mental health, cultural differences and domestic violence, domestic violence and welfare reform, and domestic violence and undocumented women |
Studies that are ‘empirically weak’ | 43 | 17,243 | No | Poor |
| Murphy et al., 200164 | To determine the strength of association between low birthweight (LBW) and physical, sexual or emotional abuse during pregnancy | MEDLINE (1966–1999), CINAHL (1982–1997) |
Published studies measuring pregnancy outcomes Case–control or cohort studies English abstract Focused on women abused during pregnancy or pregnant women living in a relationship that was abusive in the past, or both. Studies were chosen regardless of the relationship of the perpetrator to the victim, if they included clear definitions of physical, sexual or emotional abuse, or some combination of these, and examined the outcome of mean or low birthweight |
8 in the meta-analysis | 16,519 | Yes | Good | |
| Nasir and Hyder, 200363 | To estimate the magnitude and prevalence of domestic violence during pregnancy in the developing world, to explore the risk factors associated with such behaviour, and to examine the impact on adverse pregnancy outcomes | Not reported | Not reported |
9 in total 3 describing adverse pregnancy outcomes |
Not reported | No | Poor | |
| Stith et al., 200470 | To identify risk factors most strongly related to intimate partner physical abuse perpetration and victimisation | 1980–2000 |
Study must examine the relationship between the identified risk factor and intimate partner violence Must include distinct data on physical violence Must include the quantitative data necessary for the calculation of at least one effect size Sample size must be greater than 20 Sample must include heterosexual married and/or cohabiting couples Each study must use an original sample |
Unpublished master’s theses and dissertations Studies on dating violence |
94 in total 6 for depression 11 for alcohol use |
899 for depression 7084 for alcohol use |
Yes | Medium |
| Impact on children’s health | ||||||||
| Attala et al., 199568 | To examine the effects on children of witnessing domestic violence | 1974–1995 |
Primary research published in refereed journals in the last two decades Focused on children (0–18 years) who had witnessed domestic violence |
14 3 of these were qualitative, and one had qualitative components |
912 children and their parents | No | Poor | |
| Bair-Merritt et al., 200666 | To examine the association between childhood IPV exposure and physical health | 1966–2003 |
No language restriction Trials investigating postneonatal physical health outcomes related to exposure to IPV |
Studies without a contemporaneous control Studies including direct trauma from a parent to the child Studies that included sibling violence, and did not have a strict definition of IPV |
22 | Not reported | No | Medium |
| Buehler et al., 199765 | To examine whether interparental conflict is associated with internalising and externalising problems in children aged 5–18 years |
Not reported Manual search of 10 relevant journals was conducted for the last 15 years |
Published and non-published studies Sample needed to include married or divorced families who had children somewhere between the ages of 5 and18 years Target child must be a product of the marriage of focus Published in English Study must have statistical data available to calculate an effect size. Reports of non-significant findings were included |
Data on stepfamilies | 68 | Not reported | Yes | Medium |
| Kitzmann et al., 200367 | To examine the psychosocial outcomes of children exposed to interparental violence | Not reported |
Dissertations were included Studies reported empirical data Studies examined the effects of witnessing interadult physical aggression in the home Study reported on psychosocial outcomes, including psychological, emotional and behavioural, social and academic Study examined the association between interadult physical aggression and child psychosocial outcomes either in (1) correlational or multiple regression analyses or (2) group comparisons, in which a group of child witnesses was compared with one or more control groups Study sample restricted to children. Adolescent samples that included 19-year-olds were included if most of the sample was 18 or younger, but college samples of 19-year-olds were excluded Published in 2000 or earlier Reported in English |
Case studies, qualitative studies Studies examining the effects of witnessing verbal aggression, parent–sibling violence or community violence Studies with outcomes relating to physical health, intelligence, parenting competence and general family functioning Studies with group formation based on a dimension other than exposure to domestic violence |
118 | Not reported | Yes | Medium |
| Kolbo et al., 199669 | To examine the initial effect of witnessing domestic violence on children’s functioning | Not reported | Not reported | 29 | 2626 | No | Poor | |
Appendix 5 Screening tool studies
Appendix 5.1 Summary of partner violence screening tools included in the review
The tools are divided into three sections: the first describes all the instruments used as comparators; the second section describes all the index tools; and the third section describes those tools used as both index tools and comparators.
Tools used as comparators
Abuse Risk Inventory (ARI)
This is a 25-item self-report measure using a four-point Likert scale ranging from ‘rarely or never’ to ‘always’. A score of 50 or higher suggests the respondent may be in an abusive situation or at risk for abuse. The ARI has demonstrated a reliability of 0.91. 217
Composite Abuse Scale (CAS)
The CAS consists of 30 items taken from the Conflict Tactics Scale (CTS), Measures of Wife Abuse, Inventory of Spouse Abuse and the Psychological Maltreatment of Women Inventory, and is designed to assess physical, emotional and sexual abuse. The tool has four dimensions: severe combined abuse, emotional abuse, physical abuse and harassment. Hegarty et al. 218 report an internal reliability (Cronbach’s alpha) of 0.90 or more for each subscale, and all item–total score correlations of 0.6 or above. When compared with the CTS, concurrent validity between the subscales of each tool ranged from r = 0.46 to 0.91. The psychometric validation is further supported by Hegarty et al. 219
Conflict Tactics Scale (CTS)
This 19-item scale assesses abuse within the past year. Answered on a seven-point frequency scale (never, once, twice, 3–5 times, 6–10 times, 11–20 times, > 20 times), the items range in severity from ‘low in coerciveness’ to ‘physical violence’, total scores ranging from 15 to 105. Three subscales measure verbal reasoning (three items, alpha = 0.69), verbal aggression (seven items, alpha = 0.84), and violence (nine items, alpha = 0.93). 220
Conflict Tactics Scale – Revised (CTS2)
Based on the CTS, the CTS2 includes more items for the three subscales and has two extra subscales (sexual coercion and physical injury from assault), totalling 78 items encompassing five subscales (each question is asked twice, one for the respondent and the other for the respondent’s partner). Other alterations include improving certain items, such as changing ‘his/her’ or ‘him/her’ to ‘my partner’, utilising an improved distinction between minor and severe acts, simplifying the answering format, and interspersing the order of items to reduce answering in response sets. Good internal consistency was found across all five subscales (alphas for negotiation = 0.86; psychological aggression = 0.79; physical assault = 0.86; sexual coercion = 0.87 and injury = 0.95). 221
Danger Assessment Scale (DAS)
Used to assess an abused women’s potential for homicide, this tool consists of 14 dichotomous items. No time reference is given in the instructions, although some items do specifically refer to the past year. Campbell222 demonstrated a good reliability of 0.71 and moderate to strong construct validity when DAS was compared with the CTS (r = 0.43, p < 0.000) and the severity of injury scale adapted from Berk et al. 223 (r = 0.50, p < 0.000).
Index of Spousal Abuse (ISA)
The ISA has 30 questions, which can be administered in written or oral formats. It assesses for physical (ISA-P, 11 items, alpha = 0.91) and non-physical (ISA-NP, 19 items, alpha = 0.93) abuse, using a Likert scale of 1 (never) to 5 (very frequently). Items are weighted, summed and standardised for each scale, then a complex weighted calculation is required to tally a score. Scores range from 0 to 100, the higher scores representing more severe abuse. Cut-scores are 25 for non-physical abuse and 10 for physical abuse. 224 Hudson225 developed a modified version of the ISA-P, which consisted of 15 items, demonstrating a Cronbach’s alpha of 0.93.
Index tools
Abuse Assessment Screen (AAS)
This five-item tool assesses sexual coercion and emotional and physical abuse. Questions refer to time periods (lifetime, preceding 12 months and pregnancy period), severity, perpetrator and body sites. The majority of questions are asked in a yes/no format; positive answers are explored further with multiple-choice options and frequency. The AAS was developed by Parker and McFarlane. 226 Two validation papers currently exist for the AAS, by McFarlane et al. 89 (included in this review) and Soeken et al. 227
Behavioural Risk Factor Surveillance Survey (BRFSS)
This is a five-item tool using a yes/no response scale. The questions focus on women’s exposure to physical violence, forced intercourse, sexual contact without intercourse, fear because of a partner’s anger or threats and put-downs, name-calling or controlling behaviour. Typically, the respondent is asked if they have ever experienced any of the IPV types listed, although the questions can be modified to ask about their most recent partner. A single affirmative answer is indicative of ‘any abuse’; affirmative answers for the other questions are indicative of physical, sexual or psychological abuse. These questions are included in a larger questionnaire used in a population survey in the USA. 228
Hurt, Insulted, Threatened with harm and Screamed at (HITS)
Originally developed from a family physician focus group study,229 HITS contains four questions: (1) ‘How often does your partner physically hurt you?’ (2) ‘How often does your partner insult you or talk down to you?’ (3) ‘How often does your partner threaten you with harm?’ and (4) ‘How often does your partner scream or curse at you?’ Women answer each of these questions using a five-point scale from 1 (never) to 5 (frequently). Answers were summed to form an interval scale of the total HITS score, ranging from 4 to 20; a cut-score of 10 suggests abuse.
Ongoing Violence Assessment Tool (OVAT)
Developed by Weiss et al.,230,231 the OVAT consists of four questions measuring both physical and non-physical violence. Based on the ISA, three questions are answered using true/false responses, the other uses a five-point Likert response from 1 (never) to 5 (very frequently). The OVAT takes 1 minute or less to administer and can be scored immediately.
Partner Violence Screen (PVS)
Using a yes/no response, three brief questions ask about two dimensions, one item on physical violence within the past year, and two items on safety. Measuring safety is believed to be a short-term measure of risk for further violence and need for counselling. 232,233
Perinatal Self-Administered Inventory (PSAI)
Developed as an intake measure to be used on the first obstetric appointment, this tool consists of several components including substance use, pregnancy complaints, pregnancy history, personal medical and family histories, genetic history and psychosocial history. It is under the latter section that questions of current mental or physical abuse and mental and physical abuse as a child are asked. If a yes is given to any question, the nurse probes further for more detailed information which is recorded on the form. 90
Slapped, Threatened or Thrown (STaT)
This is a brief three-question tool using a yes/no response. 234 The questions are ‘Have you ever been in a relationship where a) your partner has pushed or slapped you; b) your partner threatened you with violence; c) your partner has thrown, broken or punched things?’ The total of affirmative responses is summed; respondents scoring 1 or above are considered positive for domestic abuse.
Tools used as both a comparator and index
Woman Abuse Screening Tool (WAST)
The WAST is an eight-item questionnaire that was originally developed for use in a general practice setting. Women respond on a three-point response set, then the answers are summed to form an interval scale. Brown et al. 235 report a coefficient alpha estimated at 0.95 revealing good reliability. Regarding construct validity, the evidence is again supportive. Corrected item–total correlations ranged from r = 0.81 to 0.89 (p < 0.001), individual WAST items were highly correlated with the ARI (r = 0.80 to 0.85, p < 0.001), and overall ARI and WAST scores were also highly correlated, at r = 0.96, p < 0.00.
Women’s Experience with Battering Scale (WEB)
The WEB is a 10-item tool that measures battering by characterising women’s perceptions of their vulnerability to physical and psychological danger or loss of control in relationships. A six-point Likert scale of 1 (strongly agree) to 6 (strongly disagree) is used for this tool. Smith et al. 236 reported that the WEB has moderate to good construct validity when compared with the physical violence subscale of the CTS (r = 0.71, p < 0.0001) and psychological abuse (ISA-NP) (r = 0.88, p < 0.0001), as well as other measures such as belief in a just world, self-esteem, marital satisfaction, locus of control, depression, anxiety, perceived health status, injury, chronic pain and number of visits to a physician or hospital. Good reliability has been shown for the WEB, with a Cronbach’s alpha of 0.93.
Appendix 5.2 Summary of partner violence screening tools not included in the review
Below are lists of various tools used to identify domestic abuse. The studies that utilised these tools were excluded from the review as they did not fulfil the validation study criteria, that is: either the tool comprised 13 items or more; an inappropriate comparator was used, such as a clinical interview; or a comparator was absent. This is not an exhaustive list of all the tools used from all of the excluded studies, because many studies were excluded for other reasons such as including males in the sample or using a non-health-care sample.
Stand-alone tools
Abuse Assessment Questionnaire (AAQ)
Consisting of six items, this tools screens for physical and sexual abuse during the past year. Comparison of this tool with a clinical interview showed this tool to have good diagnostic accuracy. The overall sensitivity and specificity varied from 85.7% to 95.8% and from 89.7% to 99.6% respectively. The overall positive and negative predictive value varied from 91.9% to 97.7% and 97.05 to 99.3% respectively. 237
Abuse Assessment Screen-Disability (AAS-D)
This four-item tool is designed to detect abuse towards women with physical disabilities. The first two questions of the AAS-D are taken directly from the Abuse Assessment Scale (AAS). 226 The other two questions are: ‘Within the last year, has anyone prevented you from using a wheelchair, cane, respirator, or other assistive devices?’ and ‘Within the last year, has anyone you depend on refused to help you with an important personal need, such as taking your medicine, getting to the bathroom, getting out of bed, bathing, getting dressed, or getting food or drink?’ The items are answered using yes or no. 238
Dartmouth COOP Charts – the Relationship Chart
The charts consist of picture and word questions developed for general health screening. The Relationship Chart evaluates intimate partner violence with the following question: ‘During the past four weeks, how often have problems in your household led to: insulting or swearing? yelling? threatening? hitting and pushing?’ The chart is scored on a Likert scale of 1 – ‘none of the time’ – to 5 – ‘all of the time’. 239
Intimate Partner Violence (IPV) Assessment Icon Form
Based on the five-item Abuse Assessment Scale (AAS),226 each of the questions is present in both written and pictorial format, thus an individual can complete the tool regardless of their literacy level. Inter-rater reliability and criterion-related validity of the tool have been found to be adequate for literate and semiliterate participants. 240
Life History Calendar of Domestic Violence (LHC-DV)
Based on the assumption that personally experienced events that are thematically similar and/or sequentially proximal are stored together, the recall of easily accessible information helps the recall of more detailed, associated events. This tool involves a semistructured interview format to elicit memorable and/or easily recalled information of a personal nature, such as places of residence, family members and occupational history. The information elicited is laid out in a calendar format. This information is then used as a memory aid to elicit information about domestic violence victimisation. The interview obtains information on the occurrence and timing of not only domestic violence but also events that affect the relationship between domestic violence and women’s well-being. The interview takes approximately 40–60 minutes to administer, with an additional 20–30 minutes if the interviewer asks about health and sociodemographic characteristics. 241
Partner Abuse Scale: Physical (PASPH) and Partner Abuse Scale: Non-Physical (PASNP)
These instruments were designed to measure self-reports of physical and non-physical partner abuse. 225 Each questionnaire consists of 25 questions, which are scored on a seven-point Likert scale ranging from ‘never’ to ‘all the time’. The raw scores for each questionnaire are rescaled into scaled scores, which range from 0 (never abused) to a maximum score of 100. Attala et al. 242 report good reliability for both of these questionnaires (Cronbach’s alpha: PASPH = 0.97 and PASNP = 0.98).
Partner Violence Interview (PVI)
This instrument is a 26-item structured assessment, adapted from the CTS,243 which asks subjects to report on the various levels of violence that they have experienced or perpetrated in their lifetime. The measure asks about physical and sexual abuse and takes approximately 25 minutes to complete. The tool focuses on three separate areas – violence inflicted by current partners (current partner scale); violence inflicted by previous partners (ex-partner scale); and violence inflicted by a subject towards a partner (towards partner scale). Re-test reliability ranged from 0.70 to 0.85 for ex-partner and current partner scales respectively. Internal consistency was assessed using Kuder–Richardson formula 20 (KR-20) and ranged from 0.78 to 0.93 across the three scales. 244
Psychological Maltreatment of Women Inventory (PMWI)
This is a 58-item instrument designed to measure the level of psychological maltreatment of women by their male partners in intimate relationships. Two subscales are used in this tool, Dominance-Isolation and Emotional-Verbal. Questions are answered on a five-point Likert scale ranging from never (1) to very frequently (5). Good construct validity has been shown between this tool and the ISA (non-physical subscale r = 0.89–0.94; physical subscale r = 0.78–0.85) and CTS (r = 0.64–0.68). 245
Psychological Maltreatment of Women Inventory – Short Version (PMWI-Short)
This is a 14-item version of the above tool. The subscales and items are scored in the same way. Good construct validity has been shown between the short version and the ISA (non-physical subscale r = 0.88–0.90; physical subscale r = 0.80–0.86) and CTS (r = 0.65–0.68) although the correlations tend to be slightly lower. 246
Severity of Violence Against Women Scales (SVAW)
This is a 46-item tool designed to measure threats of violence, acts of violence and sexual aggression. Respondents answer on a four-point Likert scale to indicate how often the specified behaviour has occurred. Threats of violence are scored as symbolic, mild, moderate or serious, whereas acts of violence are scored as mild, minor, moderate or serious. This tool also detects sexual aggression. Good reliability has been shown for this tool, with values ranging from 0.89 to 0.96. 247
Trauma Questionnaire (TQ)
This is a 10-item self-report questionnaire that assesses a women’s history of childhood and adult sexual trauma, sexual harassment and domestic violence, and measures her desire for mental health help. Comparison of this tool with a clinical interview revealed good to excellent k values (0.41–0.88) with no systematic bias. 248
Victimisation Assessment Tool (VAT)
The purpose of this tool is to ascertain the level of trauma a subject has experienced due to domestic violence. The interviewer asks various screening questions about any abuse that may have occurred, then the interviewer scores the reported abuse on a five-point Likert scale, ranging from 1 – ‘no experience of physical violence or abuse’, to 5 – ‘life-threatening or prolonged violence/abuse with very severe physical and or emotional trauma’. This tool has shown average to good internal consistency (kappa), ranging from 94.7 for experiences of child physical abuse to 57.5 for being mugged. 249
Wife Abuse Inventory (WAI)
This is a three-page questionnaire, page one consisting of 17 items that ask about biographical data on the respondent and their partner. 250 Pages two and three contain the 34 scale items, which ask about family management and abuse. This tool has been shown to have high internal consistency: for coefficient alpha, 0.90 and for split halves, 0.90. 251
Hospital screening tools/screening protocols/flowcharts/intake questionnaires
Department of Emergency Medicine, West Virginia University Domestic Violence Screening Questionnaire
This questionnaire was developed as an extremely brief screening tool for domestic violence in a university-affiliated emergency department. There are nine questions answered in a yes/no fashion. The questionnaire focuses on physical and emotional abuse and safety. 252
Domestic Violence Screen used in four Los Angeles hospitals
A screening tool consisting of five questions that ask about physical and emotional abuse was developed in order to identify victims of domestic abuse. This tool also asks questions about the nature of the injury, if advice/referral was given and if mandatory reports were completed. 253
Flowchart Domestic Violence Questioning
This study used a flowchart to screen women for domestic violence. The first step requires obtaining consent to ask some questions about domestic violence. If consent is given, a short paragraph is then read to the women describing physical, emotional and sexual abuse, and asking if the individual has ever experienced any of these. If a positive response is given, the woman is then asked if she would like to talk about it. The flowchart details various organisations and leaflets to give to anyone who discloses abuse. 254
IPV Questionnaire, Karachi
This questionnaire was designed to screen for physical, verbal and sexual abuse during pregnancy or marital life. The screen consisted of 14 questions and took approximately 40 minutes to administer in an interview format. 255
Kentucky Paediatric Practice Screen
Two screens were used in this study. The first was a six-item screen that included the following questions: ‘Are you in a relationship now or have you ever been in a relationship in which you have been harmed or felt afraid of your partner?’ and ‘Are you afraid of your current partner?’. The second screen consisted of a 72-item general intake questionnaire that included one DV-related question: ‘Are you or your child being hurt, hit, or frightened by anyone in your house?’. No psychometric or diagnostic accuracy data were presented for this screen. 256
Magee-Women’s Hospital Outpatients Obstetrics and Gynaecology Clinic Screening Form
Used as a screen during prenatal visits. The domestic violence-related questions were: ‘Have you had any partner(s) or family members who have been abusive to you throughout your lifetime?’. ‘Are you currently in a relationship in which you are physically hurt, threatened, or made to feel afraid?’ and ‘Are you safe?’. No psychometric or diagnostic accuracy data were presented for this screen. 257
Maternity Social Support Scale – The Royal Brisbane and Women’s Hospital
Used as part of the registration process, all new obstetric patients were asked to complete the six-item self-report questionnaire. Two of the questions relate to domestic violence: ‘I feel controlled by my husband/partner’ and ‘There is conflict with my husband/partner’. Respondents answer on a five-point Likert scale ranging from never (1) to always (5). A score of 3 or more on either of these questions indicates a case of abuse. 258
Paediatric Safety Questionnaire
This questionnaire consists of ten questions, four of which relate to domestic violence. These questions are: ‘Do you feel safe in your current relationship with your partner?’, ‘Have you been hit, kicked, punched, or otherwise hurt by a partner within the last year?’, ‘Is there a partner from a previous relationship who is making you feel unsafe now?’ and ‘Within the past year, has a partner repeatedly used words, yelled, or screamed at you in a way that frightened you, threatened you, put you down, or made you feel rejected?’. Responses to these questions were rated on a five-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. 259
Queensland Health’s Domestic Violence Initiative Form
This questionnaire consists of six questions, which ask about threats of abuse, physical and psychological abuse, and, if an affirmative response has been given, whether the respondent would like any help. All the questions are answered in a yes/no format, and one or more affirmative responses indicate a case of abuse. 258
Social History Questionnaire
Four abuse assessment questions were added to one of the general intake questions of health centres in Texas. The questions focus on physical and sexual abuse and are answered with a yes/no response. 260
Sutherland Hospital ED Domestic Violence Screen
As part of a domestic violence screening pilot, all women presenting to the emergency department were asked the following three abuse questions: ‘Within the last 12 months, have you ever been hit, slapped, kicked, or other ways hurt by your partner or ex-partner?’, ‘Are you frightened of your partner or ex-partner?’ and ‘Are you safe to go home when you leave here?’. 261
The Mount Sinai Hospital Risk Screening Questionnaire
This is a 20-item questionnaire that is used to screen new patients for risk of domestic violence. The questions focus mainly on emotional and psychological abuse and the health consequences of such abuse. The first five questions are scored as yes/no responses, the rest of the questions are scored on a three-, four- or five-point Likert scale to indicate the degree to which the respondents worry about specific behaviours, the frequency with which they experienced specific risk phenomena or the extent to which they agree with statements. A positive response on any of the items indicates the individual to be ‘at risk’ of abuse. 262
Two-Question Abuse Screen
Women entering an emergency department with vaginal bleeding were asked the following abuse screening question: ‘Have you ever been hit, slapped, kicked, or otherwise physically hurt by your male partner?’. Women who answered ‘yes’ were then asked ‘Have you ever been forced to have sexual activities?’. 263
Universal Violence Prevention Screening Protocol
This measure includes five questions related to intimate partner violence for the previous 12 months and the past month. Each question is answered with a yes/no response, an affirmative answer indicating abuse. 264
Appendix 5.3 Characteristics of included screening tool studies
| Study details | Study design | Number of participants | Participants |
|---|---|---|---|
| Bonomi et al., 200687 |
Index tool: Women’s Experience with Battering (WEB) Comparator tool: Behavioural Risk Factor Surveillance Survey (BRFSS) Inclusion criteria: Women enrolled for at least 3 years in a Group Health Cooperative (GHC) in Washington State, aged 18–64 years Exclusion criteria: Women who had never been in an intimate partner relationship, or who resided outside Washington State Sample: Abused and non-abused women Type of study: Validation study Setting: USA Telephone survey of randomly selected women Tool presentation: WAST was administered first by doctor, then a researcher administered ARI. The format has not been stated |
Eligible: 2504 Declining: 0 Recruited: 2504 |
Age (mean, SD, range): 46.2, 11.6, not stated Ethnicity: White: 82.7% Hispanic: 4% SES: < $25,000: 10.9% $25,000–50,000: 28.2% $50,000–75,000: 26.5% > $75,000: 34.5% |
| Brown et al.,200091 |
Index tool: Woman Abuse Screening Tool (WAST) Comparator tool: Abuse Risk Inventory (ARI) Inclusion criteria: Using a stratified random sampling frame, 20 physicians needed to be selected from 400 in London, Ontario, Canada. Women needed to be 18 or older, attending for a periodic health examination, for prenatal care or acute symptoms of illness, be English speaking, unaccompanied by another person, currently involved in an intimate relationship (married or common law) and they had to consider the attending physician as their primary care physician Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Validation study Setting: Canada Family practice site Tool presentation: WAST was administered first by a doctor, then a researcher administered ARI. The format has not been stated |
Eligible: 399 patients; 44 physicians Declining: 92 patients; 24 physicians Recruited: 307 patients; 20 physicians |
Age (mean, SD, range): 46.2; not stated; 18–86 Ethnicity: White: 97.6% SES: > $30,000: 58.7% |
| Brown et al., 200193 |
Index tool: Women Abuse Screening Tool (WAST) WAST-Short (WAST-S) Comparator tool: Abuse Risk Inventory (ARI) Inclusion criteria: 18 years of age (not adhered to). In a couple relationship for the last 12 months Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Validation study Setting: France Refuge and private homes Tool presentation: Tools presented in an interview (suggested) by both researchers and refuge workers |
Eligible: Not stated Declining: Not stated Recruited: 4625 abused 21 non-abused |
Age (mean, SD, range): Abused mean: 35.6 Abused range: 17–58 Non-abused mean: 37.8 Non-abused range: 27–54 SD not stated Ethnicity: Not stated SES: > Can$30,000: 15%/94.7% Abused:15% Non-abused: 94.7% |
| Chen et al., 200581 |
Index tool: Hurts, Insults, Threatens and Screams (HITS) Comparator tool: Index of Spouse Abuse – Physical (ISA-P) Woman Abuse Screening Tool (WAST) English and Spanish versions of both index and comparator were used Inclusion criteria: Women attending an urban family practice site who were 18 years or older and were currently involved in an ongoing relationship Exclusion criteria: Not stated Sample: Abused and non-abused women, predominantly Hispanic Type of study: Validation study Setting: USA Urban family practice site Tool presentation: Single structured interview with trained medical students |
Eligible: 386 Declining: 128 refused; 56 did not complete questionnaire due to long waiting period for a private room Recruited: 202 |
Age (mean, SD, range): 35.8 (SD and range not stated) Ethnicity: Total (%) English/Spanish/Non-Hisp white/Non-Hisp black/Non-Hisp other/Hispanic 20.3/36.3/NA/6.4/11.5/NA Spoken language (%) English/Spanish/Non-Hisp white/Non-Hisp black/Non-Hisp other/ Hispanic 1/1.8/NA/72.3/50.4/100 SES: Income (mean $) Spanish: 10,757 English: 14,142 |
| Coker et al., 200179 |
Index tool: Women’s Experience with Battering Scale (WEB) Comparator tool: Index of Spouse Abuse – Physical (ISA-P) Inclusion criteria: Women seeking medical care in one of two university-associated family practice clinics, aged between 18 and 65 and who were insured by a managed care organisation and/or Medicaid and had ever been in an intimate sexual relationship with a man for a least 3 months Exclusion criteria: Women whose partners would not leave them alone were not recruited Sample: Abused and non-abused women Type of study: Validation study Setting: USA Two university-associated family practice clinics Tool presentation: Tools given in an interview and followed up with a telephone survey by trained graduates |
Eligible: 1503 Declining: 174 refused 97 did not complete health assessment interview 80 had missing data on several response variables Recruited: 1152 |
Age (mean, SD, range): Not stated Ethnicity: African American: 62% White: 38% SES: Not stated |
| Connelly et al., 200092 |
Index tool: Single question hospital screen ‘Are you in a relationship in which you have been threatened, scared or hurt by someone?’ If yes, whom? Comparator tool: Conflict Tactics Scale (CTS) Inclusion criteria: Mothers giving birth between Feb 1996 and Mar 1997 who participated in a randomised clinical trial of paraprofessional home visitation services. High-risk mothers were identified 24 hours after birth using 15-item screen Furthermore, participants had to be English- or Spanish-speaking, not active to child protective services and referenced ‘baby’s father’ for the CTS Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Validation study, part of a larger clinical trial Setting: Not entirely clear where tools were administered, i.e. at hospital or home visit Tool presentation: Single question was embedded in admission protocol, CTS was administered as an interview by a trained paraprofessional interviewer |
Eligible: Not stated Declining: Not stated Recruited: 436 |
Age (mean, SD, range): 23.4, 6.2, 14–42 46% were 21 years or younger Ethnicity: Hispanic: 40% African American: 23% Caucasian: 27% Asian, Pacific Islander, Native American/other: 9% SES: Not stated |
| Ernst et al., 200480 |
Index tool: Ongoing Violence Assessment Tool (OVAT) Comparator tool: Index of Spouse Abuse (ISA) Inclusion criteria: English-speaking patients entering emergency department and completing both the OVAT and ISA Exclusion criteria: Under the age of 18, had no current partner, had an altered mental state, had an underlying psychiatric diagnosis, were too ill to participate or drug or alcohol intoxicated Sample: Abused and non-abused women Type of study: Validation study Setting: USA A&E department Tool presentation: Self-complete questionnaire administered by a researcher |
Eligible: 362 Declining: 46 10 did not complete forms Recruited: 306 |
Age (mean, SD, range): 34, 10, range not stated (includes males) Ethnicity: Caucasian: 49% African American: 16% Hispanic: 20% Asian or other: 15% (this includes males) SES: Not stated |
| Feldhaus et al., 199784 |
Index tool: Partner Violence Screen (PVS) Comparator tool: Index of Spouse Abuse (ISA) Conflict Tactics Scale (CTS) Inclusion criteria: Non-critical, English-speaking women presenting to one of two urban emergency departments Exclusion criteria: Under the age of 18, had an altered mental status or primary psychiatric disorder Sample: Abused and non-abused women Type of study: Validation study Setting: USATwo urban, hospital-based A&E departments Tool presentation: First researcher administered verbal PVS, then the written self-completed ISA Second researcher administered the verbal CTS and four further questions |
Eligible: 426 Declining: 47 Another 57 missed due to heavy volume of patients Recruited: 322 |
Age (mean, SD, range): 36, 16, range not stated Ethnicity: Black: 19% White: 45% Hispanic: 30% Other: 6% SES: < $15,000: 64% |
| MacMillan et al., 200685 |
Index tool: Partner Violence Screen (PVS); Woman Abuse Screening Tool (WAST) Comparator tool: Composite Abuse Scale (CAS) Inclusion criteria: All women presenting for an appointment at the included sites (EDs, family practices or women’s health clinics), aged 18–64 years, at a site for their own health-care visit, able to separate themselves from individuals who accompanied them, able to speak and read English, were not too ill to participate and could provide informed consent Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Validation study: primary aim was to test presentation effects of tools Setting: Canada, Ontario: 2 × ED; 2 × Family practices; 2 × Women’s health clinics Tool presentation: This study looked at one of three presentation methods: Computer-based self-complete method: PVS and WAST (randomly ordered) on table computer followed by CAS and demographics on paper. Written self-complete method: demographics, PVS, WAST (both randomly ordered) then CAS on paper Face-to-face interview with health-care provider: used one of two indexes (randomly selected), then gave written version of demographics and CAS |
Eligible: 2602 Declining: 141 Recruited: 2461 |
Age (mean, SD, range): 37.1, 11.9, not stated Ethnicity: Born in Canada: 87.4% SES: < $24,000: 17.6%Woman was the main source of income, wages or salary: 57.8% |
| McFarlane et al., 199289 |
Index tool: Abuse Assessment Screen (AAS) Comparator tool: Conflict Tactics Scale (CTS); Index of Spouse Abuse (ISA); Danger Assessment Screen (DAS) Inclusion criteria: Women entering one of two perinatal clinics Sample: Abused and non-abused women Type of study: Validation study Setting: USA Two perinatal clinics Tool presentation: Self-report questionnaires administered by primary care provider |
Eligible: 691 Declining: 0 Recruited: 691 |
Age (mean, SD, range): Age ranged from 13 to 30+ years 13 to 19 years: 31% 20 to 29 years: 57% > 30 years: 12% Ethnicity: Black: 39%White: 27%Hispanic: 34% SES: Below poverty level (not stated): 95% |
| Paranjape et al., 200686 |
Index tool: Slapped, Threatened or Thrown (STaT) Comparator tool: Index of Spousal Abuse (ISA) Inclusion criteria: Women aged 18–65 years, English speaking, and seen a medical provider within the centre on that day Exclusion criteria: Patients who could not be interviewed alone Sample: Abused and non-abused women Type of study: Validation study Setting: USA Urgent care centre in an inner city hospital that provides primary care Tool presentation: Single interview questionnaire administered by half-trained interviewers |
Eligible: 324 Declining: 84 Recruited: 240 |
Age (mean, SD, range): 38, 10, not stated Ethnicity: African American: 91.3% SES: Median monthly income: $800 |
| Peralta and Fleming, 200388 |
Index tool: One question: ‘Do you feel safe at home?’ Comparator tool: Modified Conflict Tactics Scale (CTS) (6 items) Inclusion criteria: All women within the waiting room of the urban family practice clinic in Madison, Wisconsin, who were English-speaking and aged between 18 and 36 years Exclusion criteria: Non-English speakers Sample: Abused and non-abused women Type of study: Validation study Setting: USA, urban family practice clinic Tool presentation: Self-report questionnaire administered by researchers |
Eligible: Declining: 12% Recruited: 399 |
Age (mean, SD, range): Mean and SD not stated; range 18–36 Ethnicity: Abuse status (%)Abused/non-abusedBlack: 44.2/55.8White: 43.9/56.1Other: 45.2/54.8 SES: Not stated |
| Reichenheim and Moraes, 200383 |
Index tool: Abuse Assessment Screen (AAS) Comparator tool: Revised Conflict Tactics Scale (CTS2) Inclusion criteria: Case of premature birth within 6-month period. Given birth within 24 hours; interviews conducted in first 48 hours postpartum Exclusion criteria: Diabetes mellitus, systematic arterial hypertension, or given birth to neonates with severe congenital malformations, infections associated with prematurity, or twins Sample: Abused and non-abused women Type of study: Validation study Setting: Brazil, Rio de%%Janeiro, three public sector maternity wards Tool presentation: Interview questionnaire administered by five trained interviewers |
Eligible: 3800 Declining: 3; 23 excluded Recruited: 748; 233 abused, 515 non-abused |
Age (mean, SD, range): 23.9, 6.5, range not stated Ethnicity: Brazilian SES: Median monthly income per capita of US$96.7 (95%CI 26.5–346.4) |
| Sagrestano et al., 200290 |
Index tool: Perinatal Self-Administered Inventory (PSAI): contains two questions on DV Comparator tool: Conflict Tactics Scale (CTS) Inclusion criteria: Women in a waiting room of a women’s care centre scheduled for routine prenatal care Exclusion criteria: Less than 20 weeks pregnant; were accompanied by small children who could not leave the waiting room with another relative; did not speak English or Spanish Sample: Abused and non-abused women Type of study: Validation study Setting: Mid-Western USA, university-affiliated women’s care centre Tool presentation: Interview conducted by researcher |
Eligible: 196 Declining: 0 Recruited: 196, but only 166 entered into analysis |
Age (mean, SD, range): 25.7, 6.0, 14–41 Ethnicity: African American: 48%Hispanic: 46%White or other: 6% SES: Median annual income was $10,000–20,000 49.4% earned less than$10,000 |
| Sherin et al., 199882 |
Index tool: ‘Hurts, Insults, Threatens and Screams at her’ (HITS) Comparator tool: Conflict Tactics Scale (CTS) Inclusion criteria: Phase 1: Female patients of the Family Practice Centre of Christ Hospital Medical Centre (Advocate) who attended between April and June 1996, were aged 21 or over and had lived with the same partner for at least 12 monthsPhase 2: Self-identified victims of domestic violence at either a crisis shelter or ER Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Validation study Setting: USA, phase 1: Family practice centre; phase 2: DV crisis shelter and an emergency room Tool presentation: Phase 1: Nurses administered self-report questionnaires Phase 2: Staff at the shelter/agency staff working in the emergency room administered self-report questionnaires |
Eligible: Not stated Declining: Not stated Recruited: Phase 1: 160 Phase 2: 99 (54 from crisis shelter; 45 from emergency room) |
Age (mean, SD, range): Not stated Ethnicity: Not stated SES: Not stated |
Appendix 5.4 Results of included screening tool studies
| Study | Evaluated tools | Outcomes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence | Reliability | Concurrent validity | Construct validity (diagnostic accuracy) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Comparison | Sen | Spe | PPV | NPV | LR+ | LR– | DOR | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Bonomi et al., 200687 |
Index tool: Women’s Experience with Battering (WEB) Comparator Tool: Behavioural Risk Factor Surveillance Survey (BRFSS) |
WEB: 7% BRFSS: 14.7% |
Not stated | Not stated | BRFSS any | 72.4 | 89.7 | 34.4 | 97.7 | 7.0 | 0.3 | 22.8 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| BRFSS sexual | 21.3 | 99.4 | 72.5 | 94.4 | 35.3 | 0.8 | 44.6 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| BRFSS physical | 42 | 94.7 | 37.1 | 95.6 | 7.9 | 0.6 | 12.8 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Fear due to threats | 48.3 | 96.5 | 50.9 | 96.1 | 13.7 | 0.5 | 25.9 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Controlling behaviour | 64.9 | 94.3 | 46.1 | 97.3 | 11.4 | 0.4 | 30.8 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Brown et al., 200091 |
Index: Woman Abuse Screening Tool (WAST) Comparator: Abuse Risk Inventory (ARI) |
Period: WAST: 8.5% | Coefficient alpha 0.75 | Correlation between WAST and ARI: r = 0.69, p = 0.01 | Not stated | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Brown et al., 200193 |
Index: Women Abuse Screening Tool (WAST) and WAST-Short (WAST-S) Comparator: Abuse Risk Inventory (ARI) |
Not stated | Coefficient alpha 0.95 | Not stated | Not stated | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chen et al., 200581 |
Index: HITS (English and Spanish versions) Comparator: Index of Spouse Abuse – Physical (ISA-P); Woman Abuse Screening Tool (WAST) (English and Spanish versions) |
ISA-P: 5.4% WAST: 9.9% ISA-P or WAST: 10.9% |
Presentation effects of instruments: English language: interviews were of similar reliability, regardless of tool order Spanish language: HITS and WAST then ISA-P scored higher reliability (Cronbach’s alpha 0.71) than ISA-P then HITS and WAST (Cronbach’s alpha 0.49)* Presentation method not significantly associated with total scores of any tool after controlling for demographics Presentation effects for Spanish version of HITS did not change construct validity or accuracy of the Spanish version of HITS (p > 0.05) Cronbach’s alpha: English HITS: 0.76 English ISA-P: 0.80 English WAST: 0.78 Spanish HITS: 0.61* Spanish ISA-P: 0.77 Spanish WAST: 0.80 Overall HITS: 0.71 Overall ISA-P: 0.78 Overall WAST: 0.78 *Reliability varies depending upon presentation of tools |
Correlations (r) between English HITS & ISA-P = 0.76 English HITS & WAST = 0.75 Spanish HITS & ISA-P = 0.81 Spanish HITS & WAST = 0.81 Overall HITS & ISA-P = 0.77 Overall HITS & WAST = 0.76 (p < 0.001 for all correlations) |
HITS | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| English | 86 | 99 | 86 | 99 | 90.7 | 0.1 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Spanish | 100 | 86 | 45 | 100 | 7.3 | 0.0 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coker et al., 200179 |
Index: Women’s Experience with Battering Scale (WEB) Comparator: Index of Spouse Abuse- Physical (ISA-P) |
Period: WEB:19.8%; ISA-P: 11% | Cohen’s kappa: 0.60 | Correlation between WEB and ISA-P: r = 0.67 | WEB | 85.9 | 91.1 | 51.6 | 98.3 | 9.7 | 0.2 | 64.4 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Connelly et al., 200092 |
Index: Single-question hospital screen: ‘Are you in a relationship in which you have been threatened, scared or hurt by someone? If yes, whom?’ Comparator: Conflict Tactics Scale (CTS) |
Single question: 4% CTS: 18.6% |
Not stated | Not stated | Not stated | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ernst et al., 200480 |
Index: Ongoing Violence Assessment Tool (OVAT) Comparator: Index of Spouse Abuse (ISA) |
OVAT: 33% ISA: 21% |
Cronbach’s alpha = 0.6* kappa = 0.58 (95% CI 0.53–0.63)* *Based on male and female data |
Inter-item correlation of 0.38 (variance 0.03)* *Based on male and female data |
OVAT | 85.7 | 83.1 | 56.8 | 95.7 | 5.1 | 0.2 | 29.8 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Feldhaus et al., 199784 |
Index: Partner Violence Screen (PVS) Comparator: Index of Spouse Abuse (ISA); Conflict Tactics Scale (CTS) |
Current PVS: 29.5% (95% CI: 24.6–34.8%) ISA: 24.3% (95% CI: 19.2–30.1%) CTS: 27.4%* (95% CI: 21.7–33.6%) *Of the 36 women with only a previous relationship and no current partner, prevalence was 43% |
Not stated | Not stated | PVS vs ISAPhysical violence (1 PVS question)53.289.161.185.64.90.59.2Safety (2 PVS questions)48.487.655.684.13.90.66.6Combined64.580.351.387.63.30.47.4PVS vs CTSPhysical violence (1 PVS question)68.294.682.788.812.60.337.2Safety (2 PVS questions)39.787.454.479.43.20.74.6Combined71.484.463.488.74.60.313.5 | PVS vs ISA | Physical violence (1 PVS question) | 53.2 | 89.1 | 61.1 | 85.6 | 4.9 | 0.5 | 9.2 | Safety (2 PVS questions) | 48.4 | 87.6 | 55.6 | 84.1 | 3.9 | 0.6 | 6.6 | Combined | 64.5 | 80.3 | 51.3 | 87.6 | 3.3 | 0.4 | 7.4 | PVS vs CTS | Physical violence (1 PVS question) | 68.2 | 94.6 | 82.7 | 88.8 | 12.6 | 0.3 | 37.2 | Safety (2 PVS questions) | 39.7 | 87.4 | 54.4 | 79.4 | 3.2 | 0.7 | 4.6 | Combined | 71.4 | 84.4 | 63.4 | 88.7 | 4.6 | 0.3 | 13.5 | |||||||||||||||||||||
| PVS vs ISA | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Physical violence (1 PVS question) | 53.2 | 89.1 | 61.1 | 85.6 | 4.9 | 0.5 | 9.2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Safety (2 PVS questions) | 48.4 | 87.6 | 55.6 | 84.1 | 3.9 | 0.6 | 6.6 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Combined | 64.5 | 80.3 | 51.3 | 87.6 | 3.3 | 0.4 | 7.4 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| PVS vs CTS | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Physical violence (1 PVS question) | 68.2 | 94.6 | 82.7 | 88.8 | 12.6 | 0.3 | 37.2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Safety (2 PVS questions) | 39.7 | 87.4 | 54.4 | 79.4 | 3.2 | 0.7 | 4.6 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Combined | 71.4 | 84.4 | 63.4 | 88.7 | 4.6 | 0.3 | 13.5 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| MacMillan et al., 200685 |
Index tool: Partner Violence Screen (PVS); Woman Abuse Screening Tool (WAST) Comparator tool: Composite Abuse Scale (CAS) |
CAS: 10.3% Presentation (95% CI) Computerised: PVS: 11.2% (8.8–13.5) WAST: 10.1% (7.9–12.3) Face-to-face: PVS: 8.7% (5.9–11.4) WAST: 10.5% (7.5–13.4) Written: PVS: 11.2% (9.0–13.3) WAST: 7.0% (5.3–8.8) |
Not stated | Not stated | PVS | 49.2 | 93.7 | 55.3 | 94.2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
WAST Overall accuracy of PVS = 89.2% Overall accuracy of WAST = 90.6% |
47.0 | 95.6 | 47.0 | 94.0 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| McFarlane et al., 199289 |
Index: Abuse Assessment Screen (AAS) Comparator: Conflict Tactics Scale (CTS); Index of Spouse Abuse (ISA); Danger Assessment Screen (DAS) |
ASS: Physical and sexual violence Within last year 26% During pregnancy 17% Combined 55% |
Not stated | Not stated | Not stated | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Paranjape et al., 200686 |
Index Tool: Slapped, Threatened or Thrown (STaT) Comparator Tool: Index of Spousal Abuse (ISA) |
ISA Most recent relationship 32.9% Current IPV 15.4% |
Not stated | Not stated | STaT scores | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≥ 1 | 94.9 | 36.6 | 42.3 | 93.6 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≥ 2 | 84.8 | 54.0 | 47.5 | 87.9 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | 62.0 | 65.8 | 47.0 | 77.9 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Peralta and Fleming (2003)88 |
Index: One question: ‘Do you feel safe at home?’ Comparator: Modified Conflict Tactics Scale (CTS) (6 items) |
Period (90 days) CTS: 44.3% |
Not stated | Not stated | ‘Do you feel safe at home?’Any violence8.895.862.556.82.11.01.9Mainly physical violence with some psychological violence15.094.725.090.52.90.93.2Mainly psychological violence with some physical violence8.895.962.557.62.21.02.3AAS vs CTS2Minor cases (5 items of CTS2)31.999.088.013.531.90.746.2Severe cases (7 items of CTS2)61.497.870.00.027.90.471.6Both (all 12 items on CTS2)31.799.290.013.939.60.757.4 | ‘Do you feel safe at home?’ | Any violence | 8.8 | 95.8 | 62.5 | 56.8 | 2.1 | 1.0 | 1.9 | Mainly physical violence with some psychological violence | 15.0 | 94.7 | 25.0 | 90.5 | 2.9 | 0.9 | 3.2 | Mainly psychological violence with some physical violence | 8.8 | 95.9 | 62.5 | 57.6 | 2.2 | 1.0 | 2.3 | AAS vs CTS2 | Minor cases (5 items of CTS2) | 31.9 | 99.0 | 88.0 | 13.5 | 31.9 | 0.7 | 46.2 | Severe cases (7 items of CTS2) | 61.4 | 97.8 | 70.0 | 0.0 | 27.9 | 0.4 | 71.6 | Both (all 12 items on CTS2) | 31.7 | 99.2 | 90.0 | 13.9 | 39.6 | 0.7 | 57.4 | |||||||||||||||||||||
| ‘Do you feel safe at home?’ | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Any violence | 8.8 | 95.8 | 62.5 | 56.8 | 2.1 | 1.0 | 1.9 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mainly physical violence with some psychological violence | 15.0 | 94.7 | 25.0 | 90.5 | 2.9 | 0.9 | 3.2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Mainly psychological violence with some physical violence | 8.8 | 95.9 | 62.5 | 57.6 | 2.2 | 1.0 | 2.3 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| AAS vs CTS2 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Minor cases (5 items of CTS2) | 31.9 | 99.0 | 88.0 | 13.5 | 31.9 | 0.7 | 46.2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Severe cases (7 items of CTS2) | 61.4 | 97.8 | 70.0 | 0.0 | 27.9 | 0.4 | 71.6 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Both (all 12 items on CTS2) | 31.7 | 99.2 | 90.0 | 13.9 | 39.6 | 0.7 | 57.4 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Reichenheim and Moraes, 200383 |
Index: Abuse Assessment Screen (AAS) Comparator: Revised Conflicts Tactics Scales (CTS2) |
ASS : 6.7% (95% CI: 5–8.7) CTS2 : Minor : 18.4% (95% CI: 15.7–21.4) Major: 7.6% (95% CI: 5.8–9.8) Overall: 18.9% (95% CI: 16.2–22.0) |
Not stated | Not stated | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sagrestano et al., 200290 |
Index: Perinatal Self-Administered Inventory (PSAI): contains two questions on DV Comparator: Conflict Tactics Scale (CTS) |
CTS: Verbal aggression: 84.3%, 17% experienced violence in past year During the current pregnancy, verbal abuse: 68.1%, violence 13.3% |
Not stated |
Correlations PSAI: ‘Are you experiencing severe conflicts with anyone in your home?’ and PSAI: ‘Are you suffering mental or physical abuse now?’ and |
Not stated | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sherin et al., 199882 |
Index: ‘Hurts, Insults, Threatens and Screams at her’ (HITS) Comparator: Conflict Tactics Scale (CTS) |
Not stated |
HITS Cronbach’s alpha: 0.80 Presentation effects: Median HITS score was 5 for those who completed it first and second, z = 23, p > 0.05 Median CTS score was 19.64 for first completers, 20 for second time completers, z = 0.26, p > 0.05 |
Correlation of HITS and CTS: r = 0.85 Subscores – physical violence: r = 0.8; verbal violence: r = 0.81 |
HITS (simulated data from statistical modelling using cut scores to differentiate cases and non-cases) | 96 | 91 | 87 | 97 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Appendix 5.5 Assessment of quality of screening tool studies
| Study | Assessment criteriaa | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
| Bonomi et al., 200687 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes |
| Brown et al., 200091 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No |
| Chen et al., 200581 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes |
| Coker et al., 200179 | No | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | Yes | Yes |
| Connelly et al., 200092 | No | Yes | No | No | Yes | Yes | Yes | No | No | No | No | Yes | No | No |
| Ernst et al., 200480 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | No | No | Yes | Yes | No |
| Feldhaus et al., 199784 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| MacMillan et al., 200685 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes |
| McFarlane, et al.,199289 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No |
| Paranjape et al., 200686 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes |
| Peralta and Fleming, 200388 | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | No | Yes |
| Reichenheim and Moraes, 200383 | Yes | Unclear | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes |
| Sagrestano et al., 200290 | Yes | Yes | No | No | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes |
| Sherin et al., 199882 | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No |
Appendix 5.6 Bias in screening tool studies
| Study | Bias | Decreasing quality |
|---|---|---|
| aFeldhaus et al., 199784 | Blind analysis | ↓ |
| aChen et al., 200581 | Blind analysis | |
| Incorporation bias | ||
| Brown et al., 200091 | Blind analysis | |
| Withdrawals | ||
| aMacMillan et al., 200685 | Blind analysis | |
| Uninterpretable results | ||
| aParanjape et al., 200686 | Blind analysis | |
| Incorporation bias | ||
| aBonomi et al., 200687 | Blind analysis | |
| Reference standard | ||
| Interpretation bias | ||
| aReichenheim and Moraes, 200383 | Spectrum biasb | |
| Blind analysis | ||
| Incorporation bias | ||
| aCoker et al., 200179 | Spectrum bias | |
| Blind analysis | ||
| Incorporation biasb | ||
| McFarlane et al., 199289 | Spectrum bias | |
| Withdrawals | ||
| Blind analysis | ||
| Sagrestano et al., 200290 | Reference standard | |
| Blind analysis | ||
| Incorporation bias | ||
| Sherin et al., 199882 | Reference standard | |
| Withdrawals | ||
| Blind analysis | ||
| aPeralta and Fleming, 200388 | Reference standard | |
| Blind analysis | ||
| Indeterminable results | ||
| Incorporation bias | ||
| aErnst et al., 200480 | Spectrum biasb | |
| Blind analysis | ||
| Test executionb | ||
| Withdrawals | ||
| Connelly et al., 200092 | Spectrum bias | |
| Test execution | ||
| Reference standard | ||
| Blind analysis | ||
| Indeterminate results | ||
| Withdrawals | ||
| Disease progression bias |
Appendix 6 Acceptability of screening studies to women
Appendix 6.2 Characteristics of quantitative (survey) studies
| Study details | Study design | Number of participants | Participants | Quality score (CASP total) |
|---|---|---|---|---|
| Bacchus et al., 2002119 |
Sample: abused and non-abused women Interview setting: women’s houses and general practitioner’s surgeries Data collection: semistructured interviews |
Approached: 781 Recruited: 717: 32 interviewed Response rate (%): 91.8 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated |
33 |
| Belknap and Sayeed, 200395 |
Sample: abused women Interview setting: home or at the agency Data collection: open-ended questions |
Approached: 7 Recruited: 7 Response rate (%): 100 |
Age (mean, SD, range): 30 (19–38) Ethnicity (%): Mexican American: 100 No SD stated |
21 |
| Chang et al., 2003265 |
Sample: abused women Interview setting: locations where women attended their support groups Data collection: semistructured focus group interviews |
Approached: not stated Recruited: 41 Response rate (%): not stated |
Age (mean, SD, range): 30 (19–38) Ethnicity (%): White: 29.3 Black: 34.1 Latino: 36.6 No SD stated |
30 |
| Chang et al., 200599 |
Sample: abused women Interview setting: shelter, women’s hospital, general internal medicine clinic Data collection: semistructured interviews |
Approached: not stated Recruited: 21 Response rate (%): not stated |
Age (mean, SD, range): 44.2 (22–62) Ethnicity (%): White: 81 Black: 19 |
34 |
| Chang et al., 200598 |
Sample: abused women Interview setting: locations where women attended their support groups Data collection: focus groups |
Approached: not stated Recruited: 41 Response rate (%): not stated |
Age (mean, SD, range): 37 (22–77) Ethnicity (%): White: 29.2 Black: 34.1 Latina: 36.6 |
34 |
| Dowd et al., 2002120 |
Sample: abused and non-abused women Interview setting: non-clinical meeting room of hospital property Data collection: focus groups |
Approached: not stated Recruited: 59 Response rate (%): not stated |
Age (mean, SD, range): 37 (22–77) Ethnicity (%): White: 32.2 African American: 33.9 Latina: 33.9 |
27 |
| Hathaway et al., 200297 |
Sample: abused women Interview setting: hospital or heart clinic where customer received advocacy service, except for two phone interviews Data collection: semistructured interviews |
Approached: 186 Recruited: 138; 49 interviewed Response rate (%): 74.2 |
Age (mean, SD, range): 21–81 Ethnicity (%): White: 51 Latina: 35 Asian: 6 Other: 8 |
20 |
| Lutenbacher et al., 2003266 |
Sample: abused women Interview setting: living room area of a nursing school Data collection: focus groups |
Approached: 40 Recruited: 24 Response rate (%): 60 |
Age (mean, SD, range): 35 (21–51) Ethnicity (%): White: 67 African American: 20 |
27 |
| Lutz, 2005100 |
Sample: abused women Interview setting: private safe place Data collection: in-depth, open-ended interviews |
Approached: not stated Recruited: 12 Response rate (%): not stated |
Age (mean, SD, range): 29.7 (18–43) Ethnicity (%): White: 50 Black: 33.3 Arab American: 16.7 |
27 |
| Stenson et al., 200196 |
Sample: abused and non-abused women Interview setting: private examination room in antenatal clinic Data collection: one open-ended question |
Approached: 1074 Recruited: 879 Response rate (%): 82 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated |
32 |
| Taket et al., 2004211 |
Sample: abused women Interview setting: privately Minority Birmingham: refuges Salford: Salford Women’s Aid Wakefield: S&S, GP practice Data collection: interviews |
Approached: 697 Recruited: 44 Response rate (%): not stated |
Age (mean, SD, range): 18–68 Ethnicity (%): Minority Birmingham: 13.9 Salford: 3.9 Wakefield: 2.3 |
32 |
| Zeitler et al., 2006115 |
Sample: abused women Interview setting: family planning clinic Data collection: one open-ended question |
Approached: 697 Recruited: 372, 120 interviewed Response rate (%): 53.4 |
Age (mean, SD, range): 15–24 Ethnicity (%): White: 22 Black: 31 Hispanic: 30 Asian: 11 Other: 6 |
31 |
| Zink and Jacobson, 2003267 |
Sample: abused women Interview setting: women from shelter: private room; women from support group: the interviewer’s room or private room outside the support group location Data collection: focus groups |
Approached: not stated Recruited: 32 Response rate (%): not stated |
Age (mean, SD, range): 32 (18–45) Ethnicity (%): White: 50 African American: 50 |
32 |
| Zink et al., 2004268 |
Sample: abused women Interview setting: privately Data collection: interviews |
Approached: not stated Recruited: 32 Response rate (%): not stated |
Age (mean, SD, range): 32 (18–45) Ethnicity (%): White: 50 African American: 50 |
27 |
Appendix 6.2 Results of quantitative studies and quality scores
| Study details | Study design | Number of participants | Participants |
|---|---|---|---|
| Bair-Merritt et al., 2006108 |
Inclusion criteria: Female caregivers, aged 18 and older or emancipated minors if they were not accompanied by another adult, if the child or children with them were all younger than 3 years and if their child was not critically ill, as determined by a physician Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Cross-sectional survey |
Approached: 281, 139 in the pre-group and 142 in the post-group Recruited: 269;133 in the pre-group and 136 in the post-group Response rate (%): 96 |
Age (mean, SD, range): 28.6 ± 8.7 in the pre-group 28.5 ± 9.9 in the post-group Ethnicity (%): Pre-group: White: 22 Black: 77 Other: 1 Post group: White: 18 Black: 79 White: 18 Asian: 3 Other: 0 |
| Brzank et al., 2002269 |
Inclusion criteria: Female A&E outpatients between 18 and 60 years of age Exclusion criteria: Excluded were those patients who could not be approached due to the severity of their injury or condition, danger of infection, intoxication, mental confusion, language barriers or where the interview could not take place in a secure environment without escort Sample: Abused and non-abused women Type of study: Cross-sectional survey: self-report |
Approached: 1557 Recruited: 806 Response rate (%): 70 |
Age (mean, SD, range): 18–60 years (no mean or SD) Ethnicity: Not stated |
| Caralis and Musialowski, 1997109 |
Inclusion criteria: All female patients who came daily during the 4-hour time blocks of the clinic Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Cross-sectional survey |
Approached: 516 Recruited: 406 Response rate (%): 78.7 |
Age (mean, SD, range): 50.4 ± 16 Ethnicity (%): White: 57 Black: 26 Hispanic: 17 |
| Friedman et al., 1992110 |
Inclusion criteria: Not stated Exclusion criteria: Age less than 18, inability to understand the English language, and unwillingness to give consent Sample: Abused and non-abused women Type of study: Cross-sectional survey |
Approached: Not stated Recruited: 164 Response rate (%): Not stated |
Age (mean, SD, range): < 50: 52% > 50: 48% Ethnicity (%): White: 55 Black: 30 Hispanic: 6 Caribbean: 4 Other: 5 |
| Glass et al., 2001105 |
Inclusion criteria: All women > 18 years who were attending an ED on selected shifts; not to ill to respond; English or Spanish speaking Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Cross-sectional survey- self report |
Approached: 4641 Recruited: 3455 Response rate (%): 74 |
Age (mean, SD, range): 18–65 years (no mean or SD) Ethnicity: Not stated |
| Gielen et al., 2000111 |
Inclusion criteria: Women were selected for the mailing if they were between the ages of 21 and 55 years at the time of the recruitment and had been enrolled continuously in the HMO from 1995 through 1997 Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Case–control study |
Approached: 442 Recruited: 406 Response rate (%): 87.4 – cases 90.9 – controls |
Age (mean, SD, range): 21–55 years (no mean or SD) Ethnicity (%): White: 53.4 |
| Hurley et al., 2005103 |
Inclusion criteria: Subjects included non-critically ill patients, aged 16–95 years, who presented to the ED during specified data collection time frames. All potentially eligible patients in the waiting room were approached individually during these time frames Exclusion criteria: Subjects who refused or were in distress were not included Sample: Abused and non-abused women Type of study: Self-report survey |
Approached: 304 women Recruited: 304 women Response rate (%): 100 |
Age (mean, SD, range): 16–95 years (39.4) Ethnicity: Not stated |
| McCaw et al., 2001101 |
Inclusion criteria: Health plan members were eligible to participate in the study if they were female, aged 18–60 years, and had a medical visit designated ‘routine’ by the clinician in the internal medicine or obstetrics/gynaecology departments Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Cross-sectional survey following an intervention |
Approached: Not clear Recruited: 397 (190 pre- and 207 post-intervention) Response rate (%): Not clear |
Age (mean, SD, range): 18–60 years Ethnicity (pre-intervention) (%): White: 32.6 Black: 43.6 Hispanic: 12.7 Asian: 4.4 Other: 6.6 |
| McDonnell et al.,2006112 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Verbal questionnaire |
Approached: 481 women Recruited: 478 women Response rate (%): 99.4 |
Age (mean, SD, range): Not stated Ethnicity: Not stated |
| McNutt et al., 1999113 |
Inclusion criteria: 18–44 years old, had an obstetric, gynaecology, general physical or other extended examination between 15 March and 25 April 1996; spoke English; were determined by nursing staff to be physically capable of participating; were unaccompanied in the examination room by anyone over the age of 3 years Exclusion criteria: Not stated Sample: PCT (abused and non-abused) patients, DV programme patients and shelter residents Type of study: Cross-sectional survey, self-report and interview |
Approached: 124 Recruited: 161 at PCT Response rate (%): 64.5 PCT95.5 for DV programme 100 for shelter residents |
Age (mean, SD, range): 18–45+ years Ethnicity (%): White: 47 Black: 33 Other: 20 |
| Newman et al., 2005114 |
Inclusion criteria: All English- and Spanish-speaking women who brought their children for emergency care between the hours of 7pm and 3am, Sundays to Fridays Exclusion criteria: Women who did not speak English or Spanish, were accompanied into the treatment rooms with a male partner, or had a child with illness and injury managed in the resuscitation area Sample: Abused and non-abused women Type of study: Cross-sectional survey |
Approached: 781 Recruited: 451 Response rate (%): 97.83 |
Age (mean, SD, range): 32 ± 10 years Ethnicity (%): White: 25 Black: 29 Hispanic: 42 Other: 3 Unknown: 0.2 |
| Renker and Tonkin, 2006102 |
Inclusion criteria: Given birth within last 72 hours; be in satisfactory condition; speak and read English; 18 years or older; capable of giving informed consent, delivered infant in a stable condition Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: Cross-sectional survey using anonymous computer-based self-report |
Approached: 1069 Recruited: 519 Response rate (%): 48.55 |
Age (mean, SD, range): Not stated Ethnicity (%): White: 73 Black: 20 American Indian/Alaskan Native: 2.8 Asian: 1 Native Hawaiian/Pacific Islander: 0.4 Mixed race: 1.8 No response: 1.2 |
| Richardson et al., 200241 |
Inclusion criteria: Women were eligible to participate if they were registered with the practice, were over 15 years old, and were able to read English, Turkish, or Bengali (the three languages in which the questionnaire was available) Exclusion criteria: Those who were holding an infant or who were too unwell to complete the questionnaire were ineligible Sample: Abused and non-abused women Type of study: Self-administered questionnaire survey. Review of medical records |
Approached: 2192 Recruited: 1207 Response rate (%): 55 |
Age (mean, SD, range): 16–45+ (39.4) years Ethnicity (%): White British: 41 Irish: 4 Other: 9 Black African: 6 British: 8 Caribbean: 10 Other: 1 Asian Bagladeshi: 1 Indian: 3 Pakistani: 1 Turkish: 7 Other: 10 |
| Romito et al., 2004107 |
Inclusion criteria: All women over 17 years of age attending one of six family practice sites Exclusion criteria: If patient was too ill or confused Sample: Abused and non-abused women Type of study: Cross-sectional survey, self-report |
Approached: 542 Recruited: 426 Response rate (%): 78.6 |
Age (mean, SD, range): 17–85 years (no mean or SD) Ethnicity: Not stated |
| Sethi et al., 200448 |
Inclusion criteria: Women within waiting room on chosen shift Exclusion criteria: Aged under 18 or over 80 years; too ill, distressed, intoxicated or confused to respond to the question or unable to speak English; requiring psychiatric assessment Sample: Abused and non-abused women Type of study: Cross-sectional study, researcher interview |
Approached: 228 Recruited: 198 Response rate (%): 86.8 |
Age (mean, SD, range): 18–80 years (no mean or SD) Ethnicity: Not stated |
| Zeitler et al., 2006115 |
Inclusion criteria: Adolescent and young adult females aged 15–24 years who presented for family planning services at Planned Parenthood of New York City’s Margaret Sanger clinic between April and August 2004 were eligible to participate in this study Exclusion criteria: Not stated Sample: Abused and non-abused women Type of study: A cross-sectional quantitative and qualitative survey |
Approached: 697 Recruited: 645 Response rate (%): 92.54 |
Age (mean, SD, range): 15–24 years (no mean or SD) Ethnicity (%): Hispanic: 33 White: 22 Black: 28 Asian: 12 Other: 5 |
| Webster et al., 2001116 |
Inclusion criteria: Not stated Exclusion criteria: Those who could not read or write English were excluded, unless they had responded to the original questions through an interpreter and an interpreter was available to assist with the evaluation Sample: Abused and non-abused women Type of study: Cross-sectional study |
Approached: 1500 Recruited: 1313 Response rate (%): 87.5 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated |
| Weinsheimer et al., 2005104 |
Inclusion criteria: All women aged 18–80 admitted to the Trauma Service were tracked for inclusion. Eligible participants included those who spoke English and were able to read an introductory letter regarding the survey Exclusion criteria: Patients with a head injury or psychiatric disorder precluding informed consent Sample: Abused and non-abused women Type of study: In-person survey |
Approached: 105 Recruited: 95 Response rate (%): 90 |
Age (mean, SD, range): 18–79 (38.9) years Ethnicity (%): White: 37.9 Black: 1.1 Hispanic: 32.6 Native American: 28.4 |
| Witting et al., 2006117 |
Inclusion criteria: The study participants were all English-speaking adults (older than age 18 years) in the hospitals’ ED waiting rooms (not hospital employees) Exclusion criteria: Patients too ill to participate Sample: Abused and non-abused women Type of study: A self-administered questionnaire |
Approached: 146 Recruited: 146 Response rate (%): 100 |
Age (mean, SD, range): 37.3 (12.3) Ethnicity (%): Non-white: 60 |
Appendix 6.3 Results of quantitative studies and quality scores
| Author, publication year | Results | Quality score (STROBE total) |
|---|---|---|
| Bair-Merritt et al., 2006108 |
The two groups (pre, n = 133; post, n = 136) did not significantly differ with respect to age, race, education, or personal intimate partner violence history The post group was less likely to prefer pediatric emergency department intimate partner violence screening (pre, 76%; post, 63%; OR, 0.5; 95% CI, 0.3–0.9) and tended to be less likely to say that they would divulge (pre, 85%; post, 75%; OR, 0.6; 95% CI, 0.3–1.1) In both groups, women with a history of intimate partner violence were less likely than women without this history to say that they would disclose intimate partner violence to their pediatric emergency department provider (p < 0.001) No difference existed between previously abused and non-abused women with regard to the acceptability of displaying resources or routine screening |
17 |
| Brzank et al., 2004269 |
Sixty-seven percent of interviewed women considered physicians contact persons after experiencing domestic violence. However, only 8% had ever been asked about domestic violence experiences by their physicians Thirty-two percent of all interviewees would have wanted to be asked. This number increased to 41% in case of experienced sexual violence, and to 44% in case of experienced physical or emotional violence Sixty-four percent of interviewees think that generally questions about domestic violence experience should be part of the general anamnesis |
9 |
| Caralis and Musialowski, 1997109 | Overall, the majority of women (85%) agreed that doctors should, in their practices, routinely screen for abuse (77% of non-abused women and 70% of the abused women), and 50% strongly agreed | 16 |
| Friedman et al., 1992110 |
Among the 164 participating patients, routine physical abuse inquiry was favoured by 78% and routine sexual abuse inquiry was favored by 68% Older patients were more in favour of routine physical abuse inquiry. Age, however, did not influence the desire for routine sexual abuse inquiry Regardless of site, patients with less than a high school education were more in favour of routine inquiry about physical abuse and sexual abuse Eighty percent of those who reported sexual abuse favoured routine physician inquiry about sexual abuse compared with 64% of those who reported never being sexually abused (p < 0.05) In regard to physical abuse, patients who reported abuse were just as likely as patients who reported never being abused to volunteer a history of abuse and favour routine inquiry |
19 |
| Glass et al., 2001105 | Women who were acutely abused or who were physically or sexually abused in the past year were significantly less likely to agree with either routine screening (80% vs 89%, p < 0.01) or mandatory reporting of intimate partner violence (76% vs 90%, p < 0.01) than were women who reported a lifetime history of abuse or who reported no intimate partner violence | 14 |
| Gielen et al., 2000111 |
Forty-eight percent of the sample agreed that health-care providers should routinely screen all women, with abused women more likely than non-abused women to support this policy (54% vs 42%) Women thought it would be easier for abused women to get help with screening (86%), although concerns were raised about increased risk of abuse with screening (43%) |
16 |
| Hurley et al., 2005103 | The study showed that universal screening of female patients for intimate partner violence was supported by 86% of patients, with no differences in opinion in relation to age or sex. However, from the 304 women participating in the survey, 263 approved universal screening, 32 disapproved and 9 had no opinion | 16 |
| McCaw et al., 2001101 | The majority of women (80%) felt that clinicians should screen all their women patients for domestic abuseResponses to questions about the appropriateness of clinicians screening all women patients did not reflect a substantial change between the pre- and post-intervention periods | 19 |
| McDonnell et al., 2006112 |
Of the 471 women who answered the questions regarding acceptability, 468 (99%) found the questions acceptable and considered that all women should be asked these questions There were no differences in acceptability across age groups and no differences between those who reported abuse and those who did not as to whether these questions were acceptable. The three patients who said the questions were not acceptable did not report any abuse |
13 |
| McNutt et al., 1999113 | When asked if physicians should ask all female patients about intimate partner violence, less than half of all groups (40%), except women in shelters (64%), agreed | 16 |
| Newman et al., 2005114 |
When asked if it was appropriate to screen them for intimate partner violence when they sought care for their children, 75% of women stated it was Method of screening: 44% chose direct verbal questioning, 36% written questionnaire, 20% suggested other |
16 |
| Renker and Tonkin, 2006270 |
The great majority of women screened by their prenatal care providers (97%, SE 0.01%, n = 195) stated that they were not embarrassed, angry, or offended when they were screened for domestic violence There were no differences in acceptability of screening by health-care setting (public compared with private) or income, but women aged younger than 21 years were more likely (p = 0.018) than those older than 21 years to say they were embarrassed by the violence questions (13%, SE 0.4%, n = 4 compared with 1%, SE 0.2%, n = 2), although the small total (n = 6) for this subgroup should be noted when interpreting this finding Of the 66 women who reported abuse on the computer self-interview and who were screened during their pregnancies, only 11 (17%, SE 1.5%) women stated that they acknowledged their abuse to their health-care providers. There were no significant differences for this group (n = 66) in disclosure by age, race, income, prenatal care setting (public compared with private), or relationship with their neonate’s father |
16 |
| Richardson et al., 200241 |
In total, 82 (8%) women reported that they would mind ‘in general’ if their doctor asked whether they had ever been threatened, hit or hurt by a partner or former partner, with 114 (11%) minding a similar inquiry about forced sexIf the same questions were asked by a practice nurse, 119 (12%) and 136 (13%) women, respectively, said they would mind being asked In total, 202 (20%) women reported that they would mind being asked by their general practitioner about abuse or violence in their relationship if they had come about something else, with 234 (23%) objecting to a nurse asking the same question (3% difference, 1–5%) The acceptability of being asked was not significantly different between women who were and were not currently experiencing domestic violence (data not shown). Overall, 432 (42%) women reported that they would find it easier to discuss these issues with a female doctor and 31 (3%) with a male doctor |
19 |
| Romito et al., 2004107 |
Eighty-five per cent of the respondents answered that the family doctor should ask all women about violence, 7% thought he/she should not, and 8% were uncertain Although a higher percentage of women experiencing current violence gave a positive answer than women not experiencing current violence, the association was not significant However, younger women were significantly less likely to think that doctors should ask all patients (data not shown). When asked with whom they would like to talk about violence, if needed (more than one answer was possible): 54% chose the family doctor; 28% a psychologist; 22% other women with the same experience; 9% a social worker and 7% the police (data not shown) |
20 |
| Sethi et al., 200448 |
When questioned about how often they should be asked about domestic violence in the accident and emergency department, 35% felt that this should be always and 26% felt it should be usually asked, 38% felt it should be seldom asked, and only 1% felt that they should never be askedInterestingly, a higher proportion of women who had been abused (43%) suggested that women should always be asked about experience of domestic violence, compared with 30% among those who had not been abused. Many women justified their answers by commenting on the need for privacy and safety, but felt that it would be acceptable and appropriate to ask direct questions in women presenting with injuries Of those responding, 122 (9%) stated that they were not asked the questions at their first visit, a further 5 (0.4%) indicated that they were probably not asked because their partner was present, and 52 women (4%) stated that they could not remember whether they had been asked about domestic violence or not |
18 |
| Zeitler et al., 2006115 |
The vast majority of women responded favorably to the attitude questions about violence screening. Almost 90% said they would not mind being asked When respondents were categorised according to how much they minded being asked about violence, we did not detect differences in race, school enrolment, parity, family violence, or lifetime dating violence experience. However, women aged 15–18 years as compared with women aged 19–21 years were 2.9 times more likely to voice some to much concern with violence screening by a provider (36%, p < 01) Willingness to be screened also varied depending on women’s violence experiences. Women who were victims of physical violence and women who were victims or perpetrators of sexual violence were most likely to mind being screened Almost 90% of those surveyed felt that universal screening by health-care providers is a ‘very good’ or ‘somewhat good idea’. Women who had experienced physical violence in the last year were significantly less likely (p < 0.05) to report that they felt it was a good idea for health-care providers to ask all women about violence, but even so, 80% of this group was in favour of all women being asked Multivariate analyses found three factors to be associated with young women who expressed some concern with violence screening as compared with those who did not report any concern. Those young women who reported severe physical victimisation in the last year, categorised as ‘often’ as compared with ‘none’, reported experiencing early sexual abuse and were younger than 19 years were more likely to have some to high levels of concern with screening |
19 |
| Webster et al., 2001116 |
Most of the respondents, 1263 (98%), believed it was a good idea to ask women about domestic violence when visiting a hospital. There was no difference in the responses from rural, remote or inner city sites (range 98.6 ± 95.5%, χ2 = 7.38, df 4, p = 0.117) Nor were there differences between sites in terms of how women felt when asked domestic violence questions (χ2 = 8.68, df 8, p = 0.37). Three responses were possible: 1197 (96%) felt OK about being asked, 18 (1%) felt relieved to be able to talk to someone about their problem, and 30 (3%) felt uncomfortable. Twenty-three (77%) of the women who felt uncomfortable, still agreed that it was a good idea to ask about domestic violence When asked about which health-care professionals should screen for domestic violence, multiple responses were possible: 1068 (65%) of the women nominated midwives, 1055 (64%) nominated general practitioners, 809 (49%) selected social workers and 771 (47%) selected hospital doctors. Only 42 (2%) thought no one should ask. A number of women wrote comments such as ‘anyone who cares should ask’ When analysed by hospital, respondents from the remote area site were less likely to select the hospital midwife (χ2 = 17.2, df 4, p = 0.002) or the general practitioner (χ2 = 18.2, df 4, p = 0.001) than those from either rural or city hospitals Of those responding, 122 (9%) stated that they were not asked the questions at their first visit, a further 5 (0.4%) indicated that they were probably not asked because their partner was present, and 52 women (4%) stated that they could not remember whether they had been asked about domestic violence or not |
16 |
| Weinsheimer et al., 2005104 |
Although 18% of women thought screening infringed on their privacy, the overwhelming majority (> 90%) felt that it was appropriate to ask about intimate partner violence and that women should be asked about it when in the health-care setting Nearly all (93%) of the 44 women who reported a history of IPV thought a trauma centre health-care provider could assist them with a safety plan, but about one in four abused women thought reporting would increase their chances of further harm |
19 |
| Witting et al., 2006117 |
Visitors and providers supported screening, with increasing prevalence as the scenarios increased in severity, with visitors showing a fivefold increase for the high-risk (86%) versus the low-risk (17%) scenario. Although providers showed greater support for the goal of intimate partner violence screening than visitors, the tendency to screen in practice was lower; actually, estimates of screening practice were similar to the proportion of visitors expecting screening in each scenario. As the scenarios increased in severity, the differences between providers and visitors decreased The majority of visitors and providers felt that a physician, rather than a nurse, should have the primary responsibility for intimate partner violence screening, with visitors expressing this view almost 50% more frequently than providers Neither group felt that the gender of the screener was important Among visitors, those with lower educational attainment supported ED IPV screening more frequently than those with higher education |
15 |
Appendix 7 Interventions after disclosure of partner violence
Appendix 7.1 Characteristics of intervention studies
| Author(s), publication year | Setting | Inclusion criteria | Intervention | Data monitoring periods | Primary outcome measures | Number of participants | Participants |
|---|---|---|---|---|---|---|---|
| Advocacy studies | |||||||
|
Bybee and Sullivan, 2005130 RCT |
USA DV shelter |
Abused women who stayed at least one night in refuge and intended to stay in area for at least 3 months post-refuge |
Individual advocacy to help women leaving a DV refuge to devise safety plan and access community resources: 4–6 hours planned contact per week for first 10 weeks after leaving refuge, actually provided mean 7 hours per week contact Control care: Standard shelter services provided to all residents, and then usual after-refuge care (if any) |
Baseline, and 10 weeks, 6, 12, 18, 24 months post-intervention, and 3-year post-intervention follow-up for the original sample |
Validated: Abuse (CTS – modified) Psychological abuse (IPA, developed for study) Resources (EOR and DOR) Depression (CES-D) Locus of control (IPC) Fear and anxiety (RAST) Self-efficacy (developed for study) Non-validated: Independence from assailant 3–year follow-up: Abuse (CTS – modified) Quality of life Social support Resources (DOR) |
n eligible: 157 n participants: 146 n completing intervention: 141 (97% of recruited) Intervention: 71 Control: 70 n completing follow-up (% of participants): 6 months 131 (90% of recruited; 93% of intervention group who completed 3+ sessions and all control group) |
Age range: 17–61 Mean = 28 (Not stated if any between-group differences) Ethnic origin: 42% African American 46% White 7% Latina 2% Asian American 3% other (Not stated if any between-group differences) SES: 61% unemployed 81% receive government aid 64% educated to high-school level 34% some college education (Not stated if any between-group differences) Features of abuse: Severe abuse occurring once a month or less Relationship with abuser (at study entry): 77% married or cohabiting and living with assailant 6% involved but not living with assailant 15% single, divorced, separated |
|
Constantino et al. , 2005122 RCT |
USA DV shelter |
None stated explicitly but women were first-time residents of a DV shelter, no explicit definition of abuse but talks about abuse being the intentional violence or controlling behaviour of a current or ex-intimate partner (and in this study the perpetrator being male) |
A social support intervention provided by a trained nurse to provide resources and include information on resources, time to access resources, and an environment in which to chat with a counsellor and friends. Based on theory that there are four separate functions of social support: belonging, evaluation, self-esteem, and tangible support (BEST). Belonging was generated through listening and responding to other abused women. Evaluation or appraisal was incorporated into sessions by helping women to see themselves as others do. Self-esteem was promoted by focusing on each woman’s strengths and accomplishments in surviving IPV. Tangible support included discussion of resources in the community. 90-minutes sessions, once a week for 8 weeks Control care: The control group gathered in a room with the principal investigator for a free-flowing chat session with no structure. They also continued to receive the standard shelter services provided to all residents |
Baseline and immediate post-intervention |
Validated: Social support (ISEL) Distress (BSI) Health-care utilisation (HSQ) |
n eligible: Not stated n participants: 30 n completing intervention: 24 (80% of recruited) n completing follow-up (% of participants): Not applicable, no post-intervention follow-up |
Age range: 28–43 Mean = 35 (n/s between-group differences) Ethnic origin: 71% White 29% Black (n/s between-group differences) SES: Income 58% < $10,000 17% $10,000–19,999 21% $20,000–29,999 4% > $30,000 Education 12% junior high 67% high school 4% trade school 17% degree (n/s between group differences) Features of abuse: No explicit definition but talks about abuse being the intentional violence or controlling behaviour of a current or ex-intimate partner (and in this study the perpetrator being male) Relationship with abuser (at study entry): 17% married 21% divorced 17% separated 4% widowed 21% cohabiting 21% single |
|
McFarlane et al. , 2006123 RCT |
USA Two primary care public health clinics and two women, infants, and children clinics (WICs) |
Women aged 18–44 years, English or Spanish speaking, identified by nurse as physically or sexually abused by an intimate partner within last 12 months (AAS) |
A nurse case management intervention empowering abused women by increasing independence/control, based on Dutton’s empowerment model: focus on protection/safety, enhanced choice-making/problem-solving. An underlying feature of the model is that each woman knows what is best for her and her children, and the nurse is simply facilitating this (by listening, encouraging discussion), giving anticipatory guidance, and guided referrals tailored to the woman’s individual needs. All project nurses received a 40-hour training programme. Case management sessions lasted for 20 minutes, on average Control care: A referral card listing a safety plan and sources for IPV services. No counselling, education, referrals or other services were offered |
Baseline, 6, 12, 18 and 24 months |
Validated measures: Abuse (SVAWS) Homicide risk (DAS) Harassment at work (EHQ) Non-validated: Resource use (CRC) Use of safety behaviours |
n eligible: 433 n participants: 360 Intervention: 180 Control: 180 n completing intervention: Not applicable, one-off session?? n completing follow-up (% of participants): 319 (89% of recruited) |
Age range: Intervention Mean = 30 Control Mean = 31 Significant difference (p = 0.003) (n/s between-group differences) Ethnic origin: Intervention 9% White 22% Black 67% Hispanic 1% other Control 15% White 33% Black 52% Hispanic (p = 0.01) SES: Income 31% < $5000 21% $5000–10,000 31% $10,000–20,000 17% > $20,000 Education 49% < High school 29% High school grad 22% > High school (n/s between-group differences) Features of abuse: Physical sexual abuse Relationship with abuser (at study entry): 65% Current spouse 5% Former spouse 16% Current boyfriend 14% Former boyfriend |
|
Sullivan et al. , 2002124 RCT |
USA Community – working in the family’s home |
Females had to have at least one child aged 7–11 living with them, intended to stay in the area for 8 months, with at least one of their children aged 7–11 required to participate; mother had to have experienced some type of physical violence from an intimate partner or ex-partner in the previous 4 months |
Intervention to improve well-being in mothers and self-confidence in children, and to serve as a protective factor against continued violence. Three components: (1) a trained paraprofessional helped mothers generate, mobilise and access community resources; (2) similar advocacy for the children; (3) children attended a 10-week support and education group. Intervention was based on the needs of the individual mother and child, but all advocates were instructed to focus on actively assisting mothers and children to access resources and take children to a 10-week support and education group All advocacy had five phases: assessment, implementation, monitoring, secondary implementation, and termination, also tried to ensure that advocate no longer needed after 16 weeks. Details about child intervention not reported here. Intervention lasted 16 weeks, families saw advocates for a mean 9 hours per week (median 8, SD = 2.5), averaging 5 hours with children and an additional 3 hours with the women Control care: Does not give any information about the control group women |
Baseline, immediate post-intervention, 4 months post-intervention |
Validated: Abuse (IPA, CTS – modified) Depression (CES-D) Self-esteem (RSEI) Non-validated: Quality of life Social support Child measures not included here |
n eligible: Not stated n participants: 80 (cannot calculate response rate) Breakdown by group not stated n completing intervention: Not stated n completing follow-up (% of participants): 76 (95% of recruited) Breakdown by group not stated |
Age range: Mean = 31 (77% < 35 years) (Not stated if any between-group differences) Ethnic origin: 49% Non-Hispanic white 39% African American 5% Hispanic/Latina 5% Multiracial 1% Asian 1% Native American (Not stated if any between-group differences) SES: Income Mean income $1200 per month, 88% receiving government aid Employment 44% employed (Not stated if any between-group differences) Features of abuse: Physical abuse (in last 4 months) Relationship with abuser (at study entry): 79% no longer involved with abuser 14% living with abuser 7% involved with abuser but not living together |
|
Tiwari et al. , 2005121 RCT |
Hong Kong Public hospital antenatal clinic |
Pregnant women aged 18+ years, < 30 weeks’ gestation, attending first antenatal appointment, identified as physically, psychologically or sexually abused by an intimate partner within last 12 months |
Intervention based on an empowerment protocol to enhance abused women’s independence and control: safety advice, choice-making, problem-solving. Some items in the protocol were modified to ensure cultural congruence. A component of empathic understanding, derived from client-centred therapy, was also added. Empathic understanding emphasised the need to take in and accept the woman’s perceptions and feelings. It was designed to help women positively value themselves and their own feelings. Session lasted about 30 minutes, women given a reinforcing brochure at end Control care: Standard care: a wallet-sized card with information on community resources, including shelter hotlines, law enforcement, social services and non-government organisations |
Baseline and 6 weeks post-delivery |
Validated (although not for telephone administration): Abuse (CTS – modified) Depression (EPDS) Quality of life (SF36) |
n eligible: 117 n participants: 110 n completing intervention: Not applicable, one-off session n completing follow-up (% of participants): 106 (96% of recruited women) |
Age range: Intervention mean = 30 Control mean = 31 (No information on group differences, but look non-significant) Ethnic origin: All Chinese SES: Income (HK$11,000 average wage): Intervention 13% < $10,000 28% $10,000–20,000 55% > $20,000 Control 19% < $10,000 39% $10,000–20,000 37% > $20,000 (No information on group differences, but control group look to be somewhat poorer) Features of abuse: Physical, sexual or psychological abuse Relationship with abuser (at study entry) All women stayed with their partners for the pre- and post-test period |
| Support group studies | |||||||
|
Fry and Barker, 2002139 Case–control study |
USA DV shelter |
Not reported |
‘Tell Us Your Story’ sessions: each woman narrated a story about six salient events that she had experienced in the last 4–6 months. Group facilitator offered encouragement, directed questions, and steered the contents. Sessions ranged from 30 to 90 minutes Control care: Women attended information-giving support groups at women’s shelters |
Baseline and post-intervention (at 4 months) |
Validated: Abuse (ISA, modified) Depression (BDI) Self-esteem (SES) Non-validated: Fry’s 25-item measure of Global and Domain-Specific Efficacy Scale, the Ego-strength scale |
n eligible: Not reported n participants: 39 Intervention: 21 Controls: 18 n completing intervention: Not applicable, one-off session n completing follow-up (% of participants): 38 (97.4% of recruited women) |
Age range: Not reported Ethnic origin: Not reported SES: Not reported Features of abuse: Intervention group ‘had experienced abuse in the previous 6 months or so’ Control group not reported Relationship with abuser (at study entry): Not reported |
| Psychological intervention studies | |||||||
|
Arinero and Crespo, 2004151 Case–control study |
Spain Intervention conducted in a health-care setting Women were referred from social services, counsellors and the judiciary |
Women aged over 18 years presenting with at least one post-traumatic symptom but not meeting the diagnostic criteria for PTSD at least a month after the first abusive episode. Women were excluded if they were alcohol or drug users or if they did not speak Castellano |
The intervention included psychoeducation, breathing control techniques, self-esteem improvement procedures, cognitive therapy, problem-solving, communication skills training, as well as specific strategies for relapse prevention Control care: Waiting list |
Baseline, 1, 3 and 6 months |
Validated: Depression (BDI) Self-esteem (Rosenberg scale) Post-traumatic stress symptoms (post-traumatic cognitions inventory) Scale of maladaptation |
n eligible: 17 n participants: 17 Intervention: 12 Controls: 5 n completing intervention: 12 Intervention women completed n completing follow-up (% of participants): 17 Intervention: 12 Controls: 5 |
Age range: Intervention Mean = 47.33 (SD = 8.15) Control Mean = 38.8 (SD = 9.81) Ethnic origin: Not reported SES: Income 50% of the intervention group were economically dependent on their partner Education Intervention: 8.3% had not completed primary education 58.3% completed primary education 25% completed secondary education 8.3% had a university degree Control: 40% had not completed primary education 40% completed primary education 0% completed secondary education 20% had a university degree Features of abuse: Intervention: 16.7% psychological 66.7% physical and psychological 16.7% physical, psychological and sexual Control: 20% psychological 80% physical and psychological 0% physical, psychological and sexual Relationship with abuser (at study entry): Intervention: 58.3% had denounced partner 25% had left home Control: 60% had denounced partner 80% had left home |
|
Cruz and Sanchez, 2006152 Before-and-after study |
Mexico Community |
Women who had completed at least six grades of elementary education, lived with a problem-drinker spouse and suffered some degree of marital abuse or neglect. Women were excluded if they had been referred to psychiatric treatment due to depression, or if they were dependent on alcohol or participating in support groups during the study or receiving psychological or psychiatric treatment | Group cognitive behavioural therapy to promote self-esteem, coping strategies and assertiveness: three main components: (1) identifying and correcting cognitive biases and defective information; (2) establishing emotional regulation strategies; and (3) acquiring assertive interpersonal skills. Women received 18 150-minute weekly group sessions | Baseline, 3, 6 and 18 months |
Validated: Assertion (Assertion Inventory) Self-esteem (Self-esteem inventory) Non-validated: Coping (The Birmingham coping inventory) |
n eligible: 18 n participants: 18 n completing intervention: 18 n completing follow-up (% of participants): 18 at 3- and 6-month follow-ups 15 (83%) at 18 months |
Age range: 25–50 Ethnic origin: Not reported SES Ranged from low to middle Education – ranged from completing elementary school to college education Features of abuse: Not reported Relationship with abuser (at study entry) All women were still living with the abuser |
|
Gilbert et al. , 2006150 RCT |
USA Methadone Maintenance Treatment Programs (MMTPs) |
Women aged 18 or older currently enrolled in an outpatient MMTP, who reported using any illicit drug in the past 90 days and reported physical aggression, sexual coercion, injury-related abuse or severe psychological IPV by an intimate partner in the past 90 days. Women were excluded if they had a cognitive impairment that would prevent comprehension of the assessment or intervention or did not speak and understand English at a conversational level |
A relapse prevention and relationship safety intervention to help women reduce drug use and IPV: 11 2-hour group sessions and 1 individual session. Sessions were held twice weekly for 6 weeks. Women attended a mean of 11 out of 12 sessions, half of the women attended all 12 sessions and the remaining half attended between 9 and 11 sessions Control care: An informational session was provided for the control group and consisted of a 1-hour didactic presentation of a wide range of local community services that women in MMTPs can access, tips on help-seeking, and a comprehensive directory of local IPV-related services |
Baseline and 3-month follow-up |
Validated: Abuse (CTS2) Depression (BSI) Drug and alcohol use (Drug and alcohol use behaviour questionnaire) Non-validated: Sexual risk behaviour (SRBQ) PTSD (PTSD Checklist-Civilian) |
n eligible: 40 n participants: 34 n completing intervention: 31 n completing follow-up (% of participants): 31 (91%) |
Age range: Mean 41.8 years (SD = 6.6) Ethnic origin: 59.3% Latina 20.6% White 15.6% African American SES: Education: 54.5% graduated from high school Employment: 21.8% were currently employed Features of abuse: Physical aggression, sexual coercion, injury-related abuse or severe psychological IPV 63% of the intervention group and 44% of the control group had experienced severe physical or sexual abuse Relationship with abuser (at study entry): Not reported |
|
Koopman et al. , 2005142 RCT |
USA Community |
Women over 18 years, who had experienced IPV. Able to converse and write in English and living in conditions that the women judged as safe from abuse. |
Individual expressive writing sessions used to write about the most stressful events of a woman’s life, exploring her deepest emotions and feelings Control care: Neutral writing task. Women wrote as objectively as possible about their daily schedule, and how they used their time |
Baseline and post-intervention (at 4 months) |
Validated: Pain (Bodily Pain Scale of the SF36 Health Survey) Depression (BDI) PTSD (PCL-S) |
n eligible: Not reported n participants: 59 Not known how many in each group n completing intervention: Not applicable, one-off session n completing follow-up (% of participants): 47 (80% of recruited women) |
Age range: 21–56 Mean = 36.5 (SD = 8.9) (No between-group differences) Ethnic origin: White/European American 68%, Latina/Hispanic 13%, Middle Eastern 6%, African American 6%, Asian American 2% and other 4% (No between-group differences) SES: 43% of the women were employed full-time, with an additional 21% employed part time and 36% not employed. No between-group differences 60% of the sample reported a household income under US$40,000. No between-group differences Education ranged from high school to completing graduate school, a median had completed some college. Intervention women completed more years (16.8 years) than controls (mean 14.8 years), but not related to the outcome measures. Features of abuse: Abuse was ‘quite severe’: 83% had been slapped, hit or punched, 79% had been pushed or shoved, 50% had been choked, 46% had been kicked, 46% had been raped and 16% had been threatened with a weapon Relationship with abuser (at study entry): Not living with abuser. On average, women had left abuser 5 years earlier. |
|
Labrador et al. , 2006144 Case–control study |
Spain University and centres where women were contacted Women were referred from the municipal centre for women, judges of the first instance, women’s counsellors for women’s housing and victim support centres |
Women who had experienced domestic violence and who were diagnosed with chronic post-traumatic stress disorder according to the ‘DSM-IV-TR’ criteria. Women were excluded if they had a previous diagnosis of a mental disorder, were likely to commit suicide, misused drugs or alcohol. or were already receiving therapy for the problem |
The intervention group was split in half, the first group (GE-1) received (1) self-evaluation and problem-solving, (2) breathing control, (3) exposure therapy (which involved recalling past events and confronting flashbacks), and (4) cognitive therapy. The second group (GE-2) received (1) self-evaluation and problem-solving, (2) breathing control, (3) cognitive therapy and (4) exposure therapy (in that order). There were eight sessions of 60 minutes, delivered weekly Control care: Waiting list |
Baseline and post-test (2 months after the start of the intervention) |
Validated: Depression (BDI) Self-esteem (Rosenberg scale) Scale of maladaptation Post-traumatic Cognition Inventory |
n eligible: Not reported n participants: 20 (10 intervention, 10 control) n completing intervention: 18 (8 intervention, 10 control) n completing follow-up (% of participants): Not applicable: 80% had post-treatment data, no follow-up was conducted after post-treatment |
Age range: 19–50 years Mean 35 Ethnic origin: Not reported SES: Education Intervention: 0% Primary not completed 40% Primary completed 50% Secondary 10% University Control: 20% Primary not completed 50% Primary completed 30% Secondary 0% University Employment Intervention: 50% Service sector 30% Administrative sector 10% Housewife 10% Unemployed Control: 60% Service sector 0% Administrative sector 10% Housewife 30% Unemployed Class Intervention: 40% Medium-low 60% Medium Control: 100% Medium-low Features of abuse: Median length of abuse 7.6 years 15% Physical 10% Psychological 35% Harassment 40% Needed medical attention Relationship with abuser (at study entry): Not reported |
|
Reed and Enright, 2006143 RCT |
USA Not reported Women were all self-selecting volunteers: 10% responded to recruitment flyers (posted in domestic abuse resource centres) and 90% responded to newspaper advertisements |
Women between the ages of 25 and 55 who had experienced spousal psychological abuse but not physical abuse and who had been permanently separated for at least 2 years. Women were excluded if they were currently involved in an abusive relationship, had a history of childhood physical abuse, or had a significant ongoing psychiatric illness, such as suicidal ideation or psychosis |
Forgiveness therapy based on the Enright forgiveness process model. Participants determined the time spent on each forgiveness topic. Sessions were held weekly and the mean treatment time (one 1-hour session per week) was 7.95 months (SD = 2.61), with a minimum of 5 months and a maximum of 12 months. There was no prescheduled number of sessions, therapy ended when the woman reported the work was complete Control care: Alternative treatment (AT): participants engaged in 1-hour weekly participant-initiated discussion of current life concerns (considering the impact of past abuse) and in intervener-facilitated therapeutic discussions about the validity of anger regarding the injustice of past abuse, present strategies for healthy assertive choices, and interpersonal relationship skills. Participants determined the time spent on each participant-initiated concern. The AT was designed and delivered to match as closely as possible the basic elements of the therapy approach (anger, validation with mourning, assertiveness strategies, and interpersonal skills) |
Baseline, post-test and follow-up (the length of the follow-up period was not reported). |
Validated: Forgiveness (EFI) Self-esteem (CSEI) Anxiety (STAI) Depression (BDI-II) Environmental mastery (Environmental Mastery Scale) Finding meaning in suffering (Reed Finding Meaning in Suffering Scale) Post-traumatic stress (DSM-IV criteria checklist) Non-validated: Role of the abuse in women’s lives (story measure) |
n eligible: Not reported n participants: 20 (10 intervention, 10 control) n completing intervention: 20 (10 intervention, 10 control) n completing follow-up (% of participants): 20 (10 intervention, 10 control) 100% |
Age range: 32–54 years Mean 44.95 (SD = 7.01) Ethnic origin: 90% European American 5% Hispanic American 5% Native American SES: Education – 20% had a high-school diploma or general equivalency diploma, 30% had some college education or an associate’s degree, 20% were college graduates, 15% had some postgraduate degrees Employment – 15% were unemployed, 25% had part-time employment, 60% had full-time employment. Features of abuse: Psychological abuse without physical abuse. All women had experienced serious emotional abuse. Relationship with abuser (at study entry) Participants had been divorced or separated for at least 2 years from their partner. |
| Children’s studies | |||||||
|
Ducharme et al., 2000166 Parallel group study |
Canada Women’s homes Mother–child dyads were referred from child welfare agencies, school boards, women’s shelters and other social service agencies as well as directly from potential participants |
Women had experienced family violence and had children aged 3–10 with severe behaviour problems. |
The intervention aimed to improve parent–child cooperation through the use of ‘errorless compliance training’, a success-based, non-coercive intervention involving the hierarchical introduction of more demanding parental requests at a gradual pace, which lasted between 14 and 28 weeks Control care: Delayed treatment |
Request compliance was observed throughout treatment. All other outcomes were baseline and follow-up (6 months) only |
Validated: Child behaviour (CBCL) Parental stress (PSI) Non-validated: Compliance probability checklist Observational measures of compliance |
n eligible: Not reported n participants: 22 families (22 mothers, not stated how many children) Not stated how many were in intervention and control groups n completing intervention: 9 mothers (and their 15 children) n completing follow-up (% of participants): 9 mothers (and their 15 children) 41% |
Age range: 21–56 Mean = 36.5 (SD = 8.9) (No between-group differences) Ethnic origin: Not reported SES: All mothers were receiving welfare assistance. All had received some high-school education, but only one had some college education. Features of abuse: Mean Conflict Tactics Scale score represented a minimum of 38.6 physically aggressive acts and 77.7 verbally aggressive episodes Relationship with abuser (at study entry): Women were no longer living with the abuser |
|
Jouriles et al., 2001162 McDonald et al., 2006 (24-month follow-up)163 RCT |
USA DV shelter/women’s homes |
Preliminary requirements: mothers had to (1) report the occurrence of at least one physically violent act from a male partner during the previous 12 months and (2) have at least one child in the 4–9-year-old range who met DSM-IV criteria for oppositional defiant disorder or conduct disorder. For families in which more than one child met initial eligibility criteria, the youngest child to do so was selected as the target child Post-shelter requirements: (1) mother and target child had to be living together; (2) they had to be in a residence in which the former partner was not a member of the household; (3) the residence had to be within 50 miles of the shelter; and (4) the residence had to be safe enough for project staff to visit |
Two components: (1) provided mothers and children with social and instrumental support and mothers with problem-solving skills; and (2) taught mothers to use certain child management skills designed to help reduce their children’s conduct problems. Students served as mentors for the children. Therapists and mentors provided emotional support to the women during their transition from the shelter and helped them obtain physical resources and social support. The intervention was designed to include weekly sessions of 1–1.5 hours and began after shelter departure and continued for up to 8 months Control care: Families were contacted monthly either in person or by telephone. Families were encouraged to use existing community or shelter services. With the exception of immediate safety concerns, the families in the comparison condition received no clinical services through the programme or from the therapists, other than referrals and the tangible goods |
Assessment sessions lasted 2–3 hours and consisted of mother’s completion of questionnaires and a videotaped 45-minute family interaction. Assessments were repeated every 4 months resulting in a total of five assessments over a 16-month period. |
Validated: Child behaviour (CBCL) Mother’s psychological distress (SCL-90-R) Recurrence of abuse (CTS) Child’s oppositional defiant disorder and conduct disorder symptoms (DSM-IV diagnostic criteria) Children’s happiness/social relationships (Gesten’s Health Resources Inventory) Maternal aggression towards children (CTS-R) Non-validated: Child management skills Contact with partner |
n eligible: 73 Post-shelter eligibility 40 n participants: 36 (18 intervention, 18 control) n completing intervention: 31 n completing follow-up (% of participants): 31, 86% at 8-month follow-up 32, 83% at 24-month follow-up |
Age range: Mother’s mean: 27.97 (SD = 4.90) (24-month follow-up mean 28.7, SD = 4.9) Children’s mean: 5.67 (SD = 1.88) (24-month follow-up mean 5.5, SD = 1.7) Ethnic origin: 11 African American, 10 Caucasian, 12 Latino, 1 Asian American, and 2 other 24-month follow-up: 9 Caucasian, 11 African American, 8 Latino, 1 Asian American and 1 other SES: All participants were on low income: mothers reported a mean pre-shelter income of $7500 (SD = $7100) and 89% reported receiving some form of public financial assistance during the year prior to their shelter residence Mother’s education: mean 11.03 years, SD 2.19 24-month follow-up: All of the families could accurately be described as living in poverty: mothers reported a mean pre-shelter annual income of $7100 (SD = $6130), with 64% having received some form of financial assistance during the year prior to shelter entry. Immediately after shelter departure, 84% were receiving public assistance. Over the course of the 24-month follow-up period 13% were unemployed the whole time. Features of abuse: Mean number of acts of violence perpetrated toward the women during the year prior to coming to the shelter was estimated at 68.38 (SD = 53.65) Relationship with abuser (at study entry): Women were not living with the abuser |
|
Lieberman et al. , 2005160 Lieberman et al. , 2006161 RCT |
USA Not reported |
Child–mother dyads were recruited if the child was 3 to 5 years old, had been exposed to marital violence as confirmed by mother’s report on the Conflict Tactics Scale 2, and the perpetrator was not living at home | Child–parent psychotherapy (CPP): weekly joint child–parent sessions were interspersed with individual sessions with the mother. The intervention aimed to change maladaptive behaviours and support developmentally appropriate interactions. The treatment group attended a mean of 32.09 CPP sessions (SD 15.20) | Dyads were assessed at intake, 6 months into treatment, at the conclusion of 12 months’ treatment, and 6 months post-treatment. The Symptoms Checklist-90 Revised was the only mother-related measure administered at 6 months’ follow-up |
Validated: Child behaviour (CBCL) Children’s traumatic stress disorder (semistructured interview for diagnostic classification DC: 0–3 for clinicians) Mother’s stress (life stressor checklist-revised) Psychiatric symptoms (Symptoms Checklist-90 Revised) Mother’s PTSD, re-experiencing, avoidance and hyperarousal symptoms (CAPS) |
n eligible: Not reported n participants: 75 children and their mothers 2006 paper: 42 were in the intervention group and 33 in the control group n completing intervention: 65 (87% of recruited) n completing follow-up (% of participants): 2006 paper: 6-month follow-up: 50 (27 in the intervention group and 23 in the comparison), 67% |
Age range: 3–5 years Mean: 4.06 (SD = 0.82) Mothers’ ages not reported Ethnic origin: Children: 38.7% had mixed ethnicity (predominantly Latino/white) and the rest were 28% Latino, 14.7% African American, 9.3% White, 6.7% Asian and 2.6% Other Mothers: 37.3% Latina, 24% white, 14.7% African American, 10.7% Asian, and the rest were mixed or other ethnicities SES: Mean monthly family income was $1817 (SD = $1460; range $417–$8333). Public assistance was received by 23% of the families and 41% had incomes below the federal poverty level according to the Department of Health and Human Services Guidelines. Mean duration of maternal education was 12.51 years (SD = 3.96). Features of abuse: Not reported Relationship with abuser (at study entry): Women were not living with their abusers at the start of the study. However, 17% of mothers either returned to their violent partners or entered a new violent relationship during the study |
|
McFarlane et al. , 2005 (baseline and 1-year follow-up)165 McFarlane et al. , 2005 (2-year follow-up)164 RCT |
USA Two primary care public health clinics and two women, infants, and children clinics (WICs) |
Women aged 18–44 years, English or Spanish speaking, identified by nurse as physically or sexually abused by an intimate partner (including girlfriends and ex-girlfriends) within last 12 months (AAS). Women had a child aged 18 months to 18 years who lived with them |
A nurse case management intervention empowering abused women by increasing independence/control, based on Dutton’s empowerment model: focus on protection/safety, enhanced choice-making/problem-solving. An underlying feature of the model is that each woman knows what is best for her and her children, and the nurse is simply facilitating this (by listening, encouraging discussion), giving anticipatory guidance, and guided referrals tailored to the woman’s individual needs. All project nurses received a 40-hour training programme. Case management sessions lasted for 20 minutes, on average Control care: A referral card listing a safety plan and sources for IPV services. No counselling, education, referrals or other services were offered |
Baseline, 6, 12, 18 and 24 months |
Validated measures: Child behaviour (CBCL) |
n eligible: 360 n participants: 258 n completing intervention: Not applicable, one-off session?? n completing follow-up (% of participants): 12-month follow-up: 80% 24-month follow-up: 233 90% |
Age range: Intervention: Mean = 30 Control: Mean = 31 Significant difference p = 0.003 (n/s between-group differences) Ethnic origin: 67% of the children were Hispanic, 26% African American, 7% Caucasian SES: Income: 31% < $5000 21% $5000–10,000 31% $10,000–20,000 17% > $20,000 Education: 49% < high school 29% high-school graduate 22% > high school (n/s between-group differences) Features of abuse: Physical sexual abuse Relationship with abuser (at study entry): 65% current spouse 5% former spouse 16% current boyfriend 14% former boyfriend |
|
Sullivan et al., 2002124 RCT |
USA Community – working in the family’s home |
Females had to have at least one child aged 7–11 years living with them, intended to stay in the area for 8 months, and at least one of their children aged 7–11 was required to participate; mother had to have experienced some type of physical violence from an intimate partner or ex-partner in the previous 4 months |
Intervention to improve well-being in mothers and self-confidence in children, and to serve as a protective factor against continued violence. Three components: (1) a trained paraprofessional helped mothers generate, mobilise, and access community resources; (2) similar advocacy for the children; (3) children attended a 10-week support and education group. Intervention was based on the needs of the individual mother and child, but all advocates instructed to focus on actively assisting mothers and children to access resources and take children to a 10-week support and education group. All advocacy had five phases: assessment, implementation, monitoring, secondary implementation, and termination, and also tried to ensure that the advocate was no longer needed after 16 weeks. Intervention lasted 16 weeks, families saw advocates for a mean 9 hours week (median 8, SD = 2.5), averaging 5 hours with children and an additional 3 hours with the women Control care: No information about the control group women |
Baseline, immediate post-intervention, 4 months post-intervention |
Validated: Abuse (IPA, CTS – modified) Depression (CES-D) Self-esteem (RSEI) Child’s self-competence (self-perception profile for children) Non-validated: Quality of life Social support Child’s contact with assailant Child’s witnessing abuse (mother’s responses) Assailant’s abuse of child (average of emotional abuse of child, injury of child and overall abuse of child) |
n eligible: Not reported n participants: 80 Breakdown by group not stated n completing intervention: Not reported n completing follow-up (% of participants): 76 (95% of recruited) Breakdown by group not stated |
Age range: Mean = 31 (77% < 35 years) Children ranged from 6.5 to 11 years, with the mean at 8.3 Ethnic origin: 49% Non-Hispanic white 39% African American 5% Hispanic/Latina 5% Multiracial 1% Asian 1% Native American Children: 44% were African American, 40% were non-Hispanic white, 10% were multiracial, 5% were Hispanic and 1% were Asian (Not stated if any between-group differences) SES: Income: Mean income $1200 per month, 88% receiving government aid Employment: 44% employed (Not stated if any between-group differences) Features of abuse: Physical abuse (in last 4 months) Relationship with abuser (at study entry): 79% no longer involved with abuser 14% living with abuser 7% involved with abuser but not living together |
Appendix 7.2 Results of intervention studies and quality scores
| Author(s), publication year | Outcomes including any multivariate analysis/adjustment for confounders | Quality scores (USPSTF, Jadad) |
|---|---|---|
| Advocacy studies | ||
|
Bybee and Sullivan, 2005130 |
These results are based on the findings as reported in the 2005 paper (3-year follow-up of the original sample recruited in 1992) Contact with original assailant: 19% still involved with the man and 50% had had contact in last 6 months. No data by condition Assault by perpetrator over last year: 19% (n = 23). Of these, 65% (n = 15) were still in a relationship with the man. Mean severity of assaults = 2.00 (severe abuse occurring once a month or less). No data about if there was any condition effect Harassment and intimidation over last 6 months: 22% no longer reported such behaviour. No significant condition effects New relationships: 81% had new relationship some time over the 3 years. 19% (n = 23) of the total sample had been assaulted by new partner in last 6 months. Mean severity of assaults = 2.13 (severe abuse occurring once a month or less). No data about if any condition effect Condition effects at 3 years MANOVA (physical abuse, quality of life, social support, difficulty accessing resources) was significant, p = 0.089 (alpha had been set at > 0.10 to avoid type II errors), suggesting that there were modest overall differences between conditions at 3 years Univariate one-way ANOVAs also conducted and two attained significance: quality of life (p = 0.058), social support (p = 0.016); the two non-significant findings related to physical abuse (p = 0.18) and DOR (p = 0.13) (Race was also added into a second analysis, but there was no main effect for race or any interaction with condition) Physical abuse at 3-year follow-up and change from 2-year follow-up 36% (n = 44) experienced some level of physical abuse by a partner or ex-partner during past 6 months 28% (n = 34) experienced severe physical abuse by a partner or ex-partner during past 6 months These percentages were similar to those at 2-year follow-up, but there was a correlation of only 0.53, so some women improved whereas others became re-abused. Only 53% (n = 66) of the women reported no abuse at either 2- or 3-year follow-up There was a slight increase for women in advocacy intervention (up from 31% to 36%) and a slight decline in the control group (down from 43.55% to 35.5%), but these changes did not differ significantly by condition (p = 0.44) Continued abuse risk predicted by: prior abuse (last 6 months), difficulties accessing resources, problems with state welfare system, social contacts making life more difficult Reduced risk predicted by: being employed, higher quality of life, social contacts providing practical help or available to talk |
Fair, Greatest Jadad 1 |
| Constantino et al., 2005122 |
Social support (ISEL) Total score: A trend towards significance (p = 0.060). Control group pre- to post-intervention means 19.54 to 29.00. Intervention group pre- to post-intervention means 20.64 to 21.91 Belonging subscale: Intervention group had a statistically significantly greater improvement post-treatment than control group (p = 0.016). Control group pre- to post-intervention means of 4.54 to 7.54. Intervention group pre- to post-intervention means of 6.00 to 4.82 Tangible subscale: A trend towards significance (p = 0.084). Control group pre- to post-intervention means 4.31 to 7.23. Intervention group pre- to post-intervention means 4.82 to 5.55 Appraisal subscale: no trend found Self-esteem subscale: no trend found Psychological distress (BSI): Intervention group had statistically significantly greater improvement (p = 0.013). Control group pre- to post-intervention means of 152.15 to 108.38. Intervention group pre- to post- means of 159.73 to 151.36 Health-care utilisation (HSQ): Intervention group showed statistically significant less health-care utilisation (p = 0.032). Control group pre- to post-intervention means of 0.82 to 0.21. Intervention group showed pre- to post- means of 0.36 to 0.29 |
Fair, Greatest Jadad 2 |
| McFarlane et al., 2006123 |
For a like-with-like analysis, combined 6 and 12 months, and 18 and 24 months’ Main finding is that there was no effect for the intervention; all outcomes improved over time, regardless of group allocation: Both groups reported significantly (p < 0.001) fewer threats of abuse, assaults, danger risks for homicide, events of work harassment Both groups reported significantly (p < 0.001) more safety behaviours but community resource use declined Subgroup analyses – abuse scores were stratified into tertiles; again there was no differential effect of the intervention (no statistics reported) Adverse effects: none reported by study participants |
Fair, Greatest Jadad 2 |
|
Sullivan et al., 2002124 |
Analysis based on 76/78 (97.5%) as missing follow-up data imputed Abuse (no effect): For intervention women, mean abuse steeply declined from baseline to post-intervention and then remained relatively stable when tested again at 4 months’ follow-up; for control group women, there was a less steep decline from baseline to post-intervention, but this then increased until they were very similar to the intervention women at 4 months’ follow-up (quadratic relationship, p < 0.05) Well-being (no significant effect): Effect of intervention on mothers’ overall general well-being (quality of life, social support, depression, self-esteem) over time was marginally significant (p < 0.08) Quality of life (no significant effect): mean increased from baseline to 4 months’ follow-up for intervention women, whereas it slightly decreased for control group women (linear relationship, p < 0.10) Social support (no effect): mean increased from baseline to post-intervention but reverted to baseline at 4 months’ follow-up for intervention women, whereas it worsened from baseline to post-intervention but reverted to baseline at 4 months’ follow-up for control group women (quadratic relationship, p < 0.10) Depression: mean declined from baseline to 4 months’ follow-up for intervention women, whereas it slightly increased for control group women (linear relationship, p < 0.05) Self-esteem: mean increased from baseline to 4 months’ follow-up for intervention women, whereas it stayed the same for control group women (linear relationship, p < 0.05) |
Fair, Greatest Jadad 2 |
|
Tiwari et al., 2005121 |
The analysis was conducted on an ‘intention-to-treat’ basis. In addition, a per-protocol analysis was conducted on the 106 participants who completed. There were no differences when comparing the results of the two analyses. N.B. It is not reported if they tested for baseline differences between groups for outcome measures and demographic measures, although – with the possible exception of income and there being more sexual abuse in the control group at baseline – the baseline outcome measures look very similar Abuse (CTS): Following the intervention, the experimental group reported significantly less psychological abuse (mean difference 1.1, 95% CI –2.2 to 0.04, p<0.05) and less minor physical violence (mean difference –1.0, 95% CI –1.8 to 0.17, p<0.05. Severe abuse and sexual abuse did not differ between groups Quality of life (SF36): Following the intervention, the experimental group had significantly higher physical functioning (mean difference 10, 95% CI 2.5–18, p < 0.05) and significantly improved scores on the role limitation measures for both physical (mean difference 19, 95% CI 1.5–37, p < 0.05) and emotional problems (mean difference 28, 95% CI 9–47, p < 0.05). There was, however, more bodily pain reported in this group. General health, vitality, social functioning, and mental health did not differ between groups Depression (EPDS): Significantly fewer women in the intervention group had postnatal depression at follow-up. Twenty-five controls scored ≥ 10 compared with nine interventions (RR 0.36, 95% CI 0.15–0.88) Adverse events: At follow-up, women asked if the frequency of violence had increased since the last interview, and if so, whether it was the result of their taking part in this study. No adverse events were reported by the women in the experimental or control group as a result of receiving the intervention or standard care |
Good, Greatest Jadad 4 |
| Support group studies | ||
| Fry and Barker, 2002139 |
Main finding is that there was no effect for the intervention; all outcomes improved over time, regardless of group allocation: Depression: Both the intervention group and the control group experienced significant reductions in depression (p < 0.001), but the reductions in the intervention group were greater Ego Strength Scale: Both the intervention group and the control group experienced significant improvements in the ability to share feelings, feelings of personal adequacy, and a sense of reality (measured by the Ego Strength Scale) (p < 0.001), but the improvements in the intervention group were greater Self-efficacy: Both the intervention group and the control group experienced significant improvements in global self-efficacy scores (p < 0.001), but the improvements in the intervention group were much greater Self-esteem: Both the intervention group and the control group experienced significant improvements in self-esteem scores (p < 0.001), but the improvements in the intervention group were greater |
Poor, Greatest Jadad not applicable |
| Psychological intervention studies | ||
| Arinero and Crespo, 2004151 |
Main finding is that there was a significant decrease in post-traumatic and depressive symptoms and an improvement in adaptation levels, which was maintained at 6-month follow-up. There were no significant improvements in self-esteem Depression: There were significant decreases in depression for the intervention group post-treatment (p ≤ 0.01), the authors state this was still significant at 6 months but no data were presented. The effect size post-treatment was 0.95 and at the 1-month follow-up it was 0.66, but effect sizes for the 3- and 6-month follow-ups were not presented Self-esteem: There was a small increase in self-esteem for both the intervention and control groups but this was not significant at any time point Maladaptation: The intervention group had significant decreases in scores on the global scale of maladaptation post-treatment (p ≤ 0.01), at 1- and 3-month follow-ups (p ≤ 0.05), and at 6-month follow-up (p ≤ 0.01). The effect size at post-treatment was 1, and at 6-month follow-up it was 1.26 PTSD: The intervention group had significant decreases on the avoidance subscale, which were maintained at 6-month follow-up (p ≤ 0.01), with an effect size of 1.12. Decreases on the hyperarousal subscale were significant at 1- and 3-month follow-up (p ≤ 0.05), but not the 6-month follow-up. Decreases on the re-experiencing subscale were significant only at the 1-month follow-up (p ≤ 0.05). The intervention group had decreases in the total post-traumatic thoughts scale but this only reached significance at the 6-month follow-up (p ≤ 0.01). The effect size for total post-traumatic thoughts at post-treatment was 0.36, and at 6-month follow-up it was 0.53 |
Poor, Greatest Jadad not applicable |
| Cruz and Sanchez, 2006152 |
Self-esteem: Increases in self-esteem were significant at all three follow-up periods (3, 6 and 18 months), but there were no significant changes from pre-test to immediate post-test Coping strategies: Differences were statistically significant from pre-test to all three follow-ups. Non-significant differences were obtained from pre-test to post-test Assertiveness: The likelihood to act showed statistically significant increases from both pre-test to follow-ups 1 and 2 along with pre-test to 2, but no significant changes were found between pre- and post-test, or at the third follow-up Degree of discomfort differences from pre-test to follow-up 2 revealed only a marginal significance (p < 0.10). Differences from pre-test to immediate post-test and follow-ups 1 and 3 showed non-significant statistical differences |
Poor, Moderate Jadad not applicable |
| Gilbert et al., 2006150 |
Abuse: Women in the intervention group were 7.1 times more likely than women in the information group to report a decrease in experiencing minor physical, sexual and/or injurious IPV in the past 90 days at the follow-up assessment (p = 0.05) Women in the intervention group were more likely than women in the information group to report a decrease in both minor psychological IPV (OR = 5.3, p = 0.03) and severe psychological IPV (OR = 6.07, p = 0.03) Women in the intervention group were 5.3 times more likely than women in the information group to report a decrease in experiencing any physical, sexual and/or injurious IPV at the 3-month follow-up assessment, but this was not significant (p = 0.10) Compared to women in the information group, women receiving the intervention were also 7.1 times more likely to report a decrease in experiencing severe physical IPV, but this was not significant (p = 0.07) No significant differences were found between women in the intervention and information groups with respect to sexual IPV or injurious IPV outcomes Substance use: Women in the intervention group were 3.3 times more likely than women in the control group to report a decrease in any drug use in the past 90 days at follow-up, but the difference was not significant (p = 0.08) Women in the intervention group were more likely to report a decrease in binge drinking and crack cocaine use, but the difference was not significant No significant differences were found between the groups with respect to their heroin or marijuana use at follow-up Depression: Women in the intervention group were 5.7 times more likely than women assigned to the control group to report a decrease in their level of depression at 3 months’ follow-up (p = 0.01) PTSD: Women in the intervention group were 4.6 times more likely than women assigned to the control group to report a decrease in avoidance PTSD symptoms, but the difference was not significant (p = 0.06). No significant differences were found between women in the intervention and control groups with respect to changes in their hyperarousal or re-experiencing PTSD symptoms at the 3-month follow-up Sexual HIV risk behaviour: Women in the intervention group were 6.1 times more likely than women in the control group to report a decrease in having sex while high on illicit drugs (p = 0.04). Women in the intervention group were also more likely than the control group to report a decrease in having multiple sex partners, but the difference was not significant at a 95% level (OR = 2.77, p = 0.09) No significant differences were found between groups with respect to changes in the number and proportion of protected sexual acts at the 3-month follow-up Adverse events: None of the potential adverse events identified by the authors or other adverse events were detected |
Fair, Greatest Jadad 2 |
| Koopman et al., 2005142 |
Depression and PTSD: At baseline, 40% of women reported significant levels of pain, 53% met criteria for likely PTSD, and 40% met screening criteria for clinical depression Intervention group had reduced depression at follow-up [difference scores intervention group mean – 5.8 (10.3), control group mean – 2.6 (6.7)]. The mean difference score for PTSD in the treatment group was – 6.6 (10.3) and in the control group – 6.2 (12.4). The mean difference score for bodily pain in the treatment group was 0.1 (1.7) and in the control group 0.3 (2.7) Women who were more severely depressed at baseline and allocated to the intervention fared significantly better in terms of follow-up depression scores when compared with their similarly baseline depressed control counterparts (interaction p = 0.05) Paradoxically, the reverse was true for bodily pain; here women in greater pain at baseline benefited more if allocated to the control condition (interaction p < 0.05) There was no group × time interaction for PTSD Adverse effects: None, as the safety net of referral to the clinical psychologist was not needed |
Fair, Greatest Jadad 3 |
| Labrador et al., 2006144 |
Depression: The intervention group had reductions in their mean level of depression from 23.63 (7.17) pre-treatment to 11.13 (9.17) post-treatment. The control group’s mean level of depression pre-treatment was 29.8 (10.92) and post-treatment it was 30.2 (12.14). An ANOVA (2 × 2) showed that along with the significant time effect there was also a significant condition effect (p < 0.05) Self-esteem: The intervention group showed increases in their mean level of self-esteem from 24 (4.1) pre-treatment to 30.13 (3.6) post-treatment. The control group’s mean level of self-esteem pre-treatment was 23.6 (4.81) and post-treatment it was 22 (3.62). An ANOVA (2 × 2) showed that along with the significant time effect there was also a significant condition effect (p < 0.05) Maladaptation The intervention group showed reductions in their mean level of maladaptation from 20.38 (4.5) pre-treatment to 12.73 (7.17) post-treatment. The control group’s mean level of maladaptation pre-treatment was 21.4 (5.12) and post-treatment it was 21.7 (6.03). An ANOVA (2 × 2) showed that along with the significant time effect there was also a significant condition effect (p < 0.05) PTSD: The intervention group experienced reductions in their mean level of PTSD on the inventory of post-traumatic cognitions from 14.64 (3.16) pre-treatment to 9.62 (3.59) post-treatment. The control group’s mean level of PTSD on the inventory of post-traumatic cognitions pre-treatment was 14.38 (3.66) and post-treatment it was 14.19 (3.86). An ANOVA (2 × 2) showed that there was no significant condition effect (p > 0.05). There was a significant condition effect on one item of the inventory of post-traumatic cognitions on which the intervention group displayed reductions: negative cognitions (p < 0.05) |
Fair, Greatest Jadad not applicable |
| Reed and Enright, 2006143 |
Comparison of mean change from pre-test to post-test: Statistical significance was demonstrated on all the dependent variables, with the exception of state anxiety Women in the intervention group demonstrated a significantly greater increase in forgiving the former abusive partner (p < 0.001), in self-esteem (p < 0.05), in environmental mastery (everyday decisions; p < 0.05), in finding meaning in suffering (moral decisions; p < 0.05) and in new stories (survivor status; p < 0.01) The intervention group also demonstrated a significantly greater reduction in trait anxiety (p < 0.05), depression (p < 0.05), in post-traumatic stress symptoms (p < 0.05), and in old stories (victim status; p < 0.001) There was within-group statistical significance (in the intervention group from pre-test to post-test) for improvements in state anxiety scores (p < 0.05) Comparison of mean change from pre-test to post-test and from pre-test to follow-up for intervention women: The intervention group had significant improvements in self-esteem, state anxiety and trait anxiety between post-test and follow-up (p < 0.05) The improvements experienced by the intervention group on forgiveness, depression, environmental mastery (everyday decisions), finding meaning in suffering (moral decisions) and in new stories (survivor status) were maintained at follow-up |
Fair, Greatest Jadad 2 |
| Children’s studies | ||
|
Ducharme et al., 2000166 |
N.B. The results reported are across groups, i.e. interventions and controls combined – presumably with the latter having received the intervention (so only a before-and-after analysis) Compliance Baseline: high compliance for level I requests (89.4%) graduating downwards to 36.9% for level 4 requests Treatment (progressive difficulty of requests): Level 1 requests: high compliance (86.9%), similar to baseline Level 2 requests: high compliance (86.6%), an increase of 12% over baseline Level 3 requests: high compliance (85.7%), an increase of 25% over baseline Level 4 requests: high compliance (86.1%), an increase of 49% over baseline Follow-up for level 4 requests: high compliance (82.9% at 1 month, 89.1% at 3 months, 81.2% at 6 months) Across all children mean compliance to phase 1 requests was 86.9% (similar to the high compliance levels demonstrated to level 1 requests in baseline). Mean compliance across all children in phase 2 was 86.6% (an increase of 12 percentage points over baseline). Mean compliance to level 3 requests was 85.7% (an increase of 25 percentage points over baseline levels). In phase 4 the mean compliance score across all children was 86.1% (an increase of 49 percentage points over baseline). Mean compliance across all children for 1-month follow-up was 82.9%, for 3-month follow-up 89.1%, and for 6-month follow-up was 81.2% Generalisation Comparable with treatment data Level 3 requests: high compliance (91%), an increase of 30% over baseline Level 4 requests: high compliance (85%), an increase of 47% over baseline Maternal responses Mothers rated their children significantly more cooperative after treatment. There were also significant improvements in maternal perceptions of externalising, internalising, and total behaviour problems and significant positive change on the Parent Characteristics and Child Characteristics scales. Effect sizes (represented by both r and BSED statistics) showed that all changes in maternal perception were substantial (p < 0.05) Maternal perception of externalising, internalising and total behaviour problems (measured by the CBCL): Internal problems decreased from a mean of 16.85 pre-treatment to a mean of 9.92 post-treatment with an effect size of 0.58 External problems decreased from a mean of 22.08 pre-treatment to a mean of 14.54 post-treatment with an effect size of 0.58 Total problems decreased from a mean of 62.00 pre-treatment to a mean of 37.32 post-treatment with an effect size of 0.70 Maternal responses on the Parent Characteristics and Child Characteristics scales: Child characteristic scores decreased from a mean of 137.20 pre-treatment to a mean of 112.73 post-treatment with an effect size of 0.55, and parent characteristic scores decreased from a mean of 173.27 pre-treatment to a mean of 152.00 post-treatment with an effect size of 0.67 Maternal perception of the child’s compliance to specific requests: Scores on the compliance probability checklist decreased from a mean of 312.83 pre-treatment to a mean of 215.75 post-treatment with an effect size of 0.91 Consumer satisfaction: The mean satisfaction score was 4.4 for the programme and 4.8 for the therapist (out of 5) |
Fair, Greatest Jadad not applicable |
|
Jouriles et al., 2001162 McDonald et al., 2006 (24-month follow-up)163 |
Externalising problems CBCL: Intervention group: Baseline mean 66.28, SD 10.00; 4-month mean 58.69, SD 9.41; 8-month mean 57.00, SD 11.10; 12-month mean 54.80, SD 12.95; 16-month mean 49.79, SD 9.17 Control group: Baseline mean 65.56, SD 9.13; 4-month mean 61.61, SD 12.01; 8-month mean 60.11, SD 10.81; 12-month mean 55.47, SD 10.39; 16-month mean 58.59, SD 13.62 Externalising problems improved in both groups, but at a faster rate in the intervention group At the fifth assessment (16 months) the intervention group’s mean level of externalising problems did not differ from the mean of the normative population, suggesting the results were clinically significant. The mean level of externalising problems in the control group continued to differ significantly from the mean of the normative population Internalizing problems CBCL: Intervention group: Baseline mean 62.28, SD 8.94; 4-month mean 53.06, SD 9.38; 8-month mean 52.07, SD 9.71; 12-month mean 53.20, SD 9.79; 16-month mean 48.07, SD 7.98 Control group: Baseline mean 58.72, SD 11.96; 4-month mean 55.06, SD 12.35; 8-month mean 55.41, SD 10.43; 12-month mean 50.94, SD 9.28; 16-month mean 51.59, SD 9.66 Children’s internalising problems diminished over time, with similar rates of change in both groups Child management skills: Intervention group: Baseline mean 3.58, SD 0.53; 4-month mean 4.03, SD 0.40; 8-month mean 4.04, SD 0.34; 12-month mean 4.02, SD 0.36; 16-month mean 3.88, SD 0.39 Control group: Baseline mean 3.75, SD 0.43; 4-month mean 3.67, SD 0.54; 8-month mean 3.80, SD 0.47; 12-month mean 3.66, SD 0.38; 16-month mean 3.83, SD 0.41 There was a significantly higher mean level of child management skills at assessment 3 (8 months) in the intervention group and the intervention group improved faster than the control group Mother’s psychological distress, SCL-90-GSI: Intervention group: Baseline mean 67.78, SD 8.85; 4-month mean 59.94, SD 13.66; 8-month mean 53.40, SD 12.55; 12-month mean 58.87, SD 14.27; 16-month mean 52.38, SD 8.15 Control group: Baseline mean 67.44, SD 9.49; 4-month mean 64.28, SD 11.17; 8-month mean 59.83, SD 11.08; 12-month mean 54.00, SD 13.74; 16-month mean 55.94, SD 11.31 The mothers’ psychological distress diminished over time but there was no significant difference between the comparison and intervention groups Recurrent abuse: Intervention group 31% reported yes Comparison group 44% reported yes Chi-squared test shows no significant difference between groups Mean number of moves was 3.7 (SD = 1.7, mode = 3); no difference between groups Mean number of job changes was 1.8 (SD = 1.7, mode = 0); no difference between groups Results at 24 months’ follow-up: Reductions in conduct problems: At baseline all the children met DSM-IV criteria for either oppositional defiant disorder or conduct disorder. Two years after the termination of services 2 of the 13 children (15%) in the intervention group and 9 of the 17 children (53%) in the control group were classified as meeting DSM-IV criteria for either oppositional defiant disorder or conduct disorder (p < 0.05) Two of the 13 children (15%) in the intervention group and 9 of the 17 children (53%) in the control group were reported to have externalising problems at clinical levels 2 years after the end of treatment (p < 0.05) In 12 of the 17 (71%) families in the control group, the child was reported to be at clinical levels of conduct problems (using CBCL data) at either the 8-month or 24-month follow-up. In contrast, in only 4 of the 13 (31%) families in the intervention group was the child reported to be at clinical levels at one of these assessment points. These differences are statistically significant (p < 0.05) Mean CBCL externalising scale scores for children in the intervention and control groups did not differ significantly from one another at the 24-month follow-up; however, the t-test was rerun without an outlier from the intervention group and this new analysis showed a significant difference: intervention group mean = 52.1, SD = 8.4; control group mean = 60.0, SD = 14.7 (p = 0.05) Internalising problems and happiness/social relationships: Mean levels of internalising problems did not differ significantly between the intervention and control groups at the 24-month follow-up. However, there were differences in the proportion of children in each group exhibiting clinical levels of internalising problems. In the control group 35% of the children were reported to exhibit clinical levels of internalising problems compared with 0% in the intervention group (p < 0.05) A comparison of children’s happiness/social relationships scale scores revealed a significant difference between the intervention group (M = 3.9, SD = 0.8) and the control group (M = 3.5, SD = 0.8) (p < 0.05) Maternal aggression towards children: Twenty-three percent of the mothers in the intervention group and 53% of the mothers in the comparison group returned to their partners, this difference was not found to be significant (p < 0.10). There was not a significant association between child conduct problems at the outset of the study (first assessment) and mother’s return to partner over the course of the study, nor was there a significant association between mother’s return to partner and children’s conduct problems at the 24-month follow-up Recurrence of physical violence: In the intervention group 38% reported recurrence of violence and in the control group 47% reported recurrence of violence. This difference was not significant. Recurrence of violence was not found to be associated with the mother’s return to partners N.B. There are some discrepancies within the text and table as to the significance of a mother’s return to her partner and children’s happiness/social relationships. In the text, a mother’s return to partner has a significance level of p < 0.10, but the table says p < 0.05. Children’s happiness/social relationships does not appear to be significant in the table, but is significant (p < 0.05) in the text |
Fair, Greatest Jadad 1 |
|
Lieberman et al., 2005160 Lieberman et al., 2006161 |
Child functioning: At intake, there was no group difference, with 50% (n = 18) of the CPP group and 39% (n = 11) of the comparison group meeting criteria for TSD. At post-test there was a statistically significant group difference (p<0.01) with 6% (n = 2) of children in the CPP group and 36% (n = 10) children in the comparison group meeting criteria for TSD There was a significant group × time interaction for the total number of TSD symptoms (p < 0.001). Follow-up analyses indicated that the CPP group had a significant intake post test reduction in the number of TSD symptoms (p < 0.001), whereas the comparison group did not Analyses of CBCL total scores showed a significant group × time interaction (p < 0.05) with follow-up analyses revealing that only the CPP group evidenced significant intake-post-test reductions (p < 0.01). Analyses were repeated with only the children who completed the CBCL at intake and post-test (to examine whether error was introduced because some children completed the CBCL 2–3 at intake and the CBCL 4–18 at post-test). These analyses also resulted in a significant interaction effect (p < 0.05), with follow-up analyses confirming that only the CPP group showed significant reductions in behaviour problems (p < 0.01). There were no significant age effects when the original analyses with the TSD and CBCL were repeated using age as a covariate Maternal symptoms: The CAPS scores revealed a significant group × time interaction for avoidance (p < 0.05). Follow-up analyses showed significant intake-outcome reductions in avoidant symptoms for the CPP group only (p < 0.001). For total CAPS scores and the GSI there were significant main effects for time (p < 0.001) and trends for group × time (p = 0.07) For total CAPS scores both the CPP and comparison groups showed significant intake-outcome reductions (CPP p < 0.001; comparison p < 0.05). The interaction was not significant. For GSI scores, the CPP group showed statistically significant reductions (p < 0.001) whereas the comparison group showed a trend in this direction (p = 0.06) Re-experiencing and hyperarousal showed significant effects for time (re-experiencing p < 0.001, hyperarousal p < 0.001) but not group × time (re-experiencing p = NS, hyperarousal p = NS) Clinical significance of treatment effects on maternal symptoms (determined by examining the percentage of mothers in each group who were diagnosed with PTSD): At intake, there was no group difference, with 47% (n = 16) of the CPP group and 46% (n = 12) of the comparison group meeting PTSD criteria At outcome there was a decline in PTSD diagnosis for mothers in both groups, with 12% (n = 4) of CPP mothers and 27% (n = 7) of comparison mothers meeting criteria for PTSD. This difference was not statistically significant Key results and explanations at 6-month follow-up: Child functioning: For completers analysis and ITT analysis, there were significant group × time interactions. Further analyses showed that the intervention group had significant reductions in CBCL Total Behaviour Problem scores (completer p < 0.001; ITT p < 0.001). The reduction was not significant for the control group Maternal symptoms: For completers analysis and ITT analysis, there were significant group × time interactions. Further analyses showed that the intervention group improved significantly on distress scores (GSI), but the control group did not (p < 0.001); ITT analyses showed only a significant main effect for time (p < 0.001) The immediate post-intervention analyses showed that mothers in both the CPP and the control groups had declined in the severity of their global symptoms. Although there was not a significant group × time interaction immediately after treatment completion, the decline in symptom severity was statistically significant only for the CPP mothers, with the control group showing a trend in that direction The follow-up assessment revealed a significant symptom decline only for the CPP mothers, with no comparable movement in the control group. The finding suggests that mothers in the CPP group continued to improve after the termination of treatment, whereas the control group did not |
Fair, Greatest Jadad 2 Fair, Greatest Jadad 3 |
|
McFarlane et al., 2005 (baseline and 1-year follow-up)165 McFarlane et al., 2005 (2-year follow-up)164 |
Main finding is that there was no effect for the intervention; outcomes improved over time, regardless of group allocation Other analyses: When study children were compared with a clinically referred sample, there were few differences re baseline scores, but by 24 months’ the majority (stratified by age and gender for 6+) had scores significantly less than the referred norms, but this did not differ by allocation arm. The scores of the children aged 5 and under improved the most, the scores of teenagers improved the least (with their internal behaviour scores never significantly differing from scores of clinically referred youth). So, this too shows only the positive effect of time (not the intervention) This analysis takes no account of allocation group. When study children’s scores were dichotomised into what would be referral and non-referral categories at entry and at 24 months’, approximately 30% of the young children (18 months–5 years) had moved out of the clinical range by the end of the study, less pronounced improvements were found for ages 6–18 years, and 41% remained in the clinical range for referral in terms of their internal behaviours at 24 months’ One-year follow-up paper: Both groups of children improved significantly on CBCL scores from intake to 1 year, irrespective of which treatment protocol their mothers received Normative scores, for both the clinically referred and non-referred samples of children, were obtained from the CBCL manual. At intake, most scores of children from the abused women were not significantly different from the scores of clinically referred children. However, at 1 year, with the exception of internal behaviour scores for girls aged 12–18, all scores of children from treated abused mothers were significantly lower than the scores of non-referred children. Additionally, at intake, all scores of children from the abused women were significantly higher than those of the non-referred children. At 1 year, only scores for boys aged 6–11 years and girls aged 12–18 years remained significantly higher than the scores of non-referred children. |
|
|
Sullivan et al., 2002124 |
Well-being (MANCOVA) Effect of intervention on mothers’ overall general well-being (quality of life, social support, depression, self-esteem) over time was marginally significant (p < 0.08) The following are ANOVA analyses on individual outcomes: Abuse: For intervention women, mean abuse steeply declined from baseline to post-intervention and then remained relatively stable when tested again at 4 months’ follow-up; for control group women, there was a less steep decline from baseline to post-intervention, but this then increased until they were very similar to the intervention women at 4 months’ follow-up (quadratic relationship, p < 0.05) Assailant’s overall abuse of child: Mean scale scores were 1.44 (SD = 0.90) at pre-intervention and 0.66 (SD = 0.63) at 4-month follow-up; individual scores ranged from 0.00 (indicating no abuse experienced during the time interval) to 4.96 Child’s witnessing abuse: Mean scale scores were 1.51 (SD = 0.85) at pre-intervention and 0.51 (SD = 0.73) at 4-month follow-up; individual scores ranged from 0.00 (indicating no witnessing of abuse during the time period) to 3.39 Child’s contact with assailant: Although the conditions did not differ on contact at baseline, by the 4-month follow-up, significantly fewer children in the intervention group were in daily contact with their mother’s assailant (11.1% vs 27.3%) Child’s self-competence: Pre-intervention mean scale scores were given, but no post-intervention scores were given in the text, and the means and SDs were not given by group. Table 1 in the paper gives means by group and post-intervention and 4-month follow-up, but no SDs Mother’s quality of life: Mean increased from baseline to 4 months’ follow-up for intervention women, whereas it slightly decreased for control group women (linear relationship, p < 0.10) Mother’s social support: Mean increased from baseline to post-intervention but reverted to baseline at 4-month follow-up for intervention women, whereas it worsened baseline to post-intervention but reverted to baseline at 4-month follow-up for control group women (quadratic relationship, p < 0.10) Mother’s depression: Mean declined from baseline to 4 months’ follow-up for intervention women, whereas it slightly increased for control group women (linear relationship, p < 0.05) Mother’s self-esteem: Mean increased from baseline to 4 months’ follow-up for intervention women, whereas it stayed the same for control group women (linear relationship, p < 0.05) |
Fair, Greatest Jadad 2 |
Appendix 7.3 USPSTF assessment of execution of intervention studies
| Type of intervention | Author(s), publication year | RCTs: adequate randomisation (other designs: consideration of potential confounders; if no consideration of any confounders, score as poor) | Maintenance of comparable groups (includes crossovers, adherence, contamination) (if baselines not matched, score paper as poor, if contamination only, score as fair) | No important differential loss to follow-up or overall high loss to follow-up (> 20%) | Measurements: equal, reliable and valid (if measurements so poor as to be unacceptable, score study as poor) | Clear definition of interventions (individualised interventions allowed if within a structured format) | All important outcomes considered or good match of outcomes to goals | RCT: intention-to-treat analysis (other designs: adjustment for potential confounders) | Quality rating (see Appendix 3) | Statistics |
|---|---|---|---|---|---|---|---|---|---|---|
| Advocacy | Constantino et al., 2005122 | No | No | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given |
| McFarlane et al., 2006123 | No | No | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Sullivan et al., 2002124 | No | No | Yes |
Mixed CTS is poor, others are fine |
Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Tiwari et al., 2005121 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Good Greatest |
No effect sizes given | |
| Advocacy total ‘yes’ out of 4 | 1 | 1 | 4 | 4 | 4 | 4 | 1 | – | – | |
| Support groups | Fry and Barker, 2002139 | Not applicable | No | Yes | No Cronbach’s alpha given | Yes | Yes | No |
Poor Greatest |
No effect sizes given |
| Individual psychological interventions | Koopman et al., 2005142 | No | No | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given |
| Labrador et al., 2006144 | No | No | Yes | Yes | Yes | Yes | Yes |
Poor Greatest |
No effect sizes given | |
| Reed and Enright, 2006143 | No | Yes | Yes | Yes | Yes | Yes | Yes |
Fair Greatest |
No effect sizes given | |
| Individual psychological total ‘yes’ out of 3 | 0 | 1 | 3 | 3 | 3 | 3 | 2 | – | – | |
| Group psychological interventions | Arinero and Crespo, 2004151 | No | No | Yes | Yes | Yes | Yes | No |
Poor Greatest |
Gives effect sizes |
| Cruz and Sanchez, 2006152 | Not applicable | Not applicable | Yes | Yes | Yes | Yes | No |
Poor Moderate |
No effect sizes given | |
| Gilbert et al., 2006150 | Yes | Yes | Yes | No data on reliability | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Group psychological total ‘yes’ out of 3 |
1 |
1 | 3 | 2 | 3 | 3 | 0 | – | – | |
| Interventions with children | Ducharme et al., 2000166 | Not applicable | Yes | No (59%) | No data on reliability | Yes | Yes | No |
Poor Least |
Gives effect sizes |
| Jouriles et al., 2001162 | No | Yes | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Lieberman et al., 2006;161 Lieberman et al., 2005160 | No details on randomisation | Yes | Yes | Yes | Yes | Yes | Yes |
Fair Greatest |
No effect sizes given | |
| McFarlane et al., 2005;165 McFarlane et al., 2005164 | No | No | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Sullivan et al., 2002124 | No | No | Yes | Yes | Yes | Yes | No ITT |
Fair Greatest |
No effect sizes given | |
| Interventions with children total ‘yes’ out of 5 | 0 | 3 | 4 | 4 | 5 | 5 | 1 | – | – |
Appendix 7.4 USPSTF assessment of execution of intervention studies
| Jadad score calculation | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | Score | Constantino et al., 2005122 | Jouriles et al., 2001162 | Liebermanet al., 2005,160 2006161 | Gilbert et al., 2006150 | Reed and Enright, 2006143 | Koopman et al., 2005142 | Bybee and Sullivan, 2005130 | Tiwari et al., 2005121 | Sullivan et al., 2002124 | McFarlane et al., 2006123 |
| Was the study described as randomised (this includes words such as randomly, random, and randomisation)? | 0/1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Was the method used to generate the sequence of randomisation described and appropriate (table of random numbers, computer-generated, etc.)? | 0/1 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 |
| Was there a description of withdrawals and dropouts (need demographic data or use of ITT)? | 0/1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 |
| SUBPOINT: Deduct one point if the method used to generate the sequence of randomisation was described and it was inappropriate (patients were allocated alternately, or according to date of birth, hospital number, etc.) | 0/–1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Blinded assessment of outcomes | 0/1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 |
| Total (out of 4) | 4 | 2 | 1 | 3 | 2 | 2 | 3 | 4 | 4 | 2 | 2 |
| Jadad score calculation | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Item | Score | Kubany et al., 2004146 | Kubany et al., 2003145 | Mancoske et al., 1994147 | Melendez et al., 2003156 | McFarlane et al., 2004136 | McFarlane et al., 2000134 | Sullivan and Bybee, 1999126 | Sullivan and Davidson, 1991129 |
| Was the study described as randomised (this includes words such as randomly, random, and randomisation)? | 0/1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Was the method used to generate the sequence of randomisation described and appropriate (table of random numbers, computer-generated, etc.)? | 0/1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Was there a description of withdrawals and dropouts (need demographic data or use of ITT)? | 0/1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 |
| SUBPOINT: Deduct one point if the method used to generate the sequence of randomisation was described and it was inappropriate (patients were allocated alternately, or according to date of birth, hospital number, etc.) | 0/–1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Blinded assessment of outcomes | 0/1 | 0 | 0 | 0 | 1 | – 1 | – 1 | 1 | 0 |
| Total (out of 4) | 4 | 2 | 2 | 1 | 3 | 1 | 1 | 4 | 1 |
Appendix 7.5 Sensitivity analysis for intervention studies
| Studies ranked by effect size (largest first) | Setting | Intervention | Studies ranked by quality (best first) |
|---|---|---|---|
| PTSD | |||
|
Labrador et al. , 2006144 Post-test 1.23 Large |
Spain Targeted at women with PTSD who were referred from women’s centre, judges, counsellors and victim support centres |
Individual psychological intervention Exposure and cognitive therapy |
Koopman et al. , 2005142 Fair, Greatest Jadad 3 |
|
Reed and Enright, 2006143 Post-test 2.33 Large |
Urban USA Responded to flyers |
Individual Psychological (forgiveness therapy) |
Liebermanet al., 2005,160 2006161 Fair, Greatest Jadad 3 |
|
Kubany et al. , 2003,145 2004146 Immediate post-therapy 2003 paper 0.90 Large 2004 paper 0.33 Small |
Targeted at women with PTSD |
Individual psychological intervention Cognitive behavioural therapy (CBT) |
Kubanyet al., 2003,145 2004146 Fair, Greatest Jadad 2 |
|
Lieberman et al. , 2005,160 2006161 Post-test 0.41 Small |
USA Not reported |
Child–parent psychotherapy (CPP) |
Reed and Enright, 2006143 Fair, Greatest Jadad 2 |
|
Koopman et al. , 2005142 4-month follow-up 0.10 Small |
USA Community |
Individual Psychological (expressive writing) |
Labradoret al., 2006144 Fair, Greatest Jadad not applicable |
| Depression | |||
|
Labrador et al. , 2006144 Post-test 1.77 Large |
Spain Targeted at women with PTSD who were referred from women’s centre, judges, counsellors and victim support centres. |
Individual psychological intervention Exposure and cognitive therapy |
Sullivan and Bybee, 1999126 Fair, Greatest Jadad 4 |
|
Reed and Enright, 2006143 1.55 Large |
Urban USA Responded to flyers |
Individual Psychological (forgiveness therapy) |
Koopmanet al., 2005142 Fair, Greatest Jadad 3 |
|
Kubany et al. , 2003,145 2004146 Immediate post-therapy 2003 paper 0.42 Small 2004 paper 0.25 Small |
Targeted at women with PTSD |
Individual psychological intervention CBT |
Kubanyet al., 2003,145 2004146 Fair, Greatest Jadad 2 |
|
Sullivan and Bybee, 1999126 10 weeks post-intervention 0.29 Small |
USA Women exiting shelters |
Advocacy 10 weeks community advocacy |
Reed and Enright, 2006143 Fair, Greatest Jadad 2 |
|
Koopman et al. , 2005142 4-month follow-up 0.16 Small |
USA Community |
Individual Psychological (expressive writing) |
Labradoret al., 2006144 Fair, Greatest Jadad not applicable |
| Self-esteem | |||
|
Labrador et al. , 2006144 Post-test 2.25 Large |
Spain Targeted at women with PTSD who were referred from women’s centre, judges, counsellors and victim support centres |
Individual psychological intervention Exposure and cognitive therapy |
Kubanyet al., 2003,145 2004146 Fair, Greatest Jadad 2 |
|
Reed and Enright, 2006143 Post-test 1.81 Large |
Urban USA Responded to flyers |
Individual Psychological (forgiveness therapy) |
Reed and Enright, 2006143 Fair, Greatest Jadad 2 |
|
Cox and Stoltenberg, 1991153 Post-test Intervention group 1 and control: 0.11 Small Intervention group 2 and control: 0.88 Large |
New shelter residents | Group psychological intervention including CBT, skills-building and problem-solving |
Labradoret al., 2006144 Fair, Greatest Jadad not applicable |
|
Kubany et al. , 2003,145 2004146 Immediate post-therapy 2003 paper 0.48 Small 2004 paper 0.10 Small |
Targeted at women with PTSD |
Individual psychological intervention CBT |
Cox and Stoltenberg, 1991153 Poor, Greatest Jadad not applicable |
| Physical abuse | |||
|
Tiwari et al. , 2005121 Minor physical abuse 6 weeks post-delivery 0.48 Small Severe physical abuse 6 weeks post-delivery 0.09 Small |
Hong Kong Public hospital antenatal clinic |
Advocacy |
Tiwari et al., 2005121 Good, Greatest Jadad 4 |
|
Sullivan and Bybee, 1999126 10 weeks post-intervention 0.26 Small |
USA Women exiting shelters |
Advocacy 10 weeks community advocacy |
Sullivan and Bybee, 1999126 Fair, Greatest Jadad 4 |
|
McFarlane et al. , 2006123 12-month follow-up: Assault 0.07 Small Danger risk for homicide 0.03 Small 24-month follow-up: Assault 0.02 Small Danger risk for homicide 0.09 Small |
USA Two primary care public health clinics and two women, infants and children clinics (WICs) |
Advocacy |
McFarlane et al. , 2006123 Fair, Greatest Jadad 2 |
Appendix 8 Morbidity and mortality outcomes of screening studies
Appendix 8.1 Characteristics of studies
| Study details | Study design | Intervention | Number of participants | Participants |
|---|---|---|---|---|
| Coyer et al., 2006170 |
Inclusion criteria: Women aged 18 or older who attended the rural health-care clinic Exclusion criteria: Not stated Setting: USA, rural health-care clinic Target group of intervention: Nurses Design: Before-and-after Sampling time frame: 12 months pre-intervention and 12 months post-intervention Data source: Medical notes |
Framework: Not stated Programme: Discussion with nursing staff identified a need for improving their knowledge of local community resources. Due to staff interest, two local agencies that support women in violent situations in-serviced the members of the clinic in order to provide background information, local statistics, resources available and the processes of referrals. Policies on how to manage patients giving a ‘yes’ response to ‘Is anyone hurting you?’ were developed Duration and frequency: Not stated Comparison care: Usual pre-intervention care |
Pre-intervention: 1690 Post-intervention: 859 |
Only given for those identified as abused post-intervention Age: Mean 45.5, range 27–57 Ethnicity: White: 4; Hispanic: 2 SES: Not stated Scope of abuse: Abuse. Screening question was ‘Is anyone hurting you?’ |
| Harwell et al., 1998168 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Setting: USA; four community health centres Target group of intervention: Physicians/nurses/social workers/psychologists Design: Before/after, historical controls Sampling time frame: 6 months pre- and 6 months post-intervention Data source: Medical records |
Framework: trauma theory, RADAR Programme: Training/support package for health providers to increase referrals, included step-by-step and ‘where to turn for help’ pocket guides Duration and frequency: Single session of 3–6 hours didactic training (video presentation) for all staff, with tailored follow-up training for some staff Comparison care: Usual pre-RADAR management |
Intervention: 255 Comparison: 251 |
Age: Mean = 30 (no significant differences between groups) Ethnicity: 52% Latina; 47% African American; 1% other (no significant differences between groups) SES: 97% public health insurance (no significant differences between groups) Scope of abuse: Physical and emotional abuse |
| McCaw et al., 2001101 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Setting: USA HMO Target group of intervention: Nurses, medical assistants, physical therapists, receptionists Design: Before/after, historical controls Sampling time frame: 12 months pre- and 9 months post-intervention Data source: Medical records |
Framework: Systems model approach, with links to the community Programme: Several brief training and information sessions for clinical staff, receptionists; sought improved links with community services, informed patients about domestic violence (mailings, materials in waiting room) and services, provided clinicians with information and prompts, employing on-site domestic violence specialist Duration and frequency: ‘Several brief training and information sessions’ Comparison care: Usual pre-intervention management |
Not stated |
Age: Not stated, but of local HMO patient population, about 25% aged 20–60 Ethnicity: Not stated, but of local HMO patient population: white 45%; African American 22%; Latino 15%; Asian 16%; other 2% SES: Not stated, but of local HMO patient population Income: < $25 000 – 37%; $25,000–50,000 – 34%; > $50 000 – 29% Education: 92% high-school graduates Scope of abuse: Implies that women asked about physical and emotional abuse (and maybe sexual) |
| Ramsden and Bonner, 2002173 |
Inclusion criteria: All women over 16 years of age presenting to the ED Exclusion criteria: Not stated Setting: Australia; Emergency Department (AED) Target group of intervention: AED staff Design: Before/after, historical controls Sampling time frame: 3 months pre-intervention, no time span stated for post-intervention study period Data source: Medical records |
Framework: Not stated Programme: Training on domestic violence, screening protocols and referral pathway. Resources on local services and contact numbers were provided Duration and frequency: Not stated Comparison care: Usual pre-intervention care |
245 screened in intervention group. No other details |
Age: Not stated Ethnicity: Not stated, but catchment area predominantly Anglo-Saxon, 25% born in non-English-speaking countries, 0.7% indigenous Australians SES: Not stated, but catchment area ranged from affluent to very low income Scope of abuse: Not stated, but two of the three screening questions refer to physical abuse |
| Shepard et al., 1999174 |
Inclusion criteria: Women who received home visits from county PHNs as part of a maternal and child health home visiting programme Exclusion criteria: Not stated Setting: USA; homes of women Target group of intervention: Social workers (public health nurses) Design: Before/after, historical controls Sampling time frame: pre-intervention 12 months preceding; post-intervention subsequent 12 and 24 months Data source: Medical records |
Framework: Duluth feminist model Programme: Use of protocol to increase referrals (to refuge/women’s group, arranging transport to refuge/safe housing) and information giving (booklet on abuse, information on community resources, calling police/seeking protection order) Duration and frequency: Not stated Comparison care: Usual pre-protocol management |
Intervention: 814 (52% with documented DV assessment) Comparison: 546 |
Age: > 50% aged 21–30 Ethnicity: Not stated SES: Not stated but many likely to be on low incomes Scope of abuse: Physical abuse |
| Thompson et al., 2000169 |
Inclusion criteria: Members of adult care team in primary care clinics at least half time Medical records of cases of DV between current or former intimate partners or parent or adult child; aged > 18 years; continuously enrolled at one of the clinics throughout study period; at least one clinic visit for one of four ‘sentinel’ diagnoses (depression, physical injury, pelvic pain or physical examination) Exclusion criteria: Paediatricians or receptionists or any clinical staff not based in the 5 practices Setting: USA. Five primary care clinics of Group Health Cooperative (a large HMO) Target group of intervention: Physicians, nurse practitioners, physician assistants, registered nurses, licensed practical nurses and medical assistants Design: Randomised controlled trial Sampling time frame: Baseline and 6 months post-intervention (staff asked about their responses to abused women in the previous 3 months) Data source: Staff self-reports |
Framework: Precede/proceed Programme: Focuses on changing practitioner predisposing factors, (knowledge, beliefs, barriers and attitudes), enabling factors (environmental and infrastructure processes supporting the intervention) and reinforcing factors (i.e. the use of feedback) Duration and frequency: Two separate half-day training sessions and four educational sessions. Opinion leaders attended three extra training sessions. System support included posters in waiting areas, cue cards for care providers, and screening questionnaires and newsletters for the clinical teams were all supplied Comparison care: Usual pre-intervention management |
Health-care providers 179: Intervention site: Pre-intervention: 1590 Post-intervention : 1372 Comparison site : Pre-intervention : 2205 Post-intervention: 2020 |
No demographic information stated for medical records |
| Ulbrich and Stockdale, 2002172 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Setting: USA. Four rural family planning clinics Target group of intervention: All staff, but results relate only to nurse practitioners (NPs) and registered nurses Design: Before/after, historical controls Sampling time frame: Baseline and 6 months post-intervention (staff asked about their responses to abused women in the previous 3 months) Data source: Staff self-reports |
Framework: RADAR Programme: Didactic training with RADAR pocket cue cards, plus a learning module, a presentation by DV advocacy programme, use of a screening/referral protocol; on-site advocate provided 1 day per week at one clinic, in others an advocate on-site as needed by women with crises, otherwise off-site Duration and frequency: Initial session (duration not known), with additional training and support over 2 years (also 5-hour quarterly meetings attended by one NP and DV Coordinator from each clinic, and 1-hour workshops every 6 months) Comparison care: Usual pre-intervention management |
Staff: 40 |
Age: Majority of attending women were aged 15–34 Ethnicity: Not stated, but in three of the four clinics, the catchment area was 90% white SES: In three clinics, 55% of the attending women were at or below poverty level; other clinic not stated Scope of abuse: Physical and sexual abuse |
| Wiist and McFarlane, 1999171 |
Inclusion criteria: For medical records, all prenatal patients identified at first visit as abused in year prior to or since pregnancy, perpetrator likely to be partner but not necessarily Exclusion criteria: Not stated Setting: US antenatal clinics Target group of intervention: Nurses, physicians, nutritionists, counsellors, clerical staff Design: Before/after, parallel groups Sampling time frame: Baseline, 3 and 12 months (total 15 months) post-intervention Data source: Medical records |
Framework: Not stated Programme: Use of ‘Mardi of Dimes’ protocol to increase referrals Duration and frequency: Single session of 90 minutes didactic training, additional weekly visits from nurse-trainer to provide support/instruct new staff Comparison care: Usual care, no protocol management |
Pre-protocol: 540 (both groups) Post-protocol: intervention 360; comparison 180 |
Age: Pre-protocol not stated (both groups) Post-protocol 60% aged 20–29 (both groups) Ethnicity: Pre-protocol at least 97% Latina (both groups) Post-protocol 96% Latina (both groups) SES: Pre-protocol not stated (both groups) Post-protocol 97% income < $20,000 (both groups) Scope of abuse: Not stated, but screening tool includes questions on physical and sexual abuse |
Appendix 8.2 Results of studies and quality scores
| Study details | Number identified as abused | Outcomes including any multivariate analysis/adjustment for confounders | Quality score (USPSTF) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coyer et al., 2006170 | 6 |
Identification of DV No statistics were stated |
Poor, Moderate | ||||||||||||||||||||||||
| Harwellet al., 1998168 |
Intervention: 13 confirmed abuse; 14 suspected abuse Comparison: 5 confirmed abuse; 5 suspected abuse |
DV screening performed Baseline 5%, 25% after training RR = 1.87 (95% CI = 1.61–2.16) DV confirmed DV abuse assessment completed
Safety assessment completed Abused women referred to community health centre staff Abused women referred to outside agency Two predictors for screening during the intervention period were having more than one clinic visit (OR = 1.56, 95% CI = 1.12–3.41) and being married (OR = 0.62, 95% CI = 0.40–0.92) |
Poor, Moderate | ||||||||||||||||||||||||
| McCawet al., 2001101 | Not stated |
Referrals to a DV specialist BaselinePost interventionMedicine2546Obstetrics/gynaecology825Psychiatry424AED314Social services27Unknown70Self-referrals718 |
Baseline | Post intervention | Medicine | 25 | 46 | Obstetrics/gynaecology | 8 | 25 | Psychiatry | 4 | 24 | AED | 3 | 14 | Social services | 2 | 7 | Unknown | 7 | 0 | Self-referrals | 7 | 18 | Poor, Moderate | |
| Baseline | Post intervention | ||||||||||||||||||||||||||
| Medicine | 25 | 46 | |||||||||||||||||||||||||
| Obstetrics/gynaecology | 8 | 25 | |||||||||||||||||||||||||
| Psychiatry | 4 | 24 | |||||||||||||||||||||||||
| AED | 3 | 14 | |||||||||||||||||||||||||
| Social services | 2 | 7 | |||||||||||||||||||||||||
| Unknown | 7 | 0 | |||||||||||||||||||||||||
| Self-referrals | 7 | 18 | |||||||||||||||||||||||||
| Ramsden and Bonner, 2002173 |
Intervention: 36 Comparison: not known |
Referrals to a social worker or police |
Poor, Moderate | ||||||||||||||||||||||||
| Shepardet al., 1999174 |
Intervention: 41 Comparison: 31 |
Percentage of women identified as experiencing domestic violence Percentage of women referred directly to domestic violence services Percentage of women given information |
Poor, Moderate | ||||||||||||||||||||||||
| Thompsonet al., 2000169 |
Intervention : pre-intervention 25: post-intervention 35 Comparison : pre-intervention 29; post-intervention 30 |
Identification of DV victims Proxy measures for DV – case findings by diagnosis |
Fair, Greatest Jadad score 3 |
||||||||||||||||||||||||
| Ulbrich and Stockdale, 2002172 | Not measured |
Self-reported referrals to community-based domestic violence advocacy programmes in last 3 months (%) Pre-training6-month follow-upLess than once a month46.742.91 to 3 times per month53.335.7Once a week0.021.4 Frequency of discussing domestic violence with patients in past 3 months (%) Pre-training6-month follow-upLess than once a month50.021.41 to 3 times per month31.37.1Once a week18.857.1 Only descriptive statistics given due to small sample sizes |
Pre-training | 6-month follow-up | Less than once a month | 46.7 | 42.9 | 1 to 3 times per month | 53.3 | 35.7 | Once a week | 0.0 | 21.4 | Pre-training | 6-month follow-up | Less than once a month | 50.0 | 21.4 | 1 to 3 times per month | 31.3 | 7.1 | Once a week | 18.8 | 57.1 | Poor, Moderate | ||
| Pre-training | 6-month follow-up | ||||||||||||||||||||||||||
| Less than once a month | 46.7 | 42.9 | |||||||||||||||||||||||||
| 1 to 3 times per month | 53.3 | 35.7 | |||||||||||||||||||||||||
| Once a week | 0.0 | 21.4 | |||||||||||||||||||||||||
| Pre-training | 6-month follow-up | ||||||||||||||||||||||||||
| Less than once a month | 50.0 | 21.4 | |||||||||||||||||||||||||
| 1 to 3 times per month | 31.3 | 7.1 | |||||||||||||||||||||||||
| Once a week | 18.8 | 57.1 | |||||||||||||||||||||||||
| Wiist and McFarlane, 1999171 |
Intervention: 29 (26 post-protocol and 3 pre-protocol) Comparison: 1 (0 post-protocol and 1 pre-protocol) |
Women identified as abused Referrals Pre-protocol: Post-protocol: |
Poor, Moderate |
Appendix 8.3 USPSTF assessment of execution of studies
| Author(s), publication year | RCTs: adequate randomisation; other designs: consideration of potential confounders (if no consideration of any confounders, score as poor) | Maintenance of comparable groups (includes crossovers, adherence, contamination) (if baselines not matched, score paper as poor, if contamination only, score as fair) | No important differential loss to follow-up or overall high loss to follow-up (> 20%) | Measurements: equal, reliable and valid (if measurements so poor as to be unacceptable, score study as poor) | Clear definition of interventions (individualised interventions allowed if within a structured format) | All important outcomes considered or good match of outcomes to goals | RCT: intention-to-treat analysis; other designs: adjustment for potential confounders | Quality rating (see Appendix 3) | Statistics |
|---|---|---|---|---|---|---|---|---|---|
| Coyer et al., 2006170 | No | Yes | n/a | Yes | Yes | Yes | No |
Poor Moderate |
No statistics |
| Harwellet al., 1998168 | No | Yes | n/a | No | Yes | Yes | No (only age) |
Poor Moderate |
Correct paired analysis not used No effect size |
| McCawet al., 2001101 | No | Yes (historical control) | No | Yes | Yes | Yes | No |
Poor Moderate |
No effect size |
| Ramsden and Bonner, 2002173 | No | No | n/a | No | No | Yes | No |
Poor Moderate |
No statistics |
| Shepardet al., 1999174 | No | Yes | n/a | Yes | No | Yes | Yes |
Poor Moderate |
No effect size |
| Thompsonet al., 2000169 | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Fair Greatest |
No effect size |
| Ulbrich and Stockdale, 2002172 | No | No | Yes | No | Yes | Yes | Yes |
Poor Moderate |
No statistics |
| Wiist and McFarlane, 1999171 | No | No | Yes | No | No | Yes | Yes |
Poor Moderate |
No effect size |
| Heath-care training total ‘yes’ out of 10 | 1 | 4 | 2/5 | 4 | 5 | 8 | 9 | – | – |
Appendix 9 Studies of acceptability of screening to health-care professionals
Appendix 9.1 Characteristics of qualitative studies and quality scores
| Study details | Study design | Number of participants | Participants | Quality score (CASP) |
|---|---|---|---|---|
| Dowd et al., 2002120 | Focus groups |
Approached: Not stated Recruited: 38 Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender: Female – physicians, 10; nurses, 19 HCP training/expertise: physicians, 17; nurses, 21 |
27 |
| Edin and Högberg, 2002175 | Qualitative interviews + questionnaires |
Approached: 18 (qualitative interviews) and 51 (questionnaires) Recruited: 5 (qualitative interviews) and 42 (questionnaires) Response rate (%): 27.77 (qualitative interviews) and 82 (questionnaires) |
Age (mean, SD, range): Not stated Gender (%): Female, 100 HCP training/expertise: Midwives |
37 |
| Hindin, 2006182 | Open-ended questions |
Approached: 150 Recruited: 8 Response rate (%): Not stated |
Age (mean, SD, range): 41 (30–56) Gender (%): Female, 100 HCP training/expertise: Certified nurse-midwives |
33 |
| Loughlin et al., 2000180 | In-depth interviews |
Approached: Not stated Recruited: 13 Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender (%): Not stated HCP training/expertise: Emergency department staff, 13 medical staff, 2 nursing staff, 10 administrator, 1 |
35 |
| McCosker et al., 2005179 | Focus groups |
Approached: Not stated Recruited: Not stated Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender (%): Not stated HCP training/expertise: Midwives |
31 |
| Mezey et al., 2003177 | Focus groups and semistructured interviews |
Approached: Not stated Recruited: 28 Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender (%): Female, 100 HCP training/expertise: Midwives |
31 |
| Minsky-Kelly et al., 2005181 | Focus groups |
Approached: Not stated Recruited: 39 Response rate (%): Not stated |
Age (mean, SD, range): 42 Gender (%): Female, 15 HCP training/expertise (%): Nurses, 80; mental health service providers, 20 |
32 |
| Price et al., 2005183 | Individual and focus group interviews |
Approached: Not stated Recruited: 34 Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender (%): Female, 100 HCP training/expertise: Midwives |
19 |
| Stenson et al., 2005176 | Focus groups |
Approached: 28 Recruited: 21 Response rate (%): 75 |
Age (mean, SD, range): 42–62 (54) Gender (%): Female, 100 HCP training/expertise: Midwives |
31 |
| Taket et al., 2004211 | Qualitative interviews |
Approached: Not stated Recruited: 124 Response rate (%): Not stated |
Age (mean, SD, range): Not stated Gender (%): Not stated HCP training/expertise (%): Project staff, 8; key stakeholders, 32; Womens' aid outreach workers, 3; Victim Support volunteers, 3 health service staff, 78 |
32 |
| Taylor et al., 2006178 | Focus groups and individual semistructured telephone interviews |
Approached: 38 for focus groups; 30 for interviews Recruited: 28 for focus groups; 8 for interviews Response rate (%): 73.7% focus groups; 26.6% interviews |
Age (mean, SD, range): Not stated Gender (%): Not stated HCP training/expertise: Physicians who provide obstetric care |
31 |
Appendix 9.2 Characteristics of quantitative (survey) studies
| Study details | Study design | Number of participants | Nature of participants |
|---|---|---|---|
| Bair-Merritt et al., 2004184 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 194 Recruited: 127 Response rate (%): 68 |
Age (mean, SD, range, %): < 30: 43 30–34: 51 35–40: 2 Ethnicity (%): White: 73 Black: 3 East Asian/Pacific Islander: 9 South Asian: 5 Hispanic American: 8 Other: 2 HCP gender (%): Female, 68 HCP training/expertise (%): Free-standing children’s hospital, 38 Paediatric programme in a university-based hospital, 36 Paediatric programme in a community-based general hospital, 22 |
| Bair-Merritt et al., 2006185 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional questionnaire |
Approached: 158 Recruited: 151 Response rate (%): 96 |
Age (mean, SD, range,%): Physicians: 31.5; Nurses: 32.5; Other: 31.5 Ethnicity (%): White: 77 Black: 8 Asian: 12 Other: 3 HCP gender (%): Physicians: Female 26%, male 18% Nurses: Female 30%, male 6% Other: Female 14%, male 6% HCP training/expertise (%): Physicians, 30; Nurses, 53; Paramedics, 10; Other, 7 |
| Baig et al., 2006186 |
Inclusion criteria: Residents across six residency programmes Exclusion criteria: Not stated Type of study: Self-report online questionnaire |
Approached: 309 Recruited: 167 Response rate (%): 54 |
Age (mean, SD, range, %): Not stated Ethnicity (%): Minority, 20 HCP gender (%): Female, 60 HCP training/expertise (%): Internal medicine, 42; Obs./Gyn., 8; Paediatrics, 13; Emergency medicine,16; Family medicine, 9; Medicine/paediatrics, 13 |
| Baird, 2005187 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 39 Recruited: 29 Response rate (%): 76 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated HCP gender (%): Not stated HCP training/expertise (%): Midwives |
| Barnett, 2005188 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 236 Recruited: 132 Response rate (%): 55.9 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated HCP gender (%): Not stated HCP training/expertise (%): Midwives |
| Ellis, 1999189 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 101 Recruited: 40 Response rate (%): 39.6 |
Age (mean, SD, range): 24–59 years (mean = 39) Ethnicity (%): Not stated HCP gender (%): Female, 92.5 HCP training/expertise (%): Nurses, by total years in nursing: 1–9: 32.5 10–19: 60 20–29: 5 30–39: 2.5 Educational backgrounds: High school diplomas: 17.5 Associate’s degrees: 27.5 Bachelor’s degrees: 40 Master’s degrees: 15 |
| Fikree et al., 2004190 |
Inclusion criteria: Eligibility criteria were determined by area of residence, enrolment in obstetrics residency training, and work experience Exclusion criteria: Not meeting the inclusion criteria Type of study: Self-report questionnaire |
Approached: 100 Recruited: 100 Response rate (%): 100 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated HCP gender (%): Not stated HCP training/expertise (%): 100 obstetricians: 48 seniors; 29 juniors; 23 trainees |
| Friedman et al., 1992110 |
Inclusion criteria: Not stated Exclusion criteria: Age less than 18, inability to understand the English language, and unwillingness to give consent Type of study: Cross-sectional survey |
Approached: 15 from Boston City Hospital and 18 from Lahey Clinic Recruited: 11 from Boston City Hospital and 16 from Lahey Clinic Response rate (%): 73 for Boston City Hospital and 89 for Lahey Clinic |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated HCP gender (%): Not stated HCP training/expertise (%): Primary care attending physicians |
| Goff et al., 2001191 |
Inclusion criteria: Participants’ names were selected from the Texas State Board of Medical Examiners, and the American Academy of Nurse Practitioners. No explicit inclusion criteria stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: Physicians in primary care specialties (emergency medicine, psychiatry, family practice, general practice, gynaecology, internal medicine, obstetrics/gynaecology): 345 General dentists: 177 Nurse practitioners: 84 Total: 606 Response rate (%): Physicians in primary care specialties: 27.3 General dentists: 43.5 Nurse practitioners: 43.4 Total: 34.4 NOTE: figures (p. 42) do not add up – values come to 221 (114%), which is not what is stated! |
Age (mean, SD, range): Not stated Ethnicity (pre-intervention) (%): Not stated Recruited: Physicians in primary care specialties: 315 General dentists: 170 Nurse practitioners: 76 Total: 561 HCP gender (%): Nurse practitioners, F: 91 Physicians, F: 27 Dentists, F: 8 HCP training/expertise (%): Years in practice: range 1–49, mean 16.7 years |
| Knapp et al., 2006271 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Self-administered questionnaire |
Approached (pre, post, follow-up): Not stated Recruited (pre, post, follow-up): 79/87/48 Attending physician: 20/17/17 Nurse: 42/48/18 Social worker: 14/16/12 Response rate (%) (pre, post, follow-up): Attending physician: 25.3/19.5/35.4 Nurse: 53.2/55.2/37.5 Social worker: 17.4/19.8/25.0 |
Age (mean, SD, range) (pre, post, follow-up): 36.8/32.9/33.5 Ethnicity (pre-intervention) (%): Not stated HCP gender (%) (pre, post, follow-up): F: 89.5/88.5/83.3 HCP training/expertise (%) (pre, post, follow-up): Attending physician: 25.3/19.5/35.4 Nurse: 53.2/55.2/37.5 Social worker: 17.4/19.8/25.0 |
| Lazenbatt et al., 2005192 |
Inclusion criteria: Not stated Exclusion criteria: Exclusion of midwives who were on maternity leave, career break or long-term sick leave Type of study: Self-report postal questionnaire |
Approached: 861 Recruited: 488 Response rate (%): 57 |
Age (mean, SD, range): 20–25: 1.4 26–30: 9 31–35: 29.5 36–40: 27.7 41–45: 16.2 46–50: 10.5 51–55: 5.1 56–60: 0.4 61–65: 0.2 Ethnicity (%): Not stated HCP gender (%): Female, 95 HCP training/expertise (%): Hospital midwives: 80 Community midwives: 20 |
| Nayak, 2000193 |
Inclusion criteria: Students from 4th (preclinical), 5th and 6th (clinical) years at a medical faculty in the year 1996–1997 Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 192 Recruited: 106 Response rate (%): 66.24 |
Age (mean, SD, range): Year 4: 21.53 (1.42) Year 5: 23.31 (1.33) Year 6: 24.50 (1.04) Ethnicity: Kuwaiti nationals of Arab descent Gender (%): Female, 57.8 HCP training/expertise : Medical students |
| Nicolaidis et al., 2005194 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Cross-sectional survey |
Approached: 90 practices Recruited: 31 practices; 278 HCP Response rate (%): 34.4 practicest |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated Gender (%): Female, 91 HCP training/expertise: 123 (62%) had prior IPV training Professional role: Primary care providers: 25 Medical support staff: 44 Administrative staff: 20 Other employees: 8 Unknown: 3 Medical specialty (providers only): Family medicine: 46 Internal medicine: 27 Obstetrics/gynaecology: 17 Other: 10 |
| Price and Baird, 2003195 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Audit questionnaire |
Approached: 250 Recruited: 126 Response rate (%): 50.4 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated Gender (%): Not stated HCP training/expertise (%): Midwives |
| Richardson et al., 2001196 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Anonymous questionnaire survey |
Approached: 700 Recruited: 401 Response rate (%): 57.3 |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated Gender: Higher proportion of women GPs than national average F: More women HCP training/expertise (%): GP, 48.6; nurses, 27.9; health visitors, 23.5 |
| Roelens et al., 2006197 |
Inclusion criteria: All members of the Flemish College of Obstetricians and Gynaecologists – Board Certified Exclusion criteria: Not stated Type of study: Self-report questionnaire |
Approached: 478 Recruited: 249 Response rate (%): 52.1 |
Age (mean, SD, range): 43.5 (37.0; 52.8) Ethnicity: Not stated Gender (%): Female, 30.8 HCP training/expertise (%): Public hospital: 24.2 Private hospital: 65.9 University hospital: 17.0 |
| Salmon et al., 2006198 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Pre-, post- and follow-up survey |
Approached: 79 Recruited: 70 Response rate (%): 89 |
Age (mean, SD, range): 14.8 (9.6) Ethnicity: Not stated Gender (%): Female, 100 HCP training/expertise (%): Diploma: 43 Certificate: 39 Degree: 12 Master’s: 5 |
| Shye et al., 2004199 |
Inclusion criteria: Not stated Exclusion criteria: Not stated Type of study: Survey questionnaire |
Approached: 273 Recruited: 203 Response rate (%): 74.4% |
Age (mean, SD, range): Not stated Ethnicity (%): Not stated Gender (%): Not stated HCP training/expertise (%): Subjects included all internal medicine, GPs, health appraisal, paediatric and Obs/Gyn physicians, physician assistants and nurse practitioners in the HMO’s main metropolitan area |
Appendix 9.3 Results and quality scores of quantitative studies
| Author, publication year | Results | Quality scores (Strobe) |
|---|---|---|
| Bair-Merritt et al., 2004184 | Ninety-three percent of chief residents felt that paediatricians should screen for domestic violence, but only 21% screen every patient | 15 |
| Seventy-one percent agreed or strongly agreed that paediatricians do not screen secondary to lack of training | ||
| Bair-Merritt et al., 2006185 | Most providers (65%) responded definitively yes or probably yes when asked if, in addition to the posters, paediatric emergency department health-care professionals should screen for intimate partner violence | 17 |
| Age, gender and role in the emergency department did not affect opinions about screening | ||
| Screening appropriate: total: 97/149; men: 31/44; women: 66/105; OR = 1.41 (0.66–3.01) | ||
| Baig et al., 2006186 | One hundred and eight residents thought domestic violence screening was ‘very important’, 51 ‘somewhat important’, five ‘neutral’, one ‘low importance’, and zero ‘not important’. In total, 95.2% of residents felt that domestic violence screening is important | 18 |
| Resident characteristics, such as gender, year in residency and personal history of abuse, were not independently associated with importance placed on screening or on stated intention to screen for domestic violence | ||
| Residents who had taken care of a domestic violence victim were more likely to report that domestic violence screening was very important than those who thought they had never taken care of a domestic violence victim | ||
| In the multivariate logistic regressions, emergency medicine residents remained less likely to report domestic violence screening as being important than Obs/Gyn residents | ||
| Some paediatric residents did not screen because of privacy concerns and thus may miss domestic violence among their adolescent patients. Residents reported lack of time, personal discomfort and forgetting to ask as personal barriers to domestic violence screening. Although residents stated no or poor training in domestic violence as a barrier, training in residency was not independently associated with priority placed either on screening or on stated intention to screen | ||
| Baird, 2005187 | Only 52% of respondents felt it was the midwife’s role routinely to enquire about domestic violence; 38% were unsure, whereas 10% felt there was no role for the midwife | 11 |
| When asked ‘Do you believe that a midwife enquiring about domestic violence may offend a pregnant woman’, 68% responded ‘Yes’, whereas 21% were unsure and 11% responded ‘No’ | ||
| Barnett, 2005188 | Sixty-six percent thought that midwives should ask women about domestic violence. However, a quarter were unconvinced and a further 7.1% believed that it was inappropriate | 13 |
| The majority said that it should be a multidisciplinary task with general practitioners and health visitors (who would know the whole family) asking routinely about domestic violence | ||
| Midwives’ experience of abuse and comments (20% experienced personal abuse) | ||
| Midwives felt strongly (91.7%) that robust referral systems should be in place before they ask women about domestic violence and feared that if this was not the case then questioning could in fact make a woman’s situation worse | ||
| Ellis, 1999189 |
Although 35 (88%) of the respondents had attended some type of in-service training on domestic violence, only 21 (53%) felt that nurses should screen all women for domestic violence |
12 |
| Also, 63% of nurses felt prepared to ask routine questions about domestic violence, 33% felt somewhat prepared and 5% felt not prepared | ||
| Fikree et al., 2004190 | Despite encountering physically abused victims during clinical practice, only eight obstetricians mentioned that they had ever received any training on identification or management of victims of domestic abuse. However, most (83%) thought that it was important to receive appropriate training, irrespective of marital status or gender. Interestingly, several obstetricians verbalised the desire of human rights issues training as an important component of a domestic violence screening and management programme | 16 |
| Almost half of the respondents were favourably inclined routinely to screen patients. Among the three categories of obstetricians interviewed, junior obstetricians (59%) were more likely to be favourably inclined for routine screening compared with either senior (42%) or trainee (43%) obstetricians | ||
| Emotional harm (77%), physical harm (60%) and pregnancy complications (49%) suffered by abused women were considered the most common reasons for perceiving routine screening as important | ||
| However, reasons articulated by those obstetricians who did not consider it important to screen routinely included no solution to the problem (30%), inquiring was an invasion of privacy (19%), and there was not enough time to enquire (9%). All respondents considered it important to inquire about domestic violence upon suspecting abuse | ||
| Friedman et al., 1992110 | Among physicians, one-third believed that physical abuse and sexual abuse questions should be asked routinely | 19 |
| However, sexual abuse inquiries were never made by 89% at initial visits or by 85% at annual visits. Physical abuse inquiries were never made by 67% at initial visits, or by 60% at annual visits | ||
| Eighty-one percent believed they could help with problems associated with physical abuse and 74% with sexual abuse | ||
| Goff et al., 2001191 | Twenty-five percent of physicians, 2.7% of dentists and 45.5% of nurse practitioners believed that women should be asked as part of routine exam | 16 |
| Overall, 20% of the health-care professionals believed women should be screened | ||
| Knapp et al., 2006271 | For four statements, there were no measurable changes in attitudes and beliefs between the baseline and both post-training evaluations. These included ‘It is inappropriate to ask about IPV in the pediatric setting’ (baseline: 4.3, 43% agreed; post-training: 4.3, 70% agreed; 6-month follow-up: 4.6, 65% agreed) | 17 |
| Lazenbatt et al., 2005192 |
Fifty-three percent (n = 254) felt that every woman should be screened for domestic violence |
16 |
| When midwives were asked if they had ever raised the issue of domestic violence with a client, only 28% (n = 135) reported to have done so. From the 28% of midwives who reported raising the issue of domestic violence with a client, 45.9% (n = 62) reported to have asked a direct question, with 7.4% (n = 10) reporting to have asked both a direct and indirect question | ||
| Nayak, 2000193 | Although most of the students (93%) felt that training in issues related to interpersonal violence is necessary, only 25% agreed that patients should be routinely assessed for a history of victimisation | 18 |
| Nicolaidis et al., 2005194 | Majority agreed it is the primary care provider’s responsibility to ask about domestic violence when seeing patients for health maintenance visits (66%), chronic pain (56%) or injuries (62%) | 17 |
| Fifteen percent agreed with screening for intimate partner violence at every visit | ||
| Price and Baird, 2003195 | Fourteen percent of the audit respondents did not believe it was the role of the health-care professionals to screen at all, with an even larger number (39%) feeling that routine screening should not occur within professional practice | 11 |
| From the responses it would appear that only a small number of hospital midwives screen routinely, with the majority of those who do screen being community-based midwives | ||
| When asked who should screen, a wide range of responses was given, from ‘any one who is in contact with women to specialists’. A large majority of hospital staff felt that it was the responsibility of the primary health-care team, specifically naming relevant individuals or by responses such as ‘any health professional that [sic] has an ongoing relationship with the woman, i.e. a community midwife’ | ||
| Richardson et al., 2001196 | Thirty-two percent thought that health visitors should routinely ask about domestic violence, 15% thought this for practice nurses, and 14% for general practitioners | 15 |
| Practice nurses were significantly less likely than health visitors (or general practitioners) to think that routine enquiry about domestic violence should take place (OR = 0.46, 95% CI = 0.27–0.77, p = 0.003). Other predictor variables had no significant effect | ||
| Roelens et al., 2006197 | Agreement with the incentive to screen: In the main survey participants declined universal and systematic screening (69.5%) and also refuted the common view of pregnancy as a window of opportunity to screen (48.6%). Rather, obstetrician/gynaecologists favoured direct questioning of the patient by means of the Abuse Assessment Screen in case of suspected abuse (82.7%) | 16 |
| Motivation: Most physicians surveyed considered directed screening (79.6%) although not universal screening (15.2%) as an issue of medical liability | ||
| Perceived self-efficacy: The preponderance of survey participants felt insufficiently skilled to discuss partner abuse in a straightforward manner and to manage abuse-related issues with putative victims of domestic violence (51.4%). Similarly, physicians surveyed felt insufficiently acquainted with referral practices in case of partner abuse (59.8%) | ||
| Outcome expectancy: A majority of obstetrician/gynaecologists believed that screening for intimate partner violence may be an effective means to counteract such abusive behaviours (65.4%). Yet, about half of all survey respondents were also convinced that there is a defined lack of referral services and specialised care facilities for women suffering from domestic violence | ||
| Salmon et al., 2006198 | At baseline participating community midwives thought that screening for domestic violence is important (88.6%); post-test this proportion increased to 97.5%, and at 6-month follow-up it was 97.3% | 17 |
| Agreement on the importance of midwives in such routine enquiry demonstrated a significant increase at post-test (97.6%) compared with baseline (83.6%), but this declined to a non-significant level at follow-up (94.5%) | ||
| No significant changes were found for views on the role of other health professionals enquiring about domestic violence | ||
| Shye et al., 2004199 | Clinicians’ opinions about the best approach to screening women for domestic violence exposure showed that 75% would prefer to routinely ask patients at health maintenance visits, 8% would prefer to ask only women who are at high risk, 15% would let a clinician decide who to ask, and 2% would let the woman bring the subject up herself | 17 |
Appendix 10 Cost-effectiveness of screening for partner violence
Appendix 10.1 Summary of data sources and assumptions used in the model
| Literature review | Service use data | Assumption | |
|---|---|---|---|
| Intervention unit costs | ✗ | Thirty percent of all programme steering group meetings contributed towards the management of the intervention | |
| Partner violence unit costs | ✗ |
Fifty percent of divorce proceedings arising from IPV involve children and property The average stay in a shelter in England and Wales is 6 weeks (information from Refuge) Twenty percent of IPV cases have child-care needs (based on the Women and Equity Unit figures). We assumed that this child care is for 6 weeks Women who are not abused incur civil justice and temporary housing costs. These costs are assumed to be in proportion to the divorce figures between IPV and non-IPV populations Women whose abuse is unidentified have lower costs, because their needs are not recognised or addressed. We assume their criminal justice, civil justice and temporary housing costs are half those for IPV Women undergoing advocacy and/or psychology treatment are assumed to have the same criminal justice costs, etc. as those who have disclosed and are not seeking an intervention Women in medium-term improvement have reduced costs. Their civil justice, temporary housing and mental health costs are the average of no abuse costs and the costs associated with those who have disclosed and are not seeking treatment. Their employment costs are half those of the disclosed – not seeking treatment group. The criminal justice costs are the same as in the abuse unidentified group |
|
| Transitional probabilities | ✗ |
The rate of recorded assessments must be inflated by 1.25 for intervention practices and by 3.33 for the control practice to get a true rate of assessments, with a standard error of 0.174 and 1 respectively The rate of assessing abused women to rate of assessing non-abused is 1.5 for both the intervention and control practices, with a standard error of 0.125 Fourteen percent experienced abuse in the past year In England and Wales two women die per week from domestic violence |
|
| Quality of life | ✗ | Wittenberg et al.272 estimated a quality of life of between 0.58 and 0.63 on a scale of 0 (equivalent to death) and 1 (equivalent to optimal health). We assume a quality of life of 1 when there is no abuse, 0.63 where abuse is ongoing, and 0.65 when women are experiencing medium-term improvement |
Appendix 10.2 Transition probabilities
| Control (standard error) | Intervention (standard error) | Source | Period | |
|---|---|---|---|---|
| No abuse to no abuse | 0.997 | 0.997 | Assumption | 6-monthly |
| No abuse to abuse unidentifieda | 0.0027 | 0.0027 | Complementary figure | 6-monthly |
| No abuse to death | 0.00029 | 0.00029 | Office of National Statistics all-cause mortality rate848 | 6-monthly |
| 1 | 1 | |||
| Abuse unidentified to no abuse | 0.005 | 0.005 | Assumption | 6-monthly |
| Abuse unidentified to abuse unidentified | 0.97143 | 0.94048 | Complementary figure | 6-monthly |
| Abuse unidentified to GP assessment | 0.023 (0.016) | 0.054 (0.04) | PreDoVe study | Instantaneous |
| Abuse unidentified to abuse identified (through other means) | 0 | 0 | PreDoVe study | 6-monthly |
| Abuse unidentified to death | 0.000385 | 0.000385 | Violent deaths273 and all-cause mortality848 | 6-monthly |
| 1 | 1 | |||
| GP assessment to abuse identified (true positive) | 0.21 | 0.42 | PreDoVe study. Assume control half as effective | Instantaneous |
| GP assessment to abuse unidentified (false negative) | 0.79 | 0.58 | Complementary figure | Instantaneous |
| 1 | 1 | |||
| Identified to accept referral | 0.75 | 0.95 | Assumption | Instantaneous |
| Identified to decline referralb | 0.25 | 0.05 | Complementary figure | Instantaneous |
| 1 | 1 | |||
| Accept referral to advocate | 0.67 | 0.67 | PreDoVe study | Instantaneous |
| Accept referral to psychologist | 0.29 | 0.29 | PreDoVe study | Instantaneous |
| Accept referral to both | 0.04 | 0.04 | PreDoVe study | Instantaneous |
| 1 | 1 | |||
| Advocate to psychologist | 0.05 | 0.05 | PreDoVe study | 6-monthly |
| Advocate to medium-term improvement | 0.3 | 0.3 | Assumption | 6-monthly |
| Advocate to disclosed – not seeking intervention | 0.6496 | 0.6496 | Complementary figure | 6-monthly |
| Advocate to death | 0.000385 | 0.000385 | Violent deaths273 and all-cause mortality | 6-monthly |
| 1 | 1 | |||
| Psychologist to advocate | 0.05 | 0.05 | PreDoVe study | 6-monthly |
| Psychologist to medium-term improvement | 0.3 | 0.3 | Assume same impact as advocate | 6-monthly |
| Psychologist to disclosed – not seeking intervention | 0.6496 | 0.6496 | Complementary figure | 6-monthly |
| Psychologist to death | 0.000385 | 0.000385 | Violent deaths273 and all-cause mortality | |
| 1 | 1 | |||
| Both to medium-term improvement | 0.3 | 0.3 | Assume same impact as advocate | 6-monthly |
| Both to disclosed – not seeking intervention | 0.6996 | 0.6996 | Complementary figure | 6-monthly |
| Both to death | 0.000385 | 0.000385 | Violent deaths273 and all-cause mortality | 6-monthly |
| 1 | 1 | |||
| Disclosed – not seeking intervention to accept referral | 0.2 | 0.2 | Assumption | 6-monthly |
| Disclosed – not seeking intervention to IEV | 0.7946 | 0.7946 | Complementary | 6-monthly |
| Disclosed – not seeking intervention to no abuse | 0.005 | 0.005 | Assume same rate as abuse unidentified to no abuse | 6-monthly |
| Disclosed – not seeking intervention to death | 0.000385 | 0.000385 | Violent deaths273 and all-cause mortality | 6-monthly |
| 1 | 1 | |||
| Medium-term improvement to medium-term improvement | 0.59971 | 0.59971 | Complementary | 6-monthly |
| Medium-term improvement to disclosed – not seeking intervention | 0.2 | 0.2 | Assumption | 6-monthly |
| Medium-term improvement to no abuse | 0.2 | 0.2 | Assumption | 6-monthly |
| Medium-term improvement to death | 0.00029 | 0.00029 | All-cause mortality | 6-monthly |
Appendix 10.3 Treatment costs in 2005 prices (£ sterling)
| Cost per person | Source | |
|---|---|---|
| Cost of advocacy | 164 | PreDoVe |
| Cost of psychologist | 305 | PreDoVe |
| Cost of advocate and psychologist | 469 | PreDoVe |
| Administration costs | 5 | PreDoVe |
| Use of HARK by doctor or nurse | 24 | Netten et al274 |
Appendix 10.4 Sensitivity analyses (varying cost and benefit by 25%)
| Examples of what costs are covered | No abuse | Abuse unidentified | Advocate | IEV | Medium-term improvement | |
|---|---|---|---|---|---|---|
| Criminal justice | Violence against a person | 0 | £436 | £873 | £873 | £436 |
| Civil justice | Injunctions, divorce proceedings, children and property | £18 | £93 | £185 | £186 | £101 |
| Employment loss of output | Fatalities, serious wounding | £0 | £1628 | £1628 | £1628 | £814 |
| Temporary housing | Shelters, hostel accommodation, local authority housing, friends and family | £111 | £379 | £757 | £757 | £434 |
| Social services and child care | Children looked after or in need | £0 | £432 | £432 | £432 | £0 |
| Medical services | Family medicine consultations, emergency room visits, health visitor (public health nurse) visits | £0 | £164 | £164 | £164 | £0 |
| Mental health | £52 | £209 | £209 | £209 | £131 | |
| Treatment costs | Advocate’s visits | £0 | £0 | £164 | £0 | £0 |
| Administration costs | Central administration of the intervention | £0 | £0 | £5 | £5 | £0 |
| Total 6-monthly costs | £181 | £3340 | £4416 | £4253 | £1916 | |
| Annual quality of life | 1 | 0.63 | 0.63 | 0.63 | 0.65 |
Appendix 10.5 Sensitivity analyses (varying cost and benefit by 25%)
| Variable | Base case value | Upper value | Upper value ICER | Lower value | Lower value ICER |
|---|---|---|---|---|---|
| ICER | 2450 | ||||
| No abuse to no abuse | 0.997 | 0.999 | 2078 | 0.994 | 2976 |
| No abuse to abuse unidentified | 0.003 | 0.004 | 2266 | 0.002 | 2630 |
| No abuse to GP assessment (intervention) | 0.037 | 0.046 | 2628 | 0.028 | 2284 |
| No abuse to GP assessment (control) | 0.018 | 0.023 | 2532 | 0.014 | 2362 |
| Abuse unidentified to no abuse | 0.005 | 0.006 | 2728 | 0.004 | 2172 |
| Abuse unidentified to abuse unidentified (intervention) | 0.941 | 0.972 | 1368 | 0.706 | 648 |
| Abuse unidentified to abuse unidentified (control) | 0.972 | 0.999 | 3278 | 0.941 | 54 |
| Abuse unidentified to GP assessment (intervention) | 0.054 | 0.068 | 2420 | 0.023 | 1350 |
| Abuse unidentified to GP assessment (control) | 0.023 | 0.054 | 54 | 0.017 | 2780 |
| GP assessment to identified (true positive) (intervention) | 0.420 | 0.525 | 2372 | 0.315 | 2452 |
| GP assessment to identified (true positive) (control) | 0.210 | 0.263 | 2140 | 0.158 | 2726 |
| Identified to accept referral (intervention) | 0.950 | 1.000 | 1514 | 0.750 | 6872 |
| Identified to accept referral (control) | 0.750 | 0.950 | 3390 | 0.563 | 1620 |
| Accept referral to advocate | 0.670 | 0.838 | 2294 | 0.503 | 2604 |
| Accept referral to psychologist | 0.290 | 0.363 | 2518 | 0.218 | 2384 |
| Accept both | 0.040 | 0.050 | 2476 | 0.030 | 2424 |
| Advocate and/or psychologist to disclosed – not seeking intervention (changing both together) | 0.650 | 0.813 | 41,466 | 0.488 | – 8066 (cost saving) |
| Advocate and/or psychologist to medium-term improvement (changing together) | 0.300 | 0.375 | – 3594 (cost saving) | 0.225 | 12,872 |
| Disclosed – not seeking intervention to accept referral | 0.200 | 0.250 | 512 | 0.150 | 4936 |
| Disclosed – not seeking intervention to disclosed – not seeking intervention | 0.795 | 0.994 | 19,324 | 0.596 | – 3334 (cost saving) |
| Disclosed – not seeking intervention to no abuse | 0.005 | 0.006 | 2024 | 0.004 | 2894 |
| Medium-term improvement to medium-term improvement | 0.600 | 0.750 | 2778 | 0.450 | 2286 |
| Medium-term improvement to disclosed – not seeking intervention | 0.200 | 0.250 | 5286 | 0.150 | – 366 (cost saving) |
| Medium-term improvement to no abuse | 0.200 | 0.250 | 80 | 0.150 | 6426 |
| Discount rate | 3.5% for costs and benefits | No discount | 1754 | 5% for costs and benefits | 2766 |
| Abuse unidentified | 0.630 | 0.680 | 18,542 | 0.580 | 1312 |
| Advocate | 0.630 | 0.680 | 2192 | 0.580 | 2776 |
| Psychologist | 0.630 | 0.680 | 2322 | 0.580 | 2594 |
| Advocate and psychologist | 0.630 | 0.680 | 2434 | 0.580 | 2468 |
| Disclosed – not seeking intervention | 0.630 | 0.680 | 1690 | 0.580 | 4448 |
| Medium-term improvement | 0.650 | 0.700 | 2208 | 0.630 | 2562 |
| Hark (one-off cost of administration) | 23.80 | 47.60 | 2938 | 0.000 | 1962 |
| Advocacy | 164 | 205 | 2656 | 123 | 2246 |
| Psychologist | 305 | 381 | 2640 | 229 | 2262 |
| Extra cost of mental health services when abused | 157 | 196 | 2164 | 118 | 2738 |
| Extra criminal justice cost when abused | 873 | 1091 | 4636 | 655 | 274 |
| Extra civil justice costs when abused | 168 | 210 | 2870 | 126 | 2030 |
| Extra employment costs when abused | 1628 | 2035 | – 548 (cost saving) | 1221 | 5440 |
| Extra housing costs when abused | 646 | 808 | 4070 | 485 | 830 |
| Extra medical (non-mental health) costs when abused | 164 | 205 | 2062 | 123 | 2846 |
| Extra child-care costs when abused | 432 | 540 | 1418 | 324 | 3482 |
Appendix 11 Self-appraisal of reviews
Appendix 11.1 The MOOSE criteria applied to review of prevalence studies
| Main heading | Subheading | Done |
|---|---|---|
| Reporting of background should include | ||
| Problem definition | Yes | |
| Hypothesis statement | Not applicable | |
| Description of study outcome(s) | Yes | |
| Type of exposure or intervention used | Not applicable | |
| Type of study designs used | Yes | |
| Study populations | Yes | |
| Reporting of search strategy should include | ||
| Qualifications of searchers (e.g. librarians and investigators) | Yes, although not in the text. The searchers had master’s level training that included searching bibliographic databases | |
| Search strategy, including time period included in the synthesis and keywords | Yes | |
| Databases and registries searched | Yes | |
| Effort to include all available studies, including contact with authors | Yes | |
| Search software used, name and version, including special features used (e.g. explosion) | No | |
| Use of hand searching (e.g. reference lists of obtained articles) | Yes | |
| List of citations located and those excluded, including justification | No – the inclusion/exclusion criteria were unambiguous for this review | |
| Method of addressing articles published in languages other than English | Yes | |
| Method of handling abstracts and unpublished studies | Excluded | |
| Description of any contact with authors | Yes | |
| Reporting of methods should include | ||
| Description of relevance or appropriateness | Yes | |
| Rationale for the selection and coding of data (e.g. sound clinical principles or convenience) | Yes | |
| Documentation of how data were classified and coded (e.g. multiple raters, blinding and inter-rater reliability) | Yes (as only a single, unblinded rater, test of inter-rater reliability not applicable) | |
| Assessment of confounding (e.g. comparability of cases and controls in studies where appropriate) | Yes | |
| Assessment of study quality, including blinding of quality assessors; stratification or regression on possible predictors of study results | Yes, but assessor not blinded | |
| Assessment of heterogeneity | Qualitative | |
| Description of statistical methods | Not applicable as studies not meta-analysed | |
| Provision of appropriate tables and graphics | Yes | |
| Reporting of results should include | ||
| Graphic summarising individual study estimates and overall estimate | Yes, although only included study estimates, not pooled prevalence | |
| Table giving descriptive information for each study included | Yes | |
| Results of sensitivity testing (e.g. subgroup analysis) | Yes | |
| Indication of statistical uncertainty of findings | Yes, although only confidence intervals on included study estimates | |
| Reporting of discussion should include | ||
| Quantitative assessment of bias (e.g. publication bias) | No | |
| Justification for exclusion (e.g. exclusion of non-English language citations) | Not applicable – all studies of UK prevalence were included | |
| Assessment of quality of included studies | Yes | |
| Reporting of conclusions should include | ||
| Consideration of alternative explanations for observed results | Yes | |
| Generalisation of the conclusions (i.e. appropriate for the data presented and within the domain of the literature review) | Yes | |
| Guidelines for future research | Yes | |
| Disclosure of funding source | Yes | |
Appendix 11.2 Flow diagram of inclusion/exclusion for health impact review
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
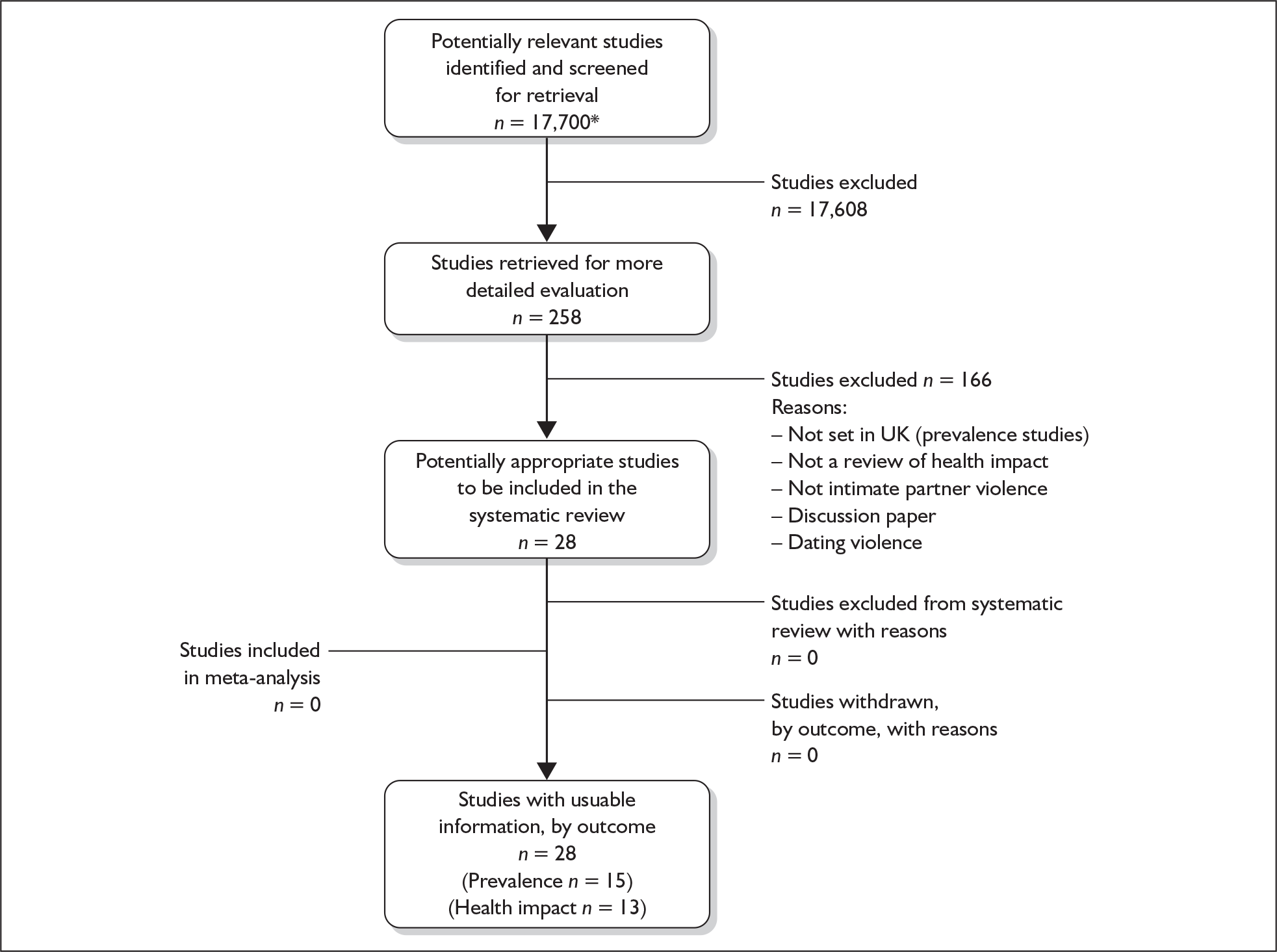
Appendix 11.3 Modified QUORUM statement checklist and flow diagram for screening tool review
QUORUM statement checklist
| Heading | Subheading | Descriptor | Reported? | Page number |
|---|---|---|---|---|
| Title | Identify the report as a systematic review | Yes | In report title | |
| Abstract | Use a structured format | Yes | iii–iv | |
| Describe | ||||
| Objectives | The clinical question explicitly | |||
| Data sources | The databases (i.e. list) and other information sources | |||
| Review methods | The selection criteria (i.e. population, intervention, outcome and study design); methods for validity assessment, data abstraction and study characteristics, and quantitative data synthesis in sufficient detail to permit replication | |||
| Results | Characteristics of the studies included and excluded; qualitative and quantitative findings (i.e. point estimates and confidence intervals); and subgroup analyses | |||
| Conclusion | The main results | |||
| Describe | ||||
| Introduction | The explicit clinical problem and rationale for review | Yes | 1–6 | |
| Methods | Searching | The information sources in detail (e.g. databases, registers, personal files, expert informants, agencies, hand-searching), and any restrictions (years considered, publication status, language of publication) | Yes | 12 |
| Selection | The inclusion and exclusion criteria (defining population, intervention, principal outcomes and study design | Yes | 8–11 | |
| Validity assessment | The criteria and process used (e.g. masked conditions, quality assessment and their findings) | Yes | 15, Appendix 5.4 | |
| Data abstraction | The process or processes used (e.g. completed independently, in duplicate) | Yes | 12–13 | |
| Study characteristics | The type of study design, participants’ characteristics, details of intervention, outcome definitions and how clinical heterogeneity was assessed | Yes | 8–11, 13 | |
| Data synthesis | The principal measures of effect (e.g. relative risk), method of combining results (statistical testing and confidence intervals), handling of missing data; how statistical heterogeneity was assessed; a rationale for any a priori sensitivity and subgroup analyses and any assessment of publication bias | Yes | 13 | |
| Results | Trial flow | Provide a meta-analysis profile summarising trial flow (see figure) | Yes | |
| Study characteristics | Present descriptive data for each study (e.g. age, sample size, intervention, dose, duration, follow-up period) | Yes | 29–33, Appendix 5.2 | |
| Quantitative data synthesis | Report agreement on the selection and validity assessment; present simple summary results | Yes | 33–36, Appendices 5.3 and 5.4 | |
| Discussion | Summarise key findings; discuss clinical inferences based on internal and external validity; interpret the results in light of the totality of available evidence; describe potential biases in the review process (e.g. publication bias); and suggest a future research agenda | Yes | 36–37, 73–77 |
QUORUM statement flow diagram
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
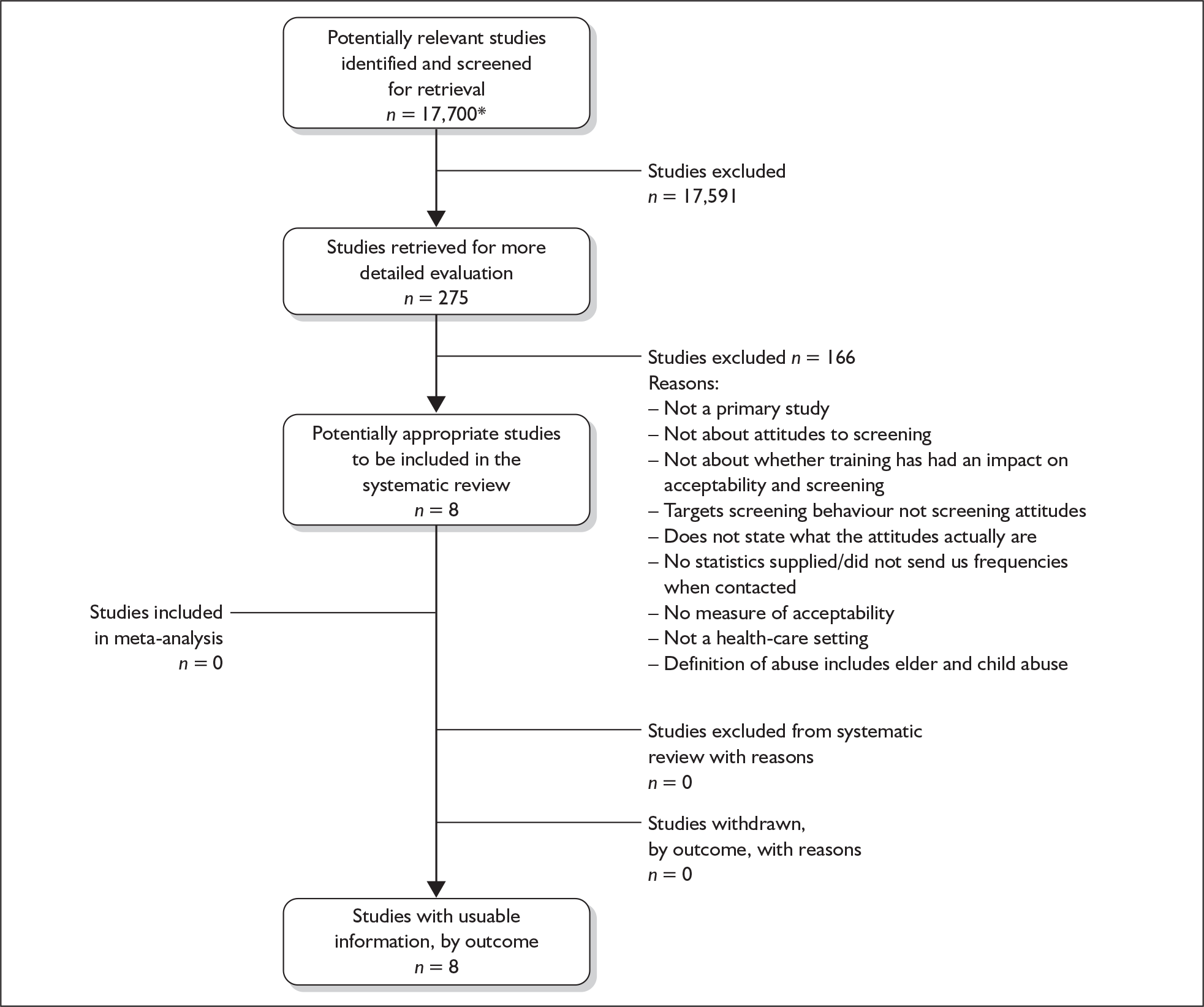
Appendix 11.4 Modified QUORUM statement checklist and flow diagram for acceptability of screening to women review
QUORUM statement checklist
| Heading | Subheading | Descriptor | Reported? | Page number |
|---|---|---|---|---|
| Title | Identify the report as a systematic review | Yes | In report title | |
| Abstract | Use a structured format | Yes | iii–iv | |
| Describe | ||||
| Objectives | The clinical question explicitly | |||
| Data sources | The databases (i.e. list) and other information sources | |||
| Review methods | The selection criteria (i.e. population, intervention, outcome and study design); methods for validity assessment, data abstraction and study characteristics, and quantitative data synthesis in sufficient detail to permit replication | |||
| Results | Characteristics of the studies included and excluded; qualitative and quantitative findings (i.e. point estimates and confidence intervals); and subgroup analyses | |||
| Conclusion | The main results | |||
| Describe | ||||
| Introduction | The explicit clinical problem and rationale for review | Yes | 1–6 | |
| Methods | Searching | The information sources in detail (e.g. databases, registers, personal files, expert informants, agencies, hand searching), and any restrictions (years considered, publication status, language of publication) | Yes | 12 |
| Selection | The inclusion and exclusion criteria (defining population, intervention, principal outcomes and study design | Yes | 8–11 | |
| Validity assessment | The criteria and process used (e.g. masked conditions, quality assessment and their findings) | Yes | 15–16, Appendices 6.1 and 6.2 | |
| Data abstraction | The process or processes used (e.g. completed independently, in duplicate) | Yes | 12 | |
| Study characteristics | The type of study design, participants’ characteristics, details of intervention, outcome definitions and how clinical heterogeneity was assessed | Yes | 8–11, 12–13 | |
| Data synthesis | The principal measures of effect (e.g. relative risk), method of combining results (statistical testing and confidence intervals), handling of missing data; how statistical heterogeneity was assessed; a rationale for any a priori sensitivity and subgroup analyses and any assessment of publication bias | Yes | 13–14 | |
| Results | Trial flow | Provide a meta-analysis profile summarising trial flow (see figure) | Yes | |
| Study characteristics | Present descriptive data for each study (e.g. age, sample size, intervention, dose, duration, follow-up period) | Yes | 39–44, Appendix 6.3 | |
| Quantitative data synthesis | Report agreement on the selection and validity assessment; present simple summary results (for each treatment group in each trial, for each primary outcome); present data needed to calculate effect sizes and confidence intervals in intention-to-treat analyses (e.g. 2 × 2 tables of counts, means and SDs, proportions) | Yes | 43–44 | |
| Discussion | Summarise key findings; discuss clinical inferences based on internal and external validity; interpret the results in light of the totality of available evidence; describe potential biases in the review process (e.g. publication bias); and suggest a future research agenda | Yes | 45, 73–77 |
QUOROM statement flow diagram for studies
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
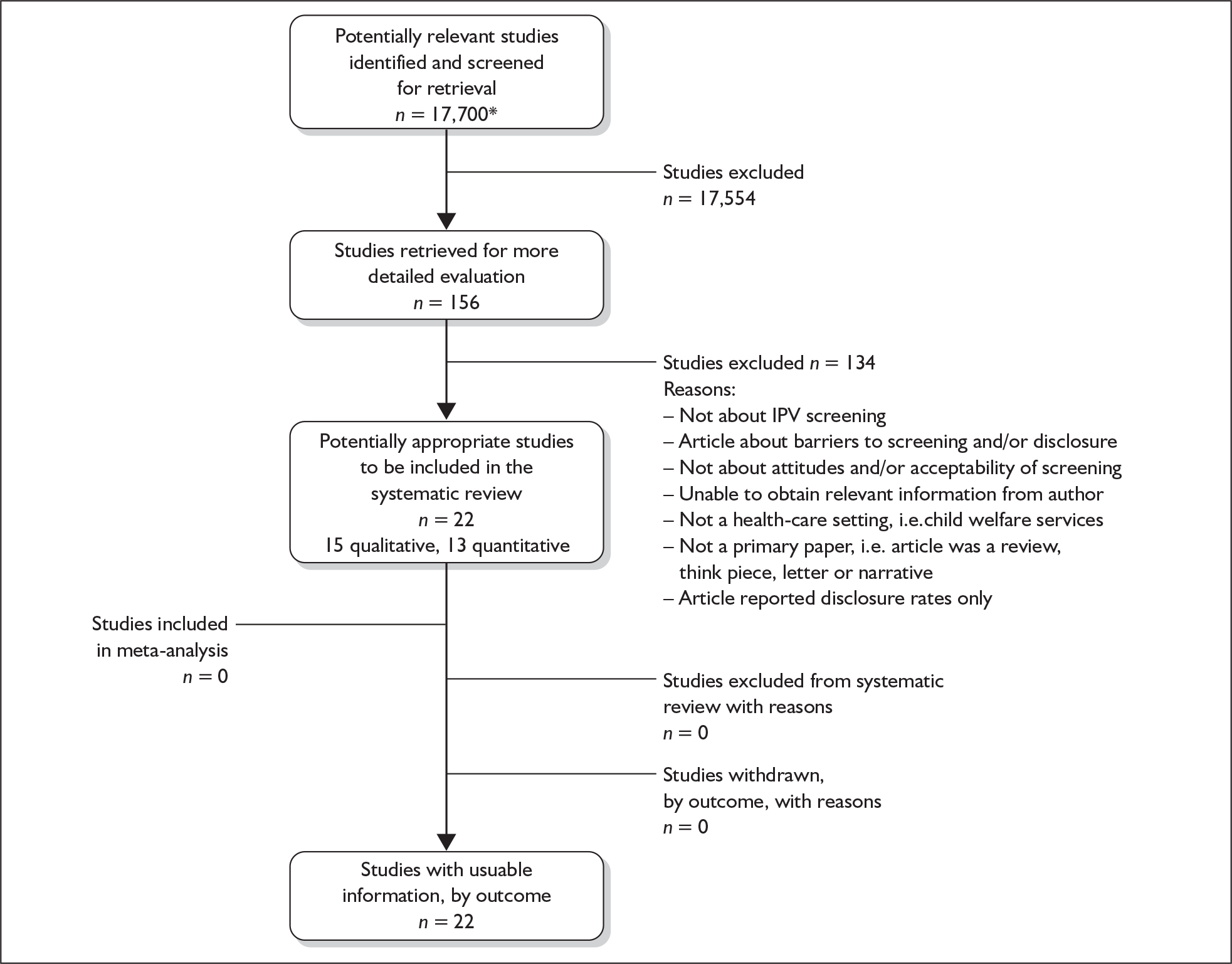
Appendix 11.5 Modified QUORUM statement checklist and flow diagram for intervention studies
QUORUM statement checklist
| Heading | Subheading | Descriptor | Reported? | Page number |
|---|---|---|---|---|
| Title | Identify the report as a systematic review | Yes | In report title | |
| Abstract | Use a structured format | Yes | iii–iv | |
| Describe | ||||
| Objectives | The clinical question explicitly | |||
| Data sources | The databases (i.e. list) and other information sources | |||
| Review methods | The selection criteria (i.e. population, intervention, outcome and study design); methods for validity assessment, data abstraction and study characteristics, and quantitative data synthesis in sufficient detail to permit replication | |||
| Results | Characteristics of the studies included and excluded; qualitative and quantitative findings (i.e. point estimates and confidence intervals); and subgroup analyses | |||
| Conclusion | The main results | |||
| Describe | ||||
| Introduction | The explicit clinical problem and rationale for review | Yes | 1–6 | |
| Methods | Searching | The information sources in detail (e.g. databases, registers, personal files, expert informants, agencies, hand searching), and any restrictions (years considered, publication status, language of publication) | Yes | 12 |
| Selection | The inclusion and exclusion criteria (defining population, intervention, principal outcomes and study design | Yes | 8–11 | |
| Validity assessment | The criteria and process used (e.g. masked conditions, quality assessment and their findings) | Yes | 15–16, Appendices 7.2 and 7.3 | |
| Data abstraction | The process or processes used (e.g. completed independently, in duplicate) | Yes | 12 | |
| Study characteristics | The type of study design, participants’ characteristics, details of intervention, outcome definitions and how clinical heterogeneity was assessed | Yes | 8–11, Appendix 7.1 | |
| Data synthesis | The principal measures of effect (e.g. relative risk), method of combining results (statistical testing and confidence intervals), handling of missing data; how statistical heterogeneity was assessed; a rationale for any a priori sensitivity and subgroup analyses and any assessment of publication bias | Yes | 12–13 | |
| Results | Trial flow | Provide a meta-analysis profile summarising trial flow (see figure) | Yes | |
| Study characteristics | Present descriptive data for each study (e.g. age, sample size, intervention, dose, duration, follow-up period) | Yes | 47–56, Appendix 7.1 | |
| Quantitative data synthesis | Report agreement on the selection and validity assessment; present simple summary results (for each treatment group in each trial, for each primary outcome); present data needed to calculate effect sizes and confidence intervals in intention-to-treat analyses (e.g. 2 × 2 tables of counts, means and SDs, proportions) | Yes | Appendices 7.2 and 7.4 | |
| Discussion | Summarise key findings; discuss clinical inferences based on internal and external validity; interpret the results in light of the totality of available evidence; describe potential biases in the review process (e.g. publication bias); and suggest a future research agenda | Yes | 56–58, 73–77 |
QUORUM statement flow diagram
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
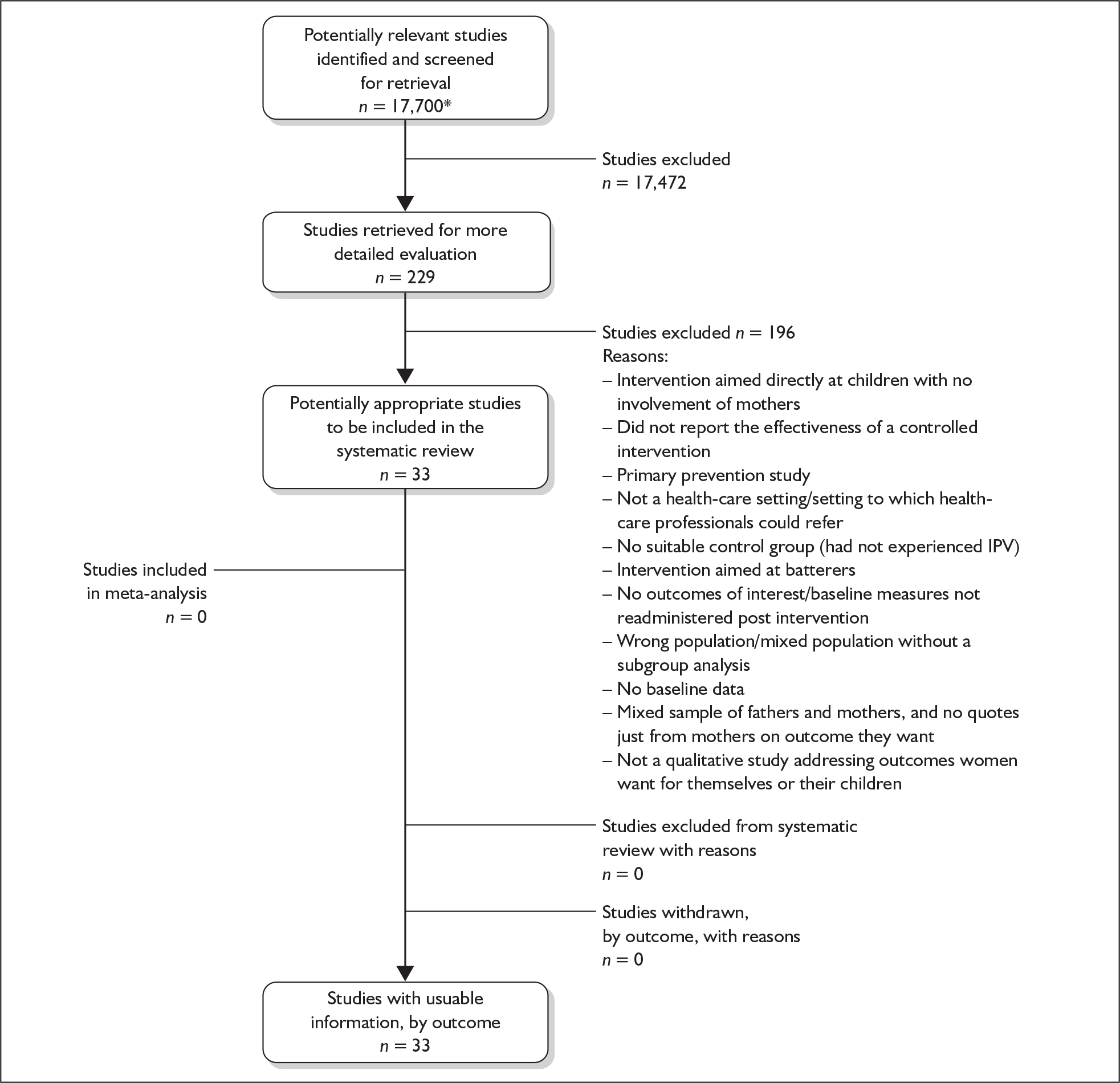
Appendix 11.6 Modified QUORUM statement checklist and flow diagram for morbidity and mortality outcomes of screening studies
QUORUM statement checklist
| Heading | Subheading | Descriptor | Reported? | Page number |
|---|---|---|---|---|
| Title | Identify the report as a systematic review | Yes | In report title | |
| Abstract | Use a structured format | Yes | iii–iv | |
| Describe | ||||
| Objectives | The clinical question explicitly | |||
| Data sources | The databases (i.e. list) and other information sources | |||
| Review methods | The selection criteria (i.e. population, intervention, outcome and study design); methods for validity assessment, data abstraction and study characteristics, and quantitative data synthesis in sufficient detail to permit replication | |||
| Results | Characteristics of the studies included and excluded; qualitative and quantitative findings (i.e. point estimates and confidence intervals); and subgroup analyses | |||
| Conclusion | The main results | |||
| Describe | ||||
| Introduction | The explicit clinical problem and rationale for review | Yes | 1–6 | |
| Methods | Searching | The information sources in detail (e.g. databases, registers, personal files, expert informants, agencies, hand searching), and any restrictions (years considered, publication status, language of publication) | Yes | 12 |
| Selection | The inclusion and exclusion criteria (defining population, intervention, principal outcomes and study design | Yes | 8–11 | |
| Validity assessment | The criteria and process used (e.g. masked conditions, quality assessment and their findings) | Yes | 15–16, Appendix 8.3 | |
| Data abstraction | The process or processes used (e.g. completed independently, in duplicate) | Yes | 12 | |
| Study characteristics | The type of study design, participants’ characteristics, details of intervention, outcome definitions and how clinical heterogeneity was assessed | Yes | 8–11, Appendix 8.1 | |
| Data synthesis | The principal measures of effect (e.g. relative risk), method of combining results (statistical testing and confidence intervals), handling of missing data; how statistical heterogeneity was assessed; a rationale for any a priori sensitivity and subgroup analyses and any assessment of publication bias | Yes | 12–13 | |
| Results | Trial flow | Provide a meta-analysis profile summarising trial flow (see figure) | Yes | |
| Study characteristics | Present descriptive data for each study (e.g. age, sample size, intervention, dose, duration, follow-up period) | Yes | 59–60, Appendix 8.2 | |
| Quantitative data synthesis | Report agreement on the selection and validity assessment; present simple summary results (for each treatment group in each trial, for each primary outcome); present data needed to calculate effect sizes and confidence intervals in intention-to-treat analyses (e.g. 2 × 2 tables of counts, means and SDs, proportions) | Yes | Appendix 8.2 | |
| Discussion | Summarise key findings; discuss clinical inferences based on internal and external validity; interpret the results in light of the totality of available evidence; describe potential biases in the review process (e.g. publication bias); and suggest a future research agenda | Yes | 61–62, 73–77 |
QUORUM statement flow diagram
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
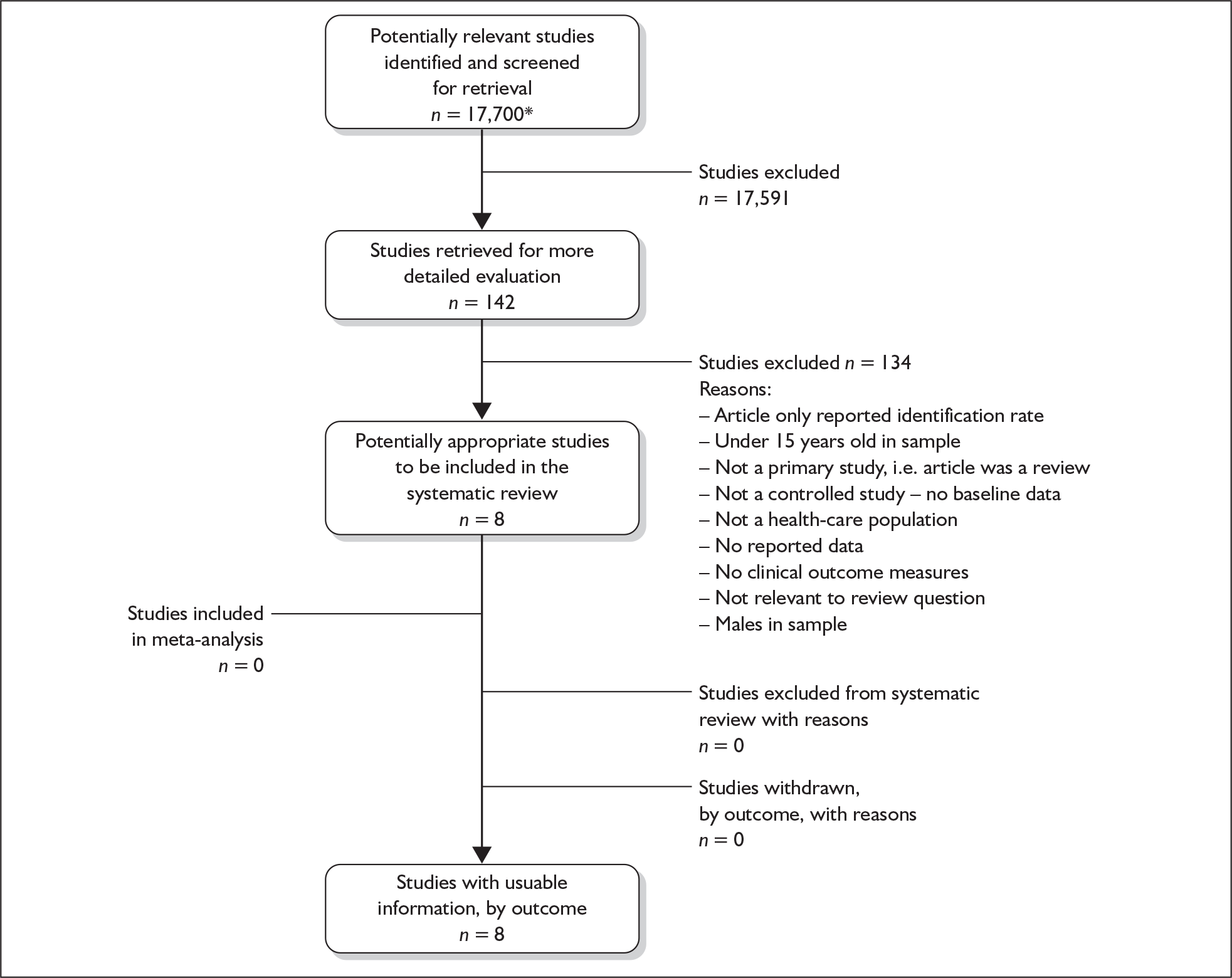
Appendix 11.7 Modified QUORUM statement checklist and flow diagram for acceptability of screening to health-care professionals
QUORUM statement checklist
| Heading | Subheading | Descriptor | Reported? | Page number |
|---|---|---|---|---|
| Title | Identify the report as a systematic review | Yes | In report title | |
| Abstract | Use a structured format | Yes | iii–iv | |
| Describe | ||||
| Objectives | The clinical question explicitly | |||
| Data sources | The databases (i.e. list) and other information sources | |||
| Review methods | The selection criteria (i.e. population, intervention, outcome and study design); methods for validity assessment, data abstraction and study characteristics, and quantitative data synthesis in sufficient detail to permit replication | |||
| Results | Characteristics of the studies included and excluded; qualitative and quantitative findings (i.e. point estimates and confidence intervals); and subgroup analyses | |||
| Conclusion | The main results | |||
| Describe | ||||
| Introduction | The explicit clinical problem and rationale for review | Yes | 1–6 | |
| Methods | Searching | The information sources in detail (e.g. databases, registers, personal files, expert informants, agencies, hand searching), and any restrictions (years considered, publication status, language of publication) | Yes | 12 |
| Selection | The inclusion and exclusion criteria (defining population, intervention, principal outcomes and study design | Yes | 8–11 | |
| Validity assessment | The criteria and process used (e.g. masked conditions, quality assessment and their findings) | Yes | 15–16, Appendix 9.3 | |
| Data abstraction | The process or processes used (e.g. completed independently, in duplicate) | Yes | 12 | |
| Study characteristics | The type of study design, participants’ characteristics, details of intervention, outcome definitions and how clinical heterogeneity was assessed | Yes | 8–11, 12–13 Appendices 9.1 and 9.2 | |
| Quantitative data synthesis | The principal measures of effect (e.g. relative risk), method of combining results (statistical testing and confidence intervals), handling of missing data; how statistical heterogeneity was assessed; a rationale for any a priori sensitivity and subgroup analyses and any assessment of publication bias | Yes | 13–14 | |
| Results | Trial flow | Provide a meta-analysis profile summarising trial flow (see figure) | Yes | |
| Study characteristics | Present descriptive data for each study (e.g. age, sample size, intervention, dose, duration, follow-up period) | Yes | 63–67, Appendices 9.1 and 9.2 | |
| Quantitative data synthesis | Report agreement on the selection and validity assessment; present simple summary results (for each treatment group in each trial, for each primary outcome); present data needed to calculate effect sizes and confidence intervals in intention-to-treat analyses (e.g. 2 × 2 tables of counts, means and SDs, proportions) | Yes | 67, Appendix 9.2 | |
| Discussion | Summarise key findings; discuss clinical inferences based on internal and external validity; interpret the results in light of the totality of available evidence; describe potential biases in the review process (e.g. publication bias); and suggest a future research agenda | Yes | 67–68, 73–77 |
QUORUM statement flow diagram
This figure* represents the total number of abstracts identified by search string. It is not possible to separate abstracts according to review questions as the search string identified all potentially relevant studies for each review question at the same time. Furthermore, the true number of abstracts is likely to be less than 17,700 because some abstracts were duplicated across databases.
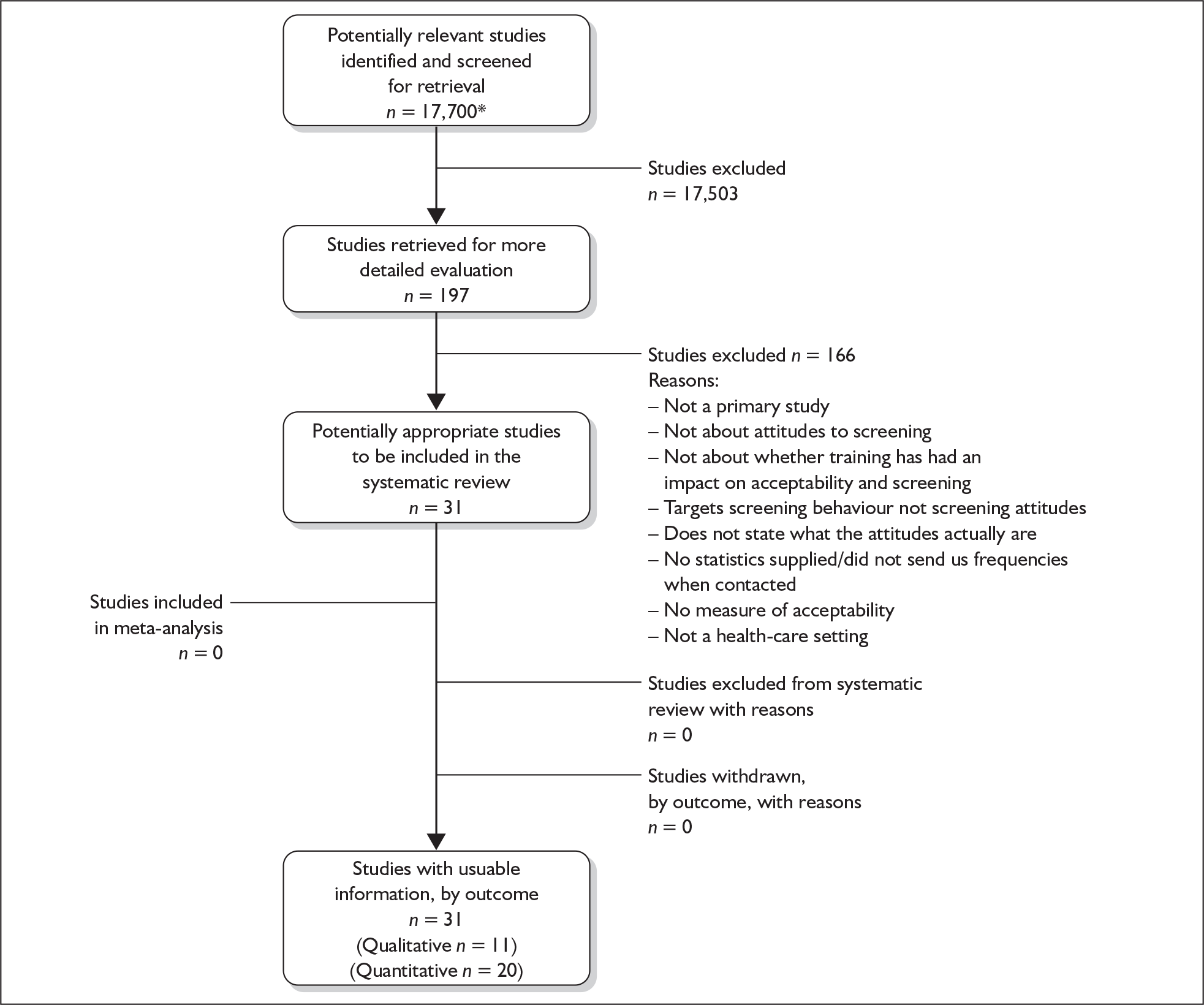
Appendix 12 Studies excluded from the reviews
| Author and year | Study title | Reason for exclusion | Paper relevant to another question? |
|---|---|---|---|
| Question I | |||
| Schiff and Zeira, 2005275 | Dating violence and sexual risk behaviours in a sample of at-risk Israeli youth | Not set in UK | QII – No age of children |
| Jain et al., 2004276 | Violence against women in India: evidence from rural Maharashtra, India | Not set in UK | |
| Mahony and Campbell, 1998277 | Children witnessing DV: a developmental approach | Health impact but not a review | |
| Wiebe and Janssen, 2001278 | Universal screening for DV in abortion | Not in the UK | |
| Coid et al., 2006279 | Violence and psychiatric morbidity in a national household population – a report from the British Household Survey | Not intimate partner violence | |
| Duxbury, 2006280 | Recognising domestic violence in clinical practice using the diagnoses of post-traumatic stress disorder, depression and low self-esteem | A discussion paper – does not review literature on health impact, just discusses it | |
| Garcia-Moreno et al., 2006212 | Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence | Not set in UK | |
| Duffy et al., 1999281 | Mothers with histories of domestic violence in a paediatric emergency department | Not set in UK | |
| Stark and Flitcraft, 1995282 | Killing the beast within: woman battering and female suicidality | A discussion paper – does not review literature on health impact, just discusses it | |
| Question II | |||
| Perrin et al., 1997283 | Validation of the Keane MMPI-PTSD scale against DSM-III-R criteria in a sample of battered women | Does not address study question | |
| Anetzberger, 2001284 | Elder abuse identification and referral: the importance of screening tools and referral protocols | Elder abuse, not specially DV | |
| Champion, 1996285 | Women abuse, assimilation, and self-concept in a rural Mexican American community | Psychometric/psychosocial measures | |
| Ejaz et al., 2001286 | Evaluating the Ohio elder abuse scale and DV in late life screening tools and referral protocol | Not a validation study | |
| Punukollu, 2003287 | DV screening made practical | Not a primary validation study | |
| Schofield et al., 2002288 | Screening for vulnerability to abuse amongst older women: Women’s Health Australia study | Elder abuse, not DV | |
| Falk et al., 2002289 | Evaluation of a DV assessment protocol used by employee assistance counsellors | Employee-based sample | |
| Peace et al., 2003290 | Translation of DV instruments for use in research | Translation and validation study | |
| Lewis, 1985251 | The wife abuse inventory: a screening device for the identification of abuse women | No gold standard | |
| Harris et al., 200134 | Current methods of the US Preventive Services Task Force | Not a primary study | |
| Straus, 2005220 | Measuring intrafamily conflict and violence: Conflict Tactics Scale | Not a primary study | |
| Waltermauer, 2005291 | Measuring IPV: You may only get what you ask for | Not a primary study | |
| Scholle et al., 2003257 | Routine screening for IPV in an obstetrics and gynaecology clinic | No gold standard | QV – No baseline measure |
| Straus and Douglas, 2004292 | A short form of the revised conflicts scales and typologies for severity and mutuality | No gold standard | |
| Straus et al., 1996221 | The revised Conflict Tactics Scale (CTS2) –- development and preliminary psychometric data | No gold standard | |
| Ross et al., 2004262 | Screening risks for IPV and primary care settings: implications for future abuse | Not a validation study | |
| Short and Rodriguez, 2002240 | Testing an IPV assessment icon form with battered migrant and seasonal farm workers | No gold standard | |
| Anderst et al., 2004256 | A comparison of DV screening methods in a paediatric setting | Three different groups using three tools | |
| Prospero, 2006293 | The role of perceptions in dating violence among young adolescents | Children aged 12–15 years in sample | |
| Sisley et al., 1999294 | Violence in America: a public health crisis – domestic violence | Not a primary study | |
| Rhodes et al., 2002295 | Between me and the computer: increased detection of intimate partner violence using a computer questionnaire | Females in sample | |
| Furbee et al., 1998252 | Comparison of domestic violence screening methods: a pilot study | No gold standard | |
| Canterino et al., 1999296 | Domestic abuse in pregnancy: a comparison of a self-completed domestic abuse questionnaire with a directed interview | Not clear if two tools used or one tool but presented differently | |
| Moraes et al., 2002297 | Portuguese-language cross-cultural adaptation of the revised Conflict Tactics Scale (CTS2), an instrument used to identify violence in couples | Translation study | |
| Meneghel et al., 2000298 | Women caring for women: a study on the ‘Viva Maria’ shelter, Port Alegre, Rio Gande do Sul, Brazil | Not a validation study | |
| Saltzman et al., 1997299 | Public health screening for intimate violence | Not a health-care population | |
| Reichenheim et al., 2000300 | Semantic equivalence of the Portuguese version of the abuse assessment screen tool used for the screening of violence against pregnant women | Translation study | |
| Tolman, 1999246 | The validation of the psychological maltreatment of women inventory | Not validating a screening tool | |
| Weiss et al., 2003230 | The out-of-hospital use of a domestic violence screen for assessing patient risk | Males in sample | |
| Ernst et al., 2002301 | Comparison of three instruments for assessing ongoing intimate partner violence | Males in sample | |
| Weiss et al., 2003230 | Development of a screen for ongoing intimate partner violence | Males in sample | |
| Wetmore and Fairbairn, 2003253 | A regional Californian programme to screen adolescent patients for intimate partner violence | Not a validation study | |
| Houry et al., 2004302 | A positive DV screen predicts future DV | Not a cross-sectional comparison | QVI – Not an objective/standardised/interview measure |
| Bonomi et al., 2005303 | Ascertainment of IPV in women seeking legal advice | Not a health-care setting: police/legal | |
| Waller et al., 1996304 | Development and validation of an ED screening and referral protocol for victims of DV | Not a full validation study – included on screen positives (triage screen positive) | QVI – Not an objective/standardised/interview measure |
| Hilton et al., 2004305 | A brief actuarial assessment for the prediction of wife assault recidivism: the Ontario domestic assault risk assessment | Recruited from police/legal population | |
| Heckert and Gondolf, 2004306 | Battered women’s perceptions of risk versus risk factors and instruments in predicting repeat reassault | Sample of batterers | |
| Sprecher et al., 2004307 | A neural network model analysis to identify victims of intimate partner violence | Not a validation study | |
| Parker et al., 1993308 | Physical and emotional abuse in pregnancy: a comparison of adult and teenage women | 13-year-olds in sample | |
| Cecil and Matson, 2006309 | Sexual victimisation among African American adolescent females | Not a DV screening tool | |
| Lazzaro and McFarlane, 1991310 | Establishing a screening programme for abused women | Not a primary study | |
| Hoff and Rosenbaum, 1994249 | A victimisation assessment tool: instrument development and clinical implications | Not a validation study | |
| Norton et al., 1995311 | Battering in pregnancy: an assessment of two screening methods | Not a validation study | |
| Lavoie and Vezina, 2001312 | Violence faite aux filles dans le contexte des frequentations à l’adolescence: elaboration d’un instrument | No gold standard, age group for women | |
| Majdalani et al., 2005313 | Validacion de un cuestionario breve para detector situaciones de violencia de genero en las consultas clinicas | No gold standard; no attitudes about screening | |
| McFarlene et al., 2001238 | Abuse Assessment Screen-Disability (AAS-D) measuring frequency, type and perpetrator of abuse towards women with physical disabilities | Not a validation study | |
| Swahnberg and Wijma, 2003314 | The NorVold Abuse questionnaire | Not a health-care population | |
| Wolfe et al., 2001315 | Development and validation of the Conflict in Adolescent Dating Relationships Inventory | Sample contains <15-year-olds | |
| Yost et al., 2005316 | A prospective observational study of domestic violence during pregnancy | Epidemiological study; no gold standard | |
| Higgins and Hawkins, 2005317 | Screening for abuse during pregnancy – implementing a multi-site programme | Not a validation study | QIV – Not a test of efficacy; QVI – No data given |
| Wasson et al., 2000239 | Routine, single-item screening to identify abusive relationships in women | No gold standard | |
| Campbell et al., 2001318 | Family issues and dangerousness: 8. risk assessment for intimate partner homicide | Not a primary study | |
| Yoshihama et al., 2002241 | Measuring the lifetime experience of domestic violence: application of the history calendar method | Not a validation study | |
| Moraes and Reichenheim, 2002319 | Cross-cultural measurement equivalence of the revised Conflict Tactics Scale (CTS2) Portuguese version used to identify violence within couples | Not a validation study | |
| Mears et al., 2005320 | Routine history as compared with audio computer-assisted self-interview for prenatal care history-taking | No valid comparator | |
| Webster and Holt, 2004258 | Screening for partner violence: direct questioning or self-report? | Not a validation study; invalid comparator | |
| McFarlane et al., 1995321 | Abuse during pregnancy: frequency, severity, perpetrator and risk factors of homicide | Not about screening | |
| Jory, 2004322 | The Intimate Justice Scale: an instrument to screen for psychological abuse and physical violence in clinical practice | No valid comparator | |
| Ramsden and Bonner, 2002261 | A realistic view of domestic violence screening in an emergency department | Not a controlled study | |
| Hegarty et al., 1999218 | A multidimensional definition of partner abuse: development and preliminary validation of the composite abuse scale | 30-item comparator | |
| Heyman et al., 2001323 | Can questionnaire reports correctly classify relationship distress and partner physical abuse? | 30-item comparator | |
| Flowers et al., 2002324 | Validation of a screening instrument for the exposure to violence in African American children | Not a DV screening tool | |
| Fals-Stewart et al., 2003325 | The timeline follow-back spousal violence interview to assess physical aggression between intimate partners: reliability and validity | Not a DV screening tool | |
| Janssen et al., 2002326 | Introducing domestic violence assessment in a postpartum clinical setting | Not a validation study | QV – Identification rates only |
| Lo et al., 1998327 | Screening for domestic violence in the emergency department | Not a validation study | QV – Not a controlled study |
| McFarlane et al., 1995260 | Identification of abuse in the emergency departments: effectiveness of a two-question screening tool | Not valid comparator | QV – No additional outcomes |
| Campbell et al., 1994328 | The reliability and factor structure of the index of spouse abuse with African American women | No comparator | |
| Bass et al., 2001329 | Screening tools and referral protocol for stopping abuse against older Ohioans: a guide for service providers | Not a validation study | |
| Anderson et al., 2002330 | Identifying intimate partner violence at entry to prenatal care: clustering routine clinical information | No valid comparator | |
| Wahl et al., 2004331 | Clinic-based screening for domestic violence: use of a child safety questionnaire | Children under 15 in sample | |
| Benight et al., 2004332 | Development and psychometric validation of a domestic violence coping self-efficacy measure (DV-CSE) | No valid comparator | |
| Schofield et al., 2003333 | Validity of self-report screening scale for elder abuse: Women’s Health Australia study | Not a DV screening tool | |
| Mohr et al., 2000334 | Children exposed to violence: measurement considerations within an ecological framework | Not a primary study | |
| Kubany et al., 2000335 | Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire | Not a DV screening tool | |
| McNamara and Fields, 2001336 | The Abuse Disability Questionnaire: internal consistency and validity considerations in two samples | Not a DV screening tool | |
| Varvaro, 1998337 | Violence against women: the role of orthopaedic nurses in the identification, assessment, treatment and care for abused women | Review paper | QIV – Not relevant, narrative |
| Gerard, 2000338 | Domestic violence: how to screen and intervene | Guidelines | |
| Fishwick, 1998339 | Assessment for women for partner abuse | Think piece | QIII – Quotes taken from a dissertation |
| Ward and Spence, 2002340 | Training midwives to screen for domestic violence | Not a primary study | |
| Babcock et al., 2004341 | What situations induce IPV? A reliability and validity study of the Proximal Antecedents to Violent Episodes (PAVE) scale | Sample consisted of batterers | |
| Shackelford and Goetz, 2004342 | Men’s sexual coercion in intimate relationships: development and initial validation of the Sexual Coercion in Intimate Relationships scale | Not a screening tool | |
| Gregg and Parks, 1995343 | Selected Minnesota Multiphasic Personality Inventory No.2 scales for identifying women with a history of sexual abuse | Not a DV screening tool | |
| Covington et al., 1997344 | Assessing for violence during pregnancy using a systematic approach | Sample split into two groups | QV – Only identification rate |
| Covington et al., 1997345 | Improving detection of violence among pregnant adolescents | Children < 15 years old | QV – Only identification rate |
| Attala et al., 1994242 | A partial validation of two short-form partner abuse scales | No valid comparator | |
| McFarlane et al., 1991263 | Assessing for abuse: self-report vs nurse interview | Two separate samples of women | |
| Cascardi et al., 1999346 | Factor structure and convergent validity of the Conflict Tactics Scale in high-school students | Males in sample | |
| Berlinger, 2004347 | Taking an intimate look at domestic violence | Not a validation study | |
| Datner et al., 1999348 | Utilisation of the 911 system as an identifier of domestic violence | No relevance to any review question | |
| Soeken et al., 1998227 | The Abuse Assessment Screen: a clinical instrument to measure frequency, severity and perpetrator of abuse against women | Psychometric validation only | |
| Brown et al., 1996235 | Development of the Women Abuse Screening Tool for use in family practice | No data on comparator | QIII – ‘Comfort’ not relevant |
| Paranjape and Liebschutz, 2003234 | STaT: a three-question screen for IPV | Uses clinical interview as comparator | |
| Moonesinghe et al., 2004237 | Development of a screening instrument to detect physical abuse and its use in a cohort of pregnant women in Sri Lanka | Uses clinical interview as comparator | |
| McIntyre et al., 1999248 | Validation of a trauma questionnaire in veteran women | Uses clinical interview as comparator | |
| Gagan, 1998349 | Correlates of nurse practitioners’ diagnostic and intervention performance for DV | Not a validation study | QVI – Looks at barriers |
| Bair-Merritt et al., 2006259 | Screening for IPV using an audiotape questionnaire | Compares presentation of tool | QIII – Not about acceptability of screening |
| Hilton and Harris, 2005 350 | Predicting wife assault: a critical review and implications for policy and practice | Not a primary study | |
| Halpern et al., 2005351 | Injury location and screening questionnaires as markers for IPV | Not a (true) validation study | |
| Boris et al., 2002244 | Partner violence among homeless young adults: measurement issues and associations | PVI (index test) has 26 items | |
| Williams et al., 2003352 | Violence against pregnant women | Not enough data present | |
| Koziol et al., 2001353 | Predictive validity of a screen for partner violence against women | Not a health-care population | |
| Gendron, 1991354 | Elaboration d’un questionnaire d’identication des femmes violentées en milieu conjugal | No comparator | |
| Dub et al., 2005355 | Etude exploratoire du point de vue des femmes et des hommes sur les services utilises en matière de violence conjugale | Not about screening | |
| Szafran and Fossion, 2005356 | La conjugale violence | Opinion piece | |
| Rinfret et al., 2002357 | Un protocole de depistage systematique de la violence congugale. Mesure de l’efficacite | Not about screening | |
| Hasselmann and Reichenheim, 2003358 | Adatacao transcultural da versao em portugues da conflict tactics scale f=Form R (CTS-1), usada para afeire violencia no casal: equivalencias semantica e de mensuracao | Adaptation of the CTS into Portuguese | |
| Heron et al., 2003359 | Do responses to an IPV screen predict scores on a comprehensive measure of IPV in low-income black women? | Only screen positives on index were recruited | |
| Nelson et al., 20045 | Screening women and elderly adults for family and IPV | Review – not primary studies | |
| O’Leary, 1999360 | Psychological abuse: a variable deserving critical attention in domestic violence | Review –- not primary studies | |
| Fogarty et al., 200294 | Communicating with patients about IPV: screening and interviewing approaches | Review – not primary studies | |
| Miscellaneous, 2002361 | Assessment for IPV in clinical practice | Resource pack | |
| Rodriguez, 1998362 | Clinical interventions with battered migrant farm worker women | Not a validation study | |
| Barthauer, 1999363 | Domestic violence in the psychiatric emergency service | Not a primary study | |
| Chuang et al., 2002364 | Screening for IPV in the primary care setting: a critical review | Not a primary study | QV – Not a primary study |
| Wyszynski, 2000365 | Screening women for family violence in the maternal child health-care setting | Think piece | |
| King and Ryan, 1996366 | Women abuse: the role of nurse-midwives in assessment | Think piece | |
| Coulthard et al., 2006367 | DV screening and intervention programmes for adults with dental or facial injury | Review – not primary studies | |
| Pontecorvo et al., 2004368 | Violencia domestica contra la mujer una encuesta en consultorios de atencion primaria | No gold standard | |
| Cook and Goodman, 2006369 | Beyond frequency and severity – development and validation of the brief coercion and conflict scales | Prison population | |
| Goetz et al., 2006370 | Adding insult to injury: development and initial validation of the Partner-directed Insults Scale | Index tool has 47 items | |
| Williams and Grant, 2006371 | Empirically examining the risk of IPV: the revised Domestic Violence Screening Instrument (DVSI-R) | Legal population | |
| Fikree et al., 2006255 | IPV before and during pregnancy: experiences of postpartum women in Karachi, Pakistan | No comparator | QIII – Asks about ‘a good time to enquire’, not about routine screening |
| Parmar et al., 2005372 | Tackling domestic violence: providing advocacy and support to survivors from black and other minority ethnic communities | None given | |
| Bateman and Whitehead, 2004254 | Health visitors’ domestic violence routine questioning tool: an exploration of women’s experience, effectiveness and acceptability | None given | QIII – None given |
| Fogarty and Brown, 2002373 | Screening for abuse in Spanish-speaking women | No gold standard | QIII – Not about attitudes to screening |
| Perry et al., 1998374 | Voices from an Afghan community | Not validation study | QIII – Not specific to screening for DV |
| Freund et al., 1996375 | Identifying domestic violence in primary care practice | No gold standard | QIII – Refusal to answer questions; QV – Only identification rate given |
| McHugo et al., 2005376 | The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence | No gold standard | QVI – Not about acceptability of routine screening |
| Kramer, 2002377 | Domestic violence: how to ask and how to listen | Not a validation study, not primary data | QVI – Not a validation study, not primary data |
| Question III | |||
| Keeling and Birch, 2004378 | Asking pregnant women about domestic abuse | Not about screening, but asking about DV | |
| McCauley et al., 1998379 | Inside ‘Pandora’s box’. Abused women’s experiences with clinicians and health services | Barriers to screening | |
| Thurston et al., 1998380 | Building a feminist theoretical framework for screening of wife-battering: key issues to be addressed | Not about acceptability of screening | QVI – Not about acceptability of screening |
| Kramer et al., 2004381 | Prevalence of IPV and health implications for women using emergency departments and primary care clinics | Unable to obtain relevant information from author | |
| Magen et al., 2000382 | Domestic violence in child welfare preventative services: results from an intake screening questionnaire | Not a health-care setting (child welfare services, so was borderline) | |
| Sleutel, 1998383 | Women’s experiences of abuse, a review of qualitative research | Literature review | |
| Hamberger et al., 2005384 | TANF workers’ responses to battered women and the impact of brief worker training | Not about attitudes to screening | QVI – Not about attitudes to screening |
| Curnow, 1997385 | The open window phase: help-seeking and reality behaviours by battered women | Not about attitudes to screening | |
| Hamberger et al., 1998386 | Physician interaction with battered women | Not about attitudes to screening | |
| Moracco et al., 2005387 | Knowledge and attitudes about intimate partner violence among immigrant Latinos in rural north Carolina | Not about attitudes to screening | |
| Panchanadeswaran and Koverola, 2005 388 | The voices of battered women in India | Not about attitudes to screening | QIV – Not about attitudes to screening |
| Lewis et al., 2005389 | Perceptions of service providers and community members on intimate partner violence within a Latino community | Not attributable to screening | QIV – Not attributable to screening |
| Sankar and Jones, 2005390 | To tell or not to tell | Not about attitudes to screening | |
| Weisz and Black, 2001391 | Evaluating a sexual assault and dating violence prevention programme for urban youths | Not about attitudes to screening | |
| Yoshioka et al., 2003392 | Social support and disclosure of abuse: comparing south Asian, African American and Hispanic battered women | Not about attitudes to screening | |
| O’Donnell, 2000393 | Abuse in pregnancy – the experience of women | Just disclosure rates | |
| Jackson, 2002394 | Abuse in dating relationships: young people’s accounts of disclosure, non-disclosure, help-seeking and prevention education | Not about attitudes to screening | |
| Zweig et al., 2002395 | Assisting women victims of violence who experience multiple barriers to services | Not about attitudes to screening | |
| Cord-Duncan et al., 2006396 | Detecting potential intimate partner violence: which approach do women want? | Not about screening methods | |
| Boyle and Jones, 2006397 | The acceptability of routine inquiry about domestic violence towards women, a survey in three health-care settings | Because of the way the authors formulated the question regarding attitudes to screening – ‘I wouldn’t mind if a doctor would ask me’ | |
| Jones and Bonner, 2002398 | Screening for domestic violence in an antenatal clinic | Is a discussion paper rather than a report of a proper examination into attitudes to screening | QVI – No statistics |
| Hester and Westmarland, 2005399 | Tackling domestic violence: effective interventions and approaches | Not really about attitudes to screening | |
| Bateman and Whitehead, 2004254 | Health visitors’ domestic violence routine questioning tool: an exploration of women’s experience, effectiveness and acceptability | None given | QII – None given |
| Varcoe, 2001400 | Abuse obscured: an ethnographic account of emergency nursing in relation to violence against women | Not really about attitudes to screening | QVI – Not really about attitudes to screening |
| Coid et al., 200354 | Sexual violence against adult women primary care attenders in east London | None given | |
| Bates et al., 2001401 | ‘A little encouragement’: health services and domestic violence | It does not seem to include anything about attitudes to screening | |
| Rodriguez et al., 1996402 | Breaking the silence: battered women’s perspectives on medical care | Not really about attitudes to screening but opinions about asking directly | |
| Dienemann et al., 2005403 | Survivor preferences for response to IPV disclosure | Unclear | |
| Peterson et al., 2003404 | Women’s perspective on IPV services: a hope in Pandora’s box | Unclear | |
| Curry et al., 2003405 | Development of an abuse screening tool for women with disabilities | Not about attitudes to screening | |
| Liang et al., 2005406 | A theoretical framework for understanding help-seeking processes among survivors of intimate partner violence | Not about screening | |
| Taylor and Sorenson, 2004407 | Injunctive social norms of adults regarding teen dating violence | Not about screening | |
| Crandall et al., 2005408 | No way out: Russian-speaking women’s experiences with domestic violence | Not about screening | |
| Sullivan et al., 2005409 | For us it is like living in the dark: Ethiopian women’s experiences with domestic violence | Not about attitudes | |
| Mattson et al., 2002410 | Exploring tele-health opportunities in domestic violence shelters | Not about attitudes to screening | |
| Battaglia et al., 2003411 | Survivors of intimate partner violence speak out | Not about attitudes to screening | |
| McNutt et al., 2000412 | Partner violence and medical encounters | Not screening attitudes | |
| O’Connor, 2002413 | Consequences and outcomes of disclosure for abused women | Letters | |
| Renker, 2002414 | Keeping safe: teenagers’ strategies for dealing with perinatal violence | Not about screening | |
| Burke et al., 2004415 | Ending intimate partner violence: an application of the transtheoretical model | Not about attitudes to screening | |
| Taylor, 2004415 | Moving from surviving to thriving: African American women recovering from intimate male partner abuse | Not about attitudes to screening | |
| Koziol-McLain et al., 2004416 | Prevalence of intimate partner violence among women presenting to an urban adult and paediatric emergency care department | Prevalence study, not about attitudes to screening | |
| Davis and Taylor, 2002417 | Voices from the margins part 2: narrative accounts of the support needs of indigenous families experiencing violence | Not about attitudes to screening | |
| Washington, 2001418 | Disclosure patterns of black female sexual assault survivors | Not about attitudes to screening | |
| McMurray and Moore, 1994419 | Domestic violence: are we listening? Do we see? | Not about attitudes to screening | |
| Gerbert et al., 1996420 | Experiences of battered women in the health setting: a qualitative study | Not about attitudes to screening | |
| Kearsey, 2002421 | Listening for silent screams | Not a primary study. Discussion type paper – with no real empirical data | |
| McCarraher et al., 2003422 | Are reproductive health services a good place to screen for intimate partner violence? | Not about attitudes to screening | |
| Campbell and Soeken, 1999423 | Women’s responses to battering: a test of the model | Not about attitudes to screening | |
| Plichta et al., 1996424 | Spouse abuse – patient–physician communication | Not about attitudes to screening | |
| Weingourt, 1985425 | Wife rape: barriers to identification and treatment | Not about attitudes to screening | |
| Rodriguez et al., 1998426 | Factors affecting patient–physician communication for abused Latina and Asian immigrant women | Not about attitudes to screening | |
| Hayden et al., 1997427 | Domestic violence in the emergency department: how do women prefer to disclose and discuss the issues? | No question on routine questioning/screening | |
| Bacchus et al., 2003428 | Experiences of seeking help from health professionals in a sample of women who experienced domestic violence | None given | |
| Hou et al., 2005429 | Domestic violence against women in Taiwan: their life-threatening situations, post-traumatic responses, and psychophysiological symptoms. An interview study | Not about attitudes towards screening | |
| Peckover, 2003430 | ‘I could just have done with a little more help’ – an analysis of women’s help-seeking from health visitors in the context of domestic violence | Not really about acceptability of routine screening | |
| Scheiman and Zeoli, 2003431 | Adolescents’ experiences of dating and intimate partner violence: once is not enough | Narrative | |
| McCosker et al., 1999432 | Evaluation of a self-paced education package on violence against women for rural community-based health workers | Not about acceptability of routine screening | |
| Flinck et al., 2005433 | Survival of intimate partner violence as experienced by women | Not about acceptability of routine screening | |
| De Mendoza, 2001434 | Culturally appropriate care for pregnant Latina women who are victims of domestic violence | Narrative | |
| Feder et al., 200633 | Women exposed to intimate partner violence | Not a primary study | |
| Choi and Harwood, 2004435 | A hypothesised model of Korean women’s responses to abuse | Not about acceptability of routine screening | |
| Brendtro and Bowker, 1989436 | Battered women: how can nurses help? | Not about attitudes towards screening | |
| Petersen et al., 2004437 | Moving beyond disclosure: women’s perspectives on barriers and motivators to seeking assistance for intimate partner violence | Not about acceptability of routine screening | |
| Grynbaum et al., 2001438 | Domestic violence: prevalence among women in a primary care centre – a pilot study | No questions about screening | |
| Fugate et al., 2005439 | Barriers to domestic violence help-seeking | Not about screening | QIV – Not about outcomes women want from an intervention |
| Bauer et al., 2000440 | Barriers to health care for abused Latina and Asian immigrant women | Not about acceptability of routine screening | |
| Bair-Merritt et al., 2006259 | Screening for intimate partner violence using an audiotape questionnaire | Not about acceptability of routine screening | |
| Gerbert et al., 1999441 | When asked, patients tell: disclosure of sensitive health-risk behaviours | Not really about acceptability of routine screening | |
| Chatzifotiou, 2003442 | Violence against women and institutional responses: the case of Greece | Not about attitudes to screening | |
| Freund et al., 1996375 | Identifying domestic violence in primary care practice | Because 3% refused to answer searching questions | QII – No gold standard; QVI – Only identification rate given |
| Edwards, 2005443 | Raising the subject of domestic violence | Not a primary study | QVI – Not a primary study |
| Fraser et al., 2002444 | Social support choices for help with abusive relationships: perceptions of African American women | Not about attitudes to screening | |
| Perry et al., 1998374 | Voices from an Afghan community | Not specific to screening for DV | QII – Not validation study |
| Richardson and Feder, 1996445 | Domestic violence: a hidden problem for general practice | Not a primary study | |
| Fogarty and Brown, 2002373 | Screening for abuse in Spanish-speaking women | Not about attitudes to screening | QII – No gold standard |
| Campbell et al., 1994446 | Battered women’s experiences in the emergency department | Not about attitudes to screening | |
| Sethi et al., 2001447 | Experience of ‘screening’ for domestic violence in women’s services | Not about attitudes to screening | |
| Milberger et al., 2003448 | Violence against women with physical disabilities | Not about attitudes to screening | |
| Dienemann et al., 2002449 | A critical pathway for intimate partner violence across the continuum of care | Maybe for QII, not really discussing attitudes to screening | |
| Yam and Oradell, 2000450 | Seen but not heard – battered women’s perceptions of the emergency department experience | Not really about attitudes to screening | |
| El-Khoury et al., 2004451 | Ethnic differences in battered women’s formal help-seeking strategies: a focus on health, mental health and spirituality | Not about screening | |
| Goodyear-Smith, 2002452 | National screening policies in general practice: a case study of routine screening for partner abuse | Literature review, very good for references | QVI – No gold standard |
| Brown et al., 1996235 | Development of the woman abuse screening tool for use in family practice | None given | QII – No comparator group as such |
| McCloskey et al., 2005453 | Intimate partner violence and patient screening across medical specialities | Women’s behaviour | |
| Busch et al., 2002454 | Battered women speak out | Barriers to disclosure | QVI – Not a longitudinal study, doesn’t meet inclusion criteria |
| Gill, 2004455 | Voicing the silent fear: south Asian women’s experiences of domestic violence | Barriers to disclosure but not attitudes to screening | |
| Edwardsen et al., 2004456 | Pilot educational outreach project on partner violence | Not only about screening rates | |
| Rodriguez et al., 2001457 | Factors affecting patient–physician communication for abused Latina and Asian immigrant women | Not about attitudes to screening | |
| Gerbert et al., 1999458 | How HCP help battered women: the survivors’ perspective | Not about attitudes to screening | |
| Burge et al., 2005459 | Parents advice to physicians about intervening in family contact | Doesn’t have subgroup analysis for women’s attitudes | |
| Zink et al., 2004460 | Hidden victims: the health-care needs and experiences of older women in abusive relationships | Not about attitudes to screening | |
| Hegarty and Taft, 2001461 | Overcoming barriers to disclosure and inquiry of partner abuse for women attending general practice | Not about attitudes to screening | |
| Romito and Gerin, 2002462 | Asking patients about violence: a survey of 510 women attending social and health services in Trieste, Italy | Not about attitudes to screening | |
| Larsen et al., 1985463 | Vold mod kvinder i samlivsforhold | Not relevant. Violence against women in their partnerships. Pattern of contact with public institutions | |
| Stenius and Veysey, 2005464 | It’s the little things – women, trauma and strategies for healing | Views on interventions, not screening | |
| Question IV | |||
| Savage and Russell, 2005465 | Tangled in a web of affiliation. Social support networks of dually diagnosed women who are trauma survivors | Baseline comparisons only | |
| Reed and Mazelis, 2005466 | Scholarship, collaboration, struggle and learning in the WCDVS: introduction to the 6-month outcome papers | Not an intervention study | |
| Finkelstein et al., 2005467 | Building resilience in children of mothers who have co-occurring disorders and histories of violence | Intervention is aimed directly at children | |
| Jaffe et al., 1986468 | Promoting changes in attitudes and understanding of conflict resolution among child witnesses of family violence | Intervention is aimed directly at children | |
| McCaw et al., 2002469 | Women referred for on-site DV services in a managed care organisation | Not reporting a controlled intervention | |
| Foshee et al., 2005470 | Assessing the effects of the dating violence prevention programme ‘Safe Dates2’ using random coefficient regression modelling | Primary prevention | |
| Riesen and Porath, 2004471 | Perceived social support of maritally abused women and their children’s global self-worth | Not assessing the effectiveness of an intervention | |
| Sullivan et al., 1992472 | After the crisis: a needs assessment of women leaving a domestic violence shelter | Not qualitative | |
| Foshee et al., 2004473 | Assessing the long-term effects of the ‘Safe Dates’ programme and a booster in preventing and reducing adolescent dating violence victimisation and perpetration | Primary prevention | |
| Davies, 1991474 | Intervention with male toddlers who have witnessed parental violence | Not an intervention study (single case study) | |
| Khemka et al., 2005475 | Evaluation of a decision-making curriculum designed to empower women with mental retardation to resist abuse | Primary prevention | |
| Weisz, 2005476 | Reaching African American battered women: increasing the effectiveness of advocacy | Not a health-care setting | |
| Panchanadeswaran and Koverola, 2005388 | The voices of battered women in India | Not reporting the effectiveness of an intervention | |
| Cannon and Sparks, 1989477 | Shelters – an alternative to violence: a psychosocial case study | Case study | |
| McBride and Korell, 2005478 | Wilderness therapy for abused women | Descriptive paper | |
| Rhodes and Zelman, 1986479 | An ongoing multifamily group in a women’s shelter | Not assessing the effectiveness of an intervention | |
| Angless et al., 1998480 | Battered women seeking solutions. A South African study | Not assessing the effectiveness of an intervention | |
| Attala and Warmington, 1996481 | Client’s evaluation of health-care services in a battered women’s shelter | No controls | |
| Frick-Helms, 1997482 | ‘Boys cry better than girls’: play therapy behaviours of children residing in a shelter for battered women | Descriptive paper | |
| Evans and Shaw, 1993483 | A social group work model for latency-aged children from violent homes | Not a controlled intervention study | |
| Grusznski et al., 1988484 | Support and education groups for children of battered women | Descriptive, not a controlled evaluation | |
| Walker, 2001485 | DV: analysis of a community safety alarm system | Not women-centred outcomes | QVII– Not screening cost-effectiveness |
| Thomas et al., 2005486 | Telepsychiatry programme for rural victims of DV | No controls | |
| Drotar et al., 2003487 | Identifying and responding to the mental health service needs of children who have experienced violence: a community-based approach | No controls | |
| Kozlowska and Hanney, 2001488 | An art therapy group for children traumatised by parental violence and separation | Not a controlled study | |
| Hillard, 1985489 | Physical abuse in pregnancy | Not assessing the effectiveness of an intervention | QV – No baseline measure |
| Short et al., 2002490 | Assessing the success of the WomanKind programme: an integrated model of 24-hour health-care response to DV | No women-based outcomes | QV – No baseline measure; QVI – Doesn’t measure the acceptability of routine screening |
| Bennett et al., 1999491 | Children’s needs in shelters: mothers’ perceptions | Not a health-care intervention; needs addressed are for the shelter not a health-care intervention | |
| Sullivan, 2003492 | Using the ESID model to reduce intimate male violence against women | Trial data published elsewhere | |
| Vives et al., 2006493 | Deteccion temprana de la violencia del companero intima en el sector sanitario. Una intervencion basada en la evidencia? | Systematic review | |
| Few, 2005494 | The voices of black and white rural battered women in DV shelters | Qualitative, but does not look at health-care services | |
| Kerig et al., 2000495 | Assessment and intervention for PTSD in children exposed to violence | Guidelines and review of PTSD in children | |
| Cook and Frantz-Cook, 1984496 | A systematic treatment approach to wife battering | Not woman-centred intervention | |
| Gehart and Morales, 2000497 | Reclaiming one’s voice: a narrative intervention for women who have been battered | Descriptive, not evaluative of a therapy for abused women | |
| Yoshihama, 2002498 | Policies and services addressing DV in Japan: from non-interference to incremental changes | Narrative | |
| Webb, 1992499 | Treatment issues and CBT with battered women | Narrative | |
| Milner, 2004500 | From ‘ disappearing’ to ‘demonized’: the effects on men and women of professional interventions based on challenging men who are violent | Wrong population | |
| Martin, 1993501 | Psychotherapy with abused women in a women’s agency | Narrative | |
| Datner et al., 2004502 | Universal screening for IPV: inability to prove universal screening improves provision of services | Observational study, not an intervention | |
| Scott-Tilley, 1999503 | Nursing interventions for DV | Not assessing the effectiveness of an intervention | |
| Van Dalen and Glasserman, 1997504 | My father, Frankenstein | No quantitative data | |
| Usdin et al., 2005505 | Achieving social change on gender-based violence: a report on the impact evaluation of Soul City’s fourth series | Primary prevention at a community/national level | |
| Coker et al., 2003506 | Social support protects against the negative effects of partner violence on mental health | Cross-sectional study, not an intervention | |
| Frohmann, 2005507 | The framing safety project. Photographs and narratives by battered women | Discussion of a qualitative study, but not about what is needed re health outcomes from an intervention | |
| Mueller and Thomas, 2001508 | The effectiveness of public health interventions to reduce or prevent spousal abuse towards women | Systematic review, but check references | |
| Jones et al., 2005509 | Family support and mental health in pregnant women experiencing IPV: an analysis of ethnic differences | No intervention | |
| Rosen and Stith, 1993510 | Intervention strategies for treating women in violent dating relationships | Qualitative, but not outcomes women want from interventions | |
| Kataoka et al., 2006511 | A community participatory research partnership: the development of a faith-based intervention for children exposed to violence | Not IPV | |
| Silvern et al., 1995512 | Individual psychotherapy for the traumatised children of abused women | Narrative and only about intervening with children not the mother | |
| Kerig et al., 2000495 | Assessment and intervention for PTSD in children exposed to violence | Narrative | |
| Rabenstein and Lehmann, 2000513 | Mothers and children together: a family group treatment approach | No control group, only discussion and no evaluation | |
| Ahmed, 2005514 | IPV against women: experiences from a woman-focused development programme in Matlab, Bangladesh | Not an evaluation of an intervention aimed at abused women, and not relevant to health care | Q1 – Not UK prevalence |
| Becker and Gatz, 2005515 | Introduction to the impact of co-occurring disorders and violence study | Background to the other studies, no data | |
| Coker et al., 2003506 | Social support reduces the impact of partner violence on health: application of structural equation models | Not an evaluation of an intervention | Q1 – Not a review |
| Kheder and VandenBosch, 2001516 | IPV: a health system’s response | Protocol, not a controlled intervention | |
| Rhodes and Levinson, 2003517 | Interventions for IPV against women | Case studies around screening | |
| Datner et al., 2004502 | Universal screening for DV. Inability to prove JCAHO-mandated screening makes an immediate impact | Observational study, not about post-identification intervention | |
| Ambuel et al., 1996518 | Partner violence: a systematic approach to identification and intervention in outpatient health care | Guidelines, not an intervention | |
| Campbell et al., 2003519 | Medical lethality assessment and safety planning in DV cases | Narrative, guidelines | |
| Berkowitz, 2005520 | Recognising and responding to DV | Narrative | |
| Duggan et al., 2004521 | Randomised trial of a statewide home visiting programme: impact in preventing child abuse and neglect | Child abuse, not IPV | |
| Varvaro, 1998337 | Violence against women: the role of orthopaedic nurses in the identification, assessment, treatment and care for the abused woman | Not relevant, narrative | |
| Mattson and Ruiz, 2005522 | IPV in the Latino community and its effect on children | Descriptive and intervention is aimed directly at children. Qualitative focus groups, but not about outcomes of interest | |
| Webb et al., 2001523 | The health of children in refuges for women victims of DV: a cross-sectional descriptive survey | No evaluation of an intervention | |
| Ham et al., 2005524 | Life constraints and psychological well-being of DV shelter graduates | Not a controlled intervention | |
| Goodkind et al., 2004525 | A contextual analysis of battered women’s safety planning | Not a quantitative evaluation of an intervention | |
| Vinton, 2003526 | A model collaborative project toward making DV centres elder ready | Narrative, no data | |
| Stein et al., 2003527 | A mental health intervention for school children exposed to violence. A randomised controlled trial | Mothers are not involved in the treatment | |
| Quinlivan and Evans, 2005528 | Impact of DV and drug abuse in pregnancy on maternal attachment and infant temperament in teenage mothers in the setting of best clinical practice | Not suitable control group (had not experienced IPV) | |
| McDermott, 2004529 | When advocacy for DV victims backfires. Types and sources of victim disempowerment | Narrative | |
| Peled, 1997530 | Intervention with children of battered women | Narrative | |
| Walton-Moss and Campbell, 2002531 | IPV: implications for nursing | Review | |
| Hotch et al., 1996532 | An ED-based DV intervention programme: findings after one year | Not an intervention study | |
| Breton and Nosko, 2005533 | Group work with women who have experienced abuse | Narrative | |
| Sudermann et al., 2000534 | Evaluation of the London (Ontario) Community Group Treatment Programme for Children who have Witnessed Woman Abuse | Intervention is directed at the children, rather than mothers | |
| Pynoos and Eth, 1986535 | Special intervention programmes for child witnesses to violence | Narrative, child-centred intervention | |
| Foshee et al., 1998536 | An evaluation of Safe Dates, an adolescent dating violence prevention programme | No health outcomes | |
| Goodman et al., 2005537 | Women’s resources and use of strategies as risk and protective factors for reabuse over time | Not an intervention | |
| Bybee and Sullivan, 2002538 | The process through which an advocacy intervention resulted in a positive change for battered women over time | Not a primary study | |
| MacMillan and Wathen, 200118 | Prevention and treatment of violence against women. Systematic review and recommendations | Review. Check why excluded Berk et al., 1996 | |
| Allen et al., 2004539 | Battered women’s multitude of needs. Evidence supporting the need for comprehensive advocacy | Expanding on findings published in another paper. Outcomes not health related | |
| Statham, 2004540 | Effective services to support children in special circumstances | Review | |
| Groves, 1999541 | Mental health services for children who witness DV | Narrative. Check references | |
| Tutty et al., 1999542 | Residents’ views of the efficacy of shelter services for assaulted women | Women’s views on shelters are too removed from health-care settings | |
| Graham-Bermann and Hughes, 2003543 | Intervention for children exposed to IPV: assessment of needs and research priorities | Review | |
| Haggerty and Goodman, 2003544 | Stages of change-based nursing interventions for victims of IPV | Narrative | |
| Hender, 20018 | Is therapy/counselling/group work more effective than no treatment for women who are victims of DV? | Not primary study | |
| Ogle and Baer, 2003545 | Addressing the service linkage problem. Increasing substance abuse treatment engagement using personalised feedback interventions in heavy-using female domestic violence shelter residents | Wrong outcomes, doesn’t measure change in abuse or health | |
| Davis et al., 2001546 | Narrative accounts of tracking the rural DV survivors’ journey: a feminist approach | Not related to health-care settings | |
| Gutman et al., 2004547 | Enhancing independence in women experiencing DV and possible brain injury: an assessment of an occupational therapy intervention | No DV survivors subgroup analysis | |
| Norton and Schauer, 1997548 | Hospital-based DV group | Not qualitative, wrong outcomes (looks at satisfaction) | |
| Chalk, 2000549 | Assessing family violence interventions: linking programmes to research-based strategies | Not a primary study | |
| Wathen and MacMillan, 2003550 | Interventions for violence against women: scientific review | Review | |
| Noether et al., 2005551 | Design strengths and issues of SAMHSA’s Women Co-occurring Disorders, and Violence Study | Not assessing the effectiveness of an intervention | |
| McFarlane et al., 2004136 | Protection orders and IPV: an 18-month study of 150 black, Hispanic and white women | Not a health-care setting | |
| Sullivan and Allen, 2001552 | Evaluating coordinated community responses for abused women and their children | Narrative | |
| Peled and Edleson, 1998553 | Predicting children’s DV service participation and completion | Intervention is child-centred | |
| Bullock, 1998554 | Nursing interventions for abused women on obstetrical units | Narrative | |
| Stone, 1984555 | Shelters for battered women: a temporary escape from danger or the first step toward divorce? | Not assessing the effectiveness of an intervention (descriptive study) | |
| Chambers, 1988556 | Group work with women from refuges | Narrative, no quantitative data | |
| Barber et al., 2000557 | A survivor’s group for women who have a learning disability | Not IPV, childhood abuse | |
| Gilson, 1997558 | The YWCA women’s advocacy programme: a case study of DV and sexual assault services | Not an intervention, service evaluation | |
| Gondolf, 1999559 | Characteristics of court-mandated batterers in four cities | Intervention aimed at batterers | |
| Zust, 2000560 | Effect of cognitive therapy on depression in rural, battered women | No usable data | |
| Veysey and Clark, 2004561 | Responding to physical and sexual abuse in women with alcohol and other drug and mental disorders: programme building. Introduction | Not assessing the effectiveness of an intervention | |
| McHugo et al., 2005562 | Women, Co-occurring Disorders, and Violence Study: evaluation design and study population | Not a primary study | |
| Preston, 2002563 | Claiming our place: women with serious mental health issues and support groups for abused women | Examines what women want from an intervention, but not outcomes they want for themselves or their children | |
| McFarlane et al., 1997133 | Resource use by abused women following an intervention programme: associated severity of abuse and reports of abuse ending | Pre-2003 | |
| Mullender et al., 1998564 | Working with children in women’s refuges | Qualitative, but doesn’t address outcomes abused women want for themselves or their children | |
| Brown and Languedoc, 2004565 | Components of an aboriginal-based family violence intervention programme | Wrong population (senior staff in national and provincial family violence divisions), not outcomes women want | QIII – Exclude, nothing on acceptability of screening |
| Ulrich, 1993566 | What helped most in leaving spouse abuse: implications for interventions | Narrative | |
| Shavers et al., 2005567 | DV research: methodological issues related to a community-based intervention with a vulnerable population | Narrative | |
| Parker et al., 1999131 | Testing an intervention to prevent further abuse to pregnant women | Is in PRP review | QV – Not just about screening but a full intervention |
| Seagull and Seagull, 1991568 | Healing the wound that must not heal: psychotherapy with survivors of DV | Narrative | |
| Clapp, 2000569 | Ending DV is everyone’s responsibility: an integrated approach to DV treatment | Narrative | |
| Campbell, 1986570 | A survivor group for battered women | Narrative | |
| Gorgen and Nagele, 2005571 | Nahraumgewalt gegen alte Menschen | Wrong population – older abused people without a subgroup analysis | |
| Morrissey et al., 2005572 | Outcomes for women with co-occurring disorders and trauma: programme and person-level effects | Not all participants experienced IPV | |
| Krishnan et al., 2004573 | From respite to transition: women’s use of DV shelters in rural New Mexico | Not assessing the effectiveness of an intervention | |
| Dutton-Douglas and Dionne, 1991574 | Counselling and shelter services for battered women | Narrative | |
| Anglin and Sachs, 2003575 | Preventive care in the ED: screening for DV in the ED | Review | |
| Crockford et al., 1993576 | Play friendly and safe: a therapeutic group model for young children (5–8 years old) who have witnessed wife assault | Descriptive rather than evaluative | |
| Jaffe et al., 1988577 | Specific assessment and intervention strategies for children exposed to wife battering: preliminary empirical investigations | Child-centred study | |
| Whipple and Lindsey, 1999578 | Music for the soul: a music therapy programme for battered women | No baseline data | |
| Peled and Edleson, 1992579 | Multiple perspectives on groupwork with children of battered women | Mixed sample of fathers and mothers, and no quotes just from mothers on outcomes they want for their children. | |
| Morrissey et al., 2005580 | Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders | Not all participants had experienced IPV and no breakdown of results | QV – No data on referrals, identification, etc. |
| Curry et al., 2006581 | Nurse care management for pregnant women experiencing or at risk for abuse | Not all participants had experienced IPV, some were just at risk, and no breakdown of results | |
| Padala et al., 2006582 | Risperidone monotherapy for post-traumatic stress disorder related to sexual assault and domestic abuse in women | Not all participants had experienced IPV and no breakdown of results | |
| Kane, 2006583 | The phenomenology of meditation for female survivors of intimate partner violence | No control group | |
| Shim and Haight, 2006584 | Supporting battered women and their children: perspectives of battered mothers and child welfare professionals | Not outcomes women want for themselves from interventions | QIII – Nothing related to screening |
| Bullock et al., 2006585 | Abuse disclosure in privately and Medicaid-funded pregnant women | Not all women experienced IPV | QV – Disclosure only |
| Katz et al., 2006586 | Domestic violence, emotion coaching and child adjustment | Not assessing the effectiveness of an intervention | |
| Parker and Stewart, 2006587 | Research and intervention with adolescents exposed to domestic violence | The intervention does not include an element for abused mothers | |
| Zust, 2006588 | Meaning of insight participation among women who have experienced intimate partner violence | Not about outcomes women want for themselves from an intervention | |
| Ford-Gilboe et al., 2006589 | Developing an evidence-based health advocacy intervention for women who have left an abusive partner | Not assessing the effectiveness of an intervention | QV – No outcomes of interest |
| Buschel and Madsen, 2006590 | Strengthening connections between mothers and children: art therapy in a domestic violence shelter | Not a controlled trial | |
| Bergeron and Herbert, 2006591 | Evaluation d’ une intervention de groupe d’approche feministe auprès de femmes victims d’aggression sexuelle | No separate data for IPV only | |
| Lewis et al., 2005389 | Perceptions of service providers and community members on intimate partner violence within a Latino community | Not attributable to screening | QIII – Not attitude to screening |
| Brienza et al., 2005592 | Evaluation of a women’s safe shelter experience to teach internal medicine residents about intimate partner violence | Not an intervention with battered women | QV – Not about changes in referral, etc. from screening; QVI – Not about whether training has had any impact on acceptability and screening |
| Fugate et al., 2006439 | Barriers to domestic violence help-seeking | Not about outcomes women want from an intervention | QIII – Not about barriers to screening |
| Thompson et al., 2000169 | Identification and management of DV, a randomised trial | No outcomes other than identification | QVI – No measure of acceptability |
| Ramsay et al., 20022 | Should health professionals screen women for domestic violence? Systematic review | Review | QVI – Review |
| Question V | |||
| Coonrod et al., 2000593 | A randomised controlled study of brief interventions to teach residents about domestic violence | Identification rate only | |
| Coonrod et al., 2000593 | The effectiveness of an ED-based violence prevention programme | Under 15-year-olds in sample | |
| Larkin et al., 2000594 | Effect of an administrative intervention on rates of screening for domestic violence in an urban emergency department | Identification rate only | |
| Holtrop et al., 2004595 | Screening for DV in a general paediatric clinic: Be prepared! | Identification rate only | |
| Olson et al., 1996596 | Increasing emergency physician recognition of domestic violence | Identification rate only | |
| Morrison et al., 2000597 | Improving the ED detection rate of DV using direct questioning | Identification rate only | |
| Wenzel et al., 2004598 | DV prevalence and detection in a family medicine residency clinic | Identification rate only | QV, QVI |
| McFarlane and Wiist, 1996599 | Documentation of abuse to pregnant women: a medical chart audit in public health clinics | Identification rate only | |
| Ernst and Weiss, 2002600 | IPV from the emergency medicine perspective | Not a primary study | |
| Richter et al., 2003601 | Detecting and documenting IPV | Not a controlled study – no baseline data | |
| Du Mont et al., 2005602 | Changing help-seeking rates for IPV in Canada | Not a health-care population | |
| Spinola et al., 1998603 | Developing and implementing an intervention | No data given | |
| Campbell et al., 2001604 | An evaluation of a system-change training model to improve emergency department response to battered women | No data given | |
| Perrin et al., 2000605 | Continuing education about physically abusive relationships: does education change the perceptions of health-care practitioners? | No clinical outcome measures – not about morbidity or mortality | |
| Siegel et al., 2003606 | Screening for DV in the paediatric office: a multi-practice experience | Prevalence study | |
| Stenson et al., 2001607 | The prevalence of violence investigated in a pregnant population in Sweden | No data on morbidity or mortality, e.g. referrals | |
| Morrissey et al., 2005580 | Twelve-month outcomes of trauma-informed interventions for women with co-occuring disorders | No data on morbidity or mortality, e.g. referrals | QIV – Included |
| Dodge et al., 2002608 | Improving IPV protocols for ED | Identification rate only; documentation not in sufficient detail | |
| Garcia and Parson, 2002609 | Effective screening for DV in the inpatient obstetric setting | Identification rate only | |
| Kothari and Rhodes, 2006610 | Missed opportunities: ED visits by police-identified victims of IPV | Not a health-care population | |
| Coker et al., 2002611 | Missed opportunities: IPV in family practice settings | Documentation not in sufficient detail, Identification rate only | QII – Medical records not a valid comparator |
| Sixsmith et al., 1997612 | Telephone follow-up for case findings of DV in an ED | Identification rate only | |
| Korenstein et al., 2003613 | An evidence-based DV education programme for internal medicine residents | Not about morbidity or mortality | |
| Hollander et al., 2001614 | The effects of written informed consent on detection of violence in the home | Looks at methodological design; Identification rate only | |
| Garcia-Moreno, 2002615 | Dilemmas and opportunities for an appropriate health-service response to violence against women | Not a primary study | |
| Agar et al., 2002616 | Identification of abuse histories in community mental health care: the need for policies and training | Males in sample | |
| Paluzzi et al., 2000617 | The American College of Nurse-Midwives’ DV education project: evaluation and results | Not about morbidity or mortality | |
| Shields et al., 1998618 | Interdisciplinary health care and female victims of DV | Not about mortality or morbidity | |
| Porcerelli et al., 2003619 | Violent victimisation of women and men: physical and psychiatric symptoms | Identification rates only | |
| Espinosa and Osborne, 2002620 | DV during pregnancy: implications for practice | Not a primary study | |
| Berenson, 1994621 | Perinatal morbidity associated with violence experienced by pregnant women | Not relevant to any review question | |
| Wallace, 2002622 | DV: an education programme for hospital staff | Not about effect of screening on morbidity or mortality | |
| Shattuck, 2002623 | A DV screening programme in the public health department | Identification rate only | |
| Matevia et al., 2002624 | Detection of IPV among members of a managed behavioural health organisation | Not a health-care setting | |
| Tilden and Shepherd, 1987625 | Increasing the rate of identification of battered women in an ED: use of a nursing protocol | Identification rate only | |
| Roberts et al., 1997626 | DV in the ED: 2. Detection by doctors and nurses | Males in sample | |
| Bergman and Brismar, 1991627 | A 5-year follow-up study of 177 battered women | Not about morbidity or mortality | |
| Tutty, 1996138 | Post-shelter services: the efficacy of follow-up programmes for abused women | Not about screening | QIV – Pre-2003 |
| Muelleman and Feighny, 1999628 | Effects of an ED-based advocacy programme for battered women on community resource utilisation | Not relevant to QIV | QIV – Pre-2003 |
| Wessel and Campbell, 1997629 | Providing sanctuary for battered women: Nicaragua’s Casas de la Mujer | Not about screening | QIV – Not about outcomes women want for themselves (outcomes are intervention-centred) |
| Vives et al., 2004630 | Temporal analysis of mortality due to intimate partner violence in Spain | Not about screening | |
| Allert et al., 1996631 | Domestic violence: efficacy of health provider training in Utah | Cross-sectional survey, plus no baseline data | QVI – Not about attitudes to screening |
| Glowa et al., 2003632 | What happens after we identify IPV? The family physician’s perspective | Cross-sectional survey, not a longitudinal or RCT design | QVI – Does not report attitudes to screening |
| Thompson et al., 1998633 | A training programme to improve domestic violence identification and management in primary care: preliminary results | Not investigating mortality or morbidity | QVI – No information on attitudes to screening |
| Davis et al., 2003634 | Victims of DV on the trauma service: unrecognised and under-reported | Definition of abuse includes elder and child abuse + males in sample | QVI – Same |
| Kohl et al., 2005635 | Child welfare as a gateway to domestic violence services | Epidemiological study in associated factors of DV services | |
| Rodriguez et al., 2001457 | The factors associated with disclosure of IP abuse to clinicians | Cross-sectional survey | QIII – Not about attitudes to screening |
| Davila, 2006636 | Increasing nurses’ knowledge and skills for enhanced response to IPV | No clinical outcomes or Identification rate | |
| McNulty et al., 2006637 | Can screening for domestic violence be introduced successfully in a sexual health clinic? | Identification rate only | |
| McCaw and Kotz, 2005638 | Family violence prevention programme: another way to save a life | Narrative | |
| Duncan et al., 2006639 | Individualised performance feedback to increase prenatal domestic violence screening | Screening rate only, no other clinical outcomes | |
| Short et al., 2006640 | A community-based trial of an online IPV CME programme | No clinical outcomes | |
| Wong et al., 2006641 | Increased awareness of IPA abuse after training: a randomised controlled trial | Identification rate only | |
| Hsieh et al., 2006642 | Changing dentists’ knowledge, attitudes and behaviour regarding domestic violence through an interactive multimedia tutorial | Intended behaviour as opposed to actual behaviour taken from medical records, etc. | QVI – Not routine enquiry/screening |
| Jonassen and Mazor, 2003643 | Identification of physician and patient attributes that influence the likelihood of screening for intimate partner violence | Not longitudinal design | QVI – Not attributable to screening, but behaviour |
| Rodriguez et al., 1999644 | Screening and intervention for intimate partner abuse: practices and attitudes of primary care physicians | Not a longitudinal design | QVI – Not about attitudes to screening; it is about behaviours |
| Brienza et al., 2005592 | Evaluation of a women’s state shelter experience to teach internal medicine residents about intimate partner violence | Not about changes in referral, etc. from screening | QIV – Not an intervention with battered women; QVI – Not about whether training has had an impact on acceptability and screening |
| Wenzel et al., 2004598 | Domestic violence: prevalence and detection in a family medicine residence clinic | None given | QVI – Not about attitudes to screening |
| Harris et al., 2002645 | Can internet-based education improve physician confidence in dealing with domestic violence? | Not based on rates or identification | QVI – Not about attitudes to screening |
| Gerber et al., 2005646 | How and why community hospital clinicians document a positive screen for intimate partner violence: a cross-sectional study | Not a controlled study | QVI – None given |
| D’Avolio et al., 2001647 | Screening for abuse: barriers and opportunities | No baseline data | |
| Kripke et al., 1998648 | Domestic violence training programme for residents | Not a longitudinal study | QVI – Does not state what the attitudes actually are |
| Danis, 2003649 | Social work response to domestic violence: encouraging news from a new look | One-shot survey, not a controlled trial or longitudinal study | |
| Freund et al., 1996375 | Identifying domestic violence in primary care practice | Only identification rate given | QII – No gold standard; QIII – Refusal to answer questions |
| Gunn et al., 2006650 | Putting women-centred care into practice: a new approach to psychosocial risk assessment during pregnancy | No measure of identification rate, only depression (self-reported), proxy measure by itself not enough | QVI – Not about screening |
| Busch et al., 2002454 | Battered women speak out | Not a longitudinal study, doesn’t meet inclusion criteria | QIII – Barriers to disclosure |
| Ramsay et al., 20022 | Should health professionals screen for domestic violence? Systematic review | Review | QIV, QVI – Review |
| Question VI | |||
| Valdez et al., 2004651 | Experiencia de la parteras en la identificacion de mujeres maltratades durante el embarazo | Not about screening | |
| Krueger and Schafer, 2000652 | Physician awareness of domestic violence: does continuing medical education have an impact? | Screening behaviour | |
| Lavoie and Martin, 1991653 | L’aide psycho-sociale offerte par les medecins à la femme violentee par son conjoint | Not about screening | |
| Leblanc and Ouellet, 2004654 | Depistage de la violence conjugale: le role de l’infirmière | Literature review | |
| MMWR, 2000655 | Role of victims’ services in improving IPV screening by trained maternal and child health-care providers – Boston, MA, 1994–1995 | Not about attitudes to screening | |
| Zink et al., 2003656 | How children affect the mother/victim’s process in intimate partner violence | Not about attitudes to screening | |
| Saunders et al., 2005657 | TANF workers’ responses to battered women and the impact of brief worker training | Not about attitudes to screening | |
| Scobie and McGuire, 1999658 | The silent enemy – domestic violence in pregnancy | None given | |
| D’Avolio et al., 2001647 | Screening for abuse – barriers and opportunities | None given | |
| Zink et al., 2005659 | Physician knowledge and management of children exposed to domestic violence in Ohio: a comparison of paediatricians and family physicians | None given | |
| Borowsky and Ireland, 2002660 | Parental screening by paediatricians and family physicians for intimate partner violence | None given | |
| Lapidus et al., 2002661 | A statewide survey of domestic violence screening behaviours among paediatricians and family physicians | None given | |
| Glaister and Kesling, 2002662 | A survey of practising nurses’ perspectives on interpersonal violence screening and intervention | None given | |
| Gerbert et al., 2002663 | Domestic violence compared to other health risks | None given | |
| Gadomski et al., 2001664 | Changes in health-care providers’ knowledge, attitudes, beliefs and behaviours regarding domestic violence following a multifaceted intervention | None given | |
| Chamberlain and Perham, 2002665 | The impact of perceived barriers on primary care physicians’ screening practices for female partner abuse | None given | |
| Goff et al., 2003666 | Preparedness of health-care practitioners to screen women for domestic violence in a border community | None given | |
| McGrath et al., 1997667 | Violence against women: provider barriers to intervention in emergency departments | Not specific enough to screening | |
| Zink et al., 2004668 | Intimate partner violence: what are physicians’ perceptions? | None given | |
| Steen and Bharj, 2003669 | Midwives’ reflections: exploring attitudes, feelings and experiences when caring for women who are being abused | Not a research study | |
| Price and Baird, 2001670 | Domestic violence in pregnancy | Does not address our review questions | |
| Moore et al., 1998671 | Attitudes and practices of registered nurses toward women who have experienced abuse/domestic violence | None given | |
| Brown and Sas, 1994229 | Focus groups in family practice research | None given | |
| Brown et al., 1993672 | Identifying and treating wife abuse | Does not address attitudes towards screening | |
| Dickson and Tutty, 1996673 | The role of public health nurses in responding to abused women | No attitudes to screening question | |
| Horan et al., 1998674 | Domestic violence screening practices of obstetrician/gynaecologists | Not about attitudes to screening | |
| Ortiz and Ford, 2005675 | Existence of staff barriers to partner violence screening and screening practices in military prenatal settings | None given | |
| Ferris, 1994676 | Canadian family physicians’ and general practitioners’ perceptions of their effectiveness in identifying and treating wife abuse | No attitude to screening question | |
| Janssen et al., 2003677 | Assessing for domestic violence exposure in primary care settings | Not about attitudes to screening | |
| Brienza et al., 2005592 | Evaluation of a women’s safe shelter experience to teach internal medicine residents about intimate partner violence | Not about whether training has had an impact on acceptability and screening | |
| Lanzilotti et al., 1999678 | EMS and the domestic violence patient: a report care of existing policy, protocol and training | Not about attitudes to screening | |
| Rodriguez et al., 1999644 | Screening and intervention for intimate partner abuse | Not about attitudes to screening but about behaviours | |
| Jonassen and Mazor, 2003643 | Identification of physician and patient attributes that influence the likelihood of screening for intimate partner violence | Not about attitudes to screening but about behaviours | |
| Harris and Kutob, 2002645 | Can internet-based education improve physician confidence in dealing with domestic violence? | Not about attitudes to screening | |
| Wenzel et al., 2004598 | Domestic violence: prevalence and detection in a family medicine residency clinic | Not about attitudes to screening | |
| Williams et al., 2000679 | Health promotion practices of emergency physicians | Not about attitudes to screening | |
| Gerber et al., 2005646 | How and why community hospital clinicians document a positive screen for intimate partner violence: a cross-sectional study | None given | |
| Tower, 2006680 | Barriers in screening women for domestic violence: a survey of social workers, family practitioners and obstetrician-gynaecologists | Because it targets screening behaviour not screening attitudes | |
| Kripke et al., 1998648 | Domestic violence training programme for residents | Does not state what the attitudes actually are | |
| Jones and Bonner, 2002398 | Screening for domestic violence in an antenatal clinic | No statistics | |
| Chamberlain and Perham-Hester, 2000681 | Physicians’ screening practices for female partner abuse during prenatal visits | Not about attitudes to screening | |
| Guedes et al., 2002682 | Integrating systematic screening for gender-based violence into sexual and reproductive health services: results of a baseline study by the International Planned Parenthood Federation, western hemisphere region | None given | |
| Ahmed et al., 2003683 | Response of Sudanese doctors to domestic violence | Talks about behaviour and barriers not attitudes to screening | |
| Smith et al., 1998684 | Changing the health-care response to battered women: a health-care education approach | Only measures screening behaviour | |
| Derk, 1998685 | Rural health-care providers’ attitudes, practices and training experience regarding intimate partner violence – West Virginia, March 1997 | No measures of attitudes towards screening | |
| Borowsky and Ireland, 1999686 | National survey of paediatricians violence prevention counselling | Not about attitudes to screening | |
| Garimella et al., 2002687 | How physicians feel about assisting female victims of intimate partner violence | Not about attitudes to screening | |
| Pakieser et al., 1998688 | Battered women – where they go for help | Not about attitudes to screening | |
| Bacigalupe, 2000689 | Family violence in Chile – exploring prevalence and clinical dimensions | Literature review | |
| Tilden, 1989690 | Response of the health-care delivery system to battered women | Literature review | |
| Weiss et al., 2000691 | EMT domestic violence knowledge and the results of an educational intervention | Not about attitudes to screening | |
| Sugg and Inui, 1992692 | Primary care physicians’ response to domestic violence | Not about attitudes to screening | |
| Tudiver and Permaul-Woods, 1996693 | Physicians’ perceptions of and approaches to woman abuse | Not about attitudes to screening | |
| Melvin, 1995694 | Domestic violence: the physician’s role | Clinical cases, nothing about attitudes to screening | |
| Chescheir, 1996695 | Violence against women; response from clinicians | Letters, not a primary study | |
| Plichta et al., 1996424 | Spouse abuse, patient–physician communication, and patient satisfaction | Not about attitudes to screening | |
| Limandri and Tildren, 1996696 | Nurses’ reasoning in the assessment of family violence | Not about attitudes to screening | |
| Parmar et al., 2005372 | Tackling domestic violence: providing advocacy and support to survivors from black and other ethnic minority communities | None given | |
| Director and Linden, 2004697 | Domestic violence: an approach to identification and intervention | Literature review, good for references | |
| Chez,1988698 | Woman battering | Not a primary study | |
| Jones, 1993699 | Domestic violence: let our voices be heard | Not a primary study, not about attitudes to screening | |
| Forcier et al., 2003700 | Paediatric residents’ attitudes and practices regarding adolescent dating violence | Not about attitudes to screening, about behaviours, barriers | |
| Groth et al., 2001701 | Domestic violence: level of training, knowledge base and practice among Milwaukee physicians | Nothing specific to screening attitudes | |
| Varjavand et al., 2004702 | A survey of residents’ attitudes and practices in screening for, managing and documenting domestic violence | About behaviour and barriers not attitudes | |
| Currier et al., 1996703 | Training and experience of psychiatric residents in identifying domestic violence | Not about attitudes to screening | |
| Gerbert et al., 1999704 | A qualitative analysis of how physicians with expertise in domestic violence approach the identification of victims | Only one vague result, which seems to be more of a barrier than an attitude per se. And only one sentence – not the main (or even secondary) focus of the study | |
| Larkin et al., 1999705 | Universal screening for intimate partner violence in the emergency department: importance of patient and provider factors | Nothing on attitudes | |
| Parsons et al., 1995706 | Methods of and attitudes toward screening obstetrics and gynaecology patients for domestic violence | Behaviour and barriers but not attitudes | |
| Erickson et al., 2001707 | Barriers to domestic violence screening in the paediatric setting | It is about actual behaviour and perceived barriers to screening, no mention of attitudes | |
| Haggblom et al., 2005708 | Nurses’ attitudes and practices towards abused women | Nought on attitudes, only behaviour and barriers | |
| Knapp et al., 2006271 | Evaluation of a curriculum for intimate partner violence screening in a paediatric emergency department | Cannot see anything specific to screening | |
| Davis and Harsh, 2001709 | Confronting barriers to universal screening for domestic violence | It’s about barriers mostly | |
| Ferris and Tudiver, 1992710 | Family physicians’ approach to wife abuse: a study of Ontario, Canada, practices | Does not refer to attitudes towards screening | |
| Heinzer and Krimm, 2002711 | Barriers to screening for domestic violence in an emergency department | No data about screening | |
| Varvaro and Gesmond, 1997712 | ED physician house staff response to training on domestic violence | Not about attitudes to screening | |
| De Wit and Davis, 2004713 | Nurses’ knowledge and learning experiences in relation to the effects of domestic abuse on the mental health of children and adolescents | Not about attitudes to screening | |
| Shearer et al., 2006714 | Chiropractors’ perceptions about intimate partner violence: a cross-sectional study | None given | |
| Renker, 2006715 | Perinatal violence assessment: teenagers’ rationale for denying violence when asked | Not really about attitudes to screening | |
| Rodriguez-Bolanos et al., 2005716 | Violencia de genero: actitud y conocimiento del personal de salud de Nicaragua | None given | |
| Mendez et al., 2003717 | Violencia contra la mujer: conocimiento y actitud del personal medico del Instituto Mexicano del Seguro Social, Morelos, Mexico | None given | |
| Tower, 2003718 | Domestic violence screening: education and institutional support correlates | Exclude – behaviour | |
| Short et al., 2002490 | Assessing the success of the Womankind Program: an integrated model of 24-hour health-care response to domestic violence | Not about attitudes to screening | |
| Janssen et al., 2002326 | Introducing domestic violence assessment in a postpartum clinical setting | Not about attitudes to screening | |
| Bryant and Spencer, 2002719 | Domestic violence: what do nurse practitioners think? | Screening behaviour | |
| Cann et al., 2001720 | Domestic violence: a comparative survey of levels of detection, knowledge, and attitudes in health-care workers | No screening attitudes question | |
| Varcoe, 2001400 | Abuse obscured: an ethnographic account of emergency nursing in relation to violence against women | Not really about attitudes to screening | |
| Elliott et al., 2002721 | Barriers to screening for domestic violence | Did not send us frequencies | |
| Hinderliter et al., 2003722 | The effect of intimate partner violence education on nurse practitioner feelings of competence and ability to screen patients | It is behaviour | |
| Ramsay et al., 200511 | Interventions to reduce violence and promote the physical and psychosocial well-being of women who experience partner violence: a systematic review of controlled evaluations | None given | |
| Edwards, 2005443 | Raising the subject of domestic violence | Not a primary study | |
| Gunn et al., 2006650 | Putting woman-centred care into practice: a new approach to psychosocial risk assessment during pregnancy | Not screening | |
| Schoening et al., 2004723 | Effect of an intimate partner violence educational programme on the attitudes of nurses | Not about screening | |
| Davies et al., 1996724 | Community health workers’ response to violence against women | Not about acceptability of screening | |
| Glowa et al., 2002725 | Increasing physician comfort level in screening and counselling patients for intimate partner violence: hands-on practice | No investigation of acceptability of screening | |
| Kurz, 1987726 | Emergency department responses to battered women: resistance to medicalisation | Does not directly address acceptability of screening | |
| Kelso, 1996727 | Selections from current literature: clinical detection of abuse | Literature review | |
| Krimm and Heinzer, 2002728 | Domestic violence screening in the emergency department of an urban hospital | Only screening rates | |
| Krantz et al., 2005729 | Intimate partner violence: forms, consequences and preparedness to act as perceived by health-care staff and district and community leaders in a rural district in northern Vietnam | Not about attitudes to screening | |
| Cohen et al., 1997730 | Barriers to physician identification and treatment of family violence: lessons from five communities | Not about screening | |
| Johnson and Benight, 2003731 | Effects of trauma-focused research on recent DV survivors | Not about screening | |
| Thompson et al., 2000169 | Identification and management of DV, a randomised trial | No measure of acceptability | |
| Gremillion and Kanof, 1996732 | Overcoming barriers to physician involvement in identifying and referring victims of domestic violence | Narrative | |
| Coeling and Harman, 1997733 | Learning to ask about domestic violence | Not about attitudes to screening | |
| Shadigian, 1996734 | Domestic violence: identification and management for the clinician | Narrative, overview | |
| Stayton and Duncan, 2005735 | Mutable influences on intimate partner abuse screening in health-care settings | Review | |
| Neufeld, 1996233 | SAFE questions: overcoming barriers to the detection of domestic violence | Narrative | |
| Kim and Motsei, 2002736 | ‘Women enjoy punishment’: attitudes and experiences of gender-based violence among PHC nurses in rural South Africa | Not about acceptability of routine screening | |
| Durant et al., 2000737 | Opportunities for intervention: discussing physical abuse during prenatal care visits | Not about factors that affect acceptability of screening | |
| Waalen et al., 20003 | Screening for intimate partner violence by health-care providers | Review | |
| Ronnberg and Hammarstrom, 2000738 | Barriers within the health-care system to dealing with sexualised violence: a literature review | Literature review | |
| Protheroe et al., 2003739 | An interview study of the impact of domestic violence training on midwives | Not about attitudes to screening | |
| Krugman et al., 2004740 | Perceptions of help resources for victims of intimate partner violence | Not about attitudes to screening | |
| Loring and Smith, 1994741 | Health-care barriers and interventions for battered women | Literature review | |
| Reid and Glasser, 1997742 | Primary care physicians’ recognition of and attitudes toward domestic violence | Not about attitudes to screening | |
| Gerbert et al., 2000743 | Interventions that help victims of domestic violence | No data about screening | |
| Larance and Porter, 2004744 | Observations from practice: support group membership as a process of social capital formation among female survivors of domestic violence | Not about attitudes to screening | |
| Ferris, 1994745 | Detection and treatment of wife abuse in aboriginal communities by primary care physicians: preliminary findings | Not about attitudes to screening | |
| Shea, 1997746 | Breaking through the barriers to domestic violence intervention | Not really about attitudes to screening | |
| Mortlock, 1996747 | The battered woman in the accident and emergency department | Letter | |
| Chung, 1996748 | Wife battering in Hong Kong: accident and emergency nurses’ attitudes and beliefs | Not really about screening | |
| Goodyear-Smith, 2002452 | National screening policies in general practice: a case study of routine screening for partner abuse | Literature review | |
| McHugo et al., 2005376 | The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence | Not about acceptability of routine screening | |
| Peltzer et al., 2003749 | Attitudes and practices of doctors towards domestic violence victims in South Africa | Not about attitudes to screening | |
| Peckover, 2002750 | Focusing upon children and men in situations of domestic violence: an analysis of the gendered nature of British health visiting | Not about attitudes to screening | |
| Hamberger, 2004751 | Evaluation of a health-care provider training programme to identify and help partner violence victims | Not about acceptability of screening | |
| Zachary et al., 2002752 | Provider evaluation of a multifaceted system of care to improve recognition and management of pregnant women experiencing domestic violence | Not about screening | |
| Kramer, 2002377 | Domestic violence – how to ask and how to listen | Narrative – not a validation study | |
| Carbonell et al., 1995753 | Florida physician and nurse education and practice related to domestic violence | None given | |
| Ramsay et al., 20022 | Should health professionals screen women for domestic violence? Systematic review | Review | |
| Bryant and Spencer, 2002719 | Domestic violence: what do nurse practitioners think? | Not about attitudes to screening but about behaviours | |
| Protheroe et al., 2004739 | An interview study of the impact of domestic violence training on midwives | Not about screening | |
| Taft et al., 2004754 | General practitioner management of intimate partner abuse and the whole family: qualitative study | Not about attitudes to screening | |
| Steen, 2000755 | Developing midwifery responses to women in their care who are living with violent men | Not really about attitudes to screening | |
| McKie et al., 2002756 | Time to disclose | Unclear | |
| McCosker et al., 1999432 | Evaluation of a self-paced education package on violence against women for rural community-based health workers | Nothing specific about screening attitudes | |
| Trute et al., 1988757 | Medical response to wife abuse: a survey of physicians’ attitudes and practices | Is it about screening? | |
| Davidson et al., 2001758 | Training programmes for health-care professionals in domestic violence | Good for references: it is a review | |
| Bessette and Peterson, 2002759 | Attitudes of adult nurse practitioner students towards women experiencing domestic violence | Not about screening attitudes | |
| Wright, 2003760 | Asking about domestic violence | Literature review, maybe for references | |
| Bates and Brown, 1998761 | Domestic violence: examining nurses’ and doctors’ management, attitudes and knowledge in an accident and emergency setting | No screening attitudes question | |
| Marchant et al., 2001762 | Addressing domestic violence through maternity services: policy and practice | It is about policies and practice related to DV | |
| Corbally, 2001763 | Factors affecting nurses’ attitudes towards the screening and care of battered women in Dublin A&E departments: a literature review | Literature review, good for references | |
| Frost, 1999764 | Health visitors’ perceptions of domestic violence: the private nature of the problem | Not about attitudes to screening | |
| Question unknown | |||
| Boyle et al., 200449 | Domestic violence in emergency medicine patients | Narrative | |
| Scales, 2004765 | Domestic violence awareness in the perianaesthesia setting | Narrative – not relevant to any questions | |
| Sullivan et al., 2005766 | Participatory action research in practice | Not relevant to any questions | |
| McAfee, 2001767 | Domestic violence as a women’s health issue | Narrative | |
| Dowd, 2004768 | The emerging role of the paediatric emergency department in IPV | Narrative/guidelines | |
| Shadigian and Bauer, 2004769 | Screening for partner violence during pregnancy | Narrative | |
| Ely, 2004770 | Domestic violence and immigrant communities in the USA: a review of women’s unique needs and recommendations for social work practice and research | Narrative | |
| Daniels, 2005771 | IPV and depression: a deadly comorbidity | Narrative | |
| Jaeger, 2000772 | Screening for DV | Narrative | |
| Lehrman and Berner, 1997773 | Physician as detective: discerning and recording DV injuries | Guidelines | |
| Cox, 2003774 | Synergy in practice: caring for victims of IPV | Not a primary study | |
| Koziol-McLain and Campbell, 2001775 | Universal screening and mandatory reporting: an update of two important issues for victims/survivors of IPV | Not a primary study | |
| Klein, 2001776 | Screening for risk of DV within HIV partner notification: evolving practice and emerging issues | Commentary | |
| Goodman and Epstein, 2005777 | Refocusing on women: a new direction for policy and research on IPV | Narrative | |
| Resick, 2004778 | A suggested research agenda on treatment-outcome research for female victims of violence | Narrative | |
| Watts, 2004779 | Screening for DV: a team approach for maternal/newborn nurses | Narrative | |
| Biroscak et al., 2006780 | IPV against women: findings from one state’s ED surveillance system | Not relevant to any review question | |
| Zlotnick et al., 2006781 | IPV and long-term psychosocial functioning in a national sample of US women | Q1 – not a review, not a health-care population | |
| Eisenstat and Bancroft, 1999782 | Domestic violence | Narrative | |
| Heath, 2001783 | DV as a women’s health issue | Not a primary study | |
| MMWR, 1994784 | Physical violence during the 12 months preceding childbirth – Alaska, Maine, Oklahoma, and West Virginia, 1990–1991 | Prevalence study | |
| Carlson, 2005785 | The most important things learned about violence and trauma in the past 20 years | Not a primary study | |
| Ferris et al., 1997786 | Documenting wife abuse: a guide for physicians | Guidelines | |
| Mayer and Liebschutz, 1998787 | DV in the pregnant patient: obstetric and behavioural interventions | Narrative | |
| Attala et al., 1999788 | An analysis of nurses’ communications in a shelter setting | Not about screening and not an intervention | |
| Nelms, 1999789 | An educational programme to examine emergency nurses’ attitudes and enhance caring intervention with battered women | Not about screening | |
| Jezierski, 1999790 | Family violence screening: opportunities in prehospital settings | Guidelines/think piece | |
| Campbell and Sheridan, 1989791 | Emergency nursing interventions with battered women | Narrative, guidelines | |
| Williams-Evans and Sheridan, 2004792 | Exploring barriers to leaving violent intimate partner relationships | Protocol for pilot, not about screening | |
| Loraine, 1981793 | Battered women. The ways you can help | Guidelines | |
| Short et al., 1997794 | Family violence: an intervention model for dental professionals | Model/guidelines | |
| Goldner, 1999795 | Morality and multiplicity: perspectives on the treatment of violence in intimate life | Narrative | |
| Davidhizar and Giger, 2002796 | Domestic violence | Narrative | |
| Humphreys et al., 2001797 | IPV against women | Narrative | |
| Schiavone and Salber, 1994798 | Hitting close to home. DV and the EMS responder | Guidelines | |
| Stark, 2004799 | Insults, injury and injustice | Narrative | |
| Thompson and Krugman, 2001800 | Screening for IPA at well-baby care visits. The right thing to do | Commentary | |
| Griffin and Koss, 2002801 | Clinical screening and intervention in cases of partner violence | Narrative | |
| Gantt and Bickford, 1999802 | Screening for DV | Guidelines | |
| El-Bayoumi et al., 1998803 | DV in women | Narrative | |
| Weiss, 2005804 | Domestic violence | Narrative | |
| Hannigan, 1999805 | DV: the response of health care | Guidelines | |
| Cassidy, 1999806 | How to assess and intervene in DV situations | Narrative | |
| Davidhizar et al., 1998807 | Recognising abuse in culturally diverse clients | Narrative | |
| Chiodo et al., 1998808 | The dentist and family violence | Narrative | |
| Butler, 1995809 | DV: a nursing imperative | Narrative | |
| Cattaneo and Goodman, 2005810 | Risk factors for re-abuse in IPV | Narrative | |
| Rickert et al., 2002811 | Adolescent dating violence and date rape | Review | |
| King, 1993812 | Changing women’s lives: the primary prevention of violence against women | Narrative | |
| Lundy and Grossman, 2001813 | Clinical research and practice with battered women. What we know, what we need to know | Review | |
| Ford-Gilboe et al., 2005814 | Strengthening capacity to limit intrusion: theorising family health promotion in the aftermath of woman abuse | Not about screening or interventions | |
| Coombes, 2004815 | Making a fist of it | Narrative | |
| Helton et al., 1987816 | Prevention of battering during pregnancy: focus on behavioural change | No data | |
| Belinger, 2001817 | Domestic violence: how you can make a difference | Narrative/guidelines | |
| Harris et al., 1997818 | The road to freedom: ending violence against women | No data | |
| Taket and Mann, 2005819 | Clinical effectiveness: information bulletin 18 | Information source | |
| Evans, 2001820 | Children living with domestic violence | Narrative | |
| Garcia and Davidson, 2002821 | Researching domestic violence and health: national perinatal epidemiology unit | Review | |
| Henderson and Ericksen, 1994822 | Enhancing nurses’ effectiveness with abused women | Not a primary study | |
| Hoff, 1993823 | Battered women: intervention and prevention | Narrative | |
| Wescott, 1995824 | Help for the hurting: when pregnant women are battered | Narrative | |
| Germain, 1984825 | Sheltering abused women: a nursing perspective | Narrative | |
| Baird et al., 2005826 | Learning from the Bristol Pregnancy and DV programme | Not about screening | |
| Hardacre, 2005827 | Routine enquiry into domestic abuse – the All-Wales Clinical Pathway | Narrative | |
| Powers, 2004828 | DV: what can nurses do? | Guidelines | |
| Kipps, 2005829 | Sexual health needs of women in violent relationships | Narrative/guidelines | |
| Willis and Porche, 2004830 | Male battering of intimate partners: theoretical underpinnings, intervention approaches and implications | Narrative | |
| Attala, 1996831 | Danger signs: detecting abuse against women in the home | Narrative | |
| McFarlane and Goodmark, 1998832 | Preventing abuse during pregnancy: a clinical protocol | Narrative | |
| Rhodes and Levinson, 2003517 | Interventions for IPV against women | Case studies and guidelines with not enough data | |
| Harris et al., 2005833 | Qualitative interviews on substance abuse relapse and prevention among female trauma survivors | Not relevant to any question | |
| Hassouneh Phillips, 2005834 | Understanding abuse of women with physical disabilities: an overview of the abuse pathway model | Not about screening | |
| Taket et al., 200316 | Routinely asking women about DV in health settings | Not a primary study | |
| Peled and Edleson, 1994835 | Advocacy for battered women: a national survey | Not really about screening | |
| Mohr et al., 2001836 | Safeguarding themselves and their children: mothers share their strategies | Not a health-care population | |
| Weitlauf et al., 2000837 | Generalisation effects of coping-skills training: influences of self-defence training on women’s efficacy beliefs, assertiveness and aggression | Not relevant to any question | |
| Turnbull, 2001838 | Domestic violence | Narrative | |
| Onyskiw, 2001839 | Research on violence and abuse in Canada: challenges and opportunities | Narrative | |
| Ryan and King, 1998840 | Scanning for violence | Narrative | |
| Belfiglio, 2001841 | Should primary care providers screen for DV? | Narrative | |
| Hague and Malos, 1996842 | Tackling DV: a guide to developing multiagency initiatives | Guidelines | |
| Henrion, 2005843 | Les violences conjugales pendant la grossesse: depistage et orientation par les soignants | Not about screening | |
| Chez, 1995844 | Aider les victims de la violence domestique: traces de coups | Not a primary study | |
| Nicolaidis and Touhouliotis, 2006845 | Addressing IPV in primary care: lessons from chronic illness management | Narrative | |
| Roberts and Roberts, 2005846 | Ending intimate abuse. Practical guidance and survival strategies | Narrative and case studies | |
Glossary
- Accident and emergency (A&E) department
- Hospital department providing emergency care.
- Advocacy
- Advocacy generally refers to the provision of support and access to resources in the community. In the UK, advocates tend to be employed outside the health system and are not qualified professionals. In the USA, advocates may be employed in health and community settings and are often qualified social workers.
- Counselling
- A form of psychological treatment, using a range of models. In the UK, this term is more generally used to denote formal psychological treatment provided by a qualified professional. In the USA, counselling may refer to empathetic support in the context of education and referrals (what would be termed ‘advocacy’ in the UK), or formal psychological treatment.
- Emergency department (ED)
- Non-UK term for accident and emergency department (see above).
- Integrative review
- Integrative reviews summarise past research and draw overall conclusions from the body of literature on a particular topic. They can include editorials and letters in addition to journal articles. They tend not to conduct secondary statistical analyses on identified studies.
- Matched, yoked and randomised design
- Design of a trial in which participants are matched (or yoked) together on specified variables (such as age), then one member of each grouping is randomly assigned to the intervention group and the other acts as a control.
- Nursing studies
- Studies published in nursing journals or studies whose authors have nursing credentials.
- Refuge
- A safe house where women experiencing domestic abuse can live free from violence.
- System-centred interventions
- Interventions that are designed to improve the response of the organisations and professionals that come into contact with abused women. The ultimate goal of these interventions is to improve outcomes for abused women, although such outcomes may not be measured directly. They include staff training interventions and the provision of more resources.
- Survivors of domestic violence
- Women who have experienced or are currently experiencing physical, sexual or emotional abuse from a husband or partner or ex-husband or ex-partner.
- Trauma centre
- A non-UK term for accident and emergency department (see above).
- Woman-centred interventions
- Interventions that are targeted directly at abused women with the aim of reducing abuse or improving the health of the women. They include advocacy and psychological interventions, including all forms of therapy and counselling.
List of abbreviations
- AAS
- Abuse Assessment Screen
- ANOVA
- analysis of variance
- ARI
- Abuse Risk Inventory
- ASI-A
- Addiction Severity Index Alcohol composite score
- ASI-D
- Addiction Severity Index Drug composite score
- AUC
- area under curve
- BDI
- Beck Depression Inventory
- BRFSS
- Behavioural Risk Factor Surveillance Survey
- BSI
- Brief Symptom Inventory
- CAPS
- Clinician Administered PTSD Scale
- CAS
- Composite Abuse Scale
- CASP
- Critical Appraisal Skills Programme
- CBCL
- Child Behaviour Checklist
- CBT
- cognitive behavioural therapy
- CES-D
- Center for Epidemiologic Studies Depression Scale
- CME
- continuing medical education
- CPP
- child–parent psychotherapy
- CRC
- Community Resources Checklist
- CSEI
- Coopersmith Self-esteem Inventory
- CTS (CTS2)
- Conflict Tactics Scale (Conflict Tactics Scale-Revised)
- DAS
- Danger Assessment Scale
- DC 0-3 TSD
- Diagnostic Classification 0-3 Traumatic stress disorder
- DOR
- diagnostic odds ratio
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders IV
- DV
- domestic violence
- ED
- emergency department
- EFI
- Enright Forgiveness Inventory
- EHQ
- Employment Harassment Questionnaire
- EMS
- emergency medical services
- EMT
- emergency medical technician
- EOR
- effectiveness in obtaining resources
- EPDS
- Edinburgh Postnatal Depression Scale
- ESID
- Experimental Social Innovation and Dissemination
- GP
- general practitioner
- GSI
- Global Severity Index
- HARK
- Humiliation, Afraid, Rape and Kick Screening Tool
- HCP
- health-care professional
- HEVAN
- Health Ending Violence and Abuse Now
- HITS
- Hurts, Insults, Threatens and Screams scale
- HMO
- health management organisation
- HSQ
- Health Screening Questionnaire
- ICER
- incremental cost-effectiveness ratio
- IPA
- intimate partner abuse
- IPC
- Internal-Powerful Others-Chance
- IPV
- intimate partner violence
- ISA (ISA-P, ISA-NP)
- Index of Spouse Abuse (Index of Spouse Abuse Physical and Non-Physical subscales)
- ISEL
- Interpersonal Support Evaluation List
- ITT
- intention to treat
- JCAHO
- Joint Commission on the Accreditation of Healthcare Organizations
- LBW
- low birth weight
- LR
- likelihood ratio
- MMPI-PTSD
- Minnesota Multiphasic Personality Inventory–Post-traumatic Stress Disorder
- MMTP
- Methadone Maintenance Treatment Programme
- MOOSE
- Meta-analysis of Observational Studies in Epidemiology
- NICE
- National Institute for Health and Clinical Excellence
- NPV
- negative predictive value
- NSC
- National Screening Committee
- ONS
- Office of National Statistics
- OR
- odds ratio
- OVAT
- Ongoing Violence Assessment Tool
- PCL-S
- PTSD Checklist Stressor Specific version
- PCT
- primary care trust
- PHC
- primary health care
- PHN
- public health nurse
- PPV
- positive predictive value
- PreDoVe
- Prevention of Domestic Violence study
- PSAI
- Perinatal Self-Administered Inventory
- PSS
- Post-traumatic Stress Disorder Symptom Scale
- PTSD
- post-traumatic stress disorder
- PVI
- Partner Violence Interview
- PVS
- Partner Violence Screen
- QALY
- quality-adjusted life-year
- QUADAS
- Quality Assessment of Diagnostic Accuracy Studies
- QUORUM
- Quality of Reporting of Meta-analyses of Randomised Controlled Trials (criteria)
- RADAR
- Routine screening; Ask direct questions; Document your findings; Assess patient safety; Review patient options and referrals (project)
- RAST
- Rape Aftermath Symptom Test
- RCT
- randomised controlled trial
- ROC
- receiver operating characteristic
- RPRS
- Relapse Prevention and Relationship Safety Programme
- RR
- relative risk
- RSEI
- Rosenberg Self-esteem Inventory
- S&S
- support and survival
- SAFE
- Stop Abuse for Everyone
- SAMHSA
- Substance Abuse and Mental Heralth Services Administration
- SCL-90-R
- Symptoms Checklist-90 Revised (psychiatric symptoms)
- SD
- standard deviation
- SE
- standard error
- SES
- socioeconomic status
- SF-36
- Short Form (36) Health Survey
- SRBQ
- Sexual Risk Behaviour Questionnaire
- STAI
- State–Trait Anxiety Inventory
- STaT
- Slapped, Threatened or Thrown scale
- STROBE
- Strengthening the Reporting of Observational Studies in Epidemiology
- SVAWS
- Severity of Violence Against Women Scale
- SWA
- Salford Women’s Aid
- TANF
- Temporary Assistance for Needy Families
- USPSTF
- United States Preventative Services Task Force
- VAWA
- Violence Against Women Act (of 1994)
- WAST
- Woman Abuse Screening Tool
- WCDVS
- Women, Co-occurring Disorders and Violence Study
- WEB
- Women’s Experience with Battering scale
- WHO
- World Health Organization
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
Health Technology Assessment Programme
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NCCHTA
-
Dr Andrew Cook, Consultant Advisor, NCCHTA
-
Dr Peter Davidson, Director of Science Support, NCCHTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NCCHTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NCCHTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NCCHTA
HTA Commissioning Board
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programmes, Research and Development Directorate, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington