Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 08/114/01. The contractual start date was in February 2009. The draft report began editorial review in August 2009 and was accepted for publication in October 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Poorly controlled severe postoperative pain can result in a number of cardiovascular, respiratory, gastrointestinal, genitourinary, metabolic, musculoskeletal and psychological adverse effects. These can lead to an increased risk of postoperative complications, including prolonged inpatient stay and reduced mobility. Furthermore, poorly controlled postoperative pain is associated with a higher incidence of development of chronic pain. 1,2 Effective pain relief may limit these consequences; however, the use of analgesics, especially morphine, is associated with adverse effects. In order to achieve optimal analgesia with minimum analgesic-related adverse effects, multimodal analgesia can be used. This is where the patient receives a combination of opioid analgesics, most commonly morphine, and non-opioid analgesics, such as paracetamol (acetaminophen), non-steroidal anti-inflammatory drugs (NSAIDs) or cyclo-oxygenase 2 (COX-2) inhibitors. The aim is that the additional and synergistic effects between morphine and non-opioid analgesics allows for optimum analgesia to be maintained, a lower dose of morphine to be used and therefore a lower incidence of morphine-related adverse effects. 3–5
The objective of this review was to evaluate the effectiveness of paracetamol and NSAIDs, including COX-2 inhibitors, in reducing morphine consumption and associated adverse effects when used as part of multimodal analgesia following major surgery. However, it should be noted that there are other non-opioid analgesics that are used as part of multimodal analgesia after major surgery. These include N-methyl-d-aspartate (NMDA) antagonists, such as ketamine and dextromethorphan; alpha-2 adrenergic antagonists including clonidine and dexmedetomidine; and adenosine, droperidol, magnesium, neostigmine and gabapentin. There is clinical evidence that these non-opioids are effective in reducing morphine consumption after major surgery although, as with all drugs, each has its own adverse effect profile. 6
Morphine
Morphine is the most valuable opioid for severe postoperative pain relief. It is the gold standard against which the effectiveness of all other analgesics is compared. 7 Although there are several modes of administration, patient-controlled analgesia (PCA) has become the standard method of administering morphine after major surgery. 5 PCA involves the patient self-administering small doses of morphine by pressing a button connected to a programmable pump. The PCA device is programmed by the health-care provider to deliver a specific amount of medication (a ‘bolus’) upon each request by the patient. A continuous ‘background’ infusion may be administered in addition to patient-controlled bolus doses. In order to prevent an overdose of morphine, bolus doses are limited by a programmed ‘lockout interval’ during which subsequent requests are ignored. 7 PCA has been shown to provide marginally superior analgesia in comparison to other modes of administration, and patients report greater satisfaction with, and in general prefer, PCA. 8
Morphine exerts its analgesic effect by binding to specific opioid receptors in the brain and spinal cord that are involved in the perception of pain. This mode of action can also result in significant adverse effects. These include: respiratory depression, postoperative nausea and vomiting (PONV), sedation, bowel dysfunction (delayed gastric emptying, inhibition of bowel motility and constipation), urinary retention and pruritus. 1,9
Respiratory depression, though uncommon, is a potentially life-threatening adverse effect and of most concern to health-care professionals. 10 Meanwhile PONV, although self-limiting, is common, having an incidence of 30–67%, and is of most concern to patients. 1,11,12 Furthermore, PONV can delay postoperative recovery, which has consequences for the patient and also has an economic impact on health-care resources. 13
Paracetamol
Paracetamol (acetaminophen) is an analgesic and antipyretic with little anti-inflammatory effect, whose exact mode of action is currently unknown. It is the most widely used drug for pain relief. In order of increasing effectiveness, paracetamol can be administered rectally, orally and intravenously. 14 While all three modes of administration can achieve adequate plasma concentrations, there are differences in absorption and time to reach peak plasma levels. With rectal administration, absorption can be unpredictable with bioavailability ranging from 24% to 98%, varying with factors such as formulation of the suppositories, number used and the particle size of the paracetamol. 15 Paracetamol, at therapeutic doses, rarely results in adverse effects and, unlike NSAIDs, does not cause gastrointestinal ulceration or bleeding. 1 Propacetamol hydrochloride, an injectable prodrug of paracetamol, was the first form of paracetamol developed to be administered intravenously. 14,16 It is hydrolysed to paracetamol in the blood, with 2 g of propacetamol releasing 1 g of paracetamol. Propacetamol, though effective and generally well tolerated, is notable for adverse effects of localised pain at the injection site and contact dermatitis. Although licensed and available in other countries, including France and Belgium, it is not licensed in the UK (Table 1). However, an intravenous form of active paracetamol, Perfalgan®, has been available in the UK since 2004. Studies have shown that compared to intravenous (i.v.) propacetamol, i.v. paracetamol is associated with a reduction in incidence of localised pain at the injection site and contact dermatitis. However, there is no significant difference in the incidence of other adverse effects. 14
| Generic name | Licensed in UK | Licensed indication for use |
|---|---|---|
| Paracetamol (acetaminophen) | ||
| Paracetamol | ✓ | Severe postoperative pain |
| Propacetamol | ✗ | ✗ |
| NSAID | ||
| Diclofenac | ✓ | Pain relief from minor surgery |
| Ibuprofen | ✓ | Mild to moderate pain |
| Dexibuprofen | Mild to moderate pain | |
| Indometacin (indomethacin) | ✓ | Severe postoperative pain |
| Ketoprofena | ✓ | Severe postoperative pain |
| Dexketoprofen | ✓ | Mild to moderate pain |
| Ketorolacb | ✓ | Severe postoperative pain |
| Lornoxicam | ✓ | Moderate postoperative pain, OA, RA |
| Mefanamic acid | ✓ | Severe postoperative pain |
| Meloxicam | ✓ | RA and AS |
| Nabumetone | ✓ | RA and AS |
| Naproxen | ✓ | Severe postoperative pain |
| Piroxicam | ✓ | RA, OA, AS |
| Tenoxicam | ✓ | RA, OA, soft tissue injuries |
| Tiaprofenic acid | ✓ | Severe postoperative pain |
| COX-2 inhibitors | ||
| Celecoxib | ✓ | RA, OA, AS |
| Etoricoxib | ✓ | RA, OA, AS, acute gouty arthritis |
| Lumiracoxib | ✗ | ✗ |
| Parecoxib | ✓ | Severe postoperative pain |
| Rofecoxib | ✗ | ✗ |
| Valdecoxib | ✗ | ✗ |
Non-steroidal anti-inflammatory drugs (NSAIDs) and cyclo-oxygenase 2 (COX-2) inhibitors
Non-steroidal anti-inflammatory drugs are analgesic, anti-inflammatory, antiplatelet and antipyretic. In comparison to paracetamol, NSAIDs have been shown to offer superior postoperative pain relief. 17 They exert their analgesic effect by reducing the production of prostaglandins responsible for pain and inflammation. NSAIDs achieve this by inhibiting the enzyme COX-2, which is essential in the synthesis of these prostaglandins. NSAIDs vary in whether they selectively inhibit COX-2. Non-selective NSAIDs, such as ibuprofen and diclofenac, inhibit not only COX-2 but also cyclo-oxygenase 1 (COX-1). COX-1 is involved in the synthesis of prostaglandins that have a role in the maintenance and protection of the gastrointestinal (GI) tract, platelet adhesion and renal function. Non-selective NSAIDs are therefore associated with adverse GI effects, renal toxicity, prolonged bleeding time, bronchospasm and oedema. 1 Several NSAIDs are available for use in the postoperative setting (see Table 1).
Non-steroidal anti-inflammatory drugs, even when used in the short term, can cause GI adverse effects ranging from abdominal pain, dyspepsia and superficial erosions to serious GI complications such as perforated gastric ulcers and life-threatening GI haemorrhage. 18 Furthermore, the risk of a GI adverse event varies between NSAIDs, with the lowest risk associated with ibuprofen and the highest with ketorolac. 19 Renal toxicity is a noted adverse effect of NSAIDs. However, a systematic review found that the use of NSAIDs for postoperative pain relief in adults with normal renal function causes only a small, temporary effect on renal function. 20
A systematic review examining the use of NSAIDs after tonsillectomy, where perioperative bleeding is a serious complication, found that NSAIDs were statistically significantly associated with the need for reoperation due to bleeding [odds ratio (OR) 2.3; 95% confidence interval (CI) 1.12 to 4.83]. However, NSAIDs were not statistically significantly associated with intraoperative blood loss, postoperative bleeding and hospital admission. 21
Cyclo-oxygenase 2 inhibitors, also referred to as ‘COXIBs’ or ‘Cox-2 selective NSAIDs’ (see Table 1), were designed to selectively inhibit COX-2 only, thereby reducing GI bleeding and renal adverse effects. 4 However, the long-term use of COX-2 inhibitors is associated with increased incidence of thromboembolic events such as myocardial infarction and stroke, and they are as likely as non-selective NSAIDs to cause impaired renal function and oedema. 1,9 Over the past 5 years, two COX-2 inhibitors have been withdrawn from use worldwide: rofecoxib due to an increased risk of cardiovascular adverse effects, and valdecoxib due to an increased risk of severe skin reactions. 22,23
Previous systematic reviews
There are a number of previous relevant reviews assessing the effectiveness of adding a non-opioid to PCA morphine for pain relief and reduction of morphine-related side effects following surgery. Some reviews have focused on specific types of surgery, for example cardiothoracic surgery24 and lumbar spine surgery. 25 We have identified three previous systematic reviews that are not procedure specific and were all published in 2005: Remy et al. 26 investigated the effects of paracetamol on morphine consumption and associated adverse effects after surgery; Marret et al. ,27 from the same research group, investigated the effects of NSAIDs (including COX-2 inhibitors); and Elia et al. 28 investigated paracetamol, NSAIDs and COX-2 inhibitors.
The reviews by Remy et al. 26 and Elia et al. 28 both showed that paracetamol (including propacetamol) combined with PCA morphine results in a statistically significant reduction in morphine consumption in the first 24 hours following surgery: there was a pooled mean reduction of 9 mg and 8.3 mg respectively compared to PCA morphine alone (Tables 2 and 3). However, there was not a statistically significant reduction in the incidence of any morphine-related adverse effects including PONV, urinary retention, sedation, pruritus, apnoea or respiratory depression in either study. 26,28
| Intervention | 24-hour morphine consumption (mg) MD (95% CI) | Nausea RR (95% CI) | Vomiting RR (95% CI) | PONV RR (95% CI) | Sedation RR (95% CI) |
|---|---|---|---|---|---|
| Paracetamol | –8.3 (–10.9 to –5.7) | 0.8 (0.6 to 1.1) | 0.9 (0.5 to 1.4) | ||
| NSAID | 0.9 (0.8 to 1.0) | 0.8 (0.7 to 1.0) | 0.7 (0.6 to 0.9) | 0.7 (0.5 to 0.9) | |
| Single dose | –10.3 (–18.3 to –2.3) | ||||
| Multiple dose | –19.7 (–26.3 to –13.0) | ||||
| Continuous | –18.3 (–26.8 to –9.7) | ||||
| COX-2 | 1.1 (1.0 to 1.3) | 1.1 (0.9 to 1.5) | 0.7 (0.4 to 1.3) | 0.8 (0.5 to 1.2) | |
| Single dosea | –7.2 (–10.6 to –3.8) | ||||
| Single doseb | –27.8 (–44.3 to –11.4) | ||||
| Multiple low dosec | –10.0 (–13.4 to –6.6) | ||||
| Multiple high dosed | –13.3 (–17.8 to –8.8) |
| Intervention | 24-hour morphine consumption (mg) MD (95% CI) | Nausea | Vomiting | PONV | Sedation |
|---|---|---|---|---|---|
| Paracetamol26 | –9.0 (–15.0 to –3.0) | OR 1.0 (0.6 to 1.6) | OR 1.3 (0.8 to 2.2) | ||
| NSAID27 | RR 0.7 (0.6 to 0.8) | RR 0.7 (0.5 to 1.0) | |||
| NSAID + COX-227 | RR 0.9 (0.8 to 1.0) | RR 0.7 (0.5 to 0.9) |
Marret et al. 27 reported that, compared to PCA morphine alone, there was a statistically significant reduction in PONV, nausea alone, vomiting alone and sedation with NSAIDs in combination with PCA morphine (see Table 3). Non-selective NSAIDs and COX-2 inhibitors were combined for some analyses. Furthermore, regression analysis indicated a positive correlation between morphine consumption and the incidence of postoperative nausea or vomiting, though the size of the correlation was small (r2 = 0.37 for nausea and r2 = 0.27 for vomiting). There was no statistically significant decrease in the incidence of pruritus, urinary retention or respiratory depression when NSAIDs were added to PCA morphine. Data were not pooled for morphine consumption.
The review by Elia et al. 28 assessed the effect of the non-selective NSAIDs and COX-2 inhibitors separately. There was a statistically significant reduction in morphine consumption with NSAIDs in combination with PCA morphine compared to PCA morphine alone (10.3 mg with single doses, 18.3 mg with continuous infusion, and 19.7 mg with multiple dose regimens). There was also a statistically significant reduction in sedation and PONV but not for nausea or vomiting alone, though the trend was towards reduction (see Table 2). 28 In contrast, whilst COX-2 inhibitors in combination with PCA morphine resulted in a statistically significant reduction in morphine consumption compared to PCA morphine alone, there was no statistically significant reduction in any morphine-related adverse effects (Table 2). 28
Any reduction in morphine-related adverse effects needs to be balanced against the possible adverse effects of the non-opioid analgesic. The reviews by Marret et al. 27 and Remy et al. 26 did not consider this issue. In the review by Elia et al. 28 the use of NSAIDs was associated with a statistically significant increase in the incidence of surgical bleeding complications (Table 4). COX-2 inhibitors were associated with a statistically significant increase in renal failure, but not surgical bleeding complications (Table 4).
| Intervention | GI bleeding OR (95% CI) | Oliguria OR (95% CI) | Renal failure OR (95% CI) | Any bleeding OR (95% CI) | Severe bleeding OR (95% CI) |
|---|---|---|---|---|---|
| NSAID | 5.1 (0.7 to 40.6) | 1.7 (0.8 to 3.5) | 7.0 (0.1 to 35.5) | 4.5 (1.5 to 13.4) | 6.1 (1.3 to 27.9) |
| COX-2 | 4.5 (0.4 to 50.0) | 1.5 (0.9 to 2.5) | 4.9 (1.0 to 23.4) |
In summary, the existing systematic reviews suggest that paracetamol, NSAIDs and COX-2 inhibitors all reduce morphine consumption in the first 24 hours following surgery, but only NSAIDs appear to reduce morphine-related adverse effects. However, the relative effects of the non-opioids are unclear.
Definition of decision problem
The problem faced by decision-makers in health care is which class of non-opioid analgesic (paracetamol, NSAID or COX-2 inhibitor) is the most effective at reducing morphine consumption and associated adverse effects when used as part of multimodal analgesia following major surgery. Any benefits in terms of reduction in morphine-related adverse effects need to be balanced against the potential risk of adverse effects of the non-opioid analgesic.
The scope of the review
We were commissioned to undertake a short report, building on earlier reviews of paracetamol and NSAIDs, to conduct an analysis comparing the morphine-sparing effects of these drugs following major surgery.
Of the available reviews we elected to update the Elia et al. 28 review. This was a good-quality review with appropriate searches and clearly defined inclusion criteria that used appropriate methods to reduce error and bias in study selection and data extraction. Study quality was assessed and taken into consideration in the synthesis. The search date for the Elia review is more recent by 7 months than the other two reviews and as a result captured more trials from 2003 and 2004. The Remy and Marret reviews used a quality score as an inclusion criterion for their review; however, we preferred to include all the randomised evidence, as Elia had done, to maximise the evidence available. In addition, we also had access to the individual trial data from the Elia review, which included the adverse effects of the non-opioid analgesics as well as morphine-related adverse effects.
The earlier three reviews, including the Elia review, did not compare the three classes of non-opioid analgesics to each other, possibly a reflection of the limited number of trials making direct comparisons. The main aim of the current review was to assess the relative effectiveness of paracetamol, NSAIDs and COX-2 inhibitors. The focus was the relative effectiveness of the drug classes and not individual drugs within the classes. The ideal evidence to address the decision problem posed would be a synthesis of three-arm trials comparing paracetamol versus NSAID versus COX-2 inhibitor. In terms of the current review, we were aware that although there was a reasonable body of evidence comparing each of the three analgesic classes to placebo, it was likely that the quantity of evidence directly comparing the three drug classes would be limited. We therefore undertook a mixed treatment comparison (MTC) to derive results for the relative effectiveness of the three non-opioid analgesics in the first 24 hours following surgery.
An MTC is an extension or generalisation of traditional meta-analysis in which trials comparing the same intervention and same comparator are pooled to estimate an overall treatment effect. An MTC overcomes the limitations of standard meta-analysis in cases where there are no or limited trials making the relevant head-to-head comparison or where the decision problem requires the comparison of several interventions. 29,30 In addition, a ranking of interventions based on the probability that each treatment is best can be produced,31 which can be of particular value where several treatment options are under consideration.
Chapter 2 Methods
The primary objective of this project was to assess the relative effectiveness of paracetamol, non-selective NSAIDs and COX-2 inhibitors in reducing morphine consumption and related adverse effects after major surgery. A systematic review of the evidence for clinical effectiveness was undertaken to update a previous review28 and to extend the earlier analysis.
Search strategy
MEDLINE, EMBASE and the Cochrane Central Register of Controlled trials (CENTRAL) were searched for the period January 2003 to February 2009. The search strategy for each database is reported in Appendix 1. The start search date was January 2003 to overlap with Elia et al. 28 (search end July 2004) to allow for late indexing of studies. Published and unpublished studies were eligible and no language restrictions were applied. In addition, the reference lists of relevant systematic reviews were checked to identify relevant studies.
Titles and abstracts were examined for relevance by two researchers, and all papers identified by either researcher as potentially relevant were ordered. Full papers were examined for relevance by two researchers independently, based on the inclusion criteria below. Disagreements were resolved by consensus and if necessary through discussion with a third researcher.
Inclusion and exclusion criteria
The inclusion criteria followed those of Elia et al. 28 except where indicated below. Studies were included if they met the following criteria:
Population Adults who had undergone major surgery and were receiving PCA morphine for postoperative pain were included. Studies using PCA opioids other than morphine, intrathecal opioids or peripheral nerve blocks were excluded.
Interventions Studies of paracetamol (including propacetamol), non-selective NSAID or COX-2 inhibitor given in addition to PCA morphine were included. The COX-2 inhibitors rofecoxib and valdecoxib were not included as these are no longer licensed in the UK. Although propacetamol is not licensed in the UK it was included as it is a prodrug of paracetamol and we anticipated that there would be few trials available of paracetamol used as licensed in the UK.
Comparator treatment PCA morphine plus placebo or PCA morphine plus a different non-opioid class (paracetamol, NSAID or COX-2 inhibitor) were included. Studies using a no treatment comparator were excluded.
Outcomes Only studies that reported cumulative morphine consumption for the first 24 hours following surgery were included. The other outcomes of interest were: morphine-related adverse effects (respiratory depression, nausea, vomiting, PONV, urinary retention, pruritus, dizziness, sedation, including drowsiness or somnolence, and bowel dysfunction) and non-opioid-related adverse effects. The presumption was made that pain was adequately controlled with PCA morphine in both arms of the trial; therefore pain was not included as an outcome.
Study design Randomised controlled trials (RCTs) with at least 10 participants per treatment group were included.
Criteria that differed from the Elia et al.review
Unlike the current review, studies of rofecoxib and valdecoxib were included by Elia et al. 28 In addition the earlier review included studies with a no-treatment comparison group, which were excluded from the current review. Studies conducted by Dr Scott S Reuben were also excluded from the current review because, whilst the review was under way, much of the research undertaken by Dr Reuben came under question, due to evidence of fraud and falsification of data.
Data extraction
The data previously extracted by Elia et al. 28 formed the basis for the update (http://anesthesiologie.hug-ge.ch/data.htm). The data from the earlier review were not available as data files, therefore the data were extracted directly from the papers. These were then checked by a second researcher against the original paper and the data extracted by Elia et al. 28 Where Elia et al. had obtained data directly from authors, these data were used for the current review. For some of the studies from the earlier review, missing data could not be obtained directly from the authors and data were then estimated from a graph. New studies were also extracted by one researcher and checked by a second. Authors of trials published since the review by Elia et al. were contacted for additional information where necessary. The data extracted from the individual studies are provided in Appendix 9.
For 24-hour morphine consumption (i.e. morphine consumption in the first 24 hours following surgery), the mean and standard deviation (SD) were extracted for the intervention and comparator. The number of events was extracted for morphine-related and non-opioid analgesic-related adverse effects. Where the denominator for adverse effects reported by the primary study authors was the number of patients in the analysis, this was extracted. This replicated the approach by Elia et al. 28 Some of the studies reported adverse effects beyond the immediate 24-hour period or were not explicit about the cut-off used. In these instances adverse events for the whole period were recorded to avoid loss of data from these studies.
Study quality
Study quality was assessed using the same modified seven-point four-item Oxford scale32 used by Elia et al. 28 This scale assesses whether randomisation, concealment of allocation, double blinding and the flow of patients within a study are adequately described or not (see Appendix 5). The minimum score attainable on the scale is zero and the maximum score is seven.
Methods for synthesis
Overview
Key study characteristics, patient outcomes and study quality were summarised in narrative and tables. Relative treatment effects for the outcomes of interest of the different classes of analgesics were estimated using an MTC. 29,30
Main analysis
In the base-case MTC analysis, four treatments were compared: placebo, paracetamol (including propacetamol), NSAIDs and COX-2 inhibitors. There are several beneficial and adverse outcomes from taking paracetamol, NSAIDs and COX-2 inhibitors. The primary outcomes of interest were 24-hour morphine consumption and morphine-related nausea and vomiting and sedation as well as surgical bleeding. Ideally for the MTC we would have selected a single primary outcome, as using multiple outcomes has the potential to create such a complex synthesis that it is difficult to interpret. However, given the conflicting evidence from previous reviews about whether or not a reduction in morphine consumption translates into a reduction in related adverse effects,27,28 it was necessary to include at least one adverse effect in addition to morphine consumption. We used nausea and vomiting as it is a common adverse effect and is of particular concern for patients, as well as sedation. Given that these outcomes cannot be considered markers for the other potential morphine-related adverse effects, we also conducted an MTC of the remaining outcomes (respiratory depression, bowel dysfunction, urinary retention, pruritus and dizziness) to provide as complete a picture of the evidence as possible. These additional outcomes are summarised in Chapter 3 (Results), and the full results are detailed in Appendix 8. Surgical bleeding associated with NSAIDs was the main non-opioid-related outcome of interest. Priority was given to the primary outcomes in the interpretation of the MTC. These were identified as primary outcomes at the protocol stage.
Sensitivity analyses
Sensitivity analyses based on study quality and drug type were undertaken for 24-hour morphine consumption. For quality, studies were classified based on whether or not they were appropriately blinded, i.e. whether or not they scored 2 for blinding on the modified Jadad scale (see Appendix 5). Blinding and allocation concealment have been identified as of particular importance where there is any subjectivity in measurement of outcomes, as is the case for the outcomes in this review. 33 The adequacy of blinding was used for the sensitivity analysis as reporting of this aspect of quality is generally better than for allocation concealment and it would be possible to have a full network for the analysis.
The sensitivity analysis by drug type did not take into consideration mode of administration or dose of the individual drugs. In the protocol we had originally planned to undertake a sensitivity analysis based on the dosing schedule as had been done in the review we were updating. 28 However, we were concerned that dosing schedule would be confounded by type of drug and that it would be more clinically meaningful to use a sensitivity analysis by individual drug, and also to allow some exploration of the appropriateness of undertaking the main analysis based on drug class.
In addition we undertook a post hoc sensitivity analysis exploring the effect of baseline morphine consumption on the results. Further details of the synthesis are given below under ‘Details of mixed treatment comparison’.
Direct comparisons
In addition, standard meta-analyses were undertaken of head-to-head comparisons between the active interventions. These were undertaken for the main morphine-related outcomes of interest (24-hour morphine consumption, sedation and PONV) and side effects related to the non-opioid analgesic. The purpose of this was to explore the consistency of the direct evidence with the results of the MTC. A random effects model was used and the analysis was undertaken in revman 5. 34 Heterogeneity was explored through consideration of the study populations, methods and interventions, by visualisation of results and, in statistical terms, by the chi-squared test for homogeneity and the I2statistic. 35
Details of mixed treatment comparison
An MTC analysis is an extension of a meta-analysis, but where a meta-analysis includes only direct evidence an MTC analysis draws on both direct and indirect evidence. The results from studies that compare interventions A and B are considered to be direct evidence for the treatment effect dAB. If a study X compares treatments A and C and a study Y compares treatments B and C, and a treatment effect dAB is calculated from these two studies, then this result is referred to as indirect evidence. As in a meta-analysis, it is the summary treatment effect from each study that is utilised in the MTC analysis, hence the benefit of randomisation in each study is retained.
A standard meta-analysis combines the results from two or more studies that have comparable populations, interventions, comparators and outcomes. Study quality and other study characteristics are also assumed to be similar. Similarly, to make indirect comparisons, it is assumed that the study characteristics are comparable. This is known as exchangeability, which can be investigated through the consistency of the direct and indirect evidence. 36 It assumes that, had treatment C been included in the study comparing A and B, then the treatment effect dAC would be the same as that found from the study of A and C. 31 Assuming consistency, the treatment effect dAC is the sum of the treatment effects dAB and dBC:
An MTC analysis can combine both the direct evidence and the indirect evidence for dAC. 31
An MTC requires a ‘network of evidence’ between all the treatments of interest. In the context of the present review this would mean that the network is required to comprise trials of paracetamol, NSAIDs, COX-2 inhibitors and placebo, where each treatment has been compared either directly or indirectly with every other. For example, although NSAIDs and COX-2 inhibitors may not have been directly compared within a single trial, they can be compared indirectly as both have been assessed against a common comparator, placebo. The common comparator need not be placebo and, within an MTC, there can be more than one common comparator. Within an MTC all the available trials’ data on a treatment for the specified indication should be included.
Interventions
The main analyses evaluated the relative effects of four classes of intervention: paracetamol, NSAIDs, COX-2 inhibitors and placebo. Several trials investigated variations of the same class of drug in different arms, such as different specific drugs, doses, or mode of delivery. In such studies the different regimens of the intervention were combined into one group. For dichotomous outcomes the number of events and the number of people with events were summed. For continuous data, the means and standard deviations were pooled using the methods described in the Cochrane Handbook. 37
Clinical outcomes
The analysis focused on four main outcomes (see ‘Overview’ above). These were 24-hour morphine consumption, sedation, nausea and vomiting, and surgical bleeding. The trials varied in how nausea and vomiting were recorded. Some recorded nausea as a single outcome and vomiting as a single outcome and other studies recorded nausea and/or vomiting combined in a single outcome (PONV). As none of the trials that recorded nausea and vomiting as single outcomes also recorded PONV, it was decided to combine the nausea outcome and PONV outcomes in one analysis to maximise the evidence available in the network for this outcome. Nausea rather than vomiting was selected as the single outcome to combine with PONV because nausea was a more prevalent adverse effect than vomiting and nausea is the most clinically relevant of the two. It was also considered likely that the relative effects of treatments on the nausea outcome and the PONV outcome were similar. Separate analyses were also performed for each of the three outcomes individually.
Networks and study inclusion
An MTC analysis can only be performed on a connected network where a direct or indirect comparison can be made between every intervention included in the analysis for a specific outcome. For every outcome, network tables were produced listing the trials that recorded that outcome. These network tables are presented in Appendix 6, Tables 22–30. Network diagrams were also produced for the 24-hour morphine consumption, nausea and PONV, and sedation outcomes, showing the number of studies in which each pair of treatments are compared. These are reported in Chapter 3 (Results). If a study compared three treatments, it will be counted three times, e.g. NSAID versus placebo, paracetamol versus placebo, and NSAID versus paracetamol. The majority of trials had a placebo comparator. An MTC analysis was performed for every outcome including only the interventions that formed a connected network. Trials that recorded a median and a range or an interquartile range were excluded from the MTC analysis for 24-hour morphine consumption because of uncertainty surrounding the accuracy of any derived mean and standard deviation.
Consistency
It was assumed that the population, intervention protocols, outcomes and other study characteristics were sufficiently similar for the included trials. Standard meta-analyses of head-to-head comparisons between the active interventions were conducted to explore consistency with the results of the MTC.
The models
The analysis was undertaken using winbugs, a Bayesian analysis software that calculates posterior distributions for the parameters of interest given likelihood functions derived from data and prior probabilities. The winbugs codes for the different analyses are presented in Appendix 2a–e.
Two different models were produced for dichotomous and continuous outcomes. Likelihood functions and models are specified for every arm of every trial. Utilising the model reported in Cooper et al. ,38 for the dichotomous adverse event outcomes, a binomial likelihood function was specified for the number of events in each arm. In the model, for the control group trial arms, on the log-odds scale, the probability of an event in each arm was related to the control group treatment effect. For the treatment group trial arms, on the log-odds scale, the probability of an event in each arm was related to the control group treatment effect and the treatment effect difference between the trial arms.
In this model, placebo is the default baseline treatment, but if there is no placebo in the trial, then another treatment such as paracetamol becomes the baseline.
For the continuous 24-hour morphine consumption outcome, a normal likelihood function was specified. In the model, for the control group trial arms, the 24-hour morphine consumption was related to the control group morphine consumption. For the treatment group trial arms, the 24-hour morphine consumption was related to the control group morphine consumption and the treatment effect difference. Random effects models were used throughout.
The trial-specific log-odds ratios in multi-arm trials will be correlated. 29,38,39 To adjust for this, the winbugs code published on the Bristol University MTC analysis webpage (https://www.bris.ac.uk/cobm/research/mpes/mtc.html) was used.
Bayesian models require prior probability distributions to be specified for every unknown parameter. Non-informative priors were assumed for each analysis. These were non-informative normal distributions for means and uniform distributions for standard deviations.
The basic model calculates the relative treatment effect of each treatment compared to the baseline treatment, placebo in this case. To calculate the absolute treatment effects for each treatment, the adverse event rate or the mean morphine consumption, the absolute treatment effect of the baseline treatment (placebo) was calculated for every outcome using a random effects model, using all the placebo arms included in each analysis. The absolute treatment effects were then calculated by adding the relative treatment effects to the treatment effect of placebo.
Selection of model and model fit
The winbugs software uses a Markov Chain Monte Carlo (MCMC) simulation, which begins the simulation with an approximate distribution and, if the model is good, the distribution converges to the true distribution. The model progress was checked for convergence. Although convergence was rapid, the first 5000 iterations were excluded and a further 100,000 iterations were performed in order to calculate the results.
Models were compared using the device information criterion (DIC) statistic,38 which combines model deviance and the effective number of parameters, and these are reported in the results. The residual deviance was used to indicate if an individual model was a good fit to the data, and these values are also reported. A residual deviance close to the number of arms in an analysis is considered to be a good fit.
Model outcomes
For the binary outcomes, the pairwise odds ratios for each pair of comparisons and the event rate for each intervention were calculated. For the continuous outcome, the mean differences between each pair of treatments and the mean outcome for each intervention were calculated. Uncertainty was presented using the upper and lower limits of 95% credibility intervals, which describe the bounds within which it is believed there is a 95% chance that the true value lies. The non-informative priors ensure that the results are dominated by the data.
The probability of each intervention being the best was also calculated, and interventions were then ranked according to the probability of being the most effective. These probabilities were derived from the posterior probability distributions derived for each of the treatment effect estimates from the simulation in winbugs. These probabilities describe the possibility of each treatment being the best given the relative treatment effect estimates and their uncertainty as expressed by the credibility interval. The probability of being best statistic summarises the uncertainty across all the pairwise comparisons. Probabilities of less than 95% should be interpreted with some caution as they indicate uncertainty. If a treatment is statistically significantly better than all the other comparators, then the probability of being the most effective treatment will be at least 95%. A probability of being best of less than 95% indicates that the best treatment is not statistically significantly better (at 95% level) than at least one of the other treatments.
Sensitivity analyses
Adjustment for baseline 24-hour morphine consumption
There was considerable variation in the placebo 24-hour morphine consumption results. The average across the placebo arms was 45.26 mg and the standard deviation was 22.23 mg. The intervention with the most trial arms other than placebo was the NSAID class of drugs. The correlation between the reduction in 24-hour morphine consumption due to NSAIDs compared to placebo and the placebo 24-hour consumption was –0.8. If the average placebo 24-hour consumption for the set of trials varied by drug class, then the results could be biased. Consequently, a model was run to estimate the baseline morphine consumption coefficients and to estimate the treatment effect differences at an average morphine consumption. This was a post hoc analysis. Details are given in Appendix 2f.
By individual drug
A sensitivity analysis was performed for all the individual paracetamol, NSAID and COX-2 inhibitor drugs that form a connected network for the 24-hour morphine consumption outcome. Only the mean difference of each drug compared to placebo was recorded as there are 120 pairwise comparisons in total. This analysis also estimated the effect of baseline morphine consumption on the treatment effect and estimated the treatment effects at an average morphine consumption. Because there were few studies for each individual drug, only the assumption of a common treatment and baseline morphine consumption interaction was assumed.
By trial quality
Another sensitivity analysis was performed evaluating the impact of study quality on the results for the 24-hour morphine consumption outcome.
The analysis was performed in two ways. Firstly, the model was run on a subset of trials that only included trials with adequate quality as defined above under ‘Overview’. This analysis included adjustment for baseline variation in morphine consumption. Secondly, study quality was added as a dummy variable in the MTC model with a covariate for baseline morphine consumption. Details are given in Appendix 2g.
Chapter 3 Results
Quantity and quality of research available
The searches identified 4357 potentially relevant references (Figure 1). On the basis of screening titles and abstracts, 147 full papers were ordered for further assessment. In addition 52 papers from the Elia et al. 28 review were ordered for screening making a total of 199 full papers. Of the 199 full papers, 139 were excluded because they did not meet the inclusion criteria; reasons for exclusion are reported in Appendix 3. One hundred and twenty-seven of these papers were new studies, of which two40,41 were excluded due to retraction by the respective journals early in 2009 because of falsification of data. 42,43 We were not able properly to assess for inclusion one Turkish language study due to problems in getting a translator,44 and one Bulgarian language study45 as the journal was not held by the British Library. Twenty new studies met the inclusion criteria.
FIGURE 1.
Selection of studies.
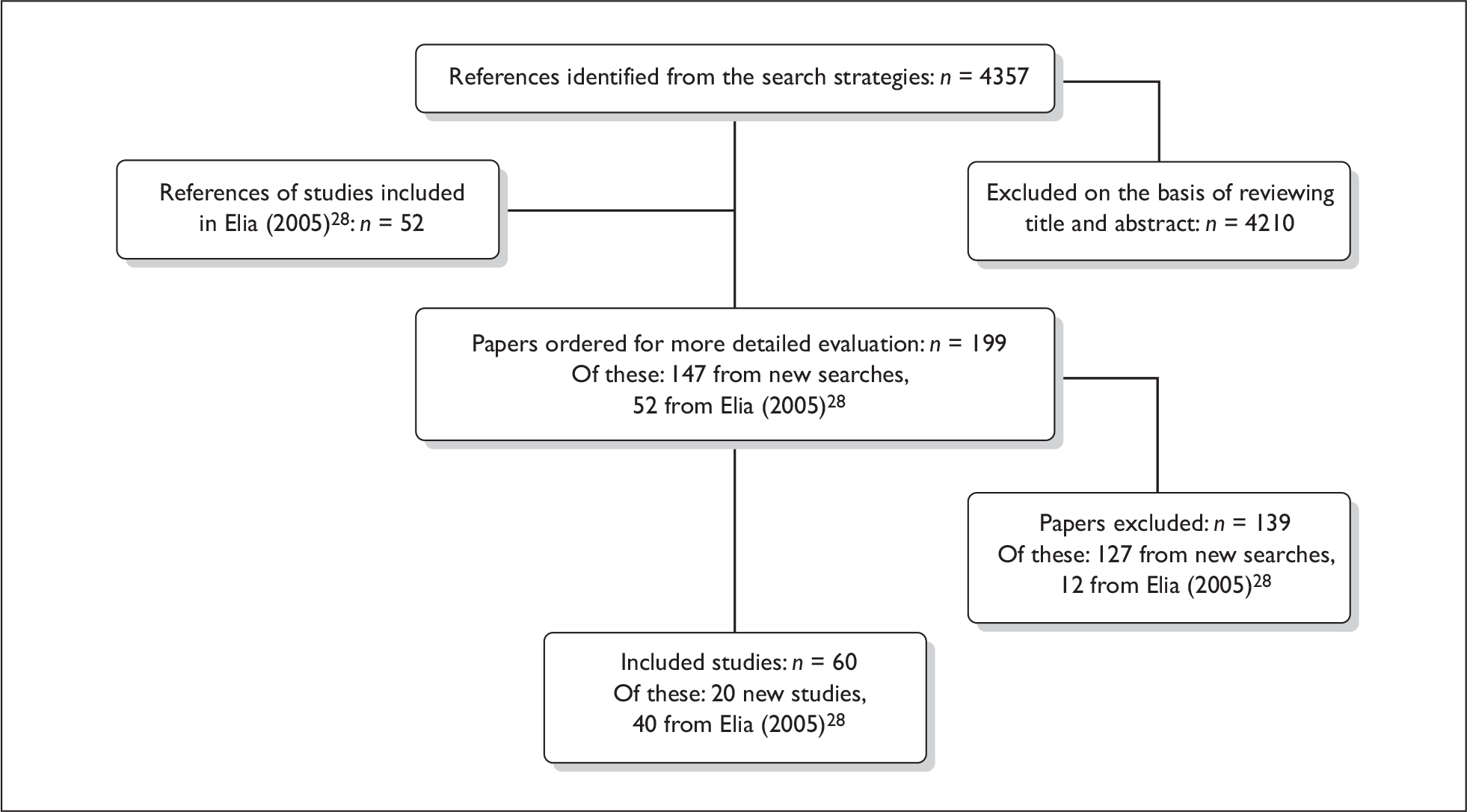
Twelve of the 52 studies included in the earlier review were excluded from the current review. Four were of valdecoxib or rofecoxib, which are no longer licensed in the UK;46–49 three had a no treatment comparison group (i.e. no placebo or active intervention);50–52 in one the NSAID was given in conjunction with another analgesic;53 in one a variety of opioids were administered via PCA;54 one was based upon an abstract for which a full paper was published since the searches undertaken by Elia;28 and one by Reuben55 was excluded as it was retracted by the journal early in 2009 due to falsification of data. 42 We also decided to exclude a further paper by this author. 56 This paper has not been retracted but, because we were aware of at least 12 papers by Reuben that had definitely been withdrawn, and at the time of the analysis were unable to establish with certainty the veracity of this second paper, we excluded it from the review. 57
When the relevant studies from the earlier review (n = 40) and those identified from our own searches (n = 20) were combined there were a total of 60 included studies. Two of the included studies were non-English language, one being Greek and the other German. 58,59
Study characteristics
There were no studies located that directly compared all three classes of drug (NSAID, COX-2 inhibitor and paracetamol) and none that compared COX-2 to paracetamol (Table 5). One study directly compared COX-2 inhibitor to NSAID (and placebo);60 and there were five studies that directly compared NSAID and paracetamol (three also had a placebo arm61–63 and two did not64,65). Placebo was the only comparator in 15 studies of COX-2 inhibitors, in 32 studies of NSAIDs and in seven studies of paracetamol (Table 5).
| Comparison | Number of studies |
|---|---|
| COX-2 vs NSAID vs paracetamol | 0 |
| COX-2 vs NSAID | 0 |
| COX 2 vs NSAID vs placebo | 160 |
| COX-2 vs paracetamol | 0 |
| COX-2 vs paracetamol vs placebo | 0 |
| NSAID vs paracetamol | 264,65 |
| NSAID vs paracetamol vs placebo | 361–63 |
| COX-2 vs placebo | 1558,66–79 |
| NSAID vs placebo | 3259,80–110 |
| Paracetamol vs placebo | 716,111–116 |
The characteristics of the included studies are summarised in Table 6. All of the participants were receiving PCA morphine for at least 24 hours following major surgery. A range of different surgeries were undertaken across the studies, and sometimes within studies, including thoracic, orthopaedic, gynaecological, obstetric and general surgery. General anaesthesia was most commonly used (see Appendix 9 for further details of anaesthesia). The number of participants in the included studies ranged from 20 to 514, and over 40% of studies had 20 or fewer participants in each comparison group.
| Study | Surgery and anaesthesia | COX-2 (type, number randomised; mode of administration; dose) | NSAID (type, number randomised; mode of administration; dose) | Paracetamol (type, number randomised; mode of administration; dose) | Placebo (number randomised) |
|---|---|---|---|---|---|
| Alexander 200280 |
Knee or hip arthroplasty GA |
1) Diclofenac, 36 i.v.; 75-mg single dose 2) Ketorlac, 33 i.v.; 60-mg single dose |
33 | ||
| Alhashemi 200664 |
Caesarean section SA |
Ibuprofen, 23 p.o.; 400 mg/6 h |
Paracetamol n = 22 i.v.; 1 g/6 h for 48 h |
||
| Argyriadou 200758 |
Thoracotomy Unclear |
Parecoxib, 20 i.v.; 20 mg after commencement of procedure and after completion |
20 | ||
| Balestrieri 199781 |
Hysterectomy Myomectomy GA |
1) Ketorolac, 83 i.v.; 60 mg postop. + 30 mg/6 h 2) Ketorolac, 83 i.v.; 60 mg intraop. + 30 mg/6 h |
82 | ||
| Blackburn 199582 |
Abdominal hysterectomy GA |
Ketorolac, 30 i.v.; 100 mg/h (15 min) + 4 mg/h (24 h) |
30 | ||
| Burns 199183 |
Upper abdominal GA |
1) Ketorolac, 22 i.m.; 12.5 mg/h (30 min) + 2.5 mg/h 2) Ketorolac, 24 i.m.; 10 mg/4 h |
21 | ||
| Cakan 2008111 |
Lumbar laminectomy and discectomy GA |
Paracetamol n = 20 i.v.; 1 g/6 h |
20 | ||
| Cassinelli 200884 |
Lumbar decompression GA |
Ketorolac, 13 i.v.; 30 mg/6 h for 12 h |
12 | ||
| Celik 200385 |
Abdominal hysterectomy GA |
Naproxen, 20 p.o.; 550-mg single dose |
20 | ||
| Chau-in 200866 |
Abdominal hysterectomy GA |
1) Etoricoxib, 17 p.o.; 120 mg single dose 2) Etoricoxib, 17 p.o.; 180-mg single dose |
15 | ||
| Cheng 200467 |
Laparoscopic cholecystectomy GA |
Celecoxib, 30 p.o.; 200-mg single dose |
30 | ||
| Cobby 199961 |
Abdominal hysterectomy GA |
Diclofenac, 24 Rectal; 50 mg/8 h |
Paracetamol n = 24 Rectal; 1.3 g/8 h |
24 | |
| aColquhoun 198986 |
Open cholecystectomy GA |
Diclofenac, 15 Rectal; 100-mg single dose |
15 | ||
| De Decker 200187 |
Spine surgery GA |
1) Piroxicam, 15 i.m.; 40-mg single dose 2) Tenoxicam, 15 i.v.; 40-mg single dose 3) Tenoxicam, 15 i.m.; 40-mg single dose |
15 | ||
| Delbos 199516 |
Knee ligamentoplasty GA |
Propacetamol n = 30 i.v.; four infusions 2 g/6 h | 30 | ||
| Durmus 200368 |
Abdominal hysterectomy GA |
1) Celecoxib, 20 p.o.; 200-mg single dose |
20 | ||
| El-Halafawy 200469 |
CABG GA |
Parecoxib, 30 i.v.; 40 mg/12 h for 72 h |
30 | ||
| Etches 199588 |
Knee or hip arthroplasty GA |
Ketorolac, 86 i.v.; 30 mg + 5 mg/h (24 h) |
88 | ||
| Fayaz 2004110 |
CABG GA |
Diclofenac, 20 Rectal; 100 mg/18 h |
20 | ||
| Fletcher 199762 |
Lumbar disc GA |
Ketoprofen, 16 i.v.; 50 mg/6 h |
Propacetamol n = 16 i.v.; 2 g/6 h |
15 | |
| Fong 200870 |
Caesarean section Spinal |
1) Celecoxib, 20 p.o.; 400-mg single dose before surgery 2) Celecoxib, 20 p.o.; 400-mg single dose after surgery |
20 | ||
| Gillies 198790 |
Upper abdominal GA |
1) Ketorolac, 21 i.m.; 6 mg + 1.5 mg/h 2) Ketorolac, 20 i.m.; 12 mg + 3 mg/h (24 h) |
20 | ||
| Hanna 200391 |
Knee or hip arthroplasty GA |
1) Dexketoprofen, 50 i.m.; 50 mg/12 h 2) Ketoprofen, 58 i.m.; 100 mg/12 h |
55 | ||
| Hegazy 200360 |
Cervical disc GA |
Parecoxib, 15 i.v.; 40 mg/6 h |
Ketorolac, 15 i.v.; 30 mg/6 h |
15 | |
| Hernandez-Palazon 2001112 |
Spinal fusion GA |
Propacetamol, 22 i.v.; 2 g/6 h |
22 | ||
| Hodsman 198792 |
Abdominal GA |
Diclofenac, 33 i.m.; 75 mg/12 h |
32 | ||
| Hsu 200393 |
Caesarean section Spinal |
Tenoxicam, 49 i.v.; 20-mg single dose |
54 | ||
| Hubbard 200371 |
Knee arthroplasty Spinal + sedation |
1) Parecoxib, 65 i.v.; 20 mg/12 h 2) Parecoxib, 67 i.v.; 40 mg/12 h |
63 | ||
| Inan 200794 |
Total knee replacement GA |
Lornoxicam, 23 i.v.; 16 mg before surgery and 8 mg/12 h |
23 | ||
| Jirarattanaphochai 200872 |
Lumbar spine surgery GA |
Parecoxib, 60 i.v.; 40 mg before surgery and 40 mg/12 h |
60 | ||
| Karaman 200695 |
Abdominal hysterectomy GA |
1) Lornoxicam, 20 i.m.; 8-mg single dose 2) Ketoprofen, 20 i.m.; 100-mg single dose |
20 | ||
| Kvalsvik 2003113 |
Abdominal hysterectomy GA |
Paracetamol, 38 rectal; 1 g/6 h for 60 h | 40 | ||
| Lee 200879 |
Open colorectal surgery GA |
1) Parecoxib, 20 i.v.; 40 mg before surgery 2) Parecoxib, 20 i.v.; 40 mg at skin closure |
20 | ||
| Mack 200189 |
Microsurgical lumbar discectomy GA |
Ketorolac, 10 i.v.; 30 mg over 4 min |
10 | ||
| Malan 200373 |
Hip arthroplasty GA or spinal |
1) Parecoxib, 67 i.v.; 20 mg/12 h 2) Parecoxib, 64 i.v.; 40 mg/12 h |
70 | ||
| Martinez 200774 |
Total hip arthroplasty GA |
1)Parecoxib, 22 i.v.; 40 mg at induction and 12 h 2) Parecoxib, 19 i.v.; 40 mg at wound closure and 12 h |
21 | ||
| cMoodie 200896 |
Major surgery GA with or without spinal |
1) Ketorolac, 43 Intranasal; 10 mg/8 h for 40 h 2) Ketorolac, 42 Intranasal; 30 mg/8 h for 40 h |
42 | ||
| Munishankar 200865 |
Caesarean section Spinal + sedation |
Diclofenac, 26 100 mg rectal then 50 mg/8 h p.o. |
Paracetamol, 26 1 g rectal then 1 g/h p.o. |
||
| Munro 199897 |
Laparoscopic cholecystectomy GA |
Tenoxicam, 20 i.v.; 40-mg single dose |
20 | ||
| Ng 200298 |
Abdominal hysterectomy GA |
Diclofenac, 20 Rectal; 75 mg twice daily |
20 | ||
| bNg 200375 |
Hysterectomy GA |
Parecoxib, 23 i.v.; 40-mg single dose |
23 | ||
| Owen 198699 |
Gynaecology GA |
Ibuprofen, 29 Rectal; 500 mg/8 h |
31 | ||
| Peduto 1998114 |
Hip arthroplasty GA |
Propacetamol, 46 i.v.; 2 g/6 h |
51 | ||
| Perttunen 1992100 |
Thoracotomy GA |
Diclofenac, 15 i.v.; 2 mg/kg/h (48 h) |
15 | ||
| Plummer 1996101 |
Gynaecology GA |
Ibuprofen, 57 p.o.; 1600 mg before surgery and at 24 h |
58 | ||
| Rao 2000102 |
Abdominal GA |
Ketoprofen, 20 i.v.; 100 mg/12 h |
20 | ||
| Ready 1994103 |
Orthopaedic Gynaecology General GA and spinal |
1) Ketorolac, 66 i.v.; 30 mg + 5 mg/h 2) Ketorolac, 70 i.v.; 30 mg + 15 mg/3 h |
71 | ||
| Riest 200876 |
Discectomy GA |
1) Parecoxib, 80 i.v.; 40 mg before surgery and after 40 mg/12 h for 72 h 2) Parecoxib, 80 i.v.; 40 mg/12 h after surgery for 72 h 3) Parecoxib, 80 i.v.; single 40-mg dose before surgery |
80 | ||
| Rowe 1992104 |
Lumbar laminectomy GA |
Indometacin, 14 p.o.; 75-mg single dose |
16 | ||
| Schug 1998115 |
Orthopaedic emergencies GA |
Paracetamol, 28 p.o.; 1 g/4 h |
33 | ||
| Sevarino 1992105 |
Gynaecology GA |
1) Ketorolac, 12 i.m.; 30 mg + 15 mg/6 h 2) Ketorolac, 12 i.m.; 60 mg + 30 mg/6 h |
11 | ||
| Siddik 200163 |
Caesarean section Spinal |
Diclofenac, 20 rectal; 100 mg/8 h |
Propacetamol, 20 i.v.; 2 g/6 h |
20 | |
| Siddiqui 200877 |
Upper or lower limb fracture fixation GA |
Etoricoxib, 100 p.o.; single 120-mg dose |
100 | ||
| Sinatra 2005116 |
Total hip or knee replacement GA spinal or epidural |
1) Propacetamol, 52 i.v.; 2 g/6 h 2) Paracetamol, 51 i.v.; 1 g/6 h |
52 | ||
| Tang 200278 |
Abdominal hysterectomy or myomectomy GA |
1) Parecoxib, 19 i.v.; 20 mg/12 h 2) Parecoxib, 18 i.v.; 40 mg/12 h |
18 | ||
| Thompson 2000106 |
Abdominal hysterectomy GA |
Meloxicam, 18 rectal; 15-mg single dose |
18 | ||
| Trampitsch 200359 |
Gynaecological surgery GA |
Lornoxicam, 22 i.v.; 8 mg/8 h |
22 | ||
| Vandermeulen 1997107 |
Abdominal orthopaedic GA |
Tenoxicam, 256 i.v.; 40 mg at 0 and 24 h |
258 | ||
| Varrassi 1994108 |
Cholecystectomy GA |
Ketorolac, 50 i.m.; 30 mg + i.v. continuous infusion 2 mg/h |
50 | ||
| Xuerong 2008109 |
Abdominal hysterectomy Spinal |
Lornoxicam, 15 i.v.; 8 mg continuous infusion during surgery |
15 |
The type of drug, dosing regimen and mode of administration of COX-2 inhibitors and NSAIDs varied between studies. The dosing regimen for each study is provided in Table 6, and details of the dosing regimen, by drug type, are provided in Appendix 4.
The COX-2 inhibitors investigated were parecoxib (11 studies),58,60,69,71–76,78,79 celecoxib (three studies),67,68,70 and etoricoxib (two studies). 66,77 In four COX-2 inhibitor studies, participants were randomised to different doses of COX-2 (dose ranging studies),66,71,73,78 and in four they were randomised to receive the COX-2 at different times such as before or after surgery (timing studies). 70,74,76,79 Celecoxib and etoricoxib were both administered orally as single doses; celecoxib at a dose of 200 mg or 400 mg and etoricoxib at a dose of 120 mg or 180 mg. In all the studies of parecoxib, the drug was administered intravenously; lower dose studies used a single dose of 40 mg or 20 mg at 12-hourly intervals, higer dose studies used 40 mg at 6-hourly intervals or 40 mg at 12-hourly intervals (see Table 6 and Appendix 4).
There were 11 different NSAIDs: ketorolac (13 studies),60,80–84,88–90,96,103,105,108 diclofenac (nine studies),61,63,65,80,86,92,98,100,110 tenoxicam (four studies),87,93,97,107 ketoprofen (four studies),62,91,95,102 lornoxicam (four studies),59,94,95,109 ibuprofen (three studies),64,99,101 indometacin (one study),104 meloxicam (one study),106 naproxen (one study),85 dexketoprofen (one study),91 and piroxicam (one study). 87 There were five NSAID dose-ranging studies;83,90,96,103,105 one timing study;81 and four studies that compared different NSAIDs. 81,87,91,95
Ketorolac was administered using intravenous, intranasal and intramuscular methods and was predominantly given in multiple doses or by continuous infusion. A single dose (30 mg and 60 mg) of ketorolac was used in two studies. The multidose regimen for ketorolac varied widely (see Appendix 4); intravenous doses ranged from 15 mg at 6-hourly intervals to 60 mg starting dose plus 30 mg every 6 hours; intranasal doses ranged from 10 mg to 30 mg every 8 hours; and intramuscular doses ranged from 1.5 mg every 6 hours (plus a starting dose of 6 mg) to 30 mg every 6 hours (plus a starting dose of 60 mg). The continuous infusion dose also varied (see Appendix 4).
There was less variability within the remaining NSAIDs. Diclofenac was most commonly administered rectally, using a multiple dose regimen, but some studies also used oral, intravenous and intramuscular methods. The rectal doses ranged from 75 mg at 12-hour intervals to 100 mg at 8-hour intervals but were mainly at the lower dose (see Appendix 4) and did not vary widely. Tenoxicam was administered as a single dose in three studies, ranging from 20 to 40 mg and in the fourth study 40 mg every 24 hours. Administration was predominantly intravenous. Ketoprofen was administered using a multiple dose regimen of 50 mg every 6 hours or 100 mg every 12 hours or in one study a single 100-mg dose. Administration was intravenous and intramuscular. Lornoxicam was administered as a single dose of 8 mg, 8 mg every 8 hours, and 8 mg every 12 hours following an initial 16-mg dose. Administration was intravenous and intramuscular. Ibuprofen was administered as a 1600-mg dose before surgery and at 24 hours, 400 mg every 6 hours, and 500 mg every 8 hours. The remaining NSAIDs were investigated in single trials only. With the exception of dexketoprofen (50 mg every 12 hours), they were given as single doses: indometacin 75 mg; meloxicam 15 mg (rectal); naproxen 550 mg; and piroxicam (40 mg).
There were 12 studies of paracetamol and the prodrug propacetamol: seven of paracetamol61,64,65,111,113,115,116 and six of propacetamol16,62,63,112,114,116 (one of which compared propacetamol and paracetamol116). In all the studies, propacetamol was administered intravenously in doses of 2 g (which releases 1 g of paracetamol) every 6 hours. The paracetamol doses were 0.5 g every 4 hours (oral administration), 1.0 g every 6 hours (oral and rectal administration) and 1.3 g every 8 hours (rectal administration).
Study quality
All the included studies were RCTs with a placebo or active comparator. Full details of the validity assessment are presented in Appendix 5. The quality of reporting was variable between studies and across the criteria. Seven studies received the maximum possible score for each of the criteria: randomisation, allocation concealment, double blinding and description of flow of participants through the study. 63–65,72,79,94,109 The method of randomisation was described and adequate in 57% of studies and mentioned in the remaining studies (this was a minimum criterion for inclusion). Allocation concealment was the most poorly reported criterion: 60% of studies did not describe allocation concealment and 40% did so. No mention was made of blinding in 10% of studies; 48% mentioned double blinding and 42% described an adequate method of blinding. There was no description of flow of participants in 20% of studies, it was described but incomplete in 32% and described and adequate in 48%.
Assessment of effectiveness
Morphine consumption
There was considerable variability in the baseline morphine consumption: the simple mean in the placebo group was 45.26 mg (SD 22.23), and ranged from a minimum of 8.6 mg (SD 5.2) to a maximum of 141.5 mg (SD 74.9). There were five studies where the placebo group had a 24-hour morphine consumption of less than 20 mg67,89,94,109,111 and five with morphine consumption greater than 70 mg. 75,79,85,90,100 There was no apparent pattern amongst these studies in terms of age of participants, type of surgery, size of morphine bolus or length of lockout.
Mixed treatment comparison
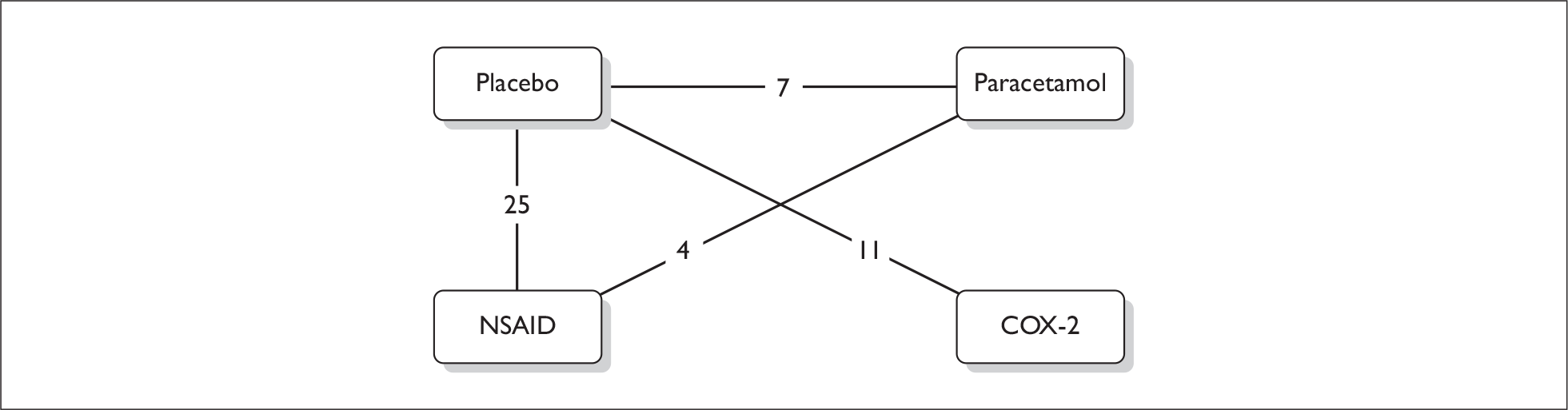
A connected network for the four treatment classes was formed for cumulative 24-hour morphine consumption, allowing a comparison between all four classes to be made for this outcome (Figure 2). There were 56 studies in the network, which included comparisons with both placebo and other active treatments. Table 22 in Appendix 6 contains details of the specific studies included in the network. Two studies were excluded because they reported median morphine consumption,83,98 one because a variance was not available from the paper,91 and one because the number analysed was unclear. 58
FIGURE 2.
Network for 24-hour morphine consumption
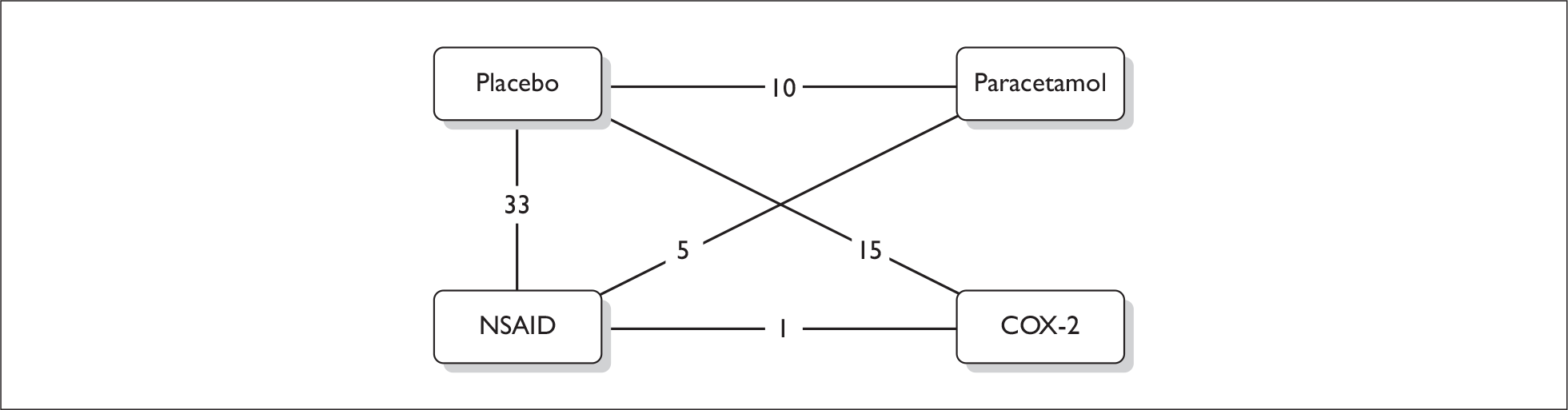
In Figure 2the numbers represent the number of studies in which the two treatments were compared. If a study compared three treatments, it will be counted three times.
The pooled mean baseline morphine consumption was 37.43 mg (SE 2.0). There was a statistically significant reduction (5% level) in mean cumulative 24-hour morphine consumption with paracetamol, NSAIDs and COX-2 inhibitors compared to placebo; that is, the credibility intervals did not cross the line of no effect (zero) (see column 3 in Table 7). The difference ranged from a mean reduction of 6.34 mg for paracetamol to 10.92 mg for COX-2 inhibitors compared to placebo. The mean reduction compared to placebo for NSAIDs was similar to that of COX-2 inhibitors. Comparison of the active treatments shows that although NSAIDs and COX-2 inhibitors were both significantly better than paracetamol, there was no statistically significant difference between NSAIDs and COX-2 inhibitors (MD –0.74; 95% CrI –3.03 to 1.56).
| Comparison | Baseline morphine consumption: mean mg (SE) | Mean difference: mg (95% CrI) |
|---|---|---|
| Placebo | 37.43 (2.00)a | 0 |
| Paracetamol vs placebo | –6.34 (–9.02 to –3.65) | |
| NSAID vs placebo | –10.18 (–11.65 to –8.72) | |
| COX-2 vs placebo | –10.92 (–12.77 to –9.08) | |
| NSAID vs paracetamol | –3.85 (–6.80 to –0.89) | |
| COX-2 vs paracetamol | –4.58 (–7.83 to –1.35) | |
| COX-2 vs NSAID | –0.74 (–3.03 to 1.56) |
The MTC analysis also produced data on the probability of each intervention being the most effective. Based on these data, COX-2 inhibitors had the highest probability of being the best (Table 8): there was a 74% chance that this drug class is the most effective treatment for reducing 24-hour morphine consumption. A probability of less than 95% indicated some uncertainty and reflected the finding of no statistically significant difference between COX-2 inhibitors and NSAIDs. The residual deviance (186) was larger than the number of study arms indicating that the model is not a perfect fit to the data.
| Treatment (n of studies) | p best (%) |
|---|---|
| Placebo (54) | 0 |
| Paracetamol (12) | 0 |
| NSAID (35) | 26 |
| COX-2 (15) | 74 |
Sensitivity analyses
Baseline morphine consumption
Sensitivity analyses were run that included a covariate to adjust for baseline morphine consumption using the network of 56 studies. The analyses evaluated the impact of baseline morphine consumption on the treatment effect for each treatment compared to placebo, and calculated the treatment effect at a placebo morphine consumption level of 37.43 mg.
Three models were run that involved independent, exchangeable and common interaction assumptions. The number of trial arms, the DIC and the residual deviance (RD) are reported in Appendix 7, Table 31. The residual deviance shows that the models with a covariate are close to the number of arms in the study and are a good fit. The DIC is considerably lower for each of the models adjusting for baseline morphine consumption than the DIC for the model with no adjustment (Appendix 7, Table 31). There is little difference in the DIC between the three models adjusting for baseline morphine consumption. As the model with an exchangeable interaction assumption had the lowest DIC, the mean pairwise differences for this model are reported in Table 9 along with those for the model with no baseline adjustment. The covariate coefficients were all statistically significantly different from zero at a 5% level (Appendix 7, Table 31).
| Comparison | Unadjusted mean difference, mg (95% CrI) | Adjusted (exchangeable interaction) mean difference, mg (95% CrI) |
|---|---|---|
| Paracetamol vs placebo | –6.34 (–9.02 to –3.65) | –8.68 (–11.43 to –5.94) |
| NSAID vs placebo | –10.18 (–11.65 to –8.72) | –9.45 (–10.90 to –8.01) |
| COX-2 vs placebo | –10.92 (–12.77 to –9.08) | –10.67 (–12.42 to –8.94) |
| NSAID vs paracetamol | –3.85 (–6.80 to –0.89) | –0.77 (–3.75 to 2.21) |
| COX-2 vs paracetamol | –4.58 (–7.83 to –1.35) | –1.99 (–5.24 to 1.24) |
| COX-2 vs NSAID | –0.74 (–3.03 to 1.56) | –1.22 (–3.43 to 1.00) |
When the model was adjusted for baseline morphine consumption, the results were broadly similar to those of the unadjusted model indicating that the results were robust. COX-2 inhibitors still had the highest probability of being the most effective treatment for reducing 24-hour morphine consumption (Table 10). The main change was that whilst there was still a statistically significant reduction in morphine consumption with all three drugs compared to placebo, the mean difference for paracetamol compared to placebo was larger than in the unadjusted analysis. Any benefits of NSAIDs and COX-2 inhibitors over paracetamol were marginal and no longer statistically significant (see Table 9) and the probabilities for NSAIDs and paracetamol being best were now similar (Table 10).
| Treatment (n of studies) | Unadjusted, p best (%) | Adjusted, p best (%) |
|---|---|---|
| Placebo (54) | 0 | 0 |
| Paracetamol (12) | 0 | 10 |
| NSAID (35) | 26 | 11 |
| COX-2 (15) | 74 | 79 |
Individual drugs
The main purpose of the review was to compare the three classes of analgesic: paracetamol, NSAIDs and COX-2 inhibitors. An MTC was also conducted by individual drug to explore the appropriateness of the assumption made when grouping all types of NSAIDs together, all types of COX-2 inhibitors, and grouping paracetamol with propacetamol. This sensitivity analysis used the single outcome of 24-hour morphine consumption. A connected network was formed consisting of the same 56 studies that were in the main analysis for 24-hour morphine consumption. The model was also adjusted for baseline morphine consumption and hence the treatment effect results are calculated for a placebo morphine consumption of 37.43 mg. There were 15 individual drugs in the analysis plus placebo: two paracetamol (paracetamol and propacetamol), 10 NSAIDs and three COX-2 inhibitors. The residual deviance (130.2) was greater than the number of trial arms (120 arms) in the analysis indicating that the model is not a perfect fit to the data: this may be due to the large number of treatments in the analysis and the fact that four of the drugs were only included in one trial each.
The drug with the best effectiveness estimate was naproxen, although the probability of it being the most effective, 41%, is very low (Table 11). This reflects the degree to which the 95% credibility intervals of the drugs overlap, particularly for naproxen, diclofenac, indometacin, piroxicam, meloxicam and celecoxib.
| Treatment (n of studies) | Mean difference, mg (95% CrI) | p best (%) |
|---|---|---|
| Placebo (54) | ||
| Paracetamol | ||
| Paracetamol (7) | –7.96 (–11.59 to –4.35) | 0 |
| Propacetamol (6) | –8.73 (–12.24 to –5.20) | 0 |
| NSAIDs | ||
| Diclofenac (8) | –16.05 (–20.41 to –11.75) | 27 |
| Ibuprofen (3) | –7.30 (–13.36 to –1.27) | 0 |
| Indometacin (1) | –11.32 (–30.64 to 7.41) | 24 |
| Ketoprofen (3) | –8.11 (–11.52 to –4.78) | 0 |
| Ketorolac (12) | –10.58 (–13.55 to –7.60) | 0 |
| Lornoxicam (4) | –7.86 (–10.39 to –5.40) | 0 |
| Meloxicam (1) | –4.81 (–17.13 to 7.77) | 2 |
| Naproxen (1) | –16.73 (–23.48 to –9.78) | 41 |
| Piroxicam (1) | –8.05 (–17.99 to 1.80) | 3 |
| Tenoxicam (4) | –8.38 (–12.45 to –4.35) | 0 |
| COX-2 inhibitor | ||
| Celecoxib (3) | –12.55 (–15.74 to –9.33) | 2 |
| Etoricoxib (2) | –8.13 (–11.50 to –4.79) | 0 |
| Parecoxib (10) | –10.94 (–13.64 to – 8.22) | 0 |
The results indicate that the decision to group together propacetamol and paracetamol in one class seems to have been reasonable: the mean difference in morphine consumption was similar for the two drugs and the credibility intervals overlapped (Table 11). This would be expected given that propacetamol is a prodrug of paracetamol. Similarly, the decision to group together COX-2 inhibitors is also shown to be reasonable: the mean reduction in morphine consumption ranged from 8.13 to 12.55 mg and the credibility intervals for celecoxib, etoricoxib and parecoxib overlapped (Table 11). The performance of individual NSAIDs was more variable than within the other two classes. For four of the drugs the analysis is based on single trials and for three of these there was no statistically significant difference between the drug and placebo. The reduction in morphine consumption compared to placebo ranged from 4.81 to 16.73 mg for individual NSAIDs and the credibility interval (CrI) for some NSAIDs barely overlapped. These findings suggest that there may be variability in the effectiveness of individual NSAIDs.
Quality
A sensitivity analysis was conducted to evaluate the impact of study quality on the results, as defined in Chapter 2 (Methods). This was done in two ways, both of which also adjusted for baseline morphine consumption. Firstly, the MTC analysis was run on the subset of studies that were recorded as good quality, i.e. studies reporting an adequate method of blinding (see Appendix 7, Table 33, for results). Secondly, a model was run using all of the studies and adding a dummy variable to account for study quality. When the dummy variable was 0 this represented a quality study. Three assumptions were again tested regarding the interaction of the dummy variable with the treatments. None of the models adjusting for study quality are an improvement over the model adjusted for baseline morphine consumption alone based on the DIC (Appendix 7, Table 32). The exchangeable interaction model had the lowest DIC (Appendix 7, Table 32) and the results from this model are reported in Tables 12 and 13. The covariate coefficients were not statistically significantly different from zero at a 5% level (Appendix 7, Table 32).
| Comparison | Unadjusted results: mean difference, mg (95% CrI) | Adjusted for quality and baseline morphine consumption: mean difference, mg (95% CrI) |
|---|---|---|
| Placebo | ||
| Paracetamol vs placebo | –6.34 (–9.02 to –3.65) | –9.01 (–12.01 to –6.01) |
| NSAID vs placebo | –10.18 (–11.65 to –8.72) | –10.17 (–12.37 to –7.99) |
| COX-2 vs placebo | –10.92 (–12.77 to –9.08) | –12.03 (–15.73 to –8.46) |
| NSAID vs paracetamol | –3.85 (–6.80 to –0.89) | –1.17 (–4.31 to 1.98) |
| COX-2 vs paracetamol | –4.58 (–7.83 to –1.35) | –3.02 (–7.24 to 1.02) |
| COX-2 vs NSAID | –0.74 (–3.03 to 1.56) | –1.86 (–5.34 to 1.39) |
| Treatment (n of studies) | Unadjusted, p best (%) | Adjusted for quality and baseline morphine consumption, p best (%) |
|---|---|---|
| Placebo (54) | 0 | 0 |
| Paracetamol (12) | 0 | 5 |
| NSAID (35) | 29 | 11 |
| COX-2 (15) | 71 | 84 |
The results were broadly similar to those of the unadjusted model indicating that the results from the main analysis are reasonably robust (Tables 12 and 13). Based on the pairwise comparisons (Table 12) there was still a statistically significant reduction in morphine consumption with all three drugs compared to placebo, though the mean difference for paracetamol compared to placebo was larger than in the unadjusted analysis. The difference between NSAIDs and COX-2 inhibitors remained small and not statistically significant, and the benefits of NSAIDs and COX-2 inhibitors over paracetamol were marginal and no longer statistically significant. These differences were apparent in the first sensitivity analysis using baseline morphine consumption only, therefore the impact of quality was minimal.
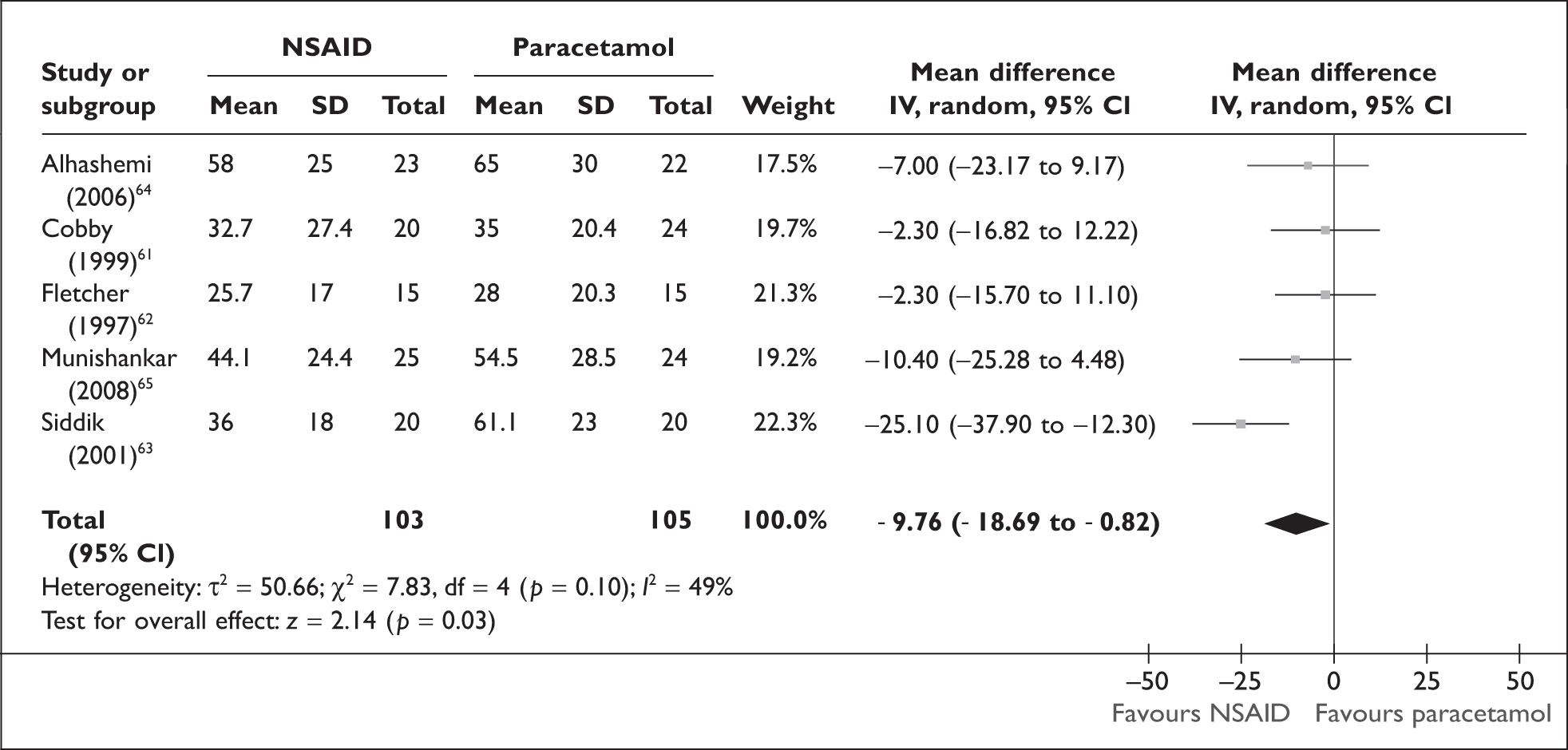
Direct comparisons
Data on cumulative mean morphine consumption were available from five studies that directly compared paracetamol and NSAIDs,61–65 and for one study that directly compared COX-2 inhibitors and NSAIDs. 60 Cumulative 24-hour morphine consumption was statistically significantly lower with NSAIDs compared to paracetamol, with a mean reduction of 9.76 mg (95% CI –18.69 to –0.82) (Figure 3). However, there was evidence of moderate statistical heterogeneity (I2 = 49%).
FIGURE 3.
Cumulative 24-hour morphine consumption (non-steroidal anti-inflammatory drug vs paracetamol).
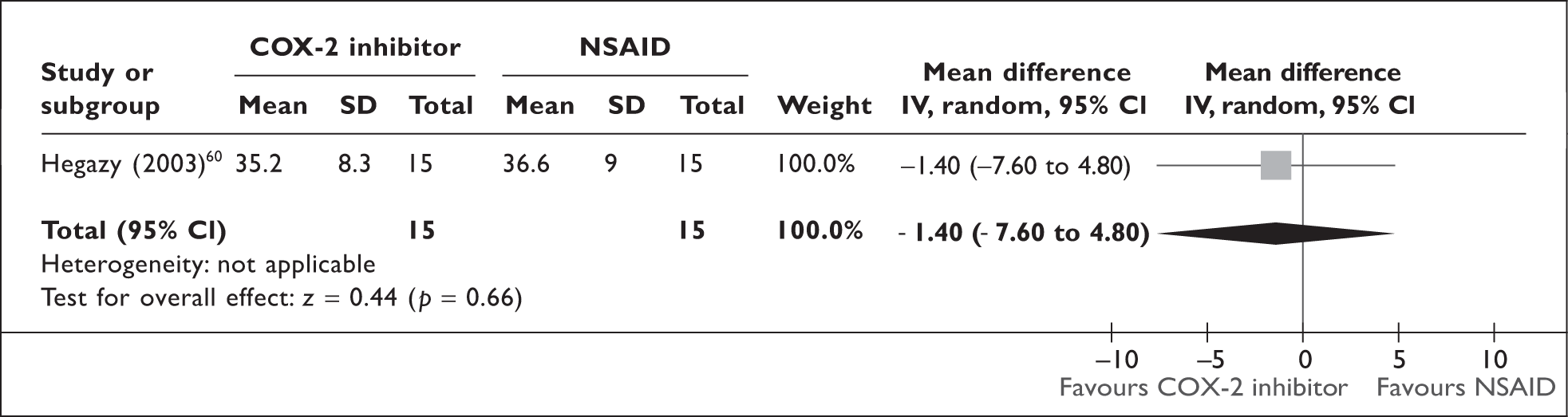
Based on a single study,60 there was no statistically significant difference in cumulative 24-hour morphine consumption between COX-2 inhibitors and NSAIDs (MD –1.40; 95% CI –7.60 to 4.80) (Figure 4).
FIGURE 4.
Cumulative 24-hour morphine consumption (cyclo-oxgenase 2 inhibitor vs non-steroidal anti-inflammatory drugs).
Morphine-related adverse effects
Nausea and postoperative nausea and vomiting (PONV)
Mixed treatment comparison
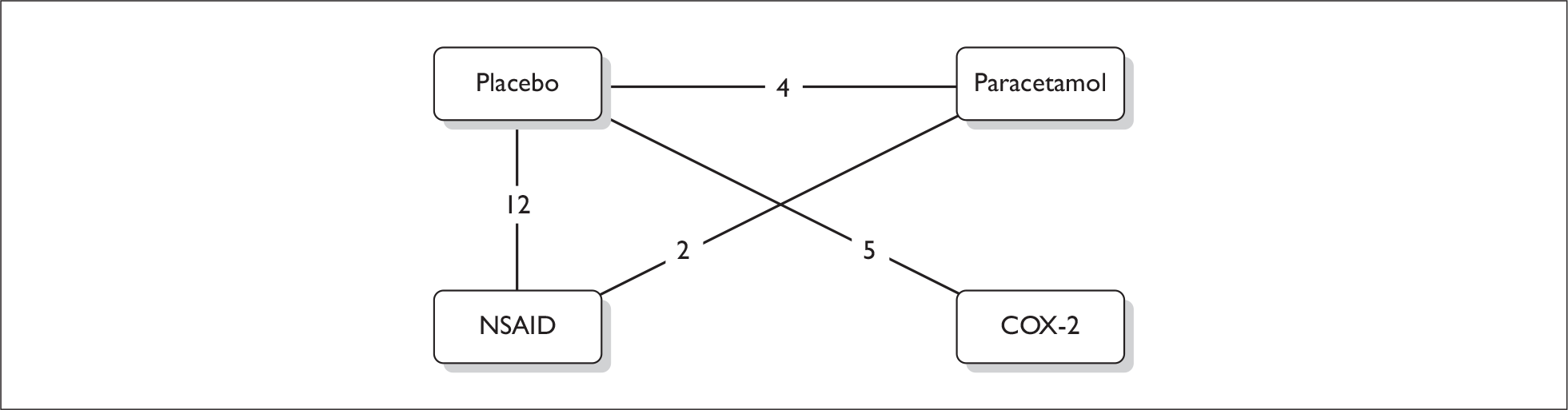
Studies reporting postoperative nausea alone were pooled with studies that reported nausea and/or vomiting (PONV) as a combined outcome. A connected network for the four classes of drugs was formed, which consisted of 43 trials (Figure 5). Details of the studies included in the network are provided in Appendix 6, Table 23.
FIGURE 5.
Network for nausea and postoperative nausea and vomiting.
The pairwise ORs and the 95% CrI are reported in Table 14, where the first treatment in the first column is the intervention and the second is the control. An OR of less than 1.0 indicates that the intervention performed better than the control.
| Comparison | Pairwise odds ratio (OR) and 95% CrI |
|---|---|
| Paracetamol vs placebo | 1.00 (0.60 to 1.53) |
| NSAID vs placebo | 0.70 (0.53 to 0.88) |
| COX-2 vs placebo | 0.88 (0.61 to 1.25) |
| NSAID vs paracetamol | 0.74 (0.44 to 1.17) |
| COX-2 vs paracetamol | 0.93 (0.51 to 1.63) |
| COX-2 vs NSAID | 1.28 (0.81 to 1.97) |
Non-steroidal anti-inflammatory drugs performed best for this outcome compared to placebo, with an odds ratio of 0.70, and this was the only comparison that was statistically significant. COX-2 inhibitors were slightly less effective than NSAIDs, and there was almost no difference between paracetamol and placebo (Table 14). These results are reflected in the probability of NSAIDs being the most effective treatment for reducing nausea or PONV: there was a 78% chance that this was the most effective treatment for this outcome (Table 15). In total, 88 trial arms were included in the analysis, of which 86 had at least one outcome event. The residual deviance (96.64) was similar to the number of arms that had at least one event, which indicates a good model fit.
| Treatment (n of studies) | p best (%) |
|---|---|
| Placebo (41) | 0 |
| Paracetamol (9) | 7 |
| NSAID (27) | 78 |
| COX-2 (11) | 15 |
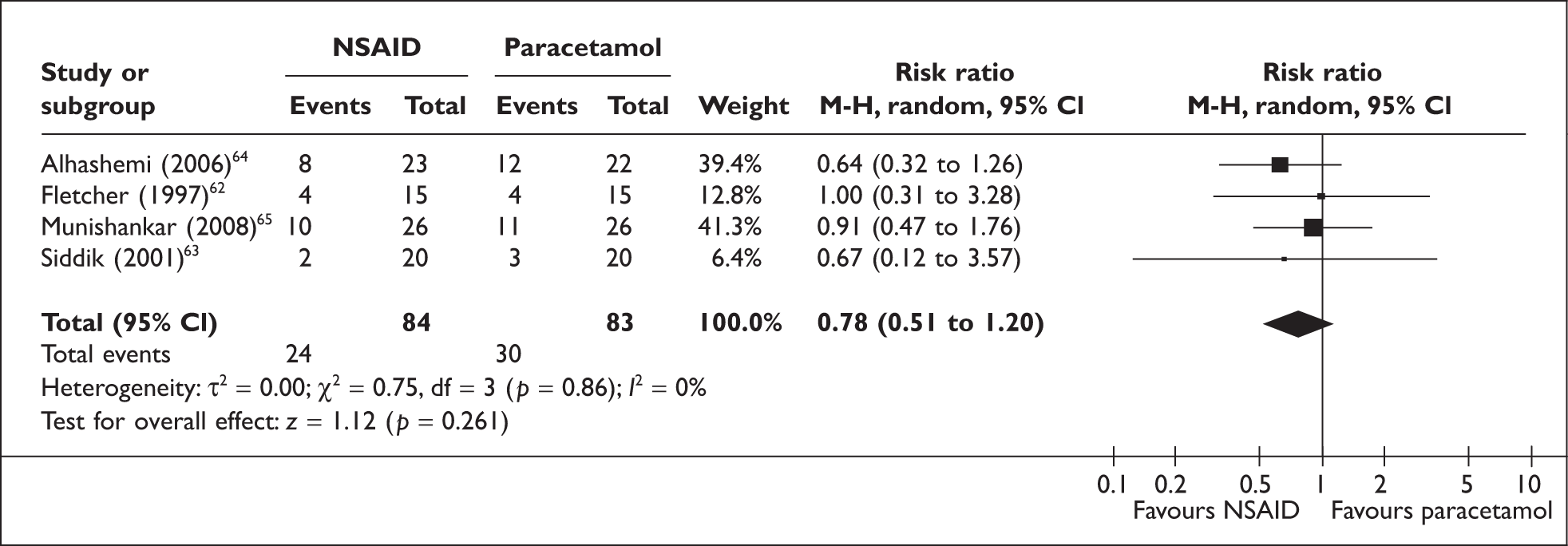
Direct comparisons
Data on nausea or PONV were available from four studies that directly compared paracetamol and NSAID. 62–65 Data from the sole study reporting postoperative nausea alone,64 was pooled with those from the three studies that reported PONV. 62,63,65 NSAIDs were slightly more effective than paracetamol in reducing nausea and PONV [risk ratio (RR) 0.78]; however, this was not statistically significant (95% CI 0.51 to 1.20). There was no statistical heterogeneity (I2 = 0%) (Figure 6).
FIGURE 6.
Nausea and postoperative nausea and vomiting (non-steroidal anti-inflammatory drugs vs paracetamol).
Sensitivity analysis
As a sensitivity analysis, an MTC was undertaken for nausea alone, vomiting alone and PONV alone, and the results were similar. In each of these separate analyses NSAIDs had the highest probability of being the most effective treatment (ranging from 50% to 84%) (Appendix 8, Table 34). There were differences in the size of the OR for some of the comparisons, and the benefit with NSAIDs compared to placebo was statistically significant for PONV but not nausea alone or vomiting alone (Appendix 8, Table 35).
Sedation
Mixed treatment comparison
A connected network for the four classes of drugs was formed for sedation, which consisted of 19 studies (Figure 7). Details of the studies included in the network are provided in Appendix 6, Table 25.
FIGURE 7.
Network for sedation.
The pairwise ORs (95% CrI) are reported in Table 16. There was no statistically significant difference between any intervention and control in reducing morphine-related sedation: there was a trend towards paracetamol performing more poorly than placebo, and COX-2 inhibitors more poorly than NSAIDs, with wide CrIs indicating considerable uncertainty, and NSAIDs and COX-2 inhibitors performing better than placebo and paracetamol.
| Comparison | Pairwise odds ratio (OR) and 95% CrI |
|---|---|
| Paracetamol vs placebo | 1.62 (0.32 to 5.02) |
| NSAID vs placebo | 0.53 (0.20 to 1.01) |
| COX-2 vs placebo | 0.63 (0.18 to 1.49) |
| NSAID vs paracetamol | 0.51 (0.08 to 1.63) |
| COX-2 vs paracetamol | 0.63 (0.07 to 2.33) |
| COX-2 vs NSAID | 1.40 (0.30 to 4.31) |
Non-steroidal anti-inflammatory drugs performed best for this outcome: there was a 53% chance that NSAIDs are the most effective treatment for reducing sedation (Table 17). This is a low probability, which reflects the considerable overlap in the CrIs for the treatment effect estimates (Table 16).
| Treatment (n of studies) | p best (%) |
|---|---|
| Placebo (19) | 0 |
| Paracetamol (4) | 6 |
| NSAID (12) | 53 |
| COX-2 (9) | 41 |
In total, 40 arms were included in the analysis, of which 31 had at least one outcome event. The residual deviance was 41.44. This was similar to the number of data points with at least one event (31), therefore demonstrating a good fit of the model to the data.
Direct comparisons
Data were available on sedation from two studies that directly compared paracetamol and NSAIDs. 62,63 There was a trend towards NSAIDs being more effective than paracetamol in reducing sedation (RR 0.35); however, this was not statistically significant (95% CI 0.04 to 3.00) (Figure 8). Statistical heterogeneity was low (I2 = 17%).
FIGURE 8.
Sedation (non-steroidal anti-inflammatory drugs vs paracetamol).
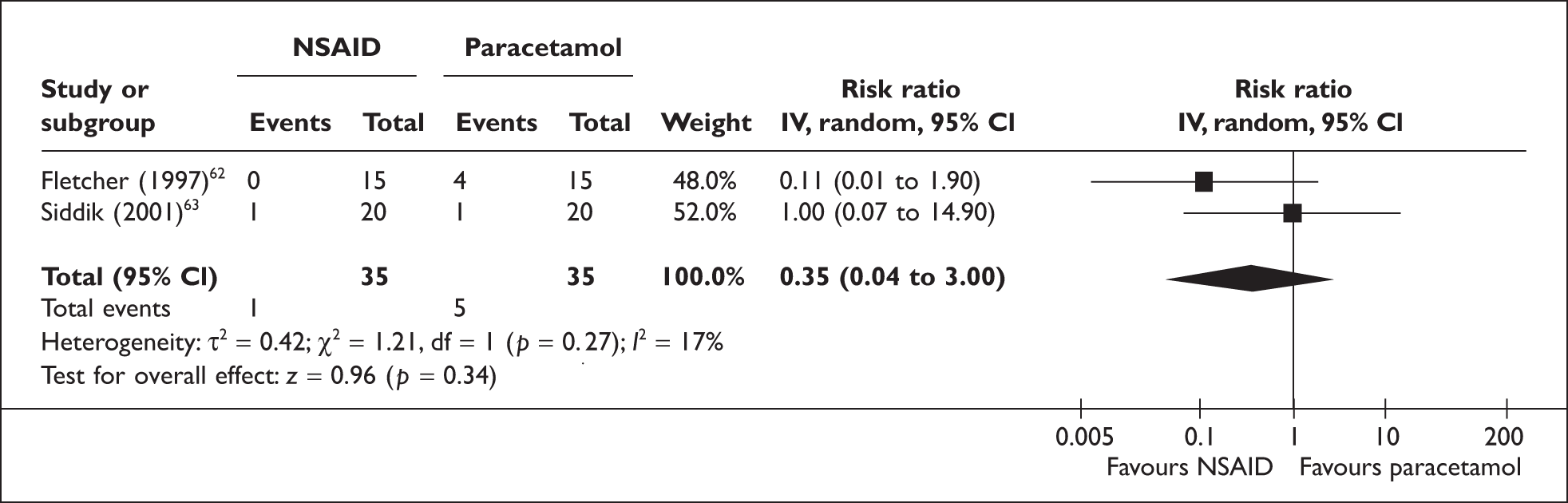
Other morphine-related side effects
In addition to the main morphine-related outcomes reported above, the effect of adding any of the three classes of non-opioid analgesics to PCA morphine, on reduction of respiratory depression, urinary retention, pruritus, bowel dysfunction and dizziness were also investigated. The full results of these analyses are reported in Appendix 8, and a summary is provided in Table 18. When taken together, these results present a complex picture of which drug was the most effective in reducing morphine-related side effects. Based on the pairwise comparisons, there were no statistically significant differences between intervention and control with the exception of pruritus, where there was a statistically significant improvement with paracetamol and NSAIDs compared to placebo (Appendix 8, Table 40). This is reflected in the low probabilities for the outcomes, which ranged from 43% to 73% (Table 18); a probability of being best of less than 95% indicates no statistically significant difference at a 95% level between the best treatment and at least one comparator.
| Outcome | Placebo | Paracetamol | NSAID | COX-2 | Comments |
|---|---|---|---|---|---|
| Respiratory depression | ✓ (43%) | One COX-2 study in network | |||
| Urinary retention | ✓ (61%) | ||||
| Pruritus | ✓ (73%) | ||||
| Bowel dysfunction | ✓ (58%) | No COX-2 studies in network | |||
| Dizziness | ✓ (56%) |
Summary of results for morphine consumption and related side effects
All three classes of non-opioid analgesic were associated with a statistically significant reduction in morphine consumption compared to placebo (i.e. the CrIs did not cross the line of no effect, zero). Based on the main analysis, compared to placebo, the mean reduction was largest for COX-2 inhibitors at 10.9 mg, followed by 10.2 mg for NSAIDs and 6.3 mg for paracetamol. Based on the pairwise comparisons of the active treatments, NSAIDs and COX-2 inhibitors were both superior to paracetamol (and this was statistically significant) but there was no statistically significant difference between NSAIDs and COX-2 inhibitors. The mean reduction in morphine consumption with COX-2 inhibitors compared to NSAIDs was 0.7 mg, and there was a 95% probability that this could fall between a reduction of 3.0 mg and an increase in morphine consumption of 1.6 mg. COX-2 inhibitors had the highest probability of being the most effective intervention to reduce 24-hour PCA morphine consumption following major surgery (Table 19), though this probability was less than 95%, reflecting the fact that COX-2 inhibitors were not statistically significantly better than all the other comparators. Therefore, the finding that COX-2 inhibitors were the ‘best’ treatment should be interpreted with some caution and in light of the very modest difference in reduced morphine consumption between COX-2 inhibitors and NSAIDs.
| Outcome | Placebo | Paracetamol | NSAID | COX-2 |
|---|---|---|---|---|
| 24-hour morphine consumption | ✓ (74%) | |||
| Nausea, PONV | ✓ (78%) | |||
| Sedation | ✓ (53%) |
Sensitivity analyses were conducted on the 24-hour morphine consumption outcome. The analysis of individual drugs (as opposed to drug class) suggested that it was reasonable to group drugs into three classes, though there appeared to be possible inconsistency across different NSAIDs. Study quality, defined as having adequate double blinding, was not shown to have a significant effect on the results. The adjustment of the model for baseline morphine consumption did not alter which drug class had the highest probability of being most effective. The adjusted results did show a greater reduction in morphine consumption with paracetamol compared to placebo, and the differences between the active interventions in the pairwise comparisons were no longer statistically significant: the reduction in morphine consumption with NSAIDs and COX-2 inhibitors compared to paracetamol were smaller, though the direction of the effect continued to favour these two drugs over paracetamol. Based on the limited direct evidence available from the included studies, the results of the MTC and the direct comparison analyses were consistent.
The impact of the analgesics on morphine-related side effects was not consistent with the findings for morphine consumption. NSAIDs had the highest probability of reducing nausea and vomiting following surgery, as well as reducing sedation (Table 19). However, although NSAIDs reduced sedation compared to placebo, paracetamol and COX-2 inhibitors, none of these comparisons were statistically significant. This is reflected in the fact that the probabilities of NSAID being the most effective were lower than 95% and in the case of sedation considerably lower (Table 19). The evidence was mixed for the secondary morphine-related side effects.
Adverse effects of non-opioid analgesics
As would be expected it was not possible to form a network for the analgesic-related adverse effects. The most commonly reported adverse effects were those associated with NSAIDs. Studies reported adverse events for the first 24–48 hours after surgery.
Bleeding
The primary analgesic-related adverse effect of interest was surgical bleeding. This outcome was not reported in any of the paracetamol studies; and although it was reported in a single study comparing COX-2 inhibitor to placebo, there were zero events in each group. Five of the remaining six studies,69,72,78–80,89 all comparing an NSAID to placebo, reported zero events in each of the placebo arms therefore a pooled estimate could not be calculated. In addition, this outcome was defined differently across studies and the number of events overall was small. In the NSAID group 2.4% of participants experienced surgery-related bleeding, compared to 0.4% in the placebo group (Table 20).
| Study | Definition of bleeding event | Placebo: number of events/number analysed | NSAID: number of events/number analysed | COX-2: number of events/number analysed |
|---|---|---|---|---|
| Balestrieri 199781 | Clinically significant bleeding | 0/82 | 4/166 | |
| Cassinelli 200884 | Epidural hematoma | 1/12 | 0/13 | |
| Gillies 198790 | Postoperative bleeding | 0/18 | 1/39 | |
| Hanna 200391 | Postoperative haemorrhage | 0/54 | 1/114 | |
| Hodsman 198792 | Reoperation due to bleeding | 0/32 | 2/33 | |
| Plummer 1996101 | Intraoperative bleeding | 0/57 | 2/57 | |
| Tang 200278 | Bleeding problems | 0/18 | 0/37 | |
| Total | 1/273 (0.4%) | 10/422 (2.4%) | 0/37 (0%) |
It was also not possible to construct a network for gastrointestinal bleed. This outcome was not reported in any paracetamol studies. For the three studies available with this outcome there were zero events in four of the six arms. 66,79,89 Among participants in the NSAID group, 2.3% experienced GI bleeding compared to 0% with placebo (Table 21).
| Study | Definition of bleeding event | Placebo: number of events/number analysed | NSAID: number of events/number analysed | COX-2: number of events/number analysed |
|---|---|---|---|---|
| Hanna 200391 | GI bleeding | 0/54 | 3/114 | |
| Plummer 1996101 | GI haemorrhage | 0/57 | 1/57 | |
| Siddiqui 200877 | GI bleeding | 0/100 | 0/100 | |
| Total | 0/211 (0%) | 4/171 (2.3%) | 0/100 (0%) |
Oliguria and renal failure
Six studies (535 participants) reported on renal dysfunction; five compared NSAID to placebo48,72,79,85,90 and one compared COX-2 to placebo. 66 There was a single event, described as transient oliguric renal failure, in a patient receiving NSAID. 97
Four studies reported on oliguria;69,91,95,98 all comparing NSAID to placebo. There was no statistically significant difference between NSAID and placebo, though there was a trend towards an increase in oliguria with NSAID (Figure 9).
FIGURE 9.
Oliguria (non-steroidal anti-inflammatory drugs vs placebo).
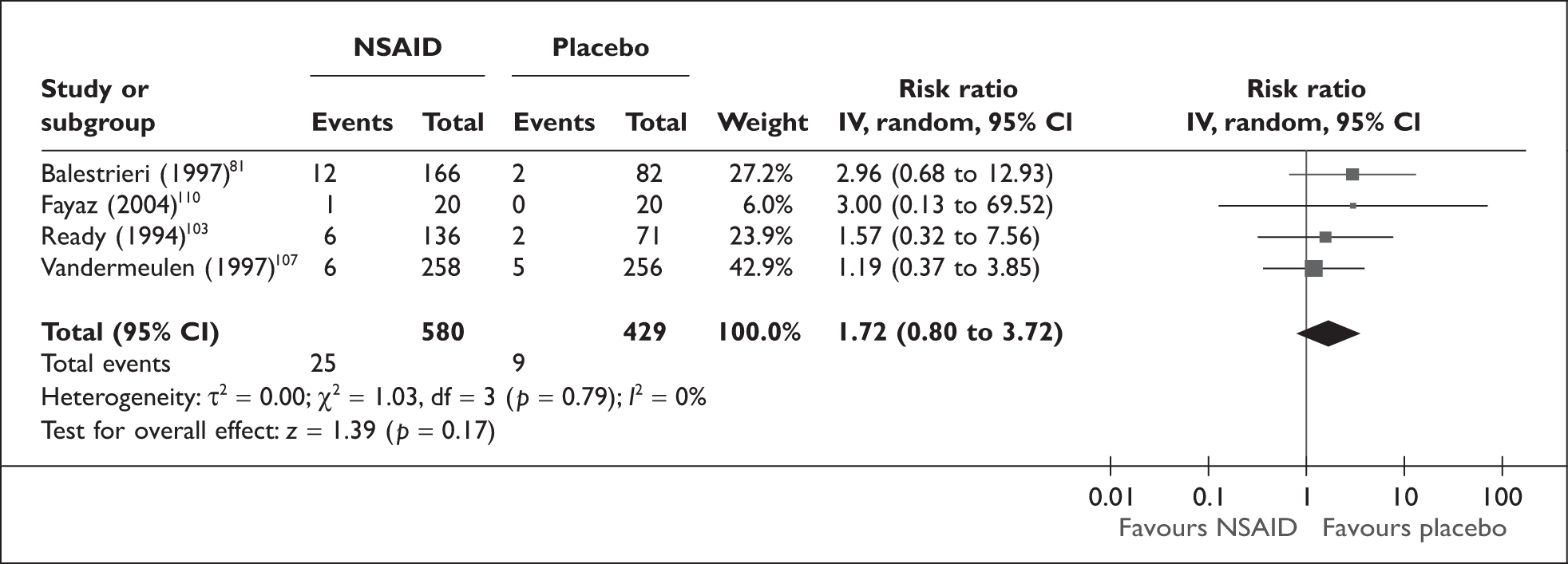
Summary of analgesic-related adverse effects
The most commonly reported adverse effects were those associated with NSAIDs. It was not possible to form a network for an MTC. There were a small number of surgical bleeding and GI bleeding events in the NSAID group as well as oliguria and a single case of renal dysfunction in the postoperative period.
Chapter 4 Discussion
Multimodal analgesia is used following major surgery to achieve optimal analgesia while reducing opioid consumption and related adverse effects. Paracetamol, NSAIDs and COX-2 inhibitors are commonly used in conjunction with morphine following major surgery to achieve these objectives. The decision problem addressed in our review was which class of non-opioid analgesic (paracetamol, NSAID or COX-2 inhibitor) is most effective at reducing morphine consumption and associated adverse effects following major surgery. The focus was the relative effectiveness of the drug classes and not individual drugs within the classes. There was very little evidence available directly comparing the three drug classes. An MTC was therefore undertaken using both direct and indirect evidence. The primary outcomes were mean cumulative morphine consumption in the first 24 hours following surgery, nausea and vomiting and sedation as well as surgical bleeding.
Principal findings
All three classes of non-opioid analgesic reduced mean cumulative morphine consumption. From the main analysis, PCA morphine with COX-2 inhibitors reduced morphine consumption by 10.9 mg, followed by NSAIDs with a 10.2 mg reduction and paracetamol with a 6.3 mg reduction compared to PCA morphine alone; these all had narrow CrIs (unadjusted results). Based on the average baseline morphine consumption of 37.43 mg, this equates to a 29.2% (COX-2 inhibitors), 27.2% (NSAIDs) and 16.9% (paracetamol) reduction in morphine consumption in the 24 hours immediately following surgery. However, from a clinical perspective, the actual reduction in morphine consumption seems modest and arguably of questionable clinical significance.
Although NSAIDs and COX-2 inhibitors were both superior to paracetamol in the main analysis, the reduction in morphine consumption with COX-2 inhibitors compared to NSAIDs was marginal, with a mean difference of less than 1 mg of morphine (mean difference –0.74 mg; 95% CrI –3.03 to 1.56) which is not of clinical significance. This is reflected in the finding that, although COX-2 inhibitors had the highest probability of being most effective, this probability (74%) was lower than 95%, thereby indicating uncertainty. The sensitivity analyses for 24-hour morphine consumption, taking into account study quality and baseline morphine consumption, showed the results of the main analysis to be robust. The analysis of individual drugs (as opposed to drug class) suggested that it was reasonable to group the drugs into three classes, though there appeared to be possible inconsistency across different NSAIDs. The sensitivity analyses are discussed in further detail below (see Strengths and limitations of the assessment).
Non-steroidal anti-inflammatory drugs had the highest probability (78%) of reducing nausea or PONV. There was a statistically significant improvement for this outcome with NSAIDs added to PCA morphine compared to PCA morphine alone (OR 0.7; 95% CrI 0.53 to 0.88). However, the credibility intervals for the comparisons between NSAIDs and paracetamol and NSAIDs and COX-2 inhibitors covered the possibility of an increase in nausea and vomiting as well as a decrease with NSAIDs. For example, the OR for NSAIDs compared to paracetamol was 0.74 (indicating a reduction with NSAIDs) but there was a 95% probability that this would fall between a reduction (0.44) and a small increase in nausea and vomiting (1.17). This is reflected in the result that the probability of NSAIDs being best, 78%, was less than 95%. Similarly, for sedation NSAIDs had the highest probability of being the most effective at reducing sedation but the probability of it being best was low, 53%, reflecting the CrIs for the pairwise comparisons between NSAIDs and the other interventions, which allowed for the possibility of an increase in sedation as well as a decrease.
When secondary morphine-related outcomes were considered, the drug that had the highest probability of being the most effective varied by outcome. NSAIDs had the highest probability of being the best in reducing respiratory depression, paracetamol had the highest probability of reducing pruritus and bowel dysfunction, and COX-2 inhibitors had the highest probability of being best in reducing urinary retention and dizziness. The probabilities that these drugs were best were low. As with the primary morphine-related adverse effects, generally, the CrIs for many of the individual pairwise comparisons were broad and covered the possibility of an increase in the particular adverse event, as well as a reduction, for the drug with the highest probability of being best.
Any benefits in reduction of morphine-related adverse effects must be balanced against any potential adverse effects associated with the non-opioid analgesics. The review could only explore this in a limited way. Given the different adverse event profiles of the three drug classes, it was not possible to form a network to carry out a comparison similar to that undertaken for the other outcomes. Many studies did not report adverse effects associated with the analgesics. As would be expected, few studies of paracetamol reported adverse events because at therapeutic doses such effects are rare. Most of the adverse events reported were from NSAID studies. Approximately 2% of study participants treated with NSAIDs experienced some type of bleeding event, and a similar proportion experienced GI bleeding. Oliguria was reported for 4% of NSAID patients, and there was one case of transient renal failure. However, it needs to be kept in mind that these figures are based on trials with a selected population and therefore may underestimate the number of events that might occur in a general population. In addition, the included studies were powered (where reported) to detect a difference in morphine consumption and not differences in analgesic-related adverse effects.
Consistency with direct comparisons
The results from the MTC are consistent with the direct evidence synthesis and the direct evidence available from previous reviews. Two previous reviews comparing paracetamol to placebo found that while paracetamol combined with PCA morphine reduced 24-hour morphine consumption compared to PCA morphine alone, there was no benefit in terms of a reduction in morphine-related adverse effects. 21,23 The reduction in morphine consumption with paracetamol in the current review was slightly smaller than the two earlier reviews but the confidence intervals from the three reviews have a good overlap. A previous review found that there was a statistically significant reduction in morphine consumption when NSAIDs and COX-2 inhibitors were added to PCA morphine compared to PCA morphine alone. 23 There was a reduction in PONV and sedation with NSAIDs but there was no statistically significant difference in any morphine-related adverse effects with COX-2 inhibitors.
It is not surprising that we did not find any studies directly comparing all three non-opioid analgesics. There were also few studies available that directly compared any two of the three analgesics. There were five comparing NSAIDs and paracetamol, and a single study comparing a COX-2 inhibitor to an NSAID. We did not find any studies comparing a COX-2 inhibitor and paracetamol. The results from the synthesis of the direct comparison studies were consistent with the results of the MTC. There was a statistically significant reduction in morphine consumption and a trend towards improvement in nausea and vomiting and sedation with NSAID compared to paracetamol, which was not statistically significant. The single study comparing a COX-2 inhibitor and an NSAID reported no statistically significant difference in 24-hour morphine consumption; data on morphine-related side effects were not available.
Strengths and limitations of the assessment
Previous reviews have investigated the effectiveness of paracetamol, NSAIDs and COX-2 inhibitors compared to placebo19,21–23,106 but we are not aware of any previous systematic reviews that have investigated the relative effectiveness of these non-opioid analgesics using appropriate statistical methods. By using currently developing methods of synthesis of direct and indirect evidence to investigate the relative effectiveness of the drug classes, the current review extends the work undertaken in a previous systematic review.
As expected, we found limited direct evidence comparing the three non-opioid analgesics. Therefore, the MTC allowed us to maximise the usefulness of the available network of evidence. This review has also provided an opportunity to update the evidence on multimodal analgesia following major surgery. Twenty new trials were included and we were able to exclude trials by Scott S Reuben from the analysis, which were based on falsified data, as well as COX-2 inhibitors that are no longer licensed for use.
A key factor to consider in evaluating the strengths and limitations of the assessment undertaken is whether the assumption that there were no systematic differences between the trials that investigated each analgesic (exchangeability) was reasonable. Based on a qualitative examination of the trials we believe this was a reasonable assumption: the inclusion criteria for the review were narrow and all the participants were adults undergoing major surgery and receiving PCA morphine in the 24 hours following surgery. We also used a random effects model to allow for any possible heterogeneity. However, this approach does not explain heterogeneity and we found considerable variability across the trials in baseline morphine consumption (based on placebo control group), which had not been anticipated. This variation may be due to differences in surgery, the exact regimen under which morphine was administered or study population such as ethnicity or age. If an interaction did exist between drug class and morphine consumption then the main results could be misleading as the exchangeability assumption would not be met. An interaction could arise, for example, where a particular drug class was used in trials where it was anticipated that pain levels could be high (and therefore morphine consumption high) due to the severity of pain anticipated. We therefore conducted a post hoc sensitivity analysis to explore this further. This replaced the originally planned sensitivity analysis based on type of surgery.
The adjustment of the 24-hour morphine consumption model, for baseline morphine consumption, did not alter the results in terms of which drug class had the highest probability of being most effective. The treatment effect estimates of NSAIDs and paracetamol became closer but COX-2 inhibitors still had the highest treatment effect estimate with a similar probability of being the most effective, 79%. This adjusted analysis did show a greater reduction in morphine consumption with paracetamol compared to placebo, and the differences between the active interventions in the pairwise comparisons were no longer statistically significant. The reduction in morphine consumption with NSAIDs and COX-2 inhibitors compared to paracetamol were smaller and non-significant, though the direction of the effect continued to favour these two drugs over paracetamol. This sensitivity analysis showed the results of the main analysis to be robust to variation in baseline morphine consumption.
Although the sensitivity analysis we undertook does support the robustness of the results of the main analysis, it was only undertaken as an exploratory analysis and the results should not be considered definitive. The feasibility of incorporating covariates in a mixed treatment comparison has been demonstrated,38 though the approach is not in common use and the methods are continually being developed. First, the analysis is based on summary data and the comparisons are not based on randomised groups as in a trial. There may be unknown confounding factors that influence the relationship between the covariates used and 24-hour morphine consumption. This is a limitation of all meta-analyses based on aggregate data and can only be resolved through the analysis of independent patient data from the included studies. Second, because morphine consumption is both an outcome and a covariate in this analysis, there is a risk of regression to the mean:117,118 the regression model made the assumption that there was no uncertainty in the measurement of baseline morphine consumption and the baseline morphine consumption, derived from the placebo control group, also formed part of the outcome (morphine consumption). 117 Third, two of the studies included in the model did not have a placebo control group; therefore, it was necessary to make an estimate of the baseline morphine consumption for these two trials.
The third point above contributes to the difficulty in accounting for regression to the mean in the model. Paracetamol was the comparator in the two trials without placebo. If placebo had been included in these trials, then the difference in morphine consumption between placebo and paracetamol could be calculated using estimates of the paracetamol treatment effect difference compared to placebo and the paracetamol covariate interaction. These were estimated by running the model without these two studies. These estimates were considered likely to be reasonably good because they were estimated using 54 trials that included placebo out of a total of 56 trials, which included 10 trials comparing paracetamol with placebo. That is, most of the data available were included and adequate paracetamol versus placebo data were available. However, the two trials were excluded in deriving these estimates and ideally the baselines for these two studies would be determined within the model including all trials. The best way to address the problem of trials not having a placebo control group is an area of ongoing work. 38
A final point to consider in the interpretation of the adjusted results is that the results presented are the mean values for the covariate, i.e. for the overall mean value of morphine consumption. This allows comparison of the results with those for the base-case model that did not adjust for baseline morphine consumption. However, the baseline morphine covariate was statistically significant, indicating that the higher the expected baseline morphine consumption, the greater the reduction in morphine will be. Effect differences at different levels of baseline morphine consumption have not been evaluated.
The main analysis was based on the assumption that it was reasonable to group individual drugs into classes. In many respects this was necessary to address the decision problem presented. There was variability between the three drug classes in the number of drugs investigated, and for some of the individual drugs there was variability in total dose, methods of administration timing and number of doses. In particular there were a large number of different NSAIDs. By pooling these as one class the assumption was made that the different NSAIDs used equivalent and optimal doses, which may not be the case. Even within some of the NSAIDs, particularly ketorolac, there was considerable variability. This was less of an issue with the COX-2 inhibitors and paracetamol. There were only three COX-2 inhibitors and the paracetamol class was made up of paracetamol and propacetamol. There was also less variability in dosage. The sensitivity analysis by individual drug (also adjusted for morphine consumption) suggested variability between NSAIDs in the size of the reduction in morphine consumption. The mean reduction in morphine consumption ranged from 4.1 mg for meloxicam to 16.7 mg for naproxen, and the CrIs for some NSAIDs barely overlapped. Due to time constraints we were not able to investigate whether this also applied to the morphine-related adverse effects and this would benefit from further investigation, though such an analysis may be constrained by the network available. The treatment effect across COX-2 inhibitors was consistent, indicating that the decision to treat them as a class was reasonable: the mean reduction in morphine consumption ranged from 8.1 mg to 12.6 mg and the CrIs for celecoxib, etoricoxib and celecoxib overlapped. Similarly the decision to group propacetamol and paracetamol was reasonable: the mean reduction in morphine consumption was 8.0 mg for paracetamol and 8.7 mg for propacetamol and there was good overlap in the CrIs.
Taking the evidence as a whole, a key finding was the disparity between the results for morphine consumption and morphine-related adverse effects. There was robust evidence of a reduction in morphine consumption with the addition of any of the non-opioid analgesics to PCA morphine but the evidence for reduction in morphine-related adverse effects was more equivocal. This dissonance between morphine consumption and related adverse effects has been noted in previous reviews. 20,23,107 A number of reasons have been suggested. One possibility is that the size of the reduction in morphine consumption was not sufficient to decrease morphine-related adverse effects. 23 The poor quality of adverse event data in many trials and the possibility that the trials are underpowered to detect a reduction in adverse events may be other factors. 107 There is a possibility that the analyses for morphine-related adverse effects were underpowered as the trials included in the review were generally powered to detect a difference in morphine consumption or, in a few instances, pain. However, against this, there was a reasonable body of evidence available for nausea and vomiting at least. Given that morphine consumption alone is not a clinically meaningful outcome, future trials should use one or more morphine-related adverse effects as the primary outcome and power calculations for the trial should be based on these outcomes and not morphine consumption alone. Also, due to time constraints we limited our sensitivity analyses to the outcome for which we had the most substantial set of data (24-hour morphine consumption) and therefore most complete network. There would be value in exploring whether taking baseline morphine consumption into account alters the results for morphine-related adverse effects. Furthermore, time constraints prevented us from evaluating the individual drug treatment effects for the morphine-related adverse effects. Given the variability in the treatment effects of individual NSAIDs in reducing morphine consumption, it is possible that the difference in the mix of individual drugs between the analyses (the relative number of studies per individual drug) may partly explain this dissonance in the results. This may warrant further investigation.
Finally, this review focused specifically on the morphine-sparing effects of the three analgesics. For the purposes of the review, the assumption was made that, because patients were receiving PCA morphine, optimum analgesia should be maintained and pain control should be the same in all arms of a trial. This does not take into account any differences there may be in the synergistic action between morphine and the three drug classes which may result in differences in pain control. Regardless of any reduction in morphine consumption, the improvement of analgesia post-surgery through the addition of a non-opioid to PCA morphine post-surgery is of clinical importance. This is likely to be of value to the patient beyond the immediate 24 hours following surgery and is itself an important research question.
Chapter 5 Conclusions
Implications for service provision
Non-steroidal anti-inflammatory drugs, COX-2 inhibitors and paracetamol reduced PCA morphine consumption by 6.3 mg to 10.9 mg, compared to placebo, in the first 24 hours following major surgery. However, the reduction was modest for all three drug classes and probably of limited clinical significance. The difference between NSAIDs and COX-2 inhibitors was marginal and not statistically significant. Although NSAIDs and COX-2 inhibitors were both more effective than paracetamol the differences in morphine consumption compared to paracetamol were small, especially when baseline morphine consumption was taken into consideration: the adjusted results suggest a mean difference of less than 2 mg of morphine when each of the drug classes was compared to each other.
Non-steroidal anti-inflammatory drugs were ranked best for reducing nausea and vomiting and sedation, and for the former there was a statistically significant improvement over placebo. However, the confidence intervals for the difference between NSAIDs and paracetamol and COX-2 inhibitors for these outcomes indicate the possibility of an increase in incidence of these outcomes as well as a decrease. Although NSAIDs were marginally better at reducing the primary morphine-related adverse effects of interest, the results do not strongly favour one class of non-opioid analgesic. Paracetamol was ranked lower than NSAIDs and COX-2 inhibitors for each of the primary outcomes, therefore NSAIDs or COX-2 inhibitors might arguably be considered a preferential option. However, any benefit provided by these analgesics in terms of morphine sparing needs to be balanced against any adverse effects related to the analgesics themselves. There was a small number of surgical bleeding, GI bleeding events and oliguria for participants treated with an NSAID.
Taking the evidence as a whole, the uncertainty suggested by the size of the probabilities of being most effective, the small reductions in morphine consumption, and the wide CIs for the adverse effects outcomes, there does not appear to be a strong case for suggesting routine addition of any of the three non-opioids to PCA morphine in the 24 hours immediately after surgery. In addition, there does not appear to be a strong case for favouring one drug class above the others.
Suggested research priorities
There would be value in extending the analyses undertaken in this review to explore whether taking baseline morphine consumption into account alters the results for morphine-related adverse effects. Given the evidence that there may be variability in the effects of individual NSAIDs, further evidence synthesis on the NSAID data would be helpful, in particular exploration of any variation in the impact on morphine-related adverse effects.
There does not appear to be a compelling case for a further trial comparing these three analgesic classes, given the overlap between the non-opioid analgesics and their different benefits. It is likely that such a trial would have to be very large to detect statistically significant differences between the treatments and any differences might not be clinically meaningful. However, any future trials testing new analgesics in conjunction with morphine should focus on morphine-related adverse effects, ensuring that the power calculation is based on key morphine-related adverse effects rather than morphine consumption.
Acknowledgements
Thanks to Dr Nadia Elia for providing information from her review, to Huiqin Yang for help provided in extracting data, and to Professor Alex Sutton for statistical advice on the MTC.
Contribution of authors
Catriona McDaid (Research Fellow) was involved in writing the protocol, study selection, data extraction, quality assessment, data analysis and report writing. Emma Maund (Research Fellow) was involved in writing the protocol, study selection, data extraction, quality assessment, data analysis and report writing. Stephen Rice (Research Fellow) contributed to the protocol, conducted the MTC analysis and was involved in writing sections of the report. Kath Wright (Information Specialist) devised the research strategy, carried out the literature searches and wrote the search methodology sections of the report. Brian Jenkins (Senior Lecturer in Anaesthetics) provided clinical input throughout the project, and commented on the protocol and drafts of the report. Nerys Woolacott (Senior Research Fellow) provided input at all stages of the review and commented on the protocol and drafts of the report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Macintyre PE, Schug SA. Acute pain management – a practical guide. Edinburgh: Elsevier; 2007.
- Breivik H, Stubhaug A. Management of acute postoperative pain: still a long way to go!. Pain 2008;137:233-4.
- Kehlet H, Dahl JB. The value of ‘multimodal’ or ‘balanced’ analgesia in postoperative pain treatment. Anesth Analg 1993;77:1048-56.
- Beaulieu P. Non-opioid strategies for acute pain management. Can J Anaesth 2007;54:481-5.
- Tan TY, Schug SA. Safety aspects of postoperative pain management. Rev Analg 2006;9:45-53.
- White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg 2005;101:S5-S22.
- Macintyre PE, Ready BL. Acute pain management: a practical guide. London: WB Saunders; 2001.
- Hudcova J, McNicol E, Quah C, Lau J, Carr DB. Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev 2006;4.
- Grahame-Smith DG, Aronson JK. Oxford textbook of clinical pharmacology and drug therapy. Oxford: Oxford University Press; 2002.
- Stannard C, Booth S. Pain. Edinburgh: Churchill Livingstone; 2004.
- Walder B, Schafer M, Henzl I, Tramer M. Efficacy and safety of patient-controlled opioid analgesia for acute postoperative pain: a quantitative systematic review. Acta Anaesthesiol Scand 2001;15:795-804.
- Tramer M, Walder B. Efficacy and adverse affects of prophylactic anti-emetics during patient-controlled analgesia therapy. A quantitative systematic review. Anesth Analg 1999;88:1354-61.
- Tramer M, Tramer M. Evidence-based resource in anaesthesia and analgesia. London: BMJ Books; 2003.
- Malaise O, Bruyere O, Reginster JY. Intravenous paracetamol: a review of efficacy and safety in therapeutic use. Future Neurol 2007;2:673-88.
- Oscier C, Bosley N, Milner Q. Paracetamol: a review of three routes of administration. Update Anaesth 2007;23:112-14.
- Delbos A, Boccard E. The morphine-sparing effect of propacetamol in orthopedic postoperative pain. J Pain Symptom Manag 1995;10:279-86.
- Hyllested J, Pedersen K. Comparative effect of paracetamol, NSAIDs or their combination in postoperative pain management: a qualitative review. Br J Anaesth 2002;88:199-214.
- Bateman N, Kerr S, Lee A. Adverse drugs reactions. London: Pharmaceutical Press; 2006.
- García Rodríguez L, Cattaruzzi C, Troncon M, Agostinis L. Risk of hospitalisation for upper gastrointestinal tract bleeding associated with ketorolac, other non-steroidal anti-inflammatory drugs, calcium antagonist, and other antihypertensive drugs. Arch Intern Med 1998;158:33-9.
- Lee A, Cooper MG, Craig JC, Knight JF, Keneally JP. Effects of nonsteroidal anti-inflammatory drugs on postoperative renal function in adults with normal renal function. Cochrane Database Syst Rev 2007;2.
- Moiniche S, Romsing J, Dahl JB, Tramer MR. Nonsteroidal antiinflammatory drugs and the risk of operative site bleeding after tonsillectomy: a quantitative systematic review. Anesth Analg 2003;96:68-77.
- EMEA public statement on the suspension of the marketing authorisation for Bextra (valdecoxib) in the European Union. European Medicines Agency; 2005.
- Merck Announces Voluntary Worldwide Withdrawal of VIOXX® Merck n.d. http://www.merck.com/newsroom/vioxx/pdf/vioxx_press_release_final.pdf.
- Bainbridge D, Cheng DC, Martin JE, Novick R. Evidence-Based Perioperative Clinical Outcomes Research Group . NSAID-analgesia, pain control and morbidity in cardiothoracic surgery. Can J Anaesth 2006;53:46-59.
- Jirarattanaphochai K, Jung S. Nonsteroidal antiinflammatory drugs for postoperative pain management after lumbar spine surgery: a meta-analysis of randomized controlled trials. J Neurosurg Spine 2008;9:22-31.
- Remy C, Marret E, Bonnet F. Effects of acetaminophen on morphine side-effects and consumption after major surgery: meta-analysis of randomized controlled trials. Br J Anaesth 2005;94:505-13.
- Marret E, Kurdi O, Zufferey P, Bonnet F. Effects of nonsteroidal antiinflammatory drugs on patient-controlled analgesia morphine side effects: meta-analysis of randomized controlled trials. Anesthesiology 2005;102:1249-60.
- Elia N, Lysakowski C, Tramer MR. Does multimodal analgesia with acetaminophen, nonsteroidal antiinflammatory drugs, or selective cyclooxygenase-2 inhibitors and patient-controlled analgesia morphine offer advantages over morphine alone? Meta-analyses of randomized trials. Anesthesiology 2005;103:1296-304.
- Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 2004;23:3105-24.
- Caldwell D, Ades A, Higgins J. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ 2005;331:897-900.
- Sutton A, Ades A, Cooper N, Abrams K. Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics 2008;26:753-67.
- Jadad A, Moore R, Carroll D, Jenkinson C, Reynolds D, Gavaghan D, et al. Assessing the quality of reports of randomised clinical trials: is blinding necessary?. Control Clin Trials 1996;17:1-12.
- Wood L, Egger M, Gluud L, Schulz K, Jüni P, Altman D, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ [Internet] 2008;336:601-5.
- Review Manager (REVMAN). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2008.
- Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2008.
- Ades AE, Welton NJ, Caldwell D, Price M, Goubar A, Lu G. Multiparameter evidence synthesis in epidemiology and medical decision-making. J Health Serv Res Policy 2008;13:12-2.
- Higgins J, Deeks J, Higgins JPT GS. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration; 2008.
- Cooper N, Sutton A, Morris D, Ades A, Welton N. Addressing between study heterogeneity and inconsistency in mixed treatment comparisons: application to stroke prevention treatments in individuals with non-rheumatic atrial fibrillation. Stat Med 2009;28:1861-81.
- Higgins J, Whitehead A. Borrowing strength from external trials in a meta-analysis. Stat Med 1996;15:2733-49.
- Reuben SS, Buvanendran A, Kroin JS, Raghunathan K. The analgesic efficacy of celecoxib, pregabalin, and their combination for spinal fusion surgery. Anesth Analg 2006;103:1271-7.
- Reuben SS, Ekman EF. The effect of cyclooxygenase-2 inhibition on analgesia and spinal fusion. J Bone Joint Surg Am 2005;87:536-42.
- Shafer SL. Notice of retraction. Anesth Analg 2009;108.
- Heckman JD. Notice of retraction. J Bone Joint Surg Am 2009;91.
- Kayacan T, Guzelmeric F, Ogus H, Yaltirik R, Barutcuoglu O, Erentug V, et al. The effects of application of rectal naproxen on postoperative analgesia, sedation and morphine use in heart surgery operations. Agri Dergisi 2004;16:47-50.
- Tablov B, Tablov V, Popov J, Radev R, Cvetkov D. Use of dexketoprofen (Dexofen) after gynecological laparoscopy. Anaesthesiol Intensive Care 2008;35:18-21.
- Camu F, Beecher T, Recker D, Verburg K. Valdecoxib, a COX-2-specific inhibitor, is an efficacious, opioid-sparing analgesic in patients undergoing hip arthroplasty. Am J Ther 2002;9:43-51.
- Huang JJ, Taguchi A, Hsu H, Andriole GL, Kurz A. Preoperative oral rofecoxib does not decrease postoperative pain or morphine consumption in patients after radical prostatectomy: a prospective, randomized, double-blinded, placebo-controlled trial. J Clin Anesth 2001;13:94-7.
- Reynolds LW, Hoo RK, Brill RJ, North J, Recker DP, Verburg KM. The COX-2 specific inhibitor, valdecoxib, is an effective, opioid-sparing analgesic in patients undergoing total knee arthroplasty. J Pain Symptom Manag 2003;25:133-41.
- Sinatra RS, Shen QJ, Halaszynski T, Luther MA, Shaheen Y. Preoperative rofecoxib oral suspension as an analgesic adjunct after lower abdominal surgery: the effects on effort-dependent pain and pulmonary function. Anesth Analg 2004;98:135-40.
- Cataldo P, Senagore A, Kilbride M. Ketorolac and patient controlled analgesia in the treatment of postoperative pain. Surg Gynecol Obstet 1993;176:435-8.
- Mimoz O, Incagnoli P, Josse C, Gillon MC, Kuhlman L, Mirand A, et al. Analgesic efficacy and safety of nefopam vs. propacetamol following hepatic resection. Anaesthesia 2001;56:520-5.
- Ott E, Nussmeier NA, Duke PC, Feneck RO, Alston RP, Snabes MC, et al. Efficacy and safety of the cyclooxygenase 2 inhibitors parecoxib and valdecoxib in patients undergoing coronary artery bypass surgery. J Thorac Cardiovasc Surg 2003;125:1481-92.
- Aubrun F, Langeron O, Heitz D, Coriat P, Riou B. Randomised, placebo-controlled study of the postoperative analgesic effects of ketoprofen after spinal fusion surgery. Acta Anaesthesiol Scand 2000;44:934-9.
- Lowder JL, Shackelford DP, Holbert D, Beste TM. A randomized, controlled trial to compare ketorolac tromethamine versus placebo after cesarean section to reduce pain and narcotic usage. Am J Obstet Gynecol 2003;189:1559-62.
- Reuben S, Connelly N. Postoperative analgesic effects of celecoxib or rofecoxib after spinal fusion surgery. Anesth Analg 2000;91:1221-5.
- Reuben SS, Connelly NR, Lurie S, Klatt M, Gibson CS. Dose-response of ketorolac as an adjunct to patient-controlled analgesia morphine in patients after spinal fusion surgery. Anesth Analg 1998;87:98-102.
- Marcus A. Fraud case rocks anesthesiology community. Anesthesiol News 2009;35.
- Argyriadou E, Amaniti E, Pourzitaki C, Zaralidou A, Karakoulas K, Vasilakos D. Intravenous parecoxib during postoperative multimodal analgesia after thoracotomy: impact on opioid needs and postoperative complications. Epitheorese Klinikes Farmakologias Farmakokinetikes 2007;25:14-6.
- Trampitsch E, Pipam W, Moertl M, Sadjak A, Dorn C, Sittl R, et al. Preemptive randomized, double-blind study with lornoxicam in gynecological surgery. Schmerz 2003;17:4-10.
- Hegazy EM, El-Hady NA, Abdallah MW. Comparative study of postoperative analgesic effects of parecoxib versus ketorolac and placebo in cervical disc surgery. Egypt J Anaesth 2003;19:179-82.
- Cobby T, Crighton I, Kyriakides K, Hobb G. Rectal paracetamol has a signficant morphine-sparing effect after hysterectomy. Br J Anaesth 1999;83:253-6.
- Fletcher D, Negre I, Barbin C, Francois A, Carreres C, Falgueirettes C, et al. Postoperative analgesia with i.v. propacetamol and ketoprofen combination after disc surgery. Can J Anaesth 1997;44:479-85.
- Siddik SM, Aouad MT, Jalbout MI, Rizk LB, Kamar GH, Baraka AS. Diclofenac and/or propacetamol for postoperative pain management after cesarean delivery in patients receiving patient controlled analgesia morphine. Reg Anesth Pain Med 2001;26:310-5.
- Alhashemi JA, Alotaibi QA, Mashaat MS, Kaid TM, Mujallid RH, Kaki AM. Intravenous acetaminophen vs oral ibuprofen in combination with morphine PCIA after Cesarean delivery. Can J Anaesth 2006;53:1200-6.
- Munishankar B, Fettes P, Moore C, McLeod GA. A double-blind randomised controlled trial of paracetamol, diclofenac or the combination for pain relief after caesarean section. Int J Obstet Anesth 2008;17:9-14.
- Chau-in W, Thienthong S, Pulnitiporn A, Tantanatewin W, Prasertcharoensuk W, Sriraj W. Prevention of post operative pain after abdominal hysterectomy by single dose etoricoxib. J Med Assoc Thai 2008;91:68-73.
- Cheng PGB, Lim MJ, Onsiong MK, Chiu KYW, Chan MK, Li KWM, et al. Celecoxib premedication in post-operative analgesia for laparoscopic cholecystectomy. Acute Pain 2004;6:23-8.
- Durmus M, Koroglu A, Demirbilek S, Ozgul U, Ersoy M. Total abdominal histerektomide rofekosib ve selekoksibin postoperatif analjesik etkinligi. Turk Anest Rean Der Dergisi 2003;31:363-7.
- El-Halafawy YM, Abu-El-Kasem O. Parecoxib for pain management after off-pump coronary artery bypass grafting. Egypt J Anaesth 2004;20:245-51.
- Fong WP, Yang LC, Wu JI, Chen HS, Tan PH. Does celecoxib have pre-emptive analgesic effect after Caesarean section surgery?. Br J Anaesth 2008;100:861-2.
- Hubbard RC, Naumann TM, Traylor L, Dhadda S. Parecoxib sodium has opioid-sparing effects in patients undergoing total knee arthroplasty under spinal anaesthesia. Br J Anaesth 2003;90:166-72.
- Jirarattanaphochai K, Thienthong S, Sriraj W, Jung S, Pulnitiporn A, Lertsinudom S, et al. Effect of parecoxib on postoperative pain after lumbar spine surgery: a bicenter, randomized, double-blinded, placebo-controlled trial. Spine 2008;33:132-9.
- Malan TP, Marsh G, Hakki SI, Grossman E, Traylor L, Hubbard RC. Parecoxib sodium, a parenteral cyclooxygenase 2 selective inhibitor, improves morphine analgesia and is opioid-sparing following total hip arthroplasty. Anesthesiology 2003;98:950-6.
- Martinez V, Belbachir A, Jaber A, Cherif K, Jamal A, Ozier Y, et al. The influence of timing of administration on the analgesic efficacy of parecoxib in orthopedic surgery. Anesth Analg 2007;104:1521-7.
- Ng A, Smith G, Davidson AC. Analgesic effects of parecoxib following total abdominal hysterectomy. Br J Anaesth 2003;90:746-9.
- Riest G, Peters J, Weiss M, Dreyer S, Klassen PD, Stegen B, et al. Preventive effects of perioperative parecoxib on post-discectomy pain. Br J Anaesth 2008;100:256-62.
- Siddiqui AK, Sadat-Ali M, Al-Ghamdi AA, Mowafi HA, Ismail SA, Al-Dakheel DA. The effect of etoricoxib premedication on postoperative analgesia requirement in orthopedic and trauma patients. Saudi Med J 2008;29:966-70.
- Tang J, Li S, White PF, Chen X, Wender RH, Quon R, et al. Effect of parecoxib, a novel intravenous cyclooxygenase type-2 inhibitor, on the postoperative opioid requirement and quality of pain control. Anesthesiology 2002;96:1305-9.
- Lee LH, Irwin MG, Yao TJ, Yuen MK, Cheung CW. Timing of intraoperative parecoxib analgesia in colorectal surgery. Acute Pain 2008;10:123-30.
- Alexander R, El-Moalem HE, Gan TJ. Comparison of the morphine-sparing effects of diclofenac sodium and ketorolac tromethamine after major orthopedic surgery. J Clin Anesth 2002;14:187-92.
- Balestrieri P, Simmons G, Hill D, Brown J, Jackson A, Brull SJ, et al. The effect of intravenous ketorolac given intraoperatively versus postoperatively on outcome from gynecologic abdominal surgery. J Clin Anesth 1997;9:358-64.
- Blackburn A, Stevens J, Wheatley R, Madej T, Hunter D. Balanced analgesia with intravenous ketorolac and patient-controlled morphine following lower abdominal surgery. J Clin Anesth 1995;7:103-8.
- Burns JW, Aitken HA, Bullingham RE, McArdle CS, Kenny GN. Double-blind comparison of the morphine sparing effect of continuous and intermittent i.m. administration of ketorolac. Br J Anaesth 1991;67:235-8.
- Cassinelli EH, Dean CL, Garcia RM, Furey CG, Bohlman HH. Ketorolac use for postoperative pain management following lumbar decompression surgery: a prospective, randomized, double-blinded, placebo-controlled trial. Spine 2008;33:1313-7.
- Celik JB, Tuncer S, Reisli R, Sarkilar G, Celik C, Akyurek C. A comparative study of the effect of rofecoxib (a COX 2 inhibitor) and naproxen sodium on analgesic requirements after abdominal hysterectomy. Arch Gynecol Obstet 2003;268:297-300.
- Colquhoun A, Fell D. Failure of rectal diclofenac to augment opioid analgesia after cholecystectomy. Anaesthesia 1989;44:57-60.
- De Decker K, Vercauteren M, Hoffmann V, Lasters B, Adriaensen H. Piroxicam versus tenoxicam in spine surgery: a placebo controlled study. Acta Anaesthesiol Belg 2001;52:265-9.
- Etches RC, Warriner CB, Badner N, Buckley DN, Beattie WS, Chan VW, et al. Continuous intravenous administration of ketorolac reduces pain and morphine consumption after total hip or knee arthroplasty. Anesth Analg 1995;81:1175-80.
- Mack P, Hass D, Lavyne M, Snow R, Lien C. Postoperative narcotic requirement after microscopic lumbar discectomy is not affected by intraoperative ketorolac or bupivacaine. Spine 2001;26:658-61.
- Gillies G, Kenny G, Bullingham R, McArdle C. The morphine sparing effect of ketorolac tromethamine: a study of a new, parenteral non-steroidal anti-inflammatory agent after abdominal surgery. Anaesthesia 1987;42:727-31.
- Hanna MH, Elliott KM, Stuart-Taylor ME, Roberts DR, Buggy D, Arthurs GJ. Comparative study of analgesic efficacy and morphine-sparing effect of intramuscular dexketoprofen trometamol with ketoprofen or placebo after major orthopaedic surgery. Br J Clin Pharmacol 2003;55:126-33.
- Hodsman NB, Burns J, Blyth A, Kenny GN, McArdle CS, Rotman H. The morphine sparing effects of diclofenac sodium following abdominal surgery. Anaesthesia 1987;42:1005-8.
- Hsu H-W, Cheng Y-J, Chen L-K, Wang Y-P, Lin C-J, Lee C-N, et al. Differential analgesic effect of tenoxicam on the wound pain and uterine cramping pain after cesarean section. Clin J Pain 2003;19:55-8.
- Inan N, Ozcan N, Takmaz SA, Ozcan A, Erdogan I, Baltaci B. Efficacy of lornoxicam in postoperative analgesia after total knee replacement surgery. Agri Dergisi 2007;19:38-45.
- Karaman S, Gunusen I, Uyar M, Firat V. The effect of pre-operative lornoxicam and ketoprofen application on the morphine consumption of post-operative patient-controlled analgesia. J Int Med Res 2006;34:168-75.
- Moodie JE, Brown CR, Bisley EJ, Weber HU, Bynum L. The safety and analgesic efficacy of intranasal ketorolac in patients with postoperative pain. Anesth Analg 2008;107:2025-31.
- Munro F, Young S, Broome I, Robb H, Wardall G. Intravenous tenoxicam for analgesia following laparoscopic cholecystectomy. Anaesth Intensive Care 1998;26:56-60.
- Ng A, Parker J, Toogood L, Cotton B, Smith G. Does the opioid-sparing effect of rectal diclofenac following total abdominal hysterectomy benefit the patient?. Br J Anaesth 2002;88:714-16.
- Owen H, Glavin R, Shaw N. Ibuprofen in the management of postoperative pain. Br J Anaesth 1986;58:1371-5.
- Perttunen K, Kalso E, Heinonen J, Salo J. IV diclofenac in post-thoracotomy pain. Br J Anaesth 1992;68:474-80.
- Plummer JL, Owen H, Ilsley AH, Tordoff K. Sustained-release ibuprofen as an adjunct to morphine patient-controlled analgesia. Anesth Analg 1996;83:92-6.
- Rao AS, Cardosa M, Inbasegaran K. Morphine-sparing effect of ketoprofen after abdominal surgery. Anaesth Intensive Care 2000;28:22-6.
- Ready LB, Brown CR, Stahlgren LH, Egan KJ, Ross B, Wild L, et al. Evaluation of intravenous ketorolac administered by bolus or infusion for treatment of postoperative pain. A double-blind, placebo-controlled, multicenter study. Anesthesiology 1994;80:1277-86.
- Rowe W, Goodwin A, Miller A. The efficacy of pre-operative controlled-release indomethacin in the treatment of post-operative pain. Curr Med Res Opin 1992;12:662-7.
- Sevarino FB, Sinatra RS, Paige D, Ning T, Brull SJ, Silverman DG. The efficacy of intramuscular ketorolac in combination with intravenous PCA morphine for postoperative pain relief. J Clin Anesth 1992;4:285-8.
- Thompson J, Sharpe P, Kiani S, Owen-Smith O. Effect of meloxicam on postoperative pain after abdominal hysterectomy. Br J Anaesth 2000;84:151-4.
- Vandermeulen EP, Van Aken H, Scholtes JL, Singelyn F, Buelens A, Haazen L. Intravenous administration of tenoxicam 40 mg for post-operative analgesia: a double-blind, placebo-controlled multicentre study. Eur J Anaesthesiol 1997;14:250-7.
- Varrassi G, Panella L, Piroli A, Marinangeli F, Varrassi S, Wolman I, et al. The effects of perioperative ketorolac infusion on postoperative pain and endocrine-metabolic response. Anesth Analg 1994;78:514-9.
- Xuerong Y, Yuguang H, Xia J, Hailan W. Ketamine and lornoxicam for preventing a fentanyl-induced increase in postoperative morphine requirement. Anesth Analg 2008;107:2032-7.
- Fayaz MK, Abel RJ, Pugh SC, Hall JE, Djaiani G, Mecklenburgh JS. Opioid-sparing effects of diclofenac and paracetamol lead to improved outcomes after cardiac surgery. J Cardiothorac Vasc Anesth 2004;18:742-7.
- Cakan T, Inan N, Culhaoglu S, Bakkal K, Basar H. Intravenous paracetamol improves the quality of postoperative analgesia but does not decrease narcotic requirements. J Neurosurg Anesthesiol 2008;20:169-73.
- Hernandez-Palazon J, Tortosa JA, Martinez-Lage JF, Perez-Flores D. Intravenous administration of propacetamol reduces morphine consumption after spinal fusion surgery. Anesth Analg 2001;92:1473-6.
- Kvalsvik O, Borchgrevink PC, Hagen L, Dale O. Randomized, double-blind, placebo-controlled study of the effect of rectal paracetamol on morphine consumption after abdominal hysterectomy. Acta Anaesthesiol Scand 2003;47:451-6.
- Peduto VA, Ballabio M, Stefanini S. Efficacy of propacetamol in the treatment of postoperative pain. Morphine-sparing effect in orthopedic surgery. Acta Anaesthesiol Scand 1998;42:293-8.
- Schug SA, Sidebotham DA, McGuinnety M, Thomas J, Fox L. Acetaminophen as an adjunct to morphine by patient-controlled analgesia in the management of acute postoperative pain. Anesth Analg 1998;87:368-72.
- Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C. Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology 2005;102:822-31.
- Sharp S, Thompson SG. Analysing the relationship between treatment effect and underlying risk in meta-analysis: comparison and development of approaches. Stat Med 2000;19:3251-74.
- Thompson G, Smith T, Sharp S. Investigating underlying risk as a source of heterogeneity in meta-analysis. Stat Med 1997;16:2741-58.
- Adachi YU, Nishino J, Suzuki K, Obata Y, Doi M, Sato S. Preemptive analgesia by preoperative administration of nonsteroidal anti-inflammatory drugs. J Anesth 2007;21.
- Akca T, Colak T, Kanik A, Yaylak F, Caglikulekci M, Aydin S. The effect of preoperative intravenous use of tenoxicam: a prospective, double-blind, placebo-controlled study. J Invest Surg 2004;17:333-8.
- Antonetti M, Kirton O, Bui P, Ademi A, Staff I, Hudson-Civetta JA, et al. The effects of preoperative rofecoxib, metoclopramide, dexamethasone, and ondansetron on postoperative pain and nausea in patients undergoing elective laparoscopic cholecystectomy. Surg Endosc 2007;21:1855-61.
- Anwari JS, Anjum S, Al-Khunain S. Placebo controlled comparison of the opioid sparing effect of meloxicam and diclofenac after abdominal hysterectomy. Saudi Med J 2008;29:379-83.
- Atallah F, Khedis M, Seguin P, Fourcade O, Samii K. Postoperative analgesia and recovery after open and laparoscopic prostatectomy. Anesth Analg 2004;99:1878-9.
- Aubrun F, Kalfon F, Mottet P, Bellanger A, Langeron O, Coriat P, et al. Adjunctive analgesia with intravenous propacetamol does not reduce morphine-related adverse effects. Br J Anaesth 2003;90:314-9.
- Babul N, Sloan P, Lipman AG. Postsurgical safety of opioid-sparing cyclooxygenase-2 inhibitors. Anesthesiology 2006;104.
- Bajaj P, Ballary CC, Dongre NA, Baliga VP, Desai AA. Comparison of the effects of parecoxib and diclofenac in preemptive analgesia: a prospective, randomized, assessor-blind, single-dose, parallel-group study in patients undergoing elective general surgery. Curr Ther Res Clinical Exptl 2004;65:383-97.
- Beaulicu P. Non-opioid strategies for acute pain management. Can J Anaesth 2007;54:481-5.
- Beaussier M, Weickmans H, Paugam C, Lavazais S, Baechle JP, Goater P, et al. A randomized, double-blind comparison between parecoxib sodium and propacetamol for parenteral postoperative analgesia after inguinal hernia repair in adult patients. Anesth Analg 2005;100:1309-15.
- Belzarena SD, Alves MT, Cucco MLD, D’Avila VD. Multimodal analgesia in outpatient videolaparoscopic gynecologic surgery. Comparison between parecoxib and tenoxicam. Rev Bras Otorrinolaringol 2005;55:158-64.
- Bianchin A, De Luca A, Caminiti A. Postoperative vomiting reduction after laparoscopic cholecystectomy with single dose of dexamethasone. Minerva Anestesiol 2007;73:343-46.
- Binhas M, Decailliot F, Rezaiguia-Delclaux S, Suen P, Dumerat M, Francois V, et al. Comparative effect of intraoperative propacetamol versus placebo on morphine consumption after elective reduction mammoplasty under remifentanil-based anesthesia: A randomized control trial [ISRCTN71723173]. BMC Anesthesiol 2004;4.
- Binning A. Nimesulide in the treatment of postoperative pain: a double-blind, comparative study in patients undergoing arthroscopic knee surgery. Clin J Pain 2007;23:565-70.
- Boccara G, Chaumeron A, Pouzeratte Y, Mann C. The preoperative administration of ketoprofen improves analgesia after laparoscopic cholecystectomy in comparison with propacetamol or postoperative ketoprofen. Br J Anaesth 2005;94:347-51.
- Bolcal C, Iyem H, Sargin M, Mataraci I, Yildirim V, Doganci S, et al. Comparison of magnesium sulfate with opioid and NSAIDs on postoperative pain management after coronary artery bypass surgery. J Cardiothorac Vasc Anesth 2005;19:714-8.
- Bourlert A. Diclofenac intramuscular single dose to decrease pain in post operative Caesarean section: a double blind randomized controlled trial. J Med Assoc Thai 2005;88:15-9.
- Boussofara M, Mtaallah MH, Bracco D, Sellam MR, Raucoles M. Co-analgesic effect of ketorolac after thoracic surgery. Tunis Med 2006;84:427-31.
- Bugter MLT, Dirksen R, Jhamandas K, Slappendel R, Weber EWG, Milne B. Prior ibuprofen exposure does not augment opioid drug potency or modify opioid requirements for pain inhibition in total hip surgery. Can J Anaesth 2003;50:445-9.
- Buvanendran A, Kroin JS, Tuman KJ, Lubenow TR, Elmofty D, Moric M, et al. Effects of perioperative administration of a selective cyclooxygenase 2 inhibitor on pain management and recovery of function after knee replacement: a randomized controlled trial. JAMA 2003;290:2411-8.
- Cabrera MC, Schmied S, Derderian T, White PF, Vega R, Santelices E, et al. Efficacy of oral rofecoxib versus intravenous ketoprofen as an adjuvant to PCA morphine after urologic surgery. Acta Anaesthesiol Scand 2004;48:1190-3.
- Carvalho B, Chu L, Fuller A, Cohen SE, Riley ET. Valdecoxib for postoperative pain management after cesarean delivery: a randomized, double-blind, placebo-controlled study. Anesth Analg 2006;103:664-70.
- Cattabriga I, Pacini D, Lamazza G, Talarico F, Di Bartolomeo R, Grillone G, et al. Intravenous paracetamol as adjunctive treatment for postoperative pain after cardiac surgery: a double blind randomized controlled trial. Eur J Cardiothorac Surg 2007;32:527-31.
- Chan VWS, Clark AJ, Davis JC, Wolf RS, Kellstein D, Jayawardene S. The post-operative analgesic efficacy and tolerability of lumiracoxib compared with placebo and naproxen after total knee or hip arthroplasty. Acta Anaesthesiol Scand 2005;49:1491-500.
- Chelly JE, Nissen CW, Rodgers AJ, Smugar SS, Tershakovec AM. The efficacy of rofecoxib 50 mg and hydrocodone/acetaminophen 7.5/750 mg in patients with post-arthroscopic pain. Curr Med Res Opin 2007;23:195-206.
- Chen JY, Wu GJ, Mok MS, Chou YH, Sun WZ, Chen PL, et al. Effect of adding ketorolac to intravenous morphine patient-controlled analgesia on bowel function in colorectal surgery patients – a prospective, randomized, double-blind study. Acta Anaesthesiol Scand 2005;49:546-51.
- Daniels SE, Desjardins PJ, Bird SR, Smugar SS, Tershakovec AM. Rofecoxib 50 mg and valdecoxib 20 or 40 mg in adults and adolescents with postoperative pain after third molar extraction: results of two randomized, double-blind, placebo-controlled, single-dose studies. Clin Ther 2006;28:1022-34.
- De Leon-Casasola OA. Multimodal therapy for abdominal surgery. Tech Reg Anesth Pain Manag 2003;7:235-41.
- Desjardins PJ, Black PM, Daniels S, Bird SR, Fitzgerald BJ, Petruschke RA, et al. A randomized controlled study comparing rofecoxib, diclofenac sodium, and placebo in post-bunionectomy pain. Curr Med Res Opin 2004;20:1523-37.
- Engelman E, Salengros J-C. Safety of parecoxib and valdecoxib after noncardiac surgery: lack of demonstration. Anesthesiology 2007;106:193-4.
- Feld JM, Laurito CE, Beckerman M, Vincent J, Hoffman WE. Non-opioid analgesia improves pain relief and decreases sedation after gastric bypass surgery. Can J Anaesth 2003;50:336-41.
- Feng Y, Ju H, Yang B, An H. Effects of a selective cyclooxygenase-2 inhibitor on postoperative inflammatory reaction and pain after total knee replacement. J Pain 2008;9:45-52.
- Feng Y, Ju H, Yang B-x, An H-y, Zhou Y-y. Postoperative analgesic and anti-inflammatory effects of rofecoxib after total knee replacement. Chung Hua Wai Ko Tsa Chih 2004;42:617-21.
- Fijalkowska A, Trela-Stachurska K, Rechberger T. Efficacy of intravenous paracetamol for early postoperative analgesia after gynaecological surgery. Anestezjologia Intensywna Terapia 2006;38:66-8.
- Gan TJ, Joshi GP, Viscusi E, Cheung RY, Dodge W, Fort JG, et al. Preoperative parenteral parecoxib and follow-up oral valdecoxib reduce length of stay and improve quality of patient recovery after laparoscopic cholecystectomy surgery. Anesth Analg 2004;98:1665-73.
- Gan TJ, Joshi GP, Zhao SZ, Hanna DB, Cheung RY, Chen C. Presurgical intravenous parecoxib sodium and follow-up oral valdecoxib for pain management after laparoscopic cholecystectomy surgery reduces opioid requirements and opioid-related adverse effects. Acta Anaesthesiol Scand 2004;48:1194-207.
- Gartner R, Kroman N, Callesen T, Kehlet H. Multimodal treatment of pain and nausea in breast cancer surgery. Ugeskr Laeger 2008;170:2035-8.
- Gilron I, Orr E, Tu D, O’Neill JP, Zamora JE, Bell AC. A placebo-controlled randomized clinical trial of perioperative administration of gabapentin, rofecoxib and their combination for spontaneous and movement-evoked pain after abdominal hysterectomy. Pain 2005;113:191-200.
- Goodman SB. Multimodal analgesia for orthopedic procedures. Anesth Analg 2007;105:19-20.
- Harney DF, Dooley M, Harhen B, McGuiness N, Cagney G, McCrory C, et al. Nimesulide 90 mg orally twice daily does not influence postoperative morphine requirements after major chest surgery. Anesth Analg 2008;106:294-300.
- Hegi TR, Bombeli T, Seifert B, Baumann PC, Haller U, Zalunardo MP, et al. Effect of rofecoxib on platelet aggregation and blood loss in gynaecological and breast surgery compared with diclofenac. Br J Anaesth 2004;92:523-31.
- Hepaguslar H, Ozzeybek D, Ozkardesler S, Tasdogen A, Duru S, Elar Z. Propofol and sevoflurane during epidural/general anesthesia: comparison of early recovery characteristics and pain relief. Middle East J Anesthesiol 2004;17:819-32.
- Horattas MC, Evans S, Sloan-Stakleff KD, Lee C, Snoke JW. Does preoperative rofecoxib (VIOXX) decrease postoperative pain with laparoscopic cholecystectomy?. Am J Surg 2004;188:271-6.
- Huang Y-M, Wang C-M, Wang C-T, Lin W-P, Horng L-C, Jiang C-C. Perioperative celecoxib administration for pain management after total knee arthroplasty – a randomized, controlled study. BMC Musculoskelet Disord 2008;9.
- Hynes D, McCarroll M, Hiesse-Provost O. Analgesic efficacy of parenteral paracetamol (propacetamol) and diclofenac in post-operative orthopaedic pain. Acta Anaesthesiol Scand 2006;50:374-81.
- Immer FF, Immer-Bansi AS, Trachsel N, Berdat PA, Eigenmann V, Curatolo M, et al. Pain treatment with a COX-2 inhibitor after coronary artery bypass operation: a randomized trial. Ann Thorac Surg 2003;75:490-5.
- Jacobson E, Assareh H, Cannerfelt R, Renstrom P, Jakobsson J. Pain after elective arthroscopy of the knee: a prospective, randomised, study comparing conventional NSAID to coxib. Knee Surg Sports Traumatol Arthrosc 2006;14:1166-70.
- Jones SJ, Cormack J, Murphy MA, Scott DA. Parecoxib for analgesia after craniotomy. Br J Anaesth 2009;102:76-9.
- Joong HA, Mi RK, Ki HK. Effect of i.v. dexamethasone on postoperative dizziness, nausea and pain during canal wall-up mastoidectomy. Acta Otolaryngol 2005;125:1176-9.
- Joshi GP, Viscusi ER, Gan TJ, Minkowitz H, Cippolle M, Schuller R, et al. Effective treatment of laparoscopic cholecystectomy pain with intravenous followed by oral COX-2 specific inhibitor. Anesth Analg 2004;98:336-42.
- Kardash KJ, Garzon J, Velly AM, Tessler MJ. Ketorolac analgesia for inguinal hernia repair is not improved by peripheral administration. Can J Anaesth 2005;52:613-7.
- Katz N, Mangano DT. Reporting of clinical trials of analgesia. J Thorac Cardiovasc Surg 2004;127:605-6.
- Khajavi MR, Najafi A, PanahKhani M, Moharari RS. Propacetamol and morphine in postoperative pain therapy after renal transplantation. Int J Pharmacology 2007;3:183-6.
- Khalil MW, Chaterjee A, Macbryde G, Sarkar PK, Marks RRD. Single dose parecoxib significantly improves ventilatory function in early extubation coronary artery bypass surgery: a prospective randomized double blind placebo controlled trial. Br J Anaesth 2006;96:171-8.
- Kocaayan E, Ozkardesler S, Ozzeybek D, Bayindir S, Akan M. Comparison of effects of preoperatively administered lornoxicam and tenoxicam on morphine consumption after laparoscopic cholecystectomy. Eur J Anaesthesiol 2007;24:714-9.
- Kovac AL. The prophylactic treatment of postoperative nausea and vomiting in oral and maxillofacial surgery. J Oral Maxillofac Surg 2005;63:1531-5.
- Kuhne J, Vanarase MY, Pandit HG, Dodd CAF, Murray DW, Popat MT, et al. Perioperative analgesia for knee arthroplasty. Br J Anaesth 2005;94:393-5.
- Kulik A, Ruel M, Bourke ME, Sawyer L, Penning J, Nathan HJ, et al. Postoperative naproxen after coronary artery bypass surgery: a double-blind randomized controlled trial. Eur J Cardiothorac Surg 2004;26:694-700.
- Landwehr S, Kiencke P, Giesecke T, Eggert D, Thumann G, Kampe S. A comparison between IV paracetamol and IV metamizol for postoperative analgesia after retinal surgery. Curr Med Res Opin 2005;21:1569-75.
- Lavand’homme PM, Roelants F, Waterloos H, De Kock MF. Postoperative analgesic effects of continuous wound infiltration with diclofenac after elective cesarean delivery. Anesthesiology 2007;106:1220-5.
- Lee L-A, Wang P-C, Chen N-H, Fang T-J, Huang H-C, Lo C-C, et al. Alleviation of wound pain after surgeries for obstructive sleep apnea. Laryngoscope 2007;117:1689-94.
- Legeby M, Sandelin K, Wickman M, Olofsson C. Analgesic efficacy of diclofenac in combination with morphine and paracetamol after mastectomy and immediate breast reconstruction. Acta Anaesthesiol Scand 2005;49:1360-6.
- Leykin Y, Casati A, Rapotec A, Dal Sasso M, Barzan L, Fanelli G, et al. A prospective, randomized, double-blind comparison between parecoxib and ketorolac for early postoperative analgesia following nasal surgery. Minerva Anestesiol 2008;74:475-9.
- Leykin Y, Casati A, Rapotec A, Dalsasso M, Barzan L, Fanelli G, et al. Comparison of parecoxib and proparacetamol in endoscopic nasal surgery patients. Yonsei Med J 2008;49:383-8.
- Lu C-H, Liu J-Y, Lee M-S, Borel CO, Yeh C-C, Wong C-S, et al. Preoperative cotreatment with dextromethorphan and ketorolac provides an enhancement of pain relief after laparoscopic-assisted vaginal hysterectomy. Clin J Pain 2006;22:799-804.
- Maxwell M, Nathanson M. Parecoxib – getting to the heart of the matter. Anaesthesia 2006;61:823-5.
- Mazaris EM, Varkarakis I, Chrisofos M, Skolarikos A, Ioannidis K, Dellis A, et al. Use of nonsteroidal anti-inflammatory drugs after radical retropubic prostatectomy: a prospective, randomized trial. Urology 2008;72:1293-7.
- Mebazaa MS, Frikha N, Hammouda NB, Mestiri T, Mestiri H, Khalfallah T, et al. Postoperative analgesia after laparoscopic cholecystectomy: comparison of the preoperatice administration of celecoxib with paracetamol?. Tunis Med 2008;86:869-73.
- Meunier A, Lisander B, Good L. Effects of celecoxib on blood loss, pain, and recovery of function after total knee replacement: a randomized placebo-controlled trial. Acta Orthop 2007;78:661-7.
- Motamed C, Merle JC, Combes X, Yakhou L, Vodinh J, Duvaldestin P. The effect of fentanyl and remifentanil, with or without ketoprofen, on pain after thyroid surgery: a randomized-controlled trial. Eur J Anaesthesiol 2006;23:665-9.
- Mui WL-M, Kwong W-H, Li ACN, Au Yeung ACM, Poon C-M, Chiu PW-Y, et al. Premedication with intravenous ketorolac trometamol (Toradol) in colonoscopy: a randomized controlled trial. Am J Gastroenterol 2005;100:2669-73.
- Myles PS, Power I. Clinical update: postoperative analgesia. Lancet 2007;369:810-2.
- Naesh O, Niles LA, Gilbert JG, Ammar MM, Phibbs PW, Phillips AM, et al. A randomized, placebo-controlled study of rofecoxib with paracetamol in early post-tonsillectomy pain in adults. Eur J Anaesthesiol 2005;22:768-73.
- Newcomb W, Lincourt A, Hope W, Schmelzer T, Sing R, Kercher K, et al. Prospective, double-blinded, randomized, placebo-controlled comparison of local anesthetic and nonsteroidal anti-inflammatory drugs for postoperative pain management after laparoscopic surgery. Am Surg 2007;73:618-24.
- Newton SE, Robinson J, Kozac J. Balanced analgesia after hysterectomy: the effect on outcomes. MEDSURG Nursing 2004;13:176-80.
- Ng A, Swanevelder J. Does the opioid-sparing effect of NSAIDS benefit the patient in the postoperative period?. J Opioid Manag 2005;1:67-9.
- Nikanne E, Kokki H, Salo J, Linna T-J. Celecoxib and ketoprofen for pain management during tonsillectomy: a placebo-controlled clinical trial. Otolaryngol Head Neck Surg 2005;132:287-94.
- Nussmeier NA, Whelton AA, Brown MT, Joshi GP, Langford RM, Singla NK, et al. Safety and efficacy of the cyclooxygenase-2 inhibitors parecoxib and valdecoxib after noncardiac surgery. Anesthesiology 2006;104:518-26.
- Nussmeier NA, Whelton AA, Brown MT, Langford RM, Hoeft A, Parlow JL, et al. Complications of the COX-2 inhibitors parecoxib and valdecoxib after cardiac surgery. N Engl J Med 2005;352:1081-91.
- Pan PH. Post cesarean delivery pain management: multimodal approach. Int J Obstet Anesth 2006;15:185-88.
- Parsa AA, Soon CWM, Parsa FD. The use of celecoxib for reduction of pain after subpectoral breast augmentation. Aesthetic Plast Surg 2005;29:441-4.
- Patrocinio LG, Rangel MdO, Marques Miziara GS, Rodrigues AM, Patrocinio JA, Patrocinio TG. A comparative study between ketorolac and ketoprofen in postoperative pain after uvulopalatopharyngoplasty. Rev Bras Otorrinolaringol 2007;73:339-42.
- Pettersson PH, Jakobsson J, Owall A. Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. J Cardiothorac Vasc Anesth 2005;19:306-9.
- Phittayawechwiwat W, Thanantaseth C, Ayudhya NIN, O-Prasertsawat P, Kongprasert J. Oral etoricoxib for pain relief during fractional curettage: a randomized controlled trial. J Med Assoc Thai 2007;90:1053-7.
- Pollak R, Raymond GA, Jay RM, Hillstrom HJ, Mahan KT, Riff D, et al. Analgesic efficacy of valdecoxib for acute postoperative pain after bunionectomy. J Am Podiatr Med Assoc 2006;96:393-407.
- Rahimi SY, Vender JR, Macomson SD, French A, Smith JR, Alleyne CH. Postoperative pain management after craniotomy: evaluation and cost analysis. Neurosurgery 2006;59:852-7.
- Rao SK, Rao PS. Comparison of intra-articular analgesics for analgesia after arthroscopic knee surgery. Med J Malaysia 2005;60:560-2.
- Rasmussen GL, Malmstrom K, Bourne MH, Jove M, Rhondeau SM, Kotey P, et al. Etoricoxib provides analgesic efficacy to patients after knee or hip replacement surgery: a randomized, double-blind, placebo-controlled study. Anesth Analg 2005;101:1104-11.
- Reuben SS, Buvenandran A, Katz B, Kroin JS. A prospective randomized trial on the role of perioperative celecoxib administration for total knee arthroplasty: improving clinical outcomes. Anesth Analg 2008;106:1258-64.
- Reuben SS, Ekman EF, Charron D. Evaluating the analgesic efficacy of administering celecoxib as a component of multimodal analgesia for outpatient anterior cruciate ligament reconstruction surgery. Anesth Analg 2007;105:222-7.
- Reuben SS, Ekman EF, Raghunathan K, Steinberg RB, Blinder JL, Adesioye J. The effect of cyclooxygenase-2 inhibition on acute and chronic donor-site pain after spinal-fusion surgery. Reg Anesth Pain Med 2006;31:6-13.
- Shafer SL. Retraction notice. Anesth Analg 2009. http://www.aaeditor.org/HWP/Retraction.Notice.pdf.
- Riest G, Peters J, Weiss M, Pospiech J, Hoffmann O, Neuhauser M, et al. Does perioperative administration of rofecoxib improve analgesia after spine, breast and orthopaedic surgery?. Eur J Anaesthesiol 2006;23:219-26.
- Romsing J, Moiniche S, Mathiesen O, Dahl JB. Reduction of opioid-related adverse events using opioid-sparing analgesia with COX-2 inhibitors lacks documentation: a systematic review. Acta Anaesthesiol Scand 2005;49:133-42.
- Romundstad L, Breivik H, Roald H, Skolleborg K, Haugen T, Narum J, et al. Methylprednisolone reduces pain, emesis, and fatigue after breast augmentation surgery: a single-dose, randomized, parallel-group study with methylprednisolone 125 mg, parecoxib 40 mg, and placebo. Anesth Analg 2006;102:418-25.
- Rosenberg J, Harvald T. Severe complications with diclofenac after colonic resection. Dis Colon Rectum 2007;50.
- Rouse DJ. Valdecoxib for postoperative pain management after cesarean delivery: a randomized, double-blind, placebo-controlled study. Obstet Gynecol Surv 2007;62:87-8.
- Rugyte D, Kokki H. Intravenous ketoprofen as an adjunct to patient-controlled analgesia morphine in adolescents with thoracic surgery: a placebo controlled double-blinded study. Eur J Pain 2007;11:694-9.
- Schlachta CM, Burpee SE, Fernandez C, Chan B, Mamazza J, Poulin EC. Optimizing recovery after laparoscopic colon surgery (ORAL-CS): effect of intravenous ketorolac on length of hospital stay. Surg Endosc 2007;21:2212-9.
- Schuster R, Stewart D, Schuster L, Greaney G, Waxman K. Preoperative oral rofecoxib and postoperative pain in patients after laparoscopic cholecystectomy: a prospective, randomized, double-blinded, placebo-controlled trial. Am Surg 2005;71:827-9.
- Shaikh N, Kettern MA, Ali Ahmed AH, Louon A. Morphine sparing effect of proparacetamol in surgical and trauma intensive care. Middle East J Emerg Med 2006;6:28-30.
- Silvanto M, Munsterhjelm E, Savolainen S, Tiainen P, Niemi T, Ylikorkala O, et al. Effect of 3 g of intravenous paracetamol on post-operative analgesia, platelet function and liver enzymes in patients undergoing tonsillectomy under local anaesthesia. Acta Anaesthesiol Scand 2007;51:1147-54.
- Sim R, Cheong DM, Wong KS, Lee BMK, Liew QY. Prospective randomized, double-blind, placebo-controlled study of pre- and postoperative administration of a COX-2-specific inhibitor as opioid-sparing analgesia in major colorectal surgery. Colorectal Dis 2007;9:52-60.
- Singla N, Pong A, Newman K, Group MDS. Combination oxycodone 5 mg/ibuprofen 400 mg for the treatment of pain after abdominal or pelvic surgery in women: a randomized, double-blind, placebo- and active-controlled parallel-group study. Clin Ther 2005;27:45-57.
- Snabes MC, Jakimiuk AJ, Kotarski J, Katz TK, Brown MT, Verburg KM. Parecoxib sodium administered over several days reduces pain after gynecologic surgery via laparotomy. J Clin Anesth 2007;19:448-55.
- Sun T, Sacan O, White PF, Coleman J, Rohrich RJ, Kenkel JM. Perioperative versus postoperative celecoxib on patient outcomes after major plastic surgery procedures. Anesth Analg 2008;106:950-8.
- Tablov B, Tablov V, Popov I, Stoikov S. Usage of the new parenteral selective cox-2 inhibitor dynastat in the gynecologic practice. Akush Ginekol 2006;45:10-3.
- Tan J, Sim R, Cheong D, Rao J. Prospective randomized study of pre- and postoperative administration of valdecoxib, a COX-2-specific inhibitor, as opioid-sparing analgesia in patients undergoing major colorectal resections. Colorectal Dis 2005;7.
- Thienthong S, Jirarattanaphochai K, Krisanaprakornkit W, Simajareuk S, Tantanatewin W, Sathitkarnmanee A. Treatment of pain after spinal surgery in the recovery room by single dose lornoxicam: a randomized, double blind, placebo-controlled trial. J Med Assoc Thai 2004;87:650-5.
- Tilleul P, Weickmans H, Sean PT, Lienhart A, Beaussier M. Cost analysis applied to postoperative analgesia regimens: a comparison between parecoxib and propacetamol. Pharm World Sci 2007;29:374-9.
- Tornero-Campello G. Placebo use to compare the analgesic efficacy of parenteral paracetamol and diclofenac in post-operative orthopaedic pain. Acta Anaesthesiol Scand 2006;50.
- Torres LM, Cabrera J, Martinez J, Calderon E, Fernandez S, Chaves J. The specific cox-2 inhibitor valdecoxib provides effective analgesia after inguinal hernia surgery. Rev Esp Anestesiol Reanim 2004;51:576-82.
- Toshiko Hirahara JT, Bliacheriene S, Yamaguchi ET, Rizzo Rosa MC, Capel Cardoso MMS. Post-Cesarean section analgesia with low spinal morphine doses and systemic nonsteroidal anti-inflammatory drug: diclofenac versus ketoprofen. Rev Bras Otorrinolaringol 2003;53:737-42.
- Tuncer S, Tavlan A, Kostekci H, Reisli R, Otelcioglu S. Postoperatif agrida deksketoprofen kullanimi. Agri Dergisi 2006;18:30-5.
- Turaga K, Wright A, Lee R, Dias WPC, Destache C, Christian R, et al. A randomized trial of the peri-operative use of COX-2 inhibitors in Lichtenstein herniorrhaphy. Hernia 2008;12:515-19.
- Turan A, White PF, Karamanlioglu B, Memis D, Tasdogan M, Pamukcu Z, et al. Gabapentin: an alternative to the cyclooxygenase-2 inhibitors for perioperative pain management. Anesth Analg 2006;102:175-81.
- Tuzuner AM, Ucok C, Kucukyavuz Z, Alkis N, Alanoglu Z. Preoperative diclofenac sodium and tramadol for pain relief after bimaxillary osteotomy. J Oral Maxillofac Surg 2007;65:2453-8.
- Vintar N, Rawal N, Veselko M. Intraarticular patient-controlled regional anesthesia after arthroscopically assisted anterior cruciate ligament reconstruction: ropivacaine/morphine/ketorolac versus ropivacaine/morphine. Anesth Analg 2005;101:573-8.
- Vlajkovic G, Sindjelic R, Stefanovic I. Ketorolac as a pre-emptive analgesic in retinal detachment surgery: a prospective, randomized clinical trial. Int J Clin Pharmacol Ther 2007;45:259-63.
- White PF, Sacan O, Tufanogullari B, Eng M, Nuangchamnong N, Ogunnaike B. Effect of short-term postoperative celecoxib administration on patient outcome after outpatient laparoscopic surgery. Can J Anaesth 2007;54:342-8.
- Xu Y, Tan Z, Chen J, Lou F, Chen W. Intravenous flurbiprofen axetil accelerates restoration of bowel function after colorectal surgery. Can J Anaesth 2008;55:414-22.
- Yamazaki E, Murao K, Asai T, Matsumoto S, Shingu K. Comparison of analgesic effects of intravenous flurbiprofen and suppository indomethacin after laparoscopic cholecystectomy. Jpn J Anesthesiol 2003;52:1186-90.
- Zippel H, Wagenitz A. Comparison of the efficacy and safety of intravenously administered dexketoprofen trometamol and ketoprofen in the management of pain after orthopaedic surgery: A multicentre, double-blind, randomised, parallel-group clinical trial. Clin Drug Investig 2006;26:517-28.
- Ziolkowski R, Srebrzynski A, Kaczka K, Butwicka A, Kuzdak K, Pomorski L. Assessment of postoperative analgesia using intravenous paracetamol during first day following thyroid surgery for goiter. Clin Exp Med Letters 2008;49:41-6.
Appendix 1 Search strategy
The following databases were searched to identify relevant studies:
MEDLINE
Used Ovid MEDLINE® on 3 February 2009 to carry out two searches, one to identify studies using NSAIDs, including cyclo-oxygenase 2 inhibitors (COXIBs), and another to identify studies using paracetamol. The searches were limited to 2003 to 2009. Details of the strategies are given below.
EMBASE
Used Ovid EMBASE® on 3 February 2009 to carry out two searches, one to identify studies using NSAIDs, including cyclo-oxygenase 2 inhibitors (COXIBs), and another to identify studies using paracetamol. The searches were limited to 2003 to 2009. Details of the strategies are given below.
Cochrane Central Register of Controlled Trials
Used CENTRAL via the Cochrane Library Issue 1 2009 on 3 February 2009 to carry out one search to identify studies using either NSAIDs, including cyclo-oxygenase 2 inhibitors (COXIBs), or paracetamol. The searches were limited to 2003 to 2009.
Details of the search strategies used are given below.
MEDLINE (to identify studies using NSAIDs)
Database: Ovid MEDLINE
Search strategy
-
exp Surgical Procedures, Operative/(824244)
-
(surgery or surgical or operat$).ti,ab. (600931)
-
1 or 2 (1115468)
-
Pain, Postoperative/or pain.ti,ab. (162287)
-
3 and 4 (64003)
-
(post surgical pain or post-surgical pain).ti,ab. (69)
-
(post operative pain or post-operative pain or postoperative pain).ti,ab. (7168)
-
(pain after surgery or pain after surgical or pain after operat$).ti,ab. (247)
-
(pain following surgery or pain following operat$).ti,ab. (38)
-
5 or 6 or 7 or 8 or 9 (64648)
-
exp anti-inflammatory agents, non-steroidal/(56171)
-
(non-steroidal anti inflammatory agent$or non-steroidal anti-inflammatory agent$).ti,ab. (316)
-
(non steroidal anti inflammatory agent$or non steroidal anti-inflammatory agent$).ti,ab. (316)
-
nsaid$.ti,ab. (8876)
-
11 or 12 or 13 or 14 (57995)
-
Diclofenac/(2833)
-
15307–86–5.rn. (2833)
-
(diclofenac or diclophenac or dicrofenac or dichlofenal).ti,ab. (3555)
-
(diclofenac sodium or sodium diclofenac or diclonate p).ti,ab. (826)
-
(feloran or voltarol or novapirina or orthofen or ortofen or orthophen).ti,ab. (15)
-
(sr-38 or sr 38 or sr38).ti,ab. (8)
-
(voltaren or diclofenac potassium).ti,ab. (116)
-
21 or 19 or 16 or 18 or 22 or 17 or 20 (4186)
-
Ibuprofen/(2567)
-
15687–27–1.rn. (2567)
-
(ibuprofen or brufen or ibumetin or motrin or nuprin or rufen or salprofen).ti,ab. (3560)
-
benzeneacetic acid.ti,ab. (23)
-
(ip-82 or ip 82 or ip82).ti,ab. (2)
-
(trauma-dolgit gel or trauma dolgit gel or traumadolgit gel).ti,ab. (0)
-
26 or 28 or 25 or 24 or 27 or 29 (4010)
-
dexibuprofen.ti,ab. (25)
-
Indomethacin/(6407)
-
53–86–1.rn. (6407)
-
(indomethacin or indometacin or indocid or osmosin).ti,ab. (9923)
-
(indomet$metindol or amuno or indocin).ti,ab. (12)
-
33 or 34 or 32 or 35 (10976)
-
Ketoprofen/(1022)
-
(ketoprofen or benzoylhydratropic acid or profenid or alrheumum or orudis or alrheumat).ti,ab. (1299)
-
(rp-19583 or rp 19583 or rp19583).ti,ab. (0)
-
22071–15–4.rn. (1022)
-
40 or 37 or 39 or 38 (1436)
-
dexketoprofen.ti,ab. (55)
-
Ketorolac/(612)
-
66635–83–4.rn. (612)
-
ketorolac.ti,ab. (991)
-
43 or 44 or 45 (1075)
-
mefanamic acid.ti,ab. (2)
-
meloxicam.ti,ab. (709)
-
nabumetone.ti,ab. (180)
-
Naproxen/(1157)
-
22204–53–1.rn. (1157)
-
(naproxen or mnpa or methoxypropiocin or anaprox or proxen or synflex or aleve or naprosin or naprosyn).ti,ab. (1705)
-
50 or 51 or 52 (1949)
-
Piroxicam/(818)
-
36322–90–4.rn. (818)
-
(piroxicam or feldene or cp-16171 or cp 16171 or cp16171).ti,ab. (900)
-
55 or 56 or 54 (1187)
-
tenoxicam.ti,ab. (208)
-
tiaprofenic acid.ti,ab. (86)
-
Cyclooxygenase 2 Inhibitors/(5054)
-
(cyclooxygenase 2 inhibitor$or cox2 inhibitor$or cyclooxygenase-2 inhibitor$or cyclooxygenase-2 or cox-2 inhibitor$or cox 2 inhibitor$or coxib$).ti,ab. (11466)
-
celecoxib.ti,ab. (2390)
-
etoricoxib.ti,ab. (235)
-
parecoxib.ti,ab. (194)
-
60 or 63 or 64 or 61 or 62 (13873)
-
53 or 48 or 42 or 46 or 30 or 23 or 65 or 36 or 57 or 41 or 58 or 15 or 47 or 59 or 49 or 31 (68537)
-
66 and 10 (2823)
-
exp Morphine/(12838)
-
(morphine adj2 (pca or less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1605)
-
(opioid$adj2 (pca or less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1073)
-
68 or 69 or 70 (13925)
-
67 and 71 (595)
-
(post surgical analges$or post-surgical analges$or postsurgical analges$).ti,ab. (32)
-
(post operative analges$or post-operative analges$or postoperative analges$).ti,ab. (2849)
-
patient controlled analges$.ti,ab. (1528)
-
analgesia, patient controlled/(2002)
-
73 or 74 or 75 or 76 (4822)
-
71 and 77 (1462)
-
(pca morphine or pca opioid$).ti,ab. (178)
-
67 or 78 or 79 (3998)
-
randomized controlled trial.pt. (166208)
-
controlled clinical trial.pt. (32474)
-
randomized.ab. (128908)
-
placebo.ab. (65964)
-
drug therapy.fs. (631837)
-
randomly.ab. (88084)
-
trial.ab. (124483)
-
groups.ab. (528986)
-
81 or 87 or 86 or 82 or 88 or 84 or 83 or 85 (1273344)
-
humans.sh. (4807787)
-
89 and 90 (1048145)
-
91 and 80 (3102)
-
limit 92 to yr=“2003 – 2009” (1607)
MEDLINE (to identify studies using paracetamol)
Database: Ovid MEDLINE
Search strategy
-
exp Surgical Procedures, Operative/(824244)
-
(surgery or surgical or operat$).ti,ab. (600931)
-
(1 or 2) and pain.ti,ab. (61812)
-
Pain, Postoperative/(11958)
-
(post surgical pain or post-surgical pain).ti,ab. (69)
-
(post operative pain or post-operative pain or postoperative pain).ti,ab. (7168)
-
(pain after surgery or pain after surgical or pain after operat$).ti,ab. (247)
-
(pain following surgery or pain following operat$).ti,ab. (38)
-
3 or 4 or 5 or 6 or 7 or 8 (65655)
-
Acetaminophen/(5251)
-
paracetamol.ti,ab. (2957)
-
propacetamol.ti,ab. (122)
-
10 or 11 or 12 (6355)
-
9 and 13 (799)
-
exp Morphine/(12838)
-
(morphine adj2 (pca or less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1605)
-
(opioid$adj2 (pca or less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1073)
-
15 or 16 or 17 (13925)
-
14 and 18 (282)
-
(post surgical analges$or post-surgical analges$or postsurgical analges$).ti,ab. (32)
-
(post operative analges$or post-operative analges$or postoperative analges$).ti,ab. (2849)
-
patient controlled analges$.ti,ab. (1528)
-
analgesia, patient controlled/(2002)
-
20 or 21 or 22 or 23 (4822)
-
24 and 18 (1462)
-
(pca morphine or pca opioid$).ti,ab. (178)
-
19 or 25 or 26 (1647)
-
randomized controlled trial.pt. (166208)
-
controlled clinical trial.pt. (32474)
-
randomized.ab. (128908)
-
placebo.ab. (65964)
-
drug therapy.fs. (631837)
-
randomly.ab. (88084)
-
trial.ab. (124483)
-
groups.ab. (528986)
-
28 or 34 or 33 or 29 or 35 or 31 or 30 or 32 (1273344)
-
humans.sh. (4807787)
-
36 and 37 (1048145)
-
38 and 27 (1487)
-
limit 39 to yr=“2003 – 2009” (730)
EMBASE (to identify studies using NSAIDs)
Database: Ovid EMBASE
Search strategy
The search strategy was originally run on 2 February 2009. It was subsequently re-run on 26 May 2009 after a minor typographical error was identified. Additional records that would have been in the database at the time of the original search were considered for inclusion.
-
exp surgery/(1046728)
-
(surgery or surgical or operat$).ti,ab. (604439)
-
1 or 2 (1252921)
-
Postoperative Pain/or pain.ti,ab. (174055)
-
4 and 3 (75739)
-
(post surgical pain or post-surgical pain).ti,ab. (95)
-
(post operative pain or post-operative pain or postoperative pain).ti,ab. (7575)
-
(pain after surgery or pain after surgical or pain after operat$).ti,ab. (259)
-
(pain following surgery or pain following operat$).ti,ab. (36)
-
8 or 6 or 7 or 9 or 5 (76205)
-
Nonsteroid Antiinflammatory Agent/(46608)
-
(nsaid$or non-steroidal anti inflammatory agent$or non-steroidal anti-inflammatory agent$or non steroidal anti inflammatory agent$or non steroidal anti-inflammatory agent$).ti,ab. (10435)
-
Diclofenac/(13371)
-
15307–79–6.rn. (13371)
-
(Abitren or Artrenac or Assaren or Athrofen).ti,ab. (0)
-
(Clofen or Delphinac or Diclo Basan or Diclobasan).ti,ab. (1)
-
(Diclofenac Rekur or Diclofenac Resin or Diclofenac Resinate or Diclofenac Sodium or Diclophenac Sodium).ti,ab. (1009)
-
(Diclo Puren or Diclopuren or Diclo Recip or Diclorecip or Dicloreum).ti,ab. (2)
-
(Dioxaflex or Dioxaflex Retard or Dolotren Retard or Doragon or Duravolten).ti,ab. (0)
-
(Ecofenac or Effekton or Effekton Retard or Feloran or Flameril or Flector).ti,ab. (15)
-
(GP 45840 or Grofenac or Inflamac or Isv 205 or Isv205).ti,ab. (2)
-
(Kriplex or Monoflam or Naclof or Novapirina).ti,ab. (3)
-
(Olfen or Orthophen or Rewodina or Rheufenac or Rheumafen or Rhumalgan).ti,ab. (7)
-
(Sodium Diclofenac or Solaraze or Sr 318t).ti,ab. (164)
-
(Tabiflex or Veral or Voldal or Voltaren or Voltarene or Voltarol or Voltral or Voveran or Xenid).ti,ab. (128)
-
18 or 23 or 15 or 19 or 21 or 24 or 14 or 20 or 13 or 16 or 25 or 22 or 17 (13411)
-
Ibuprofen/(15848)
-
15687–27–1.rn. (15848)
-
(Advil or Aktren or Algifor or Algofen or Analgyl or Anco or Attritin).ti,ab. (29)
-
(Balkaprofen or Brufen or Brufort or Bufohexal or Burana).ti,ab. (11)
-
(Contraneural or Dc 7034 or Dc7034 or Dg 7034 or Dg7034 or Dolgit or Dolocyl or Dolodolgit).ti,ab. (7)
-
(Ecoprofen or Emflam or Exidol or Femapirin or Fenalgic or Fenbid).ti,ab. (7)
-
(Halprin or Haltran or Ibofen or Ibudak or Ibufen or Ibugel or Ibugesic or Ibulgan or Ibumetin or Ibuprin).ti,ab. (6)
-
(Ibuprofen Klinge 600 or Ibu Slow or Ibusynth or Ibutop Irfen).ti,ab. (3)
-
(Junifen or Kontraneural or Lidifen or Maxagesic or MCN R 1451 or Medipren).ti,ab. (1)
-
(Mediprin or Mensoton or Midol 200 or Motrin).ti,ab. (7)
-
(Neobrufen or Nerofen or Novogent N or Nugin or Nuprin or Nureflex or Nurofen).ti,ab. (12)
-
(Optifen or Opturem or Paduden or Pedea or Proflex).ti,ab. (4)
-
(Rebugen or Reuvol or Rufen or Seclodin or Tabalon or Trendar or Unipro or Urem).ti,ab. (5)
-
39 or 37 or 33 or 38 or 29 or 32 or 27 or 34 or 30 or 36 or 28 or 31 or 35 (15875)
-
Dexibuprofen/(87)
-
51146–56–6.rn. (87)
-
(dexibuprofen or Deltaran or Seractil).ti,ab. (47)
-
42 or 43 or 41 (89)
-
Indometacin/(19624)
-
(53–86–1 or 74252–25–8 or 7681–54–1).rn. (19624)
-
(Algiflam or Algometacin or Amuno or Amuno Retard or Arthrexin or Artracin or Artrocid).ti,ab. (3)
-
(Bonidon or Boutycin or Chrono Indocid or Chronoindocid or Confortid).ti,ab. (1)
-
(Dolazol or Dolcidium or Dometin or Durametacin or Elmetacin or Endometacin or Flexin Continus or Helvecin).ti,ab. (1)
-
(Inacid or Indacin or Inderapollon or Indicin or Indocid or Indocid Retard or Indocin or Indocin Sr).ti,ab. (20)
-
(Indocollyre or Indolemmon or Indomed or Indomee or Indomelol or Indometacine or Indometacin Sodium Trihydrate).ti,ab. (25)
-
(Indomethacin or Indomethacine or Indomethacinum or Indometin Depot or Indomet Retard or Indomexum).ti,ab. (10330)
-
(Indo Phlogont or Indoptic or Indoptol or Indorektal or Indos or Indosmos or Indotard or Indoxen or Indren or Inmetsin or Inteban).ti,ab. (4)
-
(Luiflex or Lyo Indometacin Trihydrate or MCN R 1166 or MCN R1166 or Metacen or Methindol or Methindole or Metindol).ti,ab. (0)
-
(Mezolin or Miometacen or Mk 615 or Mk615 or Mobilan or Osmogit or Osmosin or Servimeta or Tannex or Taye).ti,ab. (6)
-
1 P Chlorobenzylidene 5 Methoxy 2 Methyl 3 Indoneacetic Acid.ti,ab. (0)
-
47 or 45 or 51 or 52 or 48 or 53 or 54 or 50 or 46 or 49 or 55 or 56 (20688)
-
Ketoprofen/(4465)
-
(22071–15–4 or 57495–14–4).rn. (4465)
-
(Alrhemun or Alrheumat or Alrheumin or Alrheumun or Alrhumat).ti,ab. (0)
-
(Biprofenid or Capisten or Cetoprofen or Fastum or Iso K or Ketofen or Ketoprofen Sodium).ti,ab. (15)
-
(Ketorin or Ketum or Knavon or Kpl 202).ti,ab. (8)
-
(Orudis or Oruvail or Oscorel or Oxoprofene or Profenid or 19583 Rp or Sodium Ketoprofen).ti,ab. (14)
-
62 or 61 or 58 or 63 or 60 or 59 (4467)
-
Dexketoprofen/(170)
-
22161–81–5.rn. (170)
-
(Dexketoprofen Trometamol or Enantyum or Keral or Ketesse or Nosatel or Quiralam or Sympal or Viaxal).ti,ab. (49)
-
65 or 67 or 66 (170)
-
Ketorolac/(3425)
-
74103–06–3.rn. (3425)
-
(Droal or Ketocol or Rs 37619 or Taradyl or Toradol or Toratex).ti,ab. (30)
-
71 or 69 or 70 (3428)
-
Mefenamic Acid/(1449)
-
61–68–7.rn. (1449)
-
(Ci 473 or Ci473 or Cn 35355 or Cn35355 or Coslan).ti,ab. (20)
-
(Fendol or Inf 3355 or Inf3355 or Mefacit or Mefanamic Acid or Mefenamate or Mefenamate Sodium).ti,ab. (19)
-
(Meftal or Mephenamate or Mephenamic Acid or Mephenaminic Acid).ti,ab. (3)
-
(Parkemed or Ponalar or Ponlar or Ponstan or Ponstel or Ponstel Kapseals or Ponstyl or Pontal or Sodium Mefenamate).ti,ab. (12)
-
75 or 76 or 78 or 73 or 77 or 74 (1481)
-
Meloxicam/(2379)
-
71125–38–7.rn. (2379)
-
(Mesoxicam or Metacam or Mobec or Mobic or Movalis or Movicox or Parocin).ti,ab. (31)
-
81 or 82 or 80 (2379)
-
Nabumetone/(1046)
-
42924–53–8.rn. (1046)
-
(Arthaxan or Balmox or Brl 14777 or Brl14777 or Consolan or Diosmal or Listran or Nabucox or Nabumeton or Nabuser or Relafen or Relifen or Relifex or Reliflex).ti,ab. (20)
-
86 or 84 or 85 (1047)
-
Naproxen/(9362)
-
(22204–53–1 or 26159–34–2).rn. (9362)
-
(Agilex or Aleve or Alpoxen or Anaprox or Apranax or Artroxen or Axer Alfa).ti,ab. (8)
-
(Daprox Entero or Dextro Naproxen or Dysmenalgit or Equiproxen).ti,ab. (0)
-
(Femex or Flanax or Floginax or Floxene or Levo Naproxen).ti,ab. (0)
-
6 Methoxy Alpha Methyl 2 Naphthaleneacetic Acid.ti,ab. (6)
-
(Methoxypropiocin or Naixan).ti,ab. (0)
-
(Naprelan or Napren or Naprontag or Naprosyn or Naprosyne or Naprovite or Naproxen Sodium or Naproxyn).ti,ab. (186)
-
(Naprozyne or Narox or Naxyn or Neprossin or Novuran or Nycopren or Pactens or Primeral or Proxen).ti,ab. (2)
-
(Rs 3540 or Rs 3650 or Rs3540 or Rs3650 or Sodium Naproxen or Synaprosyn or Synflex or Xenar).ti,ab. (24)
-
96 or 97 or 95 or 92 or 90 or 91 or 93 or 89 or 88 or 94 (9374)
-
Piroxicam/(3983)
-
36322–90–4.rn. (3983)
-
(Alganpar or Apopiroxicam or Artroxicam or Baxo or Brexic).ti,ab. (0)
-
(Cp 16171 or Cp16171 or Erazon or Felden or Feldene or Flogobene).ti,ab. (19)
-
(Hotemin or Inflamene or Leciva or Novopirocam or Osteral).ti,ab. (13)
-
(Pirkam or Piroftal or Piroxene or Proxicam or Riacen or Roxal or Roxicam).ti,ab. (2)
-
104 or 99 or 102 or 100 or 101 or 103 (3996)
-
Tenoxicam/(853)
-
59804–37–4.rn. (853)
-
(Liman or Mobiflex or “Ro 12 0068” or Tenoxicam Milk Formulation or Tilatil or Tilcotil).ti,ab. (9)
-
107 or 106 or 108 (855)
-
Tiaprofenic Acid/(452)
-
33005–95–7.rn. (452)
-
(Artiflam or Ru 15060 or Suralgan or Surgam or Surgam 300 or Surgam Forte or Surgamic or Surgamyl or Thiaprofenic Acid or Tiaprofen).ti,ab. (14)
-
111 or 110 or 112 (453)
-
79 or 44 or 40 or 87 or 83 or 109 or 26 or 64 or 72 or 105 or 68 or 113 or 57 or 98 (51235)
-
Cyclooxygenase 2 Inhibitor/(12458)
-
(cyclooxygenase 2 inhibitor$or cox2 inhibitor$or cyclooxygenase-2 inhibitor$or cyclooxygenase-2 or cox-2 inhibitor$or cox 2 inhibitor$or coxib$).ti,ab. (12060)
-
Celecoxib/(9313)
-
169590–42–5.rn. (9313)
-
(Celebra or Celebrex or Onsenal or SC 58635 or Sc58635 or Ym 177 or Ym177 or Zycel).ti,ab. (157)
-
Etoricoxib/(1071)
-
(202409–33–4 or 202409–40–3).rn. (1071)
-
(Arcoxia or Etoricoxib Hydrochloride or L 791456 or L791456 or “Mk 0663” or Mk 663 or Mk0663 or Mk663 or Nucoxia).ti,ab. (18)
-
Parecoxib/(846)
-
(198470–84–7 or 198470–85–8).rn. (846)
-
(Dynastat or Parecoxib Sodium or Rayzon or SC 69124 or Sc69124 or SC 69124a or Sc69124a or Xapit).ti,ab. (68)
-
116 or 123 or 120 or 119 or 124 or 121 or 115 or 118 or 117 or 125 or 122 (23654)
-
114 or 126 (67454)
-
127 or 11 or 12 (96276)
-
128 and 10 (7531)
-
morphine/(26987)
-
(morphine adj2 (less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1610)
-
(opioid$adj2 (less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1135)
-
130 or 131 or 132 (27828)
-
129 and 133 (2232)
-
(post surgical analges$or post-surgical analges$or postsurgical analges$).ti,ab. (32)
-
(post operative analges$or post-operative analges$or postoperative analges$).ti,ab. (3381)
-
patient controlled analges$.ti,ab. (1634)
-
analgesia, patient controlled/(3213)
-
138 or 136 or 137 or 135 (6287)
-
129 and 139 (1357)
-
(pca morphine or pca opioid$).ti,ab. (196)
-
129 or 140 or 141 (7678)
-
random.tw. (59417)
-
clinical trial.mp. (457186)
-
exp Health Care Quality/(762726)
-
144 or 143 or 145 (1118500)
-
142 and 146 (4636)
-
limit 147 to yr=“2003 – 2009” (3253)
EMBASE (to identify studies using paracetamol)
Database: Ovid EMBASE
Search strategy
-
exp surgery/(1014647)
-
(surgery or surgical or operat$).ti,ab. (587030)
-
1 or 2 (1215514)
-
Postoperative Pain/or pain.ti,ab. (168694)
-
3 and 4 (73423)
-
(post surgical pain or post-surgical pain).ti,ab. (87)
-
(post operative pain or post-operative pain or postoperative pain).ti,ab. (7359)
-
(pain after surgery or pain after surgical or pain after operat$).ti,ab. (252)
-
(pain following surgery or pain following operat$).ti,ab. (36)
-
5 or 6 or 7 or 8 or 9 (73862)
-
Paracetamol/(25273)
-
(acetaminophen or propacetamol).ti,ab. (4392)
-
11 or 12 (25728)
-
13 and 10 (3496)
-
MORPHINE/(26227)
-
(morphine adj2 (less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1564)
-
(opioid$adj2 (less or demand or consum$or spar$or reduc$or decreas$)).ti,ab. (1099)
-
15 or 16 or 17 (27041)
-
14 and 18 (1495)
-
(post surgical analges$or post-surgical analges$or postsurgical analges$).ti,ab. (30)
-
(post operative analges$or post-operative analges$or postoperative analges$).ti,ab. (3311)
-
patient controlled analges$.ti,ab. (1602)
-
analgesia, patient controlled/(3144)
-
20 or 21 or 22 or 23 (6148)
-
19 and 24 (489)
-
(pca morphine or pca opioid$).ti,ab. (193)
-
14 and 26 (26)
-
19 or 25 or 27 (1496)
-
random.tw. (57923)
-
clinical trial.mp. (443528)
-
exp Health Care Quality/(738047)
-
29 or 30 or 31 (1084232)
-
32 and 28 (980)
-
limit 33 to yr=“2003 – 2009” (745)
-
from 34 keep 1–745 (745)
CENTRAL (to identify studies using either NSAIDs or paracetamol)
Search
-
#1 MeSH descriptor Surgical Procedures, Operative explode all trees
-
#2 (surgery or surgical or operat*):ti,ab,kw in Clinical Trials
-
#3 (#1 OR #2)
-
#4 MeSH descriptor Pain, Postoperative explode all trees
-
#5 (pain):ti,ab,kw
-
#6 (#4 OR #5)
-
#7 (#3 AND #6)
-
#8 “post surgical pain” or “post-surgical pain”:ti or “post surgical pain” or “post-surgical pain”:ab or “post operative pain” or “post-operative pain” or “postoperative pain”:ti or “post operative pain” or “post-operative pain” or “postoperative pain”:ab
-
#9 “pain after surgery” or “pain after surgical” or “pain after operat*” or “pain after surgery” or “pain after surgical” or “pain after operat*”:ab or “pain following surgery” or “pain following surgical” or “pain following operat*”:ti or “pain following surgery” or “pain following surgical” or “pain following operat*”:ab
-
#10 (#7 OR #8 OR #9)
-
#11 MeSH descriptor Acetaminophen explode all trees
-
#12 (paracetamol or propacetamol):ti or (paracetamol or propacetamol):ab
-
#13 (#11 OR #12)
-
#14 MeSH descriptor Anti-Inflammatory Agents, Non-Steroidal explode all trees
-
#15 “non-steroidal anti inflammatory agent*” or “non-steroidal anti-inflammatory agent*”:ti or “non-steroidal anti inflammatory agent*” or “non-steroidal anti-inflammatory agent*”:ab or “non steroidal anti inflammatory agent*” or “non steroidal anti-inflammatory agent*”:ti or “non steroidal anti inflammatory agent*” or “non steroidal anti-inflammatory agent*”:ab
-
#16 (nsaid*):ti or (nsaid*):ab
-
#17 MeSH descriptor Diclofenac explode all trees
-
#18 (diclofenac or diclophenac or dicrofenac or dichlofenal):ti or (diclofenac or diclophenac or dicrofenac or dichlofenal):ab or “diclonate p”:ti or “diclonate p”:ab
-
#19 (feloran or voltarol or novapirina or orthofen or ortofen or orthophen):ti or (feloran or voltarol or novapirina or orthofen or ortofen or orthophen):ab or (sr-38 or “sr 38” or sr38):ti or (sr-38 or “sr 38” or sr38):ab
-
#20 (voltaren or “diclofenac potassium”):ti or (voltaren or “diclofenac potassium”):ab
-
#21 (sr-38 or “sr 38” or sr38):ti or (sr-38 or “sr 38” or sr38):ab
-
#22 MeSH descriptor Ibuprofen explode all trees
-
#23 (ibuprofen or brufen or ibumetin or motrin or nuprin or rufen or salprofen):ti or (ibuprofen or brufen or ibumetin or motrin or nuprin or rufen or salprofen):ab or “benzeneacetic acid”:ti or “benzeneacetic acid”:ab
-
#24 (ip-82 or “ip 82” or ip82):ti or (ip-82 or “ip 82” or ip82):ab or “trauma-dolgit gel” or “trauma dolgit gel” or “traumadolgit gel”:ti or “trauma-dolgit gel” or “trauma dolgit gel” or “traumadolgit gel”:ab
-
#25 (dexibuprofen):ti or (dexibuprofen):ab
-
#26 MeSH descriptor Indomethacin explode all trees
-
#27 (indomethacin or indometacin or indocid or osmosin):ti or (indomethacin or indometacin or indocid or osmosin):ab or “indomet* metindol” or amuno or indocin:ti or “indomet* metindol” or amuno or indocin:ab
-
#28 MeSH descriptor Ketoprofen explode all trees
-
#29 (ketoprofen or “benzoylhydratropic acid” or profenid or alrheumum or orudis or alrheumat):ti or (ketoprofen or “benzoylhydratropic acid” or profenid or alrheumum or orudis or alrheumat):ab or (rp-19583 or “rp 19583” or rp19583):ti or (rp-19583 or “rp 19583” or rp19583):ab
-
#30 (dexketoprofen):ti or (dexketoprofen):ab
-
#31 MeSH descriptor Ketorolac explode all trees
-
#32 (ketorolac):ti or (ketorolac):ab or “mefanamic acid” or meloxicam or nabumetone:ti or “mefanamic acid” or meloxicam or nabumetone:ab
-
#33 MeSH descriptor Naproxen explode all trees
-
#34 (naproxen or mnpa or methoxypropiocin or anaprox or proxen or synflex or aleve or naprosin or naprosyn):ti or (naproxen or mnpa or methoxypropiocin or anaprox or proxen or synflex or aleve or naprosin or naprosyn):ab
-
#35 MeSH descriptor Piroxicam explode all trees
-
#36 (piroxicam or feldene or cp-16171 or “cp 16171” or cp16171):ti or (piroxicam or feldene or cp-16171 or cp 16171 or cp16171):ab or (tenoxicam or “tiaprofenic acid”):ti or (tenoxicam or “tiaprofenic acid”):ab
-
#37 MeSH descriptor Cyclooxygenase 2 Inhibitors explode all trees
-
#38 “cyclooxygenase 2 inhibitor*” or “cox2 inhibitor*” or “cyclooxygenase-2 inhibitor*” or cyclooxygenase-2 or “cox-2 inhibitor*” or “cox 2 inhibitor*” or coxib*:ti or “cyclooxygenase 2 inhibitor*” or “cox2 inhibitor*” or “cyclooxygenase-2 inhibitor*” or cyclooxygenase-2 or “cox-2 inhibitor*” or “cox 2 inhibitor*” or coxib*:ab or (celecoxib or abetoricoxib or parecoxib):ti or (celecoxib or abetoricoxib or parecoxib):ab
-
#39 (#13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38)
-
#40 (#10 AND #39)
-
#41 MeSH descriptor Morphine explode all trees
-
#42 (morphine NEAR/2 (pca or less or demand or consum* or spar* or reduc* or decreas*)):ti or (morphine NEAR/2 (pca or less or demand or consum* or spar* or reduc* or decreas*)):ab or (opioid NEAR/2 (pca or less or demand or consum* or spar* or reduc* or decreas*)):ti or (opioid NEAR/2 (pca or less or demand or consum* or spar* or reduc* or decreas*)):ab
-
#43 (#41 AND #42)
-
#44 “post surgical analgesia” or “post-surgical analgesia” or “postsurgical analgesia”:ti or “post surgical analgesia” or “post-surgical analgesia” or “postsurgical analgesia”:ab or “post operative analgesia” or “post-operative analgesia” or “postoperative analgesia”:ti or “post operative analgesia” or “post-operative analgesia”:ab
-
#45 “patient controlled analgesia”:ti or “patient controlled analgesia”:ab
-
#46 MeSH descriptor Analgesia, Patient-Controlled explode all trees
-
#47 “post surgical analgesic” or “post-surgical analgesic” or “postsurgical analgesic”:ti or “post surgical analgesic” or “post-surgical analgesic” or “postsurgical analgesic”:ab or “post operative analgesic” or “post-operative analgesic” or “postoperative analgesic”:ti or “post operative analgesic” or “post-operative analgesic”:ab
-
#48 “patient controlled analgesic”:ti or “patient controlled analgesic”:ab
-
#49 (#44 OR #45 OR #46 OR #47 OR #48)
-
#50 (#40 AND #43)
-
#51 (#40 AND #49)
-
#52 “pca morphine” or “pca opioid*”:ti or “pca morphine” or “pca opioid*”
-
#53 (#50 OR #51 OR #52), from 2003 to 2009
Appendix 2 winbugs codes
(a) Random effects model to calculate the baseline treatment effect for adverse event outcomes
model {
for (i in 1:N) {
r[i]∼dbin(p[i],n[i])
logit(p[i])<-mu[i]
mu[i]∼dnorm(d,prec)
}
d∼dnorm(0,0.0001)
prec<-1/(sd*sd)
sd∼dunif(0,2)
}
(b) Random effects model to calculate the baseline treatment effect for the morphine consumption outcome
model {
for (i in 1:N) {
prec.y[i]<-n[i]/(sd[i]*sd[i])
y[i] ∼ dnorm(mu[i],prec.y[i])
mu[i] ∼ dnorm(d,prec)
}
d ∼ dnorm(0,0.0001)
prec<-1/(rho*rho)
rho ∼ dunif(0,2)
}
(c) Model for adverse event outcomes
model{
sw[1] <- 0
for(i in 1:N) {
# model
logit(p[i])<-mu[s[i]]+ delta[i] * (1-equals(t[i],b[i]))
r[i]∼dbin(p[i],n[i]) # binomial likelihood
delta[i] ∼ dnorm(md[i],taud[i]) # trial-specific LOR distributions
# precisions of LOR distributions: adjusts for correlation in three-armed trials
taud[i] <- tau * (1 + equals(m[i],3)/3)
# means of LOR distribution
md[i] <- d[t[i]] - d[b[i]] + equals(m[i],3) * sw[i]
#calculating the residual deviance
rhat[i]<-p[i] * n[i]
dev[i]<-2 * (r[i] * (log(r[i]/rhat[i])) + (n[i] – r[i]) * (log((n[i] - r[i])/(n[i] - rhat[i]))))
}
resdev<-sum(dev[])
# adjustment for 3-arm trials
for (i in 2:N) {sw[i] <- (delta[i-1] - d[t[i-1]] + d[b[i-1]])/2}
# vague priors for 24 trial baselines
for(j in 1:NS){mu[j]∼dnorm(0,.0001)}
# vague priors for basic parameters
d[1]<-0
for (k in 2:NT) {d[k] ∼ dnorm(0,.0001)}
# vague prior for random effects standard deviation
sd∼dunif(0,2) tau<-1/pow(sd,2)
# Absolute log odds(success) on Treatment A, based on a separate model on the baseline treatment arms.
mA ∼ dnorm(-1.888,0.4652)
# Absolute pr(success) Treatments B,C,D based on T[1] and the MEAN Relative treatment effects
for (k in 1:NT) {logit(T[k])<- mA + d[k]}
# Ranking and prob{treatment k is best}
for (k in 1:NT) {rk[k]<- NT+1 - rank(T[],k)
best[k]<-equals(rk[k],1)}
# Pairwise ORs
for (c in 1:(NT-1))
{for (k in (c+1):NT)
{lor[c,k] <- d[k] – d[c]
log(or[c,k]) <- lor[c,k]
}
}
(d) Model for morphine consumption outcome
model{
sw[1]<-0
for(i in 1:N) {
prec.y[i]<-n[i]/(sd[i]*sd[i])
# normal likelihood
y[i] ∼ dnorm(my[i],prec.y[i])
# the model
my[i]<-mu[s[i]] + delta[i] * (1-equals(t[i],b[i]))
delta[i] ∼ dnorm(md[i],prec.d[i])
# adjustment for correlation between arms in a three-armed trial
prec.d[i]<-precd * (1 + equals(m[i],3)/3)
md[i]<-d[t[i]] - d[b[i]] + equals(m[i],3) * sw[i]
# calculates the residual deviance
dev[i]<-(y[i]-my[i])*(y[i]-my[i]) * prec.y[i]
}
resdev<-sum(dev[])
# adjustment for correlation between arms in a three-armed trial
for (i in 2:N) {sw[i] <- (delta[i-1] - d[t[i-1]] + d[b[i-1]])/2}
for(j in 1:NS){mu[j]∼dnorm(0,.0001)}
d[1]<-0
for (k in 2:NT) {d[k] ∼ dnorm(0,.0001)}
# The range for the standard deviation of the random effect distribution for the effect difference is shown below. This was set narrowly and as a post hoc sensitivity analysis the effect of widening this was investigated. With a distribution of dunif(0,100), the treatment effects increased slightly and at a higher baseline morphine consumption, but results did not change (available from the authors).
rho ∼ dunif(0,2)
precd<-1/pow(rho,2)
mA ∼ dnorm(37.36,0.2507)
# MEAN Relative treatment effects
for (k in 1:NT) {T[k]<- mA + d[k]}
# Ranking and prob{treatment k is best}
for (k in 1:NT) {rk[k]<- NT+1 - rank(T[],k)
best[k]<-equals(rk[k],1)}
}
(e) Adjustment for baseline morphine consumption
model{
sw[1]<-0
for(i in 1:N) {
prec.y[i]<-n[i]/(sd[i]*sd[i])
y[i] ∼ dnorm(my[i],prec.y[i])
my[i]<-mu[s[i]] + delta[i] * (1-equals(t[i],b[i]))
delta[i] ∼ dnorm(md[i],prec.d[i])
prec.d[i]<-precd * (1 + equals(m[i],3)/3)
# the independent variable is morph[i]. This line is appropriate for either independent or exchangeable interaction assumptions for each treatment
md[i]<-d[t[i]] - d[b[i]] + (beta[t[i]] - beta[b[i]]) * morph[i] + equals(m[i],3) * sw[i]
# or this line is appropriate for a common interaction assumption
md[i]<-d[t[i]] - d[b[i]] + beta * morph[i] + equals(m[i],3) * sw[i]
dev[i]<-(y[i]-my[i])*(y[i]-my[i]) * prec.y[i]
}
resdev<-sum(dev[])
for (i in 2:N) {sw[i] <- (delta[i-1] - d[t[i-1]] + d[b[i-1]])/2}
# the following is appropriate for an independent interaction assumption
beta[1]<–0
for(k in 2:NT){
beta[k]∼dnorm(0,0.0001)}
# or the following is appropriate for an exchangeable interaction assumption
beta[1]<–0
for(k in 2:NT){
beta[k]∼dnorm(m.beta,tau.beta)}
m.beta∼dnorm(0,0.0001)
sd.beta∼dunif(0,2)
tau.beta<-1/pow(sd.beta,2)
# or the following is appropriate for a common interaction assumption
beta∼dnorm(0,0.0001)
(f) Description of the sensitivity analysis for baseline morphine consumption
A covariate M was added to the regression model in the MTC analysis, which was the difference M between the placebo 24-hour consumption for each trial, yp, and mean placebo 24-hour consumption, y¯, derived from the baseline random-effects meta-analysis.
If M > 0 then the treatment effectiveness would be reduced in the model, and if M < 0 then the treatment effectiveness would be increased in the model.
The difference between the treatment and placebo is denoted dt, the effectiveness difference between the baseline treatment of the trial and placebo is denoted db, and the difference in 24-hour morphine consumption between the arms of each trial is denoted δi. For trial arm i, the difference in 24-hour morphine consumption between the arms of each trial (δi) was related to the difference in effectiveness of the treatments in the arms compared to placebo (dt – db) and to the difference in placebo 24 hour morphine consumption from the mean (M). 38
Three different assumptions were made for the treatment and baseline morphine consumption interaction. The first was that there was a common interaction for all the treatments. This is the model presented in Equation 1. The second is that there is an exchangeable interaction between the treatments and study quality, where each treatment t has its own interaction, βt, as in Equation 2, each of which derives from the same normal distribution of interactions, which means that each treatment and study quality interaction is heavily influenced by the others. The third assumption is that there is an independent interaction between the treatments and study quality, where each treatment t has its own interaction βt and these are independent; they do not come from a common distribution. The term βb refers to the interaction of the baseline treatment in the trial including arm i. The DIC statistic and the residual deviance would be used to compare model assumptions.
Two studies did not have placebo as a comparator. 64,65 Ideally, the baseline for these two studies would be accounted for within one model; however, to our knowledge no such methods have been published. Consequently, the model was run first without these two studies in order to derive an estimate for βb and db for the baseline treatments t in the studies. This was considered to result in a reasonable estimate as only 2 out of 56 trials were lacking placebo. M was then calculated for these two studies as follows:
The analysis was then rerun including the two studies.
(g) Description of the sensitivity analysis for study quality
For trial arm i, the difference in 24-hour morphine consumption between the arms of each trial (δi) was related to the difference in effectiveness of the treatments in the arms compared to placebo (dt – db) and to the centred baseline morphine consumption (M) and the study quality (Q).
The dummy variable, Q, was set to 0 if the study quality was good to ensure that the absolute 24-hour morphine consumption estimate for each drug produced by the MTC analysis was the result for the good quality studies.
The same three assumptions regarding the interaction between treatment effect and the covariate were investigated for study quality. The DIC statistic and comparison with the analysis on the subset of trials were used to identify the most appropriate assumption.
Appendix 3 Excluded studies
| Author | Inappropriate participants | Inappropriate intervention | Inappropriate comparator | Inappropriate outcome measure | Inappropriate study design | Other reason for exclusion |
|---|---|---|---|---|---|---|
| Adachi 2007119 | ✗ | |||||
| Akca 2004120 | ✗ | |||||
| Antonetti 2007121 | ✗ | |||||
| Anwari 2008122 | ✗a | |||||
| Atallah 2004123 | ✗ | |||||
| Aubrun 2003124 | ✗ | |||||
| Babul 2006125 | ✗b | |||||
| Bajaj 2004126 | ✗ | |||||
| Beaulieu 2007127 | ✗c | |||||
| Beaussier 2005128 | ✗ | |||||
| Belzarena 2005129 | ✗ | |||||
| Bianchin 2007130 | ✗ | |||||
| Binhas 2004131 | ✗ | |||||
| Binning 2007132 | ✗ | |||||
| Boccara 2004133 | ✗ | |||||
| Bolcal 2005134 | ✗ | |||||
| Bourlert 2005135 | ✗d | |||||
| Boussofara 2006136 | ✗ | |||||
| Bugter 2003137 | ✗e | |||||
| Buvanendran 2003138 | ✗f | |||||
| Cabrera 2004139 | ✗f | |||||
| Carvalho 2006140 | ✗g | |||||
| Cattabriga 2007141 | ✗ | |||||
| Chan 2005142 | ✗ | |||||
| Chelly 2007143 | ✗ | |||||
| Chen 2005144 | ✗ | |||||
| Daniels 2006145 | ✗ | |||||
| De Leon-Casasola 2003146 | ✗ | |||||
| Desjardins 2004147 | ✗ | |||||
| Engelman 2007148 | ✗h | |||||
| Feld 2003149 | ✗ | |||||
| Feng 2008150 | ✗f | |||||
| Feng 2004 151 | ✗f | |||||
| Fijalkowska 2006152 | ✗ | |||||
| Gan 2004153 | ✗ | |||||
| Gan 2004154 | ✗i | |||||
| Gartner 2008155 | ✗j | |||||
| Gilron 2005156 | ✗f | |||||
| Goodman 2007157 | ✗k | |||||
| Harney 2008 158 | ✗l | |||||
| Hegi 2004 159 | ✗ | |||||
| Hepaguslar 2004160 | ✗ | |||||
| Horattas 2004161 | ✗ | |||||
| Huang 2008162 | ✗ | |||||
| Hynes 2006163 | ✗ | |||||
| Immer 2003164 | ✗ | |||||
| Jacobson 2006165 | ✗ | |||||
| Jones 2009166 | ✗ | |||||
| Joong 2005167 | ✗ | |||||
| Joshi 2004168 | ✗ | |||||
| Kardash 2005169 | ✗ | |||||
| Katz 2004170 | ✗ | |||||
| Kayacan 200444 | ✗m | |||||
| Khajavi 2007171 | ✗ | |||||
| Khalil 2006172 | ✗ | |||||
| Kocaayan 2007173 | ✗ | |||||
| Kovac 2005174 | ✗ | |||||
| Kuhne 2005175 | ✗n | |||||
| Kulik 2004176 | ✗ | |||||
| Landwehr 2005177 | ✗ | |||||
| Lavand’homme 2007178 | ✗o | |||||
| Lee 2007179 | ✗ | |||||
| Legeby 2005180 | ✗p | |||||
| Leykin 2008181 | ✗ | |||||
| Leykin 2008182 | ✗ | |||||
| Lu 2006183 | ✗q | |||||
| Maxwell 2006184 | ✗r | |||||
| Mazaris 2007185 | ✗ | |||||
| Mebazaa 2008186 | ✗ | |||||
| Meunier 2007187 | ✗ | |||||
| Motamed 2006188 | ✗ | |||||
| Mui 2005189 | ✗ | |||||
| Myles 2007190 | ✗s | |||||
| Naesh 2005191 | ✗ | |||||
| Newcomb 2007192 | ✗ | |||||
| Newton 2004193 | ✗t | |||||
| Ng 2005194 | ✗r | |||||
| Nikanne 2005195 | ✗ | |||||
| Nussmeier 2006196 | ✗ | |||||
| Nussmeier 2005197 | ✗ | |||||
| Pan 2006198 | ✗r | |||||
| Parsa 2005199 | ✗ | |||||
| Patrocinio 2007200 | ✗ | |||||
| Pettersson 2005201 | ✗ | |||||
| Phittayawechwiwat 2007202 | ✗ | |||||
| Pollak 2006203 | ✗ | |||||
| Rahimi 2006 204 | ✗ | |||||
| Rao 2005205 | ✗ | |||||
| Rasmussen 2005206 | ✗ | |||||
| Reuben 2008207 | ✗u | |||||
| Reuben 2007208 | ✗ | |||||
| Reuben 2006209 | Duplicate of data from Reuben et al. 200541 | |||||
| Reuben 200640 | Falsified data210 | |||||
| Reuben 200541 | Falsified data210 | |||||
| Riest 2006211 | ✗f | |||||
| Romsing 2005212 | ✗v | |||||
| Romundstad 2006213 | ✗ | |||||
| Rosenberg 2007214 | ✗w | |||||
| Rouse 2006215 | ✗x | |||||
| Rugyte 2007216 | ✗y | |||||
| Schlachta 2007217 | ✗d | |||||
| Schuster 2005218 | ✗f | |||||
| Shaikh 2006219 | ✗z | |||||
| Silvanto 2007220 | ✗ | |||||
| Sim 2007221 | ✗g | |||||
| Singla 2005222 | ✗ | |||||
| Snabes 2007223 | ✗ | |||||
| Sun 2008224 | ✗ | |||||
| Tablov 200845 | Journal not held by the British Library | |||||
| Tablov 2006225 | ✗aa | |||||
| Tan 2005226 | ✗g | |||||
| Thienthong 2004227 | ✗ | |||||
| Tilleul 2007228 | ✗bb | |||||
| Tornero-Campello 2006229 | ✗cc | |||||
| Torres 2004230 | ✗ | |||||
| Toshiko-Hirahara 2003231 | ✗ | |||||
| Tuncer 2006 232 | ✗ | |||||
| Turaga 2008233 | ✗ | |||||
| Turan 2006234 | ✗f | |||||
| Tuzuner 2007235 | ✗ | |||||
| Vintar 2005236 | ✗dd | |||||
| Vlajkovic 2007237 | ✗ | |||||
| White 2007238 | ✗ | |||||
| Xu 2008239 | ✗ | |||||
| Yamazaki 2003240 | ✗ | |||||
| Zippel 2006 241 | ✗ | |||||
| Ziolkowski 2008242 | ✗ |
Appendix 4 Drug regimens
| Paracetamol (acetaminophen) | |||
|---|---|---|---|
| Multiple dose | |||
| Paracetamol |
1.3 g/8 h p.r. 0.5 g/4 h p.o. 1.0 g/6 h i.v. 1.0 g p.r. + 1.0 g/6 h p.o. 1.0 g/6 h p.r. |
||
| Propacetamol | 2.0 g/6 h i.v. | ||
| Non-steroidal anti-inflammatory drugs | |||
| Multiple dose | Continuous infusion | Single dose | |
| Dexketoprofen | 50 mg/12 h i.m. | ||
| Diclofenac |
75 mg/12 h i.m. 75 mg/12 h p.r. 100 mg/16 h p.r. 50 mg/8 h p.r. 100 mg/8 h p.r. 100 mg p.r.+ 50 mg/8 h p.o. |
25 mg + 2 mg/kg/h i.v. |
100 mg p.r. 75 mg i.v. |
| Ibuprofen |
500 mg/8 h p.r. 1600 mg/24 h p.o. 400 mg/6 h p.o. |
||
| Indometacin (indomethacin) | 75 mg p.o. | ||
| Ketoprofen |
100 mg/12 h i.v. 100 mg/12 h i.m. 50 mg/6 h i.v. |
100 mg i.m. | |
| Ketorolac |
15 mg/6 h i.v. 30 mg/6 h i.v. 10 mg/8 h intranasal 30 mg/8 h intranasal 60 mg + 30 mg/6 h i.v. 10 mg/4 h i.m. 30 mg + 15 mg/3 h i.v. 30 mg + 15 mg/6 h i.m. 6 mg + 1.5 mg/h i.m. 60 mg + 30 mg/6 h i.m. 12 mg + 3 mg/h i.m. |
12.5 mg/h + 2.5 mg/h i.v. 100 mg/h+ 4 mg/h i.v. 30 mg + 5 mg/h i.v. 30 mg i.m. + 2 mg/h i.v. |
30 mg i.v. 60 mg i.v. |
| Multiple dose | Continuous infusion | Single dose | |
| Lornoxicam |
16 mg + 8 mg/12 h i.v. 8 mg/8 h i.v. |
8 mg i.m. 8 mg i.v. |
|
| Meloxicam | 15 mg p.r. | ||
| Naproxen | 550 mg p.o. | ||
| Piroxicam | 40 mg i.m. | ||
| Tenoxicam | 40 mg/24 h i.v. |
20 mg i.v. 40 mg i.v. 40 mg i.m. |
|
| Selective cyclo-oxygenase 2 inhibitors | |||
| Multiple low dose | Multiple high dose | Single dose | |
| Celecoxib |
200 mg p.o. 400 mg p.o. |
||
| Etoricoxib |
120 mg p.o. 180 mg p.o. |
||
| Parecoxib | 20 mg/12 h i.v. |
40 mg/6 h i.v. 40 mg/12 h i.v. |
40 mg i.v. |
Appendix 5 Validity assessment
| Study details | Randomisation 0 None 1 Mentioned 2 Described and adequate |
Allocation concealment 0 None 1 Yes |
Double blinding 0 None 1 Mentioned 2 Described and adequate |
Flow of participants 0 None 1 Described but incomplete 2 Described and adequate |
|---|---|---|---|---|
| Alexander 200280 | 2 | 0 | 2 | 2 |
| Alhashemi 200664 | 2 | 1 | 2 | 2 |
| Argyriadou 200758 | 1 | 0 | 0 | 0 |
| Balestrieri 199781 | 2 | 1 | 1 | 1 |
| Blackburn 199582 | 2 | 0 | 1 | 0 |
| Burns 199183 | 1 | 0 | 1 | 2 |
| Cakan 2008111 | 2 | 1 | 2 | 0 |
| Cassinelli 200884 | 2 | 1 | 1 | 1 |
| Celik 200385 | 2 | 0 | 1 | 0 |
| Chau-in 200866 | 2 | 1 | 1 | 2 |
| Cheng 200467 | 2 | 1 | 1 | 1 |
| Cobby 199961 | 1 | 1 | 2 | 2 |
| Colquhoun 198986 | 1 | 0 | 1 | 1 |
| De Decker 200187 | 2 | 0 | 0 | 0 |
| Delbos 199516 | 1 | 0 | 1 | 0 |
| Durmus 200368 | 1 | 1 | 1 | 1 |
| El-Halafawy 200469 | 1 | 0 | 0 | 0 |
| Etches 199588 | 1 | 1 | 1 | 1 |
| Fayaz 2004110 | 1 | 0 | 1 | 2 |
| Fletcher 199762 | 2 | 0 | 2 | 2 |
| Fong 200870 | 1 | 0 | 1 | 0 |
| Gillies 198790 | 1 | 0 | 1 | 2 |
| Hanna 200391 | 1 | 0 | 2 | 2 |
| Hegazy 200360 | 1 | 0 | 0 | 0 |
| Hernandez-Palazon 2001112 | 2 | 0 | 1 | 2 |
| Hodsman 198792 | 1 | 0 | 1 | 2 |
| Hsu 200393 | 2 | 0 | 2 | 2 |
| Hubbard 200371 | 2 | 0 | 1 | 1 |
| Inan 200794 | 2 | 1 | 2 | 2 |
| Jirarattanaphochai 200872 | 2 | 1 | 2 | 2 |
| Karaman 200695 | 2 | 1 | 1 | 0 |
| Kvalsvik 2003113 | 2 | 1 | 2 | 1 |
| Lee 200879 | 2 | 1 | 2 | 2 |
| Mack 200189 | 2 | 0 | 2 | 2 |
| Malan 200373 | 2 | 1 | 1 | 1 |
| Martinez 200774 | 2 | 1 | 0 | 2 |
| Moodie 200896 | 1 | 0 | 2 | 2 |
| Munishankar 200865 | 2 | 1 | 2 | 2 |
| Munro 199897 | 1 | 0 | 1 | 2 |
| Ng 200298 | 1 | 0 | 2 | 2 |
| Ng 200375 | 2 | 1 | 2 | 1 |
| Owen 198699 | 1 | 0 | 1 | 1 |
| Peduto 1998114 | 2 | 0 | 2 | 1 |
| Perttunen 1992100 | 1 | 0 | 2 | 0 |
| Plummer 1996101 | 1 | 0 | 1 | 1 |
| Rao 2000102 | 2 | 0 | 2 | 2 |
| Ready 1994103 | 2 | 1 | 2 | 1 |
| Riest 200876 | 2 | 1 | 1 | 1 |
| Rowe 1992104 | 1 | 0 | 0 | 2 |
| Schug 1998115 | 2 | 0 | 2 | 2 |
| Sevarino 1992105 | 1 | 0 | 1 | 1 |
| Siddik 200163 | 2 | 1 | 2 | 2 |
| Siddiqui 200877 | 2 | 1 | 1 | 2 |
| Sinatra 2005116 | 1 | 0 | 1 | 2 |
| Tang 200278 | 2 | 0 | 2 | 1 |
| Thompson 2000106 | 1 | 0 | 1 | 0 |
| Trampitsch 200359 | 1 | 0 | 1 | 1 |
| Vandermeulen 1997107 | 2 | 1 | 2 | 1 |
| Varrassi 1994108 | 1 | 0 | 1 | 2 |
| Xuerong 2008109 | 2 | 1 | 2 | 2 |
Appendix 6 Network tables
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Alexander 200280 | • | • | ||
| Alhashemi 200664 | • | • | ||
| Balestrieri 199781 | • | • | ||
| Blackburn 199582 | • | • | ||
| Cakan 2008111 | • | • | ||
| Cassinelli 200884 | • | • | ||
| Celik 200385 | • | • | ||
| Chau-in 200866 | • | • | ||
| Cheng 200467 | • | • | ||
| Cobby 199961 | • | • | • | |
| Colquhoun 198986 | • | • | ||
| De Decker 200187 | • | • | ||
| Delbos 199516 | • | • | ||
| Durmus 200368 | • | • | ||
| El-Halafawy 200469 | • | • | ||
| Etches 199588 | • | • | ||
| Fayaz 2004110 | • | • | ||
| Fletcher 199762 | • | • | • | |
| Fong 200870 | • | • | ||
| Gillies 198790 | • | • | ||
| Hegazy 200360 | • | • | • | |
| Hernandez-Palazon 2001112 | • | • | ||
| Hodsman 198792 | • | • | ||
| Hsu 200393 | • | • | ||
| Hubbard 200371 | • | • | ||
| Inan 200794 | • | • | ||
| Jirarattanaphochai 200872 | • | • | ||
| Karaman 200695 | • | • | ||
| Kvalsvik 2003113 | • | • | ||
| Lee 2008 79 | • | • | ||
| Malan 200373 | • | • | ||
| Mack 200189 | • | • | ||
| Martinez 200774 | • | • | ||
| Moodie 200896 | • | • | ||
| Munishankar 200865 | • | • | ||
| Munro 199897 | • | • | ||
| Ng 200375 | • | • | ||
| Owen 198699 | • | • | ||
| Peduto 1998114 | • | • | ||
| Perttunen 1992100 | • | • | ||
| Plummer 1996101 | • | • | ||
| Rao 2000102 | • | • | ||
| Ready 1994103 | • | • | ||
| Riest 200876 | • | • | ||
| Rowe 1992104 | • | • | ||
| Schug 1998115 | • | • | ||
| Sevarino 1992105 | • | • | ||
| Siddik 200163 | • | • | • | |
| Siddiqui 200877 | • | • | ||
| Sinatra 2005116 | • | • | ||
| Tang 200278 | • | • | ||
| Thompson 2000106 | • | • | ||
| Trampitsch 200359 | • | • | ||
| Vandermeulen 1997107 | • | • | ||
| Varrassi 1994108 | • | • | ||
| Xuerong 2008109 | • | • |
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Nausea | ||||
| Alhashemi 200664 | • | • | ||
| Balestrieri 199781 | • | • | ||
| Blackburn 199582 | • | • | ||
| Cakan 2008111 | • | • | ||
| De Decker 200187 | • | • | ||
| El-Halafawy 200469 | • | • | ||
| Etches 199588 | • | • | ||
| Hsu 200393 | • | • | ||
| Hubbard 200371 | • | • | ||
| Inan 200794 | • | • | ||
| Karaman 200695 | • | • | ||
| Malan 200373 | • | • | ||
| Mack 200189 | • | • | ||
| Moodie 200896 | • | • | ||
| Munro 199897 | • | • | ||
| Owen 198699 | • | • | ||
| Perttunen 1992100 | • | • | ||
| Ready 1994103 | • | • | ||
| Sinatra 2005116 | • | • | ||
| Tang 200278 | • | • | ||
| Thompson 2000106 | • | • | ||
| Trampitsch 200359 | • | • | ||
| PONV | ||||
| Alexander 200280 | • | • | ||
| Burns 199183 | • | • | ||
| Celik 200385 | • | • | ||
| Chau-in 200866 | • | • | ||
| Durmus 200368 | • | • | ||
| Fletcher 199762 | • | • | • | |
| Fong 200870 | • | • | ||
| Hernandez-Palazon 2001112 | • | • | ||
| Jirarattanaphochai 200872 | • | • | ||
| Kvalsvik 2003113 | • | • | ||
| Lee 2008 79 | • | • | ||
| Martinez 200774 | • | • | ||
| Munishankar 200865 | • | • | ||
| Peduto 1998114 | • | • | ||
| Plummer 1996101 | • | • | ||
| Sevarino 1992105 | • | • | ||
| Siddik 200163 | • | • | • | |
| Siddiqui 200877 | • | • | ||
| Vandermeulen 1997107 | • | • | ||
| Varrassi 1994108 | • | • | ||
| Xuerong 2008109 | • | • | ||
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Alhashemi 200664 | • | • | ||
| Balestrieri 199781 | • | • | ||
| Blackburn 199582 | • | • | ||
| Cakan 2008111 | • | • | ||
| Cobby 199961 | • | • | • | |
| De Decker 200187 | • | • | ||
| El-Halafawy 200469 | • | • | ||
| Etches 199588 | • | • | ||
| Hsu 200393 | • | • | ||
| Hubbard 200371 | • | • | ||
| Karaman 200695 | • | • | ||
| Malan 200373 | • | • | ||
| Moodie 200896 | • | • | ||
| Munro 199897 | • | • | ||
| Ng 200375 | • | • | ||
| Owen 198699 | • | • | ||
| Perttunen 1992100 | • | • | ||
| Ready 1994103 | • | • | ||
| Sinatra 2005116 | • | • | ||
| Tang 200278 | • | • | ||
| Thompson 2000106 | • | • | ||
| Trampitsch 200359 | • | • |
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Balestrieri 199781 | • | • | ||
| Cakan 2008111 | • | • | ||
| Celik 200385 | • | • | ||
| Chau-in 200866 | • | • | ||
| El-Halafawy 200469 | • | • | ||
| Fletcher 199762 | • | • | • | |
| Fong 200870 | • | • | ||
| Gillies 198790 | • | • | ||
| Jirarattanaphochai 200872 | • | • | ||
| Martinez 200774 | • | • | ||
| Moodie 200896 | • | • | ||
| Munro 199897 | • | • | ||
| Perttunen 1992100 | • | • | ||
| Rao 2000102 | • | • | ||
| Ready 1994103 | • | • | ||
| Schug 1998115 | • | • | ||
| Siddik 200163 | • | • | • | |
| Vandermeulen 1997107 | • | • | ||
| Varrassi 1994108 | • | • |
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Balestrieri 199781 | • | • | ||
| Blackburn 199582 | • | • | ||
| Cakan 2008111 | • | • | ||
| Delbos 199516 | • | • | ||
| Fletcher 199762 | • | • | • | |
| Gillies 198790 | • | • | ||
| Hernandez-Palazon 2001112 | • | • | ||
| Hsu 200393 | • | • | ||
| Jirarattanaphochai 200872 | • | • | ||
| Kvalsvik 2003113 | • | • | ||
| Munro 199897 | • | • | ||
| Rao 2000102 | • | • | ||
| Siddik 200163 | • | • | • | |
| Varrassi 1994108 | • | • |
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Burns 199183 | • | • | ||
| Cakan 2008111 | • | • | ||
| Cassinelli 200884 | • | • | ||
| Durmus 200368 | • | • | ||
| Etches 199588 | • | • | ||
| Fletcher 199762 | • | • | • | |
| Fong 200870 | • | • | ||
| Hernandez-Palazon 2001112 | • | • | ||
| Hubbard 200371 | • | • | ||
| Martinez 200774 | • | • | ||
| Peduto 1998114 | • | • | ||
| Ready 1994103 | • | • | ||
| Schug 1998115 | • | • | ||
| Varrassi 1994108 | • | • |
| Study | Placebo | Paracetamol | NSAID | COX-2 inhibitor |
|---|---|---|---|---|
| Alexander 200280 | • | • | ||
| Alhashemi 200664 | • | • | ||
| Balestrieri 199781 | • | • | ||
| Celik 200385 | • | • | ||
| Durmus 200368 | • | • | ||
| El-Halafawy 200469 | • | • | ||
| Fong 200870 | • | • | ||
| Hernandez-Palazon 2001112 | • | • | ||
| Hsu 200393 | • | • | ||
| Inan 200794 | • | • | ||
| Jirarattanaphochai 200872 | • | • | ||
| Kvalsvik 2003113 | • | • | ||
| Lee 200879 | • | • | ||
| Malan 200373 | • | • | ||
| Moodie 200896 | • | • | ||
| Ready 1994103 | • | • | ||
| Sevarino 1992105 | • | • | ||
| Siddik 200163 | • | • | • | |
| Sinatra 2005116 | • | • | ||
| Tang 200278 | • | • | ||
| Vandermeulen 1997107 | • | • | ||
| Varrassi 1994108 | • | • |
Appendix 7 Additional tables for sensitivity analyses
| Unadjusted | Independent interaction model | Exchangeable interaction model | Common interaction model | |
|---|---|---|---|---|
| DIC | 732.005 | 661.103 | 660.626 | 660.735 |
| Arms | 116 | 116 | 116 | 116 |
| RD | 186 | 114.4 | 114 | 115.3 |
| Coefficient (95% CrI) | Coefficient (95% CrI) | Coefficient (95% CrI) | ||
| Common interaction | –0.32 (–0.38 to –0.26) | |||
| Paracetamol interaction | –0.21 (–0.35 to –0.07) | –0.24 (–0.36 to –0.10) | ||
| NSAIDs interaction | –0.35 (–0.42 to –0.29) | –0.35 (–0.41 to –0.28) | ||
| COX-2 interaction | –0.25 (–0.40 to –0.11) | –0.27 (–0.39 to –0.13) |
| Quality studies subset baseline adjusted | Independent interaction model | Exchangeable interaction model | Common interaction model | |
|---|---|---|---|---|
| DIC | 301.474 | 663.229 | 662.26 | 662.468 |
| Arms | 49 | 116 | 116 | 116 |
| RD | 52.14 | 114.4 | 114.8 | 115.2 |
| Coefficient (95% CrI) | Coefficient (95% CrI) | Coefficient (95% CrI) | ||
| Common interaction | 1.19 (–1.51 to 3.79) | |||
| Paracetamol interaction | –3.64 (–10.65 to 3.31) | 0.70 (–3.08 to 4.09) | ||
| NSAIDs interaction | 1.10 (–2.01 to 4.18) | 1.20 (–1.51 to 3.92) | ||
| COX-2 interaction | 4.73 (–1.88 to 11.41) | 1.47 (–1.88 to 5.01) |
| Treatment | Quality study subset: mean difference, mg (95% CrI) | Exchangeable interaction: mean difference, mg (95% CrI) |
|---|---|---|
| Placebo | ||
| Paracetamol vs placebo | –6.17 (–9.17 to –3.25) | –9.01 (–12.01 to –6.01) |
| NSAID vs placebo | –7.46 (–9.66 to –5.25) | –10.17 (–12.37 to –7.99) |
| COX-2 vs placebo | –11.32 (–19.39 to –2.39) | –12.03 (–15.73 to –8.46) |
| NSAID vs paracetamol | –1.29 (–4.70 to 2.10) | –1.17 (–4.31 to 1.98) |
| COX-2 vs paracetamol | –5.15 (–13.99 to 4.23) | –3.02 (–7.24 to 1.02) |
| COX-2 vs NSAID | –3.86 (–12.32 to 5.16) | –1.86 (–5.34 to 1.39) |
Appendix 8 Mixed treatment comparison analyses for additional morphine-related outcomes
| Comparison | Nausea: pairwise OR and 95% CrI | Vomiting: pairwise OR and 95% CrI | PONV: pairwise OR and 95% CrI |
|---|---|---|---|
| Paracetamol vs placebo | 1.29 (0.54 to 2.56) | 1.21 (0.45 to 2.76) | 0.83 (0.40 to 1.51) |
| NSAID vs placebo | 0.81 (0.59 to 1.10) | 0.82 (0.52 to 1.25) | 0.51 (0.28 to 0.79) |
| COX-2 vs placebo | 0.98 (0.54 to 1.65) | 1.08 (0.43 to 2.24) | 0.85 (0.47 to 1.44) |
| NSAID vs paracetamol | 0.73 (0.31 to 1.52) | 0.83 (0.28 to 1.87) | 0.67 (0.30 to 1.28) |
| COX-2 vs paracetamol | 0.89 (0.31 to 2.12) | 1.11 (0.25 to 3.02) | 1.15 (0.45 to 2.53) |
| COX-2 vs NSAID | 1.23 (0.62 to 2.24) | 1.38 (0.47 to 3.08) | 1.79 (0.81 to3.71) |
| Treatment | Nausea | Vomiting | PONV | |||
|---|---|---|---|---|---|---|
| No. of studies | p best (%) | No. of studies | p best (%) | No. of studies | p best (%) | |
| Placebo | 21 | 2 | 21 | 5 | 20 | 0 |
| Paracetamol | 3 | 13 | 4 | 20 | 6 | 9 |
| NSAID | 16 | 58 | 15 | 50 | 11 | 84 |
| COX-2 inhibitor | 4 | 27 | 5 | 25 | 7 | 7 |
| 44 arms;a residual deviance 47.83 | 40 arms; residual deviance 43.04 | 42 arms; residual deviance 44.02 | ||||
A complete network for the four classes of drugs was formed for respiratory depression, which consisted of 14 trials (see Appendix 6, Table 26), though only one study was for COX-2 inhibitors. The pairwise odds ratios and the 95% CrI are reported in Table 36. There was no statistically significant difference between intervention and control for any of the comparisons (i.e. the CrI for all the comparisons crossed the line of no difference, 1.0). The size of the OR varied for different comparisons. Paracetamol, NSAIDs and COX-2 inhibitors performed better than placebo with NSAIDs performing the best. Reduction in respiratory depression was greatest with NSAIDs, but the probability of it being the best was very low at 43% (Table 37).
| Comparison | Pairwise OR and 95% CrI |
|---|---|
| Paracetamol vs placebo | 0.50 (0.08 to 2.59) |
| NSAID vs placebo | 0.38 (0.08 to 1.12) |
| COX-2 vs placebo | 0.63 (0.04 to 8.25) |
| NSAID vs paracetamol | 0.75 (0.08 to 5.91) |
| COX-2 vs paracetamol | 1.25 (0.05 to 30.11) |
| COX-2 vs NSAID | 1.64 (0.09 to 35.52) |
| Treatment (no. of studies) | p best (%) |
|---|---|
| Placebo (14) | 0 |
| Paracetamol (6) | 28 |
| NSAID (9) | 43 |
| COX-2 (1) | 29 |
In total, 30 trial arms were included in the analysis, of which 14 had at least one outcome. The residual deviance (16.01) was similar to the number of arms that had at least one event, which indicates a good model fit.
A complete network for the four classes of drugs was formed for urinary retention, which consisted of 14 trials (see Appendix 6, Table 27). The pairwise odds ratios and the 95% CrI are reported in Table 38. There was no statistically significant difference between intervention and control for any of the comparisons. Reduction in urinary retention was greatest with COX-2 inhibitors, but the probability of being the most effective, 61%, was low indicating a great overlap of the CrIs (Table 39).
| Comparison | Pairwise OR and 95% CrI |
|---|---|
| Paracetamol vs placebo | 0.81 (0.16 to 4.11) |
| NSAID vs placebo | 0.97 (0.30 to 3.34) |
| COX-2 vs placebo | 0.50 (0.14 to 2.21) |
| NSAID vs paracetamol | 1.20 (0.19 to 7.58) |
| COX-2 vs paracetamol | 0.62 (0.08 to 5.54) |
| COX-2 vs NSAID | 0.52 (0.09 to 3.45) |
| Treatment (no. of studies) | p best (%) |
|---|---|
| Placebo (14) | 3 |
| Paracetamol (5) | 25 |
| NSAID (6) | 11 |
| COX-2 (4) | 61 |
In total 29 arms were included in the analysis, of which 20 had at least one event. The residual deviance (19.96) was similar to the number of arms that had at least one event, which indicates a good model fit.
A complete network for the four classes of drugs was formed for pruritus, which consisted of 22 trials (see Appendix 6, Table 28). The pairwise odds ratios and the 95% CrI are reported in Table 40. Paracetamol and NSAIDs both performed better than placebo for this outcome, and this was statistically significant for both. COX-2 inhibitors also performed better than placebo, though this was not statistically significant. Reduction in pruritus was greatest with paracetamol. The probability that it was the most effective, 73%, was less than 95% because of the overlapping CrIs (Table 41).
| Comparison | Pairwise OR and 95% CrI |
|---|---|
| Paracetamol vs placebo | 0.45 (0.22 to 0.82) |
| NSAID vs placebo | 0.64 (0.40 to 0.94) |
| COX-2 vs placebo | 0.64 (0.34 to 1.09) |
| NSAID vs paracetamol | 1.56 (0.71 to 2.92) |
| COX-2 vs paracetamol | 1.58 (0.60 to 3.42) |
| COX-2 vs NSAID | 1.05 (0.48 to 2.04) |
| Treatment (no. of studies) | p best (%) |
|---|---|
| Placebo (21) | 0 |
| Paracetamol (5) | 73 |
| NSAID (12) | 9 |
| COX-2 (7) | 17 |
In total, 45 trial arms were included in the analysis, of which 42 had at least one outcome event. The residual deviance was similar to the number of arms that had at least one event, which indicates a good model fit.
COX-2 inhibitors were missing from the network for bowel dysfunction. A network was formed for placebo, paracetamol and NSAID, which consisted of four trials (see Appendix 6, Table 30). The pairwise odds ratios and the 95% CrI are reported in Table 42. Paracetamol performed slightly better than placebo, and NSAIDs performed more poorly than placebo for this outcome, though neither comparison was statistically significant (see Table 42). Paracetamol had the greatest treatment effect estimate, but the probability that it was the most effect was low, 58%, because of considerable overlap in the CrIs (Table 43).
| Comparison | Pairwise OR and 95% CrI |
|---|---|
| Paracetamol vs placebo | 0.75 (0.05 to 11.01) |
| NSAID vs placebo | 1.89 (0.35 to 33.83) |
| NSAID vs paracetamol | 2.48 (0.14 to 158.20) |
| Treatment (no. of studies) | p best (%) |
|---|---|
| Placebo (4) | 30 |
| Paracetamol (1) | 58 |
| NSAID (3) | 13 |
| COX-2 (0) |
In total eight arms were included in the analysis, of which six had at least one event. The residual deviance (8.163) was similar to the number of arms that had at least one event, which indicates a good model fit. However, the analysis was based on a small number of studies (n = 4), only one of which was paracetamol and none were available for COX-2 inhibitors.
A complete network for the four classes of drugs was formed for dizziness, which consisted of 22 trials (see Table 29). The pairwise odds ratios and the 95% CrI are reported in Table 44. There was no statistically significant difference between intervention and control for any of the comparisons though there was a trend towards COX-2 inhibitors performing better than placebo and NSAIDs in reducing morphine-related dizziness, but more poorly than paracetamol. Reduction in dizziness was greatest with COX-2 inhibitors, but the probability of them being the most effective class was low, at 56%, because of considerable overlap in the CrIs (Table 45).
| Comparison | Pairwise OR and 95% CrI |
|---|---|
| Paracetamol vs placebo | 1.17 (0.08 to 4.98) |
| NSAID vs placebo | 1.01 (0.51 to 1.77) |
| COX-2 vs placebo | 0.57 (0.19 to 1.33) |
| NSAID vs paracetamol | 2.77 (0.17 to 12.71) |
| COX-2 vs paracetamol | 1.61 (0.08 to 7.54) |
| COX-2 vs NSAID | 0.62 (0.17 to 1.68) |
| Treatment (no. of studies) | p best (%) |
|---|---|
| Placebo (12) | 1 |
| Paracetamol (1) | 38 |
| NSAID (8) | 5 |
| COX-2 (3) | 56 |
In total 24 arms were included in the analysis, of which 21 had at least one event. The residual deviance (22.41) was similar to the number of arms that had at least one event, which indicates a good model fit. However, the network was made up of predominantly NSAID and placebo treatment arms; there was only one paracetamol treatment arm and two of COX-2 inhibitors.
Appendix 9 Data extraction
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alexander 200280 |
Preoperatively Diclofenac 75 mg i.v. |
Preoperatively Ketorolac 60 mg i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 36 | 36.3a | 16.9b | 31 | 47.2a | 34.9b | 32 | 51.6a | 22.2b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 36 | 9 | 31 | 8 | 32 | 19 | ||||||
| Pruritus | 36 | 3 | 31 | 4 | 32 | 11 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Alhashemi 200664 |
Preoperatively Paracetamol 1 g (100 ml) infusion over 15 min and 1 placebo tablet 30 min before surgery, each repeated every 6 h for 48 h i.v. |
Preoperatively Ibuprofen 400-mg tablet and normal saline 100 ml infused over 15 min 30 min before surgery, each repeated every 6 h for 48 h Oral |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 22 | 65a | 30b | 23 | 58a | 25b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 22 | 12 | 23 | 8 | ||||
| PONV | ||||||||
| Pruritus | 22 | 10 | 23 | 19 | ||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | 22 | 4 | 23 | 1 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Argyriadou 200758 |
Postoperatively Parecoxib 30 min and 12 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | NA | 10.6a | 3.4b | NA | 13.9a | 4.72b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Balestrieri 199781 |
Postoperatively Ketorolac Postoperatively: 60 mg on awakening, 30 mg 6, 12 and 18 h i.v. |
Intraoperatively Ketorolac 60 mg 30 min before end surgery, 30 mg 6, 12 and 18 h post-awakening i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 68 | 46.6a | 27.7b | 65 | 41.3a | 19.9b | 66 | 58.1a | 24.9b | |||
| Bowel dysfunction | 83 | 0 | 83 | 2 | 82 | 0 | ||||||
| Dizziness | 83 | 8 | 83 | 6 | 82 | 3 | ||||||
| Nausea | 83 | 56 | 83 | 54 | 82 | 64 | ||||||
| PONV | ||||||||||||
| Pruritus | 83 | 10 | 83 | 12 | 82 | 10 | ||||||
| Respiratory depression | 83 | 2 | 83 | 3 | 82 | 3 | ||||||
| Sedation | 83 | 3 | 83 | 7 | 82 | 15 | ||||||
| Urinary retention | ||||||||||||
| Vomiting | 83 | 16 | 83 | 17 | 82 | 22 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Blackburn 199582 |
Postoperatively Ketorolac 100 mg/h for first 15 min then 4 mg/h for 23 h 45 min i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 30 | 43a | 17b | 29 | 55a | 22b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 30 | 19 | 29 | 18 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | 30 | 10 | 29 | 15 | ||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | 30 | 11 | 29 | 11 | ||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Burns 199183 |
Postoperatively Ketorolac Continuous infusion of 12.5 mg/h for 30 min and 2.5 mg/h for remainder of study and intermittent injections of saline every 4 h i.m. |
Postoperatively Ketorolac 10 mg every 4 h and continuous infusion of saline i.m. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or Median | SD/IQR/range | Number analysed | Number of events | Mean or Median | SD/IQR/range | Number analysed | Number of events | Mean or Median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 19 | 48a | 25–137b | 23 | 74a | 22–130b | 21 | 95a | 22–198b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 19 | 3 | 23 | 5 | 21 | 4 | ||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | 19 | 3 | 23 | 1 | 21 | 2 | ||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Cakan 2008111 |
Intraoperatively Paracetamol 1 g (10 mg/ml) infused over 15 min during wound closure and at 6-hourly intervals for 24 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 20 | 11.25a | 8.42b | 20 | 12.45a | 7.02b | ||
| Bowel dysfunction | ||||||||
| Dizziness | 20 | 3 | 20 | 4 | ||||
| Nausea | 20 | 12 | 20 | 17 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | 20 | 0 | 20 | 0 | ||||
| Sedation | 20 | 4 | 20 | 0 | ||||
| Urinary retention | 20 | 0 | 20 | 0 | ||||
| Vomiting | 20 | 7 | 20 | 14 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Cassinelli 200884 |
Postoperatively Ketorolac (1) Patient age > 65: 15 mg at 0, 6, 12 h; (2) patient age ≤ 65: 30 mg at 0, 6, 12 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 13 | 8a | 7.5b | 12 | 22.1a | 18b | ||
| Bowel dysfunction | 13 | 1 | 12 | 0 | ||||
| Dizziness | 13 | 0 | 12 | 0 | ||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | 13 | 0 | 12 | 0 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Celik 200385 |
Preoperatively Naproxen 550 mg once Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 20 | 63a | 6b | 20 | 93a | 6b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 20 | 0 | 20 | 4 | ||||
| Pruritus | 20 | 0 | 20 | 3 | ||||
| Respiratory depression | ||||||||
| Sedation | 20 | 0 | 20 | 0 | ||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chau-in 200866 |
Preoperatively Etoricoxib 120 mg once Oral |
Preoperatively Etoricoxib 180 mg once Oral |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 17 | 26.4a | 11.2b | 17 | 27.2a | 9.9b | 15 | 36.6a | 8.9b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | 17 | 5 | 17 | 4 | 15 | 7 | ||||||
| Nausea | ||||||||||||
| PONV | 17 | 3 | 17 | 2 | 15 | 4 | ||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | 17 | 7 | 17 | 7 | 15 | 10 | ||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Cheng 200467 |
Preoperatively Celecoxib 200 mg once Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 30 | 12.6a | 6.5b | 29 | 17.4a | 8.8b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cobby 199961 |
Postoperatively Paracetamol 1.3 g at 0, 8 and 16 h Rectal |
Postoperatively Diclofenac 50 mg at 0, 8 and 16 h Rectal |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 24 | 35a | 20.4b | 20 | 32.7a | 27.4b | 21 | 54.9a | 28.3b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 24 | 5 | 20 | 2 | 21 | 3 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Colquhoun 198986 |
Postoperatively Diclofenac 100-mg single dose Rectal |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 15 | 44.6a | 20.7b | 15 | 44.8a | 24b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | Intervention D | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| De Decker 200187 | Placebo |
Preoperatively Piroxicam 40 mg i.m. |
Preoperatively Tenoxicam 40 mg i.v. |
Preoperatively Tenoxicam 40 mg i.m. |
||||||||||||
| No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||||||
| 24-h morphine consumption (mg) | 15 | 36.5a | 20.3b | 15 | 24.6a | 15b | 15 | 21.7a | 11.3b | 15 | 24.3a | 20.7b | ||||
| Bowel dysfunction | ||||||||||||||||
| Dizziness | ||||||||||||||||
| Nausea | 15 | 5 | 15 | 1 | 15 | 4 | 15 | 2 | ||||||||
| PONV | ||||||||||||||||
| Pruritus | ||||||||||||||||
| Respiratory depression | ||||||||||||||||
| Sedation | ||||||||||||||||
| Urinary retention | ||||||||||||||||
| Vomiting | 15 | 0 | 15 | 1 | 15 | 4 | 15 | 1 | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Delbos 199516 |
Postoperatively Propacetamol 2 g every 6 h (dextrose 5%, 125 ml in 15 min) i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 30 | 34.5a | 12.7b | 30 | 43.1a | 15.9b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | 30 | 1 | 30 | 1 | ||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Durmus 200368 |
Preoperatively Celecoxib 200 mg once Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 20 | 25.6a | 5.92b | 20 | 34.9a | 10.35b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 20 | 3 | 20 | 4 | ||||
| Pruritus | 20 | 1 | 20 | 3 | ||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | 20 | 1 | 20 | 0 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| El-Halafawy 200469 |
Postoperatively Parecoxib 40 mg at 0, 12, 24, 36, 48, 60, 72 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 30 | 25.5a | 8.3b | 30 | 35.5a | 12.6b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 30 | 3 | 30 | 4 | ||||
| PONV | ||||||||
| Pruritus | 30 | 0 | 30 | 1 | ||||
| Respiratory depression | ||||||||
| Sedation | 30 | 0 | 30 | 1 | ||||
| Urinary retention | ||||||||
| Vomiting | 30 | 2 | 30 | 3 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Etches 199588 |
Postoperatively Ketorolac 30-mg bolus over 15–30 s then 5 mg/h for 24 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 79 | 39.6a | 26.7b | 78 | 64.2a | 38.6b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 79 | 48 | 78 | 45 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | 79 | 16 | 78 | 22 | ||||
| Vomiting | 79 | 22 | 78 | 22 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Fayaz 2004110 |
Postoperatively Diclofenac 100-mg suppository 2 h and 18 h after surgery Rectal |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 17 | 27a | 12b | 20 | 37a | 15b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 17 | 18 | 20 | 37 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fletcher 199762 | Placebo |
Intraoperatively Propacetamol 2 g at skin closure and repeated every 6 h for 48 h i.v. |
Intraoperatively Ketoprofen 50 mg at skin closure and repeated every 6 h for 48 h i.v. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 15 | 32.9a | 25.2b | 15 | 28a | 20.3b | 15 | 25.7a | 17b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 15 | 3 | 15 | 4 | 15 | 4 | ||||||
| Pruritus | ||||||||||||
| Respiratory depression | 15 | 1 | 15 | 0 | 15 | 0 | ||||||
| Sedation | 15 | 2 | 15 | 4 | 15 | 0 | ||||||
| Urinary retention | 15 | 3 | 15 | 4 | 15 | 3 | ||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fong 200870 |
Preoperatively Celecoxib 400 mg 30 min before anaesthesia and placebo tablet after wound closure Oral |
Postoperatively Celecoxib Placebo tablet 30 min before anaesthesia and 400 mg after wound closure Oral |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 20 | 13a | 6.2b | 20 | 12a | 5.4b | 20 | 27a | 7.2b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 20 | 5 | 20 | 5 | 20 | 7 | ||||||
| Pruritus | 20 | 10 | 20 | 11 | 20 | 13 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | 20 | 3 | 20 | 4 | 20 | 6 | ||||||
| Urinary retention | 20 | 4 | 20 | 5 | 20 | 7 | ||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gillies 198790 | Placebo |
Postoperatively Ketorolac 8 times maintenance dose for first 30 min, then 1.5 mg/h for rest of 24-h period i.m. |
Postoperatively Ketorolac 8 times maintenance dose for first 30 min, then 3 mg/h for rest of 24-h period i.m. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 18 | 78a | 38.18b | 20 | 53a | 31.3b | 19 | 55a | 30.51b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | 18 | 2 | 20 | 0 | 19 | 1 | ||||||
| Sedation | 18 | 2 | 20 | 0 | 19 | 1 | ||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hanna 200391 |
Postoperatively Dexketoprofen 50 mg at 0 and 12 h i.m. |
Postoperatively Ketoprofen 100 mg at 0 and 12 h i.m. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 64.83a | |||||||||||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hegazy 200360 |
Unclear Parecoxib 40 mg every 6 h i.v. |
Unclear Ketorolac 30 mg every 6 h i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 15 | 35.2a | 8.3b | 15 | 36.6a | 9b | 15 | 55.1a | 12b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Hernandez-Palazon 2001112 |
Intraoperatively Propacetamol 2 g every 6 h for 72 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 21 | 26a | 12.2b | 21 | 43.3a | 15.3b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 21 | 9 | 21 | 11 | ||||
| Pruritus | 21 | 3 | 21 | 5 | ||||
| Respiratory depression | 21 | 0 | 21 | 0 | ||||
| Sedation | ||||||||
| Urinary retention | 21 | 2 | 21 | 5 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Hodsman 198792 |
Postoperatively Diclofenac 75 mg/12 h i.m. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 31 | 38a | 22.27b | 31 | 59a | 27.84b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Hsu 200393 |
Intraoperatively Tenoxicam 20 mg in 4 ml solution i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 45 | 20.9a | 14.9b | 48 | 30.8a | 19.4b | ||
| Bowel dysfunction | ||||||||
| Dizziness | 45 | 13 | 48 | 14 | ||||
| Nausea | 45 | 17 | 48 | 18 | ||||
| PONV | ||||||||
| Pruritus | 45 | 15 | 48 | 23 | ||||
| Respiratory depression | 45 | 0 | 48 | 0 | ||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | 45 | 5 | 48 | 11 | ||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hubbard 200371 | Placebo |
Postoperatively Parecoxib 20 mg at completion of surgery and every 12 h for 36 h i.v. |
Postoperatively Parecoxib 40 mg at completion of surgery and every 12 h for 36 h i.v. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 63 | 43.5a | 18.7b | 61 | 36.7a | 16.9b | 65 | 31.4a | 18.3b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | 63 | 22 | 65 | 18 | 67 | 31 | ||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | 63 | 5 | 65 | 1 | 67 | 2 | ||||||
| Vomiting | 63 | 12 | 65 | 14 | 67 | 19 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Inan 200794 |
Preoperatively Lornoxicam 16 mg 15 min before surgery and 8 mg 12 and 24 h after surgery. Syringe covered with black paper i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 20 | 5.4a | 4.3b | 20 | 8.55a | 5.18b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 20 | 3 | 20 | 9 | ||||
| PONV | ||||||||
| Pruritus | 20 | 1 | 20 | 3 | ||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Jirarattanaphochai 200872 |
Preoperatively Parecoxib 40 mg (2 ml) 30 min before surgery and then 40 mg every 12 h for 48 h after surgery i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 60 | 28a | 14.1b | 60 | 45.2a | 21b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 60 | 17 | 60 | 20 | ||||
| Pruritus | 60 | 17 | 60 | 20 | ||||
| Respiratory depression | 60 | 2 | 60 | 3 | ||||
| Sedation | 60 | 45 | 60 | 44 | ||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Karaman 200695 |
Preoperatively Lornoxicam 8 mg once i.m. |
Preoperatively Ketoprofen 100 mg once i.m. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 20 | 22.9a | 3.4b | 20 | 23.1a | 3.5b | 20 | 29.7a | 3.8b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | 20 | 6 | 20 | 5 | 20 | 9 | ||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 20 | 2 | 20 | 1 | 20 | 3 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Kvalsvik 2003113 | Placebo |
Postoperatively Paracetamol 10 × 1-g suppositories over 60 h and 5 in first 24 h Rectal |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 30 | 21.1a | 11b | 30 | 16.8a | 8.4b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 40 | 12 | 38 | 11 | ||||
| Pruritus | 40 | 13 | 38 | 8 | ||||
| Respiratory depression | 40 | 7 | 38 | 4 | ||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee 200879 |
Preoperatively Parecoxib 40 mg once i.v. |
Postoperatively Parecoxib 40 mg once i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 18 | 82.4a | 60.3b | 20 | 65.6a | 59b | 18 | 141.5a | 74.9b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | 20 | 3 | 20 | 4 | 20 | 6 | ||||||
| Nausea | ||||||||||||
| PONV | 20 | 10 | 20 | 11 | 20 | 5 | ||||||
| Pruritus | 20 | 1 | 20 | 1 | 20 | 1 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Mack 200189 |
Unclear Ketorolac 1 cc (30 mg) over 4 min i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 10 | 17.4a | 12.7b | 10 | 14.9a | 15.1b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 10 | 1 | 10 | 3 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Malan 200373 | Placebo |
Postoperatively Parecoxib 20 mg at 0, 12 and 24 h i.v. |
Postoperatively Parecoxib 40 mg at 0, 12 and 24 h i.v. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 65 | 57.5a | 31.83b | 61 | 45a | 29.91b | 55 | 35.2a | 40.71b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | 70 | 4 | 67 | 2 | 64 | 3 | ||||||
| Nausea | 70 | 32 | 67 | 26 | 64 | 25 | ||||||
| PONV | ||||||||||||
| Pruritus | 70 | 8 | 67 | 3 | 64 | 6 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 70 | 11 | 67 | 13 | 64 | 3 | ||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Martinez 200774 | Placebo |
Intraoperatively Parecoxib 40 mg at induction, and then at 12 h after induction i.v. |
Postoperatively Parecoxib 40 mg at wound closure, and then at 12 h after induction i.v. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 21 | 47a | 27b | 22 | 26a | 12b | 19 | 25a | 13b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 21 | 5 | 22 | 6 | 19 | 6 | ||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | 21 | 7 | 22 | 5 | 19 | 4 | ||||||
| Urinary retention | 21 | 5 | 22 | 3 | 19 | 2 | ||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moodie 200896 |
Postoperatively Ketorolac 10 mg at 0 h, and then 8, 16, 24, 32, 40 h Other (intranasal) |
Postoperatively Ketorolac 30 mg at 0 h, and then 8, 16, 24, 32, 40 h Other (intranasal) |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 41 | 54.3a | 40.98b | 41 | 37.8a | 32.02b | 41 | 56.5a | 30.73b | |||
| Bowel dysfunction | 43 | 8 | 42 | 11 | 42 | 10 | ||||||
| Dizziness | 43 | 7 | 42 | 6 | 42 | 5 | ||||||
| Nausea | 43 | 25 | 42 | 19 | 42 | 20 | ||||||
| PONV | ||||||||||||
| Pruritus | 43 | 8 | 42 | 4 | 42 | 10 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | 43 | 9 | 42 | 1 | 42 | 5 | ||||||
| Urinary retention | ||||||||||||
| Vomiting | 43 | 12 | 42 | 12 | 42 | 11 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Munishankar 200865 |
Postoperatively Paracetamol 1 g at 0 h (rectal), and then 1 g at 6, 12, 18, 24 h (oral) Oral |
Postoperatively Diclofenac 100 mg at 0 h (rectal), and then 50 mg at 8, 16, 24 h (oral) Oral |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 24 | 54.5a | 28.5b | 25 | 44.1a | 24.4b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 26 | 11 | 26 | 10 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Munro 199897 |
Postoperatively Tenoxicam 40 mg i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 18 | 17.4a | 15.5b | 19 | 30.9a | 22.6b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 18 | 5 | 19 | 7 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | 18 | 0 | 19 | 0 | ||||
| Sedation | 18 | 0 | 19 | 0 | ||||
| Urinary retention | ||||||||
| Vomiting | 18 | 12 | 19 | 15 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Ng 200298 |
Intraoperatively Diclofenac 75 mg at 0, 12, 24, 36 h Rectal |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 18 | 31a | 14–65b | 16 | 59a | 45–85b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Ng 200375 | Placebo |
Intraoperatively Parecoxib 40 mg in 2 ml solution i.v. |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 17 | 72a | 27.22b | 19 | 54a | 23.86b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | 23 | 0 | 23 | 0 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Owen 198699 |
Preoperatively Ibuprofen 500 mg 60–90 min preop. and then every 8 h for 24 h Rectal |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 29 | 39.1a | 17.1b | 31 | 48.2a | 25.1b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 29 | 9 | 31 | 5 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | 29 | 23 | 31 | 18 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Peduto 1998114 |
Postoperatively Propacetamol 2 g after extubation, four times at 6-h intervals i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 42 | 12.1a | 9.9b | 47 | 20.1a | 12.8b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 46 | 3 | 51 | 3 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | 46 | 1 | 51 | 0 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Perttunen 1992100 |
Postoperatively Diclofenac 400 mg in 0.9% NaCl 400 ml. Bolus of 25 ml for first 15 min continued at a constant rate of 2 ml/kg/24 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 15 | 32.4a | 25.17b | 15 | 80.4a | 43.37b | ||
| Bowel dysfunction | ||||||||
| Dizziness | 15 | 6 | 15 | 4 | ||||
| Nausea | 15 | 6 | 15 | 2 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | 15 | 9 | 15 | 6 | ||||
| Urinary retention | ||||||||
| Vomiting | 15 | 2 | 15 | 1 | ||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Plummer 1996101 |
Preoperatively Ibuprofen Sustained release 2 × 800 mg 2–4 h preop. and then again 24 h after first dose Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 55 | 32a | 18b | 49 | 38a | 20b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 57 | 0 | 57 | 3 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Rao 2000102 |
Intraoperatively Ketoprofen 100 mg over 10 min at 30 min before end of surgery and 100 mg at 12 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 20 | 33a | 16.03b | 19 | 51a | 23.86b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | 20 | 0 | 19 | 0 | ||||
| Sedation | 20 | 0 | 19 | 1 | ||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ready 1994103 |
Postoperatively Ketorolac 30 mg at 0 h and then 5 mg/h for 24 h i.v. |
Postoperatively Ketorolac 30 mg at 0 h and then 15 mg every 3 h for 24 h i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 46 | 33a | 28b | 50 | 31a | 18b | 45 | 44a | 26b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | 66 | 5 | 70 | 3 | 71 | 9 | ||||||
| Nausea | 66 | 29 | 70 | 36 | 71 | 42 | ||||||
| PONV | ||||||||||||
| Pruritus | 66 | 6 | 70 | 13 | 71 | 9 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | 66 | 23 | 70 | 31 | 71 | 29 | ||||||
| Urinary retention | 66 | 6 | 70 | 3 | 71 | 0 | ||||||
| Vomiting | 66 | 8 | 70 | 6 | 71 | 19 | ||||||
| Study | Intervention A | Intervention B | Intervention C | Intervention D | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Riest 200876 |
Preoperatively Parecoxib 40 mg 45 min before surgery and every 12 h after surgery for 72 h i.v. |
Postoperatively Parecoxib Placebo 45 min before operation, 40 mg every 12 h after surgery for 72 h i.v. |
Preoperatively Parecoxib 40 mg 45 min before surgery, placebo every 12 h after surgery for 72 h i.v. |
Placebo | ||||||||||||
| No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | No. analysed | No. of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||||||
| 24-h morphine consumption (mg) | 80 | 22.8a | 19.2b | 80 | 30.1a | 23.6b | 80 | 24.9a | 18.6b | 80 | 31.3a | 21.8b | ||||
| Bowel dysfunction | ||||||||||||||||
| Dizziness | ||||||||||||||||
| Nausea | ||||||||||||||||
| PONV | ||||||||||||||||
| Pruritus | ||||||||||||||||
| Respiratory depression | ||||||||||||||||
| Sedation | ||||||||||||||||
| Urinary retention | ||||||||||||||||
| Vomiting | ||||||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Rowe 1992104 |
Preoperatively Indometacin 75 mg once Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 13 | 36.3a | 23.82b | 14 | 51.6a | 28.1b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Schug 1998115 |
Postoperatively Paracetamol Two 500-mg tablets every 4 h Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 25 | 50.3a | 40.1b | 26 | 59.5a | 42.3b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | 28 | 0 | 33 | 4 | ||||
| Urinary retention | 28 | 0 | 33 | 1 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sevarino 1992105 | Placebo |
Postoperatively Ketorolac 30 mg at 0 h and then 15 mg every 6 h for 24 h i.m. |
Postoperatively Ketorolac 60 mg at 0 h and then 30 mg every 6 h for 24 h i.m. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 12 | 58.75a | 58.89b | 12 | 30a | 38.97b | 11 | 30a | 53.89b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 12 | 8 | 11 | 7 | 11 | 4 | ||||||
| Pruritus | 12 | 2 | 11 | 0 | 11 | 1 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Siddik 200163 | Placebo |
Postoperatively Diclofenac 100 mg every 8 h for 24 h (0, 8, 16, 24 h) Rectal |
Postoperatively Propacetamol 2 g every 6 h for 24 h (0, 6, 12, 18, 24 h) Rectal |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 20 | 66.7a | 20b | 20 | 36a | 18b | 20 | 61.1a | 23b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | ||||||||||||
| PONV | 20 | 4 | 20 | 2 | 20 | 3 | ||||||
| Pruritus | 20 | 8 | 20 | 5 | 20 | 4 | ||||||
| Respiratory depression | 20 | 0 | 20 | 0 | 20 | 0 | ||||||
| Sedation | 20 | 3 | 20 | 1 | 20 | 1 | ||||||
| Urinary retention | ||||||||||||
| Vomiting | ||||||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Siddiqui 200877 |
Preoperatively Etoricoxib 120 mg 90 min before surgery Oral |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption | 100 | 35.1a | 7b | 100 | 44.2a | 8.2b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 100 | 9 | 100 | 20 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sinatra 2005116 |
Postoperatively Paracetamol 1 g in 100 ml solution infused over 15 min every 6 h i.v. |
Postoperatively Propacetamol 2 g in 100 ml solution infused over 15 min every 6 h i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption | 49 | 38.3a | 35.1b | 50 | 40.8a | 30.2b | 52 | 57.4a | 52.3b | |||
| Bowel dysfunction | 49 | 10 | 50 | 8 | 52 | 12 | ||||||
| Dizziness | ||||||||||||
| Nausea | 49 | 13 | 50 | 9 | 52 | 7 | ||||||
| PONV | ||||||||||||
| Pruritus | 49 | 5 | 50 | 4 | 52 | 5 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 49 | 6 | 50 | 3 | 52 | 3 | ||||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tang 200278 | Placebo |
Postoperatively Parecoxib 20 mg in PACU and then at 12 h and 24 h i.v. |
Postoperatively Parecoxib 40 mg in PACU and then at 12 h and 24 h i.v. |
|||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 18 | 51a | 27b | 19 | 34a | 20b | 18 | 33a | 21b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | 18 | 10 | 19 | 12 | 18 | 11 | ||||||
| PONV | ||||||||||||
| Pruritus | 18 | 5 | 19 | 4 | 18 | 3 | ||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 18 | 1 | 19 | 2 | 18 | 0 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Thompson 2000106 | Placebo |
Intraoperatively Meloxicam 15 mg after induction of anaesthesia Rectal |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 18 | 38.2a | 20.8b | 18 | 33.2a | 16.9b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | 18 | 11 | 18 | 8 | ||||
| PONV | ||||||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | 18 | 20 | 18 | 13 | ||||
| Urinary retention | ||||||||
| Vomiting | 18 | 0 | 18 | 0 | ||||
| Study | Intervention A | Intervention B | Intervention C | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trampitsch 200359 |
Preoperatively Lornoxicam 8 mg every 8 h (1st dose 20 min before incision). NaCl infusion before close of incision i.v. |
Intraoperatively Lornoxicam Placebo (NaCl) 20 min before operation, 8 mg before close of incision and then every 8 h i.v. |
Placebo | |||||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||||||
| 24-h morphine consumption (mg) | 22 | 25.15a | 2.36b | 22 | 31.5a | 3.19b | 22 | 31.6a | 3.91b | |||
| Bowel dysfunction | ||||||||||||
| Dizziness | ||||||||||||
| Nausea | 22 | 8 | 22 | 10 | 22 | 6 | ||||||
| PONV | ||||||||||||
| Pruritus | ||||||||||||
| Respiratory depression | ||||||||||||
| Sedation | ||||||||||||
| Urinary retention | ||||||||||||
| Vomiting | 22 | 5 | 22 | 5 | 22 | 4 | ||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Vandermeulen 1997107 | Placebo |
Postoperatively Tenoxicam 40 mg adminstered at end of surgery and at 24 h i.v. |
||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 256 | 39.2a | 27.6b | 258 | 34.6a | 25.9b | ||
| Bowel dysfunction | ||||||||
| Dizziness | 256 | 6 | 258 | 4 | ||||
| Nausea | ||||||||
| PONV | 256 | 76 | 258 | 67 | ||||
| Pruritus | 256 | 5 | 258 | 3 | ||||
| Respiratory depression | ||||||||
| Sedation | 256 | 6 | 258 | 3 | ||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Varrassi 1994108 |
Preoperatively Ketorolac 30 mg intramuscularly with predmedication followed by 2 mg/h continuous infusion for 24 h i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption (mg) | 48 | 15a | 13.2b | 47 | 21.7a | 19.88b | ||
| Bowel dysfunction | ||||||||
| Dizziness | 48 | 0 | 47 | 2 | ||||
| Nausea | ||||||||
| PONV | 48 | 3 | 47 | 6 | ||||
| Pruritus | 48 | 0 | 47 | 1 | ||||
| Respiratory depression | 48 | 0 | 47 | 2 | ||||
| Sedation | 48 | 1 | 47 | 5 | ||||
| Urinary retention | 48 | 0 | 47 | 2 | ||||
| Vomiting | ||||||||
| Study | Intervention A | Intervention B | ||||||
|---|---|---|---|---|---|---|---|---|
| Xuerong 2008109 |
Intraoperatively Lornoxicam 8 mg in 2-ml (4 mg/ml) bolus 5 min before skin incision, continuous infusion of normal saline from skin incision until 20 min before end of surgery, and from 5 min after skin incision 3 boluses of saline at 15-min intervals i.v. |
Placebo | ||||||
| Number analysed | Number of events | Mean or median | SD/IQR/range | Number analysed | Number of events | Mean or median | SD/IQR/range | |
| OUTCOME | ||||||||
| 24-h morphine consumption | 15 | 16.9a | 6.5b | 15 | 19.5a | 8.3b | ||
| Bowel dysfunction | ||||||||
| Dizziness | ||||||||
| Nausea | ||||||||
| PONV | 15 | 7 | 15 | 12 | ||||
| Pruritus | ||||||||
| Respiratory depression | ||||||||
| Sedation | ||||||||
| Urinary retention | ||||||||
| Vomiting | ||||||||
Glossary
- 95% credibility interval
- From the Bayesian approach. There is a 95% probability that the true treatment effect (odds ratio) lies within the interval.
- Mixed treatment comparison
- This is an extension of a traditional meta-analysis. Whereas a traditional meta-analysis includes only trials making direct comparisons between an intervention and comparator, a mixed treatment comparison analysis also includes indirect evidence. This approach overcomes the limitations of the traditional approach in cases where there are no or limited trials making the relevant head-to-head comparison.
- Morphine
- Opioid used for the relief of severe postoperative pain.
- Opioid
- Drug having morphine-like action.
- Patient-controlled analgesia
- Small doses of analgesic drugs are administered via an intravenous pump controlled by the patient. When the patient presses a hand-held button a pre-set dose (bolus) of the analgesic is delivered. The administered dose is limited by setting both the dose and the time interval between doses.
- Pruritus
- Itching.
- Respiratory depression
- The rate and/or depth of respiration is insufficient to maintain adequate gas exchange in the lungs.
List of abbreviations
- AE
- adverse event
- CI
- confidence interval
- COX
- cyclo-oxygenase
- CrI
- credibility interval (also known as credible interval)
- DIC
- deviance information criterion
- GI
- gastrointestinal
- i.m.
- intramuscular
- IQR
- interquartile range
- i.v.
- intravenous
- MD
- mean difference
- MTC
- mixed treatment comparison
- NSAID
- non-steroidal anti-inflammatory drug
- OR
- odds ratio
- PCA
- patient-controlled analgesia
- PONV
- postoperative nausea and vomiting
- RCT
- randomised controlled trial
- RD
- residual deviance
- RR
- risk ratio or relative risk
- SD
- standard deviation
- SE
- standard error
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington