Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 05/24/01. The protocol was agreed in March 2007. The assessment report began editorial review in December 2007 and was accepted for publication in December 2008. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
During the last 2 years JSRG has been a member of the Advisory Board for Actelion Pharmaceuticals, Encysive Pharmaceuticals, GlaxoSmithKline and Pfizer; an Expert European Scientific Adviser to the European Medicines Agency (EMEA) Committee for Orphan Medicinal Products; a member of the Medical Advisory Board of PHA-UK (patients’ association) for which no renumeration is paid; and a director of Breathing, a company (charity) limited by guarantee; and has received honoraria for lecturing from Actelion, Glaxo SmithKline and Schering. Clinical Service at Hammersmith Hospital has received support from Actelion and United Therapeutics. JPZ has received honorariums from Actelion, Encysive and Glaxo SmithKline; lecture fees from Actelion and Schering; a joint educational grant from Actelion, Pfizer, Lung Rx and Schering; and travelling grants from Actelion and Encysive. Many honorariums have been paid to Papworth Hospital NHS Foundation Trust. JPZ is also a member of the Steering Committee for the multicentre randomised controlled trial sponsored by Actelion and Encysive, and member of the Scientific Committee for European Register for CTEPH sponsored by the educational grant from Actelion.
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of the health problem
Pulmonary arterial hypertension (PAH) is a diverse group of diseases of similar pathophysiology and clinical presentation characterised by a progressive increase of pulmonary vascular resistance (PVR), which leads to right ventricular heart failure and premature death. PAH is a subset of pulmonary hypertension. It is defined by a mean pulmonary artery pressure (PAP) > 25 mmHg at rest or > 30 mmHg with exercise, a mean pulmonary capillary wedge pressure (PCWP) of < 15 mmHg and a raised PVR of ≥ 240 dyn s/cm5. 1 The pathology of the disease is complex, but involves pulmonary artery vasoconstriction, smooth muscle cell and endothelial cell proliferation and pulmonary thrombosis. Symptoms of PAH include dyspnoea (breathlessness), fatigue, chest pain, syncope (fainting) and oedema, all of which can worsen as the disease progresses and heart failure develops.
Classification
PAH is classified according to clinical features. In addition, patients with PAH are classified according to their functional capacity. The following paragraphs describe the clinical classification and functional classification of PAH that are referred to throughout this report.
Clinical classification
PAH is one of five differing subtypes of pulmonary hypertension.
Pulmonary hypertension was traditionally classified into two categories, primary pulmonary hypertension (PPH) or secondary pulmonary hypertension, depending on the absence or presence of identifiable causes or risk factors. In 1998 the World Health Organization (WHO) co-sponsored a symposium on pulmonary hypertension, which took place in Evian, France. A new clinical classification of pulmonary hypertension based on pathophysiological mechanism, clinical presentation and therapeutic options was proposed in the symposium. This ‘Evian classification’ (or sometimes referred to as the WHO 1998 classification) includes five major categories, with PAH being one of the categories. The term ‘primary pulmonary hypertension’ was retained within this category and included subcategories of sporadic PAH and familial PAH (FPAH). It was agreed that the term ‘secondary pulmonary hypertension’ should be abandoned. In a subsequent symposium that took place in Venice, Italy, in 2003, the Evian classification was further modified. The term ‘primary pulmonary hypertension’ was removed and the subcategory of sporadic PAH was replaced by idiopathic PAH (IPAH). The details of the Venice 2003 clinical classification are listed in Table 1. 1
As PPH was widely used before the advent of the Venice 2003 classification a decision was made to retain this term in this report if it was used in the original publications/reports of individual studies. Where PPH is retained it is regarded as being interchangeable with IPAH.
|
Functional classification
Traditionally, patients with PAH are classified according to the classification of functional capacity developed by the New York Heart Association (NYHA) for patients with cardiac diseases based on clinical severity and prognosis. An adaptation of the NYHA functional classification specifically for patients with pulmonary hypertension was proposed in the aforementioned WHO symposium in Evian. The WHO classification and the NYHA classification are nearly identical and are sometimes referred to as the NYHA/WHO classification, which is listed in Table 2. 1
| Class | Description |
|---|---|
| I | Patients with pulmonary hypertension in whom there is no limitation of usual physical activity; ordinary physical activity does not cause increased dyspnoea, fatigue, chest pain or presyncope |
| II | Patients with pulmonary hypertension who have mild limitation of physical activity. There is no discomfort at rest, but normal physical activity causes increased dyspnoea, fatigue, chest pain or presyncope |
| III | Patients with pulmonary hypertension who have a marked limitation of physical activity. There is no discomfort at rest, but less than ordinary activity causes increased dyspnoea, fatigue, chest pain or presyncope |
| IV | Patients with pulmonary hypertension who are unable to perform any physical activity and who may have signs of right ventricular failure at rest. Dyspnoea and/or fatigue may be present at rest and symptoms are increased by almost any physical activity |
Aetiology
The pulmonary vasculature is normally a low pressure system with little resistance to flow. 2 In pulmonary hypertension pulmonary arterial pressure is elevated. As indicated in the clinical classification system above, PAH frequently originates as the result of an underlying condition (disease, genetic disposition) or interaction with an inciting stimuli (e.g. toxins) or a combination of both. Whatever the underlying trigger, pathological mechanisms are activated that lead to constriction, cellular proliferation and potentially elevated blood clotting in the pulmonary microcirculation. This results in progressively increased pulmonary vascular resistance, elevated PAP and the clinical sequelae of PAH, ultimately leading to right ventricular failure and premature death. 1,2 The molecular mechanisms behind these changes are still being investigated and thus will only be briefly mentioned when necessary in this report.
Significance for patients in terms of ill health
People with PAH may remain relatively asymptomatic until the underlying disease process is advanced. The key initial symptoms are breathlessness on exertion, and possibly chest pain (angina) and fainting (syncope). Accurate diagnosis can often be difficult as symptoms may appear non-specific, and therefore there is often a long delay from the onset of symptoms to definitive diagnosis. This delay can be several years and thus patients can have severe disease (and possibly signs and symptoms of right heart failure) by the time that appropriate treatment is commenced. Loss of exercise capacity and latterly capacity for daily living can be devastating to a patient’s quality of life and can also lead to depression and further deterioration in the quality of remaining life. Oedema and ascites are associated with severe PAH and in situ thromboses may occur in the pulmonary circulation.
PAH and IPAH in particular can occur at a relatively young age, elevating the impact of the disease on the patient and carers.
Heart–lung transplantation is an option for severe PAH; however, the number of available donors is very small and thus very few patients receive such transplants (probably less than 10 patients per year in the UK).
Significance to the NHS
Given the severity of PAH and its relatively rapid progression from diagnosis to premature death there is a considerable impact on the NHS, particularly towards the end of life when patients enter right heart failure.
According to UK Hospital Episode Statistics,3 in 2005–6 IPAH accounted for nearly 4000 hospital admissions, nearly 4500 consultant episodes and over 17,000 bed days.
Because of the severity of the disease, including the risk of early death, close monitoring and expert care are required, and it is recommended that this is undertaken at specialist centres (see Current guideline for use in the NHS).
Risk factors
Numerous factors have been identified as possibly increasing the risk of developing PAH. Table 3 provides information on the risk factors, including conditions that might be associated with PAH and an indication of the strength of the likelihood of an association between the factor and PAH. This table is adapted from an article by Galiè et al. 1 Some of these risk factors are considered sufficiently important contributors to the spectrum of PAH that they have been incorporated into the clinical classification system of PAH outlined in Table 1. Some of the main issues around risk factors are discussed in the following sections.
|
Drugs and toxins
Exposure to certain drugs and toxins might increase the risk of PAH. Evidence has been provided to associate the use of appetite suppressants structurally derived from amphetamine (aminorex, fenfluramine and dexfenfluramine) with a sixfold increase in the risk of developing PAH. Because of this adverse effect such suppressants have been removed from the market. 2
No significant difference has been reported between patients with PAH and the general population with regard to smoking habits. 4
Demographic and medical conditions
There is fairly clear evidence that, in adults, women tend to be more likely to develop PAH than men. Although the ratio of women to men varies from study to study it is of the order of 1.3:1 to 2.2:1. 4–6 In most trials women constitute the majority of patients.
No significant difference between PAH patients and the general population with regard to number of births per woman has been demonstrated. 4
Diseases
PAH is frequently associated with a number of other diseases. These associations are reflected in the subclassifications of PAH (see Table 1).
A relationship between HIV infection and PAH has been clearly demonstrated. 1 About 0.5% of patients infected with HIV will develop PAH. 2
Associated PAH (APAH) occurs in connective tissue diseases (CTD) and most commonly in scleroderma; around 12% of a hospital population of scleroderma patients suffer from PAH. 7 Despite similar haemodynamics survival in scleroderma APAH is worse than in IPAH, with a median survival of 1.2 years. 8
Congenital heart disease (CHD) with non-restrictive systemic to pulmonary shunts, such as ventricular septal defects, patent ductus arteriosus and large atrial septal defects, may lead to PAH. Eisenmenger syndrome develops when such patients develop severe PAH with reversal of flow across the shunt and cyanosis. Survival in untreated Eisenmenger syndrome is much longer than in IPAH although it is still markedly reduced compared with that in the normal population. 9
Portopulmonary hypertension, associated with liver disease and portal hypertension, is observed in 4–15% of patients who are evaluated for liver transplantation. 2
Hereditary
In 6–10% of patients PAH is suspected or proven to be of hereditary origin. In total, 50–90% of patients diagnosed with FPAH have mutations of the bone morphogenetic protein receptor, type II (BMPR2) gene. Patients with FPAH tend to suffer from more severe and quickly progressing disease. 2 In 2001 in the UK there were at least 20 families known to have FPAH. 10
Prognosis and prognostic factors
The prognosis for patients with PAH on supportive care (see Current service provision) is considered to be poor. In the 1980s median survival at the time of diagnosis for patients with IPAH (PPH) receiving supportive care was 2.8 years. 5 Percentages of patients surviving a specified period were estimated as 68% [95% confidence interval (CI) 61–75%] at 1 year, 48% (95% CI 41–55%) at 3 years and 34% (95% CI 24–44%) at 5 years. 5 One of the key factors influencing prognosis is functional class (FC). Patients with FCI or FCII PAH in the 1980s cohort had a median survival of 58.6 months, whereas those with FCIII had a median survival of 31.5 months. An extremely low median survival of 6 months was observed in patients with FCIV. 5 Given the greater awareness of PAH, the development of specialised PAH services and treatment algorithms and the potential for earlier diagnosis, median survival times from diagnosis may be longer today.
Haemodynamic variables related to decreased survival have been identified: increased mean (m)PAP, increased mean right arterial pressure (RAP)and decreased cardiac index. These variables also appeared in an equation predicting patient survival based on the results of a multivariate analysis of data from a registry established in the 1980s by the National Institutes of Health (USA). 5 The applicability of survival rates predicted by this equation, however, is questionable given the changes in medical practice as well as in other socioeconomic factors over the past few decades.
Exercise endurance, usually measured with the 6-minute walk test (6MWT), is also considered to be an important prognostic factor. One of the earliest drug trials for PAH demonstrated that the 6-minute walk distance (6MWD) was a predicator of survival, independent of treatment. 2,11
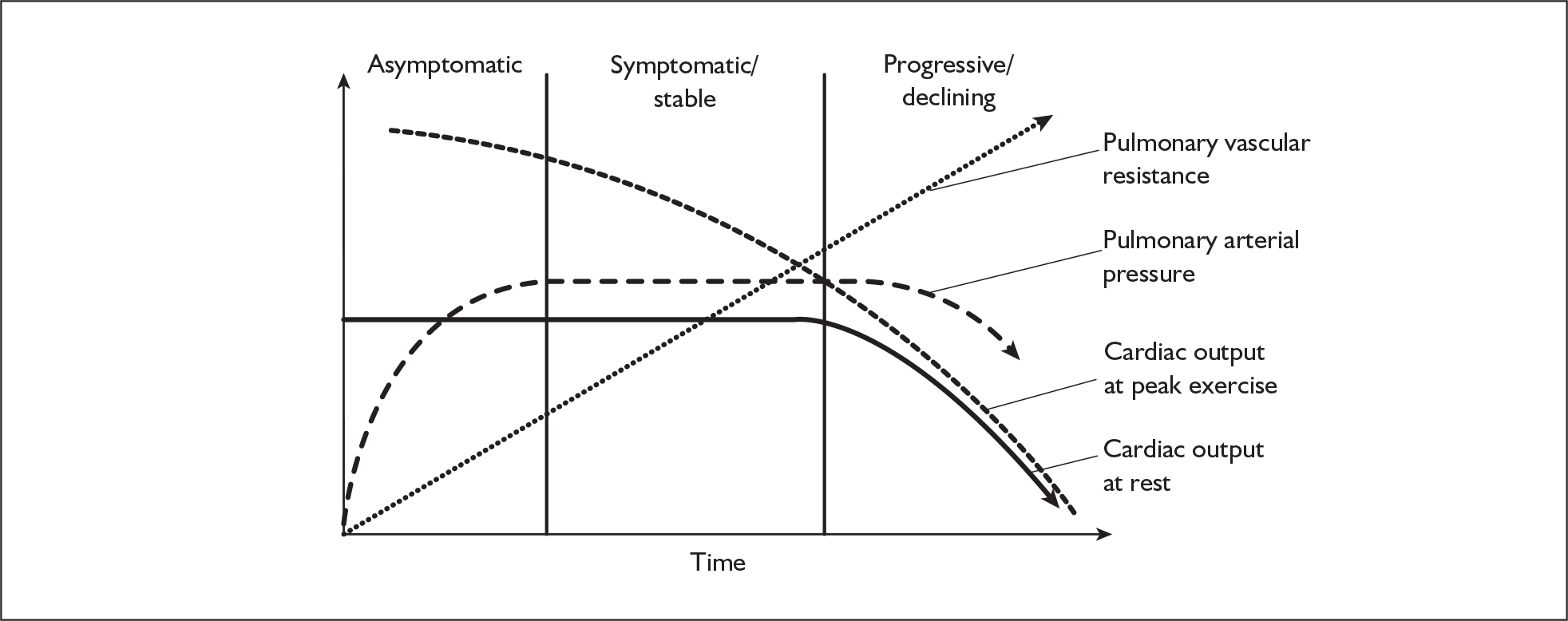
The progression of PAH symptoms in the context of change in clinical parameters is shown schematically in Figure 1.
FIGURE 1.
Schematic of progression of pulmonary arterial hypertension and change in clinical parameters. Adapted from Rich S. Primary pulmonary hypertension. Prog Cardiovasc Dis 1988;31:205–38. Copyright 1988, with permission from Elsevier.
Incidence and prevalence
PAH is a rare condition and as with such conditions the incidence and prevalence have been fairly difficult to assess. Often quoted figures for the incidence are 1–2 cases per million general population per year for IPAH and a further 1–2 cases per million population per year for other PAH aetiologies. 4,12 The likely prevalence has been estimated to be 15–50 patients per million population in the UK, with a suggestion that the estimate may be towards the upper end of the range. 6,12,13 Prevalence by FC is difficult to assess as many patients in lower FCs may not have been diagnosed yet. Thus the figures above are likely to be skewed to the more severe FCs. Assuming an adult population in England and Wales of 43.3 million this would give an approximate upper estimate of 2165 patients with PAH.
Measurement of disease
A number of measures are used clinically to monitor the severity, progression and response to treatment of PAH. Many of these can be related to exercise capacity, haemodynamics and/or cardiac performance. Clinically no single measure or composite measure is utilised to measure the disease. Severity, progression and response to treatment are assessed utilising a combination of measures. Some of the key measures are outlined in the following sections.
6-Minute walk test
The 6MWT measures the distance that a patient can walk unencouraged on a flat, hard surface in 6 minutes. 14 The absolute value of the 6MWD is predictive of survival and correlated with NYHA FC. A change from baseline is often used to assess treatment effect or patient deterioration. Conditions such as joint problems, not directly related to the pathophysiology of the pulmonary/cardiac circulation, might influence a patient’s ability to walk and the results of the test.
Dyspnoea scores
A number of measures of dyspnoea are used to measure PAH. These can be related to perceived exertion and/or a combination of magnitude of task and perceived effort. These are often subjective scales, but some have been shown to correlate with physiological parameters. Examples are the Borg and Mahler scales.
Pulmonary artery pressure
PAP is measured directly during right heart catheterisation. A mPAP > 25 mmHg at rest or > 30 mmHg with exercise is one of the criteria for PAH diagnosis. Elevated mPAP, together with other haemodynamic variables, indicates patients with a poor prognosis. 1
Right atrial pressure
Right atrial pressure is measured at cardiac catheterisation. RAP measures the filling pressure of the right ventricle and rises progressively as the right ventricle fails. High RAP thus identifies a failing right ventricle and a poor prognosis. The normal value of RAP is up to 5 mmHg.
Pulmonary capillary wedge pressure
Pulmonary capillary wedge pressure provides an indirect estimate of left atrial pressure. The measurement is made with a balloon-tipped, multilumen catheter inserted into a peripheral vein and then advanced into the right atrium, right ventricle and pulmonary artery and into a branch of the pulmonary artery. The normal value of PCWP is 8–10 mmHg. A PCWP ≤ 15 mmHg is one of the PAH diagnostic criteria. Elevated PCWP normally indicates left heart disease.
Pulmonary vascular resistance
PVR is a measure of the resistance of the pulmonary vascular circulation to flow. It is calculated as:
A PVR > 240 dyn s/cm5 is one of the diagnostic criteria for PAH. 15
Cardiac output/cardiac index
Cardiac output measures the amount of blood pumped around the circulation per minute. It is usually measured by cardiac catheterisation in PAH. Non-invasive methods of measuring cardiac output are also available. The cardiac index is calculated by dividing cardiac output by body surface area, thus relating it to the individual patient. It is usually expressed in l/min/m2.
Current service provision
Until 10 years ago PAH was managed mainly by supportive care alone. Since this time many patients have been enrolled in trials of new technologies that aim to be disease modifying rather than only tackling symptoms, and many of these drugs have been licensed for use in the UK. Thus, there is not a clear distinction between the current service provision and the technologies of this assessment. Given the uptake of the new technologies and their disease-modifying strategies they have become a routine part of clinical practice. Information on what is commonly referred to as supportive care and the technologies covered by this assessment are given in separate sections below.
Supportive treatment
A variety of treatments have been used in the management of PAH prior to the advance of the five technologies under assessment. These include anticoagulation therapy, diuretics, oxygen, digoxin and calcium channel blockers. They are commonly referred to as conventional therapy or background therapy and are used in clinical practice in addition to the technologies under assessment. Each of the treatments is briefly described below.
Anticoagulation
The aim of treatment with anticoagulants is to reduce the risk of venous thromboembolism, the risk of which is increased by PAH. 16 Usually, a target of an international normalised ratio (INR) ranging between 2.0 and 3.0 in Europe (and 1.5–2.5 in North America) is assumed. 1
The effectiveness of oral anticoagulants was originally demonstrated in retrospective single centre studies including only patients with IPAH and PAH related to anorexigens. Anticoagulation is also used in patients with other aetiologies of PAH, but all contraindications (such as a high risk of gastrointestinal bleeding in patients with CTD) have to be carefully considered. If there are no contraindications, patients treated with intravenous medication (e.g. epoprostenol; see Prostanoids, Epoprostenol) are also treated with anticoagulants, as they are at an increased risk of thrombosis associated with the use of a catheter. 1
In recent PAH randomised controlled trials (RCTs) the use of anticoagulants was reported in 51–86% of patients. 1 Warfarin is frequently the anticoagulant used in the treatment of PAH and, as with its use in other diseases, patients require frequent monitoring to reduce serious adverse effects such as haemorrhage.
Diuretics
Diuretics are used to prevent or reduce fluid retention. The aim of using diuretics in patients with PAH is to treat oedema or fluid retention connected with right heart failure, such as ankle swelling or ascites. 16 There are several classes of diuretics, including thiazides, loop diuretics and potassium-sparing diuretics. In recent PAH RCTs 49–70% of patients were treated with diuretics. Because of the lack of trials including specific classes of these drugs the choice of type and dose of medication are left to the decision of the physician. Monitoring of serum electrolytes and indices of renal function is advised in patients undergoing diuretic therapy. 1
Examples of diuretics used in the treatment of PAH include furosemide, amiloride and spironolactone.
Oxygen
Oxygen is used in patients with hypoxaemia, an abnormal deficiency of oxygen in arterial blood. 16 Hypoxaemia at rest is usually mild in patients with PAH. Some patients experience improvement in PAH with low-flow supplemental oxygen. Although the effect has not been proven in controlled studies it is considered important to maintain an oxygen saturation greater than 90% in patients with PAH. 1
The use of oxygen in patients suffering from PAH associated with some underlying conditions, such as cardiac shunts, can be controversial. A clinical trial1 assessing the efficacy of nocturnal use of oxygen in patients with PAH associated with Eisenmenger syndrome found no effect of oxygen therapy on haematological variables, quality of life or survival.
The need for oxygen often decreases in patients treated with epoprostenol. Patients without targeted treatment require more oxygen therapy.
Digoxin
The progression of right heart failure often results in depression of myocardial contractility. This condition can be treated with inotropic agents, for example agents that affect the force of muscle contraction.
Digoxin is used in patients with refractory right heart failure in sinus rhythm. 1 Digoxin is available in tablet form or as an injection. An increase in cardiac output, as well as a reduction in circulating noradrenaline levels, can be obtained by short-term intravenous use of digoxin. There is no evidence indicating the long-term efficiency of this drug. 1 Digoxin may be prescribed for improvement of cardiac output; however, now it is considered useful in rare cases of atrial fibrillation or atrial flutter to slow the ventricular rate. 16 It was used in 18–53% of patients taking part in recent PAH RCTs. 1
Calcium channel blockers
Calcium channel blockers are used in PAH patients with no right heart failure for reduction of PVR.
No more than 10% of IPAH patients respond acutely to vasodilator therapy. 17 Treatment of paediatric IPAH with calcium channel blockers has also shown some favourable results. It is less clear if therapy in patients suffering from PAH associated with other conditions is effective.
Only patients responding substantially in the short term to this therapy are considered for treatment with calcium channel blockers alone. 1 They are identified by means of an acute vasodilator challenge using short-acting agents, such as intravenous prostacyclin (see Description of technology under assessment, Prostanoids), adenosine or inhaled nitric oxide during right heart catheterisation. 18 As a result of a retrospective analysis of 557 patients tested with intravenous epoprostenol and inhaled nitric oxide, response criteria have been accepted of a fall in mPAP of 10 mmHg to an absolute mPAP ≤ 40 mmHg with an unchanged or increased cardiac output. 2
Nifedipine and diltiazem are the vasodilators most frequently used in clinical trials. There are also new-generation calcium channel blockers (e.g. amlodipine and felodopine). Limited reports on efficacy, tolerability and dosage are available.
The choice of a calcium channel blocker can be based on the patient’s heart rate, with relative bradycardia indicating nifedipine and relative tachycardia favouring diltiazem. The effective daily doses of these drugs tend to be high, ranging from 120 to 240 mg for nifedipine and from 240 to 720 mg for diltiazem. The advised procedure is to start with lower doses and gradually increase them to the highest tolerated ones. Usually, systemic hypotension and lower limb peripheral oedema limit the dose increase. The side effects can at times be decreased by the use of digoxin and/or diuretics (see earlier sections on these treatments). 1 This therapy requires close monitoring as the positive effect is not always maintained over time. 19
Description of technology under assessment
Five technologies are under assessment in this report. These are:
-
epoprostenol sodium (Flolan®, GlaxoSmithKline), administered by continuous intravenous infusion (hereafter referred to as epoprostenol)
-
iloprost (Ventavis®, Schering Health Care), administered by inhalation through a nebuliser (hereafter referred to as iloprost or inhaled iloprost)
-
bosentan (Tracleer®, Actelion Pharmaceuticals), administered orally (hereafter referred to as bosentan)
-
sitaxentan, sitaxsentan (Thelin®, Encysive Pharmaceuticals), administered orally (hereafter referred to as sitaxentan)
-
sildenafil (Revatio®, Pfizer), administered orally (hereafter referred to as sildenafil).
All have marketing authorisation in the UK/EU. All apart from epoprostenol have orphan disease medicinal products designation within the EU. These technologies can be grouped into three categories based on pharmacological mechanism of action: prostanoids, endothelin receptor antagonists and phosphodiesterase inhibitors. Further details on each technology is given in the following sections and a summary of the technologies, including licensed indication, pharmacological action and mode of delivery, is given in Table 4.
| Technology | Pharmacology | Licensed indicationa | Route of administration | ||
|---|---|---|---|---|---|
| Population | Functional class | Other | |||
| Epoprostenol (Flolan®, GlaxoSmithKline)20 | Prostacyclin (synthetic) | Primary pulmonary hypertension | III and IVb | Continuous intravenous infusion | |
| Iloprost (Ventavis®, Schering Health Care)21 | Prostacyclin (analogue) | Primary pulmonary hypertension | IIIb | To improve exercise capacity and symptoms | Inhaled via nebuliser |
| Bosentan (Tracleer®, Actelion Pharmaceuticals)22 | Endothelin receptor antagonist (non-selective) | Pulmonary arterial hypertension | IIIc | To improve exercise capacity and symptoms | Oral |
| Sitaxentan (Thelin®, Encysive Pharmaceuticals)23 | Endothelin receptor antagonist (selective) | Pulmonary arterial hypertension | IIId | To improve exercise capacity | Oral |
| Sildenafil (Revatio®, Pfizer)24 | Phosphodiesterase-5 inhibitor | Pulmonary arterial hypertension | IIId | To improve exercise capacity | Oral |
Prostanoids
Prostacyclin is mainly produced in the vascular endothelium. It is a powerful vasodilator of both the pulmonary circulation and the systemic circulation, inhibits platelet aggregation and inhibits smooth muscle growth. A relative deficiency of endogenous prostacyclin, as indicated by a deficiency of prostacyclin synthase expression in pulmonary arteries and of prostacyclin urinary metabolites, may be involved in the pathology of PAH. 1,18,19 Whether deficiency is causative or a consequence of PAH is unclear, but it has presented a justification for the use of prostacyclin to treat PAH patients. Prostacyclin is not very stable in solution at room temperature and is rapidly metabolised in the circulation. The prostanoids epoprostenol and iloprost (inhaled) are under assessment here. Other prostanoids [beraprost, treprostinil and iloprost (intravenous)] are not licensed in the UK and are thus not considered in this assessment report.
Epoprostenol
Epoprostenol is a synthetic sodium salt of prostacyclin. It is indicated for the intravenous treatment of PPH in NYHA FCIII and FCIV patients who do not respond adequately to conventional/background therapy. 20 For this indication epoprostenol is licensed in vial sizes of 1.5 mg. (1.5-mg vials along with 0.5-mg vials are also licensed for renal dialysis when the use of heparin is otherwise contraindicated or heparin use carries a high risk of causing or exacerbating bleeding. 20,25) Conventional/background therapy, although not explicitly defined, can be considered to be those treatments not classed as interventions in this assessment and as specified in the section on current service provision.
Epoprostenol is contraindicated in patients with known hypersensitivity to the drug, with congestive heart failure from severe left ventricular dysfunction and/or who develop pulmonary oedema during dose ranging. 20
Epoprostenol has a short half-life in the circulation (3–5 minutes) and therefore is administered continuously via pump into a central venous catheter (Hickman line). 1 Furthermore, once in solution epoprostenol is only stable for 8 hours at room temperature, requiring it to be kept cool before infusion with ice packs. Given the route of delivery, continuous administration and limited stability the treatment is not without complications. Not all patients are suitable for epoprostenol treatment as a great deal of self- or carer-ability and commitment is required to prepare and administer the drug under sterile conditions and to maintain sterility of the permanent central venous catheter. Ongoing patient/carer education and training are vital and these are delivered regularly by a specialist nurse.
Treatment must be initiated as an inpatient under specialist care because of the intensive training of patients and/or their carers and the close monitoring and emergency backup required. Initiation of treatment is by short-term dosing to determine the patient-specific infusion rate (this process can also be undertaken using a peripheral rather than a central line). Initially the infusion rate is 1–2 ng/kg/min and this is increased until maximum benefit on haemodynamic parameters is achieved and/or dose-limiting pharmacological effects occur.
Patients well enough to return home do so after this period, which usually lasts 1–2 weeks. Not all patients can safely manage epoprostenol treatment without help from carers.
Patients require two serviceable pumps at home in case one fails. These, along with a regular supply of sterile and other consumables and epoprostenol, are usually delivered by home care services to the patient. Patients have access to telephone support from the specialist centre, usually immediate access to outpatient and inpatient care and district nursing services.
Over time the infusion rate is gradually increased by 1–2 ng/kg/min steps to assess the clinical response and, overall, gradual dose increases are to be expected in most patients to arrest a deterioration in symptoms. 20 Typical doses might be in the range of 15–50 ng/kg/min (higher upper doses have been used in the USA) depending on the length of time on treatment, the resistance of the disease to adequate control and the severity of any adverse effects.
Patients who deteriorate appreciably while on treatment and/or who are not fit/able to return home after initiation of treatment usually require full-time hospitalisation.
Once initiated, withdrawal of epoprostenol treatment is problematic because of rebound pulmonary hypertension and rapid clinical deterioration, which may result in death. For this reason, once initiated, epoprostenol treatment is considered to be lifelong by many.
Because of the difficulties associated with epoprostenol treatment it is a very considered decision by both the patient/carer and clinical team whether and when to initiate treatment. For this reason the other interventions outlined in the following sections will be considered or utilised initially in preference. However, epoprostenol is considered to be the last defence against deterioration of the disease. It is therefore added to treatment regimes when other treatments begin to fail. Thus, many patients will be receiving epoprostenol, usually in combination with an oral treatment (see Endothelin receptor antagonists, phosphodiesterase-5 inhibitors and Current usage of technologies in the NHS). Patients presenting with aggressive disease and/or in FCIV will receive epoprostenol.
The price of epoprostenol is approximately £130–390 per day (15–45 ng/kg/min per 70-kg patient; one to three vials per day; net price). 26 This price only includes the epoprostenol powder and diluent and not the pumps, consumables, delivery or any other costs associated with administration (insertion of Hickman line), monitoring, inpatient time and training. The price for some of these items is difficult to ascertain and/or contained in confidential service agreements.
Iloprost (inhaled)
Iloprost is a stable prostacyclin analogue that has been developed for intravenous, oral and inhaled administration. Only administration by inhalation is part of this assessment.
Inhaled iloprost has EU marketing authorisation for the treatment of PPH patients in NYHA FCIII to improve exercise capacity and symptoms. 21 Two vial sizes, 1 ml and 2 ml, are licensed.
The administration of iloprost by inhalation is an attractive idea as potentially it is selectively delivered to the pulmonary circulation. To ensure distribution to the alveoli a delivery system is required to produce small enough aerosol particles. Three types of delivery systems (nebulisers) are available: compressed air, ultrasonic and vibrating mesh nebulisers. The recommended dose is 2.5 ∝g or 5.0 ∝g of iloprost (as delivered at the mouthpiece of the nebuliser) per inhalation session according to individual need and tolerability. One vial is sufficient for each inhalation session. Each inhalation session takes 3–10 minutes depending on the dose, the nebuliser and the patient breathing pattern. 21 The serum half-life of iloprost is about 20–25 minutes and this short duration requires six to nine inhalation sessions per day.
Treatment is usually initiated under specialist care with the patient admitted to hospital for about 3 days for training, education and monitoring of self-delivery. Patients can return home once stabilised and trained. Patients receive two nebulisers (one as backup) and consumables are delivered regularly to their home. Nebulisers are replaced approximately every 2 years. Support from the specialist centre is readily available.
Length of treatment is patient specific and unless discontinued for other reasons will continue until the patient’s condition deteriorates and epoprostenol treatment (see Epoprostenol) is accepted by the patient and initiated.
Inhaled iloprost is often seen as an additional treatment to the oral therapies in this assessment, bridging the gap for those patients in whom oral interventions do not adequately reduce progression of disease, but who are either not so severely affected that epoprostenol treatment is indicated or not suitable for epoprostenol treatment.
Iloprost is contraindicated in patients with known hypersensitivity to the drug, conditions in which activity on platelets might be undesirable (e.g. active peptic ulcers, intracranial bleeds, trauma), severe coronary disease events (e.g. severe artery disease, angina, recent myocardial infarction), recent cerebrovascular events (e.g. stroke), pulmonary hypertension due to veno-occlusive disease, valvular defects with clinically relevant myocardial function disorders unrelated to pulmonary hypertension, pregnancy and lactation. Furthermore, iloprost is not recommended in patients with unstable pulmonary hypertension, with advanced right heart failure. 21
The cost of iloprost nebuliser solution is approximately £85–127 per day (one vial six to nine times per day; net price same for each vial size). 26 This price is for the solution only and does not include the nebulisers, consumables, service, delivery, inpatient time and training. The price for some of these items is difficult to ascertain and/or contained in confidential service agreements.
Endothelin receptor antagonists
Endothelin-1 (ET-1), which is produced primarily in vascular endothelial cells, is a potent vasoconstrictor and mitogen (promoter of cell proliferation) in smooth muscle. ET-1 expression and concentration in plasma and lung tissue are elevated in PAH. 1,19 It is unclear whether increases in ET-1 are a consequence or a cause of PAH. Irrespectively, the ET-1 system is a target for the treatment of PAH.
ET-1 action is mediated through two types of receptors: ETA and ETB. ETA receptors are found in smooth muscle cells and ETB receptors in endothelial cells and smooth muscle cells. ET-1 interaction with ETA and ETB receptors in smooth muscle cells promotes sustained vasoconstriction and proliferation of vascular smooth muscle cells. 1,19 ET-1 stimulation of ETB receptors promotes ET-1 clearance and release of nitric oxide and prostacyclin. Blocking ET-1 interaction with ETA and/or ETB receptors therefore has a theoretical basis in the treatment of PAH and has led to the development of agents that bind to the receptors without eliciting a biological response, thus blocking binding of ET-1. Such agents are commonly referred to as receptor antagonists. Three endothelin receptor antagonists are available: bosentan and sitaxentan are covered by this assessment, whereas ambrisentan (Volibris/Letairis®) is not as it was not licensed in the UK when the technology assessment was carried out in 2007. Ambrisentan was approved in the USA for PAH in June 2007 and received marketing authorisation in the EU in April 2008. 27,28
Bosentan
Bosentan is an orally administered dual ETA and ETB receptor antagonist. It has UK marketing authorisation for PAH to improve exercise capacity and symptoms in patients in FCIII. 22 Two tablet sizes are available: 62.5 mg and 125 mg.
Treatment should be initiated and monitored under specialist care. Initially, dosing is 62.5 mg twice daily (morning and evening with or without food) for 4 weeks, increased thereafter to a maintenance dose of 125 mg twice daily. Doses for some patients may be increased to 250 mg twice daily but this is rare.
Patients are usually admitted to hospital as day cases under specialist care for the initiation of treatment. Some education is also given. Patients return home and drugs are usually delivered to them at regular intervals.
Length of treatment is patient specific. Limited or no response after 8–16 weeks of treatment or a deterioration of condition at any time requires re-evaluation of treatment. This usually entails either the addition of, or the replacement with, other treatments. Withdrawal of bosentan requires careful management.
Bosentan is metabolised by the liver and has been associated with a dose-dependant increase in the liver enzymes aspartate aminotransferase and alanine aminotransferase (more than eight times the upper limit of normal in some cases). Such elevation can be the marker of potentially serious liver injury. This is reflected in the recommended maintenance dose of 125 mg twice daily rather than 250 mg twice daily. This is not a unique feature of bosentan as it also occurs with sitaxentan. Regular monitoring of hepatic enzymes (usually monthly) is required for as long as the drug is taken.
Bosentan is not indicated in patients with a known hypersensitivity to the drug, those with hepatic impairment (including aminotransferase levels more than three times the upper limit of normal) and those taking ciclosporin A (amplifies the plasma concentration of bosentan by an unknown mechanism). Bosentan is contraindicated in pregnancy as it is assumed to be teratogenic and therefore women with childbearing potential should not receive bosentan unless using reliable contraception (bosentan may interact and lessen the effectiveness of hormonal contraception).
The cost of bosentan tablets is approximately £55 per day (2 · 62.5 or 2 · 125 mg as the net price is the same for each tablet size). 26 This price is for the drug only and does not include delivery, monitoring of liver function or inpatient time, etc.
Sitaxentan
Sitaxentan is an orally administered selective receptor antagonist for ETA (but not ETB). It has EU marketing authorisation for PAH to improve exercise capacity in FCIII. 23 One tablet size is available: 100mg.
Treatment should be initiated and monitored under specialist care. Dosing is 100 mg once a day with or without food. Patients are usually admitted to hospital as a day case under specialist care for the initiation of treatment. Some education is also given. Patients return home and drugs are usually delivered to them at regular intervals.
Length of treatment is patient specific. Limited response after 24 weeks of treatment or a deterioration of condition at any time requires re-evaluation of treatment. 23 This usually entails either the addition of, or the replacement with, other treatments. Withdrawal of treatment requires careful management.
As with bosentan, sitaxentan is associated with effects on liver enzymes and these require regular monitoring, with subsequent treatment adjustment if elevated more than three times the upper limit of normal. 23
Contraindications are similar to those of bosentan. There is significant drug interaction between sitaxentan and warfarin. Reducing the dose of warfarin upon starting sitaxentan and regular monitoring of the INR is required to reduce the risk of bleeding.
The cost of sitaxentan is approximately £55 per day (1 · 100 mg; net price). 26 This price is for the drug only and does not include delivery, monitoring of liver function or inpatient time, etc.
Phosphodiesterase-5 inhibitors
PAH is associated with a defect in the production of nitric oxide. 1,18,19 Nitric oxide is an endogenous pulmonary arterial vasodilator that acts by relaxing vascular smooth muscle through its stimulation of increased production of intracellular cyclic guanosine monophosphate (cGMP). Thus, dilation through this mechanism is reduced in PAH. cGMP is a short-lived molecule because of its rapid degradation by phosphodiesterases. Phosphodiesterase-5 is strongly expressed in the lung and its expression and activity are elevated in chronic pulmonary hypertension. 19 Thus, inhibitors of phospodiesterase-5 will decrease cGMP degradation, enhancing nitric oxide-dependant cGMP-mediated pulmonary vasodilation. 1,18,19
Sildenafil
Sildenafil is an orally administered specific inhibitor of phosphodiesterase-5. It has UK/EU marketing authorisation for PAH to improve exercise capacity in patients in FCIII. 24 It is available as 20-mg tablets.
Treatment should be initiated and monitored under specialist care. Dosing is 20 mg three times per day (6–8 hours apart) with or without food. 24
Patients are usually admitted to hospital as a day case under specialist care for the initiation of treatment. Some education is also given. Patients return home and drugs are usually delivered to them at regular intervals.
Length of treatment is patient specific. Deterioration of condition at any time requires a re-evaluation of treatment. 24 This usually entails either the addition of, or the replacement with, other treatments. Withdrawal of treatment requires careful management.
Contraindications for sildenafil include hypersensitivity to the drug; use with nitric oxide-producing treatment or nitrates is not recommended as sildenafil potentiates the hypotensive effects of these agents. It is also contraindicated in patients with severe hepatic impairment, recent history of stroke or myocardial infarction, and severe hypotension at initiation. Furthermore it is contraindicated in some specific eye conditions. 24
The cost of sildenafil is approximately £12.45 per day (20 mg · 3; net price). 26 This price is for the drug only and does not include delivery, inpatient time and training, etc.
Current guideline for use in the NHS
Since 2001, patients in the UK with PAH have been referred to and managed at specialist centres. There are seven centres in England designated by the Department of Health through the National Commissioning Group (NCG) (formerly known as the National Specialist Commissioning Advisory Group or NSCAG). 29 There is one centre in Scotland designated by the National Service Division of NHS Scotland. There are no centres in Wales and Northern Ireland and patients are seen at English centres. The centres are:
-
London: Hammersmith Hospital, Royal Free Hospital, Royal Brompton Hospital, Great Ormond Street Hospital (Children)
-
Newcastle-upon-Tyne: Freeman Hospital
-
Papworth/Cambridge: Papworth Hospital
-
Sheffield: Royal Hallamshire Hospital
-
Scotland: Western Infirmary Glasgow.
The cost of the service at the English centres is not funded through NSCAG but by the NHS, except for the designated children’s centre. 29
Treatment guidelines
In 2001, the British Cardiac Society sought for the first time to gain a consensus on the treatment of pulmonary hypertension. 10 The resulting recommendations set out criteria for the use of disease-targeting therapies, such as the technologies in this assessment, primarily based on cardiac catheterisation. Given the findings of many trials published more recently in which patients were enrolled based on NYHA/WHO FC and the granting of marketing authorisation for new technologies, the recommendations are considered by many to be out of date. 30 An update to the recommendations, including new treatment algorithms, has been published. 31
Guidelines published by the European Society of Cardiology (ESC) in 20041 are considered the most current with regard to practice in the UK at the time of writing (August 2007). Guidelines have also been produced by the American College of Chest Physicians. Both organisations are believed to be updating their guidelines for 2008. 30
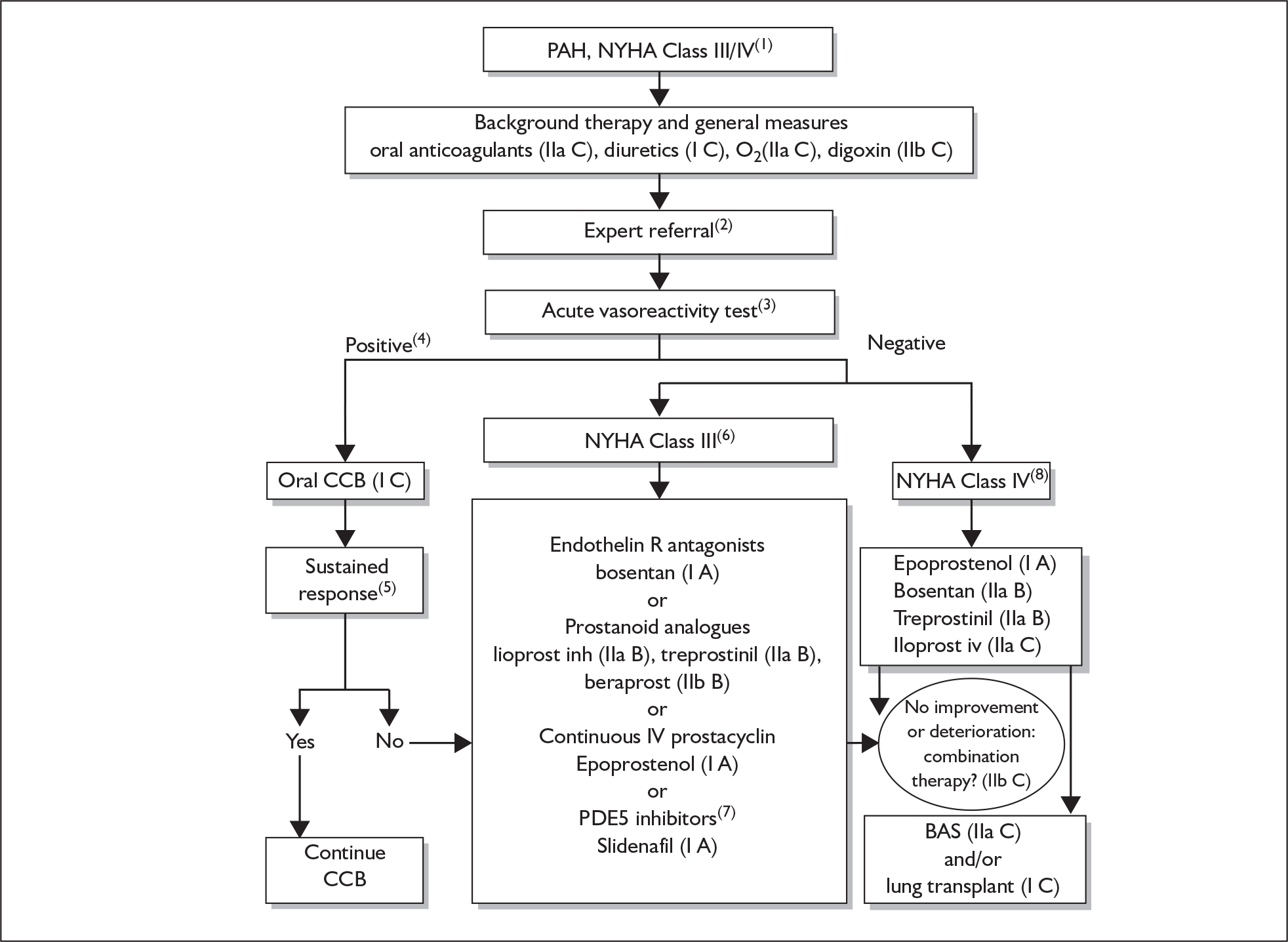
The ESC guidelines cover all aspects of the diagnosis, monitoring and treatment of PAH. They contain an evidence-based algorithm for the treatment of PAH FCIII and FCIV. This algorithm is reproduced in Figure 2 along with a complete description.
FIGURE 2.
European Society of Cardiology (ESC) evidence-based treatment algorithm. (1) The algorithm is restricted to patients in NYHA functional class III or IV because they represent the largest population included in controlled clinical trials. For NYHA functional class I or II very few data are available. In addition, the different treatments have been evaluated mainly in sporadic idiopathic pulmonary hypertension (IPAH) and in patients with PAH associated with scleroderma or anorexigen use. Extrapolation of these recommendations to other PAH subgroups should be carried out with caution. (2) Because of the complexity of the acute vasoreactivity tests, and of the treatment options available, it is strongly recommended that consideration be given to referral of patients with PAH to specialised centres. (3) Acute vasoreactivity tests should be performed in all patients with PAH even if the greater incidence of a positive response is achieved in patients with IPAH and PAH associated with anorexigen use. (4) A positive acute response to vasodilators is defined as a fall in mean pulmonary artery pressure of at least 10 mmHg to ≤ 40 mmHg with an increase or unchanged cardiac output during acute challenge with inhaled nitric oxide, intravenous (i.v.) epoprostenol or i.v. adenosine. (5) Sustained response to calcium channel blockers (CCB) is defined as patients being in NYHA class I or II with near-normal haemodynamics after several months of treatment. (6) In patients in NYHA functional class III first-line therapy may include oral endothelin receptor antagonists, chronic i.v. epoprostenol or prostanoid analogues. (7) At the time of writing sildenafil is not approved for PAH by any regulatory agency. (8) Most experts consider that NYHA functional Class IV patients in an unstable condition should be treated with iv epoprostenol (survival improvement, worldwide experience and rapidity of action). A, B, C grading according to definitions in Tables 4 and 5 of the ESC guidelines. BAS, balloon atrial septostomy; inh, inhaled; PDE, phosphodiesterase; R, receptor. Reproduced from Galiè et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. European Heart Journal (2004;25:2243–78) by kind permission of the European Society of Cardiology. 1
Current usage of technologies in the NHS
All five technologies are currently being utilised within the NHS. Perhaps the best information on uptake comes from the submission from the Royal College of Physicians30 for this appraisal, which contains year-on-year utilisation of the technologies from 2004 to 2007 collated by the National Pulmonary Hypertension Service of the UK and Ireland. The data are available for all pulmonary hypertension patients and thus the census is likely to cover a wider population than just PAH patients. The number of patients with pulmonary hypertension who received disease-targeted therapy in the UK designated centres (in both clinical practice and clinical trials) on 31 March was 638 in 2004, 912 in 2005, 1242 in 2006 and 1499 in 2007. 31 It has been requested that further data from this utilisation survey remains academic-in-confidence. A small number of patients may not be seen at the Pulmonary Hypertension Service and therefore will be missing from the census.
[Academic-in-confidence information has been removed]. The 2007 census contains data from [Academic-in-confidence information has been removed] UK designated centres [Academic-in-confidence information has been removed]. This data is reproduced in Appendix 1 (Tables 64–67) and outlined as follows and summarised in Table 5. There are currently about [Academic-in-confidence information has been removed] UK patients attending the Pulmonary Hypertension Service. Of these just under [Academic-in-confidence information has been removed] are children. Of the adult patients nearly [Academic-in-confidence information has been removed] are in Scotland. The remaining [Academic-in-confidence information has been removed] patients are seen in England (there are no Welsh or Northern Irish Pulmonary Hypertension Service centres).
| Name of therapy | English patientsa |
|---|---|
| Monotherapy | |
| Epoprostenol (i.v.) | [Academic-in-confidence information has been removed] |
| Treprostinil (s.c.) | [Academic-in-confidence information has been removed] |
| Treprostinil (i.v.) | [Academic-in-confidence information has been removed] |
| Iloprost (i.v.) | [Academic-in-confidence information has been removed] |
| Iloprost (nebulised) | [Academic-in-confidence information has been removed] |
| Bosentan | [Academic-in-confidence information has been removed] |
| Sitaxentan | [Academic-in-confidence information has been removed] |
| Sildenafil | [Academic-in-confidence information has been removed] |
| Trial drugb | [Academic-in-confidence information has been removed] |
| Monotherapy total | [Academic-in-confidence information has been removed] |
| Dual therapy | |
| Bosentan and sildenafil | [Academic-in-confidence information has been removed] |
| Sitaxentan and sildenafil | [Academic-in-confidence information has been removed] |
| Bosentan + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] |
| Bosentan + iloprost (i.v. or nebulised) | [Academic-in-confidence information has been removed] |
| Bosentan + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] |
| Sildenafil + iloprost (i.v. or nebulised) | [Academic-in-confidence information has been removed] |
| Sildenafil + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] |
| Sildenafil + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] |
| Trial drugb | [Academic-in-confidence information has been removed] |
| Dual therapy total | [Academic-in-confidence information has been removed] |
| Triple therapy | |
| Bosentan + sildenafil + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] |
| Bosentan + sildenafil + iloprost (i.v. or nebulised) | [Academic-in-confidence information has been removed] |
| Bosentan + sildenafil + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] |
| Treprostinil (s.c.) + bosentan + sildenafil + iloprost (nebulised) | [Academic-in-confidence information has been removed] |
| Triple therapy total | [Academic-in-confidence information has been removed] |
In England, over [Academic-in-confidence information has been removed]. A small number of patients are on unspecified trial drugs (see Table 5). [Academic-in-confidence information has been removed].
Chapter 2 Definition of the decision problem
Decision problem
According to the final scope issued by the National Institute for Health and Clinical Excellence (NICE) for this technology appraisal the decision problems were:
-
Whether epoprostenol, iloprost, bosentan, sitaxentan and sildenafil, when used within their licensed indications, are clinically effective and cost-effective compared with supportive treatments (see Chapter 1, Supportive treatment) in adults with PAH for whom calcium channel blockers are inappropriate or no longer effective.
-
Whether the interventions being considered are clinically more effective, or more cost-effective, in patients with certain subpopulations of PAH according to the Venice 2003 clinical classification (see Chapter 1, Classification).
-
Whether significant differences in clinical and cost-effectiveness exist between the interventions being considered (either used alone or in combination) when compared with each other and/or intravenous iloprost.
It was clear that this assessment report would be able to address only some of the issues surrounding these decision problems for the following reasons:
-
Although the Venice 2003 clinical classification provides a significantly improved framework for the diagnosis and management of PAH, patients with PAH represent diverse populations that vary greatly in aetiology, disease progression and prognosis. Cases being grouped under each of the Venice subcategories can still be heterogeneous in terms of severity, the choice and response to treatment and prognosis. For example, within the Venice subcategory 1.3.1, scleroderma has distinct features that may warrant it being considered separately from other forms of CTD (see Chapter 1, Clinical classification).
-
The five interventions being considered in this technology appraisal have different routes of administration, demands on patients’ self-management, speeds of action, adverse effect profiles and contraindications. The selection of treatment is to some extent dependent on the nature of the underlying condition, the clinical circumstances and patient ability and acceptance. As such the choice of treatment and appropriate comparators is dependent on all of these factors.
-
PAH is a rare condition. The number of patients included in clinical studies is relatively small. There was unlikely to be sufficient data to allow meaningful comparison between many of the subpopulations of PAH and between different treatments (or combinations of treatments).
-
The resources available to undertake this assessment report were comparable to those for other assessment reports and therefore not limitless.
-
Bearing these in mind the assessment group planned to undertake a systematic review of RCTs and a review of manufacturer submissions to establish the underlying evidence base that is available to answer the above decision problems and to highlight issues that are unlikely to be addressed because of the paucity of evidence. Then a model-based economic evaluation was to be carried out to address refined and focused decision problem(s) that take into account the availability of evidence, the appropriateness of combining different populations of PAH in terms of underlying cause (e.g. whether the model can include all PAH populations or the modelling can be reasonably carried out only for a specific population according to the evidence) and disease severity (e.g. it may be necessary to model patients in FCIII and FCIV separately), and the most appropriate place in the treatment pathway for each of the interventions being considered (e.g. oral treatments would not be considered as alternative, competing interventions against intravenous epoprostenol for patients in NYHA/WHO FCIV).
Population and relevant subgroups
The population considered is adults with PAH (category 1 of the Venice 2003 clinical classification) in NYHA/WHO FCIII (and also FCIV for epoprostenol) for whom calcium channel blockers are inappropriate or no longer effective.
Potentially relevant subgroups include:
-
subcategories of PAH (e.g. IPAH) under category 1 of the Venice 2003 clinical classification
-
NYHA/WHO functional classes.
Subcategories are best perceived as different patient populations that share similar clinical manifestations of PAH rather than as ‘subgroups’ of a well-characterised disease. Given the likely volume of available evidence and the resources available for this technology assessment, the key specific subgroup to be examined was patients with IPAH in FCIII.
Definition of the interventions
For patients in FCIII, interventions being considered are:
-
epoprostenol (Flolan®, GlaxoSmithKline), administered by continuous intravenous infusion
-
iloprost (Ventavis®, Schering Health Care), administered by inhalation through a nebuliser, 2.5–5.0 ∝g as delivered at the mouthpiece per inhalation session
-
bosentan (Tracleer®, Actelion Pharmaceuticals), administered orally, 62.5–250 mg twice daily
-
sitaxentan (Thelin®, Encysive Pharmaceuticals), administered orally, 100 mg once daily
-
sildenafil (Revatio®, Pfizer), administered orally, 20 mg three times daily.
For patients in FCIV:
-
epoprostenol administered by continuous intravenous infusion was the only intervention considered.
Relevant comparators
-
Supportive treatments – these include digoxin, diuretics, anticoagulants and oxygen (see Chapter 1, Supportive treatment).
-
Placebo or no treatment – although the above supportive treatments are used for preventing/treating conditions and symptoms associated with PAH, the goals and mechanisms of these treatments are generally different from those of the interventions being considered. As these supportive treatments usually start earlier in the treatment pathway and are usually continued when introducing the interventions, studies in which the interventions were compared with placebo or no treatment are clinically relevant provided that supportive treatments were continued in all study arms.
-
The interventions being considered, either used alone or in combination, were to be compared with each other if evidence was available from RCTs.
-
Intravenous iloprost was considered as a comparator if evidence was available from RCTs.
Outcomes
The key outcomes to be examined for the technology assessment include changes in survival and quality of life with treatment; change in FC; time to clinical deterioration (including switch of drug therapy and lung transplantation); serious adverse events (SAEs); and incremental cost-effectiveness ratios (ICERs) for the interventions compared with supportive treatments.
Place of the intervention in the treatment pathway(s)
Based on the final scope the interventions being considered were to be used when conventional supportive treatments and calcium channel blockers either are inappropriate or have failed to control symptoms and maintain functional capacity.
For this technology assessment, only the first use of listed interventions was considered. Use of any of the interventions after failure of another listed intervention was not considered in the economic evaluation section, but was described in the clinical effectiveness section for information only (when evidence was available from RCTs). One exception to this was for epoprostenol as second-line treatment for patients progressing to FCIV as many such patients would have received other listed interventions first.
Key issues
Potentially problematic factors
-
Trials including patients with mixed functional classes. Given that none of the interventions were licensed for FCII and only one of them (epoprostenol) was licensed for FCIV the main focus of the technology assessment was on patients in FCIII. Nevertheless, existing trials have included patients of various functional classes (e.g. FCII–IV)(see Chapter 1, Functional classification). Data for the specific subgroup of patients in FCIII were believed in many cases to be unlikely to be readily available and therefore were to be requested from the sponsors/investigators of the trials.
-
Trials including patients of mixed clinical classification of PAH. Existing trials may include types of PAH of a very different nature. Separate data for specific patient clinical classifications (see Chapter 1, Clinical classification) may not be available and therefore were to be requested from the sponsors/investigators of the trials.
-
Insufficiency of data for subgroup analysis. As described already, the volume of existing evidence may not be sufficient for the exploration of treatment effects in subcategories of PAH or PAH associated with specific conditions even if the data were (made) available.
-
Lack of long-term survival data from RCTs. Survival is one of the key outcomes that affect the cost-effectiveness of the interventions. The short duration of the trials was likely to restrict the availability of survival data from well-controlled studies. Economic modelling based on comparisons involving historical control subjects or data from non-randomised studies was inevitable. Prediction of survival had been based on patients’ risk factors and/or surrogate outcomes such as haemodynamic assessment in many of the studies.
-
Rapid and continuing development of treatment algorithms and patient pathways. Different treatment guidelines have been drawn up by various organisations and are being updated rapidly. For example, we are aware that the guidelines issued by the ESC are being updated and new guidelines are expected to be issued in 2009. It was unlikely that there would be sufficient evidence to deal with the issues around the sequencing of the technologies and, as stated already [see Place of the intervention in the treatment pathway(s)], only the first use of the technologies was considered, except for epoprostenol for which second-line use for patients in FCIV was considered.
-
Co-morbidity and functional capacity can affect treatment choice, for example bosentan and sitaxentan cannot be considered in patients with moderate to severe hepatic impairment; epoprostenol cannot be considered in outpatients who are unable and/or unwilling to have this treatment administered by themselves or a carer.
-
Request for data from manufacturers/sponsors. Because of the low prevalence of PAH it was likely that there would be a discrepancy between the patient groups included in clinical trials and the patient groups for whom the interventions are licensed. Furthermore it was unlikely that published trial data would be available purely for the licensed populations (clinical and functional classification) and on the licensed dose of the interventions. Such data for published and unpublished studies were to be requested from individual trial sponsors and therefore the assessment report was somewhat reliant on the availability of such data.
Areas that are considered outside the scope of the appraisal
The assessment group was aware of the emerging evidence that suggests a potential benefit of early treatment in patients with PAH who have mild symptoms and mild functional limitation. However, this group of patients was excluded from the final scope as none of the interventions being considered were licensed for PAH patients of FCII.
Drugs and preparations that were not licensed for treating PAH in the UK in 2007, such as treprostinil (Remodulin®, United Therapeutics), Beraprost® (United Therapeutics), ambrisentan (Volibris®/Letaris®, GlaxoSmithKline) and iloprost intravenous infusion (Ilomedin(e)®, Schering Health Care), were not considered as an intervention, even though they may be being used in clinical practice. However, intravenous iloprost was considered as a comparator when evidence permitted according to the final scope of the appraisal.
The assessment concentrated on the treatment of adults and, therefore, the treatment of children was not considered specifically.
Overall aims and objectives of assessment
The aims of this technology assessment were :
-
to assess whether epoprostenol, iloprost, bosentan, sitaxentan and sildenafil (alone or in combination) are clinically effective and cost-effective when used within their licensed indications for the treatment of adults with PAH for whom calcium channel blockers are inappropriate or no longer effective compared with supportive treatment (and/or intravenous iloprost)
-
to assess, as far as available clinical data from RCTs would allow, whether epoprostenol, iloprost, bosentan, sitaxentan and sildenafil (alone or in combination) are clinically effective and cost-effective when used within their licensed indications for the treatment of adults with IPAH for whom calcium channel blockers are inappropriate or no longer effective compared with supportive treatment (and/or intravenous iloprost)
-
if head-to-head RCTs exist, to assess whether one technology is significantly more or less clinically effective and cost-effective than another (alone or in combination) when used within their licensed indications for the treatment of adults with PAH for whom calcium channel blockers are inappropriate or no longer effective.
These aims were to be achieved by:
-
a systematic review of RCTs that investigated the effectiveness of the technologies in PAH; variations in effectiveness between the drugs and/or between different PAH populations were to be explored if evidence from RCTs permitted
-
a systematic review of published studies on the costs and cost-effectiveness of the technologies in PAH
-
a review of the dossiers submitted to NICE by the manufacturers of the technologies
-
a focused, model-based economic evaluation of the cost-effectiveness of the technologies from the perspective of the UK NHS.
Chapter 3 Assessment of clinical effectiveness
Methods for reviewing effectiveness
Search strategy
The following resources were searched for relevant primary studies:
-
Bibliographic databases: Cochrane Library (CENTRAL) 2007 Issue 1, MEDLINE (Ovid) 1950 to February 2007, MEDLINE In-Process & Other Non-Indexed Citations (Ovid) and EMBASE (Ovid) 1980 to February 2007. Searches used index and text words that encompassed the condition (pulmonary arterial hypertension) and the interventions [epoprostenol, iloprost, bosentan, sitaxentan (and sitaxsentan) and sildenafil]. When the databases allowed, a methodological ‘filter’ was applied to identify trials.
-
Citations of relevant studies were examined.
-
Further information was sought from clinical experts.
-
Research registers of ongoing trials including the National Research Register 2007 Issue 1, Current Controlled Trials and ClinicalTrials.gov.
-
Manufacturer submissions.
Searches were not limited by date and neither were there language restrictions. Full search strategies can be found in Appendix 2.1.
Search results were entered into an electronic bibliographic database (reference manager version 11; Thomson ISI ResearchSoft) and duplicate entries were removed.
Study selection
One reviewer screened all titles and abstracts for relevance and a subset of approximately half were checked by a second reviewer for quality assurance purposes. Full papers of potentially relevant studies were obtained and assessed for inclusion by two reviewers independently. Disagreements were resolved by consensus or referral to a third reviewer when necessary.
Studies that met all of the following criteria were included in the clinical effectiveness review:
-
Study design – an RCT or article including data from one or more RCTs [e.g. systematic reviews or additional analyses of data from RCT(s)] in which the duration of the RCT(s) was greater than 1 week.
-
Intervention(s) – any of epoprostenol (intravenous), iloprost (inhaled), bosentan (oral), sitaxentan (oral), sildenafil (oral).
-
Comparator(s) – any treatment(s) other than different doses, formulations or methods of administration of the intervention itself. These could be placebo, conventional supportive treatments, other interventions listed above, other treatments not currently licensed in the UK (see Chapter 2, Areas that are considered outside the scope of the appraisal) or any combination of these.
-
Population – adult patients diagnosed with PAH (even if not all of the patients enrolled had PAH or were adults).
-
Outcomes – any.
A list of excluded studies and the reason for exclusion were recorded.
Included systematic reviews were not themselves systematically reviewed, but were utilised to identify further RCTs.
Data extraction strategy
Data extraction for published papers was performed independently by two reviewers into a specific proforma. Disagreements were resolved by consensus or by referral to a third reviewer when necessary. Additional data from manufacturer submissions, unpublished manuscripts and clinical study reports were extracted by only one reviewer because of time constraints.
Data were extracted on study design, patient characteristics, method of data analysis and results.
Critical appraisal strategy
The quality of each of the included studies was assessed by one reviewer and checked by another. Disagreements were resolved by consensus and a third reviewer was available to resolve any disagreements. The criteria on which studies were assessed were:
-
Randomisation – whether allocation was truly random. Randomisation using computer or random number tables was considered adequate whereas the use of alternation, case record numbers or dates of birth and day of the week was considered inadequate. Strata for randomisation (if used) were recorded for information.
-
Allocation concealment – whether allocation concealment was adequate. Any of the following methods was considered adequate: centralised (e.g. allocation by a central office unaware of subject characteristics) or pharmacy-controlled randomisation; prenumbered or coded identical containers that are administered serially to participants; on-site computer system combined with allocations kept in a locked unreadable computer file that can be accessed only after the characteristics of an enrolled participant have been entered; sequentially numbered, sealed, opaque envelopes.
-
Blinding – use of blinding and who was blinded.
-
Intention-to-treat (ITT) analysis – whether ITT analysis was used. During data extraction it became apparent that trials may have used ITT analysis for some of the outcomes but not others. Use of ITT analysis for each of the main outcomes (survival analysis, clinical worsening, change in FC, 6MWD, haemodynamic measures and quality of life measures) was therefore checked in detail for each trial by one reviewer.
-
Follow-up – proportion (%) of patients completing the trial in each study arm.
The information from quality assessment was tabulated and utilised in a narrative assessment of the studies.
Methods of data synthesis
Outcomes of interest
Selected outcomes of interest were specified in the review protocol, based upon the final scope issued by NICE for this technology appraisal. They were:
-
survival
-
time to clinical deterioration (including switch of drug therapy and lung transplantation)
-
health-related quality of life
-
exercise capacity (6MWT)
-
symptomatic improvement
-
frequency and duration of hospitalisation and outpatient/GP visits
-
SAEs
-
adverse events that are considered as being clinically relevant or having a potential impact on tolerability
-
withdrawal for any reason
-
withdrawal because of lack of efficacy
-
withdrawal because of adverse events
-
haemodynamic assessment, e.g. cardiac index, RAP, pulmonary arterial oxygen saturation, PAP and PVR.
Of these, sufficient data were available from the included trials and meta-analyses were carried out for the following outcomes:
-
dichotomous outcomes: death, clinical worsening (as defined in individual trials), symptomatic improvement (change in functional class), SAEs and withdrawal for any reason
-
continuous outcomes: exercise capacity (6MWT), haemodynamic assessment including mPAP, RAP, PVR and cardiac index.
When data were available, narrative summaries were also provided in this review for time-to-event analyses of survival and clinical deterioration, and for other outcomes related to symptomatic relief (such as dyspnoea or fatigue) and health-related quality of life.
Individual adverse events were not meta-analysed as adverse event profiles varied between the interventions being assessed, and data on the severity or seriousness of specific adverse events were usually not provided. Withdrawal because of lack of efficacy and withdrawal because of adverse events were not separately analysed as it became apparent during data extraction that lack of efficacy of treatment in PAH naturally leads to adverse events associated with disease worsening. It was therefore not possible to attribute withdrawal to either lack of efficacy or adverse events in many cases and withdrawal for any reason would be a more appropriate outcome covering both. None of the included RCTs reported the frequency and duration of hospitalisation and outpatient/GP visits and pulmonary arterial oxygen saturation.
Handling of data and presentation of results
For dichotomous outcomes, results are presented as RRs. For continuous outcomes, results are presented as weighted mean differences (WMD).
Relative risks for ‘FC improved or maintained’ were initially calculated to provide more stable estimates as the proportion of patients with FC either improved or deteriorated was expected to be small. However, it was felt that ‘FC improved’ alone was also clinically important and thus RRs for this outcome were also calculated and presented. In addition, when data specifically for FCIII patients were available from the RCTs, odd ratios were compiled for ‘FC improved’ and ‘FC worsened’ at 12 weeks to inform the independent economic assessment (see Chapter 4).
For outcomes with continuous data the values of mean change from baseline (i.e. mean value measured at the end of the trial minus the mean value measured at baseline) were used in meta-analysis. When possible the standard deviation (SD) was taken directly from the reported results or derived from the standard error of the mean (SEM) or CIs. For the 6MWD data of Barst et al. ,11 SDs for mean change from baseline were imputed using the SDs of baseline values and SDs of post-treatment values assuming an intercorrelation coefficient of 0.5. 32 For the 6MWD data of Badesch et al. ,33 for which only the SD for the post-treatment value was available, it was used as the SD for the mean change from baseline.
Approaches for meta-analysis
Meta-analyses were carried out using review manager version 4.2. Separate analyses were performed for each of the interventions being considered for the outcomes specified above. The primary analysis included data for licensed doses only (where appropriate) for patients with PAH (all subcategories in category 1 of the Venice 2003 clinical classification excluding the subcategory 1.5, persistent pulmonary hypertension of the newborn) in NYHA/WHO FCIII (and FCIV for epoprostenol) using the latest follow-up data available from the randomised controlled period of each trial. A random-effects model was used given the heterogeneous populations within PAH. Comparisons were made separately for:
-
each of the interventions versus placebo/nothing with ongoing supportive treatments
-
each of the interventions versus placebo/nothing with another ongoing intervention and ongoing supportive treatment (trials were available for iloprost versus placebo/nothing with ongoing bosentan and supportive treatment; and sildenafil versus placebo with ongoing epoprostenol and supportive treatment)
-
comparison of the interventions against each other (trials were available for sitaxentan versus bosentan and sildenafil versus bosentan)
-
comparison between different combinations of interventions (one trial was available for epoprostenol plus bosentan versus epoprostenol).
No indirect comparisons or mixed treatment comparisons were planned or performed.
Given the expected discrepancy between the scope of this technology appraisal (specific types of PAH, FC and dose for each of the drugs within their licensed indication) and the heterogeneous trial evidence actually available for each drug, several sensitivity analyses taking into account the population mix in terms of FC and pulmonary hypertension categories, intervention doses, trial design and data status, as well as subgroup analyses for IPAH and PAH associated with connective tissue disease (CTD-APAH), were planned. The primary analysis (analysis A) and other planned analyses (analyses B–H) are listed in Table 6. Whether each of the listed analyses was actually carried out depended on the availability of data, and this is stated in an analyses checklist within each of the specific comparisons. The aims of these analyses were to ensure that available evidence that was directly applicable to this technology appraisal (or the lack of such evidence) was highlighted, while allowing other potentially relevant evidence to also be considered.
| Planned analysis | Population/doses/data to be included | |
|---|---|---|
| A | Primary analysis | All PAH, FCIII,a licensed dose(s) |
| B | Sensitivity analysis – mixed FC | All PAH, all FC, licensed dose(s) |
| C | Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed dose(s) |
| D | Sensitivity analysis – including above licensed dose(s) | All PAH, all FC, licensed dose(s) and above licensed dose(s) |
| E | Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data |
| F | Sensitivity analysis – excluding open-label trial(s) | All PAH, all FC, licensed dose(s), excluding open-label trials |
| G | Subgroup analysis – IPAH | IPAH, FCIII (or all FC), licensed dose(s) |
| H | Subgroup analysis – CTD-APAH | CTD-APAH, FCIII (or all FC), licensed dose(s) |
Assessment of heterogeneity
Statistical heterogeneity between studies was assessed with the chi-squared test and I2. The I2 is a measure of inconsistency in studies’ results in meta-analysis. 34 It describes the percentage of the total variation across studies that is due to heterogeneity rather than to chance (sampling error), and lies between 0% (no observed heterogeneity) and 100% (significant heterogeneity). An I2 of 25%, 50% and 75% would indicate low, moderate and high heterogeneity respectively. When there was evidence of statistical heterogeneity (p ≤ 0.10 for chi-squared test for heterogeneity or I2 ≥ 50%), the values of I2 were shown besides the pooled estimates within the results tables and the heterogeneity was discussed in the text. I2 was reported for all of the pooled estimates quoted in the texts, irrespective of its value.
Assessment of publication bias
All manufacturers were requested to provide a list of all company-sponsored RCTs that were relevant to this appraisal. Requests were also made for reports of unpublished trials and data that are potentially available but not reported in published papers. Given that the lists of RCTs were provided by all of the companies and the number of trials for each of the technologies was small, publication bias was not formally assessed.
Ongoing studies
Ongoing studies (RCTs/open-label studies) were identified as already described in the search strategy. These were not included in the systematic review, but were tabulated separately for information.
Long-term follow-up studies
A systematic review of follow-up studies of the long-term use of the technologies was not undertaken. However, long-term studies were identified from scrutiny of the manufacturer submissions in order to inform the economic assessment. Information in these studies was tabulated.
Results
Overall quantity of research available
The searches resulted in the identification of 1354 articles after duplicates had been removed. Screening of the titles and abstracts of these articles indicated that 1307 were not directly relevant to the clinical effectiveness section of this report. Inclusion criteria were applied to the remaining 47 articles. Of these 16 were excluded for not meeting one or more of the criteria. Details of these studies can be found in Appendix 3.
Of the 31 articles meeting the criteria, 23 were papers documenting 16 RCTs, and eight were reports of systematic reviews. The systematic reviews were only utilised to identify further RCTs. A list of these systematic reviews can be found in Appendix 4. One additional published RCT35 was identified from the systematic reviews. A further three unpublished RCTs36–38 were identified through screening of the five manufacturer submissions for this assessment. All of these met the inclusion criteria. This resulted in 20 RCTs being included in the review. Figure 3 documents the selection process.
FIGURE 3.
Flow chart of clinical effectiveness study selection.
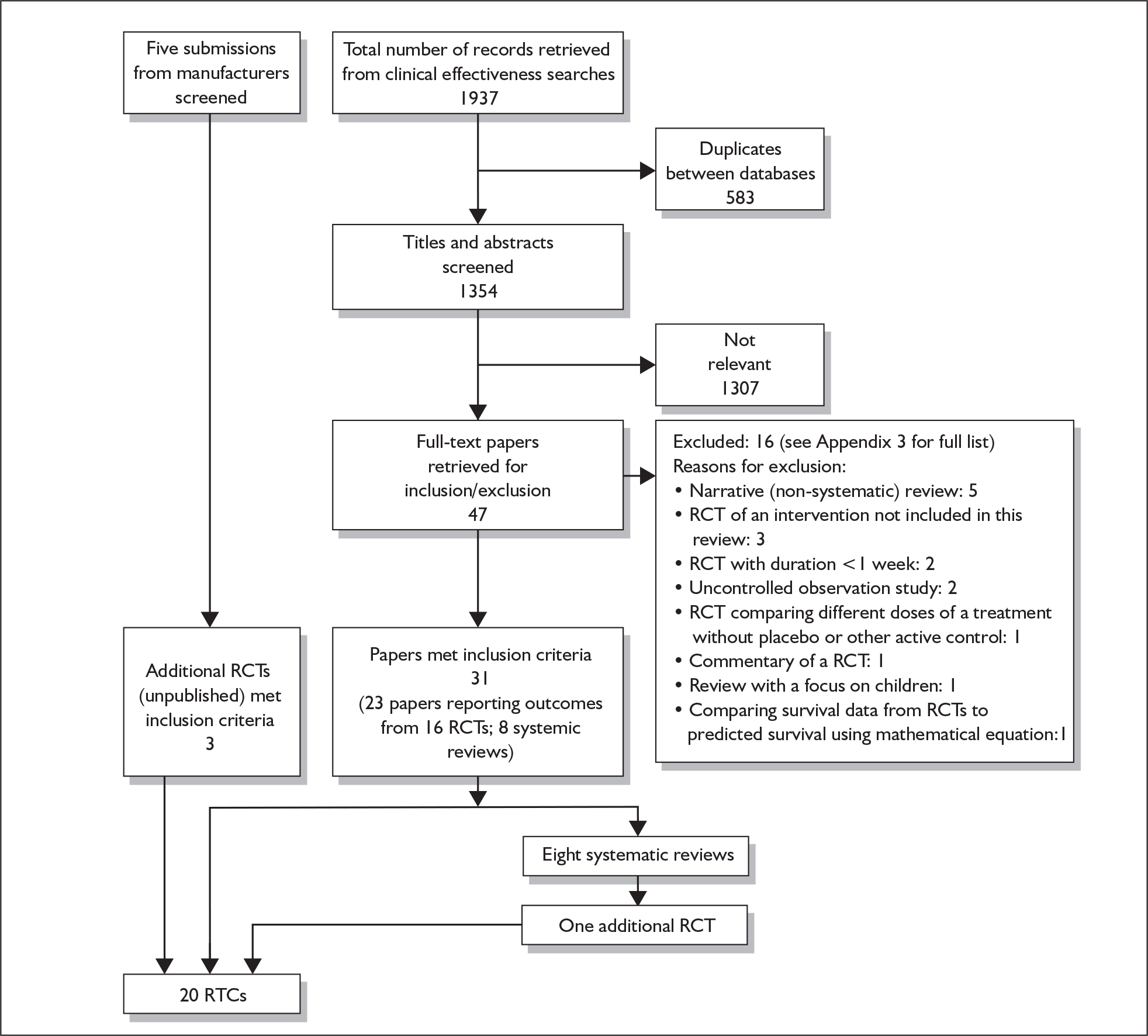
There were RCTs on all of the five technologies for this assessment. The distribution of the RCTs across the technologies and the respective comparisons undertaken in them are shown in Table 7. Most RCTs compared one technology plus supportive care against placebo and/or supportive care. There were few head-to-head comparisons of the technologies and few RCTs comparing a single technology with combination technologies. There were no RCTs comparing any of the technologies with unlicensed drugs for PAH [e.g. treprostinil, iloprost (intravenous), beraprost, ambrisentan].
The assessment of effectiveness of the technologies is reported in the following six sections, one for each of the technologies and one on head-to-head comparisons. When RCTs assessed a combination of the technologies this is addressed as a subsection of the main technology under assessment.
| Epoprostenol | Iloprost | Bosentan | Sitaxentan | Sildenafil | Bosentan + epoprostenol | Iloprost + (ongoing) bosentan | Sildenafil + (ongoing) epoprostenol | |
|---|---|---|---|---|---|---|---|---|
| Placebo/existing treatment | n = 3; Rubin 1990,39 Barst 1996,11,40 Badesch 200033 | n = 2; Olschewski 2002 (AIR),41,42 unpublished (AIR-2)36 | n = 4; Channick 2001,15,43,44 Rubin 2002 (BREATHE-1),44–46 Galiè 2006 (BREATHE-5),47 Barst 2006 (STRIDE-2)48 | n = 3; Barst 2004 (STRIDE-1),49–51 Barst 2006 (STRIDE-2),48 Barst 2007 (STRIDE-4)37,52 | n = 4; Galiè 2005 (SUPER-1),53 Bharani 2003,35 Sastry 2004,54 Singh 200655 | n = 0 | n = 0 | n = 0 |
| Epoprostenola | n/a | n = 0 | n = 0 | n = 0 | n = 0 | n = 1; Humbert 2004 (BREATHE-2)56 | n = 0 | n = 1; unpublished (PACES-1)38 |
| Iloprost | n/a | n/a | n = 0 | n = 0 | n = 0 | n = 0 | n = 0 | n = 0 |
| Bosentanb | n/a | n/a | n/a | n = 1; Barst 2006 (STRIDE-2)48 | n = 1; Wilkins 2005 (SERAPH)57 | n = 0 | n = 2; Hoeper 2006 (COMBI),58 McLaughlin 2006 (STEP)59 | n = 0 |
| Sitaxentan | n/a | n/a | n/a | n/a | n = 0 | n = 0 | n = 0 | n = 0 |
| Sildenafil | n/a | n/a | n/a | n/a | n/a | n = 0 | n = 0 | n = 0 |
Epoprostenol
Quantity and quality of included studies
Three RCTs11,33,39,40 compared epoprostenol (added to supportive treatment) with supportive treatment. [An additional study (BREATHE-2; Bosetan Randomised Trial of Endothelin Antagonist Therapy)56 that compared the initiation of bosentan–epoprostenol combination with epoprostenol alone will be described in the bosentan section and a further study (PACES-1)36 that compared sildenafil with placebo in patients who were stable on epoprostenol treatment will be described in the sildenafil section.] In addition to the main publications associated with these trials, further data not included in these publications were available from the Cochrane review by Paramothayan and colleagues. 60 The clinical study report for one of the RCTs11 was made available to the assessment group by GlaxoSmithKline.
The characteristics of the three trials are summarised in Table 8. All were industry-sponsored multicentre studies conducted in the USA. The number of patients randomised ranged from 2339 to 11133 and study duration was between 839 and 1211,33 weeks. Rubin et al. 39 and Barst et al. 11 recruited exclusively patients with PPH, whereas Badesch et al. 33 recruited exclusively PAH patients with a scleroderma spectrum of disease. All three trials included patients with mixed FC, with 65–78% of patients in FCIII and 17–26% of patients in FCIV at baseline. The mean/median 6MWD at baseline was less than 300 metres in all three trials. The primary end point was change in 6MWD for Barst et al. 11 and Badesch et al. ,33 and was not stated for Rubin et al. 39
| Trial name/key paper; location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD); % female | Baseline exercise capacity and haemodynamic measures, mean (SD)b |
|---|---|---|---|---|---|---|---|
| Rubin et al., 1990;39 USA, four centres | 8 weeks; open-label, parallel; n = 23 | Epoprostenol (i.v. infusion) individualised dose (n = 11) | None (n = 12) | PPH (100%) | II (9%), III (65%), IV (26%) | 36 (14); 70% | 6MWD (n = 19): 227 (NR); cardiac index: NR; mPAP: 61.3 (NR); PVR: NR; RAP: NR; SvO2: NR |
| Barst et al., 1996;11 USA, multicentre | 12 weeks; open-label, parallel; n = 81 | Epoprostenol (i.v. infusion) individualised dose (n = 41) | None (n = 40) | PPH (100%) | III (74%), IV (26%) | 40 (15); 73% | 6MWD: 294 (126); cardiac index: 2.1 (0.8); mPAP: 60 (13); PVR: 1280 (560);c RAP: 12 (7); SvO2: 61 (13) |
| Badesch et al., 2000;33 USA, 17 centres | 12 weeks, open-label, parallel; n = 111 | Epoprostenol (i.v. infusion) individualised dose (n = 56) | None (n = 55) | Scleroderma spectrum of disease (100%) | II (5%), III (78%), IV (17%) | 55 (12); 86% | 6MWD: 272/240;d cardiac index: 2.0 (0.7); mPAP: 50 (10); PVR: 1016 (504);c RAP: 12 (5); SvO2: 58.1 (10.4) |
Quality assessment of these trials is summarised in Table 9. All of the trials were open-label studies as a double-blind, placebo-controlled design was not considered possible because of the known incidence of sepsis caused by central venous catheters and the unique or highly predictable symptoms during long-term epoprostenol treatment. 11 However, assessors for the 6MWT were blinded in Barst et al. 11 and Badesch et al. 33 With the exception of survival and 6MWD in Barst et al. 11 and 6MWD in Badesch et al. ,33 ITT analysis was not used. Treatment withdrawal/loss to follow-up was not clearly reported in Rubin et al. 39 and Badesch et al. 33
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| Rubin et al., 1990;39 8 weeks | Yes (FC, pre-existing drug therapy) | Yes | Open-label | Survival analysis: N/A; clinical worsening: N/A; functional class: no (19/23); 6MWD: no (19–21/23); haemodynamics: no (19–21/23); quality of life: N/A | Not reported | Patients who died during the trial (n = 1 for epoprostenol; n = 3 for control) were excluded from analysis. Additional data were available from Paramothayan 200560 (Cochrane review) |
| Barst et al., 1996;11 12 weeks | Yes (FC, study centre, baseline vasodilator use) | Unclear | Open-label (assessor for 6MWT and quality of life blinded) | Survival analysis: yes; clinical worsening: N/A; functional class: no (71/81); 6MWD: yes; haemodynamics; no (44–68/81); quality of life: no (73/81) | Control: 75% (30/40); epoprostenol: 93% (38/41) | |
| Badesch et al., 2000;33 12 weeks | Yes (vasodilator use and exercise capacity at baseline) | Yes | Open-label (assessor for 6MWT blinded) | Survival analysis: unclear; clinical worsening: N/A; functional class; unclear; 6MWD: yes; haemodynamics: unclear; quality of life: N/A | Not reported |
Epoprostenol (added to supportive treatment) versus supportive treatment
Planned meta-analyses for this comparison and those actually carried out are summarised in Table 10.
As outcome data stratified by FC were available neither from published papers nor from the clinical study report it was not possible to perform the planned primary analyses [analysis for PAH, by FC (FCIII and FCIV), treated with licensed doses]. Furthermore, some other planned analyses were also not possible or not required. The reasons for these are also given in Table 10.
| Planned analyses | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A1. Primary analysis | All PAH, FCIII, licensed doses | No | All trials included patients with mixed FC but data stratified by FC were not available |
| A2. Primary analysis | All PAH, FCIV, licensed doses | No | All trials included patients with mixed FC but data stratified by FC were not available |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed doses | Yes | Data from all three trials11,33,39 were included |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed doses | No | None of the epoprostenol trials included pulmonary hypertension other than PAH |
| D. Sensitivity analysis – including above licensed dose | All PAH, all FC, licensed doses and above licensed doses | No | The dose for epoprostenol was individualised and no maximum dose was specified in its license |
| E. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed doses, excluding commercial-in-confidence and academic-in-confidence data | No | The amount of data classified as confidential was small and unlikely to have a significant impact on the results |
| F. Sensitivity analysis – excluding open-label trials | All PAH, all FC, licensed doses, excluding open-label trials | No | Not applicable – all of the epoprostenol trials were open label |
| G. Subgroup analysis – IPAH | IPAH (PPH), mixed FC, licensed doses | Yes | Data from Rubin et al.39 and Barst et al.11 were included. This analysis matches most closely with epoprostenol’s licensed indication (FCIII and FCIV, PPH), although two patients from Rubin et al.39 were in FCII at baseline |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, mixed FC, licensed doses | Yes | Data from Badesch et al.33 were included |
All of the findings presented in this section are on analyses that could be performed and these are associated with patient populations of mixed FC (III and IV). The results of meta-analyses (or of individual trials when only one trial provided the data) are listed in Table 11. Results for individual outcomes are summarised in the following subsections.
| Analysis (see Table 10) A1/A2: Primary analyses |
B: Sensitivity analysis – mixed FC | G: Subgroup analysis – IPAH | H: Subgroup analysis – CTD-APAH | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PAH population | All PAH subcategories | All PAH subcategories | IPAH only | CTD-APAH only | |||||
| Functional class (FC) | A1: FCIII; A2: FCIV | All FC (II–IV) | All FC (II–IV) | All FC (II–IV) | |||||
| Doses | Licensed doses | Licensed doses | Licensed doses | Licensed doses | |||||
| Total no. eligible for analysis | 16211,33,39 | 21511,33,39 | 10411,39 | 11133 | |||||
| No. included in analysis | 0 (none of the trials reported data stratified by FC) | 85–215 (data from all three trials were included) | 65–104 (data from Rubin et al.39 and Barst et al.11 were included) | ≤ 111 (data from Badesch et al.33 were included) | |||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||||
| Death | RR | 0 | Data not available | 21511,33,39 | 0.37 (0.09–1.57) | 10411,39 | 0.18 (0.03–1.18) | 11133 | 0.79 (0.22–2.77) |
| Clinical worsening | RR | 0 | Data not available | 0 | Data not available | 0 | Data not available | 0 | Data not available |
| FC improved | RR | 0 | Data not available | 21511,33,39 | 10.58 (3.07–36.50) a | 10411,39 | 7.45 (2.55–21.77) a | 11133 | 42.25 (2.62–680.61) a |
| FC maintained or improved | RR | 0 | Data not available | 8111 | 1.22 (0.96–1.55)b | 8111 | 1.22 (0.96–1.55)a | 0 | Data not available |
| Withdrawal for any reason | RR | 0 | Data not available | 8111 | 0.29 (0.09–0.99) a | 8111 | 0.29 (0.09–0.99) a | 0 | Data not available |
| 6-minute walk distance (metres)c | WMD | 0 | Data not available | 21311,33,39 | 81 (45–117) a | 10211,39 | 58 (6–110) a | 11133 | 100 (55–144) a |
| Haemodynamics | |||||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 0 | Data not available | 20011,33,39 | –6.3 (–8.7 to –3.9) a | 8911,39 | –6.8 (–10.6 to –3.0) a | 11133d | –6.0 (–9.0 to –2.9) a |
| Right atrial pressure (RAP) (mmHg)c | WMD | 0 | Data not available | 17611,33 | –2.4 (–4.1 to –0.7) a | 6511 | –2.3 (–5.1 to 0.5) | 11133d | –2.5 (–4.6 to –0.4) a |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)d | WMD | 0 | Data not available | 17611,33,39 | –427 (–548 to –306) a | 6511,39 | –401 (–613 to –189) a | 11133d | –440 (–588 to –292) a |
| Cardiac index (l/min/m2)e | WMD | 0 | Data not available | 17911,33 | 0.6 (0.4–0.8) a | 6811 | 0.6 (0.2–0.9) | 11133d | 0.6 (0.4–0.8) a |
| Safety | |||||||||
| Serious adverse events | RR | 0 | Data not available | 0 | Data not available | 0 | Data not available | 0 | Data not available |
Survival
A total of 21 deaths (five for epoprostenol, 16 for supportive treatment) were reported in the three trials. 11,33,39 A significant decrease in the risk of death was reported in Barst et al. ,11 in which eight deaths occurred in the control group versus none in the epoprostenol group (RR = 0.06, 95% CI 0.00–0.96). The pooled RR favours epoprostenol although it does not reach statistical significance (RR = 0.37, 95% CI 0.09–1.57, I2 = 39%).
Time to clinical worsening
This outcome was not reported in any of the epoprostenol trials.
Functional class
The proportion of patients who had their FC unchanged/worsened was not reported in Rubin et al. 39 or Badesch et al. 33
Results from Barst et al. 11 showed a non-significant RR of 1.22 (95% CI 0.96–1.55) for having FC improved or maintained (the planned dichotomous outcome for FC) for the epoprostenol group compared with the control group.
A significantly higher proportion of patients in the epoprostenol group had their FC improved compared with those in the control group in all three trials11,33,39 (pooled RR = 10.58, 95% CI 3.07–36.50, I2 = 25%).
Exercise capacity
The mean changes from baseline for the 6MWD for the three trials11,33,39 are shown in Figure 4. Improvements were seen in all three trials and the pooled result for the WMD was an increase of 81 metres (95% CI 45–117, I2 = 25%) for epoprostenol groups compared with control groups.
FIGURE 4.
Forest plot: epoprostenol added to supportive treatment versus supportive treatment alone – change in 6-minute walk distance. Note: The standard deviations for Barst et al.11 and Badesch et al.33 were not reported and were imputed using the methods described in the section on handling of data and presentation of results. CI, confidence interval; CTD, connective tissue disease; IPAH, idiopathic pulmonary arterial hypertension; PAH, pulmonary arterial hypertension; SD, standard deviation; WMD, weighted mean difference.
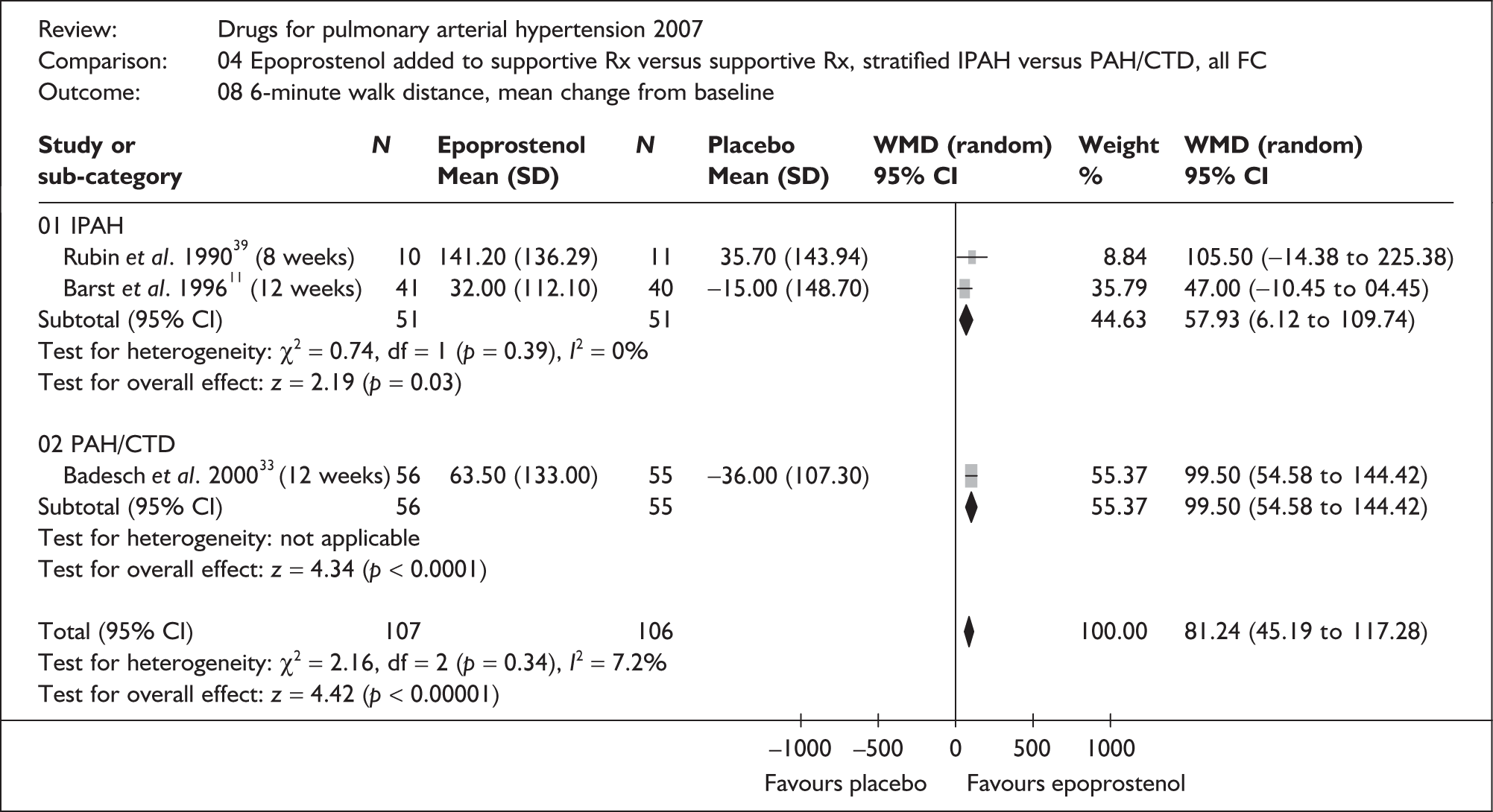
Quality of life
This outcome was reported only in Barst et al. 11 Patients who died during the trial (0/41 in the epoprostenol group and 8/40 in the control group) were excluded from the analysis. A significant improvement for the epoprostenol group compared with the control group was observed for all four parts of the Chronic Heart Failure Questionnaire (dyspnoea, fatigue, emotional function and mastery) and for two (emotional reaction and sleep), but not four (energy, pain, physical mobility and social isolation) of the six parts of the Nottingham Health Profile.
Haemodynamic measures
The pooled results shown in Table 11 demonstrate that epoprostenol significantly reduced mPAP, RAP and PVR and increased the cardiac index compared with supportive treatment. The results were consistent across the trials with little heterogeneity between them.
Other effectiveness measures
Both Barst et al. 11 and Badesch et al. 33 reported a significant improvement in the dyspnoea–fatigue rating for the epoprostenol group compared with the control group. A significant improvement in the Borg dyspnoea index in favour of epoprostenol was also observed in Badesch et al. 33
Serious adverse events and other adverse events
SAEs were not described separately from other adverse events in the three trials and the total number of SAEs was not reported. However, serious complications due to the delivery system including catheter-related sepsis, pneumothorax and paradoxical embolism were observed in the trials. 11,33,39 Common adverse events occurred more frequently in patients receiving epoprostenol including jaw pain, diarrhoea, nausea, flushing and headache.
Subgroup analysis – PAH subcategories
As the existing epoprostenol RCTs included either patients with PPH only or patients with scleroderma only, no within-trial comparisons between PAH subcategories can be made. Little heterogeneity was observed between the pooled results of the two trials in patients with PPH11,39 and the results of the trial in patients with scleroderma. 33
Summary and discussion
-
Three open-label RCTs11,33,39 comparing epoprostenol (added to supportive treatment) with supportive treatment alone were identified. The duration of the studies ranged from 8 to 12 weeks.
-
Except for Barst et al. ,11 in which allocation concealment was not clear, methods of randomisation and allocation concealment were adequate in the trials. The reporting of treatment withdrawal and SAEs was poor. ITT analysis was not used for many of the outcomes reported. The potential bias, however, is likely to be in favour of control groups as most patients who were excluded from analyses were those who died or withdrew from the trials because of deterioration, and this occurred more frequently in the control groups.
-
The trials included predominantly FCIII and FCIV patients, who were likely to be the sickest of any PAH trial participants judging from a mean 6MWD of less than 300 metres at baseline and other haemodynamic measures.
-
Data stratified by FC were not available from published literature and were not provided by the manufacturer. Results were summarised based on patient populations with mixed FC.
-
Compared with supportive treatment alone, epoprostenol significantly improved exercise capacity (6MWD) and haemodynamic measures (mPAP, RAP, PVR, cardiac index), and increased the proportion of patients with improved FC during 8–12 weeks of treatment in patients with PPH (licensed indication) and scleroderma spectrum of disease (unlicensed indication). Significant improvements in survival, PAH-associated symptoms (dyspnoea) and certain domains of quality of life measures were also observed in individual trials.
-
No significant differences were observed in any of the outcomes examined in this review between the trials in patients with PPH11,39 and the trial in patients with scleroderma. 33
Iloprost
Quantity and quality of included studies
Two RCTs [AIR (Aerosolized Iloprost Randomised study),41 AIR-236] compared iloprost (added to supportive treatment) with supportive treatment. The AIR-2 study36 was identified through industry submission and Schering Health Care provided the assessment group with an unpublished manuscript. The study had not been published at the completion of this report and data from the manuscript are considered academic-in-confidence. Two further RCTs [COMBI (Combination Therapy of Bosetan and Aerosolized Iloprost in Idiopathic Pulmonary Arterial Hypertension),58 STEP (Safety and Pilot Efficacy Trial in Combination with Bosetan for Evaluation in PAH)59] compared iloprost (added to ongoing bosentan therapy and supportive treatment) with ongoing bosentan therapy and supportive treatment.
The characteristics of these four trials are summarised in Table 12. All were industry-sponsored multicentre studies (COMBI58 was investigator-initiated, but was supported by the manufacturer58). The AIR study41 was a multinational study conducted in Europe and was the pivotal trial for iloprost. The AIR-236 and COMBI58 trials were conducted in Germany and the STEP study59 was conducted in the USA. The number of patients randomised ranged from 4058 to 20341 and the duration of study was 12 weeks for all four trials.
| Trial name/key paper (protocol number); location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures, mean (SD)b |
|---|---|---|---|---|---|---|---|
| AIR/Olschewski et al., 200241 (A02997); Europe, 37 centres | 12 weeks; double-blind, parallel; n = 203 | Iloprost (inhalation) 2.5 or 5.0 µg six or nine times dailyc (n = 101) | Placebo (inhalation) (n = 102) | PPH (50%),d collagen vascular disease (17%), appetite suppressant (4%), non-PAHe (28%) | III (59%), IV (41%) | 52 (13, 20–70); 68% | 6MWD: 323 (95); cardiac index: NR; mPAP: 53 (13); PVR (n = 187): 1035 (446); RAP: NR; SvO2 (n = 169): 60.5 (7.9) |
| AIR-2/Olschewski et al.,36 (A02237); Germany, multicentre | 12 weeks, open-label, parallel; n = 63 | Iloprost (inhalation) 24 µg daily divided into six or nine dosesf (n = 30) | None (n = 33) | PPH (63%), [Academic-in-confidence information has been removed]g | II (33%), III (48%), IV (19%) | 46 (12, 24–78); 70% | 6MWD: [Academic-in-confidence information has been removed]; cardiac index: NR; mPAP: 56 (14); PVR: [Academic-in-confidence information has been removed]; RAP: NR; SvO2: [Academic-in-confidence information has been removed] |
| COMBI/Hoeper et al., 2006;58 Germany, multicentre | 12 weeks, open-label, parallel; n = 40 | Iloprost (inhalation) 5 µg six times daily + ongoing bosentan (oral) 125 mg b.d. (n = 19) | Ongoing bosentan (oral) 125 mg b.d. (n = 21) | IPAH (100%) | III (100%) | 52 (NR); 78% | 6MWD: 306 (77); cardiac index: 2.1 (0.6); mPAP: 57 (16); PVR: 1056 (536);h RAP: 9 (5); SvO2: 62 (9) |
| STEP/McLaughlin et al., 2006;59 USA, multicentre | 12 weeks, double-blind, parallel; n = 67 | Iloprost (inhalation) 5 µg six to nine times daily + ongoing bosentan (oral) 125 mg b.d. (n = 34) | Placebo + ongoing bosentan (oral) 125 mg b.d. (n = 33) | IPAH (55%), associated PAH including scleroderma, other connective tissue diseases, repaired congenital heart disease, HIV infection and anorexigen use (45%) | II (1.5%), III (94%), IV (4.5%) | 50 (14, 10–77); 79% | 6MWD: 335 (67); cardiac index: NR; mPAP (n = 57): 52 (12); PVR: 799 (381); RAP: NR; SvO2: 63.8 (7.7) |
Both the AIR and the AIR-2 studies were carried out in mixed populations including IPAH and other PAH within category 1 of the Venice classification, as well as other pulmonary hypertension (mainly chronic thrombolic, Venice category 4). The COMBI study recruited exclusively IPAH patients and the STEP study included mixed PAH populations (all within Venice category 1). The trials were also different in the mix of patients in terms of baseline FC: the AIR study had mixed FCIII and FCIV patients, whereas the AIR-2 study also included patients in FCII. The COMBI study recruited exclusively patients in FCIII. The vast majority of patients in the STEP trial were also in FCIII at baseline. Mean 6MWD at baseline was lowest in the COMBI study (306 metres)58 and was highest [Academic-in-confidence information has been removed].
With regard to end points, the AIR study41 used a composite end point of ‘at least a 10% increase in 6MWD and improvement in FC without deterioration’ as the primary outcome. Change in 6MWD was the primary outcome for the COMBI study,58 whereas the AIR-236 and the STEP59 trials did not clearly state their primary end points.
Quality assessment of these trials is summarised in Table 13. The AIR and the STEP studies were double-blind, placebo-controlled trials, whereas the AIR-2 and the COMBI trials were open-label studies. Methods of randomisation and allocation concealment were adequate except in the COMBI study in which the method of randomisation was unclear. Neither of the open-label studies36,58 mentioned blinding of outcome assessors. Only the COMBI study used ITT analysis across all of the outcomes examined. The AIR study used ITT analysis for its primary composite end point, clinical worsening and 6MWD, but not for changes in FC and other measures. ITT analysis was not used in the AIR-2 and the STEP trials. As more patients from the iloprost arms than from the control arms were excluded from the analysis in these two studies there was a potential bias in favour of iloprost (if excluded patients had poorer outcomes) in these studies.
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| AIR/Olschewski et al., 2002;41 12 weeks | Yes (FCIII or FCIV; PPH or non-PPH) | Yes | Double-blind | Survival analysis: N/A; clinical worsening: yes; functional class: no (184/203); 6MWD: yes; haemodynamic: unclear; quality of life: no (177/203) | Placebo: 86% (88/102); iloprost: 96% (97/101) | |
| AIR-2/Olschewski et al.;36 12 weeks | Yes (PPH or non-PPH; use of calcium channel blocker; baseline 6MWD) | Yes | Open-label | Survival analysis: N/A; clinical worsening: N/A; functional class: no (54/63); 6MWD: no (49/63); haemodynamic: no (43–50/63); quality of life: no (49/63) | Control: 79% (26/33); iloprost: 73% (22/30) | |
| COMBI/Hoeper et al., 2006;58 12 weeks | Unclear | Yes | Open-label | Survival analysis: no death; clinical worsening: yes; functional class: yes; 6MWD: yes; haemodynamic: N/A; quality of life: yes | Control: 100% (21/21); iloprost: 100% (19/19) | |
| STEP/McLaughlin et al., 2006;59 12 weeks | Yes | Yes | Double-blind | Survival analysis: no death; clinical worsening: no (65/67); functional class: no (64/67); 6MWD: no (65/67); haemodynamic: no (57/67); quality of life: N/A | Placebo: 85% (28/33); iloprost: 88% (30/34) | Two patients in the iloprost group had no post-baseline data (reason not stated) and were excluded from efficacy analysis |
The results of the AIR and AIR-2 studies, and of the COMBI and STEP studies are described separately in the following sections given the different nature of the comparisons between the trials. Because of the relatively short half-life of iloprost (hence short acute effect) and the intermittent nature of drug inhalation (as opposed to continuous infusion in the case of epoprostenol), studies of iloprost frequently measure treatment effect both before and after iloprost inhalation, which corresponds to the expected trough and peak drug concentration/effect. The post-inhalation measures (which represent acute effects) are used in the analysis in this review, although relevant findings from preinhalation measures (which represent chronic effects) are also discussed.
Iloprost added to supportive treatment versus supportive treatment alone
This comparison was investigated in the AIR and AIR-2 studies. Planned meta-analyses for the comparison and those actually carried out are summarised in Table 14. Because both trials included non-PAH patients, and outcome data excluding these patients and stratified by FC were not available, it was not possible to perform the planned primary analysis (all PAH, FCIII). However, various sensitivity analyses and limited subgroup analysis were carried out to summarise the available evidence, which may help inform the technology appraisal. The results of meta-analyses (or of individual trials when only one trial provided the data) are listed in Table 15. Results for individual outcomes are summarised in the following subsections. As there was a paucity of results that were directly applicable to iloprost’s licensed indication (PPH, FCIII), findings presented here were mainly based on the overall results of the AIR and AIR-2 studies, which included patients with mixed pulmonary hypertension and FC.
| Planned analyses | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FC III, licensed doses | No | Both the AIR41 and AIR-236 studies included non-PAH patients (categories 2–5 of the Venice 2003 classification). Data separating out these patients and stratified by FC were not available |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed doses (only IPAH actually available/included) | Yes | Both the AIR41 and AIR-236 studies included non-PAH patients (categories 2–5 of the Venice 2003 classification). Separate data including only PAH patients (all those in category 1) were not available; however, limited data specifically for IPAH patients were available form the AIR study41 |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed doses | Yes | This analysis allows the inclusion of all participants from both the AIR41 and AIR-236 studies |
| D. Sensitivity analysis – including above licensed doses | All PAH, all FC, licensed doses and above licensed doses | No | The doses for iloprost were individualised and doses used in the trials were in line with its license |
| E. Sensitivity analysis – excluding data designated as confidential | All pulmonary hypertension, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data | Yes | Data designated as academic-in-confidence from the AIR-2 study36 were excluded. This analysis was, however, not separately described as the results were identical to those in analysis F (excluding open-label trial) |
| F. Sensitivity analysis – excluding open-label trial(s) | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed doses, excluding open-label trial(s) | Yes | This analysis included data only from the AIR study41 and excluded data from the AIR-2 study,36 which was an open-label trial. This analysis also serves as a sensitivity analysis of excluding confidential information as most data from the AIR-2 study were academic-in-confidence |
| G. Subgroup analysis – IPAH | IPAH (PPH), FCIII, licensed doses | Yes | This analysis matches iloprost’s licensed indication. Data were available only for the outcome of change in FC from the AIR41 and AIR-236 studies |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, FCIII, licensed dose(s) | No | No data available |
| Analysis (see analysis checklist) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| B. Sensitivity analysis – mixed FC | C. Sensitivity analysis – mixed pulmonary hypertension | F. Sensitivity analysis – excluding open-label study | G. Subgroup analysis | ||||||
| PAH population | All PAH subcategories (only IPAH actually included) | All pulmonary hypertension (Venice categories 1–5) | All pulmonary hypertension (Venice categories 1–5) | IPAH only | |||||
| Functional class (FC) | All FC (II–IV) | All FC (II–IV) | All FC (II–IV) | FCIII | |||||
| Doses | Licensed doses | Licensed doses | Licensed doses | Licensed doses | |||||
| Total no. eligible for analysis | [Academic-in-confidence information has been removed]36,41 | 26636,41 | 20341 | 8936,41 | |||||
| No. included in analysis | 101–108 (only data for IPAH from the AIR study41 were available and were included) | 187–266 (data from both the AIR41 and AIR-236 studies were included) | 187–203 (only data from the AIR41 were included) | 70 (subgroup data were available only from the AIR study41 for changes in FC) | |||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||||
| Death | RR | 10841 | 0.52 (0.05 to 5.55) | 26636,41 | 0.58 (0.14 to 2.46) | 20341 | 0.25 (0.03 to 2.22) | 0 | Data not available |
| Clinical worsening | RR | 0 | Data not available | 20341 | 0.42 (0.15 to 1.15) | 20341 | 0.42 (0.15 to 1.15) | 0 | Data not available |
| FC improved | RR | 10141 | 3.19 (1.11 to 9.11) a | 25236,41 | 1.98 (1.13 to 3.48) | 18941 | 1.82 (0.99 to 3.35) | 7041 | 3.71 (0.83 to 16.61) |
| FC maintained or improved | RR | 10141 | 1.12 (0.97 to 1.29)c | [Academic-in-confidence information has been removed]36,41 | 1.05 (0.96 to 1.15) | 18941 | 1.07 (0.97 to 1.18) | 7041 | 1.22 (0.98 to 1.51) |
| Withdrawal for any reason | RR | 10841 | 0.30 (0.06 to 1.36) | 26636,41 | 0.62 (0.14 to 2.70); I2 78% | 20341 | 0.29 (0.10 to 0.85) a | 0 | Data not available |
| 6-minute walk distance (metres)b | WMD | 0 | Data not available | 20341 | 36 (12 to 60) a | 20341 | 36 (12 to 60) a | 0 | Data not available |
| Haemodynamics | |||||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 0 | Data not available | 20141d | –4.4 (–6.7 to –2.1) a | 20141d | –4.4 (–6.7 to –2.1) a | 0 | Data not available |
| Right atrial pressure (RAP)c (mmHg) | WMD | 0 | Data not available | 20341d | –2.2 (–3.5 to –0.9) a | 20341d | –2.2 (–3.5 to –0.9) a | 0 | Data not available |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)c | WMD | 0 | Data not available | 18741d | –335 (–421 to –249) a | 18741d | –335 (–421 to –249) a | 0 | Data not available |
| Cardiac indexb (l/min/m2) | WMD | 0 | Data not available | 0 | Data not available | 0 | Data not available | 0 | Data not available |
| Safety | |||||||||
| Serious adverse events | RR | 0 | Data not available | 26636,41 | 1.16 (0.77 to 1.75) | 20341c | 1.13 (0.71 to 1.80) | 0 | Data not available |
Survival
A total of nine deaths (three for iloprost and six for supportive treatment) were reported in the AIR41 and AIR-236 studies. The numbers are too small to draw any firm conclusions.
Time to clinical worsening
No time-to-event analysis of this outcome was reported.
Deterioration was defined as two or more of the following in the AIR study:41 refractory systolic arterial hypotension (blood pressure < 85 mmHg); worsening right ventricular failure (e.g. as indicated by the development of refractory oedema or ascites); rapidly progressing cardiogenic, hepatic or renal failure; a decrease of at least 30% in the 6MWD; and a decline in measures of haemodynamic function, such as central venous pressure and mixed venous oxygen saturation. Fewer patients in the iloprost arm (5/101) died or deteriorated compared with the control arm (12/102), but this did not reach statistical significance (RR = 0.42, 95% CI 0.15–1.15). This outcome was not reported in the AIR-2 study. 36
Functional class
Both the AIR41 and AIR-236 trials failed to report this outcome according to the ITT principle. In the AIR trial41 patients who did not complete the study were excluded (n = 14 for placebo and n = 5 for iloprost). In the AIR-2 trial36 [Academic-in-confidence information has been removed]. In both studies the proportion of patients (non-ITT population) who maintained or improved FC was not significantly different between the iloprost and control arms, although there was a trend approaching statistical significance in favour of iloprost in the AIR study41 (RR = 1.07, 95% CI 0.97–1.18), which was also observed in the subgroup of patients with PPH in FCIII (RR = 1.22, 95% CI 0.98–1.51). The proportion of patients who had their FC improved was significantly higher for iloprost-treated patients according to the pooled estimate of the two trials36,41 (RR = 1.98, 95% CI 1.13–3.48, I2 = 0).
Exercise capacity
The mean changes from baseline for the 6MWD for the two trials36,41 are shown in Figure 5. The post-inhalation measurement from AIR-2 was not available, hence results from the two trials were not pooled. In addition, the analysis in the AIR-2 study [Academic-in-confidence information has been removed], hence the data shown for this study needs to be interpreted with great caution. A significant improvement in 6MWD of 36 metres (95% CI 12–60) was seen for the iloprost group compared with the placebo group in the post-inhalation measurement of the AIR study (mixed pulmonary hypertension and FC). 41 On the contrary, [Academic-in-confidence information has been removed]. 36 No data specifically for PPH, FCIII were available.
FIGURE 5.
Forest plot: iloprost added to supportive treatment versus supportive treatment – change in 6-minute walk distance. Note that the data shown were measured post inhalation for the AIR study (top) and preinhalation for the AIR-2 study (bottom). [Academic-in-confidence information has been removed].
Quality of life
Both trials36,41 reported improvement in the EuroQol visual analogue scale (VAS; 0–100) for the iloprost group compared with the control group (WMD = [Academic-in-confidence information has been removed], I2 = 0%, non-ITT). An improvement of 0.09 in the EuroQol health state score in the iloprost group compared with no change in the placebo group was also reported in the AIR study41 but the difference was not statistically significant (p = 0.11 by analysis of covariance). None of the other measures (12-item Medical Outcomes Study Short-Form General Health Survey) of the quality of life were significantly different between treatment groups in this study. No data specifically for PPH, FCIII were available.
Haemodynamic measures
The results of the post-inhalation measures from the AIR study,41 shown in Table 15, demonstrated that iloprost significantly reduced mPAP, RAP and PVR compared with supportive treatment although it is unclear if ITT analysis was used. Preinhalation values measured before the first morning dose of iloprost were largely unchanged from baseline in the iloprost group and were either unchanged or worsened in the placebo group. For mPAP and RAP the differences in preinhalation values between groups were not significantly different, but for PVR the difference was significantly in favour of iloprost (–105 dyn s/cm5, 95% CI –191 to –19).
[Academic-in-confidence information has been removed].
No data specifically for PPH, FCIII were available.
Other effectiveness measures
The AIR study41 reported a significant improvement in the Mahler dyspnoea index transition score for the iloprost group compared with the placebo group.
Serious adverse events and other adverse events
There was no significant difference in the risk of SAEs between the iloprost and control groups in the two trials (pooled RR = 1.16, 95% CI 0.77–1.75, I2 = 0%). Significantly more syncope classified as a SAE was reported in the iloprost group than in the placebo group (5 versus 0). Common adverse events that occurred more frequently in the iloprost group included flushing, jaw pain, increased cough and headache. 41
Subgroup analysis – PAH subcategories
No randomised comparison between iloprost and supportive treatment in PAH subcategories other than those in the PPH population mentioned above was identified.
Summary and discussion
-
Two RCTs (AIR,41 which was double-blind, and AIR-2,36 which was open-label) comparing iloprost (added to supportive treatment) with supportive treatment alone were identified. The duration of study was 12 weeks for both trials.
-
The trials appeared to be well conducted, although whether [Academic-in-confidence information has been removed]. ITT was not used for the change in FC measure in the AIR study, and [Academic-in-confidence information has been removed]. 36 The potential bias was likely to be in favour of the control group in the AIR study [Academic-in-confidence information has been removed]. Despite this the AIR study demonstrated favourable outcomes for iloprost treatment [Academic-in-confidence information has been removed]. The results from the AIR-2 study needed to be interpreted with great caution, particularly because of the potential bias in the exclusion of patients from analysis and the weakness of open-label study.
-
The trials included populations of mixed pulmonary hypertension, including non-PAH (chronic thromboembolic pulmonary hypertension), and mixed FC. Patients had a mean 6MWD of 323 metres and [Academic-in-confidence information has been removed] at baseline in the AIR41 and AIR-236 studies respectively. Only 34% of the patients in the AIR study and 30% in the AIR-2 study had PPH in FCIII at baseline (licensed indication for iloprost).
-
Few data for patients with PAH only (category 1 of the Venice classification) stratified by FC were available from published literature and manufacturer submissions.Results were summarised mainly based on patient populations with mixed pulmonary hypertension and FC.
-
Given the cautions with respect to the AIR-2 study already highlighted, the following results were mainly based on findings from a single trial, the AIR study. 41 Compared with supportive treatment alone, iloprost significantly improved exercise capacity (6MWD) and haemodynamic outcomes (mPAP, RAP and PVR) when measured post inhalation, and increased the proportion of patients with improved FC during 12 weeks of treatment in a patient population of mixed pulmonary hypertension and FC. Significant improvements in a PAH-associated symptom (dyspnoea) and in the EuroQol VAS were also observed. The paucity of data prevents any inference specific to PPH, FCIII being made.
-
Outcomes measured immediately after inhalation demonstrate acute effects of inhaled iloprost. Whether these represent overall treatment effects is debatable, as outcomes measured preinhalation showed much smaller effects (within the duration of the trials).
-
No randomised comparison between iloprost and supportive treatment in PAH subcategories other than the PPH population was identified.
Iloprost added to ongoing bosentan and supportive treatment versus ongoing bosentan and supportive treatment
This comparison was investigated in the COMBI58 and STEP59 studies. Planned meta-analyses for this comparison and those actually carried out are summarised in Table 16. Because all patients in the COMBI study and the vast majority of patients in the STEP study were in FCIII at baseline, both studies were included in the primary analysis (all PAH, FCIII) and no sensitivity analysis including mixed FC was performed. The results of meta-analyses (or of individual trials when only one trial provided the data) are listed in Table 17. Results for individual outcomes are summarised in the following subsections.
| Planned analyses | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FCIII, licensed doses | Yes | Both the COMBI58 and STEP59 studies were included. Note that, although the STEP study59 included patients with mixed FC, the vast majority (94%, 63/67) of the patients were in FCIII at baseline and thus this study was included in this analysis |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed doses | No | See above. Only a minority of patients were not in FCIII at baseline and the impact on the results is expected to be very small |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed doses | No | Neither of the two trials included patients outside category 1 of the Venice 2003 classification |
| D. Sensitivity analysis – including above licensed doses | All PAH, all FC, licensed doses and above licensed doses | No | The doses for iloprost were individualised and doses used in the trials were in line with its license |
| E. Sensitivity analysis – excluding open-label trials | All PAH, all FC, licensed doses, excluding open-label trials | Yes | This analysis excluded data from the COMBI study,58 which was open-label, and included only data from the STEP study59 |
| F. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed doses, excluding commercial-in-confidence and academic-in-confidence data | No | All available data were from published literature |
| G. Subgroup analysis – IPAH | IPAH (PPH), all FC licensed doses | Yes | All data from the COMBI study58 and IPAH subgroup data from the STEP study59 were included. This analysis matches closely with iloprost’s licensed indication (PPH, FCIII), as the vast majority of the participants in these two trials were in FCIII |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, FCIII, licensed dose(s) | No | Data were not available |
| Analysis (see analysis checklist) | |||||||
|---|---|---|---|---|---|---|---|
| A. Primary analyses | E. Sensitivity analysis – excluding open-label trial | G. Subgroup analysis – IPAH | |||||
| PAH population | All PAH subcategories | All PAH subcategories | IPAH only | ||||
| Functional class (FC) | FCIII | All FC (data mainly on FCIII) | All FC (data mainly on FCIII) | ||||
| Doses | Licensed doses | Licensed doses | Licensed doses | ||||
| Total no. eligible for analysis | 10758,59 | 67 (only data from the STEP trial59 were included) | 7758,59 | ||||
| No. included in analysis | 0–107 | 0–67 | 0–77 (all data available from COMBI58 were included; STEP trial59 provided IPAH data only for the outcome of ‘FC improved’) | ||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||
| Death | RR | 10758,59 | Not estimable (no death) | 6759 | Not estimable (no death) | 7758,59 | Not estimable (no death) |
| Clinical worsening | RR | 10558,59 | 0.39 (0.04 to 3.45),I2 = 53% | 6559 | 0.09 (0.01 to 1.63) | 4058 | 0.83 (0.21 to 3.24) |
| FC improved | RR | 6459 | 5.85 (1.41 to 24.34) a | 6459 | 5.85 (1.41 to 24.34) a | 3659 | 7.50 (1.00 to 56.11) |
| FC maintained or improved | RR | 6459 | 1.03 (0.95 to 1.12) | 6459 | 1.03 (0.95 to 1.12) | 0 | No data available |
| Withdrawal for any reason | RR | 10758,59 | 0.94 (0.30 to 2.94) | 6759 | 0.78 (0.23 to 2.64) | 4058 | 3.30 (0.14 to 76.46) |
| 6-minute walk distance (metres)b | WMD | 10558,59 | 13 (–21 to 47) | 6559 | 26 (–3 to 55) | 4058 | –10 (–56 to 36) |
| Haemodynamics | |||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 5759 | –8.0 (–11.4 to –4.6) a | 5759 | –8.0 (–11.4 to –4.6) a | 0 | No data available |
| Right atrial pressure (RAP) (mmHg)c | WMD | 0 | No data available | 0 | No data available | 0 | No data available |
| Pulmonary vascular resistance (PVR)(dyn s/cm5)c | WMD | 5759 | –245 (–373 to –117) a | 5759 | –245 (–373 to –117) a | 0 | No data available |
| Cardiac indexb (l/min/m2) | WMD | 0 | No data available | 0 | No data available | 0 | No data available |
| Safety | |||||||
| Serious adverse events | RR | 6759 | 0.65 (0.23 to 1.85) | 6759 | 0.65 (0.23 to 1.85) | 0 | No data available |
Time to clinical worsening
The pooled RR indicated a trend in favour of iloprost, but this did not reach statistical significance (RR = 0.39, 95% CI 0.04–3.45) and showed moderate heterogeneity between the studies (I2 = 53%). Sensitivity analyses excluding the open-label RCT (COMBI) increased the effect size but this was also not a statistically significant finding (see Table 17, analyses A and E) (the STEP trial used the log rank test for time to clinical worsening and reported a statistically significant finding in favour of iloprost; as individual patient data were not available for this assessment this measure could not be used for the pooled or sensitivity analysis).
Functional class
Changes in FC were reported as a continuous outcome in the COMBI study. 58 No significant difference between treatment groups was found. The STEP study59 provided sufficient data for calculating RRs and the results are shown in Table 17. The proportion of patients who had their FC improved or maintained was not significantly different between the iloprost and placebo groups. Significantly more patients in the iloprost group than in the placebo group had their FC improved (11/31 versus 2/33, RR = 5.85, 95% CI 1.41–24.34); however, three patients randomised to the iloprost group (and none randomised to the placebo group) were excluded from the analysis.
Exercise capacity
The mean changes from baseline for the 6MWD (post inhalation) for the two trials are shown in Figure 6. The mean 6WMD for the iloprost group compared with the placebo/control group increased by 26 metres in the STEP trial,59 but decreased by 10 metres in the COMBI trial. 58 Neither difference was statistically significant. The difference between treatment groups was smaller (18 metres) when 6MWD was measured preinhalation in the STEP trial. 59
FIGURE 6.
Iloprost added to ongoing bosentan and supportive treatment versus ongoing bosentan and supportive treatment – change in 6-minute walk distance. CI, confidence interval; FC, functional class; PAH, pulmonary arterial hypertension; SD, standard deviation; WMD, weighted mean difference.
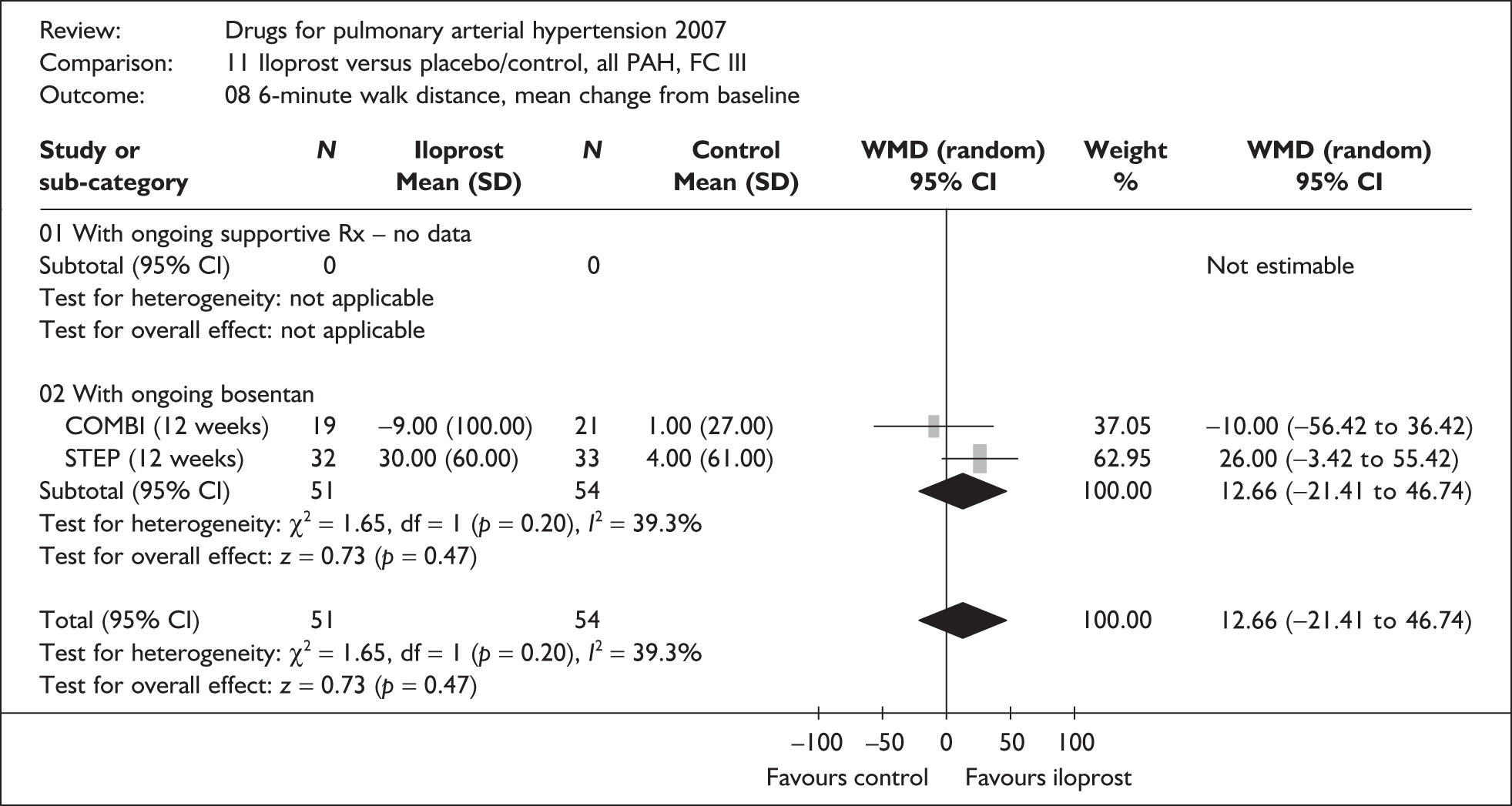
Quality of life
This outcome was reported only in the COMBI study. 58 No significant difference in the EuroQoL questionnaire (0–100 scale) was observed between the treatment groups (+7 for the iloprost group versus –3 for the control group, p = 0.14).
Haemodynamic measures
Haemodynamic outcomes were measured in the STEP study,59 but not in the COMBI study. 58 Results (post inhalation) from the STEP study (see Table 17) showed that iloprost significantly reduced mPAP and PVR compared with placebo. When measured preinhalation the between-group differences were in the same direction but were smaller and not statistically significant.
Other effectiveness measures
The change in Borg dyspnoea index from baseline was not significantly different between treatment groups (–0.5 for iloprost versus no change for placebo, p = 0.16) in the STEP study. 59
Serious adverse events and other adverse events
SAEs were not described separately from other adverse events in the COMBI study. 58 One patient in the iloprost arm stopped treatment because of intractable coughing. 58 Similar numbers of patients experienced at least one SAE in the two treatment groups in the STEP study59 (5/35 for iloprost versus 7/32 for placebo). The SAEs included worsening PAH requiring hospitalisation and right heart failure in the placebo group, and headache and rectal bleeding in the iloprost group. Common adverse events that occurred more frequently in patients receiving iloprost included jaw pain, headache and flushing. 59
Subgroup analysis – PAH subcategories
The proportions of patients having their FC improved were similar between the subgroups of IPAH patients (6/16 in the iloprost group versus 1/20 in the placebo group) and patients with other PAH (iloprost 5/16 versus placebo 1/13) in the STEP trial59 (test for heterogeneity: χ2 = 0.18, df = 1, p = 0.67). The improvement in 6MWD was also similar between these two subgroups (25 metres for IPAH versus 30 metres for other PAH).
Summary and discussion
-
Two RCTs, one double-blind (STEP59) and one open-label (COMBI58), compared inhaled iloprost with placebo/control with ongoing bosentan and supportive treatment. The duration of both trials was 12 weeks.
-
The method of randomisation and SAEs were not clearly reported in the COMBI study. 58 The methodology and outcomes were well reported in the STEP study. 59 ITT analysis was used in the COMBI study,58 but not in the STEP study. 59 The potential bias in the latter may be in favour of the iloprost group.
-
The trials included predominantly FCIII patients. The COMBI trial recruited exclusively patients with IPAH,58 whereas the STEP trial included patients with IPAH (55%) as well as PAH of various causes. The mean 6MWD at baseline was 306 metres for the COMBI study and 335 for the STEP study.
-
In the COMBI study no significant differences between the iloprost group and the control group were observed for any of the outcome measures examined. 58 By contrast, the STEP study showed a significant reduction in the risk of clinical worsening and an increased likelihood of FC improvement for iloprost-treated patients compared with placebo-treated patients (with ongoing bosentan and supportive treatment), and also a significant improvement in post-inhalation haemodynamic measures (mPAP and PVR). 59 The changes in 6MWD between treatment groups were not statistically significant in either trial.
-
The differences between treatment groups were generally smaller and not statistically significant for measures taken preinhalation. This is consistent with results from the AIR study (iloprost versus placebo with ongoing supportive treatment). 41
-
Compared with the COMBI study the STEP study had the advantage of being a multicentre, double-blind trial and having a slightly larger sample size. However, the failure to use ITT analysis in the STEP study was a potential threat to the credibility of its results. Patients included in the COMBI study appeared to have more severe disease than those in the STEP study according to the mean 6MWD at baseline. It is not clear whether the inconsistent results between the two studies can be attributed to any of these factors.
-
No significant differences in the improvements in 6MWD and FC were observed in the STEP study between patients with IPAH and those with PAH of other causes. 59
Bosentan
Quantity and quality of included studies
Bosentan was investigated in six of the included RCTs. Four of these [Channick et al. ,15,43 BREATHE-1,45,46 BREATHE-547 and STRIDE (Sitaxsentan to Relieve Impaired Exercise study)-248] allowed the comparison between bosentan and placebo with ongoing background therapy. Another trial (BREATHE-256) compared the combination of epoprostenol plus bosentan with epoprostenol alone. The characteristics of these five studies are summarised in Table 18.
| Trial name/key paper (protocol number); location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures,b mean (SD) |
|---|---|---|---|---|---|---|---|
| Bosentan vs placebo | |||||||
| Channick et al., 2001 (AC-052–351);43 USA and France, six centres | 12 weeks; double-blind, parallel; n = 32 | Bosentan (oral) 125 mg b.d.c (n = 21) | Placebo (n = 11) | PPH (84%), scleroderma (16%) | III (100%) | 51 (13); 88% | 6MWD: 358 (85); cardiac index (n=30): 2.4 (0.8); mPAP (n=30): 55 (12); PVR (n=29): 912 (427); RAP (n=29): 9.8 (5.1); SvO2: NR |
| BREATHE-1/Rubin et al., 2002;45 international, 27 centres | 16 weeks;d double-blind, parallel; n = 213 | Bosentan (oral) 125 mg b.d.c (n = 74), 250 mg b.d.c (n = 70) | Placebo (n = 69) | PPH (70%), CTD (30%) | III (92%), IV (8%) | 48 (16); 79% | 6MWD: 334 (75); cardiac index (n=208): 2.4 (0.8); mPAP: 54 (16); PVR (n=200): 970 (628); RAP (n=210): 9.5 (5.7); SvO2: NR |
| BREATHE-5/Galiè et al., 2006;47 international, 15 centres | 16 weeks; double-blind, parallel; n = 54 | Bosentan (oral) 125 mg b.d.c (n = 37) | Placebo (n = 17) | Eisenmenger syndrome (100%) | III (100%) | 39 (11); 61% | 6MWD: 343 (78); cardiac index: NR; mPAP: 76 (17); PVR: 3250 (1352); RAP: 5.8 (3.5); SvO2: NR |
| STRIDE-2/Barst et al., 200648 (FPH02); international, 55 centres | 18 weeks; double-blind (open-label for bosentan), parallel; n = 247 | Bosentan (oral) 125 mg b.d.c (n = 60); sitaxentan (oral) 50 mg o.d. (n = 62), 100 mg o.d. (n = 61) | Placebo (n = 62) | IPAH (59%), CTD (30%), congenital heart disease (11%) | II (37%), III (59%), IV (4%) | 54 (15); 78% | 6MWD: 337 (80); cardiac index: 2.4 (0.8); mPAP: 48 (14); PVR: 880 (560);e RAP: NR; SvO2: NR |
| Bosentan + epoprostenol vs epoprostenol | |||||||
| BREATHE-2/Humbert et al., 2004;56 USA and Europe, seven centres | 16 weeks; double-blind, parallel; n = 33 | Bosentan (oral) 125 mg b.d.c + epoprostenol (i.v. infusion) started with 2 ng/kg/min and increased to 12–16 ng/kg/min between weeks 14 and 16 (n = 22) | Placebo + epoprostenol (i.v. infusion) started with 2 ng/kg/min and increased to 12–16 ng/kg/min between weeks 14 and 16 (n = 11) | PPH (82%), CTD (18%) | III (76%), IV (24%) | 46 (18, 15–69); 70% | 6MWD: NR; cardiac index: 1.7 (0.5); mPAP: 60 (16); PVR: 1483 (537); RAP: 11.9 (5.9); SvO2: NR |
Bosentan was compared with sitaxentan in STRIDE-248 and with sildenafil in a further study by Wilkins and colleagues. 57 These direct comparisons will be described separately.
All of the five studies shown in Table 18 were industry-sponsored international studies (STRIDE-2 was sponsored by the manufacturer of sitaxentan). The number of patients randomised (excluding the sitaxentan arms in STRIDE-2) ranged from 3243 to 21345 and the duration of study was 12 weeks,43 18 weeks48 or 16 weeks. 45,47,56 The bosentan dose of 125 mg twice daily was used in all of the trials. In addition, BREATHE-1 also included the dose of 250 mg twice daily. In line with bosentan’s license, an initiation dose of 62.5 mg twice daily for the first 4 weeks was used before patients were uptitrated to the targeted doses in all trials.
The patient populations varied between trials in terms of PAH subcategories and FC. With the exception of BREATHE-5,47 which recruited exclusively patients with Eisenmenger syndrome, all of the trials included a mixed population of IPAH (59–84% within each trial) and CTD-APAH (16–30% within each trial). STRIDE-2 also included 11% of patients with CHD. The submission to NICE by Actelion indicates that patients with PAH associated with CHD (postsurgically corrected) were enrolled in BREATHE-1, although this was not stated in the published papers. 45,46 The Actelion submission also states that:
… as the post-surgical CHD patient numbers were small and since they are believed by clinicians to act like IPAH patients, the CHD patients were grouped with the IPAH patients for all analyses. Within this submission, the CHD group is never separated out from the IPAH sub-group, but is implicitly included.
Two43,47 of the five trials recruited exclusively patients in FCIII. Most of the patients in the other three studies were also in FCIII. STRIDE-248 and BREATHE-145 included a small proportion of patients in FCIV (4% and 8% respectively), whereas nearly one-quarter of patients in BREATHE-256 were in FCIV at baseline. STRIDE-248 also included a significant proportion of patients in FCII at baseline (37%). Baseline 6MWD was not reported in BREATHE-2 and was fairly similar for the other four trials (range 334–358 metres) despite the differences in FC mix. The primary outcome measure was change in 6MWD for Channick et al. ,43 BREATHE-145 and STRIDE-2;48 change in total pulmonary resistance (determined by right heart catheterisation) for BREATHE-2;56 and change in systemic pulse oximetry for BREATHE-5. 47
Quality assessment of the five trials is summarised in Table 19. The method of randomisation was adequate in Channick et al. ,43 BREATHE-547 and STRIDE-248 and was not clearly described in the published papers for BREATHE-145,46 and BREATHE-2. 56 Allocation concealment was also adequate in BREATHE-547 and STRIDE-248 and was not clearly described in the other three trials. All of the five trials were double-blind studies, except that the bosentan arm in the STRIDE-2 trial was open-label (the only open-label arm in the trial). The investigators stated that this was because ‘bosentan was only available commercially on a named-patient basis and blinded drug supplies were not available’. Nevertheless, the assessors for 6MWT, FC assessments and Borg dyspnoea scores were blinded. ITT analysis was used in all trials for most outcomes, but not for haemodynamic measures. The proportion of patients completing each study was slightly lower in the placebo group than in the bosentan group, except for the BREATHE-2 study in which a slightly lower proportion of patients treated with bosentan (plus epoprostenol) completed the trial compared with those treated with placebo (plus epoprostenol).
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| Bosentan vs placebo | ||||||
| Channick et al., 2001;43 12 weeks | Yes | Unclear | Double-blind | Survival analysis: no death; clinical worsening: yes; functional class: yes; 6MWD: yes; haemodynamic: no (29–30/32); quality of life: N/A | Placebo: 82% (9/11); bosentan: 100% (21/21) | |
| BREATHE-1/Rubin et al., 2002;45 16 weeks | Unclear | Unclear | Double-blind | Survival analysis: N/A; clinical worsening: yes; functional class: yes; 6MWD: yes; haemodynamic: N/A; quality of life: N/A | Not reported | |
| BREATHE-5/Galiè et al., 2006;47 16 weeks | Yes | Yes | Double-blind | Survival analysis: no death; clinical worsening: N/A; functional class: yes; 6MWD: yes; haemodynamic: no (unclearb); quality of life: N/A | Placebo: 88% (15/17); bosentan: 95% (35/37) | |
| STRIDE-2/Barst et al., 2006;48 18 weeks | Yes | Yes | Double-blind for placebo (and sitaxentan); open-label for bosentan | Survival analysis: N/A; clinical worsening: yes; functional class: no (120/122); 6MWD: no (120/122); haemodynamic: N/A; quality of life: N/A | Placebo: 82% (51/62); bosentan: 87% (52/60) | Seven randomised patients (two did not receive treatment, five did not have a valid post-baseline 6MWT) were excluded from efficacy analyses |
| Bosentan + epoprostenol vs epoprostenol | ||||||
| BREATHE-2/Humbert et al., 2004;56 16 weeks | Unclear | Unclear | Double-blind | Survival analysis: N/A; clinical worsening: yes; functional class: yes; 6MWD: no (29/33); haemodynamic: yes except PVR; quality of life: N/A | Epoprostenol: 91% (10/11); epoprostenol + bosentan: 82% (18/22) | |
Given the different nature of the comparisons between the trials, the results of Channick et al. 43 and the BREATHE-1,45 BREATHE-547 and STRIDE-2 (bosentan versus placebo only)48 studies will be described separately from the results of the BREATHE-2 study.
Bosentan added to supportive treatment versus supportive treatment alone
This comparison was investigated in Channick et al. ,43 BREATHE-1,45 BREATHE-547 and STRIDE-2. 48 Planned meta-analyses for the comparison and those actually carried out are summarised in Table 20. As no data stratified by FC were available from BREATHE-1 (the largest among the bosentan trials) and the only stratified data available from STRIDE-2 were for change in FC, the planned primary analysis (all PAH, FCIII) included data only from Channick et al. 43 and BREATHE-547 for most outcomes. If the stratified data were available, 195 out of 213 patients in BREATHE-1 and 72 out of 122 patients in STRIDE-2 receiving either bosentan or placebo would have also been included in this analysis. However, sensitivity analyses including populations of mixed FC from these two trials were carried out. The results of meta-analyses (or of individual trials when only one trial provided the data) are listed in Table 21. Results for individual outcomes are summarised in the following subsections. Given the relatively small number of patients included in the primary analysis, results presented are mainly drawn from data of mixed FC. Findings specifically for FCIII are stated separately when appropriate.
| Planned analysis | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FCIII, licensed dose(s) | Yes | Data from Channick et al.43 (n = 32) and BREATHE-547 (n = 54) were included. STRIDE-248 only provided data (commercial-in-confidence) for change in FC. BREATHE-145 was not included as data stratified by FC were not available |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed dose(s) | Yes | Data from Channick et al.43 (n = 32), BREATHE-145 (n = 213), BREATHE-547 (n = 54) and STRIDE-248 (n = 122) were included |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed dose(s) | No | None of the bosentan trials included pulmonary hypertension other than PAH |
| D. Sensitivity analysis – including above licensed dose | All PAH, all FC, licensed doses and above licensed dose | No | None of the bosentan trials used above licensed doses |
| E. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data | No | No confidential data were provided |
| F. Sensitivity analysis – excluding open-label trial | All PAH, all FC, licensed dose(s), excluding open-label trial (STRIDE-2) | Yes | Data from Channick et al.43 (n = 32), BREATHE-145 (n = 213) and BREATHE-547 (n = 54) were included. STRIDE-248 was excluded as the bosentan arm was open-label |
| G. Subgroup analysis – IPAH | IPAH, all FC, licensed dose | No | Stratified data were not available |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, all FC, licensed dose(s) | Yes | Subgroup analyses reported by Denton and colleagues44 were included. See texts for detail |
When data from BREATHE-145 were included, the results from the two bosentan arms (125 mg twice daily and 250 mg twice daily) in the trial were combined unless otherwise specified. When STRIDE-248 is mentioned in this section it is only referred to with regard to data from the placebo and bosentan arms.
Survival
A total of five deaths (one from the bosentan groups, four from the placebo groups) were reported in the four trials. 43,45,47,48 An additional three deaths from the bosentan group (250 mg twice daily) occurred within 4 weeks after withdrawal from or completion of the BREATHE-1 trial. The number is too small to draw any firm conclusions.
Time to clinical worsening
Clinical worsening was not reported in BREATHE-547 and was defined differently in Channick et al. 43 (right ventricular heart failure or aggravated pulmonary hypertension), BREATHE-145 (death, lung transplantation, hospitalisation for pulmonary hypertension, lack of clinical improvement or worsening leading to discontinuation, need for epoprostenol therapy, or atrial septostomy) and STRIDE-248 (hospitalisation for PAH, death, transplantation, atrial septostomy, initiation of new chronic PAH treatment, or combined WHO FC deterioration and ≥ 15% decrease in 6MWD from baseline). Time-to-event analysis was carried out in all three trials, although hazard ratios were not reported. Two of these reported a significant increase in time to clinical worsening for the bosentan group(s) compared with the placebo groups (p = 0.033 in Channick et al. ;43 p = 0.01 for both doses of bosentan in BREATHE-145). No difference in time to clinical worsening between the bosentan group (open-label) and the placebo group was found in the STRIDE-2 study (p = 0.80). Table 21 shows that, when analysed as a binary outcome, the pooled RR of clinical worsening for the Channick et al. 43 and BREATHE-145 trials significantly favours bosentan (analysis F: RR = 0.28, 95% CI 0.13–0.60, I2 = 0%). Inclusion of data from STRIDE-2 introduced substantial statistical heterogeneity and the pooled result was no longer statistically significant (analysis B: RR = 0.43, 95% CI 0.15–1.24, I2 = 62%).
| Analysis (see analysis checklist) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| A. Primary analysis | B. Sensitivity analysis – mixed FC | F. Sensitivity analysis – excluding open-label trial | H. Subgroup analysis – CTD-APAH | ||||||
| PAH population | All PAH subcategories | All PAH subcategories | All PAH subcategories | CTD-APAH only | |||||
| Functional class (FC) | FCIII | All FC | All FC | All FC | |||||
| Doses | Licensed dose (125–250 mg twice daily) | Licensed dose (125–250 mg twice daily) | Licensed dose (125–250 mg twice daily) | Licensed dose (125–250 mg twice daily) | |||||
| Total no. eligible for analysis | 35343,45,47,48 | 42143,45,47,48 | 29943,45,47 (data from STRIDE-248 were excluded) | 6643,45 | |||||
| No. included in analysis | 29–156 (data stratified by FC were not available from BREATHE-145) | 29–421 | 29–299 | 0–66 | |||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||||
| Death | RR | 8643,47 | Not estimated (no death) | 42143,45,47,48 | 0.23 (0.03 to 1.47) | 29943,45,47 | 0.24 (0.02 to 2.60) | 0 | Data not available |
| Clinical worsening | RR | 3243 | 0.08 (0.00 to 1.39) | 36743,45,48 | 0.43 (0.15 to 1.24), I2 62% | 24543,45 | 0.28 (0.13 to 0.60) a | 0 | Data not available |
| FC improved | RR | 15643,47,48 | 2.08 (0.97 to 4.46) | 41943,45,47,48 | 1.51 (1.05 to 2.15) a | 29943,45,47 | 1.80 (0.93 to 3.47) | 0 | Data not available |
| FC maintained or improved | RR | 15643,47,48 | 1.05 (0.96 to 1.15) | 20643,47,48 | 1.06 (0.97 to 1.15) | 8643,47 | 1.09 (0.91 to 1.30) | 0 | Data not available |
| Withdrawal for any reason | RR | 8643,47 | 0.30 (0.06 to 1.48) | 20843,47,48 | 0.62 (0.29 to 1.29) | 8643,47 | 0.30 (0.06 to 1.48) | 0 | Data not available |
| 6-minute walk distance (metres)b | WMD | 8643,47 | 59 (20 to 99) a | 42143,45,47,48 | 41 (24 to 58) a | 29943,45,47 | 49 (27 to 70) a | 6643,45 | 22 (–32 to 76) |
| Haemodynamics | |||||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 8443,47 | –5.9 (–9.3 to –2.5) a | 8443,47 | –5.9 (–9.3 to –2.5) a | 8443,47 | –5.9 (–9.3 to –2.5) a | 0 | Data not available |
| Right atrial pressure (RAP) (mmHg)c | WMD | 8343,47 | –3.0 (–9.0 to 3.0), I2 89% | 8343,47 | –3.0 (–9.0 to 3.0), I2 89% | 8343,47 | –3.0 (–9.0 to 3.0), I2 89% | 0 | Data not available |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)c | WMD | 2943 | –414 (–596 to –232) a | 2943 | –414 (–596 to –232) a | 2943 | –414 (–596 to –232) a | 0 | Data not available |
| Cardiac index (l/min/m2)b | WMD | 3043 | 1.0 (0.7 to 1.3) a | 3043 | 1.0 (0.7 to 1.3) a | 3043 | 1.0 (0.7 to 1.3) a | 0 | Data not available |
| Safety | |||||||||
| Serious adverse events | RR | 5447 | 0.77 (0.21 to 2.84) | 17747,48 | 0.45 (0.23 to 0.89) a | 5447 | 0.77 (0.21 to 2.84) | 0 | Data not available |
Functional class
Table 21 shows that the proportion of patients who maintained or improved FC was not significantly different between the bosentan and placebo groups. BREATHE-145 could not be included in the analysis as it only reported the proportion of patients whose FC was improved but did not report the proportion of patients whose FC was unchanged or worsened. The pooled result including data from all four trials43,45,47,48 for having FC improved significantly favours bosentan (mixed FC, RR = 1.51, 95% CI 1.05–2.15, I2 = 0%). The pooled result from three trials43,47,48 specifically for FCIII (excluding BREATHE-1, data not available) also favours bosentan, but just fails to reach statistical significance (RR = 2.08, 95% CI 0.97–4.46, I2 = 0%).
Exercise capacity
The mean changes from baseline for the 6MWD for the four trials43,45,47,48 (mixed FC) are shown in Figure 7. A significant increase in 6MWD for the bosentan groups compared with the placebo groups was observed in all trials, including those by Channick et al. 43 and BREATHE-5,47 which recruited only patients in FCIII. The pooled result from these two studies (analysis A, Table 21) was 59 metres in favour of bosentan (95% CI 20–99, I2 = 0%).
FIGURE 7.
Forest plot: bosentan added to supportive treatment versus supportive treatment – change in 6-minute walk distance. CI, confidence interval; SD, standard deviation; WMD, weighted mean difference.
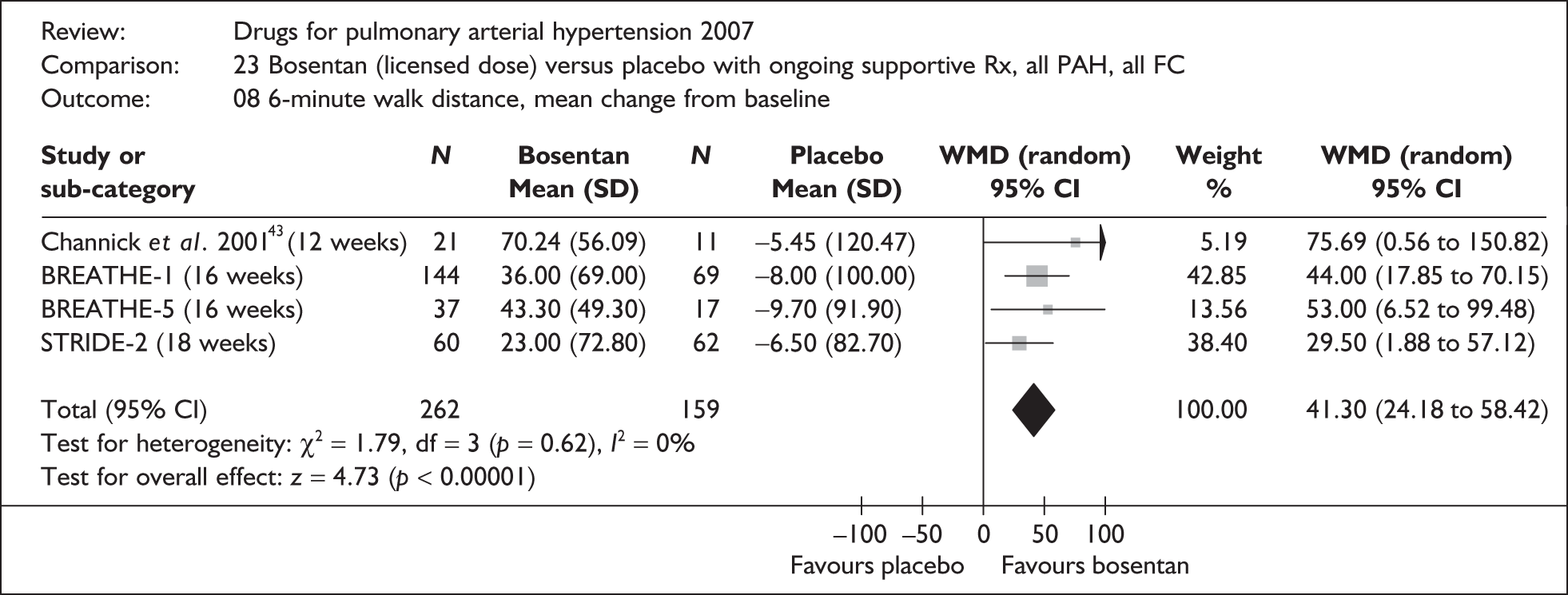
Quality of life
No trial reported quality of life outcomes.
Haemodynamic measures
As post-treatment haemodynamic outcomes were measured only in Channick et al. 43 and BREATHE-5,47 which recruited exclusively patients in FCIII, the results shown in Table 21 for haemodynamic outcomes were identical for analyses A, B and F. Compared with placebo, bosentan significantly reduced mPAP and PVR and increased the cardiac index. A significant difference in the change of RAP between the bosentan and placebo groups was observed in Channick et al. 43 (–6.2 mmHg, 95% CI –9.6 to –2.8), but not in BREATHE-5 (–0.1, 95% CI –2.1 to 1.9). In Channick et al. the RAP reduced by 1.3 mmHg in the bosentan group, whereas it increased by 4.9 mmHg in the placebo group. RAP increased slightly in both the bosentan and placebo groups (0.3 and 0.4 mmHg respectively) in BREATHE-5.
Other effectiveness measures
A significant decrease (improvement) in the Borg dyspnoea index for the bosentan groups compared with the placebo group was observed in BREATHE-145 (mean difference –0.6, 95% CI –1.2 to –0.1) and Channick et al. 43 (–1.6, 95% CI –3.1 to 0.0); however, no significant difference between the bosentan and placebo groups was observed in STRIDE-2. 48
Serious adverse events and other adverse events
The total number of patients who experienced at least one SAE was not reported in Channick et al. 43 and BREATHE-1. 45 The pooled result (mixed FC) for BREATHE-5 and STRIDE-2 showed a significant decreased risk for bosentan-treated patients compared with placebo-treated patients (RR = 0.45, 95% CI 0.23–0.89, I2 = 0%). Common adverse events that occurred more frequently in the bosentan group include abnormal liver function,45 peripheral oedema and palpitation. 47
Subgroup analysis – PAH subcategories
Denton and colleagues44 reported post hoc analyses of data from two of the bosentan trials43,45 for the subgroup of PAH patients with CTD. Data from the two trials were pooled together before analyses were carried out and thus initial randomisation was not preserved; however, the number of patients with CTD-APAH in Channick et al. would have been too small to be analysed separately (n = 5 for the bosentan group and n = 1 for the placebo group).
The baseline characteristics for the CTD-APAH patients (n = 66) indicated that patients treated with bosentan may have had more severe disease than those treated with placebo (6MWD 312 metres versus 361 metres, p = 0.01). The change in 6MWD from baseline was +19.5 metres in patients treated with bosentan and –3 metres in patients treated with placebo. The difference between groups was not statistically significant (22.5 metres, 95% CI –32 to 76). The Kaplan–Meier estimates of the percentage of patients not experiencing clinical worsening also showed a non-significant trend in favour of bosentan compared with placebo: 95.4% versus 90.9% at 12 weeks, and 90.3% versus 86.4% at 16 weeks. Dizziness, lower limb oedema and fatigue occurred more frequently in bosentan-treated patients.
Subgroup analysis within the BREATHE-1 trial45 showed no significant difference between PPH (51 metres) and PAH associated with scleroderma (43 metres) in the change of 6MWD from baseline for bosentan-treated groups compared with the placebo group. Nevertheless, the treatment effect was mainly associated with increased 6MWD in PPH (+46 for bosentan group versus –5 for placebo group), but was related to the prevention of worsening in PAH associated with scleroderma (+3 for bosentan group versus –40 for placebo group).
The results from BREATHE-5,47 which recruited exclusively patients with PAH associated with Eisenmenger syndrome, were similar to those of the other bosentan trials. No heterogeneity attributed to this trial was observed in the outcomes examined in this review, with the exception of right atrial pressure. A significant treatment effect was found in Channick et al. ,43 but not in BREATHE-547 (see Haemodynamic measures subsection).
Summary and discussion
-
Four RCTs comparing bosentan (added to supportive treatment) with supportive treatment alone were identified. Three of them (Channick et al. 43, BREATHE-145 and BREATHE-547) were double-blind studies, whereas the bosentan arm in the STRIDE-2 trial48 was open-label. The duration of study ranged from 12 to 18 weeks.
-
Methods of randomisation and allocation concealment were not clearly described in some bosentan trials. 43,45,47 ITT analysis was used in most trials except for STRIDE-2. The potential bias from non-ITT analysis was expected to be small in STRIDE-2 as the number excluded from analysis in each treatment group was very small; however, the interpretation of results from this study for outcomes not blindly assessed (such as clinical worsening, treatment withdrawal and adverse events) requires greater caution because of its open-label design.
-
There was heterogeneity with regard to the populations enrolled in the trials. For example, BREATHE-5 enrolled exclusively those with Eisenmenger syndrome, whereas the other trials enrolled mixed IPAH and CTD-APAH populations. The mean 6MWD at baseline ranged from 334 metres to 358 metres.
-
Few data stratified by FC were available from the two larger trials with mixed FC (BREATHE-1 and STRIDE-2), although two smaller trials (Channick et al. and BREATHE-5) provided some data specific to FCIII.
-
Compared with supportive treatment alone, bosentan added to supportive treatment has demonstrated significant improvements in exercise capacity (6MWD) and haemodynamic outcomes (mPAP, PVR and cardiac index), both in PAH populations with mixed FC and specifically in FCIII. A significant increase in time to clinical worsening, improvements in FC and a PAH symptom (dyspnoea), and a decreased risk of SAEs were also observed among bosentan-treated patients compared with placebo-treated patients in PAH populations with mixed FC.
-
Subgroup analysis of CTD-APAH patients in Channick et al. 43 and BREATHE-145 showed similar results to those of the whole trial population (mixed IPAH and CTD-APAH).
Bosentan plus epoprostenol versus epoprostenol
This comparison was investigated in the BREATHE-2 trial. 56 This trial was the only study included in this review that genuinely compared the initiation of a drug combination with a single drug (rather than comparing the addition of a drug to placebo with another ongoing drug). The characteristics and quality assessment of the study are shown in Tables 18 and 19 respectively. Methods of randomisation and allocation concealment were not clearly reported, and ITT analysis was not used for 6MWD (patients who were unable to or who did not perform the assessment were excluded from the analysis). Although the majority of patients included in this study were in FCIII at baseline, nearly one-quarter of the patients (8/33) were in FCIV. As data stratified by FC were only available for FC improvement, results described in this section were mainly based on patients with mixed FC. Given that the findings were from a single trial with a relatively small sample size (n = 33), only a narrative summary of the study findings will be provided.
Findings
Two patients died during this 16-week study (one of acute cardiopulmonary failure, the other of anaemia and pneumonia with rapidly progressing right heart failure). A third patient died after being withdrawn from the study for worsening PAH. All three patients received the epoprostenol/bosentan combination; however, the number was too small to make any firm conclusions. Worsening pulmonary hypertension was reported as an adverse event in two patients in the epoprostenol group and one patient in the combination group. These figures obviously do not include deaths and thus are not comparable to the composite outcome of clinical worsening reported in other studies.
No significant difference was observed between the treatment groups in the proportion of patients who had their FC improved (13/22 for the combination group and 5/11 for the epoprostenol group; RR = 1.30, 95% CI 0.62–2.71). Results specifically for patients in FCIII at baseline showed little difference (9/17 for the combination group and 4/8 for the epoprostenol group; RR = 1.06, 95% CI 0.46–2.42). The proportion of patients with FC unchanged or worsened was not reported. Improvement in 6MWD and the dyspnoea–fatigue rating was similar between treatment groups (median increase 68 metres versus 74 metres, median improvement 0 versus 1.0 unit, for the combination group and epoprostenol group respectively). No quality of life data were reported. Improvement in haemodynamic outcomes from baseline was observed in both treatment groups and was generally larger (in terms of percentage improvement) in the combination group than in the epoprostenol group. None of the differences between groups, however, was statistically significant.
The proportion of patients who experienced at least one SAE in each treatment group was not reported. Common adverse events that occurred in higher proportions of patients in the combination group included leg oedema and diarrhoea. Four patients (out of 22) in the combination group versus one patient (out of 11) in the epoprostenol group withdrew from the study (RR = 2.00, 95% CI 0.25–15.82).
Summary and discussion
-
One double-blind, placebo-controlled trial (BREATHE-156) compared the initiation of epoprostenol plus bosentan with epoprostenol alone in mixed PAH populations (IPAH and CTD-APAH) with mixed FC (III and IV).
-
Methods of randomisation and allocation concealment were not clearly described in the published paper for this trial,56 and ITT analysis was not used for 6MWD.
-
No significant differences between the group treated with the epoprostenol/bosentan combination and the group treated with epoprostenol were observed for any of the outcomes assessed in the trial.
Sitaxentan
Quantity and quality of included studies
Sitaxentan was investigated in three of the included RCTs. All three of the trials (STRIDE-1,49 STRIDE-2,48 STRIDE-437) compared sitaxentan with placebo in patients with ongoing supportive treatment. The STRIDE-2 trial48 also included an open-label bosentan arm. The bosentan–placebo comparison from this trial has already been described; the bosentan–sitaxentan comparison is described later in this chapter [see Direct (head-to-head) comparisons]. This section focuses on the comparison of sitaxentan added to supportive treatment versus supportive treatment alone. The characteristics of the three studies are summarised in Table 22. The STRIDE-2 trial48 has been listed in relevant tables in the section on bosentan, but is also listed in this section for the convenience of readers.
| Trial name/key paper (protocol number); location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures,b mean (SD) |
|---|---|---|---|---|---|---|---|
| STRIDE-1/Barst et al., 200449 (FPH01); USA and Canada, 23 centres | 12 weeks; double-blind, parallel; n = 178 | Sitaxentan (oral) 100 mg o.d. (n = 55), 300 mg o.d. (n = 63) | Placebo (n = 60) | IPAH (53%), CTD (24%), congenital S–P shunts (24%) | II (33%), III (66%), IV (1%) | 46 (13, 17–74); 79% | 6MWD: 398 (110); cardiac index: 2.4 (0.8); mPAP: 54 (15); PVR: 958 (560); RAP: 8 (5); SvO2: NR |
| STRIDE-2/Barst et al., 200648 (FPH02); international, 55 centres | 18 weeks; double-blind (open-label for bosentan), parallel; n = 247 | Bosentan (oral) 125 mg b.d.c (n = 60); sitaxentan (oral) 50 mg o.d. (n = 62), 100 mg o.d. (n = 61) | Placebo (n = 62) | IPAH (59%), CTD (30%), congenital heart disease (11%) | II (37%), III (59%), IV (4%) | 54 (15); 78% | 6MWD: 337 (80); cardiac index: 2.4 (0.8); mPAP: 48 (14); PVR: 880 (560);g RAP: NR; SvO2: NR |
| STRIDE-4/Barst, 200737 (FPH04); Latin America, Poland, Spain | 18 weeks; double-blind, parallel; n = 98 | Sitaxentan (oral) 50 mg o.d. (n = 32), 100 mg o.d. (n = 32) | Placebo (n = 34) | IPAH (68%), CTD (15%), congenital heart disease (16%) | II (61%), III (38%), IV (1%) | 41 (14); 84% | 6MWD: 345 (80); cardiac index: NR; mPAP: 61 (18); PVR: 1148 (752); RAP: NR; SvO2: NR |
All three studies37,48,49 were industry-sponsored multicentre trials that randomised between 98 and 247 patients. The STRIDE-1 study was conducted in North America. The STRIDE-2 study was an international study and the STRIDE-4 trial was conducted mainly in South America, but also in Spain and Poland. The clinical study reports (commercial-in-confidence) for all three trials were made available to the assessment group by Encysive. The study duration was 12 weeks for STRIDE-149 and 18 weeks for STRIDE-248 and STRIDE-4. 37 The licensed dose (100 mg once daily) for sitaxentan was investigated in all three trials. In addition, STRIDE-149 included an above licensed dose of 300 mg once daily (included only in the relevant sensitivity analysis in this review) and STRIDE-248 and STRIDE-437 included a sublicensed dose of 50 mg once daily (not considered in this review).
All three trials recruited mixed PAH populations of IPAH (ranging from 53% in STRIDE-1 to 68% in STRIDE-4), CTD-APAH (15–30% within each trial) and CHD (11–24% within each trial). The majority of patients in STRIDE-1 and STRIDE-2 were in FCIII at baseline (66% and 59% respectively), whereas in STRIDE-4 only 38% were in FCIII at baseline (the majority being in FCII: 61%). The primary end point was per cent of predicted peak oxygen uptake (VO2) in STRIDE-1 and change in 6MWD in STRIDE-2 and STRIDE-4.
Quality assessment of the three trials is summarised in Table 23 (only information relevant to the placebo and sitaxentan arms is listed). Methods of randomisation and allocation concealment were adequate in all three trials. 37,48,49 ITT analysis was used for most of the outcomes in STRIDE-149 and STRIDE-4. 37 STRIDE-248 excluded a small number of patients ([Academic-in-confidence information has been removed]) without a valid post-baseline 6MWT.
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| STRIDE-1/Barst et al., 2004;49 12 weeks | Yes (centre) | Yes | Double-blind | Survival analysis: N/A; clinical worsening: yes; functional class: yes; 6MWD: yes; haemodynamic: yes; quality of life: no (176–177/178) | Placebo: 92% (55/60); sitaxentan 100 mg o.d.: 100% (55/55), sitaxentan 300 mg o.d.: 89% (56/63) | |
| STRIDE-2/Barst et al., 2006;48 18 weeks | Yes | Yes | Double-blind for sitaxentan and placebo; open-label for bosentan | Survival analysis: N/A; clinical worsening: yes; functional class: no [Academic-in-confidence information has been removed];b 6MWD: no [Academic-in-confidence information has been removed];b haemodynamic: not measured; quality of life: not measured | Placebo: 82% (51/62); sitaxentan 50 mg o.d.: 87% (54/62), sitaxentan 100 mg o.d.: 93% (57/61) | Patients who did not have a valid post-baseline 6MWT were excluded from efficacy analysis |
| STRIDE-4/Barst, 2007;37 18 weeks | Yes (baseline 6MWD) | Yes | Double-blind | Survival analysis: no death; clinical worsening: yes; functional class: yes; 6MWD: yes; haemodynamic: not measured; quality of life: not measured | Placebo: 88% (30/34); sitaxentan 50 mg o.d.: 88% (28/32), sitaxentan 100 mg o.d.: 91% (29/32) |
Sitaxentan (added to supportive treatment) versus supportive treatment
This comparison was investigated in all three trials. 37,48,49 Planned analyses and those actually carried out are summarised in Table 24. Results of the meta-analysis are listed in Table 25 according to planned comparisons. Results for individual outcomes are described in the following subsections. As all three trials included patients with mixed FC, and data stratified by FC were available only for the outcome of change in FC, the findings presented in this section are mainly based on meta-analysis results of mixed PAH populations. Findings specifically for FCIII are stated separately when appropriate.
| Planned analysis | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FCIII, licensed dose | Yes | Data stratified by FC were available only for the outcome of change in FC from STRIDE-248 and STRIDE-437 |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed dose | Yes | Data from STRIDE-1,49 STRIDE-248 and STRIDE-437 were included |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed dose(s) | No | None of the sitaxentan trials included patients outside category 1 of the Venice 2003 classification |
| D. Sensitivity analysis – including above licensed dose | All PAH, all FC, licensed dose and above licensed dose | Yes | Data from the sitaxentan 300-mg arm were combined with data from the 100-mg arm and included in this analysis |
| E. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data | Yes | Confidential data that were included in analysis B were excluded from this analysis |
| F. Sensitivity analysis – excluding open-label trial | All PAH, all FC, licensed dose(s), excluding open-label trial | No | Not applicable (only bosentan arm in STRIDE-248 was open-label) |
| G. Subgroup analysis – IPAH | IPAH, all FC, licensed dose and above | No | Only limited data were available from STRIDE-1,61 described in the text |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, all FC, licensed dose and above | No | Only limited data were available from STRIDE-1,61 described in the text |
Survival
A total of three deaths were reported in the three trials, one in STRIDE-1 (sitaxentan 300-mg arm)49 and two in STRIDE-2 (both in placebo arm). 48 The number is too small to draw any conclusions.
Time to clinical worsening
Clinical worsening was defined as death, epoprostenol use, atrial septostomy or transplantation in STRIDE-1. 49 A broader definition was used in STRIDE-248 and STRIDE-4,37 which included hospitalisation for PAH, death, transplantation, atrial septostomy, initiation of new chronic PAH treatment, or combined WHO FC deterioration and ≥ 15% decrease in 6MWD from baseline. Time-to-event analysis for individual trials did not identify a statistically significant difference between any doses of sitaxentan and placebo. However, clinical worsening occurred more frequently in the placebo arm than in the sitaxentan arms across all three trials, and the pooled RR (mixed FC) for experiencing one or more clinical worsening events was significantly in favour of sitaxentan at the licensed dose (100 mg once daily) compared with placebo (RR = 0.33, 95% CI 0.12–0.87, I2 = 0%). Inclusion of the above licensed dose had little impact on the estimate.
Functional class
Table 25 shows that the proportion of patients who maintained or improved FC was significantly higher among patients treated with sitaxentan (licensed dose) than among those treated with placebo (RR = 1.10, 95% CI 1.04–1.16, I2 = 0%). The proportion of patients having FC improved was also significantly higher among sitaxentan (licensed dose)-treated patients than among placebo-treated patients (RR = 1.74, 95% CI 1.12–2.70, I2 = 0%). Inclusion of the above licensed dose had little impact on the estimates. The results specifically for FCIII patients for both outcomes were in the same direction, but did not reach statistical significance (see analysis A, Table 25).
| Analysis (see analysis checklist) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| A. Primary analysis | B. Sensitivity analysis – mixed FC | D. Sensitivity analysis – including above licensed doses | E. Sensitivity analysis – excluding data designated as confidential | ||||||
| PAH population | All PAH subcategories | All PAH subcategories | All PAH subcategories | All PAH subcategories | |||||
| Functional class (FC) | FCIII | All FC | All FC | All FC | |||||
| Doses | Licensed dose (100 mg once daily) | Licensed dose (100 mg once daily) | Licensed dose and above (100 mg, 300 mg once daily) | Licensed dose (100 mg once daily) | |||||
| Total no. eligible for analysis | 17237,48,49 | 30437,48,49 | 36737,48,49 | 30437,48,49 | |||||
| No. included in analysis | 95 (data stratified by FC were not available from STRIDE-149) | 66–304 (haemodynamic outcomes were measured only in STRIDE-149) | 178–367 (haemodynamic outcomes were measured only in STRIDE-149) | 115–304 (confidential data from clinical trial reports were excluded) | |||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||||
| Death | RR | 0 | Data not available | 30437,48,49 | 0.20 (0.01 to 4.15) | 36737,48,49 | 0.53 (0.06 to 4.73) | 30437,48,49 | 0.20 (0.01 to 4.15) |
| Clinical worsening | RR | 0 | Data not available | 30437,48,49 | 0.33 (0.12 to 0.87) a | 36737,48,49 | 0.32 (0.12 to 0.81) a | 30437,48,49 | 0.33 (0.12 to 0.87) a |
| FC improved | RR | 9537,48 | 1.53 (0.74 to 3.17) | 30237,48,49 | 1.74 (1.12 to 2.70) a | 36537,48,49 | 1.76 (1.15 to 2.70) a | 30237,48,49 | 1.74 (1.12 to 2.70) a |
| FC maintained or improved | RR | 9537,48 | 1.11 (1.00 to 1.23) | 30237,48,49 | 1.10 (1.04 to 1.16) a | 36537,48,49 | 1.09 (1.03 to 1.15) a | 30237,48,49 | 1.10 (1.04 to 1.16) a |
| Withdrawal for any reason | RR | 0 | Data not available | 30437,48,49 | 0.43 (0.19 to 0.98) a | 36737,48,49 | 0.57 (0.29 to 1.12) | 23848,49 | 0.31 (0.11 to 0.87) a |
| 6-minute walk distance (metres)b | WMD | 0 | Data not available | 30237,48,49 | 32 (18 to 47) a | 36537,48,49 | 32 (18 to 46) a | 30237,48,49 | 32 (18 to 47) a |
| Haemodynamics | |||||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 0 | Data not available | 11549 | –3.0 (–5.9 to –0.1) a | 17849 | –4.0 (–6.7 to –1.3) a | 11549 | –3.0 (–5.9 to –0.1) a |
| Right atrial pressure (RAP) (mmHg)c | WMD | 0 | Data not available | 11549 | –1.0 (–2.5 to 0.5) | 17849 | –1.5 (–2.8 to –0.3) a | 11549 | –1.0 (–2.5 to 0.5) |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)c | WMD | 0 | Data not available | 11549 | –270 (–402 to –138) a | 17849 | –256 (–349 to –163) a | 11549 | –270 (–402 to –138) a |
| Cardiac index (l/min/m2)b | WMD | 0 | Data not available | 11549 | 0.3 (0.1 to 0.5) a | 17849 | 0.4 (0.2 to 0.5) a | 11549 | 0.3 (0.1 to 0.5) a |
| Safety | |||||||||
| Serious adverse events | RR | 0 | Data not available | 30437,48,49 | 0.55 (0.27 to 1.12) | 36737,48,49 | 0.65 (0.37 to 1.15) | 11549 | 0.35 (0.10 to 1.23) |
Exercise capacity
The mean changes from baseline for 6MWD for the three trials37,48,49 are shown in Figure 8. Sitaxentan at the licensed dose significantly increased the 6MWD compared with placebo (32 metres, 95% CI 18–47, I2 = 0%) in patients with mixed FC. Data specifically for FCIII patients were not available.
FIGURE 8.
Sitaxentan added to supportive treatment versus supportive treatment alone – change in 6-minute walk distance. CI, confidence interval; FC, functional class; PAH, pulmonary arterial hypertension; WMD, weighted mean difference.
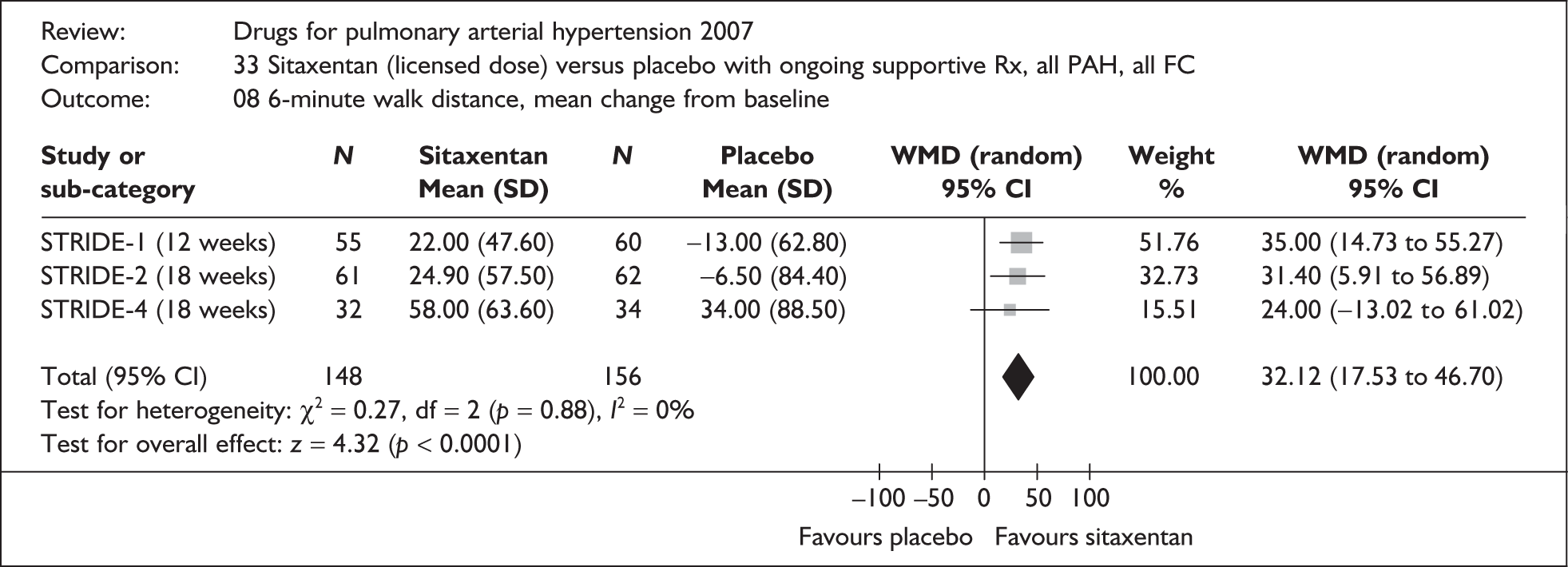
Quality of life
Quality of life outcomes were measured only in the STRIDE-1 study49 using the Short-Form 36 (SF-36). No significant differences between treatment groups were found.
Haemodynamic measures
Haemodynamic outcomes were measured only in the STRIDE-1 study. 49 The results, summarised in Table 25, show that sitaxentan at its licensed dose significantly reduced mPAP (–3.0 mmHg, 95% CI –5.9 to –0.1) and PVR (–270 dyn s/cm5, 95% CI –402 to –138) and improved the cardiac index (0.3, 95% CI 0.1–0.5) compared with placebo in patients with mixed FC. Inclusion of the above licensed dose appeared to slightly increase the treatment effects (except PVR), and the reduction in RAP also reached statistical significance.
Other effectiveness measures
The Borg dyspnoea index was measured in STRIDE-248 and STRIDE-4. 37 There was no significant difference between the sitaxentan groups and the placebo groups.
Serious adverse events and other adverse events
Significantly fewer patients treated with sitaxentan (licensed dose) experienced one or more SAEs than those treated with placebo in the STRIDE-2 study (8/61 versus 19/62). 48 The pooled RR of the three trials was not statistically significant (mixed FC, RR = 0.55, 95% CI 0.27–1.12, I2 = 31%). The above licensed dose (300 mg once daily) appears to be associated with increased liver toxicity. 49 Common adverse events that occurred more frequently in the sitaxentan groups included: headache, peripheral oedema, nasal congestion and increased INR and/or prothrombin time prolonged (interaction with warfarin). 48,49
Subgroup analysis – PAH subcategories
Results for the subgroup of patients with connective tissue disease (CTD-APAH) within the STRIDE-1 study were reported by Girgis and colleagues. 61 Data from the sitaxentan 100-mg and 300-mg arms were combined in this post hoc analysis. The mean 6MWD increased by 20 metres (SD 52) from baseline in the combined sitaxentan group (n = 33) and decreased by 38 metres (SD 84) in the placebo group (n = 9) after 12 weeks of treatment (p = 0.027). Significant improvements for sitaxentan-treated patients compared with placebo-treated patients were also observed in haemodynamic measures, including RAP, PVR and cardiac index. More sitaxentan-treated patients improved FC than placebo-treated patients (8/33 versus 1/9, p = 0.14). In contrast to the overall trial results, which showed no significant treatment effect in all six domains of the SF-36, significant improvements in the physical functioning and role–physical domains were observed.
The authors also compared data from the CTD-APAH population with data from the IPAH population within the trial. 61 No significant differences between the two cohorts were observed in any of the efficacy measures. Significant improvements in the physical functioning domain of the SF-36 were also observed in the IPAH subgroup.
Summary and discussion
-
Three RCTs comparing sitaxentan with placebo with ongoing supportive treatment were identified. All three trials (STRIDE-1,49 STRIDE-2,48 STRIDE-437) were industry-sponsored, international, double-blind studies with a study duration of 12–18 weeks. The licensed dose for sitaxentan (100 mg once daily) was investigated in all of the trials.
-
Methods of randomisation and allocation concealment were adequate in all three trials. ITT analysis was used in STRIDE-149 and STRIDE-4,37 but not in STRIDE-2. 48 The potential bias due to exclusion of a small number of patients from efficacy analysis in STRIDE-248 was unclear, but the impact on the pooled results of the meta-analysis is likely to be small.
-
All three trials included mixed populations of patients with IPAH, CTD-APAH and PAH associated with CHD. The mean 6MWD at baseline ranged from 337 metres48 to 398 metres. 49 Patients were of mixed FC, with 66% and 59% in FCIII at baseline for STRIDE-149 and STRIDE-248 respectively. The majority of patients (61%) in STRIDE-4 were in FCII at baseline.
-
Data stratified by FC were available only for the outcome of change in FC. Results presented in this section were largely based on a patient population with mixed FC.
-
Compared with supportive treatment alone, sitaxentan at its licensed dose (added to supportive treatment) significantly reduced the risk of clinical worsening, increased exercise capacity (6MWD), and improved FC and haemodynamic outcomes (mPAP, PVR and cardiac index) in PAH populations with mixed FC. Improvement in FC was observed in FCIII patients, but this did not reach statistical significance.
-
Post hoc analysis suggested that the treatment effects of sitaxentan observed in the subgroup of CTD-APAH were similar to those observed in the whole trial population. 61 No significant differences were found between the IPAH and CTD-APAH subgroups across various efficacy outcomes. The additional positive finding in physical health-related quality of life in the post hoc analysis needs to be interpreted with caution and requires further confirmation in future studies with prospectively planned analysis.
Sildenafil
Quantity and quality of included studies
Sildenafil was investigated in six of the included RCTs. Four of these [SUPER-1 (Sildenafil Use in Pulmonary Arterial Hypertension study),53 Bharani et al. ,35 Sastry et al. ,54 Singh et al. 55] compared sildenafil with placebo in patients with ongoing supportive treatment (patients in Bharani et al. 35 appeared to have stopped previous vasodilator therapy before entering the study). Another trial (PACES-138), identified through manufacturer submission, compared sildenafil with placebo in patients with ongoing epoprostenol and supportive treatment. The characteristics of these five studies are summarised in Table 26. Sildenafil was compared with bosentan in a further study by Wilkins and colleagues (SERAPH),57 which will be described later in this chapter [see Direct (head-to-head) comparisons].
| Trial name/key paper (protocol number); location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures,b mean (SD) |
|---|---|---|---|---|---|---|---|
| Sildenafil vs placebo with ongoing supportive treatment | |||||||
| SUPER-1/Galiè et al., 200553 (A1481140); international, 53 centres | 12 weeks; double-blind, parallel; n = 278 | Sildenafil (oral) 20 mg t.i.d. (n = 69), 40 mg t.i.d. (n = 67), 80 mg t.i.d. (n = 71) | Placebo (n = 70) | IPAH (63%), CTD (30%), repaired congenital S–P shunts (6%) | I (0.4%), II (39%), III (58%), IV (3%) | 49 (15); 75% | 6MWD: 344 (81); cardiac index: 2.4 (0.7); mPAP: 53 (15); PVR: 957 (509); RAP: 9 (5); SvO2: NR |
| Bharani et al., 2003;35 India, single centre | 2 × 2 weeks (with washout period of ≥ 2 weeks); double-blind, cross-over; n = 10 | Sildenafil (oral) 25 mg t.i.d. | Placebo | PPH (30%), Eisenmenger syndrome (30%), non-PAH (30%)c | II (33%), III (56%), IV (11%) | 32 (15, 18–60); 56% | 6MWD: 164; cardiac index: NR; mPAP: NR; PVR: NR; RAP: NR; SvO2: NR |
| Sastry et al., 2004;54 India, single centre | 2 × 6 weeks (no washout period); double-blind, cross-over; n = 22 | Sildenafil (oral) 25–100 mg t.i.d. depending on body weightd (n = 10 receiving sildenafil first) | Placebo (n = 12 receiving placebo first) | PPH (100%) | II (82%), III (18%) | NR (16–55); 55% | 6MWD: NR; cardiac index: 2.8 (1.1); mPAP: NR; PVR: NR; RAP: NR; SvO2: NR |
| Singh et al., 2006;55 India, single centre | 2 × 6 weeks with a 2-week washout period; double-blind, cross-over; n = 20 | Sildenafil (oral) 25–100 mg t.i.d. depending on body weight | Placebo | IPAH (50%), Eisenmenger syndrome (50%) | II (40%), III (55%), IV (5%) | NR (3–45); 75% | 6MWD: 262 (99); cardiac index: NR; mPAP: NR; PVR: NR; RAP: NR; SvO2: NR |
| Sildenafil vs placebo with ongoing epoprostenol and supportive treatment | |||||||
| PACES-1 (A1481141);38 international, multicentre | 16 weeks; double-blind, parallel; n = 267 | Sildenafil (oral) started 20 mg t.i.d., uptitrated to 80 mg t.i.d. by week 8 if tolerated + ongoing epoprostenol (individualised optimal dose) (n = 134) | Placebo + ongoing epoprostenol (individualised optimal dose) (n = 133e) | PPH (79%), CTD (21%) | n = 257; I (1%), II (26%), III (67%), IV (5%) | 48 (13, 18–75); 80% | 6MWD: NR; cardiac index: NR; mPAP: NR; PVR (n = 164): [Commercial-in-confidence information has been removed]; RAP: [Commercial-in-confidence information has been removed]; SvO2: [Commercial-in-confidence information has been removed] |
The SUPER-153 and PACES-138 trials were industry-sponsored international studies that randomised 278 and 267 patients respectively. The clinical study reports (commercial-in-confidence) for both trials were made available to the assessment group by Pfizer. The study duration was 12 weeks for SUPER-153 and 16 weeks for PACES-1. The studies by Bharani et al. ,35 Sastry et al. 54 and Singh et al. 55 were small (n = 10, 22 and 20 respectively) single-centre, cross-over trials conducted in India. The study by Sastry and colleagues54 was sponsored by a not-for-profit organisation and the sponsorship for Bharain et al. 35 and Singh et al. 55 was not reported. The cross-over trials had a duration of 235–654,55 weeks for each treatment period. The doses investigated in these trials varied, but only the SUPER-1 study53 included a treatment arm using the licensed dose (20 mg three times daily). Above licensed doses of up to 80 mg three times daily were also investigated in the SUPER-1 trial53 and in all of the other trials (see Table 26).
Both the SUPER-153 and PACES-138 trials recruited mixed PAH populations of IPAH and CTD-APAH. The SUPER-1 study also included 6% of patients with CHD. The majority of patients in both trials were in FCIII at baseline; there were 39% and 26% of patients in FCII at baseline for the SUPER-1 and PACES-1 trials respectively. The primary end point was change in 6MWD for both trials. Bharani et al. 35 recruited patients in FCII–IV at baseline with various types of pulmonary hypertension including PPH, PAH associated with Eisenmenger syndrome and other forms of pulmonary hypertension. Sastry et al. recruited exclusively PPH patients, the majority of which (82%) were in FCII at baseline. 54 Singh et al. 55 recruited mixed populations of IPAH and Eisenmenger syndrome patients and the study included a significant proportion of children (as young as 3 years old). Given the large proportion of the study populations being outside sildenafil’s licensed indication in Bharani et al. ,35 Sastry et al. 54 and Singh et al. ,55 and their small sample sizes, the characteristics and study results of these three trials are only briefly listed/mentioned in the following sections and data from these studies were not meta-analysed.
Quality assessment of the five trials is summarised in Table 27. Both SUPER-153 and PACES-138 used adequate methods of randomisation and allocation concealment. ITT analysis was not used as the primary analysis, but was used as sensitivity analysis for a few outcomes. The proportion of patients who completed the trials was similar between treatment arms in SUPER-1, and was [Commercial-in-confidence information has been removed].
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| Sildenafil vs placebo with ongoing supportive treatment | ||||||
| SUPER-1/Galiè et al., 2005;53 12 weeks | Yes (baseline 6MWD and cause of PAH) | Yes | Double-blind | Survival: yes; clinical worsening: yes; functional class: no (273/277); 6MWD: yes; haemodynamic: no (258/277); quality of life: N/A | Placebo: 97% (68/70); sildenafil 20 mg t.i.d.: 97% (67/69), 40 mg t.i.d.: 97% (65/67), 80 mg t.i.d.: 92% (65/71) | Primary analysis for 6MWD excluded patients without baseline and at least one post-baseline measurement (n = 266), but ITT analysis was performed as a sensitivity analysis |
| Bharani et al., 2003;35 2 × 2 weeks | Unclear | Unclear | Double-blind | Survival: no death; clinical worsening: N/A; functional class: unclear; 6MWD: unclear; haemodynamic: unclear; quality of life: N/A | 90% (9/10) | |
| Sastry et al., 2004;54 2 × 6 weeks | Yes | Unclear | Double-blind | Survival: yes; clinical worsening: N/A; functional class: N/A; 6MWD: N/A; haemodynamic: N/A; quality of life: yes | At week 6: placebo: 92% (11/12); sildenafil: 90% (9/10) | |
| Singh et al., 2006;55 2 × 6 weeks | Unclear | Yes | Double-blind | Survival: N/A; clinical worsening: N/A; functional class: unclear; 6MWD: unclear; haemodynamic: unclear; quality of life: N/A | Not reported | |
| Sildenafil vs placebo with ongoing epoprostenol and supportive treatment | ||||||
| PACES-1;38 16 weeks | Yes (baseline 6MWD, PAH subcategory) | Yes | Double-blind | Survival: yes; clinical worsening: yes; functional class: no (257/265); 6MWD: no (250–[Commercial-in-confidence information has been removed]/265); haemodynamic: no ([Commercial-in-confidence information has been removed]/265); quality of life: no (234–242/265) | Placebo: 82% (108/131); sildenafil: 91% (122/134) | Patients with missing baseline 6MWT or no post-baseline 6MWT were excluded from the 6MWD analysis |
Because of the different nature of the comparisons between the trials, the results of SUPER-1 and PACES-1 will be described separately [see Direct (head-to-head) comparisons].
Sildenafil added to supportive treatment versus supportive treatment alone
This comparison was investigated in SUPER-1,53 Bharani et al. ,35 Sastry et al. 54 and Singh et al. 55 As previously stated, results from the last three trials will only be briefly mentioned and will not be combined with results from SUPER-153 because of the minimal relevance of their study populations to this technology appraisal. The findings presented in this section are therefore mainly based on a single trial (SUPER-153) rather than meta-analysis, but results will be presented in a format similar to previous sections. Planned comparisons and those actually available are summarised in Table 28. The results from SUPER-1 are listed in Table 29 according to planned comparisons. Results for individual outcomes are described in the following subsections. As data stratified by FC were only available for the outcome of change in FC, results described were mainly drawn from data of mixed FC. Findings specifically for FCIII are stated separately when appropriate.
| Planned comparison | Population/doses/data to be included | Comparison listed | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FCIII, licensed dose | Yes | Data stratified by FC were available only for the outcome of change in FC |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed dose | Yes | The comparison between sildenafil 20 mg three times daily and placebo from the SUPER-1 study53 was included |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed dose(s) | No | SUPER-153 did not include pulmonary hypertension other than PAH |
| D. Sensitivity analysis – including above licensed doses | All PAH, all FC, licensed dose and above licensed doses | Yes | Data from all three sildenafil arms (20 mg, 40 mg and 80 mg three time daily) in the SUPER-1 study53 were combined |
| E. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data | No | Not applicable (results from a single trial – data designated as confidential are highlighted) |
| F. Sensitivity analysis – excluding open-label trial | All PAH, all FC, licensed dose(s), excluding open-label trial | No | Not applicable |
| G. Subgroup analysis –IPAH | IPAH, all FC, licensed dose | No | Stratified data were not available. Data for mixed FC were available for 6MWD and were described in the text |
| H. Subgroup analysis – CTD-APAH | CTD-APAH, all FC, licensed dose | No | Stratified data were not available. Data for mixed FC were available for 6MWD and were described in the text |
Survival
A total of four deaths were reported in the SUPER-1 trial (one in the placebo arm, one in the 20-mg arm and two in the 80-mg arm). 53 The number was too small to draw any conclusions.
Time to clinical worsening
Clinical worsening was defined in the SUPER-1 trial53 as death, transplantation, hospitalisation for PAH or initiation of additional therapies for PAH, such as intravenous epoprostenol or oral bosentan. Time-to-event analysis was carried out. No significant increase in time to clinical worsening or decrease in the incidence of clinical worsening was found in the sildenafil groups compared with the placebo group.
Functional class
Table 29 shows that the difference in the proportion of patients who maintained or improved FC between the placebo group and the sildenafil group(s) (20 mg three times daily or three doses combined) was in favour of sildenafil, but just failed to reach statistical significance. The proportion of patients having FC improved was significantly higher in the sildenafil 20 mg three times daily group than in the placebo group (mixed FC, RR = 3.91, 95% CI 1.55–9.88). The RR increased further when the two higher-dose sildenafil groups were included (mixed FC, RR = 4.97, 95% CI 2.09–11.79). The result of having FC improved specifically for FCIII patients [Commercial-in-confidence information removed].
| Analysis (see comparison checklist) | |||||||
|---|---|---|---|---|---|---|---|
| A. Primary analysis | B. Sensitivity analysis – mixed FC | D. Sensitivity analysis – including above licensed doses | |||||
| PAH population | All PAH subcategories | All PAH subcategories | All PAH subcategories | ||||
| Functional class (FC) | FCIII | All FC | All FC | ||||
| Doses | Licensed dose (20 mg three times daily) | Licensed dose (20 mg three times daily) | Licensed dose and above (20 mg, 40 mg and 80 mg three times daily) | ||||
| Total no. eligible for analysis | 7453 | 13953 | 27753 | ||||
| No. included in analysis | 0–74 | 130–139 | 258–277 | ||||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||||
| Death | RR | 0 | Data not available | 13953 | 1.01 (0.06 to 15.90) | 27753 | 1.01 (0.11 to 9.60) |
| Clinical worsening | RR | 0 | Data not available | 13953 | 0.43 (0.12 to 1.61) | 27753 | 0.48 (0.19 to 1.22) |
| Functional class improved | RR | 7453 | [Commercial-in-confidence data has been removed] | 13853 | 3.91 (1.55 to 9.88) a | 27353 | 4.97 (2.09 to 11.79) a |
| Functional class maintained or improved | RR | 7453 | [Commercial-in-confidence data has been removed] | 13853 | 1.08 (0.99 to 1.18) | 27353 | 1.08 (0.99 to 1.17) |
| Withdrawal for any reason | RR | 0 | Data not available | 13953 | [Commercial-in-confidence data has been removed] | 27753 | [Commercial-in-confidence data has been removed] |
| 6-minute walk distance (metres)b | WMD | 0 | Data not available | 13953 | 38 (12 to 64) a | 14153d | 42 (9 to 75) a , d |
| Haemodynamics | |||||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)c | WMD | 0 | Data not available | 13053 | –2.7 (–5.3 to –0.1) a | 25853 | –3.7 (–5.5 to –1.9) a |
| Right atrial pressure (RAP) (mmHg)c | WMD | 0 | Data not available | 13053 | –1.1 (–2.7 to 0.5) | 25853 | –1.3 (–2.7 to 0.1) |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)c | WMD | 0 | Data not available | 13053 | –171 (–311 to –31) a | 25853 | –225 (–341 to –109) a |
| Cardiac index (l/min/m2)c | WMD | 0 | Data not available | 13053 | 0.2 (0.0 to 0.5) | 25853 | 0.3 (0.1 to 0.5) a |
| Safety | |||||||
| Serious adverse events | RR | 0 | Data not available | 13953 | 0.85 (0.39 to 1.83) | 27753 | 0.82 (0.44 to 1.51) |
Exercise capacity
A significant increase in 6MWD for the sildenafil 20 mg three times daily group compared with the placebo group was observed (38 metres, 95% CI 12–64). The increase appeared to be slightly larger with high doses, although the differences between doses were not statistically significant.
Quality of life
Quality of life outcomes were not reported in the published paper for SUPER-153 but were reported in Pfizer’s submission to NICE. It stated that improvements in all domains of the SF-36 (physical functioning, role–physical, bodily pain, general health, vitality, social functioning, role–emotional and mental health) were observed in the sildenafil groups compared with the placebo group with the exception of role–physical for sildenafil 20 mg three times daily and role–emotional for sildenafil 40 mg three times daily. Statistical testing for these comparisons was not performed according to the study protocol, but the differences may not have been statistically significant in the bodily pain and role–emotional domains for any of the three doses according to the data presented. There appears to be no consistent pattern between the sildenafil doses and their effects on the various domains of the SF-36. The EuroQol 5 dimensions (EQ-5D) utility index was unchanged in the placebo and sildenafil 40 mg three times daily groups (mean change from baseline 0.0, 95% CI 0.0–0.1) and was slightly increased in the sildenafil 20 mg and 80 mg three times daily groups (0.1, 95% CI 0.1–0.2). Data specifically for FCIII patients were not available.
Haemodynamic measures
Table 29 shows that sildenafil at its licensed dose significantly reduced mPAP (–2.7 mmHg, 95% CI –5.3 to –0.1) and PVR (–171 dyn s/cm5, 95% CI –311 to –31) compared with placebo in patients with mixed FC. Inclusion of above licensed doses consistently increased treatment effects across the haemodynamic measures and the increase in cardiac output also reached statistical significance.
Other effectiveness measures
There was no significant difference in the change in Borg dyspnoea index for the sildenafil groups compared with the placebo group.
Serious adverse events and other adverse events
The risk of experiencing at least one SAE was similar between treatment groups (mixed FC, RR = 0.82, 95% CI 0.44–1.51 for sildenafil groups combined versus placebo). Common adverse events that occurred more frequently in the sildenafil groups include: headache, flushing, diarrhoea, dyspepsia, pain in limb, myalgia and pyrexia. 53
Subgroup analysis – PAH subcategories
Treatment effects on 6MWD among various subgroups of patients, defined according to demographic features, disease characteristics and baseline variables, were examined descriptively in the SUPER-1 study. 53 The treatment effect at the licensed dose did not differ significantly between PPH and CTD-APAH subgroups: 40 metres (95% CI 14–66) versus 55 metres (95% CI 25–85) respectively (test for heterogeneity: χ2 = 0.55, df = 1, p = 0.46).
Results from cross-over trials
All three short-term cross-over trials35,54,55 reported significant improvements in exercise capacity and haemodynamic measures for sildenafil (at above licensed doses) compared with placebo.
Summary and discussion
-
Four RCTs comparing sildenafil (added to supportive treatment) with supportive treatment alone were identified. The SUPER-1 study53 was the pivotal trial for this comparison and was the only trial that investigated the licensed dose for sildenafil (20 mg three times daily). It was an international, double-blind study with a duration of 12 weeks. Three further single-centre, cross-over trials35,54,62 included predominantly patients outside the scope of this technology appraisal and used sildenafil only at above licensed doses.
-
Methods of randomisation and allocation concealment were adequate in SUPER-1. 53 The primary analyses reported in this study excluded some patients with missing data and thus were not based on the ITT principle. However, ITT analyses were performed as sensitivity analyses and the results were consistent with the primary analyses.
-
The majority of patients included in the SUPER-1 study had IPAH. Patients with CTD-APAH and PAH associated with CHD were also included. The mean 6MWD at baseline was 344 metres. Patients were of mixed FC; 58% were in FCIII and 39% in FCII at baseline.
-
Data stratified by FC were available only for the outcome of change in FC. Results presented below were largely based on a patient population of mixed FC.
-
Compared with supportive treatment alone, sildenafil at its licensed dose (added to supportive treatment) demonstrated significant improvements in exercise capacity (6MWD), haemodynamic outcomes (mPAP and PVR) and certain domains of quality of life measures and improvement in FC in PAH populations with mixed FC. Above licensed doses up to 80 mg three times daily appear to increase the treatment effect for these outcomes, although the differences between doses were not statistically significant in the trial. No significant improvement in time to clinical worsening and the symptom of dyspnoea was observed.
-
The treatment effect of sildenafil on 6MWD was similar in the PPH and CTD-APAH groups.
Sildenafil added to ongoing epoprostenol versus ongoing epoprostenol
This comparison was investigated in the PACES-1 trial. 38 This study remained unpublished at the time of completion of this technology assessment. Data presented in this section were largely obtained from Pfizer’s submission to NICE for this technology appraisal. Additional data were sought from the clinical study report (commercial-in-confidence) of this study, which was made available to the assessment group by Pfizer. The characteristics and quality assessment of the PACES-1 study are shown in Tables 26 and 27 respectively.
As the results presented in this section were based on a single trial and the dose of sildenafil used (80 mg three times daily) was above its licensed dose, only a narrative summary of the study findings is provided. Most of the findings were based on the whole trial population, which included mixed types of PAH (IPAH and CTD-APAH) and mixed FC (I–IV).
Findings
Seven deaths occurred in the placebo group and one in the sildenafil group. The difference between groups just failed to reach statistical significance (RR = 0.14, 95% CI 0.02–1.12). Clinical worsening was defined in this trial as death, lung transplantation, hospitalisation due to PAH, initiation of bosentan therapy or change in epoprostenol dose because of clinical deterioration. Time-to-event analysis showed that a significantly lower proportion of patients treated with sildenafil 80 mg three times daily compared with those treated with placebo experienced clinical worsening (stratified log-rank test p = 0.012). The difference was also significant when analysed as a dichotomous outcome (RR = 0.36, 95% CI 0.16–0.77). Significantly fewer patients in the sildenafil group withdrew from the study compared with the placebo group (RR = 0.51, 95% CI 0.26–0.98).
The proportion of patients with FC improved or maintained was not significantly different between the sildenafil group and the placebo group (mixed FC, RR = 1.06, 95% CI 0.98–1.15; FCIII only, RR = 1.04, 95% CI 0.96–1.12), but significantly more patients treated with sildenafil had their FC improved (mixed FC, RR = 2.47, 95% CI 1.52–4.02; FCIII only, RR = 1.95, 95% CI 1.16–3.29). Patients treated with sildenafil also had a greater improvement in 6MWD (mean difference 26 metres, 95% CI 11–41) and in various domains (physical functioning, role limitation due to physical problems, bodily pain, general health, vitality, social functioning and mental health) of the SF-36 questionnaire (but not role limitation due to emotional problems). No significant differences were found between treatment groups in the change from baseline in Borg dyspnoea score (no change in median score in both groups) and the EQ-5D utility index (increased by 0.052 for the sildenafil group and by 0.022 for the placebo group). Significant reductions in mPAP, RAP and PVR were also observed in the sildenafil group compared with the placebo group. The analyses of all of the above outcomes (FC, 6MWD, Borg dyspnoea index, quality of life and haemodynamic measures) were not based on the ITT principle, and more patients in the placebo group than in the sildenafil group were excluded from the analyses.
SAEs were experienced by 29/134 patients in the sildenafil group and 39/131 in the placebo group (RR = 0.73, 95% CI 0.48–1.10). Common adverse events that occurred more frequently in the sildenafil group than in the placebo group included: headache, diarrhoea, nausea, flushing, dyspepsia and nasal congestion.
The mean change from baseline in 6MWD appeared to be greater in the subgroup of patients with IPAH (31 metres, 95% CI 14–49) than in the subgroup of patients with CTD-APAH (8 metres, –23 to 38); however, the difference was not statistically significant (test for heterogeneity χ2 = 1.80, df = 1, p = 0.18).
Summary and discussion
-
One double-blind RCT (PACES-138) compared sildenafil 80 mg three times daily (above licensed dose) with placebo in patients who were receiving ongoing epoprostenol and supportive treatment.
-
Methods of randomisation and allocation concealment were adequate in PACES-1. ITT analysis was not used for most outcomes. More patients in the placebo group than in the sildenafil group were excluded from analyses because of missing data. The potential bias would be in favour of placebo if the excluded patients had worse outcomes.
-
Results from PACES-1 indicated that patients treated with sildenafil 80 mg three times daily had a significantly lower risk of clinical worsening and a greater improvement in FC, 6MWD, some domains of quality of life measures and haemodynamic measures (mPAP, RAP and PVR). There were no significant differences between the sildenafil and placebo groups in changes in Borg dyspnoea score, the EQ-5D utility index and risk of SAEs.
-
The trial included mixed PAH populations (IPAH and CTD-APAH) with mixed FC (67% FCIII). Changes in 6MWD were not significantly different between the IPAH and CTD-APAH groups. Results of changes in FC for patients in FCIII at baseline were similar to results of the overall trial population.
Direct (head-to-head) comparisons
Quantity and quality of included studies
Direct comparisons between the five technologies under assessment in this review were made in two of the included RCTs. Bosentan was compared with sitaxentan (both at the licensed dose) in the STRIDE-2 study. 48 The comparisons in this trial of both drugs with placebo have been included in the bosentan and sitaxentan sections respectively. Bosentan (licensed dose) was compared with sildenafil (above licensed dose) in a further study (SERAPH) by Wilkins and colleagues. 57 The characteristics of these two studies are summarised in Table 30 (STRIDE-248 is listed again for the convenience of readers; only relevant treatment arms are listed). Additional comparisons involving combinations of the technologies under assessment (iloprost added to ongoing bosentan versus ongoing bosentan; epoprostenol plus bosentan versus epoprostenol alone) have been described in the iloprost and bosentan sections respectively.
| Trial name/key paper (protocol number); location/centres | Duration; design; number of patients randomised | Interventiona | Comparatora | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures,b mean (SD) |
|---|---|---|---|---|---|---|---|
| STRIDE-2/Barst et al., 200648 (FPH02); international, 55 centres | 18 weeks; double-blind (open-label for bosentan), parallel; n = 247 | Bosentan (oral) 125 mg b.d.c (n = 60); | Sitaxentan (oral) 100 mg o.d. (n = 61) | IPAH (59%), CTD (30%), congenital heart disease (11%) | II (37%), III (59%), IV (4%) | 54 (15); 78% | 6MWD: 337 (80); cardiac index: 2.4 (0.8); mPAP: 48 (14); PVR: 880 (560);e RAP: NR; SvO2: NR |
| SERAPH/Wilkins et al., 2005;57 UK, single centre | 16 weeks; double-blind, parallel; n = 26 | Bosentan (oral) 125 mg b.d.c (n = 12) | Sildenafil (oral) 50 mg t.i.d.d (n = 14) | IPAH (88%), CTD (12%) | III (100%) | 43 (NR, 27–62); 81% | 6MWD: 297 (82); cardiac index: 2.3 (0.1); mPAP: NR; PVR: NR; RAP: NR; SvO2: NR |
The study characteristics and quality assessment of the STRIDE-2 study48 have been described in previous sections. The SERAPH study57 was a 16-week, single-centre trial that randomised 26 patients. It was conducted in the Hammersmith Hospital, London and was funded by the British Heart Foundation. The dose of sildenafil used was 50 mg twice daily for the first 4 weeks, uptitrated to 50 mg three times daily thereafter (above licensed dose). The trial recruited exclusively patients in FCIII at baseline and the majority of patients had IPAH (23/26) with the rest having CTD-APAH. The mean 6MWD at baseline was 297 metres. The primary end point for SERAPH was change in right ventricular mass from baseline as measured by cardiovascular magnetic resonance. 57
The methods of randomisation and allocation concealment in the SERAPH study were adequate. Both ITT analysis and per-protocol analysis (including patients who completed the trial) were used. Except for one patient who died during the study, no patient was withdrawn from treatment. 57 The quality assessment for STRIDE-2 and SERAPH is summarised in Table 31.
| Study; duration | Truly random allocation (strata for randomisation) | Adequate allocation concealment | Blinding | Use of ITT analysisa (n included in analysis/N randomised) | % of patients completing the trial | Comments |
|---|---|---|---|---|---|---|
| STRIDE-2/Barst et al., 2006;48 18 weeks | Yes | Yes | Double-blind for sitaxentan and open-label for bosentan (outcome assessor blinded) | Survival analysis: N/A; clinical worsening: yes; functional class: no [Commercial-in-confidence information has been removed];b 6MWD: no [Commercial-in-confidence information has been removed];a haemodynamic: not measured; quality of life: not measured | Bosentan: 87% (52/60); sitaxentan 100 mg: 93% (57/61) | Patients who did not have a valid post-baseline 6MWT were excluded from efficacy analysis [Commercial-in-confidence information has ben removed] |
| SERAPH/Wilkins et al., 2005;57 16 weeks | Yes | Yes | Double-blind | Survival analysis: N/A; clinical worsening: N/A; functional class: N/A; 6MWD: yes; haemodynamic: yes; quality of life: yes | Bosentan: 100% (12/12); sildenafil: 93% (13/14) | ITT analysis was performed and reported, although the main results table in the paper excluded the patient who died during the trial |
Sitaxentan versus bosentan with ongoing supportive treatment
The results presented in this section are from STRIDE-248 rather than from meta-analysis, as this study was the only one that investigated this comparison. Planned comparisons and those actually performed are summarised in Table 32. Results are listed in Table 33 according to the planned comparisons, followed by a paragraph summarising the findings. As STRIDE-2 included patients with mixed FC, and data stratified by FC were available only for the outcome of change in FC, the findings presented are mainly based on the results of mixed PAH populations. Findings specifically for FCIII are stated separately when appropriate.
| Planned comparison | Population/doses/data to be included | Analysis carried out | Comments and source of data |
|---|---|---|---|
| A. Primary analysis | All PAH, FCIII, licensed dose | Yes | Data stratified by FC were available only for the outcome of change in FC |
| B. Sensitivity analysis – mixed FC | All PAH, all FC, licensed dose | Yes | All data from relevant treatment arms were included |
| C. Sensitivity analysis – mixed pulmonary hypertension | All pulmonary hypertension including categories 1–5 of the Venice 2003 classification, all FC, licensed dose(s) | No | STRIDE-248 did not include patients outside category 1 of the Venice 2003 classification |
| D. Sensitivity analysis – including above licensed doses | All PAH, all FC, licensed dose and above licensed doses | No | No above licensed dose was used in STRIDE-248 |
| E. Sensitivity analysis – excluding data designated as confidential | All PAH, all FC, licensed dose(s), excluding commercial-in-confidence and academic-in-confidence data | No | Not applicable. Data were from only one trial. Confidential data are highlighted |
| F. Sensitivity analysis – excluding open-label trial | All PAH, all FC, licensed dose(s), excluding open-label trial | No | Not applicable (the bosentan arm was open-label in STRIDE-248) |
| G. Subgroup analysis –IPAH | IPAH, FCIII, licensed dose(s) | No | No data specifically for patients with IPAH were available |
| H. Subgroup analysis –CTD-APAH | CTD-APAH, FCIII, licensed dose(s) | No | No data specifically for CTD-APAH were available |
| Analysis (see comparison checklist) | |||||
|---|---|---|---|---|---|
| A. Primary analysis | B. Sensitivity analysis – mixed FC | ||||
| PAH population | All PAH subcategories | All PAH subcategories | |||
| Functional class (FC) | FCIII | All FC | |||
| Doses | Licensed dose (sitaxentan 100 mg once daily; bosentan 125 mg twice daily) | Licensed dose (sitaxentan 100 mg once daily; bosentan 125 mg twice daily) | |||
| Total no. eligible for analysis | 7148 | 12448 | |||
| No. included in analysis | 69 | [Commercial-in-confidence information has been removed]–12248 | |||
| Outcomes | Statistics | n | Effect size (95% CI) | n | Effect size (95% CI) |
| Efficacy | |||||
| Deatha | RR | 0 | Data not available | 12148 | Not estimable (no death) |
| Clinical worseninga | RR | 0 | Data not available | 12148 | 0.44 (0.14 to 1.34) |
| Functional class maintained or improvedb | RR | 6948 | 1.06 (0.96 to 1.16) | 12148 | 1.07 (0.99 to 1.17) |
| Functional class improvedb | RR | 6948 | 0.78 (0.27 to 2.22) | [Commercial-in-confidence information has been removed]48 | [Commercial-in-confidence information has been removed] |
| Withdrawal for any reasona | RR | 0 | Data not available | [Commercial-in-confidence information has been removed]48 | 0.49 (0.16 to 1.55) |
| 6-minute walk distance (metres)c | WMD | 0 | Data not available | [Commercial-in-confidence information has been removed]48 | 2 (–22 to 26) |
| Borg dyspnoea indexd | WMD | 0 | Data not available | [Commercial-in-confidence information has been removed]48 | [Commercial-in-confidence information has been removed] |
| Haemodynamics | |||||
| Mean pulmonary arterial pressure (mPAP) (mmHg)d | WMD | 0 | Not measured | 0 | Not measured |
| Right atrial pressure (RAP) (mmHg)d | WMD | 0 | Not measured | 0 | Not measured |
| Pulmonary vascular resistance (PVR) (dyn s/cm5)d | WMD | 0 | Not measured | 0 | Not measured |
| Cardiac index (l/min/m2)c | WMD | 0 | Not measured | 0 | Not measured |
| Safety | |||||
| Serious adverse eventsa | RR | 0 | Data not available | 12248 | [Commercial-in-confidence information has been removed] |
Findings
No deaths occurred in either treatment group. The number of patients with the following events was larger in the bosentan arm than in the sitaxentan 100-mg arm: clinical worsening (9/60 versus 4/61), withdrawal for any reason (8/60 versus 4/61) and FC worsened (5/[Commercial-in-confidence information has been removed] versus 1/[Commercial-in-confidence information has been removed]). However, these numbers were small and the differences between groups were not statistically significant. The numbers of patients having FC improved and experiencing at least one SAE were similar between the two groups; in addition, the changes in 6MWD and Borg dyspnoea index were also similar between the two groups. Change in FC did not differ significantly between groups for patients in FCIII at baseline. Quality of life and haemodynamic outcomes were not measured in STRIDE-2. 48
Sildenafil versus bosentan with ongoing supportive treatment
This comparison was investigated in the SERAPH study. 57 As the dose used in the study was above the licensed dose and the number of patients randomised was small (n = 26), only a narrative summary is provided below.
Findings
One death occurred in this trial. The patient who was assigned to sildenafil died suddenly at week 14. Clinical worsening and changes in FC were not reported in this trial. ITT analysis, in which the patient who died was assigned a 6MWD of 0 metres at week 16, showed no significant difference in the mean change from baseline in 6MWD between the sildenafil group (increased by 75 metres) and the bosentan group (increased by 59 metres) at week 16 (end of trial). The improvement in the sildenafil group increased to 114 metres in a per-protocol analysis excluding the patient who died, and the between-group difference became statistically significant (p = 0.044). The total number of patients who experienced at least one SAE was not reported. Hospital admissions or unscheduled visits were required for three patients in the bosentan group and one patient in the sildenafil group. Right ventricular mass (the primary end point) was reduced in both groups, but only significantly in the sildenafil group compared with baseline. The differences between the two groups in right ventricular mass and all other measures including haemodynamic, hormonal and quality of life (Kansas City Cardiomyopathy Questionnaire) measures were not statistically significant.
Summary and discussion
-
Two RCTs included a direct comparison between the technologies under assessment in this report. The STRIDE-2 trial48 was an 18-week, international study sponsored by the manufacturer of sitaxentan and compared sitaxentan (licensed dose) with bosentan (licensed dose) with ongoing supportive treatment. The SERAPH study57 was a 16-week, single-centre UK study sponsored by the British Heart Foundation and compared sildenafil (above licensed dose) with bosentan (licensed dose) with ongoing supportive treatment. The bosentan arm in STRIDE-2 was open-label, whereas SERAPH was a double-blind study.
-
Methods of randomisation and allocation concealment were adequate in both trials. ITT analysis was used in SERAPH57 but not in STRIDE-2. 48 The potential bias due to exclusion of a small number of patients from the efficacy analysis in STRIDE-248 was unclear, but the impact is likely to be small.
-
STRIDE-2 included mixed populations of patients with IPAH, CTD-APAH and PAH associated with CHD with mixed FC (59% FCIII). 48 SERAPH included exclusively patients in FCIII predominantly with IPAH.
-
For the comparison between sitaxentan and bosentan at licensed doses, no significant differences between the two treatment groups were found in any of the outcomes examined. Data stratified by FC were available only for the outcome of change in FC, and the results for FCIII patients only were similar to the overall trial results.
-
For the comparison between sildenafil (above licensed dose) and bosentan (licensed dose), no significant differences between the two treatment groups were found in any of the outcomes examined. However, the sample size for this trial was small (n = 26) and it might not be sufficiently powered to detect clinically important differences.
-
Results from SERAPH57 demonstrated the importance of using ITT analysis and the potential impact of excluding randomised patients from analysis, particularly when the sample size is small.
Ongoing studies
Several ongoing studies were identified through the formal searches and scrutiny of the manufacturer submissions. These are documented for information in Appendix 6, Table 74.
More evidence from RCTs regarding the use of combination therapy will become available in the next few years. This includes the addition of inhaled iloprost to sildenafil (NCT00302211), bosentan to sildenafil (NCT00303459), and sildenafil to bosentan (NCT00323297). This review should be updated when the results from these trials are reported.
In addition, an RCT (NCT00091715) of bosentan versus placebo in patients with mild PAH (FCII at baseline) has been completed. There are also RCTs of other emerging treatments for PAH that have recently been completed or are ongoing. More treatments for PAH may become available and the licensed indications for existing treatments may be amended in view of the emerging evidence. The scope of any future review may need to be changed accordingly.
Long-term studies
Scrutiny of the manufacturer submissions revealed a number of long-term follow-up studies. These are documented in Appendix 7, Tables 75 and 76. Those studies that reported data for change/no change in FC and/or mortality data stratified by FC were utilised to inform the independent economic assessment (see Chapter 4).
Overview and discussion of clinical effectiveness
Comparison of each of the five technologies with placebo/control with ongoing supportive treatment
This comparison is the main focus of this technology assessment and is also where the vast majority of RCT evidence lies. Table 34 summarises the results of relevant meta-analyses and individual studies (when only one trial provided relevant data) for each of the five technologies under assessment for selected key outcomes. The results show that significant improvements in FC, 6MWD and haemodynamic measures have been clearly demonstrated in PAH populations for each of the technologies compared with placebo/control, although the volume of evidence varies between technologies. The findings for the other outcomes were less clear-cut. The main findings for this comparison are discussed below.
| Drug and population | Death, RR (95% CI) | Clinical worsening, RR (95% CI) | FC improvement, RR (95% CI); NNT (95% CI) | 6MWD, WMDa (95% CI) | Quality of lifeb | Haemodynamics, WMDc (95% CI) |
|---|---|---|---|---|---|---|
| Epoprostenol | ||||||
| Mixed PAH, mixed FC | 0.37 (0.09 to 1.57) [3] | No data | 10.58 (3.07 to 36.50); 2.2 (1.6 to 3.6, I2 = 69%)d [3] | 81 (45 to 117)d [3] | Chronic Heart Failure Questionnaire (+) [1]; Nottingham Health Profile (+/–) [1] | mPAP: –6.3 (–8.7 to –3.9)d [3]; RAP: –2.4 (–4.1 to –0.7)d [2]; PVR: –427 (–548 to –306)d [3]; cardiac index: 0.6 (0.4 to 0.8)d [2] |
| PPH, mixed FC | 0.18 (0.03 to 1.18) [1] | No data | 7.45 (2.55 to 21.77); 1.9 (1.1 to 5.9, I2 = 82%)d [2] | 58 (6 to 110)d [2] | Same as above | mPAP: –6.8 (–10.6 to –3.0)d [2]; RAP: –2.3 (–5.1 to 0.5) [1]; PVR: –401 (–613 to –189)d [2]; cardiac index: 0.6 (0.2 to 0.9)d [1] |
| PPH, FCIII | No stratified data | No data | No stratified data | No stratified data | No stratified data | No stratified data |
| PPH, FCIV | No stratified data | No data | No stratified data | No stratified data | No stratified data | No stratified data |
| CTD-APAH, mixed FC | 0.79 (0.22 to 2.77) [1] | No data | 42.25 (2.62 to 680.61); 2.6 (2.0 to 4.0)d [1] | 100 (55 to 144)d [1] | No data | mPAP: –6.0 (–9.0 to –2.9)d [1]; RAP: –2.5 (–4.6 to –0.4)d [1]; PVR: –440 (–588 to –292)d [1]; cardiac index: 0.6 (0.4 to 0.8)d [1] |
| Iloprost | ||||||
| Mixed PH, mixed FC | 0.58 (0.14 to 2.46) [2] | 0.42 (0.15 to 1.15) [1] | 1.98 (1.13 to 3.48); 8.3 (4.5 to 33.3, I2 = 0%)d [2] | 36 (12 to 60)d [1] | EQ-5D VAS (+) [2]; EQ-5D health state score (–) [1]; SF-12 (–) [1]; MLHF Questionnaire (–) [1] | mPAP: –4.4 (–6.7 to –2.1)d [1]; RAP: –2.2 (–3.5 to –0.9)d [1];PVR: –335 (–421 to –249)d [1]; cardiac index: no data |
| PPH, mixed FC | 0.52 (0.05 to 5.55) [1] | No stratified data | 3.19 (1.11 to 9.11); 5.9 (3.1 to 33.3)d [1] | No stratified data | No stratified data | No stratified data |
| PPH, FCIII | No stratified data | No stratified data | 3.71 (0.83 to 16.61) [1] | No stratified data | No stratified data | No stratified data |
| CTD-APAH, mixed FC | No stratified data | No stratified data | No stratified data | No stratified data | No stratified data | No stratified data |
| Bosentan | ||||||
| Mixed PAH, mixed FC | 0.23 (0.03 to 1.47) [4] | 0.43 (0.15 to 1.24) [3], I2 = 62% | 1.51 (1.05 to 2.15); 7.1 (4.0 to 50.0, I2 = 46%)d [4] | 41 (24 to 58) [4] | No data | mPAP: –5.9 (–9.3 to –2.5)d [2]; RAP: –3.0 (–9.0 to 3.0) [2], I2 = 89%; PVR: –414 (–596 to –232)d [1];cardiac index: 1.0 (0.7 to 1.3)d [1] |
| Mixed PAH, FCIII | No death [2] | 0.08 (0.00 to 1.39) [1] | 2.08 (0.97 to 4.46) [3] | 59 (20 to 99) [2] | No data | Same as above |
| IPAH, mixed FC | No stratified data | No stratified data | No stratified data | No stratified data | No stratified data | No stratified data |
| CTD-APAH, mixed FC | No stratified data | No stratified data | No stratified data | 22 (–32 to 76) [2] | No stratified data | No stratified data |
| Sitaxentan | ||||||
| Mixed PAH, mixed FC | 0.20 (0.01 to 4.15) [3] | 0.33 (0.12 to 0.87)d [3] | 1.74 (1.12 to 2.70); 10 (5 to infinity, I2 = 21%)d [3] | 32 (18 to 47) [3] | SF-36 (–) [1] | mPAP: –3.0 (–5.9 to –0.1)d [1]; RAP: –1.0 (–2.5 to 0.5) [1]; PVR: –270 (–402 to –138)d [1];cardiac index: 0.3 (0.1 to 0.5)d [1] |
| Mixed PAH, FCIII | No stratified data | No stratified data | 1.53 (0.74 to 3.17) [2] | No stratified data | No stratified data | No stratified data |
| IPAH, mixed FC | No stratified data | No stratified data | 2.02 (0.88 to 4.60) [1]a | 34 (7 to 61) d,e [1] | No stratified data | No stratified data |
| CTD-APAH, mixed FC | No stratified data | No stratified data | 2.18 (0.31 to 15.24) [1]a | 58 (0 to 116)d,e [1] | No stratified data | No stratified data |
| Sildenafil | ||||||
| Mixed PAH, Mixed FC | 1.01 (0.06 to 15.90) [1] | 0.43 (0.12 to 1.61) [1] | 3.91 (1.55 to 9.88); 4.8 (3.0 to 11.1)d [1] | 38 (12 to 64)d [1] | SF-36 (+/–) [1]; EQ-5D current health state VAS (+) [1]; EQ-5D utility index (?) [1] | mPAP: –2.7 (–5.3 to –0.1)d [1]; RAP: –1.1 (–2.7 to 0.5) [1]; PVR: –171 (–311 to –31)d [1]; cardiac index: 0.2 (0.0 to 0.5) [1] |
| Mixed PAH, FCIII | No stratified data | No stratified data | 2.55 (0.91 to 7.18) [1] | No stratified data | No stratified data | No stratified data |
| IPAH, mixed FC | No stratified data | No stratified data | No stratified data | 40 (14 to 66)d [1] | No stratified data | No stratified data |
| CTD-APAH, mixed FC | No stratified data | No stratified data | No stratified data | 55 (25 to 85)d [1] | No stratified data | No stratified data |
Survival
All of the RCTs included in this review were of a duration of 18 weeks or less. Death generally occurred more frequently in the placebo/control groups than in the treatment groups, but the numbers were very small within each trial. The epoprostenol trial by Barst and colleagues11 was an exception and was the only RCT that demonstrated a significant survival benefit within a trial. The pooled RRs for death were in favour of each of the technologies (except for sildenafil for which the result was based on two deaths in a single trial), but did not reach statistical significance as confidence intervals were wide.
A recent meta-analysis63 of treatments for pulmonary hypertension (i.e. a wider population than just PAH) reported a RR of death of 0.70 (95% CI 0.41–1.22) compared with control. The analysis pooled all disease-modifying technologies for pulmonary hypertension including those outside this technology assessment. The merits of this are debatable. However, the estimated non-significant 30% reduction in mortality led the authors to question the survival benefit offered by the technologies for pulmonary hypertension, and in particular whether the trials were adequately powered or of a long enough duration to adequately measure survival. The findings of this assessment report are in agreement with this conclusion.
Despite some methodological issues with this meta-analysis63 (e.g. the head-to-head trial SERAPH57 was included in the analysis with the bosentan arm being treated as a control), its finding is consistent with the finding of this technology assessment in that the overall direction of effect was in favour of active treatments and was consistent across different types of drugs. The key questions are therefore whether the magnitude of the effect varies between drugs and whether it changes over time. Unfortunately these questions are unlikely to be answerable with existing evidence because of the small numbers of deaths that occurred in the RCTs and their short duration. Increasing evidence from long-term observational studies (see Appendix 7) agrees with the potential survival benefit of these treatments observed during short-term trials, but unbiased comparison between drugs using observational data is difficult to achieve because of differences in patient populations, entry criteria, treatments offered and methods of follow-up.
In addition to the small numbers of patients/events and short duration of study, interpretation of results from RCTs in relation to mortality as well as other outcomes needs to take into account the following issues.
Patient populations
Trials varied in their population mix in terms of types of PAH and FC at baseline. Although limited within- and between-trial comparisons shown in this assessment report did not demonstrate significant differences between subcategories of PAH, these comparisons were limited by the small number of patients within each subcategory and thus the low statistical power to detect genuine differences between the subgroups. It should be noted that baseline mortality rates between different subcategories of PAH are different. Very limited data from trials included in this report have also shown that results from the subset of patients in FCIII at baseline were generally similar to the overall trial results, which included patients with mixed FC. From a statistical point of view it is worth emphasising that a certain level of association between data sets is to be expected when one set of data (i.e. FCIII only) is compared with another set of data that includes the former (i.e. data for the whole trial population including that for FCIII and other FC). Conclusive results with regard to whether the treatment effect varied by FC can only be obtained from comparisons between mutually exclusive subgroups (e.g. FCII versus FCIII) or analysis of individual patient data using appropriate statistical tests. These were not carried out in this assessment report as evaluating the clinical effectiveness of the treatments outside their licensed indications (in terms of FC) is beyond the scope of the assessment. Nevertheless, similar problems of (lack of) availability of data stratified by FC and small patient numbers within each FC would have prevented such comparisons in most cases.
Although there appears to be limited statistical heterogeneity within many of the pooled analyses, there was considerable clinical heterogeneity between some of the populations enrolled in and between trials.
In addition to the varied population mix within each trial, the awareness of the condition of PAH within the medical community has risen in the past few years. Consequently, patients enrolled in the trials conducted in 1990s were likely to have been at different stages of the disease from those enrolled in the trials conducted in the past few years, even if they were designated the same FC at baseline. This is apparent when the mean age, baseline 6MWD and haemodynamic measures are compared between trials (particularly for epoprostenol trials compared with others). However, it is still clear that patients are generally being diagnosed well after the onset of symptoms64 and thus there is a considerable delay in patients being first seen at a designated centre.
One further issue relates to the inclusion criteria of the trials. Again, the major difference was between epoprostenol trials and other trials, but important differences also existed between some of the other trials in terms of use of baseline FC and 6MWD as inclusion criteria. A common feature for nearly all trials was the requirement of patients to be stable on supportive treatment for a certain period of time (usually 4 weeks or longer) before study entry. The trials therefore essentially excluded unstable and therefore potentially sicker patients whom are frequently seen in clinical practice. This could have an implication for the generalisability of the results from the trials.
Comparator
Although supportive treatment was the common comparator across the trials, the standard of care is likely to have changed over time and may vary between countries. Consequently the results of the trials may not be directly comparable. In terms of survival benefit, if epoprostenol did reduce mortality, as the limited evidence suggests, it would be more difficult for the other trials to demonstrate a reduction in mortality as patients who deteriorated in the control groups would have been given epoprostenol as a rescue therapy, which may have prevented/delayed death.
Whether a placebo was used in the control arm may also have affected the response in control groups because of the placebo effect (when placebo was used) and possible bias in the provision of care and assessment of outcome (when placebo was not used), although this would be less of an issue for the outcome of survival.
In brief, limited evidence from RCTs (and observational studies) suggests that various treatments for PAH confer survival benefit, although it is difficult to quantify the treatment effects and to ascertain whether differences exist between drugs. However, it is unlikely that the survival benefit demonstrated in the epoprostenol trial by Barst and colleagues11 [prevention of eight deaths over 12 weeks for every 40 patients treated, number needed to treat (NNT) = 5, 95% CI 3–14] would be replicated in future trials because epoprostenol has since been used as a standard treatment for severe PAH. Interpretation of results from RCTs needs to take into account the relatively small sample sizes and short duration of these studies, and differences in patient populations and comparators (supportive treatment) between trials and over time.
Clinical worsening
Clinical worsening events were not defined or reported in any of the epoprostenol trials. A significant reduction in clinical worsening events and/or an increase in time to clinical worsening was demonstrated in individual trials of bosentan,43,45 the pooled results of sitaxentan trials and the pooled results of bosentan trials (excluding STRIDE-248). Fewer clinical worsening events occurred in the active treatment arms than in the placebo arms in the pivotal trials for iloprost (AIR study41) and sildenafil (SUPER-153), but the results did not reach statistical significance.
Most points already discussed in relation to survival are also applicable to clinical worsening events. An additional issue for this outcome is that different definitions of clinical worsening have been used in different trials. It is likely that both the severity of disease in study participants at baseline and the definition of clinical worsening adopted in the trials had an impact (in addition to the treatment effect) on the event rates for clinical worsening. Standardisation of the definition in future trials would be helpful for comparison of results between trials.
Changes in functional class
All five technologies demonstrated a significant benefit compared with placebo/control with regard to having an improved FC on treatment. One issue that needs to be highlighted in relation to this outcome is the substantial variations between trials in the response rates in the placebo/control groups. The differences between trials may partly be attributable to the differences in the mix of FC at baseline. However, even when limiting the data to patients in FCIII at baseline, the proportion of patients having their FC improved still ranged from 29% (19/65) in BREATHE-145 (bosentan trial) to 6% (2/36) in the AIR study41 (iloprost trial). Again, the differences in trial populations and standard of (supportive) care need to be considered when interpreting the results. Within the context of RCTs, the nature of FC being a subjective outcome means that there was a possibility of misclassification of FC at baseline. Interpretation of baseline FC and outcomes related to FC changes should therefore be made in conjunction with objective outcome measures such as 6MWD.
The variations in the response rates in the placebo/control groups between trials mean that calculating the NNT, assuming a common ‘baseline risk’ across different technologies or even within a drug, may be problematic. The NNTs presented in Table 34 were calculated according to the pooled risk differences of the trials contributing to the data for each technology. Therefore they should not be compared against each other and should be interpreted with great caution, particularly when substantial heterogeneity in risk differences is shown (I2 ≥ 50%).
In contrast to the significant effect on improving FC, most technologies, except sitaxentan, failed to demonstrate a statistically significant effect on having FC improved or maintained (i.e. not worsened). This was unexpected and was in part due to some of the trials failing to report changes in FC other than improvement (i.e. proportion of patients having FC maintained or worsened), and consequently the smaller number of patients included in the analysis of this outcome. Furthermore, it is likely that the exclusion of patients with unstable conditions from these trials made it more difficult for these studies to demonstrate the benefit of reducing FC deterioration within the short duration of the trials.
6-Minute walk distance
All five technologies demonstrated a significant effect compared with placebo/control on increasing exercise capacity as measured by 6MWT. The mean difference between the treatment and placebo/control groups appeared to be greatest in two of the epoprostenol trials33,39 (approximately 100 metres). The between-group difference varied from approximately 30 to 75 metres in the other trials, with wide confidence intervals because of the high variability between individual patients. Again, values from different trials are not directly comparable because of differences in patient populations in terms of types of PAH, baseline FC and exercise capacity. For example, a ceiling effect in 6MWD (those patients with milder disease/higher baseline 6MWD had less scope for improvement) was observed in a post hoc analysis of the STRIDE-1 study (sitaxentan trial). 50,51
Whether ITT analysis was used and the methods for imputing missing data can also have a substantial impact on the reported group means and differences for 6MWD, particularly in trials of small sample size. Excluding patients who had no post-baseline 6MWT would almost certainly bias the results. Different methods of imputing data (e.g. last observation carried forward; assuming no change compared with baseline; assuming a 6MWD of 0 for missing observations), however, could produce different results. Interpretation of trial results and comparison between studies therefore requires great caution.
Quality of life
The volume of evidence from RCTs with regard to the impact of treatment on health-related quality of life varied between technologies. No data were reported in the trials for bosentan. Other trials used different tools and the findings seemed inconclusive (see Table 34). Two studies measured the EQ-5D utility index (AIR study for iloprost;41 SUPER-1 study for sildenafil53); there was an improvement of approximately 0.1 (on a scale of 0–1) compared with placebo in both trials.
Haemodynamic measures
All five technologies demonstrated significant effects on haemodynamic measures, which are important indicators of PAH disease progression and/or survival. 5,65,66 In the context of clinical trials these measures were most susceptible to missing observations and were usually not analysed by ITT. Consequently, statistically significant findings in these outcomes may better be treated as ‘proof of concept’ for PAH treatment. The magnitude of the reported group means and differences, however, may not be clinically useful.
Serious adverse events and withdrawal for any reasons
The potential harm associated with any treatment for PAH needs to be weighed against the potential worsening of the disease without treatment. Worsening of PAH frequently incurs events that are classified as SAEs and may require withdrawal from RCTs. Effective treatments for PAH with an acceptable safety profile would therefore be expected to demonstrate a reduced risk of SAEs and withdrawal for any reason compared with placebo/control.
Data on the total number of patients experiencing at least one SAE were not available for the three epoprostenol trials11,33,39 and two of the bosentan trials. 43,45 The pooled data for the other two bosentan trials47,48 showed a significant reduction in the risk of experiencing at least one SAE for bosentan compared with placebo, but the pooled results (or result from the only trial) for other technologies failed to demonstrate a significant risk reduction. A significant reduction in the risk of withdrawal for any reason was observed in individual trials for epoprostenol11 and iloprost41 and in the pooled results for sitaxentan.
Poor reporting of the outcomes and the small number of patients with the events are possible reasons for the lack of consistent findings for these outcomes across technologies (contrary to some of the efficacy outcomes). Further evidence from comparative trials is needed as these drugs have different adverse effect profiles and differences between drugs in the maintenance of patients on treatment and the overall risk–benefit profile cannot be ruled out.
Direct comparisons between the five technologies under assessment
Only two of the included RCTs directly compared one of the technologies under assessment against another. The STRIDE-2 trial48 was the only trial that used licensed doses for both treatments being compared. No statistically significant difference was found between sitaxentan and bosentan for all major outcomes. The main concern in interpreting the results from this study was the lack of blinding for the bosentan arm only. Although assessors for efficacy outcomes were blinded, potential bias introduced by the differential blinding of investigators and patients could not be ruled out. Another head-to-head trial (SERAPH57) compared an above licensed dose for sildenafil with bosentan at its licensed dose and was relatively small in its sample size. Again, no significant differences were found for any of the outcomes measured in the trial when ITT analysis was used.
A total of 10 different head-to-head comparisons would have been possible for the five technologies under assessment when used as monotherapy. The number of possible comparisons would increase further if combinations of these drugs are also considered. However, given the influence of routes of administration, the speediness of action and potential adverse effects of different technologies (plus costs) on patients’ and physicians’ preferences, direct comparisons between epoprostenol/iloprost and the three oral treatments are likely to be neither feasible nor clinically relevant.
Although very limited data from the aforementioned trials did not identify significant differences between sitaxentan and bosentan, and between sildenafil and bosentan, these trials may have been underpowered to detect clinically relevant differences because of their sample sizes and duration. Indeed, [Commercial-in-confidence information has been removed] were reported in the long-term extension of the STRIDE-2 trial (which was not included in this review as the patients in each of the treatment groups had varied durations of exposure to the drugs because of the study design). Sufficiently powered, long-term, head-to-head RCTs (preferably double-blind and independently funded) of the three oral treatments therefore remain a high priority for future research. However, the limited patient pool may make undertaking such trials difficult.
No indirect comparisons or mixed treatment comparisons between the five technologies were planned or performed in this review. Many issues that would affect comparability between results of individual trials have been highlighted in the previous section. In addition, there appeared to be no single outcome measure that could adequately represent the overall effectiveness of individual treatments. Together with the relatively small volume of available evidence, indirect comparisons and mixed treatment comparisons are unlikely to provide conclusive results and could potentially generate misleading findings.
Treatment involving combination of the technologies under assessment
A few RCTs have explored the use of combinations of the technologies under assessment. The BREATHE-2 study compared the combination of epoprostenol plus bosentan with epoprostenol alone in patients who required the initiation of epoprostenol treatment. 47 No significant differences were observed between groups. The sample size for this study was not large (n = 54) and the results were not conclusive. However, they do suggest caution in assuming greater benefit for combination therapy versus monotherapy.
Two trials (COMBI58 and STEP59) compared iloprost with control/placebo in patients who were stable on bosentan and supportive treatment, but who remained symptomatic. Given the general preference of oral treatment over other routes, results from these two studies were probably more relevant to the actual use of inhaled iloprost in clinical practice than the results from studies that compared inhaled iloprost with supportive treatment in patients who had not received oral treatments. Inhaled iloprost demonstrated significant benefit compared with placebo in the STEP study,59 but failed to demonstrate such benefit compared with control in the COMBI study58 for all outcomes including 6MWD and changes in FC. It was difficult to determine whether the inconsistency arose from differences in study population, location, study design, the combination of these or any other factors.
Finally, results from the PACES-1 study38 demonstrated a significant benefit of giving sildenafil to patients who were stable on epoprostenol. However, the dose used in this study was much higher than the licensed dose of sildenafil.
Specific issues related to this technology appraisal
Several potential problems that might affect our ability to address the decision problems outlined in the final scope of this technology appraisal were expected at the inception of the project and were highlighted in the review protocol as well as in Chapter 2 of this report. The major difficulty was that this assessment was undertaken for the licensed indications of individual technologies, and there was a mismatch between the license and available evidence. To this end this assessment report presents findings for whole trial populations (usually mixed populations of different PAH subcategories and/or FC), but also, when possible, evidence that is directly applicable to the licensed indication and evidence for specific subcategories of PAH (IPAH and CTD-APAH) (see Table 34 and also results tables for individual technologies in Chapter 3).
It can be seen that, although the most inclusive (whole trial data) evidence is sufficiently robust for all of the technologies, the volume of available evidence reduces dramatically when only evidence directly applicable to the licensed indications is included (PPH FCIII and FCIV for epoprostenol; PPH FCIII for iloprost; PAH FCIII for bosentan, sitaxentan and sildenafil). When evidence is available the confidence intervals tend to be wider than those for the inclusive evidence and the results may no longer be significant. There are few data for specific subcategories of PAH and little scope for comparison between them. In addition to the volume of evidence, all of the data were restrictive to a duration of 18 weeks or shorter. A possible lesson learned (amongst other explanations) from a 1-year trial of beraprost (not included in this assessment) suggests that observations made at 3 months may not last beyond this time. 67
Furthermore, there are specific issues related to the evidence for individual technologies. For epoprostenol, all of the trials were conducted in the USA and in the 1990s. There is therefore a potential issue of the generalisability of the study results to the current UK context. For inhaled iloprost there is a fluctuation of drug effects because of the method of administration. Whether some of the outcomes measured immediately after inhalation can present the overall treatment benefit is questionable. In addition, conflicting results between some of the iloprost trials have been observed. For bosentan, the exceptionally high response for FC improvement in the placebo group in its pivotal trial (BREATHE-145) and lack of stratified data from this trial for various outcomes increases the uncertainty of the pooled estimate presented in this report. For sildenafil, the bulk of its trial evidence is related to doses that are higher than the licensed dose (this also applies to evidence from observational studies). Beyond all this there is also a possible mismatch between the licensed indication of each drug and the actual use in clinical practice.
Chapter 4 Assessment of cost-effectiveness
Systematic review of existing cost-effectiveness evidence
Searches
A comprehensive search for literature on the cost and cost-effectiveness of drugs for PAH was carried out.
The searches identified existing economic models and information on cost-effectiveness, costs and quality of life from the following sources:
-
bibliographic databases: MEDLINE (Ovid) 1950 to February 2007, EMBASE (Ovid) 1980 to February 2007, Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO) 1982 to February 2007, Cochrane Library [Database of Abstracts of Reviews of Effects (DARE) and NHS Economic Evaluation Database (NHS EED)] 2007 Issue 1, and Health Economic Evaluation Database (HEED) February 2007
-
manufacturer submissions
-
internet sites of national economic units.
Searches were not limited by date neither were there language restrictions. Full search strategies can be found in Appendix 2.2.
Study selection, data extraction and quality assessment strategy
The inclusion and exclusion criteria applied to the economic searches are shown in Table 35.
An experienced health economist applied the inclusion and exclusion criteria to papers, with checking by a second health economist. The quality of the eligible economic evaluation studies was assessed using the Consensus on Health Economic Criteria (CHEC)-list68 and an adapted version of the Drummond and Jefferson BMJ criteria for economic evaluations. 69 Papers remaining in the review were read in detail and data extracted using a predesigned data extraction form. Data on the following were sought:
-
study characteristics such as the study question, form of economic analysis, population, interventions, comparators, perspective, time horizon and modelling used
-
clinical effectiveness and cost parameters, such as effectiveness data, health state valuations (utilities), resource use data, unit cost data, price year, discounting, key assumptions and productivity costs
-
results and sensitivity analysis.
In addition, any papers related to quality of life of patients with PAH were read and, where relevant, utility data for PAH-related health states were extracted.
| Study design | Cost–consequence analysis, cost–benefit analysis, cost-effectiveness analysis, cost–utility analysis, cost studies (UK only), quality of life studies |
| Population | Pulmonary arterial hypertension patients |
| Intervention | Intravenous epoprostenol, inhaled iloprost, bosentan, sitaxentan, sildenafil |
| Comparator | Placebo, supportive therapy, any intervention drug |
| Outcome | Quality of life estimates, cost estimates, cost-effectiveness |
Results
Economic evaluations
A total of four economic evaluations meeting the inclusion criteria were identified, none of which were a UK study. All four evaluations met at least eight of the 10 Drummond and Jefferson quality assessment criteria and 16 of the 19 CHEC-list criteria. Full details can be found in Appendix 8. The characteristics and the main results of the economic evaluations are summarised in Table 36. Einarson et al. 70 and Narine et al. 71 both compared treprostinil with epoprostenol, and several of the authors were involved in both papers. In essence, the same model was used; however, one study considered Canadian costs70 and the other considered US costs. 71 For simplicity these papers will be discussed in tandem as the model structure and data inputs are essentially the same. However, it should be noted that treprostinil is not a technology being evaluated as part of this assessment. The Highland et al. paper,72 a US-based study, compared bosentan with treprostinil or epoprostenol, and Wlodarczyk and colleagues73 from Australia also considered bosentan but in comparison to conventional therapy. Three out of the four studies had connections with industry; the exception was the study by Highland et al. 72 in which no reference was made to funding or conflicts of interests stated.
| Economic analysis features | Einarson, 200570 | Highland, 200372 | Narine, 200571 | Wlodarczyk, 200673 |
|---|---|---|---|---|
| Country | Canada | USA | USA | Australia |
| Sponsor | Northern Therapeutics (distributor of treprostinil in Canada) | Not stated | United Therapeutics | Submissions to PBAC funded by Actelion Pharmaceuticals Australia |
| Choice of therapy | Treprostinil | Bosentan | Treprostinil | Bosentan |
| Comparator(s) | Epoprostenol | Treprostinil, epoprostenol | Epoprostenol | Conventional therapy |
| Patient characteristics | Two cohorts of patients of FCIII and FCIV | Cohort of 100 PAH patients | Two cohorts of 270 patients of FCIII and FCIV who have failed or who are not candidates for bosentan | Patients of FCIII or FCIV |
| Form of analysis | Cost-minimisation | Cost–utility | Cost-minimisation | Cost-effectiveness (cost per life-year gained) |
| Model used | Microsoft excel spreadsheet | Markov model | Microsoft excel spreadsheet | Individual patient level simulation |
| Time horizon of model | 3 years | 1 year | 3 years | 15 years |
| Cost year and currency | 2003, Canadian $ | 2002, US $ | 2003, US $ | 2001/2, Australian $ |
| Base-case results | Treprostinil gave savings of C$2,610,642 (60 patients over 3 years) (£1,364,959, 2006) and an average annual saving of C$14,504 (per patient per year) (£7583, 2006) from a health-care perspective | Bosentan less costly (cost savings of US$3,631,900) (£2,990,169, 2006) with a QALY gain (11 QALYs) for 100 patients | Treprostinil gave savings of US$37,433 (£27,252, 2006) per patient (over 3 years) and the average cost saving per patient per year was $12,478 (£9084, 2006) | ICER: A$55,927 per life-year gained (£23,657, 2006) |
All four studies were model-based analyses. In the studies by Einarson et al. and Narine et al. a cost-minimisation analysis was conducted as they assumed that treprostinil and epoprostenol were clinically equivalent. 70,71 The Wlodarczyk et al. study, which describes the process of the Australian Pharmaceutical Benefits Scheme (PBS) listing for bosentan, conducted a cost-effectiveness analysis using survival as the outcome. 73 Only the model by Highland et al. 72 conducted a cost–utility analysis. This paper was not explicit about the population modelled in terms of FC, with the population described as a cohort of 100 PAH patients. The other papers all considered patients of FCIII and FCIV, although the Narine and Einarson model only considered patients who were non-responders to oral therapy.
The model presented in the Narine et al. and Einarson et al. papers was a decision-analytical spreadsheet model built in Microsoft excel. This model followed a cohort of patients over a 3-year period and was built to represent a logical sequence of clinical practice for PAH patients. Highland et al. presented a Markov cohort model that followed patients over a 1-year period with a cycle length of 3 months, with health states based on FC. The model in the Wlodarczyk et al. study was an individual patient level simulation, run over a time horizon of 15 years with a cycle length of 6 months. Within the model patients could improve, stabilise or not respond to a therapy.
The effectiveness data used in the model presented by both Narine et al. and Einarson et al. were obtained from preliminary data analysis, expert clinical opinion and also non-comparative studies. The two therapies in question were assumed to be clinically equivalent, based on results of a 3-year clinical trial showing equal survival. Highland et al. obtained transition probabilities for bosentan from Rubin et al. 45 Values for treprostinil and epoprostenol were based on bosentan probabilities and adjusted by the RR of improvement in the 6MWT for each therapy obtained from other trials. The model presented by Wlodarczyk and colleagues obtained effectiveness data from two clinical trials43,45 and a long-term open-label extension study provided by industry. Mortality data for conventional therapy were estimated using clinical data on haemodynamic parameters from a trial with long-term follow-up. 43,45 The data were entered into the NIH equation and mortality estimated using the survival model proposed by D’Alonzo et al. 5 Bosentan mortality data were obtained from the two clinical trials. In addition, data on withdrawal rates and the probability of hospitalisation were also estimated using trial data.
The analysis in Narine et al. was from a health-care perspective, with Einarson et al. widening the perspective that the analysis considered by including societal costs. Both models discounted costs only at a rate of 3%, as no measure of effectiveness was used. The models presented in the Wlodarczyk and Highland papers considered a health-care perspective only, with the former discounting costs and life-years at 5%. The Highland model did not require discounting as the time horizon was 1 year.
All four studies considered appropriate resource use items. These typically were the cost of the drugs, initiation of therapy, medical supplies, particularly those associated with the delivery of the drugs, primary and secondary care consultations, surgical and diagnostic procedures, including liver function tests for bosentan, and treatment of SAEs, in particular sepsis. Wlodarczyk et al. considered conventional therapy as the comparator, and this consisted of diuretics, oral anticoagulants, calcium channel blockers, oxygen therapy and digoxin. Unit costs were obtained from standard sources in all studies.
The model presented by both Einarson et al. and Narine et al. did not consider outcomes as the two therapies were considered to be of equal efficacy. The Wlodarczyk model considered outcomes in life-years and only the Highland model measured outcomes in quality-adjusted life-years (QALYs). The health state valuations were obtained from clinical experts. Using the EQ-5D questionnaire, a consensus was achieved on the extent of limitations in each of the five dimensions for each FC. Then the health state descriptions were adjusted for expected side effects associated with the treatments. An alternative set of values was also estimated by increasing FCI estimates by 0.04 and other estimates by this factor plus a further 0.02. A minimum of 0.1 was allowed for FCIV. The values produced are presented in Table 37.
| Keogh et al., 200784 | Kirsch, 200076 | Highland et al., 200372 | |||
|---|---|---|---|---|---|
| Source | SF-36; n = 177, PAH patients on bosentan | 2-year TTO; n = 64, general population | 10-year TTO; n = 64, general population | Clinician consensus using EQ-5D | |
| Health state | Mean (± SD) | Mean (SD) | Mean (SD) | Bosentan | Epoprostenol |
| FCI | 0.73 (± 0.09) | 0.934 (0.093) | 0.930 (0.093) | Base: 0.92; alternative: 0.96 | Base: 0.68; alternative: 0.72 |
| FCII | 0.67 (± 0.10) | 0.782 (0.244) | 0.765 (0.183) | Base: 0.75; alternative: 0.81 | Base: 0.63; alternative: 0.69 |
| FCIII | 0.60 (± 0.10) | 0.553 (0.361) | 0.509 (0.351) | Base: 0.27; alternative: 0.35 | Base: 0.18; alternative: 0.26 |
| FCIV | 0.52 (± 0.09) | 0.371 (0.407) | 0.284 (0.404) | Base: 0; alternative: 0.1 | Base: 0; alternative: 0.1 |
The model used by the Einarson and Narine papers demonstrated savings when using treprostinil compared with epoprostenol. The analysis by Einarson et al. from a US perspective gave savings of US$37,433 over the 3-year time horizon, with an expected average cost saving per patient per year of US$12,478. The greatest savings were attributed to reducing hospitalisation for dose titration and treatment of adverse events, particularly sepsis. The savings reported from a Canadian perspective by Einarson et al. were C$2,610,642 overall, with an average annual saving of C$14,504 from a health-care perspective and C$15,452 from a societal perspective. Again, savings were attributed to reduced hospitalisations. Probabilistic sensitivity analysis (PSA) presented in both papers demonstrated almost a 100% probability of cost savings.
The results of the Highland et al. analysis, from a US perspective, showed bosentan to be dominant over epoprostenol. For a cohort of 100 patients, cost savings were US$3,631,900 with a QALY difference of 11. Sensitivity analyses included changing the RR of improvement and also using alternative utility values, but bosentan still remained cheaper and with greater QALYs. The Australian study by Wlodarczyk et al. demonstrated greater survival on bosentan than on conventional therapy, with 6.7 discounted life-years after 15 years for bosentan compared with 2.8 for conventional therapy. The discounted mean cost was A$234,618 for bosentan and A$18,287 for conventional therapy, giving an ICER of A$55,927 per QALY gained. After 5 years the ICER was a much higher A$84,231 per QALY gained. Sensitivity analyses considered issues such as continuation rules (addition of or switching to epoprostenol), and a series of one-way sensitivity analyses were conducted on many of the model parameters. Mortality was found to be a key variable that reduced the ICER, as was the inclusion of epoprostenol for a small proportion of patients.
Quality of life
A total of 16 quality of life studies (excluding the economic evaluation papers presenting quality of life) were identified; however, two of these74,75 were subsequently found to be general commentary papers that did not present empirical data. Five papers presented values using standard tools to elicit health state utilities. The remaining nine papers considered generic or disease-specific quality of life measures, the most common being the SF-36. One further published paper76 was identified from the manufacturer submissions, giving health state valuations for NYHA FCI–IV. This section will briefly describe the studies considering generic and disease-specific quality of life measures, and will concentrate on those studies containing utility values for health states.
Excluding those studies converting SF-36 values into utility values, quality of life was assessed using the SF-36 in a total of seven studies. 9,49,77–81 Chua et al. 81 also used the Minnesota Living with Heart Failure (MLHF) questionnaire and the Assessment of Quality of Life (AQoL) instruments. The MLHF tool was also used by Cenedese et al. 82 A paper published in 2006 by McKenna et al. 83 reported on the development of the disease-specific Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR) questionnaire, the first PAH-specific tool. The EQ-5D was also administered in the validation stage; however, only correlations between the tools were presented.
Keogh et al. 84 considered the SF-36 and AQoL questionnaire in 177 patients receiving bosentan. Responses to certain items in the SF-36 were used to produce utility values for each FC. Two papers generated values using the EQ-5D. Olschewski et al. 41 conducted a study to evaluate the use of inhaled iloprost in patients with severe pulmonary hypertension compared with placebo. The questionnaire was administered at baseline and after 12 weeks, demonstrating an improvement in health state for patients on active therapy. However, utility values were not presented by FC, and at baseline there was a mix of FCIII and FCIV patients. Sitbon et al. 85 considered both the EQ-5D and SF-36 in 16 patients with HIV-associated PAH receiving bosentan for a total of 16 weeks. As in the previous study the questionnaire was administered at baseline and at the end of follow-up and demonstrated an improvement in quality of life on treatment.
Shafazand et al. 86 described quality of life in 53 patients with PAH, of whom 53% received epoprostenol and 75% were in FCIII or FCIV. The tools administered in the study were the Nottingham Health Profile, the Congestive Heart Failure Questionnaire and the Hospital Anxiety and Depression Scale. In addition, the authors used the VAS and standard gamble methods to elicit preferences for current health. Results were presented for all patients and those taking and not taking epoprostenol. The standard gamble results showed little difference between the epoprostenol and non-epoprostenol groups; however, the VAS score gave a slightly lower value with no epoprostenol, and overall the VAS values were lower. One drawback of the utilities gained in the study is that they were directly elicited from patients rather than from the general population.
The paper by Groen et al. 87 presented a model of lung transplantation for patients with end-stage pulmonary disease, which included pulmonary hypertension. Utility values were derived from the EQ-5D questionnaire administered to patients on the waiting list of a lung transplantation programme every 3 months and after transplantation; however, the values for different periods of time on the waiting list were not related to any health state, for example FC or specific condition. Kirsch76 considered the feasibility of defining a QALY from disease-specific data using the NYHA classifications using the time trade-off method (TTO) associated with the EQ-5D valuation method. The TTO valuations were conducted over a 2-year and a 10-year period for each of the health states (FC), and were elicited from a general population sample of 64 people via interview. Health state valuations by FC were also given in the paper by Highland et al. ,72 described earlier in this chapter, which presented a decision model comparing three treatments. For completeness the values used in this paper are presented in Table 37 alongside all of the utility values presented in the other papers for each FC. Table 38 presents the utility values for the other health states outlined in the papers.
| Olschewski et al., 200241 | Sitbon et al., 200485 | Shafazand et al., 200486 | Groen et al., 200487 | |
|---|---|---|---|---|
| Source | EQ-5D; n = 203, PAH patients on iloprost or placebo | EQ-5D; n = 16, HIV-related PAH patients on bosentan | VAS, SG; n = 53, PAH patients, 53% taking epoprostenol | |
| Health state | Mean (± SD) | Mean (± SD) | Mean (95% CI) | |
| Iloprost baseline | 0.49 (± 0.28) | |||
| Iloprost week 12 | 0.58 (± 0.27) | |||
| Placebo baseline | 0.56 (± 0.29) | |||
| Placebo week 12 | 0.56 (± 0.31) | |||
| Bosentan baseline | 0.37 (± 0.43) | |||
| Bosentan week 16 | 0.63 (± 0.21) | |||
| PAH patients, mix FC | SG: 0.71 (0.64–0.78); VAS: 0.58 (0.54–0.62) | |||
| PAH patients, epoprostenol | SG: 0.72 (0.61–0.82); VAS: 0.60 (0.54–0.66) | |||
| PAH patients, non–epoprostenol | SG: 0.71 (0.61–0.81); VAS: 0.56 (0.50–0.62) | |||
| Pretransplantation: | ||||
| First 6 months | 0.55 | |||
| 6–9 months | 0.50 | |||
| 9–12 months | 0.45 | |||
| 1 year | 0.40 |
Although four cost studies were identified, three88–90 were not UK studies. The remaining study91 concerned epoprostenol treatment in children alone and presented costs in US dollars. This population group is outside the remit of the appraisal and therefore this paper was also omitted.
Summary
The published economic evaluations used three different approaches to modelling, and none of the models produced results that are generalisable to the NHS. None of the studies were UK based, and only one considered QALYs as the outcome, with two studies only considering a cost-minimisation analysis. Two studies considered an intervention (treprostinil) that was not part of this appraisal and only one used conventional therapy as a comparator. However, the review of quality of life studies yielded several sets of health state utility values appropriate for use in the economic evaluation of intervention therapies for PAH.
Review of manufacturer cost-effectiveness submissions
A submission was received from each company; however, only four manufacturers included a model-based economic analysis. Table 39 provides a brief summary of the four economic analyses provided.
| Submission features | Schering Health Care; iloprost trometamol (Ventavis®) | Actelion Pharmaceuticals; bosentan (Tracleer®) | Encysive Pharmaceuticals; sitaxentan sodium (Thelin®) | Pfizer; sildenafil (Revatio®) |
|---|---|---|---|---|
| Choice of therapy | Inhaled iloprost with switch to intravenous epoprostenol on reaching FCIV | Bosentan as first-line treatment | Sitaxentan as first-line treatment | Sildenafil as first-line treatment followed by iloprost or epoprostenol on failure |
| Comparator(s) | Intravenous epoprostenol | Historical care (30% intravenous prostaglandins, 70% supportive therapy); supportive therapy alone; intravenous prostaglandins | Bosentan; supportive care | Background therapy; each of the other four intervention therapies |
| Patient characteristics | Patients with primary pulmonary hypertension, FCIII, who are unable to tolerate oral therapy. Age on initiation 52 years | FCIII, age sampled from distribution. Separate analyses for IPAH patients and those with CTD | FCIII, age 18+years (STRIDE trial populations48,95) | FCIII. Age 18+ years with primary or secondary PAH from SUPER-153 and SUPER-296 studies. Age on initiation 49 years |
| Form of analysis | Cost–utility analysis | Cost–utility analysis | Cost-effectiveness analysis (life-years gained) | Cost–utility analysis (vs background therapy); cost-minimisation analysis (vs four other intervention therapies) |
| Model used | Markov model (with cohort of 100 patients and cycle length of 3 months) | Discrete event simulation (run for 10,000 hypothetical patients) | Markov model (with cycle length of 1 week) | Markov model of two distinct parts: year 1; year 2 onwards (with cycle length of 12 weeks (×3) and 16 weeks (×1) for year 1 and yearly cycle for year 2 onwards) |
| Time horizon of model | 20 years | Length of time on bosentan before ‘clinical worsening’ (i.e. death, change in treatment or need for transplantation) | 5 years | 30 years |
| Base-case results | Iloprost dominates epoprostenol alone (cost difference: £348,000; QALY difference: 0.04 per person) |
IPAH: vs historical care, £21,000 per QALY; vs epoprostenol, bosentan dominates; vs supportive therapy, £84,000 per QALY CTD: vs historical care, £15,000 per QALY; vs epoprostenol, bosentan dominates; vs supportive therapy, £78,000 per QALY |
Sitaxentan: vs bosentan, £19,531 per life-year gained; vs supportive care, £94,631 per life-year gained |
Sildenafil vs background therapy, £22,058 per QALY CMA result: lowest cost for sildenafil |
GlaxoSmithKline submission (epoprostenol)
The submission for epoprostenol did not include any economic modelling. The report states that ‘no formal cost-effectiveness analysis is available for epoprostenol’. However, information was given with regards to the pricing of the technology. The submission states that the drug is available at a discount [Commercial-in-confidence information has been removed] for this indication. [Commercial-in-confidence information has been removed].
Schering Health Care submission (iloprost)
A Markov model with a cohort of 100 patients was built to evaluate the cost-effectiveness of inhaled iloprost versus intravenous epoprostenol, with no supportive therapy comparator included in the model. The type of evaluation undertaken was a cost–utility analysis with outcomes measured in QALYs. The model had a time horizon of 20 years, with a cycle length of 3 months. The patient group modelled included those with a diagnosis of PPH of FCIII who had failed or were unable to tolerate oral therapy and who would otherwise have required intravenous epoprostenol. Age on initiation of treatment was 52 years.
Health states were based on the NYHA functional classification, with a starting state of FCIII and transitions to FCII or FCIV or death, or patients could remain in FCIII. In addition, there were also health states representing transplantation and post transplantation. In the first cycle of therapy no transition to transplantation or post transplantation was possible, and improvement of FC was only allowed in this cycle. When patients reached FCIV there was a switch of therapy to intravenous epoprostenol. The justification given for this was that it is the only licensed therapy for this indication.
Data on effectiveness were considered separately for the initial and subsequent periods. The initial period was set at 12 weeks, in line with randomised studies that followed patients for this time period. The base-case analysis used data from the AIR trial,41 which was the largest randomised trial comparing iloprost with placebo. The trial reported FC change with treatment, and included a range of patients with primary or secondary pulmonary hypertension. Data on epoprostenol versus usual care were obtained from Barst et al. 11 However, as findings for the subgroup of patients in FCIII at baseline were not available, the percentage with improvement or deterioration from baseline in a mixed population of FCIII and FCIV was used. Additional analyses were undertaken using pooled data, using additional data from studies identified in their systematic review.
For subsequent periods of treatment, the D’Alonzo et al. study5 was used as it reported the long-term survival of patients preceding widespread use of epoprostenol. Several studies on long-term survival were also identified for epoprostenol and iloprost and for each therapy this information was pooled. Using this data the rate of progression for actively treated patients was reduced to 69% of the rate of progression in untreated patients, so that survival after 5 years equalled that observed in the pooled analysis.
In the base-case analysis the utility values employed were those obtained from the AIR study. 41 The mean EQ-5D tariff was calculated for patients in FCII, FCIII and FCIV, using a repeated assessments model to take into account that individuals in the study provided multiple estimates. Values for transplant and post transplant were taken from an economic evaluation of lung transplantation. 92 Sensitivity analysis was undertaken on values derived from an alternative analysis of the AIR study data and on data obtained from two studies identified in a literature review. 72,76
Resource use was estimated from a review of the literature and a panel of five experts from four specialist centres in the UK. Results were presented for each FC separately. Clinicians were asked about the conventional therapies they prescribed, the average doses and the proportion taking each therapy. Information was collected on NHS contacts such as the number of contacts with doctors and nurses at specialist and non-specialist centres, GP contacts and visits to A&E. In addition, rates and length of hospital admissions and use of day, residential and home care were collected. The frequency of adverse events during the first cycle of treatment was taken from the literature and unit costs attached to each event. It was assumed that, in subsequent cycles, adverse events would result in discontinuation of medication or be managed during routine consultations. Finally, the submission refers to a fixed fee system in which iloprost is provided at a fixed cost irrespective of the dose, thus allowing patients to be treated in a more ‘economical manner’. This cost was included in the base-case analysis with the NHS price included in a sensitivity analysis. An NHS/personal social services (PSS) cost perspective was used and all costs were updated to 2006 prices. Costs and QALYs were discounted at 3.5%.
The base-case results showed that, for a cohort of 100 patients, treatment with inhaled iloprost (followed by intravenous epoprostenol in FCIV) compared with treatment with epoprostenol alone reduced costs by £34.8 million (£348,000 per person) and increased QALYs by 4 (0.04 QALYs per person). Therefore, iloprost was dominant versus epoprostenol alone. The authors noted that, although the reduction in costs was statistically significant, the difference in outcomes was close to zero. The PSA results demonstrated that, at a threshold of £30,000 per QALY gained, the probability of iloprost being cost-effective was 100%. Additional one-way sensitivity analyses were undertaken, with findings most sensitive to assumptions made about the proportion of patients improving with usual care. Results were also sensitive to the cost of drugs, but were less sensitive when the costs of managing PAH were included.
A number of limitations were discussed in the submission including problems with the evidence base, the paucity of direct comparisons in trials and the small number of patients involved. In addition, it was suggested that the assumption of no improvement in FC after the first cycle may not be realistic as ‘some patients are maintained very well on active treatment’.
In conclusion, the key issue in this submission relates to the choice of comparator. Although the model results in the submission point to the cost-effectiveness of iloprost compared with epoprostenol, no comparison with supportive therapy was made. The submission argues that a comparator of epoprostenol is appropriate with the claim that it is consistent with UK clinical practice. This claim is, however, not substantiated and is not consistent with the position adopted by other manufacturers. The drug pricing assumptions are also noteworthy; as discussed, iloprost is assumed to have a fixed price regardless of dose.
Actelion submission (bosentan)
The model presented in this submission was a discrete event simulation, constructed in simul8 software, which compared bosentan (as first-line treatment) with three comparators: ‘historical care’, supportive therapy and intravenous prostaglandins. Historical care is defined as 30% of patients receiving the lowest cost intravenous prostaglandins and the remaining 70% receiving supportive care. This definition was based on audit data from specialised PAH centres before the launch of bosentan. The submission states that ‘treatment with supportive care alone is no longer a reasonable option’. The authors state that intravenous iloprost is historically the intravenous prostaglandin of choice but, because epoprostenol is cheaper, this is used in the model. In addition, epoprostenol efficacy data is also used for intravenous prostaglandins because of limited intravenous iloprost data.
The model considered 10,000 hypothetical FCIII PAH patients, with patients remaining in the model until ‘clinical worsening’ occurred, defined as death, a change in treatment through addition of or substitution of another intervention or the need for transplantation. Thus, costs and QALYs were not counted after a patient was deemed to have reached clinical worsening. If a patient achieved their life expectancy age without clinical worsening they were assumed to die from other causes. Two types of PAH were considered separately by the model: IPAH and CTD-APAH. Starting age was sampled from a distribution.
The model used data on the mean length of time on bosentan therapy before clinical worsening, using a combined data set of two pivotal RCTs43,45 plus data on long-term follow-up and a data set associated with additional papers by Williams et al. 93 and Denton et al. 44 Time on supportive therapy was calculated using the equation in the paper by D’Alonzo et al. 5 Survival models were constructed to consider time to clinical worsening by FC for IPAH and CTD-APAH. A Kaplan–Meier analysis was used, utilising all data irrespective of FC and type of PAH, using a Weibull model. The nature of the model meant that the time to clinical worsening and the time to death were sampled for each patient.
Utility data were obtained from two sources. Utilities from Keogh et al. 84 provided values in relation to FC, derived from SF-36 responses for bosentan treatment. Meads et al. 94 provided additional data on utilities, collected alongside the CAMPHOR disease-specific quality of life scale. Data were derived from a broad spectrum of PAH patients and, although about 60% were using bosentan, the remaining patients were taking alternative therapies. However, the assumption was made that the utilities applied regardless of treatment. They noted that this may overestimate the utility of patients on supportive therapy alone. No disutility associated with taking intravenous prostaglandins was included, which was likely to be favourable for this type of therapy. The Keogh data were used in the base case with results using the CAMPHOR utilities presented in the sensitivity analyses. Further analysis of the CAMPHOR data suggested an [Commercial-in-confidence information has been removed] in utility [Commercial-in-confidence information has been removed] in FCIII from taking no treatment to taking bosentan, and this was also included in the sensitivity analyses.
Resource use was assessed by an empirical costing study of bosentan use in 2006, which is currently unpublished. Information was obtained from multiple sources, including protocols, and much was obtained from a retrospective record review of patients from two specialist PAH centres. Costs were grouped into three periods: initiation of therapy, first year follow-up and second year follow-up. In the initiation of therapy period, resource use associated with diagnostic tests and procedures, hospitalisations, outpatient visits, equipment and consumables and other therapies was ascertained. For the follow-up periods the same items were assessed, with the exception of the exclusion of the diagnostic tests and procedures and the addition of home care delivery. Home care delivery costs were assumed to be 8% of the advanced therapy acquisition costs, based on input from one of the specialist centres. However, it was stated that this cost is negotiated centre by centre. A breakdown of the therapies forming the supportive care comparator was not given. In addition, it was not clear if the cost of a monthly liver function test is included in the costs for bosentan. Costs were for 2006 and a discount rate of 3.5% was applied to both costs and QALYs. It is assumed that the analysis was from an NHS/PSS perspective, although this was not explicitly stated.
In the base-case results for the IPAH group, the ICER for bosentan versus historical care was £21,000 per QALY gained. This rose to £84,000 per QALY for supportive therapy, and bosentan dominated when compared with intravenous prostaglandins (epoprostenol). The therapy was more cost-effective when considered in the CTD group alone, with an ICER of £15,000 per QALY versus historical care and £78,000 per QALY versus supportive therapy. Again, bosentan dominated intravenous prostaglandins. Results of the PSA for IPAH patients showed bosentan to have a 40% chance of being cost-effective compared with historical care at £20,000 per QALY, and a 90% chance of being cost-effective compared with historical care at £30,000; however, it was not cost-effective at either threshold when compared with supportive care. Analysis for CTD patients versus historical care gave 90% and 100% probabilities of bosentan being cost-effective for £20,000 and £30,000 per QALY thresholds, respectively; again, bosentan was not cost-effective at either threshold when the comparator was supportive therapy.
Use of the CAMPHOR utility data only marginally changed the overall results. However, bosentan did appear more cost-effective when the differential utility between patients on active treatment and patients not on active treatment was included. Additional sensitivity analyses considered the proportion of patients on intravenous prostaglandins, with bosentan becoming more cost-effective with a higher proportion and less cost-effective with lower proportions.
The submission concluded that treatment with supportive care is no longer a reasonable option. Therefore, taking historical care as the comparator, the submission argues that bosentan is cost-effective in the IPAH and CTD subgroups, which represent the majority of patients considered reflective of the entire Venice category 1 group.
In conclusion, the comparator issue again clearly comes through as being central to the cost-effectiveness result. The sensitivity analyses undertaken as part of this submission (reported on page 42 of the submission) highlight this well. If the higher cost comparator of intravenous iloprost is used then, as expected, bosentan begins to look much more attractive. Another interesting issue in this submission relates to the modelling approach of counting costs and benefits only up until ‘clinical worsening’. This will have understated the costs and QALY estimates, but it is not clear whether serious bias is introduced as a result of doing this.
Encysive submission (sitaxentan)
A Markov model was built to determine the cost-effectiveness of sitaxentan as first-line treatment when compared with supportive care and bosentan. The type of evaluation undertaken was a cost-effectiveness analysis with outcomes measured in life-years rather than QALYs. A cost–utility analysis was not undertaken, the justification being that ‘there is limited information on quality of life in patients with PAH in the literature’. The model time horizon was 5 years with a cycle length of 1 week. The model followed a population of PAH patients of FCIII over the age of 18 years, based on trial populations from STRIDE-248 and STRIDE-2X. 95 Patients started in a predeterioration state and could remain in that state, deteriorate and move into a post-deterioration state, or die.
Data for STRIDE-2 and STRIDE-2X were pooled and two Weibull survival regressions (using an accelerated failure time model) were fitted to estimate the rates of FC deterioration and death of patients. Survival in the supportive care arm was obtained using the NIH survival equation in which mortality was related to haemodynamic measures. 5 This equation applied to IPAH and was derived from 3-year data. The rationale behind the short time horizon of 5 years was that the survival equation used for supportive care was derived from 3-year data, and so the authors did not consider it valid beyond 5 years. Deterioration in supportive care was handled in the accelerated failure time model by including treatment as a dummy variable, thus indicating when the treatment effect (from active treatment) should be applied in the equation.
Costs included in the analysis were drug costs and hospitalisation costs, with rate of hospitalisation and length of state for each health state determined from both STRIDE trials. As too little data were available in the bosentan arm to determine resource use post deterioration, sitaxentan data were used. Costs of supportive care were not included, and no description of what supportive care contained was provided. In addition, adverse event costs were not taken into account and, even though both bosentan and sitaxentan require monthly liver function monitoring, the cost of these additional tests was not included. All costs and life-years were discounted at a rate of 3.5% and an NHS/PSS perspective was stated, although no PSS costs were included. As the model only considered life-years gained, no utility values were required.
Base-case results showed sitaxentan to be more effective (3.32 life-years) than supportive care (2.70 life-years) or bosentan (2.45 life-years) but more expensive. The ICER was £94,631 per life-year gained for sitaxentan compared with supportive care, and £19,531 per life-year gained for sitaxentan compared with bosentan. PSA was also undertaken, with the results showing considerable uncertainty, particularly versus supportive care when sitaxentan had only a 44% chance of being cost-effective at £80,000 per life-year gained. The authors highlighted the uncertainty around the accuracy of the NIH equation as a predictive measure of survival for supportive care, and that little data were available for this therapy option. In addition, they also pointed out that the STRIDE trial data included patients with CTD and that this subgroup have a poorer prognosis, whereas the NIH equation uses data for IPAH patients who have a better prognosis.
The authors conclude that sitaxentan is at least as cost-effective as bosentan and that longer-term bosentan data suggest cost-effectiveness; thus, the submission therefore argues that sitaxentan is also likely to be so.
It is important to remember that the ICERs reported here relate to life-years gained and not QALYs. This is the only economic submission that failed to report results using QALYs. The model is described only briefly and the justification for some aspects of the analysis (e.g. the distributions used in the PSA) was not provided. The lack of comprehensiveness cost analysis data (e.g. the failure to include costs of supportive care or adverse events) was another negative. The choice of comparator again comes through as a key issue in considering cost-effectiveness – the ICERs are dramatically different depending on whether supportive care or bosentan is used as the comparator.
Pfizer submission (sildenafil)
The economic analysis conducted in this submission considered two types of analysis. The first analysis was a cost–utility analysis of sildenafil compared with background therapy. The second was a cost-minimisation analysis comparing all five interventions considered in the appraisal. The premise behind the cost-minimisation analysis was the ‘absence of evidence that there any clinically meaningful efficacy differences’ between the five intervention therapies.
The model presented was a Markov model with two distinct parts. In the first year the first three cycles were 12 weeks each, followed by one cycle of 16 weeks. From year 2 onwards a yearly cycle was used. The model population was patients aged 18 years and over with primary or secondary PAH in FCIII, conforming to the inclusion/exclusion criteria of the SUPER-153 and SUPER-296 studies. The start age of patients in the model was 49 years, which was the average age of patients in the SUPER-1 trial. Base-case results were presented for a time horizon of 30 years, representing remaining lifetime, and all patients had died by the age of 79 years.
Patients received initial treatment and switched to alternative therapy when that treatment failed and they deteriorated. Alternative treatment was iloprost or epoprostenol and patients remained on that therapy even if they deteriorated. Events and health states were based on changes in the 6MWD, with states representing improvement, no change and deterioration in 6MWD and death. An improvement in 6MWD was more than 39 metres compared with baseline, no change in 6MWD was between 0 and 39 metres greater than baseline and deterioration represented a reduction in distance walked. Health states also took into account whether patients were on the initial therapy or alternative therapy.
The main sources of data on clinical effectiveness and mortality for sildenafil were the SUPER-1 and SUPER-2 trials, with death rates extrapolated from unpublished clinical trial data. 97 Placebo-specific probabilities were used for supportive care. As all other therapies (except for supportive care) were assumed to be equally efficacious, sildenafil transition probabilities were used for all therapies.
Utility data were also obtained from the SUPER-1 and SUPER-2 trials, with values at baseline, week 12 and week 24 used for improvement, no change and deterioration. The data for week 24 were used for weeks 36 and 52. The submission points out that the value for deterioration at 12 weeks (0.62) was in fact higher than the baseline value (0.57) and stated that this was an ‘apparent anomaly derived from the nature of utility measurement over time’. Therefore ‘the utility value was averaged among all the patients in that particular health state at either baseline, 12 and 24 weeks’.
Resource use data were collected by a questionnaire administered by telephone interview with PAH experts, and the data were validated by a clinical expert with the use of patient profiles for the average FCIII patient. The resource use included was comprehensive and included adverse events, medication and co-medication, laboratory tests, diagnostic and therapeutic procedures, visits and consultations and ward admissions, all dependent on therapy and whether the patient was taking first-line therapy or in a state of deterioration. The cost of equipment required by the patient for inhalation was not included ‘as the BNF mentions that it is on loan’. Supportive care was defined as use of warfarin and furosemide by 100% of patients. Intervention therapies were taken alongside standard co-medication with alternative therapy regimens depending on the intervention therapy and FC. Unit costs were obtained from standard sources, and the cost year was 2007. Cost and QALYs were discounted at 3.5%. The costs considered were NHS only, as the authors stated that there were no robust data for PSS resource use.
The results of the base-case analyses gave an ICER of £22,058 per QALY gained for sildenafil versus background therapy. The PSA, run for 1000 iterations, suggested that sildenafil had an 84% probability of being cost-effective at £30,000 per QALY gained and a 66% probability of being cost-effective at £20,000. In the cost-minimisation analysis, QALYs were assumed to be equivalent across intervention therapies as efficacy was assumed to be the same. Therefore total costs and an ‘average cost per QALY’ were presented for each therapy, with the lowest costs demonstrated by sildenafil. The sensitivity analysis considered results over a 1-year period, and the ICER for sildenafil compared with background therapy was lower at £15,252 per QALY gained. Total costs and average cost per QALY when compared with other intervention therapies also demonstrated sildenafil to be of lowest costs.
This submission does not provide adequate detail of the model structure, the data inputs or the analysis methods to allow a detailed critique of the economic model to be undertaken. Thus, it is difficult to have confidence in the results of the cost–utility analyses. For example, the definition of ‘background therapy’, the comparator for the main analysis, is not precisely defined. However, in its favour, this is the only submission that has attempted a head-to-head comparison of all of the newer treatments, although the strong assumption was made of no effectiveness differences between treatments and so the analysis was simply a search for the lowest cost alternative. This assumption does not consider the absence of long-term published data for sildenafil at the licensed dose.
Summary of manufacturer submissions
The disparity in methods used between the different manufacturer submissions highlights the fact that there is as yet no consensus as to the most appropriate model to use for the current technology assessment. This partly reflects the fact that the technologies are aimed at somewhat different groups of patients. There is some variability in the modelling approach, but more importantly in the type of economic evaluation used, with cost per QALY and cost per life-year being offered as efficiency measures. One submission has performed a cost-minimisation analysis.
There is also wide variation in the methods used and sources of data for important model inputs such as survival estimates, quality of life (utility) scores and cost estimates.
Finally, a key issue is that of the appropriate comparator to be used. The various manufacturer submissions are, in effect, not all addressing the same policy question.
Independent economic assessment
This section provides details of a model developed by the assessment team and used to evaluate the cost-effectiveness of each active therapy within its licensed indication compared with supportive care over the effective lifetime of PAH patients (30 years).
Methods
Model description
A Markov model built in treeage pro® was developed to determine the cost-effectiveness of each intervention therapy with supportive care for PAH compared with supportive care alone. The population considered was adults with PAH (category 1 of the Venice 2003 clinical classification1) in NYHA/WHO FCIII (and NYHA/WHO FCIV for epoprostenol) for whom calcium channel blockers were inappropriate or no longer effective. One reference case analysis was conducted using data on all category 1 PAH patients. A separate analysis for idiopathic PAH alone was proposed but a lack of data prevented this.
The five intervention therapies considered within their licensed indications for FCIII were epoprostenol (administered by continuous intravenous infusion), iloprost (administered by inhalation) and the oral therapies of bosentan, sitaxentan and sildenafil, with epoprostenol also considered for FCIV. Only the first use of the interventions was considered, and initiation of any of the interventions after failure of another listed intervention was not considered, with the exception of epoprostenol for patients in FCIV. Therefore, for all treatments the starting state was FCIII with a further analysis conducted with a starting state of FCIV for epoprostenol.
The time horizon of the model was the effective lifetime of patients (30 years), and a starting age of 50 years was used to represent the average age of patients with the disease. The general mortality data were weighted to take into account the ratio of women to men with the disease (1.5:1). A time cycle of 12 weeks was chosen as being sufficiently short enough to capture the effect of treatment, and this time period was in line with that used in the trials for measurement of treatment effect. Health states were based on FC, with a starting health state of FCIII for all therapies and FCIV when the model was run for intravenous epoprostenol for this patient population.
In the first cycle of treatment patients could improve from their starting state FC to the adjacent FC. In all cycles patients could also remain in the same health state or deteriorate and move to the next FC. In addition, patients were also at risk from PAH-related mortality or an age-related death due to other causes. In the intervention arm, once a patient deteriorated and moved to FCIV, the patient switched to intravenous epoprostenol alone, with the first-line therapy discontinued. Although in clinical practice the first-line therapy is unlikely to be stopped, this appraisal considers the treatments within their licensed indications only and therefore this was the only option considered. Data on the effectiveness of combination therapies was not available and therefore inclusion of combinations in FCIV would only have an impact on cost. In the supportive care arm, once deterioration to FCIV was reached, patients switched to intravenous epoprostenol. The only exception was for the model run concerning epoprostenol in FCIV patients and here the comparator was supportive care alone. For all active therapies patients also received supportive therapy.
As the model ran, costs and QALYs were accumulated dependent on the transitions between health states determining FC, therapy and survival. A half-cycle correction was applied. All costs and QALYS were discounted at the rate of 3.5% per year. The model is presented in Figure 9.
FIGURE 9.
Diagram of the decision model. PAH, pulmonary arterial hypertension.
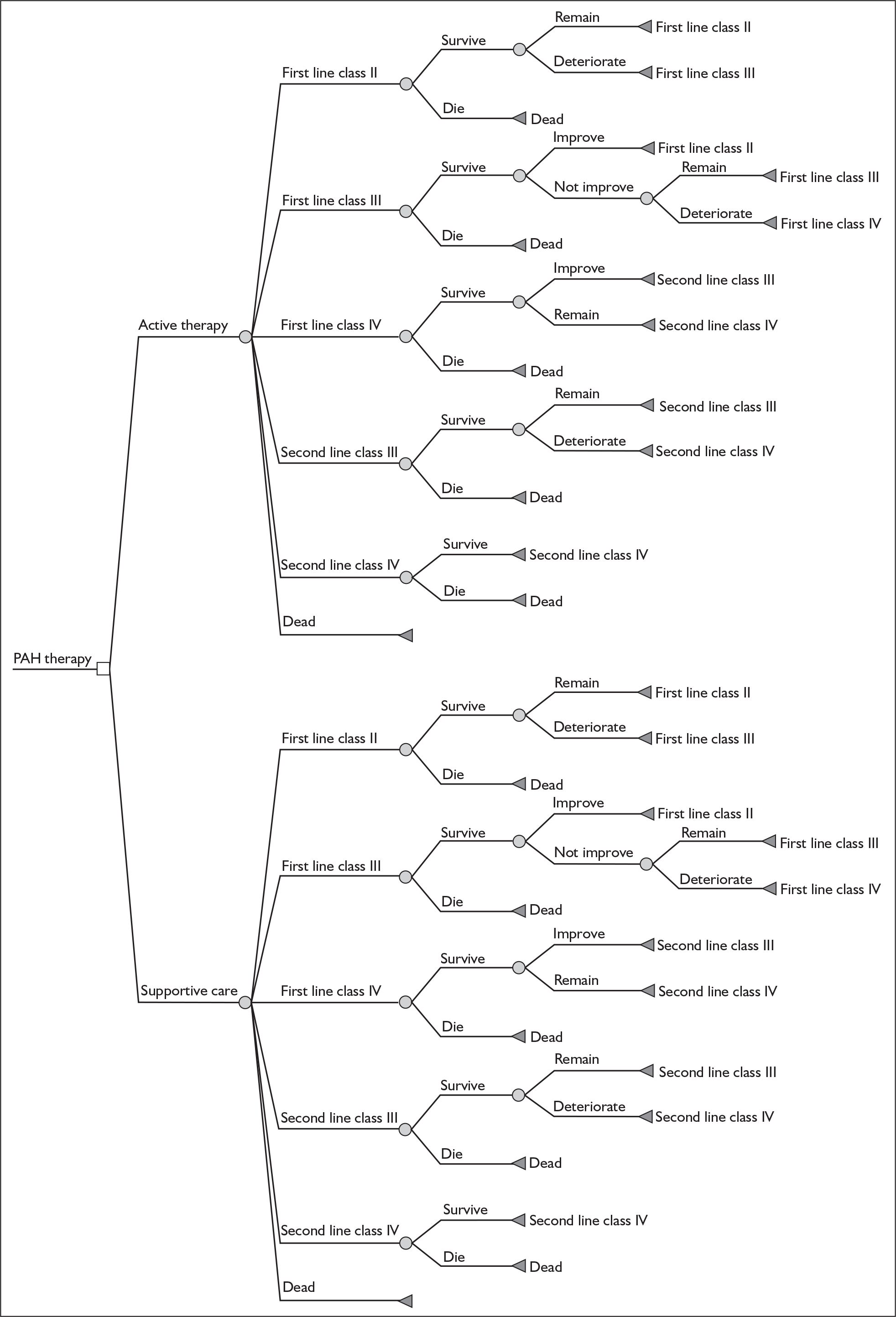
Estimation of model parameters
Treatment effect
Transition probabilities on supportive care were directly related to the intervention, with separate probabilities for epoprostenol, iloprost and the three oral therapies. The rationale behind this was that the supportive care group in question may have been different in the epoprostenol, iloprost and oral therapy trials and patient prognosis may have been less favourable in the epoprostenol and iloprost trials. For each therapy the effect of treatment was incorporated into a transition probability by applying the odds ratio for change in FC on treatment to the respective supportive care transition probability.
For the first cycle of 12 weeks, the transition probabilities and odds ratios for iloprost were obtained from data for the subset of FCIII, PPH patients in the AIR study41 provided within the manufacturer submission. No appropriate transition data stratified by FC were available for epoprostenol. Of the three epoprostenol trials, data from Barst et al. 11 (PPH only, mixed FC) were regarded as the best option given that the study by Rubin et al. 39 was only of 8 weeks duration and that by Badesch et al. 33 included exclusively PAH patients with scleroderma, which is outside epoprostenol’s license. Data from Barst et al. 11 were therefore used, but it had to be assumed that values from the whole trial population (74% FCIII, 26% FCIV) can be applied to both FCIII and FCIV (i.e. transition probabilities and odds ratios for improvement of at least one FC based on the whole trial population are used for both FCIII to FCII and FCIV to FCIII; the values for deterioration of at least one FC including deterioration to death based on the whole trial population are used for FCIII to FCIV). Similar rules were applied for other drugs for which FC-specific transition probabilities and odds ratios were not available (i.e. assuming same value for FCIV to FCIII and FCIII to FCII; for FCII to FCIII and FCIII to FCIV).
Transition probabilities for the supportive care for models of oral therapies were calculated using combined data from the placebo arms of Channick et al. 43 (bosentan), BREATHE-547 (bosentan), STRIDE-248 (sitaxentan and bosentan) and SUPER-153 (sildenafil). Apart from these trials, data for FCIII patients receiving supportive care were also available from the placebo arms of BREATHE-145 and STRIDE-4. 37 However, these data were not included as FC improvement (from FCIII to FCII) in the placebo arms of these two trials was exceptionally high (> 20%) at 12 weeks and was considered unrealistic in clinical practice according to the advice from clinical experts.
The source of odds ratios for bosentan treatment relative to supportive care was a pooled analysis that included data from Channick et al. 43 and BREATHE-5,47 but excluded data from STRIDE-248 (bosentan arm only was open-label) and BREATHE-145 (data stratified by FC were not available for bosentan arms). The odds ratios for sitaxentan were obtained from a pooled analysis using data from STRIDE-248 and STRIDE-4,37 but excluding data from STRIDE-149 (data stratified by FC were not available). The odds ratios for sildenafil were available from the SUPER-1 trial. 53
Because of the paucity of data, the same values for the transition probabilities and odds ratios for FC improvement and FC deterioration were used for the first 12 weeks on treatment and beyond 12 weeks. Twelve-week data for FC deterioration in FCII patients in the placebo arms of the STRIDE-248 and SUPER-153 trials were used as an approximation of the transition probability for deterioration from FCII to FCIII beyond 12 weeks on supportive care.
Transition probabilities were entered into the model as beta distributions (Tables 40 and 41). Odds ratios were entered as lognormal distributions (Tables 42 and 43).
| Intervention | Functional class (FC) transition (r/n) (lower and upper confidence limits) | ||
|---|---|---|---|
| FCIII to FCII | FCIII to FCIVa | FCIV to FCIII | |
| Epoprostenol (Barst et al., 199611) | 0.025 (1/40) (0.001–0.090) | 0.300 (12/40) (0.170–0.449) | 0.025 (1/40) (0.001–0.090) |
| Iloprost (AIR41) | 0.056 (2/36) (0.007–0.149) | 0.250 (9/36) (0.125–0.401) | – |
| Oral therapy (pooled Channick et al., 2001,43 BREATHE-5,47 STRIDE-248 and SUPER-153) | 0.125 ([Commercial-in-confidence information has been removed]) (0.067–0.198) | 0.094 ([Commercial-in-confidence information has been removed]) (0.044–0.159) | – |
| Intervention | Functional class (FC) transition (r/n) (lower and upper confidence limits) | ||
|---|---|---|---|
| FCII to FCIIIa | FCIII to FCIV | FCIV to FCIII | |
| Epoprostenol (Barst et al., 199611) | 0.300 (12/40); (0.170–0.449) | 0.300 (12/40); (0.170–0.449) | 0.025 (1/40); (0.001–0.090) |
| Iloprost (AIR41) | 0.250 (9/36); (0.125–0.401) | 0.250 (9/36); (0.125–0.401) | – |
| Oral therapy (STRIDE-248 and SUPER-153 for FCII to FCIII; Channick et al., 2001,43 BREATHE-5,47 STRIDE-248 and SUPER-153 for FCIII to FCIV) | 0.127 ([Commercial-in-confidence information has been removed]); (0.054–0.226) | 0.094 ([Commercial-in-confidence information has been removed]); (0.044–0.159) | – |
| Intervention | Functional class transition (FC), odds ratio (lower and upper confidence limits) | ||
|---|---|---|---|
| FCIII to FCII | FCIII to FCIVa | FCIV to FCIII | |
| Epoprostenol (Barst et al., 199611) | 24.96 (3.11–200.14) | 0.40 (0.13–1.20) | 24.96 (3.11–200.14) |
| Iloprost (AIR41) | 4.41 (0.85–22.97) | 0.29 (0.07–1.18) | – |
| Bosentan (pooled data from Channick et al., 200143 and BREATHE-547) | 5.02 (1.35–18.65) | 0.21 (0.03–1.76) | – |
| Sitaxentan (pooled data from STRIDE-248 and STRIDE-437) | 2.08 (0.46–9.44) | 0.18 (0.02–1.64) | – |
| Sildenafil (SUPER-153) | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | – |
| Intervention | Functional class (FC) transition, odds ratio (lower and upper confidence limits) | ||
|---|---|---|---|
| FCII to FCIII (using same as FCIII to FCIV) | FCIII to FCIV | FCIV to FCIII | |
| Epoprostenol (Barst et al., 199611) | 0.40 (0.13–1.20) | 0.40 (0.13–1.20) | 24.96 (3.11–200.14) |
| Iloprost (AIR41) | 0.29 (0.07–1.18) | 0.29 (0.07–1.18) | – |
| Bosentan (pooled data from Channick et al., 200143 and BREATHE-547) | 0.21 (0.03–1.76) | 0.21 (0.03–1.76) | – |
| Sitaxentan (pooled data from STRIDE-248 and STRIDE-437) | 0.18 (0.02–1.64) | 0.18 (0.02–1.64) | – |
| Sildenafil (SUPER-153) | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | – |
Mortality
Mortality comprised two components: age-related general population mortality and PAH-related mortality. It was assumed that there was an additional mortality due to PAH, dependent on FC and treatment. This was assumed to be constant for each cycle. Mortality in FCII was assumed to be the general population mortality only. Details of the method used and uncertainty around it appear in Appendix 9. Transition probabilities for PAH-related mortality were entered in the model as beta distributions. The 12-week mortality rates for the intervention therapies are presented in Table 44. The corresponding mortality rates for supportive care are presented in Table 45.
| Treatment | FC | Per-cycle mortality (95% CI) | Beta distribution |
|---|---|---|---|
| Epoprostenol, iloprost (pooled data from Sitbon et al., 2002,66 Sitbon et al.,2005,98 McLaughlin et al., 200265) | III | 0.021 (0.017–0.025) | n = 5000, r = 105 |
| Epoprostenol (pooled data from Sitbon et al., 2002,66 McLaughlin et al., 200265) | IV | 0.056 (0.044–0.069) | n = 1250, r = 70 |
| Bosentan (Sitbon et al., 200598) | III | 0.010 (0.006–0.015) | n = 1600, r = 16 |
| Sitaxentan, sildenafil (pooled data from STRIDE-1X99 and STRIDE-2X100 | III | 0.011 (0.004–0.023) | n = 450, r = 5 |
| Treatment | FC | Mortality on supportive care (95% CI) | Beta distribution |
|---|---|---|---|
| Epoprostenol | III | 0.051 (0.041–0.069) | n = 950, r = 48 |
| Epoprostenol | IV | 0.129 (0.103–0.156) | n = 600, r = 77.5 |
| Iloprost | III | 0.069 (0.056–0.093) | n = 700, r = 48 |
| Oral therapies | III | 0.058 (0.006–0.116) | n = 66, r = 3.84 |
Resource use and costs
The resource use was broadly concerned with the initiation and ongoing costs of each therapy, contacts with primary and secondary health care, adverse events and use of wider social services including palliative care. The perspective adopted for the reference case is that of the NHS/PSS, and a price year of 2006 was applied.
The cost of each of the therapies in question was calculated using British National Formulary (BNF) prices for March 2007,26 using the licensed dose (Table 46). For bosentan, in the first month of treatment it was assumed that the dose was 62.5 mg twice a day, with a dose of 125 mg twice a day for subsequent months. For inhaled iloprost and intravenous epoprostenol, for which the actual doses vary, estimates of average doses from clinical opinion were used. The amount of inhaled iloprost varies from patient to patient; however, as one vial is 10 ∝g and a patient opens a vial each time they nebulise, the cost of a 10-∝g vial (£14.15) was used for each inhalation. It was assumed that a patient nebulised seven times a day. The amount of epoprostenol required for infusion was approximately 15–20 ng/kg/min at the end of the first year, and an average of 17.5 ng/kg/min was used for the first year. Although it was assumed that the dose in the first months would be much lower (the iloprost manufacturer submission uses values of 2.2 ng/kg/min at baseline and 14.1 ng/kg/min at 3 months), comparison with this industry data demonstrated that using this mean over the whole year would not be inappropriate. An average dose of 40 ng/kg/min was used for the second and subsequent years as the range was between 30 and 50 ng/kg/min. A standard deviation around the point estimate was estimated by assuming that the difference between the mean and an upper (or lower) limit equalled two standard deviations. The cost per mg of the drug was £86.71 and an average patient weight of 70 kg was applied.
| Therapy | Dose, mean (range) | Unit cost (per 4 weeks) (£) (SD) |
|---|---|---|
| Epoprostenol: | ||
| Year 1 | 17.5 (15–20) ng/kg/min | 4282.94 (305.92) |
| Year 2 | 40 (30–50) ng/kg/min | 9789.59 (1223.70) |
| Iloprost | 10-µg vial seven times a day | 2773.40 |
| Bosentan | 125 mg twice daily | 1541.00 |
| Sitaxentan | 100 mg once daily | 1540.00 |
| Sildenafil | 20 mg three times daily | 348.60 |
Further information was provided by the manufacturers with regards to the cost contract with the NHS. GlaxoSmithKline stated that epoprostenol was available at a discount [Commercial-in-confidence information has been removed] for this indication, [Commercial-in-confidence information has been removed]. Schering Health Care referred to a fixed fee system called VENTafee, in which iloprost was provided at a fixed cost of £7400 (excluding VAT) per quarter irrespective of the dose. For both drugs the BNF price was included in the reference case, with the price of the alternative arrangements included in a sensitivity analysis. This equates to £2269.13 for 4 weeks of iloprost and [Commercial-in-confidence information has been removed] per 4 weeks for the first and subsequent years of epoprostenol respectively.
The therapies included in the definition of supportive care were warfarin, furosemide, digoxin and oxygen and it was assumed that all patients would be on each therapy. This is likely to be an overestimate; however, the costs of supportive therapies are small in comparison with the intervention therapies. In addition, when supportive care was not used in conjunction with an active therapy, it was assumed that the patient was hospitalised until death in FCIV. Supportive therapy was assumed to be given to patients irrespective of being on active therapy, but the intensity of supportive therapy was dependent on FC, particularly oxygen therapy. The proportion of patients requiring oxygen in each FC was obtained from the iloprost manufacturer submission, with rates of 5%, 27% and 71% for FCII, FCIII and FCIV respectively. An assumption was made that all patients in FCIV taking supportive therapies would only be on oxygen. The intensity of oral supportive therapies may also increase with worsening FC; however, this level of detail was not available and therefore a standard dose for each drug was used. As the cost of these oral therapies was deemed very low, the impact of dose changes would be negligible. All units and costs are presented in Table 47.
| Therapy | Average dose per day | Cost per 4 weeks (£) |
|---|---|---|
| Warfarin | 5 mg once daily | 1.47 |
| Furosemide | 100 mg once daily | 3.59 |
| Digoxin | 125 mg once daily | 2.40 |
| Oxygen: | 0.66 per unit | |
| FCII (5% uptake) | 2 ml | 1.84 |
| FCIII (27% uptake) | 2 ml | 9.94 |
| FCIV (71% uptake) | 2.3 ml | 30.06 |
| FCIV (100% uptake, supportive therapy only) | 2.3 ml | 42.34 |
The cost of warfarin therapy includes not only the drug but also regular monitoring to ensure that the patient lies within their therapeutic INR range, thus reducing the risk of thrombolic or haemorrhagic events. As there are different models of care for monitoring, an average cost per visit was used from a trial of 617 patients101 and applied to an assumed average frequency of a monitoring visit every 4 weeks.
For each active therapy an initiation cost was required. In the case of the three oral therapies the model assumed that the patient was on a day ward as a day case and any education by a nurse was assumed to be part of this day case cost. The unit cost used was that of a day case with cardiac catheterisation as this procedure would take place at this visit. An additional initiation cost for bosentan and sitaxentan was a liver function test. Patients commencing inhaled iloprost or intravenous epoprostenol therapy required a longer period of time in hospital and training in order to use the drug delivery system safely. For inhaled iloprost it was assumed that patients were admitted for 3 days with a specialist nurse spending 2 hours a day with the patient for training. Initiation costs for intravenous epoprostenol were higher as it was assumed that a patient would spend approximately 12 days in hospital. Much training is required to ensure that patients are familiar with mixing the drugs and keeping all equipment sterile to reduce the risk of infection. Therefore it was assumed that a specialist nurse would spend 2 hours a day, 5 days a week training the patient. In addition, the cost of the insertion of a central venous catheter for intravenous administration of epoprostenol was also included. The unit cost used here was an elective inpatient stay for catheterisation of 2 days. Therefore the cost of the additional 10 days was calculated using the daily inpatient rate. Other costs may be applicable to patients at initiation of therapy, particularly with regard to standard tests for PAH patients; however, these were not included as they were assumed to apply for all therapies.
Ongoing costs were attributed to each drug to take into account a service fee, which includes delivery of the drug and providing any equipment required for drug delivery. Costs presented here are strictly confidential. Because of the possibility of liver toxicity when taking bosentan or sitaxentan it was assumed that patients had a liver function test every 4 weeks. In addition, each therapy was associated with a number of adverse events, varying in severity and most common in the first period of taking therapy. However, it was decided that the model should only consider the most severe (and therefore costly) adverse events. Therefore only line infection and sepsis while on intravenous epoprostenol were considered, with 17% (line infection) and 4% (sepsis) of patients suffering these events over a 3-month period. 11,39
Primary and secondary care resource use was assumed to be related to FC. Social care and palliative care were also included in resource use, again related to FC. No published data were available on resource use; however, information was available in the iloprost industry submission, obtained from the research carried out by Schering Health Care. The overall costs per FC are presented in Table 48. NHS contacts included seeing hospital physicians and nurses, GP visits and A&E attendance. Personal and social services included residential, day and home care and hospice visits. Hospitalisations considered stays in general wards and intensive care and coronary care units and associated A&E attendance. Full details of resource use and unit costs used by this industry submission are presented in the Appendix 10. As the model assumes that patients on supportive care alone in FCIV will be hospitalised until death, the same resource use for FCIV was used except that the average hospitalisation costs were excluded and replaced by a cost of ongoing inpatient care for all patients at £188 a day.
| Functional class | NHS contacts | Hospitalisations | Personal and social services | Total |
|---|---|---|---|---|
| II | 42.44 | 19.01 | 4.91 | 66.36 |
| III | 68.87 | 85.86 | 54.83 | 209.56 |
| IV | 89.05 | 601.93 | 709.38 | 1400.36 |
Unit costs were obtained from a number of standard sources and are presented in Table 49. Drug costs were obtained from the most recent BNF (March 2007). 26 Staff costs and the cost of an inpatient stay were obtained from the Unit Costs of Health and Social Care. 102 Costs of procedures were obtained from NHS reference costs for 2005/6. 103 Warfarin monitoring costs were obtained from a trial dataset presented in Jowett et al. 101 and were inflated to 2006 costs. Other costs, for example liver function tests, were obtained from estimates used in the industry submissions.
| Resource item | Unit cost (£) | Source |
|---|---|---|
| Initiation costs | ||
| Day ward | 838 | NHS reference costs 2005/6103 [day cases, cardiac catheterisation and angiography without complications (HRG code E14)] |
| Inpatient day | 188 | Curtis and Netten102 (patient rehabilitation, general inpatient cost, cost per bed day) |
| Specialist nurse (per hour) | 37 | Curtis and Netten102 [nurse advanced (including clinical nurse specialist) (including qualifications)] |
| Central venous catheter insertion for intravenous therapy | 1648 | NHS reference costs 2005/6103 [elective inpatient, cardiac catheterisation and angiography without complications (2-day stay) (HRG code E14)] |
| Additional costs | ||
| Service contracts (per year): | ||
| Epoprostenol | 9464 | Costs estimated through expert contact |
| Iloprost | 5512 | |
| Bosentan, sitaxentan, sildenafil | 542 | |
| Liver function test | 22.47 | London Clinic pathology price list 2003–4 (from sildenafil submission) |
| Sepsis | 2011 | NHS reference costs 2005/6103 [non-elective inpatient, septicaemia (HRG code S12)] |
| Catheter site infection | 1321 | NHS reference costs 2005/6103 [non-elective inpatient, other non-viral infections (HRG code S15)] |
| Warfarin monitoring visit | 10.39 | Jowett et al.101 |
Estimation of quality-adjusted life-years
As the model health states were based on FC, utility values also based on FC were sought from the literature and manufacturer submissions. Valuations based on FC were available from two quality of life studies,76,84 one economic evaluation72 and the iloprost and bosentan manufacturer submissions. 41,94 The data in the AIR study were analysed further to provide utility scores by FC, and values presented in the iloprost submission. The data presented here are from the simple pooling analysis. The data from Meads et al. 94 remains academic-in-confidence. The values used in the Highland et al. model72 were not utilised here as the values were gained by clinical consensus and a valuation of 0 was given for FCIV, i.e. the same as death, which was not deemed to be appropriate for this cost-effectiveness analysis. The values from Keogh et al. 84 were used in the base case as this study has the largest sample size and is not academic-in-confidence. However, it should be noted that, although the patient population comprised bosentan patients, the model assumes that these values are applicable for all therapies. The utility values were entered into the model as beta distributions (Table 50). Alternative values were used in the sensitivity analysis to investigate the impact on overall results (Table 51).
| Health state | Mean (SD) | α | β |
|---|---|---|---|
| Functional class II | 0.67 (0.1) | 14.144 | 6.966 |
| Functional class III | 0.60 (0.1) | 13.800 | 9.200 |
| Functional class IV | 0.52 (0.09) | 15.504 | 14.311 |
| Health state | Meads et al.94 | Kirsch 2000,76 2-year TTO | Kirsch 2000,76 10-year TTO | Olschewski et al., 200241 |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Functional class II | [Academic-in-confidence information has been removed] | 0.782 (0.031) | 0.765 (0.023) | 0.75 (0.193) |
| Functional class III | [Academic-in-confidence information has been removed] | 0.553 (0.045) | 0.509 (0.044) | 0.61 (0.254) |
| Functional class IV | [Academic-in-confidence information has been removed] | 0.371 (0.051) | 0.284 (0.051) | 0.44 (0.291) |
Model assumptions
Odds ratios were calculated for the deterioration from FCIII to FCIV for each therapy, to be applied to supportive care transition probabilities. In the absence of suitable mortality data for supportive care alone, it was assumed that the odds ratios for deterioration could also be used as odds ratios for mortality.
Although lung transplantation is an option available to PAH patients in FCIV, this was not included as an event in this model as very few PAH patients actually have a transplant
Bosentan is licensed at 125 mg twice daily and 250 mg twice daily, and consideration of the dose taken was required for the drug costs. Advice from clinical experts indicated that very few patients are on the 250-mg twice daily dose, as liver toxicity is greater and no significant improvement is seen on this higher dose. Accordingly, the model assumed that all patients were taking 125 mg twice daily.
Assessment of cost-effectiveness
The main results are presented as mean costs and QALYs from 10,000 simulations for the alternative policy options considered. Incremental costs and QALYs and, when appropriate, an estimate of the incremental cost per QALY are shown. Cost-effectiveness acceptability curves (CEACs) are included to give a measure of the uncertainty reflected in the model. Some exploration of the contribution of individual model parameters to this uncertainty is reported.
Non-reference case analyses
Additional model runs were undertaken to consider the three main issues. First, there was an investigation of the effect on the results of running the model for shorter time horizons of 10 and 20 years. Second, alternative therapy costs supplied by the manufacturers for inhaled iloprost and intravenous epoprostenol were incorporated. Finally, as there was more than one set of utility values to apply to the health states, those values not used in the reference case were explored.
Results
A separate comparison is presented for each intervention therapy in addition to supportive care versus supportive care alone (with switching to epoprostenol in FCIV) for FCIII, and for epoprostenol in addition to supportive care versus supportive care alone in FCIV. All model results are presented separately for each therapy, with the reference case results presented first followed by the non-reference case analyses.
As discussed, non-reference case analyses considered three main issues: time horizon, alternative drug price and alternative health state utility values. The reference case analysis had a time horizon of 30 years to represent effective lifetime and therefore shorter time horizons of 20 years and 10 years were also considered. The reference case analysis used the list price for drugs and therefore alternative model runs were undertaken to consider the lower price of epoprostenol, as stated in the industry submission for this drug, and the fixed fee scheme for iloprost, again as stated in the relevant manufacturer submission. Finally, four alternative sets of health states values were used so that values used in the manufacturer models were also used in the assessment group model. The full results of these analyses can be found in Appendix 12.
Epoprostenol in addition to supportive care versus supportive care alone, functional class III
Reference case
Table 52 presents the results of the analysis for epoprostenol in FCIII. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £277,000 per QALY gained. The CEAC presented in Figure 10 shows that at willingness to pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 479,000 | 2.056 | |||
| Epoprostenol | 697,000 | 218,000 | 2.843 | 0.787 | 277,000 |
FIGURE 10.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class III. Inset graph shows a larger x-axis scale. QALY, quality-adjusted life-year.
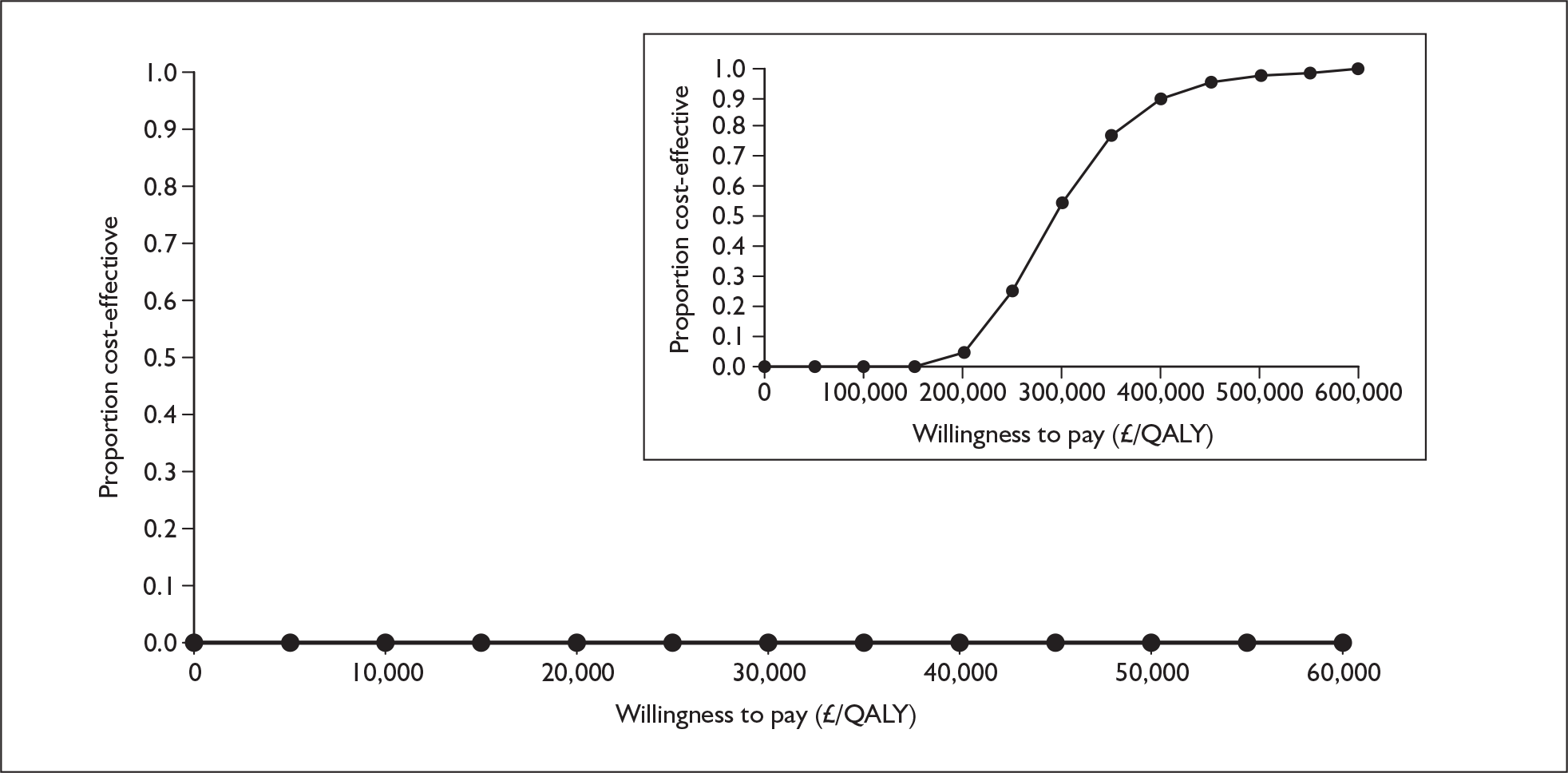
Analysis of the effect of single parameters in the reference case shows that in many cases the cost and QALY differences change significantly, but in the same direction, so that the difference in ICER is small. Full details are in Appendix 11.1.
Non-reference case analyses
Table 53 presents the results of the additional analyses undertaken. The only variable that affected the ICER was the alternative (and lower) epoprostenol price, which reduced the ICER from £277,000 per QALY to £106,000 per QALY.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | 218,000 | 0.787 | 277,000 | 0 | 0 |
| Alternative time horizon: | |||||
| 20 years | 216,000 | 0.779 | 277,000 | 0 | 0 |
| 10 years | 189,000 | 0.683 | 277,000 | 0 | 0 |
| Alternative epoprostenol price | 83,000 | 0.787 | 106,000 | 0 | 0 |
| Alternative health state utility values: | |||||
| Meads et al.94 | 218,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0 | 0 |
| Kirsch 2000,76 2-year TTO | 218,000 | 0.831 | 262,000 | 0 | 0 |
| Kirsch 2000,76 10-year TTO | 218,000 | 0.799 | 272,000 | 0 | 0 |
| Olschewski et al. 200241 | 218,000 | 0.853 | 256,000 | 0 | 0 |
Epoprostenol with supportive care versus supportive care alone, functional class IV
Reference case
In FCIV, epoprostenol has a much greater cost than supportive care alone and produces just over one extra QALY, resulting in an ICER of £343,000 per QALY gained (Table 54). At the £20,000 and £30,000 per QALY thresholds, the probability of epoprostenol being cost-effective is zero in both cases (Figure 11).
Analysis of the effect of single parameters in the reference case shows that in most cases the cost and QALY differences change noticeably, but in the same direction, so that the difference in ICER is small. Full details are in Appendix 11.2.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.829 | |||
| Epoprostenol | 531,000 | 403,000 | 2.003 | 1.174 | 343,000 |
FIGURE 11.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class IV. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
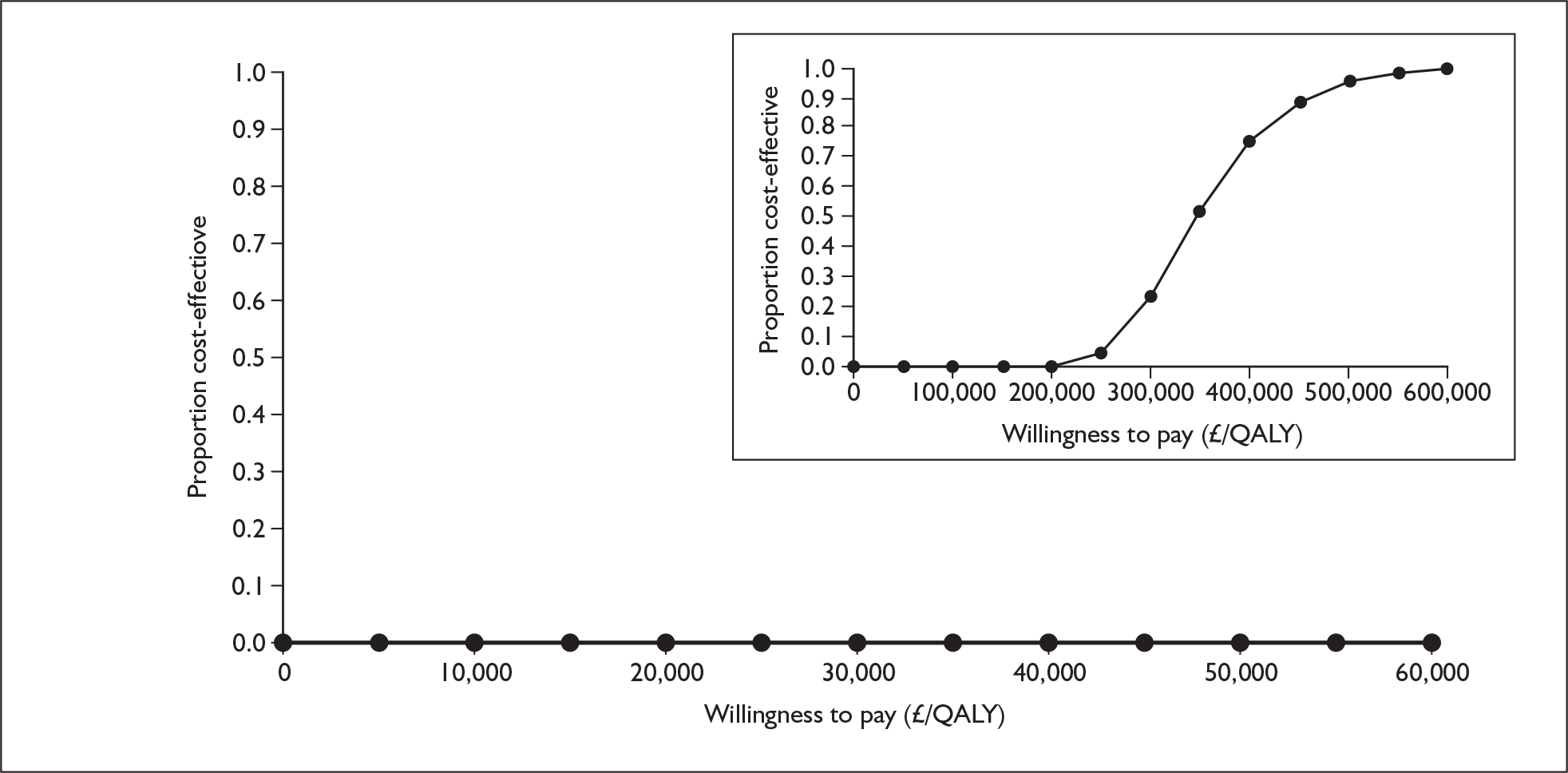
Non-reference case analyses
Table 55 presents the results of the additional non-reference case analyses. The majority of analyses made very little impact to the overall ICER. The two alternative health state data sets presented in Kirsch et al. 76 gave a much higher ICER for epoprostenol in FCIV, and using the lower price as stated by the manufacturer reduced the ICER to £96,000 per QALY gained.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | 403,000 | 1.174 | 343,000 | 0 | 0 |
| Alternative time horizon: | |||||
| 20 years | 401,000 | 1.167 | 344,000 | 0 | 0 |
| 10 years | 368,000 | 1.058 | 348,000 | 0 | 0 |
| Alternative epoprostenol price | 113,000 | 1.174 | 96,000 | 0 | 0 |
| Alternative health state utility values: | |||||
| Meads et al.94 | 403,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0 | 0 |
| Kirsch 2000,76 2-year TTOa | 402,000 | 0.895 | 449,000 | 0 | 0 |
| Kirsch 2000,76 10-year TTOa | 402,000 | 0.726 | 554,000 | 0 | 0 |
| Olschewski et al. 200241 | 403,000 | 1.049 | 384,000 | 0 | 0 |
Iloprost with supportive care versus supportive care alone, functional class III
Reference case
Table 56 presents the results of the analysis for iloprost in FCIII. Iloprost alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £101,000 per QALY gained. The CEAC presented in Figure 12 shows that at willingness to pay thresholds of £20,000 and £30,000 per QALY gained, iloprost has a probability of being cost-effective of 3% and 5% respectively.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | 1.958 | |||
| Iloprost | 537,000 | 103,000 | 2.975 | 1.017 | 101,000 |
Analysis of the effect of single parameters in the reference case shows that the odds ratio for deterioration from FCIII to FCIV after the first cycle makes the most difference to the ICER. Even so, the lowest ICER for any decile group in this parameter is over £30,000 per QALY. Full details are in Appendix 11.3.
FIGURE 12.
Cost-effectiveness acceptability curve for iloprost with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
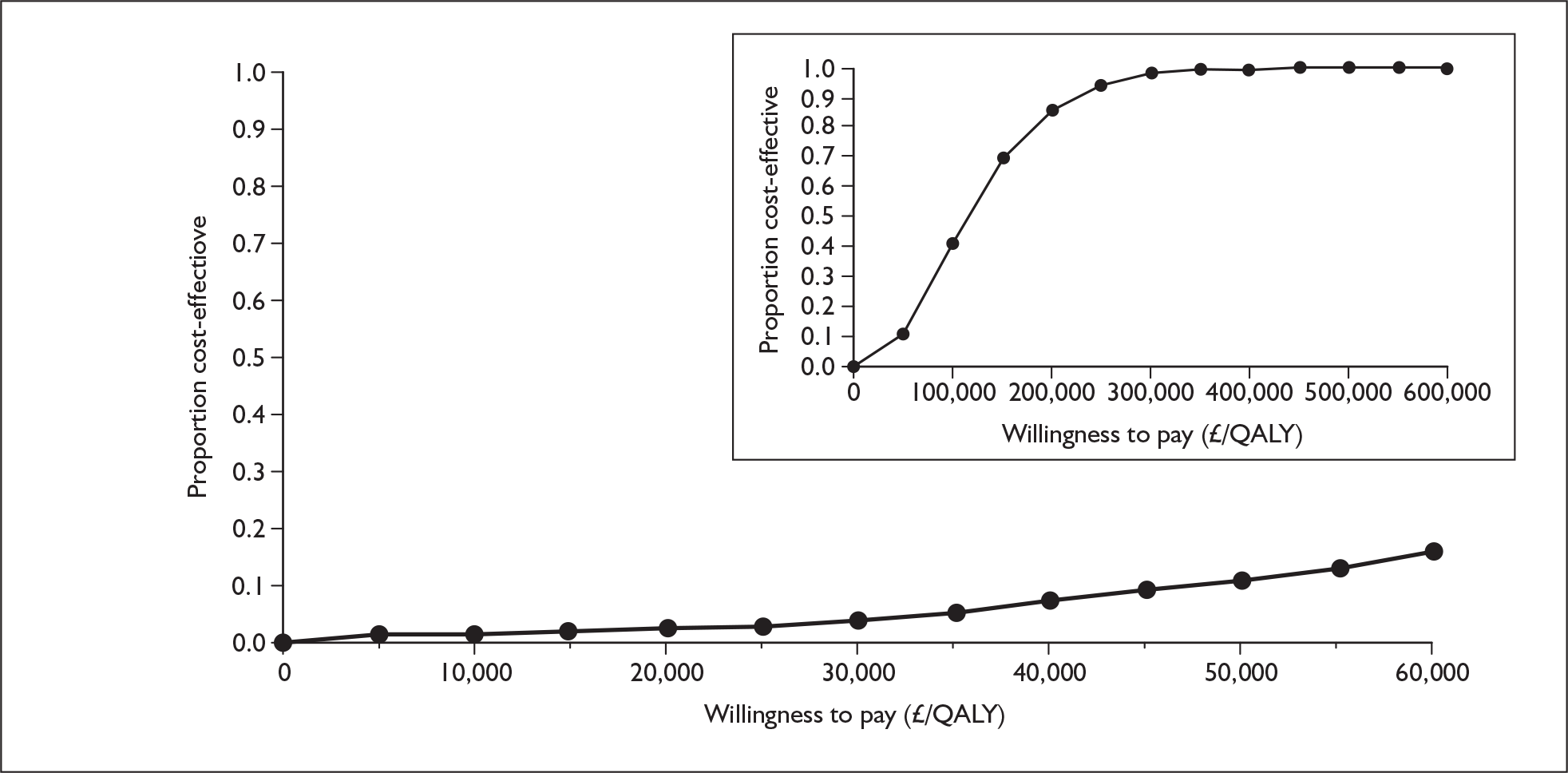
Non-reference case analyses
The results of the additional analyses, presented in Table 57, show that none has a significant effect on the overall ICER. Reducing the time horizon to 10 years changed the ICER to £81,000 per QALY, and using the lower price for iloprost reduced the ICER to £85,000 per QALY.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | 103,000 | 1.017 | 101,000 | 0.03 | 0.05 |
| Alternative time horizon: | |||||
| 20 years | 99,000 | 0.999 | 99,000 | 0.03 | 0.06 |
| 10 years | 68,000 | 0.844 | 81,000 | 0.12 | 0.16 |
| Alternative epoprostenol price | 102,000 | 1.017 | 101,000 | 0 | 0 |
| Alternative iloprost price | 87,000 | 1.017 | 85,000 | 0.06 | 0.10 |
| Alternative iloprost and epoprostenol prices | 86,000 | 1.017 | 85,000 | 0 | 0 |
| Alternative health state utility values: | |||||
| Meads et al.94 | 103,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0.03 | 0.04 |
| Kirsch 2000,76 2-year TTOa | 102,000 | 1.030 | 99,000 | 0.03 | 0.05 |
| Kirsch 2000,76 10-year TTOa | 102,000 | 0.975 | 104,000 | 0.03 | 0.05 |
| Olschewski et al. 200241 | 103,000 | 1.074 | 96,000 | 0.03 | 0.06 |
Bosentan in addition to supportive care versus supportive care alone, functional class III
Reference case
Table 58 presents the reference case results for bosentan, with the intervention more expensive than supportive care alone and producing a greater amount of QALYs, resulting in an ICER of £27,000 per QALY gained. The CEAC in Figure 13 demonstrates that bosentan has a 41% chance of being cost-effective at £20,000 per QALY and a 54% chance at £30,000 per QALY.
| Strategy | Cost(£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 2.201 | |||
| Bosentan | 436,000 | 93,000 | 5.696 | 3.494 | 27,000 |
FIGURE 13.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
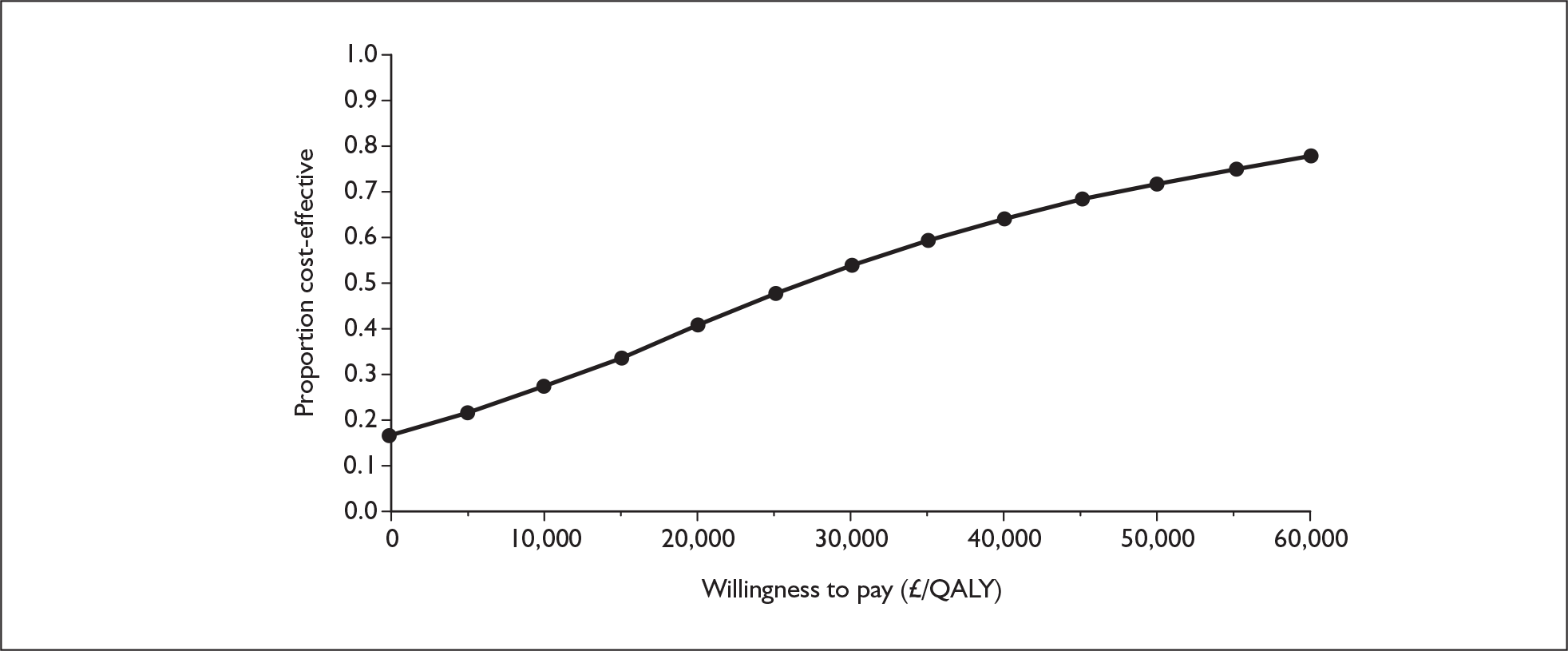
Analysis of the effect of single parameters in the reference case shows that the result is highly sensitive to two parameters. Full details are in Appendix 11.4.
The results relating to the odds ratio for deterioration from FCIII to FCIV after the first cycle vary from bosentan dominating the comparator in the most favourable decile group (in which the odds ratio is < 0.053) to an ICER of £90,000 per QALY in the least favourable (odds ratio > 0.86). The ICER was greater than £30,000 per QALY in the top five decile groups (odds ratio > 0.21).
The higher the mortality rate in FCIII on supportive care the greater the difference in both costs and QALYs between bosentan and the comparator. The variation in costs is far higher than the variation in QALYs. This is probably because, comparatively, more people are surviving to be treated with epoprostenol in FCIV in the bosentan arm. The higher the mortality rate on supportive care the greater this difference becomes. The effect is that the results also vary from dominance in the most favourable decile group (mortality per cycle less than 0.0254, corresponding to annual mortality less than 10.5 per cent) up to £49,000 per QALY in the least favourable group (annual mortality rate > 35.5%). The ICER was greater than £30,000 per QALY in the top five decile groups (annual mortality rate > 21.3%).
Non-reference case analyses
Additional analyses for bosentan are presented in Table 59. Reducing the time horizon to 20 years changed the ICER from £27,000 to £21,000 per QALY, and a further reduction in the time horizon to 10 years meant that bosentan was cheaper and therefore dominated supportive care alone. Here, the probability of bosentan being cost-effective at £20,000 per QALY increased to 70%. Reducing the price of epoprostenol increased the cost difference substantially, therefore making bosentan less cost-effective at £39,000 per QALY, with only a 3% chance of it being cost-effective at £20,000 per QALY and a 20% chance at £30,000 per QALY. Changing the set of utility values used has very little impact on the overall result.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | 93,000 | 3.494 | 27,000 | 0.41 | 0.54 |
| Alternative time horizon: | |||||
| 20 years | 66,000 | 3.108 | 21,000 | 0.49 | 0.60 |
| 10 years | –8,000 | 1.964 | Dominates | 0.70 | 0.76 |
| Alternative epoprostenol price | 137,000 | 3.494 | 39,000 | 0.03 | 0.20 |
| Alternative health state utility values: | |||||
| Meads et al. 94 | 93,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0.40 | 0.52 |
| Kirsch 2000,76 2-year TTOa | 92,000 | 3.700 | 25,000 | 0.43 | 0.56 |
| Kirsch 2000,76 10-year TTOa | 92,000 | 3.549 | 26,000 | 0.42 | 0.55 |
| Olschewski et al. 200241 | 93,000 | 3.774 | 25,000 | 0.43 | 0.55 |
Sitaxentan in addition to supportive care versus supportive care alone, functional class III
Reference case
Compared with supportive care alone, sitaxentan provided an additional 3 QALYs but at greater cost, resulting in an ICER of £25,000 per QALY gained (Table 60). The CEAC presented in Figure 14 demonstrates that, at thresholds of £20,000 and £30,000 per QALY gained, the probability of sitaxentan being cost-effective is 45% and 56% respectively.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 2.201 | |||
| Sitaxentan | 419,000 | 76,000 | 5.289 | 3.087 | 25,000 |
FIGURE 14.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year
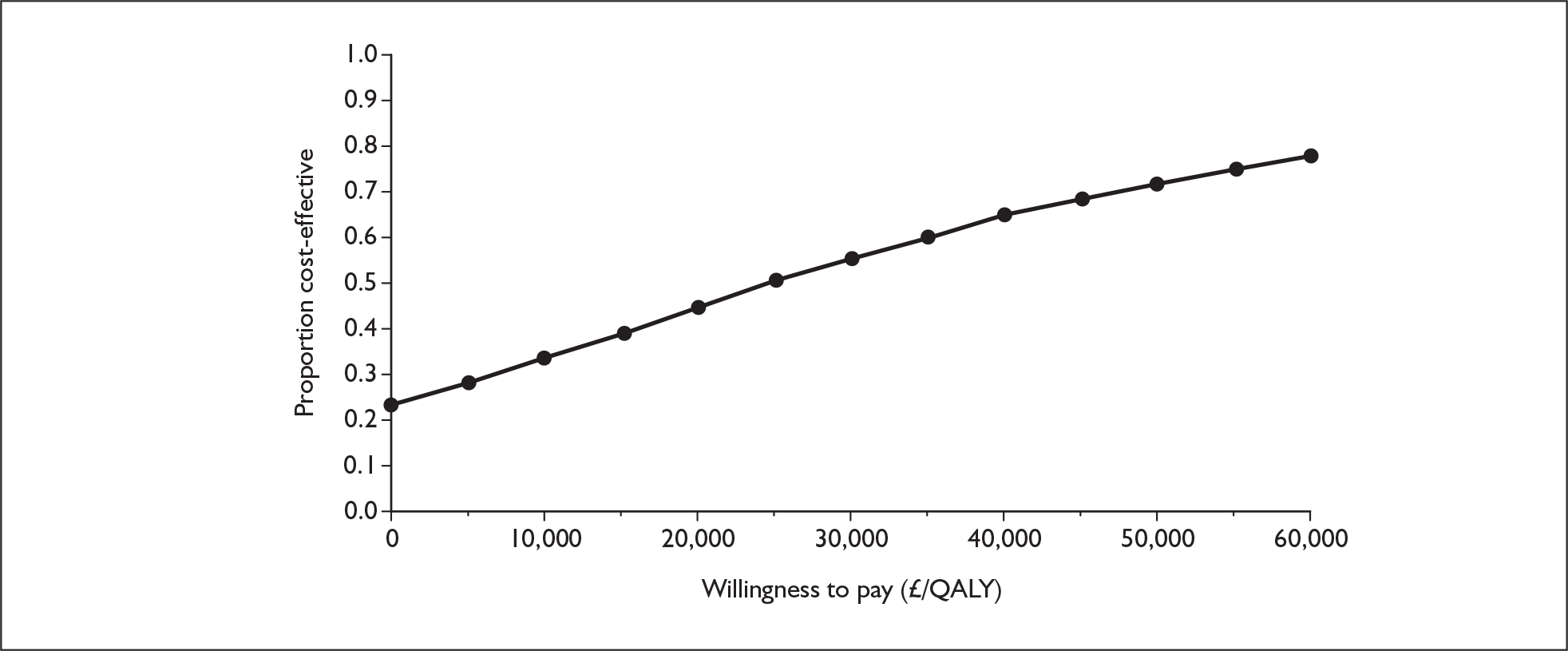
Analysis of the effect of single parameters in the reference case shows that the result is highly sensitive to three parameters. Full details are in Appendix 11.5.
The results relating to the odds ratio for deterioration from FCIII to FCIV after the first cycle vary from sitaxentan dominating the comparator in the most favourable decile group (in which the odds ratio is < 0.042) to an ICER of £120,000 per QALY in the least favourable (odds ratio > 0.76). The ICER was over £30,000 per QALY in the top four decile groups (odds ratio > 0.24).
The lower the mortality rate in FCIII on treatment, the greater the difference in both costs and QALYs between sitaxentan and the comparator. The variation in costs is far higher than the variation in QALYs, with the effect that the results vary from an ICER of £2500 per QALY in the most favourable decile group (mortality per cycle > 0.0176, corresponding to annual mortality rate > 7.4%) up to £37,000 per QALY in the least favourable group (annual mortality rate < 2.3%). The ICER was over £30,000 per QALY in the worst three decile groups (annual mortality rate < 3.5%).
Similarly, the higher the mortality rate in FCIII on supportive care, the greater the difference in both costs and QALYs between sitaxentan and the comparator. The variation in costs is again far higher than the variation in QALYs, with the effect that the results vary from dominance in the most favourable decile group (mortality per cycle less than 0.0254, corresponding to annual mortality rate < 10.5%) up to £50,000 per QALY in the least favourable group (annual mortality rate > 35.5%). The ICER was over £30,000 per QALY in the top four decile groups (annual mortality rate > 23.9%).
Non-reference case analyses
The additional analyses presented in Table 61 show the same trend for sitaxentan as previously demonstrated for bosentan. Reducing the time horizon to 20 years reduced the ICER from £25,000 per QALY to £19,000 per QALY, and running the model for 10 years further changed the result and sitaxentan was dominant. Incorporating a reduced price for epoprostenol resulted in a much larger ICER of £40,000 per QALY. Again, changing the set of utility values used has little impact on the ICER.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | 76,000 | 3.087 | 25,000 | 0.45 | 0.56 |
| Alternative time horizon: | |||||
| 20 years | 52,000 | 2.755 | 19,000 | 0.51 | 0.61 |
| 10 years | –11,000 | 1.754 | Dominates | 0.69 | 0.74 |
| Alternative epoprostenol price | 122,000 | 3.087 | 40,000 | 0.06 | 0.23 |
| Alternative health state utility values: | |||||
| Meads et al.94 | 76,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0.44 | 0.54 |
| Kirsch 2000,76 2-year TTOa | 75,000 | 3.700 | 24,000 | 0.45 | 0.56 |
| Kirsch 2000,76 10-year TTOa | 75,000 | 2.997 | 25,000 | 0.44 | 0.54 |
| Olschewski et al. 200241 | 76,000 | 3.294 | 23,000 | 0.46 | 0.56 |
Sildenafil in addition to supportive care versus supportive care alone, functional class III
Reference case
Compared with supportive care alone, sildenafil is less costly and more effective and therefore dominates supportive care (Table 62). The CEAC presented in Figure 15 shows that, at all threshold values, sildenafil is at least 60% cost-effective, and has a probability of being cost-effective of 75% at £20,000 per QALY and 78% at £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 2.201 | |||
| Sildenafil | 307,000 | –36,000 | 5.436 | 3.235 | Dominates |
FIGURE 15.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year
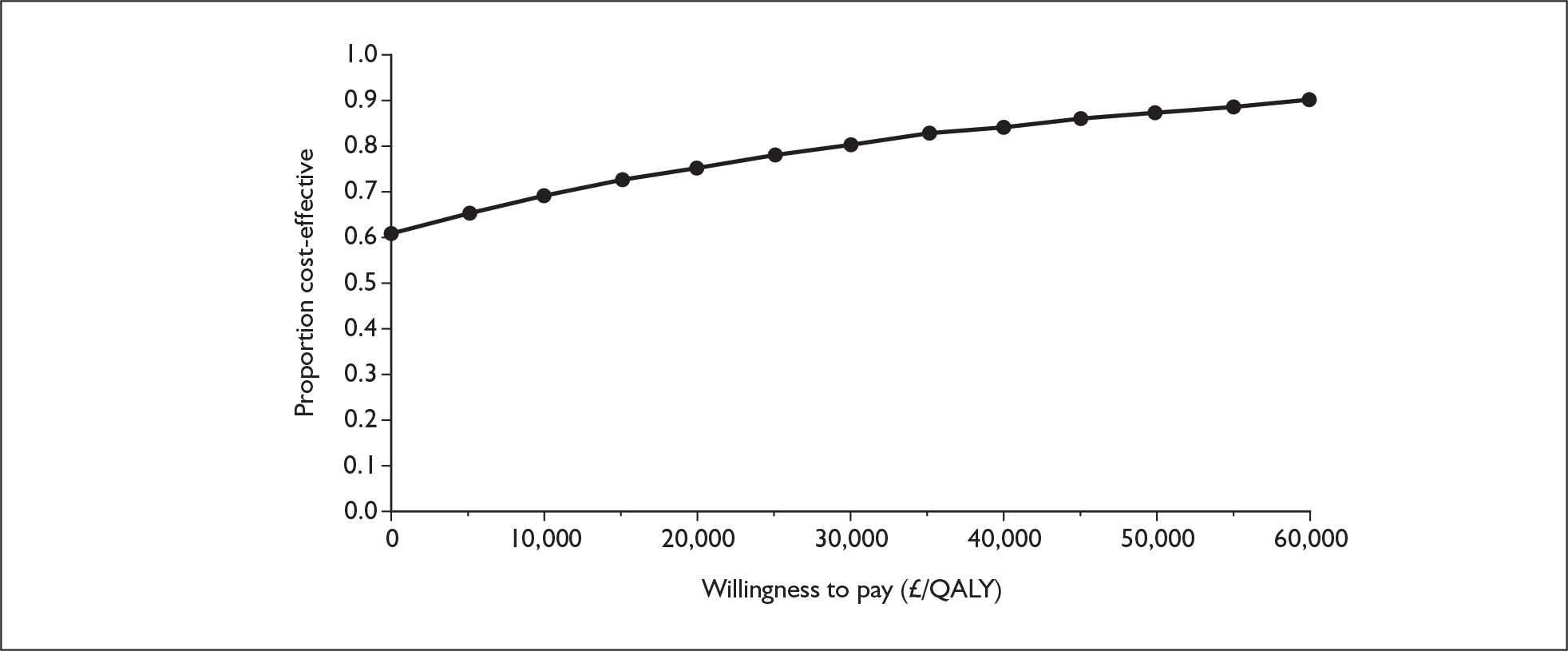
Analysis of the effect of single parameters in the reference case shows that the sildenafil option remained dominant over its comparator except for variation in three parameters. Full details are in Appendix 11.6.
In the case of the odds ratio for deterioration from FCIII to FCIV after the first cycle, sildenafil remained dominant in six decile groups (in which the odds ratio is < 0.26), but the ICER reached £70,000 per QALY in the least favourable decile group (odds ratio > 0.83). The ICER was over £30,000 per QALY in the top two decile groups (odds ratio > 0.50).
The lower the mortality rate in FCIII on treatment, the greater the difference in both costs and QALYs between sildenafil and the comparator. In this case sildenafil remained dominant over the comparator in all but the least favourable decile group, in which the ICER was still below £2000 per QALY.
Similarly, the higher the mortality rate in FCIII on supportive care, the greater the difference in both costs and QALYs between sildenafil and the comparator. In this case sildenafil ceased to dominate the comparator in the top three decile groups, but the ICER still remained below £20,000 per QALY in all groups.
Non-reference case analyses
The results of the additional analyses included in Table 63 show that, for almost all scenarios, sildenafil remains dominant over supportive care alone. Reducing the time horizon to 20 years and 10 years increases the cost saving with sildenafil and therefore increases the probability of the intervention being cost-effective. Running the model with alternative health state utility values had no impact on the overall result. The scenario incorporating the lower price for epoprostenol gave an ICER of £3700.
| Scenario | Cost difference (£) | QALY difference | ICER (£/QALY) | Probability cost-effective at £20,000/QALY | Probability cost-effective at £30,000/QALY |
|---|---|---|---|---|---|
| Reference case | –36,000 | 3.235 | Dominates | 0.75 | 0.78 |
| Alternative time horizon: | |||||
| 20 years | –53,000 | 2.878 | Dominates | 0.78 | 0.82 |
| 10 years | –95,000 | 1.823 | Dominates | 0.86 | 0.88 |
| Alternative epoprostenol price | 12,000 | 3.235 | 3700 | 0.79 | 0.87 |
| Alternative health state utility values: | |||||
| Meads et al.94 | –36,000 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 0.75 | 0.80 |
| Kirsch 2000,76 2-year TTOa | –34,000 | 3.376 | Dominates | 0.76 | 0.81 |
| Kirsch 2000,76 10-year TTOa | –34,000 | 3.227 | Dominates | 0.75 | 0.80 |
| Olschewski et al. 200241 | –36,000 | 3.480 | Dominates | 0.75 | 0.81 |
Discussion
All intervention therapies alongside supportive care led to a QALY improvement compared with supportive care alone; however, the cost-effectiveness ratios vary considerably. It should be emphasised that, as the interventions are largely used in different populations, comparison between therapies is not appropriate.
Sensitivity of modelling results and non-reference case analyses
As described earlier, the model was run for a number of non-reference case scenarios, with time horizon appearing to have the greatest impact on results. All drugs other than epoprostenol showed more favourable results when the time horizon was shortened. This is likely to be because the downstream effects omitted are greater on the active treatment arm, in which overall survival is greater.
The ICERs for bosentan, sitaxentan and sildenafil, but not iloprost, are sensitive to the price of epoprostenol. The price of epoprostenol is particularly important when a technology is compared with supportive care in FCIII. If the technology was effective (delaying transition to FCIV) and much cheaper than epoprostenol, reducing the price of epoprostenol will make the technology less cost-effective as the cost of supportive care will greatly reduce and the cost of the technology (including epoprostenol in FCIV) will reduce but much less so (as less patients are going to FCIV). Iloprost is more expensive than the oral therapies but results in a smaller QALY difference; patients on iloprost get to FCIV quicker than on oral therapies, but slightly less so than on supportive care. Therefore the price of epoprostenol has a significant impact on the cost of both the iloprost and supportive care arms. Thus, while the cost in both arms is reduced, there is little overall impact on the difference in cost.
In addition to the non-reference case analyses described and discussed above, further analyses were undertaken at the request of the NICE Appraisal Committee to explore various non-reference case scenarios. These included:
-
assuming that patients in FCIV (for both the active treatment and supportive care arms) receive supportive care only (without epoprostenol)
-
for the three oral treatments assuming the same mortality rates on treatment and on supportive care as those for epoprostenol in FCIII
-
for the three oral treatments exploring the minimal survival benefit (in terms of the odds ratio for the risk of death on treatment over the risk of death on supportive care) required to meet incremental cost-effectiveness thresholds of £20,000, £30,000 and £40,000 per QALY
-
assuming that no death occurs while patients stay in FCIII
-
assuming that patients on supportive care alone in FCIV receive only intermittent care as required for respite until death rather than hospitalisation until death
-
for the three oral treatments combining the above assumptions 1 and 2
-
for the three oral treatments combining the above assumptions 1, 2 and 5.
These additional analyses were carried out based on the reference case, with the specific assumption(s) altered in each scenario. Further descriptions of these additional analyses, their results and brief comments on the results are presented in Appendix 13.
Overall, these additional analyses further confirmed the crucial impact of the cost associated with epoprostenol use in FCIV on the cost-effectiveness of the oral treatments for FCIII patients. The assumption with regard to whether patients in FCIV on supportive care alone (without epoprostenol) are hospitalised until death or receive intermittent care has a very small impact on ICERs. Paradoxically, the analyses also suggested that survival benefits conferred by the oral treatments were inversely related to their cost-effectiveness in most instances (i.e. the greater the reduction in the odds of death on treatment compared with the odds of death on supportive care, the less cost-effective the treatment is). These results, while needing to be interpreted within the context and limitation of the model, are not unexpected: if a treatment reduces death in FCIII, more patients will live longer and eventually enter FCIV, which incurs substantial treatment costs that impact on the overall cost-effectiveness of the treatment. When the cost of epoprostenol in FCIV is taken out of the equation, however, the ICERs appear to be no longer sensitive to assumptions regarding survival benefits of the oral treatments according to the result of additional analysis 6.
Limitations and uncertainties associated with the choice of outcome measure, availability of data and model assumptions
The challenge in assessing the cost-effectiveness of the technologies for the treatment of PAH is well acknowledged for a number of reasons, but most notably because of the lack of appropriate data. The approach of using change in FC as the key outcome measure along with the need for making various assumptions and extrapolating short-term data are some practical solutions in the absence of better alternatives. These assumptions are explicitly stated and extensive sensitivity analyses have been carried out as described in the previous sections. There are additional limitations and uncertainties that may not be fully captured in the sensitivity analyses. These will be discussed below.
The transition probabilities for supportive care and the odds ratios for the relative treatment effects of individual drugs used in the model require data related to change of FC stratified by patients’ initial FC at the start of treatments. Despite the request from the assessment group to the companies for such data for all eligible trials, stratified data were not supplied for many trials. In some cases data were completely absent and various assumptions have to be made (such as using equal values for FCII to FCIII and FCIII to FCIV and for FCIV to FCIII and FCIII to FCII; and use of first cycle values for subsequent cycles). The direction of potential bias introduced by these assumptions is difficult to predict. In other cases data were available from only some, but not all of the trials that would have been included. This could also introduce bias towards the estimation of model parameters. For example, BREATHE-145 was not included in the estimation of pooled odds ratios for bosentan as FCIII data for the bosentan arms were not available for this trial. Given the high response rate for FC improvement in its placebo arm, inclusion of this trial would have reduced the pooled odds ratio for FC improvement with resultant less favourable ICERs.
While determining the transition probabilities of FC improvement/worsening for FCIII patients receiving supportive care alone (the comparator in the base case), data were sought from the control groups in the trials of the technologies under assessment. Separate data for FCIII and FCIV were not available for epoprostenol and data from a trial with a mixed FCIII and FCIV population was used instead. For the remaining four drugs, FC-specific data were available. Despite all being in FCIII at baseline, the proportion of patients who had their FC improved at 12 weeks varied widely between studies, from 5.6% (2/36) in the AIR study (iloprost)41 and 9.1% (1/11) in Channick et al. 43 (bosentan) to [Commercial-in-confidence information has been removed] in STRIDE-437 (sitaxentan) and 29.2% (19/65) in BREATHE-1 (bosentan). The differences may reflect the varied severity (within FCIII) of patient populations included in the trials, particularly between the epoprostenol and iloprost trials and the trials of the three oral treatments. The different mix of subcategories of PAH within each trial and the relatively small numbers upon which the proportions were based may also contribute to the apparent variation. However, it is likely that the exceptionally high responses observed in the BREATHE-1 and STRIDE-4 studies were partly attributable to the Hawthorne effect (patients who enter a trial perform better irrespective of treatment received because of increased attention/standard of care) and possibly misclassification of FC (into a more severe FC) at study screening so that patients could be entered into a trial. Data from these two trials were therefore not used in the calculation of transition probabilities for supportive care. Sensitivity analysis shows that the results are not sensitive to the response rate in the supportive care arm; rather, it is the odds ratio between treatment and comparator (supportive care) that is critical.
The model assumes that improvement in FC occurs only in the first cycle (12 weeks). In the industry submission by the manufacturer of sitaxentan, a ‘delayed first efficacy response beyond the 12-week study’ in the STRIDE-1X study was mentioned. Such phenomenon, however, did not appear to have been observed in subsequent sitaxentan long-term studies. Similarly, few patients who were classified as FCIII after 4 months of bosentan treatment subsequently improved to FCII during long-term follow-up. 104 The assumption that no FC improvement occurs beyond the first cycle therefore seems reasonable and was agreed by our clinical experts.
The model is based on the use of FC alone as the description of a patient’s current health state. Even with such a limited set of health states it has been difficult to populate the model with appropriate data for the transition probabilities within the model.
It would be highly desirable to use a more refined classification of health states. In a model-based cost–utility analysis it is desirable that the health states used are reasonable for both prognostic value and measurement of utility scores. Probably the most appropriate measure for this purpose would be to group patients into bands by 6MWD. This would, however, require the collection of appropriate data. Such data were not available to the assessment team; accordingly, any analysis based on such a model would be highly speculative in nature.
It should be noted that data such as mean improvement in walking distance or proportion improving from a varied starting point are of limited use for a realistic model. What would be needed for such a model is a longitudinal data set of sufficient size to allow a serious attempt to measure transition probabilities between states over an appropriately long period of time.
There is also the problem that the very short randomisation period of the trials has necessitated the assumption that treatment effects are preserved far beyond the timing of the trials.
For the above reasons the PSA is likely to have considerably underestimated the full uncertainty in the decision to be made. No attempt has been made to impose a correlation structure on the parameter distributions used in the model. Finally, any attempt at value of information analysis would lead to results that would not be meaningful.
Chapter 5 Assessment of factors relevant to the NHS and other parties
The technologies in this assessment report are already being widely used for the treatment of PAH in the NHS and are seen as key interventions in the process of stabilising the deterioration in patient health.
Designated specialist centres
Services for PAH are provided through the NCG designated centres. As most PAH patients are already seen at these centres, and the technologies of this assessment are already in use for PAH patients, there should be limited impact on the centres.
Primary care trusts
Apart from services for children, drug costs are not funded by the NCG services but locally by, for example, application to patients’ primary care trusts (PCTs). National guidance recommending the use of disinvestments from the technologies in this assessment will add clarity to this funding process.
There is some information to suggest that the concentration of PAH patients may be higher closer to the designated centres. Whether this is related to more ready identification of patients who live in the proximity of a centre or the fact that patients move to be closer to a centre is unclear. However, it could mean that a greater financial burden for funding PAH drug treatment occurs close to as opposed to distant from a centre.
National guidelines
A consensus statement on the management of pulmonary hypertension in the UK and Ireland has recently been published. 31 In addition, the ESC is in the process of updating their guidelines for publication in 2009. These guidelines are likely to have a wider scope and include drugs outside this technology appraisal. Although this technology assessment report aims to critically appraise and synthesise the best available evidence pertinent to the decision problems defined in Chapter 2 (see Decision problem), it is beyond the report’s remit to make any recommendations regarding treatment choices and service provisions for the technologies being assessed.
Disinvestment
A potential difficulty is that the five technologies of this assessment are currently being used within the NCG centers to treat PAH. If a decision is made not to recommend the use of one or more of the technologies then this disinvestment will need to be carefully managed. This is particularly important given the uncertainties around the clinical risk and the effects of withdrawal of the technologies on the patient.
Other interventions
Several other technologies targeted at modifying the PAH disease process are in development or are already available, but have yet to be licensed in the UK. Some of these are already being used in the designated PAH centres. To ensure equity these technologies, once licensed, may need to be assessed in updates to this assessment report. These technologies are likely to be included in the UK/EU guidelines being drawn up by expert groups.
Budget impact
The budget impact of each technology is difficult to accurately assess because of the absence of information on the number of PAH patients in England and Wales, the number in each FC, the numbers in each FC likely to be administered a given intervention, the doses given and also the fact that some of the fees associated with delivery of some of the interventions are commercially sensitive. However, accepting these uncertainties it is possible to indicate the magnitude of the annual impact for each technology for a range of patient population sizes. These are highlighted in Appendix 14 (Figures 142–144). The values presented do take drug (licensed doses) and administration costs into consideration, but not additional monitoring and underlying supportive care as these were considered to be of relatively minimal cost compared with the technologies.
The data on current English (including Welsh) usage of the technologies (see Chapter 1, Current usage of technologies in the NHS, and Appendix 1) were considered to represent the approximate total number of patients likely to receive epoprostenol, iloprost inhaled or an oral technology. Using this data the magnitude of the budgetary impacts for each technology per annum is:
-
[Commercial-in-confidence information has been removed]
Many patients are receiving treprostinil off licence at present, which may be reducing the number of patients on epoprostenol.
It should be remembered that for oral treatments the total pool of currently treated patients is approximately [Commercial-in-confidence information has been removed] and thus if all three oral technologies are utilised the total budget impact will be considerably less than the sum of the individual budgetary impacts above as most patients are receiving monotherapy and a smaller number dual and triple therapy.
Chapter 6 Discussion
Statement of principal findings
Clinical effectiveness
Overall quantity and quality of evidence
A total of 20 RCTs, most of good quality, were included in this assessment. The majority of them had a duration of 12–18 weeks and compared one of the technologies (intravenous epoprostenol, inhaled iloprost, bosentan, sitaxentan and sildenafil) added to supportive treatment with supportive treatment alone. Only a small number of trials compared the technologies against each other or investigated the use of combinations of these technologies.
Many of the trials included patient populations (in terms of FC and types of PAH) and doses that were outside the licensed indications of the technologies. Only very limited data examining specific types (subcategories) of PAH were available. Existing data do not suggest significant differences in treatment effects between subcategories of PAH, but studies are likely to be underpowered to detect clinically important differences.
Data stratified by FC were scant. Assessment of treatment effects stratified by FC could not be reliably conducted with the available evidence. This is particularly problematic when findings from the clinical effectiveness review were to be used to inform the economic modelling, which requires FC-specific data.
Monotherapy added to supportive treatment versus supportive treatment
All of the technologies, when added to supportive treatment at their licensed doses, have for the most part been shown to be more effective than supportive treatment alone in improving exercise capacity, symptoms of PAH and haemodynamic measures. The volume of evidence and patient populations included in the trials, however, varied between technologies.
The clinical effectiveness of intravenous epoprostenol (added to supportive treatment) compared with supportive treatment alone was demonstrated in open-label RCTs that included patients of mixed FC (mainly FCIII and FCIV). 11,33,39 Effectiveness has been shown in both patients with PPH11,39 and patients with scleroderma. 33
The clinical effectiveness of inhaled iloprost (added to supportive treatment) compared with supportive treatment alone was shown in a double-blind RCT41 that included patients of mixed FC (FCIII and FCIV) with mixed types of pulmonary hypertension including non-PAH. An additional open-label RCT36 also demonstrated effectiveness, but only for some of the measured outcomes.
The clinical effectiveness of bosentan (added to supportive treatment) compared with supportive treatment alone was demonstrated in double-blind RCTs43,45,47 that included patients predominantly of FCIII and in an additional sitaxentan RCT that included open-label bosentan. 48 The effectiveness of bosentan has been shown in mixed PAH populations of IPAH and CTD-APAH43,45 and in patients with PAH associated with Eisenmenger syndrome. 47
The clinical effectiveness of sitaxentan (added to supportive treatment) compared with supportive treatment alone was demonstrated in double-blind RCTs37,48,49 that included patients of mixed FC (predominantly FCII and FCIII) with mixed types of PAH including IPAH, CTD-APAH and PAH associated with CHD.
The clinical effectiveness of sildenafil (added to supportive treatment) compared with supportive treatment alone was demonstrated in a double-blind RCT53 that included patients of mixed FC (predominantly FCII and FCIII) with mixed types of PAH including IPAH, CTD-APAH and PAH associated with CHD. For sildenafil in particular there is more data for above licensed doses than for the licensed dose.
Direct comparison
Only two RCTs have directly compared the technologies against each other. The STRIDE-2 study48 compared sitaxentan with bosentan (both at licensed dose) for 18 weeks. The SERAPH study57 compared sildenafil (above licensed dose) with bosentan (licensed dose). No significant difference between the drugs was observed in any outcome in both trials. However, the sample size for SERAPH was small and there was an issue of differential blinding in STRIDE-2 (bosentan being the only open-label arm).
Combination therapy
Use of combinations of the technologies (including adding one to another) was investigated in four RCTs. 38,56,58,59 A double-blind RCT56 showed no benefit of using the combination of bosentan plus intravenous epoprostenol compared with intravenous epoprostenol alone in patients of mixed FC (FCIII and FCIV) with mixed types of PAH (IPAH, CTD-APAH).
One double-blind RCT41 showed that inhaled iloprost added to ongoing bosentan and supportive treatment was more effective than ongoing bosentan and supportive treatment in patients (mainly FCIII) with mixed types of PAH. However another open-label RCT58 that included patients of FCIII with IPAH failed to demonstrate this.
A further double-blinded RCT38 showed that sildenafil 80 mg three times daily (above licensed dose) added to ongoing epoprostenol and supportive care was more effective than ongoing epoprostenol and supportive care in patients of mixed FC (predominantly FCII and FCIII) with mixed types of PAH (IPAH and CTD-APAH).
Cost-effectiveness
None of the four published economic evaluations produced results that were generalisable to the NHS, as none were UK based, only one considered QALYs and only one compared the intervention with supportive care alone.
There was no consensus in the manufacturer submissions on the most appropriate model structure for the technology assessment, with variability seen in the type of economic evaluation, the methods used and the data sources. In addition, the same comparator was not used in all submissions and therefore they were not all addressing the same policy question.
The independent economic assessment demonstrated that all intervention therapies led to an improvement in QALYs, but the cost-effectiveness ratios varied considerably. The reference case analysis gave an ICER of £277,000 per QALY for intravenous epoprostenol with supportive care versus supportive care alone in FCIII and an ICER of £343,000 in FCIV. For FCIII only, the ICER was £101,000 per QALY for inhaled iloprost, £27,000 per QALY for bosentan and £25,000 per QALY for sitaxentan. Sildenafil with supportive care dominated supportive care alone (i.e. more effective and less costly). The analyses for iloprost, bosentan, sitaxentan and sildenafil were based on an assumption that all patients switch to intravenous epoprostenol upon deterioration to FCIV. Comparison between intervention therapies is not appropriate because of different target populations.
The reference case represents the full drug cost of epoprostenol. Sensitivity analyses were carried out using a reduced epoprostenol cost, which appears to be the price paid by the designated centres. The ICERs for the three oral treatments, but not for iloprost, were sensitive to the costs of epoprostenol. The lower the cost was for epoprostenol, the less favourable the ICERs were for bosentan and sitaxentan. Sildenafil no longer dominated supportive care when the cost for epoprostenol was lowered. These analyses suggest that the key driver of cost-effectiveness for the use of oral treatments in FCIII patients is the avoidance or delay of the high treatment costs that would be incurred when patients reach FCIV.
Because of the lack of stratified data to populate the model, and in some cases a complete absence of data, a number of assumptions had to be made and therefore bias may have been introduced by these assumptions. In addition, the data used for the model were from trials of short duration containing few patients. Therefore a longitudinal data set of a sufficient number of patients would be of great benefit to future modelling in this clinical condition.
Strengths and limitations of the assessment
Strengths of the assessment
-
This assessment strictly adhered to its remit and did not cover technologies outside the scope of the technology appraisal, but which are being used in clinical practice, such as subcutaneous treprostinil and intravenous iloprost. Nor did it include technologies under development such as ambrisentan. Furthermore this assessment only considered each technology within its licensed indication. Evidence in relation to the use of these technologies outside their current licensed indications such as treating patients with milder disease (FCII) was not assessed.
-
This assessment focused on evidence from RCTs, which were considered to be the most robust and the least subject to bias.
-
A comprehensive literature search was performed. Submissions from the manufacturer were scrutinised and several unpublished trials were included. Additional data were obtained from clinical study reports. The assessment is likely to be the most up-to-date and comprehensive compared with the existing literature.
-
Extensive reporting of the RCTs was undertaken and comprehensive analyses were carried out to highlight the mismatches between the licensed indications (the scope of the technology appraisal) and the available evidence.
-
There was considerable clinical input into the model.
-
Evidence from meta-analyses of RCTs (or individual RCTs when only one trial was available) was used to inform the parameters of the treatment effects in economic modelling.
-
Trials included in the assessment were of short duration. Long-term observational studies were not systematically reviewed because of time/resource constraints; however, data were sought from all such studies cited in manufacturer submissions to inform the economic evaluation. In part, clinicians often make treatment decisions based on available long-term data rather than solely on the RCTs. The duration of the trials may be too short to demonstrate some of the possible biologically plausible effects of the technologies on disease processes.
-
For both clinical effectiveness and cost-effectiveness considerable sensitivity analyses were undertaken.
Limitations of the assessment
-
Although the assessment group requested and had access to unpublished trial data, the provision of such data stratified by FC and PAH subcategory was voluntary. The assessment was therefore limited by what was made available to the assessment group.
-
This assessment report focused mainly on outcome measures for effectiveness. Only very limited outcomes related to safety were investigated as reporting of adverse events in the RCTs according to seriousness was relatively poor, and analysis of specific adverse events irrespective of seriousness was considered of little use in technology assessment given the seriousness of the disease itself.
-
The primary purpose of this report was to provide an independent evaluation of the evidence to inform the NICE technology appraisal. As such, the scope of this report has to be in keeping with the scope of the technology appraisal. It is therefore inappropriate for this report to consider issues that are beyond the scope of the technology appraisal, such as the use of drugs or doses not currently licensed.
Uncertainties
-
Whether the improvements in FC, exercise capacity and haemodynamic measures on treatment shown in the RCTs last beyond the duration of these trials, and whether these improvements translate into long-term benefits for survival and quality of life, remain uncertain. Although an increasing volume of evidence from observational studies supports the possibility of long-term benefits from the use of these technologies, the possibility of attenuation of treatment effect over time cannot be ruled out.
-
Because of the lack of data stratified by FC, several assumptions with regard to change in FC had to be made for both the technologies and the comparator (supportive care) in the economic model. These include assuming the same treatment effects (odds ratios) for patients in different FC in terms of FC improvement and deterioration, and assuming that the treatment effect in preventing FC deterioration (from FCIII to FCIV) was the same as the treatment effect in preventing death. These assumptions require further validation.
-
There is also considerable uncertainty with regard to whether the changes in FC sufficiently capture the overall impact of treatment on patients’ quality of life. FC is a very blunt and to an extent subjective tool.
-
The vast majority of the RCTs undertaken are placebo controlled and therefore unable to answer questions regarding which technologies are better. Thus, there is a need for head-to-head comparisons for patients in FCIII and in particular for the three oral technologies (bosentan, sitaxentan and sildenafil).
Generalisability
-
Most trials excluded patients with unstable conditions. The patients who are seen in clinical practice are likely to be sicker and more unstable than those included in the trials.
-
Finding the costs of the technologies (including associated services) for this assessment was not without difficulty. Variations in the costs between regions/centres inevitably affect the cost-effectiveness. Furthermore, the economic modelling suggested that the cost-effectiveness of the three oral treatments depends to some extent on the cost of epoprostenol. For example, as epoprostenol is the treatment of choice when patients deteriorate to FCIV, patients on less effective treatment (such as supportive care) will on average go on to epoprostenol earlier than those on more effective treatment (technologies). Thus, the time spent on epoprostenol will be different between the technologies and the total cost attributable to epoprostenol will be different between them. The unit cost of epoprostenol can therefore influence the ICER of compared treatments/technologies.
-
This assessment considers only the use of the technologies for intentional long-term treatment in PAH. It does not consider the use of the technologies for treatment in other specific circumstances, such as bridging treatment for those patients who are awaiting a heart/lung transplantation but deteriorating on other treatment(s).
Other relevant factors
-
Interpretation of results from RCTs needs to take into account the relatively small sample sizes and short duration of these studies, and differences in patient populations and comparator (supportive treatment) between trials and over time.
-
Indirect comparisons and mixed treatment comparisons between the five technologies were not undertaken. These were unlikely to produce any conclusive results given the amount of evidence currently available, and could be potentially inappropriate because of the differences in trial design and study population between the technologies, and their different places in the treatment pathway.
Chapter 7 Conclusions
All five of the technologies (intravenous epoprostenol, inhaled iloprost, bosentan, sitaxentan and sildenafil), when added to supportive treatment and used at the licensed dose(s), have been shown to be more effective than supportive treatment alone in RCTs that included patients of mixed FC with mixed types of PAH. The volume of evidence and patient populations included in the trials varied between the technologies. Current evidence does not allow adequate comparisons between the technologies nor for the use of combinations of the technologies.
Independent economic evaluation suggests that bosentan, sitaxentan and sildenafil may be cost-effective by standard thresholds and that iloprost and epoprostenol may not.
Implications for service provision
Given the uncertainties listed in Chapter 6 there is evidence from the clinical effectiveness and cost-effectiveness analysis that may be sufficiently robust to allow a decision to be made on whether to recommend the use or otherwise of each of the five technologies as an adjunct to supportive care (compared with supportive care alone). There is insufficient evidence because of the lack of head-to-head comparisons to undertake the same for the merits of one technology over another.
All five technologies are currently used in the NHS. As requests for funding for the technologies for adult patients are currently made on an individual patient basis to the respective PCT any recommendation about the use of the technologies will impact on this process; a positive recommendation should make positive funding decisions easier, and a negative recommendation the opposite.
There is insufficient evidence with regard to whether any of the treatments are more effective for specific subcategories of PAH and on the effectiveness of combinations of technologies, the benefits of which cannot be assumed without being adequately tested in RCTs.
The findings of the review of cost-effectiveness of these technologies may require further confirmation as substantial uncertainty exists because of the paucity of data and consequently the large number of assumptions that need to be made. In particular, the differential cost-effectiveness between the oral treatments needs to be confirmed as current analysis was not designed for comparison between the technologies. If confirmed the use of the most cost-effective oral treatment(s) could potentially reduce overall treatment costs to the NHS. On the other hand, if technologies that are not considered as cost-effective according to the generally accepted threshold are withdrawn it would have a substantial impact on patients who are currently treated with these technologies and would also raise ethical issues as it could be argued that there is no exchangeable alternative treatment available for patients who require these treatments after failing oral therapies. Furthermore, as the findings suggested that the cost-effectiveness of oral treatments is highly dependent upon the cost of epoprostenol, any changes in the cost and/or availability of epoprostenol and the licensing of new treatments that occupy a similar place in the treatment pathway (i.e. if cheaper treatments with similar effectiveness to epoprostenol were licensed for patients in FCIV) would have knock-on effects on the cost-effectiveness of the other technologies.
Suggested research priorities
Being a very rare disease there is only a very limited pool of patients with PAH that can be enrolled in trials. There are always going to be more research priorities than available numbers of patients to investigate them and this is always going to limit the power of any study. Furthermore, there is also going to be competition for patients for the investigation of even newer technologies than are included in this assessment. These issues need to be considered alongside the research priorities listed below:
-
Trials are required of the comparative effectiveness of the technologies. This seems most pressing for the three oral therapies (bosentan, sitaxentan and sildenafil) given their similar places in the treatment pathway and the possibility of differential clinical effectiveness/cost-effectiveness between them. Such trials would allow for direct clinical effectiveness and cost-effectiveness analyses.
-
Trials are required of mono- versus dual and triple therapy across all of the technologies. Some of these are already in progress.
-
Any future RCTs should ideally have a longer duration and measure clinically meaningful outcomes (see point below). The RCTs to date have been relatively short term, typically 12–18 weeks, and this is a relatively short period over which to measure any benefit on survival. However, recruitment to such trials with the possibility of patients receiving placebo may be difficult and raises ethical issues. Ethical issues should not be a problem though for well-designed head-to-head comparisons.
-
6MWT and other parameters routinely measured in the trials as the key end points have not been adequately evaluated and it is unclear how clinically meaningful any changes in them are. Further work is required in this area including the exploration and validation of existing and new end points
-
Trials should report data in a disaggregated manner. Many trials report only aggregate data for change in parameters, usually for the whole trial population and often for mixed FC. The availability of data collected at baseline and subsequent follow-ups (and data on changes from baseline to follow-ups) stratified by subpopulation of PAH and by FC or the availability of individual patient data would greatly help future analyses. Data in this format from existing trials were requested for this assessment report, but for the most part were not provided/available.
-
There is a great deal of variability between some of the existing trials with regard to improvement while receiving supportive care alone. Such variability needs to be explored to ascertain the underlying cause so that this can be fed into the design of future studies.
-
There is no information currently available on sequencing of technologies. Although probably a lower priority than the above this is still an important research question. Therefore, studies assessing the feasibility of replacing an ongoing treatment that failed to provide adequate control of the disease with a new treatment rather than adding the new treatment to the existing treatment are required.
-
In the absence of trials and prospective long-term controlled studies, data from well-run comprehensive national patient registries may be helpful in understanding further disease progression, the long-term response to treatment and survival.
Acknowledgements
The authors wish to thank the following: Linda Briscoe for invaluable administrative support; Professor Stirling Bryan and Lazaros Andronis for assisting with the review of industry dossiers; Dr Amanda Burls for advice at the early stages of the assessment; Dr Catherine Meads for advice on drafts of this manuscript; and our colleagues at NICE and the HTA programme for support and guidance.
This report was commissioned by the HTA programme as project number 05/24/06 on behalf of NICE. The views expressed in this report are those of the authors and not necessarily those of the HTA Programme. Any errors are the responsibility of the authors.
Contribution of authors
YFC was lead reviewer for the clinical effectiveness section of this report and also contributed to the discussion, conclusions and other sections. SJ reviewed existing economic evaluations and manufacturer submissions and undertook the independent economic evaluation along with PB. Both wrote and edited the economic sections of the report. KM contributed to the background section, identified clinical effectiveness data for the economic model from long-term studies and assisted in other areas of the clinical effectiveness section. CH acted as a methodological advisor and deputised for DM. SG and JPZ acted as clinical experts giving extensive advice and contributed to the drafting of the report. AFS devised and undertook all searches. JR undertook study selection (with YFC and DM) and assisted with data extraction for the clinical effectiveness sections. DM acted as project manager and senior reviewer on the report, wrote and edited sections of the report and takes responsibility for the overall content.
About the ‘home unit’
The West Midlands Health Technology Assessment Collaboration (WMHTAC) is an organisation involving several universities and academic groups who collaboratively undertake research synthesis to produce health technology assessments. Most of our members are based in the Public Health, Epidemiology and Biostatistics Unit, University of Birmingham; however, other members are drawn from a wide field of expertise including economists and mathematical modellers from the Health Economics Unit, University of Birmingham.
WMHTAC produces systematic reviews, health technology assessments and economic evaluations for NETSCC, HTA, NICE and the health service in the West Midlands. WMHTAC also undertakes methodological research on research synthesis and provides training in systematic reviews and health technology assessment.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Galiè N, Torbicki A, Barst R, Dartevelle P, Haworth S, Higenbottam T, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension: the Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 2004;25:2243-78.
- McLaughlin VV, Mcgoon MD. Pulmonary arterial hypertension. Circulation 2006;114:1417-31.
- Department of Health . Hospital Episode Statistics n.d. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937 (accessed 15 July 2007).
- Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Primary pulmonary hypertension: a national prospective study. Ann Intern Med 1987;107:216-23.
- D’Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Survival in patients with primary pulmonary hypertension: results from a national prospective registry. Ann Intern Med 1991;115:343-9.
- Peacock AJ, Murphy NF, McMurray JJC, Caballero L, Stewart S. An epidemiological study of pulmonary arterial hypertension in Scotland. Eur Respir J 2007;30:104-9.
- Mukerjee D, St George D, Coleiro B, Knight C, Denton CP, Davar J, et al. Prevalence and outcome in systemic sclerosis associated pulmonary arterial hypertension: application of a registry approach. Ann Rheum Dis 2003;62:1088-93.
- Kawut SM, Taichman DB, Archer-Chicko CL, Palevsky HI, Kimmel SE. Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest 2003;123:344-50.
- Archibald CJ, Auger WR, Fedullo PF, Channick RN, Kerr KM, Jamieson SW, et al. Long-term outcome after pulmonary thromboendarterectomy. Am J Respir Crit Care Med 1999;160:523-8.
- Gibbs JSR, Higenbottam TW. Recommendations on the management of pulmonary hypertension in clinical practice. Heart 2001;86:i1-13.
- Barst RJ, Rubin LJ, Long WA, Mcgoon MD, Rich S, Badesch DB, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. The Primary Pulmonary Hypertension Study Group. N Eng J Med 1996;334:296-302.
- Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med 2006;173:1023-30.
- Evans TW, Gatzoulis MA, Gibbs JSR. A national pulmonary hypertension service for England and Wales: an orphan disease is adopted?. Thorax 2002;57:471-2.
- American Thoracic Society . ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-17.
- Badesch DB, Bodin F, Channick RN, Frost A, Rainisio M, Robbins IM, et al. Complete results of the first randomized, placebo-controlled study of bosentan, a dual endothelin receptor antagonist, in pulmonary arterial hypertension. Curr Ther Res Clin Exp 2002;63:227-46.
- Hamilton N, Elliot C. Pulmonary hypertension – treatment options. Hosp Pharm 2006;13:10-4.
- Sitbon O, Humbert M, Jais X, Ioos V, Hamid AM, Provencher S, et al. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation 2005;111:3105-11.
- Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Eng J Med 2004;351.
- Rubin LJ, Badesch DB. Evaluation and management of the patient with pulmonary arterial hypertension. Ann Intern Med 2005;143:282-92.
- GlaxoSmithKline UK. Summary of Product Characteristics. Flolan Injection 1.5 Mg n.d. http://emc.medicines.org.uk/ (accessed 10 July 2007).
- Schering AG. Summary of Product Characteristics. Ventavis n.d. http://emc.medicines.org.uk (accessed 11 July 2007).
- Actelion Pharmaceuticals UK. Summary of Product Characteristics. Tracleer n.d. http://emc.medicines.org.uk/ (accessed 12 July 2007).
- Encysive (UK) Limited . Summary of Product Characteristics. Thelin n.d. www.emea.europa.eu/humandocs/PDFs/EPAR/thelin/H-679-PI-en.pdf (accessed 12 July 2007).
- Pfizer Ltd . Summary of Product Characteristics. Revatio n.d. http://emc.medicines.org.uk/ (accessed 13 July 2007).
- GlaxoSmithKline UK. Summary of Product Characteristics. Flolan Injection 0.5 Mg n.d. http://emc.medicines.org.uk/ (accessed 10 July 2007).
- British Medical Association and the Royal Pharmaceutical Society of Great Britain . British National Formulary 53 n.d. www.bnf.org (accessed 15 July 2007).
- US Food and Drug Administration . FDA Approves New Orphan Drug for Treatment of Pulmonary Arterial Hypertension n.d. www.fda.gov/bbs/topics/NEWS/2007/NEW01653.html (accessed 12 July 2007).
- European Medicines Agency . European Public Assessment Report (EPAR): Volibris. EPAR Summary for the Public n.d. http://www.europa.eu/humandocs/PDFs/EPAR/volibris/H-839-en1.pdf (accessed 30 April 2009).
- National Specialist Commissioning Advisory Group (NSCAG) . Pulmonary Hypertension (PH) Service for Adults n.d. www.advisorybodies.doh.gov.uk/NSCAG/services/pulmo-hypertension.htm (accessed 21 July 2007).
- Royal College of Physicians . Drugs for the Treatment of Pulmonary Arterial Hypertension 2007.
- National Pulmonary Hypertension Centres of the UK and Ireland . Consensus statement on the management of pulmonary hypertension in clinical practice in the UK and Ireland. Heart 2008;94:i1-4.
- Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 1992;45:769-73.
- Badesch DB, Tapson VF, Mcgoon MD, Brundage BH, Rubin LJ, Wigley FM, et al. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease. A randomized, controlled trial. Ann Intern Med 2000;132:425-34.
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J 2003;327:557-60.
- Bharani A, Mathew V, Sahu A, Lunia B. The efficacy and tolerability of sildenafil in patients with moderate-to-severe pulmonary hypertension. Indian Heart J 2003;55:55-9.
- Olschewski H, Hoper MM, Behr J, Ewert R, Meyer A, Borst M, et al. Long-Term Therapy With Inhaled Iloprost in Patients With Pulmonary Hypertension (AIR-2 study). A Randomized Controlled 3-Month Trial Followed by Open Label Long-Term Treatment n.d.
- Barst RJ. Sitaxsentan: a selective endothelin-A receptor antagonist, for the treatment of pulmonary arterial hypertension. Expert Opin Pharmacother 2007;8:95-109.
- Pfizer . PACES-1 Clinical Study Report (protocol A1481141) 2006.
- Rubin LJ, Mendoza J, Hood M, McGoon M, Barst R, Williams WB, et al. Treatment of primary pulmonary hypertension with continuous intravenous prostacyclin (epoprostenol). Results of a randomized trial. Ann Intern Med 1990;112:485-91.
- Hinderliter AL, Willis PW, Barst RJ, Rich S, Rubin LJ, Badesch DB, et al. Effects of long-term infusion of prostacyclin (epoprostenol) on echocardiographic measures of right ventricular structure and function in primary pulmonary hypertension. Primary Pulmonary Hypertension Study Group. Circulation 1997;95:1479-86.
- Olschewski H, Simonneau G, Galiè N, Higenbottam T, Naeije R, Rubin LJ, et al. Inhaled iloprost for severe pulmonary hypertension. N Eng J Med 2002;347:322-9.
- Ghofrani A. Positive outcome of the Aerosolized Iloprost Randomized study in primary and non-primary pulmonary hypertension (AIR study). J Anasthesie Intensivbehandlung 2002;9.
- Channick RN, Simonneau G, Sitbon O, Robbins IM, Frost A, Tapson VF, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet 2001;358:1119-23.
- Denton CP, Humbert M, Rubin L, Black CM. Bosentan treatment for pulmonary arterial hypertension related to connective tissue disease: a subgroup analysis of the pivotal clinical trials and their open-label extensions. Ann Rheum Dis 2006;65:1336-40.
- Rubin LJ, Badesch DB, Barst RJ, Galiè N, Black CM, Keogh A, et al. Bosentan therapy for pulmonary arterial hypertension [erratum appears in N Engl J Med 2002; 346: 1258]. N Eng J Med 2002;346:896-903.
- Galiè N, Hinderliter AL, Torbicki A, Fourme T, Simonneau G, Pulido T, et al. Effects of the oral endothelin-receptor antagonist bosentan on echocardiographic and doppler measures in patients with pulmonary arterial hypertension. J Am Coll Cardiol 2003;41:1380-6.
- Galiè N, Beghetti M, Gatzoulis MA, Granton J, Berger RM, Lauer A, et al. Bosentan therapy in patients with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation 2006;114:48-54.
- Barst RJ, Langleben D, Badesch D, Frost A, Lawrence EC, Shapiro S, et al. Treatment of pulmonary arterial hypertension with the selective endothelin-A receptor antagonist sitaxsentan. J Am Coll Cardiol 2006;47:2049-56.
- Barst RJ, Langleben D, Frost A, Horn EM, Oudiz R, Shapiro S, et al. Sitaxsentan therapy for pulmonary arterial hypertension. Am J Respir Crit Care Med 2004;169:441-7.
- Langleben D, Brock T, Dixon R, Barst R. STRIDE 1: effects of the selective ET receptor antagonist sitaxsentan sodium, in a patient population with pulmonary arterial hypertension that meets traditional inclusion criteria of previous pulmonary arterial hypertension trials. J Cardiovasc Pharmacol 2004;44:S80-84.
- Frost AE, Langleben D, Oudiz R, Hill N, Horn E, McLaughlin V, et al. The 6-min walk test (6MW) as an efficacy endpoint in pulmonary arterial hypertension clinical trials: demonstration of a ceiling effect. Vascul Pharmacol 2005;43:36-9.
- Pulido T, Kurzyna M, Souza R, Ramirez A, Sandoval J. STRIDE-4 investigators . Sitaxsentan 100 mg proves more effective than sitaxentan 50 mg in patients with pulmonary arterial hypertension (PAH). Proc Am Thorac Soc 2006;3.
- Galiè N, Ghofrani HA, Torbicki A, Barst RJ, Rubin LJ, Badesch D, et al. Sildenafil citrate therapy for pulmonary arterial hypertension [erratum appears in N Engl J Med 2006; 354: 2400– 1]. N Eng J Med 2005;353:2148-57.
- Sastry BK, Narasimhan C, Reddy NK, Raju BS. Clinical efficacy of sildenafil in primary pulmonary hypertension: a randomized, placebo-controlled, double-blind, crossover study. J Am Coll Cardiol 2004;43:1149-53.
- Singh TP, Rohit M, Grover A, Malhotra S, Vijayvergiya R. A randomized, placebo-controlled, double-blind, crossover study to evaluate the efficacy of oral sildenafil therapy in severe pulmonary artery hypertension. Am Heart J 2006;151:e1-5.
- Humbert M, Barst RJ, Robbins IM, Channick RN, Galiè N, Boonstra A, et al. Combination of bosentan with epoprostenol in pulmonary arterial hypertension: BREATHE-2. Eur Respir J 2004;24:353-9.
- Wilkins MR, Paul GA, Strange JW, Tunariu N, Gin-Sing W, Banya WA, et al. Sildenafil versus Endothelin Receptor Antagonist for Pulmonary Hypertension (SERAPH) study. Am J Respir Crit Care Med 2005;171:1292-7.
- Hoeper MM, Leuchte H, Halank M, Wilkens H, Meyer FJ, Seyfarth HJ, et al. Combining inhaled iloprost with bosentan in patients with idiopathic pulmonary arterial hypertension. Eur Respir J 2006;28:691-4.
- McLaughlin VV, Oudiz RJ, Frost A, Tapson VF, Murali S, Channick RN, et al. Randomized study of adding inhaled iloprost to existing bosentan in pulmonary arterial hypertension. Am J Respir Crit Care Med 2006;174:1257-63.
- Paramothayan NS, Lasserson TJ, Wells AU, Walters EH. Prostacyclin for pulmonary hypertension in adults [update of Cochrane Database Syst Rev 2003; 2:CD002994]. Cochrane Database Syst Rev 2005;2.
- Girgis RE, Frost AE, Hill NS, Horn EM, Langleben D, McLaughlin VV, et al. Selective endothelin A receptor antagonism with sitaxsentan for pulmonary arterial hypertension associated with connective tissue disease. Ann Rheum Dis 2007.
- Summary for patients . Sildenafil (Viagra) may help improve control of pulmonary hypertension. Ann Intern Med 2002;136.
- Macchia A, Marchioli R, Marfisi R, Scarano M, Levantesi G, Tavazzi L, et al. A meta-analysis of trials of pulmonary hypertension: a clinical condition looking for drugs and research methodology. Am Heart J 2007;153:1037-47.
- Pulmonary Hypertension Association UK . Impact Survey 2002 n.d. www.pha-uk.com/research.asp# (accessed 13 August 2007).
- McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation 2002;106:1477-82.
- Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Herve P, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol 2002;40:780-8.
- Barst RJ, McGoon M, McLaughlin V, Tapson V, Rich S, Rubin L, et al. Beraprost therapy for pulmonary arterial hypertension [erratum appears in J Am Coll Cardiol 2003; 42: 591]. J Am Coll Cardiol 2003;41:2119-25.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care 2005;21:240-5.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. Br Med J 1996;313:275-83.
- Einarson TR, Granton JT, Vicente C, Walker JH, Engel G, Iskedjian M. Cost-effectiveness of treprostinil versus epoprostenol in patients with pulmonary arterial hypertension: a Canadian analysis. Can Respir J 2005;12:419-25.
- Narine L, Hague LK, Walker JH, Vicente C, Schilz R, Desjardins O, et al. Cost-minimization analysis of treprostinil vs. epoprostenol as an alternate to oral therapy non-responders for the treatment of pulmonary arterial hypertension. Curr Med Res Opin 2005;21:2007-16.
- Highland KB, Strange C, Mazur J, Simpson KN. Treatment of pulmonary arterial hypertension: a preliminary decision analysis. Chest 2003;124:2087-92.
- Wlodarczyk JH, Cleland LG, Keogh AM, McNeil KD, Perl K, Weintraub RG, et al. Public funding of bosentan for the treatment of pulmonary artery hypertension in Australia: cost effectiveness and risk sharing. Pharmacoeconomics 2006;24:903-15.
- Keogh A, Wlodarczyk J. Idiopathic- and scleroderma-related pulmonary arterial hypertension: outcomes and QOL on bosentan. Expert Rev Pharmacoeconomics Outcomes Res 2004;4:505-13.
- Hoeper MM, Oudiz RJ, Peacock A, Tapson VF, Haworth SG, Frost AE, et al. End points and clinical trial designs in pulmonary arterial hypertension: clinical and regulatory perspectives. J Am Coll Cardiol 2004;43:48S-55S.
- Kirsch J MA. Establishing health state valuations for disease specific states: an example from heart disease. Health Econ 2000;9:149-58.
- Mikhail GW, Prasad SK, Li W, Rogers P, Chester AH, Bayne S, et al. Clinical and haemodynamic effects of sildenafil in pulmonary hypertension: acute and mid-term effects. Eur Heart J 2004;25:431-6.
- Taichman DB, Shin J, Hud L, Archer-Chicko C, Kaplan S, Sager JS, et al. Health-related quality of life in patients with pulmonary arterial hypertension. Respir Res 2005;6.
- Mereles D, Ehlken N, Kreuscher S, Ghofrani S, Hoeper MM, Halank M, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation 2006;114:1482-9.
- White J, Hopkins RO, Glissmeyer EW, Kitterman N, Elliott CG. Cognitive, emotional, and quality of life outcomes in patients with pulmonary arterial hypertension. Respir Res 2006;7.
- Chua R, Keogh AM, Byth K, O’Loughlin A. Comparison and validation of three measures of quality of life in patients with pulmonary hypertension. Intern Med J 2006;36:705-10.
- Cenedese E, Speich R, Dorschner L, Ulrich S, Maggiorini M, Jenni R, et al. Measurement of quality of life in pulmonary hypertension and its significance. Eur Respir J 2006;28:808-15.
- McKenna SP, Doughty N, Meads DM, Doward LC, Pepke-Zaba J. The Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR): a measure of health-related quality of life and quality of life for patients with pulmonary hypertension. Qual Life Res 2006;15:103-15.
- Keogh AM, McNeil KD, Wlodarczyk J, Gabbay E, Williams TJ. Quality of life in pulmonary arterial hypertension: improvement and maintenance with bosentan. J Heart Lung Transplant 2007;26:181-7.
- Sitbon O, Gressin V, Speich R, Macdonald PS, Opravil M, Cooper DA, et al. Bosentan for the treatment of human immunodeficiency virus-associated pulmonary arterial hypertension. Am J Respir Crit Care Med 2004;170:1212-17.
- Shafazand S, Goldstein MK, Doyle RL, Hlatky MA, Gould MK. Health-related quality of life in patient with pulmonary arterial hypertension. Chest 2004;126:1452-9.
- Groen H, van der Bijb W, Koëter GH, TenVergert EM. Cost effectiveness of lung transplantation in relation to type of end-stage pulmonary disease. Am J Transplant 2004;4:1155-62.
- Boquet EM, Prats VM, Merino AC, Marin MRPM, San MC. Estimate of the cost of the treatment of primary pulmonary hypertension with epoprostenol in continuous infusion. Impact of the commercial presentation. Farmacia E Clinica 1997;14:622-6.
- Cortijo CS, Garcia RM, Escobar RI, Herreros De Tejada YL-C. Analysis of the evolution in the treatment of pulmonary hypertension. Atencion Farmaceutica 2005;7:54-62.
- De Wet CJ, Affleck DG, Jacobsohn E, Avidan MS, Tymkew H, Hill LL, et al. Inhaled prostacyclin is safe, effective, and affordable in patients with pulmonary hypertension, right heart dysfunction, and refractory hypoxemia after cardiothoracic surgery. J Thorac Cardiovasc Surg 2004;127:1058-67.
- Petros AJ, Turner SC, Nunn AJ. Cost implications of using inhaled nitric oxide compared with epoprostenol for pulmonary hypertension. J Pharm Technol 1995;11:163-6.
- Anyanwu A, McGuire A, Rogers C, Murday A. An economic evaluation of lung transplantation. J Thorac Cardiovasc Surg 2002;123:411-20.
- Williams MH, Das C, Handler CE, Akram MR, Davar J, Denton CP, et al. Systemic sclerosis associated pulmonary hypertension: improved survival in the current era. Heart 2006;92:926-32.
- Meads DM, Doughty N, Pepke-Zaba J, . Validity and Responsiveness of the Cambridge Pulmonary Hypertension Outcome Review (CAMPHOR) Utility Index n.d.
- Benza RL, Barst RJ, Galie N, Frost A, Girgis RE, Highland KB, et al. Sitaxsentan for the treatment of pulmonary arterial hypertension. Chest 2008;134:775-82.
- Pfizer . SUPER-2 Clinical Study Report (protocol A1481142) 2007.
- Pfizer . SUPER-1 Clinical Study Report (protocol A1481140) 2004.
- Sitbon O, McLaughlin VV, Badesch DB, Barst RJ, Black C, Galiè N, et al. Survival in patients with class III idiopathic pulmonary arterial hypertension treated with first line oral bosentan compared with an historical cohort of patients started on intravenous epoprostenol. Thorax 2005;60:1025-30.
- Encysive (UK) . STRIDE-1X Clinical Study Report 2005.
- Encysive (UK) . STRIDE-2X Clinical Study Report 2005.
- Jowett S, Bryan S, Murray E, McCahon D, Raftery J, Hobbs F, et al. Patient self-management of anticoagulation therapy: a trial-based cost-effectiveness analysis. Br J Haematol 2006;134:632-9.
- Curtis L, Netten A. Unit costs of health and social care 2006. Canterbury: Personal Social Services Research Unit, University of Kent; 2006.
- Department of Health . NHS Reference Costs 2005 6 n.d. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4133221 (accessed 24 July 2007).
- Provencher S, Sitbon O, Humbert M, Cabrol S, Jais X, Simonneau G. Long-term outcome with first-line bosentan therapy in idiopathic pulmonary arterial hypertension. Eur Heart J 2006;27:589-95.
- Archer SL, Michelakis ED. An evidence-based approach to the management of pulmonary arterial hypertension. Curr Opin Cardiol 2006;21:385-92.
- Battistini B, Berthiaume N, Kelland NF, Webb DJ, Kohan DE. Profile of past and current clinical trials involving endothelin receptor antagonists: the novel ‘-sentan’ class of drug. Exp Biol Med 2006;231:653-95.
- Bell A, Davis M, Close F, Honeywell M, Branch IE. Sildenafil citrate (revatio) for the treatment of pulmonary arterial hypertension. P &Amp; T 2006;31:135-8.
- Benza RL, Mehta S, Keogh A, Lawrence EC, Oudiz RJ, Barst RJ, et al. Sitaxsentan treatment for patients with pulmonary arterial hypertension discontinuing bosentan. J Heart Lung Transplant 2007;26:63-9.
- Castro G. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomized placebo-controlled study. Rev Port Cardiol 2001;20:1151-2.
- Galiè N, Seeger W, Naeije R, Simonneau G, Rubin LJ. Comparative analysis of clinical trials and evidence-based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol 2004;43:81S-88S.
- Ghofrani HA, Wiedemann R, Rose F, Schermuly RT, Olschewski H, Weissmann N, et al. Sildenafil for treatment of lung fibrosis and pulmonary hypertension: a randomised controlled trial. Lancet 2002;360:895-900.
- Ghofrani HA, Wiedemann R, Rose F, Olschewski H, Schermuly RT, Weissmann N, et al. Combination therapy with oral sildenafil and inhaled iloprost for severe pulmonary hypertension. Ann Intern Med 2002;136:515-22.
- Goldsmith DR, Wagstaff AJ. Inhaled iloprost: in primary pulmonary hypertension. Drugs 2004;64:763-73.
- Hughes RJ, Jais X, Bonderman D, Suntharalingam J, Humbert M, Lang I, et al. The efficacy of bosentan in inoperable chronic thromboembolic pulmonary hypertension: a 1-year follow-up study. Eur Respir J 2006;28:138-43.
- McLaughlin VV, Sitbon O, Badesch DB, Barst RJ, Black C, Galiè N, et al. Survival with first-line bosentan in patients with primary pulmonary hypertension [erratum appears in Eur Respir J 2005; 25: 942]. Eur Respir J 2005;25:244-9.
- Oudiz RJ, Schilz RJ, Barst RJ, Galiè N, Rich S, Rubin LJ, et al. Treprostinil, a prostacyclin analogue, in pulmonary arterial hypertension associated with connective tissue disease. Chest 2004;126:420-7.
- Ricachinevsky CP, Amantea SL. Treatment of pulmonary arterial hypertension. J Pediatr (Rio J) 2006;82:S153-S165.
- Simonneau G, Barst RJ, Galiè N, Naeije R, Rich S, Bourge RC, et al. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension: a double-blind, randomized, placebo-controlled trial. Am J Respir Crit Care Med 2002;165:800-4.
- Voswinckel R, Enke B, Reichenberger F, Kohstall M, Kreckel A, Krick S, et al. Favorable effects of inhaled treprostinil in severe pulmonary hypertension: results from randomized controlled pilot studies. J Am Coll Cardiol 2006;48:1672-81.
- Kenyon KW, Nappi JM. Bosentan for the treatment of pulmonary arterial hypertension. Ann Pharmacother 2003;37:1055-62.
- Fung SM, Ferrill MJ. Treatment of pulmonary arterial hypertension with sildenafil. Hosp Pharm 2004;39:243-53.
- Kanthapillai P, Lasserson T, Walters E. Sildenafil for pulmonary hypertension. Cochrane Database Syst Rev 2004;4.
- Baker SE, Hockman RH. Inhaled iloprost in pulmonary arterial hypertension. Ann Pharmacother 2005;39:1265-74.
- Lee AJ, Chiao TB, Tsang MP. Sildenafil for pulmonary hypertension. Ann Pharmacother 2005;39:869-84.
- Liu C, Chen J. Endothelin receptor antagonists for pulmonary arterial hypertension [update of Cochrane Database Syst Rev 2005; 1:CD004434]. Cochrane Database Syst Rev 2006;3.
- Wittbrodt ET, Abubakar A. Sitaxsentan for treatment of pulmonary hypertension. Ann Pharmacother 2007;41:100-5.
- Barst RJ, Rubin LJ, Mcgoon MD, Caldwell EJ, Long WA, Levy PS. Survival in primary pulmonary hypertension with long-term continuous intravenous prostacyclin. Ann Intern Med 1994;121:409-15.
- Kuhn KP, Byrne DW, Arbogast PG, Doyle TP, Loyd JE, Robbins IM. Outcome in 91 consecutive patients with pulmonary arterial hypertension receiving epoprostenol. Am J Respir Crit Care Med 2003;167:580-6.
- Hoeper MM, Schwarze M, Ehlerding S, dler-Schuermeyer A, Spiekerkoetter E, Niedermeyer J, et al. Long-term treatment of primary pulmonary hypertension with aerosolized iloprost, a prostacyclin analogue. N Eng J Med 2000;342:1866-70.
- Sitbon O, Channick R, McLaughin VV. First-Line Bosentan in Pulmonary Arterial Hypertension: Survival and Prognostic Factors n.d.
- Langleben D, Hirsch AM, Shalit E, Lesenko L, Barst RJ, Langleben D, et al. Sustained symptomatic, functional, and hemodynamic benefit with the selective endothelin-A receptor antagonist, sitaxsentan, in patients with pulmonary arterial hypertension: a 1-year follow-up study. Chest 2004;126:1377-81.
- Pfizer . PACES-2 Clinical Study Report 2006.
- Shapiro SM, Oudiz RJ, Cao T, Romano MA, Beckmann XJ, Georgiou D, et al. Primary pulmonary hypertension: improved long-term effects and survival with continuous intravenous epoprostenol infusion. J Am Coll Cardiol 1997;30:343-9.
- McLaughlin VV, Genthner DE, Panella MM, Rich S. Reduction in pulmonary vascular resistance with long-term epoprostenol (prostacyclin) therapy in primary pulmonary hypertension. N Eng J Med 1998;338:273-7.
- Opitz CF, Wensel R, Winkler J, Halank M, Bruch L, Kleber F-X, et al. Clinical efficacy and survival with first-line inhaled iloprost therapy in patients with idiopathic pulmonary arterial hypertension. Eur Heart J 2005;26:1895-902.
- Schering Health Care . Inhaled Iloprost Trometamol (Ventavis®) for the Treatment of Primary Pulmonary Hypertension 2007.
- Nikkho S, Seeger W, Baumgartner R, Behr J, Borst M, Ewert R, et al. One-year observation of iloprost inhalation therapy in patients with pulmonary hypertension. Eur Respir J 2001;18.
- Nikkho S, Seeger W, Behr J, Borst M, Ewert R, Ghofrani A, et al. Two-Year Survival in Patients With Pulmonary Hypertension Inhaling Iloprost [Abstract] n.d.
- Olschewski H, Nikkho S, Behr J, Borst M, Ewert R, Höper M, et al. Long-term survival in patients with pulmonary hypertension inhaling iloprost. Eur Heart J 2003;24.
- Olschewski H, Hoeper MM, Behr J, Borst M, Ewert R, Hetzer R, et al. Safety, Dosing, and Clinical Benefit of 2-Year Therapy With Inhaled Iloprost [Abstract] n.d.
- Sitbon O, Badesch DB, Channick RN, Frost A, Robbins IM, Simonneau G, et al. Effects of the dual endothelin receptor antagonist bosentan in patients with pulmonary arterial hypertension: a 1-year follow-up study. Chest 2003;124:247-54.
- Gatzoulis MA, Beghetti M, Galie N, Granton J, Berger R, Lauer A, et al. Bosentan shows persistent benefit in functional class and exercise capacity amongst Eisenmenger patients in the BREATHE-5 open label extension study. Eur Heart J 2006;27.
- Denton CP, Pope JE, Peter HH, Gabriellli A, Boonstra A, Van Den Hoogen FHJ, et al. Long-term effects of bosentan on quality of life, survival, safety and tolerability in pulmonary arterial hypertension related to connective tissue diseases. Ann Rheum Dis 2007.
Appendix 1 National Pulmonary Hypertension Service census. Distribution of patients and current UK usage of the technologies
Current usage data are taken from the National Pulmonary Hypertension Service census submitted as part of the submission for this technology appraisal by the Royal College of Physicians. 30 The data in this census are confidential. The census provides data on year-on-year numbers of patients under the care of the service centres and utilisation of the technologies. The census covers all types of pulmonary hypertension not only PAH and therefore figures may be greater than those for the PAH population. Conversely, not all PAH patients may be being seen at a designated centre. Further details about the designated centres can be found in Chapter 1 (see Current usage of technologies in the NHS).
Figure 16 details the total number of patients seen at designated pulmonary hypertension centres in England and Scotland by year since 2004.
Key summary data (Table 64) and data on mono-, dual and triple therapy utilisation by adults and children in England and Scotland (Tables 65–67 respectively) are selectively reproduced below for the year 2006–7.
FIGURE 16.
Total numbers of patients under the care of the National Pulmonary Hypertension Service. Data from [Academic-in-confidence information has been removed] UK centres. [Academic-in-confidence information has been removed]. Data was collected to the 31 March each year and excluded patients who had been discharged, died or not been seen since 1 April of the previous year. [Academic-in-confidence information has been removed].
| Summary data | English patientsa | Scottish patients | UK children | Total UK patientsa |
|---|---|---|---|---|
| Patients attending the National Pulmonary Hypertension Service | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Patients on disease-targeted monotherapy | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Patients on disease-targeted dual/triple therapy | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Patients on any disease-targeted therapy | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Transplants | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Name of therapy | English patientsa | Scottish patients | UK children | Total UK patients |
|---|---|---|---|---|
| Epoprostenol (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Treprostinil (s.c.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Treprostinil (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Iloprost (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Iloprost (nebulised) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sildenafil | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Trial drugb | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Total | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Name of therapy | Total English patientsa | Total Scottish patients | UK children | Total UK patientsa |
|---|---|---|---|---|
| Bosentan and sildenafil | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan and sildenafil | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan + iloprost (i.v. or nebuliser) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sildenafil + iloprost (i.v. or nebuliser) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sildenafil + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sildenafil + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Trial drugb | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Total | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Name of therapy | English patientsa | Scottish patients | UK children | Total UK patientsa |
|---|---|---|---|---|
| Bosentan + sildenafil + epoprostenol (i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan + sildenafil + iloprost (i.v. or nebuliser) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Bosentan + sildenafil + treprostinil (s.c. or i.v.) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Treprostinil (s.c.) + bosentan + sildenafil + iloprost (nebuliser) | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Total | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
Appendix 2 Literature search strategies
Appendix 2.1 Clinical effectiveness searches
Source – Ovid MEDLINE(R), 1950 to February Week 2 2007
-
hypertension pulmonary/(15980)
-
pah.mp. (6334)
-
pulmonary hypertension.mp. (15783)
-
pulmonary arterial hypertension.mp. (1610)
-
pulmonary artery hypertension.mp. (459)
-
or/1–5 (27823)
-
(epoprostenol or flolan or prostacyclin).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (15446)
-
(iloprost or ventavis).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1817)
-
(bosentan or tracleer).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1012)
-
(sitaxentan or thelin).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (7)
-
(sildenafil or revatio).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (2706)
-
or/7–11 (19556)
-
6 and 12 (1582)
-
randomized controlled trial.pt. (229118)
-
controlled clinical trial.pt. (74075)
-
randomized controlled trials.sh. (46851)
-
random allocation.sh. (56772)
-
double blind method.sh. (89402)
-
single blind method.sh. (10586)
-
or/14–19 (388897)
-
(animals not human).sh. (3987213)
-
20 not 21 (356739)
-
clinical trial.pt. (431735)
-
exp clinical trials/(186384)
-
(clin$adj25 trial$).ti,ab. (125601)
-
((singl$or doubl$or trebl$or tripl$) adj25 (blind$or mask$)).ti,ab. (88641)
-
placebo$.ti,ab. (99696)
-
random$.ti,ab. (359511)
-
placebos.sh. (25756)
-
research design.sh. (45986)
-
or/23–30 (823215)
-
31 not 21 (723790)
-
32 not 22 (382729)
-
22 or 33 (739468)
-
13 and 34 (329)
Source – Ovid MEDLINE(R), 1950 to February Week 2 2007
Additional search to account for alternative spelling of sitaxentan/sitaxsentan.
-
hypertension pulmonary/(16015)
-
pah.mp. (6358)
-
pulmonary hypertension.mp. (15802)
-
pulmonary arterial hypertension.mp. (1630)
-
pulmonary artery hypertension.mp. (460)
-
or/1–5 (27871)
-
sitaxsentan.mp. (48)
-
6 and 7 (32)
-
randomized controlled trial.pt. (229481)
-
controlled clinical trial.pt. (74116)
-
randomized controlled trials.sh. (46944)
-
random allocation.sh. (56812)
-
double blind method.sh. (89516)
-
single blind method.sh. (10609)
-
or/9–14 (389441)
-
(animals not human).sh. (3990282)
-
15 not 16 (357227)
-
clinical trial.pt. (431918)
-
exp clinical trials/(186631)
-
(clin$adj25 trial$).ti,ab. (125889)
-
((singl$or doubl$or trebl$or tripl$) adj25 (blind$or mask$)).ti,ab. (88764)
-
placebo$.ti,ab. (99860)
-
random$.ti,ab. (360222)
-
placebos.sh. (25762)
-
research design.sh. (46062)
-
or/18–25 (824452)
-
26 not 16 (724876)
-
27 not 17 (383417)
-
17 or 28 (740644)
-
8 and 29 (23)
Source – EMBASE (Ovid), 1980 to 2007 Week 8
-
(epoprostenol or flolan or prostacyclin).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (19059)
-
(iloprost or ventavis).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (3222)
-
(bosentan or tracleer).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (2059)
-
(sitaxentan or thelin).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (20)
-
(sildenafil or revatio).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (5736)
-
or/1–5 (26908)
-
pah.mp. (7544)
-
pulmonary hypertension.mp. (18439)
-
pulmonary arterial hypertension.mp. (1394)
-
pulmonary artery hypertension.mp. (373)
-
pulmonary hypertension/(16068)
-
or/7–11 (25738)
-
6 and 12 (2854)
-
randomized controlled trial/(114078)
-
exp clinical trial/(422654)
-
exp controlled study/(2359146)
-
double blind procedure/(62924)
-
randomization/(21582)
-
placebo/(94966)
-
single blind procedure/(6391)
-
(control$adj (trial$or stud$or evaluation$or experiment$)).mp. (2398474)
-
((singl$or doubl$or trebl$or tripl$) adj5 (blind$or mask$)).mp. (105032)
-
(placebo$or matched communities or matched schools or matched populations).mp. (143199)
-
(comparison group$or control group$).mp. (141821)
-
(clinical trial$or random$).mp. (675397)
-
(quasiexperimental or quasi experimental or pseudo experimental).mp. (1498)
-
matched pairs.mp. (1904)
-
or/14–27 (2810149)
-
13 and 28 (1306)
-
limit 29 to human (1158)
Source – EMBASE (Ovid), 1980 to 2007 Week 8
Additional search to account for alternative spelling of sitaxentan/sitaxsentan.
-
pah.mp. (7569)
-
pulmonary hypertension.mp. (18495)
-
pulmonary arterial hypertension.mp. (1408)
-
pulmonary artery hypertension.mp. (375)
-
pulmonary hypertension/(16121)
-
or/1–5 (25814)
-
sitaxsentan.mp. (289)
-
6 and 7 (240)
-
randomized controlled trial/(114430)
-
exp clinical trial/(423797)
-
exp controlled study/(2365454)
-
double blind procedure/(62995)
-
randomization/(21692)
-
placebo/(95340)
-
single blind procedure/(6412)
-
(control$adj (trial$or stud$or evaluation$or experiment$)).mp. (2404868)
-
((singl$or doubl$or trebl$or tripl$) adj5 (blind$or mask$)).mp. (105168)
-
(placebo$or matched communities or matched schools or matched populations).mp. (143619)
-
(comparison group$or control group$).mp. (142366)
-
(clinical trial$or random$).mp. (677217)
-
(quasiexperimental or quasi experimental or pseudo experimental).mp. (1502)
-
matched pairs.mp. (1910)
-
or/9–22 (2817435)
-
8 and 23 (196)
Cochrane Library (CENTRAL), 2007 Issue 1
-
#1 pulmonary next arterial next hypertension 83
-
#2 pah 147
-
#3 pulmonary next hypertension 516
-
#4 pulmonary next artery next hypertension 15
-
#5 MeSH descriptor Hypertension, Pulmonary, this term only 264
-
#6 (#1 OR #2 OR #3 OR #4 OR #5) 714
-
#7 epoprostenol or prostacyclin or flolan 898
-
#8 iloprost or ventavis 223
-
#9 bosentan or tracleer 57
-
#10 sitaxentan or thelin or sitaxsentan 25
-
#11 sildenafil or revatio 398
-
#12 (#7 OR #8 OR #9 OR #10 OR #11) 1450
-
#13 (#6 AND #12) 137
Source – Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, 27 February 2007
-
pah.mp. (392)
-
pulmonary hypertension.mp. (364)
-
pulmonary arterial hypertension.mp. (109)
-
pulmonary artery hypertension.mp. (19)
-
or/1–4 (776)
-
(epoprostenol or flolan or prostacyclin).mp. (142)
-
(iloprost or ventavis).mp. (25)
-
(bosentan or tracleer).mp. (56)
-
(sitaxentan or thelin).mp. (1)
-
(sildenafil or revatio).mp. (169)
-
or/6–10 (342)
-
5 and 11 (93)
Source – Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, 27 February 2007
-
Additional search to account for alternative spelling of sitaxentan/sitaxsentan.
-
pah.mp. (368)
-
pulmonary hypertension.mp. (357)
-
pulmonary arterial hypertension.mp. (99)
-
pulmonary artery hypertension.mp. (20)
-
sitaxsentan.mp. (8)
-
or/1–4 (748)
-
5 and 6 (6)
Appendix 2.2 Economic evaluation searches
Source – Ovid MEDLINE(R), 1950 to February Week 3 2007
-
hypertension pulmonary/(16015)
-
pah.mp. (6358)
-
pulmonary hypertension.mp. (15802)
-
pulmonary arterial hypertension.mp. (1630)
-
pulmonary artery hypertension.mp. (460)
-
or/1–5 (27871)
-
(epoprostenol or flolan or prostacyclin).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (15459)
-
(iloprost or ventavis).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1821)
-
(bosentan or tracleer).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (1029)
-
(sitaxentan or sitaxsentan or thelin).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (55)
-
(sildenafil or revatio).mp. [mp=title, original title, abstract, name of substance word, subject heading word] (2720)
-
or/7–11 (19615)
-
6 and 12 (1620)
-
economics/(24681)
-
exp “costs and cost analysis”/(126798)
-
cost of illness/(8780)
-
exp health care costs/(27787)
-
economic value of life/(4800)
-
exp economics medical/(11276)
-
exp economics hospital/(14542)
-
economics pharmaceutical/(1717)
-
exp “fees and charges”/(22697)
-
(econom$or cost or costs or costly or costing or price or pricing or pharmacoeconomic$).tw. (238018)
-
(expenditure$not energy).tw. (10144)
-
(value adj1 money).tw. (10)
-
budget$.tw. (10446)
-
or/14–26 (349667)
-
13 and 27 (38)
-
quality of life/(57413)
-
life style/(25231)
-
health status/(32068)
-
health status indicators/(10696)
-
value of life/(4800)
-
quality adjusted life.mp. (3745)
-
or/29–34 (120619)
-
6 and 35 (116)
Source – Cochrane Library (DARE and NHS EED), 2007 Issue 1
See above Cochrane Library clinical effectiveness search strategy.
Source – HEED, February 2007
Search terms: epoprostenol or flolan or prostacyclin; iloprost or ventavis; bosentan or tracleer sitaxentan or sitaxsentan or thelin; sildenafil or revatio. References were selected when they also included the terms pulmonary artery hypertension or pulmonary hypertension.
Source – EMBASE (Ovid), 1980 to 2007 Week 9
-
(epoprostenol or flolan or prostacyclin).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (19083)
-
(iloprost or ventavis).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (3235)
-
(bosentan or tracleer).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (2072)
-
(sitaxentan or sitaxsentan or thelin).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (292)
-
(sildenafil or revatio).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (5764)
-
or/1–5 (27002)
-
pah.mp. (7569)
-
pulmonary hypertension.mp. (18495)
-
pulmonary arterial hypertension.mp. (1408)
-
pulmonary artery hypertension.mp. (375)
-
pulmonary hypertension/(16121)
-
or/7–11 (25814)
-
6 and 12 (2890)
-
cost benefit analysis/(25543)
-
cost effectiveness analysis/(47494)
-
cost minimization analysis/(1092)
-
cost utility analysis/(1869)
-
economic evaluation/(3519)
-
(cost or costs or costed or costly or costing).tw. (143239)
-
(economic$or pharmacoeconomic$or price$or pricing).tw. (68823)
-
(technology adj assessment$).tw. (1319)
-
or/14–21 (218757)
-
13 and 22 (69)
-
“quality of life”/or quality adjusted life year/(74702)
-
health status/(30678)
-
health status indicator$.mp. (127)
-
or/24–26 (100428)
-
12 and 27 (317)
-
23 or 28 (372)
Source – CINAHL (EBSCO), 1982 to February 2007
S1 TX (epoprostenol OR flolan OR prostacyclin) AND DE Hypertension, pulmonary, drug therapy
S2 TX (iloprost OR ventavis) AND DE Hypertension, pulmonary, drug therapy
S3 TX (bosentan OR tracleer) AND DE Hypertension, pulmonary, drug therapy
S4 TX (sitaxentan OR sitaxsentan OR thelin) AND DE Hypertension, pulmonary, drug therapy
S5 TX (sildenafil OR revation) AND DE Hypertension, pulmonary, drug therapy
S6 S1 OR S2 OR S3 OR S4 OR S5
Appendix 2.3 Ongoing studies
Source – National Research Register, 2007 Issue 1
See above Cochrane Library clinical effectiveness search strategy
Sources – Current Controlled Trials and ClinicalTrials.gov
Search terms: epoprostenol or flolan or prostacyclin; iloprost or ventavis; bosentan or tracleer sitaxentan or sitaxsentan or thelin; sildenafil or revatio. References were selected when they also included the terms pulmonary artery hypertension or pulmonary hypertension.
Appendix 3 Table of excluded studies with rationale
| Study | Inclusion criteria not met/reasons for exclusion |
|---|---|
| Archer 2006105 | Study design/narrative review |
| Battistini 2006106 | Study design/narrative review |
| Bell 2006107 | Study design/narrative review |
| Benza 2007108 | Comparator/comparison of two doses of sitaxentan without placebo or other active control |
| Castro 2001109 | Study design/Spanish commentary on Channick 200143 |
| Galiè 2004110 | Study design/narrative review |
| Ghofrani 2002111 | Study design/< 1 week duration |
| Ghofrani 2002112 | Study design/< 1 week duration |
| Goldsmith 2004113 | Study design/narrative review |
| Hughes 2006114 | Study design/uncontrolled study |
| Keogh 200784 | Study design/uncontrolled study |
| McLaughlin 2005115 | Comparator/comparison of survival data from RCT with predicted survival using mathematical equation |
| Oudiz 2004116 | Intervention/treprostinil not included in this review |
| Ricachinevsky 2006117 | Population/review of treatment of PAH in children |
| Simonneau 2002118 | Intervention/treprostinil not included in this review |
| Voswinckel 2006119 | Intervention/treprostinil not included in this review |
Appendix 4 Included systematic reviews
Systematic reviews included in this assessment were utilised to identify relevant RCTs and for background information. A list of these reviews is presented in Table 69.
| Study | Description |
|---|---|
| Kenyon 2003120 | Bosentan for the treatment of PAH |
| Fung 2004121 | Sildenafil for the treatment of PAH |
| Kanthapillai 2004122 | Sildenafil for pulmonary hypertension (Cochrane review) |
| Baker 2005123 | Inhaled iloprost in PAH |
| Lee 2005124 | Sildenafil for pulmonary hypertension |
| Paramothayan 200560 | Prostacyclin for pulmonary hypertension in adults (Cochrane review) |
| Liu 2006125 | Endothelin receptor antagonists for PAH (Cochrane review) |
| Wittbrodt 2007126 | Sitaxentan for treatment of pulmonary hypertension |
Appendix 5 Extracted data from included randomised controlled trials for outcomes included in meta-analysis
| Death | Clinical worsening | Withdrawal for any reason | Change in functional class | SAEs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n/N | Life table estimates: proportion died (95% CI) | n/N | Life table estimates: proportion worsened (95% CI) | n/N | N | Improved | Unchanged | Worsened | n/N | |
| Epoprostenol | ||||||||||
| Rubin 1990,39 8 weeks | ||||||||||
| Control | 3/12 | NR | NR | NR | NR | 9 | 2 | NR | NR | NR |
| Epoprostenol | 1/11 | NR | NR | NR | NR | 10 | 10 | 0 | 0 | NR |
| Barst 1996,11 12 weeks | ||||||||||
| Control | 8/40 | 0.2a | NR | NR | 10b/40 | 31 | 1 | 27 | 3 | NR |
| Epoprostenol | 0/41 | 0 | NR | NR | 3b/41 | 40 | 16 | 19 | 5 | NR |
| ITT population (used in analysis) assuming worsening FC for patients who died or who had transplantation: | ||||||||||
| Control | NR | NR | NR | NR | NR | 40 | 1 | 27 | 12 | NR |
| Epoprostenol | NR | NR | NR | NR | NR | 41 | 16 | 19 | 6 | NR |
| Badesch 2000,33 12 weeks | ||||||||||
| Control | 5/55 | NR | NR | NR | NR | 55 | 0 | NR | NR | NR |
| Epoprostenol | 4/56 | NR | NR | NR | NR | 56 | 21 | NR | NR | NR |
| Iloprost | ||||||||||
| AIR-1/Olschewski 2002,41 12 weeks | ||||||||||
| Placebo | 4/102 | NR | 12/102c | NR | 14/102 | 92 | 13 | 67 | 12d | 25/102 |
| Iloprost | 1/101 | NR | 5/101c | NR | 4/101 | 97 | 25 | 65 | 7d | 28/101 |
| PPH, all FC: | ||||||||||
| Placebo | 2/55 | NR | NR | NR | 7/55 | 50 | 4 | 38 | 8e | NR |
| Iloprost | 1/53 | NR | NR | NR | 2/53 | 51 | 13 | 35 | 3e | NR |
| PPH, FC III (from industry submission): | ||||||||||
| Placebo | NR | NR | NR | NR | NR | 36 | 2 | 25 | 9 | NR |
| Iloprost | NR | NR | NR | NR | NR | 34 | 7 | 24 | 3 | NR |
| AIR-2/Olschewski,36 12 weeks [data from industry submission or unpublished manuscript (academic-in-confidence)] | ||||||||||
| Control | 2f/33 | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 2/33g | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 7/33 |
| Iloprost | 2/30 | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 6/30g | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 8h/30 |
| COMBI/Hoeper 2006,58 12 weeks | ||||||||||
| Ongoing bosentan | 0/21 | Not applicable | 4/21 | NR | 0/21 | NR | NR | NR | NR | NR |
| Iloprost + ongoing bosentan | 0/19 | Not applicable | 3/19 | NR | 1i/19 | NR | NR | NR | NR | NR |
| STEP/McLaughlin 2006,59 12 weeks | ||||||||||
| Placebo + ongoing bosentan | 0/33 | Not applicable | 5/33 | 0.16a | 5/33 | 33 | 2 | 30 | 1 | 7/32 |
| Iloprost + ongoing bosentan | 0/34 | Not applicable | 0/32 | 0 | 4/34 | 31 | 11 | 20 | 0 | 5/35 |
| IPAH only, mixed FC: | ||||||||||
| Placebo + ongoing bosentan | 0/20 | Not applicable | NR | NR | NR | 20 | 1 | NR | NR | NR |
| Iloprost + ongoing bosentan | 0/17 | Not applicable | NR | NR | NR | 16 | 6 | NR | NR | NR |
| Bosentan | ||||||||||
| Channick et al., 2001,43 12 weeks | ||||||||||
| Placebo | 0/11 | Not applicable | 3/11 | NR | 2/11 | 11 | 1 | 8 | 2 | NR |
| Bosentan 125 mg b.d. | 0/21 | Not applicable | 0/21 | NR | 0/21 | 21 | 9 | 12 | 0 | NR |
| BREATHE-1/Rubin 2002,45 16 weeks | ||||||||||
| Placebo | 2/69 | NR | 14/69 | 0.15a | NR | 69 | 21 | NR | NR | NR |
| Bosentan 125 mg b.d. | 1/74 | NR | 5/74 | 0.06a | NR | 74 | }60j | NR | NR | NR |
| Bosentan 250 mg b.d. | 0 (3?)/70 | NR | 4/70 | 0.06a | NR | 70 | NR | NR | NR | |
| BREATHE-2/Humbert 2004,56 16 weeks | ||||||||||
| Placebo + epoprostenol | 0/11 | NR | NR | NR | 1/11 | 11 | 5 | NR | NR | NR |
| Bosentan + epoprostenol | 2 (3?)/22 | NR | NR | NR | 4/22 | 22 | 13 | NR | NR | NR |
| BREATHE-5/Galiè 2006,47 16 weeks | ||||||||||
| Placebo | 0/17 | Not applicable | NR | NR | 2/17 | 17 | 2 | 14 | 1 | 3/17 |
| Bosentan 125 mg b.d. | 0/37 | Not applicable | NR | NR | 2/37 | 37 | 13 | 23 | 1 | 5/37 |
| Sitaxentan | ||||||||||
| STRIDE-1/Barst 2004,49 12 weeks | ||||||||||
| Placebo | 0/60 | NR | 3/60 | Proportion with no event: [Academic-in-confidence information has been removed] | 5/60 | 60 | 9 | 47 | 4 | 9/59 |
| Sitaxentan 100 mg o.d. | 0/55 | NR | 0/55 | [Academic-in-confidence information has been removed] | 0/55 | 55 | 16 | 39 | 0 | 3/56 |
| Sitaxentan 300 mg o.d. | 1/63 | NR | 1/63 | [Academic-in-confidence information has been removed] | 7/63 | 63 | 19 | 43 | 1 | 10/63 |
| IPAH, mixed FC:61 | ||||||||||
| Placebo | NR | NR | NR | NR | NR | 37 | 6 | 28 | 3 | NR |
| Sitaxentan 100 mg and 300 mg | NR | NR | NR | NR | NR | 55 | 18 | 36 | 1 | NR |
| CTD-APAH, mixed FC:61 | ||||||||||
| Placebo | NR | NR | NR | NR | NR | 9 | 1 | 7 | 1 | NR |
| Sitaxentan 100 mg and 300 mg | NR | NR | NR | NR | NR | 33 | 8 | 25 | 0 | NR |
| STRIDE-2/Barst 2006,48 18 weeks | ||||||||||
| Placebo | 2/62 | NR | 10/62 | NR | 11/62 | [Academic-in-confidence information has been removed] | 6 | [Academic-in-confidence information has been removed] | 8 | 19/62 |
| Bosentan 125 mg b.d. | 0/60 | NR | 9/60 | p = 0.80 vs placebo | 8/60 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 5 | [Academic-in-confidence information has been removed] |
| Sitaxentan 50 mg o.d. | 0/62 | NR | 6/62 | p = 0.27 vs placebo | 8/62 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 8 | [Academic-in-confidence information has been removed] |
| Sitaxentan 100 mg o.d. | 0/61 | NR | 4/61 | p = 0.08 vs placebo | 4/61 | [Academic-in-confidence information has been removed] | 8 | [Academic-in-confidence information has been removed] | 1 | 8/61 |
| FCIII only, mixed PAH: | ||||||||||
| Placebo | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Bosentan 125 mg b.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sitaxentan 50 mg o.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sitaxentan 100 mg o.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| STRIDE-4/Barst 2007,37 18 weeks | ||||||||||
| Placebo | 0/34 | NR | 3/34 | NR | [Academic-in-confidence information has been removed] | 34 | 9 | 21 | 4 | [Academic-in-confidence information has been removed] |
| Sitaxentan 50 mg o.d. | 0/32 | NR | 1/32 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | 32 | 8 | 22 | 2 | [Academic-in-confidence information has been removed] |
| Sitaxentan 100 mg o.d. | 0/32 | NR | 0/32 | p = 0.0898 vs placebo | [Academic-in-confidence information has been removed] | 32 | 15 | 17 | 0 | [Academic-in-confidence information has been removed] |
| FCIII only, mixed PAH: | ||||||||||
| Placebo | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sitaxentan 50 mg o.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sitaxentan 100 mg o.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sildenafil | ||||||||||
| SUPER-1/Galiè 2005,53 12 weeks | ||||||||||
| Placebo | 1/70 | NR | 7/70 | 0.100 (0.03–0.17) | [Academic-in-confidence information has been removed] | 70 | 5 | 58 | 7 | 12/70 |
| Sildenafil 20 mg t.i.d. | 1/69 | NR | 3/69 | 0.044 (0–0.093) | [Academic-in-confidence information has been removed] | 68 | 19 | 47 | 2 | 10/69 |
| Sildenafil 40 mg t.i.d. | 0/67 | NR | 2/67 | 0.030 (0–0.071) | [Academic-in-confidence information has been removed] | 66 | 24 | 40 | 2 | 10/67 |
| Sildenafil 80 mg t.i.d. | 2/71 | NR | 5/71 | 0.071 (0.011–0.132) | [Academic-in-confidence information has been removed] | 69 | 29 | 38 | 2 | 9/71 |
| FCIII only, mixed PAH: | ||||||||||
| Placebo | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sildenafil 20 mg t.i.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sildenafil 40 mg t.i.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| Sildenafil 80 mg t.i.d. | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR |
| PACES-1,38 16 weeks | ||||||||||
| Placebo + ongoing epoprostenol | 7/131 | NR | 22/131 | 0.180 (0.110–0.249) | [Academic-in-confidence information has been removed]/131 | 125 | 18 | 92 | 15 | 39/131 |
| Sildenafil + ongoing epoprostenol | 1/134 | NR | 8/134 | 0.062 (0.020–0.104) | [Academic-in-confidence information has been removed]/134 | 132 | 47 | 76 | 9 | 29/134 |
| FCIII only, mixed PAH: | ||||||||||
| Placebo + ongoing epoprostenol | NR | NR | NR | NR | NR | 85 | 16 | 62 | 7 | NR |
| Sildenafil + ongoing epoprostenol | NR | NR | NR | NR | NR | 87 | 32 | 51 | 4 | NR |
| Head-to-head trial | ||||||||||
| SERAPH/Wilkins 2005,57 16 weeks | ||||||||||
| Bosentan 125 mg b.d. | 0/12 | NR | NR | NR | 0/12 | NR | NR | NR | NR | NR |
| Sildenafil 50 mg t.i.d. | 1/14 | NR | NR | NR | 1/14 | NR | NR | NR | NR | NR |
| 6MWD (metres) | Borg dyspnoea index | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | |
| Epoprostenol | ||||||||||||||||||
| Rubin 1990,39 8 weeks | ||||||||||||||||||
| Control | 9 | 205 | NR | 9 | 292 | NR | 9 | 79a | 87.3a | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Epoprostenol | 10 | 246 | NR | 10 | 378 | NR | 10 | 131a | 131.3a | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Additional data from Cochrane review60 and used in analysis: | ||||||||||||||||||
| Control | NR | NR | NR | NR | NR | NR | 11 | 35.70 | 143.94 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Epoprostenol | NR | NR | NR | NR | NR | NR | 10 | 141.20 | 136.29 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Barst 1996,11 12 weeks | ||||||||||||||||||
| Control | 40 | 272 | 145.5b | 40 | 257 | 151.8b | 40 | –15 | 148.7c | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Epoprostenol | 41 | 316 | 115.3b | 41 | 348 | 108.9b | 41 | 32 | 112.1c | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Badesch 2000,33 12 weeks | ||||||||||||||||||
| Control | 55 | 240.0 (median) | NR | 44d | 233.6d | 107.3d | 55 | –36.0 | NR | NR | NR | NR | NR | NR | NR | NR | 1.0 (median) | NR |
| Epoprostenol | 56 | 271.5 (median) | NR | 50d | 317.0d | 133.0d | 56 | 63.5 | NR | NR | NR | NR | NR | NR | NR | NR | –2.0 (median) | NR |
| Iloprost | ||||||||||||||||||
| AIR/Olschewski 2002,41 12 weeks | ||||||||||||||||||
| Placebo | 102 | 315 | 96 | NR | NR | NR | 102 | –19e | 81b,e | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Iloprost | 101 | 332 | 93 | NR | NR | NR | 101 | 17e | 90b,e | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| AIR-2/Olschewski,36 12 weeks | ||||||||||||||||||
| Control | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Iloprost | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| COMBI/Hoeper 2006,58 12 weeks | ||||||||||||||||||
| Ongoing bosentan | 21 | 296 | 79 | 21 | 297 | 94 | 21 | 1 | 27 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Iloprost + ongoing bosentan | 19 | 317 | 74 | 19 | 309 | 124 | 19 | –9 | 100 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| STEP/McLaughlin 2006,59 12 weeks | ||||||||||||||||||
| Placebo + ongoing bosentan | 33 | 340 | 73 | 33 | 343f | 99f | 33 | 4f | 61f | 33 | 3.5 | 2.1 | 33 | 3.6f | 2.5f | 33 | 0.0f | 1.5f |
| Iloprost + ongoing bosentan | 34 | 331 | 64 | 32 | 367f | 84f | 32 | 30f | 60f | 32 | 3.9 | 1.7 | 32 | 3.4f | 1.7f | 32 | –0.5f | 1.2f |
| Bosentan | ||||||||||||||||||
| Channick 2001,43 12 weeks | ||||||||||||||||||
| Placebo | 11 | 355.09 | 81.96 | 11 | 349.64 | 147.12 | 11 | –5.45 | 120.47 | 11 | 3.82 | 1.72 | 11 | 4.91 | 2.91 | 11 | 1.09 | 2.66 |
| Bosentan 125 mg b.d. | 21 | 360.29 | 86.05 | 21 | 430.52 | 66.43 | 21 | 70.24 | 56.09 | 21 | 4.38 | 1.80 | 21 | 4.19 | 2.42 | 21 | –0.19 | 1.66 |
| BREATHE-1/Rubin 2002,45 16 weeks | ||||||||||||||||||
| Placebo | 69 | 344 | 76 | NR | NR | NR | 69 | –8 | 100b,e | 69 | 3.8 | 2.0 | 69 | 4.2 | 2.5b | 69 | 0.3 | 1.7b |
| Bosentan 125 mg b.d. | 74 | 326 | 73 | NR | NR | NR | 74 | 27 | 77b,e | 74 | 3.3 | 2.2 | 74 | 3.2 | 2.6b | 74 | –0.1 | 1.7b |
| Bosentan 250 mg b.d. | 70 | 333 | 75 | NR | NR | NR | 70 | 46 | 59b,e | 70 | 3.8 | 1.9 | 70 | 3.3 | 2.5b | 70 | –0.6 | 1.7b |
| BREATHE-2/Humbert 2004,56 16 weeks | ||||||||||||||||||
| Placebo + epoprostenol | 11 | NR | NR | NR | NR | NR | 10 | 74 (median) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bosentan + epoprostenol | 22 | NR | NR | NR | NR | NR | 19 | 68 (median) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| BREATHE-5/Galiè 2006,47 16 weeks | ||||||||||||||||||
| Placebo | 17 | 366.4 | 67.5 | NR | NR | NR | 17 | –9.7 | 91.9b | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bosentan 125 mg b.d. | 37 | 331.9 | 82.8 | NR | NR | NR | 37 | 43.3 | 49.3b | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan | ||||||||||||||||||
| STRIDE-1/Barst 2004,49 12 weeks | ||||||||||||||||||
| Placebo | 60 | 413 | 105 | NR | NR | NR | 60 | –13 | 62.8 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg o.d. | 55 | 394 | 114 | NR | NR | NR | 55 | 22 | 47.6 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 300 mg o.d. | 63 | 387 | 110 | NR | NR | NR | 63 | 20 | 67.8 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| IPAH, mixed FC:61 | ||||||||||||||||||
| Placebo | NR | NR | NR | NR | NR | NR | 37 | –10 | 65 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg and 300 mg | NR | NR | NR | NR | NR | NR | 57 | 24 | 68 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| CTD-APAH, mixed FC:61 | ||||||||||||||||||
| Placebo | NR | NR | NR | NR | NR | NR | 9 | –38 | 84 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg and 300 mg | NR | NR | NR | NR | NR | NR | 33 | 20 | 52 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| STRIDE-2/Barst 2006,48 18 weeks | ||||||||||||||||||
| Placebo | 62 | 321 | 85 | NR | NR | NR | [Academic-in-confidence information has been removed] | –6.5 | 84.4 | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | 0.19 | 2.15 |
| Bosentan 125 mg b.d. | 60 | 337 | 78 | NR | NR | NR | [Academic-in-confidence information has been removed] | 23.0 | 76.4 | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan 50 mg o.d. | 62 | 328 | 80 | NR | NR | NR | [Academic-in-confidence information has been removed] | 17.8 | 58.3 | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan 100 mg o.d. | 61 | 360 | 72 | NR | NR | NR | [Academic-in-confidence information has been removed] | 24.9 | 57.5 | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | –0.01 | 1.91 |
| STRIDE-4/Barst 2007,37 18 weeks | ||||||||||||||||||
| Placebo | 34 | 342 | 82 | NR | NR | NR | 34 | 34 | 88.5 | 34 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | 34 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan 50 mg o.d. | 32 | 350 | 73 | NR | NR | NR | 32 | 22 | 48.6 | 32 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | 32 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sitaxentan 100 mg o.d. | 32 | 344 | 83 | NR | NR | NR | 32 | 58 | 63.6 | 32 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | 32 | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Sildenafil | ||||||||||||||||||
| SUPER-1/Galiè 2005,53 12 weeks | ||||||||||||||||||
| Placebo | 70 | 344 | 79 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sildenafil 20 mg t.i.d. | 69 | 347 | 90 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | –1 (median) | NR |
| Sildenafil 40 mg t.i.d. | 67 | 345 | 77 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 0 (median) | NR |
| Sildenafil 80 mg t.i.d. | 71 | 339 | 79 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | –1 (median) | NR |
| PACES-1,38 16 weeks | ||||||||||||||||||
| Placebo + ongoing epoprostenol | 119 | NR | NR | NR | NR | NR | 119 | 4.1 | NR | 119 | 3 (median) | NR | 119 | 3 (median) | NR | NR | NR | NR |
| Sildenafil + ongoing epoprostenol | 131 | NR | NR | NR | NR | NR | 131 | 30.1 | NR | 131 | 3 (median) | NR | 131 | 3 (median) | NR | NR | NR | NR |
| Mean pulmonary arterial pressure (mPAP) (mmHg) | Right atrial pressure (RAP) (mmHg) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | |
| Epoprostenol | ||||||||||||||||||
| Rubin 1990,39 8 weeks | ||||||||||||||||||
| Control | 9 | 62.2 | NR | 9 | 62.2 | NR | 9 | 0a | 13.6a | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Epoprostenol | 10 | 58.6 | NR | 10 | 49.3 | NR | 10 | –8.4a | 15.0a | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Additional data from Cochrane review60 and used in analysis: | ||||||||||||||||||
| Control | NR | NR | NR | NR | NR | NR | 11 | 0.30 | 13.50 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Epoprostenol | NR | NR | NR | NR | NR | NR | 10 | –7.57 | 14.14 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Barst 1996,11 12 weeks | ||||||||||||||||||
| Control | 40 | 59 | 12.6b | NR | NR | NR | 30 | 1.87 | 8.49b | 40 | 12 | 6.3 | NR | NR | NR | 29 | 0.09 | 4.95b |
| Epoprostenol | 41 | 61 | 12.8b | NR | NR | NR | 38 | –4.82 | 8.14b | 41 | 13 | 6.4 | NR | NR | NR | 36 | –2.17 | 6.54b |
| Badesch 2000,33 12 weeks | ||||||||||||||||||
| Control | 55 | 49.1 | 10.2 | NR | NR | NR | NR | 0.94 | 8.16b | 55 | 11.1 | 5.5 | NR | NR | NR | NR | 1.20 | 5.12b |
| Epoprostenol | 56 | 50.9 | 10.6 | NR | NR | NR | NR | –5.03 | 8.16b | 56 | 13.1 | 5.0 | NR | NR | NR | NR | –1.26 | 6.14b |
| Iloprost | ||||||||||||||||||
| AIR-1/Olschewski 2002,41 12 weeks | ||||||||||||||||||
| Placebo | 101 | 53.8 | 14.1 | NR | NR | NR | NR | –0.2 | 6.9 | NR | NR | NR | NR | NR | NR | NR | 1.4 | 4.8 |
| Iloprost (post inhalation) | 100 | 52.8 | 11.5 | NR | NR | NR | NR | –4.6c | 9.3c | NR | NR | NR | NR | NR | NR | NR | –0.8c | 4.6c |
| Iloprost (preinhalation) | NR | NR | NR | NR | NR | NR | NR | –0.1d | 7.3d | NR | NR | NR | NR | NR | NR | NR | 0.5d | 4.6d |
| AIR-2/Olschewski,36 12 weeks | ||||||||||||||||||
| Control | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Iloprost | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| COMBI/Hoeper 2006,58 12 weeks | ||||||||||||||||||
| Ongoing bosentan | 59 | 19 | NR | NR | NR | NR | NR | NR | NR | 9 | 5 | NR | NR | NR | NR | NR | NR | NR |
| Iloprost + ongoing bosentan | 54 | 12 | NR | NR | NR | NR | NR | NR | NR | 9 | 6 | NR | NR | NR | NR | NR | NR | NR |
| STEP/McLaughlin 2006,59 12 weeks | ||||||||||||||||||
| Placebo + ongoing bosentan | 28 | 52 | 13 | 28 | 55c | 16c | 28 | 2c | 6c | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Iloprost + ongoing bosentan | 29 | 51 | 11 | 29 | 46c | 13c | 29 | –6c | 7c | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bosentan | ||||||||||||||||||
| Channick 2001,43 12 weeks | ||||||||||||||||||
| Placebo | 10 | 56 | 10 | NR | NR | NR | 10 | 5.1 | 8.9 | 10 | 9.9 | 4.1 | NR | NR | NR | 10 | 4.9 | 4.7 |
| Bosentan 125 mg b.d. | 20 | 54 | 13 | NR | NR | NR | 20 | –1.6 | 5.4 | 19 | 9.7 | 5.6 | NR | NR | NR | 19 | –1.3 | 3.9 |
| BREATHE-1/Rubin 2002,45 16 weeks | ||||||||||||||||||
| Placebo | 69 | 53 | 17 | NR | NR | NR | NR | NR | NR | 67 | 8.9 | 5.1 | NR | NR | NR | NR | NR | NR |
| Bosentan 125 mg b.d. | 74 | 53 | 14 | NR | NR | NR | NR | NR | NR | 74 | 9.7 | 5.4 | NR | NR | NR | NR | NR | NR |
| Bosentan 250 mg b.d. | 70 | 57 | 17 | NR | NR | NR | NR | NR | NR | 69 | 9.9 | 6.5 | NR | NR | NR | NR | NR | NR |
| BREATHE-2/Humbert 2004,56 16 weeks | ||||||||||||||||||
| Placebo + epoprostenol | 11 | 60.9 | 9.6b | 11 | 59.2 | 10.6b | 11 | –2.2% | SE 3.6% | 11 | 11.9 | 7.3b | 11 | 12.2 | 6.0b | 11 | 0.3 | 4.3b |
| Bosentan + epoprostenol | 22 | 59.2 | 18.8b | 22 | 52.5 | 11.3b | 22 | –9.0% | SE 6.0% | 22 | 11.9 | 5.2b | 22 | 10.0 | 5.6b | 22 | –1.9 | 6.6b |
| BREATHE-5/Galiè 2006,47 16 weeks | ||||||||||||||||||
| Placebo | 17 | 72.1 | 19.4 | NR | NR | NR | 17 | 0.5 | 5.8b | 17 | 5.0 | 3.7 | NR | NR | NR | 17 | 0.4 | 3.7b |
| Bosentan 125 mg b.d. | 37 | 77.8 | 15.2 | NR | NR | NR | 37 | –5.0 | 9.7b | 37 | 6.1 | 3.4 | NR | NR | NR | 37 | 0.3 | 3.0b |
| Sitaxentan | ||||||||||||||||||
| STRIDE-1/Barst 2004,49 12 weeks | ||||||||||||||||||
| Placebo | 60 | 52 | 16 | 60 | 53 | 15 | 60 | 0 | 8 | 60 | 8 | 5 | NR | NR | NR | 60 | 1 | 4 |
| Sitaxentan 100 mg o.d. | 55 | 54 | 17 | 55 | 51 | 16 | 55 | –3 | 8 | 55 | 7 | 5 | NR | NR | NR | 55 | 0 | 4 |
| Sitaxentan 300 mg o.d. | 63 | 54 | 14 | 63 | 49 | 15 | 63 | –5 | 11 | 63 | 9 | 5 | NR | NR | NR | 63 | –1 | 4 |
| STRIDE-2/Barst 2006,48 18 weeks | ||||||||||||||||||
| Placebo | 62 | 49 | 14 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bosentan 125 mg b.d. | 60 | 50 | 15 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 50 mg o.d. | 62 | 48 | 15 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg o.d. | 61 | 45 | 12 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| STRIDE-4/Barst 2007,37 18 weeks | ||||||||||||||||||
| Placebo | 34 | 64 | 14 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 50 mg o.d. | 32 | 56 | 17 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg o.d. | 32 | 63 | 23 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sildenafil | ||||||||||||||||||
| SUPER-1/Galiè 2005,53 12 weeks | ||||||||||||||||||
| Placebo | 70 | 56 | 16 | NR | NR | NR | 65 | 0.6 | 5.8a | 70 | 9 | 4 | NR | NR | NR | 65 | 0.3 | 4.9a |
| Sildenafil 20 mg t.i.d. | 69 | 54 | 13 | NR | NR | NR | 65 | –2.1 | 8.8a | 69 | 8 | 5 | NR | NR | NR | 65 | –0.8 | 4.5a |
| Sildenafil 40 mg t.i.d. | 67 | 49 | 13 | NR | NR | NR | 63 | –2.6 | 7.1a | 67 | 9 | 6 | NR | NR | NR | 63 | –1.1 | 5.3a |
| Sildenafil 80 mg t.i.d. | 71 | 52 | 16 | NR | NR | NR | 65 | –4.7 | 8.0a | 71 | 9 | 5 | NR | NR | NR | 65 | –1.0 | 4.5a |
| PACES-1,38 16 weeks | ||||||||||||||||||
| Placebo + ongoing epoprostenol | NR | NR | NR | NR | NR | NR | 102 | 0.2 | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | NR | NR | NR |
| Sildenafil + ongoing epoprostenol | NR | NR | NR | NR | NR | NR | 117 | –3.6 | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | NR | NR | NR |
| Cardiac index (l/min/m2) | Pulmonary vascular resistance (dyn s/cm5) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | Baseline n | Mean | SD | Post-Rx n | Mean | SD | Change n | Mean | SD | |
| Epoprostenol | ||||||||||||||||||
| Rubin 1990,39 8 weeks | ||||||||||||||||||
| Data from Cochrane review:60 | ||||||||||||||||||
| Control | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 11 | –23.2a | 878.4a |
| Epoprostenol | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 10 | –473.6a | 680.8a |
| Barst 1996,11 12 weeks | ||||||||||||||||||
| Control | 40 | 2.1 | 1.3b | NR | NR | NR | 30 | –0.23 | 0.88b | 40 | 1280b | 504a,b | NR | NR | NR | 17 | 121.6b | 405.6a,b |
| Epoprostenol | 41 | 2.0 | 0.6b | NR | NR | NR | 38 | 0.33 | 0.62b | 41 | 1280b | 512a,b | NR | NR | NR | 27 | –273.6b | 299.2a,b |
| Badesch 2000,33 12 weeks | ||||||||||||||||||
| Control | 55 | 2.2 | 0.7 | NR | NR | NR | NR | –0.10 | 0.59b | 55 | 896a | 424a | NR | NR | NR | NR | 73.6a | 332.0a,b |
| Epoprostenol | 56 | 1.9 | 0.6 | NR | NR | NR | NR | 0.50 | 0.60b | 56 | 1136a | 568a | NR | NR | NR | NR | –366.4a | 455.2a,b |
| Iloprost | ||||||||||||||||||
| AIR/Olschewski 2002,41 12 weeks | ||||||||||||||||||
| Placebo | NR | NR | NR | NR | NR | NR | NR | NR | NR | 96 | 1041 | 493 | NR | NR | NR | NR | 96 | 322 |
| Iloprost (post inhalation) | NR | NR | NR | NR | NR | NR | NR | NR | NR | 91 | 1029 | 390 | NR | NR | NR | NR | –239 | 279 |
| Iloprost (preinhalation) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | –9 | 275 |
| AIR-2/Olschewski,36 12 weeks | ||||||||||||||||||
| Control | NR | NR | NR | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| Iloprost | NR | NR | NR | NR | NR | NR | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | NR | NR | NR | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| COMBI/Hoeper 2006,58 12 weeks | ||||||||||||||||||
| Ongoing bosentan | 21 | 2.1 | 0.5 | NR | NR | NR | NR | NR | NR | 21 | 1032a | 536a | NR | NR | NR | NR | NR | NR |
| Iloprost + ongoing bosentan | 19 | 2.1 | 0.7 | NR | NR | NR | NR | NR | NR | 19 | 1080a | 528a | NR | NR | NR | NR | NR | NR |
| STEP/McLaughlin 2006,59 12 weeks | ||||||||||||||||||
| Placebo + ongoing bosentan | NR | NR | NR | NR | NR | NR | NR | NR | NR | 28 | 783 | 378 | 28 | 867c | 496c | 28 | 81c | 267c |
| Iloprost + ongoing bosentan | NR | NR | NR | NR | NR | NR | NR | NR | NR | 29 | 821 | 389 | 29 | 676c | 404c | 29 | –164c | 223c |
| Bosentan | ||||||||||||||||||
| Channick 2001,43 12 weeks | ||||||||||||||||||
| Placebo | 10 | 2.5 | 1.0 | NR | NR | NR | 10 | –0.5 | 0.3 | 10 | 942 | 430 | NR | NR | NR | 10 | 191 | 234 |
| Bosentan 125 mg b.d. | 20 | 2.4 | 0.7 | NR | NR | NR | 20 | 0.5 | 0.4 | 19 | 896 | 425 | NR | NR | NR | 19 | –223 | 244 |
| BREATHE-1/Rubin 2002,45 16 weeks | ||||||||||||||||||
| Placebo | 68 | 2.4 | 0.7 | NR | NR | NR | NR | NR | NR | 66 | 880 | 540 | NR | NR | NR | NR | NR | NR |
| Bosentan 125 mg b.d. | 70 | 2.5 | 0.8 | NR | NR | NR | NR | NR | NR | 73 | 884 | 412 | NR | NR | NR | NR | NR | NR |
| Bosentan 250 mg b.d. | 70 | 2.2 | 0.8 | NR | NR | NR | NR | NR | NR | 62 | 1167 | 875 | NR | NR | NR | NR | NR | NR |
| BREATHE-2/Humbert 2004,56 16 weeks | ||||||||||||||||||
| Placebo + epoprostenol | 11 | 1.7 | 0.7b | 11 | 2.3 | 0.7b | 11 | 37.9% | SE 13.3% | 10 | 1426 | 443b | 10 | 1050 | 487b | 10 | –25.7% | SE 7.2% |
| Bosentan + epoprostenol | 22 | 1.7 | 0.5b | 22 | 2.5 | 0.5b | 22 | 48.7% | SE 11.0% | 20 | 1511 | 577b | 20 | 947 | 465b | 20 | –35.2% | SE 5.4% |
| BREATHE-5/Galiè 2006,47 16 weeks | ||||||||||||||||||
| Placebo | NR | NR | NR | NR | NR | NR | NR | NR | NR | 17 | 2870.0d | 1209.3d | NR | NR | NR | 17 | 155.1d | 552.5b,d |
| Bosentan 125 mg b.d. | NR | NR | NR | NR | NR | NR | NR | NR | NR | 37 | 3425.1d | 1410.5d | NR | NR | NR | 37 | –316.9d | 841.3b,d |
| Sitaxentan | ||||||||||||||||||
| STRIDE-1/Barst 2004,49 12 weeks | ||||||||||||||||||
| Placebo | 60 | 2.4 | 0.8 | 60 | 2.4 | 0.9 | 60 | 0.0 | 0.5 | 60 | 911 | 504 (484 in text) | 60 | 960 | 535 | 60 | 49 | 244 |
| Sitaxentan 100 mg o.d. | 55 | 2.4 | 0.8 | 55 | 2.7 | 0.8 | 55 | 0.3 | 0.6 | 55 | 1026 (1025 in text) | 694 | 55 | 805 | 553 | 55 | –221 | 442 |
| Sitaxentan 300 mg o.d. | 63 | 2.3 | 0.7 | 63 | 2.7 | 0.9 | 63 | 0.4 | 0.6 | 63 | 946 | 484 | 63 | 753 | 524 | 63 | –194 | 330 |
| STRIDE-2/Barst 2006,48 18 weeks | ||||||||||||||||||
| Placebo | 62 | 2.4 | 0.7 | NR | NR | NR | NR | NR | NR | 62 | 880a | 640a | NR | NR | NR | NR | NR | NR |
| Bosentan 125 mg b.d. | 60 | 2.4 | 0.6 | NR | NR | NR | NR | NR | NR | 60 | 880a | 400a | NR | NR | NR | NR | NR | NR |
| Sitaxentan 50 mg o.d. | 62 | 2.7 | 1.0 | NR | NR | NR | NR | NR | NR | 62 | 800a | 560a | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg o.d. | 61 | 2.4 | 0.6 | NR | NR | NR | NR | NR | NR | 61 | 800a | 560a | NR | NR | NR | NR | NR | NR |
| STRIDE-4/Barst 2007,37 18 weeks | ||||||||||||||||||
| Placebo | NR | NR | NR | NR | NR | NR | NR | NR | NR | 34 | 1200a | 800a | NR | NR | NR | NR | NR | NR |
| Sitaxentan 50 mg o.d. | NR | NR | NR | NR | NR | NR | NR | NR | NR | 32 | 1120a | 800a | NR | NR | NR | NR | NR | NR |
| Sitaxentan 100 mg o.d. | NR | NR | NR | NR | NR | NR | NR | NR | NR | 32 | 1129a | 640a | NR | NR | NR | NR | NR | NR |
| Sildenafil | ||||||||||||||||||
| SUPER-1/Galiè 2005,53 12 weeks | ||||||||||||||||||
| Placebo | 70 | 2.2 | 0.6 | NR | NR | NR | 65 | –0.02 | 0.62e | 70 | 1051 | 512 | NR | NR | NR | 65 | 49 | 425.7e |
| Sildenafil 20 mg t.i.d. | 69 | 2.4 | 0.7 | NR | NR | NR | 65 | 0.21 | 0.70e | 69 | 987 | 464 | NR | NR | NR | 65 | –122 | 390.8e |
| Sildenafil 40 mg t.i.d. | 67 | 2.3 | 0.7 | NR | NR | NR | 63 | 0.24 | 0.75e | 67 | 869 | 438 | NR | NR | NR | 63 | –143 | 301.7e |
| Sildenafil 80 mg t.i.d. | 71 | 2.5 | 0.8 | NR | NR | NR | 65 | 0.37 | 0.72e | 71 | 918 | 601 | NR | NR | NR | 65 | –261 | 427.8e |
| PACES-1,38 16 weeks | ||||||||||||||||||
| Placebo + ongoing epoprostenol | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Sildenafil + ongoing epoprostenol | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
Appendix 6 Ongoing trials of the technologies in pulmonary arterial hypertension patients
A number of ongoing studies were identified. These are tabulated in Table 74.
| Clinical trial identifier; location (centres) | PICO | (Expected) enrolment | Study design | Time frame | Status | Sponsor | Comments |
|---|---|---|---|---|---|---|---|
| NCT00004754; centres not stated | P: severe PAH, able to self-administer medication; I: epoprostenol; C: not stated; O: safety, economic resource consumption | Not stated | Open-label | Start: August 1993 | Completed | National Center for Research Resources, Baylor College of Medicine | Unclear if published increasing dose until target is reached or at least one dose-limiting effect occurs |
| NCT00250640; multicentre (international) | P: NYHA FCIII familial or IPAH, no previous active treatment within 6 weeks of study inclusion; I: inhaled iloprost; C: none; O: continued effectiveness | 54 | Prospective, observational | Start: April 2005; follow-up: up to 4 years | Recruiting | Schering AG, Germany | |
| NCT00086463; multicentre (USA) | P: PAH, NYHA FCIII–FCIV, receiving conventional therapy and bosentan; I: inhaled iloprost at frequency of six to nine inhalations per day added to bosentan; C: placebo added to bosentan; O: safety and efficacy | 60 | Double-blind RCT | Start: June 2004; follow-up:12 weeks | Completed | Combination therapy (possibly included trial – McLaughlin 2006)59 | |
| NCT00302211; multicentre (USA) | P: IPAH or FPAH, age 12–80 years, on sildenafil; I: inhaled iloprost added to sildenafil; C: placebo added to sildenafil; O: 6MWT, safety and effectiveness | 180 | Double-blind RCT | Start: March 2006 | Recruiting | CoTherix | Combination therapy; ‘VISION’ trial |
| NCT00266162; multicentre (Germany) | P: PAH secondary to Eisenmenger syndrome, age ≥ 18 years; I: bosentan; C: none; O: 6MWD, haemodynamic outcomes, NYHA FC, increase in pulmonary reagibility, normalisation of vasoactive mediators | 60 | Open-label, prospective | Start: August 2004; expected completion: November 2007 | No longer recruiting | Competence Network for Congenital Heart Defects, German Federal Ministry of Education and Research, Actelion | |
| NCT00091715; multicentre (international) | P: PAH, NYHA FCII, age ≥ 12 years; I: bosentan; C: placebo; O: exercise capacity, cardiac haemodynamics | 170 | Double-blind RCT | Start: September 2004; completion: December 2006 | Completed | Actelion | EARLY study |
| NCT00303459; multicentre (international) | P: symptomatic PAH, WHO FCI, age ≥ 12 years, on sildenafil; I: bosentan added to sildenafil; C: placebo added to sildenafil; O: morbidity/mortality events, 6MWT, WHO FC, Borg dyspnoea index, EQ-5D, patient global self-assessment, time to hospitalisation or worsening or complication of PAH or initiation of prostanoids, atrial septostomy, lung transplantation or death from baseline until end of study, time to death of all causes from baseline until end of study | 600 | Double-blind RCT | Start: April 2006; expected completion: June 2010; follow-up: 16 weeks | Recruiting | Actelion | Combination therapy |
| NCT00352482; single-centre (Los Angeles, USA) | P: idiopathic pulmonary fibrosis and pulmonary hypertension; age ≥ 19 years; I: sildenafil (50 mg); C: placebo; O: 6MWD, haemodynamic parameters | 20 | Double-blind, cross-over RCT | Start: November 2004; follow-up: 3 weeks | Recruiting | National Heart, Lung, and Blood Institute | |
| NCT00323297; multicentre (international) | P: PAH, age ≥ 18 years, on bosentan; I: sildenafil added to bosentan; C: placebo added to bosentan; O: 6MWT, safety, clinical worsening, Borg dyspnoea score, FC, pharmacokinetic outcomes | 106 | Double-blind RCT + open-label extension | Start: September 2006; follow-up: 12 weeks (extension: 12 months) | Recruiting | Pfizer | Combination therapy |
Appendix 7 Long-term follow-up studies
Long-term follow-up studies on the technologies in this assessment were identified from the manufacturer submissions for the purpose of providing further information, in particular for the independent economic evaluation (see Chapter 4). The identified studies are documented below and in Table 75. The key requirement was for data to be provided by FC for the outcomes of change (or no change) in FC and/or survival. Studies containing such data are indicated and further details provided in Table 76.
Studies were included based on their duration and number of patients enrolled. Data stratified by NYHA/WHO FC were extracted on change in NYHA/WHO FC and survival. As a rule summary data were used, but for STRIDE-1X and STRIDE-2X it was necessary to use individual patient data.
Supportive care/standard treatment
One study of patients treated only with supportive care was identified. 5 No information applicable to the economic model was found as data on deterioration in FC were not presented. Although data on survival were provided they were also not stratified by FC and were therefore not very useful.
Epoprostenol
In total, six long-term studies were identified for epoprostenol. Four of these stratified data in some way by FC for the outcomes of change in FC and survival. These were the studies by Barst et al. ,127 McLaughlin et al. ,65 Sitbon et al. 66 and Kuhn et al. 128 Barst et al. 127 used a prospective design and all the other studies were retrospective.
Iloprost
Four long-term studies were identified. Only one of these, that by Hoeper et al. ,129 provided any data stratified by FC and this was for survival. It was an open-label, prospective study of 24 patients.
Bosentan
For bosentan a total of nine studies were identified, three of which93,98,130 were used to obtain data for the model. Also, data from STRIDE-2X,100 which compared sitaxentan and bosentan, were included for the long-term analysis of bosentan. Although Keogh et al. 84 provided data on deaths stratified by FC, the numbers were given for the end of study, without specifying the length of follow-up. It is worth mentioning that the study by Sitbon et al. 98 is an analysis of an IPAH subgroup of patients from the same population that was analysed in the study by Sitbon et al. 130
Sitaxentan
For sitaxentan two long-term extensions of RCTs were identified: STRIDE-1X99 and STRIDE-2X. 100 An article131 describing the Canadian subpopulation of the STRIDE-1X trial was also found. Both STRIDE-1X and STRIDE-2X contained data stratified by FC.
Sildenafil
The manufacturer submission for sildenafil mentioned two long-term studies on treatment of PAH with sildenafil: SUPER-296 and PACES-2. 132 Both studies were described as ongoing and no data stratified by FC were provided.
| Name of study | Duration/follow-up; number of participants | Type of PAH | Functional class (FC) | Design | FC assessed (FC specific) | Survival assessed (FC specific) | 6MWT assessed | Data on adverse events | Comments |
|---|---|---|---|---|---|---|---|---|---|
| Conventional treatment | |||||||||
| D’Alonzo 19915 | Up to 5 years; 194 patients | IPAH | I, II, III, IV (% not stated) | Registry with prospective follow-up | No | Yes* | No | No | *Median survival for FCIII and FCIV; D’Alonzo equation |
| Epoprostenol | |||||||||
| Barst 1994127 | 3 years; 18 patients | IPAH | II (6%), III (72%), IV (22%) | Open-label multicentre extension to Rubin 1990;39 matched with historic control subjects for survival | No | Yes | Yes | Yes | Time to transplantation |
| Shapiro 1997133 | 330–700 days; 69 patients (18 followed up > 330 days) | IPAH | III, IV (% not stated) | Open-label, prospective | No | Yes (no) | No | No | Mainly haemodynamic variables |
| McLaughlin 1998134 | 2 years (16.7 ± 5.2 months); 27 patients | IPAH | III (63%), IV (37%)* | Open-label, retrospective | Yes (no) | No | No | Yes |
Treadmill exercise *Unclear if the % applies to 27 included patients or 38 treated |
| McLaughlin 200265 | 5 years (36.3 months); 162 patients | IPAH | III (46%), IV (54%) | Open-label, retrospective | Yes (yes) | Yes (yes) | No | Yes | Treadmill exercise |
| Sitbon 200266 | 5 years (26 ± 21 months); 313 patients (178 epoprostenol, 135 control) | IPAH | Epoprostenol: III (67%), IV (33%) | Open-label, retrospective | Yes (no) | Yes (yes) | Yes | Yes | Control used for survival only, FC not stated |
| Kuhn 2003128 | 3 years; 91 patients | IPAH, scleroderma, CHD, HIV, systemic lupus erythematous, portopulmonary, pulmonary veno-occlusive disease | III (52%), IV (48%) | Retrospective cohort | Yes (yes) | Yes (yes)* | Yes | No | *1 year |
| Iloprost | |||||||||
| Hoeper 2000129 | 1 year; 24 patients | IPAH | III (83%), IV (17%) | Open-label, prospective | No | Yes (yes) | Yes | Yes | |
| Opitz 2005135 | 5 years (median 535 ± 61 days); 76 patients | IPAH | II, III, IV | Prospective | No | Yes (no) | No | No | Cardiopulmonary exercise test |
| AIR follow-up, study report 303045136 | Up to 5 years; 71 patients | III, IV (no % given) | Open-label extension of AIR | Yes (no) | Yes (no) | – | Yes | Based on submission; data not stratified by FC | |
| AIR-2; Olschewski,36 Nikkho 2001,137 Nikkho 2003,138 Olschewski 2003,139 Olschewski 2005140 | 2 years; 52 patients | IPAH, secondary | II (33.3%), III (47.6%), IV (19%)* | Prospective, open-label, active controlled | Yes [Academic-in-confidence information has been removed] | Yes [Academic-in-confidence information has been removed] | Yes | Yes |
[Academic-in-confidence information has been removed] *At baseline of RCT |
| Bosentan | |||||||||
| Sitbon 2003141 | 1 year; 29 patients | IPAH, scleroderma | – | Open-label extension to Channick 200143 | Yes | – | Yes | - | No article |
| McLaughlin 2005115 | 2.1 ± 0.5 years; 169 patients | IPAH | I (1%), II (8%), III (82%), IV (9%) | Prospective extension of two RCTs: BREATHE-145 and Channick 200143 | No | Yes (no) | No | Yes | |
| Sitbon 200598 (bosentan vs epoprostenol) | 3 years; 485 patients (139 bosentan, 346 epoprostenol) | IPAH | III (100%) | Prospective extension of two RCTs, BREATHE-145 and Channick 2001,43 matched with historic control subjects | No | Yes (yes) | No | Yes | Includes subgroup survival analysis for 83 patients plus 83 matched patients from both cohorts |
| Denton 200644 | 2 years (1.8 ± 0.2); 64 patients | CTD | III (95.5%)*, IV (4.5%)* | Prospective extension of two RCTs: BREATHE-145 and Channick 2001;43 subgroup | Yes | Yes (no) | Yes | No |
Data on time to clinical worsening *Data on beginning of RCTs, two did not enter extensions |
| Gatzoulis 2006142 | 6–10 months (6-month results reported); 37 patients | Eisenmenger syndrome | II (30%), III (70%) | Open-label extension of BREATHE-547 | Yes (yes) | Yes | Yes | Yes | Based on industry submission and conference abstract; |
| Provencher 2006104 | 1 year; 103 patients | IPAH | III (88%), IV (12%) | Retrospective single centre | Yes (yes)* | Yes (no) | Yes | Yes | *4 months |
| Williams 200693 | 2 years; 92 patients (45 bosentan, 47 control) | Systemic sclerosis | Bosentan: III (58%), IV (42%); control: III (77%), IV (23%) | Prospective experimental, historic control subjects | Yes (yes) | Yes (no) | No | No | |
| Koegh 200784 | Follow-up: up to 21 months; 177 patients | IPAH, CTD | III, IV (% not stated) | Multicentre, prospective, open-label study | Yes (no) | Yes (yes) | No | Yes | QoL; FC and survival data provided for end of study – patients followed up for different periods |
| Sitbon 2007130 | [Academic-in-confidence information has been removed]; [Academic-in-confidence information has been removed] | IPAH, CTD | [Academic-in-confidence information has been removed] | Prospective extension of two RCTs: BREATHE-145 and Channick 200143 | [Academic-in-confidence information has been removed] | Yes [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | |
| Denton 2007143 | 48 weeks; 53 patients | CTD | III (100%) | Open-label prospective | Yes | Yes | No | Yes | QoL data, time to clinical worsening |
| Sitaxentan | |||||||||
| STRIDE-1X99 | 58 weeks; [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | Randomised, double-blind prospective extension of STRIDE-149 (two doses) | Yes (yes) | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
| STRIDE-1X; Langleben 2004131 | 1 year; 11 (10) patients | IPAH, CTD, CHD | II (10%), III (90%)* | Open-label prospective extension of STRIDE-149 (Canadian) | Yes (yes) | Yes (yes) | Yes | Yes |
One patient discontinued because of deterioration at 7 months not included later *For 10 patients |
| Stride-2X100 | |||||||||
| (sitaxentan vs bosentan) |
1 year [Commercial-in-confidence information removed] |
[Commercial-in-confidence information removed] | [Commercial-in-confidence information removed] | Prospective, randomised, multi-centre, open label extension study of STRIDE-2 | Yes (yes) | Yes (yes) | [Commercial-in-confidence information removed] | Yes | [Commercial-in-confidence information removed] |
| Sildenafil | |||||||||
| SUPER-296 | |||||||||
| Ongoing (design: 3 years or proven ineffectiveness/unsafe): 259 patients | IPAH, CTD |
I (0.04%) II (39%) III (58%) IV (3%)a |
Prospective extension of SUPER-1 | Yes (no) | Yes (no) | Yes | Yes | Based on manufacturer submission:data for 1-year survival; QOL | |
| PACES-2144 | |||||||||
| Ongoing (design: 3 years): 242 patients | IPAH, CTD | (I–IV); mostly II and III | Open-label prospective extension of PACES-1 | Yes | Yes | Yes | Yes | Based on sildenafil industry submission; QOL | |
| Study name/key paper (protocol number); location/ centres | Duration/follow-up; design (retrospective or prospective); number of patients included | Intervention (and comparator if applicable) | Type of PAH | Functional class | Age (years), mean (SD, range); % female | Baseline exercise capacity and haemodynamic measures, mean (SD) | Comments (inclusion criteria) |
|---|---|---|---|---|---|---|---|
| D’Alonzo 1991;5 32 clinical centres in USA | Up to 5 years; registry with prospective follow-up; 194 patients | Long-term drug therapy in 19% at study entry and 83% on hospital discharge; therapy included vasodilators, digitalis, diuretics, anticoagulants, oxygen and other drugs | IPAH (100%) | I, II, III, IV (% not stated) | No data on age; 56% | No data | Inclusion: PPH; criteria described in Rich 19874 |
| Barst 1994;127 four referral centres | Up to 70 months; open-label, multicentre, uncontrolled; 18 patients |
Epoprostenol started at 2 ng/kg/min and increased by 2 ng/kg/min every 10–15 minutes; dose increased no further when one or more of the following occurred: (1) > 40% decrease in systemic arterial pressure, (2) > 40% increase in heart rate, (3) nausea, vomiting, headache; afterwards dose decreased to one not causing adverse effects Background: warfarin; five patients oral vasodilator therapy |
IPAH (100%) | II (6%), III (72%), IV (22%) | 35.9 (13.4); 67% | 6MWT: 264 (160) metres; mPAP: 60.9 (15) mmHg; PVR: no data |
Inclusion: PPH diagnosis based on NIH registry criteria Exclusion: patients with associated conditions such as portal hypertension, HIV, collagen vascular diseases, pulmonary vasculitides |
| McLaughlin 2002;65 Rush Heart Institute, Centre for Pulmonary Heart Disease database | Mean follow-up 36.3 ± 27.1 months; retrospective database analysis; 162 patients |
Epoprostenol started at 2 ng/kg/min and gradually increased to maximum tolerated dose; additionally increased on outpatient basis, depending on symptoms of PAH and side effects of epoprostenol; from 1998 doses readjusted based on cardiac index Background (according to patient state and needs): warfarin, diuretics, digoxin, continuous nasal oxygen |
IPAH (100%) | III 46%, IV 54% | 42.2; 75% | Mean treadmill exercise time: 192 ± 183 seconds (127 patients); mPAP: 61 (13) mmHg; PVR: 17.5 (8.1) Wood units | Inclusion: FCIII or FCIV; treated with calcium channel blockers previously and failed to improve or with limited response (predicting failure of calcium channel blocker therapy) |
| Sitbon 2002;66 Clamart, France | 5 years (26 ± 21 months); retrospective; 178 epoprostenol patients, 135 historic control subjects matched for NYHA FC for survival analysis – not FC stratified |
Epoprostenol started at 1 ng/kg/min and increased every 12 hours by 1 ng/kg/min up to 10 ng/kg/min; dose adjustments made systematically to reach mean level of 14 ± 4 ng/kg/min at 3 months Background (according to patient state and needs): warfarin, diuretics, digoxin, continuous nasal oxygen |
IPAH (100%) | III 67%, IV 33% | 43 (13); 76% | 6MWT: 240 (146) metres; mPAP: 67 (14) mmHg; PVR: no data |
Inclusion: age > 15 years, PPH diagnosis based on NIH registry criteria Exclusion: (1) CTD, CHD, portal hypertension, HIV; (2) distal chronic thromboembolic pulmonary hypertension, (3) chronic pulmonary disease; (4) acute pulmonary vasodilator response that predicted response to calcium channel blockers |
| Kuhn 2003;128 one centre; Vanderbilt University Medical Center, USA | Follow-up: up to 3 years; 1 year for FC; retrospective cohort study; 91 patients |
Epoprostenol on discharge from hospital at 4–6 ng/kg/min as limited by side effects with a goal of 20 ng/kg/min at 4–6 months; regimen did not change significantly during study period; mean dose at 1 year was 23 (18) ng/kg/min Background: anticoagulants (84%), calcium channel blockers (25%), digoxin (23%), diuretics (78%), additional vasoactive medications (31%) |
IPAH (54.5%), scleroderma (21%), CHD (12%), systemic lupus erythematous (5.5%), HIV (2%), portopulmonary (3%), pulmonary veno-occlusive disease (2%) | III (52%), III (48%); | 43 (15); 70% | 6MWD: 296 (111) metres*; haemodynamics reported by aetiology for 57 patients |
Inclusion: IPAH, scleroderma, systemic lupus erythematous; patients with scleroderma were eligible if they did not have significant restrictive lung disease *Data for 25 patients |
| Hoeper 2000;129 one centre; Hannover, Germany | 12 months; open-label, prospective; 24 patients |
Iloprost daily dose was 100 µg; subsequently increased to 150 µg in patients whose exercise capacity did not increase after 3 months Background: anticoagulants; some were receiving diuretics, digitalis, calcium channel blockers |
IPAH (100%) | III (83%), IV (17%) | 38 (12, 22–65); 63% | 6MWT: 278 (96) metres; mPAP: 59 (10) mmHg; PVR: 1205 (467) dyn s/cm5 (preinhalation data) |
Inclusion: PPH according to NIH Registry criteria; FCIII or FCIV; non-responders to conventional treatment Exclusion: secondary pulmonary hypertension; severe right heart failure who were receiving catecholamines at time of presentation, lost to follow-up |
| Sitbon 2005;98 multicentre, international; records from referral centres: Clamart, France; Chicago; Denver; New York; San Diego | 36 months; prospective extension of two RCTs: BREATHE-145 and Channick 200143 (subgroup); matched with historic control subjects; 485 patients (139 bosentan, 346 control) | Intervention: bosentan as first-line treatment; control: epoprostenol | IPAH (100%) | III (100%) |
Experimental: 46 (16, 13–80); 80% Control: 41 (14, 10–75); 74% |
Experimental: 6MWT: 351 (80) metres; mPAP: 56 (15) mmHg; PVR: 12 (6) Wood units Control: 6MWT: 335 (106) metres; mPAP: 66 (18); PVR: 18 (10) Wood units |
Inclusion, bosentan: age at least 12 years; symptomatic FCIII IPAH; primary or secondary to CTD; resting mPAP > 25 mmHg; PVR > 3 Wood units; pulmonary capillary wedge pressure < 15 mmHg; 6MWT 150–450 metres Inclusion, epoprostenol: FCIII IPAH at start of epoprostenol; more than zero survival time; known survival status; started epoprostenol on or after January 1995 |
| Williams 2006;93 Royal Free Hospital, London | Up to 6 years; data for 2 years; prospective experimental, historic control subjects; 92 patients (45 bosentan, 47 control: 27 prostanoids) |
Intervention: bosentan 62.5 mg twice a day for 4 weeks, increased to 125 mg twice a day; deterioration: prostanoids (combination or on their own) Control: intravenous iloprost (predominant) or epoprostenol, inhaled iloprost, treprostinil Basic treatment: diuretics (loop diuretics and spironolactone), digoxin, oxygen (at least 16 hours in every 24 hours) if resting oxygen saturation < 90%, warfarin, calcium channel blockers (nifedipine, diltiazem, almodipine) for Raynaud’s phenomenon – continued, high-dose calcium channel blockers rarely used and withdrawn after 6 months |
Secondary to systemic sclerosis (100%) |
Experimental: III (58%), IV (42%) Control: III (77%), IV (23%) (11) |
Experimental: 60 (11.3); 84% Control: 58 (11.1); 85% |
Experimental: 6MWT: median 207 (range 0–538) metres; mPAP: 40 (11.8) mmHg; PVR: 613 (345) dyn s/cm5 Control: 6MWT: median 179 (range 0–471) metres*; mPAP: 40 (11.4) mmHg; PVR: 613 (345) dyn s/cm5 |
Inclusion: mPAP > 25 mmHg; pulmonary capillary wedge pressure < 15 mmHg; PVR > 240 dyn s/cm5; FCIII or FCIV, conventional treatment; 6MWT < 450 metres Exclusion: FCI or FCII; interstitial pulmonary fibrosis resulting in total lung capacity of < 60% and either mPAP < 35 mmHg or oxygen saturation at rest on air of < 85% or both; substitutes for 6MWT < 150 metres: cardiac index < 2.1 l/min/m2, right arterial pressure > 11 mmHg, mixed venous oxygen saturation < 63% *Data on 30 patients of whom majority in FCIV |
| Sitbon 2007;130 multicentre, international | [Academic-in-confidence information has been removed]; prospective extension of two RCTs: BREATHE-145 and Channick 2001;43 [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] | [Academic-in-confidence information has been removed] |
| STRIDE-1X (FPH01-X);99 [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
| STRIDE-2X (FPH02-X);100 [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
Appendix 8 Review of economic evaluations
| Highland 200372 | Einarson 200570 | Narine 200571 | Wlodarczyk 200673 | |
|---|---|---|---|---|
| 1. Was a well-defined question posed in an answerable form? | Yes | Yes | Yes | Yes |
| 2. Was a comprehensive description of the competing alternatives given? | Yes | Yes | Yes | Yes |
| 3. Was there evidence that the programmes effectiveness was established? | Yes | Yes | Yes | Yes |
| 4. Were all of the important and relevant costs and consequences for each alternative identified? | Yes | Yes (costs) | Yes (costs) | Yes |
| 5. Were costs and consequences measured accurately in appropriate physical units? | Yes | Yes (costs) | Yes (costs) | Yes |
| 6. Were costs and consequences valued credibly? | Yes | Yes (costs) | Yes (costs) | Yes |
| 7. Were costs and consequences adjusted for differential timing? | Yes | Yes (costs) | Yes (costs) | Yes |
| 8. Was an incremental analysis of costs and consequences of alternatives performed? | Yes | No | No | Yes |
| 9. Was allowance made for uncertainty in the estimates of costs and consequences? | Yes | Yes (costs) | Yes (costs) | Yes |
| 10. Did the presentation and discussion of study results include all issues of concern to users? | Yes | No | No | Yes |
| Highland 200372 | Einarson 200570 | Narine 200571 | Wlodarczyk 200673 | |
|---|---|---|---|---|
| 1. Is the study population clearly described? | Yes | Yes | Yes | Yes |
| 2. Are competing alternatives clearly described? | Yes | Yes | Yes | Yes |
| 3. Is a well-defined research question posed in answerable form? | Yes | Yes | Yes | Yes |
| 4. Is the economic study design appropriate to the stated objective? | Yes | Yes | Yes | Yes |
| 5. Is the chosen time horizon appropriate to include relevant costs and consequences? | Yes | Yes | Yes | Yes |
| 6. Is the actual perspective chosen appropriate? | Yes | Yes | Yes | Yes |
| 7. Are all important and relevant costs for each alternative identified? | Yes | Yes | Yes | Yes |
| 8. Are all costs measured appropriately in physical units? | Yes | Yes | Yes | Yes |
| 9. Are costs valued appropriately? | Yes | Yes | Yes | Yes |
| 10. Are all important and relevant outcomes for each alternative identified? | Yes | Yes | Yes | Yes |
| 11. Are all outcomes measured appropriately? | Unclear | Not applicable | Not applicable | Yes |
| 12. Are outcomes valued appropriately? | No | Not applicable | Not applicable | Yes |
| 13. Is an incremental analysis of costs and outcomes of alternatives performed? | Yes | Not applicable | Not applicable | Yes |
| 14. Are all future costs and outcomes discounted appropriately? | Yes | Yes (costs) | Yes (costs) | Yes |
| 15. Are all important variables, whose values are uncertain, appropriately subjected to sensitivity analysis? | Yes | Yes | Yes | Yes |
| 16. Do the conclusions follow from the data reported? | Yes | Yes | Yes | Yes |
| 17. Does the study discuss the generalisability of the results to other settings and patient/client groups? | Yes | No | No | Yes |
| 18. Does the article indicate that there is no potential conflict of interest of study researcher(s) and funder(s)? | No | No | No | No |
| 19. Are ethical and distributional issues discussed appropriately? | Yes | No | No | Yes |
Appendix 9 Mortality parameters for the model
Other-cause mortality
This was based on general population mortality assuming a starting age of 50 years and a ratio of women to men of 1.5:1. Annual survival figures were based on actuarial data (www.gad.gov.uk; accessed 1 August 2007). Linear interpolation was used to estimate the survival probability at the end of each cycle. This was converted to a conditional probability of dying in each cycle. These were entered as constants.
Mortality due to pulmonary arterial hypertension
This was assumed to be an independent competing risk, dependent on FC and treatment but not age (such data that were available were consistent with this assumption). The per-cycle mortality probabilities were entered as samples from beta distributions. The explanation here gives the calculations used for epoprostenol in FCIII. The same method was used for other treatments. It was assumed that there was no additional mortality in FCII.
| Treatment | FC | Time | Survival (95% CI) | Per cycle mortality (95% CI) | Beta distribution |
|---|---|---|---|---|---|
| Epoprostenol, iloprost | III | 3 years | 0.75 (0.71–0.79) | 0.021 (0.017–0.025) | n = 5000, r = 105 |
| Epoprostenol | IV | 3 years | 0.47 (0.39–0.55) | 0.056 (0.044–0.069) | n = 1250, r = 70 |
| Bosentan | III | 3 years | 0.87 (0.81–0.92) | 0.010 (0.006–0.015) | n = 1600, r = 16 |
| Sitaxentan, sildenafil | III | 1 year | 0.95 (0.90–0.98) | 0.011 (0.004–0.023) | n = 450, r = 5 |
Overall survival at 3 years was given as 0.75 (95% CI 0.71–0.79). Taking the central estimate of 0.75, this was compared with a general population mortality of 0.9901 to give a PAH-related survival of 0.75/0.9901 = 0.7575. This is the PAH-related survival over 13 cycles of the model (13 × 12 weeks equals 3 years). Survival in one cycle was found by solving the equation x13 = 0.7575 to give x = 0.979, or a probability of PAH-related mortality in one cycle of 0.021. Similar calculations give a 95% CI of 0.017–0.025. These numbers fit to a beta distribution with n = 5000 and r = 105.
Applying the same method to all of the other treatments gave the following result:
Mortality when on supportive care
In the absence of better data we have used the odds ratios for deterioration from FCIII to FCIV to give us the effect of treatment on reducing mortality. Again, using epoprostenol in FCIII as the example, the odds ratio of 0.4 in favour of epoprostenol gives us per-cycle mortality on supportive care of 0.051 (95% CI 0.041–0.069). Beta distributions were fitted to the correct mean and width of confidence interval. In this case this gives n = 950 and r = 48.
As with transitions for supportive care we have used a single figure for oral therapies, but separate figures for epoprostenol and iloprost. The figures used are shown in the following table:
| Treatments | FC | Mortality on treatment (95% CI) | Odds ratio | Mortality on supportive care (95% CI) | Beta distribution |
|---|---|---|---|---|---|
| Epoprostenol | III | 0.021 (0.017–0.025) | 0.4 | 0.051 (0.041–0.069) | n = 950, r = 48 |
| Epoprostenol | IV | 0.056 (0.044–0.069) | 0.4 | 0.129 (0.103–0.156) | n = 600, r = 77.5 |
| Iloprost | III | 0.021 (0.017–0.025) | 0.29 | 0.069 (0.056–0.093) | n = 700, r = 48 |
| Oral therapies | III | 0.011 (0.004–0.023) | 0.18 | 0.058 (0.006–0.116) | n = 66, r = 3.84 |
Appendix 10 Resource use information provided by Schering Health Care
New York Heart Association (NYHA) functional class II
| NHS contacts | Mean number per year | SD | Frequency per 3 months | % patients | Mean cost | Total cost per 3 months |
|---|---|---|---|---|---|---|
| Physician at specialist PAH centre | 2.800 | 0.8 | 0.7 | 100% | £51.1 | £138.4 |
| Specialist nurse at PAH centre | 2.750 | 2.8 | 0.7 | 100% | £19.9 | |
| Physician at non-specialist centre | 2.500 | 1.1 | 0.6 | 100% | £45.6 | |
| Nurse at non-specialist centre | 1.000 | 1.7 | 0.3 | 100% | £5.5 | |
| GP | 2.600 | 1.6 | 0.7 | 100% | £16.3 | |
| A&E | 0.002 | 0.0 | 0.0 | 100% | £0.0 | |
| Personal and social services | Mean days per week | SD | Frequency per 3 months | % patients | Mean cost | Total cost per 3 months |
| Residential care | 1.750 | 3.5 | 21.0 | 0% | £0.0 | £16.0 |
| Day care | 1.250 | 2.5 | 15.0 | 2% | £5.6 | |
| Home care | 0.500 | 1.0 | 6.0 | 10% | £10.3 |
| Mean number per year | SD | Average LOS | SD | % patients | Total cost per 3 months | |
|---|---|---|---|---|---|---|
| Overall hospitalisation | 0.8 | 0.4 | 6.5 | 6.3 | 18% | £62 |
| General ward | 96% | £46 | ||||
| ICU | 3% | £9 | ||||
| CCU | 1% | £3 | ||||
| A&E | 50% | £4 |
New York Heart Association (NYHA) functional class III
| NHS contacts | Mean number per year | SD | Frequency per 3 months | % patients | Mean cost | Total cost per 3 months |
|---|---|---|---|---|---|---|
| Physician at specialist PAH centre | 4.200 | 1.1 | 1.1 | 100% | £76.6 | £224.6 |
| Specialist nurse at PAH centre | 5.500 | 4.4 | 1.4 | 100% | £39.9 | |
| Physician at non-specialist centre | 2.300 | 1.1 | 0.6 | 100% | £42.0 | |
| Nurse at non-specialist centre | 0.800 | 1.8 | 0.2 | 100% | £4.4 | |
| GP | 3.800 | 1.6 | 1.0 | 100% | £23.8 | |
| A&E | 0.730 | 0.6 | 1.2 | 100% | £38.0 | |
| Personal and social services | Mean days per week | SD | Frequency per 3 months | % patients | Mean cost | Total cost per 3 months |
| Residential care | 3.500 | 4.0 | 42.0 | 6% | £50.5 | £178.8 |
| Day care | 3.750 | 2.5 | 45.0 | 8% | £67.4 | |
| Home care, hospice | 1.400 | 0.9 | 16.8 | 28% | £60.8 |
| Mean number per year | SD | Average LOS | SD | % patients | Total cost per 3 months | |
|---|---|---|---|---|---|---|
| Overall hospitalisation | 1.40 | 0.22 | 7.60 | 5.19 | 38% | £280 |
| General ward | 97% | £199 | ||||
| ICU | 4% | £53 | ||||
| CCU | 1% | £13 | ||||
| A&E | 43% | £14 |
New York Heart Association (NYHA) functional class IV
| NHS contacts | Mean number per year | SD | Frequency per 3 months | % patient | Mean cost | Total cost per 3 months |
|---|---|---|---|---|---|---|
| Physician at specialist PAH centre | 7.100 | 2.9 | 1.8 | 100% | £129.6 | £290.4 |
| Specialist nurse at PAH centre | 8.750 | 2.8 | 2.2 | 100% | £63.4 | |
| Physician at non-specialist centre | 1.900 | 1.5 | 0.5 | 100% | £34.7 | |
| Nurse at non-specialist centre | 0.800 | 1.1 | 0.2 | 100% | £4.4 | |
| GP | 5.900 | 1.2 | 1.5 | 100% | £36.9 | |
| A&E | 2.600 | 1.2 | 0.7 | 100% | £21.5 | |
| Personal and social services | Mean days per week | SD | Frequency per 3 months | % patient | Mean cost | Total cost per 3 months |
| Residential care | 7.000 | 0.0 | 84.0 | 13% | £529.6 | £2313.4 |
| Day care | 5.667 | 1.2 | 68.0 | 25% | £321.4 | |
| Home care | 4.600 | 2.5 | 55.2 | 61% | £580.4 | |
| Hospice | 5.000 | 3.5 | 60.0 | 18% | £882 |
| Mean number per year | SD | Average LOS | SD | % patients | Total cost per 3 months | |
|---|---|---|---|---|---|---|
| Overall hospitalisation | 2.6 | 1.2 | 9.5 | 4.1 | 70% | £1963 |
| General ward | 86% | £755 | ||||
| ICU | 16% | £909 | ||||
| CCU | 4% | £227 | ||||
| A&E | 50% | £71 |
Appendix 11 Effects of single parameter values on model outputs
The graphs shown in Figures 17–71 were obtained as follows. The results from the 10,000 replications of the model used for the reference case PSA were sorted in order according to the value of one of the model parameters. These sorted results were then divided into decile groups. For each group the mean cost and QALY difference, and corresponding ICER, were calculated. These results are plotted on the various graphs shown. To assist visual comparison the same scales are used throughout each section of this appendix.
When the parameter in question makes a clear difference to the outcome, the points lie close to a smooth curve. When the parameter makes little or no difference, the randomness in the selection of other parameters becomes more apparent. As the purpose of this analysis is to determine whether or not a particular parameter is important to the outcome of the model, no attempt has been made to remove this randomness; to do so would require unfeasibly large numbers of runs of the model.
In some cases negative ICERs are shown. These invariably result from points in the south-east quadrant of the cost-effectiveness plane, where the treatment option dominates the comparator. Although the numerical value of a negative ICER is never relevant to a decision, the values are shown on the graph to preserve the smoothness of the curves. The ICER graph is omitted in cases in which all ICERs are negative.
Appendix 11.1 Epoprostenol starting in functional class III
FIGURE 17.
Epoprostenol functional class III variation by odds ratio of improvement from functional class III to functional class II. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
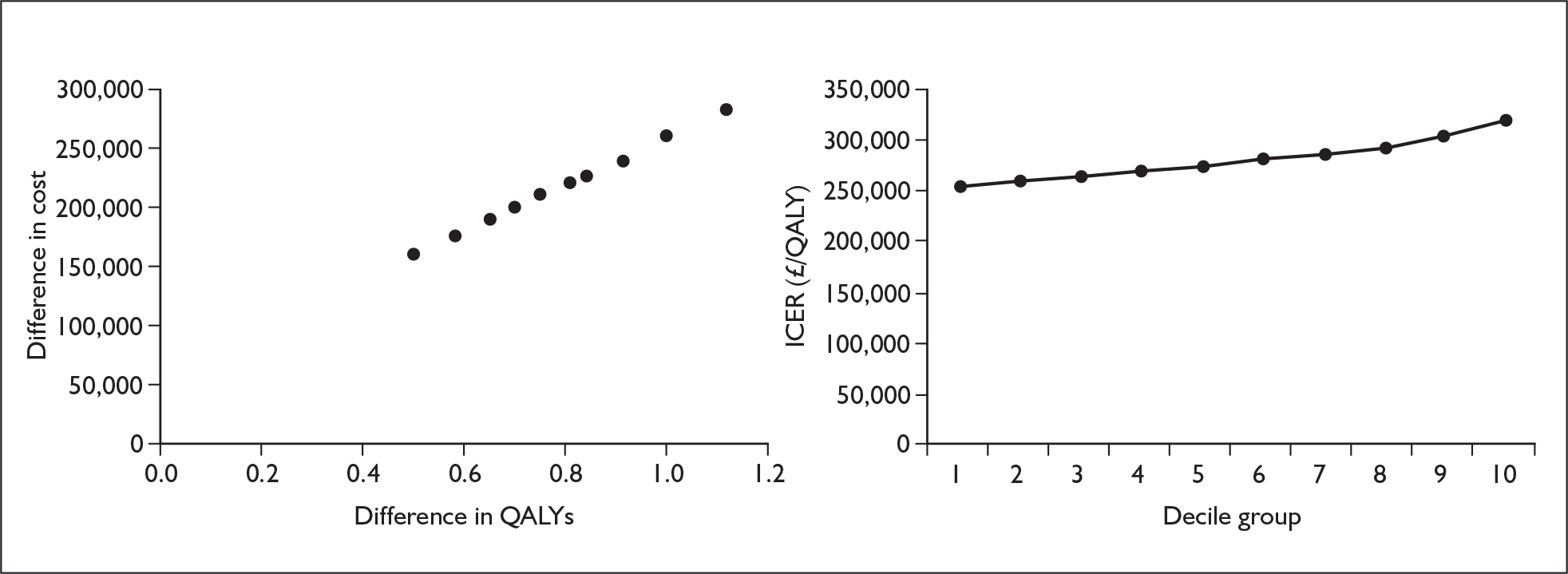
FIGURE 18.
Epoprostenol functional class III variation by odds ratio of deterioration from functional class II to functional class III. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
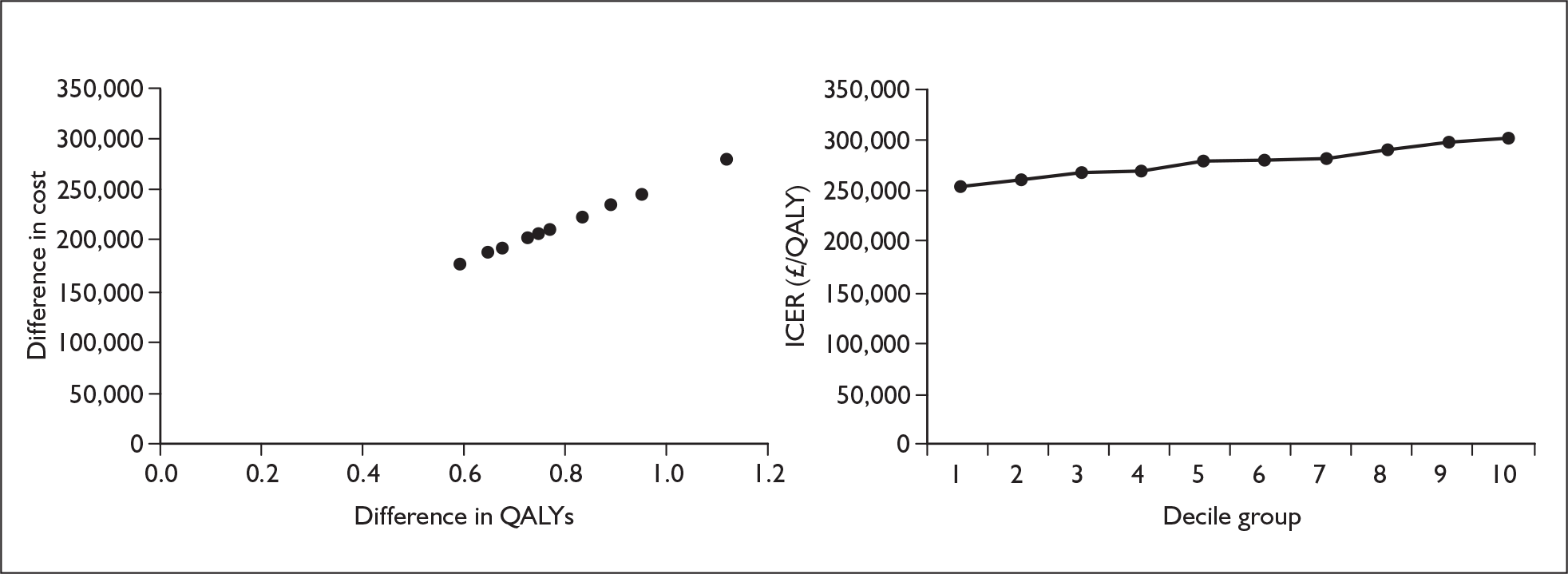
FIGURE 19.
Epoprostenol functional class III variation by odds ratio of deterioration from functional class III to functional class IV. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
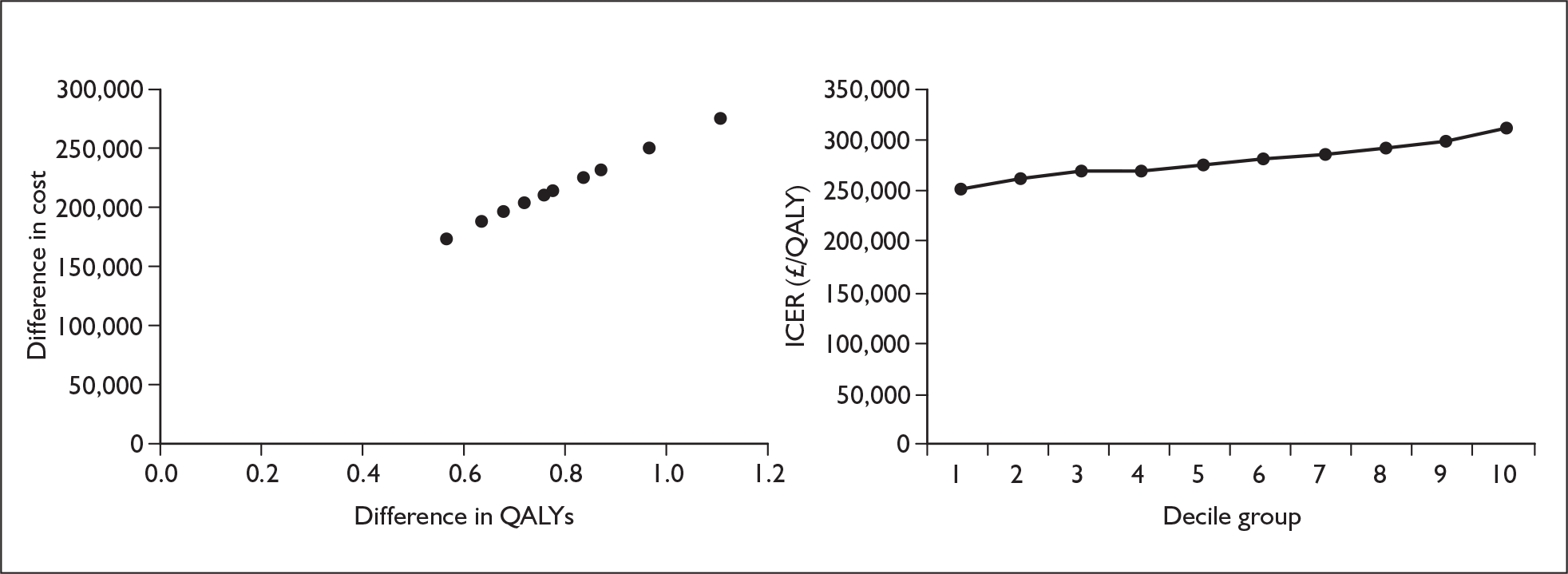
FIGURE 20.
Epoprostenol functional class III variation by probability of improvement from functional class III to functional class II on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
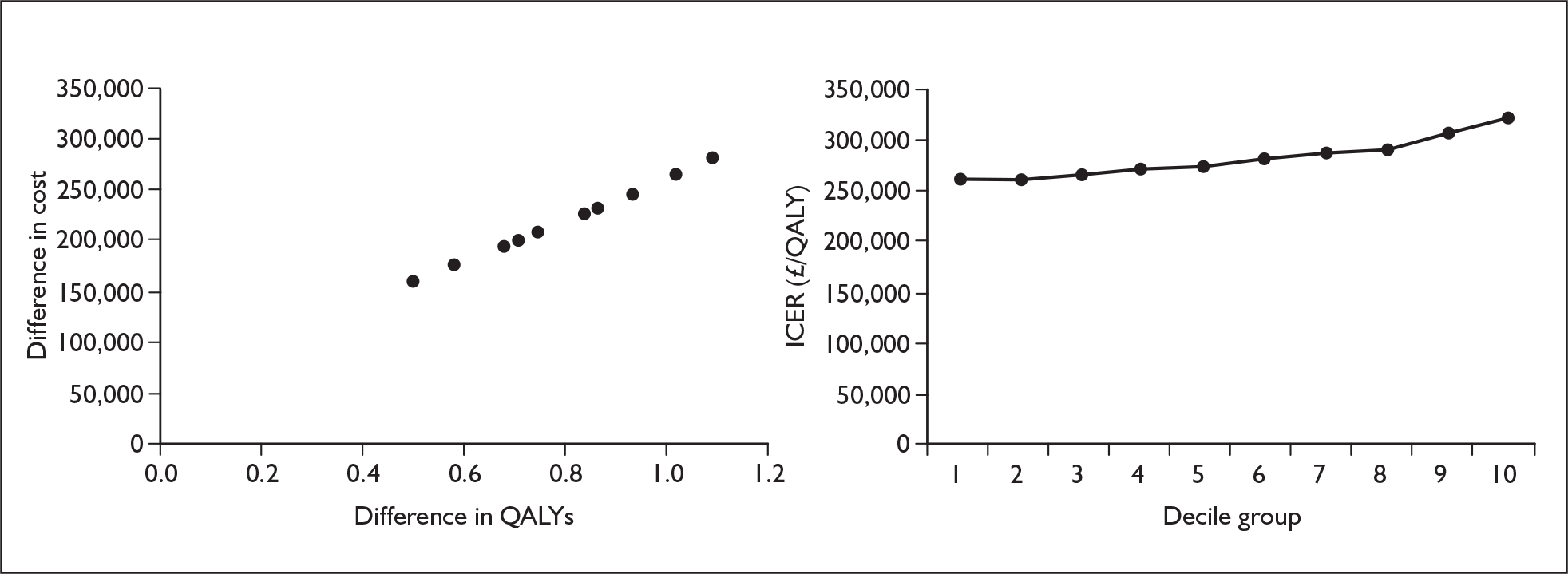
FIGURE 21.
Epoprostenol functional class III variation by probability of deterioration from functional class II to functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
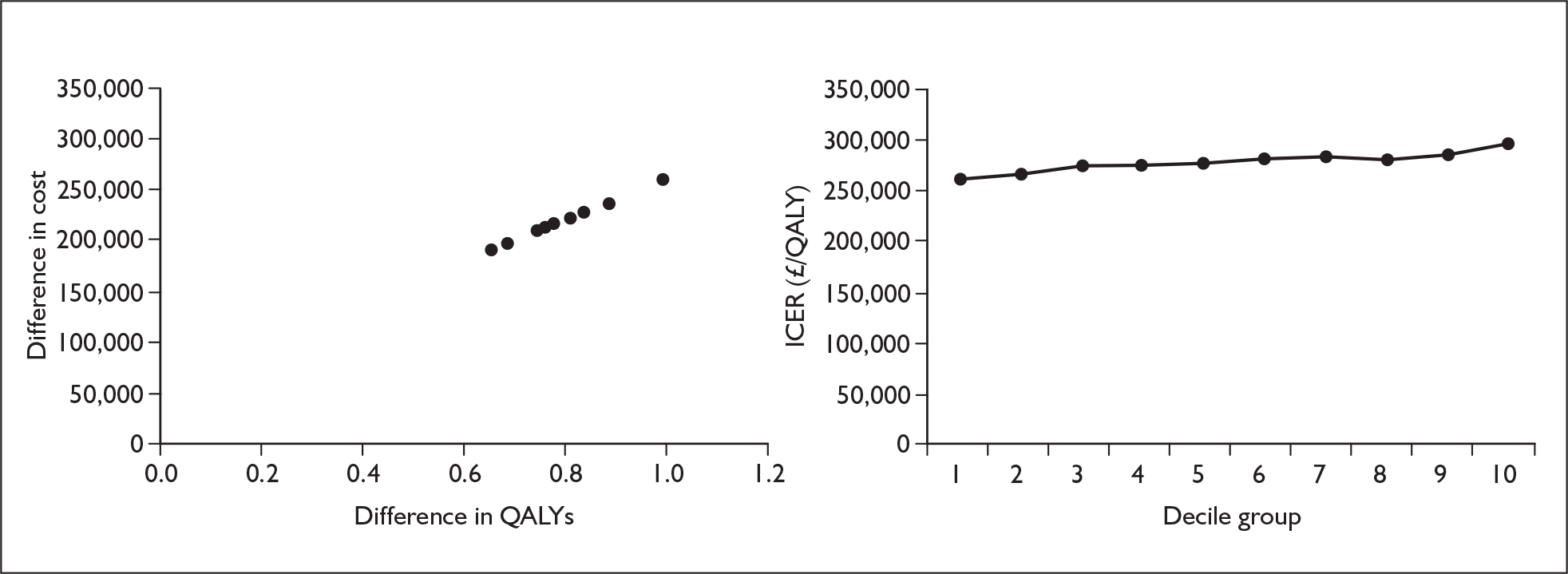
FIGURE 22.
Epoprostenol functional class III variation by probability of deterioration from functional class III to functional class IV in the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
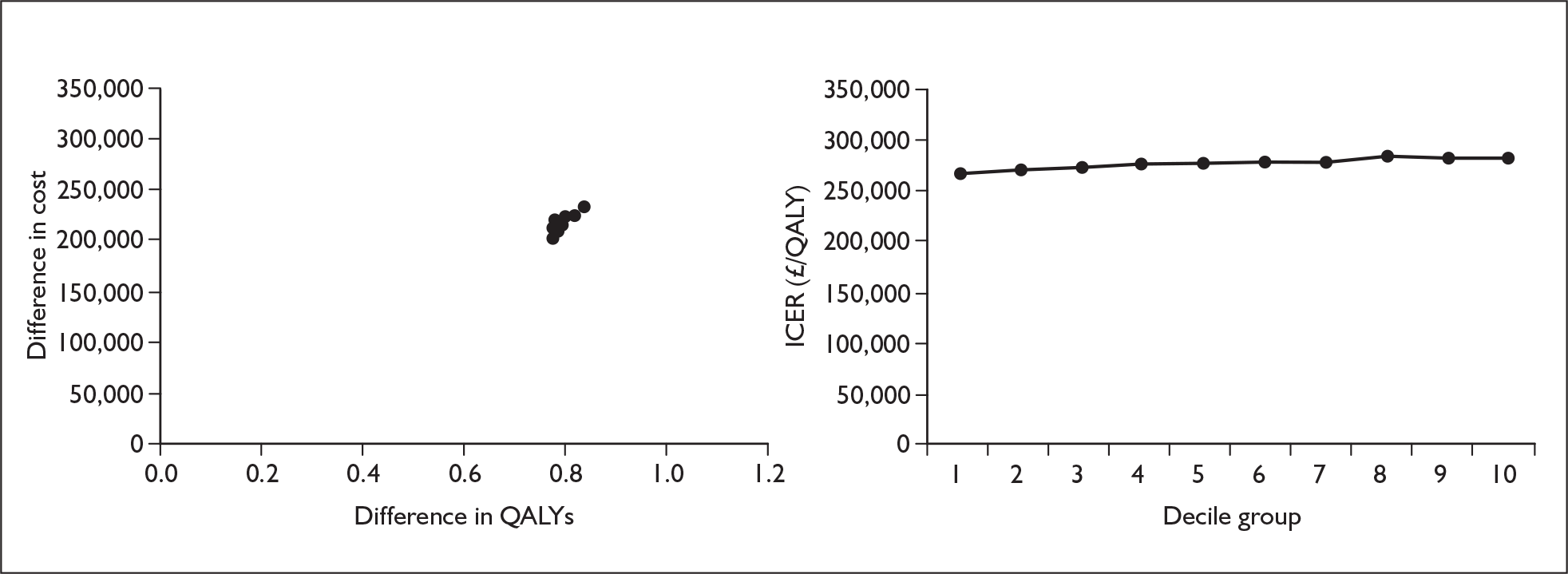
FIGURE 23.
Epoprostenol functional class III variation by probability of deterioration from functional class III to functional class IV after the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
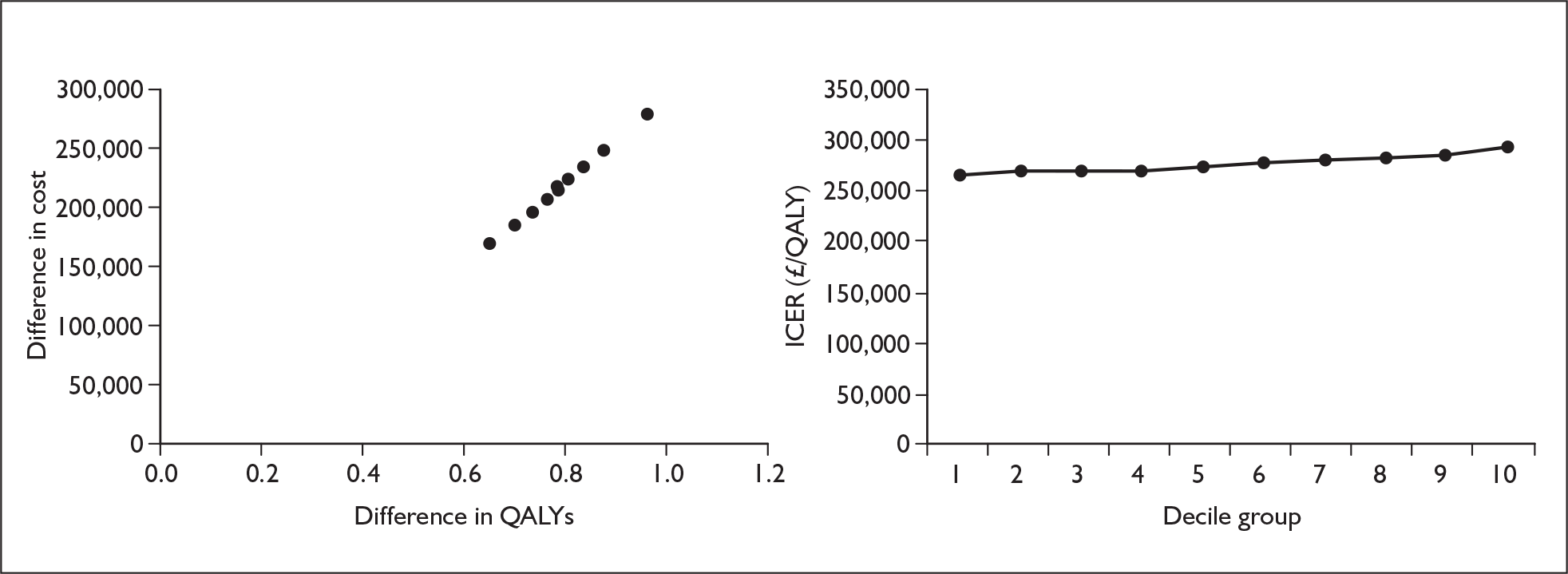
FIGURE 24.
Epoprostenol functional class III variation by mortality in functional class III on treatment. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
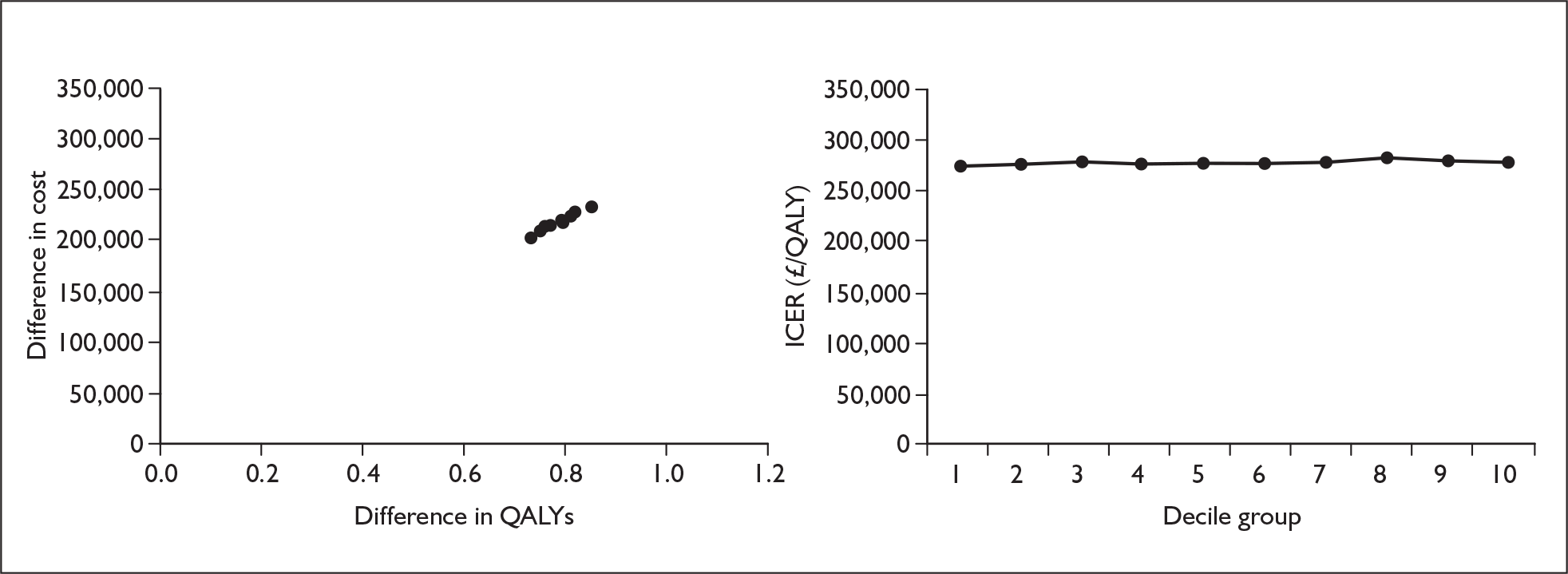
FIGURE 25.
Epoprostenol functional class III variation by mortality in functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
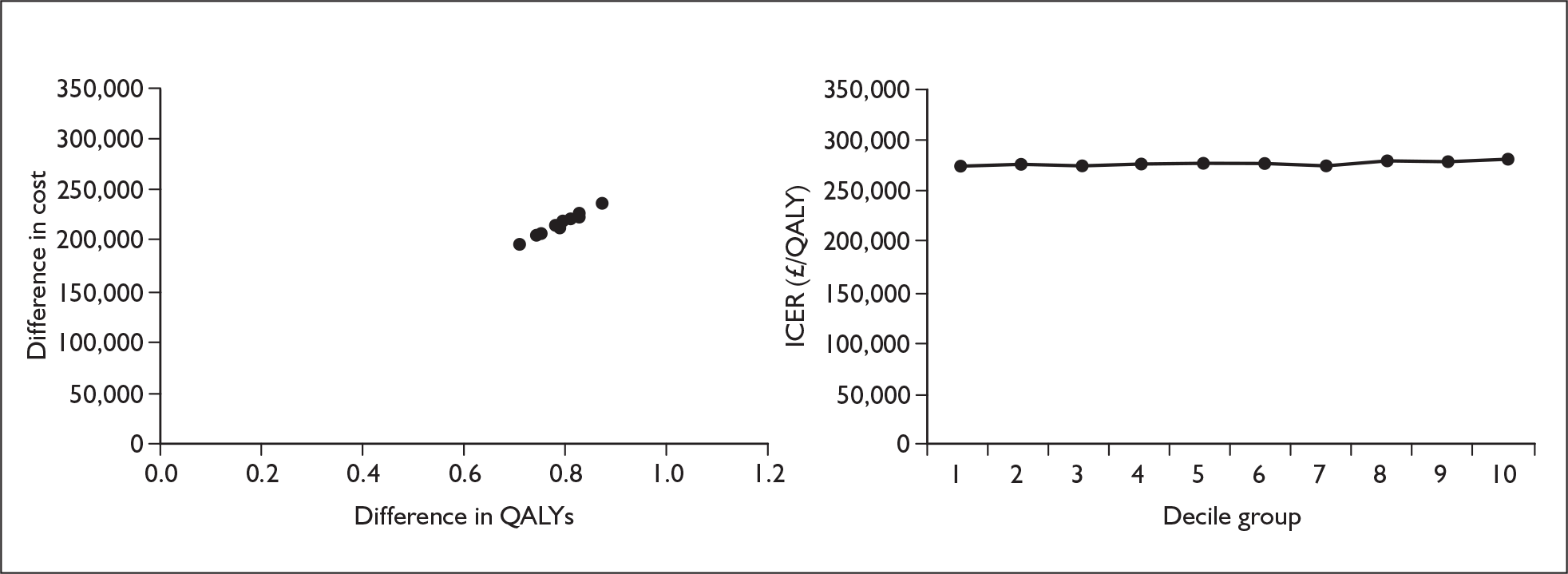
Appendix 11.2 Epoprostenol starting in functional class IV
FIGURE 26.
Epoprostenol functional class IV variation by odds ratio of improvement from functional class IV to functional class III. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
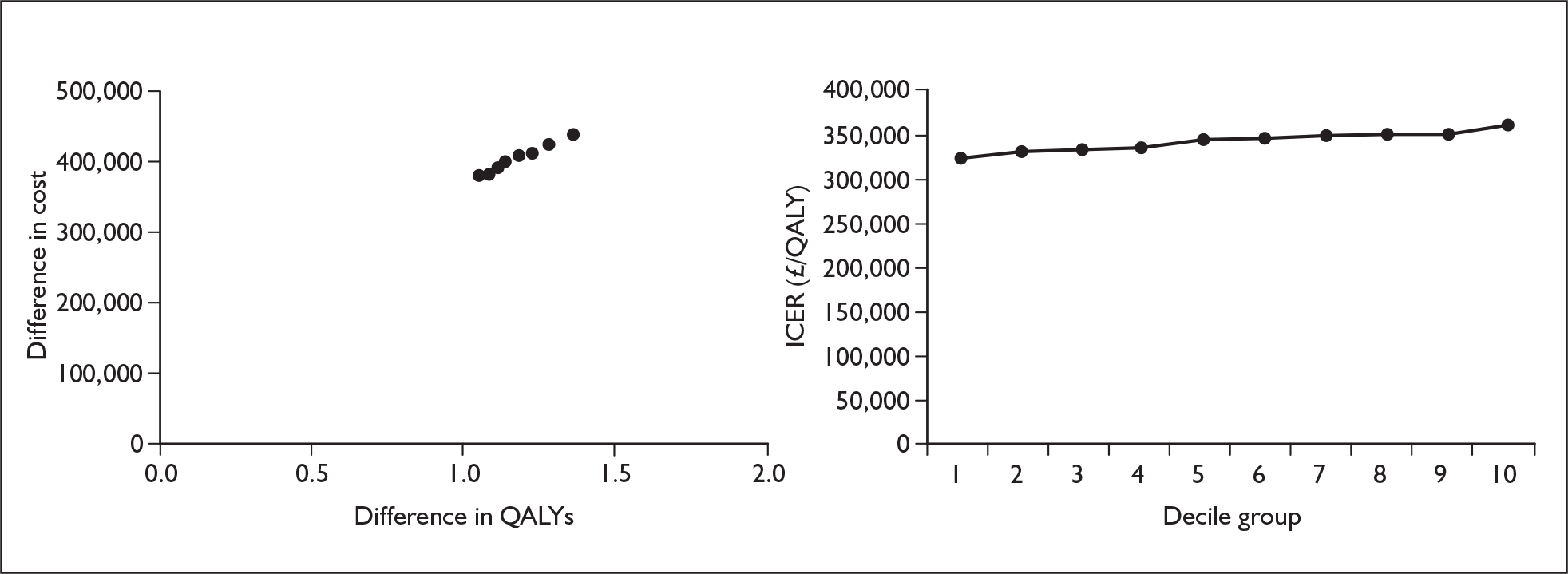
FIGURE 27.
Epoprostenol functional class IV variation by odds ratio of deterioration from functional class III to functional class IV. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
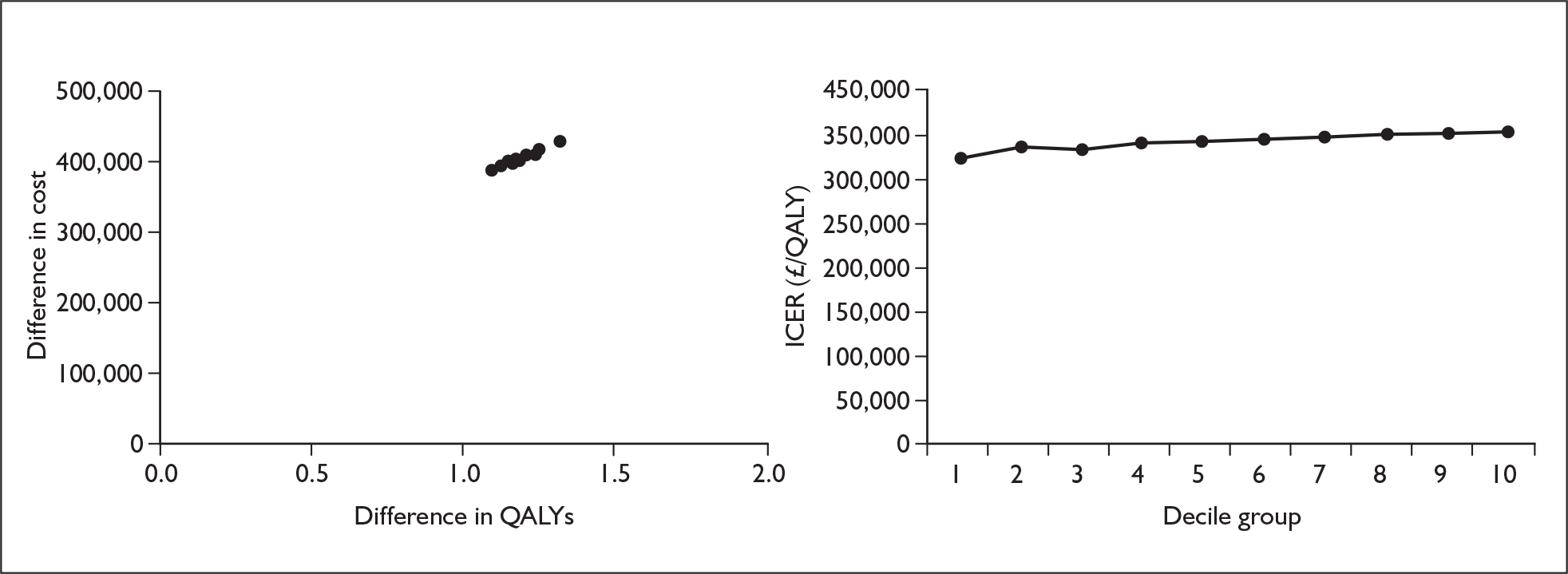
FIGURE 28.
Epoprostenol functional class IV variation by probability of improvement from functional class IV to functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
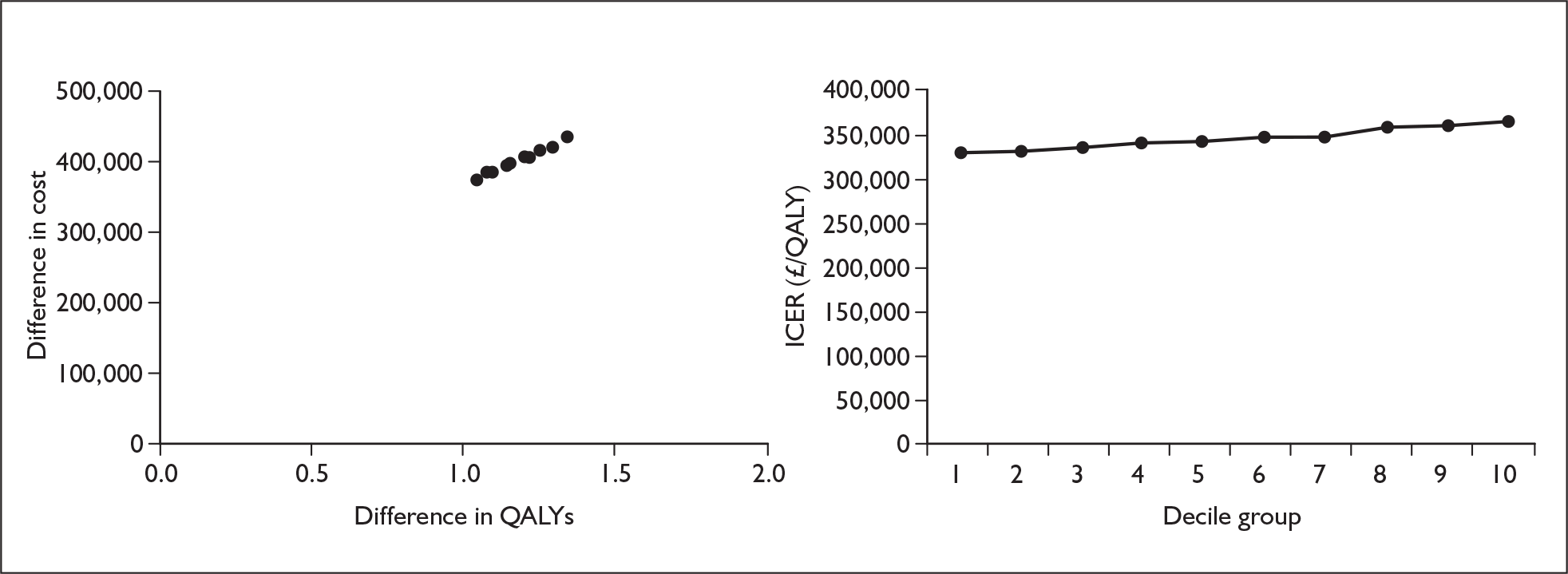
FIGURE 29.
Epoprostenol functional class IV variation by probability of deterioration from functional class III to functional class IV on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
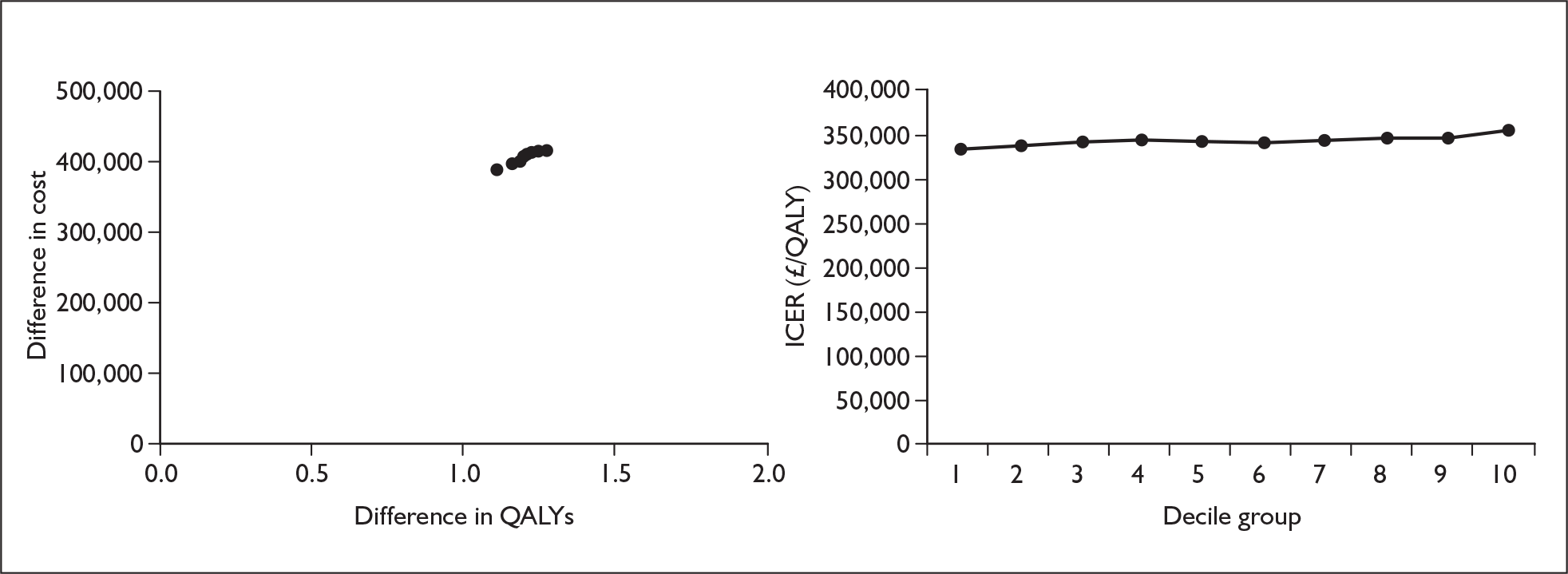
FIGURE 30.
Epoprostenol functional class IV variation by mortality in functional class IV on treatment. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
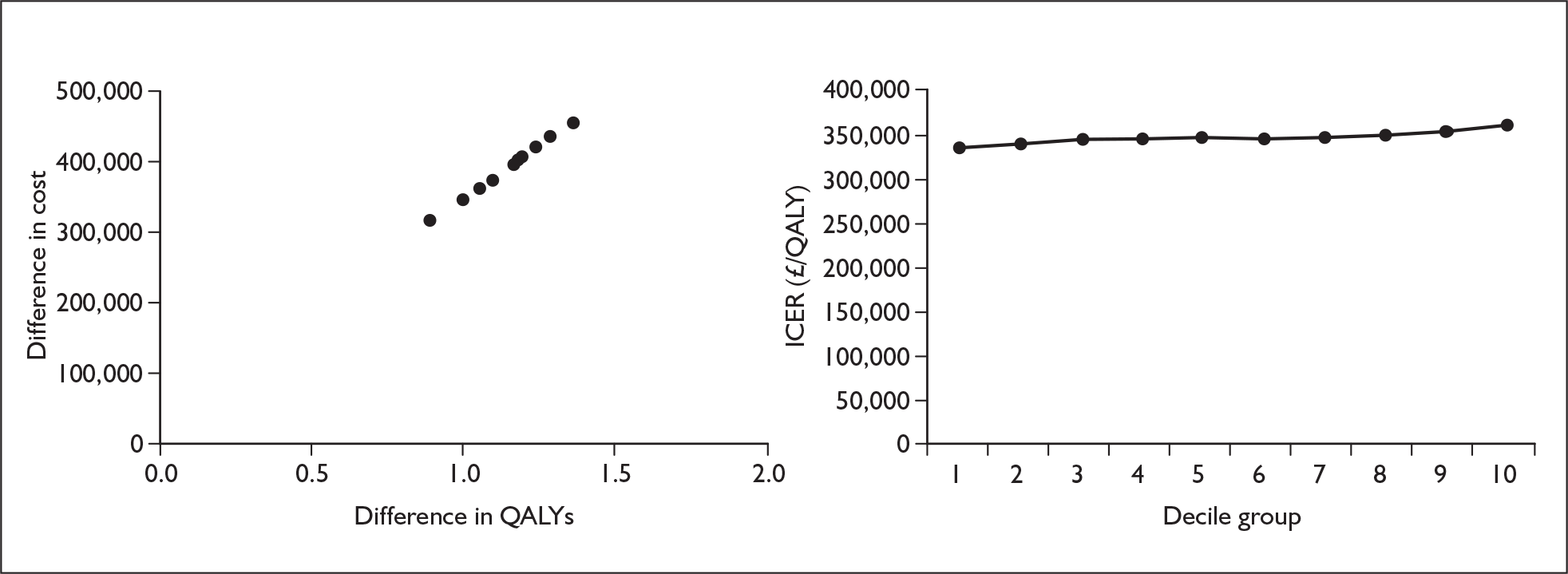
FIGURE 31.
Epoprostenol functional class IV variation by mortality in functional class IV on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
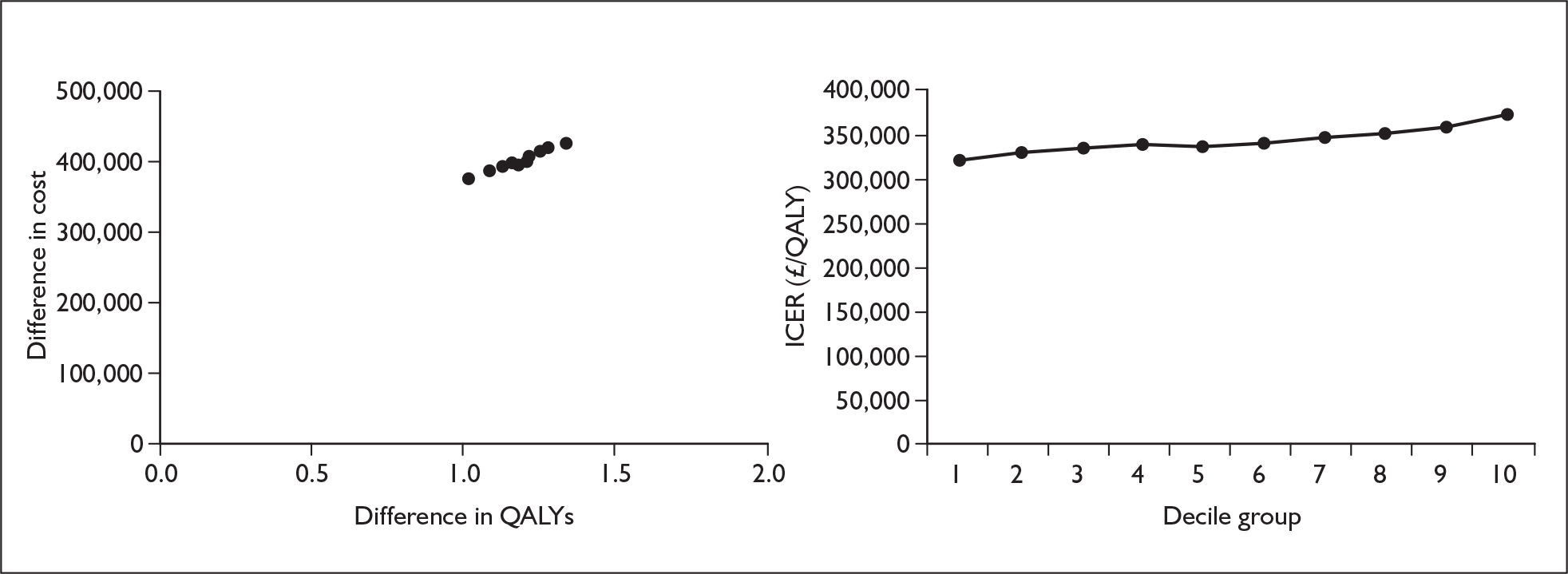
Appendix 11.3 Iloprost
FIGURE 32.
Iloprost variation by odds ratio of improvement from functional class III to functional class II. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
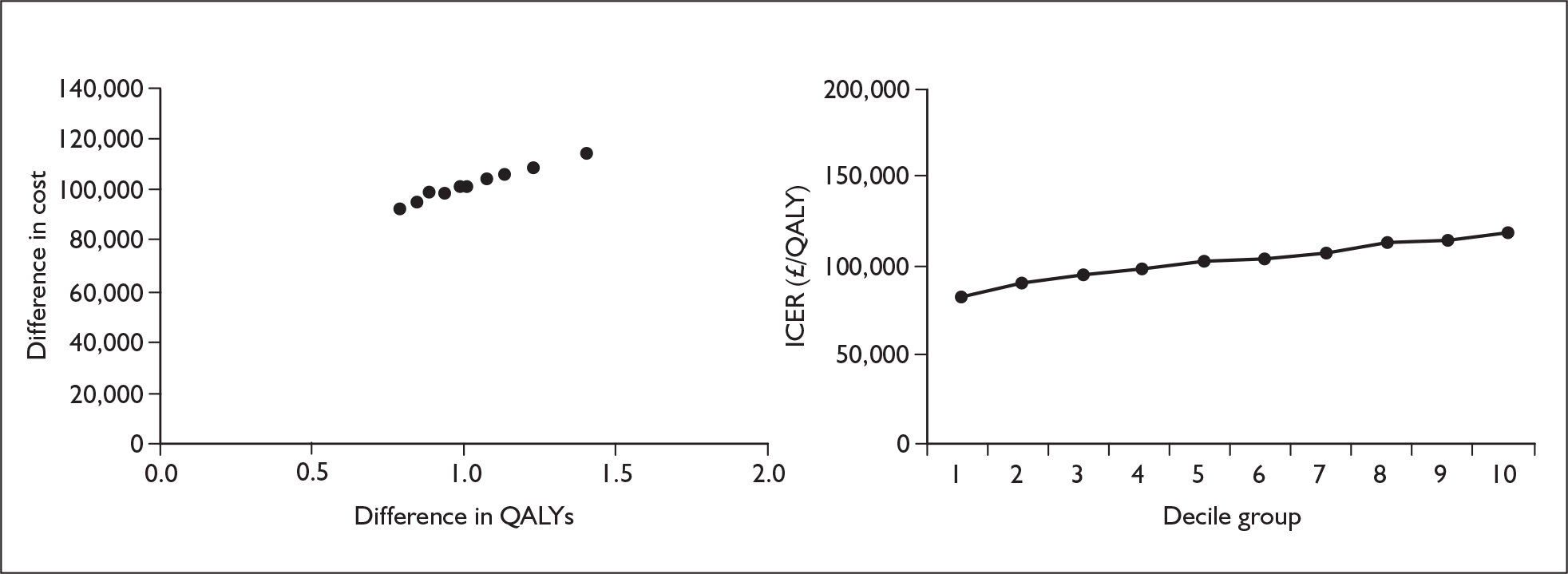
FIGURE 33.
Iloprost variation by odds ratio of deterioration from functional class II to functional class III. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
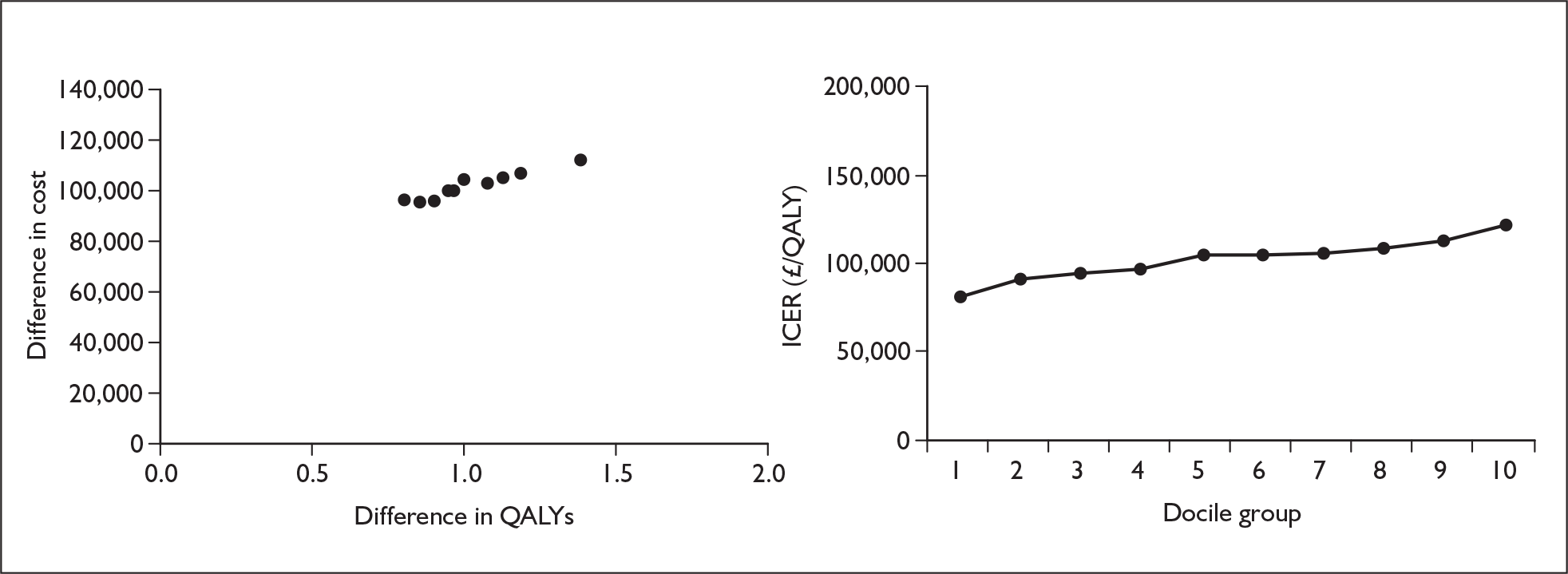
FIGURE 34.
Iloprost variation by odds ratio of deterioration from functional class III to functional class IV in the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
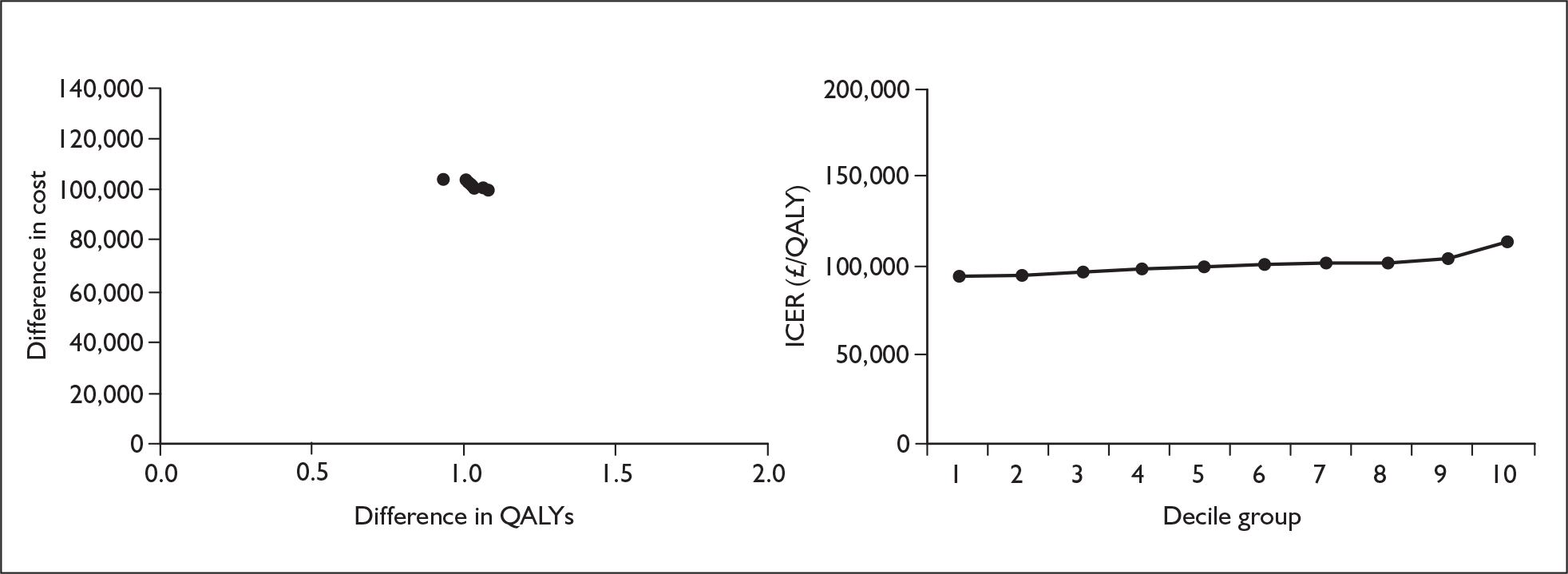
FIGURE 35.
Iloprost variation by odds ratio of deterioration from functional class III to functional class IV after the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
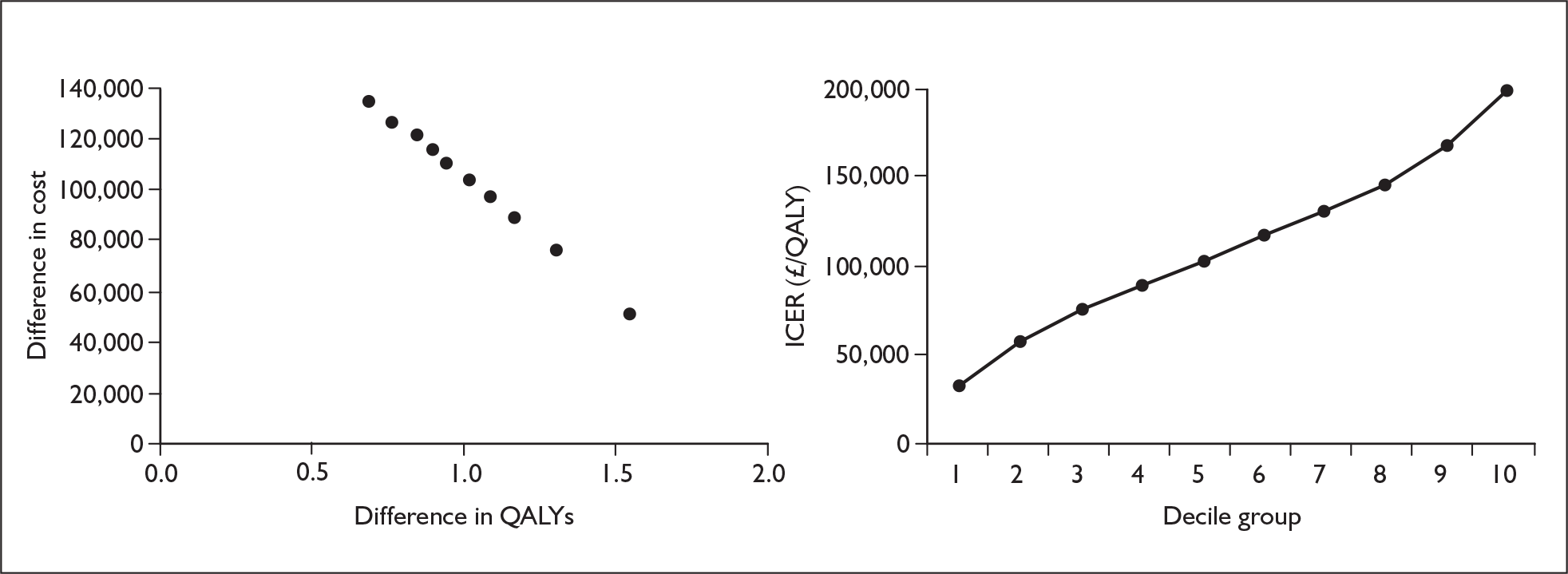
FIGURE 36.
Iloprost variation by probability of improvement from functional class III to functional class II on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
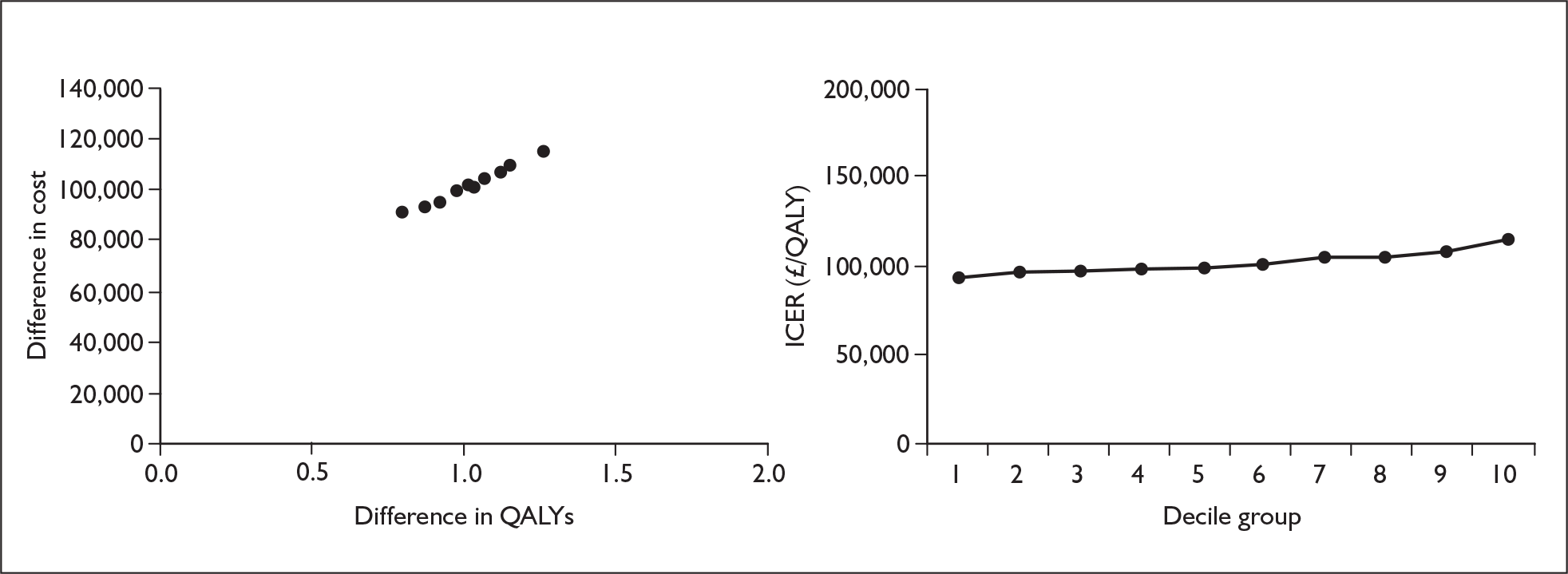
FIGURE 37.
Iloprost variation by probability of deterioration from functional class II to functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
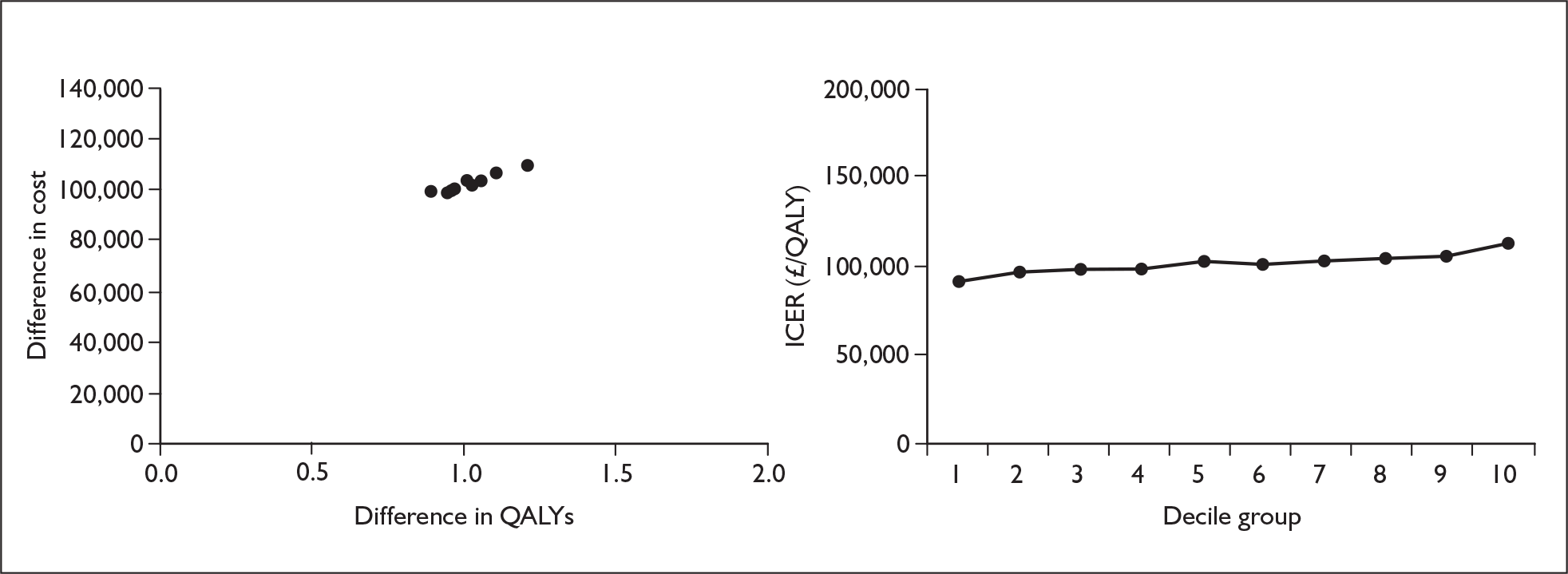
FIGURE 38.
Iloprost variation by probability of deterioration from functional class III to functional class IV in the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
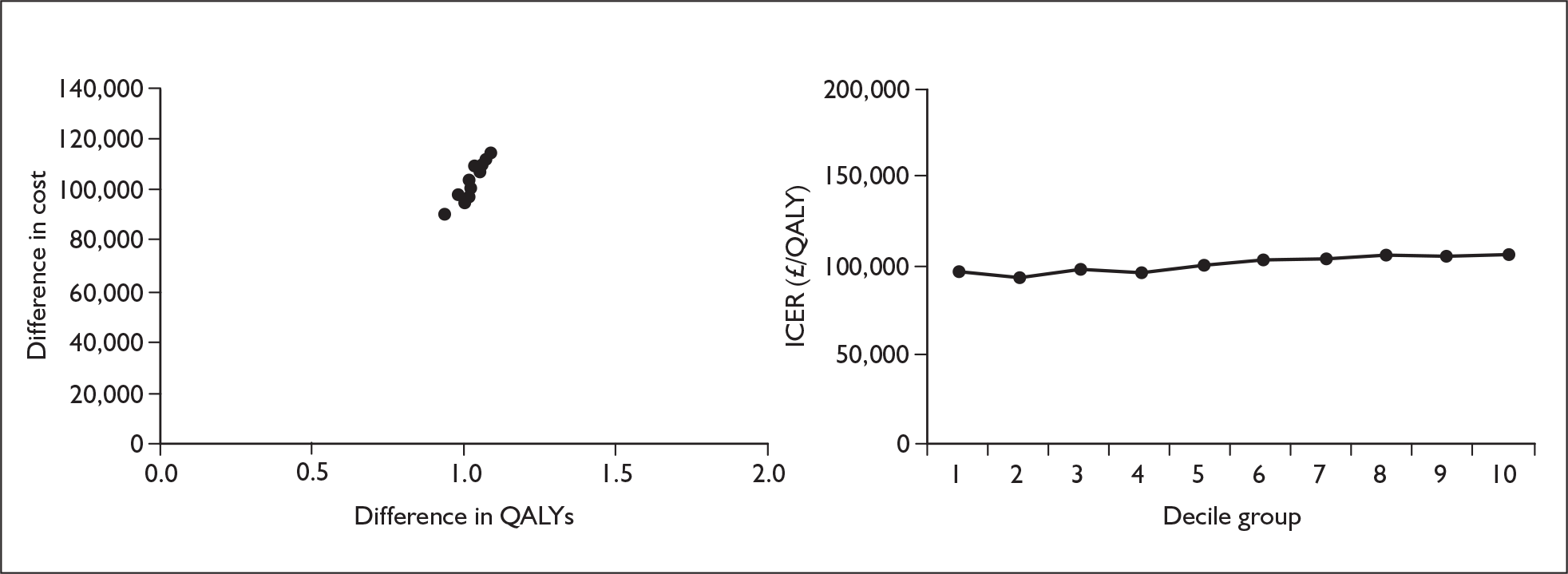
FIGURE 39.
Iloprost variation by probability of deterioration from functional class III to functional class IV after the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
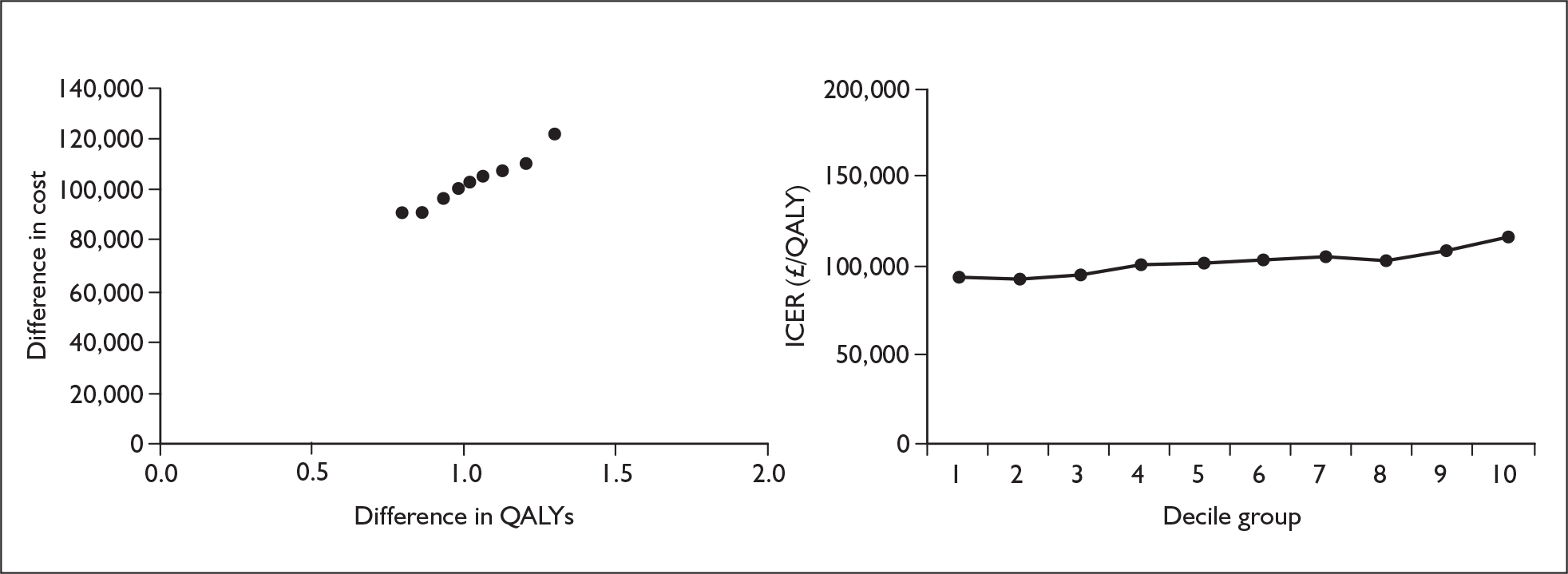
FIGURE 40.
Iloprost variation by mortality in functional class III on treatment. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
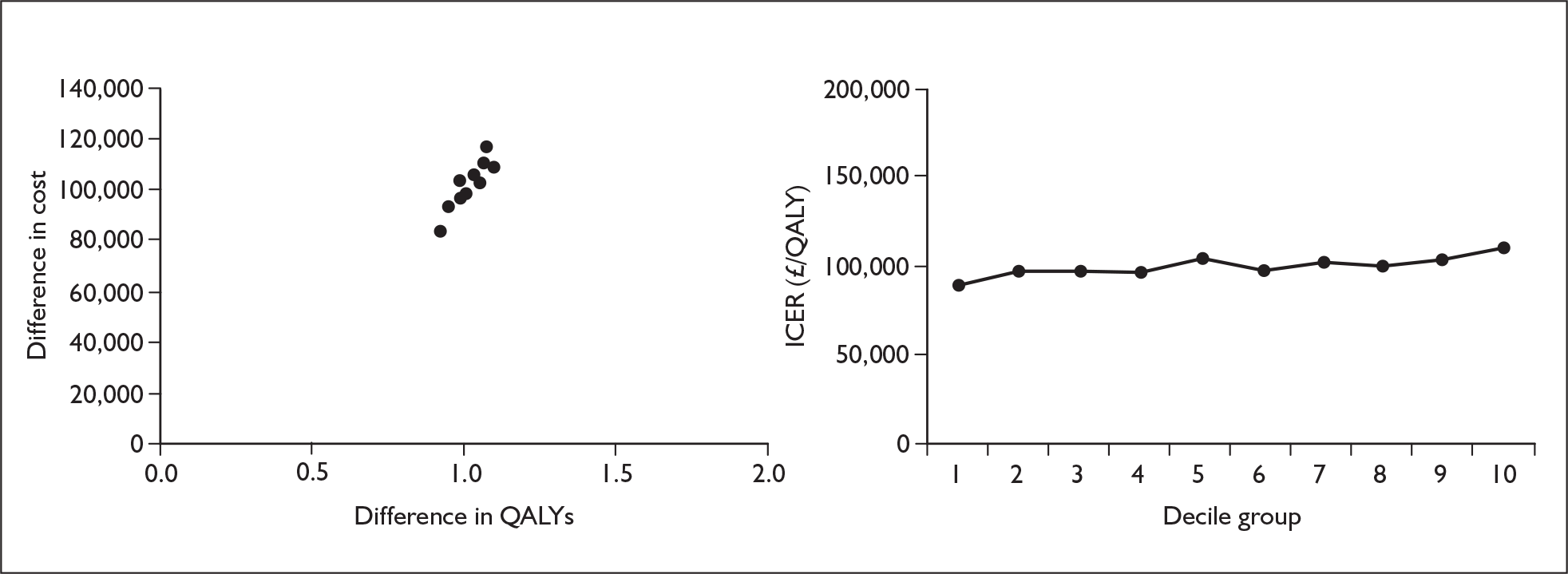
FIGURE 41.
Iloprost variation by mortality in functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
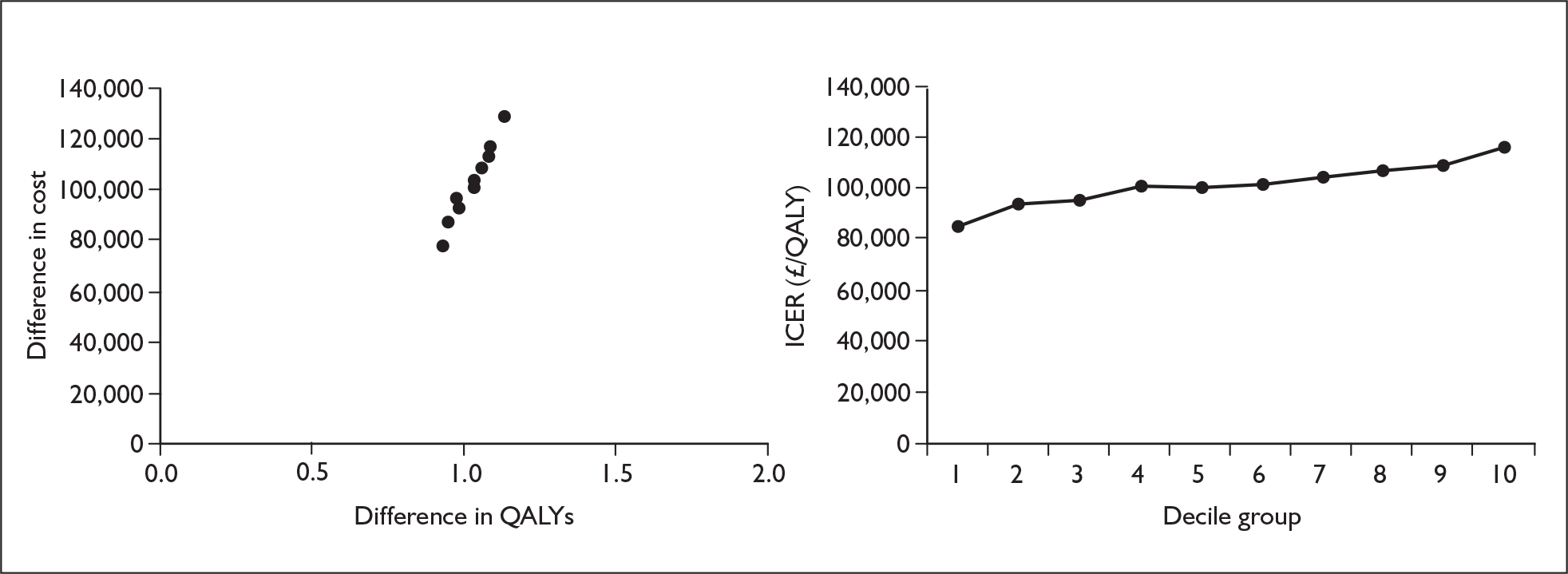
Appendix 11.4 Bosentan
FIGURE 42.
Bosentan variation by odds ratio of improvement from functional class III to functional class II. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
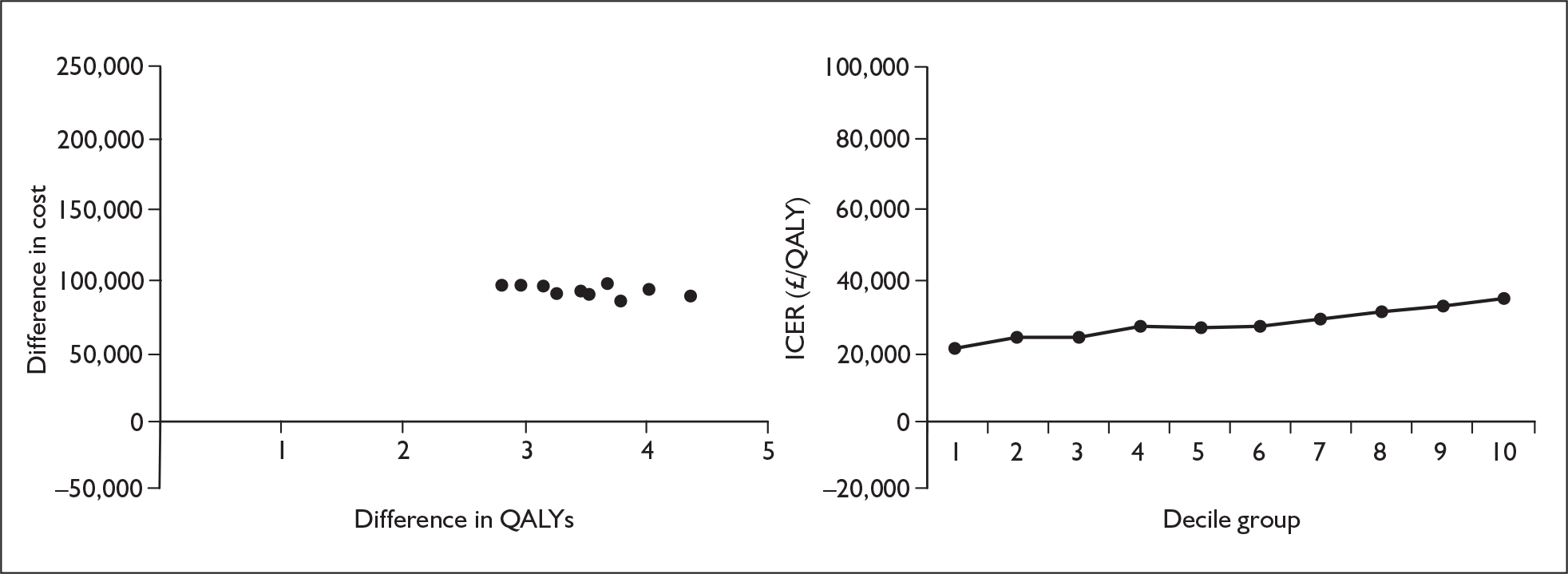
FIGURE 43.
Bosentan variation by odds ratio of deterioration from functional class II to functional class III. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
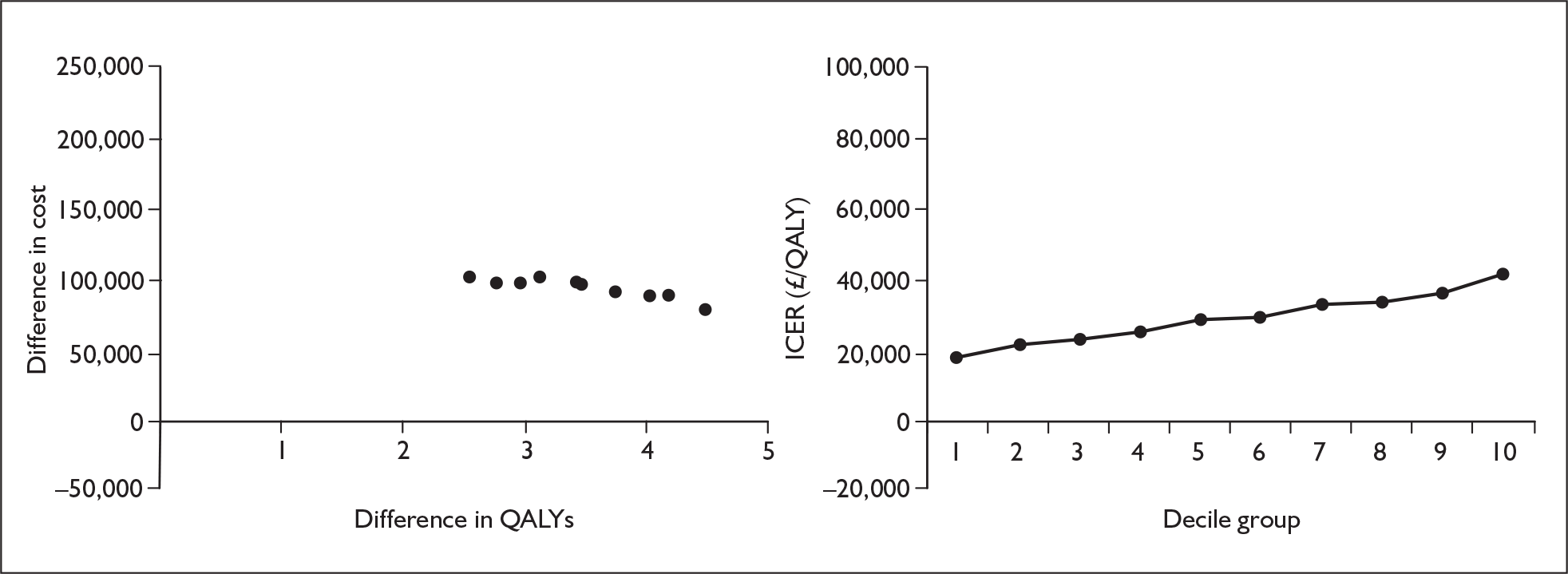
FIGURE 44.
Bosentan variation by odds ratio of deterioration from functional class III to functional class IV in the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
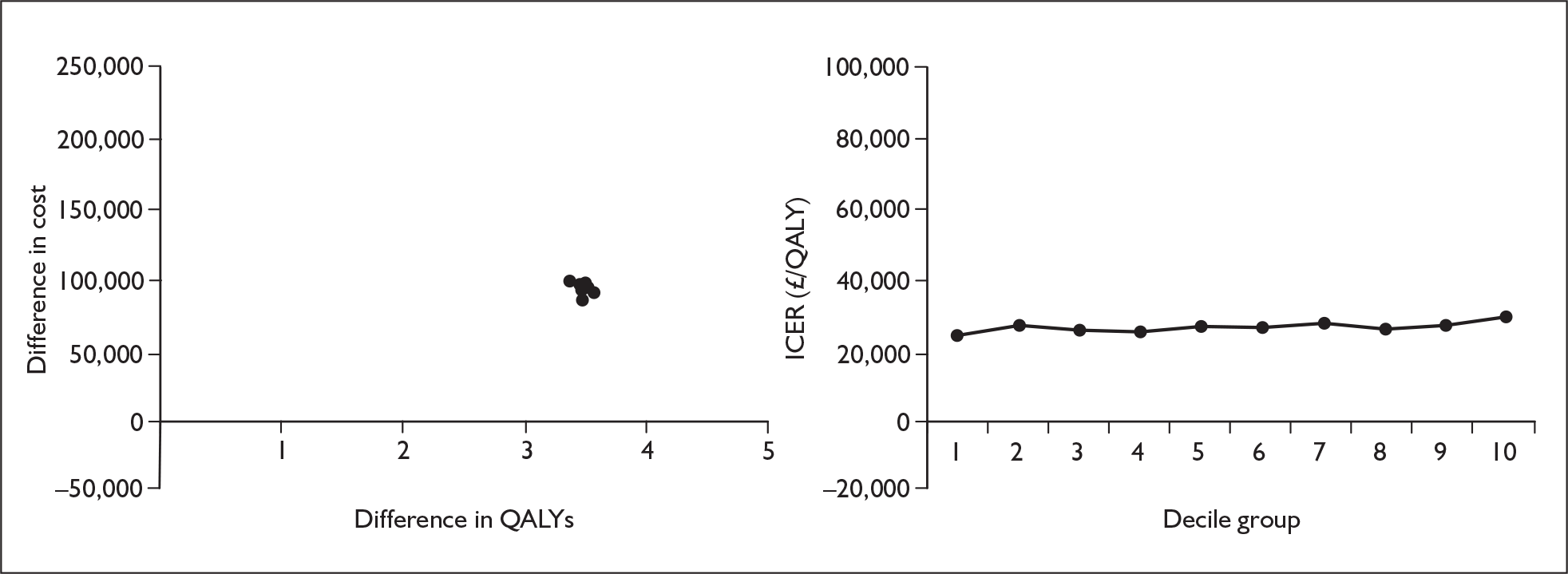
FIGURE 45.
Bosentan variation by odds ratio of deterioration from functional class III to functional class IV after the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
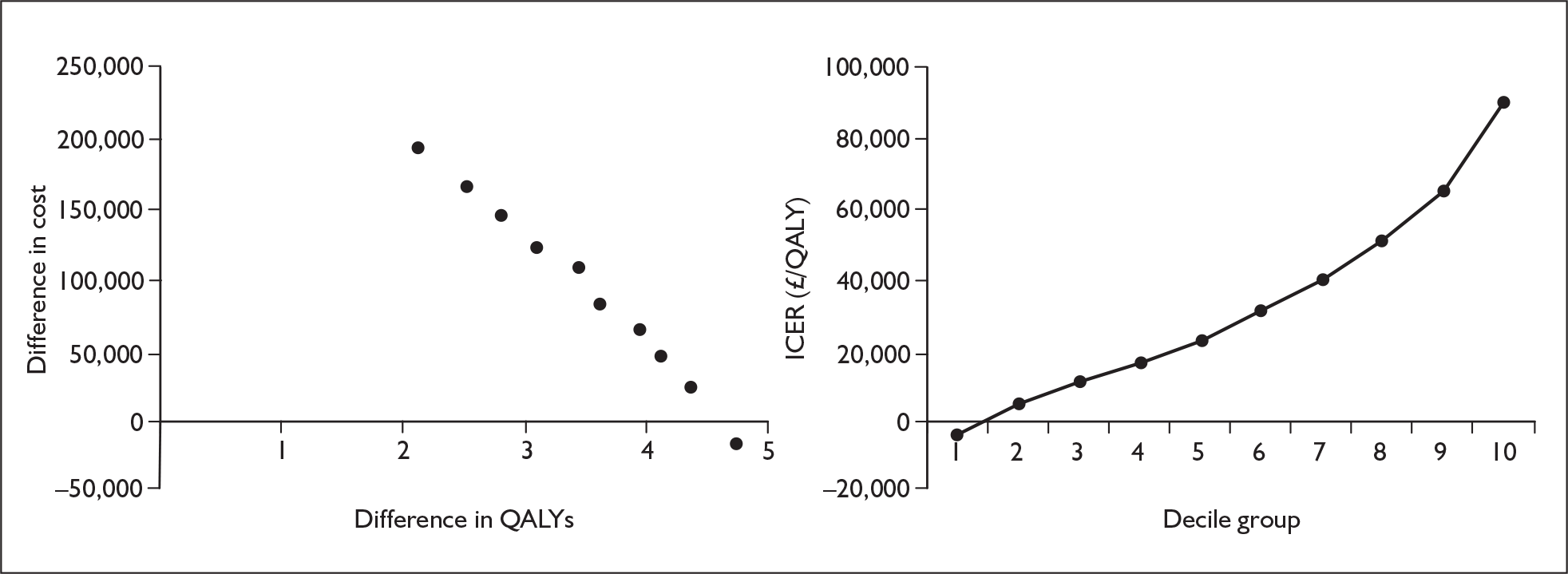
FIGURE 46.
Bosentan variation by probability of improvement from functional class III to functional class II on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
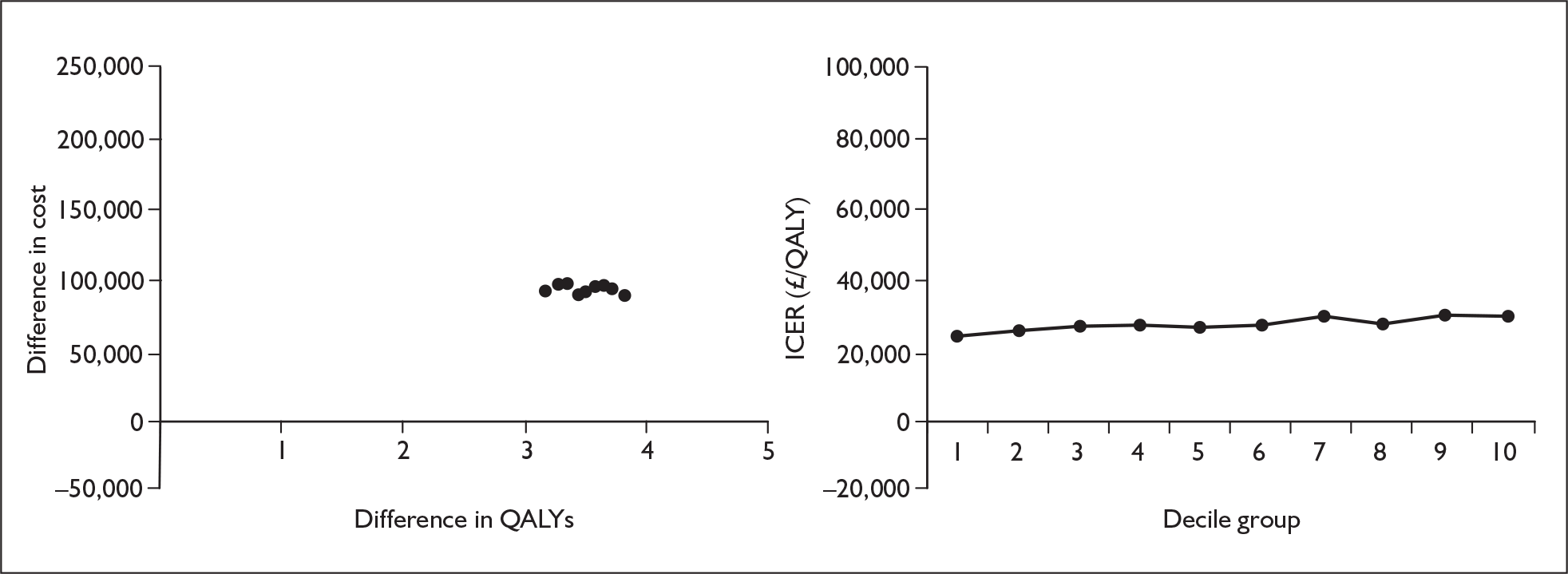
FIGURE 47.
Bosentan variation by probability of deterioration from functional class II to functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
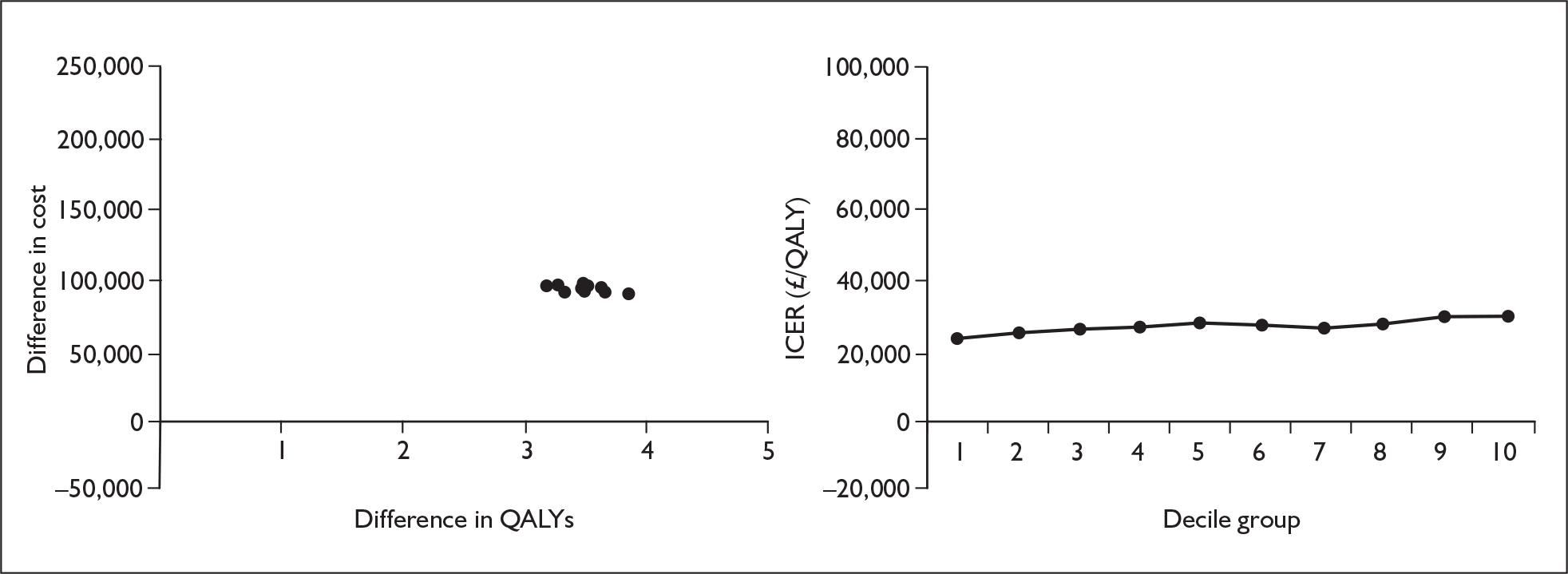
FIGURE 48.
Bosentan variation by probability of deterioration from functional class III to functional class IV in the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
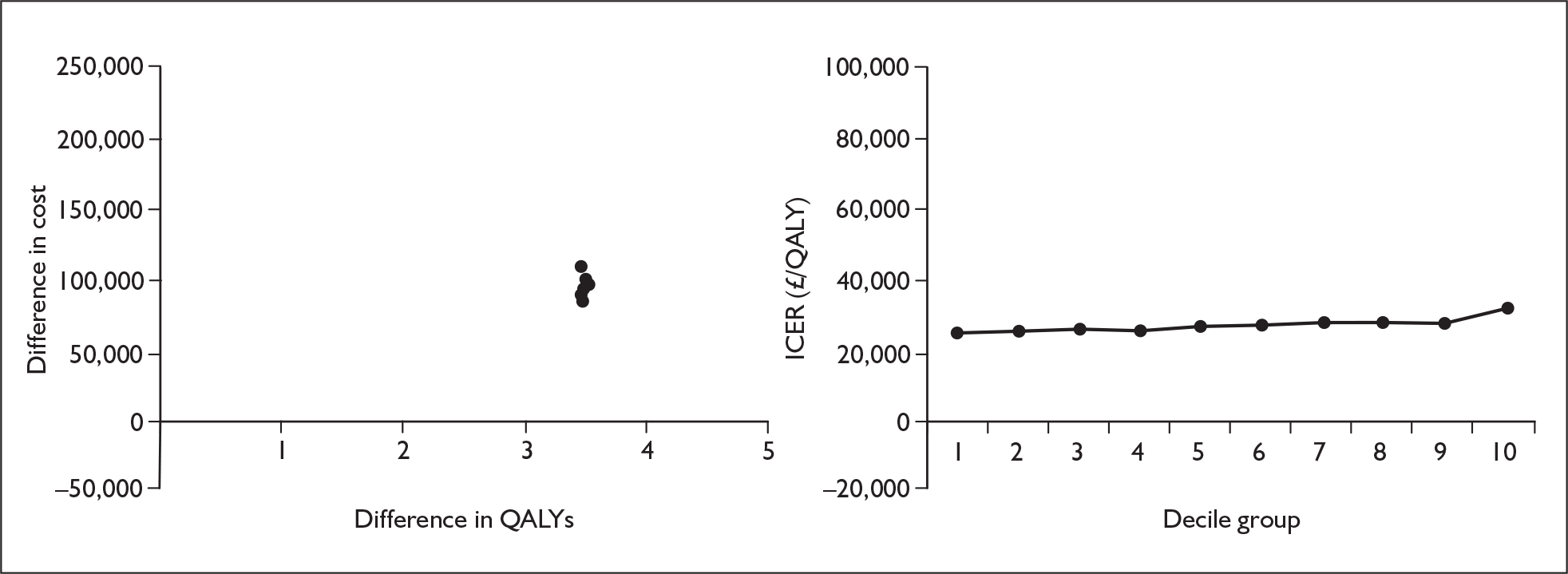
FIGURE 49.
Bosentan variation by probability of deterioration from functional class III to functional class IV after the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
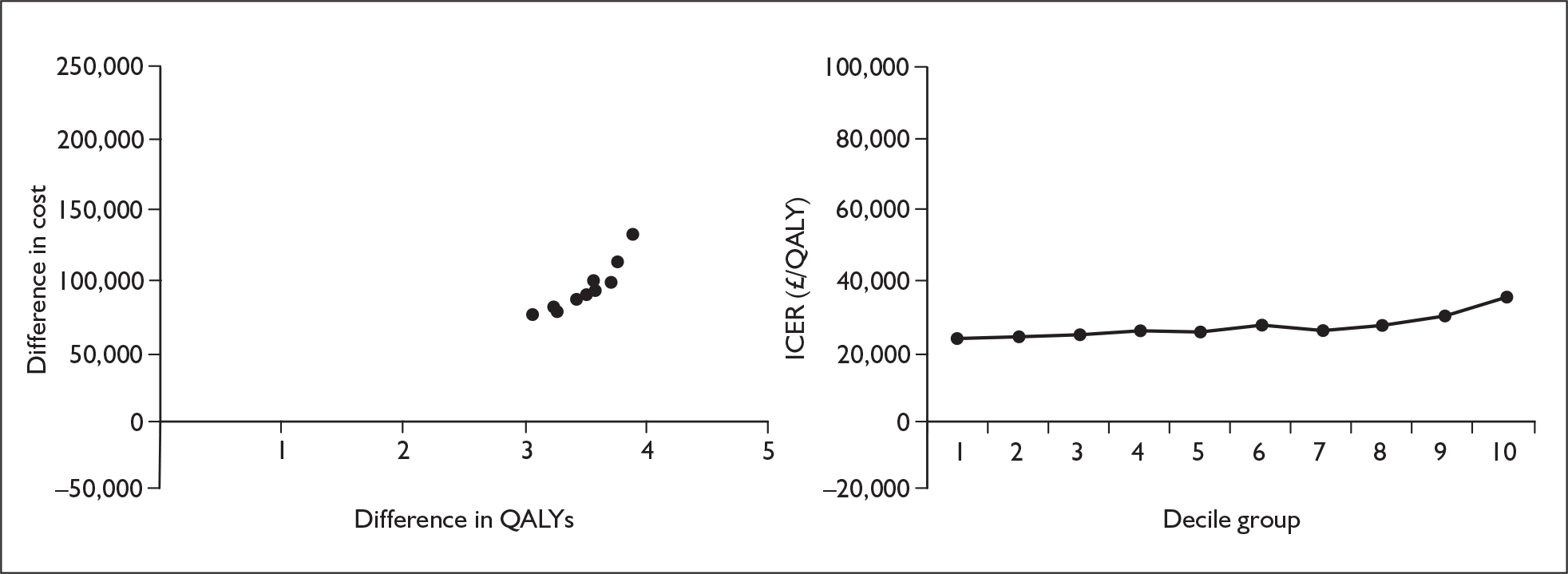
FIGURE 50.
Bosentan variation by mortality in functional class III on treatment. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
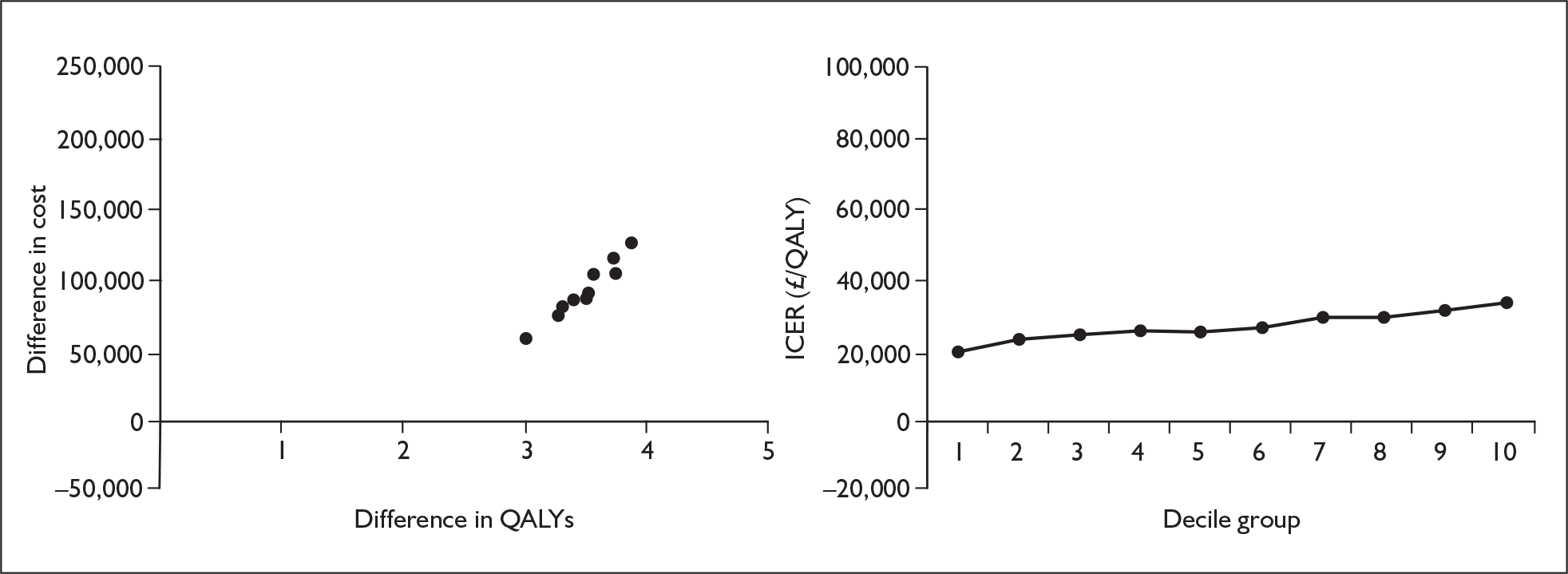
FIGURE 51.
Bosentan variation by mortality in functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
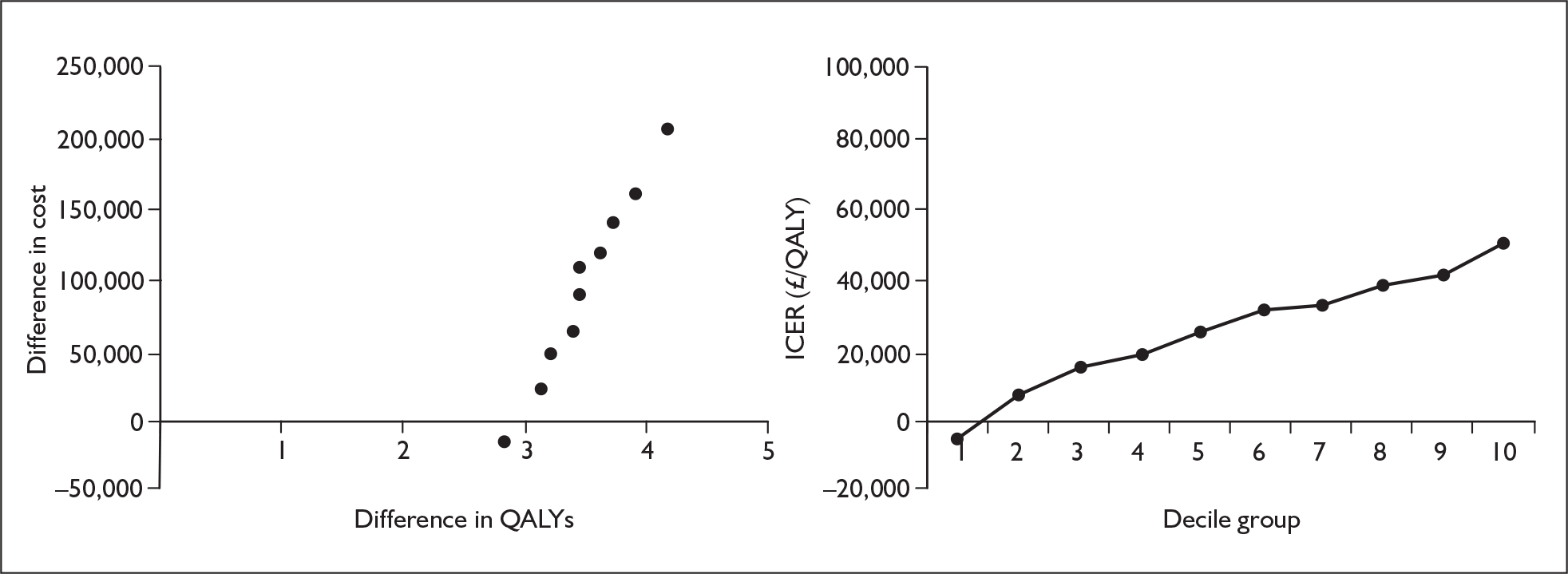
Appendix 11.5 Sitaxentan
FIGURE 52.
Sitaxentan variation by odds ratio of improvement from functional class III to functional class II. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
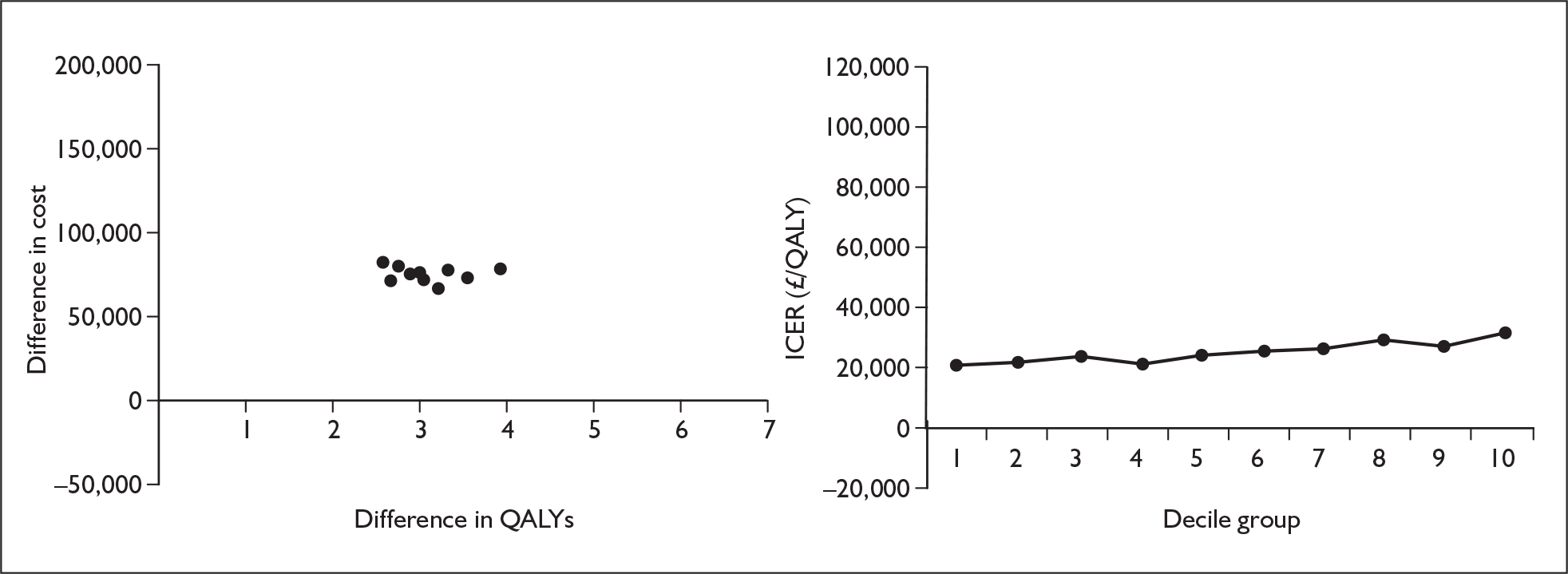
FIGURE 53.
Sitaxentan variation by odds ratio of deterioration from functional class II to functional class III. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
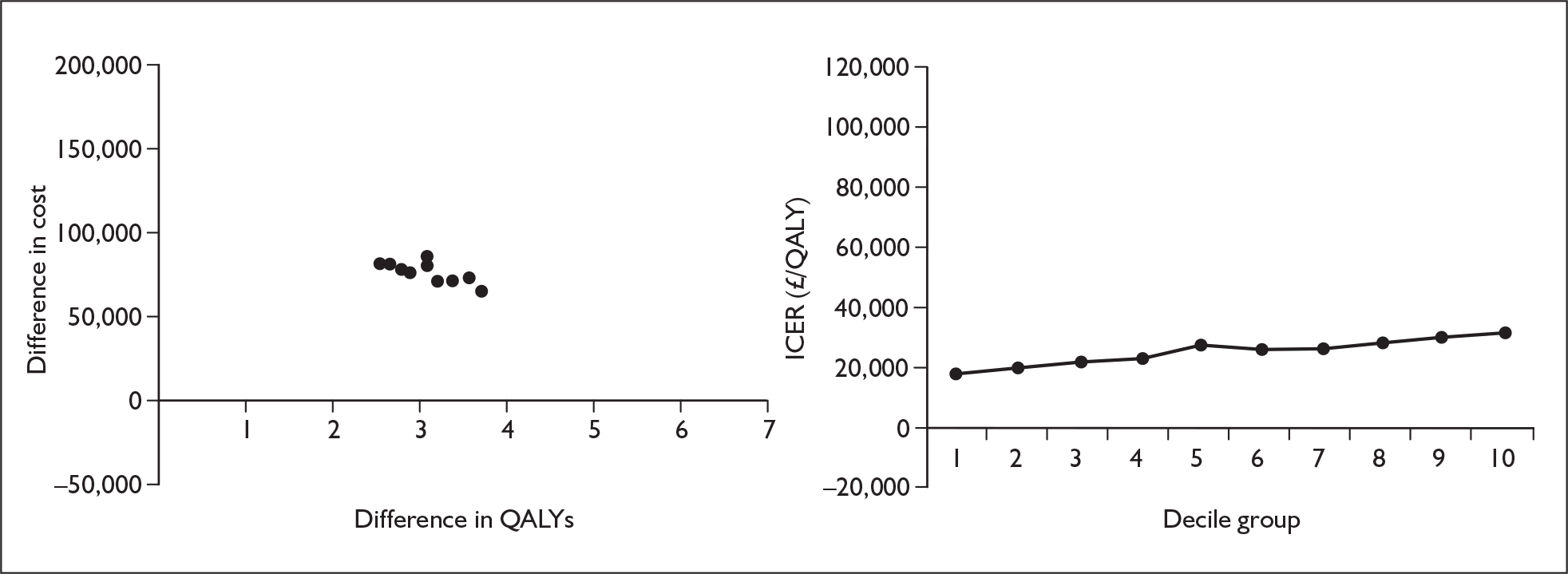
FIGURE 54.
Sitaxentan variation by odds ratio of deterioration from functional class III to functional class IV in the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
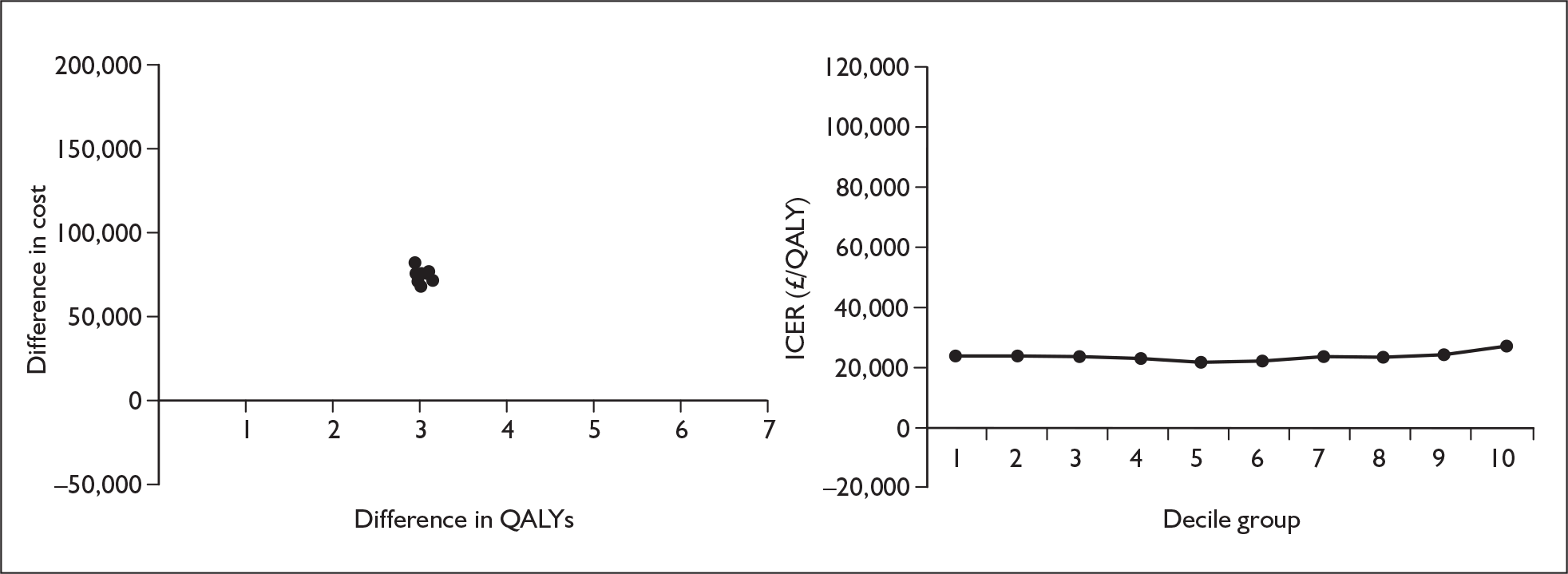
FIGURE 55.
Sitaxentan variation by odds ratio of deterioration from functional class III to functional class IV after the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
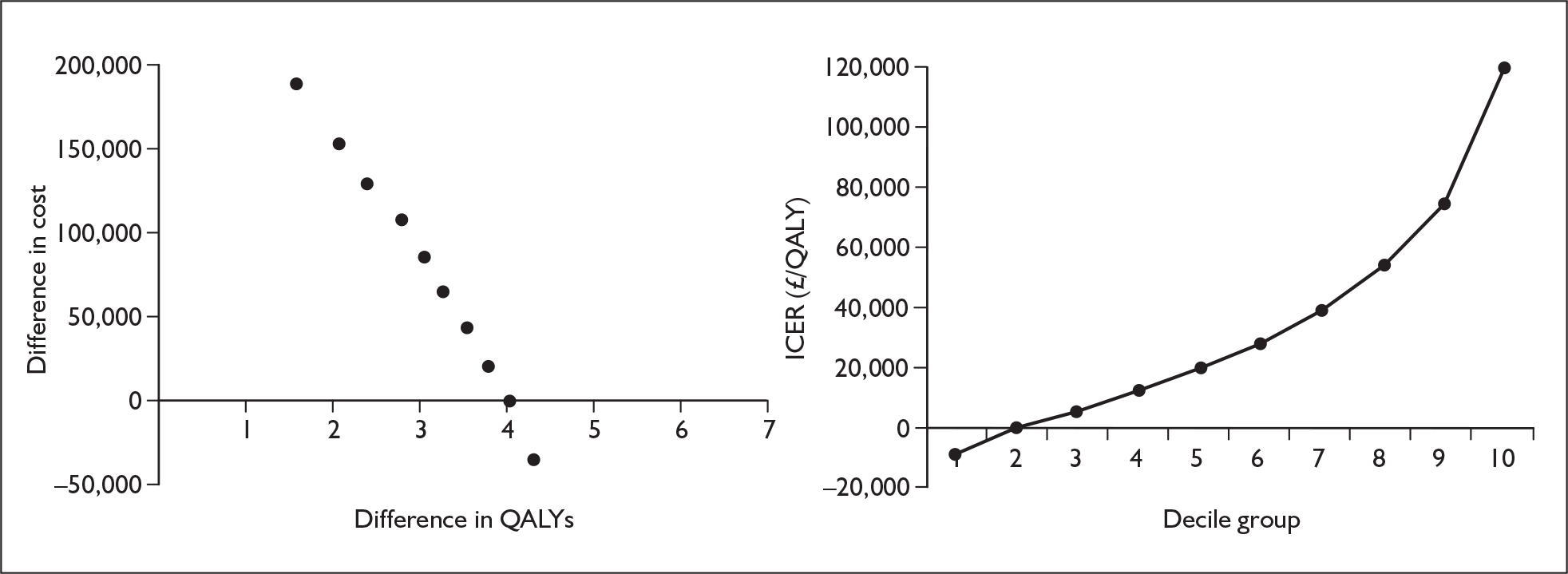
FIGURE 56.
Sitaxentan variation by probability of improvement from functional class III to functional class II on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
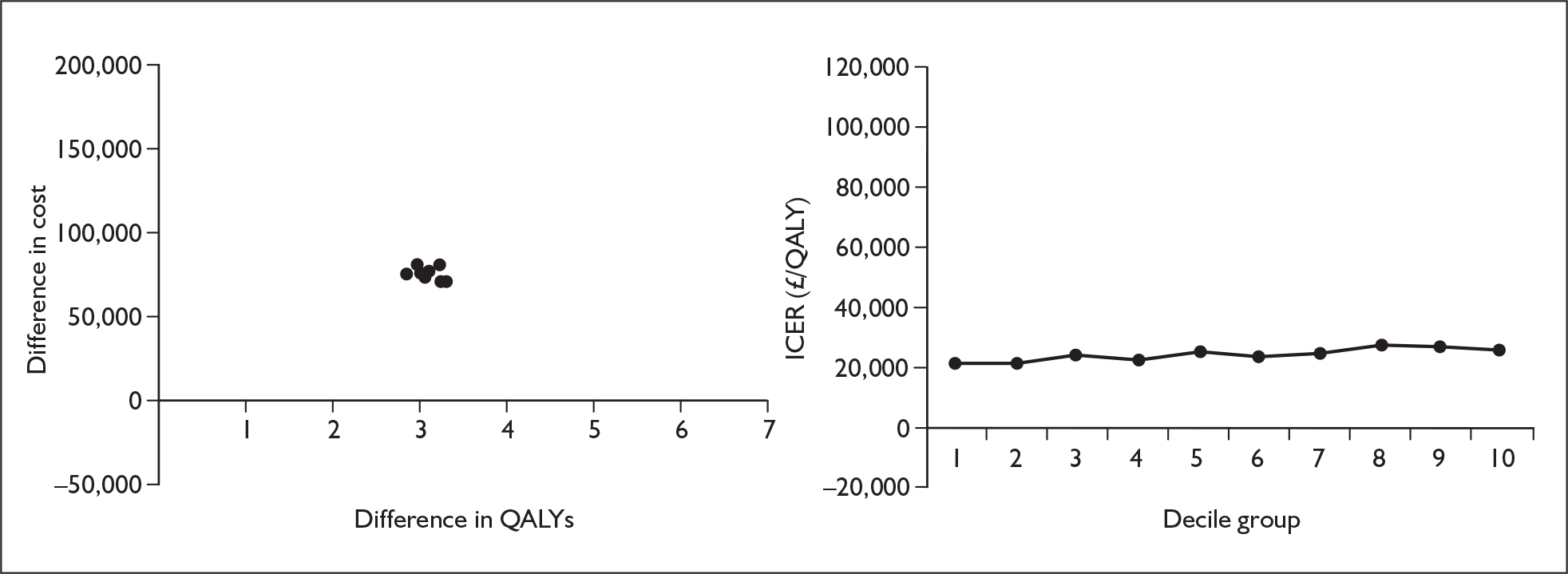
FIGURE 57.
Sitaxentan variation by probability of deterioration from functional class II to functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
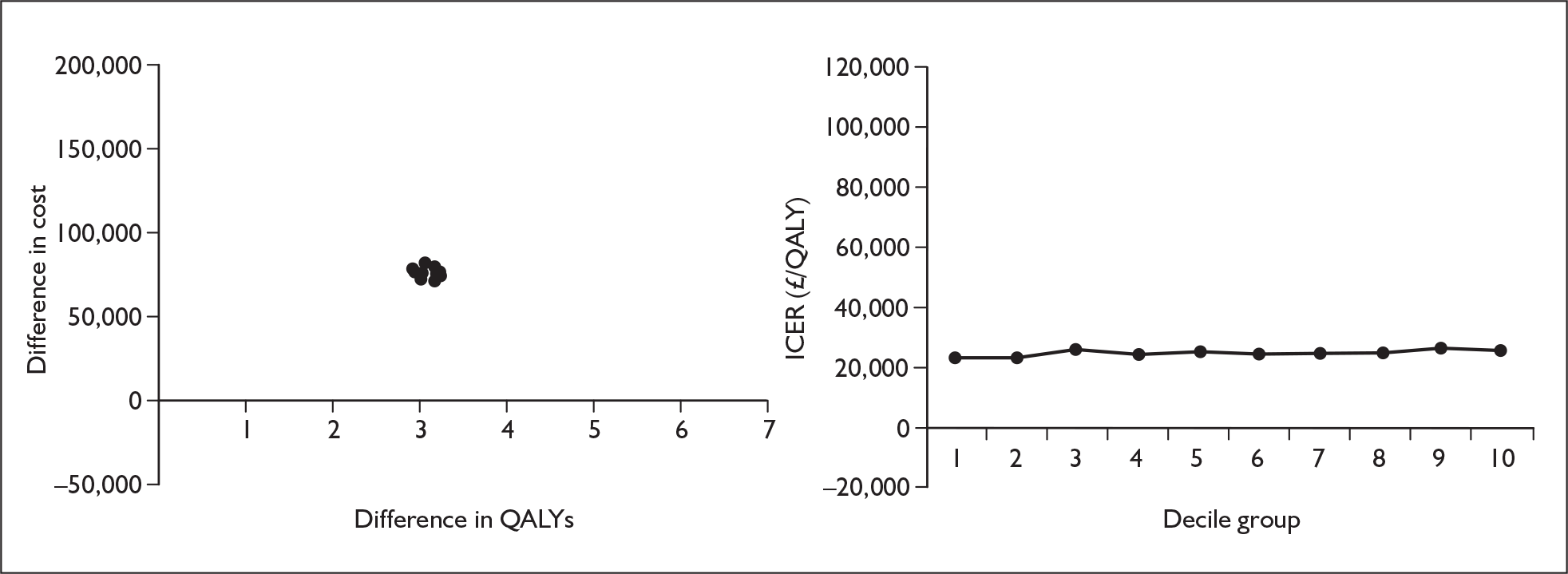
FIGURE 58.
Sitaxentan variation by probability of deterioration from functional class III to functional class IV in the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
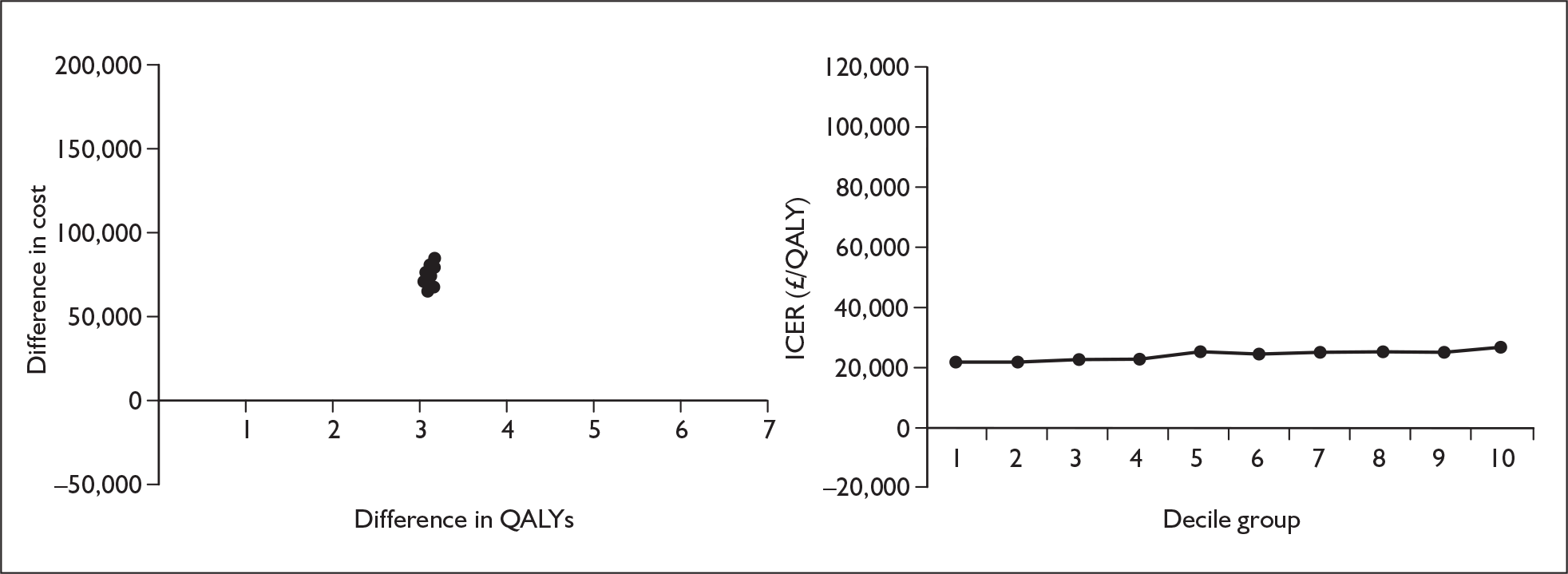
FIGURE 59.
Sitaxentan variation by probability of deterioration from functional class III to functional class IV after the first cycle on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
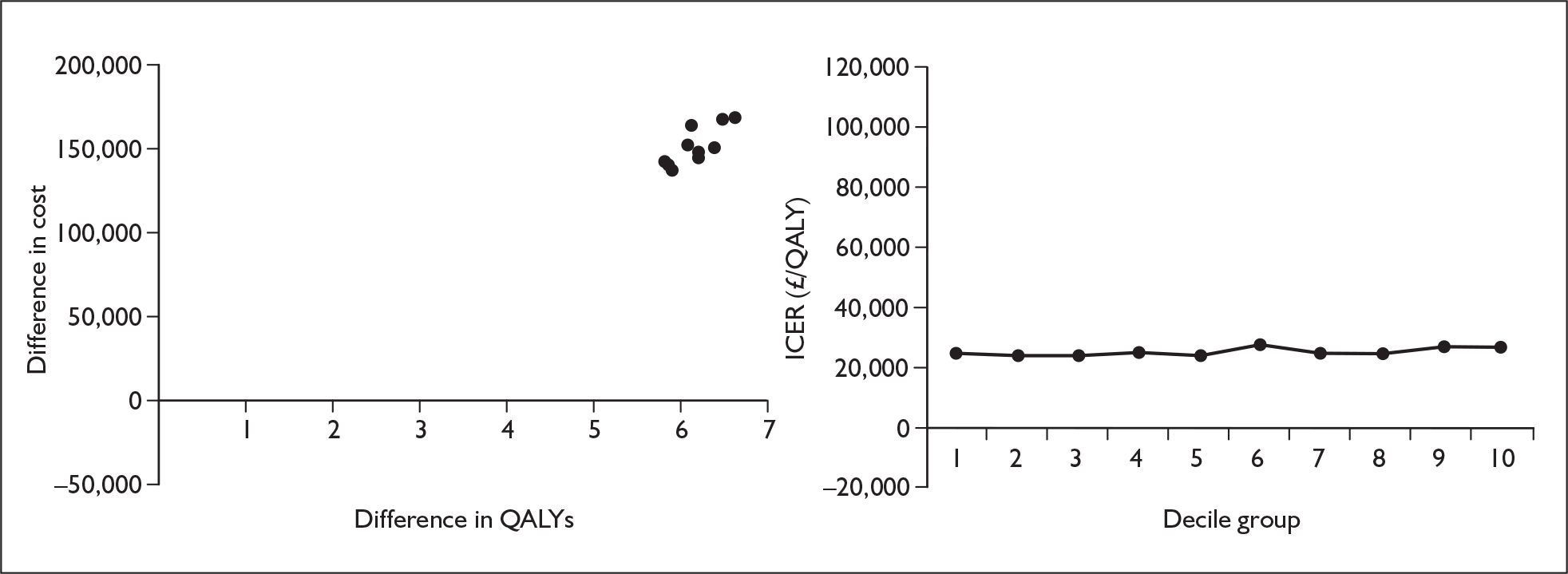
FIGURE 60.
Sitaxentan variation by mortality in functional class III on treatment. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
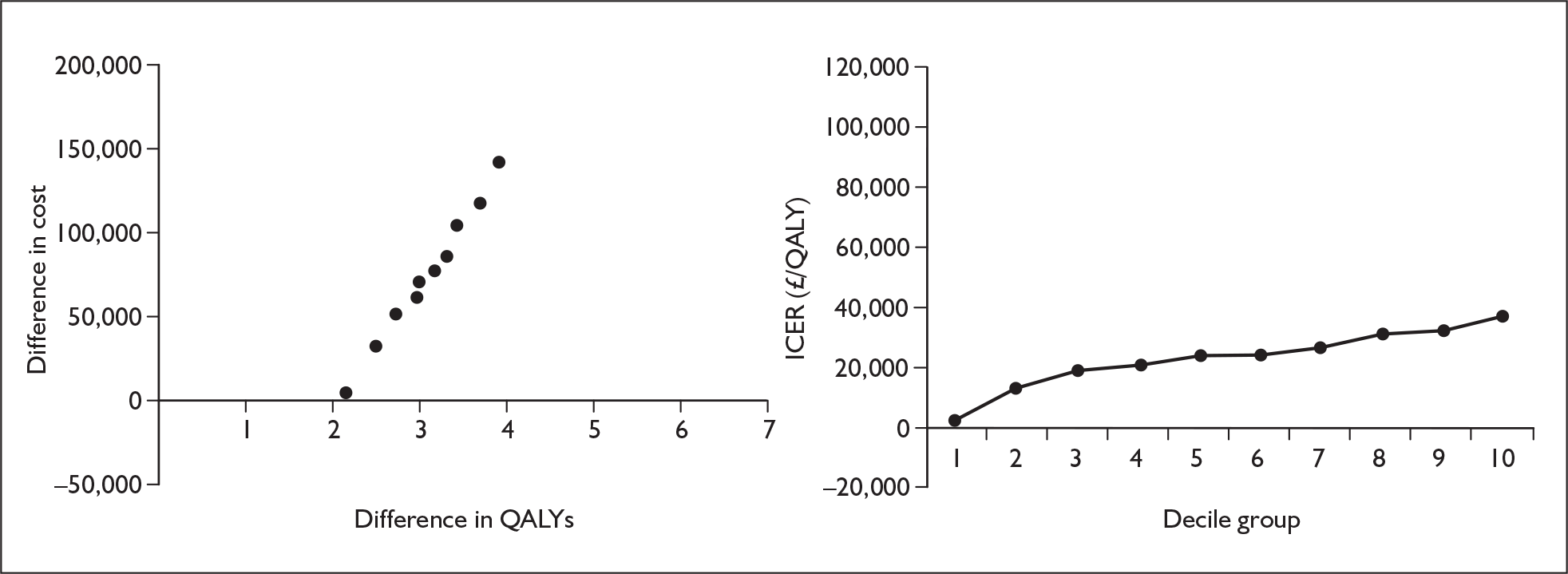
FIGURE 61.
Sitaxentan variation by mortality in functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
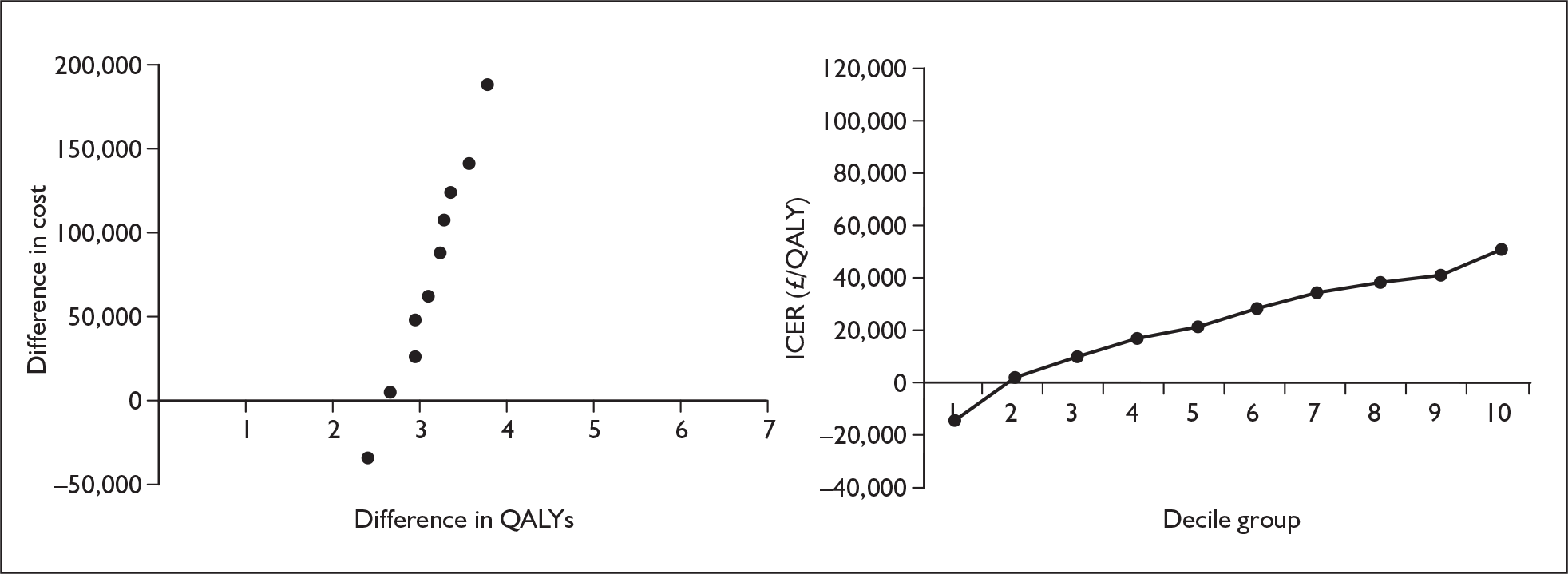
Appendix 11.6 Sildenafil
FIGURE 62.
Sildenafil variation by odds ratio of improvement from functional class III to functional class II. QALYs, quality-adjusted life-years.
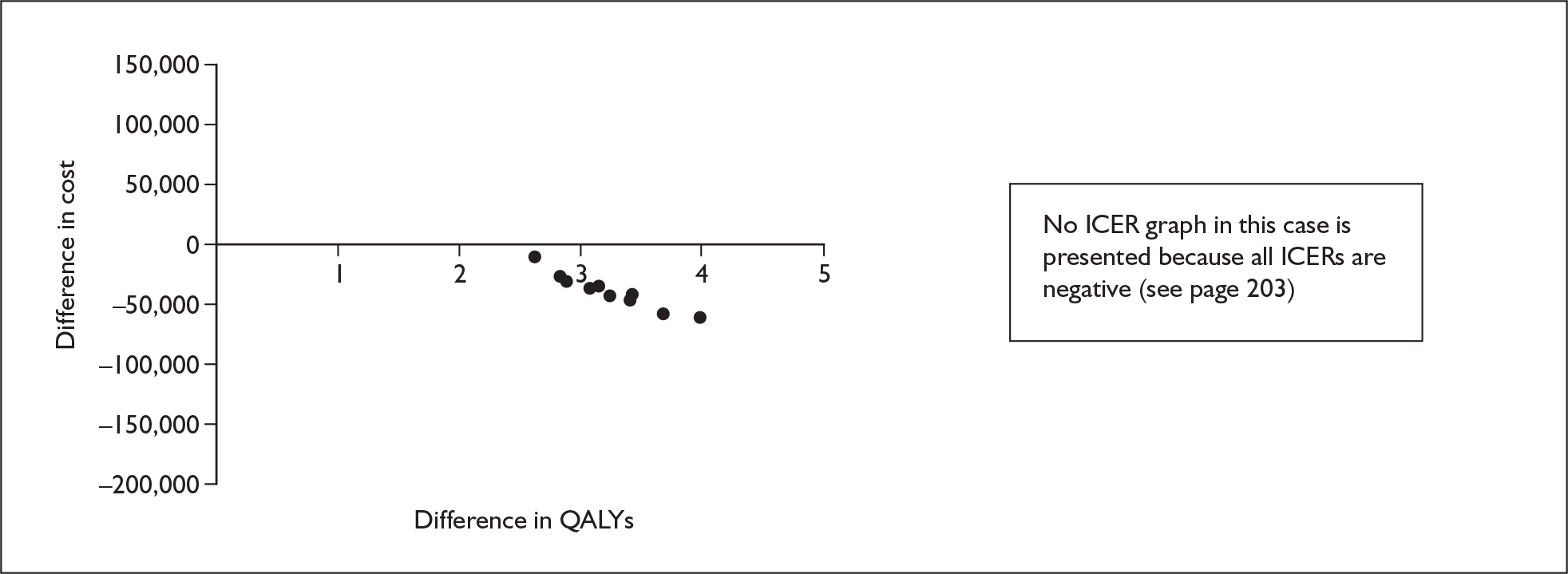
FIGURE 63.
Sildenafil variation by odds ratio of deterioration from functional class II to functional class III. QALYs, quality-adjusted life-years.
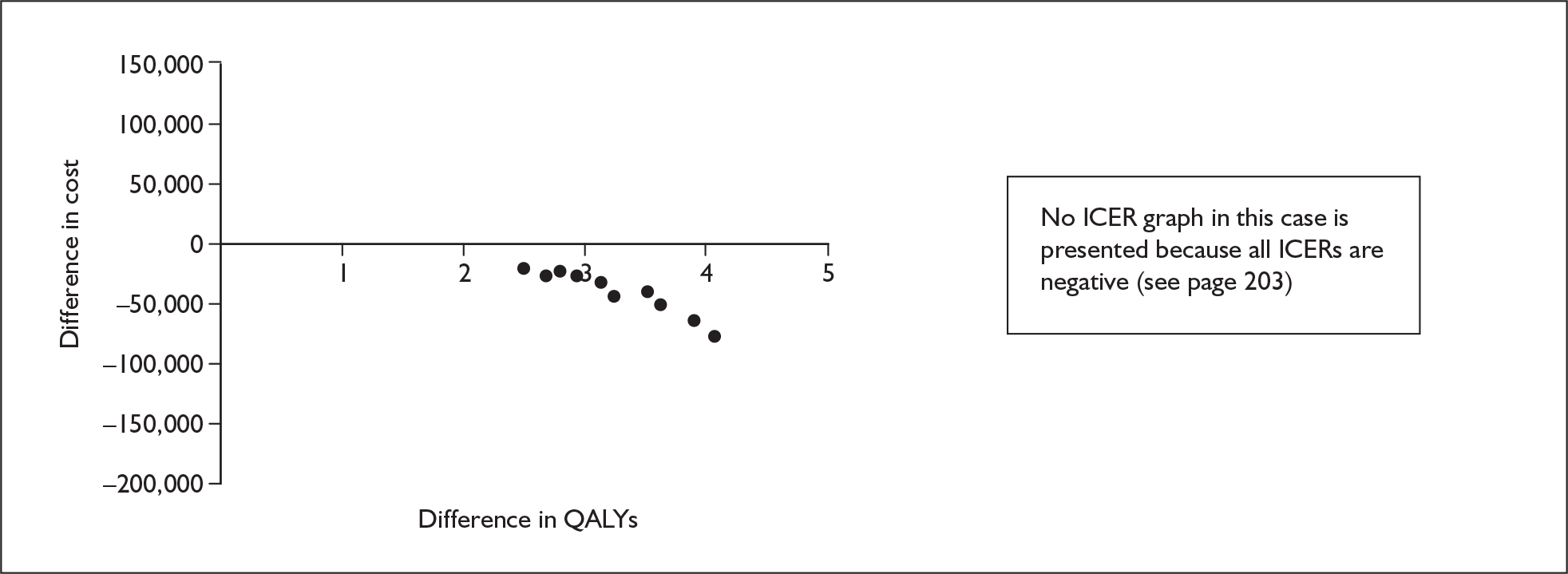
FIGURE 64.
Sildenafil variation by odds ratio of deterioration from functional class III to functional class IV in the first cycle. QALYs, quality-adjusted life-years.
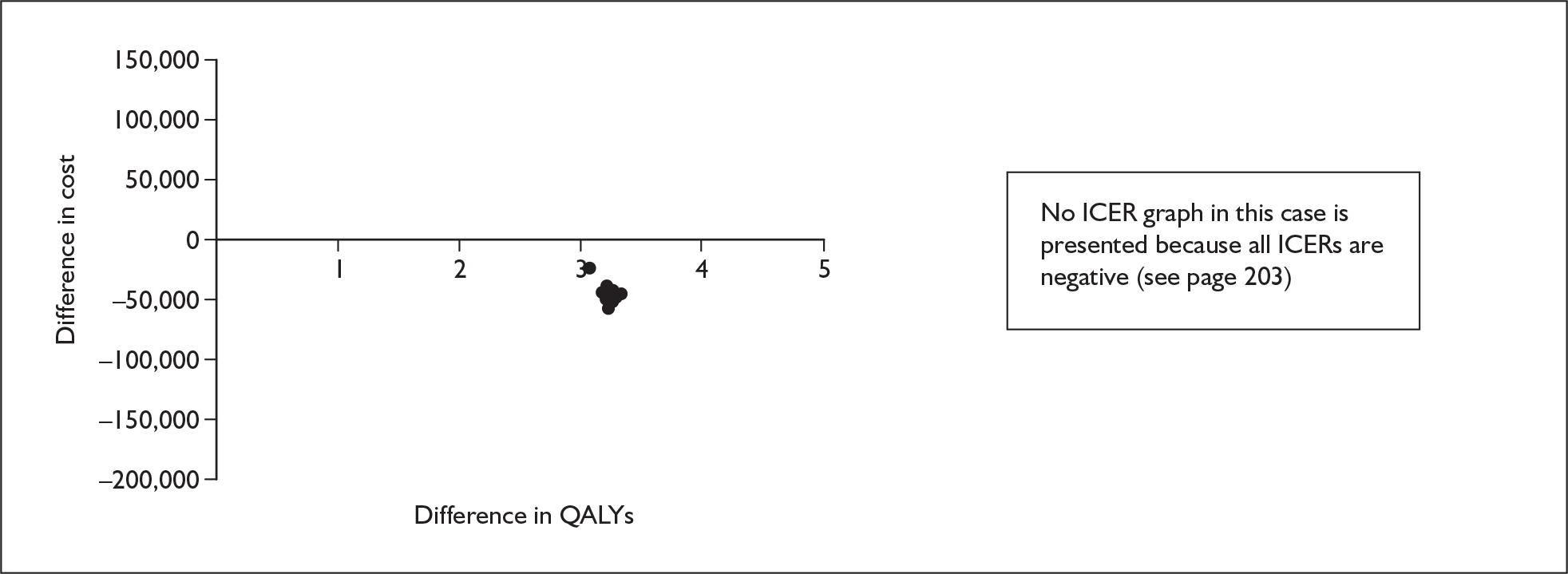
FIGURE 65.
Sildenafil variation by odds ratio of deterioration from functional class III to functional class IV after the first cycle. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
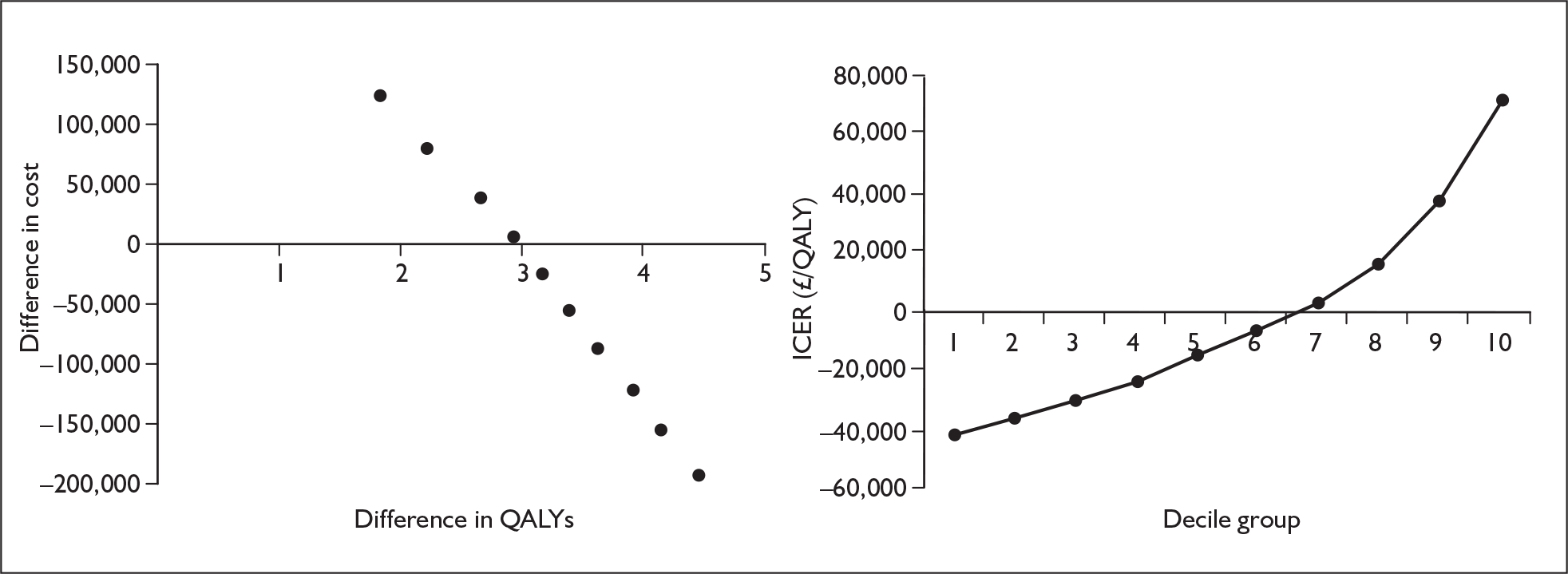
FIGURE 66.
Sildenafil variation by probability of improvement from functional class III to functional class II on supportive care. QALYs, quality-adjusted life-years.
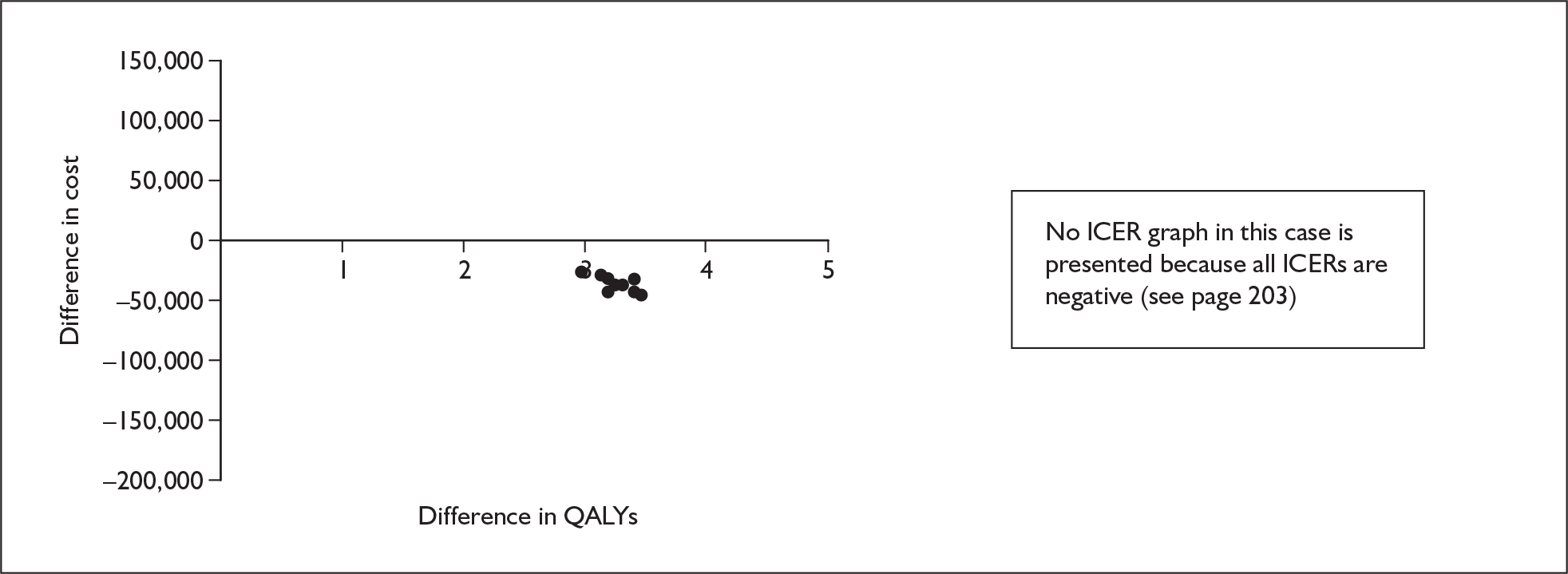
FIGURE 67.
Sildenafil variation by probability of deterioration from functional class II to functional class III on supportive care. QALYs , quality-adjusted life-years.
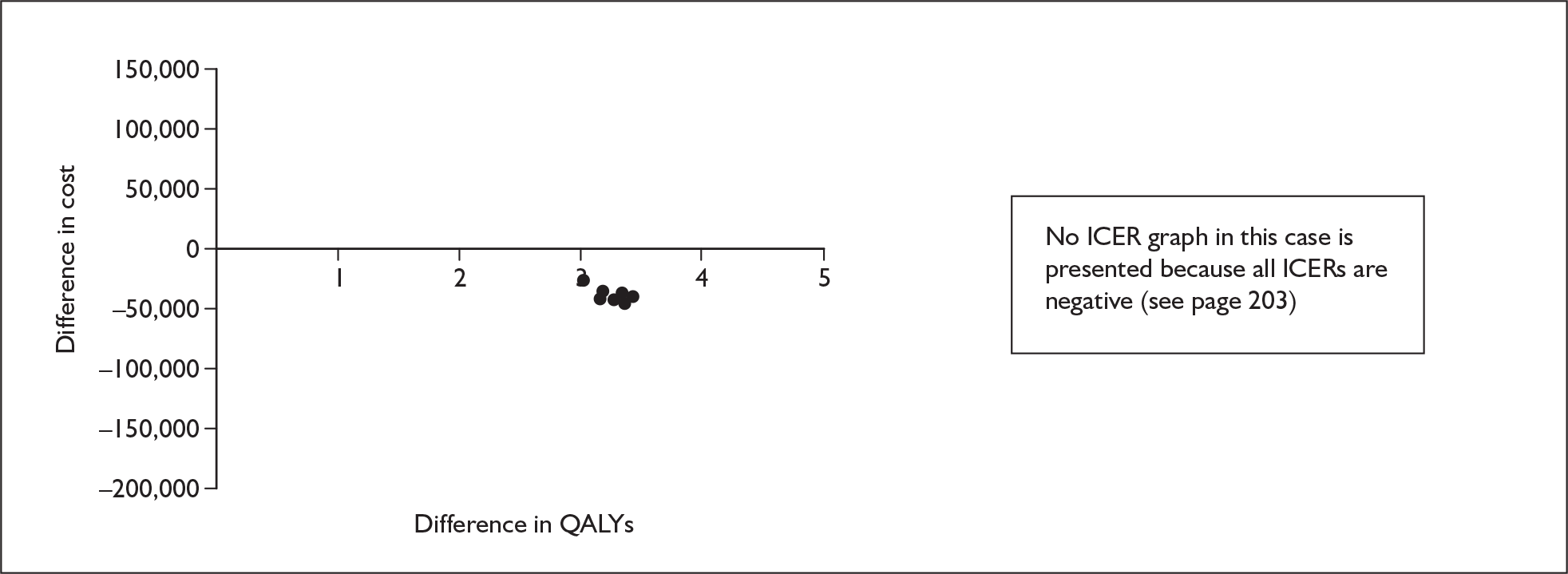
FIGURE 68.
Sildenafil variation by probability of deterioration from functional class III to functional class IV in the first cycle on supportive care. QALYs, quality-adjusted life-years.
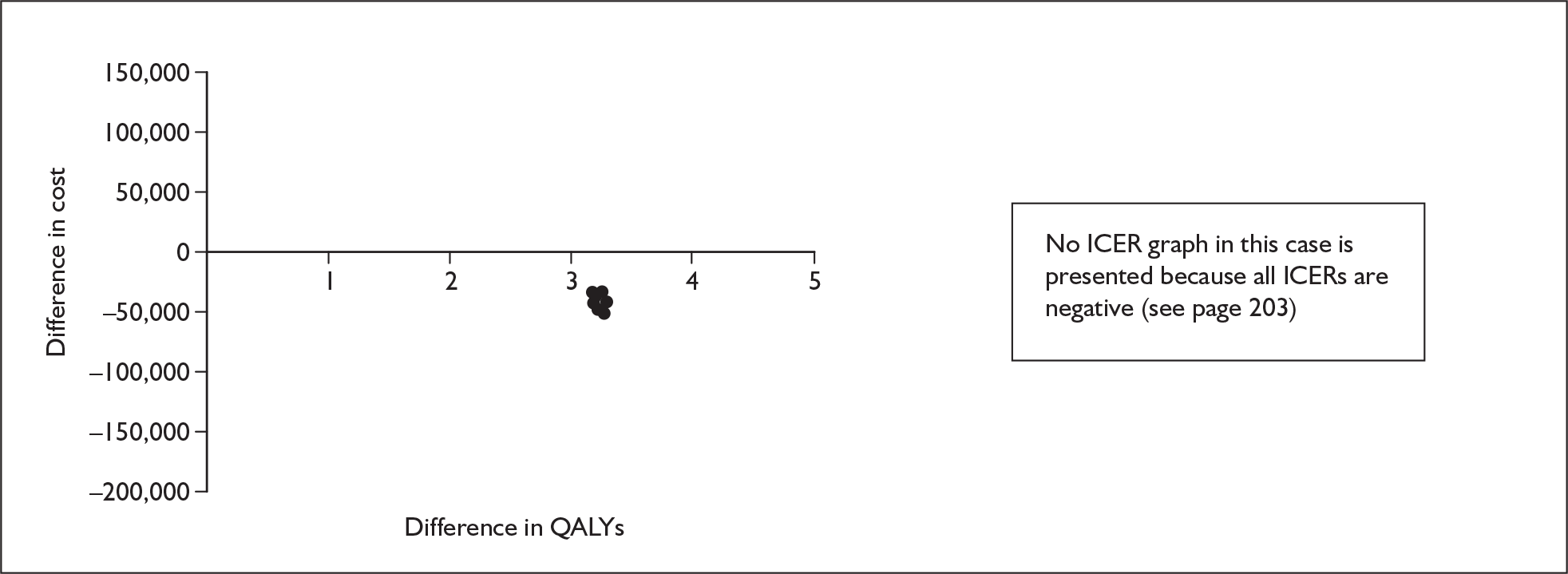
FIGURE 69.
Sildenafil variation by probability of deterioration from functional class III to functional class IV after the first cycle on supportive care. QALYs, quality-adjusted life-years.
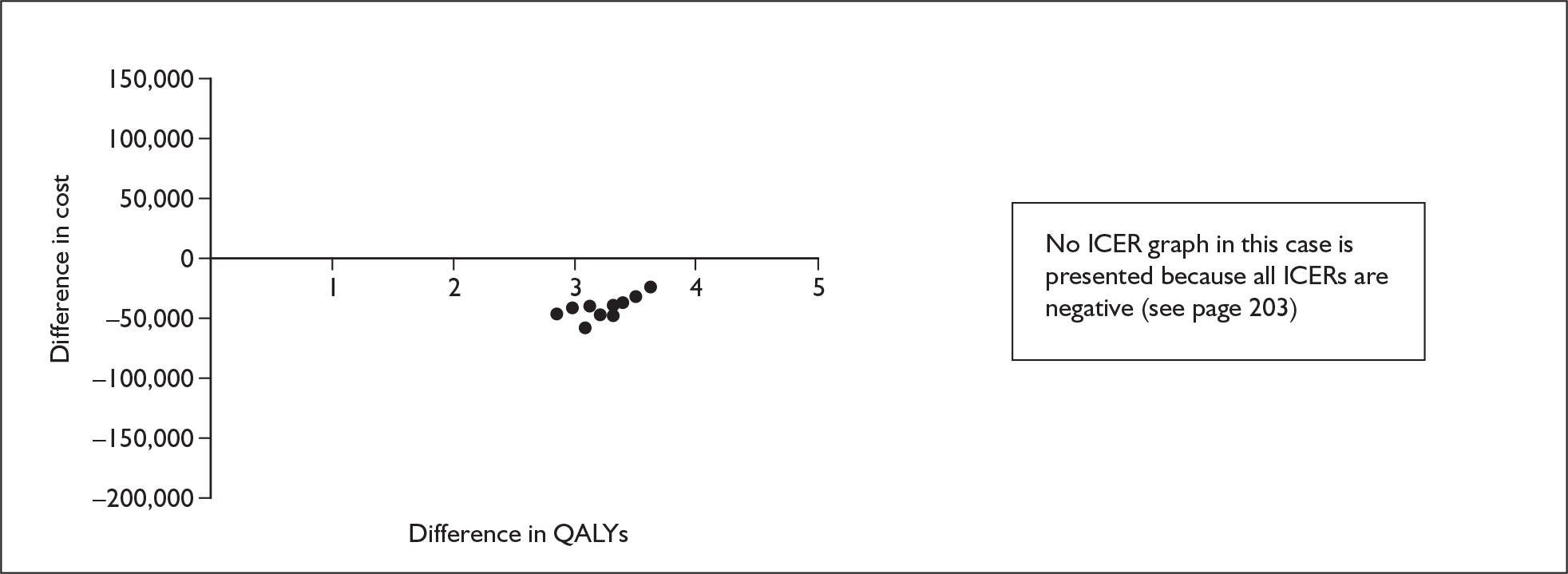
FIGURE 70.
Sildenafil variation by mortality in functional class III on treatment. ICER, incremental cost-effectiveness ratio; ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
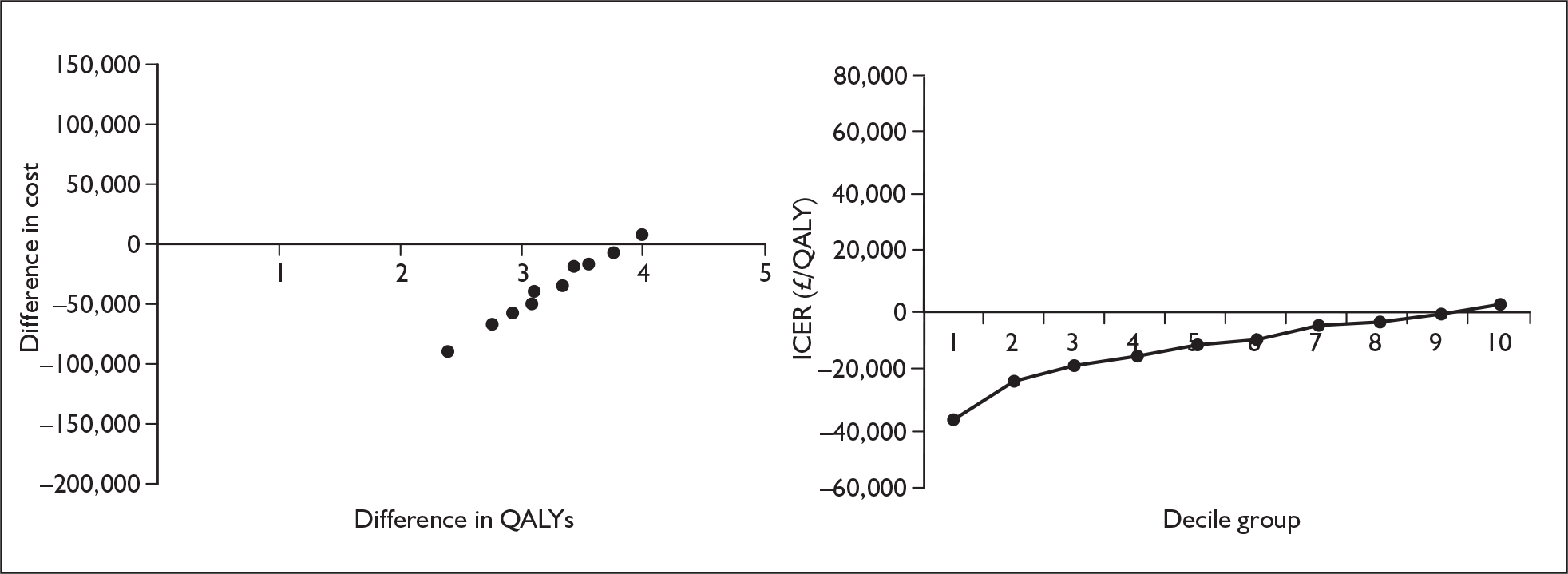
FIGURE 71.
Sildenafil variation by mortality in functional class III on supportive care. ICER, incremental cost-effectiveness ratio; QALY(s), quality-adjusted life-year(s).
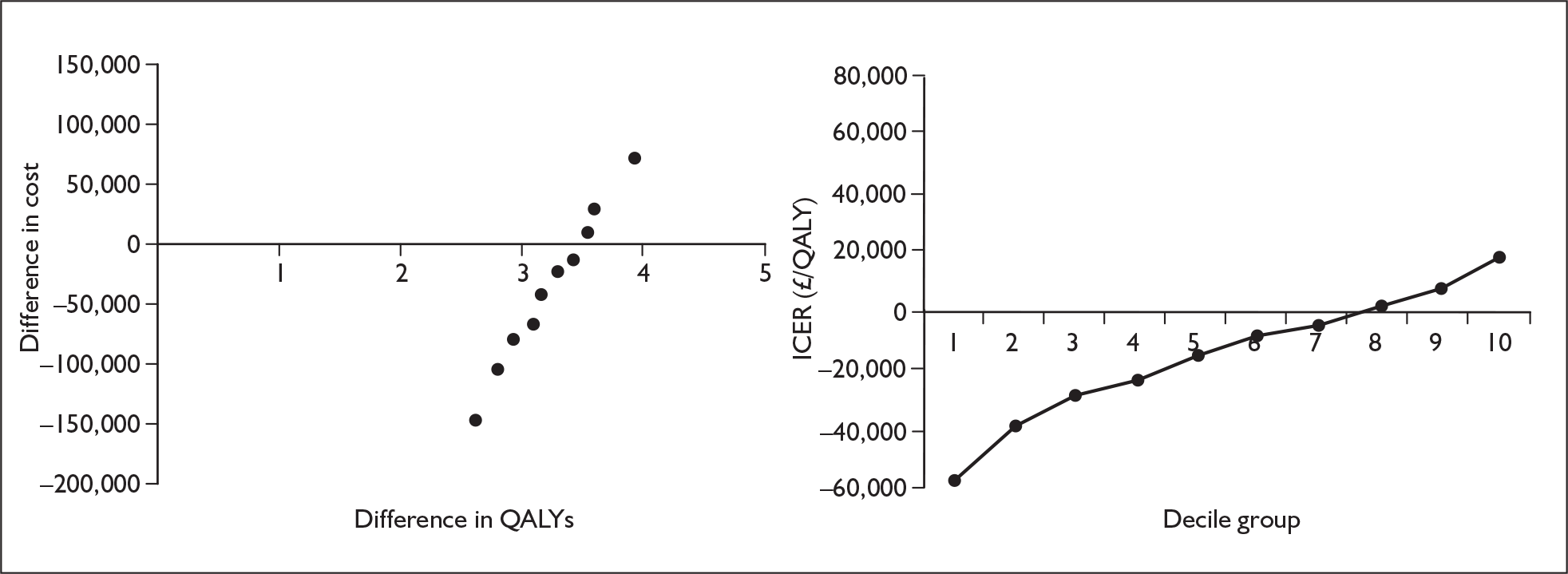
Appendix 12 Non-reference case model runs
The following tables and cost-effectiveness acceptability curves are for the non-reference case analyses conducted to consider alternative time horizons, pricing and health state utility value sets. The analyses are presented therapy-by-therapy.
Appendix 12.1 Epoprostenol with supportive care versus supportive care alone, functional class III
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 477,000 | 2.049 | |||
| Epoprostenol | 693,000 | 216,000 | 2.828 | 0.779 | 277,000 |
FIGURE 72.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: time horizon of 20 years. QALY, quality-adjusted life-year.
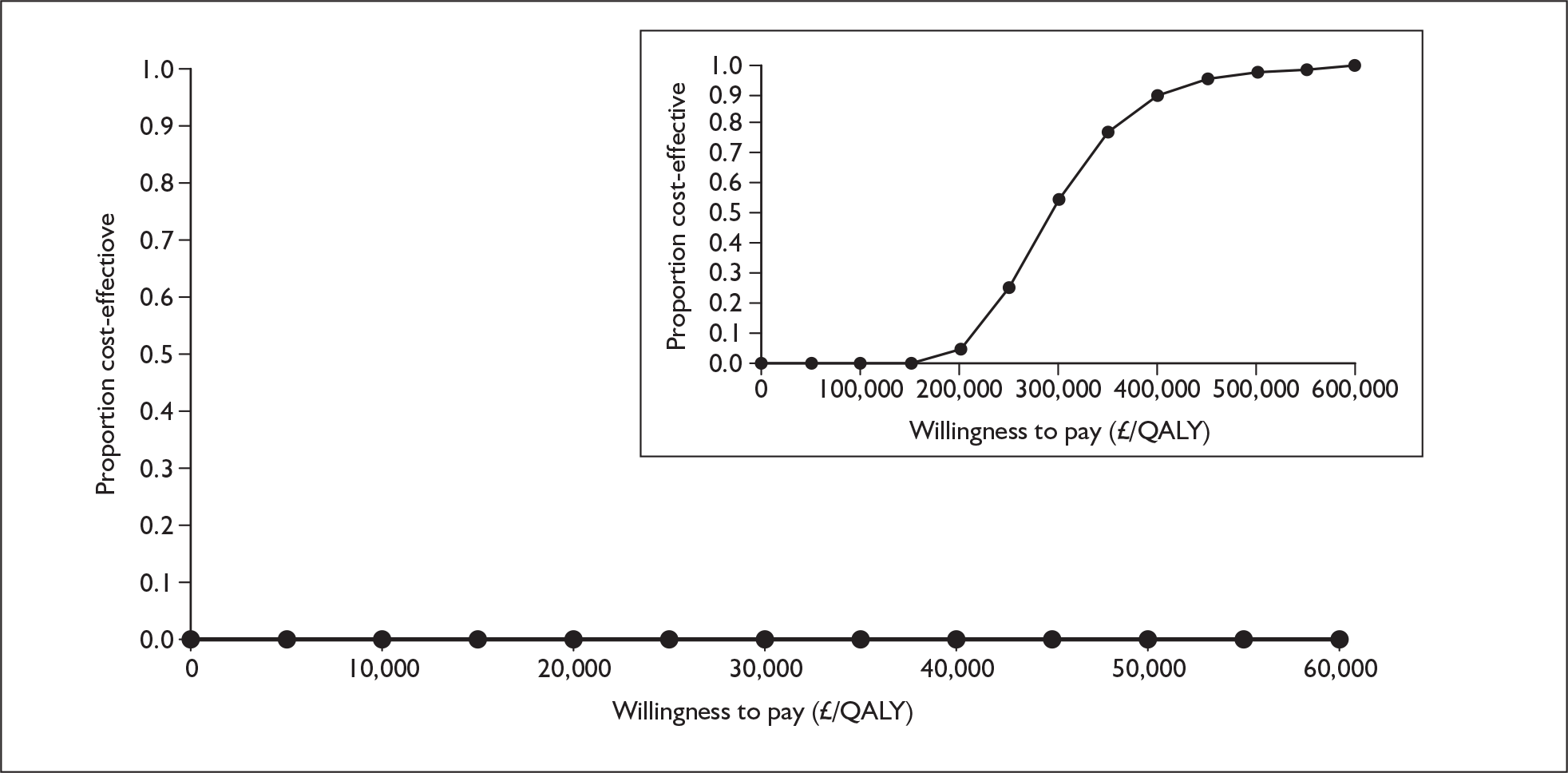
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 443,000 | 1.936 | |||
| Epoprostenol | 632,000 | 189,000 | 2.619 | 0.683 | 277,000 |
FIGURE 73.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: time horizon of 10 years. QALY, quality-adjusted life-year.
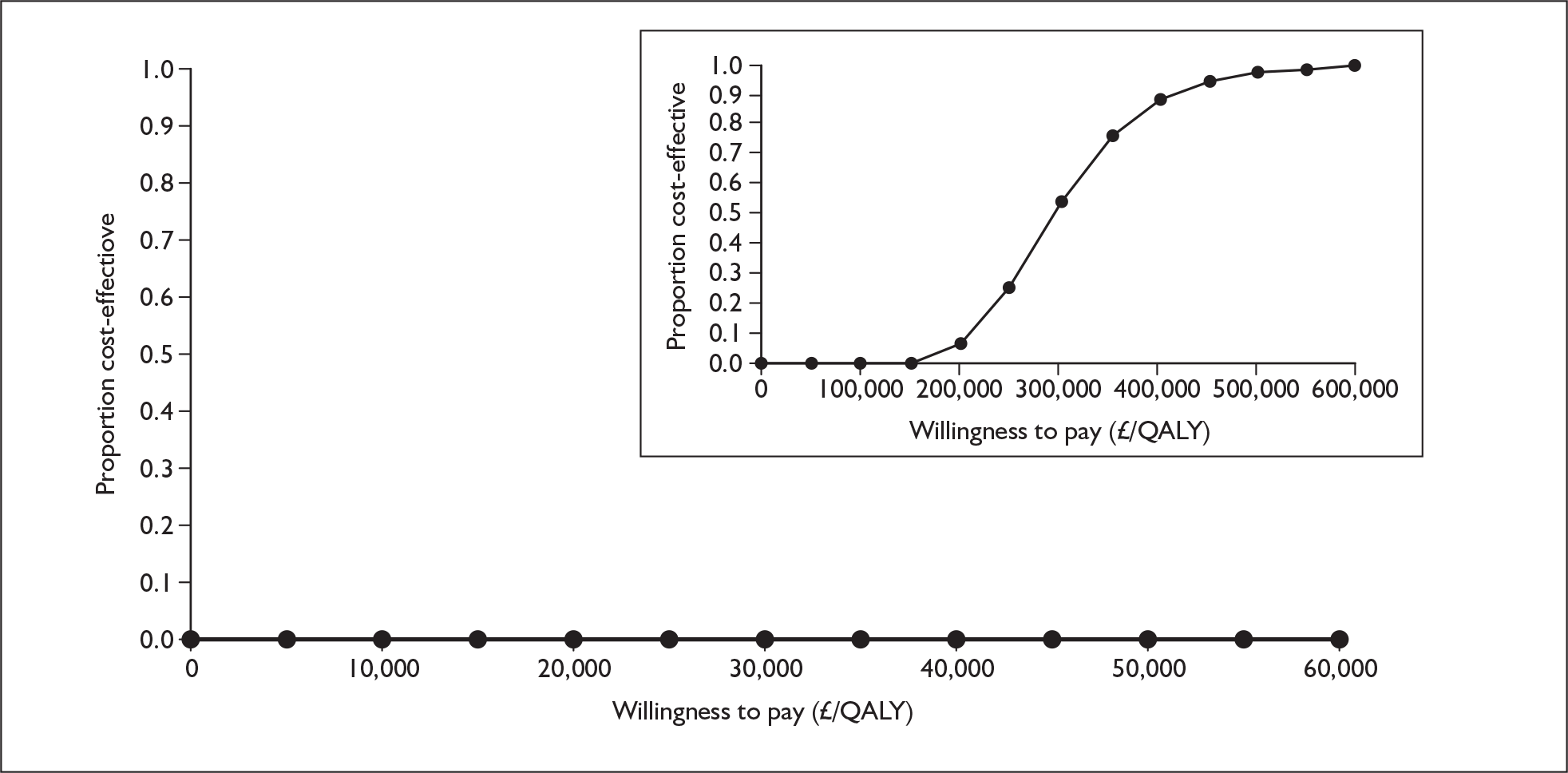
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 217,000 | 2.056 | |||
| Epoprostenol | 301,000 | 83,000 | 2.843 | 0.787 | 106,000 |
FIGURE 74.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: alternative price for epoprostenol. QALY, quality-adjusted life-year.
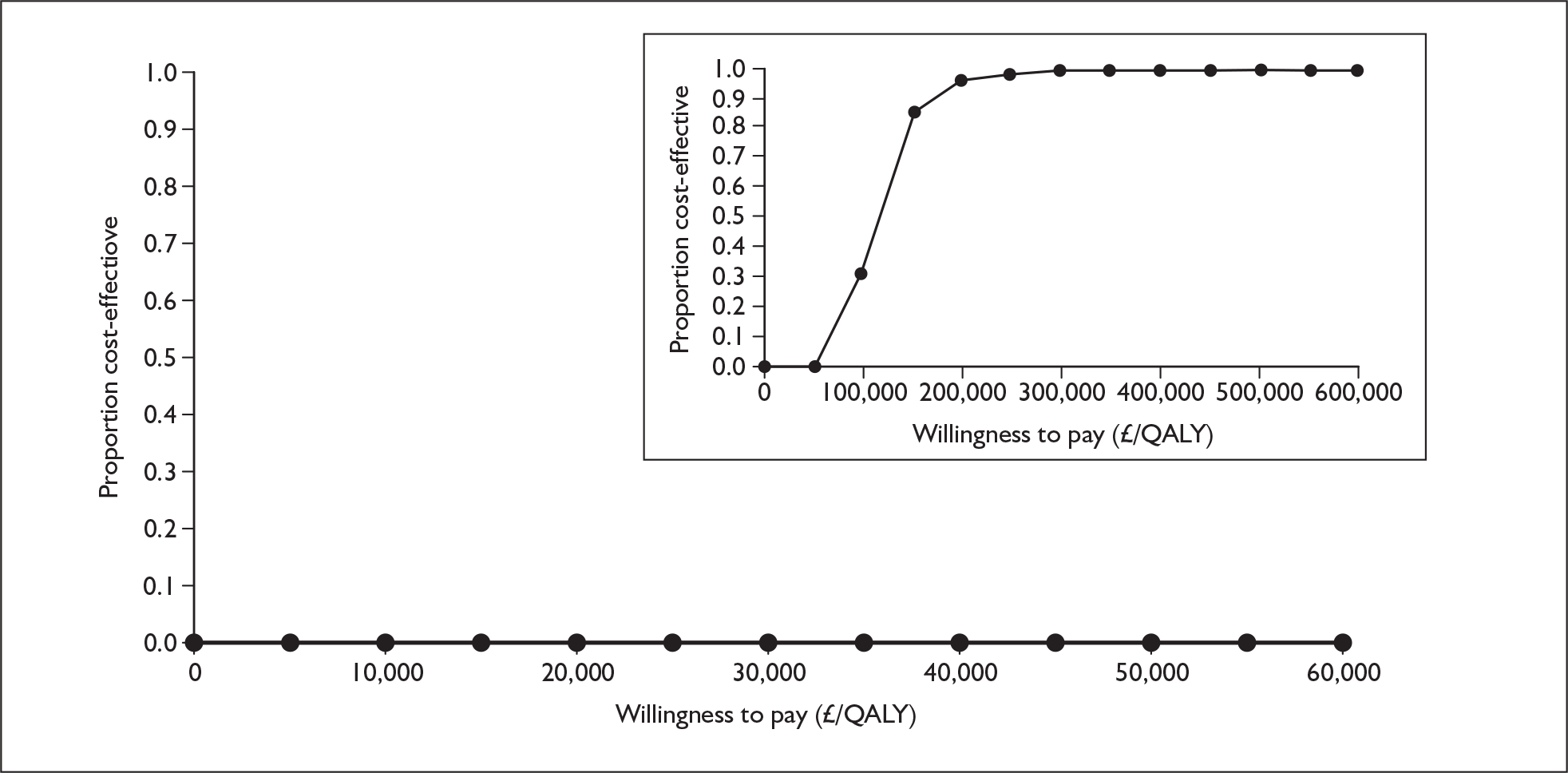
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 479,000 | [Commercial-in-confidence information has been removed] | |||
| Epoprostenol | 697,000 | 218,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 75.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: alternative health state utility values (Meads et al. ). 94 [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 478,000 | 1.590 | |||
| Epoprostenol | 696,000 | 218,000 | 2.422 | 0.831 | 262,000 |
FIGURE 76.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
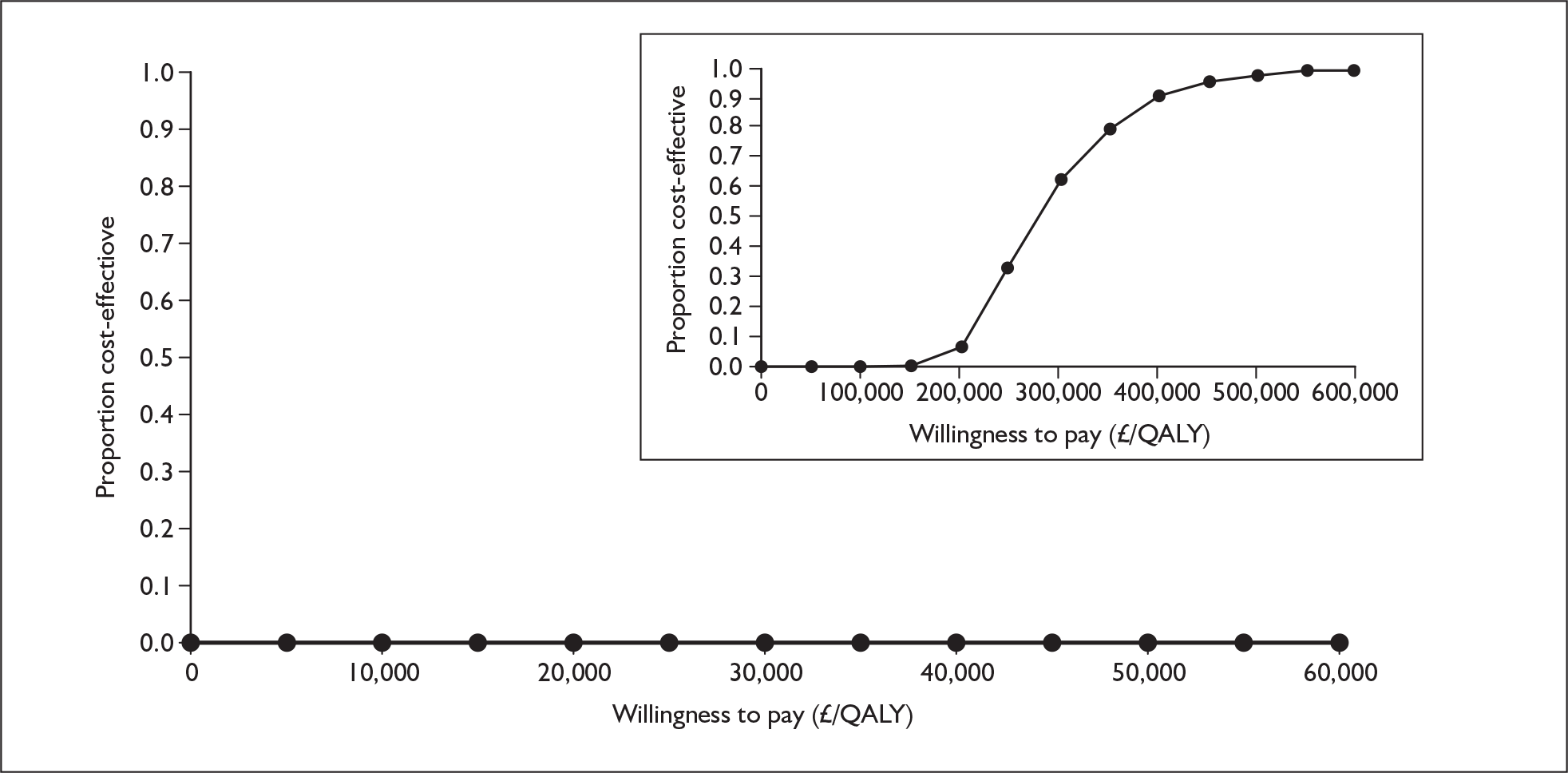
Utilities from Kirsch,76 10-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 478,000 | 1.303 | |||
| Epoprostenol | 696,000 | 218,000 | 2.102 | 0.799 | 272,000 |
FIGURE 77.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: alternative health state utility values (Kirsch76, 10-year time trade-off). QALY, quality-adjusted life-year.
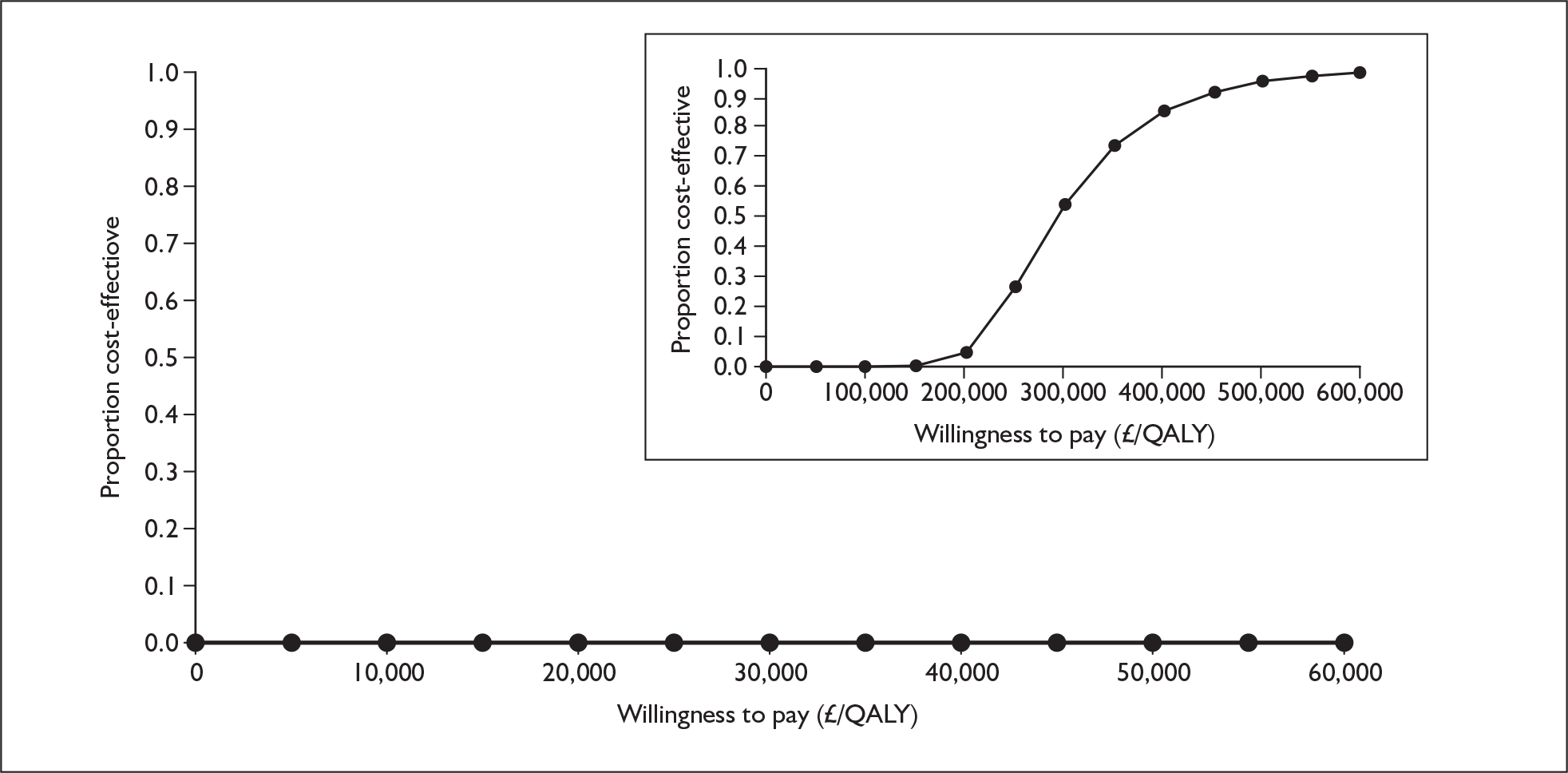
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 479,000 | 1.853 | |||
| Epoprostenol | 697,000 | 218,000 | 2.706 | 0.853 | 256,000 |
FIGURE 78.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class III: alternative health state utility values (Olschewski et al. ). 41 QALY, quality-adjusted life-year.
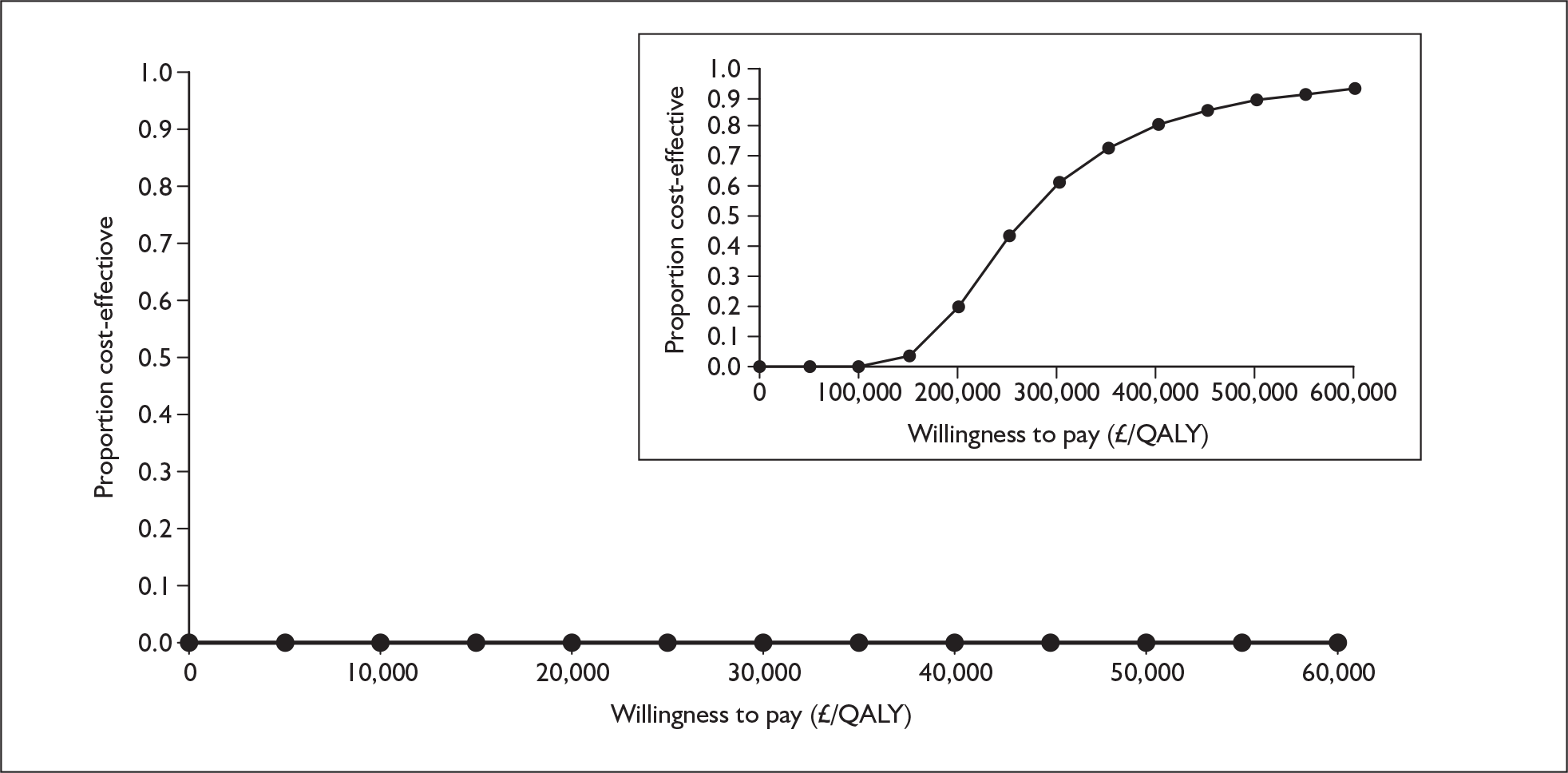
Appendix 12.2 Epoprostenol with supportive care versus supportive care alone, functional class IV
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.829 | |||
| Epoprostenol | 529,000 | 401,000 | 1.996 | 1.167 | 344,000 |
FIGURE 79.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: time horizon of 20 years. QALY, quality-adjusted life-year.
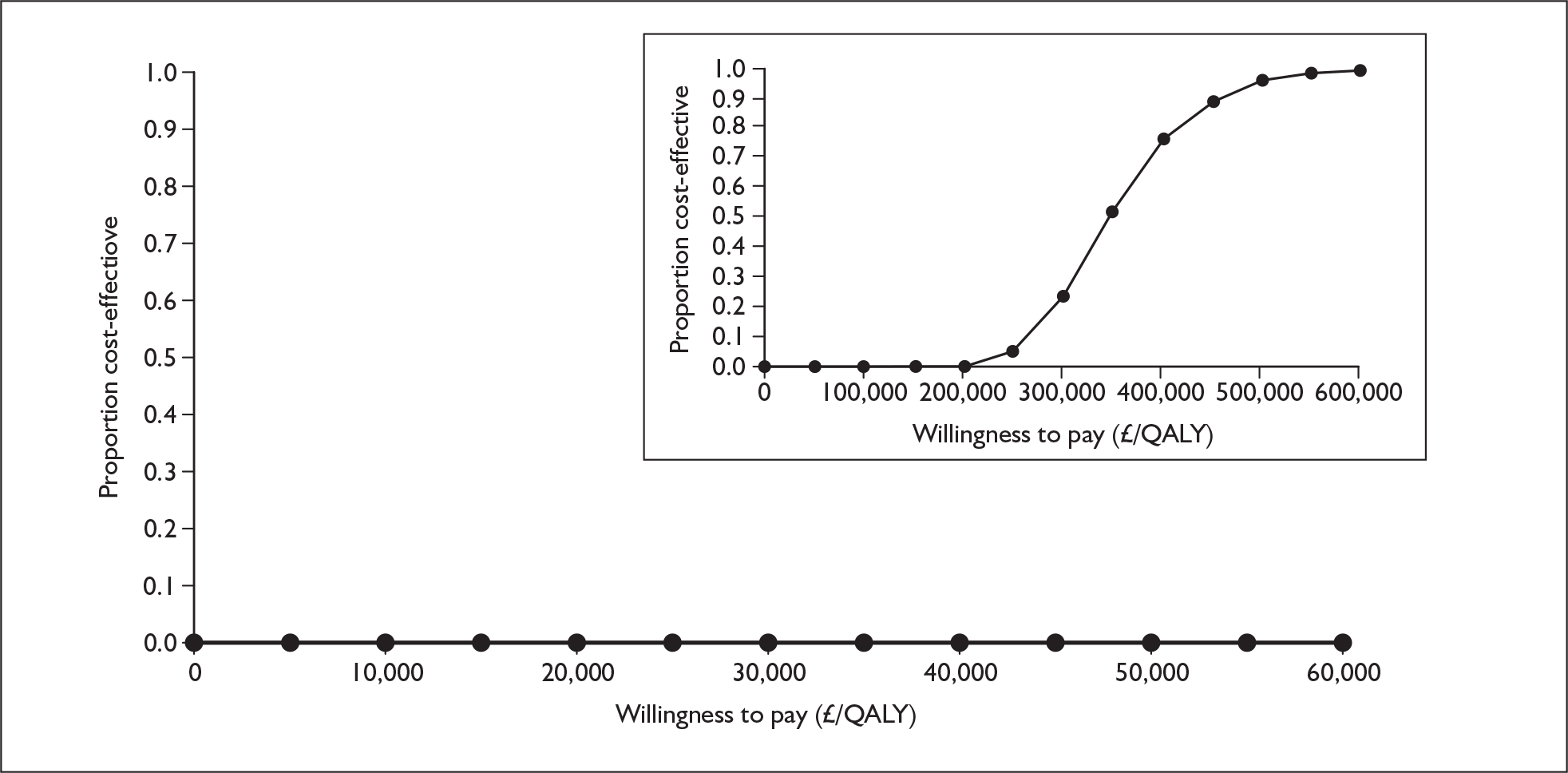
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 127,000 | 0.827 | |||
| Epoprostenol | 495,000 | 368,000 | 1.885 | 1.058 | 348,000 |
FIGURE 80.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: time horizon of 10 years. QALY, quality-adjusted life-year.
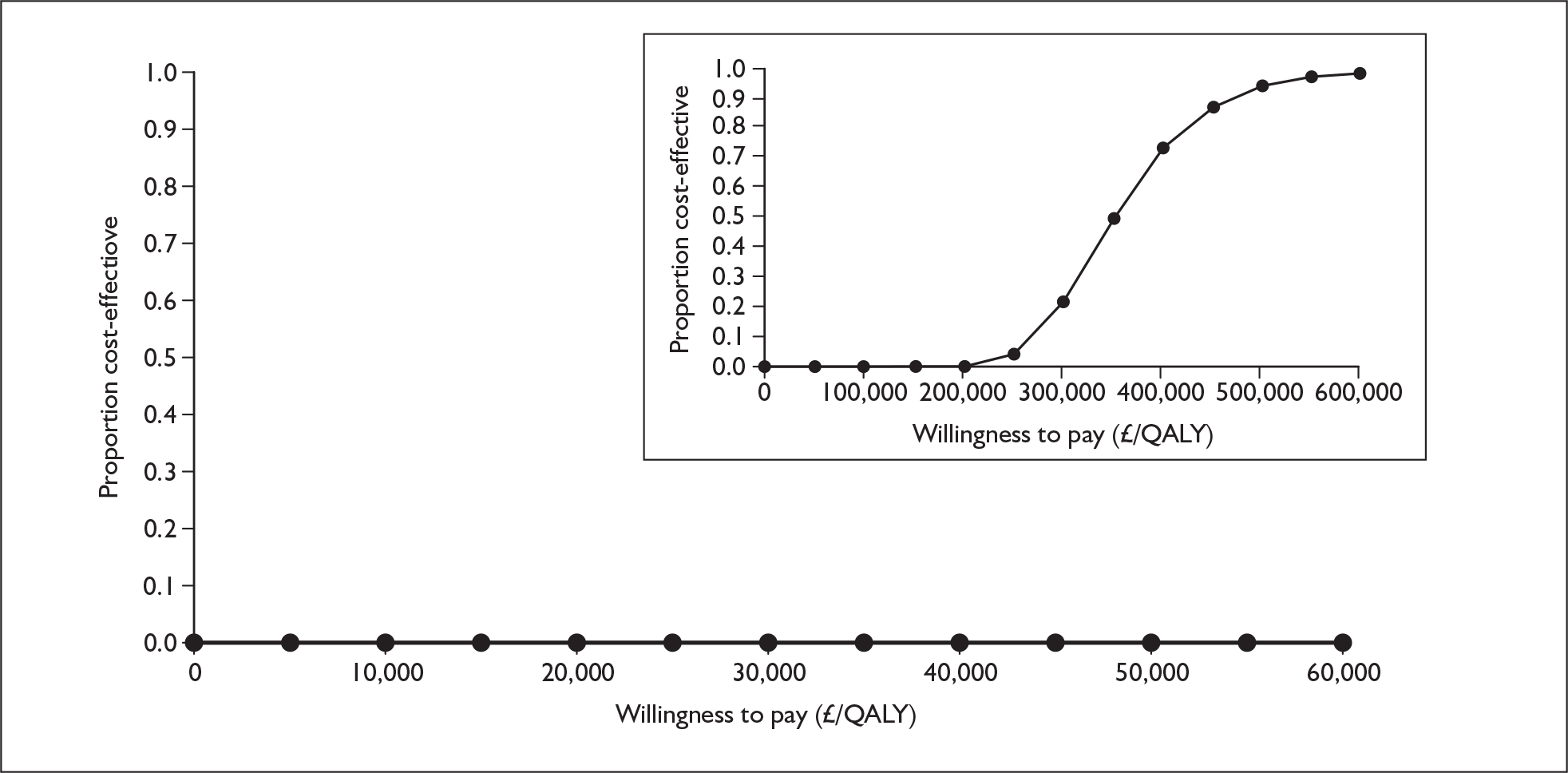
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.829 | |||
| Epoprostenol | 240,000 | 113,000 | 2.003 | 1.174 | 96,000 |
FIGURE 81.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: alternative price for epoprostenol. QALY, quality-adjusted life-year.
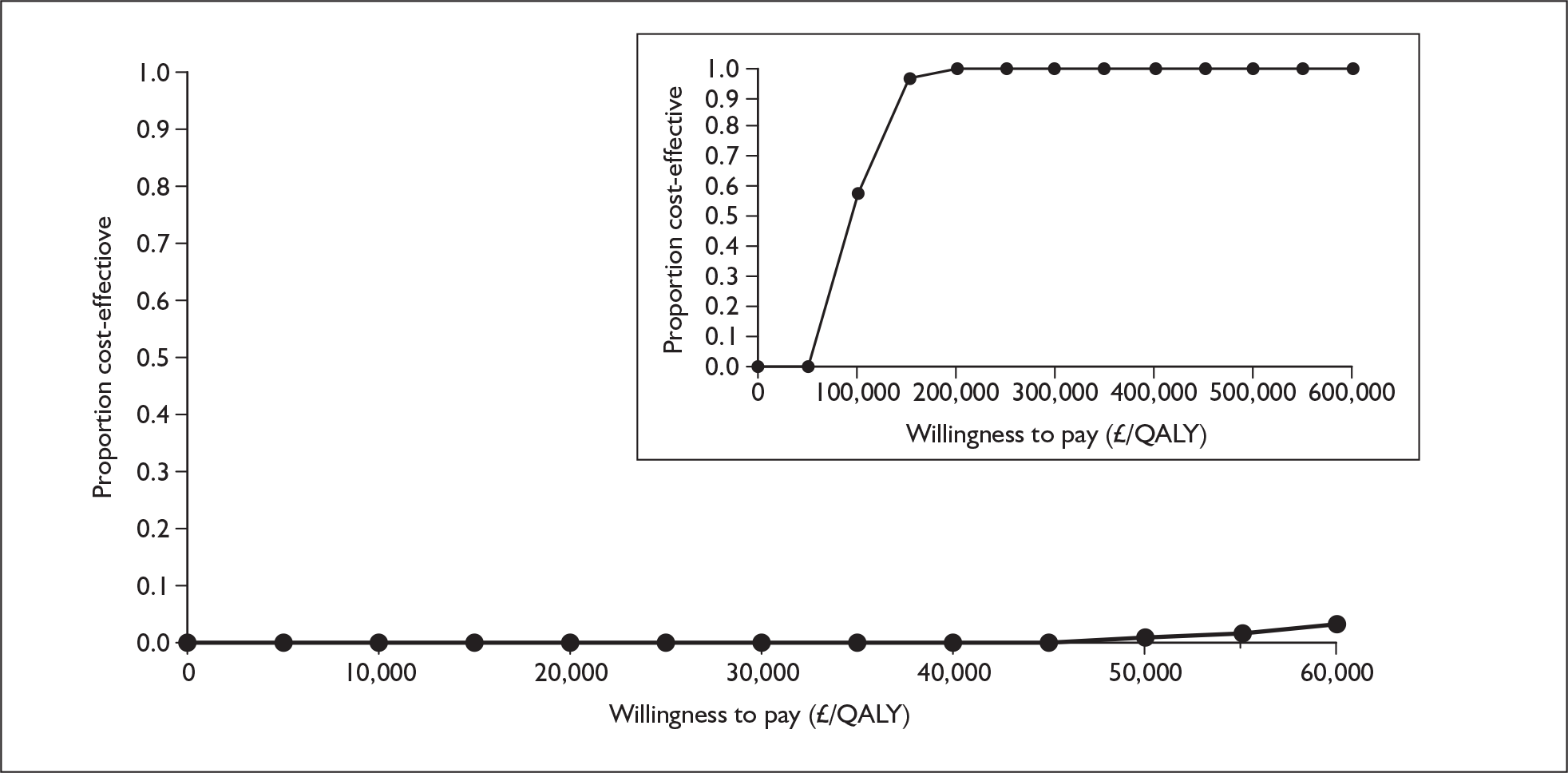
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | [Commercial-in-confidence information has been removed] | |||
| Epoprostenol | 531,000 | 403,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 82.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: alternative health state utility values (Meads et al. ). 94 [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.590 | |||
| Epoprostenol | 530,000 | 402,000 | 1.485 | 0.895 | 449,000 |
FIGURE 83.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
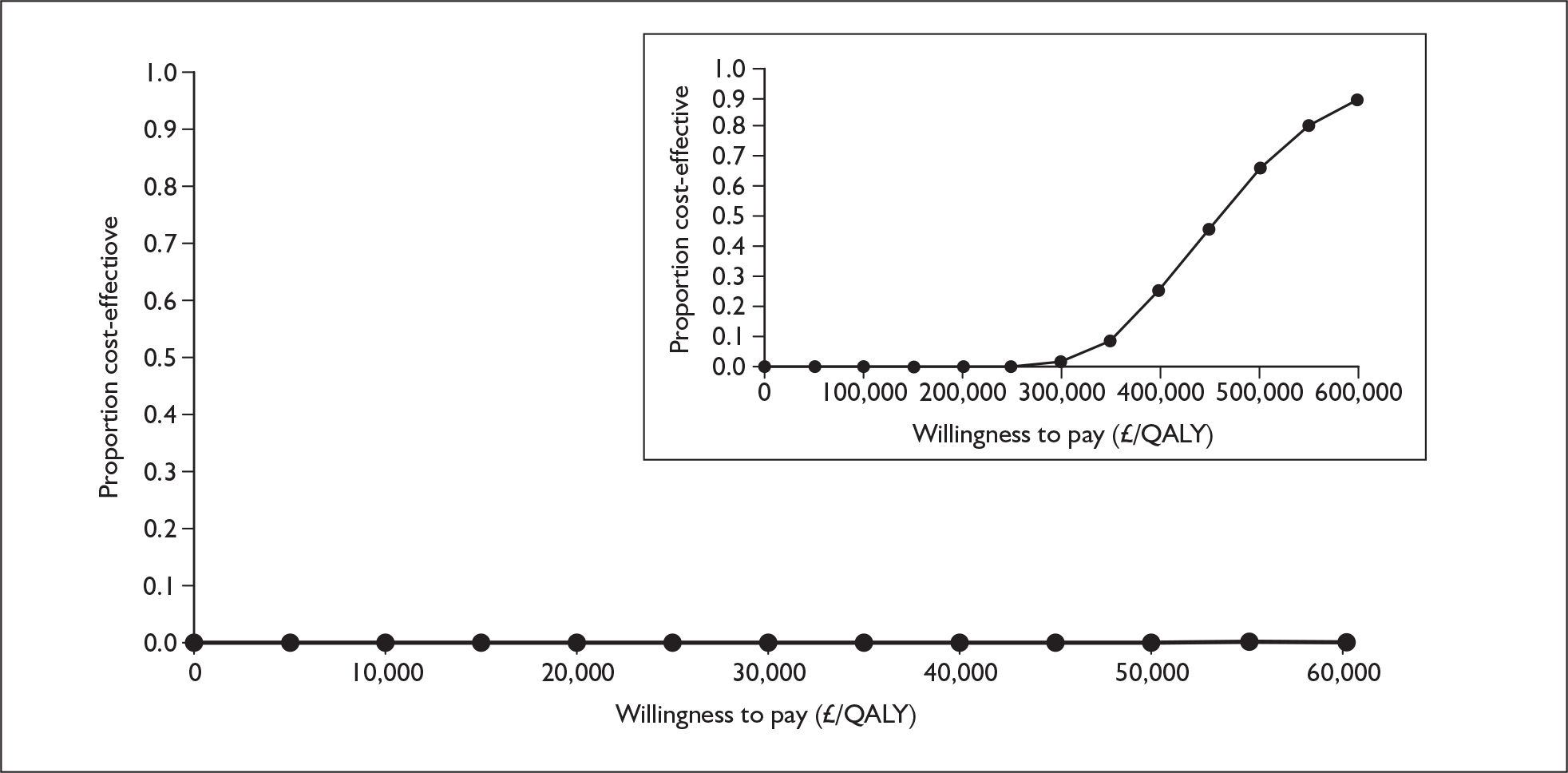
Utilities from Kirsch,76 10-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.451 | |||
| Epoprostenol | 530,000 | 402,000 | 1.177 | 0.726 | 554,000 |
FIGURE 84.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: alternative health state utility values (Kirsch,76 10-year time trade-off). QALY, quality-adjusted life-year.
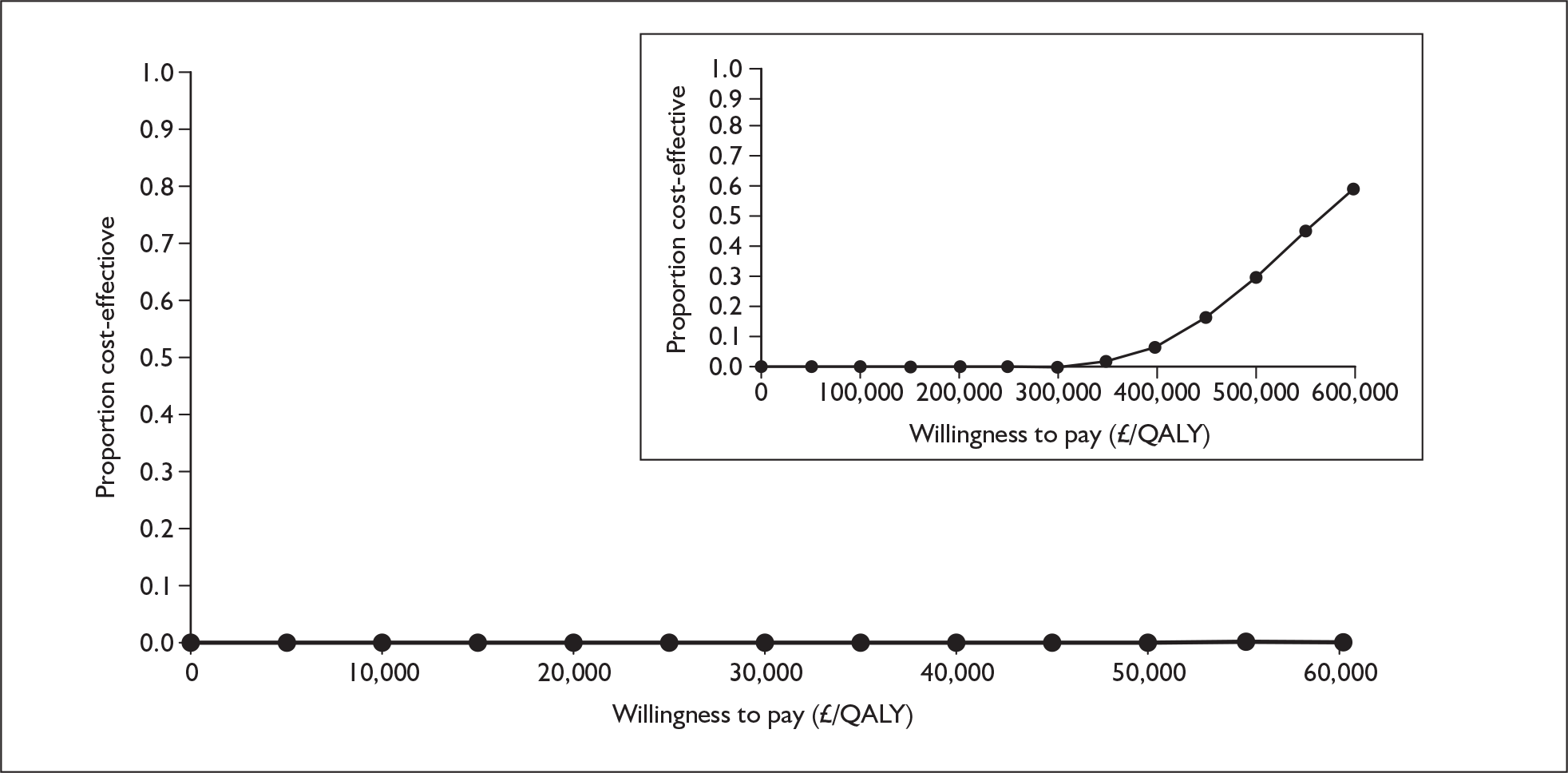
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.705 | |||
| Epoprostenol | 531,000 | 403,000 | 1.754 | 1.049 | 384,000 |
FIGURE 85.
Cost-effectiveness acceptability curve for epoprostenol versus supportive care, functional class IV: alternative health state utility values (Olschewski). 41 QALY, quality-adjusted life-year.
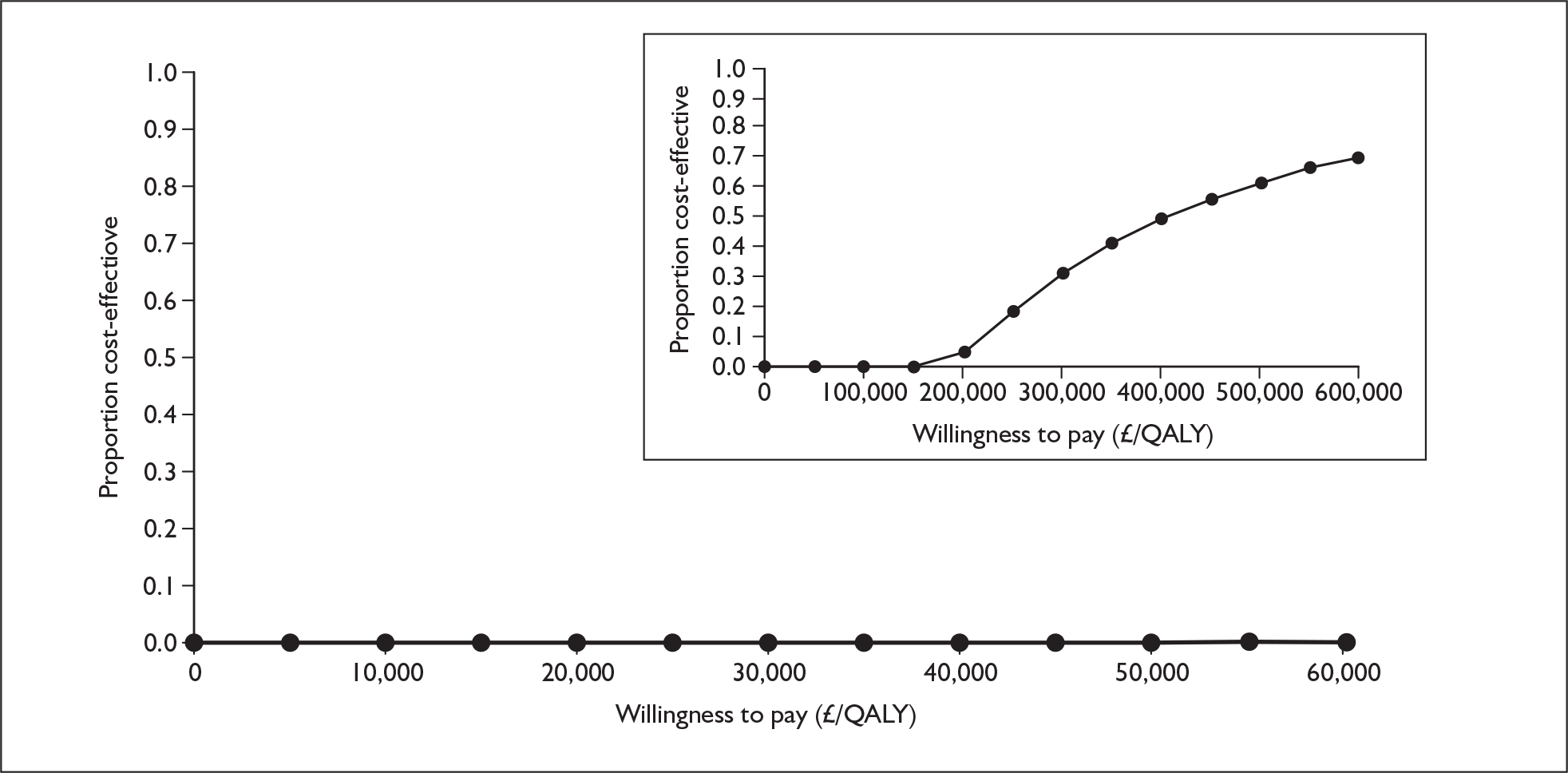
Appendix 12.3 Iloprost with supportive care versus supportive care alone, functional class III
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 432,000 | 1.952 | |||
| Iloprost | 531,000 | 99,000 | 2.951 | 0.999 | 99,000 |
FIGURE 86.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: time horizon of 20 years. QALY, quality-adjusted life-year.
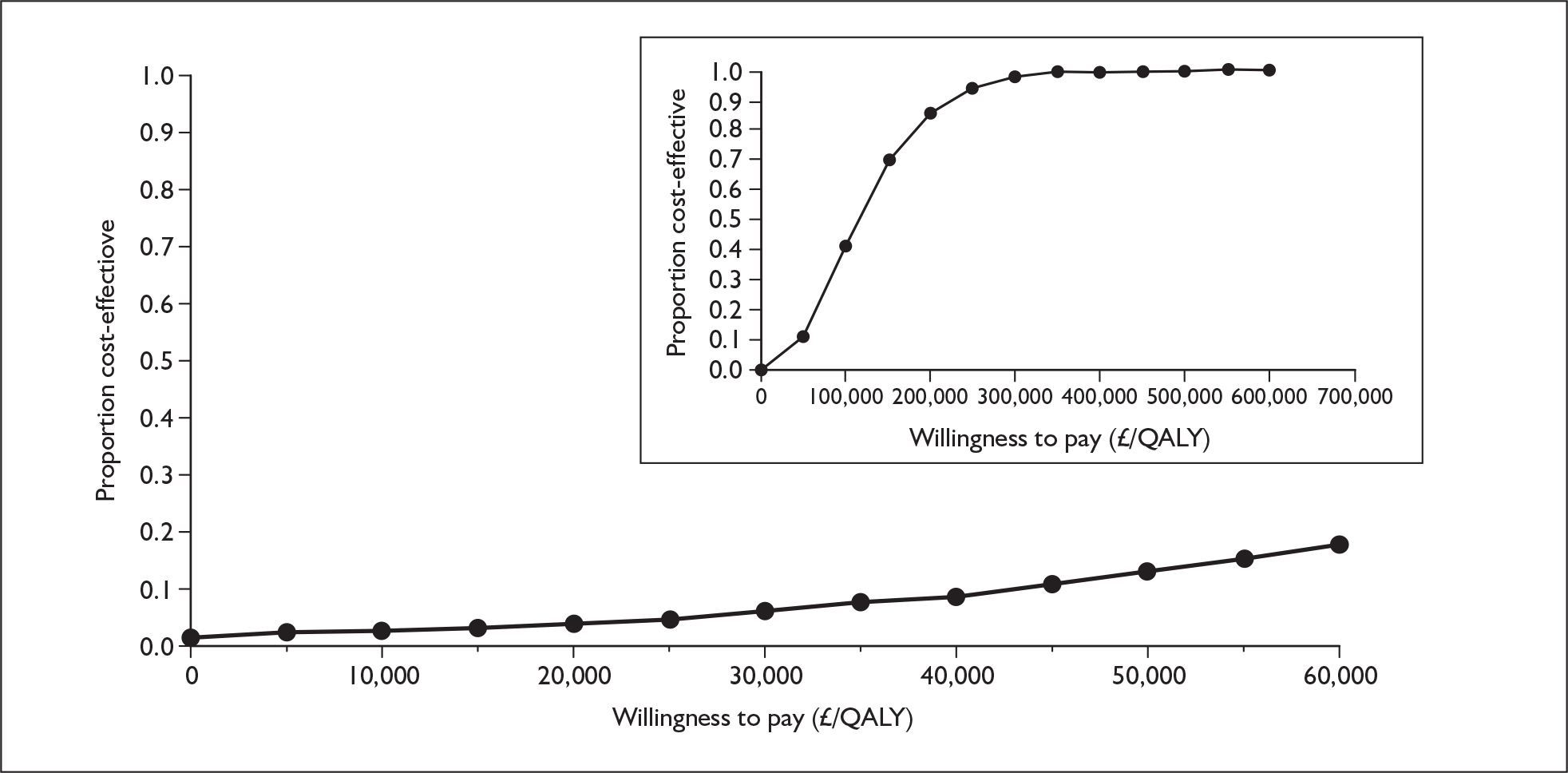
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 400,000 | 1.846 | |||
| Iloprost | 469,000 | 68,000 | 2.690 | 0.844 | 81,000 |
FIGURE 87.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: time horizon of 10 years. QALY, quality-adjusted life-year.
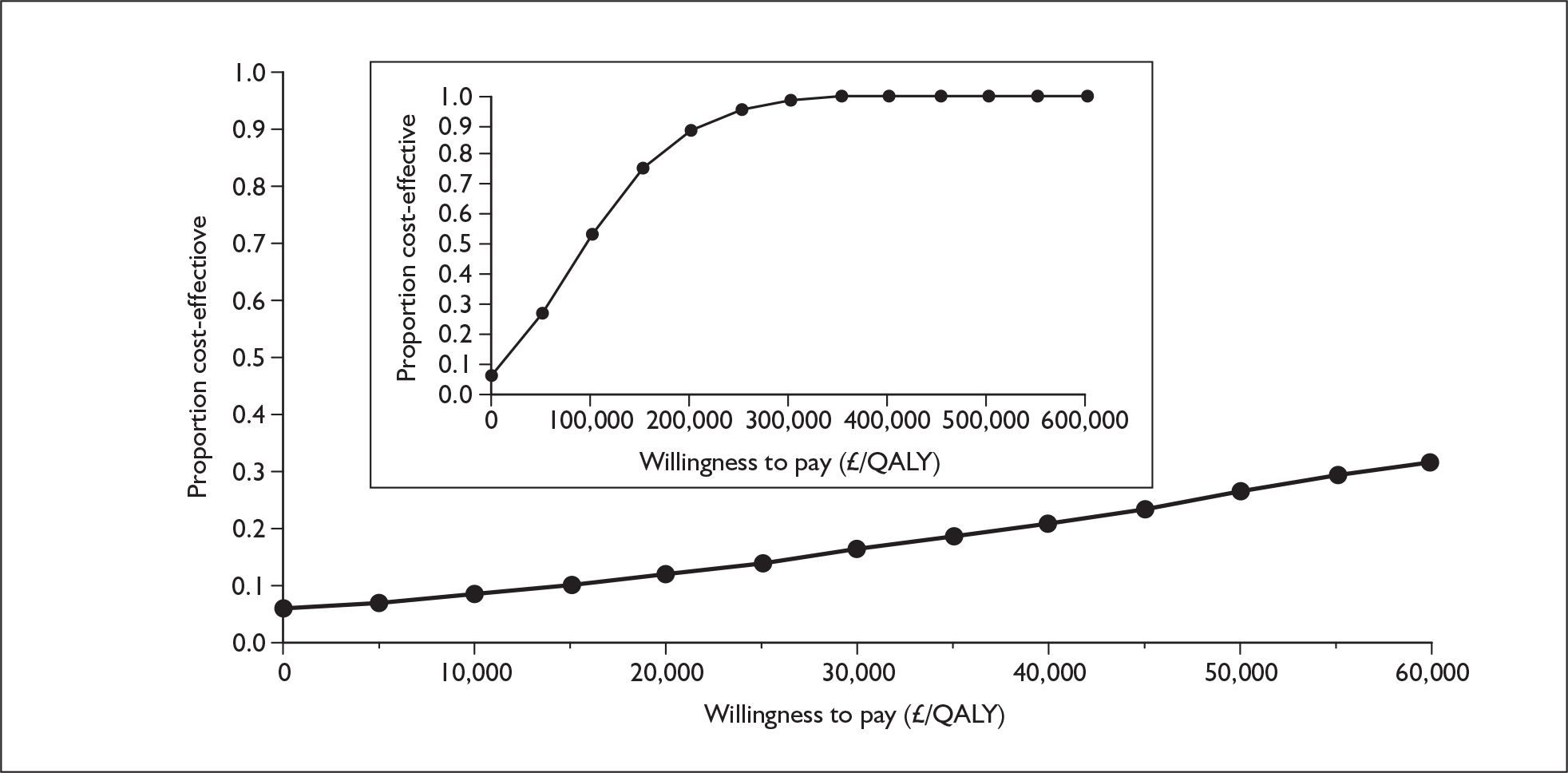
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 197,000 | 1.958 | |||
| Iloprost | 299,000 | 102,000 | 2.975 | 1.017 | 101,000 |
FIGURE 88.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative price for epoprostenol. QALY, quality-adjusted life-year.
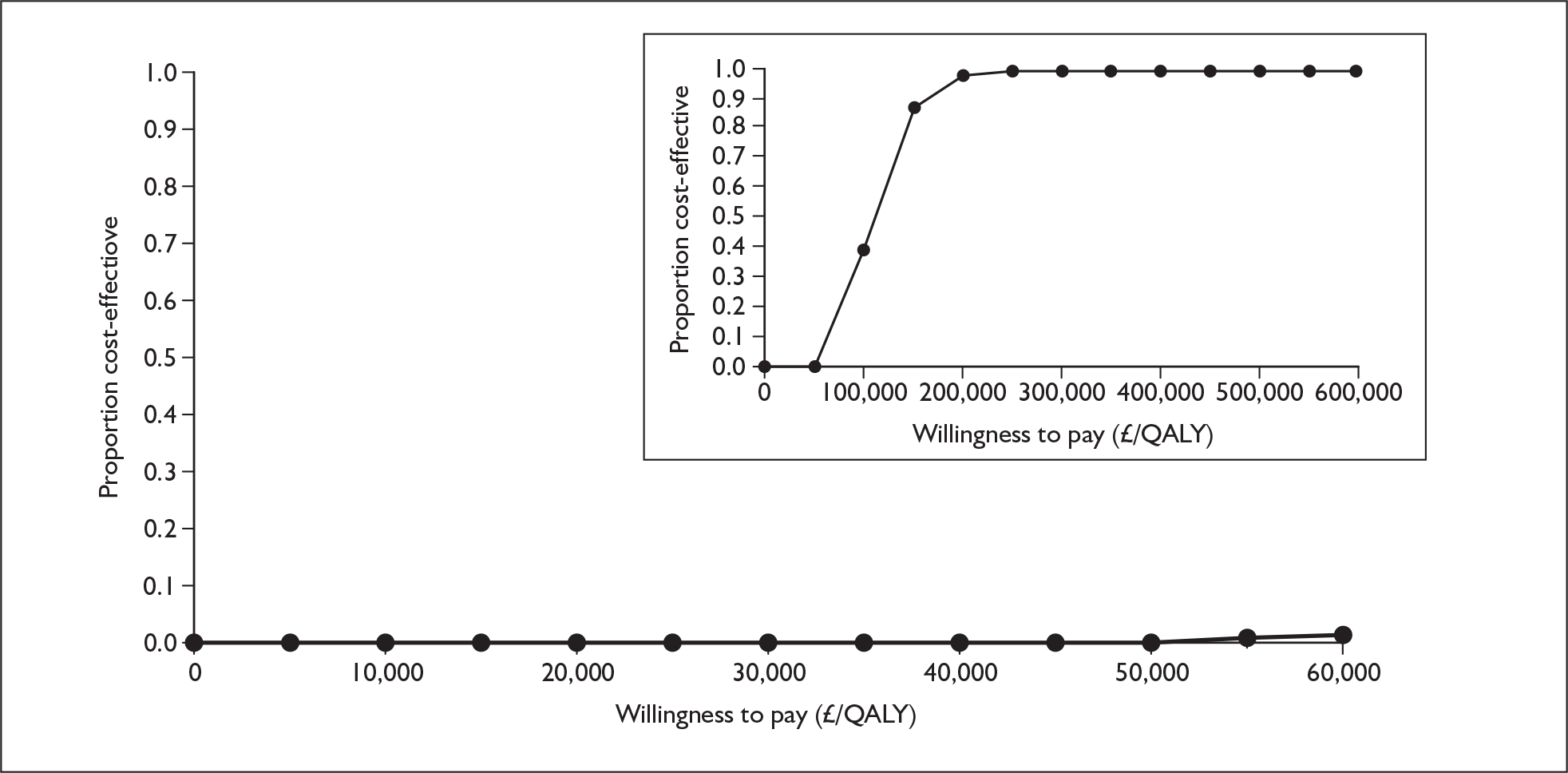
Alternative iloprost price, reference case epoprostenol price
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | 1.958 | |||
| Iloprost | 521,000 | 87,000 | 2.975 | 1.017 | 85,000 |
FIGURE 89.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative iloprost price, reference case epoprostenol price. QALY, quality-adjusted life-year.
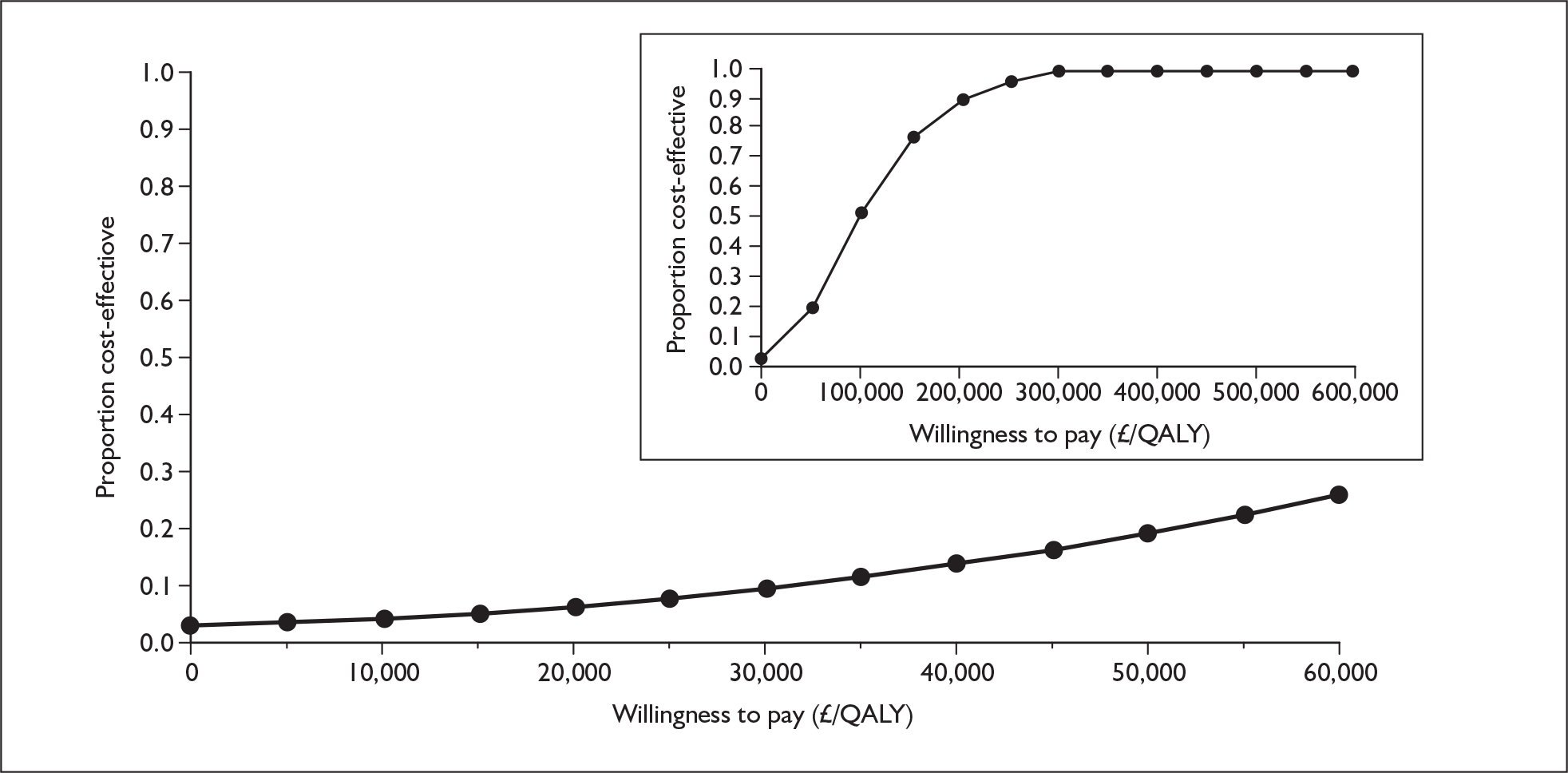
Alternative iloprost and epoprostenol prices
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 197,000 | 1.958 | |||
| Iloprost | 283,000 | 86,000 | 2.975 | 1.017 | 85,000 |
FIGURE 90.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative iloprost and epoprostenol prices. QALY, quality-adjusted life-year.
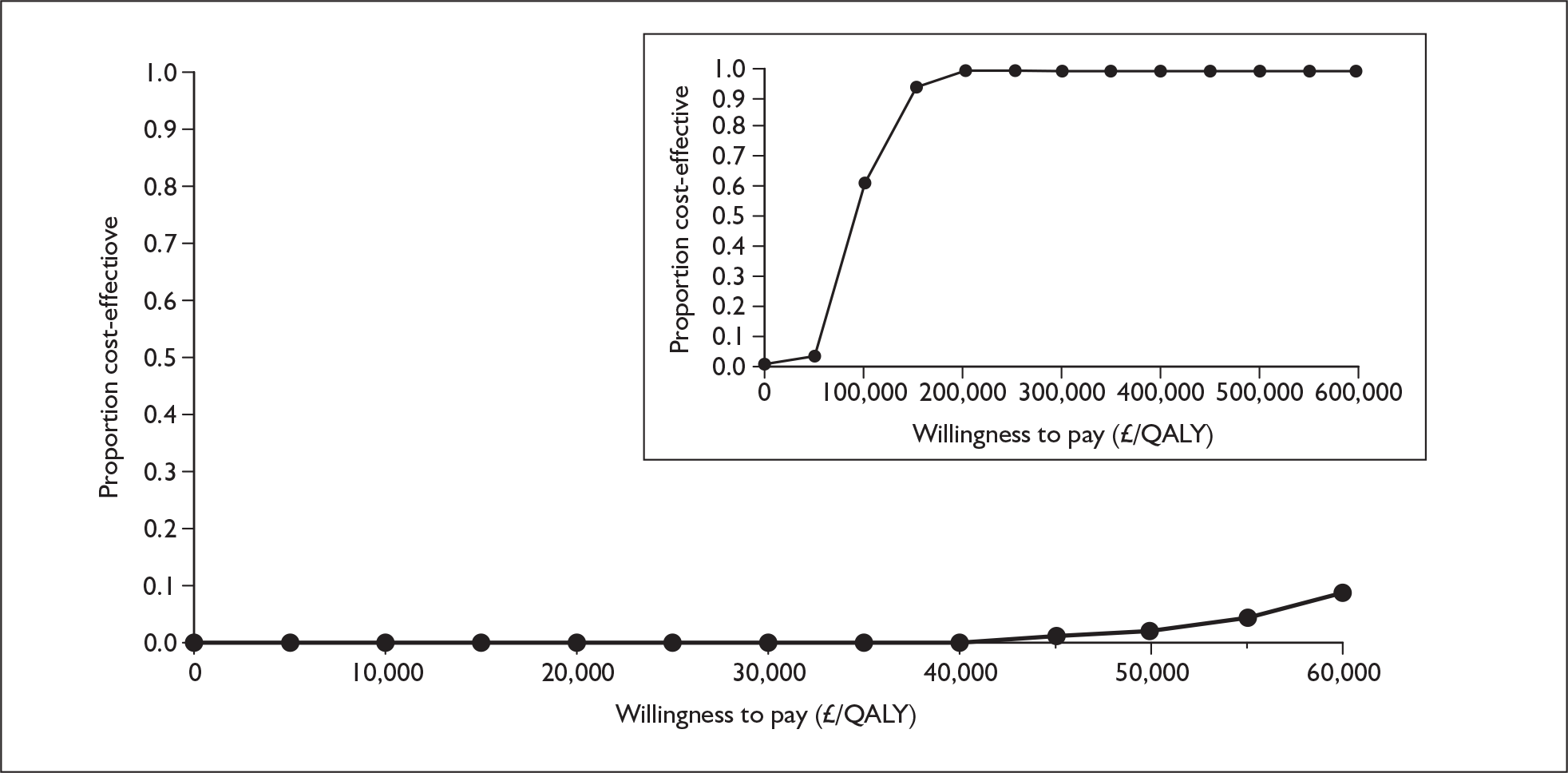
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | [Commercial-in-confidence information has been removed] | |||
| Iloprost | 537,000 | 103,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 91.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative health state utility values (Meads et al. ). 94 [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | 1.535 | |||
| Iloprost | 535,000 | 102,000 | 2.564 | 1.030 | 99,000 |
FIGURE 92.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
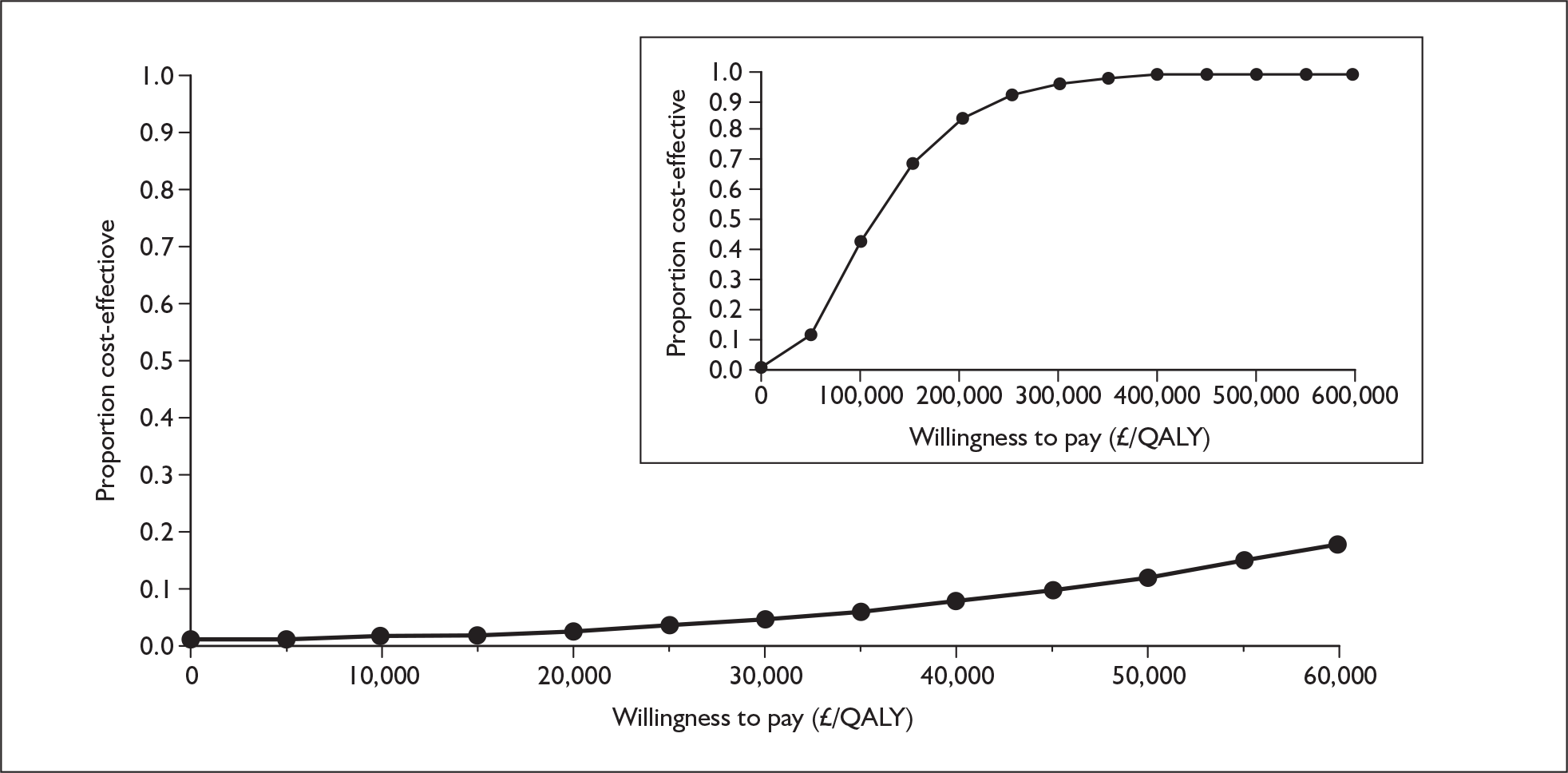
Utilities from Kirsch,76 10-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | 1.269 | |||
| Iloprost | 535,000 | 102,000 | 2.244 | 0.975 | 104,000 |
FIGURE 93.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative health state utility values (Kirsch,76 10-year time trade-off). QALY, quality-adjusted life-year.
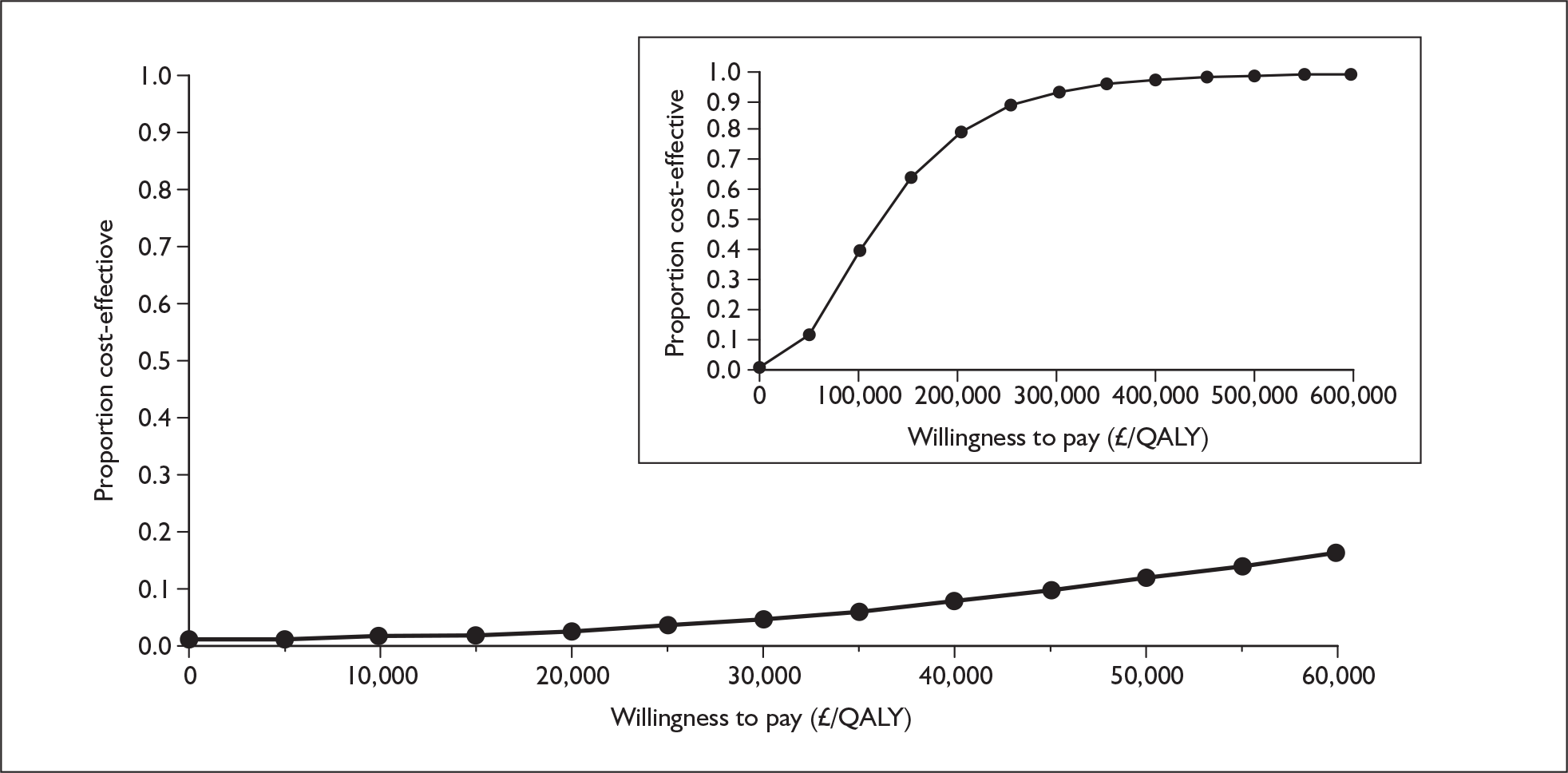
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 434,000 | 1.781 | |||
| Iloprost | 537,000 | 103,000 | 2.854 | 1.074 | 96,000 |
FIGURE 94.
Cost-effectiveness acceptability curve for iloprost versus supportive care, functional class III: alternative health state utility values (Olschewski et al. ). 41
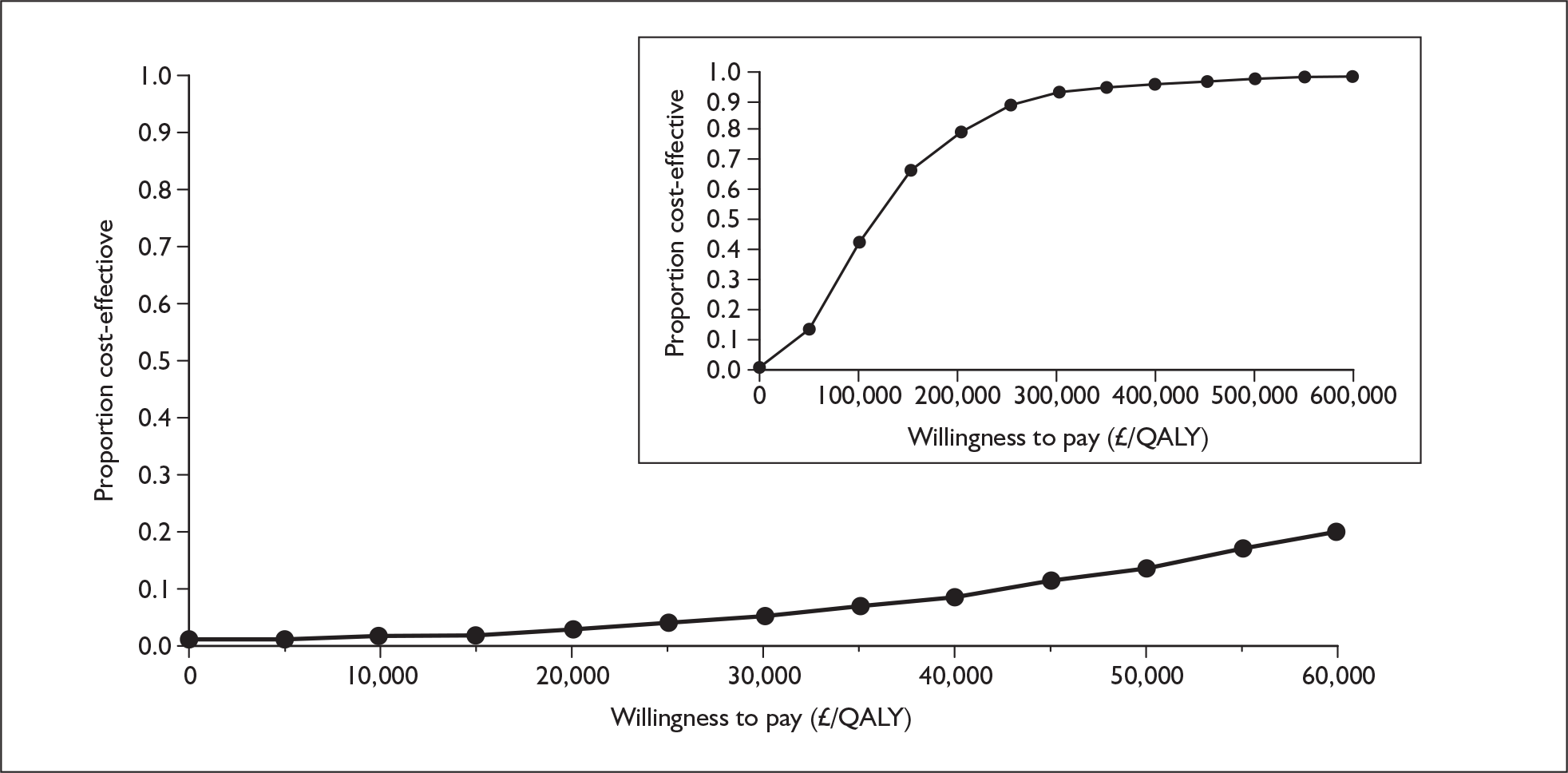
Appendix 12.4 Bosentan with supportive care versus supportive care alone, functional class III
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 341,000 | 2.193 | |||
| Bosentan | 406,000 | 66,000 | 5.301 | 3.108 | 21,000 |
FIGURE 95.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: time horizon of 20 years. QALY, quality-adjusted life-year.
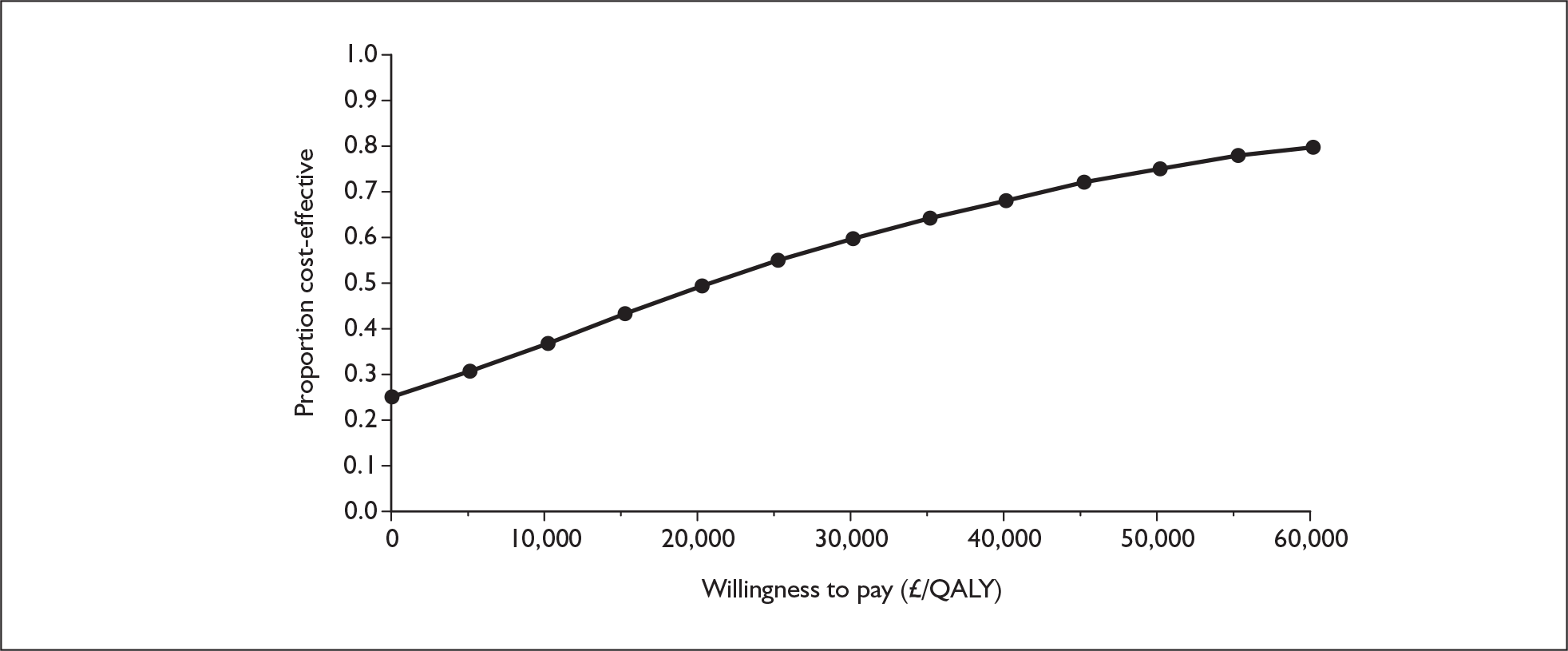
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 304,000 | 2.063 | |||
| Bosentan | 296,000 | –8,000 | 4.027 | 1.964 | Dominates |
FIGURE 96.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: time horizon of 10 years. QALY, quality-adjusted life-year.
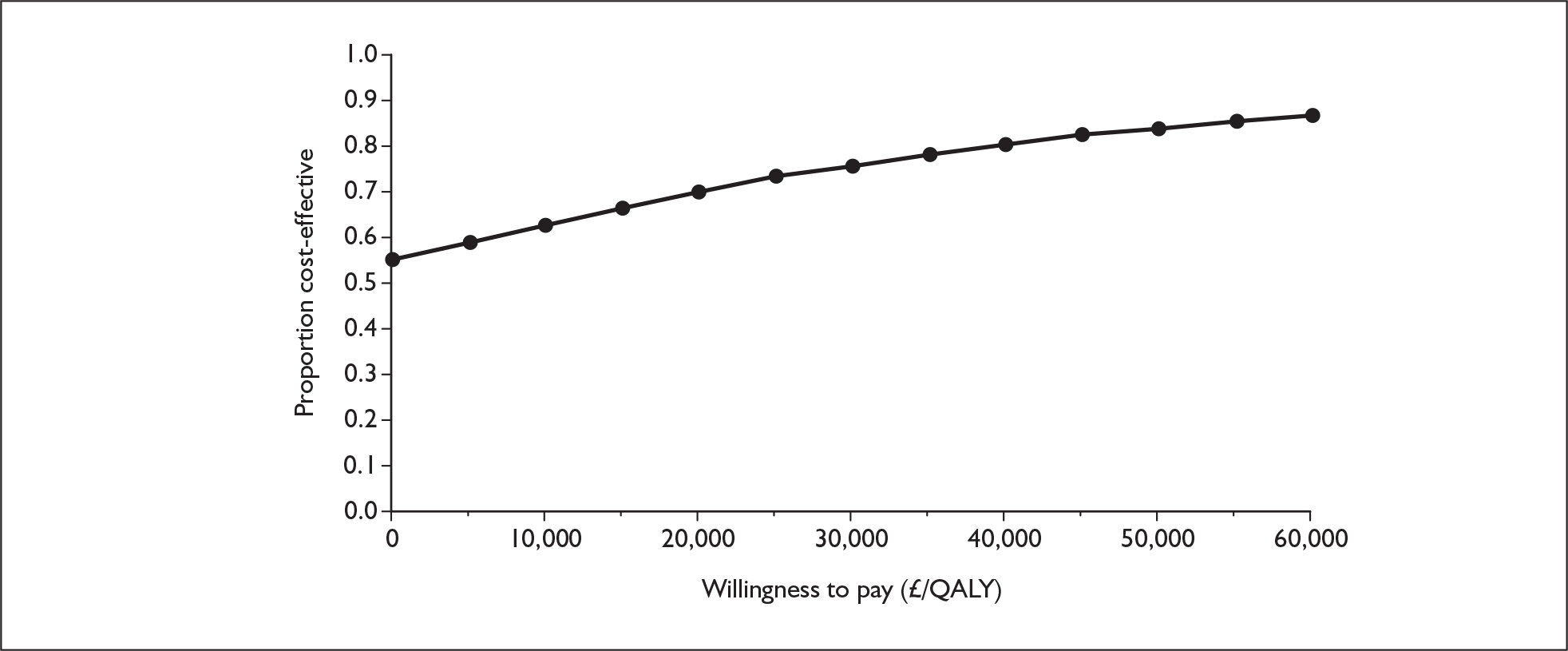
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 156,000 | 2.201 | |||
| Bosentan | 294,000 | 137,000 | 5.696 | 3.494 | 39,000 |
FIGURE 97.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: alternative price for epoprostenol. QALY, quality-adjusted life-year.
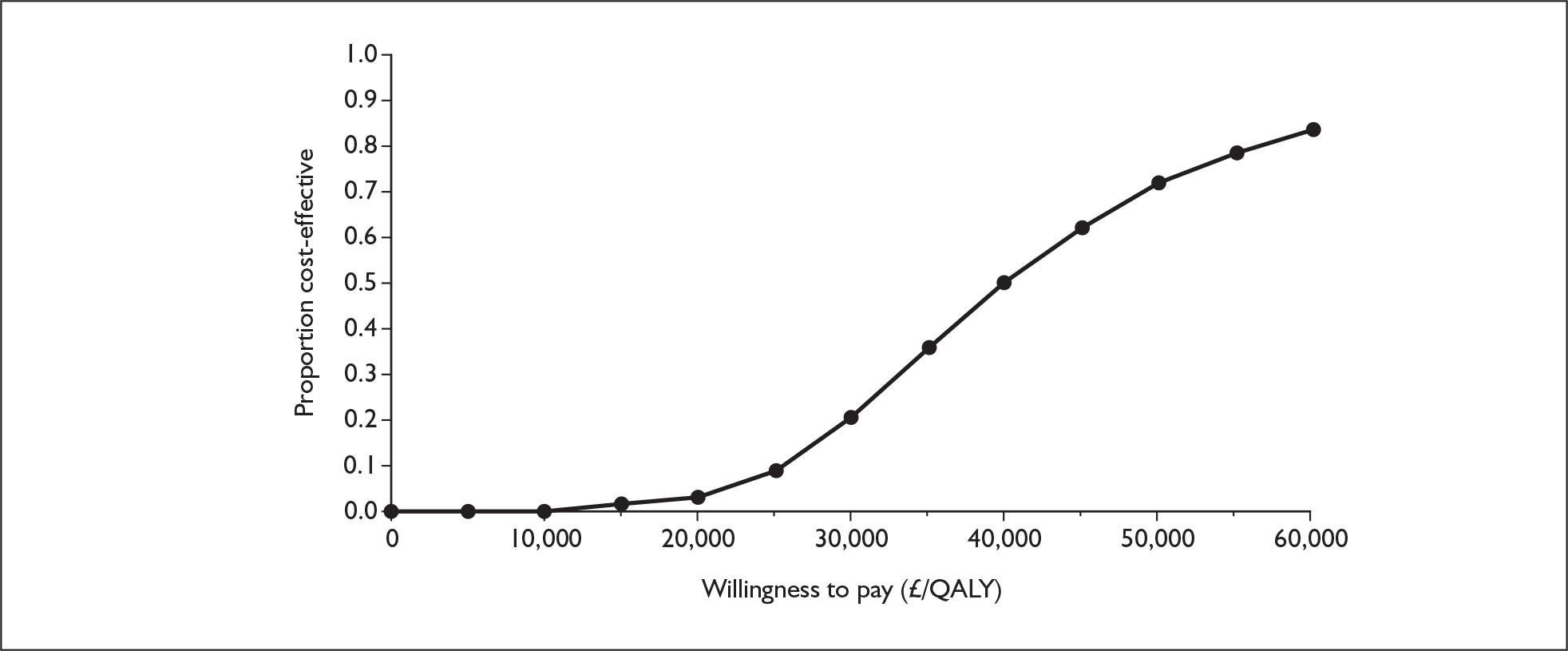
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | [Commercial-in-confidence information has been removed] | |||
| Bosentan | 436,000 | 93,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 98.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: alternative health state utility values (Meads et al. )94. [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 1.852 | |||
| Bosentan | 435,000 | 92,000 | 5.552 | 3.700 | 25,000 |
FIGURE 99.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
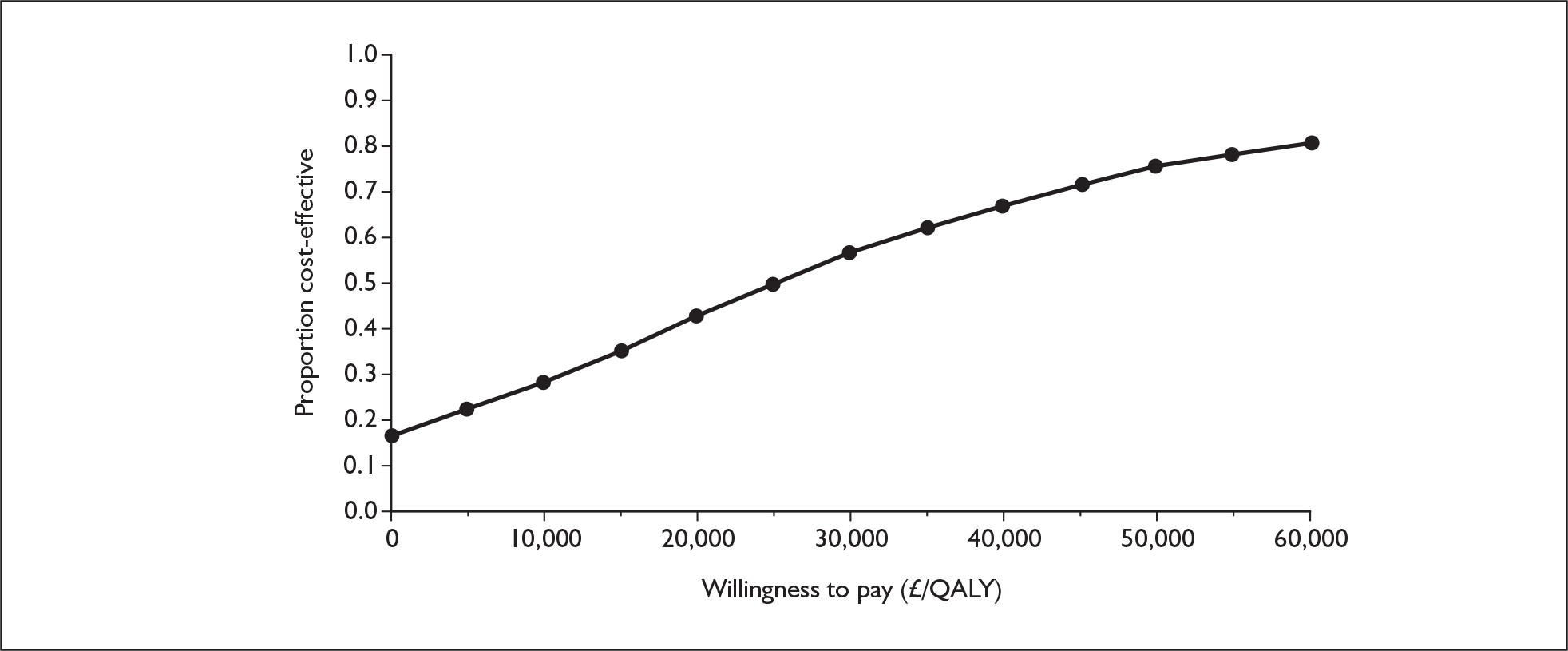
Utilities from Kirsch,76 10 year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 1.602 | |||
| Bosentan | 435,000 | 92,000 | 5.151 | 3.549 | 26,000 |
FIGURE 100.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: alternative health state utility values (Kirsch,76 10-year time trade-off). QALY, quality-adjusted life-year.
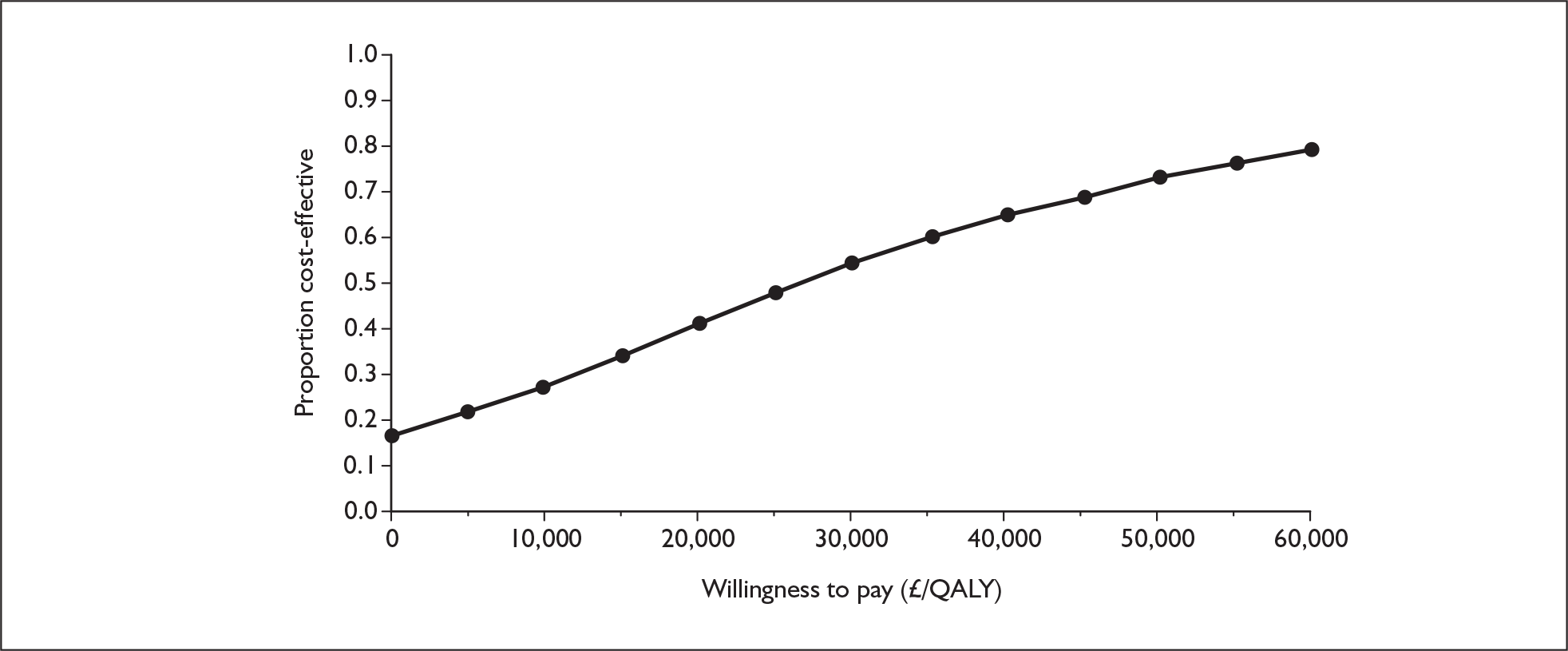
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 2.092 | |||
| Bosentan | 436,000 | 93,000 | 5.866 | 3.774 | 25,000 |
FIGURE 101.
Cost-effectiveness acceptability curve for bosentan versus supportive care, functional class III: alternative health state utility values (Olschewski et al. ). 41 QALY, quality-adjusted life-year.
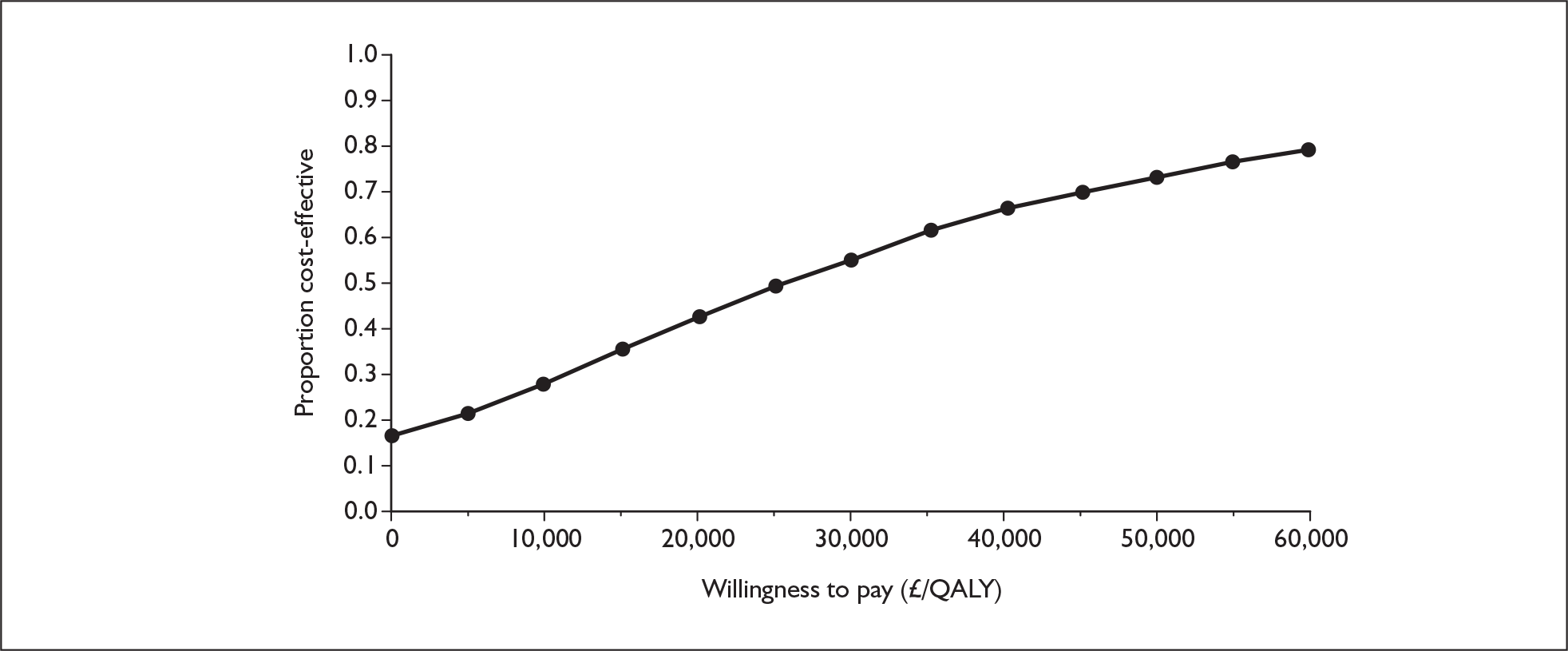
Appendix 12.5 Sitaxentan with supportive care versus supportive care alone, functional class III
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 341,000 | 2.193 | |||
| Sitaxentan | 393,000 | 52,000 | 4.949 | 2.755 | 19,000 |
FIGURE 102.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: time horizon of 20 years. QALY, quality-adjusted life-year. QALY, quality-adjusted life-year.
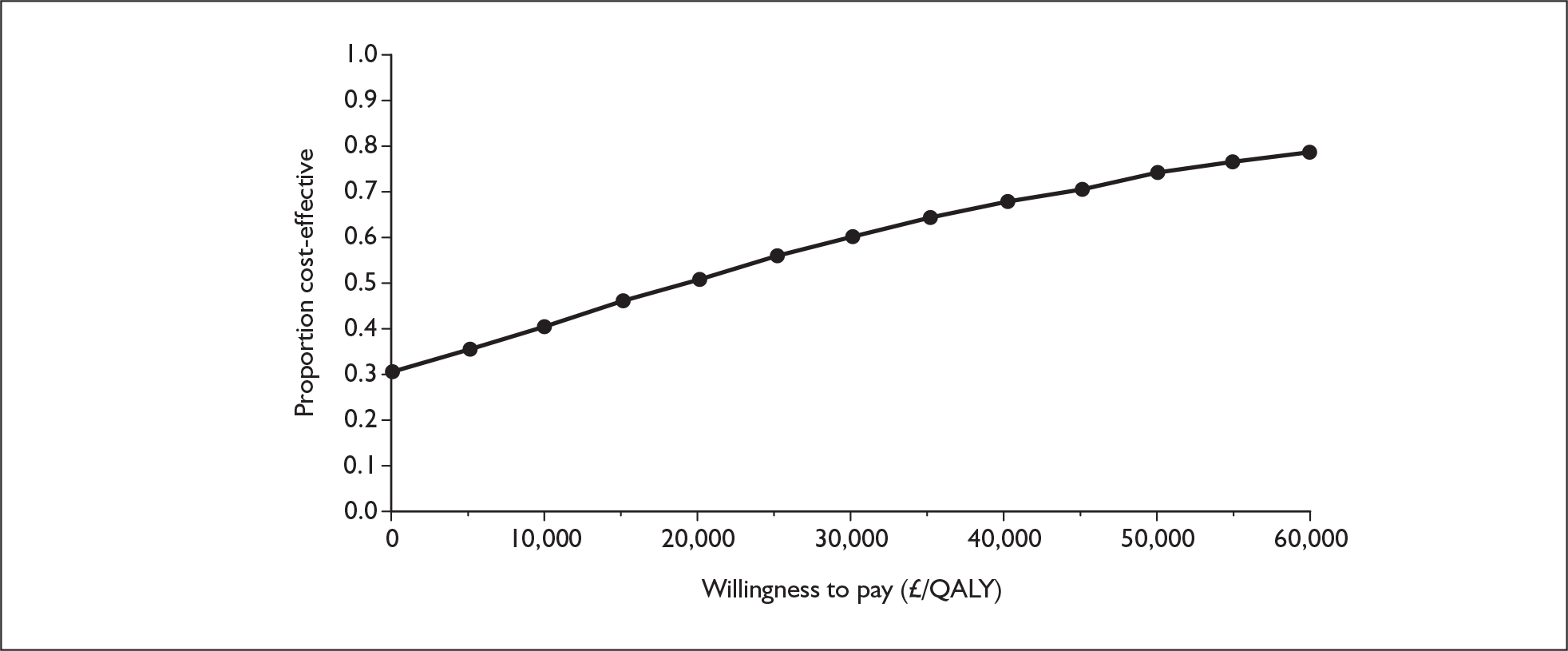
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 304,000 | 2.063 | |||
| Sitaxentan | 293,000 | –11,000 | 3.817 | 1.754 | Dominates |
FIGURE 103.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: time horizon of 10 years. QALY, quality-adjusted life-year.
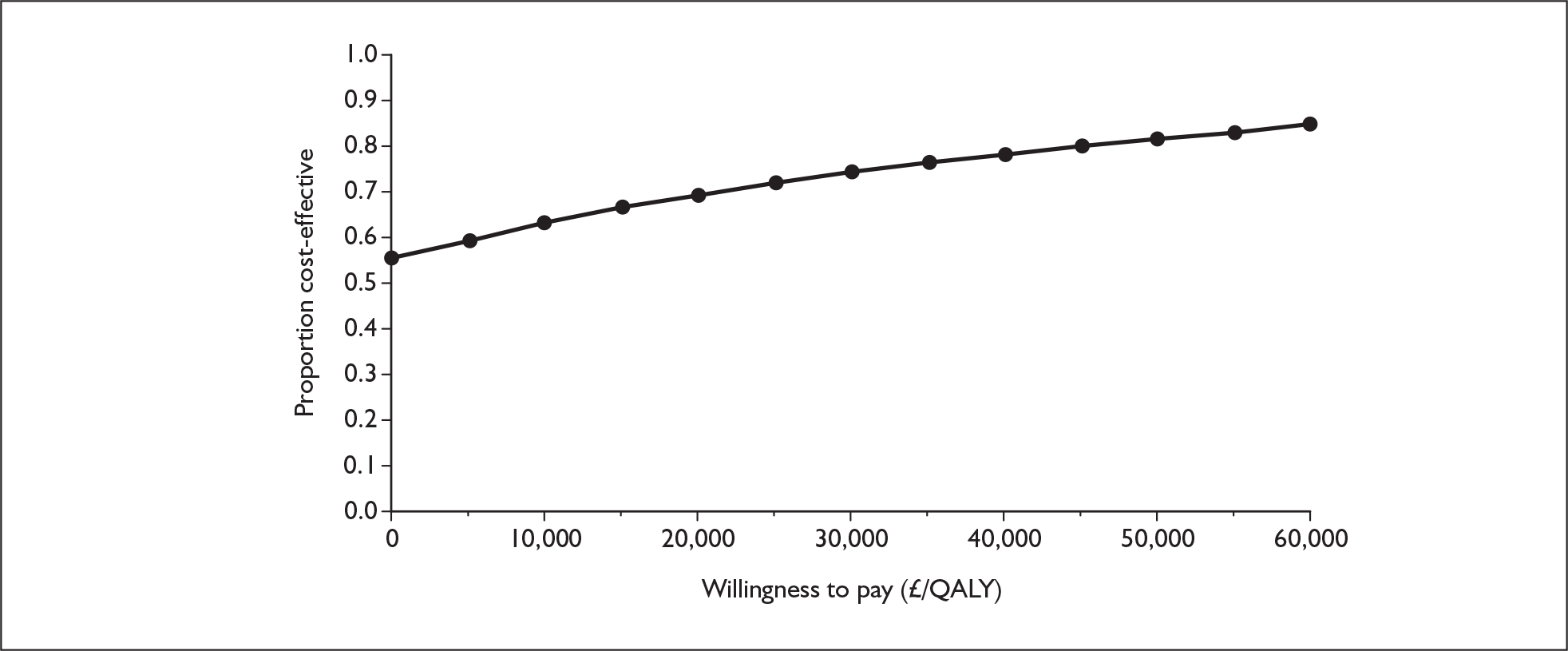
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 156,000 | 2.201 | |||
| Sitaxentan | 279,000 | 122,000 | 5.289 | 3.087 | 40,000 |
FIGURE 104.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: alternative price for epoprostenol. QALY, quality-adjusted life-year.
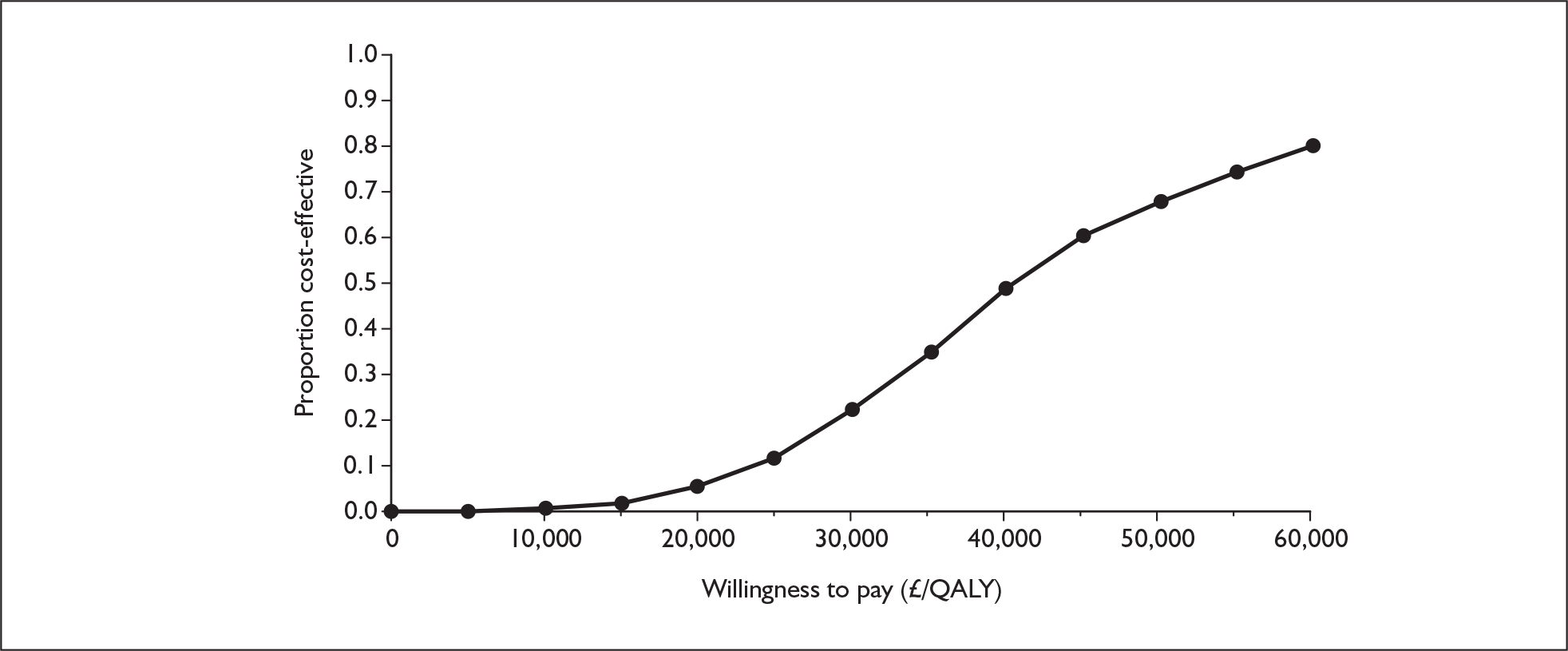
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | [Commercial-in-confidence information has been removed] | |||
| Sitaxentan | 419,000 | 76,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 105.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: alternative health state utility values (Meads et al. ). 94 [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 1.852 | |||
| Sitaxentan | 418,000 | 75,000 | 4.998 | 3.146 | 24,000 |
FIGURE 106.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
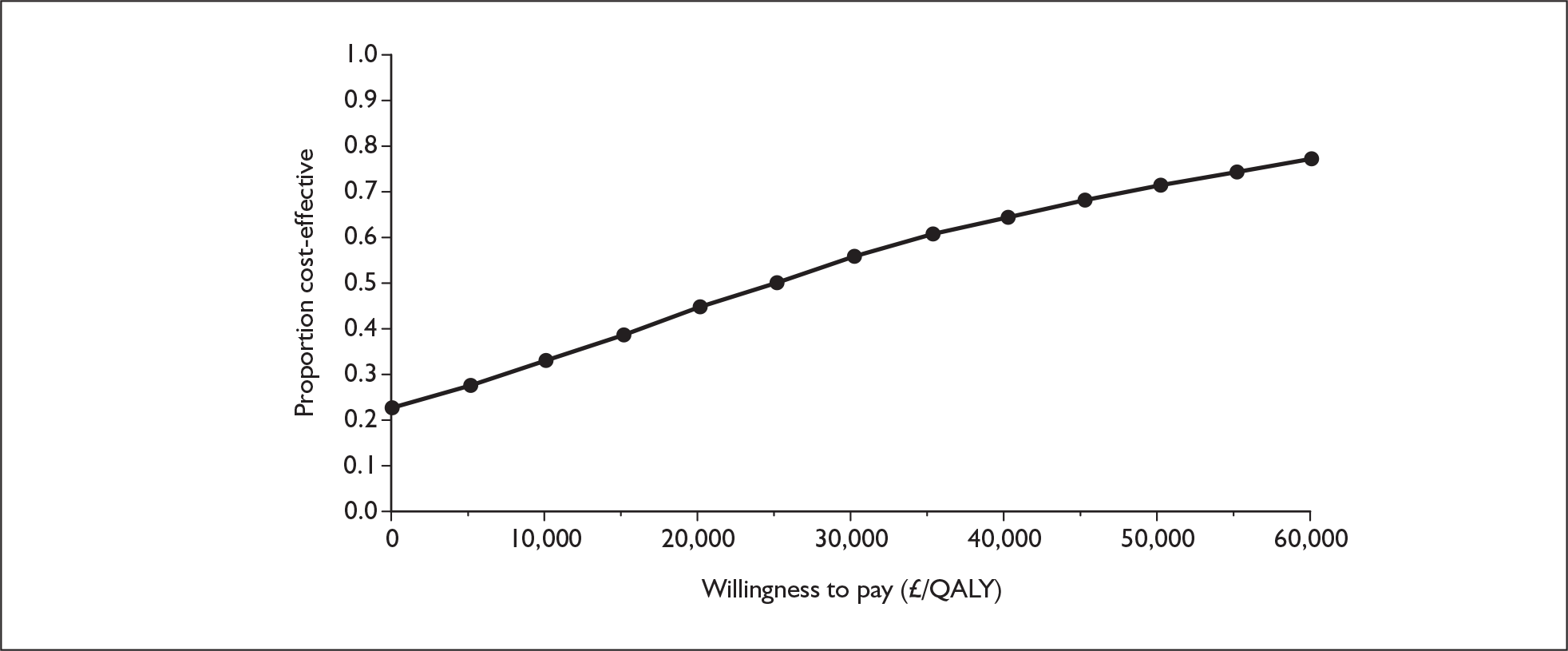
Utilities from Kirsch,76 10-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 1.602 | |||
| Sitaxentan | 418,000 | 75,000 | 4.600 | 2.997 | 25,000 |
FIGURE 107.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: alternative health state utility values (Kirsch,76 10-year time trade-off).
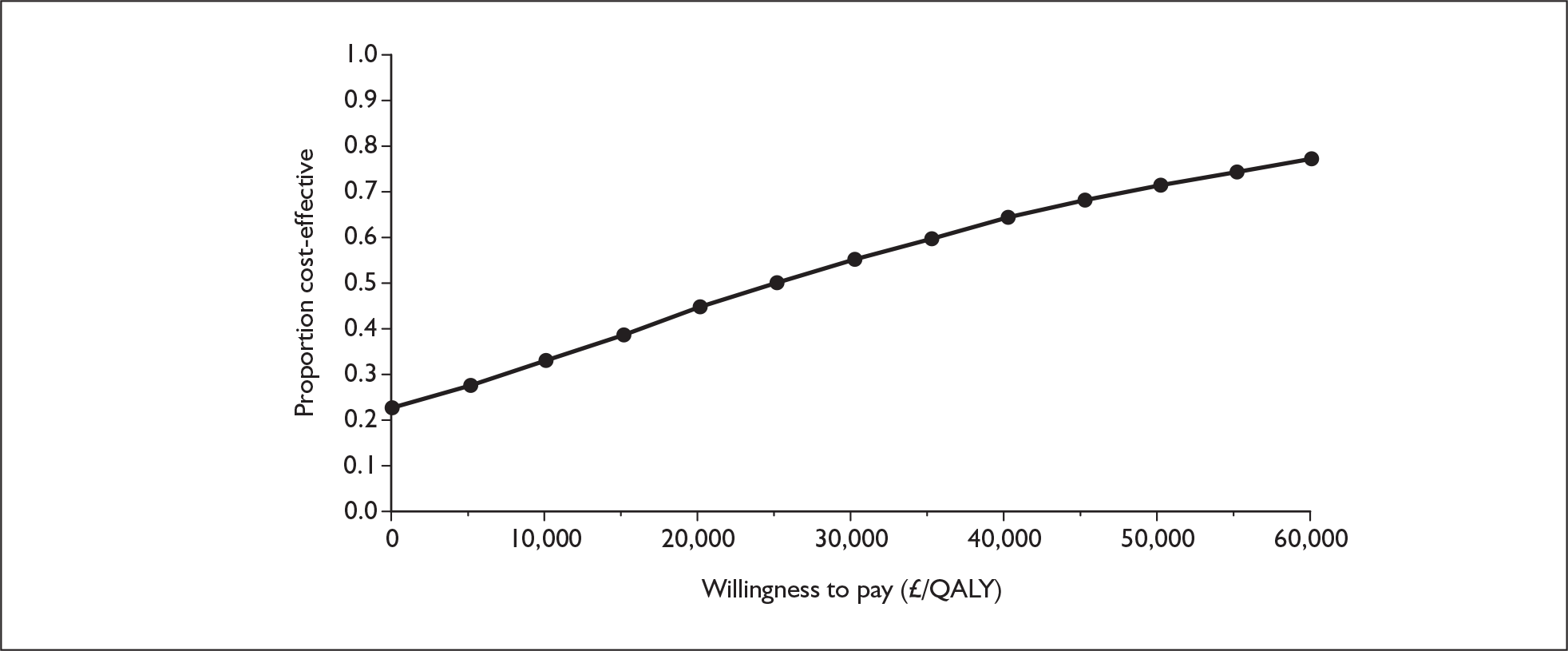
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 2.092 | |||
| Sitaxentan | 419,000 | 76,000 | 5.385 | 3.294 | 23,000 |
FIGURE 108.
Cost-effectiveness acceptability curve for sitaxentan versus supportive care, functional class III: alternative health state utility values (Olschewski et al. ). 41 QALY, quality-adjusted life-year.
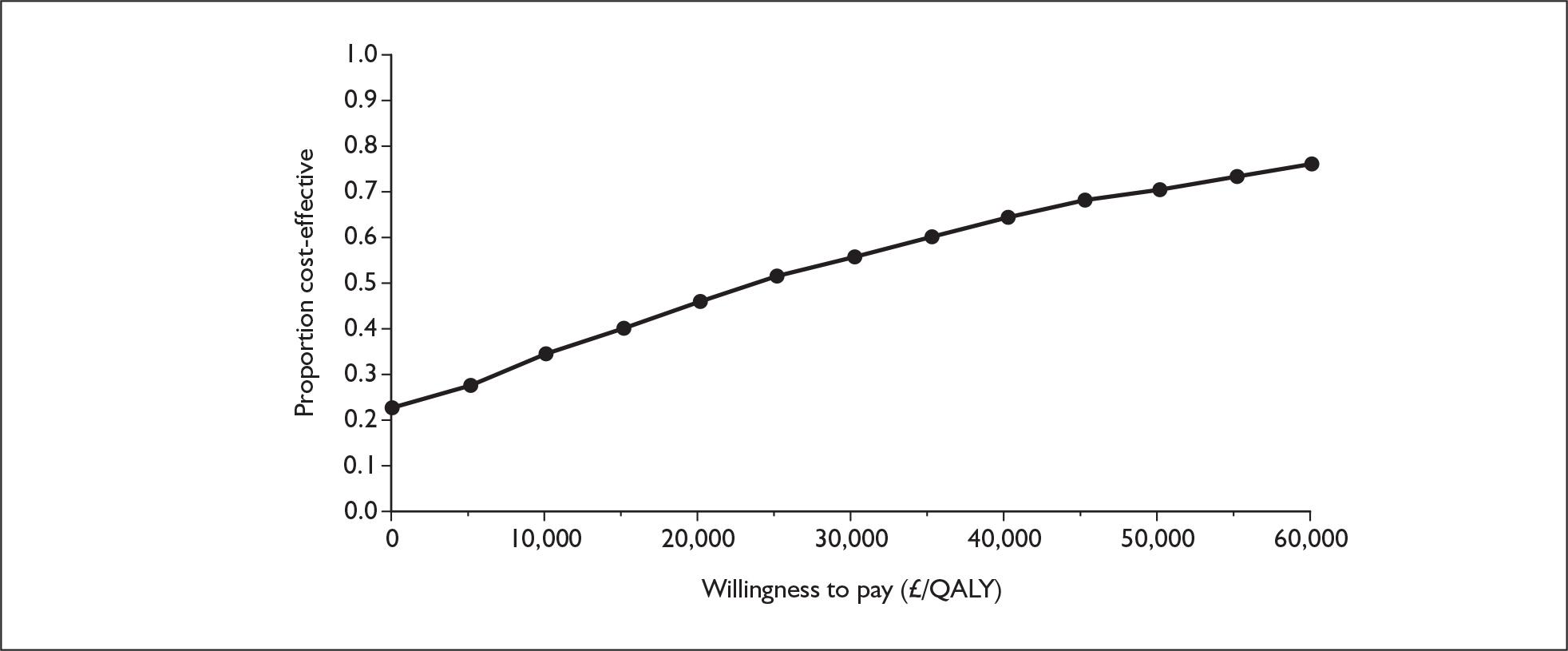
Appendix 12.6 Sildenafil with supportive care versus supportive care alone, functional class III
Alternative time horizon
Time horizon of 20 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 341,000 | 2.193 | |||
| Sildenafil | 288,000 | –53,000 | 5.071 | 2.878 | Dominates |
FIGURE 109.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: time horizon of 20 years. QALY, quality-adjusted life-year.
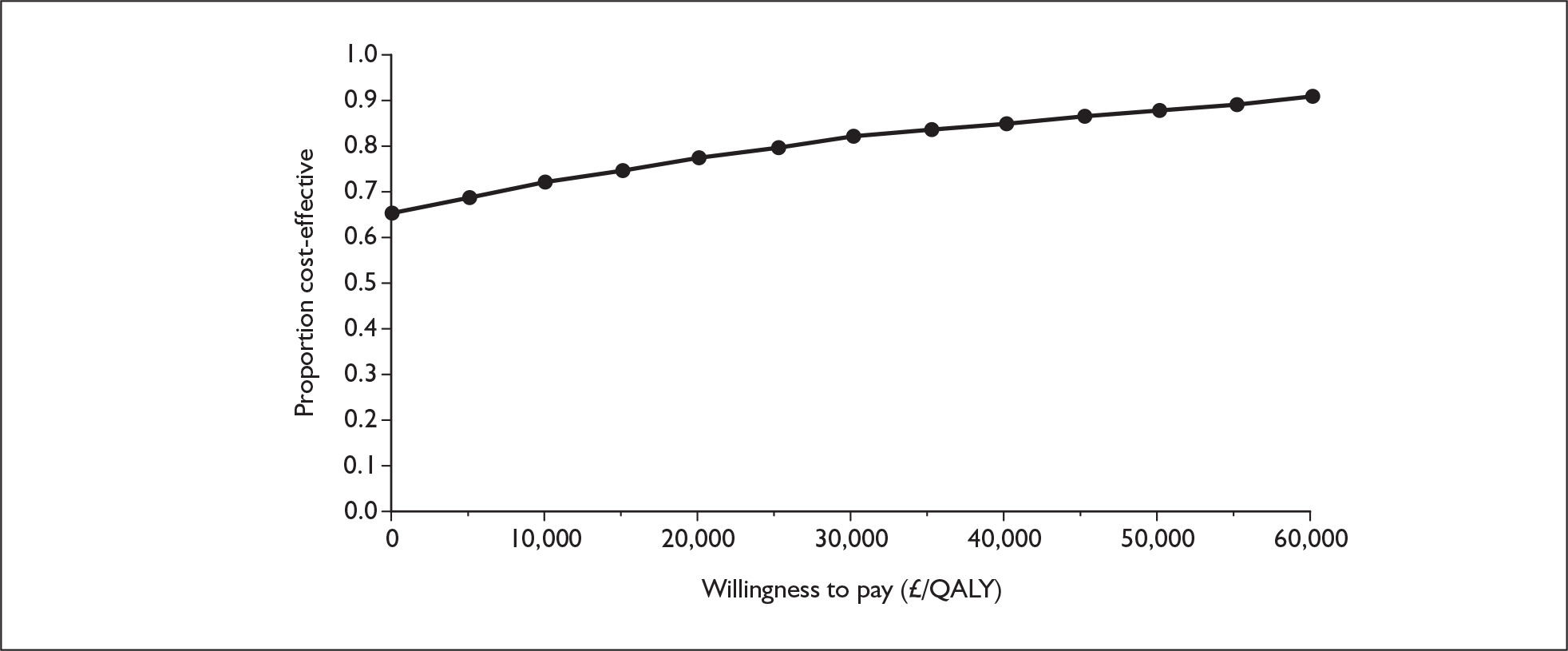
Time horizon of 10 years
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 304,000 | 2.063 | |||
| Sildenafil | 209,000 | –95,000 | 3.887 | 1.823 | Dominates |
FIGURE 110.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: time horizon of 10 years. QALY, quality-adjusted life-year.
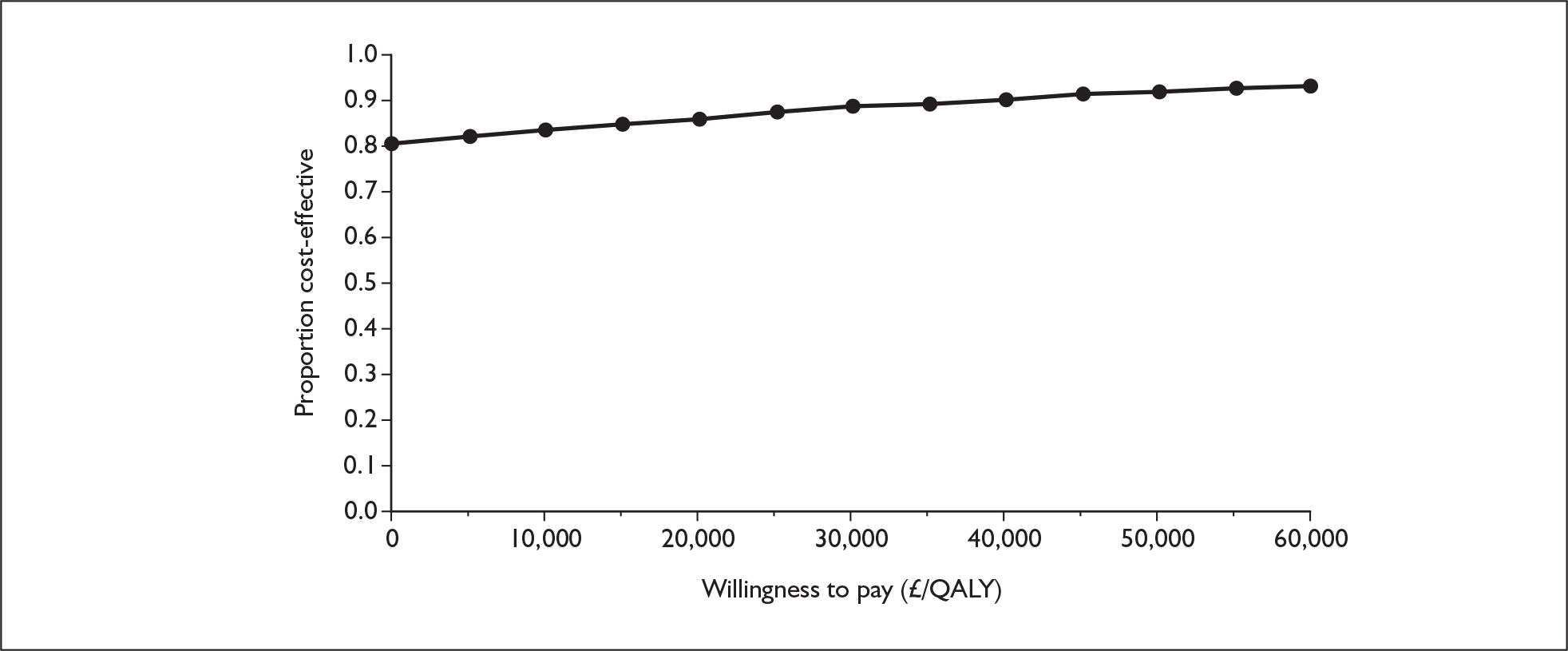
Alternative prices
Alternative price for epoprostenol
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 156,000 | 2.201 | |||
| Sildenafil | 168,000 | 12,000 | 5.436 | 3.235 | 3700 |
FIGURE 111.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: alternative price for epoprostenol. QALY, quality-adjusted life-year.
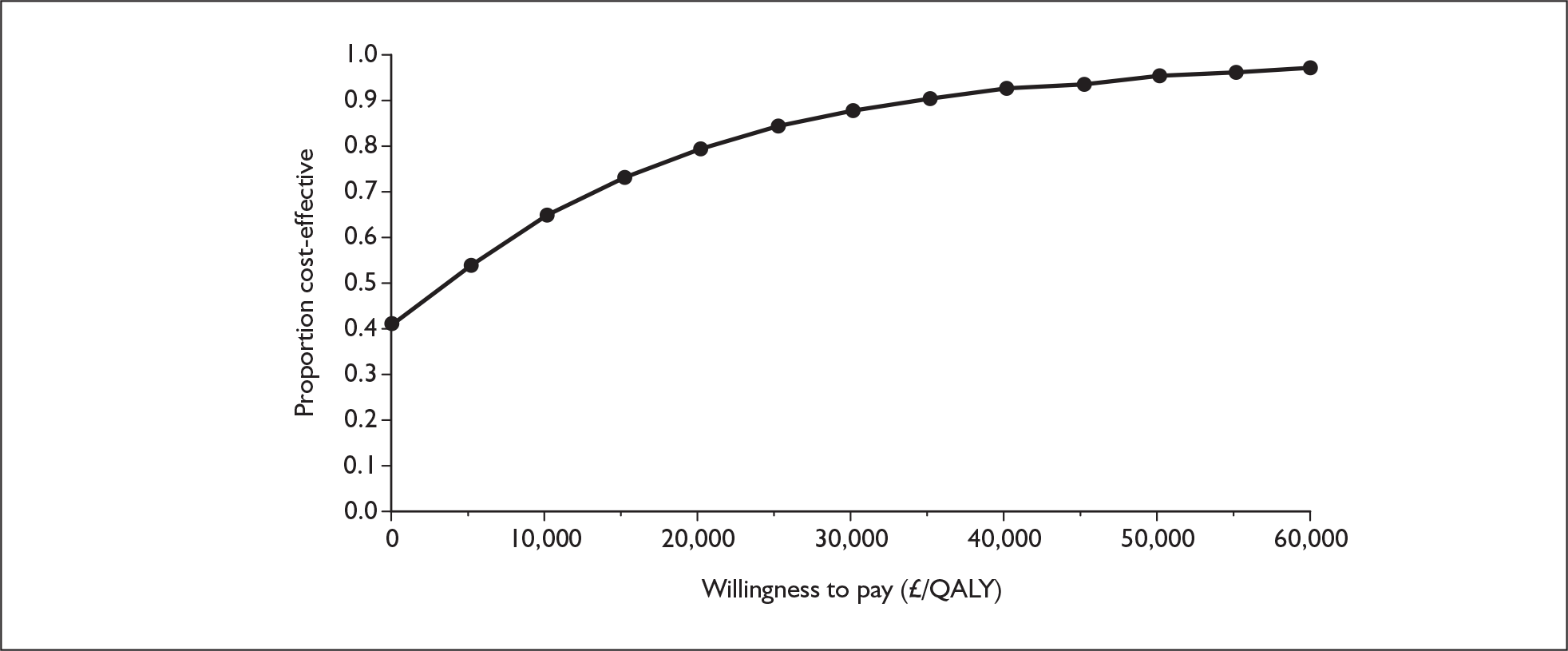
Alternative health state utility values
Utilities from Meads et al.94
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | [Commercial-in-confidence information has been removed] | |||
| Sildenafil | 307,000 | –36,000 | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] | [Commercial-in-confidence information has been removed] |
FIGURE 112.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: alternative health state utility values (Meads et al. ). 94 [Commercial-in-confidence information has been removed].
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 1.852 | |||
| Sildenafil | 309,000 | –34,000 | 5.228 | 3.376 | Dominates |
FIGURE 113.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: alternative health state utility values (Kirsch,76 2-year time trade-off). QALY, quality-adjusted life-year.
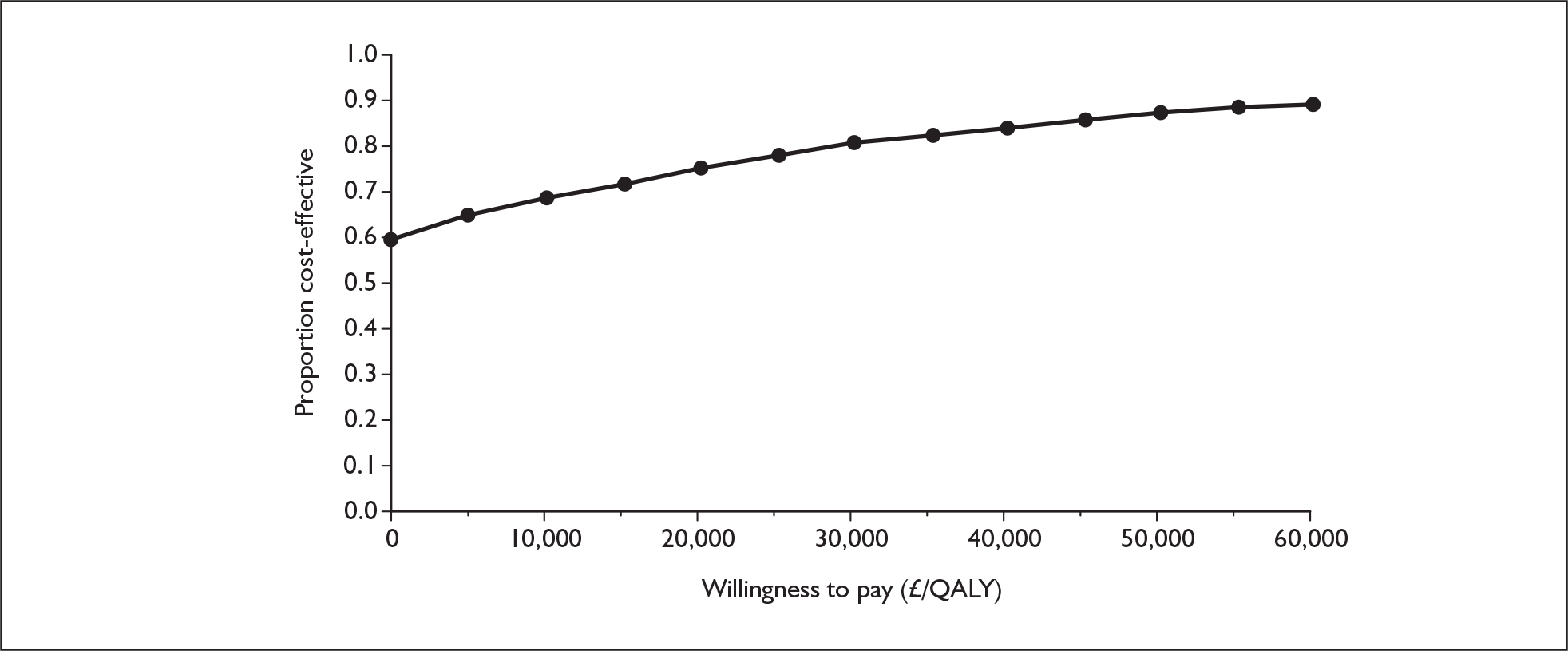
Utilities from Kirsch,76 2-year time trade-off
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 4.830 | |||
| Sildenafil | 309,000 | –34,000 | 1.602 | 3.227 | Dominates |
FIGURE 114.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: alternative health state utility values (Kirsch,76 10-year time trade-off).
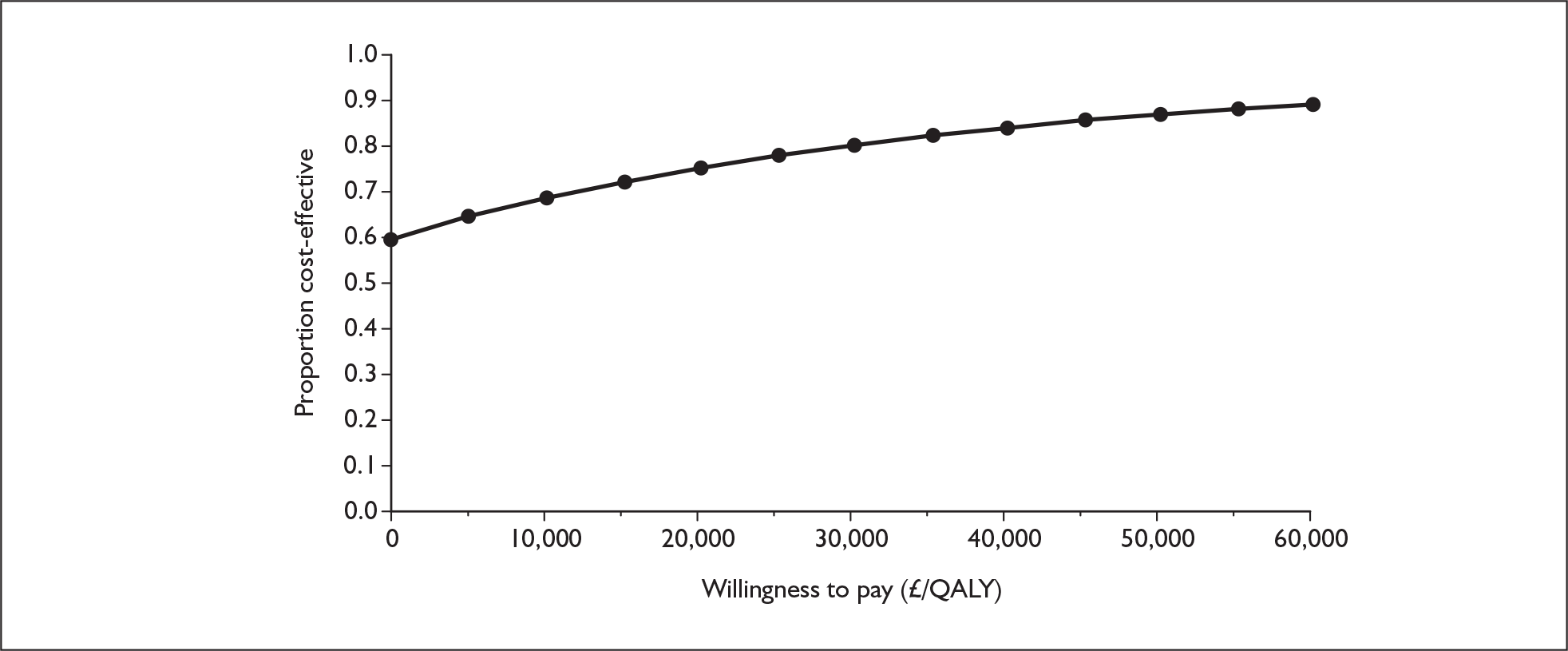
Utilities from Olschewski et al.41
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 343,000 | 5.572 | |||
| Sildenafil | 307,000 | –36,000 | 2.092 | 3.480 | Dominates |
FIGURE 115.
Cost-effectiveness acceptability curve for sildenafil versus supportive care, functional class III: alternative health state utility values (Olschewski et al. ). QALY, quality-adjusted life-year.
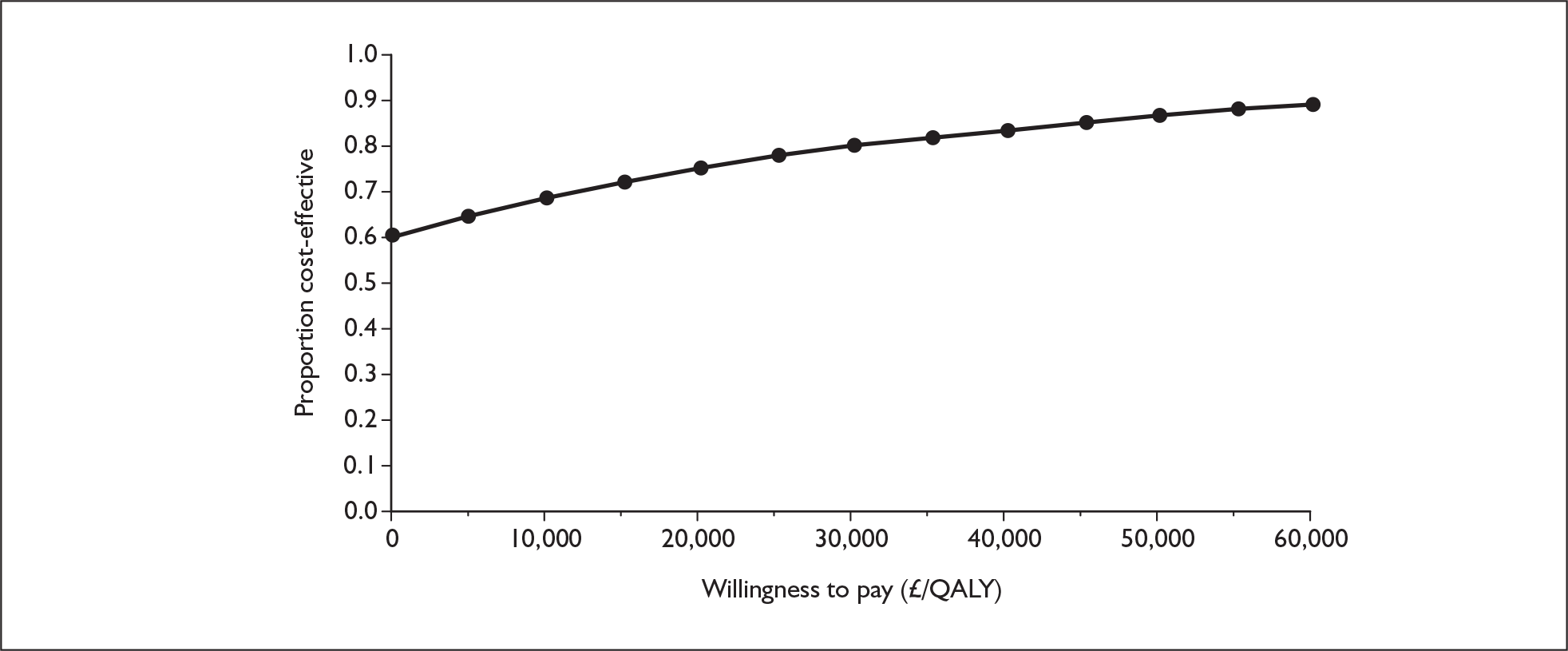
Appendix 13 Additional analyses requested by the NICE Appraisal Committee
Appendix 13.1 Assuming that patients in functional class IV (for both active treatment and supportive care arms) receive supportive care only (without epoprostenol)
Question: What is the effect on cost-effectiveness of altering the assumption that patients receive supportive care including epoprostenol once they have progressed to FCIV in both the active and supportive care arms of the model?
Analysis requested by NICE: Based on the reference case in the assessment report conduct an extreme case analysis (for all five technologies) by modifying the model to remove epoprostenol from supportive care in the FCIV state for the active treatment and supportive treatment arms. Thus, patients in FCIV only receive supportive care.
To explore this, the assessment model was run for all therapies assuming that patients receive supportive care alone in FCIV. This is in contrast to the reference case in which epoprostenol is assumed to be prescribed. The findings are presented below. No analysis is presented for epoprostenol in FCIV as the reference case analysis already assumes supportive care only in the comparator arm.
Epoprostenol in addition to supportive care versus supportive care alone, functional class III
Table 129 shows the results of the analysis for epoprostenol in FCIII. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £273,000 per QALY gained. The CEAC presented in Figure 116 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 115,000 | 1.091 | |||
| Epoprostenol | 344,000 | 229,000 | 1.927 | 0.837 | 273,000 |
FIGURE 116.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
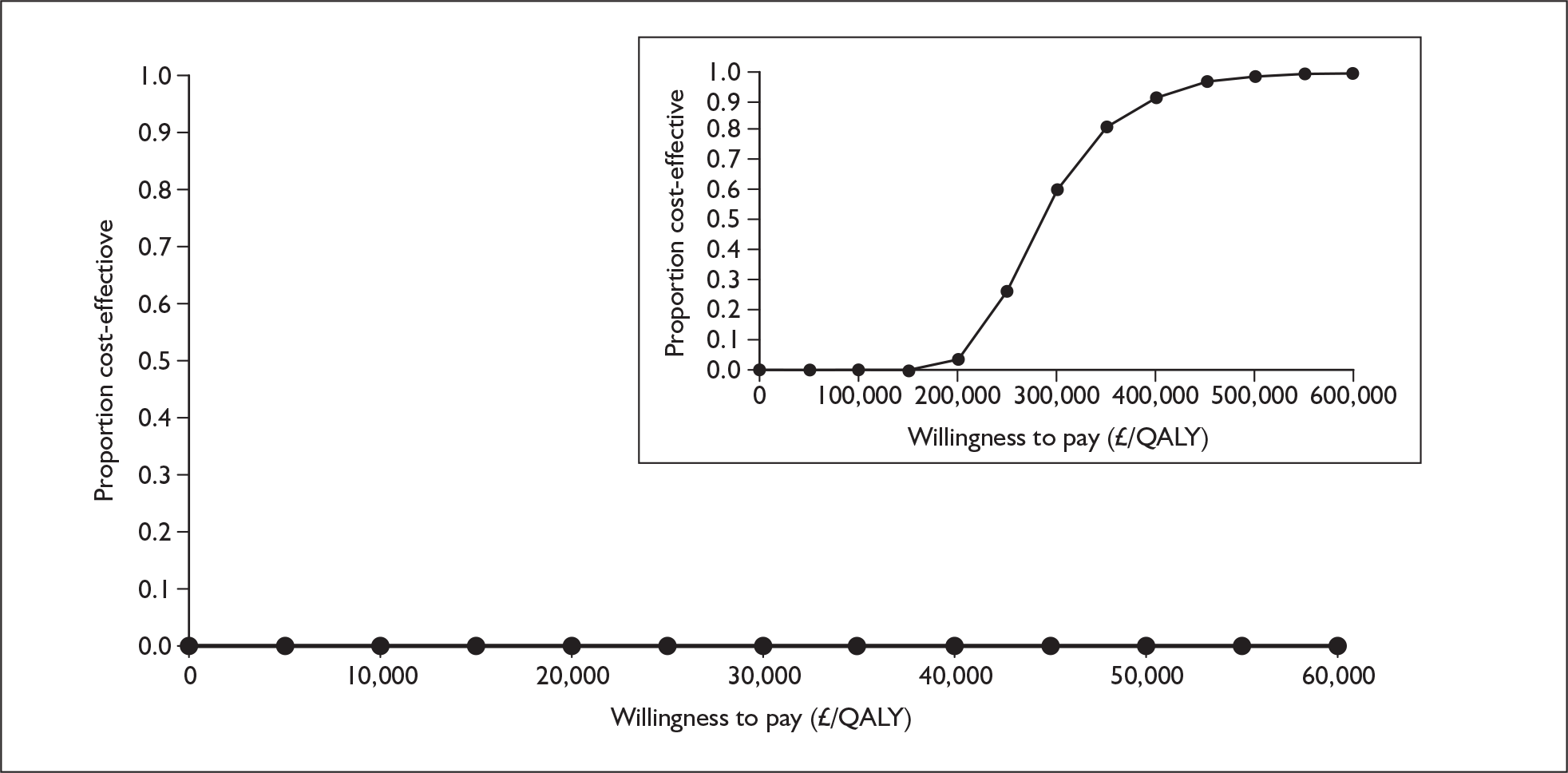
Iloprost with supportive care versus supportive care alone, functional class III
Table 130 shows the results of the analysis for iloprost in FCIII. Iloprost alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £98,000 per QALY gained. The CEAC presented in Figure 117 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, iloprost has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 105,000 | 1.086 | |||
| Iloprost | 207,000 | 102,000 | 2.131 | 1.045 | 98,000 |
FIGURE 117.
Cost-effectiveness acceptability curve for iloprost with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
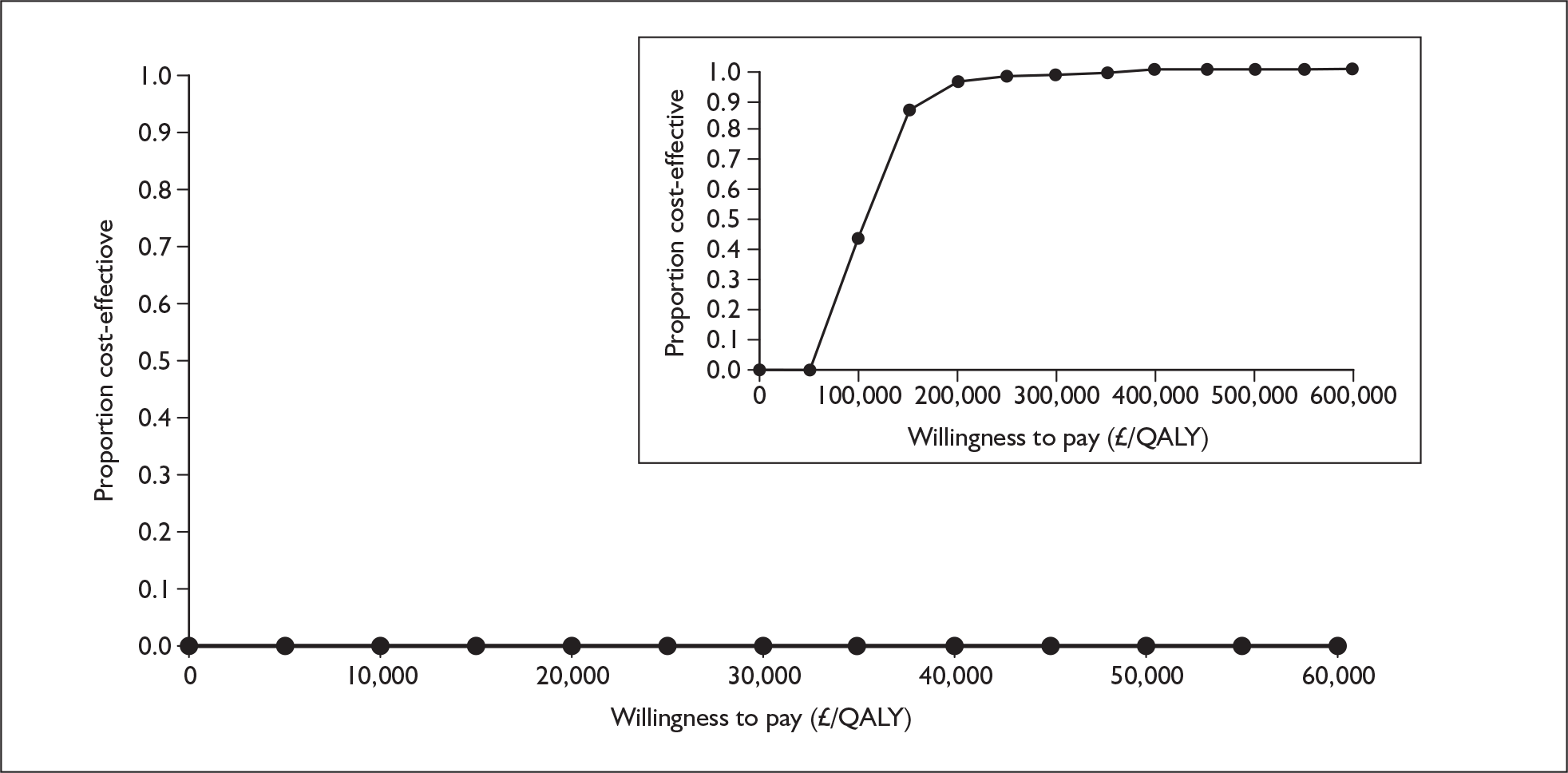
Bosentan in addition to supportive care versus supportive care alone, functional class III
Table 131 shows the results for bosentan, with the intervention more expensive than supportive care alone and producing a greater amount of QALYs, resulting in an ICER of £42,000 per QALY gained. The CEAC in Figure 118 demonstrates that bosentan has a zero chance of being cost-effective at £20,000 per QALY and a 3% chance at £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 84,000 | 1.532 | |||
| Bosentan | 239,000 | 155,000 | 5.209 | 3.677 | 42,000 |
FIGURE 118.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
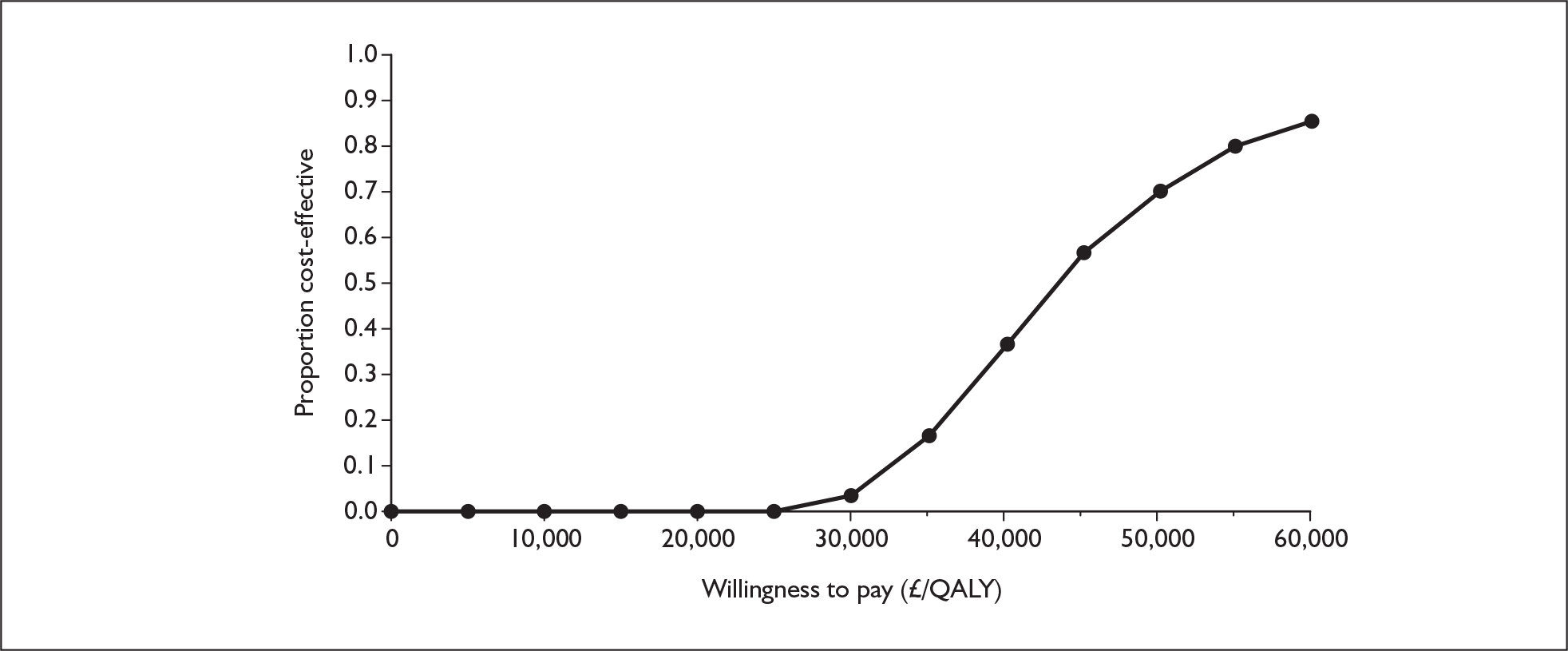
Sitaxentan in addition to supportive care versus supportive care alone, functional class III
Table 132 shows the results for sitaxentan, with the intervention more expensive than supportive care alone and producing a greater amount of QALYs, resulting in an ICER of £44,000 per QALY gained. The CEAC presented in Figure 119 demonstrates that at thresholds of £20,000 and £30,000 per QALY gained, the probability of sitaxentan being cost-effective is 0% and 3% respectively.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 84,000 | 1.532 | |||
| Sitaxentan | 226,000 | 142,000 | 4.780 | 3.248 | 44,000 |
FIGURE 119.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
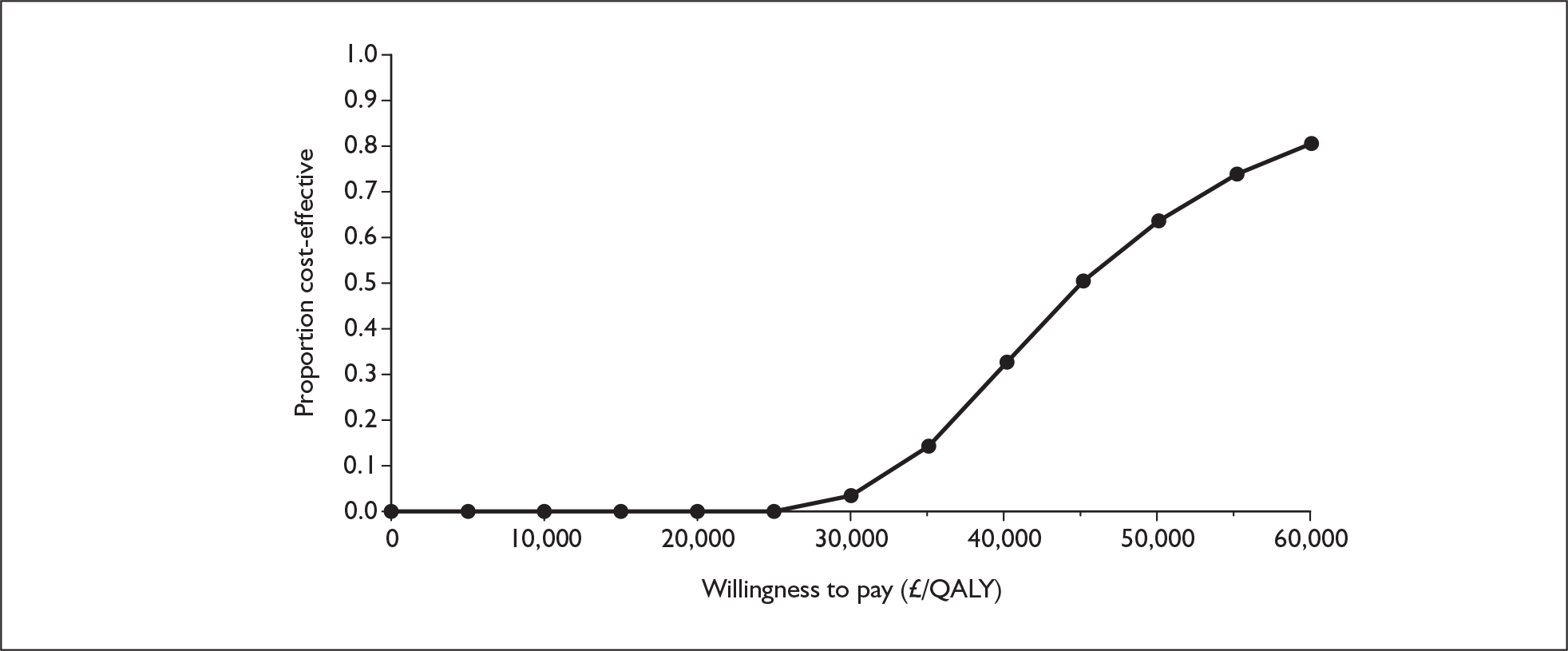
Sildenafil in addition to supportive care versus supportive care alone, functional class III
Table 133 shows the results for sildenafil, with the intervention more expensive than supportive care alone and producing a greater amount of QALYs, resulting in an ICER of £9000 per QALY gained. The CEAC presented in Figure 120 shows that sildenafil has a probability of being cost-effective of 83% at £20,000 per QALY and 92% at £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 84,000 | 1.532 | |||
| Sildenafil | 115,000 | 31,000 | 4.950 | 3.418 | 9000 |
FIGURE 120.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
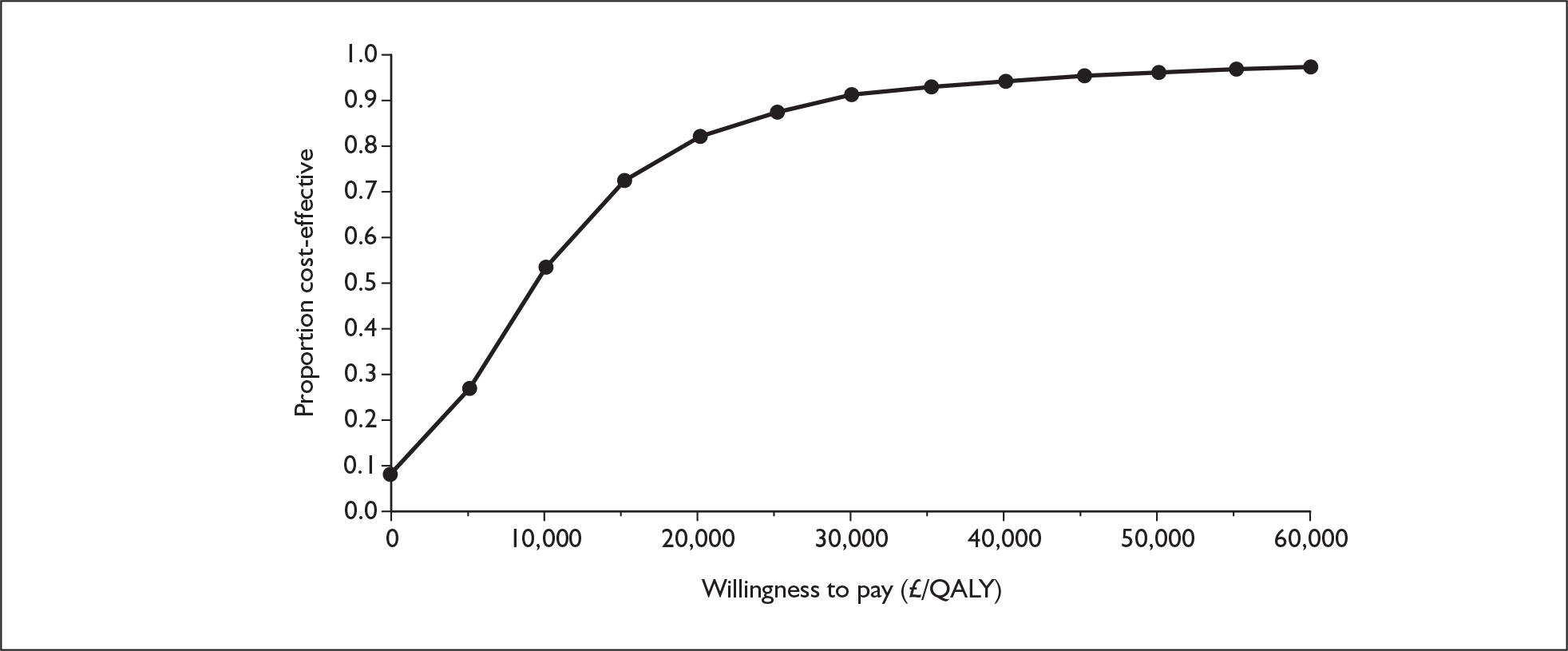
Summary of results – comparison with reference case
-
The ICER for epoprostenol reduced very slightly from £277,000 per QALY gained to £273,000. Although the difference in costs increases, the difference in QALYs also increases.
-
The ICER for iloprost reduced very slightly from £101,000 per QALY gained to £98,000. The difference in costs changes very little, but the difference in benefits is greater.
-
The ICER for bosentan increased from £27,000 per QALY gained to £42,000. Although the difference in QALYs increases slightly, the difference in costs is much greater.
-
The ICER for sitaxentan increased from £25,000 per QALY gained to £44,000. Although the difference in QALYs increases slightly, the difference in costs is much greater.
-
The ICER for sildenafil was £9000 per QALY gained compared with being dominant in the reference case. The difference in QALYs increases; however, the direction on the difference in costs changes and so costs are now greater in the sildenafil arm.
Explanation of results
When comparing treatments that start in FCIII patients, in the reference case the main driver of cost in both the treatment and supportive care arms was epoprostenol for patients subsequently reaching FCIV. Removal of epoprostenol from FCIV substantially reduced the costs in both arms, but more so in the supportive care arm as in this arm more patients reach FCIV and they do so quicker compared with the treatment arm (i.e. treatment of FCIII patients reduces progression to FCIV). The supportive care option therefore became relatively cheap. The removal of epoprostenol also meant that there was a greater loss of QALYs (which would be saved by using epoprostenol) in the supportive care arm, but this had less impact on the ICERs than the change in costs.
This scenario may not reflect clinical practice as other prostaglandins (which may not have been licensed in the UK) may be used if epoprostenol is not available for treating FCIV patients.
Appendix 13.2 Assuming that the three oral treatments result in the same mortality rates on treatment and on supportive care as those used for epoprostenol in functional class III
Question: What is the effect on cost-effectiveness of the oral drugs if the same assumptions for mortality on treatment and best supportive care are used as are used for epoprostenol in FCIII?
Analysis requested by NICE: Based on the reference case in the assessment report conduct a sensitivity analysis (for the three oral drugs) by applying the same mortality rates on treatment and on supportive care as are used for epoprostenol in FCIII.
The data on mortality for epoprostenol (0.021 per cycle, 95% CI 0.017–0.025) and the corresponding data on mortality for supportive care (0.051 per cycle, 95% CI 0.041–0.069) were used in the model, replacing those mortalities used in the reference case analysis for each intervention (see Appendix 9).
Bosentan in addition to supportive care versus supportive care alone, functional class III
Table 134 shows the results of the analysis for bosentan in FCIII. Bosentan alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £6000 per QALY gained. The CEAC presented in Figure 121 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, bosentan has a 67% and 75% probability, respectively, of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 349,000 | 2.236 | |||
| Bosentan | 364,000 | 14,000 | 4.857 | 2.620 | 6000 |
FIGURE 121.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
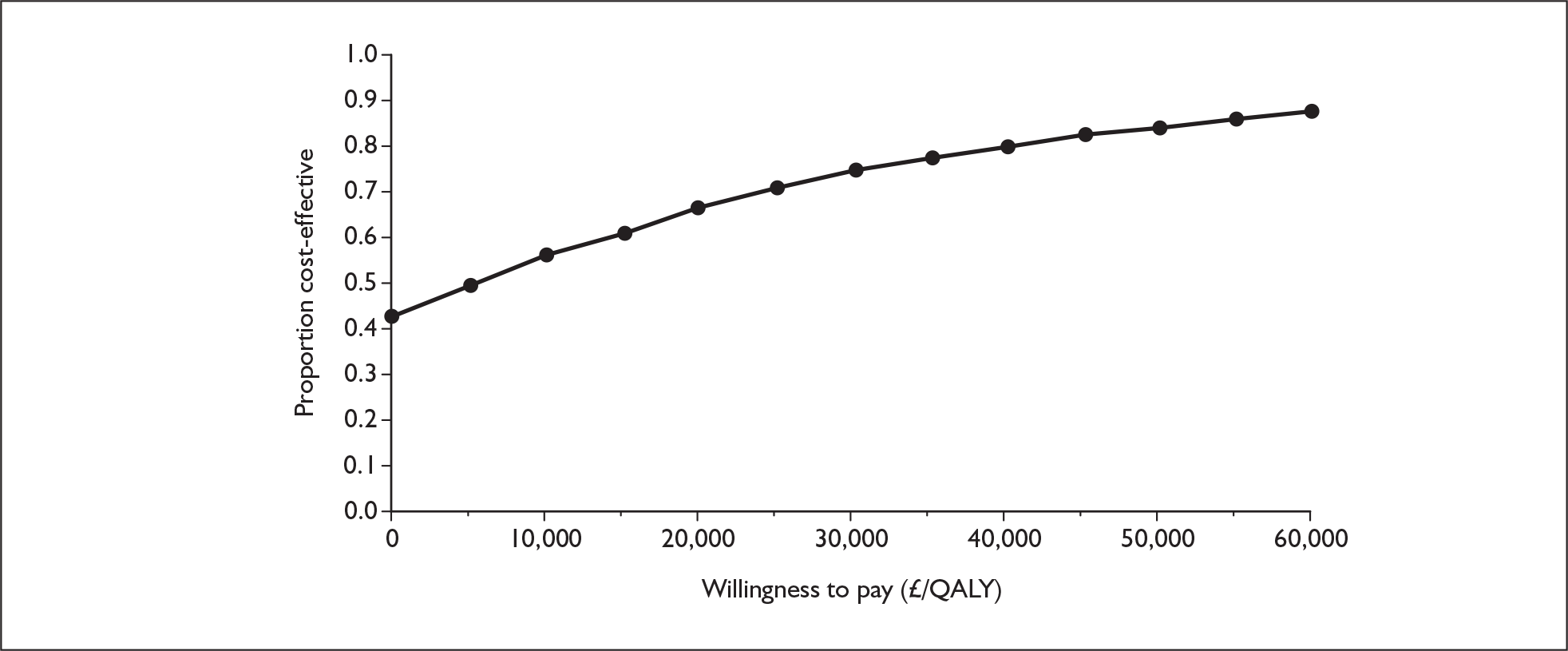
Sitaxentan in addition to supportive care versus supportive care alone, functional class III
Table 135 shows the results of the analysis for sitaxentan in FCIII. Sitaxentan alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £1400 per QALY gained. The CEAC presented in Figure 122 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, bosentan has a 67% and 73% probability, respectively, of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 349,000 | 2.236 | |||
| Sitaxentan | 352,000 | 3000 | 4.409 | 2.173 | 1400 |
FIGURE 122.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
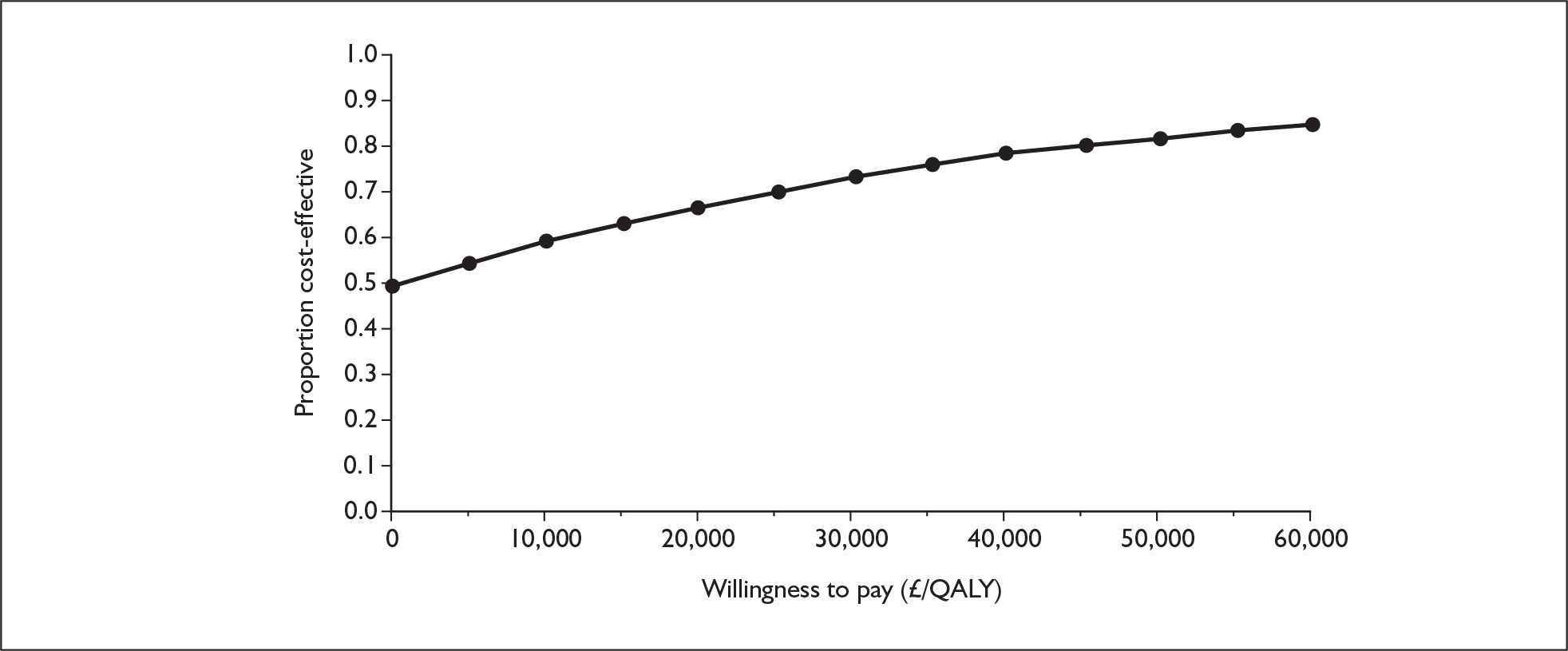
Sildenafil in addition to supportive care versus supportive care alone, functional class III
Compared with supportive care alone, sildenafil is less costly and more effective resulting in dominance for the intervention (Table 136). The CEAC presented in Figure 123 shows that sildenafil has a probability of being cost-effective of 86% at £20,000 per QALY and 89% at £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 349,000 | 2.236 | |||
| Sildenafil | 259,000 | –90,000 | 4.618 | 2.381 | Dominant |
FIGURE 123.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
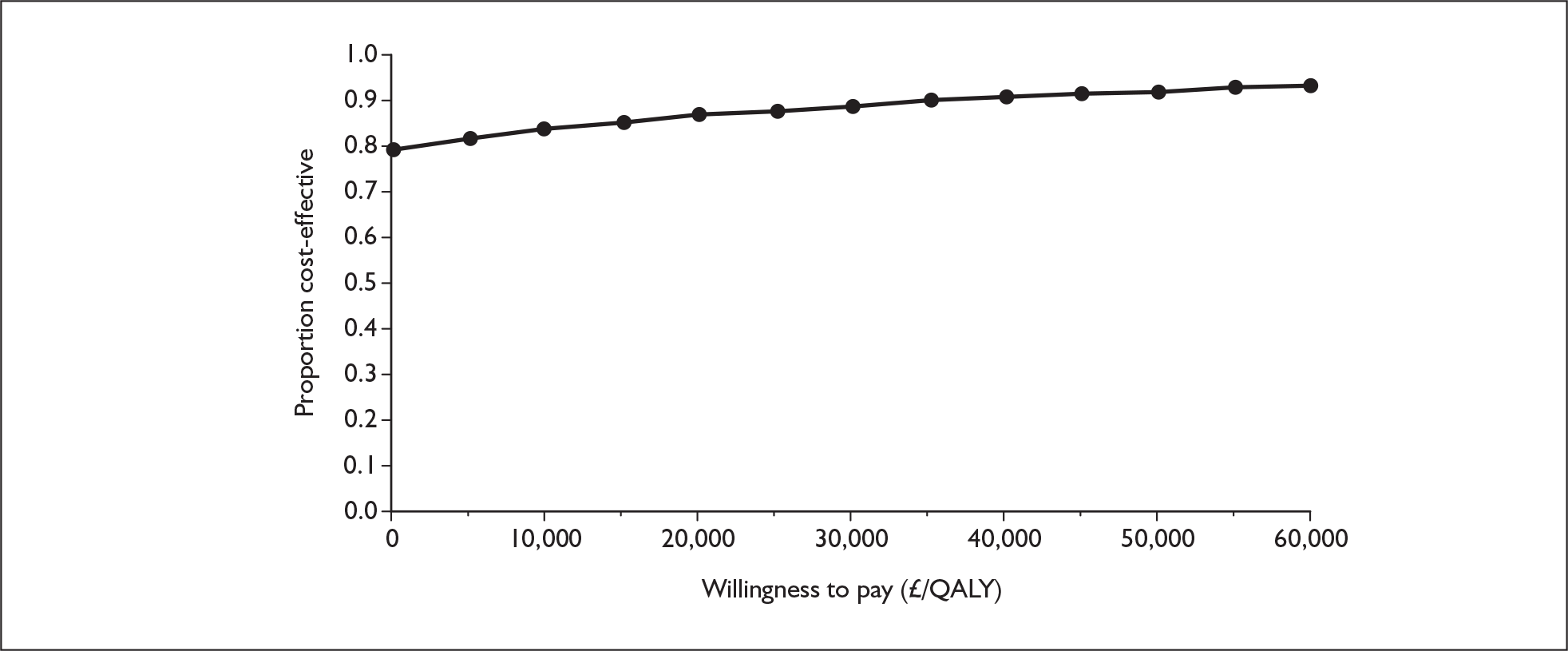
Summary of results – comparison with reference case
-
The ICER for bosentan is much lower, dropping from £27,000 per QALY gained in the reference case to £6000. Although the difference in QALYs decreases, the difference in costs is much reduced.
-
The ICER for sitaxentan is greatly reduced from £25,000 per QALY gained to £1400. Although the difference in QALYs decreases, the difference in costs is now very small.
-
In both the reference case and this additional analysis, sildenafil is dominant when compared with supportive care. However, the probability of being cost-effective at thresholds of £20,000 and £30,000 per QALY gained is greater in the additional analysis than in the reference case.
Explanation of results
This sensitivity analysis explored a scenario in which the mortality rate on treatment and the mortality rate on supportive care in FCIII for the three oral treatments are the same as those for epoprostenol, i.e. these treatments offer the same survival benefit and there is no difference in ‘baseline mortality’ between patients treated with different drugs. Compared with the reference case the mortality rate in the treatment arm for the oral treatments was almost doubled (per-cycle mortality on treatment in FCIII was increased from 0.011 to 0.021), whereas the mortality rate in the supportive care arm was slightly reduced (from 0.058 to 0.051). This reduced the proportion of patients surviving to reach FCIV (which would incur expensive epoprostenol treatment) in the oral treatment arms whist slightly increasing the proportion of patients surviving to reach FCIV in the supportive care arms. The oral treatment options therefore became comparatively cheaper compared with the reference case. Although the QALY gain in the oral treatment groups was reduced and the QALY gain in the supportive care arms was slightly increased compared with the reference case the changes in cost appear to have a greater impact than the changes in QALYs.
Appendix 13.3 Exploring the minimal survival benefit required to meet incremental cost-effectiveness thresholds of £20,000, £30,000 and £40,000 per QALY
Question: What would be the minimum survival benefit required for the oral drugs to meet cost-effectiveness thresholds of £20,000, £30,000 and £40,000 per QALY?
Analysis requested by NICE: Based on the reference case in the assessment report conduct a sensitivity analysis (for the three oral drugs) on the minimum survival benefit (in terms of the odds ratio for the risk of death on treatment over the risk of death on supportive care) required to meet incremental cost effectiveness thresholds of £20,000, £30,000 and £40,000 per QALY.
Data for mortality on treatment were available for some oral therapies from long-term observational studies. There is a lack of data in the literature with regard to long-term mortality for patients who receive supportive care alone because it is considered unethical to withhold active treatments that have proven to be effective. In the model, to account for this absence of data, mortality on supportive care was derived by applying an odds ratio to the mortality on oral treatment. The odds ratio used was the same as the odds ratio for deterioration from FCIII to FCIV for each treatment relative to supportive care. This odds ratio was obtained from the RCTs on the effectiveness of the oral therapies and used under the assumption that a treatment which delays deterioration in FC in the short term would also reduce mortality proportionately in the long term.
In this threshold analysis the odds ratio (which approximates the survival benefit) was varied to determine at what level of survival benefit the oral drugs reached the suggested cost-effectiveness thresholds. A smaller odds ratio (further away from 1 and towards 0) corresponds to a larger survival benefit for the active treatment; conversely, a larger odds ratio (closer to 1) corresponds to a smaller survival benefit for the active treatment compared with supportive care.
Model runs have been conducted as per the reference case, with epoprostenol available for patients in FCIV. Results are presented for odds ratios of 0.1, 0.2 and 0.3 and for the odds ratios giving ICERs in the region of £20,000, £30,000 and £40,000 per QALY gained. As can been seen in Tables 137–139 the ICERs increase (the treatments become less cost-effective) as the survival benefits increase (the odds ratios become smaller).
| Odds ratio | 12-week cycle mortality on supportive carea | Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|---|---|
| 0.1 | 0.100 | Comparator | 264,000 | 1.731 | |||
| Active therapy | 434,000 | 170,000 | 5.689 | 3.959 | 43,000 | ||
| 0.115 | 0.088 | Comparator | 282,000 | 1.838 | |||
| Active therapy | 434,000 | 153,000 | 5.688 | 3.849 | 40,000 | ||
| 0.165 | 0.063 | Comparator | 328,000 | 2.111 | |||
| Active therapy | 434,000 | 106,000 | 5.687 | 3.577 | 30,000 | ||
| 0.18b | 0.058 | Comparator | 343,000 | 2.201 | |||
| Active therapy | 436,000c | 93,000 | 5.969 | 3.494 | 27,000 | ||
| 0.2 | 0.053 | Comparator | 351,000 | 2.246 | |||
| Active therapy | 434,000 | 83,000 | 5.680 | 3.434 | 24,000 | ||
| 0.23 | 0.046 | Comparator | 367,000 | 2.342 | |||
| Active therapy | 434,000 | 67,000 | 5.683 | 3.341 | 20,000 | ||
| 0.3 | 0.036 | Comparator | 396,000 | 2.512 | |||
| Active therapy | 434,000 | 39,000 | 5.683 | 3.171 | 12,000 |
| Odds ratio | 12-week cycle mortality on supportive carea | Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|---|---|
| 0.1 | 0.100 | Comparator | 264,000 | 1.731 | |||
| Active therapy | 420,000 | 157,000 | 5.254 | 3.523 | 44,000 | ||
| 0.118 | 0.086 | Comparator | 284,000 | 1.855 | |||
| Active therapy | 421,000 | 136,000 | 5.255 | 3.400 | 40,000 | ||
| 0.165 | 0.063 | Comparator | 328,000 | 2.111 | |||
| Active therapy | 421,000 | 93,000 | 5.262 | 3.151 | 30,000 | ||
| 0.18b | 0.058 | Comparator | 343,000 | 2.201 | |||
| Active therapy | 419,000c | 76,000 | 5.289 | 3.087 | 25,000 | ||
| 0.2 | 0.053 | Comparator | 351,000 | 2.246 | |||
| Active therapy | 421,000 | 70,000 | 5.268 | 3.022 | 23,000 | ||
| 0.22 | 0.048 | Comparator | 362,000 | 2.312 | |||
| Active therapy | 421,000 | 59,000 | 5.266 | 2.954 | 20,000 | ||
| 0.3 | 0.036 | Comparator | 396,000 | 2.512 | |||
| Active therapy | 421,000 | 25,000 | 5.263 | 2.751 | 9000 |
| Odds ratio | 12-week cycle mortality on supportive carea | Strategy | Cost (£)c | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|---|---|
| 0.03 | 0.270 | Comparator | 124,000 | 0.895 | |||
| Active therapy | 305,000 | 182,000 | 5.459 | 4.563 | 40,000 | ||
| 0.05 | 0.182 | Comparator | 178,000 | 1.222 | |||
| Active therapy | 306,000 | 128,000 | 5.445 | 4.223 | 30,000 | ||
| 0.075 | 0.129 | Comparator | 227,000 | 1.514 | |||
| Active therapy | 307,000 | 80,000 | 5.432 | 3.918 | 20,000 | ||
| 0.1 | 0.100 | Comparator | 264,000 | 1.731 | |||
| Active therapy | 307,000 | 43,000 | 5.432 | 3.702 | 12,000 | ||
| 0.18b | 0.058 | Comparator | 343,000 | 2.201 | |||
| Active therapy | 307,000 | –36,000 | 5.436 | 3.235 | Dominates | ||
| 0.2 | 0.053 | Comparator | 351,000 | 2.246 | |||
| Active therapy | 307,000 | –44,000 | 5.428 | 3.182 | Dominates | ||
| 0.3 | 0.036 | Comparator | 396,000 | 2.512 | |||
| Active therapy | 308,000 | –88,000 | 5.427 | 2.915 | Dominates |
Explanation of results
The results are consistent with those from the sensitivity analysis described in Appendix 13.2. Both analyses show that by reducing the survival benefit of the active treatment, either by increasing the mortality on treatment (as in Appendix 13.2) or by increasing the odds ratio towards 1 (hence reducing the mortality on supportive care as in this section), the active treatment becomes more cost-effective. This is because, when survival benefit is reduced compared with the reference case, either a smaller proportion of patients in the oral treatment arm survive to reach FCIV (which would incur expensive epoprostenol treatment) or a larger proportion of patients in the supportive care arm survive to reach FCIV. The oral treatment options therefore became comparatively cheaper. Although the QALY gain in the oral treatment groups was reduced and the QALY gain in the supportive care group was increased compared with the reference case, the changes in costs appear to have a greater impact on the ICERs than the changes in QALYs.
Appendix 13.4 Assuming that no death occurs while patients stay in functional class III
Question: What is the effect on cost-effectiveness of altering the assumption on mortality in FCIII, i.e. that people in the model go straight from FCIII to death rather than go through FCIV first for all drugs in this appraisal?
Analysis requested by NICE: Based on the reference case in the assessment report conduct an extreme case analysis (for all five technologies) which assumes that no deaths occur while patients stay in FCIII.
The assessment model was run including the assumption that no PAH-related mortality was possible in FCIII; patients had to be in FCIV before this type of mortality was possible.
Epoprostenol in addition to supportive care versus supportive care alone, functional class III
Table 140 shows the results of the analysis for epoprostenol in FCIII. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £285,000 per QALY gained. The CEAC presented in Figure 124 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 600,000 | 2.530 | |||
| Epoprostenol | 838,000 | 238,000 | 3.367 | 0.837 | 285,000 |
FIGURE 124.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
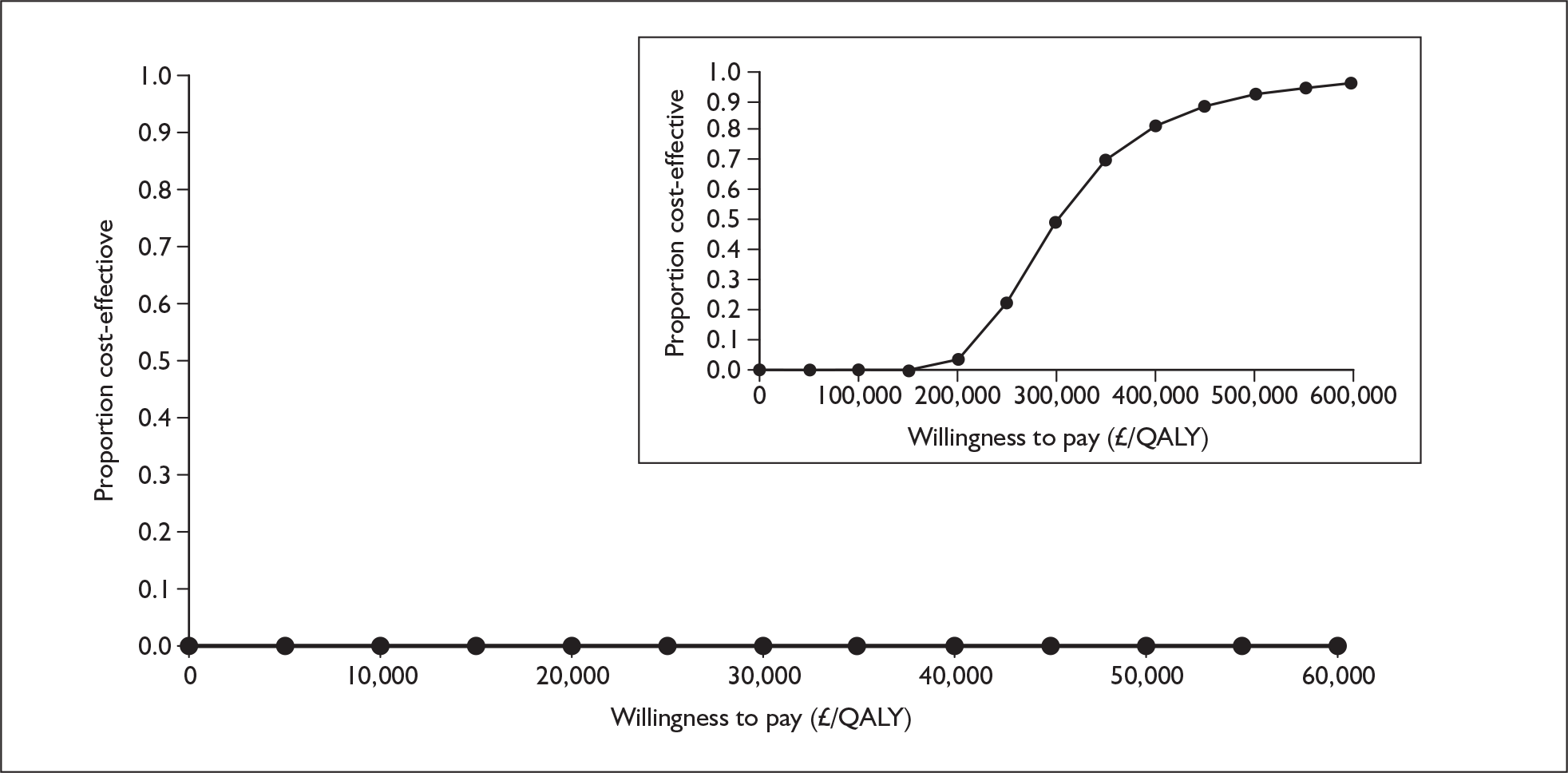
Epoprostenol in addition to supportive care versus supportive care alone, functional class IV
Table 141 shows the results of the analysis for epoprostenol in FCIV. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £337,000 per QALY gained. The CEAC presented in Figure 125 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 128,000 | 0.826 | |||
| Epoprostenol | 565,000 | 437,000 | 2.121 | 1.295 | 337,000 |
FIGURE 125.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class IV. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
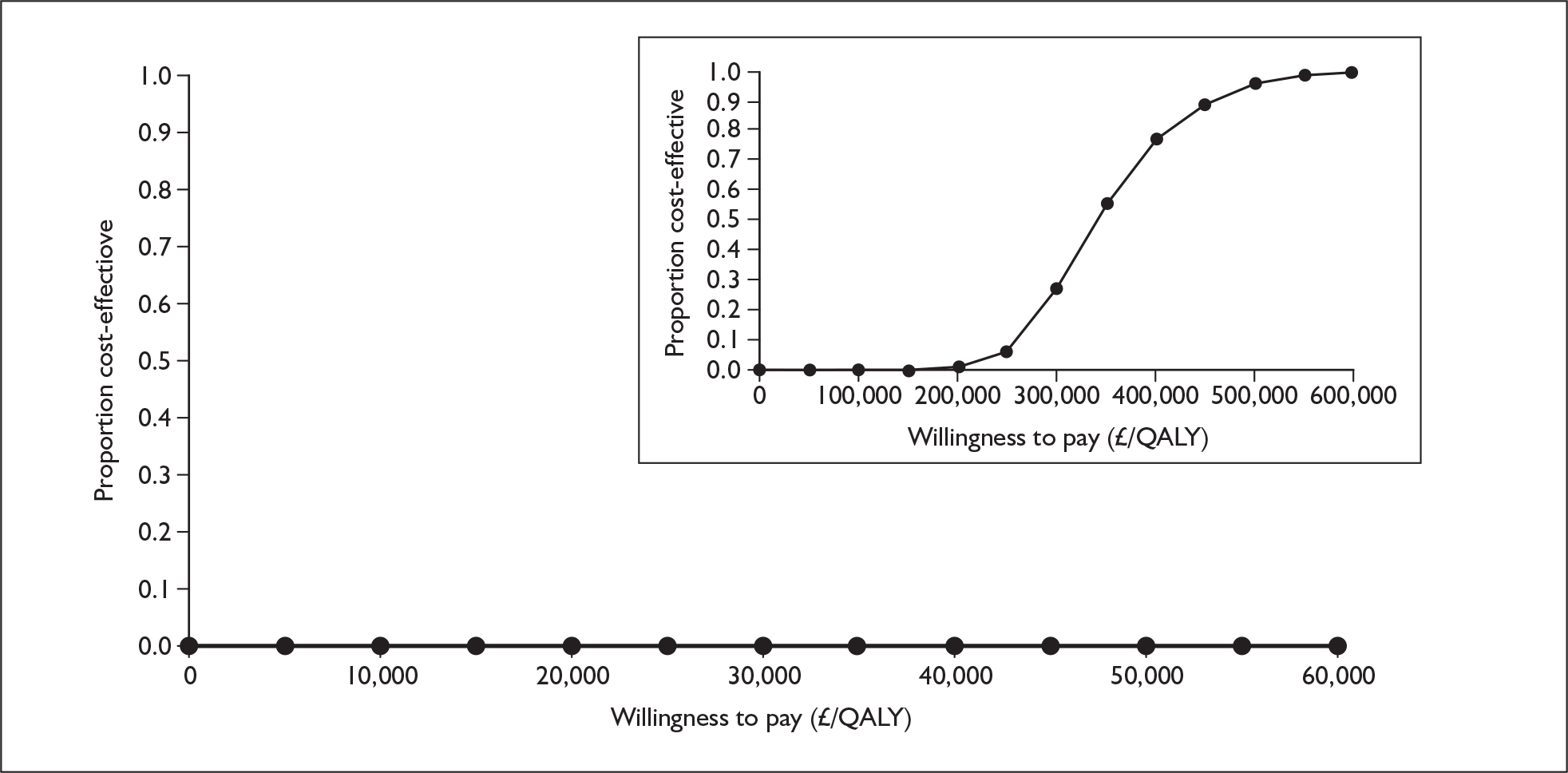
Iloprost with supportive care versus supportive care alone, functional class III
Table 142 shows the results of the analysis for iloprost in FCIII. Iloprost alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £76,000 per QALY gained. The CEAC presented in Figure 126 shows that at willingness to pay thresholds of £20,000 and £30,000 per QALY gained, iloprost has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 599,000 | 2.635 | |||
| Iloprost | 682,000 | 83,000 | 3.733 | 1.098 | 76,000 |
FIGURE 126.
Cost-effectiveness acceptability curve for iloprost with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
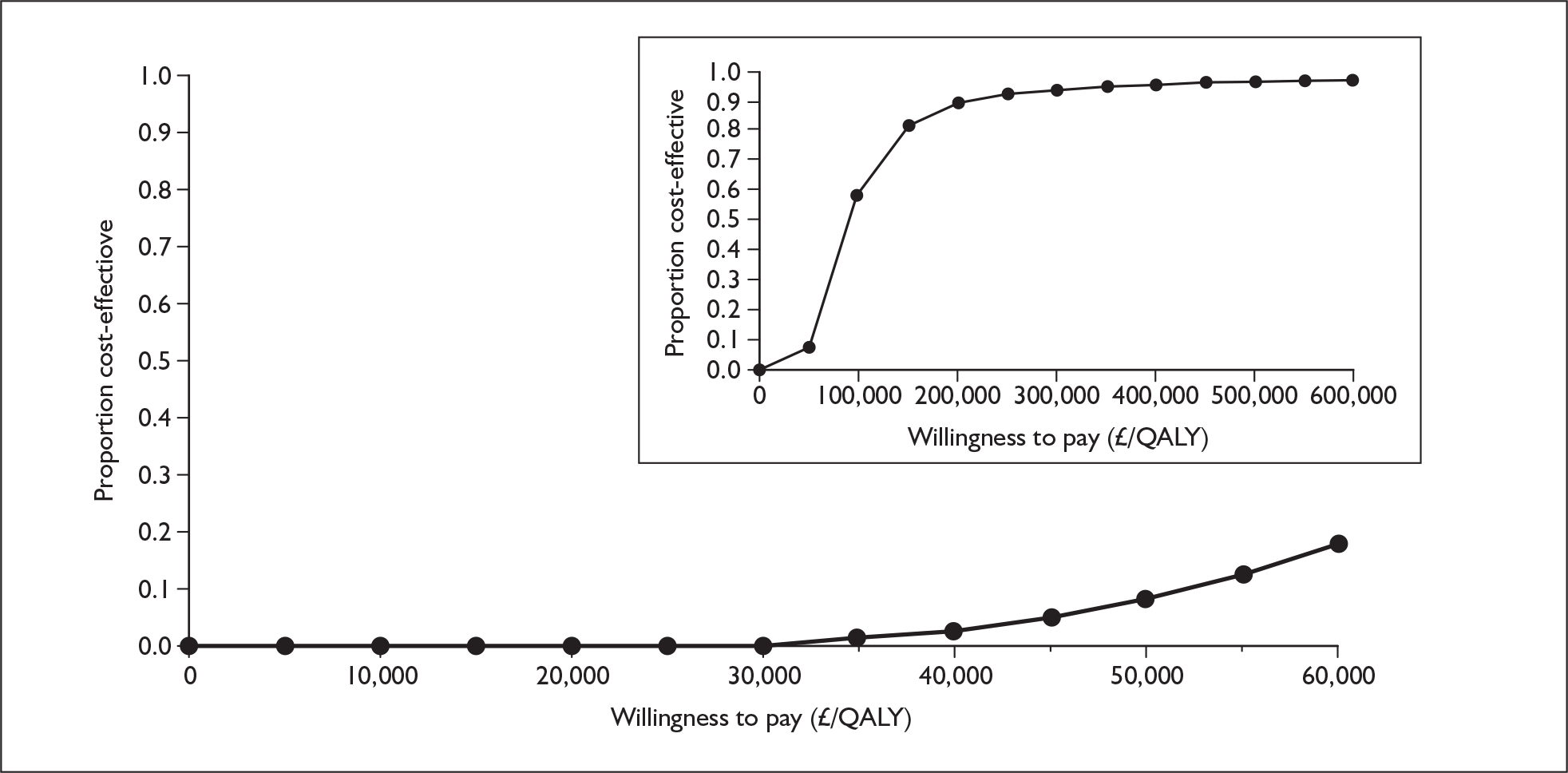
Bosentan in addition to supportive care versus supportive care alone, functional class III
Table 143 shows the results for bosentan, with the intervention less expensive than supportive care alone and producing a greater amount of QALYs, resulting in bosentan being dominant over supportive care. The CEAC in Figure 127 demonstrates that bosentan has an 82% chance of being cost-effective at £20,000 per QALY and an 88% chance at £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 572,000 | 3.494 | |||
| Bosentan | 551,000 | –21,000 | 6.992 | 3.498 | Dominant |
FIGURE 127.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
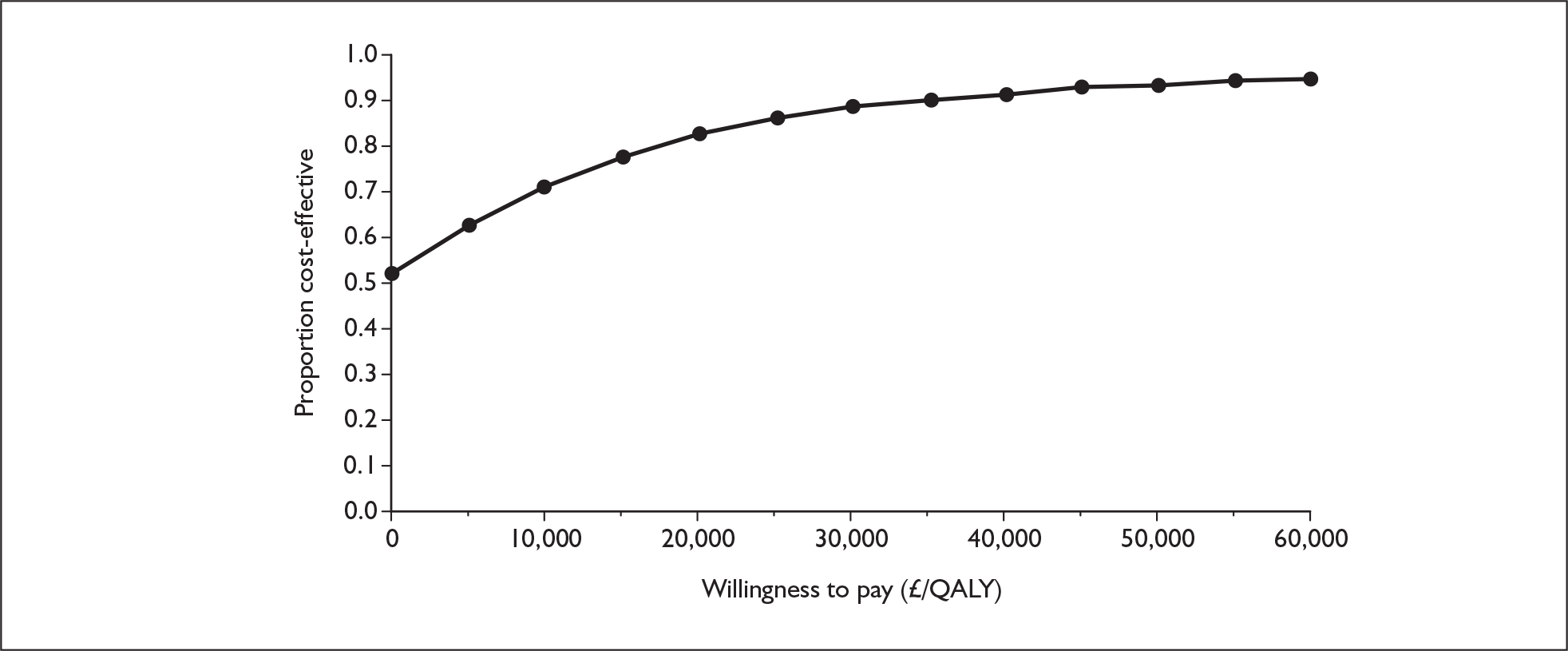
Sitaxentan in addition to supportive care versus supportive care alone, functional class III
Table 144 shows the results for sitaxentan, with the intervention less expensive than supportive care alone and producing a greater amount of QALYs, resulting in sitaxentan being dominant over supportive care. The CEAC presented in Figure 128 demonstrates that at thresholds of £20,000 and £30,000 per QALY gained, the probability of sitaxentan being cost-effective is 79% and 85% respectively.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 572,000 | 3.494 | |||
| Sitaxentan | 553,000 | –19,000 | 6.812 | 3.318 | Dominant |
FIGURE 128.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
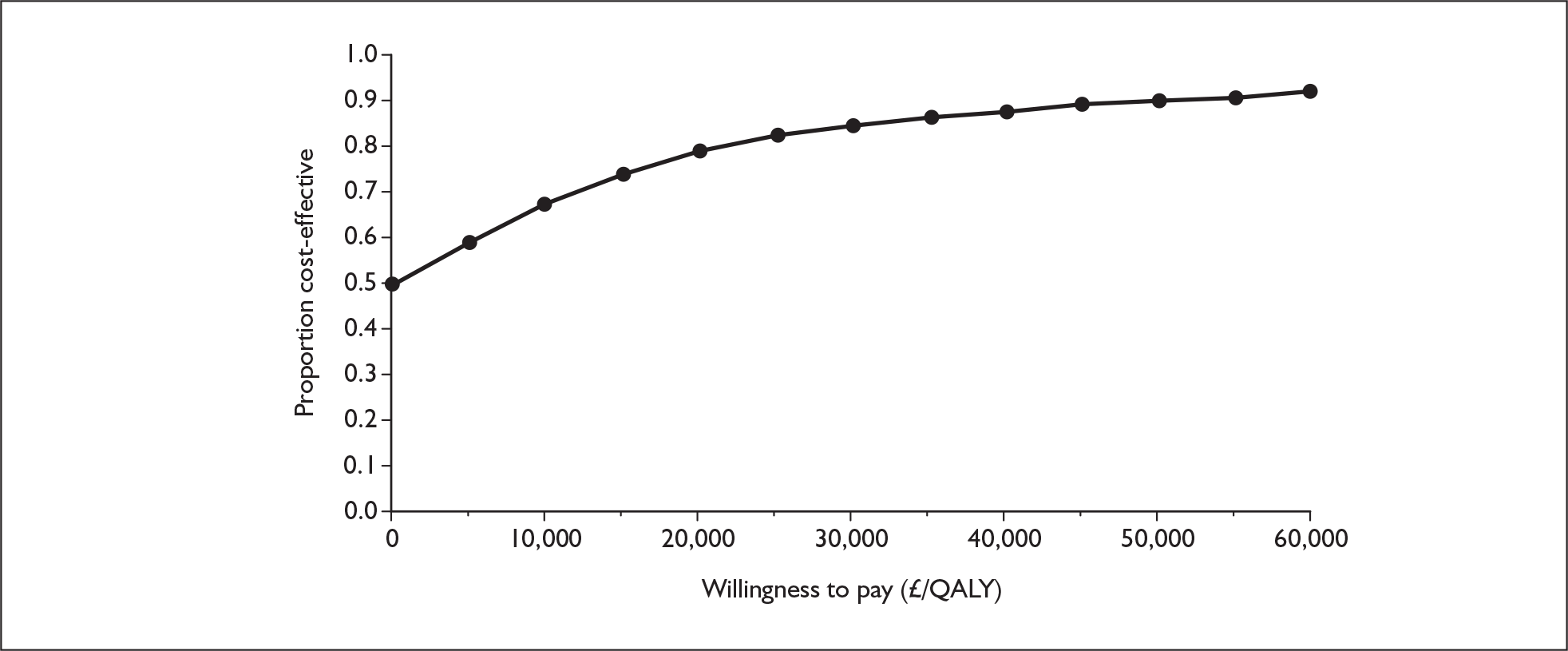
Sildenafil in addition to supportive care versus supportive care alone, functional class III
Table 145 shows the results for sildenafil, with the intervention less expensive than supportive care alone and producing a greater amount of QALYs, resulting in dominance over supportive care. The CEAC presented in Figure 129 shows that sildenafil has a probability of being cost-effective of 98% at both £20,000 and £30,000 per QALY.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 572,000 | 3.494 | |||
| Sildenafil | 404,000 | –168,000 | 6.893 | 3.399 | Dominant |
FIGURE 129.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
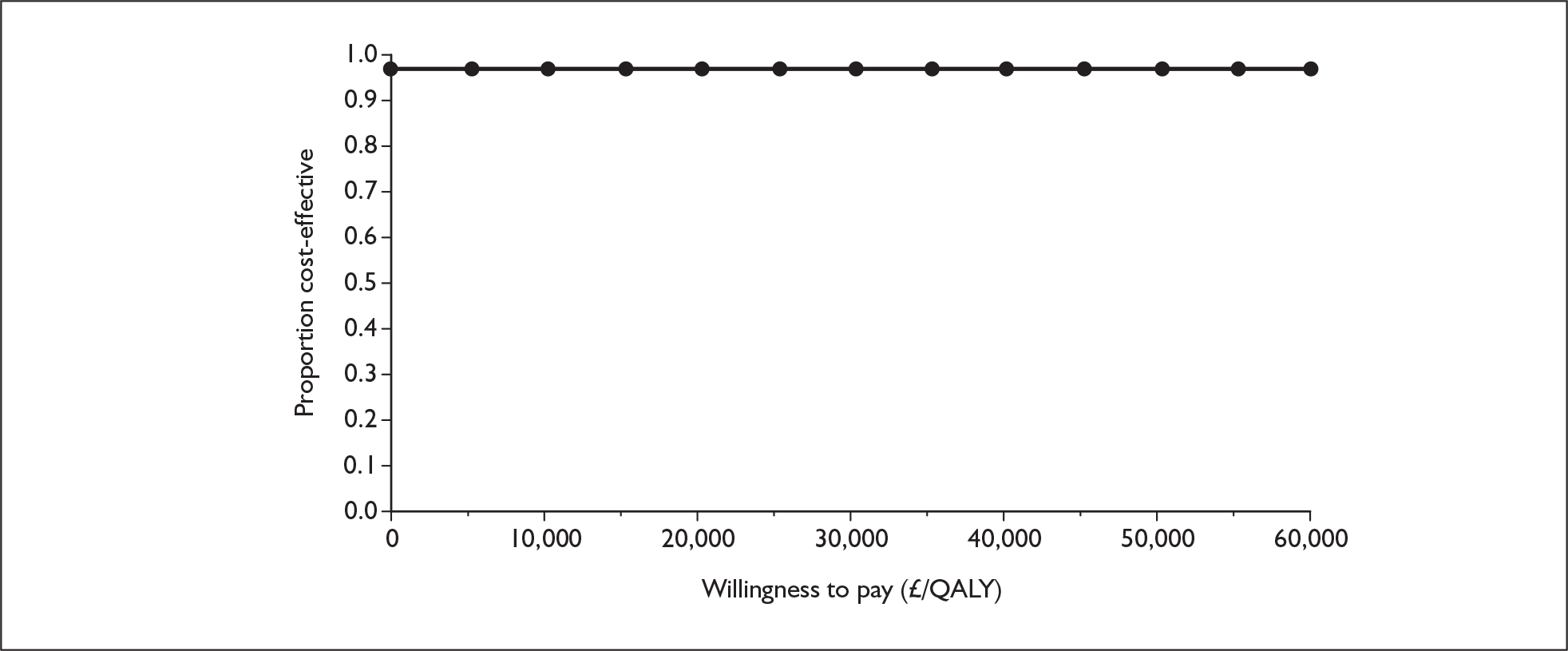
Summary of results – comparison with reference case
-
The ICER for epoprostenol in FCIII increased from £277,000 per QALY gained in the reference case to £285,000. Although the difference in QALYs increases, the difference in costs also increases.
-
The ICER for epoprostenol in FCIV decreased slightly from £343,000 per QALY gained to £337,000. Although the difference in costs increases, the difference in QALYs also increases.
-
The ICER for iloprost reduces from £101,000 per QALY gained in the reference case to £76,000. The differences in costs and benefits are both reduced, but more so for the costs.
-
The result for bosentan changes from an ICER of £27,000 per QALY gained in the reference case to being dominant over supportive care. The difference in QALYs changes very little, but costs are now lower for the intervention arm than for supportive care.
-
The result for sitaxentan changes from an ICER of £25,000 per QALY to being dominant over supportive care. The difference in QALYs is slightly larger and the costs are now lower for the intervention arm than for supportive care.
-
In both the reference case and additional analysis, sildenafil is dominant compared with supportive care; however, the probability of sildenafil being cost-effective at thresholds of £20,000 and £30,000 per QALY gained is greater in this additional analysis.
Explanation of results
In this extreme analysis in which patients cannot die from PAH-related causes in FCIII the oral therapies become much more cost-effective.
In the reference case the mortality rates on individual treatments for patients in FCIII were obtained from observational studies. In these studies patients started treatment in FCIII and were followed up for a certain period of time (e.g. 1 year or 3 years). PAH-specific mortality was calculated according to the number of patients who were followed up and the number of deaths observed during this period, taking into account the general population mortality (see Appendix 9). The estimated PAH-specific mortality assumed that all of the observed deaths occurred while the patients were in FCIII and did not take into account the possibility that some of the patients might have deteriorated to FCIV (and incurred the associated cost of epoprostenol treatment) before death. The mortality on treatment for FCIII patients in the model might therefore have been overestimated as some of the deaths would have been accounted for through deterioration to FCIV and subsequent death in this FC.
Because of the lack of data it is not clear what proportion of patients would die within a 12-week cycle in FCIII and what proportion would go through FCIV before death in the model. This sensitivity analysis therefore explored an extreme scenario in which all deaths in FCIII were removed and only deaths in FCIV were allowed. In this scenario all patients who would have died in FCIII in the reference case survived and incurred epoprostenol treatment in FCIV. The impact was greater for the supportive care arm (given its higher mortality in the reference case), making it a much more expensive option. The active treatment therefore became comparatively more cost-effective. There was a greater QALY gain for the supportive care arm because of a proportionately greater reduction in mortality for this arm than for the active treatment arm under this assumption, but the impact due to changes in costs outweighs the impact due to changes in QALYs.
Appendix 13.5 Assuming that patients on supportive care alone in functional class IV receive only intermittent care rather than hospitalisation until death
Question: What is the impact on cost-effectiveness of altering the assumption that patients are hospitalised until death to only intermittent care as required for respite, etc. (assumption relating to costing for patients on supportive care alone in FCIV) for all drugs in this appraisal?
Analysis requested by NICE: Based on the reference case in the assessment report conduct a sensitivity analysis (for all five technologies) which assumes that patients on supportive care alone in FCIV receive only intermittent care as required for respite until death rather than hospitalisation until death.
In the reference case it was assumed that patients in FCIV on supportive care plus epoprostenol receive intermittent care, whereas patients on supportive care alone are hospitalised until death. For this additional analysis intermittent care rather than continuous hospitalisation is assumed for patients in FCIV on supportive care alone.
Supportive care alone in FCIV only occurs in the model as a comparator to epoprostenol plus supportive care in FCIV. This is because the reference case assumes that for all of the other analyses patients are given epoprostenol plus supportive care when they reach FCIV. Consequently, only the results for epoprostenol in FCIV are presented for this additional analysis.
The only other time that altering the assumption regarding continuous hospitalisation would impact on analysis is in the additional analysis presented in Appendix 13.1 in which it is assumed that epoprostenol is not available and hence supportive care alone is available in FCIV. The assumption of intermittent care rather than hospitalisation to death was applied to this additional analysis and the results are also presented below.
Alternative supportive care costs in FCIV: epoprostenol available in functional class IV
Epoprostenol in addition to supportive care versus supportive care alone, functional class IV
Table 146 shows the results of the analysis for epoprostenol in FCIV. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £427,000 per QALY gained. The CEAC presented in Figure 130 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 31,000 | 0.826 | |||
| Epoprostenol | 530,000 | 498,000 | 1.994 | 1.167 | 427,000 |
FIGURE 130.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class IV. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
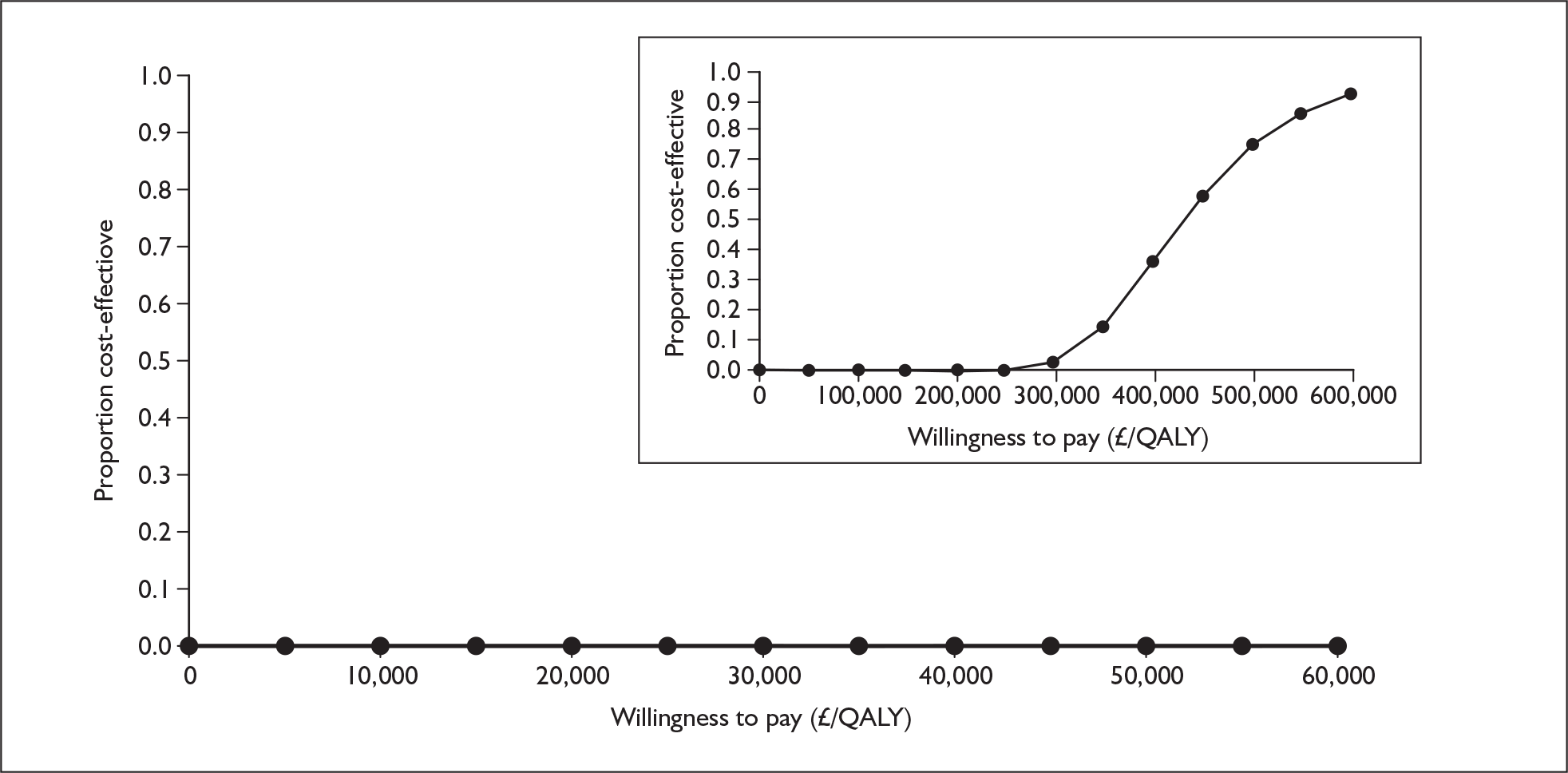
Alternative supportive care costs in FCIV: supportive care only in functional class IV
Epoprostenol in addition to supportive care versus supportive care alone, functional class III
Table 147 shows the results of the analysis for epoprostenol in FCIII. Compared with supportive care alone, epoprostenol alongside supportive care is more expensive but generates more QALYs, giving an ICER of £278,000 per QALY gained. The CEAC presented in Figure 131 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, epoprostenol has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 30,000 | 1.091 | |||
| Epoprostenol | 263,000 | 232,000 | 1.927 | 0.837 | 278,000 |
FIGURE 131.
Cost-effectiveness acceptability curve for epoprostenol with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
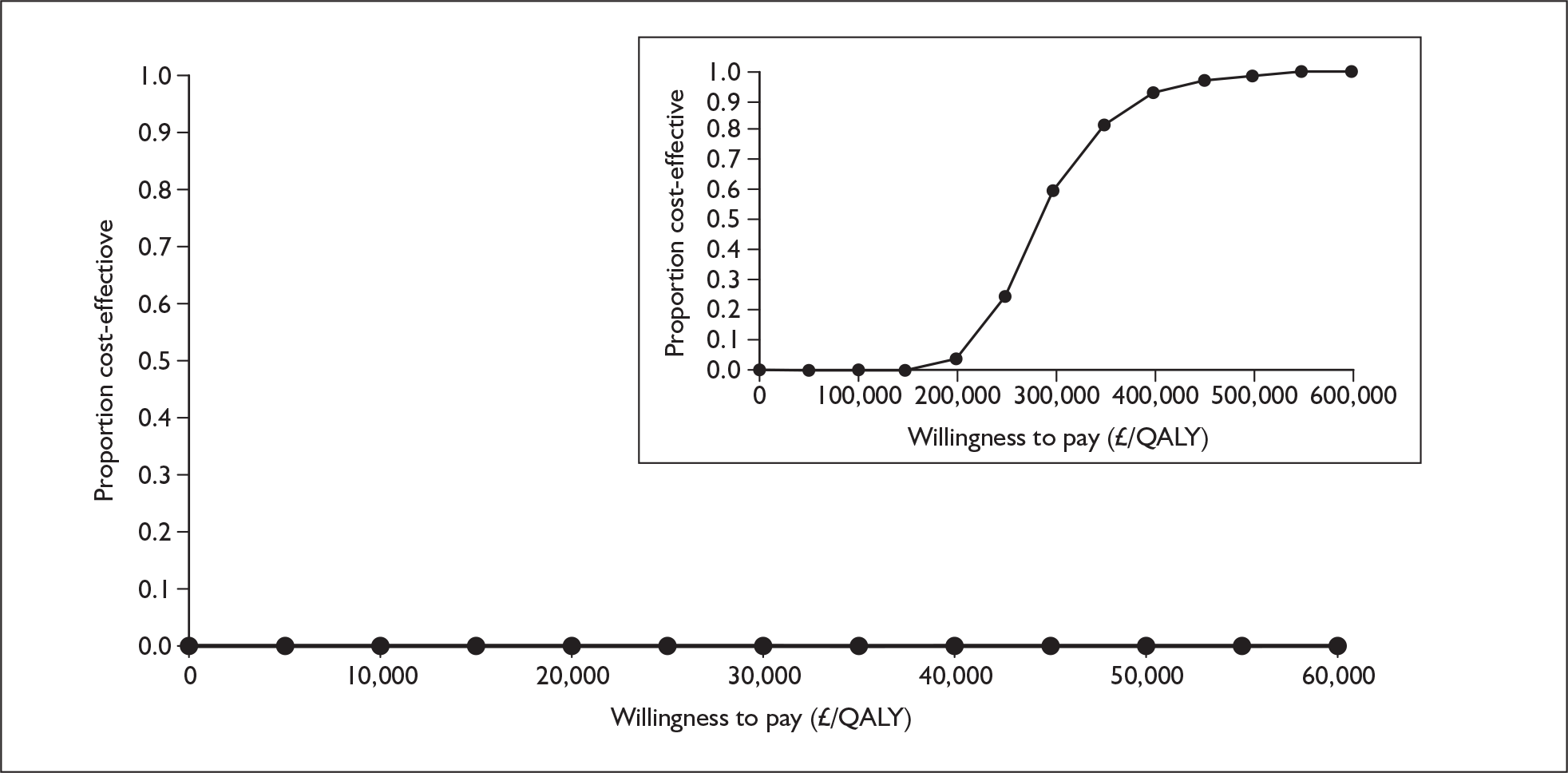
Iloprost in addition to supportive care versus supportive care alone, functional class III
Table 148 shows the results of the analysis for iloprost in FCIII. Iloprost alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £99,000 per QALY gained. The CEAC presented in Figure 132 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, iloprost has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 28,000 | 1.086 | |||
| Iloprost | 132,000 | 104,000 | 2.131 | 1.045 | 99,000 |
FIGURE 132.
Cost-effectiveness acceptability curve for iloprost with supportive care versus supportive care alone, functional class III. Inset graph shows larger x-axis scale. QALY, quality-adjusted life-year.
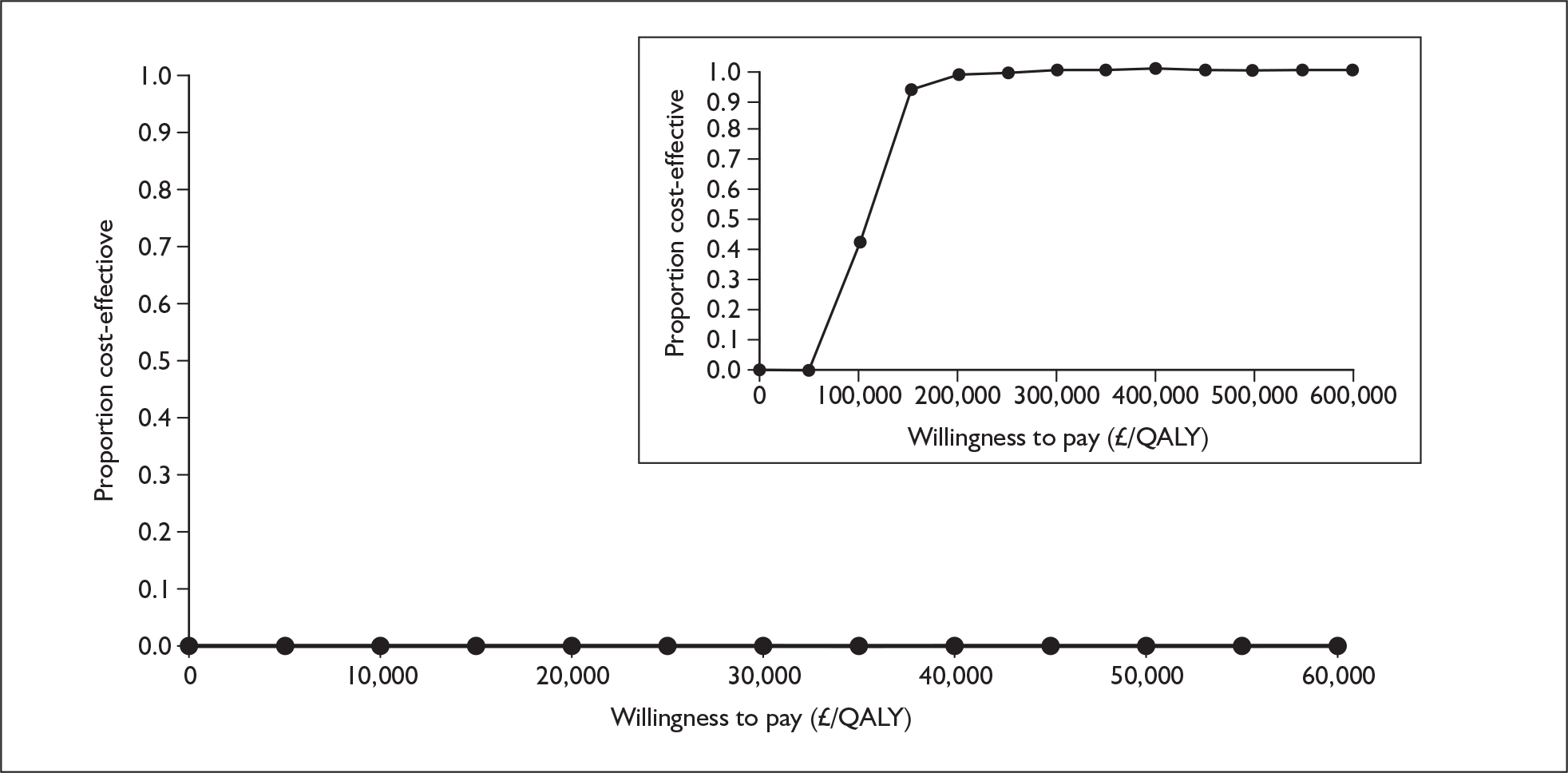
Bosentan in addition to supportive care versus supportive care alone, functional class III
Table 149 shows the results for bosentan, with the intervention more expensive than supportive care alone and producing a greater amount of QALYs, resulting in bosentan having an ICER of £46,000 per QALY gained. The CEAC in Figure 133 demonstrates that bosentan has a zero probability of being cost-effective at both £20,000 and £30,000 per QALY gained.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.532 | |||
| Bosentan | 195,000 | 170,000 | 5.209 | 3.677 | 46,000 |
FIGURE 133.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
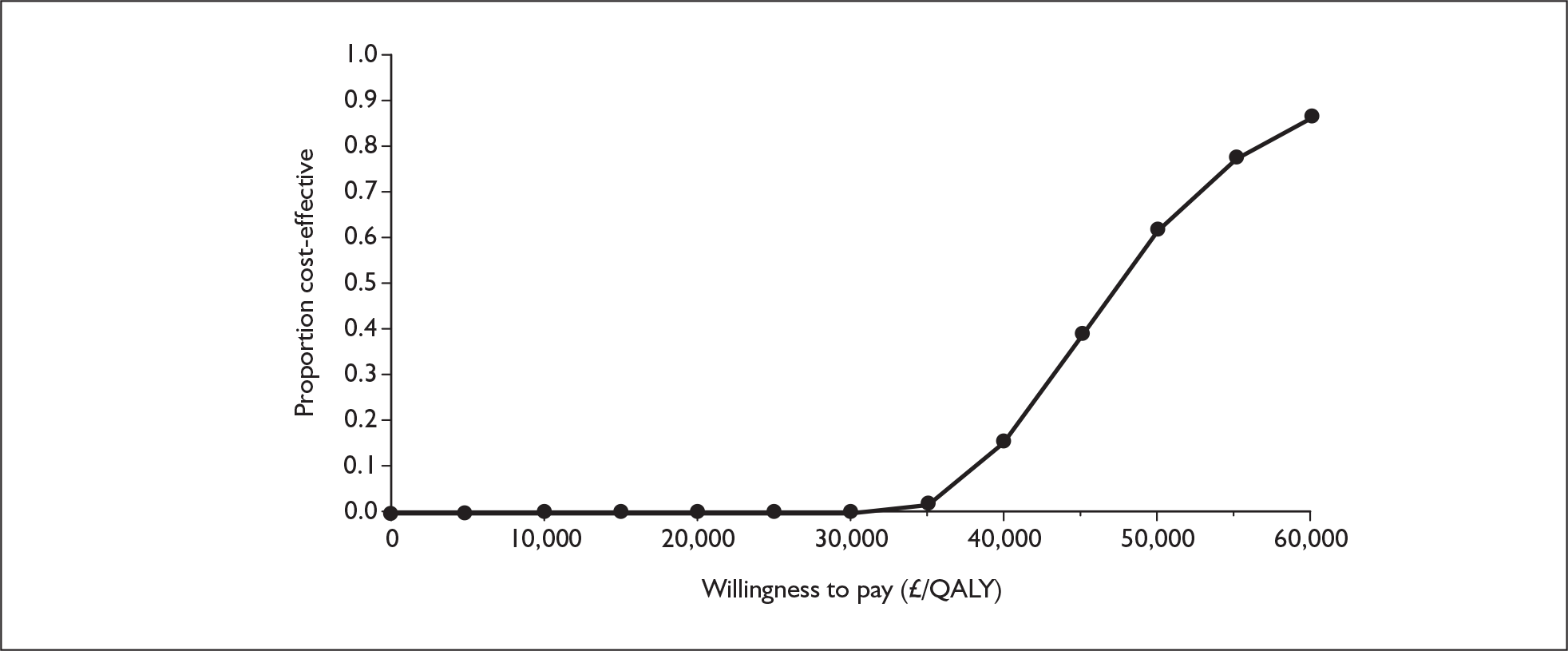
Sitaxentan in addition to supportive care versus supportive care alone, functional class III
Table 150 shows the results of the analysis for sitaxentan in FCIII. Sitaxentan alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £48,000 per QALY gained. The CEAC presented in Figure 134 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, sitaxentan has a zero probability of being cost-effective.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.532 | |||
| Sitaxentan | 182,000 | 157,000 | 4.780 | 3.248 | 48,000 |
FIGURE 134.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
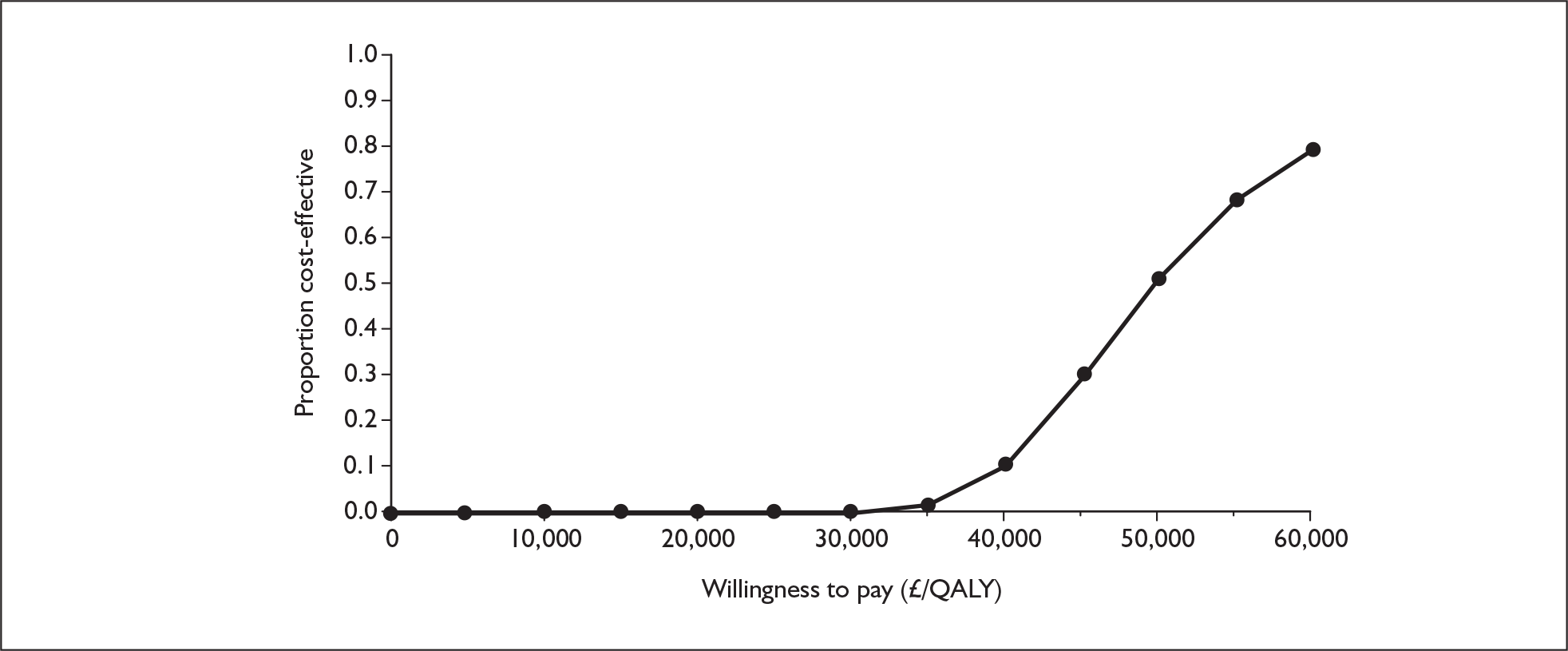
Sildenafil in addition to supportive care versus supportive care alone, functional class III
Table 151 shows the results of the analysis for sildenafil in FCIII. Sildenafil alongside supportive care is more costly than supportive care alone but yields more QALYs, giving an ICER of £13,000 per QALY gained. The CEAC presented in Figure 135 shows that at willingness-to-pay thresholds of £20,000 and £30,000 per QALY gained, sildenafil has probabilities of being cost-effective of 90% and 98% respectively.
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.532 | |||
| Sildenafil | 71,000 | 46,000 | 4.950 | 3.418 | 13,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 85,000 | 1.559 | |||
| Bosentan | 201,000 | 116,000 | 4.447 | 2.888 | 40,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 85,000 | 1.559 | |||
| Sitaxentan | 188,000 | 103,000 | 3.995 | 2.435 | 42,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 85,000 | 1.559 | |||
| Sildenafil | 96,000 | 11,000 | 4.206 | 2.647 | 4,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.559 | |||
| Bosentan | 164,000 | 139,000 | 4.447 | 2.888 | 48,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.559 | |||
| Sitaxentan | 151,000 | 13,000 | 3.995 | 2.435 | 52,000 |
| Strategy | Cost (£) | Cost difference (£) | QALYs | QALY difference | ICER (£/QALY) |
|---|---|---|---|---|---|
| Supportive care | 25,000 | 1.559 | |||
| Sildenafil | 59,000 | 34,000 | 4.206 | 2.647 | 13,000 |
FIGURE 135.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
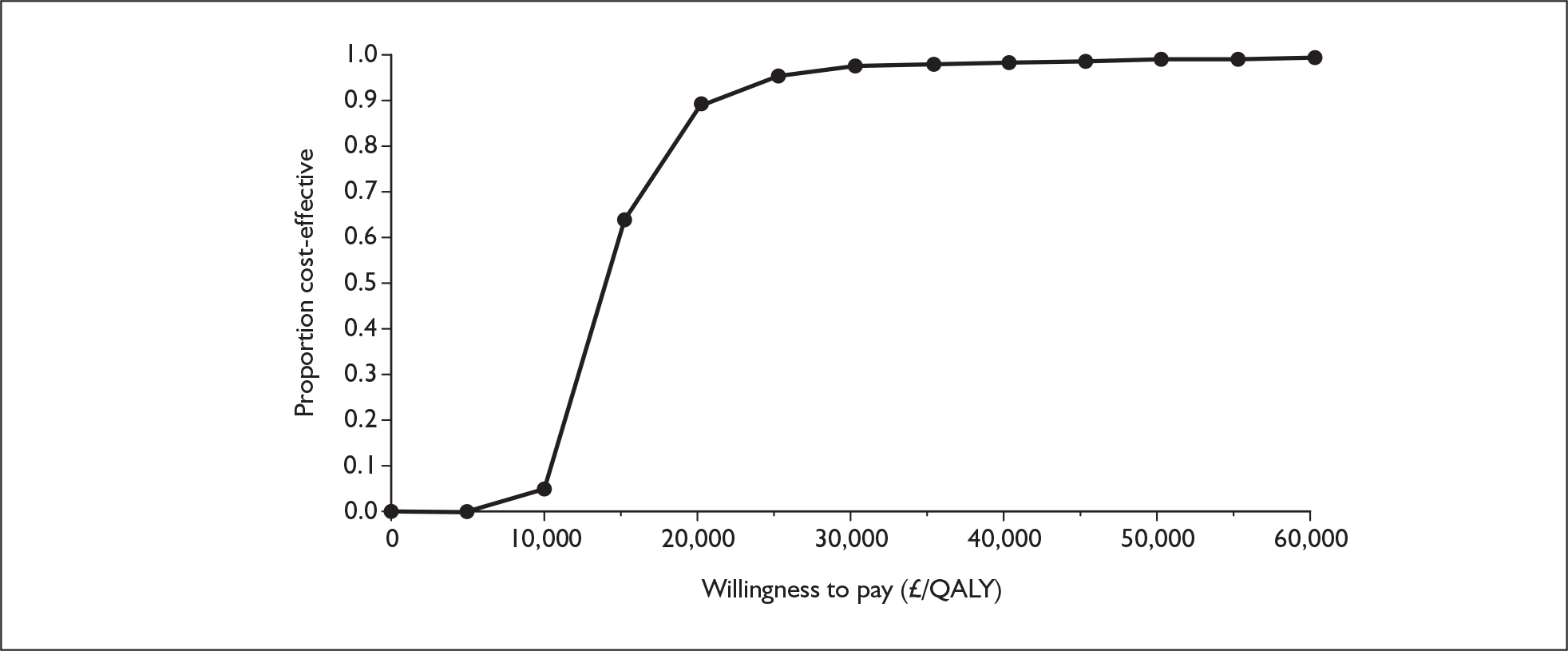
FIGURE 136.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
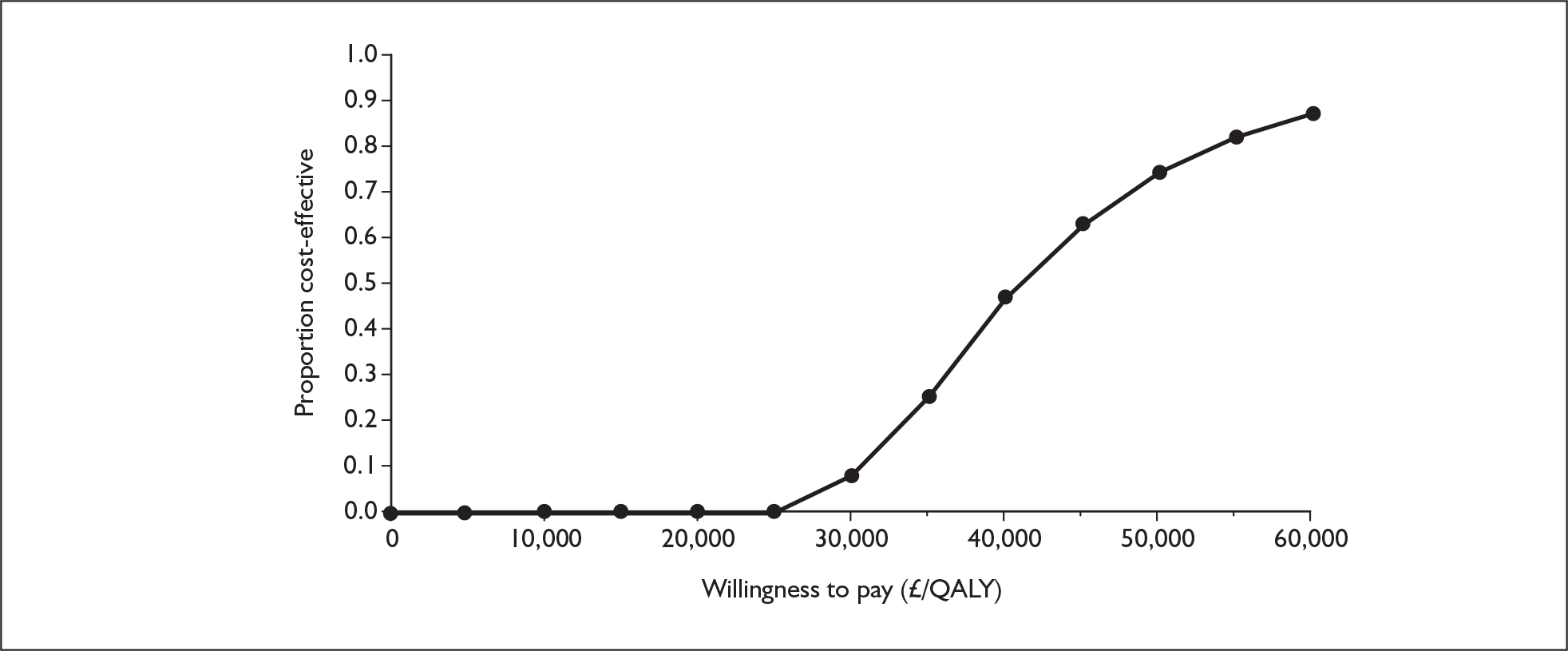
FIGURE 137.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
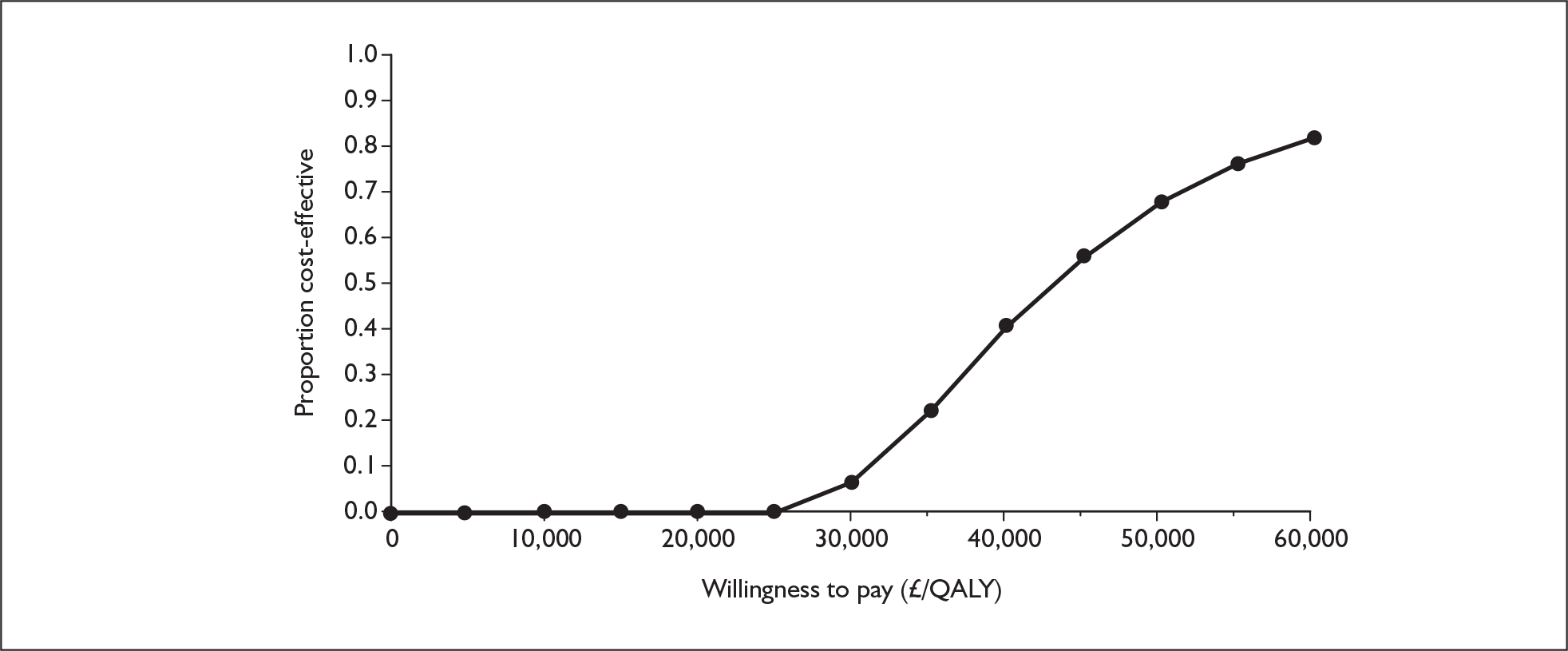
FIGURE 138.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
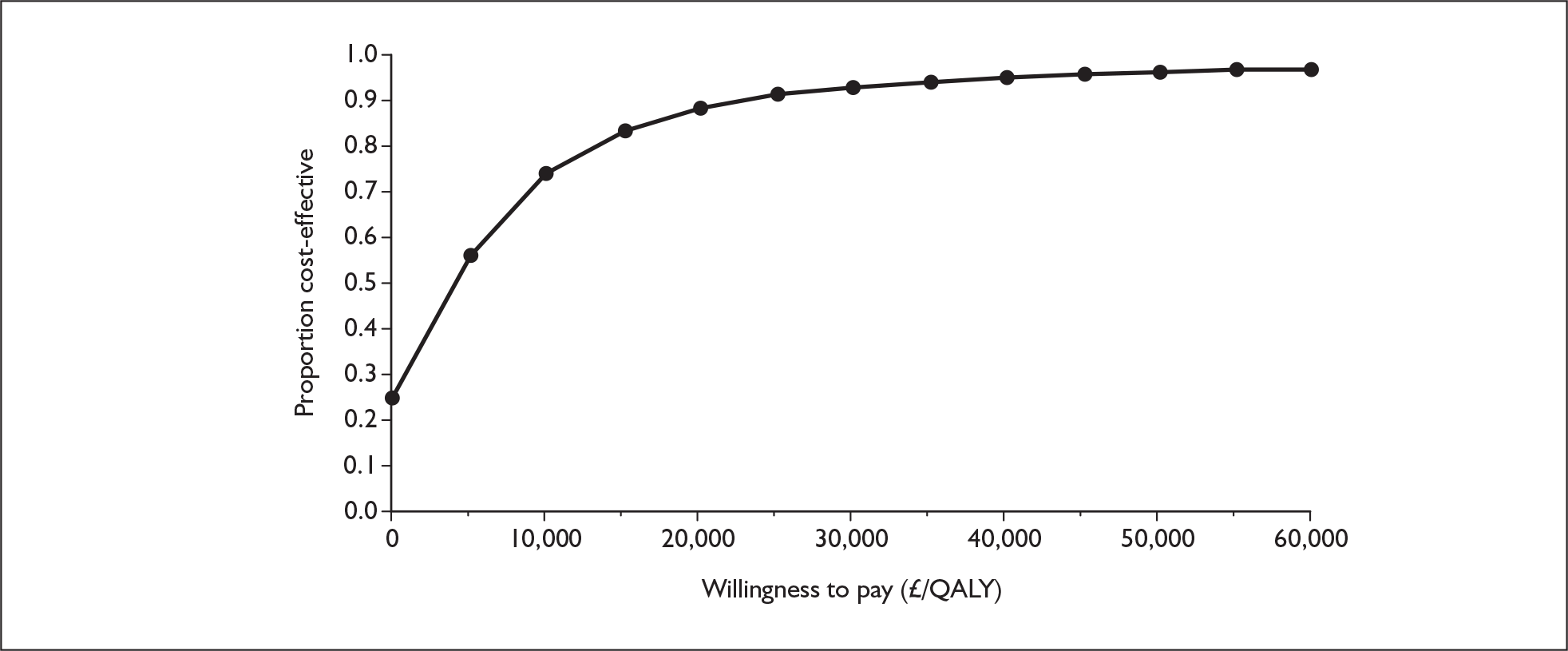
FIGURE 139.
Cost-effectiveness acceptability curve for bosentan with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
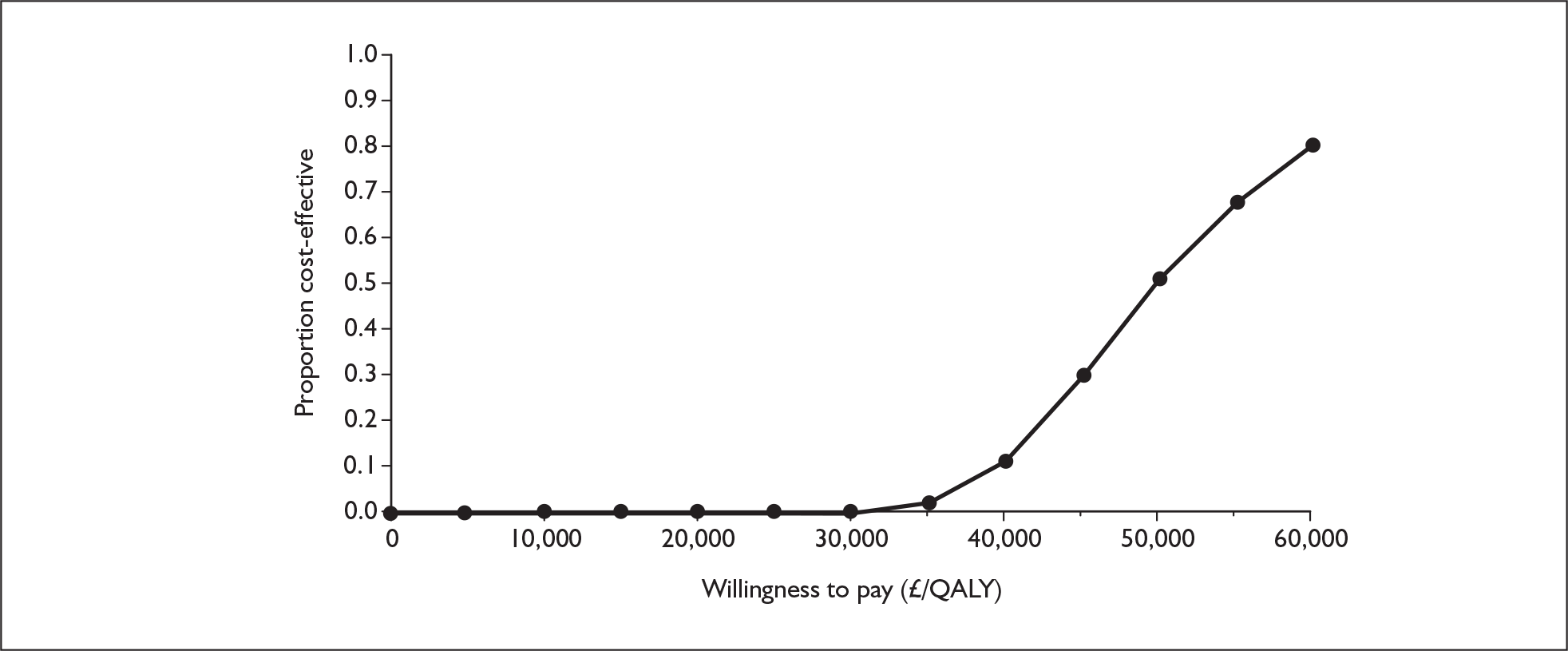
FIGURE 140.
Cost-effectiveness acceptability curve for sitaxentan with supportive care versus supportive care alone, functional class III.QALY, quality-adjusted life-year.
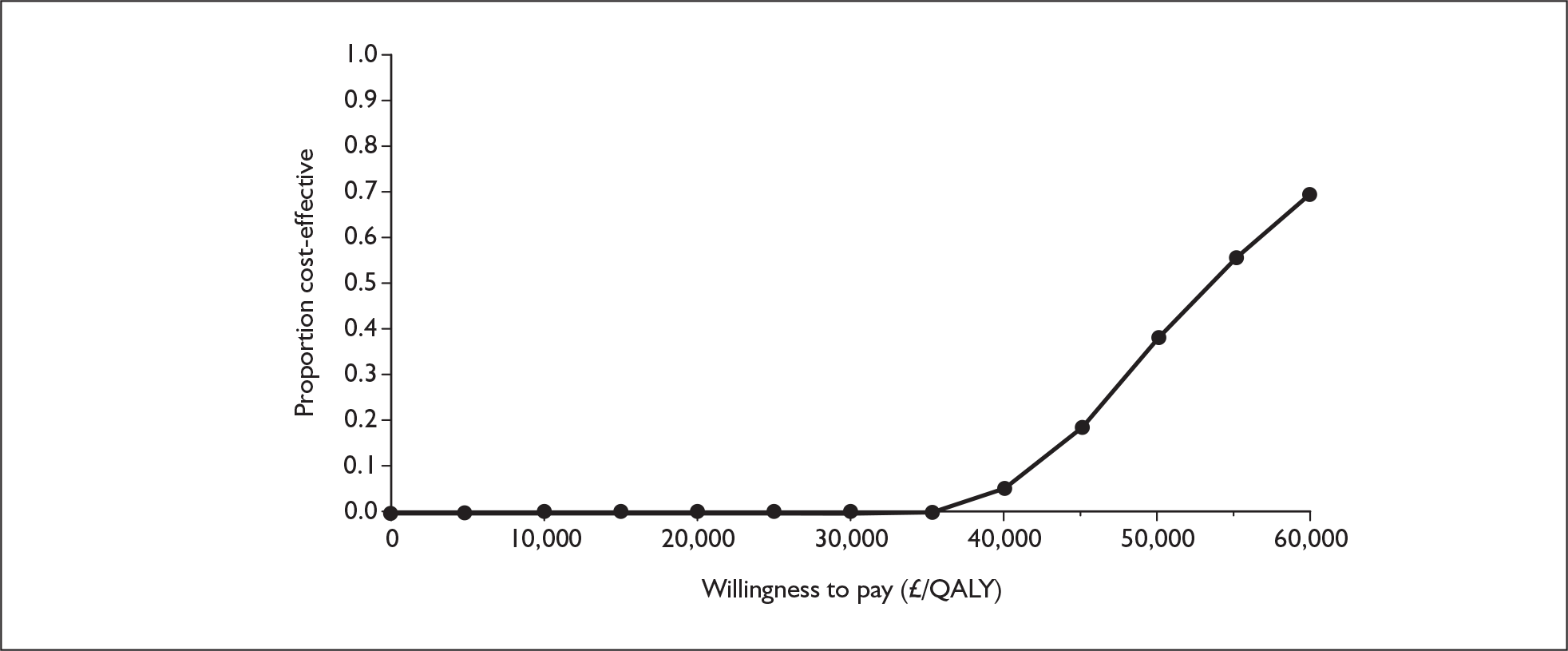
FIGURE 141.
Cost-effectiveness acceptability curve for sildenafil with supportive care versus supportive care alone, functional class III. QALY, quality-adjusted life-year.
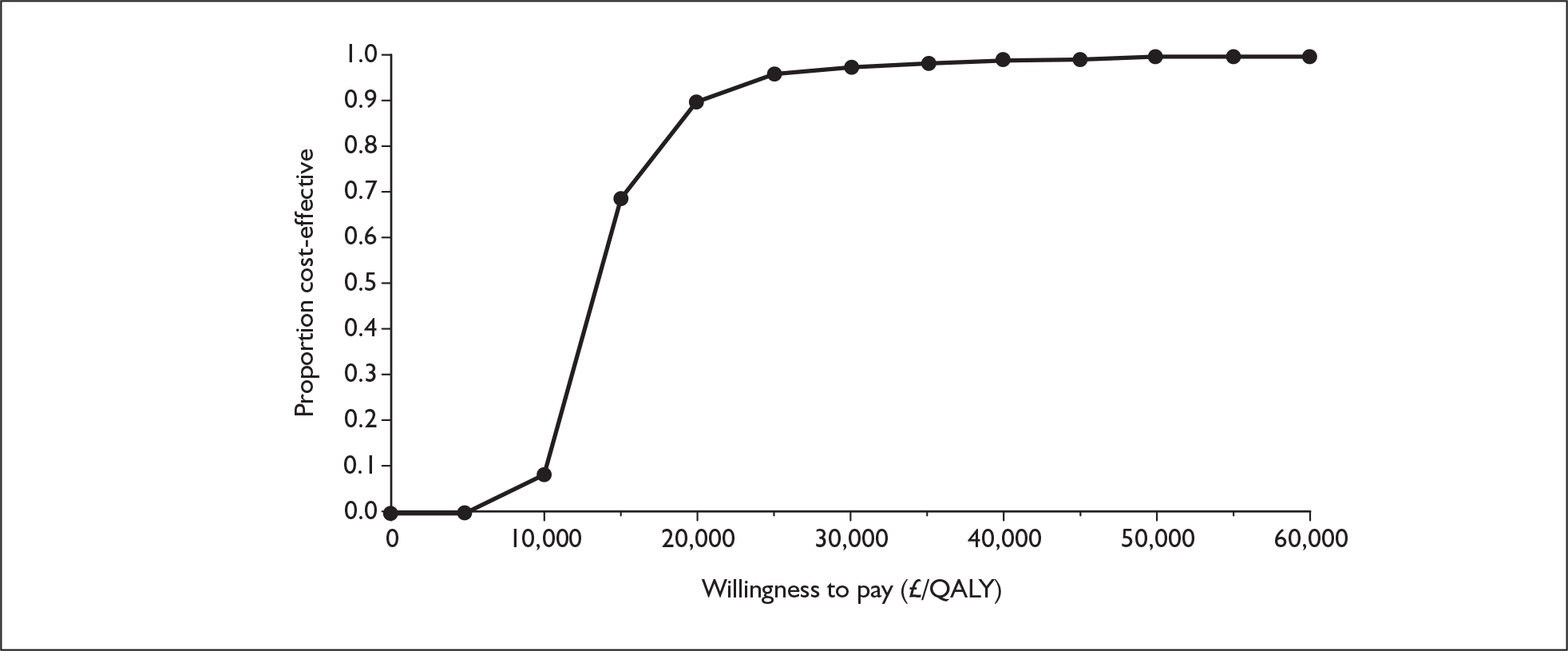
Summary of results
Comparison with the reference case
-
The ICER for epoprostenol in FCIV increases from the reference case value of £343,000 per QALY gained to £427,000 per QALY gained as the difference in costs increases.
Comparison of results with analysis in which epoprostenol is not available in functional class IV (Appendix 13.1)
-
The ICER for epoprostenol in FCIII increases from £273,000 per QALY gained to £278,000 per QALY gained as the difference in costs increases very slightly.
-
The ICER for iloprost increases marginally from £98,000 per QALY gained to £99,000 per QALY gained as the difference in costs increases very slightly.
-
The result for bosentan increases from an ICER of £42,000 per QALY gained to £46,000 per QALY gained as there is a rise in the difference in costs.
-
The result for bosentan increases from an ICER of £44,000 per QALY gained to £48,000 per QALY gained as there is a rise in the difference in costs.
-
The ICER for sildenafil increases from £9000 per QALY gained to £13,000 per QALY gained, again because the difference in costs increases.
Explanation of results
As explained at the beginning of this section this sensitivity analysis is applicable only to scenarios in which epoprostenol is not used in FCIV. The assumption of intermittent care instead of hospitalisation until death reduced costs associated with patients in FCIV for both the treatment and supportive care arms, but the reduction in costs was greater in supportive care arms as patients reached FCIV faster. The supportive care option thus became relatively cheap and active treatments became less cost-effective. The ICERs, however, only increased slightly compared with the results of the additional analysis described in Appendix 13.1. This is because the differential costs between treatment options accrued in FCIV under these scenarios (without epoprostenol) were small compared with the differential costs accrued in FCIII (costs of active treatment versus costs of supportive care), which drive the ICERs.
Appendix 13.6 Combining the assumptions of no epoprostenol in functional class IV (Appendix 13.1) and equal mortality between epoprostenol and oral treatments (Appendix 13.2)
Appendix 13.7 Combining the assumptions of no epoprostenol in functional class IV (Appendix 13.1), equal mortality between epoprostenol and oral treatments (Appendix 13.2) and intermittent care for functional class IV patients on supportive care alone (Appendix 13.5)
Appendix 13.8 Overall summary of additional analyses
-
A summary of the ICERs for the reference case and various sensitivity analyses is shown in Table 158.
-
By assuming that patients receive supportive care alone in FCIV, the ICERs reduce slightly for epoprostenol and iloprost compared with reference case ICERs but are in excess of £90,000 per QALY gained. Conversely, the ICERs for bosentan and sitaxentan increase to above £40,000 per QALY gained, and sildenafil is no longer dominant but still has an ICER below £10,000 per QALY gained.
-
Applying data on mortality for epoprostenol in FCIII to the oral therapies reduces the ICERs for all oral therapies to below £10,000 per QALY gained.
-
When considering a scenario of no patients suffering PAH-related mortality in FCIII, the ICERs for epoprostenol in FCIII and FCIV increase and the ICER for iloprost decreases but is still in excess of £70,000 per QALY gained. All oral therapies become dominant over supportive care alone.
-
Reducing the costs on supportive care alone in FCIV by reducing the intensity of hospitalisation (when treatment in FCIV is supportive care alone) increases the ICERs for all therapies, and sildenafil is the only therapy with an ICER below £40,000 per QALY gained.
| FCIV | FCIII | |||||
|---|---|---|---|---|---|---|
| Epoprostenol | Epoprostenol | Iloprost | Bosentan | Sitaxentan | Sildenafil | |
| Original analyses | ||||||
| Reference case | 343,000 | 277,000 | 101,000 | 27,000 | 25,000 | Dominates |
| Alternative epoprostenol price | 96,000 | 106,000 | 101,000 | 39,000 | 40,000 | 3700 |
| Additional analyses | ||||||
| Supportive care without epoprostenol in FCIV | Same as base case | 273,000 | 98,000 | 42,000 | 44,000 | 9000 |
| Assume epoprostenol mortality on supportive care and on treatment | – | – | – | 6000 | 1400 | Dominates |
| No PAH-specific death in FCIII | 337,000 | 285,000 | 76,000 | Dominates | Dominates | Dominates |
| Supportive care without epoprostenol in FCIV, intermittent care | 427,000 | 278,000 | 99,000 | 46,000 | 48,000 | 13,000 |
Appendix 14 Budget impact
The annual budgetary impact of uptake of the five technologies was assessed using the drug (licensed dose) and service fee cost for each intervention, as outlined in Table 159, multiplied by the number of patients likely to be receiving the intervention. Additional care was presumed to be already funded and therefore was not considered. No consideration was given to any drug-specific monitoring of patients as such costs were presumed to be small in comparison to drug costs. Where different costs for a technology were known these were also used, for example the iloprost VENTafee scheme. Different costs for the first year and subsequent years of use of epoprostenol were also used to reflect the likely dose escalation beyond the first year of treatment. Graphs showing the budgetary impact per annum of each technology for a range of patient uptakes were produced. The budgetary impacts per annum for epoprostenol, for iloprost and for bosentan, sitaxentan and sildenafil are shown in Figures 142–144 respectively.
FIGURE 142.
Budgetary impact per annum – epoprostenol. [Commercial-in-confidence information has been removed].
FIGURE 143.
Budgetary impact per annum – iloprost. [Commercial-in-confidence information has been removed].
FIGURE 144.
Budgetary impact per annum – bosentan, sitaxentan and sildenafil. [Commercial-in-confidence information has been removed].
| Epoprostenol year 1 | Epoprostenol year 2+ | Iloprost | Bosentan | Sitaxentan | Sildenafil | ||||
|---|---|---|---|---|---|---|---|---|---|
| List price | Reduction | List price | Reduction | List price | VENTafee | ||||
| Drug | 55,869 | [Commercial-in-confidence information has been removed] | 127,702 | [Commercial-in-confidence information has been removed] | 36,178 | 29,600 | 20,102 | 20,089 | 4547 |
| Service fee | 9464 | 9464 | 9464 | 9464 | 5512 | 5512 | 542 | 542 | 542 |
| Total | 65,333 | [Commercial-in-confidence information has been removed] | 137,166 | [Commercial-in-confidence information has been removed] | 41,690 | 35,112 | 20,644 | 20,631 | 5089 |
Glossary
Technical terms and abbreviations are used throughout this report. The meaning is usually clear from the content, but a glossary and list of abbreviations are provided for the non-specialist reader.
- 6MWT – 6-minute walk test
- The 6MWT measures the distance that a patient can walk unencouraged on a flat, hard surface in a time of 6 minutes.
- Borg dyspnoea index
- A measure of perceived breathlessness on a scale of 0–10, in which 0 = no breathlessness. Initially designed to measure exertion.
- Cardiac index
- The cardiac index relates the volume of blood pumped by the heart in a unit of time (cardiac output) to the body surface area. It is calculated as: (stroke volume · heart rate)/body surface area. The cardiac index is usually expressed in l/min/m2.
- Functional class (FC)
- A classification of functional capacity initially developed by the New York Heart Association (NYHA) for patients with cardiac diseases based on clinical severity and prognosis. It was later adapted specifically for patients with pulmonary hypertension (see Chapter 1, Clinical classification). Briefly, patients are classified into one of the following four categories: FCI (asymptomatic), FCII (mild), FCIII (moderate), FCIV (severe).
- Pulmonary arterial hypertension (PAH)
- Throughout this report PAH refers to category 1 (excluding subcategory 1.5) of the Venice 2003 classification for pulmonary hypertension (see Chapter 1, Clinical classification). Subcategories of PAH, such as idiopathic PAH (IPAH) and associated PAH (APAH), were defined in line with this classification. However, it is acknowledged that the term primary pulmonary hypertension (PPH) was widely used before the advent of the Venice 2003 classification and a decision was made to retain this term in this report if it was used in the original publications/reports of individual studies. When the term PPH is retained it is regarded as being interchangeable with IPAH.
- Pulmonary artery pressure (PAP)
- Measured directly during right heart catheterisation. Mean pulmonary artery pressure (mPAP) > 25 mmHg at rest or > 30 mmHg with exercise is one of the criteria of PAH diagnosis.
- Pulmonary capillary wedge pressure (PCWP)
- PCWP provides an indirect estimate of left atrial pressure. The measurement is made with a balloon-tipped, multilumen catheter (Swan–Granz catheter), inserted into a peripheral vein and then advanced into the right atrium, right ventricle, pulmonary artery and into a branch of the pulmonary artery. The normal value of the PCWP is 8–10 mmHg. A PCWP ≤ 15 mmHg is one of the PAH diagnostic criteria. PCWP is used to calculate pulmonary vascular resistance.
- Pulmonary hypertension
- When the term ‘pulmonary hypertension’ is used in this report it refers to all categories (1–5) of the Venice 2003 classification for pulmonary hypertension (see Chapter 1, Clinical classification). This is therefore a broader term that encompasses PAH and other forms of pulmonary hypertension.
- Pulmonary vascular resistance (PVR)
- PVR = [mean pulmonary artery pressure (mmHg) – pulmonary capillary wedge pressure (mmHg)]/cardiac output (l/min) · 80. Units are dyn s/cm5. A PVR > 240 dyn s/cm5 is one of the diagnostic criteria of PAH.
- Right atrial pressure (RAP)
- RAP is measured at right heart catheterisation. It measures the filling pressure of the right ventricle, and rises progressively as the right ventricle fails. High RAP thus identifies a failing right ventricle and a poor prognosis. Normal value is up to 5 mmHg.
- Supportive treatment(s)
- Supportive treatment(s) or supportive care refers to anticoagulation therapy, diuretics, oxygen, digoxin and calcium channel blockers (see Chapter 1, Supportive treatment). It was commonly referred to as conventional therapy or background therapy in the literature.
- Venice 2003 classification
- This is a clinical-based classification that groups pulmonary hypertension into five major categories based on pathophysiological mechanisms, clinical presentation and therapeutic options. PAH is one of the categories. See Chapter 1 (Clinical classification) for the full list of categories and subcategories.
Abbreviations
- 6MWD
- 6-minute walk distance
- 6MWT
- 6-minute walk test
- AIR
- Aerosolized Iloprost Randomized study
- APAH
- associated pulmonary arterial hypertension
- AQoL instrument
- Assessment of Quality of Life instrument
- BNF
- British National Formulary
- BREATHE
- Bosentan Randomized Trial of Endothelin Antagonist Therapy
- CAMPHOR
- Cambridge Pulmonary Hypertension Outcome Review
- CEAC
- cost-effectiveness acceptability curve
- cGMP
- cyclic guanosine monophosphate
- CHD
- congenital heart disease
- CHEC
- Consensus on Health Economic Criteria
- CI(s)
- confidence interval(s)
- CTD
- connective tissue disease
- CTD-APAH
- pulmonary arterial hypertension associated with connective tissue disease
- COMBI trial
- Combination Therapy of Bosentan and Aerosolised Iloprost in Idiopathic Pulmonary Arterial Hypertension trial
- ESC
- European Society of Cardiology
- ET-1
- endothelin-1
- ETA, ETB
- endothelin receptor type A, type B
- FCII, FCIII, FCIV
- functional class II, III, IV
- FPAH
- familial pulmonary arterial hypertension
- ICER(s)
- incremental cost-effectiveness ratio(s)
- IPAH
- idiopathic pulmonary arterial hypertension
- INR
- international normalised ratio
- ITT
- intention to treat
- MLHF questionnaire
- Minnesota Living with Heart Failure questionnaire
- mPAP
- mean pulmonary arterial pressure
- NCG
- National Commissioning Group, formerly known as NSCAG.
- NICE
- National Institute for Health and Clinical Excellence
- NNT
- number needed to treat
- NSCAG
- National Specialist Commissioning Advisory Group
- NYHA
- New York Heart Association
- PAH
- pulmonary arterial hypertension
- PAP
- pulmonary artery pressure
- PCTs
- primary care trusts
- PCWP
- pulmonary capillary wedge pressure
- PPH
- primary pulmonary hypertension
- PSA
- probabilistic sensitivity analysis
- PSS
- personal social services
- PVR
- pulmonary vascular resistance
- QALY(s)
- quality-adjusted life-year(s)
- RAP
- right atrial pressure
- RCT
- randomised controlled trial
- RR(s)
- relative risk(s)
- SAE(s)
- serious adverse event(s)
- SEM
- standard error of the mean
- SD(s)
- standard deviation(s)
- SF-36
- Short-Form 36
- STEP
- Safety and Pilot Efficacy Trial in Combination with Bosentan for Evaluation in PAH
- STRIDE
- Sitaxsentan to Relieve Impaired Exercise study
- SUPER
- Sildenafil Use in Pulmonary Arterial Hypertension study
- TTO
- time trade-off
- VAS
- visual analogue scale
- WHO
- World Health Organization
- WMD
- weighted mean differences
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Note
This monograph is based on the Technology Assessment Report produced for NICE. The full report contained a considerable amount of data that was deemed commercial-in-confidence or academic-in-confidence. The full report was used by the Appraisal Committee at NICE in their deliberations. The full report with each piece of commercial-in-confidence or academic-in-confidence data removed and replaced by the statement ‘commercial-in-confidence removed’ or ‘academic-in-confidence removed’ and is available on the NICE website www.nice.org.uk.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all of the data considered in the original full NICE report.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and costeffectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebocontrolled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and costeffectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington