Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 97/42/02. The contractual start date was in January 2000. The draft report began editorial review in July 2009 and was accepted for publication in October 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Anorexia nervosa in young people
Anorexia nervosa (AN) is a complex eating disorder, generally developing in adolescence or young adulthood but sometimes in late childhood. It is relatively rare at 12 years, but the prevalence rises with age, reportedly reaching about one in 200 adolescent girls at 16 years. The highest incidence rates are for females aged 15–19 years, who represent approximately 40% of all identified cases. 1 Incidence and prevalence rates of AN in males are more rarely reported, but it has been noted that where they are, the female to male ratio is around 11 : 1 overall1 but it appears to be somewhat lower in adolescents,2 with a more equal sex ratio at the younger end of the spectrum.
Anorexia nervosa appears to have become more common over recent decades, but the apparent increase could well be the result of greater help-seeking, better detection and changes in diagnostic practice rather than of any true increase in the incidence of the disorder. 3 The best evidence for this comes from Rochester, MN, USA. 4 This study suggested an increase in incidence of 36% in adolescent females every 5 years from 1950 to 1984. Anorexia nervosa is currently the most prevalent disorder within inpatient child and adolescent mental health services. 5
It is thought that eating disorders may have changed over time, particularly in the increasing ratio of the purging form of AN to the restricting form. Anorexia nervosa used to be seen as a middle-class disorder of the white, western world. This is no longer the case, although uncertainties exist as to whether there has been a change in identification of cases in different cultures or whether the condition has spread to black and ethnic minority populations and to developing nations as they have taken on western culture and lifestyles.
Anorexia nervosa has the highest mortality rate of any psychiatric disorder in the UK; with patients with AN being 12 times more likely to die than women of a similar age in the general population. 6 The mortality rate among adolescents is low. Most deaths are either a direct result of medical complications or due to suicide.
Clinical features
Anorexia nervosa is a syndrome comprising a range of physical, psychological and behavioural features. These usually have an impact on social functioning and eventually their effects pervade most areas of the young person’s life.
Four features are required to make a diagnosis:
-
overevaluation of the importance of weight and shape (this is often expressed as an intense fear of becoming fat and is sometimes referred to as a distortion of body image)
-
maintenance of an unduly low bodyweight [that is less than 85% of that expected, or a body mass index (BMI) below the second percentile for age]
-
active control of weight by dietary restriction, exercise, vomiting or purging
-
a widespread endocrine disturbance involving the hypothalamic–pituitary–gonadal axis (this is manifest as amenorrhoea in postpubertal females, as pubertal delay in pubescent females and as impotence and lack of sexual interest in males).
The central features are essentially the same in both sexes; those with AN judge their self-worth largely, or even exclusively, in terms of their shape and weight and their ability to control them. This results in a pursuit of weight loss and an intense fear of weight gain and fatness. Most of the other features are secondary to this cognitive abnormality and its consequences and there is a complex relationship between cognition, behaviour and the physical features. To the extent that this pursuit of a low weight is successful, weight control is seen as necessary rather than problematic. Successful dieting therefore tends to be viewed positively and, as a consequence, young people with AN generally have low motivation to change.
In AN a very low weight may be attained through severe and selective restriction of food intake with self-induced vomiting and other forms of weight-control behaviour (such as the misuse of laxatives or diuretics) practised by a subgroup. Depressive and anxiety features, irritability, lability of mood, impaired concentration, loss of sexual interest and obsessional symptoms are frequently present. Typically these features get worse as weight is lost and improve to a large extent with weight restoration. Interest in the outside world also declines with the result that most become socially withdrawn and isolated. As bodyweight is maintained at least 15% below that expected, pubertal development is stunted or reversed. This results in either a delay in the menarche or secondary amenorrhoea in those who have completed puberty.
Negative physical outcomes such as failure to reach expected height, stunted breast development and reduced bone density are often reported. In the longer term, eating disorders may have an impact on pregnancy and motherhood. In those recovering from AN, fertility problems, spontaneous abortion, prematurity and small-for-gestational-age babies are regularly reported, as are elevated rates of infant mortality. 7,8
A systematic review of 119 outcome studies of patients across the age range,9 found high rates of anxiety disorders and affective disorders at long-term follow-up as well as substance misuse. Full long-term recovery was reported for 45.1%, a fair outcome for 35%, whereas 19.8% had a chronic course.
Treatment of anorexia nervosa
There has been surprisingly little research on the treatment of AN but most of this work has concerned adolescents. 10,11. Recent systematic reviews11–13 have drawn attention to the shortage of quality, adequately-powered treatment trials for anorexia nervosa. The National Institute for Clinical Excellence [now National Institute for Health and Clinical Excellence (NICE)] guidelines made treatment recommendations classified from A (the strongest) to C (the weakest), based on the strength of evidence. In considering the full range of psychological therapies, physical (including pharmacological) treatment and service settings, it was unable to make a single Grade A treatment recommendation across the age range. 11 Guidelines on the management of child and adolescent eating disorders are therefore based mainly on expert clinical opinion and cohort studies rather than on randomised clinical trials. A number of academic bodies have published consensus guidelines, some specifically in relation to the management of children and adolescents. There is much greater emphasis in these on physical rather than other aspects of management.
Physical management
In AN, guidelines refer to the potentially irreversible effects on physical growth and development and argue that the threshold for medical intervention in adolescents should be lower than in adults. Of particular importance, is the potential for permanent growth retardation if the disorder occurs before fusion of the epiphyses, and impaired bone calcification and mass during the second decade of life, predisposing to osteoporosis and increased fracture risk later in life. These features emphasise the importance of immediate medical management and ongoing monitoring by physicians who understand normal adolescent growth and development. There is a lack of consensus regarding oral feeding requirements. A weight gain of around 1 kg per week is generally recommended for inpatients and 0.5 kg per week for outpatients. After an initial safe weight has been achieved, the young person’s food intake should be adjusted to ensure that growth is in keeping with normal weight and height trajectories. Weight restoration should use the least invasive procedures possible and should be provided within a caring age-appropriate setting. Nasogastric feeding should only be resorted to in the face of persistent refusal to eat normally. Strict behavioural regimes in which young people have to earn privileges through eating and weight gain are not desirable or acceptable because they militate against the therapeutic alliance and there is no evidence that these approaches work, other than by achieving short-term weight gain. In the long term, undue coercion may be perceived by the young person either as a recapitulation of abuse or neglect that they may have suffered previously, or it may reinforce low self-esteem and feelings of ineffectiveness, both of which are common antecedents of AN.
Pharmacological treatment
The use of psychotropic medication is not considered a first-line treatment for AN. A lack of studies and negative findings have led to the widely held view that the use of drugs is not justified in the first-line management and should be reserved for cases complicated by comorbid diagnoses. However, a recent survey of seven specialist eating disorder services for children and adolescents in the UK,14 showed that psychotropic medication is commonly prescribed (chiefly selective serotonin reuptake inhibitors antidepressants and major tranquillisers), and with apparently beneficial symptomatic benefit.
Psychological therapies
Although there are a considerable number of studies of psychological therapies in the recent eating disorder literature, a number of methodological issues make for difficulties in combining results in meta-analysis and reaching firm conclusions about the merits of different therapies. These include:
-
heterogeneity within therapies of the same name
-
the wide range of outcome measures used
-
differences in timing of follow-up
-
entry criteria
-
other therapies given concurrently.
The NICE guideline concluded that there was limited evidence that a range of specific psychological treatments for AN with more therapeutic contact was superior to ‘treatment as usual’ (with a lower rate of contact) in terms of mean weight gain and the proportion of patients recovered. There was insufficient evidence from six small randomised controlled trials (RCTs) to suggest that any particular specialist psychotherapy [cognitive analytic therapy, cognitive behavioural therapy (CBT), interpersonal therapy, family therapy, or focal psychodynamic therapy] was superior to others.
Cognitive behavioural therapy
A number of cognitive behavioural models have been described for the development and maintenance of eating disorders (generally within the adult field); perhaps the most validated one being the model of Fairburn et al. 15 for bulimia nervosa, which has since been adapted to form a ‘transdiagnostic’ model of eating disorders. 16 This proposes that the restriction of food intake that characterises the onset of eating disorders has two main origins. The first is a need to feel ‘in control’ of life, which becomes displaced onto controlling eating. This need for control may be greatest in those who are constitutionally anxious, perfectionist or lacking in self-esteem. The second is an overevaluation of shape and weight in those who have been sensitised to their appearance, either by prior experiences (e.g. childhood obesity, parental concerns about eating) or by the changes in shape that occur during puberty. In both instances, the resulting dietary restriction and weight loss are highly reinforcing. Subsequently, other processes serve to maintain the eating disorder. In patients who are severely underweight, certain physical symptoms of starvation, particularly the preoccupation with food and eating, heightened fullness as the result of delayed gastric emptying, and social withdrawal have this effect.
A handful of small studies have examined the efficacy of CBT in AN in adults. 11 These suggest that it may be moderately effective, although there is insufficient evidence to recommend it over other therapies. Some suggest that CBT may be effective at the symptomatic level, e.g. in improving self-esteem, but studies lack power. More recently, Fairburn’s Oxford group have trialled their transdiagnostic modification of the well-researched CBT for bulimia nervosa programme. This form of CBT is showing good results in older adolescents and adults presenting with a BMI above 15.
Family-based therapies
The psychosomatic conceptual model of Minuchin et al. 17 stimulated considerable interest in the use of family interventions in AN, particularly in adolescents. Initially the rationale was based on the notion of the ‘anorexogenic family’, but empirical study has failed to support the aetiological role of family dysfunction and the model fuels concern about blaming parents. Family interventions have therefore developed as treatments which mobilise family resources, whether delivered as ‘conjoint’ family therapy, separated family therapy (in which parents and the child or adolescent patient are seen separately) or ‘parental counselling’. There have been a number of RCTs, although the results are somewhat inconsistent. To date, several studies have compared different forms of family intervention in child and adolescent AN, but only two have compared family therapy with forms of individual therapy.
Russell et al. 18 in a trial of patients whose weight had been restored in a specialist inpatient service before randomisation, found that for a small group of adolescents (n = 21) with short duration of illness, family therapy was superior to individual therapy. The findings in relation to those who had been ill for more than 3 years were inconclusive and the outcomes were generally poor. Robin et al. 19 compared the effect of Behavioural Family Systems Therapy (BFST) with Ego-Oriented Individual Therapy (EOIT) in 37 adolescents with AN. Parents in the EOIT group received separate parental counselling. There was no significant difference between groups for weight gained or for psychological measures; however, the BFST group had a greater change in BMI over time, although this probably reflected different baseline values between groups. By the 1-year follow-up 94% of the BFST group had resumed menstruation compared with 66% of the EOIT group; however, 43% of the series had also been hospitalised when their weight fell below 77% ideal body weight (IBW).
Two further studies20,21 at the Maudsley Hospital (Denmark Hill, London, UK) compared conjoint family therapy with separated family therapy in which patients were seen on their own and parents were seen separately by the same therapist. The overall results were similar in the two trials, with a trend towards a superior outcome for the separated form of therapy. A small subgroup with high maternal expressed emotion did markedly better with separated family therapy.
Multiple family group therapy
The apparent effectiveness of family interventions with children and adolescents with AN and the need to develop more intensive family-based interventions for those who require it, led to the development of this treatment approach. The therapy aims to help family members learn by identifying with members of other families with the same condition, by analogy. 22 It is generally delivered within a day-hospital programme, in which up to 10 families with a child with AN, attend a mixture of whole family group discussions, parallel meetings of parents and adolescents and creative activities. Preparation of lunch and communal eating is a central part of the programme. There is generally a 4- to 5-day block of therapy followed by a limited number of day attendances at approximately monthly intervals. 23,24 This treatment is at an early stage of evaluation, but preliminary findings suggest a high degree of acceptability and promising outcomes particularly in terms of a reduced need for hospitalisation. 23
Service issues
Various treatment settings have been used to manage AN. The main ones being outpatient, day-patient or partial hospitalisation, and inpatient treatment; and within these settings a variety of interventions may be provided, physical, psychological or both. To complicate matters, patients may move from one setting to another, and within any one setting often more than one treatment is employed.
Inpatient treatment is used differently in different places; for example, it is common in some countries but unusual in others, and length of stay also varies markedly. 25 Such differences are not evidence-based because inpatient treatment has received scant research attention. For example, not only are the indications for hospitalisation not established, but the specific goals are not agreed nor is it known how best to achieve them. At best, there is modest evidence from cohort studies to support a focus on eating and an emphasis on weight regain. Comparisons of flexible behavioural programmes with more rigid ones have either yielded no significant differences in the rate of weight regain or have favoured the more flexible regimes. There is no evidence that drug treatment significantly enhances weight regain.
Whatever the place of inpatient and day-patient treatment, outpatient treatment is the mainstay of the treatment of AN. Outpatient treatment is the sole treatment for many patients, and even if patients receive inpatient or day-patient treatment, it is usually followed by outpatient treatment. The choice of setting used to treat young people with AN has tended to be based on clinical judgement and the availability of different models of service rather than research evidence. Debate about the merits of inpatient management frequently fails to distinguish between (often brief) medical admission and longer psychiatric admission, aimed at a combination of weight restoration, normal eating and psychological change. Most young people with AN can be managed on an outpatient basis, with inpatient care being only required for a minority, where there are serious complications related to comorbid diagnoses, or where there is high physical or psychiatric risk. 26 When admission is deemed necessary this may be to a paediatric ward, a general child or adolescent psychiatric unit, or to a specialist eating disorder service.
Research in the area of service provision is limited. There is one systematic review summarising what is known about the relative effectiveness of inpatient and outpatient care across the age range. 27 However, the review was based on only one small RCT with a 5-year follow-up, often referred to as the St Georges study,28,29 plus a number of very varied cohort series, making it difficult to draw meaningful conclusions. The main conclusions of the systematic review are that outpatient treatment for AN at a specialist tertiary referral eating disorder service was as effective as inpatient treatment in those not so severely ill as to warrant emergency intervention, and that outpatient care is in general cheaper than inpatient care.
It is widely believed that there are advantages in treating severe AN within a specialised tertiary eating disorder service compared with less specialised secondary services. Both competence and confidence tend to develop in settings where such treatment is a regular and ongoing activity.
User satisfaction
A crucial issue in AN concerns the patient’s attitude to the disorder. There is generally some ambivalence and at times determined opposition to treatment. Controversy also exists over the role of treatments given without the patient’s consent. Patients may in certain circumstances be detained under the Mental Health Act (1983) but the NICE guideline expressed concern about the lack of clarity and openness around the treatment of young people when given on the basis of parental consent alone. 11
Patient satisfaction has become increasingly important to the UK health-care industry and evaluation of the quality of health-care provision is essential for the improvement of services. However, there is a lack of clarity with regards to the definitions of service quality and satisfaction. Service quality and patient satisfaction are linked, indeed a South Korean study30 recently found that 62% of the total variation in patient satisfaction was explained by service quality dimensions. Clearly when expectations of a service are greater than perceived performance, then quality will be judged as less satisfactory and dissatisfaction will be high. Those with eating disorders have been said to represent a unique group of health-care consumers among whom dissatisfaction tends to be high. 31 Furthermore, the source of negative commentary is often around activities and structures viewed as essential to traditional treatments. 32
Economic aspects
As well as being associated with severe physical, psychological and social impairments and high levels of mortality,11 AN places a significant cost-burden on young people, their families, health services and the wider society. 33,34 Inpatient admission for young people with AN is particularly disruptive to school, family and social life, and is an expensive option, yet evidence to support its cost-effectiveness is lacking. 11,35
Rationale for the current trial
The recent research literature (confirmed during the course of the study by the NICE guideline) suggested that despite lengthy inpatient psychiatric treatment being commonly recommended as the ‘gold standard’ treatment for the condition,36 there was little evidence to support this practice. The one small RCT of service setting showed no advantage of inpatient management over outpatient care for adults,29 whereas our earlier cohort study37 showed poor outcomes for adolescent inpatients. It seemed likely that inpatient management might be cost-ineffective. We were also aware of the low levels of satisfaction reported in some studies with inpatient management. Although, (in the course of this study) the NICE guideline recommended treatment in specialist settings, this has often been confused with treatment in homogeneous units in which all patients have the same condition. We therefore wished to explore the effectiveness of specialist services as described by the Eating Disorders section of the Royal College of Psychiatrists; that is, services with a dedicated, trained, multidisciplinary team treating a significant number of cases each year.
We report here a large population-based RCT of the three most common treatments available for adolescents with AN in the UK to compare the relative merits of inpatient psychiatric treatment and two forms of outpatient management, namely ‘treatment as usual’ in generic CAMHS, and a specialist multimodal multidisciplinary programme developed for the study.
Aims and objectives
The Treatment Outcome for Child and Adolescent Anorexia Nervosa (TOuCAN) trial aimed to compare the clinical effectiveness of inpatient against outpatient treatment and of generalist against specialist management, using a randomised design of three treatment approaches. The study also aimed to examine the cost-effectiveness of each approach, and user and carer satisfaction with each treatment. Subsidiary aims were to measure the medium-term to long-term outcomes of the condition in a population-based cohort and identify predictors of outcome.
Hypotheses
The main hypotheses were:
Clinical
-
The more intensive inpatient treatment would be more effective than outpatient treatment.
-
Specialist treatment would be more effective than general CAMHS treatment.
Health economics
-
Outpatient treatment (especially a specialist outpatient programme) would be more cost-effective than inpatient management.
-
Specialist outpatient services would be more cost-effective than general treatment.
Satisfaction
-
Carers (generally parents) would have higher expectations of treatment and would be more satisfied with it than young people with the disorder.
-
Satisfaction would be higher with specialist treatment than with generalist treatment.
Subsidiary hypotheses
-
For the total series, few patients would fully recover by 1 year after the start of treatment, but overall outcomes would improve at the 2-year and 5-year time points.
-
For those in remission, subsequent relapse would be unusual during the course of the study.
Chapter 2 Methods
Trial procedures
Study population and participants
The trial took place in the north-west of England. The population (total 7.5 million) is served by 38 community CAMHS and four inpatient psychiatric units. The study aimed to recruit as complete a series as possible of consecutive cases of AN referred to community CAMHS. Thirty-five of the 38 CAMHS agreed to refer to the trial.
Inclusion criteria
Inclusion criteria were as follows:
Adolescents (male or female), age 12 to 18 years with a diagnosis of AN according to the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV) criteria modified for this age group as follows:
-
food restriction +/– compensatory behaviours
-
weight below 85% of that expected within 1 month of assessment, based on age and current height or previous height centile
-
intense fear of gaining weight or undue influence of weight or shape on self-evaluation
-
primary or secondary amenorrhoea for 3 months (in females), or menstruation only while on the contraceptive pill.
Exclusion criteria
Exclusion criteria were:
-
those with severe learning difficulties
-
presence of severe, chronic comorbid physical conditions affecting digestion or metabolism.
No exclusions were made on grounds of clinical severity, but the responsible clinician reserved the right to refer for acute medical management if required.
Recruitment and follow-up strategy
The CAMHS identified cases of probable AN and invited them to meet a representative of the research team. The researcher, supported by a clinician, then interviewed the young person (usually with a parental informant), confirmed the diagnosis and obtained informed consent to take part in the randomisation, along with completion of baseline measures. Those agreeing were sent an appointment at the allocated treatment facility closest to their home. The recruitment and consent strategy was approved by the north-west Multicentre Research Ethics Committee (ref no: MREC 99/8/21).
Follow-up interviews took place approximately 1, 2 and 5 years after baseline either at a local CAMHS or at the subject’s home according to their preference. All interviews were carried out blind to treatment allocation by a research worker who had not been involved in recruitment and did not have access to the baseline database or recruitment file. Where the subject declined an interview, information was provided (with consent) by a relative (usually parent), a health-service professional involved in their care or (rarely) by telephone interview.
Randomisation and blinding
Treatment allocation was carried out by an independent randomisation service, by telephone, using stochastic minimisation controlling for sex, age above and below 16 years and BMI above and below 15.5.
Measures
Baseline
Interviewer-based measures
Clinical diagnosis (modified DSM-IV)
The use of the DSM-IV clinical diagnosis38,39 as an entry criterion is described above.
Morgan–Russell Average Outcome Scale
The Morgan–Russell Average Outcome Scale (MRAOS)40 adjusted for adolescents and used as a severity measure. This provides a quantitative score from 0 to 12 and a categorical measure (good, intermediate and poor), in which a good outcome represents weight restoration, return of menstruation and absence of bulimia, a poor outcome represents continuing AN and an intermediate outcome represents weight restoration without resumption of normal hormone functioning or frequent engagement in bingeing or purging. It has been widely used in AN research. 18,21,28,40,41
Health of the Nation Outcome Scale for Children and Adolescents
The 13-item clinician-rated measure Health of the Nation Outcome Scale for Children and Adolescents (HoNOSCA-CR)42 yields a total severity and outcome score and has been shown to be reliable, valid and sensitive to change. 43,44 It has been used as the main outcome measure in treatment trials in adolescent mental health. 45
Subject ratings
Eating Disorder Inventory-2
The Eating Disorder Inventory-2 is a self-rated questionnaire covering 12 domains of eating cognitions, behaviours and social functioning. 46 Total and subscale scores can be generated, with satisfactory validity and sensitivity to change.
HoNOSCA-SR
The adolescent self-rated (i.e. SR) version of HoNOSCA, covers the same 13 generic items as the clinician-rated measure. 47
Family Assessment Device
The Family Assessment Device (FAD)48 is a self-report questionnaire designed to evaluate family functioning based on the seven subscales of the McMaster model.
Follow-up (1, 2 and 5 years)
The same measures were completed at follow-up, (the main outcome measure being the MRAOS) and with the addition of the Eating Disorder Examination (EDE) at 5 years.
Eating Disorder Examination
The EDE is a semi-structured interview that has been developed as a measure of the specific psychopathology of AN and bulimia nervosa. 53 It comprises five subscales covering eating, weight concern, shape concern, restraint and binge eating.
Satisfaction measures
Satisfaction questionnaires
Two questionnaires designed for the purpose of the study asked young people and their carers (independently) about any of the researched treatments they had received (randomised or not), at the 1-year and 2-year follow-up. They were asked to rate on a seven-point Likert scale (from very positive to very negative) their prior expectations of the treatment and subsequently (on the same scale) their satisfaction with it. Space was allocated for any further free comments about any treatment received.
Focus groups
All participants at 2-year follow-up were invited to attend focus groups in Chester or Manchester to expand on their experiences.
Sample size
The sample size was calculated using the main outcome measure, the MRAOS. Based on our previous findings,40 an effect size of 1.5 units on this primary outcome was considered to be a clinically important difference. This also suggested a within-group standard deviation (SD) of 2.3 units on the MRAOS, a 2.5% two-sided significance level to adjust for two treatment group comparisons. Samples comprising 62 and 46 subjects per treatment arm would have 90% and 80% power, respectively, to detect this effect size. Initially, it was proposed to recruit 72 subjects per arm, but at a Health Technology Assessment review this was reduced to 57 subjects in each of the three groups. The study therefore had 80% power to detect a difference of this magnitude assuming an 85% follow-up rate.
Reliability of assessment measures:
Inter-rater reliability series involving 154 subjects and three ratings per subject were carried out within research site and between sites at baseline. For MRAOS the intraclass correlation coefficients were as follows: within-site: Manchester 0.93, Liverpool 0.97, between-sites: 0.96, and the inter-rater reliability was 0.93 at 1 year and 0.90 at 2 years. For HoNOSCA the intraclass correlations were: within-site: Manchester 0.83, Liverpool 0.98, between-sites: 0.87, and the inter-rater reliability was 0.89 at both 1 and 2 years.
Case ascertainment
Cases were diagnosed on clinical grounds by a qualified child and adolescent psychiatrist using the inclusion diagnostic criteria above. The researcher checked the recorded clinical features against a checklist and essential features (e.g. low weight for height, presence of amenorrhoea, weight concern) were confirmed by completion of the global MRAOS, which includes these clinical features.
Treatments
Inpatient psychiatric treatment – four services
This was provided within the regional children’s or adolescent psychiatric inpatient units. All four services had substantial experience and expertise in treating eating disorders. They were not however exclusive eating disorder services. In keeping with the national census findings,5 AN often comprised the most prevalent diagnosis within the units. Treatment lasted 6 weeks in the first instance, extended as clinically indicated and determined by the treating service. The treatment was not manualised, but services met at the outset to identify core elements in treatment. They all used a multidisciplinary psychiatric approach with the aim of normalising eating, restoring healthy weight and facilitating psychological (cognitive) change. Each subject received both individual supportive or cognitive therapies and family therapy. All services had staff who were trained and experienced in family therapy, but not necessarily family interventions specifically for eating disorders. There was a high expectation of early behavioural change and services employed a weight restoration programme with an expected weight increase of 800–1000 g per week. Patients were ambulant and attended the unit school subject to medical stability. Nasogastric feeding was rarely employed and the services aimed to avoid coercive treatment practices.
Specialised outpatient treatment – two services
This programme was manualised and devised for the trial. It comprised an initial motivational interview, individual CBT plus parental feedback (12 sessions), parental counselling with the patient (minimum four sessions, increasing to eight for younger patients), dietary therapy (four sessions, with parental involvement as required), and multimodal feedback (weight, self-report and clinician-rated questionnaire) and monitoring (four sessions). The treatment was designed to last 6 months. The CBT programme and parental counselling were provided by a trained member of the eating disorder team, with good experience of behavioural management of eating disorders and addressing the typical cognitions. They had pilot experience of the manualised treatment, but they represented a range of disciplines and their formal training in CBT was variable and sometimes only at foundation level. The same therapist provided feedback to the patient every 6 weeks, reviewing the physical and self-report questionnaire data. The aim was to demonstrate an association between weight gain and reduced self-reported psychopathology, to motivate the patient to take the next steps to recovery. Dietetic therapy was provided by a trained dietician working as a fully integrated member of the team. This treatment has been described in detail52 along with the rationale behind it. 55 Checks of treatment fidelity were made at weekly joint meetings between the clinical and research teams. Travel times to the specialist services were generally under 90 minutes, by either car or public transport.
Treatment as usual in general community CAMHS
This was not a manualised treatment, but comprised the usual first-line treatment approach that young people in the UK receive. The 35 services provided (generally) a multidisciplinary, family-based approach, with variable dietetic, individual supportive therapy and paediatric (medical) liaison. As the study aimed to compare the specialised treatment with ‘treatment as usual’, the latter was not prescriptive and the outpatient arms were not matched for intensity; however, the duration of therapy was set at 6 months.
Data analytic strategy and methods
Comparison of randomised treatment groups
Statistical analysis of the three randomised treatment groups was based on the intention-to-treat principle subject to the availability of data. Clinical outcome was measured at 1, 2 and 5 years. Preliminary analysis investigated the pattern of missing outcome data comparing baseline characteristics of subjects with and without follow-up data.
Longitudinal modelling of treatment effects for quantitative outcomes
Statistical analysis of continuous clinical outcome measures combined the data from the 1-, 2- and 5-year assessments in a longitudinal analysis using a linear mixed model. 56 Unlike some forms of longitudinal analysis, such as repeated measures analysis of variance, a linear mixed model does not require complete follow-up data for all subjects. In a longitudinal analysis of trial data the treatment effect, by which one means a difference between randomised groups, can be a treatment group with time interaction, that is the difference between treatment groups changes over time during the follow-up period. Alternatively, there may be a constant difference in the mean value of the outcome measure throughout the follow-up period, sometimes called the main effect of treatment. As a result of the unequal spacing (1, 2, 5 years) the assessment number, rather than the time to follow-up assessment, was included as the time covariate. This was chosen to prevent the 5-year assessment having undue influence on the analyses. Hence, the time effect was assessed by the assessment number with the treatment-group interaction term and the main effect by the covariate for treatment group.
Where there is evidence of an assessment with treatment-group interaction, the covariate of treatment group cannot be easily interpreted because the treatment effect is changing between assessments. In this case, the separate analysis for each assessment (1, 2 or 5 years) provides a method of interpretation. Hence, where there is an interaction, the p-value for the cross-sectional analysis at the 1-, 2- and 5-year assessments has been given in the relevant summary table. If there is no evidence of an assessment with treatment-group interaction, the model was refitted without the interaction term to estimate the main effect of treatment, and a p-value has not been given for the cross-sectional analysis. The distributional assumptions of the model were checked using normal probability plots for assessment and subject level residuals.
Analysis of diagnostic outcome category
Diagnostic outcome category (poor, intermediate, good) was modelled using ordinal logistic regression with the same covariates. 57 In this case, the longitudinal data analysis was carried out estimating the marginal effect of treatment rather than the subject-specific effect using a standard ordinal logistic regression with robust standard errors.
Baseline covariates
For the analysis of each variable, the baseline values of that measure, and the variables in minimisation (age at randomisation, gender, age, baseline MFQ and baseline MRAOS) were included as covariates in the model.
Multiplicity
One issue in quantitative studies is multiplicity, as the result of either multiple groups or multiple outcome measures. An option is to adjust p-values or significance levels for this. Such procedures can be highly conservative, particularly with multiple outcomes because these tend to be correlated.
Where more than two treatment groups are employed, various comparisons can be made between treatment groups. With three treatment groups there are six possible contrasts that can be made. Following the studies objectives, two contrasts were considered to be of primary interest, first a comparison of outpatient treatments with inpatient treatment and second a comparison of specialist treatments with routine CAMHS treatment.
Sample size used a significance level of 2.5% to allow for multiplicity. A Bonferroni correction has not therefore been made to p-values, but readers may wish to use a 2.5% significance level instead of the conventional 5% level.
Baseline predictors of clinical outcome and service use
Secondary analyses investigated baseline predictors of clinical outcome measures and service use. Clinical outcome measures considered were:
-
% weight for height
-
self-reports of morbidity [Eating Disorders Inventory second edition (EDI-2) total score, MFQ, HoNOSCA-SR]
-
researcher-assessed morbidity (MRAOS, HoNOSCA-CR)
-
family functioning [FAD-General Functioning(-GF)]
-
separate analyses were carried out for 1-, 2- and 5-year follow-up data.
Service use measures considered were:
-
hospital admissions within 2 years
-
time until first hospital admission
-
number of hospital admissions
-
number of inpatient days for admitted patients
-
still in treatment at 1 and 2 years.
The following baseline variables were considered as potential predictors:
-
age of patient at outset of study
-
gender
-
length of history of eating disorder (< 15 months, ≥ 15 months)
-
diagnostic subtype (restrictor, binge–purger)
-
site (Mersey/north-west)
-
% weight for height
-
self-reports of morbidity (EDI-2 total score, MFQ, HoNOSCA-SR)
-
research-assessed morbidity (MRAOS, HoNOSCA-CR)
-
family functioning (FAD-GF).
One approach to identifying predictor variables is to apply backward stepwise selection procedures to a pool of candidate variables. A limitation of this method is that the estimated coefficients of any selected variable may overestimate the effect of that variable. Correlations between variables, mean that the coefficients of variables finally selected for the model may include the causal effect of other variables that have been excluded from the model. (Suppose two variables A and B predict outcome Y, and suppose that A is a stronger predictor of Y than B. If A and B are correlated and if B is dropped from the model, the coefficient for A may increase because it may now include some of the effect of B.)
Two analyses are therefore presented. The first gives the coefficients of a model where the variables have been selected by backward stepwise selection. The second gives the corresponding coefficient for the selected variables from the full-model, including all covariates, to give an indication of the overprediction caused by stepwise selection.
For quantitative clinical outcome measures, standardised beta-coefficients are given as a measure of the effect of a variable. These express the effect on a dimensionless scale thereby enabling comparison of effect between different predictor variables. For binary outcome variables, the adjusted odds is given. For ordered categorical outcome variables, the adjusted odds common odds ratios are given. These are estimated using binary or ordinal logistic regression models. The adjusted hazard ratio, estimated using a Cox proportional hazard model, is used for modelling time until admission.
Inclusion of highly correlated predictor variables can give contradictory results symptomatic of overfitting the data. Some predictor variables were strongly correlated. For example EDI-2 total score, MFQ and HoNOSCA-SR at baseline were quite strongly correlated, with correlation coefficients ranging from 0.69 to 0.80. Where there is correlation between predictor variables, models with different variables may have very similar fit. For example when EDI-total score at 1 year was considered, models including either MFQ or EDI-total score at baseline had very similar values of r-squared. Results of the predictor analyses should therefore be interpreted with care. Hence, inclusion of any one of MFQ, EDI or HoNOSCA-SR is perhaps best interpreted as suggesting any self-assessed morbidity is important, rather than as a prediction due to specific measure of morbidity.
Economic evaluation methods
Perspective and data collection
At the 2-year follow-up, the economic evaluation took a broad service-providing perspective, including costs to the health, social services, education, voluntary and private sectors. Resource use data were collected in interview at the 1- and 2-year follow-up assessments using the Child and Adolescent Service Use Schedule (CA-SUS), developed by the authors in previous research with young people and adapted for the purpose of the current study. 58–60 Information on hospital contacts were collected from clinical records to avoid patients un-blinding research assessors in follow-up interviews. In addition, the use of primary and secondary hospital and community health-care services (including NHS, private and voluntary sectors) by the young person’s primary carer were collected at the 1- and 2-year follow-ups using the Carer Service Use Schedule (CARER-SUS), which was developed and used by the authors previously in similar research. 46
At the 5-year follow-up, a brief version of the CA-SUS was used to collect resource use information on the participant’s use of services for the 3-year period between the 2-year and final 5-year follow-up interviews. The CA-SUS was limited to use of key resources (high cost and/or high probability of use) anticipated to be relatively easy to recall over this period of time, including hospital services, information on accommodation and employment and use of benefits. The decision to focus on key services was taken: (1) to reduce the problem of inaccurate recollection of less significant service contacts and (2) because the relative expense of these key services is likely to over-ride any differences in less resource-intensive services; hence, although absolute costs may be underestimated, relative costs are unlikely to be greatly affected. The brief CA-SUS was completed by participant self-report in the final follow-up interview.
Unit cost calculation
All unit costs were for the financial year 2003–4. A summary of the unit costs applied is provided in Table 1. Local unit costs were applied to hospital data and data on schools attended. Nationally applicable unit costs were applied to services that make a much smaller contribution to total costs, such as community health and social services and medication. Trust-specific costs for NHS hospital contacts, including the trial interventions, were sourced from NHS reference costs. 61 Unit costs for inpatient stays and outpatient appointments in private sector services were collected through direct personal communication with each facility. Community health and social services costs were taken from national publications. 62 The costs of mainstream and specialist schooling came from a number of sources including various OFSTED reports (the inspectorate and regulatory body for schools in England – see www.ofsted.gov.uk) and published documents. 63 The cost of medications was calculated using the British National Formulary. 64 Where necessary, unit costs were inflated to 2003–4 costs using the Hospital and Community Health Services inflation indices. 61 For the economic evaluation carried out at the 2-year follow-up, costs in the second year were discounted at a rate of 3.5%, as recommended by NICE. 65 The rate was varied from 0% to 6% in sensitivity analysis. For the economic analyses carried out at the 5-year follow-up point, costs are presented in 2003–4 prices.
| Service | Unit cost (£) | Source |
|---|---|---|
| Hospital | ||
| Inpatient (night) | 195.00–520.00 | Department of Health (2004)59 |
| Outpatient (appointment) | 31.00–307.00 | |
| Day patient (attendance) | 89.00–381.00 | |
| Accident and emergency (attendance) | 97.00 | |
| Community | ||
| General practitioner (per minute contact) | 1.73 | Curtis and Netten (2004)60 |
| Practice nurse (per minute contact) | 0.42 | |
| Dietician (per minute contact) | 0.87 | |
| District nurse (per minute contact) | 0.78 | |
| Health visitor (per minute contact) | 1.08 | |
| Community paediatrician (per minute contact) | 1.73 | |
| Community nurse (per minute contact) | 0.42 | |
| Clinical psychologist (per minute contact) | 0.68 | |
| Counsellor (per minute contact) | 0.55 | |
| Family therapist (per minute contact) | 0.55 | |
| Dentist (per examination) | 6.49 | |
| School doctor (per minute contact) | 1.73 | |
| School nurse (per minute contact) | 0.42 | |
| Social worker (per minute contact) | 0.53 | |
| Foster care (per night) | 66.00 | |
| Education | ||
| Day school (per day) | 15.50–19.94 | Curtis and Netten (2004)60, Independent Schools Council (2004)61 |
| Boarding school (per day) | 27.00 | |
| Hospital school (per day) | 129.60 | |
| Home tuition (per hour) | 34.34 | |
| School counsellor (per minute contact) | 0.55 | |
| Education welfare officer (per minute contact) | 0.45 | |
Economic evaluation at 2-year follow-up
Economic analyses were carried out on an intention-to-treat basis using a statistical analysis plan drawn up before the analysis of the data. The primary analysis was of total costs over 2 years for the sample of young people with complete service use data who entered the RCT.
Differences in service use are reported descriptively and are not compared statistically to avoid problems associated with multiple testing, and because the focus of the economic evaluation was on costs and cost-effectiveness. As is common in such data sets, costs were not normally distributed. Analyses compared mean costs in the three groups using analysis of covariance with covariates for prespecified baseline characteristics: site (Liverpool and Manchester), gender, age at baseline, baseline BMI and baseline MRAOS score. Because of the non-normal distribution of the data, the robustness of the parametric tests was confirmed using bootstrapping,66 as recommended by Barber and Thompson. 67 The primary analysis was of the sample of young people with complete service use data; the impact of dropout was assessed by comparing the baseline characteristics of patients who had missing data with those of patients who had full economic data.
Cost-effectiveness was assessed through the calculation of incremental cost-effectiveness ratios (ICERs) – the additional costs of one intervention compared with another, divided by the additional effects of one intervention compared with another,68 in this case using the MRAOS measure of effectiveness. When more than two strategies are compared, as is the case in this study, ICERs are calculated using rules of dominance and extended dominance. 69 In this approach, strategies are ranked by cost, from the least expensive to the most expensive, and if a strategy is more expensive and less effective than the previous strategy, it is said to be dominated and is excluded from the calculation of ICERs. Hence, this process compares strategies in terms of observed differences in costs and effects, regardless of the statistical significance of the difference.
Uncertainty around the cost and effectiveness estimates was represented by plotting cost-effectiveness acceptability curves. 68,70. Repeat resampling from the costs and effectiveness data (bootstrapping) was used to generate a distribution of mean costs and effects for the three treatments. These distributions were used to calculate the probability that each of the treatments is the optimal choice, subject to a range of possible maximum values (a ceiling ratio, λ) and that a decision-maker might be willing to pay for a unit improvement in MRAOS score. The cost-effectiveness acceptability curves are presented by plotting these probabilities for a range of possible values of the ceiling ratio and so they incorporate (1) the uncertainty that exists around the estimates of mean costs and effects as a result of sampling variation and (2) the uncertainty regarding the maximum cost-effectiveness ratio that a decision-maker would consider acceptable. 71
Missing data were explored in three sensitivity analyses using the following data: (1) hospital cost data collected from clinical records and available for a larger sample of young people than full economic data from the CA-SUS; (2) hospital cost data collected from records plus missing non-hospital cost data imputed using the last value carried forward approach for participants with missing year 2 data; and (3) hospital cost data collected from records plus mean imputation by randomised group of missing non-hospital cost data.
Economic evaluation at 5-year follow-up
No analysis of cost-effectiveness between randomised groups was carried out using the 5-year data because of the substantial amount of further treatments received in this period and the small sample sizes. However, differences in the use of hospital services between randomised groups are explored. Use of accommodation and rates of employment over the 3-year period between 2-year and final follow-up are reported descriptively for the cohort as a whole, including both randomised and preference groups.
Total hospital costs for the full cohort (randomised plus preference) over the 5-year follow-up period (1-year plus 2-year plus 5-year data) were calculated, and a regression analysis was carried out to explore baseline characteristics that predict high or low costs in terms of use of hospital services over the full 5-year follow-up period. To identify possible predictors, we examined studies that had previously explored the impact of baseline characteristics on service use and costs in adolescents with mental health problems,45,72 although we did not identify any relevant papers in eating disorders. The list of possible predictors was then developed and discussed with the TOuCAN research team.
Univariate associations between each of the specified predictors and total hospital costs over 5 years were explored first in a linear regression. For continuous variables, although analyses were carried out on continuous data, results are presented in two groups split at the median. Multiple regression was then used to reduce the variable set to those factors independently associated with costs. The multiple regression initially included all variables that had significant univariate associations with cost, discarding from the model all variables that were no longer found to be important. Variables that did not have a univariate association were then added and retained if they added significantly to the model, or otherwise discarded. The model arrived at was checked to ensure that no variables excluded would add significantly to it. 73 A significance level of around 10% was used though not strictly applied.
Chapter 3 Results
Baseline characteristics
Demographic characteristics of randomised subjects
Subjects were aged between 11 years 11 months and 17 years 11 months, mean age 14 years 11 months. One hundred and fifty-three (92%) were female; 127 (78%) experienced the restricting subtype, 40 (24%) and had the binge–purging subtype of AN. Mean length of history was 13 months. One hundred and four (64.3%) lived with both biological parents, 32 with mother (19.2%) and six (3.6%) with the father. Eleven (6.6%) lived with mother and stepfather and 13 (7.8%) in other arrangements (one case not known). There were no significant differences between the samples recruited from the Manchester site (n = 80) and the Liverpool site (n = 87).
Clinical features
Table 2 and Table 3 show the presenting features of the three randomised treatment arms and the preference group. They were generally a moderately to severely ill group (mean weight for height 80.0%, lowest 59.9%). Eight cases had a weight for height above the diagnostic threshold for AN. Of these, four were included because they lost significant weight in the 4 weeks following assessment, or they had previously attained a greater height percentile, suggesting stunting of growth. While four others with borderline weights were included because they fulfilled the other criteria plus significant (> 15% and generally > 20%) weight loss with amenorrhoea. Five cases were sporadically menstruating, but at < 85% weight for height.
| General CAMHS (n = 55) | Specialist outpatient (n = 55) | Specialist inpatient (n = 57) | Preference (n = 48) | |
|---|---|---|---|---|
| Site | ||||
| Mersey | 29 (53) | 25 (45) | 33 (58) | 31 (65) |
| North-west | 26 (47) | 30 (55) | 24 (42) | 17 (35) |
| Female | 51 (93) | 51 (93) | 51 (89) | 46 (96) |
| Subtype | ||||
| Restrictor | 44 (80) | 42 (76) | 41 (72) | 35 (73) |
| Binge–purger | 11 (20) | 13 (24) | 16 (28) | 13 (27) |
| History (months) | ||||
| < 15 | 36 (65) | 34 (62) | 41 (72) | 19 (40) |
| > 15 | 18 (33) | 16 (29) | 13 (23) | 26 (54) |
| Not known | 1 (2) | 5 (9) | 3 (5) | 3 (6) |
| General CAMHS | Specialist outpatient | Specialist inpatient | Preference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | n | Mean | (SD) | n | Mean | (SD) | n | Mean | (SD) | n | |
| Age (years) | 14.97 | (1.40) | 55 | 15.09 | (1.22) | 55 | 14.88 | (1.46) | 57 | 15.40 | (1.76) | 48 |
| Morgan–Russell Scales | ||||||||||||
| A (Food intake) | 3.09 | (1.63) | 55 | 3.36 | (1.99) | 55 | 3.30 | (1.74) | 57 | 2.67 | (2.16) | 48 |
| B (Menstruation) | 1.00 | (2.41) | 48 | 0.80 | (2.14) | 50 | 0.87 | (2.52) | 46 | 0.74 | (2.00) | 43 |
| C (Mental state) | 5.31 | (2.18) | 55 | 5.24 | (1.87) | 55 | 5.47 | (1.95) | 57 | 5.33 | (2.08) | 48 |
| D (Psychosexual state) | 5.53 | (2.65) | 55 | 5.84 | (2.82) | 55 | 6.57 | (2.87) | 56 | 5.64 | (3.26) | 45 |
| E (Socioeconomic state) | 7.84 | (1.98) | 55 | 7.21 | (2.99) | 55 | 8.11 | (2.17) | 57 | 7.17 | (2.68) | 48 |
| MRAOS (average of all scales)a | 4.67 | (1.27) | 55 | 4.56 | (1.46) | 55 | 5.05 | (1.46) | 57 | 4.38 | (1.59) | 48 |
| Weight for height (%) | 78.80 | (7.86) | 55 | 77.14 | (8.10) | 55 | 78.16 | (8.08) | 57 | 74.82 | (9.30) | 48 |
| Body mass index | 15.48 | (1.60) | 55 | 15.25 | (1.58) | 55 | 15.29 | (1.65) | 57 | 14.85 | (1.78) | 48 |
| EDI-2 total | 88.48 | (51.36) | 52 | 86.52 | (47.53) | 54 | 89.61 | (44.52) | 56 | 89.76 | (45.76) | 41 |
| MFQ total | 32.36 | (16.12) | 53 | 30.09 | (14.70) | 54 | 32.55 | (14.60) | 56 | 32.20 | (14.67) | 44 |
| FAD-GF | 2.13 | (0.59) | 52 | 2.12 | (0.53) | 54 | 2.08 | (0.49) | 56 | 2.08 | (0.58) | 41 |
| HoNOSCA | ||||||||||||
| Clinician-rated | 20.04 | (5.72) | 55 | 20.71 | (7.50) | 55 | 20.04 | (5.63) | 57 | 20.98 | (5.94) | 48 |
| Self-rated | 16.46 | (9.95) | 54 | 17.40 | (9.88) | 53 | 15.64 | (9.54) | 53 | 15.70 | (9.89) | 43 |
There were no significant differences between groups on any variable including length of history. For the EDI, MFQ, FAD and HoNOSCA a higher score indicates greater difficulty, whereas the Morgan–Russell Scales indicate greater clinical severity by a lower score. Characteristics of all four groups were similar, although the non-randomised preference group was slightly older, contained more patients with a longer history of eating disorder and tended to have worse morbidity at baseline with a lower % weight for height and MRAOS.
Adherence to treatment allocation and withdrawals
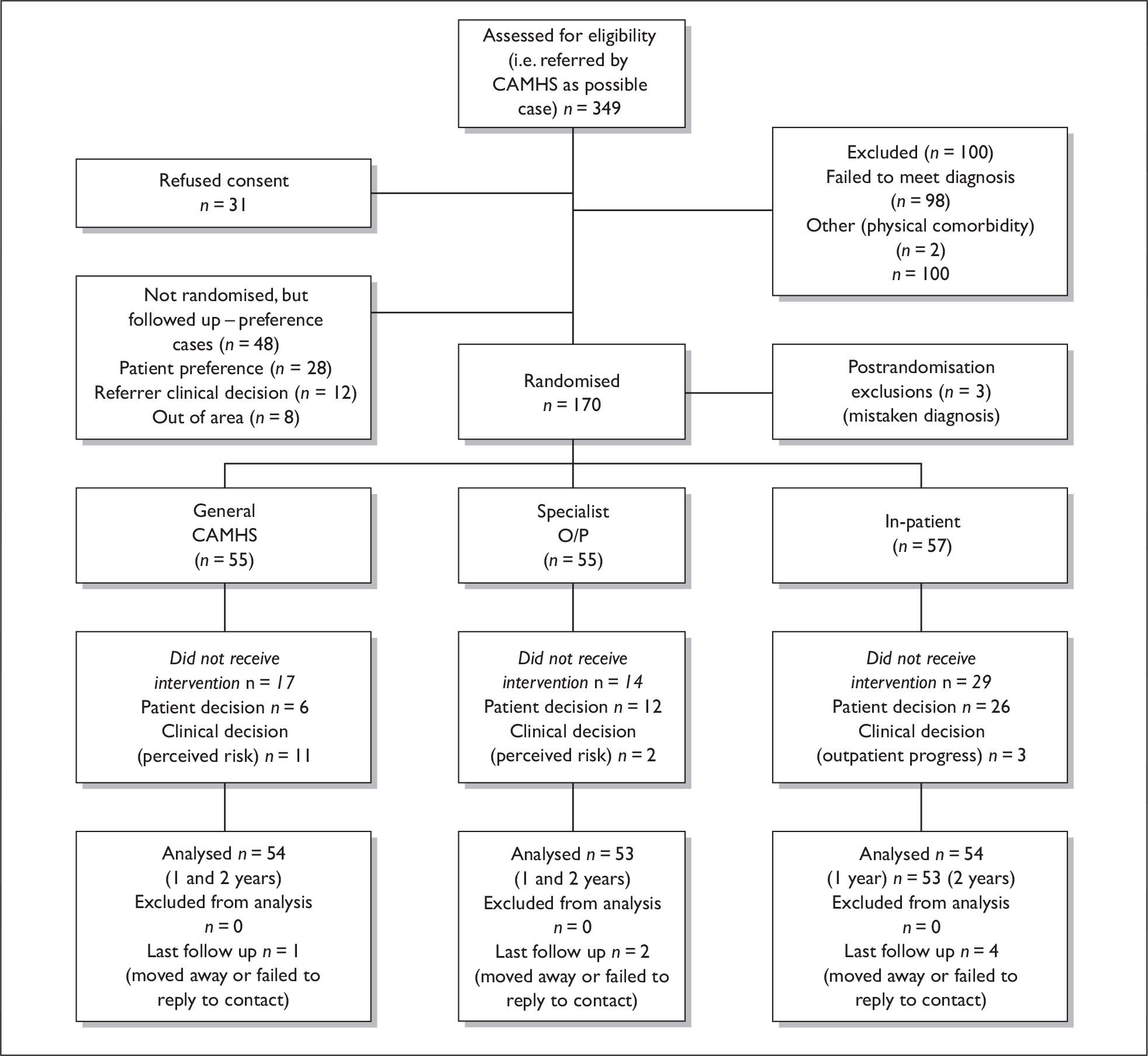
Despite all randomised subjects agreeing to randomisation at the point of giving signed informed consent, adherence to allocated treatment was only 67% and varied between groups (Figure 1). To a large extent this lack of adherence is in the nature of the condition and the attitude of patients with AN to treatment. Explanation of the failure of adherence was as follows:
-
Inpatient treatment adherence rate = 28/59 (49.1%) (defined as a minimum 4-week inpatient stay). In most cases, those failing to adhere agreed initially to admission and then bargained their way out by achieving a small weight gain in the short time between randomisation and admission. Mean length of stay for those admitted was 15.2 weeks.
-
Specialist outpatient adherence rate = 41/57 (76.5%) (defined as a minimum of six attendances). Of the remainder, 10 changed their mind and opted for general CAMHS treatment (generally because of travelling distance), three were admitted before treatment could start and one dropped out of all treatment.
-
General CAMHS adherence rate = 38/57 (71.1%) [defined as attending general CAMHS and no other treatment (beyond possibly specialist second opinion) in the initial 6-month phase]. Two of the remainder had no treatment, four opted for specialist outpatient treatment, while 11 were referred to an alternative by clinician preference (10 inpatient, one specialist outpatient).
FIGURE 1.
TOuCAN trial – recruitment.
Clinical outcomes
Tracing and completion of follow-up assessments
The main outcome point determined at the start of the trial was 2 years. To this point, every subject was traced, with the main outcome measures completed as follows: diagnostic outcome and outcome category 164 (98%) at 1 year, 160 (96%) at 2 years; MRAOS 157 (94%) at 1 year, 155 (93%) at 2 years; BMI/weight for height 154 (92%) at 1 year, 150 (90%) at 2 years; HoNOSCA 154 (92%) at 1 year, 155 (93%) at 2 years. These were achieved by face-to-face interview in 129 (79%) at 1 year and 121 (75%) at 2 years. Outcome data were obtained by telephone interview or interview with a health professional informant with recent knowledge of the case in 34 (20%) at 1 year and 40 (24%) at 2 years. The remaining four at 1 year and six at 2 years were all traced (alive) but little or no information was obtained on their health status.
At 5 years, the rate of completion of follow-up was much lower, largely because of refusals to take part, but also because subjects were not traced. In large part, this was likely to be because the mean age of subjects at 5 years was 20 years. Many would have left home to attend higher education and they were no longer likely to be persuaded by parents to take part. The number followed up at 5 years was: diagnostic outcome and outcome category 97 (60%), MRAOS 81 (47%). Similar levels of follow-up were seen for HoNOSCA-CR and % weight for height. Lower levels of follow-up were observed for patient-completed outcomes (MFQ, EDI-2 and HoNOSCA-SR). For the MFQ the follow-up rate at 1, 2 and 5 years was 81%, 77% and 43%, respectively. Two patients died during the course of the study (and are included at the relevant time point as having a poor outcome) – one died by 2 years of an apparently unrelated physical illness, the other at 5 years of a drug overdose.
Baseline characteristics of patients with and without follow-up are given in Table 4 and Table 5. The proportion of subjects with follow-up assessments for the primary outcome were similar between treatment groups for the year 1 and year 2 assessments, but at 5 years a smaller proportion of subjects in the general CAMHS treatment group (35%) were followed up, compared with specialist outpatient treatment (58%) and specialist inpatient treatment (53%). Quantitative characteristics of the groups were similar, although at 5 years followed up subjects tended to have a lower baseline HoNOSCA-SR, and a higher MRAOS, i.e. were slightly healthier at baseline.
| (n) | Year 1 | Year 2 | Year 5 | |||||
|---|---|---|---|---|---|---|---|---|
| Followed up | (%) | Followed up | (%) | Followed up | (%) | |||
| Site | Mersey | (87) | 84 | 97% | 81 | 93% | 46 | 53% |
| North-west | (80) | 73 | 91% | 74 | 93% | 33 | 41% | |
| Gender | Male | (14) | 13 | 93% | 13 | 93% | 4 | 29% |
| Female | (153) | 144 | 94% | 142 | 93% | 75 | 49% | |
| Type | Restrictor | (127) | 119 | 94% | 117 | 92% | 61 | 48% |
| Binge–purger | (40) | 38 | 95% | 38 | 95% | 18 | 45% | |
| History | < 15 months | (111) | 104 | 94% | 103 | 93% | 58 | 52% |
| ≥ 15 months | (47) | 44 | 94% | 43 | 91% | 18 | 38% | |
| Treatment arm | General CAMHS | (55) | 53 | 96% | 52 | 95% | 19 | 35% |
| Specialised outpatient | (55) | 52 | 95% | 51 | 93% | 31 | 56% | |
| Specialised inpatient | (57) | 52 | 91% | 52 | 91% | 29 | 51% | |
| Without follow-up | With follow-up | |||||
|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |
| Year 1 | ||||||
| Age (years) | 14.86 | 1.50 | 10 | 14.99 | 1.35 | 157 |
| MRAOS (average of all scales) | 4.30 | 1.38 | 10 | 4.79 | 1.41 | 157 |
| Weight for height (%) | 80.00 | 7.19 | 10 | 77.91 | 8.05 | 157 |
| EDI-2 total | 88.22 | 70.07 | 9 | 88.22 | 46.19 | 153 |
| MFQ total | 2.12 | 0.54 | 9 | 2.11 | 0.54 | 153 |
| FAD – general functioning | 32.22 | 15.34 | 9 | 31.64 | 15.13 | 154 |
| HoNOSCA-CR | 21.70 | 6.04 | 10 | 20.17 | 6.33 | 157 |
| HoNOSCA-SR | 19.78 | 12.73 | 9 | 16.30 | 9.57 | 151 |
| Year 2 | ||||||
| Age (years) | 14.35 | 1.41 | 12 | 15.03 | 1.35 | 155 |
| MRAOS (average of all scales) | 4.25 | 1.42 | 12 | 4.80 | 1.41 | 155 |
| Weight for height (%) | 77.07 | 8.86 | 12 | 78.11 | 7.95 | 155 |
| EDI-2 total | 61.00 | 40.52 | 11 | 90.20 | 47.49 | 151 |
| MFQ total | 2.15 | 0.52 | 11 | 2.11 | 0.54 | 151 |
| FAD – general functioning | 28.55 | 16.68 | 11 | 31.90 | 15.01 | 152 |
| HoNOSCA-CR | 22.75 | 7.64 | 12 | 20.06 | 6.17 | 155 |
| HoNOSCA-SR | 17.18 | 10.21 | 11 | 16.45 | 9.76 | 149 |
| Year 5 | ||||||
| Age (years) | 14.86 | 1.39 | 88 | 15.11 | 1.32 | 79 |
| MRAOS (average of all scales) | 4.65 | 1.47 | 88 | 4.89 | 1.34 | 79 |
| Weight for height (%) | 77.79 | 7.87 | 88 | 78.31 | 8.17 | 79 |
| EDI-2 total | 86.37 | 49.84 | 86 | 90.30 | 44.98 | 76 |
| MFQ total | 2.18 | 0.50 | 86 | 2.04 | 0.57 | 76 |
| FAD – general functioning | 32.51 | 15.04 | 86 | 30.74 | 15.19 | 77 |
| HoNOSCA-CR | 20.85 | 5.89 | 88 | 19.59 | 6.71 | 79 |
| HoNOSCA-SR | 18.33 | 10.08 | 84 | 14.47 | 9.03 | 76 |
All groups made substantial mean improvements in terms of weight, global measures and self-reported psychopathology by 1 year, with further significant improvement by 2 years. Table 6 and Table 7 summarise the quantitative outcomes at 1, 2 and 5 years. By intention-to-treat there are no statistically significant differences between the three groups at 1 year or 2 years. In particular, the mean values on the MRAOS were remarkably similar across the treatments. Confidence intervals are also presented for the comparison of inpatient treatment with outpatient and for general CAMHS treatment with specialist treatment for 1 year, 2 years and 5 years.
| Assessment | General CAMHS | Specialist outpatient | Specialist inpatient | Inpatient–Outpatient | Specialist–General | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | n | Mean | (SD) | n | Mean | (SD) | n | Diff.a | (95% CI) | Diff.a | (95% CI) | ||
| A (Food intake) | Baseline | 3.09 | (1.63) | 55 | 3.36 | (1.99) | 55 | 3.30 | (1.74) | 57 | ||||
| 1 year | 7.78 | (2.65) | 53 | 7.43 | (2.77) | 52 | 6.98 | (2.95) | 52 | – 0.77 | (– 1.73 to 0.18) | – 0.53 | (– 1.46 to 0.41) | |
| 2 years | 7.88 | (2.75) | 52 | 8.11 | (2.63) | 51 | 7.49 | (3.25) | 52 | – 0.55 | (– 1.58 to 0.47) | – 0.11 | (– 1.11 to 0.89)0 | |
| 5 years | 8.42 | (3.25) | 19 | 8.28 | (3.20) | 31 | 9.19 | (2.96) | 29 | 0.72 | (– 0.75 to 2.19) | 0.78 | (– 0.86 to 2.42) | |
| B (Menstruation) | Baseline | 1.00 | (2.41) | 48 | 0.80 | (2.14) | 50 | 0.87 | (2.52) | 46 | ||||
| 1 year | 5.62 | (5.25) | 47 | 5.42 | (5.06) | 45 | 6.04 | (5.50) | 45 | 0.68 | (– 1.26 to 2.62) | 0.22 | (– 1.68 to 2.12) | |
| 2 years | 7.24 | (5.46) | 42 | 7.14 | (5.41) | 42 | 7.52 | (5.17) | 42 | 0.66 | (– 1.31 to 2.63) | 0.32 | (– 1.61 to 2.25) | |
| 5 years | 9.43 | (4.60) | 14 | 9.90 | (3.71) | 21 | 10.29 | (3.41) | 14 | 0.73 | (– 1.73 to 3.18) | 0.81 | (– 1.64 to 3.26) | |
| C (Mental state) | Baseline | 5.31 | (2.18) | 55 | 5.24 | (1.87) | 55 | 5.47 | (1.95) | 57 | ||||
| 1 year | 7.32 | (2.91) | 53 | 7.31 | (2.93) | 52 | 7.00 | (2.84) | 52 | – 0.57 | (– 1.52 to 0.37) | – 0.32 | (– 1.24 to 0.60) | |
| 2 years | 8.00 | (3.17) | 52 | 8.08 | (2.83) | 51 | 8.00 | (3.17) | 52 | – 0.27 | (– 1.28 to 0.75) | – 0.08 | (– 1.07 to 0.90) | |
| 5 years | 9.47 | (2.74) | 19 | 9.68 | (2.88) | 31 | 10.76 | (2.17) | 29 | 1.27 | (0.01 to 2.53) | 1.02 | (– 0.37 to 2.40) | |
| D (Psychosexual state) | Baseline | 5.53 | (2.65) | 55 | 5.84 | (2.82) | 55 | 6.57 | (2.87) | 56 | ||||
| 1 year | 7.76 | (3.28) | 52 | 7.86 | (3.56) | 51 | 7.61 | (3.38) | 51 | – 0.16 | (– 1.27 to 0.95) | – 0.13 | (– 1.23 to 0.96) | |
| 2 years | 8.19 | (3.49) | 52 | 8.84 | (3.21) | 51 | 8.70 | (3.47) | 52 | 0.06 | (– 1.08 to 1.20) | 0.49 | (– 0.62 to 1.60) | |
| 5 years | 10.56 | (2.36) | 19 | 9.80 | (3.10) | 31 | 10.80 | (2.32) | 29 | 0.86 | (– 0.44 to 2.15) | 0.09 | (– 1.33 to 1.51) | |
| E (Socioeconomic state) | Baseline | 7.84 | (1.98) | 55 | 7.21 | (2.99) | 55 | 8.11 | (2.17) | 57 | ||||
| 1 year | 9.30 | (2.65) | 53 | 8.61 | (3.19) | 52 | 9.40 | (2.19) | 52 | 0.11 | (– 0.80 to 1.01) | – 0.35 | (– 1.30 to 0.60) | |
| 2 years | 9.58 | (2.71) | 52 | 9.30 | (2.73) | 51 | 9.34 | (2.77) | 52 | – 0.35 | (– 1.30 to 0.60) | – 0.33 | (– 1.26 to 0.60) | |
| 5 years | 10.32 | (1.64) | 19 | 9.68 | (2.50) | 31 | 10.51 | (1.95) | 29 | 0.57 | (– 0.49 to 1.63) | – 0.10 | (– 1.26 to 1.06) | |
| MRAOS (Average of all scales) | Baseline | 4.67 | (1.27) | 55 | 4.56 | (1.46) | 55 | 5.05 | (1.46) | 57 | ||||
| 1 year | 7.61 | (2.22) | 53 | 7.34 | (2.27) | 52 | 7.50 | (2.43) | 52 | – 0.09 | (– 0.88 to 0.70) | – 0.26 | (– 1.03 to 0.50) | |
| 2 years | 8.25 | (2.61) | 52 | 8.36 | (2.38) | 51 | 8.25 | (2.58) | 52 | – 0.20 | (– 1.07 to 0.68) | 0.00 | (– 0.85 to 0.84) | |
| 5 years | 9.60 | (2.01) | 19 | 9.44 | (2.26) | 31 | 10.34 | (1.81) | 29 | 0.87 | (– 0.12 to 1.85) | 0.46 | (– 0.62 to 1.53) | |
| Assessment | General CAMHS | Specialist outpatient | Specialist inpatient | Inpatient–Outpatient | Specialist–General | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | n | Mean | (SD) | n | Mean | (SD) | n | Diffa | (95% CI) | Diffa | (95% CI) | p-value | ||
| Weight for height (%) | Baseline | 78.80 | (7.86) | 55 | 77.14 | (8.10) | 55 | 78.16 | (8.08) | 57 | |||||
| 1 year | 90.89 | (13.34) | 50 | 88.15 | (10.63) | 52 | 86.67 | (9.90) | 52 | – 2.24 | (– 5.93 to 1.46) | – 2.33 | (– 6.00 to 1.35) | 0.21 | |
| 2 years | 94.17 | (12.98) | 46 | 90.10 | (9.78) | 50 | 90.45 | (13.35) | 51 | – 1.74 | (– 5.85 to 2.38) | – 2.85 | (– 7.00 to 1.30) | 0.18 | |
| 5 years | 88.71 | (10.43) | 20 | 96.01 | (12.00) | 31 | 95.65 | (12.14) | 24 | 4.31 | (– 1.69 to 10.31) | 7.64 | (1.45 to 13.83) | 0.02 | |
| EDI-2 total | Baseline | 88.48 | (51.36) | 52 | 86.52 | (47.53) | 54 | 89.61 | (44.52) | 56 | |||||
| 1 year | 69.38 | (53.32) | 45 | 57.64 | (54.02) | 44 | 60.60 | (52.91) | 43 | – 1.09 | (– 18.44 to 16.26) | – 4.28 | (– 21.39 to 12.83) | 0.62 | |
| 2 years | 60.98 | (51.97) | 40 | 52.50 | (49.15) | 42 | 40.33 | (36.36) | 43 | – 12.15 | (– 28.98 to 4.68) | – 11.71 | (– 28.53 to 5.11) | 0.17 | |
| 5 years | 56.09 | (44.44) | 22 | 51.76 | (45.53) | 25 | 42.00 | (35.66) | 25 | – 11.56 | (– 32.30 to 9.17) | – 10.07 | (– 31.43 to 11.29) | 0.35 | |
| FAD-General functioning | Baseline | 2.13 | (0.59) | 52 | 2.12 | (0.53) | 54 | 2.08 | (0.49) | 56 | |||||
| 1 year | 1.97 | (0.57) | 46 | 2.08 | (0.55) | 45 | 1.95 | (0.49) | 43 | – 0.08 | (– 0.25 to 0.10) | 0.05 | (– 0.12 to 0.22) | 0.57 | |
| 2 years | 2.02 | (0.65) | 41 | 1.99 | (0.59) | 39 | 1.99 | (0.52) | 42 | 0.05 | (– 0.16 to 0.26) | – 0.01 | (– 0.21 to 0.20) | 0.93 | |
| 5 years | 2.03 | (0.65) | 22 | 1.92 | (0.45) | 24 | 1.85 | (0.55) | 23 | – 0.13 | (– 0.42 to 0.16) | – 0.16 | (– 0.46 to 0.13) | 0.27 | |
| MFQ total | Baseline | 32.36 | (16.12) | 53 | 30.09 | (14.70) | 54 | 32.55 | (14.60) | 56 | |||||
| 1 year | 23.85 | (17.71) | 46 | 19.28 | (16.70) | 46 | 18.16 | (15.65) | 43 | – 3.11 | (– 8.82 to 2.61) | – 3.64 | (– 9.19 to 1.92) | 0.20 | |
| 2 years | 24.19 | (20.18) | 42 | 17.14 | (15.14) | 42 | 15.83 | (14.51) | 42 | – 3.36 | (– 9.45 to 2.74) | – 5.71 | (– 11.61 to 0.19) | 0.06 | |
| 5 years | 22.32 | (17.32) | 22 | 18.08 | (15.45) | 25 | 14.00 | (11.70) | 25 | – 7.24 | (– 14.92 to 0.45) | – 7.23 | (– 15.15 to 0.68) | 0.07 | |
| HoNOSCA | |||||||||||||||
| Clinician-rated | Baseline | 20.04 | (5.72) | 55 | 20.71 | (7.50) | 55 | 20.04 | (5.63) | 57 | |||||
| 1 year | 15.02 | (9.09) | 53 | 16.84 | (9.69) | 49 | 14.19 | (7.40) | 52 | – 1.29 | (– 4.18 to 1.60) | 0.51 | (– 2.32 to 3.33) | 0.72 | |
| 2 years | 13.75 | (9.76) | 52 | 13.69 | (8.92) | 51 | 14.25 | (9.14) | 52 | 0.96 | (– 2.14 to 4.07)0.07 | 0.44 | (– 2.60 to 3.47) | 0.78 | |
| 5 years | 9.11 | (7.04) | 19 | 10.55 | (8.22) | 31 | 6.72 | (4.87) | 29 | – 3.38 | (– 6.69 to 0.07) | – 1.07 | (– 4.70 to 2.56) | 0.56 | |
| Self-rated | Baseline | 16.46 | (9.95) | 54 | 17.40 | (9.88) | 53 | 15.64 | (9.54) | 53 | |||||
| 1 year | 10.53 | (10.03) | 45 | 11.70 | (9.03) | 44 | 8.62 | (8.15) | 42 | – 1.55 | (– 4.75 to 1.65) | 0.92 | (– 2.20 to 4.04) | 0.56 | |
| 2 years | 9.97 | (9.84) | 37 | 8.88 | (8.11) | 43 | 7.65 | (8.58) | 43 | – 0.42 | (– 3.56 to 2.73) | – 0.92 | (– 4.13 to 2.29) | 0.57 | |
| 5 years | 6.74 | (4.15) | 19 | 7.34 | (8.09) | 29 | 4.38 | (4.78) | 24 | – 2.68 | (– 5.61 to 0.26) | – 1.31 | (– 4.31 to 1.68) | 0.38 | |
Mixed Model Analysis of Quantitative Outcome
As outlined in the analysis plan, two comparisons were made between the three randomised groups. First, between inpatient treatment and outpatient treatment (general CAMHS and specialist) and second between general CAMHS and specialist treatment (outpatient and inpatient).
Comparison of inpatient with outpatient treatment
Table 6 and Table 7 summarise the outcome for the quantitative outcome measures and give confidence intervals for the two planned comparisons.
When a linear mixed model was fitted including the assessment point (1, 2, 5 years) with treatment–group interaction, there were no interactions between assessment and treatment for the primary outcome measure (MRAOS), nor for the secondary outcome measures (Table 8) for this comparison. When the model was refitted without an interaction there was no main effect of inpatient treatment for MRAOS or the secondary measures. In a further analysis, not presented here, there was no treatment by site interaction. No further subgroup analyses of potential moderators have been carried out.
| Coefficient | 95% CI | p-value | |
|---|---|---|---|
| MRAOS | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | 0.12 | (– 0.60 to 0.83) | 0.752 |
| Treatment main effectb | 0.15 | (– 0.86 to 1.16) | 0.770 |
| Specialist–Generalist | |||
| Treatment with session interaction | 0.42 | (– 0.09 to 0.94) | 0.104 |
| Treatment main effectb | – 0.01 | (– 0.67 to 0.64) | 0.965 |
| % Weight for height | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | – 0..86 | (– 4.37 to 2.64) | 0.629 |
| Treatment main effectb | – 0.46 | (– 5.57 to 4.66) | 0.862 |
| Specialist–Generalist | |||
| Treatment with session interactiona | 2.80 | (0.31 to 5.29) | 0.027 |
| Treatment main effect | – 2.16 | (– 5.47 to 1.115) | 0.200 |
| EDI-2 total | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | – 4.51 | (– 19.10 to 10.09) | 0.545 |
| Treatment main effectb | 0.24 | (– 19.87 to 20.35) | 0.981 |
| Specialist–Generalist | |||
| Treatment with session interaction | – 2.95 | (– 12.72 to 6.82) | 0.553 |
| Treatment main effectb | – 10.26 | (– 23.39 to 2.87) | 0.126 |
| FAD-GF | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | 0.102 | (– 0.094 to 0.297) | 0.309 |
| Treatment main effectb | – 0.080 | (– 0.31 to 0.15) | 0.494 |
| Specialist–Generalist | |||
| Treatment with session interactiona | – 0.13 | (– 0.26 to 0.00) | 0.047 |
| Treatment main effect | – 0.01 | (– 0.16 to 0.14) | 0.929 |
| MFQ | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | 0.09 | (– 5.77 to 5.96) | 0.975 |
| Treatment main effectb | 0.72 | (– 6.07 to 7.52) | 0.835 |
| Specialist–Generalist | |||
| Treatment with session interaction | – 1.68 | (– 5.60 to 2.24) | 0.400 |
| Treatment main effectb | – 5.94 | (– 10.35 to – 1.54) | 0.008 |
| HoNOSCA-CR | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | 0.82 | (– 1.76 to 3.39) | 0.534 |
| Treatment main effectb | – 1.29 | (– 4.92 to 2.35) | 0.488 |
| Specialist–Generalist | |||
| Treatment with session interaction | – 1.55 | (– 3.36 to 0.26) | 0.094 |
| Treatment main effectb | – 0.19 | (– 2.54 to 2.17) | 0.876 |
| HoNOSCA-SR | |||
| Inpatient–Outpatient | |||
| Treatment with session interaction | 1.17 | (– 1.37 to 3.71) | 0.367 |
| Treatment main effectb | – 1.46 | (– 4.89 to 1.97) | 0.404 |
| Specialist–Generalist | |||
| Treatment with session interaction | – 1.14 | (– 2.89 to 0.61) | 0.202 |
| Treatment main effectb | – 0.63 | (– 2.94 to 1.68) | 0.593 |
The analyses suggest no advantage for inpatient over outpatient treatment.
Comparison of specialist treatment with general CAMHS
In the comparison of specialist services with general CAMHS, there was no interaction between assessment and treatment in the linear mixed model analyses for the primary outcome measure except for the secondary outcome measures % weight for height and FAD-GF. In both cases, the direction of the interactions suggested that the outcome for specialist treatments tended to improve relative to general CAMHS over time. There was an increased effect of specialist treatment relative to general CAMHS between consecutive assessments of 2.80 (95% CI 0.31 to 5.29 p = 0.027). At the 1-year and 2-year follow-ups the general CAMHS treatment gave slightly better (but non-significant) outcomes than the two specialist treatments for % weight for height.
Patients in the specialist treatments reported better outcomes at 5 years than those on CAMHS treatment (p = 0.02, see Table 7). For FAD-GF specialist treatments reported a better outcome at 5 years, but this finding was not statistically significant. It should be noted, that the proportion of subjects followed up to 5 years is low and varied between treatment arms [general CAMHS 36% (20/57), specialist outpatient 58% (31/57), specialist inpatient 42% (24/59)], so that differences between treatments at 5 years may therefore be based on selection effects with the follow-up influenced by randomisation; as the reduced follow-up in the CAMHS arm may arise because of the reduced contact of trial subjects with specialist services.
When the model was refitted without an interaction there was a significant main effect of specialist treatment compared with general CAMHS treatment for MFQ. Averaging across follow-up assessments MFQ was 5.94 points (95% CI 1.56 to 10.35, p = 0.008) lower (better outcome) in specialist services than general CAMHS. This difference is also apparent in Table 7 with the difference between specialist treatment and general CAMHS being 3.6, 5.7 and 7.2 at 1, 2 and 5 years follow-up, respectively. There were no other differences between groups.
There was no treatment by site interaction and no other subgroup analyses were carried out.
Diagnostic outcome category
Table 9 and Figure 2 show the diagnostic outcome category at years 1, 2 and 5. These are based on the categories employed in the Maudsley studies18,21,37 employing a high threshold for assigning recovery. A good outcome indicates a full recovery from AN (weight above 85% of expected, return of menstruation, bingeing/purging no greater than once per month). A poor outcome was indicated if weight was not above 85% or the young person was still being treated as an inpatient for AN. The intermediate category comprises those whose weight had risen to within the normal range, but without return of menstruation, with bingeing–purging at a frequency greater than monthly, or considerable residual concerns about weight and shape scored on Morgan–Russell scale A. At 1 year, 18% had fully recovered, 38% still had diagnostic AN. By 2 years there was an overall good outcome for 33%, but 27% still had the condition.
| General CAMHS | Specialist outpatient | Specialist inpatient | Odds ratio | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| n = 55 | n = 55 | n = 57 | ||||
| 1 year | ||||||
| Poor | 13 | 24 | 26 | Inpatient–Outpatient | ||
| 24% | 44% | 46% | 0.70 | (0.37 to 1.34) | ||
| Intermediate | 31 | 22 | 18 | |||
| 57% | 41% | 32% | Specialist–General | |||
| Good | 10 | 8 | 12 | 0.54 | (0.29 to 1.01) | 0.05 |
| 19% | 15% | 21% | ||||
| Followed up | 54 | 54 | 56 | |||
| Alive but no further info. | 1 | 1 | 1 | |||
| 2 year | ||||||
| Poor | 14 | 12 | 17 | Inpatient–Outpatient | ||
| 26% | 23% | 32% | 0.86 | (0.45 to 1.64) | ||
| Intermediate | 20 | 28 | 17 | |||
| 37% | 53% | 32% | Specialist–General | |||
| Good | 20 | 13 | 19 | 0.84 | (0.45 to 1.56) | 0.58 |
| 37% | 25% | 36% | ||||
| Followed up | 54 | 53 | 53 | |||
| Alive but no further info. | 1 | 1 | 3 | |||
| No info. | 0 | 1 | 1 | |||
| 5 year | ||||||
| Poor | 5 | 2 | 3 | Inpatient–Outpatient | ||
| 18% | 6% | 9% | 1.56 | (0.61 to 4.02) | ||
| Intermediate | 6 | 13 | 8 | |||
| 21% | 37% | 24% | Specialist–General | |||
| Good | 17 | 20 | 22 | 1.52 | (0.59 to 3.93) | 0.39 |
| 61% | 57% | 67% | ||||
| Followed up | 28 | 35 | 33 | |||
| Alive but no further info. | 6 | 3 | 7 | |||
| No info. | 21 | 17 | 17 | |||
FIGURE 2.
Percentage good outcome (cases with known outcome).
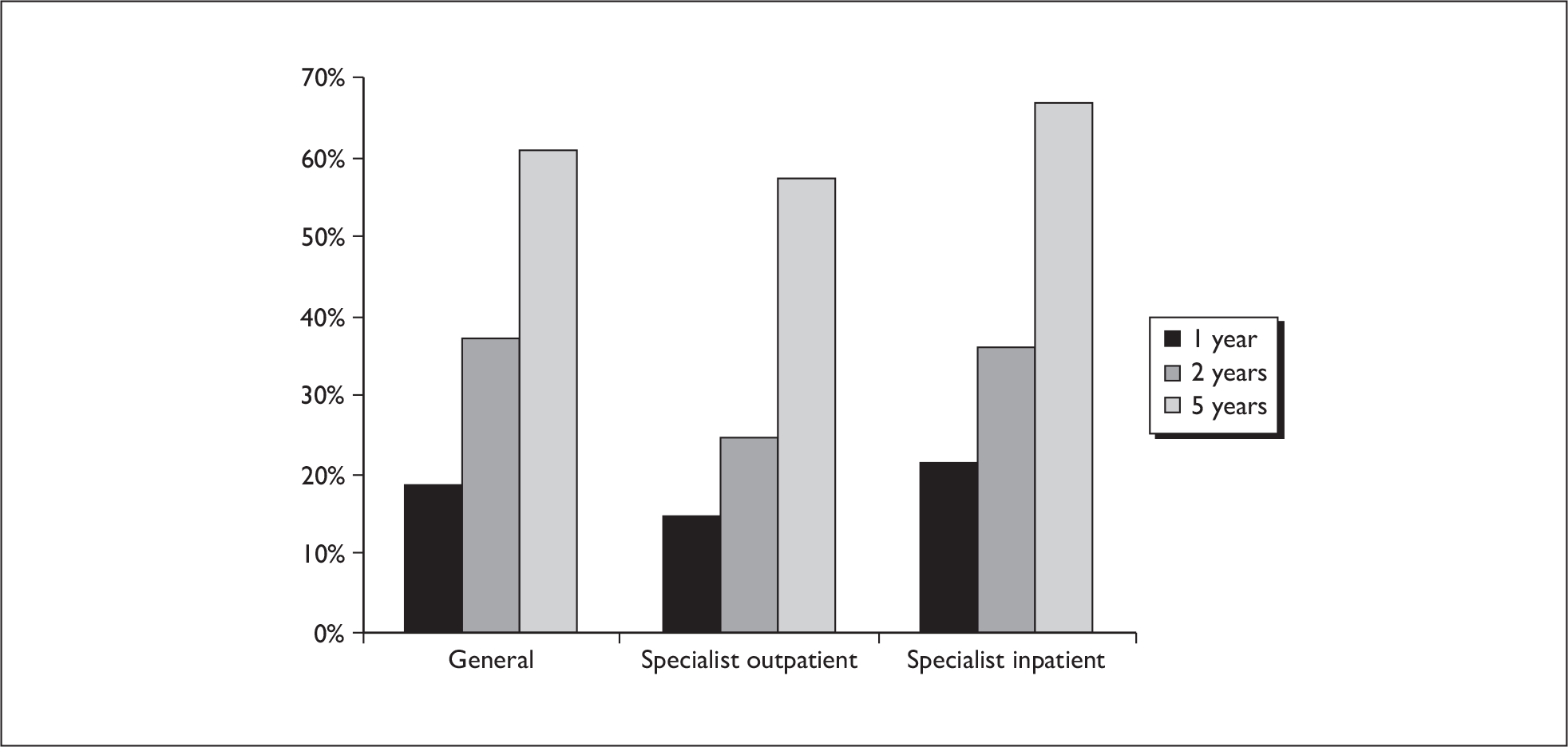
Table 10 summaries the longitudinal marginal model analysis using robust standard errors. There were no statistically significant differences between inpatient and outpatient treatments. In the comparison of specialist treatment with general CAMHS treatment there was slight evidence of a time with treatment interaction (0 = 0.66). From Table 10 it can be seen that general CAMHS did better than specialist treatments at 1 year (Common Odds Ratio 0.56, 95% CI 0.29 to 1.01 p = 0.05), having fewer poor outcomes, whereas at 5 years the Common Odds Ratio tended to favour specialist treatment (1.54, 95% CI 0.61 to 3.93) although not significantly (p = 0.39). There was no treatment by site interaction and no other subgroup analyses were carried out.
| Odds ratio | 95% CI | p-value | |
|---|---|---|---|
| Inpatient–Outpatient | |||
| Treatment with session interaction | 0.91 | (0.48 to 1.73) | 0.769 |
| Main effect | 1.16 | (0.54 to 2.48) | 0.705 |
| Specialist–General | |||
| Treatment with session interaction | 1.57 | (0.97 to 2.52) | 0.064 |
| Main effect | 0.78 | (0.47 to 1.29) | 0.327 |
Clinical course
On the whole, patients made a steady improvement over the 5 years. Table 11 shows the movement between outcome category by each of the four groups between 2-year and 5-year outcomes. Overall, the outcome category is known for 131 subjects at both the 2-year and 5-year time points. Of 54 with a good outcome at 2 years, only two had a poor outcome at 5 years (one with AN and one who had died). Only eight with a good outcome at 2 years had slipped back into an intermediate outcome, suggesting that when full recovery is achieved, relapse is relatively unlikely. This pattern is seen for each of the treatment groups with no notable differences between them. Meanwhile, the outcome at 5 years for the 28 in the poor category at 2 years is much more mixed, with equal numbers having recovered as remain with AN at 5 years (10 in each category).
| 5 years | 2 years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Poor | (%) | Inter. | (%) | Good | (%) | Not known | (%) | No info. | (%) | Total | (%) | |
| General CAMHS | ||||||||||||
| Poor | 3 | (21) | 2 | (10) | 0 | (0) | 0 | (0) | – | – | 5 | (9) |
| Intermediate | 2 | (14) | 2 | (10) | 2 | (10) | 0 | (0) | – | – | 6 | (11) |
| Good | 1 | (7) | 6 | (30) | 9 | (45) | 1 | (100) | – | – | 17 | (31) |
| Alive – no further information | 2 | (14) | 1 | (5) | 3 | (15) | 0 | (0) | – | – | 6 | (11) |
| No information | 6 | (43) | 9 | (45) | 6 | (30) | 0 | (0) | – | – | 21 | (38) |
| Total | 14 | 20 | 20 | 1 | – | – | 55 | |||||
| Specialist outpatient | ||||||||||||
| Poor | 0 | (0) | 1 | (4) | 1 | (8) | 0 | (0) | 0 | (0) | 2 | (4) |
| Intermediate | 2 | (17) | 9 | (32) | 2 | (15) | 0 | (0) | 0 | (0) | 13 | (24) |
| Good | 5 | (42) | 6 | (21) | 9 | (69) | 0 | (0) | 0 | (0) | 20 | (36) |
| Alive – no further information | 0 | (0) | 3 | (11) | 0 | (0) | 0 | (0) | 0 | (0) | 3 | (5) |
| No information | 5 | (42) | 9 | (32) | 1 | (8) | 1 | (100) | 1 | (100) | 17 | (31) |
| Total | 12 | 28 | 13 | 1 | 1 | 55 | ||||||
| Specialist inpatient | ||||||||||||
| Poor | 2 | (12) | 1 | (6) | 0 | (0) | 0 | (0) | 0 | (0) | 3 | (5) |
| Intermediate | 4 | (24) | 2 | (12) | 2 | (11) | 0 | (0) | 0 | (0) | 8 | (14) |
| Good | 2 | (12) | 7 | (41) | 12 | (63) | 1 | (33) | 0 | (0) | 22 | (39) |
| Alive – no further information | 3 | (18) | 2 | (12) | 2 | (11) | 0 | (0) | 0 | (0) | 7 | (12) |
| No information | 6 | (35) | 5 | (29) | 3 | (16) | 2 | (67) | 1 | (100) | 17 | (30) |
| Total | 17 | 17 | 19 | 3 | 1 | 57 | ||||||
| Patient preference | ||||||||||||
| Poor | 5 | (45) | 1 | (5) | 1 | (6) | 0 | (0) | – | – | 7 | (15) |
| Intermediate | 0 | (0) | 5 | (26) | 2 | (12) | 0 | (0) | – | – | 7 | (15) |
| Good | 2 | (18) | 9 | (47) | 12 | (71) | 0 | (0) | – | – | 23 | (48) |
| Alive – no further information | 0 | (0) | 1 | (5) | 0 | (0) | 0 | (0) | – | – | 1 | (2) |
| No information | 4 | (36) | 3 | (16) | 2 | (12) | 1 | (100) | – | – | 10 | (21) |
| Total | 11 | 19 | 17 | 1 | – | – | 48 | |||||
| Total | ||||||||||||
| Poor | 10 | (19) | 5 | (6) | 2 | (3) | 0 | (0) | 0 | (0) | 17 | (8) |
| Intermediate | 8 | (15) | 18 | (21) | 8 | (12) | 0 | (0) | 0 | (0) | 34 | (16) |
| Good | 10 | (19) | 28 | (33) | 42 | (61) | 2 | (33) | 0 | (0) | 82 | (38) |
| Alive – no further information | 5 | (9) | 7 | (8) | 5 | (7) | 0 | (0) | 0 | (0) | 17 | (8) |
| No information | 21 | (39) | 26 | (31) | 12 | (17) | 4 | (67) | 2 | (100) | 65 | (30) |
| Total | 54 | 84 | 69 | 6 | 2 | 215 | ||||||
The course of every patient through the four assessment points for the main outcome measure (MRAOS) is shown in Figure 8 in Appendix 1 to the last assessment point achieved for that patient. It can be seen that in general (though not exclusively) the trends of the graphs are generally upwards with time. Similarly, Figure 9 in Appendix 2 shows individual patient progress in terms of percentage weight for height.
Adherence to treatment allocation and outcome
The trial aimed to compare randomisation to specialist inpatient treatment and specialist outpatient treatment with randomisation to general CAMHS treatment. However, as we have discussed, adherence to the allocated treatment was poor for the inpatient arm. In the first year of the trial, specialist inpatient treatment at one of the four centres was received by 49% (28/59) of subjects randomised to this treatment and 20% (23/110) of those randomised to general CAMHS or specialist treatment. Assuming that there are no subjects who will always opt for the opposite of their randomly assigned treatment, one can argue that only 29% of patients (49% minus 20%) accepted randomisation to specialist inpatient treatment because 20% would have received this irrespective of random allocation and 53% (29/59) did not receive it.
Of those patients randomised to specialist outpatient treatment at the two specialist outpatient centres, 75% (41/57) received specialist outpatient treatment, whereas only 18% (20/112) of patients randomised to either general CAMHS or specialist inpatient received this. Hence, randomisation to specialist outpatient treatment was more likely to be determined by randomisation than specialist inpatient treatment, with 57% (75% minus 18%) accepting randomisation of this option. Allocation to specialist outpatient treatment led to 77% of the sample receiving some form of specialist treatment whereas only half of those assigned to specialist inpatient treatment received it.
Adherence to allocated treatment did have a significant bearing on outcome, though a number of issues, including those above, mean that caution is advised in interpreting the findings.
Examining the outcome of those allocated to inpatient treatment reveals that adherence to this treatment was poor (49%, 28 out of 59) and so in theory this might have compromised the effectiveness of this intervention. At baseline, Table 12 demonstrates that, on the measures used, there was little difference between the two subgroups (adherers and non-adherers), though those who were admitted were on average 6 months younger and showed a reduced food intake (Morgan–Russell Scale A).
| Outcome measure | Baseline | 1 year | 2 years | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adherers (n = 28) | Non-adherers (n = 29) | Adherers (n = 26) | Non-adherers (n = 26) | Difference between non-adherers and adherers | Adherers (n = 25) | Non-adherers (n = 27) | Difference between non-adherers and adherers | ||||||||||||
| Mean | (SD) | Mean | (SD) | p | Mean | (SD) | Mean | (SD) | Diff.a | 95% CI | p | Mean | (SD) | Mean | (SD) | Diffa | 95% CI | p | |
| Body mass index (BMI) | 14.8 | (1.8) | 15.8 | (1.4) | 0.026 | 17.2 | (2.2) | 17.9 | (2.1) | 0.02 | (– 1.07 to 1.11) | 0.97 | 18.3 | (3.0) | 19.0 | (2.6) | 0.39 | (– 1.20 to 1.97) | 0.63 |
| % Weight for height | 76.5 | (8.3) | 79.7 | (7.6) | 0.134 | 85.8 | (9.6) | 87.5 | (10.3) | –0.06 | (– 5.15 to 5.04) | 0.98 | 88.9 | (14.4) | 91.9 | (12.4) | 1.82 | (– 5.79 to 9.44) | 0.63 |
| EDI-2 | |||||||||||||||||||
| Drive for thinness | 11.0 | (7.1) | 11.1 | (7.5) | 0.985 | 9.6 | (8.4) | 4.5 | (5.6) | –4.47 | (– 8.65 to – 0.28) | 0.04 | 3.5 | (4.1) | 4.6 | (6.1) | 1.45 | (– 1.59 to 4.49) | 0.34 |
| Body dissatisfaction | 14.1 | (8.9) | 16.3 | (7.5) | 0.317 | 15.0 | (11.4) | 8.7 | (8.6) | –6.78 | (– 12.31 to – 1.24) | 0.02 | 8.4 | (9.2) | 8.6 | (9.3) | –0.82 | (– 6.09 to 4.45) | 0.76 |
| Total | 89.9 | (47.0) | 89.3 | (42.7) | 0.962 | 74.6 | (55.0) | 48.5 | (49.0) | –21.99 | (– 52.31 to 8.33) | 0.15 | 43.1 | (33.2) | 38.2 | (39.3) | –4.66 | (– 25.7 to 16.4) | 0.66 |
| MFQ Total | 33.9 | (13.8) | 31.3 | (15.5) | 0.509 | 24.5 | (17.0) | 12.7 | (12.3) | –10.28 | (– 19.03 to – 1.52) | 0.03 | 20.1 | (14.2) | 12.3 | (14.1) | –7.10 | (– 15.2 to 1.00) | 0.08 |
| HoNOSCA | |||||||||||||||||||
| Clinician-rated | 21.0 | (6.7) | 19.1 | (4.3) | 0.224 | 17.2 | (7.0) | 11.4 | (6.7) | –5.27 | (– 9.07 to –1.47) | 0.01 | 16.8 | (9.9) | 11.9 | (7.9) | –3.48 | (– 8.17 to 1.21) | 0.14 |
| Self-rated | 17.3 | (10.2) | 13.8 | (8.6) | 0.177 | 12.3 | (8.8) | 5.3 | (6.0) | –5.67 | (– 10.71 to – 0.63) | 0.03 | 9.3 | (9.7) | 6.2 | (7.3) | –1.59 | (– 6.41 to 3.24) | 0.51 |
| Morgan–Russell Scales | |||||||||||||||||||
| Scale A (Food intake) | 2.7 | (1.5) | 3.9 | (1.8) | 0.009 | 5.8 | (2.9) | 8.1 | (2.6) | 1.61 | (0.10 to 3.13) | 0.04 | 6.5 | (3.5) | 8.4 | (2.8) | 1.62 | (– 0.25 to 3.48) | 0.09 |
| Scale B (Menstruation) | 0.7 | (2.0) | 1.0 | (3.0) | 0.645 | 4.6 | (5.3) | 7.3 | (5.5) | 3.24 | (– 0.24 to 6.72) | 0.07 | 6.2 | (5.5) | 9.0 | (4.5) | 2.67 | (– 0.50 to 5.84) | 0.10 |
| Scale C (Mental state) | 5.0 | (1.8) | 5.9 | (2.0) | 0.071 | 5.8 | (2.8) | 8.1 | (2.3) | 1.89 | (0.49 to 3.28) | 0.01 | 7.0 | (2.9) | 8.9 | (3.2) | 1.03 | (– 0.57 to 2.63) | 0.20 |
| Scale D (Psychosexual) | 6.6 | (3.3) | 6.5 | (2.4) | 0.870 | 6.7 | (3.7) | 8.4 | (2.9) | 1.66 | (– 0.20 to 3.52) | 0.08 | 8.0 | (3.8) | 9.3 | (3.1) | 1.31 | (– 0.60 to 3.22) | 0.17 |
| Scale E (Socioeconomic state) | 7.8 | (2.2) | 8.4 | (2.1) | 0.336 | 8.4 | (2.1) | 10.4 | (1.8) | 1.90 | (0.81 to 2.98) | 0.001 | 9.1 | (2.9) | 9.6 | (2.7) | 0.35 | (– 1.21 to 1.92) | 0.65 |
| Average outcome (Average of all scales) | 4.8 | (1.5) | 5.3 | (1.4) | 0.127 | 6.3 | (2.5) | 8.6 | (1.8) | 2.02 | (0.83 to 3.22) | 0.001 | 7.4 | (2.6) | 9.0 | (2.3) | 1.46 | (0.05 to 2.87) | 0.04 |
For the two outpatient treatment arms there was a notably better outcome for those who fully adhered to treatment compared with those failing to adhere or later transferring away from the allocated treatment. Specifically, for general CAMHS treatment, only one out of 17 admitted for inpatient treatment had a good outcome at 1 year, whereas for the specialist outpatient programme, none of the 14 who initially failed to adhere to the allocated programme had a good outcome, nor any of 14 subsequently admitted to inpatient treatment (Table 13). At 2 years, of 17 allocated to CAMHS who were admitted to hospital, two had a good outcome whereas for the specialist outpatient programme, 13 found their way into inpatient management, of whom only one had a good outcome.
| 1 year | 2 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Good | Intermediate | Poor | Not known (alive) | Good | Intermediate | Poor | Not known (alive) | |
| General CAMHS | ||||||||
| Adherers | ||||||||
| Full | 8 | 19 | 4 | 15 | 12 | 3 | 1 | |
| Subsequently admitted | 0 | 3 | 4 | 0 | 0 | 7 | ||
| Total (n = 38) | 8 | 22 | 8 | 15 | 12 | 10 | 1 | |
| Non-adherers | ||||||||
| Treated as outpatient | 1 | 2 | 1 | 1 | 2 | 2 | 1 | |
| Treated as inpatient | 1 | 6 | 3 | 2 | 6 | 2 | ||
| Untreated | 0 | 1 | 1 | 1 | 0 | 1 | ||
| Total (n = 17) | 2 | 9 | 5 | 1 | 5 | 8 | 4 | |
| Total | 10 (18%) | 31 (56%) | 13 (24%) | 1(2%) | 20(36%) | 20(36%) | 14 (26%) | 1 (2%) |
| Specialist outpatient | ||||||||
| Adherers | ||||||||
| Full | 8 | 12 | 11 | 11 | 15 | 5 | ||
| Subsequently admitted | 0 | 3 | 7 | 0 | 7 | 2 | 1 | |
| Total (n = 41) | 8 | 15 | 18 | 11 | 22 | 7 | 1 | |
| Non-adherers | ||||||||
| Treated as outpatient | 0 | 6 | 3 | 1 | 5 | 3 | ||
| Treated as inpatient | 0 | 1 | 3 | 1 | 1 | 1 | 2 | 1 |
| Total (n = 14) | 0 | 7 | 6 | 1 | 2 | 6 | 5 | 1 |
| Total | 8 (15%) | 22 (40%) | 24 (44%) | 1 (2%) | 13(24%) | 28(51%) | 12 (22%) | 2 (4%) |
| Inpatient | ||||||||
| Adherers (n = 28) | 3 | 9 | 15 | 1 | 6 | 9 | 11 | 2 |
| Non-adherers (n = 29) | 9 | 9 | 11 | 13 | 8 | 6 | 2 | |
| Total | 12 (21%) | 18 (32%) | 26 (46%) | 1 (2%) | 19(33%) | 17 (30%) | 17 (30%) | 4 (7%) |
Below, a predictor model is developed for prediction of admission in year 1 among subjects not randomised to inpatient treatment. This can be applied to subjects randomised to inpatient treatment to estimate the probability that each subject would have been admitted. Figure 3 illustrates the probability of admission according to initial adherence to randomisation to admission. Without randomisation, those subjects who initially adhere to allocation to hospital treatment had a high probability of receiving inpatient treatment. Thirty-eight per cent of adherers would have been admitted whereas only 24% of non-adherers would have been admitted (Wilcoxon p = 0.007). Initial adherers to hospital treatment had a higher propensity to receive it, suggesting that they had a different prognosis. Tables 12 and 13 cannot therefore be interpreted as providing a valid comparison of inpatient and outpatient treatment and should be interpreted with caution.
FIGURE 3.
Graphs by initial adherence.
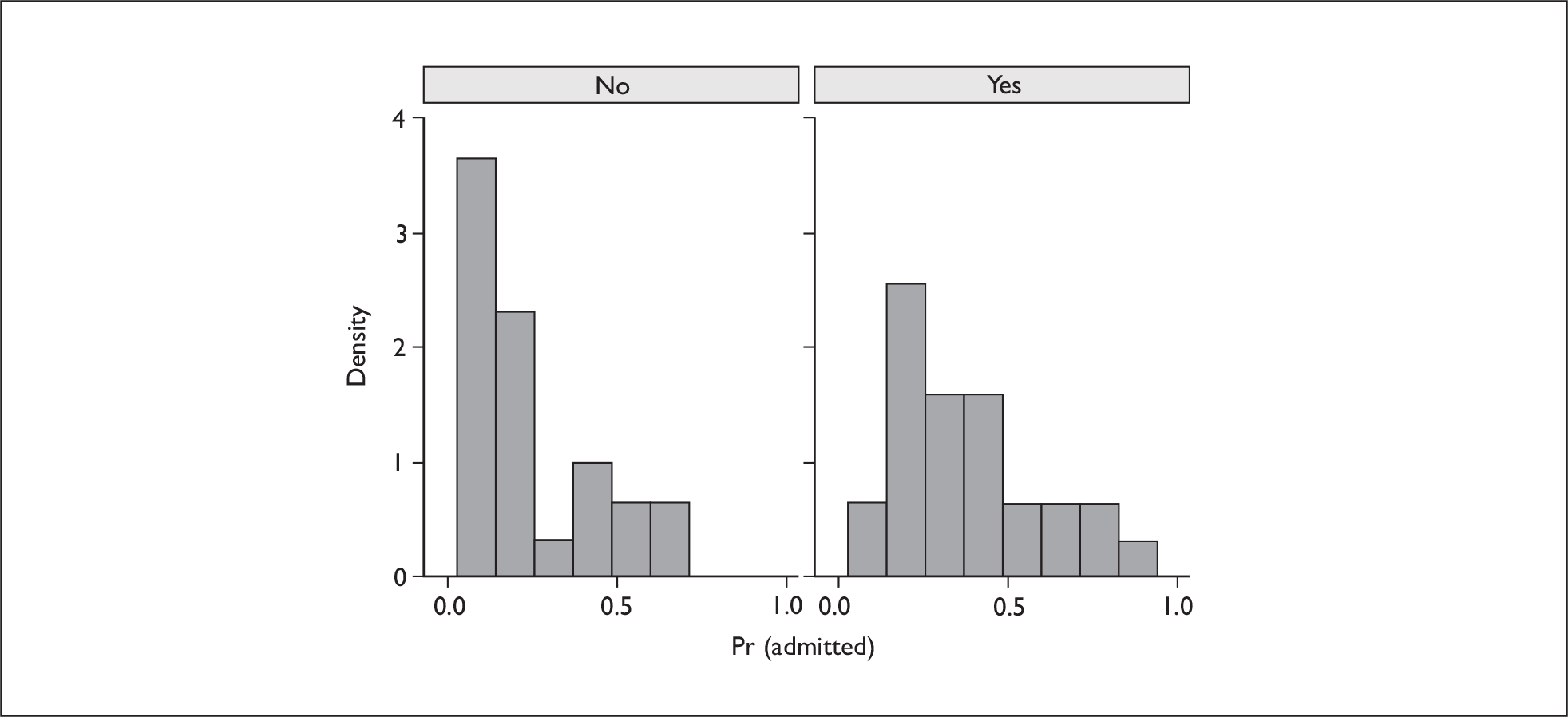
Table 13 demonstrates the relatively better outcome of non-adherers in terms of outcome category. By 2 years, there is a general improvement from the 1-year time point, but this is more marked for those who declined admission. There remains a better outcome on the main outcome measure for those declining admission compared with those who were admitted, even controlling for baseline variables (Table 12).
At 1-year follow-up, those not admitted were doing significantly better on the MRAOS (mean difference 2.0, 95% CI 0.8 to 3.2, p = 0.001) and virtually all self-report measures of psychopathology, including mood (all change scores controlled for baseline values).
Inpatient admission appears to be associated with continuing high rates of core abnormal cognitions, such as body dissatisfaction and drive for thinness, whereas those who declined admission made improvements in these areas, suggestive of early cognitive improvement in this subgroup.
Predictors of outcome
The TOuCAN project provides a large population-based cohort of adolescents with AN, representative of those presenting to UK CAMHS. Irrespective of the RCT component of the study it provides an opportunity to examine prognostic variables and in particular (given the aim of the trial to explore the value of different forms of service provision) those related to service usage.
The following variables were selected for this analysis: gender, age, subtype, length of history, site, % weight for height, MRAOS, HoNOSCA, HoNOSCA-SR, EDI-2 total, MFQ and FAD-GF.
Table 14 shows that a number of these variables are correlated at baseline, notably the global measures (MRAOS and HoNOSCA). It should be noted that the MRAOS–HoNOSCA correlation is negative, given that these items are scored in opposite directions to indicate severity. There is also a strong correlation between the self-report items (EDI-2, MFQ and HoNOSCA-SR).
| Gender | Age | Subtype | History | Site | % Weight for height | Morgan–Russell total | HoNOSCA-CR | HoNOSCA-SR | EDI-2 Total | MFQ Total | FAD-GF | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1.000 | |||||||||||
| Age | 0.095 | 1.000 | ||||||||||
| Subtype | – 0.019 | 0.085 | 1.000 | |||||||||
| History | 0.000 | 0.222 | 0.090 | 1.000 | ||||||||
| Site | 0.019 | – 0.277 | 0.148 | – 0.060 | 1.000 | |||||||
| % Weight for height | – 0.117 | – 0.176 | 0.174 | – 0.019 | 0.034 | 1.000 | ||||||
| Morgan–Russell total | – 0.177 | 0.176 | 0.136 | 0.079 | – 0.163 | 0.366 | 1.000 | |||||
| HoNOSCA-CR | 0.077 | – 0.021 | 0.201 | 0.028 | 0.076 | – 0.131 | – 0.580 | 1.000 | ||||
| HoNOSCA-SR | 0.077 | – 0.053 | 0.388 | 0.043 | 0.194 | 0.125 | – 0.343 | 0.613 | 1.000 | |||
| EDI-2 Total | 0.113 | 0.080 | 0.264 | 0.047 | 0.012 | 0.277 | – 0.193 | 0.383 | 0.682 | 1.000 | ||
| M & FQ Total | 0.138 | 0.035 | 0.278 | – 0.040 | 0.053 | 0.175 | – 0.206 | 0.411 | 0.666 | 0.784 | 1.000 | |
| FAD-GF | 0.060 | 0.036 | 0.200 | 0.003 | 0.075 | 0.071 | – 0.106 | 0.224 | 0.376 | 0.409 | 0.345 | 1.000 |
Table 15 shows the baseline variable selected to predict outcome at each of the time points by outcome variable. Only significant predictors are given. For example, in terms of the main outcome measure (MRAOS), this outcome at 1 and 2 years is predicted by the baseline MRAOS, but at 5 years it is best predicted by weight for height at baseline (i.e. higher weight at baseline predicts better outcome on MRAOS at 5 years). The EDI-2 negatively predicts 5-year outcome on this measure [i.e. a lower (healthier) EDI score at baseline predicts healthier MRAOS score at 5 years]. Percentage weight for height is predicted best by baseline weight for height at each of the time points, i.e. extreme thinness at presentation is a predictor of thinness 5 years later. It is also of note that there is consistency in assessment of family functioning across the four time points. It should be noted also that for quantitative variables, the effects, as measured by the standardised beta coefficient, were mainly small (approximately 0.2), and so the effects are quite weak.
| Outcome | Year | Baseline | Reduced modela | Full modelb | ||
|---|---|---|---|---|---|---|
| Beta | p-value | Beta | p-value | |||
| Morgan–Russell Scales | 1 | Morgan–Russell | 0.290 | < 0.001 | 0.302 | 0.014 |
| Global Score | 2 | Morgan–Russell | 0.246 | < 0.001 | 0.209 | 0.045 |
| 5 | Weight for height | 0.343 | < 0.001 | 0.290 | 0.005 | |
| EDI-2 Total | –0.400 | < 0.001 | – 0.461 | 0.004 | ||
| Weight for height (%) | 1 | Weight for height | 0.329 | < 0.001 | 0.366 | 0.000 |
| 2 | Weight for height | 0.335 | < 0.001 | 0.351 | 0.000 | |
| 5 | Weight for height | 0.273 | 0.004 | 0.266 | 0.005 | |
| EDI-2 Total | 1 | MFQ Total | 0.380 | < 0.001 | 0.221 | 0.075 |
| Weight for height | 0.237 | 0.002 | 0.161 | 0.068 | ||
| History | 0.193 | 0.005 | 0.158 | 0.037 | ||
| Morgan–Russell | – 0.156 | 0.025 | – 0.281 | 0.011 | ||
| Age | 0.153 | 0.036 | 0.105 | 0.186 | ||
| 2 | EDI-2 Total | 0.391 | < 0.001 | 0.237 | 0.093 | |
| 5 | EDI-2 Total | 0.472 | < 0.001 | 0.480 | 0.012 | |
| Weight for height | – 0.224 | 0.023 | – 0.151 | 0.252 | ||
| FAD-GF | 1 | FAD | 0.506 | < 0.001 | 0.534 | 0.000 |
| Morgan–Russell | – 0.225 | 0.008 | – 0.174 | 0.097 | ||
| HoNOSCA-CR | – 0.190 | 0.025 | – 0.145 | 0.169 | ||
| History | 0.170 | 0.012 | 0.139 | 0.066 | ||
| 2 | FAD | 0.451 | < 0.001 | 0.433 | < 0.001 | |
| 5 | FAD | 0.371 | < 0.001 | 0.383 | 0.001 | |
| Morgan–Russell | – 0.274 | 0.003 | – 0.370 | 0.020 | ||
| MFQ Total | 1 | MFQ Total | 0.412 | < 0.001 | 0.331 | 0.009 |
| Morgan–Russell | – 0.176 | 0.012 | – 0.238 | 0.026 | ||
| History | 0.206 | 0.003 | 0.161 | 0.036 | ||
| 2 | MFQ Total | 0.389 | < 0.001 | 0.210 | 0.116 | |
| 5 | EDI-2 Total | 0.384 | <0.001 | 0.435 | 0.028 | |
| Weight for Height | – 0.258 | 0.011 | – 0.291 | 0.036 | ||
| HoNOSCA-CR | 1 | HoNOSCA-SR | 0.296 | < 0.001 | 0.245 | 0.055 |
| Morgan–Russell | – 0.154 | 0.034 | – 0.163 | 0.129 | ||
| 2 | HoNOSCA-SR | 0.379 | 0.001 | 0.404 | 0.002 | |
| 5 | EDI-2 Total | 0.427 | < 0.001 | 0.343 | 0.040 | |
| Weight for height | – 0.289 | 0.002 | – 0.225 | 0.054 | ||
| HoNOSCA-SR | 1 | HoNOSCA-SR | 0.340 | 0.005 | 0.316 | 0.017 |
| Morgan–Russell | – 0.156 | 0.039 | – 0.316 | 0.006 | ||
| 2 | HoNOSCA-SR | 0.404 | < 0.001 | 0.357 | 0.012 | |
| 5 | HoNOSCA-SR | 0.326 | < 0.001 | 0.339 | 0.025 | |
| Age | 0.273 | 0.002 | 0.245 | 0.027 | ||
| Morgan–Russell | – 0.206 | 0.023 | – 0.179 | 0.174 | ||
Baseline predictors of service usage
As only 18% of cases had fully recovered by 1 year and clinical judgement was used to determine treatment beyond the initial 6 months of the trial; we were interested to explore what predicted non-randomised admission to hospital and the use of inpatient beds within the first 2 years, irrespective of treatment allocation and predictors of still being in treatment 1 and 2 years after assessment. Table 16 shows some of the categorical features of those 102 patients admitted to hospital. Admission was more likely in the Manchester site, for binge–purgers and for those with a longer history of illness. Table 17 shows that those admitted had a lower presenting MRAOS and % weight for height and higher self-rated measures of psychopathology. Table 18 provides the statistical analysis showing that % weight for height and self-rated mood were powerful predictors of admission, and that weight for height and EDI-2 total score predicted a shorter time to admission and a greater number of admissions. Table 19 and the associated scatter plot (Figure 4) show that there is a modest but significant association between presenting MRAOS and number of inpatient days in the first 2 years. This illustrates that 15 subjects spent more than 1 year in the first 2 years in hospital, all with a presenting MRAOS of less than four.
| Frequency | % | |
|---|---|---|
| Gender | ||
| Male | 9/16 | 56% |
| Female | 93/193 | 47% |
| Type | ||
| Restrictor | 71/162 | 44% |
| Binge–purger | 31/53 | 58% |
| History | ||
| < 18 months | 64/142 | 45% |
| ≥ 18 months | 38/73 | 52% |
| Baseline characteristic | Not admitted | Admitted | ||||
|---|---|---|---|---|---|---|
| Mean | SD | n | Mean | SD | n | |
| Age | 15.17 | 1.32 | 89 | 15.10 | 1.64 | 69 |
| MRAOS | 4.95 | 1.31 | 89 | 4.02 | 1.43 | 69 |
| Weight for height | 78.8 | 7.1 | 89 | 74.7 | 9.6 | 69 |
| EDI-2 Total | 79.0 | 43.2 | 85 | 100.7 | 51.9 | 62 |
| FAD-GF | 2.07 | 0.55 | 85 | 2.18 | 0.58 | 62 |
| MFQ Total | 27.8 | 14.5 | 89 | 36.8 | 14.5 | 62 |
| HoNOSCA-CR | 18.9 | 6.4 | 89 | 22.7 | 5.8 | 69 |
| HoNOSCA-SR | 14.2 | 8.5 | 87 | 19.8 | 10.8 | 63 |
| Admission | Reduced model | Full model | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| Site | 2.768 | (1.308 to 5.855) | 0.008 | 3.545 | (1.406 to 8.939) | 0.007 |
| Weight for height | 0.916 | (0.873 to 0.961) | < 0.001 | 0.914 | (0.857 to 0.975) | 0.007 |
| MFQ Total | 1.056 | (1.029 to 1.085) | < 0.001 | 1.031 | (0.988 to 1.076) | 0.161 |
| Time to first admission | Hazard ratio | 95% CI | p-value | Hazard ratio | 95% CI | p-value |
| Site | 3.630 | (1.821 to 7.237) | < 0.001 | 3.899 | (1.706 to 8.913) | 0.001 |
| Weight for height | 0.905 | (0.865 to 0.947) | < 0.001 | 0.907 | (0.853 to 0.963) | 0.002 |
| EDI-2 Total | 1.013 | (1.006 to 1.020) | < 0.001 | 1.009 | (0.997 to 1.022) | 0.128 |
| Number of inpatient admissions | Common odds | 95% CI | p-value | Common odds | 95% CI | p-value |
| Site | 2.062 | (1.056 to 4.027) | 0.034 | 2.234 | (0.995 to 5.013) | 0.051 |
| Weight for height | 0.919 | (0.880 to 0.959) | < 0.001 | 0.944 | (0.895 to 0.996) | 0.036 |
| EDI-2 Total | 1.012 | (1.005 to 1.019) | 0.001 | 1.005 | (0.993 to 1.017) | 0.458 |
| Inpatient days | Reduced model | Full model | ||||
|---|---|---|---|---|---|---|
| Common odds ratio | 95% CI | p-value | Common odds ratio | 95% CI | p-value | |
| MRAOS | 0.667 | (0.484 to 0.918) | 0.013 | 0.652 | (0.371 to 1.146) | 0.138 |
FIGURE 4.
Predictors of inpatient days within first 2 years from MRAOS.
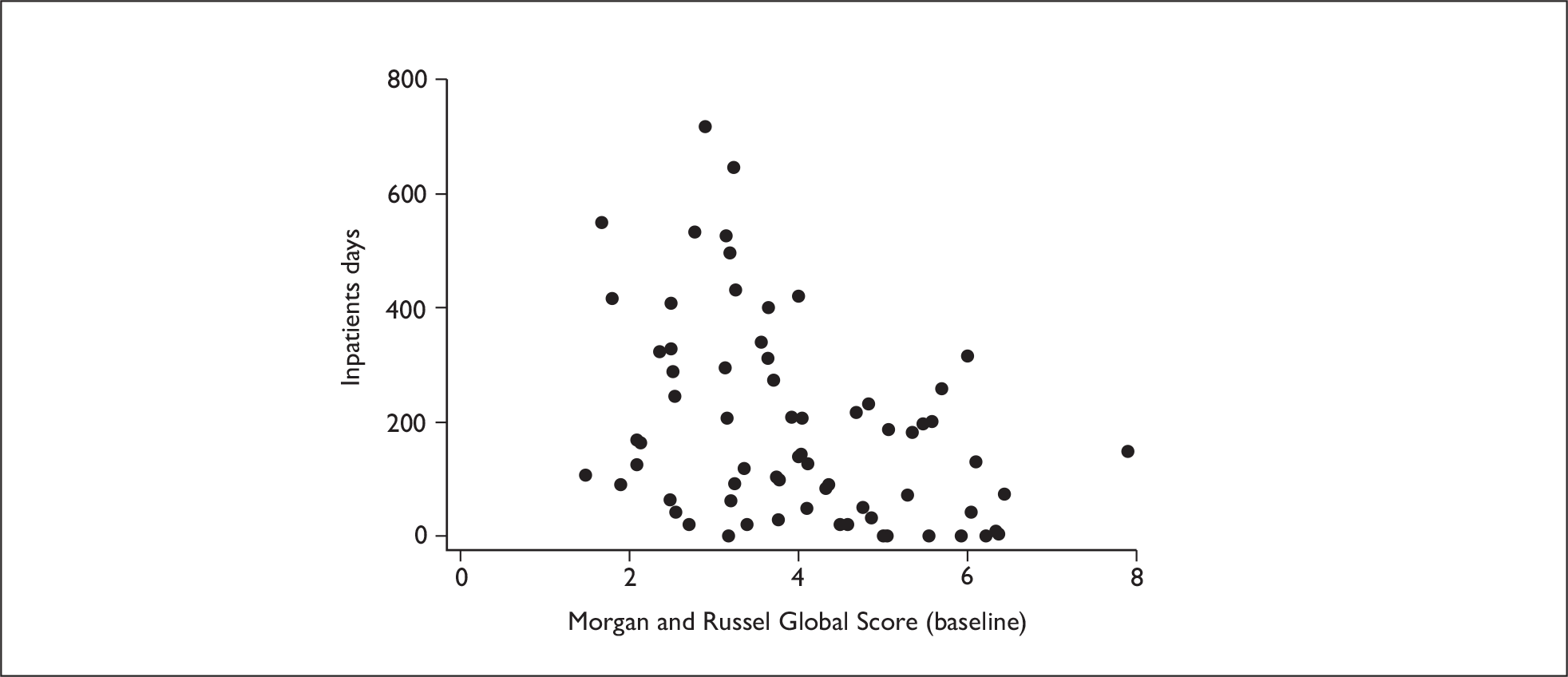
At 1 year, 130 cases were still in treatment and at 2 years this number was 64. Table 20 shows the categorical breakdown of these cases, Table 21 shows the baseline values of those who are in treatment at the two time points and Table 22 the baseline predictors of still being in treatment. In particular, those who were the thinnest and had the highest self-rated cognitions on the EDI-2 at presentation were likely to be still in treatment at 2 years.
| 1 year | 2 years | |||
|---|---|---|---|---|
| n | % | n | % | |
| Site | ||||
| Mersey | 58/116 | 50% | 31/115 | 27% |
| North-west | 55/96 | 57% | 31/96 | 32% |
| Gender | ||||
| Male | 8/16 | 50% | 3/16 | 19% |
| Female | 105/196 | 54% | 59/195 | 30% |
| Type | ||||
| Restrictor | 92/160 | 58% | 49/159 | 31% |
| Binge–purger | 21/52 | 40% | 13/52 | 25% |
| History | ||||
| < 18 months | 78/142 | 55% | 45/141 | 32% |
| ≥ 18 months | 35/70 | 50% | 17/70 | 24% |
| 1 year | 2 years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | |||||||||
| Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | n | |
| Age | 15.37 | 1.35 | 99 | 14.79 | 1.52 | 113 | 15.27 | 1.40 | 149 | 14.53 | 1.52 | 62 |
| MRAOS | 5.20 | 1.40 | 99 | 4.23 | 1.34 | 113 | 4.91 | 1.39 | 149 | 4.12 | 1.46 | 62 |
| Weight for height | 78.5 | 7.6 | 99 | 76.4 | 9.0 | 113 | 78.0 | 8.0 | 149 | 75.7 | 9.3 | 62 |
| EDI-2 Total | 83.3 | 47.4 | 95 | 93.4 | 46.8 | 106 | 86.3 | 46.8 | 143 | 95.7 | 47.5 | 57 |
| FAD-GF | 2.07 | 0.55 | 95 | 2.13 | 0.55 | 106 | 2.11 | 0.53 | 143 | 2.10 | 0.59 | 57 |
| MFQ Total | 28.6 | 14.4 | 96 | 34.8 | 14.9 | 108 | 31.0 | 14.7 | 145 | 34.3 | 15.3 | 58 |
| HoNOSCA-CR | 18.8 | 6.0 | 99 | 21.7 | 6.1 | 113 | 20.0 | 6.2 | 149 | 21.3 | 6.3 | 62 |
| HoNOSCA-SR | 14.4 | 9.2 | 94 | 18.0 | 10.0 | 107 | 15.7 | 9.4 | 141 | 18.0 | 10.6 | 59 |
| Reduced model | Full model | |||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Odds ratio | 95% CI | p-value | |
| 1 year | ||||||
| Age | 0.805 | (0.648 to 1.001) | 0.051 | 0.774 | (0.599 to 1.001) | 0.051 |
| Subtype | 0.429 | (0.201 to 0.916) | 0.029 | 0.402 | (0.171 to 0.945) | 0.037 |
| MRAOS | 0.642 | (0.505 to 0.816) | <0.001 | 0.740 | (0.532 to 1.029) | 0.073 |
| MFQ Total | 1.034 | (1.010 to 1.059) | 0.005 | 1.042 | (1.004 to 1.083) | 0.032 |
| 2 years | ||||||
| Age | 0.661 | (0.521 to 0.840) | 0.001 | 0.700 | (0.536 to 0.914) | 0.009 |
| Weight for height | 0.947 | (0.909 to 0.986) | 0.008 | 0.961 | (0.915 to 1.008) | 0.105 |
| EDI-2 Total | 1.009 | (1.002 to 1.016) | 0.018 | 1.008 | (0.995 to 1.020) | 0.232 |
Economic evaluation results
Economic evaluation at 2 years
Data availability
Full economic data for the 2-year follow-up period were available for 135 young people (81%), 47 in the inpatient group, 45 in the specialist outpatient group and 43 in the general CAMHS group. A comparison of baseline characteristics (site, age, gender, BMI and MRAOS) revealed no significant differences between those included in the economic evaluation and those who were missing and there was no difference overall in missing data between the three treatment groups. Length of follow-up varied somewhat (range 99 to 118 weeks); however, there was no significant difference in length of follow-up between the three treatment groups on average (mean 105 weeks in the inpatient and general CAMHS groups and 106 in the specialist group).
Resource use
The mean number of contacts the young people had with all services over the 2-year follow-up period is detailed in Table 23. Service use differed little between the randomised groups except for use of hospital inpatient and outpatient services. The general CAMHS group spent more time in hospital and had a greater number of outpatient attendances on average than the specialist outpatient or inpatient groups and the specialist outpatient group spent the least amount of time in hospital. Exploring hospital contacts over the 1-year, 2-year and 5-year follow-up periods revealed a reduction in the use of hospital services over time: a larger proportion of days were spent in hospital in the first year (inpatient group 64 days, specialist outpatient 35 days, general CAMHS 67 days) than the second year (inpatient group 12 days, specialist outpatient 20 days, general CAMHS 24 days). By 3–5 years, the average number of inpatient days per annum fell further (inpatient group 5 days, specialist outpatient 9 days, general CAMHS 8 days) (see Table 29). When study participants in one of the outpatient groups received inpatient treatment, this generally occurred after assigned treatment had ended. Details of adherence to treatment have been discussed and are given in Tables 12 and 13.
| Service | General CAMHS (n = 43) | Specialist outpatient (n = 45) | Specialist inpatient (n = 47) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Secondary health services | |||
| Inpatient nights | 89 (159) | 55 (114) | 73 (124) |
| Outpatient appointments | 31 (24) | 26 (22) | 23 (20) |
| Day patient contacts | 1 (5) | 1 (7) | 4 (12) |
| Accident and emergency | 0 (1) | 1 (2) | 0 (1) |
| Community health and social services | |||
| General practitioner | 6 (8) | 7 (9) | 7 (9) |
| Practice nurse | 1 (4) | 3 (10) | 2 (5) |
| Medication | 63% | 58% | 60% |
| Dietician | 0 (0) | 0 (0) | 0 (3) |
| District nurse | 0 (0) | 0 (2) | 0 (0) |
| Health visitor | 0 (0) | 0 (0) | 0 (1) |
| Community paediatrician | 0 (3) | 0 (0) | 0 (1) |
| Community psychiatric nurse | 1 (5) | 1 (7) | 0 (1) |
| Clinical psychologist | 0 (0) | 0 (1) | 1 (8) |
| Counsellor | 0 (1) | 0 (2) | 0 (1) |
| Family therapist | 0 (2) | 0 (0) | 1 (8) |
| Dentist | 0 (0) | 0 (1) | 0 (0) |
| School doctor | 0 (0) | 0 (0) | 0 (2) |
| School nurse | 1 (2) | 1 (2) | 1 (6) |
| Social worker | 0 (1) | 1 (4) | 1 (2) |
| Foster care | 2 (13) | 0 (0) | 0 (0) |
| Eating disorders association | 0 (0) | 0 (1) | 0 (1) |
| Family therapy | 0 (0) | 0 (1) | 0 (1) |
| Education | |||
| State day school months | 12 (10) | 10 (9) | 11 (9) |
| Independent day school months | 1 (5) | 2 (6) | 1 (4) |
| Independent boarding school months | 0 (2) | 0 (0) | 0 (1) |
| Hospital school months | 2 (4) | 1 (2) | 1 (3) |
| Home tuition months | 1 (4) | 1 (3) | 0 (1) |
| School counsellor | 0 (0) | 1 (7) | 1 (7) |
| Education welfare officer | 0 (1) | 0 (1) | 0 (0) |
Although the hospital contacts reported in Table 23 include all medical specialties, the vast majority of contacts were psychiatric (73% of inpatient admissions and 90% of inpatient days) or paediatric (20% of admissions and 10% of inpatient days). Other medical specialties used by the young people (9% of admissions and 0.2% of inpatient days) included gastroenterology, general medicine, haematology, intensive care unit, obstetrics, orthopaedics, plastic surgery and urology.
Time spent by the young people in education was similar across the three groups with evidence of substantial periods out of education in this sample; on average, participants spent a significant proportion of the 2-year follow-up period not in education (approximately 10 out of the 24 months follow-up).
Use of resources by the young person’s primary carer is reported in Table 24. Very few differences between randomised groups are evident.
| Service | General CAMHS (n = 14) | Specialist outpatient (n = 20) | Specialist inpatient (n = 16) |
|---|---|---|---|
| Mean | Mean | Mean (SD) | |
| Secondary-care services | |||
| Inpatient nights | 1 (2) | 0 (2) | 0 (2) |
| Outpatient appointments | 2 (3) | 2 (3) | 4 (7) |
| Day patient attendances | 0 (0) | 0 (0) | 0 (1) |
| Accident and emergency | 0 (0) | 0 (1) | 0 (0) |
| Primary-care services | |||
| General practitioner | 8 (13) | 4 (5) | 7 (8) |
| Practice nurse | 1 (1) | 2 (3) | 1 (2) |
| Counsellor/therapist | 1 (4) | 4 (15) | 5 (18) |
| Medication (%) | 64% | 40% | 56% |
Costs
Mean total costs over the 2-year follow-up are detailed in Table 25. Analysis of covariance demonstrated that there were no statistically significant differences between the three groups. In terms of observed differences, the specialist outpatient group was consistently cheaper than the other two groups and the general CAMHS group was the most expensive of the three. The bootstrapped results differed little from the analyses using the raw data and are therefore not reported here. Hospital costs constitute the greatest proportion of total costs (93% in each group), with relatively few community health and social services being used. In Table 26, the individual service contributions to total costs over the 2-year follow-up are reported. It shows that inpatient and outpatient hospital costs make up 81% and 10% of total costs respectively and that the remaining costs constitute a much smaller proportion of total costs.
| Sector | General CAMHS (n = 43) | Specialist outpatient (n = 45) | Specialist inpatient (n = 47) | ANOVAa | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Min | Max | Mean (SD) | Min | Max | Mean (SD) | Min | Max | p-value | |
| Secondary health care | 37,746 (62,046) | 68 | 269,236 | 24,724 (46,231) | 103 | 244,043 | 32,015 (51,541) | 69 | 280,580 | 0.456 |
| Primary health care | 245 (361) | 0 | 2078 | 385 (873) | 0 | 4325 | 380 (640) | 4 | 2773 | 0.503 |
| Education | 2654 (2228) | 0 | 12,093 | 1595 (1456) | 0 | 6393 | 2098 (2115) | 0 | 8783 | 0.088 |
| Other community servicesb | 150 (806) | 0 | 5244 | 35 (104) | 0 | 445 | 37 (110) | 0 | 513 | 0.504 |
| Total 2-year cost | 40,794 (63,652) | 1483 | 274,838 | 26,738 (46,809) | 462 | 244,174 | 34,531 (52,439) | 86 | 282,508 | 0.426 |
| Total cost per week | 386 (600) | 14 | 2603 | 253 (442) | 4 | 2288 | 325 (487) | 1 | 2588 | 0.423 |
| Service | % of total costs | Cumulative % |
|---|---|---|
| Inpatient | 81.34 | 81.34 |
| Outpatient | 10.33 | 91.67 |
| State day school | 3.03 | 94.70 |
| Hospital school | 2.67 | 97.37 |
| Day patient | 0.76 | 98.13 |
| General practitioner | 0.38 | 98.52 |
| Independent day school | 0.37 | 98.89 |
| Medication | 0.28 | 99.17 |
| Accident and Emergency | 0.15 | 99.32 |
| Community psychiatric nurse | 0.12 | 99.44 |
Figure 5 illustrates change in costs over time, over the 2-year follow-up. It shows the total cost per participant separated by year and clearly demonstrates that the majority of the costs were incurred in the first year after entry to the study, with much lower costs incurred in the second year.
FIGURE 5.
Total cost per young person by year.
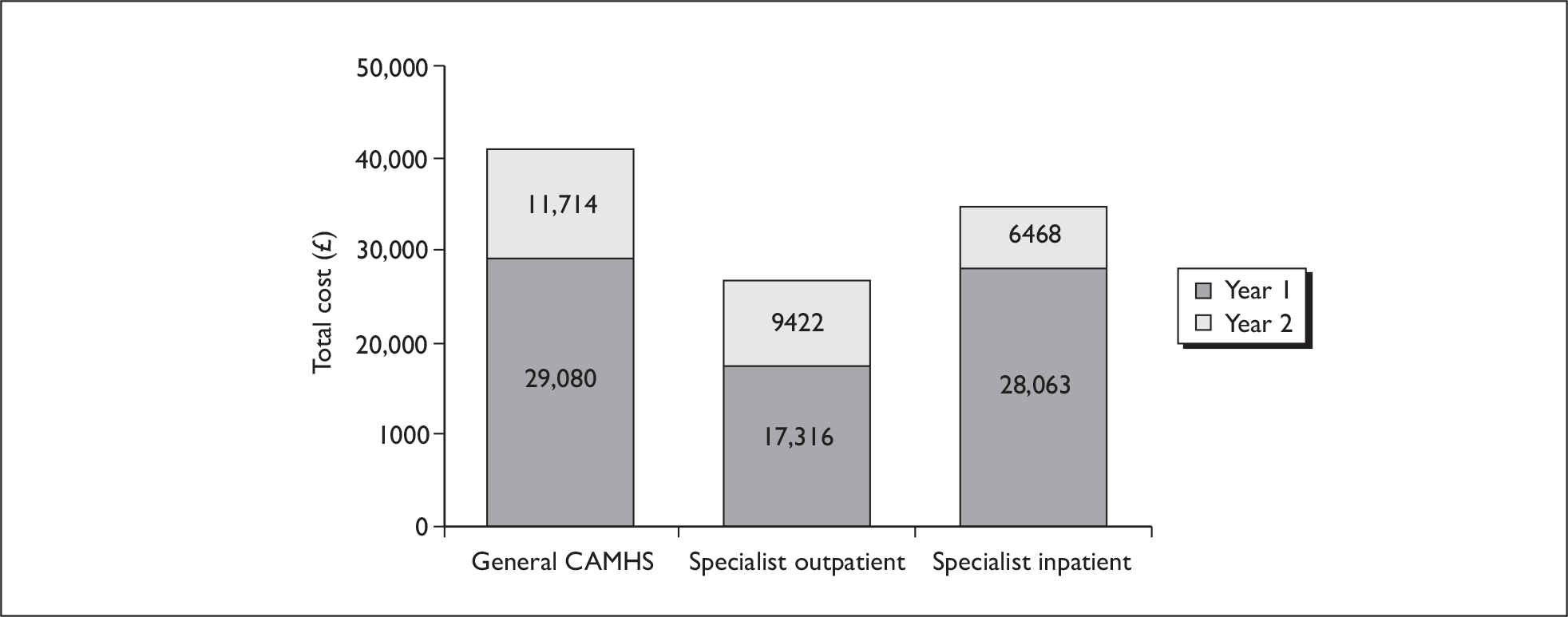
Mean total costs of health services used by the young person’s primary carer are reported in Table 27. Overall the primary carers of the specialist outpatient group cost slightly less than those of the inpatient and general CAMHS groups, but this difference was not statistically significant.
| Service | General CAMHS (n = 14) | Specialist outpatient (n = 20) | Specialist inpatient (n = 16) | ANOVAa |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p-value | |
| Community health services | 297 (670) | 196 (514) | 223 (382) | |
| Hospital services | 258 (335) | 218 (311) | 440 (805) | |
| Medication | 152 (424) | 77 (113) | 87 (252) | |
| Total cost | 707 (840) | 491 (772) | 750 (1199) | 0.68 |
Cost-effectiveness analysis
The cost-effectiveness analysis at the 2-year follow-up point employed the rules of dominance and found that the specialist outpatient treatment (bootstrapped mean cost per patient £26,797; bootstrapped mean MRAOS effect 8.35) dominates the inpatient group (£34,371; 8.26) and the general CAMHS group (£40,520; 8.26) because it is both cheaper and more effective. The cost-effectiveness acceptability curve in Figure 6 illustrates the uncertainty associated with the costs and effects of the three treatments at 2 years. It demonstrates that if decision-makers were willing to pay nothing for a unit increase in MRAOS score, then there would be a 80% chance of specialist outpatient services being the most cost-effective strategy, 16% for inpatient services and only 6% for general CAMHS. The probability of specialist outpatient services being the most cost-effective strategy decreases with increasing levels of willingness to pay for gains in effectiveness. This levels out at around 47%, but remains higher than the other two strategies over the full range of willingness-to-pay values shown, and beyond.
FIGURE 6.
Cost-effectiveness acceptability curve for MRAOS score – three arms.
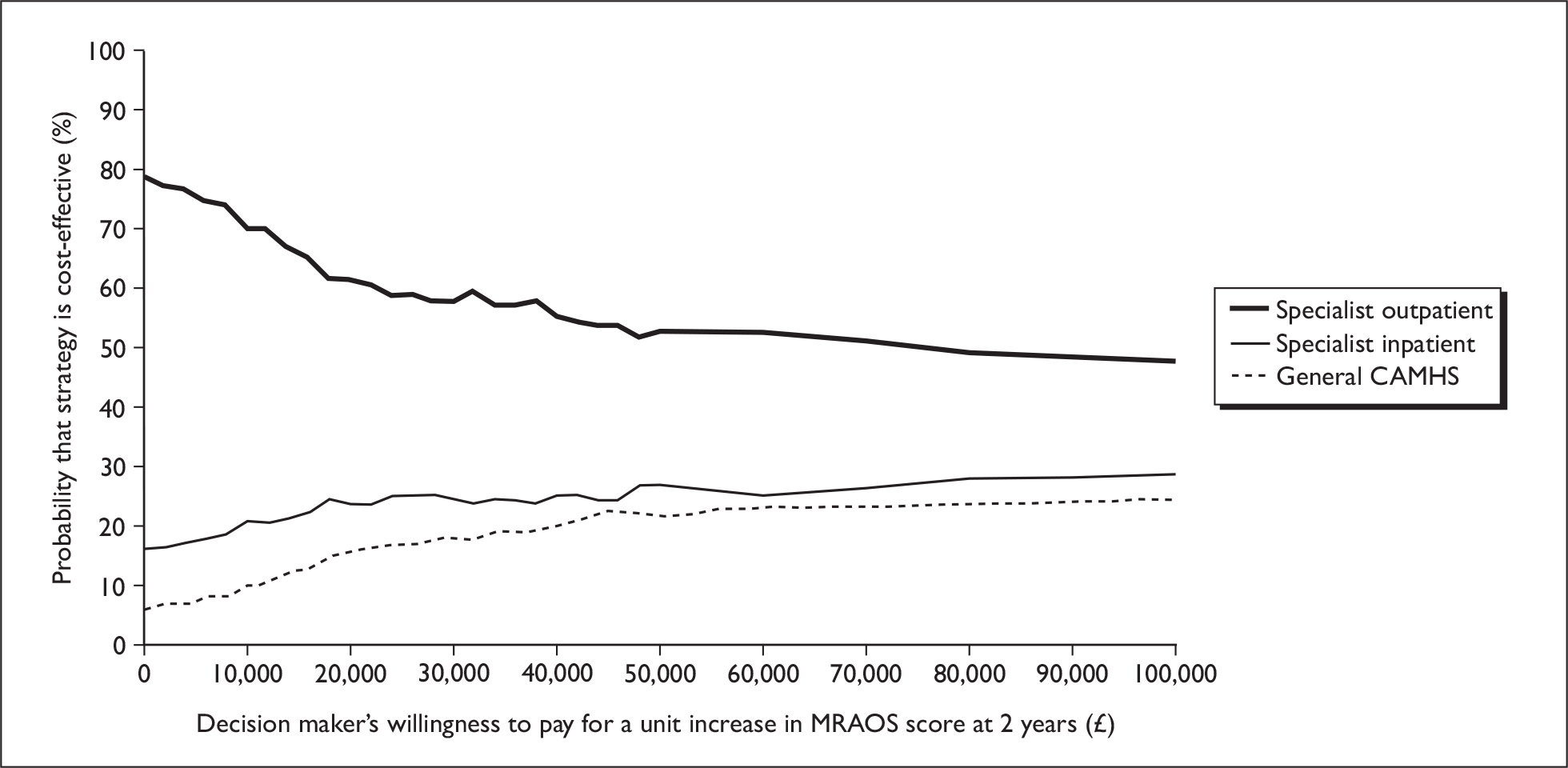
Figure 6 suggests that the probability of our first hypothesis being true is high, i.e. that specialist outpatient services are more cost-effective than general outpatient services. Figure 7 depicts the cost-effectiveness acceptability curve for the second hypothesis – that outpatient services (specialist combined with general CAMHS) are more cost-effective than inpatient services. It shows that there is a greater probability of outpatient services being more cost-effective than inpatient services for the full range of values of willingness to pay.
FIGURE 7.
Cost-effectiveness acceptability curve for MRAOS score – inpatient versus outpatient.
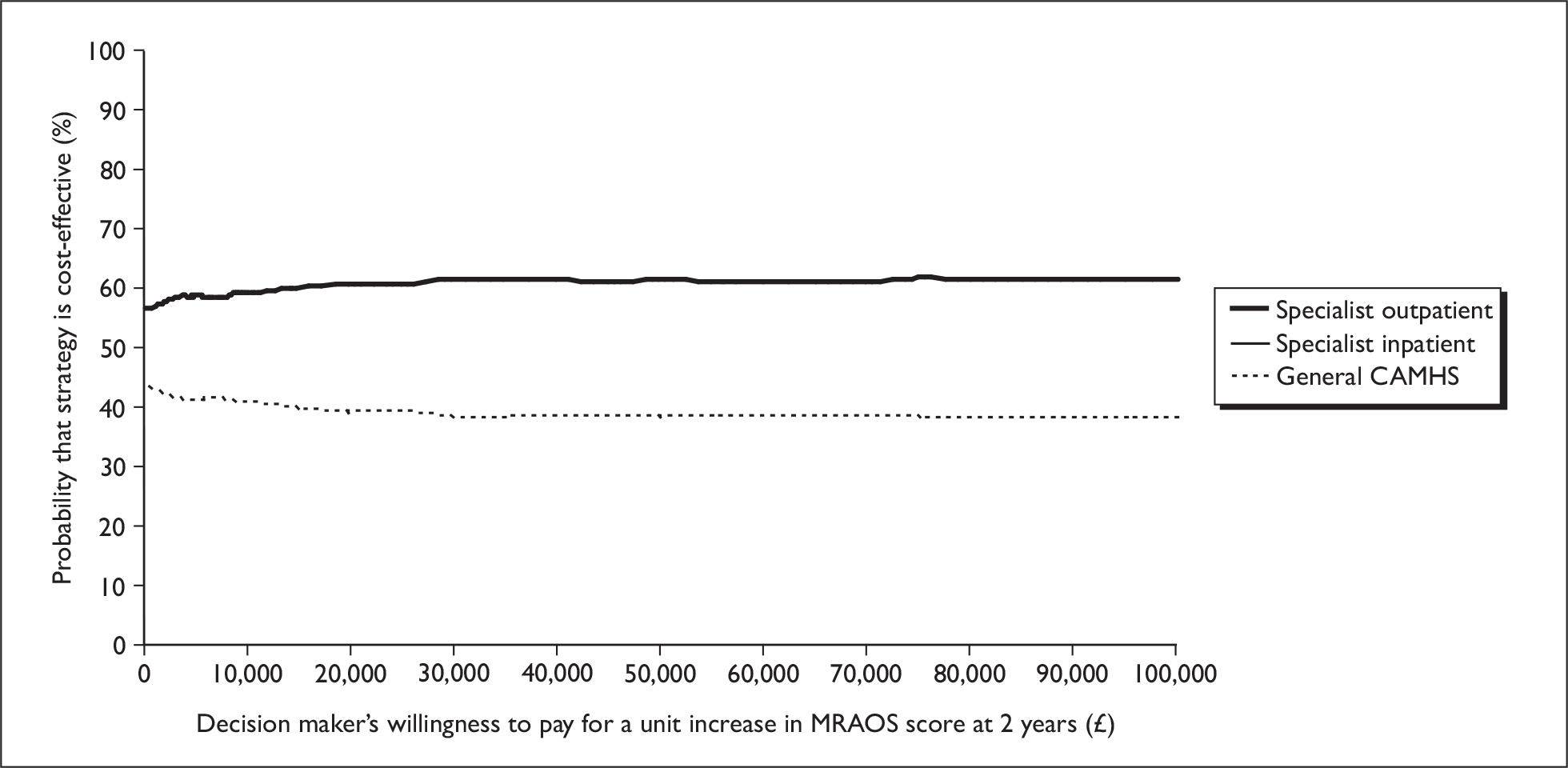
Sensitivity analyses explored the impact of missing data on the results of the cost-effectiveness analysis. Similar relationships between the three arms of the study were found, with specialist outpatient services having a higher probability of being cost-effective than the other groups over a wide range of willingness-to-pay values, using both last-value-carried-forward and mean imputation techniques. At a zero level of willingness to pay for effectiveness gains, the probability of being the most cost-effective option ranged between 72 and 80% for specialist outpatient services, 13 and 14% for inpatient services and 7 and 16% for general CAMHS. The probability of general CAMHS being the most cost-effective option remains low for all values of willingness to pay. The probability of inpatient services being the most cost-effective option increases as willingness to pay increases, whereas the probability for specialist outpatient services falls. At values of willingness to pay over £100,000, the probability for inpatient services overtakes that for specialist outpatient services but only for the last-value-carried-forward imputation. In all other missing data sensitivity analyses, the specialist outpatient service dominates across the full range of values of willingness to pay.
The cost of education received by study participants was included to explore the additional costs associated with greater disruption as a result of longer admissions to hospital or greater illness severity, such as hospital school attendance or home tuition. However, it is also the case that education may be more expensive because a young person has better attendance (a good outcome). For this reason, we undertook a further sensitivity test, which excluded the cost of education. This analysis left the results of the base-case cost-effectiveness analysis unchanged.
Economic evaluation at 5 years
Data availability
Full economic data for the 5-year follow-up period were available for 102 young people (49%). Of those cases randomised, full economic data were available for 71 (41%), 23 in the inpatient group, 28 in the specialist outpatient group and 18 in the general CAMHS group. A comparison of baseline characteristics (site, age, gender, BMI and MRAOS) revealed some differences between those included in the 5-year analysis and those who were missing. Although there was no difference overall in missing data between the three treatment groups, those in the preference arm were more likely to have been followed up than those in the randomised groups. In addition, the young people for whom data were available at follow-up were slightly older than those for whom data were missing. Length of follow-up varied (range 131–223 weeks); however, there was no significant difference in length of follow-up between the three treatment groups on average (mean 168 weeks in the inpatient group, 165 weeks in the general CAMHS group and 166 weeks in the specialist outpatient group).
Accommodation and employment
The type of accommodation and employment status of the young people 3–5 years after baseline is detailed in Table 28. During this period, the young people tended to live at home with their parents or independently and there was little use of supported accommodation or residential care.
| Service (n = 102) | Mean (SD) |
|---|---|
| Domestic accommodation (months) | 27 (11) |
| Independent living (months) | 8 (11) |
| Residential care (months) | 0 (1) |
| Supported accommodation (months) | 0 (2) |
| Hostel (months) | 0 (1) |
| Currently employed (%) | 61% |
| Months employed | 17 (14) |
| Days off sick | 10 (28) |
| Months on benefits | 3 (9) |
Almost two-thirds of the participants were employed at some point during the 3 years of follow-up, for an average of 17 months. Self-reported time off work due to illness was low, at only 10 days on average, whereas the average length of time on benefits was 3 months.
Hospital use and cost
Use and total cost of hospital services during the 3–5 years after baseline for the randomised groups is detailed in Table 29. There appear to be some quite substantial differences in the use of hospital services between randomised groups, for example the mean number of inpatient nights in both the specialist outpatient and general CAMHS groups is much higher than that in the inpatient group. In addition, the mean number of day-patient attendances in the specialist outpatient group is far higher than attendances in the inpatient and general CAMHS group. Closer inspection of the data reveals that these differences are the result of a skewed dataset where a small number of young people in each group made substantial use of hospital services. For example, two young people in the specialist outpatient group spent very long periods of a year or more in inpatient services and one young person in the specialist outpatient group attended a day-patient service on 730 occasions. Despite these differences in service use, there are no overall differences in total costs between the randomised groups at 5 years. This is largely because of the higher unit costs of inpatient and day-patient attendances at private facilities, which were observed more often in the general CAMHS and inpatient groups than in the specialist outpatient group.
| General CAMHS (n = 18) | Specialist outpatient (n = 28) | Specialist inpatient (n = 23) | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Service use | |||
| Inpatient nights | 25 (106) | 28 (89) | 14 (62) |
| Outpatient appointments | 6 (11) | 14 (29) | 5 (11) |
| Day-patient attendances | 1 (3) | 26 (138) | 10 (50) |
| Accident and emergency | 1 (1) | 1 (5) | 0 (1) |
| Costs (£) | |||
| Inpatient nights | 13,758 (58,233) | 10,874 (35,128) | 8867 (41,561) |
| Outpatient appointments | 1005 (2153) | 2263 (5339) | 652 (1860) |
| Day-patient attendances | 376 (1553) | 2356 (12,399) | 5743 (27,523) |
| Accident and emergency | 63 (125) | 142 (473) | 42 (117) |
| Total costs | 15,203 (61,275) | 15,636 (46,545) | 15,304 (69,083) |
Regression analysis
Variables examined in the regression analysis are reported in Table 30. Univariate analysis revealed that higher total costs were significantly associated with lower baseline percentage weight for height ratio, lower MRAOS score, higher MFQ scores and higher HoNOSCA-CR, all in the anticipated direction (i.e. higher costs associated with greater morbidity). Weight for height ratio remained the only variable significantly and independently related to cost in multiple regression analysis (Table 31). The results demonstrate that for a unit reduction in the weight for height ratio, total costs over the full 5-year follow-up period increased by £4024. The regression model was able to account for less than 10% of the variation in total costs (adjusted R2 = 0.080), suggesting substantial unexplained variation in this group of young people.
| n | Mean cost (£) | p-value | |
|---|---|---|---|
| Sex | |||
| Male | 6 | 25,105 | 0.520 |
| Female | 96 | 56,013 | |
| Age | |||
| ≤ 15 years | 71 | 48,118 | 0.915 |
| > 15 years | 31 | 68,113 | |
| ED type | |||
| Restrictor | 75 | 57,037 | 0.676 |
| Binge–purger | 27 | 46,303 | |
| Length of history of eating disorder | |||
| ≤ 15 months | 62 | 44,776 | 0.280 |
| > 15 months | 38 | 70,401 | |
| Percentage weight for height | |||
| ≤ 78 | 51 | 74,913 | 0.002 |
| > 78 | 51 | 33,478 | |
| MRAOS | |||
| ≤ 5 | 51 | 84,106 | 0.003 |
| > 5 | 51 | 24,285 | |
| MFQ score | |||
| ≤ 25 | 42 | 25,363 | 0.104 |
| > 25 | 57 | 75,978 | |
| HoNOSCA-CR | |||
| ≤ 19 | 53 | 26,543 | 0.014 |
| > 19 | 49 | 84,105 | |
| Home situation | |||
| Living with both parents | 72 | 52,850 | 0.854 |
| All other home situations | 30 | 57,425 | |
Chapter 4 User and carer satisfaction
Method
All 215 participants and their parents (randomised and non-randomised) were contacted at 1 year for a full clinical assessment. At this point they were given a satisfaction questionnaire to return anonymously by post. This asked them to rate their prior expectations of any treatment they had received (randomised or not) on a seven-point Likert scale (from very positive, to very negative). It then asked them their subsequent level of satisfaction with each treatment received over the course of the year. Participants were also invited to give free comments about any aspect of the services they had received. Many subjects received further treatment during year 2 of the trial. If this included one of the three treatment options not received in year 1, their views on this were elicited, by way of further quantitative ratings and comments by questionnaire at the 2-year follow-up. The quantitative (Likert scale) ratings were collated and simple frequencies were compared across treatment groups.
The qualitative evaluation comprised an analysis of the free comments from the questionnaire supported by data derived from a subsequent series of focus groups.
The authors were familiar with the eating disorder satisfaction literature but a process for data analysis was chosen that aimed to minimise the effect of any preconceptions. The free comments were analysed with the aim of establishing common satisfaction themes through a series of steps, following the established qualitative methodologies described by Mason. 74 First, the comments were collected and coded according to treatment option and whether by parent or child. Then comments from one of the two sites (n approximately 200) were reviewed separately by the three authors who proposed their own series of themes (open coding). These themes were then extensively discussed between coders, resulting in a consensus and a provisional set of agreed themes.
The printed comments were then reduced to individual elements, coded by whether they were positive or negative about the service in question and collated according to the provisional themes. The comments allocated to each theme were reread and the themes were modified several times until there was agreement on the minimum number that reflected the content of the comments. The rest of the data were then allocated according to these themes (focused coding) with no new themes emerging from these data.
In the second qualitative stage, focus groups for parents and adolescents were arranged in the two main sites to further explore the themes and identify any other important issues that were not highlighted in the questionnaires. Purposive sampling was used to select a varied group of participants, receiving each of the treatments but only a relatively small number (n = 21) were able to take part. Incidental expenses were offered.
A questioning route was developed for the focus groups that included general questions about satisfaction and specific questions related to the themes we had identified from the questionnaires and that allowed time for other themes to be raised by participants, following prescribed conventions. 75
The sessions were audio-taped, transcribed, coded and analysed for thematic content in a similar manner to the questionnaire data. 74 Themes were developed, the materials in the focus group were aggregated and the themes were reviewed and modified several times. Other members of the research team then reviewed the themes and the illustrative quotes to reach a consensus that they could be justified from the transcribed material.
To ascertain the independent validity of the themes, an external researcher was given a structured recoding task to match all 430 comments from the questionnaires and focus groups to a list of 10 themes or identify additional themes not covered.
Results
The questionnaire response rate was 76% (160 out of 215) for adolescents and 71.8% (150 out of 215) for parents. The rate of response by treatment group was proportional to the numbers receiving it, suggesting that there was no response bias by treatment received. As some participants received more than one treatment, the total number giving an opinion of each treatment option exceeded the number of participants in the trial. For the purposes of analysis, the three negative categories and the three positive categories were collapsed for both expectation and satisfaction.
Prior expectation
Parents had very positive expectations of all treatment options, significantly higher than those of their children (see Table 32). There were no statistically significant differences in parental expectations between treatments but adolescents’ expectations of general CAMHS treatment were lower than of the more specialist options.
| Inpatient | General CAMHS | Specialist outpatient | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adolescent (n = 46) | Parent (n = 48) | Adolescent (n = 83) | Parent (n = 83) | Adolescent (n = 82) | Parent (n = 74) | ||||||
| Expectation (n = 46) | Satisfaction (n = 40) | Expectation (n = 47) | Satisfaction (n = 44) | Expectation (n = 80) | Satisfaction (n = 80) | Expectation (n = 77) | Satisfaction (n = 76) | Expectation (n = 80) | Satisfaction (n = 78) | Expectation (n = 69) | Satisfaction (n = 68) |
| 11 | 12 | 1 | 7 | 29 | 30 | 7 | 19 | 20 | 17 | 3 | 8 |
| 6 | 3 | 1 | 6 | 23 | 8 | 4 | 10 | 13 | 11 | 2 | 4 |
| 29 | 25 | 45 | 31 | 28 | 42 | 66 | 47 | 47 | 50 | 64 | 56 |
Satisfaction
Parents reported being generally satisfied with all treatments but were significantly more satisfied with specialist outpatient treatment than with general CAMHS (Table 32), inpatient treatment showing intermediate levels of satisfaction. However, overall satisfaction levels were notably lower than their very high prior expectations.
Adolescents had more mixed experiences of treatment, with significantly lower overall levels of satisfaction than parents. Many young people rated the treatments negatively. However, as with their parents, adolescents appeared more satisfied with specialist outpatient treatment than general CAMHS but this finding was not statistically significant. Whereas parents’ expectations appeared unrealistically high, the adolescents’ expectations seemed borne out by their subsequent experience.
Qualitative results
General
Most of the questionnaire respondents added at least one comment. In total 375 responses from the questionnaires were analysed as follows:
-
adolescent inpatient = 40
-
adolescent general CAMHS = 67
-
adolescent specialist outpatient= 64
-
adolescent other treatment = 14
-
parent inpatient = 48
-
parent general CAMHS = 66
-
parent specialist outpatient = 65
-
parent other treatment = 19.
Some responses incorporated more than one comment and were therefore split, yielding a total of 430 comments.
There were slightly more positive than negative comments. The 10 most common themes relating to treatment satisfaction are presented in Table 33; 71% of the comments fitted into these themes. A large number of the remainder comprised general appraisals of services (repeating the Likert scale ratings) or comments about the outcome of treatment. The independent rater’s validity check revealed a very high level of agreement for the major themes and resulted in even more examples of comments about clinician expertise being identified. An extra theme emerged from this exercise of the perceived value of developing insight into the condition.
| Theme | Number of comments |
|---|---|
| Importance of an individual relationship | 101 |
| Importance of expertise | 48 |
| Parental involvement in treatment | 39 |
| Communication with parents and other agencies | 28 |
| Mixing with other patients | 22 |
| Importance of dietary therapy | 19 |
| Access and flexibility of treatment | 12 |
| Delay or lack of intensity of treatment | 10 |
| Too much focus on psychological factors (motivation or talking) | 10 |
| Too much focus on weight | 7 |
Themes highlighting differences between treatment groups
The importance of expertise (48 comments)
‘I think the trouble with CAMHS is that they do have a working knowledge of adolescence and mental health disorders but not necessarily with the anorexia side of it…Yeah I mean they tried their best but…’ [parents’ focus group]
The highest number of negative comments and some of the most strongly worded comments were related to this theme and were almost exclusively made in relation to a perceived lack of expertise in general CAMHS. We wondered why specialist knowledge should be so important, if the things that were most frequently identified as helpful were generic skills that should be found in all services. In the focus groups it appeared that a combination of these qualities was considered essential. Therapists needed to gain the trust of parents and young people by demonstrating their familiarity and understanding of what people with eating disorders may go through.
‘The most helpful aspect of the treatment was that my daughter trusted the people she was working with and was therefore more ready to follow their advice. I think she trusted them because they were experienced and sympathetic’ [parent questionnaire]
This expertise also needs to be used sensitively (or expertly). It was not appreciated if it was conveyed in the form of too much direct advice giving or comparison with previous patients:
‘They say “Yeah well I’ve seen one girl who did this and did this and now she’s better so now you can do it” but I’m not her’ [adolescent focus group]
Availability of dietetic therapy (19 comments)
The only professional role the importance of which was repeatedly singled out was the dietician’s. This was highly valued and there was some concern when this service was not available. Both of the specialist services involved had dedicated specialist dietetic input. This is often not available for CAMHS teams without such high patient flows.
Themes highlighting differences between parents and young people
Overall parents made more comments related to service delivery issues, availability of services, communication, access and flexibility, and in the focus groups raised major concerns about the difficulties of getting the eating disorder recognised in primary care.
Family therapy and parental involvement (39 comments)
Parent and family support was very often highlighted.
As parents we did get a lot of support and helpful advice on how to cope and manage our daughter’s illness [parent questionnaire]
Parents greatly valued family work and wanted to be kept informed and to be able to ask questions. There was unease about being excluded from some aspects of treatment because of confidentiality issues or a perceived need to protect the therapeutic relationship. On the other hand, there was an appreciation that some degree of separation from parents had its place in helping the young person to talk. In the focus groups there was strong advocacy for parent support groups and strong views that siblings were not well catered for.
Young people appreciated the need for family work but were not as enthusiastic about it as their parents. In the focus groups it was apparent that young people thought it vital that their parents receive support themselves but found the joint sessions to be challenging and often unhelpful.
Contrary to our preconception that some forms of family therapy might be perceived as blaming of parents, there were no comments about this. This issue was specifically addressed in the focus groups where a number of parents reported that they valued professionals actively helping them to disabuse themselves of feeling guilty that their child had AN.
You think it yourself ‘did I do something wrong?’ as a parent…I think all parents do with a lot of illnesses but I think they were very clear here that it’s a lot of issues, it’s a lot of things, it’s complex, it’s genetic, it’s personality it’s partly this…you haven’t to blame yourself [parents’ focus group]
Common themes across treatment groups
Many of the satisfaction comments applied to all treatment options.
Importance of an individual therapeutic relationship (101 comments)
The most prominent theme that emerged was the important impact of individual therapeutic relationships. Around 80% of these comments spoke in positive terms about the helpfulness of specific clinicians.
It was good to go and talk to a specialist who understood my feelings and fears. [A]’s understanding and friendliness was very useful to me and it was good that she listened [adolescent questionnaire]
More than 50 comments named clinicians who were appreciated, mostly for generic interpersonal and psychotherapeutic skills such as listening, understanding, seeing the whole person and forming a good relationship with them.
Themes eliciting polarised views
Mixing with other inpatients (22 comments)
An area where there were strongly polarised views among both young people and parents, was the helpfulness, or otherwise, of mixing with other patients in inpatient units. There were many comments about this in the questionnaires, which were explored further in the focus groups. Some extolled the benefits of mixing with non-eating-disordered patients to gain broader perspectives, share common difficulties and obtain distance from other patients with eating disorders. Others had very negative views on the stress of being on a mixed unit with young people with serious mental disorders and felt the influence of other eating-disordered patients was supportive.
Focus on weight and physical issues (seven comments)
We had expected, on the basis of the existing literature, to find a number of comments about there being too much focus on weight and other physical factors. There were only seven comments to this effect and in contrast there were 10 comments about there being too much focus on psychological issues such as motivation.
Chapter 5 Summaries of findings
Summary of clinical trial
The TOuCAN trial was successful in recruiting in excess of the required number of cases as calculated by the power estimate. As such, this trial represents the largest RCT of AN carried out to date; successfully recruiting the vast majority of new cases known to CAMHS during the recruitment phase. It is a population-based pragmatic, effectiveness RCT based on the range of NHS treatments available in the north-west of England and probably typical of the rest of the country. One of these treatments (the specialist outpatient programme) was manualised, with fidelity checks; the other two arms represented treatment ‘as usual’ in generic CAMHS and the four regional inpatient units.
Tracing and follow-up were also satisfactory and almost complete to the 2-year time point but less so at 5 years. Reliable and robust outcome measures were used.
Adherence to treatment allocation was less than optimal, reflecting the real world of services and in particular attitudes of patients with AN and their families to treatment. Nevertheless, the data collected and its analysis are adequate to answer the clinical hypotheses:
-
Inpatient treatment is not more clinically effective than outpatient treatment.
-
Specialist treatment was not found in this study to be more effective than general CAMHS treatment – at least in the short term but it may possibly be in the longer term.
The subanalysis of those allocated to inpatient treatment, examining adherence, suggests poorer outcomes for those actually admitted, even taking into account the baseline levels of measured psychopathology. However, these findings should be treated cautiously given that the two subgroups (adhering and not), may differ on significant but unmeasured variables such as motivation and ability to respond to the assessment interview in the immediate days before admission was available.
The analysis of prognostic indicators reveals that baseline levels of morbidity (chiefly the main outcome measure – MRAOS) and degree of thinness (percentage weight for height) are powerful predictors of service use and medium-term to long-term outcome. Self-reported eating psychopathology at baseline is also a notable predictor of long-term outcome based on the main outcome measure.
Anorexia nervosa is often a chronic disorder in which a number of young people are still ill with the condition at 5-year follow-up. However, it is not primarily a remitting and relapsing disorder, with those who managed to achieve recovery tending to stay well.
Summary of economic analysis
This study represents the first economic evaluation of alternative strategies for the treatment of AN using primary data collected from an RCT.
At 2 years, the specialist outpatient group were the least costly and the general CAMHS group was the most costly, although these results were not statistically significant. These findings were robust to sensitivity analysis of the discount rate and in analyses of missing data. Observed differences in total mean cost per patient were almost entirely the result of differences in the length of time spent in hospital.
The majority of inpatient admissions took place during the first year and there was substantial cross-contamination of groups. For example, although not randomised to psychiatric inpatient services, the general CAMHS group spent almost as much time in hospital as the inpatient group. This finding suggests that general CAMHS were less successful at maintaining the young people in the community than the specialist outpatient services.
With the exception of CAMHS, participants used very few community health and social services. The number of months in education was similar across the groups on average, though the relatively low mean number of months in this adolescent population highlighted the significant proportion of time participants spent out of education, presumably as a result of their illness.
The annual service costs of caring for this group of young people, £17,000, are substantial and much higher than the cost of conditions generally treated in the community – for example, conduct disorder with annual service cost estimates varying between £1300 and £3200. 58,72 However, the annual cost is similar to the cost of a cohort of young people with mental health problems that led to them being treated in child and adolescent psychiatric inpatient wards, estimated to be £24,000 per admission. 76 The slightly higher costs in this case were the result of longer mean lengths of stay, on average.
The results of the cost-effectiveness analysis reveal that specialist outpatient services were the dominant treatment option in terms of incremental cost-effectiveness, as they were more effective and less costly. The cost-effectiveness acceptability curves, which consider associated uncertainty, support this finding. In terms of our hypotheses, the data suggest that specialist outpatient services have a higher probability of being cost-effective than general CAMHS and that outpatient services (specialist combined with general) have a higher probability of being cost-effective than inpatient services.
By the 5-year follow-up, hospital-use information was available for less than half of the randomised cases, and the skewed nature of the data (because of a small number of young people with lengthy hospital or day-case admissions) makes it difficult to reach conclusions on differences in resource use and costs. Some clear findings do emerge however. First, the trend in reductions in hospital use between years 1 and 2 was maintained over the longer term with, on average, much lower use of hospital services by 5 years follow-up. Second, there were no differences in average total cost per young person between randomised groups.
Univariate regression analysis at 5-years demonstrated that more severe cases of anorexia nervosa at baseline, including those with lower percentage weight for height and lower MRAOS scores (poorer health), cost significantly more in terms of hospital costs over the 5-year follow-up. In addition, those with more severe mental health problems, as measured by the MFQ and the HoNOSCA-CR, cost significantly more in terms of hospital costs over the 5-year follow-up. However, when these variables were included in a multiple regression analysis, only weight for height remained significant, suggesting that thinness at baseline was the most important factor predicting high costs in terms of hospital services over 5 years.
Summary of satisfaction study
This study provided a wealth of information from both users and carers in relation to their experience of the range of treatment approaches.
Overall, levels of satisfaction with services were good with young people being twice as likely to express positive as negative views of their treatment. Parents were much more satisfied with about five times as many expressing positive as negative views of treatment. Parents were consistently more satisfied than young people with each treatment, but both parents and young people were more satisfied with specialist than general treatments. The satisfaction of both young people and their parents was largely based on their confidence in ‘expertise’ and forging a good relationship with an individual therapist working on either an inpatient or an outpatient basis.
Chapter 6 Conclusions
-
Lengthy inpatient psychiatric treatment, although commonly employed for adolescent AN, offers no advantage over good-quality outpatient care and is more expensive.
-
Treatment in specialist services offers little advantage over good-quality multidisciplinary care delivered in generic CAMHS with a family approach, although both young people and their parents prefer it.
-
Treatment in a specialist outpatient programme is likely to be the most cost-effective treatment approach for adolescent AN, chiefly because it reduces the need for later inpatient care.
-
The traditional model of stepped care from outpatient to inpatient care for those who fail to respond is not supported by this trial, as transfer from outpatient to inpatient care after the study period generally yielded poor outcomes.
-
As AN is associated with serious physical and psychological risk, inpatient admission is probably unavoidable because approximately 50% of patients expecting to be treated as outpatients were admitted in the first 2 years of the study. This trial was unable to reach conclusions about the best setting or length of admission, for such unplanned admissions.
-
Anorexia nervosa in adolescents is commonly a chronic condition lasting a number of years, in which any one episode of care is unlikely to result in a complete cure.
-
Nevertheless, at 2 years from presentation to CAMHS only 26% have the full syndrome, whereas 33% have gone into remission, often with recovery lasting to 5 years.
-
Achieving a very low weight (as a % of expected weight) in the early stages of the illness and severity, as measured by a global assessment measure for eating disorders comprising psychosocial as well as physical aspects, is a good predictor of long-term outcome as well as use of services.
-
Achieving a very low weight (as a % of expected weight) in the early stages of the illness is also a good predictor of long-term total costs.
-
Young people and to some extent their parents have low expectations that generic CAMHS will meet their treatment needs and they want treatment in specialist centres, delivered by staff with expertise in managing the condition.
-
Young people’s experience of treatment is mixed but they tend to be satisfied with treatment in specialist services. Parents are generally quite satisfied, particularly with specialist care, even when outcomes are poor.
-
There are a number of areas in which there is a lack of consensus among service users about aspects of care which are valued and disliked. Examples include the balance in emphasis between physical and psychological aspects of care and the desirability or otherwise of mixing with other young people with eating disorders.
Discussion
This pragmatic treatment trial has attempted to address the issues posed by the brief concerning the merits of different models of care for adolescent AN. Specifically, little was previously known of the relative clinical effectiveness and cost-effectiveness of different service settings or young people’s and their parents’ satisfaction with these. 11 The brief was an important one because of the extremely high cost of inpatient care,35,61 when stays commonly last several months and when AN makes a major demand on adolescent inpatient services. 5 The facility to offer long-term psychiatric (as opposed to medical) treatment in the UK has often been highly valued, clinical intuition suggesting that more intensive treatments should be more effective than briefer, non-specialist treatment for a condition that is often chronic and has a high morbidity and mortality.
Previous cohort and treatment studies28,37,41 have raised questions about the value of inpatient care, but without a randomised allocation to inpatient care it has been difficult to evaluate the benefits of admission over and above outpatient management; although the one systematic review concluded that outpatient treatment in a specialist eating disorder service was as effective as inpatient treatment in those not so severely ill as to warrant emergency admission. Furthermore, these reviewers estimated the costs of outpatient treatment to be approximately one-tenth the cost of inpatient treatment. 27
Not surprisingly, given the ambivalence of young people with AN to treatment and the large personal and family investment required of those admitted to inpatient care, adherence to this arm of the trial was unavoidably less than optimal. In addition, given the often chronic nature of the condition, it was not possible to keep patients treatment-free between the treatment and follow-up phases. It might be argued that a 6-month follow-up assessment point would have been useful to assess the trial interventions before the picture became blurred by subsequent treatment. However, we deliberately avoided doing this as recommendations in this field11 suggest 2 years as a minimum useful follow-up point and because it is well known that inpatient gains are often short-lived (for example in the St George’s and Maudsley trials28,41) and so such an assessment point would be likely to favour this treatment arm.
Nevertheless, this trial has reached some important conclusions, particularly given the recruitment design, which was highly inclusive, population-based and used readily available CAMHS. This study is much larger than those reported in the literature to date and includes around four-fifths of incident cases known to child and adolescent mental health services in the north-west of England over a 3-year period. We achieved a high follow-up rate with demonstrably reliable outcome measures.
The findings challenge a number of notions about care for this disorder. In particular, psychiatric inpatient treatment does not confer advantages over outpatient care, and is associated with a lower probability of being cost-effective than the combined outpatient groups. Although adherence to inpatient care was only 50%, the subanalysis reveals that rather than the outcome of this arm being adversely affected by a lack of adherence, in fact, the overall (intention-to-treat) outcomes are improved by the better outcomes of those declining admission once offered it. The subanalysis of those accepting or declining admission within the inpatient arm should, however, be interpreted with caution. It may be that the decision to accept randomised admission is based on a number of negative prognostic variables, rather than it reflecting on the inpatient treatment itself. Based on the predictive model for admission developed among patients not admitted, one can see that those adhering to admission had a higher probability of admission based on baseline characteristics. Possibly some unmeasured variables such as motivation or family resources may have accounted for the difference in response.
This finding does not deny the necessity of emergency medical management of physical complications in an inpatient setting, which may on occasions be life-saving, but our results do suggest that inpatient management is rarely associated with comprehensive recovery, as opposed to improvement or stability within the condition.
The finding that specialist care offers few advantages requires clarification. In some respects the findings mirror the results from the New Zealand trial,77 in which an adult (and probably less severely unwell) series did as well with non-specific supportive clinical management as with two specialist psychological therapies. As with this trial, it is important not to underestimate the quality of the ‘control’ or generic intervention. General CAMHS (as opposed to adult Community Mental Health Teams, for example) commonly offer psychological therapies (often based on CBT) and family-based treatments in the context of a developmental perspective – an approach which suits this condition well. However, the greater success of specialist outpatient services at maintaining young people in the community resulted in a poorer performance in terms of cost-effectiveness for general CAMHS. This relative cost-effectiveness of specialist care may be the result of the inexperience of managing AN in the CAMHS teams and the resulting anxiety which may have led to the more frequent hospital admissions and costs of this treatment. This anxiety may in turn have transmitted itself to the families involved, leading to lower levels of satisfaction.
It is also of note that the specialist outpatient arm was the only manualised treatment and also incorporated fidelity checks. This may have added to its effectiveness and these components are essential in comparing findings across different studies.
Our study suggested that there was a reasonably high level of satisfaction for each of the treatment groups in this trial, by parent and, to a lesser extent, patient perspective. The overall response rate (over 72%) would appear good for a satisfaction measure, but we are unable to say whether non-responders would have been less satisfied over all, or with one particular treatment option. As in a Norwegian study,78 this was in spite of the clinical outcomes. When expectations of a service are greater than perceived performance, then quality will be judged as less satisfactory and dissatisfaction will be high. Although definitions of satisfaction vary, satisfaction has been defined as being about ‘the appraisal of the extent to which the care provided has met the individual’s expectations and preferences’. 79 In our study, parental expectations were very high, rendering them liable to dissatisfaction when the experience was less than anticipated.
The literature often reveals negative experiences of inpatient treatment. A postal survey of members of the Eating Disorders Association78 revealed mixed experiences, with slightly more respondents feeling this made the situation worse than found it very helpful. These findings were largely replicated in a Norwegian survey that showed patients were relatively satisfied with outpatient individual and group therapies (and to a lesser extent with family therapy) and dissatisfied with inpatient treatment. 81 This survey showed that patients particularly valued therapist expertise, results duplicated in a survey of 300 patients from the Netherlands. 80
The most reported theme in our series – the importance of a relationship with an individual professional – replicates findings from previous research in the eating disorder field and within mental health more generally. Good generic psychotherapeutic skills are seen as very important by service users. All three treatment modalities in the study generally aimed to provide these and there was no perception that therapy was overly focused on physical aspects.
General CAMHS compared unfavourably with specialist outpatient and inpatient services, mainly because of a perceived lack of expertise with eating disorders. It may be that when parents and adolescents are accessing specialist services, they feel reassured that they are in the right hands because of the ‘specialist’ status even if they are not making significant clinical progress. This view was borne out by the quantitative data, which suggested that adolescents had lower expectations of CAMHS, than other treatments, though strikingly 86% of parents had positive expectations of CAMHS treatment. During the TOuCAN study, a survey of the local CAMHS teams found that the average number of AN presentations to CAMHS was around two or three cases a year. It may well be that generic clinicians do not become familiar with working with what can be a particularly demanding condition and at particularly worrying stages of the treatment; professionals without experience of eating disorders may therefore find it harder to maintain the positive aspects of their therapeutic relationship. Experienced specialists working with colleagues with similar expertise may be more able to maintain warmth, hope and positivity in the face of uncertain outcomes and the chronic nature of the condition, and also possibly avoid the hospital admissions which drive up costs. Greater patient flows also enable specialist services to incorporate dietetics and creative therapies into their treatment programmes.
It is encouraging that unlike previous reports, we did not find that families reported feeling blamed by services for the condition of their daughter or son. In fact they greatly valued the support that they received and their involvement in treatment. A strong message was given in the focus groups about the impact of eating disorders on siblings. This should encourage services to continue to offer parental and family therapies in keeping with NICE recommendations.
Limitations of the trial
It could be argued that the inpatient services in the study were not truly specialised because they were not exclusive eating disorder facilities. However, all four units had extensive experience and tradition of treating such cases. Indeed 17 cases entered other (often exclusive) specialist inpatient services in the follow-up period of the study and nevertheless, had (generally) poor outcomes at 2 years.
The present study was devised before the more recent positive outcomes of family-based treatment81 were published and it is of note that our findings suggest poorer outcomes. We had been impressed by the preliminary outcomes of CBT-Enhanced16 in addressing the core psychopathology of eating and weight concerns, and questioned the power of family-based treatment to address these as opposed to behavioural aspects of the condition.
The outcome of our individual CBT was poorer than reported for family-based treatment – a direct comparison is required on a similar population to clarify this further.
In the cost-effectiveness analysis, despite substantial observed differences in costs between groups, the differences did not reach statistical significance at 2 years. This may be because of inadequate sample sizes for the economic evaluation because sample size calculations were based on the primary outcome measure, the MRAOS. Calculations on the basis of cost or cost-effectiveness were not feasible at the design stage because of the lack of any relevant published cost data, but it is possible that a sample calculated in this way may have required a much larger sample. Although acknowledging this limitation, the use of a decision-making approach to the economic evaluation provides probabilistic evidence of the cost-effectiveness of the alternative treatment strategies, given the data currently available. Larger trials may be considered in the future, but this must be balanced against the cost of additional research in a disease area where low prevalence rates necessitate large and resource intensive multicentre evaluation.
Analysis of patients excluded because of missing economic data at both 2 and 5 years did not suggest any bias; patients included in the economic evaluation did not differ significantly from those excluded and there was no evidence to suggest any bias in missing data between the three treatment groups. On the whole, exploration of missing data in sensitivity analysis supported the results of the main analysis.
This study was able to demonstrate the value of economic evidence as a decision-making tool in situations where clinical differences between treatments are minimal. However, the value of the results presented is more limited in a broader decision-making context because of the lack of a generic, preference-based measure of outcome. NICE guidelines, for example, require evidence of cost-effectiveness (to be presented in terms of cost per quality-adjusted life-year) to allow comparison across diverse disease areas to support the allocation of scarce societal health and personal social services resources. 65 Future studies should consider the inclusion of such measures so as to place services for adolescents with AN within this broader decision-making context.
Implications for health care
For moderately to severely ill adolescents with AN, outpatient services delivered by experienced, expert professionals, supported by medical management of physical complications as required, offer the most cost-effective treatments. Lengthy psychiatric inpatient treatment does little to add to positive outcomes and is cost-ineffective. Treatment in specialist services, with experience and expertise in managing the condition, is to be preferred because of its cost-effectiveness and higher levels of both young people’s and carer’s satisfaction. Where young people with AN are managed in community CAMHS, a consultation and advice link with a specialist service may enable the CAMHS to contain anxiety and reduce unnecessary hospital admissions, thereby leading to greater user satisfaction. This needs further investigation.
The findings are broadly consistent with the NICE guidelines on the treatment of AN. Although physical risk should not be underestimated and may require urgent and active intervention, this trial does not lend support to the advantages of managing this within a psychiatric service.
Recommendations for future research
Further research is recommended in the following areas.
Clarify the positive and negative aspects of inpatient care
Physical and psychological risk, parental anxiety and social and educational withdrawal often result in inpatient admission. The opportunities for intensive psychological therapies, general support, refeeding and respite from external stresses make specialist inpatient care a logical step. Satisfaction (particularly among parents) is quite good. However, research outcomes are consistently disappointing, suggesting that adverse effects are under-recognised. Some are likely to be associated with the specifics of inpatient care, such as reinforcement of feelings of ineffectiveness; some to do with difficulties negotiating discharge and continuity of care. These need further clarification.
Clarify the optimum length of stay for inpatient care
Some of the adverse effects of inpatient care may relate to ‘institutionalisation’, reinforcement of the sick role, or a deskilling effect on both young people and their carers. A study comparing brief stays to stabilise physical health and initiate normal eating, with longer more comprehensive treatment, would help to clarify these issues. Again user views and a health economic component should be incorporated into such a study, given the high cost of inpatient care.
Evaluation of the efficacy and cost-effectiveness of individual psychological therapies
The current findings lent only modest support to the specialist programme used in this study comprising CBT with dietary therapy and parental counselling. As AN is a psychological disorder based on abnormal cognitions, further research is required to evaluate the effect of different approaches on the specific (weight and shape) and non-specific cognitions underlying the disorder. This research in adults is ongoing, but untested in (particularly younger) adolescents.
Evaluation of co-ordinated individual psychological therapies with family-based treatments
Since this project started, research into family-based treatments has been productive and indicated that these can be effective. However, they have not been adequately tested against individual approaches. For pragmatic as well as theoretical reasons, (supported by our user views), adolescents should receive individual therapies and the family should be involved. The specific components of combined therapies and how these should be co-ordinated to produce cognitive as well as behavioural change, requires further testing.
Acknowledgements
The authors are grateful to the following people: Dr Asha Bhatt, the clinical lead at the specialist outpatient programme (Manchester) for recruitment; Irene Cohen for data management; Dr Tania Stanway for recruitment and follow up; Kandy Giles from the specialist outpatient programme (Manchester); Sheeba Ehsan, Rachel Charlesworth, Matilda Moffatt and Sarah Bailey-Rogers for recruitment, data management and follow-up; Mary Claxton for the 5-year follow-up interviews and data entry; Drs Anandhi Inbasagaran and Nishi Puri for calculating predictors of outcome; Linda Rhodes for help with finance and for preparation of the report and Professor Richard Harrington (deceased) for the initial design and supervision of the Manchester site.
Contributions of authors
Simon G. Gowers was the principal investigator and designed the study and was lead author of the report. Andrew F. Clark led the research at the Manchester site and contributed to writing and editing the report. Chris Roberts, lead statistician, helped in the statistical design, analysis and report writing and editing. Sarah Byford and Barbara Barrett were responsible for health economic design, analysis, report writing and editing. Alison Griffiths, Vanessa Edwards, Claudine Bryan and Nicola Smethurst were project trial managers and contributed to clinical support, data management, tracing and report editing. Laura Rowlands, a project trial manager, helped with clinical support, data management, tracing, the satisfaction study and the report editing and Peter Roots lead the satisfaction study and contributed to editing the report.
Publications
Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatment for anorexia nervosa in adolescents – Randomised controlled trial. Br J Psychiatry 2007:191;427–35.
Byford S, Barrett B, Roberts C, Clark A, Edwards V, Smethurst N, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007:191;436–40.
Roots P, Rowlands L, Gowers S. User satisfaction with services in a randomized controlled trial of adolescent anorexia nervosa. Eur Eat Disord Rev 2009:17;331–37.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- van Hoeken D, Seidell J, Hoek H, Treasure J, Schmidt U, Van Furth E. Handbook of eating disorders. Chichester: Wiley; 2003.
- Doyle J, Bryant-Waugh R, Lask B, Bryant-Waugh R. Anorexia nervosa and related eating disorders in childhood and adolescence. Hove: Psychology Press; 2000.
- van Son GE, van Hoeken D, Bartelds AIM, van Furth EF, Hoek HW. Time trends in the incidence of eating disorders: a primary care study in the Netherlands. Int J Eat Disord 2006;39:565-9.
- Lucas AR, Beard CM, O’Fallon WM, Kurland LT. 50-year trends in the incidence of anorexia nervosa in Rochester, Mn – a population-based study. Am J Psychiatry 1991;148:917-22.
- O’Herlihy A, Worrall A, Lelliott P, Jaffa T, Hill B, Banerjee S. Distribution and characteristics of in-patient child and adolescent mental health services in England and Wales. Br J Psychiatry 2003;183:547-53.
- Keel PK, Dorer DJ, Eddy KT, Franko D, Charatan DL, Herzog DB. Predictors of mortality in eating disorders. Arch Gen Psychiatry 2003;62:179-83.
- Zipfel S, Reas DL, Thornton C, Olmsted MP, Williamson DA, Gerlinghoff M, et al. Day hospitalization programs for eating disorders: A systematic review of the literature. Int J Eat Disord 2002;31:105-17.
- Key A, Mason H, Bolton J. Reproduction and eating disorders: a fruitless union. Eur Eat Disord Rev 2000;8:81-9.
- Steinhausen HC. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry 2002;159:1284-93.
- Evans DL, Foa EB, Gur RE, Hendin H, O’Brien CP, Seligman MEP, et al. Treating and Preventing Adolescent Mental Health Disorders. New York: Oxford University Press; 2005.
- National Collaborating Centre for Mental Health (NCCMH) . Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder 2004.
- Gowers SG, Bryant-Waugh R. Management of child and adolescent eating disorders: the current evidence base and future directions. J Child Psychol Psychiatry 2004;45:65-83.
- Treasure J, Schmidt U. Anorexia nervosa. Clin Evid 2002;7:824-33.
- Gowers S, Claxton M, Rowlands L, Inbasagaran A, Wood D, Yi I, et al. Drug prescribing in child and adolescent eating disorder services (CAMH). Child Adolesc Ment Health 2005;10:170-8.
- Fairburn CG, Marcus MD, Wilson GT, Fairburn CG, Wilson GT. Binge eating: nature, assessment and treatment. New York, NY: Guilford Press; 1993.
- Fairburn C, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders; a ‘transdiagnostic’ theory and treatment. Behav Res Ther 2003;41:509-28.
- Minuchin S, Baker L, Rosman BL, Liebman R, Milman L, Todd TC. Conceptual model of psychosomatic illness in children: family organization and family therapy. Arch Gen Psychiatry 1975;32:1031-8.
- Russell GF, Szmukler GI, Dare C, Eisler I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch Gen Psychiatry 1987;44:1047-58.
- Robin A, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1999;38:1482-9.
- Le Grange D, Eisler I, Dare C, Russell GFM. Evaluation of family therapy in anorexia nervosa: a pilot study. Int J Eat Disord 1992;12:347-59.
- Eisler I, Dare C, Hodes M, Russell GFM, Dodge E, Le Grange D. Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. J Child Psychol Psychiatry 2000;41:727-36.
- Asen KE. Developments in multiple family therapy. J Family Ther 2002;24:3-16.
- Scholtz M, Asen E. Multiple family therapy with eating disordered adolescents. Eur Eat Disord Rev 2001;9:33-42.
- Dare C, Eisler I. A multi-family group day treatment programme for adolescent eating disorder. Eur Eat Disord Rev 2000;8:4-18.
- Gowers SG, Edwards V, Fleminger S, Massoubre C, Wallin U, Canalda G, et al. Treatment aims and philosophy in the treatment of adolescent anorexia nervosa in Europe. Eur Eat Disord Rev 2002;10:271-80.
- Nicholls D, Bryant-Waugh R, Treasure J, Schmidt U, Van Furth E. Handbook of eating disorders. Chichester: Wiley; 2003.
- Meads C, Gold L, Burls A. How effective is outpatient compared to inpatient care for treatment of anorexia nervosa? A systematic review. Eur Eat Disord Rev 2001;9:229-41.
- Crisp AH, Norton KWR, Gowers SG, Halek C, Levett G, Yeldham D, et al. A controlled study of the effect of therapies aimed at adolescent and family psychopathology in anorexia nervosa. Br J Psychiatry 1991;159:325-33.
- Gowers S, Norton K, Halek C, Crisp AH. Outcome of outpatient psychotherapy in a random allocation treatment study of anorexia nervosa. Int J Eat Disord 1994;15:165-79.
- Cho WH, Lee H, Kim C, Lee S, Choi K-S. The impact of visit frequency on the relationship between service quality and outpatient satisfaction: a South Korean study. Health Serv Res 2004;39:13-3.
- Bell L. What can we learn from consumer studies and qualitative research in the treatment of eating disorders?. Eat Weight Disord 2003;8:181-7.
- Swain-Campbell NR, Surgenor LJ, Snell DL. An analysis of consumer perspectives following contact with an eating disorders service. Aust NZ J Psychiatry 2001;35:99-103.
- Simon J, Schmidt U, Pilling S. The health service use and cost of eating disorders. Psychol Med 2005;35:1543-53.
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA. One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: evidence from a national database of health insurance claims. Int J Eat Disord 2000;27:381-9.
- Romeo R, Byford S, Knapp M. Economic evaluations of child and adolescent mental health interventions: a systematic review. J Child Psychol Psychiatry 2005;46:919-30.
- Crisp AH. Anorexia nervosa; let me be. London: Lawrence Erlbaum Associates; 1995.
- Gowers SG, Weetman J, Shore A, Hossain F, Elvins R. The impact of hospitalisation on the outcome of adolescent anorexia nervosa. Br J Psychiatry 2000;45:138-41.
- North C, Gowers SG. Anorexia nervosa, psychopathology and outcome. Int J Eat Disord 1999;26:386-91.
- American Psychiatric Association . Diagnostic and Statistical Manual for Mental Disorders-Fourth Edition (DSM-IV) 1994.
- Morgan HG, Hayward AE. Clinical assessment of anorexia nervosa. The Morgan–Russell Outcome Assessment Schedule. Br J Psychiatry 1988;152:367-74.
- Eisler I, Dare C, Russell GFM, Szmukler G, Le Grange D, Dodge E. Family and individual therapy in anorexia nervosa. A 5-year follow-up. Arch Gen Psychiatry 1997;56:1025-30.
- Gowers SG, Harrington R, Whitton A, Lelliott P, Wing J, Beevor A, et al. A brief scale for measuring the outcomes of emotional and behavioural disorders in children: HoNOSCA. Br J Psychiatry 1999;174:413-16.
- Garralda ME, Yates P, Higginson I. Child and adolescent mental health service use; HoNOSCA as an outcome measure. Br J Psychiatry 2000;177:54-8.
- Yates P, Garralda ME, Higginson I. The PCS and HoNOSCA as measures of child mental health service intakes. Br J Psychiatry 1999;174:417-23.
- Goodyer I, Dubicka B, Wilkinson P, Kelvin RG, Roberts C, Byford S, et al. A randomised controlled trial of cognitive behavioural therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. Health Technol Assess 2008;12.
- Garner DM. Eating Disorder Inventory–2. Odessa, FL: Psychological Assessment Resources; 1991.
- Gowers SG, Levine W, Bailey-Rogers S, Shore A, Burhouse E. The use of a routine self report outcome measure (HoNOSCA-Sr) in two adolescent mental health services. Br J Psychiatry 2002;180:266-9.
- Epstein N, Bishop D, Levin S. The McMaster Family Assessment Device. J Marital Fam Ther 1983;9:171-80.
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Wood A, Kroll L, Moore A, Harrington R. Properties of the mood and feelings questionnaire in adolescent psychiatric outpatients: a research note. J Child Psychol Psychiatry 1995;36:327-34.
- Bryant-Waugh R, Cooper P, Taylor C, Lask B. The use of the eating disorder examination with children: a pilot study. Int J Eat Disord 1996;19:391-8.
- Gowers S, Smyth B. The impact of a motivational assessment interview on initial response to treatment in adolescent anorexia nervosa. Eur Eat Disord Rev 2004;12:87-93.
- Gowers SG. Evidence based research in CBT with adolescent eating disorders. Child Adolescent Mental Health 2006;11:9-12.
- Diggle PJ, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford: Oxford Scientific Publications; 1994.
- McCullagh P. Regression models for ordinal data (with discussion). JRSS Series B 1980;42:109-42.
- Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry 1999;174:58-64.
- Harrington RC, Peters P, Green J, Byford S, Woods J, McGowan R. Randomised comparison of the effectiveness and costs of community and hospital based mental health services for children with behavioural disorders. BMJ 2000;321:1047-50.
- Barrett B, Byford S, Chitsabesan P, Kenning C. Mental health provision for young offenders: service use and cost. Br J Psychiatry 2006;188:541-6.
- Department of Health . NHS Reference Costs 2004.
- Curtis L, Netten A. Unit costs of health and social care. Canterbury: University of Kent; 2004.
- Independent Schools Council . ISC Census 2004.
- British Medical Association, Royal Pharmaceutical Society of Great Britain . British National Formulary 47 2004.
- National Institute for Clinical Excellence . Guide to the Methods of Technology Appraisal 2004.
- Efron B, Tibshirani R. An introduction to the bootstrap. New York, NY: Chapman and Hall; 1993.
- Barber JA, Thompson SG. Analysis and interpretation of cost data in randomised controlled trials: review of published studies. BMJ 1998;317:1195-200.
- Van Hout BA, Al MJ, Gordon GS, Rutten FH. Costs, effects and cost-effectiveness ratios alongside a clinical trial. Health Econ 1994;3:309-19.
- Johannesson M, Weinsten MC. On the decision rules of cost-effectiveness analysis. J Health Econ 1993;12:459-69.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8.
- Clark A, O’Malley A, Woodham A, Barrett B, Byford S. Children with complex mental health problems: needs costs and predictors over one year. Child and Adolescent Mental Health 2005;10:170-8.
- Byford S, Barber JA, Fiander M, Marshall S, Green J. Factors that influence the cost of caring for patients with severe psychotic illness: report from the UK700 trial. Br J Psychiatry 2001;178:441-7.
- Mason J. Qualitative researching. New York, NY: Sage Publications Ltd; 2002.
- Krueger RA, Casey M. Focus groups – a practical guide for applied research. New York: Sage Publications; 2000.
- Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, et al. Inpatient treatment in child and adolescent psychiatry – an exploratory prospective study of health gain and costs. J Child Psychol Psychiatry 2007;48:1259-69.
- McIntosh VVW, Jordan J, Carter FA, Luty SE, McKenzie JM, Bulik CM, et al. Three psychotherapies for anorexia nervosa: a randomised controlled trial. Am J Psychiatry 2005;162:741-7.
- Halvorsen I, Heyerdahl S. Treatment perception in adolescent onset anorexia nervosa: retrospective views of patients and parents. Int J Eating Disord 2007;40:629-39.
- Brennan PF. Patient satisfaction and normative decision theory. J Am Med Inform Assoc 1995;2:250-9.
- Newton T, Robinson P, Hartley P. Treatment for eating disorders in the United Kingdom. Part II. Experiences of treatment: a survey of members of Eating Disorders Association. Eur Eat Disord Rev 1993;1:10-21.
- Rosenvinge JH, Khulefelt Klusmeier A. Treatment for eating disorders from a patient satisfaction perspective. Eur Eat Disord Rev 2000;8:293-300.
- De la Rie S, Noordenbos G, Donker M, van Furth E. Evaluating the treatment of eating disorders from the patient’s perspective. Int J Eat Disord 2006;39:667-78.
- Lock J, Agras WS, Bryson S, Kraemer HC. A comparison of short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry 2005;7:632-39.
Appendix 1 Case-by-case 2-year course – general (MRAOS)
FIGURE 8.
Individual longitudinal profiles for Morgan and Russell Average Outcome Score by treatment. a, general CAMHS; b, specialist outpatient; c, specialist inpatient; and d, preference.
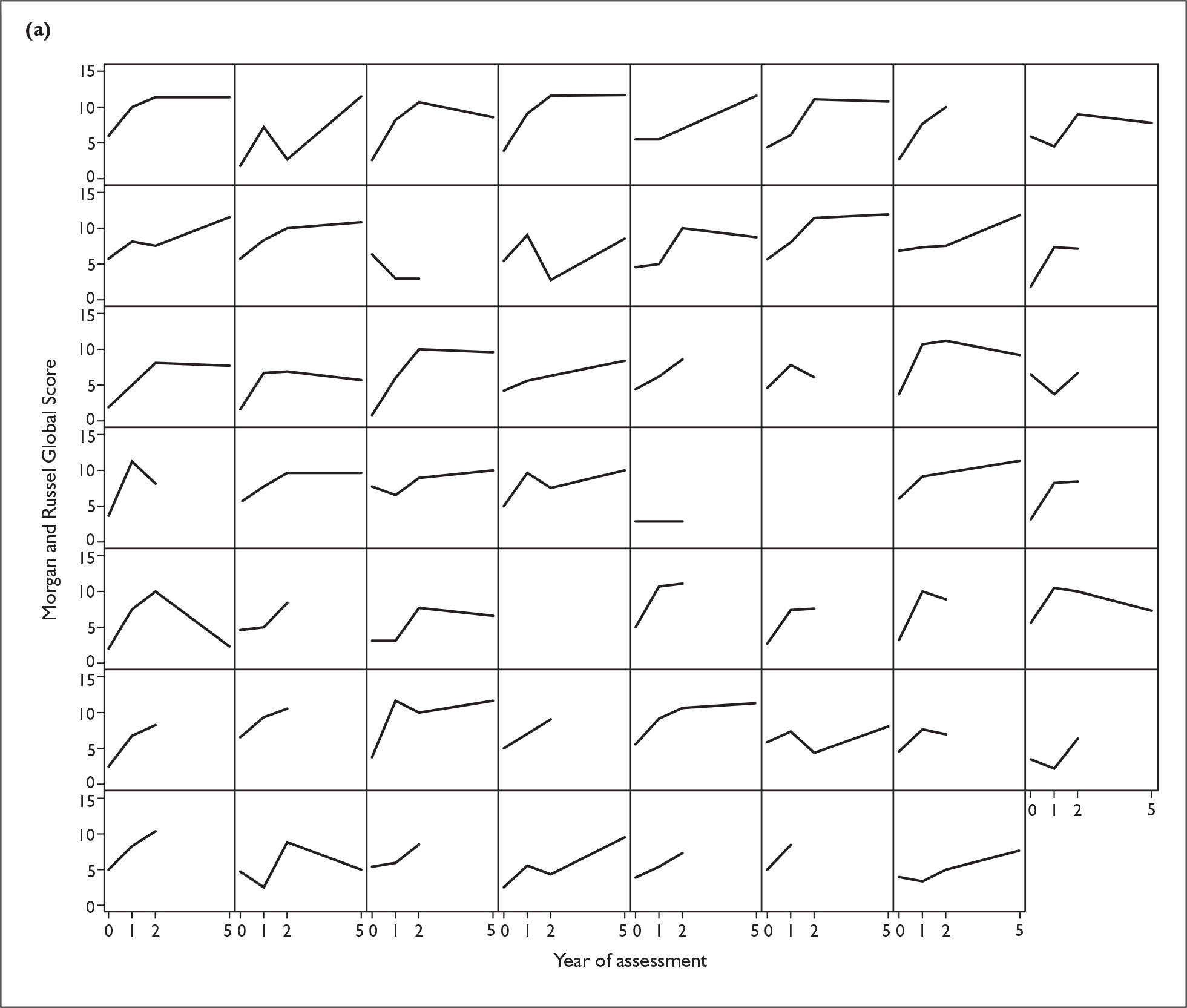
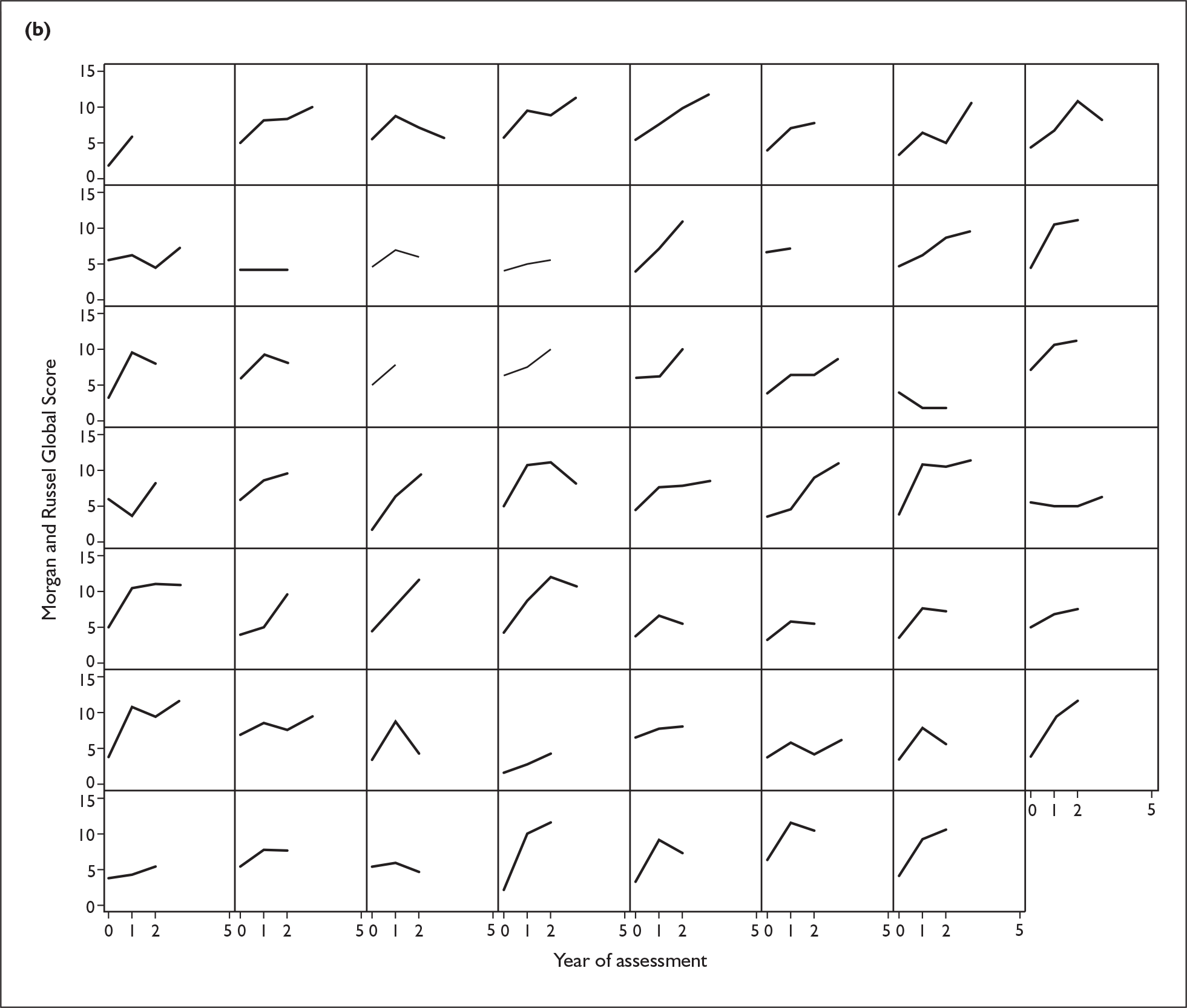
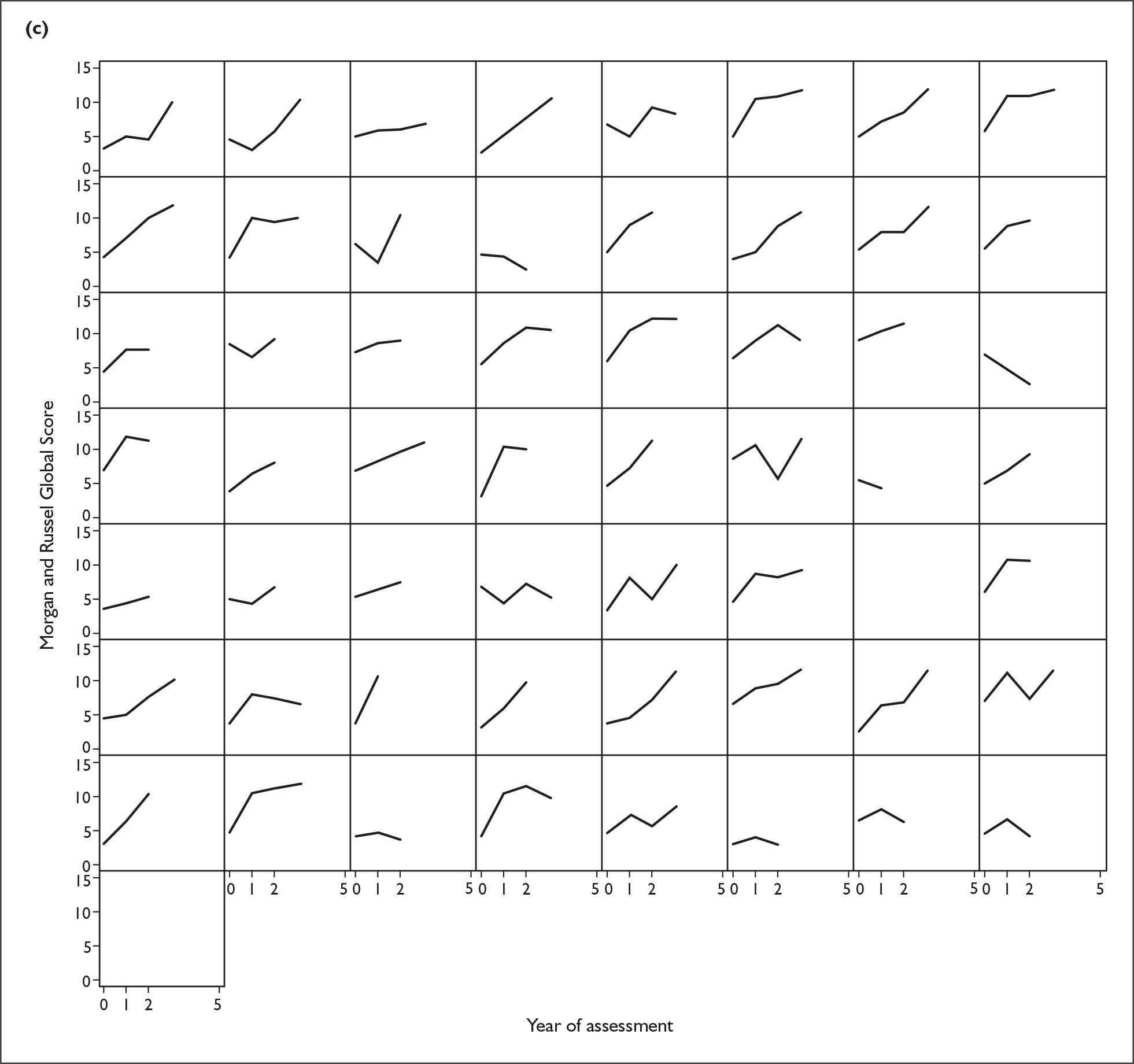
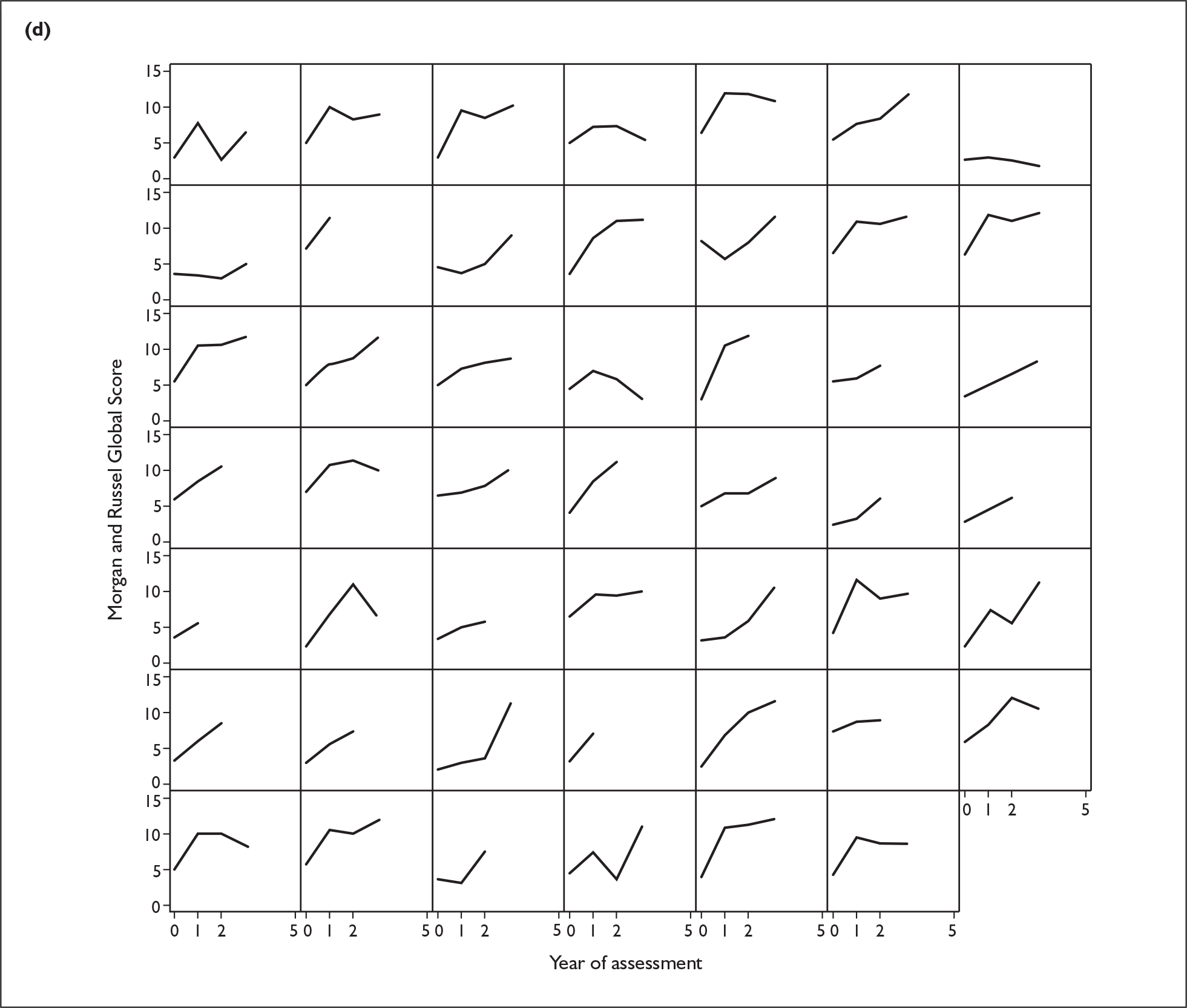
Appendix 2 Case-by-case 2-year course – percentage weight for height
FIGURE 9.
Individual longitudinal profiles for % weight for height by treatment. a, general CAMHS; b, specialist outpatient; c, specialist inpatient; and d, preference.
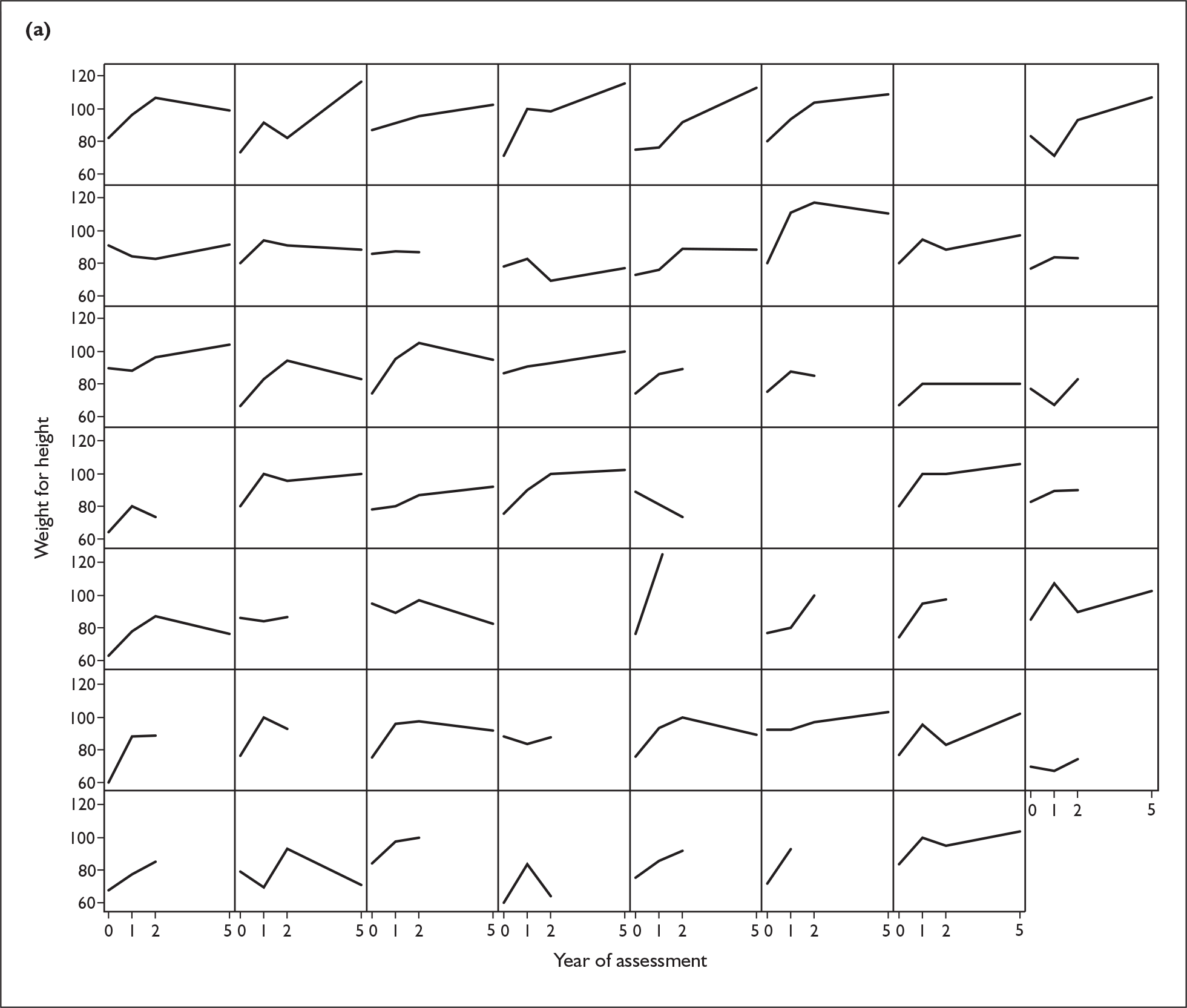
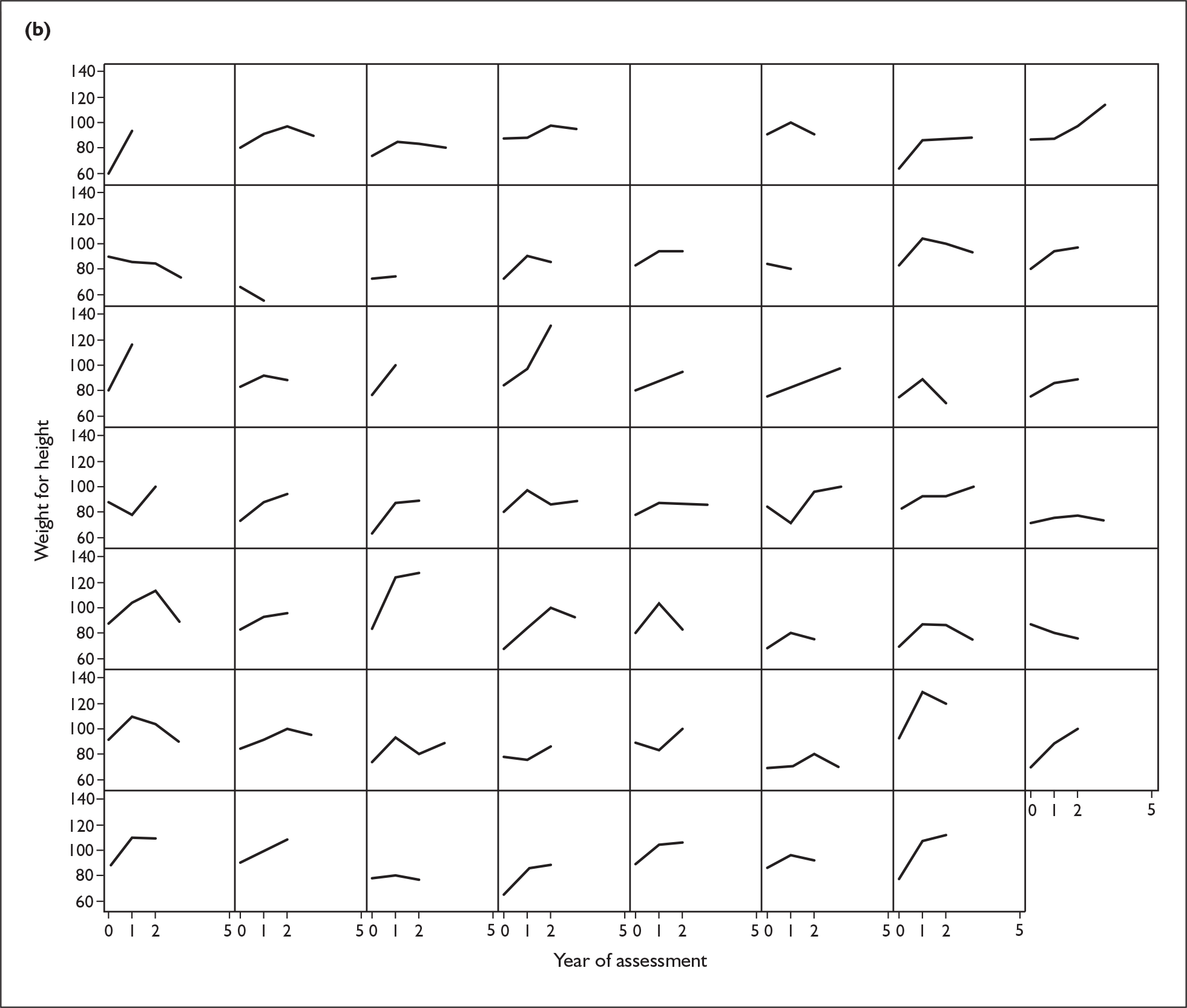
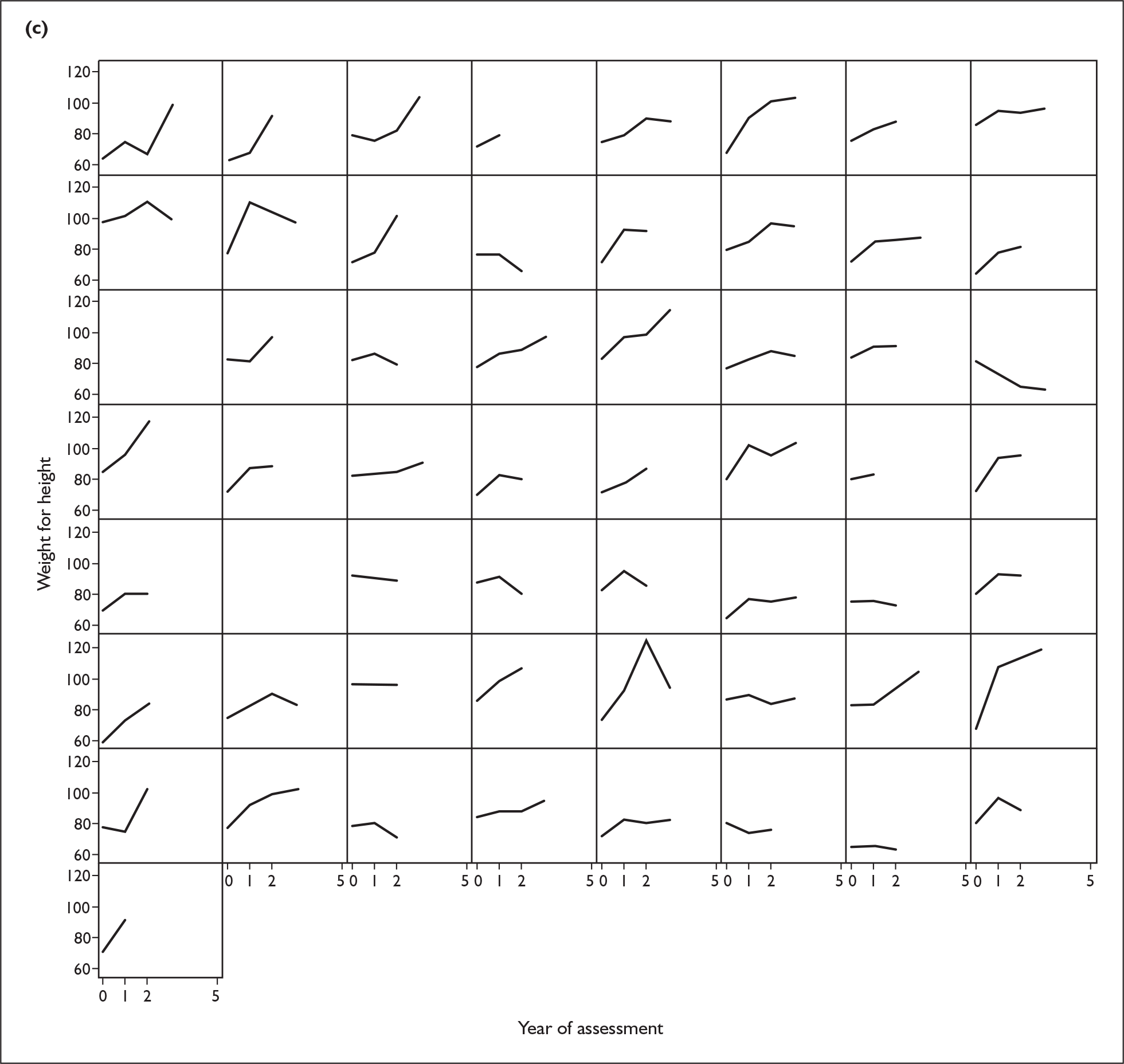
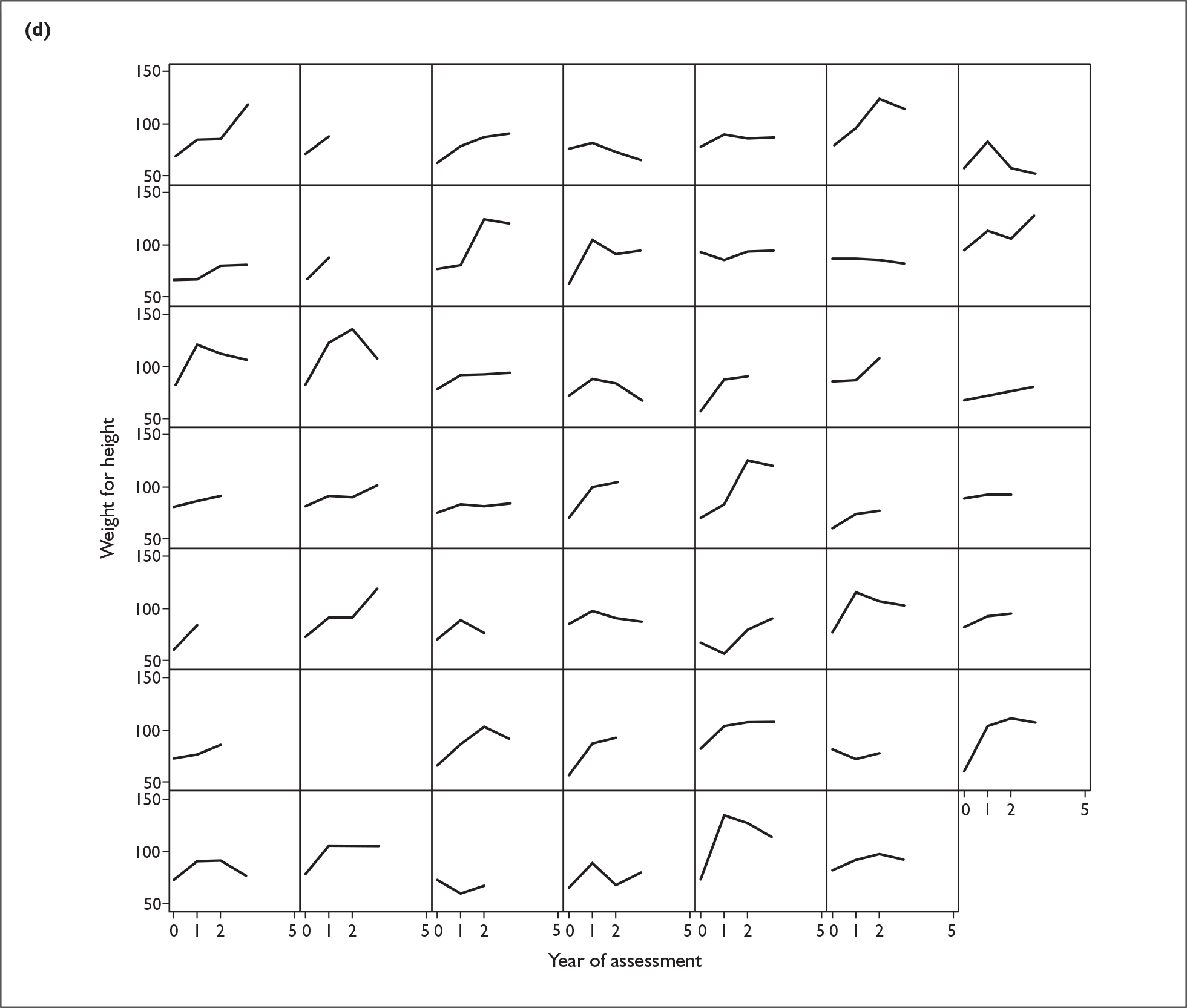
List of abbreviations
- AN
- anorexia nervosa
- BFST
- Behavioural Family Systems Therapy
- BMI
- body mass index
- CAMHS
- Child and Adolescent Mental Health Services
- CA-SUS
- Child and Adolescent Service Use Schedule
- CARER-SUS
- Carer Service Use Schedule
- CBT
- cognitive behaviour therapy
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders 4th Edition
- EDE
- Eating Disorder Examination
- EDI-2
- Eating Disorders Inventory second edition
- EOIT
- Ego-Oriented Individual Therapy
- FAD-GF
- Family Assessment Device–General Functioning
- HoNOSCA-CR
- clinician-rated Health of the Nation Outcome Scale for Children and Adolescents
- HoNOSCA-SR
- self-rated Health of the Nation Outcome Scale for Children and Adolescents
- IBW
- ideal body weight
- ICER
- incremental cost-effectiveness ratio
- MFQ
- Mood and Feelings Questionnaire
- MRAOS
- Morgan–Russell Average Outcome Scale
- NICE
- National Institute for Clinical Excellence (now National Institute for Health and Clinical Excellence)
- RCT
- randomised controlled trial
- SD
- standard deviation
- TOuCAN
- Treatment Outcome of Child and Adolescent Anorexia Nervosa
All abbreviations that have been used in this report are listed here unless the abbreviation is well-known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington