Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 04/07/06. The contractual start date was in June 2005. The draft report began editorial review in January 2007 and was accepted for publication in June 2008. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Aim of the review
The aim was to provide a systematic literature review of the effectiveness and cost-effectiveness of breaks in care for informal carers of frail and disabled older people living in the community. The review includes a synthesis of both quantitative and qualitative data pertaining to the impact of respite care on users and carers.
Background
The ageing population
In 2002 4,464,000 people in the UK were aged 75 years and over1 and it is projected that the number of people over pensionable age will increase to over 15 million by 2040. 2 This will impact on health-care systems as age-related conditions become more common. In 2001 46% of people over the age of 75 years reported having a limiting long-standing illness. 3 The most frequently reported chronic conditions in people aged 65 years and over in 2001 were heart and circulatory diseases and musculoskeletal ailments. 4 Dementia is a particularly debilitating problem associated with ageing, with around one in 20 people aged 65 years and over having the condition, rising to around one in five people over 80 years of age. 5 Stroke is also one of the most prevalent causes of morbidity in older people. In the UK around 110,000 people per year experience a first stroke and a further 30,000 have recurrent strokes. 6
Provision of care for people with disabilities
Many older people with chronic conditions are cared for in the community, with their main source of support coming from informal carers. Such informal carers of the frail and elderly are frequently in mid- to later life themselves, being spouses or adult children of the care recipient. In 2001 almost 2.8 million people in England and Wales aged 50 years and over provided unpaid care for family members, friends or neighbours. In total, 24% of carers in the 50- to 60-year age group spend 50 hours per week or more on caring activities. 3,4 Although people from white British or white Irish backgrounds were more likely to be carers than other ethnic groups, this probably reflects the older age structure of the white UK-born population. However, Bangladeshi and Pakistani carers were just as likely to spend 50 hours a week or more on caring activities as their white UK counterparts, and numbers of ethnic minority carers will increase in the future as these populations age.
According to the General Household Survey3 women were more likely to be carers than men and have a heavy caring commitment of over 20 hours per week. About one-third of carers were the only means of support for the care recipient. In total, 21% of carers had been in a caring role for at least 10 years and 45% for 5 years or more; 62% of carers were looking after someone with a physical disability only, 6% with a mental disability only and 18% with both physical and mental disabilities; 14% reported caring for a person simply because they were ‘old’.
The types of help given by informal carers consisted mainly of practical help with activities of daily living (ADL) such as meal preparation, shopping and household tasks. A total of 60% reported that they ‘kept an eye’ on the person they cared for and 55% reported providing company; 26% gave more personal care such as personal hygiene and 35% reported helping with mobility.
Impact of caring on carers’ health and well-being
Caring can have a direct effect on health, such as physical strain and musculoskeletal problems, as well as causing emotional strain. It can also have an indirect effect on health status through lower earnings or income or increased costs when the recipient of care takes up residence with the carer. 7 As a result, carers tend to report poorer health than their peers who are not carers. Health is particularly poor among those who devote at least 20 hours a week to caring, with around half reporting a long-standing illness. 4 In many cases poor health is directly attributed to the caring role. In total, 39% of carers report that their physical or mental health has been impaired as a result of caregiving. Other complaints include tiredness, depression, loss of appetite, disturbed sleep, stress and short temper. Such complaints were higher in those caring for someone who lived in the same household than in those caring for someone living elsewhere, probably reflecting the number of hours spent caring and the level of care needed. 3,8,9
The impact of caring on mental health was explored in a survey carried out by the Office for National Statistics (ONS) for the Department of Health. 10 Neurotic symptoms were measured using the revised version of the Clinical Interview Schedule (CIS-R). Psychiatric morbidity was related to hours spent caring, with only 13% of those caring for less than 20 hours a week having a CIS-R score of 12 or more, compared with 27% of those spending 20–34 hours caring. Sole carers were more likely to have mental health problems than those not having the main responsibility for the care recipient. Mental health was also related to the ability to take a break from caring, with 36% of carers who had not had a break experiencing high levels of neurotic symptoms, compared with 17% of those able to take a break. Over half of the carers reported worrying about their caring responsibilities and one-third felt that caring had made them depressed. Relationships and social life were also adversely affected in around one-third of carers, which again was related to high levels of neurotic symptoms.
To capture the caring impacts on these different aspects of health and well-being, research studies have focused on the concept of ‘carer burden’. This is an all-encompassing term that refers to the financial, physical and emotional impact of caring. It may include factors such as restrictions to social activity of the carer, lack of privacy, impaired sleep, feelings of stress, satisfaction with the caregiving relationship, effects on family/job, etc. Carer outcome measures often include a general health measure and/or a standard measure of anxiety and depression. But it should also be noted that not all outcomes of caring are negative. Qualitative studies have reported positive feelings related to caring such as pride, gratification and a sense of closeness to the person being cared for. 8
The concept of carer burden is complex and is mediated by many factors. It is not necessarily the case that the carers of the most impaired patients experience the greatest stress and burden. 11 Factors such as age, gender and ethnicity play a role. Female carers experience greater burden than male carers. White carers have been reported to experience greater burden than African American carers. However, relationship may be a confounding factor in this context as white carers are more likely to be spouses and African Americans tend to be adult children of the care recipient, and it has been reported that spouses experience greater burden. 12 Other factors include carer support, carer health status, coping abilities and quality of the previous relationship with the care recipient. The type of problems displayed by the care recipient are also an important factor as it is suggested that carers of dementia patients experience greater stress than carers of individuals with physical disabilities, and it is specifically behaviour problems rather than cognitive impairment that cause most stress. 13
Definition of respite care
Respite care is traditionally defined as the provision of a temporary break in caregiving activities for the informal carer to reduce carer distress and promote well-being. 14 Respite care can be provided in a number of different ways. These include care as an inpatient of a care home or hospice, typically for 1 or 2 weeks, or adult day care (ADC) or in-home or sitting services. There are also some night-sitting services available. Care may be provided by a variety of bodies including voluntary services, social services or the NHS. However, operationalising a definition of respite care in a review is not straightforward. There are a number of situations when the carer may be physically separated from the caring role and the care recipient but the aim is not to achieve respite. For example, if the care recipient is admitted to hospital for medical treatment this may provide ‘respite’ for the carer; however, the aim of the intervention is to deal with a health event of the care recipient. The intervention will be focused on changing the health state of the care recipient and not the carer. The health and well-being of the carer may also be improved but it is difficult to determine to what extent this is due to a temporary relief in the caring responsibility or to an improvement in the care recipient’s health, functional abilities or dependence.
In an attempt to identify the specific effects of respite itself rather than interventions aimed at changing the state of the care recipient, this review takes a fairly restricted definition of respite care. The view is taken that respite is aimed at changing the well-being of the carer and so focuses on studies that explicitly state that the intervention is designed to provide respite for the carer and that assess carer outcomes. This also includes studies which evaluate interventions that have the potential to provide respite (such as day care or in-home service provision) without explicitly expressing the aim as being respite, but which focus on carer outcomes. It excludes studies that provide interventions whose primary purpose is to change the health state of the care recipient (e.g. rehabilitation interventions or highly medicalised interventions as in some palliative care contexts), as in this case it is more difficult to distinguish the effects of confounding factors. The aim was to include studies in which the normal care carried out by the informal carer is taken over for a set period of time by another person to allow the carer a break. However, it does not require the care recipient to be physically removed from the informal care context; for example, in-home care may provide respite without the carer actually leaving the home.
Definition of frail elderly
Frail elderly was defined as anyone over the age of 65 years in receipt of informal care from a relative or friend. In defining the older care recipient a cut-off of 65 years is common and most likely to be identified in studies of respite care. Frailty is not a concept that is consistently reported or defined in the relevant literature and so in this instance, with the focus on carers, it is assumed that anyone over the age of 65 years identified as having an informal carer can be defined as frail. The need for informal care suggests a certain level of disability whether it be cognitive or physical.
Questions addressed by the review
The questions addressed by the review are as follows.
-
How effective and cost-effective are respite interventions compared with no respite or other interventions?
-
What is the impact of respite interventions on care recipients?
-
What are the barriers to uptake of respite care?
-
What are carers’ expressed needs in relation to respite care?
Chapter 2 Review methods
The primary aims of the review were to identify and evaluate the quantitative and qualitative evidence base for the effectiveness of respite care for community resident frail elderly and to estimate the cost-effectiveness of respite care provided in various settings. The methods used to achieve these aims are outlined in the following sections and are based on guidance provided by the Centre for Reviews and Dissemination (CRD). 15
Operational definition of respite care in the frail elderly
Based on the discussion in Chapter 1 on the definition of respite care, the following operational definition will be used in the review (Box 1).
| Definition | Implications for the review |
|---|---|
| Care that aims to improve the well-being of the carer by providing substitution for the normal caring duties of the informal carer and not care that is aimed primarily at providing therapeutic intervention for the care recipient | Studies must report carer outcomes |
| Studies must explicitly state that the intervention aims to provide respite for the carer or the intervention provides substitution of care and carer outcomes are measured, e.g. day care | |
| Interventions intended to change the health state of the care recipient are excluded, e.g. rehabilitation | |
| Care is provided for a set period of time | |
| Care can be provided in the home or in day or institutional care settings | All care contexts included, i.e. day care, home care and institutional |
| Care recipient is aged 65 years or older and is identified as having an informal carer | Outcomes for carers of care recipients aged 65 years or older must be discernible in the findings |
The definition of respite care focused primarily on the benefits to the carer and considered the outcome for carer well-being as not only the primary outcome but also the defining criterion for respite care. This placed some limitations on measuring outcomes for the care recipient, as only studies that reported carer outcomes were included. There is the possibility that a paper examining a respite intervention may report outcomes for the care recipient only (as in some cases in which studies are ‘salami sliced’). However, the inclusion of all studies that report only care recipient outcomes (for example, of day care) would prove problematic as it would be unclear whether all recipients of the service actually had or depended on an informal carer. It would therefore be difficult to establish if these samples were equivalent to those who were reported as having informal carers. It was felt most appropriate, therefore, to accept the possible loss of a small number of studies, rather than have broader inclusion criteria and include a potentially large number of articles of dubious relevance.
It must also be acknowledged that not all included interventions are ‘pure respite’ in that formal care provision will never map exactly to care provided by the informal carer. There may be activities undertaken that are designed to benefit the care recipient (for example, directed group activities such as reminiscence or occupational therapy), but there may also be changes in care that may prove to be a disbenefit (such as lack of exercise and mobility). These are confounders that are poorly described in studies and are not measurable and cannot therefore be accounted for in study selection or analysis, although the selection criteria aimed to exclude studies in which the intervention predominantly provided individual treatments (usually of a medical nature) to the care recipient.
Study inclusion and exclusion criteria
Inclusion criteria for quantitative studies
Inclusion criteria for quantitative studies were as follows:
-
study mentions an intervention designed to provide the carer with a break from caring
-
care recipient population is aged 65 years or over (or analyses carried out on a subsample of population aged 65 years or over)
-
carer outcomes are measured
-
respite intervention is compared with either no respite or another intervention (this included regression analyses in which respite was used as a predictor of carer outcome such as carer burden, and within-group longitudinal comparisons that reported carer outcomes before and after the delivery of a respite intervention)
-
articles written in any language.
Two additional criteria were used to identify any quantitative papers including cost data:
-
include all papers costing informal care, respite, carer outcomes or service usage (even if respite component not specifically costed)
-
include above only if costs are directly measured.
Exclusion criteria for quantitative studies
-
Exclude studies in which the intervention is designed to change the state of the care recipient (e.g. stroke rehabilitation).
-
Palliative care/hospital-at-home interventions to be excluded unless stated aim is to provide respite for carer and carer outcomes are measured.
-
Exclude if care recipient population is under 65 years, age of care recipient population is not discernible or outcome data cannot be identified for those in the care recipient sample who are aged 65 years and over.
-
Exclude if only care recipient outcomes are measured.
-
Exclude qualitative studies and observational studies having no comparison group, e.g. surveys providing descriptive data only.
Inclusion criteria for qualitative studies
A broader set of inclusion criteria were devised for assessing qualitative studies as it was felt important to assess both care recipient and carer views of their needs and preferences for respite care even if they were not actually in receipt of respite. Inclusion criteria for qualitative studies were as follows:
-
study employs qualitative methods (face-to-face semistructured/in-depth interviews; focus groups; open questions in questionnaires)
-
care recipients have a mean age of 65 years or over (or analyses carried out on a subsample aged 65 or over)
-
study reports views of carers and/or recipients
and either:
-
study reports views of respite care or study reports respite as a theme in relation to other types of care, e.g. care aimed to change the state of the care recipient
or:
-
views of respite include:
-
respite care service provision/satisfaction with services
-
impact of respite on the carer and/or care recipient
-
unmet needs/perceived needs for respite care
-
reasons for utilising or not utilising respite care.
-
Exclusion criteria for qualitative studies
-
Quantitative data reported as part of a qualitative or quantitative study, e.g. descriptive statistics.
-
Data not reporting themes or concepts related to views of respite care, respite needs, use of respite or impact of respite care on carer and/or care recipient, e.g. data reporting general experiences of caring.
-
Studies using direct observation methods, e.g. participant observation.
-
Care recipients are under 65 years of age or data relating to those over 65 years are not discernible in the study findings.
-
Non-English language papers.
In the qualitative synthesis all foreign language papers were excluded as the issue of translation and interpretation is of greater significance and would have a potential impact on the findings. It was felt that these difficulties outweighed the potential limitation of excluding relevant studies. The impact of these exclusions would depend on the similarity of the different health-care systems and any cultural differences. Although many of the good-quality European studies are published in English journals there is the possibility of relevant studies being published in the language of origin.
Qualitative studies involving direct observation were excluded to maintain comparability of the type of data included in the synthesis,15 i.e. self-reported views rather than inferences made from observation. However, no observational studies were identified in the searches.
Year of publication
The year of publication was defined by the databases searched. All years were searched for each database.
Data sources and search strategy
Search strategy
The remit of the current review is very broad: respite care might feasibly occur within both community and institutional settings and across many different conditions (e.g. dementia, palliative care, stroke, etc.). In addition, interventions or services designed to give carers a break from their caring role may not be explicitly labelled as respite care. Therefore, an inclusive and broad search strategy was felt most appropriate to capture all potentially relevant literature and specificity was sacrificed to some degree to maximise sensitivity.
The final search strategy was developed iteratively following discussion with the review management group (all investigators, listed as authors of this review) and carer representatives (Carers Wales). This was based on the most appropriate definitions of respite care, the target population (i.e. frail elderly) and possible respite settings. The search strategy comprised three distinct blocks: the first set of terms were designed to capture all studies reporting respite care; the remaining two sets were included to limit results to studies carried out within elderly populations and those specifically citing carers or the caring role respectively. Words and phrases within each set were combined using the Boolean OR operator; the three sets were then combined using the AND operator. Search terms were trialled initially on MEDLINE, mapping words and phrases to MeSH headings (using the .mp operator). Keywords using the .mp operator were used either in addition to MeSH headings or in place of them when they produced the same or additional hits. Input on the appropriateness and comprehensiveness of the search terms was sought from an information specialist, all members of the review group and user representatives from two UK charities. The final MEDLINE search terms are shown in Figure 1.
FIGURE 1.
MEDLINE search terms.
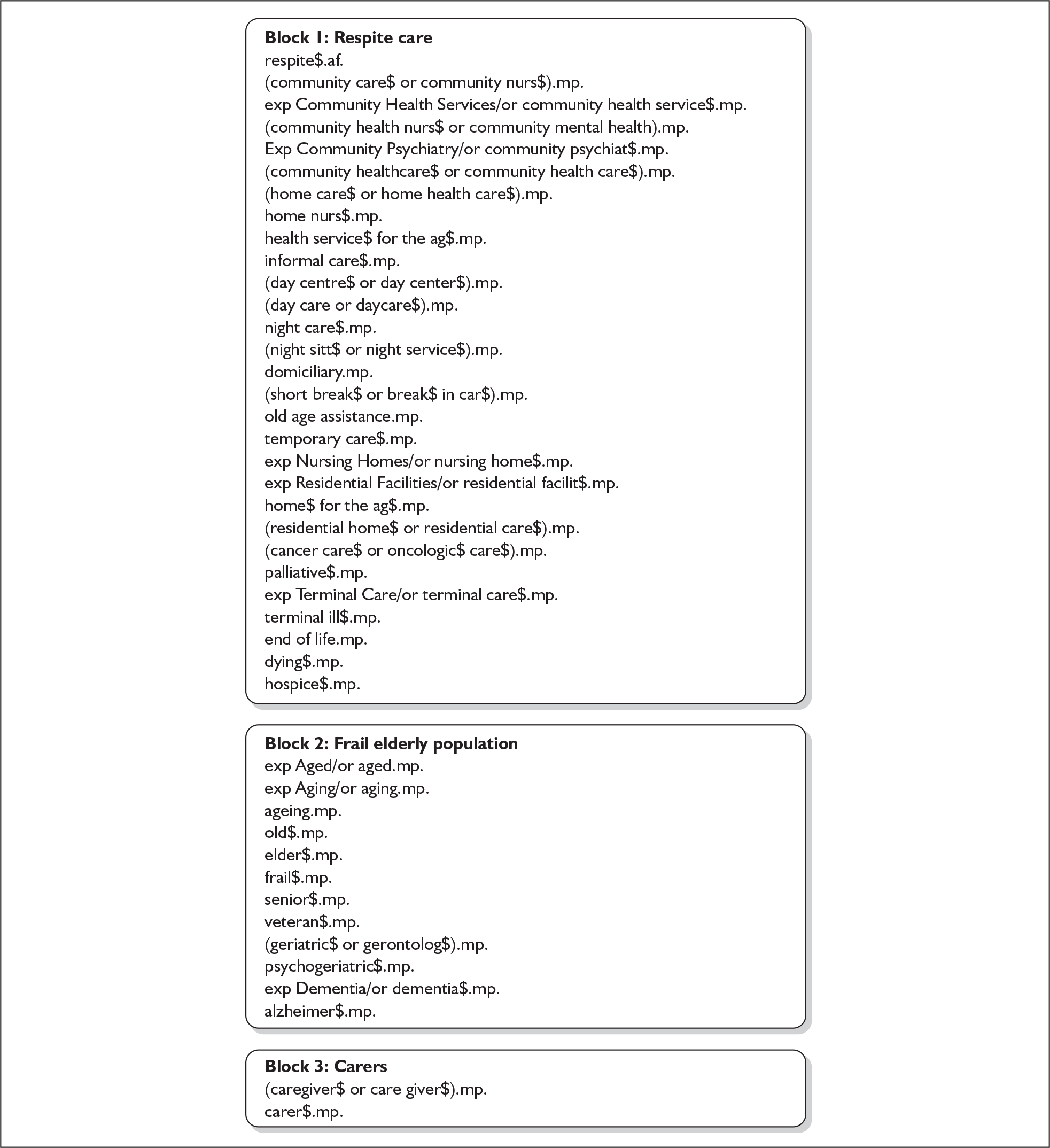
Data sources
The terms provided in Figure 1 were adapted as appropriate to search an additional 24 electronic databases from the earliest possible date to the end of September 2005. Searches were rerun until the end of 2005, resulting in an additional 332 references not previously identified. All databases searched (and number of hits retrieved from each) are shown in Table 1.
| Electronic data source | Hits |
|---|---|
| Allied and Complementary Medicine (AMED) | 278 |
| Applied Social Sciences Index and Abstracts (ASSIA) | 599 |
| BIDS International Bibliography of the Social Sciences (IBSS) | 59 |
| British Nursing Index (BNI) | 284 |
| Cochrane Database of Methodology Reviews | 1494 |
| Cochrane Database of Systematic Reviews (CDSR) | |
| Cochrane Methodology Register (CMR) | |
| Cochrane Register of Controlled Trials (CENTRAL) | |
| Database of Abstracts of Reviews of Effects (DARE) | |
| Health Technology Assessment Database (HTA) | |
| NHS Economic Evaluation Databasea | |
| Cumulative Index to Nursing and Allied Health Literature (CINAHL) | 3467 |
| Computer Retrieval of Information on Scientific Projects (CRISP)a | 28 |
| EconLit | 22 |
| EMBASE | 2402 |
| Health Management Information Consortium (HMIC, including King’s Fund) | 1024 |
| MEDLINE | 5118 |
| MEDLINE (in progress and non-indexed citations) | 81 |
| National Research Register (NRR)a | 478 |
| PsychInfo | 2662 |
| PubMed Cancer Citations (maintained by NCI/NLM – formerly CancerLit) | 631 |
| Scopus | 1210 |
| Social Care Online (previously CareData) | 782 |
| Sociological Abstracts | 302 |
| Web of Science (including Social Science Citation Index) | 523 |
Once duplicates were removed a total of 12,992 unique references were identified. Overlap between databases was substantial. Taking four of the major electronic data sources as an example, 64% of citations were identified on MEDLINE and original citations on EMBASE accounted for a further 24%, PsychInfo for 11% and the British Nursing Index for just 1%.
Hand searching of the following journals was also undertaken from the earliest possible date to the end of 2005: Gerontologist, Journal of Gerontology, Age and Ageing, International Psychogeriatrics, Journal of Palliative Medicine and Stroke.
Study selection
A preliminary title sift of all 12,992 references was undertaken by two reviewers. Obviously irrelevant titles such as those relating to respite for carers of children or pharmacological interventions were excluded at this stage. For any titles on which disagreements occurred the abstracts were assessed, along with all of the remaining abstracts, by two reviewers. When disagreements occurred papers were selected for full retrieval. Inter-rater agreement ranged from fair to moderate (kappa coefficient range 38–52). 16 At the full paper stage all exclusions were checked by a second reviewer selected from within the project management team. Inclusions of papers in the meta-analysis were checked by group discussion of the statistical team (RM, KH, KA), and inclusions of papers in the narrative syntheses (longitudinal and cross-sectional observational studies and qualitative studies) were checked by CS. The number of studies included at each of these stages is shown in Table 2.
| Sift stage | Number of articles |
|---|---|
| Initial search (duplicates removed) | 12,992 |
| Irrelevant titles excluded | 8042 |
| Included articles following abstract sift | 928 |
Before full paper retrieval all quantitative, qualitative and cost papers were grouped together. Following full paper retrieval papers were categorised according to their content (i.e. quantitative/qualitative). All full papers were assessed against the inclusion criteria by a single reviewer, with any excluded papers checked by a second reviewer. The number of papers categorised into each component of the review on full paper retrieval and second-stage inclusion assessment are shown in Table 3.
| Review component | Papers retrieved | Included at second-stage assessment |
|---|---|---|
| Quantitative | 374 | 104 |
| Qualitative | 226 | 71 |
| Cost | 125 | |
| Reviews | 59 | N/A |
| Grey literature | 144 | N/A |
| Total | 928 |
A much greater number of qualitative studies was retrieved than originally anticipated. This is due in part to the wider remit and less stringent inclusion criteria adopted for qualitative studies and in part to reliance on qualitative methods in an area in which it is difficult to carry out controlled trials for ethical reasons.
Quality assessment
Methods for assessing the quality of both quantitative and qualitative studies are outlined in the following sections.
Quality assessment of quantitative studies
Numerous tools are available for the quality assessment of randomised controlled trials (RCTs), with at least 25 currently in use. 17 However, a MEDLINE search from 1990 to 1997 did not identify any quality checklists for assessing cohort and case–control studies. 18 A brief review of the literature by the current authors to the end of 2005 indicated that this situation has changed very little. Given the broad and inclusive nature of the current review it was important to identify a tool that could be used to assess the quality of varied quantitative designs simultaneously (i.e. RCTs and cohort and case–control studies).
Two particularly relevant quality checklists were identified from a brief review of the available literature. 18,19 Downs and Black18 developed a tool to assess the quality of both randomised and non-randomised designs. The tool comprises a 27-item checklist and an overall score pertaining to the quality of the study. Checklist items relate to the appropriateness and adequate description of the hypotheses, study design, intervention, main outcomes and methods of analysis. The checklist demonstrated good inter-rater reliability, although further development and testing of the tool was recommended. The tool devised by Kmet et al. 19 was also intended for quality assessment of both randomised and non-randomised designs and was produced following a review of the relevant literature and discussion of issues central to internal validity. The checklist provides an overall summary score, although the authors acknowledge this approach is inherently prone to bias. In addition, inter-rater reliability appeared somewhat limited (a subsample of 10 studies scored by two reviewers). The Kmet et al. 19 checklist contains 14 items relating to study design, intervention, outcome measurement and methods of analysis.
Within the context of the current effectiveness review both tools were felt to contain useful elements but each had particular drawbacks. For example, the Downs and Black18 checklist is heavily weighted towards randomised designs (likely to be small in number in the current review) and is also lengthy at 27 items. Although more concise, comprising just 14 items, the Kmet et al. 19 checklist is less detailed (e.g. adequate description of the intervention is not included). In addition, previously developed tools did not accommodate particular issues relevant to this review, such as the presence of two samples of interest (carer and care recipient). A single quality checklist was therefore created, in line with CRD recommendations,15 specifically designed for the current review (see Appendix 1) but likely to be of value in reviews of similarly complex areas encompassing few randomised trials.
The current tool was also developed within the framework recommended by the US Preventive Services Task Force. 20 The first of three strata within this framework relates to quality assessment at the individual study level. The framework does not give a quantifiable score but provides an indication of quality based on certain parameters. Study designs are first organised into a hierarchy [RCT, non-RCT, cohort, case–control, observational (i.e. multiple time series, case studies, opinion of experts)] and are then classified as ‘good’, ‘fair’ and ‘poor’ according to criteria specific to the particular study design.
The final checklist contains 18 items, with three levels of quality assessment: good (2), fair (1) or poor (0). Some items within the list are relevant only to RCTs; therefore, a ‘non-applicable’ option is provided for other study designs. Scores across items are summed to create a quality score, which is represented as a percentage to account for any non-applicable (i.e. missing) items.
Quality assessment of qualitative studies
There is some debate as to the appropriateness of formal quality assessment in qualitative research and the use of such tools is comparatively new. Qualitative research is extremely useful in addressing patient-centred views in health-care research and as such is a valuable and often expected study component. Controversy relating to the appropriateness of quantifiable quality assessment arises from the belief that this serves to stem the interpretative and creative aspects of qualitative study. 21 Nonetheless, many believe that some form of quality assessment is necessary if qualitative research is to be taken seriously within the wider research community. 22–24 Within the context of the current review, equal weight and importance are given to both the quantitative and the qualitative components and therefore a common approach to assessing study quality was needed.
To maximise consistency across these two aspects of the review, the aim was to develop a quality tool similar in structure to that of the quantitative tool previously described, keeping in mind the different aims of qualitative and quantitative research. Quantitative research seeks to eliminate bias to render results generalisable to the wider population, whereas qualitative research is context bound and seeks to expose and discuss bias. For these reasons it has been proposed that a common language may be misleading. 22 Alternatives to terms such as internal and external validity, reliability and objectivity have been proposed, for example credibility, dependability, transferability and confirmability. 25 Others, however, feel that issues of validity and relevance are appropriate to qualitative research even though the concepts supporting them may be dissimilar to those pertaining to quantitative research. 22,23
However, it has been pointed out that there is a need to qualify this by ensuring that the different paradigms within qualitative research are acknowledged. 26 Qualitative research is not a unitary activity and aims and methods will vary according to the philosophical underpinnings and requirements of the study. This could be considered similar to the varied approaches in quantitative research with the resultant difficulty of establishing a quality assessment tool that is appropriate to all types of study. However, a number of concepts are relevant across study types, if interpreted somewhat differently. To identify items for inclusion in the assessment tool, a review was undertaken of papers that presented either a quality checklist or a narrative account of quality assessment. This scoping review followed a similar approach to that used by Walsh et al. ,27 who adopted such a scoping method designed to assess commonalities between quality assessment tools and eliminate redundant items. The review by Walsh et al. 27 was based on seven existing checklists: the checklist that they produced was included in the present scope.
The scope of the quality assessment literature revealed considerable overlap and agreement between studies in terms of the relevant criteria for assessing quality. Items to be included in the tool were chosen based on their frequency of occurrence in the articles reviewed, their appropriateness to the requirements of the current review and their generalisability across different qualitative methods. However, the types of study likely to occur within the context of respite care will largely comprise thematic analysis, such as grounded theory or phenomenology (direct observational studies or data from sources other than focus groups, interviews or open-ended questions were excluded). Some quality checklists were quite broad and vague although they had the advantage of appearing shorter and more succinct than others. A more detailed and structured approach was preferred in order to give clear definitions to facilitate interpretation and increase inter-rater reliability. The rating format was based on the checklist developed by Kmet et al. 19 for quality assessment of qualitative research, in line with the format used for the quantitative tool. The tool was piloted and amended; items included in the final version are shown in Appendix 2. Three levels were assigned to each item in the tool, which were scored from 2 to 0. The scores could then be summed to produce an overall quality rating.
Data extraction
Data extraction was carried out as a two-stage process for both the quantitative and qualitative sections of the review. These stages are outlined in the following sections.
Data extraction for quantitative studies
A paper version of a quantitative data extraction form was circulated to all members of the review group for comment and revised appropriately. Members of the study team could use either a paper or an electronic version of the data extraction form at this stage. The electronic version comprised an Access database with identical fields to the paper version. When extraction was completed using the paper version the information extracted was entered into the Access database to enable a direct comparison of all data. The use of Access forms for data entry also aided in ensuring consistency of the extracted data by allowing only certain types of options to be entered in any one field, thus ensuring that all data were categorised in a similar way.
At the first stage of data extraction detailed information relating to study methods was extracted, which included information about the intervention (e.g. type, setting, duration and length of follow-up), carer and recipient characteristics, and types of outcomes measured (including information on the tool used to measure each outcome). The first-stage data extraction form is given in Appendix 3.
The second stage involved more detailed extraction of appropriate numerical data for all studies categorised as either randomised trials or quasi-experimental designs into an Excel spreadsheet. The same procedure was followed for all longitudinal studies in which participants served as their own control (i.e. outcomes measured before and after an intervention in a single group). Summary tables detailing the observational studies (both longitudinal and cross-sectional) were also created (see Appendices 6 and 7 respectively)
Data extraction for qualitative studies
The qualitative review followed a similar pattern with an initial meta-methods analysis in which data were extracted to a summary table (see Appendix 9). A meta-data analysis was then carried out on a subsample of papers; the findings from the qualitative papers were extracted into a software package specifically designed for qualitative analysis (NUDIST version 6). Data extracted comprised the concepts identified in the results sections of the papers but not the themes defined by the researchers or their conclusions derived from their analyses, usually presented in the discussion sections of the papers.
Data analysis and synthesis
Methods of analysis and approaches to data synthesis for the quantitative and qualitative components of the review are outlined in the following sections.
Quantitative data synthesis
When appropriate and possible, quantitative results from individual studies were synthesised using meta-analysis techniques, taking account of statistical, clinical and methodological heterogeneity. 28 To account for the variety of ways in which some outcomes such as carer burden and depression are measured, standardised effect sizes were used.
Initially, between-study heterogeneity was investigated within randomised and quasi-experimental studies. Separate meta-analyses were carried out for each carer outcome using the following study-level covariates when possible: length of follow-up, length of intervention (i.e. brief versus sustained) and respite setting (e.g. day versus home care). A number of studies measured outcomes at two or more follow-up periods; therefore, additional separate meta-analyses were carried out splitting studies into short- and longer-term follow-up groups.
Meta-analyses were carried out both on follow-up data only and on change scores. However, standard deviations for change scores (change SDs) were rarely provided. Change SDs were therefore estimated using two previous assumptions: first, that the correlation between baseline and follow-up scores is zero and, second, that the correlation between baseline and follow-up scores is likely to be 0.6, based on data from the Rothman et al. 29 study. This study reported correlation coefficients for a large number of outcomes from baseline to both short- and long-term follow-up. Outcomes for carers were the primary focus of the meta-analyses: however, likelihood of institutionalisation was also assessed to represent a patient outcome relative to either positive or negative effects of a respite intervention. This was felt to be an important step as a preliminary scoping of the qualitative literature indicated that a common reason for non-uptake of services is concern on the part of the carer that respite may be detrimental to the care recipient. All meta-analyses were carried out in Stata (version 9).
Studies in which outcomes were measured in a single group before and after delivery of an intervention were analysed separately.
It was intended to assess negative publication bias by funnel plots but there were few studies eventually included in each analysis and so this was not feasible. To assess any potential for publication biases the country of origin and year of publication were examined across the different types of study design.
Observational studies identified by the review (both cross-sectional and longitudinal) formed the basis of a narrative synthesis, with particular reference to the rate of institutionalisation amongst those accessing respite compared with non-users and the impact on carer burden and mental health. However, much of the observational work in the area tends to focus on use of respite as a generic, dichotomous outcome and so differentiating between the effects of diverse respite settings (i.e. home care, day care) is problematic.
Qualitative data synthesis
The methods used to review the qualitative literature followed those used in carrying out primary qualitative research and were based on the methods of meta-study described by Paterson et al. 30 The synthesis aimed to be both interpretive, to provide further explanation of the research findings in the quantitative review, and aggregative, to identify the extent of the literature and gaps that need to be addressed. To do this a three-stage process was adopted by, first, carrying out a meta-method analysis, second, a meta-data analysis and, finally, meta-synthesis.
Meta-method analysis assesses both the quality of the research methods of the primary research papers and the ways in which the methodological context may have influenced the study findings. 31 Each paper was summarised into a table under the headings shown in Appendix 9. Separate tables were constructed depending on the country in which the research was conducted, and the factors influencing study findings could then be explored. For example, as well as differences in sampling procedures, variation in data collection methods might have an impact on study findings, such as data collected by face-to-face interview versus focus groups. Such tables may also provide information about the generalisability of findings if consistent results are found across samples and contexts (such as place of care) and also about the extent of the literature and any gaps for future research. The listing of sampling procedures could reveal the types of carers and care recipients whose views were not sought, giving an indication of the representativeness of the findings. These tables also give a view of the literature over time, as preferred methods have changed and developed, and how the field of research is likely to develop in the future.
Because of the large number of studies identified in the qualitative literature search, a purposive sampling technique was used in the meta-data analysis stage. At the outset of the study we had intended to sample according to type of respite provision (e.g. institutional care, day care, home care) and characteristics of the care recipients (e.g. dementia, physically impaired, palliative care). However, such categorisations were not possible as the majority of studies reported a mix of respite use and often a mix of care recipients. We therefore decided, in the first instance, to focus on the organisational context of studies and relevance to UK policy. Accordingly, all UK studies were included. Although there were a substantial number of studies carried out in the UK, studies carried out in the USA were also prominent and tended to be of higher quality, with a more direct focus on respite care issues. We considered that the concerns of carers of older people in the USA would be similar, within the Medicare system, to those of carers in the UK and so these too were included, along with all studies conducted in Canada, where the health-care system is more similar to that in the UK. Also included were studies carried out in Australia and New Zealand, where there are similarities with the UK in culture and health-care systems.
The meta-data analysis stage was carried out using similar methods to those used in primary qualitative studies,31 with each study representing a case. This was based on a grounded theory approach31 although certain aspects of the study had limitations in relation to grounded theory methodology. Because a discrete set of studies was available, theoretical sampling could not be carried out, and therefore data saturation may not necessarily have been achieved for all categories and themes. In addition, although a wide range of studies was included, representing general views of respite care, and coding aimed to focus on emergent themes rather than themes identified a priori, it is likely that the coding process was influenced by the main research question related to identifying barriers to uptake. However, there were no previous assumptions concerning the nature of barriers or other views of respite care.
The findings from each study (the concepts as reported by the authors) were extracted. Category codes were developed using a constant comparative technique. 31 Common categories were extracted from the studies by comparing for similarities and differences between the concepts expressed in each study. As concepts emerged that did not fit the coding frame a new category was instigated. The data within each category code were then compared to identify subcategories describing the range of the general properties of each main category. Characteristics of the studies were coded as base data, for example quality rating, type of data collection, characteristic of care recipient, etc. A sample of texts was coded by two reviewers to assess the reliability of the coding framework. The coding demonstrated a high level of concordance, showing good reliability. By comparing the data in the categories across groups of cases (i.e. studies) and in relation to other categories, hypotheses concerning the causal, contextual and intervening relationships between categories and subcategories were developed in a process of ‘axial coding’. 31 Data were then sought across the different studies that either supported or refuted these hypotheses.
Finally, in the meta-synthesis stage of the analysis ‘selective coding’31 was carried out, whereby a core category was identified (i.e. barriers to respite), which became the central focus of the analysis, and a theory developed concerning the causal relationships between this and the other major categories. This core category was to some extent defined by the research question as studies were selected based on their ability to answer this question. However, the category ‘barriers to respite’ did fulfil the criteria for a core category31 and related to all of the other major categories apart from three, which are reported separately (i.e. ethnicity, positive aspects of respite and palliative care). In addition to this, and for completeness, a descriptive analysis of the data occurring under the category ‘carer needs’ is reported separately although these data also related to the core category.
The final stage of the analysis described above provides a theory of the barriers to the uptake of respite over and above that described in individual studies. It is based on integration and interpretation of the data (rather than merely aggregation) and takes account of the methodological aspects of the studies reviewed by including design features, such as carer and care recipient characteristics and quality ratings, as categories within the coding frame. As such it can be considered to represent a synthesis of the data, although there are limitations concerning the contribution of meta-theory analysis (analysis of the theoretical approaches underpinning primary studies) prescribed by Paterson et al. 30 for meta-synthesis.
These findings were then integrated with the findings of the quantitative review. One important feature was to identify whether the outcomes addressed in the quantitative studies were consistent with those identified in the qualitative studies as being important for both care recipients and carers. The findings from the qualitative review were used to shed further light on findings in the quantitative review and aid interpretation.
Chapter 3 Quantitative synthesis
Organisation of the presentation of results
The results will be presented under headings according to the level of evidence, i.e. RCTs and quasi-experimental studies, single-group longitudinal before-and-after studies, observational longitudinal studies and cross-sectional studies. Meta-analyses are carried out on RCTs and quasi-experimental studies and the longitudinal before-and-after studies and so these two levels of evidence will be presented together and form the main source of evidence related to the effectiveness of respite care. Before presentation of the meta-analyses narrative summaries are provided of studies unsuitable for inclusion in the meta-analyses, pertaining to both trials and longitudinal before-and-after studies.
Following the meta-analyses narrative summaries of all of the observational studies (longitudinal and cross-sectional) are presented. A narrative synthesis will also be presented of care recipient outcomes across the different types of study. No meta-analyses were carried out on care recipient outcomes because the inclusion/exclusion criteria for the review were based on studies reporting carer outcomes; there may be studies focusing only on care recipient outcomes of respite services that are not included in this review and so meta-analysis was not felt to be appropriate. A section relating to the economic review follows the quantitative synthesis and, finally, the synthesis of qualitative studies is presented.
Within each section the evidence relating to particular outcomes will be presented separately, for example carer burden, carer depression. The review focuses on outcomes reported by more than one study, which mainly includes carer burden, carer depression and institutionalisation. A discussion relating to each outcome across all of the levels of evidence, in combination with how this relates to findings from the qualitative review, will be presented in the discussion section.
Studies included in the review
A total of 374 full quantitative papers were selected for retrieval following the abstract and title screening stages (including one identified from bibliographies); 270 of these were excluded following screening of the full papers.
A total of 104 quantitative papers met the inclusion criteria for the review. 29,32–134 These are summarised in tabular format in Appendices 4–7, classified according to study design (26 RCT/quasi-experimental papers;29,32–56 14 longitudinal before-and-after papers;57–70 19 longitudinal papers;71–89 and 45 cross-sectional observational papers90–134). In some cases more than one paper refers to the same study and so the number of studies at each level of evidence was seven RCTs, 12 quasi-experimental studies, 13 longitudinal before-and-after studies, 13 observational longitudinal studies and 40 observational cross-sectional studies. Figure 2 shows the numbers of papers identified at each level of evidence.
FIGURE 2.
Number of papers retrieved and identified as eligible for inclusion in the quantitative review. MA, meta-analysis; RCT, randomised controlled trial.
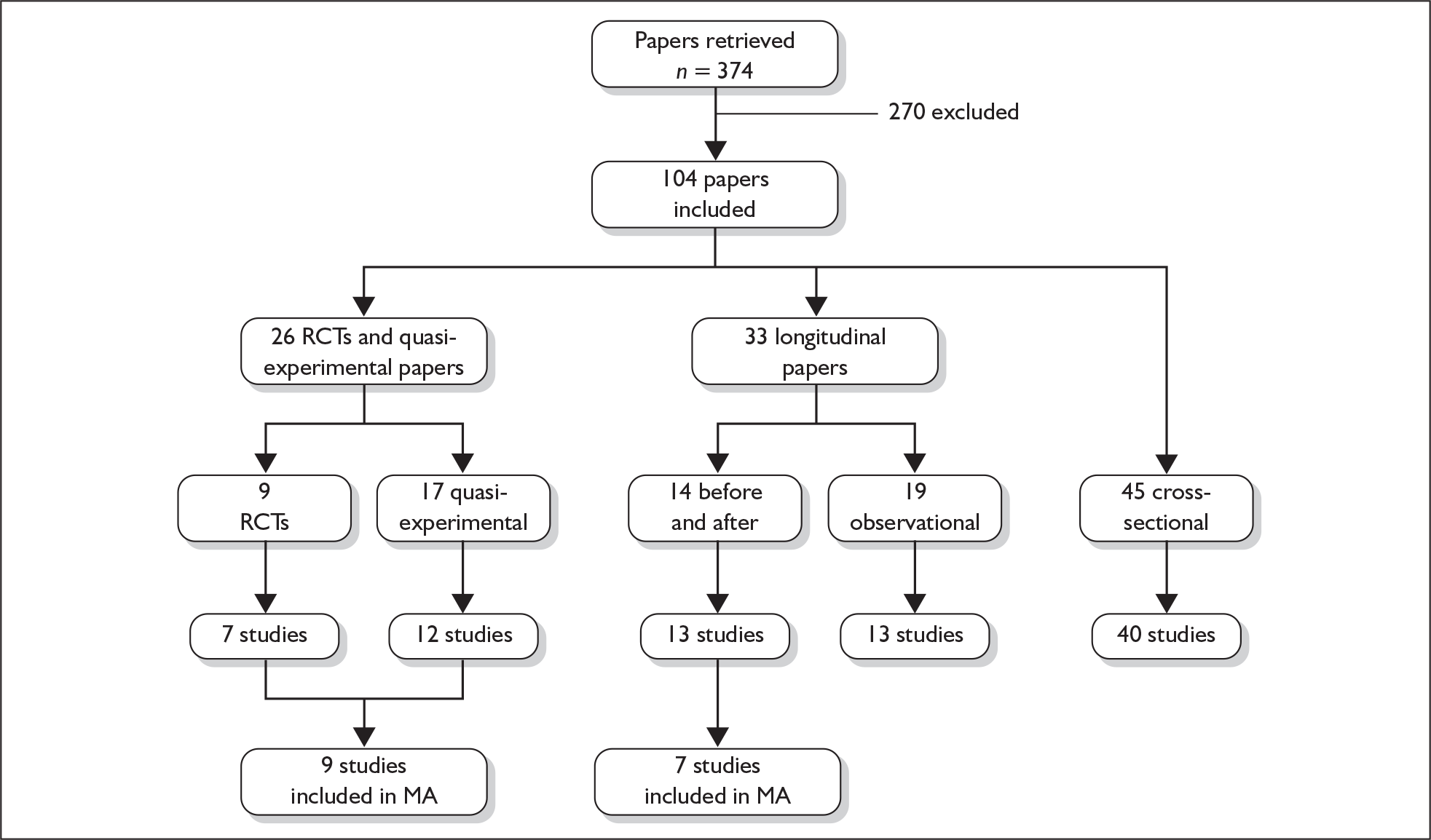
A subset of these papers was included in a series of meta-analyses (split by outcomes). A number of studies have been excluded from the meta-analyses as it was not always possible to extract appropriate data. A total of nine RCTs and quasi-experimental studies (detailed by 14 papers) and seven longitudinal before-and-after studies were included in the meta-analyses. When studies could not be included the reasons for exclusion are indicated in the final column of the summary tables in Appendices 4 and 5; the reasons for exclusion are also listed in Table 6.
Quality assessment
The previously described quality checklist was used to assess the quality of all of the 104 included quantitative papers (quality scores are given in the appropriate tables). Quality scores were divided into tertiles (low, moderate, high) to allow the relative quality of included studies to be assessed; this is discussed in more detail in the appropriate sections.
First and second level of evidence: RCTs/quasi-experimental studies and longitudinal before-and-after studies
Characteristics of RCTs/quasi-experimental studies and longitudinal before-and-after studies
The majority of randomised and quasi-experimental studies assessed day care and mixed respite care interventions, followed by in-home care and then institutional care (Table 4). Most studies were carried out in the USA or UK, with the USA having nine studies and the UK having five; none of these studies assessed institutional care. The remaining studies were carried out in Canada, Australia, New Zealand and Germany.
| Country | Type of respite care | ||||
|---|---|---|---|---|---|
| Day care | Institutional | In-home | Mixed | Total | |
| UK | 2 | 2 | 1 | 5 | |
| USA | 3 | 2 | 4 | 9 | |
| Canada | 1 | 1 | 2 | ||
| Australia | 1 | 1 | |||
| New Zealand | 1 | 1 | |||
| Germany | 1 | 1 | |||
| Total | 7 | 3 | 4 | 5 | 19 |
Similarly, the majority of longitudinal before-and-after studies were carried out in the USA and UK. These studies were more evenly spread across the different types of respite, although only one study (carried out in the UK) assessed in-home respite (Table 5).
| Country | Type of respite care | ||||
|---|---|---|---|---|---|
| Day care | Institutional | In-home | Mixed | Total | |
| UK | 1 | 1 | 1 | 1 | 4 |
| USA | 1 | 1 | 3 | 5 | |
| Canada | 2 | 2 | |||
| Australia | 1 | 1 | |||
| Hong Kong | 1 | 1 | |||
| Total | 5 | 3 | 1 | 4 | 13 |
Studies excluded from the meta-analyses
Table 6 summarises the reasons why RCTs and quasi-experimental studies and longitudinal before-and-after studies (identified for inclusion in the review) were excluded from the meta-analyses. Ten randomised and quasi-experimental studies were excluded, as well as six longitudinal before-and-after studies. A narrative summary of the studies excluded from the meta-analyses is presented first, followed by the meta-analyses according to each outcome.
| Study | Reason for exclusion from meta-analyses |
|---|---|
| Randomised and quasi-experimental studies | |
| Brodaty et al. 199733 | No other studies measuring mean time to institutionalisation identified |
| Burch et al. 199934 | Could not derive mean values |
| Burdz et al. 198835 | Could not derive mean values |
| Lawton et al. 198942; Lawton et al. 199143 | No follow-up data provided |
| Montgomery and Borgatta 198945; Montgomery 198846 | Not possible to extract means |
| Riordan and Bennett 199849 | No SDs |
| Rolleston and Ball 199450 | Study assessing effect of temporary closure of existing service |
| Schwarz and Blixen 199752 | Data not given for experimental and control groups separately |
| Wells and Jorm 198753 | Comparison of respite vs institutional care (comparison group not appropriate) |
| Zank and Schacke 200254 | Not possible to extract means |
| Longitudinal before-and-after studies | |
| Adler et al. 199357 | No means given |
| Chi and Wong 199458 | Outcomes not measured in any other study (attitudes to care recipient and caring) |
| Cox 199859 | No SDs |
| Deimling 199260 | No SDs |
| Gilleard 198762; Gilleard et al. 198463 | No suitable comparison group |
| Johnson and Maguire 198968 | No SDs |
Narrative review of randomised and quasi-experimental studies excluded from the meta-analyses
The effectiveness of respite for carer well-being
Zank and Schacke54 evaluated the effects of specialist geriatric day care on the well-being of carers. After 15 months of service use no significant differences between the respite and control groups were observed in terms of well-being and burden. However, semistructured interviews indicated that carers of day care recipients reported a more positive change than those in the control group. Conlin et al. 36 demonstrated a positive effect of respite (either in-home or day care) on carer stress levels at both 5 and 10 weeks following service use. Carers not receiving respite reported greater stress at follow-up. However, no difference in the rate of institutionalisation (included in meta-analysis) between respite and control groups was observed, although the follow-up period is likely to be too short to detect any meaningful difference.
In contrast, Lawton and colleagues42,43 did not find that the use of a mixed respite service significantly impacted on carer burden or psychological health. However, satisfaction with the service at 12 months was reported to be high, and families accessing respite services maintained the care recipient in the community for significantly longer (22 days on average) than those not accessing such a service. Schwarz and Blixen52 also failed to detect any positive effects of in-home respite services on depression and strain relative to the control group at 3 months. No significant differences in positive caregiving appraisal were found between the two groups.
Riordan and Bennett49 examined the effectiveness of a dementia-specific augmented domiciliary service on levels of psychological well-being and carer strain after 6 months of service use. Use of the service was not found to be of significant benefit to carers in terms of psychological well-being; however, service users remained in the community significantly longer than matched control subjects.
The interaction of respite effectiveness and reason for frailty
Burdz et al. 35 examined the effects of inpatient respite care on carer strain after 5 weeks of service use. Although it was hypothesised that non-dementia patients and their carers would benefit most from the respite intervention, results indicated a significant decrease in carer burden in the respite condition (relative to a waiting list control group) regardless of diagnosis.
The effectiveness of respite care relative to other supportive interventions
Montgomery and Borgatta45,46 followed up carers of frail elderly receiving several different service interventions, one of which comprised a mixed respite intervention (day care, home care, night inpatient care), after 12 months of service eligibility. It was not possible to include the results in the meta-analysis (means not given) but results suggest that subjective burden was significantly reduced in all intervention groups at 12 months relative to the control group who received no intervention. However, there were no significant differences in subjective burden between any of the intervention groups, indicating that various other supportive interventions (i.e. educational interventions and support groups) are just as effective in reducing burden as respite care.
Comparison of two or more respite interventions
Burch et al. 34 carried out a RCT comparing day hospital and day centre interventions. Although carer strain was reduced in both groups at 3 months, no significant differences were found between the two interventions in terms of outcomes for carers.
The impact of service closure on carer well-being
Rolleston and Ball50 measured levels of general carer well-being before and following a 2-week closure of a psychiatric day hospital. The results indicate that the removal of existing respite services is detrimental to carer well-being, although well-being regressed to preclosure levels on assessment at 3 weeks following reopening of the unit.
Comparison of respite and institutional care
Wells and Jorm53 carried out a randomised comparison of permanent institutional care and periodic respite care in terms of carer outcomes. Levels of anxiety and depression were significantly reduced in carers who institutionalised the care recipient, whereas those accessing periodic respite care continued to demonstrate high levels of emotional distress. Wells and Jorm53 also noted no detrimental effects of institutionalisation on care recipients (all dementia sufferers) in terms of behavioural symptoms.
Respite as a predictor of institutionalisation
Brodaty et al. 33 carried out a randomised trial comparing a carer training programme (either immediate or waiting list control subjects) with a 10-day respite intervention with no training. The 8-year survival analysis indicated that carer training delayed both death and institutionalisation; the respite intervention, in comparison, although coupled with memory retraining for dementia patients, was associated with a shorter mean time to institutionalisation.
Narrative review of longitudinal (before-and-after) studies excluded from the meta-analyses
Six studies (reported in seven papers) were excluded from the meta-analyses of single-group longitudinal comparisons (i.e. before-and-after studies).
Adler et al. 57 found that levels of carer burden and depression were reduced during a 2-week inpatient respite intervention, but that levels returned to baseline once patients had returned home, which suggests that the effects of respite may be short-lived in some instances.
Johnson and Maguire68 examined the impact of the use of day care on a range of carer outcomes and found no difference in carer stress between baseline and follow-up (2 and 4 months).
Chi and Wong58 studied the effect of institutional respite on carer attitudes at 1 month. They found that carers were less likely to express a wish to institutionalise recipients following respite; however, perceptions of the caring role as stressful actually increased following respite.
Gilleard and colleagues[62,63] examined the effects of carers’ psychological well-being and self-reported strain and also the number of care recipient problems on community status after 3 and 6–7 months of day care. Institutionalisation was predicted by the number of patient problems and carer psychological distress. Day care itself was associated with reduced distress for the majority of carers; for those in whom day care did not help to alleviate psychological distress, institutionalisation had a significant positive impact in terms of this outcome.
Cox59 examined a mixed respite programme for carers of dementia sufferers, which allowed families to buy up to 164 hours of respite, consisting of in-home care, institutional care (4–5 days) or day care. Follow-up was carried out at 6 months and African American participants were compared to white participants. There was no reduction in anxiety or depression in either group but there was a decline in carer burden in both groups.
Deimling60 also examined a mixed respite programme for dementia carers, consisting of short institutional stays, day care and home health aides. Follow-up was carried out at 4–6 months and assessed depression, symptoms of health problems and relationship strain. Comparisons were made between carers of those with stable conditions and carers of those with declining conditions. Carers of stable recipients had decreases in depression, health problems and relationship strain whereas outcomes for carers of recipients with declining conditions either stabilised or deteriorated.
Summary
Two of the studies reported respite to be associated with a delay in institutionalisation whilst having no effect on carer well-being. One of these studies, however, had too short a follow-up to give a meaningful result. In addition, one further study found respite to be associated with a shorter time to institutionalisation when compared with carer training interventions. There was no clear effect of type of respite in these studies.
The results pertaining to the impact of respite on carers’ well-being were variable although it would appear that, in the main, there was not a substantial effect on carer well-being; effects that were seen were beneficial with no evidence for negative effects. The longest length of follow-up was around 12–15 months. Studies that did show a positive effect of respite tended to be either short term or studies comparing respite with other types of intervention. In these studies respite reduced burden to a similar extent as the other interventions. It was not clear whether any particular type of respite was more effective than another, although the two studies examining mixed respite showed beneficial effects.
Meta-analysis: the effectiveness of respite care on carer well-being
The effectiveness evidence for respite care in terms of carer well-being is outlined in the following sections, presented for each outcome separately. Meta-analyses of randomised and quasi-experimental studies are given first, followed (when applicable) by the results from meta-analyses of single-group comparisons (longitudinal before-and-after studies) to examine any differences in terms of effects. All results from meta-analyses (Cohen’s method) are based on change scores and, when the change standard deviation is missing, a 0.6 correlation between baseline and follow-up is assumed. 29 Fixed models were initially fitted, except when tests for heterogeneity were statistically significant at the 5% level. In this instance a more conservative random-effects model is presented and resulting changes discussed. When significance was between the 5% and 10% levels both fixed and random models are shown. Appropriate descriptive findings are also summarised at the end of each section (outcome). Results are therefore presented in terms of a hierarchy of evidence quality; the relative quality of included studies is also discussed within each outcome.
Carer burden
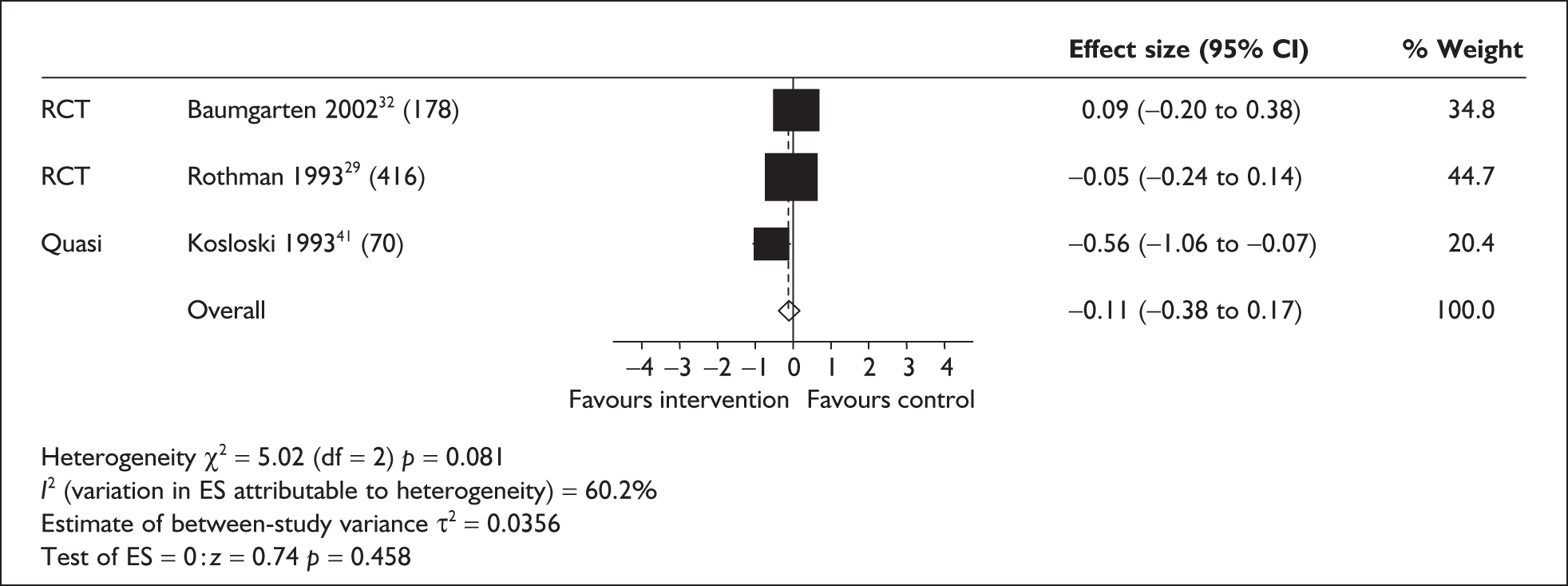
Carer burden in randomised and quasi-experimental studies
Three studies provided sufficient data on carer burden for inclusion in the meta-analysis: two RCTs29,32 and a single quasi-experimental study. 41 Two studies29,32 assessed day care interventions and the other41 both day and home care. Care recipients were frail elders,29 elders with dementia41 and elders experiencing mixed problems. 32 Two of the studies were carried out in the USA29,41 and one in Canada. 32 Carers in one study29 were followed up at 6 and 12 months; the length of follow-up for the other two studies32,41 was 3 and 6 months and, therefore, only the 6-month follow-up period in the Rothman et al. 29 study was included in the meta-analysis. All interventions comprised day care and were delivered continuously over the respective follow-up periods. No significant effects of respite care on carer burden were observed (Figures 3 and 4) in either fixed or random models. The two RCTs can be seen to be closer to the line of no effect than the quasi-experimental study.
FIGURE 3.
Carer burden in randomised controlled trials/quasi-experimental studies (fixed model) – 6-month follow-up (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
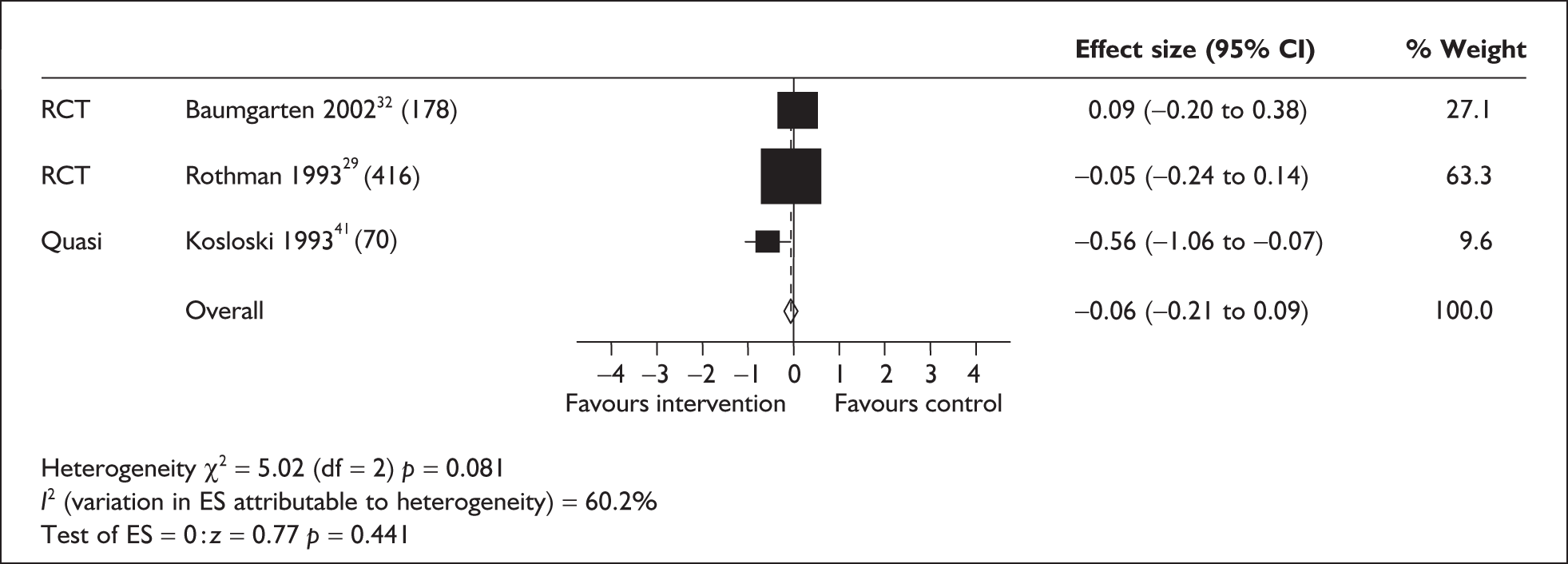
FIGURE 4.
Carer burden in randomised controlled trials/quasi-experimental studies (random model) – 6-month follow-up (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
Carer burden in longitudinal before-and-after studies
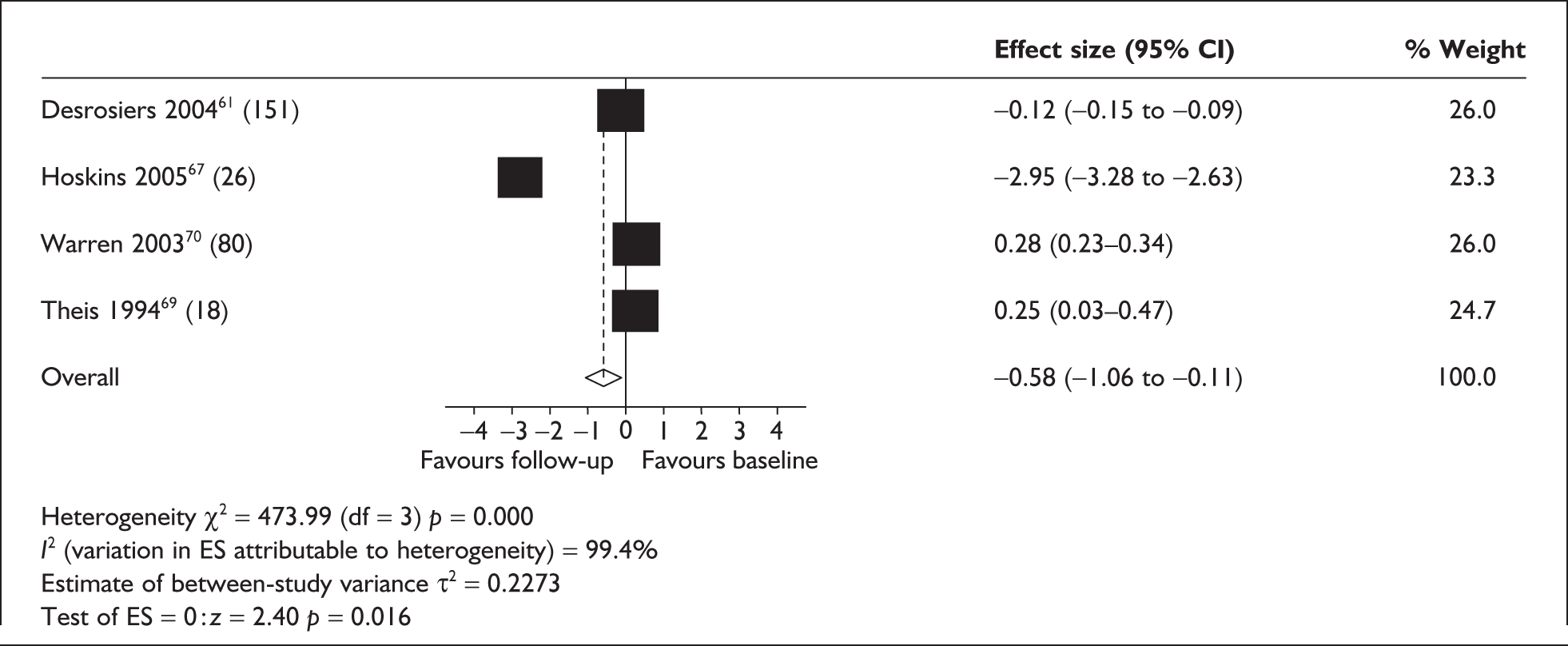
Four longitudinal studies comprising a single-group (before-and-after studies) were included in a meta-analysis of carer burden. 61,67,69,70 Two studies were carried out in Canada using a day care intervention;61,70 one in the UK on a combination of institutional and day care;67 and one in the USA on a combination of home and institutional care. 69 The two studies focusing on day care gave similar levels of respite of around 2 days per week, but the study using a combination of day and institutional care did not give any information on the amount of respite provided. Three of the studies focused on frail elders61,69,70 and one on care recipients with dementia. 67 All studies measured burden at multiple time points (3 and 6 months;61,67 2 and 6 months;70 6 and 12 months69). Warren et al. 70 also measured burden at 2 weeks post-respite; this follow-up measurement was excluded from the meta-analysis. Therefore, two meta-analyses were carried out, one at short-term follow-up (2–3 months) and one at longer-term follow-up (6 months); the 12-month follow-up69 was not included in the meta-analysis. At both short- and longer-term follow-up tests for heterogeneity fitting a fixed model were significant (p = 0.0000); therefore, results of random models are presented (Figures 5 and 6). The only individual study with a positive significant effect at either follow-up67 was focused on care recipients with dementia rather than frail elderly more generally and used a combination of institutional and day care.
FIGURE 5.
Carer burden in longitudinal before-and-after studies at 2–3 months’ follow-up (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size.
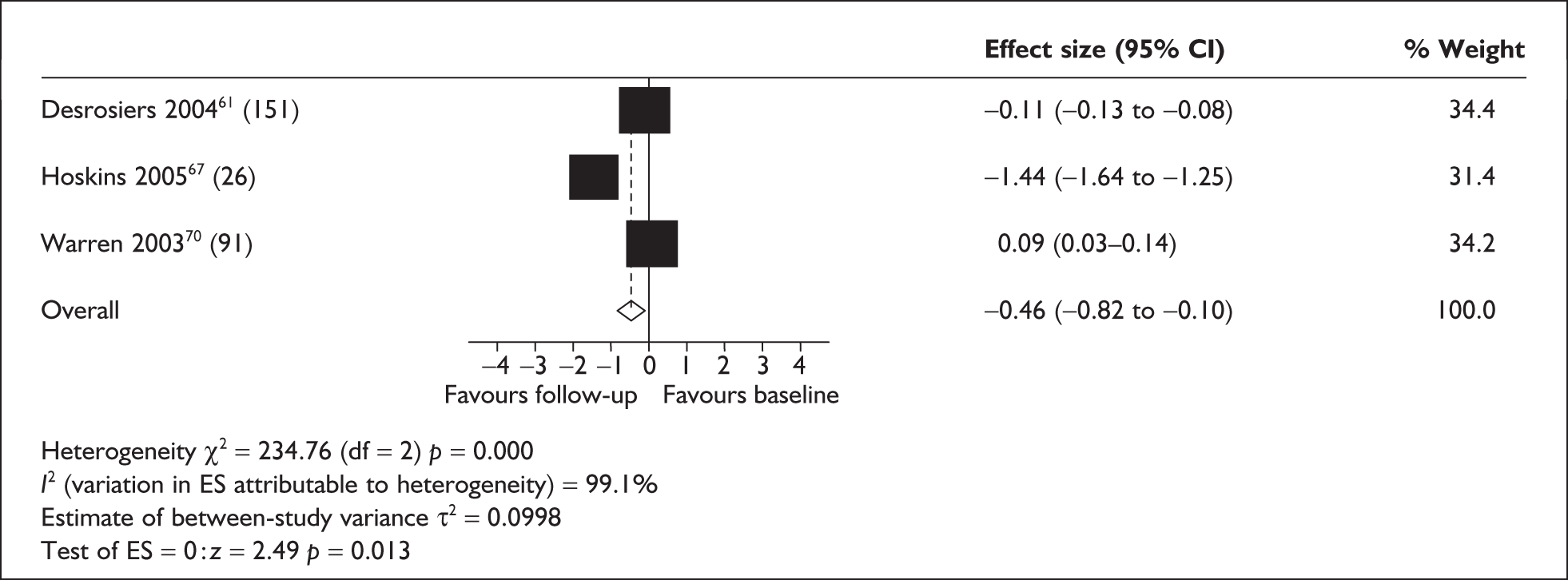
FIGURE 6.
Carer burden in longitudinal before-and-after studies at 6 months’ follow-up (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size.
Quality and design characteristics of studies included in the meta-analysis of carer burden
As seen in the analysis presented above, only two RCTs29,32 assessed carer burden. Neither of these studies found a significant effect of day care on carer burden. Only one of these trials was rated as high quality,32 having scored highly on all attributes on the quality assessment. This study examined a day care programme that included some functional and psychosocial activities, although these were group based, which is common in many day care facilities. The day centres did have access to a range of staff such as nurses, recreation technicians, special care counsellors and drivers, with possibly a rehabilitation technician, occupational therapist and psychosocial worker in some facilities. The intervention was fairly active but the main aim was of support rather than medical intervention. In addition, any attendees who required individual intervention were excluded from the analysis, thus excluding those who were having more treatment-focused interventions. However, there were some limitations in relation to external validity as only 34% of participants attended the facility at least once a week. The majority, therefore, had low exposure to the intervention, which may have been insufficient to exert any effects on carers. A subgroup analysis was carried out of high attendees (those attending at least once a week) and those attending less often. Carers of high attendees were substantially less burdened post-intervention whereas carers of low attendees had a slight increase in burden, although the difference was not statistically significant. Although the authors acknowledge that little weight can be placed on conclusions as there may be confounding factors in such an analysis, they suggest that future studies should aim to encourage a level of attendance that would be felt to be of consequence for carers. In addition to this, both intervention and control groups could access other services involving respite if they desired, but this was not measured or accounted for in the analysis.
The other RCT29 was of moderate quality and details had to be gleaned from a number of papers reporting different aspects of this large study. The sample in the analysis included here was not representative of the carer population generally as the trial was carried out in Veteran Administration facilities; the majority of care recipients (96%) were therefore men. The care recipient population further differed from a general community population in that 66% were in hospital at recruitment and were at high risk of nursing home placement on discharge, with the intervention being offered as an alternative to residential care. There were limited details of care recipients’ characteristics or context, but it is likely that there were more carer and care recipient dyads in crisis situation than in the population in general. There was little description of the services provided although, as in the previous study, some additional services were offered such as occupational, physical and recreational therapy. There were also some more individualised services, such as monitoring of complex medications. However, the overall aim of the intervention was focused on support, to allow people to remain at home by providing respite, motivation for self-care and stabilisation of health status. Uptake of the intervention was said to vary considerably with some not attending at all or for very few days; however, actual uptake in the group was not specified, and neither was use of other support services during the time period of the study. The control group received customary care but it was unclear what this involved, although it was apparent that this could be nursing home as well as community care.
The only study in this particular analysis reporting a positive effect of respite on carer burden was a quasi-experimental study,41 which was rated to be of high quality. The main difference between this and the other two studies is that the intervention included more flexibility of respite options. At three sites in-home and day care respite were offered with no limitations on access; two sites offered in-home care, both day and evening with a flexible schedule, and two sites offered only day care on weekdays from 8am to 5pm. It was reported that respite workers received special training but beyond this there was no further definition of the intervention. A further notable difference in this study is that all participants used the respite services, with mean use being 220 hours over the period of the study (range 4–1137 hours). A major issue with quasi-experimental studies is the potential for bias in sampling. In this study waiting list control subjects were used but the majority were recruited from just one site. This had an impact on comparability of the intervention and control groups as they differed on race and income (the control group had more ethnic minorities and a lower income). There were no other statistically significant differences between the groups. Consequently, race and household income were controlled in the analysis, and the positive effect of respite remained. Use of other services was not restricted but was also controlled in the analysis. Finally, the sample of care recipients in this study were people with dementia, whereas care recipients in the other two studies had a range of physical and cognitive disabilities.
Four before-and-after studies assessed carer burden, only one of which was rated as being of high quality and which found no effect of day care. 61 One was rated as being of moderate quality67 and demonstrated a positive effect of institutional and day care, and two were rated as being of lower quality,69,70 both showing no effect. The high-quality study61 assessed burden following ADC in a geriatric day hospital. The aim of the programme was to maintain people in their living environments, but being a day hospital as opposed to a day centre participants had access to a more medicalised support team of nurses, physicians, physical therapists, occupational therapists, recreational therapists, a neuropsychologist and a gerontopsychiatrist. All participants in the study had received services from at least two of these categories, which may or may not have involved medical intervention. However, description of the study intervention was incomplete, which was reflected in the quality assessment scoring. Whereas this study assessed a range of physical and cognitive disorders, the study rated as being of moderate quality67 focused on care recipients with dementia. This study showed a positive impact of the intervention on carer burden but again the intervention was poorly described, which in this instance was more problematic, as a range of services were offered, not all of which necessarily involved a respite element. Those specifically aimed at respite provision involved day care and institutional care; 50% of participants received institutional respite and 69% day care, although these were not received in isolation. Other interventions included a social care worker scheme, home help, inpatient access, carers group and B-grade nurse. Participants were assessed by a social worker or community psychiatric nurse on entry to the intervention and an individualised programme of care was devised. As well as poor description of the intervention characteristics and the amount and type of intervention received by participants, other aspects rated on the quality assessment form received only moderate scores (i.e. caregiver characteristics poorly described, incomplete control for population characteristics and methods of analysis inadequately described). As it was not possible to identify which particular aspects of the intervention had a positive effect, a logistic regression analysis was carried out, which suggested that only institutional respite had a positive effect. Those receiving day care appeared to be negatively affected. It is not clear if any other factors were included in this analysis and so there may be some confounding.
Of the studies rated as low quality, one assessed day care70 and the other69 in-home and institutional care; neither of these studies showed any effect of the respective interventions. Warren et al. 70 included both day hospitals (nine sites) and day support programmes (five sites); the majority (69%) of the sample was recruited from the day support programmes and received on average 10.4 hours of respite per week. No differences were detected in any of the outcomes between those attending day hospital and those attending day support and so the sample was analysed as one group. There were no details about the structure or content of the intervention programmes and the characteristics of care recipients were not described. Other aspects of the study receiving low ratings on the quality assessment form were selection methods (not completely described), population characteristics (not controlled for), intention to treat analysis (no attempt made) and conclusions (not all supported by the study).
The other study of low quality,69 which assessed in-home and institutional care, had a large and significant problem of attrition. Details of the carer sample were given for the 130 participants for whom data were available at baseline, but follow-up data at 6 months were only available for 18 carers. The intervention was a nurse-managed co-ordination of the available services. Trained volunteers provided up to 4 hours a week of in-home respite and institutional care was provided in a long-term care facility, but further details of the use and process of the intervention were lacking. However, the maximum potential usage of respite was low. The study design was generally poorly described, as were the selection criteria for the sample, and potential confounders were not addressed in the analysis.
Summary of studies assessing the impact of respite care on carer burden (studies included and excluded from the meta-analysis)
The analysis involving RCTs and quasi-experimental studies failed to show any evidence of an impact of respite care on carer burden. Although the two RCTs included in the analysis were of high and moderate quality, it must be noted that the sample characteristics of one were not generalisable to the population of carers as a whole29 and the other32 acknowledged difficulties in interpretation as uptake of respite was low in the sample. It is possible, therefore, that respite use was insufficient to show any effect in that particular study. The only study included in this analysis to show a positive effect of respite was a quasi-experimental study,41 which was also of high quality. A notable difference between this and the other two studies was the type of respite provision, which involved a range of day care and in-home provision as opposed to day care alone.
Before-and-after studies, on the other hand, demonstrated a positive impact of respite on carer burden. Two of the studies included in this analysis were of low quality;69,70 only one was rated as being of high quality61 and the other was rated as being of moderate quality. 67 The interventions used in these studies, again, consisted mainly of day care provision. However, one study stood out as reporting a large positive impact of respite,67 and this involved a combined intervention of day and institutional care and also a number of other services such as home help, which may also have provided some respite, as well as interventions not providing respite. Although this study offers some consideration of combined approaches to respite provision it also poses some difficulty in interpretation as it is not possible to determine the specific effects of those interventions providing respite.
None of the studies in this analysis was without problems in its applicability to the research question of this review. The range of methods, interventions and sampling used leaves no clear conclusions other than to say that evidence is lacking.
The narrative synthesis of studies not included in the meta-analysis indicates that day care54,68 and home care52 alone may have little or no significant impact on carer burden or self-perceived caring-related stress. At longer-term (6–12 months’) follow-up a number of studies42,43,49 also failed to detect a significant effect of a mixed service on burden. Further evidence for the short-term effects of respite on burden is indicated by the finding57 that burden decreased during a period of inpatient respite, but that levels returned to baseline when care recipients returned home. Some research58 asserts that levels of carer stress may actually increase following a period of respite. A number of studies reported a positive effect of respite on burden35,36 compared with controls, yet follow-up periods were less than 2 months.
In studies evaluating the effects of different types of day care (day care/day hospital34), or mixed respite relative to other interventions (e.g. support groups, education45,46), no differences were observed between groups in terms of burden.
Carer depression and psychological well-being
Carer depression in randomised and quasi-experimental studies
A total of six studies (of which two were RCTs) were included in a meta-analysis of the effects of respite on depression. 29,40,44,47,48,55 Two studies29,55 measured depression at two follow-up times (6 and 12 months and 3 and 12 months respectively). Two separate analyses were therefore carried out examining the effects of both short- and long-term follow-up.
Five studies were included in the analysis for short-term follow-up. 29,40,44,47,55 Four of the studies were carried out in the USA29,40,47,55 (three assessing day care29,47,55 and one home care40). Only one was carried out in the UK,44 assessing home care. 44 Three of the studies focused on care recipients with dementia40,47,55 and two focused on frail elderly care recipients. 29,44 Length of follow-up ranged from 1 to 6 months. As the test for heterogeneity was significant in this instance, the effect of fitting a random model was evaluated (Figure 7); the effect just fails to reach significance in favour of respite care. The studies reporting the largest effects in favour of the intervention were quasi-experimental rather than trials.
FIGURE 7.
Carer depression in randomised controlled trials/quasi-experimental studies – short-term follow-up (1–6 months) (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
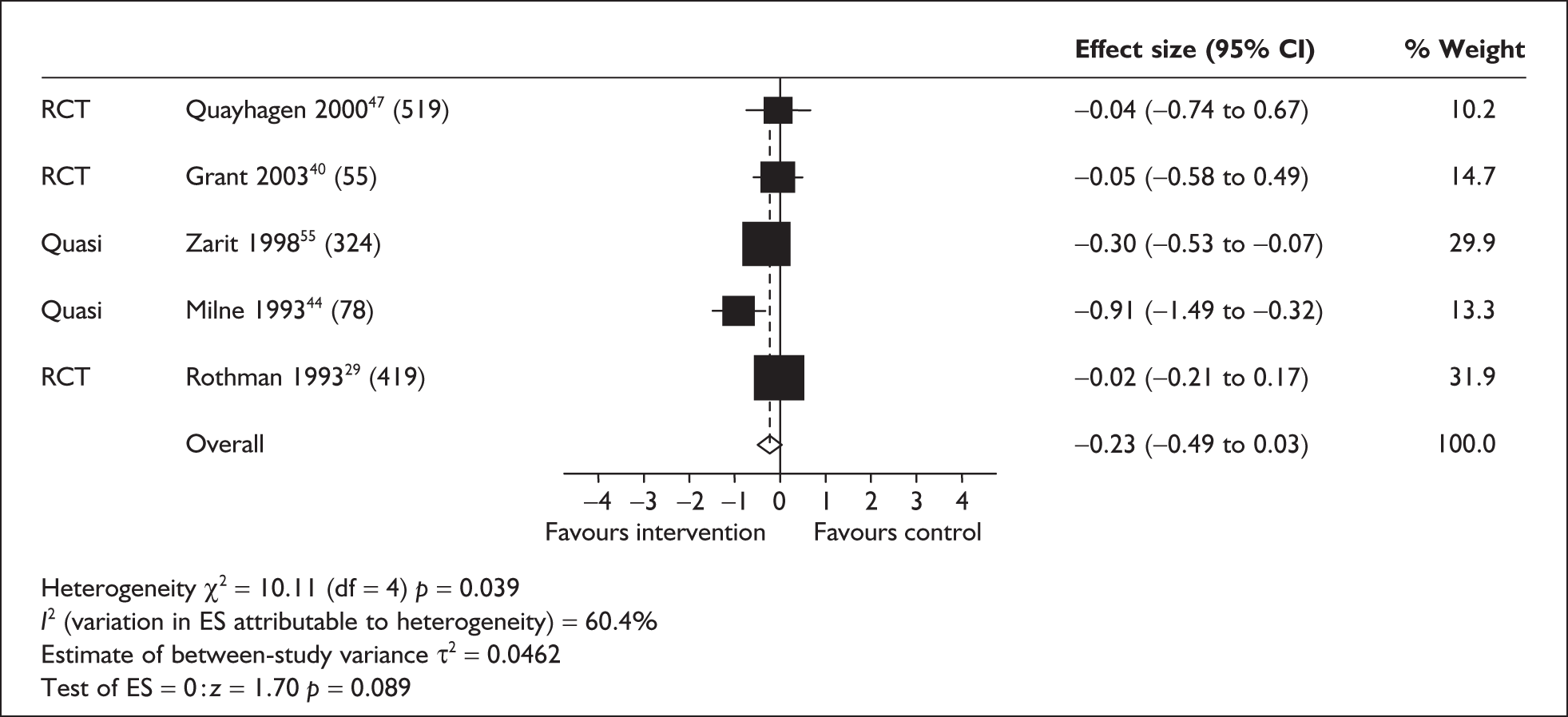
Three studies were included in the meta-analysis of depression at longer-term follow-up. 29,48,55 Two studies were carried out in the USA,29,55 assessing day care in the frail elderly29 and in care recipients with dementia. 55 The third study assessed a combined day and home care intervention for dementia care recipients in the UK. 48 The follow-up period for all studies was 12 months. As the test for heterogeneity was significant in this instance, the effect of fitting a random model was evaluated (Figure 8), which showed a non-significant overall effect.
FIGURE 8.
Carer depression in randomised controlled trials/quasi-experimental studies – long-term follow-up (12 months) (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
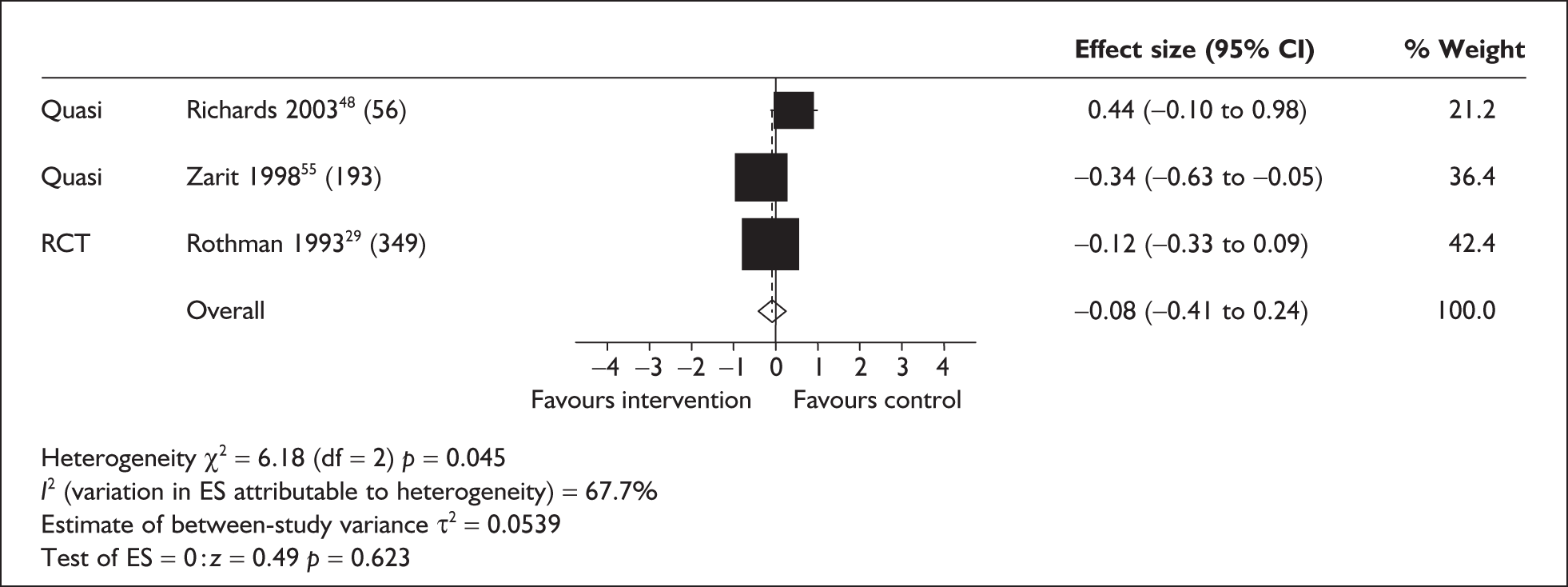
Depression and respite setting
Separate meta-analyses were carried out to determine the relative influence of day and home care. Four studies evaluated day care services29,47,48,55 and two home care. 40,44 Using a fixed-effects model significant effects in terms of a reduction in depression were not observed for day care services (Figure 9).
FIGURE 9.
Carer depression in randomised controlled trials/quasi-experimental studies day care (fixed model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
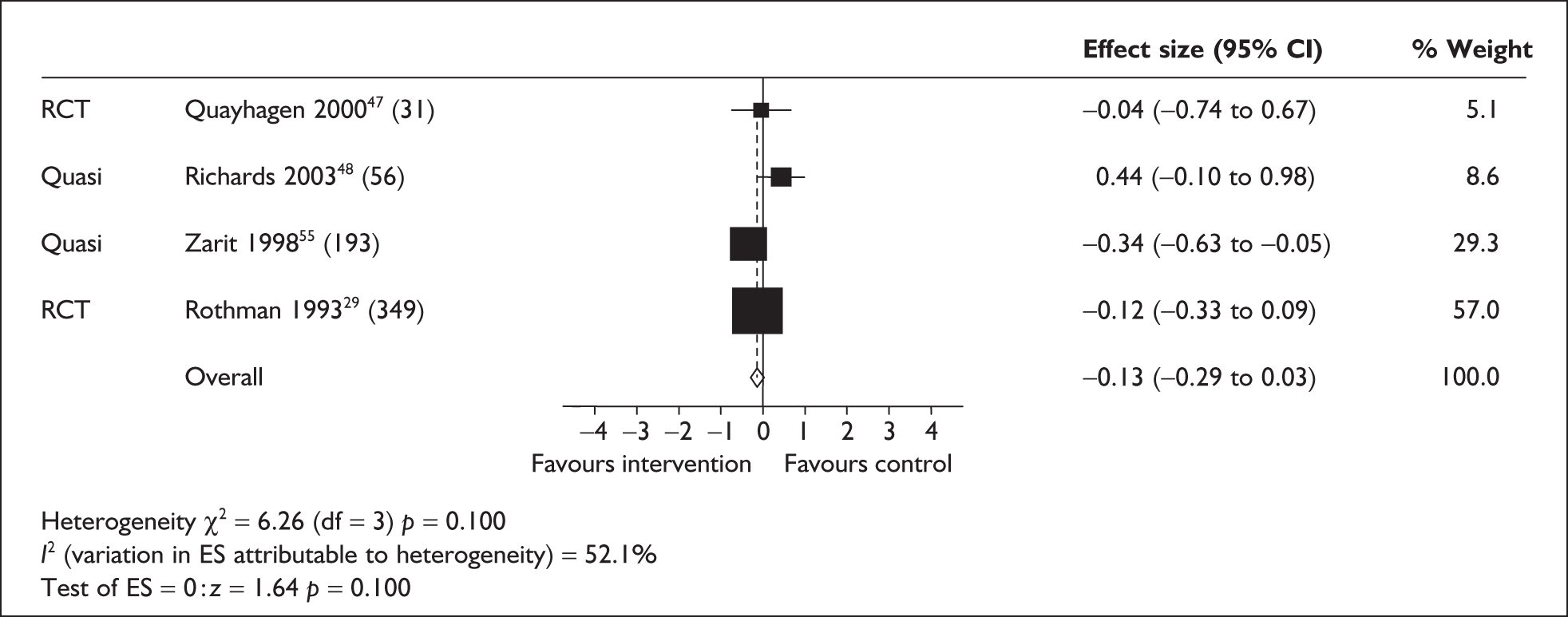
As the test for heterogeneity was significant, a random-effects model was used in assessing the effects of home care on carer depression (Figure 10). This resulted in a slighter larger but non-significant effect size.
FIGURE 10.
Carer depression in randomised controlled trials/quasi-experimental studies – home care (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
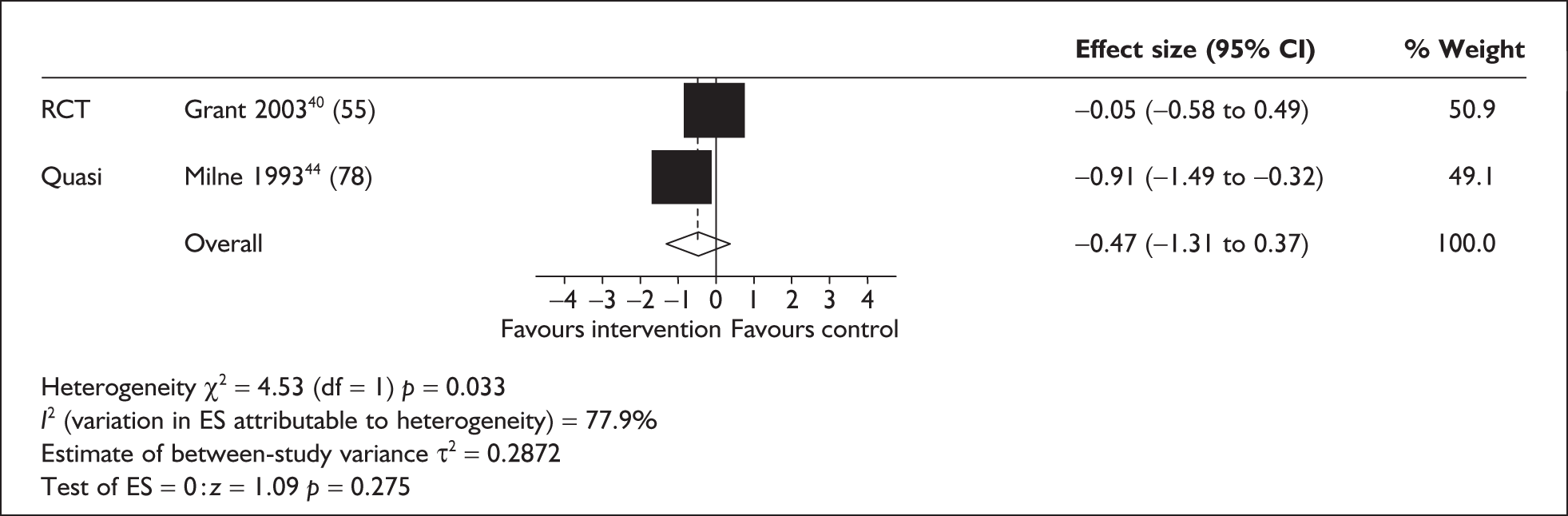
Carer depression and length of intervention
Three of the studies evaluated the effects of a long-term intervention (as opposed to long-term follow-up of a shorter intervention) provided over a 12-month period29,48,55 and two of the studies40,47 evaluated the effects of short-term respite interventions (the former for 2–8 weeks). Neither long-term (random model; Figure 11) nor short-term (fixed model; Figure 12) interventions were found to significantly impact on depression.
FIGURE 11.
Carer depression in randomised controlled trials and quasi-experimental studies: long-term intervention (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
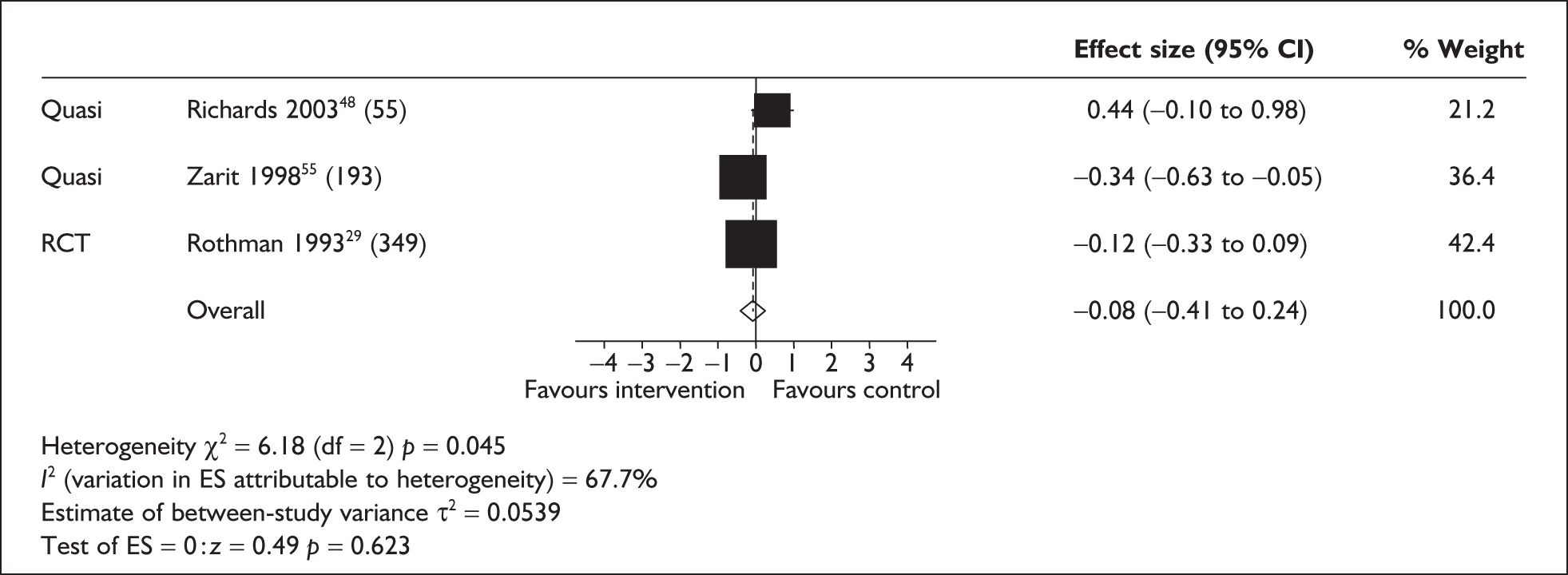
FIGURE 12.
Carer depression in randomised controlled trials/quasi-experimental studies: short-term intervention (fixed model) (sample sizes in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
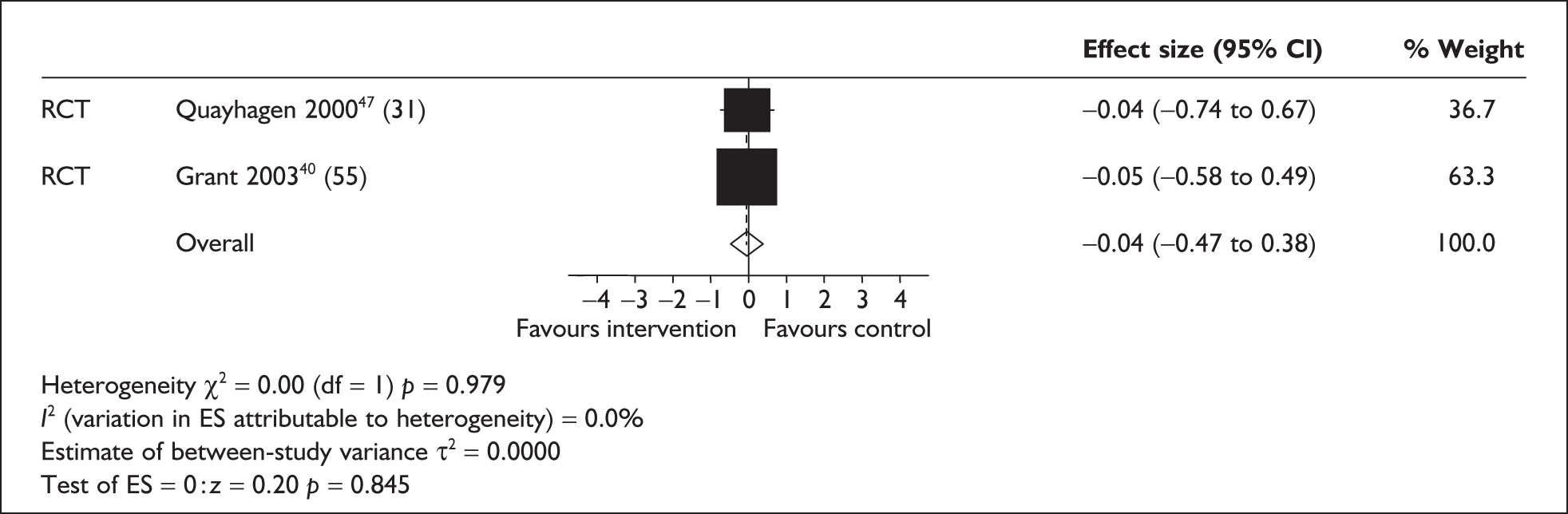
Carer depression in longitudinal before-and-after studies
Three single-group longitudinal studies were included in a meta-analysis of depression (all continuously available interventions: 3-month follow-up of home care;64 depression measured during an inpatient respite intervention;66 6-month follow-up of a mixed respite programme69). Two of these studies were carried out in the UK66,69 and one in the USA. 64 The impact of respite on depression is not statistically significant when a random-effects model is fitted (Figure 13).
FIGURE 13.
Carer depression in longitudinal before-and-after studies (0–6 months) (random model) (sample sizes in brackets). CI, confidence interval; ES, effect size.
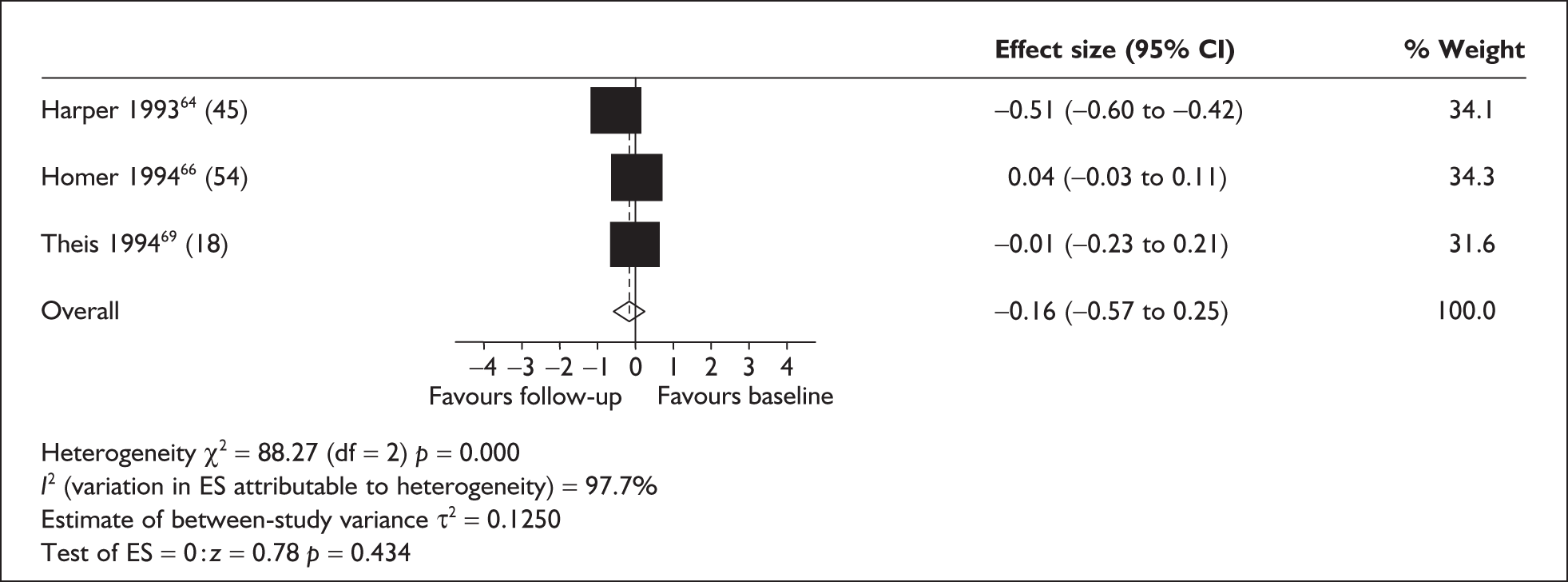
Quality and design characteristics of studies included in the meta-analysis assessing the impact of respite on carer depression
Three studies used RCT methodology29,40,47 and three a quasi-experimental approach. 44,48,55 The RCTs were rated as being of moderate quality; two assessed day care and one assessed home care. None of these studies showed any significant effect of respite on carer depression. The Rothman et al. study29 has already been discussed in relation to carer burden. Although a fairly well-conducted RCT, the main issues in this study concerned the generalisability of the sample (being nearly all men attending Veteran Administration facilities); the majority being hospital inpatients at the time of recruitment; and the potentially low rate of uptake of day care services (although insufficient details given on this).
The Quayhagen et al. study47 was of moderate quality and compared a range of support interventions for a group of carers of care recipients with dementia with a waiting list control group. Day care was provided as one of the interventions with the main aim of providing respite. Two support group sessions for the carer were also included in this arm of the trial. Care recipients received 4 hours a week of day care over a period of 8 weeks, which is a low level of respite provision and which may have been insufficient to have a significant impact on outcomes. The intervention included structured activities designed to stimulate the participant cognitively and socially. The quality assessment identified poor definition of carer characteristics, randomisation methods and whether allocation concealment took place. In addition, it was unclear whether there was any other use of respite services in either the intervention or control groups.
The final RCT40 examined home care and was more specifically focused on respite by providing trained respite carers for up to 6 hours a day for 10 days in a 2-week period. Therefore, although the amount of respite offered was fairly substantial, the length of the intervention was very short. It is debatable whether an intervention of only 2 weeks would impact on depression ratings. In-home care was chosen in this study by assessing preferences for type of care beforehand. The use of other services was controlled during sample selection by including only those who received other respite services for less than 8 hours per week. The sample was considered in relation to level of vulnerability, based on the number of hours a day spent caring and the level of respite received. Vulnerable carers took up more of the respite offered in the intervention (56 hours) whereas non-vulnerable carers took up about half the amount (27.6 hours), although the levels were similar in the two groups when five carers were excluded who did not take up respite at all. A number of physiological measures of stress were also carried out, with the finding that plasma adrenaline declined significantly in the vulnerable carers who received respite but rose in those in the control group. The quality assessment form showed low or moderate ratings for information on care recipient characteristics and incomplete control/description of population characteristics in the analysis.
The only study to be rated as high quality was a quasi-experimental study,55 which demonstrated a positive effect of respite (day care). This study rigorously controlled the amount of respite used during the study to ensure adequate exposure in the intervention group and to ensure that both the intervention and the control group used only minimal amounts of other formal services. The intervention group had to use the service at least twice a week for a period of 3 months. However, being a quasi-experimental study there was the potential for selection bias, as the intervention group was recruited from one area of New Jersey whereas the control group was recruited in Ohio. Although care was taken to choose the sites based on similarities of the populations, the control subjects were recruited via advertisements and were self-selecting. Some differences were identified between the groups at baseline, although these were taken account of in the analysis strategy; although the difference between groups was not significant before controlling for these factors, it was after adjusting the means to take account of the differences. All attributes on the quality assessment were scored highly in this study.
The remaining two quasi-experimental studies44,48 were of low quality. One assessed home care and was the only study to show a positive effect of respite. 44 The intervention provided a care attendant to replace the informal carer duties for an agreed time up to a few hours; however, there was little further detail about the intervention or the number of hours that respite was used, and no indication of the extent of use of other services. Participants in the study were those referred to an Age Concern carer support scheme; the control group elected not to use services for a variety of unreported reasons, giving the potential for significant selection bias. There were inadequate details given in the study concerning participant selection or participant characteristics and so it was difficult to assess this further. No account was taken of any population characteristics in the analysis and it is possible that these may have seriously influenced the results.
The final quasi-experimental study48 assessed day care in the context of specialist dementia services. The comparison groups consisted of a memory clinic, a community mental health team and a day hospital. These interventions were intended to represent the care pathways for dementia patients with different levels of need. In the present analysis the day hospital was compared with the memory clinic, although people attending the memory clinic had mild dementia whereas those attending the day hospital had moderate to severe dementia. As well as having more severe memory problems the day hospital group also had a greater frequency of problem behaviours. The study scored poorly on a number of quality assessment criteria: description of care recipients, carers and the intervention; characteristics of loss to follow-up (likely to affect results); population characteristics (not controlled for); analysis methods (not reported but probably appropriate); intention to treat analysis (no attempt to carry out); and conclusions (some not supported by the data).
Three before-and-after studies assessed carer depression. 64,66,69 Only one64 reported a positive effect of respite. This study assessed a home-based care aide service for care recipients with dementia and was of a moderate quality rating. There was some flexibility in this service as carers decided whether they wanted frequent but short periods of help or less frequent but longer periods of help, so that they could tailor the respite to suit their needs. In addition, continuity was maintained by keeping, as far as possible, the same care aide/care recipient combination. The aide provided help with bathing, dressing, continence care, medication, shopping, preparing meals, household tasks and social activities in and outside the home. There was further flexibility in the programme as the aides themselves could define their role and carry out tasks other than personal care at their own discretion. Once a week the care aides and care recipients all met to provide mutual support, and the carers met monthly for information provision activities. The paper reports an average number of hours of care provided by the service as 15.8 per month, but it is unclear if this figure refers to the sample involved in the study or the average service provision before commencement of the study. Again, details of other service use are lacking. In addition, the quality assessment identified that incomplete carer details were provided and no account was taken of any sample characteristics in the analysis; that variance estimates were provided for some but not all outcomes; and that the selection criteria were not described. Losses to follow-up were also fairly substantial although these were addressed in the analysis. From these observations it was likely that there was some selection bias in the sampling.
The remaining two studies were of low quality. One, that by Theis et al. ,69 was discussed in relation to carer burden. This study had a substantial problem of attrition and the characteristics of both the carer and care recipient samples are unclear. Respite provision (home and institutional) at home was low (up to 4 hours a week) and the level of usage of either in-home or institutional respite is unclear. The final study66 assessed geriatric services providing inpatient respite care; however, the structure of and process involved in the intervention is not described. Limited details of the characteristics of the carer sample are given and no details of the characteristics of the care recipient sample are given. Outcome measures were carried out in the middle of the respite provision, which appeared to be in the middle of a 2-week inpatient stay. It is unlikely that there would be a significant impact on depression scores after this level of respite provision, although there is no information concerning the number of times respite had been utilised, for how long or whether any other services were being accessed. The quality assessment score also identified poor description of aims, study design and analysis.
Summary of studies assessing the impact of respite care on carer depression (studies included and excluded from the meta-analysis)
At short-term follow-up the meta-analysis of the impact of respite care on carer depression was in favour of respite care, although this just failed to reach significance. No effect of respite was seen in the longer term. The RCTs in these analyses were of moderate quality but none found an effect of respite. One was a study carried out in a Veterans’ facility in the US29 and the sample was poorly generalisable, and the other two40,47 had low levels of respite provision, which may be unlikely to have any impact. Only one study was of high quality,55 a quasi-experimental study, which demonstrated a positive effect of day care. The other quasi-experimental studies44,48 showed no significant effects and were of low quality with poor descriptions of methodology and potential sample bias.
Longitudinal before-and-after studies also failed to demonstrate any effects of respite care on carer depression in the meta-analysis. One study included in this analysis was of moderate quality,64 which on its own reported a positive effect of home care, whereas the other two studies were rated as low quality and failed to show any effects. 66,69 The study reporting a positive effect64 assessed a home aide service that incorporated some flexibility for carers to tailor the intervention to suit their needs. Of the two studies reporting no effect, one assessed both home and institutional care69 and the other inpatient respite. 66 These studies were poorly reported and, in one,69 attrition and sample bias were significant problems. The other had limited information from which to assess the reliability of the findings, although it is likely that outcomes were assessed after minimal respite provision. 66
In terms of respite setting there were no significant effects of either day care or home care, although they were in a direction favouring respite. Longer-term interventions seemed to have a greater impact on depression, although this effect was marginal.
Evidence from individual randomised and quasi-experimental studies not included in the meta-analysis largely indicates that respite does not have a significant impact on psychological well-being42,43,54 or depression49,52 when compared with normal care. However, these findings may reflect the type of intervention or the length of follow-up. In a study comparing respite with permanent institutional care, levels of depression were reduced amongst carers who institutionalised the care recipient but not amongst those receiving respite. However, removal of an existing respite service appears to result in increased levels of depression. 50
Two longitudinal before-and-after studies did, however, report a positive effect of respite care on carer depression. 57,[62,63] Significant effects were observed at relatively short follow-up periods (≤ 3 months).
Carer anxiety
Carer anxiety in randomised and quasi-experimental studies
Four randomised/quasi-experimental studies measured carer anxiety as an outcome. 29,40,47,48 One of these studies was carried out in the UK,48 the remaining three in the USA. Two focused on day care,29,47 one on frail elders29 and one on care recipients with dementia. 47 One assessed home care in care recipients with dementia40 and one both day and home care, again in care recipients with dementia. 48 No significant effects of respite on anxiety were observed at either short-term (1–6 months) or long-term (12 months) follow-up. Fixed-effects models for both short- and long-term follow-up are shown in Figures 14 and 15, respectively, and a random-effects model for long-term follow-up is shown in Figure 16.
FIGURE 14.
Carer anxiety in randomised controlled trials/quasi-experimental studies – short-term follow-up (1–6 months) (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
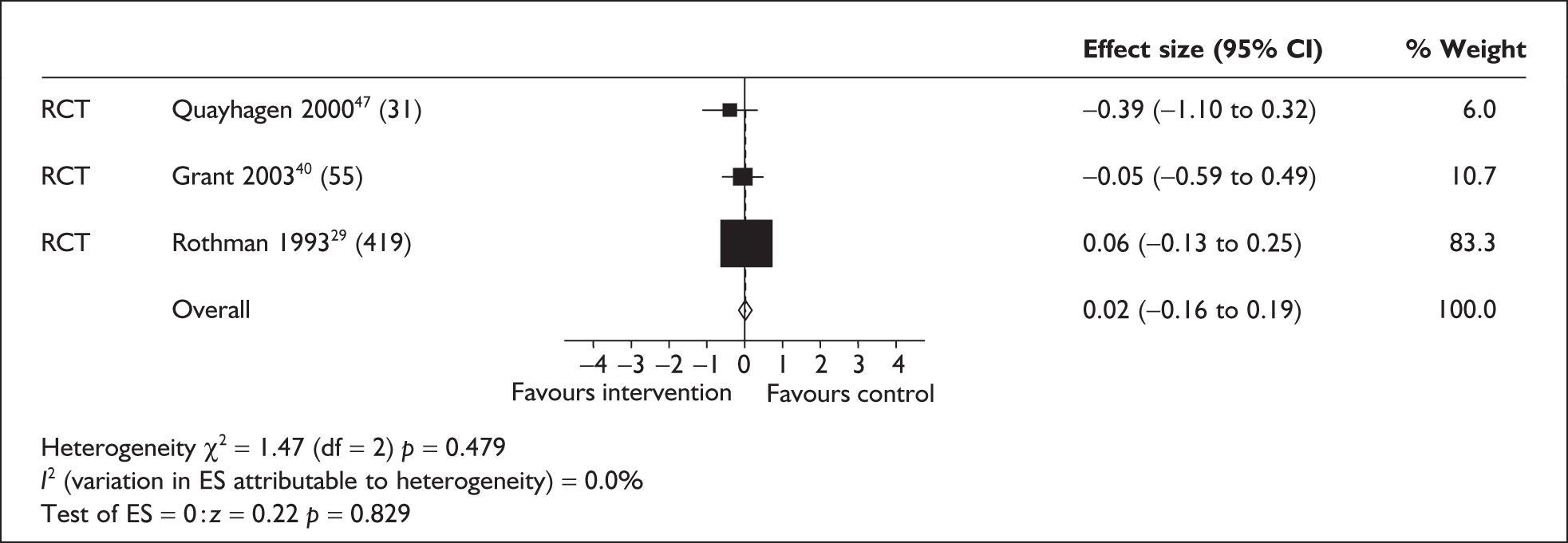
FIGURE 15.
Carer anxiety in randomised controlled trials/quasi-experimental studies – long-term follow-up (12 months) (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
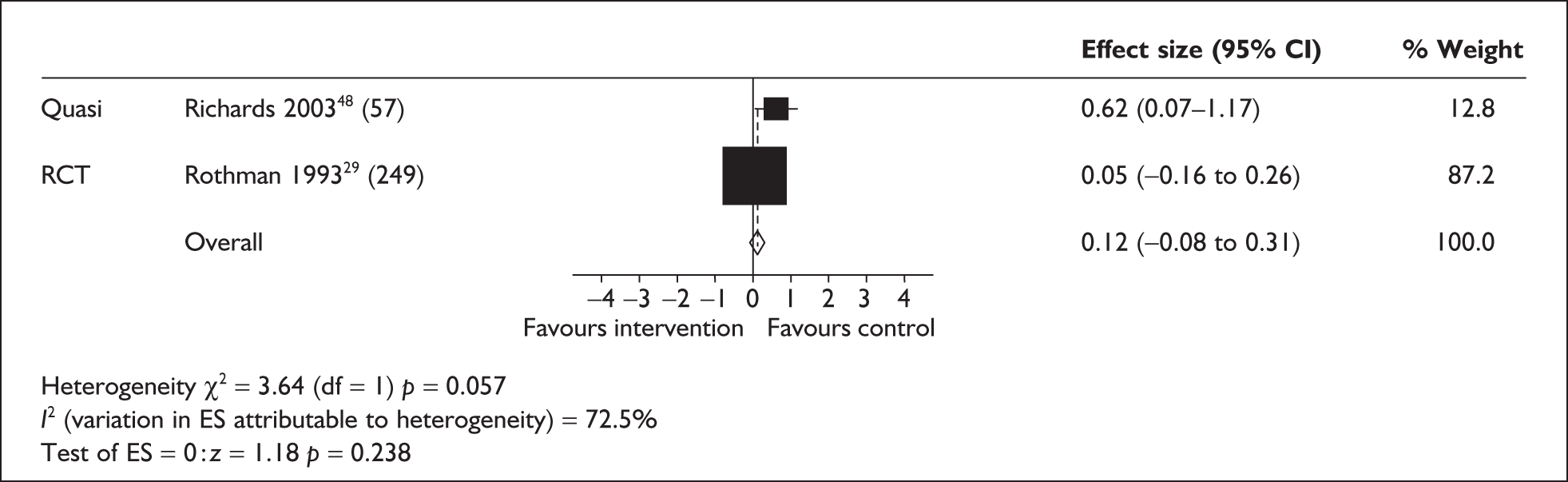
FIGURE 16.
Carer anxiety in randomised controlled trials/quasi-experimental studies – long-term follow-up (12 months) (random model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
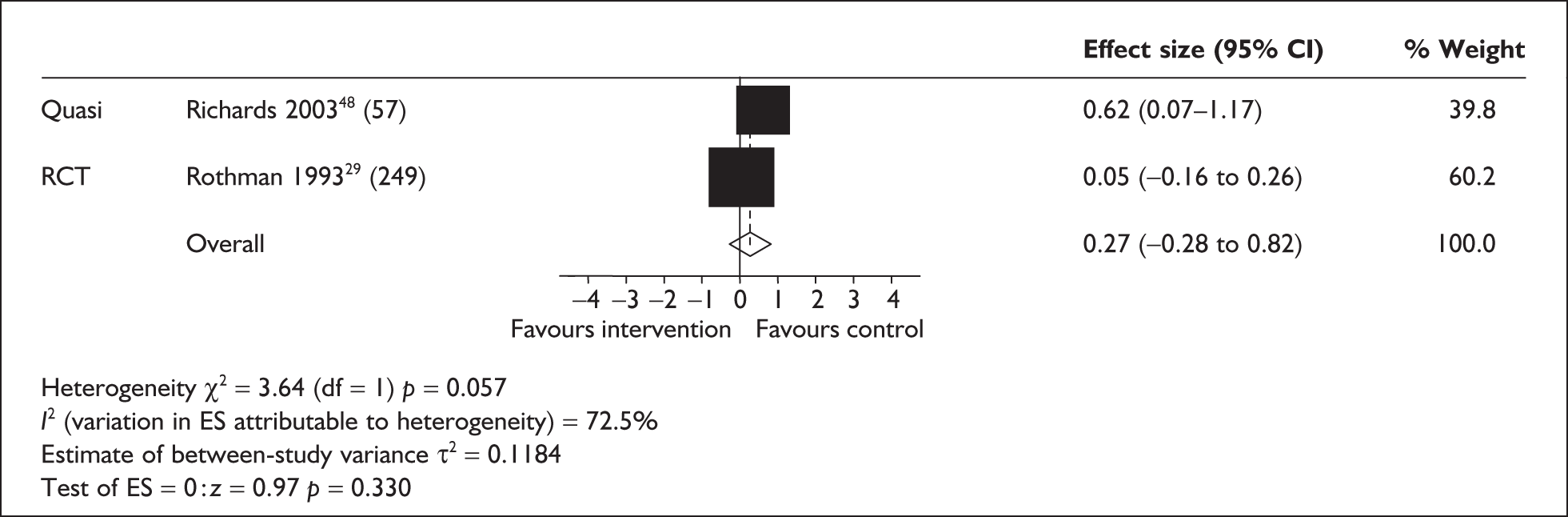
Respite setting (day care29,47,48) did not significantly predict anxiety (separate analysis for day care only shown in Figures 17 and 18 for fixed and random effects respectively).
FIGURE 17.
Carer anxiety in randomised controlled trials/quasi-experimental studies – day care (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
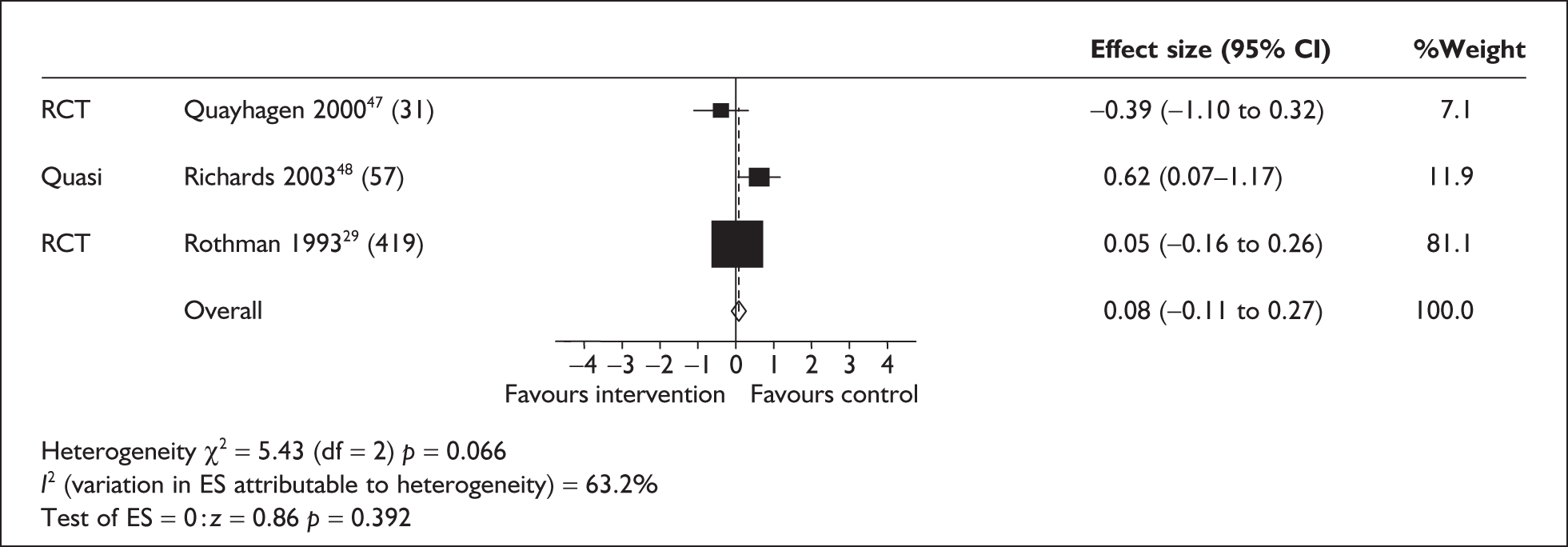
FIGURE 18.
Carer anxiety in randomised controlled trials/quasi-experimental studies – day care (random model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
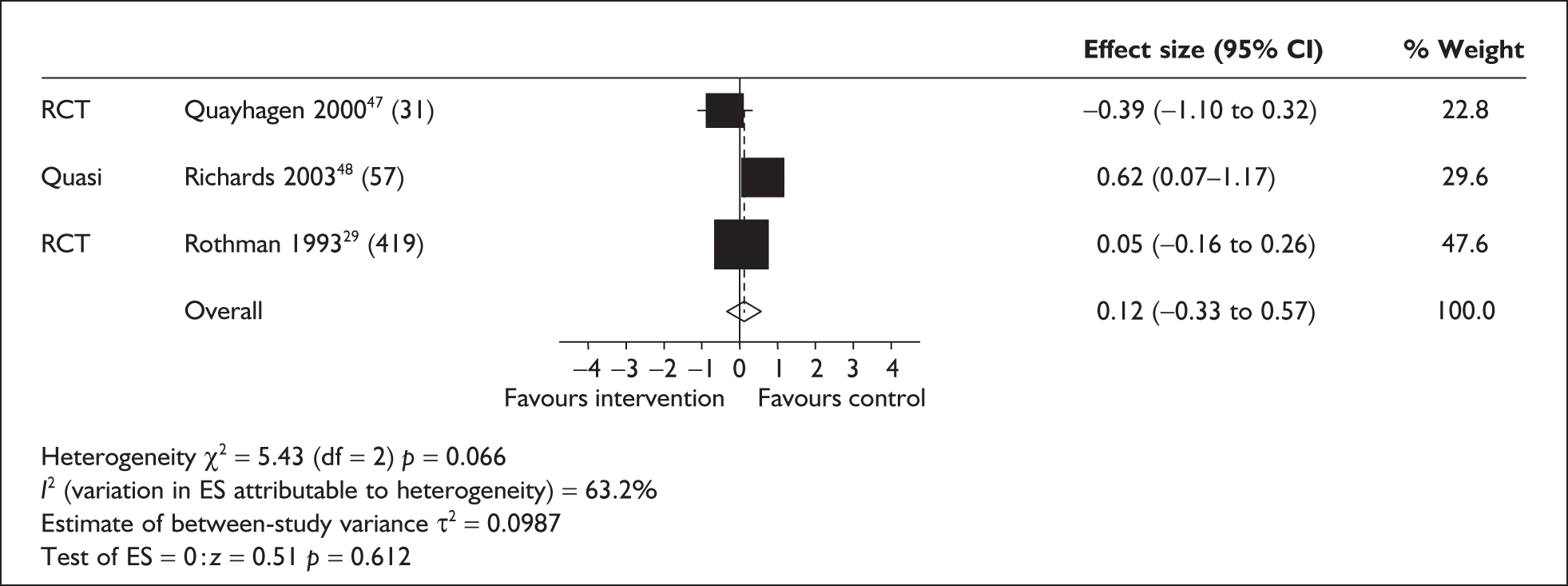
Length of intervention (short, i.e. 2–8 weeks,40,47 or continuous29,48) also did not significantly predict carer anxiety (Figures 19–21).
FIGURE 19.
Carer anxiety in randomised controlled trials/quasi-experimental studies – short-term intervention (2–8 weeks) (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
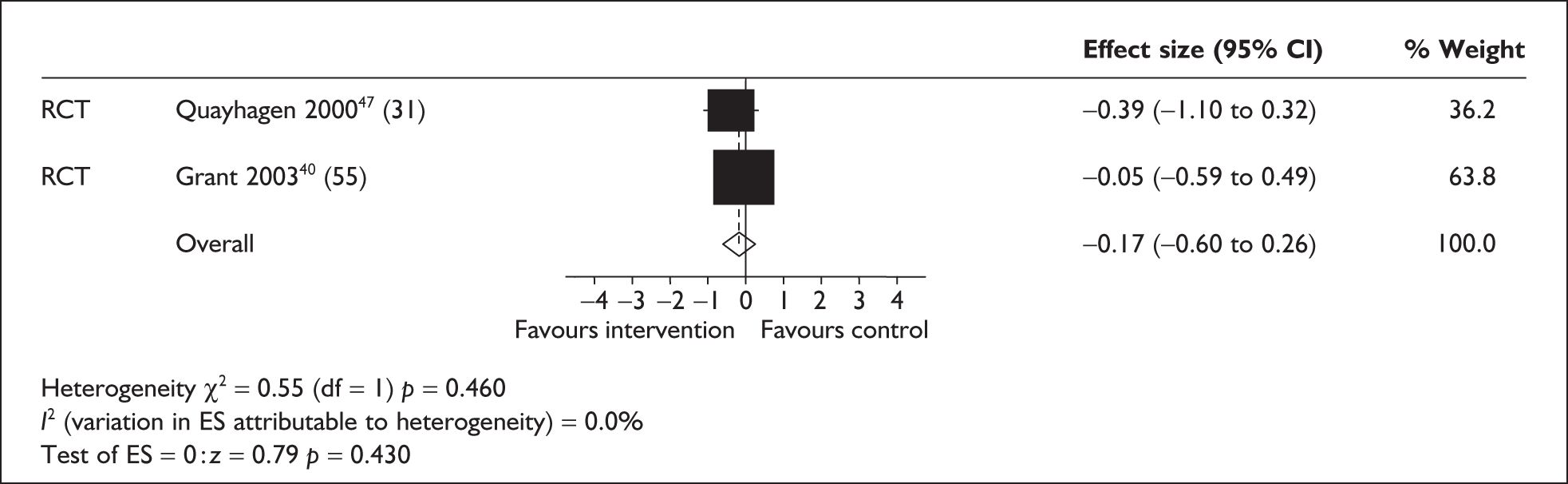
FIGURE 20.
Carer anxiety in randomised controlled trials/quasi-experimental studies – long-term intervention (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
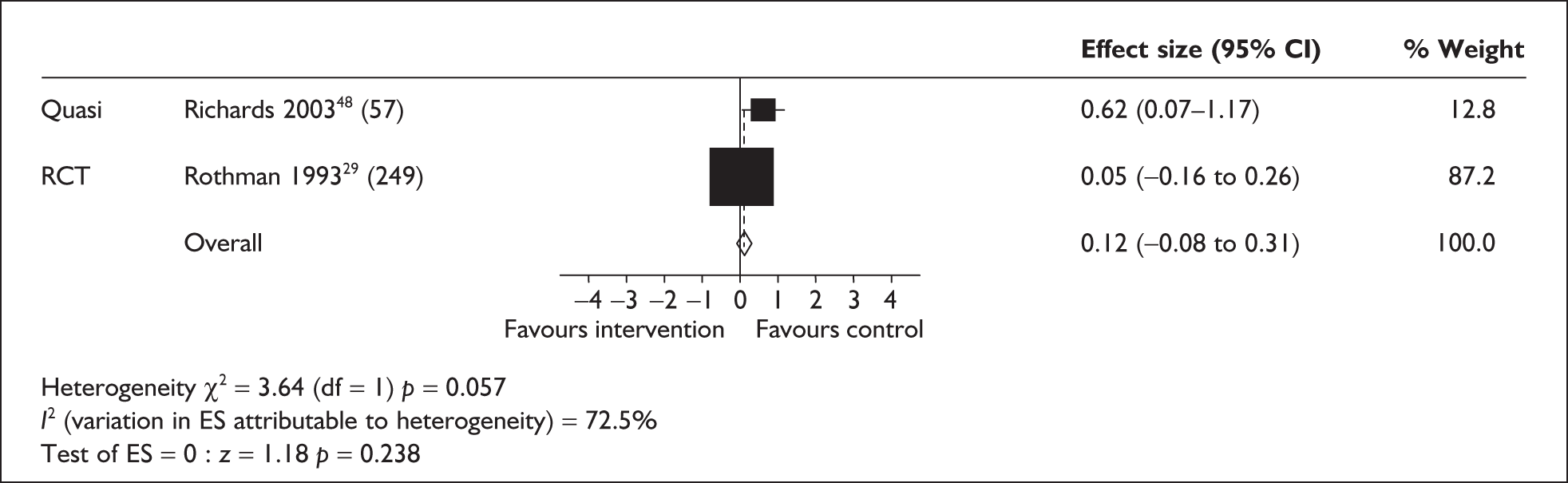
FIGURE 21.
Carer anxiety in randomised controlled trials/quasi-experimental studies – long-term intervention (random model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
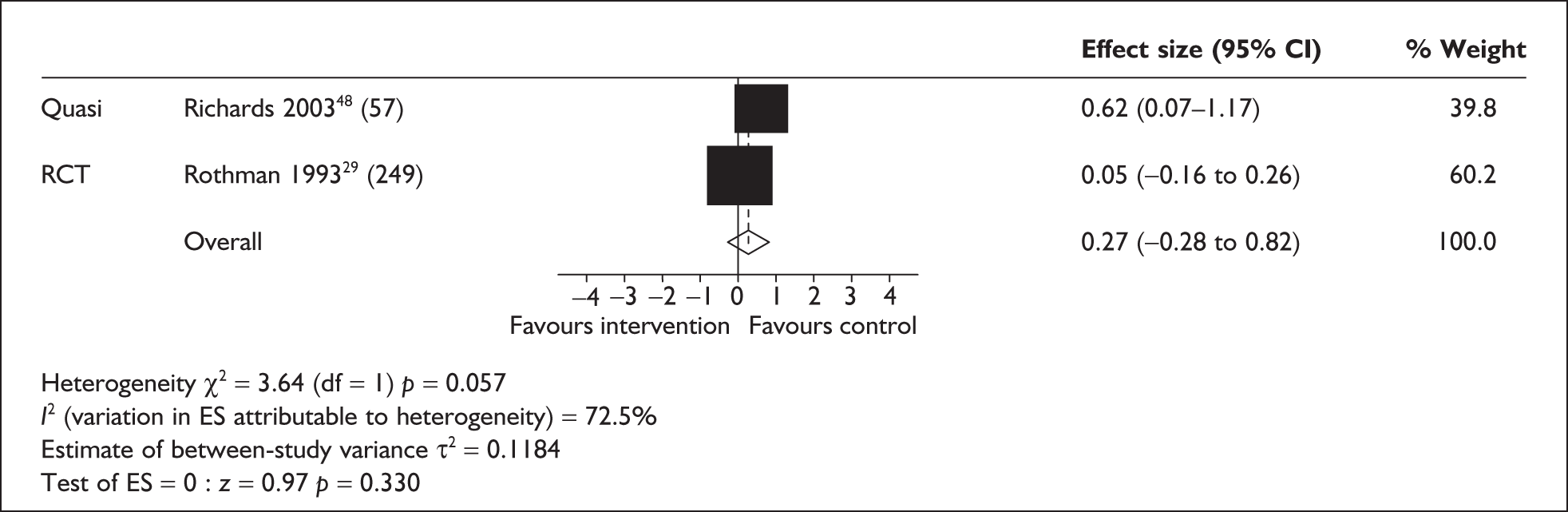
Quality and study design characteristics of studies included in the meta-analysis assessing the impact of respite care on carers’ anxiety
Three RCTs29,40,47 and one quasi-experimental study48 were included in this analysis. These were all described previously in relation to the analysis of carer depression. The three RCTs were of moderate quality. One47 provided early-stage day care for care recipients with mild to moderate dementia. Day care was provided for 4 hours a week for 8 weeks and involved a range of psychosocial activities. Although the day care group was less anxious at follow-up than a waiting list control group, this was not statistically significant. There were some problems of reporting in this study as carer characteristics and randomisation were poorly reported and it was unclear if allocation concealment had taken place at consent. Rothman et al. 29 also assessed day care but, as discussed previously, this was carried out in a veteran’s facility resulting in poor generalisability in the sampling. The final RCT assessed home care in dementia care recipients and provided in-home help for up to 6 hours a day for a period of 2 weeks. As mentioned previously, this represents a relatively short duration of respite provision, although it was provided fairly intensively in that time. Sample characteristics were poorly reported in this study and no consideration was given to potential sample biases in the analysis.
One quasi-experimental study48 was included, also described previously in relation to carer depression. This study was of low quality and reported a negative effect of day care on carer anxiety at 12 months. The study also found that the interpersonal dimension of the patient–carer dyad deteriorated, which may have some impact on carer anxiety. It is unclear why this occurred as the physical and self-care needs and the demanding and disturbing behaviours remained stable in this day care group.
Summary: evidence for the effectiveness of respite in reducing carer anxiety
The meta-analysis of randomised/quasi-experimental studies measuring carer anxiety as an outcome did not demonstrate any significant effects of respite. The RCTs included in the analysis were of moderate quality but either provided little respite or had problems with generalisability of the sample. The quasi-experimental study found a negative effect of respite on carer anxiety but this study was of low quality.
Subgroup analyses were carried out to assess home care, day care and long and short interventions but no significant effects were found. No longitudinal before-and-after studies measuring carer anxiety were identified.
A single quasi-experimental study measuring carer anxiety as an outcome was not included in the meta-analysis as comparison groups were institutional care versus respite. Results indicate that levels of anxiety were reduced for carers who institutionalised the care recipient but remained high for those receiving respite. 53
Carer morale
Carer morale in randomised and quasi-experimental studies
Two studies41,47 measured morale as an outcome in relation to respite care. Quayhagen et al. 47 assessed day care in care recipients with dementia, whereas the study by Kosloski and Montgomery41 assessed combined home and day care. Both studies were carried out in the USA with dementia care recipients. Length of follow-up was 3 and 6 months respectively. There was a positive effect of respite on morale, although this was not statistically significant (Figure 22).
FIGURE 22.
Carer morale in randomised controlled trials/quasi-experimental studies (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
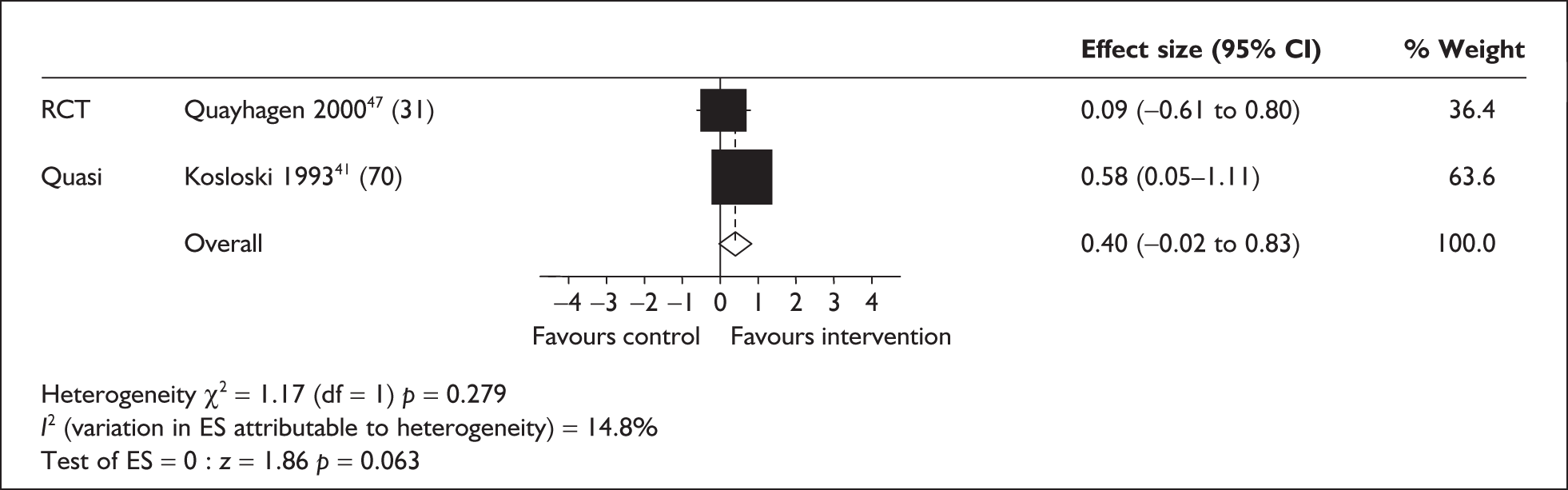
Quality and design characteristics of studies included in the meta-analysis assessing the effects of respite care on carer morale
One RCT47 rated as moderate quality and one quasi-experimental study41 rated as high quality assessed carer morale. Both have been discussed previously in relation to carer burden41 and carer depression47 and both examined care recipients with dementia. The RCT47 provided a low amount of respite (4 hours of day care per week for 8 weeks). There was poor definition of carer characteristics, randomisation methods and allocation concealment, and it was unclear whether there was any other use of respite services in either the intervention or the control groups.
The quasi-experimental study41 showed a trend towards a positive impact of respite care on carer morale although this failed to reach statistical significance. This study also reported a positive effect on carer burden. The intervention included both home and day care and provided some flexibility of service provision with the potential for high usage. Although there were differences between the intervention and control group characteristics at baseline, these were controlled for in the analysis. However, further differences may have been present, but not accounted for, because of the quasi-experimental nature of the study.
Summary of studies assessing the effects of respite on carer morale (included and excluded from the meta-analysis)
Only two studies measuring carer morale were identified, one of which was a randomised trial of moderate quality, the other a high-quality quasi-experimental comparison. Both interventions comprised day care delivered over a 3- to 6-month period, but the quasi-experimental study also included home care with a greater degree of flexibility in the programme. The RCT intervention provided a low amount of respite only. Results of the meta-analysis favoured the respite intervention but were marginally non-significant.
Carer anger/hostility
Carer anger in randomised and quasi-experimental studies
Two studies measured anger or hostility as an outcome following a respite intervention. 47,55 Length of follow-up was 3 months, and 3 and 12 months respectively. Follow-up data at 3 months were used for the meta-analysis. Day care comprised the respite setting in both studies (length of intervention was 8 weeks and 3 months respectively). Day care was found to significantly reduce levels of anger/hostility (Figure 23).
FIGURE 23.
Carer anger/hostility in randomised controlled trials/quasi-experimental studies (fixed model) (sample size in brackets). CI, confidence interval; ES, effect size; RCT, randomised controlled trial.
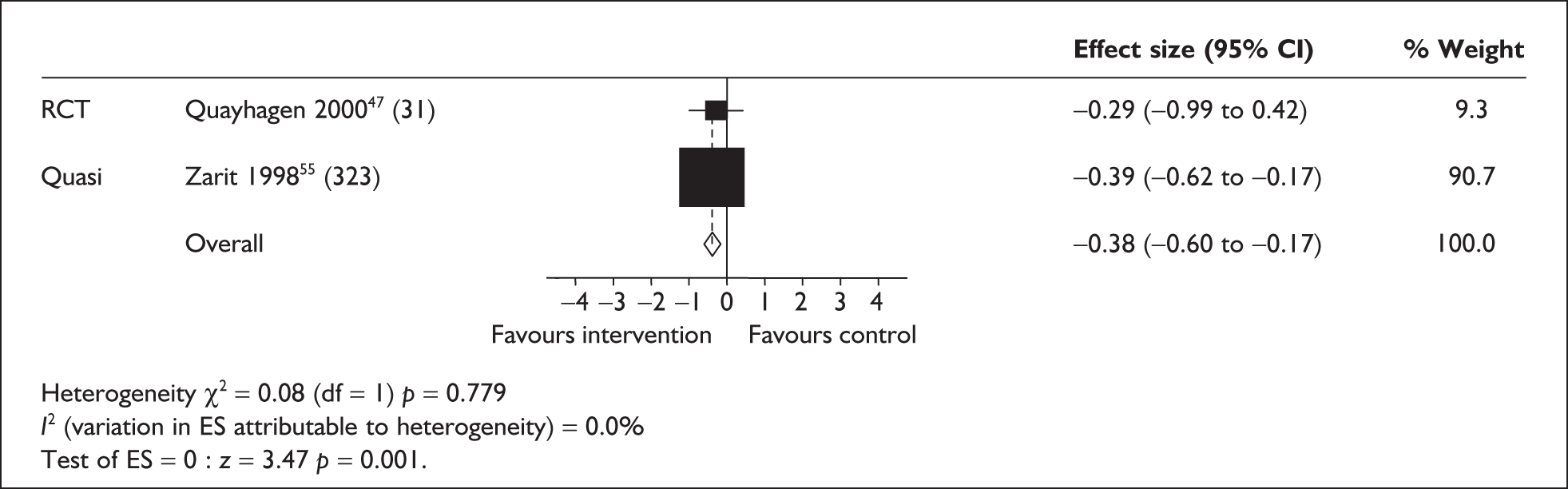
Quality and design characteristics of studies assessing the effects of respite care on carer anger and hostility
Of the two studies assessing anger and hostility, one was a moderate-quality RCT47 and one a high-quality quasi-experimental study. 55 Both have been discussed previously in relation to carer depression. The RCT was of moderate quality because of poor definition of carer characteristics, randomisation methods and allocation concealment. In addition, respite provision was low.
The quasi-experimental study55 rated well on all criteria in the quality assessment tool. It also controlled the amount of respite provision to ensure adequate exposure to the intervention and limited exposure to other types of respite. The control group was recruited via advertisement and so was self-selecting. As a result there were differences between the intervention and control groups. However, anger was significantly lower at 3 months post intervention in the intervention group (although not at 12 months) when adjusting for differences between groups at baseline.
Summary: evidence for the effectiveness of respite in reducing carer anger
Only two studies measuring carer anger/hostility were identified, one of which was a randomised trial of moderate quality, the other a high-quality quasi-experimental comparison. The randomised trial provided limited respite care whereas the quasi-experimental study controlled the amount of respite provision within the intervention and from other sources. Both interventions comprised day care and findings from the meta-analysis showed a significant positive impact on self-reports of carer anger/hostility towards the care recipient.
Quality of life
Carer quality of life in randomised and quasi-experimental studies
No trials or quasi-experimental studies measuring carer quality of life as an outcome were identified.
Carer quality of life in single-group longitudinal studies
Three single-group (longitudinal before-and-after) studies measuring quality of life post respite were included in a meta-analysis. 65,69,70 Two of the studies were carried out in the USA65,69 and one in Canada. 70 Two assessed day care65,70 and the other a combination of home care and institutional care. 69 Two69,70 focused on frail elders and one on dementia care recipients. 65
Two separate models were studied, to account for different follow-up periods: the first comprised two studies followed up at 6 months65,70 and a third at 12 months,69 and the second comprised two studies followed up at 12 months65,69 and a third at 6 months. 70 The result of these analyses are shown in Figures 24 and 25 respectively (random-effects and fixed-effects models respectively).
FIGURE 24.
Carer quality of life in longitudinal before-and-after studies (two studies at 6 months’ follow-up and one at 12 months’ follow-up) (sample sizes in brackets). CI, confidence interval; ES, effect size.
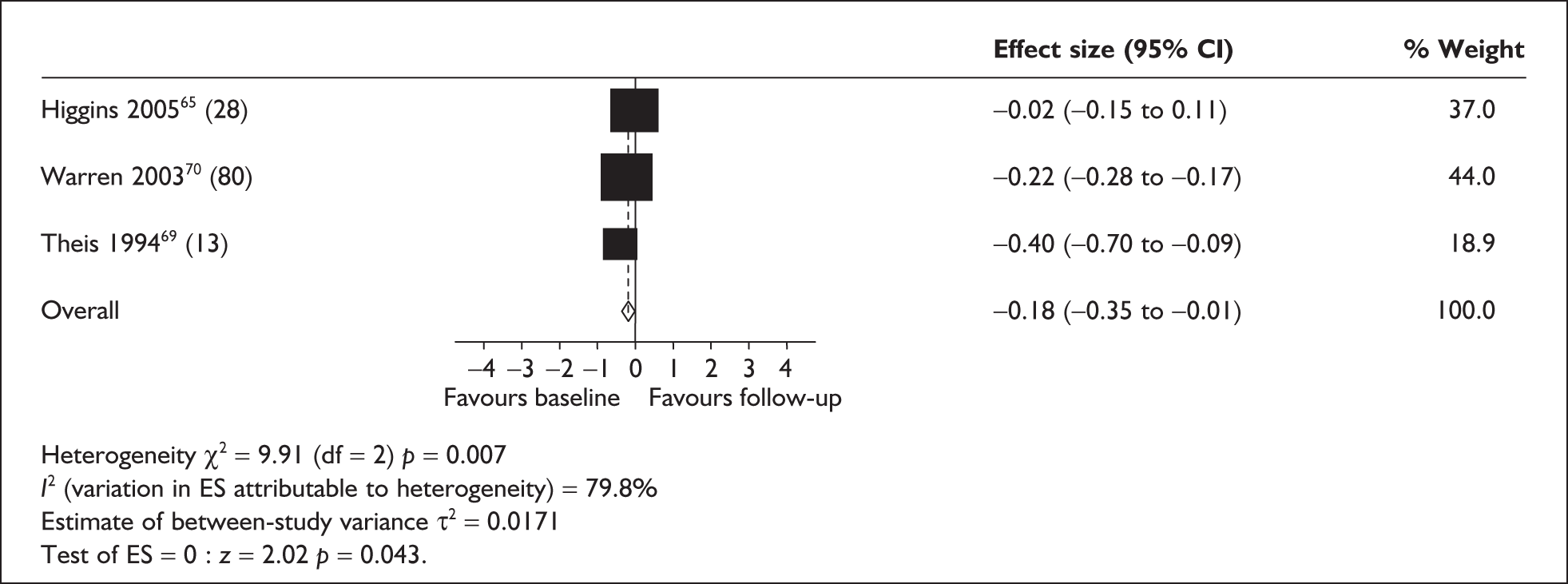
FIGURE 25.
Carer quality of life in longitudinal before-and-after studies (two studies at 12 months’ follow-up and one at 6 months’ follow-up) (sample sizes in brackets). CI, confidence interval; ES, effect size.
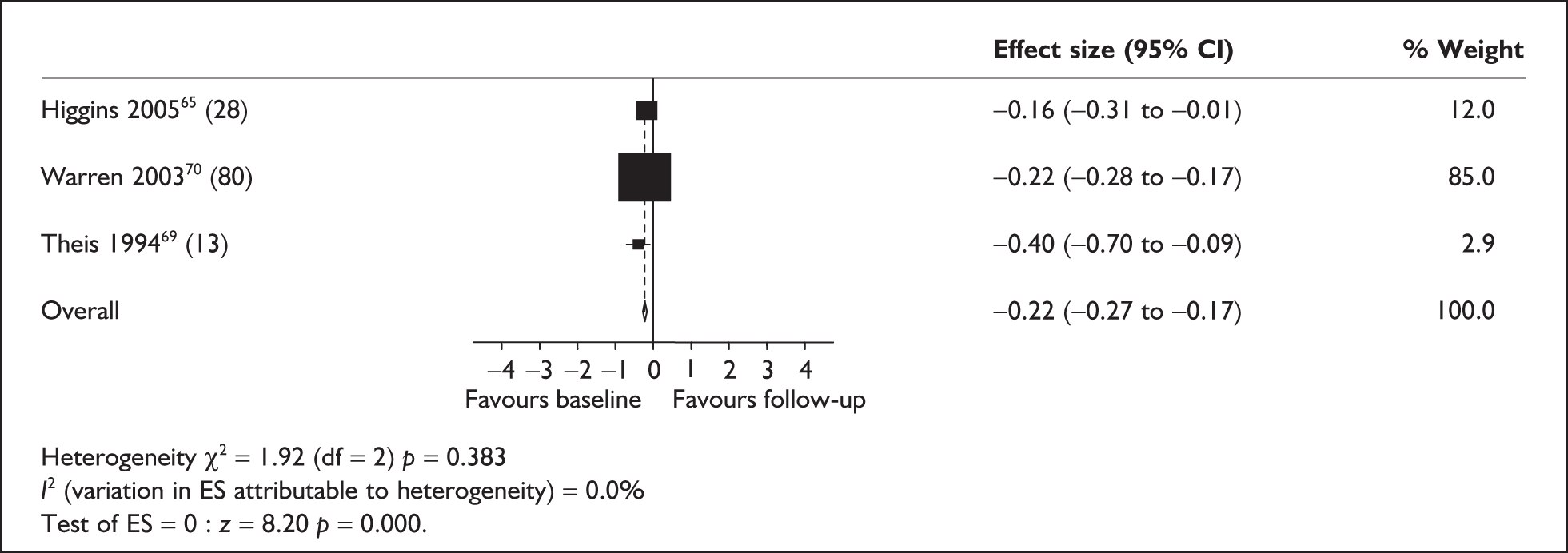
Quality and design characteristics of studies included in the meta-analysis assessing the effects of respite care on carer quality of life
Two of the studies were rated as low quality,69,70 both of which have been discussed previously in relation to carer burden. Both of these studies report a negative effect of respite care on quality of life (in relation to day care at 6 months70 and home and institutional care at 12 months69). In general, the study by Warren et al. 70 was poorly described with limited details of population selection and characteristics and so there was a possibility of selection bias. The other study had a significant problem with attrition, which probably did influence the findings.
The study rated as moderate quality65 measured outcomes at both 6 and 12 months. Unlike the other two studies, which focused on frail elders, this study provided a day care facility for care recipients with mild to moderate dementia. Day care was provided for 1 day per week from 9.30am to 2pm. An educational programme was also provided for carers as part of the package. There was no difference in carer quality of life between baseline and 6 months but quality of life was significantly worse at 12 months. However, the condition of the care recipient deteriorated significantly over the study period with both mini-mental state examination (MMSE) scores and behavioural ratings showing decline. In addition, although the patients themselves rated their own quality of life similarly at the end of the study as at baseline, the carers rated their care recipient’s quality of life as lower, showing that they also perceived there to be a decline in the care recipient’s status. No attempt was made to control for patient decline in the analysis. Use of other support services also increased over the study period, including housekeeping assistance and in-home help with care recipient care. Without an appropriate control group comparison it is difficult to assess whether the decline in quality of life is a result of the use of respite or of other factors.
Summary: evidence for the effectiveness of respite in improving carer quality of life
Only three studies measuring carer quality of life following respite care were identified, and all comprised longitudinal before-and-after evaluations. Two included day care65,70 whereas the third was a mixed respite service. 69 Respite interventions were delivered continuously until follow-up (6–12 months). Carer self-reports of quality of life were actually significantly lower following receipt of respite than before the interventions. The quality of the studies was low to moderate. Two of the studies were poorly described with the potential for selection bias, particularly in one study, which had significant attrition problems. The other study, of moderate quality, showed a significant decline in the condition of care recipients over the period of the study and failed to take account of this in the analysis. As these studies have no comparison groups and are generally of low quality they represent very weak evidence in support of a decline in quality of life after respite care.
Institutionalisation
Rates of institutionalisation were considered when this information was provided alongside carer outcomes.
Recipient institutionalisation in randomised and quasi-experimental studies
Three studies provided information on rates of recipient institutionalisation at follow-up, in addition to carer outcomes. 36,41,55 One study55 provided rates of institutionalisation at 3 and 12 months’ follow-up; separate meta-analyses were therefore carried out to determine the effect of respite on institutionalisation in both the long and short term. Results indicate that carers who had received respite were more likely to institutionalise care recipients at short-term follow-up (10 weeks,36 3 months;55 Figure 26). No care recipients died between baseline and follow-up in either of these studies.
FIGURE 26.
Recipient institutionalisation in quasi-experimental studies: short-term follow-up (10 weeks and 3 months) (fixed model) (sample sizes in brackets). CI, confidence interval; OR, odds ratio.
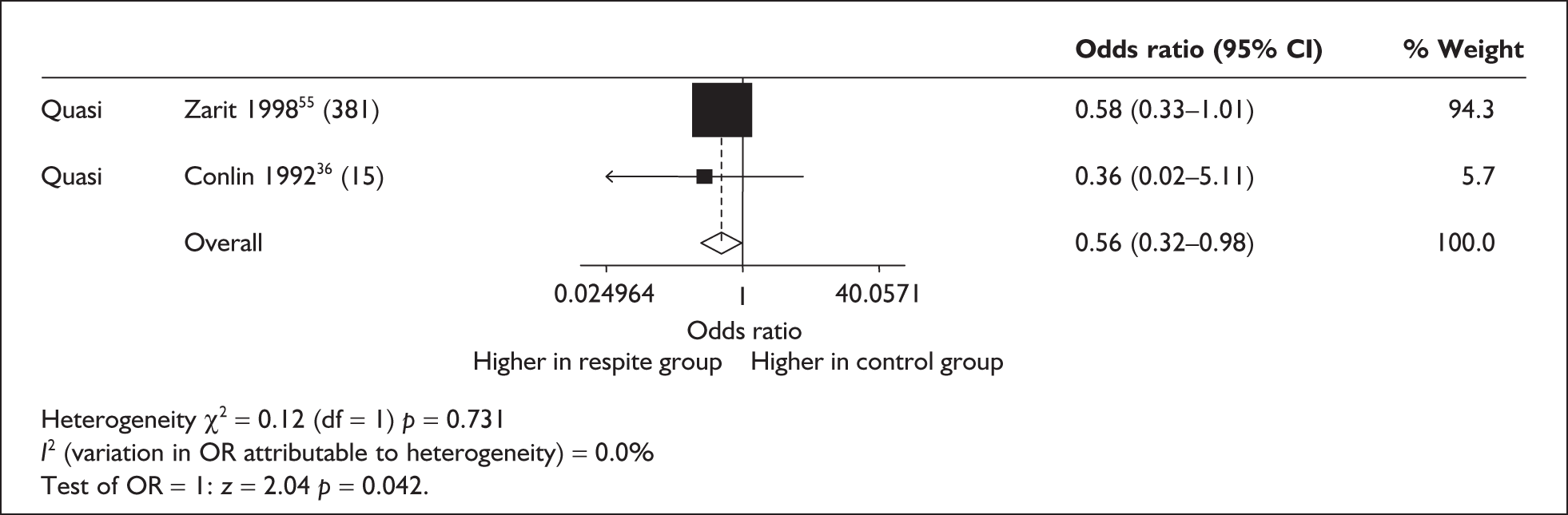
Rates of institutionalisation at longer-term follow-up (6 months,41 12 months55) were analysed compared with rates in those remaining in the community, including care recipients who had died as well as those institutionalised (Figure 27). It is evident from Figure 27 that death or institutionalisation was more likely in the intervention groups.
FIGURE 27.
Recipient institutionalisation and death in quasi-experimental studies: long-term follow-up (fixed model) (sample sizes in brackets). CI, confidence interval; OR, odds ratio.
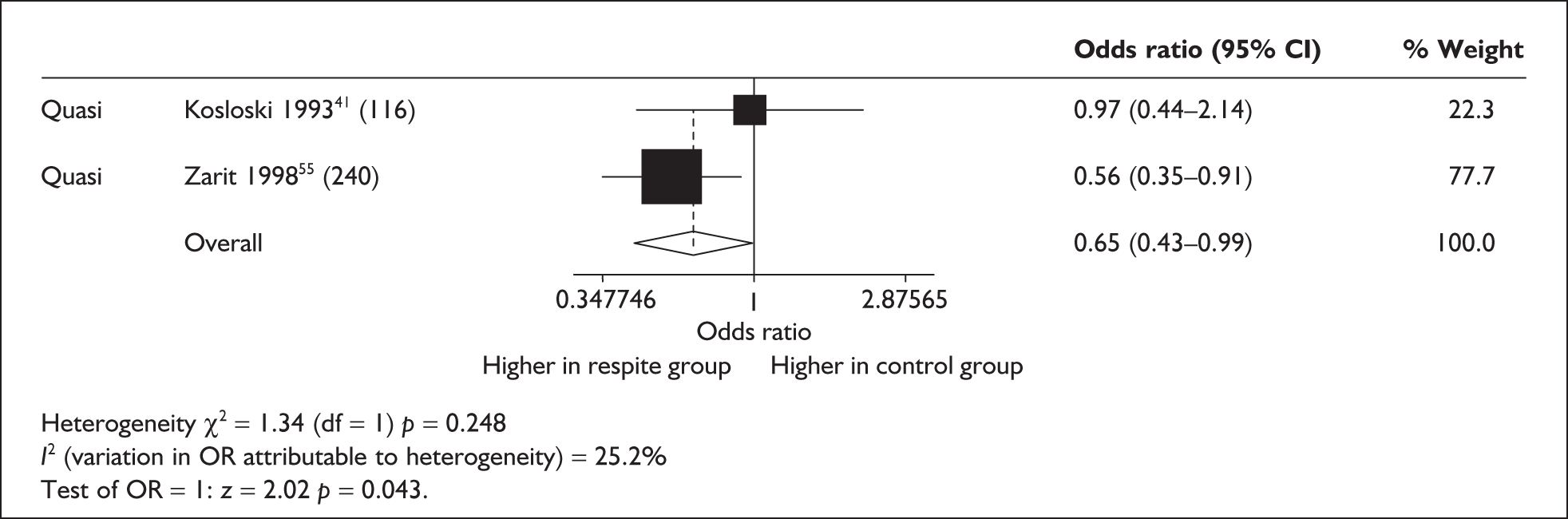
Quality and design characteristics of studies included in the meta-analysis assessing institutionalisation after respite care
Two of the studies reporting institutionalisation were quasi-experimental studies of high quality,41,55 both of which have been discussed previously in relation to carer burden and depression. Overall, the analysis found that care recipients were more likely to be institutionalised in the longer term after using respite services, although one study reported that the intervention group were not more likely to be institutionalised after a respite programme involving both home and day care. 41 In this study the programme offered different interventions at different sites but tended to offer a fairly flexible schedule. A positive aspect of this study was that all participants did take up respite services and use of other services was accounted for. The main problem with this study was potential selection bias resulting from the quasi-experimental nature of the study design, particularly as the control group was recruited from one site only. However, known differences between the intervention and control groups were accounted for in the analyses.
The other study55 assessing institutionalisation in the longer term suffered from similar selection bias as, again, control subjects were recruited from one site, which was in a different geographical area to that of the intervention group; however, again, known differences were accounted for in the analysis. This study demonstrated an increased likelihood of institutionalisation after day care. Both this and the previous study recruited care recipients with dementia, and carers spent similar amounts of time per week caring for their relatives. Because of the long timescale of the study it was felt inappropriate to randomise participants to a control group and so control subjects were recruited from areas where day care provision was limited. One significant difference between the characteristics of the treatment and control groups was the relationship of the carers to the care recipients. A total of 55% of carers were adult children in the intervention group compared with 38% of the control group. A larger percentage of carers in the control group were spouses. In the study by Kosloski and Montgomery,41 discussed above, the majority of carers were spouses. It is possible that the relationship between carer and care recipient impacted on the decision to institutionalise. The Zarit et al. 55 study also provided data on institutionalisation at a shorter term of 3 months but found no greater likelihood of placing the care recipient in long-term care after using respite services, although overall the analysis found an increased likelihood of institutionalisation.
Another study assessing institutionalisation in the short term gave carers the choice of respite care, either in an assisted-living facility or at home. 36 Care was provided for 6–8 hours a day, 2 days a week for 10 weeks. On average, participants received 15.3 hours per week of respite. The quality rating of this study, however, was low. Participants were assigned to either intervention or control and sampling was stratified based on dementia severity. Randomisation was not mentioned, although it would have been feasible to randomly allocate participants to the two groups. However, there were only seven and eight participants in each of the groups and so it is likely that randomisation would not have avoided differences in the characteristics of the samples. Recruitment procedures were not clear and reporting of the characteristics of the carer and care recipient samples was incomplete. It was not clear if there were any differences between the groups and no account was taken of any differences in the analyses. There was incomplete description of the statistics and variance estimates were not reported for all results.
Summary: the impact of respite on care recipient institutionalisation
Three quasi-experimental studies were included in the meta-analysis of recipient institutionalisation. Results suggest that a negative outcome for the care recipient in terms of institutionalisation or death is more likely following a period of respite. Two of the studies were rated as being of high quality and one as being of low quality. No single-group longitudinal studies reporting rates of institutionalisation were identified. Individual studies varied in their findings, with one study having more adult children as carers reporting an increased likelihood of institutionalisation after respite. Carers in the high-quality study who showed no increase in the risk of institutionalisation after respite were mainly spouses.
Narrative evidence also suggests that institutionalisation may be more likely after a period of respite. One study reported that, compared with a carer training programme,33 carers in receipt of respite tended to institutionalise care recipients faster. In contrast, Riordan and Bennett49 found that respite users tended to keep the care recipient in the community for significantly longer than matched control subjects. In a study of preferences for community or institutional care,58 carers were less likely to express a wish to institutionalise the care recipient following respite than before receipt of the service.
Sensitivity analysis
A further set of meta-analyses were carried out as a sensitivity analysis. Results presented in this chapter are based on the assumption that the correlation between baseline and follow-up scores (used to estimate change SDs) is 0.6. However, all analyses were repeated assuming the most extreme situation of a zero correlation between baseline and follow-up; the impact of this assumption on results was evaluated, although the assumption of a non-significant relationship between baseline and follow-up scores would seem unlikely. Adopting this model for randomised and quasi-experimental studies resulted in reduced effect sizes, which were not statistically significant (tests for heterogeneity were almost exclusively non-significant). Carer anger/hostility proved an exception, however, in that the overall effect size was marginally reduced but remained significant when assuming a zero correlation between baseline and follow-up. In terms of single-group (longitudinal before-and-after) studies, fixed models assuming a zero correlation generally resulted in larger but non-significant effect sizes. Tests for heterogeneity were still significant for burden but not for depression and quality of life.
Third level of evidence: observational longitudinal studies
Characteristics of longitudinal observational studies
A total of 19 papers reported a longitudinal observational design, representing 13 studies. Seven papers all referred to the Medicare Alzheimer’s Disease Demonstration Evaluation (MADDE) study, but each gave data on different samples taking part in the MADDE. 77–83 The majority of the research (nine studies) was carried out in the USA with one study carried out in the UK,71 one in Canada72 and two in Australia73,87 (Table 7). All except two examined mixed respite provision; the remaining two examined in-home care. Four studies focused on frail elderly with mixed disabilities and the remainder were specific to dementia care recipients. All studies assessed a range of formal service provision including respite and non-respite services, and some also included informal support. It was not possible, therefore, to categorise according to type of respite provision. Length of follow-up ranged from 3 months to 5+ years with the majority being between 1 and 2 years. Although many of the studies used multiple measures, there were generally only one or two related to service use in each analysis. The results of these studies are discussed according to the various outcomes measured.
| Country | Type of respite care | ||||
|---|---|---|---|---|---|
| Day care | Institutional | In-home | Mixed | Total | |
| UK | 1 | 1 | |||
| USA | 2 | 7 | 9 | ||
| Canada | 1 | 1 | |||
| Australia | 2 | 2 | |||
| Total | 2 | 11 | 13 | ||
Institutionalisation
A meta-analysis of institutionalisation in quasi-experimental studies was presented in the previous section. The analysis found institutionalisation and death to be more likely following respite use. This section summarises the evidence from observational longitudinal studies.
Six papers examined the relationship between formal service use and institutionalisation; however, the measure of service use included a range of personal care and support services of varying types and it was difficult to identify the impact of respite. 74,77,84–86,88 The methods and results of these studies were heterogeneous and it is difficult, therefore, to draw any firm conclusions because of the lack of definitions and the variation in study contexts. One further study87 reported on institutionalisation but did not have data linking respite and institutionalisation.
The papers that had a more distinct focus on respite care are summarised below. Seven referred to the same study (the MADDE study) although data were reported for different subsamples. 77–83
The MADDE study77–83
These papers, carried out in the USA, report on the MADDE project and explore the relationship between service use and institutionalisation in dementia care recipients. The service of most interest to the present review is ADC. Care recipients were recruited who had a physician diagnosis of dementia and who were enrolled or eligible for Parts A and B of the Medicare programme and had service needs.
Participants were randomly assigned to a treatment group, receiving reimbursable case management services, or to a control group, who purchased their own community services. This intervention itself was not found to have significant effects on institutionalisation or burden and depression for carers. Samples focused on in these papers were the control group, carers early in the caregiving career, the treatment and the control groups combined, and African Americans. More detailed findings suggest that early use of in-home help was associated with a delay in institutionalisation,80 and carers were less likely to institutionalise when family members provided overnight help and assisted with activities of daily living. 77 An unmet need for ADC and an overnight hospital stay was also reported to be a predictor of institutionalisation. 81
One of the papers78 reported that, over a 3-year period, both low use of ADC (1–30 days in a 6-month period) and high use (78+ days) gave a 30% increased likelihood of institutionalisation compared with no use of ADC, whereas moderate use did not show any relationship. The authors pointed to the complex relationship between service use and institutionalisation. For those with a low use of ADC the amount of service provision may not be sufficient to alleviate burden. For those accessing high levels of ADC institutionalisation may be confounded by other factors, such as timing, symptom severity, behaviour problems, personal preferences and the relationship between the carer and the care recipient; alternatively, accessing high levels of ADC may be a precursor to institutionalisation in a deteriorating symptom trajectory. In addition, one of the papers reported an analysis focused on behavioural problems,79 which found that care recipients with behavioural problems such as aggression and delusional or mood disruptive behaviours were more likely to be institutionalised earlier. These problems also resulted in increased levels of burden and depression for carers.
Bond and Clark73
In support of the MADDE study this study, again in dementia carers, found that greater use of respite services (a variety of day and nursing home respite) was associated with institutionalisation but that this relationship was non-significant when adjusted for dementia severity. This study was carried out in Australia and followed up 158 spouse carers registered with the Alzheimer’s Association for 2 years.
Andrew et al.71
Similarly, the study by Andrew et al. 71 reported a statistically significant relationship between severity of cognitive impairment and time to institutionalisation; the severely impaired had significantly shorter times to institutionalisation than those with mild or moderate impairment. There was no significant difference between the mild and moderately impaired. This study found that those using day care or home care were less likely to be institutionalised at follow-up of around 1 year. What appeared to be important was whether day care was used or not rather than the amount, whereas an additional hour or day per week of home care decreased the likelihood of institutionalisation. Not using home care increased the likelihood of institutionalisation by nearly two and a half times, and not using day care increased the odds by nearly six times. This study also demonstrated the importance of the relationship between carer and care recipient in any study attempting to establish predictors of institutionalisation. Care recipients with mild or moderate impairment who had a spouse or daughter carer were half as likely to have entered long-term care over the study period. Although these confounders (relationship and severity of dementia) were controlled for in this study the authors suggested that there could still be possible confounders in the characteristics of those using and not using services (such as behavioural problems).
Summary
Although the findings of the meta-analyses showed a greater level of institutionalisation after respite care, the observational studies found some support for the benefits of respite and suggested that severity of dementia may be an important confounding factor in institutionalisation. Relationships between respite and institutionalisation were reduced when dementia severity was taken into account. In one study78 those having both low use and high use of ADC were more likely to institutionalise, whereas another study found that amount of day care use was not related to institutionalisation71 but that those having day care were less likely to institutionalise. However, increases in the amount of home care gave added benefit in terms of institutionalisation. These findings may all be influenced by factors such as the severity of the care recipients’ underlying conditions (particularly in relation to dementia and behavioural problems).
The predictors of institutionalisation are complex and other confounders such as the relationship between carer and care recipient were found to be important, as spouses and daughter carers were more likely to maintain the care recipient at home when dementia severity was moderate as opposed to severe.
The quality of studies was rated as high to moderate.
Depression
The evidence discussed so far in relation to carer depression was provided by randomised and quasi-randomised studies, representing the highest level of evidence, although the quality of individual studies within this group was generally moderate. Although not all analyses were statistically significant, the direction of the effect was in favour of respite care, with carers having reduced levels of depression. This section summarises the longitudinal observational data in relation to carer depression.
Three studies (all carried out in the USA) examined the relationship between formal help and carer depression. 75,76,83
Cox75
This study aimed to explore the factors associated with use of respite care and recruited a sample (n = 228) from Maryland’s Alzheimer’s Demonstration Grant, which focused on increasing services among underserved populations in the state through financial reimbursement that allowed participants to purchase up to 164 hours of respite care per year. Eligibility for the programme was based on low income. Respite consisted of in-home care provided by a trained worker, a short nursing home stay or day care. Over the 6-month period of the study there was no change in carers’ mean anxiety or depression scores but there was a significant decrease in burden scores.
Cox and Monk76
This study compared 31 black and 19 Hispanic dementia carers on measures of carer distress and use of formal and informal support at baseline and 6 months. Sampling was carried out via hospital clinics, senior centres, community organisations, family support groups and day care centres. Formal support was defined as use of specific services although the extent of respite is not detailed. Informal support consisted of the presence of a confidante and their availability to help with particular caregiving tasks. Therefore, again, it is not clear to what extent this provides respite. Correlations were calculated between support and carer depression measured by the Centre for Epidemiological Studies Depression Scale (CES-D), but no significant associations were found in either group.
Jarrott et al.83
The study by Jarrott et al. 83 carried out regression analyses of predictors of carer distress at two time points 3 months apart. Participants were taking part in a larger quasi-experimental study of carers enrolling a care recipient into an ADC programme compared with a control group of carers not enrolling a care recipient into an ADC programme. The carers (n = 405) were caring for dementia relatives and the study assessed formal and informal help with activities of daily living and also respite activities such as sitting with the care recipient or taking the care recipient out of the house. At baseline there was no relationship between formal or informal help and depression, but at 3 months increases in formal help were associated with decreases in depression. This analysis controlled for factors such as carer and care recipient gender, relationship to care recipient, months caring for relative, income, education, baseline and change in memory and behavioural problems, change in activities of daily living and change in informal help.
Summary
Contrary to findings in the meta-analyses the three studies examining the impact of respite on depression failed to show any positive effects, although one study reported that respite was not a predictor of depression at time point one but that increases in respite predicted depression at time point two.
The quality of two of the studies was high with one rated as being of lower quality.
Burden
Meta-analyses found weak evidence of a positive impact of respite care on carer burden, as significant effects were found only in longitudinal before-and-after studies but not in randomised and quasi-randomised trials. This section assesses the evidence from longitudinal observational studies of the impact of respite on carer burden.
Five studies72,75,76,83,89 looked at the relationship between formal support and measures of burden. In three of the studies there was no clear distinction between respite care and other forms of support service, whereas the study by Cox75 focused specifically on respite care with carers having in-home care, short stay institutional respite care or day care available to them.
Jarrott et al.83
This study, described above, assessed depression but also carer anger, overload and worry/strain. Feelings of anger and irritation were measured using four items from the Hopkins Symptom Checklist and overload using seven items based on the work of Zarit (see Appendix 11 for references for measures). Worry and strain was assessed using an eight-item measure developed by the authors for the study. Change in overload was predicted in a multivariate regression analysis by change in formal help only, controlling for carer age, carer gender, care recipient gender, duration of caring, memory and behavioural problems, change in activities of daily living problems and change in informal help. Change in carer anger was predicted by spousal relationship, baseline and change in memory/behavioural problems, change in activities of daily living and change in formal help. Worry and strain was predicted only by change in activities of daily living and change in formal help. Change in formal help, therefore, predicted a decrease in all measures of carer burden.
Zarit et al.89
This study followed up 64 dementia carers (33 wives and 31 husbands of the care recipient) for 2 years (with data for 32 couples available at 2 years). The sample was drawn from a clinic offering counselling and support for carers and also from an Alzheimer’s advocacy group. Formal support was measured as the frequency of services provided by agencies or other paid helpers, and informal support as the frequency of contact with family and friends and what assistance they provided. There was not any clear indication of the extent or nature of respite provision from these sources. In addition, the sample was small and the sampling strategy quite likely to introduce bias. No significant correlations were found between either type of support and carer burden.
Cox and Monk76
This study, described above under depression, also assessed carer burden in relation to formal and informal supports. No details are given concerning the burden scale used and no significant correlations were found between burden and formal or informal supports (not clear to what extent respite is provided as part of the support services).
Cox75
This study also assessed depression (discussed above) and found that, although there was no change in depression over the study period of 6 months, carer burden was significantly reduced. Burden was measured using a six-item scale concerning the restrictions on activities and personal time experienced by the carer. This type of measure may only reflect the reduction in time spent caring as a consequence of respite use and may not include psychological or physical impacts resulting from reduced caring time. Multivariate analyses were carried out to assess predictors of respite use but the analyses looking at the outcomes for carers and care recipients over time were univariate statistics only, assessing each outcome separately. No account was therefore taken of confounding factors.
Armstrong-Esther et al.72
This Canadian study measured carer stress, which included items related to feelings of grief, guilt, depression, exhaustion and being overburdened, isolated and frustrated, and to experiencing lack of sleep, feeling that they cannot respond to care recipients’ needs, feeling like striking out and failing to look after their basic needs, which are similar to the concepts measured in burden. The study was conducted over a 30-month period and assessments made on three occasions at 9-monthly intervals. A total of 210 carers were non-randomly selected and enrolled to take part in the study from a list of home-care clients. In a multiple regression analysis, receiving more respite was reported to be predictive of carer stress, although no actual data were supplied to support this. A number of factors were included in the model (e.g. client gender and age, carer age, scores of health and mental status, levels of disability, relationship and financial variables, and access to respite). Seven were found to contribute significantly to carer stress (carer financial difficulties, younger carer age, taking care of spouse rather than other people, providing more hours of caregiving a day, greater mental disability, higher MMSE scores, receiving more respite). However, they also reported significant differences in stress scores in those receiving regular daily respite (15.2), occasional respite (14.1) and those receiving no respite (17.7). From this it would appear that those receiving occasional respite are the least stressed, although severity of impairment is likely to be a confounding variable here. There is also no indication of the time point at which these measures were taken.
Summary
Results from the observational longitudinal studies do not provide consistent evidence of the effects of respite on burden to either support or refute the findings of the meta-analyses. There were mixed results, but in studies showing no effect of respite on burden the extent of respite provision is unclear. One study showing a positive effect used a non-standard measure and failed to control for confounders; in the other study showing a positive effect there was a decrease in overload, carer anger, worry and strain. The final study highlighted the complex relationship between factors, as those receiving occasional respite were less burdened than those receiving regular respite or no respite and, in the multivariate analysis, carer stress was predicted by receipt of more respite (controlling for level of disability).
The quality of three of the studies was high, with two rated as being of lower quality.
Fourth level of evidence: observational cross-sectional studies
Characteristics of observational cross-sectional studies
This section provides a narrative synthesis of the cross-sectional studies that were identified as being relevant to the review but not of an appropriate design to be included in a meta-analysis. Again, they are considered according to each particular outcome, but because of the larger number of studies in this group they are broken down further according to the type of service provision. Depression and anxiety are discussed together in this narrative synthesis as the measures used are frequently combination measures such as the Hospital Anxiety and Depression Scale, which consists of two subscales measuring anxiety and depression, as well as an overall measure of mental health.
A total of 45 papers90–134 with a cross-sectional study design were included in the review (see Appendix 7). These 45 papers represented 40 studies. In five of these studies service use was the outcome variable and the carer and care recipient variables were analysed as predictors of respite use in multivariate analyses. These have been excluded from the following narrative summary but may be found in the summary table in Appendix 7.
The remaining 35 studies are summarised in Table 8 by country of origin, condition of care recipient and outcomes assessed. The majority of papers were published since 1995 (n = 34) with 11 published before 1995. The main outcomes were mental health and burden. The following narrative review will focus on these two outcomes.
| Number of studies | Outcomes assessed | Care recipient condition | |||||
|---|---|---|---|---|---|---|---|
| Mental health (anxiety and depression) | Burden/stress | Othera | Care recipient outcomes | Dementia | Frail elderly and physically impaired | ||
| USA | 15 | 5 | 8 | 2 | 6 | 9 | |
| UK | 5 | 3 | 4 | 1 | 3 | 2 | |
| Canada | 3 | 1 | 2 | 1 | 3 | ||
| Australia | 2 | 1 | 1 | 1 | 1 | 1 | |
| Other European | 4 | 2 | 4 | 4 | |||
| Japan | 5 | 2 | 3 | 1 | 4 | ||
| Korea | 1 | 1 | 1 | 1 | |||
| Total | 35 | 15 | 23 | 4 | 1 | 15 | 20 |
Mental health outcomes: observational cross-sectional studies
Depression and anxiety were included in the meta-analyses and depression was also discussed as an outcome in the longitudinal observational studies. There were positive effects of respite care on depression in the meta-analyses of randomised and quasi-randomised studies but there was little support within the longitudinal observational studies. Randomised studies showed no positive effects of respite care on anxiety and there was no further evidence from longitudinal before-and-after or longitudinal observational studies.
In the main this category focused on depression, although some measurement tools also assessed anxiety, for example the Hospital Anxiety and Depression Scale (HADS) (see Appendix 11 for references for measures used in studies). Table 9 shows the direction of association of studies assessing mental health in relation to service use and respite. The service contexts are categorised as being ADC, in-home care, respite (this could include a range of services that are specifically aimed at providing respite) and general service provision (which includes a range of community services, some of which provide respite). This last category may include personal care services, homemaker services or even information provision, legal advice or carer counselling. The studies categorised as providing general services do not usually define the amount and type of services that potentially provide respite.
| Study | Findings related to relationship between service use and depression | Type of service | Direction of associationa |
|---|---|---|---|
| Arai et al. 199891 | Use of services associated with decrease in depression | General | + |
| Bass et al. 199693 | Personal care services and household help moderate effect of care recipient problem behaviour on depression | General | + |
| Mittelman et al. 1995121 | Neither formal services nor amounts of paid help related to depression | General | 0 |
| Tennstedt et al. 1992128 | Neither informal nor formal support associated with depression | General | 0 |
| Wailing et al. 1997129 | Carer support did not have a main or buffering effect on depression | General | 0 |
| Washio and Arai 1999131 | No association between help or time to oneself and depression | General | 0 |
| Williams 2005133 | Use of formal support predicted more depressive symptoms | General | _ |
| Colvez et al. 2002101 | Hospital respite group had more depression than those in expert centre programme | Respite | _ |
| Cossette and Levesque 1993102 | Carers who received respite more likely to use psychotropic medication. Adequacy of informal social support had no significant impact on mental health outcomes | Respite | _ |
| Fell et al. 2001104 | No difference in psychological distress between users and non-users of day care | ADC | 0 |
| Gilhooly 1986,108 1984107 | No correlation between day hospital and mental health or morale | ADC | 0 |
| Park 2003124 | No effect of day care on depression | ADC | 0 |
| Lorensini and Bates 1997118 | Carers not using adult day care more depressed | ADC | + |
| Warrington and Eagles 1996130 | Carers of day hospital attendees more depressed than carers of day care attendees | ADC | _ |
| Rosa et al. 2004127 | Depression significantly lower with immigrant carer helper | Home | + |
All studies measuring mental health outcomes (n = 15) used a standard validated depression scale, the most common being the CES-D (used by eight studies).
Provision of general services
Nearly half of the studies (n = 7) explored the general use of formal services, assessing the number of formal services utilised by carers and recipients. This included a wide variety of different types of service such as respite care, day care, personal care services, household help, transport and nurse visits and also carer-specific interventions such as counselling and carer support groups. It is therefore difficult to identify the impact of respite in the context of these many confounding interventions. Of the studies examining general service use, four failed to show an association of service use with carer depression;121,128,129,131 one showed a negative effect of respite133 and two a positive effect. 91,93 As well as looking at formal service use, some of the studies also combined this with an assessment of informal support, which could involve respite provision, help with personal care activities or emotional support. There were no clear definitions of the amount or type of care received and whether respite was a specific aspect of this support.
Respite provision
Two studies examined respite specifically. One study101 compared different types of elderly care centre programmes in five different countries in Europe. In this study hospital respite was the comparator and all of the other programmes showed benefits over this service (home social services, day centres, group living and expert centres). Depression was significantly better for carers using the expert centre compared with those using hospital respite. The expert centre provided medical treatment and diagnosis and follow-up for medical and social care. However, the hospital respite also had elements of medical treatment. Again it is difficult to assess the relative contributions of respite and medical intervention to the findings.
The study by Cossette and Levesque102 also focused on respite but this was informally provided respite as well as tangible and emotional support provided by family and friends. Carers receiving more respite were taking more psychotropic medication, but it is quite possible that those taking medication are acknowledged to have problems by family and friends, who consequently offer respite support.
Adult day care
Five studies examined ADC in relation to carer depressive symptoms. Three104[107,108],124 found no significant associations between day care use and carer depression, one118 found a positive effect of day care and one130 found a negative effect. The study showing a negative effect was a comparison between day hospital attendees and day care attendees with the result that carers of those attending the day hospital were more depressed than carers of those attending day care. This does not give any information concerning the impact of respite compared with no respite and so does not truly represent a negative effect. In addition, the higher levels of depression amongst carers of care recipients attending day hospital may be indicative of more severe conditions of the care recipients using this type of service, resulting in greater demands on the carer.
The study by Lorensini and Bates,118 which reported a positive effect of day care, was small with 45 care recipients attending day care compared with 40 not using day care. Also included was a control group of older people not requiring care but who nominated a person who might provide informal care if needed. There was no information on how the participants were selected for this study. There is no indication of random selection and it is not clear if those in the non-day care group were potential day care attendees or not. The groups did differ in age and this was controlled for in the analysis, but no other factors were included as covariates and so the severity of the care recipients’ dementia was a likely confounder.
The three studies reporting no effect of day care on depression represented a range of care recipients: dementia,107,108 frail elderly104 and stroke patients. 124 All were small studies, with sample sizes of 48, 40 and 101 respectively. The study by Gilhooly108 did not compare users with non-users of day care but carried out a correlational analysis between the days per week that the care recipient attended day care and the score on the depression scale, thus examining whether increasing amounts of respite will have a corresponding effect on alleviation of depressive symptoms. The study by Fell et al. 104 compared users with non-users on the waiting list for day care, which controls for need for help, but the level of use was fairly minimal, being only 1 day per week for 7 weeks. It is quite possible that any benefits of day care in relation to depression were not apparent at such a short interval or for such a minimal level of use. Park124 also compared users with non-users of day care, but in this study the level of service use is unclear and, although a number of possible confounders were measured based on a hypothesised theoretical relationship between the variables, only univariate statistics were presented.
Home care
Only one study127 examined home care (apart from the range of home-care services contained in the general measures of service support discussed above). The intervention of interest was a paid immigrant home aide, which is not a typical home-care context and is not widely generalisable.
Burden
Adult day care
A total of 23 studies examined carer burden in relation to service use (Table 10). Nine of these studies examined use of ADC,[92,95,110],94,97,103–105,118,124,130 five showing a positive effect of day care on burden94,97,103,118,124 and four no effect. [92,95,110],104,105,130
| Study | Findings related to relationship between service use and burden | Type of service | Direction of associationa |
|---|---|---|---|
| Dziegielewski and Ricks 2000103 | Carers reported less stress but increased feelings of guilt | ADC | + |
| Park 2003124 | Significantly more burden in non-day care group | ADC | + |
| Lorensini and Bates 1997118 | Carers not using ADC had higher stress arousal and lower life satisfaction and social activities | ADC | + |
| Biegel et al. 199394 | Carers using out-of-home care (includes ADC) or combined out-of-home and in-home care had less burden than those using in-home care or no services | ADC | + |
| Cefalu et al. 199697 | Carers in a social ADC group had less burden than carers in a medical ADC group | ADC | + |
| Artaso et al. 2003;92 Biurrun Unzue et al. 2003;95 Gon-i Sarries et al. 2003110 | No difference in burden between those attending ADC and those not | ADC | 0 |
| Fell et al. 2001104 | No difference in burden between users and non-users of day care | ADC | 0 |
| Furness et al. 2000105 | No difference in burden between different day care settings | ADC | 0 |
| Warrington and Eagles 1996130 | No difference in stress of carers of day hospital vs day care attendees | ADC | 0 |
| Arai et al. 199891 | Use of services associated with decrease in burden | General | + |
| Lechner 1993116 | Service use predicted impact of caring but not role strain, mental strain or physical strain | General | + |
| Gaugler et al. 2004106 | No relationship between carer stress and resource use | General | 0 |
| Washio and Arai 1999131 | No association between help or time to oneself and burden | General | 0 |
| Caserta et al. 198796 | No difference in burden between those who do and those who do not use services (those not ready to use services less burdened) | General | 0 |
| Chappell and Reid 200298 | Formal service use did not impact on burden | General | 0 |
| Gilleard et al. 1984109 | More formal support (weekly home help) less strain, but no association with burden | Home | + |
| Rosa et al. 2004127 | Burden significantly lower with immigrant carer helper | Home | + |
| Marks 1987;119 Marks 1987120 | Carer stress significantly lower in those receiving services | Home | + |
| Jutras and Veilleux 1991113 | As assistance increases the burden experienced by the carer decreases | Home/informal support | + |
| Kuwahara et al. 2001115 | Lightly burdened more likely to be able to go out without patient and to have help with care | Respite | 0 |
| Mui 1992122 | Perceived availability of respite support had strong impact on role strain of black carers but not that of white carers | Respite, ?type | + |
| Grasel 1997111 | Burden higher in those who used respite in last 12 months | Institutional respite | _ |
| Colvez et al. 2002101 | Hospital respite group had more burden than those using expert centre programme, group living and home social services | Respite | _ |
Two of the studies reporting no effect compared different types of day care. Furness et al. 105 compared psychiatric day hospital with social service day centres and Age Concern day centres and found no difference between settings. Warrington and Eagles130 also found no difference in carer stress when comparing day hospital attendees with day care attendees. However, Cefalu et al. 97 reported that carers of recipients attending a social care day centre were less burdened than those with care recipients attending a medical ADC centre. In this study the characteristics of the care recipients using the two types of day care provision were very similar, but patients in the medical subgroup were more dependent, having less total function and requiring more assistance with personal care. They also had more problem behaviours. These differences just failed to reach statistical significance but are nevertheless confounders and are likely to have some impact on the experience of burden in the medical care group. Another study comparing different types of service provision found a positive effect for day care. Biegel et al. 94 compared out-of-home services (including day care) with in-home and no services. As well as demonstrating a positive effect for day care compared with no services there was also a lower burden in those using out-of-home care than in those using in-home care. Home care consisted of health aide services, housekeeping, nursing care and delivered meals. Out-of-home services consisted of ADC, senior centre meals and transportation. The numbers in each of the groups were small (27 in-home, 26 out-of-home, 30 using both and 87 non-users). It is unclear to what extent the in-home services provided respite; the out-of-home services were more directly linked to respite provision as the majority of carers (66%) were co-resident with the care recipient, suggesting that the respite elements were important in this particular comparison.
The two remaining studies that reported no effect of day care on burden were both small studies having 40 participants104 and 80 participants. [92,95,110] Fell et al. 104 reported on a day care programme that involved care for 1 day a week for a period of 7 weeks. The carer burden of those attending and those on the waiting list was compared. Although not statistically significant, burden scores were higher in the waiting list group than in the attending group. Attenders, however, had been caring for longer and were more likely to be spouses (60% versus 30%). Qualitative data, also collected as part of the study, suggested that 1 day per week was felt to be too short a time period and, coupled with the time-limited provision of the respite (7-week blocks), this may have been insufficient to have any impact on burden. In the group of papers by Artaso et al. ,[92,95,110] although there was no impact of day care, less social support was associated with greater burden. The level of informal social support, therefore, was probably acting as a confounder to the day care attendance analysis.
There were three remaining studies reporting a positive effect of day care on burden. 103,118,124 The study by Dziegielewski and Ricks103 was a small pilot study that surveyed only 26 carers of attendees of a dementia day care establishment. There are no details of how sampling was conducted although the authors do acknowledge that the sample is probably unrepresentative. The measure of carer stress was not a validated measure and so the results from this study should be viewed with caution. The studies by Park124 and Lorensini and Bates118 are slightly larger, having 101 and 85 participants respectively. As mentioned above, in relation to the mental health outcomes the study by Park124 presents only univariate analyses, no confounders being accounted for, and the extent of day care use is unclear. This is a Korean study that was unusual in that it focused specifically on stroke survivors. The Australian study by Lorensini and Bates118 compares carers of people with dementia using and not using day care. The authors of this study did not use a standard measure of burden but a stress-arousal checklist and life satisfaction and social interaction questionnaires and so measured slightly different concepts to the more standard burden assessment tools, which focus more on carer restrictions.
Respite provision
Four studies examined the use of respite care. 101,111,115,122 One showed no effect of respite on burden,115 one a positive effect122 and two a negative effect. 101,111 The study by Kuwahara et al. 115 was carried out in Japan and assessed burden in relation to the ability to go out without the care recipient, which in this review is considered to constitute respite, and also the number of social services used. The formal service support measure gives no detail of the types of services used and so it is unclear to what extent respite is a component. The question concerning the ability to go out alone is a more direct link to respite but there is no information as to what this actually means. It is possible that the care recipient can be left alone without supervision, which could thus represent a less burdensome situation, or it may indicate more extensive social networks and the provision of informal respite support. Although there was a trend towards respite alleviating burden this was not significant in a multivariate analysis controlling for time spent looking after patients, time spent consulting a physician, patient gender and location. Again, this study is small with only 58 participants and consisted of care recipients with varying problems.
The studies reporting negative effects of respite included the study by Colvez et al. 101 discussed above, which compared hospital respite with several other types of care (day centre, home social services, expert centres, group living) across five European countries. It is difficult to distinguish the respite elements in these studies and without a clear control group it is difficult to assess the results concerning the impact of respite. The other study,111 carried out in Germany, was a much larger study that surveyed 1272 carers to establish utilisation of institutional respite during the preceding 12 months. However, recruitment was by advertisement in two magazines distributed via contact addresses by the German Association for Alzheimer’s Disease and district nursing organisations, producing a response rate of 25% (although it was not possible to establish the exact denominator). The sample, therefore, although large, is probably not without bias. In addition, univariate analyses were used and so there was no control for confounders. Without controlling for the severity of the care recipient condition it is difficult to establish whether those utilising services represent a more severely impaired and thus more burdensome group.
Finally, the only study reporting a positive effect of specific respite services on burden was the study by Mui122 carried out in the USA, which assessed the availability of respite and secondary help for carers of frail elders. This was part of a much larger study and focused on black and white daughter carers in the sample, yielding 581 respondents. Although the study assessed respite support the question was hypothetical, asking who would be available if needed rather than how much or how often respite was available. The positive effect was experienced only by the black participants and not the white group.
Provision of general services
Six studies reported the use of formal services in general, which included both in-home and out-of-home services. 91,96,98,106,116,131 Two studies reported a positive effect of service use on burden91,116 and four no effect. 96,98,106,131 Of the two studies finding a positive effect of service use, the study by Arai et al. 91 was small, having only 24 participants, and thus gives little weight to the evidence. Lechner116 also demonstrated a positive effect of service use. This was a slightly larger study, surveying 133 employed carers. The number of services used was assessed. In multiple regression models the number of agency services used predicted the impact of caring, mental strain and physical strain but not caregiver role strain. The impact of caring consisted of measures of how much the carers’ lives had changed as a result of caregiving in the domains of financial, personal, interpersonal and leisure time. As these were employed carers they are probably not representative of carers in general or carers of more impaired elderly relatives.
Studies showing no effect of service use included a small study by Washio and Arai,131 which recruited 45 participants. The larger studies96,98,106 had sample sizes of 344, 597 and 243 respectively. Two of the samples were recruited from an Alzheimer’s Research Centre106 and a mailing list of a local support group,96 both of which have potential biases. Only the Chappell and Reid98 study recruited a random sample via a telephone random dialling procedure, but this also has potential biases. Resource use was assessed in the three studies by the number of times services were used in the last 6 months, the number of services used and a comparison of users/non-users. Both Gaugler et al. 106 and Chappell and Reid98 carried out a path analysis and examined various predictors of burden whereas Caserta et al. 96 carried out a group comparison of users and non-users of services. However, within the general service use studies it remains difficult to determine the contribution of the respite components and the amount and type of respite, if any.
In-home support
All four studies focusing on home care reported positive effects of service use. 109,113,[119,120],127 Jutras and Veilleux113 concentrated on informal support rather than formal services and Rosa et al. 127 assessed the use of paid immigrant help in Italy, which is not representative of the types of services generally available but which may have increasing significance with the influx of migrant workers to the UK from EU accession countries. Gilleard et al. 109 did find a weak but significant positive effect of weekly home help on strain but not burden, although items were very similar to those used in burden measures (sleep disturbance, worry, depression, frustration, health, disruption to household routine, embarrassment, demand for attention, lack of pleasure in caring, fear of accidents). This positive effect was found only in older carers over the age of 65 years and not in those under 65 years. Home help in this study covered a wide range of services (district nurse, health visitor, general practitioner, social worker, home help, meals on wheels, chiropodist, hairdresser, volunteer, other), few of which were related to respite provision specifically. Marks119,120 defined service provision as 4–8 hours per week of health and personal services, socialisation and home management activities. Although defining this as respite care, the extent to which these services were utilised as respite is unclear. The study was also small, having only 25 carers in the group receiving services and 25 in the group selected from the waiting list for services. Both the service use group and the control group were, however, selected randomly.
Summary of cross-sectional studies
The main outcomes assessed in the cross-sectional studies related to mental health and carer burden. The majority of studies assessing carer mental health focused on general service provision giving a range of personal care and respite services, which are difficult to compare and for which it is difficult to identify the impact of respite. Those examining day care provided heterogeneous methods and results. Studies were small and frequently either did not take account of confounding factors or had limited or no information on levels of service provision. The two studies focusing specifically on respite included one examining informal care and the other examining different types of respite in different European countries, neither of which provide information that is suitable for establishing generalisable conclusions.
Studies measuring the impact of ADC on burden give varying results. A number make comparisons between different types of service provision and do not include a comparison group having no respite care. Studies that did make the appropriate comparisons and which showed no effect of day care were small and provided limited amounts of respite, which could account for the lack of effects. Two of the studies showing a positive effect were larger, although one suffered from possible confounding effects that were not taken into account in the analysis. Again, the extent and quality of the evidence are insufficient to come to any firm conclusions concerning the impact of day care on carer burden.
Studies focusing on the impact on burden of the use of services specifically designed to provide respite do not, however, clearly define the type of respite. Some focus on informal support and some include comparisons of different types of respite service provision or frame the availability of respite hypothetically. The samples used had the potential for considerable bias and, again, there is insufficient evidence to draw firm conclusions.
Studies of the impact of general service provision again suffered from difficulties of definition and the identification of the constituent elements of respite. Studies of the use of in-home support faced similar difficulties in that in-home services tended also to include personal care service provision and home-maker services, with no clear indication of the extent of respite that these services provided. There was also considerable variation in the methods used, making interpretation difficult.
Cross-sectional studies do not, therefore, provide consistent or clear evidence concerning the impact of respite care on carer burden or mental health to support any of the previous findings, although the majority of studies reported either a positive effect or no effect, with little support for negative effects of respite.
The quality ratings of the cross-sectional studies were mixed, with a fair proportion of studies having either high- or lower-quality ratings.
The effects of respite on the care recipient
Randomised and quasi-randomised trials: characteristics of studies
Because the search strategy focused on carer outcomes it was not felt that it was appropriate to combine care recipient outcomes quantitatively. Therefore, studies reporting care recipient outcomes are summarised in the following section. Table 11 summarises the outcomes for both carer and care recipient within the randomised and quasi-experimental studies. Further details of the studies can be found in Appendix 4.
| Care recipient outcomes measureda | Care recipient results and direction of effectb | Carer resultsc and direction of effectb | |||
|---|---|---|---|---|---|
| Baumgarten et al. 200232 | Functional status (OARS); depression (CES-D); anxiety (STAI) | Difference between time point one and time point two was small and there was no significant difference between the groups on magnitude of change (day care vs waiting list). Measured at 3 months | 0 | No difference in carer burden | 0 |
| Burch et al. 199934 | Functional abilities (Barthel); morale (Philadelphia Geriatric Morale Scale) | No difference between day hospital and day care on change in functional abilities at 3 months | 0 | Carer strain: no effect | 0 |
| Burdz et al. 198835 | Problems (Memory and Behaviour Problems Checklist; Zarit and Zarit 1983) | Significant interaction between treatment group (respite vs waiting list) and occasion (pre- and post-intervention) for problems (behaviour decreased in treatment group and increased in control group). Measured at 6 weeks and 3 months | + | Burden: significant decrease in burden in respite condition | + |
| Quayhagen et al. 200047 | Measures of cognitive function (memory, problem solving, verbal fluency) | Cognitive stimulation group showed improvements in these measures. No effect in respite group | 0 | Decrease in hostility for carers with patients in the day care group. None of the groups differed on perceived stress | + |
| Richards et al. 200348 | Cognition (MMSE); problem behaviours (PC) | Cognition remained stable but behaviour problem frequency increased in the day hospital group compared with the memory clinic group and the community mental health service for older people. This was due to worsening in the subscale related to apathy problems at home. Measured at 12 months | – | Carer coping and carer mood (HADS): in day hospital group anxiety and depression increased over 12 months’ intervention | – |
| Riordan and Bennett 199849 | Cognitive function (MMSE); behaviour (Crichton Royal Behaviour Rating Scale; Robinson 1977); institutionalisation |
Experimental group (home support service): at 6 months mental status deteriorated while behaviour remained stable Control group (standard care): decline in mental status but an increase in behavioural dysfunction. No statistical analysis reported Significantly increased rate of institutionalisation in control group at 6 and 12 months but no difference at 18 months |
+ |
Psychological well-being (GHQ); Carer Problem Checklist and Machin Strain Scale (Gilleard 1984) No difference in carer stress and problem checklist although no statistical analysis reported |
0 |
| Rolleston and Ball 199450 | Well-being measured by questionnaire developed for the study | Well-being not affected by closure and reopening of respite facility (strong trends for improved well-being on reopening but not statistically significant) | 0 | Closure of respite detrimental to well-being but returned to preclosure levels at 3 weeks after reopening | 0 |
| Rothman et al. 199329,51 | SIP; Psychological Distress Scale; MMSE; health perception | Significant difference between contract ADC (more impaired) and customary care at 12 months on physical dimension of SIP and total score. No difference between groups on the other outcomes | – | No difference in burden or health perceptions between groups | 0 |
| Wells and Jorm 198753 | Cognitive function (MMSE); Memory and Behaviour Problems Checklist; Adaptive Behaviour Scale | Deterioration in both groups over time (respite group and institutional care group) with no difference between the groups. Measured at 3 months | 0 |
GHQ; DSSI; anxiety and depression, quality of life; grief and guilt Quality of life, GHQ and DSSI significantly better in institutional group at 3 months compared with respite group |
0 |
| Zank and Schacke 200254 | Life satisfaction (LSQ); perceived social support (Fydrich et al. 1987); depression (MADRS); self-esteem (Silbereisen and Zank 1984); cognitive impairment (MMSE); non-cognitive dementia symptoms (Memory and Behaviour Problems Checklist); activities of daily living (Nuremberg Aging Observation Scale) | Significant effects (measured at 9 months): perceived social support and life satisfaction: treatment group (day care) stabilised whereas control group (no day care) declined; depression: decrease in treatment group and increase in control group; self-esteem: no significant difference between groups; cognitive function: treatment group improved and control group worse on recognition of words; non-cognitive dementia symptoms: agitation and memory and behaviour problems – stabilisation of the treatment group and increase in agitation symptoms in the control group, no effect on the Memory and Behaviour Problems Checklist | + | No significant effect on subjective well-being (measured by life satisfaction), perceived social support, self-esteem and depression or on carer burden, but positive effect in day care group in qualitative interviews | 0 |
| Zarit et al. 1998;55 | Behaviour problems (Teri et al. 1992) | Day service users significantly fewer behavioural problems than non-users over the 3-month study period | + | Reduced feelings of role overload in day care users. In multiple regression models with role overload, role captivity, worry and strain, depression and anger, ADC use was predictive of role overload only | + |
Eleven randomised or quasi-randomised studies included care recipient outcomes in the design. The majority were carried out in the UK (n = 4)34,48,49,50 and the USA (n = 3),[29,51],47,55 with two from Canada,32,35 one from New Zealand53 and one from Germany54 (Table 12). Six were carried out between 1990 and 2000, two between 1985 and 1989, and three between 2000 and 2002. Six of the 11 studies focused on dementia care recipients,35,47,48,49,53,55 three on frail elderly,[29,51],50,54 one on physical disability34 and one on mental health. 32
| Dementia | Frail elderly | Physical | Mental health | Total | |
|---|---|---|---|---|---|
| UK | 2 | 1 | 1 | 4 | |
| USA | 2 | 1 | 3 | ||
| Canada | 1 | 1 | 2 | ||
| New Zealand | 1 | 1 | |||
| Germany | 1 | 1 | |||
| Total | 6 | 3 | 1 | 1 | 11 |
Outcomes included cognitive function, behaviour problems, functional ability, psychological distress and well-being, self-esteem, health perception, social support and institutionalisation. Five32,34,47,50,53 of the studies showed no effect of respite care, four an effect in favour of respite care35,49,54,55 and two an effect in favour of other interventions or the control group. [29,51],48
Sample sizes were generally small across all of the studies with only three[29,51],32,55 having sample sizes greater than 50 per group. Follow-up was short term at around 3 months, although two assessed outcomes at 12 months and one at 9 months.
Studies showing no effect of respite
Outcomes assessed amongst the ‘no effect’ studies included functional status, depression and anxiety, cognitive function, behaviour problems and well-being. Only one study32 compared respite users with non-respite users and was carried out in the context of ADC. This study, which was carried out in Canada, was a moderately large study, having 89 and 93 participants in the ADC and control groups, respectively, and was rated as being of high quality. Day care was received for 6 hours per day on 1–2 days per week. Outcomes measured included functional status, depression and anxiety. Although it may be unrealistic to expect day care to have any significant impact on functional status in a deteriorating condition, the authors felt that depression and anxiety were appropriate outcomes for this group. The study also failed to show any effect on carer burden. However, the short follow-up time and the relatively limited provision of weekly respite may be responsible for any lack of effect. Indeed, the authors reported that there was a trend for higher-level users to have greater benefit than low-level users.
The remaining studies showing no beneficial effect of respite care were designed to compare different types of service provision rather than respite versus no respite47,50,53 and so it is difficult to interpret the findings for respite per se.
Studies showing a negative effect of respite
Two of the studies reporting a significant association between respite and care recipient outcomes showed a negative effect. [29,51],48 One quasi-experimental study48 rated as low quality compared day hospital with a memory clinic and a community mental health team intervention, with those in the day hospital intervention having significantly more behavioural problems than those in the memory clinic group. However, because of selection criteria those entering the day hospital arm of the study were a distinct group in comparison to the memory clinic group, having differences in cognition and behaviour at baseline and being in the early stages of the disease compared with moderate to severe impairment in those in the memory clinic arm. These interventions obviously included much more than respite care. The other negative study[29,51] was of moderate quality and this also provided a range of activities, although in this case day care was compared with usual care. Services included in the day care facility were medical monitoring, occupational, physical and recreational therapy, personal care and social services. This was one of the larger studies, having 259 participants in the intervention group and 251 in the control group. However, the participants were not randomly assigned and there were differences between groups at baseline showing selection bias. It was also unclear as to what services the standard care group received.
Studies showing positive effects of respite
Studies favouring respite care included two day care evaluations,54,55 one institutional respite intervention35 and one providing in-home support services,49 which were tailored to individual needs and consisted of a range of personal care and respite services additional to usual dementia support (home help and home care, day care and day hospital, and Meals on Wheels). This last study was a small pilot study and had just 19 participants in each group (intervention and control). The control group was found to have increased behavioural dysfunction compared with the intervention group at 6 months although only eight of the 19 control subjects remained in the community at 6 months and so statistical significance was not calculated. This study, therefore, was too small to draw any firm conclusions. The study examining institutional respite also found a positive effect on behavioural problems35 over a short time frame of 6 weeks and 3 months. The study hypothesised that dementia patients would react negatively to relocation for respite in a nursing home, but contrary to expectations both dementia and non-dementia patients showed improvements in behaviour relative to the control group. This study was also small and non-randomised, using the waiting list as the control group, and although there were differences between the characteristics of the participants in the two groups at baseline, there were no statistical differences. However, the assessment of behavioural problems is a subjective assessment by the carer and this may not have been affected by alleviation of carer burden as there was no treatment effect on burden scores.
One of the studies assessing day care use compared with non-use55 also found a positive effect of day care use on behaviour problems at 3 months and 12 months. The study by Zank and Schacke reported decreased depression and agitation and an increase in cognitive function. This study used longer follow-up times of 6 months and 9 months compared with the study by Baumgarten et al. ,32 which did not find any effect of day care respite on care recipient depression, which may account for the difference in outcome. There appeared to be a similar level of day care provision in both studies although in the Zank study participants also received home care in the mornings and evenings.
Summary
The results of care recipient outcomes in the randomised and non-randomised trials are variable and so it is difficult to draw clear conclusions. Many of the studies were too small to provide reliable data, and some compared different forms of respite provision or included a variety of interventions in the respite interval, which did not give clear outcomes for respite itself. The range of different types of respite (day care, in-home, institutional) and different types of care recipients did not allow results to be categorised according to these factors. The majority of studies measured the outcomes at short follow-up times of around 3 months, although two used a 12-month follow-up period and one a 9-month follow-up period. The evidence, in the main, suggested that respite did not have any negative impact on care recipients.
Care recipient outcomes: longitudinal before-and-after studies
Nine before-and-after studies (presented in 10 papers) included care recipient outcomes57–63,65,66,68 (see summary table of before-and-after studies in Appendix 5). Four of the studies were from the USA,57,59,60,65 two from the UK,[62,63],66 one from Canada,61 one from Australia68 and one from Hong Kong. 58 The majority of studies were carried out after 1990 (all except two). There was a fairly even split of studies focusing on dementia (n = 5) and the frail elderly (n = 4). The dementia studies were carried out mainly in the USA (n = 4) with one in the UK (see summary table in Appendix 5). Overall, four studies reported a positive effect of respite on the care recipient,59,61,66,68 four no effect57,60[62,63],65 and one a negative effect58 (Table 13).
| Care recipient outcomes measureda | Care recipient results and direction of effectb | Carer resultsc and direction of effectb | |||
|---|---|---|---|---|---|
| Adler et al. 199357 | Behaviour problems (Behavioural Assessment Instrument); ADL (PSMS) | After 2 weeks of in-hospital respite behaviour and ADL did not exceed expected normal deterioration | 0 | An improvement in burden (BI) on discharge, which returned to baseline levels at 2 weeks post discharge | 0 |
| Chi and Wong 199458 | Attitudes to carer | More clients reported negative attitudes towards the carer after respite. They thought that the carers were impatient, not very helpful and trying to get rid of them | – | In 3 out of 10 statements the carers had a more negative attitude after using the service; in 2 statements they had a more positive attitude | – |
| Cox 199859 | ADL (Memory and Behavior Problems Checklist); behaviour (Pearlin et al. 1990); cognition (Pearlin et al. 1990) | Strong decline in ADL for white but not black group. Deterioration in both groups for cognitive status. Black but not white group had improvement in behaviour | + | Neither black nor white carers reported any change in anxiety or depression whereas both groups had significant reductions in feelings of burden | + |
| Deimling 199260 | ADL (PSMS); cognitive ability (Poulshock and Deimling 1984) | On average there was little impact on the care recipient’s functioning after respite | 0 |
Depression (CES-D): depression declined in carers of stable care recipients but stabilised in carers of declining care recipients. Carers of stable care recipients showed a significant decline in health problems Relationship strain decreased in carers of stable care recipients but increased in carers of declining care recipients Respite did not decrease carer activity restriction in families with stable care recipients but there was lower activity restriction in carers of declining care recipients |
+ |
| Desrosiers et al. 200461 | ADL (SMAF); well-being (General Well-being Schedule); psychiatric profile (SCL-90); perception of social support (Social Provisions Scale); other physical measures (pain, nutrition, balance, walking, etc.) | At T2 (3 months): general well-being, psychiatric profile, ADL and all physical measures except nutritional risk improved. T2–T3 (6 months) change scores: ADL declined, other measures no statistically significant changes | + | No statistically significant effects at T1 or T2 | 0 |
| Gilleard 1987; Gilleard et al. 198462,63 | Carer Problem Checklist and Machin Strain Scale (Gilleard et al. 1982) | No impact on care recipient problems | 0 | Carer burden (Machin Strain Scale) and psychological distress (GHQ) reduced | + |
| Higgins et al. 200565 | Quality of life (QOL-AD); behaviour (CERAD); cognitive function (MMSE) | Care recipient’s own rating of quality of life not significantly different but carer ratings of care recipient’s quality of life significantly worse. Cognitive function and behavioural symptoms significantly worse over the 12 months of the study | 0 | Quality of life (QOL-AD): no significant difference over study | 0 |
| Homer and Gilleard 199466 | Behaviour Rating Scale (CAPE) | Significant reduction in overall dependency during the respite period, with marked reduction in both the physical disability and social disturbance subscale scores | + | Psychological distress: no evidence of any improvement in total GHQ score during the respite period, but significant reduction in depression and social dysfunction subscales | + |
| Johnson and Maguire 198968 | Anxiety, suspiciousness and helplessness (Katz Adjustment and Social Behaviour Scale) | A significant reduction in anxiety and suspiciousness but no difference in helplessness | + | Carer Stress Scale: no reduction in carer stress | 0 |
Studies showing a positive effect
One study showing a positive effect examined hospital inpatient respite for frail elderly clients in the UK. 66 The measures were taken before respite admission and during the respite stay. The assessment of the care recipient’s behavioural functioning was carried out by the carer at baseline and by the nurse during the hospital stay but it is unclear if there were any systematic differences in the assessments made by informal and formal carers. There was no information concerning any activities or interventions received whilst in respite or of extent of service use.
Two studies carried out in Canada and Australia reported a positive outcome for frail elderly care recipients of day care. 61,68 The clients in the Johnson and Maguire68 study attended a day care centre for between 1 and 3 days a week giving 8–24 hours of care. The study was small, having 46 carer/care recipient dyads, and outcomes were measured at short time frames of 2 and 4 months. There was a significant reduction in anxiety and suspiciousness but no difference in measures of helplessness. Dropout was substantial with only 28 pairs completing the 4-month follow-up but regression analyses were used to produce a complete data set for the 46 subjects. There was no detail of the content or activities of the day care programme. The Desrosiers et al. 61 study reported a similar level of respite care (2 days per week), which was received for a period of 12 weeks. This was carried out in a specialist geriatric outpatient facility and was therefore designed to provide some medical intervention and rehabilitation. Assessments were carried out at similar time periods (3 and 6 months). This was a larger study with 171 participants recruited and 126 completing the final assessments. There was evidence of positive effects on general well-being, the psychiatric profile, ADL and all physical measures at the 3-month follow-up, which then stabilised with no further changes at 6 months. This day care intervention is, however, likely to be focused more on improving health outcomes for care recipients than on providing respite benefit for carers.
The final study59 showing a positive outcome (although in this study outcomes were mixed) was carried out in the USA and included a range of respite services. Carers were given the option to buy up to 164 hours of respite care, which included in-home care by a trained worker, nursing home care for 4–5 days at a time or day care. Care recipients all experienced dementia and outcomes were assessed at 6 months. The study focused on comparing the respite needs of African American and white carers. Behaviour, ADL and cognition measures were assessed at 6 months. There was a strong decline in ADL for white but not black participants and there was a deterioration in cognitive status in both groups, which would be expected in relation to normal deterioration of the condition; however, the black participants showed some improvement in behaviour whereas white participants did not.
Studies showing no effect
A similar range of respite interventions had no effect on care recipients: two day care studies,[62,63],65 one institutional care study57 and one study in which a range of respite was given. 60
The study examining institutional care57 gave dementia care recipients an inpatient stay in a Veterans’ hospital for 2 weeks every 6 months. Participants in the study were first-time and repeat respite users. This study assessed pure respite in as much as no activity programmes or medical care were provided, although participants were encouraged to function at their highest level. Outcomes measured at 14 days post discharge were behaviour problems and ADL, which did not exceed expected normal deterioration for dementia sufferers. This gives only immediate outcomes of the particular 2-week respite period and does not give any indication of longer-term outcomes of repeated respite admission, although more appropriate outcomes would be required for this type of evaluation, along with some control for condition-associated decline. The study was also very small, having only 37 participants.
The study by Gilleard et al. [62,63] reported no effect of day hospital admittance on everyday problems experienced by care recipients. Follow-up was carried out at 3 and 6 months and respite was provided in four psychogeriatric day hospitals, but there was no information concerning the level of day care support. However, carers’ views of the benefits for their dependants of their participation in respite care were greater for those still attending day care at 6 months than for those who were institutionalised or discharged. The extent of the care recipient’s problems was significantly correlated with the carer’s rating of the impact of respite on the care recipient, suggesting that the differences in the severity of the care recipient’s condition was a possible confounder. The carers’ ratings may have been affected by many issues in this comparison and interpretation is difficult.
The other study examining day care65 provided day care respite for dementia carers for 1 day per week. The day care programme provided activities such as cognitive stimulation exercises and physical exercise but did not include medical intervention. The outcomes in this study were somewhat mixed in that care recipient ratings of their quality of life were not significantly different at follow-up (up to 12 months) but carer ratings of their dependents quality of life were worse. Cognitive and behavioural functioning had also declined, which may be a result of the natural history of the condition (dementia sufferers). For the purposes of this narrative the quality of life ratings of the care recipients themselves are considered the main outcome measure. This study was small with only 37 participants recruited and 21 completing the study.
Deimling60 reported a respite programme providing a range of respite services to dementia patients including short institutional stays, day care and a home health aide service. A total of 78 care recipients were recruited to the study who had taken part in the programme for a 4-month period. There was no detail given of the extent of respite received by individual carers and their dependants. Overall, there was little indication of any impact on care recipients’ physical or cognitive functioning after respite.
Studies showing negative effect
Only one study58 reported a negative effect of respite care on the care recipient. This study evaluated institutional respite in either elderly hostels for more capable care recipients or care homes for those in frail health. A total of 43 carer/care recipient dyads were recruited to the study and followed up for 1 month (after the care recipient returned home). Outcomes reported were the care recipient’s attitudes towards the carer after respite use. More of the care recipients expressed negative attitudes towards their carers after respite. Specific items showing an increase in responses were ‘the carer is very impatient’ and ‘the carer is trying to get rid of me’. There was a decrease in responses to the item ‘the carer is very helpful’; however, there was also an increase in the item ‘the carer is a very good companion’. After respite the carers also had more negative views concerning their dependants, particularly ‘the elderly are very impatient’ and ‘taking care of the elderly is a stressful job for me’. However, there was a stronger commitment to maintaining the care recipient at home.
Summary
The majority of these studies reported either a positive effect or no effect of respite care on the care recipient. There were similarities in outcomes across the range of different respite contexts. Outcomes tended to focus on ADL, behaviour, which was often a version of ADL, and cognitive function. These are aspects that will vary with the natural history of the condition and which will depend to some extent on the nature of the samples recruited to the studies, i.e. the severity of the condition and the duration and stage of decline. Studies were small and dropout rates were high. Account was not always taken of confounding factors in multivariate analyses. However, the results of the studies would suggest that there are no strong negative impacts on care recipients at relatively short follow-up intervals from respite provision.
Care recipient outcomes in relation to carer outcomes
The direction of the effects for carers and care recipients were in the same direction for the majority of randomised and quasi-experimental studies. Only two studies47,54 showed different effects for carers and care recipients. In the study by Quayhagen et al. 47 there was no effect of respite on the care recipient whereas the carer had a decrease in hostility. Respite, however, did not affect perceived stress. The study by Zank and Schacke54 measured a number of outcomes for care recipients, showing positive effects in both psychosocial and cognitive tests. Similarly, a number of outcomes were assessed for the carer but no significant effects were found in any of the burden or mental health outcomes.
There was greater disagreement in outcomes for carers and care recipients in the longitudinal before-and-after studies. In two studies there was no effect of respite on care recipient outcomes and a positive effect on carer outcomes;60,[62,63] in one study61 there was a positive effect for care recipients but no effect for carers.
It would appear from these comparisons that respite, although often designed to be an intervention aimed at carers, does not necessarily provide benefit to carers to the detriment of care recipients. The consistency of the effects on carers and care recipients suggests that the design of the study and the intervention is likely to be responsible for the types of effects seen, rather than there being differences in outcomes for the two groups of participants.
Longitudinal observational studies: care recipient outcomes
Although a number of the studies measured care recipient characteristics such as severity of mental impairment and functional abilities they generally were not related in any meaningful way to service supports. Only the following studies provided relevant data.
Cox 199775
This study also assessed depression and burden in the carer and has been described in the relative sections above. There was deterioration in the care recipient outcomes of ADL and cognition over the 6-month period of the study, reflecting the deteriorating nature of the condition, but carers felt that care recipients’ behaviour did improve over the study. This is a subjective view and it is possible that this judgement is affected by the decreased burden of carers demonstrated in the study, thus giving them greater capacity to deal with problem behaviours.
Cox and Monk 199076
This study (described above) examined carer-rated ADL and mental impairment (memory and behaviour problems) of the care recipient in relation to formal and informal supports in black and Hispanic groups. There was a significant correlation between informal support and memory/behaviour in the black care recipients but not in the Hispanic care recipients. Physical impairment measured by ADL was also correlated with informal support, with a lesser correlation with formal support. This longitudinal study made assessments at baseline (n = 50) and at 6 months (n = 43). It is not clear, but it would appear that the correlations reported above were measured at baseline and so they do not identify the direction of the relationship between formal/informal support and care recipient health.
Summary
Only two observational longitudinal studies provided data on care recipient outcomes. In both studies there were felt to be benefits of respite care for care recipients in relation to behaviour problems and ADL, although in one study the data were probably cross-sectional.
Update of systematic review for period December 2005–April 2008
A modified update of the systematic review was carried out for the period December 2005–April 2008. The search strategy remained the same but was carried out only in the main databases, i.e. MEDLINE, CINAHL and PsychInfo. A total of 1995 hits were achieved. The titles and abstracts were scrutinized for inclusion/exclusion and 73 full papers were then acquired for assessment. From these, seven quantitative studies were identified as being eligible for inclusion based on the criteria established in the main review. These studies are discussed below and are summarised in Appendix 8.
None of the quantitative studies identified was carried out in the UK. Two were carried out in the US,135,136 two in Japan137,138 and three in Europe. 139–141 Two136,141 compared two different models of respite care. In the study by Droes et al. 141 users of a programme that involved day care plus extra support for the carer in terms of information, discussion groups and social activities were compared to users of day care only without the added support. No differences were found between the groups on psychological and psychosomatic symptoms (GHQ) but after 7 months significantly fewer people in the experimental group were institutionalised (4%) compared with the control group (29%). The other study compared direct-pay home respite to agency provision of in-home respite care. In the direct-pay group carers were included who used their payments to recruit family and friends to carry out respite care for them. There were no differences between the two groups on carer depression (CES-D) although carers who hired family and friends were slightly more satisfied with their respite provision. Both of these studies focused on care recipients with cognitive impairment.
Three studies135,137,138 took an observational approach to look at predictors of carer outcomes, with use of service being one of the predictors. Both Japanese studies137,138 were of this design and also the study by Kang135 carried out in the US. The Japanese studies137,138 used the number of services accessed as their predictive measure. In one,137 use of services was found to have a negative relationship with carer burden (more services, less burden), whereas the other138 found no significant relationship between use of services and carer depression (GHQ12). Both studies focused on a mixed group of frail elders.
Only two studies139,140 used a quasi-experimental design using a comparison group of non-users of respite services. Both of these studies were carried out in Europe (Spain and Germany). One focused on home respite services for frail elderly139 and the other on day care for people with dementia. 140 The study of in-home services139 found no difference between groups on carer burden. Although this intervention was a home help service providing assistance with ADLs, particularly personal hygiene and domestic tasks, it is presented by the authors as the main respite service available for carers in Spain. The service was used by participants in the experimental group for an average of 3 days per week for 4 hours per day but it is unclear whether carers actually took advantage of this for respite. The other experimental study140 was quite small, having only 18 and 19 participants in the experimental and control groups respectively (having had an attrition of just under 50% from baseline). There were differences in carer stress favouring the experimental group on some aspects of the measure, i.e. stress associated with care recipients’ aversive behaviours, carers’ restrictions in personal needs, and job–caregiving and family–caregiving conflicts. The authors suggested that other dimensions of stress may have been alleviated in the first days of care use as it had not been possible to carry out the baseline measures before commencement of day care but only shortly after starting day care. The measure of stress was not a standardised measure but one developed specifically for the study and so the level of validity and reliability of the instrument is unclear. However, unlike many other studies care was taken to control the level of use of services in both the experimental and control groups. Eligibility criteria in the experimental group included use of day care at least twice a week although actual use was not given. Day care was delivered by staff specially trained in dementia care and offered group activities such as cognitive stimulation, ADL training or gymnastics. Meals were given and appointments with the doctor, hairdresser or pedicurist could be organised and personal tasks such as bathing or dental care could be provided.
These additional quantitative papers do not provide any conclusive evidence over and above that found in the main review and the findings of the main review still stand.
Chapter 4 Health economics
Background
There are an estimated 6.8 million informal carers in the UK. Three-quarters of these carers look after an older person, typically devoting a minimum of 20 hours per week to caring activities. 142,143 Consequently, the opportunity costs of the time and resources associated with informal care activities are substantial in terms of the indirect costs accruing to carers and their families. National estimates of the costs of informal care vary widely, ranging between £34 and £57 billion per year. 144–146 Without informal carers much of this burden would be placed upon statutory providers. In recognition of this there has been increasing policy focus on informal carers, advocating their support to enable them to maintain care of dependants at home for as long as possible and delay or avoid placement in institutional settings. Encouraging respite through the provision of short-term breaks to improve the well-being of informal carers has recently been promoted with the government pledging £140 million over 3 years (recently extended to £185 million) to support this. 147 Consequently, establishing priorities and ensuring efficient utilisation of the scarce resources available to provide respite has become a main concern. The economic component of this research aims to inform these choices.
Aim and objectives of the economic analysis
The aim of the economic analysis outlined in this section was to build on the synthesis of the literature previously outlined by estimating the cost-effectiveness of respite care provided across various settings.
The objectives of the economic analysis were to review the economic evidence relating to key respite care models, identifying the key cost drivers within them and disentangling their impact on health outcomes. For example, it was hoped to be able to evaluate the economic effectiveness of respite care differentiated according to a number of factors hypothesised to impact on outcomes, including recipient group (age, extent of frailty, disease group); care setting (inpatient, home, hospice, day care, etc.); provider type and local market conditions (voluntary, social services, NHS, private); length of respite (hours, days, weeks); and type of respite programme (proactive, aiming to anticipate problems, or reactive emergency management schemes).
Methods
Literature review
Review of the literature to facilitate the economic analysis was incorporated into the search strategy previously identified above. Abstracts yielded from the search that included any economic component were passed to the economists on the research team for further scrutiny and consideration for inclusion or exclusion. A total of 125 papers were identified making reference to economic issues pertaining to respite care. In addition, reference lists of papers were reviewed to identify any further potentially relevant papers to consider for inclusion. This generated a further 30 papers. Relevant web pages (e.g. PSSRU, HTA, Department of Health and health economics research centres) were also reviewed, yielding a further 17 relevant references, one a draft report by a team at the University of York investigating a very similar topic. 148 In total, therefore, 155 peer-reviewed publications, 16 public documents and one draft report were considered for inclusion.
Initial review classified identified papers into two groups: those reporting both costs and consequences and those reporting either costs or consequences but not both. To be included in the economic review studies had to have either a controlled or a matched design, compare at least two options and measure and report both costs and consequences.
Economic evaluation methods
The existence of scarcity and thus opportunity cost considerations underpins the need to undertake economic evaluations. Economic evaluation methods are applied to evaluate the relative efficiency of different methods of providing health-care services, assessing the relationship between resource use, processes and outcomes. 149 The basic task of economic evaluation is to identify, measure and compare the costs and consequences of the alternatives being considered. 149
Three main economic evaluation methodologies exist: (1) cost-effectiveness analysis (CEA) incorporating cost–minimisation analysis and cost–consequences analysis; (2) cost–utility analysis (CUA); and (3) cost–benefit analysis (CBA). All three methodologies adopt a common approach in that they all seek to compare the costs and consequences of health-care interventions. Further, they all deal with costs in very similar ways. The primary difference between them is the differing, although sometimes subtle, ways in which they measure and value consequences. Table 14 presents the three main techniques of economic evaluation and summarises the key differences in their approaches to identifying, measuring and valuing consequences. 149
| Type of study | Measurement/valuation of costs in both alternatives | Identification of consequences | Measurement/valuation of consequences |
|---|---|---|---|
| Cost-effectiveness analysis (CEA)b | Monetary | Single effect of interest, common to both alternatives, but achieved to different degrees | Natural units |
| Cost–utility analysis (CUA) | Monetary | Single or multiple effects, not necessarily common to both alternatives | Healthy years or quality-adjusted life-years |
| Cost–benefit analysis (CBA) | Monetary | Single or multiple effects, not necessarily common to both alternatives | Monetary |
There has been considerable debate among health economists in recent years regarding encouraging ‘good practice’ in the conduct of economic evaluations within health-care settings. Benchmark standards have been identified in the UK, which recognise the key considerations in the design conduct and critique of economic evaluations. 149 These key considerations were incorporated into the abstraction instrument for synthesis and appraisal of the economic evaluations included in this study.
Results
The main result of this review is that there is a paucity of economic evaluation evidence pertaining to respite care services. Of the 155 papers identified as potentially relevant, only five32,[150,151],152–154 met the study inclusion criteria. All of the included studies reported on respite provided through day care programmes only. The limited number of studies and focus on only one type of respite precluded comment on alternative types of respite provision and the range of factors potentially impacting on outcomes.
Detailed abstraction of the included papers was undertaken. Table 15 summarises the main study features with a narrative synthesis highlighting the key findings presented in the text.
| Study | Country, respite setting, design and type of economic evaluation | Description of intervention/s | n | Health problem | Demographics | Carer outcomes (and length of follow-up) | Resources (and length of follow-up) | Results |
|---|---|---|---|---|---|---|---|---|
|
Artaso Irigoyen et al. 2002150,151 Data collected 1995 |
Spain Day care Quasi-experimental Cost–consequences analysis |
Attendance at day care centre | 80 (40 experimental group; 40 control group) | Dementia |
Recipients: mean age 79.64 years Carers: mean age 54.5 years; female 100%; 30% spouse, 70% adult child |
Caregiver: burden (ZBI Spanish version); quality of Life (CCV); satisfaction (ATTKISSON) Care recipient: cognitive function (MEC); behavioural test (BEHAVE); functional capacity (RITCHIE) Follow-up: baseline and 6 and 12 months |
Public sector and patient/carer perspective Ingredients: use of health, local authority resources. Costs to carers of providing informal care, patient out-of-pocket expenses The average cost per patient was 1754 Euros and 1238 Euros for the intervention and control groups respectively Follow-up: baseline and 12 months |
Apart from satisfaction, no difference was detected in any other outcome measure The intervention group sustained higher average costs; this did not reach statistical significance |
|
Baumgarten et al. 200232 Data collected 1991 |
Canada Day care RCT Cost–consequences analysis |
Intervention group received immediate admission to moderate-intensity, adult day care within multipurpose centres; 6 hours a day, once or twice a week; free Control group placed on 3-month waiting list to receive day care services |
212 (108 experimental group; 104 control group) |
Frail elderly Mental health (anxiety, depression, insecurity, loneliness) |
Recipients (experimental/control): mean age 76.4/78 years; female 74.1%/73.1% Carers (experimental/control): mean age 54.2/58.4 years; female 73%/71%; 25%/28.9% spouse, 46.6%/44.4% child |
Caregiver: burden (CBI) Care recipient: depression (CES-D); anxiety (STAI); functional status (OARS) Follow-up: baseline and 3 months |
Public sector perspective Ingredients: hospital, physician, and home care; long-term and day care; outpatient, day hospital and transport services The mean cost per patient was C$2935 (SD C$5536) in the experimental group and C$2138 (SD C$4530) in the control group Follow-up: baseline and 3 months |
No effect detected. No statistically significant differences in either average total costs or individual service costs Included in meta-analysis |
|
Donaldson and Gregson 1989152 Data collected 1987 |
UK Day care Quasi-experimental Cost-effectiveness analysis |
A family support unit (FSU) providing day and respite care for confused elderly people | 105 (35 experimental group; 70 control group) |
Confused elderly Dementia |
Recipients: reported for combined FSU and control groups; age: 94% 65+ years; 60% female Carers: not reported |
Caregiver: burden on carers (not based on validated instruments) Care recipient: none Time spent in community; reduction in use of long-term care beds; costs of care; carer costs incurred Follow-up: reported at end of 3-year study |
Public sector and patient/carer perspective Ingredients: use of health, local authority and voluntary agency resources. Costs to carers of providing informal care The mean cost per patient was £4400 in the experimental group and £1200 in the control group Follow-up: reported at end of 3-year study |
Intervention three times more expensive than usual care but increased days at home and reduced use of long-term care beds |
|
Gaugler et al. 2003153 Data collected 1993 |
USA Day care Quasi-experimental Cost-effectiveness analysis |
Intervention group accessing subsidised adult day care at least twice per week. Control group did not use day care service |
Short term 385 (154 experimental group; 231 control group) Long term 233 (80 experimental group; 153 control group) |
Dementia |
Recipients (treatment/control): mean age 78.2/76.2 years; 63.6% female; 76%/57% spouse Carers (treatment/control): mean age 56.7/60.8 years; 69.7% female; 75%/78% spouse |
Caregiver: overload (Role Overload Scale); depression(CES-D) Care recipient: behaviour (Behaviour Problem Scale); ADL dependency Follow-up: reported at baseline and 3 and 12 months |
Public sector perspective Ingredients: adult day care, formal and informal services and employment costs At 12 months the total cost per adult day services was US$54 in the intervention group and US$47 in the control group Follow-up: reported at baseline and 3 and 12 months |
Favourable incremental cost-effectiveness ratios for carer role overload and depression, with daily costs of these benefits reducing over the year |
|
Hedrick et al. 1993154 Data collected 1986–9 |
USA Day care RCT and prospective cohort Cost–consequences analysis |
Phase1: intervention group received individually tailored programme of adult day care within four Veteran Administration (VA) medical centres; control group received customary (nursing home) care Phase 2: intervention group received individually tailored programme of adult day care within four VA medical centres; control group received adult day care provided by community-based contractors |
Phase 1: 826 Phase 2: 163 |
Frail elderly at risk of nursing home placement | Recipients: 82% dependent in at least one ADL, with an average of 2.4 dependencies |
Caregiver: distress (Psychological Distress Scale); life satisfaction; ADHC Social Support Scale; Caregiver Impact Scale; behavioural problems; caregiver versions of ADHC; patient satisfaction questionnaire Care recipient: survival; Sickness Impact Profile; psychological distress; cognitive status; health perceptions; satisfaction with care Follow-up: reported at 12 months |
Public sector perspective Ingredients: use of hospital, clinics, nursing homes, day care, home care, rehabilitation and pharmacy/laboratory The average cost of the intervention group was US$2500 higher than the average cost of the control group Follow-up: reported at 12 months |
Phase 1: intervention group had a significantly higher average cost with no apparent incremental health benefits to patients or caregivers Phase 2: total mean costs were not significantly higher for contract as opposed to VA-provided day care |
All of the included economic evaluations investigated the provision of day care interventions compared with customary care. Of the five evaluations identified, only one152 was conducted in the UK; two were undertaken in the USA,153,154 one in Canada32 and one in Spain[150,151]. The studies included two cost-effectiveness analyses and three cost–consequences analyses, with two based on RCT designs and three quasi-experimental matched designs.
Synthesis of the clinical and cost-effectiveness results reported in the five economic evaluations presented is frustrated by the lack of common outcome measures applied, making aggregation and comparison of results difficult. Overall, few discernible benefits were found to be associated with the day care interventions reported. Three studies32,92,150,151,154 reported no benefits associated with day care. Donaldson and Gregson152 reported that day care participants were able to spend more days at home and Gaugler et al. 153 reported improvements in role overload and depression for caregivers.
Average total costs were higher among the day care intervention groups in all five economic evaluations (reaching statistical significance in the Donaldson and Gregson,152 Gaugler et al. 153 and Hedrick et al. 154 studies). Evidence linking costs to effectiveness is, however, relatively weak. Only two studies reported favourable cost-effectiveness results. Donaldson and Gregson152 conclude that day care is cost-effective because of savings accrued via reduced utilisation of long-term care beds and Gaugler et al. 153 report favourable incremental cost-effectiveness ratios for carer role overload and depression.
Moreover, the robustness of the evidence presented is further affected by a number of limitations in the study design and execution, which in one way or another affected all of the five studies. Relatively little information was provided on the nature of the interventions and routine care, specifically the extent and type of respite care available within the day care programmes evaluated and the heterogeneity or otherwise between them. Measures of dispersion (SD, range) of the cost data were not always reported and, often, even if they were reported they were not discussed. A top-down approach was used to cost the resources, which inevitably leads to problems in terms of the accuracy and generalisability of cost estimates. The period of follow-up was in some cases very short to properly account for the resources and most importantly the clinical effectiveness effects. The strength of the results is further affected by the small sample sizes in some of the studies. None of the studies reported a clear description of the key cost drivers or performed any sensitivity analysis to test the robustness of the results.
Only one of the studies is UK based, raising inevitable concerns about the transferability and salience of the other study findings within the current UK context. Sculpher et al. 155 explore methods to model the transferability of results across countries; the quality of the studies in the present review, however, was not sufficient to allow any such modelling exercise to be undertaken. In addition, only two RCT designs are included and, despite matching, bias cannot be ruled out in the three quasi-experimental studies. The lack of common outcome measures reported alongside limited efforts to link costs to effectiveness frustrates robust comparisons between the studies. Typically, there is inadequate reporting of the economic outcomes and their methods of derivation, with even less attention given to economic outcomes for carers. Further, although four of the five studies were published relatively recently, the data on which they are based are considerably older (range 11–20 years). Finally, the Baumgarten et al. 32 RCT was the only economic evaluation identified to also be included within the meta-analysis, and even then it was analysed with reference to carer burden only. For this reason it was not possible to link the results of the economic synthesis to those of the meta-analysis overall. In conclusion, there is a dearth of evidence to assess the efficiency, or otherwise, of providing respite to carers of older people through day care programmes.
Although there is potentially an endless number of respite care schemes, hence the same definition of customary care might be hard to find (Von Behren156 identified 2000 care schemes operating in the USA in the 1980s), future evidence should be based on robust designs with a clear description of both intervention and customary care and should include a longer period of follow-up and a range of sensitivity analyses to assess the generalisability of the results. Future research should also explore the possibility of using gold standard evidence-based data to model the long-term effects of important resource drivers (e.g. effect on institutionalisation).
Chapter 5 Qualitative synthesis
Review of the methods used in the included qualitative studies
Country of origin
A total of 70 papers96,103,157–222,235,236 were identified for inclusion in the qualitative review, representing 69 studies. The majority of studies were carried out in the UK and USA (25 and 22 studies respectively). Of the remaining studies, ten were from Canada, three from Australia, two from New Zealand, two from Japan, one from Iceland and four from Sweden.
Note that in the following discussion when the number of studies is referred to these will total 69, whereas when referring to the number of papers or articles the total will be 70.
Condition of the care recipient
Just over half of the studies (n = 38) focused on care recipients who had dementia (see Appendix 9). The other 31 studies focused on frail elders who had a mixed aetiology of both physical and cognitive impairments; those with specific physical disabilities such as stroke; respite care in a palliative care context; or frail older groups for whom it is unclear whether their disabilities were physical or cognitive or both. For this last group of studies it is likely that at least some of the care recipients will experience some combination of both cognitive and physical disability.
Year of publication
The majority of the articles were published relatively recently, 42 being published since 2000 and only six published before 1995. This pattern was consistent across the countries of origin, with only the UK and USA having published studies before 1995.
Sampling and data collection methods
The preferred method of data collection was by individual interview (46 studies). Eleven studies used focus group methodology and five a case study approach. Seven studies used a qualitative approach within a structured survey by reporting on responses to open-ended questions. Two of these were included in the previous quantitative synthesis. 96,103
There was limited information concerning data collection beyond the type of interview and whether it was audio recorded, although some studies did outline the questions posed and the length and location of interviews. Few detailed the approach and recruitment of participants. There was also little justification of data collection methods in relation to an overall qualitative framework. A total of 15 studies did not describe the sampling strategy, four used a random sample, 15 mentioned either purposive or theoretical sampling and 35 used a convenience sample. These last 35 papers included studies in which all users of a particular service were recruited consecutively and studies using volunteers or participants identified by service providers. Those studies using purposive sampling were very variable in the level of detail concerning the criteria used in the sampling and the justification for the criteria.
Theoretical framework and analysis
The use of a theoretical framework to guide data collection and analysis was poorly reported and/or infrequently used. The summary table in Appendix 9 lists the types of framework reported in the articles, although not all represent a theoretical underpinning to qualitative methodology but either a theoretical perspective (such as feminism) or an approach to analysis (such as constant comparative technique). In total, 46 papers did not report any theoretical framework at all; seven reported using a grounded theory approach, five phenomenology and one critical discourse analysis. Two studies claimed to use an interpretivist approach but did not give further details as to which type of interpretivist approach they were adopting. One study claimed to be using content analysis but the analysis was actually thematic. Others (n = 3) reported using a combination of content and thematic analysis although, again, these took mainly a thematic approach. One study proposed a feminist perspective but did not go further to describe the methodological framework. The majority of studies were thematically analysed allowing further integration and thematic synthesis within the present review.
Focus of the study
The papers were categorised according to their main aims, as proposed by the authors. These fell broadly into five categories: views of respite care (n = 28), views of wider community services (n = 14), experiences of caring (n = 6), carer needs (n = 13) and evaluation of specific respite interventions (n = 9). Studies exploring the experience of caring provided information related to carer needs and, to a lesser extent, barriers to uptake of services. Studies examining carer views of community services gave some specific mention of respite services, including views of service use or expressions of need or preferences for types of service provision. The studies explicitly focusing on respite care gave similar information. The studies designed to form an evaluation or part of an evaluation of a specific programme focused on the following.
-
Provision of day care (compared with domiciliary stroke team) for stroke survivors; this was an addition to an RCT. 190 Also a pilot study evaluating an ADC programme103 in which open questions were included in the quantitative survey.
-
Evaluations of multiservice respite programmes,96,165 in one of which participants were given a choice of a range of services to respond to: unexpected circumstances, routine periodic relief or for special purposes such as short family vacations or outings. 165
-
Two evaluations of case management interventions providing respite relief. 180,192
-
Evaluation of a weekend respite programme geared to individual needs and preferences. 200
-
An action research study to develop and evaluate a palliative care night respite service. 183
-
Evaluation of a continuous intermittent care programme. 163
-
Evaluation of a hospital night respite service. 214
-
Reporting of the context of the research
Description of the context of service provision within the studies was generally poor. Participants were frequently in receipt of a variety of services but these were often not described. However, as this was not always the focus of a study this is not surprising and does not detract from the quality of the study. But many studies focusing specifically on respite care and those in which participants were recruited by particular respite services failed to describe the characteristics of the services in detail, or the extent of use of the service (duration and/or frequency). Many of the studies discussed ‘formal service use’ or ‘community service provision’ covering a wide variety of home care services designed to support either the carer (e.g. respite) or the care recipient (e.g. personal care). This reflects the difficulty in defining respite care in relation to specific services, as carers often talked about the respite achieved by the input of home health aides, whose main purpose was to provide personal care to the care recipient. Many of the studies were interested in any service likely to provide support to both carer and care recipient.
There was also great variability in the range of participant characteristics reported. The unit of interest in most of these studies in relation to the present review is the carer/care recipient dyad, but authors frequently did not report the characteristics of both parties. As the carers were generally the ones taking part in the interviews their characteristics had greater emphasis. Around half of the studies were designed to explore issues around dementia care, with others aimed at palliative care or physical disabilities such as stroke. For many of the remainder it was often not apparent what disabilities were experienced by the care recipients. Cognitive impairments present particular difficulties in relation to informal care as well as formal services, and defining these characteristics would enable the reader to assess generalisability of the findings.
Overall quality rating
Despite the reservations listed above the majority of the studies were of moderate quality. The scores on the quality ratings were categorised as low, medium or high based on a division of scores into tertiles. This is in line with the method used in the quantitative review, and gives a relative quality rating rather than an absolute quality. The total possible score for any individual study was 30; scores of 8–13 were categorised as low, scores of 14–18 as moderate and scores over 18 as high. Many of the papers scored in the mid-range for the individual items in the scoring system (each item scored from 0–2 – see Appendix 2 for quality assessment instrument). This was because the reports generally gave some information concerning the criteria being assessed, for example context, sampling, data collection and data analysis, whilst not giving full details, thus scoring 1 on individual items. For example, those studies using a purposive or theoretical sampling procedure would state this, while frequently giving little information concerning the basis of the purposive sampling. Some assumptions were then made as to whether the sample included the full range of possible cases based on the characteristics of the sample. Included in the studies using convenience sampling were those that had recruited all participants taking part in a particular service, which, if justified, would receive higher scores than those studies using purposive sampling that was not fully explained.
As few studies reported the use of an underlying methodological framework it was difficult to relate the methods used to a particular typology of qualitative research, and so a general thematic approach was assumed and the requirements for sampling, data collection and analysis, as set out in the quality assessment, were expected. It was also necessary to judge each study on its own terms and assess the reporting in relation to the stated aims. As mentioned previously, the provision of respite was perhaps a subsidiary concern and so detail concerning the types of service received may not be expected to be given in the context of a particular study. This means that little information is available concerning the context of the research for the purposes of the review but does not necessarily mean that a particular study will be assessed as being of poor quality.
When a more quantitative approach was taken and open questions were included in a survey, the quality assessment was not scored on all items. In such cases the scores given were prorated so that they could be compared with the quality assessments of the other studies. Ratings were very dependent on how the authors reported the study; for example, two papers207,208 reporting on the same study scored 19 and 22, respectively, based on differences in reporting. However, with scores of more than 18 both of these papers fall within the category of high quality. It is for this reason that a categorisation approach of low, medium and high was taken rather than giving undue weight to a continuous score on a measure that is not fully validated. Table 16 shows the quality ratings of the qualitative papers by country. Studies carried out in the UK tended to be of lower quality than studies carried out elsewhere. The majority of studies carried out in the UK (60%) were categorised as low quality. Studies carried out in the USA were more evenly distributed across the categories, whereas those carried out in Canada were of generally higher quality. The lower quality studies in the UK tended to be earlier studies, eight out of the 15 having been carried out before 2000, five between 2000 and 2003 and only two after 2003.
| Quality rating | |||
|---|---|---|---|
| Low | Medium | High | |
| UK | 15 | 6 | 4 |
| USA | 7 | 8 | 7 |
| Canada | 2 | 1 | 8 |
| Australia/New Zealand | 0 | 5 | 0 |
| Other | 3 | 1 | 3 |
Synthesis of qualitative data
The main aim of this review was to assess barriers to respite care and also to identify needs for service provision. From the data it emerged that these two concepts were closely linked, each providing two sides to the same issue: what was seen as a barrier was considered a need. Consequently, the core category identified in this analysis was ‘barriers to uptake of respite care’ (see Appendix 12 for a list of codes used in the analysis). The other codes were examined in relation to this category to identify an explanatory framework of the context surrounding barriers to respite use.
Because the aim of this part of the review is to identify barriers to uptake of services the discussion will tend to emphasise the negative aspects of experiences. It should be borne in mind whilst reading this section that these negative experiences do not represent all views. To provide balance, a discussion of the theme representing positive aspects of respite is also included in a later section. In addition, the analysis aims to further the state of knowledge by integrating findings from the various studies in a framework of explanatory relationships not evident in any single study. The emphasis here is on identification of relationships between themes and, as the primary aims of included studies were heterogeneous, it is not possible to comment on the prevalence of either positive or negative views.
Barriers to uptake of respite care
Figure 28 shows a proposed model of the barriers to uptake of respite care emerging from the review of the qualitative studies. It identifies aspects of the carer and the care recipient and the characteristics of service provision that may influence uptake of respite. Personal and cultural attitudes to the caring role and to the function and purpose of respite services may impact on the carers’ perceptions of their needs for respite. The nature of the carer/care recipient relationship may contribute to attitudes to the caring role and the extent and nature of perceived responsibility for care. Guilt is a significant emotion in the uptake and use of respite care and is influenced by the caregiving relationship as well as the actual or anticipated reactions of the care recipient to participation in respite.
FIGURE 28.
Barriers to uptake of respite services.
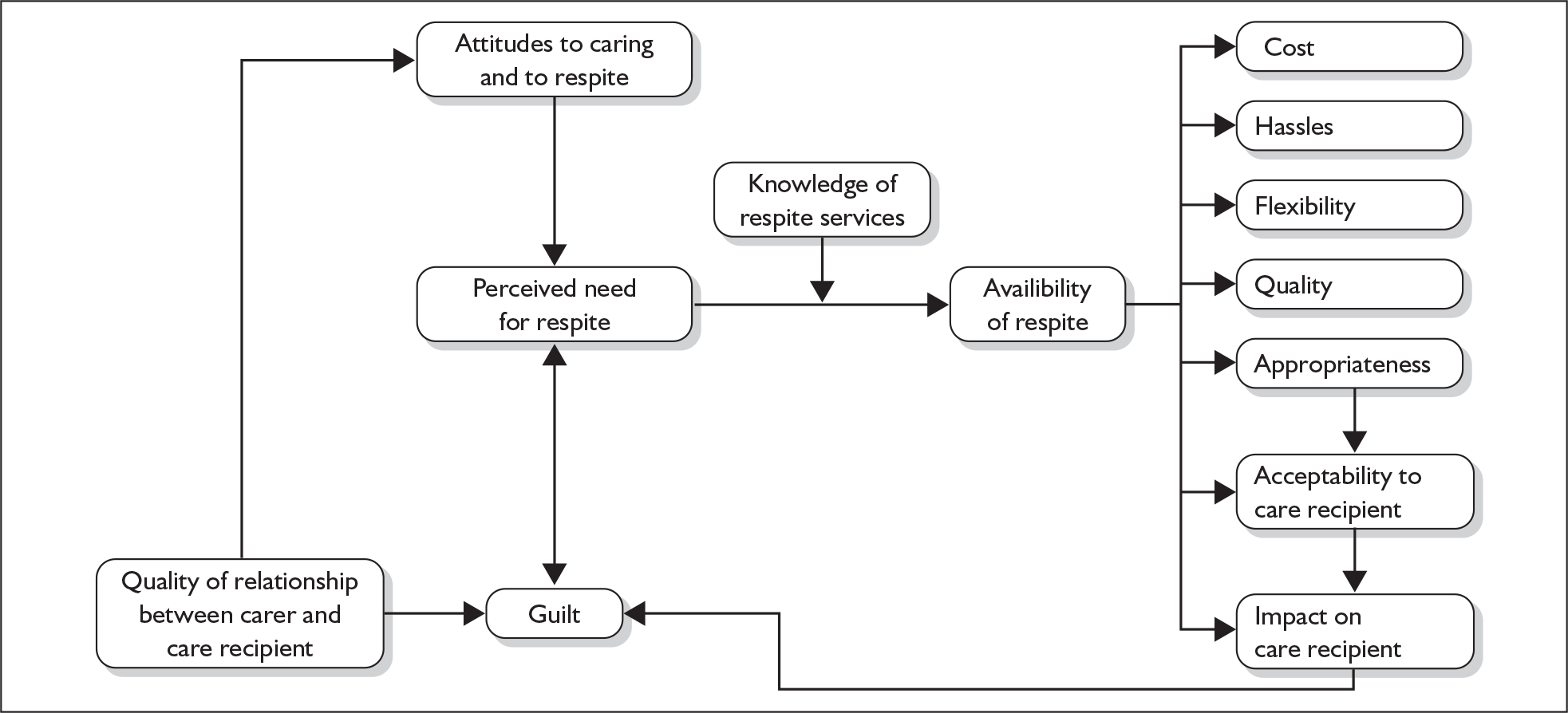
Once a need for respite is acknowledged, services must be available and the carer must be aware of them for respite to be utilised. A host of other issues more directly related to service provision, such as the appropriateness of service provision and the quality of care, may then be potential barriers to the uptake of services. A change in any one item shown in the model could potentially affect other relationships and the eventual outcome. It must be noted that this is not necessarily a comprehensive model but portrays the findings of the literature to date.
Each of the potential barriers is discussed below.
Attitudes to caring and respite and the caregiving relationship
The studies reviewed suggested that carers had a strong desire to continue caring and to maintain their care recipient in the community. 179 This desire resulted from a number of factors, one being a strong sense of commitment to the care recipient based on the quality of the relationship between carer and care recipient both past and present. 193,198,207,211 This was particularly true of spouse carers who maintained a strong bond of love and companionship:
Marilyn talked fondly of the good life she and her husband had together and that, even though her present circumstances were difficult, she seemed content. She could not conceive of doing anything but take care of her husband. This contentment and acceptance of her role as carer was exemplified when she said ‘he’s lucky he’s here and I’m lucky he’s here . . . I just think I’m very lucky that I still have him.’
Strang and Haughey207
Sometimes the caring relationship itself engendered a closeness that would not otherwise have been possible:
In offering positive feelings about caring, the carers mostly (six out of nine) based this on the sense of closeness to the person being cared for: ‘she’s (still) the apple of my eye’. This closeness was itself part of the reward for caring and was seen as a product of caring as if it could not have occurred without the existence of a degree of dependency.
Ashworth and Baker157
As a result it was often difficult for carers to relinquish the caring role:
One carer thought that the closer the caring relationship, the greater the adjustment required in coming to terms with the fact that they would no longer be the sole provider of care.
Ashworth and Baker157
The carer can become so bound up in the caring role that they are unable to distinguish their own needs from those of their care recipient. Such carers were portrayed as older, isolated women who had been caring for their spouses for many years. It was suggested that they became unable to differentiate the physical aspects of caring from the emotional support they provided within a loving relationship. 165 This results in a feeling that they are the only ones who can provide the right sort of care for their loved ones, which was an attitude reported in varying degrees by a number of authors.
A sense of commitment to caring was not, however, exclusive to those who had a good relationship:
By contrast, several carers had experienced unsatisfactory and sometimes very unhappy past spousal relationships often resulting in perceptions of long-standing ‘lovelessness’, frequently devoid of mutual warmth and togetherness. For these carers the drive to cope was expressed in terms of duty, responsibility, pity and compassion seemingly discharged on the altruistic principle of ‘do unto others as you would have them do unto you’.
Upton and Reid211
Yet another carer, whose 55yr marriage had been difficult and full of conflict, stayed with her husband and cared for him as his dementia progressed because ‘for better or for worst, I promised’.
Strang206
The discussion around this sense of obligation was often gendered, with a view frequently expressed that women have a long history of commitment to caring for the family and putting the needs of others first:
The carer had taken full responsibility for all aspects of raising her family and had always made decisions to maximize the benefit of other family members but not herself. Faced with caring for a husband with dementia, she was resentful and bitter. She needed a break, she said, yet was almost immobilized in making the decision to use a 2-week respite service.
Strang and Haughey208
These issues were compounded by a feminine subservience to a male-dominated relationship common in the older generation:
Another study carer stated ‘there are a lot of things you think you could do and should do but they [men] won’t let you. And you can’t do things against their will all the time . . . , you can’t. And I think that’s how a lot of us women feel you know.’
Strang206
There was a strong sense of stoicism and desire for privacy in many reports of carer attitudes,184 with a view that there were many worse off who were in greater need of help. 193
The types of attitudes discussed above that drive the desire to maintain the care recipient at home can lead to a sense of failure when a need for support is acknowledged, particularly in the presence of negative attitudes to respite care itself:
One group of carers seemed to associate day care with institutionalization. One spouse commented, ‘Once you move them out of the environment it’s a give-up . . .’ Other caregivers associated the use of day care with words such as abandonment, rejection, and warehousing.
Cotrell167
Other negative attitudes towards respite included the view that it is demeaning for the care recipient, with its connotations of babysitting. This was not helped by experiences of a perceived lack of respect for the care recipient from formal care staff. Carers of recipients with dementia felt that day care, for example, was more appropriate for more severely demented people who were unaware of their surroundings. In the early stages it was felt by carers that attendance at day care could confront a care recipient’s denial of their condition, and so a pretence of normality is maintained as long as possible to maintain the integrity of the care recipient’s self-image.
Guilt
The outcome in relation to many of the issues described above is the carer’s feeling of guilt. The strong commitment to caring and eventual realisation that they cannot cope on their own leads not only to feelings of failure but also to feelings of guilt. The negative connotations of respite and the feelings of abandonment also contribute to guilt. If respite is seen as benefiting only the carer this will be viewed in a selfish light, which can trigger guilt, particularly in women who have spent their lives caring for others. These strong feelings of guilt can be sufficient to prevent uptake of respite care:
One study carer openly stated she had always considered the family’s needs before her own. And now she had great difficulty making the decision to use respite services which might benefit only herself. When asked why she cancelled the service which could have given her some time for personal enjoyment she stated: ‘. . . guilt. I didn’t sleep that night hardly any at all and in the morning I got up and . . . cancelled.’
Strang206
In addition, many assumptions were made about how the care recipient might perceive respite care, and if this was considered to be negative the ensuing guilt could be a sufficient deterrent to the uptake of respite. 167 These types of assumptions moderated carers’ perceptions of need, but there were also many examples quoted of active resistance to participation in respite care by care recipients, as well as negative impacts on care recipients and examples of poor service quality or inappropriate respite care, which contributed further to carers’ feelings of guilt. These are discussed more fully in the following sections.
Knowledge of and availability of services
Once carers acknowledge a need for support they are often at a loss as to what is available and how to access help.
Caregivers expressed frustration and hopelessness arising from a lack of information and the inadequacy of statutory respite care and other support services. ‘I have asked what kind of help is available and I still haven’t got any real answers.’ A number of caregivers reported a lack of awareness regarding government financial schemes such as the Carers Allowance: ‘I find nobody tells you anything, what you are entitled to’, while another caregiver asked, ‘Would you have to pay for them? [day care services]’.
Lane et al. 185
The most accessible location for advice is the primary health-care centre, but it was suggested by more than one study that GPs do not appear to be providing appropriate support and information (this was reported in a Canadian study and not in the UK):
In the home, GPs can play a supportive and reassuring role for caregivers especially when they make home visits willingly or are attentive to the specific needs of the family. Therefore, it was somewhat surprising to learn from caregivers that, in many cases, their GP had not known about services or at least not mentioned them to caregivers, or even had been an obstacle in getting support.
Wiles216
It would appear that information is sometimes only given in response to a crisis event:
Family carers explained that information about respite care in reality is crisis-orientated, ‘it often takes an emergency to get the ball rolling’.
Hanson et al. 172
A lack of awareness of services was attributed, in part, to a lack of recognition of the status of ‘carer’. 198 In a long-term relationship, in which probably the health of both partners is failing, at what point does one become a carer?
In terms of availability of services there were perceptions of rationing and delay in reports from UK studies:
There appeared to be general perceptions of delay, rationing and inequity in service provision. Patients/carers often commented about the restricted number of times a particular service could be provided, for example, such as the number of sessions provided by Marie Curie nurses or hours of domestic help provided by social services in a week.
Jarrett et al. 177
This was not, however, restricted to the UK, with poor knowledge and availability reported in other studies in all geographical locations. 161,216,219 In the UK it was reported that sometimes the long waiting lists for social services meant that support came too late, the care recipient having been institutionalised or died. 215 Most discussions related to service availability, however, focused on the inflexibility of services and the failure to meet carers’ individual needs, which is discussed in a later section.
The acceptability of respite care to care recipients
There were a number of reports of the reluctance of care recipients to be involved in respite care, particularly in relation to day care:
One caregiver reported, ‘I set it up, got ready to go and then he refused. I tried three times.’ Some recipients refused to get into the car, while others refused to return the following day.
Cotrell167
Reluctance may stem from the care recipients’ previous personality and social preferences:
Others assumed that their spouse would resist because of his or her personality or state of mind, i.e. the care recipient had never enjoyed social activities, was ‘home oriented,’ or did not like strangers.
Cotrell167
Values of self-sufficiency, privacy and independence that were displayed by carers were also held by the care recipients themselves, which contributed to resistance to service use:
Concern for the beliefs of her mother and her comfort with assistance from outside the family became the dominant value influencing one caregiver who reported: ‘Even in her demented [sic] stage she is hesitant and is leery of strangers and by nature does not accept freely any help. My parents were very much their own people and very private – fiercely private.’
King and Parsons180
Many strategies were used to persuade the care recipient to take part in respite, from cajoling to trickery:
But he will never go [to adult day care]. I mean, you know, he’s just not into arts and crafty things. But I learned from one of the gals in one of the support groups, just ask them if they would like to volunteer. He loves to help, so I think that would work.
Teitelman and Watts210
Because of difficulties with day care many carers in the studies reported a preference for in-home care as being less disruptive for the care recipient. However, sitters were sometimes rejected by care recipients and not allowed into the home. 167,197 It may be more difficult for care recipients with dementia to feel comfortable with strangers in the home as they are more likely to feel suspicious of them and ill at ease. Indeed, this was mentioned by carers in several of the studies – the trust that is required of people coming into the home in this capacity.
The impact of respite care on the care recipient
There were a number of possible negative impacts on the care recipient that could act as a deterrent to the use of respite care. Beisecker et al. 161 reports that ‘perceptions about patient unhappiness, safety, physical health, functional levels and behaviour were viewed as barriers to ADC use’. Care recipient distress was a commonly reported impact, which frequently took some time to recover from after return home:
Mrs C, although she takes advantage of respite services, admits it distresses her husband: ‘. . . they’re very good to him, honest, but when he comes home he’s very withdrawn . . . he won’t talk at all. By the time he goes I’m just getting him into my way when he has to go and I don’t like him going, but they say I’ve got to let him go.’
Pickard and Glendinning201
For those with dementia it tended to exacerbate their confusion:
confusion of the dependant on admission to a residential home and confusion on return home such that, ‘he didn’t even recognize me, like he didn’t know . . .’
Ashworth and Baker157
With confusion comes inappropriate behaviours, which were difficult for both in-home and institutional respite carers to accommodate, resulting in exclusion of the care recipient from the service.
Physical impacts included loss of mobility when exercise was not maintained during respite:
‘All that hard work and two days in bed for her and that’s the length of the hall gone.’
Gilmour171
Regaining this and other health losses created more burden on carers:219
The fact that those being cared for experienced weight loss, constipation and decreased mobility as a consequence of their admission concerned the caregivers greatly. Furthermore, extra care was required at home to help the person regain their previous level of health.
Gilmour171
Being away from the one-to-one care given by the informal carer could also lead to loss of continence, which is a significant factor in the ability of carers to maintain the care recipient in the home environment. Other more serious health impacts included reports of a hip fracture resulting from a fall that went unnoticed and the need to admit one man to hospital because of a blocked catheter. 201
Hassles
There were many hassles (i.e. inconveniences, irritations and frustrations that were troublesome to deal with) involved in the preparation for respite care. These hassles were costly in terms of the physical and emotional energy involved in dealing with them, and these costs were weighed against the benefits received from respite. 200 Worcester and Hedrick220 talk about this as conservation of limited energy and social resources:
As caregivers talked about the need for time away, they struggled with what needed to be done prior to leaving, what would occur during their absence, and what effect being away would have on receivers.
Worcester and Hedrick220
The need for preparation began with the identification of appropriate services to meet a particular need:
These hassles included red tape in obtaining services, lack of time to obtain services, family conflict over what services should be used, information overload from service providers . . .
Winslow218
Once a service had been identified the preparation for the respite event could be a burden in itself:
An additional barrier is that preparation for a nursing home stay is generally complicated with many forms to be filled out, medical information to be secured from doctors, clothing and personal effects to be labeled and packed, and most importantly the short term stay had to be explained to the mentally impaired person.
Brody et al. 165
Gaining the care recipient’s co-operation was one of the major hassles involved, which was reported particularly in relation to day care. The issue had to be approached sensitively in care recipients who were cognitively impaired or resistant to outside care. Worcester and Hedrick220 report words such as ‘testing, timing, setting things up, concealing and tricking’. Even once the respite had been agreed with the care recipient there could still be difficulties in getting them ready for day care and getting to the necessary transport service:
Too much physical and emotional effort may be required to get the impaired member willing to leave the home and to complete the task involved in getting them on the bus.
Brody et al. 165
Transport itself may prove to be difficult. There were a number of reports of complaints concerning transport, which included lack of transport in rural areas197 and a general unreliability of transport services. Carers complained that they did not know what time the transport service would pick up or drop off. 157 In addition, Butterworth166 related how one carer’s mother was dropped off in the street on each occasion and because she could not remember which was her own house she would wander off. This carer gave up using day care for this reason.
One other major area of difficulty was related to the lack of continuity of care and the high turnover of staff in support services. This required repeated information exchange by the carer, especially for in-home carers. 180,217
Quality of care
A barrier to the uptake of respite services was a concern about the quality of care provided and this concern was most notable in relation to nursing homes, although home care was also sometimes problematic:
There were three types of problems: incompetence, dependability, and personality conflicts between worker and elderly client. Caregivers defined incompetence as workers that allowed care recipients to do things not in their best interest health wise, such as skipping meals or refusing baths, or as workers that failed to provide adequate treatment. These situations resulted in more work for family caregivers. Some caregivers increased their monitoring of the paid providers, which resulted in loss of desired respite or increased emotional stress.
Piercy and Dunkley202
Concerns about quality of care have also been demonstrated to some extent in concerns about the negative impacts of respite on the care recipients, which could, in some instances, reflect poor quality of care. The reverse is also true in that:
Concerns about the variable quality of care also lead to concerns for the safety of the care recipient on the part of the caregiver.
Wiles216
Specific aspects of institutional care were inadequate staffing levels161,217,219 and frequent staff changes resulting in a lack of continuity,216 which can be particularly problematic for care recipients who are cognitively impaired184 although it is an issue for all care recipients and carers in establishing a relationship that allows trust to be built. 159,203 Also mentioned by several studies was the low level of knowledge concerning dementia in both home care staff and institutional carers. 161,219 Also mentioned by more than one study was a concern that staff did not treat care recipients with a respectful attitude,159,161,203,207 which was extremely distressing for some carers.
One final issue related to communication between the formal and informal carers and sensitivity of the formal carer to the knowledge and expertise of the informal carer and also to the care recipient’s routine. Carers feel that it is important for care recipients to maintain their established routines to avoid losing functional abilities. However, nurses in institutional settings often did not seek information concerning the normal routine of the care recipient, and if it was offered by the carer it was disregarded:
She expressed frustration about communication processes between her and nurses, believing that her written notes to them were put in the rubbish bin.
. . . disregarding the knowledge and expertise of the family. In the caregivers’ representations, the care of the person with dementia is delivered on the nurses’ terms within a medical model, and the family caregiver is excluded from decision making.
Gilmour171
The perception of the quality of service provision is central to a carer’s decision to take up respite care, and impacts on many of the other issues discussed here. Even if respite use continues in the face of a perceived lack of quality the carer may not achieve an effective respite experience, as one carer in the Strang205 study clearly states:
Respite care is only respite if the same quality of care is offered to the patient in a respite facility that is offered at home.
Strang205
With poor-quality care the carer will continue to worry about the care recipient; will not have peace of mind; will not be able to relax; will experience greater guilt; and will subsequently reduce respite to a minimum, if not completely. Carers who lack confidence in the care are likely to visit the care recipient frequently in the respite facility to carry out care tasks such as help with meals or to provide company. 205 This was one of the most fundamental themes that occurred regularly throughout the studies in the review.
Responding to needs: appropriateness and flexibility
For respite to be acceptable it must respond to both the carer’s and the care recipient’s needs. Innes et al. 175 reported that 26 out of 45 participants in their study had refused services as they were not suitable to their needs. Response to care recipient needs is encapsulated in the ‘appropriateness’ category. It was felt to be important to place care recipients with people of a similar level of disability, as demonstrated in the following extract:
. . . respite in the local hospital. The hospital let us down. I was shown a ward where she would stay for a week, I thought it was reasonable, I thought she could survive but when we arrived in the ambulance they said: ‘We’ve changed our minds’ and they put her in a different ward with people who were much worse than herself. It was very depressing for her and friends who I had asked to go and visit her whilst I was away met me with very reproachful looks when I returned and said they couldn’t understand why I had put her through such a dreadful experience. So I felt guilty and decided ‘never again’.
Butterworth166
Several studies focused on the activities carried out in ADC. Ritchie203 reported that it was important to develop ADC programmes that:
support and promote the self-esteem of older persons through activities that are meaningful to them.
Ritchie203
Although craft activities may be enjoyable for many day care users, for some it was felt to be demeaning or lacking in purpose. 203 Some older people may wish to feel that they are contributing something more worthwhile and in line with previous experiences:
It seems to me that people in this age group like to have practical activities, not just cutting and pasting, but they need to do things that they always did – useful things such as peeling potatoes.
Ritchie203
The communal nature of day care activities can also be difficult for some more reserved participants. Strang205 reported on one care recipient who became extremely distressed on being encouraged to take part in a group activity:
He was so upset . . . he started to cry . . . we tried to calm him down and he cried so hard . . . well, I never can take him back there again.
Strang205
A major barrier to the uptake of respite services was a lack of response to carer needs in terms of timing and flexibility of service provision:
The most prominent of the barriers reported by both the users (48%) and nonusers (42%) related to convenience issues, including program availability, hours of operation, location of the ADC, and access to ADC services during times of caregiver need.
Beisecker et al. 161
The type of respite that was felt to be the most flexible and convenient varied by study and by context as there was no consistency in organisation of services. Brody et al. 165 suggest that in-home respite is most flexible as it:
can be adjusted more readily to the amounts and specific times that relief is wanted – for short periods of time, at night or during the day, or on weekends, for example. Finally, in-home respite can be used for patients with varying degrees of impairment, levels of functioning, and different behaviours and personalities.
Brody et al. 165
Other studies cited problems with in-home respite as users were restricted to 1 hour three times a week, which did not allow enough time for the carer to go shopping. 175 Other carers just preferred respite to take place out of the home as they did not relish strangers in the home, or felt that they would only experience respite if the care recipient was physically in a different place. Problems with day care were the lack of weekend and evening provision. 165,191 In another study day care was only offered for 3 days a week and finished at 3pm, which did not accommodate the needs of working carers. 221 Day care provision that was longer, providing 8 hours care during the day, still did not allow enough time for the carer to get to and from their workplace.
Waiting lists proved to be an issue for nursing home care216 and night care. 183 Long waiting lists and respite that had to be booked months in advance compromised the opportunity for spontaneity. 213 Even within the restrictions outlined, carers generally were unable to exert any control over the timing of respite provision. Situations in which carers were granted some flexibility and control by being able to choose when their limited hours could be used gave a sense of empowerment that was greatly appreciated. 180,216 Other areas demonstrating a lack of flexibility were a lack of responsiveness to changes in a patient’s condition and the exclusion of care recipients with more severe disabilities from certain types of service. 191 There was also a lack of flexibility in relation to crisis care.
Leong et al. 186 suggested that carers’ preferences would be for the provision of a range of services designed to be more responsive to varying needs:
What this study indicates is that those caring for people with dementia at home feel a need for a variety of respite services, including day, overnight and weekend care accessible at short notice. It is evident that current services need to be more flexible and responsive to the actual needs of those who use them.
Leong et al. 186
Cost
Because of the different organisational processes involved in the different countries, cost issues may vary. However, loss of earnings because of caregiving responsibilities was a concern voiced in studies in the UK, USA and Canada. 157,203 Carers reported giving up work entirely to carry out caring duties or reducing hours from full- to part-time. This resulted not only in financial hardships but also in a loss of emotional independence:
she said, seven years later [after giving up work to care for her husband], at the time of the study, she regretted this decision because she felt she had lost her personal identity, autonomy and financial resources.
Strang206
UK studies placed more emphasis on informational needs in relation to finances. 172,179,185 Carers in these studies expressed a need for adequate financial support and information about what allowances they were entitled to, as many did not received allowances through poor knowledge. However, there was also a reluctance to divulge financial information, which acted as a barrier to seeking services. 177
Studies carried out in Canada and the USA more overtly expressed cost as a barrier to the use of services. 165,188,197 Costs frequently affected the choice of type of respite provision with costs of day care weighed against those of institutional and home care. 165 Canadian studies reported on the inadequate provision of publicly funded respite, and financial issues either acted as a deterrent to acquiring further services or allowed the better off to acquire extra help from the private sector. 197,216 One US study reported that when services were experienced via Medicare carers often found less expensive alternatives once the provision ended. 167 There was also an attitude of conservation, not only of financial resources but also emotionally and physically. In relation to financial resources carers were unsure whether to use money for respite ‘now’ or save it until later, as they did not know how long the caring situation would go on for. 220 In relation to conserving resources, some carers were reluctant to spend money on relief for themselves, feeling that they should be able to cope. 197
One issue, common across UK and Canadian studies, was a concern over the cost of transport. 175 This was a particular issue for those living in rural locations. It was also an issue if publicly funded services, such as buses or specific transport services, were unreliable. 216
Reasons for uptake of services
A commonly reported reason for the use of respite services is carer fatigue. However, this was often reported as a last resort, when fatigue had become exhaustion and the carer could no longer cope and was in crisis:
many families delayed using respite until they really needed it, first extending themselves to the point of mental and physical exhaustion.
Brody et al. 165
When formal help had been sought it was usually only when the carer was no longer able to cope, sometimes in response to a crisis or when all other possibilities had been exhausted.
McGarry and Arthur193
Occasionally carers were given the impression by health-care professionals that help would only be available once they had reached the ‘limits of their resilience’:
The doctor told me some of [the diagnosis] and said if you can’t cope with it any longer we will get her into a day clinic and that will give you a day’s rest.
Gillies170
Crisis events could be health events of either the carer or the care recipient, but often the services instituted to deal with sudden health events were continued afterwards if they had proved acceptable:
These caregivers sustained a number of health problems that prevented them from caring for the recipient, including cardiovascular events, cancer, and orthopaedic problems. In some cases, the services that were initiated during their hospitalisation or convalescence were retained.
One male caregiver who sustained a mild stroke experienced a particularly good fit with the sitter acquired by a social worker during his illness. Although he regained his pre-morbid level of functioning, he described the sitter’s on-going role as a companion to his wife and a friend to him, an integral part of the family.
Cotrell167
The experience expressed in the last quote was common not only of respite used during a crisis but also for other situations of one-off pragmatic use that break down the barriers to acceptance of service use. The need for respite for particular social events or occasions such as conferences, weddings and holidays triggered the use of respite, and once the benefit was experienced and proved successful it was used again on a more regular basis. 167 However, it could be a long process of acceptance of the need for relief, and one study165 reported on a counselling intervention that helped carers to identify and accept a need for leisure time and helped them to work out problems preceding the use of respite such as finances, patient management and conflicted relationships. The tendency to delay take-up of respite was sometimes related to cost, which prevented carers using respite until absolutely necessary or prevented the optimum use of services. 165
As well as the need to promote physical well-being, respite was also used to address emotional needs. Some studies reported on carers who recognised their need to distance themselves emotionally to maintain control:
They sought respite to place some emotional distance between them and the care situation because thy perceived that they were becoming irritable and ineffective in their care.
Cotrell167
This was often in response to behaviour problems. Deterioration in the care recipient’s condition was reported as a trigger to the instigation of respite care and was often a precursor to institutionalisation:
Two months later, the situation had deteriorated. A home visit revealed that the mother was incontinent of both bowel and bladder. Mrs J. was overwhelmed, exhausted and depressed. She could not keep up with the house and her mother. In-home respite was immediately arranged and the worker began to discuss with Mrs J. the possibility of institutionalizing.
Brody et al. 165
Apart from the needs of carers there were a number of care recipient issues identified as the focus of the uptake of services. As the care recipient’s condition deteriorates carers express concern for safety and the need for a sitter may be expressed. There are also concerns about maintaining care recipient health in relation to maintaining adequate nutrition. As well as consideration of care recipient physical health, respite was also seen as a means of providing socialisation and stimulation for the care recipient and of facilitating emotional health. Day care was often viewed as an activity centre for elders that could provide socialisation. In-home care, however, also provided an opportunity for stimulation:
she realised that the sitter could provide her husband with the stimulation and supervision he needed and which she herself could not physically provide.
Cotrell167
Positive aspects of respite care
Although some carers had negative experiences with respite care, or had low expectations or fears about the outcome, which acted as barriers to the take-up of services, there were also many reports concerning the positive aspects of respite. These were often the ‘other side of the coin’ to the barriers reported above and illustrate how a positive respite experience could have real benefits for carers and their care recipients.
Shorter-term respite such as day care was felt to give structure to the carer’s week157 along with a sense of normality as the free time matched the ebb and flow of caregiving activities. The respite time gained through this type of care tended to be used for necessary everyday chores:
Analysis highlighted how respite was not a time of relaxation rather an opportunity for cleaning, cooking, shopping, gardening, ironing, etc. and attending to his/her own health/social needs, i.e. the time and space were reinvested into sustaining the overall coping experience.
Upton and Reed211
This focus on catching up with chores was echoed by a number of studies in the review. 161,175,194,199 However, as the above quote suggests, respite was also used to carry out pleasurable activities on a regular basis such as playing golf,205 personal shopping, bowling and sewing,208 participating in religious or diversional activities,161 going to the gym, going for walks and socialising with friends157,171,199 and provided time to devote to the needs of the carer’s own family. 212 Day care also allowed some carers to remain in employment, either paid or voluntary. 175
Longer periods of respite such as institutional care were most associated with ‘recuperating and restoring of batteries’. 207 This type of care, often consisting of around 2 weeks of inpatient care for the care recipient, allowed the carer to take a vacation or visit relatives. Some preferred to stay at home to have uninterrupted time to relax. 161,195 This type of respite was also used for health-care needs such as surgery or emergency hospitalisation. 161
A recurring theme throughout the studies in the review was the essential nature of respite for maintaining and continuing the caring role:
Most of the caregivers perceived that respite enabled them to endure in the caring for their relatives instead of becoming fatigued and burned out.
Piercy and Dunkley202
Several studies reported respite to be instrumental in maintaining carer physical and mental health157,161,186,199 with carers in these studies quoted as saying that without respite they would have had a nervous breakdown. The result of such breakdowns in care would be institutionalisation of the care recipient. 157 These positive effects on mental and physical health were achieved by improved sleep,175 physical relief and the chance to rest and relax,161 the release of the build-up of stress and tension209 and rejuvenation from a sense of freedom. 161 The experience of positive respite was dependent on many of the issues already discussed, such as quality of care and the well-being of the care recipient, which allowed freedom from worry and confidence in the respite event.
There was some disagreement as to whether the positive aspects of respite were framed as being for the benefit of the carer158 or the benefit of the care recipient,170 although the two were frequently viewed as interdependent. One of the main benefits for the care recipient was perceived as the opportunity for socialisation,194 which was felt to play an important role in health improvements, particularly in relation to mental health and well-being:
Overwhelmingly, carers considered socialization the predominant factor for the improvement in their elderly relative’s mental health and overall outlook on life.
Valadez et al. 212
Other physical health improvements were attributed to consistent diet, exercise programmes, daily activities and mental stimulation exercises. 212 The positive effects of stimulation of care recipients from appropriate activities undertaken at respite was a consistent finding in the review:
Some participants stressed the way that services tried to motivate and maintain mental, physical and social awareness through using games and activities.
Innes et al. 175
The process criteria that caregivers identified (for evaluating care) were opportunities for socializing, meaningful interaction, and sensory stimulation.
Perry and Bontinen200
Socialisation and stimulation had benefits for the relationship between carer and care recipient. It enhanced communication by providing topics of conversation as both carer and care recipient felt they had more individual experiences to talk about, and resulted in an enhanced mood in both parties on return from respite. But the relief of strain of the carer also had positive impacts on the relationship as carers felt more tolerant after the respite break. Some carers reported that they did not lose their temper as much after respite. 205 This has obvious implications for the prevention of elder abuse although none of the studies addressed this issue directly.
The relationship between the service provider and both the care recipient and the carer played an important role in providing support:
Several caregivers cited the supportive relationships, even friendships they developed with their relative’s providers, as helpful to their caregiving performance.
Piercy and Dunkley202
This support could result from the passing on of expert knowledge, empathy for the carer’s situation and social support. It was important for carers that the care recipient got on well with the service provider, particularly if care was in-home. This provided the care recipient with the social stimulation gained at day care by other care recipients. It also enhanced the co-operation of the care recipient, which in turn made the carer’s life much easier. It also gave the carer peace of mind when leaving the care recipient with the service provider. This was a consistent theme running through all of the studies, which:
supports the idea of a relationship between the caregiver’s ability to experience relief and the caregiver’s perception that his or her relative is comfortable and safe.
Perry and Bontinen200
As seen in the barriers to the uptake of services the carer’s perception of the quality of care and the acceptability of respite to the care recipient was extremely important and when these aspects were favourable it contributed to a very positive experience for both carer and care recipient.
Ethnicity
Few studies addressed issues of ethnic minority carers. Notably, Bowes and Wilkinson164 carried out case studies of Indian and Pakistani carers; Wykle and Segal222 interviewed 20 white and 20 black carers of people with dementia; Netto198 interviewed 15 Chinese, 15 Pakistani, eight Indian, three Bangladeshi, two Afro-Caribbean and two other Asian ethnicities. Several other studies had small numbers of ethnic minority groups in their samples. On the whole, general issues related to respite care were very similar to those reported in the white populations and were consistent with the model of uptake of services shown in Figure 28. Some of the detail, however, was specific to ethnic minorities.
There was a stronger cultural obligation to care for older relatives amongst ethnic minorities. The study by Bowes and Wilkinson164 portrayed the prevalent view of the extended family in South Asian populations that was supportive of the caring role. In some cases the wider family network took a share in care with the older person staying with different relatives in turn. Netto,198 on the other hand, proposed that the view of ethnic carers as having all the support that they require from within the extended family is a myth. More than one-third of participants in this study received no support from family members:
one of the important findings of this study is that the proportion of sole carers in these communities is, in fact, larger than the proportion of sole carers in the general population, which the GHS recorded as less than a quarter (23 per cent). Dispelling the myth of the supportive family network further and underlining the need for respite services, nearly half (46.7 per cent; 21/45) reported that they had no time off from caring.
Netto198
There was a greater tendency for a lack of relief from the caring role as there was a cultural obligation for older relatives to be co-resident with their adult children compared with white populations, in which many care recipients were not co-resident. As in the white population the majority of carers were female, but the average age of carers tended to be younger, with more carers having the added responsibility of childcare. Burden, therefore, is considered high. However, few used any form of respite, although there were indications in all of the studies of an expressed need by ethnic minority carers for respite. 164,198,222 Not only was there evidence of limited access to respite services but also there was a low awareness of the availability of services. This was coupled with poor knowledge of conditions such as dementia. There is a general issue of information provision to communities who may have language difficulties and whose carers are isolated within the home in a caring role and who do not have access to normal channels of information.
When questioned about the types of service need there were similar requirements as those expressed in the studies of the white population, with particular importance being placed on the appropriateness of care. In this context this referred to ensuring that carers were of the same ethnic group, spoke the same language and were preferably of the same gender as the care recipient. Other important considerations for carers were that food was appropriate for their religion, for example vegetarian, and that the service was sensitive to other cultural and religious differences. Incontinence was a particularly problematic issue as this created a ‘dirty’ environment, preventing the rest of the family from prayer at home; without respite for the care recipient family members would be unable to access other facilities such as the mosque.
Carer needs
The need for a mental break
Some studies distinguished between a physical break and a mental break,180 proposing that respite was not merely the physical separation of carer and care recipient, that caring is a cognitive and emotional activity and that relief from it necessarily involves cognitive and emotional processes.
Caregivers described respite as a ‘mental state’ which resulted in feelings of freedom from responsibility for and worry about caregiving. This type of respite was rarely achieved.
McGrath et al. 194
Many of the studies talked about respite as a feeling of freedom from worry, responsibility or carer strain although not directly identifying a distinction between a mental and physical break. It was thus a theme running throughout the studies. As demonstrated in previous sections, respite use and experience were dependent on a number of psychological processes such as trust in carers, satisfaction that the care recipient was happy and safe, and feelings of guilt, etc., which have the potential to get in the way of the actual experience of respite even if someone else is taking over the physical caring. The carer has difficulty relinquishing emotional caring. To achieve this it is proposed that carers must cultivate activities that allow them this mental break. 210 This involves activities that take them away from the situation, that are totally absorbing and that are within their own personal world.
It’s a mind set. My mind is completely on something that I am doing and not subliminally on somebody’s needs.
Strang206
The time and type of activity required to achieve this break varied between carers. Some could catch it momentarily by taking a long leisurely bath while the care recipient was resting. Others made use of short respite periods to allow them to take exercise classes, go to a movie or see friends, whereas some required more than a few hours of time. 194 Other strategies involved:
… arranging or adapting to the physical, social, and/or task environment of the care recipient, allowing the caregiver to have a less vigilant mental state.
… relaxation of expectations of how things ‘should’ be, and taking advantage of any small opportunities for a mental break.
Teitelman and Watts210
Other needs
Most of the needs related to respite services have been outlined in the previous sections. Table 17 summarises carer needs in relation to respite service provision.
| Respite needs |
|---|
| Active provision of information on the availability of services, how to access them and what they provide |
| Support offered early in the caring career in a planned way and not as crisis management |
| Access to a variety of services, e.g. day care, home care and institutional care, to cater for different needs at different times |
| Flexibility of service provision – respite at short notice, at times to suit (including evening and weekends) and for the duration required |
| Reliable transport services (particularly in rural areas) |
| Continuity of care: particularly for home care services |
| Good-quality care: well-trained staff (trained in care of the elderly and dementia care); sensitive and respectful attitudes; care ensuring the safety of care recipients; care aimed at maintaining functional abilities and health of care recipients; good communication between formal and informal carers |
| Environment appropriate for the purpose, providing safety |
| Continuity of care between home and institution: formal carers seek information on the care recipient’s routine and take on board carer knowledge of care recipient’s abilities and needs |
| Care that provides benefits for care recipients as well as respite for carers: opportunity for socialisation; activities that provide mental stimulation; good nutrition |
| Appropriate care: right mix of service users (similar levels of cognitive abilities, cultural and language similarities); flexibility of activities to suit individual preferences, with activities also accessible for people with physical or sensory impairments |
Palliative care
Five studies177,183,189,204,209 focused on respite care in a palliative care context. Although many of the issues identified in these studies were similar to those already discussed there were some differences. These studies have been included in the thematic analysis already described; however, the differences are discussed here to include the more general findings in the overall synthesis. One of the main differences is in the approach to caring, which has some impact on the attitudes to respite. Because of the expectation of the impending death of the care recipient the caring experience was more intense. Carers in this situation wanted to spend as much time as possible with the care recipient. This highlighted to a greater extent the distinction between a physical and a mental break. Mental breaks were sought in closer proximity to the care recipient as physical separation could cause anxiety. 209 This is probably very much dependent on how imminent death is seen to be, as the study by Skilbeck et al. 204 did not report these types of views. In this study respite was provided in a hospice for 2 weeks twice a year, which suggests that death was not expected within weeks or months as in the Strang et al. study. 209 Some of the patients in the Skilbeck et al. 204 study had suffered from neurological conditions for many years and so the caring trajectory would be more similar to the long-term caring situations found in most of the studies included in the review.
The mental breaks reported by Strang et al. 209 were achieved by taking part in absorbing activities such as reading a book or watching television. A mental break was also couched in terms of regaining the previous relationship rather than being in the role of carer/care recipient, which helped the carer to forget the gravity of the situation and the impending bereavement. Physical respite was important, however, to allow the carer to catch up on sleep or to carry out chores such as grocery shopping, echoing the needs of carers in general. What was, perhaps, more important to the carers as a form of respite was the sharing of responsibility with both formal and informal respite providers.
Being able to take a break wasn’t as important as being able to have someone share in the responsibility or ease the responsibility.
Strang et al. 209
Related to this and in common with the studies in general was the feeling that respite could only be achieved through peace of mind, achieved when the care recipient was being well looked after. In the palliative care context this required more medical input and well-trained staff as the respite providers were required to have greater specialist knowledge. So, for example, in the study by Jarrett et al. 177 carers received support from Marie Curie nurses but considered their input purely as provision of respite because the specialist training of the nurses gave carers sufficient peace of mind to experience respite. In fact, palliative respite care was viewed as an opportunity to access specialist information and therapies such as complementary therapies.
Views of the service mirrored those already identified. For example, continuity of care was an issue when large numbers of nurses were entering the home. Continuity between home and hospital was also commented on, although in this context it was commented on more positively as the hospice nurses visited the care recipient at home to carry out treatment. However, there was also dissatisfaction with failure to maintain routines, as one carer reported that her father had become incontinent at night since admission to the hospice and another that their relative had not been mobilised sufficiently.
Service users felt considerable benefits of respite. It gave them the opportunity to socialise and talk to people in similar circumstances about issues that they felt their carers could not handle. It also increased self-esteem through being taken at face value rather than as a cancer diagnosis.
The impact of location of study, condition of care recipient and methodological quality rating of study on the findings
The country of origin of the study was one of the criteria used for sampling in the second-stage synthesis of qualitative data; countries were chosen that were culturally similar to the UK and which had service delivery organisation with similarities to that of the UK. As many of the issues raised as barriers to the uptake of respite services were culturally determined issues, such as the relationship between carer and care recipient and the nature of the extended family, relationships with formal carers, the practicalities of dealing with physical and mental disability, attitudes to caring and attitudes to respite, the findings were consistent across locations. The relationship with services is one area in which differences may arise because of the different nature of health and social care provision. However, in sampling these particular countries it was felt that this would not have substantial implications; for example, the existence of Medicare in the USA results in a similar system of services for frail elders as in the UK. However, there is still the potential for differences to exist in relation to the quality of service provision and the interaction between service providers and informal carers and care recipients. The findings, however, showed that the views expressed of service provision were similar across these different contexts. For example, there were similar concerns about continuity in both home care and institutional care, reliability of home care staff, training of staff (particularly in relation to dementia care), staff to patient ratios in nursing homes, the sensitivity of staff and the appropriateness of programming in day care facilities. A major issue for all participants in studies in all countries was the provision of flexible services that are appropriate to carer and care recipient needs.
Underprovision of respite care was a prominent theme across the board with little choice or control available, within generally limited resources. The level of resources and the cost implications were mentioned more frequently in studies outside the UK. There are probably greater limitations in what is covered by Medicare services in the USA and there was more discussion in this country of the difficulties of finding appropriate services even when the carer is willing to pay. This is, however, also an issue in the UK because if carers need to top up limited service provision for particular needs they must seek this support in the private sector. UK studies tended to talk about financial aspects in relation to the needs of carers for information concerning entitlements to allowances, such as attendance allowance, and for financial support generally. Care of the elderly in the UK was viewed as a responsibility of the state and carers viewed their role as deserving acknowledgement of the contribution that they make by receiving better financial support to carry out this role. Many carers lose out financially by giving up employment or reducing employment to undertake their caring responsibilities. However, apart from issues such as costs, the consistency across studies supports the approach of combining the data from studies carried out in different countries to aid understanding of the barriers to uptake of respite services.
Some specific issues have been identified in relation to the characteristics of the care recipients. Palliative care represents a particular aspect of the provision of respite care and this has been considered separately, as have the needs of ethnic minority carers. The remaining major defining characteristic of the care recipient is that of cognitive impairment as opposed to physical impairment. A number of studies have focused specifically on people with dementia or on particular physical conditions such as stroke survivors. Others have included mixed groups of both cognitively and physically disabled care recipients. Other studies have been more vague in their sampling and have included ‘frail elders’ who are likely to comprise care recipients with some degree of both physical and cognitive disability. Many issues are similar in these groups but when there are particular concerns these have been pointed out. For example, continuity of care has been held to be particularly important for cognitively impaired care recipients as constant changes of staff are more difficult for those care recipients who are confused. Similarly, it was pointed out that other changes, such as a change of environment, also add to confusion. Consequently, many carers of cognitively impaired elders prefer in-home respite, although this does not hold for all cases. Training of staff was found to be particularly deficient in relation to dementia, although a perceived lack of training in the care of bed-bound and physically frail patients was also felt to be a barrier to the take-up of services. The difficult behaviour of demented care recipients also caused particular problems for accessing services as it was reported that some services excluded care recipients when they became more severely impaired.
The majority of studies used individual interviews, with fewer studies using focus groups. Although the concepts identified were similar, one-to-one interviews tended to address more sensitive and personal issues whereas focus groups identified more general issues such as needs. There were several studies that used open questions in more structured approaches. Again, the concepts identified were consistent with other approaches but the data tended to be broader rather than focusing in-depth on particular issues. This was advantageous in some respects as these studies tended to access both positive and negative views of respite. However, the majority of studies using open questions addressed views of a particular service. Although addressing a very narrow context they provide useful information about practical needs related to service delivery, highlighting practical issues that may make respite difficult for carers to use.
No systematic differences were found in the issues raised in studies having different quality ratings. The findings of lower-quality studies were consistent with those of higher-quality studies and there was also consistency between those that did and those that did not focus directly on respite care issues.
Update of systematic review for period December 2005–April 2008
The modified update of the systematic review for the period December 2005–April 2008 identified seven additional qualitative studies eligible for inclusion based on the criteria established in the main review. These studies are discussed below and are summarised in Appendix 9
Only one study had been carried out in the UK,223 with three carried out in the US,224–226 one in Canada,227 one in Australia228 and one in Finland. 229 In the main, the studies were of mixed groups of demented and physically frail older people; however, two studies focused on people with mild dementia,224,226 one of which involved African American carers only,226 and two studies examined palliative care. 223,228 The two studies of palliative care were concerned with carer needs and identified respite as one of the main needs, along with information and support. Respite at home was the most commonly requested.
Similar issues arose in these studies to those described in the main review. This included a reluctance to use services with concerns about quality of care, poor awareness of services, resistance of the care recipient to use formal services and difficulties in letting go of the caring role. Difficulties with respite were expressed in the Finnish study,229 which described the guilt and loneliness that carers experienced when the care recipient was no longer there. One study that focused on ethnic minority groups in the US pointed to the lack of cultural sensitivity in formal services and a mistrust of government agencies.
There were no new concepts emerging from these studies over and above those identified in the main review.
Chapter 6 Discussion
Outcomes are discussed in relation to the level of evidence provided by the type of study design, with randomised and quasi-experimental studies considered the highest level of evidence, followed by (in order) longitudinal before-and-after studies, longitudinal observational studies and cross-sectional studies. Qualitative studies are not included as part of the hierarchy of evidence but are considered to operate in parallel, shedding light on the findings of the quantitative review, providing further explanation and informing conclusions.
The evidence related to carer burden
Evidence from randomised and quasi-randomised trials found no effect of respite on carer burden. Only three trials were identified to include in a meta-analysis. 29,32,41 Of these three studies, the two showing no effect focused on ADC as the respite intervention,29,32 whereas the study having a positive effect provided unlimited day and home care,41 which may have provided greater flexibility and more of an opportunity to address carer needs. Flexibility of services and the ability to respond to carer needs, often at short notice, were demonstrated to be important aspects of carer needs and significant barriers to the uptake of respite care in the qualitative review.
This analysis was based on follow-up periods of 6 months. Trials excluded from the meta-analysis because of a lack of appropriate data did not give consistent findings, although studies of mixed respite at 6- to 12-months’ follow-up failed to detect significant effects of respite, thus failing to support the beneficial effects of a mixed respite service. On the other hand, studies examining day care and home care alone also failed to show a significant effect.
The meta-analysis of longitudinal before-and-after studies constituted the next level of evidence in the hierarchy. In this analysis a significant effect in favour of respite was found at a follow-up of both 2–3 months61,67,70 and 6 months. 61,67,69,70 Examination of the relative impact of mixed respite and day care in these studies found that the study67 showing a marked improvement in burden for participants provided a package of interventions that was delivered in a more individualised manner, thus having greater potential to meet carer needs. Two studies of mixed respite, not included in the meta-analysis, both showed beneficial effects on carer burden. 59,60 However, the other study in this group that provided mixed respite care69 (in-home and institutional respite) did not show any benefit to the carer. The in-home care was given for up to 4 hours per week, which is minimal and has the potential to exacerbate stress rather than reduce it. Reports in the qualitative review describe how carers in receipt of short (a few hours) in-home respite used the time to carry out chores, such as shopping, and frequently found the time insufficient to provide the relaxation that they needed. They were, in fact, rushed to complete chores in the time period and were under pressure to return home to allow the formal carer to leave on time. Few reported using the time for leisure or social activities.
Although the above studies represent the highest level of evidence in terms of study design, this has to be qualified by consideration of the quality of individual studies included in the analyses. There were few studies of high quality based on relative ratings, but most were of moderate quality allowing some confidence in the findings. The only two RCTs in this analysis were of high and moderate quality, but although internal validity was high there were problems of external validity. In the high-quality study the uptake of respite was low, resulting in limited exposure to the intervention; the sample in the other study was recruited from a veteran’s facility and so consisted mainly of men who were hospitalised at the time of recruitment. The quasi-experimental studies experienced some bias in sampling with differences detected between the intervention and control groups. The quality of the before-and-after studies tended to be lower. There was poor definition of the intervention and the participant characteristics in these studies, with the potential for sampling bias. One of the lower quality studies in this group had a substantial problem of attrition, which would have had a significant impact on the findings.
The next level of evidence to be considered was the longitudinal observational studies. Well-conducted and relevant longitudinal studies could provide useful information on the evidence for effectiveness; however, relatively few longitudinal studies were identified. Out of five studies,72,75,76,83,89 three focused on the provision of formal support services but did not describe in sufficient detail the specific contribution of respite to the outcomes. This was a difficulty encountered throughout the review. Although respite was probably a component of these interventions the findings are difficult to interpret. Two studies found no relationship between formal support and carer burden,76,89 one found burden to be significantly reduced over a 6-month period,75 one found amount of respite predicted carer stress,72 and one found formal support to predict change in overload, anger, worry and strain over the period of the study. 83 This study was of high quality and controlled for a number of factors including carer age, carer gender, duration of caring, care recipient memory, behaviour problems, spousal relationship and change in care recipient ADL. The relationship between carer and care recipient has been suggested to be an important factor in a number of studies of outcomes of caring in that spouse or daughter carers have a greater commitment to caring and maintaining the care recipient at home. 117 The qualitative data reported that spouses had a sense of commitment irrespective of whether their previous marital relationship was good or not, as commitment could be based on a feeling of obligation as well as a genuine desire to care for a loved one. The commitment and endurance of daughters was suggested by the qualitative data to be a gender issue, with women continuing with long-standing caring roles begun earlier in life in relation to care of family. However, these issues were not consistently pursued in the quantitative studies as carer groups were generally mixed; relationships were infrequently included in analyses as covariates and certainly no account was taken of the quality of relationships.
Only one study had a specific focus on respite in the form of in-home respite, short institutional respite and day care, thus covering a range of services. Contrary to expectations, receiving more respite was found to predict carer stress, alongside a number of other predictors, including spousal relationship and amount of daily caregiving. This finding was a result of those receiving occasional respite being less stressed than those receiving daily respite, with them also being less stressed than those receiving no respite. 72 Those receiving no respite were, in fact, the most stressed group. Although the level of dementia severity of the care recipient was controlled for in this analysis by MMSE score and mental disability, there may be other confounders related to the severity of the condition that were not taken into account, for example behavioural problems, night-time disturbance or incontinence. Those receiving more respite may be those who have a greater variety and extent of these non-cognitive difficulties. In addition, the study by Deimling,60 a longitudinal before-and-after study, found outcomes to differ depending on whether the care recipient was in a stable condition or declining, with carers of stable care recipients having better outcomes than those with care recipients in decline. This also demonstrates the importance of measuring all relevant confounders in these studies. Cognitive impairment is frequently measured as an indicator of the severity of the condition, but behavioural problems perhaps have the greatest impact on the carer. The qualitative review highlighted the difficulties experienced by carers with unco-operative care recipients in relation to preparing for respite, with respite frequently being discontinued or withdrawn because of care recipient behaviour; however, it is precisely these carers who are in most need of respite care.
Longitudinal studies, therefore, did not provide consistent evidence to support a conclusion on the impact of respite care on carer burden but pointed to the complexity of relationships and the possible confounders that may be operating in relation to findings.
There were many more cross-sectional studies examining service use and carer burden. Results from these studies are very variable and their relevance to this review is frequently difficult to determine. A large proportion of the studies focused on formal service support of a very general nature, in which it is difficult to determine the type and quantity of respite, if any, that are provided within the study context. Even those purporting to examine respite use do not clearly define the type of respite. Adult day care was a more specific intervention that could be clearly defined as providing respite by its very nature. However, the results of these studies were not consistent, with half reporting no effect and half reporting a positive effect. Those reporting no effect either had small sample sizes or compared different types of day care. These may, therefore, have had insufficient power to detect any significant effects. Those reporting a positive effect were not without design difficulties, having small sample sizes, a lack of standardised outcome measures, a lack of control for confounders in the analysis, or sampling subject to potential biases. Few cross-sectional studies sampled randomly but rather tended to use either volunteer samples or samples recruited via service providers or voluntary support agencies. Carers and care recipients known to such agencies may be quite different from those not known to services who are caring unsupported or using informal or privately obtained respite support. The quality ratings of these studies are also variable with a fairly even proportion of high- and low-quality studies and few of moderate quality. There are, therefore, few consistent data available from cross-sectional studies to inform the evidence on the impact of respite on carer burden, apart from there being no evidence of a negative impact of respite on carer burden.
In conclusion, the evidence for a positive impact of respite care on carer burden is limited, coming mainly from longitudinal before-and-after studies, not all of which were of high quality. There was no evidence to support beneficial effects of respite from the highest level of evidence, that is, randomised or quasi-experimental studies, and supporting evidence from observational studies was mixed and inconsistent. However, there were significant issues relating to the design of randomised and quasi-experimental studies that limit their applicability.
The evidence relating to carer depression
Evidence from randomised and quasi-experimental studies showed a positive effect of respite on carer depression although this was not statistically significant. At a follow-up of 1–6 months an effect favouring respite interventions just failed to reach significance in a random-effects model. In the longer term (12 months) the effect was not significant. In comparisons of home care and day care separately the effect for day care was again non-significant but was in the direction of a benefit for respite, as was the finding for home care, although not to the same extent. Categorising studies by the length of the intervention did not reveal any significant effects.
Longitudinal before-and-after studies failed to show a significant effect of respite, although again the effects were in the direction favouring respite interventions.
The randomised and quasi-experimental studies were categorised generally as moderate to high quality whereas the longitudinal studies were generally moderate to low quality. One longitudinal study of high quality55 provided day care continuously for the 12 months of the study period for an average of 3 days per week for 6 hours per day, but failed to show a positive effect of respite. Other studies included in the review provided either small amounts of respite, for example 4 hours per week, or short-term respite, for example 10 days of in-home help for up to 6 hours a day, or compared a range of services that included education and training for the carer, memory clinics, community mental health teams and counselling. In addition, uptake of the intervention was sometimes low.
The amount of day care provision was proposed in the qualitative review to be an important consideration for carers. Day care is often unavailable at times when respite is most needed, for example evenings and weekends, or for long enough intervals to allow carers to get to and from work, or during the working day. It may not, therefore, be only the amount of ADC provision but also the flexibility of service provision to fit with the circumstances of the carer which is the important component that is lacking. Studies of the effectiveness of respite do not, however, measure the extent to which these services meet carer needs. Also identified in the qualitative review as important is the quality of service provision, but there is little information concerning process in the studies reviewed. Some of the participants in studies reported in the qualitative review expressed a preference for home care, as this avoids the hassles involved in getting the care recipient ready for day care and also maintains them in a familiar environment, and results from this analysis support this (although preferences are also related to other factors such as the carer/care recipient relationship). One study that stands out as having a larger positive effect size in favour of respite is the study by Milne et al. ,44 which examined an Age Concern intervention that provided a care attendant for a few hours. Although this is an intervention providing limited time for respite there is the potential for greater flexibility within this type of service, as well as it being in-home care.
Although some of the studies provided care for a fairly long period (outcome measures up to 12 months with respite provided for the duration of this follow-up), other studies provided respite interventions of limited duration. For example, Grant et al. 40 assessed an intervention of 10 days of in-home help. Although no statistically significant effects could be found for length of intervention in the meta-analysis, the qualitative review highlighted the caution with which carers approach support services, with suggestions that they are wary of short-term interventions. They are concerned about becoming dependent on help that might be removed, because they are aware that having support removed may have a rebound effect and make it difficult to cope in the longer term. This was demonstrated in studies examining the impact of institutional respite on burden. Burden was reduced during the respite period but returned to normal levels on return home57 or resulted in a more negative perception of the caring role after experiencing respite. 58 Rolleston and Ball50 also found that removal of an existing institutional respite service was detrimental to carer well-being. This points to a need for respite to be consistent, with varying implications for the timing and regularity with which services are provided, depending on the type of respite. However, flexibility was also desired to allow for changes in circumstances and changes in need.
Little evidence was available from longitudinal observational studies concerning carer depression with only three studies identified. 75,76,83 Two assessed formal service use with poor definition of respite76,83 and one75 assessed a mixed package of respite (in-home, nursing home stay and day care), which would be expected, based on the previous discussion, to have a positive impact. There was no change, however, in depression or anxiety in this study although there was a significant decrease in burden. The follow-up period was only 6 months, with the possibility of more positive effects in the longer term.
Cross-sectional studies contribute little to the evidence concerning the impact of respite on depression. It is difficult to identify the role of respite in the majority of studies as they focus on general service use, informal support and comparisons of different types of service provision. They also suffer from small, potentially biased samples and interventions that are not generalisable. There is little consistency in the reported results, reflecting the heterogeneous nature of the study methods.
In conclusion, studies at the highest level of evidence showed trends for respite to have beneficial effects on carer depression, which was not supported in the weaker before-and-after longitudinal studies. From the randomised studies there was no clear evidence in support of day care versus home care, or long versus short interventions. Evidence from the qualitative synthesis, however, suggested that the amount and flexibility of respite are important in alleviating carer distress, as well as the appropriateness and quality of care. These factors are important in ensuring that services respond to carer needs. It is unclear to what extent the interventions assessed in the randomised and quasi-experimental studies, and the before-and-after studies, were responding to individual carer needs.
Carer anxiety, morale, quality of life and anger and hostility
The meta-analysis found no effect of respite care on anxiety in the short or long term or of day care specifically. Anxiety was not considered separately from depression and mental health in the narrative syntheses of the observational studies and so no further evidence is available from that group of studies.
Although anxiety is often a consequence of health threats, in this context the nature of caring appears to have a longer and more pervasive impact on the carers’ way of life, resulting frequently in social isolation. Caring for a failing spouse or parent with dementia also creates a grieving situation, with the loss of the relative as they were previously known as the personality deteriorates. In addition, for some carers there appears to be a certain amount of cognitive dissonance resulting in feelings of guilt. The qualitative review proposed that carers experience feelings of guilt in relation to respite care if their relative is not happy about going to day care, or they feel that it is demeaning to employ a ‘sitter’ or that they are letting their loved one down by committing them to day care in an institutional setting. There is also guilt stemming from the desire to be rid of their burden, which would result only from either death or institutionalisation. These are major life event issues that must rate alongside other major life events and consequently it is not surprising that depression is an appropriate outcome to measure in evaluating interventions designed to alleviate carer distress.
A positive effect of respite care was found in the meta-analysis in relation to morale. Both studies in this analysis assessed day care. 41,47 There was little evidence available in any of the other types of literature, apart from a study by Gilhooly,108 which assessed morale in relation to day hospital care and home help services. Only the home help service showed a significant correlation with morale (and also mental health) although carers frequently mentioned the day hospital as a great source of help. However, use of the day hospital was low and it lacked variation, which was proposed by the authors as a possible reason for the lack of significance.
A surprising finding, in the light of the potential benefits in relation to depression and carer burden, was that quality of life was worse after respite at both 6 and 12 months’ follow-up. Three longitudinal before-and-after studies65,69,70 were included in this analysis: two focused on day care and one on mixed in-home and inpatient respite. No other evidence is available to support this finding. The reasons for this negative effect on quality of life are unclear. One possible reason is the natural deterioration of the care recipient’s condition over time with accompanying difficulties and a greater likelihood of utilising respite services. It is not always clear what stage the care recipient has reached in the natural history of the condition. One of the studies included nine day hospital sites as well as day care centres. Those attending day hospitals are possibly more disabled than those attending for day care alone. Another issue is a heightened awareness of the impact of caring on an individual’s quality of life after experiencing respite. There is the potential for respite to not only provide relief but also to increase dissatisfaction if the level of respite provision is not adequate to provide a balance between caring for the recipient and caring for the self. Studies assessing quality of life were rated as low to moderate quality and so should be viewed with some caution.
Two randomised and quasi-experimental studies were combined in a meta-analysis to assess the impact of day care on carer anger and hostility. 47,55 These studies were of moderate to high quality and found a beneficial effect of day care. This is supported by the qualitative data in which carers talked about the positive impacts of respite care. Respite was felt to relieve strain and enhance the relationship between carer and care recipient. Carers reported feeling more tolerant after a respite break with some reporting that they did not lose their temper as much. These are important issues in relation to elder abuse. This was not addressed directly in the qualitative literature or indeed in the quantitative papers. There is limited evidence available but estimates suggest that around 500,000 older people are being abused at any one time in the UK and around 60% of this abuse takes place in the home environment. 230 This estimate is based on data collected in 1992. Considering the time since data collection and the sensitive nature of the question it is possible that this is an underestimate of the extent of the problem. Good-quality research is required not only to obtain more accurate figures but also to assess the potential effects of carer support on alleviating this problem.
Institutionalisation
One of the assumptions of providing support for carers is that it improves their well-being and thus enables them to continue to care for their relative and avoid the need for institutionalisation. The meta-analysis, however, found increased rates of institutionalisation in respite users both in the short term (6 months) and the longer term (12 months). The quality ratings of the studies in the meta-analysis were variable, ranging from high to low.
Longitudinal observational studies supported this finding in the main but did point to the complex relationships between caring variables and institutionalisation. The MADDE study77–83 found that both high and low users of day care were more likely to institutionalise, but this, the authors felt, probably reflects the characteristics of carers and care recipients. Low users may have had insufficient respite support and high users may have more severe problems. This was supported by Bond and Clark73 who found that adjustment for dementia severity eliminated significant associations with institutionalisation. Other possible confounders include the relationship between carer and care recipient, as spouse and daughter carers are less likely to institutionalise their care recipient. 71 This was true for care recipients with moderate impairment but was no longer apparent for those with severe dementia, highlighting the importance of need factors and the limited capacity of carers, no matter how committed they are to the caring relationship.
Contrary to this finding, the qualitative review found that carers had a strong desire and commitment to maintain their relatives at home and felt that one of the positive aspects of respite was the benefits it provided in achieving this aim. However, the view was also expressed that respite use is sometimes a means of trying out institutional care when carers are feeling that they can no longer cope and are beginning to consider institutionalisation as an option. Carers holding negative views of institutional care will often change their attitudes once respite has been experienced, and especially if the care recipient responds positively also. Some also expressed the view that once the care recipient became unaware of their surroundings there was less motivation to keep them in their own home and so respite was more likely to be used in more severe conditions. There was a sense that, although some carers are determined to maintain the care recipient at home until the end, for others there is an inevitable progression towards institutional care and the acceptance that they will not be able to cope indefinitely. This is often expedited by failing health of the carer. Institutionalisation is therefore seen as a last resort and respite care can be an immediate precursor to this, resulting from negative views of respite and also the commitments towards caring obligations that were expressed in the qualitative review. It is likely, then, that many of the samples recruited to studies of respite care are at a relatively late stage in the caregiving career and respite is unlikely to have a substantial impact on institutionalisation rates. Many of the attitudes preventing early use of respite are not only a result of cultural values but also result from poor knowledge of the availability and content of respite programmes, and the need for better information provision concerning entitlements and availability of services was a finding of the qualitative review.
Care recipient outcomes
The outcomes of respite care for care recipients were assessed but the data were not combined statistically because of the way that respite was defined and searched. Respite provision was defined as any intervention designed to take over the care normally provided by the carer in order to provide relief for the carer. Therefore, only studies that measured carer outcomes were included. This search strategy may have excluded studies that assessed only care recipient outcomes of a genuine respite intervention. Therefore, as the data were potentially incomplete statistical combination of results was not felt to be appropriate. However, in the studies included in this review there was little evidence for any negative effects of respite care on care recipients. The outcomes measured were mainly assessments of functional ability, ADL and cognitive status. Many of the studies used problem checklists that frequently covered similar items to functional ability scales. It would be anticipated that these types of measures would show decline over time in conditions characterised by deterioration in physical and/or cognitive abilities and so it would be difficult to interpret longitudinal studies having no control group. The randomised and quasi-experimental studies tended to show either a positive effect or no effect of respite on behaviour problems when compared with other groups. Only two studies assessed depression in care recipients attending day care compared with that in a group not attending day care. One32 found no difference between the groups (day care and waiting list) and the other54 found a positive difference in favour of the treatment group attending day care at 9 months’ follow-up. Zank and Schacke54 also found a positive effect for life satisfaction but no effect for self-esteem. Which measures are most appropriate for assessing outcomes in care recipients is not clear, although this will obviously vary with the aims of the intervention and the degree to which active intervention is offered to care recipients. But this is an important question for consideration as the qualitative study found that carers were concerned that any respite provision should have benefits for the care recipient and certainly not have any negative impacts. The carers were concerned that care recipients received cognitive stimulation and socialisation and so consideration must be given to how these needs can be translated into measured outcomes.
Outcome measurement
The above discussion of the results of the review has highlighted the difficulties in identifying appropriate outcomes in studies assessing the effectiveness of respite care. The standard measure used in these studies is carer burden, which was not found to be affected by respite use in RCTs and quasi-experimental studies; however, carer depression, a less frequently measured outcome, was found to be positively affected by respite. Carer burden, however, produced more consistently positive results in before-and-after studies. Other possible outcomes of interest were measured even less frequently, for example anger and hostility, morale and quality of life.
A number of standard measures were used to assess carer burden as well as a number of compilations of items from various scales, which were not generally validated for use in this way. Several of the more frequently used scales were not developed from first principles, that is, qualitative exploration of the views of carers themselves. For example, items for the Zarit Burden Interview were developed from a combination of clinical experience and previous studies. 231 This is a unidimensional scale covering the carer’s health, psychological well-being, finances and social life and the relationship between the carer and care recipient. Another frequently used unidimensional scale is the Carer Strain Index,232 which assesses convenience, confinement, family adjustments, changes in personal plans, competing demands on time, emotional adjustments, and feelings of being completely overwhelmed. Novak and Guest,233 however, proposed that multidimensional scales were more appropriate as carers can have different patterns of responses across the different constructs, which has the advantage of informing an individualised approach to interventions. They developed the Carer Burden Inventory consisting of five factors: time dependence burden, developmental burden, physical burden, social burden and emotional burden. Another commonly used multidimensional scale (the Caregiver Burden Questionnaire) is based on a theoretical underpinning of caregiver appraisal234 and measures the constructs subjective caregiving burden, impact of caregiving, caregiving mastery and caregiving satisfaction. The measures, therefore, have many similarities as they frequently borrow items from other scales but they also have different combinations of items and approaches. Psychometric validation of the measures in general is variable in quality and unconvincing, and further work is required to identify the most appropriate measure of burden, rigorously validated in the contexts of interest.
Similarly, outcomes for care recipients need to be more thoughtfully considered. Assessing functional ability and cognitive function may not be very informative in a naturally deteriorating condition except for detecting any gross negative impacts or perhaps no change when compared with control groups. Care recipient outcomes that fit more closely with carer wishes for positive effects of respite interventions would be more appropriate, and research should be aimed at identifying the most informative outcomes.
The timing of the assessment of outcomes varied from immediately following respite provision to around 12 months’ follow-up, although some studies did use longer time frames. The length of follow-up in these studies was closely linked to the length of the intervention. It is quite possible that any benefits of respite will take time to manifest as the carer and care recipient gradually adapt to respite care and find a routine that best suits them. To assess this hypothesis and the duration of respite that one would expect to achieve most benefit requires a more systematic approach to research in this area.
Problems of definition of respite care
In carrying out the review there were obvious difficulties in defining respite care. The approach taken in this review was to focus on the role of respite for the carer by including only studies that assessed carer outcomes. Interventions such as rehabilitation programmes, designed to alter the health state of the care recipient, were excluded. However, the content of the interventions was not clearly described in many studies and it was difficult to determine the extent of any active interventions included in the services that were being evaluated. As this is a difficult area in which to carry out RCTs the review did not exclude observational studies. Many of these studies were difficult to interpret as they included a wide range of services such as home care involving personal care services and housekeeping, as well as other services such as training or counselling for the carer, Meals on Wheels, transport services, etc. These represented more general support, some of which had the potential to provide respite, but there was little information concerning the amount of respite afforded to participants.
Even within intervention type categories there was considerable variation in the activities undertaken as part of a respite service. This was particularly notable in relation to day care, which varied in the type of activity carried out with the care recipient. This ranged from purely personal care to access to group interventions delivered by highly trained staff (and possibly individual interventions in some cases although this was not always clear). Provision of respite services was also carried out in a range of settings from hospital to in-home. This reflects the range of services existing in the community in relation to respite and suggests that there is, potentially, a range of respite provision that is not always acknowledged as such, which may represent a level of ‘hidden’ respite. For example, there is frequently more to health-care provision than changing health status, and acute and rehabilitation admissions may be responding to crisis situations in place of appropriate respite provision. The research difficulties encountered in defining respite, therefore, reflect service providers’ difficulties in defining the characteristics of a respite service.
Issues of defining respite are compounded by the finding that consideration of carer needs cannot be easily disentangled from the needs of the care recipient. It became clear from the qualitative data that carers themselves wanted more than merely carer substitution from respite facilities. Carers expressed a need for relief for themselves to enable them to continue caring but also wished to obtain benefit for the care recipient in the form of socialisation and stimulation that would improve the care recipient’s quality of life and promote self-esteem. Not seeing some positive aspects of the service for the care recipient presented a barrier to the uptake of respite care. This demonstrates the importance of assessing care recipient outcomes alongside carer outcomes in studies of respite care, as well as designing interventions with both carer and care recipient needs in mind. The different types of respite provision will vary in the extent to which care recipient benefits are considered a specific aim. For example, night-sitting services would not be viewed in this way, although the relationship between the sitter and the care recipient was still important. In-home services did provide a change of company for the care recipient, which was felt to be stimulating, and day care and institutional care provided more structured programmes designed to engage the care recipient. It was particularly important for institutional care to be of good quality as poor care could result in loss of mobility or even threats to safety. Although the review could not draw any firm conclusions as to the best location or type of provider for respite care, quality was probably an over-riding factor and it was clear that, wherever services were provided, staff needed to be appropriately equipped in terms of knowledge and skills to deal with the disabilities of the particular care recipient population.
The qualitative review also pointed out that a physical break from the care recipient was probably not sufficient in itself to provide the mental break that was needed by most carers to improve their well-being. A mental break meant freedom from worry and total disengagement from the caring role. This was only achieved in the knowledge that the care recipient was happy, safe and well cared for. In addition, this was sometimes only achieved through having support and advice to enable carers to acknowledge and address their needs and the difficulties that they faced in achieving them.
Why don’t carers take up respite care?
It is a concern that carers do not take up respite care services even when available to them. The qualitative review identified quite clearly the factors affecting the uptake of respite. Many of these issues were service orientated, which can be addressed by ensuring that services respond more closely to carer needs. Some issues could be easily addressed by the provision of better information concerning the availability of services and entitlements and how to access them. Others are probably more difficult to address, such as attitudes to respite care and to caring obligations. Many of these attitudes are deeply ingrained, which would require more intensive counselling approaches to enable change on an individual basis. Other approaches could address the stigma attached to some respite services. Some carers, reported in the qualitative review, attempted to do this for their dependants themselves by reframing the purpose of day care, for example to embody a more useful or active role for the care recipient. However, no quantitative data on the effectiveness of interventions designed to address barriers to uptake were identified in this review.
Economics
Although it would be of considerable importance to the NHS and personal social services to quantify the overall impact that the introduction of a respite service for a specific patient population, in terms of both clinical and cost-effectiveness, would have, both the paucity and heterogeneity of the data identified as part of the systematic review preclude such an undertaking at this stage. Specifically, some of the largest observational studies have been conducted outside the UK, which means, for example, that UK age-specific baseline rates of institutionalisation are unavailable. In addition, the heterogeneity of the scales and instruments used in the assessment of carer outcomes, including a lack of appropriate utility data, means that incorporating the impact of respite care on carers is also problematic.
Conclusions
Implications for care
The evidence suggests that the provision of respite care is, under certain circumstances, of benefit to carers’ well-being. However, the evidence did not identify the relative merits of all of the different types of respite provision, although home care emerged as a preference in a number of qualitative studies and also had some benefits over day care in relation to carer depression. Preferences were dependent on a number of factors and perhaps more important than any particular type of respite provision was a need for flexible respite services that are responsive to changing carer needs, which might include a range of different services. A number of studies in the review provided a range of services such as day care and home care, day care and institutional care, as well as a range of other services likely to provide some respite such as domestic help and personal care services. It would be appropriate for service providers to carry out assessments of needs and preferences before developing services.
The outcomes that arose as indicators of the positive impact of respite on carer well-being were depression, burden, morale, anger and hostility. Anxiety was unaffected by respite provision and quality of life was worse after respite care. Rates of institutionalisation were higher after respite provision but this is likely to be a result of the characteristics of those accessing respite rather than an outcome of respite per se.
There was some evidence to suggest that longer interventions had greater benefits for carers.
The review did not find any evidence of negative effects of respite on care recipients or any consistent evidence for positive effects, although outcome measurement for care recipients is inadequately addressed and requires further definition.
Further issues of prominence arising mainly in the qualitative review that have implications for care provision are as follows.
-
The need for information. This is a need that came across in many of the qualitative studies and was identified as a barrier to the uptake of respite. Without the knowledge of the availability of services and how to access them, carers cannot make informed choices of how best to carry out their caregiving role. It is an issue for care provision of how to identify and inform carers of the availability of services.
-
Provision of respite early in the caregiving career. The review pointed to the potential for respite only to be offered or accessed at a late stage in the caregiving career, as a result of a crisis situation or immediately before institutionalisation. This relates to point 1 above, in that information provided earlier about respite availability may delay or avoid crisis situations and maintain carer well-being for longer. To achieve this the relevant health professionals need to be knowledgeable about the available options to support and inform carers appropriately.
-
Training of formal carers. Quality of care was an important issue for carers and a number of papers in the qualitative review highlighted poor skills of care staff, particularly in relation to dementia care. Carers expressed a wish for a sensitive approach as opposed to demeaning attitudes sometimes held by care staff towards care recipients. Training and monitoring of staff is an issue for consideration by service providers.
-
Continuity of care. Continuity of care was an important issue in avoiding the disorientation of care recipients but also in avoiding unnecessary stress for carers who may be in a position of repeatedly having to inform new care staff.
-
Benefits for care recipients. Carers placed importance on the benefits of respite care for care recipients, which required good-quality care with appropriate activities and opportunities for socialisation and stimulation.
-
Transport services. Difficulties with transport arose as an issue in many of the qualitative studies, particularly in relation to day care and in more rural communities.
Recommendations for future research
This is an expanding area of research with the majority of studies carried out in the last 10–15 years. However, there were few good-quality RCTs or quasi-experimental studies available for statistical synthesis. Many of the studies reviewed had small sample sizes with inadequate definitions of respite care. However, before larger-scale trials are carried out further developmental work is required to:
-
classify available respite services and settings
-
quantify carer and care recipient needs and preferences for respite care, taking account of the variations in the characteristics of the carer and care recipient
-
define the characteristics of an appropriate intervention (e.g. the type and location, e.g. day care, home care; extent of activities provided within the intervention; duration; range of responsiveness to individual needs)
-
define (and validate) outcomes for the care recipient based on type of intervention
-
review the robustness of outcome measures for measuring carer burden and well-being
-
develop process measures to assess the quality of the interventions.
From the studies reviewed it is not clear that any one type of respite intervention is better than another, but rather that different interventions are appropriate for different types of carer under different circumstances and that flexibility is important. This review has identified some of the factors that affect need, but further qualitative and quantitative work is needed to ensure that these are comprehensive.
Further large-scale trials should ensure that the following factors are considered in the design and execution of the studies:
-
use of randomisation and/or appropriate control group comparisons
-
outcomes mapped over both the short and long term including and accounting for mortality
-
adequate service provision ensured, i.e. in terms of length and duration
-
account taken of the uptake of respite and use of other services
-
characterisation of the care recipient, i.e. type of disability, severity of condition from a cognitive, physical, affective and behavioural point of view, demographics
-
characterisation of the carer and the caring situation, i.e. duration of caring, number of hours per day spent caring, type of caring activities, history of respite use, relationship to care recipient, demographics
-
clear and detailed definitions of the intervention used, including skill mix, activities involved, location, duration
-
a mixed-methods approach used to assess user views
-
process measures utilised to assess the quality of the intervention
-
an economic evaluation included
-
an assessment of both carer and care recipient outcomes using well-validated measures and measures of utility.
The research should attempt to identify the particular components of the intervention that are likely to provide benefit for carers and care recipients so that they can be replicated in future service development. This will include not only the activities provided as part of the respite package but also the timing and duration of respite provision and the training and skill mix of the care providers. That is, it should address the questions of when respite is best provided in the caregiving career and what amount and duration would be expected to provide optimum benefit, as well as the types of intervention that might be appropriate for different types of carer. Defining these relationships will allow service providers to map services to their populations of carers.
All of the issues mentioned apply equally to ethnic minority groups who will have specific needs distinct from those of the white population. Only a small number of studies were available exploring the needs of ethnic minority groups and examining how culturally sensitive services may be developed. There are a limited number of ethnic-specific services available and research must address how this growing group of carers can be accommodated in the future.
Although the ability of an intervention to provide the carer with a mental break from care is an outcome for development and use in a large study as described above, qualitative work is needed to address and define the concept in more detail. A relatively small number of the studies in the qualitative review addressed this issue but there was some suggestion that a mental break could be achieved in other ways than by physical separation from the care recipient (e.g. by helping the carer to organise the caregiving schedule to allow some regular time to themselves or perhaps by more innovative methods such as cognitive behavioural intervention). The meaning of a mental break and how this can be achieved should be explored more fully.
There is a burgeoning amount of qualitative research in the areas that explore barriers to service use, the views of services and carer needs, and the impact of caring. The findings in relation to identifying barriers to uptake of respite are fairly consistent and future work should focus on identifying how the barriers can be overcome in order to develop interventions designed to break down these barriers. This qualitative work should lead to quantitative investigations and randomised trials of specific interventions. It is likely that there are a number of different types of intervention in this area ranging from individual-level to organisational and community-level interventions.
Related to interventions to overcome barriers to uptake is the need for further research identifying how information can best be provided concerning respite services. What information do carers require and at what point in time and who should deliver it? As part of this it is necessary to assess not only the knowledge of carers but also that of professionals who are likely to be in a position of supporting carers, particularly within the primary care context, which is likely to be the first port of call for many carers. Particular consideration should be given within this research to the needs of ethnic minority groups. From the little information that was available it appeared that ethnic minorities had less access to information than white populations and had less access to respite.
Finally, there was little research available concerning respite care in the palliative care context. The needs and issues that arose had some similarities to those relating to general respite care but they were also quite different in a number of ways. Respite was provided within the remit of palliative care teams, either in a domiciliary setting or in a hospice setting. Research is needed to address the specific respite needs of carers involved in terminal care and how these might be best incorporated into the range of services that are already available.
Acknowledgements
Contribution of authors
The review management group consisted of all of the investigators who are listed as authors of this study. All investigators contributed to the identification of studies for inclusion/exclusion, data extraction and quality assessment.
Chris Shaw (Reader in Nursing Research) was the principal investigator and was responsible for overall project management under the guidance of the management group. She carried out data extraction, analysis and quality assessment of the qualitative data and wrote the narrative reviews of the quantitative and qualitative data and the introduction, qualitative methods, discussion and executive summary sections of the report.
Rachel McNamara (Research Fellow) co-ordinated the project and devised and carried out the search strategy, managed the data collection, carried out the quantitative analyses and contributed to the preparation of the report (quantitative methods and meta-analysis section).
Keith Abrams (Professor of Statistics) provided statistical and economic advice and advice on the review methods and the design and interpretation of the study.
Rebecca Cannings-John (Research Fellow in Statistics) contributed to the identification of studies and provided statistical support in the early phases of the study.
Kerenza Hood (Reader in Statistics and Director of South East Wales Trials Unit) supervised the statistical analysis and contributed to the design, interpretation and management of the study.
Susan Myles and Mirella Longo carried out the economic review and prepared the chapter on health economics for the report.
Sinead O’Mahony (Senior Lecturer Geriatric Medicine) provided advice on definitions, interpretation and clinical implications.
Brenda Roe (Professor of Health Research) contributed to the identification of studies, gave advice on systematic review methods and elderly care perspectives and also advised on qualitative methods and contributed to the reliability assessment of the coding frame.
Kate Williams (Senior Research Fellow in Nursing) contributed to the identification of studies and gave advice on systematic review methods and elderly care perspectives.
Francesca Montemaggi and Beth Evans (Carers’ Wales) and Sarah Stone (Age Concern) gave user perspectives for the design and implications of the study.
All investigators have seen and approved the final version of the report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Office for National Statistics . Population Trends 2003.
- Office for National Statistics . Population Trends 2003.
- Office for National Statistics . General Household Survey. Living in Britain, Results from the 2001 General Household Survey n.d.
- Office for National Statistics . Census 2001 n.d. www.statistics.gov.uk/census2001/.
- Alzheimer’s Disease Society n.d. www.alzheimers.org.uk.
- Bath P, Lees KR. Acute stroke. Br Med J 2000;320:920-3.
- Royal Commission on Long Term Care . With Respect to Old Age: Long Term Care – Rights and Responsibilities 1999.
- Ashworth M, Baker AH. ‘Time and space’: carers’ views about respite care. Health Soc Care Community 2000;8:50-6.
- Wimo A, von Strauss E, Norberg G, Sassi F, Johansson L. Time spent on informal and formal care giving for persons with dementia in Sweden. Health Policy 2002;6:255-68.
- Office for National Statistics . Mental Health of Carers 2002.
- Scholte OP, Reimer WJM, de Haan RJ, Rijnders PT, Limburg M, van den Bos GA. The burden of caregiving in partners of long-term stroke survivors. Stroke 1998;29:1605-11.
- Dunkin JJ, Anderson-Hanley C. Dementia caregiver burden: a review of the literature and guidelines for assessment and intervention. Neurology 1998;51:S53-S.
- Robinson KM, Adkisson P, Weinrich S. Problem behaviour, caregiver reactions, and impact among caregivers of persons with Alzheimer’s disease. J Adv Nurs 2001;36:573-82.
- Hanson EJ, Tetley J, Clarke A. Respite care for older people and their family carers: concept analysis and user focus group findings of a pan-European nursing research project. J Adv Nur 1999;30:1396-407.
- Khan K, ter Riet G, Glanville J, Sowden AJ, Kleijnen J. Undertaking systematic reviews of research on effectiveness. CRD’s guidance for those carrying out or commissioning reviews. York: NHS Centre for Reviews and Dissemination, University of York; 2001.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74.
- Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S. Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Control Clin Trials 1995;16:62-73.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377-84.
- Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton, Canada: Heritage Foundation for Medical Research; 2004.
- Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Methods Work Group, Third US Preventive Services Task Force . Current methods of the US Preventive Services Task Force. A review of the process. Am J Prev Med 2001;20:21-35.
- Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Qual Saf Health Care 2004;13:223-5.
- Fade SA. Communicating and judging the quality of qualitative research: the need for a new language. J Hum Nutr Diet 2003;16:139-49.
- Mays N, Pope C. Qualitative research in health care: assessing quality in qualitative research. Br Med J 2000;320:50-2.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51.
- Lincoln Y. Emerging criteria for quality in qualitative and interpretive research. Qual Inq 1995;1:275-89.
- Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry 2002;36:717-32.
- Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs 2005;50:204-11.
- Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for meta-analysis in medical research. Chichester: Wiley and Sons; 2000.
- Rothman ML, Hedrick SC, Bulcroft KA, Erdly WW, Nickinovich DG. Effects of VA adult day health care on health outcomes and satisfaction with care. Med Care 1993;31:SS38-49.
- Paterson B, Thorne SE, Canam C, Jillings C. Meta-study of qualitative health research. A practical guide to meta-analysis and meta-synthesis. London: Sage Publications; 2001.
- Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. London: Sage Publications; 1998.
- Baumgarten M, Lebel P, Laprise H, Leclerc C, Quinn C. Adult day care for the frail elderly: outcomes, satisfaction, and cost. J Aging Health 2002;14:237-59.
- Brodaty H, Gresham M, Luscombe G. The Prince Henry Hospital dementia caregivers’ training programme. Int J Geriatr Psychiatry 1997;12:183-92.
- Burch S, Longbottom J, McKay M, Borland C, Prevost T. A randomized controlled trial of day hospital and day centre therapy. Clin Rehabil 1999;13:105-12.
- Burdz MP, Eaton WO, Bond JB. Effect of respite care on dementia and nondementia patients and their caregivers. Psychol Aging 1988;3:38-42.
- Conlin MM, Caranasos GJ, Davidson RA. Reduction of caregiver stress by respite care: a pilot study. South Med J 1992;85:1096-100.
- Gaugler JE, Jarrott SE, Zarit SH, Stephens MA, Townsend A, Greene R. Respite for dementia caregivers: the effects of adult day service use on caregiving hours and care demands. Int Psychogeriatr 2003;15:37-58.
- Gaugler JE, Jarrott SE, Zarit SH, Stephens MA, Townsend A, Greene R. Adult day service use and reductions in caregiving hours: effects on stress and psychological well-being for dementia caregivers. Int J Geriatr Psychiatry 2003;18:55-62.
- Leitsch SA, Zarit SH, Townsend A, Green R. Medical and social adult day service programs. Res Aging 2001;23:473-98.
- Grant I, McKibbin CL, Taylor MJ, Mills P, Dimsdale J, Ziegler M, et al. In-home respite intervention reduces plasma epinephrine in stressed Alzheimer caregivers. Am J Geriatr Psychiatry 2003;11:62-7.
- Kosloski K, Montgomery RJ. The effects of respite on caregivers of Alzheimer’s patients: one-year evaluation of the Michigan Model Respite Programs. J Appl Gerontol 1993;12:4-17.
- Lawton MP, Brody EM, Saperstein AR. A controlled study of respite service for caregivers of Alzheimer’s patients. Gerontologist 1989;29:8-16.
- Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol 1991;46:P181-9.
- Milne D, Pitt I, Sabin N. Evaluation of a carer support scheme for elderly people: the importance of ‘coping’. Br J Social Work 1993;23:157-68.
- Montgomery RJ, Borgatta EF. The effects of alternative support strategies on family caregiving. Gerontologist 1989;29:457-64.
- Montgomery RJV. Respite care: lessons from a controlled design study. Health Care Financ Rev 1988;9:133-8.
- Quayhagen MP, Quayhagen M, Corbeil RR, Hendrix RC, Jackson JE, Snyder L, et al. Coping with dementia: evaluation of four nonpharmacologic interventions. Int Psychogeriatr 2000;12:249-65.
- Richards K, Moniz-Cook E, Duggan P, Carr I, Wang M. Defining ‘early dementia’ and monitoring intervention: what measures are useful in family caregiving?. Aging Ment Health 2003;7:7-14.
- Riordan JM, Bennett AV. An evaluation of an augmented domiciliary service to older people with dementia and their carers. Aging Ment Health 1998;2:137-43.
- Rolleston M, Ball C. Evaluating the effects of brief day hospital closure. Int J Geriatr Psychiatry 1994;9:51-3.
- Rothman ML, Diehr P, Hedrick SC, Erdly WW, Nickinovich DG. Effects of contract adult day health care on health outcomes and satisfaction with care. Med Care 1993;31:SS75-83.
- Schwarz KA, Blixen CE. Does home health care affect strain and depressive symptomatology for caregivers of impaired older adults?. J Community Health Nurs 1997;14:39-48.
- Wells Y, Jorm AF. Evaluation of a special nursing home unit for dementia sufferers: a randomised controlled comparison with community care. Aust N Z J Psychiatry 1987;21:524-31.
- Zank S, Schacke C. Evaluation of geriatric day care units: effects on patients and caregivers. J Gerontol B Psychol Sci Soc Sci 2002;57:P348-57.
- Zarit SH, Stephens MA, Townsend A, Greene R. Stress reduction for family caregivers: effects of adult day care use. J Gerontol B Psychol Sci Soc 1998;53:S267-77.
- Zarit SH, Stephens MAP, Townsend A, Greene R, Leitsch SA. Patterns of adult day service use by family caregivers: a comparison of brief versus sustained use. Fam Relat 1999;48:355-61.
- Adler G, Ott L, Jelinski M, Mortimer J, Christensen R. Institutional respite care: benefits and risks for dementia patients and caregivers. Int Psychogeriatr 1993;5:67-7.
- Chi I, Wong SF. Respite service for the elderly in Hong Kong: evaluation of a pilot project. J Gerontol Soc Work 1994;22:201-10.
- Cox C. The experience of respite: meeting the needs of African American and white caregivers in a statewide program. J Gerontol Soc Work 1998;30:59-72.
- Deimling GT. Respite use and caregiver well-being in families caring for stable and declining AD patients. J Gerontol Soc Work 1992;18:117-34.
- Desrosiers J, Hebert R, Payette H, Roy P-M, Tousignant M, Cote S, et al. Geriatric day hospital: who improves the most?. Can J Aging 2004;23:217-29.
- Gilleard CJ. Influence of emotional distress among supporters on the outcome of psychogeriatric day care. Br J Psychiatry 1987;150:219-23.
- Gilleard CJ, Gilleard E, Whittick JE. Impact of psychogeriatric day hospital care on the patient’s family. Br J Psychiatry 1984;145:487-92.
- Harper DJ, Manasse PR, James O, Newton J. Intervening to reduce distress in caregivers of impaired elderly people: a preliminary evaluation. Int J Geriatr Psychiatry 1993;8:139-45.
- Higgins M, Koch K, Hynan LS, Carr S, Byrnes K, Weiner MF. Impact of an activities-based adult dementia care program. Neuropsychiatr Dis Treat 2005;1:165-9.
- Homer AC, Gilleard CJ. The effect of inpatient respite care on elderly patients and their carers. Age Ageing 1994;23:274-6.
- Hoskins S, Coleman M, McNeely D. Stress in carers of individuals with dementia and community mental health teams: an uncontrolled evaluation study. J Adv Nurs 2005;50:325-33.
- Johnson M, Maguire M. Give me a break – benefits of a caregiver support service. J Gerontol Nurs 1989;15:22-6.
- Theis SL, Moss JH, Pearson MA. Respite for caregivers: an evaluation study. J Community Health Nurs 1994;11:31-44.
- Warren S, Kerr JR, Smith D, Schalm C. The impact of adult day programs on family caregivers of elderly relatives. J Community Health Nurs 2003;20:209-21.
- Andrew T, Moriarty J, Levin E, Webb S. Outcome of referral to social services departments for people with cognitive impairment. Int J Geriatr Psychiatry 2000;15:406-14.
- Armstrong-Esther C, Hagen B, Sandilands M, Williams R, Smith C. A longitudinal study of home care clients and their informal carers. Br J Community Nurs 2005;10:284-91.
- Bond MJ, Clark MS. Predictors of the decision to yield care of a person with dementia. Aust J Ageing 2002;21:86-91.
- Cohen CA, Gold DP, Shulman KI, Wortley JT, McDonald G, Wargon M. Factors determining the decision to institutionalize dementing individuals: a prospective study. Gerontologist 1993;33:714-20.
- Cox C. Findings from a statewide program of respite care: a comparison of service users, stoppers, and nonusers. Gerontologist 1997;37:511-7.
- Cox C, Monk A. Minority caregivers of dementia victims: a comparison of black and Hispanic families. J Appl Gerontol 1990;9:340-54.
- Gaugler JE, Edwards AB, Femia EE, Zarit SH, Stephens MP, Townsend A, et al. Predictors of institutionalization of cognitively impaired elders: family help and the timing of placement. J Gerontol B Psychol Sci Soc Sci 2000:P247-55.
- Gaugler JE, Kane RL, Kane RA, Clay T, Newcomer R. Caregiving and institutionalization of cognitively impaired older people: utilizing dynamic predictors of change. Gerontologist 2003;43:219-29.
- Gaugler JE, Kane RL, Kane RA, Newcomer R. The longitudinal effects of early behavior problems in the dementia caregiving career. Psychol Aging 2005;20:100-16.
- Gaugler JE, Kane RL, Kane RA, Newcomer R. Early community-based service utilization and its effects on institutionalization in dementia caregiving. Gerontologist 2005;45:177-85.
- Gaugler JE, Kane RL, Kane RA, Newcomer R. Unmet care needs and key outcomes in dementia. J Am Geriatr Soc 2005;53:2098-105.
- Gaugler JE, Leach CR, Clay T, Newcomer RC. Predictors of nursing home placement in African Americans with dementia. J Am Geriatr Soc 2004;52:445-52.
- Jarrott SE, Zarit SH, Stephens MAP, Townsend A, Greene R. Instrumental help and caregivers’ distress: effects of change in informal and formal help. Am J Alzheimers Dis Other Dement 2005;20:181-90.
- Jette AM, Tennstedt S, Crawford S. How does formal and informal community care affect nursing home use?. J Gerontol B Psychol Sci Soc Sci 1995;50:S4-12.
- McFall S, Miller BH. Caregiver burden and nursing home admission of frail elderly persons. J Gerontol 1992;47:S73-9.
- Pruchno RA, Michaels JE, Potashnik SL. Predictors of institutionalization among Alzheimer disease victims with caregiving spouses. J Gerontol 1990;45:S259-66.
- Wells YD, Kendig HL. Changes in carers’ capacity and motivation to provide care. J Fam Stud 1996;2:15-28.
- Winslow BW. Effects of formal supports on stress outcomes in family caregivers of Alzheimer’s patients. Res Nurs Health 1997;20:27-3.
- Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 1986;26:260-6.
- Arai Y, Kumamoto K, Washio M, Ueda T, Miura H, Kudo K. Factors related to feelings of burden among caregivers looking after impaired elderly in Japan under the long-term care insurance system. Psychiatry Clin Neurosci 2004;58:396-402.
- Arai Y, Miura H, Washio M, Kudo K. Depression among caregivers of the elderly in need of care and their service utilization: a pilot study. Psychiatry Clin Neurosci 1998;52:463-5.
- Artaso B, Gon-i A, Biurrun A. Informal care in dementia: prediction of burden in female family caregivers. Revista Espanola De Geriatria Y Gerontologia 2003;38:212-8.
- Bass DM, Noelker LS, Rechlin LR. The moderating influence of service use on negative caregiving consequences. J Gerontol B Psychol Sci Soc Sci 1996;51:S121-31.
- Biegel DE, Bass DM, Schulz R, Morycz R. Predictors of in-home and out-of-home service use by family caregivers of Alzheimer’s disease patients. J Aging Health 1993;5:419-38.
- Biurrun Unzue A, Artaso Irigoyen B, Gon-i Sarries IA. Social support in family female caregivers of dementia patients. Geriatrika 2003;19:37-43.
- Caserta MS, Lund DA, Wright SD, Redburn DE. Caregivers to dementia patients: the utilization of community services. Gerontologist 1987;27:209-14.
- Cefalu CA, Ettinger WH, Espeland M. A study of the characteristics of the dementia patients and caregivers in dementia-nonspecific adult day care programs. J Am Geriatr Soc 1996;44:654-9.
- Chappell NL, Reid RC. Burden and well-being among caregivers: examining the distinction. Gerontologist 2002;42:772-80.
- Clark MS, Bond MJ. The effect on lifestyle activities of caring for a person with dementia. Psychol Health Med 2000;5:13-27.
- Clarke RM, Finucane P. Care-receivers’ and care-givers’ experience and perceptions of respite care: implications for service provision. Aust J Ageing 1995;14:183-7.
- Colvez A, Joel ME, Ponton-Sanchez A, Royer AC. Health status and work burden of Alzheimer patients’ informal caregivers: comparisons of five different care programs in the European Union. Health Policy 2002;60:219-33.
- Cossette S, Levesque L. Caregiving tasks as predictors of mental health of wife caregivers of men with chronic obstructive pulmonary disease. Res Nurs Health 1993;16:251-63.
- Dziegielewski SF, Ricks JL. Adult day programs for elderly who are mentally impaired and the measurement of caregiver satisfaction. Activ Adapt Aging 2000;24:51-64.
- Fell M, Kenny G, MacLachan M. Caring for older people: does day care benefit carers?. Ir J Psychol 2001;22:23-37.
- Furness L, Simpson R, Chakrabarti S, Dennis MS. A comparison of elderly day care and day hospital attenders in Leicestershire: client profile, carer stress and unmet need. Aging Mental Health 2000;4:324-9.
- Gaugler JE, Anderson KA, Leach MS, Smith CD, Schmitt FA, Mendiondo M. The emotional ramifications of unmet need in dementia caregiving. Am J Alzheimer’s Dis Other Demen 2004;19:369-80.
- Gilhooly ML. The impact of care-giving on care-givers: factors associated with the psychological well-being of people supporting a dementing relative in the community. Br J Med Psychol 1984;57:35-44.
- Gilhooly ML. Senile dementia: factors associated with caregivers’ preference for institutional care. Br J Med Psychol 1986;59:165-71.
- Gilleard CJ, Gilleard E, Gledhill K, Whittick J. Caring for the elderly mentally infirm at home: a survey of the supporters. J Epidemiol Community Health 1984;38:319-25.
- Gon-i Sarries A, Biurrun Unzue A, Artaso Irigoyen B. Assistance in a day care center or at home: differences between demented patients and their caregivers. Geriatrika 2003;19:36-41.
- Grasel E. Temporary institutional respite in dementia cases: who utilizes this form of respite care and what effect does it have?. Int Psychogeriatr 1997;9:437-48.
- Henry ME, Capitman JA. Finding satisfaction in adult day care: analysis of a national demonstration of dementia care and respite services. J Appl Gerontol 1995;14:302-20.
- Jutras S, Veilleux F. Informal caregiving: correlates of perceived burden. Can J Aging 1991;10:40-55.
- Kosloski K, Montgomery RJV, Youngbauer JG. Utilization of respite services: a comparison of users, seekers, and nonseekers. J Appl Gerontol 2001;20:111-32.
- Kuwahara Y, Washio M, Arai Y. Burden among caregivers of frail elderly in Japan. Fukuoka Igaku Zasshi 2001;92:326-33.
- Lechner VM. Support systems and stress reduction among workers caring for dependent parents. Soc Work 1993;38:461-9.
- Leddy Barnes C, Given CW. Parent caregivers: a comparison of employed and not employed daughters. Social Work 1995;40:375-81.
- Lorensini S, Bates GW. The health, psychological and social consequences of caring for a person with dementia. Aust J Ageing 1997;16:198-202.
- Marks R. Stress in families providing care to frail elderly relatives and the effects of receiving in-home respite services. Home Health Care Serv Q 1987;8:103-30.
- Marks R. The family dimension in long term care: an assessment of stress and intervention. Pride Inst J Long Term Home Health Care 1987;6:18-26.
- Mittelman MS, Ferris SH, Shulman E, Steinberg G, Ambinder A, Mackell JA, et al. A comprehensive support program: effect on depression in spouse-caregivers of AD patients. Gerontologist 1995;35:792-80.
- Mui AC. Caregiver strain among black and white daughter caregivers: a role theory perspective. Gerontologist 1992;32:203-12.
- Noelker LS, Bass DM. Service use by caregivers of elderly receiving case management. J Case Manag 1995;4:142-9.
- Park YH. The effects of the day care service program for the elderly and family with the stroke: compared with the elderly and family in home. Taehan Kanho Hakhoe Chi 2003;33:990-8.
- Penning MJ. Cognitive impairment, caregiver burden, and the utilization of home health services. J Aging Health 1995;7:233-53.
- Ramirez M, Teresi J, Holmes D, Orzechowska L. Institutional risk among African-American and white adult day health care participants. J Soc Work Long-Term Care 2002;1:57-75.
- Rosa E, Ambrogio M, Binetti G, Zanetti O. Immigrant paid caregivers’ and primary caregivers’ burden. Int J Geriatr Psychiatry 2004;19:1103-4.
- Tennstedt S, Cafferata GL, Sullivan L. Depression among caregivers of impaired elders. J Aging Health 1992;4:58-76.
- Wailing Li L, Seltzer MM, Greenberg JS. Social support and depressive symptoms: differential patterns in wife and daughter caregivers. J Gerontol Soc Sci 1997;52:S200-10.
- Warrington J, Eagles JM. A comparison of cognitively impaired attenders and their coresident carers at day hospitals and day centres in Aberdeen. Int J Geriatr Psychiatry 1996;11:251-6.
- Washio M, Arai Y. Depression among caregivers of the disabled elderly in southern Japan. Psychiatry Clin Neurosci 1999;53:407-12.
- Washio M, Arai Y, Kuwahara Y, Yoshimasu K, Kobayashi K, Sakauchi F, et al. Burden among family caregivers of the frail elderly with tumors. Tumor Res 2002;37:17-22.
- Williams I. Emotional health of black and white dementia caregivers: a contextual examination. J Gerontol 2005;60B:P287-95.
- Yates ME, Tennstedt S, Chang BH. Contributors to and mediators of psychological well-being for informal caregivers. J Gerontol B Psychol Sci Soc Sci 1999;54:P12-22.
- Kang S-Y. Predictors of emotional strain among spouse and adult child caregivers. J Gerontol Soc Work 2006;47:107-31.
- Whitlatch CJ, Feinberg LF. Family and friends as respite providers. J Aging Soc Policy 2006;18:127-39.
- Kumamoto K, Arai Y, Zarit SH. Use of home care services effectively reduces feelings of burden among family caregivers of disabled elderly in Japan: preliminary results. Int J Geriatr Psychiatry 2006;21:163-70.
- Yajima Y, Tsutsui T, Nakajima K, Li H-Y, Takigawa T, Want D-H, et al. The effects of caregiving resources on the incidence of depression over one year in family caregivers of disabled elderly. Acta Med Okayama 2007;61:71-80.
- Carretero S, Garcés J, Ródenas F. Evaluation of the home help service and its impact on the informal caregiver’s burden of dependent elders. Int J Geriatr Psychiatry 2007;22:738-49.
- Schacke C, Zank SR. Measuring the effectiveness of adult day care as a facility to support family caregivers of dementia patients. J Appl Gerontol 2006;25:65-81.
- Droes RM, Meiland FJM, Schmitz MJ, van Tilburg W. Effect of the meeting centres support program on informal carers of people with dementia: results from a multi-centre study. Aging Ment Health 2006;10:112-24.
- Pickard L, Pickard L. The effectiveness and cost-effectiveness of support and services to informal carers of older people. London: Audit Commission and PSSRU; 2004.
- Pickard L. The effectiveness and cost-effectiveness of support and services to informal carers of older people. London: Audit Commission and PSSRU; 2004.
- Nuttall SR, Blackwood RJL, Bussell BMH, Cliff JP, Cornall MJ, Cowley A, et al. Financing longterm care in Great Britain. J Inst Actuaries 1994;121:1-53.
- Laing W. Financing long-term care. London: Age Concern; 1993.
- Carers UK . Without Us . . .? Calculating the Value of carers’ Support 2002.
- Department of Health . Caring about Carers: A National Strategy for Carers 1999.
- Mason A, Weatherly H, Spilsbury K, Golder S, Adamson J, Drummond M, et al. Respite care for frail older people. A Systematic Review of the Effectiveness and Cost-Effectiveness of Different Models of Community-Based Respite Care for Frail Older People and Their Carers 2006.
- Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
- Artaso Irigoyen B, Martin Carrasco M, Cabases Hita JM. The cost of care of elderly patients with psychogeriatric pathology in the community. Actas Espanolas De Psiquiatria 2002;30:135-41.
- Artaso Irigoyen B, Martin Carrasco M, Cabases Hita JM. Análisis coste-consecuencia de un centro de día psicogeriátrico. Rev Espanolas Geriatric Gerontol 2002;37:291-7.
- Donaldson C, Gregson B. Prolonging life at home: what is the cost?. Community Med 1989;2:200-9.
- Gaugler JE, Zarit SH, Townsend A, Stephens M, Greene R. Evaluating community-based programs for dementia caregivers: the cost implications of adult day services. J Applied Gerontol 2003;22:118-33.
- Hedrick SC, Rothman ML, Chapko M, Ehreth J, Diehr P, Inui TS, et al. Summary and discussion of methods and results of the adult day heath care evaluation study. Med Care 1993;31:SS94-103.
- Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al. Generalisability in economic evaluation studies in healthcare: a review of case studies. Health Technol Assess 2004;8.
- Von Behren R. Adult day care: a decade of growth. Perspect Aging 1989;18:14-9.
- Ashworth M, Baker AH. ‘Time and space’: carers’ views about respite care. Health Soc Care Community 2000;8:50-6.
- Ashworth M, Nafisa M, Corkery M. Respite care in an intermediate care centre: the views of patients and carers. Health Soc Care Community 1996;4:241-5.
- Bamford C, Bruce F. Defining the outcomes of community care: the perspectives of older people with dementia and their carers. Ageing Soc 2000;20:543-70.
- Bedini LA, Guinan DM. The leisure of caregivers of older adults: implications for CTRS’s in non-traditional settings. Ther Recreation J 1996;30:274-88.
- Beisecker AE, Wright LJ, Chrisman SK, Ashworth J. Family caregiver perceptions of benefits and barriers to the use of adult day care for individuals with Alzheimer’s disease. Res Aging 1996;18:430-50.
- Bergs D. ‘The hidden client’ – women caring for husbands with COPD: their experience of quality of life. J Clin Nurs 2002;11:613-21.
- Berthold H, Landahl S, Svanborg A. Intermittent care and caregivers at home. Aging Clin 1991;3:51-6.
- Bowes A, Wilkinson H. ‘We didn’t know it would get that bad’: South Asian experiences of dementia and the service response. Health Soc Care Community 2003;11:387-96.
- Brody EM, Saperstein AR, Lawton M. A multi-service respite program for caregivers of Alzheimer’s patients. J Gerontol Soc Work 1989;14:41-74.
- Butterworth M. Dementia: the family caregiver’s perspective. J Ment Health 1995;4:125-32.
- Cotrell V. Respite use by dementia caregivers: preferences and reasons for initial use. J Gerontol Soc Work 1996;26:35-5.
- Ericson I, Hellstrom I, Lundh U, Nolan M. What constitutes good care for people with dementia?. Br J Nurs 2001;10:710-4.
- Farran CJ, Loukissa D, Perraud S, Paun O. Alzheimer’s disease caregiving information and skills. Part I: care recipient issues and concerns. Res Nurs Health 2003;26:366-75.
- Gillies B. Acting up: role ambiguity and the legal recognition of carers. Ageing Soc 2000;20:429-44.
- Gilmour JA. Dis/integrated care: family caregivers and in-hospital respite care. J Adv Nurs 2002;39:546-53.
- Hanson EJ, Tetley J, Clarke A. Respite care for frail older people and their family carers: concept analysis and user focus group findings of a pan-European nursing research project. J Adv Nurs 1999;30:1396-407.
- Heenan D. Informal care in farming families in Northern Ireland: some considerations for social work. Br J Soc Work 2000;30:855-66.
- Hennessy CH, John R. American Indian family caregivers’ perceptions of burden and needed support services. J Appl Gerontol 1996;15:275-93.
- Innes A, Blackstock K, Mason A, Smith A, Cox S. Dementia care provision in rural Scotland: service users’ and carers’ experiences. Health Soc Care Community 2005;13:354-65.
- Jansson W, Almberg B, Grafstrom M, Winblad B. The Circle Model – support for relatives of people with dementia. Int J Geriatr Psychiatry 1998;13:674-81.
- Jarrett NJ, Payne SA, Wiles RA. Terminally ill patients’ and lay-carers’ perceptions and experiences of community-based services. J Adv Nurs 1999;29:476-83.
- Johansson L. Informal care of dependent elderly at home – some Swedish experiences. Ageing Soc 1991;11:41-58.
- Kerr SM, Smith LN. Stroke: an exploration of the experience of informal caregiving. Clin Rehabil 2001;15:428-36.
- King A, Parsons M. An evaluation of two respite models for older people and their informal caregivers [see comment]. N Z Med J 2005;118.
- King S, Collins C, Liken M. Values and the use of community services. Qual Health Res 1995;5:332-47.
- Koffman J, Taylor S. The needs of caregivers. Elder Care 1997;9:16-9.
- Kristjanson LJ, Cousins K, White K, Andrews L, Lewin G, Tinnelly C, et al. Evaluation of a night respite community palliative care service. Int J Palliat Nurs 2004;10:84-90.
- Lampley-Dallas VT, Mold JW, Flori DE. Perceived needs of African-American caregivers of elders with dementia. J Natl Med Assoc 2001;93:47-5.
- Lane P, McKenna H, Ryan A, Fleming P. The experience of the family caregivers’ role: a qualitative study. Res Theory Nurs Pract 2003;17:137-51.
- Leong J, Madjar I, Fiveash B. Needs of family carers of elderly people with dementia living in the community. Aust J Ageing 2001;20:133-8.
- Lewis MB, Curtis MP, Lundy KS. ‘He calls me his angel of mercy’: the experience of caring for elderly parents in the home. Holist Nurs Pract 1995;9:54-65.
- Liken MA, King SK. Home health aide services: barriers perceived by dementia family caregivers. Home Healthcare Nurse 1995;13:60-8.
- Low J, Perry R, Wilkinson S. A qualitative evaluation of the impact of palliative care day services: the experiences of patients, informal carers, day unit managers and volunteer staff. Palliat Med 2005;19:65-70.
- Low JT, Roderick P, Payne S. An exploration looking at the impact of domiciliary and day hospital delivery of stroke rehabilitation on informal carers. Clin Rehabil 2004;18:776-84.
- MaloneBeach EE, Zarit SH, Spore DL. Caregivers’ perceptions of case management and community-based services: barriers to service use. J Appl Gerontol 1992;11:146-59.
- Martin-Cook K, Trimmer C, Svetlik D, Weiner MF. Caregiver burden in Alzheimer’s disease: case studies. Am J Alzheimers Dis 2000;15:47-52.
- McGarry J, Arthur A. Informal caring in late life: a qualitative study of the experiences of older carers. J Adv Nurs 2001;33:182-9.
- McGrath WL, Mueller MM, Brown C, Teitelman J, Watts J. Caregivers of persons with Alzheimer’s disease: an exploratory study of occupational performance and respite. Phys Occupational Ther Geriatrics 2000;18:51-69.
- McLean J, Roper-Hall A, Mayer P, Main A. Service needs of stroke survivors and their informal carers: a pilot study. J Adv Nurs 1991;16:559-64.
- Michallet B, Le Dorze G, Tetreault S. The needs of spouses caring for severely aphasic persons. Aphasiology 2001;15:731-47.
- Morgan DG, Semchuk KM, Stewart NJ, D’Arcy C. Rural families caring for a relative with dementia: barriers to use of formal services [see comment]. Soc Sci Med 2002;55:1129-42.
- Netto G. ‘I forget myself’: the case for the provision of culturally sensitive respite services for minority ethnic carers of older people. J Public Health Med 1998;20:221-6.
- Pearson ND. An assessment of relief hospital admissions for elderly patients with dementia. Health Trends 1988;20:120-1.
- Perry J, Bontinen K. Evaluation of a weekend respite program for persons with Alzheimer disease. Can J Nurs Res 2001;33:81-95.
- Pickard S, Glendinning C. Caring for a relative with dementia: the perceptions of carers and CPNs. Qual Ageing 2001;2:3-11.
- Piercy KW, Dunkley GJ. What quality paid home care means to family caregivers. J Appl Gerontol 2004;23:175-92.
- Ritchie L. Adult day care: northern perspectives. Public Health Nurs 2003;20:120-31.
- Skilbeck J, Payne S, Ingleton M, Nolan M, Carey I, Hanson A. An exploration of family carers’ experience of respite services in one specialist palliative care unit. Palliat Med 2005;19:610-8.
- Strang VR. Caregiver respite: coming back after being away. Perspectives 2000;24:10-2.
- Strang VR. Family caregiver respite and leisure: a feminist perspective. Scand J Caring Sci 2001;15:74-81.
- Strang VR, Haughey M. Factors influencing the caregiver’s ability to experience respite. J Fam Nurs 1998;4:231-54.
- Strang VR, Haughey M. Respite – a coping strategy for family caregivers. West J Nurs Res 1999;21:450-71.
- Strang VR, Koop PM, Peden J. The experience of respite during home-based family caregiving for persons with advanced cancer. J Palliat Care 2002;18:97-104.
- Teitelman J, Watts JH. Family members’ recommendations for achieving a mental break from caring for a loved one with Alzheimer’s disease. Alzheimer’s Care Q 2004;5:252-60.
- Upton N, Reed V. Caregiver coping in dementing illness – implications for short-term respite care. Int J Psychiatr Nurs Res 2005;10:1180-96.
- Valadez AA, Lumadue C, Gutierrez B, de Vries-Kell S. Family caregivers of impoverished Mexican American elderly women: the perceived impact of adult day care centers. Fam Soc 2005;86:384-92.
- Ward H, Cavanagh J. A descriptive study of the self-perceived needs of carers for dependants with a range of long-term problems. J Public Health Med 1997;19:281-7.
- Watkins M, Redfern SJ. Evaluation of a new night service for elderly people suffering from dementia. J Clin Nurs 1997;6:485-94.
- Wenger GC, Scott A, Seddon D. The experience of caring for older people with dementia in a rural area: using services. Aging Ment Health 2002;6:30-8.
- Wiles J. Informal caregivers’ experiences of formal support in a changing context. Health Soc Care Community 2003;11:189-207.
- Winslow BW. Family caregivers’ experiences with community services: a qualitative analysis. Public Health Nurs 2003;20:341-8.
- Winslow BW. Family caregiving and the use of formal community support services: a qualitative case study. Issues Ment Health Nurs 1998;19:11-27.
- Witt E, Chenoweth L, Jeon Y. Respite services for older persons and their family carers in southern Sydney. Collegian 2004;11:31-5.
- Worcester M, Hedrick S. Dilemmas in using respite for family caregivers of frail elders. Fam Community Health 1997;19:31-48.
- Wuest J, Ericson PK, Stern PN, Irwin GW. Connected and disconnected support: the impact on the caregiving process in Alzheimer’s disease. Health Care Women Int 2001;22:115-30.
- Wykle M, Segal M. A comparison of black and white family caregivers’ experience with dementia. J Natl Black Nurses Assoc 1991;5:29-41.
- McIlfatrick S. Assessing palliative care needs: views of patients, informal carers and healthcare professionals. J Adv Nurs 2006;57:77-86.
- Adams KB. The transition to caregiving: the experience of family members embarking on the dementia caregiving career. J Gerontol Soc Work 2006;47:3-29.
- Scharlach AE, Kellam R, Ong N, Baskin A, Goldstein C, Fox PJ. Cultural attitudes and caregiver service use: lessons from focus groups with racially and ethnically diverse family caregivers. J Gerontol Soc Work 2006;47:133-56.
- Gerdner LA, Tripp-Reimer T, Simpson HC. Hard lives, God’s help, and struggling through: caregiving in Arkansas Delta. J Cross Cult Gerontol 2007;22:355-74.
- Hawranik PG, Strain LA. Giving voice to informal caregivers of older adults. Can J Nurs Res 2007;39:156-72.
- Zapart S, Kenny P, Hall J, Servis B, Wiley S. Home-based palliative care in Sydney, Australia: the carer’s perspective on the provision of informal care. Health Soc Care Community 2007;15:97-107.
- Salin S, Åstedt-Kurki P. Women’s views of caring for family members. J Gerontol Nurs 2007;33:37-45.
- House of Commons Health Committee . Elder Abuse 2004.
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649-55.
- Robinson BC. Validation of a caregiver strain index. J Gerontol 1983;38:344-8.
- Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist 1989;29:798-803.
- Lawton MP, Kleban MH, Moss M, Rovine M, Glicksman A. Measuring caregiver appraisal. J Gerontol Psychol Sci 1989;44:61-7.
- Yamamoto N, Wallhagen MI. Service use by family caregivers in Japan. Soc Sci Med 1998;47:677-91.
- Young HM, McCormick WM, Vitaliano PP. Attitudes toward community-based services among Japanese American families. Gerontologist 2002;42:814-25.
Appendix 1 Quality assessment of quantitative studies
| Criteria | Yes (2/good) | Partial (1/fair) | No (0/poor) | N/A | |
|---|---|---|---|---|---|
| Study aims | |||||
| 1 | Is the hypothesis/aim/objective of the study clearly and sufficiently described? | Easily identified in introduction/methods. Specifies: purpose; subjects/target population; and specific interventions/associations under investigation | Vague/incomplete reporting or some information has to be gathered from parts of the paper other than the introduction/background/objective sections | Question or objective not reported/incomprehensible | |
| Study design and sample characteristics | |||||
| 2 |
Is the study design well described and appropriate? (If study question not given, infer from conclusions) |
Design easily identified, well described and appropriate | Design and/or study question not clearly described or design only partially addresses study question | Design does not answer study question or design is poorly described | |
| 3 | Is the method of patient/control group selection described and appropriate? | Described and appropriate. Inclusion/exclusion criteria described and defined | Selection methods (and inclusion/exclusion criteria) not completely described but no obvious inappropriateness or selection strategy likely introduces bias but not enough to seriously distort results | No information/inappropriate information provided or selection bias that likely distorts results | |
| 4 | Are the characteristics of patient/control group(s) clearly described (i.e. age range, health characteristic/s)? | Sufficient relevant demographic information. Reproducible criteria used to categorise participants clearly defined | Poorly defined criteria or incomplete demographic information | No baseline/demographic information provided | |
| 5 | Are caregiver characteristics clearly described (i.e. age, gender, relationship to care recipient, time spent caring)? | Sufficient relevant demographic information. Reproducible criteria used to categorise participants clearly defined | Poorly defined criteria or incomplete demographic information | No baseline/demographic information provided | |
| 6 | Were patients/participants randomised to intervention groups? | If randomisation appropriate: evidence of randomisation with a description of the method used (e.g. random number tables, block design) | Randomisation mentioned but method is not (i.e. may be possible that randomisation was not carried out) | Random allocation not mentioned although it would have been feasible and appropriate (and was possibly carried out) | Study has no control group, i.e. observational/survey/case–control study, or adequate justification for non-randomisation given |
| 7 |
For RCTs only Was randomisation/allocation concealed from patients? |
Evidence that next allocation was concealed from both parties (recruiter and patient/carer) at the point of consent (e.g. remote randomisation) | Allocation concealment reported but not described | Allocation concealment would have been possible (and was possibly carried out) but not reported | Allocation concealment not possible because of study design (e.g. cluster randomised trial) |
| 8 | Have the characteristics of patients lost to follow-up been described? | Losses adequately reported and not likely to affect results | Losses not well reported, but small and not likely to affect results | No information or losses large and likely to affect results | No patients lost to follow-up |
| 9 | Are intervention(s) clearly described? | Defined and reproducible | Partially defined but insufficient detail to reproduce design | Not described | |
| Data analysis and results | |||||
| 10 | Are the main outcomes to be measured clearly described in the introduction/methods? | Defined and measured according to reproducible criteria | Definition leaves room for subjectivity or not sure (i.e. not reported in detail, but probably acceptable) or precise definition(s) are missing, but no evidence of major problems or instrument/mode of assessment(s) not reported | Main outcomes first mentioned in results section or measures not defined/inconsistent/poorly defined | |
| 11 | If possible, was an attempt made to blind those measuring the main outcomes of the intervention? | Assessor blind to intervention/study group | Inadequate blinding, i.e. assessor may have been aware of the group that the participant was assigned to | No attempt made to blind assessor | Not possible/appropriate, e.g. observational/before-and-after study |
| 12 | Are population characteristics (if measured and described) controlled for and adequately described? | Appropriate control at design/analysis stage or randomised study with comparable baseline characteristics | Incomplete control/description or not considered but unlikely to seriously influence results | Not controlled for and likely to seriously influence results | |
| 13 | Are the main findings clearly described? | Simple outcome data (e.g. mean/prevalence) reported for all major findings | Incomplete or inappropriate descriptive statistics | No/inadequate descriptive statistics | |
| 14 | Are methods of analysis adequately described and appropriate? | Described and appropriate | Not reported but probably appropriate or some tests appropriate, some not | Methods not described and cannot be determined | |
| 15 | Are estimates of variance reported for the main results? | Appropriate estimates provided (SD/SE, confidence intervals) | Undefined or estimates provided for some but not all outcomes | No information | |
| 16 | In trials/cohort studies do analyses adjust for different lengths of follow-up, or in case–control studies is the time between intervention and outcome the same for cases/controls? | Different lengths of follow-up adjusted for (e.g. survival analysis) and adequately described | Different lengths of follow-up probably adjusted for but not adequately described | Differences in follow-up ignored | Cross-sectional design or same length of follow-up |
| 17 | If appropriate, were data analysed according to ITT (intention to treat) principle? | All participant data analysed regardless of adherence to protocol or continuation in trial | Attempt made to analyse data according to ITT principle, but inappropriate method or some participants not included | No attempt made to carry out ITT analysis | Design not appropriate for ITT (e.g. cross-sectional data) |
| Conclusions | |||||
| 18 | Are the conclusions supported by the results? | All conclusions supported by data | Some of the major conclusions supported by data, some not or speculative interpretations are not indicated as such | None/few of the major conclusions supported by the data | |
Appendix 2 Quality assessment checklist for qualitative studies
| Criteria | Yes (2/good) | Partial (1/fair) | No (0/poor) | |
|---|---|---|---|---|
| Study aims and context | ||||
| 1 | Is the research question sufficiently described? | Research question clearly identified by the end of the research process, if not at the outset | Research question or objective is vaguely/incompletely reported | Question or objective is not reported or is incomprehensible |
| 2 | Is qualitative method appropriate? | Qualitative method is appropriate for the aims and the qualitative framework is identified and justified | Qualitative method appropriate but the methodological framework unclear or not adequately justified | Qualitative methods inappropriate for the aims |
| 3 | Is the setting/context clearly described? | *Context/setting is clearly described, permitting the reader to relate the findings to other settings | The context/setting is partially described | The context/setting is not described |
| Sampling | ||||
| 4 | Is the sampling strategy clearly described? | Sampling strategy and rationale clearly described and justified | Sampling strategy not clearly described or not fully justified | Sampling not described |
| 5 | Is sampling method likely to recruit all relevant cases? (purposive, theoretical sampling) | Sample includes the full range of relevant, possible cases (more than simple convenience sample) permitting conceptual (rather than statistical) generalisations | Sampling was purposive but does not include the full range of possible cases | No attempt made to sample purposively or theoretically or sampling strategy not described |
| 6 | Are relevant characteristics of the sample given? | Relevant details of the characteristics of the sample given | Incomplete details of sample characteristics given | No details of sample characteristics given |
| 7 | Is rationale for sample size (e.g. data saturation) given? | Gives rationale for termination of data collection, e.g. data saturation | Reasons for sample size implied or no firm rationale | No reason given for sample size |
| Data collection | ||||
| 8 | Are methods of data collection clearly described? | Data collection methods are systematic and clearly described allowing an audit trail such that procedures could be replicated | Data collection methods not clearly described. Difficult to determine if systematic or replicable | Data collection procedures are not described |
| 9 | Is method of data collection appropriate for the research question and paradigm? | Data collection methods are appropriate for the research aims and the methodological and analytical framework | The appropriateness of the data collection methods is unclear | Data collection inappropriate for the aims and methodological framework |
| 10 | Has the researcher verified the data (e.g. by triangulation)? | More than one method of data collection carried out or more than one analyst involved or other methods of verification employed (e.g. member checking or line of questioning during interview) | Unclear whether triangulation or other types of verification used | No triangulation or other methods of verification described |
| Data analysis | ||||
| 11 | Are data analysis methods clearly described? | Systematic analytic method clearly described such that procedures could be replicated | Analytic methods not clearly described | Analytic methods not described |
| 12 | Are data analysis methods appropriate? | Analytic methods seem appropriate and are well described | Analytic methods only partially described and/or some concerns about appropriateness | Analytic methods not described and/or appropriate |
| 13 | Are competing accounts/deviant data taken into account? | Account given of negative or deviant cases in the analysis | Analysis of deviant or negative cases not clearly described | No account given of negative or deviant cases |
| Reflexivity | ||||
| 14 | To what extent is the researcher reflective? | The researcher explicitly assessed the likely impact of their own personal characteristics and the methods used on the data obtained | Possible sources of influence on the data obtained were mentioned, but the likely impact of the influence was not discussed | No evidence of reflexivity in the report |
| Conclusions | ||||
| 15 | Are the interpretations and conclusions supported by the data? | The interpretations are clearly described and supported by the data and are evidenced by sufficient participant quotes | The conclusions are unclear or only partially supported by the data or there are insufficient raw data to support conclusions | Conclusions are not identified or are felt not to be supported by the data or conclusions are absent |
Appendix 3 Data extraction form – quantitative
1. Administration details
1.1 Paper reference number: ____________
1.2 Extractor initials: __________
1.3 Date information extracted: __________
2. Study identification details
Title: ____________________________________________________________________________
_____________________________________________________________________________________
_____________________________________________________________________________________
2.2 First author (surname, initials): _______________________
2.3 Date of publication: __________
2.4 Country of origin: UK □0
Other □1
_____________________ (specify)
2.5 Language of publication: English □0
Other □1
_____________________ (specify)
2.6 Primary source: Database □0
Hand searching □1
Provided by user group □2
3. Study design details
3.1 Type of study (tick more than one option if applicable): (a) RCT □1
(b) Quasi-experimental □1
(c) Cohort □1
(d) Observational □1
(e) Qualitative □1
(f) Description of services □1
(g) Other □1
(specify)__________________
3.2 Review category
(tick more than one option if applicable): (a) Quantitative synthesis □1
(b) Qualitative synthesis □1
(c) Economic synthesis □1
3.3 Setting in which respite mostly provided
(tick more than one option if applicable: if intervention compared with another form of respite indicate in text option):
(a) Inpatient □1
(b) Community □1
(c) Home □1
(d) Day care □1
(e) Hospice □1
(f) Other □1
_______________________________________________________________________________________
3.4 Description of intervention or respite category (including location and duration):
(a) Intervention 1: _________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
(b) Intervention 2:_________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
(c) Intervention 3:_________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
(d) Intervention 4:_________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
3.5 (a) Was the intervention delivered by health-care professional/s?
Intervention 1: Yes □1 No □0 No information □2
Intervention 2: Yes □1 No □0 No information □2
Intervention 3: Yes □1 No □0 No information □2
Intervention 4: Yes □1 No □0 No information □2
(b) If yes, was the health-care team multidisciplinary?
Intervention 1: Yes □1 No □0 No information □2
Intervention 2: Yes □1 No □0 No information □2
Intervention 3: Yes □1 No □0 No information □2
Intervention 4: Yes □1 No □0 No information □2
3.6 Control group receiving no intervention? Yes □1 No □0
3.7 Planned vs ‘crisis’ respite (a) Planned □0
(b) Crisis □1
(c) No information □2
4. Participant details
4.1 Sampling method: (a) Random □0
(b) Convenience □1
(c) Population □2
(d) Other □3
(specify)_____________________
4.2 Inclusion/exclusion criteria:
(a) Intervention/respite group/s: __________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
(b) Control group: _________________________________________________________________
_______________________________________________________________________________________
OR:
(c) Total sample: ________________________________________________________________________
_______________________________________________________________________________________
4.3 Total number recruited:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: ________________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.4 Total number completing study:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.5 (a) Were participants lost to follow-up? Yes □1 No □0
(b) If yes, were sufficient details regarding the reasons for dropout given? Yes □1 No □0
(additional information)__________________________________________________________________
Population characteristics – frail elderly
4.6 Defining characteristic/health problem of frail elderly population:
| (a) Intervention group/s | (b) Control group | OR | (c) Total sample | ||
| Alzheimer’s/dementia | □0 | Alzheimer’s/dementia | □0 | Alzheimer’s/dementia | □0 |
| Mental health – other | □1 | Mental health – other | □1 | Mental health – other | □1 |
| Physical disability | □2 | Physical disability | □2 | Physical disability | □2 |
| Chronic illness | □3 | Chronic illness | □3 | Chronic illness | □3 |
| Terminal illness | □4 | Terminal illness | □4 | Terminal illness | □4 |
| Other | □5 | Other | □5 | Other | □5 |
(d) Additional details (e.g. functional health status): ___________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
4.7 Gender:
(a) Intervention group:
Intervention 1: females ______ (n) or _______ (%)
Intervention 2: females ______ (n) or _______ (%)
Intervention 3: females ______ (n) or _______ (%)
Intervention 4: females ______ (n) or _______ (%)
(b) Control group:
Females ______ (n) or _______ (%)
OR:
(c) Total sample:
Females ______ (n) or _______ (%)
4.8 Age range: if given, indicate whether sample or subsample likely to be ≥ 65 years
(a) Intervention 1: _____________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.9 Mean age (and SD):
(a) Intervention 1: _____________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.10 Ethnicity:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
Population characteristics – carers
4.11 Age range:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.12 Mean age (and SD):
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.13 Ethnicity:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.14 SES:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.15 Education:
(a) Intervention 1: _______________ Intervention 2: _______________
Intervention 3: _______________ Intervention 4: _______________
(b) Control: _______________
OR:
(c) Total sample: _______________
4.16 Information regarding caregiver health status provided
(including self-reported): Yes □1 No □0
(If yes, give details)
(a) Intervention 1: ______________________________________________________
Intervention 2: ______________________________________________________
Intervention 3: ______________________________________________________
Intervention 4: ______________________________________________________
(b) Control: ______________________________________________________
OR:
(c) Total sample: ______________________________________________________
4.17 Currently working:
(a) Intervention 1: n/% _______ No information □0
Intervention 2: n/% _______ No information □0
Intervention 3: n/% _______ No information □0
Intervention 4: n/% _______ No information □0
(b) Control: n/% _______ No information □0
OR:
(c) Total sample: n/% _______ No information □0
4.18 Gender:
(a) Intervention group:
Intervention 1: females ______ (n) or _______ (%)
Intervention 2: females ______ (n) or _______ (%)
Intervention 3: females ______ (n) or _______ (%)
Intervention 4: females ______ (n) or _______ (%)
(b) Control group:
Females ______ (n) or _______ (%)
OR:
(c) Total sample:
Females ______ (n) or _______ (%)
4.19 (a) Relationship to care recipient – intervention group 1:
Spouse _______ (n) or _______ (%)
Child _______ (n) or _______ (%)
Relative – other _______ (n) or _______ (%) __________ (specify)
Friend/neighbour _______ (n) or _______ (%)
Other _______ (n) or _______ (%) __________ (specify)
Relationship to care recipient – intervention group 2:
Spouse _______ (n) or _______ (%)
Child _______ (n) or _______ (%)
Relative – other _______ (n) or _______ (%) __________ (specify)
Friend/neighbour _______ (n) or _______ (%)
Other _______ (n) or _______ (%) __________ (specify)
Relationship to care recipient – intervention group 3:
Spouse _______ (n) or _______ (%)
Child _______ (n) or _______ (%)
Relative – other _______ (n) or _______ (%) __________ (specify)
Friend/neighbour _______ (n) or _______ (%)
Other _______ (n) or _______ (%) __________ (specify)
Relationship to care recipient – intervention group 4:
Spouse _______ (n) or _______ (%)
Child _______ (n) or _______ (%)
Relative – other _______ (n) or _______ (%) __________ (specify)
Friend/neighbour _______ (n) or _______ (%)
Other _______ (n) or _______ (%) __________ (specify)
(b) Relationship to care recipient – control group:
Spouse _______ (n) or _______ (%)
Child _______ (n) or _______ (%)
Relative – other _______ (n) or _______ (%) __________ (specify)
Friend/neighbour _______ (n) or _______ (%)
Other _______ (n) or _______ (%) __________ (specify)
OR:
(c) Relationship to care recipient – total sample:
Spouse _______ (n) _______ (%)
Child _______ (n) _______ (%)
Relative – other _______ (n) ______ (%) __________ (specify)
Friend/neighbour _______ (n) ______ (%)
Other _______ (n) _______ (%) __________ (specify)
4.20 (a) Lives with care recipient:
Intervention 1: ______ (n) ______ (%) No information □0
Intervention 2: ______ (n) ______ (%) No information □0
Intervention 3: ______ (n) ______ (%) No information □0
Intervention 4: ______ (n) ______ (%) No information □0
(b) Lives with care recipient:
Control: ______ (n) ______ (%) No information □0
OR:
(c) Lives with care recipient:
Total sample: ______ (n) ______ (%) No information □0
4.21 (a) Number of months spent caring:
Intervention 1: mean ______ No information □0
Intervention 2: mean ______ No information □0
Intervention 3: mean ______ No information □0
Intervention 4: mean ______ No information □0
(b) Number of months spent caring:
Control: mean ______ No information □0
(c) Number of months spent caring:
Total sample: mean ______ No information □0
4.22 (a) Hours per day/week spent caring:
Intervention 1: mean ______ No information □0
Intervention 2: mean ______ No information □0
Intervention 3: mean ______ No information □0
Intervention 4: mean ______ No information □0
(b) Hours per day/week spent caring:
Control: mean ______ No information □0
OR:
(c) Hours per day/week spent caring:
Total sample: mean ______ No information □0
5. Outcomes
Intervention 1:
5.1 Number of outcomes measured for:
(a) caregiver _____%/n reported _____
(b) care recipient _____%/n reported _____
5.2 Number of measurement/time points for:
(a) caregiver _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
(b) care recipient _________________________
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
5.3 Caregiver outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.4 Care recipient outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.5 (a) Service outcomes measured (i.e. outcome/s not solely attributable to either care recipient or carer)?
Yes □1 No □0
(b) If yes, please specify: Service outcome 1 ________________________________
Service outcome 2 ________________________________
Service outcome 3 ________________________________
Service outcome 4 ________________________________
5.6 Additional comments:
___________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
Intervention 2:
5.7 Number of outcomes measured for: (a) caregiver _____%/n reported _____
(b) care recipient _____%/n reported _____
5.8 Number of measurement/time points for:
(a) caregiver _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
(b) care recipient _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
5.9 Caregiver outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.10 Care recipient outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.11 (a) Service outcomes measured (i.e. outcome/s not solely attributable to either care recipient or carer)?
Yes □1 No □0
(b) If yes, please specify: Service outcome 1 ________________________________
Service outcome 2 ________________________________
Service outcome 3 ________________________________
Service outcome 4 ________________________________
5.12 Additional comments:
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
Intervention 3:
5.13 Number of outcomes measured for: (a) caregiver _____%/n reported _____
(b) care recipient _____%/n reported _____
5.14 Number of measurement/time points for:
(a) caregiver _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
(b) care recipient _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
5.15 Caregiver outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.16 Care recipient outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.17 (a) Service outcomes measured (i.e. outcome/s not solely attributable to either care recipient or carer)?
Yes □1 No □0
(b) If yes, please specify: Service outcome 1 ________________________________
Service outcome 2 ________________________________
Service outcome 3 ________________________________
Service outcome 4 ________________________________
5.18 Additional comments:
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
Intervention 4:
5.19 Number of outcomes measured for: (a) caregiver _____%/n reported _____
(b) care recipient _____%/n reported _____
5.20 Number of measurement/time points for:
(a) caregiver _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
(b) care recipient _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
5.21 Caregiver outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.22 Care recipient outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.23 (a) Service outcomes measured (i.e. outcome/s not solely attributable to either care recipient or carer)?
Yes □1 No □0
(b) If yes, please specify: Service outcome 1 ________________________________
Service outcome 2 ________________________________
Service outcome 3 ________________________________
Service outcome 4 ________________________________
5.24 Additional comments:
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
No intervention control:
5.25 Number of outcomes measured for: (a) caregiver _____%/n reported _____
(b) care recipient _____%/n reported _____
5.26 Number of measurement/time points for:
(a) caregiver _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
(b) care recipient _____
T1 (details) _________________________ n ______
T2 (details) _________________________ n ______
T3 (details) _________________________ n ______
T4 (details) _________________________ n ______
5.27 Caregiver outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.28 Care recipient outcomes:
Outcome 1 ______________________ Scale used ___________________________
Outcome 2 ______________________ Scale used ___________________________
Outcome 3 ______________________ Scale used ___________________________
Outcome 4 ______________________ Scale used ___________________________
Outcome 5 ______________________ Scale used ___________________________
Outcome 6 ______________________ Scale used ___________________________
Outcome 7 ______________________ Scale used ___________________________
Outcome 8 ______________________ Scale used ___________________________
Outcome 9 ______________________ Scale used ___________________________
Outcome 10 ______________________ Scale used ___________________________
Outcome 11 ______________________ Scale used ___________________________
Outcome 12 ______________________ Scale used ___________________________
Outcome 13 ______________________ Scale used ___________________________
Outcome 14 ______________________ Scale used ___________________________
Outcome 15 ______________________ Scale used ___________________________
5.29 (a) Service outcomes measured (i.e. outcome/s not solely attributable to either care recipient or carer)?
Yes □1 No □0
(b) If yes, please specify: Service outcome 1 ________________________________
Service outcome 2 ________________________________
Service outcome 3 ________________________________
Service outcome 4 ________________________________
5.30 Additional comments:
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
6. Economic modelling
6.1 Are any cost data provided?
Yes □1 No □0 (If yes, please give details)
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
6.2 Is information regarding health service usage provided (e.g. number of GP visits)?
Yes □1 No □0 (If yes, please give details)
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
6.3 Is information regarding other service usage provided (e.g. caregiver time)?
Yes □1 No □0 (If yes, please give details)
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
6.4 Does the paper provide a good description of respite services?
Yes □1 No □0
6.5 Additional information/model used:
_______________________________________________________________________________________
_______________________________________________________________________________________
_______________________________________________________________________________________
Appendix 4 Table of randomised controlled and quasi-randomised trials
| Study and quality scorea | Country, respite setting and design | Description of intervention/s | Inclusion criteria | n | Health problem | Demographics | Carer outcomes (and length of follow-up)b |
|---|---|---|---|---|---|---|---|
|
Baumgarten et al. 200232 High |
Canada Day care RCT |
1. Clients randomised to experimental group eligible for immediate admission to day centre. Clients and carers interviewed after randomisation and before admission (T2 = 3 months). Recommended participation is 6 hours per day, 1–2 days per week | Age > 60 years; English or French speaking; not too cognitively impaired to be interviewed; presence of primary carer; those referred to day care for specialist treatments excluded (e.g. rehabilitation for Parkinson’s disease) | 251 recruited; 212 completed (108 intervention: 104 control). Carers at T2 = 89 experimental and 93 control | Mental health (anxiety, depression, insecurity, loneliness) |
Recipients (experimental/control): mean age 76.4/78 years; female 74.1%/73.1% Carers (experimental/control): mean age 54.2/58.4 years; 73%/71% female; 25%/28.9% spouse; 46.6%/44.4% child |
Baseline and 3 months: burden (CBI) No difference in carer burden Included in meta-analysis |
|
Brodaty et al. 199733 Moderate |
Australia Inpatient respite RCT |
1. Carer training (10-day programme including input from occupational therapists/psychiatrists/psychologists) 2. Memory retraining for recipient (respite for carer) |
Carer/recipient dyads: recipient was required to have progressive mild/moderate dementia (diagnosed using standard criteria) | 96: 33 carer training, 31 memory training and 32 controls | Alzheimer’s disease/dementia |
Recipients: 48.4% female; mean age 70.1 years Carers: 53.8% female; mean age 67.5 years; 93% spouse |
Time to institutionalisation Survival analysis for time until outcome (death or institutionalisation) for all three groups. Length of follow-up: training and respite groups for 7.8 (0.56) years; waiting list group for 7.4 (0.37) years Shorter time to institutionalisation in respite group Excluded from meta-analysis: no other studies measuring mean time to institutionalisation identified |
|
Burch et al. 199934 High |
UK Day care RCT |
1. Day hospital (not stated) 2. Day centre (2 fixed days per week) |
Referred for day hospital within catchment area. Excluded if suffered from dysphasia, required nursing/medical procedure/drug monitoring/treatment more than twice per week or if focus is occupational therapy | 105 recruited (50 day hospital and 55 day centre); 72 completed (34 day hospital and 38 day centre) | Physical disability |
Recipients (day hospital/day centre): 60%/67% female; mean age 80.9/79.8 years No carer data |
Baseline and 3 months: Burden (Zarit) stress of memory/behaviour problems; perceptions of respite (assistance, burden and problems prerespite; burden, problems and perceptions postrespite) No difference between groups Excluded from meta-analysis: comparison of two respite interventions (no control) |
|
Burdz et al. 198835 Low |
Canada Inpatient Quasi-experimental |
1. Respite beds in nursing homes [mean = 15.3 (5.6) days] | Recruited through respite programme and scheduled to enter respite care | 74 recruited; 55 completed | Alzheimer’s disease/dementia |
Recipients (experimental/control): 60%/70% female; mean age 80.9/78.6 years Carers (experimental/control): 89%/75% female; mean age 56.5/62.4 years; 23%/50% spouse; 43%/30% child |
Baseline, 6 weeks, 3 months: strain (CSI) Significant decrease in burden in respite group Excluded from meta-analysis: could not derive mean values |
|
Conlin et al. 199236 Low |
USA Home care/inpatient care Quasi-experimental |
1. Respite for 6 hours per day, 2 days per week for 10 weeks. Either in-home or in an assisted-living facility (decided by carer) consisting of supervision and assistance with ADLs. Control group received respite care at end of study | Primary informal carers of persons aged 60+ years with Alzheimer’s disease/related dementia | 15 recruited and completed: 7 intervention, 8 control | Alzheimer’s disease/dementia | Experimental group: 7 women, mean age 50.3 years; control group: 6 women, mean age 69.3 years. All carers spouses |
At entry and 5 weeks: stress (Relatives Stress Scale) Less stress in respite group Excluded from meta-analysis: all SDs missing |
|
Grant et al. 200340 Moderate |
USA Home care Quasi-experimental |
1. 10 days in-home help (up to 6 hours per day) over a 2-week period | Diagnosis possible/probable dementia. Carers had to be caring for spouse at home and receiving < 8 hours respite per week | 55 recruited/completed | Alzheimer’s disease/dementia | Recipients 65+ years. Carers split into vulnerable (n = 27; age 72.07 years; 44.4% female) and non-vulnerable (n = 28; age 74.54 years; 32.1% female). All spouses |
Baseline and 1 month: anxiety, depression (Hamilton Depression Rating Scale), psychological symptoms (BSI), peripheral nervous system activation (catecholamines), blood pressure, heart rate No effect Included in meta-analysis |
|
Kosloski and Montgomery 199341 High |
USA Home and day care Quasi-experimental |
1. Two sites providing ADC 8am–5pm on weekdays; two sites providing in-home care (day/evening throughout week); three sites offering ADC and in-home care (states six programmes but only describes five?). Amount of respite available not limited. Compared with control group not receiving respite | None stated | 116 recruited (76 experimental and 40 control) and 72 completed (47 experimental and 25 control) | Alzheimer’s disease/dementia |
Recipients: 24 females in experimental group, 14 in control group Carers: 36 females in experimental group, 17 in control group; all aged 38–89 years. Experimental group: 28 spouse, 15 child; control group: 17 spouse, 7 child |
Before programme and at 6 months: burden (Zarit) and morale (Montgomery and Borgatta 1987) Lower burden and higher morale in respite group Included in meta-analysis |
|
Lawton et al. 1989;42 Lawton et al. 199143 Low; moderate |
USA Inpatient, home and day care RCT |
1. Respite programme: institutional, day care or in-home (the last either regular or occasional, during the day or evening, weekday or weekend). Respite embedded in context that included assessment, carer education, case management and counselling. Informal respite (from friends/family) also measured | Family carers of mentally impaired older persons | 632 | Likely dementia suffers but not specifically stated |
Recipients (experimental/control): 55.9%/63.4% female; mean age 76.1/76.4 years Carers (experimental/control): 80.8%/77.9% female; mean age 60.4/59.4 years; 41.8%/40.4% spouse; 40%/46% child |
Baseline and 12 months: burden, caregiver uplifts, caregiving impact, competence, ideology, physical health (MAI), depression (CES-D), positive and negative affect No effect on burden or psychological health Excluded from meta-analysis: no follow-up data provided |
|
Milne et al. 199344 Low |
UK Home care Quasi-experimental |
1. Provided by Age Concern – care attendant replaces carer for agreed periods up to a few hours, undertaking all tasks normally carried out by carer. Control group normal care | All carers of elderly (65+ years) referred to Age Concern Northumberland’s carer support scheme during a full calendar year | 136 recruited; 78 completed | Frail elderly |
Recipients (experimental/control): 67%/47% female; mean age 76.2/75.2 years Carers (experimental/control): 73% female; mean age 56.6/62.3 years; 48%/73% spouse; 50%/27% child |
Baseline and 3 months: stress, coping, psychological well-being (GHQ) Less strain in intervention group Included in meta-analysis |
|
Montgomery and Borgatta 1989;45 Montgomery 198846 Low |
USA Inpatient, day and community care Quasi-experimental |
1. Carer seminars (6 weeks, 2 hours per week; support groups; family consultation and respite 2. Family consultation service, carer seminars and support 3. Carer seminars and support groups. G4: family consultation 4. Respite only. Chose from home care, ADC or overnight in nursing home |
Self-referred to project: family units comprising impaired elderly person and at least one family member providing regular care/assistance | 541 recruited; 486 completed | Frail elderly (carers reported 28% had cognitive impairment) |
Recipients: 67% female; mean age 81.6 years Carers: 79% female; 167 spouse; 321 child |
Baseline, 12 and 20 months: subjective and objective burden (Montgomery et al. 1985) Burden significantly reduced in all intervention groups but no difference between intervention groups Exclude from meta-analysis: not possible to extract means |
|
Quayhagen et al. 200047 Moderate |
USA Day care RCT |
1. Cognitive stimulation 1 hour daily for 5 days (8 weeks) 2. Dyadic counselling 1.5 hours (8 weeks) 3. Dual supportive seminar groups (1.5 hours per week for 8 weeks) 4. Early-stage day care – respite and education/training for carers and stimulating environment for patients (4 hours per week). Carers met monthly for counselling support (8 weeks) |
Physically capable of participating in interventions; diagnosis of dementia (mild–moderate; Reisberg 1988) and score +100 on Mattis Dementia Rating Scale (1988) | 103 recruited and completed (21 cognitive stimulation; 29 dyadic counselling; 22 seminar groups; 16 day care; 15 control group) | Alzheimer’s disease/dementia |
Recipients: 38% female; mean age 74.51 years Carers: 65% female; mean age 71.83 years; 100% spouse |
Pre- and post-intervention: depression (BSI), hostility, anxiety, morale, physical health status, stress Decrease in hostility for carers with patients in the day care group None of the groups differed on perceived stress Included in meta-analysis |
|
Richards et al. 200348 Low |
UK Day and community care Quasi-experimental |
1. Memory clinic: all those (over 16-month period) referred to memory clinic by GP. Trial of early psychosocial intervention in dementia 2. CMHTs: old age psychiatry community teams 3. Specialist dementia day hospital |
Intervention 1: MMSE of > 16; duration of memory problems < 4 years Intervention 2: Supported by carer and had diagnosis of dementia based on DSM-IV Intervention 3: Moderate to severe need; required specialist mental health services not provided by CMHT |
216 recruited (group 1 = 48, group 2 = 113, group 3 = 55) and 91 completed (group 1 = 35, group 2 = 34, group 3 = 22) | Alzheimer’s disease/dementia | Recipient: mean ages 76.9/77.2/78.76 years intervention groups 1/2/3 |
Baseline and 12 months: anxiety, depression (HADS), coping with behaviour problems (PC) Day hospital group: anxiety and depression increased Included in meta-analysis |
| Riordan and Bennett 199849 |
UK Home care Quasi-experimental |
1. Home support service tailored to individual need (included assistance with ADLs, some household chores, outings, respite for carer) Matched control (possibly receiving standard domiciliary services) |
Carers need not be co-resident but had to engage in personal care at least three times per week. Recipients otherwise likely to be institutionalised. Dementia only | 19 receiving augmented home support; 19 matched control subjects | Alzheimer’s disease/dementia |
Recipients: mean age 79.8 years, 19 women Carers: mean age 61 years, 33 women; 14 spouse, 19 adult child |
Baseline and 6 months: psychological well-being, strain (GHQ, Carer Problem Checklist and Machin Strain Scale) No effect of respite Excluded from meta-analysis: no SDs |
| Rolleston and Ball 199450 |
UK Day hospital Quasi-experimental |
1. Evaluated effects of short-term closure (2 weeks) of old age psychiatric day hospital | Physically and cognitively impaired elderly (65+ years) | 36 carers (47 attendees) | Frail elderly | No information |
Baseline (closure) and at reopening: general well-being (non-standard questionnaire) Closure of respite detrimental to well-being but returned to preclosure levels at 3 weeks after reopening Excluded from meta-analysis |
|
Rothman et al. 199351 Rothman et al. 199329 Moderate |
USA Day care RCT |
1. 4–8 hours per day, 1–5 days per week in day care facility (continuous and assessed at 6 and 12 months). Services included: medical (monitoring only); occupational; physical and recreational therapy; personal care and social services (four medical centres) | At least one of: residing in/admitted to hospital from nursing home; use of personal assistance/supervision for personal care tasks; bowel incontinence; or significant cognitive impairment (MMSE) | 729 recruited; 510 completed (259 intervention and 251 control subjects) | Frail elderly |
Recipients: mean age 72.3 years; 4% female Carers: mean age 62.5 years; 76% spouse |
Baseline, 6 and 12 months: psychological distress scale (Veit and Ware 1983), burden (CBI) No difference between groups on burden or health perceptions Included in meta-analysis |
|
Schwarz and Blixen 199752 Low |
USA Home care Quasi-experimental |
1. Home health care following hospital discharge for 3-month period (amount used/type determined by carer and recipient according to personal preference, physician referral and beliefs about individual needs). Mean number of visits = 55.3 (41.7). Home health aides provided most visits followed by nurses. 13% received additional services, e.g. mobile meals, respite, day care and outpatient physical therapy | Age 65+ years, living with carer and needing assistance with at least three ADLs/IADLs | 148 recruited; 100 completed (49 intervention: 51 controls) | Frail elderly |
Recipients: 52% female; mean age 76.5 years Carers: mean age 64.7 years; 74% female; spouse n = 64 |
Baseline and 3 months: depression (CES-D); strain (Caregiver Strain Questionnaire), physical health No effect Excluded from meta-analysis: data not given for experimental and control groups separately |
| Wells and Jorm 198753 |
New Zealand Inpatient care RCT |
1. Permanent institutional care in specialist dementia unit, compared with: 2. Periodic respite care |
Cognitively impaired elderly in reasonable physical health; diagnosis of dementia (psychiatrist) | 26 randomised; 12 completed follow-up in institutionalised group, 10 in respite group | Alzheimer’s disease/dementia | None given |
Baseline and 3 months: psychological well-being (GHQ), anxiety, depression (DSSI), QOL, grief, guilt (developed for study) Quality of life, GHQ and DSSI significantly better in institutional group but not in respite group at 3 months Excluded from meta-analysis: comparison of respite vs permanent institutional care |
|
Zank and Schacke 200254 Moderate |
Germany Day care Quasi-experimental |
1. Day care patients (six day care centres in Berlin) compared with control subjects (selected for similarity on age, gender, physical and mental health, SES). Measurement at T1 (10 days), T2 (6 months) and T3 (9 months) – follow-up 6 months post T3 carers. Twice per week for 3 months |
Intervention: patients visiting one of the centres twice per week intending to stay more than 3 months Control: did not use day care but received home-based community care (household/dressing assistance). Day care attendees also received home-based community care in mornings/evenings |
151 recruited (83 intervention; 68 controls) and 83 completed (43 intervention, 40 controls) | Frail elderly; majority with dementia (79% day care; 63% control) |
Recipient (experimental/control): 79%/68% female; mean age 79.3/79.8 years Carers (experimental/control): 85%/83% female; mean age 55/59 years; 25%/39% spouse, 45%/52% child |
For carers: 6 months post T3 (n = 20): life satisfaction (LSQ), self-esteem, depression (CES-D), burden (Zarit), family conflict, job/caring conflict, positive and negative effects No effect of respite Excluded from meta-analysis: not possible to extract means |
|
Zarit et al. 1998;55 Zarit et al. 1999;56 Gaugler et al. 2003;37 Gaugler et al. 2003;38 Leitsch 200139 High; moderate; high; high; high |
USA Day care Quasi-experimental |
1. Day care in 45 centres in New Jersey (at least twice per week and for a period of 3 months before T2, 12 months before T3). Average of 3.07 days per week for 6.01 hours in first 3 months (baseline immediately before service use and at 3 months and 1 year) (Leitsch et al. 2001 provides a comparison of medical/social day care subgroups) | Diagnosis of dementia; primary carer and not currently using ADC; not used ADC in previous 3 months; not using more than 8 hours other paid help per week; relative independently mobile (with or without devices). Note: all descriptions at T1 for T3 sample | Recruited: intervention group 261 and control group 305; completed: intervention group 73 and control group 120 | Alzheimer’s disease/dementia |
Recipient (experimental/control): 61.2%/60.1% female; mean age 78.2/77.3 years Carers (experimental/control): 80.2%/80.8% female; mean age 59.4/60.5 years; 41.3%/45.3% spouse; 45.5%/40.4% child |
Baseline, 3 and 12 months: role captivity, overload, worry and strain, depression (CES-D), anger, positive affect Reduction in role overload only Included in meta-analysis |
Appendix 5 Summary table of before-and-after studies
| Study and quality scorea | Country and respite setting | Description of intervention/s | Inclusion criteria | n | Health problem | Demographics | Carer outcomes (and length of follow-up)b |
|---|---|---|---|---|---|---|---|
|
Adler et al. 199357 Moderate |
USA Institutional |
Before-and-after study of in-hospital respite (2 weeks – Minneapolis Veterans Affairs Center). No special care or activity programs for recipients, just normal care on non-acute geriatric ward | Recipients had DSM-III-R diagnosis of dementia; lived in community. Carer defined as family member living with/having primary responsibility for recipient | 37 recruited and completed | Alzheimer’s disease/non-Alzheimer’s dementia |
Recipients: all male; mean age 73.6 years Carers: 92% female; mean age 64 years; 81% spouse |
On discharge and at 2 weeks: burden (ZBI), depression (GDS) Outcomes reduced during inpatient respite but returned to baseline on return home |
|
Chi and Wong 199458 Low |
Hong Kong Institutional |
Elderly hostels if capable of self-care; care homes if in frail health and limited self-care abilities | No information. All care and care recipient dyads applying to the service | 43 recruited and completed | Frail elderly |
Recipients: 70% female; mean age 78.3 years Carers: 81% female; mean age 50.2 years; 26% spouse; 37% child |
1 month: stress (attitude statements); non-standard measure Less likely to wish to institutionalise but perceptions of stress increased |
|
Cox 199859 Low |
USA Home, day care and institutional |
Respite programme in Maryland: allows families to buy up to 164 hours respite (maximum rate US$6.4/hour). In-home care by trained worker; nursing homes with beds for dementia patients (4–5 days); day care but no information given | Carer a relative and recipient with diagnosis of Alzheimer’s disease. Restricted to those with incomes < 150% of state’s median income adjusted for family size |
265 recruited; 103 completed Compared African American (AA) carers with white carers |
Alzheimer’s disease/dementia |
Recipients: mean age 80.89 years Carers (white/AA): 84%/87% female; mean age 58.35/58.37 years; spouse n = 30/23; childn = 55/43 |
6 months: anxiety (BSI), depression (CES-D), burden (Montgomery and Borgatta 1989). Neither black nor white carers reported any change in anxiety or depression but both groups had significant reductions in burden |
|
Deimling 199260 Low |
USA Home, day care and institutional |
‘Time off promotes strength’ respite programme in Cuyahoga County, USA. Three types of respite offered: short institutional stays (178-bed nursing home); day care; and home health aide | Alzheimer’s disease patients and carers; took part in service for minimum of 4 months | 78 recruited and completed | Alzheimer’s disease/dementia | Carers: 59% spouse |
4–6 months: depression (CES-D), symptoms of health problems, relationship strain (Poulshock and Deimling 1984), restriction of activity Carers of stable care recipients had positive effects on all outcomes whereas carers of declining care recipients did not |
|
Desrosiers et al. 200461 Moderate |
Canada Day care |
Day care at specialised geriatric outpatient service; does include medical intervention/rehabilitation component for some patients. Usual care is 2 days per week for 12 weeks | Client had to receive services from at least two disciplines, attend for minimum of 4 days and have been discussed during at least one meeting of multidisciplinary team. All clients aged 65 years and over. All clients attending for over 1 year | 171 recruited; at T2 151 completed; at T3 126 evaluated | Frail elderly |
Recipients: n = 89 female; mean age 77.63 years Carers: n = 50 spouse; n = 44 child |
3 and 6 months: burden (ZBI) No statistically significant effects at T1 or T2 Included in meta-analysis |
|
Gilleard 1987;62 Gilleard et al. 198463 Low |
UK Day care |
Day hospital care: four psychogeriatric day hospitals attached to an independent psychiatric hospital in Lothian | Referred from community; no previous inpatient care in last 6 months; lived with or visited by carer at least three times per week; carer identified by patient willing to be interviewed | 129 recruited; 81 completed | Majority dementia sufferers |
Recipients: n = 84 female Carers: n = 49 spouse; n = 49 adult child |
3 and 6–7 months: psychological well-being (GHQ) (compared still attending day care, discharged to community and institutionalised), carer strain (Machin Strain Scale) Reduced distress in majority of carers Excluded from meta-analysis |
|
Harper et al. 199364 Moderate |
UK Home care |
Home-based care aide service – nursing assistants to give carers a break by spending a few hours a week with recipients: 4–15.8 hours per month over 2-year period. Either frequent/short or less frequent/longer. Also help with ADL tasks | Carers of impaired elderly | 82 recruited; 45 completed | Frail elderly |
Recipients: n = 49 female; mean age 81.3 years Carers: n = 64 female; 29.3% spouse; 42.7% child |
3 months: psychological health (GHQ) Reduction in carer distress after intervention Included in meta-analysis |
|
Higgins et al. 200565 Moderate |
USA Day care |
Day care (also includes education sessions for carers – confounding factor??); 1 day per week including word games, exercise, games, singing. Attendance from 35–50 sessions (mean 44.6; 91% attendance) | Medical diagnosis of dementia; community dwelling; continent; independently mobile/with assistive devices. Carers fluent in English and able to complete questionnaires with minimum 3-month commitment. Excluded if patient physical threat/attending other ADC | 37 recruited; 21 completed | Alzheimer’s disease/dementia | Recipients: n = 43 female; mean age 77.3 years |
3, 6, 9 and 12 months: quality of life (QOL-AD) QOL unchanged after intervention Included in meta-analysis |
|
Homer and Gilleard 199466 Low |
UK Institutional |
Inpatient (hospital) respite | Referred to two geriatric services in London | 108 recruited; 54 completed | Frail elderly | Carers: n = 77 female; mean age 66 years |
During respite: psychological health (GHQ) No evidence of any improvement in total GHQ score during the respite period, but significant reduction in depression and social dysfunction subscales Included in meta-analysis |
|
Hoskins et al. 200567 Moderate |
UK Institutional and day care |
Respite beds in hospitals/residential homes – no information on duration Day care |
Dementia/clearly identified memory problems, living at home only | 45 recruited; 26 completed | Alzheimer’s disease/dementia |
Recipients: n = 19 female; mean age 81.04 years Carers: n = 19 female; mean age 64 years; spouse 10; child 13 |
3 and 6 months: strain (CSI) Significant reduction in carer strain Included in meta-analysis |
|
Johnson and Maguire 198968 Low |
Australia Day care |
Day care: 80% attended once per week, 1% three times per week; 8–24 hours carer relief | Carers of geriatric and psychogeriatric patients at day care centre, New South Wales | 46 | Frail elderly | Carers: mean age 75 years; 50% female |
2 and 4 months: burden No difference in carer burden Excluded from meta-analysis |
|
Theis et al. 199469 Low |
USA Home and inpatient respite |
Respite Care Project (nurse-managed service providing continuum of care). Services included a referral centre, in-home care (up to 4 hours per week) and inpatient respite (long-term facility for short-term stay) | Carers providing care to persons aged 65 years and over and co-resident | 130 recruited; 18 completed 6-month follow-up; 10–13 at 12 months | Frail elderly |
Recipients: mean age 83 years; 55% male Carers: mean age 68.5 years; 89% female |
6 and 12 months: depression (POMS), burden (ZBI), QOL (Quality of Life Index) No statistically significant change Included in meta-analysis |
|
Warren et al. 200370 Low |
Canada Day care |
14 sites: nine day hospital (focused on rehabilitation) and five ADC mainly providing respite support. Mean attendance 1.8 days or 10.4 hours per week | 10 pairs per site (carer and recipient). Excluded if cognitive impairment | 140 recruited; 80 completed | Frail elderly | Carers: 72% female; mean age 61.6 years; 56% spouse; 20% child |
2 weeks, 2 and 6 months: burden (CBI), quality of life (SASS), health status, opinion of institutionalisation, satisfaction No significant change Included in meta-analysis |
Appendix 6 Summary table of observational longitudinal studies
| Study and quality scorea | Country and respite setting | Description of intervention/s | Inclusion criteria | n and length of follow-up | Health problem | Demographics | Outcomes assessedb |
|---|---|---|---|---|---|---|---|
|
Andrew et al. 200071 Moderate |
UK Home, day and short stays |
Use of home care and/or day care; short stays | Recipient 65 years and over; had received needs assessment by social services; had signs of cognitive impairment suggestive of dementia |
141 recruited over 4-month period (34 had no carer) Mean follow-up 11 months (SD ± 103 days) |
Dementia |
Recipients: mean age 83 years; 69% female Carers: 33% spouse |
Institutionalisation: those using day or home care less likely to be institutionalised at 1 year |
|
Armstrong-Esther et al. 200572 Low |
Canada Respite use |
Regular/daily or occasional respite | Home care clients aged 75+ years; 3–9 (moderate–high) on HCCC | Baseline = 210 (care recipients = 330); 9 months = 133 (288); 18 months = 81 (234) | Frail elderly |
Recipients: mean age 85 years; female n = 187 Carers: mean age 63.2 years; 69% female |
Psychological burden (ICA) More respite predictive of more carer stress Also found higher levels of stress in those receiving no respite, and higher levels in regular users compared with occasional users |
|
Bond and Clark 200273 Low |
Australia Day care and institutional |
Use of respite in last 3 months [day care/activity centres and extended respite (nursing home/hostel)]; n and % | Alzheimer’s disease diagnosed by geriatrician; patient and carer aged 65+ years; coresident and carer spouse. Carers sampled in three groups: < 1 year, 1–4 years and > 4 years since diagnosis | 163 recruited; 158 completed 2-year follow-up (5 died) | Dementia |
Recipients: mean age 73.1 years; 50% female Carers: mean age 71.7 years; 57.7% female; 100% spouse |
Institutionalisation 98 (62%) of 158 institutionalised; greater use of respite associated with institutionalisation: not significant when adjusted for dementia severity |
|
Cohen et al. 199374 High |
USA Formal/informal supports |
Number and frequency of community services used from list of public/private health and social services and number of additional carers | Diagnosis of dementia according to DSM-III for at least 1 year; community resident; carer present; absence of other disabling medical conditions of a severity threatening physical independence | Baseline = 196 participants; 6 months = 119 (9 died, 49 institutionalised, 19 lost to follow-up); 1 year = 74 (7 died, 27 institutionalised, 11 lost to follow-up); 1.5 years = 37 (3 died, 24 institutionalised, 10 lost to follow-up) | Dementia |
Recipients: mean age 77.46 years Carers: mean age 54.41 years; 76% female; 59% spouse; 27% child |
Institutionalisation Carers who used more community services at initial assessment more likely to institutionalise |
|
Cox 199775 High |
USA Level of formal/informal service use |
Informal help (percent reporting and hours per week); formal service use (percent reporting day care and home help) | Carer’s annual income ≤ 150% of state’s median income (adjusted to family size) and medical certification that relative had Alzheimer’s disease or related disorder. Baseline telephone interviews with carers at time of application to wider respite programme | n = 228, with follow-up 6 months later (n = 123) | Dementia |
Recipients: mean age 79.6 years Carers: mean age 58 years, 85% female; 26% spouse; 50% adult child |
Anxiety (Brief Symptom Inventory), depression (CES-D): no change with respite use Burden (Montgomery and Borgatta 1989): significant decrease in burden over 6 months of respite use Care recipient outcomes: ADL and cognitive status declined but carers felt that care recipient behaviour improved |
|
Cox and Monk 199076 Low |
USA Formal/informal supports |
Use of formal and informal supports (frequency) | Black and Hispanic carers of older people with dementia only | Baseline = 50; 6-month follow-up (n = 43) | Dementia |
Recipients: mean age 77.5 years Carers: mean age 63.5 years; 75.5% female; 29% spouse; 29% child |
Depression (CES-D): no association with service use Burden: no association with service use Recipient ADL positively correlated with informal and formal supports and between informal support and memory/behaviour problems in the black group only |
|
Gaugler et al. 200378 High |
USA Home care |
Chore services: none/low 1–36/medium 37–103/high 104+/increased hours in previous 6 months; personal services (as chore services); day care: none/low 1–30/medium 61–207/high 78+/increased days in previous 6 months | Diagnosis of irreversible dementia; enrolled for A/B Medicare; had service needs and community resident in MADDE catchment area |
3994 MADDE control subjects; 3 year follow-up 1 year: 386 institutionalised, 283 died/lost to follow-up; 2 years: 251 institutionalised, 195 died/lost to follow-up; 3 years: 142 institutionalised, 1149 died/lost to follow-up |
Dementia | Carers: 59.7% > 70 years; n = 1832 spouse; n = 1570 child |
Institutionalisation More likely to institutionalise with low and high use of community services compared with moderate use |
|
Gaugler et al. 200579 High |
USA Formal/informal services |
Personal care (number of services in previous 6 months); adult day care days in previous 6 months; overnight hospital stays in previous 6 months; (all mean values) and secondary care-giving hours in a typical week | As above |
804 early-career carers (MADDE experimental group); 3 year follow-up 1 year = 555 (33 died; 193 institutionalised; 23 lost to follow-up); 2 years = 350 (50 died; 123 institutionalised; 32 lost to follow-up); 3 years = 221 (29 died; 84 institutionalised; 16 lost to follow-up) |
Dementia |
Recipients: mean age 78.53 years; 60% female Carers: mean age 60.07 years; 74.6% female; 40.8% spouse |
Institutionalisation Severe behaviour problems predicted institutionalisation |
|
Gaugler et al. 200580 High |
USA Formal services |
Either hours of home help or days of day centre use in previous 6 months or timing of service use in terms of duration of care (months) | (1) doctor-diagnosed dementia; (2) enrolled/eligible for Medicare A/B; (3) had service needs; (4) lived at home in appropriate catchment area. Carer defined as relative who provided most assistance | MADDE treatment and control groups: 4761; 3-year follow-up | Dementia |
Recipients: mean age 78.53; 59.3% female Carers: mean age 62.63 years; 73% female; 49.7% spouse |
Institutionalisation Those who utilised in-home help earlier in their dementia caregiving career were more likely to delay institutionalisation |
|
Gaugler et al. 200482 High |
USA Formal and informal services |
Which services used in last 6 months and how often: chores, personal care, day centres | As above | MADDE treatment and control groups: African American only, n = 667 (265 died during 3-year period) | Dementia |
Recipients: 90.4% 65–89 years; 68.5% female Carers: 26.1% spouse; 41.1% child |
Institutionalisation No association between ADC and institutionalisation |
|
Gaugler et al. 200077 High |
USA Formal and informal in-home help |
Paid help and family help (support with ADLs; sitting; taking relative out; overnight respite) | Diagnosis of dementia; carer willing to use day care but not during study and no more than 8 hours paid service per week | 304 recruited and completed 3-year follow-up; 87 remained in study; 60 died; 41 lost to follow-up | Dementia |
Recipients: mean age 77.96 years; n = 195 female Carers: mean age 59.37 years; 80.6% female; 40.1% spouse; 53.4% child |
Institutionalisation Carers less likely to institutionalise when family members provided overnight help and assisted with ADL |
|
Gaugler et al. 200581 High |
USA Home and day care |
Services used in last 6 months (times chores and personal care; days ADC and hours per week help from family/friends) | Larger MADDE study criteria: doctor-diagnosed irreversible dementia; eligible for Medicare; community resident in one of eight catchment areas. Carer defined as person who provided most assistance | Baseline = 5831; 6 months = 4719 (240 died, 695 institutionalised, 177 lost to follow-up); 1 year = 3740 (279 died, 582 institutionalised, 118 lost to follow-up); 1.5 years = 2996 (210 died, 444 institutionalised, 90 lost to follow-up) | Dementia |
Recipients: mean age 78.6 years; 59.9% female Carers: mean age 63 years; 72.2% female; 49.1% spouse |
Institutionalisation Nursing home admission; death and loss to follow-up as outcomes (multivariate logistic regression) Unmet need for ADC; an overnight hospital stay a predictor of institutionalisation |
|
Jarrott et al. 200583 High |
USA Home help |
Formal or informal in-home help (help with ADLs/IADLs; sitting with care recipient/taking recipient out of house) – asked how many hours of each in last month | In larger study: primary carer; recipient had diagnosis of dementia; no more than 8 hours per week formal help in month before baseline; carer not currently using ADC; care recipient mobile | 432 at baseline and 3 months; 27 excluded because of institutionalisation/loss to follow-up, etc. (n = 405) | Dementia |
Recipients: mean age 77.69 years; 60% female Carers: mean age 60 years; 81% female; 43.9% spouse |
Depression (CES-D) Increases in formal help associated with decrease in depression, anger, overload, worry and strain |
|
Jette et al. 199584 Moderate |
USA Formal and informal service use |
Hours per week informal and formal service use, i.e. care provided for personal care, housekeeping, meals, transportation and financial management | Age 70 years and over; identified as disabled based on a disability index |
634 recruited T2 (4–5 years): 284 continued, 208 died, 94 institutionalised, 48 lost to follow-up; T3 (1.5 years since T2 = 284): 206 continued, 33 died, 30 institutionalised, 15 lost to follow-up; T4 (1.2 years since T3 = 206): 152 continued, 18 died, 19 institutionalised, 17 lost to follow-up |
Frail elderly | Recipients: 45.6% aged 70–79 years |
Institutionalisation Increasing amount of formal service use associated with reduced risk of institutionalisation. Service use did not buffer the effects of severity of disability on institutionalisation |
|
McFall and Miller 199285 Moderate |
USA Use of formal services |
Use of formal help (yes/no). Does not define the type of help | Frail elderly with sole spouse/adult child carer | Analysis sample n = 940; 2-year follow-up | Frail elderly |
Recipients: mean age 68–85 years; 56.9% female Carers: 69.7% female; 58.9% spouse; 41.1% spouse |
Institutionalisation Use of formal help predicted institutionalisation |
|
Pruchno et al. 199086 Moderate |
USA Either formal or informal help |
Informal help: number of family/friends who provided hands-on assistance (range = 0–4; mean = 0.77). Formal services: count of total formal/informal programs including Meals on Wheels; counselling; legal services; home-maker services; self-help groups (range = 0–11; mean = 3.7) | Carers providing community care to spouse with Alzheimer’s disease or related disorder | 315 recruited; 220 completed 1-year follow-up (72 dropped out; 23 died before follow-up) | Dementia | Carers: mean age 70.2 years; 67.9% female; 100% spouse |
Institutionalisation Use of formal and informal help not associated with institutionalisation |
|
Wells and Kendig 199687 Low |
Australia Formal service use |
Used respite (yes/no) | Clients with complex needs at risk of institutionalisation | 498 recruited; completed? (unclear); 18- to 22-month follow-up | Frail elderly |
Recipients: mean age 79.5 years; 69% female Carers: 35% spouse; 32% child |
Institutionalisation No direct data linking service use and institutionalisation |
|
Winslow 199788 High |
USA Formal service use |
Use of formal support services: asked carers which of 11 services they had used in the past year and how often per week, e.g. home health care/visiting nurse; housekeeper; ADC. Amount of service use was rated from 5 (use four or more times per week) to 0 (do not use) | Carers of relatives with family-reported diagnosis of dementia | Convenience sample 452; 1-year follow-up | Dementia |
Recipients: mean age 75 years Carers: mean age 61 years; n = 310 female; n = 260 spouse; n = 192 child |
Institutionalisation Predicted by more use of formal supports |
|
Zarit et al. 198689 High |
USA Formal/informal supports |
Formal and informal social supports: informal: how often contact with family/friends and what assistance received; formal: frequency of services provided by agencies/paid helpers. Combined total for weekly frequencies of formal/informal help. Carers rated quality of support on 4-point scale | Carer with dementia patient at home (demographics for husband and wife patients/carers respectively) |
64 at baseline (33 wife carers; 31 husbands); 2-year follow-up At 2 years = 32 (15 died; 11 institutionalised; 6 lost to follow-up) |
Dementia |
Recipients: mean age males 69.3 years; mean age females 70.53 years Carers: mean age males 72.27 years; mean age females 63.37 years |
Burden (ZBI) No relationship between formal/informal support and carer burden |
Appendix 7 Summary table of cross-sectional studies
| Study and quality scorea | Country and respite setting | Description of intervention/s | Inclusion criteria | Health problem and n | Demographics | Carer outcomesb |
|---|---|---|---|---|---|---|
|
Arai et al. 199891 High |
Japan Level of formal service use |
Number of services used of home help, seminars on caregiving, respite care, visiting nurses, renting special equipment, home dental treatment, day care, counselling, home bathing services, rehabilitation sessions | Informal carers of frail elderly. All elderly in need of care registered at town welfare centre |
Frail elderly 24 pairs of carer and care recipient |
Recipients: mean age 77.5 years; n = 17 female Carers: mean age 56.7 years; 80% female; n = 11 spouses (5 husbands, 6 wives) |
Depression (CES-D) Compared depressed (n = 12) with non-depressed (n = 12) carers. Non-depressed used significantly more services |
|
Arai et al. 200490 High |
Japan Hours of respite received |
Hours per day caregiving relieved: 2 or less/3 or more | Impaired elderly registered with practice nurse clinic attached to hospital |
Dementia 46 |
Recipients: mean age 79.8 years; n = 30 female Carers: mean age 60.5 years; n = 35 female; n = 17 spouse; n = 26 adult child |
Burden (ZBI) Compared burdened (n = 23) with non-burdened (n = 23). Those relieved of care for 3 or more hours a day less burdened |
|
Artaso et al. 2003;92 Biurrun Unzue et al. 2003;95 Gon-i Sarries et al. 2003110 Quality rating not carried out |
Spain Day care |
Attendance at day care centre | Female spouse/daughter Carers living with recipient and being principal carer |
Dementia 80 (40 experimental group; 40 control group) |
Recipients: mean age 79.64 years Carers: mean age 54.5 years; 100% female; 30% spouse; 70% adult child |
Burden (ZBI Spanish version) No difference in burden between those attending a day centre and those not Less social support more burden |
|
Bass et al. 199693 High |
USA Level of formal service use |
Single interviews with carers. Service categories were personal care; household help; escort services; health care identified by factor analysis of 43 tasks – emphasis on formal services | Recipient 65 years or over; community resident; received case management services for at least 1 month before study. Carer as friend/family member (unpaid) who assists with at least one personal care or daily living task |
Frail elderly 401 (58.7% of those eligible to take part) |
Recipients: mean age 79.1 years; 79.6% female Carers: mean age 58.6 years; 75.6% female; 18.7% spouse; 44.9% adult child |
Depression (CES-D), subjective health deterioration, social isolation Personal care services (which includes respite) modified the effects of care recipient problem behaviour on carer depression, health deterioration and social isolation. Household help moderated the effects on depression |
|
Biegel et al. 199394 Moderate |
USA Level of formal service use |
In-person interviews with carers (yes/no): use of in-home services (housekeeping, nursing care, delivered meals); use of out-of-home services (adult day care, senior centre meals, transportation) | Carers of family members with diagnosed/probable Alzheimer’s disease. Non-institutionalised and scoring 12–27 on MMSE. Recruited via Alzheimer’s disease diagnostic centres |
Dementia 170 (71% RR) (27 receiving in-home help; 26 out-of-home help; 30 combined services and 87 receiving no help) |
Carers: mean age 58 years; 70% female; 41.5% spouse; 49.1% adult child; 66% coresident |
Relationship strain, emotional strain (developed for the study) (depression, guilt, isolation, fear of the future and feeling of helplessness) Care recipients who do not use services or who use in-home services have inadequate informal support and more strained carers and are more functionally impaired than those using out-of-home and combined services |
|
Caserta et al. 198796 Moderate |
USA Level of formal/informal service use |
Informal support measured by network size, ease of contact and satisfaction (single score). Respondents also categorised into users/non-users of formal services: respite accounted for 62.5% of services; used regularly by 57%. Also includes day care and in-home care | Carers of community-resident elderly identified through mailing lists of various local support groups |
Frail elderly 597 (67.2% of original sample) (cross-sectional survey) |
Recipients: mean age 73 years; 55% female Carers: mean age 60 years; 74% female; 57% spouse; 27% adult child |
Burden (ZBI) Those not ready to utilise services had lower burden, functional dementia and higher social support than those who did use services or who did not for other reasons. Those who did not for other reasons had similar burden to those who did use services |
|
Cefalu et al. 199697 Moderate |
USA Day care and level of formal/informal service use |
Telephone interviews with carers: length of stay/number of days Compared attendees at social and medical day care centres Level of paid/non-paid help |
Diagnosis of dementia: patients who had left day care more than 3 years before were excluded. Recruited from three medical and three social day care units |
Dementia 206 completed interviews |
Recipients: mean age 77.9 years; 68.4% female Carers: mean age 57.7 years; n = 156 female; 40.4% spouse |
Burden (Relatives Stress Scale) Carers in the medical ADC group had greater burden and significantly more paid help than those using social ADC |
|
Chappell and Reid 200298 High |
Canada Level of formal service use |
Interviews with carers: frequency of getting a break and number of formal services used in home and out of home, e.g. homemaker and ADC | Recruited by randomly generated telephone numbers to identify households with a carer |
Frail elderly 243 (82.7% of eligible sample) |
Recipients: mean age 80.4 years; 68% female Carers: mean age 51.1 years; 69% female |
Burden (ZBI) Burden decreased by more frequent breaks. Hours of care and care recipient behaviour increased burden. Well-being not affected by getting a break. Formal service use did not impact on burden or well-being |
| Clark and Bond 200099 |
Australia Formal service use (day care and inpatient services) |
Respite use in previous 3 months (distinguished between day care and extended periods of respite). Use/non-use and frequency | Diagnosis of Alzheimer’s disease by geriatrician; patient and carer at least 65 years; coresident; spouse carer actively providing care at time of study. Recruited via Alzheimer’s Association (randomly) |
Dementia 163 couples (83.9% RR) |
Recipients: mean age 74.5 years; n = 69 female Carers: mean age 71.7 years; n = 94 female; 100% spouse |
Examined predictors of respite use Respite use associated with higher levels of domestic chores Excluded from the narrative |
|
Clarke and Finucane 1995100 Low |
Australia Level of formal/informal service use |
In-person interviews with carers: 36% of care recipients and 45% of carers had received a respite break defined as a break of a week or more | Age 60+ years and non-institutionalised; carer providing help for one or more ADLs |
Frail elderly 71 carers and 67 care recipients |
Recipients: 66% female Carers: 77% female |
Views of respite Fewer care recipients than carers felt positive about respite or felt that respite had benefited them. Both groups showed a preference for at-home respite and care recipients were much less positive about residential care |
| Colvez et al. 2002101 |
France Formal service use |
Service use (compared five groups having day centre, home social services, expert centres, group living, respite hospitalisation) across four countries in Europe | Age 55+ years; MMSE < 26; cared for at the centre for > 3 months |
Dementia 50 patients chosen randomly at each centre – 302 replies |
Recipients: mean age 80.4 years; mean MMSE 10.0 Carer: mean age 61 years; mean 62% female across the centres |
Burden (ZBI) Hospital respite group higher burden than home social services, group living, expert centre programme groups Depression (NHP) Hospital respite group more depression than expert centre programme group |
|
Cossette and Levesque 1993102 Moderate |
Canada Informal support |
Three forms of social support from friends/family: tangible assistance; emotional support; respite | Wife carers of men with COPD. Men had to have a confirmed COPD diagnosis from pneumologist and severity between moderately impaired (grade III) and severely impaired (grade V). Convenience sample |
Physically frail (COPD) 89 |
Recipients: mean age 68.6 years; 100% male Carers: 100% spouse |
Mental health outcomes (SCL-90 and use of psychotropic medication) Adequacy of informal social support had no significant impact on the mental health outcomes, but carers who received respite were three times more likely to use psychotropic medication |
|
Dziegielewski and Ricks 2000103 Low |
USA Day care |
Cross-sectional survey of carers: adult day care programme in Florida | All those attending day care |
Dementia 39 questionnaires sent out; 26 received |
Carers: 65.4% female; 57.7% spouse, 34.6% adult child |
Stress and guilt (developed for the study) Carers reported less stress but increased feelings of guilt |
|
Fell et al. 2001104 Low |
Ireland Day care |
Day centre: 1 day per week for 7 weeks. Compared those attending ADC with those on waiting list | Primary carers who lived with recipient |
Frail elderly 40 (20 receiving day care; 20 on waiting list) |
Carers (experimental/control): mean age 64.7/57.75 years; 65%/85% female; 60%/30% spouse |
Psychological distress (GHQ12), burden (CWS) No difference between users and non-users on psychological distress or burden |
|
Furness et al. 2000105 Low |
UK Day care Quasi-experimental |
1. Three psychiatric day hospitals; mainly for elderly with mental health problems/had days allocated for those with functional/cognitive impairment 2. Three social services day centres 3. Four voluntary agency (Age Concern) day centres |
Elderly clients attending day centres in Leicestershire |
Alzheimer’s disease/dementia 129 recruited (50 intervention 1; 36 intervention 2; 43 intervention 3); 74 completed (23 intervention 1; 28 intervention 2; 23 intervention 3) |
Recipients: mean age 77 years Carers: 61% female; 53% spouse |
Carer outcomes for cognitively impaired only (n = 23/32/43) Burden (CSI) No difference between settings; severity of care recipient depression greater in Age Concern day centres |
|
Gaugler et al. 2004106 Moderate |
USA Level of formal/informal service use |
Cross-sectional survey of use of community resources, e.g. bed days in hospital, nursing home stays, adult care days and in-home help days, secondary caregiving hours (i.e. help from family/friends) – all how many times per days in last 6 months | Carers of dementia patients. Recruited from the database of the University of Kentucky Alzheimer’s Research Centre. Responses from community-dwelling care recipients and carers only in this paper |
Dementia 344 |
Recipients: mean age 76.4 years; 63.6% female Carers: mean age 62.2 years; 69.7% female; 48.3% spouse |
Carer stress (loss of intimate exchange, role overload, role captivity) Greater unmet need for confidante support predicted carer stress. No relationship with resource use reported |
|
Gilhooly 1986;108 Gilhooly 1984107 High; moderate |
UK Day hospital and home care |
Semistructured interviews with carers: day hospital (days per week); home help (visits per week) Recruited from records of two Scottish day hospitals |
Primary diagnosis of senile dementia; carers living in city or within easy access |
Dementia 48 |
Recipients: mean age 78.6 years; n = 36 female Carers: mean age 57.9 years; n = 39 female; n = 11 spouse; n = 29 adult child |
Morale (Kutner Morale Scale); mental health (OARS) Correlations between day hospital and morale and mental health and between home help and morale and mental health not significant |
|
Gilleard et al. 1984109 Low |
UK Level of formal/informal service use |
In-person interviews with carers: informal (family member visits: none/occasional/frequent) or formal support (none vs weekly home help) | Carers of patients referred and accepted for day care in their own home. Carer coresident or visits patient at least three times per week |
Frail elderly (majority with dementia) 129 |
Recipients: n = 83 female Carers: mean age 61 years; n = 102 female; n = 49 spouse; n = 62 child |
Burden and strain (developed for the study) Informal support not associated with burden or strain. Professional support correlated weakly but significantly with strain but not burden in older carers but not younger (more support less strain) |
|
Grasel 1997111 Low |
Germany Inpatient care |
Utilised temporary institutional respite in last 12 months or not |
Carers in own home; care needs covered at least four ADLs (hygiene, eating, toileting, mobility) Recruited from adverts in magazines |
Dementia 1272 (RR 25%) |
Recipients: used respite: 75.8% female; did not use respite: 65.6% female Carers: used respite: mean age 56.4 years, 90.9% female, 54% adult child; did not use respite: mean age 58.1 years, 83.3% female, 45% adult child |
Burden Subjective burden higher in those who used respite in last 12 months compared with those who did not |
|
Henry and Capitman 1995112 Moderate |
USA Day care |
Cross-sectional survey: length of respite ADC attendance (months); average attendance days during 6 months of study | Active recipients of ADC services from 10 study sites |
Frail elderly (sample split into dementia vs non-dementia) 312 |
Carers: mean age dementia carers 59 years; mean age non-dementia carers 57 years |
Well-being (positive attitudes to caring; developed for study) No associations found between service use and well-being. Predictors of well-being were situational factors and personality traits |
|
Jutras and Veilleux 1991113 Low |
Canada Informal support |
Telephone interviews with carers: amount of help provided by personal network – e.g. spouse, other family, friends, neighbours) – scale = 0–29 (mean 5.99) | Carers had to help the elderly person very/fairly often with at least two of 12 ADLs; elderly person had to be functionally dependent because of physical handicap, memory loss, depression, anxiety. Recruited by random telephone dialling |
Frail elderly 294 |
Carers: mean age 40.6 years; 67.2% female |
Burden (psychological and physical difficulties, impact on personal life and professional life; developed for study) As assistance increases the burden experienced by the carer decreases |
|
Kosloski et al. 2001114 Moderate |
USA Home and day care |
Users and non-users of in-home respite or day care | Primary carers of Alzheimer’s disease patients. Demographics grouped by user, seeker and non-seeker |
Dementia 176 respite users; 282 non-users |
Recipients: mean age 77 years; 54% female Carers: 78.3% female |
Examined predictors of respite use Excluded from the narrative |
|
Kuwahara et al. 2001115 High |
Japan Use of formal/informal services |
Cross-sectional survey: had someone to help with care (yes/no); had time to go out without patient (yes/no); number of family members and number of social services used Compared heavily burdened with lightly burdened |
Disabled elderly and carers who received regular visits from community nurses (with and without dementia) |
Frail elderly 58 |
Recipients: mean age 78.5 years; 58.6% female Carers: mean age 61.2 years; 88% female; n = 23 spouse; n = 22 adult child |
Burden (ZBI) Although lightly burdened were more likely to have someone to help with care or to be able to go out, it was not statistically significant. Heavily burdened group used more social services but this failed to be a significant factor in multivariate analysis |
|
Lechner 1993116 High |
USA Level of formal/informal service use |
Cross-sectional survey of agency service use (e.g. homemaker, home health aide, skilled nurse, hot meals, telephone support, counsellor, transport, senior day care and other) and level of support from family/friends | Employed carers of dependent parents (sampled via three unions and three hospitals in New York) |
Frail elderly 133/177 questionnaires returned |
Recipients: 73% aged over 74 years; 84% female Carers: mean age 49 years; 86% female; 100% children of dependent |
Impact of caring, role strain, mental strain and physical strain (items from various scales) Service use predicted impact of caring but not role strain, mental strain or physical strain. Support from family and friends predicted impact of caring and role strain |
|
Leddy-Barnes et al. 1995 Low |
USA Level of formal/informal service use |
Formal and informal service use (mean number used daily); split by employed, never employed and terminated employment | Recipient 64 years or over; dependent on at least two ADLs/IADLs; family member as primary carer. Recruited via a larger longitudinal study |
Frail elderly 118 |
Recipients: mean age 83.3 years Carers: mean age 54.6 years; 100% adult child (daughters) |
Caregiver reaction (CRA) (impact of self-esteem, impact on health, impact on schedule, financial impact) Excluded: does not relate service use to outcomes |
|
Lorensini and Bates 1997118 Moderate |
Australia Day care |
Day care centres in Victoria. Mean attendance = 3.42 days per week (1.25) | Lived with carer; age 70+ years; clinical diagnosis of dementia (DSM) of at least 6 months duration; Barthel Index at least 60/100 |
Dementia 85 (RR 90%) (45 day care, 40 control subjects) |
Recipients: all aged 70+ years Carers: age 50–80+years; 75.6% female for attendees, 66.7% adult child; 75% female for control group, 47.5% adult child |
Depression (BDI), stress arousal (SACL), life satisfaction (SLS), social interactions Carers not using ADC were significantly more depressed and had higher stress arousal and lower life satisfaction and social activities |
|
Low; high |
USA Home care |
In-home respite: 4–8 hours per week, e.g. health and personal services, socialisation and home management activities | Family carers providing full-time in-home care to frail elderly. Selected randomly |
Frail elderly 50 (25 experimental group receiving respite; 25 control subjects from waiting list) |
Recipients: mean age 79.04 years Carers: mean age 60.3 years; 82% female; 38% spouse; 50% adult child |
Stress and strain (CSI) Carer stress was significantly lower in those receiving respite than in those not when carer age, hours per week caring, carer’s health, amount of household work and carer’s perception of relatives’ satisfaction were controlled for |
|
Mittelman et al. 1995121 Moderate |
USA Level of formal/informal service use |
Number of formal services (not defined) used; amount of paid help (none – day and night); number of days per month help and/or help from family/friends (visits, telephone calls and patient sitting) | Primary carer married; coresident; patient with clinical diagnosis of Alzheimer’s disease. Carers receiving support group or counselling ineligible. Recruited via NYU Aging and Dementia Research Centre and referral from Alzheimer’s Association |
Dementia 206 (baseline interview with carers before supportive intervention) |
Carers: 58% female; 100% spouse |
Depression (GDS) Neither the number of formal services nor the amounts of paid help were related to depression |
|
Mui 1992122 High |
USA Formal/informal service use |
Availability of respite (no information on type or amount) and secondary help (number of people) | Frail elderly: severe impairment in ADLs; referred by service providers or family members. Carers identified by recipients. Baseline of larger study, sample recruited via case management agencies |
Frail elderly 581 |
Recipients: age range 64–90 years; 82.4% female Carers: age range 40–80 years; 100% female; 100% daughters; n = 117 black and n = 464 white |
Role strain (rating 1–5) Black and white carers analysed separately. Perceived unavailability of respite support had a very strong impact on the role strain of black but not white carers |
| Noelker and Bass 1995123 |
USA Level of formal/informal service use |
Use of respite (formal or informal) but also help finding/arranging services, emotional support/counselling, education/training, assistance with other responsibilities | Recipient aged 65 years or over with informal carer, community resident and received case management for at least 1 month. Participants in wider case management programme |
Frail elderly 401 |
Carers: mean age 58.6 years; 75% female; 45% adult child |
Depression (CES-D), health deterioration, relationship strain, social isolation Excluded from narrative; service use the outcome variable |
| Park 2003124 |
Korea Day care |
Use of day care services | Elderly stroke patient with family carer |
Stroke 50 receiving day care, 51 control subjects |
Recipients: mean age 68.8 years; n = 34 female Carers: mean age 58.8 years |
Burden (CBI) Significantly more burden in non-day care group Depression (CES-D) No effect of day care on depression |
|
Penning 1995125 Moderate |
Canada Level of formal service use. |
In-person interviews with carers: number of formal services used: Meals on Wheels; day centre use; hospital/nursing home as respite. Information on use of home help (cleaning and home help for ADLs) | Diagnosis of dementia; carer most responsible for day-to-day decision-making and care. Recruited from Canadian Study of Health and Aging and used cluster sampling; random samples drawn from three age strata |
Dementia 327 |
Recipients: mean age 82 years; 61% female Carers: mean age 62 years; 79% female; 32% spouse; 44% adult child |
Burden (ZBI) Excluded from narrative; service use the outcome variable |
|
Ramirez et al. 2002126 Low |
USA Day care |
12 adult day health-care programmes in New York state | None other than participating in relevant programmes |
Frail elderly 331 |
Recipients: mean age 75.8 years; 73% female Carers: 82% female; 15.8% spouse; 44% child |
Institutionalisation risk Formal support was not associated with readiness to institutionalise the care recipient |
|
Rosa et al. 2004127 Low |
Italy Home care |
Paid home help from immigrant paid carer | Carers of dementia patients (moderate to severe; mean MMSE 14 ± 7). Recruited from patients admitted to Alzheimer’s Research and Care Unit, Memory Clinic, Brescia, Italy |
Dementia 51 |
Carers: mean age 57 years; n = 68 female |
Burden (CBI) Significant reduction in physical, emotional and developmental burden in families with an immigrant carer Depression (CES-D) Carer depression significantly lower with immigrant carer |
|
Tennstedt et al. 1992128 Moderate Same study as Yates et al. 1999134 but phase 1 sample |
USA Level of formal service use |
Use of formal support, e.g. assistance with meals or housekeeping, home health care, transportation or ADC Informal support – whether secondary carers provided any hours of care or any emotional or instrumental support from secondary carer |
Frail elderly (difficulty performing at least two ADLs; difficulty with one ADL and mobility aid; or difficulty with any of above and difficulty with either dressing/health limitation of normal activity or restricted mobility outside home) and primary carers |
Frail elderly 415 |
Recipients: age range 70+ years; 74.7% female Carers: age range 50–70 years; 70% female |
Depression (CES-D) Neither informal support nor the use of formal services mediated depression. In fact, use of formal services was associated with higher levels of depressive symptoms |
|
Wailing Li et al. 1997129 High |
USA Level of formal/informal service use |
Caregiving support: help from informal sources (relatives/friends) and formal sources (aides/service providers). Help with 14 ADLs (yes/no) | Wife/daughter providing assistance to husband/parent with ADLs. Probability sample using random digit dialling techniques |
Frail elderly 252 |
Recipients: mean age 75.8 years Carers: age range 50–80+ years; 100% female (103 wives, 149 daughters) |
Depression (CES-D) Carer support did not have a main or a buffering effect on depression |
|
Warrington and Eagles 1996130 Low |
UK Day care |
Cross-sectional comparison between local authority ‘generic’ day centres (median 2 days per week, 16 months) and NHS day hospitals (dementia specific and carer oriented: median 3 days per week, 11 months) | Coresident carers: MMSE cut-off 23 (or more) |
Dementia 33 day hospital (DH) attendees; 27 day centre (DC) attendees |
Recipients: mean age 81.5 years in DH, 78 years in DC; n = 20 female in DH, n = 16 female in DC Carers: DH mean age 63.5 years, DC mean age 74 years; n = 17 female in DH, n = 21 female in DC; n = 31 spouse; n = 24 adult child |
Anxiety and Depression (HADS), stress (Relatives Stress Scale) No difference between carers of DH vs DC attendees for anxiety or stress. Carers of DH attendees significantly more depressed than DC attendees |
|
Washio et al. 2002132 High |
Japan Level of service use |
Hours per day go out not accompanied by recipient; presence of additional family carer to help. Use of social services not specified | Pairs of carers/disabled elders receiving regular nurse visits | Physical disability (cancer diagnosis) but some with dementia |
Recipients: mean age 79.7 years; n = 9 female Carers: mean age 62.3 years; n = 16 female; 40% spouse; 60% adult child 20 diagnosed as having tumours (five brain tumours, three oesophageal cancers, three colon cancers, two stomach cancers, seven others) |
Burden (ZBI) No relationship between time going out without care recipient and burden or presence of family support and burden, but heavily burdened used more social services |
|
Washio and Arai 1999131 High |
Japan Level of formal/informal support |
Cross-sectional survey: number of hours per day able to be temporarily relieved of care | Carers of disabled elderly who received twice-weekly visits from the practice nurse clinic; age 65+ years; coresident with carer |
Frail elderly 45 carers |
Carers: mean age 60.3 years; n = 35 female; n = 20 spouse; n = 19 child; n = 1 sister; n = 1 daughter-in-law Recipients: mean age 78.6 years; n = 25 female; n = 20 with dementia |
Depression (CES-D) No significant difference between groups (depressed vs not depressed) on time to go out or having someone to help |
| Williams 2005133 |
USA Level of formal/informal service use |
Number of formal services in previous month (homemaker, home health aide, transportation, CT scans, MRI scans, etc.); social support (tangible, emotional and informational support) | Dementia carers. Recruited from larger longitudinal study |
Dementia 720 |
Recipients: mean age 79.2 years Carers: mean age 61.6 years; 78% female. |
Depression (CES-D) Use of formal support predicted more depressive symptoms |
|
Yates et al. 1999134 High |
USA Home care |
Hours per week formal service use – home care, Meals on Wheels, homemaker services, transportation, financial and case management and social work | Carers of functionally disabled elderly. Data from single time point but part of longitudinal Massachusetts Elder Health Project |
Frail elderly 204 |
Recipients: mean age 86.6 years; 75% female Carers: mean age 62.1 years; 68.6% female; 49% adult child; 21% spouse |
Depression (CES-D) Service use not related to depression. Hours of care related to depression and was mediated by carer/care recipient relationship |
Appendix 8 Summary table of quantitative studies published between December 2005 and April 2008
| Study | Country, respite setting and type of study | Description of intervention/s | Inclusion criteria | Health problem and n | Demographics | Carer outcomesa |
|---|---|---|---|---|---|---|
| Carretero et al.139 |
Spain Cross-sectional comparison of users and non-users of home respite services |
Home help service providing support with ADLs. Delivered in the morning for an average of 3 days per week (4 hours per day) | Random selection of users of home help services and those on the waiting list |
Frail elderly 117 users of services and 36 non-users |
Carers: mean age 62 years (16.1); 67% low education, 17% high and 15% no education; 83% not working | No difference between the two groups on carer burden (Zarit Burden Interview) |
| Schacke and Zank140 |
Germany Compared longitudinal changes in day care users vs non-day care users |
Five day care units having staff specially trained in dementia care. Programme offered cognitive stimulation, ADL training or gymnastics. Aimed to stabilise ADLs and promote social activities |
Recipients: medical diagnosis of dementia; ambulant Carers: provide support at least once a week; treatment group used day care at least twice per week and not used in previous year; control group not using day care during study |
Dementia At T2 (9 months) n = 18 in the experimental group and n = 19 in the control group |
Carers: mean age 58 years; 87% female; 41% employed, 46% retired; 57% adult children, 32% spouses, 11% other Recipients: mean age 80 years; 73% female; majority severely demented; mean MMSE 12.7 |
Care-related stress: no effect on assistance with IADL, ADL, psychosocial support and supervision. Significant difference favouring the treatment group for stress associated with patients’ aversive behaviours, carers’ restrictions in personal needs and job–caregiving and family–caregiving conflicts |
| Kumamoto et al.137 |
Japan Use of services provided by LTC insurance system Cross-sectional observational study using structural equation modelling |
Six public services available for long-term care: home help, home nurse, overnight respite, bathing service, adult day services and day care centre. Measured number of services used | Care recipients registered disabled elderly from Matsuyama town in northern Japan, who had applied for services under the long-term care insurance scheme and who were residing with family carers |
Frail elderly n = 82 |
Carers: mean age 60.5 years (13.2); 77% female, 33 daughters-in-law, 16 wives, 12 husbands, nine daughters, six sons; 62% gave 3 hours or less care per day; 70% had some assistance from family; 58% used less than 30% of services available and 27% 30–50% Recipients: mean age 80.2 years (8.8); 60 female; 36 had behavioural disturbance |
Utilisation of services had a negative relation to caregiver burden |
| Yajima et al.138 |
Japan Use of formal services Longitudinal study using logistic regression to predict depression |
Number of services used of home help, day care and short-stay respite |
Female family carers of the disabled elderly, registered at the municipal offices as insured by public long-term care insurance in a large city in Japan Identified as non-depressed (GHQ < 3) |
Frail elderly 235 carers |
Carers: wives 30%, daughters 36% and daughters-in-law 34%; mean age 59.6 years (11.1) Recipients: 60% female; mean age 81.9 years (8.1); 50% married |
Depression using GHQ12 Use of formal services did not predict incidence of depression when adjusting for age, duration of caring, care recipient ADL and behaviour problems. The analyses were stratified by kin relationship (wives, daughters and daughters-in-law) |
| Kang135 |
US Availability of respite Cross-sectional study using logistic regression to predict carer strain |
Yes/no response to the availability of respite |
Spouse and adult child carers providing care to elders with ADL or IADL impairments living in the community Sample recruited via the National Long Term Care Survey (sampled from Medicare files) |
Frail elderly (mixed physically and cognitively impaired) 956 carers |
249 wives, 192 husbands, 386 daughters, 129 sons |
Adult child – predictors were care recipients’ race, disruptive behaviours, perceived overload, family disagreement, limitations on carer’s life, personal coping strategies and availability of respite Spouse carers: similar but not elders race or availability of respite |
| Droes et al.141 |
Holland Carers of dementia patients attending the programme compared with carers of patients just attending day care Quasi-experimental longitudinal design |
Social day club 3 days per week for the care recipient to provide respite, and support for the carer in the form of informative meetings, discussion groups and social activities to improve knowledge and sense of competence and emotional support | Caring for person with moderate to severe dementia at least 1 day per week and willingness to use the support offered |
Dementia 71 carers in the experimental group and 13 in the control group |
Carers (experimental/control): 16%/23% male; mean age 64/60 years; 93%/69% married/cohabiting; 16%/30% employed; 64%/38% partners; 26%/53% daughters Recipients (experimental/control): 21%/61% moderately severe to severe dementia |
Outcome GHQ12 No significant effect Significant interaction between loneliness and group: carers who felt lonely at the start of the support befitted significantly more from the intervention than normal day care Significant effect on time to institutionalisation: significantly fewer in the intervention group were institutionalized at 7 months |
| Whitlatch and Feinberg136 |
US Agency-based and direct-pay in-home respite Cross-sectional comparison of two types of respite provision |
Direct pay: vouchers given to carers to hire and manage their own respite workers Agency: agency provided in-home respite |
Carer the person primarily responsible for day-to-day care of a cognitively impaired adult living in the community receiving in-home respite provision from one of 11 caregiver resource centres. Direct-pay clients receiving respite from family or friends |
Cognitively impaired 116 carers: direct pay n = 39; agency n = 77 |
Carers: 75% female; 16% employed full time; mean age 59 years (range 22–96 years); 79% spouses; 95% cohabiting with care recipient; 90% married; 83% Caucasian Recipients: mean age 65 years; 42% female |
No difference in levels of depression (CES-D) between groups Caregivers who hired family or friends were slightly more satisfied than carers who hired service providers |
Appendix 9 Summary tables of qualitative studies
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Bamford and Bruce 2000159 Moderate |
15 care recipients and six carers from resource centre for older people with mental health problems (dementia but excluding severe cases). All attending for day or respite care. Six carers also interviewed |
Convenience Focus groups (up to five) and informal discussions with recipients and (semistructured?) interviews for carers |
Six carers: three daughters, one son, one granddaughter; one spouse, four employed, one retired 14 female care recipients; aged 60–90+ years; eight lived alone; 14 used day care; five had regular respite; and seven used home care |
Purpose: to identify desired outcomes of community care |
English UK |
No theoretical framework Thematic analysis |
Having a say in type of service provision and by whom an important outcome for recipients and carers. Service users need to feel valued and respected, and be treated as individuals Social contact and integration; meaningful activity and stimulation (for care recipients). Maintaining sense of autonomy and personal identity; feeling safe and secure; clean and comfortable |
|
Bowes and Wilkinson 2003164 Low |
Four case studies: South Asian families of people with dementia One had home help and one had attended day care |
Purposive Semistructured interview |
Three female care recipients and one male having diagnosis of dementia Indian and Pakistani |
Views of dementia care |
English Scotland, UK |
Multiple case study Thematic analysis |
One had received day care, otherwise not in receipt of respite. Access to support limited Expressed need for home respite. Residential care seen as insensitive to South Asian needs |
|
Butterworth 1995166 Low |
Case study of daughter caring for mother with dementia who used various respite services |
Case study Transcript of participant’s own version of experience of caring |
Daughter carer for 15 years – no details of characteristics | Experiences of caring and support services |
English UK |
Case study No details of analysis |
Difficulty in accessing appropriate service. Poor training of support workers in relation to dementia. Lack of continuity – confusing. Transport to day care problematic – long waits, patient left at gate. Deterioration in condition after in-hospital respite Essential that respite should be a good experience for both care recipient and carer. Bad experiences result in guilt and reluctance to use respite. Professionals need to understand needs of carers and make allowances |
|
Gillies 2000170 Low |
20 carers of people with dementia attending day care |
Sampling strategy not given Not clear what type of interview |
No systematic details on the sample | Examines the experiences of carers who have accepted help in order to maintain their caring activities |
English UK |
No theoretical framework Thematic analysis |
When there is a conflict of need (care recipients may not want to go to day care) this results in emotional turmoil. Efforts to get the care recipient to day care result in stress and guilt in the absence of more flexible forms of respite There is ambiguity about who is expected to be the beneficiary of day care. Relationship with carers unspecified and more informal |
|
Innes et al. 2005175 High |
15 service users with dementia and 16 carers (+ focus groups with further 14 carers) in rural Scotland. Recruited via voluntary sector |
Purposive Semistructured interview and focus group |
Service users: four males, 11 females; 14 aged 60–99 years. Carers: eight male, 22 female (aged 40–89 years) | Views of dementia care (mainly respite) |
English Scotland, UK |
No theoretical framework given Thematic analysis |
Transport and practical difficulties involved in getting to respite, e.g. day care. Expression of unmet need for flexible respite services that suit carer and home care. Respite benefits for recipient (social life, stimulation) and for carer (free time, peace of mind) |
|
Koffman and Taylor 1997182 Low |
12 dementia carers Sample recruited from respite service provider lists, so all current or recent respite users |
No details of sampling strategy Focus group |
None given | Views of respite services and carers needs |
English UK |
No theoretical framework and analysis not described |
Criticisms of lack of flexibility and quality of services. Ignoring carer’s specific needs can contribute to rather than ameliorate stress. These negative factors can prevent service use Positive views – respite can enhance the quality of life of dependents |
|
Pearson 1988199 Low |
25 carers of older people with a diagnosis of dementia admitted for preplanned respite care (68% severely impaired) to a psychogeriatric unit |
25 consecutive admissions Survey and semistructured interview |
Carers’ mean age 65 years (31–83 years); eight men; 56% spouses and 28% offspring; 72% lived alone with care recipient; 40% attended day care; 8% had sitting service | Advantages and disadvantages of respite for carers |
English UK |
No theoretical framework to the study and no details of analysis of qualitative data |
Advantages: made care easier – either could not continue care without respite or prevented a nervous breakdown. Most wished to continue caring Time used for domestic chores, holidays or outings. Most saw it as a relief of strain Disadvantages: just under half saw no disadvantages. Of the rest, reports of difficulties visiting; change in the patient; feeling sad or lonely; feeling guilty; criticism from friends and relatives |
|
Pickard and Glendinning 2001201 Low |
12 carers of family members with dementia recruited from CPN home nursing service Three attended day care and also respite, two used respite only |
Random sample Semistructured interview |
All coresident; all caring for spouses except one caring for brother | To examine the caregiving experience and support from CPNs |
English UK |
No theoretical framework No details of analysis |
All had reservations about respite; those who used it felt that it had a negative impact on the care recipient in terms of a deterioration in their mental condition, distress and physical adverse consequences, e.g. falls. Concerns about the quality of care |
|
Upton and Reed 2005211 Moderate |
46 spouse carers of demented elderly: nine received residential respite, 21 day care and 17 had no respite (one received both day and residential care). Recruited by three CPNs |
Convenience sampling Semistructured interview |
Mean age of carers 77.3 years. Mean duration of caring 3 years | Carer perceptions of day and short-term residential respite care |
English UK |
Phenomenology Thematic analysis |
A desire for some relief from caring was expressed by all carers but all were also wary of respite. There was a fear of dependency (third-party reliance), fear of making spouse worse, fear of upsetting spouse and fear of making decisions There was a direct relationship between the duration of respite and sufferer decline |
|
Watkins and Redfern 1997214 Low |
26 carers of patients attending CREST, a night institutional respite service. Attended for 1–4 nights per week |
All carers of dementia patients attending CREST Semistructured interview within 1 week of first attendance and 6 weeks, 12 weeks and 6 months |
13 wives, three husbands, seven daughters, one son, one sister, one male friend. Median age of patients 80 years. All suffered from dementia | To evaluate the night hospital service |
English UK |
No theoretical framework Analysis not described |
Positive feelings about CREST were attributed to feelings of both respite and the quality of care received. For those emotionally attached to the care recipient the advantages were being better able to cope with the carer role and to go on supporting the care recipient at home. Benefit to non-emotionally attached was respite (these carers were more likely to consider admission to long-term care) |
|
Wenger et al. 2002215 Low |
40 carers identified in a larger study screening for people with dementia Respite: nine day care, five planned hospital respite, nine emergency hospital respite, five day hospital |
All carers of dementia sufferers identified in a screening questionnaire Semistructured |
31 female carers (35% daughters, 18% wives, 15% other relatives, 10% non-relatives); nine male carers (13% husbands, 10% sons); 77% of all carers over 50 years; 27 co-resident; 23% received respite |
1. Problems faced by carers 2. Impact of caring 3. Experiences of formal and informal support |
English UK |
No theoretical framework Type of analysis not described |
Sometimes services not utilised because of refusal of care recipient. Day care valued and considered by some as the most useful service, followed by respite. Respite more important to adult children to meet other family responsibilities. Delays in receiving services, e.g. home sitters, resulted in receiving them too late. Most carers satisfied with services except for a few instances of poor quality (quality = timeliness and sensitivity) |
| Author | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Ashworth and Baker 2000157 High |
23 carers utilising a range of respite care services: day care, residential care and care provided by social services and NHS, and a sitting service provided by voluntary sector. Recruited via these services |
Purposive Semistructured interviews |
14 female; age range 14–85 years; mean 65 years; all but one coresident; 26% Black African; mean years caring = 12 Mean age of care recipients 72 years |
Views of caring and respite care |
English UK |
Grounded theory and thematic analysis |
Respite important for a sense of normality – time used to do everyday things. Respite gave a sense of freedom and space – releasing from the ties of the carer role. Respite viewed as an admission of failure Concern on quality of care – particular problem with transport services. Planning involved in preparing for respite a burden in itself. Respite care enabled the carer to continue caring |
|
Ashworth et al. 1996158 Low |
21 carers of physically impaired users of respite services (mean use of 1 week inpatient care per 8 weeks) |
All patients accessing service approached; 21/42 carers responded Open questions on postal survey |
12 female, mean age 56 years (22–72 years) Mean age of care recipient 72 years |
Evaluation of respite care for physically dependent people |
English UK |
Analysis not described |
Satisfaction with the service was high. Problems encountered were disengagement from care recipient; guilt; visiting found tiring; respite too short; care recipient did not look forward to admission; food poor Benefits were rest and relief from strain; enabled continuation of caring; benefits to care recipient such as physiotherapy and companionship |
|
Hanson et al. 1999172 Moderate |
A group of 6 family carers of frail elderly, both demented and non-demented. Some recruited via carers organisations. Some used respite |
Purposive sampling Focus group using semistructured interview |
Five female; age 58–83 years, all co-habiting; all retired; duration of caring 11 months–47 years; two wives, one husband, three daughters | Explores respite needs in relation to information, education and support |
English UK |
Constant comparative technique Content and thematic analysis |
Carers need education about respite care before specific information about services, they had difficulty determining what services are available Carers had positive feelings about respite care but also felt guilty and at a loss as to what to do with respite time |
|
Heenan 2000173 Low |
13 farmer’s wives caring for elderly relatives. None receiving formal respite |
Sampling strategy not given In-depth interviews |
13 carers Care recipients: 12 mothers-in-law and one father-in-law, nine coresiding, four independent and four frail elderly with variety of disabilities |
Dynamics of family caregiving in this particular culture |
English Northern Ireland |
None given and no details of analysis | Assistance from social services was stigmatising and an admission of failure. Respite schemes were dismissed as irrelevant. Respondents felt that it would not be acceptable to the care recipient, and there were concerns about the quality of care |
|
Jarrett et al. 1999177 Moderate |
12 carers and nine care recipients. Interviews focused on the experiences of 12 terminally ill care recipients, 11 with cancer and one with motor neurone disease, receiving a variety of community-based services |
Carer and care recipient interviewed separately in all but four interviews, which were joint. Convenience sample recruited by community nurses Semistructured face-to-face and telephone interviews |
Carers: six wives, one husband, one mother, one father, one daughter, one son, one neice Care recipients: mean age 67 years (range 38–81), eight male, 11 white, one south Asian; four prostate cancer, four lung cancer, one bladder cancer, one tongue cancer, one glioma, one motor neurone disease |
To examine ways that effective community-based support was, and could be, provided for terminally ill patients and their lay carers |
English UK |
Thematic analysis. No underlying theoretical framework | Marie Curie nurses were considered mainly a form of respite (for a night’s sleep or to get out during the day). There were perceptions of delay, rationing and inequity of service and problems with continuity. There was a belief that the state should provide help, but for some there was a reluctance to ask for help and to be a ‘burden on the state’ |
|
Kerr and Smith 2001179 Moderate |
22 carers (16 > 60 years) of stroke survivors (1 year post stroke) who were not dependent on a carer prior to stroke One used sitting service, one used regular respite |
Convenience sample All patients meeting inclusion criteria identified from hospital records In-depth interview |
Median age 61 years; 13 female; 18 married; 15 spouses/partners; one son, five daughters; one daughter-in-law Care recipients: 10 female |
Exploring the carer’s experience of caregiving |
English Scotland |
Not stated Thematic analysis |
Few carers had received a break and there was obviously a physical and emotional toll Carers felt it important to maintain their own health in order to continue caring and that a break from care was important, but most preferred to have additional support in their own home rather than institutional respite |
|
Lane et al. 2003185 Moderate |
10 carers recruited via social services. Not clear what services received |
Random sample following survey In-depth unstructured interview |
Three urban and seven rural dwelling carers. No further details | To explore the perceived health and social care needs of family carers of older people and their experiences of home care |
English Ireland |
No theoretical framework Thematic analysis using framework analysis format |
Participants expressed the importance of maintaining care recipient in the home and a preference for home respite. Respite was considered vital in sustaining the carer role but there was little information available and some had never been offered respite. Respite and other support services considered inadequate |
|
Low et al. 2004190 Low |
40 carers of stroke survivor car recipients taking part in an RCT of day care vs domiciliary stroke team |
All identified carers of stroke survivors taking part in the RCT (n = 106) were approached Semistructured interviews |
Carer mean age 68 years (13.1); 72% female; 78% retired; majority were wives and most lived with care recipient who were generally mildly to moderately disabled with a large minority severely disabled | To assess carer views and preferences of day care and domiciliary stroke teams, and how these affect quality of life |
English UK |
Content analysis followed by thematic analysis on 15 transcripts | Advantages of domiciliary team mainly therapeutic whereas advantages of day care mainly in terms of respite and social advantages. There were feelings of guilt but use of day hospital was justified in terms of benefits to care recipient. Carers also saw it as a social opportunity for car recipient and therefore of therapeutic benefit |
|
Low et al. 2005189 Low |
12 carers of patients attending a palliative care day centre |
Purposive sampling Focus groups |
Mainly female: median age 69 years; age of care recipients not given | Assess perceived benefit and impact of PCDS on quality of life |
English UK |
Thematic analysis | Respite the main benefit. Carers felt confident that patients were well cared for, which gave them peace of mind |
|
McGarry and Arthur 2001193 High |
14 carers taking part in > 75 year health check in Melton Mowbray, Leics | Semistructured interview | 10 (71%) female; age 76–92 years; 13 spouses and one sibling | To identify needs of carers and impact of caring |
English UK |
No theoretical framework Thematic analysis |
Fear that care recipient would feel rejected and so home respite preferred Feeling that only carer could provide appropriate standard of care Carers place their own needs second Would prefer home respite but no formal services available. Voluntary service available but did not meet needs (insufficient time) |
|
McLean et al. 1991195 Low |
20 carers of stroke survivors. Not clear how recruited Five used day hospital, three used hospital respite |
Sampling strategy not given Semistructured interview |
15 female and 5 male; Mean age 59 and 52 years respectively, 17 coresident; three employed part-time | To discover areas of perceived need of stroke survivors and their carers |
English UK |
No theoretical framework ‘Content analysis’ but no details on process |
Majority of carers said that they would use a sitting service (service available but not known about). Day hospital much appreciated Seven carers felt tied down due to lack of temporary relief. Those who received respite felt it helped them cope although they still continued to visit spouse daily rather than take a holiday |
|
Netto 1998198 Low |
45 minority ethnic carers of sick, handicapped or elderly person; sample identified through voluntary organisations and home care providers None used respite |
Convenience sample In-depth interview |
15 Chinese, 15 Pakistani, eight Indian, three Bangladeshi, two Afro-Caribbean, two other Asian | Needs for respite and preferences for service delivery |
Study in English, but interviews used interpreters when necessary Scotland |
None given, but semiquantitative (proportions given) | None used respite. One-third would as long as the sitter spoke the same language. Gender matching also important. Most reacted negatively to residential respite. Concern that care recipient would be unwilling, that they would be unable to communicate with others and would not have access to appropriate food |
|
Skilbeck et al. 2005204 High |
25 carers of care recipients with cancer or neurological conditions recruited via a palliative care unit. All receiving 2 weeks’ inpatient respite |
All people accessing the service approached Semistructured interviews before and after respite |
23 female; age 38–78 years, mean 61 years: two-thirds of care recipients over 65 years, 16 married, duration of care 6 months– 20 years, mean 6.5 years, 16 spouses 15 had cancer and 12 had neurological conditions |
Explore carer expectations and experiences of respite |
English UK |
Constant comparison, thematic analysis | For the majority, expectations of respite were met. Satisfaction with high standard of care, although small number dissatisfied with administration of drugs and mobilising. A large number required more information about respite provision. There was some difficulty with the negative connotations of hospice care, but hospices were considered to provide higher quality of respite care than other options |
|
Ward and Cavanagh 1997213 Low |
103 known to voluntary services (48 carers of frail elderly or those with dementia, the rest younger care recipients) |
Systematic non-probablistic Focus groups |
Not given | Needs of carers |
English Scotland |
Not given Analysis not clear |
Barriers: some care recipients reluctant to use respite, and some carers felt guilt Respite a vital need, common to all carers. Respite had to be flexible i.e. available in emergencies, over weekends, and during holiday periods, and not requiring booking months in advance |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Beisecker et al. 1996161 Low |
104 carers of people with Alzheimer’s disease who had used ADC (52) or not (52) |
Volunteers to flyers and adverts Semistructured telephone interview |
Mean age of carers 64 years; 71% female; 62% spouses; 14 years of education; 15 using ADC at the time of interview and 37 discontinued Care recipients’ mean age 77 years; 56 female |
Benefits of and barriers to use of ADC |
English USA |
No theoretical framework Analysis depended on coding and reporting of frequencies of codes and to some extent thematic analysis |
Benefits to carer were respite, preservation of physical health and emotional relief; allow carer to give better care and for a longer time; freedom from worry. Felt that care recipient benefited from stimulation, socialisation, safety, physical health, self-esteem and enjoyment. Staff knowledge seen as benefit Barriers: lack of convenience; hours of operation; location; difficulty in getting care recipient ready and transport problems; perceptions of patient unhappiness, safety, physical health, functional levels and behaviour; lack of information |
|
Brody et al. 1989165 Low |
305 carers of Alzheimer’s disease patients taking part in a study to evaluate a multiservice respite programme and case management | Recruited via support groups and local service agencies, advertisement and word of mouth to an RCT. Case studies reported and qualitative descriptive report of assessments |
Carers: mean age 60 years; 45% spouses; 39% children; 72% married; 78% women; 34% employed; 25% black Recipients: mean age 76 years; 60% female; 50% married; 8% lived alone |
Evaluation of Philadelphia multiservice respite project using a case management approach |
English USA |
Analysis strategy not given |
Just over half took up respite, two-thirds using home care. Reasons for reluctance to use respite: difficulties preparing care recipient for respite; transportation problems; lack of availability; carers felt that it was their responsibility to care; reluctance to allow strangers into home; care recipient distress; care recipient behaviour problems; quality of care In-home respite most popular, institutional least. Most carers put the needs of the care recipient before their own |
|
Cotrell 1996167 Moderate |
100 carers of dementia sufferers recruited through agencies and organisations such as Alzheimer’s Association 52 received various respite provision |
Convenience sample Open-ended questions concerning service preference, reasons for initiating or not using services, as part of structured interview |
52 (16 male) spouses; 48 (three male) adult children; most (except 17 adult children) resided with care recipient |
1. Why do carers use/not use respite? 2. Carers’ perceptions of services and preferences for delivery |
English USA |
No qualitative framework Responses coded according to common categories |
In-home respite preferred by spouses, day care by residing children and no strong preference by non-residing children. Spouses tended to feel more guilt on using day care and were more sensitive to care recipients’ wishes and needs. There was a dislike of strangers in the home and familiar people often utilised. Formally provided overnight respite least used and understood by spouses. Adult children more positive about overnight respite Data also given on reasons for initiating respite |
|
Dziegielewski and Ricks 2000103 Low |
26 carers of dementia care recipients taking part in an ADC programme | Carers taking part in ADC programme. Survey – open-ended question | Carers: 31% male; mean age 62 years; 80% white; caring for 3–10 years | To investigate the effects of ADC on carers |
English USA |
Open question on survey No theoretical or analytical framework |
Dislikes: cost; lack of transport and limited hours. Likes: gave them free time; relative was well cared for; relative had the opportunity to socialise; caring and supportive staff; safe environment; relieved carer stress |
|
Farran et al. 2003169 Moderate |
16 carers of care recipients with dementia taking part in an RCT of carer skill building vs information and support Some using various respite facilities |
Purposive Typed facilitator comments made after the weekly group intervention sessions based on open discussion and questions |
Majority of carers female, married, living with care recipient, spouses or daughters/in-law, white; mean age approx 64 years | To explore carer issues |
English USA |
Content analysis |
Major concern was how to locate and utilise services such as day care and respite, but had mixed feelings about using them – feelings of guilt Recognised the need for self-care and getting a break was an important aspect of self-care |
|
King et al. 1995181 Moderate |
34 carers of people with dementia, some of whom received respite and some not 32% used day care, 6% had used day care, 65% used or had used a home health aide, 59% used or had used a support group |
Convenience sample from non-random longitudinal survey Semistructured interview |
79% of carers female; 50% daughters or daughters-in-law (mean age 52 years); 50% spouses (mean age 71 years); 26% worked full time, 11% part time and the remainder did not work; caring for 1–10 years, mean 3.7 years | To describe values of carers and how they relate to service use |
English USA |
No theoretical framework Content and thematic analysis |
Barrier to service use is need to trust the carer to be honest and to provide good-quality care. Need to be able to reciprocate for help received so sometimes formal help more acceptable. Fear of dependence on others. Family attitudes of self-sufficiency and keeping difficulties within the family |
|
Lampley-Dallas et al. 2001184 Moderate |
13 carers of dementia sufferers recruited via day care, nursing home staff, local churches, families and friends using a variety of services |
Convenience sample Focus groups |
11 female (three wives, eight daughters), two male (sons); mean age 54 years; six had been caring for > 5 years; eight were employed; seven married, four widowed, two divorced; seven co-residents |
1. Carers’ needs and expectations of health-care system 2. Stress experienced in interacting with the health care system |
English USA |
No theoretical framework Thematic analysis |
Barriers to use were lack of knowledge and negative experiences such as demeaning attitudes of staff Day care most utilised service. Primary expectation was for respectful and dignified treatment, described as ‘sensitive’ and ‘good-quality care’. Expressed a need for well-trained staff, with specific training in dementia care. General dissatisfaction with nursing home care |
|
Liken and King 1995188 Moderate |
32 carers of dementia sufferers aged 50 years or older; recruited via Alzheimer’s Association and primary care; using home health-care service 16 used home health aide, three used in the past, 13 never used |
Convenience sample recruited from larger survey Semistructured interviews |
25 female, seven male; 16 spouses, 15 daughters, one sibling; 11 working; age 40–85 years; caring for 1–10 years; 19 used home health-care service | To identify structural barriers to use of home health-care nurses |
English USA |
No theoretical framework Type of analysis not specified |
Feeling that the cost of home health-care services was high and that the service did not meet expectations. There were hassles in obtaining and managing home health care. There was a discrepancy between the type of help needed and the type available. Quality of service – workers not adequately trained in care of dementia. However, many benefits as some found the service invaluable if the worker was caring and conscientious |
|
MaloneBeach et al. 1992191 Low |
46 dementia carers using case management; 14 used respite, 11 used day care, 13 used respite from informal sources |
Convenience Semistructured interviews |
18 spouses, 23 adult children, five other relative; mean age 55 (14.5) years; 29 reside with care recipient | Views of case management and use of and satisfaction with community-based services |
English USA |
No theoretical framework and no details of analysis | Concerns raised over quality of care, lack of control over scheduling, and system inflexibility. Preferred in-home care, with little interest in day care. Important that respite directly benefited care recipient also |
|
Martin-Cook et al. 2000192 Low |
Four carers of care recipients with Alzheimer’s disease taking part in a needs-based case management intervention. Various respite provision | Case studies of participants in the intervention programme | All female; ages 69, 57, 37 and 76 years; two daughters and two wives | Descriptive assessment of the programme for needs-based assessment of care needs for carers |
English USA |
Analysis strategy not given | Participants generally reluctant to relinquish care; one viewed it as her responsibility to look after her husband and another felt that the care recipient’s behaviour would be an embarrassment to her and a barrier to him taking up day care. Once participants had experienced respite they gained benefit |
|
McGrath et al. 2000194 High |
Five carers recruited through support groups for Alzheimer’s disease Varied respite provision |
Convenience sample of volunteers Semistructured interview |
Four females (two adult children, two wives), one male (husband), age 57–72 years; age of care recipients 68–84 years; all white |
1. To assess perceived influence of respite on self-care, leisure and work 2. Reasons for use/non-use of respite |
English USA |
Phenomenology Content analysis and cross-cases analysis |
Respite only sought if beneficial to both carer and care recipient. Ability to get a mental break seen as crucial to coping with other issues in carers’ lives. Short regular respite allowed this mental break. Chores such as shopping, etc. were prioritised during respite time over leisure pursuits |
|
Teitelman and Watts 2004210 Moderate |
15 dementia carers caregiving for at least 6 months; no details of respite provision |
Purposive In-depth guided interview |
13 female; nine spouses; three African American; mean age 63 years (range 47–88 years) | How carers achieved a mental break from caregiving |
English USA |
Phenomenological Thematic analysis |
Barriers to respite: belief that seeking relief or assistance is selfish and that nobody else can provide high-quality care; not trusting that loved one is safe; feeling rushed for time even when care recipient is in the care of others; care recipient’s negative emotional responses when carer is away |
|
Winslow 2003210 High |
21 carers of elderly diagnosed with dementia, attending support groups in California |
Convenience Semistructured interview |
14 women; 15 spouses, six adult children; mean age 69 years (mean age of recipient 79 years) | Experience of community services (not just respite) |
English USA |
None?? |
Refusal of recipient to leave house, feeling of guilt/worry/shame on part of carer, worry about cost of community services, concerns about quality of care and being too tired to access services/too much bureaucracy Sense of support from shared experiences (although not respite?). Time for themselves, being able to relax and recognising benefits to care recipient, e.g. stimulation/companionship |
|
Winslow 1998218 High |
Case study of wife caring for husband with dementia in receipt of formal support services (day care) |
Participant chosen as revelatory case from interviews with seven carers Unstructured in-depth interviews |
Carer 76 years, care recipient 81 years; no family support; financially secure; married 31 years; caring for 8 years | Exploration of experiences of formal support services |
English USA |
Case study approach Thematic analysis |
Outcomes of day care for carer were a sense of freedom, relief and renewal – only possible because of the quality of care and effect of formal support on care recipient (care recipient enjoyed day care). Negative effects were guilt. Reluctance to use home care. The day care acted as a stepping stone to residential care |
|
Wykle and Segal 1991222 Moderate |
40 carers of Alzheimer’s disease sufferers (aged 60+ years) who were receiving day care |
Sample identified by directors of day care; non-random and non-purposive Structured interview with additional open questions |
Carers: 20 black and 20 Caucasian; mean ages 57 years (range 29–82 years) and 64 years (range 28–87 years) respectively; 90% women; 70% married; 25 daughters; 37% employed; caring 10 hours a day, duration 3 years Recipient: median age 79 years; 73% female; more than moderately impaired (Blessed scale) |
What are the problems and stresses for black and Caucasian carers? How do coping strategies of black and Caucasian carers differ? |
English USA |
No theoretical framework Analysis of open questions based on frequency of responses |
Inadequate respite was the most frequent response by black carers to a question concerning the single most difficult problem in caring. This resulted in inability to get away for socialisation, fatigue and lack of sleep. Only 10% of white carers said that they needed more respite Both groups felt that the hours and days available at day care needed to be increased |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Bedini and Guinan 1996160 High |
16 carers of older people recruited through adult day care centres and support groups |
Theoretical sampling Semistructured interview |
All female; all coresident; age range 34–77 years; eight employed; 10 daughters, two daughters-in-law, one great niece, two wives; duration of caring 1–11 years | Views on perceptions and caregiving and leisure |
English USA |
Constant comparative technique Thematic analysis |
Fear of leaving care recipient and of the quality of respite care. Services such as day care did not fit in with needs for leisure Reasons for not using the service – bad experiences or concerns about finance or quality of care |
|
Caserta et al. 198796 Low |
597 carers of mixed group (community dwelling) taking part in a survey | Sample identified via support groups |
Carers: 74% female; 87% married; 94% white; mean age 60 years; 57% spouses, 27% adult daughters; caring for mean of 4.3 years; 50% caring for at least 16 hours per day Recipients: 55% female; 73% married; 69% Alzheimer’s disease |
Identification of service utilisation patterns and factors associated with service use |
English USA |
Open question on a survey. Content analysed | Reasons for not using services – a lack of immediate need; carers did not want to leave care recipient with a stranger; care recipient presented too many behavioural and emotional problems; or services such as day care, respite or home care were too expensive |
|
Hennessy and John 1996174 Low |
33 carers of impaired elders from five reservation-dwelling American Indian tribes; no details of respite |
Convenience sample? Focus groups |
88% women: spouses, siblings, in-laws, adult children, grandchildren | Views of their situation and need for support services |
English USA |
Grounded theory? Thematic analysis |
Participants felt that their well-being depended on the availability of respite (particularly those with heavy care demands). Those who did not get a break had highest burden Carers preferred long-term care services that supplemented family support |
|
Lewis et al. 1995187 Moderate |
Five carers of older parents aged 65+ years recruited via a home health-care agency |
Sampling strategy not given Semistructured interviews |
All women, aged 35–73 years; three employed, one retired and one unemployed Recipients – four fathers, two mothers; age of care recipients 67–93 years |
To explore and validate the needs of carers of elder parents |
English USA |
Ethnography Thematic analysis |
Need for time off but services not available. Expressed a need for a sitter service, of people appropriately trained, within financial constraints, flexible to respond at short notice |
|
Piercy and Dunkley 2004202 High |
35 carers of care recipients with ADL limitations in receipt of home care services at least once a week |
Theoretical sampling Unstructured interview |
Four spouses, 30 adult children, one other; mean age 55 years | Meaning of quality home care services to carers. Respite reported as a theme |
English USA |
McCracken’s (1988) multistage process for analysis | Home care provided free time to do other things but the kinds of relief were usually of short-term duration. The respite enabled carers to endure in caring and prevented burnout. Also provided relief from emotional stress. Negative experiences with workers resulted in loss of respite and increased emotional distress |
|
Valadez et al. 2005212 High |
15 Mexican Americans with elderly mothers attending a day centre for a minimum of 3 years at least three times per week. None had dementia |
Convenience sample recruited by directors of day care centres Semistructured interviews |
14 female carers and one male; aged 24–55 years; all employed and earning over US$10,000 per year | Carers’ views of how ADC centres might buffer stress |
Interviews mainly in English with some utterances in Spanish Southern Texas |
None given Thematic analysis |
Day care relieved guilt of leaving parent on their own for long hours whilst in work. Allowed carers to spend more time with their families; care recipient’s demands less intense as health was better and carer did not feel obliged to spend every hour off work with the care recipient Care recipient’s mental and physical health improved |
|
Worcester and Hedrick 1997220 High |
30 carers of physically impaired (15) and cognitively impaired (15) (no mixed) recipients; carers coresident; six used day care – for four it was a one-time use because of refusal by the care recipient |
Theoretical Semistructured interview Sample recruited via Veterans’ clinic in US |
28 female; mean age 68 years; 76% spouse; all caring for at least past 6 months | Aim was to explore feelings associated with using respite/reasons for non-uptake |
English USA |
Grounded theory using constant comparative analysis | Dilemmas in using respite: knowing (i.e. worries that formal carers will not understand receiver and hence not give proper care); imposing (on carers and also of being imposed on, i.e. in-home help); matching (concerns that carer is likely to get on with recipient). Conservation of energy/resources (e.g. financial and hassles) |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Morgan et al. 2002197 High |
Four dementia carers (all adult children) in rural Canada |
Convenience Focus group |
No information | Barriers to use of respite |
English Canada |
None | Stigma of dementia, lack of privacy in rural communities, not wanting to admit they needed help, accessibility of services all barriers to use |
|
Perry and Bontinen 2001200 High |
19 carers of dementia patients who used a weekend respite programme |
Sampled all users of the programme over 6 months Semistructured telephone interviews |
14 females (eight wives, three daughters, one granddaughter and two sisters), five male (two husbands, three sons); age 28–80 years, median age 65 years; programme used 1–12 times | To evaluate a weekend respite care programme |
English Canada |
No theoretical framework given Thematic analysis using a constant comparative technique |
Carers used respite to fulfil their own needs but could only achieve respite if they felt that care recipients were also benefiting. Used respite to rest, deal with their own health issues, socialise, give time to family |
|
Strang and Haughey 1998207 High |
10 carers of dementing elderly; eight used ADC, three institutional respite, eight personal care at home, two in-home day sitter, one in-home night sitter; one used no formal services |
Sampling strategy not given Two unstructured interviews per person |
Eight female; all spouses except for one son; mean age 70 years; caring for 1–10 years | To describe carers’ experiences of respite |
English Canada |
Grounded theory Thematic analysis |
Factors affecting take-up of respite – nature of pre-illness relationship (e.g. giving in to care recipient wishes); role expectation; attributes of respite services (acceptability of the service to the care recipient); time (length of time caring and extent of behavioural deterioration of the care recipient) |
|
Strang and Haughey 1999208 Same study as Strang and Haughey207 above |
10 carers of demented elderly receiving respite; recruited via voluntary self-help groups |
Volunteer sample from self-help groups and home care agencies In-depth loosely structured interviews |
Eight female, two male carers; mean age 70 years (range 47–82 years); all retired (except one); mean time caring 5 years (6 months–10 years); all care recipients had dementia | How carers experience respite |
English Canada |
Interpretivist Thematic analysis |
Three phases to accepting respite – recognition of need for respite, coming to the resolution that it is acceptable behaviour, and realising the availability and adequacy of social support resources. Short intervals, e.g. day care often, only allowed chores to be carried out; longer respite more rejuvenating. Sometimes respite viewed more as a cognitive process than an actual one |
|
Strang 2000205 High |
20 carers of people with dementia recruited from home care agencies and informal community connections; no details of respite service provision |
Sampling strategy not given In-depth unstructured interviews |
16 female; age range 45–85 years, mean 67 years; 13 spouses, six adult children, one niece; 18 coresident | How do respite experiences influence the return of carers to the caregiving situation? |
English Canada |
Qualitative interpretivist research perspective Thematic analysis |
Factors influencing the experience of return to caring: duration and quality of respite interval; nature and quality of respite service; condition of care recipient on return Outcomes included improved relationship; having more energy; greater tolerance; improved sense of humour Negative outcomes: short-term despondency; guilt; emotional devastation |
|
Strang 2001206 High |
Eight female spouses of dementia patients in a city in western Canada |
Convenience Unstructured interview |
Age range 66–82 years (mean 73 years); all coresident | To examine the respite experience |
English Canada |
Feminist theory relating to leisure?? Thematic analysis using integrative diagramming |
Commitment/sense of duty: belief that no-one else would be able to provide adequate care. Guilt regarding accessing services that only benefit carer Positive effects on emotional well-being; free time for leisure; removal of worry |
|
Wuest et al. 2001221 Low |
15 dementia carers recruited through community care agency Use of various services: day care, respite care and homemaker services |
Convenience and snowball sampling Interviews |
11 women and four men; one sibling, eight spouses, six adult children | Explores the impact of connected and disconnected social support (helpful and unhelpful support) |
English Canada |
Grounded theory Continuous comparative analysis |
Day care seen as a good respite service with some carers learning new ways of caring from it. Did not fit with employed carers’ hours. Residential respite was not always readily accepted by care recipient and carers not always satisfied with the care given. Most important is that service provision is matched to need |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Michallet et al. 2001196 Low |
Six spouses of stroke survivors with severe aphasia; not clear how recruited No detail of respite services |
Sampling strategy not given Semistructured interview |
Carers: five female; age range 59–71 years Recipients: five male; age range 64–77 years |
To identify the perceived needs of carers of aphasic people |
English Canada |
No theoretical framework Thematic analysis |
Carers expressed a clear need for respite to include physical rest and psychological distance |
|
Ritchie 2003203 Moderate |
Seven carers of older people (mixed disabilities); only one had experience of day care use |
Sample were all members of a carer group; convenience sample One individual interview and remaining participants took part in a focus group |
Seven females; mean age 65 years; two present carers and five past carers | To explore perceptions of quality day care provision and explanations for programme underuse |
English North America |
Thematic analysis | Day care viewed as a much-needed respite for carers that also enhances well-being of the care recipient. Carers talked about the stress and economic strain resulting from lack of day care. Several carers had either given up their job or reduced hours. Need for flexible and relevant activities that support self-esteem of care recipients. Reasons for non-uptake – lack of awareness, stigma, difficult bureaucracy |
|
Strang et al. 2002209 High |
15 carers of patients who had died from cancer, not in the context of formal respite care | Sampling purposive via palliative home care programme. Participants interviewed twice | Carer age 58.5 years (range 37–81 years); 11 women; nine spouses, three daughters, one daughter-in-law, one son, one sister; duration of caring 1–11 months | To explore the meaning and experience of respite |
English Canada |
Phenomenological framework using a thematic analysis | Discusses the distinction between a mental and physical break. Carers reluctant to take breaks as they wanted to spend as much time as possible with the care recipient, but brief mental breaks were important. Physical breaks tended to increase anxiety |
|
Wiles 2003216 High |
30 carers looking after an elderly person at home using various services; 24 had received some formal support but not specified and six no formal support at all |
Self-selecting sample recruited from advert, support groups, formal support services and snowballing In-depth interview |
23 female; 14 aged 70 years and above; 19 spouses; 23 co-resident | Experiences of accessing and negotiating formal support services |
English Canada |
Thematic analysis and narrative analysis |
Reluctance to get help because of desire to maintain independence and a sense of personal responsibility and pride. Felt that support for care recipient more important than care for themselves. Care recipients were reluctant to have strangers in their homes Confusion about formal support system. Inflexibility of respite a problem (2-week blocks only) and long waiting lists for respite. Many preferred short breaks at shorter notice. Difficult to get respite at home. High turnover of staff resulted in poor continuity |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Gilmour 2002171 Moderate |
Nine carers of people with dementia using hospital respite care from a few months to 7 years; predetermined periods of respite of 12 consecutive days |
No sampling strategy given Interviews |
Carers: six children, two wives, one husband; six female; age range 36–85 years Recipients: age range 65–94 years |
Perceptions of respite care, impact on care recipient and ability to take advantage of it |
English NZ |
Critical discourse analysis | Three approaches to respite: (1) good continuity between hospital and home care – nurses actively seek information from carer; (2) caregiving only partly relinquished because of concerns over quality of care, but no impact on care recipient; information not actively sought by nurses; (3) carers ambivalent about respite as detrimental impact on care recipient – information from carer disregarded |
|
Leong et al. 2001186 Moderate |
10 carers of dementia sufferers recruited from a survey sampled via a community nursing service, using a variety of services |
Purposive sample Semistructured interviews |
Age range 45–97 years; caring for 1–20 years; three retired, one semiretired, one receiving disability, three housewives, two unemployed; all coresident | To explore carer needs that are poorly met |
English Australia |
No theoretical framework Content and thematic analysis |
Carers felt that health and state of mind depended on time to themselves. Respite one of the most frequently mentioned needs. Accessing respite on short notice not usually possible. There was a need for a variety of respite services, including day, night and weekend care accessible at short notice. Services need to be more flexible and responsive to carer needs |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
King and Parsons 2005180 Moderate |
Two carers of dementia sufferers utilising respite for 50 days or more per year. Given a choice of home-based respite, residential care or an increase in support services or a combination of all three |
Sample recruited by respite co-ordinator Semistructured interviews |
Not given | Evaluation of two case management models of respite relief care |
English NZ |
No theoretical framework Thematic analysis |
Respite provided a physical but not a mental break. For some, the care recipient’s condition deteriorated with respite. Expressed a need for continuity of care with home respite |
|
Kristjanson et al. 2004183 Moderate |
13 carers of terminally ill relatives in receipt of a night respite service |
Purposive sampling Open-ended self-completed evaluation form |
10 spouses, one sibling, three adult children; age unclear although majority between ages of 55 and 75 years; received respite for 1–6 nights per week | Action research study developing a palliative care night respite service and qualitative study to assess views of the service |
English Australia |
No theoretical framework Thematic analysis |
Service was of benefit to both care recipient and carer. Allowed care recipient to die at home and carer to continue to support care recipient through last stages of life |
|
Witt et al. 2004219 Moderate |
18 carers of older people with chronic degenerative diseases and who were users of community health services – no details given |
Random sampling Semistructured interviews |
Carers: 83% female; aged 49–86 years; caring for < 1 year–45 years Recipients aged 62–95 years; had dementia, Parkinson’s disease, hypertension, deafness, blindness, glaucoma, arthritis, incontinence and Paget’s disease |
To assess availability, suitability and utilisation of respite services for older people in southern Sydney |
English Australia |
Content analysed for themes No theoretical framework |
Little knowledge of respite availability and scope. Demand greater than availability. Not adequately meeting clients’ needs – long waiting and booking times. Difficulty in obtaining unplanned respite. Limited times and days of service provision. Staff unskilled and inadequate staffing levels. Respite referral services inefficient and not user friendly. Difficulty in managing care recipients post respite |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Yamamoto and Wallhagen 1998235 High |
26 carers of dementia patients in Japan; recruited via service organisations; had used various formal services (home helper, bath services, day care, short stay) |
Theoretical Unstructured interviews |
13 daughters and 13 daughters-in-law; age range 32–63 years; 18 living with recipient, five independently and three in institutions | How carers make decisions about using formal services |
Japanese Japan |
Design and analysis using a grounded theory approach | Issues regarding availability of services (quality, distance, stigma/financial sanction, information); authority level within family and ability to negotiate. Carers only use services/institutionalise when they have reached saturation point |
|
Young et al. 2002236 High |
Japanese American sample including 26 carers (half of recipients cognitively impaired) and four recipients (no cognitive impairment); nine used day care, 13 used multiple services, eight home help, 10 nursing home, six no services |
Theoretical (states random, then purposive) Semistructured interviews |
Carers: 18 co-resident; mean age 69.8 years; majority female; 35% spouses and 50% adult children Recipients: three female; age range 73–88 years (mean 79.3 years) |
Attitudes towards community-based long-term care and factors influencing formal service use |
Japanese and English USA (Japanese language papers excluded) |
Grounded theory and constant comparative method | Attitudes towards services (ability to meet care needs, autonomy for carer, quality of care and staff, cost, emotional connotations, e.g. loneliness of recipient in nursing homes, physical and social environment). Barriers to service use: availability and confusion regarding entitlements and services offered; positive/negative views of particular services. Carers sometimes able to overcome negative feelings towards care by augmenting services (e.g. taking food to nursing home) |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Ericson et al. 2001168 Low |
20 family carers of dementia patients recruited via existing service users (day/respite care) |
Convenience Semistructured interviews?? |
15 spouses, three children, two siblings | Views of best care |
Swedish Sweden |
None Content analysis to identify main themes |
Importance of familiar environment; provision of stimulating/rewarding activity; intimate knowledge of person with dementia and providing support for carers |
|
Jansson et al. 1998176 Moderate |
27 dementia carers taking part in an intervention designed to provide in-home respite by volunteers; recruited via church |
Convenience? Semistructured interviews? |
22 spouses, four adult children, one friend; mean age 69 years (range 39–86 years); 23 lived with recipient | Views of a support and education service |
Swedish (paper in English) Sweden |
None Thematic analysis |
Feelings of security and relaxation |
| Study and quality ratinga | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
|
Bergs 2002162 High |
Six wives (< 70 years) caring for husbands who had had COPD for at least 2 years living in Reykjavik; recruited via pulmonary unit |
Convenience sample – all identified who met inclusion criteria Unstructured? |
Age < 70 years No other details given |
Participants asked to describe their experiences of caring and quality of life |
Icelandic Iceland |
Phenomenological Thematic analysis |
Desire to care for as long as required but need for increased support (respite) to do so. Need to stay healthy in order to care. Employment provides some respite |
|
Berthold et al. 1991163 Low |
19 relatives of care recipients receiving continuous intermittent care in a nursing home; recruited via evaluation study of the programme |
No details on sampling; 16 face-to-face and three telephone interviews Structured with open questions |
12 cohabiting relatives (three husbands, seven wives, two sisters); seven relatives of care recipients living alone (one sister, five children, one daughter-in-law) | Views of a continuous intermittent care programme |
Swedish (paper in English) Sweden |
Semiquantitative method No details on qualitative analysis |
The regular respite was of great importance to carers, allowing rest and relief from burden. One felt lonely and a few felt guilt. Majority of carers felt that it was valuable for the care recipient enabling them to meet people and receive good food, therapy, activation and medical care. Negative aspects were patients’ worries about moving, boredom, being disturbed by other patients. Carers felt that care recipients could not have remained at home without this respite care |
|
Johansson 1991178 Low |
39 carers of people over the age of 75 years; half received home help services and two received more extensive help |
Chosen randomly from sample taking part in a larger study Semistructured interview |
Carer age range 41–86 years; 28 female; seven spouses, 29 offspring, two sisters, one friend; nine cohabited; one-third received payment for help | Burden of caring and the role of formal support |
Swedish (paper in English) Sweden |
No theoretical framework and no details of analysis of qualitative data |
Those cohabiting felt socially isolated because they could not leave their partners unattended. Carers were reluctant to ask for help, as they felt they would be betraying their partners. Concentrated on the positive aspects and the close bond with their partners Carers in shared households also found it difficult to get away, limiting social life, but were more accepting of formal support Those living nearby: care taxing and a tie, but formal help seldom taken up. Did not know much about or have much faith in formal help |
| Study | Study design | Summary of study findings | |||||
|---|---|---|---|---|---|---|---|
| Sample and setting | Sampling and type of interview | Sample characteristics | Focus of study | Language of original study | Theoretical framework and/or type of analysis | ||
| Hawranick and Strain 2007227 | 30 carers of older people living in the community; recruited via advert, snowballing and services |
Purposive sampling (male and female, employed and not, users and non-users of home care services) Focus group and individual interviews |
24 female/6 male; median age 59 years (range 38–88 years); 14 spouses, 13 children and three other; 11 employed; 18 co-resident; median duration of care 60 months (range 1–240 months) | To explore the experience of caring and how factors such as employment and use of home care services impact on this |
English Canada |
No theoretical framework Thematic analysis |
Some care recipients reluctant to use services. Carers also reluctant and service not sought until a crisis. There was a lack of knowledge of services. There was inadequate training of staff (particularly for dementia care) and lack of continuity. Carers monitored that services met the needs of care recipients and also felt it important to be involved in care by service providers |
| Adams 2006224 | 20 carers of people with mild cognitive impairment or diagnosis of dementia recruited from a research registry |
Sampling strategy not given Individual interviews |
10 male/10 female; 10 husbands, six wives, four daughters; 18 white; MMSE mean 23.8 (range 13–29) | Subjective experience of early caregiving; needs and concerns of carers |
English US |
Phenomenology and grounded theory Thematic analysis |
Reluctance to use formal services. Many thought it too soon and did not want to face the issue but wanted to maintain the status quo as long as they were able to manage. Concerns about other people’s disapproval and acceptability to the care recipient. Some were dubious of the benefits that they might experience |
| Scharlach 2006 et al.225 | Carers of older people from eight non-white populations (African American, Chinese, Filipino, Korean, Native American, Hispanic, Russian, Vietnamese) |
Recruited through community organisations serving each of the eight ethnic populations Focus groups |
Age range early 20s–early 70s; approximately 66% female; majority providing care for parent, with some for spouses, family members, neighbours or friends | Reasons for restricted service use |
English US |
Thematic analysis for focus groups |
Low use of formal support. Reasons: cultural preference for family care; low knowledge of formal support services; mistrust of government agencies; services not culturally appropriate; economic factors Needs: training, respite care. Carers typically described services to alleviate care recipients’ needs rather than their own |
| Zapart 2007 et al.228 | 82 carers of care recipients receiving palliative care at home |
Recruited through two specialist community palliative care services Individual semistructured interviews |
Carers: mean age 57 years; majority female, the spouse or partner, and living with care recipient Recipients: mean age 69 years, majority > 60 years; most had metastatic cancer |
Investigation of the contribution of carers, impact and needs for support |
English Australia |
No theoretical framework Thematic analysis |
Carers most frequently identified needs for information, financial assistance, respite care and assistance with household tasks. Respite at home most commonly requested, the period required ranging from a few hours to 1 week. Four carers wanted overnight respite; 18% did not want respite and 10% thought that care recipient would not like it |
| Salin Astedt-Kurki 2007229 | 17 women caring for a family member who used residential respite at least three times per year |
Sampling strategy not given Individual interviews |
Carers: 13 wives/four daughters; mean age 71 years (range 46–83 years); 16 co-resident; duration of caring 5 years (range 1.5–10 years) Recipients: mean age 78.5 years (range 58–96 years); four had dementia |
Examination of relationship between carer and care recipient and the impact of respite use |
Finnish Finland |
No theoretical framework Thematic analysis |
Respite was both a relief and heartrending. Doing personal things without scheduling was a relief. Taking care of themselves often postponed until respite. It took several days to get out of the programme of care. There were feelings of guilt, emptiness and loneliness during respite. Some experienced anxiety and worry about quality of care, and it was difficult to let go. Some visited daily. The reaction was dependent on the relationship between carer and care recipient |
| McIlfatrick 2006223 | Eight carers and care recipients; receiving palliative care during preceding year with diagnosis of circulatory, respiratory or nervous system disease |
Participants identified by a GP Individual interviews |
Recipients: all aged 60 years and over except for one aged 50 years; five female Carers: mean age 62.5 years; three daughters, three wives, two husbands |
A palliative care needs assessment |
English UK |
No theoretical framework given Thematic analysis |
Main needs expressed were for respite care, psychological support and information and choice. There was a lack of information about financial benefits and the processes for obtaining formal social support |
| Gerdner 2007 et al.226 | 15 carers of confused older people living in the Arkansas Delta |
Individual interviews Recruitment aided by community leaders; sampling strategy not given |
Carers: 11 male; mean age 57 years (range 44–84 years) Recipients: all female; mean age 80 years (range 64–92 years) |
The experience of family caregiving of African American carers of elder family members with chronic confusion |
English US |
Ethnography Thematic analysis |
Carers were reluctant to use long-term care facilities having concerns about the well-being of care recipients. Six carers used day care saying that it allowed them to continue caring. Others recognised the need but did not use it because of care recipient resistance. There was lack of awareness of some available services |
Appendix 10 Economics data extraction
Study 1
Reference
Artaso Irigoyen B, Martin Carrasco M, Cabases Hita JM. The cost of care of elderly patients with psychogeriatric pathology in the community. Actas Espanolas de Psiquiatria 2002;30:135–41.
Artaso Irigoyen B, Martin Carrasco M, Cabases Hita JM. Análisis coste-consecuencia de un centro de día psicogeriátrico. Rev Espanolas Geriatric Gerontol 2002;37:291–7.
Intervention
A psychogeriatric day care centre. The intervention was delivered by a multidisciplinary team of health-care professionals and included a series of treatments: physical and cognitive rehabilitation, behavioural skills training, reality orientation therapy, pharmaceutical care and support to families (e.g. respite care). The control group received normal care; here this included both national health system (primary and secondary care) and community care (home visits).
Key findings
The cognitive, behavioural and functional status of the care recipients were measured at baseline and at 6 and 12 months, with no differences found between the two groups. Quality of life, burden and satisfaction were measured at baseline and at 6 and 12 months; only satisfaction showed a statistical significance in favour of the control group.
In terms of resource implications, in the intervention group 42% of the cost was attributable to the use of the day centre, whereas 71% of the control group costs were imputable to informal care. The intervention group was most costly but it did not reach statistical significance. Subgroup analysis showed that costs increased with age and functional status of the care recipient and burden of the caregiver.
Objectives of the economic evaluation/analysis
To estimate the cost and cost variability of psychogeriatric care in the community and to identify the key cost components.
Type of economic evaluation
Costs and consequences.
Appropriate economic evaluation methodology selected? (yes/no)
Yes, the effectiveness looked at both the caregiver and the care recipient outcomes (which might go in opposite directions); these could be accounted for together either by generating a common utility score or by using a cost–benefit analysis approach (which implied the need to estimate all of the costs and benefits carried by caregivers and care recipients).
Country/currency/year data relate to
Spain, Euros, 1995.
Evaluation perspective
Societal.
Organisation/context for the study
-
National health system.
-
Social care.
-
Community.
Setting in which respite intervention mostly provided (provider type)
Day care.
Respite type
Proactive; aiming to anticipate problems.
New resources devoted or existing resources
The study assessed the costs and consequences of an existing psychiatric day centre and compared them with the costs associated with a group of elderly receiving routine community care; the groups were matched by age, gender and functional capacity.
Data collection methods
Sociodemographic, clinic and resource data were collected at baseline and at 6 and 12 months.
Design
Prospective resource utilisation.
Costs
Source of cost data
-
Hospital records.
-
Patient records.
-
Literature.
Data analysis
The data analysis covered baseline and the end of the follow-up period. The loss to follow-up was accounted for. A subgroup analysis of the intervention group was performed by comparing incident (those admitted to the day centre within the last month) with those admitted over a month before. No statistical significance was detected. Baseline characteristics were compared using the chi-squared test or Student’s t-test depending on the nature of the variable. Outcome measures were analysed using analysis of variance (ANOVA) and costs were analysed using both non-parametric and multiple linear regression methods.
Types of costs
National health system costs, direct costs borne by the patient (care recipient/caregiver), cost of formal caring and opportunity costs of informal caring were retrieved. The unit cost data used were retrieved from local health authorities, local government and market prices. A bottom-up approach was used to identify the total cost per participant (Table 30).
| Ingredient costs | Units | Valuation method | Credible | Year |
|---|---|---|---|---|
| Medication | Estimated by patients | Health authority tariffs, market price | Yes | 1995 |
| Tests and investigations | Estimated by patients | Yes | 1995 | |
| Formal care | Hours estimated by the participants | Yes | 1995 | |
| Patient-borne costs | Patient self-report | Yes | 1995 | |
| Informal care | Patient self-report | |||
| Loss of productivity | Patient self-report |
Were all important and relevant costs for each alternative identified?
Yes.
Were there any special circumstances regarding resource use (e.g. joint use of resources)?
No.
Time horizon of costs appropriate?
Similarly to the other studies, the length of follow-up should have been longer (Table 31).
| T0 | T1 | T2 | T3 | |
|---|---|---|---|---|
| Data provided | ✓ | ✓ | ||
| Months since baseline | 0 | 12 | ||
| Control: mean % or rate | 1238 Euros | |||
| Intervention: mean % or rate | 1754 Euros | |||
| p-value | Not significant |
The authors do not report the standard deviations, which would have been very useful information to assess the dispersion of the participants’ costs.
Were costs adjusted for differential timing?
The length of follow-up did not require discounting.
Were allowances made for uncertainty?
No sensitivity analysis was performed.
Cost outcomes interpretation
As expected, the intervention group was more costly.
Benefits/effectiveness
Burden (Zarit), quality of life and satisfaction with care were the caregiver outcomes collected. Cognitive status, behavioural assessment scale (Behave-AD), Katz index of ADL and physical status were measured for the care recipient.
Source of effectiveness data
Primary data.
Estimation of health state/benefits
Validated questionnaires.
Were all important and relevant benefits for each alternative identified?
Yes.
Time horizon of benefits appropriate?
As for costs, the follow-up should have been longer (Table 32).
| T0 | T1 | T2 | T3 | |
|---|---|---|---|---|
| Data provided | ✓ | ✓ | ✓ | |
| Months since baseline | 0 | 6 | 12 | |
| Control: mean % or rate | ||||
| Intervention: mean % or rate | ||||
| p-value |
Careagivers in the intervention group had higher levels of satisfaction than those in the control group, which continued throughout the study [intervention = 28.70, control = 26.22 (baseline); intervention = 29.32, control = 26.57 (at 6 months); intervention = 29.20, control = 26.97 (at 12 months)]. The paper includes the standard deviations of the outcome estimates.
Were benefits adjusted for differential timing?
Discounting was not necessary.
Effectiveness outcomes interpretation
Very limited.
Summary information
-
Total cost.
-
Total effectiveness.
Strength of link between costs and effectiveness data?
Prospective concurrent (strongest).
Synthesis and direction of results
-
Positive effect statistically significant.
-
Positive effect statistically insignificant.
-
Negative effect statistically insignificant.
Study limitations
The major limitation of the study is the design. The two groups were not comparable; the intervention group included participants with higher levels of income and the caregivers had better quality of life scores. This, together with the relatively small sample, diminishes the quality of the results.
Implications for practice
Before any conclusions are drawn on the effectiveness of psychiatric day care, larger and longer RCTs should be performed.
Relevance of the study for specific policy questions or decisions
The study is relevant; however, it must be pointed out that the intervention does not explicitly indicate the use of respite care as the core of the intervention.
Study 2
Reference
Baumgarten M, Lebel P, Laprise H, Leclerc C, Quinn C. Adult day care for the frail elderly: outcomes, satisfaction, and cost. J Aging Health 2002;14:237–59.
Intervention
Adult day care provided in six multipurpose day centres (general purpose, providing moderate intensity clinical and social care). Service offered to frail older persons on an outpatient basis, with a personalised programme of therapeutic and preventive activities. The recommended minimum level of participation was 6 hours a day once or twice a week. Once admitted to the programme the service is free.
The intervention group (n = 108) was given immediate admission to an adult day centre and the control group (n = 104) was placed on a waiting list for 3 months.
The mean age of clients in the intervention and control groups was 76.4 (SD 7.6) and 78 (SD 6.9) years respectively. The mean age of caregivers in the intervention and control groups was 54.2 (SD 16.2) and 58.4 (SD 15.3) years respectively.
Key findings
Participants’ and caregivers’ subjective perceptions of the day centre effects were positive. However, using standard research instruments there was no evidence of an effect of day centre attendance on the client’s anxiety, depression or functional status; on caregiver burden; or on the cost of health services.
Objectives of the economic evaluation/analysis
To assess outcomes and satisfaction among frail elderly day care clients and their informal caregivers and the impact of adult day care on the cost of health services.
Type of economic evaluation
Not stated but a cost–consequence analysis.
Appropriate economic evaluation methodology selected?
Yes.
Country/currency/year data relate to
Canada, Canadian dollars, 1991.
Evaluation perspective
Public services (health and social services) in Canada.
Organisation/context for the study
International publicly funded care system.
Setting in which respite intervention mostly provided (provider type)
Day care centre.
Respite type
Proactive; aiming to anticipate problems.
New resources devoted or existing resources
Existing.
Data collection methods
Interviews with clients and informal caregivers before admission to the day centre and at the end of the 3-month study period. Day centre records regarding client attendances also reviewed.
Design
Prospective RCT.
Costs
Source of cost data
-
Day centre records.
-
Patient and carer records; information on frequency and utilisation of services obtained from client and caregiver interviews.
Data analysis
-
Multiple linear regressions to test for heterogeneity in results across sites and to predict outcome variables.
-
All results analysed at the end of the 3-month study period.
-
Intention to treat analysis planned; however, because a substantial number of clients had little or no attendance a secondary analysis to examine the effect of attendance on outcome variables was also undertaken (high and low attenders if more than or less than 13 visits respectively).
Types of costs (Table 33):
-
Direct.
-
Indirect.
-
Top-down.
-
Capital (except for home care services).
-
Operational.
-
Total average direct health and social care costs.
-
Total charges for private services.
| Ingredient costs | Units (hourly, daily, weekly) | Valuation method | Credible | Year |
|---|---|---|---|---|
| Hospital care | Unit costs, published sources, rate schedules, interviews, market prices | Yes | 1991 | |
| Physician care | ||||
| Home care | ||||
| Outpatient services | ||||
| Day hospital services | ||||
| Long-term care | ||||
| Transportation | ||||
| Adult day care (intervention group) |
Were all important and relevant costs for each alternative identified?
Carer costs not reported.
Were there any special circumstances regarding resource use (e.g. joint use of resources)?
None specified.
Time horizon of costs appropriate?
Very short at 3 months only.
Were costs adjusted for differential timing?
Not applicable as only a 3-month study.
Were allowances made for uncertainty?
No.
Cost outcomes interpretation
No effect detected. No statistically significant differences in either average total costs or individual service category costs identified between the intervention and control groups.
Benefits/effectiveness
Outcomes measured included depression, anxiety, functional status, caregiver burden and cognitive status.
Source of effectiveness data
Single study.
Estimation of health state/benefits
Direct based on primary study
Were all important and relevant benefits for each alternative identified?
Yes.
Time horizon of benefits appropriate?
Very short at 3 months only.
Were benefits adjusted for differential timing?
Not applicable as only a 3-month study.
Effectiveness outcomes interpretation
-
Little discernible effect.
-
For all variables change between intake and 3 months was small and insignificant in magnitude.
-
Mean burden score much higher among caregivers of high attendees (32.1) than among caregivers of low attendees (17.5). After controlling for confounding this was not statistically significant.
-
Participants’ and caregivers’ subjective perceptions of the benefits of day care were positive. Two-thirds reported that it reduced their loneliness and around half reported feeling less anxious and depressed.
-
Also perceived that burden decreased more among caregivers of high attendees than among caregivers of low attendees.
Summary information
-
Total average cost.
-
Individual effectiveness results reported.
Strength of link between costs and effectiveness data?
Prospective concurrent (strongest).
Synthesis and direction of results
No detectible effect.
Study limitations
Very short study period – only 3 months. Very few details on what ‘respite’ component involved and the extent to which there was heterogeneity of provision across the different day centres.
Study 3
Reference
Donaldson C, Gregson B. Prolonging life at home: what is the cost? Community Med 1989;2:200–9.
Intervention
A family support unit (FSU) to assist carers to enable confused elderly persons to remain at home for as long as possible. FSU provides day care and respite care. Evening care and special occasional residential care can also be provided.
Key findings
Community support provided through a FSU is almost three times more costly than that which would otherwise be provided. The FSU prolonged life at home, saving costly long-term care beds. If life at home is preferable to long-term care, a FSU can be judged cost-effective.
Objectives of the economic evaluation/analysis
-
To compare the effect on clients of a mix of community services, including the FSU, with the effect of a mix of community services that does not include the FSU in terms of the length of time elapsed between assessment and either admission to long-term care or death whilst living at home.
-
To assess if the advent of the FSU results in extra days at home in the community and to compare the costs of these extra days at home with the cost of an equivalent period in long-term care.
-
To compare the costs and benefits to relatives of clients consuming the two packages of community services evaluated.
Type of economic evaluation
Not stated but a cost-effectiveness analysis.
Appropriate economic evaluation methodology selected?
Yes.
Country/currency/year data relate to
UK, pounds sterling, 1986–7.
Evaluation perspective
Public services (health and local authority); however, capital, transport and housing costs were excluded.
Patient-/carer-borne costs.
Organisation/context for the study
Community (mixed NHS and local authority care).
Setting in which respite intervention mostly provided (provider type)
Community-based FSU providing day care and respite care. Evening care and special occasional residential care can also be provided.
Respite type
Proactive; aiming to anticipate problems; however, very few details given on the respite provision offered per se.
New resources devoted or existing resources
New.
Data collection methods
Review of agency records and interviews with carers.
Design
Matched sample – n = 35 in the FSU group and n = 70 in the usual-care group. Matched on the basis of age, sex, psychiatric diagnosis, physical state, behavioural ability and whether live alone or not; however, the characteristics of the two groups were not reported separately so it is not possible to establish the effectiveness of the matching.
Outcome measures:
-
time spent in the community to either death or admission to long-term care
-
cost of care and support services utilised whilst living in the community
-
costs and benefits to carers.
Costs
Source of cost data
-
Local authority client data file (services and frequency used).
-
Health authority medical records (inpatient and day care use).
-
Voluntary agencies’ records on client use.
-
Cost data on cost per patient day (1986/87 prices).
-
Carer interviews.
Data analysis
Reporting at the end of a 3-year period. No interim analysis presented.
Types of costs
Costs.
Cost of care and support services utilised whilst living in the community
Basic ‘ingredients’ costing identifying local unit costs and units of utilisation:
-
direct – heath and local authority and voluntary agencies
-
indirect – costs to carers of providing informal care
-
top-down from agency costs (based on 100% occupancy)
-
capital, transport and housing costs excluded.
Total cost of all services consumed £4400 in the FSU group (n = 35) and £1200 in the control group (n = 367) (difference £3200). Cost per person per day maintained in the community was £6.60 in the FSU group and £2.30 in the control group. Costs were almost three times higher for the FSU group. Cost per extra day spent in the community by the FSU group was £18.80 (compared with £46.00 per person per day in a long-term hospital bed).
Costs to carers
Interview with carers (n = 24 in FSU and n = 29 in control group). There was no difference in terms of time spent caring for dependent relatives.
Were all important and relevant costs for each alternative identified?
Difficult to ascertain.
Were there any special circumstances regarding resource use (e.g. joint use of resources)?
None specified.
Time horizon of costs appropriate?
Point (average cost) estimates only.
Were costs adjusted for differential timing?
No.
Were allowances made for uncertainty?
No.
Cost outcomes interpretation
Community support provided through a FSU is almost three times more costly than that which would otherwise be provided. The FSU prolonged life at home, saving costly long-term care beds.
Benefits/effectiveness
Time spent at home in the community to either death or admission to long-term care
The FSU group spent more time in the community than the control group: mean number of days spent at home was 664 for the FSU group and 492 for the control group (difference of 172 days; significant at the p < 0.05 level; Mann–Whitney U test).
Costs and benefits to carers
Negative effects: the FSU group reported that their ability to have visitors and rest was more adversely affected than in the control group (p < 0.001; Fisher’s exact test). No statistically significant differences in terms of the financial or opportunity costs of caring emerged between the two groups.
Source of effectiveness data
Single study.
Estimation of health state/benefits
Direct, based on primary study.
Were all important and relevant benefits for each alternative identified?
Difficult to ascertain.
Time horizon of benefits appropriate?
Point estimates only.
Were benefits adjusted for differential timing?
No.
Effectiveness outcomes interpretation
Positive.
The FSU prolonged life at home, saving costly long-term care beds. If life at home is preferable to long-term care, a FSU can be judged cost-effective.
Summary information
Total utilisation and cost figures only reported.
Strength of link between costs and effectiveness data?
-
Prospective concurrent (strongest).
-
Retrospective disconnected (weakest).
-
Other.
Synthesis and direction of results
Positive effect; no statistical analysis of cost data undertaken.
Study limitations
Few details on the precise nature of the respite care provided by the FSU. No randomisation to intervention and control groups. Respite services were provided to some subjects in each group through local authority day care and hospital schemes; this may have impacted on the results.
Study 4
Reference
Gaugler JE, Zarit SH, Townsend A, Stephens M, Greene R. Evaluating community-based programs for dementia caregivers: the cost implications of adult day services. J Applied Gerontol 2003;22:118–33.
Intervention
Intervention group – 45 subsidised adult day care programmes in New Jersey for dementia clients. Participants had to use day care at least twice per week for around 8 hours.
Control group – recruited from northeast Ohio, a similar region where day care services were not widely available. This group did not use day care services.
Mean age of participants in the short-term (0–3 months) cohort was 59.1 (SD 14.6) and 60.3 (SD 13.1) years in the intervention and control groups respectively. Mean age of participants in the long-term (0–12 months) cohort was 56.7 (SD 13.6) and 60.8 (SD 12.6) years in the intervention and control groups respectively.
Statistically significant differences did exist between the intervention and control groups at the different data capture points, including the percentage living with relatives, the percentage of spouse caregivers, family income, age, the presence of behaviour problems, the number of ADL dependencies, the number of primary and secondary caregiving hours, and caregiver outcomes (role overload and depression). To adjust for these differences the indicators were included in subsequent analyses as covariates.
Key findings
Daily costs to reduce caregiver role overload and depression decreased with adult day service utilisation over a 1-year period. The findings emphasise that adult day programmes are most effective for dementia caregivers who use these services consistently and for longer periods of time. As adult day service use assuages role overload and depression, the daily cost of these benefits was reduced over a 1-year period.
Objectives of the economic evaluation/analysis
To analyse the short- (3 months) and long-term (1 year) cost implications of adult day care on a community-based programme for dementia caregivers.
Type of economic evaluation
Not stated but a cost–consequence analysis.
Appropriate economic evaluation methodology selected?
Yes.
Country/currency/year data relate to
USA (New Jersey and Ohio), US dollars, 1993.
Evaluation perspective
-
Public services (health and social services).
-
Patient and carer.
Organisation/context for the study
International mixed publicly/privately funded care system.
Setting in which respite intervention mostly provided (provider type)
Day care, community based.
Respite type
Proactive; aiming to anticipate problems.
New resources devoted or existing resources
Existing.
Data collection methods
Data were collected via interviews with caregivers at baseline, 3 months and 1 year asking about utilisation of services in the last month.
Design
-
Cross-sectional quasi-experimental study.
-
Retrospective resource utilisation.
Two regions that were similar across key sociodemographic indicators were selected; one where subsidised adult day care was available (New Jersey) and one where it was not (Ohio).
Costs
Source of cost data
-
Provider records.
-
Patient records.
-
Literature.
Data analysis
-
Three data capture points (baseline, 3 and 12 months).
-
Interim analysis at 3 months.
-
Logistic regression investigating factors indicating attrition.
-
Short-term cost analysis applying one-way ANOVA and chi-squared test statistics to ascertain if the intervention and control groups differed on important baseline variables. If significant differences emerged, variables included as covariates when estimating costs and outcomes via analysis of covariance (ANCOVA).
Types of costs
Costed adult day services, formal service use, informal sources of care and employment changes; n = 367 (n = 154 and n = 213 intervention and control groups respectively) at 3 months; n = 201 (n = 80 and n = 21 intervention and control groups respectively) at 12 months.
Costs (Table 34):
-
direct
-
indirect
-
top-down, e.g. provider charges
-
bottom-up, e.g. employment costs
-
total direct health-care costs
-
charges.
| Ingredient costs | Units (hourly, daily, weekly) | Valuation methoda | Credible | Year |
|---|---|---|---|---|
| Adult day care | Programme costs, caregiver estimates | Yes | 1993 | |
| Formal services | ||||
| Informal assistance | ||||
| Employment costs |
Short-term cost analysis (0–3 months):
-
on average, total costs per day were higher (by US$7.53) among the intervention group (US$54.32 versus US$46.79; p < 0.05)
-
employment costs were significantly higher for the intervention group (US$1.78 versus US$1.39; p < 0.05).
Long-term cost analysis (0–12 months):
-
average cost per day over the year was higher among the intervention group (US$47.10 versus US$41.15; p < 0.05)
-
daily formal service costs were significantly higher among the intervention group (US$2.01 versus US$0.41; p < 0.05) as were secondary caregiving costs (US$6.12 versus US$4.08; p < 0.05)
-
however, in contrast to short-term analysis, primary caregiving and employment costs were significantly lower for the intervention group (US$32.42 versus US$35.61 and US$0.30 versus US$1.05 respectively).
Were all important and relevant costs for each alternative identified?
Resource use and cost data are not clearly reported.
Were there any special circumstances regarding resource use (e.g. joint use of resources)?
None specified.
Time horizon of costs appropriate?
Yes although fairly brief (3 and 12 months only): short term 0–3 months; long term 0–12 months.
Were costs adjusted for differential timing?
Not applicable as only 12-month study period.
Were allowances made for uncertainty?
No.
Cost outcomes interpretation
Positive. Authors note that the most important finding is that, even as adult day service use assuages role overload and depression, the daily costs of these benefits are reduced over a 1-year period.
Benefits/effectiveness
Short-term analysis (0–3 months):
-
role overload (20.14 versus 21.32; p < 0.05) and depression (19.96 versus 21.28; p < 0.05) were significantly lower among the adult day service intervention group.
Long-term analysis (0–12 months):
-
the effectiveness of adult day services in alleviating role overload and depression was maintained long term (19.96 versus 21.28 and 12.77 versus 15.74 respectively).
Source of effectiveness data
Single study.
Estimation of health state/benefits
Direct, based on primary study.
Were all important and relevant benefits for each alternative identified?
Yes.
Time horizon of benefits appropriate?
Yes although fairly brief (3 and 12 months only): short term 0–3 months; long term 0–12 months.
Were benefits adjusted for differential timing?
Not applicable as only 12-month study period.
Effectiveness outcomes interpretation
Positive. Adult day care appeared to alleviate role overload and depression among caregivers.
Summary information
-
Total average cost.
-
Individual effectiveness results reported.
-
Incremental costs per unit change in caregiver outcomes of depression and role overload were reported.
Strength of link between costs and effectiveness data?
Retrospective.
Synthesis and direction of results
Some positiveve effects and statistically significant.
Study limitations
Matching between the two geographical cohorts at baseline was not great with several statistically significant differences identified between the intervention and control groups at both short- and long-term time data points. Generally, resource use and cost data are not clearly presented.
Study 5
Reference
Hedrick SC, Rothman ML, Chapko M, Ehreth J, Diehr P, Inui TS, et al. Summary and discussion of methods and results of the adult day health care evaluation study. Med Care 1993;31:SS94–103.
Intervention
Phase 1 – comparing client and carer outcomes associated with adult day health care (ADHC) provided within four medical centres in the US VA (Veterans’) care system (VA-ADHC) with outcomes of those receiving customary (nursing home) care (n = 826). The VA-ADHC programme offered the intensive health and social care services likely to be required by severely disabled patients at risk of nursing home placement. On average, 45 visits were made over 12 months; 15% of the sample made no visits.
Phase 2 – prospective cohort study comparing client and carer outcomes associated with ADHC provided within four medical centres in the US VA (Veterans’) care system (VA-ADHC) with outcomes of those associated with ADHC provided under contract to community agencies in four different VA medical centres (n = 163). The contract ADHC programme offered fewer services than the VA-ADHC. On average, 58 visits were made over 12 months; 8% of the sample made no visits.
ADHC programmes were serving frail elderly populations that frequently used health-care services before the study began. Sickness Impact Profiles (SIPs) indicated that the intervention sample was much more impaired than the non-veteran sample and only slightly less impaired than the sample of veterans within the customary care (nursing home) setting. In total, 82% of the sample exhibited dependency in at least one ADL, with an average 2.4 dependencies overall; 19% of the sample died during the 12-month follow-up period.
Key findings
Patients who were offered VA-ADHC in the first phase of the study had significantly higher VA costs on average than patients assigned to customary care, with no apparent incremental health benefits to themselves or their caregivers. The second phase of the study evaluating contract ADHC provided no evidence that contract ADHC was any better or worse than VA-ADHC.
Objectives of the economic evaluation/analysis
To determine the effect of ADHC on health status and utilisation and cost of care and whether this differs by type of programme, site or type of patient.
Type of economic evaluation
Not stated but a cost–consequences analysis.
Appropriate economic evaluation methodology selected?
Yes.
Country/currency/year data relate to
USA, US dollars, 1986–9.
Evaluation perspective
Public services (health and social services); US Veterans’ Administration (VA).
Organisation/context for the study
International mixed publicly/privately funded care system.
Setting in which respite intervention mostly provided (provider type)
Day care – community based.
Respite type
Proactive; aiming to anticipate problems.
New resources devoted or existing resources
Existing.
Data collection methods
Interviews; interrogation of VA computer database; fiscal reports; reports from ADHC personnel and non-VA providers.
Design
Prospective. Phase 1 RCT comparing VA-ADHC with customary (nursing home) care and phase 2 prospective cohort study comparing community-contracted ADHC with VA-ADHC. All three groups also compared.
Costs
Source of cost data
VA and non-VA providers and data gathered during interviews.
Data analysis
-
Data capture at four points (intake, 6 months, 12 months and discharge); however, analysis presented compared utilisation and cost over the total 3-year study period.
-
Subgroup analysis identified (based on previous research) before overall comparisons undertaken; t-tests used to compare ADHC and customary care in each subgroup for each outcome.
Types of costs
-
Direct.
-
Top-down.
-
Charges.
-
Total VA costs.
-
Total non-VA costs.
-
Total VA and non-VA costs.
Mean cost per day for contract ADHC and VA-ADHC care reported in the range of US$36–43 and US$48–103 respectively (Table 35).
| Ingredient costs | Units (hourly, daily, weekly | Valuation method | Credible | Year |
|---|---|---|---|---|
| Hospital | Unclear | Unclear | ||
| Clinics | ||||
| ADHC | ||||
| Home care | ||||
| Rehabilitation | ||||
| Pharamacy/laboratory |
Were all important and relevant costs for each alternative identified?
No costs to carers reported.
Were there any special circumstances regarding resource use (e.g. joint use of resources)?
None specified.
Time horizon of costs appropriate?
Relatively short (12 months).
Were costs adjusted for differential timing?
Not applicable as only 12 months of data.
Were allowances made for uncertainty?
No sensitivity analysis reported.
Cost outcomes interpretation
-
Positive.
-
Patients offered VA-ADHC in the first-phase RCT had significantly higher VA health-care costs on average than patients assigned to customary care.
-
ADHC increased the cost of care in the VA by 15% above the cost of customary care: an average of US$2152 per patient per year (95% CI US$25–US$4279).
-
High cost of ADHC care indicated that it was substituting for other services (e.g. outpatient and clinic visits).
-
The number of nursing home days was marginally significantly lower by 8 days (p < 0.055) for VA-ADHC patients.
-
For VA-ADHC patients there was a non-significant reduction (US$733) in the cost of nursing home care.
-
When costs were adjusted for intake differences, the total mean VA cost for contract ADHC patients was not significantly higher than that for VA-ADHC patients (US$816 difference).
-
The VA cost for contract ADHC patients was significantly higher than that for customary care patients (US$2500 difference).
Benefits/effectiveness
Health status measured included survival, SIP, psychological distress, cognitive status, health perceptions and satisfaction with care.
-
VA-ADHC patients had the same health status outcomes as patients assigned to customary care.
-
Three subgroups for whom VA-ADHC may have improved health outcomes: unmarried patients; patients not in hospital at intake; and those satisfied with help received before intake.
-
Patients in the VA-ADHC programme were more satisfied with their care than those receiving customary care.
-
Caregivers of patients assigned to VA-ADHC had the same health outcomes as caregivers of patients in customary care.
-
Contract ADHC patients were significantly more impaired in health status than the customary care group at intake and at 12 months.
-
No differences were found in physical or psychosocial health status between caregivers of patients in contract ADHC, VA-ADHC and customary care at 6 or 12 months.
-
Patients receiving contract ADHC care were less satisfied than those receiving VA-ADHC but more satisfied than the customary care group.
Source of effectiveness data
Single study.
Estimation of health state/benefits
Direct, based on primary study.
Were all important and relevant benefits for each alternative identified?
Limited caregiver benefits identified.
Time horizon of benefits appropriate?
Relatively short (12 months).
Were benefits adjusted for differential timing?
Not applicable as only 12 months of data.
Effectiveness outcomes interpretation
Very little discernible effect across outcome measures.
Summary information
-
Total cost.
-
Individual effectiveness results reported.
Strength of link between costs and effectiveness data?
Prospective concurrent.
Synthesis and direction of results
No detectible effect.
Study limitations
Veterans are a very specific population, typically higher dependency than comparable non-veteran populations. The higher level of use of health-care services by patients at intake indicates that ADHC was used as a substitute for other services. None of the customary care group received VA-ADHC but 8% did arrange day care at their own expense. The two studies are not totally concurrent regarding the timeline – only a few months of overlap. The data were collected and reported for 1986–9, meaning that they are approximately 20 years old.
Appendix 11 Outcome measures used in the included quantitative studies – abbreviations and references
Activities of daily living (ADL): Nuremberg Aging Observation Scale: Oswald WD, Fleischmann UM. Das Nurnberger Alters-Inventar NAI. Kurzbeschreibung, Testanweisung, Normwerte, Testmaterial [The Nuremberg Aging Inventory. Short description, manual and norms]. Nurnberg, Germany: Universitat Erlangen-Nurnberg; 1982.
BA (Behavioural Assessment Instrument): Reisberg B, Borenstein J, Salob S, Feris S, Franssen E, Georgotas A. Behavioural symptoms in Alzheimer’s disease: phenomenology and treatment. J Clin Psychiatry 1987;48:9–15.
Behavioural problems: Teri L, Truaz P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioural problems in dementia: the revised memory and behaviour problems checklist. Psychol Aging 1992;7:622–31.
Barthel Index: Mahoney F, Barthel DW. Functional evaluation: the Barthel Index. Maryland State Med J 1965;14:61–5.
BDI (Beck Depression Inventory): Beck A, Rush A, Shaw C, Emery G. Beck Depression Inventory. San Antonio, TX: Harcourt Brace; 1979.
Behavioral Assessment Instrument: see BA above.
Burden: Montgomery R, Borgatta E. The effects of support strategies on family caregiving. Gerontologist 1989;29:457–64.
Burden: Montgomery RJV, Gonyea JG, Hooyman NR. Caregiving and the experience of subjective and objective burden. Fam Relations 1985;34:19–26.
Burden: Zarit SH, Zarit JM. Families under stress: interventions for caregivers of senile dementia patients. Psychother Theory Res Pract 1982;19:461–71.
BSI (Brief Symptom Inventory): Derogatis L. The Hopkins symptom checklist: a self-report symptom inventory. Behav Sci 1974;19:1–15.
CBI (Caregiver Burden Inventory): Novak M, Guest C. Application of multidimensional Caregiver Burden Inventory. Gerontologist 1989;29:798–803.
Caregiver Burden Questionnaire: Hooyman N, Gonyea J, Montgomery R. The impact of in-home services termination on family caregivers. Gerontologist 1985;25:141.
CRA (Caregiver Reaction Assessment): Given CW, Given B, Stommel M, Collins C, King S, Franklin S. The Caregiver Reaction Assessment (CRA) for caregivers to persons with chronic physical and mental impairments. Res Nurs Health 1992;15:271–83.
CSI (Caregiver Strain Index): Robinson B. Validation of the Caregiver Strain Index. J Gerontol 1983;38:344–8.
Caregiver Strain Questionnaire: England MM. Test of a model for caregiver strain. Dissert Abstr Int 1990;51(09):4271B. University Microfilms No. AA19103871.
Carer Problem Checklist and Machin Strain Scale: Gilleard C. Living with dementia: community care of the elderly mentally infirm. London: Croom Helm; 1984.
CERAD Behaviour Rating Scale for Dementia: Tariot PN, Mack JL, Patterson MB, Edland SD, Weiner MF, Fillenbaum G. The CERAD Behavior Rating Scale for Dementia. Am J Psychiatry 1995;152:1349–57.
Crichton Royal Behavioural Rating Scale: Robinson R. Differential diagnosis and assessment in brain failure. Age Ageing 1977;6:42–9.
CAPE Behaviour Rating Scale: Pattie AH, Gilleard CJ. Clifton assessment procedures for the elderly manual. Sevenoaks, Kent: Hodder and Stoughton; 1979.
CES-D: Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measur 1977;1:385–401.
Cognitive ability: Poulshock SW, Deimling GT. Families caring for elders in residence: issues in the measurement of burden. J Gerontol 1984;39:230–9.
CWS (Care Work Strain Scale): Orbell S, Hopkins N, Gillies B. Measuring the impact of informal caring. J Community Appl Soc Psychol 1993;3:149–63.
DSSI (Delusions–Symptoms–States Inventory): Bedford A, Foulds GA, Sheffield BF. A new personal disturbance scale (DSSIsAD). Br J Soc Clin Psychol 1976;15:387–94.
General Well-being Schedule: Bravo G, Gaulin P, Dubois MR. Validation d’une échelle de bien-être général auprès d’une population francophone âgée de 50 à 75 ans. Revue Canadienne du Bieillissement 1996;15:112–28.
GDS (Geriatric Depression Scale): Yesavage JA, Brink TL, Rose RL, Lum O, Huang V, Adey M. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17:37–49.
GHQ (General Health Questionnaire): Goldberg DP. Manual for the General Health Questionnaire. Windsor: NFER-Nelson; 1978.
Global Deterioration Scale: Reisberg B, Ferris SH, DeLeon MJ, Crook T. The Global Deterioration Scale (GDS). Psychopharmacol Bull 1988;24:661–9.
HADS (Hospital Anxiety and Depression Scale): Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361–70.
Hamilton Depression Rating Scale: Williams JBW. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry 1988;45:742–7.
Hopkins Symptom Checklist: Derogatis LR, Lipman RS, Covi L, Rickels K. Neurotic symptom dimensions. Arch Gen Psychiatry 1971;24:454–64.
ICA (Informal Caregiver Assessment): Armstrong-Esther CA, Sandilands M. Informal Caregiver Assessment Schedule. Alberta: Department of Health Sciences, University of Lethbridge; 1997.
Katz Adjustment and Social Behaviour Scale: Katz MM, Lyerley SB. Methods for measuring adjustment and social behaviour in the community: rationale, description, discriminative validity and senile development. Psychol Rep 1963;13:503–35.
LSQ (Life Satisfaction Questionnaire): Closs C, Kempe P. Eine differenzierende Betrachtung und Validierung des Konstruktes Lebenszufriedenheit: Analyse bewahrter Verfahren und Vorschlage fur ein methodisch fundiertes Vorgehen bei der Messung der Dimnesion dieses Konstruktes [A differential view and validation of the construct of life satisfaction: analysis of proven methods and proposals for a methodologically based procedure for measuring construct dimensions]. Zeitschrift fur Gerontologie 1986;19:47–55.
Machin Strain Scale: Machin E. A survey of the behaviour of the elderly and their supporters at home. MSc thesis. Birmingham: Department of Psychology, University of Birmingham; 1980.
MADRS (depression scale): Montgomery RJV, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979;134:382–9.
MAI (Philadelphia Geriatric Center Multilevel Assessment Instrument): Lawton MP, Moss M, Fulcomer MC, Kleban MH. A research and service oriented multilevel assessment instrument. J Gerontol 1982;27:91–9.
MAI: McCracken G. The Long Interview. Newbury Park, CA: Sage, 1988.
Memory and Behavior Problems Checklist: Zarit SH, Zarit JM. The Memory and Behavior Problems Checklist and the Burden Interview. Pennsylvania: University Park, Pennsylvania State University, Gerontology Center; reprint series 1983/1990.
Morale (Kutner Morale Scale): Kutner B, Fanshel D, Togo AM, Langer TS. Five hundred over sixty. New York: Russell Sage Foundation; 1956.
Morale: Montgomery RJ, Borgatta EF. Effects of alternative support strategies. Final report to the Health Care Financing Administration. Detroit, MI: Wayne State University, Institute of Gerontology; 1987.
(Mini Mental Sate Examination) MMSE: Folstein MF, Folstein S, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189.
NHP (Nottingham Health Profile): The European Group for Quality of Life in Health Measurement. European Guide to the Nottingham Health Profile. Montpellier: Sarl-Escubase; 1992.
OARS (OARS Multidimensional Functional Assessment Questionnaire): Duke University Center for the Study of Aging and Human Development. Multidimensional functional assessment: the OARS methodology, a manual. Durham, NC: Center for the Study of Aging and Human Development; 1978.
Pearlin L, Mullan J, Semple S, Skaff. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990;30:583–91.
Perceived Social Support (PSS): Fydrich T, Sommer G, Menzel U, Holl B. Fragebigeb zur Sozialen Unterstutzung [Questionnaire of social support]. Zeitschrift fur Klinische Psychologie 1987;16:434–6.
Phildelphia Geriatric Center Morale Scale: Powell-Lawton M. The Philadelphia Geriatric Center Morale Scale: a revision. J Gerontol 1975;30:85–9.
POMS (Profile of Mood States): McNair DM, Lorr M, Droppelman LF. Profile of Mood States. San Diego: Educational and Industrial Testing Service; 1981.
PC (Problem Checklist): Gilleard CJ, Boyd WD, Watt G. Problems in caring for the elderly mentally infirm at home. Arch Gerontol Geriatr 1982;1:151–8.
PSMS (Physical Self-maintenance Scale): Lawton M, Brody E. Physical Self-maintenance Scale (PSMS). In: Mangen DJ, Peterson WA, editors. Research instruments in social gerontology. Volume 3: health programs and demography. Minneapolis, MN: University of Minnesota Press; 1984. pp. 274–8.
Psychological Distress Scale: Veit C, Ware J. The structure of psychological distress and well-being in general populations. J Consulting Clin Psychol 1993;31:730.
QoL-AD (Quality of life in Alxheimer’s disease): Logsdon RG, Gibbons LE, McCurry SM, Teri L. Quality of life in Alzheimer’s disease: patient and caregiver reports. J Ment Health Aging 1999;5:21–32.
Quality of Life Index: Ferrans CE, Powers MJ. Quality of Life Index: development and psychometric properties. Adv Nurs Sci 1985;26:253–9.
Relationship strain: Poulshock SW, Deimling GT. Families caring for elders in residence: issues in the measurement of burden. J Gerontol 1984;39:230–9.
Relatives Stress Scale: Greene JG, Smith R, Gardiner M, Timbury GC. Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives. A factor analytic study. Age Ageing 1982;11:121–6.
Role captivity: Pearlin LI, Mullan JT, Semple SJ, Sjaff MM. Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 1990;30:583–94.
Role overload: Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: effects of adult day care use. J Gerontol 1998;5:S267–78.
SACL (Stress and Arousal Checklist): Gotts GH, Cox T. Stress and arousal checklist: a manual for its scoring and interpretation. Melbourne: Swinburn University of Technology Press; 1986.
SASS (Self-anchoring Striving Scale): Cantril H. The pattern of human concerns. New Brunswick, NJ: Rutgers University Press; 1965.
SCL-90 (Symptom Checklist 90): Derogatis LR. SCL-90-R (revised) version administration, scoring and procedures, manual 1. Baltimore, MD: John Hopkins University School of Medicine; 1977.
Self-esteem: Silbereisen RK, Zank S. Development of self-related cognition in adolescence. In: Schwarzer R, editor. The self in anxiety, stress and depression. Amsterdam: ESP, North Holland; 1984. pp. 49–60.
SIP (Sickness Impact Profile): Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981;19;787.
SLS (Satisfaction with Life Scale): Diener E, Emmons R, Larsen R, Griffin S. The Satisfaction with Life Scale. J Personal Assess 1985;29:71–5.
SMAF (Systeme de Mesure de l’Autonomie Fonctionnelle): Hebert R, Carrier R, Bilodeau A. Le Systeme di Mesure de l’Autonomie Fonctionnelle (SMAF). Revue de Geriatrie 1988;13:161–7.
Social Provisions Scale: Cutrona CE. Objective determinants of perceived social support. J Personal Soc Psychol 1986;50:349–55.
STAI (Spielberger’s State-Trait Anxiety Inventory): Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y). Palo Alto, CA: Consulting Psychologists Press; 1983.
Subjective and objective burden: Montgomery RJV, Gonyea JG, Hooyman N. Caregiving and the experience of subjective and objective burden. Fam Relat 1985;34:19–26.
Worry and strain: Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: effects of adult day care use. J Gerontol 1998;5:S267–78.
ZBI (Zarit Burden Interview): Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist 1980;20:649–55.
ZBI (Zarit Burden Interview): Arai Y, Kudo K, Hosokawa T, Washio M, Miura H, Hisamichi S. Reliability and validity of the Japanese version of Zarit Caregiver Burden. Psychiatry Clin Neurosci 1997;51:281–7.
Appendix 12 Coding framework for qualitative synthesis
| 1. Barriers to respite | Includes organisational and perceived barriers; reasons for non-uptake; and reasons for reluctance to use |
| 2. Positive aspects | Positive aspects of respite care |
| 3. Negative aspects | Negative aspects of respite care |
| 4. Reasons for uptake | Stated or implied reasons for taking up respite care |
| 5. Service provision | Any views or reports of service provision not coded in the subcodes below |
| 5.1. Quality of care | Any quality issues not coded under Skills of carers or Confidence |
| 5.1.1. Skills of carers | Any reports, either positive or negative, of aspects of the skills of respite carers |
| 5.1.2. Confidence | Mention of confidence in the service, or trust of carers |
| 5.2. Transport | Difficulties of transport to respite care, or of respite carers travelling to carry out in-home respite |
| 5.3. Appropriateness | Whether the service responds to cultural needs or specific physical/cognitive/emotional/behavioural needs of the condition or individual |
| 5.4. Availability | Whether service was available or not. Also responses of services, e.g. withdrawal of services because of difficulties |
| 5.5. Flexibility/timing | Flexibility of service provision in response to carer/care recipient needs, which included issues related to timing of service provision. Also expressions of needs in relation to flexibility of service provision |
| 6. Carer needs | Any expression of needs in relation to the caring role or respite care. These were not specific to carer needs but also carer views of the needs of care recipients or other helpers |
| 7. Type of respite | Specific mention of particular types of respite care, e.g. day care, institutional, in-home. This code includes stated preferences for different types of respite |
| 8. Attitudes to caring | This code captures expressed views of the caring role and indications of underlying individual and cultural attitudes to caring for older people |
| 9. Consequences of caring | The physical and emotional outcomes of caring for an older person |
| 10. Attitudes to respite | Views of the different types of respite and the meaning of respite in general for carers. General positive or negative perceptions of respite care and expectations of the service. Perceptions of care recipient feelings about respite |
| 11. Ethnic minority groups | Any issues related directly to ethnic minority groups |
| 12. Caring relationship | Reference to the quality of the past or present relationship between carer and care recipient that impacts on attitudes to the caring role and to uptake of respite services |
| 13. Care recipient | Any issues related to the care recipient perspective not coded under the subcodes of Reluctance or Reaction, or under code 19 related to views of the need for respite to provide stimulation of the care recipient |
| 13.1. Reluctance | This code captures reports of care recipient reluctance to co-operate with respite care |
| 13.2. Reaction | Reactions to or outcomes of respite care for the care recipient |
| 14. Preparation | Difficulties encountered in preparing for respite care. This includes the actual preparation of the care recipient for the respite event, e.g. getting the care recipient to day care, or the preparation required in engaging a respite service |
| 15. Knowledge | Knowledge of service availability; knowledge of formal carers |
| 16. Mental break | Any discussion of the quality of respite as being a cognitive process rather than a physical separation from the caring role |
| 17. Base data | Base data included coding of country of origin of study; quality rating; condition of care recipient, i.e. dementia/physical/mixed; type of interview, i.e. individual or focus group |
| 18. Activities | Activities carried out during the respite period |
| 19. Stimulation of care recipient | Discussions of the importance of stimulation of the care recipient as a component of the respite experience |
| 20. Informal respite | Any discussion of the use of family/friends as a substitute for more formal respite service provision |
| 21. Cost | Financial aspects of respite care |
List of abbreviations
- ADC
- adult day care
- ADL
- activities of daily living
- AMED
- Allied and Complementary Medicine Database
- ASSIA
- Applied Social Sciences Index and Abstracts
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Register of Controlled Trials
- CES-D
- Centre for Epidemiological Studies Depression Scale
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CIS-R
- Clinical Interview Schedule – revised
- CMR
- Cochrane Methodology Register
- CRISP
- Computer Retrieval of Information on Scientific Projects
- DARE
- Database of Abstracts of Reviews of Effects
- HADS
- Hospital Anxiety and Depression Scale
- IADL
- instrumental activities of daily living
- IBSS
- BIDS International Bibliography of the Social Sciences
- MADDE
- Medicare Alzheimer’s Disease Demonstration Evaluation
- MMSE
- mini-mental state examination
- RCT
- randomised controlled trial
- SD
- standard deviation
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table. Abbreviations for outcome measures used (reported in tables) can be found in Appendix 11 along with references for the measures as cited in the articles.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and costeffectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programmes, Research and Development Directorate, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington