Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 07/28/02. The contractual start date was in October 2007. The draft report began editorial review in October 2008 and was accepted for publication in May 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Background
The aetiology, prevalence and diagnosis of diabetic retinopathy
Diabetic retinopathy (DR) is caused by pathological changes in the blood vessels of the retina, which can lead to blindness. The European Grading Protocol defines five levels of DR: (1) no evidence of retinopathy; (2) background retinopathy (development of microaneurysms, formation of hard exudates and/or mild retinal haemorrhage); (3) preproliferative retinopathy (multiple microvascular abnormalities, venous loops, cotton-wool spots, venous bleeding and severe retinal haemorrhage); (4) proliferative retinopathy (abnormal new vessel growth, preretinal or vitreous haemorrhage, preretinal fibrosis); and (5) maculopathy (retinal thickening and hard exudates near the centre of the macula). 1 The early stages of retinopathy are usually asymptomatic with respect to the quality of vision experienced by the patient. However, the changes observed in the early stages have been shown to be predictive of progression to sight-threatening proliferative retinopathy and maculopathy. 2 The Early Treatment of Diabetic Retinopathy Study (ETDRS) showed the benefits of laser panretinal photocoagulation on long-term visual outcomes for patients with high-risk proliferative retinopathy (although photocoagulation was considered inappropriate, and potentially detrimental, in mild to moderate retinopathy). 3 Therefore, early identification and monitoring of retinopathy is crucial for successful management.
All patients with diabetes mellitus (DM) are at risk of DR and generally risk increases with duration of diabetes. Data collected during the 1970s indicated that the earliest stages of retinopathy may develop as early as during the first 5 years after onset of type 1 diabetes in young patients. However, eyesight-threatening proliferative retinopathy is unusual until at least 7 years approximately after onset of type 1 diabetes. 4 Type 2 diabetes is frequently diagnosed some years after its onset and as a result up to 39% of patients with type 2 diabetes have retinopathy at diagnosis and this is sight threatening in 4–8% of cases;5,6 it is estimated that more than 60% of patients have DR 20 years after diagnosis of type 2 diabetes. 7
Risk factors for the development and progression of DR include poor glycaemic control, hypertension, duration of diabetes, microalbuminuria and proteinuria, elevated tryglycerides and a low haematocrit level. 4,8–15
Despite advances in the management of DM, visual impairment due to DR remains a significant complication, in terms of both its consequences for the functioning and quality of life of individual patients and its wider socioeconomic impacts. DR remains the commonest cause of blindness in the working age population. 16 The incidence of blindness in the European diabetes population is estimated at between 50 and 65 per 100,000 per year. 17–19 Regular screening examinations for sight-threatening retinopathy are an essential part of effective diabetes care. As new methods of screening are developed it is important that these be evaluated rigorously, applying the best available methodology.
A systematic review,20 conducted for the National Institute of Clinical Excellence (NICE), reported limited evidence on the effectiveness of screening and monitoring tests for DR. No randomised controlled trials were identified, but analysis of the available diagnostic accuracy studies suggested that retinal photography through dilated pupils provides the most sensitive method of screening for sight-threatening retinopathy. The report further stated that sensitivities in excess of 80%, the acceptable threshold defined by Diabetes UK,21 should be achievable in a screening programme. Longitudinal studies have shown a decrease in the annual incidence of blindness and partial sightedness arising from diabetes since the introduction of screening programmes. 22 Existing evidence therefore suggests that the recognition of early fundal changes in diabetes may provide opportunities for the delivery of effective interventions and an ultimate reduction in the negative impacts of diabetic eye disease. Current UK national guidance7,23,24 recommends annual screening by trained individuals using retinal photography or slit-lamp biomicroscopy; screening is recommended from diagnosis in type 2 diabetes and from age 12 years (or 3 years post diagnosis if onset is post puberty) in type 1 diabetes.
Current service provision
In 2001/2 the Diabetes National Service Framework25 set a target of inviting 80% of people with diabetes in England to retinopathy screening by 2006, rising to 100% by the end of 2007. By December 2007, 85.7% of people diagnosed with diabetes were offered screening for DR. 26
The Department of Health have prioritised quality and safety over chasing the 100% target and will continue to work with partners in Government, the NHS and the voluntary sector to improve the standard and quality of screening programmes across the country. 26 Colour vision testing (CVT) is not currently part of the national DR screening programme.
Description of technology under assessment
A group of tests have been assessed that all examine the colour vision of patients with diabetes as a means of differentiating between those people with and without retinopathy, and the different grades of the disease. For the purpose of this report we have grouped the tests into categories according to the different methods that they use. These groups are pseudoisochromatic plates, arrangement tests, automated/computerised hue discrimination tests and anomaloscopes.
Colour deficiencies can be congenital or acquired, and these two forms typically differ in several ways. Congenital colour deficiency is stable throughout life and affects both eyes equally, whereas acquired deficiency changes in severity over time, differs between eyes and is frequently more difficult to classify. Also, unlike congenital deficiency, acquired colour deficiency is often associated with reduced visual acuity and the occurrence of visual field defects. 27
Acquired colour deficiency can be classified into three main types: acquired type 1 red–green defects, which resemble congenital protan deficiency and are associated with central retinal dystrophies; acquired type 2 red–green defects, which resemble congenital deutan deficiency and are associated with some lesions of the optic nerve; and acquired type 3 tritan (often referred to as ‘blue-yellow’) defects, which closely resemble congenital tritan defects.
The severity of colour deficiency has been seen to correspond with visual field loss and with the extent of macular involvement in diabetes patients with type 3 acquired defects. In proliferative retinopathy and maculopathy the patient is functionally tritanopic but all three colour mechanisms are affected and red–green errors as well as tritan errors are made on clinical tests. 27
Pseudoisochromatic plates
The Ishihara pseudoisochromatic test has long been established as the most widely used test for screening for red–green colour vision deficiency. The test consists of a series of plates that require the participant to distinguish a coloured numeral from a coloured background. Depending upon the plate presented, the colour-deficient observer will either fail to distinguish the numeral or see a different numeral than would be seen by a normal trichromat. Other types of pseudoisochromatic plates that test for protan, deutan and tritan deficits, such as the Hardy, Rand and Rittler (HRR) plates, have also been developed.
Arrangement tests
Arrangement tests typically consist of a range of coloured caps that incrementally vary in hue. Test participants are required to place these caps in order of hue. Test scores are derived from the number and pattern of errors made in this procedure. These tests can generally be used to detect protan, deutan and tritan colour vision deficiencies.
Farnsworth–Munsell 100 hue test
The most comprehensive colour arrangement test, the Farnsworth–Munsell 100 hue test (FM-100), consists of four trays containing a total of 85 reference caps spanning the visible colour spectrum. The test is intended to evaluate hue discrimination ability (or colour vision aptitude). Hue discrimination ability is ascertained from the total error score, and the type of colour vision deficiency is established by interpreting a graphical illustration of the results.
Farnsworth D-15 and Lanthony desaturated D-15 tests
The Farnsworth D-15 test is an abridged version of the FM-100, consisting of 15 loose coloured caps and a single reference cap. Rather than measure overall hue discrimination ability, the original D-15 was developed to detect moderate and severe colour deficiencies and separate these from normal colour vision or more slight deficiencies. The Lanthony desaturated D-15 test is an arrangement test that is similar to the original D-15 but it has a Munsell value of 8 and chroma of 2 and should be presented under high levels of illumination (> 500 lux). 27
Lanthony New Colour Test
The Lanthony New Colour Test (NCT) contains 70 Munsell samples – four series of 15 colours with Munsell value 6 and chroma of 2, 4, 6, and 8, and 10 grey caps representing a lightness scale. For each series participants must first separate the coloured caps from the grey caps before arranging the coloured caps in colour order and the grey caps in lightness scale. As with other arrangement tests the results are plotted graphically and an error score is calculated. The NCT is intended to distinguish between slight, moderate and severe colour deficiency. 27
Mollon–Reffin Minimalist Test
Initially, participants must identify an orange ‘demonstration’ chip from among five grey chips of varying lightness. If successful, the participant must select a probe chip from the middle of a protan, deutan or tritan series. If successful, the participant is presented with a less saturated probe chip. If unsuccessful, a more saturated probe chip is presented. Participants are scored on the number of reliably identified coloured chips for each confusion line.
Automated/computerised tests
More recently, technological advances have permitted the development of computerised CVTs, which in some cases dispense with the need for an operator to be present at the time of testing, as required with traditional arrangement tests. These automated systems may be based on colour contrast sensitivity or on variations of the principles used in colour arrangement tests. For example, the Sussex Gratings Machine (SGM) and its variants produce equiluminant, sinusoidal, chromatic gratings on a colour cathode ray tube monitor. The chromaticity of these gratings can be systematically altered along a red–green or tritan confusion axis until the value at which a participant can just perceive coloured stripes is established. Another automated system, the ChromaTest, uses a similar colour contrast sensitivity test procedure but with alphabetical letters being presented on an equiluminant background.
Anomaloscopes
The spectral anomaloscope is typically used to distinguish between normal vision and red–green deficits and to diagnose the type of colour deficiency, although newer instruments provide a colour match for classifying tritan defects. 27 In the traditional Nagel anomaloscope, two halves of a 3-degree circular bipartite field are respectively illuminated by monochromatic yellow and a mixture of red and green wavelengths. The testing procedure requires the participant first to make colour matches by adjusting both the red–green ratio and the luminance of the yellow field. The participant is then required to determine whether adjustments in the luminance of the yellow field can or cannot produce exact matches to red–green ratios set by the examiner. Normal trichromats make a precise colour match within a narrow range of red–green ratios. Participants with colour deficiencies show distinctively different colour-matching distributions.
Chapter 2 Research questions
Relevance of colour vision testing for diabetic retinopathy in the NHS
The existing screening programme for DR is based on retinal photography, the performance of which is known to be dependent upon the experience of the examiners and techniques used; Sharp et al. reported sensitivities of 83–85% and specificities of 71–83%. 28 The introduction of a combination of screening tests, used in parallel or sequentially, might improve performance but has significant cost implications. 29,30 The reference standard examination of fluorescein angiography is invasive and does not form part of the initial testing used in screening programmes. Consequently, there remains a potential role for a screening test that is inexpensive and simple to conduct, whilst giving reliably good diagnostic performance across different examiners. As uptake of retinopathy screening remains a challenge, non-invasive tests that could be performed with minimal discomfort and inconvenience to patients are particularly desirable. Recent studies31,32 have proposed that CVT could be used for the detection of sight-threatening retinopathy. A thorough evaluation of the diagnostic performance of CVT in the context of DR screening, particularly in relation to its ability to detect the earlier stages of retinopathy and to predict progression, is therefore the goal of the current project.
Overall aims and objectives of assessment
This project has been divided into three elements that have the combined aim of assessing the usefulness of CVT as a diagnostic tool to be used by the National Screening Programme for Diabetic Retinopathy (NSPDR):
-
a systematic literature review of all studies reporting results on the diagnostic accuracy of CVT for DR
-
a survey sent to the clinical leads and programme managers of the NSPDR, which aimed to determine the current use of CVT and other screening modalities in the NSPDR and the future research priorities in this field
-
a systematic review to identify previous economic evaluations of CVT in screening for DR and development of an independent decision-analytic model of potential cost-effectiveness.
Methods for reviewing diagnostic accuracy
The systematic review was undertaken in accordance with the Centre for Reviews and Dissemination (CRD) guidelines for undertaking systematic reviews33 and published guidelines on the meta-analysis of diagnostic tests. 34
Search strategy
Studies were identified by searching the following databases: MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Pascal, Science Citation Index, BIOSIS, Latin American and Caribbean Health Sciences (LILACS), Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), Database of Abstracts of Reviews of Effects (DARE) and Health Technology Assessment (HTA) database. In addition, information on studies in progress, unpublished research or research reported in the grey literature were identified by searching Inside Conferences, Dissertation Abstracts, NTIS, ClinicalTrials.gov, ReFeR, ClinicalStudyResults.org and Clinical Trial Results. All resources were searched from their inception to October 2007, with update searches conducted on the 17 September 2008. There was no restriction of study by country of origin, language or publication date.
Internet searches were carried out using the specialist search gateways intute (www.intute.ac.uk) and MedlinePlus (www.nlm.nih.gov/medlineplus/) to identify relevant resources. Potentially relevant websites identified during the initial internet gateway searches were then searched and browsed. The organisation websites searched were Diabetes UK, American Diabetes Association, Royal College of Ophthalmologists, College of Optometrists, American Academy of Ophthalmology, Association of Optometrists and the US National Eye Institute. In addition, the following websites were searched: NSPDR, British Association for Retinal Screeners, National Library for Health (NLH) Diabetes Specialist Library and the NLH Screening Specialist Library.
The following conference proceedings were searched: American Academy of Ophthalmology annual meeting (1999–2006), American Diabetic Association annual scientific sessions (2003–7), European Association for the Study of Diabetes annual meeting (2001–7) and Royal College of Ophthalmologists annual congress (2004–7).
Search alerts (details of newly published articles retrieved using a saved search sent by email) were set up in a number of journals: American Journal of Ophthalmology, British Journal of Ophthalmology, Clinical and Experimental Ophthalmology, Diabetes, Diabetes Care, Diabetic Medicine, Investigative Ophthalmology and Visual Science, and Ophthalmology. Search alerts were also set up to run weekly in MEDLINE and EMBASE.
Full details of the search strategies are given in Appendix 1.
Inclusion and exclusion criteria
Two reviewers independently screened titles and abstracts for relevance; disagreements were resolved by consensus. Full papers of potentially relevant studies were obtained and assessed for inclusion by one reviewer and checked by a second. Articles were selected according to the following criteria:
-
Population Patients of any age with type 1 or type 2 DM with or without existing DR.
-
Index test Any test of colour vision.
-
Reference standard Fundus examination by fluorescein angiography, digital retinal photography, biomicroscopy or ophthalmoscopy (either at the time of colour vision screening for diagnostic detection studies or at follow-up for predictive studies).
-
Target condition DR or grading of retinopathy status. Previous research20 suggests that grading method is poorly reported in diagnostic accuracy studies of retinopathy screening. Grading method was therefore not used to exclude studies.
-
Outcomes Sufficient data to construct 2 · 2 tables of test performance [numbers of true-positives (TPs), false-negatives (FPs), false-positives (FPs) and true-negatives (TNs); or sufficient data to allow their calculation]. In addition, ‘phase I’ studies comparing the range of test results in patients with and without retinopathy, or across stages of retinopathy, were included. Studies not reporting these outcomes were identified but not incorporated into the analyses.
-
Study designs Diagnostic cohort studies or diagnostic case–control studies with a minimum of 20 participants, at least five of whom had evidence of retinopathy (any stage), or phase I diagnostic studies with a minimum of 20 participants with diabetes.
-
Preference studies Any studies of attitudes or preferences of patients with diabetes in relation to CVT were included.
Data extraction strategy
Data extraction was performed by one reviewer and checked by a second using EPPI-Reviewer. Data extraction forms were piloted on a small selection of studies. Foreign language papers were extracted by one reviewer, accompanied by a speaker of that language, and the data were entered directly into the EPPI-Reviewer database. Data extraction of non-English language studies was not checked by a second reviewer.
The following information was extracted for all studies when reported: study details (identifier, aim, study design, location), participant details (age, sex, comorbidities, red–green colour vision status, treatment status, inclusion criteria), test details, reference standard details, 2 × 2 or correlation data on test performance, test result ranges (phase I studies only).
Quality assessment strategy
Diagnostic accuracy studies were assessed by one reviewer and checked by another for methodological quality using the 14-item QUADAS (Quality for Assessing Diagnostic Accuracy Studies) tool. 35 Detailed guidance specific to the review was produced on how to score QUADAS (Appendix 2).
Data analysis
Results were analysed by type of CVT. Within these groups tests were examined according to the specific CVTs or test combinations reported in the literature. For each test the range in sensitivity, specificity and likelihood ratios (of both positive and negative tests results) with 95% confidence intervals (CIs) were calculated and discussed.
Insufficient data were reported in the studies to allow for the statistical pooling of diagnostic data. Therefore results were presented in a narrative synthesis with sensitivity and specificity estimates plotted in receiver operating characteristic (ROC) space for illustration.
Chapter 3 Results of review of diagnostic accuracy
Studies included in the review
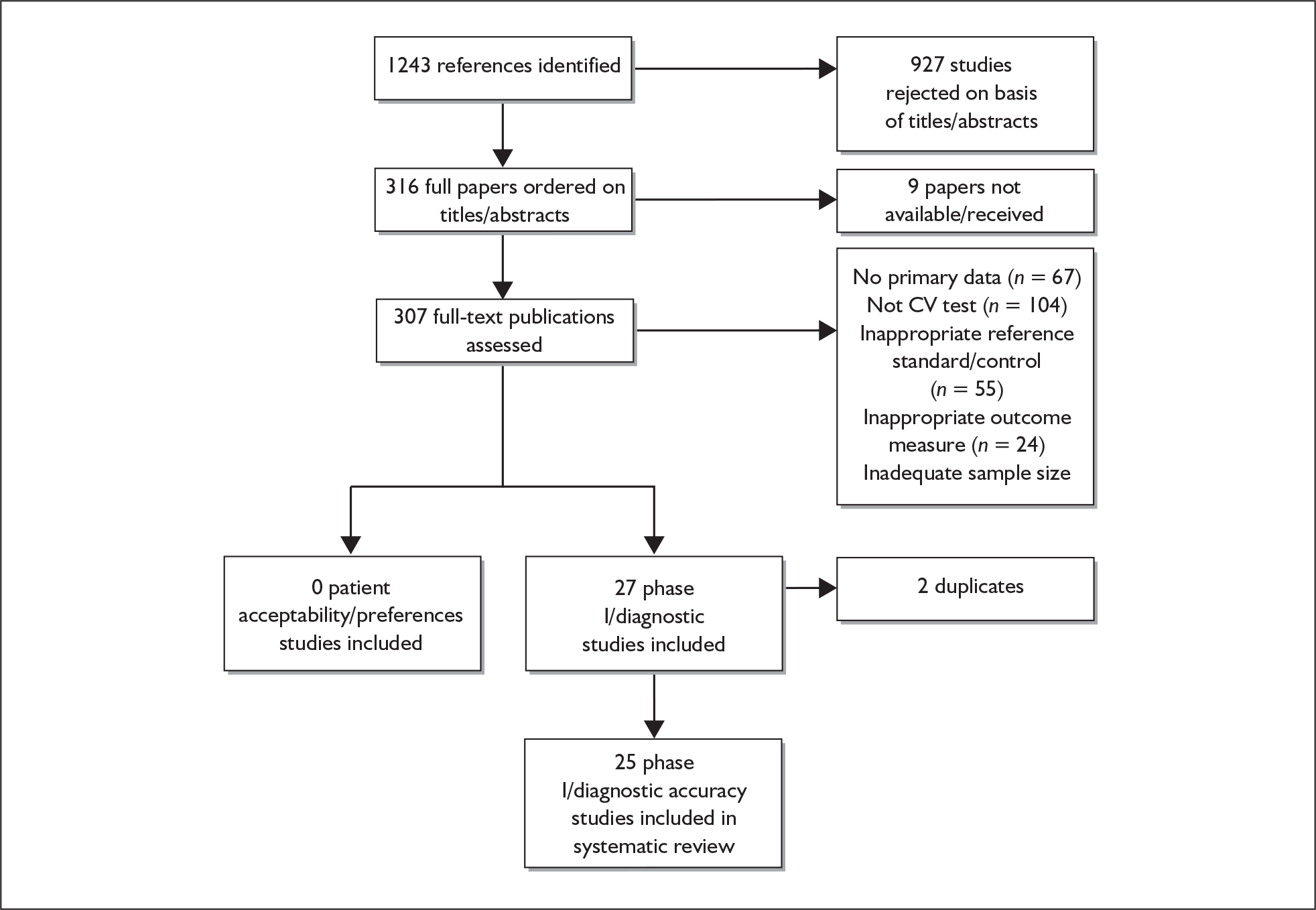
The literature searches identified 1243 references. These were screened for relevance and 316 were ordered for further evaluation. Figure 1 shows the flow of studies through the review process and the numbers of studies excluded at each stage. A total of 25 studies evaluating the relationship between colour vision and retinopathy status in patients with diabetes met the inclusion criteria. Table 1 shows the number of studies included per colour vision test. No relevant studies on the preferences of patients in relation to incorporating CVT were identified. Studies excluded from the review are listed in Appendix 4.
FIGURE 1.
Flow diagram showing study selection process. CV, colour vision.
| Colour vision test | Number of included studies (some studies evaluated more than one test) |
|---|---|
| Pseudoisochromatic plates | 3 |
| Farnsworth–Munsell 100 hue test | 10 |
| Lanthony desaturated D-15 test | 6 |
| Lanthony New Colour Test | 2 |
| Mollon–Reffin Minimalist Test | 1 |
| Automated/computerised tests | 6 |
| Anomaloscopes | 2 |
Quality of included studies
Study quality was generally poor, with the majority of studies explicitly failing to meet QUADAS criteria or reporting insufficient data to allow an assessment to be made (e.g. only one study clearly reported an appropriate patient spectrum). Other aspects of study conduct, such as justification for the selection of particular reference standards, were typically unreported. None of the included studies evaluated the reproducibility of CVT.
Pseudoisochromatic plates
Although all three studies of pseudoisochromatic plates in patients with diabetes used an appropriate reference standard, independent of the index test in all participants, there remained the potential for a range of biases, including those relating to patient spectrum (e.g. including only patients with established signs of retinopathy), disease progression (e.g. long or unspecified time between the index test and reference standard), clinical review (e.g. when different/additional data were available to aid diagnosis than would be available in practice) and attrition (Table 2).
| Studya | Appropriate spectrum composition | Selection criteria described | Appropriate reference standard | Disease progression bias avoided | Partial verification bias avoided | Differential verification bias avoided | Incorporation bias avoided | Adequate test execution details | Adequate reference standard execution details | Test review bias avoided | Diagnostic review bias avoided | Clinical review bias avoided | Uninterpretable results reported | Withdrawals accounted for |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pseudoisochromatic plates | ||||||||||||||
| Bernardczyk-Meller 200147 | ✗ | ✗ | ? | ? | ✓ | ✓ | ✓ | ? | ✗ | ? | ? | ? | ✗ | ? |
| Mirkiewicz-Sieradzka 198657 | ✗ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? | ? |
| Sinha 197958 | ? | ✗ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ? | ? | ? |
| Farnsworth–Munsell 100 hue test | ||||||||||||||
| Aspinall 198336 | ? | ? | ✓ | ✗ | ✗ | ? | ✓ | ? | ✗ | ? | ? | ? | ? | ✗ |
| Ayed 199037 | ? | | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ✓ | ✓ |
| Barton 198738 | ? | ✗ | ? | ? | ? | ? | ? | ? | ✗ | ? | ? | ? | ✗ | ✗ |
| Fong 199939 | ✓ | ? | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ? | ✓ |
| Green 198540 | ? | ✗ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ? | ✗ |
| Greenstein 199041 | ✗ | ✗ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ✓ | ✗ |
| Ismail 199842 | ? | ✗ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ? | ? |
| Jeddi 199443 | ? | ✗ | ✓ | ? | ✓ | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ? | ? |
| Lombrail 198344 | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ✗ | ✗ |
| Trick 198845 | ✗ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ? |
| Lanthony desaturated D-15 test | ||||||||||||||
| Bernardczyk-Meller 200147 | ✗ | ✗ | ? | ? | ✓ | ✓ | ✓ | ? | ✗ | ? | ? | ? | ✗ | ? |
| Doucet 199148 | ? | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ | ✓ |
| Maár 200132 | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ✓ | ✓ | ✓ |
| Mäntyjärvi 199546 | ✗ | ? | ? | ? | ? | ? | ? | ✗ | ✗ | ? | ? | ? | ✗ | ✓ |
| Mecca 198849 | ? | ? | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ✓ | ✓ |
| Saracco 198050 | ? | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✗ | ✗ | ? | ? | ? | ✗ | ✓ |
| Lanthony New Colour Test | ||||||||||||||
| Matsuo 199051 | ? | ? | ? | ? | ? | ? | ? | ✓ | ✗ | ? | ? | ? | ✗ | ✗ |
| Mecca 198849 | ? | ? | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✗ | ? | ? | ? | ✓ | ✓ |
| Mollon–Reffin Minimalist Test | ||||||||||||||
| Maár 200132 | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ |
| Computerised/automated tests | ||||||||||||||
| De Alwis 199452 | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✗ |
| Findl 200053 | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✓ | ✗ | ? |
| Knowles 199654 | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ? | ? | ✓ | ✗ | ? |
| Ong 200431 | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✓ |
| Tregear 199755 | ? | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ? | | ✓ |
| Wong 200856 | ✗ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | ? | ✗ | ✗ |
| Anomaloscopes | ||||||||||||||
| Aspinall 198336 | ? | ? | ✓ | ✗ | ✗ | ? | ✓ | ? | ✗ | ? | ? | ? | ? | ✗ |
| Mäntyjärvi 199546 | ✗ | ? | ? | ? | ? | ? | ? | ✗ | ✗ | ? | ? | ? | ✗ | ✓ |
Arrangement tests
Farnsworth–Munsell 100 hue test
A total of 10 studies36–45 evaluated FM-100 CVT in diabetes patients.
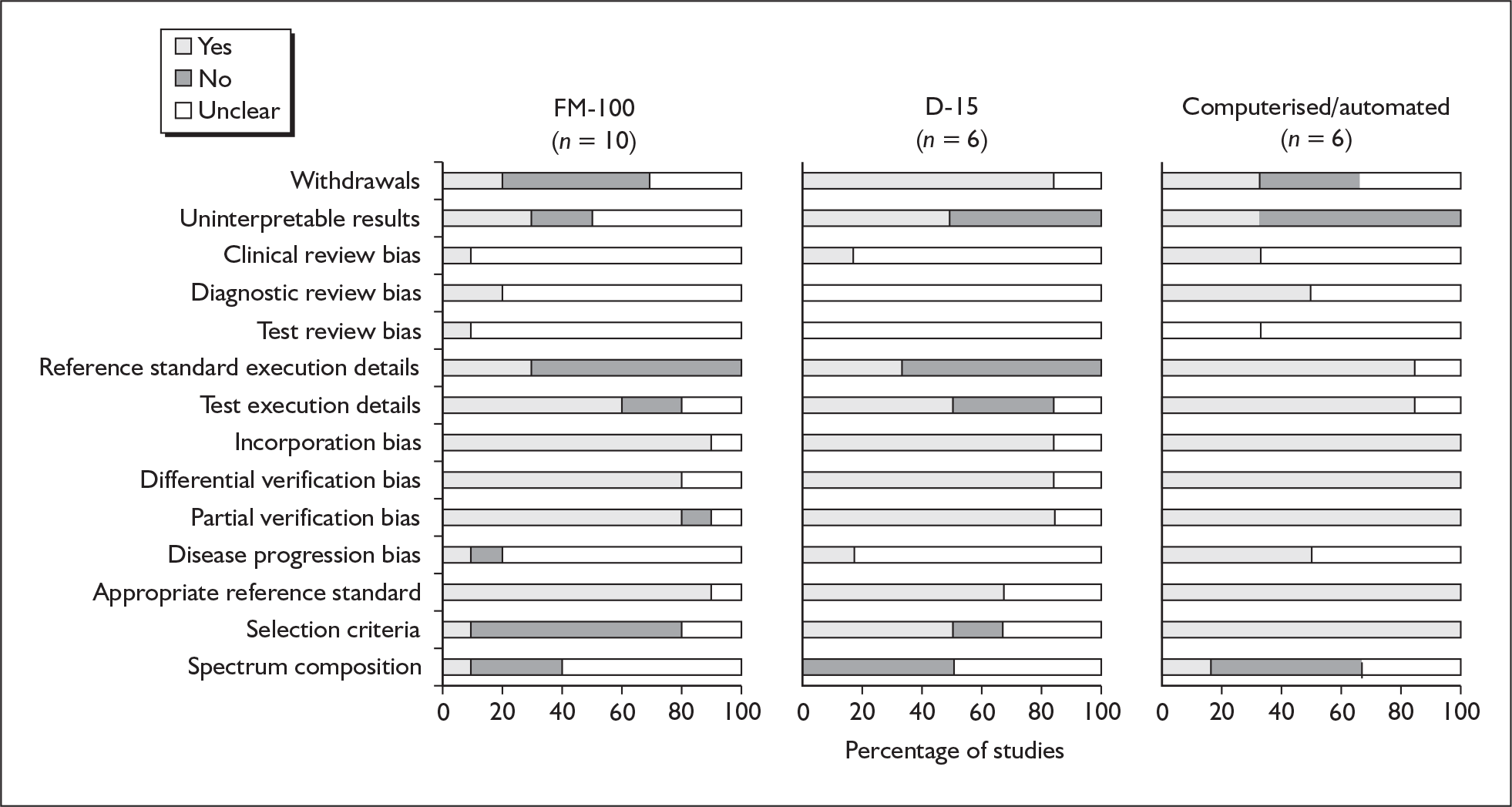
Five36,38,39,42,44 of these studies compared mean error scores on the FM-100. The quality of reporting among these studies was generally low. Only one39 of the five papers had a representative spectrum of patients and reported the reference standard and index test in detail, and none of the papers reported the participant selection criteria that were used (Table 2 and Figure 2).
FIGURE 2.
Proportion of studies rated as yes, no or unclear for each of the QUADAS items for all tests evaluated in five or more studies. D-15, Lanthony desaturated D-15 test; FM-100, Farnsworth–Munsell 100 hue test.
The remaining five studies provided diagnostic accuracy data on the FM-100 test. QUADAS assessment indicated that the quality of reporting among these studies was generally poor (Table 2). The spectrum of patients included in each study was not representative of the general population in practice. In four studies37,41,43,45 patients were excluded if they did not have good visual acuity, whereas one study excluded patients with soft exudates. The English National Screening Programme states that all diabetes patients should be offered retinopathy screening regardless of how good their sight is, therefore these studies are not representative of the entire population who will be offered screening in practice. Only the paper by Trick et al. 45 described the patient selection criteria clearly.
Lanthony desaturated D-15 test
Six studies33,46–50 evaluated the Lanthony desaturated D-15 test in patients with diabetes. QUADAS assessment indicated that the quality of reporting among these studies was generally poor (Table 2 and Figure 2). None of the studies provided any information on blinding of outcome assessors, and only one indicated whether the clinical data available during the interpretation of test results reflected that which would be available in practice. Therefore the potential for test, diagnostic and clinical review biases among this group of studies cannot be ruled out. In addition, the participant inclusion criteria applied to these studies means that their results cannot necessarily be generalised to a diabetic screening population. In two studies46,47 participants were predominantly children and younger adults.
Lanthony New Colour Test
Two studies49,51 evaluated the NCT in diabetes patients. The quality of reporting of both studies was poor (Table 2). It was not possible to distinguish poor reporting of methods from poor methodological quality, but it is likely that there were limitations in both the internal and external validity of these studies as neither adequately reported the patient spectrum or any attempts to avoid review biases.
Mollon–Reffin Minimalist Test
One study32 evaluated the Mollon–Reffin Minimalist Test. The study was generally well reported, although no information on blinding of outcome assessors was given. In addition, only patients less than 50 years of age with type 1 diabetes were included, thereby limiting the generalisability of the study’s findings to a screening population (Table 2).
Automated/computerised tests
Six studies31,52–56 evaluated computerised CVTs in patients with diabetes. The quality of reporting, as rated by QUADAS, was generally better for this group of studies than for studies evaluating other types of CVT (Table 2 and Figure 2). All of the evaluations of computerised/automated tests clearly described their inclusion criteria and used an appropriate reference standard in all participants, independently of the index test. Most studies described the tests in sufficient detail to permit their replication. However, these studies were conducted within a spectrum of patients typical of that which might be seen in a screening setting (i.e. participant inclusion was restricted by age, visual acuity or other reasons excluding them from CVT investigation).
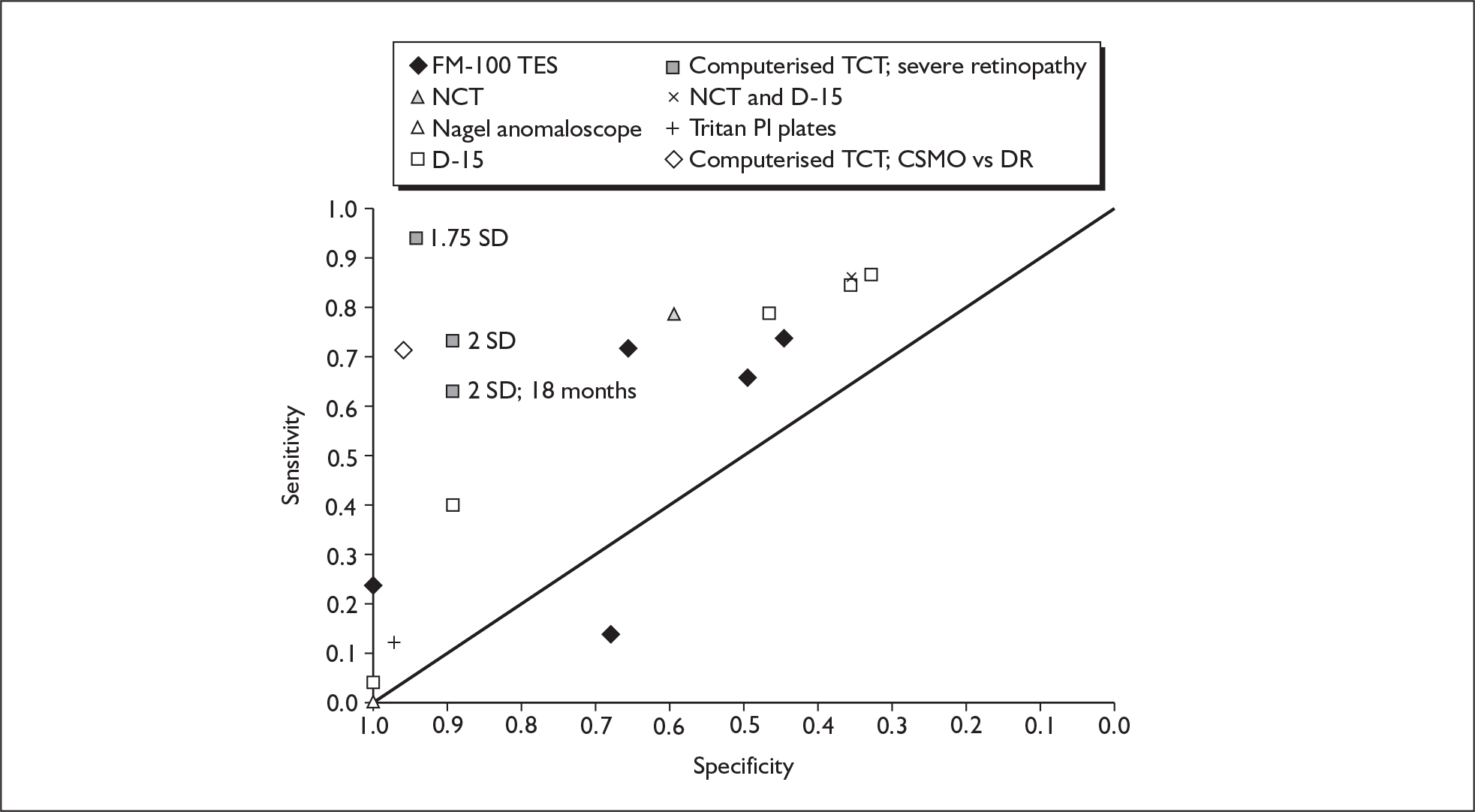
Summary of test accuracy results
Figure 3 brings together the estimates for all of the different tests evaluated in the included studies. When more than one threshold was reported for the same test in the same study, the ‘best performing’ thresholds in terms of overall sensitivity and specificity are presented. Detailed results of all studies, according to type of test evaluated, are presented in subsequent sections.
FIGURE 3.
All studies plotted in receiver operating characteristic (ROC) space (see section on quality of included studies for methodological limitations of plotted studies). 18 months, retinopathy assessed 18 months after baseline colour vision measurement; CSMO, clinically significant macular oedema; D-15, Lanthony desaturated D-15 test; DR, diabetic retinopathy; FM-100, Farnsworth–Munsell 100 hue test; NCT, Lanthony New Colour Test; PI, pseudoisochromatic; SD, diagnostic threshold in standard deviations above mean normal score; TCT, tritan contrast threshold; TES, total error score.
Pseudoisochromatic plates
Three studies evaluated pseudoisochromatic plates in diabetes patients; two47,57 evaluating the Ishihara test and one58 a combination of the Ishihara and Tokyo Medical College tests (Table 3). One study47 did not report any outcomes for the Ishihara test and so will not be discussed further here.
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Bernardczyk-Meller 200147 |
Inclusion criteria: patients for whom long-term follow-up data were available Exclusion criteria: congenital colour vision deficiencies |
Mean age: 17 years 100% type 1 DMa |
Normal vs ‘pathological’ CV test scores |
Ophthalmoscopy Pathological changes vs no pathological changes |
D-15 desaturated (threshold: ‘pathological results’): TP: unclear; FP: 9; FN: unclear; TN: 21 | Not reported | Not reported | |
| Mirkiewicz-Sieradzka 198657 |
Inclusion criteria: diabetes patients with signs of retinopathy Exclusion criteria: patients with congenital red–green colour deficits; patients who had previously undergone photocoagulation |
50.9% male | Pass vs fail (no threshold reported) |
Ophthalmoscopy: (I) microaneurysms and yellow spots; (II) microaneurysms, yellow spots and ‘wybroczyn?’; (III) massive yellow spots; (IV) oedema Fluorescein angiography: (I) single leak; (II) larger leaks; (III) limited oedema; (IV) diffuse oedema |
Not reported | Not reported | Not reported |
Ophthalmoscopy as reference standard (n pass CV test, n fail CV test): (I) microaneurysms and yellow spots (39 eyes, 7 eyes); (II) microaneurysms, yellow spots and ‘wybroczyn’ (19 eyes, 5 eyes); (III) massive yellow spots (1 eye, 2 eyes); (IV) oedema (2 eyes, 15 eyes) Angiography as reference standard (n pass CV test, n fail CV test): (I) single leak (34 eyes, 3 eyes); (II) larger leaks (25 eyes, 11 eyes); (III) limited oedema (2 eyes, 9 eyes); (IV) diffuse oedema (6 eyes in total, CV results unclear) |
| Sinha 197958 |
Inclusion criteria: diabetes patients Exclusion criteria: patients giving the mildest indications about colour defects in family and/or growth impairment of vision |
Mean age: 52.9 years | Normal colour vision; protan deficit; deutan deficit; tritan deficit |
Slit-lamp biomicroscopy DR vs no DR |
Protan deficit: 0; 0; 33; 40 Deutan deficit: 0; 0; 33; 40 Tritan deficit: 4; 1; 29; 39 |
Protan deficit: 0 Deutan deficit: 0 Tritan deficit: 12% |
Protan deficit: 100% Deutan deficit: 100% Tritan deficit: 100% |
One study57 graded retinal status according to both ophthalmoscopy and fluoroscein angiography, and the other58 reported presence or absence of retinopathy on biomicroscopy as the reference standard. The first study57 rated colour vision as a pass or fail on the Ishihara test; the second58 defined patients as normal or protan-, deutan- or tritan-deficient on the combination of the Ishihara and Tokyo Medical College tests.
For the Ishihara test, Mirkiewicz-Sieradzka et al. 57 reported sensitivities of 15% and 8%, respectively, for detecting the background retinopathy on ophthalmoscopy and detecting a single leak on angiography. These sensitivities increased to 88% and 82% for detecting oedema compared with ophthalmology and angiography respectively. The authors did not report sufficient data to permit the calculation of specificity values.
Sinha et al. 58 reported a sensitivity of 12% (95% CI 3% to 28%) and a specificity of 97.5% (95% CI 87% to 100%) in detecting retinopathy for a ‘tritan-deficit’ result on the combined Ishihara/Tokyo Medical College test. This equates to a positive likelihood ratio (LR+) of 4.85 (95% CI 0.57 to 41.3) and a negative likelihood ratio (LR–) of 0.90 (95% CI 0.79 to 1.03), indicating that detection of a tritan deficit on these tests cannot be reliably used to rule in or rule out retinopathy. None of the participants was shown to have a protan- or deutan-deficit result on the CVT.
Arrangement tests
Farnsworth–Munsell 100 hue test
Five studies36,38,39,42,44 compared mean error scores on the FM-100 as opposed to investigating diagnostic accuracy (Table 4). One of these studies44 reported mean FM-100 scores and standard deviations for six grades of retinopathy, reporting an overall trend towards deterioration of colour vision (i.e. higher mean error scores) with increasing retinopathy grade (p < 0.05). However, FM-100 scores did not differ significantly among the less severe grades. A second study42 similarly found that FM-100 scores had some value in discriminating advanced retinopathy from no retinopathy but could not be used to detect early retinopathy. Two papers38,39 came from the ETDRS, one39 of which reported a significant correlation between FM-100 error score and the following factors: presence of clinically significant macular oedema (CSMO) involving the centre of the macula (p = 0.0001); presence of new vessels (p = 0.0001); presence of fluorescein leakage in centre of the macula (p = 0.0001); presence of cystoid changes in the centre of the macula (p = 0.003); and presence of focal leakage (p = 0.002). The second study38 briefly reported that there was no difference in mean FM-100 scores by level of retinopathy.
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Diagnostic accuracy studies | ||||||||
| Ayed 199037 | Inclusion criteria: visual acuity ≥ 5/10 |
Mean age: 44 years 37% male 39% type 1 DM |
‘Abnormal’ if TES is greater than the 95th percentile for participant’s age, according to Verriest curves; ‘normal’ if TES is participant’s age in years plus 30; ‘weak discrimination’ if TES is participant’s age in years multiplied by two, plus 30 (axis not well defined); ‘dyschromatopsia’ if TES is ≥ participant’s age in years multiplied by two, plus 30 (with B-Y or R-G axis). |
Fluorescein angiography Graded: (1) retinopathy absent; (2) beginnings of retinopathy; (3) oedemic; (4) ischaemic with or without new vessels DR vs no DR |
Abnormal colour vision: 70, 58, 25, 47 Abnormal colour vision with dyschromatopsia: 46, 42, 49, 63 Abnormal colour vision with weak discrimination: 25, 16, 70, 89 R-G deficits: 29, 30, 66, 75 |
Abnormal colour vision: 74% Abnormal colour vision with dyschromatopsia: 48% Abnormal colour vision with weak discrimination: 26% R-G deficits: 31% |
Abnormal colour vision: 45% Abnormal colour vision with dyschromatopsia: 52% Abnormal colour vision with weak discrimination: 85% R-G deficits: 71% |
|
| Green 198540 |
Inclusion criteria: diabetes patients attending for routine ocular screening Exclusion criteria: patients with soft exudates |
Dichotomous: abnormal TES vs normal score |
Ophthalmoscopy Dichotomous: serious vs non-serious |
40, 46, 22, 124 | 72% | 66% | ||
| Jeddi 199443 | Inclusion criteria: visual acuity 10/10 |
Mean age: 43.5 years 48% male 52% type 1 DM |
Categorical: normal, weak discrimination, dyschromatopsia |
Ophthalmoscopy DR vs no DR |
25, 11, 13, 11 | 66% | 50% | |
| Trick 198845 |
Inclusion criteria: DM patients with no or mild to moderate background retinopathy; visual acuity of at least 20/30 and intraocular pressure < 21 mmHg in the eye to be tested Exclusion criteria: patients with macular oedema detected in either the ophthalmoscopic examination or the fundus photographs |
Mean age: 37.2 years 68% type 1 DM |
Continuous/average: square root of TES (SQRT TES) and partial error scores (B-Y, R-G) Dichotomous: total/partial error score > 2 SD above the normal mean |
Conventional retinal photography Dichotomous: no retinopathy vs preproliferative background retinopathy |
Total error score: 5, 7, 30, 15 B-Y partial error score: 4, 5, 32, 16 R-G partial error score: 4, 7, 16, 30 |
Total error score: 14% B-Y partial error score: 11% R-G partial error score: 20% |
Total error score: 68% B-Y partial error score: 76% R-G partial error score: 81% |
|
| Studies comparing mean values | ||||||||
| Aspinall 198336 |
Inclusion criteria: diabetes patients < 70 years old with normal fundi Exclusion criteria: congenital colour vision defects; cataracts |
Dichotomous |
Ophthalmoscopy No retinopathy vs retinopathy |
Not reported | Not reported | Not reported | No FM-100 data reported | |
| Barton 198738 | Continuous/average: SQRT TES for deferred eyes is presented for each grade of macular oedema |
Method not stated/final diagnosis Graded: no macular oedema; not clinically significant macular oedema; clinically significant macular oedema |
Comparison of scores in two groups (t-test; Mann–Whitney) No macular oedema (n = 1000), SQRT TES = 12 (SD ± 4); not clinically significant macular oedema (n = 609), SQRT TES = 13 (SD ± 4); clinically significant macular oedema (n = 1248), SQRT TES = 17 (SD ± 5) |
|||||
| Fong 199939 | Inclusion criteria: no attempt was made to eliminate cases of congenital R-G colour deficiency or other known colour vision defects | 55% male | Continuous/average: SQRT TES |
Conventional retinal photography ETDRS graded |
Association between clinical characteristics and outcomes (multivariate regression) Multiple linear regression for SQRT of 100 hue scores: presence of CSMO involving the centre of the macula: beta = 1.36, p-value = 0.0001; presence of new vessels: beta = 1.26, p-value = 0.0001; presence of fluorescein leakage in centre of the macula: beta = 0.48, p-value = 0.0001; presence of cystoid changes in the centre of the macula: beta = 0.87, p-value = 0.003; presence of focal leakage: beta = –0.54, p-value = 0.002 |
|||
| Greenstein 199041 | Inclusion criteria: diabetes mellitus patients requiring insulin therapy; Snellen visual acuity ≥ 20/30 in the tested eye; patients showing either no sign of background retinopathy or only early background retinopathy; no history of hypertension or other metabolic disorders; no significant lens opacities or glaucoma |
Mean age: 45.8 years 100% type I DM |
Dichotomous: though not explicitly stated in the paper, a 2-SD threshold in FM-100 corrected difference score was considered a positive colour vision abnormality test result |
Ophthalmoscopy/conventional retinal photography/fluorescein angiography Graded: modified Airlie House classification: graded levels 1 to 4 Dichotomous: no retinopathy = level 1; background retinopathy ≥ level 2 |
4, 0, 7, 13 | 24% | 100% | |
| Ismail 199842 | Exclusion criteria: any sign of cataracts on ophthalmoscopy; congenital colour deficiency; major systemic pathology other than DM |
Mean age: 57.7 years 0% type 1 DM |
Continuous/average: total and partial (B-Y axis and R-G axis) error scores were calculated; SQRT transformation was used before parametric analysis |
Ophthalmoscopy Conventional retinal photography Graded: modified Airlie House classification: DRL10, DRL30 |
TES (estimated from figure): DRL10: 9.7; DRL20: 9.9; DRL30: 14.0 Partial error scores: B-Y: DRL10: 6.9; DRL20: 7.8 |
|||
| Lombrail 198344 | Inclusion criteria: type 1 DM patients | Continuous/average: FM-100 hue score |
Fluorescein angiography Graded: (A) no retinopathy; (B) only angiographic retinopathy; (C) background retinopathy; (D) preproliferative retinopathy; (E) proliferative retinopathy; (F) retinopathy at incurable stage |
Comparison of multiple groups (ANOVA) Grade A (n = 24), mean (SD) FM-100 score: 107 (50); grade B (n = 15), FM-100: 144 (109); grade C (n = 48), FM-100: 124 (78); grade D (n = 12), FM-100: 182 (96); grade E (n = 2), FM-100: 189 (21); grade F (n = 2), FM-100: 234 (89) |
||||
Five studies provided diagnostic accuracy data on the FM-100 test (Table 4). Figure 4 shows results from these studies plotted in ROC space. Patient spectrums were not representative of the general population who would be screened in practice; four studies37,41,43,45 excluded patients who did not have good visual acuity and one study excluded patients with soft exudates. 40
FIGURE 4.
FM-100 studies reporting 2 × 2 data plotted in receiver operating characteristic (ROC) space (see section on quality of included studies for methodological limitations of plotted studies). B-Y, blue-yellow partial error score; CV, colour vision; R-G, red–green partial error score; TES, total error score.
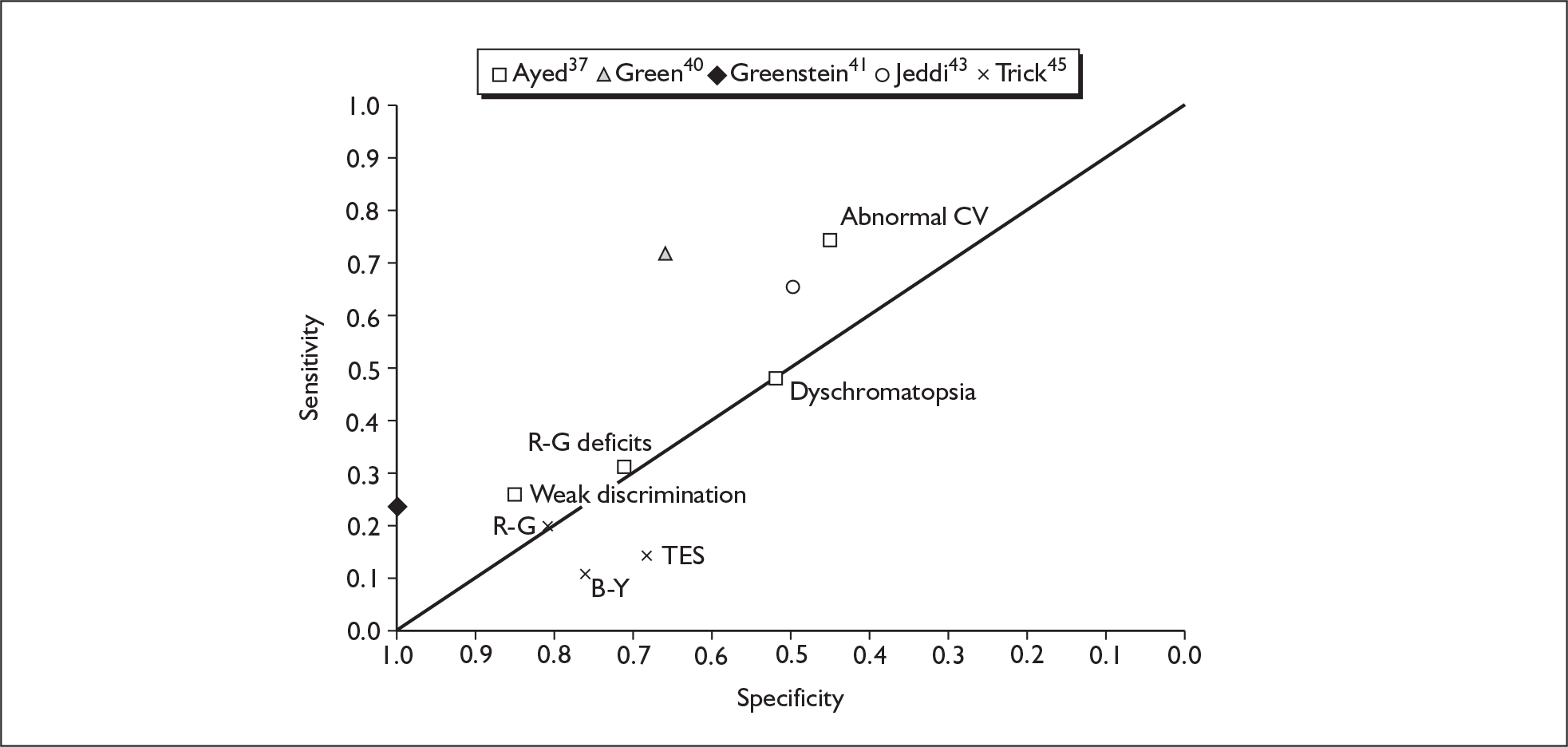
Thresholds to define a positive FM-100 score varied between studies. Sensitivity ranged from 11% to 74% and specificity ranged from 45% to 100%. The study reporting a specificity of 100% reported a sensitivity of only 24%. 41 The reference standard in all of the diagnostic accuracy studies was used to distinguish between patients with retinopathy and those without. One40 of these studies made the additional distinction between those with no or background retinopathy and those with more serious retinopathy. Three studies40,41,43 used the reference standard to establish the grade of retinopathy in line with the Airlie House classification system. The study40 distinguishing between those with no or background retinopathy and those with more serious retinopathy reported a sensitivity of 65% (95% CI 51% to 76%) and a specificity of 73% (95% CI 66% to 79%). One study40 reported a LR+ of 2.38 (95% CI 1.75 to 3.24). The remaining comparisons all reported even smaller LR+, with confidence intervals incorporating 1. Therefore, the available evidence does not suggest that FM-100 testing alone could be used to rule in or rule out retinopathy in diabetes patients, or to discriminate between no or background retinopathy and more serious disease.
Lanthony desaturated D-15 test
Six studies32,46–50 evaluated the Lanthony desaturated D-15 test in patients with diabetes, all of which provided diagnostic accuracy data (Table 5).
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Bernardczyk-Meller 200147 |
Inclusion criteria: patients for whom long-term follow-up data were available Exclusion criteria: congenital colour vision deficiencies |
Mean age: 17 years 100% type 1 DM Mean diabetes duration: 7.8 years (range 3–18 years) |
Normal vs ‘pathological’ CV test scores |
Ophthalmoscopy Pathological changes (non-proliferative DR, preproliferative DR, cataract) vs no pathological changes |
Pathological changes (non-proliferative DR, pre-proliferative DR, cataract) vs no pathological changes: TP: unclear; FP: 9; FN: unclear; TN: 21 | |||
| Doucet 199148 | Exclusion criteria: people aged > 65 years; visual acuity < 4/10; cataract or glaucoma; known congenital dyschromatopsia; deterioration in mental functioning; using medicines that could alter colour vision |
Mean (SD) age: 43.4 (14.4) years 62% male 88% type 1 DM Mean (SD) diabetes duration: 134 (106) months |
Score of 0–2 given for each eye: 0 = dyschromatopsia with one or several axes; 1 = dyschromatopsia without an axis; 2 = normal (three simple inversions at any age, or four inversions/diametrical inversions over age 45 years, or minimum of five inversions or two diametrical inversions over age 60 years) |
Fundoscopy ETDRS grading Retinopathy vs no retinopathy |
26, 47, 4, 23 | 87% | 33% | |
| Maár 200132 |
Inclusion criteria: type 1 DM; best corrected visual acuity of at least 0.4 LogMAR (0.4 Snellen value); < 50 years; no lens opacities Exclusion criteria: congenital CV deficiencies; cataract; glaucoma; retinopathy, new vessels or chorioretinal scars in the macula; more than mild proliferative retinopathy; history of intraocular surgery or laser therapy |
Mean age: 29.5 years 41% male 100% type 1 DM |
D-15: total colour difference score (TCDS) |
Slit-lamp biomicroscopy Conventional retinal photography Fluorescein angiography CSMO vs without CSMO |
4, 3, 6, 26 | 40% | 90% | |
| Mäntyjärvi 199546 | Inclusion criteria: schoolchildren with diabetes and healthy eyes at recruitment |
Mean (SD) age: 14 (2) years 46.3% male Mean (SD) diabetes duration: 6 (4) years |
Pass/fail for each test |
Method not stated/final diagnosis Retinopathy vs no retinopathy |
1, 0, 22, 31 | 4% | 10% | |
| Mecca 198849 |
Inclusion criteria: all patients had duration > 4 years; all patients had visual acuity 8/10 or better Exclusion criteria: participants with congenital colour vision deficits; patients with maculopathy or macular oedema of mixed or proliferative retinopathy and participants with retinopathy of an advanced degenerative stage (large or numerous haemorrhages with exudate ‘confluents’) |
Altered colour vision vs normal |
Ophthalmoscopy Fluorescein angiography With retinopathy vs without retinopathy |
72, 45, 13, 25 | 85% | 34% | ||
| Saracco 198050 |
Inclusion criteria: included patients with visual acuity ≥ 6/10. Exclusion criteria: excluded those with congenital dyschromatism, those with retinal or general problems (unspecified) that could affect the interpretation of colour vision; diabetes patients who had had laser eye correction were also excluded |
Mean age: 51.1years | Normal colour vision vs abnormal colour vision |
Fluorescein angiography Dichotomous: normal (grade 0) vs pathological (grades 1, 2 and 3) Also angiography grade 0 vs grade 1 |
All angiography: 63, 49, 17, 43 Angiography grade 1: 42, 49, 12, 43 |
All angiography: 79% Angiography grade 1: 78% |
All angiography: 47% Angiography grade 1: 47% |
Stand-alone reference standards included ophthalmoscopy47,48 and fluorescein angiography. 50 Combined reference standards included ophthalmoscopy with fluorescein angiography49 and combined biomicroscopy/photography/angiography. 32 Only one study46 did not specify a reference standard.
Although they applied different measures, most studies used the reference standard to distinguish between diabetes patients with and without retinopathy. Retinopathy, when defined, was typically characterised by the presence of microaneurysms, haemorrhages and hard exudates. One study32 specifically evaluated the accuracy of the desaturated D-15 test in detecting ‘clinically significant macular oedema’ as opposed to any presence of retinopathy. Colour vision deficiency was generally defined as a ‘pathological’ or ‘abnormal’ desaturated D-15 score, although the specific threshold – when reported – was not consistent between studies (Table 5).
The studies investigating the presence or absence of retinopathy in adults with diabetes48–50 reported sensitivities between 79% and 87% and specificities between 33% and 47% (Figure 5). The study evaluating the D-15 test for the detection of CSMO in adults32 reported a sensitivity of 36% and a specificity of 88%.
FIGURE 5.
D-15 studies reporting 2 × 2 data plotted in receiver operating characteristic (ROC) space (see section on quality of included studies for methodological limitations of plotted studies). Grades 1–3, all ‘pathology’ on angiography; grade 1, angiography grade 1 (‘dry retinopathy’) only; 6-years, retinopathy assessed 6 years after baseline colour vision measurement.
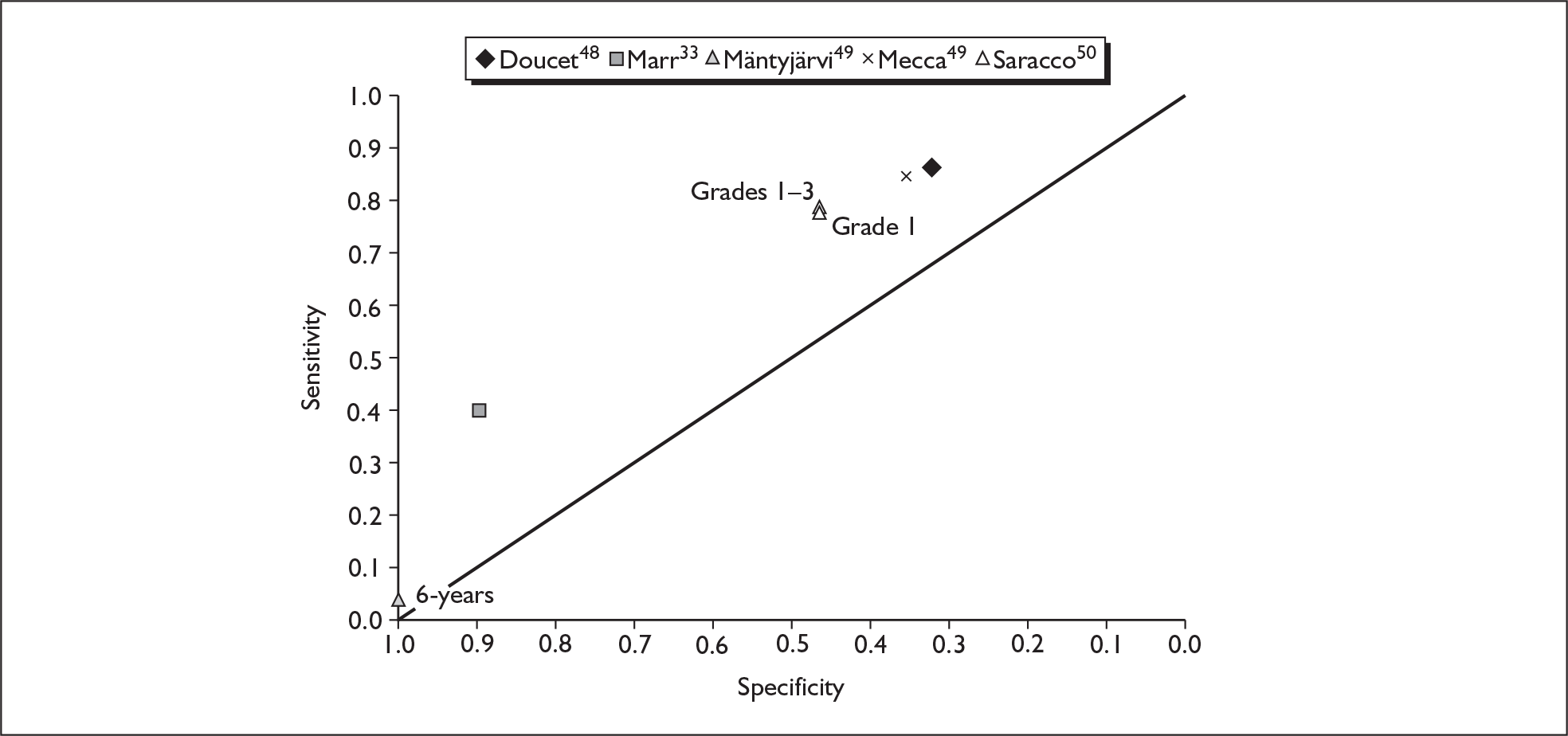
Of the two studies investigating DR in younger patients, one47 reported a specificity of 70% (95% CI 51% to 85%) in patients with a mean age of 17 years, but provided insufficient data to calculate a sensitivity value. The second study46 administered the D-15 test in participants with a mean age of 14 years and assessed their retinopathy status 6 years later, reporting a sensitivity of 4% (95% CI 0% to 22%) and a specificity of 100% (95% CI 89% to 100%), which equates to a LR+ of 4.0 (95% CI 0.17 to 94.0) and a LR– of 0.95 (95% CI 0.85 to 1.07). On this basis there is little evidence to suggest that the D-15 test could be used to detect or predict retinopathy in young people with diabetes.
Likelihood ratios among the cross-sectional studies in adults were poor, with LR+ ranging from 1.29 to 3.87 and LR– ranging from 0.67 to 0.41, suggesting that there is little evidence to support the use of the desaturated D-15 test for detecting retinopathy in adults with diabetes. LRs were not calculable for the study investigating CSMO.
Lanthony New Colour Test
Two studies49,51 evaluated the NCT in diabetes patients (Table 6).
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Matsuo 199051,59 |
Inclusion criteria: visual acuity score > 0.5 Exclusion criteria: participants with eyesight problems |
Mean age: 57.4 years 54% male |
Total error score (TES) |
Method not stated/final diagnosis Graded |
Retinopathy: mean TES = 7.9 (SD 1.51); no retinopathy: mean TES = 3.03 (SD 0.56) | |||
| Mecca 198849 |
Inclusion criteria: all patients had duration > 4 years; all patients had visual acuity ≥ 8/10 Exclusion criteria: participants with congenital colour vision deficits; patients with maculopathy or macular oedema of mixed or proliferative retinopathy and participants with retinopathy of an advanced degenerative stage (large or numerous haemorrhages with exudate ‘confluents’) |
NCT Altered colour vision (anything above zero) vs normal (no errors) |
Ophthalmoscopy Fluorescein angiography With DR vs without retinopathy |
NCT alone: 67, 28, 18, 42 NCT and D-15: 73, 45, 12, 25 |
NCT alone: 79% NCT and D-15: 86% |
NCT alone: 60% NCT and D-15: 34% |
One study49 used a reference standard of combined ophthalmoscopy with fluorescein angiography, whereas the second51 did not specify a reference standard. Both studies aimed to differentiate between patients with and without DR. Mecca et al. 49 defined retinopathy as the presence of at least 10 microaneurysms and small haemorrhages, whereas Matsuo et al. 51 did not define retinopathy.
Both studies collected total error scores on the NCT, with Mecca et al. 49 dichotomising participants as having either ‘normal colour vision’ (no errors) or ‘altered colour vision’ (any score above 0).
The study by Matsuo et al. 51 did not present diagnostic accuracy estimates but reported that total error scores on the NCT were significantly greater among participants with DR than in those without retinopathy (p < 0.01), suggesting a possible correlation between colour vision deficits and the presence of retinopathy (Table 6).
Mecca et al. 49 reported an overall sensitivity of 79% (95% CI 69% to 87%) and specificity of 60% (95% CI 48% to 72%) for the NCT. The authors reported that combining the NCT results with findings of the D-15 test (how these were combined was not clear) increased overall sensitivity (86%) but decreased specificity (36%). Both positive and negative LRs were better for NCT alone: LR+ 1.97 (95% CI 1.45 to 2.68), LR– 0.35 (95% CI 0.22 to 0.55). Although these values are slightly more promising than for some other arrangement tests, they still indicate a poor ability to rule in or rule out disease, and it should be noted that they are derived from the results of a single, small, poor-quality study.
Mollon–Reffin Minimalist Test
One study32 evaluated the Mollon–Reffin Minimalist Test (Table 7).
| Study | Patient selection criteria | Clinical characteristics (mean age,% male,% Type 1 DM) | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Maár 200132 |
Inclusion criteria: type 1 DM; best corrected visual acuity of at least 0.4 LogMAR (0.4 Snellen value); < 50 years; no lens opacities Exclusion criteria: congenital CV deficiencies; cataract; glaucoma; retinopathy, new vessels or chorioretinal scars in the macula; more than mild proliferative retinopathy; history of intraocular surgery or laser therapy |
Mean age: 29.5 years 41% male 100% type 1 DM |
Number of reliably identified coloured chips for each confusion line |
Slit-lamp biomicroscopy Conventional retinal photography Fluorescein angiography Clinically significant macular oedema (CSMO) vs without CSMO |
Not reported | Not reported | Not reported |
Tritan axis; threshold error score of 1: sensitivity: 88.9%, specificity: 93.3% Tritan axis; error score: CSMO (n = 10): 2.1 (0.74), no CSMO (n = 29): 1.03 (0.19) Logistic regression: patients with CSMO had non-significantly higher total colour difference score (TCDS) on the D-15 (p = 0.345) and significantly higher Mollon–Reffin tritan score (p = 0.0015; r2 = 0.565) |
A combination of slit-lamp biomicroscopy, retinal photography and fluorescein angiography was used to identify CSMO. An error score greater than 1 was considered a ‘fail’ on the Mollon-Reffin test.
Although exact numbers of patients required to calculate diagnostic accuracy measures were not reported, the authors stated that no errors were made on the protan or deutan axes by any patient. The overall sensitivity and specificity of the Mollon-Reffin test were reported to be 89% and 93% respectively. These values would suggest a LR+ of 12.7 and a LR– of 0.12. Despite the positive conclusions of this study, there is no further evidence to corroborate these findings on the diagnostic accuracy of the Mollon-Reffin test for the detection of CSMO.
Automated/computerised hue discrimination tests
Six studies31,52–56 evaluated computerised CVTs in patients with diabetes (Table 8). Four of these studies evaluated variants of the SGM and one evaluated the ChromaTest56 (see Chapter 1, Automated/computerised tests), all of which were co-authored by developers of the system itself. A sixth study53 evaluated a similar kind of colour monitor system to measure colour contrast sensitivity, whereby the system determines the threshold chrominance of a coloured grating in which there is no change in luminance.
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| De Alwis 199452 |
Inclusion criteria: proven diagnosis of DM; visual acuity 6/12 or better Exclusion criteria: any other eye disease including glaucoma; visual acuity 6/18 or worse; previous laser treatment for retinopathy; elevated intraocular pressure in the absence of frank glaucoma |
Mean age: 53.9 years (range 18–84 years) | z-score thresholds based on standard deviations from –3.0 to 0 |
Slit-lamp biomicroscopy Dichotomous: severe retinopathy vs non-severe retinopathy |
Overall score: 3 SD: 11, 2, 19, 105; 2.5 SD: 17, 5, 13, 102; 2 SD: 22, 11, 8, 96; 1.5 SD: 23, 21, 7, 86; 1 SD: 24, 27, 6, 80; 0.5 SD: 25, 40, 5, 67; 0 SD: 29, 64, 1, 43 Tritan score: 2 SD: 22, 11, 8, 96 |
Overall score: 3 SD: 37%; 2.5 SD: 57%; 2 SD: 73%; 1.5 SD: 77%; 1 SD: 80%; 0.5 SD: 83%; 0 SD: 97% Tritan score: 2 SD: 73% |
Overall score: 3 SD: 98%; 2.5 SD: 95%; 2 SD: 90%; 1.5 SD: 80%; 1 SD: 75%; 0.5 SD: 63%; 0 SD: 40% Tritan score: 2 SD: 90% |
Right eye tritan: maculopathy grade p < 0.001, ischaemic grade p < 0.005 Left eye tritan: maculopathy grade p < 0.001, ischaemic grade p < 0.002 Right eye R-G: maculopathy grade p < 0.001, ischaemic grade p < 0.002 Left eye R-G: maculopathy grade p < 0.001, ischaemic grade p < 0.002 |
| Findl 200053 |
Inclusion criteria: insulin-dependent type 1 diabetes patients; age < 32 years; diabetes duration between 12 and 17 years Exclusion criteria: systemic hypertension or any sign of non-diabetes-induced vascular complications; excluded patients if any ocular disease except diabetic retinopathy was evident at pre-study ophthalmic examination |
Mean (SD) age: 23.1 (4.3) years 66% male Mean diabetes duration: 12–17 years |
The threshold chrominance of a coloured optotype without changes in luminance compared with the surrounding expressed as a percentage |
Slit-lamp biomicroscopy Retinal photography Fundoscopy Graded Modified Airlie House classification |
Not reported | Not reported | Not reported |
Level 1: 7.1% (1.7) (n = 20) Level 2: 7.3%, (1.9) (n = 27) Level 3: 10.1%, (3.0) (n = 12) p = 0.02 |
| Knowles 199654 |
Inclusion criteria: diabetic pseudophakes with/without retinopathy and age-matched phakic diabetic controls; pseudophakes were examined at least 3 months after cataract surgery Exclusion criteria: visual acuity < 6/12; previous laser eye treatment; other eye disease likely to affect CV (e.g. glaucoma/macular degeneration); significant cataract; observable posterior capsular opacity |
Mean age: 74.2 years | R-G or tritan discrimination sensitivity |
Slit-lamp biomicroscopy Dichotomous: no retinopathy vs background retinopathy |
Not reported | Not reported | Not reported |
Mean R-G discrimination sensitivity: no retinopathy: 0.610; background retinopathy: 0.789; p = 0.035 Mean tritan discrimination sensitivity: no retinopathy: 0.660; background retinopathy: 0.806; p = 0.307 Mean R-G discrimination sensitivity (controls): no retinopathy: 0.537; background retinopathy: 0.601 Mean tritan discrimination sensitivity (controls): no retinopathy: 0.786; background retinopathy: 0.823 |
| Ong 200431 |
Inclusion criteria: consenting diabetes patients attending photographic screening Exclusion criteria: corrected visual acuity < 6/9; previous history of photocoagulation therapy; history of eye disease known to affect colour vision (e.g. glaucoma); signs and symptoms of significant media opacification; inability to complete the test satisfactorily |
Mean age: 60.9 years 21% (107/510) type 1 DM Mean diabetes duration: 10.4 years |
Using the weighted kappa coefficient of association analysis technique, the optimal pass/fail criterion to detect sight-threatening diabetic retinopathy (STDR) was z = –1.75 |
Slit-lamp biomicroscopy Dichotomous: STDR vs non-STDR |
Any retinopathy: 24, 103, 18, 365 Maculopathy: 12, 30, 0, 468 STDR: 16, 26, 1, 467 STDR TCT + photography: 15, 2, 2, 491 |
Any retinopathy: 57% Maculopathy: 94% STDR: 94% STDR TCT + photography: 88% |
Any retinopathy: 78% Maculopathy: 100% STDR: 95% STDR TCT + photography: 99% |
Mean (SD) TCT score: no retinopathy (n = 383): 42.5 (6.3); background retinopathy (n = 110): 41.7 (7.1); preproliferative retinopathy (n = 3): 29.6 (8.5); proliferative retinopathy (n = 2): 21.7 (3.3); maculopathy (n = 12): 24.0 (7.2) |
| Tregear 199755 |
Inclusion criteria: type 1 and type 2 diabetes patients; those taking any form of medication other than those used to control glucose levels deliberately not excluded Exclusion criteria: previous laser treatment; signs of significant lens opacification as determined by slit-lamp examination through dilated pupil; corrected visual acuity worse than 6/18 |
Mean age: 56 years 30% type 1 DM Mean (SD) diabetes duration: 14 years (range 1.5–60 years) |
Longitudinal subgroup only: threshold scores +2 SDs above the lens equated mean |
Slit-lamp biomicroscopy Graded: no retinopathy, background, preproliferative, proliferative, maculopathy, ischaemia or maculopathy |
12, 7, 7, 62 | 63% | 90% | |
| Wong 200856 |
Inclusion criteria: type 2 diabetic patients with untreated NPDR and untreated CSMO Exclusion criteria: type 1 diabetes; proliferative DR; previous laser photocoagulation; current ocular pathology including infection, trauma; amblyopia; glaucoma; and/or vascular occlusion |
Median 60 years (range 31–82 years) 0% type 1 DM |
ChromaTest Pass/fail criterion for tritan colour contrast threshold (TCCT) given for each age group: 11.0 (30–49 years); 23.0 (50–69 years); 32.0 (70–89 years) |
Slit-lamp biomicroscopy Grading according to the Early Treatment Diabetic Retinopathy Study extension of the Airlie House classification; no clinical retinopathy, NPDR and CSMO |
TCCT detection of CSMO (NPDR used as control group): TP = 25, FP = 35, FN = 10, TN = 80 Subjects with LogMAR: NPDR vs no DR: TP = 35, FP = 1, FN = 80, TN = 29, LR+ 9.13, LR– 0.72 CSMO vs no DR: TP = 25, FP = 1, FN = 10, TN = 29 CSMO vs NPDR: TP = 25, FP = 35, FN = 10, TN = 80 |
TCCT detection of CSMO (NPDR used as control group): 71% (53–83%) NPDR vs no DR: 30% CSMO vs NPDR: 71% |
TCCT detection of CSMO (NPDR used as control group): 70% (60–78%) NPDR vs no DR: 97% CSMO vs NPDR: 70% |
All six studies used slit-lamp biomicroscopy as the reference standard to ascertain retinopathy status. One study53 additionally evaluated participants with indirect fundoscopy and retinal photography. The Findl et al. study53 indicated that colour contrast sensitivity thresholds on the tritan axis significantly increased with the level of retinopathy as determined by the modified Airlie House classification (p = 0.02).
Knowles et al. ,54 however, found no significant difference in tritan discrimination using the SGM between background retinopathy and no retinopathy in patients with diabetes either with (p = 0.6) or without (p = 0.3) phakic eyes. The only significant difference in colour vision between patients with and without retinopathy reported in this study was on the red–green axis in those participants with phakic eyes (p = 0.035). The only study reporting diagnostic accuracy data for the red–green contrast threshold55 indicated a sensitivity of 33% and specificity of 93% in detecting macular oedema or ischaemia (Table 8).
A total of four studies31,52,55,56 provided diagnostic accuracy data, one of which evaluated the ChromaTest56 and three31,52,55 of which evaluated a variant of the SGM.
The ChromaTest study56 included 150 patients with type 2 diabetes, 115 of whom had untreated non-proliferative diabetic retinopathy (NPDR) and 35 of whom had untreated CSMO, confirmed by slit-lamp biomicroscopy. Sensitivity and specificity of the tritan colour contrast threshold (TCCT) part of the ChromaTest for screening of CSMO in this group were 71% (95% CI 53% to 85%) and 70% (95% CI 60% to 78%) respectively. These equate to positive and negative LRs of 2.35 and 0.41 respectively. The study also reported ChromaTest scores for 30 diabetes patients without retinopathy. Using the thresholds suggested by the authors, the ChromaTest TCCT score yielded a sensitivity of 30% for distinguishing NPDR from no retinopathy and a sensitivity of 71% for distinguishing CSMO from no retinopathy. In both of these cases, the specificity of the ChromaTest was 97%. Positive and negative LRs were better for distinguishing the presence of CSMO (21.4 and 0.30 respectively) than of NPDR (9.13 and 0.72 respectively). The study’s authors acknowledge that their findings may be biased (in favour of the ChromaTest) because the test was evaluated in the same data set that was used to derive positive and negative threshold levels.
One31 of the SGM studies specifically evaluated the machine’s tritan contrast threshold (TCT) test alongside retinal photography. This study reported a z-score of –1.75 (i.e. 1.75 standard deviations from the mean) as the optimum pass/fail criterion for distinguishing sight-threatening from non-sight-threatening retinopathy, with a sensitivity for TCT alone of 94% (95% CI 71% to 100%) and specificity of 95% (95% CI 92% to 97%). Positive and negative LRs were 17.9 (95% CI 12.1 to 26.4) and 0.06 (95% CI 0.01 to 0.42) respectively. For detecting the presence of retinopathy of any severity (anything above and including background DR), sensitivity of TCT was 57% (95% CI 41% to 72%) and specificity 78% (95% CI 74% to 82%), equating to a LR+ of 2.60 (95% CI 1.90 to 3.55) and a LR– of 0.55 (95% CI 0.39 to 0.78). Using the same threshold of z = –1.75 for sight-threatening CSMO, sensitivity for TCT alone was 100% (95% CI 70% to 100%) and specificity was 94% (95% CI 91% to 96%). Positive and negative LRs were 16.6 (95% CI 11.7 to 23.5) and 0 respectively. These data tend to indicate that, although TCT may be useful for ruling in higher grades of retinopathy, its performance is likely to be inadequate for the early detection of lower levels of disease.
TCT appeared to be slightly more sensitive than photography alone [94% (95% CI 69% to 100%) versus 88% (95% CI 62% to 98%)], with identical specificity [95% (95% CI for TCT, 92% to 96%; for photography, 93% to 97%). The values reported for photography alone appeared to be consistent with those reported elsewhere in the literature. 20 The authors also reported the diagnostic accuracy of TCT combined with fundus photography for detecting sight-threatening diabetic retinopathy (STDR), in which a positive test result was defined as STDR on photography and colour deficit on TCT. For combined TCT/fundus photography, sensitivity was similar to that of photography alone [88% (95% CI 64% to 99%)] and specificity increased to 100% (95% CI 99% to 100%). Combining the tests did not influence the LR– [0.12 (95% CI 0.03 to 0.43) for both combined TCT/photography and photography alone]; however, because specificity was increased to 100%, the LR+ dramatically increased from 18.9 (95% CI 12.2 to 29.2) for photography to 218 (95% CI 54.0 to 877) for the combined test. In practice, to minimise administration and travel costs, it would be most efficient to conduct CVT and photography at the same screening appointment. Given the general acceptance of retinal photography as the standard method of screening, it seems likely that, in the short term, all individuals would be screened with retinal photography and any with sight-threatening retinopathy would be referred for assessment by an ophthalmologist. Therefore, one potentially viable combination of CVT and retinal photography, not evaluated in this paper,31,60 would be referral for assessment of any individual with sight-threatening retinopathy visualised by photography or tritan colour vision deficit. It should also be noted that, as in the ChromaTest study, the TCT thresholds used here appear to be derived from the same data set in which the test’s accuracy was evaluated, thereby potentially biasing the accuracy results in favour of the TCT.
De Awis52 reported the accuracy of a tritan pass/fail criterion for a range of thresholds: a threshold of 2 standard deviations above the mean to detect severe/advanced retinopathy had a sensitivity of 73% (95% CI 54% to 88%) and a specificity of 90% (95% CI 82% to 95%) (this provided a better balance of sensitivities and specificities than other thresholds;52,55 Figure 6). Positive and negative LRs for this threshold were 7.13 (95% CI 3.92 to 13.0) and 0.30 (95% CI 0.16 to 0.54) respectively. The same threshold used to detect the broader grouping of ‘moderate and severe’ retinopathy had a sensitivity of 55% (95% CI 41% to 68%) and a specificity of 95% (95% CI 89% to 99%), equating to a LR+ of 12.0 (95%CI: 4.47 to 32.2) and a LR– of 0.48 (95% CI 0.36, 0.64). 52
FIGURE 6.
Studies of computerised/automated tests reporting 2 × 2 data plotted in receiver operating characteristic (ROC) space (see section on quality of included studies for methodological limitations of plotted studies). CSMO, clinically significant macular oedema; DR, diabetic retinopathy; NPDR, non-proliferative diabetic retinopathy; SD, diagnostic threshold in standard deviations above mean normal score; SGM, Sussex Gratings Machine; STDR, sight-threatening diabetic retinopathy; TCT, tritan contrast threshold.
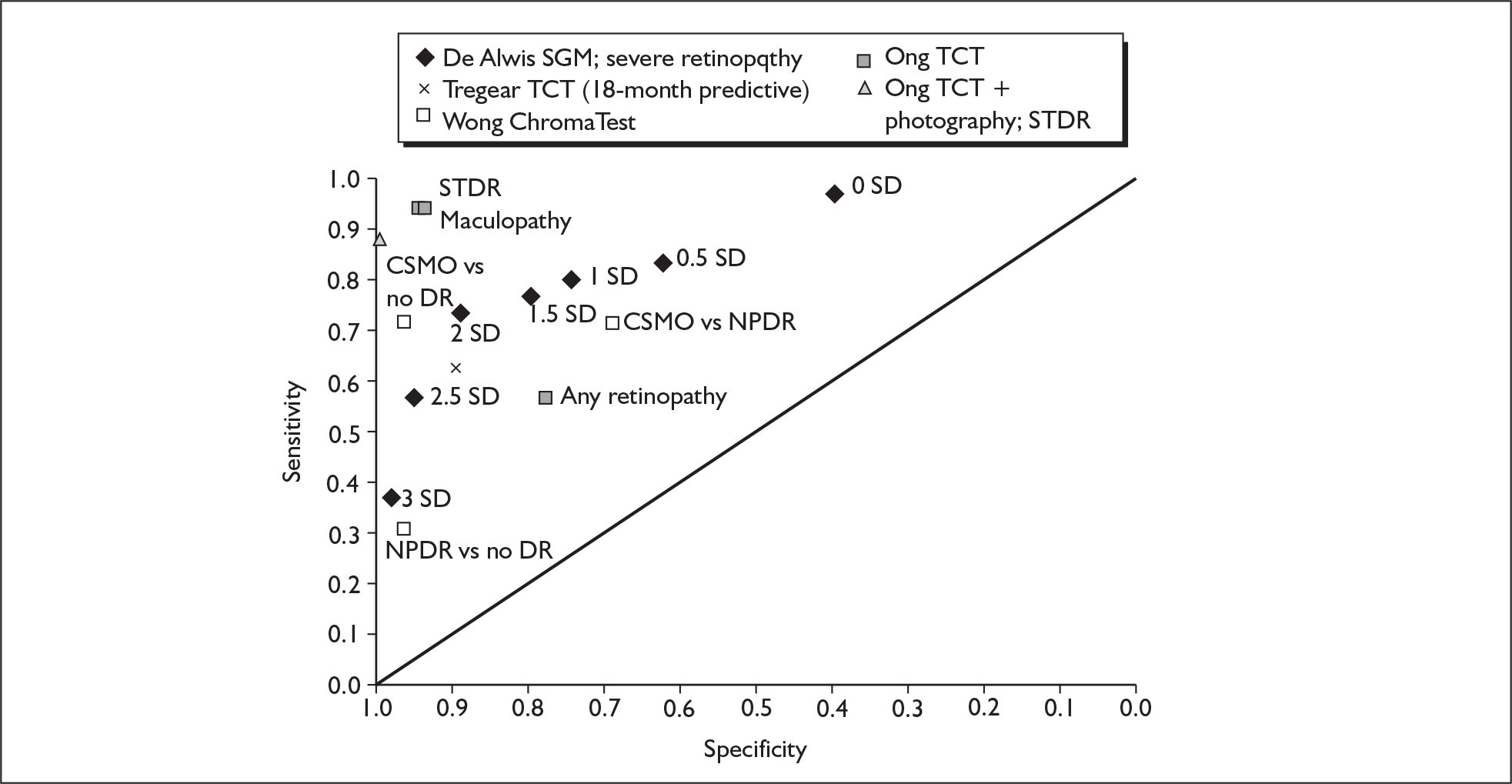
Tregear et al. 55 looked specifically at the ability of the SGM to predict macular oedema or ischaemia in a subgroup of patients who were reassessed using slit-lamp biomicroscopy 18 months after baseline TCT evaluation. At follow-up this gave a sensitivity of 63% (95% CI 38% to 84%) and a specificity of 90% (95% CI 80% to 96%). Positive and negative LRs were 6.23 (95% CI 2.85 to 13.6) and 0.41 (95% CI 0.23 to 0.74) respectively.
These data suggest that the automated TCT test might have some value in ruling in more advanced retinopathy, particularly when used in combination with retinal photography. However, it should be noted that the data for combined TCT/photography are derived from a single study with a very small number of cases with sight-threatening retinopathy, and that all of the available evaluations of the TCT were conducted in conjunction with its developers. Similarly there are no data available on the potential of this test for predicting DR.
Anomaloscopes
Two studies36,46 evaluated anomaloscopes in patients with diabetes (Table 9).
| Study | Patient selection criteria | Clinical characteristics | Colour vision test (grading method) | Reference standard (grading method) | TP, FP, TN, FN | Sensitivity | Specificity | Other outcome data |
|---|---|---|---|---|---|---|---|---|
| Aspinall 198336 |
Inclusion criteria: diabetes patients < 70 years old with normal fundi Exclusion criteria: congenital colour vision defects; cataracts |
Not stated |
N: normal fundus, fundi still showing no signs of retinopathy in either eye R: retinopathy, fundi showing signs, however slight, in one or both eyes |
Ophthalmoscopy Dichotomous |
Yellow–blue colour discrimination (anomaloscope units JND) coefficient = 5.113 × 10–2, standard error = 1.39 × 10–2, t = 3.67 | |||
| Mäntyjärvi 199546 | Inclusion criteria: schoolchildren with diabetes and healthy eyes at recruitment |
Mean age: 14 years (SD 2; range 9–19) 46.3% male Mean diabetes duration: 6 years (SD 4; range 1 month–15 years) |
Retinopathy vs no retinopathy |
Method not stated/final diagnosis Dichotomous |
0, 0, 22, 31 | 0% | 100% |
Both studies investigated anomaloscope testing to distinguish between participants with signs of retinopathy and those without. Definitions of retinopathy were not clearly specified, and one study46 did not specify the reference standard beyond final diagnosis.
Aspinall et al. 36 evaluated the Pickford–Nicolson anomaloscope and measured colour matching ratios and colour discrimination ranges for red–green, yellow–blue, and green–blue colour equations. A range of test and disease parameters was measured and analysed. Yellow–blue discrimination was found to be the best single factor for establishing retinopathy; when the population was divided at age 40 years, yellow–blue discrimination remained the best single factor in the over 40s and duration of diabetes was found to be the best factor in the under 40s.
Mäntyjärvi et al. 46 evaluated the traditional Nagel anomaloscope and a newer ‘colour vision meter’ (CVM) anomaloscope (which included a blue equation). All participants (with and without retinopathy) scored within normal limits on the Nagel anomaloscope (sensitivity of 0%, specificity of 100%), and the authors reported that mean CVM scores did not significantly differ between groups.
Neither study therefore provided evidence to support the use of these particular anomaloscopes in testing for DR.
Chapter 4 Assessment of cost-effectiveness evidence
Review of existing cost-effectiveness evidence
Methods
Search strategy
MEDLINE, EMBASE, CINAHL, NHS Economic Evaluation Database (NHS EED) and the Health Economic Evaluation Database (HEED) were searched for economic evaluations of CVT for the diagnosis of DR. Searches were performed on 15 November 2007. The full search strategy is described in Appendix 1. In brief, the search strategy for the systematic review of CVT diagnostic accuracy was adapted by including economics search filter terms and excluding diagnostic accuracy terms. In total, after excluding duplicate articles, we identified 356 potentially relevant publications.
Results
Our search identified several economic evaluations of DR screening, including some in NHS settings. 61–63 However, there were no economic evaluations describing the cost and effects of any type of CVT for DR screening. Therefore, we reviewed the existing DR screening economic evaluations to inform parameter estimates for our independent economic assessment of CVT.
Independent economic assessment
Methods of independent economic assessment
Model structure
We developed a decision tree and Markov model to estimate the costs and effects of adding CVT to the current NSPDR using digital photography of the retina. An NHS perspective was taken for the cost-effectiveness analysis. The model was developed in Microsoft excel 2000 and run with 1-year cycles for a time horizon of 50 years. The time horizon of 50 years was felt adequate to represent a lifetime horizon of the vast majority of the cohort. Half-cycle corrections have been used to improve the precision of cost-effectiveness estimates. To represent the uncertainty surrounding our base-case estimates of cost-effectiveness we used probabilistic sensitivity analyses (PSA), based on 1000 Monte Carlo second-order simulations, to estimate the possible distribution of cost-effectiveness. PSA results are presented graphically on the cost-effectiveness plane and cost-effectiveness acceptability curve (CEAC). 64
The hypothetical cohort consisted of patients over the age of 12 years with a recorded diagnosis of diabetes, on a centralised register and invited for screening by the English NSPDR. Two models were created, one each for type 1 diabetes and type 2 diabetes.
Grading diabetes-related eye disease
Three stages of diabetes-related eye disease have been assigned based on those suggested in the English National Screening Committee (NSC) report65 (Table 10). In the Markov model, the preproliferative and proliferative retinopathy states as well as maculopathy are collectively referred to as STDR as all three diagnoses follow similar referral and treatment pathways. Table 10 also compares the NSC retinopathy grades with grades used by the ETDRS,66 which have been used by several large epidemiological studies of disease incidence and progression.
| Retinopathy grade (English NSC) | Description of NSC grades | Modified ETDRS grades and descriptions | Clinical pathway |
|---|---|---|---|
| No retinopathy (R0, M0) | No visible haemorrhage or aneurysm on the fovea | Level 10: no retinopathy | Annual rescreen |
| Background retinopathy (R1) | Microaneurysm(s); retinal haemorrhage(s) ± any exudate not within the definition of maculopathy | Level 20 or 30: haemorrhages/microaneurysms ETDRS STD 2A, and/or < 6 CWS | Annual rescreen |
| Preproliferative retinopathy (R2) | Venous beading; venous loop or reduplication; intraretinal microvascular abnormality (IRMA); multiple deep, round or blot haemorrhages | Level 40 or 50: IRMA ETDRS STD 8A, and/or two or more quadrants venous change | Refer to hospital eye service |
| Proliferative retinopathy (R3) | New vessels on disc (NVD); new vessels elsewhere (NVE); preretinal or vitreous haemorrhage; preretinal fibrosis ± tractional retinal detachment | ≥ Level 60: fibrovascular proliferation, proliferative retinopathy. DRS high-risk characteristics | Refer to hospital eye service |
| Maculopathy (M1) | Exudate within 1 disc diameter (DD) of the centre of the fovea; circinate or group of exudates within the macula; retinal thickening within 1 DD of the centre of the fovea (if stereo available); any microaneurysm or haemorrhage within 1 DD of the centre of the fovea only if associated with a best visual acuity of ≤ 6/12 (if no stereo) | Level 3 or 4: exudate > 1 DD from centre of macula | Refer to hospital eye service |
Patient cohort
The average age of a patient with type 1 diabetes attending retinopathy screening for the first time is approximately 33 years, compared with 65 years for a patient with type 2 diabetes. 67 Because the patient age, prevalence and incidence of eye disease differ substantially between these clinical subgroups, we elected to develop a separate model for each.
Current screening
The current English national screening programme invites eligible individuals with diabetes to referral units typically based at hospitals although they can also be based in mobile units, GP surgeries or optometrists offices. 65 Patients are invited for screening at annual intervals. Screening is performed by a trained and accredited technician68 using a digital non-mydriatic fundus 45-degree field camera with ophthalmological grading. If screening indicates STDR then patients are referred to an ophthalmologist for further assessment and treatment planning. If screening indicates no retinopathy or background retinopathy the individual is invited back for screening at the next annual appointment (Figure 7). In practice, policy varies by region: in some areas individuals graded with background retinopathy may be referred to an ophthalmologist.
FIGURE 7.
Screening pathway. STDR, sight-threatening diabetic retinopathy.
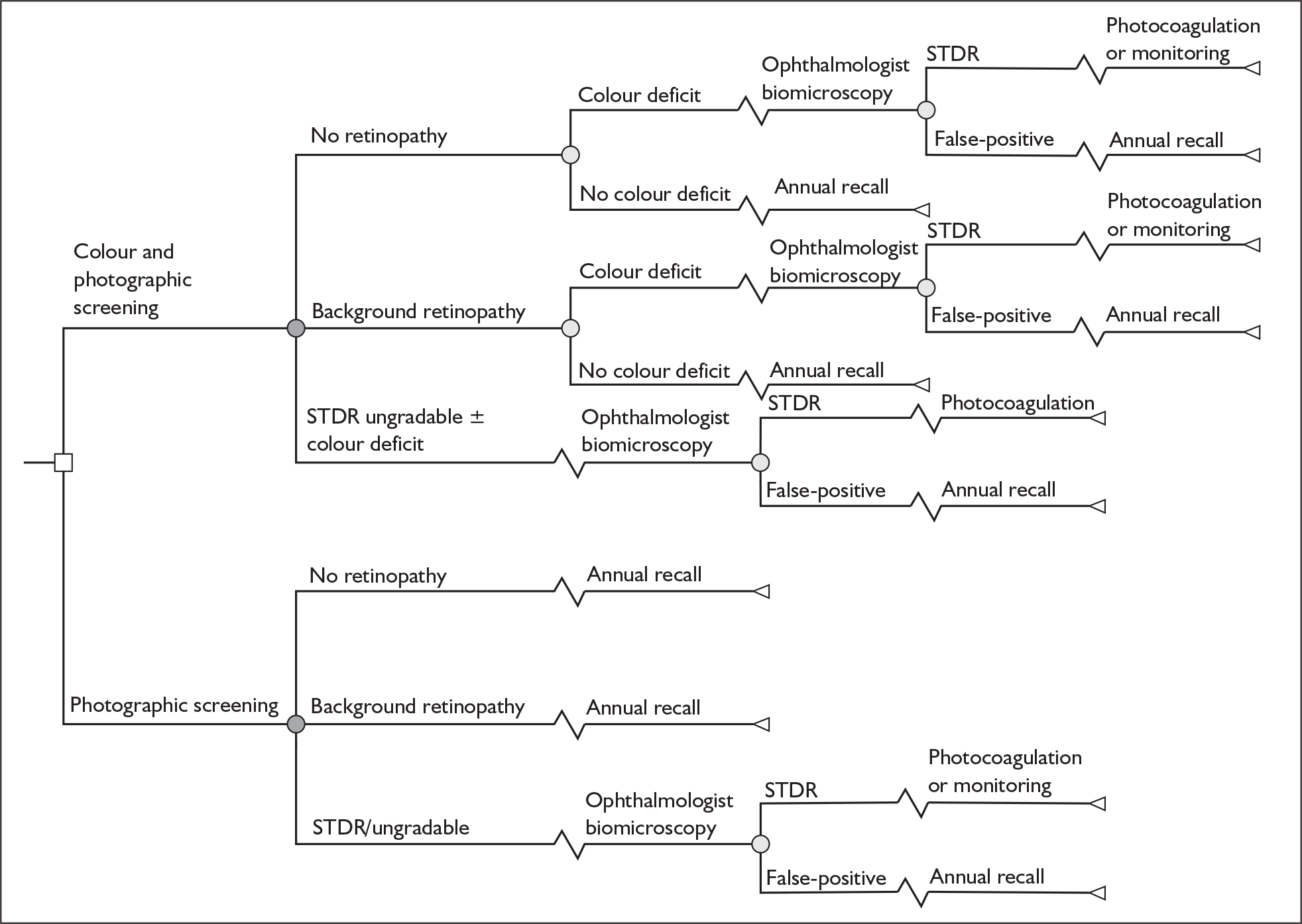
Colour vision testing
CVT may be a useful adjunct to current retinopathy screening methods. It is hypothesised that CVT may be able to detect nascent DR earlier than conventional photographic screening as it measures visual function as opposed to physiological findings associated with visual loss. 60 However, it is currently unclear to what extent this could affect treatment and patient outcomes. There are many methods for CVT (e.g. TCT,31 D-15,69 Mollon–Reffin Minimalist Test,32 FM-10070).
In theory, CVT could be combined with retinal photography screening in many different ways including parallel testing (e.g. refer patient if both tests suggest eye disease) and serial testing (e.g. use the CVT to select patients for, or select the frequency of, retinal photography). Ong and colleagues,31 in the only diagnostic accuracy study combining colour vision and retinal photography screening modalities identified by our systematic review, estimate the sensitivity and specificity of retinal photography only versus retinal photography plus CVT (TCT) with referral if both tests indicate possible eye disease or if retinal photography is ungradable in the presence of colour vision deficit.
In practice, given the acceptance of retinal photography in the NHS retinopathy screening programme, we believe that the most likely current role for CVT is in increasing the sensitivity of screening by identifying individuals with colour vision deficits who do not yet have retinopathy evident on retinal photography. Therefore, the initial structural assumption in our model is that an individual with no or background retinopathy on retinal photography but with colour vision deficit will be referred to the hospital eye clinic for a definitive diagnosis (Figure 7). In our model, an individual with STDR or an ungradable retinal photography result was referred to the hospital eye clinic regardless of the CVT findings. However, the CVT would be performed at the same screening appointment before the results of retinal photography were available and therefore the costs of both tests would be incurred.
Ophthalmologist diagnosis
Patients who screen positive for referable retinopathy or macular oedema are referred to an ophthalmologist for further examination using slit-lamp biomicroscopy. If the ophthalmologist confirms a diagnosis of proliferative retinopathy or macular oedema, the patient is offered laser therapy. Patients with preproliferative retinopathy are kept under ophthalmological surveillance until they either progress to proliferative retinopathy and are suitable for laser photocoagulation, or become blind or die. If the slit-lamp biomicroscopy indicates that the initial screening result was a false-positive finding, the patient will be referred back to the annual screening programme.
Treatment
Photocoagulation targets an argon laser at aneurysms or haemorrhages within the retina. Laser treatment has been shown to be effective in preventing further diabetes-related loss of vision. 71 It is assumed that individuals diagnosed with proliferative STDR are treated with laser photocoagulation and then are recalled for ophthalmological consultation annually.
Disease progression
The possible health state (Markov) transitions are depicted in Figure 8. We assumed that the eyesight of patients with diabetes progresses through the various stages of retinopathy, in some cases leading to blindness. Treatment of STDR with laser photocoagulation slows down the progression from STDR to blindness, but regression from more severe to less severe retinopathy or visual impairment is assumed not to occur.
FIGURE 8.
Markov transitions. STDR, sight-threatening diabetic retinopathy.
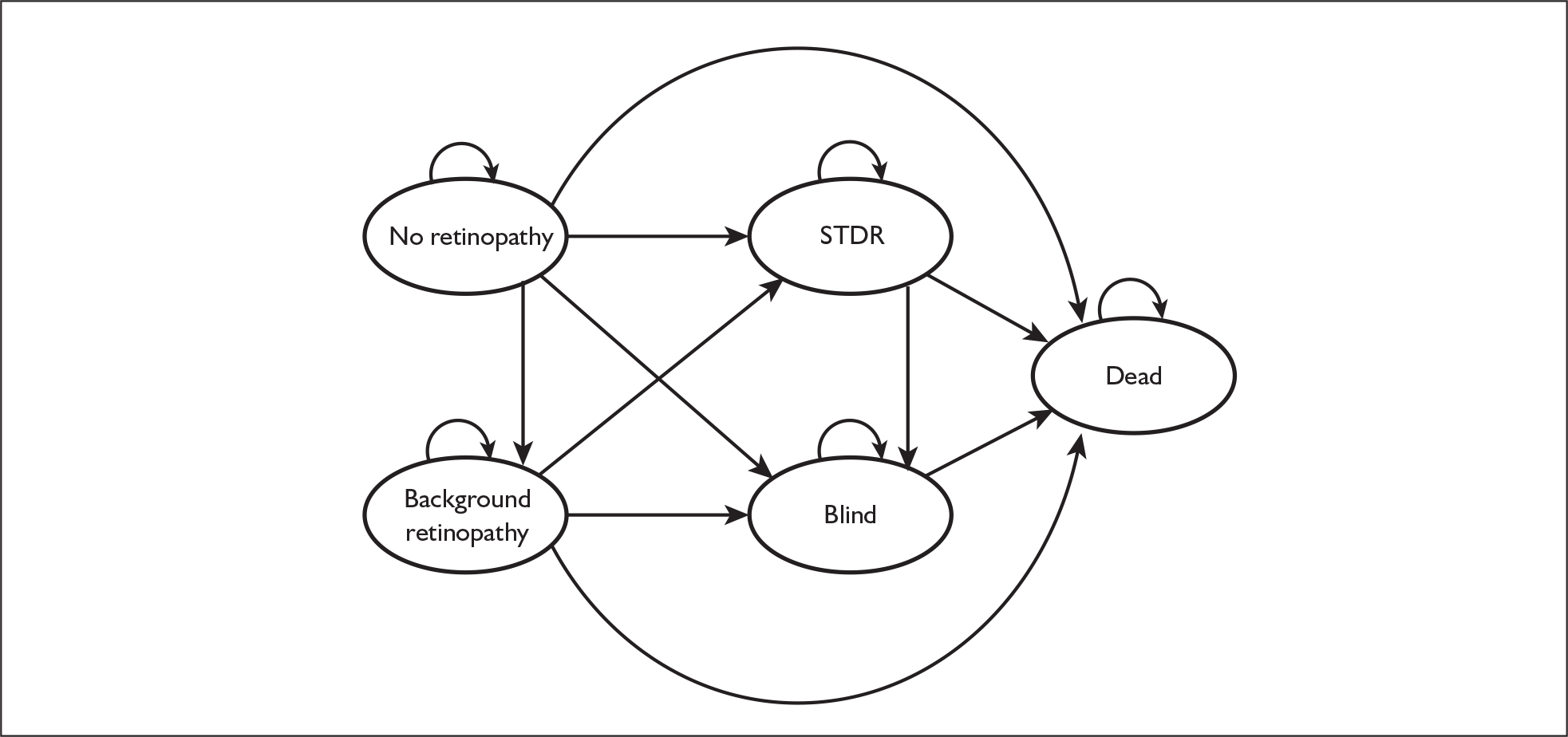
Source data
Screening attendance
The base-case estimate of screening attendance rates was based on the Younis et al. 67 study, which reported that 79% of type 1 and 77% of type 2 patients responded to the invitation and attended screening. 72,73 However, estimates of response rates to retinal photography screening invitations in the UK vary widely. 74,75 Nearly all studies of attendance at systematic screening are based on single centres. The characteristics of patients and methods of inviting individuals for screening differ between centres accounting for the wide variability in the literature. Therefore, we varied attendance rates in the PSA over a uniform distribution between 50% and 100% (Table 11). In the absence of evidence to the contrary, it was assumed that the inclusion of CVT in addition to retinal photography would not alter screening attendance rates.
| Variables | Point estimate | Lower bound | Upper bound | Source | PSA distribution |
|---|---|---|---|---|---|
| Screening attendance:a | |||||
| Type 1 | 0.79 | 0.50 | 1 | Younis 200267 | Uniform (0.5,1)b |
| Type 2 | 0.77 | 0.50 | 1 | Uniform (0.5,1)b | |
| Diagnostic accuracy | |||||
| Photography | Ong 200431 | ||||
| Specificity no retinopathy | 0.95 | 0.93 | 0.97 | Beta (435.97, 23.89)c | |
| Specificity background retinopathy | 0.95 | 0.93 | 0.97 | Beta (435.97, 23.89)c | |
| Sensitivity STDR | 0.88 | 0.64 | 0.99 | Beta (11.49, 2.43)c | |
| Photography with colour vision | |||||
| Specificity no retinopathy | 0.90 | 0.86 | 0.94 | Beta (191.25, 22.14)c | |
| Specificity background retinopathy | 0.90 | 0.86 | 0.94 | Beta (191.25, 22.14)c | |
| Sensitivity STDR | 0.94 | 0.71 | 1 | Beta (12.11, 1.71)c | |
| Ophthalmologista | |||||
| Specificity no retinopathy | 1 | 0.98 | 1 | Assumption | Uniform (0.98, 1)b |
| Specificity background retinopathy | 1 | 0.98 | 1 | ||
| Sensitivity STDR | 1 | 0.98 | 1 | ||
| Prevalenceb | |||||
| Type 1 | Younis 200267 | ||||
| No retinopathy | 0.538 | Dirichleta | |||
| Background retinopathy | 0.365 | ||||
| STDR | 0.097 | ||||
| Technical failure | 0.044 | ||||
| Type 2 | |||||
| No retinopathy | 0.741 | Dirichleta | |||
| Background retinopathy | 0.234 | ||||
| STDR | 0.077 | ||||
| Technical failure | 0.110 | ||||
| Age (years) | |||||
| Type 1 | 33.4 | Younis 200267 | Fixed | ||
| Type 2 | 64.9 | Fixed | |||
| Utility valuesd | |||||
| No retinopathy | 0.83 | 0.63 | 1 | Lloyd 200876 | Normal (0.83, 0.10)d |
| Background retinopathy | 0.83 | 0.63 | 1 | Normal (0.83, 0.10)d | |
| STDR | 0.83 | 0.63 | 1 | Normal (0.83, 0.10)d | |
| Blind | 0.34 | –0.02 | 0.70 | Normal (0.34, 0.18)d | |
| Dead | 0 | Fixed | |||
| Mortality hazard ratios (by diabetes type)e | |||||
| Type 1 vs no diabetes | 3.70 | Soedamah-Muthu 200677 | Fixed | ||
| Type 2 vs no diabetes | 1.93 | Mulnier 200678 | Fixed | ||
| Mortality hazard ratios (by retinopathy grade)e | |||||
| No retinopathy | Reference | Klein 199979 | |||
| Background retinopathy | 1.02 | 0.52 | 1.99 | Lognormal (1.02, 0.34)e | |
| STDR/blind | 1.28 | 0.62 | 2.62 | Lognormal (1.28, 0.37)e | |
| Treatment compliance | |||||
| Attendance at ophthalmologist | 1 | 0.95 | 1 | Assumption | Uniform (0.95, 1)b |
| % of STDR receiving immediate photocoagulation | 20.8% | 10.4% | 41% | Harvey 200680 | Uniform (0.104, 0.410)b |
| % of preproliferative STDR (type 1) who develop proliferative STDR and have photocoagulation | 13.5% | 4.2% | 22.7% | Younis 200372 | Uniform (0.042, 0.227)b |
| % of preproliferative STDR (type 2) who develop proliferative STDR and have photocoagulation | 15% | 10.2% | 19.8% | Younis 200373 | Uniform (0.102, 0.198)b |
| Compliance with photocoagulation | 1 | 0.95 | 1 | Assumption | Uniform (0.95, 1)b |
| Discount rate | |||||
| Costs | 3.5% | NICE | Fixed | ||
| QALYs | 3.5% | Fixed | |||
| Costsc | |||||
| Additional cost colour screening | £7.80 | £3.90 | £29 | Calculated in Table 20 | Uniform (£3.90, £29)b |
| Photographic screening | £29 | £14.50 | £58 | Garvican 200468 | Uniform (£14.50, £58)b |
| Ophthalmologist appointment | £65 | £32.50 | £130 | Garvican 200468 | Uniform (£32.50, £130)b |
| Photocoagulation | £815 | £407.50 | £1630 | Garvican 200468 | Uniform (£407.50, £1630)b |
| Annual NHS cost of blindness | £872 | £526 | £1299 | Clarke 200381 | Normal (872, 197.20)d |
Diagnostic accuracy
Sensitivity and specificity data for the screening methods are shown in Table 11. The base-case estimates of the diagnostic accuracy of retinal photography and CVT are taken from Ong et al. 31 This was a prospective, comparative study of a type of CVT (TCT) compared with non-mydriatic fundus 45-degree field camera with ophthalmological grading.
In this study, 510 patients with diabetes attended a hospital-based screening centre. All patients had their eyes individually tested on the TCT followed by photographic testing in both eyes. Slit-lamp examination by an experienced ophthalmologist (considered the gold standard) was also carried out on each patient. Retinopathy grades were assessed for each test in a masked and independent manner. Ong et al. report that the sensitivity and specificity of retinal photography alone for the detection of STDR are 88% (15/17) and 95% (470/493) respectively. CVT alone had higher sensitivity 94% (16/17) and similar specificity 95% (467/493). 31 Ong et al. do not report the sensitivity and specificity of a strategy of using CVT only in patients with negative (i.e. no retinopathy or background retinopathy) retinal photography results. In the absence of this information, in the base case we assumed that the sensitivity of the combined screening strategy could increase to 94%, but specificity would be lower at 90% (assuming independence of test specificity). Therefore, CVT could potentially lead to earlier detection of DR, but would also result in more referrals to the hospital eye service. We note, however, that our estimate is based on only one study, using one type of CVT that is not readily available in clinical practice, in a very small number of patients with STDR. In sensitivity analyses we explore the thresholds of sensitivity and specificity at which CVT potentially becomes cost-effective.
Because of a paucity of evidence, any potential predictive ability of including CVT in the screening workup has not been included in our modelling approach.
As slit-lamp biomicroscopy performed by an ophthalmologist is considered to be the reference standard for diagnosing diabetic eye disease, the sensitivity and specificity of this test are assumed to be 100%. In our PSA we varied this assumption by assuming a uniform distribution for both sensitivity and specificity between 98% and 100%.
Initial prevalence
The initial prevalence of diabetic eye disease in patients with type 1 and type 2 diabetes (Table 11) was taken from a large study of individuals attending a primary care-based DR screening programme. 67 The study was based in Liverpool and included patients with diabetes who were not under the continuing care of an ophthalmologist and who, at baseline, had not been in the systematic screening program before. Patients with type 1 (n = 831) and type 2 (n = 7231) diabetes were recruited between 1991 and 1999. Retinopathy and maculopathy were graded from dilated three-field non-stereoscopic photography by trained graders. Younis et al. 67 reported diabetes-related eye disease using an adaptation of the ETDRS gradings,66 which we mapped to the English NSC Retinopathy Grading Standard65 so that all grading definitions are consistent across the model (Table 10). For example, 442 out of 822 individuals (i.e. 53.8%) with type 1 diabetes and gradable biomicroscopy had no retinopathy (level 10).
Images from photographic screening may, because of technical failures, be ungradable. In these circumstances individuals are automatically referred to the hospital eye service for ophthalmologist grading. Data on the rate of technical failure have been taken from the Younis et al. study,67 in which 36 out of 822 (4.4%) images were ungradable for type 1 patients and 796 out of 7231 (11%) for type 2. The higher rate of ungradable images in the type 2 population reflects the older age of patients. It was assumed that ungradable images are equally likely to occur across all DR grades. The impact of uncertainty about the prevalence of retinopathy was assessed in our PSA; prevalence probabilities were assumed to follow a Dirichlet distribution based on the source data in the Younis et al. 67 study.
Disease transition
Annual transition rates for the progression through the various stages of DR, within a screened population, have been calculated separately for type 1 (Table 12) and type 2 diabetes (Table 13). 72,73 Type 1 (n = 501) and type 2 (n = 4770) patients from the Liverpool Diabetic Eye Study were screened at annual intervals for up to 6 years after first entering the screening programme. We converted the 6-year cumulative incidences of DR reported in the Liverpool study into annual transition probabilities using a standard conversion formula. 83 For example, the 6-year cumulative incidence of STDR in patients with type 1 diabetes and initially no retinopathy was 5.4%. This is equivalent to an annual transition probability of 0.92%. 83 These transition probabilities have been deflated to take account of transitions to mortality and blindness detailed below.
A proportion of patients with preproliferative STDR are not initially offered laser photocoagulation80 but remain under ophthalmologist monitoring until they develop proliferative retinopathy. We used data from the Liverpool study to estimate the annual transition from preproliferative to proliferative STDR72,73 (Table 11).
Data for the annual probabilities of transition to blindness from either no retinopathy or background retinopathy were taken from the economic evaluation of DR screening of Dasbach et al. 84 and used data from the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR). Dasbach et al differentiated the severity of DR into high risk and low risk of progression to blindness. For our model, no retinopathy and background retinopathy have been considered equivalent to low risk in the Dasbach model.
Effectiveness of laser photocoagulation
The transition probabilities from STDR to blindness in treated and untreated patients have been taken from Odland et al. 71 This study was a randomised controlled trial involving 107 patients with a similar degree of STDR in both eyes, followed for 5–7 years after treatment, testing the efficacy of photocoagulation. One eye chosen at random was treated whilst the other was used as a control. In total, 77 individuals completed the 5-year follow-up. At follow-up, 44% (34/77) of eyes in the control group were legally blind compared with 13% (10/77) in the treatment group, suggesting annual transition probabilities of 10.9% and 2.7% respectively (see Tables 12 and 13). Odland et al. did not differentiate between individuals with type 1 and type 2 diabetes and so, in our model, both have an identical transition probability before deflating for mortality.
| NR | BR | STDR | Blind | Dead | |
|---|---|---|---|---|---|
| NR | 0.9021 | 0.0809 | 0.0091 | 0.000 | 0.0074 |
| BR | 0 | 0.8659 | 0.1266 | 0.000 | 0.0075 |
| STDR | 0 | 0 | 0.8826 | 0.1080b | 0.0095 |
| Blind | 0 | 0 | 0 | 0.9905 | 0.0095 |
| Death | 0 | 0 | 0 | 0 | 1 |
| NR | BR | STDR | Blind | Dead | |
|---|---|---|---|---|---|
| NR | 0.8757 | 0.0789 | 0.0141 | 0.000 | 0.0312 |
| BR | 0 | 0.8447 | 0.1234 | 0.000 | 0.0319 |
| STDR | 0 | 0 | 0.8554 | 0.1046b | 0.0400 |
| Blind | 0 | 0 | 0 | 0.9600 | 0.0400 |
| Death | 0 | 0 | 0 | 0 | 1 |
Health-related quality of life
Utility values have been taken from Lloyd et al. 76 (Table 11). Utilities in this study were obtained from a group of patients with type 1 or type 2 diabetes and retinopathy in the UK (n = 122). Patients rated their current health using the EuroQol 5 dimensions (EQ-5D) questionnaire, which provides a single utility score [anchored at 1 (best health) and 0 (health state as bad as death)] for current health. Lloyd et al. found a mean utility score of 0.83 in patients with no DR and a utility score of 0.34 for patients with severe vision loss (counting fingers – hand motion). We assumed that most patients attending screening would be asymptomatic (0.83 utility score) and that the benefit of screening and treatment is through reducing the probability that a patient with STDR becomes legally blind (0.34 utility score).
Although it would have been more realistic to model differing severities of vision loss, we were unable to do so. The randomised controlled trial of photocoagulation71 did not report results in sufficient detail to be combined with the utility scores for imperfect vision estimated by Lloyd et al. 76
Mortality
Age-specific mortality rates are based on general population UK life tables (ONS, 2008, www.statistics.gov.uk/) and have been inflated to reflect the higher mortality rates of individuals with diabetes. Mortality rates gradually increase throughout the lifetime of the modelled cohort as it ages. We adjusted general population mortality rates using hazard ratios taken from Soedamah-Muthu et al. 77 for type 1 diabetes and Mulnier et al. 78 for type 2 diabetes (Table 11). Both studies were prospective cohort studies following patients from 1992 to 1999 matching a cohort with diabetes (n = 7713,77 n = 44,23078) to an age and sex-matched cohort with no history of diabetes (n = 38,518,77 n = 219,79778). Mortality hazard ratios between the two groups were calculated using Cox proportional hazard models. The mortality hazard ratio in type 1 diabetes was 3.7 times higher than that in the matched general population and for type 2 diabetes the hazard ratio was 1.93 times higher.
These mortality rates were then adjusted further to reflect positive correlation between the severity of diabetes-related eye disease and mortality based on Klein et al. 79 (Table 11). This was a population-based cohort study following 996 younger-onset and 1370 older-onset patients. Klein et al. reported the mortality hazard ratios for patients with mild retinopathy and proliferative retinopathy compared with a reference group with diabetes but no retinopathy. In our model we assumed that the relative mortality of patients with background retinopathy was equal to that of patients with ‘mild retinopathy’ and the mortality of patients with STDR was equal to that of patients with proliferative retinopathy. As there is no evidence to suggest that photocoagulation affects mortality, we assumed that mortality did not increase in patients with STDR who subsequently became blind.
Attendance at hospital eye clinics and compliance with therapy
Previous decision-analytical models have often assumed that 100% of patients who have positive screening results will attend the ophthalmology clinic for further diagnostic workup and, if indicated, undergo therapy for retinopathy. 62,85,86 We have also assumed in our base case that there is 100% attendance for both, but have used a uniform distribution between 95% and 100% to assess the impact of imperfect compliance on our conclusions in the sensitivity analysis.
Costs
All current screening costs have been taken from the 2004 costings of diabetic retinal photography screening in England of Garvican. 68 That paper estimated a cost of £23 per patient on a diabetes register and £29 per patient screened if we assume an attendance rate of 80% for registered patients at screening appointments (similar to the attendance levels used in the base-case estimate). This is made with the assumption of a geographic region containing 15,000 individuals with diabetes eligible for screening and included all costs associated with equipment (e.g. cameras, eye drops), staffing, screening invitation, administration and quality assurance. A full breakdown of the costs is shown in Table 14.
| Cost per year | |
|---|---|
| Administration: salaries (office manager and two part-time clerical assistants), postage, maintenance | £105,000 |
| Photography: camera (n = 4) maintenance, technician salary 3.5 WTE, storage | £140,000 |
| Grading costs: salary 1.5 WTE of ‘expert grader’ | £45,000 |
| Quality assurance: consultant ophthalmologist 1–2 sessions per week, 0.5 WTE ‘expert grader’ | £30,000 |
| Management: (0.5 WTE programme manager) session consultant time | £32,000 |
| Total | £354,000a |
| Cost per test (80% attendance) | £29 |
We are not aware of any studies on the costing or resource use of any CVT in a clinical setting. To minimise administrative and patient burden, we have assumed that the CVT is conducted during the same screening appointment as the retinal photography. Therefore, administration and management costs would not increase greatly. Many of the automated CVTs, including the TCT used by Ong et al. ,31,60 are not commercially available. Therefore, as an example of the likely cost of CVT, we have estimated the cost of including the FM-100 test alongside retinal photography screening. We vary the cost of CVT widely in our sensitivity analysis to establish a threshold cost at which CVT might be cost-effective.
The capital cost of a FM-100 test kit is £350 (Richmond Products), and a lamp to provide the appropriate lighting costs £140 (Macbeth Lighting). It is assumed that, at most, four CVT sets and lamps would be purchased each year to be used alongside the four retinal cameras. Over time, and through use, the testing kit hues degrade; therefore, we have assumed that the kits need replacing each year. The introduction of the test would lead to an increase in staff time because of extra time spent administering the CVTs and automated recording of the results. We have made the assumption that additional staff time would be equivalent to 3.5 full-time technicians. Effectively, the introduction of CVT would double the amount of technician time compared with a screening programme based solely on retinal photography.
The extra costs associated with using the FM-100 test alongside photographic screening are presented in Table 15. For a geographical area of 15,000 people eligible for screening this will lead to an increased cost of £7.80 per patient screened. The FM-100 probably represents a lower bound for the cost of CVT. For automated CVTs, the equipment and maintenance costs are likely to be much higher, although technician costs could be lower.
| Cost | |
|---|---|
| FM-100 tests (n = 4) | £1400 |
| Macbeth Easel lamp (n = 4) | £560 |
| 3.5 WTE screening technicians | £91,000 |
| Total | £92,960 |
| Cost per test (80% attendance) | £7.80 |
Based on previous work,68 the cost for a referral to an ophthalmologist is estimated to be £65 and bilateral photocoagulation costs are £815, which is made up of 1.5 treatments (average number of treatments needed per patient) and 8 outpatient follow-ups. Those who are screened as having preproliferative retinopathy are assumed to be recalled to an ophthalmologist annually, incurring an ophthalmologist cost of £65. This is incurred until the patient progresses to proliferative retinopathy or until they go blind or die. All patients who are blind also incur an annual cost of £872. 81 An annual ophthalmologist cost of £65 has been added to post laser photocoagulation patients to represent the cost of continued monitoring. All costs have been varied in the PSA, assuming uniform distributions from 50% to 200% of the primary estimate. This is to reflect the large uncertainties regarding the costs.
All costs have been inflated to 2007 prices using the hospital and community health services price indices. All costs and quality-adjusted life-years (QALYs) after the first year of the model have been discounted at 3.5% per annum.
Analysis
We calculated the incremental cost-effectiveness ratio (ICER) of screening using CVT as an adjunct to retinal photography versus retinal photography alone. Although there is no uniformly accepted ICER threshold defining cost-effective care, NICE87 has cited a £20,000–30,000 per QALY threshold below which an intervention is generally accepted as cost-effective.
Results of independent economic assessment
The costs and QALYs of both current photographic screening and photographic screening with CVT, using our baseline assumptions, are shown in Table 16 for type 1 diabetes and Table 17 for type 2 diabetes. Adding the CVT to the screening workup adds a lifetime discounted cost of £105 per person for type 1 diabetes with a marginal increase in lifetime discounted QALYs (0.017) and years of sight (0.068). For type 2 diabetes there is an increase in cost of £177 for adding CVT with an increase in QALYs and years of sight of 0.006 and 0.022 respectively.
| Photographic screening | Photographic screening with adjunct CVT | |
|---|---|---|
| Percentage of patients who attend screening given a correct screening diagnosis in year 1 | 87.0% | 83.2% |
| Percentage of cases of STDR identified by screening | 70.1% | 74.6% |
| Total ophthalmologist appointments (15,000 people over 50 years) | 36,826 | 44,127 |
| Lifetime costsa | £2422 | £2527 |
| Lifetime QALYsa | 12.900 | 12.917 |
| Average years of lifeb | 31.185 | 31.185 |
| Average years of sightb | 21.739 | 21.807 |
| ICERa | £6364/QALY |
| Photographic screening | Photographic screening with adjunct CVT | |
|---|---|---|
| Percentage of patients who attend screening given a correct screening diagnosis in year 1 | 80.0% | 77.4% |
| Percentage of cases of STDR identified by screening | 68.9% | 73% |
| Total ophthalmologist appointments (15,000 people over 50 years) | 33,750 | 39,585 |
| Lifetime costsa | £1049 | £1226 |
| Lifetime QALYsa | 9.013 | 9.019 |
| Average years of lifeb | 16.908 | 16.908 |
| Average years of sightb | 14.111 | 14.133 |
| ICERa | £12,432/QALY |
In all patients, CVT increases the lifetime costs per individual because of higher screening costs and also through the increase in ophthalmologist appointments and treatment because of the increased numbers of true-positives for STDR and false-positives. Overall, the proportion of patients with a correct screening diagnosis is lower when CVT is combined with retinal photography, because of the increase in false-positives. In our model, the addition of CVT increased ophthalmologist workload by approximately 7300 appointments during the lifetime of the cohort for the type 1 diabetes cohort and by 6000 appointments for the type 2 cohort.
CVT increases the number of lifetime QALYs and years of sight by increasing the number of patients with STDR who ultimately receive an ophthalmologist appointment and treatment. In total, 74.6% of patients with type 1 diabetes and STDR are correctly identified by CVT combined with retinal photography, compared with 70.1% of the same patients screened with retinal photography alone. A similar increase in true-positives is evident in patients with type 2 diabetes. The results of the base-case analysis show an ICER of £6364 per QALY and £12,432 per QALY for type 1 and type 2 diabetes respectively. This suggests that the addition of CVT in the screening workup can be cost-effective (i.e. below £20,000 per QALY) if the additional testing method adequately increases sensitivity and is relatively inexpensive.
Threshold/scenario analysis
Figures 9 and 10 depict the impact of different levels of sensitivity of CVT on the ICER, keeping all other base-case estimates constant. The ICER rises sharply as the sensitivity of combined CVT and retinal photography falls towards 0.88 (the sensitivity of retinal photography alone). However, because CVT screening is relatively cheap and photocoagulation is effective at reducing progression to blindness, the sensitivity of CVT and retinal photography screening has to fall to 0.896 (type 1 diabetes) or 0.916 (type 2 diabetes) before the ICER for type 1 diabetes exceeds the £20,000 threshold.
FIGURE 9.
Two-way threshold analysis of the sensitivity and cost of colour vision testing for sight-threatening diabetic retinopathy (STDR)versus the incremental cost-effectiveness ratio (ICER) (type 1 diabetes).
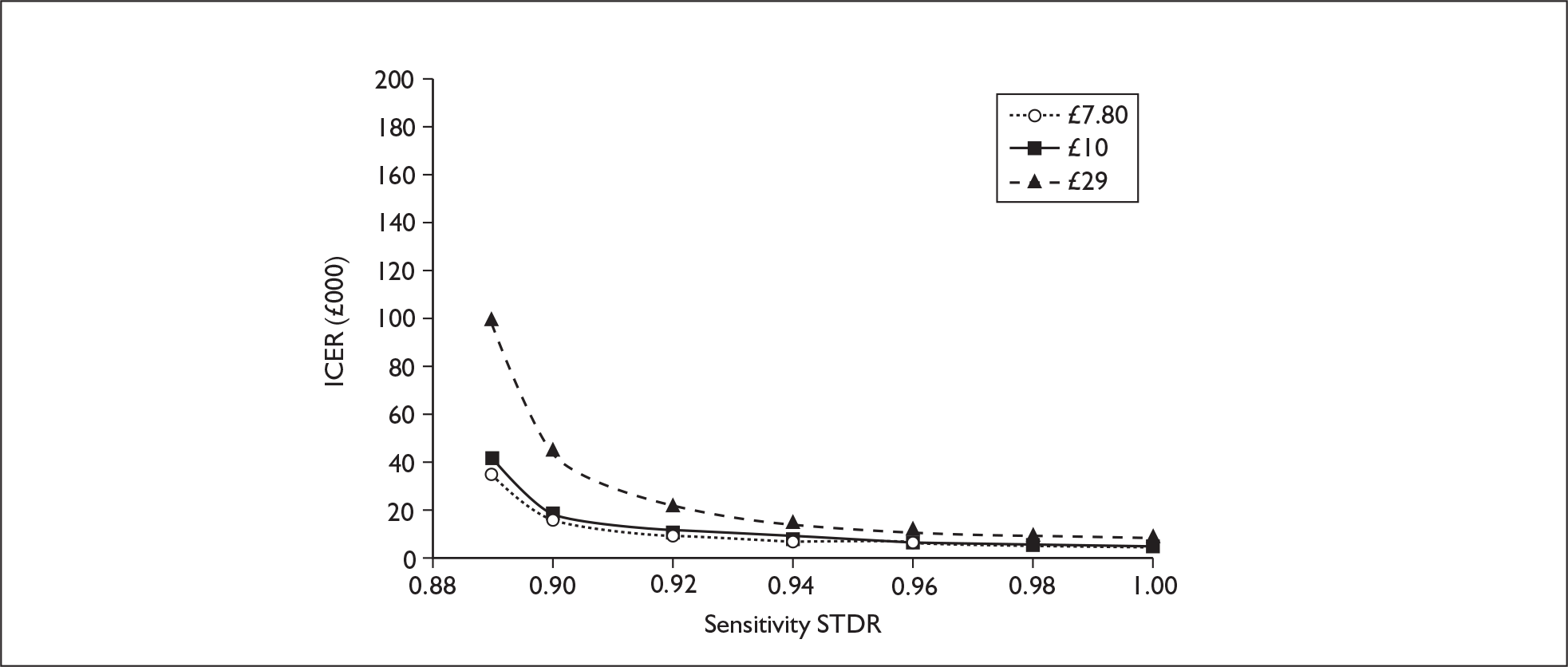
FIGURE 10.
Two-way threshold analysis of the sensitivity and cost of colour vision testing for sight-threatening diabetic retinopathy (STDR) versus the incremental cost-effectiveness ratio (ICER) (type 2 diabetes).
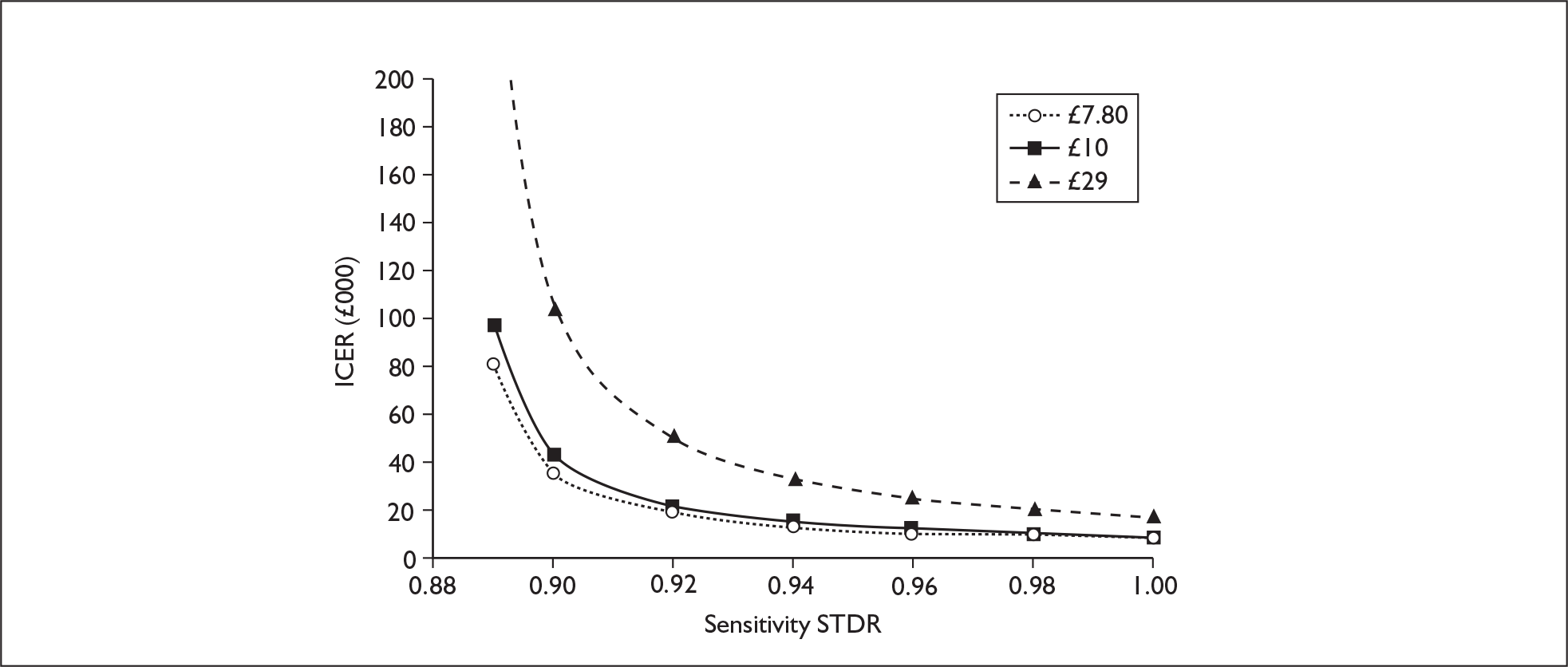
At an additional cost of CVT testing of £29, doubling the overall cost of the screening workup, the ICER still remains below the £20,000 threshold for our base case of 94% sensitivity for STDR in type 1 diabetes (Figure 9). However at this cost a small reduction in sensitivity below the base case 94% (0.924 for type 1 diabetes) would render the use of CVT not cost-effective. If CVT costs £29, the ICER for type 2 diabetes is not below the £20,000 threshold unless the sensitivity is increased to 0.984 (Figure 10).
Probabilistic sensitivity analysis
The cost-effectiveness planes in Figures 11 and 12 show that, under our structural assumptions, the inclusion of CVT in screening always results in increased costs and is as effective or more effective than retinal photography screening alone. This is because the results of CVT only affect the management of patients with negative retinal photography screening results, in effect increasing the sensitivity and reducing the specificity of screening. The increased sensitivity leads to increased effectiveness, but the cost of the CVT itself and the additional ophthalmologist visits because of reduced specificity lead to increased costs overall. The increased number of false-positive cases referred to the ophthalmologist may also increase unnecessary anxiety, although this is difficult to quantify and is not included in our QALY calculations. The uncertainty about whether CVT is more accurate than current retinal photography screening, because of the paucity of diagnostic accuracy studies, is depicted by the number of points that lie on or very close to the vertical axis (where the CVT strategy is not effective).
FIGURE 11.
Cost-effectiveness plane – type 1 diabetes.
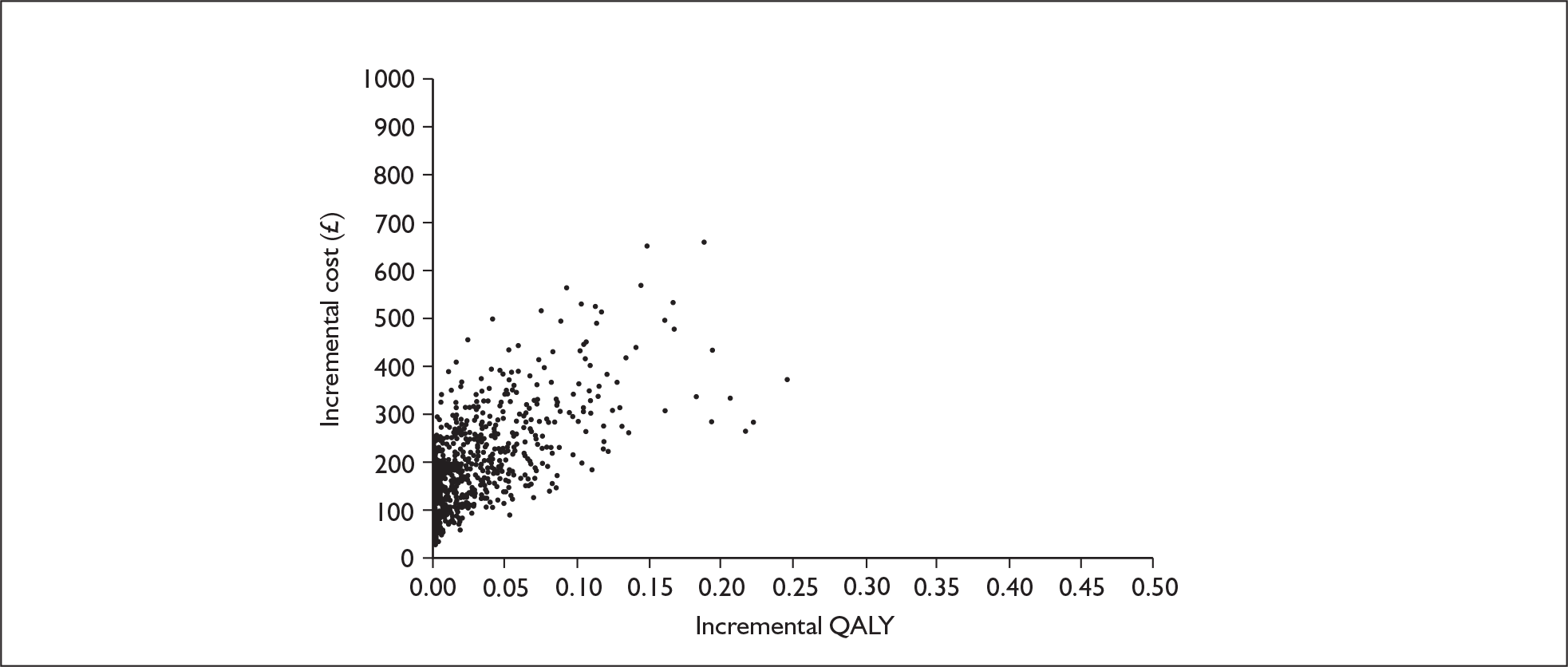
FIGURE 12.
Cost-effectiveness plane – type 2 diabetes.
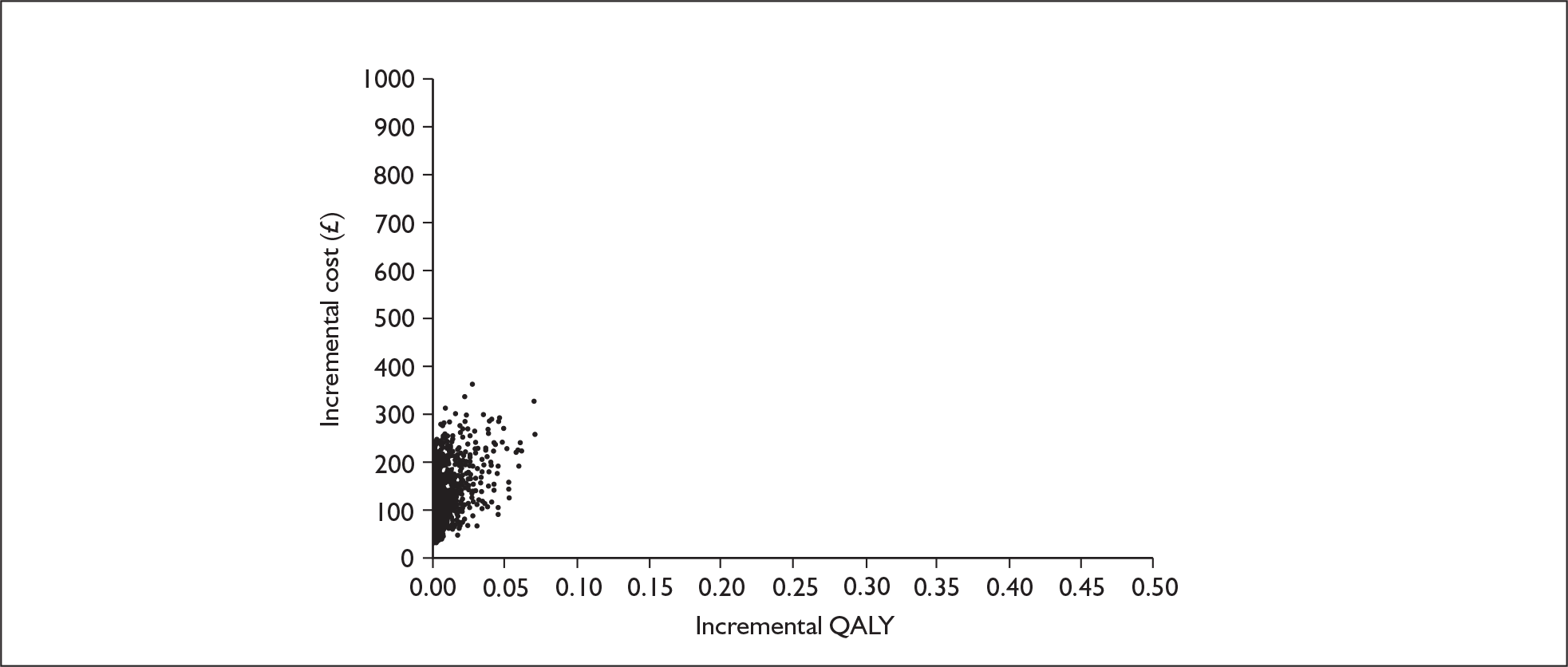
The CEACs (Figures 13 and 14) derived from the PSA indicate a 52.9% probability (type 1) or 39% probability (type 2) that the addition of CVT to retinal photography will be cost-effective at a cost per QALY threshold of £20,000. The fact that the probability of cost-effectiveness depicted in the CEACs never increases beyond 70%, no matter how much society is willing to pay for a QALY, reflects the considerable uncertainty that CVT combined with retinal photography is more sensitive than retinal photography alone. If CVT combined with retinal photography is not more sensitive, it is unlikely to be effective or cost-effective in improving patient outcomes.
FIGURE 13.
Cost-effectiveness acceptability curve – type 1 diabetes.
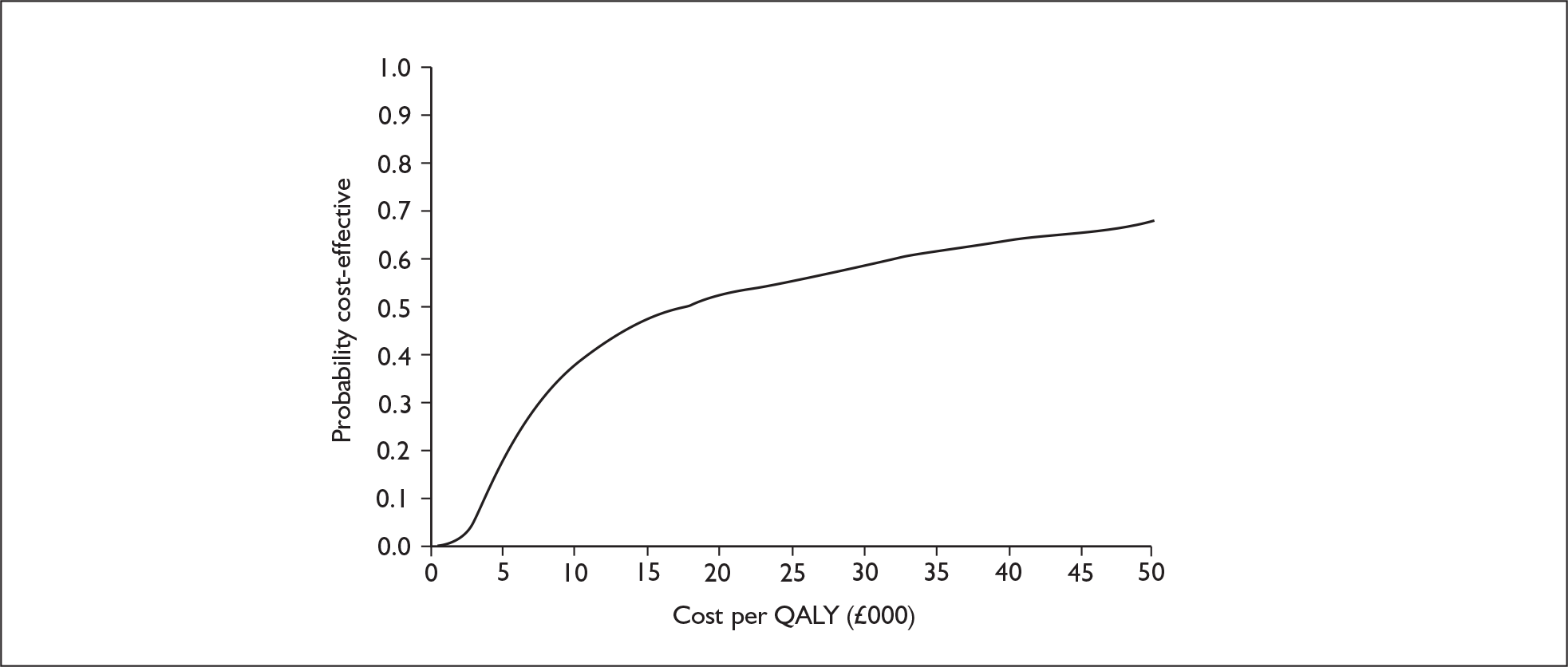
FIGURE 14.
Cost-effectiveness acceptability curve – type 2 diabetes.
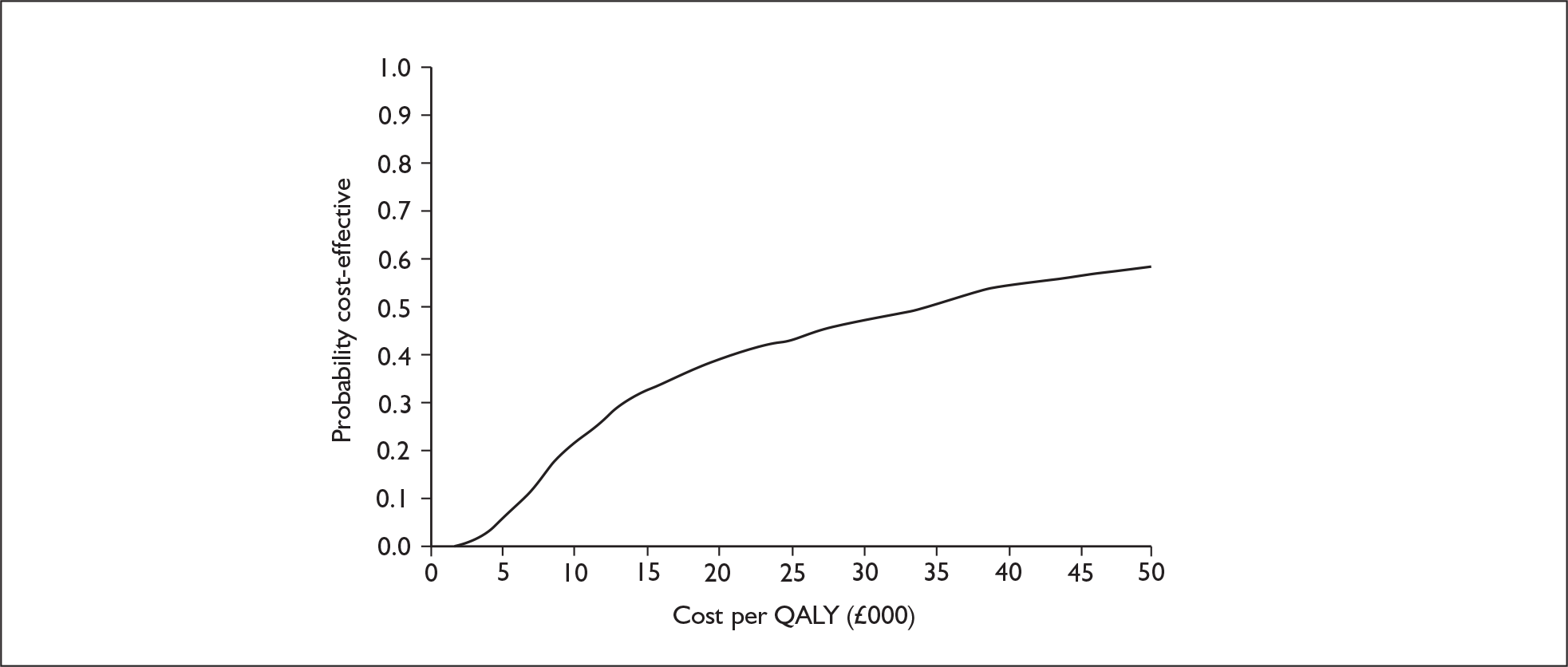
Chapter 5 Survey of current practice
Methods
The aim of the survey was to determine which tests are currently used in the detection and management of DR, over and above the requirements of the national screening programme, to gather views of practitioners on the potential role of CVT.
The English NSC was set up to provide advice, support and facilitation to strategic health authorities, primary care trusts and local programmes implementing systematic DR screening programmes. The aim of the programme is to reduce the risk of sight loss among people with diabetes, by the prompt identification and effective treatment of sight-threatening retinopathy, at the appropriate stage during the disease process. 88 We consulted the NSC for their input before survey development, and contacted national screening programme clinical leads and project managers through the committee.
The survey was created using the online software Survey Monkey (www.surveymonkey.com/). A link to the online survey was sent to the target respondents.
Questionnaire specification
Participants were asked general identification questions, which geographical region they were from and how many primary care trusts are covered by their local programme. Participants were then asked to select from several options the primary methods of retinal screening that their programme currently uses and if any additional tests are routinely used. The following questions concerned who receives the additional tests, be it all patients screened or a specific subgroup. An open question at the end of the survey asked respondents to list and give details on any screening tests that they felt deserved to be a future research priority (see Appendix 5).
When composing the survey we avoided the use of leading questions that might prompt respondents to discuss colour vision specifically. A combination of tick box and open questions were used when appropriate.
Sample selection and data collection
All NSPDR clinical leads and project managers at 96 local programme centres in England were invited to take part in the online survey. These participants were contacted via the NSC. To maximise the response rate, potential participants were sent a reminder email 1 month after receiving the initial survey.
Data analysis
The survey data were cleaned and deduplicated to remove multiple responses from the same individual. Proportions were calculated across different responses.
Results of the survey
Clinical leads and project managers from 48 of a possible 96 centres responded to the survey, giving a response rate of 50%. Respondents were evenly spread over the geographical regions of England. The southwest had the highest proportion of respondents (18.9%) and Yorkshire and the Humber had the smallest (5.7%).
The National Service Framework for diabetes was set up to ensure that all patients with diabetes were offered retinopathy screening by December 2007. Therefore it was anticipated that respondent centres would have at least one method of screening for all patients in the local area covered by their programme. The results show that retinal photography is the primary method of screening used in all of the responding local DR screening programmes, and that none of these local programmes routinely uses CVT, nor is it used for research purposes. In total, 2% of respondents reported contrast sensitivity, 6% slit-lamp biomicroscopy and 2% ophthalmoscopy as other routinely used tests.
Only 8% of the respondents believed that CVT should be a future research priority for the NSPDR. These respondents were from Lincolnshire, Nottingham, Shropshire and Southampton. Although CVT is not high on the research agenda of many of the clinical leads or programme managers, it is interesting to note that optical coherence tomography was listed by 32% of the respondents as being a test that should be a future research priority. An optical coherence tomography scan is an optical analogue of ultrasound imaging, which uses low coherence interferometry to acquire cross-sectional images of the retina. 89
Chapter 6 Discussion
Statement of principal findings
Clinical evaluation
Quantity and quality of evidence
The limited available evidence on the diagnostic accuracy of CVT in DR is generally of poor methodological quality. With a few exceptions, the potential for multiple biases could not be excluded. For example, spectrum of disease is an important consideration in the evaluation of diagnostic accuracy, yet on the QUADAS evaluation only one included study met the ‘appropriate spectrum composition’ criterion. In addition, the majority of studies excluded groups of patients (i.e. those with poorer visual acuity) that form part of the typical diabetes screening population, thereby limiting the generalisability of these findings to a screening context.
Pseudoisochromatic plates
A very small amount of poorly reported evidence is available on the diagnostic accuracy of pseudoisochromatic plates. Ishihara plates are not designed to detect tritan defects, and the available evidence suggests that they are of little value in screening for DR.
Arrangement tests
A small number of studies show a correlation between FM-100 score and degree or stage of retinopathy; however, diagnostic accuracy estimates were highly variable and no consistent cut-off value for FM-100 score was identified among the included studies. Even for the detection of more advanced retinopathy, accuracy estimates were poor, which suggests that FM-100 alone would not be useful as a screening tool for the detection of DR.
Although diagnostic accuracy estimates in adults with diabetes were more consistent across studies of the D-15 than across those of the FM-100, specificities were generally low and, on the basis of the available evidence, the D-15 alone does not appear to be a promising screening tool for the detection of DR.
The NCT showed little promise as a screening test and, although a single study reported promising results for the Mollon–Reffin Minimalist Test in detecting CSMO, no data were available on its ability to detect less severe forms of retinopathy. In addition, this test is not currently commercially available.
Computerised/automated tests
Of the six studies evaluating computerised or automated CVTs, four focused on tritan testing using the ChromaTest or variants of the SGM. Specificities were generally good for detecting more advanced retinopathy and CSMO, although sensitivities were more variable. As with the surface arrangement tests, these methods appear less sensitive and specific in detecting milder forms of retinopathy. In one study, the combination of positive results on both TCT and retinal photography produced an extremely high positive likelihood ratio for the detection of sight-threatening retinopathy, but did not appear to improve the ability of retinal photography alone to rule out disease. The optimal performance thresholds reported for these tests were derived from the data collected in the evaluation, thereby potentially biasing the diagnostic accuracy results in favour of the test. It should also be noted that these studies were all conducted in collaboration with the developers of the ChromaTest/SGM tests; there is no independent evaluative evidence available.
Anomaloscopes
Although generally considered the gold standard for detecting (typically red–green) colour deficiencies, the evidence on anomaloscopes was limited in both quality and quantity. The two available studies gave conflicting findings, one reporting that yellow–blue discrimination was the best single predictive factor of retinopathy and the other reporting no differences in anomaloscope performance between diabetes patients with and without retinopathy. Therefore these methods cannot currently be recommended as a tool for screening for DR.
Economic evaluation
The results of the base-case analysis give an ICER of £6364 and £12,432 for type 1 and type 2 diabetes, respectively, suggesting that the addition of CVT to the screening workup can be cost-effective if it adequately increases sensitivity (compared with retinal photography alone) and is relatively inexpensive.
However, as noted in the systematic review of diagnostic accuracy, the direct evidence on diagnostic accuracy of CVT alone is scant and studies evaluating the accuracy of combining CVT with retinal photography are even more rare. Therefore the results of our base-case analysis indicate what CVT might achieve if larger, independent diagnostic accuracy studies confirm the preliminary findings of Ong et al. 31,60 that it can increase the sensitivity of retinal photography alone. Our PSA highlighted the uncertainty in the literature on the diagnostic accuracy of CVT. There is still a substantial probability that CVT is not diagnostically accurate enough to be either an effective or a cost-effective addition to current screening methods.
Survey
Our survey of national screening programme clinical leads and project managers indicated the following:
-
retinal photography is universally employed as the primary method for retinal screening
-
a small minority of local programmes also incorporate slit-lamp biomicroscopy and contrast sensitivity testing
-
no centres responding to the survey reported using CVT as part of their retinopathy programme, and few considered CVT to be a research priority
-
a substantial proportion of respondents considered optical coherence tomography to be a research priority.
Strengths and limitations of the assessment
Clinical evaluation
We searched a wide range of electronic databases and other sources to identify relevant studies for the systematic review. However, despite using a search strategy designed for maximum sensitivity, only a small amount of evidence on CVT in diabetes was found. We included relevant studies regardless of language of publication or publication status to avoid publication and language biases; 32% (n = 8) of studies were published in a language other than English and 20% (n = 5) were not full-length peer-reviewed journal articles. Although not as straightforward to assess as for intervention studies, publication bias can be an issue for reviews of diagnostic accuracy studies. We therefore excluded studies including very small numbers of patients. To obtain the maximum available evidence, we included phase I-type studies measuring the correlation of CVT scores with retinopathy status, as well as studies measuring diagnostic accuracy. Nevertheless, only a total of 25 relevant studies fulfilled criteria for inclusion in the systematic review. The majority of these studies were relatively old, with 79% (n = 19) being published at least 10 years before this report and 38% (n = 9) being published at least 20 years ago.
To prevent errors or bias in the selection, quality assessment and data extraction of studies, two reviewers undertook each of these processes independently. We used the validated QUADAS criteria to assess study quality, although, in many cases, when studies failed QUADAS criteria it was impossible to determine which had clear methodological flaws and which failed because of poor reporting of methods.
As the included studies were highly heterogeneous, it was considered inappropriate to statistically pool their findings. We therefore presented the results in a narrative synthesis, according to the test evaluated, with sensitivities and specificities plotted in ROC space for illustration. ROC plots provide an easy to interpret visual summary of all of the studies included in a review. They enable the reader to assess quickly the variability between studies, the accuracy of the test and whether there appears to be a threshold effect, without the potentially misleading effect of pooling using a summary ROC when there is significant between-study heterogeneity. In addition, we provided the corresponding likelihood ratios, as these allow clinicians to calculate post-test probabilities of disease from pretest probabilities. It should be noted, however, that the number of studies included for each CVT was small, and not all studies reported data to allow the calculation of diagnostic accuracy estimates.
Economic evaluation
The economic evaluation is strengthened by the recent publication of several large epidemiological studies67,72,73,90 detailing the prevalence and incidence of DR in the UK population eligible for screening.
The main limitations of the economic evaluation relate to the lack of evidence on the diagnostic accuracy of CVT and the cost-effectiveness of photocoagulation therapy. Diagnostic accuracy data on CVT were taken from one paper that looked at TCT, a test that has seldom been used in a clinical setting. Only 17 patients in this study had STDR and therefore the confidence intervals surrounding the estimate for sensitivity are wide, resulting in the wide range in cost-effectiveness estimates found in our PSA. Although this paper did report the sensitivity and specificity of CVT and retinal photography combined, it did not directly evaluate the accuracy of CVT in patients with no STDR evident on screening retinal photography. Therefore, we had to make assumptions about the independence of CVT and retinal photography tests in order to estimate the sensitivity and specificity of CVT combined with retinal photography in our analysis. For these reasons, the cost-effectiveness results describe what CVT could achieve if these initial diagnostic accuracy results are confirmed in larger studies examining different ways of combining the results of CVT and retinal photography.
No detailed costings of any type of CVT were identified. Furthermore, many types of CVT used in research settings are not available commercially, making cost estimation difficult. We included a wide range of costs in our sensitivity analysis to address this limitation and recognise the likely cost differences between relatively simple colour arrangement tests and more technically complex computer-based tests. In fact, our results did not vary greatly at plausible test costs (from £7.80 to £29). Nevertheless, before any type of CVT could be included in routine screening, it would be important to precisely measure the fixed and variable costs of implementation.
The effectiveness of treatment is important in analysing the cost-effectiveness of systematic screening programmes. Treatment efficacy for our model was taken from a randomised controlled trial published in 1984. 71 If treatment has improved over time then results from this paper will underestimate the effectiveness of photocoagulation as used in clinical settings today. More recent trials are not available as this treatment is now the standard of care. The randomised trial also did not report any details on the incremental costs of photocoagulation or any generic outcome that could be used to calculate QALYs. Therefore, we estimated costs and patient utility scores based on observational data collected in other studies. This limitation, which is common in decision-analysis models, could lead to bias in our conclusions if photocoagulation is more or less cost-effective than estimated.
Survey of current practice
To ensure the relevance of the survey and to contact an appropriate sample population, we approached the English NSC who consulted on the content of the survey and contacted all of the programme managers and clinical leads in England. Further attempts to maximise response were made by keeping the survey brief and providing it online, as well as sending a brief follow-up reminder to potential responders. Ultimately, these efforts resulted in a response rate of 50%, higher than typically achieved in postal and email surveys. No further attempts were made to contact the 50% who did not respond. There would be potential for bias in the findings of the survey if the non-responders were systematically different from the responders on factors that might influence their responses. We considered this unlikely in this case but, as the possibility cannot be entirely ruled out, appropriate caution must be exercised when interpreting the findings of the survey. The phrasing of the survey introduction and questions was specifically designed to avoid unduly biasing responses in favour of, or against, CVT.
Uncertainties
There are several CVTs (e.g. Harvey–Rand–Ritter and tritan-based pseudoisochromatic plates) that have been developed but not evaluated in the context of detecting or predicting retinopathy in patients with diabetes. Consequently, direct conclusions cannot be drawn about the diagnostic accuracy of these tests.
The NSC has developed a list of criteria for the viability, effectiveness and appropriateness of a screening programme. These criteria relate to the condition and test of interest, the available treatments and the proposed screening programme itself. As a national retinopathy screening programme has already been implemented, only the subset of criteria relating to the test is relevant to the appropriateness of CVT in DR. The first of these criteria states that any potential screening test should be simple, safe, precise and validated. Most of the tests evaluated in the review were both relatively safe and simple to conduct (although scoring and interpretation of the non-automated arrangement tests can be relatively complex). As discussed previously, not all CVTs have been validated and, for those that have, data on their precision are limited and/or heterogeneous.
The second criterion states that the distribution of test values in the target population should be known and a suitable cut-off level defined and agreed. When more than one study evaluated the same CVT, cut-offs used to define a positive result varied considerably and the method to establish these cut-offs was rarely reported.
The NSC criteria state that the test should be acceptable to the screening population. However, our extensive search found no evidence on this issue. In the context of introducing CVT as a component of screening for DR, patient concerns, if any, might relate to the potential additional time required for attending screening appointments. Patients may also be concerned about the consequences of any false-positive results, such as additional follow-up appointments.
The final NSC criterion mandates that there should be an agreed policy on the further diagnostic investigation of individuals with a positive test result and on the choices available to these individuals. In our model, patients who screen positive for referable retinopathy or macular oedema are referred to an ophthalmologist for further examination using slit-lamp biomicroscopy. If the ophthalmologist confirms the diagnosis of preproliferative retinopathy, proliferative retinopathy or macular oedema, the patient is offered laser therapy. If the slit-lamp biomicroscopy indicates that the initial screening result was a false-positive finding, the patient will be referred back to the annual screening programme.
The available evidence suggests that CVT alone would not be sufficiently accurate to screen for DR. Unlike mydriatic retinal photography, CVT has not consistently been shown to have sensitivity values exceeding 80%. 20 If CVT was to be used in retinopathy screening, this would most likely be as an adjunct to the existing programme, which is based on retinal photography. However, the only available direct evidence on the combination of retinal photography and CVT comes from a single study31,60 and would require confirmation from further studies before CVT could be considered an effective adjunct in retinal screening.
There is insufficient evidence to draw any clear conclusions on the ability of CVT to predict the risk of future DR among patients without evidence of retinal damage at assessment. The value of any test to predict DR depends upon the availability and effectiveness of strategies to act on a positive result to prevent or delay the occurrence of clinically significant retinopathy. Such strategies might include more intensive monitoring of metabolic control and blood pressure among patients identified as being at risk. In the absence of data on the predictive value of CVT, there is currently little to support this approach for opportunistic detection of early-stage DR in primary care, as incipient retinopathy is screened for on an annual basis.
Our survey of local retinopathy screening programmes showed that there is limited interest in CVT as an adjunct to retinal photography as a screening tool. However, some respondents did report an interest in optical coherence tomography. The evaluation of optical coherence tomography was outside the scope of this report, but its role in detecting DR is the subject of an HTA-funded research project (ongoing at the time of publication). 89,91
As stated previously, restricted inclusion criteria mean that some kinds of patients who would be seen routinely in DR screening were excluded from the majority of studies, thereby limiting the generalisability of their findings.
The primary uncertainty in the economic evaluation related to how CVT could be incorporated into a screening programme currently using retinal photography. As described previously in this report, the test could be used in parallel with retinal photography or serially to filter patients before or after retinal photography. The stage at which the test is incorporated will determine which diagnostic properties are most crucial. For example, if the objective was to avoid the need for patients to undergo retinal photography, the test would need to be highly sensitive. Alternatively, if a test was used to confirm a positive result on retinal photography, it would need to be highly specific. The diagnostic accuracy studies identified in our review provided little guidance on this vital issue. Most studies evaluated the accuracy of CVT in isolation and did not explore whether it would improve the sensitivity and specificity of current screening methods. In consultation with clinical colleagues on our research team, we developed a structural model (Figure 7) describing how CVT might be incorporated into current screening. Based on this structural model we were able to estimate cost-effectiveness. However, if CVT is considered a potentially useful adjunct to the current screening programme, there will clearly be a need for further evaluations in large cohorts who are eligible for screening, demonstrating how it can be combined with retinal photography to improve diagnostic accuracy, targeting of treatment and patient outcomes.
There is also likely to be clinical variation in the treatment of patients with STDR identified by screening, which cannot be adequately represented by a decision-analysis model. Some patients at the early stages of STDR may not receive laser photocoagulation immediately after ophthalmologist confirmation of the disease. Instead, a period of close monitoring may occur until treatment is deemed suitable. It is therefore possible that a screening test such as CVT, which may detect some cases of STDR earlier, merely prolongs the time spent under ophthalmological monitoring without reducing the time until definitive therapy. If this is the case, our model would overestimate the cost-effectiveness of adding CVT to current screening. We did not identify any studies examining the therapeutic impact of CVT and therefore we did not quantify this uncertainty in the model.
Other relevant factors
The majority of CVTs developed to detect acquired colour vision defects such as DR do so by evaluating tritan colour deficits. However, there has been some debate as to whether the performance of participants on tritan-based colour vision tests might be influenced by age-related lens yellowing. 92,93 There is evidence that lenses of patients with diabetes may ‘yellow’ more quickly than those in non-diabetes control subjects. 92 Only one31,60 of the included studies explicitly accounted for this potential confounding factor. Some authors93 have suggested that iris colour and macular pigment density should also be taken into consideration when interpreting CVT performance. None of these variables was explicitly addressed in the evidence identified in this review.
Assessment of factors relevant to the NHS and other parties
The current NHS screening programme is based on providing people with diabetes the opportunity for annual retinal screening, predominantly based on retinal photography. Any changes in the structure or delivery of the DR screening programme need to take into account several factors, including the likely ongoing increase in the prevalence of diabetes corresponding to the increased prevalence of obesity and an aging population. The relative costs and benefits of any potentially competing adjunct tests (e.g. CVT versus optical coherence tomography) need to be considered explicitly. Should any future evidence support the use of CVT, this will need to be sufficiently robust to impact on clinical opinion, which at present does not appear to consider CVT worthy of further attention in a screening context.
Chapter 7 Conclusions
Implications for service provision
-
There is insufficient evidence to support the use of CVT alone as a method of screening for retinopathy in patients with diabetes. The evidence that is available is limited in quantity and is of generally poor quality.
-
Pseudoisochromatic plates, anomaloscopes and colour arrangement tests (including FM-100, D-15 and NCT) all showed unacceptably poor diagnostic accuracy estimates for screening for milder forms of retinopathy (the Exeter Standards of the British Diabetic Association require screening levels of at least 80% sensitivity and 95% specificity). 21 These estimates generally improved for advanced forms of retinopathy, but remained poor.
-
A single study reported that sensitivity and specificity for detecting advanced retinopathy exceeded 90% for certain variations on the automated SGM when combined with retinal photography such that presence of disease was defined as failure of both tests; this represents a small, but not statistically significant, improvement in sensitivity over retinal photography alone. However, this single study was conducted by the test developers and the technology has not been independently evaluated. As for CVT alone, the available evidence on combination testing is extremely limited.
-
If these initial results on diagnostic accuracy for the automated SGM are confirmed in larger independent studies then the addition of CVT to current screening using retinal photography could be cost-effective. However, better quality diagnostic accuracy studies directly comparing the incremental value of CVT in addition to retinal photography are needed before drawing conclusions on cost-effectiveness.
-
There is no published evidence on patient preferences in relation to colour vision screening for DR.
-
Retinal photography is universally employed as the primary method for retinal screening by centres responding to a survey of current practice; none used CVT.
Suggested research priorities
-
A total of 32% of survey respondents considered optical coherence tomography to be a research priority. CVT was not identified as a research priority by survey respondents. Therefore, optical coherence tomography may be a greater priority for future research than CVT. An ongoing HTA-funded study is investigating the value of adding optical coherence tomography to retinal photography to identify macular oedema.
-
Information about the sensitivity and specificity of CVT alone, which is the focus of most previous studies, is less useful than estimates of the diagnostic accuracy of CVT combined with retinal photography as this is the most likely mode of use in the NHS. Uncertainties in the CVT literature could be resolved by further research evaluating the addition of different CVT modalities to retinal photographic screening, either to improve accuracy of detection or to establish any predictive ability. Any such study would have to be conducted prospectively, in a sample generalisable to the wider screening population, be independent of the test developers, account for the potential effects of lens yellowing, iris colour and macular pigment density alongside other clinical factors, and follow STARD reporting guidelines for reporting diagnostic accuracy studies.
-
Ideally, as well as measuring diagnostic accuracy, any future studies of screening for DR should consider the consequences of positive and negative results in terms of costs, subsequent treatment/prevention options and participant outcomes.
-
Activity-based cost analyses detailing the resource use of the various manual and automated CVT strategies are also necessary. These studies should estimate the capital and labour costs of implementing CVT in typical primary care trust diabetes populations.
Acknowledgements
We would like to acknowledge the assistance of Dr Peter Scanlon and Donna Prentis of the National Screening Programme for Retinopathy in conducting the national survey, Dr Lionel Ripley of the University of Sussex for providing details and clarifications on published studies, and Steve Chaffey of the Department of Social Medicine, University of Bristol for project support.
Contribution of authors
Mark Rodgers, Rebecca Hodges, James Hawkins and Will Hollingworth were responsible for conception and design, acquisition of data, analysis and interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published.
Steven Duffy was responsible for conception and design, acquisition of data, interpretation of data, drafting and revision of the manuscript, and final approval of the version to be published.
Martin McKibbin and Michael Mansfield were responsible for analysis and interpretation of data, revision of the manuscript, and final approval of the version to be published.
Roger Harbord was responsible for acquisition of data, analysis and interpretation of data, revision of the manuscript, and final approval of the version to be published.
Jonathan Sterne was responsible for conception and design, interpretation of data, revision of the manuscript, and final approval of the version to be published.
Paul Glasziou was responsible for conception and design, interpretation of data, revision of the manuscript, and final approval of the version to be published
Penny Whiting and Marie Westwood were responsible for conception and design, interpretation of data, revision of the manuscript, and final approval of the version to be published.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Kohner EM, Porta M. Protocols for screening and treatment of diabetic retinopathy in Europe. Eur J Ophthalmol 1991;1:45-54.
- Klein R, Meuer SM, Moss SE, Klein BE. Retinal microaneurysm counts and 10-year progression of diabetic retinopathy. Arch Ophthalmol 1995;113:1386-91.
- Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991;98:766-85.
- Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol 1984;102:520-6.
- UK Prospective Diabetes Study Group . Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53.
- Kohner EM, Aldington SJ, Stratton IM, Manley SE, Holman RR, Matthews DR, et al. United Kingdom Prospective Diabetes Study, 30: diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factors. Arch Ophthalmol 1998;116:297-303.
- National Institute for Clinical Excellence . Inherited Clinical Guideline E. Management of Type 2 Diabetes: Retinopathy – Screening and Early Management 2002.
- Diabetes Control and Complications Trial Group . Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Arch Ophthalmol 1998;116:874-86.
- The Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977-86.
- UK Prospective Diabetes Study Group . Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703-13.
- Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol 1984;102:527-32.
- Mathiesen ER, Rønn B, Storm B, Foght H, Deckert T. The natural course of microalbuminuria in insulin-dependent diabetes: a 10-year prospective study. Diabet Med 1995;12:485-7.
- Savage S, Estacio RO, Jeffers B, Schrier RW. Urinary albumin excretion as a predictor of diabetic retinopathy, neuropathy, and cardiovascular disease in NIDDM. Diabetes Care 1996;19:1243-8.
- Davis MD, Fisher MR, Gangnon RE, Barton F, Aiello LM, Chew EY, et al. Risk factors for high-risk proliferative diabetic retinopathy and severe visual loss: Early Treatment Diabetic Retinopathy Study Report No. 18. Invest Ophthalmol Vis Sci 1998;39:233-52.
- Klein BE, Moss SE, Klein R. Effect of pregnancy on progression of diabetic retinopathy. Diabetes Care 1990;13:34-40.
- Bunce C, Wormald R. Leading causes of certification for blindness and partial sight in England & Wales. BMC Public Health 2006;6.
- Rhatigan MC, Leese GP, Ellis J, Ellingford A, Morris AD, Newton RW, et al. Blindness in patients with diabetes who have been screened for eye disease. Eye 1999;13:166-9.
- Trautner C, Icks A, Haastert B, Plum F, Berger M. Incidence of blindness in relation to diabetes. A population-based study. Diabetes Care 1997;20:1147-53.
- Cormack TG, Grant B, Macdonald MJ, Steel J, Campbell IW. Incidence of blindness due to diabetic eye disease in Fife 1990–9. Br J Ophthalmol 2001;85:354-6.
- Hutchinson A, McIntosh A, Peters J, O’Keeffe C, Khunti K, Baker R, et al. Effectiveness of screening and monitoring tests for diabetic retinopathy – a systematic review. Diabet Med 2000;17:495-506.
- British Diabetic Association . Retinal Photography Screening for Diabetic Eye Disease: A British Diabetic Association Report 1997.
- Arun CS, Ngugi N, Lovelock L, Taylor R. Effectiveness of screening in preventing blindness due to diabetic retinopathy. Diabet Med 2003;20:186-90.
- Scottish Intercollegiate Guidelines Network . Management of Diabetes. A National Clinical Guideline 2001.
- National Institute for Clinical Excellence . Diagnosis and Management of Type 1 Diabetes in Children, Young People and Adults 2004.
- Department of Health . National Service Framework for Diabetes 2001.
- Department of Health . Diabetic Retinopathy Screening Statement 2008.
- Birch J. Diagnosis of defective colour vision. Oxford: Oxford University Press; 1993.
- Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M. The value of digital imaging in diabetic retinopathy. Health Technol Assess 2003;7:1-132.
- Sculpher MJ, Buxton MJ, Ferguson BA, Spiegelhalter DJ, Kirby AJ. Screening for diabetic retinopathy: a relative cost-effectiveness analysis of alternative modalities and strategies. Health Econ 1992;1:39-51.
- Buxton MJ, Sculpher MJ, Ferguson BA, Humphreys JE, Altman JF, Spiegelhalter DJ, et al. Screening for treatable diabetic retinopathy: a comparison of different methods. Diabet Med 1991;8:371-7.
- Ong GL, Ripley LG, Newsom RS, Cooper M, Casswell AG. Screening for sight-threatening diabetic retinopathy: comparison of fundus photography with automated color contrast threshold test. Am J Ophthalmol 2004;137:445-52.
- Maár N, Tittl M, Stur M, Zajic B, Reitner A. A new colour vision arrangement test to detect functional changes in diabetic macular oedema. Br J Ophthalmol 2001;85:47-51.
- Centre for Reviews and Dissemination . Systematic Reviews of Clinical Tests. Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2008.
- Cochrane Diagnostic Test Accuracy Working Group . Cochrane Handbook for Diagnostic Test Accuracy Reviews n.d.
- Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3.
- Aspinall PA, Kinnear PR, Duncan LJ, Clarke BF. Prediction of diabetic retinopathy from clinical variables and color vision data. Diabetes Care 1983;6:144-8.
- Ayed S, Jeddi A, Kallal Z. Diabetes and color vision disorder detected by the Farnsworth 100 Hue test. Diabetic dyschromatopsia. J Fr Opthalmol 1990;13:506-10.
- Barton FB, Bresnick GH, Garcia CA, Benson W, Knatterud GL. ETDRS baseline color vision test results. Invest Ophthalmol Vis Sci 1987;28.
- Fong DS, Barton FB, Bresnick GH. Impaired color vision associated with diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report No. 15. Am J Ophthalmol 1999;128:612-17.
- Green FD, Ghafour IM, Allan D, Barrie T, McClure E, Foulds WS. Colour vision of diabetics. Br J Ophthalmol 1985;69:533-6.
- Greenstein V, Sarter B, Hood D, Noble K, Carr R. Hue discrimination and S cone pathway sensitivity in early diabetic retinopathy. Invest Ophthalmol Vis Sci 1990;31:1008-14.
- Ismail GM, Whitaker D. Early detection of changes in visual function in diabetes mellitus. Ophthalmic and Physiol Opt 1998;18:3-12.
- Jeddi A, Ben Osman N, Daghfous F, Kaoueche M, Baccar M, Gaigi S, et al. Methods for screening and surveillance of diabetic retinopathy. J Fr Opthalmol 1994;17:769-73.
- Lombrail P, Gervais P, Cathelineau G. Prediction of diabetic retinopathy from color vision data. Diabetes Care 1983;6:621-2.
- Trick GL, Burde RM, Gordon MO, Santiago JV, Kilo C. The relationship between hue discrimination and contrast sensitivity deficits in patients with diabetes mellitus. Ophthalmology 1988;95:693-8.
- Mäntyjärvi M, Tuppurainen K. Could colour vision tests predict or find retinopathy in diabetic schoolchildren?. Br J Ophthalmol 1995;79:711-2.
- Bernardczyk-Meller J, Siwiec J, Kielczewska-Mrozikiewicz D, Pecold K, Korman E. Color vision in diagnosis of early ocular changes in young patients with type 1 diabetes mellitus. Diabetol Polska 2001;8:270-3.
- Doucet J, Retout A, Poutrain JR, Ozenne G, Leprince MP, Parain D, et al. A multifactorial etiologic approach to diabetic dyschromatopsia. Study of 100 diabetics. Diabete Metab 1991;17:31-7.
- Mecca E, Tovena G, Marchini G, Manganotti A, Marraffa M, Bonomi L. Study of color perception using a new color test and desaturated panel D 15 in normal subjects and diabetics. J Fr Opthalmol 1988;11:493-500.
- Saracco JB, Gastaud P, Estachy G, Trani JC, Leid J. Value of desaturated Panel D 15 in the detection of diabetic retinopathy. Bull Soc Ophtalmol France 1980;80:969-73.
- Matsuo H, Sakamoto K, Toratani Y, Ueda Y, Mikuni E, Nishimura S, et al. The significance of color vision defects in diabetics. J Japan Diabetol Soc 1990;33:675-80.
- De Alwis DV. The role of automated chromatic contrast sensitivity tests in the management of diabetic retinopathy. University of Sussex; 1994.
- Findl O, Dallinger S, Rami B, Polak K, Schober E, Wedrich A, et al. Ocular haemodynamics and colour contrast sensitivity in patients with type 1 diabetes. Br J Ophthalmol 2000;84:493-8.
- Knowles PJ, Tregear SJ, Ripley LG, Casswell AG. Colour vision in diabetic and normal pseudophakes is worse than expected. Eye 1996;10:113-16.
- Tregear SJ, Knowles PJ, Ripley LG, Casswell AG. Chromatic-contrast threshold impairment in diabetes. Eye 1997;11:537-46.
- Wong R, Khan J, Adewoyin T, Sivaprasad S, Arden GB, Chong V. The ChromaTest, a digital color contrast sensitivity analyzer, for diabetic maculopathy: a pilot study. BMC Ophthalmol 2008;8.
- Mirkiewicz-Sieradzka B, Zygulska-Machowa H, Romanowska B. Evaluation of macular function in patients with diabetic retinopathy. Klin Oczna 1986;88:209-11.
- Sinha AK, Bhatia RP. Colour vision in diabetes mellitus. Indian J Ophthalmol 1979;27:6-8.
- Matsuo H, Sakamoto K, Toratani Y, Ueda Y, Mikuni E, Kondo M, et al. Significance of color vision defect in patients with non-insulin-dependent diabetes (NIDDM). Diabetes Res Clin Pract 1988;5.
- Ong GL, Ripley LG, Newsom RSB, Casswell AG. Assessment of colour vision as a screening test for sight threatening diabetic retinopathy before loss of vision. Br J Ophthalmol 2003;87:747-52.
- Davies R, Roderick P, Canning C, Brailsford S. The evaluation of screening policies for diabetic retinopathy using simulation. Diabet Med 2002;19:762-70.
- Scotland GS, McNamee P, Philip S, Fleming AD, Goatman KA, Prescott GJ, et al. Cost-effectiveness of implementing automated grading within the national screening programme for diabetic retinopathy in Scotland. Br J Ophthalmol 2007;91:1518-23.
- James M, Turner DA, Broadbent DM, Vora J, Harding SP. Cost effectiveness analysis of screening for sight threatening diabetic eye disease. BMJ 2000;320:1627-31.
- Fenwick E, O’Brien B, Briggs A. Cost-effectiveness acceptability curves – facts, fallacies and frequently asked questions. Health Econ 2004;13:405-15.
- United Kingdom National Screening Committee . Essential Elements in Developing a Diabetic Retinopathy Screening Programme: Work Book 4 2007.
- Early Treatment Diabetic Retinopathy Study Research Group . Grading diabetic retinopathy from stereoscopic color fundus photographs – an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 1991;98:786-80.
- Younis N, Broadbent DM, Harding SP, Vora JR. Prevalence of diabetic eye disease in patients entering a systematic primary care-based eye screening programme. Diabet Med 2002;19:1014-21.
- Garvican L. Resources Required for a Local Service in the National Diabetic Retiopathy Screening Programme 2004. www.retinalscreening.nhs.uk/.
- Meller M, Karolczak-Kulesza M, Bernardczyk-Meller J. Diagnosis and surgical treatment of idiopathic macular holes. Klin Oczna 2001;103:39-42.
- Hidajat RR, Hidayat JR, McLay JL, Elder MJ, Goode DH, Pointon RC. A fast system for reporting the Farnsworth–Munsell 100-hue colour vision test. Doc Ophthalmol 2004;109:109-14.
- Odland M, Blach RK, Hamilton AM, Leaver EK, Townsend C. Photocoagulation for proliferative diabetic retinopathy: a randomised controlled clinical trial using the xenon-arc. Diabetologia 1984;26:109-15.
- Younis N, Broadbent DM, Harding SP, Vora JP. Incidence of sight-threatening retinopathy in type 1 diabetes in a systematic screening programme. Diabet Med 2003;20:758-65.
- Younis N, Broadbent DM, Vora JP, Harding SP. Incidence of sight-threatening retinopathy in patients with type 2 diabetes in the Liverpool Diabetic Eye Study: a cohort study. Lancet 2003;361:195-200.
- Leese GP, Morris AD, Swaminathan K, Petrie JR, Sinharay R, Ellingford A, et al. Implementation of national diabetes retinal screening programme is associated with a lower proportion of patients referred to ophthalmology. Diabet Med 2005;22:1112-15.
- Buch HN, Barton DM, Varughese GI, Bradbury S, Scarpello JHB, Walker AB. An assessment of the coverage of a district-wide diabetic retinopathy screening service. Diabet Med 2005;22:840-1.
- Lloyd A, Nafees B, Gavriel S, Rousculp MD, Boye KS, Ahmad A. Health utility values associated with diabetic retinopathy. Diabet Med 2008;25:618-24.
- Soedamah-Muthu SS, Fuller JH, Mulnier HE, Raleigh VS, Lawrenson RA, Colhoun HM. All-cause mortality rates in patients with type 1 diabetes mellitus compared with a non-diabetic population from the UK general practice research database, 1992–1999. Diabetologia 2006;49:660-6.
- Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA. Mortality in people with type 2 diabetes in the UK. Diabet Med 2006;23:516-21.
- Klein R, Klein BE, Moss SE, Cruickshanks KJ. Association of ocular disease and mortality in a diabetic population. Arch Ophthalmol 1999;117:1487-95.
- Harvey JN, Craney L, Nagendran S, Ng CS. Towards comprehensive population-based screening for diabetic retinopathy: operation of the North Wales diabetic retinopathy screening programme using a central patient register and various screening methods. J Med Screen 2006;13:87-92.
- Clarke P, Gray A, Legood R, Briggs A, Holman R. The impact of diabetes-related complications on healthcare costs: results from the United Kingdom Prospective Diabetes Study (UKPDS Study No. 65). Diabet Med 2003;20:442-50.
- Briggs AH, Ades AE, Price MJ. Probabilistic sensitivity analysis for decision trees with multiple branches: use of the Dirichlet distribution in a Bayesian framework. Med Decis Mak 2003;23:341-50.
- Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics 1998;13:397-409.
- Dasbach EJ, Fryback DG, Newcomb PA, Klein R, Klein BE. Cost-effectiveness of strategies for detecting diabetic retinopathy. Med Care 1991;29:20-39.
- Javitt JC. Cost savings associated with detection and treatment of diabetic eye disease. Pharmacoeconomics 1995;8:33-9.
- Javitt JC, Aiello LP, Chiang Y, Ferris FL, Canner JK, Greenfield S. Preventive eye care in people with diabetes is cost-saving to the federal government. Implications for health-care reform. Diabetes Care 1994;17:909-17.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2008.
- National Screening Programme for Diabetic Retinopathy . English National Screening Programme for Diabetic Retinopathy n.d. www.retinalscreening.nhs.uk/pages/.
- Virgili G, Menchini F, Dimastrogiovanni E, Rapizzi E, Menchini U, Bandello F, et al. Optical coherence tomography versus stereoscopic fundus photography or biomicroscopy for diagnosing diabetic macular edema: a systematic review. Invest Ophthalmol Vis Sci 2007;48:4963-73.
- Younis N, Broadbent DM, James M, Harding SP, Vora JP. Current status of screening for diabetic retinopathy in the UK. Diabet Med 2002;19:44-9.
- Olsen JA. Improving the Value of Screening for Diabetic Macular Oedema Using Surrogate Photographic Markers n.d. www.hta.ac.uk/1703.
- Lutze M, Bresnick GH. Lenses of diabetic patients ‘yellow’ at an accelerated rate similar to older normals. Invest Ophthalmol Vis Sci 1991;32:194-9.
- Beirne RO, McIlreavy L, Gore S, Zlatkova MB. Age-related lens yellowing per se contributes little to the increase in Farnsworth-Munsell 100 hue error scores with age. Ophthalmic Physiol Opt 2008;28.
- Verriest G, Laethem GV, Uvijls A. A new assessment of the Farnsworth Munsell 100 Hue test scores. Am J Opthalmol 1982;93:635-42.
Appendix 1 Literature search strategies
Systematic review search strategies
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OVID gateway) 1950 to September Week 3 2007
Searched 4 October 2007.
643 records were retrieved in MEDLINE and 6 in MEDLINE In-Process & Other Non-Indexed Citations.
-
Color Vision Defects/
-
Color Perception/
-
Color Perception Tests/
-
Vision Screening/
-
Vision Tests/
-
Contrast Sensitivity/
-
((color$or colour$or vision or visual) adj3 (test$or screen$)).ti,ab.
-
((color$or colour$) adj3 (blind$or deficien$or defect$or loss or impair$or perception)).ti,ab.
-
(monochromatopsia or achromatopsia or deutan or protan).ti,ab.
-
anomaloscop$.ti,ab.
-
pseudoisochromatic$.ti,ab.
-
hue$discrimination$.ti,ab.
-
lantern$.ti,ab.
-
(tritan or TCT).ti,ab.
-
Ishihara$.ti,ab.
-
Kojima$.ti,ab.
-
Ohkuma$.ti,ab.
-
Matsubara$.ti,ab.
-
Dvorine$.ti,ab.
-
cvtmet.ti,ab.
-
(Hardy Rand Rittler$or AOHRR or AO H-R-R).ti,ab.
-
Lanthony$.ti,ab.
-
(panel d 15 or panel d15 or d 15 panel or d15 panel).ti,ab.
-
Farnsworth$.ti,ab.
-
((color$or colour$) adj plate).ti,ab.
-
Mollon Reffin$.ti,ab.
-
Pease Allen$.ti,ab.
-
Giles Archer$.ti,ab.
-
Adams Desaturated.ti,ab.
-
(City University or CUCVT).ti,ab.
-
Velhagen Pflugertrident$.ti,ab.
-
(contrast adj3 sensitivit$).ti,ab.
-
or/1–32
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.
-
or/34–36
-
33 and 37
-
exp Diabetic Retinopathy/
-
retinopath$.ti,ab.
-
exp Macular Degeneration/
-
Retinal Hemorrhage/
-
Retinal Neovascularization/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/39–47
-
38 and 48
-
Animals/
-
Humans/
-
50 not (50 and 51)
-
49 not 52
EMBASE (OVID gateway) 1980 to 2007 Week 39
Searched 4 October 2007.
419 records were retrieved.
-
Color Vision Defect/
-
Color Vision/
-
Color Vision Test/
-
Vision Test/
-
Color Blindness/
-
Contrast Sensitivity/
-
((color$or colour$or vision or visual) adj3 (test$or screen$)).ti,ab.
-
((color$or colour$) adj3 (blind$or deficien$or defect$or loss or impair$or perception)).ti,ab.
-
(monochromatopsia or achromatopsia or deutan or protan).ti,ab.
-
anomaloscop$.ti,ab.
-
pseudoisochromatic$.ti,ab.
-
hue$discrimination$.ti,ab.
-
lantern$.ti,ab.
-
(tritan or TCT).ti,ab.
-
Ishihara$.ti,ab.
-
Kojima$.ti,ab.
-
Ohkuma$.ti,ab.
-
Matsubara$.ti,ab.
-
Dvorine$.ti,ab.
-
cvtmet.ti,ab.
-
(Hardy Rand Rittler$or AOHRR or AO H-R-R).ti,ab.
-
Lanthony$.ti,ab.
-
(panel d 15 or panel d15 or d 15 panel or d15 panel).ti,ab.
-
Farnsworth$.ti,ab.
-
((color$or colour$) adj plate).ti,ab.
-
Mollon Reffin$.ti,ab.
-
Pease Allen$.ti,ab.
-
Giles Archer$.ti,ab.
-
Adams Desaturated.ti,ab.
-
(City University or CUCVT).ti,ab.
-
Velhagen Pflugertrident$.ti,ab.
-
(contrast adj3 sensitivit$).ti,ab.
-
or/1–32
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.).ti,ab.
-
or/34–36
-
33 and 37
-
exp Retinopathy/
-
retinopath$.ti,ab.
-
Retina Maculopathy/
-
Retina Edema/
-
Retina Hemorrhage/
-
Retina Neovascularization/
-
Retina Macula Degeneration/
-
Microaneurysm/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/39–50
-
38 and 51
-
Animal/or Animal Experiment/or Nonhuman/
-
(rat or rats or mouse or mice or murine or rodent or rodents or hamster or hamsters or pig or pigs or porcine or rabbit or rabbits or animal or animals or dogs or dog or cats or cow or bovine or sheep or ovine or monkey or monkeys).ti,ab,sh.
-
or/53–54
-
exp Human/or Human Experiment/
-
55 not (55 and 56)
-
52 not 57
CINAHL (OVID gateway) 1982 to September Week 4 2007
Searched 4 October 2007.
115 records were retrieved.
-
Color Perception/
-
Color Perception Tests/
-
Color Vision Defects/
-
Vision Screening/
-
Vision Tests/
-
((color$or colour$or vision or visual) adj3 (test$or screen$)).ti,ab.
-
((color$or colour$) adj3 (blind$or deficien$or defect$or loss or impair$or perception)).ti,ab.
-
(monochromatopsia or achromatopsia or deutan or protan).ti,ab.
-
anomaloscop$.ti,ab.
-
pseudoisochromatic$.ti,ab.
-
hue$discrimination$.ti,ab.
-
lantern$.ti,ab.
-
(tritan or TCT).ti,ab.
-
Ishihara$.ti,ab.
-
Kojima$.ti,ab.
-
Ohkuma$.ti,ab.
-
Matsubara$.ti,ab.
-
Dvorine$.ti,ab.
-
cvtmet.ti,ab.
-
(Hardy Rand Rittler$or AOHRR or AO H-R-R).ti,ab.
-
Lanthony$.ti,ab.
-
(panel d 15 or panel d15 or d 15 panel or d15 panel).ti,ab.
-
Farnsworth$.ti,ab.
-
((color$or colour$) adj plate).ti,ab.
-
Mollon Reffin$.ti,ab.
-
Pease Allen$.ti,ab.
-
Giles Archer$.ti,ab.
-
Adams Desaturated.ti,ab.
-
(City University or CUCVT).ti,ab.
-
Velhagen Pflugertrident$.ti,ab.
-
(contrast adj3 sensitivit$).ti,ab.
-
or/1–31
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.
-
or/33–35
-
32 and 36
-
Diabetic Retinopathy/
-
retinopath$.ti,ab.
-
Macular Degeneration/
-
Eye Hemorrhage/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/38–45
-
37 and 46
Science Citation Index (Web of Science) 1900 to 30 September 2007
Searched 4 October 2007.
463 records were retrieved.
TS=(color* SAME test*) or TS=(color* SAME screen*) or TS=(colour* SAME test*) or TS=(colour* SAME screen*) or TS=(vision SAME test*) or TS=(vision SAME screen*) or TS=(visual SAME test*) or TS=(visual SAME screen*)
TS=(color* SAME blind*) or TS=(color* SAME deficien*) or TS=(color* SAME defect*) or TS=(color* SAME loss*) or TS=(color* SAME impair*) or TS-(color* SAME perception) or TS=(colour* SAME blind*) or TS=(colour* SAME deficien*) or TS=(colour* SAME defect*) or TS=(colour* SAME loss*) or TS=(colour* SAME impair*) or TS=(colour* SAME perception)
TS=(monochromatopsia or achromatopsia or deutan or protan)
TS=(anomaloscop* or pseudoisochromatic*) or TS=(hue* discrimination*) or TS=(lantern* or tritan or TCT or Ishihara* or Kojima* or Ohkuma* or Matsubara* or Dvorine* or cvtmet)
TS=(Hardy Rand Rittler*) or TS=(AOHRR or AO H-R-R or Lanthony*) or TS=(panel d 15) or TS=(panel d15) or TS=(d 15 panel) or TS=(d15 panel) or TS=(Farnsworth*)
TS=(color* plate) or TS=(colour* plate) or TS=(Mollon Reffin*) or TS=(Pease Allen*) or TS=(Giles Archer*) or TS=(Adams Desaturated) or TS=(City University) or TS=(CUCVT) or TS=(Velhagen Pflugertrident*) or TS=(contrast SAME sensitivit*)
#1 or #2 or #3 or #4 or #5 or #6
TS=(diabet* or IDDM or NIDDM or T2DM)
#7 and #8
TS=(retinopath*) or TS=(macula* SAME edema*) or TS=(macula* SAME oedema*) or TS=(retina* SAME edema*) or TS=(retina* SAME oedema*) or TS=(optic* SAME edema*) or TS=(ocular* SAME edema*) or TS=(optic* SAME oedema*) or TS=(ocular* SAME oedema*)or TS=(intraocular* SAME edema*) or TS=(intraocular* SAME oedema*) or TS=(maculopath*) or TS=(microaneurysm*) or TS=(micro aneurysm*) or TS=(microaneurism*) or TS=(micro aneurism*) or TS= (retina* SAME hemorrhag*) or TS=(retina* SAME haemorrhage*) or TS=(retina* SAME neovascular*) or TS=(retina* SAME leak*) or TS=(retina* SAME perme*) or TS=(retina* SAME bleed*) or TS= (eye* SAME hemorrhag*) or TS=(eye* SAME haemorrhage*) or TS=(eye* SAME neovascular*) or TS=(eye* SAME leak*) or TS=(eye* SAME perme*) or TS=(eye* SAME bleed*)
TS= (ocular* SAME hemorrhag*) or TS=(ocular* SAME haemorrhage*) or TS=(ocular* SAME neovascular*) or TS=(ocular* SAME leak*) or TS=(ocular* SAME perme*) or TS=(ocular SAME bleed*) or TS= (intraocular* SAME hemorrhag*) or TS=(intraocular* SAME haemorrhage*) or TS=(intraocular* SAME neovascular*) or TS=(intraocular* SAME leak*) or TS=(intraocular* SAME perme*) or TS=(intraocular* SAME bleed*) or TS= (optic* SAME hemorrhag*) or TS=(optic* SAME haemorrhage*) or TS=(optic* SAME neovascular*) or TS=(intraocular* SAME leak*) or TS=(optic* SAME perme*) or TS=(optic* SAME bleed*)
#10 or #11
#9 and #12
TS=(rat or rats or mouse or mice or murine or rodent or rodents or hamster or hamsters or pig or pigs or porcine or rabbit or rabbits or animal or animals or dogs or dog or cats or cow or bovine or sheep or ovine or monkey or monkeys)
#13 NOT #14
CDSR and CENTRAL (Cochrane Library) 2007 Issue 3
Searched 4 October 2007.
38 reviews were retrieved in CDSR and 84 records in CENTRAL.
-
#1 MeSH descriptor Color Vision Defects explode all trees
-
#2 MeSH descriptor Color Perception explode all trees
-
#3 MeSH descriptor Color Perception Tests explode all trees
-
#4 MeSH descriptor Vision Screening explode all trees
-
#5 MeSH descriptor Vision Tests explode all trees
-
#6 MeSH descriptor Contrast Sensitivity explode all trees
-
#7 (color* NEAR/3 test*) or (colour* NEAR/3 test*) or (color* NEAR/3 screen*) or (colour* NEAR/3 screen*) or (vision NEAR/3 test*) or (vision NEAR/3 screen*) or (visual NEAR/3 test*) or (visual NEAR/3 screen*)
-
#8 (color* NEAR/3 blind*) or (color* NEAR/3 deficien*) or (color* NEAR/3 defect*) or (color* NEAR/3 loss) or (color* NEAR/3 impair*) or (colour* NEAR/3 blind*) or (colour* NEAR/3 deficien*) or (colour* NEAR/3 defect*) or (colour* NEAR/3 loss) or (colour* NEAR/3 impair*)
-
#9 monochromatopsia or achromatopsia or deutan or protan or anomaloscop* or pseudoisochromatic* or “hue* discrimination*” or lantern* or tritan or TCT
-
#10 ishihara* or kojima* or ohkuma* or matsubara* or dvorine* or cvtmet or “hardy rand rittler*” or AOHRR or AO H-R-R or lanthony* or “panel d 15” or “panel d15” or “d 15 panel” or “d15 panel” or farnsworth* or “color* plate” or “colour* plate” or “mollon reffin*” or “pease allen*” or “giles archer*” or “adams desaturated” or “City University” or CUCVT or “velhagen pflugertrident*” or (contrast NEAR/3 sensitivit*)
-
#11 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10)
-
#12 MeSH descriptor Diabetes Mellitus explode all trees
-
#13 (diabet* or IDDM or NIDDM or T2DM)
-
#14 (#12 OR #13)
-
#15 (#11 AND #14)
-
#16 MeSH descriptor Diabetic Retinopathy explode all trees
-
#17 (retinopath*)
-
#18 MeSH descriptor Macular Degeneration explode all trees
-
#19 MeSH descriptor Retinal Hemorrhage explode all trees
-
#20 MeSH descriptor Retinal Neovascularization explode all trees
-
#21 (macula* NEAR/3 edema*) or (macula* NEAR/3 oedema*) or (retina* NEAR/3 edema*) or (retina* NEAR/3 oedema*) or (optic* NEAR/3 edema*) or (optic NEAR/3 oedema*) or (ocular* NEAR/3 edema*) or (ocular* NEAR/3 oedema*) or (intraocular* NEAR/3 edema*)
-
#22 (maculopath* or microaneurysm* or “micro aneurysm*” or microaneurism* or “micro aneurism*” or (retina* NEAR/3 hemorrhag*) or (retina* NEAR/3 haemorrhag*) or (retina* NEAR/3 neovascular*) or (retina* NEAR/3 leak) or (retina* NEAR/3 perme*) or (eye* NEAR/3 hemorrhag*) or (eye* NEAR/3 haemorrhag*) or (eye* NEAR/3 neovascular*) or (eye* NEAR/3 leak) or (eye* NEAR/3 perme*) or (ocular* NEAR/3hemorrhag*) or (ocular* NEAR/3 haemorrhag*) or (ocular* NEAR/3 neovascular*) or (ocular* NEAR/3 leak*) or (ocular* NEAR/3 perme*) or (ocular* NEAR/3 bleed*) or (intraocular* NEAR/3hemorrhag*) or (intraocular* NEAR/3 haemorrhag*) or (intraocular* NEAR/3 neovascular*) or (intraocular* NEAR/3 leak*) or (intraocular* NEAR/3 perme*) or (intraocular* NEAR/3 bleed*)
-
#23 (#16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22)
-
#24 (#15 AND #23)
DARE and HTA (CRD internal databases) 1994 to September 2007
Searched 4 October 2007.
0 records were retrieved in DARE and 1 record was retrieved in HTA.
s (color$or colour$or vision or visual)(w3)(test$or screen$)
s (color$or colour$)(w3)(blind$or deficien$or defect$or loss or impair$or perception)
s monochromatopsia or achromatopsia or deutan or protan or anomaloscop$or pseudoisochromatic$or hue$(w)discrimination$or lantern$or tritan or TCT
s ishihara$or kojima$or ohkuma$or matsubara$or dvorine$or cvtmet or hardy(w)rand(w)rittler$or AOHRR or AO(w)H(w)R(w)R or lanthony$or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or farnsworth$or (color$or colour$)(w)plate or mollon(w)reffin$or pease(w)allen$or giles(w)archer$or adams(w)desaturated or City(w)University or CUCVT or velhagen(w)pflugertrident$or contrast(w3)sensitivit$
s s1 OR s2 OR s3 OR s4
s diabet$or IDDM or NIDDM or T2DM
s s5 and s6
s retinopath$
s (optic$or ocular$or intraocular$or macula$or retina$)(w3)(edema$or oedema$)
s maculopath$or microaneurysm$or micro(w)aneurysm$or microaneurism$or micro(w)aneurism$or (ocular$or intraocular$or optic$or retina$or eye$)(w3)(hemorrhag$or haemorrhag$or neovascular$or leak or perme$or bleed$or neo(w)vascular$)
s s8 OR s9 OR s10
s s7 AND s11
LILACS (Birme Virtual Health Library) 1982 to September 2007
Searched 4 October 2007.
1 record was retrieved.
(color test$) OR (color screen$) OR (colour test$) OR (colour screen$) OR (vision test$) OR (vision screen$) OR (visual test$) OR (visual screen$) OR (color blind$) OR (colour blind$) OR monochromatopsia OR achromatopsia OR deutan OR protan OR anomaloscop$OR pseudoisochromatic$OR (hue$discrimination$) OR lantern$or tritan OR TCT OR ishihara$OR kojima$OR ohkuma$OR matsubara$OR dvorine$OR cvtmet OR (hardy rand rittler$) OR AOHRR OR lanthony$OR (panel d 15) OR (panel d15) OR (d 15 panel) OR (d15 panel) OR farnsworth$OR (color plate) OR (colour plate) OR (mollon reffin$) OR (pease allen$) OR (giles archer$) OR (adams desaturated) OR (City University) OR CUCVT OR (velhagen pflugertrident$) OR (contrast sensitivit$)[words]
AND
diabet$OR IDDM OR NIDDM OR T2DM[words]
AND
retinopath$OR (macula$edema$) OR (macula$oedema$) OR (retina$edema$) OR (retina$oedema$) OR maculopath$OR microaneurysm$OR (micro aneurysm$) OR microaneurism$OR (micro aneurism$) OR (retina$hemorrag$) OR (retina$haemorrhage$) OR (retina$neovascular$) OR (retina$leak) OR (retina$perme$) OR (eye$hemorrhag$) OR (eye$haemorrhag$) OR (eye$neovascular$) OR (eye$leak) OR (eye$perme$)[words]
BIOSIS (Dialog) 1926 to September Week 5 2007
Searched 5 October 2007.
325 records were retrieved.
s (color? or colour? or vision or visual)(3n)(test or tests or testing or tested or screen or screens or screening or screened)
s (color? or colour?)(3n)(blind or blindness or deficient or deficiency or defect or defects or defection or loss or impair or impaired or impairment or perception)
s monochromatopsia or achromatopsia or deutan or protan
s anomaloscop? or pseudoisochromatic? or hue(w)discrimination? or lantern? or tritan or TCT or Ishihara? or Kojima? or ohkuma? or Matsubara? or Dvorine? or cvtmet or Hardy(w)Rand(w)Rittler? or AOHRR or Lanthony? or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or Farnsworth? or color?(w)plate or colour?(w)plate or Mollon(w)Reffin? or Pease(w)Allen? or Giles(w)Archer? or Adams(w)Desaturated or City(w)University or CUCVT or Velhagen(w)Pflugertrident? or contrast(3n)sensitivit?
s s1:s4
s diabet? or IDDM or NIDDM or T2DM
s retinopath? or macula?(3n)edema? or macula?(3n)oedema? or retina?(3n)edema? or retina?(3n)oedema? or optic?(3n)edema? or optic?(3n)oedema? or ocular?(3n)edema? or ocular?(3n)oedema? or intraocular?(3n)edema? or intraocular?(3n)oedema? or maculopath? or microaneurysm? or micro(w)aneurysm? or microaneurism? or micro(w)aneurism? or retina?(3n)hemorrhag? or retina?(3n)haemorrhage? or retina?(3n)neovascular? or retina?(3n)leak or retina?(3n)perme? or eye?(3n)hemorrhag? or eye?(3n)haemorrhag? or eye?(3n)neovascular? or eye?(3n)leak or eye?(3n)perme? or ocular?(3n)hemorrhag? or ocular?(3n)haemorrhag? or ocular?(3n)neovascular? or ocular?(3n)leak? or ocular?(3n)perme? or ocular?(3n)bleed? or intraocular?(3n)hemorrhag? or intraocular?(3n)haemorrhag? or intraocular?(3n)neovascular? or intraocular?(3n)leak? or intraocular?(3n)perme? or intraocular?(3n)bleed? or optic?(3n)hemorrhag? or optic?(3n)haemorrhag? or optic?(3n)neovascular? or optic?(3n)leak? or optic?(3n)perme? or optic?(3n)bleed?
s s5 and s6 and s7
Pascal (Dialog) 1973 to September Week 4 2007
Searched 5 October 2007.
83 records were retrieved.
s (color? or colour? or vision or visual)(3n)(test or tests or testing or tested or screen or screens or screening or screened)
s (color? or colour?)(3n)(blind or blindness or deficient or deficiency or defect or defects or defection or loss or impair or impaired or impairment or perception)
s monochromatopsia or achromatopsia or deutan or protan
s anomaloscop? or pseudoisochromatic? or hue(w)discrimination? or lantern? or tritan or TCT or Ishihara? or Kojima? or ohkuma? or Matsubara? or Dvorine? or cvtmet or Hardy(w)Rand(w)Rittler? or AOHRR or Lanthony? or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or Farnsworth? or color?(w)plate or colour?(w)plate or Mollon(w)Reffin? or Pease(w)Allen? or Giles(w)Archer? or Adams(w)Desaturated or City(w)University or CUCVT or Velhagen(w)Pflugertrident? or contrast(3n)sensitivit?
s s1:s4
s diabet? or IDDM or NIDDM or T2DM
s retinopath? or macula?(3n)edema? or macula?(3n)oedema? or retina?(3n)edema? or retina?(3n)oedema? or optic?(3n)edema? or optic?(3n)oedema? or ocular?(3n)edema? or ocular?(3n)oedema? or intraocular?(3n)edema? or intraocular?(3n)oedema? or maculopath? or microaneurysm? or micro(w)aneurysm? or microaneurism? or micro(w)aneurism? or retina?(3n)hemorrhag? or retina?(3n)haemorrhage? or retina?(3n)neovascular? or retina?(3n)leak or retina?(3n)perme? or eye?(3n)hemorrhag? or eye?(3n)haemorrhag? or eye?(3n)neovascular? or eye?(3n)leak or eye?(3n)perme? or ocular?(3n)hemorrhag? or ocular?(3n)haemorrhag? or ocular?(3n)neovascular? or ocular?(3n)leak? or ocular?(3n)perme? or ocular?(3n)bleed? or intraocular?(3n)hemorrhag? or intraocular?(3n)haemorrhag? or intraocular?(3n)neovascular? or intraocular?(3n)leak? or intraocular?(3n)perme? or intraocular?(3n)bleed? or optic?(3n)hemorrhag? or optic?(3n)haemorrhag? or optic?(3n)neovascular? or optic?(3n)leak? or optic?(3n)perme? or optic?(3n)bleed?
s s5 and s6 and s7
Dissertation Abstracts (Dialog) 1861 to July 2007
Searched 5 October 2007.
4 records were retrieved.
s (color? or colour? or vision or visual)(3n)(test or tests or testing or tested or screen or screens or screening or screened)
s (color? or colour?)(3n)(blind or blindness or deficient or deficiency or defect or defects or defection or loss or impair or impaired or impairment or perception)
s monochromatopsia or achromatopsia or deutan or protan
s anomaloscop? or pseudoisochromatic? or hue(w)discrimination? or lantern? or tritan or TCT or Ishihara? or Kojima? or ohkuma? or Matsubara? or Dvorine? or cvtmet or Hardy(w)Rand(w)Rittler? or AOHRR or Lanthony? or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or Farnsworth? or color?(w)plate or colour?(w)plate or Mollon(w)Reffin? or Pease(w)Allen? or Giles(w)Archer? or Adams(w)Desaturated or City(w)University or CUCVT or Velhagen(w)Pflugertrident? or contrast(3n)sensitivit?
s s1:s4
s diabet? or IDDM or NIDDM or T2DM
s retinopath? or macula?(3n)edema? or macula?(3n)oedema? or retina?(3n)edema? or retina?(3n)oedema? or optic?(3n)edema? or optic?(3n)oedema? or ocular?(3n)edema? or ocular?(3n)oedema? or intraocular?(3n)edema? or intraocular?(3n)oedema? or maculopath? or microaneurysm? or micro(w)aneurysm? or microaneurism? or micro(w)aneurism? or retina?(3n)hemorrhag? or retina?(3n)haemorrhage? or retina?(3n)neovascular? or retina?(3n)leak or retina?(3n)perme? or eye?(3n)hemorrhag? or eye?(3n)haemorrhag? or eye?(3n)neovascular? or eye?(3n)leak or eye?(3n)perme? or ocular?(3n)hemorrhag? or ocular?(3n)haemorrhag? or ocular?(3n)neovascular? or ocular?(3n)leak? or ocular?(3n)perme? or ocular?(3n)bleed? or intraocular?(3n)hemorrhag? or intraocular?(3n)haemorrhag? or intraocular?(3n)neovascular? or intraocular?(3n)leak? or intraocular?(3n)perme? or intraocular?(3n)bleed? or optic?(3n)hemorrhag? or optic?(3n)haemorrhag? or optic?(3n)neovascular? or optic?(3n)leak? or optic?(3n)perme? or optic?(3n)bleed?
s s5 and s6 and s7
Inside Conferences (Dialog) 1993 to 3 October 2007
Searched 5 October 2007.
0 records were retrieved.
s (color? or colour? or vision or visual)(3n)(test or tests or testing or tested or screen or screens or screening or screened)
s (color? or colour?)(3n)(blind or blindness or deficient or deficiency or defect or defects or defection or loss or impair or impaired or impairment or perception)
s monochromatopsia or achromatopsia or deutan or protan
s anomaloscop? or pseudoisochromatic? or hue(w)discrimination? or lantern? or tritan or TCT or Ishihara? or Kojima? or ohkuma? or Matsubara? or Dvorine? or cvtmet or Hardy(w)Rand(w)Rittler? or AOHRR or Lanthony? or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or Farnsworth? or color?(w)plate or colour?(w)plate or Mollon(w)Reffin? or Pease(w)Allen? or Giles(w)Archer? or Adams(w)Desaturated or City(w)University or CUCVT or Velhagen(w)Pflugertrident? or contrast(3n)sensitivit?
s s1:s4
s diabet? or IDDM or NIDDM or T2DM
s retinopath? or macula?(3n)edema? or macula?(3n)oedema? or retina?(3n)edema? or retina?(3n)oedema? or optic?(3n)edema? or optic?(3n)oedema? or ocular?(3n)edema? or ocular?(3n)oedema? or intraocular?(3n)edema? or intraocular?(3n)oedema? or maculopath? or microaneurysm? or micro(w)aneurysm? or microaneurism? or micro(w)aneurism? or retina?(3n)hemorrhag? or retina?(3n)haemorrhage? or retina?(3n)neovascular? or retina?(3n)leak or retina?(3n)perme? or eye?(3n)hemorrhag? or eye?(3n)haemorrhag? or eye?(3n)neovascular? or eye?(3n)leak or eye?(3n)perme? or ocular?(3n)hemorrhag? or ocular?(3n)haemorrhag? or ocular?(3n)neovascular? or ocular?(3n)leak? or ocular?(3n)perme? or ocular?(3n)bleed? or intraocular?(3n)hemorrhag? or intraocular?(3n)haemorrhag? or intraocular?(3n)neovascular? or intraocular?(3n)leak? or intraocular?(3n)perme? or intraocular?(3n)bleed? or optic?(3n)hemorrhag? or optic?(3n)haemorrhag? or optic?(3n)neovascular? or optic?(3n)leak? or optic?(3n)perme? or optic?(3n)bleed?
s s5 and s6 and s7
NTIS (National Technical Information Service) (US Department of Commerce) 1990 to September 2007
Searched 5 October 2007.
0 records were retrieved.
Each line searched separately:
color test diabetic [With all of the words]
color test diabetes [With all of the words]
color testing diabetic [With all of the words]
color testing diabetes [With all of the words]
color screen diabetic [With all of the words]
color screen diabetes [With all of the words]
color screening diabetic [With all of the words]
color screening diabetes [With all of the words]
colour test diabetic [With all of the words]
colour test diabetes [With all of the words]
colour testing diabetic [With all of the words]
colour testing diabetes [With all of the words]
colour screen diabetic [With all of the words]
colour screen diabetes [With all of the words]
colour screening diabetic [With all of the words]
colour screening diabetes [With all of the words]
color retinopathy diabetes [With all of the words]
color retinopathy diabetic [With all of the words]
colour retinopathy diabetes [With all of the words]
colour retinopathy diabetic [With all of the words]
ReFer (Research Findings electronic Register) (ReFer website) September 2007
Searched 5 October 2007.
0 records were retrieved.
Each line searched separately:
color AND diabetic AND retinopathy
color AND diabetes AND retinopathy
colour AND diabetic AND retinopathy
colour AND diabetes AND retinopathy
ClinicalTrials.gov (US National Library of Medicine) September 2007
Searched 5 October 2007.
0 records were retrieved.
Each line searched separately:
color, diabetic, retinopathy
color, diabetes, retinopathy
colour, diabetic, retinopathy
colour, diabetes, retinopathy
Current Controlled Trials (MetaRegister of Current Controlled Trials – mRCT) September 2007
Searched 5 October 2007.
0 records were retrieved.
Each line searched separately:
retinopathy AND colour
retinopathies AND colour
retinopathy AND color
retinopathies AND color
screening AND color
screen AND color
screening AND colour
screen AND colour
ClinicalStudyResults.org (ClinicalStudyResults website) September 2007
5 October 2007.
0 records were retrieved.
Each line searched separately:
color, diabetes, retinopathy
retinopathy
retinopathies
ClinicalTrialResults.org (Clinical Trial Results website) September 2007
5 October 2007.
0 records were retrieved.
Each line searched separately:
retinopathy
retinopathies
NHS EED (CRD internal databases) 1994 to September 2007
5 October 2007.
0 records were retrieved.
s (color$or colour$or vision or visual)(w3)(test$or screen$)
s (color$or colour$)(w3)(blind$or deficien$or defect$or loss or impair$)
s monochromatopsia or achromatopsia or deutan or protan or anomaloscop$or pseudoisochromatic$or hue$(w)discrimination$or lantern$or tritan or TCT
s ishihara$or kojima$or ohkuma$or matsubara$or dvorine$or cvtmet or hardy(w)rand(w)rittler$or AOHRR or AO(w)H(w)R(w)R or lanthony$or panel(w)d(w)15 or panel(w)d15 or d(w)15(w)panel or d15(w)panel or farnsworth$or (color$or colour$)(w)plate or mollon(w)reffin$or pease(w)allen$or giles(w)archer$or adams(w)desaturated or City(w)University or CUCVT or velhagen(w)pflugertrident$or contrast(w3)sensitivit$
s s1 OR s2 OR s3 OR s4
s diabet$or IDDM or NIDDM or T2DM
s s5 and s6
s retinopath$
s (optic$or ocular$or intraocular$or macula$or retina$)(w3)(edema$or oedema$)
s maculopath$or microaneurysm$or micro(w)aneurysm$or microaneurism$or micro(w)aneurism$or (ocular$or intraocular$or optic$or retina$or eye$)(w3)(hemorrhag$or haemorrhag$or neovascular$or leak or perme$or bleed$or neo(w)vascular$)
s s8 OR s9 OR s10
s s7 AND s11
HEED (Wiley online) September 2007
5 October 2007.
2 records were retrieved.
AX=‘color test’ within 3 OR ‘color testing’ within 3 OR ‘color tests’ within 3 OR ‘color screen’ within 3 OR ‘color screening’ within 3 OR ‘color screened’ within 3 OR ‘colour test’ within 3 OR ‘colour testing’ within 3 OR ‘colour tests’ within 3 OR ‘colour screen’ within 3 OR ‘colour screening’ within 3 OR ‘colour screened’ within 3
AX=‘vision test’ within 3 OR ‘vision testing’ within 3 OR ‘vision tests’ within 3 OR ‘vision screen’ within 3 OR ‘vision screening’ within 3 OR ‘vision screened’ within 3 OR ‘visual test’ within 3 OR ‘visual testing’ within 3 OR ‘visual tests’ within 3 OR ‘visual screen’ within 3 OR ‘visual screening’ within 3 OR ‘visual screened’ within 3
CS=1 or 2
AX=diabetes or diabetic or IDDM or NIDDM or T2DM
AX=retinopathy or retinopathies or (macular edema) or (macular oedema) or (retina edema) or (retina oedema) or (macular edemas) or (macular oedemas) or (retina edemas) or (retina oedemas) or maculopathy or microaneurysm or (micro aneurysm) or microaneurism or (micro aneurism) or (retina hemorrhage) or (retina haemorrhage) or (eye hemorrhage) or (eye haemorrhage)
CS=3 and 4 and 5
Internet sites searched
Websites were browsed (publications and research) and searched using a variety of combinations of the following terms: ‘colour vision screening’, ‘color vision screening’, ‘colour vision’, ‘color vision’, ‘colour screening’, ‘color screening’, ‘retinopathy’, ‘diabetes’, ‘diabetic’.
MedlinePlus: www.nlm.nih.gov/medlineplus/medlineplus.html
intute: www.intute.ac.uk/
National Library for Health (NLH) Diabetes Specialist Library: www.library.nhs.uk/diabetes/
National Library for Health (NLH) Screening Specialist Library: www.library.nhs.uk/screening/
National Screening Programme for Sight-threatening Diabetic Retinopathy: www.nscretinopathy.org.uk/
British Association for Retinal Screeners: www.eyescreening.org.uk/
Diabetes UK: www.diabetes.org.uk/
American Diabetic Association (US): www.diabetes.org/home.jsp
Royal College of Ophthalmologists: www.rcophth.ac.uk/
American Academy of Ophthalmology (US): www.aao.org/
College of Optometrists: www.college-optometrists.org/
Association of Optometrists: www.assoc-optometrists.org/
National Eye Institute (US): www.nei.nih.gov/
Conference proceedings
American Academy of Ophthalmology annual meeting (1999–2006) (www.aao.org/meetings/annual_meeting/) – Searchable archive available: posters 1999–2006; programs 2001–6. Searched using various combinations of the following terms: ‘color’, ‘colour’, ‘color vision’, ‘colour vision’ and ‘retinopathy’.
American Diabetic Association Annual Scientific Sessions (2003–7) (www.diabetes.org/for-health-professionals-and-scientists/profed.jsp) – Searchable archive available: 2003–7. Searched using various combinations of the following terms: ‘color vision’, ‘colour vision’, ‘retinopathy screening’ and ‘retinopathy testing’. Browsed results for potentially relevant abstracts.
European Association for the Study of Diabetes annual meeting (2001–7) (www.easd.org/) – Abstracts available in a variety of PDF, web page and searchable formats: 2001–7. Browsed/searched: ‘color’, ‘colour’, ‘retinopathy’.
Royal College of Ophthalmologists Annual Congress (2004–7) (www.rcophth.ac.uk/scientific/) – Abstracts available in PDF format: 2004–7. Browsed PDFs using search facility: ‘color’, ‘colour’, ‘retinopathy’.
Search alerts
Search alerts were set up in MEDLINE and EMBASE to run every time the databases were updated (usually weekly). The following strategy was used:
(colo?r vision and retinopathy).ti,ab.
Search alerts were also created in the following journals:
American Journal of Ophthalmology (http://archopht.ama-assn.org/) – Alert criteria: Title or Abstract: (color or colour) and vision and retinopathy.
British Journal of Ophthalmology (http://bjo.bmj.com/) – Alert criteria: Title or Abstract: (color or colour) and vision and retinopathy.
Clinical and Experimental Ophthalmology (www.blackwell-synergy.com/loi/ceo) – Alert criteria: Full text: (color or colour) and vision and retinopathy.
Diabetes (http://diabetes.diabetesjournals.org/) – Alert criteria: Anywhere: (color or colour) and vision and retinopathy.
Diabetes Care (http://care.diabetesjournals.org/) – Alert criteria: Anywhere: (color or colour) and vision and retinopathy
Diabetic Medicine (www.blackwell-synergy.com/toc/dme/0/0) – Alert criteria: Full text: (color or colour) and vision and retinopathy
Investigative Ophthalmology and Visual Science (www.iovs.org/) – Alert criteria: Title or Abstract: (color or colour) and vision and retinopathy.
Ophthalmology (www.sciencedirect.com/science/journal/01616420) – Alert criteria: Title-Abstr-Key: ((color or colour) and vision and retinopathy)
Economics search strategies
Diabetic retinopathy screening (economic/cost) search strategies
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OVID gateway) 1950 to November Week 1 2007
15 November 2007.
209 records were retrieved in MEDLINE and 5 in MEDLINE In-Process & Other Non-Indexed Citations.
-
economics/
-
exp “costs and cost analysis”/
-
economics, dental/
-
exp “economics, hospital”/
-
economics, medical/
-
economics, nursing/
-
economics, pharmaceutical/
-
(economic$or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).tw.
-
(expenditure$not energy).tw.
-
(value adj1 money).tw.
-
budget$.tw.
-
or/1–11
-
((energy or oxygen) adj cost).ti,ab.
-
(metabolic adj cost).ti,ab.
-
((energy or oxygen) adj expenditure).ti,ab.
-
or/13–15
-
12 not 16
-
Vision Screening/
-
Vision Tests/
-
exp Mass Screening/
-
screen$.ti,ab.
-
((optic$or ocular$or intraocular$or eye$or retina$or vision$or visual$) adj2 (test$or exam$)).ti,ab.
-
Fluorescein Angiography/
-
Ophthalmoscopy/
-
Fluorophotometry/
-
Electroretinography/
-
Retinoscopy/
-
(fluoresence or fluorescein).ti,ab.
-
(fundoscop$or electroretin$or electro retin$or fluorophotometr$or retinoscop$or biomicroscop$or ophthalmoscop$).ti,ab.
-
Photography/
-
Image Processing, Computer-Assisted/
-
Angiography/
-
(digital$or imag$or camer$or photograph$or polaroid$or angiograph$).ti,ab.
-
Ophthalmology/
-
Optometry/
-
(optomet$or optician$or ophthalm$).ti,ab.
-
or/18–36
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.
-
or/38–40
-
exp Diabetic Retinopathy/
-
retinopath$.ti,ab.
-
exp Macular Degeneration/
-
Retinal Hemorrhage/
-
Retinal Neovascularization/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/42–50
-
17 and 37 and 41 and 51
-
Animals/
-
Humans/
-
53 not (53 and 54)
-
52 not 55
EMBASE (OVID gateway) 1980 to 2007 Week 45
Searched 15 November 2007.
240 records were retrieved.
-
Health Economics/
-
exp Economic Evaluation/
-
exp Health Care Cost/
-
exp PHARMACOECONOMICS/
-
or/1–4
-
(econom$or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab.
-
(expenditure$not energy).ti,ab.
-
(value adj2 money).ti,ab.
-
budget$.ti,ab.
-
or/6–9
-
5 or 10
-
(metabolic adj cost).ti,ab.
-
((energy or oxygen) adj cost).ti,ab.
-
((energy or oxygen) adj expenditure).ti,ab.
-
or/12–14
-
11 not 15
-
editorial.pt.
-
note.pt.
-
letter.pt.
-
or/17–19
-
16 not 20
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dogs or dog or cats or bovine or sheep).ti,ab,sh.
-
exp animal/
-
Nonhuman/
-
or/22–24
-
exp human/
-
exp human experiment/
-
26 or 27
-
25 not (25 and 28)
-
21 not 29
-
exp vision test/
-
exp SCREENING/
-
screen$.ti,ab.
-
((eye$or retina$or vision$or visual$) adj2 (test$or exam$)).ti,ab.
-
Fluorescence Angiography/
-
OPHTHALMOSCOPY/
-
FLUOROPHOTOMETRY/
-
ELECTRORETINOGRAPHY/
-
RETINOSCOPY/
-
(fluoresence or fluorescein).ti,ab.
-
(fundoscop$or electroretin$or fluorophotometr$or retinoscop$or biomicroscop$or ophthalmoscop$).ti,ab.
-
PHOTOGRAPHY/
-
digital imaging/or image processing/
-
Retina Angiography/
-
(digital$or imag$or camer$or photograph$or polaroid$or angiograph$).ti,ab.
-
OPHTHALMOLOGY/
-
OPTOMETRY/
-
(optomet$or optician$or ophthalm$).ti,ab.
-
or/31–48
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.
-
or/50–52
-
exp Retinopathy/
-
retinopath$.ti,ab.
-
Retina Maculopathy/
-
Retina Edema/
-
Retina Hemorrhage/
-
Retina Neovascularization/
-
Retina Macula Degeneration/
-
Microaneurysm/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/54–65
-
30 and 49 and 53 and 66
CINAHL (OVID gateway) 1982 to November Week 2 2007
Searched 15 November 2007.
24 records were retrieved.
-
exp “costs and cost analysis”/or “economic aspects of illness”/or “economic value of life”/or economics, pharmaceutical/
-
((cost or costs or costed or costly or costing) adj (utilit$or benefit$or effective$or stud$or minimi$or analys$)).ti,ab.
-
(economic$or pharmacoeconomic$or price$or pricing).ti,ab.
-
(expenditure$not energy).ti,ab.
-
(value adj1 money).ti,ab.
-
budget$.ti,ab.
-
or/1–6
-
exp Vision Tests/
-
exp Health Screening/
-
screen$.ti,ab.
-
((eye$or retina$or vision$or visual$) adj2 (test$or exam$)).ti,ab.
-
OPHTHALMOSCOPY/
-
(fluoresence or fluorescein).ti,ab.
-
(fundoscop$or electroretin$or fluorophotometr$or retinoscop$or biomicroscop$or ophthalmoscop$).ti,ab.
-
PHOTOGRAPHY/
-
Digital Imaging/
-
Image Processing, Computer Assisted/
-
Angiography/
-
(digital$or imag$or camer$or photograph$or polaroid$or angiograph$).ti,ab.
-
OPHTHALMOLOGY/
-
OPTOMETRY/
-
(optomet$or optician$or ophthalm$).ti,ab.
-
or/8–22
-
exp Diabetes Mellitus/
-
diabet$.ti,ab.
-
(IDDM or NIDDM or T2DM).ti,ab.
-
or/24–26
-
Diabetic Retinopathy/
-
Macular Degeneration/
-
Eye Hemorrhage/
-
((optic$or ocular$or intraocular$or macula$or retina$) adj3 (edema$or oedema$)).ti,ab.
-
maculopath$.ti,ab.
-
(microaneurism$or micro aneurism$or microaneurysm$or micro aneurysm$).ti,ab.
-
((ocular$or intraocular$or optic$or retina$or eye$) adj3 (hemorrhag$or haemorrhag$or neovascular$or leak$or perme$or bleed$or neo vascular$)).ti,ab.
-
or/28–34
-
7 and 23 and 27 and 35
NHS EED (CRD internal databases) 1994 to October 2007
Searched 15 November 2007.
41 records were retrieved.
s screen$
s screening/xti
s (eye$or retina$or vision$or visual$)(w2)(test$or exam$)
s fluoresence or fluorescein
s fundoscop$or electroretin$or fluorophotometr$or retinoscop$or biomicroscop$or ophthalmoscop$
s digital$or imag$or camer$or photograph$or polaroid$or angiograph$
s optomet$or optician$or ophthalm$
s s1 or s2 or s3 or s4 or s5 or s6 or s7
s diabet$or IDDM or NIDDM or T2DM
s retinopath$
s (optic$or ocular$or intraocular$or macula$or retina$)(w3)(edema$or oedema$)
s maculopath$or microaneurysm$or micro(w)aneurysm$or microaneurism$or micro(w)aneurism$or (ocular$or intraocular$or optic$or retina$or eye$)(w3)(hemorrhag$or haemorrhag$or neovascular$or leak or perme$or bleed$or neo(w)vascular$)
s s10 OR s11 OR s12
s s8 AND s9 AND s13
HEED (Wiley online). 2007/Nov. 15th November 2007.
64 records were retrieved.
AX=screen or screened or screening
AX=‘eye test’ within 2 or ‘eye exam’ within 2 or ‘eye examination’ within 2
AX=‘retina test’ within 2 or ‘retinal test’ within 2 or ‘retina exam’ within 2 or ‘retinal exam’ within 2 or ‘retina examination’ within 2 or ‘retinal examination’ within 2
AX=‘vision test’ within 2 or ‘visual test’ within 2 or ‘vision exam’ within 2 or ‘visual exam’ within 2 or ‘vision examination’ within 2 or ‘visual examination’ within 2
AX=fluoresence or fluorescein or s fundoscopy or electroretinography or fluorophotometry or retinoscopy or biomicroscopy or ophthalmoscopy or ophthalmoscope
AX=digital or image or imaging or camera or photograph or polaroid or angiography
AX=optometrist or optician or ophthalmologist
CS=1 or 2 or 3 or 4 or 5 or 6 or 7
AX=diabetes or diabetic or IDDM or NIDDM or T2DM
AX=retinopathy
AX=(macular edema) or (macular oedema) or (retinal edema) or (retinal oedema) or (macular edemas) or (macular oedemas) or (retinal edemas) or (retinal oedemas)
AX=maculopathy or microaneurysm or (micro aneurysm) or microaneurism or (micro aneurism)
CS=10 or 11 or 12
CS=8 and 9 and 13
Appendix 2 The QUADAS tool for methodological assessment of diagnostic studies
| QUADAS criterion | Criterion met? | |
|---|---|---|
| 1. | Was the spectrum of patients representative of the patients who will receive the test in practice? | Yes/no/unclear |
| 2. | Were selection criteria clearly described? | Yes/no/unclear |
| 3. | Is the reference standard likely to correctly classify the target condition? | Yes/no/unclear |
| 4. | Is the time period between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests (i.e. under 1 month)? | Yes/no/unclear |
| 5. | Did the whole sample or a random selection of the sample receive verification using a reference standard of diagnosis? | Yes/no/unclear |
| 6. | Did patients receive the same reference standard regardless of the index test result? | Yes/no/unclear |
| 7. | Was the reference standard independent of the index test (i.e. the index test did not form part of the reference standard)? | Yes/no/unclear |
| 8. | Was the execution of the index test described in sufficient detail to permit replication of the test? | Yes/no/unclear |
| 9. | Was the execution of the reference standard described in sufficient detail to permit its replication? | Yes/no/unclear |
| 10. | Were the index test results interpreted without knowledge of the results of the reference standard? | Yes/no/unclear |
| 11. | Were the reference standard results interpreted without knowledge of the results of the index test? | Yes/no/unclear |
| 12. | Were the same clinical data available when test results were interpreted as would be available when the test is used in practice (i.e. duration of diabetes, hypertension, renal disease, HbA1c, smoking, visual acuity)? | Yes/no/unclear |
| 13. | Were uninterpretable/intermediate test results reported? | Yes/no/unclear |
| 14. | Were withdrawals from the study explained? | Yes/no/unclear |
Appendix 3 Data extraction tables
| Bibliographic details | |
|---|---|
| Author | Aspinall36 |
| Year | 1983 |
| Study characteristics | |
| Study design |
Longitudinal Over 7 years follow-up; recruitment 1963–5, follow-up to 1972 |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: diabetics < 70 years with normal fundi |
| Exclusion criteria: congenital colour vision defects; cataracts | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Ophthalmoscopy |
| Retinopathy grading (reference standard) |
Dichotomous N: normal fundus, fundi still showing no signs of retinopathy in either eye R: retinopathy, fundi showing signs, however slight, in one or both eyes |
| For which eye was retinopathy assessed? |
Random/quasi-randomly selected Patients’ preferred eye |
| Colour vision test(s) |
FM-100 Anomaloscope |
| Colour vision grading | Dichotomous |
| Participant characteristics | |
| Number of participants | Number of participants included in study: N: n = 209; R: n = 86 |
| Number of participants included in analysis: N: n = 209; R: n = 86 | |
| Age | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Association between clinical characteristics and outcomes (multivariate regression): Yellow–blue colour discrimination (anomaloscope units JND) coefficient = 5.113 × 10–2, standard error = 1.39 × 10–2, t = 3.67 The single variable with the greatest discriminating power between the two groups was colour discrimination along the yellow–blue axis Following division of the population into two groups at 40 years, duration was found to be the best single predictive parameter for the under 40s and yellow–blue colour discrimination was the best single predictive parameter for the over 40s (see Figures 1 and 2) The model, which also includes blood glucose control, duration of diabetes, proteinuria and colour discrimination, has a negative predictive value of 0.82 and a positive predictive value of 0.54 |
| Bibliographic details | |
|---|---|
| Author | Ayed37 |
| Year | 1990 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: visual acuity ≥ 5/10 |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Fluorescein angiography |
| Retinopathy grading (reference standard) | Graded
|
| For which eye was retinopathy assessed? | Both |
| Colour vision test(s) | FM-100; presented under luminance of 600 lux |
| Colour vision grading |
Continuous/average Total error score (TES) |
|
Dichotomous ‘Abnormal’ if TES is greater than the 95th percentile for participants age, according to Verriest curves |
|
Categorical
|
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: 100 (200 eyes) |
| Number of participants included in analysis: 100 (200 eyes) | |
| Age | Mean: 44 years (range 14–70 years) |
| Sex | 37% male |
| Clinical characteristics | 39% insulin-dependent DM |
| Mean diabetes duration: 9 years (range 3–22 years) | |
| Other relevant clinical measures: tested urinary and blood glucose; data not reported | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? | Diagnostic data (2 × 2; sensitivity, specificity)
|
|
Association between clinical characteristics and outcomes (multivariate regression): 80% of participants aged 30+ years and 52.5% of participants aged < 30 years had colour vision impairment 63% of patients with 10 years’ duration of DM, 69% of patients with 10–20 years’ duration, and 75% of patients with 20+ years’ duration had CV impairment 61% CV impairment in well-controlled diabetes and 69% in poorly controlled diabetes |
|
| Notes |
36% of patients made errors on reading urinary glucose dipsticks, and 31% made errors on blood glucose dipsticks. All of these patients were found to have dyschromatopsia on the FM-100 30% of patients had different CV results for each eye The authors concluded that colour vision impairment is frequent in DM and can occur in the absence of retinopathy |
| Bibliographic details | |
|---|---|
| Author | Barton38 |
| Year | 1987 |
| Related papers | Fong 199939 |
| Study characteristics | |
| Study design | Cross-sectional |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Method not stated/final diagnosis |
| Retinopathy grading (reference standard) |
Graded No macular oedema; not clinically significant macular oedema; clinically significant macular oedema |
| For which eye was retinopathy assessed? | Unclear |
| Colour vision test(s) | FM-100 |
| Colour vision grading |
Continuous/average Square root of total error score (SQRT TES) for deferred eyes is presented for each grade of macular oedema |
| Participant characteristics | |
| Number of participants | Number of participants included in study: no macular oedema: n = 1000; not clinically significant macular oedema: n = 609; clinically significant macular oedema: n = 1248 |
| Number of participants included in analysis: no macular oedema: n = 1000; not clinically significant macular oedema: n = 609; clinically significant macular oedema: n = 1248 | |
| Results | |
| What data/analysis is presented in the study? |
Comparison of scores in two groups (t-test; Mann–Whitney): No macular oedema (n = 1000), SQRT TES = 12 (SD ±4) Not clinically significant macular oedema (n = 609), SQRT TES = 13(SD ±4) Clinically significant macular oedema (n = 1248), SQRT TES = 17(SD ±5) |
|
Association between clinical characteristics and outcomes (multivariate regression): No difference in mean SQRT TES by level of retinopathy or sex |
|
| Bibliographic details | |
|---|---|
| Author | Bernardczyk-Meller47 |
| Year | 2001 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | No |
| Patient selection criteria | Inclusion criteria: patients for whom long-term follow-up data were available |
| Exclusion criteria: congenital colour vision deficiencies | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Ophthalmoscopy |
| Retinopathy grading (reference standard) |
Dichotomous Pathological changes (non-proliferative DR, preproliferative DR, cataract) vs no pathological changes |
| For which eye was retinopathy assessed? | Both |
| Colour vision test(s) | D-15, saturated and desaturated |
| Ishihara plates | |
| Colour vision grading |
Dichotomous Normal vs ‘pathological’ CV test scores |
| Participant characteristics | |
| Number of participants | Number of participants included in study: 38 |
| Number of participants included in analysis: 38 | |
| Age | 17 years (range 7–27 years) |
| Clinical characteristics | 100% insulin-dependent DM |
| Mean diabetes duration: 7.8 years (range 3–18 years) | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) D-15 desaturated (threshold: ‘pathological results’): TP = unclear; FP = 9; FN = unclear; TN = 21 |
| Bibliographic details | |
|---|---|
| Author | De Alwis52 |
| Year | 1993 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: proven diagnosis of DM; visual acuity 6/12 or better |
| Exclusion criteria: any other eye disease including glaucoma; visual acuity 6/18 or worse; previous laser treatment for retinopathy; elevated intraocular pressure in the absence of frank glaucoma | |
| Does the study include a control group of non-diabetics? | Yes (n = 69) |
| Reference standard |
Slit-lamp biomicroscopy Dilation of pupil; 90-dioptre fundus examination lens; 5 of 7 fields examined |
| Retinopathy grading (reference standard) |
Dichotomous Severe retinopathy (maculopathy grade 4 and/or ischaemic grade 4) vs non-severe retinopathy (anything below maculopathy grade 4 and/or ischaemic grade 4) |
| For which eye was retinopathy assessed? | Both |
| Colour vision test(s) |
Computerised/automated method Chromatic contrast sensitivity test (Sussex Grating Machine); computer-automated, television-based machine; red–green and tritan axes tested; performed at a distance of 2 m at an angle of 5 degrees to retina |
| Colour vision grading |
Dichotomous z-score thresholds based on standard deviations from –3.0 to 0 |
| Participant characteristics | |
| Number of participants | Number of participants included in study: non-severe retinopathy: n = 107; severe retinopathy: n = 30 |
| Number of participants included in analysis: non-severe retinopathy: n = 107; severe retinopathy: n = 30 | |
| Age | Mean overall: 53.9 years (range 18–84 years) |
| Results | |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) –3.0 SD: TP n = 11, FP n = 2, TN n = 105, FN n = 19, sens. = 37%, spec. = 98% –2.5 SD: TP n = 17, FP n = 5, TN n = 102, FN n = 13, sens. = 57%, spec. = 95% –2.0 SD: TP n = 22, FP n = 11, TN n = 96, FN n = 8, sens. = 73%, spec. = 90% –1.5 SD: TP n = 23, FP n = 21, TN n = 86, FN n = 7, sens. = 77%, spec. = 80% –1.0 SD: TP n = 24, FP n = 27, TN n = 80, FN n = 6, sens. = 80%, spec. = 75% –0.5 SD: TP n = 25, FP n = 40, TN n = 67, FN n = 5, sens. = 83%, spec. = 63% 0 SD: TP n = 29, FP n = 64, TN n = 43, FN n = 1, sens. = 97%, spec. = 40% |
|
Association between clinical characteristics and outcomes (multivariate regression): Right eye tritan: duration p < 0.001, age at onset p < 0.001, maculopathy grade p < 0.001, ischaemic grade p < 0.005 Left eye tritan: duration p < 0.001, age at onset p < 0.001, maculopathy grade p < 0.001, ischaemic grade p < 0.002 Right eye red–green: duration p < 0.001, age at onset p < 0.185, maculopathy grade p < 0.001, ischaemic grade p < 0.002 Left eye red–green: duration p < 0.002, age at onset p < 0.002, maculopathy grade p < 0.001, ischaemic grade p < 0.002 |
|
| Notes |
Grading system used: 1 = no retinopathy: no lesions seen on fundoscopy; 2 = background retinopathy: maculopathy 1 and ischaemia 1; 3 = maculopathy: ischaemia 1 and maculopathy 2–4; 4 = ischaemia: maculopathy 1 and ischaemia 2–4; 5 = mixed disease: maculopathy 2–4 and ischaemia 2–4 Each eye was assigned a diagnostic code consisting of two digits, the first corresponding to the maculopathy grade and the second to the ischaemia grade. No retinopathy and background retinopathy were combined into one group |
| Bibliographic details | |
|---|---|
| Author | Doucet48 |
| Year | 1991 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Exclusion criteria: people aged over 65 years; visual acuity < 4/10; cataract or glaucoma; known congenital dyschromatopsia; deterioration in mental functioning; using medicines that could alter colour vision |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Other: fundoscopy |
| Retinopathy grading (reference standard) |
Graded ETDRS grading: 0: no retinopathy or one or two microaneurysms; 1: background retinopathy; 2: preproliferative retinopathy; 3: proliferative retinopathy |
| Colour vision test(s) | D-15; presented under luminance of 500 lux |
| Colour vision grading |
Categorical Score of 0–2 given for each eye: 0 = dyschromatopsia with one or several axes; 1 = dyschromatopsia without an axis; 2 = normal (three simple inversions at any age, or four inversions/diametrical inversions over age 45 years, or minimum of five inversions or two diametrical inversions over age 60 years) |
| Participant characteristics | |
| Number of participants | Number of participants included in study: 100 |
| Number of participants included in analysis: 100 | |
| Age | 43.36 (14.4) years (range 16–65 years) |
| Sex | 62% male |
| Clinical characteristics | 88% insulin-dependent DM |
| Mean (SD) diabetes duration: 133.74 (105.76) months (range 1 month to 39 years) | |
|
Mean (SD) HbA1c levels: 11.38% (3.41%) (range 5.4–28.8%) 12 patients had a normal result (57.5%) |
|
| Other relevant clinical measures: tested creatinine clearance, nocturnal microalbuminuria and peripheral neuropathy | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) ETDRS grading: 0: no retinopathy or one or two microaneurysms: n = 70 1: background retinopathy: n = 14 2: preproliferative retinopathy: n = 3 3: proliferative retinopathy: n = 13 26/30 with DR had dyschromatopsia on D-15; 47/70 without DR had dyschromatopsia on D-15 (p < 0.01) |
|
Association between clinical characteristics and outcomes (multivariate regression): Numbers were small but authors noted a relationship between severity of retinopathy and FM-100 score 29/73 with dyschromatopsia on D-15 also have peripheral neuropathy; 8/27 without dyschromatopsia on D-15 have peripheral neuropathy (p < 0.01) Electrophysiology scores were significantly lower in the dyschromatopsia group (76.78, SD 38.35) than in the non-dyschromatopsia group (115.68, SD 35.85) (p < 0.001) Within non-DR patients, no significant difference in peripheral neuropathy between those with and those without dyschromatopsia Within DR patients, significant difference in peripheral neuropathy between those with (17/26) and those without (1/4)dyschromatopsia; however, the mean electrophysiological score was not significantly different Overall, patients with dyschromatopsia were significantly older (p < 0.05), with more alcohol problems (p < 0.05), more peripheral neuropathy (p < 0.05), more microalbuminuria (p < 0.01) and more hypertension (p < 0.001) |
|
| Bibliographic details | |
|---|---|
| Author | Findl53 |
| Year | 2000 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Retrospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: insulin dependent type I diabetics; age < 32 years; diabetes duration between 12 and 17 years |
| Exclusion criteria: excluded patients with systemic hypertension or any sign of non-diabetes-induced vascular complications; excluded patients if any ocular disease except DR was evident at prestudy ophthalmic examination | |
| Does the study include a control group of non-diabetics? | Yes; 25 age-matched healthy control subjects: 17 males; mean age 23.8 years |
| Reference standard | Slit-lamp biomicroscopy |
| Conventional retinal photography: colour fundus photography of seven fields | |
| Combined methods: fundoscopy, biomicroscopy and retinal photography | |
| Retinopathy grading (reference standard) |
Graded Modified Airlie House classification |
| For which eye was retinopathy assessed? | Left |
| Colour vision test(s) |
Computerised/automated method Colour contrast sensitivity along tritan axis investigated using a computer graphics device and a colour monitor system; the threshold chrominance of a coloured optotype without changes in luminance compared with the surrounding is determined |
| Colour vision grading |
Continuous/average The threshold chrominance of a coloured optotype without changes in luminance compared with the surrounding expressed as a percentage |
| Participant characteristics | |
| Number of participants | Number of participants included in study: overall: n = 59; level 1: n = 20; level 2: n = 27; level 3: n = 12 |
| Number of participants included in analysis: overall: n = 59; level 1: n = 20; level 2: n = 27; level 3: n = 12 | |
| Age | Mean (SD): overall 23.1 (4.3) years; level 1: 22.9 (4.2) years; level 2: 23.7 (4.5) years; level 3: 22.1 (4.0) years |
| Sex | 66% male |
| Clinical characteristics | Overall 100% insulin dependent |
| Diabetes duration: overall range 12–17 years | |
|
Mean (SD) LogMAR or Snellen visual acuity Snellen best-corrected visual acuity: level 1: 20/20 in all; level 2: 20/20 in all; level 3: 20/20 in 7, 20/25 in 5 |
|
| Mean (SD) fasting blood glucose: level 1: 121.3 (57.9) mg/100 ml; level 2: 164.3 (67) mg/100 ml; level 3: 194.8 (84.4) mg/100 ml | |
| Mean (SD) HbA1c levels: level 1: 7.7% (1.1%); level 2: 8.5% (1.0%); level 3: 10.7% (1.5%) | |
|
Other relevant clinical measures: Systolic blood pressure: level 1: 127.9 (7.1) mmHg; level 2: 121.1 (10.5) mmHg; level 3: 124.8 (8.0) mmHg Diastolic blood pressure: level 1: 66.3 (12.1) mmHg; level 2: 60.6 (10.1) mmHg; level 3: 60.0 (7.3) mmHg Pulse rate: level 1: 72.4 (11.4) bpm; level 2: 73.4 (11.2) bpm; level 3: 74.3 (10.5) bpm |
|
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | No; plasma glucose levels (p = 0.012) and HbA1c values (p < 0.001) were higher in the more advanced stages of DR |
| What data/analysis is presented in the study? |
Comparison of multiple groups (analysis of variance): Level 1: 7.1% (1.7), n = 20; level 2: 7.3% (1.9), n = 27; level 3: 10.1% (3.0), n = 12 (p = 0.02) |
| Bibliographic details | |
|---|---|
| Author | Fong39 |
| Year | 1999 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: no attempt was made to eliminate cases of congenital red–green colour deficiency or other known colour vision defects |
| Does the study include a control group of non-diabetics? | No |
| Reference standard |
Conventional retinal photography Stereoscopic fundus photographs of the seven standard fields taken with a 30-degree fundus camera |
| Retinopathy grading (reference standard) |
Graded ETDRS extension of the modified Airlie House classification: group A: eyes without macular oedema; group B: macular oedema not clinically significant; group C: eyes with clinically significant macular oedema with centre of macular not involved; group D: clinically significant macular oedema with centre of the macula involved |
| For which eye was retinopathy assessed? |
Random/quasi-randomly selected One eye was selected but no details on which eye or how it was selected |
| Colour vision test(s) |
FM-100 Conducted under the illumination of a Macbeth Easel lamp at a distance of 30 cm with the subjective near refraction placed in a trial frame |
| Colour vision grading |
Continuous/average Square root of total error score (SQRT TES) |
| Participant characteristics | |
| Number of participants | Number of participants included in study: group A: n = 825; group B: n = 557; group C: n = 469; group D: n = 850 |
| Number of participants included in analysis: group A: n = 825; group B: n = 557; group C: n = 469; group D: n = 850 | |
| Sex | Overall 55% male |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Association between clinical characteristics and outcomes (multivariate regression) Multiple linear regression for SQRT 100 hue scores: Age: beta = 0.11, p-value = 0.0001; type 2 diabetes: beta = 0.45, p-value = 0.0001; presence of CSMO involving the centre of the macula: beta = 1.36, p-value = 0.0001; presence of new vessels: beta = 1.26, p-value = 0.0001; presence of fluorescein leakage in centre of the macula: beta = 0.48, p-value = 0.0001; presence of cystoid changes in the centre of the macula: beta = 0.87, p-value = 0.003; presence of focal leakage: beta = –0.54, p-value = 0.002 Non-significant factors: gender, body mass index, duration of diabetes, urine glucose, urine protein, serum creatinine, HbA1c, cholesterol, haematocrit, haemoglobin, diastolic blood pressure, effort at diabetic control, years of cigarette smoking |
| Bibliographic details | |
|---|---|
| Author | Green40 |
| Year | 1985 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: diabetics attending for routine ocular screening |
| Exclusion criteria: patients with soft exudates | |
| Does the study include a control group of non-diabetics? | Yes (n = 16) |
| Reference standard | Ophthalmoscopy |
| Retinopathy grading (reference standard) |
Dichotomous Serious (proliferative and exudative maculopathy) vs non-serious (no DR and background retinopathy) |
|
Graded Group NR: no retinopathy; group B: background retinopathy; group P: proliferative retinopathy; group E: exudative maculopathy |
|
| For which eye was retinopathy assessed? | Both, monocularly performed on both eyes |
| Colour vision test(s) |
FM-100 Test performed under illuminant C lighting conditions at an illumination level of approx. 200 lux in a VeriVide light cabinet and with no time limit |
| Colour vision grading |
Dichotomous Abnormal total error score (TES) vs normal score. Abnormal defined as outside the 95th percentile as defined by Verriest et al. 94 |
| Participant characteristics | |
| Number of participants |
Number of participants included in study: Serious: n = 36; non-serious: n = 90 Normal: n = 3; no retinopathy: n = 19; background retinopathy: n = 11; proliferative retinopathy: n = 14; exudative maculopathy: n = 12 |
|
Number of participants included in analysis: Serious: n = 36; non-serious: n = 90 Normal: n = 3; no retinopathy: n = 19; background retinopathy: n = 11; proliferative retinopathy: n = 14; exudative maculopathy: n = 12 |
|
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) Number of eyes: TP = 40; FP = 46; FN = 22; TN = 124; sens. = 72%; spec. = 66% |
|
Comparison of multiple groups (analysis of variance): Number of patients: no retinopathy TES = 59; background retinopathy TES = 31; proliferative retinopathy TES = 24; exudative maculopathy TES = 12 Number of patients: no retinopathy polarity assessment = 59; background retinopathy polarity assessment = 15; proliferative retinopathy polarity assessment = 8; exudative maculopathy polarity assessment = 3 Number of patients with abnormally high 100 hue test TES: no retinopathy n = 19; background retinopathy n = 11; proliferative retinopathy n = 14; exudative maculopathy n = 12 Number of eyes: no retinopathy TES = 115; background retinopathy TES = 55; proliferative retinopathy TES = 42; exudative maculopathy TES = 20 Number of eyes: no retinopathy polarity assessment = 115; background retinopathy polarity assessment = 28; proliferative retinopathy polarity assessment = 13; exudative maculopathy polarity assessment = 5 Number of eyes with abnormally high 100 hue test TES: no retinopathy n = 28; background retinopathy n = 18; proliferative retinopathy n = 21; exudative maculopathy n = 19 |
|
| Bibliographic details | |
|---|---|
| Author | Greenstein41 |
| Year | 1990 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: DM patients requiring insulin therapy; Snellen visual acuity ≥ 20/30 in the tested eye; patients showing either no sign of background retinopathy or only early background retinopathy; no history of hypertension or other metabolic disorders; no significant lens opacities or glaucoma |
| Does the study include a control group of non-diabetics? | Yes (n = 14); mean age 38 years ± 11.6 years (range 23–61 years) |
| Reference standard | Ophthalmoscopy |
| Conventional retinal photography | |
| Fluorescein angiography | |
| Retinopathy grading (reference standard) |
Dichotomous No retinopathy level 1: n = 7; background retinopathy level 2: n = 17 |
|
Graded Modified Airlie House classification: level 1: normal fundus; level 2: one or more microaneurysms only; level 3: microaneurysms with one or more other non-proliferative lesions present of mild to moderate degree; level 4: microaneurysms with one or more other non-proliferative lesions present of severe degree |
|
| For which eye was retinopathy assessed? | Right |
| Colour vision test(s) |
FM-100 FM-100-hue test under standard illuminant C lighting conditions |
| Colour vision grading |
Dichotomous Although not explicitly stated in the paper we have applied a 2 SD threshold in FM-100 age-corrected difference score for a positive colour vision abnormality test result |
| Participant characteristics | |
| Number of participants | Number of participants included in study: level 1: n = 7; level > 1–2: n = 8; level > 2–3: n = 6; level > 3–4: n = 3; no background retinopathy is level 1 and background retinopathy > level 1 |
| Number of participants included in analysis: level 1: n = 7; level > 1–2: n = 8; level > 2–3: n = 6; level > 3–4: n = 3; no background retinopathy is level 1 and background retinopathy > level 1 | |
| Age | Mean age overall: 45.8 years ± 13.9 years (range 24–68 years) |
| Clinical characteristics | 100% insulin-dependent DM |
|
Mean duration of insulin therapy: 18.2 years ± 9.1 years (range 7–40 years) Mean age at onset of diabetes: 27.6 years ± 14.7 years (range 8–54 years) |
|
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) FM-100 hue test assuming a positive result at a threshold of 2 SD in age-corrected difference score: TP = 4; FP = 0; FN = 13; TN = 7 |
| Notes | We have assumed that ±2 SD difference in FM-100 score difference is a positive test result for background retinopathy. We have applied this to the results in Figure 1 |
| Bibliographic details | |
|---|---|
| Author | Jeddi43 |
| Year | 1994 |
| Study characteristics | |
| Study design |
Longitudinal Mean follow-up 18 months (range 12–24 months) |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: visual acuity 10/10 |
| Does the study include a control group of non-diabetics? | No |
| Reference standard |
Ophthalmoscopy All tests given every 6 months |
| Other: fundoscopy; visual field test | |
| Colour vision test(s) |
FM-100 All tests given every 6 months |
| Colour vision grading | Categorical
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: 60 |
| Number of participants included in analysis: 60 | |
| Age | Mean: 43.5 years (range 24–63 years) |
| Sex | 48% male |
| Clinical characteristics | 52% insulin-dependent DM |
| Mean diabetes duration: 10 years (range 1–18 years) | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) Of patients with normal fundoscopy (n = ?), 27% had signs of retinopathy on angiography. On angiography, 38/60 patients had beginnings of retinopathy. At follow-up, retinopathy appeared in 9% of cases and got worse, developing into the preproliferative form, in 10.5% Visual field was altered in 35% of cases: 32% of patients without retinopathy on angiography and 37% of patients with retinopathy. On follow-up, appearance of new ‘scotomes parafoveolaires’ in 27% of patients without retinopathy and 24% with background retinopathy Colour vision was abnormal in 57% of participants: weak discrimination with most areas in the blue-yellow axis in 22%, dyschromatopsia of the blue-yellow axis in 35%. In 10% of cases there is also red–green dyschromatopsia There is colour vision impairment in 50% of people without retinopathy on angiography and 65% of people with retinopathy An increase in CV error scores or individualisation of an axis was noted in 36% of cases without retinopathy and 34% with background retinopathy Overall, 37% of patients made mistakes in reading colours |
| Bibliographic details | |
|---|---|
| Author | Lombrail44 |
| Year | 1983 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: insulin dependent diabetics |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Fluorescein angiography |
| Retinopathy grading (reference standard) |
Graded Grade A: no retinopathy; grade B: only angiographic retinopathy (at least two microaneurysms at the posterior pole); grade C: background retinopathy; grade D: preproliferative retinopathy (presence of oedema or ischaemia); grade E: proliferative retinopathy (retinal or preretinal neovascularisation); grade F: retinopathy at incurable stage |
| For which eye was retinopathy assessed? | Unclear |
| Colour vision test(s) | FM-100 |
| Colour vision grading |
Continuous/average FM-100 hue score |
| Participant characteristics | |
| Number of participants | Number of participants included in study: overall: 103; grade A: 24; grade B: 15; grade C: 48; grade D: 12; grade E: 2; grade F: 2 |
| Number of participants included in analysis: overall: 103; grade A: 24; grade B: 15;grade C: 48; grade D: 12; grade E: 2; grade F: 2 | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Comparison of multiple groups (analysis of variance) Grade A: n = 24, mean (SD) FM-100 score = 107 (50); grade B: n = 15, FM-100 = 144 (109); grade C: n = 48, FM-100 = 124 (78); grade D: n = 12, FM-100 = 182 (96); grade E: n = 2, FM-100 = 189 (21); grade F: n = 2, FM-100 = 234 (89) F = 2.42, p < 0.05 |
| Bibliographic details | |
|---|---|
| Author | Maár32 |
| Year | 2001 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: type I DM; best corrected visual acuity of at least 0.4 LogMAR (0.4 Snellen value); < 50 years of age; no lens opacities |
| Exclusion criteria: congenital CV deficiencies; cataract; glaucoma; retinopathy, new vessels or chorioretinal scars in the macula; more than mild proliferative retinopathy; history of intraocular surgery or laser therapy | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Slit-lamp biomicroscopy |
| Conventional retinal photography | |
| Fluorescein angiography | |
| Retinopathy grading (reference standard) |
Dichotomous Clinically significant macular oedema (CSMO) vs without CMSO Biomicroscopic findings were graded using the ETDRS criteria; fundal photographs were graded using the modified Airlie House classification; angiograms were classified using the ETDRS fluorescein angiogram grading form |
| For which eye was retinopathy assessed? | Random/quasi-randomly selected |
| Colour vision test(s) | D-15 |
|
Other: Mollon–Reffin Minimalist Test version 6.0 Contains set of grey chips of varying lightness that serve as background chips, a set of coloured probe chips and an orange demonstration chip. Five grey chips are placed randomly on black Plexiglass. To these the examiner first adds the orange chip, which does not lie on any confusion line, mixes it with the grey chips and invites the patient to identify the ‘coloured chip’ by touching with a pointer. If the patient successfully identifies the orange chip, the examiner draws a probe chip from the middle of the protan, deutan or tritan series. After correct identification of this probe, the examiner then moves inwards along the confusion line and presents the least saturated chip; if, on the other hand, the response to the first protan probe is incorrect, the examiner moves outwards to the most saturated chip |
|
| Colour vision grading |
Continuous/average D-15: total colour difference score (TCDS) Mollon–Reffin: number of reliably identified coloured chips for each confusion line |
| Participant characteristics | |
| Number of participants | Number of participants included in study: overall: 39; CMSO: 10; no CMSO: 29 |
| Number of participants included in analysis: overall: 39; CMSO: 10; no CMSO: 29 | |
| Age | Mean (SD): overall: range 17–47 years; CMSO: 33.7 (7.75) years; no CMSO: 28.07 (5.67) years |
| Sex | Overall 41% male |
| Clinical characteristics | % insulin dependent: overall: 100%; CMSO: 100%; no CMSO: 100% |
| Mean (SD) diabetes duration: overall: not stated; CMSO: 22.8 (7.00) years; no CMSO: 12.31 (7.22) years | |
| Mean (SD) LogMAR or Snellen visual acuity: overall LogMAR: not stated; CMSO: 0.07 (2.01); no CMSO: –0.6 (0.17) | |
| Mean (SD) HbA1c levels: overall: not stated; CMSO: 6.94 (0.68); no CMSO: 7.93 (1.04) | |
|
Other relevant clinical measures Duration of intensive insulin treatment (years): CMSO: 6.22 (2.33); no CMSO: 5.95 (3.40) |
|
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? |
No Duration of diabetes was significantly longer in patients with CMSO (p = 0.0003) and more severe retinopathy (p < 0.0001). Visual acuity was poorer in the CMSO group (p = 0.692) |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) D-15 (TCDS of 116.9): sensitivity: 36%; specificity: 88% Mollon–Reffin (tritan axis; threshold error score of 1): sensitivity: 88.9%; specificity: 93.3% Values were estimated using chi-squared test |
|
Comparison of scores in two groups (t-test; Mann–Whitney) D-15 (TCDS): CSMO (n = 10): 144.8 (23.34); no CSMO (n = 29): 132.23 (28.44) Mollon–Reffin (tritan axis; error score): CSMO (n = 10): 2.1 (0.74); no CSMO (n = 29): 1.03 (0.19) There were no errors on the Mollon–Reffin protan or deutan axes by any patient |
|
|
Association between clinical characteristics and outcomes (multivariate regression) Logistic regression: patients with CSMO had non-significantly higher TCDS on the D-15 (p = 0.345) and significantly higher Mollon–Reffin tritan score (p = 0.0015; r2 = 0.565) |
|
| Notes |
Authors’ conclusions: The Mollon–Reffin Minimalist Test version 6.0 may be useful as part of the screening and follow-up for macular oedema in young patients with juvenile onset diabetes. The use of blue-yellow colour vision tests without examination of the lens in diabetic patients older than 30 years is inadvisable |
| Bibliographic details | |
|---|---|
| Author | Mäntyjärvi46 |
| Year | 1995 |
| Study characteristics | |
| Study design |
Longitudinal, cross-sectional Patients were assessed for both CV and retinopathy at follow-up |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: diabetic schoolchildren with healthy eyes at recruitment |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Method not stated/final diagnosis |
| Retinopathy grading (reference standard) |
Dichotomous Retinopathy vs no retinopathy |
| For which eye was retinopathy assessed? | Unclear |
| Colour vision test(s) | D-15 |
| Lanthony desaturated | |
| Anomaloscope; Nagel anomaloscope was administered at baseline and at follow-up; colour vision meter 712 anomaloscope (CVM) was administered at follow-up only | |
| Colour vision grading |
Dichotomous Pass/fail for each test |
| Participant characteristics | |
| Number of participants | Number of participants included in study: overall: 54; DR at follow-up: 23; no DR at follow-up: 31 |
| Number of participants included in analysis: overall: 54; DR at follow-up: 23; no DR at follow-up: 31 | |
| Age | Mean (SD): at recruitment: 14 (2) years (range 9–19 years) |
| Sex | 46.3% male |
| Clinical characteristics | Mean (SD) diabetes duration: 6 (SD 4) years (range 1 month to 15 years) |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) TP, FP, FN, TN calculated from text (no thresholds reported): |
| Notes |
Authors’ conclusion: No predictive signs of DR could be found with the CV tests, nor could these tests distinguish between DR and non-DR children |
| Bibliographic details | |
|---|---|
| Author | Matsuo51 |
| Year | 1990 |
| Related papers | Matsuo 198859 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: visual acuity score > 0.5 |
| Exclusion criteria: participants with eyesight problems | |
| Does the study include a control group of non-diabetics? | Yes |
| Reference standard | Method not stated/final diagnosis |
| Retinopathy grading (reference standard) | Graded |
| For which eye was retinopathy assessed? | Both |
| Colour vision test(s) | Other: Lanthony New Colour Test (NCT): 15 component colour arrangement test |
| Colour vision grading |
Continuous/average Total error score (TES) |
| Participant characteristics | |
| Number of participants | Number of participants included in study: total: 56; retinopathy: 20; no retinopathy: 36 |
| Age | Mean (SD): 57.4 (1.7) years |
| Sex | 54% male |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Comparison of scores in two groups (t-test; Mann–Whitney) Retinopathy: mean TES = 7.9 (SD 1.51); no retinopathy: mean TES = 3.03 (SD 0.56) (p < 0.01) |
|
Association between clinical characteristics and outcomes (multivariate regression) NCT score was positively correlated with duration of diabetes (p < 0.05) and HbA1c (p < 0.02), but negatively correlated with coefficient variation of R–R interval in electrocardiography (an index for autonomic neuropathy, p < 0.02) |
|
| Bibliographic details | |
|---|---|
| Author | Mecca49 |
| Year | 1988 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: all patients had duration greater than 4 years; all patients had visual acuity 8/10 or better |
| Exclusion criteria: participants with congenital colour vision deficits; patients with maculopathy or macular oedema of mixed or proliferative retinopathy and participants with retinopathy of an advanced degenerative stage (large or numerous haemorrhages with exudate ‘confluents’) | |
| Does the study include a control group of non-diabetics? | Yes: 80 non-diabetics, aged 18–75 years, all of whom had 10/10 vision and no alterations of the anterior segment, back of the eye or intraocular pressure |
| Reference standard | Ophthalmoscopy |
| Fluorescein angiography | |
| Retinopathy grading (reference standard) |
Dichotomous With retinopathy (with at least 10 microaneurysms and small haemorrhages and exudates that are non-‘confluents’) vs without retinopathy |
| For which eye was retinopathy assessed? | Right |
| Colour vision test(s) |
D-15 Presented under luminance of 500 lux |
| Other: Lanthony New Colour Test (NCT): conducted under luminance of 250 lux. Scored on the number of errors in each series multiplied by the saturation of the colour. Tested four figures, which together constituted the total score for the examined eye | |
| Colour vision grading |
Continuous/average NCT: error scores |
|
Dichotomous D-15: altered colour vision vs normal NCT: altered colour vision (anything above zero) vs normal (no errors) |
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: 155 |
| Number of participants included in analysis: 155 | |
| Age |
Mean (SD) Participants were divided into two groups: those aged 18–45 years and those aged 46–75 years Without retinopathy: 18–45 group: 30.1 (8.5) years; 46–75 group: 61.4 (7.0) years With retinopathy: 18–45 group: 35.6 (8.4) years; 46–75 group: 61.1 (6.9) years |
| Clinical characteristics |
Mean (SD) diabetes duration Without retinopathy: 18–45 group: 9.6 (4.9) years; 46–75 group: 9.8 (4.4) years With retinopathy: 18–45 group: 17.4 (5.2) years; 46–75 group: 12.1 (5.0) years |
| Results | |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) D-15, 18–45 group: TP = 31, TN = 20, FP = 15, FN = 9 D-15, 46–75 group: TP = 41, TN = 5, FP = 30, FN = 4 D-15, overall: TP = 72, TN = 25, FP = 45, FN = 13 NCT, 18–45 group: TP = 32, TN = 25, FP = 10, FN = 8 NCT, 46–75 group: TP = 35, TN = 17, FP = 18, FN = 10 NCT, overall: TP = 67, TN = 42, FP = 28, FN = 18 NCT + D-15 combined overall (threshold: impaired CV on one or both tests): TP = 73; TN = 25; FP = 45; FN = 12 |
|
Comparison of scores in two groups (t-test; Mann–Whitney) NCT scores: 18–45 group: without retinopathy 0.69 (1.18); with retinopathy 2.40 (1.58) 46–75 group: without retinopathy 1.60 (1.87); with retinopathy 3.24 (2.14) Chi-squared values (retinopathy vs no retinopathy): D-15 18–45 group: 9.446, p < 0.01 D-15 46–75 group: 0.574, p = not significant NCT 18–45 group: 20.037, p < 0.001 NCT 46–75 group: 6.113, p < 0.05 |
|
| Bibliographic details | |
|---|---|
| Author | Mirkiewicz-Sieradzka57 |
| Year | 1986 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: diabetic patients with signs of retinopathy |
| Exclusion criteria: patients with congenital red–green colour deficits; patients who had previously undergone photocoagulation | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Ophthalmoscopy |
| Fluorescein angiography | |
| Retinopathy grading (reference standard) |
Graded Ophthalmoscopy:Angiography: |
| For which eye was retinopathy assessed? | Unclear |
| Colour vision test(s) | Ishihara plates |
| Colour vision grading |
Dichotomous Pass vs fail (no threshold reported) |
| Participant characteristics | |
| Number of participants | Number of participants included in study: 51 |
| Age | Range 20–78 years |
| Sex | 50.9% male |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) Ophthalmoscopy as reference standard (n pass CV, n fail CV):Angiography as reference standard (n pass CV, n fail CV): |
| Notes | The authors concluded that small ophthalmoscopic changes and little leakage on the angiographic picture of the macular region are connected with colour disturbances in 15% and 8% of eyes respectively. The authors do not provide data at the level of patient |
| Bibliographic details | |
|---|---|
| Author | Ong31,60 |
| Year | 2004 |
| Related papers | Ong 200360 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: consenting diabetic patients attending photographic screening |
| Exclusion criteria: corrected visual acuity worse than 6/9; previous history of photocoagulation therapy; history of eye disease known to affect colour vision (e.g. glaucoma); signs and symptoms of significant media opacification; inability to complete the test satisfactorily | |
| Does the study include a control group of non-diabetics? | Yes: ‘lens-equated’ control subjects: n = 310; mean (SD) age: 48 (19.1) years |
| Reference standard |
Slit-lamp biomicroscopy Examinations conducted by an experience ophthalmologist |
| Retinopathy grading (reference standard) |
Dichotomous Retinopathy stage was graded using the European staging protocol and then dichotomised into ‘sight-threatening diabetic retinopathy’ (STDR; includes preproliferative retinopathy, proliferative retinopathy, maculopathy) or ‘non-sight-threatening diabetic retinopathy’ (NSTDR; includes no retinopathy and background retinopathy) |
| For which eye was retinopathy assessed? | Random/quasi-randomly selected |
| Colour vision test(s) |
Computerised/automated method Tritan contrast threshold (TCT) test: computerised cathode ray tube (CRT)-based technique – participants are scored on their ability to distinguish vertical, sinusoidal, low spatial frequency and standardised equiluminent gratings from a uniform background; chromaticity of the gratings is changed along a tritan confusion axis |
| Colour vision grading |
Continuous/average z-score: To account for the accelerated lens yellowing experienced by diabetics, standardised scores were obtained from a randomly selected eye of 310 non-diabetic control participants. The TCT scores from the diabetic participants and ‘lens-equated’ control subjects were used to calculate an overall z-score for the diabetic participants. A negative z-score indicates that a patient’s tritan vision is still worse than normal, even when both age and lens yellowing have been taken into account |
|
Dichotomous Using the weighted kappa coefficient of association analysis technique, the optimal pass/fail criterion to detect STDR was z = –1.75. This threshold was used to dichotomise patients into pass/fail on the TCT test |
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: 510 (STDR 17, NSTDR 493) |
| Number of participants included in analysis: 510 (STDR 17, NSTDR 493) | |
| Age | Mean (SD): STDR: 60.4 (11.3) years; NSTDR: 60.9 (13.9) years (p > 0.5) |
| Clinical characteristics | 21% insulin dependent (107/510) |
| Mean (SD) diabetes duration: STDR: 11.8 (6.9) years; NSTDR: 10.4 (8.6) years (p = 0.43) | |
|
Mean (SD) LogMAR or Snellen visual acuity Snellen log values: STDR: 0.1 (0.11); NSTDR: 0.06 (0.09) (p = 0.13) |
|
| Mean (SD) HbA1c levels: STDR: 9.8 (1.6); NSTDR: 8.1 (2.2) (p = 0.02) | |
|
Other relevant clinical measures: Urinary albumin counts (ml/l): STDR: 28.2 (28.7); NSTDR: 26 (47.6) (p = 0.19) |
|
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | No; STDR patients had significantly worse HbA1c levels than NSTDR patients |
| What data/analysis is presented in the study? | Diagnostic data (2 × 2; sensitivity, specificity)
|
|
Comparison of scores in two groups (t-test; Mann–Whitney) Significantly worse TCT (p < 0.0001) and HbA1c (p = 0.02) in patients with STDR than in those with NSTDR (Mann–Whitney U). Best corrected visual acuity was worse, duration of diabetes was longer and urinary albumin counts were higher in the STDR group, but these differences were not significant (Mann–Whitney U) STDR patients have significantly abnormal TCTs compared with ‘lens-equated’ control subjects (p < 0.0001; Mann–Whitney U). No significant differences in TCT were found between NSTDR patients and ‘lens-equated’ control subjects |
|
|
Comparison of multiple groups (analysis of variance) Mean (SD) TCT score: no retinopathy (n = 383): 42.5 (6.3); background retinopathy (n = 110): 41.7 (7.1); preproliferative retinopathy (n = 3): 29.6 (8.5); proliferative retinopathy (n = 2): 21.7 (3.3); maculopathy (n = 12): 24.0 (7.2) |
|
|
Association between clinical characteristics and outcomes (multivariate regression) Pearson correlation analysis found significant correlations between age and TCT (p < 0.0001), age and diabetes duration (p < 0.001), and age and HbA1c (p < 0.001). None of the other variables showed significant correlation with TCT (HbA1c: p > 0.4; urinary albumin counts: p > 0.1; duration of diabetes: p > 0.8) Logistic regression showed TCT (p < 0.001) and HbA1c (p = 0.018) significantly correlated with the presence of STDR, but not with duration of diabetes, urinary albumin counts or log best corrected visual acuity |
|
| Notes | The authors concluded that TCT had a higher sensitivity and was more cost-effective than fundus photography. They also concluded that adding the TCT test to fundus photography can also significantly improve the overall performance in screening for STDR |
| Bibliographic details | |
|---|---|
| Author | Saracco50 |
| Year | 1980 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Unclear |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: included patients with visual acuity ≥ 6/10 |
| Exclusion criteria: excluded those with congenital dyschromatism and those with retinal or general problems (unspecified) that could affect the interpretation of colour vision; diabetic patients who had had laser eye correction were also excluded | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard | Fluorescein angiography |
| Retinopathy grading (reference standard) |
Dichotomous Normal (grade 0) vs pathological (grades 1, 2 and 3) Also angiography grade 0 vs grade 1 |
Graded
|
|
| For which eye was retinopathy assessed? | Unclear |
| Colour vision test(s) | D-15 |
| Colour vision grading |
Dichotomous Normal colour vision (grades 0 and 1) vs abnormal colour vision (grades 2c, 2d and 3) |
|
Categorical Grades: |
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: 88 (172 eyes) |
| Number of participants included in analysis: 88 (172 eyes) | |
| Age |
Mean: 51.12 years 0–20 years: 8 eyes; 20–40 years: 31 eyes; 40–60 years: 76 eyes; 60+ years: 57 eyes |
| Clinical characteristics |
Mean (SD) LogMAR or Snellen visual acuity Myopia (at least 2 dioptres): 17 people (34 eyes) |
| Other relevant clinical measures: 22 people (40 eyes) beginnings of cataracts | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) Normal vs pathology: TP = 63, FP = 49,FN = 17, TN = 43 Angiographic grade 0 vs 1: TP = 42, FP = 49, FN = 12, TN = 43 |
| Bibliographic details | |
| Author | Sinha58 |
| Year | 1979 |
| Study characteristics | |
|---|---|
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: diabetics |
| Exclusion criteria: patients giving the mildest indications about colour defects in family and/or growth impairment of vision | |
| Does the study include a control group of non-diabetics? | Yes: n = 40 |
| Reference standard |
Slit-lamp biomicroscopy Biomicroscopy |
| Retinopathy grading (reference standard) |
Dichotomous Diabetics with DR vs diabetics without DR |
| For which eye was retinopathy assessed? | Both; each eye was tested on two occasions and the results averaged |
| Colour vision test(s) | Ishihara plates |
| Other: Ishihara charts and Tokyo Medical College colour vision charts | |
| Colour vision grading |
Categorical Normal colour vision; protan deficit; deutan deficit; tritan deficit |
| Participant characteristics | |
| Number of participants | Number of participants included in study: non-DR: n = 40; DR: n = 33 |
| Number of participants included in analysis: non-DR: n = 40; DR: n = 33 | |
| Age | Mean: non-DR: 51.2 years; DR: 55 years |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) TP = 4, FP = 1, FN = 29, TN = 39, sens. = 12%, spec. = 97.5% This result is for tritan deficits vs normal. No participants had a protan or deutan defect CV result |
| Bibliographic details | |
|---|---|
| Author | Tregear55 |
| Year | 1997 |
| Study characteristics | |
| Study design | Longitudinal, cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: type I and type II diabetics; diabetics taking any form of medication other than those used to control glucose levels deliberately not excluded |
| Exclusion criteria: previous laser treatment; signs of significant lens opacification as determined by slit-lamp examination through dilated pupil; corrected visual acuity worse than 6/18 | |
| Does the study include a control group of non-diabetics? | Yes: n = 347 lens-equated control subjects |
| Reference standard |
Slit-lamp biomicroscopy Dilated with 1% tropicamide |
| Retinopathy grading (reference standard) |
Graded No retinopathy: no evidence of retinopathy can be seen clinically Background: characterised by the development of microaneurysms, superficial and deep retinal haemorrhages and the formation of hard exudates Preproliferative: five or more cotton wool spots on the fundus, presence of white vessels, venous bleeding and venous loops, features associated with severe background retinopathy such as widespread blotchy dark haemorrhages Proliferative: presence of new blood vessels at the optic disc (elsewhere on the retina if more than half a disc diameter in size, less than half a disc diameter associated with vitreous haemorrhage) or by vitreous haemorrhage anywhere Maculopathy: clinically significant macular oedema as characterised by the ETDRS group, characterised by thickening of the retina within 500 µm of the centre of the macula, the presence of hard exudates associated with retinal thickening within 500 µm of the macula, and a zone of retinal thickening one disc area or larger in size within a disc diameter of the centre of the macula |
| For which eye was retinopathy assessed? | Random/quasi-randomly selected |
| Colour vision test(s) |
Computerised/automated method SGM; set up to produce low spatial frequency equiluminant, sinusoidal gratings on a high-resolution colour monitor that were randomly tritan or red–green |
| Colour vision grading |
Continuous/average (1) Tritan contrast threshold (TCT) and (2) red–green contrast threshold (RGCT) |
|
Dichotomous Longitudinal subgroup only: threshold scores +2 SDs above the lens-equated mean |
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: no retinopathy: n = 87; background retinopathy: n = 116; preproliferative: n = 26; proliferative: n = 13; maculopathy: n = 63; total: n = 305 |
| Number of participants included in analysis: no retinopathy: n = 87; background retinopathy: n = 116; preproliferative: n = 26; proliferative: n = 13; maculopathy: n = 63; total: n = 305 | |
| Age | Mean (SD): no retinopathy: 52.09 (16.89) years; background retinopathy: 55.10 (14.95) years; preproliferative: 63.04 (14.39) years; proliferative: 53.92 (18.72) years; maculopathy: 62.32 (11.94) years |
| Clinical characteristics | 30% insulin-dependent type I diabetics |
| Overall mean duration: 14 years (range 1.5–60 years) | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Unclear |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) Ability to predict macular oedema or ischaemia (longitudinal data from subgroup of 87 patients with background DR, followed up at 18 months): (1) TCT: TP = 12, FP = 7, FN = 7, TN = 62; (2) RGCT: TP = 6, FP = 5, FN = 12, TN = 64 |
|
Comparison of multiple groups (ANOVA) Main cross-sectional study results: No retinopathy RGCT: mean 0.45, SD 0.17, variance 0.03 Background RGCT: mean 0.57, SD 0.24, variance 0.06 Maculopathy RGCT: mean 0.81, SD 0.29, variance 0.08 Preproliferative RGCT: mean 0.73, SD 0.19, variance 0.08 Proliferative RGCT: mean 0.88, SD 0.34, variance 0.12 Main cross-sectional study results No retinopathy TCT: mean 0.55, SD 0.17, variance 0.05 Background TCT: mean 0.74, SD 0.29, variance 0.09 Maculopathy TCT: mean 1.14, SD 0.31, variance 0.09 Preproliferative TCT: mean 1.05, SD 0.26, variance 0.07 Proliferative TCT: mean 1.13, SD 0.31, variance 0.09 |
|
| Bibliographic details | |
|---|---|
| Author | Trick45 |
| Year | 1988 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: DM patients with no or mild to moderate background retinopathy; visual acuity of at least 20/30 and intraocular pressure < 21 mmHg in the eye to be tested |
| Exclusion criteria: patients with macular oedema detected in either the ophthalmoscopic examination or the fundus photographs | |
| Does the study include a control group of non-diabetics? | Yes: n = 35 |
| Reference standard |
Conventional retinal photography Seven-field fundus photographs |
| Retinopathy grading (reference standard) |
Dichotomous No retinopathy vs preproliferative background retinopathy (grade 1a to grade 1b lesions according to the modified Airlie House classification) |
| For which eye was retinopathy assessed? |
Random/quasi-randomly selected Monocular test but no details on how the eye was selected |
| Colour vision test(s) |
FM-100 Administered monocularly under standard illuminant C (Macbeth Easel lamp) lighting conditions with no time limit imposed. The order of presentation of the boxes was varied randomly between patients |
| Colour vision grading |
Continuous/average Square root of total error score (TES) and partial error scores (blue-yellow, red–green) |
|
Dichotomous Total/partial error score > 2 SD above the normal mean |
|
| Participant characteristics | |
| Number of participants | Number of participants included in study: no retinopathy: n = 37; background retinopathy: n = 20 |
| Number of participants included in analysis: no retinopathy: n = 37; background retinopathy: n = 20 | |
| Age | Mean (SD): no retinopathy 36.9 (11.1) years; background retinopathy 37.9 (8.6) years |
| Clinical characteristics | Overall 68% insulin dependent |
| Mean diabetes duration: retinopathy: 8.1 years (range 1–45 years); background retinopathy: 16 years (range 2–33 years) | |
| Mean (SD) fasting blood glucose: no retinopathy: 203.2 (73.9); background retinopathy: 236.0 (84.2) | |
| Mean (SD) HbA1c levels: no retinopathy 8.5 (1.8); background retinopathy: 9.2 (1.7) | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | No; groups are comparable in all characteristics other than diabetes duration. The average duration of diabetes was 8.1 years (range 1–45 years) in the group without DR and 16 years (range 2–33 years) for the patients with background retinopathy |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) TES: TP = 5, FP = 7, FN = 15, TN = 30 Blue-yellow: TP = 4, FP = 5, FN = 16, TN = 32 Red–green: TP = 4, FP = 7, FN = 30, TN = 16 |
|
Comparison of multiple groups (ANOVA) No retinopathy: square root TES 9.69 (4.16), blue-yellow error 7.6, red–green error 6.25 Background retinopathy: square root TES 11.33 (4.23), blue-yellow error 8.75, red–green error 7.5 No difference in square root TES between no retinopathy and background retinopathy diabetics (t = 1.42, df = 55, p > 0.15) |
|
|
Association between clinical characteristics and outcomes (multivariate regression) HbA1c correlated with square root TES (r = 0.30, df = 55, p < 0.05) but duration of diabetes and blood glucose did not |
|
| Notes | We calculated mean error score for blue-yellow and red–green from Figure 1 |
| Bibliographic details | |
|---|---|
| Author | Wong56 |
| Year | 2008 |
| Study characteristics | |
| Study design | Cross-sectional |
| How were the data collected? | Prospectively |
| Were participants recruited consecutively? | Unclear |
| Patient selection criteria | Inclusion criteria: type 2 diabetic patients with untreated non-proliferative DR and untreated clinically significant macular oedema (CSMO); cataract and pseudophakia were not excluded as both are more common in diabetics and exclusion would have limited the usefulness of the ChromaTest screening |
| Exclusion criteria: type 1 diabetes; proliferative DR; previous laser photocoagulation; current ocular pathology including infection, trauma; amblyopia; glaucoma; and/or vascular occlusion | |
| Does the study include a control group of non-diabetics? | No |
| Reference standard |
Slit-lamp biomicroscopy Dilated fundoscopy with slit-lamp biomicroscopy and 78 D lens was performed by a specialist registrar |
| Retinopathy grading (reference standard) |
Graded Grading according to the ETDRS extension of the Airlie House classification: no clinical retinopathy, non-proliferative diabetic retinopathy (NPDR) and CSMO |
| For which eye was retinopathy assessed? |
Unclear Text says that both eyes were tested but the results are for 150 eyes from 150 patients? |
| Colour vision test(s) |
Computerised/automated method ChromaTest: the subject is seated at a fixed distance from the monitor so that the alphabetical letter displayed on the computer screen subtends a constant angle on the retina. The letter size creates an image that tests the central 6.5 degrees of the retina. The letters are displayed on a background of equiluminance. The operator has no influence on the contrast of the test letter given. The computer finds the end point of the test by a modified binary search method; if a response is correct, on the next presentation the colour difference between letter and background is halved; if the response is incorrect, the colour contrast is doubled |
| Colour vision grading |
Dichotomous Pass/fail criterion for tritan colour contrast threshold (TCCT) given for each age group: 11.0 (30–49 years); 23.0 (50–69 years); 32.0 (70–89 years) Pass/fail criterion for protan colour contrast threshold (PCCT) not given |
| Participant characteristics | |
| Number of participants | Number of participants included in study: no clinical retinopathy: n = 30; NPDR: n = 115; CSMO: n = 35 |
| Number of participants included in analysis: no clinical retinopathy: n = 30; NPDR: n = 115; CSMO: n = 35 | |
| Age | Median age of all groups: 60 years (range 31–82 years) |
| Sex | % male not stated |
| Clinical characteristics | % insulin dependent not stated |
| Median duration of diabetes: 16.0 years | |
| Best corrected LogMAR visual acuity (BCVA) median for NPDR = 0.2; BCVA median for CSMO = 0.2; interquartile range for visual acuity NPDR = 0.20; interquartile range for visual acuity CSMO = 0.30 | |
| Results | |
| Were groups comparable in terms of demographic and clinical characteristics? | Yes |
| What data/analysis is presented in the study? |
Diagnostic data (2 × 2; sensitivity, specificity) TCCT detection of CSMO (NPDR used as control group): TP = 25, FP = 35, FN = 10, TN = 80, sens. = 71% (95% CI 53% to 83%), spec. = 70% (95% CI 60% to 78%) (p < 0.0001) Subjects with LogMAR BCVA ≥ 0.1, sens. to detect CSMO improves to 75% (95% CI 47–91%) and spec. to 85% (95% CI 67% to 89%) (p = 0.0002) Subjects with CSMO with central macular thickening, sens. to detect CSMO improves to 83.3% (95% CI 58% to 96%) (p < 0.0001) NPDR vs no DR: TP = 35, FP = 1, FN = 80, TN = 29, sens. = 30%, spec. = 97%, LR+ 9.13, LR– 0.72 CSMO vs no DR: TP = 25, FP = 1, FN = 10, TN = 29, sens. = 71%, spec. = 97%, LR+ 21.43, LR– 0.30 CSMO vs NPDR: TP = 25, FP = 35, FN = 10, TN = 80, sens. = 71%, spec. = 70%, LR+ 2.35, LR– 0.41 |
|
Comparison of scores in two groups (t-test; Mann–Whitney) Median PCCT for NPDR = 3.9%, CSMO = 5.6%; Wilcoxon Rank sum test p = 0.01 PCCT difference between no DR and NPDR: p = 0.15; no DR and CSMO: p = 0.002 Median TCCT for NPDR = 15.4%, CSMO = 29.6%; Wilcoxon Rank sum test p = 0.0002 TCCT difference between no DR and NPDR: p < 0.001; no DR and CSMO: p < 0.001 |
|
Appendix 4 Table of excluded studies with rationale
| Study | Reason for exclusiona |
|---|---|
| Abraham FA, Haimovitz J, Berezin M. (1988) The photopic and scotopic visual thresholds in diabetics without diabetic retinopathy | 2, 5 |
| Adab P. (1996) Screening for sight-threatening eye disease. Cost-effectiveness of screening modalities must be determined | 1 |
| Adams AJ. (1982) Chromaticity and luminosity changes in glaucoma and diabetes | 3 |
| Adams AJ, Huie K, Schefrin BE, Bresnick GH, Zisman F. (1986) A simple clinical test of blue cone sensitivity in early eye disease | 2, 3, 5 |
| Adams AJ, Schefrin B, Huie K. (1987) New clinical color threshold test for eye disease | 1 |
| Afrashi F, Erakgun T, Kose S, Ardic K, Mente J. (2003) Blue-on-yellow perimetry vs achromatic perimetry in type 1 diabetes patients without retinopathy | 4, 5 |
| Agardh E, Agardh CD, Hansson-Lundblad C. (1993) The five-year incidence of blindness after introducing a screening programme for early detection of treatable diabetic retinopathy | 2 |
| Agardh E, Agardh CD, Koul S, Torffvit O. (1994) A four-year follow-up study on the incidence of diabetic retinopathy in older onset diabetes mellitus | 2 |
| Ahmed J, Ward TP, Bursell SE, Aiello LM, Cavallerano JD, Vigersky RA. (2006) The sensitivity and specificity of nonmydriatic digital stereoscopic retinal imaging in detecting diabetic retinopathy | 2 |
| Alexander MM, Canning CR. (1995) A telephone study of diabetic retinopathy and the diabetes miniclinic in general practice: a regional study in Wessex | 2 |
| Anderson RM, Wolf FM, Musch DC, Fitzgerald JT, Johnson MW, Nwankwo RB, et al. (2002) Conducting community-based, culturally specific, eye disease screening clinics for urban African Americans with diabetes | 2 |
| Anderson S, Broadbent DM, Swain JYS, Vora JP, Harding SP. (2003) Ambulatory photographic screening for diabetic retinopathy in nursing homes | 2 |
| Apostol S, Carstocea B. (1994) [Color vision in diabetics] | 1 |
| Arden G, Gunduz K, Perry S. (1988) Color vision testing with a computer graphics system: preliminary results | 5 |
| Arden GB, Gündüz K, Perry S. (1988) Color vision testing with a computer graphics system: preliminary results | 3 |
| Arden GB, Wolf JE, Tsang Y. (1998) Does dark adaptation exacerbate diabetic retinopathy? Evidence and a linking hypothesis | 3 |
| Arend O, Remky A, Evans D, Stüber R, Harris A. (1997) Contrast sensitivity loss is coupled with capillary dropout in patients with diabetes | 2 |
| Ariyasu RG, Lee PP, Linton KP, LaBree LD, Azen SP, Siu AL. (1996) Sensitivity, specificity and predictive values of screening tests for eye conditions in a clinic-based population | 2 |
| Arun CS, Ngugi N, Lovelock L, Taylor R. (2003) Effectiveness of screening in preventing blindness due to diabetic retinopathy | 2 |
| Author not found. (1992) Screening guidelines for diabetic retinopathy. American College of Physicians, American Diabetes Association, and American Academy of Ophthalmology | 1 |
| Bachmann MO, Nelson SJ. (1998) Impact of diabetic retinopathy screening on a British district population: case detection and blindness prevention in an evidence-based model | 1 |
| Bailey CC, Sparrow JM. (2001) Visual symptomatology in patients with sight-threatening diabetic retinopathy | 2 |
| Baker R, Grimshaw G, Thompson JR, Wilson A. (1999) Services for diabetic retinopathy screening in England and Wales: a survey of ophthalmologists | 2 |
| Banford D, North RV, Dolben J, Butler G, Owens DR. (1994) Longitudinal study of visual functions in young insulin-dependent diabetics | 4 |
| Bangstad HJ, Brinchmann-Hansen O, Hultgren S, Dahl-Jorgensen K, Hanssen KF. (1994) Impaired contrast sensitivity in adolescents and young type 1 (insulin-dependent) diabetic patients with microalbuminuria | 2 |
| Barca L, Vaccari G. (1978) Diabetic retinopathy and colour discrimination under various illuminants | 1 |
| Barton FB, Bresnick GH, Knatterud GL, Fisher MR, Early Treatment Diabetic Retinopathy Study Research Group. (1988) Classification of Farnsworth-Munsell 100-hue test results by pattern of error scores [meeting abstract] | 4 |
| Barton FB, Fong DS, Knatterud GL, Group ER. (2004) Classification of Farnsworth-Munsell 100-hue test results in the Early Treatment Diabetic Retinopathy Study | 4 |
| Basch CE, Walker EA, Howard CJ, Schmoon H, Zybert P. (1999) The effect of health education on the rate of ophthalmic examinations among African Americans with diabetes mellitus | 2 |
| Bensinger RE. (1992) Color vision and color vision testing | 1 |
| Benson WH, Farber ME. (1988) Clinical screening for diabetic retinopathy using Lanthony’s desaturated D-15 [meeting abstract] | 4 |
| Bernardczyk-Meller J, Kielczewska-Mrozikiewicz D, Meller M, Pecold K. (2000) [Diagnostics of the early retinal and optic nerve changes in long-standing type 1 diabetes mellitus] | 1 |
| Bernardczyk-Meller J, Siwiec-Prociska J, Stankiewicz W, Fichna P, Pecold K, Korman E. (2004) [Influence of Eqb 761 on the function of the retina in children and adolescent with long lasting diabetes mellitus – preliminary report] | 5 |
| Birbeck JA. (1972) Studies of colour vision in juvenile diabetes [meeting abstract] | 1 |
| Birch J. (1993) Diagnosis of defective colour vision | 1 |
| Birch J. (1997) Acquired tritanopia in diabetic maculopathy | 3, 5 |
| Birch J, Ariffin AE, Kurtz A. (1991) Colour vision screening for the detection of diabetic retinopathy | 3 |
| Birch J, Chisholm IA, Kinear P, Marre M, Pinckers AJLG, Pokorny J, et al. (1979) Acquired colour vision defects | 1 |
| Birch J, Dain SJ. (1987) An averaging method for the interpretation of the Farnsworth-Munsell 100-Hue Test. II. Colour vision defects acquired in diabetic retinopathy | 3 |
| Bischoff P. (1993) [Frequency of ophthalmological examinations in diabetic retinopathy] | 2 |
| Bonvin ER, Dosso AA, Baglivo E. (1994) Contrast sensitivity in diabetics with and without background retinopathy [meeting abstract] | 2 |
| Booth AJ, Sinclair NE, Clover A, Luff AJ, Leatherdale A, Newsom RSB. (2004) Does retinal screening improve the visual outcome of diabetic maculopathy treatment? | 2 |
| Boucher MC, Nguyen QT, Angioi K. (2005) Mass community screening for diabetic retinopathy using a nonmydriatic camera with telemedicine | 2 |
| Bowman KJ. (1982) A method for quantitative scoring of the Farnsworth panel D-15 | 3 |
| Brash PD, Ripley L, De Alwis D, Tooke JE. (1995) Tritan colour vision impairment is evident in the pre-diabetic state [meeting abstract] | 3, 5 |
| Bresnick GH, Condit RS, Palta M, Korth K, Groo A, Syrjala S. (1985) Association of hue discrimination loss and diabetic retinopathy | 2, 4 |
| Bresnick GH, Mukamel DB, Dickinson JC, Cole DR. (2000) A screening approach to the surveillance of patients with diabetes for the presence of vision-threatening retinopathy | 2 |
| Broadbent DM, Scott JA, Vora JP, Harding SP. (1999) Prevalence of diabetic eye disease in an inner city population: the Liverpool Diabetic Eye Study | 2 |
| Bronte-Stewart JM, Cant JS, Craig JO. (1984) Colour vision in young diabetics | 3, 4 |
| Bryant VM, Wilson A, Jones TH, Hague RV. (1999) A high uptake eye and foot screening service for an urban population | 2 |
| Bucher MB, Leuenberger PM, Roth A. (1983) [Diabetes and color vision] | 3 |
| Buckingham TJ, Young SA. (1993) Changes in retinal function with duration of diabetes mellitus | 2 |
| Buonaccorso KM. (1999) Diabetic retinopathy screening: a clinical quality improvement project | 2 |
| Buxton MJ, Sculpher MJ, Ferguson BA, Humphreys JE, Altman JF, Spiegelhalter DJ, et al. (1991) Screening for treatable diabetic retinopathy: a comparison of different methods | 2 |
| Cameron BL. (2002) Making diabetes management routine: how often do you and your patients screen for complications? | 1, 2 |
| Cathelineau G, Cathelineau BV. (1991) Diabetic retinopathy: methodologies in practice | 2 |
| Cathelineau G, Villatte-Cathelineau B, Lombrail P. (1986) [Color vision and diabetes] | 1 |
| Cirillo D, Gonfiantini E, De Grandis D, Bongiovanni L, Robert JJ, Pinelli L. (1984) Visual evoked potentials in diabetic children and adolescents | 2 |
| Clark JB, Grey RH, Lim KK, Burns-Cox CJ. (1994) Loss of vision before ophthalmic referral in blind and partially sighted diabetics in Bristol | 2 |
| Collier A, Mitchell JD, Clarke BF. (1985) Visual evoked potential and contrast sensitivity function in diabetic retinopathy | 2, 5 |
| Condit R, Bresnick G, Korth K, Mattson D, Syrjala S. (1982) Hue discrimination loss and retinopathy severity in diabetes mellitus [meeting abstract] | 1, 4 |
| Conrath J, Giorgi R, Raccah D, Ridings B. (2005) Foveal avascular zone in diabetic retinopathy: quantitative vs qualitative assessment | 2 |
| Cranston IC. (2002) Bexley diabetes retinal screening programme | 1 |
| Crognale MA, Switkes E, Rabin J, Schneck ME, Haegerstrom-Portnoy G, Adams AJ. (1993) Application of the spatiochromatic visual evoked potential to detection of congenital and acquired color-vision deficiencies | 1, 5 |
| d’Annunzio G, Malvezzi F, Vitali L, Barone C, Giacchero R, Klersy C, et al. (1997) A 3–19 year follow up study on diabetic retinopathy in patients diagnosed in childhood and treated with conventional therapy | 2 |
| Dain SJ. (2004) Clinical colour vision tests | 1 |
| Dain SJ, Saunders JE. (1987) F-M 100 hue total error scores have discrete values | 1, 3 |
| Daley ML, Watzke RC, Riddle MC. (1987) Early loss of blue-sensitive color vision in patients with type 1 diabetes | 3, 5 |
| Danne T, Kordonouri O, Enders I, Hövener G. (1998) Monitoring for retinopathy in children and adolescents with type 1 diabetes | 1, 2 |
| Davies NP, Morland AB. (2002) Chromatic and achromatic spectral sensitivity in diabetes mellitus | 3, 5 |
| Davies R, Roderick P, Canning C, Brailsford S. (2002) The evaluation of screening policies for diabetic retinopathy using simulation | 1, 2 |
| De Marco R, Capasso L, Magli A, Franzese A, Gasparini N, Ambrosio G. (1996) Measuring contrast sensitivity in aretinopathic patients with insulin dependent diabetes mellitus | 2 |
| Deb-Joardar N, Germain N, Thuret G, Garcin AF, Manoli P, Defreyn A, et al. (2007) Systematic screening for diabetic retinopathy with a digital fundus camera following pupillary dilatation in a university diabetes department | 2 |
| Del Beato P, Tanzilli P, Giusti C, Pannarale L, Vingolo EM. (1995) Acquired dyschromatopsia in diabetes without diabetic retinopathy [meeting abstract] | 4 |
| Della Sala S, Bertoni G, Somazzi L, Stubbe F, Wilkins AJ. (1985) Impaired contrast sensitivity in diabetic patients with and without retinopathy: a new technique for rapid assessment | 2 |
| Dhanesha U, Gilchrist J, Miles D, Bradford N, Weatherill J. (1991) Loss of visual function associated with microalbuminuria in diabetes mellitus: a pilot study | 2 |
| Di Leo MA, Caputo S, Falsini B, Porciatti V, Greco AV, Ghirlanda G. (1994) Presence and further development of retinal dysfunction after 3-years follow-up in IDDM patients without angiographically documented vasculopathy | 2 |
| Di Leo MA, Caputo S, Falsini B, Porciatti V, Minnella A, Greco AV, et al. (1992) Nonselective loss of contrast sensitivity in visual system testing in early type 1 diabetes | 2 |
| Dickson PR, McCarty CA, Keeffe JE, Baxter R, Harper CA, Taylor HR. (1996) Diabetic retinopathy: examination practices and referral patterns of general practitioners | 2 |
| Doucet J, Chassagne P, Poutrain JR, Ozenne G, Denis P, Bercoff E, et al. (1992) [Dyschromatopsia: a manifestation of diabetic neuropathy] | 4 |
| Doucet J, Chassagne P, Trivalle C, Ozenne G, Retout A, Parain D, et al. (1994) [Dyschromatopsia: manifestation or epiphenomenon in the course of diabetic neuropathy] | 3 |
| Drum B, Armaly MF, Huppert WE. (1987) Sources of short wavelength sensitivity loss in glaucoma | 3 |
| Dunn NR, Bough P. (1996) Standards of care of diabetic patients in a typical English community | 2 |
| Elia Y. (2004) Is poor glucose control associated with colour vision deficiencies before retinopathy in pre-teen children with type 1 diabetes? | 5 |
| Elliott M, Plehwe W, Kearns M, Yue DK, Turtle JR. (1988) Visual contrast sensitivity in diabetes using a simple screening test [meeting abstract] | 2 |
| Erb C, Fahle M. (2006) [Colour vision and acquired colour vision disturbances. I. basic aspects] | 1 |
| Esbester M. (2002) The Portsmouth retinopathy screening scheme | 1 |
| Facey K, Cummins E, Macpherson K, Morris A, Reay L, Slattery J. (2002) Organisation of services for diabetic retinopathy screening. Health Technology Assessment Report 1 | 1, 2 |
| Farber ME, Lotshaw RR. (1986) Screening for diabetic retinopathy contrast sensitivity function [meeting abstract] | 4 |
| Faria de Abreu JR, Neves F, Reis J. (1981) [Functional retinal abnormalities in diabetic patients with no retinopathy] | 5 |
| Farnsworth D. (1957) The Farnsworth-Munsell 100-hue test manual | 1 |
| Feigl B, Brown B, Lovie-Kitchin J, Swann P. (2005) Monitoring retinal function in early age-related maculopathy: visual performance after 1 year | 3 |
| Feitosa-Santana C, Oiwa NN, Paramei GV, Bimler D, Costa MF, Lago M, et al. (2006) Color space distortions in patients with type 2 diabetes mellitus | 3, 5 |
| Fendrick AM, Javitt JC, Chiang YP. (1992) Cost-effectiveness of the screening and treatment of diabetic retinopathy. What are the costs of underutilization? | 1, 2 |
| Fong DS, Gottlieb J, Ferris FL, III, Klein R. (2001) Understanding the value of diabetic retinopathy screening | 1 |
| Fontana M, Verriest G. (1986) Modification by fluoangiography of color vision in diabetic patients | 3 |
| Foster DT, Wylie-Rosett J, Walker EA. (1996) Local survey of optometrists about dilated fundoscopic examinations for patients with diabetes: making use of phone book yellow-page listings | 2 |
| Foulds WS, McCuish A, Barrie T, Green F, Scobie IN, Ghafour IM, et al. (1983) Diabetic retinopathy in the west of Scotland: its detection and prevalence and the cost-effectiveness of a proposed screening programme | 2 |
| Fristrom B. (1998) Peripheral and central colour contrast sensitivity in diabetes | 5 |
| Gartaganis SP, Psyrojannis AJ, Koliopoulos JX, Mela EK. (2001) Contrast sensitivity function in patients with impaired oral glucose tolerance | 2 |
| Garvican L, Clowes J, Gillow T. (2000) Preservation of sight in diabetes: developing a national risk reduction programme | 2 |
| Gatling W, Howie AJ, Hill RD. (1995) An optical practice-based diabetic eye screening programme | 2 |
| Gerkowicz M. (1989) [Color vision in patients with juvenile-onset diabetes mellitus] | 4 |
| Ghafour IM, Foulds WS, Allan D. (1984) Short-term effect of slit-lamp illumination and argon laser light on visual function of diabetic and non-diabetic subjects | 3 |
| Ghafour IM, Foulds WS, Allan D, McClure E. (1982) Contrast sensitivity in diabetic subjects with and without retinopathy | 2 |
| Gillibrand WP, Broadbent DM, Swain JY, Harding SP, Vora JP. (2000) Knowledge levels of diabetic eye disease in people with diabetes: results of a descriptive survey | 2 |
| Ginsberg AP. (1984) A new contrast sensitivity vision test chart | 2 |
| Ginsburg AP, Cannon MW. (1983) Comparison of three methods for rapid determination of threshold contrast sensitivity | 3 |
| Giusti C. (2001) Lanthony 15-Hue Desaturated Test for screening of early color vision defects in uncomplicated juvenile diabetes | 3, 5 |
| Giusti C. (2002) Novel diagnostic and therapeutic approaches to the diabetic retinopathy | 1 |
| Glenn S. (2000) Risk factors screening and treatment of diabetic eye disease | 1 |
| Gruben C, Zrenner E. (1990) Contrast sensitivity loss in early diabetic retinopathy [meeting abstract] | 2 |
| Gualtieri M, Nishi M, Lago M, Ventura DF. (2005) Color discrimination and chromatic contrast sensitivity assessed in type 2 diabetic patients without retinopathy | 3, 5 |
| Gunduz K, Arden GB, Perry S. (1988) Color-contrast thresholds are elevated in mild disease though other color tests give normal results [meeting abstract] | 1 |
| Hampson S. (2001) Experience of setting up a retinal screening service | 2 |
| Hardy KJ, Fisher C, Heath P, Foster DH, Scarpello JH. (1995) Comparison of colour discrimination and electroretinography in evaluation of visual pathway dysfunction in aretinopathic IDDM patients | 3 |
| Hardy KJ, Lipton J, Scase MO, Foster DH, Scarpello JH. (1992) Detection of colour vision abnormalities in uncomplicated type 1 diabetic patients with angiographically normal retinas | 3 |
| Hardy KJ, Scarpello JH, Foster DH. (1995) Relation between blood glucose control over 3 months and colour discrimination in insulin dependent diabetic patients without retinopathy | 3, 4 |
| Harvey JN, Craney L, Nagendran S, Ng CS. (2006) Towards comprehensive population-based screening for diabetic retinopathy: operation of the North Wales diabetic retinopathy screening programme using a central patient register and various screening methods | 2 |
| Heitz R, Heitz-Wackermann RM. (1987) [The Haguenau automatized Farnsworth 100 hue test] | 1 |
| Hellstedt T, Kaaja R, Teramo K, Immonen I. (1997) Contrast sensitivity in diabetic pregnancy | 2 |
| Henricsson M, Nyström L, Blohmé G, Ostman J, Kullberg C, Svensson M, et al. (2003) The incidence of retinopathy 10 years after diagnosis in young adult people with diabetes | 2 |
| Hood DC, Benimoff NI, Greenstein VC. (1984) The response range of the blue-cone pathways: a source of vulnerability to disease | 2, 3 |
| Howes SC, Caelli T, Mitchell P. (1982) Contrast sensitivity in diabetics with retinopathy and cataract | 2, 5 |
| Ichikawa H, Hukami K, Tanabe S. (1983) Standard pseudoisochromatic plates. 2. For acquired color vision defects | 2 |
| Immonen IJ, Hellstedt T, Teramo K, Kaaja R. (1996) Contrast sensitivity during pregnancy in diabetics with minimal retinopathy [meeting abstract] | 2 |
| James M, Turner DA, Broadbent DM, Vora J, Harding SP. (2000) Cost effectiveness analysis of screening for sight threatening diabetic eye disease | 2 |
| Javitt JC, Aiello LP. (1996) Cost-effectiveness of detecting and treating diabetic retinopathy | 1, 2 |
| Javitt JC, Canner JK, Frank RG, Steinwachs DM, Sommer A. (1990) Detecting and treating retinopathy in patients with type 1 diabetes mellitus. A health policy model | 2 |
| Karadeniz S, Kir N, Yilmaz MT, Ongor E, Dinccag N, Baar D, et al. (1996) Alteration of visual function in impaired glucose tolerance | 3 |
| Kawasaki K, Yonemura K, Yokogawa Y, Saito N, Kawakita S. (1986) Correlation between ERG oscillatory potential and psychophysical contrast sensitivity in diabetes | 2 |
| Kergoat H, Lovasik JV. (1991) Accommodative performance for chromatic targets in diabetes mellitus: a preliminary report | 5 |
| Kessel L, Alsing A, Larsen M. (1999) Diabetic vs non-diabetic colour vision after cataract surgery | 5 |
| Khosla PK, Talwar D, Tewari HK. (1991) Contrast sensitivity changes in background diabetic retinopathy | 2 |
| Kinnear PR. (1970) Proposals for scoring and assessing the 100-hue test | 1 |
| Kinnear PR, Aspinall PA, Lakowski R. (1972) The diabetic eye and colour vision | 4 |
| Kitano S. (2005) [Grading of diabetic retinopathy from non-stereoscopic color fundus photographs: relationship to fluorescein angiography findings and three-year prognosis] | 2 |
| Klein BE, Davis MD, Segal P, Long JA, Harris WA, Haug GA, et al. (1984) Diabetic retinopathy: assessment of severity and progression | 2 |
| Klein R, Klein BE, Moss SE. (1990) The Wisconsin epidemiologic study of diabetic retinopathy: an update | 2 |
| Klemperer I, Yassur Y. (1987) [Contrast sensitivity in testing visual functions in diabetics] | 1 |
| Knudsen LL, Andersen CU, Lervang HH, Vad J. (2002) [Screening for diabetic retinopathy in the County of North Jutland] | 2 |
| Krasny J, Cihelkova I, Dominek Z, Soucek P, Treslova L, Lebl J, et al. (2007) [Contrast sensitivity and fluorescein angiography in evaluating the ocular changes in the relation to the diabetes mellitus type 1 compensation in young adult patients | 2 |
| Kristensen JK, Sandbaek A, Bro F, Lassen JF, Lauritzen T. (2004) Routine screening for diabetic eye complications in a population based cohort of 4.438 persons with type 2 diabetes in a Danish county | 2 |
| Kumari Rani P, Raman R, Manikandan M, Mahajan S, Paul PG, Sharma T. (2006) Patient satisfaction with tele-ophthalmology vs ophthalmologist-based screening in diabetic retinopathy | 2 |
| Kurtenbach A, Erb C, Adler M, Born B. (2001) Colour vision in diabetics tested by the Farnsworth–Munsell 28-hue desaturated test | 5 |
| Kurtenbach A, Flogel W, Erb C. (2002) Anomaloscope matches in patients with diabetes mellitus | 5 |
| Kurtenbach A, Schiefer U, Neu A, Zrenner E. (1999) Development of brightness matching and colour vision deficits in juvenile diabetics | 3, 5 |
| Kurtenbach A, Schiefer U, Neu A, Zrenner E. (1999) Preretinopic changes in the colour vision of juvenile diabetics | 5 |
| Kurtenbach A, Schiefer U, Zrenner E, Neu A. (1997) Juvenile diabetics and the colour vision meter | 5 |
| Kurtenbach A, Wagner U, Neu A, Schiefer U, Ranke MB, Zrenner E. (1994) Brightness matching and colour discrimination in young diabetics without retinopathy | 5 |
| Lagerlof O. (1978) Quantitative assessment of acquired colour vision deficiency in maculopathy | 1 |
| Lagerlof O. (1999) [To test color vision is also important] | 1 |
| Lakowski R, Aspinall PA, Kinnear PR. (1972) Association between colour vision losses and diabetes mellitus | 4 |
| Lanthony P. (1978) The new color test | 1 |
| Lee SC. (1997) Screening for early diabetic retinopathy by a high resolution computer vision system [meeting abstract] | 1 |
| Lee SJ, McCarty CA, Sicari C, Livingston PM, Harper CA, Taylor HR, et al. (2000) Recruitment methods for community-based screening for diabetic retinopathy | 2 |
| Lee SJ, Sicari C, Harper CA, Livingston PM, McCarty CA, Taylor HR, et al. (2000) Examination compliance and screening for diabetic retinopathy: a 2-year follow-up study | 2 |
| Leese G, Broadbent D, Harding S, Vora J. (1995) Screening for diabetic retinopathy. Approaching 90% sensitivity with new techniques | 1 |
| Leese GP, Broadbent DM, Harding SP, Vora JP. (1996) Detection of sight threatening diabetic eye disease | 1 |
| Leese GP, Morris AD, Swaminathan K, Petrie JR, Sinharay R, Ellingford A, et al. (2005) Implementation of national diabetes retinal screening programme is associated with a lower proportion of patients referred to opthalmology | 2 |
| Leid J, Gastaud P, Vola J. (1982) Resultats d’examens de la vision color ée chez les diabétiques avec ou sans rétinopathie | 1 |
| Leid J, Gastaud P, Vola JL. (1985) [Diagnostic and prognostic significance of chromatic syndromes in diabetes] | 1 |
| Leid J, Leid V. (1990) [Medical management of diabetic retinopathy. Pathophysiologic rationale. Time-course of color vision impairment and angiography in patients treated for one year] | 4 |
| Liska V. (1999) [Contrast sensitivity in type 1 diabetics without symptoms of diabetic retinopathy] | 2 |
| Liska V, Dostalek M. (1999) Are contrast sensitivity functions impaired in insulin dependent diabetics without diabetic retinopathy? | 2 |
| Livingston PM, McCarty CA, Woods CA, Harper AC, Keeffe JE, Taylor HR. (1998) Use of focus groups to identify health promotion strategies for the early detection of diabetic retinopathy | 2 |
| Livingston PM, Wood CA, Butler M, Oh J, Keefe JE, Taylor HR. (1998) General practitioners are the most important conveyors of information to their patients regarding diabetic retinopathy | 1 |
| Lobefalo L, Verdesca G, D’Antonio E, Verrotti A, Rancitelli L, Mancini A, et al. (1996) [Chromatic perimetry in diabetics without retinopathy] | 3, 5 |
| Lobefalo L, Verrotti A, Mastropasqua L, Chiarelli F, Della Loggia G, Morgese G, et al. (1998) Colour and achromatic perimetry in diabetic children without retinopathy | 3, 5 |
| Lobefalo L, Verrotti A, Mastropasqua L, Della Loggia G, Cherubini V, Morgese G, et al. (1998) Blue-on-yellow and achromatic perimetry in diabetic children without retinopathy | 4, 5 |
| Lopez M, Martin R, Martinez R, Garcia J, Sanchez R, Lopez I, et al. (2002) What is the cause of the impaired color vision in diabetic patients? [meeting abstract] | 4 |
| Lutz M, Bresinck GH. (1989) Diabetic retinopathy and visual field sensitivity assessed with color perimetry [meeting abstract] | 5 |
| Maberley D, Walker H, Koushik A, Cruess A. (2003) Screening for diabetic retinopathy in James Bay, Ontario: a cost-effectiveness analysis | 2 |
| Maberley DAL, Koushik A, Cruess AF. (2002) Factors associated with missed eye examinations in a cohort with diabetes | 2 |
| MacCuish AC. (1993) Early detection and screening for diabetic retinopathy | 1 |
| Mackie SW, Barrie T, Maccuish AC, Walsh G. (1993) Measurement of contrast sensitivity in patients with diabetic retinopathy using the Pelli–Robson chart [meeting abstract] | 2 |
| Mailath L. (1972) The AN-59 anomaloscope in the research of acquired colour vision deficiencies | 5 |
| Maione M, Bontempelli G, Scoccianti L, Righi I. (1985) [Color vision and diabetes. Hue test results in reexamination after 5 yr] | 3 |
| Maione M, Graziosi P, Scoccianti L, Righi I, Bontempelli G, La Medica A. (1987) [Contrast sensitivity for coloured gratings in diabetic retinopathy] | 4 |
| Malagola R, Gargiulo P, Giusti C, Bosco D, Pannarale L, Scalfati M, et al. (1994) Screening of early color-vision defects in insulin-dependent diabetic-patients with background retinopathy [meeting abstract] | 4 |
| Maliszewski M, Dennis C, DeCoste KC. (1988) Prevention, detection and treatment of diabetic eye disease: an overview and demonstration project | 2 |
| Mäntyjärvi M. (1987) Screening of colour vision defects in diabetic patients | 3 |
| Mäntyjärvi M. (1989) Colour vision and dark adaptation in diabetic patients after photocoagulation | 2, 3 |
| Mäntyjärvi M. (1992) Screening of diabetics who read incorrectly colour-dependent glucose test-strips | 3, 4 |
| Mäntyjärvi M. (1993) Colour vision in diabetic patients after photocoagulation treatment. A five-year follow-up | 3, 5 |
| Mäntyjärvi M, Nielikainen S, Osmoviita J, Myohanen T. (1988) [Diabetes and color vision] | 1 |
| Marmion VJ. (1977) The results of a comparison of the hundred hue test and static color perimetry in diabetic retinopathy (short description of methods and results) | 3 |
| Mastropasqua L, Lobefalo L, Carpineto P, Ciancaglini M, Calogiuri MT, Verrotti A, et al. (1994) Study of color discrimination in insulin-dependent mellitus diabetes | 3 |
| McCarlie J, Alexander G, Sommerville J, McGettrick P, MacPherson N, Collier A. (1999) Use of collaborative audit to assist local implementation of the SIGN guideline for prevention of visual impairment in diabetes | 2 |
| Mittl R, Jindra LF, Zemon V, Ng E, Peralta M. (1989) Contrast sensitivity testing in patients with diabetic maculopathy [meeting abstract] | 2 |
| Mollon JD, Pokorny J, Knoblauch K. (2003) Normal and defective colour vision | 1 |
| Montori VM. (2001) Review: mydriatic retinal photography is the most effective test for detecting diabetic retinopathy. Commentary on Hutchinson A, McIntosh A, Peters J, O’Keefe C, Khunti K, Baker R, et al. Effectiveness of screening and monitoring tests for diabetic retinopathy | 1 |
| Mortlock KE, Chiti Z, North RV, Drasdo N, Owens DR. (2003) L/M and S-cone ERGs in subjects with no or early diabetic retinopathy [meeting abstract] | 3, 4 |
| Moss SE, Klein R, Klein BE. (1995) Factors associated with having eye examinations in persons with diabetes | 2 |
| Muise JG, Blanchard L, DesRosiers M, Caissie D, Watier C, Pelletier J. (1997) Achromatic visual backward masking of colored stimuli in type 1 diabetes | 5 |
| Mukamel DB, Bresnick GH, Wang Q, Dickey CF. (1999) Barriers to compliance with screening guidelines for diabetic retinopathy | 2 |
| Mulak M, Reniewska B, Kostu E, Balcewicz A, Misiuk-Hojlo M. (2002) [The role of color vision disturbances in diagnostics of early diabetic retinopathy] | 4 |
| Muntoni S, Serra A, Mascia C, Songini M. (1982) Dyschromatopsia in diabetes mellitus and its relation to metabolic control | 4, 5 |
| Navuluri RB. (2000) Diabetic retinopathy screening among Hispanics in Lea County New Mexico | 2 |
| New Zealand Health Technology Assessment. (1998) Colour vision screening: a critical appraisal of the literature | 2 |
| Nguyen QD, Do DV. (2003) Diabetic retinopathy: an overview for non-ophthalmologists | 1 |
| Nomura R, Terasaki H, Hirose H, Miyake Y. (2000) Blue-on-yellow perimetry to evaluate S cone sensitivity in diabetics | 5 |
| Nordmann JP, Guigui A, Laroche L, Denis P, Saraux H. (1990) [Contrast sensitivity and diabetes] | 2 |
| Norris SL, Saadine J, Chowdhury FM, Zhang X, Kanjilal S, Mangione C, et al. (2005) Interventions to promote screening for diabetic retinopathy | 1 |
| North RV, Farrell U, Banford D, Jones C, Gregory JW, Butler G, et al. (1997) Visual function in young IDDM patients over 8 years of age: a 4-year longitudinal study | 4, 5 |
| Noyori S, Hamano K, Tomonaga M, Ohta Y. (1987) [Normal values of FM-100 hue test in Japanese subjects] | 3 |
| Park KH, Shin Y, Lee M, Hwang J, Wee W, Lee J. (2004) Role of new SNU computerized color test and OCT in diabetic macular oedema | 4 |
| Parker JA. (1979) Farnsworth 100 hue scoring for acquired color vision deficiencies by weighted functions | 3 |
| Pasagian-Macaulay A, Basch CE, Zybert P, Wylie-Rosett J. (1997) Ophthalmic knowledge and beliefs among women with diabetes | 2 |
| Peduzzi M, Longanesi L, Ascari A, Cascione S, Galletti M, Roncaia R, et al. (1989) [Screening of early color vision loss in diabetic patients] | 5 |
| Phillips CJ, Harper GAD, Waheed N, Owens DR, Gibbons RL, Allen J, et al. (1997) Screening for diabetic retinopathy: the costs to patients: a pilot study | 2 |
| Pinckers A, Cruysberg JR. (1986) Farnsworth-Munsell 100-hue test and lightness discrimination test | 1 |
| Pokorny J, Smith VC. (1986) Eye disease and color defects | 1 |
| Pokorny J, Smith VC, Verriest G, Pinckers A. (1979) Congenital and acquired colour vision defects | 1 |
| Porta M, Kohner E. (1991) Screening for diabetic retinopathy in Europe | 1 |
| Porta M, Rizzitiello A, Tomalino M, Trento M, Passera P, Minonne A, et al. (1999) Comparison of the cost-effectiveness of three approaches to screening for and treating sight-threatening dibetic retinopathy | 2 |
| Puent BD, Nichols KK. (2004) Patients’ perspectives on noncompliance with diabetic retinopathy standard of care guidelines | 2 |
| Raphael BA, Galetta KM, Jacobs DA, Markowitz CE, Liu GT, Nano-Schiavi ML, et al. (2006) Validation and test characteristics of a 10-item neuro-ophthalmic supplement to the NEI-VFQ-25 | 2 |
| Regan D, Neima D. (1983) Low-contrast letter charts as a test of visual function | 2 |
| Rockett M, Anderle D, Bessman AN. (1987) Blue-yellow vision deficits in patients with diabetes | 5 |
| Roy MS, Gunkel RD, Podgor MJ. (1986) Color vision defects in early diabetic retinopathy | 3 |
| Roy MS, McCulloch C, Hanna AK, Mortimer C. (1984) Colour vision in long-standing diabetes mellitus | 5 |
| Sanchez-Thorin JC, Emanuele N, Klein R, Henderson W, Abraira C. (1997) Retinopathy and type 2 diabetes. ‘Evaluations of retinopathy in the VA Cooperative Study on Glycemic Control and Complications in Type 2 Diabetes (VA CSDM): a feasibility study by Emanuele et al. | 1 |
| Santana CF, Costa MF, Lago M, Bernick M, Nishi M, Ventura DF. (2005) Color discrimination in type 2 diabetes mellitus patients with no retinopathy [meeting abstract] | 3, 4 |
| Saracco JB, Gastaud P, Leid J, Vola JL, Lecourt-Leid V. (1982) [Two-color thresholds in diabetic: preliminary study] | 5 |
| Saracco JB, Gastaud P, Trani JC, Estachy G, Leid J, Vola JL, et al. (1981) [The role of saturation in color vision tests used for diabetics] | 1 |
| Scase MO, Foster DH, Honan WP, Heron JR, Gulliford MC, Scarpello JHB. (1990) Abnormalities in hue discrimination revealed with very brief stimuli in diabetes mellitus and in optic neuritis | 5 |
| Scase MO, Honan WP, Guillford MC, Scarpello JHB, Heron JR, Foster DH. (1987) Colour vision loss in diabetic subjects [meeting abstract] | 5 |
| Schauseil-Zipf U, Puyn U, Schulte K, Sickel W. (1984) Wavelength-dependent abnormalities of pattern evoked cortical responses in young diabetics | 2, 5 |
| Schoenfeld ER, Greene JM, Wu SY, Leske MC. (2001) Patterns of adherence to diabetes vision care guidelines: baseline findings from the Diabetic Retinopathy Awareness Program | 2 |
| Sculpher MJ, Buxton MJ, Ferguson BA, Spiegelhalter DJ, Kirby AJ. (1992) Screening for diabetic retinopathy: a relative cost-effectiveness analysis of alternative modalities and strategies | 2 |
| Shin YJ, Park KH, Hwang JM, Wee WR, Lee JH. (2007) A new color vision test to differentiate congenital and vision defects | 3 |
| Shiraishi H, Shimizu K, Ohta Y. (1989) [Color vision under different luminosity in various fundus diseases] | 4 |
| Shotliff K, Moore D, Dimock J, Feher MD. (2004) Screening for diabetic retinopathy – false-positives do occur (it could be Shagreene) | 2, 5 |
| Simader E, Kreissig I, Turmer KH, Reinauer KM. (1995) [Importance of color vision testing in diabetic patients] | 5 |
| Singer DE, Nathan DM, Fogel HA, Schachat AP. (1992) Screening for diabetic retinopathy | 1 |
| Singer DE, Schachat A, Nathan DM, Patz A, Kahn R, Aiello LM, et al. (1992) Screening guidelines for diabetic retinopathy | 1 |
| Sloan FA, Brown DS, Carlisle ES, Picone GA, Lee PP. (2004) Monitoring visual status: why patients do or do not comply with practice guidelines | 2 |
| Smith VC, Pokorny J, Pass AS. (1985) Color-axis determination on the Farnsworth–Munsell 100-hue test | 3 |
| Sokol S, Moskowitz A, Skarf B, Evans R, Molitch M, Senior B. (1985) Contrast sensitivity in diabetics with and without background retinopathy | 2 |
| Soto-Pedre E, Hernaez-Ortega MC, Pinies JA. (2007) Duration of diabetes and screening coverage for retinopathy among patients with type 2 diabetes | 2 |
| Spafford MM, Lovasik JV. (1986) Clinical evaluation of ocular and visual functions in insulin-dependent juvenile diabetics | 3 |
| Squirrell DM, Talbot JF. (2003) Screening for diabetic retinopathy | 1 |
| Stefansson E. (2004) Man vs machine: is technology a blessing or a barrier in screening for diabetic eye disease? | 1 |
| Sussman EJ, Tsiaras WG, Soper KA. (1982) Diagnosis of diabetic eye disease | 2 |
| Suzuki R, Yokota A, Seki R. (1982) [Color vision in diabetic retinopathy] | 5 |
| Tanabe S, Hukami K, Ichikawa H. (1983) New pseudoisochromatic plates for acquired color vision defects | 3 |
| Taylor SP. (1984) Acquired colour defects under restricted viewing time: a new diagnostic technique? | 3, 5 |
| Taylor WO. (1974) Problems in performance and interpretation of Farnsworth’s 100-hue test | 1 |
| Tenore A, Giardino I, Sandomenico M, Magli A, Zaccaria S, Gasparini N. (1989) Early detection of retinal damage in children with insulin dependent diabetes mellitus (IDDM) [meeting abstract] | 3,5 |
| Terasaki H, Hirose H, Miyake Y. (1996) S-cone pathway sensitivity in diabetes measured with threshold vs intensity curves on flashed backgrounds | 3, 4 |
| Thompson DG, Howarth F, Taylor H, Levy IS, Birch J. (1979) Defective color vision in diabetes: a hazard to management | 2, 4 |
| Tokuda H, Yasuma T, Ichikawa H. (1984) [Color vision defects in diabetic retinopathy. 2. Correlation with clinical findings] | 3, 5 |
| Tong L, Carkeet A. (2001) A new colour vision arrangement test to detect functional changes in diabetic macular oedema | 1 |
| Toyoguchi A, Kudo H, Rokugo T, Usui M. (1998) [Cone sensitivity measurements in diabetic retinopathy] | 5 |
| Tregear SJ, Ripley LG, Knowles PJ, Gilday RT, de Alwis DV, Reffin JP. (1994) Automated tritan discrimination sensitivity: a new clinical technique for the effective screening of severe diabetic retinopathy | 4 |
| Turner K, Bodmer C. (2004) Improving retinopathy screening: are we meeting the NSF target? | 2 |
| Urban B, Bakunowicz-Lazarczyk A, Peczyska J, Urban M. (1999) [The evaluation of contrast sensitivity in children and adolescents with insulin-dependent diabetes mellitus] | 2 |
| Utku D, Atmaca LS. (1992) Farnsworth–Munsell 100-hue test for patients with diabetes mellitus | 4 |
| Ventura DF, Nishi M, Bernicki M, Costa MF, Bonci D, Gualtieri M, et al. (2003) Early vision loss in diabetic patients assessed by the Cambridge Colour Test | 3 |
| Vermeire E, Wens J, Van Royen P, Biot Y, Hearnshaw H, Lindenmeyer A. (2005) Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus | 2 |
| Verriest G. (1963) Further studies on acquired deficiency of color discrimination | 3 |
| Verriest G. (1980) Colour deficiencies V | 1 |
| Verriest G, Caluwaerts MR. (1978) An evaluation of three new colour vision tests | 3 |
| Verriest G, Van Laethem J, Uvijls A. (1982) A new assessment of the normal ranges of the Farnsworth–Munsell 100-hue test scores | 3 |
| Verrotti A, Lobefalo L, Chiarelli F, Mastropasqua L, Ciancaglini M, Morgese G. (1995) Colour vision and persistent microalbuminuria in children with type-1 (insulin-dependent) diabetes mellitus: a longitudinal study | 3, 5 |
| Verrotti A, Lobefalo L, Petitti MT, Mastropasqua L, Morgese G, Chiarelli F, et al. (1998) Relationship between contrast sensitivity and metabolic control in diabetics with and without retinopathy | 2 |
| Vingrys AJ, King-Smith PE. (1988) A quantitative scoring technique for panel tests of colour vision | 3 |
| Walker EA, Zybert PA, Basch CE. (2002) What is the sensitivity and specificity of self-report for retinopathy screening? | 1 |
| Wall M, Collins C, May DR. (1990) Low-intensity grids improve sensitivity of amsler grid testing in diabetic patients without background retinopathy | 5 |
| Warburton T. (2003) Current status of screening for diabetic retinopathy in the UK | 1 |
| Warburton TJ, Hale PJ, Dewhurst JA. (2004) Evaluation of a local optometric diabetic retinopathy screening service | 2 |
| Weiss H, Zwas F, McKinnon P. (1979) Spectral sensitivity measurements in early diabetic retinopathy [meeting abstract] | 1 |
| Wilson A, Baker R, Thompson J, Grimshaw G. (2004) Coverage in screening for diabetic retinopathy according to screening provision: results from a national survey in England and Wales | 2 |
| Wilson J.B. (1999) Colour vision defects: the development of a computer-generated test for their diagnosis | 5 |
| Witkin SR, Bresnick GH, Friedberg M, Palta M, Adams AJ, Huie K. (1986) Blue cone sensitivity and hue discrimination in diabetic retinopathy [meeting abstract] | 4 |
| Wong R, Chong V. (2004) The ChromaTest a digital color contrast sensitivity analyzer, for diabetic maculopathy | 4 |
| Yamamoto S, Kamiyama M, Nitta K, Yamada T, Hayasaka S. (1996) Selective reduction of the S cone electroretinogram in diabetes | 5 |
| Younis N, Broadbent DM, James M, Harding SP, Vora JP. (2002) Current status of screening for diabetic retinopathy in the UK | 1 |
| Zisman F, Adams AJ. (1982) Spectral sensitivity of cone mechanisms in juvenile diabetics [meeting abstract] | 1 |
| Zwas F, Weiss H, McKinnon P. (1980) Spectral sensitivity measurements in early diabetic retinopathy | 1 |
Appendix 5 Online survey of screening programme managers and clinical leads
Appendix 6 STARD checklist for reporting of studies of diagnostic accuracy
| Section and topic | Item number | On page number | |
|---|---|---|---|
| Title/Abstract/Keywords | 1 | Identify the article as a study of diagnostic accuracy (recommend MeSH heading ‘sensitivity and specificity’) | iii |
| Introduction | 2 | State the research questions or study aims, such as estimating diagnostic accuracy or comparing accuracy between tests or across participant groups | 5 |
| Methods | |||
| Participants | 3 | The study population: The inclusion and exclusion criteria, setting and locations where data were collected | 6 |
| 4 | Participant recruitment: Was recruitment based on presenting symptoms, results from previous tests, or the fact that the participants had received the index tests or the reference standard? (Participant inclusion criteria) | 6 | |
| 5 | Participant sampling: Was the study population a consecutive series of participants defined by the selection criteria in items 3 and 4? If not, specify how participants were further selected (Study design inclusion criteria) | 6 | |
| 6 | Data collection: Was data collection planned before the index test and reference standard were performed (prospective study) or after (retrospective study)? (Study design inclusion criteria) | 6 | |
| Test methods | 7 | The reference standard and its rationale (Reference standard inclusion criteria) | 6 |
| 8 | Technical specifications of material and methods involved including how and when measurements were taken, and/or cite references for index tests and reference standard (Data extraction) | 6, Appendix 3 | |
| 9 | Definition of and rationale for the units, cut-offs and/or categories of the results of the index tests and the reference standard (Data analysis) | 7 | |
| 10 | The number, training and expertise of the persons executing and reading the index tests and the reference standard (Data extraction) | Appendix 3 | |
| 11 | Whether or not the readers of the index tests and reference standard were blind (masked) to the results of the other test and describe any other clinical information available to the readers (Quality assessment) | 6, Table 2, Figure 2 | |
| Statistical methods | 12 | Methods for calculating or comparing measures of diagnostic accuracy, and the statistical methods used to quantify uncertainty (e.g. 95% confidence intervals) (Data analysis) | 7 |
| 13 | Methods for calculating test reproducibility, if carried out | N/A | |
| Results | |||
| Participants | 14 | When study was performed, including beginning and end dates of recruitment (Data extraction) | Appendix 3 |
| 15 | Clinical and demographic characteristics of the study population (at least information on age, gender, spectrum of presenting symptoms) (Data extraction) | Appendix 3 | |
| 16 | The number of participants satisfying the criteria for inclusion who did or did not undergo the index tests and/or the reference standard; describe why participants failed to undergo either test (a flow diagram is strongly recommended) (Data extraction) |
Appendix 3 Study flow diagram p. 9 |
|
| Test results | 17 | Time interval between the index tests and the reference standard, and any treatment administered in between (Quality assessment) | Table 2, Figure 2 |
| 18 | Distribution of severity of disease (define criteria) in those with the target condition; other diagnoses in participants without the target condition (Data extraction) | Appendix 3 | |
| 19 | A cross-tabulation of the results of the index tests (including indeterminate and missing results) by the results of the reference standard; for continuous results, the distribution of the test results by the results of the reference standard (Data extraction) | Appendix 3 | |
| 20 | Any adverse events from performing the index tests or the reference standard (Data extraction) | Appendix 3 | |
| Estimates | 21 | Estimates of diagnostic accuracy and measures of statistical uncertainty (e.g. 95% confidence intervals) (Data extraction and results) | Appendix 3 |
| 22 | How indeterminate results, missing data and outliers of the index tests were handled (Data extraction) | Appendix 3 | |
| 23 | Estimates of variability of diagnostic accuracy between subgroups of participants, readers or centres, if carried out (Results) | ROC plots | |
| 24 | Estimates of test reproducibility, if carried out | N/A | |
| Discussion | 25 | Discuss the clinical applicability of the study findings | 49–53 |
Glossary
- Deutanopia
- The colour receptors (cones) in the eyes of people with deutanopia are not sensitive to medium wavelengths (i.e. greens).
- Diabetic retinopathy
- Damage to blood vessels in the retina, caused by diabetes.
- Munsell colour system
- A colour space that defines colours based on three dimensions: hue, value (lightness) and chroma (colour purity or colourfulness).
- Phakic eye
- An eye that still possesses its natural crystalline lens.
- Protanopia
- The colour receptors (cones) in the eyes of people with protanopia are not sensitive to long wavelengths (i.e. reds).
- Snellen
- Scale used to measure visual acuity. This has now been superseded by the development of the LogMAR scale.
- Tritanopia
- Insensitivity to short wavelengths (i.e. blues).
- Visual acuity
- The limit of spatial visual discrimination, commonly measured using letter or other geometric forms. Two of the scales used to measure visual acuity are the Snellen and LogMAR scales.
- Diagnostic case–control study
- Diagnostic accuracy study in which the test results of a series of patients with an established diagnosis are compared with those of a non-diseased control group.
- Diagnostic cohort study
- Diagnostic accuracy study in which a group of individuals with a suspected disease undergo both the index test and the reference standard, and the results of the two tests are compared.
- False-negative
- A test result which indicates that a person does not have a specific disease or condition when the person actually does have the disease or condition.
- False-positive
- A test result which indicates that a person does have a specific disease or condition when the person actually does not have the disease or condition.
- Likelihood ratio
- Describes how many times more likely a person with a disease is to receive a particular test result than a person without disease. A likelihood ratio of a positive test result is usually a number greater than 1; a likelihood ratio of a negative test result usually lies between 0 and 1.
- Receiver operating characteristic
- A receiver operating characteristic curve represents the relationship between ‘true-positive fraction’ (sensitivity) and ‘false-positive fraction’ (1–specificity). It displays the trade-offs between sensitivity and specificity as a result of varying the cut-off value for positivity in case of a continuous test result.
- Reference standard
- Established test(s) against which the accuracy of a new test for detecting a particular condition can be evaluated.
- Screening
- A health service in which members of a defined population, who do not necessarily perceive that they are at risk of a disease or its complications, are asked a question or offered a test to identify those individuals who are more likely to be helped than harmed by further tests or treatment.
- Sensitivity (true-positive rate)
- The proportion of individuals with the target condition in a population who are correctly identified by a diagnostic test.
- Specificity (true-negative rate)
- The proportion of individuals free of the target condition in a population who are correctly identified by a diagnostic test.
- Test accuracy
- The proportion of test results that are correctly identified by the test.
- Cost-effectiveness acceptability curve
- A way of illustrating cost-effectiveness results by plotting the probability that the intervention is cost-effective (y-axis) against the maximum that society is willing to pay for an improvement in health (x-axis).
- Cost-effectiveness plane
- A way of illustrating cost-effectiveness results by plotting the mean incremental cost and effectiveness on a four-quadrant graph. Interventions that are more costly and more effective fall in the north-east quadrant.
- Incremental cost-effectiveness ratio
- The difference in costs between one intervention and an alternative, divided by the difference in outcomes.
- Quality-adjusted life-year
- A measure of benefit of health care combining the impact of both expected length of life and quality of life.
- Whole time equivalent
- Equivalent to one individual working full time (about 40 hours per week).
List of abbreviations
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CSMO
- clinically significant macular oedema
- CVM
- colour vision meter
- CVT
- colour vision testing
- DM
- diabetes mellitus
- DR
- diabetic retinopathy
- D-15
- Lanthony desaturated D-15 test
- ETDRS
- Early Treatment of Diabetic Retinopathy Study
- FM-100
- Farnsworth–Munsell 100 hue test
- FN
- false-negative
- FP
- false-positive
- HbA1c
- glycosylated haemoglobin
- ICER
- incremental cost-effectiveness ratio
- LR+
- positive likelihood ratio
- LR–
- negative likelihood ratio
- NCT
- Lanthony New Colour Test
- NICE
- National Institute for Health and Clinical Excellence
- NSC
- National Screening Committee
- NSPDR
- National Screening Programme for Diabetic Retinopathy
- NPDR
- non-proliferative diabetic retinopathy
- PSA
- probabilistic sensitivity analysis
- QALY
- quality-adjusted life-year
- QUADAS
- Quality for Assessing Diagnostic Accuracy Studies
- ROC
- receiver operating characteristic
- SGM
- Sussex Gratings Machine
- STDR
- sight-threatening diabetic retinopathy
- TCCT
- tritan colour contrast threshold
- TCT
- tritan contrast threshold (test)
- TN
- true-negative
- TP
- true-positive
- WESDR
- Wisconsin Epidemiologic Study of Diabetic Retinopathy
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), has been used only once, or is a non-standard abbreviation used only in figures/tables/appendices in which case the abbreviation is defined in the figure legend or at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and costeffectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebocontrolled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and costeffectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington