Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 08/05/01. The protocol was agreed in May 2008. The assessment report began editorial review in September 2008 and was accepted for publication in January 2010. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Cummins provided a report commissioned by Greater Glasgow Health Board (GGHB) on the cost of the current targeted hepatitis B immunisation programme. GGHB received financial support from GlaxoSmithKline for this study. The study was undertaken between November 2005 and July 2006. Dr Philip has received funds for reimbursements for travel expenses and lecture fees from GlaxoSmithKline, Merck Sharpe & Dohme, Eli Lilly, Novo Nordisk and Sanofi-aventis.
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Type 2 diabetes
Diabetes mellitus is characterised by raised blood glucose levels. In non-diabetic people, the level of glucose in the blood is controlled by a balance of hormonal actions, principally insulin and glucagon, both of which are produced by specific types of cell in the pancreas, beta cells producing insulin and alpha cells producing glucagon. Insulin lowers blood glucose and glucagon raises it. In type 1 diabetes, the beta cells are lost because of an autoimmune process, little or no insulin is produced, and insulin treatment is required for survival. The cause, or causes, of type 1 diabetes are not known.
Type 2 diabetes is usually seen in people who are overweight or obese, particularly if inactive. They are usually insulin resistant, and therefore require higher levels of insulin in order to keep blood glucose within the normal range. The pancreatic beta cell is initially able to compensate for insulin resistance, by increasing production, thereby maintaining normal blood glucose levels. The higher than usual level of insulin is known as hyperinsulinaemia.
However, in most patients who may develop type 2 diabetes, the pancreatic beta-cell function progressively declines, leading to hyperglycaemia and clinical diabetes. 1 In the United Kingdom Prospective Diabetes Study (UKPDS),2 beta-cell function was found to be impaired at diagnosis, especially in patients who were not overweight. Individuals with type 2 diabetes may have few or none of the classic clinical symptoms (such as thirst, passing abnormally large amounts of urine) of hyperglycaemia, and may be diagnosed incidentally as seen in the UKPDS,3 where 33% were found by incidental means (for example, urine testing for an insurance medical) and 53% via symptoms.
The difficulty in maintaining metabolic control over time may be related to several behavioural factors (for example, difficulties with healthy eating, exercise, medication regimens) but primarily reflects the underlying progressive decline in beta-cell function,4 so that control deteriorated over a 9-year follow-up period. 5
Type 2 diabetes has traditionally been treated in a stepwise manner, starting with lifestyle modifications and encouragement of physical activity and, when necessary, pharmacotherapy with oral agents [National Institute for Health and Clinical Excellence (NICE) guideline, published May 2008]. 6 Several classes of oral agents are available. Until recently, these included:
-
Insulin secretagogues, which stimulate the pancreas to release more insulin, by binding to a sulfonylurea receptor The main group is the sulfonylureas. There are seven of these in the British National Formulary (BNF), but older ones such as chlorpropamide are now little used. The ones most used in the UK are gliclazide, glipizide, glimepiride and glibenclamide (glyburide). A newer group of secretagogues is the meglitinide analogues, including nateglinide and repaglinide, but these are used far less than the sulfonylureas. They bind to the same receptor but are less potent than the sulfonylureas. 7 They are shorter acting, and have been suggested for controlling postprandial hyperglycaemia, perhaps in combination with a long-acting insulin.
-
Insulin sensitizers, which make tissues such as the liver and the muscles more sensitive to insulin (i.e. they reduce the insulin resistance) The commonest one in the UK is metformin, from the group of drugs called the biguanides. A newer group called the thiazolidinediones (TZDs), or glitazones, includes rosiglitazone and pioglitazone. The balance of actions on different tissues is different between the glitazones and metformin, and they are sometimes used in combination. Metformin increases insulin sensitivity in the liver by inhibiting hepatic gluconeogenesis and thereby reducing hepatic glucose production. 8 Metformin may also increase peripheral insulin sensitivity by enhancing glucose uptake in the muscle. There have been concerns about the risk of lactic acidosis with metformin but the risk is probably much less than had been thought. 9 The TZDs decrease insulin resistance in muscle and adipose tissue by activating the peroxisome proliferator-activated receptor-g (PPAR-g), which increases production of proteins involved in glucose uptake. They also decrease hepatic glucose production by improving hepatic insulin sensitivity.
-
Drugs that delay the absorption of carbohydrates from the gastrointestinal tract, such as acarbose Acarbose, and its related drug, miglitol, are alpha-glucosidase inhibitors. These drugs reduce especially postprandial elevations in plasma glucose (PG) levels. They do not significantly lower fasting plasma glucose (FPG) levels but cause a modest reduction in glycated haemoglobin (HbA1c). 10
The Prescribing Support Unit (PSU), in collaboration with the York and Humber Public Health Observatory (YHPHO), produces data on use of diabetes drugs. The most used drug is metformin, with about 10 million prescriptions a year in England. 11 Its use has been rising steadily. Second come the sulfonylureas, with around 5 million prescriptions a year, with little change over the last 5 years. Third come the glitazones, with about 2.4 million prescriptions per year. They are newer drugs, the use of which has increased over recent years. In terms of cost per annum, the glitazones are by far the most costly, being recently introduced drugs with no generic forms.
Insulin treatment comes in different forms:
-
Short acting, with a rapid onset and short duration. There are two forms, the older soluble or ‘regular’ short-acting insulins, and the newer short-acting analogues (lispro, aspart, glulisine). These are used for mealtime injections (often called ‘bolus’, although the term is not universally popular).
-
Intermediate acting, such as isophane [or Neutral Protamine Hagedorn (NPH)].
-
Long acting, again with two types, the older forms such as ultralente, and the newer long-acting analogues, glargine and detemir. These are usually given once a day in type 2 diabetes.
Mixtures of short-acting and intermediate acting insulins are widely used. These can be mixed in the syringe by the patient prior to injection, but there are several premixed preparations available, which are more convenient. They are called biphasic.
The normal pancreas produces a little insulin throughout the 24 hours, with additional peaks of insulin after food. In recent years, in an attempt to mimic this physiological pattern, more use has been made of the combination of a long-acting insulin to provide the basal insulin with injections of short-acting insulin at mealtimes – usually referred to as a basal bolus regimen.
In the UKPDS,5 insulin treatment started with a once-daily injection of long-acting ultralente. If that was insufficient, short-acting insulin was added – in effect a form of basal bolus.
The PSU/YHPHO prescribing data11 show that the use of glargine increased very rapidly. In terms of number of prescriptions per annum, it overtook isophane insulin in the spring of 2004, and now runs at around 1 million per year, with isophane around 400,000 in the first quarter of 2007. Detemir was launched later than glargine but has now probably overtaken isophane in numbers.
Table 1 shows the range of costs of diabetes drugs.
| Drug | Cost (£) per annum (insulins assume 40 IU/day)a |
|---|---|
| Metformin 500 mg × 4/day | 39 |
| Gliclazide 80 mg twice daily | 25 |
| Glibenclamide 5 mg twice daily | 36 |
| Glimepiride 2 mg once daily | 69 |
| Soluble insulin 10-ml vial | 109 |
| Isophane insulin 10-ml vial (including mixtures) | 109 |
| Metformin modified release 4 × 500-mg tablets/day | 166 |
| Biphasic insulins, cartridges | 195–286 |
| Insulin aspart 10-ml vial | 286 |
| Glargine or detemir 10-ml vial or glargine pre-filled device | 379 |
| Metformin/pioglitazone 2 × 850 mg + 15 mg/day | 410 |
| Sitagliptin 100 mg daily | 432 |
| Pioglitazone 45 mg once daily | 480 |
| Rosiglitazone 4 mg twice daily | 643 |
| Metformin/rosiglitazone combination | 682 |
| Exenatide 10 µg twice daily | 828 |
NICE guideline
The purpose of this assessment report is to support an update of the NICE guideline on type 2 diabetes, released in May 2008. 6 That guideline covers the full range of management of type 2 diabetes, whereas the update covers only the place of the new drugs. Some key recommendations and other aspects of the guidelines are listed below:
-
Targets for control. An HbA1c level of 6.5% or under was set for people with type 2 diabetes in general, but it was recommended that targets should be tailored to the needs of the individual, and might be higher than 6.5% (Recommendation 16).
-
If HbA1c levels were above target, but pre-meal levels were well controlled (< 7.0 mmol/l) then consideration should be given to reduction of postprandial glucose levels (Recommendation 18).
-
It was recommended that treatment start with lifestyle measures, but it was accepted that these would fail in many or most cases.
-
First-line therapy (algorithm, p. 99) should be metformin for people who are overweight or obese. A sulfonylurea to be considered in those who were not overweight.
-
If monotherapy failed a sulfonylurea should be added to metformin, or vice versa. In some people, a meglitinide analogue might be considered instead of a sulfonylurea. Glitazones should be considered only if hypoglycaemia was expected to be a problem (though if it was a problem during a trial of the sulfonylurea, there could be a switch to a glitazone).
-
If on dual therapy and HbA1c remained above 7.5%, third-line treatment with a glitazone or insulin should be added. However, at this point treatment with exenatide could be considered.
-
Once insulin was started, metformin and the sulfonylurea would be continued but with reconsideration of the sulfonylurea if hypoglycaemia occurred.
-
If control deteriorated the insulin therapy would be intensified (and although not stated, it would be logical to withdraw the sulfonylurea).
-
As regards the type of insulin, Recommendation 52 stated that the first choice should be human NPH insulin, taken at bedtime or twice daily according to need. Glargine should be considered in certain situations for: those who required a carer to give the injections; those whose lifestyle is restricted by recurrent symptomatic hypoglycaemia; and those who would otherwise need twice-daily basal injections. These situations are the same as those for glargine in Technology Appraisal (TA) 53. 12 [Detemir was excluded from the Guideline Development Group (GDG) considerations because it was expected to be the subject of a technology appraisal.]
-
As regards choice of glitazone, the GDG noted concerns over cardiovascular risks with rosiglitazone, but concluded that: ‘On balance, despite reservations over rosiglitazone, it was felt not to be possible to unequivocally recommend a preference for pioglitazone in all circumstances, but rather to allow the choice of agent to rest with the person with diabetes and their advisor, taking account of the then current regulatory circumstances (which may yet change)’. 6
This is a little puzzling, as the risks appeared higher with rosiglitazone, and the economic analysis (p. 127) concluded that ‘pioglitazone was estimated to yield a greater quality-adjusted life-year (QALY) gain at lower cost than rosiglitazone’ and ‘rosiglitazone was consistently dominated by human insulin (both less effective and more expensive)’.
-
On exenatide, the guideline concluded that, on the evidence then available (p. 135, section 10.4) ‘human insulin is a consistently more cost-effective option in any patient in whom it is an acceptable form of treatment.’ And Recommendation R44 said that ‘Exenatide is not recommended for routine use in type diabetes.’ But R45 identified a situation in which exenatide might be considered, if all of the following applied: a body mass index (BMI) of over 35; ‘specific problems of a psychological, biochemical or physical nature arising from high body weight’; inadequate blood glucose control (HbA1c > 7.5%) with conventional oral agents after a trial of metformin and sulfonylurea; and other high-cost medication (such as a TZD or insulin injection therapy) would otherwise be started.
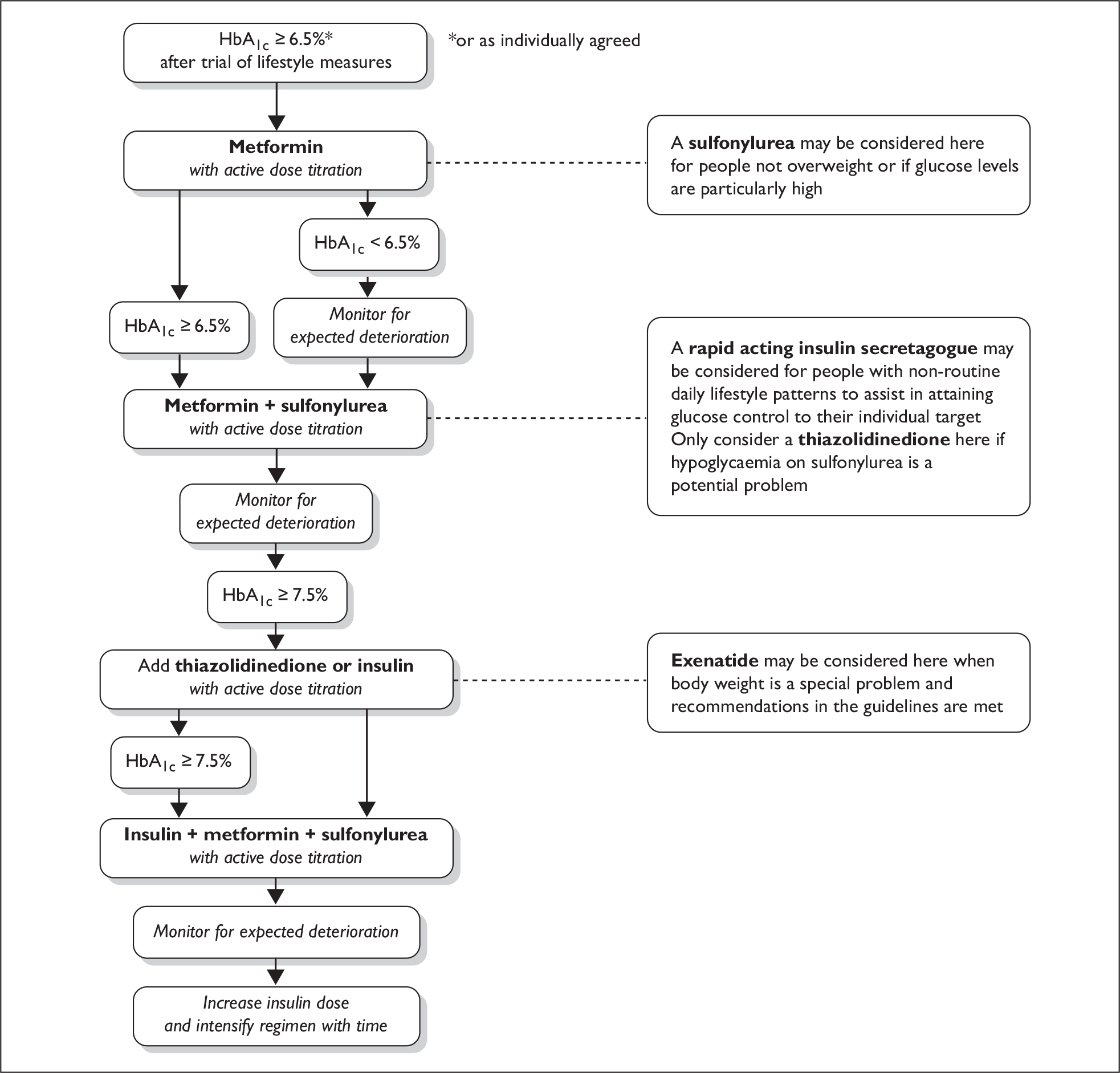
Figure 1 shows the flow chart from the NICE guideline. Please note that this may not be the final version.
FIGURE 1.
The National Institute for Health and Clinical Excellence guideline algorithm.
Use of insulin treatment
In the UK there has been reluctance to switch to insulin in patients who are failing on oral agents. Two studies have used general practice databases to examine glycaemic control and treatment.
Calvert et al. (2007)13 used data from the DIN-LINK database, from the years 1995 to 2005. DIN-LINK has anonymised data from 154 general practices. Calvert et al. obtained data on patients with type 2 diabetes, including the treatment they were on and their HbA1c levels. They were particularly interested in how long patients remained poorly controlled on oral agents before starting insulin. [The study was on behalf of Pfizer™ (Sandwich, Kent), to inform the NICE appraisal of inhaled insulin; Pfizer thought that one advantage of inhaled insulin would be to make it easier to persuade people to start insulin.]
Calvert et al. identified all patients with type 2 who were prescribed two or more types of oral agent, and looked at their HbA1c levels before and after the addition of another drug. Adding a second drug reduced HbA1c level by about 1% (95% CI 0.95 to 1.05). Adding a third reduced it by a further 0.48% (0.37 to 0.59). Adding a fourth drug gave no further benefit. [We should note that this was before the arrival of the glucagon-like peptide-1 (GLP-1) analogues and the dipeptidyl peptidase-4 (DPP-4) inhibitors.]
When insulin was prescribed for the first time to those with poor control on oral agents, the initial drop in HbA1c was 1.3%, but 73% still had levels above the NICE target of 7.5% or less. The median time from addition of the last oral agent to the start of insulin therapy, for patients on two or more oral agents, was seven years. In those with poor glycaemic control following addition of the last oral drug, only 27% were prescribed insulin during the study. The implication is that many patients were left poorly controlled rather than being switched to insulin.
Rubino et al. (2007)14 used another British general practice database, The Health Improvement Network (THIN) database, to identify patients with type 2 diabetes who were poorly controlled (at two HbA1c levels: > 8% and > 9%) on oral agents, and who had not been treated with insulin. They then followed them to see how long it was before insulin was started.
Using the cut-off for poor control of HbA1c levels of 8% or over, they found 2501 eligible patients, mostly aged 50–79 years, and with duration of diabetes usually at least 5 years. Most had been on oral glucose-lowering agents (OGLAs) for over 5 years. About 25% of these patients started insulin by 2 years, and 50% by 5 years. So transition was slow, and many were not transferred to insulin at all.
When OGLA failure was defined as HbA1c level of 9% or over, they found 1691 patients who qualified. By 4.2 years, 50% had started insulin.
The presence of complications such as retinopathy, had little effect on the time to insulin treatment. Those with retinopathy started insulin at a median of 4.6 years, those without at 5 years.
This study was also funded by Pfizer.
Why is there reluctance to use insulin?
In a previous technology assessment report (TAR) for NICE, on inhaled insulins, we pondered upon why there should be reluctance. 15 There seemed to be reluctance amongst both patients and physicians. What follows is based on that TAR. Time did not permit a systematic review.
The DAWN (Diabetes Attitude Wishes and Need) study found that 55% of patients who have never had insulin treatment are anxious about it being required. The authors, Peyrot et al. (2005)16 review previous studies of patient attitudes to insulin therapy. They note that these involve beliefs that ‘taking insulin … :
-
leads to poor outcomes including hypoglycaemia, weight gain and complications
-
means that the patient’s diabetes is worse and that the patient has failed
-
means life will be more restricted and people will treat the patient differently
-
will not make diabetes easier to manage’.
It is important to note that insulin treatment is not just about injections, but a whole package of care, including dietary adjustments, home blood glucose testing and self-adjustment of insulin doses. It is likely that, for most people, insulin injections are less troublesome than blood testing.
Changing to insulin does not mean that control will improve. Unpublished data from the Lothian audit show that the average HbA1c in patients with type 2 diabetes on insulin is about 8.5% [J McKnight, presented at the Royal College of Physicians of Edinburgh (RCPE) conference, September 2005, personal communication]. The average for those with type 2 diabetes on OGLAs is 7.5%.
Similarly, a study from seven European countries17 found that only 9.5% of patients with type 2 diabetes, who were on insulin, had HbA1c < 6.5%; another 44% had HbA1c levels of 6.5–7.5%; and 47% had HbA1c levels of over 7.6%.
One issue in insulin therapy is the provision of structured education programmes, such as DAFNE (Dose Adjustment For Normal Eating). Good education may reduce problems with insulin treatment.
What is the optimum treatment for people with type 2 diabetes inadequately controlled on oral agents?
It seems clear from the literature that there are differences of opinion on management of people with type 2 diabetes who are not adequately controlled on oral agents. A working group drawn from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) produced a consensus statement in 2006. 18 Some extracts from this statement give an impression of the problems:
The availability of the newer agents has provided an increased number of choices for practitioners and patients and heightened uncertainty regarding the most appropriate means of treating this widespread disease. Although numerous reviews on the management of type 2 diabetes have been published in recent years, practitioners are often left without a clear pathway of therapy to follow.
The most appropriate target levels for blood glucose, on a day-to-day basis, and HbA1c, as an index of chronic glycaemia, have not been systematically studied.
They noted the different target levels proposed by the various bodies, and reached a consensus that: ‘an HbA1c of over 7% should serve as a call to action to initiate or change therapy’.
They recommended that insulin should be initiated with either bedtime intermediate-acting insulin or once-daily long-acting insulin; metformin should be continued.
Goudswaard et al. (2004),19 in a Cochrane review, concluded that combinations of insulin and oral hypoglycaemic agents should be the starting point for people with type 2 diabetes who required insulin. Their review preceded the studies on long-acting analogues, such as glargine and detemir. The oral agents most commonly used in the trials they found were sulfonylureas; only 7% used metformin alone.
Douek et al. (2005)20 from the Metformin Trial Group carried out a randomised controlled trial (RCT) of adding metformin or placebo in people with type 2 diabetes who had been switched to insulin because of poor control. Continuation of metformin resulted in less weight gain, lowered insulin requirement and improved glycaemic control.
Aviles-Santa et al. (1999)21 also showed that adding metformin to an insulin regimen in people with type 2 diabetes reduced HbA1c by 0.9% compared with placebo. Insulin requirement was 29% lower, and the weight gain of 3.2 kg, seen in the placebo group, was much more than in the metformin group (0.5 kg).
Strowig and Raskin (2005)22 carried out a review of combination therapy with insulin and either metformin or a glitazone, or both. Details of methods are not given and it was probably not systematic. They also concluded that it was worthwhile continuing an insulin sensitiser in patients with type 2 diabetes who were switched to insulin. Because metformin and glitazones have different balances of sites of preferential action (acting on glucose production and glucose disposal), they also made the case that triple therapy should also be considered. Bailey (2005)23 also supported combination therapy with metformin and a glitazone for reducing insulin resistance in type 2 diabetes.
Gerstein et al. (2006)24 randomised poorly controlled (HbA1c level 7.5–11%) patients to continue oral agents or to switch to glargine, in the Canadian INSIGHT (International Nifedipine GITS Study: Intervention as a Goal in Hypertension Treatment) study. Those treated with glargine achieved lower HbA1c and non-high-density lipoprotein (HDL) cholesterol, and greater satisfaction, but more weight gain. However, only 17.5% of patients on glargine reached the target of two or more consecutive HbA1c levels of 6.5% or under. One weakness of the study was that at baseline about 17% of the patients had not been treated with any oral agent; another 40% were on oral monotherapy.
Hayward et al. (1997)25 noted that results from trials of insulin therapy in type 2 diabetes showed it to be efficacious, but thought that these results might not be replicated in routine care. In a very large study (8668 patients with type 2 diabetes) they found that ‘insulin therapy was rarely effective in achieving tight glycemic control’. Two years after starting insulin therapy, 60% still had HbA1c levels of 8% or greater; 25% had levels between 8.0% and 8.9%, 20% between 9.0% and 9.9%, and 15% had levels over 10%. These are similar to the population-based audit from Lothian (J McKnight, personal communication).
The observation that starting insulin in routine care usually fails to give good control in people with type 2 diabetes failing on oral agents is presumably one reason why the physicians in the DAWN study16 showed considerable resistance to starting insulin therapy in type 2 diabetes – only about half of the physicians thought that insulin would be useful.
Yki-Järvinen et al. (2006)26 came to similar conclusions in people with type 2 diabetes who were obese (defined in this study as BMI of over 28.1 kg/m2) – insulin did not improve control. In many of these patients, poor control is associated with overweight or obesity.
Aas et al. (2005)27 tried another approach, randomising patients with poorly controlled type 2 diabetes to insulin or to a lifestyle intervention (exercise and diet counselling). Lifestyle intervention was as effective in glycaemic control but also resulted in weight loss. In a follow-up study in 2006, the authors also noted that lowering HbA1c level by lifestyle measures had more beneficial effects on adipokine levels than when insulin therapy achieved the same lowering, which may result in a lower cardiovascular risk. 28 However, numbers in this study were small (38 in total), and the study needs to be replicated with larger numbers.
Beta-cell mass
As mentioned above, by the time of diagnosis of type 2 diabetes, beta-cell function is considerably impaired. An important issue is whether any treatments can preserve the remaining beta-cell function, or promote regeneration.
Conversely, it is important to know if any treatments might accelerate beta-cell decline. In the ADOPT (A Diabetes Outcome Progression Trial) trial, patients were randomised to monotherapy with glibenclamide, metformin or rosiglitazone. Outcomes included failure of monotherapy. By 5 years, 34% of the glibenclamide group had failed, compared with 21% on metformin and 15% on rosiglitazone. 29 Aston-Mourney et al. (2008)30 have argued, based on this trial and basic science studies, that it may be harmful to force the beta cell to produce more insulin, and that doing so may cause earlier beta-cell death. The implication might be that drugs that are insulin sensitisers, rather than insulin secretagogues, may help to preserve beta-cell function or mass, by reducing the pressure to produce more insulin. However, in the UKPDS4 the slopes of rises in blood glucose were similar for metformin and sulfonylureas, which does not support the sulfonylurea harm theory.
Meier (2008)31 has recently reviewed the evidence on beta-cell mass, and the hypothesis that ‘resting’ the beta cell would help, but concludes that: ‘as yet, there is no direct evidence for the induction of beta cell apoptosis (death) by sulfonylurea drugs or for the preservation of beta cell mass by either metformin, glitazones or exogenous insulin in patients with type 2 diabetes.’
Decision issues
This TAR is being produced to assist the NICE Short GDG, whose task is to update the 2008 NICE Guidelines for the management of type 2 diabetes. The update is required because of a number of drug developments, namely:
-
the GLP-1 analogues
-
the dipeptidyl peptidase-4 (DPP-4) inhibitors
-
the long-acting insulin analogues, which are not new, but where the current NICE guidance needs reviewed
-
safety concerns over the glitazones.
The evidence on clinical effectiveness will be dealt with separately for each drug group, in Chapters 2–6. The literature on economic studies of new drugs for diabetes will be reviewed in Chapter 7, and the cost-effectiveness modelling of the new drugs will be in Chapter 8.
Chapter 2 The GLP-1 analogue: exenatide
The GLP-1 analogues are a new class of oral glucose-lowering drugs that mimic the endogenous hormone, glucagon-like peptide. GLP-1 is an incretin, a gastrointestinal hormone that is released into the circulation in response to ingested nutrients from food. The mechanism by which food stimulates GLP-1 release from intestinal endocrine cells is not known; however, it may be under the control of neuroendocrine pathways. The effect was discovered after it was noted that the stimulation of release of insulin from the pancreas was greater after oral glucose than after an equivalent amount given intravenously. 32
Endogenous GLP-1 has a number of actions. 33 It stimulates insulin secretion34, but only in a glucose-dependent manner, so that insulin is not released if glucose is low. The incretin effect stops once the PG is down to 3 mmol/l. 32 It also suppresses glucagon secretion, delays gastric emptying35 and reduces appetite. It also increases insulin biosynthesis. 36,37 Therefore, it controls PG level in a number of ways. 38 The reduction of glucagon secretion in type 2 diabetes is also glucose dependent. 39,40
Natural GLP-1 has been shown to affect PG levels when given by subcutaneous injection. 41 However, it is rapidly broken down by the enzyme DPP-4, resulting in a half-life of 1–2 minutes. 32,33,40 So, the endogenous form could only be used via a continuous infusion, and therefore would be impractical for treatment.
The GLP-1 analogues, of which only exenatide is currently available, have the same actions as GLP-1 but are resistant to breakdown by DPP-4. This gives them a much longer half-life than endogenous GLP-1. Other drugs are coming, with liraglutide expected to be licensed in 2009.
Exenatide has the following actions:42,43
-
increasing glucose-dependent insulin release
-
suppressing glucagon secretion in situations where that is inappropriate, such as when glucose level is high
-
slowing of gastric emptying (which will slow glucose absorption after meals)
-
reducing appetite, and hence reduction of food intake
-
restoring of first-phase insulin secretion in people with type 2 diabetes.
Given these actions, it was hoped that the GLP-1 analogues would not be associated with the weight gain that is seen with some other diabetes drugs. Early reports suggested that weight loss might occur. 44,45
Exenatide
Exenatide was originally isolated from the venom of the Gila lizard (Amylin Pharmaceuticals, San Diego, CA, USA). The peptide from the lizard had similarities with GLP-1, but had greater affinity with the receptor and was resistant to DPP-4.
Exenatide is produced synthetically. It has a short half-life of about 4 hours, and has to be given (by injection) twice daily at present. The drug has been developed for diabetes treatment under the trade name Byetta (Amylin Pharmaceuticals45 and Eli Lilly,46 Indianapolis, IN, USA). A longer-acting form, exenatide long-acting release (LAR) has been developed and is currently undergoing trials. 45,47 It may have to be given only weekly.
The second GLP-1 analogue will be liraglutide, produced by Novo Nordisk (Crawley, UK). 48 It is based on human GLP-1 but has an amino acid substitution and an attached acyl chain, which fosters binding to serum albumin, thereby delaying renal excretion. It has a longer half-life, of about 11–13 hours, and so can be given once daily. (Note: Because the GLP-1 analogues are designed to act mainly at mealtimes, though they have some effect beyond those, they are not required during the night.) Again, being a digestible peptide, it has to be given by subcutaneous injection. Liraglutide has not yet received a licence for use in the UK, and will not be further discussed in this report.
Criteria for considering studies for this review
Types of evidence
For efficacy, RCTs are the gold standard. Open-label extension studies are useful to see if the effects persist, and for the development (or sometimes waning) of side effects. The dropout rate may also be a useful guide to tolerability.
For our purposes, we are interested mainly in trials that use standard UK practice as the comparator. Standard practice is set out in the current NICE guideline for type 2 diabetes (NICE 2008)6 and is shown in the flow chart in Chapter 1.
Types of interventions
Intervention consists of treatment for a minimum of 12 weeks with exenatide, exenatide long-acting or liraglutide. Twelve weeks is chosen because of the time it takes for glycaemic control to be reflected in HbA1c level, but should be regarded as the minimum acceptable rather than satisfactory. Longer-duration studies would be better.
The 2008 NICE guideline on management of type 2 diabetes (see flow chart) stated that for individuals with a BMI of over 25 kg/m2, the first choice in addition to diet was metformin, and, if that was insufficient, an insulin secretagogue should be added. In practice that would be a sulfonylurea; the other secretagogues, the meglitinide agonists, are little used in the UK.
So the most relevant comparisons are:
-
The addition of a GLP-1 analogue to standard combination therapy when that is insufficient to achieve good control, i.e. metformin + a sulfonylurea versus metformin + sulfonylurea + a GLP-1 analogue. A variant might use two insulin sensitisers: metformin + glitazone versus metformin + glitazone + GLP-1.
-
In those who cannot tolerate metformin, a glitazone might be used in combination therapy instead: sulfonylurea + a glitazone versus sulfonylurea + glitazone + GLP-1 analogue. One outcome of interest will be progression to insulin treatment.
-
Another option suggested in the NICE guideline was to add a glitazone to the metformin and sulfonylurea combination, i.e. triple therapy. If that fails, insulin treatment is the next step, usually with a long-acting basal insulin, with metformin, and perhaps the other drugs, continued. So another possible comparison would be to try a GLP-1 agonist instead of insulin: metformin + sulfonylurea + glitazone + GLP-1 agonist versus basal insulin + metformin + sulfonylurea + glitazone.
-
In those who have started insulin recently there could be a case for stopping insulin and trying a GLP-1 analogue, so a further comparison is: insulin (with or without oral agents) versus oral agents + a GLP-1 analogue. This is not a licensed use. The Food and Drug Administration (FDA) patient information sheet49 states that ‘Byetta is not a substitute for insulin in patients whose diabetes requires insulin treatment’.
-
This comparison looks at adding exenatide to metformin monotherapy, and was included at the request of the GDG, which felt that there were some overweight patients in whom the further weight gain likely with the usual second-line combinations of adding a sulfonylurea (or a glitazone) was so undesirable that a GLP-1 agonist should be considered instead, given the likelihood of weight loss.
Ideally, the comparison would be of metformin + exenatide versus metformin + a gliptin but at the time of writing, no such trials had been done, so Comparison 5 is: metformin + exenatide versus metformin alone.
Licensed indications
The licensed indications vary a little between Europe and the USA. The European Medicines Evaluation Agency (EMEA)-approved indications are: ‘Byetta is indicated for the treatment of type 2 diabetes mellitus in combination with metformin, and/or sulfonylureas in patients who have not achieved adequate glycaemia control on maximally tolerated doses of these oral therapies’.
The FDA approval includes the glitazones:49 ‘Byetta is indicated as adjunctive therapy to improve glycemic control in patients with type 2 diabetes mellitus who are taking metformin, a sulfonylurea, a TZD, a combination of metformin and a sulfonylurea, or a combination of metformin and a TZD, but have not achieved adequate glycemic control’.
Current evidence for effectiveness of GLP analogues in type 2 diabetes
Appendix 2 shows all of the trials. Most of the studies were parallel-group RCTs [Barnett et al. (2007)50 was a crossover trial]. The majority of studies appear to have been conducted in North America and/or Europe, with the exception of one that was conducted entirely in Japan [Seino et al. (2007)51]. Four studies [Barnett et al. (2007),50 Davis et al. (2007),52 Heine et al. (2006),53 Nauck et al. (2007)54] were reported as non-inferiority/equivalence trials.
Excluded studies
The studies in the Table 2, below, were excluded for the reasons given. Some of these trials provided useful information, for example showing that the GLP-1 agonists were effective in lowering PG compared with placebo, or were early dose-ranging studies, but were not relevant to our key comparisons.
| First author and year | Reason for exclusion |
|---|---|
| Exenatide trials | |
| Bunck (2007)55 | Participants were on metformin monotherapy; in addition, it is not clear from the abstract whether they remained on metformin |
| Buse (2004)56 | Participants had failed on sulfonylurea monotherapy |
| Trescoli-Serrano (2005)57 | Abstract only and few details; does not say whether oral agents continued |
| Kim (2007)47 (exenatide LAR) | No details yet and not licensed |
Included studies
Seven trials were relevant for our purposes, and are listed below, under the relevant comparisons. The quality of the trials seems reasonable, although some details were not reported, and insulin, when a comparator, may not have been optimally used. Table 3 gives the details.
| Study | Method of randomisation | Allocation concealment | Blinding | ITT data analysis | Percentage who completed trial | Power calculation | Similarity of groups at baseline | Sponsorship/author affiliation |
|---|---|---|---|---|---|---|---|---|
| Barnett (2007)50 (crossover trial) | Computer-generated central randomisation table | Yes | Open | Yes |
Exenatide/insulin glargine sequence: 80.9 Insulin glargine/exenatide sequence: 84.3 |
Yes (non-inferiority design) | Yes | Authors from Eli Lilly and Amylin Pharmaceuticals; funded by Eli Lilly |
| Davis (2007)52 | Not reported | Not reported | Open | No | Exenatide: 57.6; insulin: 93.8 | Yes | Yes | Authors from Eli Lilly and Amylin Pharmaceuticals |
| DeFronzo (2005)58 | Not reported | Not reported | Triple blind | Yes | Exenatide (10 µg): 82.3; placebo: 78.8 | Yes | Yes | Funded by Amylin Pharmaceuticals, Eli Lilly; authors from manufacturer |
| Heine (2005)53 | Central randomisation table | Yes | Open | Yes | Exenatide: 80.9; glargine: 90.6 | Yes (non-inferiority design) | Yes | Funded by Amylin Pharmaceuticals, Eli Lilly; authors from manufacturer |
| Kendall (2005)59 | Not reported | Not reported | Double blind | Yes | Exenatide (5 µg): 84.1; exenatide (10 µg): 82.6; placebo: 76.1 | Yes | Yes | Sponsorship from and author affiliation with Eli Lilly and Amylin Pharmaceuticals |
| Nauck (2007)54 | Computer-generated randomisation table | Yes | Open | Yes | Exenatide: 78.7; biphasic insulin aspart: 89.9 | Yes (non-inferiority design) | Yes | Some authors from Amylin Pharmaceuticals and Eli Lilly |
| Zinman (2007)60 | Central randomisation table | Yes | Double blind | Yes | Exenatide: 71.1; placebo: 85.7 | Yes | Yes | Sponsorship by Eli Lilly and Amylin Pharmaceuticals |
Comparison 1
Comparison 1 involved the addition of GLP-1 analogue to dual combination therapy.
Kendall (2005)
Kendall et al. 59 recruited 733 people with type 2 diabetes whose control was inadequate (HbA1c level 7.5–11%) on dual therapy with metformin and a sulfonylurea. Their average age was 55 years (range 22–77), and mean BMI was around 34 kg/m2. They were recruited from 91 centres in the USA, with an average of eight recruits per centre. Most were Caucasian, with about 11% being black people and 16% Hispanic. Mean duration of diabetes was about 9 years.
There were three arms: placebo controls, exenatide 5 µg b.i.d. (twice a day) and exenatide 10 µg b.i.d. (after 4 weeks on 5 µg).
Zinman (2007)
Zinman et al. 60 recruited 233 patients whose control was inadequate on a glitazone with or without metformin, but about 80% were on metformin. They came from 49 centres in Canada, the USA and Spain, with an average of just under five patients per centre. Mean age was 56 (range 21–75) years, and their mean BMI was 34 kg/m2.
These patients came from a larger group of 435 who were screened for entry. Discontinuation rates differed, with 71% of the exenatide group completing compared with 86% of the placebo group. The commonest reason for discontinuation was adverse events (19 out of 121 on exenatide versus 2 out of 112 on placebo). Exenatide was started at 5 µg twice daily for 4 weeks, and increased to 10 µg for the remaining 12 weeks.
Concerns about the study by Zinman et al. were raised by Malozowski (2007). 61 These included:
-
The representativeness of the included patients. Their control was inadequate, but many were not on maximal doses of other oral drugs. Also, 21% were not on any metformin, which should be first-line therapy.
-
The lack of reinforcement of lifestyle interventions, such as diet; no details were given of educational input. (So care before starting exenatide does not appear to have been optimised.)
-
There was a significant dropout rate, especially in the exenatide group which had 71% completing the trial.
-
Full details of adverse events were not published, nor details of whether there were any subgroups more susceptible to the side effects (although with their relatively small numbers, Zinman et al. would not have the power to do much in the way of subgroup analysis).
-
The study duration – 16 weeks – was too short for a chronic disease.
Comparison 2
-
Comparison 2 involved patients who were intolerant of metformin, where a sulfonylurea plus glitazone combination was the standard arm comparator, versus that plus a GLP-1 analogue. No studies were found.
Comparison 3
-
Comparison 3 consisted of insulin plus oral agents versus GLP-1 analogue plus oral agents.
Heine 2005
Heine et al. 53 recruited 551 patients in 82 centres in 13 countries, with an average of just under 7 patients per centre. Mean age was 59 (range 30–75) and mean duration of diabetes was 9.6 years. The recruits were less overweight than in some other studies, with a mean BMI of 31 kg/m2. On dual therapy with metformin and sulfonylurea (at maximum doses), HbA1c level was between 7% and 10%. Those with recent severe hypoglycaemia were excluded.
Patients were randomised to have glargine [starting at 10 units, titrated to achieve fasting blood glucose (FBG) < 5.6 mmol/l] or exenatide (10 µg b.i.d.) added to their oral agents. The dosage of the oral drugs was fixed unless hypoglycaemia was a problem, in which case the sulfonylurea dose was halved. Overall, 19% of the exenatide group and 10% of the glargine group withdrew from the study. The proportions withdrawing because of adverse events were 9.5% for exenatide and 0.7% for glargine.
Nauck 2007
Nauck et al. 54 compared twice-daily exenatide with twice-daily biphasic insulin (aspart 30 : 70) in 505 patients whose control was not good enough (mean HbA1c level 8.6%; inclusion range 7–11%) on dual therapy with optimal doses of metformin and sulfonylurea. Those with recent severe hypoglycaemia were excluded. The oral agents were continued in unchanged dosage, unless hypoglycaemia occurred, in which case the dose of sulfonylurea was halved in the exenatide group. (In the insulin group, the insulin was reduced.)
As in other studies, those randomised to exenatide started on 5 µg twice daily and increased to 10 µg (if tolerated – it was in 80%) after 4 weeks. The dosage of biphasic aspart was left to each investigator to adjust, according to glucose control and hypoglycaemia.
The study was carried out in 13 countries but the number of centres is not given. The trial was powered for equivalence, defined as a difference in HbA1c level of not more than 0.4%. Of the 505 randomised, 199 (79%) of 253 on exenatide and 223 (90%) of the 248 on insulin completed the study. The difference was mainly due to withdrawals because of side effects – 20 withdrawals in the exenatide group and none in the insulin group.
Home (2007)62 had concerns about the study by Nauck et al. , including:
-
The exenatide regimen was optimised but the biphasic insulin was not. The total daily insulin dose was lower than usually seen (it was 24 units/day at the end of 1 year).
-
Blood glucose control was relatively poor in the insulin group, with a reduction of 0.9% in HbA1c level, lower than seen in most recent treat-to-target studies of insulin in type 2 diabetes.
-
Puzzlement about the use of an aspart product, from a rival manufacturer to the sponsor of the study (Eli Lilly), when they could have used their own similar product. Exenatide is made by Eli Lilly, who also produce the Humalog biphasic insulin.
The authors63 mounted a reasonable defence against most of these points, but could not explain why insulin doses were not raised in pursuit of better control.
Barnett 2007
Strictly speaking, this study50 does not meet our inclusion criteria, because it recruited patients with inadequate control on either metformin or a sulfonylurea, but we include it in order to have more than one trial against glargine, and hence more data on relative effect size. The study was carried out in 26 places in six countries (not including the UK) and recruited 138 patients to a crossover trial of 10 µg exenatide twice daily or glargine titrated to achieve a satisfactory fasting glucose level. The baseline HbA1c level was 9%. Mean age was 55 years, and baseline BMI was 31. It was funded by the manufacturer – Eli Lilly.
Comparison 4
This involved patients already on insulin, with replacement by GLP-1. This comparison is included for completeness and interest, but note that it is not currently a licensed indication.
Davis 2007
Davis et al. 52 recruited 51 patients who were already on insulin (various forms, for about 3 years) in combination with oral agents (mostly metformin alone or with a sulfonylurea). Randomisation was 2 : 1 in favour of exenatide. Mean age was 53, mean BMI was 34 kg/m2, and mean duration was 10 years. The study was carried out in five centres in the USA (average of 10 patients per centre).
There were more withdrawals in the exenatide group (14 out of 33) than in those remaining on insulin (1 out of 16). The commonest reason was loss of glycaemic control on exenatide.
An editorial by Rosenstock and Fonseca (2007)64 made a number of criticisms, starting with the comment that ‘the scientific value is rather unclear, but the marketing appeal is obvious’. This may be a little harsh, as one aim of the study was to see if people with type 2 diabetes who had relatively recently started insulin could manage without it. More pertinent points were that insulin treatment was not optimised, and that the results were less successful than the paper implied: ‘this study raises issues about commercial bias in study design, interpretation and reporting by the pharmaceutical sponsors’.
Comparison 5
This concerned the addition of GLP-1 analogue to metformin monotherapy. DeFronzo et al. (2005)58 carried out a three-armed trial (the Exenatide–112 trial), in 336 patients, aged 19–78 years (mean age 53), who had had diabetes for an average of about 6 years, in 82 sites in the USA. Baseline mean BMI was 34 and mean HbA1c level was 8.2%. The three arms were metformin plus one of placebo, exenatide 10 µg b.i.d., and exenatide 5 µg b.i.d. Only the standard dose of 10 g b.i.d. is included here.
HbA1c results
These are shown in Tables 4A and 4B overleaf.
| Study | Study arm and number randomised | HbA1c (%) baseline | Change from baseline (%) | p-value from baseline | Difference between groups at end (exenatide–comparator 95% CI) | p-value between groups | Percentage of pts achieving HbA1c level of ≤ 7% |
|---|---|---|---|---|---|---|---|
| Barnett (2007)50 (crossover trial) | Exenatide/insulin glargine treatment sequence + MET or SU (n = 68) | 8.89 (SE 0.13) | –1.36 (SE 0.09) | p < 0.001 | NS | 37.5 (exenatide-treated pts) | |
| Insulin glargine/exenatide treatment sequence + MET or SU (n = 70) | 9.00 (SE 0.13) | –1.36 (SE 0.09) | p < 0.001 | 39.8 (glargine-treated pts) | |||
| Davis (2007)52 | Exenatide + oral medications (n = 33) | 8.0 (SD 1.2) | +0.3 (SE 1.5) | NS | 0.4% | NS | |
| Current insulin regimen + oral medications (n = 16) | 8.3 (SD 0.9) | –0.1 (SE 0.7) | NS | ||||
| DeFronzo (2005)58 | Exenatide (10 µg) + MET (n = 113) | 8.18 (SD 1.0) | –0.78 (SE 0.1) | p < 0.002 | 46 | ||
| Placebo + MET (n = 113) | 8.2 (SD 1.0) | +0.08 (SE 0.1) | 13 | ||||
| Heine (2005)53 | Exenatide + MET + SU (n = 282) | 8.18 | –1.11 | 0.017 (–0.123 to 0.157) | NS | 46 | |
| Insulin glargine + MET + SU (n = 267) | 8.23 | –1.11 | 48 | ||||
| Kendall (2005)59 | Exenatide + MET + SU 5 µg (n = 245) | 8.5 (SD 1.0) | –0.55 (SE 0.07) | p < 0.0001 | 24a | ||
| Exenatide + MET + SU 10 µg (n = 241) | 8.5 (SD 1.1) | –0.77 (SE 0.08) | 30a | ||||
| Placebo + MET + SU (n = 247) | 8.5 (SD 1.0) | +0.23 (SE 0.07) | 7a | ||||
| Nauck (2007)54 | Exenatide + MET + SU (n = 253) | 8.6 (SD 1.0) | –1.04 (SE 0.07) | p < 0.001 | –0.15 (–0.32 to 0.01) | NS (p = 0.067) | 32b |
| Biphasic insulin aspart + MET + SU (n = 248) | 8.6 (SD 1.1) | –0.89 (SE 0.06) | p < 0.001 | 24b | |||
| Zinman (2007)60 | Exenatide + MET + TZD (n = 121) | 7.89 (SE 0.9) | –0.89 | –0.98 (–1.21 to –0.74) | p < 0.001 | 62,c 30d | |
| Placebo + MET + TZD (n = 112) | 7.91 (SE 0.8) | +0.09 | 30,c 8d |
| Exenatide 5 µg | Exenatide 10 µg | Placebo | Significance | |
|---|---|---|---|---|
| Baseline A1c < 9% (read from graph, figure 2C) | –0.40 | –0.55 | 0.35 | Compared with placebo (p < 0.0001) |
| Baseline A1c ≥ 9 (read from graph, figure 2C) | –0.95 | –1.40 | 0 | Compared with placebo (p < 0.0002) |
The trials show that in those whose control is not good enough on dual therapy, addition of exenatide improved HbA1c by about 1% [Kendall (2005),59 Zinman (2007)60].
In the Kendall (2005)59 trial, the changes in HbA1c at 30 weeks were greater in those whose baseline level was higher.
When exenatide is compared with various insulin regimens, the results are similar, suggesting non-inferiority, although the issue of non-optimisation of the insulin treatment remains an issue.
Hypoglycaemia
Table 5 shows the frequency of hypoglycaemia.
| Study | Study arm and number | Incidence of hypoglycaemia (%) (n) | Overall hypoglycaemia rates (events/patient-year) | Serious hypos | Nocturnal hypo events (events/patient-year) | Daytime hypos | Severe hypos |
|---|---|---|---|---|---|---|---|
| Barnett (2007)50 (crossover trial) | Exenatide + MET or SU | 14.7 | 1.9 (95% CI 1.5% to 2.4%) | 0.4 (95% CI 0.2% to 0.7%) | Zero episodes | ||
| Insulin glargine + MET or SU | 25.2 | 2.6 (95% CI 2.2% to 3.2%) | 1.3 (95% CI 1.0% to1.7%) | Eight episodes | |||
| Davis (2007)52 | Exenatide + oral medications (n = 33) | 39 (13) | 1.72 | 0 | 11/13 | One patient treated with exenatide + SU had three severe hypos | |
| Current insulin regimen + oral medications (n = 16) | 38 (6) | 0.97 | 0 | 4/6 | |||
| DeFronzo (2005)58 | Exenatide (10 µg) + MET (n = 113) | 5.3 | 0 | ||||
| Placebo + MET (n = 113) | 5.3 | 0 | |||||
| Heine (2005)53 | Exenatide + MET + SU (n = 282) | 7.3a | 0.9b | 6.6c | Four pts | ||
| Insulin glargine + MET + SU (n = 267) | 6.3 | 2.4 | 3.9 | Four pts | |||
| Kendall (2005)59 | Exenatide + MET + SU 5 µg (n = 245) | 19.2 (47) | One case | ||||
| Exenatide + MET + SU 10 µg (n = 241) | 27.8 (67) | ||||||
| Placebo + MET + SU (n = 247) | 12.6 (31) | ||||||
| Nauck (2007)54 | Exenatide + MET + SU (n = 253) | 4.7 (SE 0.7) | 17% (44)d | ||||
| Biphasic insulin aspart + MET + SU (n = 248) | 5.6 (SE 0.7) | 25% (62) | |||||
| Zinman (2007)60 | Exenatide + MET + TZD (n = 121) | 10.7 (13)e | 0 | ||||
| Placebo + MET + TZD (n = 112) | 7.1 (8) | 0 |
Definitions of hypoglycaemia used in the included trials
-
Barnett et al. (2007)50 defined it as any sign or symptom due to hypoglycaemia, or a serum glucose concentration under 3.3 mmol/l. So, asymptomatic hypoglycaemic episodes were included.
-
Davis et al. (2007)52 included any episode in which a patient felt that they were experiencing a sign or symptom of hypoglycaemia, or a blood glucose under 3.4 mmol/l, irrespective of whether any symptoms were associated.
-
DeFronzo et al. (2005)58 based recording on symptoms that were confirmed by a PG level of under 3.3 mmol/l.
-
Heine et al. (2005)53 included both symptomatic episodes and biochemical ones.
-
Kendall et al. (2005)59 used symptoms that ‘may have been documented by a PG under 3.33 mmol/l’.
-
Nauck et al. (2007)54 included both symptomatic episodes and instances of blood glucose level under 3.4 mmol/l during self-monitoring, whether or not the monitored episode was associated with any symptoms.
-
Zinman et al. (2007)60 also defined hypoglycaemia as either symptoms or self-monitoring readings.
As expected, the frequency of hypoglycaemia varied amongst studies. Severe hypoglycaemia was uncommon. There were no severe hypos in the Nauck et al. (2007)54 and Zinman et al. (2007)60 trials, and only one in the Kendall et al. (2005)59 study.
In Barnett et al. (2007),50 three patients experienced eight episodes of severe hypoglycaemia during insulin glargine treatment, whereas there were no episodes of severe hypoglycaemia during exenatide treatment.
Also exenatide-treated patients had significantly lower mean rates of overall hypoglycaemia (p = 0.039) and nocturnal hypoglycaemia (p < 0.001) than insulin glargine-treated patients. There were also no significant differences in rates of daytime hypoglycaemia between exenatide and insulin glargine treatment.
In the Davis et al. (2007)52 trial, most hypoglycaemia occurred during daytime. Of the 13 exenatide patients who reported hypoglycaemia, 10 were also taking a sulfonylurea. Overall hypoglycaemia rates were higher in those with good control (exenatide 2.5 events per patient-year, insulin 1.2 events per patient-year).
In the Heine et al. (2005)53 trial, the overall frequencies of hypoglycaemia were similar, but nocturnal hypoglycaemia was less frequent in those on exenatide. In those who achieved good control (HbA1c level of 7% or less at week 26), 61% of the exenatide group and 68% of the glargine group reported at least one symptomatic hypoglycaemic episode, and 21% of those on exenatide and 43% of those on glargine reported at least one episode of nocturnal hypoglycaemia.
Although the nocturnal hypoglycaemia rate in the Nauck et al. (2007)54 study was significantly lower in the exenatide group (see Table 5), this was no longer statistically significant once adjusted for baseline HbA1c level. Once the sulfonylurea doses were reduced, hypoglycaemia rates fell from 27 to 6 events per patient-year.
Weight
Most studies reported weight loss with exenatide treatment. Results are shown in Table 6.
| Study | Study arm and number randomised | Weight in kg (SD) at baseline | Change in kg (SE) from baseline | p-value from baseline | Difference in kg between groups at end (exenatide–comparator 95% CI) | p-value between groups |
|---|---|---|---|---|---|---|
| Barnett (2007)50 (crossover trial) | Exenatide/insulin glargine treatment sequence + MET or SU (n = 68) | 85.6 (SE 2.0) |
Exenatide treated –1.6 (SE 0.3) |
–2.2 (SE 0.3), 95% CI –2.8 to –1.7 | p < 0.001 | |
| Insulin/glargine/exenatide treatment sequence + MET or SU (n = 70) | 84.0 (SE 2.0) |
Glargine treated +0.6 (SE 0.3) |
||||
| Davis (2007)52 | Exenatide + oral medications (n = 33) | 95 (17) | –4.2 (3) | p < 0.001 | p < 0.001 | |
| Current insulin regimen + oral medications (n = 16) | 102 (19) | +0.5 (1.7) | p = NS | |||
| DeFronzo (2005)58 | Exenatide (10 µg) + MET (n = 113) | 101 (SE 2) | –2.8 (SE 0.5) | p ≤ 0.001 | ||
| Placebo + MET (n = 113) | 100 (SE 2) | –0.3 (SE 0.3) | ||||
| Heine (2005)53 | Exenatide + MET + SU (n = 282) | 87.5 (16.9) | –2.3 | –4.1 (–4.6 to –3.5) | p < 0.0001 | |
| Insulin glargine + MET + SU (n = 267) | 88.3 (17.9) | +1.8 | ||||
| Kendall (2005)59 | Exenatide + MET + SU 5 µg (n = 245) | 97 (19) | –1.6 (0.2) | p ≤ 0.01 vs placebo | ||
| Exenatide + MET + SU 10 µg (n = 241) | 98 (21) | –1.6 (0.2) | ||||
| Placebo + MET + SU (n = 247) | 99 (19) | –0.9 (0.2) | ||||
| Nauck (2007)54 | Exenatide + MET + SU (n = 253) | 85.5 (15.7) | –2.5 (0.2) | p < 0.01 | –5.4 (–5.9 to –5.0) | p < 0.001 |
| Biphasic insulin aspart + MET + SU (n = 248) | 83.4 (15.6) | 2.9 (0.2) | p < 0.01 | |||
| Zinman (2007)60 | Exenatide + MET + TZD (n = 121) | 97.5 (18.8) | –1.75 | –1.51 (–2.15 to –0.88) | p < 0.001 | |
| Placebo + MET + TZD (n = 112) | 96.9 (19) | –0.24 |
Does nausea cause the weight loss?
Maggs et al. (2005)65 carried out an analysis of patients in three trials [Buse et al. (2004),56 DeFronzo et al. (2005),58 Kendall et al. (2005)59] to see if the weight loss with exenatide was related to the nausea. Severe nausea was found in only 4%. They found little correlation between nausea and weight loss (or HbA1c level). In the extension studies (to 52 weeks) the majority of patients had very little nausea, but lost the same amount of weight as the more nauseated subgroups.
Heine et al. (2005)53 found that although the magnitude of weight reduction tended to be greater in patients taking exenatide who experienced longer durations of nausea, patients who did not report any episodes of nausea during the trial (n = 120) still demonstrated a mean weight change of –1.9 kg (CI –2.5 to –1.4).
Adverse events other than hypoglycaemia
Table 7 shows the most frequent side effects.
| Study | Study arm and number randomised | Nausea | Vomiting | Diarrhoea | Any AE | Discontinuation due to AEs |
|---|---|---|---|---|---|---|
| Barnett (2007)50 (crossover trial) | Exenatide treatment | 42.6% | 9.6% | 65.4% | 11 | |
| Insulin glargine treatment | 3.1% | 3.1% | 52.8% | 1 | ||
| Davis (2007)52 | Exenatide + oral medications (n = 33) | 48.5% | 79% | Five pts | ||
| Current insulin regimen + oral medications (n = 16) | 12.5% | 56% | Zero pts | |||
| DeFronzo (2005)58 | Exenatide (10 µg) + MET (n = 113) | 45% | 12% | 16% | 2.7% (serious) 9.7% (severe) | 7.1% |
| Placebo + MET (n = 113) | 23% | 4% | 8% | 3.5% (serious) 8.8% (severe) | 0.9% | |
| Heine (2005)53 | Exenatide + MET + SU (n = 282) | 161 (57.1%)* | 49 (17.4%)* | 24 (8.5%)** | 9.5% | |
| Insulin glargine + MET + SU (n = 267) | 23 (8.6%) | 10 (3.7%) | 8 (3.0%) | 0.7% | ||
| Kendall (2005)59 | Exenatide + MET + SU 5 µg (n = 245) | 96 (39.2%) | 36 (14.7%) | 25 (10.2) | 14 (5.7%) | |
| Exenatide + MET + SU 10 µg (n = 241) | 117 (48.5%) | 33 (13.7%) | 42 (17.4) | 22 (9.1%) | ||
| Placebo + MET + SU (n = 247) | 51 (20.6%) | 11 (4.5%) | 16 (6.5%) | 11 (4.5%) | ||
| Nauck (2007)54 | Exenatide + MET + SU (n = 253) | 84 (33.2%) | 38 (15.0%) | 24 (9.5%) | 179 (70.8%) | Together, 5.1% of pts withdrew because of gastrointestinal-related AEs |
| Biphasic insulin aspart + MET + SU (n = 248) | 1 (0.4%) | 8 (3.2%) | 5 (2.0%) | 123 (49.6%) | ||
| Zinman (2007)60 | Exenatide + MET + TZD (n = 121) | 48 (39.7%)a | 16 (13.2%)b | 7 (5.8%)c | 92 (76.0%) pts reporting ≥ 1 AE | 19 (16%) |
| Placebo + MET + TZD (n = 112) | 17 (15.2%) | 1 (0.9%) | 3 (2.7%) | 73 (65.2%) pts reporting ≥ 1 AE | 2 (2%) |
The most striking finding is the high frequency of nausea with exenatide, with vomiting not uncommon. However, the number who had to stop exenatide because of side effects was much lower. Most nausea was mild, and the frequency decreased over time. For example, Heine et al. (2005)53 reported that 55% of patients reported nausea in the first 8 weeks, but only 13% did so in the last 8 weeks. However, 18 patients from the exenatide group withdrew because of nausea (compared with one patient in the insulin group). Heine et al. reported the frequencies of mild, moderate and severe nausea to be 33%, 20% and 5%, respectively.
Kendall et al. (2005)59 also reported that the frequency of nausea diminished over time, and only 4% had to withdraw because of it.
Zinman et al. (2007)60 reported that 9% of the exenatide group withdrew because of nausea, but that most nausea was mild (44%) or moderate (41%), and that it declined over time.
Cardiovascular risk factors
Three trials reported lipid and blood pressure data.
-
DeFronzo (2005)58 reported that exenatide treatment was not associated with an increased incidence of cardiovascular, hepatic, or renal adverse events. Also no changes in plasma lipids, laboratory safety parameters, heart rate, blood pressure, or electrocardiogram variables were observed between treatment arms.
-
Nauck et al. (2007)54 reported that HDL was higher by 0.04mmol/l with insulins, but that blood pressure fell with exenatide (systolic by 5 mmHg and diastolic by 2 mmHg), but did not change with insulin.
-
Zinman et al. (2007)60 found no significant differences in lipids and blood pressure.
Other outcomes
Patient-reported outcomes from the Barnett (2007)38 trial were reported by Secnik et al. (2006)66 in a poster presented at the International Diabetes Federation (IDF) in 2006. Responses to the following health outcome instruments were examined: the Psychological General Well-Being Index (PGWB), Diabetes Symptom Checklist-Revised (DSC-R), European Quality of Life-5 Dimensions (EQ-5D), Treatment Flexibility Scale (TFS) and Hypoglycaemia Fear Survey (HFS). No statistically significant between-group differences between twice-daily exenatide and glargine were found on any of these measured health outcomes.
Secnik et al. (2006)67 reported some patient-reported outcomes from the Heine trial, including EQ-5D, the vitality scale of the Short Form questionnaire-36 items (SF-36) health survey, the Diabetes Symptom Checklist, and the Diabetes Treatment Satisfaction Questionnaire. No differences were found, suggesting that the greater number of injections with exenatide (twice daily versus once for glargine), and the frequent (at least initially) nausea was not enough to affect overall satisfaction, perhaps because those were balanced by weight loss on exenatide (on average, 2.3 kg) versus gain on insulin (mean 1.8 kg).
An abstract from the Nauck (2006) trial by Yurgin et al. (2006)68 also reported EQ-5D and SF-36 data, stating that the exenatide group showed some improvement, whereas the biphasic aspart group showed no change.
Lower-dose exenatide
The standard dose of exenatide is 10 µg b.i.d., but there are some results on 5 µg b.i.d. from two of the trials. Table 8 shows the results for comparison of low- and standard-dose results.
| 5 µg b.i.d. | 10 µg b.i.d. | Placebo | |
|---|---|---|---|
| DeFronzo (2005)58 | |||
| HbA1c change (%) | –0.4 | –0.8 | – |
| Percentage reaching < 7% | 32 | 46 | 13 |
| Weight (kg) | –1.6 | –2.8 | –0.3 |
| Kendall (2005)59 | |||
| HbA1c change (%) | –0.55 | –0.77 | 0.23 |
| Percentage < 7% | 24 | 30 | 7 |
Hence those who can tolerate the starting dose but not the full one, still get some benefit. (Note: The cost appears to be the same, so the benefit–cost ratio is higher.)
Follow-up studies: open-label extensions
Klonoff et al. (2008)42 report results in people who had been on exenatide for at least 3 years. The participants were from the three 30-week studies [Buse et al. (2004),56 DeFronzo et al. (2005),58 Kendall et al. (2005)59], only one of which met our inclusion criteria for this review. However, the pooled open-label follow-up can provide useful data on duration of efficacy and side effects.
The withdrawal rate was high. Of 527 eligible patients, 310 withdrew. The reasons for withdrawal included adverse events (11%), poor control (3%), and patient or investigator decision (41% – reasons not given).
Weight loss was maintained amongst the 41% (217) who stayed in the follow-up study. The mean weight loss at 3 years was 5.3 kg. Overall, 84% of patients lost weight. Reductions in HbA1c level were also sustained (but this may be because those in whom it rose again left the study). Total cholesterol fell by 5% and triglycerides by 12%, presumably because of the weight loss, because there was a correlation between weight loss and cardiovascular risk factors.
The most frequent adverse effect (in 59%) was nausea, usually mild. Next came hypoglycaemia, but only in those treated with a sulfonylurea. Upper respiratory infections were common (36%) but the significance of that cannot be assessed without a control group. There were no serious side effects other than a few severe hypoglycaemic episodes. So exenatide appears safe, but the high dropout rate reduces the value of the study.
Results from routine care
Rather different results were found in routine care by Wolfe and King (2007). 69 Two hundred consecutive exenatide-treated patients included 56 treated for 12 months. The nadir of weight occurred at 6 months. Few details are given of later weight loss in this ADA conference abstract, but the suggestion is that there was a plateau after 6 months.
Loh and Clement (ADA poster 2007)70 reported a small follow-up study of 30 patients with type 2 diabetes who were treated with exenatide, some in addition of oral antidiabetic (OAD) drugs, others in addition to insulin. At 1 year, there was weight loss (mean 2 kg, p = 0.0033) but no significant reduction in HbA1c level overall. Maximum weight loss occurred by 7 months, with most patients regaining weight over months 7–12. Half the patients had stopped exenatide by 12 months, because of therapeutic failure or side effects. Loh and Clement conclude that in the ‘real world’ exenatide may not give as good results as seen in trials.
Yoon et al. (2008)71 in a conference abstract (ADA 2008), reported use of exenatide added to insulin. In a case series of 226 patients who started exenatide, 34 (15%) stopped within 3 months due to adverse effects. 71 Another 78 discontinued it later, mainly due to side effects or lack of efficacy. The final analysis of those who had used it for more than a year (116) showed weight loss of 6 kg, and a 20% reduction in insulin dosage. Eleven patients with an initial mean insulin dose of 17 units per day were able to stop insulin.
Another study from routine care, reported by Bhushan et al. 72 at the ADA 2008 conference, followed 201 patients for 16 weeks; all received exenatide in addition to previous treatment (details of which not given). Weight loss was seen in 69%, and averaged about 2 kg. Total cholesterol fell by 6 mg/dl. Blood pressure was unchanged.
It seems logical that exenatide be combined with insulin, although this is not a currently licensed indication. In an abstract from the recent EASD, Govindan et al. 73 presented a small case series from Wolverhampton, of 27 obese patients (mean BMI 43 at baseline), who were already on insulin but poorly controlled (mean HbA1c level 8.8%). About half had nausea on exenatide, but only three had to stop it. The mean weight fell from 128 kg to 115 kg after 3 months; BMI from 43 to 40; and insulin dose from a mean of 170 to 36 units/day. The average insulin dose reduction comes about because 10 patients could stop it altogether, although mean HbA1c level did not improve much (by only 0.3%; NS). Longer follow-up might show greater benefit, and it suggests that trials of combined exenatide and insulin therapy are justified.
Also from the EASD conference, Wintle et al. (from Amylin and Lilly)74 presented data from diabetic care records from the General Electric database, on 2086 patients treated with exenatide for 6 months or more. Patients had previously been on metformin, sulfonylurea or glitazone monotherapy (about 30%), or on dual therapy (38%) or triple therapy (34%), but were not well controlled (mean HbA1c level 8.4% and BMI 38.5).
Exenatide reduced HbA1c level by 0.9% in those who had been on monotherapy, but by less (0.5–0.8%) in those who had been on combination treatment.
Kendall et al. (Amylin and Lilly)75 reported a pooled analysis of 2 years of exenatide treatment. Patients were split into three groups according to pattern of weight loss: one group that lost none (they gained about 1 kg, but as their HbA1c level fell by over 1%, they were presumably taking the exenatide, suggesting that compliance was not the issue); a second group (34%), which lost weight quite quickly (about 4 kg by week 12); and a third group (46%), which lost as much weight as the second group, but who did so more slowly. Groups 2 and 3 lost on average 6 kg by 2 years.
In the group that did not lose weight, HbA1c level fell by about 1.2% but started rising again in the second year, to a drop of about 0.7% (from graph). In groups 2 and 3, the fall in HbA1c level of about 1.5% was more sustained – about 1.5% reduction at 52 weeks and 1.3% at 104 weeks.
This finding might have implications if NICE recommended a stopping rule for exenatide, as it could be stopped in those in whom it was least effective (no weight loss), thereby improving the cost-effectiveness.
Exenatide LAR
The exenatide LAR formulation has been studied in a 15-week Phase II trial [Kim (2007)]47 in patients with type 2 diabetes. The trial reported that a 2-mg dose of exenatide LAR showed a reduction in HbA1c level of 1.4% (relative to placebo), which the authors say is approximately twice as great as that seen with twice-daily injections of conventional exenatide. Preliminary results have suggested that the LAR formulation is also better tolerated than the original formulation, with less nausea, and (in the 2-mg form) is associated with greater weight loss; however, patient numbers were small. Results from other trials are awaited. The Amylin website45 reports an unpublished 30-week RCT of long-acting exenatide versus twice-daily Byetta, and states that ‘results showed that exenatide once weekly demonstrated powerful glucose efficacy, complemented by striking weight loss’.
This trial is presumably the DURATION trial, recently described in two abstracts. The ADA abstract, Drucker et al. (2008),76 reported the 30-week results in brief. They showed that once-weekly exenatide reduced HbA1c level slightly more than twice daily: 1.9% versus 1.5%. Seventy-seven per cent of the once-weekly group achieved an HbA1c level of less than 7.0%, compared with 61% for the twice daily. The trial recruited 295 patients who were poorly controlled (mean HbA1c level 8.3%), but most were on no oral drugs (15%) or monotherapy (45%). Only the 40% on two oral agents are relevant to this review. However, the trial clearly suggests that the future lies with once-weekly exenatide. No details on cost are yet available, but some economies would be expected compared with twice-daily injections.
The second abstract is from EASD77 and is a 22-week open-label follow-up of 241 of the DURATION patients by Buse et al. (2008)77 [the same team as Drucker et al. (2008)76]. Much of the abstract is about the patients who switched from twice-daily to weekly, but the 52-week HbA1c level results in the original once-weekly group are reported in brief as being sustained – reduction at 52 weeks of 2% (1.9% at 30 weeks).
GLP-1 agonists and beta-cell function
Rodent studies have reported that liraglutide can increase beta-cell mass.
Gallwitz (2006)78 has reviewed some of the animal and in vitro studies. The animal studies are mainly in rats, with a couple in mice. The evidence suggests that beta-cell growth is stimulated and that apoptosis is reduced. In isolated human islets, GLP-1 expands beta-cell mass. However, Gallwitz found no evidence regarding beta-cell mass in humans.
Xu et al. (1999)79 reported that exenatide treatment improved diabetic control in rats that were made diabetic by partial pancreatectomy, and that this was related to an increase in beta-cell mass (assessed histologically). Interestingly, the improved control was seen even after exenatide was stopped after 10 days. Gedulin et al. (2005)80 also reported an increase in beta-cell mass in rats after exenatide treatment.
Tourrel et al. (2001)81 treated newborn rats, made diabetic with streptozotocin, with exenatide and, again, noted an increase in beta-cell mass, which persisted (although the beta cells were less responsive to glucose).
If these findings are confirmed in humans, it would be of great importance, because it would suggest that the progressive nature of type 2 diabetes4,5 could be halted. Barnett (2007)38 and Holst et al. (2008)82 both note that if the GLP-1 analogues could increase beta-cell mass there would be an argument for treatment early in the disease, before too many beta cells are lost.
However, there are few data on the effect in humans – some very short experiments on islet cells in vitro, reviewed by Wajchenberg (2007),83 who concludes that there is, as yet, no clinical evidence that the GLP-1 analogues protect beta cells.
Bunck et al. (2008),84 in an ADA abstract from their RCT of exenatide versus glargine,85 reported that the beneficial effects seen on exenatide were not sustained – 5 weeks after stopping exenatide all of the improvements had gone, which may suggest that beta-cell function was not improved.
Further research is required, ideally with some means of determining at an early stage (2–3 years?) whether beta-cell mass is maintained in humans with type 2 diabetes.
Discussion
Barnett (2007)38 comments that ‘The appeal of exenatide therapy is that it provides glycaemic control with concomitant weight loss (as opposed to rapid or short-acting insulins which tend to cause weight gain), and, when not used with a drug that increases circulating insulin levels, does not cause hypoglycaemia’.
The evidence to date shows that the GLP-1 analogues can provide a useful improvement in glucose control when added to dual treatment with oral drugs, and that, at least in the short term, they can be an alternative to starting insulin. How long this effect would last, is not known. If we assume that the disease will steadily progress, as shown in UKPDS 16,4 then some of the benefit will be lost, as the beta cells will no longer be there to be release insulin. Other benefits, such as delayed gastric emptying, may continue, which may help control postprandial hyperglycaemia.
The glucose-dependent nature of the insulin release means that hypoglycaemia should be less of a problem, but the differences in the trials were not marked.
Weight loss is a useful feature in the trials, though perhaps seen less in routine care.
The drawbacks are the need for injections (twice daily with exenatide and once a day with liraglutide), the high rate of side effects (especially nausea) and the cost.
Injecting a foreign peptide could lead to antibody formation, but Barnett (2007)38 notes that such antibodies were common by 30 weeks but did not appear to reduce efficacy.
A review by the well-respected Prescrire International group from France concluded that exenatide was an alternative to starting insulin in patients with poorly controlled type 2 diabetes but that there was no evidence, as yet, that it was better, and, given the much greater experience with insulin, that should be preferred. 86
The German Institute for Quality and Efficiency in Health Care [Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG)] issued a report on exenatide in 2007. 87 Their review of exenatide addressed two questions:
-
Is it worthwhile to add exenatide to therapy with metformin and/or a sulfonylurea?
-
How does adding exenatide compare with other additional treatments?
The review identified five trials. These included the Kendall et al. (2005),59 Nauck et al. (2007),54 DeFronzo et al. (2005)58 and Heine et al. (2005)53 studies included in our TAR. The other one was Buse et al. (2004),56 excluded from this TAR, because patients had failed on sulfonylurea monotherapy but not had metformin.
The IQWiG review concluded that:
-
the reduction in HbA1c level was comparable for exenatide and insulin
-
no difference in the frequency of severe hypoglycaemia was shown in the trials against insulins
-
patients on exenatide lost weight, but those on insulin gained weight
-
the long-term benefits or harms of exenatide are unclear.
Postprandial hyperglycaemia
The slowing of gastric emptying by the incretin mimetics could, in theory, reduce postprandial hyperglycaemia.
Acute pancreatitis
There have been recent concerns about acute pancreatitis in people who have been treated with exenatide. 88 The FDA had (as at end of 2006) reviewed 30 reports of acute pancreatitis in patients on exenatide. Nearly all had other possible reasons for pancreatitis, including gallstones and alcohol use. Nearly all improved after exenatide was stopped, and a few in whom it was started again had a recurrence of symptoms. However, the improvement after the drug was stopped may be coincidental. The FDA has asked for a warning to be added to patient information and arranged enhanced monitoring, but has not restricted use. 89
The Medicines and Healthcare Products Regulatory Agency (MHRA) (Drug Safety Update May 2008)90 has called for vigilance. It notes that by September 2007 there had been 89 reports of acute pancreatitis, with, curiously, 87 in the USA and two in Germany. One case has since been reported in the UK, after only 5 µg of the drug.
Summary
In patients with inadequate control, the addition of exenatide led to a fall in HbA1c level of about 1.0%. In trials against insulins, the HbA1c level results were comparable. There was less nocturnal hypoglycaemia with exenatide than with insulin. In trials against insulin, patients on exenatide lost weight, whereas those on insulin gained weight. Nausea is very common, especially initially, but is not usually severe.
The need to inject exenatide twice daily may be a deterrent, but a long-acting once-weekly form is forthcoming.
Chapter 3 The DPP-4 inhibitors
This chapter draws on the recently published Cochrane review by Richter et al. (2008),91 but focuses on the comparisons that are relevant to this guideline.
As mentioned in the previous chapter, naturally occurring GLP-1 is broken down by the enzyme DPP-4. DPP-4 inhibitors, or ‘gliptins’, prevent GLP-1 degradation and prolong its half-life. Two inhibitors are currently on the market: – vildagliptin and sitagliptin – both for once-daily oral administration. A third, saxagliptin, is coming. 92 The manufacturer has submitted a request for regulatory approval to the FDA. 93 A new drug application for a fourth drug, alogliptin (Takeda Pharmaceutical, Osaka, Japan), was submitted in 2007. However, Takeda Pharmaceutical has recently been notified by the FDA that the cardiovascular safety data that it is in the process of reviewing for alogliptin are ‘insufficient’. The announcement is expected to delay approval of the drug.
Methods
For the review of the clinical effectiveness of the DPP-4 inhibitors, the primary sources of evidence were systematic reviews of RCTs, and recent RCTs, with other types of study such as open-label extensions being used only for data on duration of effect, side effects and continuation rates. Because the Cochrane review by Richter et al. 91 is very recent, we searched only for studies that had been published after the searches for the Cochrane review were done.
Types of interventions
Treatment for a minimum of 12 weeks with DPP-4 inhibitors (sitagliptin or vildagliptin) in combination with meglitinide analogues, metformin, a sulfonylurea or a TZD.
As with the GLP-1 analogues, the comparisons of interest for this review are based on the licensed indications, and on the standard treatment of type 2 diabetes, as set out in the NICE guideline (2008),6 the algorithm that was reproduced in Chapter 1.
The licensed indications are as follows. 94
Sitagliptin
-
In patients with type 2 diabetes, to improve glycaemic control in combination with metformin when diet and exercise plus metformin, do not provide adequate glycaemic control.
-
In combination with a sulfonylurea, in patients who cannot tolerate metformin, or in whom metformin is inappropriate, when maximally tolerated dose of a sulfonylurea does not provide adequate control.
-
For patients with type 2 diabetes in whom use of a TZD is appropriate, sitagliptin is indicated in combination with the peroxisome proliferator-activated receptor (PPAR) agonist when diet and exercise alone do not provide adequate glycaemic control.
-
To improve glycaemic control in combination with a sulfonylurea and metformin when diet and exercise plus dual therapy with these agents do not provide adequate glycaemic control.
This differs from the FDA approval,95 which allows monotherapy as well.
Vildagliptin is indicated in the treatment of type 2 diabetes, as dual oral therapy in combination with:
-
metformin, in patients with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin
-
a sulfonylurea, in patients with insufficient glycaemic control despite maximum tolerated dose of a sulfonylurea and in whom metformin is inappropriate due to contraindications or intolerance
-
a TZD, in patients with insufficient glycaemic control and for whom the use of a TZD is appropriate.
The following comparisons are relevant to this review.
-
Comparison 1 When dual therapy with metformin (or a glitazone) and a sulfonylurea have failed to achieve adequate control. The main comparisons will be:
-
– 1a. metformin + sulfonylurea versus metformin + either DPP-4 inhibitor
-
– 1b. sulfonylurea + glitazone versus sulfonylurea + either DPP-4 inhibitor
-
– 1c. sulfonylurea + glitazone versus glitazone + either DPP-4 inhibitor
-
– 1d. metformin + glitazone versus metformin + either DPP-4 inhibitor
-
– 1e. metformin + sulfonylurea versus metformin + sulfonylurea + sitagliptin.
-
-
Comparison 2 As an alternative to adding insulin to oral therapy. This would be in patients who have failed to achieve adequate control on dual or triple oral therapy. In those starting insulin, it is assumed that metformin would be continued, so the comparisons include:
-
– 2a. metformin + long-acting insulin versus metformin + a DPP-4 inhibitor.
-
-
Comparison 3 There is evidence that in patients failing on standard combination therapy, an intensive lifestyle intervention (diet and supervised exercise) can be as good as starting insulin. So it may be that rather than start a DPP-4 inhibitor, an intensive lifestyle package could be tried:
-
– 3. dual therapy + lifestyle versus dual therapy + a DPP-4 inhibitor.
-
Exclusions
-
Trials of DPP-4 monotherapy versus placebo. These can show that the DPP-4 inhibitors are pharmacologically active, but are not relevant to standard practice.
-
Trials of DPP-4 monotherapy versus monotherapy with other oral agents – not relevant to standard practice.
-
Trials of DPP-4 inhibitors in combination with insulin (not licensed).
The Cochrane review of the DPP-4 inhibitors found 29 comparisons (some of the 25 trials had more than one arm), but these included:91
-
six trials of sitagliptin monotherapy versus placebo
-
two trials of sitagliptin monotherapy versus metformin or glipizide
-
four trials of a sitagliptin combination versus metformin monotherapy
-
one trial of a sitagliptin combination versus pioglitazone monotherapy
-
one trial of a sitagliptin combination versus glimepiride monotherapy
-
two trials of a sitagliptin combination versus alternative dual therapy
-
six trials of vildagliptin monotherapy versus placebo
-
three trials of vildagliptin monotherapy versus metformin, pioglitazone or rosiglitazone monotherapies
-
two trials of vildagliptin and metformin versus metformin monotherapy
-
two trials of vildagliptin and pioglitazone versus pioglitazone alone
-
one trial of vildagliptin and insulin versus insulin alone
-
one trial of vildagliptin and metformin versus pioglitazone and metformin.
About half of all of the vildagliptin trials were in patients who had never had an oral drug, but had been treated only with diet and exercise.
Most of these studies from the Cochrane review are not relevant to this review. Table 9 shows which studies from the Cochrane review are exclusions for this HTA report, and the reasons for exclusion.
| Study | Reason for exclusion |
|---|---|
| Ahren (2004)96 | Compared with metformin monotherapy |
| Aschner (2006)97 | Compared to placebo |
| Bosi (2008)98 | Compared to metformin monotherapy |
| Charbonnel (2006)99 | Compared to metformin monotherapy |
| Dejager (2007)100 | Compared to placebo |
| Fonseca (2007)101 | Compared to metformin monotherapy |
| Garber (2007)102 | Compared to pioglitazone monotherapy |
| Goldstein (2007)103 | Compared to placebo |
| Goldstein (2007)103 | Compared with metformin monotherapy |
| Hanefeld 2007104 | Compared to placebo |
| Mimori (2006)105 | Compared to placebo |
| Nonaka (2008)106 | Compared to placebo |
| Pan (2008)107 | Compared to acarbose monotherapy |
| Pi-Sunyer (2007)108 | Compared to placebo |
| Pratley (2006)109 | Compared to placebo |
| Raz (2006)110 | Compared to placebo |
| Raz (2008)111 | Compared with metformin monotherapy |
| Ristic (2005)112 | Compared to placebo |
| Rosenstock (2006)113 | Compared to pioglitazone monotherapy |
| Rosenstock (2007)114 | Compared to rosiglitazone monotherapy |
| Rosenstock (2007)115 | Compared to pioglitazone monotherapy |
| Rosenstock (2008)116 | Compared to placebo |
| Scherbaum (2008)117,118 | Compared to placebo |
| Schweizer (2007)119 | Compared with metformin monotherapy |
| Scott (2007)120 | Compared to placebo |
| Scott (2008)121 | Compared to placebo |
What do the excluded studies tell us?
Compared to placebo, sitagliptin and vildagliptin reduced HbA1c level by around 0.7% and 0.6%, respectively. The sitagliptin versus placebo trials demonstrated substantial heterogeneity. (However, after eliminating a single study of Japanese patients only, Cochrane review noted that the heterogeneity decreased to an I2-value of 25%.) There was no weight loss advantage with the DPP-4 inhibitors.
Compared to monotherapy with other agents, neither drug showed any advantage.
There are no data on diabetic complications or mortality, but that is to be expected because of the short duration. Most included trials were 24 weeks’ duration; three were for 52 weeks.
The trials gave no data on costs or quality of life (QoL).
Both drugs were well tolerated. No severe hypoglycaemia was reported.
Inclusions
A disappointingly small number of trials met our inclusion criteria – only four. All were funded by the manufacturers, and half or m ore of the authors were from the manufacturer.
The characteristics of the included trials are shown in Appendix 3.
There were no trials for Comparisons 1b and 1c.
Comparison 1a
Nauck (2007)122 – sitagliptin + metformin vs glipizide + metformin
This 52-week trial recruited 1172 patients, mean age 57 years and mean duration 6 years, whose control was unsatisfactory (HbA1c 6.5–10%) on metformin alone. They had a period of dose titration on metformin first. They were randomised to sitagliptin (100 mg once daily) or glipizide (starting dose 5 mg/day). The latter was titrated up aiming at a target for pre-meal blood glucose of under 6.1 mmol/l, but could be reduced if hypoglycaemia was a problem. It was designed to confirm non-inferiority of sitagliptin to glipizide, and did so.
Comparison 1d
Bolli (2008)123 – vildagliptin + metformin vs pioglitazone + metformin
This 24-week trial recruited 576 patients whose control was inadequate (HbA1c 7.5–11%) on metformin alone, and randomised them to additional vildagliptin or additional pioglitazone, in a 24-week trial. Participants had poor control (HbA1c 7.5–11%), were aged 18–77 (mean about 57 years), and had had diabetes for a mean of 6.4 years. It showed that vildagliptin was not inferior to pioglitazone.
Scott (2008)121 – sitagliptin + metformin vs rosiglitazone + metformin
This 18-week trial121 also recruited 273 patients whose control was inadequate on metformin monotherapy, and randomised them to dual therapy with either sitagliptin or rosiglitazone, or to a placebo group having metformin monotherapy. Patients were 18–75 years of age, taking at least 1500 mg of metformin each day. Inadequate control was defined as an HbA1c level of 7% or over (but not more than 11%). The average duration of diabetes was 5 years (range 0.2–19 years). After 18 weeks, the mean HbA1c levels decreased by 0.22% in the placebo arm, and by 0.73% and 0.79% in the sitagliptin and rosiglitazone arms, respectively. So the net gain in HbA1c level from sitagliptin over placebo was 0.51%. There was weight gain with rosiglitazone (1.5 kg) but reductions with sitagliptin (0.4 kg) and placebo (0.9 kg).
Comparison 1e
Hermansen (2007)124 – sitagliptin + glimepiride + metformin vs glimepiride + metformin
There were four arms and 441 patients in this 24 week trial124 the two above, a glimepiride monotherapy arm, and a sitagliptin + glimepiride arm (a combination not currently licensed in Europe). The mean age at entry was around 57, and the mean duration of diabetes was around 8.5 years. They had inadequate control (HbA1c level of 7.5% or over, up to 10.5%) on a sulfonylurea alone or with metformin. Mean baseline HbA1c was 8.34%. Sitagliptin 100 mg once-daily reduced HbA1c level by 0.89% compared with placebo, in patients also treated with both glimepiride and metformin.
There were no trials for Comparisons 2 and 3.
Quality of included trials
The quality of the included trials, as shown in Table 10, was good.
| Study | Method of randomisation | Allocation concealment | Blinding | ITT analysis | Percentage completed | Power calculation | Similarity at baseline | Sponsorship by manufacturer |
|---|---|---|---|---|---|---|---|---|
| Bolli (2008)123 | Not reported; 295 allocated to vildagliptin arm vs 281 to pioglitazone | Not reported | Double blind | Per protocol | 89% and 87% | Yes | Good | Funded by Novartis and corresponding author from company |
| Hermansen (2007)124 | Computer generated | Yes | Double blind | No | 92/113 and 102/116 | Yes | Good | Funded by Merck and 4/6 authors from company |
| Nauck (2007)122 | Not reported | Not reported | Not blinded | No – per protocol | 67% and 74% | Not clear | Good | Funded by Merck with four authors from company |
| Scott (2008)121 | Not reported | Not reported | Double blind | Per protocol | 90% and 98% | Not clear | Good | Funded by Merck and 3/4 authors from company |
HbA1c results
The results for HbA1c in Table 11 show that sitagliptin and vildagliptin have similar effects to a glitazone, but an improvement of 0.9% compared with placebo.
| Study | Study arm | HbA1c (%) baseline | HbA1c (%) end | Change from baseline (%) | Difference between groups at end (DPP-4 inhibitor–comparator) | p-value between groups | Percentage achieving HbA1c < 7% |
|---|---|---|---|---|---|---|---|
| Bolli (2008)123 | Vildagliptin + metformin | 8.4 | –0.88 (± 0.5a) | 0.10 (95% CI –0.05 to –0.26) | 27 | ||
| Pioglitazone + metformin | 8.4 | –0.98 (± 0.06a) | 36 | ||||
| Hermansen (2007)124 | Sitagliptin + metformin + glimepiride | 8.27 | –0.59 | –0.89 | < 0.001 | 22.6 | |
| Metformin + glimepiride | 8.26 | +0.30 | 1.0 | ||||
| Nauck (2007)54 | Sitagliptin + metformin | 7.7% (all) | 6.86 (PP) | –0.67 | –0.02 | NS | 63 |
| Glipizide + metformin | 7.6 | 6.84 | –0.67 | 59 | |||
| Scott (2007)120 | Sitagliptin + metformin | 7.8 | 7.01 | –0.79 | +0.07 | NS | 55 |
| Rosiglitazone + metformin | 7.7 | 6.94 | –0.76 | 63 |
Weight change
Table 12 shows there was less weight gain than with the glitazones [Bolli (2008),123 Scott (2007)120] but that is mainly because people on glitazones gained weight – not because those on a DPP-4 inhibitor lost any. In the comparison with glipizide, the sitagliptin arm ended 2.6 kg lighter. In the Hermansen et al. trial (2007)124 there was more weight gain with the DPP-4 inhibitor than in the placebo control arm.
| Study | Study arm | BMI baseline | Weight in kg (SD) at baseline | Change from baseline (kg) | Difference between groups at end (DPP-4 inhibitor–comparator) | p-value between groups |
|---|---|---|---|---|---|---|
| Bolli (2008)123 | Vildagliptin + metformin | 32.2 | 91.8 (18.5) | 0.3 | –1.6 kg | < 0.001 |
| Pioglitazone + metformin | 32.1 | 91.2 (16.9) | 1.9 | |||
| Hermansen (2007)124 | Sitagliptin + metformin + glimepiride | 31.3 | 87.2 (19.7) | +0.4 | +1.1 kg | |
| Metformin + glimepiride | 30.7 | 86.7 (21.1) | –0.7 | |||
| Nauck (2007)54 | Sitagliptin + metformin | 31.2 | 89.5 | –1.5 | –2.6 kg | < 0.001 |
| Glipizide + metformin | 31.3 | 89.7 | +1.1 | |||
| Scott (2007)120 | Sitagliptin + metformin | 30.3 | 83.1 (17.1) | –0.4 | –1.9 kg (95% CI 1.3 to 2.5) | |
| Rosiglitazone + metformin | 30.4 | 84.9 (18.5) | +1.5 |
The Cochrane review91 concluded (see tables 13 and 14 under ‘Additional tables’ for details) that in trials against placebo there was greater weight loss after placebo treatment than with sitagliptin and vildagliptin. The pooled estimate for sitagliptin studies was a weighted mean difference (WMD) of 0.7 kg (95% CI 0.3 to 1.1, p = 0.0002) in favour of placebo and 0.8 kg (95% CI 0.2 to 1.3, p = 0.009), for vildagliptin studies in favour of placebo. Most active hypoglycaemic comparators also resulted in more pronounced weight losses than sitagliptin or vildagliptin treatment.
So the DPP-4 drugs do not seem to have as great a weight reduction effect as exenatide, but in most cases there is no weight gain, which, compared with sulfonylureas and glitazones, is an advantage.
Adverse events
Table 13 shows selected adverse events.
| Study | Study arm | Nausea (%) | Vomiting (%) | Diarrhoea (%) | Other GI (%) | Any AE (%) | Discontinuation due to side effects |
|---|---|---|---|---|---|---|---|
| Bolli (2008)123 | Vildagliptin + metformin | NR | NR | 3.4 | 3.1 (constipation) | 2.0 | 3.1 |
| Pioglitazone + metformin | NR | NR | 2.9 | 1.1 (constipation) | 4.6 | 3.2 | |
| Hermansen (2007)124 | Sitagliptin + metformin + glimepiride | 0.9 | 1.7 (2 patients ex 116) | 0.9 | All GI AEs 4.3 | 18 | 1.7 |
| Metformin + glimepiride | 0.9 | 0.9 (1 patient ex 113) | 3.5 | All GI AEs 7.1 | 7.1 | 1.8 | |
| Nauck (2007)54 | Metformin + sitagliptin | 2.6 | 0.4 | 5.8 | 2.7 (abdominal pain) | 71 | 2.7 |
| Metformin + glipizide | 2.7 | 1.5 | 5.5 | 2.1 | 76 | 3.6 | |
| Scott (2007)120 | Sitagliptin + metformin | 1 | 1 | 3 | Any GI event 9 | 39 | 2 |
| Rosiglitazone +metformin | 1 | 1 | 3 | Any GI event 7 | 44 | 0 |
For full details, see tables 15–27 of the Cochrane review by Richter et al. (2008). 91 As mentioned above, the drugs were well tolerated. Discontinuation due to adverse effects did not differ significantly between sitagliptin or vildagliptin intervention and control arms. The risk ratios of serious adverse events also did not show statistically significant differences between groups.
In the Cochrane review, headache was reported more often with DPP-4 inhibitors, especially following vildagliptin therapy.
Hypoglycaemia
Bolli et al. (2008)123 defined hypoglycaemia as symptoms that are suggestive of low blood glucose, confirmed by a self-monitored PG level of under 3.1 mmol/l. Hypoglycaemia was reported in only one patient in the Bolli study – in the vildagliptin group – and it was mild.
In the Hermansen et al. trial (2007),124 any hypoglycaemia was reported in 16% of the sitagliptin group versus 0.9% of the control group. In the Scott et al. study (2007),120 hypoglycaemia was reported in 1% of both groups. No severe hypoglycaemia was reported.
Nauck et al. (2007)54 defined severe hypoglycaemia as requiring medical assistance, and had another category where non-medical assistance was sufficient. Any hypoglycaemia was reported in 32% in the glipizide arm and in 5% in the sitagliptin arm; severe hypoglycaemic attacks were reported in 1.2% and 0.2%, respectively. Hypoglycaemia of the ‘non-medical assistance needed’ category was reported in 1.4% (eight patients) and 0.2% (one patient).
In the wider Cochrane review by Richter et al. (2008),91 severe hypoglycaemia was not reported in patients taking sitagliptin or vildagliptin, and there were no statistically significant differences in hypoglycaemic episodes between sitagliptin/vildagliptin and comparator groups.
Infections
The Cochrane review by Richter et al. (2008)91 reported an increase in all-cause infections.
The Merck & Co responses to the consultation mentioned the analysis by Williams-Herman et al. (2008) (who are from Merck & Co),125 and stated that this did not find any increase in infections.
There are three reviews that report infection rates in DPP-4 inhibitor trials:
-
The Cochrane review by Richter et al. (2008)91 included all RCTs in adults with type 2 diabetes, with trial duration of at least 12 weeks. It included 25 trials: 11 sitagliptin, 14 vildagliptin. Study duration ranged from 12 to 52 weeks. Searches were carried out until January 2008. All-cause infections [for example, nasopharyngitis, upper respiratory tract infection, urinary tract infection (UTI)] showed a statistically significant increase after sitagliptin treatment [relative risk (RR) 1.29, 95% CI 1.09 to 1.52, p = 0.003] but did not reach statistical significance following vildagliptin therapy (RR 1.04, 95% CI 0.87 to 1.24, p = 0.7).
-
A review by Amori et al. (2007)32 also included RCTs of at least 12 weeks’ duration. Searches were until 20 May 2007. They found eight sitagliptin studies and 12 vildagliptin studies. They found a slightly increased risk of nasopharyngitis (6.4% for DPP-4 inhibitor versus 6.1% for comparator; RR 1.17; 95% CI 0.98 to 1.40), which was significant only for sitagliptin (RR 1.38, CI 1.06 to 1.81). The risk of UTI was increased by about 50% (3.2% for DPP-4 inhibitor versus 2.4% for comparator; RR 1.5; 95% CI 1.0 to 2.2), and this was seen with both DPP-4 inhibitors, although in the individual comparisons, confidence intervals (CIs) on risk ratios were wide and overlapped with unity. Amori et al. accepted that the relative risks were small, but commented: ‘there are more than 20 million patients with diabetes in the United States who are both more likely to develop a urinary tract infection and are at higher risk of complications, including death from urosepsis. A relative risk of 1.5 increases the number of UTIs by 1 million new cases per year, placing a significant burden on the individual patient and the health-care system. Until more safety data are available, it may be prudent to avoid use of these agents in patients with a history of recurrent UTIs’.
-
The analysis by Williams-Herman et al. (2008)125 included only sitagliptin (100-mg dose). It pooled 12 large Phase IIb and Phase III RCTs, with duration at least 18 weeks (up to 2 years), based on data available in the industry database at November 2007. They reported that the only infection more common in the sitagliptin group was nasopharyngitis, with 7.1% in the sitagliptin group versus 5.9% in the comparators, but that the 95% CI for the difference overlapped with no difference (95% CI –0.1 to +2.4). They found no difference in the frequency of UTIs.
So we have two independent reports suggesting an increase in UTIs, and the manufacturer’s analysis reporting no increase.
Table 14 shows the trials included in these reviews.
| Study ID | Reviews | DPP-4 inhibitor | ||
|---|---|---|---|---|
| Richter (2008)91 | Amori (2007)32 | Williams-Herman (2008)125 | Vildagliptin (V) or sitagliptin (S) | |
| Ahren (2004)96 | ✓ | ✓ | NA | V |
| Aschner (2006)97 | ✓ | ✓ | ✓ | S |
| Bolli (2008)123 | ✓ | ✗ | NA | V |
| Bosi (2007)98 | ✓ | ✓ | NA | V |
| Charbonnel (2006)99 | ✓ | ✓ | ✓ | S |
| Dejager (2007)100 | ✓ | ✓ | NA | V |
| Dobs (2008)126 | ✗ | ✗ | ✓ | S |
| Fonseca (2007)101 | ✓ | ✓ | NA | V |
| Garber (2007)102 | ✓ | ✓ | NA | V |
| Goldstein (2007)103 | ✓ | ✗ | ✓ | S |
| Hanefeld (2005)127 | ✗ | ✓ | ✗ | S |
| Hanefield (2007)104 | ✓ | ✗ | ✓ | S |
| Hermansen (2007)124 | ✓ | ✗ | ✓ | S |
| Mimori (2006)105 | ✓ | ✓ | NA | V |
| Nauck (2007)122 | ✓ | ✓ | ✓ | S |
| Nonaka (2006, 2008)106,128 | ✓ | ✓ | ✗ | S |
| Pi-Sunyer (2007)108 | ✓ | ✓ | NA | V |
| Pratley (2006)109 | ✓ | ✓ | NA | V |
| Raz (2006)110 | ✓ | ✓ | ✗ | S |
| Raz (2008)111 | ✗ | ✗ | ✓ | S |
| Ristic (2005)112 | ✓ | ✓ | NA | V |
| Rosenstock (2006)113 | ✓ | ✓ | ✓ | S |
| Rosenstock (2007)114 | ✓ | ✓ | NA | V |
| Rosenstock (2007)115 | ✓ | ✓ | NA | V |
| Scherbaum (2008)118 | ✓ | ✗ | NA | V |
| Schweizer (2007)119 | ✓ | ✓ | NA | V |
| Scott (2007)120 | ✓ | ✓ | ✓ | S |
| Scott (2008)121 | ✓ | ✗ | ✗ | S |
| Yang (2007)129 | ✗ | ✗ | ✓ | S |
| P023 (Merck & Co, unpublished) | ✗ | ✗ | ✓ | S |
Quality of life
No publication provided data on health-related QoL.
Hypothetical adverse effects
In addition to reducing the breakdown of the incretins, GLP-1 and gastric inhibitory peptide, DPP-4 inhibitors also prolong the action of a number of neuropeptides, such as neuropeptide Y, growth hormone-releasing hormone and chemokinines, such as stromal cell-derived factor 1 and macrophage-derived chemokine. Potential side effects include neurogenic inflammation, increase in blood pressure, enhanced inflammation and allergic reactions. DPP-4 contributes to T-cell activation, raising the possibility that these compounds compromise immune function. 130 Levels of tissue DPP-4 are reduced in nasal tissue of people with chronic rhinosinusitis, and DPP-4 inhibition seems to aggravate nasopharyngitis, as could be observed in clinical studies.
Therefore, the long-term safety of DPP-4 inhibitors merits further investigation, and it seems to be important to monitor DPP-4-treated patients for the development of inflammatory conditions, such as angioedema, rhinitis and urticaria.
Costs
Both of the sitagliptin trials used 100 mg daily, which, at a cost (BNF 55131) of £33.26 for 28 tablets, comes to £432 per year.
No cost is available for vildagliptin yet. The dose used by Bolli et al. (2008)123 was also 100 mg daily.
Beta-cell function
A progressive reduction in beta-cell mass contributes significantly to gradual loss of glycaemic control in individuals with type 2 diabetes. A major goal of diabetes research is to restore the beta-cell mass typically lost during the natural progression of type 2 diabetes. Current treatments not only show no ability to reduce beta-cell loss, but also some, such as the sulfonylureas, have been shown to induce beta-cell apoptosis in cultured human islets. 132 If the DPP-4 inhibitors can enhance beta-cell survival and stimulate beta-cell growth, they may provide a means to preserve or restore functional beta-cell mass in individuals with type 2 diabetes.
The Cochrane reviewers91 found few data on measurements of beta-cell function, especially for vildagliptin. The variety of methods used also made definite conclusions on the effects of DPP-4 inhibitors on beta-cell function difficult. Inspection of the sitagliptin homeostasis model assessment beta (HOMA-beta) data seems to indicate that sitagliptin, when compared with placebo, results in increased values of beta-cell function measurements, but the effect in comparison with other hypoglycaemic agents does not seem to be clear cut.
Most studies are quite short. An exception is the 2-year extension study by Scherbaum et al. (2008). 117 This study (funded by Novartis, with the corresponding author from the company) was one of our exclusions because it compared vildagliptin with only placebo, but it does provide some data on a measure of beta-cell function, the insulin secretory rate relative to glucose level after meals. This measure reflects the responsiveness of the beta cell to glucose, rather than absolute insulin production or plasma insulin level. The extension study was undertaken in under half of those who completed the original study (108 compared with 264). All of the original recruits had HbA1c levels in the range of 6.2–7.5%. At recruitment the mean duration was 2 years.
Scherbaum et al. found that their measure of insulin secretory rate/glucose ‘tended to increase’ from the end of year 1 to the end of year 2, by which they mean that there was an increase that did not reach statistical significance. The implication is that there may be a steady improvement in beta-cell function. However, the mean HbA1c level in the vildagliptin group fell after initiation, reached a nadir of about 6.2% by around 32 weeks, and then slowly rose to about 6.4% by 110 weeks. That rise suggests that vildagliptin is not having a dramatic effect on beta-cell function. It may be slowing the progression of the disease, which has been reported by the UKPDS (16 or 17);4,5 it is worth noting that the graph shows that mean HbA1c level rose a little more steeply in the placebo group, whereas in UKPDS the lines were roughly parallel.
So far, no definite conclusions can be drawn on the effects of sitagliptin and vildagliptin on long-term beta-cell function. If beta-cell function does improve, and if that improvement is sustained over the long term (say 10–20 years), then that would be very important and there would be a case for early use, perhaps as the first drug to be used when diet fails. Or, given that diet usually fails, perhaps from the diagnosis of type 2 diabetes.
There could be an issue about the duration of diabetes at which any beta-cell preservation effect might be seen. The UKPDS study2 reported that at diagnosis, about half of beta-cell function had been lost. If patients are then treated with incretin enhancers or mimetics after they had had diabetes for many years, it may be too late to see much effect. It would be interesting to assess effects on beta-cell function by duration of known diabetes, and perhaps also in people with impaired glucose tolerance (there is one trial of the effects of a DPP-4 inhibitor on people with impaired glucose tolerance116).
Emerging studies
Another third-line trial was reported at the ADA 2008 conference, in abstract only, by Dobs et al. (2008)126 It was an 18-week RCT of adding sitagliptin to metformin and rosiglitazone. HbA1c level fell by 0.7% overall, but by 1.3% in those whose baseline HbA1c level was over 9%.
At the same meeting, Krobot et al. (2008)133 had an abstract from a second-line trial, of metformin and sitagliptin versus metformin and glipizide. The effects on HbA1c level were similar, but hypoglycaemia was less frequent with sitagliptin (any hypoglycaemic event 5%) than the sulfonylurea (32%).
At the September 2008 conference of the EASD three new gliptin trials were presented. One by Goodman et al. (2008)134 was of vildagliptin versus placebo as an add-on to metformin, and would be an exclusion under our criteria. The other two are of interest. Arjona-Ferreira et al. (2008)135 describe a Merck & Co-funded trial of adding sitagliptin in patients with inadequate control (HbA1c level 7.5–11%) on metformin and rosiglitazone. Adding sitagliptin reduced HbA1c level by 0.7% overall, but by 1.3% in those with baseline HbA1c level of over 9%.
Braceras et al. (2008)136 presented a Novartis trial comparing vildagliptin to a glitazone in patients not adequately controlled (initial HbA1c level of over 7%) on metformin, and found them to be roughly equivalent. HbA1c level fell by 0.68% on vildagliptin + metformin, and by 0.57% on glitazone + metformin.
Another new trial118 was published in full in August 2008, but is not relevant for our purposes. It compared vildagliptin and placebo in patients who had not previously had drug treatment. Their hyperglycaemia was mild (baseline HbA1c level 6.2–7.5%). After 1 year on treatment, HbA1c level fell by 0.3% in those receiving vildagliptin and rose by 0.15% in those on placebo, which was statistically significant, if not clinically so. It does provide a useful reminder that the size of reduction in HbA1c level depends on baseline level.
Conclusions
Sitagliptin and vildagliptin are clinically effective in reducing blood glucose, do not cause problems with hypoglycaemia, and are well tolerated. However, we cannot yet say what the long-term effects on diabetes complications will be, nor what long-term adverse effects may appear.
Only indirect comparisons can be made with the GLP-1 analogues, because there have been no head-to-head trials. The main differences are that the DPP-4 inhibitors are given orally, are less expensive, cause fewer adverse events in the short term (but may be slightly less potent in lowering blood glucose), and do not cause weight loss. They may not be so specific in action, and their effects on the immune system require monitoring.
Chapter 4 The long-acting insulin analogues
Objectives
In this chapter, we assess the effects of the new insulin analogues – glargine and detemir – with older long-acting (for example, ultralente) and intermediate-acting insulins (for example, NPH).
Background
An ideal basal insulin would have a flat action profile (i.e. the same level at all times of day) with no day-to-day variability in the same patient. Older long-acting insulins use a crystalline or amorphous suspension, that forms a slowly dissolving depot after subcutaneous injection. The newer long-acting analogues have adopted different approaches. Both have structural changes.
In glargine, these changes mean that it is soluble in the acidic (pH 4.0) solvent in which it is provided, but once injected into the neutral pH of the subcutaneous tissues, it forms stable hexamers which slowly release the insulin into the bloodstream. 137 In detemir, one amino acid is omitted and a long-chain (14-carbon) fatty acid, myristoyl, is attached. This facilitates binding of detemir to serum albumin. It has been suggested138 that albumin binding may facilitate transport into the brain, and that this might cause slightly less weight gain than is seen with other insulins. 139
Methods
Inclusion criteria
Types of studies
A number of high-quality systematic reviews already exist in this area, so in the first instance, we reviewed systematic reviews of RCTs. The reviews had to include at least one RCT of at least 12 weeks’ duration. We also considered any additional RCTs that were published after the last search of any relevant included review. The trials had to have a minimum duration of 12 weeks, although trials of at least 24 weeks’ duration were preferred.
Types of participants
Patients of any age and gender with type 2 diabetes.
Types of interventions
In type 2 diabetes, treatment with insulin is started when control on a combination of oral drugs is unsatisfactory. Therefore, the comparators of glargine/detemir were other basal insulins, usually NPH but, occasionally, ultralente. Metformin will now usually be continued, and other oral therapies may be used. Some trials used insulin alone. So comparisons can include:
-
glargine + oral agents versus NPH + oral agents
-
detemir + oral agents versus NPH + oral agents
-
glargine + oral agents versus ultralente + oral agents
-
detemir + oral agents versus ultralente + oral agents
-
glargine versus detemir
-
glargine or detemir alone versus NPH alone.
Overweight people with type 2 diabetes often do not achieve good glycaemic control after switching to insulin, partly because it can cause further weight gain. We set out to review one other option (but did not identify any new relevant trials): metformin + sulfonylurea + insulin versus metformin + sulfonylurea + lifestyle interventions.
The trial by Aas et al. (2005)27 (already described in Chapter 1) is relevant here.
There are trials of the long-acting analogues against short-acting insulins at mealtimes, for example once-daily glargine versus thrice-daily aspart. We excluded such trials, because they are comparing different approaches to glycaemic control, rather than the new and old basal insulins.
Types of outcomes
We planned to consider the following outcome measures:
-
HbA1c
-
frequency of hypoglycaemia, especially if severe
-
glycaemic excursions, including postprandial hyperglycaemia
-
total daily dose of insulin
-
weight gain or loss
-
complication rates: retinopathy, nephropathy, myocardial infarction (MI), angina, heart failure, stroke, amputation, death
-
adverse events
-
health-related QoL.
Search strategy
Relevant literature was identified, and comprehensiveness checked, by:
-
searches of bibliographic databases, MEDLINE, Cochrane Library and EMBASE
-
checking reference lists of retrieved studies
-
obtaining lists of published studies from manufacturers
-
our peer review process.
Searches were also carried out to identify emerging evidence, from conference abstracts and trial registers. Studies available only in abstract were included in the assessment of clinical effectiveness if there was a paucity of studies published in full in peer-reviewed journals, but they were reported with appropriate caution. Our default position is for studies available only in abstract not to be used.
Authors of previous studies were not contacted.
Quality assessment of studies
The quality of systematic reviews was assessed using the following quality criteria, based on the NICE guidelines manual:
-
appropriate and clearly focused question
-
inclusion and exclusion criteria described
-
literature search sufficiently rigorous to identify all relevant studies
-
study selection described
-
data extraction described
-
study quality assessed and taken into account
-
study flow shown
-
study characteristics of individual studies described
-
quality of individual studies given
-
results of individual studies shown
-
enough similarities between studies selected to make combining them reasonable.
Each of the items was rated as: well covered/adequately addressed/poorly addressed/not addressed/not reported/not applicable.
The overall quality of the review was rated as (++), (+) or (–).
Randomised controlled trials were assessed on the following criteria, based on the NICE guidelines manual:
-
appropriate and clearly focused question
-
method of randomisation
-
allocation concealed
-
participants blinded
-
outcome assessors blinded
-
all relevant outcomes measured in standard, valid, reliable way
-
proportion of participants excluded/lost to follow-up
-
handling of missing data
-
intention-to-treat (ITT) analysis performed
-
statistical analysis appropriate
-
only difference between groups is treatment under investigation
-
results in multicentre studies comparable for all sites
-
groups comparable at baseline.
Again, overall quality of the trials was classified as (++), (+) or (–).
Data extraction
Data extraction was carried out by one researcher and checked by another. Any disagreements were resolved through discussion, involving a third person if necessary.
Data analysis
The clinical effectiveness, relative to the key comparators, was assessed, in terms of difference in effect size. (The key question for the cost-effectiveness analysis is not whether a drug is better than the comparator, but how much better.)
Data were summarised using tables and text. In addition, we performed a meta-analysis of all relevant trial data, combining data from the previous meta-analyses with newly identified trials. Data were summarised for continuous variables (for example, HbA1c, weight change) as WMDs with 95% CIs using the inverse variance method and a random effects model. For dichotomous variables (hypoglycaemia), data were expressed as relative risks with 95% CIs (for patients with or without hypoglycaemia) and summarised using the Mantel-Haenzsel method and a random effects model. For data already used in previous meta-analyses, data were generally used as given in the meta-analyses, although some double-checking was undertaken with the original papers. Where not given directly, standard deviations (SDs) were either calculated from standard errors (SEs) or CIs, or in case of no measure of variability reported, the average of the SDs for the other studies for that outcome measure was used. If the SDs were missing for more than half of the studies, meta-analysis was considered not to be reliable and a statistical summary was not presented. Meta-analyses were generally done for end-of-study values except for weight change, as most studies reported data for weight change without giving baseline values. Heterogeneity was assessed using the chi-squared statistic.
We had set out to conduct sensitivity analyses to explore uncertainties in important parameters, and of the impact of hypoglycaemic episodes and the fear of hypoglycaemic episodes on QoL.
We did not include any indirect comparisons, for two main reasons. Firstly, such comparisons are prone to bias due to confounding variables, which may not all be apparent. Secondly, they are used mainly in technology appraisals, when seeking to decide which of two or more options is better or best. We do not expect the guideline development group will wish to make any recommendations of whether glargine should be used in preference to detemir, or vice versa, because such comparisons would be based partly on cost, which may change. Having two drugs available in each group encourages competition on price.
Systematic reviews
Search results
Fourteen papers were identified as potentially relevant systematic reviews. Of these, five fulfilled the inclusion criteria. 140–144 Most of the remainder did not use systematic review methodology, and one was only a protocol for a systematic review (Table 15). Two further systematic reviews were identified after the completion of the present analysis and these will only be summarised briefly. 145,146
| Study | Reason for exclusion |
|---|---|
| Dailey (2003)147 | Not a systematic review, abstract only |
| Garber (2007)148 | Not a systematic review |
| Glass (2008)149 | Not a systematic review |
| Hemraj (2004)150 | Not a systematic review |
| Mullins (2007)151 | Not a systematic review |
| Mullins (2007)152 | Not a systematic review, abstract only |
| Rašlová (2007)153 | Not a systematic review |
| Rosenstock (2005)154 | Not a systematic review |
| Swinnen (2007)155 | Protocol only, no full review |
Description of reviews
The characteristics of the included reviews are shown in Appendix 4. Of the five included reviews, the reviews by Duckworth et al. (2007)140 and Wang (2003)143 had only a very limited description of methodology, the review by Horvath et al. (2007)141 was a Cochrane review, and the reviews by Warren et al. (2004)144 and Tran et al. (2007)142 were Health Technology Assessments (one from the UK and one from Canada). Four of the reviews had non-industrial funding, whereas the review by Duckworth et al. (2007)140 was funded by Sanofi-aventis (New Jersey, NJ, USA).
Inclusion criteria
Only four out of the five reviews specified the study design of the studies to be included. The others included RCTs (or just ‘clinical trials’), where Warren et al. (2004)144 specified a minimum duration of 4 weeks, Horvath et al. (2007)141 24 weeks and Wang (2003)143 specified a minimum number of participants of 100. Wang also included other designs to answer different parts of their review question, but only the clinical efficacy trials are considered here.
Both Health Technology Assessments and the review by Wang included both participants with type 1 and type 2 diabetes. The remaining two reviews were concerned only with participants with type 2 diabetes. The present review only summarises parts of the included reviews that describe patients with type 2 diabetes.
The reviews by Duckworth and Davis (2007),140 Warren et al. (2004)144 and Wang (2003)143 focused on insulin glargine, whereas the reviews by Horvath et al. (2007)141 and Tran et al. (2007)142 reviewed the effects of both insulin glargine and insulin detemir. Comparison treatments were NPH insulin in the study by Duckworth and Davis, and Horvath et al. , another long-acting basal insulin in the review by Warren et al. , conventional human insulin or OAD agents in the review by Tran et al. , and comparison treatments were not specified in the review by Wang.
Outcomes that reviews set out to assess included glycaemic control (HbA1c, FPG), hypoglycaemia (overall, severe and nocturnal), other adverse events, mortality, cardiovascular morbidity, diabetic late complications and health-related QoL.
Trials included in systematic reviews
General
The reviews included reports of 14 individual trials of insulin glargine and two trials of insulin detemir, as shown in Table 16.
| Duckworth (2007)140 | Wang (2003)143 | Horvath (2007)141 | Tran (2007)142 | Warren (2004)144 | |
|---|---|---|---|---|---|
| Previous insulin – glargine vs NPH insulin | |||||
| Fonseca (2004)156–158 (subgroup analysis of Rosenstock 2001) | ✓ | ✓ | ✓ | ✓ | ✓ |
| Rosenstock (2001)159 | ✓ | ✓ | ✓ | ✓ | ✓ |
| Yokoyama (2006)160 | ✓ | ||||
| Insulin naive, oral antihyperglycaemic drugs – glargine vs NPH insulin | |||||
| Eliaschewitz (2006)161 | ✓ | ||||
| Fritsche (2003)162 | ✓ | ✓ | ✓ | ✓ | |
| HOE 901/2004 Study Investigators Group (2003)163,164 | ✓ | ✓ | ✓ | ✓ | |
| Massi Benedetti (2003)165 | ✓ | ✓ | |||
| Meneghini (2005)166 | ✓ | ||||
| Yki-Järvinen (2000)137 | ✓ | ✓ | ✓ | ✓ | |
| Yki-Järvinen (2006)26,167 | ✓ | ✓ | ✓ | ||
| Raskin (1998)168 | ✓ | ✓ | |||
| Riddle (2003)169 | ✓ | ✓ | ✓ | ✓ | |
| Rosenstock (2006)170 | ✓ | ||||
| Previous insulin – insulin detemir | |||||
| Haak (2005)171 | ✓ | ✓ | |||
| Insulin naive – insulin detemir | |||||
| Hermansen (2006)172 | ✓ | ✓ | |||
| Unclear | |||||
| Witthaus (2000)173 | ✓ | ||||
There was one main trial of insulin glargine considering patients with previous insulin treatment [Rosenstock et al. (2001)159], whereas the remainder of the glargine trials included previously insulin-naive patients who had been on oral antihyperglycaemic agents (OHAs) before the trial and continued an oral regimen during the trial (either their previous treatment or a new treatment as specified by the trial). Of the remaining glargine trials in patients with previous insulin treatment, the trial by Fonseca et al. (2004)158 was in fact a subgroup analysis of Rosenstock et al. (2001). 159 This trial included both patients using a once-daily and a twice-daily insulin regimen, and Fonseca et al. (2001)157 considered only the subgroup on a once-daily insulin regimen. The trial by Yokoyama et al. (2006)160 used two different insulin regimens – dose titration in the glargine group and an unchanged dose of NPH in the comparison group, which was considered to be an inappropriate comparison in the review by Horvath et al. (2007). 141 Although the trial was included in their review, it was not considered in detail and it was not included in any analyses. Of the trials on insulin detemir, one included patients previously on insulin and the other included insulin-naive patients.
The individual reviews included between five and nine trials of insulin glargine versus NPH insulin, and two trials of insulin detemir versus NPH insulin. Both reviews assessing insulin detemir included the same trials, whereas only two trials of insulin glargine were included in all reviews. The reviews summarised data of between around 1400 and around 4700 patients in the included trials.
Design
All included trials were open-label RCTs and many were described as multicentre trials. Some trials had a non-inferiority or equivalence design. A number of trials were published as abstracts only (especially in the older reviews). Trial duration was between 4 and 52 weeks. Most trials came from Europe or North America, two also included data from South Africa, and one was conducted in participants from Latin America. A substantial number of trials were industry funded.
Trial quality
Trial quality was generally rated as rather poor. Blinding was considered difficult or impossible by most reviews, as insulins glargine and detemir exist as a clear solution, whereas NPH insulin has a milky appearance. The review by Horvath et al. (2007)141 stresses the bias that can be introduced by lack of blinding and especially the lack of blinding of outcome assessment, which does not seem to have been mentioned or considered by any of the trials. Horvath et al. considered all of their included trials to have been of insufficient methodological quality, with poor reporting of randomisation in most trials, adequate allocation concealment in five trials, discontinuation rates of between 1.6% and 10.2% and an ITT approach in all main analyses. The studies included in the review by Tran et al. (2007)142 had a mean Jadad score of 2.4 (out of 5, but blinding being impractical, a perfect score was not possible), with adequate allocation concealment in four trials and ITT analysis in 90%. Warren et al. (2004)144 considered quality assessment to be possible for the two full publications included in their review, which both scored 2 on the Jadad score, with none of them specifying a blinded outcome assessment. The Wang review (2003)143 did not present a formal quality assessment, but suggested that there was inconsistent reporting of mean or adjusted mean changes in primary and secondary efficacy end points within and between treatment groups, and that studies were generally statistically underpowered.
Participants
Patients with type 2 diabetes included in the reviews had a mean age of between 53 and 62 years. Where reported, between 36% and 49% of participants were female, patients had a mean BMI of between 27 and 35 kg/m2, a diabetes duration of between 8 and 14 years, and a mean baseline HbA1c value of between 7.9 to 9.7%.
Interventions
As mentioned above, there was one main trial of insulin glargine156–159 and one of insulin detemir171 in patients on previous insulin therapy without concomitant OHAs. In three trials of insulin-naive patients using oral therapy,26,161,162 the patient’s previous oral therapy was stopped and replaced by glimepiride161,162 or metformin. 26 In the other trials, the previous oral therapy was continued. OHAs included metformin, acarbose, pioglitazone, rosiglitazone, sulfonylurea or other insulin secretagogues or alpha-glucosidase inhibitors. One glargine trial included pre-meal regular insulin159 and one detemir trial included pre-meal insulin aspart. 171 Most glargine trials compared bedtime glargine with bedtime NPH, but one162 compared morning glargine with bedtime glargine and bedtime NPH, and in one,159 patients received glargine at bedtime and NPH either once at bedtime or twice – at bedtime and in the morning. One of the detemir trials171 used detemir or NPH once daily at bedtime or twice daily at bedtime and in the morning, whereas the other172 used a twice-daily regimen of detemir or NPH. Trials used different dose titration targets, between 4.5 and 7.8 mmol/l for FBG, or of 7–7.5% for HbA1c level.
Outcomes
Outcomes reported included HbA1c, FPG, blood glucose profiles, hypoglycaemic episodes (overall, symptomatic, severe and nocturnal), the percentage of patients reaching the titration target, weight change, mortality, QoL and adverse events. None of the trials published diabetes secondary complication rates [although Horvath et al. (2007)41 retrieved some unpublished information], and there were no QoL data (one trial reported on patient satisfaction). Trials were underpowered to assess mortality. Weight change was not systematically reported.
Review quality
The review by Duckworth and Davis (2007)140 was of poor quality. Its search strategy was restricted to a PubMed search and English articles only, and no information was given on other methodological procedures such as study selection, quality assessment of trials, data extraction or data analysis. Inclusion criteria were briefly specified, but only for participants, interventions and outcomes, not for study design.
Both the Cochrane review by Horvath et al. (2007)41 and the Canadian HTA Assessment by Tran et al. (2007)142 were of good quality. Inclusion criteria were well described, as was study selection, quality assessment of trials, data extraction, and data analysis. A comprehensive search was carried out and described in detail. Study flow was shown. Both reviews included a meta-analysis.
The UK HTA Assessment by Warren et al. (2004)144 appears good but had some reporting omissions. Inclusion criteria were well described and the search strategy was very comprehensive. However, it is unclear whether study selection and quality assessment were done in duplicate and data extraction was only done by one reviewer. Study flow was not shown.
The review by Wang (2003)143 was of poor quality. Inclusion criteria were described and the search strategy was adequate. However, study selection, quality assessment, data extraction and data analysis were not described, nor was study flow shown. Although no details of quality assessment methodology were given, some comments on study quality were made.
Results
Main results are shown in Table 17 and subgroup analyses in Table 18.
| Study | Outcome | n (studies) | Results – magnitude of change/difference | Statistical significance |
|---|---|---|---|---|
| All studies – glargine vs NPH insulin | ||||
| HbA1c | ||||
| Horvath (2007)141 | HbA1c (%) (studies with available data) | 4 | WMD 0.1% (95% CI –0.1 to 0.2) | p = NS |
| HbA1c (%) (all studies, pooled SD) | 6 | WMD 0.00% (95% CI –0.1 to 0.1) | p = NS | |
| Tran (2007)142 | HbA1c (%) | 7 | Meta-analysis, WMD 0.05 (95% CI –0.07 to 0.16) | p = NS; no significant difference for analysis by different cointerventions |
| Hypoglycaemia | ||||
| Horvath (2007)141 | Severe hypoglycaemia | 4 | Meta-analysis, 6-month studies only, Peto OR 0.70 (95% CI 0.40 to 1.23) | p = NS; no significant difference or no statistical information for remaining three studies |
| Symptomatic hypoglycaemia | 3 | Meta-analysis, 6-month studies only, RR 0.84 (95% CI 0.75 to 0.95) | Significantly fewer with glargine, p = 0.005; for remaining four studies: three studies no significant difference, one significant in favour of glargine (p < 0.02) | |
| Overall hypoglycaemia | 1 |
Morning glargine: 74% Evening glargine: 68% Evening NPH insulin: 75% |
p = NS | |
| Nocturnal hypoglycaemia | 3 | Meta-analysis, 6-month studies only, RR 0.66 (95% CI 0.55 to 0.80) | Significantly fewer with glargine, p < 0.0001; also significant results for the three studies not included in the meta-analysis but reporting on nocturnal hypoglycaemia | |
| Tran (2007)142 | Overall hypoglycaemia | 6 | Meta-analysis, RR 0.89 (95% CI 0.83 to 0.96), NNT 14 (95% CI 9 to 33) | p = 0.002; no significant difference for analysis by different cointerventions |
| Severe hypoglycaemia | 4 | Meta-analysis, RR 1.09 (95% CI 0.56 to 2.12) | p = NS; no significant difference for analysis by different cointerventions | |
| Nocturnal hypoglycaemia | 5 | Meta-analysis, RR 0.57 (95% CI 0.44 to 0.74), NNT 8 (95% CI 6 to 11) | p < 0.0001; no significant difference for analysis by different cointerventions | |
| Glycaemic excursions | ||||
| Tran (2007)142 | Eight-point blood glucose profiles | 3 | Generally no statistically significant difference between glucose profiles for glargine vs NPH; pre-dinner values lower in two studies for glargine, and in one study for morning (but not evening) glargine vs evening NPH | |
| Total daily dose – not reported | ||||
| Weight change – not reported | ||||
| Complication rates | ||||
| Horvath (2007)141 | Mortality | 3 | Small numbers, no study adequately powered to assess this parameter | |
| New development of non-proliferative retinopathy | 1 |
Glargine: 8.4% NPH insulin: 14% |
p-value not reported | |
| Development of clinically significant macular oedema (of people with no retinopathy) | 1 |
Glargine: 1.8% NPH insulin: 2.4% |
p-value not reported | |
| Progression of retinopathy by more than three stages | 2 |
Glargine: 5.9–7.5% NPH insulin: 2.7–9.1% |
p-value not reported for one study, significantly more with glargine in the other study, p = 0.028 | |
| Development of clinically significant macular oedema | 1 | Glargine: 11.2% NPH insulin: 6.5% | p = NS | |
| Tran (2007)142 | Mortality | 4 | None of reported deaths thought to be related to study medication | |
| Adverse events | ||||
| Horvath (2007)141 | Overall AEs | 4 | Numbers comparable between groups | |
| Serious AEs | 2 | Numbers comparable between groups | ||
| AEs possibly related to treatment | 4 | Numbers comparable between groups | ||
| Patients withdrawing due to AEs | 6 | Numbers comparable between groups | ||
| Tran (2007)142 | AEs | 10 | No significant differences in AEs between glargine and NPH | |
| Health-related QoL | ||||
| Horvath (2007)141 | Diabetes Treatment and Satisfaction Questionnaire | 1 | More pronounced improvement of treatment satisfaction reported with glargine vs NPH | p < 0.05 |
| Previous insulin – glargine vs NPH insulin | ||||
| HbA1c | ||||
| Duckworth (2007)140 | HbA1c (%) | 2 |
Glargine: –0.41% NPH insulin: –0.46% to –0.59% |
Change in HbA1c similar between groups |
| Target reached (HbA1c ≤ 7.0 to ≤ 7.5; FBG ≤ 6.7 mmol/l) | 2 |
HbA1c Glargine: 18% NPH insulin: 18% FBG Glargine: 29.6% to 34% NPH insulin: 24% to 27.1% |
Similar between groups for both studies | |
| Wang (2003)143 | HbA1c (%) | 2 |
Glargine: –0.35% to –0.41% NPH insulin: –0.44% to –0.59% |
p = NS in one study, not reported for the other |
| Warren (2004)144 | HbA1c (%) | 2 |
Glargine: –0.35% NPH insulin: –0.44% Numbers reported for only one |
p = NS for both |
| Patients reaching target FBG | 1 |
Glargine: 29.6% NPH insulin: 27.1% |
p = NS | |
| Hypoglycaemia | ||||
| Duckworth (2007)141 | Overall symptomatic hypoglycaemia | 2 |
Glargine: 46% to 61.4% NPH insulin: 60% to 66.8% |
p < 0.05 in one study, p = NS in the other |
| Severe hypoglycaemia | 2 |
Glargine: 0% to 0.4% NPH insulin: 2.0% to 2.3% |
p = NS | |
| Nocturnal hypoglycaemia | 2 |
Glargine: 15% to 26.5% NPH insulin: 27 to 35.5% |
p < 0.05 in one study, p = NS in the other | |
| Wang (2003)143 | ≥ 1 episode of hypoglycaemia | 1 |
Glargine: 46.2% NPH insulin: 60.4% |
p = 0.048 |
| Reported nocturnal hypoglycaemic events | 2 |
Glargine: 15.4% to 31.3% NPH insulin: 27.1% to 40.2% |
p = NS in one study, p = 0.014 in other study | |
| Symptomatic hypoglycaemia | 2 |
Glargine: 17.3% to 61.4% NPH insulin: 31.3% to 66.8% |
p = NS in 1 study, p = 0.002 in the other | |
| Episodes of severe hypoglycaemia | 1 |
Glargine: 6.6% (–0.4%) NPH insulin: 10.4% (–2.3%) |
p = NS | |
| Warren (2004)144 | Symptomatic hypoglycaemia | 2 |
Glargine: 6.6% to 17.3% NPH insulin: 10.4% to 31.3% |
p = NS in one study, p < 0.05 in the other study |
| Nocturnal hypoglycaemia | 2 |
Glargine: 15.4% to 35% NPH insulin: 27.1% to 43.7% |
p = NS in one study, p < 0.05 in the other study | |
| Severe hypoglycaemia | 2 | Not reported separately | ||
| Glycaemic excursions – not reported | ||||
| Total daily dose | ||||
| Warren (2004)144 | Insulin use | 1 |
For patients on pre-trial once-daily NPH, slightly more insulin used at trial end than at baseline (no data presented) For patients on pre-trial more than once-daily NPH, people on glargine used slightly less at trial end (reduced by 4.4 U/day) and patients treated with NPH used about the same (no more data presented) |
Unclear |
| Weight change | ||||
| Wang (2003)143 | Weight gain | 1 |
Glargine: +0.4 kg NPH insulin: +1.4 kg p < 0.001, CIs not reported |
|
| Complication rates – not reported | ||||
| Adverse events | ||||
| Wang (2003)143 | Injection site pain | 1 |
28 weeks Greater number of patients reported injection site pain with insulin glargine compared with NPH insulin (pain usually mild and did not result in discontinuation of treatment) |
|
| Warren (2004)144 | Injection site pain | 1 |
Glargine: 10.4% NPH insulin: 7.7% |
Unclear, probably p < 0.05; but mild and no dropouts as a result |
| Insulin antibodies | 1 | No increases in either comparison group | ||
| Health-related QoL – not reported | ||||
| Insulin-naive, oral antihyperglycaemics – glargine vs NPH insulin | ||||
| HbA1c | ||||
| Duckworth (2007)141 | HbA1c (%) | 5 |
Glargine: –0.46% to –2.36% NPH insulin: –0.38% to –2.44% |
Four trials HbA1c similar between groups, one trial significantly more HbA1c reduction with morning glargine than bedtime NPH (p < 0.001) and with morning glargine vs bedtime glargine (p = 0.009) |
| Target reached (HbA1c ≤ 7.0 to ≤ 7.5; FBG ≤ 6.7 mmol/l) | 4 |
HbA1c Glargine: 33% to 58% NPH insulin: 32% to 57.3% FBG Glargine: 40.7% to 42% NPH insulin: 35.1% to 44% |
Three trials no significant difference, one trial significantly more patients reaching target with morning glargine than with bedtime glargine or NPH (p < 0.05) | |
| Wang (2003)143 | HbA1c (%) | 4 |
Glargine: –0.76% to –1.64% NPH insulin: –0.66% to –1.63% |
Three trials no significant difference between glargine and NPH, one trial significantly more HbA1c reduction with morning glargine than bedtime NPH (p < 0.001) and with morning glargine vs bedtime glargine (p = 0.009) |
| Target reached (≤ 7.0% to < 8.0%) | 2 |
Glargine: 53.8 to 57.9% NPH insulin: 43.9 to 57% |
One study p = NS, one study unclear | |
| Warren (2004)144 | HbA1c (%) | 3 |
Glargine: –0.8% NPH insulin: –0.8% Numbers only reported for one |
p = NS for all studies |
| Patients reaching target FBG | 1 |
Glargine: 7.7% NPH insulin: 7.6% |
p = NS | |
| Hypoglycaemia | ||||
| Duckworth (2007)140 | Overall symptomatic hypoglycaemia | 6 |
Glargine: 18.8% to 56%, 5.5 to 13.9 events/patient-year NPH insulin: 32.4% to 58%, 8.0 to 17.7 events/patient-year |
p < 0.05 in four studies, p = NS in two studies |
| Severe hypoglycaemia | 2 |
Glargine: 0% to 2.5% NPH insulin: 0% to 1.8% |
p = NS | |
| Nocturnal hypoglycaemia | 5 |
Glargine: 7.3% to 23%, 4.0 events/patient-year NPH insulin: 19.1% to 38%, 6.9 events/patient-year |
p < 0.05 in all studies | |
| Wang (2003)143 | Hypoglycaemic episodes (%) | 2 |
Glargine: 7.3% to 33% NPH insulin: 19.1% to 43% |
p < 0.05 for both studies |
| Nocturnal hypoglycaemia | 3 |
Glargine: 9.9% to 47% NPH insulin: 24% to 55% |
p < 0.05 for all studies | |
| Achieving HbA1c ≤ 7.0% without nocturnal hypoglycaemia | 1 |
Glargine: 33% NPH insulin: 27% |
p < 0.05 | |
| Severe hypoglycaemia | 1 |
Glargine: 2.5% NPH insulin: 2.3% |
p = NS | |
| Warren (2004)144 | Symptomatic hypoglycaemia | 2 |
Glargine: 7.3% NPH insulin: 19.1% Numbers only for one trial |
p < 0.05 for both |
| Nocturnal hypoglycaemia | 1 | No numbers reported in trial | Significantly fewer in glargine group, p = 0.0001 | |
| Severe hypoglycaemia | 0 | Not reported by studies | ||
| Glycaemic excursions | ||||
| Wang (2003)143 | 1 | Change in FPG levels significantly greater both before and after dinner with insulin glargine (p = 0.035, no details); FPG levels at 3.00 a.m. similar between groups (glargine: 133, SE 3.6 mg/dl; NPH: 131.4, SE 3.6 mg/dl) | ||
| Total daily dose | ||||
| Warren (2004)144 | Insulin use | 1 |
Glargine: 23 U/day NPH insulin: 21 U/day |
Unclear |
| Weight change | ||||
| Wang (2003)143 | 2 |
Glargine: no change to +2.57 kg NPH insulin: no change to +2.34 kg |
p = NS for both studies | |
| Complication rates – not reported | ||||
| Adverse events | ||||
| Wang (2003)143 | Injection site pain | 1 | Greater number of patients reported injection site pain with insulin glargine compared with NPH insulin (pain usually mild and did not result in discontinuation of treatment) | |
| Warren (2004)144 | Insulin antibodies | 1 | No increases in either comparison group | |
| Health-related QoL | ||||
| Wang (2003)143 | Diabetes Treatment Satisfaction Well-Being Questionnaire | 1 | No numeric data reported; increases in treatment satisfaction significantly greater for insulin glargine than NPH insulin at week 36 (p = 0.033); small increase in the perceived frequency of hypoglycaemia in both groups, but no significant difference between groups | |
| FPG (where HbA1c not reported) | ||||
| Duckworth (2007)140 | FPG | 1 | Not reported for groups separately, decrease from baseline –3.10 to –3.49 mmol/l | Similar between groups |
| Wang (2003)143 | FPG | 1 |
Glargine with 30 µg/ml of zinc: –2.8 mmol/l Glargine with 80 µg/ml of zinc: –2.6 mmol/l NPH insulin: –2.3 mmol/l |
p-value not reported |
| All studies – detemir vs NPH insulin | ||||
| HbA1c | ||||
| Horvath (2007)141 | HbA1c (%) | 2 | Meta-analysis using different ways of estimating missing SDs, WMD 0.12% (95% CI 0.01 to 0.23), WMD with pooled SD 0.15% (95% CI –0.02 to 0.32) | First calculation yields significant result (p = 0.03) in favour of NPH, but well within predefined non-inferiority margin of 0.4% HbA1c; second calculation, p = NS |
| Tran (2007)142 | HbA1c (%) | 2 | Meta-analysis, WMD 0.11% (95% CI –0.03 to 0.26) | p = NS; no significant difference for analysis by different cointerventions |
| Hypoglycaemia | ||||
| Horvath (2007)141 | Severe hypoglycaemia | 2 |
Meta-analysis Peto OR 0.5 (95% CI 0.18 to 1.38) |
p = NS |
| Symptomatic hypoglycaemia | 1 |
Detemir: 4.9 events/patient-year NPH insulin: 9.7 events/patient-year Relative risk 0.56 (95% CI 0.42 to 0.74) |
p < 0.001 | |
| Overall hypoglycaemia | 2 | Meta-analysis, RR 0.82 (95% CI 0.74 to 0.90) | p < 0.0001 | |
| Nocturnal hypoglycaemia | 2 | Meta-analysis, RR 0.63 (95% CI 0.52 to 0.76) | p < 0.00001 | |
| Tran (2007)142 | Overall hypoglycaemia | 1 | Relative risk 0.91 (95% CI 0.75 to 1.11) | p = NS |
| Nocturnal hypoglycaemia | 1 | Relative risk 0.66 (95% CI 0.45 to 0.96) | p < 0.05 | |
| Glycaemic excursions | ||||
| Tran (2007)142 | Eight-point blood glucose profiles | 2 | Glucose profiles similar for detemir vs NPH; no difference depending on cointervention (insulin aspart or OHAs) | |
| Total daily dose – not reported | ||||
| Weight change | ||||
| Horvath (2007)141 | Weight change | 2 | Difference in weight gain between detemir and NPH –0.8 to –1.6 kg | p < 0.05 |
| Complication rates | ||||
| Horvath (2007)141 | Mortality | 1 | Small numbers, no study adequately powered to assess this parameter | |
| Cardiovascular morbidity | 1 | Very small numbers, no conclusions can be drawn | ||
| Diabetic late complications | 1 | Very small numbers, no conclusions can be drawn | ||
| Tran (2007)142 | Mortality | 1 | None of reported deaths thought to be related to study medication | |
| Adverse events | ||||
| Horvath (2007)141 | AEs | 2 | No difference in frequency of AEs | |
| Tran (2007)142 | AEs | 1 | No significant differences in AEs between detemir and NPH | |
| Health-related QoL – not reported | ||||
| Study | Outcome | Factor | n (studies) | Results [of meta-analysis (95% CI) or narrative] | Statistical significance |
|---|---|---|---|---|---|
| All studies – glargine vs NPH insulin | |||||
| HbA1c | |||||
| Horvath (2007)141 | HbA1c (%) | Morning glargine vs evening glargine or NPH | 1 | Greater reduction in HbA1c from baseline in the morning group than in evening groups | p < 0.05 |
| Insulin-naive patients | 1 | No significant difference | p = NS | ||
| Patients applying insulin only once daily | 1 | No significant difference | p = NS | ||
| Hypoglycaemia | |||||
| Horvath (2007)141 | At least one episode of symptomatic hypoglycaemia | Insulin-naive patients | 1 |
Glargine: 33% NPH insulin: 43% |
p = 0.04 |
| At least one episode of symptomatic hypoglycaemia | Patients applying insulin only, once daily | 1 |
Glargine: 17% NPH insulin: 31% |
p < 0.002 [wrong numbers in Horvath (2007)141] | |
| Nocturnal hypoglycaemia | Insulin-naive patients | 1 |
Glargine: 10% NPH insulin: 24% |
p = 0.0001 | |
| Nocturnal hypoglycaemia | Patients applying insulin only, once daily | 1 |
Glargine: 15% NPH insulin: 27% |
p = NS | |
| Complication rates | |||||
| Horvath (2007)141 | Development of clinically significant macular oedema | Patients without insulin pretreatment vs patients with insulin pretreatment | 1 |
Without insulin pretreatment Glargine: 14% NPH insulin: 4% With insulin pretreatment Glargine: 1.9% NPH insulin: 12.7% |
p-value not reported |
| Insulin-naive, oral antihyperglycaemics – glargine vs NPH insulin | |||||
| Duckworth (2007)140 | HbA1c | BMI > 28 kg/m2 | 1 |
Change from baseline Glargine: –0.42% NPH insulin: –0.11% |
p = 0.0237 |
| Wang (2003)143 | Nocturnal hypoglycaemia | Patients reaching/not reaching FPG target (≤ 120 mg/dl) | 1 |
52 weeks Target reached Glargine: 12.6% NPH insulin: 28.8% Target not reached Glargine: 9.0% NPH insulin: 21.4% |
p < 0.05 for both subgroups glargine vs NPH |
Glycaemic control
Trials generally showed a reduction in HbA1c level from baseline to end of study, but without any difference between comparison groups. Horvath et al. (2007)141 carried out two meta-analyses regarding HbA1c results for insulin glargine versus NPH insulin, one including only the four for which SDs were available or could be calculated, and the other including studies where this was not the case and where a pooled SD was used (two extra studies, i.e. six in the meta-analysis). In both analyses, there was no significant difference between glargine and NPH in end-of-study level of HbA1c, with a WMD between groups of around 0 (for all six studies WMD 0.0, 95% CI –0.01, 0.1). Similarly, Tran et al. (2007)142 in their meta-analysis of seven studies found no significant difference in HbA1c values between glargine and NPH (WMD 0.05, 95% CI –0.07 to 0.16). For the remaining reviews, results were presented according to whether patients had received previous insulin treatment without oral treatment or were previously insulin naive with concomitant oral treatment. For the two trials (or rather one with subgroup analysis) of people with previous insulin treatment, HbA1c level at the end of study was similar between the glargine and NPH groups (reduction from baseline between –0.35 and –0.6%). For the trials in insulin-naive patients using concomitant oral therapy, most trials showed no significant difference between glargine and NPH at the end of the study either, except in the study by Fritsche (2003),162 where, after 24 weeks of treatment HbA1c level was significantly more reduced with morning glargine than with evening glargine or evening NPH (–1.24% versus –0.96% and –0.84%, respectively). Subgroup analyses in two trials, one of insulin-naive patients and one of patients applying insulin once rather than twice daily also showed no difference in HbA1c values between groups. However, one study found a significant effect for HbA1c in favour of glargine in a subgroup analysis of patients with a BMI of more than 28 kg/m2 (HbA1c change from baseline –0.42% with glargine and –0.11% with NPH, p = 0.024). There was no significant difference in end-of-study HbA1c values in the two studies of insulin detemir versus NPH, irrespective of previous treatment and cointerventions.
Where reported, the percentages of patients reaching the FPG or HbA1c targets were also similar between insulin glargine and NPH insulin, except in the study by Fritsche (2003),162 where significantly more patients reached the target with morning glargine than with evening glargine or evening NPH.
Hypoglycaemia
Severe hypoglycaemia
In their meta-analysis of studies of glargine versus NPH, Horvath et al. (2007)141 summarised four studies of 6 months’ duration (to avoid imbalance due to different study durations) and found no significant difference in the frequency of severe hypoglycaemia between glargine and NPH [Peto odds ratio (OR) 0.70, 95% CI 0.40 to 1.23]. There was no significant difference – or no statistical information available – for the remaining three studies assessing severe hypoglycaemia that were not included in the meta-analysis. Similarly, Tran et al. (2007)142 did a meta-analysis of severe hypoglycaemia in four studies and found no significant difference between glargine and NPH (RR 1.09, 95% CI 0.56 to 2.12) and no significant difference when analysing trials depending on their cointerventions. In the remaining reviews, no significant differences in severe hypoglycaemia were reported for patients on previous insulin therapy or for previously insulin-naive patients on oral antihyperglycaemic therapy (and continuing oral therapy). Similarly, no significant difference was found for severe hypoglycaemia for the two trials of insulin detemir versus NPH insulin.
Overall and symptomatic hypoglycaemia
Definition of ‘overall’ and ‘symptomatic’ hypoglycaemia varied, with some reviews summarising under ‘overall’ hypoglycaemia ‘overall symptomatic hypoglycaemia’ and some referring to ‘any hypoglycaemic event’. Results for this outcome were inconclusive. In their meta-analysis of three 6-month studies of glargine versus NPH, Horvath et al. (2007)141 found significantly fewer symptomatic hypoglycaemic episodes with glargine than with NPH (RR 0.84, 95% CI 0.75 to 0.95), but only one of the remaining four studies reporting this outcome found a significant effect in favour of glargine. Similarly, the one study reporting overall hypoglycaemia found no significant difference between glargine (morning or evening) and NPH.
Tran et al. (2007)142 included six trials in their meta-analysis of overall hypoglycaemia and found a significant difference in favour of glargine (RR 0.89, 95% CI 0.83 to 0.96). Considering studies in patients previously on insulin separately, the trial by Rosenstock et al. (2001)159 found no significant effect on overall symptomatic hypoglycaemia in favour of glargine, whereas the subgroup analysis of that study including patients on once daily insulin did (46.2% versus 60.4% of patients with one or more episodes). In the analyses of insulin-naive patients on oral therapy, Duckworth and Davis (2007)140 summarised data for overall symptomatic hypoglycaemia in six studies and found a significant effect in favour of glargine versus NPH in four of these (where between 10% and 13% fewer patients had symptomatic hypoglycaemias in the glargine groups, or between 2.5 and 3.8 fewer events occurred per patient-year). Warren et al. (2004)144 and Wang (2003)143 included two studies in their analyses and found significant differences in favour of glargine for both of them for hypoglycaemic episodes/symptomatic hypoglycaemia (10 or more per cent less with glargine). For insulin detemir, Horvath et al. (2007)141 found a significant difference in favour of detemir in one study for symptomatic hypoglycaemia (not reported by the other study) (4.9 versus 9.7 events per patient-year), and for overall hypoglycaemia the meta-analysis of the two included studies gave a significant result (RR 0.82, 95% CI 0.74 to 0.90, p < 0.0001).
Nocturnal hypoglycaemia
Results for nocturnal hypoglycaemias were clearly in favour of the long-acting insulin analogues. In their meta-analysis of three 6-month studies of glargine versus NPH, Horvath et al. (2007)141 obtained a RR of 0.66 (95% CI 0.55 to 0.80, p < 0.0001). The three studies not included in the meta-analysis, but reporting on nocturnal hypoglycaemia, also all found a significant result in favour of glargine. Tran et al. (2007)142 included five studies in their meta-analysis and obtained a RR for nocturnal hypoglycaemias of 0.57 (95% CI 0.44 to 0.74) in favour of glargine. Considering studies in patients previously on insulin separately, the trial by Rosenstock et al. (2001)159 found a significant effect on nocturnal hypoglycaemia (31.3 versus 40.2%, with at least one episode of nocturnal hypoglycaemia, p = 0.016), whereas the subgroup analysis of that study including patients on once-daily insulin did not. All trials of previously insulin-naive patients on oral therapy found significantly fewer nocturnal hypoglycaemias with insulin glargine than with NPH insulin (between ∼10% to 20% fewer patients with nocturnal hypoglycaemias with glargine). One trial also reported that significantly more patients using glargine reached the HbA1c target of 7% or less without nocturnal hypoglycaemias (33% versus 27% using NPH, p < 0.05). With respect to insulin detemir, the meta-analysis of nocturnal hypoglycaemia in the two trials by Horvath et al. (2007)141 obtained a RR of 0.63 (95% CI 0.52 to 0.76, p < 0.00001) in favour of detemir [similar relative risk in the review by Tran et al. (2007),142 which reported data from only one trial].
Glycaemic excursions
Data on glycaemic excursions were only systematically summarised by the review by Tran et al. (2007),142 who reported data from three studies that had measured eight-point glucose profiles. There was generally no statistically significant difference between glucose profiles for glargine versus NPH with the exception of two trials. One study showed significantly lower pre-dinner glucose levels for glargine, and the other reported significant values for morning (but not evening) glargine in comparison with evening NPH. For insulin detemir, eight-point glucose profiles were similar in comparison to NPH, irrespective of the cointervention.
Total daily insulin dose
Total daily insulin dose was not systematically reported by the systematic reviews. Warren et al. (2004)144 reported for one trial of patients with previous insulin use, that patients on pre-trial once-daily NPH used slightly more insulin at trial end than at baseline, and patients on more than once-daily NPH pre-trial used slightly less insulin in the glargine group at the end of the trial (reduced by 4.4 U/day) than patients treated with NPH, who used about the same (no more data presented). For one trial of previously insulin-naive patients on oral therapy, Warren et al. (2004)144 reported similar insulin consumption of 23 U/day for glargine and 21 U/day for NPH, but statistical information was not provided. Insulin daily doses were not provided for the trials using insulin detemir.
Weight change
Weight change was not systematically reported by the systematic reviews. Wang (2003)143 reported a significant change in weight gain for a trial of patients previously treated with insulin, with patients receiving insulin glargine gaining significantly less weight than patients on NPH insulin (+0.4 kg versus +1.4 kg, p < 0.001). In two other trials of previously insulin-naive patients on oral therapy, no significant difference in weight change was seen between the glargine and NPH insulin groups (total changes between no change and +2.6 kg). Horvath et al. (2007)141 reported significantly less weight gain with insulin detemir than NPH insulin with a weight difference of between 0.8 and 1.6 kg between the comparison groups (p < 0.05).
Diabetic complications
Data on diabetic complications were not systematically reported by the reviews – and were generally not available in the trials (and trials were underpowered for assessing such outcome parameters). Several reviews – and trials – reported mortality data, but numbers were generally small and deaths were considered to be unrelated to the trial interventions. No data on diabetic late complications were included in any of the reviews, but Horvath et al. (2007)141 found some information on diabetic retinopathy for one trial of patients with previous insulin treatment and for one trial of patients on oral therapy (some of whom had been insulin pretreated). In the trial including oral therapy, 8.4% of patients in the insulin glargine group and 14% of patients in the NPH insulin group who had had no retinopathy at baseline developed non-proliferative retinopathy, and 1.8% and 2.4%, respectively, developed clinically significant macular oedema. Progression of retinopathy by more than three stages was seen in 5.9% of patients on glargine and 9.1% of patients on NPH (no significance values reported). In the study of patients on previous insulin treatment without oral therapy, significantly more patients on glargine had a progression of retinopathy by three or more stages than with NPH (7.5 versus 2.7%, p = 0.028). In the study of patients on concomitant oral therapy, no significant difference in development of clinically significant macular oedema was seen between glargine and NPH (11.2% with glargine, 6.5% with NPH, p = NS). However, there was a marked difference in this outcome between previously insulin-naive patients and patients pretreated with insulin. In insulin-naive patients, the development of clinically significant macular oedema in 14% in the glargine group and 4% in the NPH group. In contrast, patients previously treated with insulin had incidences of 1.9% and 12.7% (no significance reported). Numbers of diabetic late complications occurring in one of the trials of insulin detemir were too small to draw any conclusions.
Adverse events
No significant differences in adverse events, number of patients with adverse events, severe adverse events, or withdrawals because of adverse events were generally seen between insulin glargine or detemir and NPH insulin. There was some indication in some trials that a greater number of patients on insulin glargine reported injection site pain than patients on NPH insulin, but pain was usually mild and did not result in discontinuation of treatment. Where reported, no differences in insulin antibodies were seen between study groups. None of the studies was long enough to assess any longer-term effects.
Health-related QoL
No data were reported on health-related QoL. Wang (2003)143 and Horvath et al. (2007)141 reported on one study each, and it was suggested that there was a significantly greater improvement of treatment satisfaction with insulin glargine than with NPH insulin.
Additional reviews identified after completion of this review
Two systematic reviews, both including meta-analyses, were identified after completion of the main analyses for this review. The review by Bazzano et al. (2008)145 focused on the safety and efficacy of glargine compared with NPH insulin in type 2 diabetes, whereas the review by Monami et al. (2008)146 considered both glargine and detemir compared with NPH insulin in type 2 diabetes. Bazzano et al. included 12 RCTs and Monami et al. included 11 RCTs of glargine versus NPH insulin and three RCTs of detemir versus NPH insulin. All of the RCTs included in the two reviews have been considered by the present review.
The review by Bazzano et al. was of good quality. The search strategy was thorough, inclusion criteria were described, as was data extraction, quality assessment and data analysis. Study flow was shown. Descriptive and quality data were given for each included RCT. The review by Monami et al. was also of good quality. Inclusion criteria, search strategies, data extraction, quality assessment and data analysis were described. Study flow was shown and descriptive and quality data were shown for each trial.
Both reviews suggested that there was no significant difference between glargine or detemir and NPH insulin for glycaemic control. Bazzano et al. reported slightly less patient-reported hypoglycaemia with glargine than with NPH insulin, and Monami et al. reported less symptomatic and nocturnal hypoglycaemia with glargine or detemir versus NPH. Bazzano et al. reported slightly less weight gain with NPH than with glargine, whereas Monami et al. reported no differences in BMI when comparing glargine and NPH, but a lower BMI with detemir than with NPH insulin.
Review conclusions and research recommendations
Review conclusions and recommendations are shown in Table 19.
| Study | Conclusions (medical effectiveness) | Recommendations for research | Comments |
|---|---|---|---|
| Bazzano (2008)145 |
HbA1c: Results indicate that there is no difference in glycaemic control between glargine and NPH insulin Hypoglycaemia: Results indicate that there is less patient-reported hypoglycaemia with glargine than NPH in patients with type 2 diabetes (absolute differences small but significant for all types, symptomatic and nocturnal hypoglycaemia; not significant for rates of hypoglycaemia) Glycaemic excursions: No relevant trial data reported Total daily dose: No significant difference between groups Weight change: Patients on NPH insulin gained slightly less weight than patients on glargine Complication rates: No relevant trial data reported Adverse events: No relevant trial data reported Health-related QoL: No relevant trial data reported |
Review financially supported by Eli Lilly and Company | |
| Duckworth (2007)140 |
HbA1c: Review suggests that insulin glargine and NPH insulin are similarly effective with respect to achieving and maintaining glucose control Hypoglycaemia: Insulin glargine is associated with a significantly lower risk of hypoglycaemia, particularly nocturnal hypoglycaemia, than NPH insulin Glycaemic excursions: No relevant trial data reported Total daily dose: No relevant trial data reported Weight change: No relevant trial data reported Complication rates: No relevant trial data reported Adverse events: No Relevant trial data reported Health-related QoL: No relevant trial data reported |
None explicit; suggested that QoL research would be useful in eliciting which insulin patients prefer | |
| Horvath (2007)141 |
HbA1c: No significant difference between insulin glargine or insulin detemir and NPH insulin (statistically significant but clinically unimportant superiority for detemir vs NPH) Hypoglycaemia: No significant difference for severe hypoglycaemia; rate of overall, symptomatic and nocturnal hypoglycaemia significantly lower with glargine or detemir than with NPH, but authors suggest that there is only a minor clinical effect Glycaemic excursions: No relevant trial data reported Total daily dose: No relevant trial data reported Weight change: No conclusions given Complication rates: Only limited information available |
Long-term follow-up data needed to assess effectiveness in terms of diabetes late complications and safety issues Studies in young and old patients (i.e. younger and older than the age range of 55–62 years in the included studies) |
|
|
Adverse events: No significant difference between glargine or detemir and NPH insulin Health-related QoL: No relevant trial data reported; limited data suggesting more treatment satisfaction with glargine than NPH insulin (but only one study and data potentially unreliable) |
More uniform and rigorous reporting of results; including definitions of different types of hypoglycaemia | ||
| Monami (2008)174 |
HbA1c: The use of long-acting insulin analogues in patients with type 2 diabetes does not seem to provide a better glycaemic control in comparison with NPH insulin Hypoglycaemia: Treatment with long-acting insulin analogues in comparison with NPH reduces the risk of nocturnal and symptomatic hypoglycaemia Glycaemic excursions: No relevant trial data reported Total daily dose: No relevant trial data reported Weight change: Detemir, but not glargine, could be associated with smaller weight gain than NPH insulin Complication rates: No relevant trial data reported Adverse events: No relevant trial data reported Health-related QoL: No relevant trial data reported |
Longer-term data are needed to assess the clinical relevance of differences in the effects on weight gain of glargine/detemir | |
| Tran (2007)142 |
HbA1c: No significant difference in HbA1c levels with insulin glargine or detemir in comparison with NPH Hypoglycaemia: Risk of nocturnal hypoglycaemia significantly reduced with insulin glargine compared with NPH, probably also with insulin detemir Glycaemic excursions: No evidence for significant difference in eight-point blood glucose profiles when comparing insulin glargine or detemir with NPH Total daily dose: No relevant trial data reported Weight change: Some trials reported increases in weight, but no differences between comparison groups were quoted Complication rates: No deaths in trials related to study medication Adverse events: No significant differences between comparison groups reported Health-related QoL: No relevant information identified |
None | Six trials in patients with type 2 diabetes were identified after the completion of the assessment; the authors conclude that the results of those trials were unlikely to change the conclusions of the review; only three of the extra trials are valid comparisons of long-acting insulin analogues with NPH and two are included in the review by Horvath (2007);141 the third is presented below |
| Wang (2003)143 |
HbA1c: Insulin glargine appears to have equal clinical efficacy as NPH insulin Hypoglycaemia: Insulin glargine is associated with significant reductions in nocturnal hypoglycaemia compared with NPH insulin Glycaemic excursions: Insulin glargine is associated with lower FPG and FBG levels than NPH insulin Total daily dose: No relevant trial data reported Weight change: No conclusions given Complication rates: No relevant trial data reported Adverse events: Insulin glargine was associated with greater pain at the injection site than NPH insulin Health-related QoL: Greater treatment satisfaction has been reported with insulin glargine than with NPH insulin |
None (only indirect – see Comments) | The authors comment that the place of insulin glargine in routine clinical practice remains to be determined; studies were limited by their open-label design, inadequate sample sizes, use of individual dose titration to achieve FPG ≤ 120 mg/dl, lack of information on cointerventions; use should be limited in patients with type 2 diabetes to those taking multiple daily injections of basal/bolus regimens who have not achieved optimal glycaemic control with NPH insulin who have episodes of symptomatic hypoglycaemia; in insulin-naive patients taking OAD agents, use of insulin glargine should be limited to those who continue to have elevated morning blood glucose levels and episodes of nocturnal hypoglycaemia while taking a combination of oral agents or a combination of bedtime NPH insulin with OAD agents |
| Warren (2004)144 |
HbA1c: Insulin glargine does not appear to improve long-term glycaemic control compared with NPH insulin Hypoglycaemia: Insulin glargine is effective in reducing the number of nocturnal hypoglycaemic episodes, especially when compared to once-daily NPH; equivocal evidence regarding control of symptomatic hypoglycaemia; no evidence of improvement on severe hypoglycaemia Glycaemic excursions: No relevant trial data reported Total daily dose: There are insufficient data to make reliable conclusions regarding insulin dose Weight change: No conclusions given Complication rates: No relevant trial data reported Adverse events: Most common adverse event was injection site pain; where reported, no significant increases in insulin antibodies in either comparison group Health-related QoL: No relevant trial data reported |
Studies of QoL required focusing on assessing both the short-term immediate impact of acute episodes of hypoglycaemia and the longer-term impact of living with a reduced fear of hypoglycaemia | Clinical relevance unclear, as trial patients may have used different regimens than patients in usual clinical practice |
Although there were some differences in assessment of the data between reviews, all reviews essentially came to the same conclusions. All reviews concluded that insulin glargine – and insulin detemir where assessed – led to a glycaemic control equivalent to that when using NPH insulin.
Regarding the occurrence of hypoglycaemia, all reviews concluded that insulin glargine – and where assessed, probably also insulin detemir – were more effective at reducing nocturnal hypoglycaemias than NPH insulin. In addition, there was no between group differences for severe hypoglycaemias, and the evidence was inconclusive regarding overall/symptomatic hypoglycaemias (with some reviews being more optimistic than others). However, the review by Horvath et al. (2007)141 suggested that even the effect on nocturnal hypoglycaemias was only minor. Only Tran et al. (2007)142 systematically assessed glycaemic excursions and concluded that, overall, there was no significant difference in glucose profiles between glargine or detemir and NPH insulin. None of the studies came to any firm conclusions regarding total insulin dose or weight change. Not enough trial information was available to make any conclusions about diabetic secondary complications or health-related QoL. Overall, reviews concluded that there were no significant differences in adverse events between glargine or detemir than with NPH insulin (although there may be slightly more injection site pain with glargine, as reported by some reviews).
In some of the reviews, it was suggested that the clinical relevance of the findings was unclear: trials were thought to have major design flaws (for example, all being open label, giving limited information on important factors such as cointerventions, etc.). In addition, Warren et al. (2004)144 suggested that trial patients may have used different regimens than patients in usual clinical practice.
Not all of the reviews included clear recommendations for research; where given, research recommendations included the need for:
-
long-term follow-up data to assess effectiveness in terms of diabetes late complications and safety issues
-
studies in young and old patients (i.e. younger and older than the age range of 55–62 years in the included studies)
-
more uniform and rigorous study design and reporting of results; including definitions of different types of hypoglycaemia
-
studies of QoL, focusing on assessing both the short-term immediate impact of acute episodes of hypoglycaemia and the longer-term impact of living with a reduced fear of hypoglycaemia; and other aspects of the impact of the different insulin on patients’ QoL.
Randomised controlled trials
Search results
Fourteen papers were identified as potentially relevant RCTs. Of these, six fulfilled the inclusion criteria, but one175 turned out to refer to a trial [Hermansen et al. (2006)172], already included in the review by Horvath et al. (2007). 141 One abstract and one full publication referred to the same trial176,177 of insulin glargine versus insulin detemir. Full data extraction was undertaken for five trials. 143,177–180 Table 20 shows the excluded trials. Trials were excluded because they did not include the comparisons of interest (for example, no comparison with another basal insulin), because data were inadequate or because no outcomes of interest were investigated.
Description of trials
Characteristics of the included trials are shown in Appendix 5.
Design
All five trials were parallel, open-label RCTs, sponsored by industry (where reported). Trial duration was between 12 and 52 weeks. The LEAD (Liraglutide Effect and Action in Diabetes) trial by Pan et al. (2007)179 was carried out in China, Korea and France; the trial by Wang et al. (2007)185 was carried out in China; the PREDICTIVE-BMI trial reported by Montanana et al. (2007)178 was carried out in Spain, and the trials by Philis-Tsimikas et al. (2006)180 and Rosenstock et al. (2008)177 were carried out in various European countries and the USA.
Participants
The trials included between 24 and 582 participants, with between 8 and 291 in each comparison group. The total number of participants was 1818. The LEAD trial (2007)179 was carried out using only Asian participants, and the trial by Wang et al. (2007)185 in Chinese participants. The LEAD trial, and the trials by Philis-Tsimikas et al. (2006),180 Wang et al. (2007)185 and Rosenstock et al. (2008)177 were carried out in insulin-naive patients with concomitant OHAs, whereas the PREDICTIVE-BMI trial (2007)178 was undertaken in participants who had been on insulin (two daily doses, at least one pre-mix) for 3 months or more. The LEAD trial did not detail any required specific previous oral therapy, while the trial by Wang et al. required previous treatment with sulfonylurea or combination treatment. The trial by Philis-Tsimikas et al. specified that previous oral therapy had to have been with metformin, an insulin secretagogue or a combination of the two; at US centres, concomitant treatment with TZDs was permitted throughout the study period, whereas at European centres TZD was to be discontinued before initiation of insulin treatment; use of an alpha-glucosidase inhibitor was permitted but only in combination with another oral agent. The trial by Rosenstock et al. required previous treatment with one or two oral agents (metformin, insulin secretagogues, alpha-glucosidase inhibitors). The PREDICTIVE-BMI trial included patients who were already overweight (BMI of between 25 and 40 kg/m2). Further details of inclusion and exclusion criteria of the trials can be found in Appendix 5. Trial participants had a mean age of between 56 and 62 years. Between 41% and 62% of women took part in the trials. Ethnicity was reported for the Asians in the LEAD trial, who came from 10 different countries of origin (the largest groups from China and South Korea); 99% of participants in the PREDICTIVE-BMI trial were white people, and between 86% and 90% of participants in the trial by Rosenstock et al. (2008) were white people. Mean diabetes duration was between 9 and 16 years. Details of previous diabetes medication for the two trials are shown in Appendix 5. Baseline BMI was between 25 kg/m2 and 32 kg/m2.
Interventions
The trial by Philis-Tsimikas et al. (2006)180 compared three intervention groups, whereas the other trials compared two groups. In the LEAD trial (2007),179 insulin glargine once daily at bedtime plus once-daily glimepiride (3 mg) in the morning was compared with NPH insulin at bedtime plus 3 mg glimepiride once daily in the morning. In both arms, insulin was titrated to a target FBG ≤ 6.7 mmol/l, starting at insulin dose of 0.15 U/kg/day. The trial included a screening phase of 3–4 weeks in which oral treatments were standardised to 3 mg of glimepiride, and patients were given training in self-administration of insulin and self-monitoring of blood glucose levels.
Wang et al. (2007)185 compared insulin glargine plus extended-release glipizide with NPH insulin plus extended-release glipizide. Glargine or NPH were injected at bedtime with an initial dose of 0.15 IU/kg/day and then titrated to reach a FBG value of < 6.7 mmol/l. Glipizide was given before breakfast (5 mg/day). During a 2-week screening phase, previous oral medication was stopped and patients were initiated on 5 mg/day extended-release glipizide. They also received diabetes education.
In the PREDICTIVE-BMI trial (2007),178 once-daily evening insulin detemir was compared with once-daily evening NPH insulin. In both groups, basal insulin was continually and individually titrated, aiming for pre-breakfast PG levels of ≤ 6.1 mmol/l without levels of hypoglycaemia considered unacceptable to the patient. In addition, all patients received insulin aspart at the main meals (individually titrated aiming for postprandial glucose levels of ≤ 10.0 mmol/l); concomitant treatment with metformin was also allowed (used by ∼50% of patients on detemir and ∼58% of patients on NPH).
In the trial by Philis-Tsimikas et al. (2006),180 insulin detemir once daily before breakfast was compared with insulin detemir once daily in the evening, as well as to human NPH insulin once daily in the evening. The initial dose of treatment was 10 IU, doses were titrated at clinic visits or by telephone at least once every 4 weeks based on the mean of three PG levels measured on three consecutive days; in patients receiving detemir in the morning, the dose was titrated to aim for pre-dinner PG concentration of ≤ 6.0 mmol/l; in patients receiving detemir or NPH in the evening, titration was aimed to achieve pre-breakfast PG concentration of ≤ 6.0 mmol/l. Oral antihyperglycaemic therapy and dose was to remain unchanged.
In the trial by Rosenstock et al. (2008),177 detemir was compared with glargine. The detemir group received an injection once daily in the evening or twice daily (morning and evening). Glargine was injected once daily in the evening. In both groups, basal insulin was initiated at once daily (evening) 12 IU and titrated according to a structured treatment algorithm; people on detemir were allowed to receive an additional morning dose, i.e. pre-dinner PG was > 7.0 mmol/l, but only if pre-breakfast PG was < 7.0 mmol/l or nocturnal hypoglycaemia (major episode or PG ≤ 4.0 mmol/l) precluded the achievement of the FPG target. Insulin was injected using a pen-injector. The FPG was ≤ 6.0 mmol/l in the absence of hypoglycaemia. Oral glucose-lowering therapy, diet and physical activity recommended to remain stable during the study; no mealtime insulin was allowed.
Outcomes
In the LEAD trial (2007),179 the trial by Philis-Tsimikas et al. (2006),180 and the trial by Rosenstock et al. (2008)177 the primary outcome measure was HbA1c level. No primary outcome measure was specified the trial by Wang et al. (2007). 185 The primary outcome in the PREDICTIVE-BMI (2007)178 trial was weight change. All trials reported outcomes related to HbA1c level, hypoglycaemia and weight change. Blood glucose profiles, total daily insulin dose, and adverse events were also reported by most of the trials. None of the trials reported health-related QoL or diabetic secondary complications.
Trial quality
Details of the quality assessment of the trials are shown in Table 21.
| Pan (2007)179 | Wang (2007)185 | Montanana (2007)178 | Philis-Tsimikas (2006)180 | Rosenstock (2008)177 | |
|---|---|---|---|---|---|
| Appropriate and clearly focused question | Yes | Yes | Yes | Yes | Yes |
| Method of randomisation | Not described | Not described | Described, adequate | Described, adequate | Described, adequate |
| Allocation concealed | Not reported | Not reported | Yes | Unclear | Yes |
| Participants blinded | No | Not reported | No | No | No |
| Outcome assessors blinded | No | Not reported | Not reported | No | Unclear |
| All relevant outcomes measured in standard, valid, reliable way | Yes | Yes | Yes | Yes | Yes |
| Proportion of participants excluded/lost to follow-up | Four patients withdrew consent after randomisation and received no study medication; one received medication but provided no outcome measures; 49 were excluded for major protocol violations; no further details | Not reported (no dropouts/withdrawals?) | Seven withdrawals in detemir group, 12 withdrawals in NPH group, reasons listed, no significant difference between groups | 18, 16 and 17 in morning detemir, evening detemir and evening NPH groups, respectively; reasons listed, no significant difference between groups | 60 withdrawn in detemir group (23 adverse events, three ineffective therapy, 10 non-compliant, 24 other reasons); 39 withdrawn in glargine group (11 adverse events, two ineffective therapy, 15 non-compliant, 11 other reasons) |
| Handling of missing data | Not reported | Not reported | Last observation carried forward | Last observation carried forward | Last observation carried forward |
| ITT analysis performed | Yes | Not reported | Yes | Yes | Yes |
| Statistical analysis appropriate | Yes | Yes | Yes | Yes, non-inferiority analysis | Yes, non-inferiority analysis |
| Only difference between groups is treatment under investigation | Yes | Yes | Yes | Yes | Yes, although detemir was dosed twice daily in some patients |
| Results in multicentre studies comparable for all sites | Not reported | Not applicable | Not reported | Not reported | Unclear |
| Groups comparable at baseline | Yes | Yes | Yes | Yes | Yes |
| Summary | |||||
| How well was study done to minimise bias (++/+/–)? | (–) | (–) | (+) | (+) | (+) |
| What is the likely direction in which bias might affect study results? | Positive effects of study drug exaggerated | Positive effects of study drug exaggerated | |||
| Taking into account clinical considerations, your evaluation of the methodology used, and the statistical power of the study, are you certain that the overall effect is due to the study intervention? | Probably | Probably | Yes | Yes | Yes |
| Are the results of this study directly applicable to the patient group targeted by this guideline? | No (Asian patients only) | No (Chinese study) | Yes | Yes | Yes |
The LEAD trial (2007)179 and the trial by Wang et al. (2007)185 had a number of quality deficits, whereas the trials by Philis-Tsimikas et al. (2006)180 and Rosenstock et al. (2008)177 and the PREDICTIVE-BMI trial (2007)178 were of better quality.
In the LEAD trial (2007),179 the method of randomisation was not described, nor was allocation concealment. Participants and outcome assessors were not blinded. As far as reported, all relevant outcomes were measured in a standard, valid, reliable way. The proportion of participants excluded/lost to follow-up was only reported for the whole study group, but not for comparison groups separately, with five patients (1%) withdrawing before receiving treatment or not providing any outcomes, and 49 excluded due to major protocol violations (11%). ITT analysis was performed, but handling of missing data was not reported. The comparison groups were comparable at baseline. The study population was 100% Asian.
The trial by Wang et al. (2007)185 was underpowered (only 24 participants); randomisation and allocation concealment were not described, and neither was blinding. As far as reported, all relevant outcomes were measured in a standard, valid, reliable way. Withdrawals or dropouts were not mentioned, and handing of missing data and ITT analysis were not reported. The study groups were comparable at baseline.
The PREDICTIVE-BMI (2007)178 trial had adequate randomisation and allocation concealment. Participants were not blinded, blinding of outcome assessors was not reported. As far as reported, all relevant outcomes were measured in a standard, valid, reliable way. The proportion of participants excluded/lost to follow-up was reported with reasons for each comparison group separately, with no significant differences between study groups (7% withdrawals/losses to follow-up). ITT analysis was performed, and handling of missing data was by last observation carried forward. The comparison groups were comparable at baseline.
In the trial by Philis-Tsimikas et al. (2006),180 the method of randomisation was described and adequate, but allocation concealment was uncertain. Participants and outcome assessors were not blinded. As far as reported, all relevant outcomes were measured in a standard, valid, reliable way. The proportion of participants excluded/lost to follow-up was reported with reasons for each comparison group separately, with no significant differences between study groups (11% withdrawals/losses to follow-up). ITT analysis was performed, and handling of missing data was by last observation carried forward. The comparison groups were comparable at baseline.
The trial by Rosenstock et al. (2008)177 had adequate randomisation and allocation concealment. Participants were not blinded, blinding of outcome assessors was not reported. As far as reported, all relevant outcomes were measured in a standard, valid, reliable way. The proportion of participants excluded/lost to follow-up was reported with reasons for each comparison group separately, with no significant differences between study groups (10% withdrawals/losses to follow-up). ITT analysis was performed, and handling of missing data was by last observation carried forward. The data were analysed in a non-inferiority analysis. The comparison groups were comparable at baseline.
Results
Results for the five trials are shown in Table 22.
| Study | Outcome | Baseline | End of study | Change from baseline/difference between groups | p-value (between groups) |
|---|---|---|---|---|---|
| Insulin-naive, oral antihyperglycaemics – glargine vs NPH insulin | |||||
| HbA1c | |||||
| Pan (2007)179 (LEAD study) | HbA1c (%) |
Glargine: 9.02, SD 0.88% NPH insulin: 9.05 SD, 0.84% |
Glargine: 8.03% NPH insulin: 8.28% |
Glargine: –0.99% NPH insulin: –0.77% Difference in ITT population 0.22 (95% CI 0.02 to 0.42) |
p = NS for per-protocol population, p = 0.0319 for ITT population |
| Patients achieving target HbA1c (< 7.5%) (%) |
Glargine: 38.1% NPH insulin: 30.3% |
p = NS | |||
| Patients achieving target HbA1c (< 7.5%) without nocturnal hypoglycaemia (%) |
Glargine: 22.9% NPH insulin: 14.0% |
p = 0.017 | |||
| Patients achieving target FBG (≤ 120 mg/dl) (%) |
Glargine: 62.3% NPH insulin: 58.7% |
p = NS | |||
| Wang (2007)185 | HbA1c (%) |
Glargine: 8.77, SD1.18% NPH insulin: 8.75, SD1.24% |
Glargine: 7.62, SD 0.98% NPH insulin: 7.43, SD 0.73% |
p = NS | |
| Hypoglycaemia | |||||
| Pan (2007)179 (LEAD study) | Number of hypoglycaemic episodes |
Glargine: 682 NPH insulin: 1019 |
p < 0.004 | ||
| Symptomatic hypoglycaemia |
Glargine: 515 NPH insulin: 908 |
p < 0.0003 | |||
| Severe hypoglycaemia |
Glargine: 5 NPH insulin: 28 |
p < 0.03 | |||
| Nocturnal hypoglycaemic episodes |
Glargine: 221 NPH insulin: 620 |
p < 0.001 | |||
| Wang (2007)185 | All hypoglycaemic events |
Glargine: 2 in 2 patients NPH insulin: 6 in 4 patients |
p = NS | ||
| Nocturnal hypoglycaemic events |
Glargine: 1 in 1 patient NPH insulin: 4 in 4 patients |
p = 0.028 | |||
| Glycaemic excursions | |||||
| Pan (2007)179 (LEAD study) | Eight-point blood glucose profiles | Eight-point blood glucose profiles similar between groups at study end, except for post dinner, where blood glucose concentration in glargine group was significantly lower than in NPH group (236 mg/dl vs 249 mg/dl; p = 0.044) | p = 0.044 | ||
| Wang (2007)185 (continuous glucose monitoring system) | Average blood glucose |
Glargine: 8.2, SD1.2 mmol/l NPH insulin: 8.0, SD 2.0 mmol/l |
p = NS | ||
| SD of blood glucose |
Glargine: 1.4, SD 0.4 mmol/l NPH insulin: 2.3, SD 0.5 mmol/l |
p < 0.05 | |||
| SD of FPG |
Glargine: 0.7, SD 0.4 mmol/l NPH insulin: 1.5, SD 0.7mmol/l |
p < 0.05 | |||
| SD of bedtime PG |
Glargine: 1.2, SD 0.4 mmol/l NPH insulin: 2.0, SD 0.7mmol/l |
p < 0.05 | |||
| Blood glucose – pre-breakfast |
Glargine: 5.5, SD 0.8 mmol/l NPH insulin: 5.8, SD 1.5 mmol/l |
p = NS | |||
| Blood glucose – 2 hours post breakfast |
Glargine: 9.8, SD 2.6 mmol/l NPH insulin: 10.4, SD 1.9 mmol/l |
p = NS | |||
| Blood glucose – pre-lunch |
Glargine: 5.9, SD 1.0 mmol/l NPH insulin: 6.6, SD 1.2 mmol/l |
p = NS | |||
| Blood glucose – 2 hours post lunch |
Glargine: 9.8, SD 1.5 mmol/l NPH insulin: 10.2, SD 1.8 mmol/l |
p = NS | |||
| Blood glucose – pre-supper |
Glargine: 6.0, SD 0.7 mmol/l NPH insulin: 7.1, SD 1.0 mmol/l |
p < 0.05 | |||
| Blood glucose – 2 hours post supper |
Glargine: 10.8, SD1.6 mmol/l NPH insulin: 11.7, SD 1.4 mmol/l |
p = NS | |||
| Blood glucose – bedtime |
Glargine: 7.8, SD 1.2 mmol/l NPH insulin: 9.2, SD 2.0 mmol/l |
p < 0.05 | |||
| Blood glucose – 3.00 a.m. |
Glargine: 5.1, SD 0.8 mmol/l NPH insulin: 4.2, SD 1.4 mmol/l |
p < 0.05 | |||
| Total daily dose | |||||
| Pan (2007)179 (LEAD study) | Daily insulin dose |
Glargine: 9.6, SD 1.5 IU NPH insulin: 9.8, SD1.9 IU |
Glargine: 32.1, SD 17.6 IU NPH insulin: 32.8, SD 18.9 IU |
p = NS | |
| Wang (2007)185 | Daily insulin dose |
Glargine: 18.5, SD 7.5 IU NPH insulin: 19.0, SD 8.4 IU |
p = NS | ||
| Weight change | |||||
| Pan (2007)179 (LEAD study) | BMI |
Glargine: 24.8, SD 3.1 kg/m2 NPH insulin: 25.1, SD 3.3 kg/m2 |
Glargine: +1.40 kg/m2 NPH insulin: +1.29 kg/m2 |
p = NS | |
| Wang (2007)185 | Weight |
Glargine: +1.47, SD 1.04 kg NPH insulin: +1.20, SD 1.17 kg |
p = NS | ||
| Complication rates – not reported | |||||
| Adverse events | |||||
| Pan (2007)179 (LEAD study) | Treatment-emergent adverse events that were possibly treatment related (66 events in 45 patients) |
Glargine: 22 patients NPH insulin: 23 patients, majority related to injection-site reactions (45 events in 31 patients) |
p-value not reported | ||
| Serious adverse events | No significant difference between groups, none of the events was considered unusual for the demographic group studied | p = NS | |||
| Health-related QoL – not reported | |||||
| Previous insulin – detemir vs NPH insulin | |||||
| HbA1c | |||||
| Montanana (2007)178 (PREDICTIVE-BMI) | HbA1c |
Detemir: 8.9, SD 0.9% NPH: 8.8, SD 1.0 % |
Detemir: 7.8, SD 1.1% NPH: 7.8, SD 1.0% |
p = NS | |
| Percentage reaching HbA1c ≤ 7.0% without hypoglycaemia |
Detemir: 27% NPH: 27% |
p = NS | |||
| Hypoglycaemia | |||||
| Montanana (2007)178 (PREDICTIVE-BMI) | All hypoglycaemic events | Not reported |
26 weeks Detemir: 256 NPH: 481 |
Significantly less in detemir group, RR 0.62 | p < 0.0001 |
| Patients reporting any hypoglycaemic events |
26 weeks Detemir: 34.7% NPH: 65.3% |
||||
| Nocturnal hypoglycaemic events | Not reported |
26 weeks Detemir: 46 NPH: 107 |
Significantly less in detemir group, RR 0.43 | p < 0.0001 | |
| Patients reporting nocturnal hypoglycaemia |
26 weeks Detemir: 30.1% NPH: 69.9% |
||||
| Severe hypoglycaemic episodes |
26 weeks Detemir: 0 NPH: 3 |
||||
| Glycaemic excursions – not reported | |||||
| Total daily dose | |||||
| Montanana (2007)178 (PREDICTIVE-BMI) | Insulin dose (IU/kg) – total (basal + bolus) |
Detemir: 0.64, SD 0.21 IU/kg NPH: 0.59, SD 0.18 IU/kg |
Detemir: 1.05, SD 0.40 IU/kg NPH: 0.85, SD 0.29 IU/kg |
p-value not reported | |
| Insulin dose (IU/kg) – basal |
Detemir: 0.30, SD 0.11 IU/kg NPH: 0.28, SD 0.09 IU/kg |
Detemir: 0.59, SD 0.25 IU/kg NPH: 0.47, SD 0.18 IU/kg |
p-value not reported | ||
| Weight change | |||||
| Montanana (2007)178 (PREDICTIVE-BMI) | Weight change |
Detemir: 79.5 kg NPH: 82.2 kg |
26 weeks Detemir: +0.4 kg NPH: +1.9 kg |
Baseline-adjusted difference 1.5 kg (95% CI 0.8 to 2.8) | p < 0.0001 |
| BMI |
Detemir: 31.6 kg/m2 NPH: 32.2 kg/m2 |
26 weeks Detemir: +0.17 kg/m2 NPH: +0.77 kg/m2 |
Baseline-adjusted difference 0.6 kg/m2 | p < 0.0001 | |
| Percentage with no change or loss of weight |
26 weeks Detemir: 46.4% NPH: 22.6% |
p-value not reported | |||
| Complication rates – not reported | |||||
| Adverse events | |||||
| Montanana (2007)178 (PREDICTIVE-BMI) | All adverse events |
26 weeks Detemir: 91 NPH: 73 |
|||
| Serious adverse events |
26 weeks Detemir: 6 NPH: 4 |
All thought to be unlikely to be related to basal insulin | |||
| Withdrawals because of adverse events |
Detemir: 3 NPH: 0 |
||||
| Health-related QoL – not reported | |||||
| Insulin-naive, oral antihyperglycaemics – detemir vs NPH insulin | |||||
| HbA1c | |||||
| Philis-Tsimikas (2006)180 | HbA1c (%) |
Morning detemir: 9.08, SD 0.97% Evening detemir: 8.88, SD 0.95% NPH insulin: 9.15, SD 1.0% |
Morning detemir: 7.50, SD 0.96% Evening detemir: 7.40, SD 0.77% NPH insulin: 7.35, SD 0.93% |
Morning detemir: –1.58, SD 1.07% Evening detemir: –1.48, SD 1.01% NPH insulin: –1.74, SD 1.08% |
p = NS |
| Hypoglycaemia | |||||
| Philis-Tsimikas (2006)180 | Major episodes |
Morning detemir: 0 Evening detemir: 2 events in 2 (1.2%) patients NPH insulin: 0 |
Too few events for statistical analysis | ||
| All confirmed episodes |
Morning detemir: 91 events in 32 (19.4%) patients Evening detemir: 82 events in 27 (16.0%) patients NPH insulin: 153 events in 53 (32.3%) patients |
Relative risk Morning vs evening detemir: 1.43 Morning detemir vs evening NPH: 0.68 Evening detemir vs evening NPH: 0.47 |
Morning detemir vs evening detemir or NPH p = NS Evening detemir vs evening NPH p = 0.019 |
||
| Nocturnal episodes |
Morning detemir: 6 events in 4 (2.4%) patients Evening detemir: 19 events in 8 (4.7%) patients NPH insulin: 47 events in 22 (13.4%) patients (no major episodes occurred) |
Relative risk Morning vs evening detemir: 0.35 Morning detemir vs evening NPH: 0.13 Evening detemir vs evening NPH: 0.35 |
Morning detemir vs evening detemir p = NS Morning detemir vs evening NPH p < 0.001 Evening detemir vs evening NPH p = 0.031 |
||
| Glycaemic excursions | |||||
| Philis-Tsimikas (2006)180 | Pre-breakfast self-measured PG (mmol/l) |
Morning detemir: 7.97, SD 1.23 mmol/l Evening detemir: 6.50, SD 1.28 mmol/l NPH insulin: 6.78, SD 1.26 mmol/l |
p < 0.001, morning detemir vs evening detemir and evening NPH | ||
| Pre-dinner self-measured PG (mmol/l) |
Morning detemir: 7.11, SD 1.91 mmol/l Evening detemir: 7.76, SD 1.84 mmol/l NPH insulin: 7.95, SD 1.98 mmol/l |
p = 0.005, morning detemir vs evening detemir; p < 0.001, morning detemir vs evening NPH | |||
| Nine-point self-measured PG profile | Similar for two evening insulin groups, mean profile of morning insulin detemir group was characterised by lower glycaemic values in the daytime and higher values overnight; p < 0.001 | ||||
| Total daily dose | |||||
| Philis-Tsimikas (2006)180 | Mean insulin dose |
Morning detemir: 0.5, SD 0.3 IU/kg Evening detemir: 0.4, SD 0.2 IU/kg NPH insulin: 0.4, SD 0.2 IU/kg |
p = NS | ||
| Weight change | |||||
| Philis-Tsimikas (2006)180 | Weight gain |
Morning detemir: +1.2 kg Evening detemir: +0.7 kg NPH insulin: +1.6 kg |
Morning detemir vs evening detemir or NPH; p = NS Evening detemir vs evening NPH; p = 0.005 |
||
| Complication rates – not reported | |||||
| Adverse events | |||||
| Philis-Tsimikas (2006)180 | Withdrawals due to adverse events |
Morning detemir: 2.4% Evening detemir: 2.4% NPH insulin: 2.4% |
|||
| Overall profiles of adverse events |
Morning detemir: 123 AEs in 70 patients Evening detemir: 150 AEs in 67 patients NPH insulin: 144 AEs in 82 patients |
Statistically similar, mostly considered unrelated to study insulins; all serious adverse events unrelated to insulins | |||
| Injection site reactions |
Morning detemir: 2 events in 2 patients Evening detemir: 7 events in 6 patients NPH insulin: 2 events in 2 patients |
p = NS | |||
| Potential allergic reactions |
Morning detemir: 2 events in 2 patients Evening detemir: 5 events in 5 patients NPH insulin: 1 event in 1 patient |
p = NS | |||
| Health-related QoL – not reported | |||||
Glycaemic control
None of the trials found any significant difference in HbA1c values between insulins glargine or detemir and NPH insulin at study end. Levels of HbA1c decreased by between 0.92% and 1.74% from baseline to study end. No significant difference between glargine and NPH was seen in the LEAD trial (2007)179 for patients reaching the HbA1c target (< 7.5%: 38% for glargine, 30% for NPH) or the FBG target (≤ 6.7 mmol/l: 62% for glargine, 59% for NPH). There was a significant difference in the proportion of patients reaching the HbA1c target (< 7.5%) without nocturnal hypoglycaemia in favour of glargine (23% for glargine, 14% for NPH, p = 0.017). There was no significant difference between detemir and NPH for patients reaching HbA1c ≤ 7.0% in the PREDICTIVE-BMI trial (2007)178 (27% of patients in each group).
The results of the meta-analysis are shown in Figure 2 for insulin glargine and in Figure 3 for insulin detemir. Baseline HbA1c values in the trials included in the meta-analysis were between 8.5% and 9.7% in the glargine versus NPH trials, and between 7.8% and 9.2% in the detemir versus NPH trials. None of the meta-analyses showed a significant effect for insulin glargine (nine studies) or insulin detemir (four studies) versus NPH for HbA1c level. The WMD was 0.00% (95% CI –0.11 to 0.10) for glargine and 0.07% (95% CI –0.03 to 0.18) for detemir. There was significant heterogeneity for the results for insulin glargine which disappeared when the only study of patients on previous insulin therapy [Rosenstock et al. (2001)]159 was excluded.
FIGURE 2.
HbA1c glargine versus Neutral Protamine Hagedorn.
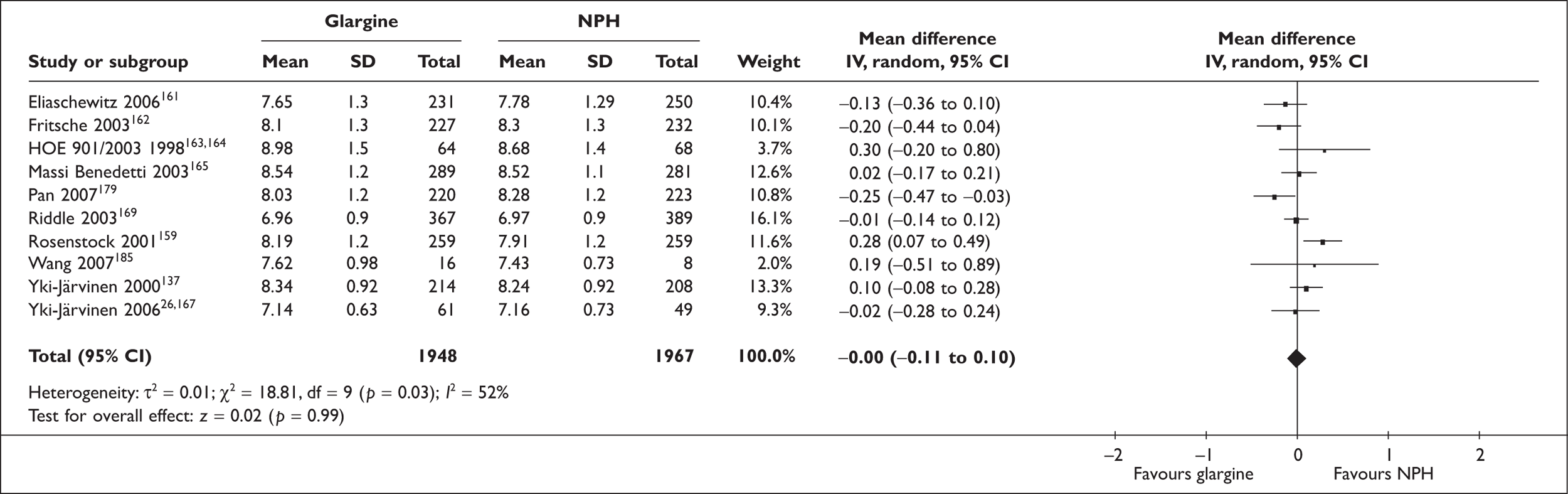
FIGURE 3.
HbA1c detemir versus Neutral Protamine Hagedorn.
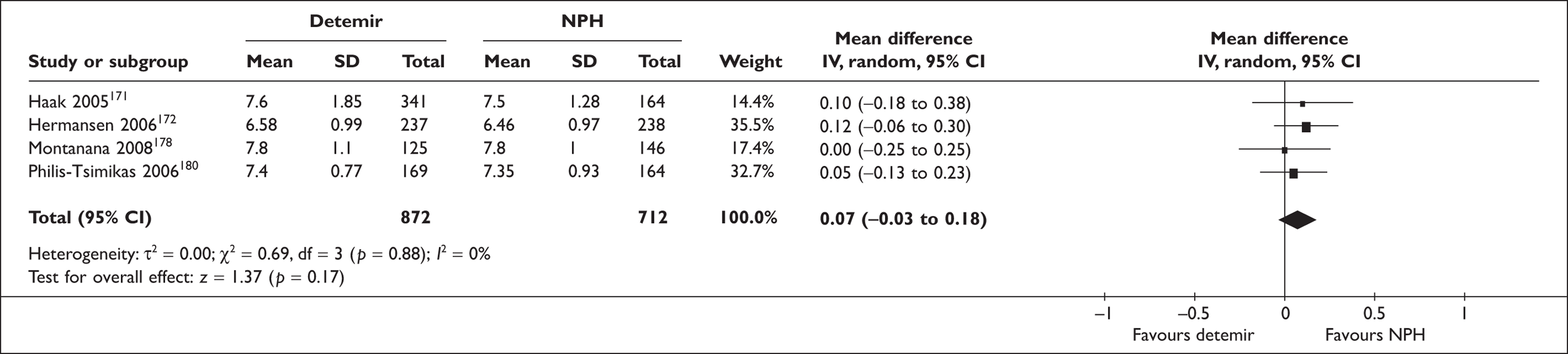
Hypoglycaemia
The LEAD trial (2007)179 and the PREDICTIVE-BMI trial (2007)178 found significant results in favour of glargine and detemir respectively in comparison with NPH for all hypoglycaemia-related outcomes reported. The trial by Wang et al. (2007)185 found significantly fewer episodes of nocturnal hypoglycaemia with glargine compared with NPH, but no significant difference for all hypoglycaemic events. The trial by Philis-Tsimikas et al. (2006)180 found significant effects in favour of detemir for all comparisons of evening detemir versus evening NPH, but not for some of the other comparisons.
In the LEAD trial (2007)179 there were 682 hypoglycaemic episodes in the glargine group compared with 1019 in the NPH group (p < 0.004). There were 515 episodes of symptomatic hypoglycaemia in the glargine group compared with 908 in the NPH group (p < 0.0003), five of severe hypoglycaemia in the glargine group compared with 28 in the NPH group (p < 0.03), and 221 episodes of nocturnal hypoglycaemia in the glargine group compared with 620 in the NPH group (p < 0.001).
In the trial by Wang et al. (2007),185 there were two hypoglycaemic events in two patients in the glargine group and six hypoglycaemic events in four patients in the NPH group (p = NS). There was one nocturnal hypoglycaemic event in one patient in the glargine group and four nocturnal hypoglycaemic events in four patients in the NPH group (p = 0.028).
The PREDICTIVE-BMI trial (2007)178 reported significantly fewer hypoglycaemic events with detemir than with NPH (256 versus 481, RR 0.62; p < 0.0001) and also significantly less nocturnal hypoglycaemia (46 versus 107, RR 0.43, p < 0.0001).
In the trial by Philis-Tsimikas et al. (2006)180 there were too few major hypoglycaemic episodes for statistical analysis (only two events in the evening detemir group). For all confirmed hypoglycaemic episodes, there were 91 events in 32 patients on morning detemir, 82 events in 27 patients on evening detemir, and 153 events in 53 patients on evening NPH, with a significant difference in favour or evening detemir versus evening NPH, but not of morning detemir versus evening detemir or NPH. For nocturnal hypoglycaemia, there were six events in four patients on morning detemir, 19 events in eight patients on evening detemir, and 47 events in 22 patients on evening NPH, with a significant difference in favour or either detemir group versus evening NPH, but not of morning detemir versus evening detemir.
The meta-analyses for severe hypoglycaemia (Figures 4 and 5) included six studies (reporting the number of patients with severe hypoglycaemia) for insulin glargine versus NPH and four studies for insulin detemir versus NPH. There was no significant difference in the number of patients with severe hypoglycaemia in the glargine or detemir groups compared with NPH insulin [RR 0.82 (95% CI 0.45 to 1.49) for glargine and RR 0.59 (95% CI 0.15 to 2.24) for detemir]. There was no significant heterogeneity.
FIGURE 4.
Severe hypoglycaemia glargine versus Neutral Protamine Hagedorn.
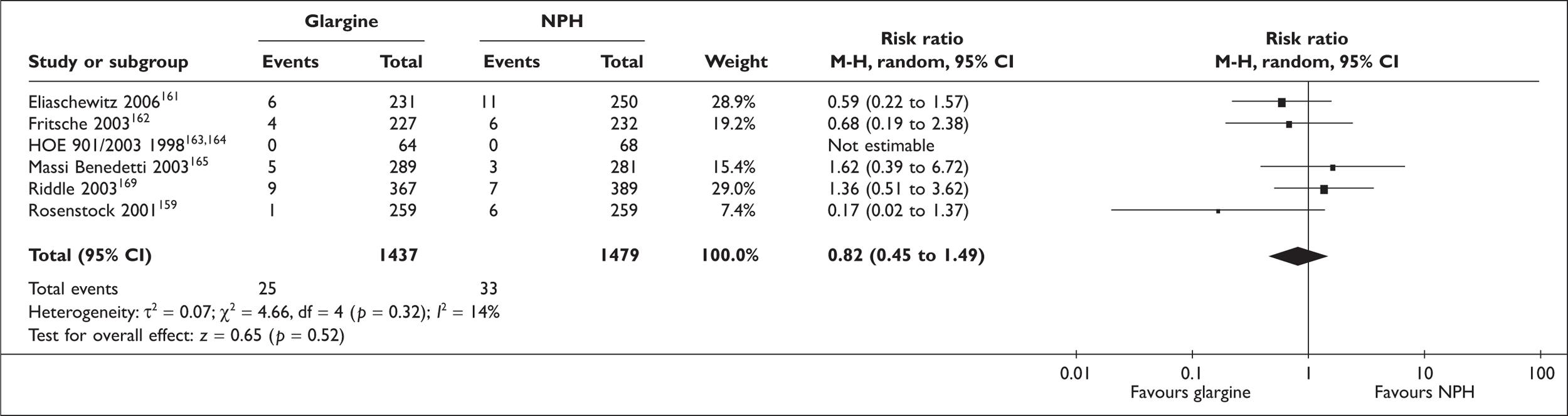
FIGURE 5.
Severe hypoglycaemia detemir versus Neutral Protamine Hagedorn.
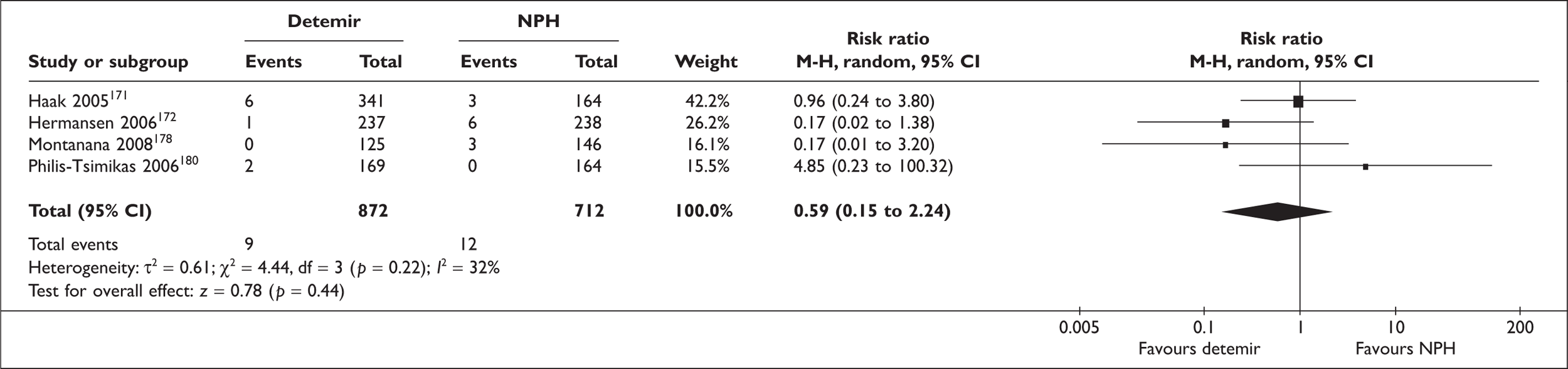
The meta-analysis for overall hypoglycaemia (Figures 6 and 7) included seven studies (reporting the number of patients with any hypoglycaemia) for insulin glargine versus NPH, and four studies for insulin detemir versus NPH. There was a significant difference in the number of patients reporting any hypoglycaemia in favour of the glargine and detemir groups compared with NPH insulin [RR 0.89 (95% CI 0.83 to 0.96, p = 0.002) for glargine, and RR 0.68 (95% CI 0.54 to 0.86, p = 0.001) for detemir]. There was no significant heterogeneity for glargine versus NPH but there was for detemir versus NPH (p = 0.002).
FIGURE 6.
Overall hypoglycaemia glargine versus Neutral Protamine Hagedorn.
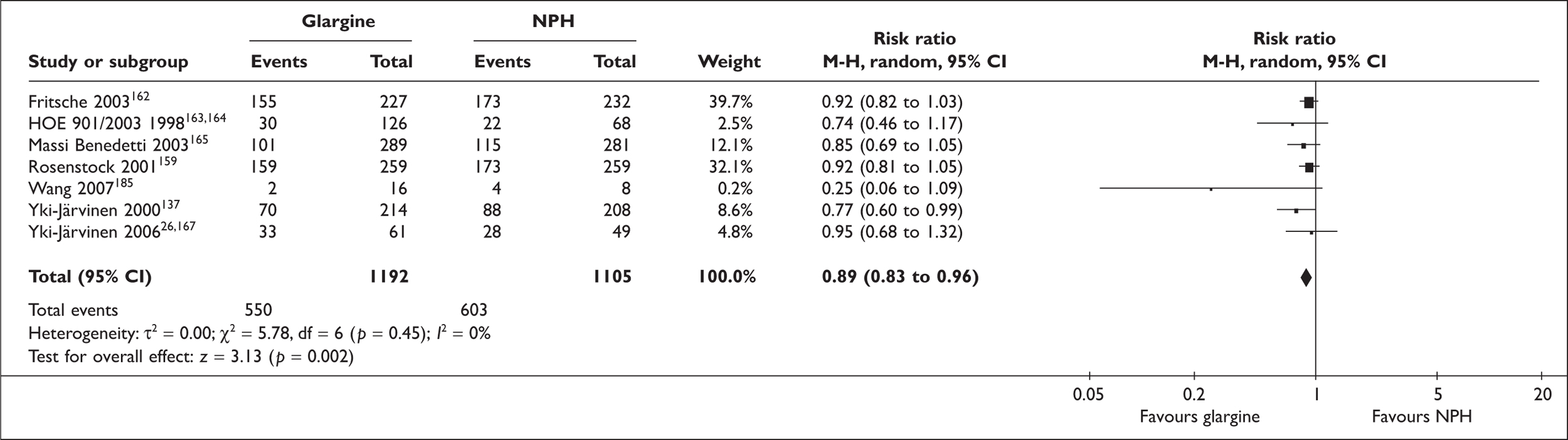
FIGURE 7.
Overall hypoglycaemia detemir versus Neutral Protamine Hagedorn.
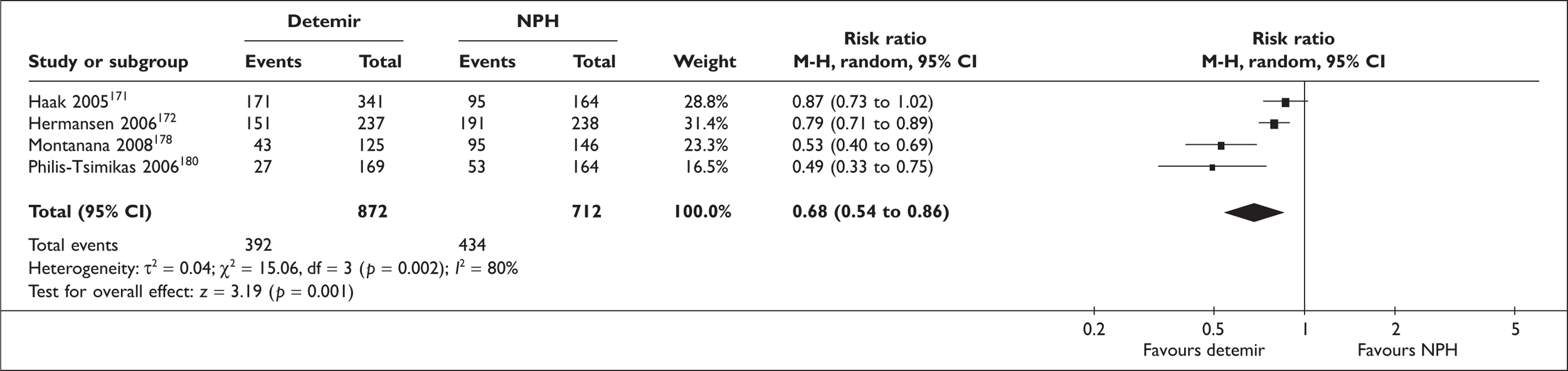
The meta-analysis for symptomatic hypoglycaemia (Figure 8) included four studies (reporting the number of patients with symptomatic hypoglycaemia) for insulin glargine versus NPH. There was a significant difference in the number of patients reporting symptomatic hypoglycaemia in favour of the glargine groups compared with NPH insulin [RR 0.80 (95% CI 0.68, 0.93, p < 0.004)]. There was significant heterogeneity (p = 0.04).
FIGURE 8.
Symptomatic hypoglycaemia glargine versus Neutral Protamine Hagedorn.
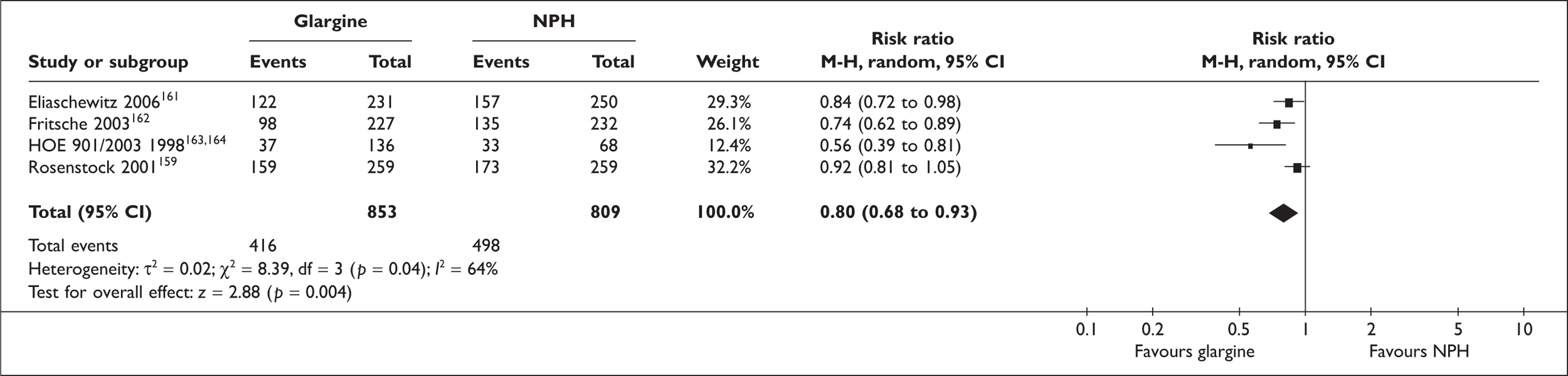
The meta-analysis for nocturnal hypoglycaemia (Figures 9 and 10) included seven studies (reporting the number of patients with nocturnal hypoglycaemia) for insulin glargine versus NPH and four studies for insulin detemir versus NPH. There was a significant difference in the number of patients reporting nocturnal hypoglycaemia in favour of the glargine and detemir groups compared with NPH insulin [RR 0.54 (95% CI 0.43 to 0.69, p < 0.00001) for glargine and RR 0.54 (95% CI 0.24 to 0.68, p < 0.00001) for detemir]. There was significant heterogeneity for glargine versus NPH (p = 0.03) but not for detemir versus NPH. The heterogeneity disappeared when the only study of patients on previous insulin therapy [Rosenstock et al. (2001)]159 was excluded.
FIGURE 9.
Nocturnal hypoglycaemia glargine versus Neutral Protamine Hagedorn.
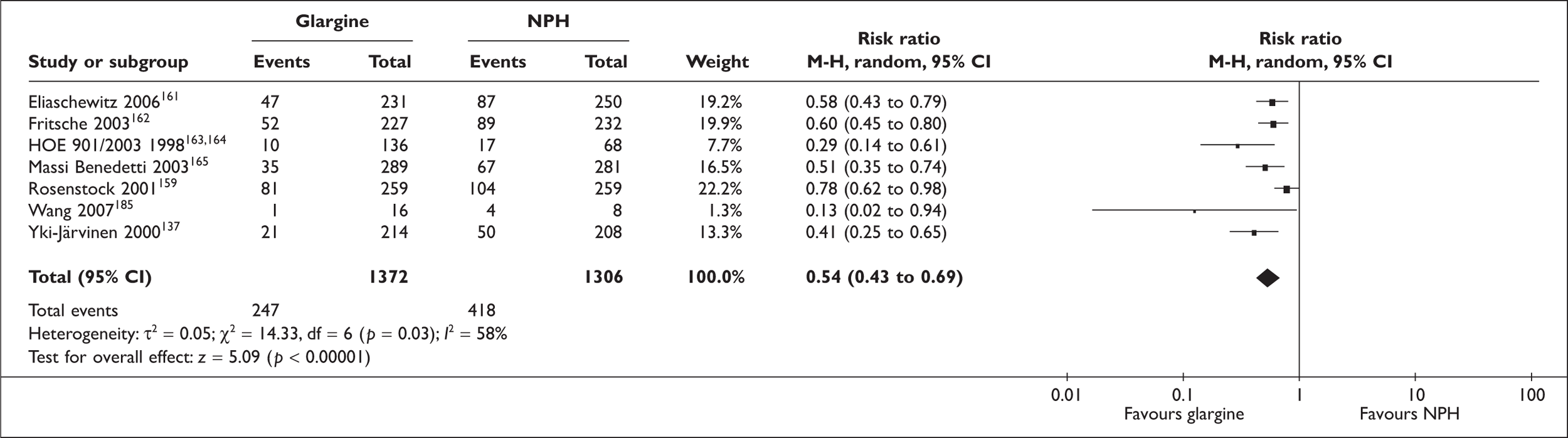
FIGURE 10.
Nocturnal hypoglycaemia detemir versus Neutral Protamine Hagedorn.
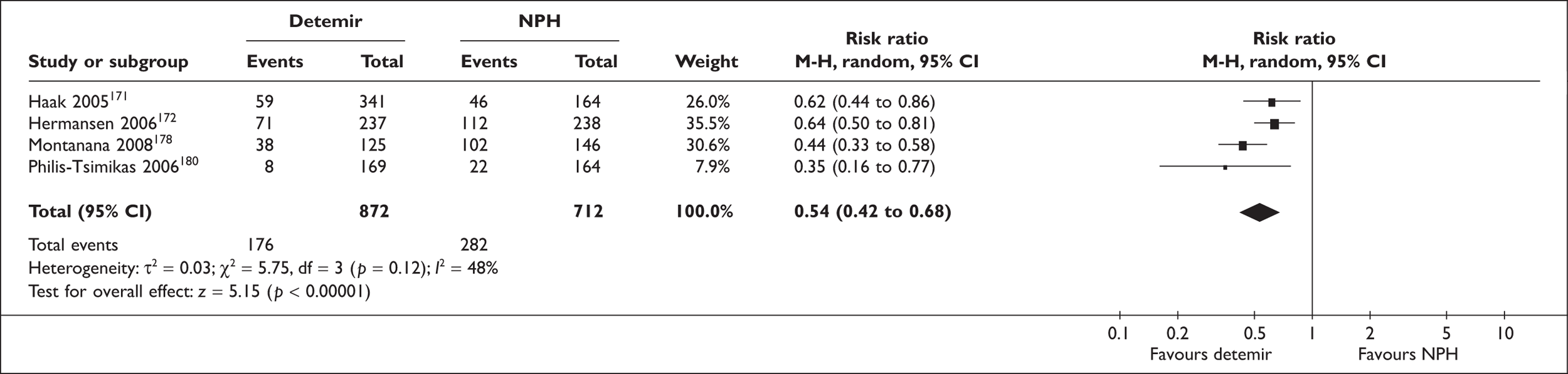
Glucose excursions
The LEAD trial (2007)179 found eight-point blood glucose profiles to be similar between groups at study end, except for postdinner values, where blood glucose concentration in the glargine group was significantly lower than in the NPH group (236 mg/dl versus 249 mg/dl, p = 0.044).
In the Wang et al. (2007)185 trial, a continuous glucose monitoring system was used. No differences between glargine and NPH were found in average blood glucose values, pre-breakfast, 2 hours post breakfast, pre-lunch, 2 hours post lunch, and 2 hours post supper blood glucose values, but the SDs of blood glucose, FPG and bedtime PG were significantly smaller with glargine than NPH, pre-supper and bedtime blood glucose values were significantly lower with glargine than NPH, and 3 a.m. blood glucose values were significantly larger with glargine than NPH.
In the trial by Philis-Tsimikas et al. (2006),180 nine-point blood glucose profiles were similar for the two evening insulin groups, whereas the mean profile of the morning insulin detemir group was characterised by lower glycaemic values in the daytime and higher values overnight (p < 0.001). Pre-breakfast PG values were between 1.19 and 1.47 mmol/l higher (p < 0.001) in the morning detemir group, and pre-dinner PG values between 0.65 and 0.84 mmol/l lower (p ≤ 0.01) in the morning detemir group than in the evening groups.
Total daily insulin dose
No significant differences in mean daily insulin doses between treatment groups were reported in the LEAD trial (2007),179 the trial by Wang et al. (2007),185 the PREDICTIVE-BMI trial (2007),178 or the trial by Philis-Tsimikas et al. (2006). 180
Weight change
In the LEAD trial (2007),179 BMI increased both in the glargine and in the NPH group to a similar extent during the course of the trial (+1.4 and +1.3 kg/m2). Similarly, in the trial by Wang et al. (2007)185 body weight increased to a similar extent in both groups (+1.47 kg with glargine and +1.20 kg with NPH).
In the PREDICTIVE-BMI trial (2007),178 significantly less weight gain was seen with insulin detemir than with NPH insulin over the course of the trial (+0.4 kg versus +1.9 kg, p < 0.0001). Similarly, patients in the detemir group had a significantly smaller increase in BMI (+0.17 kg/m2 versus +0.77 kg/m2, p < 0.0001).
In the trial by Philis-Tsimikas et al. (2006),180 patients in the morning detemir group gained a mean of 1.2 kg, patients in the evening detemir group gained a mean of 0.7 kg, and patients in the evening NPH group gained a mean of 1.6 kg, with weight gain being significantly less in the evening detemir group than in the evening NPH group (p = 0.005, no other significant differences).
Overall (eight studies), the glargine groups gained 0.23 kg less weight than the NPH groups (range –1.10 to +0.23 kg). However, a meta-analysis could not be carried out for this outcome because of too many missing SDs. The detemir groups (four studies) gained 1.20 kg less weight than the NPH groups (range –0.8 to –1.6 kg) but, again, a meta-analysis could not be carried out due to too many missing SDs.
Diabetic complications
These were not reported by any of the trials.
Adverse events
The LEAD study (2007)179 reported 66 adverse events in 45 patients that were possibly treatment related (22 patients in the glargine group and 23 patients in the NPH group). The majority was related to injection-site reactions, and, although p-values were not reported, there does not seem to have been a significant difference between groups. There was no significant difference in serious adverse events between groups, and none of the events were considered unusual for the demographic group studied (i.e. not related to the treatment).
The trial by Wang et al. (2007)185 did not report adverse events.
In the PREDICTIVE-BMI trial (2007)178 there were 91 adverse events in the detemir group and 73 in the NPH group, six of these in the detemir group and four in the NPH group were serious (but thought to be unlikely to be related to basal insulin). There were three withdrawals because of adverse events in the detemir group and none in the NPH group.
In the trial by Philis-Tsimikas et al. (2006),180 there was no significant difference in overall adverse events between comparison groups (123–144 events in 67–82 patients in each group). No serious adverse events were considered to be related to the insulins. There was no significant difference in potential allergic reactions (1–5 events in 1–5 patients per group) or injection site reactions (2–7 events in 2–6 patients per group) between the groups.
Health-related QoL
This was not reported by any of the trials.
Glargine vs detemir
The main results of the included glargine versus detemir trial are shown Table 23.
| Study | Outcome | Baseline | End of study | Change from baseline/difference between groups | p-value (between groups) |
|---|---|---|---|---|---|
| Insulin-naive – glargine vs detemir | |||||
| HbA1c | |||||
| Rosenstock (2008)177 | HbA1c (%) |
Detemir (n = 291): 8.64, SD 0.78% Glargine (n = 291): 8.62, SD 0.77% |
Detemir (n = 268): 7.16, SE 0.08% glargine (n = 275): 7.12, SE 0.08% |
Difference glargine – detemir 0.05% (95% CI 0.11 to 0.21) | p = NS |
| Patients achieving HbA1c ≤ 7.0% (%) |
Detemir (n = 248): 52% Glargine (n = 259): 52% |
p = NS | |||
| Patients achieving target HbA1c ≤ 7.0% (%) without hypoglycaemia (%) |
Detemir (n = 248): 33% Glargine (n = 259): 35% |
p = NS | |||
| Hypoglycaemia | |||||
| Rosenstock (2008)177 | All hypoglycaemic episodes |
Detemir Participants: 182 (63%) Episodes: 1521 Rate: 5.8 per patient-year Glargine Participants: 191 (66%) Episodes: 1670 Rate: 6.2 per patient-year |
Relative risk 0.94 (95% CI 0.71 to 1.25) | p = NS | |
| Nocturnal hypoglycaemic episodes |
Detemir Participants: 95 (33%) Episodes: 352 Rate: 1.3 per patient-year Glargine Participants: 93 (32%) Episodes: 350 Rate: 1.3 per patient-year |
Relative risk 1.05 (95% CI 0.69 to 1.58) | p = NS | ||
| Major hypoglycaemic episodes |
Detemir Participants: 5 (2%) Episodes: 9 Rate: 0.0 per patient-year Glargine Participants: 8 (3%) Episodes: 8 Rate: 0.0 per patient-year |
Not reported, number too small | |||
| Major nocturnal hypoglycaemic episodes |
Detemir Participants: 3 (1%) Episodes: 5 Rate: 0.0 per patient-year Glargine Participants: 4 (1%) Episodes: 4 Rate: 0.0 per patient-year |
Not reported, number too small | |||
| Minor hypoglycaemic episodes |
Detemir Participants: 135 (46%) Episodes: 737 Rate: 2.9 per patient-year Glargine Participants: 151 (52%) Episodes: 786 Rate: 2.9 per patient-year |
Relative risk 1.05 (95% CI 0.75 to 1.46) | p = NS | ||
| Minor nocturnal hypoglycaemic episodes |
Detemir Participants: 73 (25%) Episodes: 212 Rate: 0.8 per patient-year Glargine Participants: 71 (24%) Episodes: 192 Rate: 0.7 per patient-year |
Relative risk 1.17 (95% CI 0.75 to 1.83) | p = NS | ||
| Symptoms only hypoglycaemic episodes |
Detemir Participants: 137 (47%) Episodes: 760 Rate: 3.0 per patient-year Glargine Participants: 133 (46%) Episodes: 866 Rate: 3.2 per patient-year |
Relative risk 0.88 (95% CI 0.61 to 1.25) | p = NS | ||
| Symptoms only nocturnal hypoglycaemic episodes |
Detemir Participants: 48 (17%) Episodes: 128 Rate: 0.5 per patient-year Glargine Participants: 49 (17%) Episodes: 151 Rate: 0.6 per patient-year |
Relative risk 0.88 (95% CI 0.50 to 1.54) | p = NS | ||
| Glycaemic excursions | |||||
| Rosenstock (2008)177 | Within-participant variation (mmol/l) – pre-breakfast |
Detemir (n = 238): SD 1.06 Glargine (n = 257): SD 1.03 |
p = NS | ||
| Within-participant variation (mmol/l) – pre-dinner |
Detemir (n = 238): SD 1.60 Glargine (n = 258): SD 1.55 |
p = NS | |||
| Total daily dose | |||||
| Rosenstock (2008)177 | Daily insulin dose |
Detemir (n = 227): 0.78 U/kg/day (0.52 U/kg for once daily and 1.0 U/kg for twice daily, with 55% on twice daily) Glargine (n = 248): 0.44 U/kg/day |
p-value not reported | ||
| Weight change | |||||
| Rosenstock (2008)177 | Weight gain |
Detemir: 87.4, SD 16.6 kg Glargine: 87.4, SD 17.4 kg |
Detemir (n = 230): +3.0, SE 0.4 kg Glargine (n = 252): +3.9, SE 0.4 kg Confirmed in ITT analysis, but weight gain with once daily detemir was +2.3, SE 0.5 kg and with twice-daily detemir +3.7, SE 0.4 kg (no difference to glargine) |
p = 0.01 | |
| Adverse events | |||||
| Rosenstock (2008)177 | Withdrawal because of adverse events |
Detemir: 8% Glargine: 4% |
|||
| Serious adverse events |
Detemir: 42 patients with 47 events Glargine: 53 patients with 73 events, but only 5 events with detemir and 4 events with glargine considered to be (possibly) related to study medication |
||||
| Deaths |
Detemir: n = 1 (possibly MI) Glargine: n = 1 (pulmonary fibrosis) |
||||
| Injection site disorders |
Detemir: 4.5% Glargine: 1.4% |
||||
| Allergic reactions |
Detemir: n = 3 Glargine: n = 1 |
||||
| Skin disorders (including pruritus and rash) |
Detemir: n = 6 Glargine: n = 1 |
||||
The results of the trial by Rosenstock et al. (2008)177 suggest that the effects of glargine and detemir are similar. After 52 weeks of treatment, there were no significant differences in HbA1c level, percentage of patients reaching HbA1c value of ≤ 7.0% (with or without hypoglycaemia), overall hypoglycaemic events or nocturnal hypoglycaemic events. There was statistically significantly less weight gain with detemir overall than with glargine (+2.7 versus 3.5 kg, p = 0.03), but the difference of 0.8 kg is of doubtful clinical significance. However, when analysing use of detemir once or twice daily, only the once-daily detemir group was at an advantage for weight gain (+2.3 kg), whereas the weight gain in the twice-daily detemir group was similar to that of the glargine group (+3.7 kg). The mean daily dose was higher for detemir (0.52 U/kg with once-daily dosing, 1.00 U/kg with twice-daily dosing) than for glargine (0.44 U/kg). Injection site reactions were slightly more common with detemir than with glargine (4.5% versus 1.4%, p-value not reported).
Another short study, available in abstract only186 compared the effect of once daily glargine and detemir on blood glucose profiles over the course of a week, and found no significant difference.
Discussion
Taking the evidence from the systematic reviews and the RCTs as a whole, both insulin glargine and insulin detemir appear to be equivalent with respect to parameters of glycaemic control in comparison with NPH insulin. This was confirmed by our meta-analysis of trials included in previous meta-analyses and additional trials identified. A significant reduction in nocturnal hypoglycaemia was associated with both glargine and detemir treatment, but the effect size is not clear from the reviews. The reduction in nocturnal hypoglycaemia both for glargine and detemir was confirmed by our meta-analysis. Some reduction in overall or symptomatic hypoglycaemia was also seen with glargine or detemir, but this was not consistent for all trials. Our meta-analysis did however show a significant reduction in overall hypoglycaemia for both glargine and detemir and for symptomatic hypoglycaemia for glargine (not reported for detemir). In many trials, severe hypoglycaemia did not occur frequently enough to allow a meaningful statistical analysis.
Glycaemic excursions were reported infrequently but where reported, no consistent differences between glargine or detemir and NPH insulin were seen.
Total daily doses of insulin and health-related QoL (or patient satisfaction) were reported too infrequently to allow any conclusions.
Similarly, change in weight or BMI was not reported systematically enough to allow any firm conclusion. There was some indication that there may be less weight gain with the long-acting analogues than with NPH insulin (possibly dependent on previous insulin treatment), but the results on this outcome were not consistent. One study of glargine versus detemir suggested that there may be less weight gain with once daily detemir than with once daily glargine. Most trials included in this review did not provide enough information to enable a meta-analysis, but data extracted also suggest that there may be slightly less weight gain with detemir than with glargine, though the difference is of doubtful clinical significance. Any effects seen appear to have been independent of whether patients have been treated with insulins previously or not, or were on oral antihyperglycaemic therapy or not.
Reported adverse events appear to have been largely similar between the long-acting insulin analogues and NPH insulin, possibly with more injection site reactions for the analogues. However, no data on the longer term safety of the insulin analogues were available.
No information was available on diabetic complications, and the studies were underpowered to assess such outcomes or mortality reliably. Horvath et al. (2007)141 reported limited data on a possible differential effect of glargine on development of clinically significant macular oedema depending on previous treatment with insulin, suggesting that this may be a point of concern.
Conclusions
Glargine and detemir are equivalent to NPH in terms of glycaemic control as reflected in HbA1c level, but have modest advantages in terms of hypoglycaemia, especially nocturnal.
There is little to choose between the two analogues. Detemir, when used once daily, may be associated with marginally less weight gain, but this is unlikely to be clinically significant. It requires a higher daily dose than glargine which will have cost implications.
Chapter 5 The glitazones
History
There are two TZDs, or glitazones for short, used in the UK: pioglitazone and rosiglitazone. They have been the subject of technology appraisals (TAs) by NICE, starting with appraisals of the individual drugs (TAs 9 and 21), later superseded by a review of both – TA 63, issued in August 2003. 12
The guidance issued after the review in 2003 stated that:
1.1 For people with type 2 diabetes, the use of a glitazone as second-line therapy added to either metformin or a sulphonylurea – as an alternative to treatment with a combination of metformin and a sulphonylurea – is not recommended except for those who are unable to take metformin and a sulphonylurea in combination because of intolerance or a contraindication to one of the drugs.
1.3 The present UK licence does not allow the Institute to recommend the use of glitazones in triple combination therapy, as monotherapy, or in combination with insulin.
Section 1.1 was based on cost-effectiveness rather than clinical efficacy. Regarding section 1.3, the Appraisal Committee noted (paragraph 4.3.6 of the guidance) that:
The off-licence use of glitazones as part of triple combination therapy is widely practised in the UK. This use has been particularly targeted at a subset of people with diabetes for whom the combination of metformin and sulphonylurea has failed to achieve target HbA1c levels despite appropriate doses of these drugs, and for whom the conventional choice of switching to insulin therapy is not acceptable …
The Committee was aware of recent trial evidence on the clinical effectiveness of triple therapy. However, NICE is restricted to issuing guidance on licensed indications and so could not comment.
The licensed indications have changed, and are now (based on EMEA 2008):187
-
Rosiglitazone is indicated in the treatment of type 2 diabetes as:
-
– Monotherapy, in patients (particularly overweight patients) who are inadequately controlled by diet and exercise, for whom metformin is inappropriate because of contraindications or intolerance.
-
– Dual oral therapy in combination with metformin, in patients (particularly overweight ones) with insufficient glycaemic control, despite maximal tolerated dose of monotherapy with metformin.
-
– Dual oral therapy in combination with a sulfonylurea, only in patients who show intolerance to metformin, or for whom metformin is contraindicated, with insufficient glycaemic control despite sulfonylurea monotherapy.
-
– Triple oral therapy in combination with metformin, in patients with insufficient glycaemic control despite dual oral therapy.
-
-
The licence for pioglitazone is as above, but with, in addition:188
-
– Pioglitazone is also indicated for combination with insulin in type 2 diabetes patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance.
-
There are now more trials than were available at the time of NICE TA 63. The evidence base for rosiglitazone was updated in a Cochrane review published in July 2007 by Richter et al. (2007). 189 Their summary included:
Eighteen trials randomised 3888 people to rosiglitazone therapy. The longest duration of rosiglitazone treatment was 4 years. Most trials lasted around half a year. Unfortunately, the published studies of at least 24 weeks rosiglitazone treatment in people with type 2 diabetes mellitus did not provide relevant evidence that patient-orientated outcomes are positively influenced by this agent. The chance of developing oedema was approximately doubled. The single large randomised controlled trial showed evidence of raised cardiovascular risk after rosiglitazone treatment. Moreover, new safety data show increased numbers of fractures in women.
The review noted an increased risk of MI in those treated with rosiglitazone but that this was not statistically significant.
A Cochrane review of pioglitazone by the same authors190 (published Cochrane Library, Issue 4, 2006) was summarised thus:
Twenty-two trials which randomised 6200 people to pioglitazone treatment were identified. Longest duration of therapy was 34.5 months. Published studies of at least 24 weeks pioglitazone treatment in people with type 2 diabetes mellitus did not provide convincing evidence that patient oriented outcomes like mortality, morbidity, adverse effects, costs and health-related QoL are positively influenced by this compound. Metabolic control measured by HbA1c as a surrogate end point did not demonstrate clinically relevant differences to other oral antidiabetic drugs. Occurrence of oedema was significantly raised.
Comments like this would apply to most new diabetes drugs, as trials are usually short term and rely on proxy outcomes – usually HbA1c values. There are few trials, such as UKPDS, which are long enough to produce data on complications or mortality. Nor are they usually long enough to produce data on uncommon side effects.
The only exception to the short-term trials found in the Cochrane review was the PROactive study,191 a large study, with over 500 patients, which did set out to examine the effect of pioglitazone on hard outcomes, in a trial against placebo, in patients who had evidence of macrovascular disease. Patients continued their other diabetes medications, mainly metformin, sulfonylureas, insulin, or combinations thereof. The primary end point was a composite of death and non-fatal cardiovascular outcomes. The pioglitazone group had a lower risk but this did not reach statistical significance [hazard ratio (HR) 0.90, 95% CI 0.80 to 1.02, p = 0.095] despite the large numbers of recruits and events (at least one end point event in 514 of the pioglitazone group and 572 of the placebo group). A secondary end point measure of death, non-fatal MI and stroke did reach statistical significance (HR 0.84, 95% CI 0.72 to 0.98, p = 0.027). The closing statement focused on the secondary outcome, which was another composite outcome: ‘Pioglitazone reduces the composite of all-cause mortality, non-fatal MI and stroke’.
However, oedema and heart failure were commoner in the pioglitazone group, with 11% reported as having heart failure compared with 8% in the placebo group; the proportions needing hospital admission were 6% and 4%. The death rates from heart failure showed no difference. Heart failure was not defined centrally, but was ‘as judged by the investigator’. Another outcome was ‘oedema in the absence of heart failure’. Heart failure can be difficult to diagnose, and the absence of any difference in mortality from heart disease, might suggest that it could have been overdiagnosed. However, an independent group of cardiologists reviewed all of the cases of serious heart failure and concluded that it did occur more frequently in the pioglitazone group (5.5% versus 4.2% for placebo). 192
The most relevant finding from the PROactive study, in the light of today’s concerns about the safety of rosiglitazone, was that even if the reduction in cardiovascular events was small it was certainly not increased by pioglitazone.
The results have been somewhat optimistically interpreted in later publications. The economic analysis reported that:193 ‘Within trial cost-effectiveness analysis compared with pioglitazone was associated with improved life expectancy (undiscounted 0.0109 years)’.
(Note: 0.0109 years = 4 days.)
Another finding from PROactive191 was that progression to needing insulin was halved in the pioglitazone group. At the start of the study, about one-third of the patients were on insulin. Their mean age was 62 years, mean BMI = 31 and duration of diabetes 8 years. In total, 75% had a history of hypertension. Mean HbA1c level was around 7.8%. The protocol asked investigators to aim for an HbA1c level of < 6.5%. By the end of follow-up, 11% of the pioglitazone group and 21% of the placebo group were on insulin treatment. The switch to insulin started early in the trial, presumably due to investigators trying to achieve the HbA1c target.
Given that one alleged benefit of some of the new drugs for diabetes is a delay in, or avoidance of, insulin therapy, this finding seems highly relevant. The reduction in insulin use played a significant part in the economic analysis of the PROactive trial,193 where the Center for Outcomes Research (CORE) team, with co-authors from the manufacturer, reported that adding pioglitazone was cost-effective.
Rosiglitazone and safety
The glitazones situation changed in May 2007, when a meta-analysis by Nissen and Wolski (2007)194 was published in the New England Journal of Medicine. It concluded that there was an increased risk (by 40%) of cardiovascular disease with rosiglitazone compared with those on metformin or a sulfonylurea, or placebo. An editorial shortly after stated that a patient level analysis by the manufacturer of rosiglitazone had confirmed the findings. 195
Much debate followed. Another meta-analysis involving adding a new trial, the RECORD study (2007)196 to those in the meta-analysis by Nissen and Wolski, found that the risk still seemed to be increased, this time at an OR of 1.33 (95% CI 1.02 to 1.72). 197 This was because the RECORD study interim analysis reported a HR of only 1.11.
It is worth noting that the absolute risk in the studies was low.
The meta-analysis by Nissen and Wolski was criticised on various grounds, in particular that it excluded six trials which had no relevant events. With no events, it is impossible to assess the relative cardiovascular risks. However, the lack of events can tell us something about absolute risks. Interestingly, of the 42 trials that were included, 26 were unpublished, with data obtained from trials provided by GlaxoSmithKline (North Carolina, USA) to the US FDA. The FDA later (letter dated 25 March 2008)198 complained to GlaxoSmithKline about failure to pass on data from some trials and postmarketing studies.
A later meta-analysis [Diamond et al. (2007)199] applied different statistical techniques, included the six studies with no events, but excluded four studies. They then recalculated the ORs in six different ways, and showed that while there was still an increased risk for both MI and cardiovascular death, the CIs now overlapped with unity, and the ORs varied with method. For example, the OR for cardiovascular death ranged from 1.58 (95% CI 0.91 to 2.74) to 1.16 (0.75 to 1.79).
The Nissen and Wolski (2007) review194 included all trials, irrespective of duration. Most were too short-term to assess cardiovascular outcomes, but used glycaemic control as the main outcome. Singh et al. (2007)200 provided another meta-analysis, but restricted to trials with at least 12 months of follow-up, and which reported cardiovascular events. Their inclusion criteria reduced the number of trials to only four. They found that rosiglitazone increased the risk of MI (RR 1.42; 95% CI 1.06 to 1.91). It also doubled the risk of heart failure, as had been known. However, the overall cardiovascular mortality was not increased (RR 0.9, CI 0.63 to 1.26). The finding that heart failure is increased (with both glitazones), but that cardiovascular death was not, was also reported in yet another meta-analysis by Lago et al. (2007). 201
The NICE GDG reviewed the evidence up to the end of 2007, including trials and statements from regulatory bodies, the EMEA, the FDA and the MHRA. It noted that the new glycaemic control studies did not change what was already known. The main issue was safety. The GDG commented in guideline CG 666 that:
The GDG felt that there was certainly a ‘signal’ of increased risk of non-fatal myocardial infarction for rosiglitazone.
(The term ‘signal’ had been used by the FDA.)
But that:
On balance, despite reservations over rosiglitazone, it was not felt to be possible to unequivocally recommend a preference for pioglitazone in all circumstance, but rather to allow the choice of agent to rest with the person with diabetes and their advisor, taking account of the then regulatory advice (which may yet change).
The GDG continued:
However, the issues over fracture and fluid retention/cardiac failure and the costs of these drugs led the GDG to conclude that the TZDs could not generally replace sulphonylureas as second line therapy, except where sulphonylureas were contraindicated by particular risk of hypoglycaemia.
However, the GDG then went on to note that:
The health economic modelling appeared to identify that these drugs, in particular the then more highly priced rosiglitazone, were not cost-effective compared to insulin therapy.
But hypothesised that this might not apply in people of higher body weight, in whom insulin resistance was marked and weight gain common with insulin treatment.
If a patient is going to receive a glitazone, the key issue is whether pioglitazone is safer than rosiglitazone. If so, the next GDG may wish to recommend that rosiglitazone should not be used.
Recent evidence
No new trials of glitazones with hard clinical outcomes, which were not known to the previous guideline group, were found.
We did find a trial that reported proxy outcomes. In the PERISCOPE trial, Nissen et al. (2008)202 compared pioglitazone with glimepiride (a sulfonylurea) to see if there were any differences in progression of coronary artery disease. A total of 543 patients had coronary intravascular ultrasonography to measure the extent of coronary atherosclerosis, were randomised to pioglitazone or glimepiride, and had their coronary investigation repeated 18 months later. The investigators were asked to try to achieve an HbA1c level of < 7%. Baseline HbA1c levels were identical in the two groups (7.4%), but, over time the glimepiride group developed slightly higher levels – HbA1c 7.0% versus 6.9% (from the text: ‘figure 2 suggests that by study end the difference was about 0.3%’).
The main outcome measure was the mean atheroma volume. This increased by 0.73% (95% CI 0.33 to 1.12) in the glimepiride group but decreased by 0.16% (–0.57% to + 0.25%) in the pioglitazone group. The clinical significance of this small difference is uncertain, and, if the effect was due to the insulin-sensitising pioglitazone having advantages over the insulin secretagogue glimepiride, then, as the accompanying editorial points out, the more cost-effective approach would have been to compare metformin with a sulfonylurea. 203
A claim has been made recently that similar results have been obtained with rosiglitazone. These come from an unpublished trial, called VICTORY (Vein-Coronary Atherosclerosis and Rosiglitazone after bypass surgery). The results were presented at the American College of Cardiology 2008 conference, and the claim is reported in a newsletter, Heartwire (10 April 2008). 204 The data reported are of atheroma plaque volume, with a smaller percentage increase in those on rosiglitazone compared with those on placebo. Two comments are necessary. First, atheroma increased in both groups. Second, the different was not statistically significant (the p-value was 0.22). Further assessment must await full publication, but the details available at present do not justify the claim that the effect of rosiglitazone is similar to those seen with pioglitazone in PERISCOPE.
As reported in the recent guideline, a meta-analysis of the risk of cardiovascular events with pioglitazone was carried out by Lincoff et al. (2007)205 (who include Nissen and Wolski, who undertook the similar meta-analysis for rosiglitazone). Based on 19 trials with 16,930 participants, they concluded that pioglitazone was associated with a reduced risk of death, MI or stroke. They speculate that the differences in cardiovascular risk between rosiglitazone and pioglitazone are related to different effects on blood lipids (pioglitazone having a greater reduction in triglycerides and an increase in HDL cholesterol).
This meta-analysis included only trials funded by the manufacturer, because the authors used patient level data obtained from Takeda. Because most trials were short term and had relatively small numbers, around 80% of the events came from the PROactive trial.
Fractures
In the PERISCOPE trial, fractures occurred in 3% of the pioglitazone group but in none of the sulfonylurea group (p = 0.004).
Fracture risk has been reported in other studies. Kahn et al. (2006)29 in the ‘durability’ study (ADOPT) reported that 9.3% of women on rosiglitazone had fractures compared with 5.1% on metformin and 3.5% on glibenclamide. The increases were in fractures of upper limb and foot, rather than in the classical osteoporosis-associated neck of femur and vertebrae. There was no difference in men.
A case–control study by Meier et al. (2008),206 using British general practice data from General Practice Research Database, also found that use of glitazones was associated with increased fracture rates. No such increase was seen with other oral diabetes drugs.
A letter to physicians issued by Takeda Pharmaceuticals, and posted on the US FDA website207 reported an analysis of its clinical trials database on pioglitazone. They compared the incidence of fractures in over 8100 patients treated with pioglitazone compared to over 7400 patients treated with a comparator.
The fracture incidence calculated was 1.9 fractures per 100 patient-years in women treated with pioglitazone and 1.1 fractures per 100 patient-years in women treated with a comparator. The observed excess risk of fractures for women in this data set on pioglitazone is therefore 0.8 fractures per 100 patient-years of use. There was no increased risk of fracture identified in men.
The letter stated ‘the risk of fracture should be considered in the care of female patients with type 2 diabetes mellitus who are currently being treated with pioglitazone, or when initiation of pioglitazone treatment is being considered’.
What have other organisations said about rosiglitazone?
The FDA convened an advisory committee which concluded that:208 ‘The use of rosiglitazone for the treatment of type 2 diabetes was associated with a greater risk of myocardial ischemic events that placebo, metformin or sulphonylurea’.
However, the advisory committee did not recommend that rosiglitazone be removed from the market. It asked for label warnings, educational efforts and further trials.
The FDA issued a statement on 14 November 2007, with the key message being as follows:209
-
A meta-analysis of 42 clinical studies (mean duration 6 months; 14,237 total patients), most of which compared Avandia to placebo, showed Avandia to be associated with an increased risk of myocardial ischemic events such as angina or MI. Three other studies (mean duration 41 months; 14,067 patients) comparing Avandia to some other approved OAD agents, have not confirmed or excluded this risk. In their entirety, the available data on the risk of myocardial ischemia are inconclusive.
Health Canada issued a warning letter announcing new restrictions on the use of rosiglitazone on 6 November 2007, the key messages being:210
-
Rosiglitazone is no longer approved for use alone to treat type 2 diabetes, except when metformin use is contraindicated or nor tolerated.
-
Rosiglitazone is no longer approved for use with a sulfonylurea drug (such as glyburide), except when metformin is contraindicated or not tolerated.
-
Rosiglitazone should not be used if you have heart failure, or have experienced heart failure in the past.
-
Patients who are taking rosiglitazone, especially those with underlying heart disease, or those who are at high risk of heart attack or heart failure, should talk to their doctor about the benefits and risks of continuing rosiglitazone therapy.
-
Rosiglitazone should not be taken if you are using insulin.
-
Rosiglitazone should not be used in ‘triple therapy’.
These restrictions were based on advice from the Scientific Advisory Committee on metabolic and endocrine therapies (SAC-MET). The minutes of the meeting on 16 November 2007 give little detail for confidentiality reasons, but one comment was:211 ‘The Committee expressed concern that the risk data on rosiglitazone were inconclusive’.
The recommendations are curious, in that they say that rosiglitazone can be used when metformin cannot, but do not mention pioglitazone. Given that the evidence suggests cardiovascular harm with rosiglitazone but benefit with pioglitazone, they might have suggested that if metformin was not tolerated, pioglitazone should be the glitazone of choice.
The Drug and Therapeutics Bulletin reassessed the glitazones in April 2008. 212 As regards glycaemic control, the conclusions were that:
-
the glitazones were useful in dual combination with metformin or a sulfonylurea in patients who could not tolerate one or other of those
-
there was no convincing evidence of any benefits over metformin or a sulfonylurea as monotherapy
-
evidence for their use in triple therapy was weak, and that they should be reserved for patients in whom insulin was contraindicated or poorly tolerated
-
if a glitazone was thought to be necessary, pioglitazone was probably safer.
Two other UK bodies have issued advice:
The Midlands Therapeutics Reviews and Advisory Committee (MTRAC) reviewed both rosiglitazone and pioglitazone in March 2008. 213,214 They concluded that rosiglitazone should not be used: ‘Rosiglitazone cannot be recommended for prescribing, based on the current concerns about potential cardiovascular adverse effects and the lack of evidence for improved patient-oriented outcomes’.
Pioglitazone glitazone was classed as suitable for restricted prescribing, but with a low place in therapy.
The diabetes managed clinical network for Greater Glasgow and Clyde, as reported in The Scotsman of 8 May 2008,215 has recommended that no new patients should be started on rosiglitazone, and that GPs should look carefully at those already taking it. Some consultants favoured withdrawing rosiglitazone completely.
The consensus group from ADA and EASD216 issued an update about the glitazones to its algorithm on treatment for type 2 diabetes. The update reserved judgement:
At this time, we do not view as definitive the clinical trial data regarding increased or decreased risk of myocardial infarctions with rosiglitazone or pioglitazone, respectively.
On the other hand, we do believe that the weight of the new information …should prompt clinicians to consider more carefully whether to use this class of drugs versus insulin or sulfonylureas …
and
The current decision not to remove either or both of the glitazones from the algorithm represents a balance between the preservations of options to treat a challenging and progressive disease, and the recent unfavourable evidence.
The Australian National Prescribing Service issued notes on rosiglitazone in December 2007217 and on pioglitazone in March 2008. 218 They also issued a media release in December 2007 saying that:219 ‘Prescribers should also be aware of a possible increased risk of myocardial ischaemia in patients taking rosiglitazone. The same risk has not been shown with pioglitazone but the possibility cannot be dismissed’.
The December note on rosiglitazone suggested that in patients failing on dual therapy, clinicians should consider using insulin rather than rosiglitazone because:
-
Insulin reduces the risk of diabetic complications, whereas the effect of rosiglitazone on diabetes-related morbidity and mortality is still unclear.
-
The long-term safety profile of insulin is better defined. The only completed long-term trial of rosiglitazone reported significantly higher rates of heart failure, oedema and fracture among the rosiglitazone group than among those using metformin or glibenclamide.
-
Greater reductions in HbA1c levels have been reported among patients with poor glycaemic control who were treated with insulin rather than rosiglitazone.
The pioglitazone note in March 2008 was quite similar. Neither note suggested that pioglitazone should be preferred to rosiglitazone. A practice review for GPs dated February 2008 suggested that:220 ‘If metformin and a sulphonylurea no longer control blood glucose, start insulin promptly. Trialling a glitazone as part of triple oral therapy may be an option but insulin should be started if hyperglycaemia is still uncontrolled after 3 months’.
More on the safety of glitazones
As new trials are reported, they are being added to new meta-analyses. Dahabreh (2008)221 updated the Nissen and Wolski (2007)194 meta-analysis with the results from the DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication)222 and ADOPT29 trials, and the interim report from the RECORD (Rosiglitazone Evaluated for Cardiac Outcomes and Regulation of glycaemia in Diabetes) trial. 196 [Note: DREAM included patients with impaired glucose tolerance (IGT) or impaired fasting glucose (IFG), not diabetes.] He noted the debate about the methods for doing meta-analysis when some trials had no events, and carried out the analyses using methods that allowed inclusion of such trials, as well as the Peto method, which was used in the original Nissen and Wolski meta-analysis.
The results were consistent with the previous finding of an increase in MI with rosiglitazone but ORs were slightly less, and in two of the five meta-analyses their CIs sometimes just overlapped with no increase (95% CIs of 0.97 to 1.59 and 0.96 to 1.57).
It is curious that rosiglitazone appears to increase non-fatal MI but not cardiovascular death. It may simply be a function of numbers, because the CV death ORs have much wider CIs.
Another meta-analysis by Mannucci et al. (2008)174 included 84 published and 10 unpublished trials of pioglitazone compared with placebo or active comparators, but excluded the PROactive trial. They reported a reduction of all-cause mortality with pioglitazone (OR 0.30; 95% CI 0.14 to 0.63, p < 0.05), but no significant effect on non-fatal coronary events.
Several new studies have asked why rosiglitazone should increase cardiovascular events but pioglitazone does not. Most have concluded that the likely reason is that while the two glitazones have the same effects on glycaemic control, and the same side effects of fluid retention and heart failure, they have different effects on blood lipids. Berneis et al. (2008)223 (based on data from the abstract only) carried out a very small crossover trial in 9 patients, giving them all 12 weeks on pioglitazone and 12 weeks on rosiglitazone. Total cholesterol increased more on rosiglitazone (need absolute levels) than on pioglitazone (p = 0.04), and triglycerides increased on rosiglitazone but decreased on pioglitazone (p = 0.004).
Chappuis et al. (2007)224 also studied patients on both glitazones, this time with 17 patients having 12 weeks on each. The effects of HbA1c level were similar, but triglyceride and cholesterol levels were lower with pioglitazone.
Deeg et al. (2007)225 carried out a much larger comparison, with 369 randomised to pioglitazone and 366 to rosiglitazone. The two drugs had differing effects on lipids, with rosiglitazone having the more atherogenic pattern, including higher low-density lipoprotein (LDL) cholesterol levels.
Norris et al. (2007)226 carried out a systematic review of the comparative effectiveness and safety of pioglitazone and rosiglitazone. They concluded that effects of glycaemic control, weight and most adverse events were similar, but that rosiglitazone may increase total cholesterol compared with pioglitazone. However, they concluded they had insufficient evidence with which to compare cardiovascular event rates.
Data from the VADT (Veterans Affairs Diabetes Trial) have been used to assert that rosiglitazone does not cause cardiovascular harm [Duckworth (2009)227]. However, this evidence seems dubious, given that most patients in both arms were taking rosiglitazone.
The effect of all this has been that sales of rosiglitazone have fallen. A report in the newsletter Endocrine Today228 states that sales fell from US$617M worldwide in the first quarter of 2007 to US$327M in the fourth quarter (although it does not say whether the price was reduced). A Canadian report notes that there was a sudden decline in the use of rosiglitazone after the publication of the Nissen and Wolski meta-analysis,194 accompanied by an increase in the use of pioglitazone. 229
Points raised in the consultation process
In their responses to the draft guideline, GlaxoSmithKline referred to new studies that provided safety data. The studies cited were the ACCORD (Action to Control Cardiovascular Risk in Diabetes Study)230 and the VADT. 227
The ACCORD study was a trial of intensive versus standard therapy, aiming at a separation in HbA1c level. The intensive group did worse with higher mortality and no reduction in cardiovascular events. In the intensive group, 2.6% of patients died from cardiovascular causes, versus 1.8% in the standard group (p = 0.02); 91% of the intensive group were treated with rosiglitazone versus 58% of the standard group. So the ACCORD study did not provide new data on the safety of rosiglitazone.
Summary
Little new has emerged since the last guideline was produced. Pioglitazone and rosiglitazone appear to have similar effectiveness in controlling hyperglycaemia, and similar toxicity in terms of oedema, heart failure and (in women only) fractures. However, the current evidence suggests that rosiglitazone slightly increases cardiovascular mortality but that pioglitazone reduces it. Most of the regulatory and prescribing advisory bodies have asked for warnings on rosiglitazone but have allowed its continued use. Some have suggested that, in future, pioglitazone be used in preference.
Chapter 6 Clinical effectiveness of pioglitazone in combination with insulin
Objectives
In this chapter, we assess the effects of the combination of insulin treatment with pioglitazone compared with:
-
insulin treatment alone, and
-
pioglitazone treatment alone.
Methods
Inclusion criteria
Types of studies
We considered RCTs with a minimum duration of 12 weeks, although trials of at least 24 weeks’ duration were preferred.
Types of participants
Patients with type 2 diabetes, of any age and gender.
Types of interventions
Pioglitazone in combination with any insulin regimen (including insulin plus metformin).
Comparisons could include:
-
A:
-
long-acting insulin plus pioglitazone versus long-acting insulin alone
-
long-acting insulin plus metformin plus pioglitazone versus long-acting insulin plus metformin
-
twice-daily mixture plus pioglitazone versus twice-daily mixture
-
twice-daily mixture plus metformin plus pioglitazone versus twice-daily mixture plus metformin.
-
-
B:
-
long-acting insulin plus pioglitazone versus pioglitazone alone
-
long-acting insulin plus metformin plus pioglitazone versus pioglitazone plus metformin
-
twice-daily mixture plus pioglitazone versus pioglitazone alone
-
twice-daily mixture plus metformin plus pioglitazone versus pioglitazone plus metformin.
-
There may be trials of the above with sulfonylurea as well as metformin.
Types of outcomes
We planned to consider the following outcome measures:
-
HbA1c
-
frequency of hypoglycaemia, especially if severe
-
glycaemic excursions, including postprandial hyperglycaemia
-
total daily dose of insulin
-
weight gain or loss
-
complication rates – retinopathy, nephropathy, MI, angina, heart failure, stroke, amputation, death
-
adverse events
-
health-related QoL.
Search strategy
Relevant literature was identified, and comprehensiveness checked, by:
-
searches of bibliographic databases, MEDLINE, Cochrane Library, and EMBASE
-
checking reference lists of retrieved studies
-
obtaining lists of published studies from manufacturers
-
our peer review process.
Searches were also undertaken to identify emerging evidence, from conference abstracts and trial registers. Studies available only in abstract were included in the assessment of clinical effectiveness if there is a paucity of studies published in full in peer reviewed journals, but they were reported with appropriate caution. Our default position is for studies available only in abstract not to be used.
Authors of previous studies were not contacted.
Quality assessment of studies
Randomised controlled trials were assessed on the following criteria based on the NICE guidelines manual:
-
method of randomisation
-
allocation concealed
-
participants and blinded
-
outcome assessors blinded
-
ITT analysis performed
-
proportion of participants excluded/lost to follow-up
-
power calculation
-
groups comparable at baseline.
Again, overall quality of the trials was classified as good, moderate, or poor.
Data extraction
Data extraction was carried out by one researcher and a sample checked by another. Any disagreements were resolved through discussion, involving a third person if necessary.
Data analysis
The clinical effectiveness, relative to the key comparators, was assessed, in terms of difference in effect size.
Data were summarised in a meta-analysis and using tables and text. For dichotomous outcomes, ORs were calculated and a Mantel-Haenszel random effects model was used. For continuous outcomes, standardised mean differences were calculated and an inverse variance random effects model was used. Heterogeneity was assessed using the chi-squared test.
Systematic reviews
Search results
Eleven papers were identified as potentially relevant RCTs. Of these, eight fulfilled the inclusion criteria and compared pioglitazone plus insulin with insulin. 231–238 One compared pioglitazone plus insulin with pioglitazone. The remaining trials were excluded because they did not examine the comparison of interest, and one was the uncontrolled extension of a trial that seemed relevant but could not be identified (shown in Table 24).
Description of studies – insulin + pioglitazone vs insulin
Characteristics of the included trials are shown in Appendix 6.
Design
Seven trials were randomised double-blind placebo-controlled trials,231–233,235–238 while one trial was a randomised open-label trial. 234 The studies had different emphases: Asnani et al. (2006)238 and Fernandez et al. (2008)232 focused on vascular reactivity; Berhanu et al. (2007)231 focused on reduction of insulin dosage; Mattoo et al. (2005)233 focused on glycaemic control, lipids and cardiovascular risk factors; Raz et al. (2005)234 and Rosenstock (2002)235 focused on glycaemic control; Scheen and Charbonnel (2006)236 focused on secondary prevention of macrovascular events; and Shah et al. (2007)237 focused on body fat distribution. Trial duration ranged between 12 and 36 weeks. Where stated, trials were sponsored by industry. Five trials were from the USA,231,232,235,237,238 one included centres from a range of European countries,236 and two included centres worldwide. 233,234
Participants
The trials included between 20 and 1760 participants, with between 10 and 896 participants in each comparison group. The total number of patients assessed was 3092. All studies included participants with previous inadequate glucose control [with different definitions, not reported for Shah et al. (2007)237]. Inclusion criteria with respect to previous treatment varied substantially. Only five trials232,233,235,237,238 required previous insulin treatment. Three trials233,235,238 required previous insulin therapy with or without OAD agents (where reported, previous insulin monotherapy ranged between 48% and 88%). The trial by Fernandez et al. (2008)232 required previous insulin combination therapy,232 and the trials by Shah et al. (2007)237 included only insulin-treated obese patients. 237 Of the remaining trials, the trial by Berhanu et al. (2007)231 required previous combination therapy with or without insulin, and in this trial, between 90% and 93% of patients had been on sulfonylurea plus metformin therapy without insulin. The study by Raz et al. (2005)234 required previous therapy with sulfonylurea (alone or as oral combination therapy) and over 80% of patients in that trial had been on sulfonylurea plus metformin previously. The study by Scheen and Charbonnel (2006)236 included patients previously on diet alone, oral agents, or insulin plus an oral agent and in that trial, over half of the patients (53%) had been on sulfonylurea plus insulin, and the second largest group had been on sulfonylurea monotherapy (24%). Where reported, mean age of participants was between 46 and 59 years, the comparison groups included between 35% and 60% of women, mean BMI was between 29 and 37 kg/m2, and diabetes duration was between 6 and 14 years. The trial by Berhanu et al. (2007)231 included between 50% and 59% of Hispanic participants, and the study by Fernandez et al. (2008)232 included only Mexican–American participants. 232
Interventions
The trials used pioglitazone doses up to 45 mg/day. Four trials used titration schemes for pioglitazone (up to 45 mg/day, usually starting at 15 mg/day). 231,232,236,237 Three trials used fixed doses of 30 mg/day. 233,234,238 Rosenstock (2002)235 compared two pioglitazone doses: 15 and 30 mg/day.
As concerns the insulin therapy, Asnani et al. (2006),238 Rosenstock (2002)235 and Scheen and Charbonnel (2006)236 only specified that insulin therapy was continued as before. Rosenstock (2002)235 used a single-blind insulin monotherapy lead-in period. Berhanu et al. (2007)231 used a 4-week titration period for insulin (Humalog, Humulin 70/30 or Humulin N) and defined a target FPG of less than 140 mg/dl while avoiding hypoglycaemia. In the study by Fernandez et al. (2008)232 patients could choose between multiple daily injections (basal bolus therapy using combination of insulin glargine at bedtime plus premeal insulin aspart) or continuous subcutaneous infusions (basal infusion and pre-meal boluses of insulin aspart) and defined targets for blood glucose values (fasting and pre-meal capillary blood glucose 80–120 mg/dl, 2 hours post-meal glucose < 160 mg/dl, bedtime glucose < 140 mg/dl). Mattoo et al. (2005)233 used a 3-month insulin intensification period before randomisation; the insulin dose was reduced by 10% at randomisation to avoid hypoglycaemia and adjusted thereafter, based on self-monitored blood glucose levels. Raz et al. (2005)234 used biphasic insulin aspart 30/70. In the study by Scheen and Charbonnel (2006),236 concomitant therapy with metformin was used by 47–52%, sulfonylurea alone by 16%, and metformin plus sulfonylurea by 10–11%. Shah et al. (2007)237 did not give details of the insulin therapy.
Various studies specified cointerventions. Asnani et al. (2006)238 allowed stable lipid lowering therapy with statins and antihypertensive therapy (including ACE inhibitors in all patients). In the study by Berhanu et al. (2007)231 statins and metformin where continued as before. Fernandez et al. (2008)232 changed all patients previously on angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers for blood pressure control to alpha-methyl dopa. Fernandez et al. (2008)232 and Rosenstock (2002)235 allowed lipid-lowering therapy as used before the study.
Outcomes
The trials used a variety of primary end points. HbA1c level was the primary end point in the studies by Mattoo et al. (2005),233 Raz et al. (2005)234 and Rosenstock (2002). 235 The primary end point in the study by Asnani et al. (2006)238 was flow-mediated dilatation, in the study by Berhanu et al. (2007)231 it was change in insulin dosage, Fernandez et al. (2008)232 used vascular analyses as primary end point, in the study by Scheen and Charbonnel (2006)236 it was a composite macrovascular end point, and in the study by Shah et al. (2007)237 it was body fat distribution. All studies reported on end-of-study HbA1c values; six studies reported on hypoglycaemia;231–236 one study reported on glycaemic excursions;234 six studies reported on total daily dose;231–236 six studies reported on weight change;231–235,237 five studies reported on adverse events; and six studies reported on lipid parameters,231–235,238 while none of the studies reported on rates of diabetic secondary complications or health-related QoL.
Quality of studies – insulin + pioglitazone vs insulin
Details of the quality of included trials are shown in Table 25.
| Study | Method of randomisation | Allocation concealment | Blinding | ITT data analysis | Percentage who completed trial | Power calculation | Similarity of groups at baseline | Sponsorship/author affiliation |
|---|---|---|---|---|---|---|---|---|
| Asnani (2006)238 | Carried out by research pharmacist using predetermined randomisation code | Yes | Double blind | Not reported |
PIO + Ins: 80% P + Ins: 80% |
Yes (on flow-mediated dilatation) | HbA1c higher at baseline for PIO + Ins group (10% vs 8.7%) but not statistically significant | Takeda, National Institutes of Health |
| Berhanu (2007)231 | Computer-generated schedule | Yes | Double blind | Yes |
PIO + Ins: 87.3% P + Ins: 91.1% |
Yes (on mean change in insulin dose) | Insulin group had significantly higher BMI (31.8 vs 30.7 kg/m2) and longer diabetes duration (8.5 vs 7.7 years) | Takeda Global R&D Centre |
| Fernandez (2008)232 | Not reported | Not reported | Double blind | Not reported | Unclear – all? | Yes (on vascular parameters) | Yes | American Diabetes Association, Takeda Pharmaceuticals |
| Mattoo (2005)233 | Central randomisation table administered by an automated interactive voice system | Yes | Double blind | Yes |
PIO + Ins: 90% P + Ins: 92% |
Yes (on change in HbA1c) | Yes | Eli Lilly, Takeda Europe |
| Raz (2005)234 | Unclear (‘assignment of lowest available patient number’) | Not reported | No | Yes |
PIO + Ins: 78% Ins mono: 77% |
Yes (on change in HbA1c) | Yes | Novo Nordisk |
| Rosenstock (2002)235 | Not reported | Not reported | Double blind | Yes |
PIO15 + Ins: 84% PIO30 + Ins: 91% P + Ins: 88% |
Not reported | Yes | Takeda Pharmaceuticals |
| Scheen (2006)236 | Central interactive voice-response system | Not reported | Double blind | Yes | Not reported | Yes | Not reported | Takeda Europe, Eli Lilly |
| Shah (2007)237 | Not reported | Not reported | Double blind | Not reported | Not reported | Not reported – small numbers, probably underpowered | Not reported | Not reported |
For four231,233,234,238 of the eight trials, randomisation was adequate, whereas for the remaining four trials the randomisation procedure was not reported or unclear. Three trials231,233,238 had adequate allocation concealment, whereas the rest of the trials did not report on allocation concealment. All but one trial234 were described as double blind. Five trials used ITT analysis. 231,233–236 Five trials reported on follow-up rates231,233–235,238 and in those trials, between 77% and 92% of participants completed the trial, without any significant differences between comparison groups. Six of the eight trials reported that they had carried out a power calculation. 231–233,235,236,238 Two trials (reported as abstracts)236,237 did not report relevant baseline characteristics, five trials reported that there comparison groups were similar at baseline,232,233–235,238 while Berhanu et al. (2007)231 stated that participants in the placebo group had a slightly higher BMI at baseline and longer diabetes duration, but it was unclear whether these differences were significant. All but one trial237 reported on sources of funding, and all funding included industry funding.
Results – insulin + pioglitazone vs insulin
Details of the results for included trials for insulin plus pioglitzone versus insulin are shown in Table 26.
| Study | Outcome | Baseline | End of study | Change from baseline/difference between groups | p-value (between groups) |
|---|---|---|---|---|---|
| HbA1c | |||||
| Asnani (2006)238 | HbA1c (%) |
PIO + Ins: 10.0, SD 2.3% P + Ins: 8.7, SD 2.3% |
PIO + Ins: 8.4, SD 2.0% P + Ins: 8.6, SD 1.4% |
p not reported (p < 0.05 for PIO before and after) | |
| Berhanu (2007)231 | HbA1c (%) |
PIO + Ins: 8.4, SD 0.13% P + Ins: 8.6, SD 0.13% |
PIO + Ins: 6.81% P + Ins: 7.23% |
PIO + Ins: –1.6, SE 0.11% P + Ins: –1.4, SE 0.11% |
p = NS |
| Fernandez (2008)232 | HbA1c (%) |
PIO + Ins: 9.0, SD 0.7% P + Ins: 9.2, SD 0.4% |
PIO + Ins: 6.9, SD 0.3% P + Ins: 7.2, SD 0.1% |
||
| Mattoo (2005)233 | HbA1c (%) |
PIO + Ins: 8.85 SE0.11% P + Ins: 8.79 SE0.1% |
PIO + Ins: 8.11, SE 0.09% P + Ins: 8.66, SE 0.08% |
PIO + Ins difference between groups: 0.69, SE 0.09% P + Ins: –0.13% |
p < 0.002 |
| Percentage attaining HbA1c < 7.0% |
PIO + Ins: 18% P + Ins: 6.9% |
||||
| HbA1c subgroups: patients using ≤ 2 or ≥ 3 insulin injections | No significant difference | ||||
| HbA1c subgroups: previous use of OAD agents |
Previous use of oral agents PIO + Ins: –0.90, SE 0.14% P + Ins: –0.11, SE 0.13% No previous use of oral agents PIO + Ins: –0.65, SE 0.11% P + Ins: –0.2, SE 0.12% |
No significant difference for subgroups | |||
| Raz (2005)234 | HbA1c (%) |
PIO + Ins: 9.6, SD 1.3% Ins mono: 9.5, SD 1.3% |
PIO + Ins: 8.4, SD 1.2% Ins mono: 9.0, SD 1.3% |
p = 0.008 | |
| Rosenstock (2002)235 | HbA1c (%) |
PIO15 + Ins: 9.75, SE 0.1% PIO30 + Ins: 9.84, SE 0.1% P + Ins: 9.75, SE 0.1% |
PIO15 + Ins: –0.99, SE 0.08% PIO30 + Ins: –1.26, SE 0.08% P + Ins: –0.26, SE 0.08% |
p < 0.01 pioglitazone vs placebo | |
| Shah (2007)237 | HbA1c (%) |
PIO + Ins: 7.6% P + Ins: 7.8% |
PIO + Ins: 7.1% P + Ins: 7.2% |
p not reported, presumably non-significant | |
| Scheen (2006)236 | HbA1c (%) |
PIO + Ins: 8.4% P + Ins: 8.5% |
PIO + Ins: 7.47% P + Ins: 8.05% |
PIO + Ins: –0.93% P + Ins: –0.45% |
p < 0.0001 |
| Hypoglycaemia | |||||
| Berhanu (2007)231 | Patients with hypoglycaemic events |
PIO + Ins: 46% (91% mild) P + Ins: 31% (66% mild) |
p < 0.005 | ||
| Severe hypoglycaemia (episodes) |
PIO + Ins: n = 0 P + Ins: n = 4 |
p not reported | |||
| Fernandez (2008)232 | Patients with hypoglycaemic episodes |
PIO + Ins: n = 4 P + Ins: n = 6 |
|||
| Mattoo (2005)233 | Patients with subjective hypoglycaemic episodes |
PIO + Ins: 63.4% P + Ins: 51.0% |
p < 0.05 | ||
| Clinical hypoglycaemic episodes (blood glucose < 2.8 mmol/l) | No significant difference | ||||
| Raz (2005)234 | Major hypoglycaemic episodes | None | |||
| Minor hypoglycaemic episodes (% patients) |
PIO + Ins: 12% Ins mono: 15% |
p not reported | |||
| Minor hypoglycaemic episodes (episodes) |
PIO + Ins: 15 Ins mono: 47 |
p not reported | |||
| Symptoms only (% patients) |
PIO + Ins: 34% Ins mono: 40% |
p not reported | |||
| Symptoms only (episodes) |
PIO + Ins: 115 Ins mono: 171 |
p not reported | |||
| Incidence (per patient-week for all episodes) |
PIO + Ins: 0.083 Ins mono: 0.132 |
p < 0.05 | |||
| Nocturnal hypoglycaemia (episodes) |
PIO + Ins: 0 Ins mono: 8 |
p not reported | |||
| Rosenstock (2002)235 | Hypoglycaemia |
PIO15 + Ins: 8% PIO30 + Ins: 15% P + Ins: 5% (all considered mild to moderate) |
|||
| Scheen (2006)236 | Hypoglycaemia (not specified further) |
PIO + Ins: 41% P + Ins: 29% |
p < 0.0001 | ||
| Glycaemic excursions | |||||
| Raz (2005)234 | Measurements before dinner, 90 minutes after dinner and at bedtime significantly lower in PIO + Ins group than in Ins-mono group | ||||
| Total daily dose | |||||
| Berhanu (2007)231 | Daily insulin dose |
PIO + Ins: 55.8, SD 2.95 units P + Ins: 57.7, SD 2.95 units |
PIO + Ins: –12.0, SE 1.84 units P + Ins: +0.8, SE 1.84 units Adjusted mean difference between groups: 12.7 units (95% CI –17.5 to –8.0) |
p < 0.001 | |
| Fernandez (2008)232 | Daily insulin dose | All groups: ~1.2 U/kg/day |
PIO + Ins: 1.0 U/kg/day P + Ins: ~1.2 U/kg/day |
p not reported | |
| Mattoo (2005)233 | Daily insulin dose |
PIO + Ins: 0.96, SE 0.03 U/kg/day P + Ins: 0.92, SE 0.03 U/kg/day |
PIO + Ins: 0.76, SE 0.02 U/kg/day P + Ins: 0.94, SE 0.02 U/kg/day |
Difference between groups –0.18, SE 0.02 U/kg/day | p < 0.002 |
| Raz (2005)234 | Daily insulin dose |
PIO + Ins: 0.2 U/kg/day Ins mono: 0.3 U/kg/day |
PIO + Ins: 0.5 U/kg/day Ins mono: 0.7 U/kg/day |
PIO + Ins: +0.3 U/kg/day Ins mono: +0.4 U/kg/day |
p = 0.002 |
| Rosenstock (2002)235 | Daily insulin dose |
PIO15 + Ins: 70.2, SE 34.0 U/day PIO30 + Ins: 72.3, SE 38.5 U/day P + Ins: 70.7, SE 33.5 U/day |
PIO15 + Ins: 67.3, SE 33.5 U/day PIO30 + Ins: 64.2, SE 32.7 U/day P + Ins: 70.1, SE 33.9 U/day |
p not reported | |
| Scheen (2006)236 | Daily insulin dose |
PIO + Ins: 47 U/day P + Ins: 47 U/day |
PIO + Ins: 42 U/day P + Ins: 55 U/day |
p < 0.0001; at final visit, insulin discontinued in 9% of PIO group and 2% of placebo group (p < 0.0001) | |
| Weight change | |||||
| Berhanu (2007)231 | Weight (kg) |
PIO + Ins: +4.39 kg P + Ins: +2.42 kg |
p not reported | ||
| Patients reporting weight gain |
PIO + Ins: n = 10 P + Ins: n = 3 |
p not reported | |||
| Fernandez (2008)232 | Weight (kg) |
PIO + Ins: +4.4 kg P + Ins: +1.7 kg |
p not reported | ||
| Mattoo (2005)233 | Weight (kg) |
PIO + Ins: +4.05, SE 4.03 kg P + Ins: +0.20, SE 2.92 kg |
p not reported | ||
| Raz (2005)234 | Weight (kg) |
PIO + Ins: +4.0 kg Ins mono: +2.2 kg |
p not reported | ||
| Patients experiencing weight gain (%) |
PIO + Ins: 8% Ins mono: 2% |
p not reported | |||
| Rosenstock (2002)235 | Weight (kg) |
PIO15 + Ins: 95.4, SE 17.6 kg PIO30 + Ins: 98.7, SE 17.7 kg P + Ins: 95.4, SE 17.0 kg |
PIO15 + Ins: +2.3 kg PIO30 + Ins: +3.7 kg P + Ins: –0.04 kg |
p not reported; weight gain related to decreases in HbA1c; p = 0.002 | |
| Shah (2007)237 | Weight (kg) |
PIO + Ins: 107.1 kg P + Ins: 108.7 kg |
PIO + Ins: 112.0 kg P + Ins: 110.1 kg |
p not reported, presumably non-significant | |
| Complication rates | |||||
| Berhanu (2007)231 | Cardiac events |
PIO + Ins: 5.5% P + Ins: 10.7% (mostly ECG abnormalities) |
p not reported | ||
| Deaths | No deaths | ||||
| Lipid parameters | |||||
| Berhanu (2007)231 | Total cholesterol (mg/dl) |
PIO + Ins: 178, SE 3.53 mg/dl P + Ins: 183, SE 3.6 mg/dl |
PIO + Ins: +5.7, SD 2.75 mg/dl P + Ins: +4.7, SD 2.78 mg/dl |
p = NS | |
| HDL cholesterol (mg/dl) |
PIO + Ins: 44.6, SE 1.3 mg/dl P + Ins: 42, SE 1.3 mg/dl |
PIO + Ins: +4.3, SD 0.75 mg/dl P + Ins: –0.2, SD 0.77 mg/dl |
p < 0.001 | ||
| LDL cholesterol (mg/dl) |
PIO + Ins: 107, SE 3.1 mg/dl P + Ins: 111, SE 3.2 mg/dl |
PIO + Ins: +4.0, SD 2.37 mg/dl P + Ins: +0.9, SD 2.37 mg/dl |
p = NS | ||
| Triglycerides (mg/dl) |
PIO + Ins: 123, SE 7.5 mg/dl P + Ins: 141, SE 7.6 mg/dl |
PIO + Ins: –0.2, SD 9.80 mg/dl P + Ins: +43.7, SD 9.96 mg/dl |
p < 0.001 | ||
| Fernandez (2008)232 | Total cholesterol (mg/dl) |
PIO + Ins: 176, SD 9 mg/dl P + Ins: 195, SD 9 mg/dl |
PIO + Ins: 175, SD 16 mg/dl P + Ins: 180, SD 8 mg/dl |
p = NS | |
| LDL cholesterol (mg/dl) |
PIO + Ins: 107, SD 7 mg/dl P + Ins: 121, SD 8 mg/dl |
PIO + Ins: 105, SD 12 mg/dl P + Ins: 115, SD 7 mg/dl |
p = NS | ||
| HDL cholesterol (mg/dl) |
PIO + Ins: 45, SD 3 mg/dl P + Ins: 49, SD 4 mg/dl |
PIO + Ins: 51, SD 3 mg/dl P + Ins: 46, SD 3 mg/dl |
p < 0.05 pioglitazone vs baseline | ||
| VLDL cholesterol (mg/dl) |
PIO + Ins: 109, SD 16 mg/dl P + Ins: 113, SD 24 mg/dl |
PIO + Ins: 88, SD 15 mg/dl P + Ins: 93, SD 19 mg/dl |
|||
| Triglycerides (mg/dl) |
PIO + Ins: 148, SD 17 mg/dl P + Ins: 146, SD 15 mg/dl |
PIO + Ins: 123, SD 11 mg/dl P + Ins: 132, SD 18 mg/dl |
p < 0.05 pioglitazone vs baseline | ||
| Mattoo (2005)233 | HDL cholesterol (mmol/l) |
PIO + Ins: 1.23, SE 0.03 mmol/l P + Ins: 1.24, SE 0.03 mmol/l |
PIO + Ins: 1.35, SE 0.02 mmol/l P + Ins: 1.21, SE 0.02 mmol/l |
Difference between groups: 0.13, SE 0.03 mmol/l | p < 0.002 |
| LDL cholesterol (mmol/l) |
PIO + Ins: 3.20, SE 0.09 mmol/l P + Ins: 3.18, SE 0.08 mmol/l |
PIO + Ins: 3.18, SE 0.06 mmol/l P + Ins: 3.10, SE 0.06 mmol/l |
p = NS | ||
| Raz (2005)234 | Triglycerides (mg/dl) |
PIO + Ins: 149, SD 88 mg/dl Ins mono: 158, SD 88 mg/dl |
p = NS | ||
| Total cholesterol (mg/dl) |
PIO + Ins: 212 mg/dl Ins mono: 204 mg/dl |
p = NS | |||
| HDL cholesterol (mg/l) | Difference between PIO + Ins vs Ins mono: +4, SD 1 mg/dl | p < 0.01 | |||
| LDL cholesterol (mg/l) | No data shown | p = NS | |||
| Rosenstock (2002)235 | Triglycerides (mmol/l) |
PIO15 + Ins: 2.61, SE 0.2 mmol/l PIO30 + Ins: 2.96, SE 0.2 mmol/l P + Ins: 2.74, SE 0.2 mmol/l |
LS % mean change from baseline PIO15 + Ins: +5.35, SE 6.56% PIO30 + Ins: –10.35, SE 6.54% P + Ins: +13.30, SE 6.63% |
p < 0.05, PIO30 vs placebo | |
| HDL cholesterol (mg/dl) |
PIO15 + Ins: 43.42, SE 0.95 mg/dl PIO30 + Ins: 42.71, SE 0.94 mg/dl P + Ins: 42.66, SE 0.96 mg/dl |
LS % mean change from baseline PIO15 + Ins: +7.07, SE 1.58% PIO30 + Ins: +9.13, SE 1.57% P + Ins: –0.21, SE 1.59% |
p < 0.05 PIO30 vs placebo | ||
| Total cholesterol (mg/dl) |
PIO15 + Ins: 213.08, SE 3.57 mg/dl PIO30 + Ins: 207.32, SE 3.53 mg/dl P + Ins: 214.03, SE 3.58 mg/dl |
LS % mean change from baseline PIO15 + Ins: +1.40, SE 1.06% PIO30 + Ins: +0.40, SE 1.05% P + Ins: –0.66, SE 1.07% |
p = NS | ||
| LDL cholesterol (mg/dl) |
PIO15 + Ins: 127.33, SE 3.07 mg/dl PIO30 + Ins: 121.69, SE 3.06 mg/dl P + Ins: 130.95, SE 3.05 mg/dl |
LS % mean change from baseline PIO15 + Ins: +2.83, SE 1.80% PIO30 + Ins: +5.05, SE 1.71% P + Ins: –1.41, SE 1.74% |
p = NS | ||
| Adverse events | |||||
| Berhanu (2007)231 | Oedema |
PIO + Ins: n = 10 P + Ins: n = 5 (all mild to moderate) |
p not reported | ||
| Serious adverse events |
PIO + Ins: n = 4 P + Ins: n = 2 (none considered to be related to study medication) |
p not reported | |||
| Mattoo (2005)233 | Withdrawal due to adverse events |
PIO + Ins: n = 7 P + Ins: n = 3 |
p not reported | ||
| Oedema |
PIO + Ins: n = 20 (10 classified as mild) P + Ins: n = 5 (three classified as mild) |
p not reported | |||
| Raz (2005)234 | Withdrawal due to adverse events |
PIO + Ins: n = 1 Ins mono: n = 2 |
p not reported | ||
| Patients with product-related adverse events |
PIO + Ins: 28% Ins mono: 20% |
p not reported | |||
| Peripheral oedema |
PIO + Ins: 6% Ins mono: 0 |
p not reported | |||
| Serious adverse events |
PIO + Ins: n = 0 Ins mono: n = 2 (none considered to be related to study medication) |
||||
| Rosenstock (2002)235 | Withdrawal due to adverse events |
PIO15 + Ins: 1.6% PIO30 + Ins: 2.6% P + Ins: 3.2% |
p not reported | ||
| Oedema |
PIO15 + Ins: 12.6% PIO30 + Ins: 17.6% P + Ins: 7.0% |
p not reported | |||
| Cardiovascular adverse events |
PIO15 + Ins and PIO30 + Ins: 7.9% P + Ins: 7.0% |
p = NS; none considered related to study medication | |||
| Scheen (2006)236 | Oedema |
PIO + Ins: 31% P + Ins: 18% |
p < 0.0001 | ||
| Health-related QoL – not reported | |||||
HbA1c
All studies reported HbA1c values and could be included in the meta-analysis (Figure 11). Baseline HbA1c values were between 7.6% and 10% in the pioglitazone-plus-insulin groups, and between 7.8% and 9.8% in the insulin-without-pioglitazone groups. End-of-study HbA1c values were significantly lower in the groups taking pioglitazone plus insulin than in the groups taking insulin without pioglitazone (WMD –0.58%, 95% CI –0.70 to –0.46, p < 0.00001). There was no significant heterogeneity. In the study by Mattoo et al. (2005),233 18% of patients on pioglitazone plus insulin and 6.9% of patients on insulin without pioglitazone attained HbA1c values of below 7.0%. There was no significant difference between patients using two or fewer daily injections and patients using three or more. Similarly, there was no significant difference between patients who had previously been on OAD agents and those who had not. In the study by Rosenstock (2002),235 no significant difference in HbA1c level was reported for the group using 15 mg/day of pioglitazone and the group using 30 mg/day.
FIGURE 11.
Forest plot of HbA1c results – pioglitazone and insulin.
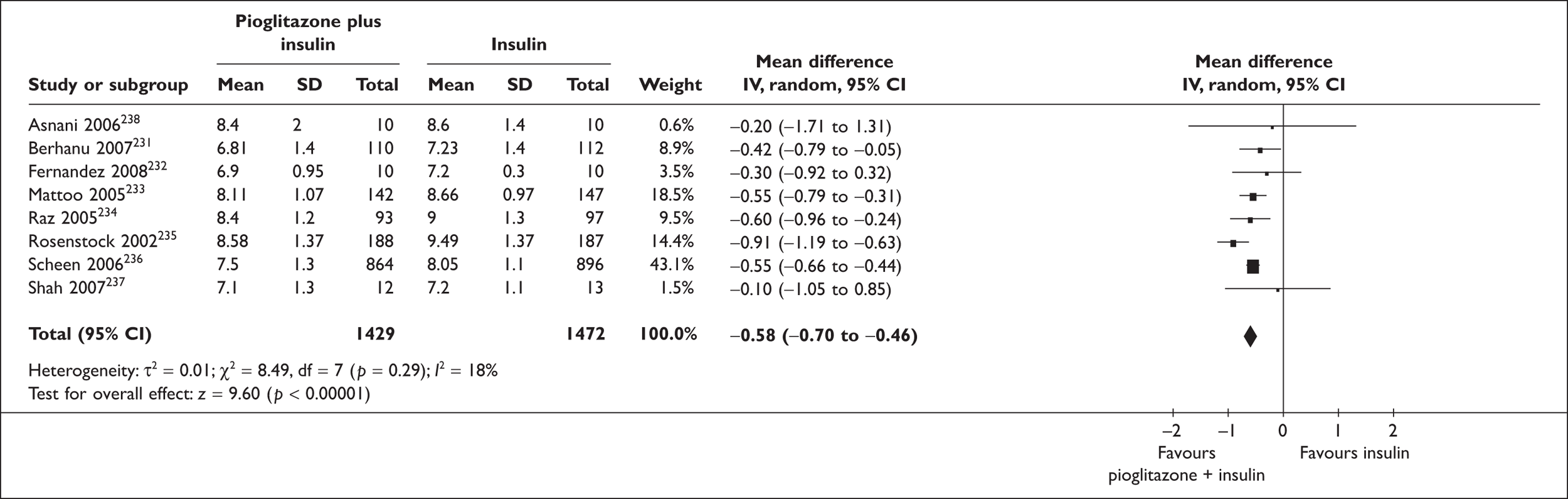
Hypoglycaemia
Six studies reported on hypoglycaemia outcomes and could be summarised in a meta-analysis (Figure 12). There were marginally more patients with hypoglycaemic episodes in the pioglitazone-plus-insulin groups than with insulin without pioglitazone (RR 1.27, 95% CI 0.99 to 1.63, p = 0.06). The results showed significant heterogeneity (p = 0.001). The study by Raz et al. (2005),234 which used biphasic insulin aspart 30 (BIAsp 30) rather than other insulin regimens contributed most to the heterogeneity. There is evidence to suggest that BIAsp 30 is associated with a reduced rate of nocturnal and major episodes of hypoglycaemia compared with other types of insulin. 241 After eliminating this study from the analysis, there remained moderate heterogeneity (I2 = 57%, p = 0.05) and there was significantly more hypoglycaemia in the pioglitazone-plus-insulin groups (RR 1.40, 95% CI 1.14 to 1.73, p = 0.002).
FIGURE 12.
Forest plot of frequency of hypoglycaemia – pioglitazone and insulin.
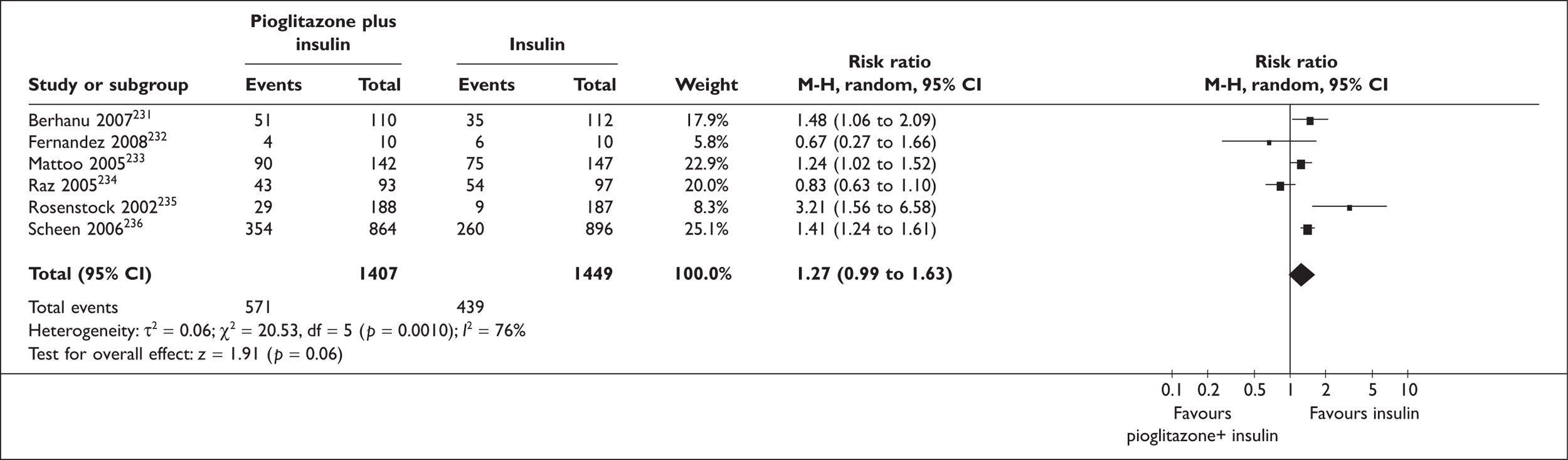
Dose
Six studies231–236 reported insulin doses (as units per kg per day or as units per day). Only two studies reported SDs, so a meta-analysis could not be carried out reliably. Of the six studies, four found that the insulin-plus-pioglitazone groups used significantly less insulin than the insulin without pioglitazone groups (WMD –0.19 U/kg/day or –12.03 U/day). The remaining two studies did not report any p-values. Insulin dose ranged between 42 and 64 U/day, or 0.5–1 U/kg/day in the pioglitazone groups, and between 55 and 70 U/day or 0.7–1.2 U/kg/day in the groups taking no pioglitazone.
Weight change
Six studies reported weight change. 231–235,237 However, only one of the studies reported a measure of variability, so a meta-analysis could not be carried out reliably. In most studies, patients in the insulin-without-pioglitazone groups gained less weight than patients in the insulin-plus-pioglitazone groups (mean difference 2.91 kg, range 3.85 to –3.50 kg), but no p-values were reported. Weight change ranged between +1.4 and +4.4 kg in the pioglitazone-plus-insulin groups, and between –0.04 and +4.9 kg in the insulin-only groups.
Lipid parameters
Four studies reported results for serum triglycerides. 231,232,234,235
Of the four studies, only two231,235 found significantly reduced triglyceride values in the pioglitazone groups (reductions of between 0.44 and 0.70 mmol/l in the pioglitazone groups compared with the insulin-only groups).
Four studies reported on total serum cholesterol. 231,232,234,235
None of the studies found any significant difference in total cholesterol between the pioglitazone-plus-insulin groups and the insulin-without-pioglitazone groups.
Four studies reported on HDL cholesterol. 231–233,235 Overall, HDL cholesterol was increased by between 0.10 and 0.18 mmol/l in the pioglitazone groups compared with the insulin-only groups.
Four studies reported on LDL cholesterol,231–233,235 with none finding any significant difference between the pioglitazone-plus-insulin groups and the insulin-without-pioglitazone groups.
Adverse events
Where reported, there did not appear to be any significant difference in withdrawals due to adverse events between the pioglitazone-plus-insulin groups and the insulin-without-pioglitazone groups. The only adverse event (apart from weight gain) reported as occurring more frequently with pioglitazone was (peripheral) oedema, which was generally classified as mild to moderate, and which would be manageable with a diuretic. However, p-values were generally not reported.
Description of studies – insulin + pioglitazone vs pioglitazone
There was only one trial, published as an abstract, comparing pioglitazone with pioglitazone plus insulin. Characteristics of the included trial are shown in Appendix 7.
The focus of the study by Raskin (2006)242,243 was on the safety and efficacy of BIAsp 30 (30% soluble and 70% protaminated insulin aspart) in insulin-naive patients with type 2 diabetes, who are taking any two OAD agents. The study was a randomised parallel-group trial with a duration of 34 weeks and was carried out in the USA.
Participants
The trial included 181 participants (93 and 88 in each comparison group). The trial included insulin-naive patients with type 2 diabetes, with a HbA1c value of between 7.5% and 12%, and who were taking any two OAD agents. No demographic characteristics were reported.
Interventions
The trial compared optimised treatment with a combination of pioglitazone and metformin with BIAsp 30 added to an optimised treatment with combination of pioglitazone and metformin. BIAsp 30 was initialised at 6 U twice per day (pre-breakfast and pre-supper) and titrated to target blood glucose values of 4.4–6.1 mmol/l by an algorithm-directed forced titration. There was an 8-week run-in phase during which treatment was changed to metformin (2500 mg/day) and pioglitazone (30 or 45 mg/day).
Outcomes
The primary end point was not reported (but was presumably HbA1c level). Apart from HbA1c level, minor hypoglycaemia (blood glucose < 3.1 mmol/l) and weight were reported.
Quality
The abstract gave no information on the method of randomisation, allocation concealment, blinding, ITT analysis, the percentage of participants who completed the trial, whether a power calculation was carried out, or whether the comparison groups were comparable at baseline. Funding was by Novo Nordisk.
Results – insulin + pioglitazone vs pioglitazone
The trial by Raskin et al. (2006)241,242 found a significantly greater reduction of HbA1c level at study end in the BIAsp 30-plus-metformin-plus-pioglitazone group than in the metformin-plus-pioglitazone group (–1.5% versus –0.2%, p < 0.0001)(Table 27). There were also larger proportions of patients reaching HbA1c values of less than 7% in the BIAsp 30-plus-metformin-plus-pioglitazone group (76.3% versus 24.1% in the metformin-plus-pioglitazone group), as well as values less than or equal to 6.5% (59.1 versus 11.5%), values less than or equal to 6% (33.3 versus 2.3%) and values less than or equal to 5.5% (14.0 versus 0%). However, the BIAsp 30-plus-metformin-plus-pioglitazone group had significantly more minor hypoglycaemic events than the metformin-plus-pioglitazone group (8.3 versus 0.1 events/year, p < 0.001). The patients in the BIAsp 30-plus-metformin-plus-pioglitazone group also gained significantly more weight than the patients in the metformin-plus-pioglitazone group (4.6 versus 0.8 kg, p < 0.05). Peripheral oedema occurred in 10% of patients in the BIAsp 30-plus-metformin-plus-pioglitazone group and in 12% of patients in the metformin-plus-pioglitazone group.
| Study | Outcome | Baseline | End of study | Change from baseline/difference between groups | p-value (between groups) |
|---|---|---|---|---|---|
| HbA1c | |||||
| Raskin (2006)241,242 | HbA1c (%) |
BIAsp 30 + MET + PIO: 8.1, SD 1.0% MET + PIO: 7.9, SD 0.9% |
BIAsp 30 + MET + PIO: 6.5, SD 1.0% MET + PIO: 7.8, SD 1.2% |
BIAsp 30 + MET + PIO: –1.5% MET + PIO: –0.2% |
p < 0.0001 |
| Percentage with HbA1c < 7.0% |
BIAsp 30 + MET + PIO: 76.3% MET + PIO: 24.1% |
p not reported | |||
| Percentage with HbA1c ≤ 6.5% |
BIAsp 30 + MET + PIO: 59.1% MET + PIO: 11.5% |
p not reported | |||
| Percentage with HbA1c ≤ 6.0% |
BIAsp 30 + MET + PIO: 33.3% MET + PIO: 2.3% |
p not reported | |||
| Percentage with HbA1c ≤ 5.5% |
BIAsp 30 + MET + PIO: 14.0% MET + PIO: 0% |
p not reported | |||
| Hypoglycaemia | |||||
| Raskin (2006)241,242 | Minor hypoglycaemia (events/year) |
BIAsp 30 + MET + PIO: 8.3 events/year MET + PIO: 0.1 events/year |
p < 0.001 | ||
| Weight | |||||
| Raskin (2006)241,242 |
BIAsp 30 + MET + PIO: +4.6, SD 4.3 kg MET + PIO: +0.8, SD 3.2 kg |
p < 0.05 | |||
| Adverse events | |||||
| Raskin (2006)241,242 | Peripheral oedema |
BIAsp 30 + MET + PIO: 10% MET + PIO: 12% |
|||
Discussion
Summary
Eight RCTs were identified comparing combinations of insulin and pioglitazone with insulin without pioglitazone regimes (two published only as abstracts). One trial (published only as abstract) was identified comparing a pioglitazone-plus-insulin regime with a pioglitazone-without-insulin regime. Compared with the insulin regimes, the pioglitazone-plus-insulin regimes reduced HbA1c level by a mean of –0.54% (95% CI –0.70 to –0.38, p < 0.00001). However, hypoglycaemic events were marginally increased with the pioglitazone regimes (RR 1.27, 95% CI 0.99 to 1.63, p = 0.06). Where reported, studies tended to find reduced insulin doses in the pioglitazone groups, as well as increased HDL cholesterol values. None of the other lipid parameters reported (triglycerides, total cholesterol, LDL cholesterol) showed any systematic differences between the comparison groups. The studies tended to show increased weight (mean difference 2.91 kg) and more peripheral oedema with pioglitazone. The one trial comparing a pioglitazone-plus-insulin (plus metformin) regime with a pioglitazone (plus metformin) regime found significantly lower HbA1c values in the groups taking insulin, but also more minor hypoglycaemic events and more weight gain. The rates of peripheral oedema appeared to have been similar between the groups.
Chapter 7 Literature review of economic studies on new drugs for diabetes
Methods
Search strategy
The databases MEDLINE, EMBASE, Science Citation Index, ISI Proceedings and the NHS Economic Evaluation Database (NHS EED) were searched, as described in Appendix 1 (see Economic searches). Articles for inclusion were retrieved and initially screened by one author and then further screened selected by the health economist for inclusion.
GLP-1: exenatide
QoL studies
Secnik et al. (2006)67 summarised the QoL effect of exenatide 10 µg twice daily and glargine once daily as observed in a 26-week Phase III trial among 455 per-protocol patients with type 2 diabetes. These were added to patients’ existing regimes of metformin and a sulfonylurea. Both the addition of exenatide and the addition of glargine demonstrated statistically significant improvements in the SF-36 vitality subscale score: from 53.18 to 56.30 for exenatide and from 55.18 to 57.62 for glargine. They were also associated with statistically significant improvements in the DSC-R (range 0–5) total score, with exenatide recording an improvement from 1.07 to 0.90, and glargine an improvement from 0.99 to 0.84. Both exenatide and glargine were reported as showing statistically significant improvements in the psychology: fatigue, psychology: cognitive, ophthalmology, hypoglycaemia and hyperglycaemia subscales of the DSC-R. Statistically significant improvements in the Diabetes Treatment Satisfaction Questionnaire were also observed: from 26.41 to 29.48 for exenatide and from 26.31 to 30.04 for glargine, with the perceived frequency of both hypoglycaemia and hyperglycaemia recording improvements for both groups. However, while the change in EQ-5D was of similar size between the two groups, for exenatide the change from 0.82 to 0.85 was not statistically significant, with p = 0.08, whereas for glargine the change from 0.84 to 0.87 was with p = 0.05.
A study by Yurgin et al. (2006),68 available only as an abstract, reported the effects of exenatide compared with biphasic insulin when added to existing regimes of metformin and a sulfonylurea from a 52-week non-inferiority trial among 505 patients with type 2 diabetes. The HbA1c effects were similar, –0.98% for exenatide and –0.88% for biphasic insulin. Exenatide led to statistically significant improvements in EQ-5D visual analogue scale (VAS) of 3.39, the SF-36 vitality scale of 3.89 and the DSC-R of –0.13. No significant effect was observed in the TFS. There were no statistically significant changes in these for biphasic insulin, although it should be noted that there was also no statistically significant difference between exenatide and biphasic insulin with the exception of the DSC-R, which recorded an increase under biphasic insulin of +0.05.
Weight, nausea, QoL and cost of treatment
Ratner et al. (2006)244 reported a progressive reduction in weight of an average around 2.4 kg by week 30 within a placebo-controlled trial of exenatide among 150 patients with type 2 diabetes. From these, 92 patients also completed a 52-week follow-up study to give a total time horizon of 82 weeks. The average weight loss at 30 weeks was –3.0 kg, this increasing to –5.3 kg by week 82.
Blonde et al. (2006)245 report similar results from a somewhat larger placebo-controlled trial in 1446 patients, of whom 1125 (or 78%) completed the initial 30-week trial. In total, 974 of these patients entered the open-label phase, 668 of these having been originally randomised to receive exenatide within the placebo-controlled trial. Only 551 of these patients could be evaluated at the 82-week point due to enrolment dates, 314 of these completing the 52-week follow-up study. The ITT group and the completer cohort had similar weights and BMIs: 98 kg and 34 kg/m2 and 99 kg and 34 kg/m2, respectively. For this 82-week completer cohort, the average change at 30 weeks was –2.1 kg, which was reportedly similar to the range of –1.6 kg to –2.8 kg reported for the 10-µg arm of the placebo-controlled trial. Unfortunately the mean change for the 10-µg arm was not stated, and it should also be noted that the placebo control group also experienced weight loss of between –0.3 kg and –0.6 kg at week 30. Among the 82-week completer cohort, at week 82 the average weight loss was 4.4 kg, with 81% of patients having lost weight. The average change in weight among the 82-week completer cohort showed a generally increasing trend with BMI: for patients of less than 25 kg/m2 the average weight loss was 2.9%, whereas for patients in increasing BMI increments of 5 kg/m2 the average weight loss was 3.6%, 4.6%, 4.3%, until those with a BMI of more than 40 kg/m2, for whom the average weight loss was 5.5%.
As summarised in Table 6, for the direct comparison with glargine, Heine et al. (2005)53 reported, among a patient population with an average BMI of 31 kg, an average 2.3-kg weight loss among those starting exenatide treatment by week 26 compared with an average weight gain of 1.8 kg for those starting glargine treatment.
The submission for exenatide to the Scottish Medicines Consortium, citing trial results for exenatide in terms of weight loss, reported an additional utility estimation exercise conducted among 129 patients with diabetes. This used standard gamble to estimate the utility for patients in their current health state, a basic representative health state for patients with type 2 diabetes, and for the representative health state plus a variety of combinations of nausea and weight loss. The average utility for patients’ current health state and the notional representative health state were 0.891 and 0.873, respectively: a difference of –0.018. The absolute utility impacts of nausea and weight change were estimated, as shown in Table 28.
| Change | |
|---|---|
| Weight (%) | Utility |
| Nausea not experienced | |
| +5 | –0.065 |
| +3 | –0.044 |
| –3 | +0.020 |
| –5 | +0.032 |
| Nausea experienced | |
| +5 | –0.095 |
| +3 | –0.073 |
| Nil | –0.043 |
| –3 | –0.028 |
| –5 | –0.010 |
Dennett et al. (2008),246 in a study funded by Eli Lilly, conducted a systematic review of the literature to evaluate the impact of weight gain on patients with or without type 2 diabetes. Utility scores for patients without diabetes who were of normal weight were between 0.71 and 0.93, whereas for obese patients without diabetes the scores ranged from 0.60 to 0.91. Utility scores were lower for patients with diabetes, ranging from 0.57 to 0.77 for those of normal weight compared with 0.33–0.70 for those who were obese. The authors concluded that older studies tended to examine changes in weight or BMI without controlling for whether weight was being gained or lost. More recent studies suggest that changes may be asymmetrical, with a percentage gain in weight or BMI having a lesser effect than the same percentage loss. However, no particular study, method of elicitation or values were arrived at or recommended for use. Within the summary of results presented by Dennett et al. it is also not clear to what extent other comorbidities have been controlled for within the estimates. Bagust and Beale (2005),247 as referenced within the Dennet et al. review, did control for other comorbidities and found, through time trade-off estimates, that for every BMI point above 25 kg/m2 utility declined by 0.0061. Coffey et al. (2002),248 also having controlled for comorbidities, found that being obese with a BMI of more than 30 kg/m2 reduced utility by 0.021.
Yu et al. (2007),249 in a study funded by Eli Lilly and Amylin Pharmaceuticals, analysed data from US Health Maintenance Organizations to assess the impact upon overall treatment costs of weight changes among 458 patients with type 2 diabetes. Over the 6 months of weight measurement, around half of patients gained weight, whereas half were described as non-weight-gainers, both groups having a similar average BMI at baseline of around 34 kg/m2. In the year subsequent to the change in weight, emergency room visits were similar between the groups at 11.6% for the weight gainers compared with 11.1% for the non-weight-gainers. Hospitalisations were higher among weight gainers, at 8.0%, compared with 4.7% for the non-weight-gainers, although this was not statistically significant, with p = 0.143.Total health-care costs were statistically significantly different, being US$3167 for the weight gainers compared with US$1852 with p = 0.003.
Regression analyses appeared to suggest about a 3–4% change in costs for every 1% change in weight. Within an additional regression analysis that controlled for patient obesity, percentage point weight losses among the non-obese were not associated with cost savings but reduced costs among the obese by 6%. Within this analysis for both the non-obese and the obese, percentage point increases in weight increase costs by between 2% and 3%, but these estimates for the subgroups were not statistically significant. These results illustrate the impact of obesity upon the overall treatment costs of diabetes, but cannot be directly appended to the modelling of exenatide given that the effects of obesity on complications and costs will be being indirectly modelled through the effect upon systolic blood pressure (SBP) and high-density lipids as a ratio of total lipids.
Cost-effectiveness studies
Edwards (2006)250 undertook a systematic literature review of the clinical effects of exenatide compared with glargine and NPH insulin, all these being additional to a regime of metformin and sulfonylurea therapy. Only one paper met their inclusion criteria: the 24 week Riddle (2003) et al. study. 169 Based upon this, they performed a simple cost-effectiveness analysis, anticipating that for every US$100 spent the reduction in HbA1c would be 0.091, 0.655 and 0.201 for exenatide, glargine and NPH, respectively. Similarly, they anticipated that for every US$100 spent there would be a 0.19 kg weight loss for exenatide. Both forms of insulin were associated with weight gain. But given the outcome measures of the analysis and that exenatide was more expensive than either of the insulin treatments, few conclusions as to the treatments’ relative cost-effectiveness can be drawn.
Shaya (2007)251 analysed manufacturer data for 5 µg and 10 µg of exenatide to evaluate the cost-effectiveness of exenatide relative to placebo using the CORE cost-effectiveness model. Unfortunately, no details of the inputs and assumptions used for the modelling were provided within the paper, but the manufacturer summary referenced suggested the following clinical inputs at 30 weeks, as shown in Table 29.
| All patients | Placebo | Exenatide 5 g | Exenatide 10 µg | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | HbA1c (%) | Weight (kg) | n | HbA1c (%) | Weight (kg) | n | HbA1c (%) | Weight (kg) | |
| With sulfonylurea | 123 | +0.1 | –0.6 | 125 | –0.5 | –0.9 | 129 | –0.9 | –1.6 |
| With metformin | 113 | +0.1 | –0.3 | 110 | –0.4 | –1.6 | 113 | –0.8 | –2.8 |
| With metformin + sulfonylurea | 247 | +0.2 | –0.9 | 245 | –0.6 | –1.6 | 241 | –0.8 | –1.6 |
This modelling yielded cost-effectiveness estimates of US$43,814 per additional life-year and US$48,921 per QALY. Curtailing the time horizon to 20 years has limited impact upon modelled outputs, but curtailing the time horizon to only 5 years increases the cost per life-year to US$359,757 and the cost per QALY to US$104,697. As would be anticipated, the effect upon the cost per life-year is somewhat larger as relatively few in either arm will have died at the 5-year point, but the increase in the cost per QALY underlines the importance of extrapolation and longer-term complications within the lifetime estimate of cost-effectiveness. The assumptions made in terms of longer-term effects upon HbA1c level and weight were not stated, and the likelihood of transferring to an insulin regime at some point for both the placebo arm and the exenatide arm was, similarly, not made clear.
Minshall et al. (2008),252 in assessing the cost-effectiveness of exenatide relative to placebo, appear to have used similar 30-week clinical effectiveness data from placebo-controlled trials to Shaya (2007),251 although in a more disaggregate form, as outlined in Table 30.
| All patients | n | Placebo | Exenatide | ||||
|---|---|---|---|---|---|---|---|
| 5 µg | 10 µg | ||||||
| HbA1c (%) | Weight (kg) | HbA1c (%) | Weight (kg) | HbA1c (%) | Weight (kg) | ||
| With sulfonylurea | 377 | +0.1 | –0.6 | –0.5 | –0.9 | –0.9 | –1.6 |
| With metformin | 336 | +0.1 | –0.3 | –0.4 | –1.6 | –0.8 | –2.8 |
| With metformin + sulfonylurea | 733 | +0.2 | –0.9 | –0.6 | –1.6 | –0.8 | –1.6 |
| For patients with HbA1c < 9% | |||||||
| With sulfonylurea | 239 | +0.1 | – | –0.4 | – | –0.7 | – |
| With metformin + sulfonylurea | 513 | +0.3 | – | –0.4 | – | –0.5 | – |
| For patients with HbA1c ≥ 9% | |||||||
| With sulfonylurea | 138 | +0.1 | – | –0.6 | – | –1.2 | – |
| With metformin + sulfonylurea | 220 | +0.0 | – | –0.9 | – | –1.4 | – |
| For patients with BMI < 30 | |||||||
| With metformin | 89 | – | +0.4 | – | –0.5 | – | –2.4 |
| For patients with BMI ≥ 30 | |||||||
| With metformin | 247 | – | –0.5 | – | –2.1 | – | –3.0 |
These 30-week data were augmented with 82-week clinical effectiveness estimates from an optional open-label extension study, within which exenatide patients had a reported sustained HbA1c level reduction of –1.1% and a progressive mean body weight reduction of 4.4 kg. The 82-week data were also used to estimate a reduction in SBP of –1.3 mmHg, a reduction in LDL cholesterol of –1.6 mg/dl, an increase in HDL cholesterol of +4.6 mg/dl and a reduction in triglycerides of 39 mg/dl. After the 82-week point the trend in these variables was assumed to follow the identified UKPDS trend, as seems likely to have been assumed for the placebo arm subsequent to the 30-week point. Medicare costs were applied to adverse events, with utilities being drawn from the European CODE-2 study EQ-5D values as reported in Bagust and Beale (2005). 247 As with the study by Shaya (2007),251 the paper used the CORE model to assess the cost-effectiveness of adding exenatide to metformin and sulfonylurea compared with patients remaining on just metformin and sulfonylurea. Despite a presumably worsening HbA1c level over time in both arms, there does not appear to have been any consideration of patients transferring to insulin therapy.
Results for exenatide among patients of average age 56, 7 years’ duration of diabetes and a baseline HbA1c level of 8.3%, SBP of 123 mmHg, a BMI of 34, HDL level of 38 mg/dl, LDL level of 115 mg/dl and triglyceride level of 239 mg/dl over a 30-year time horizon, were a discounted life expectancy of 9.63 years and a quality-adjusted life expectancy of 6.33, coupled with a lifetime cost of US$86,281. For the placebo arm the parallel estimates were 9.10 life-years, 5.81 QALYs and a cost of US$67,531, yielding a net impact from exenatide of 0.53 life-year, 0.52 QALYs and US$18,750 to yield a cost-effectiveness estimate of US$36,133 per QALY. Shortening the time horizon to 20 years had limited impact upon cost-effectiveness, although a time horizon of only 10 years worsened the anticipated cost-effectiveness to US$64,538 per QALY.
A 20% lessening of the impact of exenatide on HbA1c level from –1.1% to –0.88% had roughly proportionate impact upon cost-effectiveness, worsening it by 16% to US$41,917 per QALY. Removing the impact upon weight and SBP had reportedly little impact upon cost-effectiveness, although values were not given. Removing the lipid effects also worsened the cost-effectiveness by around 16% to US$41,738 per QALY. Subgroup analyses among those with HbA1c level < 9% at baseline and those with HbA1c level ≥ 9% suggested marked differences in cost-effectiveness: US$45,971 and US$20,548 per QALY, respectively.
The relevance of the studies of both Shaya (2007)251 and Minshall et al. (2008)252 are limited in that there appears to be no consideration of patients transferring to insulin therapy as HbA1c level worsens. Ray et al. (2007)253 in part addressed this, also having used the CORE model but to model the cost-effectiveness of exenatide relative to glargine. Exenatide was anticipated to result in a slightly lower improvement in HbA1c level than glargine, but greater improvements in a number of other outcomes with the central values as shown in Table 31, where nausea was the proportion of patients experiencing nausea, and hypoglycaemia was the average number of hypoglycaemic events per year.
| HbA1c (%) | SBP | Cholesterol | LDL | HDL | Triglyceride | BMI | Nausea (%) | Hypoglycaemia | |
|---|---|---|---|---|---|---|---|---|---|
| Exenatide | –0.99 | –4.15 | –3.47 | –1.54 | +1.54 | –15.04 | –0.80 | 57.1 | 6.94 |
| Glargine | –1.07 | –0.57 | –0.39 | +5.80 | +1.54 | –30.08 | +0.55 | 8.6 | 5.84 |
The base case cost of exenatide was drawn from the US cost converted at the prevailing exchange rate, as the UK wholesale cost for exenatide had not been formalised. The insulin dose was assumed to be 25 IU in the first year, and thereafter 40IU. Annual blood glucose monitoring costs were assumed to be £290 in the exenatide arm and £414 in the glargine arm, based upon predictions from a UK survey of health-care professionals and patients. Prices of complications were drawn from UK sources and indexed to 2004 prices, while utility values were mainly drawn from UKPDS data as reported in Clarke et al. (2002). 254 Utility gains from weight loss were also applied to the first 2 years of the simulations, the values for this being taken from CODE-2 data that jointly analysed the effect of nausea and BMI. Subsequent to the 2-year point, the CODE-2 time trade-off data of a utility loss of 0.0061 per unit of BMI above 25 kg/m2 was applied.
Results for exenatide among patients of average age 59, 10 years’ duration of diabetes and a baseline HbA1c level of 8.2%, SBP of 137 mmHg, a BMI of 32, HDL level of 47 mg/dl, LDL of 106 mg/dl and triglycerides of 199 mg/dl over a 35-year time horizon were a discounted life expectancy of 10.66 years and a quality-adjusted life expectancy of 7.39, coupled with a lifetime cost of £29,401. The parallel figures for glargine were 10.61 years, 6.95 QALYs and £19,489, yielding a net impact from exenatide of 0.06 life-years, 0.44 QALYs and an average cost increase of £9912 to yield a cost-effectiveness estimate of £22,420 per QALY.
Results were sensitive to the assumed utility gain from weight loss: the adoption of CODE-2 time trade-off utilities247 for the weight gain worsened the cost-effectiveness of exenatide to £39,763 per QALY. It was also reported in the text that results were sensitive to the utility assumed for nausea. While the impact of nausea upon cost-effectiveness was not separately quantified, it seems likely that the effect of this was encompassed within the £39,763 per QALY figure.
Note that while the Minshall et al. (2008)252 study applied long-term trends to the progression of HbA1c after a period of initial treatment success, it appears that there was no explicit allowance for progression to insulin therapy within the modelling. Fewer details were provided within the Shaya (2007)251 study, but it appears likely that it made similar assumptions.
Watkins et al. (2006)255 used the CORE model to compare the anticipated costs and outcomes among the standard UKPDS population and a modified obese population, these being identical in terms of most characteristics and an HbA1c level of 8.5% at baseline, differing only in weight and the consequences of this for the various risk factors as outlined in Table 32.
| BMI | SBP | Cholesterol | HDL | LDL | Triglycerides | |
|---|---|---|---|---|---|---|
| UKPDS population | 27.5 | 135 | 207 | 41 | 134 | 207 |
| Obese population | 35.0 | 145 | 217 | 41 | 144 | 230 |
Both patient groups were assumed to be treated with exenatide. For the UKPDS population this intensification of treatment was assumed to have the CORE default value impacts upon risk factors, with there being no change in weight, a rise of 1.3 mmHg in SBP, a rise of 1.6 mg in LDL levels and a rise of 39 mg in triglycerides. When treated with exenatide the obese population was assumed to experience a weight loss of 8.5% or 3 BMI points, a 10-mm fall in SBP, a 20-mg fall in LDL and a 59-mg fall in triglycerides. Immediately apparent from this is that it appears to have been assumed that the obese population would have a lower SBP, lower levels of LDL and lower levels of triglycerides than the UKPDS population. This raises questions as to the reliability of the modelling, or at a minimum the reporting of the conduct of it within the paper. Unfortunately, the paper was also not explicit as to whether any reduction in HbA1c was anticipated for exenatide, although in the introductory sections the authors noted an average reduction of 0.5–0.9%.
Treatment with exenatide was compared with the treatments of once-daily glargine, pioglitazone, glyburide and no additional treatment. The impact of these treatments was reductions in baseline HbA1c levels of 2.0%, 0.6%, 0.9% and 0%, respectively, which appears to be likely to have been coupled with the standard CORE reductions in other variables as reported for exenatide use among the UKPDS population. Treatments were assumed to continue for the time horizon of the model.
Among obese patients, exenatide was anticipated to result in cost savings of around US$3000 from reduced cardiovascular disease. Exenatide resulted in higher costs of renal disease by around US$1000 compared with glyburide and glargine, but savings of US$2600 and US$3800 compared with pioglitazone and no additional treatment, respectively. A similar cost pattern was observed for neurological and ophthalmic costs with exenatide being of around US$1700 higher in cost compared with glyburide and glargine, but around US$1000 lower in cost compared with pioglitazone and placebo. Cost-effectiveness estimates of US$32,000, US$13,000 and US$16,000 per QALY were reported for exenatide against glyburide, glargine and placebo, respectively; while pioglitazone was dominated, although it is not clear whether these estimates were for obese patients or for the patient group as a whole.
As is apparent from the summary above, interpreting the results of Watkins et al. (2006)255 is problematic, and it is unclear quite what the cost-effectiveness estimates relate to and their reliability is also questionable. It also does not appear that any subsequent intensification of therapy has been considered in patients as time progresses.
The Scottish Medicines Consortium (SMC) issued guidance on exenatide in June 2007, recommending it for restricted use in combination with metformin and/or sulfonylureas. The SMC appraisal was based on an industry submission that used only one trial – that of exenatide versus biphasic insulin. 256 The SMC commented that the comparator of biphasic insulin aspart was more expensive than cheaper forms of insulin, but concluded that additional sensitivity analysis suggested that the incremental cost-effectiveness ratio (ICER) against biphasic human insulin would probably be cost-effective.
DPP-4 inhibitors
Cost-effectiveness studies
Schwarz et al. (2008)257 explored the cost-effectiveness of adding second-line sitagliptin to first-line metformin for uncontrolled patients on a regime of metformin in terms of their HbA1c level rising above 6.5%. This was compared on a pair-wise basis with two main comparators: (1) adding second-line rosiglitazone to first-line metformin and (2) adding second-line sulfonylurea to first-line metformin. Those failing on these treatments would progress to metformin plus third-line basal insulin, with possible further progression to fourth-line multidose insulin. For the comparison with adding second-line sulfonylurea to first-line metformin, an additional scenario was modelled with those failing on sitagliptin or sulfonylurea progressing to a third-line combination of rosiglitazone and metformin prior to possible progression to insulin therapy as fourth line. For these later therapies, it appears that the same switching threshold in terms of HbA1c level was used, although the value for this was varied in sensitivity analyses.
Modelling was undertaken for six European countries – Austria, Finland, Portugal, Scotland, Spain and Sweden – and used the Januvia Diabetes Economic (JADE) model. While the JADE model relied extensively upon the UKPDS Outcomes Model risk equations, it will not necessarily have resulted in the same anticipated patient outcomes as had the UKPDS Outcomes Model been used. The costs of medicines, side effects, direct costs of diabetes related complications and discount rates for both costs and health-related QoL impacts were based upon country-specific data, rather than being drawn from the UKPDS Outcomes Model.
The average treatment effects upon HbA1c level when added to metformin were differentiated by baseline HbA1c level and by comparator treatment as shown in Table 33.
| Baseline HbA1c (%) | Comparison | |||
|---|---|---|---|---|
| Rosiglitazone | Sulfonylurea | |||
| Sitagliptin (%) | Rosiglitazone (%) | Sitagliptin (%) | Sulfonylurea (%) | |
| < 7 | –0.46 | –0.10 | –0.47 | –0.44 |
| 7–8 | –0.63 | –0.77 | –0.74 | –0.90 |
| 8–9 | –1.04 | –0.86 | –1.35 | –1.41 |
| > 9 | –1.64 | –1.98 | –1.89 | –2.07 |
For the comparison with rosiglitazone it was anticipated that sitagliptin would provide an incremental discounted QALY gain of between 0.016 and 0.063, with the cost impact being between a cost saving of €687 to a net cost of €208. For the UK modelling based upon Scottish data, the patient gain was anticipated to be 0.016 and the incremental cost £25.08 to yield an estimated cost-effectiveness of £1567 per QALY.
For the comparison with sulfonylurea in which failures progressed to insulin, it was anticipated that sitagliptin would provide an incremental discounted QALY gain of between 0.037 and 0.095, with the cost impact being a net cost of between €331 and €1097. For the UK modelling, the patient gain was anticipated to be 0.095 and the incremental cost £764 to yield an estimated cost-effectiveness of £8045 per QALY.
For the comparison with sulfonylurea in which failures progressed to rosiglitazone plus metformin prior to insulin it was anticipated that sitagliptin would provide an incremental discounted QALY gain of between 0.045 and 0.103, with the cost impact being a net cost of between €339 and €1130. For the UK modelling, the patient gain was anticipated to be 0.103 and the incremental cost £772 to yield an estimated cost-effectiveness of £7502 per QALY.
The average cost-effectiveness of across the modelling was estimated to be €4766 per QALY. Results relative to rosiglitazone were sensitive to the assumed effects of rosiglitazone on cholesterol, SBP and the risk of heart failure. Removing the effect upon cholesterol and SBP, and halving the increase risk of heart failure saw the cost-effectiveness estimate rise to €5012 per QALY, fall to €2630 per QALY and rise to €6677 per QALY, respectively. Varying the utility decrements associated with the long-term complications of diabetes had relatively little impact upon results, a 20% change changing the cost-effectiveness estimate by less that €100 per QALY. Varying the costs of these complications had a somewhat larger impact, a 20% change altering the cost-effectiveness estimate by less around €700 per QALY. However, for all the sensitivity analyses performed, the cost-effectiveness estimate remained below €8000 per QALY. Reducing the effectiveness of sitagliptin by 10% had the largest impact, increasing the cost-effectiveness estimate to €7548 per QALY.
While the analysis of Schwarz et al. (2008)257 did explicitly model the progression to insulin, a limitation of the study may be in considering sitagliptin as a second-line treatment rather than as a third-line addition to metformin and sulfonylurea prior to patients progressing to fourth-line insulin therapy compared with patients progressing directly to insulin therapy as a third-line treatment.
Three other papers modelling the cost-effectiveness of DPP-4 inhibitors were available only as abstracts: Minshall et al. (2007),258 Celaya et al. (2007)259 and Fon et al. (2007). 260 Minshall et al. considered the cost-effectiveness of sitagliptin relative to pioglitazone, whereas both Celaya et al. and Fon et al. considered the relative cost-effectiveness of sitagliptin, vildagliptin, rosiglitazone and pioglitazone. Minshall adopted a US perspective, while both Fon and Celaya adopted a Mexican health-care perspective, with it seeming likely that treatments under consideration were second-line treatments being added to first-line metformin for patients failing on metformin alone.
Minshall et al. (2007),258 estimated the effectiveness of sitagliptin from a separate study of the effectiveness of pioglitazone, although noted that the baseline HbA1c values were similar between the two studies, at 8.04% for sitagliptin and 7.60% for pioglitazone. Daily drug acquisition costs were also similar – US$4.86 and US$4.91, respectively. Given this, pioglitazone was associated with an incremental cost over 35 years of US$359, but also an incremental 0.075 QALYs to yield a cost-effectiveness estimate of US$4804 per QALY.
The Fon et al. and Celaya et al. studies259,260 both relied upon a meta-analysis for their estimates of the effectiveness of sitagliptin, vildagliptin, rosiglitazone and pioglitazone. It appears likely that the Celaya paper was a development of the Fon paper, given their similarities and that both lead authors are named authors of the other paper. While it is not explicit within the abstracts, it appears likely that the same meta-analysis was used by both, Celaya et al. noting that it standardised the baseline HbA1c level at 9% across treatments. Both studies adopted a 1-year perspective, estimating the direct treatment costs, outpatient visits, inpatient admissions, emergency room admissions, etc. to estimate the incremental cost-effectiveness and incremental net benefits. Few details were provided within the abstracts, to the extent that the outcome measures were not clear, although it may have been as simple as per unit of HbA1c reduction. Vildagliptin was estimated to have the lowest overall annual treatment cost – US$1434 within the Fon paper compared with US$9176 within the Celaya paper. Vildagliptin was also estimated to have the lowest cost per successful unit US$1304 in the Fon paper compared with US$8342 within the Celaya one, these figures both implying an additional 1.10 units of outcome arising from vildagliptin use. The authors concluded that vildagliptin dominated the other treatments. The reasons for the differences in cost estimates between Fon and Celaya were not clear.
The SMC issued guidance on vildagliptin in March 2008261 and on sitagliptin in September 2008. 262 The guidance on vildagliptin was based on the Novartis submission, which provided a cost-minimisation analysis comparing vildagliptin with the glitazones. The assumption was that they were equally clinically effective. Costs were over a 1-year period. The comparison used the maximum daily dose of rosiglitazone, which is not used in the majority of patients in Scotland. However, the SMC guidance concluded that using a lower dose would not change the conclusions. The SMC noted that there were limited data, at that time, on some of the assumptions. However, vildagliptin was accepted for restricted use. The guidance does not specify any costs per QALY.
The guidance on sitagliptin was based on the Merck Sharp and Dohme submission, which provided two cost-utility analyses, both with a glitazone as the comparator. One was sitagliptin added to metformin and a sulfonylurea versus a glitazone added to metformin and sulfonylurea; the other assumed that metformin was not tolerated, and compared sulfonylurea plus sitagliptin with sulfonylurea plus a glitazone. The UKPDS model was used. The SMC guidance notes that the main drivers were the congestive heart failure associated with the glitazones, and the cardiovascular risk associated with weight gain – also a feature of the glitazones. The modelling produced very low ICERs, at £5007 and £1902 for the two cost–utility analyses, respectively. The SMC identified some limitations and problems with the modelling, but accepted that the economics case had been demonstrated. The SMC guidances are quite short, and little detail is given.
Economic literature review: glargine and detemir
The previous TAR investigating the cost-effectiveness of the long-acting insulin analogues – TA53 – undertook a systematic review of the literature to January 2002 and concluded that ‘There are no published studies investigating the cost-effectiveness of insulin glargine, or indeed any other insulin analogue. In addition, there are no published studies investigating the cost-effectiveness of NPH insulin, the most likely comparator for insulin glargine’. 12
What follows reviews the cost-effectiveness studies, arising subsequent to this, of glargine, detemir and NPH among patients with type 2 diabetes, although a number of these were available in only abstract or summaries of International Society For Pharmacoeconomics and Outcomes Research (ISPOR) poster presentations. It will become obvious that most of these studies have been funded by the manufacturers, often with co-authors from the companies, and a consistent finding is that the studies funded by manufacturers find their own products cost-effective. The modelling is often well done and thorough, but will not be convincing if based on assumptions that seem unduly favourable to the product under review.
Full papers
Cost-effectiveness
The report from the Canadian Agency for Drugs and Technologies in Health (CADTH) by Tran et al. (2007)142 includes a cost-effectiveness analysis. However, it included no cost-effectiveness studies for type 2 diabetes.
Brandle et al. (2007)263 estimated the cost-effectiveness of glargine compared with NPH among patients failing on OAD agents over a 10-year time horizon, from the perspective of the Swiss health-care system. Patient characteristics were an average age of 66 years, 9 years’ duration of diabetes, a BMI of 29.4 kg/m2 and an SBP of 155 mm. Modelling was implemented through the Diabetes Mellitus Model, the main inputs being two possible effects upon HbA1c level for glargine of –0.96%, which was labelled as pessimistic, and –1.24%, which was labelled as optimistic, compared with an assumed effect for NPH of –0.84%. These values were drawn from a single study within the literature. This was the study by Fritsche et al. (2003),162 details of which are in the clinical effectiveness section of this review. As shown in Figure 2, it reported one of the bigger differences in HbA1c level. As a consequence, glargine was seen as having a superior effect on HbA1c level – of between 0.12% and 0.40%. These relative benefits appear to have been assumed to persist indefinitely, as a common annual increase of 0.1% was applied after the first 2 years to both glargine and NPH. The HbA1c effects were applied to three patient groups with differing baseline HbA1c levels: 10%, 9% and 8%. Effects upon severe hypoglycaemic events and weight were not modelled.
Within the pessimistic scenario, glargine was seen as costing Swiss francs (CHF)1532, CHF1685 and CHF1887 more per patient with net patient benefits of 0.038, 0.037 and 0.038 QALYs, respectively, resulting in cost-effectiveness estimates of CHF49,441, CHF45,701 and CHF49,468 per QALY. Within the optimistic scenario, glargine was seen as saving CHF95, costing CHF350 and costing CHF734 more per patient with net patient benefits of 0.123, 0.123 and 0.128 QALYs, respectively, resulting in cost-effectiveness estimates of dominance, CHF2853 and CHF5711 per QALY.
While these appear relatively favourable cost-effectiveness estimates for glargine, the relevance of the study is undermined through the reliance upon a single study for the estimate of glargine having a 0.12–0.40% superior HbA1c impact compared with NPH, and the assumption that this absolute benefit will be maintained through time through the application of a common 0.1% annual increase.
This analysis by Brandle et al. (2007)263 was funded by Sanofi-aventis, the manufacturer of glargine, and one of the authors was from that company.
A similar study by Maxion-Bergemann et al. (2005)264 from the German branch of Aventis Pharma and the consultancy firm, Analytica International (Lörrach, Germany), funded by Aventis, also used the Diabetes Mellitus Model, also with similarly favourable assumptions, and also concluded that glargine would give better glycaemic control, and hence reductions in complications, mortality and costs. However, they did test the effect of three different levels of improved glycaemia control with differences between NPH and glargine of 0.13%, 0.44% and 0.85%. (Note: Our meta-analysis showed no difference.) It is a careful and thorough analysis but all underpinned by what we think are unduly favourable assumptions about differences in HbA1c level.
Grima et al. (2007),265 from Sanofi-aventis and an economics consultancy, funded by the manufacturer, developed their own Markov model from data within the literature, mainly the UKPDS papers and the Diabetes Control and Complications Trial (DCCT) trial, to assess the cost-effectiveness of glargine relative to NPH for both patients with type 1 diabetes and patients with type 2 diabetes. While the paper noted that meta-analysis suggested similar effects from both glargine and NPH upon HbA1c level, it was assumed [based on analysis by Yki-Järvinen et al. (2003)266] that the lower rate of hypoglycaemia with glargine compared with NPH could be translated into an additional effect upon HbA1c level of –0.87% for glargine, over and above that observed for NPH. This relative effect was assumed to persist over a patient’s lifetime, with a common annual drift on HbA1c level of 0.135% being applied to both arms. Patients with type 2 diabetes, averaging the age of 53 years were simulated across cohorts of differing baseline HbA1c level: 7%, 8%, 9% and 10%+.
The average net cost of glargine compared with NPH among patients with type 2 diabetes was estimated as Can$1992. This varied considerably across the cohorts simulated: additional costs of C$3310, C$2160 and C$896 for those of 7%, 8% and 9% at baseline, respectively. Within the cohort of more than 10% HbA1c level at baseline, glargine was found to be cost saving at – C$320. In terms of patient impact, the net benefit from glargine was estimated to be 0.22, 0.23, 0.24 and 0.25 QALYs for the four cohorts of HbA1c levels 7%, 8%, 9% and 10%+, respectively.
Overall, glargine was estimated as conferring an additional 0.25 years’ survival and a gain of 0.23 QALYs, resulting in a cost-effectiveness estimate of C$8618 per QALY relative to NPH. While the study is interesting in terms of the de novo model structure, the applicability of the conjectured 0.87% relative absolute benefit on HbA1c from glargine over NPH may be questionable. The assumption that this absolute benefit persists over the patient lifetime is also questionable.
McEwan et al. (2006)267 in two abstracts and a full paper (funded by Sanofi-aventis and with an author from the company) evaluated the use of glargine from an NHS perspective. The first abstract by McEwan et al. 267 assumed that the main impact was on rates of severe, symptomatic and nocturnal hypoglycaemic events, with there being no difference in HbA1c level between glargine and NPH. Currie268 was listed as an author, and it seems likely that the QoL impacts of hypoglycaemic events were as previously estimated within the paper listing him as first author, and as reviewed within the cost-effectiveness modelling chapter below. Given these impacts, the authors estimated cost-effectiveness for glargine of £15,197 per QALY.
In the second abstract, of an ISPOR presentation by McEwen et al. (2007),269 glargine was anticipated to lead to a 0.21% superior HbA1c level in comparison with NPH, and also to confer benefits in terms of reduced hypoglycaemia events. Overall, the cost-effectiveness of glargine was estimated to be £5806 per QALY for insulin-naive patients, and £3415 per QALY for non-insulin-naive patients. Excluding the effects upon hypoglycaemic events raised these to £18,179 per QALY and £7973 per QALY, respectively.
In the full paper by McEwan et al. (2007),270 it is noted that the key assumption on HbA1c level comes from the same meta-analysis by Yki-Järvinen et al. (2003)266 used in the Grima et al. (2007) analysis,265 which probably overestimates the difference. However, McEwan et al. also carried out their analysis assuming no difference in HbA1c level, but only in the frequency of hypoglycaemia. But the assumptions there were derived partly from a recent meta-analysis carried out for the manufacturer, and not in the public domain. This gave a relative reduction in hypoglycaemia of 40%. But the background rates of hypoglycaemia appear to come partly from studies in type 1, such as the DCCT, which may not be relevant to patients in the situation of just starting insulin.
So, again, the underlying assumptions may favour glargine.
Only one full paper evaluating the cost-effectiveness of detemir was identified among those with type 2 diabetes: Valentine et al. (2007),271 from the IMS consultancy, and Novo Nordisk, the manufacturers of detemir. Modelling was over a 35-year time horizon for an average age at baseline of 62 years, duration of diabetes of 7 years and BMI of 30 kg/m2. It appears to have used the CORE diabetes model. The costing perspective was that of the US health-care system. Clinical effectiveness estimates were drawn from the German part of the PREDICTIVE study (2007),178 an observational study of 2000 patients who were uncontrolled on either oral hypoglycaemic agents, NPH plus oral hypoglycaemic agents or glargine plus oral hypoglycaemic agents, and who were switched to detemir. 272 This anticipated beneficial effects from switching to detemir upon both HbA1c level and BMI, and typically also upon hypoglycaemic events, as shown in Table 34.
| Switching to detemir from: | |||
|---|---|---|---|
| Oral hypoglycaemic agents | NPH | Glargine | |
| HbA1c | –1.29% | –0.60% | –0.59% |
| BMI | –0.138 | –0.382 | –0.520 |
| Hypoglycaemic events per annum | +1.17 | –6.76 | –7.28 |
Given those assumptions, modelling anticipated that switching to detemir would yield an additional 0.71, 0.35 and 0.34 undiscounted life years compared with remaining on OHAs, NPH and glargine, respectively. The impact on discounted QALYs was 0.31, 0.45 and 0.46, which, when coupled with net costs of US$2290, US$2824 and US$1834, resulted in cost-effectiveness estimates of US$7412 per QALY, US$6269 per QALY and US$3951 per QALY compared with OHA, NPH and glargine, respectively.
However, some of the improvements could be due a ‘trial effect’, even although the study was not a trial. Patients who were not well controlled on glargine might have improved their control, given more attention, even if left on glargine. The clinical effectiveness estimates for the effect of detemir on HbA1c level being superior to those of both NPH and glargine are very favourable to detemir, making the cost-effectiveness results questionable.
Comparative costs
Two studies compared the costs of care with detemir and glargine. Poole et al. (2007),273 in a study funded by Sanofi-aventis, and published in a journal supplement sponsored by Sanofi-aventis, concluded that: ‘Diabetes management with glargine results in markedly reduced costs of diabetes-related treatment compared with detemir in people with type 1 or type 2 diabetes’.
Valentine et al. (2006),274 in a study sponsored by Novo Nordisk, concluded that: ‘In comparison with glargine, detemir … reduced direct medical costs and decreased indirect costs …’.
Premixed regimens
While not the focus of the review, two full papers were identified comparing the cost-effectiveness of once-daily glargine with twice-daily premixed insulin (70 : 30) [Ray et al. (2007)275 and Goodall et al. (2008)276].
Ray et al. (2007)275 assessed the cost-effectiveness of once-daily glargine with twice-daily premixed insulin among those failing on OAD drugs from the perspective of the US health-care system, using the CORE diabetes model. Baseline patient characteristics were an average age of 52 years, 9 years’ duration of diabetes, BMI of 31 kg/m2 and a baseline HbA1c level of 9.77%. Clinical effectiveness estimates were drawn from the INITIATE trial: a 28-week randomised open-label US study. The mean reduction in HbA1c level within this was statistically significantly greater for premixed insulin than for glargine, the average changes being –2.79% and –2.36%, respectively, although premixed insulin was associated with a slightly greater increase in BMI: 1.88 kg/m2, as against 1.22 kg/m2 for glargine. Premixed insulin was associated with a greater insulin dose increase by end of study to 0.82 IU/kg compared with 0.55 IU/kg for glargine.
Results of the modelling were that premixed insulin conferred an additional 0.19 discounted years’ life expectancy, and by coincidence an identical additional 0.19 discounted QALYs. Total lifetime costs were around 9% higher with premixed insulin at a net cost of US$8824, resulting in a cost-effectiveness estimate for premixed insulin of US$46,533 per QALY relative to glargine.
Goodall et al. (2008)276 assessed the cost-effectiveness of once-daily glargine with twice-daily premixed insulin among those failing on OAD drugs within the Swedish setting, also using the CORE diabetes model. Baseline patient characteristics and clinical effectiveness estimates were drawn from the INITIATE trial and were the same as reported for Ray et al. (2007),275 above.
Results of the modelling were that premixed insulin conferred an additional 0.21 discounted years’ life expectancy, and an additional 0.21 discounted QALYs. The source of the slightly larger net patient benefits compared with the estimates of Ray et al. (2007)275 reported above is not clear, given apparently identical patient characteristics, clinical effectiveness estimates and discount rates. Total lifetime costs were also around 2.5% less with premixed insulin, a saving of Swedish kronor (SEK)10,367, resulting in the authors concluding that premixed insulin dominated glargine.
The modelling of Ray et al. (2007)275 and Goodall et al. (2008)276 was much the same, but with net costs differing due to a difference balance between the direct treatment costs and the costs of the downstream complications of diabetes. The extent to which they may overstate the relative cost-effectiveness of premixed insulin may be influenced by patients on once-daily glargine, presumably at some point progressing to mealtime insulin, which will not have been captured within the clinical trial.
While not the focus of this review, two full papers were identified comparing the costs of once-daily glargine with twice-daily premixed insulin.
Lechleitner et al. (2005)277 conducted a prospective observational study among 678 Austrian patients with type 2 diabetes being switched from oral therapy to either once-daily glargine with continued OAD agents or, typically, twice-daily conventional insulin therapy with premixed insulin, although 5% required only once-daily injections and 20% required more than twice-daily injections. The effectiveness on control of HbA1c level was the same for both groups and, as a consequence, the study undertook a cost analysis.
Within the glargine group, 93% of patients continued their oral therapy regimen, mainly of metformin (43%) and sulfonylurea (43%), while within the conventional insulin therapy group only 46% continued with their oral regime. Probably as a result of this, the median daily dose of insulin was considerably lower in the glargine group, at only 16 IU, compared with 40 IU for the conventional insulin therapy group, thereby introducing a bias. A fairer comparison of the insulins would have kept the oral agents the same, but the trialists were presumably more interested in the total regime. Not surprisingly, the median monthly use of blood monitoring strips was lower in the glargine group, at 60, than at 80 for the conventional insulin therapy group. In the light of this, the higher cost of glargine was largely offset by lower insulin test strip usage, leading to similar average costs per day: €1.90 for glargine compared with €1.99 for the conventional insulin therapy group. HbA1c results were 7.8% in both groups.
Janka and Hogy (2008)278 undertook a similar study to Lechleitner et al. (2005),277 above, estimating the cost differences between once daily glargine plus oral agents, against twice-daily premixed insulin. Glargine was estimated to have half of the annual needle costs, testing strip costs and lancet costs, at only €375, compared with €750 for premixed insulin. This helped offset the additional cost of metformin and glimepiride of €346 within the glargine arm. Insulin usage was considerably lower within the glargine arm, being less than half of that of the premixed insulin arm, resulting in an insulin cost, including pens, of around €510 for glargine compared with €735 for premixed insulin. This resulted in an average annual cost of €1259 for once-daily glargine compared with €1495 for twice-daily premixed insulin. The study was sponsored by, and the author for correspondence was from, Sanofi-aventis.
Meeting abstracts
Thompson et al. (2005)279 in an ISPOR poster (co-authors from Sanofi-aventis) present the results of cost-effectiveness modelling of glargine compared with NPH. This appears to be a precursor to the full Grima et al. (2007)265 paper reported above, as the author list is the same, with the same 0.25 QALY gain being estimated from the use of glargine. The estimated cost-effectiveness differed slightly at Can$9804 for reasons that are not clear.
Smith et al. (2004),280 in an ISPOR poster presentation from CORE and Novo Nordisk authors, estimated the cost-effectiveness of detemir compared with NPH basal bolus among UK patients with type 2 diabetes from the perspective of the NHS. Clinical effectiveness estimates were not explicitly stated, but it appears to have been assumed that the only significant difference would be in weight, with detemir leading to a 0.4-kg gain compared with 1.3 kg for NPH. It was noted that detemir has been demonstrated to be non-inferior in terms of both HbA1c level and hypoglycaemic events. The modelling predicted a survival gain of 0.13 years from detemir and a gain of 0.08 QALYs, for an additional cost of £1534: yielding a cost-effectiveness estimate of £19,218 per QALY for detemir relative to NPH.
Valentine et al. (2006)281 in an ISPOR presentation (CORE and Novo Nordisk) appear to have undertaken a similar cost-effectiveness analysis for detemir as that reported above for their full 2007 paper,282 but only for the subset of those transferring from NPH to detemir. An additional 0.30 QALYs was anticipated from the transfer to detemir, although in this analysis it was also anticipated to be cost saving by US$2416 due mainly to reduced severe hypoglycaemic events, coupled with lower rates of retinopathy and cardiovascular complications. An additional 2006 ISPOR poster presentation by the same authors283 concluded that over a 5-year time horizon detemir would result in an additional 0.17 QALYs compared with NPH, with a cost-effectiveness of US$25,368 per QALY.
A third ISPOR poster presentation by Valentine et al. (2007)271 (Novo Nordisk and the IMS consultancy, which took over CORE) considered the cost-effectiveness of patients transferring from glargine to detemir. Clinical effectiveness estimates were as for their full 2007 paper, but costs were from the German perspective. Cost savings of €1032 were anticipated from the conversion to detemir among those failing on glargine, alongside a gain of 0.29 QALYs. The reason for the lower QALY gain compared with their full 2007 paper is not apparent.
In a like manner to the poster presentations of Valentine et al. summarised above, Palmer et al. (2006)284 (CORE and Novo Nordisk) in an ISPOR poster presentation appear to have undertaken a similar cost-effectiveness analysis for detemir as that within the Valentine et al. (2007)282 full paper, but for the subset of those transferring from orals to detemir. Transferring to detemir was estimated to result in an additional 0.17 QALYs at minimal total cost to yield a cost-effectiveness estimate of US$657 per QALY. Within this, transfer to an insulin other than detemir for those failing on oral agents does not appear to have been considered, which is a major weakness.
Palmer et al. (2005)285 [sponsorship not given, but several authors also authors of the Ray et al. (2007)275 paper, from Novo Nordisk and CORE] estimated the cost-effectiveness of premixed insulin compared with glargine from the US Medicare perspective, using clinical effectiveness estimates from the INNOVATE trial. As such, it mirrors the results of the full paper of Ray et al. (2007)275 reported above, although estimates a slightly lower gain of 0.15 QALYs but also a slightly lower ICER of £39,000 per QALY for premixed insulin compared with glargine.
Chapter 8 Cost-effectiveness modelling of the new drugs
UKPDS Outcomes Model
As summarised by Clarke et al. (2004),286 the UKPDS Outcomes Model is a lifetime model that aims to estimate the first occurrence of a number of diabetes complications: MI, which may or may not be fatal, ischaemic heart disease (IHD), stroke, congestive heart failure, amputation, renal failure and blindness in one eye. The likelihoods of complications were estimated from the data of the 3642 patients with type 2 diabetes who took part in the UKPDS. The utilities and costs associated with complications and with routine ongoing care are included within the model, having also been estimated from the UKPDS population. These are discounted at rates specified by the user.
The likelihoods of complications occurring are functions of patient characteristics, some of which are time varying and projected by the model, and past complications’ history. The main time-varying factors are HbA1c, SBP and the ratio of total cholesterol to HDL cholesterol, their evolution being estimated using panel data and random effects modelling. Past complications cascade through the model, in that:
-
ischaemic heart disease increases the risk of MI
-
chronic heart failure (CHF) increases the risk of MI, stroke and death
-
blindness increases the risk of renal failure and amputation
-
myocardial infarction stroke, renal failure and amputation all increase the risk of death.
Details of the above complications are shown in Figure 13.
FIGURE 13.
The United Kingdom Prospective Diabetes Study model algorithm (taken from Clarke et al. 2004286). With kind permission of Springer Science + Business Media. AC, Afro-Caribbean; AMP, amputation; AtrFib, atrial fibrillation; BLIND, blindness; BMI, body mass index; CHF, congestive heart failure; IHD, ischaemic heart disease; Ln, logarithm; MI, myocardial infarction; PVD, peripheral vascular disease; RENAL, renal failure; SBP, systolic blood pressure; SMOK, smoking.
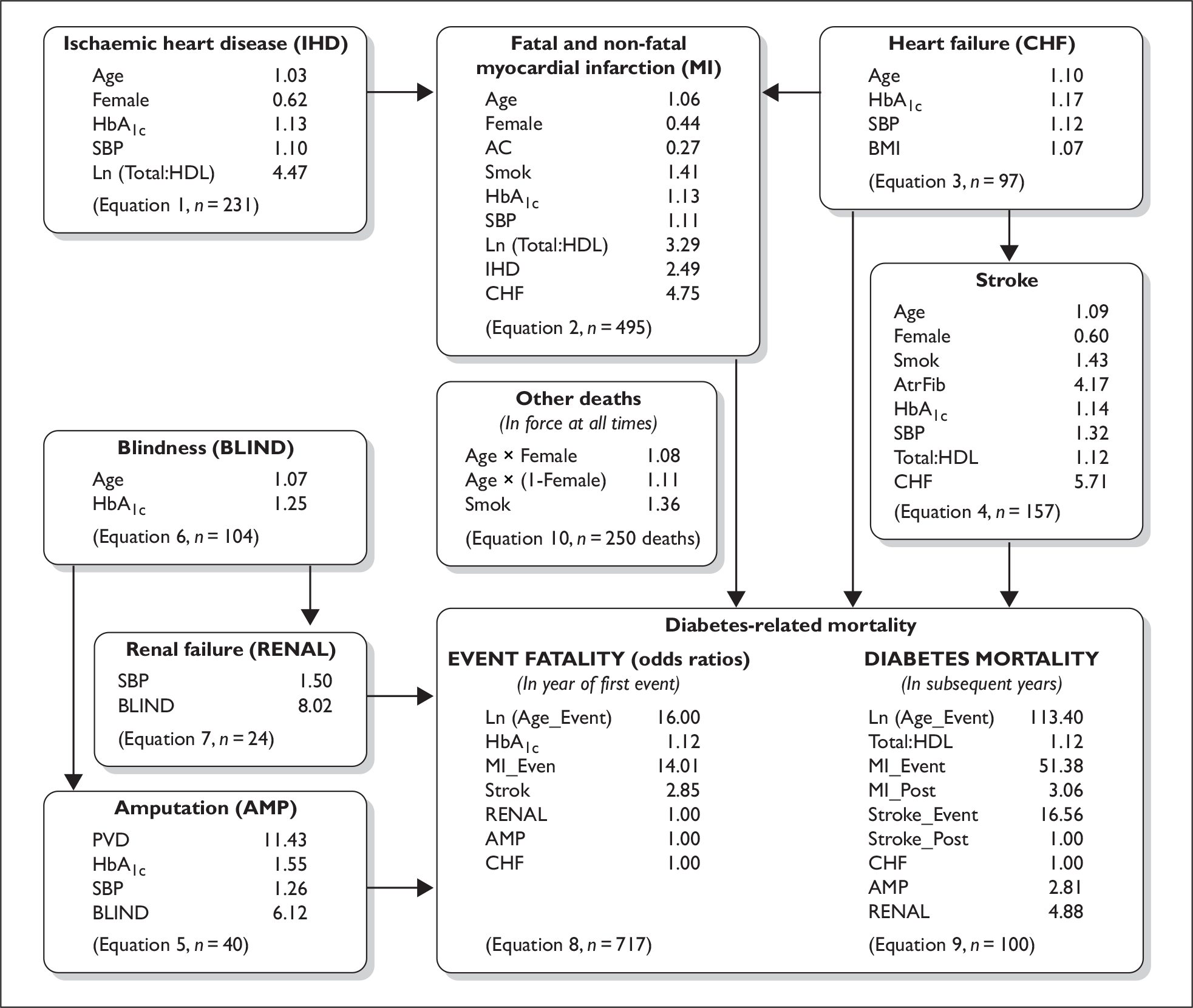
For example, a one-point increase in a patient’s BMI increases the annual risk of heart failure by a factor of 1.07, whereas a 1% point increase in a patient’s HbA1c level increases the annual risk of CHF by 1.17. As can be seen from the above, a patient’s BMI has limited direct impact, affecting only the likelihood of CHF as already outlined. However, this is because most of the effect of BMI is mediated through changes in SBP and the total ‘cholesterol–HDL cholesterol’ ratio. But should CHF occur, the effects cascade through the model, increasing the risk of MI, stroke and death.
The implementation of the model is also most easily seen through reference from the figure within Clarke et al. (2004),286 shown in Figure 14.
FIGURE 14.
The United Kingdom Prospective Diabetes Study model equations (taken from Clarke et al. 2004286). With kind permission of Springer Science + Business Media.

Limitations to the model, as noted in Clarke et al. (2004),286 are that:
-
It estimates only the first event (strictly speaking, the first new event, as patients may have had past events).
-
Not all complications are modelled, for example peripheral neuropathy.
-
Hypoglycaemic events are not modelled.
-
Quality-of-life impacts are derived only from complications.
Note that within the model it is possible to specify the evolution of risk factors such as HbA1c level through time, and, as a consequence, the effect of intensification of treatment can be specified upon these risk factors, from oral agents to basal insulin, and from basal insulin to basal bolus insulin, even if these intensifications occur some time after baseline.
Other parameters, such as weight, can be specified for the baseline as patient characteristics. For these parameters an initial treatment effect can be implemented between treatments; for example (1) for exenatide versus glargine, by specifying the baseline value for exenatide to be equal to the baseline value plus initial treatment effect for exenatide, and (2) for glargine, by specifying the baseline value for glargine to be equal to the baseline value plus initial treatment effect for glargine. But these parameters cannot be altered at any intensifications of treatment after baseline. This is also common to other models of diabetes, such as the Economic Assessment of Glycemic control and Long-Term Effects (EAGLE) model,287 and the CORE model. 288 This has implications for comparing treatments with different effects on weight.
The UKPDS Outcomes Model286 is a patient-level simulation model that provides the point estimates in terms of average life expectancy, quality-adjusted life expectancies, and the costs of complications using a set of central parameter values to predict the likelihood of diabetes-related complications occurring, given various patient characteristics. The model also outputs the central estimate of the cumulative mortality through time, this again being based upon the results of modelling using the set of central parameter values. Due to the patient-level simulation approach, a number of iterations of the model have to be performed in order to reduce variability within the estimates and achieve convergence for the point estimates, i.e. for each treatment regime simulated for a given patient the model performs a number of iterations to achieve convergence for the point estimates for that one treatment–patient combination.
To illustrate the impact of the number of iterations and their effect upon convergence of model estimates, the impact of increasing the number of iterations upon the SD as a percentage of the average value of the model outputs across 1000 identical patients can be examined as below. Within this, the patient characteristics for each of 1000 patients was taken to be as outlined for the male patient, with a BMI of 35 kg/m2, receiving exenatide followed by glargine upon the intensification to insulin at year 6, as outlined later in this chapter. For current purposes the patient characteristics are secondary to the illustration of the impact of increasing the number of iterations upon the SD of the estimated outputs, as shown in Table 35.
| Estimated outputs | Model iterations | |||
|---|---|---|---|---|
| 1000 | 10,000 | 100,000 | 250,000 | |
| SD (QALYs)/E (QALYs) (%) | 1.27 | 0.44 | 0.24 | 0.18 |
| SD (costs)/E (costs) (%) | 6.65 | 2.14 | 0.67 | 0.44 |
Given the above and computational availability, 250,000 iterations were performed in order to approach convergence. However, there remains small variability across estimates as shown above. The size of this variability should be borne in mind when examining the results of the modelling and their practical significance, even given that 250,000 iterations have been applied.
The UKPDS Outcomes Model incorporates, and allows the user to modify, the following: the immediate costs of routine care excluding the immediate drug therapy costs, the immediate and long-term costs of complications, and the QoL impact of the complications modelled. It does not provide a ready means of including other costs or effects, but it does output point estimates, through time, of the cumulative mortality for a given treatment simulation. As outlined below, there is a range of other inputs to the modelling that need to be included: the drug therapy costs and the costs of switching to insulin, and the direct QoL impacts arising from nausea, severe hypoglycaemic events and weight changes. These will be appended to the output of the UKPDS Outcomes Model in a deterministic fashion, annual quantities being conditioned by the proportion of patients remaining alive within the relevant year, prior to being discounted at the 3.5% as recommended by NICE. For ease of reference, these will be described as the ‘bolt-ons’.
It should be noted that the UKPDS Outcomes Model also has a facility to perform additional runs of the model for a set of up to 999 bootstrapped sets of parameter values. This facility can be used to characterise the second-order uncertainty around the outputs of the model, i.e. to perform a probabilistic sensitivity analysis (PSA), for a given evolution of HbA1c. This facility has not been used and a PSA has not been undertaken for the current review for two reasons:
-
First, full characterisation of second-order uncertainty as required for a PSA would also require characterisation of the second-order uncertainty around treatment effectiveness parameters. Indeed, it could be argued that the second-order uncertainty around the treatment effectiveness parameters is the most important second-order uncertainty that needs to be introduced for a PSA to be meaningfully undertaken, or at a minimum is necessary if not sufficient for a PSA. Unfortunately, this is not easily implementable within the UKPDS Outcomes Model, within which it is not possible to specify a distribution around relative treatment effects. Any attempt to introduce this might also conflict with the reliable elimination of first-order uncertainty.
-
Second, given the centrality of the point estimates of cumulative mortality and resultant survival function to the estimated effect of the ‘bolt-ons’, aligning the three aspects of the modelling: the model point estimates, the bootstraps and the ‘bolt-ons’ would be complicated. The ‘bolt-ons’ rely upon the estimated survival function, and as a consequence require that the point estimates be used.
But the main difficulty in terms of implementing a PSA within the UKPDS Outcomes Model is that there are no ready means to characterise the second-order uncertainty around the treatment effectiveness parameters for a head-to-head comparison of two treatments.
Methods
Patient population modelled
The previous clinical guideline (CG 66) drew patient baseline characteristics from expert opinion rather than the UKPDS, as this was felt to be more likely to reflect those moving on to third-line therapy. 6 These were broadly in line with the inputs to the modelling reported in the economic literature above, and will be adopted for the current modelling. Note that within this, the representative patient is assumed to have progressed from metformin, to combined metformin and sulfonylurea, but now to having poor control as defined by HbA1c level rising above 7.5%. Given this worsening of control, there is a choice as to how to intensify therapy with the newer agents – such as exenatide, vildagliptin and sitagliptin, older ones – such as rosiglitazone and pioglitazone, and the insulins – glargine, NPH and detemir – all being possible options.
Table 36 shows baseline characteristics of patient populations.
| Characteristic | Gender | |
|---|---|---|
| Male | Female | |
| Age (years) | 58 years | 58 years |
| Duration of diabetes (years) | 5 years | 5 years |
| HbA1c (%) | 7.5 | 7.5 |
| Height (cm) | 170 | 165 |
| Weight (kg) | 87 | 82 |
| BMI (kg/m2) | 30 | 30 |
| SBP (mmHg) | 140 | 140 |
| Total cholesterol (mmol/l) | 4.4 | 4.4 |
| HDL cholesterol (mmol/l) | 1.0 | 1.0 |
Note that male and female patients will be modelled separately. Being typically slightly shorter, for a given BMI the average female patient weight will be slightly less. Since the BMI modelled is the same for both male and female patients, any differences in the output of the UKPDS Outcomes Model are anticipated to be a pure gender effect.
Similarly, since insulin dosage is weight dependent and BMI has some, though limited, impact upon the outcomes of the UKPDS Outcomes Model, the impact of weight upon cost-effectiveness will also be explored through applying a BMI of 35 kg/m2.
For a given BMI and insulin dose per kilogram, women will also require a lower overall insulin requirement.
The previous guideline did not outline the background prevalences of complications associated with diabetes. The study by THIN288 outlines rates of complications for those transferring to insulin therapy, using data from a large UK general practice database. Adopting the rates of complications as reported for the HbA1c values ≥ 7% would imply prevalences, as shown in Table 37.
| Morbidity | Prevalence assumed (%) | Source |
|---|---|---|
| Congestive heart failure | 3.7 | UKPDS286 and THIN289 |
| Amputations | 0 | UKPDS |
| Neuropathy | 6.5 | THIN |
| Blindness | 0 | UKPDS |
| Retinopathy | 17.7 | THIN |
| End-stage renal failure | 0 | UKPDS |
| Nephropathy | 0.7 | THIN |
| Stroke | 4.9 | THIN |
| Myocardial infarction | 8.2 | THIN |
However, it should be noted that a proportion of patients within this group would have had somewhat worse HbA1c levels than is being assumed within the baseline UKPDS patient characteristics. There may also have been some correlation among these, with some patients having more than one complication. This is not easily accounted for within the UKPDS Outcome Model, and as a consequence the base case will first model using an assumption of no complications at entry. Since we know from the UKPDS that many (about 25%) had complications at entry, this will be followed by with an analysis assuming the above complication rates coupled with a further assumption that patients with one complication did not have another concurrently. This latter analysis may provide an upper estimate since: the rates of complications may be too high for the group modelled; and, the likelihood is that some patients had a range of comorbidities and while these patients would do relatively poorly this would be more than balanced by other patients having no comorbidities and performing rather better.
It is worth noting also that the UKPDS excluded newly diagnosed patients who had experienced recent MI, or who had angina.
Comparator treatments: direct head-to-head comparisons
As previously noted, all patients reaching this stage have failed on dual oral therapy, usually with metformin and a sulfonylurea, and so the issue is which drug to add as third line. Given the clinical effectiveness review, the comparisons chosen for modelling are:
-
exenatide and glargine [as reported above in the summary of Heine et al. (2005)53]
-
sitagliptin and rosiglitazone [as reported above in the summary of Scott et al. (2008)121]
-
vildagliptin and pioglitazone [as reported above in the summary of Bolli et al. (2008)123]
-
glargine and NPH insulin (as reported within the meta-analysis in Chapter 4)
-
detemir and NPH insulin (as reported within the meta-analysis in Chapter 4).
This gives rise to the following clinical effectiveness estimates for the modelling for the base-case male patient with a BMI of 30 kg/m2 (Table 38).
| Comparison 1 | Comparison 2 | Comparison 3 | Comparison 4 | Comparison 5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Exenatide | Glargine | Sitagliptin | Rosiglitazone | Vildagliptin | Pioglitazone | Glargine | NPH | Detemir | NPH | |
| HbA1c (%) | –1.11 | –1.11 | –0.79 | –0.76 | –0.88 | –0.98 | No difference | No difference | 0.08% higher with detemir | |
| Weight (kg) | –2.3 | +1.8 | –0.4 | +1.5 | +0.3 | +1.9 | –0.28 | –1.20 | ||
| Nausea (%) | 57 | 9 | 1 | 1 | – | – | – | – | – | – |
| Severe hypoglycaemic attacks | 0.3 p.a. | 0.3 p.a. | – | – | 0 | 0 | 0.82 RR | 0.76 RR | ||
| Nocturnal hypoglycaemic attacks | 2.67 RR | 0.56 RR | 0.61 RR | |||||||
Note that within these comparisons many of the differences in point estimates did not reach statistical significance. Also note that the comparison of exenatide and glargine is based upon the results of Heine et al. (2005). 53 The results of Barnett et al. (2007)50 would imply relatively greater effect from exenatide upon severe hypoglycaemic events but a relatively lesser effect upon patient weight. Given the results of Barnett et al. , the effect upon BMI will be taken to apply across the other patients simulated.
Insulin doses
A distinction between the newer drugs, such as exenatide and the insulins, is that the insulin dose is weight dependent. There is also evidence that the insulin dose increase with patients’ BMIs, (as shown in Figure 15) from data of the Aberdeen Diabetic Clinic (unpublished).
FIGURE 15.
Mean insulin dose per day vs body mass index.
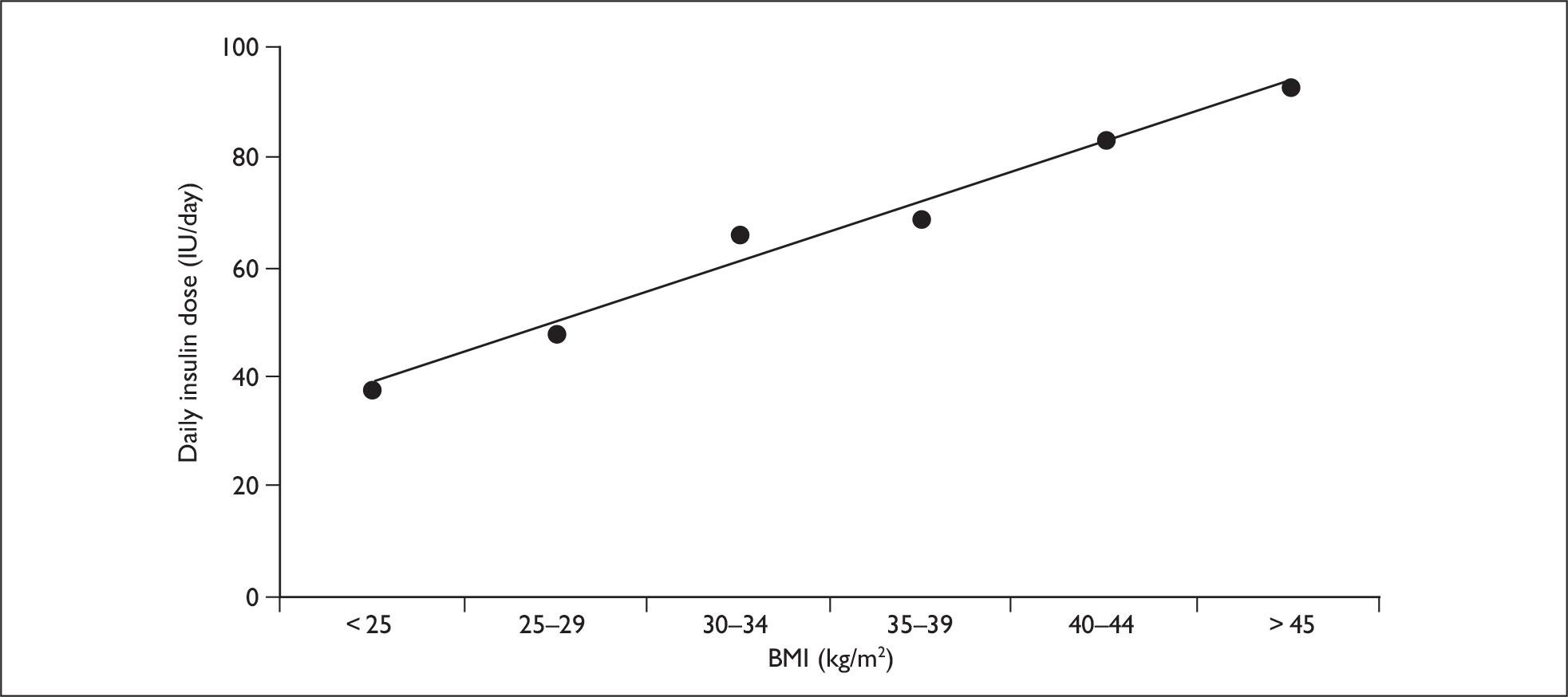
Figure 15 suggests an average requirement for the base case of around 0.55 IU/kg/day. Patients with BMIs in the mid-30s would require a higher dose of around 0.65 IU/kg/day.
Direct drug costs
The annual direct drug costs and monitoring of the various regimes are valued using BNF 56,290 resulting in costs for a male patient of BMI 30 kg/m2 as shown below in Table 39.
| Cost (£) | |
|---|---|
| Met + sulf + exenatide | |
| Metformin 2 g/day | 26.07 |
| Gliclazide 160 mg/day | 20.56 |
| Exenatide b.i.d.: | 830.25 |
| snap-on needle cost | 31.10 |
| Annual total | 907.98 |
| Met + sitagliptin | |
| Metformin 2 g/day | 26.07 |
| Sitagliptin 100 mg/day | 433.57 |
| Annual total | 459.64 |
| Met + vildagliptin | |
| Metformin 0 g/day | – |
| Vildagliptin 2 × 50 mg/1 mg Met | 386.41 |
| Annual total | 386.41 |
| Met + sulf + rosiglitazone | |
| Metformin 0 g/day | – |
| Gliclazide 160 mg/day | 20.56 |
| Rosiglitazone 8 mg + Met (2 × 4 mg/1 mg) | 481.80 |
| Annual total | 502.36 |
| Met + sulf + pioglitazone | |
| Metformin 2 g/day | 26.07 |
| Gliclazide 160 mg/day | 20.56 |
| Pioglitazone 30 mg/day | 437.22 |
| Annual total | 483.85 |
| Met + sulf + glargine | |
| Metformin 2 g/day | 26.07 |
| Gliclazide 80 mg/day | 10.28 |
| Glargine 0.55 U/kg/day: | 452.53 |
| pen | 5.15 |
| needles | 31.10 |
| Monitoring strips 1 | 109.50 |
| Annual total | 634.63 |
| Met + sulf + NPH | |
| Metformin 2 g/day | 26.07 |
| Gliclazide 80 mg/day | 10.28 |
| NPH average 0.55 U/kg/day: | 284.09 |
| pen | 6.89 |
| needles | 31.10 |
| Monitoring strips 1 | 109.50 |
| Annual total | 467.93 |
The ingredient cost per unit of detemir is the same as for glargine, but there is evidence of there being an estimated 18% higher dosing requirement for detemir in type 2 diabetes compared with glargine. With a slightly higher cost per pen, this yields a cost for detemir of £716.09 compared with the £634.63 for glargine shown above. Note that while the non-insulin regimens postpone the need for insulin, they do not prevent the need for insulin eventually. For example, the UKPDS model indicates that given the initial HbA1c effect from exenatide, the patient’s HbA1c will progressively worsen until after 5 years, the 7.5% threshold will be reached, triggering an intensification of treatment, with a switch to insulin.
For those intensifying to mealtime insulin it will be assumed that the dose of insulin increases by 0.2 IU/kg/day with the estimated regimen costs as shown in Table 40.
| Cost (£) | |
|---|---|
| Met + glargine + bolus | |
| Metformin 2 g/day | 26.07 |
| Glargine 0.55 U/kg/day: | 452.53 |
| pen | 5.15 |
| needles | 31.10 |
| Short-acting 0.2 U/kg/day: | 121.82 |
| pen | 6.19 |
| needles | 31.10 |
| Monitoring strips 1 | 109.50 |
| Annual total | 783.47 |
| Met + NPH + bolus | |
| Metformin 2 g/day | 26.07 |
| NPH 0.55 U/kg/day: | 284.09 |
| pen | 5.15 |
| needles | 31.10 |
| Short-acting 0.2 U/kg/day: | 121.82 |
| pen | 6.19 |
| needles | 31.10 |
| Monitoring strips 1 | 109.50 |
| Annual total | 615.02 |
Again, it will be assumed that detemir requires an additional 18% dose compared with glargine, leading to a cost of £864.92 compared with the £783.47 as reported above for glargine.
For a female patient of BMI 30 kg/m2, the slightly lower average weight due to slightly lesser average height slightly reduces the average costs of the insulin-containing regimes. Similarly, increasing the BMI of male and female patients to 35 kg/m2 increases the costs of the insulin-containing regimes, due to both the greater weight of the patient and the higher dose require per kilogram (Table 41).
| Cost (£) | |||
|---|---|---|---|
| Female, BMI = 30 | Male, BMI = 35 | Female, BMI = 35 | |
| Metformin + sulfonylurea + glargine | 608.41 | 806.05 | 769.88 |
| Metformin + sulfonylurea + NPH | 451.46 | 575.54 | 552.83 |
| Metformin + sulfonylurea + detemir | 685.14 | 918.36 | 875.69 |
| Metformin + glargine + bolus | 750.18 | 975.19 | 930.79 |
| Metformin + NPH + bolus | 593.24 | 744.68 | 713.74 |
| Metformin + detemir + bolus | 826.91 | 1087.50 | 1036.59 |
Other costs of treatment
In addition to the above costs, transferring to insulin requires patient education in the use of pens and titration of dosage over time, which involves specialist nursing time with an associated cost. If it is assumed that this requires an additional 15 minutes of nurse time for training in blood glucose monitoring, 30 minutes in the use of pens plus two follow-up phone calls then this would amount to roughly an additional hour of a senior nurse’s time – currently costed by the Personal Social Services Research Unit (PSSRU) at £60 per hour. 291 More conservatively, the 2006–7 reference costs state the average cost per non-consultant-led outpatient attendance for diabetic medicine as being £84, which, when combined with the additional follow-up phone calls, would suggest an overall cost of £178. This cost of £178 will be used for the base case. Note that this contrast with the fixed doses of exenatide, where the only change is the doubling from half dose to full dose to minimise early side effects.
The costs of the complications of diabetes as estimated within the UKPDS Outcomes Model are intrinsic to the model, having been estimated from UKPDS data (Table 42). These will be uprated from 2004 prices to 2007 prices using the PSSRU Hospital & Community Health Services Pay and Prices Index, showing a general inflation of 12% over the period as below. 291
| Cost | |||
|---|---|---|---|
| At time of event | Annual thereafter (£) | ||
| Fatal (£) | Non-fatal (£) | ||
| Ischaemic heart disease | – | 3020 | 998 |
| Myocardial infarction | 1530 | 5823 | 959 |
| Heart failure | 3368 | 3368 | 1180 |
| Stroke | 4492 | 3562 | 673 |
| Amputation | 11,596 | 11,596 | 670 |
| Blindness | – | 1521 | 644 |
| Renal failure | 33,600 | 33,600 | 33,600 |
Similarly, in the absence of complications the annual costs excluding the costs of therapy will be drawn from the UKPDS Outcomes Model and inflated to £419.
QoL impacts of complications within the UKPDS Outcomes Model
For the QoL impacts of the complications modelled, the UKPDS Outcomes Model applies the following decrements to a baseline average QoL of 0.785 (Table 43).
| Complication | Utility decrement |
|---|---|
| Ischaemic heart disease | –0.090 |
| Myocardial infarction | –0.055 |
| Heart failure | –0.108 |
| Stroke | –0.164 |
| Amputation | –0.280 |
| Blindness | –0.074 |
| Renal failure | –0.263 |
Evolution of HbA1c within the modelling
The new drugs such as exenatide and the gliptins may postpone the transfer of patients to insulin. However, the assumption will be one of postponement rather than avoidance. Given this, there will be a sawtooth pattern to the evolution of HbA1c from the new drugs, with their initial reduction in HbA1c being followed by a slow rise as beta-cell function declines.
The evolution of HbA1c will be that projected by the UKPDS Outcomes Model. But, as advised by the GDG, treatment will be intensified when the HbA1c level rises above 7.5%. If this implies a switch to insulin therapy, a treatment effect, as outlined in the summary of model inputs, will be assumed, depending on the insulin regimen adopted. If treatment intensification is to add mealtime insulin to basal insulin, an initial effect of a 0.5% improvement in HbA1c level will be assumed. Note that within the implementation of the UKPDS Outcomes Model, it will be assumed that patients will rise above the 7.5% intensification threshold. The HbA1c effect of treatment intensification will be assumed to apply for the year subsequent to this, with the evolution of HbA1c level being that projected by the UKPDS Outcomes Model thereafter. This gives rise to a sawtooth evolution.
The evolution of HbA1c under different treatments requires consideration, and, for some drugs, long-term data are not available.
The UKPDS showed progression of disease, irrespective of which drug was used. That study used two sulfonylureas: metformin and insulin. It has been suggested in the ‘durability’ study29 that progression might be slower on a glitazone than a sulfonylurea, but, if true, that would not be relevant here because the glitazone would be used after the sulfonylurea, and the relevant comparison would be with a gliptin or exenatide.
Despite assertions that exenatide or the gliptins might preserve beta-cell function, the evidence from studies in which these drugs have been used, and then withdrawn, show no lasting effect. We will assume, therefore, that there are no differences in progression rates amongst the glitazones, the gliptins, exenatide or the insulins. (Note: The UKPDS did not report on progression according to weight loss – those with dramatic weight loss might have been expected to show slower, or no, progression. However, dramatic weight loss is not common enough to be relevant here.)
However, the evolution of HbA1c may be different with insulins. Take, for example, the comparison of exenatide and glargine as third-line therapy (i.e. in addition to metformin and a sulfonylurea). After exenatide is started, there is a fall in HbA1c level of about 1.1%, after which the HbA1c level slowly rises because of progression of disease, and because the dose is fixed. After about 5 years, the HbA1c level reaches 7.5%, triggering intensification with a switch to long-acting insulin, with a drop in HbA1c of about 1%.
If glargine is started rather than exenatide then there is the same 1.1% fall, but with some differences. The dose needs to be titrated, so that the fall may occur more slowly. However, the dose of glargine can be increased further (unlike fixed-dose exenatide). So when the HbA1c level starts rising, the dose of glargine can be increased further, so that the rise in HbA1c level should be slower with glargine than exenatide (although possibly at the cost of further weight gain).
Hence over the first period the rising curve for HbA1c level for exenatide might be expected to stay above that for glargine. The 7.5% threshold for intensification will be reached sooner with exenatide than glargine, and the exenatide group may switch to glargine sooner than the glargine group require to intensify to a basal bolus insulin regimen. This may not apply if those on exenatide lose a lot of weight and those on glargine gain a lot.
Many of those on glargine, whether as third line, or as fourth line after a period on exenatide, will still progress to requiring intensification, because with disease progression and loss of beta-cell capacity they will be unable to control postprandial glucose with only a basal insulin (or will do so only at the cost of troublesome hypoglycaemia). When they do progress to a basal bolus insulin regimen, they will experience another ‘sawtooth’ drop in HbA1c level, after which they will be controlled by titration of the mealtime insulin.
As both of the exenatide and glargine groups are assumed to progress at the same rate, their HbA1c curves will in time come to converge. Any differences in areas under the curves will be temporary. We lack data on the difference – there may be a slightly higher curve with exenatide – and it may not be clinically significant over a lifetime.
Note that where the figure for HbA1c level during any year is only marginally less than 7.5%, but where the UKPDS Outcomes Model would project it to increase somewhat above this during the following year, the intensification of therapy will be assumed to occur during this following year. This avoids introducing what seems likely to be spurious gains from one treatment postponing the intensification of therapy by an additional year compared with another treatment when the modelled evolution of HbA1c level is only very marginally different between the two treatments.
The reductions in HbA1c level observed in the four trials in Table 11 should not be used to conclude that, for example, vildagliptin was more potent than sitagliptin, or pioglitazone than rosiglitazone, because there were no head-to-head comparisons, and the baseline HbA1c levels in the trials were different. For our base case, we have to assume that in terms of glucose-lowering effects, there are no significant differences amongst any of sitagliptin, vildagliptin, pioglitazone or rosiglitazone.
Evolution of weight within the modelling
As noted within the section describing the UKPDS Outcomes Model (Chapter 8), the weight of a patient at baseline, and as modified by the initial treatment intensification, can be specified by the user (with the necessary mechanism of assuming that weight change is immediate), but, unlike other input parameters, its evolution through time cannot. As a consequence, although HbA1c level can be specified to change as patients intensify treatment and move from, say, exenatide to glargine, to glargine plus mealtime insulin, the patient weight cannot be specified to change and remains principally determined by the value set at baseline. So, while the initial fall in weight on exenatide can be entered explicitly within the UKPDS Outcomes Model, the subsequent gain after the switch to insulin cannot.
This may tend to bias the analysis in favour of those treatments that tend to reduce patient weight from the baseline value. For example, exenatide is anticipated to give a weight loss of 2.3 kg. This will affect both the likelihood of developing CHF, as estimated through the UKPDS Outcomes Model, and the direct QoL effect of weight changes. But when the patient intensifies treatment and moves from exenatide to insulin, it is not possible to dial this weight loss effect out of the UKPDS Model. It can only be reversed for the direct QoL effect of weight change. As a consequence, a sensitivity analysis will explore the effect of equalising patient weights at baseline within the UKPDS Outcomes Model and only exploring the effects of weight differentials associated with concurrent treatments through their direct impact upon QoL as outlined below.
Impact of weight changes and nausea
Applying the estimates of the impact of weight upon QoL as reported in Bagust and Beale (2005)247 to the results of Heine et al. (2005)53 suggest that the weight loss associated with exenatide would result in a direct QoL increment of 0.005. This compares with a QoL loss of around 0.004 for the weight gain associated with glargine a net treatment effect of a gain of in QoL from the use of exenatide over glargine of a little under 0.01 arising from the weight dimension alone. At mean weight loss values, the parameter estimate of Coffey et al. (2002)248 would not anticipate any QoL impact, although this is due to the dichotomous nature of the variable, which is of only limited applicability to the scenario described.
Among the 82-week completer cohort as reported in Blonde et al. (2006),245 the changes in BMI can be inferred if a common height of 1.68 m is assumed across categories. This would imply a QoL increment of around 0.004, 0.006, 0.009, 0.010 and 0.014 for the baseline categories of BMI < 25 kg/m2, 25 kg/m2 < BMI < 30 kg/m2, 30 kg/m2 < BMI < 35 kg/m2, 35 kg/m2 < BMI < 40 kg/m2 and BMI > 40 kg/m,2 respectively.
The above does not take into account the effects of nausea as reported within Heine et al. (2005)53. At the 26-week point, 57% of patients receiving exenatide had experienced nausea compared with 9% of patients receiving glargine. Given the weight loss of 2.63%, on average (ratio of mean weight loss and baseline weight), from exenatide, and QoL increment estimates as reported within the exenatide SMC submission, this suggests that those on exenatide had a QoL increment of a little less than 0.020 for the 43% not experiencing nausea compared with a QoL decrement of a little less than 0.028 for the 57% who did have nausea, giving a net effect of an average slight utility decrement among those trialling exenatide of a little less than 0.007. The parallel utility decrements for the 91% of glargine patients not experiencing nausea but seeing an average weight gain of 2.05% would be perhaps around two-thirds of the –0.044 associated with a 3% weight loss. The remaining 9% experiencing both a 2.05% weight gain and nausea might experience a similar fraction of the –0.073 QoL decrement estimated for those gaining 3% weight and experiencing nausea, as within the SMC submission. (Note: We have accepted the frequency of nausea as reported by the study. The 9% may seem high for those on insulin use, but ‘nausea’ is probably used to cover a range of feelings, and the opinion of the GDG indicated that though the precise rate might differ according to definition, the absolute difference between exenatide and insulin appeared correct. Note that this is incident not prevalent nausea, so one episode in the 6 months is enough for patients to be included in the 9%.)
However, the QoL increments due to weight change as reported in Lilly’s SMC submission, based on the study by Matza et al. (2007),292 are considerably higher than those of Bagust and Beale (2005). 247 For instance, given a patient height of 1.68 cm and a BMI of 31 kg/m2, for patients not experiencing nausea the Bagust and Beale estimates would imply a QoL increment of around 0.006 for a 3% weight loss and of around 0.010 for a 5% weight loss, these estimates being roughly symmetric for weight gains. The QoL increments from weight loss as reported by Matza et al. (2007)292 are around three to four times those of Bagust and Beale, while weight gains are around seven to eight times those of Bagust and Beale.
It can also be noted that the economic appendix of the NICE guideline on obesity293 applied the following utility modifiers within the economic modelling, as shown in Table 44.
| BMI (kg/m2) | Male | Female |
|---|---|---|
| < 21 | 0.86 | 0.85 |
| 21–25 | 0.87 | 0.87 |
| 26–30 | 0.86 | 0.82 |
| 31–39 | 0.82 | 0.78 |
These would suggest that a move from the mid-point of the 26–30 kg/m2 to the mid point of 31–39 kg/m2, an increase of 7 points on the BMI scale, would be associated with a 0.04 loss, or around –0.0057 per BMI point. This is very similar to the –0.0061 per BMI point as estimated for those with type 2 diabetes by Bagust and Beale (2005). 247
For the base case it will be assumed that nausea is mainly experienced during the first 3 months of treatment with exenatide, which from a QoL decrement of 0.048 implies a QALY loss of 0.012. Given the results of Heine et al. (2005),53 it will be further assumed that a net 50% of patients treated with exenatide will experience nausea, implying an average QALY loss of 0.006 from treatment with exenatide.
The direct utility effect of weight changes associated with the different therapies will be assessed in the base case using the parameter estimates of Bagust and Beale (2005). 247 As noted above, the new non-insulin therapies will be assumed to postpone treatment with insulin but not prevent it. In assessing the direct utility effect of weight changes, upon transferring to insulin it will be assumed that any weight loss associated with the non-insulin will be reversed and will also be coupled with the weight gain associated with the transfer to insulin.
Note that to apply these QoL impacts from weight changes, the treatment sequences modelled and associated weight changes need to be conditioned by the survival curves as modelled by the UKPDS Outcomes Model, i.e. the QoL effect of any weight change associated with treatment is applied only to the surviving cohort. From this, it is possible to vary the QoL increments and decrements arising from weight changes to reflect the treatment sequence; for example, a patient initially using exenatide would experience the QoL impact of a 2.3-kg fall in weight while on exenatide, but, when switching to glargine, would experience the QoL impact of returning to the baseline weight and putting on an additional 1.8 kg. (Note: These trial-based data may underestimate differences in routine care and longer follow-up, which may be larger.)
Furthermore, within this calculation, in the absence of other information, the switch to mealtime insulin is assumed to cause the same weight gain as with glargine. This latter assumption may cause a slight bias against detemir within the indirect comparison with glargine, given that the weight gain from glargine as drawn from the indirect comparison appears slightly greater, although it seems unlikely to have a significant impact upon the comparisons between non-insulin regimes, being a common factor to all. But in general the possible differences between the permutations of weight gain upon the switch from basal to basal bolus insulin seems likely to be slight.
Impact of severe hypoglycaemia events
The UKPDS Outcomes Model does not permit the direct evaluation of changes to rates of severe hypoglycaemic event rates. But in the technology appraisal (TA 53) of long-acting insulin analogues (at that time only glargine), the NICE Appraisal Committee accepted that both hypoglycaemic episodes, and the fear of such episodes recurring, caused significant disutility. The relevant paragraph states:12
The Committee accepted that episodes of hypoglycaemia are potentially detrimental to an individual’s quality of life. This is partly the result of an individual’s objective fear of symptomatic hypoglycaemic attacks as indicated in the economic models reviewed in the Assessment Report. In addition, as reported by the experts who attended the appraisal meeting, individuals’ quality of life is affected by increased awareness and uncertainty of their daily blood glucose status and their recognition of the need to achieve a balance between the risk of hypoglycaemia and the benefits of longer-term glycaemic control. The Committee understood that improvement in this area of concern regarding the balance between hypoglycaemia and hyperglycaemia could have a significant effect on an individual’s quality of life.
However, the guidance did not specify the amount of utility lost because of fear of hypoglycaemic episodes, and nor did the TAR,144 because it was based on the industry submission from Aventis, which was classed as confidential. But, clearly, the utility gain from reducing the fear of hypoglycaemia was enough to change a very large cost per QALY to an affordable one. There is the probability that a reduction in the rate of severe hypoglycaemia events may reduce the fear of severe hypoglycaemia events, though the impact of this seems likely to be variable across patients. The QoL impact arising from this would be over and above the direct QoL impact of severe hypoglycaemia events in themselves.
This fear effect may only apply to a subgroup of patients, but as an illustration of the possible impact of this, the social tariffs derived by Dolan et al. (1995)294 suggest that a move from level 2 within the anxiety subscale of EQ-5D to level 1 would be associated with a 0.07 QoL gain. In a similar vein, the coefficients derived by Brazier et al. (1998)295 for the SF-6D questionnaire for the consistent model using standard gamble valuations suggest that a movement within the social dimension from health problems interfering moderately to not interfering would be associated with a 0.022 QoL improvement. Similarly, an improvement in the mental health subscale from feeling downhearted some of the time to little or none of the time would be associated with a 0.021 QoL improvement. However, the proportion of patients in whom a reduction in severe hypoglycaemic events would result in these changes to the social dimension or mental dimension is not known.
Currie et al. (2006)268 surveyed 1305 UK patients with type 1 diabetes and type 2 diabetes, using both the HFS and the EQ-5D. Each severe hypoglycaemic event avoided was associated with a change of 5.9 on the HFS. Given a further estimate that each unit change on the HFS was associated with an EQ-5D QoL change of 0.008 this led to an estimated benefit from reduced fear of severe hypoglycaemic events of 0.047 per annual event avoided. This was coupled with a direct utility loss associated with a severe hypoglycaemic event of 0.0016 to yield an overall patient benefit of 0.05 per unit reduction in annual severe hypoglycaemic events.
The 0.05 QoL increment was adopted by the previous guideline (CG 66) in its evaluation of the effects of exenatide. However, at face value this estimate may be quite high. It suggests that a patient with diabetes in less than perfect health and currently experiencing one severe hypoglycaemia event every 2 years would in effect be willing to sacrifice an annual 11 days’ survival to avoid this risk. A patient experiencing one severe hypoglycaemic event would be willing to sacrifice an annual three weeks’ survival to avoid this risk.
The findings of the study by Currie et al. (2006)268 have been given considerable weight by industry and NICE. There are weaknesses in it that need to be considered. It involved a first questionnaire survey of 1500 subjects who had received diabetes care in primary care and hospital, and, later, another 3200 who had been admitted to hospital or attended outpatient appointments. The response rate was 31%. The hypoglycaemic events were reported for the 3 months before the survey, and this could mean that the results only apply to those with recent events, fresh in the memory; 45% were treated with insulin, and about 63% of these had type 2 diabetes.
Bias might arise through the response bias, and through the effect of recent hypoglycaemic episodes. The economists amongst the authors were from industry, and the study was funded by Sanofi-aventis and Novo Nordisk.
The independent technology assessment team form Sheffield that did the assessment report for NICE considered that the disutility was overestimated.
In terms of the cost per severe hypoglycaemic event that requires medical attention, Leese et al. (2003)296 coupled TA 5312 and NHS reference costs, and suggested costs per hypoglycaemia as shown in Table 45.
| Unit cost (£) | Percentage receiving | Weighted (£) | Source | |
|---|---|---|---|---|
| Glucagon | 20 | 90 | 18 | Glargine TAR |
| Ambulance | 144 | 34 | 49 | Leese |
| A&E | 29 | 7 | 2 | Leese & NHS reference costs TA&E |
| Ambulance and A&E | 173 | 52 | 90 | Leese & NHS reference costs TA&E |
| Hospital | 631 | 28 | 176 | Leese & NHS reference costs TNELIP |
| Weighted total | 335 |
Note that using the unit costs of Leese et al. (2003)296 and indexing to the current year (2008) gives an average of £424. However, only a minority of severe hypoglycaemia events will require medical attention, and the average cost per severe hypoglycaemia event will fall proportionately with the percentage of severe hypoglycaemia events that are attended to by relatives or friends and do not require outside medical assistance. For the base case it will be assumed that 20% of severe hypoglycaemia events require outside medical assistance.
Given these uncertainties, where a difference in severe hypoglycaemic event rates has been demonstrated between two treatments, an exploratory analysis will be performed. This will append QoL increments within the ranges suggested above to the avoidance of a severe hypoglycaemic event, coupled with a range of possible cost savings per hypoglycaemic event avoided.
In terms of the baseline rate of severe hypoglycaemia events that will be assumed to model any observed differences, within the ScHARR modelling of the cost-effectiveness of glargine (TA 53)12 the cost per severe hypoglycaemic event was reported as £62 (although note that this was subsequently revised) and the 9-year cost of severe hypoglycaemic events of around £175 for both glargine and NPH. This, in turn, implied an annual incidence of severe hypoglycaemic events of 0.35 per patient-year, as drawn from the Diabetes Audit and Research in Tayside Scotland (DARTS) data. 297 This is roughly in line with the rate of severe hypoglycaemic events over 26 weeks as reported in Heine et al. (2005)53 – eight events among 549 patients, which converts to an annual rate of 0.3 per patient.
The base case will assume a 0.01 utility gain from the reduced fear associated with an annual severe hypoglycaemic event, while the baseline annual rate will be assumed to be 0.35.
Impact of nocturnal hypoglycaemic events
The Heine et al. (2005)53 and Barnett et al. (2007)50 studies reported that exenatide caused fewer nocturnal hypoglycaemic events than glargine. While these are unlikely to significantly affect costs, the GDG was of the opinion that the reduction in nocturnal hypoglycaemia would yield a significant benefit to at least a subset of patients for similar reasons as the reduced fear associated with an annual severe hypoglycaemic event outlined above. In order to address this, an additional literature search was undertaken to identify whether any concrete values for this effect could be identified. Two papers were identified that addressed QoL and nocturnal hypoglycaemic events – Davis et al. (2005)298 and Levy et al. (2007),299 though the latter was available only as an abstract.
Davis et al. (2005)298 administered a postal survey among 3200 patients with diabetes – both type 1 and type 2 – and 897 questionnaires were returned to give a response rate of only 28%: 590 patients with type 2 diabetes and 271 with type 1 diabetes. The average EQ-5D score among those with type 2 diabetes experiencing only nocturnal hypoglycaemia events, was marginally better than those experiencing daytime hypoglycaemia events that were defined as either mild or moderate. However, patient numbers falling into the only nocturnal category were small. While this was not reported for the EQ-5D results, within the 361 patients with type 2 diabetes who completed SF-36 only two patients were reported as having only nocturnal hypoglycaemia events. Within patients with type 1 diabetes a similar pattern was observed.
Across all respondents the average EQ-5D value was reported as being 0.77 for those experiencing only nocturnal hypoglycaemic events compared with 0.65 among those whose worst hypoglycaemic event was classified as mild or moderate. Again sample size may have been small with only seven respondents of the 605 respondents within the SF-36 data having only nocturnal hypoglycaemic events.
Note that the results of Davis et al. (2005)298 would not be anticipated to uncover any additional QoL impacts from the fear of nocturnal hypoglycaemia.
The abstract of Levy et al. (2007)299 summarises the paper as having undertaken a time trade off exercise among both patients with diabetes (n = 50) and patients without diabetes (n = 75) to estimate the utility loss associated with hypoglycaemic episodes. The health state descriptors were based upon the HFS. The patients with diabetes apparently reported a disutility from rare hypoglycaemic events of –0.01, from intermittent hypoglycaemic events of –0.05, from frequent hypoglycaemic events of –0.17 and from nocturnal hypoglycaemic events of –0.12. Unfortunately, the abstract was not sufficiently detailed to outline either the severity of the hypoglycaemic events or their frequency and as a consequence is of limited use. In comparison with the other estimates for hypoglycaemic events as outlined above the estimates appear to be quite large.
Given the above, the possible effects of treatments’ effects upon nocturnal hypoglycaemic events have not been formally quantified within the economic modelling, though the limited results of Davis et al. (2005)298 suggest that on average the impact of nocturnal hypoglycaemia events may be limited. Some of the impact of nocturnal hypoglycaemia on QoL will in any case be captured via the fear-of-hypoglycaemic-events aspect.
Results
Within the pair-wise comparisons that follow, the default will be to present the numerical results for the male patient with a BMI of 30 kg/m2, augmenting this with a description of results of the other modelling undertaken. The full set of results for the pair-wise comparisons for the five patients modelled – male with BMI 30 kg/m2, female with BMI 30 kg/m2, male with BMI 30 kg/m2 but excluding the weight changes from the UKPDS Outcomes Model while retaining their effect within the ‘bolt-ons’, male with BMI 35 kg/m2 and female with BMI 35 kg/m2 – can be found in Appendix 8.
Comparison 1: exenatide vs glargine
The comparison here is in people failing to achieve satisfactory control on dual therapy with metformin and sulfonylurea, and the options are to start exenatide, with the expectation of needing insulin at a later stage, or to start insulin right away. Because glargine is the market leader in basal insulins in England, we use that as the comparator here. This, in effect, assumes that glargine is cost-effective compared with NPH. The cost-effectiveness of glargine and detemir versus NPH is examined later.
No allowance is made for pancreatitis in the modelling, on the grounds that the link is as yet unproven – although, even if it is confirmed, the occurrence is probably too rare to have any effect on the modelling.
Because the trials were quite short, we lack data on the longer-term relative evolutions of HbA1c on exenatide followed by glargine, and on immediate glargine. There is probably little difference (results were similar in the trials) but differences may emerge over time for reasons given above. One could plausibly speculate that either treatment might have a slight advantage in HbA1c level, which, however, would not be the sole factor in the cost-effectiveness equations, because, as will be seen, weight changes also have effects. We give results, therefore, for both scenarios to see what happens if evolution of HbA1c is slightly better on immediate glargine (comparison 1a), and then what happens if it is slightly better on exenatide (comparison 1b).
Comparison 1a: evolution of HbA1c assumed to be slower with initial glargine
The evolution of HbA1c, and the resultant intensifications of therapy once HbA1c level rises above 7.5%, has been assumed to follow the path as projected by the UKPDS Outcomes Model.
As previously noted, glargine has the benefit of possible titration and, when compared to the fixed-dose exenatide, this may result in a slower worsening of HbA1c level through time. So when comparing the evolution of HbA1c on glargine and exenatide we might see the curve for exenatide lying above that for glargine, as shown in Figure 16. (Note: The peaks are exaggerated due to the truncated vertical scale.)
FIGURE 16.
HbA1c: exenatide versus glargine with dose titration for glargine.
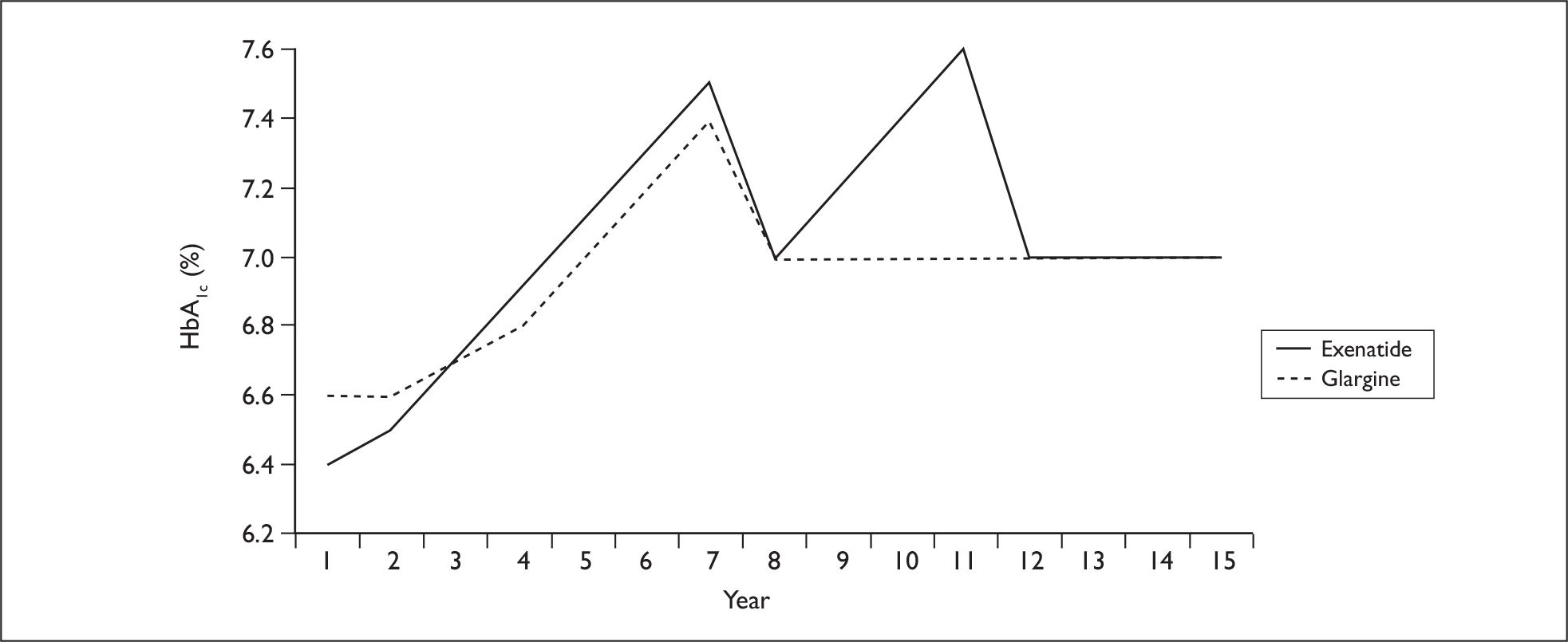
Within the above, for both first-line exenatide and first-line glargine there is assumed to be a therapy switch to second-line at the start of year 8. Those on first-line exenatide switch to basal glargine, while those on first-line basal glargine switch to a basal bolus combination involving glargine. Thereafter, those starting on first-line exenatide see a further therapy switch to a third-line basal bolus combination involving glargine at year 12.
For the base-case model of the male patient with a BMI of 30 kg/m2 the modelling anticipates the following, as shown in Table 46.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.648 | 8.638 | 0.011 | 8.432 | 8.422 | 0.010 |
| Total QALYs | 8.617 | 8.559 | 0.058 | 8.402 | 8.345 | 0.057 |
| Direct drug cost (£) | 9084 | 7814 | 1271 | 8857 | 7599 | 1257 |
| Total cost (£) | 19,128 | 17,977 | 1151 | 19,634 | 18,501 | 1133 |
| ICER (£) | 19,854 | 19,995 | ||||
Within this comparison, as before the underlying assumption is that intensification to insulin therapy uses a long-acting insulin analogue rather than NPH, with glargine used here as the current market leader.
The patient impact of treatment with exenatide compared with treatment with glargine is not large: the UKPDS Outcomes Model suggests an average gain of around 0.01 QALYs. As before, this should be read in conjunction with the section on convergence of the UKPDS Outcomes Model, and represents only a small fraction of the overall lifetime patient QALYs of one-eighth of 1%.
Paralleling this is the relative cost of treatment. The additional lifetime direct drug cost from adopting exenatide prior to glargine of around £1260 is partially offset by a relatively minor saving from a reduction in the longer-term complications of diabetes to result in an overall net total cost of around £1140. In the light of this, adopting exenatide prior to glargine is estimated to have a cost-effectiveness of between £19,000 and £20,000 per QALY.
Similar results applied for the female patient with a BMI of 30 kg/m2, (Table 47) with a similar absolute gain in QALYs being anticipated, although it should be noted that within the UKPDS Outcomes Model results there is effectively no gain from exenatide, presumably due to the superior weight profile being counterbalanced in effect by the worse HbA1c profile between years 8 and 12. But, again, these should be read in conjunction with the section on convergence of the UKPDS Outcomes Model.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 9.512 | 9.511 | 0.001 | 9.252 | 9.250 | 0.002 |
| Total QALYs | 9.476 | 9.427 | 0.049 | 9.218 | 9.168 | 0.050 |
| Direct drug cost (£) | 9206 | 8261 | 945 | 8970 | 8014 | 957 |
| Total cost (£) | 19,083 | 18,181 | 902 | 19,640 | 18,739 | 900 |
| ICER (£) | 18,408 | 18,005 | ||||
Despite the greater female life expectancy, the lower absolute patient weight results in the overall net cost falling to around £950, resulting in a slightly better cost-effectiveness estimate for the adoption of exenatide prior to glargine of £18,408 per QALY for the no-complications modelling and £18,005 per QALY for the with-complications modelling.
These results rely upon even smaller estimates of QALY gains than before, and are extremely sensitive to small absolute changes in these. Removing the direct QoL impact from weight changes from the analysis worsens the anticipated cost-effectiveness of exenatide for the male patient with a BMI of 30 kg/m2 from £19,854 per QALY to £263,100 per QALY within the no complications modelling, and from £19,995 per QALY to £293,551 per QALY within the with complications modelling.
For the female patient with a BMI of 30 kg/m2, removing the direct QoL impact from weight changes from the analysis results in the gain from exenatide disappearing. A very slight loss is anticipated due to the higher rate of nausea, but the overall effect is so small as to be inconsequential. In this circumstance, glargine would be estimated to be the more cost-effective treatment on the basis of its lower direct treatment costs.
As previously noted, the effect of weight changes after intensification from the first-line treatment cannot be cancelled or changed to those of the second-line treatment in the UKPDS Outcomes Model. A sensitivity analysis that assumed no weight changes from treatments within the UKPDS Outcomes Model, but retained the direct QoL impact of these within the ‘bolt-ons’, resulted in the following for the male patient with a BMI of 30 kg/m2 (Table 48).
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.641 | 8.645 | –0.005 | 8.425 | 8.429 | –0.004 |
| Total QALYs | 8.609 | 8.566 | 0.043 | 8.394 | 8.352 | 0.042 |
| Direct drug cost (£) | 9079 | 7819 | 1260 | 8852 | 7604 | 1248 |
| Total cost (£) | 19,156 | 17,937 | 1219 | 19,661 | 18,465 | 1196 |
| ICER (£) | 28,509 | 28,226 | ||||
The above suggests that despite the better initial HbA1c profile from exenatide, the superior profile of glargine during years 8–12 results in a very small anticipated patient loss from the use of exenatide if there are no weight effects entered into the UKPDS Outcomes Model. Despite this, the bolt-on elements to the survival curves are sufficient to still cause exenatide to result in minor patient gains and cost-effectiveness estimates of between around £28,200 and £28,500 per QALY. As would be anticipated, removing the direct QoL impacts from weight gain within this analysis would see exenatide being dominated by glargine.
For the male patient with a BMI of 35 kg/m2 the annual net drug cost of treatment with exenatide relative to glargine compared with the male patient with a BMI of 30 kg/m2 is much reduced. These results are shown in Table 49.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.577 | 8.559 | 0.018 | 8.363 | 8.353 | 0.010 |
| Total QALYs | 8.546 | 8.481 | 0.065 | 8.333 | 8.276 | 0.057 |
| Direct drug cost (£) | 9976 | 9745 | 231 | 9713 | 9487 | 226 |
| Total cost (£) | 20,180 | 20,077 | 104 | 20,648 | 20,559 | 89 |
| ICER (£) | 1602 | 1568 | ||||
The higher weight and greater dose per kilogram for glargine for the male patient with a BMI of 35 kg/m2, coupled with a slight increase in the net QALY gain from exenatide, results in exenatide having an overall lifetime additional direct drug of around £230, although this is offset from increased downstream cost savings to result in an overall net cost of only around £100. While exenatide does not dominate glargine, given the changing net drug costs and that glargine costs are increasing with weight, the adoption of exenatide prior to glargine appears to result in only a small overall cost increase. Patient gains do not have to be large to justify this and provided the direct QoL impacts from weight changes are realised, the cost-effectiveness estimates appear reasonable at around £1600 per QALY. However, if the direct QoL impacts from weight changes are not realised, these cost-effectiveness estimates worsen to £9301 per QALY for the no complications modelling and £21,531 per QALY for the with complications modelling.
Given their slightly lesser average weight for a BMI of 35 kg/m2, the results are not as dramatic for the female patient but it remains the case that the net drug costs are much reduced given the greater patient weight (as shown in Table 50).
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 9.452 | 9.457 | –0.005 | 9.200 | 9.202 | –0.003 |
| Total QALYs | 9.417 | 9.373 | 0.044 | 9.165 | 9.120 | 0.045 |
| Direct drug cost (£) | 10,719 | 10,297 | 422 | 10,421 | 9995 | 426 |
| Total cost (£) | 20,739 | 20,434 | 306 | 21,243 | 20,925 | 318 |
| ICER (£) | 7021 | 7034 | ||||
The additional direct drug cost falls to around £420, with the total net cost being only around £300. Given the direct QoL gains from weight changes, this results in cost-effectiveness estimates of around £7000 per QALY. However, if these direct QoL gains from weight changes are not realised, the UKPDS Outcomes Model estimates glargine as being very slightly more effective, and, as it is also cheaper than exenatide, it dominates.
Comparison 1b: evolution of HbA1c assumed to be slower with exenatide
The underlying assumption here is that over the period before the HbA1c lines converge, exenatide gives a small advantage to HbA1c. This gives rise to the results in Table 51.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.607 | 8.538 | 0.069 | 8.394 | 8.331 | 0.063 |
| Total QALYs | 8.567 | 8.464 | 0.103 | 8.354 | 8.258 | 0.096 |
| Direct drug cost (£) | 8813 | 7939 | 875 | 8592 | 7727 | 865 |
| Total cost (£) | 18,953 | 18,258 | 696 | 19,469 | 18,778 | 691 |
| ICER (£) | 6755 | 7180 | ||||
The QoL impact of treatment with exenatide compared with treatment with glargine is not large: the UKPDS Outcomes Model suggests an average gain of between 0.06 and 0.07 QALYs or around three-quarters of 1% of the overall lifetime patient QALYs. Due to the superior weight profile from the use of exenatide, the ‘bolt-ons’ increase this gain to around 0.10 QALYs, which is a little over 1% of the overall lifetime patient QALYs.
Paralleling this is the relative cost of treatment. The additional lifetime direct drug cost from adopting exenatide prior to glargine of around £900 is partially offset by a relatively minor saving from a reduction in the longer-term complications of diabetes to result in an overall net total cost of around £700. In the light of this, adopting exenatide prior to glargine is estimated to have a cost-effectiveness of between £6700 and £7200 per QALY.
Similar results applied for the female patient with a BMI of 30 kg/m2, with a similar absolute gain in QALYs being anticipated. However, given the greater female life expectancy, the overall net cost increased to around £1000 resulting in a slightly worse cost-effectiveness estimate for the adoption of exenatide prior to glargine of £7970 per QALY for the no complications modelling and £8653 per QALY for the with complications modelling.
These results rely upon relatively small estimates of QALY gains, and as would be anticipated are sensitive to small absolute changes in these. Removing the direct QoL impact from weight changes from the analysis worsens the anticipated cost-effectiveness of exenatide for the male patient with a BMI of 30 kg/m2 from £6755 per QALY to £11,136 per QALY within the no complications modelling, and from £7180 per QALY to £12,303 per QALY within the with complications modelling. Similarly, for the female patient with a BMI of 30 kg/m2, removing the direct QoL impact from weight changes from the analysis worsens the anticipated cost-effectiveness of exenatide from £7970 per QALY to £13,103 per QALY within the no-complications modelling, and from £8653 per QALY to £15,041 per QALY within the with-complications modelling.
Within the UKPDS Outcomes Model, it was noted that the effect of the first therapy upon weight could be modelled. But, whereas the effect of the switch to the second therapy upon HbA1c could be modelled through the risk input sheets, the effect of the first therapy upon weight could not be undone. As a consequence, additional modelling was undertaken that assumed no weight changes from treatments within the UKPDS Outcomes Model but retained the direct QoL impact of these within the ‘bolt-ons’ to the resultant estimates from the UKPDS Outcomes Model.
If we assume a slight advantage in HbA1c with exenatide, removing the differential impact upon weight from exenatide relative to glargine within the UKPDS Outcomes Model reduces, but does not eliminate, the QoL gain as estimated by the UKPDS Outcomes Model. A gain of around 0.05 QALYs remains, which, when coupled with the ‘bolt-ons’ suggests an overall QALY gain to between 0.08 and 0.09 QALYs. The overall net cost also increased slightly due to a smaller net effect upon the complications of diabetes and their associated costs, resulting in a cost-effectiveness estimate for the adoption of exenatide prior to glargine of £8967 per QALY for the no-complications modelling and £9449 per QALY for the with-complications modelling.
Whether the estimate of the cost-effectiveness for the male patient of between £6700 and £7200 per QALY from the application of weight effects within the UKPDS Outcomes Model is a more accurate estimate than the £9000–10,000 per QALY when these weight effects are excluded cannot be determined within the modelling, and relates to model structure.
For the male patient with a BMI of 35 kg/m2 the annual net drug cost of treatment with exenatide relative to glargine compared with the male patient with a BMI of 30 kg/m2 is much reduced. Similarly, though the life expectancy is shorter for the patient with a BMI of 35 kg/m2 this has the effect of slightly increasing the impact of the up-front weight loss on the total lifetime QALYs, given the assumption of the same absolute impact upon patients’ BMI from the use of exenatide and from the use of glargine. As a consequence, modelling results in the following (as shown in Table 52).
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.533 | 8.448 | 0.085 | 8.328 | 8.252 | 0.076 |
| Total QALYs | 8.493 | 8.375 | 0.118 | 8.289 | 8.180 | 0.109 |
| Direct drug cost (£) | 9958 | 9863 | 96 | 9703 | 9612 | 91 |
| Total cost (£) | 20,311 | 20,360 | –49 | 20,787 | 20,844 | –57 |
| ICER (£) | Dominant | Dominant | ||||
The higher weight and greater dose per kilogram for glargine for the male patient with a BMI of 35 kg/m2, coupled with a slight increase in the net QALY gain from exenatide, results in exenatide having a small overall lifetime additional direct drug cost of around £100. When coupled with some additional downstream cost savings the modelling suggests that exenatide is slightly cost saving when adopted prior to glargine for the heavier patient. Given this, adopting exenatide prior to glargine is estimated to dominate moving straight to glargine for the male patient with a BMI of 35 kg/m2.
This result does not quite carry over to the female patient with a BMI of 35 kg/m2, as the absolute effects upon the cost of the glargine containing regimes is slightly less for the female patient compared with the male patient. When coupled with the slightly better survival curves this leads to an anticipated lifetime total drug cost increase of around £250 for the female patient, although cost offsets reduce the overall additional cost to a little over £100. This is still a relatively marginal cost increase, and results in cost-effectiveness estimates of only around £1000 per QALY from adopting exenatide prior to glargine compared with moving straight to glargine.
The above comparisons between exenatide and glargine recognise that glargine is the market leader, but in effect assume that glargine is cost effective (relative to NPH). Previous NICE guidance and modelling has typically found glargine to be of poor or borderline cost-effectiveness unless QoL gains are anticipated from the reduced fear of severe hypoglycaemic events. In the light of this, for comparisons 2 and 3 below the default assumption will be that intensification will lead to the use of NPH insulin.
In summary, taking into account effects, side effects, costs and expected time to progression, and assuming sufficient weight is lost, exenatide, when compared with glargine, appears to give ICERs within the range usually regarded as cost-effective for patients with a BMI of 30 kg/m 2 . Provided that the effect of exenatide upon BMI is reasonably consistent across the weight range, the cost-effectiveness of exenatide relative to glargine improves as BMI worsens, due, in large part, to the increasing cost of the required total glargine dose.
Comparison 2: sitagliptin vs rosiglitazone
Table 53 shows the first comparison of sitagliptin versus rosiglitazone.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 8.566 | 8.549 | 0.017 | 8.347 | 8.342 | 0.005 |
| Total QALYs | 8.479 | 8.447 | 0.032 | 8.263 | 8.242 | 0.021 |
| Direct drug cost (£) | 5793 | 5938 | –145 | 5628 | 5779 | –151 |
| Total cost (£) | 16,083 | 16,277 | –194 | 16,650 | 16,853 | –203 |
| ICER (£) | Dominant | Dominant | ||||
The point estimates above suggest that the very slightly greater improvement in HbA1c level from the use of sitagliptin coupled with a superior weight profile results in a small net gain for patients from its use relative to rosiglitazone, as estimated by the UKPDS Outcomes Model. But the absolute gains are so small that despite the 250,000 iterations applied within the modelling, it may be more appropriate to conclude that sitagliptin is clinically equivalent to rosiglitazone, and could even be slightly less effective. However, the patient gain from sitagliptin increases to around 0.02 to 0.03 QALYs with the application of the ‘bolt-ons’ as would be anticipated given the better weight profile, but this remains a relatively small gain of only between one-quarter and one-third of 1% of the overall lifetime patient QALYs.
The more reliable results, as would be anticipated given the minor differences in treatment effect, are the differences in the direct drug costs. Sitagliptin is somewhat cheaper than rosiglitazone and, as a consequence, results in an anticipated lifetime direct drug cost saving of around £150 per patient, or around 2.7%. Note that this is the lifetime cost and includes the cost of later NPH insulin therapies, which are common to both regimes. While on first-line therapies the differences in direct drug costs are somewhat larger, at 9.4%. This net direct drug cost saving of around £150 applies with reasonable consistency across the patients modelled. But it should be borne in mind that the glitazones will shortly be coming off patent, with the likelihood of significant price reductions as generic formulations become available. Paralleling the difference in the drug costs of the two regimes, a fall of 9% in the price of rosiglitazone would equalise its regimen cost with one containing sitagliptin.
Concerns about the cardiovascular safety of rosiglitazone mean that its use is also declining, which may limit the relevance of this comparison.
Comparison 3: vildagliptin vs pioglitazone
Table 54 shows the first comparison of vildagliptin versus pioglitazone.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 8.561 | 8.590 | –0.029 | 8.353 | 8.378 | –0.025 |
| Total QALYs | 8.468 | 8.479 | –0.011 | 8.262 | 8.269 | –0.007 |
| Direct drug cost (£) | 5371 | 5824 | –453 | 5220 | 5665 | –445 |
| Total cost (£) | 15,731 | 16,180 | –449 | 16,309 | 16,756 | –446 |
| ICER (£) | 39,846 | 66,799 | ||||
The pairwise comparison of vildagliptin against pioglitazone is unusual in having the main clinical outcomes pull in opposite directions, though this recurs in the pair-wise comparison of detemir and NPH. Vildagliptin has a marginally poorer effect upon HbA1c: –0.88% as compared with –0.98% for pioglitazone, but it has a slightly better weight profile: a gain of only 0.3kg compared with a gain of 1.9 kg for pioglitazone.
Note that in the above, the move from pioglitazone to vildagliptin is anticipated to result in a slight loss of utility while also being coupled with a reduction on overall cost. In this situation, cost-effectiveness improves as cost saving increases. For instance, both the no-complications and the with-complications modelling anticipate roughly the same cost-saving of –£450, but the patient loss is greater at –0.011 QALYs within the no-complications modelling compared with –0.007 within the with-complications modelling. Both sets of modelling suggest that the cost-saving from vildagliptin is warranted as the patient loss is small in both cases, but the case for this is stronger within the with-complications modelling. However, the situation is reversed within the modelling of the female patient with a BMI of 30 kg/m2, as outlined in Table 55.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 9.428 | 9.427 | 0.000 | 9.175 | 9.176 | –0.001 |
| Total QALYs | 9.328 | 9.310 | 0.019 | 9.078 | 9.061 | 0.017 |
| Direct drug cost (£) | 5824 | 6265 | –441 | 5646 | 6082 | –437 |
| Total cost (£) | 15,959 | 16,502 | –543 | 16,581 | 17,112 | –531 |
| ICER (£) | Dominant | Dominant | ||||
The UKPDS Outcomes Model now no longer anticipates any real gain from the use of pioglitazone, and the bolt-on effects of the direct QoL impacts result in a small gain from the use of vildagliptin. Within the UKPDS Outcomes Model it appears that the greater longevity of the female patient in general may lead to the impact of BMI upon CHF having more time to lead to the resultant knock-on effects upon the other complications modelled, so causing the superior weight profile of vildagliptin to balance its marginally worse impact upon HbA1c level.
This pattern broadly repeats itself for the modelling of patients with a BMI of 35 kg/m2, the only notable change within this being that for the male patient while the UKPDS Outcomes Model still projects a vanishingly small loss from the use of vildagliptin, –0.014 QALYs per patient, the ‘bolt-ons’ are sufficient to turn the overall patient impact into an even smaller gain of 0.04 QALYs per patient.
The reliability of QALY differences of this magnitude is questionable, particularly in the light of the previous discussion as to convergence within the modelling. It may be better to conclude that there remains uncertainty as to the patient impact of vildagliptin compared with pioglitazone, with any net effect arising from the impact of changes in weight and HbA1c level being likely to be minor. The more reliable result is a fairly consistent reduction in the average direct drug cost of around £450.
As with the comparison of sitagliptin with rosiglitazone, the above will change when pioglitazone comes off patent. A fall of around 22% in the price of pioglitazone would equalise its regime cost with one containing vildagliptin.
In summary, the gliptins and the glitazones appear roughly equivalent in glycaemic effect, but the former have an advantage in avoidance of weight gain, which, together with their lower (at present) costs may give them an edge. However, given the size of the QALY estimates and uncertainties around them, it would be inappropriate to say that the glitazones were definitely less cost-effective than the gliptins. This does not take into account the side effects of the glitazones. These apply more with rosiglitazone, but pioglitazone also has problems with fractures and heart failure. However, until we have longer follow-up we will not know whether the gliptins have as yet unreported long-term side effects.
Comparison 4: glargine vs NPH
Table 56 shows a comparison of glargine versus NPH.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 8.538 | 8.540 | –0.002 | 8.331 | 8.333 | –0.003 |
| Total QALYs | 8.464 | 8.457 | 0.007 | 8.258 | 8.253 | 0.006 |
| Direct drug cost (£) | 7939 | 6111 | 1828 | 7727 | 5946 | 1780 |
| Total cost (£) | 18,258 | 16,402 | 1855 | 18,778 | 16,980 | 1798 |
| ICER (£) | 281,349 | 320,029 | ||||
In the base UKPDS Outcomes Model, for the male patient with a BMI of 30 kg/m2, there was no difference in QALYs between glargine and NPH. (Indeed one run indicated a very small loss of between –0.002 and –0.003 QALYs when compared with NPH, which, given the same effect upon HbA1c level and a slightly superior weight profile for glargine, appears to have arisen from the convergence issues alluded to previously.)
The bolt-on direct QoL impacts of the slightly superior weight profile of glargine, coupled with its 0.82 RR of severe hypoglycaemic events compared with NPH yield, a gain of 0.009 QALYs, to lead to an overall net impact gain of 0.006–0.007 QALYs from the use of glargine. This is inconsequential.
The female modelling, again for a BMI of 30 kg/m2, shows similar results, although for this the UKPDS Outcome Model results in a gain from glargine of 0.002 QALYs, which is again likely to be well within the bounds of modelling variability due to convergence, despite 250,000 iterations. The bolt-on gains are similarly small at 0.008 QALYs to take the overall net gain from the use of glargine to 0.010 QALYs for both the no-complications modelling and the with-complications modelling. While this reduces the estimate cost-effectiveness of glargine to £177,940 per QALY for the no-complications modelling, and to £179,074 per QALY for the with-complications modelling, these estimates are clearly well outside the usual bounds for cost-effectiveness.
Among patients with a BMI of 30 kg/m2 the clear result is an average net direct drug cost of between £1800 and £1900 from the use of glargine.
For patients with a BMI of 35 kg/m2 the UKPDS Outcomes Model suggests slightly larger gains of between 0.002 and 0.005 QALYs, with the ‘bolt-ons’ increasing this to between 0.010 and 0.013 QALYs. However, the greater weight and dose per kilogram increase the overall net cost and the estimated cost-effectiveness of glargine remains poor, at between £189,400 per QALY and £233,187 per QALY.
Among patients with a BMI of 35 kg/m2 glargine is estimated to result in a net direct drug cost increase from the use of glargine of around £2500.
The above calculations do not take account of any differences in mortality from severe hypoglycaemia, which might be expected to run in parallel with, for example, the frequency of nocturnal hypoglycaemia. Such mortality is not easily integrated into the UKPDS model, but data are lacking in any case.
Comparison 5: detemir vs NPH
Table 57 shows the comparison of detemir versus NPH.
| No complications | With complications | |||||
|---|---|---|---|---|---|---|
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 8.530 | 8.540 | –0.010 | 8.316 | 8.333 | –0.018 |
| Total QALYs | 8.472 | 8.457 | 0.015 | 8.259 | 8.253 | 0.006 |
| Direct drug cost (£) | 8826 | 6111 | 2715 | 8585 | 5946 | 2638 |
| Total cost (£) | 19,128 | 16,402 | 2726 | 19,621 | 16,980 | 2641 |
| ICER (£) | 187,726 | 417,625 | ||||
The results for detemir relative to NPH mirror those of glargine relative to NPH outlined above. There is a slight worsening in the anticipated net patient impact from the UKPDS Outcomes Model for detemir. While this might be anticipated given the slightly worse HbA1c profile, the overall effect is small, may have been impacted by the slightly superior weight profile for detemir and may still be subject to a degree of variability due to convergence given the size of the overall impact.
The ‘bolt-ons’ have a slightly larger effect than in the modelling of glargine relative to NPH, as would be anticipated given that detemir has a superior weight profile and a slightly better relative risk of severe hypoglycaemic events of 0.72. But the net patient impacts remain slight. The resulting estimates of the cost-effectiveness of detemir relative to NPH are well outside conventional thresholds.
Note that as in the modelling of glargine relative to NPH for the female patient of BMI 30 kg/m2, within the comparison of detemir with NPH the UKPDS Outcomes Model again suggests little to no difference in patient impact between the two treatments. The ‘bolt-ons’ in terms of the direct QoL impacts from weight changes and severe hypoglycaemic events lead to an anticipated gain of between 0.024 and 0.027 QALYs, but this still results in cost-effectiveness estimates of £102,007 per QALY for the no-complications modelling and £113,988 for the with-complications modelling.
Net costs are somewhat worse for detemir relative to NPH when compared with glargine relative to NPH. This is mainly due to the difference in dosing requirement, the cost per unit being the same. For patients with a BMI of 30 kg/m2 the net direct drug cost is anticipated to be around £2700 to £2800, while for patients with a BMI of 35 kg/m2 the net direct drug cost is anticipated to be around £3600–3800.
Caveats
For all the results above the anticipated differences in the QALYs are small given the 40-year time horizon. The differences in overall QALYs as outputted from the UKPDS Outcomes Model are small. Despite 250,000 iterations, small variations may remain between treatments due to the model not having completely converged. This should be borne in mind, as, given modelling uncertainties, even small reductions in the anticipated QALY differences could give rise to large increases in the cost-effectiveness estimates. Also note that although the utility coefficient on patients’ BMI is small, with a detriment per point of only 0.0061 QALYs, it is sufficient to drive some of the analysis, given the small differences in overall QALYs as outputted from the UKPDS Outcomes Model.
Given the findings of our review and meta-analyses of the insulins, it is not surprising that the long-acting analogues are not cost-effective compared with NPH. The cost-effectiveness analysis hinges on small differences in weight gain, the poorly quantified fear of hypoglycaemia, and the baseline BMI and hence daily dose. The price difference is larger and the clinical advantages small.
One caveat is that the results of the meta-analyses are based on averages from trials. Some patients will have more trouble with hypoglycaemia than others, either having more episodes, or having poorer control of glucose levels because of fear of hypoglycaemic events. For them, the utility gain from switching to an analogue may be greater, and hence cost-effectiveness better.
We also heard from members of the GDG that injection devices for the newer insulins were better. This might also have some effect on QoL.
A caveat is necessary when comparing detemir with glargine. In the head-to-head trial by Rosenstock et al. (2008),177 detemir was used twice daily in 55% of patients, whereas glargine was used once daily. The total daily doses were 1.0 U/kg with twice-daily detemir, 0.52 U/kg with once-daily detemir, and 0.44 U/kg with glargine. This would make detemir more expensive. However, in the very large PREDICTIVE study (2007),178 82% of over 20,000 patients on detemir took it once daily. 272
The only definite advantage of NPH is cost. (There could be other unknown advantages if the analogues have any as yet undiscovered side effects.) The cost difference may only be £170–230 per year per patient for glargine relative to NPH, although this would increase for very obese patients. However, if about 30% of the roughly 2.2 million people with type 2 diabetes in England are treated with insulin, the difference between using NPH and the analogues could be of the order of £100–150M per annum. This might have to be taken from other forms of diabetes care, such as structured education, or screening for complications.
In summary, as was recommended in the NICE Clinical Guideline CG 66, NPH should be preferred as first-line insulin, rather than a long-acting analogue. The analogues have modest advantages but at present much higher cost. In some patients, the benefits of the analogues relative to NPH may be greater, and cost-effectiveness correspondingly better.
Comparator treatments – exploratory indirect comparisons
In an ideal world, we would have direct comparisons of all the competing drugs. Unfortunately, as reported in the clinical effectiveness chapter, there are comparisons for which there are no trials, and others for which evidence is sparse. The most important example is probably the lack of trials comparing exenatide with the gliptins, since when looking for new third-line agents, these are the truly new ones.
The National Institute for Health and Clinical Excellence (NICE) therefore asked us to carry out some indirect comparisons. These involve comparing one drug with another through two or more trials against other agents, for example using one trial of drug A versus drug B, and another of drug B versus drug C, to compare A and C indirectly. There are various problems in that sort of analysis, such as selection bias. The patients in the trial may have different characteristics, which affect the outcomes. These characteristics might have different implications for the different drugs. For example, increases in BMI increase the cost of glargine but not of exenatide. If drug B was exenatide and the patients in one trial are much heavier than in the other, comparing drugs A and C could be misleading.
The problems of indirect comparisons have been reported by Glenny et al. (2005),300 who examined the results of 44 analyses in which interventions could be compared both directly and indirectly, and found that ‘There were considerable statistical discrepancies between the direct and indirect estimates, but the direction of such discrepancy was unpredictable. The relative efficacy may be overestimated or underestimated by the indirect comparison …’.
The clinical effectiveness section reports the number of drug options for clinicians to consider. For some choices, there is strong evidence from RCTs with direct head-to-head comparisons. For other choices, there are no direct comparisons at present. In order to examine possible relativities, exploratory indirect comparisons were carried out. These were regarded as hypothesis generating rather than as firm evidence, and may be a useful way of identifying comparators for future head-to-head trials. The results were provided to the GDG for discussion purposes but are not included here.
Chapter 9 Discussion
The new (and some not so new) drugs are useful additions to the therapeutic armamentarium in diabetes, and our review shows that they are clinically effective. Their cost-effectiveness depends on when they are used, and the comparators. NPH should be the insulin of first use in type 2 diabetes but has now been largely superseded. So the cost-effectiveness of exenatide depends on whether it is compared with what is used (mainly glargine) or what should be used (NPH).
The key question for drug use is where the drugs fit into the treatment pathways, but this question is an issue for the NICE GDG, not this review.
Limitations of this review
The main weaknesses are evidence gaps on clinically relevant scenarios and on long-term safety. For example, there are about 15 trials of the DPP-4 inhibitors against placebo, and almost as many against other drugs as monotherapy, but few with them as third-line agents (i.e. added to dual treatment with metformin and a sulfonylurea), and even fewer in head-to-head comparisons with other potential third-line agents.
Most trials are short term, and may not provide any indication of long-term safety issues, such as pancreatitis with exenatide. Only time will tell how often that happens, and whether (if confirmed) it is a problem only with exenatide or with all GLP-1 agonists.
When comparing drugs, one problem is that the primary effects on glycaemic control are often roughly similar, in that the drugs improve blood glucose control by similar amounts. Comparisons then depend mostly on side effects, such as weight gain or hypoglycaemia, or on QoL effects, which may be less well-defined or less well-documented than the primary outcome, which is usually HbA1c level.
Problems arose with the economic modelling, partly because of a few limitations of the UKPDS model, such as inability for weight changes to be evolved over time. This was particularly relevant to the comparison of exenatide and insulin where weight loss with the former and gain with the latter was a key difference. However, the biggest problem in economic analysis was that differences in QALYs were often very small, leading to instability of the ICERs. For example, the direct utility of weight loss though small, was sufficient to drive some analyses because of the otherwise very small QALY differences.
Compliance
People with type 2 diabetes often have comorbidities such as hypertension or hyperlipidaemia for which they receive medications. Many should be on a statin to reduce the risk of cardiovascular disease; most are overweight. Data from Aberdeen City practices (unpublished) show that 70% to 91% of people with diabetes are overweight, and that 34– 53% are obese. Many will have weight-induced osteoarthritis and will be taking medication for that too. So they may be taking several non-diabetic drugs.
The more drugs a patient has to take, the poorer the adherence. Donnan et al. (2002),301 from Dundee, found that even those on only one glucose-lowering agent have poor compliance, with adequate adherence in only one in three. Compliance is better with a single daily dose. 301 Those taking other medications had poorer compliance than those on just a hypoglycaemic agent. In another study from Dundee, Donnelly et al. (2007)302 found that adherence to prescribed insulin dose was only 71%. Poorer adherence was associated with poorer control.
Farmer et al. (2006)303 carried out a questionnaire survey in Aylesbury. Most of the 121 respondents (all with type 2 diabetes) had positive views about the benefits of taking their medications. In particular, 86% believed that taking them regularly would reduce the chance of them needing insulin treatment. The proportion worried about weight gain was small (13%) and the fear of weight gain did not appear to reduce adherence.
A systematic review of medication adherence by Odegard and Capoccia (2007)304 summarises the barriers to taking medicines, and the interventions that may help. Some of the studies are more relevant to the North American situation, where people have to pay for drugs, but much of it is relevant to the UK. The review concurs with the work of Donnan et al. (2002)301 (mentioned above), that common barriers to adherence include complexity of regimen and number of doses.
The implication for the treatment of type 2 diabetes may be that we should keep both the number of drugs and the number of tablets or injections per day as low as possible.
Research needs
The key question is that after metformin and sulfonylurea therapy has failed, what is the most effective and cost-effective next step? And for whom? Different drugs might be better for different subgroups (for example, subgroups based on weight).
We also need more data on some subgroups that are under-represented in the trials, such as the elderly, ethnic groups, obese children with type 2 diabetes, and those with renal impairment.
The main weaknesses in the evidence base at present are:
-
the lack of long-term data on the efficacy and safety of exenatide and the gliptins
-
the need for long-term data on whether the incretin-based drugs will slow the progression of disease, for example compared with progression rates on insulin
-
the lack of trials directly comparing exenatide and the gliptins
-
the need for more data on combined treatment with insulin and either exenatide or a gliptin
-
the need for a UK trial of intensive lifestyle intervention in patients with type 2 diabetes who are failing on maximal oral agents, similar to the trial by Aas et al. (2005). 27
At the Diabetes UK Annual Professional Conference 2009, there was a large batch of abstracts, mainly posters, reporting the results of case series of patients on exenatide. Most had small numbers, and follow-up was usually for only 3 months. Without control groups, we cannot say how much of the changes were ‘trial effects’, but many posters reported reductions in HbA1c level of more than 1% and in weight of more than 5 kg. The few that reported data from more than one time interval showed less impressive changes in HbA1c level at 6 months than at 3 months, but weight loss continued.
A few posters reported on the use of exenatide in combination with insulin, which as stated earlier in this review, does seem a logical combination with basal insulin targeting fasting and other preprandial hyperglycaemia, and exenatide (or other GLP-1 agonist) targeting postprandial hyperglycaemia. One poster by Vithian et al. (2009)305 reported that half of 42 obese patients with type 2 diabetes, who were previously on insulin, could stop the insulin after a mean of 19 weeks on exenatide, and another 29% could reduce the dose by 50%. The fall in HbA1c level was 0.75% and in weight, 5%.
Price et al. (2009)306 tried exenatide in 10 obese patients on over 100 units of insulin per day, and reported a mean fall in HbA1c level of 1.2% and in BMI of 0.7% at 3 months. Median insulin dose per fell by 40 U/day, from a median at baseline of 201 U/day.
Brake et al. (2009)307 tried exenatide in a mixed group of 24 patients (some on insulin, some not) and found that amongst those on insulin, HbA1c level fell by 1.55% by 3 months and weight by 9.6 kg.
So there seems to be sufficient evidence to justify larger trials of the combination of metformin, insulin and GLP-1 agonists.
Future trials are likely to use the long-acting version of exenatide. Its competitor, liraglutide, has already been tested in various trials in the LEAD studies,308 but some of these would be exclusions under our criteria. A long-acting form is now in Phase II studies.
It is unlikely that trials will be big enough or long enough to provide hard end points such as complications or mortality; they will provide intermediate outcomes such as HbA1c, BMI, QoL, hypoglycaemia, postponement of need for insulin, and adherence (the last related to complexity of regimen). Trials should use strict definitions of the different forms of hypoglycaemia.
There may be trade-offs between efficacy and adherence.
We also need more data on the fracture problem with pioglitazone (just pioglitazone because rosiglitazone use is already in decline).
Present evidence on exenatide suggests that there is no long-term preservation of beta-cell capacity by a direct effect on the pancreas, but if weight loss continued over years, would that have an indirect effect by reducing insulin resistance?
It would be useful if evidence of beta-cell mass could be obtained directly, rather than by waiting for long-term deterioration in glycaemic control (for example, 9 years as in UKPDS 17). One option might be newer forms of imaging, if these could detect changes, or lack of changes, in only a few years. The methods have been reviewed by Meier (2008). 31
This review, in line with the NICE guideline, has assumed a stepwise approach in the management of type 2 diabetes, with insulin as a late stage. We note the arguments for earlier use of insulin, but also the reality that in many patients, especially the more overweight, it often does not achieve good control.
However, recent research has suggested a radical approach to insulin treatment in type 2 diabetes. Weng et al. (2008)309 carried out a randomised trial in newly-diagnosed Chinese people with type 2 diabetes, of intensive insulin therapy [continuous subcutaneous insulin infusion (CSII) or multiple daily injection (MDI)] or oral agents for short periods, given for a few days (under 8 days in most) to achieve good glucose control, followed by 2 weeks of maintained normoglycaemia. Drug treatment was then stopped, and patients continued on diet and exercise alone. They were monitored for relapse.
At 12 months, 51% of the CSII group, 45% of the MDI group, and 27% of the OHA group were still in remission. Relapse was defined as fasting PG over 7.0 mmol/l or 2-hour postprandial PG more than 10 mmol/l.
These results suggest that a period of early tight control can produce lasting remission. It is possible that repeated short periods (say once a year) might be worthwhile.
This approach needs to be replicated in other populations. The results might not be applicable to other countries. The Chinese patients had a mean BMI of only 25 kg/m2. There were some weaknesses in the design, such as a weak method of randomisation by sealed envelopes, but the main design flaw was the absence of a diet-and-exercise-alone arm.
The results are in line with a few other smaller studies of intensive therapy in newly diagnosed type 2 diabetes, reviewed by Retnakaran and Drucker (2008)310 in an editorial that accompanied the Lancet article by Weng et al. (2008). 309
Cost-effectiveness studies
The main weakness in the literature is the number of studies funded by the manufacturers, although often carried out by commercial consultancies, which tend to find that their drug is cost-effective, often by being somewhat selective in underlying assumptions.
For assessing cost-effectiveness, we need better data on issues around the effects on QoL of changes in weight, nocturnal hypoglycaemia, and the fear of hypoglycaemia.
Alternatives to polypharmacy
Lastly, but perhaps most important of all, we need more studies of the type undertaken by Aas et al. (2005),27 on intensive lifestyle intervention in people failing on oral agents.
Recent comments from other reviewers
The Drug and Therapeutics Bulletin311 took a fairly firm line on exenatide, sitagliptin and vildagliptin: ‘While, on current evidence, we cannot recommend the routine use of these drugs, there may be individual circumstances in which they may be helpful. For example, exenatide may provide a useful alternative to insulin, particularly since it does not seem to cause weight gain. However exenatide frequently causes nausea and vomiting, and it is much more expensive than insulin therapy. There seem to be few convincing reasons for preferring sitagliptin or vildagliptin to other oral hypoglycaemic options’.
This seems a little harsh on the gliptins, as they also do not cause weight gain.
The Australian National Prescribing Service312 concluded that NPH should be the initial basal insulin therapy in type 2 diabetes, mentioning concerns about the long-term safety of glargine and detemir.
One reviewer of the NICE guidelines issued in May 2008 noted the problems when new evidence was continually emerging. In an editorial, Winocour (2008)313 commented: ‘Sadly, I expect this one will have a very limited shelf life – almost by design – … An organic web-based document, which is updated annually, could address the need for clinical guidelines where there is a rapidly progressive evidence base’.
The shelf-life was expected to be limited because NICE will issue an update early in 2009, which this TAR has been produced to support. However, we know that long-acting exenatide, liraglutide and two more gliptins will be arriving in the near future, and so the update will soon need to be updated.
Changes in costs will also change the cost-effectiveness ratios. For example, we would not recommend the use of rosiglitazone at present, because of its cardiovascular safety record and the fact that it has no advantages over pioglitazone or the gliptins. But, if the cost of rosiglitazone dropped dramatically (perhaps because generic forms arrived), the equations would change, and we might well recommend rosiglitazone, despite the slightly increased risk, because lower expenditure on oral drugs could release considerable amounts of funds for other investments in diabetes care.
However, this illustrates a tension arising from the different perspectives of clinicians, seeking the best treatment for individual patients, and those such as policy-makers or programme managers who are trying to maximise the health gains which can be achieved with limited resources.
Conclusion
The new drugs – exenatide, the gliptins – and (the not so new) detemir are all clinically effective. Their cost-effectiveness is always relative, and depends on where they are used in the therapeutic pathways.
Acknowledgements
We thank the members of the NICE Short Guideline Development Group, their expert advisor (Professor Anthony Barnett) and the technical team at NICE for useful comments and information during the iterative process that produced this report. We thank Alastair Gray of Oxford for guidance on using the UKPDS model.
Contribution of authors
Norman Waugh led the review of clinical effectiveness of DPP-4 inhibitors, assisted with cost-effectiveness section, wrote the introduction and discussion and edited the whole report. Ewen Cummins carried out the review of economics literature, and did the de novo cost-effectiveness analysis. Pam Royle led the review of clinical effectiveness of GLP-1 agonists, carried out the literature searches, and helped with editing and checking of the final draft. Christine Clar led the review of clinical effectiveness of insulins and of adding pioglitazone to insulin regimens. Meaghan Marien assisted with the review of effectiveness of insulins. Bernd Richter contributed to the review of the clinical effectiveness of DPP-4 inhibitors. Sam Philip provided clinical advice and commented on drafts.
About the Aberdeen HTA Group
The Aberdeen Health Technology Assessment Group is part of the Institute of Applied Health Sciences (IAHS), which is part of the College of Medicine and Life Sciences of the University of Aberdeen. The IAHS is made up of discrete but methodologically related research groups. The HTA Group is drawn mainly from the Health Services Research Unit, the Department of Public Health, and the Health Economics Research Unit.
The HTA Group carries out independent health technology assessments, producing technology assessment reports (TARs) for the UK HTA Programme, which commissions TARs for NICE and other bodies, such as the National Screening Committee. The group has produced previous TARs on diabetic topics, including:
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation. Health Technol Assess 2010;14(11).
-
Screening for type 2 diabetes: literature review and economic modelling. Health Technol Assess 2007;11(17).
-
Non-pharmacological prevention of diabetes in those with impaired glucose tolerance. In preparation.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation. Health Technol Assess 2007;11(33).
We also produce Cochrane reviews on diabetes topics.
About the CMED group
The Cochrane Metabolic and Endocrine Disorders Group (CMED) is one of the collaborative review groups of the Cochrane Collaboration. It is primarily concerned with the evaluation of health-care interventions for the prevention, treatment or management, and rehabilitation of metabolic, nutritional and endocrine disorders, such as diabetes.
The CMED Group aims to serve several groups of people, including:
-
health-care workers, by providing high-quality, regularly updated and easily accessible summaries of scientific knowledge
-
patients (present and potential) and relatives, directly by providing them with high-quality information; indirectly by supporting health-care workers and policy-makers
-
researchers and those who commission research, by accurately summarising present knowledge identifying research gaps; also through development of methodology for systematic reviewing
-
policy-makers, by producing accessible and reliable summaries, free of the biases that may be present in submissions by groups with a particular interest. Support to policy-makers may be indirect, via support to those who produce policy analyses for governments and others, such as health technology assessment units
-
undergraduate and postgraduate students, through the provision of concise reviews of difficult topics.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- DeFronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med 1999;131:281-303.
- UKPDS Study Group . UK Prospective Diabetes Study. V. Characteristics of newly presenting type 2 diabetic patients: estimated insulin sensitivity and islet 4-cell function. Multi-centre study. Diabet Med 1988;5:444-8.
- UKPDS Study Group . UK Prospective Diabetes Study. IV. Characteristics of newly presenting type 2 diabetic patients: male preponderance and obesity at different ages. Multi-centre study. Diabet Med 1988;5:154-9.
- UKPDS Study Group . UK Prospective Diabetes Study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. UK Prospective Diabetes Study Group. Diabetes 1995;44:1249-58.
- Turner R, Cull C, Holman R. UK Prospective Diabetes Study 17: a 9-year update of a randomized, controlled trial on the effect of improved metabolic control on complications in non-insulin-dependent diabetes mellitus. Ann Intern Med 1996;124:136-45.
- National Institute for Health and Clinical Excellence (NICE) . Type 2 Diabetes: The Management of Type 2 Diabetes (update). Clinical Guideline CG66 n.d. www.nice.org.uk/Guidance/CG66 (accessed 25 September 2008).
- Black C, Donnelly P, McIntyre L, Royle PL, Shepherd JP, Thomas S. Meglitinide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev 2007;1.
- Saenz A, Fernandez-Esteban I, Mataix A, Ausejo M, Roque M, Moher D. Metformin monotherapy for type 2 diabetes mellitus. Cochrane Database Syst Rev 2005;3.
- Salpeter S, Greyber E, Pasternak G, Salpeter E. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev 2006.
- Van de Laar FA, Lucassen PL, Akkermans RP, Van de Lisdonk EH, Rutten GE, Van WC. Alpha-glucosidase inhibitors for type 2 diabetes mellitus. Cochrane Database Syst Rev 2005;2.
- The Information Centre and Yorkshire and Humber Public Health Observatory (YHPHO) . Prescribing for Diabetes in England: An Analysis of Volume, Expenditure and Trends 2007. www.yhpho.org.uk/Download/Public/1265/1/Prescribing%20for%20Diabetes%20in%20England%20Nov%202007%20FINAL.pdf (accessed 4 May 2008).
- National Insitute for Health and Clinical Excellence (NICE) . Guidance on the Use of Long-Acting Insulin Analogues for the Treatment of Diabetes – Insulin Glargine: Technology Appraisal 53 2002. www.nice.org.uk/nicemedia/pdf/53_Insulin_analogues_full_guidance.pdf (accessed 4 May 2008).
- Calvert MJ, McManus RJ, Freemantle N. Management of type 2 diabetes with multiple oral hypoglycaemic agents or insulin in primary care: retrospective cohort study. Br J Gen Pract 2007;57:455-60.
- Rubino A, McQuay LJ, Gough SC, Kvasz M, Tennis P. Delayed initiation of subcutaneous insulin therapy after failure of oral glucose-lowering agents in patients with type 2 diabetes: a population-based analysis in the UK. Diabet Med 2007;24:1412-18.
- Black C, Cummins E, Royle P, Philip S, Waugh N. The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation. Health Technol Assess 2007;11.
- Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, et al. Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care 2005;28:2673-9.
- Alvarez GF, Mavros P, Nocea G, Alemao E, Alexander CM, Yin D. Glycaemic control among patients with type 2 diabetes mellitus in seven European countries: findings from the Real-Life Effectiveness and Care Patterns of Diabetes Management (RECAP-DM) study. Diabetes Obes Metab 2008;10:8-15.
- Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, et al. Management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia 2006;49:1711-21.
- Goudswaard AN, Furlong NJ, Rutten GE, Stolk RP, Valk GD. Insulin monotherapy versus combinations of insulin with oral hypoglycaemic agents in patients with type 2 diabetes mellitus. Cochrane Database Syst Rev 2004;4.
- Douek IF, Allen SE, Ewings P, Gale EA, Bingley PJ. Continuing metformin when starting insulin in patients with Type 2 diabetes: a double-blind randomized placebo-controlled trial. Diabet Med 2005;22:634-40.
- Aviles-Santa L, Sinding J, Raskin P. Effects of metformin in patients with poorly controlled, insulin-treated type 2 diabetes mellitus. A randomized, double-blind, placebo-controlled trial. Ann Intern Med 1999;131:182-8.
- Strowig SM, Raskin P. Combination therapy using metformin or thiazolidinediones and insulin in the treatment of diabetes mellitus. Diabetes Obes Metab 2005;7:633-41.
- Bailey CJ. Treating insulin resistance in type 2 diabetes with metformin and thiazolidinediones. Diabetes Obes Metab 2005;7:675-91.
- Gerstein HC, Yale JF, Harris SB, Issa M, Stewart JA, Dempsey E. A randomized trial of adding insulin glargine vs. avoidance of insulin in people with Type 2 diabetes on either no oral glucose-lowering agents or submaximal doses of metformin and/or sulphonylureas. The Canadian INSIGHT (Implementing New Strategies with Insulin Glargine for Hyperglycaemia Treatment) Study. Diabet Med 2006;23:736-42.
- Hayward RA, Manning WG, Kaplan SH, Wagner EH, Greenfield S. Starting insulin therapy in patients with type 2 diabetes: effectiveness, complications, and resource utilization. JAMA 1997;278:1663-9.
- Yki-Järvinen H, Kauppinen-Makelin R, Tiikkainen M, Vahatalo M, Virtamo H, Nikkila K, et al. Insulin glargine or NPH combined with metformin in type 2 diabetes: the LANMET study. Diabetologia 2006;49:442-51.
- Aas AM, Bergstad I, Thorsby PM, Johannesen O, Solberg M, Birkeland KI. An intensified lifestyle intervention programme may be superior to insulin treatment in poorly controlled type 2 diabetic patients on oral hypoglycaemic agents: results of a feasibility study. Diabet Med 2005;22:316-22.
- Aas AM, Seljeflot I, Torjesen PA, Diep LM, Thorsby PM, Birkeland KI. Blood glucose lowering by means of lifestyle intervention has different effects on adipokines as compared with insulin treatment in subjects with type 2 diabetes. Diabetologia 2006;49:872-80.
- Kahn SE, Haffner SM, Heise MA, Herman WH, Holman RR, Jones NP, et al. Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427-43.
- Aston-Mourney K, Proietto J, Morahan G, Andrikopoulos S. Too much of a good thing: why it is bad to stimulate the beta cell to secrete insulin. Diabetologia 2008;51:540-5.
- Meier JJ. Beta cell mass in diabetes: a realistic therapeutic target?. Diabetologia 2008;51:703-13.
- Amori RE, Lau J, Pittas AG. Efficacy and safety of incretin therapy in type 2 diabetes: systematic review and meta-analysis. JAMA 2007;298:194-206.
- Baggio LL, Drucker DJ. Biology of incretins: GLP-1 and GIP. Gastroenterology 2007;132:2131-57.
- Kreymann B, Williams G, Ghatei MA, Bloom SR. Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet 1987;2:1300-4.
- Meier S, Hucking K, Ritzel R, Holst JJ, Schmiegel WH, Nauck MA. Absence of a memory effect for the insulinotropic action of glucagon-like peptide 1 (GLP-1) in healthy volunteers. Horm Metab Res 2003;35:551-6.
- Drucker DJ, Philippe J, Mojsov S, Chick WL, Habener JF. Glucagon-like peptide I stimulates insulin gene expression and increases cyclic AMP levels in a rat islet cell line. Proc Natl Acad Sci U S A 1987;84:3434-8.
- Fehmann HC, Habener JF. Insulinotropic glucagonlike peptide-I(7–37)/(7–36)amide: a new incretin hormone. Trends Endocrinol Metab 1992;3:158-63.
- Barnett A. Exenatide. Expert Opin Pharmacother 2007;8:2593-608.
- Nauck MA, Walberg J, Vethacke A, El-Ouaghlidi A, Senkal M, Holst JJ, et al. Blood glucose control in healthy subject and patients receiving intravenous glucose infusion or total parenteral nutrition using glucagon-like peptide 1. Regul Pept 2004;118:89-97.
- Deacon CF. Incretin-based treatment of type 2 diabetes: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors. Diabetes Obes Metab 2007;9:23-31.
- Nauck MA, Wollschlager D, Werner J, Holst JJ, Orskov C, Creutzfeldt W, et al. Effects of subcutaneous glucagon-like peptide 1 (GLP-1 [7–36 amide]) in patients with NIDDM. Diabetologia 1996;39:1546-53.
- Klonoff DC, Buse JB, Nielsen LL, Guan X, Bowlus CL, Holcombe JH, et al. Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr Med Res Opin 2008;24:275-86.
- European Medicines Agency . Byetta: European Public Assessment Report n.d. www.emea.europa.eu/humandocs/Humans/EPAR/byetta/byetta.htm (accessed 25 March 2009).
- Zander M, Madsbad S, Madsen JL, Holst JJ. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and beta-cell function in type 2 diabetes: a parallel-group study. Lancet 2002;359:824-30.
- Amylin Pharmaceuticals 2008. www.amylin.com/ (accessed 2 June 2009).
- Eli Lilly and Company 2008. www.lilly.co.uk/ (accessed 2 June 2009).
- Kim D, MacConell L, Zhuang D, Kothare PA, Trautmann M, Fineman M, et al. Effects of once-weekly dosing of a long-acting release formulation of exenatide on glucose control and body weight in subjects with type 2 diabetes. Diabetes Care 2007;30:1487-93.
- Novo Nordisk 2008. www.novonordisk.com/ (accessed 2 June 2009).
- FDA . Byetta (Exenatide Injection) 2005. www.fda.gov/cder/foi/label/2008/021773s012lbl.pdf (accessed 4 May 2008).
- Barnett AH, Burger J, Johns D, Brodows R, Kendall DM, Roberts A, et al. Tolerability and efficacy of exenatide and titrated insulin glargine in adult patients with type 2 diabetes previously uncontrolled with metformin or a sulfonylurea: a multinational, randomized, open-label, two-period, crossover noninferiority trial. Clin Ther 2007;29:2333-48.
- Seino Y, Kaku K, Nishijima K, Rasmussen MF, Zdravkovic M, Kristensen P. The long-acting human GLP-1 analogue liraglutide given once daily significantly improves glycaemic control by reducing fasting and postprandial glucose levels in subjects of Japanese origin with type 2 diabetes. Diabetologia 2007;50.
- Davis SN, Johns D, Maggs D, Xu H, Northrup JH, Brodows RG. Exploring the substitution of exenatide for insulin in patients with type 2 diabetes treated with insulin in combination with oral antidiabetes agents. Diabetes Care 2007;30:2767-72.
- Heine RJ, Van Gaal LF, Johns D, Mihm MJ, Widel MH, Brodows RG. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: A randomized trial. Ann Intern Med 2005;143:559-69.
- Nauck MA, Duran S, Kim D, Johns D, Northrup J, Festa A, et al. A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia 2007;50:259-67.
- Bunck MC, Diamant M, Corner A, Eliasson B, Malloy JL, Shaginian RM, et al. One year treatment with exenatide improves beta cell function and glycaemic control in metformin treated type 2 diabetes patients. Diabetologia 2007;50:S111-12.
- Buse JB, Henry RR, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetes. Diabetes Care 2004;27:2628-35.
- Trescoli-Serrano C, Rivas M, Fajardo-Montanana C, Del Pino I, Garcia-Zarco M, Martorrell-Barraquet A, et al. Clinical site experience comparing insulin glargine with exenatide treatment in type 2 diabetic patients. Diabetologia 2005;48.
- DeFronzo RA, Ratner RE, Han J, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2. Diabetes Care 2005;28:1092-100.
- Kendall DM, Riddle MC, Rosenstock J, Zhuang D, Kim DD, Fineman MS, et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care 2005;28:1083-91.
- Zinman B, Hoogwerf BJ, Duran GS, Milton DR, Giaconia JM, Kim DD, et al. The effect of adding exenatide to a thiazolidinedione in suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2007;146:477-85.
- Malozowski S. Exenatide in combination therapy: small study, big market, and many unanswered questions. Ann Intern Med 2007;146:527-8.
- Home PD. Comment on: A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study [Nauck MA, Duran S, Kim D, et al. (2007), Diabetologia 50: 259– 67]. Diabetologia 2007;50:1561-2.
- Nauck MA, Trautman M, Brodows R, Johns D, Northrup J, Kim D. Response to comment on: A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study [Nauck MA, Duran S, Kim D, et al. (2007), Diabetologia 50: 259– 67]. Diabetologia 2007;50:1563-4.
- Rosenstock J, Fonseca V. Missing the point: substituting exenatide for nonoptimized insulin: going from bad to worse!. Diabetes Care 2007;30:2972-3.
- Maggs D, Kim D, Holcombe J, Han J, Shen L, Ruggles J, et al. Exenatide-induced reductions in A1C and body weight in long-term trials are not explained by gastrointestinal side effects. Diabetes 2005;54.
- Secnik K, Oglesby A, Yurgin N, Johns D, Trautman M. Exenatide Compared With Insulin Glargine: Patient Reported Outcomes Assessments in Individuals With Type 2 Diabetes n.d.
- Secnik BK, Matza LS, Oglesby A, Malley K, Kim S, Hayes RP, et al. Patient-reported outcomes in a trial of exenatide and insulin glargine for the treatment of type 2 diabetes. Health Qual Life Outcomes 2006;4.
- Yurgin N, Secnik K, Hayes C, Johns D, Trautmann M. Patient reported outcomes in patients with type 2 diabetes treated with exenatide compared to biphasic insulin aspart. Diabetologia 2006;49:474-5.
- Wolfe G, King A. Lack of continued weight loss beyond six months despite continued exenatide (EX) treatment. Diabetes 2007;56.
- Loh JA, Clement SC. Efficacy of exenatide therapy over 12 months in a ‘real world’ setting. Diabetes 2007;56.
- Yoon N, Cavaghan MK, Brunelle R, Roach P. Exenatide added to insulin therapy: clinical experience in an academic endocrinology. Diabetes 2008;57.
- Bhushan R, Elkind-Hirsh KE, Bhushan M, Butler WJ, Duncan KD, Marionneaux O. Effects of exenatide therapy in patients with type 2 diabetes include reductions in HbA1c, weight, and cardiovascular risk factors in routine clinical practice. Diabetes 2008;57.
- Govindan JP, Healey B, Kalupahana DN, Singh BM. Exenatide therapy in insulin treated patients with type 2 diabetes and obesity. Diabetologia 2008;51:S352-3.
- Wintle M, Fabunmi R, Boye K, Adam-Marx C, Ye X, Brixner D. Real-world six-month outcomes of patients initiating exenatide in a primary care electronic medical record database. Diabetologia 2008;51.
- Kendall D, Nielsen L, Han J, Brodows R, Bhole D. Metabolic improvement associated with temporal pattern of weight loss in exenatide-treated patients with type 2 diabetes. Diabetologia 2008;51:S353-4.
- Drucker DJ, Buse JB, Taylor K, Kendall D, Trautmann M, Zhuang DL, et al. Exenatide once weekly results in significantly greater improvements in glycemic control compared to exenatide twice daily in patients with type 2 diabetes. Diabetes 2008;57.
- Buse J, Drucker D, Taylor K, Kim T, Wilhelm K, Kendall D, et al. Exenatide once weekly elicits sustained glycaemic control and weight loss over 52 weeks. Diabetologia 2008;51.
- Gallwitz B. Exenatide in type 2 diabetes: treatment effects in clinical studies and animal study data. Int J Clin Pract 2006;60:1654-61.
- Xu G, Stoffers DA, Habener JF, Bonner-Weir S. Exendin-4 stimulates both beta-cell replication and neogenesis, resulting in increased beta-cell mass and improved glucose tolerance in diabetic rats. Diabetes 1999;48:2270-6.
- Gedulin BR, Nikoulina SE, Smith PA, Gedulin G, Nielsen LL, Baron AD, et al. Exenatide (exendin-4) improves insulin sensitivity and {beta}-cell mass in insulin-resistant obese fa/fa Zucker rats independent of glycemia and body weight. Endocrinology 2005;146:2069-76.
- Tourrel C, Bailbe D, Meile MJ, Kergoat M, Portha B. Glucagon-like peptide-1 and exendin-4 stimulate beta-cell neogenesis in streptozotocin-treated newborn rats resulting in persistently improved glucose homeostasis at adult age. Diabetes 2001;50:1562-70.
- Holst JJ, Deacon CF, Vilsboll T, Krarup T, Madsbad S. Glucagon-like peptide-1, glucose homeostasis and diabetes. Trends Mol Med 2008;14:161-8.
- Wajchenberg BL. Beta-cell failure in diabetes and preservation by clinical treatment. Endocr Rev 2007;28:187-218.
- Bunck MC, Diamant M, Corner A, Eliasson B, Malloy JL, Shaginian RM, et al. beta-cell function and glycemic control following one year exenatide therapy, and after 12 week wash out, in patients with type 2 diabetes. Diabetes 2008;57.
- Bunck MC, Corner A, Diamant M, Eliasson B, Malloy JL, Shaginian RM, et al. Exenatide improves postprandial hyperglycemia and dyslipidemia in metformin treated patients with type 2 diabetes. Diabetes 2008;57.
- Exenatide: new drug . Type 2 diabetes for some overweight patients. Prescrire Int 2007;16:228-31.
- Institute for Quality and Efficiency in Health Care (IQWIG) . Evaluation of Therapeutic Benefits and Harms of Exenatide 2007. www.iqwig.de/index.563.en.html (accessed 5 May 2008).
- European Medicines Agency . Exenatide. Annex 1: Summary of Product Characteristics 2008. www.emea.europa.eu/humandocs/PDFs/EPAR/byetta/H-698-PI-en.pdf (accessed 4 May 2008).
- US Food and Drug Administration (FDA) . FDA Drug Safety Newsletter n.d. www.fda.gov/cder/dsn/2008_winter/postmarketing.htm (accessed 2 June 2009).
- Medicines and Healthcare Products Regulatory Agency (MHRA) . MHRA Drug Safety Update n.d. www.mhra.gov.uk/Publications/Safetyguidance/DrugSafetyUpdate/CON015025 (accessed 25 September 2008).
- Richter B, Bandeira-Echtler E, Bergerhoff K, Lerch CL. Dipeptidyl peptidase-4 (DPP-4) inhibitors for type 2 diabetes mellitus. Cochrane Database Syst Rev 2008;2.
- European Medicines Agency . EPARS for Authorised Medicinal Products for Human Use. Onglyza 2009. www.ema.europa.eu/humandocs/Humans/EPAR/onglyza/onglyza (accessed 4 March 2010).
- US Food and Drug Administration (FDA) . Meeting of the Endocrinologic and Metabolic Drugs Advisory Committee, 10 March 2009 n.d. www.fda.gov/cder/audiences/acspage/meetings/emdac_meeting_20090402.htm (accessed 25 March 2009).
- European Medicines Agency . EPARs for Authorised Medicinal Products for Human Use 2008. www.emea.europa.eu/htms/human/epar/eparintro.htm (accessed 25 September 2008).
- US Food and Drug Administration (FDA) 2008. www.fda.gov/ (accessed 19 April 2008).
- Ahren B, Gomis R, Standl E, Mills D, Schweizer A. Twelve- and 52-week efficacy of the dipeptidyl peptidase IV inhibitor LAF237 in metformin-treated patients with type 2 diabetes. Diabetes Care 2004;27:2874-80.
- Aschner P, Kipnes MS, Lunceford JK, Sanchez M, Mickel C, Williams-Herman DE. Effect of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy on glycemic control in patients with type 2 diabetes. Diabetes Care 2006;29:2632-7.
- Bosi E, Camisasca RP, Collober C, Rochotte E, Garber AJ. Effects of vildagliptin on glucose control over 24 weeks in patients with type 2 diabetes inadequately controlled with metformin. Diabetes Care 2007;30:890-5.
- Charbonnel B, Karasik A, Liu J, Wu M, Meininger G. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes inadequately controlled with metformin alone. Diabetes Care 2006;29:2638-43.
- Dejager S, Razac S, Foley JE, Schweizer A. Vildagliptin in drug-naive patients with type 2 diabetes: a 24-week, double-blind, randomized, placebo-controlled, multiple-dose study. Horm Metab Res 2007;39:218-23.
- Fonseca V, Schweizer A, Albrecht D, Baron MA, Chang I, Dejager S. Addition of vildagliptin to insulin improves glycaemic control in type 2 diabetes. Diabetologia 2007;50:1148-55.
- Garber AJ, Schweizer A, Baron MA, Rochotte E, Dejager S. Vildagliptin in combination with pioglitazone improves glycaemic control in patients with type 2 diabetes failing thiazolidinedione monotherapy: a randomized, placebo-controlled study. Diabetes Obes Metab 2007;9:166-74.
- Goldstein BJ, Feinglos MN, Lunceford JK, Johnson J, Williams-Herman DE. Effect of initial combination therapy with sitagliptin, a dipeptidyl peptidase-4 inhibitor, and metformin on glycemic control in patients with type 2 diabetes. Diabetes Care 2007;30:1979-87.
- Hanefeld M, Herman GA, Wu M, Mickel C, Sanchez M, Stein PP. Once-daily sitagliptin, a dipeptidyl peptidase-4 inhibitor, for the treatment of patients with type 2 diabetes. Curr Med Res Opin 2007;23:1329-39.
- Mimori N, Terao S, Holmes D. Vildagliptin improves glucose control as evidenced by HbA(1c) after 12 weeks therapy in Japanese patients with type 2 diabetes. Diabetes 2006;55:A125-6.
- Nonaka K, Kakikawa T, Sato A, Okuyama K, Fujimoto G, Hayashi N, et al. Twelve-week efficacy and tolerability of sitagliptin, a dipleptidyl peptidase-IV (DPP4) inhibitor, in Japanese patients with T2DM. Diabetes 2006;55.
- Pan C, Yang W, Barona JP, Wang Y, Niggli M, Mohideen P, et al. Comparison of vildagliptin and acarbose monotherapy in patients with Type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetic Med 2008;25:435-41.
- Pi-Sunyer FX, Schweizer A, Mills D, Dejager S. Efficacy and tolerability of vildagliptin monotherapy in drug-naive patients with type 2 diabetes. Diabetes Res Clin Pract 2007;76:132-8.
- Pratley RE, Jauffret-Kamel S, Galbreath E, Holmes D. Twelve-week monotherapy with the DPP-4 inhibitor vildagliptin improves glycemic control in subjects with type 2 diabetes. Horm Metab Res 2006;38:423-8.
- Raz I, Hanefeld M, Xu L, Caria C, Williams-Herman D, Khatami H, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy in patients with type 2 diabetes mellitus. Diabetologia 2006;49:2564-71.
- Raz I, Chen Y, Wu M, Hussain S, Kaufman KD, Amatruda JM, et al. Efficacy and safety of sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes. Curr Med Res Opin 2008;24:537-50.
- Ristic S, Byiers S, Foley J, Holmes D. Improved glycaemic control with dipeptidyl peptidase-4 inhibition in patients with type 2 diabetes: vildagliptin (LAF237) dose response. Diabetes Obes Metab 2005;7:692-8.
- Rosenstock J, Brazg R, Andryuk PJ, Lu K, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing pioglitazone therapy in patients with type 2 diabetes: A 24-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Clin Ther 2006;28:1556-68.
- Rosenstock J, Baron MA, Dejager S, Mills D, Schweizer A. Comparison of vildagliptin and rosiglitazone monotherapy in patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabetes Care 2007;30:217-23.
- Rosenstock J, Baron MA, Camisasca RP, Cressier F, Couturier A, Dejager S. Efficacy and tolerability of initial combination therapy with vildagliptin and pioglitazone compared with component monotherapy in patients with type 2 diabetes. Diabetes Obes Metab 2007;9:175-85.
- Rosenstock J, Foley JE, Rendell M, Landin-Olsson M, Holst JJ, Deacon CF, et al. Effects of the dipeptidyl peptidase-IV inhibitor vildagliptin on incretin hormones, islet function, and postprandial glycemia in subjects with impaired glucose tolerance. Diabetes Care 2008;31:30-5.
- Scherbaum WA, Schweizer A, Mari A, Nilsson PM, Lalanne G, Wang Y, et al. Evidence that vildagliptin attenuates deterioration of glycaemic control during 2-year treatment of patients with type 2 diabetes and mild hyperglycaemia. Diabetes Obes Metab 2008;10:1114-24.
- Scherbaum WA, Schweizer A, Mari A, Nilsson PM, Lalanne G, Jauffret S, et al. Efficacy and tolerability of vildagliptin in drug-naive patients with type 2 diabetes and mild hyperglycaemia. Diabetes Obes Metab 2008;10:675-82.
- Schweizer A, Couturier A, Foley JE, Dejager S. Comparison between vildagliptin and metformin to sustain reductions in HbA(1c) over 1 year in drug-naive patients with Type 2 diabetes. Diabetic Med 2007;24:955-61.
- Scott R, Wu M, Sanchez M, Stein P. Efficacy and tolerability of the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy over 12 weeks in patients with type 2 diabetes. Int J Clin Prac 2007;61:171-80.
- Scott R, Loeys T, Davies MJ, Engel SS. Efficacy and safety of sitagliptin when added to ongoing metformin therapy in patients with type 2 diabetes. Diabetes Obes Metab 2008;10:959-69.
- Nauck MA, Meininger G, Sheng D, Terranella L, Stein PP. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trial. Diabetes Obes Metab 2007;9:194-205.
- Bolli G, Dotta F, Rochotte E, Cohen SE. Efficacy and tolerability of vildagliptin vs. pioglitazone when added to metformin: a 24-week, randomized, double-blind study. Diabetes Obes Metab 2008;10:82-90.
- Hermansen K, Kipnes M, Luo E, Fanurik D, Khatami H, Stein P. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab 2007;9:733-45.
- Williams-Herman D, Round E, Swern AS, Musser B, Davies MJ, Stein PP, et al. Safety and tolerability of sitagliptin in patients with type 2 diabetes: a pooled analysis. BMC Endocr Disord 2008;8.
- Dobs A, Goldstein BJ, Wieczorek L, Golm G, Davies MJ, Williams-Herman D, et al. Triple combination therapy with sitagliptin, metformin, and rosiglitazone improves glycemic control in patients with type 2 diabetes. Diabetes 2008;57:A595-6.
- Hanefeld M, Herman G, Mickej C, McGowan A, Wu M, Zhao P, et al. Effect of MK-0431, a dipeptidyl peptidase IV (DPP-IV) inhibitor, on glycemic control after 12 weeks in patients with type 2 diabetes. Diabetologia 2005;48.
- Nonaka K, Kakikawa T, Sato A, Okuyama K, Fujimoto G, Kato N, et al. Efficacy and safety of sitagliptin monotherapy in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract 2008;79:291-8.
- Yang W, Mohan V, Son HY, Liu J, Langdon RB, Stein P. Sitagliptin monotherapy significantly improves glycaemic control and beta-cell function, and is well tolerated in patients with type 2 diabetes in China, India, and Korea. ASEAN Federation of Endocrine Societies 2007;24.
- Green BD, Flatt PR, Bailey CJ. Dipeptidyl peptidase IV (DPP IV) inhibitors: A newly emerging drug class for the treatment of type 2 diabetes. Diab Vasc Dis Res 2006;3:159-65.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2008.
- Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab 2005;90:501-6.
- Krobot KJ, Stein PP, Allen S, Davies MJ, Meininger G. Lower risk of hypoglycemia with sitagliptin compared to glipizide when added to ongoing metformin therapy: an analysis based on A1C-adjusted event rates. Diabetes 2008;57.
- Goodman M, Thurston H, Minic B, Thuren T. Improved glycaemic control with vildagliptin 100 mg administered either as a morning or evening dose as add-on therapy to metformin in type 2 diabetes mellitus. Diabetologia 2008;51.
- Arjona-Ferreira JC, Dobs A, Goldstein BJ, Wieczorek L, Golm G, Davies MJ, et al. Triple combination therapy with sitagliptin, metformin, and rosiglitazone improves glycaemic control in patients with type 2 diabetes. Diabetologia 2008;51.
- Braceras R, Blonde L, Banerji M, Gogo-Jack S, Pratley R, Marcellari A, et al. Vildagliptin is as effective as TZDs in metformin failures: results of GALIANT – a primary care diabetes study. Diabetologia 2008;51.
- Yki-Järvinen H, Dressler A, Ziemen M. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime NPH insulin during insulin combination therapy in type 2 diabetes. HOE 901/3002 Study Group. Diabetes Care 2000;23:1130-6.
- Hennige AM, Sartorius T, Tschritter O, Preissl H, Fritsche A, Ruth P, et al. Tissue selectivity of insulin detemir action in vivo. Diabetologia 2006;49:1274-82.
- Hermansen K, Derezinski T, Kim H, Gall MA. Treatment with insulin detemir in combination with oral agents is associated with less risk of hypoglycaemia and less weight gain than NPH insulin at comparable levels of glycaemic improvement in people with Type 2 diabetes. Diabetologia 2004;47:A273-4.
- Duckworth W, Davis SN. Comparison of insulin glargine and NPH insulin in the treatment of type 2 diabetes: a review of clinical studies. J Diab Complications 2007;21:196-204.
- Horvath K, Jeitler K, Berghold A, Ebrahim SH, Gratzer TW, Plank J, et al. Long-acting insulin analogues versus NPH insulin (human isophane insulin) for type 2 diabetes mellitus. Cochrane Database Syst Rev 2007;2.
- Tran K, Banerjee S, Li H, Cimon K, Daneman D, Simpson SH. Short-acting insulin analogues for diabetes mellitus: meta-analysis of clinical outcomes and assessment of cost-effectiveness. Ottawa: The Canadian Agency for Drugs and Technologies in Health (CADTH); 2007.
- Wang F. Insulin glargine: a systematic review of a long-acting insulin analogue. Clin Ther 2003;25:1541-77.
- Warren E, Weatherley-Jones E, Chilcott J, Beverley C. Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine. Health Technol Assess 2004;8.
- Bazzano LA, Lee LJ, Shi L, Reynolds K, Jackson JA, Fonseca V. Safety and efficacy of glargine compared with NPH insulin for the treatment of Type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetic Med 2008;25:924-32.
- Monami M, Marchionni N, Mannucci E. Long-acting insulin analogues versus NPH human insulin in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract 2008;81:184-9.
- Dailey G, Riddle M, Benedetti MM, Fritsche A, Lin ZN, Salzman A. A meta-analysis of phase III/IIIb studies comparing insulin glargine with human NPH insulin in type 2 diabetes: severe hypoglycemia is less common with glargine. Diabetes 2003;52.
- Garber AJ, Clauson P, Pedersen CB, Kolendorf K. Lower risk of hypoglycemia with insulin detemir than with neutral protamine hagedorn insulin in older persons with type 2 diabetes: a pooled analysis of phase III trials. J Am Geriatr Soc 2007;55:1735-40.
- Glass LC, Qu YM, Lenox S, Kim D, Gates JR, Brodows R, et al. Effects of exenatide versus insulin analogues on weight change in subjects with type 2 diabetes: a pooled post-hoc analysis. Curr Med Res Opin 2008;24:639-44.
- Hemraj F, Garces K. Insulin glargine for type 2 diabetes. Issues Emerg Health Technol 2004;8:1-4.
- Mullins P, Sharplin P, Yki-Järvinen H, Riddle MC, Haring HU. Negative binomial meta-regression analysis of combined glycosylated hemoglobin and hypoglycemia outcomes across eleven Phase III and IV studies of insulin glargine compared with neutral protamine Hagedorn insulin in type 1 and type 2 diabetes mellitus. Clin Ther 2007;29:1607-19.
- Mullins P, Jarvinen HY, Sharplin PA, Riddle M. Hypoglycemia and glycemic control in type 2 diabetes: a meta-analysis of six randomized controlled trials comparing insulin NPH with insulin glargine. Diabetes 2007;56.
- Rašlová K, Tamer SC, Clauson P, Karl D. Insulin detemir results in less weight gain than NPH insulin when used in basal-bolus therapy for type 2 diabetes mellitus, and this advantage increases with baseline body mass index. Clin Drug Investig 2007;27:279-85.
- Rosenstock J, Dailey G, Massi-Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine: a meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care 2005;28:950-5.
- Swinnen SGHA, Holleman F, DeVries JH, Hoekstra JBL. Long-acting insulin analogue versus another long-acting insulin analogue for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews: Protocols. Cochrane Database Syst Rev 2007;1.
- Fonseca V, Bell D, Mecca T. Less symptomatic hypoglycemia with insulin glargine compared to NPH in patients with type 2 diabetes. Diabetologia 2001;44.
- Fonseca V, Bell D, Mecca T. Less symptomatic hypoglycemia with bedtime insulin glargine (Lantus (R)) compared to bedtime NPH insulin in patients with type 2 diabetes. Diabetes 2001;50.
- Fonseca V, Bell DS, Berger S, Thomson S, Mecca TE. A comparison of bedtime insulin glargine with bedtime neutral protamine hagedorn insulin in patients with type 2 diabetes: subgroup analysis of patients taking once-daily insulin in a multicenter, randomized, parallel group study. Am J Med Sci 2004;328:274-80.
- Rosenstock J, Schwartz SL, Clark CM, Park GD, Donley DW, Edwards MB. Basal insulin therapy in type 2 diabetes: 28-week comparison of insulin glargine (HOE 901) and NPH insulin. Diabetes Care 2001;24:631-6.
- Yokoyama H, Tada J, Kamikawa F, Kanno S, Yokota Y, Kuramitsu M. Efficacy of conversion from bedtime NPH insulin to morning insulin glargine in type 2 diabetic patients on basal-prandial insulin therapy. Diabetes Res Clin Pract 2006;73:35-40.
- Eliaschewitz FG, Calvo C, Valbuena H, Ruiz M, Aschner P, Villena J, et al. Therapy in type 2 diabetes: insulin glargine vs. NPH insulin both in combination with glimepiride. Arch Med Res 2006;37:495-501.
- Fritsche A, Schweitzer MA, Haring HU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med 2003;138:952-9.
- HOE 901 Study Investigators Group . Safety and efficacy of insulin glargine (HOE 901) versus NPH insulin in combination with oral treatment in Type 2 diabetic patients. Diabet Med 2003;20:545-51.
- Matthews DR, Pfeiffer C. Comparative clinical trial of a new long-acting insulin (HOE901) vs. protamine insulin demonstrates less nocturnal hypoglycaemia. Diabetes 1998;47.
- Massi Benedetti M, Humburg E, Dressler A, Ziemen M. A one-year, randomised, multicentre trial comparing insulin glargine with NPH insulin in combination with oral agents in patients with type 2 diabetes. Horm Metab Res 2003;35:189-96.
- Meneghini LF, Schwartz SL, Rak ES, Harris A, Strange P. Improved Glycemic Control With Insulin Glargine (GLAR) Vs Pioglitazone (PIO) As Add-on Therapy in Patients With Type 2 Diabetes (T2D) on Sulfonylurea (SU) or Metformin (MET) Monotherapy n.d.
- Ryysy L, Yki-Järvinen H, Hanninen J, Hulme S, Kauppinen-Makelin R, Lahdenpera S, et al. Simplifying treat to target: the LANMET study. Diabetologia 2004;47:A271-2.
- Raskin P, Park G, Zimmerman J. The effect of HOE 901 on glycemic control in type 2 diabetes. Diabetes 1998;47.
- Riddle MC, Rosenstock J, Gerich J. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080-6.
- Rosenstock J, Sugimoto D, Strange P, Stewart JA, Soltes RE, Dailey G. Triple therapy in type 2 diabetes: insulin glargine or rosiglitazone added to combination therapy of sulfonylurea plus metformin in insulin-naive patients. Diabetes Care 2006;29:554-9.
- Haak T, Tiengo A, Draeger E, Suntum M, Waldhausl W. Lower within-subject variability of fasting blood glucose and reduced weight gain with insulin detemir compared to NPH insulin in patients with type 2 diabetes. Diabetes Obes Metab 2005;7:56-64.
- Hermansen K, Davies M, Derezinski T, Martinez RG, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care 2006;29:1269-74.
- Witthaus E, Stewart J, Bradley C. Improved psychological outcomes after initiation of insulin treatment in patients with Type II diabetes. Diabetologia 2000;43.
- Mannucci E, Monami M, Lamanna C, Gensini GF, Marchionni N. Pioglitazone and cardiovascular risk. A comprehensive meta-analysis of randomized clinical trials. Diabetes Obes Metab 2008;10:1221-38.
- Derezinski T, Davies M, Kim H, Clauson P. No correlation between weight gain and number of hypoglycaemic events in patients with type 2 diabetes treated with insulin detemir as compared to NPH insulin. Diabetologia 2006;49.
- Rosenstock J, Davies M, Home PD, Larsen J, Tamer SC, Schernthaner G. Insulin detemir added to oral anti-diabetic drugs in type 2 diabetes provides glycemic control comparable to insulin glargine with less weight gain. Diabetes 2006;55.
- Rosenstock J, Davies M, Home PD, Larsen J, Koenen C, Schernthaner G. A randomised, 52-week, treat-to-target trial comparing insulin detemir with insulin glargine when administered as add-on to glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetologia 2008;51:408-16.
- Montanana CF, Herrero CH, Fernandez MR. Less weight gain and hypoglycaemia with once-daily insulin detemir than with NPH insulin in basal-bolus therapy of overweight type 2 diabetes patients: The PREDICTIVE-BMI trial. Diabet Med 2008;25:916-23.
- Pan CY, Sinnassamy P, Chung KD, Kim KW. LEAD-Study-Investigators-Group . Insulin glargine versus NPH insulin therapy in Asian Type 2 diabetes patients. Diabetes Research and Clinical Practice 2007;76:111-18.
- Philis-Tsimikas TA, Charpentier G, Clauson P, Ravn GM, Roberts VL, Thorsteinsson B. Comparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetes. Clin Ther 2006;28:1569-81.
- Holman RR, Thorne KI, Farmer AJ, Davies MJ, Keenan JF, Paul S, et al. Addition of biphasic, prandial, or basal insulin to oral therapy in type 2 diabetes. N Engl J Med 2007;357:1716-30.
- Hermansen K, Larsen J, Tamer SC, Mathieu C. More subjects achieve an HbA(1c) ≤ 7% without hypoglycaemia or weight gain when treated with insulin detemir in comparison with NPH insulin. Diabetologia 2007;50.
- Klein O, Lynge J, Endahl L, Damholt B, Nosek L, Heise T. Insulin detemir and insulin glargine: Similar time-action profiles in subjects with type 2 diabetes. Diabetes 2006;55.
- Kolendorf K, Kim H. Lower risk of hypoglycemia at each level of glycemic control when insulin detemir is added to oral agents compared to NPH insulin in patients with type 2 diabetes. Diabetes 2005;54.
- Wang XL, Lu JM, Pan CY, Mu YM, Dou JT, Ba JM, et al. Evaluation of the superiority of insulin glargine as basal insulin replacement by continuous glucose monitoring system. Diabetes Res Clin Pract 2007;76:30-6.
- King AB, Armstrong DU. A randomized, crossover, double-blind comparison of insulin detemir and insulin glargine daily blood glucose profiles in subjects with type 2 diabetes. Diabetes 2008;57.
- European Medicines Agency . Avandia: European Public Assessment Report 2008. www.emea.europa.eu/humandocs/Humans/EPAR/avandia/avandia.htm (accessed 13 May 2008).
- European Medicines Agency . Actos: European Public Assessment Report 2007. www.emea.europa.eu/humandocs/Humans/EPAR/actos/actos.htm (accessed 13 May 2008).
- Richter B, Bandeira-Echtler E, Bergerhoff K, Clar C, Ebrahim SH. Rosiglitazone for type 2 diabetes mellitus. Cochrane Database Syst Rev 2007;3.
- Richter B, Bandeira-Echtler E, Bergerhoff K, Clar C, Ebrahim SH. Pioglitazone for type 2 diabetes mellitus. Cochrane Database Syst Rev 2006;4.
- Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279-89.
- Erdmann E, Charbonnel B, Wilcox RG, Skene AM, Massi-Benedetti M, Yates J, et al. Pioglitazone use and heart failure in patients with type 2 diabetes and preexisting cardiovascular disease: data from the PROactive study (PROactive 08). Diabetes Care 2007;30:2773-8.
- Valentine WJ, Bottomley JM, Palmer AJ, Brandle M, Foos V, Williams R, et al. PROactive 06: cost-effectiveness of pioglitazone in Type 2 diabetes in the UK. Diabet Med 2007;24:982-1002.
- Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med 2007;356:2457-71.
- Drazen JM, Morrissey S, Curfman GD. Rosiglitazone: continued uncertainty about safety. N Engl J Med 2007;357:63-4.
- Home PD, Pocock SJ, Beck-Nielsen H, Gomis R, Hanefeld M, Jones NP, et al. Rosiglitazone evaluated for cardiovascular outcomes: an interim analysis. N Engl J Med 2007;357:28-3.
- Psaty BM, Furberg CD. The record on rosiglitazone and the risk of myocardial infarction. N Engl J Med 2007;357:67-9.
- US Food and Drug Administration (FDA) . GlaxoSmithKline Warning Letter 2008. www.fda.gov/foi/warning_letters/s6714c.htm (accessed 13 May 2008).
- Diamond GA, Bax L, Kaul S. Uncertain effects of rosiglitazone on the risk for myocardial infarction and cardiovascular death. Ann Intern Med 2007;147:578-81.
- Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA 2007;298:1189-95.
- Lago RM, Singh PP, Nesto RW. Congestive heart failure and cardiovascular death in patients with prediabetes and type 2 diabetes given thiazolidinediones: a meta-analysis of randomised clinical trials. Lancet 2007;370:1129-36.
- Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA 2008;299:1561-73.
- Steg PG, Marre M. Does PERISCOPE provide a new perspective on diabetic treatment?. JAMA 2008;299:1603-4.
- Heartwire . VICTORY: “Reassuring” Atherosclerosis Metabolic Data on Rosiglitazone 2008. www.medscape.com/viewarticle/572836 (accessed 13 May 2008).
- Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA 2007;298:1180-8.
- Meier C, Kraenzlin ME, Bodmer M, Jick SS, Jick H, Meier CR. Use of thiazolidinediones and fracture risk. Arch Intern Med 2008;168:820-5.
- Takeda Pharmaceuticals . Reobservation of an Increased Incidence of Fractures in Female Patients Who Received Long-Term Treatment With Actos (pioglitazone HCL) Tablets for Type 2 Diabetes Mellitus 2007. www.fda.gov/medwatch/safety/2007/Actosmar0807.pdf (accessed 26 March 2009).
- Rosen CJ. The rosiglitazone story: lessons from an FDA Advisory Committee meeting. N Engl J Med 2007;357:844-6.
- US Food and Drug Administration (FDA) . FDA Adds Boxed Warning for Heart-Related Risks to Anti-Diabetes Drug Avandia 2007. www.fda.gov/bbs/topics/NEWS/2007/NEW01743.html (accessed 13 May 2007).
- Health Canada, GlaxoSmithKline . New Restrictions on the Use of AVANDIA®, AVANDAMET® and AVANDARYLTM (rosiglitazone Products) Due to Cardiac Safety Concerns 2007. www.hc-sc.gc.ca/dhp-mps/alt_formats/hpfb-dgpsa/pdf/medeff/avandia_pc-cp_4_e.pdf (accessed 13 May 2008).
- Health Canada . Scientific Advisory Committee On Metabolic And Endocrine Therapies (SC-MET) 2007. www.hc-sc.gc.ca/dhp-mps/alt_formats/hpfb-dgpsa/pdf/prodpharma/sacmet_a_ccstme_o_2007–11–15_e.pdf (accessed 13 May 2008).
- Glitazones in type 2 diabetes: an update. Drug Ther Bull 2008;46:25-9.
- MTRAC (Midlands Therapeutics Review and Advisory Committee) . Rosiglitazone (Avandia): Verdict and Summary 2008. www.keele.ac.uk/schools/pharm/MTRAC/ProductInfo/verdicts/R/Rosiglitazone2.pdf (accessed 13 May 2008).
- MTRAC (Midlands Therapeutics Review and Advisory Committee) . Pioglitazone (Actos): Verdict and Summary 2008. www.keele.ac.uk/schools/pharm/MTRAC/ProductInfo/verdicts/P/Pioglitazone2.pdf (accessed 13 May 2008).
- The Scotsman. Doctors Demand Freeze on Use of Diabetes Drug for Heart Patients 2008. http://news.scotsman.com/latestnews/Doctors-demand-freeze-on-use.3953015.jp (accessed 13 May 2008).
- Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, et al. Management of hyperglycaemia in type 2 diabetes mellitus: a consensus algorithm for the initiation and adjustment of therapy: update regarding the thiazolidinediones. Diabetologia 2008;51:8-11.
- NPS RADAR . Rosiglitazone (Avandia) and Rosiglitazone With Metformin (Avandamet) for Type 2 Diabetes Mellitus 2007. www.npsradar.org.au/npsradar/content/rosiglitazone.pdf (accessed 13 May 2008).
- NPS RADAR . Pioglitazone (Actos) for Type 2 Diabetes Mellitus 2008. www.npsradar.org.au/npsradar/content/pioglitazone.pdf (accessed 13 May 2008).
- National Prescribing Service Limited . New Safety Information about Glitazones in NPS RADAR 2007. www.nps.org.au/resources/content/mediarel_glitazones_tp.pdf (accessed 13 May 2008).
- National Prescribing Service Ltd . Early Use of Insulin and Oral Antidiabetic Drugs: Prescribing Practice Review No. 40 2008. www.nps.org.au/site.php?content = /html/ppr.php%26ppr = /resources/Prescribing_Practice_Reviews/ppr40 (accessed 13 May 2008).
- Dahabreh IJ. Meta-analysis of rare events: an update and sensitivity analysis of cardiovascular events in randomized trials of rosiglitazone. Clin Trials 2008;5:116-20.
- Gerstein HC, Yusuf S, Bosch J, Pogue J, Sheridan P, Dinccag N, et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 2006;368:1096-105.
- Berneis K, Rizzo M, Stettler C, Chappuis B, Braun M, Diem P, et al. Comparative effects of rosiglitazone and pioglitazone on fasting and postprandial low-density lipoprotein size and subclasses in patients with Type 2 diabetes. Exp Opin Pharmacother 2008;9:343-9.
- Chappuis B, Braun M, Stettler C, Allemann S, Diem P, Lumb PJ, et al. Differential effect of pioglitazone (PGZ) and rosiglitazone (RGZ) on postprandial glucose and lipid metabolism in patients with type 2 diabetes mellitus: a prospective, randomized crossover study. Diabetes Metab Res Rev 2007;23:392-9.
- Deeg MA, Buse JB, Goldberg RB, Kendall DM, Zagar AJ, Jacober SJ, et al. Pioglitazone and rosiglitazone have different effects on serum lipoprotein particle concentrations and sizes in patients with type 2 diabetes and dyslipidemia. Diabetes Care 2007;30:2458-64.
- Norris SL, Carson S, Roberts C. Comparative effectiveness of pioglitazone and rosiglitazone in type 2 diabetes, prediabetes, and the metabolic syndrome: a meta-analysis. Curr Diab Rev 2007;3:127-40.
- Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129-39.
- Endocrine Today. Rosiglitazone: One Year Later 2008. http://endocrinetoday.com/view.aspx?rid = 29105 (accessed 27 July 2008).
- Shah BR, Juurlink DN, Austin PC, Mamdani MM. New use of rosiglitazone decreased following publication of a meta-analysis suggesting harm. Diabet Med 2008;25:871-4.
- Gerstein HC, Miller ME, Byington RP, Goff DC, Bigger JT, Buse JB, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545-59.
- Berhanu P, Perez A, Yu S. Effect of pioglitazone in combination with insulin therapy on glycaemic control, insulin dose requirement and lipid profile in patients with type 2 diabetes previously poorly controlled with combination therapy. Diabetes Obes Metab 2007;9:512-20.
- Fernandez M, Triplitt C, Wajcberg E, Sriwijilkamol AA, Musi N, Cusi K, et al. Addition of pioglitazone and ramipril to intensive insulin therapy in type 2 diabetic patients improves vascular dysfunction by different mechanisms. Diabetes Care 2008;31:121-7.
- Mattoo V, Eckland D, Widel M, Duran S, Fajardo C, Strand J, et al. Metabolic effects of pioglitazone in combination with insulin in patients with type 2 diabetes mellitus whose disease is not adequately controlled with insulin therapy: results of a six-month, randomized, double-blind, prospective, multicenter, parallel-group study. Clin Ther 2005;27:554-67.
- Raz I, Stranks S, Filipczak R, Joshi P, Lertoft B, Rastam J, et al. Efficacy and safety of biphasic insulin aspart 30 combined with pioglitazone in type 2 diabetes poorly controlled on glibenclamide (glyburide) monotherapy or combination therapy: an 18-week, randomized, open-label study. Clin Ther 2005;27:1432-43.
- Rosenstock J. Efficacy and safety of pioglitazone in type 2 diabetes: a randomised, placebo-controlled study in patients receiving stable insulin therapy. Int J Clin Prac 2002;56:251-7.
- Scheen A, Charbonnel B. Reduced insulin requirements and improved glycemic control with pioglitazone in insulin-treated patients with type 2 diabetes: results from PROactive. Diabetes 2006;55.
- Shah PK, Mudahar S, Aroda V, Wilson J, Chao E, Chang A, et al. Weight gain and fat distribution with pioglitazone in patients with type 2 diabetes on insulin therapy. J Inves Med 2007;55.
- Asnani S, Kunhiraman B, Jawa A, Akers D, Lumpkin D, Fonseca V. Pioglitazone restores endothelial function in patients with type 2 diabetes treated with insulin. Metab Syndr Relat Disord 2006;4:179-84.
- Davidson JA, Perez A, Zhang J, The P. Addition of pioglitazone to stable insulin therapy in patients with poorly controlled type 2 diabetes: results of a double-blind, multicentre, randomized study. Diabetes Obes Metab 2006;8:164-74.
- Rosenblatt S, Cichy S, Sanes-Miller C. Long-term pioglitazone/insulin combination therapy improves glycemic control in type 2 diabetes. Diabetologia 2001;44.
- Davidson J, Vexiau P, Cucinotta D, Vaz J, Kawamori R. Biphasic insulin aspart 30: literature review of adverse events associated with treatment. Clin Ther 2005;27:S75-88.
- Raskin P, Braceras R, Schwartz S, Chaykin L, Chu PL, Wynne A. Over 75% of patients with type 2 diabetes reached target A1C by adding biphasic insulin aspart 70/30 to optimized metformin and pioglitazone treatment. Diabetes 2006;55.
- Raskin P, Braceras R, Schwartz S, Chaykin L, Chu PL, Wynne A. Over 75% of patients with type 2 diabetes reached HbA(1c) %3C 7% by adding biphasic insulin aspart 30 to optimized metformin and pioglitazone treatment. Diabetologia 2006;49.
- Ratner RE, Maggs D, Nielsen LL, Stonehouse AH, Poon T, Zhang B, et al. Long-term effects of exenatide therapy over 82 weeks on glycaemic control and weight in over-weight metformin-treated patients with type 2 diabetes mellitus. Diabetes Obes Metab 2006;8:419-28.
- Blonde L, Klein EJ, Han J, Zhang B, Mac SM, Poon TH, et al. Interim analysis of the effects of exenatide treatment on A1C, weight and cardiovascular risk factors over 82 weeks in 314 overweight patients with type 2 diabetes. Diabetes Obes Metab 2006;8:436-47.
- Dennett SL, Boye KS, Yurgin NR. The impact of body weight on patient utilities with or without type 2 diabetes: a review of the medical literature. Value Health 2008;11:478-86.
- Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ 2005;14:217-30.
- Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, et al. Valuing health-related quality of life in diabetes. Diabetes Care 2002;25:2238-43.
- Yu AP, Wu EQ, Birnbaum HG, Emani S, Fay M, Pohl G, et al. Short-term economic impact of body weight change among patients with type 2 diabetes treated with antidiabetic agents: analysis using claims, laboratory, and medical record data. Curr Med Res Opin 2007;23:2157-69.
- Edwards KL. Cost-effectiveness of intermediate or long-acting insulin versus Exenatide in type 2 diabetes mellitus patients not optimally controlled on dual oral diabetes medications. Pharmacy Practice 2006;4:129-33.
- Shaya FT. Clinical and economic evaluation of exenatide for formulary decisions. J Med Econ 2007;10:529-37.
- Minshall ME, Oglesby AK, Wintle ME, Valentine WJ, Roze S, Palmer AJ. Estimating the long-term cost-effectiveness of exenatide in the United States: an adjunctive treatment for type 2 diabetes mellitus. Value Health 2008;11:22-33.
- Ray JA, Boye KS, Yurgin N, Valentine WJ, Roze S, McKendrick J, et al. Exenatide versus insulin glargine in patients with type 2 diabetes in the UK: a model of long-term clinical and cost outcomes. Curr Med Res Opin 2007;23:609-22.
- Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making 2002;22:340-9.
- Watkins JB, Minshall ME, Sullivan SD. Application of economic analyses in U.S. managed care formulary decisions: a private payer’s experience. J Manag Care Pharm 2006;12:726-35.
- Scottish Medicines Consortium . Exenatide 5 or 10 Micrograms, Solution for Injection, Prefilled Pen (Byetta) 2007. www.scottishmedicines.org.uk/smc/5206.html (accessed 25 March 2009).
- Schwarz B, Gouveia M, Chen J, Nocea G, Jameson K, Cook J, et al. Cost-effectiveness of sitagliptin-based treatment regimens in European patients with type 2 diabetes and haemoglobin A1c above target on metformin monotherapy. Diabetes Obes Metab 2008;10:43-55.
- Minshall M, Charles M, Pandya B, Baran RW, Bron M. The cost-effectiveness of pioglitazone compared with sitagliptin: An economic evaluation using a validated economic model from a third party payer perspective in the USA. Value Health 2007;10.
- Celaya JM, Fon F, Ayala C, Antunez O, Garcia-Contreras F. A pharmacoeconomic evaluation for diabetes type 2 (DM 2) with inhibitors of dipeptidyl peptidase-4 (DPP-4) and thiazolidinediones (TZD) in monotherapy. Value Health 2007;10.
- Fon F, Celaya JM, Ayala C, Antunez O, Garcia-Contreras F. A pharmacoeconomic evaluation for diabetes type 2 (DM 2) patients with inhibitors of dipeptidyl peptidase-4 (DPP-4) and thiazolidinediones (TZD) as add-on therapy. Value Health 2007;10.
- Scottish Medicines Consortium . Vildagliptin (Galvus) 2008. www.scottishmedicines.org.uk/smc/5473.html (accessed 24 March 2009).
- Scottish Medicines Consortium . Sitagliptin 100mg Tablets (Januvia) 2007. www.scottishmedicines.org.uk/smc/5358.html (accessed 24 March 2009).
- Brandle M, Azoulay M, Greiner RA. Cost-effectiveness and cost-utility of insulin glargine compared with NPH insulin based on a 10-year simulation of long-term complications with the Diabetes Mellitus Model in patients with type 2 diabetes in Switzerland. Int J Clin Pharmacol Ther 2007;45:203-20.
- Maxion-Bergemann S, Huppertz E, Jacobs LD, Muller E, Walleser S. Improved glycemic control with decreased hypoglycemia prevents long-term complications in type 2 diabetes patients: long-term simulation analysis using the “diabetes mellitus model”. Int J Clin Pharmacol Ther 2005;43:271-81.
- Grima DT, Thompson MF, Sauriol L. Modelling cost effectiveness of insulin glargine for the treatment of type 1 and 2 diabetes in Canada. Pharmacoeconomics 2007;25:253-66.
- Yki-Järvinen H, Haring HU, Johnson E, Robert-Engels C, Nguyen H, Zeger S, et al. The relationship between glycemic control and Hypoglycemia using insulin glargine-versus NPH insulin: a meta-regression analysis in type 2 diabetes. Diabetes 2003;52:A149-150.
- McEwan P, Tetlow AP, Holmes P, Poole CD, Currie CJ. The relative cost effectiveness of insulin glargine versus NPH insulin in the UK in people with type 2 diabetes. Value Health 2006;9:A227-8.
- Currie CJ, Morgan CL, Poole CD, Sharplin P, Lammert M, McEwan P. Multivariate models of health-related utility and the fear of hypoglycaemia in people with diabetes. Curr Med Res Opin 2006;22:1523-34.
- McEwan P, Mehin N, Ap T, Sharplin P. The relative cost effectiveness of insulin glargine versus nph insulin using UK real life data in patients with type 2 diabetes mellitus. Value Health 2007;10:A64-5.
- McEwan P, Poole CD, Tetlow T, Holmes P, Currie CJ. Evaluation of the cost-effectiveness of insulin glargine versus NPH insulin for the treatment of type 2 diabetes in the UK. Curr Med Res Opin 2007;23:S21-31.
- Valentine WJ, Erny-Albrecht KM, Ray JA, Roze S, Cobden D, Palmer AJ. Therapy conversion to insulin detemir among patients with type 2 diabetes treated with oral agents: A modeling study of cost-effectiveness in the United States. Advances Ther 2007;24:273-90.
- Dornhorst A, Luddeke HJ, Sreenan S, Kozlovski P, Hansen JB, Looij BJ, et al. Insulin detemir improves glycaemic control without weight gain in insulin-naive patients with type 2 diabetes: subgroup analysis from the PREDICTIVE study. Int J Clin Pract 2008;62:659-65.
- Poole CD, Tetlow T, McEwan P, Holmes P, Currie CJ. The prescription cost of managing people with type 1 and type 2 diabetes following initiation of treatment with either insulin glargine or insulin detemir in routine general practice in the UK: a retrospective database analysis. Curr Med Res Opin 2007;23:S41-8.
- Valentine WJ, Palmer AJ, Erny-Albrecht KM, Ray JA, Cobden D, Foos V, et al. Cost-effectiveness of basal insulin from a US health system perspective: Comparative analyses of detemir, glargine, and NPH. Advances Ther 2006;23:191-207.
- Ray JA, Valentine WJ, Roze S, Nicklasson L, Cobden D, Raskin P, et al. Insulin therapy in type 2 diabetes patients failing oral agents: cost-effectiveness of biphasic insulin aspart 70/30 vs. insulin glargine in the US. Diabetes Obes Metab 2007;9:103-13.
- Goodall G, Jendle JH, Valentine WJ, Munro V, Brandt AB, Ray JA, et al. Biphasic insulin aspart 70/30 vs. insulin glargine in insulin naive type 2 diabetes patients: modelling the long-term health economic implications in a Swedish setting. Int J Clin Pract 2008;62:869-76.
- Lechleitner M, Roden M, Haehling E, Mueller M. Insulin glargine in combination with oral antidiabetic drugs as a cost-equivalent alternative to conventional Insulin therapy in type 2 diabetes mellitus. Wien Klin Wochenschr 2005;117:593-8.
- Janka HU, Hogy B. Economic evaluation of the treatment of type 2 diabetes with insulin glargine based on the LAPTOP trial. Eur J Health Econ 2008;9:165-70.
- Thompson M, Sauriol L, Grima D. Health economic evaluation of insulin glargine for the treatment of type-1 and type-2 diabetes. Value Health 2005;8.
- Smith I, Palmer AJ, Roze S, Kennedy-Martin T. Cost-effectiveness analysis of insulin detemir compared to NPH insulin in patients with type-2 diabetes in the United Kingdom. Value Health 2004;7:735-6.
- Valentine WJ, Cobden D, Palmer AJ, Wagner S, Roze S. Therapy class conversion in patients with type 2 diabetes: Economic evaluation of insulin detemir and NPH. Value Health 2006;9.
- Valentine WJ, Goodall G, Aagren M, Nielsen S, Kotchie R. Evaluating the long-term clinical and economic implications of converting type 2 diabetes patients to insulin detemir (± oral hypoglycemic agents) from insulin glargine based regimens in Germany; Data from the predictive study. Value Health 2007;10:A263-4.
- Valentine W, Cobden D, Palmer A, Roze S. Modeling the cost-utility of reduced hypoglycemia and weight gain among type 2 diabetes patients newly initiated on basal insulin: a case study of detemir and NPH. Value Health 2006;9.
- Palmer AJ, Cobden D, Valentine WJ, Wagner S, Roze S. Economic evaluation of initiating insulin detemir among type 2 diabetes patients receiving oral medication. Value Health 2006;9.
- Palmer A, Roze S, Nicklasson L, Allen E, Garber A. Estimating the cost-effectiveness in the US of biphasic insulin aspart 70/30 vs. insulin glargine over the INITIATE trial patient’s estimated lifespan. Diabetes 2005;54.
- Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, et al. A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia 2004;47:1747-59.
- Mueller E, Maxion-Bergemann S, Gultyaev D, Walzer S, Freemantle N, Mathieu C, et al. Development and validation of the Economic Assessment of Glycemic Control and Long-Term Effects of diabetes (EAGLE) model. Diabetes Technol Ther 2006;8:219-36.
- Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM, et al. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin 2004;20:5-26.
- Rubino A, McQuay LJ, Kvasz M, Tennis P. Population-Based Study of Time to Insulin After Failure of Oral Antidiabetic Therapy in Type 2 Diabetes in the UK 2006. www.rtihs.org/request/index.cfm?fuseaction = display%26PID = 7159 (accessed 27 July 2008).
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2008.
- Personal Social Services Research Unit (PSSRU) . Unit Costs of Health and Social Care 2007. www.pssru.ac.uk/uc/uc2007contents.htm (accessed 27 May 2008).
- Matza LS, Boye KS, Yurgin N, Brewster-Jordan J, Mannix S, Shorr JM, et al. Utilities and disutilities for type 2 diabetes treatment-related attributes. Qual Life Res 2007;16:1251-65.
- National Insitute for Health and Clinical Excellence (NICE) . Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children n.d. www.nice.org.uk/Guidance/CG43 (accessed 23 March 2009).
- Dolan P, Gudex C, Kind P, Williams A. A social tariff for EuroQoL: results from a UK General Population Survey. University of York: Centre for Health Economics discussion paper 138; 1995.
- Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 Health Survey. J Clin Epidemiol 1998;51:1115-28.
- Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, et al. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care 2003;26:1176-80.
- Donnelly LA, Morris AD, Frier BM, Ellis JD, Donnan PT, Durrant R, et al. Frequency and predictors of hypoglycaemia in type 1 and insulin-treated type 2 diabetes: a population-based study. Diabet Med 2005;22:749-55.
- Davis RE, Morrissey M, Peters JR, Wittrup-Jensen K, Kennedy-Martin T, Currie CJ. Impact of hypoglycaemia on quality of life and productivity in type 1 and type 2 diabetes. Curr Med Res Opin 2005;21:1477-83.
- Levy AR, Christensen T, Bavinton H, Tabberer M, Johnson JA. Estimating health-related quality of life from hypoglycemia elicited from non-diabetic and diabetic respondents in Canada. Diabetes 2007;56.
- Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al. Indirect comparisons of competing interventions. Health Technol Assess 2005;9.
- Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with Type 2 diabetes: a retrospective cohort study [see comment]. Diabetic Med 2002;19:279-84.
- Donnelly LA, Morris AD, Evans JM. Adherence to insulin and its association with glycaemic control in patients with type 2 diabetes. QJM 2007;100:345-50.
- Farmer A, Kinmonth AL, Sutton S. Measuring beliefs about taking hypoglycaemic medication among people with Type 2 diabetes. Diabet Med 2006;23:265-70.
- Odegard PS, Capoccia K. Medication taking and diabetes: a systematic review of the literature. Diabetes Educ 2007;33:1014-29.
- Vithian K, Qureshi A, Chen B, Steer K. Exenatide replacing insulin in obese/overweight patients with type 2 diabetes; a district general hospital experience. Diabetic Med 2009;24:139-40.
- Price HC, Holman RR, Levy J, Ayyagari U. Addition of exenatide therapy to insulin treatment in individuals with type 2 diabetes. Diabetic Med 2009;24.
- Brake JA, Hopkins M, Greenwood A, Spelman S, Brame C. First three months data from an observational study in people with diabetes commenced on exenatide within a large diabetes centre in both insulin treated and insulin naive patients. Diabetic Med 2009;24.
- Novo Nordisk . Liraglutide: A Once-Daily Human GLP-1 Analogue 2009. www.novonordisk.com/science/pipeline/liraglutide.asp (accessed 23 March 2009).
- Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D, et al. Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 2008;371:1753-60.
- Retnakaran R, Drucker DJ. Intensive insulin therapy in newly diagnosed type 2 diabetes. Lancet 2008;371:1725-6.
- Three new drugs for type 2 diabetes . Drug Ther Bull 2008;46:49-52.
- National Prescribing Service Ltd . NPS News 56: Managing Hyperglycaemia in Type 2 Diabetes 2008. www.nps.org.au/health_professionals/publications/nps_news/current/nps_news_56/managing_hyperglycaemia_in_type_2_diabetes (accessed 26 September 2008).
- Winocour PH. NICE guidance on type 2 diabetes: too little, too early. Pract Diab Int 2008;25:254-6.
Appendix 1 Search strategies
Clinical effectiveness searches
GLP-1 (exenatide and liraglutide) searches
MEDLINE (Ovid) (1990–April 2008)
-
exp Glucagon-Like Peptide 1/
-
(Glucagon-Like Peptide 1 or GLP-1).tw.
-
(exenatide or liraglutide).mp.
-
1 or 2 or 3
-
randomized controlled trial.pt.
-
random$.tw.
-
meta-analysis.pt.
-
review.pt.
-
5 or 6 or 7 or 8
-
4 and 9
-
limit 10 to humans
-
limit 11 to yr = “1990 – 2008”
EMBASE (Ovid) (1990–April 2008)
-
exp Glucagon-Like Peptide 1/
-
(Glucagon-Like Peptide 1 or GLP-1).tw.
-
(exenatide or liraglutide).mp.
-
exp Glucagon-Like Peptide 1/
-
meta analysis/or randomized controlled trial/or “systematic review”/
-
random$.tw.
-
1 or 2 or 3 or 4
-
5 or 6
-
7 and 8
-
limit 11 to yr = “1990 – 2008”
Cochrane Library, Issue 2, 2008 (all sections)
(exenatide):ti,ab,kw or (liraglutide):ti,ab,kw or (GLP-1):ti,ab,kw
SCI (Science Citation Index) and ISI Proceedings (2000-April 2008)
TS = (exenatide or liraglutide) AND PY = (2000–2008)
DocType = Meeting Abstract; Language = All languages; Database = SCI-EXPANDED;
ADA (American Diabetes Association) meeting abstracts
http://scientificsessions.diabetes.org/Abstracts/index.cfm?fuseaction%20=%20Locator.SearchAbstracts
EASD (European Association for the Study of Diabetes) meeting abstracts
www.easd.org/easdwebfiles/annualmeeting/meetingmain.html#past-AM
FDA (US Food and Drug Administration)
EMEA (European Medicines Evaluation Agency)
MHRA (Medicines and Healthcare Products Regulatory Agency)
Manufacturers’ websites
-
Amylin (Exenatide and Exenatide LAR)
-
Novo Nordisk (Liraglutide)
Contact with Novo Nordisk concerning the unpublished LEAD trials
DPP-4 inhibitors searches
Ovid MEDLINE(R) (1996–April 2008)
EMBASE (1996–April 2008)
-
dipeptidyl peptidase-4 inhibitor$.mp.
-
dipeptidyl peptidase-IV inhibitor$.mp.
-
dpp-iv inhibitor$.mp.
-
dpp-4 inhibitor$.mp.
-
(vildagliptin or sitagliptin or saxagliptin).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
1 or 2 or 3 or 4 or 5
-
limit 6 to english language
SCI (meeting abstracts) 2005–8
dipeptidyl peptidase-4 inhibitor* OR dipeptidyl peptidase-IV inhibitor* OR dpp-iv inhibitor* OR dpp-4 inhibitor* OR vildagliptin or sitagliptin or saxagliptin
Cochrane Library, Issue 2, 2008 (all sections)
(dipeptidyl peptidase-4 inhibitor* OR dipeptidyl peptidase-IV inhibitor* OR dpp-iv inhibitor* OR dpp-4 inhibitor* OR vildagliptin or sitagliptin or saxagliptin):ti,ab,kw
ADA meeting abstracts
http://scientificsessions.diabetes.org/Abstracts/index.cfm?fuseaction%20=%20Locator.SearchAbstracts
EASD meeting abstracts
www.easd.org/easdwebfiles/annualmeeting/meetingmain.html#past-AM
EMEA
Insulins – glargine and detemir searches
Ovid MEDLINE(R) (1996–April 2008)
EMBASE (1996–April 2008)
-
(glargine or detemir).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
Diabetes Mellitus, Type 2/
-
type 2 diabetes.tw.
-
2 or 3
-
1 and 4
Cochrane Library Issue 2, 2008 (all sections)
(glargine or detemir):ti,ab,kw and (type 2 diabetes):ti,ab,kw
ADA meeting abstracts
http://scientificsessions.diabetes.org/Abstracts/index.cfm?fuseaction%20=%20Locator.SearchAbstracts
EASD meeting abstracts
www.easd.org/easdwebfiles/annualmeeting/meetingmain.html#past-AM
EMEA
Manufacturers
-
Detemir (Levimir) – Novo Nordisk
-
Glargine (Lantus) – sanofi-aventis
Thiazolidinediones (rosiglitazone and pioglitazone) searches
Ovid MEDLINE(R) (1996–January, week 4, 2008)
-
exp Thiazolidinediones/
-
rosiglitazone.tw.
-
pioglitazone.tw.
-
1 or 2 or 3
-
randomized controlled trial.pt.
-
meta-analysis.pt.
-
(random$or meta-analysis or systematic review).tw.
-
5 or 6 or 7
-
4 and 8
Ovid MEDLINE(R) (1996–January, week 4, 2008)
-
exp Thiazolidinediones/
-
rosiglitazone.tw.
-
pioglitazone.tw.
-
(risk or safety or adverse or harm or pharmacovigilance).tw.
-
(side-effect$or precaution$or warning$or contraindication$or contra-indication$).tw.
-
exp Thiazolidinediones/ae [Adverse Effects]
-
1 or 2 or 3
-
4 or 5
-
7 and 8
-
6 or 9
EMBASE (1996–2008, week 18)
-
exp Thiazolidinediones/
-
rosiglitazone.tw.
-
pioglitazone.tw.
-
1 or 2 or 3
-
(random$or meta-analysis or systematic review).tw.
-
Randomized Controlled Trial/
-
exp “systematic review”/
-
Meta Analysis/
-
5 or 6 or 7 or 8
-
4 and 9
-
limit 10 to english language
EMBASE (1996–2008, week 18)
-
exp Thiazolidinediones/
-
rosiglitazone.tw.
-
pioglitazone.tw.
-
exp Rosiglitazone/ae [Adverse Drug Reaction]
-
exp Pioglitazone/ae [Adverse Drug Reaction]
-
(risk or safety or adverse or harm or pharmacovigilance).tw.
-
(side-effect$or precaution$or warning$or contraindication$or contra-indication$).tw.
-
6 or 7
-
1 or 2 or 3
-
8 and 9
-
4 or 5 or 10
Cochrane Library 2008, Issue 2
(thiazolidinedione*):ti,ab,kw or (pioglitazone):ti,ab,kw or (glitazone):ti,ab,kw
Searched web sites below for safety and adverse data information
ADA meeting abstracts
http://scientificsessions.diabetes.org/Abstracts/index.cfm?fuseaction%20=%20Locator.SearchAbstracts
FDA MedWatch
EMEA
AutoAlerts
Ovid AutoAlerts were set-up for the clinical effectiveness for the rest of 2008 in order to retrieve new studies published after the initial searches (shown above) were run.
Economics searches
GLP-1 economics searches
Ovid MEDLINE (1996–May, week 1, 2008)
-
exp Glucagon-Like Peptides/
-
(Glucagon-Like Peptide 1 or GLP-1).tw.
-
(exenatide or byetta).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
liraglutide.mp.
-
1 or 2 or 3 or 4
-
“Costs and Cost Analysis”/
-
“cost of illness”/
-
exp Economics/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
exp Health Status/
-
exp health status indicators/
-
exp “Quality of Life”/
-
exp quality-adjusted life years/
-
exp Patient Satisfaction/
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18
-
5 and 19
-
from 20 keep 29,38,49
-
from 21 keep 1–3
Total retrieved = 19
Ovid EMBASE (1996 to 2008, week 19)
-
(Glucagon-Like Peptide 1 or GLP-1).tw.
-
(exenatide or byetta).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
-
liraglutide.mp.
-
exp Glucagon Like Peptide 1/
-
exp health economics/
-
exp health status/
-
exp “quality of life”/
-
exp patient satisfaction/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
-
1 or 2 or 3 or 4
-
14 and 15
Total retrieved = 47
CRD databases [DARE (Database of Abstracts of Reviews of Effectiveness), NHS-EED (NHS Economic Evaluation Database) and HTA] (April 2008)
glp-1 OR liraglutide OR exenatide
Total retrieved = 9
SCI (1980–April 2008)
Topic = ((glp-1 or liraglutide or exenatide) and (cost* or economic* or pharmacoeconomic* or pharmaco-economic*).)
Total retrieved = 19
DPP-4 inhibitors – economics searches
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) [1950 to present (May, week 3, 2008)]
-
dipeptidyl peptidase-4 inhibitor$.mp.
-
dipeptidyl peptidase-IV inhibitor$.mp.
-
Dipeptidyl-Peptidase IV Inhibitors/
-
dpp-iv inhibitor$.mp.
-
dpp-4 inhibitor$.mp.
-
(vildagliptin* or sitagliptin* or saxagliptin*).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
1 or 2 or 3 or 4 or 5 or 6
-
“Costs and Cost Analysis”/
-
“cost of illness”/
-
exp Economics/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
exp Health Status/
-
exp health status indicators/
-
exp “Quality of Life”/
-
exp quality-adjusted life years/
-
exp Patient Satisfaction/
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20
-
7 and 21
Total retrieved = 25
Ovid EMBASE (1980–2008, week 22)
-
dipeptidyl peptidase-4 inhibitor$.mp.
-
dipeptidyl peptidase-IV inhibitor$.mp.
-
dpp-iv inhibitor$.mp.
-
dpp-4 inhibitor$.mp.
-
(vildagliptin* or sitagliptin* or saxagliptin*).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
-
exp Dipeptidyl Peptidase IV Inhibitor/
-
1 or 2 or 3 or 4 or 5 or 6
-
exp health economics/
-
exp health status/
-
exp “quality of life”/
-
exp patient satisfaction/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16
-
7 and 17
Total retrieved = 180
NHS-EED (May 2008)
dipeptidyl peptidase-4 inhibitor* OR dipeptidyl peptidase-IV inhibitor* OR dpp-iv inhibitor* OR dpp-4 inhibitor* OR vildagliptin or sitagliptin or saxagliptin
Total retrieved = 0
SCI database (searched on 2 May 2008)
Topic = ((dipeptidyl peptidase-4 inhibitor* OR dipeptidyl peptidase-IV inhibitor* OR dpp-iv inhibitor* OR dpp-4 inhibitor* OR vildagliptin or sitagliptin or saxagliptin) and (cost* or economic* or pharmacoeconomic* or pharmaco-economic* or quality same life or QALY*))
Time span = All Years. Databases = SCI-EXPANDED, SSCI, A&HCI.
Total retrieved = 38
ISI Proceedings
Results Topic = ((dipeptidyl peptidase-4 inhibitor* OR dipeptidyl peptidase-IV inhibitor* OR dpp-iv inhibitor* OR dpp-4 inhibitor* OR vildagliptin or sitagliptin or saxagliptin)
and (cost* or economic* or pharmacoeconomic* or pharmaco-economic* or quality same life or QALY*))
Time span = All Years. Databases = STP.
Total retrieved = 5
Long-acting insulin analogues – economics searches
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) [1950 to present (week 4, April 2008)] and EMBASE (1996–2008, week 17)
-
(cost* or economic* or pharmacoeconomic* or pharmaco-economic*).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
(quality adj2 life).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
(treatment adj2 satisfaction).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
(glargine or detemir or levemir or lantus or NPH).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
-
1 or 3 or 2
-
4 and 5
-
limit 6 to yr = “2005 – 2008”
Total retrieved = 74 from MEDLINE and 294 from EMBASE
NHS-EED (30 May 2008)
glargine or detemir or levemir or lantus
Total retrieved = 22
SCI
Topic = ((glargine or detemir) and (cost* or economic* or pharmacoeconomic* or pharmaco-economic* or quality same life or satisfaction))
Time span = 2005–2008. Databases = SCI-EXPANDED, SSCI, A&HCI.
Total retrieved = 142
Glitazones – economics searches
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) [1950 to present (May, week 3, 2008)]
-
“Costs and Cost Analysis”/
-
“cost of illness”/
-
exp Economics/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
exp Health Status/
-
exp health status indicators/
-
exp “Quality of Life”/
-
exp quality-adjusted life years/
-
exp Patient Satisfaction/
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13
-
Thiazolidinediones/
-
(Thiazolidinedione$or pioglitazone$or rosiglitazone$).tw.
-
15 or 16
-
14 and 17
Total retrieved = 234
Ovid EMBASE 1996 to 2008 Week 22
-
pioglitazone/or rosiglitazone/
-
(Thiazolidinedione$or rosiglitazone$or pioglitazone$).tw.
-
1 or 2
-
exp health economics/
-
exp health status/
-
exp “quality of life”/
-
exp patient satisfaction/
-
(pharmacoeconomic$or pharmaco-economic$or cost$or economic$).tw.
-
(qaly$or EQ5D or EQ-5D or well-being or wellbeing or health status or satisfaction or euroqol or euro-qol or SF-36 or SF36 or hrql or hrqol).tw.
-
(markov or health utilit$or hrql or hrqol or disabilit$).tw.
-
(quality adj2 life).tw.
-
(decision adj2 model).tw.
-
4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
-
3 and 13
Total retrieved = 936
NHS EED (30 May 2008)
thiazolidinedione* or rosiglitazone* or pioglitazone*
Total retrieved = 18
Web of Science®
Topic = ((thiazolidinedione* or rosiglitazone* or pioglitazone*) and (pharmacoeconomic* or pharmaco-economic* or cost* or economic* or quality same life))
Time span = All Years. Databases = SCI-EXPANDED, SSCI, A&HCI.
Refined by: Document Type = (MEETING ABSTRACT)
Total retrieved = 45
Appendix 2 Characteristics of included trials – GLP-1 receptor agonists
| Study | Methods | Participants | Interventions | Outcomes |
|---|---|---|---|---|
| Barnett (2007) 50 |
TRIAL DESIGN: Open-label, crossover DURATION OF INTERVENTION: 16 weeks DURATION OF FOLLOW-UP: 16 weeks RUN-IN PERIOD: Not reported RANDOMISATION PROCEDURE: Computer-generated central randomisation table BLINDING: Open label OVERALL RISK OF BIAS: ++ SOURCE OF FUNDING: Eli Lilly |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: Type 2 diabetes, equal to or more than 30 years of age, receiving treatment with either a stable dose of immediate- or extended-release MET equal to or greater than 1500 mg/day or an optimally effective dose of SFU for 3 months, HbA1c level equal to, or more than, 7.1% and equal to, or less than, 11%, BMI more than 25 kg/m2 and less than 40 kg/m2, stable body weight (not varying by more than 10% for at least 3 months prior to screening) EXISTING THERAPY: Failing on MET or SFUs EXCLUSION CRITERIA: Not reported NUMBERS: 141 AGE: Mean 54 years (SD 9) DURATION OF DIABETES: EXEN first 6.5 years (4.9), INSULIN first 8.2 years (6.0) HbA1c: 8.9% (SD 1.1) GENDER: EXEN first 52.7% males, INSULIN first 45.8% males ETHNIC GROUP: Not reported COMORBIDITIES: Not stated COMEDICATIONS: Patients continued prestudy dose of MET or SFU |
NUMBER OF STUDY CENTRES: 26 sites SETTING: Unclear INTERVENTION: EXEN, subcutaneous injection, 10 µg/day for 4 weeks then 20 µg/day for 12 weeks, administered twice daily CONTROL: Insulin glargine (INSULIN), titrated to FBG ≤ 5.6 mmol/l, initiated at 10 IU and increased weekly, four times daily TREATMENT BEFORE STUDY: - Patients had been receiving treatment with either a stable dose of immediate- or extended-release MET 1500 mg/day or an optimally effective dose of SFU for 3 months - Patients continued on prestudy dose of MET or SFU |
PRIMARY OUTCOMES: HbA1c (change from baseline to end of treatment) SECONDARY OUTCOMES: Target HbA1c: bodyweight, fasting serum glucose, fasting serum lipids, 7-point SMBG; PPG excursions; safety assessment; adverse events, including hypoglycaemia |
| Davis (2007) 51 |
TRIAL DESIGN: Parallel, open-label trial DURATION OF INTERVENTION: 16 weeks DURATION OF FOLLOW-UP: 16 weeks RUN-IN PERIOD: Not reported RANDOMISATION PROCEDURE: Not reported in detail; 2 : 1 EXENATIDE–INSULIN BLINDING: None SETTING: Five centres COUNTRY: USA ITT ANALYSIS: No. Results are only for patients with sufficient data for primary efficacy analysis (n = 45 compared with n = 49 ITT) DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Inadequate; numbers vary in tables SAMPLE SIZE CALCULATION: Yes; however, powered to ‘verify probability of observing > 60% success in Exenatide group’ (?) OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Not specified but some authors declared as employees of Amylin Pharmaceuticals and/or Eli Lilly |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: Between 30 and 75 years, diagnosed within 2 years, treated with one of the following for equal to or more than 3 months to 12 years: once- or twice-daily NPH insulin; once-daily glargine; once daily or three times daily ultralente insulin or insulin mixture. All patients on immediate or extended-release MET and/or SFU for at least 3 months prior to screening; or fixed-dose SFU/MET combination therapy. At time of screening: HbA1c level equal to or less than 10.5; BMI > 27 and < 40 kg/m2; history of stable body weight EXISTING THERAPY: Insulin and oral agents EXCLUSION CRITERIA: > three episodes of severe hypoglycaemia within 6 months prior to screening, used any prescription drug to promote weight loss within 3 months, previously received EXEN or GLP-1 analogues NUMBERS: 49 (51 were randomised; one discontinued before receiving study drug and one withdrawn as found not to have type 2 diabetes) AGE: Mean – EXEN 54 years (SD 8), INSULIN 52 (SD 8) DURATION OF DIABETES: Mean EXEN 10.4 years (SD 6.2), INSULIN 11.9 years (SD 7.4) HbA1c: Mean EXEN 8% (SD 1.2), INSULIN 8.3% (SD 0.9) GENDER: EXEN 46% males, INSULIN 50% males ETHNIC GROUPS: Not reported |
INTERVENTION: EXEN, s.c., 10 µg/day for 4 weeks and 20 g/day for 12 weeks, before morning and evening meals CONTROL: Usual insulin (INSULIN) regimen for 16 weeks OTHER TREATMENT: Both groups continued oral medication and instructed to continue diet and exercise regimen |
PRIMARY OUTCOMES: 1. HbA1c *Mean HbA1c (%) change from baseline to 16 weeks 2. Fasting serum glucose *Mean fasting serum glucose (mmol/l) at baseline and 16 weeks SECONDARY OUTCOMES: 1. Blood chemistries 2. Fasting serum lipids 3. Fasting C-peptide 4. Body weight *Mean change in body weight from baseline to 16 weeks 5. Point SMBG OTHER OUTCOMES: 1. Adverse events defined as any untoward medical occurrence, without regard to the possibility of a causal relationship |
| DeFronzo (2005) 58 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 30 weeks DURATION OF FOLLOW-UP: 30 weeks RUN-IN PERIOD: 4 weeks single-blind with twice-daily s.c. injections of placebo RANDOMISATION PROCEDURE: Stratified according to screening HbA1c values (< 9% and ≥ 9%) BLINDING: Triple blinded. Except for lead-in period (single blind) and MIN or MAX SFU dose (not blinded) SETTING: 91 sites (82, DeFronzo at 30 weeks; 54, Ratner, at 82 weeks) COUNTRY: USA ITT ANALYSIS: Yes DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Yes; powered for primary outcome HbA1c OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Amylin Pharmaceuticals and Eli Lilly |
WHO PARTICIPATED: Patients with type 2 diabetes treated with MET and a SFU (those taking a SFU were excluded in DeFronzo study) INCLUSION CRITERIA: 22–77 years of age (19–78 in DeFronzo), type 2 diabetes, treated with MET, screening FPG of < 13.3 mmol/l, BMI 27–45 kg/m2, HbA1c 7.5 (7.1 in DeFronzo study) to 11%, MET dose equal to or more than 1500 mg/day for 3 months before screening, and SFU dose at least maximum effective dose for 3 months before screening; weight stable for 3 months before screening, no clinically significant abnormal laboratory test values, females postmenopausal, surgically sterile, or using contraceptives for 3 months before screening and continuing throughout study EXISTING THERAPY: Failing MET EXCLUSION CRITERIA: Use of meglitinides, TZDs, alpha-glucosidase inhibitors, exogenous insulin therapy, weight-loss drugs, any investigational drug, or evidence of clinically significant comorbid conditions NUMBERS: 733 AGE: EXEN10, 55 years (SD 9); EXEN20, 55 years (SD 10); PLACEBO, 56 years (SD 10) DURATION OF DIABETES: EXEN10, 8.7 years (SD 5.9); EXEN20, 8.7 years (SD 6.1); PLACEBO, 9.4 years (SD 6.1) HbA1c: EXEN10, 8.5 (SD 1); EXEN20, 8.5 (SD 1.1); PLACEBO 8.5 (SD 1) GENDER: EXEN10, 59.2% males; EXEN20, 59.3% males; PLACEBO, 55.9% males ETHNIC GROUPS: EXEN10 – white 69%, black 10.2%, Hispanic 15.9%; EXEN20 – white 66.4%, black 11.6%, Hispanic 16.6%; PLACEBO – white 68.4%, black 12.1%, Hispanic 15.8% |
INTERVENTION: EXEN s.c., 10 µg/day, morning and evening for 30 weeks INTERVENTION: EXEN s.c., 10 µg/day for 4 week, increasing to 20 µg/day for 26 weeks, morning and evening CONTROL: Placebo s.c. twice daily OTHER TREATMENT: All participants continued current regimen of MET. No variation of SFU dose permitted after week 12; unblinded randomisation to either maximally effective or minimum recommended doses of SFU |
PRIMARY OUTCOMES: 1. HbA1c *Mean HbA1c change from baseline 2. Safety Treatment-emergent adverse events defined as those occurring upon or after receiving the first randomised dose SECONDARY OUTCOMES: 1. HbA1c *Number (%) of patients achieving HbA1c ≤ 7% by week 30 (of ITT subjects with baseline HbA1c >7%) Change in HbA1c at 30 weeks stratified by baseline A1c 2. Effect of EXEN on fasting and postprandial (meal cohort only) PG concentrations 3. Body weight *Change in body weight (kg) from baseline to 30 weeks 4. Fasting and postprandial concentrations of blood insulin 5. Fasting proinsulin 6. Lipids |
| Heine (2005) 53 |
TRIAL DESIGN: Randomised parallel open label DURATION OF INTERVENTION: 26 weeks DURATION OF FOLLOW-UP: 26 weeks RUN-IN PERIOD: No details of any run-in period RANDOMISATION PROCEDURE: Central randomisation table administered by interactive voice-response system; randomisation stratified by investigative size (block of four) BLINDING: Open label SETTING: 82 centres COUNTRY: 13 countries ITT ANALYSIS: Yes DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Yes, powered for primary outcome HbA1c OVERALL RISK OF BIAS: ++ SOURCE OF FUNDING: Eli Lilly and Amylin Pharmaceuticals |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: 30–75 years of age, treated with stable and maximally effective doses of MET and a SFU for at least 3 months before screening, HbA1c ranging from 7% to 10%, BMI ranging from 25 to 45 kg/m2 EXISTING THERAPY: MET and SFU EXCLUSION CRITERIA: Had more than three episodes of severe hypoglycaemia within 6 months before screening; had been treated with insulin within 3 months before screening, with TZDs, within 4 months before screening, with alpha-glucosidase inhibitors within 3 months before screening, or with meglitinides within 3 months before screening NUMBERS: 551 AGE: EXEN 55 years, INSULIN 56.6 years DURATION OF DIABETES: 9.5 years HbA1c: EXEN 8.2% (SD 1), INSULIN 8.3% (SD 1) GENDER: EXEN 55% males INSULIN 56.5 males ETHNIC GROUPS: EXEN – white 79.8%, black 0.7%, Hispanic 15.6%; INSULIN – white 80.5%, black 1.1%, Hispanic 15% |
INTERVENTION: EXEN 20 µg/day s.c., morning and evening CONTROL: Insulin glargine (INSULIN), s.c., titrated to BG level < 5.6mmol/l OTHER TREATMENT: MET and SFUs fixed at prestudy levels |
PRIMARY OUTCOMES: 1. HbA1c *Mean HbA1c change from baseline to 26 weeks *Percentage patients who achieved target HbA1c level ≤ 7% (for ITT patients with HbA1c level >7% at baseline) SECONDARY OUTCOMES: 1. Body weight *Mean change in body weight from baseline to 26 weeks 2. FPG *Reduction in FPG from baseline to 26 weeks *Percentage of patients achieving FPG < 5.6 mmol/l 3. Blood glucose *Mean change in SMBG from baseline to 26 weeks 4. Patient-reported health outcome measures (Secnik Boye) |
| Kendall (2005) 59 |
TRIAL DESIGN: RCT, double-blind, parallel DURATION OF INTERVENTION: 30 weeks DURATION OF FOLLOW-UP: 30 weeks RUN-IN PERIOD: 4 weeks RANDOMISATION PROCEDURE: Randomisation stratified according to HbA1c values; no details reported BLINDING: Double blind SETTING: 91 centres COUNTRY: USA ITT ANALYSIS: Yes DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Yes, powered for primary outcome HbA1c OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Amylin Pharmaceuticals and Eli Lilly |
WHO PARTICIPATED: Patients with type 2 diabetes, treated with MET and SFU INCLUSION CRITERIA: 22–77 years of age, screening FPG < 13.3 mmol/l; BMI 27–45 kg/m2; HbA1c 7.5–11%. MET dose was ≥ 1500 mg/day and SFU dose at least maximum effective dose for 3 months before screening. Weight stable for 3 months before screening; no clinically significant abnormal lab test values (> 25% outside normal lab values). Female subjects postmenopausal, surgically sterile, or using contraceptives for 3 months before screening and continuing through study EXISTING THERAPY: MET and a SFU EXCLUSION CRITERIA: Use of meglitinides, TZDs, alpha-glucosidase inhibitors, exogenous insulin therapy, weight-loss drugs, corticosteroids, drugs known to affect GI motility, transplantation medications or any investigational drug or evidence of clinically significant comorbid conditions for 3 months before screening DIAGNOSTIC CRITERIA: Not reported NUMBERS: 733 AGE: EXEN 10 µg, 55 years (SD 9); EXEN 20 µg, 55 years (SD10); PLACEBO, 56 years (SD10) DURATION OF DIABETES: EXEN 10 µg, 8.7 years (SD 5.9), EXEN 20 µg, 8.7 years (SD 6.4), PLACEBO, 9.4 years (SD 6.2) HbA1c: EXEN 10 µg 8.5% (SD 1); EXEN 20 µg, 8.5% (SD 1.1); PLACEBO 8.5% (SD 1) GENDER: EXEN 10 µg, 59.2% males; EXEN 20 µg, 59.3% males; PLACEBO, 55.9% males ETHNIC GROUPS: EXEN 10 µg, white 69%, black 10.2%, Hispanic 15.9%; EXEN 20 µg, white 66.4%, black 11.6%, Hispanic 16.6%; PLACEBO, 68.4%, black 12.1%, Hispanic 15.8% |
INTERVENTION: EXEN10 10 µg/day, subcutaneous, morning and evening INTERVENTION: EXEN20 20 µg/day, subcutaneous, morning and evening CONTROL: Subcutaneous, titrated to BG level < 5.6mmol/l OTHER TREATMENT: MET and SFU fixed at pre-study levels |
PRIMARY OUTCOMES: 1. HbA1c *Mean HbA1c change from baseline to 30 weeks *Percentage of patients who achieved target HbA1c level ≤ 7% (for ITT patients with HbA1c level > 7% at baseline) SECONDARY OUTCOMES: 1. Body weight *Mean change in body weight from baseline to 30 weeks 2. FPG *Reduction in FPG from baseline to 30 weeks *Percentage of patients achieving FPG < 5.6 mmol/l 3. Blood glucose *Mean change in self-monitored blood glucose from baseline to 26 weeks 4. Fasting plasma lipids 5. Exenatide pharmacokinetics ADDITIONAL PUBLISHED OUTCOMES: Safety: 1. Treatment emergent adverse events 2. Hypoglycaemic events 3. Clinical laboratory tests 4. Physical examination 5. 12-lead ECG 6. Vital signs 7. Titration of anti-EXEN antibodies |
| Nauck (2007) 122 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 52 weeks DURATION OF FOLLOW-UP: 52 weeks RANDOMISATION PROCEDURE: Procedure not reported. Stratified by site, based on screening values of HbA1c BLINDING: Not reported SETTING: Multicentre (number not reported) COUNTRY: 13 countries ITT ANALYSIS: Yes DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Yes SAMPLE SIZE CALCULATION: Yes OVERALL RISK OF BIAS: ++ SOURCE OF FUNDING: Not specified but authors declared as consultants or employees of Amylin Pharmaceuticals and/or Eli Lilly |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: Between 30 and 75 years of age; had suboptimal glycaemic control despite receiving optimally effective MET and SFU therapy for at least 3 months; HbA1c levels ≥ 7% and ≤ 11%; BMI ≥ 25 and ≤ 40 kg/m2, and a history of stable body weight EXISTING THERAPY: MET and SFU EXCLUSION CRITERIA: More than three episodes of severe hypoglycaemia within 6 months prior to screening, had been treated with insulin, TZDs, alpha-glucosidase inhibitors or meglitinides for longer than 2 weeks within 3 months NUMBERS: 501 in ITT sample AGE: EXEN 59 years (SD 9), INSULIN 58 (SD 9) DURATION OF DIABETES: EXEN, 9.8 years (SD 6.3); INSULIN, 10 years (SD 6.2) HbA1c: EXEN, 8.6% (SD 1), INSULIN, 8.6 (SD 1.1) GENDER: EXEN 53% males, INSULIN 49% males ETHNIC GROUPS: Not reported |
INTERVENTION: EXEN, s.c., 10 µg/day for 4 weeks then 20 µg for 48 weeks (morning and evening doses) CONTROL: INSULIN ASPART 30/70, s.c., morning and evening doses OTHER TREATMENT: Maintenance of optimally effective prestudy MET and SFU doses |
PRIMARY OUTCOMES: 1. HbA1c *Mean change in HbA1c from baseline to week 52 SECONDARY OUTCOMES 1. Body weight *Mean reduction in body weight from baseline to week 52 2. FSG *Mean change in fasting serum glucose from baseline to week 52 3. SMBG 4. Beta-cell function *Mean change in beta-cell function from baseline to 52 weeks (HOMA-B) 5. Insulin sensitivity *Mean change in insulin sensitivity from baseline to 52 weeks (HOMA-S) 6. HDL cholesterol and fasting lipids OTHER OUTCOMES 1. Treatment-emergent adverse events |
| Zinman (2007) 60 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 16 weeks DURATION OF FOLLOW-UP: 16 weeks RUN-IN PERIOD: 2-week single-blind placebo run-in RANDOMISATION PROCEDURE: Central randomisation table; automated interactive voice-response system administered assignment; stratified by site and current treatment (TZD alone or TZD plus MET) BLINDING: Double-blind. Prefilled disposable injection pens or cartridges containing indistinguishable EXEN and placebo solutions used SETTING: 49 research clinics, hospitals and primary facilities COUNTRY: USA, Canada, Spain ITT ANALYSIS: Yes DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Yes SAMPLE SIZE CALCULATION: Yes OVERALL RISK OF BIAS: ++ SOURCE OF FUNDING: Eli Lilly and Amylin Pharmaceuticals |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: Adults; treated with stable dose of TZD for at least 4 months before screening; patients received TZD therapy alone or in combination with a stable dosage of MET for 30 days; HbA1c value between 7.1% and 10% at screening; BMI between 25 kg/m2 and 45 kg/m2, and a history of stable body weight (≤ 10% variation) for at least 3 months before screening EXISTING THERAPY: TZD alone or TZD with MET EXCLUSION CRITERIA: Not reported NUMBERS: 233 AGE: EXEN, 55.6 years (SD 10.8); PLACEBO 56.6 years (SD 10.2) DURATION OF DIABETES: EXEN, 7.3 years (SD 4.9); PLACEBO, 8.2 years (SD 5.8) HbA1c: EXEN 7.9% (SD 0.9); PLACEBO 7.9 (SD 0.8) GENDER: EXEN 53.7% males; PLACEBO 57.1% males ETHNIC GROUPS: EXEN, white 85.1%; PLACEBO white 82.1% |
INTERVENTION (ROUTE, TOTAL DOSE/DAY, FREQUENCY): EXEN, s.c., 10 µg/day for 4 weeks and 20 µg/day for 12 weeks, morning and evening doses CONTROL (ROUTE, TOTAL DOSE/DAY, FREQUENCY): Placebo, s.c., morning and evening doses OTHER TREATMENT: Doses of TZD and MET constant throughout study |
PRIMARY OUTCOMES: 1. Changes HbA1c *Mean reduction in HbA1c from baseline to 16 weeks *Percentage of patients who achieved a target HbA1c level ≤ 7% (of those patients with HbA1c level > 7% at baseline) *Percentage of patients who achieved a target HbA1c level ≤ 6.5% SECONDARY OUTCOMES: 1. Body weight *Mean reduction in body weight from baseline to 16 weeks 2. FSG *Mean reduction in fasting serum glucose from baseline to 16 weeks 3. SMBG 4. HOMA levels |
Appendix 3 Characteristics of included trials – DPP-4 inhibitors
| Study | Methods | Participants | Interventions | Outcomes |
|---|---|---|---|---|
| Bolli (2008) 123 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 24 weeks DURATION OF FOLLOW-UP: 24 weeks RUN-IN PERIOD: None reported RANDOMISATION PROCEDURE: Not reported BLINDING: Reported as ‘double-blind’ SETTING: Not clear COUNTRY: Multinational – Germany, UK, USA, Spain, Italy, Switzerland, Austria, South Africa, Australia ITT ANALYSIS: No, per-protocol analysis DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Yes, and adequately powered per protocol OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Novartis |
WHO PARTICIPATED: Patients with type 2 diabetes inadequately controlled with prior MET monotherapy INCLUSION CRITERIA: 18–77 years of age, type 2 diabetes, treated with MET ≥ 1500 mg per day, screening HbA1c 7.5–11.0%, non-fertile or using a medically approved birth control method, BMI 22–45 kg/m2, FPG < 15 mmol/l EXISTING THERAPY: Failing MET EXCLUSION CRITERIA: History of type 1 diabetes or secondary forms of diabetes, acute metabolic diabetic complications, MI, unstable angina or coronary artery bypass surgery within the previous 6 months, congestive heart failure (NYHA I–IV) and liver disease such as cirrhosis or chronic active hepatitis. Also specific abnormal lab NUMBERS: 576 randomised AGE: VILDA 100 mg + MET, 56.3 years (SD 9.3); PIO 30 mg + MET, 57.0 years (SD 9.7) DURATION OF DIABETES: VILDA 100 mg + MET, 6.4 years (SD 4.9); PIO 30 mg + MET, 6.4 years (SD 5.2) HbA1c: VILDA 100 mg + MET 8.4% (SD 1.0); PIO 30 mg + MET 8.4% (SD 0.9) GENDER: VILDA 100 mg + MET 61.7% males and PIO 30 mg + MET 64.1% males ETHNIC GROUPS: VILDA 100 mg + MET, white 82.4%, Hispanic or Latino 8.5%, Asian (non-Indian subcontinent) 4.1%, black 3.0%, other 2.0%; PIO 30 mg + MET, white 81.9%, Hispanic or Latino 10.3%, Asian (non-Indian subcontinent) 3.9%, black 2.5%, other 1.4% COMORBIDITIES: Not reported COMEDICATIONS: Not reported |
INTERVENTION: VILDA 100 mg daily, two equally divided doses CONTROL: PIO 30 mg once daily OTHER TREATMENT: Assumed that participants continued current regimen of MET |
PRIMARY: 1. HbA1c *Mean HbA1c change from baseline 2. Percentage of patients responsive to treatment (HbA1c < 7%, ≤ 6.5%, reduction ≥ 1%, ≥ 0.7%, ≥ 0.5%, meeting at least one criterion) SECONDARY: *Change in body weight (kg) from baseline to 24 weeks Safety |
| Hermansen (2007) 124 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 24 weeks DURATION OF FOLLOW-UP: 24 weeks RUN-IN PERIOD: Up to 14 weeks RANDOMISATION PROCEDURE: Not reported but 1 : 1 BLINDING: Reported as ‘double-blind’ SETTING: Not clear COUNTRY: Reported as ‘multinational’ ITT ANALYSIS: Yes, with LOCF DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Yes, but not reported if numbers achieved OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Merck |
WHO PARTICIPATED: Patients with type 2 diabetes INCLUSION CRITERIA: 18–75 years of age, type 2 diabetes, taking either glimepiride (any dose) alone or in combination with MET (any dose), or taking another oral hypoglycaemic drug mono, dual or triple therapy or not taking any oral hypoglycaemic drug during the previous 8 weeks EXISTING THERAPY: If taking glimepiride alone or with MET, entered placebo run-in. If other regime and depending on HbA1c control, discontinued and started treatment with glimepiride alone or with MET, dose titrated for 4 weeks, then run-in period 10 weeks, with placebo run-in period if HbA1c ≥ 7.5% and ≤ 10.5%. Entered for randomisation if adherence ≥ 75% EXCLUSION CRITERIA: History of type 1 diabetes, treated with insulin in prior 8 weeks, renal dysfunction, history of hypersensitivity, intolerance or contraindications to glimepiride, SFUs, MET or PIO NUMBERS: 441 randomised – SIT 100 mg + MET + SU, 116; PLACEBO + MET + SU, 113 AGE: SIT 100 mg + MET + SU, 56.5 years (SD 9.6); PLACEBO + MET + SU, 57.7 years (SD 8.9) DURATION OF DIABETES: SIT 100 mg + MET + SU, 9.3 years (SD 5.7); PLACEBO + MET + SU, 10.6 years (SD 6.8) HbA1c: SIT 100 mg + MET + SU, 8.27% (SD 0.73); PLACEBO + MET + SU 8.26% (SD 0.68) GENDER: SIT 100 mg + MET + SU 52.6% males; PLACEBO + MET + SU 59% males ETHNIC GROUPS: SIT 100 mg + MET + SU, white 64.7%, black 6.6%, Hispanic 24.5%, Asian 5.7%, other 5.7%; PLACEBO + MET + SU, white 71.7%, black 8.0%, Hispanic 6.2%, Asian 11.5%, other 2.7% COMORBIDITIES: Not reported COMEDICATIONS: Not reported |
INTERVENTION: SIT 100 mg once daily CONTROL: Placebo OTHER TREATMENT: Continued stable doses of glimepiride and MET (as established in the run-in period). Also given rescue therapy of PIO 30 mg/day (open label) if FPG not meeting specific, and progressively lower, goals after randomization. Discontinued from study if rescue therapy for more than 4 weeks and FPG still high NOTE: Only reported details for relevant comparator arms |
PRIMARY: 1. HbA1c *Mean HbA1c change from baseline. If significant then assessed treatment effects by strata SECONDARY: |
| Nauck (2007) 122 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 52 weeks DURATION OF FOLLOW-UP: 52 weeks RUN-IN PERIOD: 2 week single-blind placebo RANDOMISATION PROCEDURE: Not reported, 1 : 1 ratio BLINDING: Double blinded, except for lead-in period (single blind) SETTING: Not clear COUNTRY: Described as ‘multinational’ ITT ANALYSIS: Per-protocol and all-patients-treated analysis DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Not reported OVERALL RISK OF BIAS: – SOURCE OF FUNDING: Merck |
WHO PARTICIPATED: Patients with type 2 diabetes with inadequate control on MET INCLUSION CRITERIA: 18–78 years of age, type 2 diabetes, treated with MET (eligible if not taking any oral therapy, any oral therapy as monotherapy, any oral therapy with MET, then titrated to MET monotherapy over 8-week period) EXISTING THERAPY: Failing MET EXCLUSION CRITERIA: History of type 1 diabetes, insulin use within 8 weeks of screening, renal function impairment inconsistent with use of MET, FPG at or prior to randomisation > 15.0 mmol/l NUMBERS: 1172 randomised AGE: SIT + MET, 56.8 years (SD 9.3); SU + MET 56.6 years (SD 9.8) DURATION OF DIABETES: SIT + MET, 6.5 years (SD 6.1); SU + MET, 6.2 years (SD 5.4) HbA1c: SIT + MET, 7.7 (SD 0.9); SU + MET, 7.6 (SD 0.9) GENDER: SIT + MET 57.1% males, SU + MET 61.3% ETHNIC GROUPS: SIT + MET, white 73.5%, black 7.0%, Hispanic 7.3%, Asian 8.5%, other 3.7%; SU + MET, white 74.3%, black 6.0%, Hispanic 739%, Asian 8.4%, other 3.4% COMORBIDITIES: Not reported COMEDICATIONS: Allowed lipid lowering, antihypertensive, thyroid, medications and HRT, birth control – but expected to remain at stable doses. Other treatments for hyperglycaemia not allowed PHARMACONAIVE: SIT + MET 4.3%, SU + MET 4.8% at screening |
INTERVENTION: SIT 100 mg once daily CONTROL: Glipizide, initial dose of 5 mg with up-titration according to protocol specifications to maximum of 20 mg/day OTHER TREATMENT: Assumed that all participants continued stable regimen of MET |
PRIMARY: 1. HbA1c *Mean HbA1c change from baseline SECONDARY: 1. HbA1c *Number (%) of patients achieving HbA1c ≤ 7% or 6.5% change in HbA1c stratified by baseline A1c Safety and tolerability: Adverse experiences, lab safety parameters, body weight, vital signs, ECG data Compliance Tablet count |
| Scott (2007) 120 |
TRIAL DESIGN: RCT DURATION OF INTERVENTION: 18 weeks DURATION OF FOLLOW-UP: 18 weeks RUN-IN PERIOD: 2 week single-blind placebo RANDOMISATION PROCEDURE: Not reported, 1 : 1 : 1 ratio BLINDING: Double blinded, except for lead-in period (single blind) SETTING: Not clear COUNTRY: Described as ‘multinational’ ITT ANALYSIS: All-patients-treated analysis DESCRIPTION OF WITHDRAWALS AND LOSSES TO FOLLOW-UP: Adequate SAMPLE SIZE CALCULATION: Not reported OVERALL RISK OF BIAS: + SOURCE OF FUNDING: Merck |
WHO PARTICIPATED: Patients with type 2 diabetes treated with MET INCLUSION CRITERIA: 18–75 years of age, type 2 diabetes, treated with MET at stable dose of at least 1500 mg/day for at least 10 weeks prior to screening, HbA1c 7–11% EXISTING THERAPY: Failing MET EXCLUSION CRITERIA: Type 1 diabetes, insulin use within 8 weeks of screening, impaired renal function, contraindications for TZDs or MET NUMBERS: 273 randomised AGE: SIT100, 55.2 years (SD 9.8); ROSI8, 54.8 years (SD 10.5); PLACEBO 55.3 years (SD 9.3) DURATION OF DIABETES: SIT100, 4.9 years (SD 3.5); ROSI8, 4.6 years (SD 4.0); PLACEBO 5.4 years (SD 3.7) HbA1c: SIT100, 7.8 (SD 1.0); ROSI8, 737 (SD 0.8); PLACEBO 7.7 (SD 0.9) GENDER: SIT100 55% males, ROSI8 63% males, PLACEBO 59% males ETHNIC GROUPS: SIT100, Caucasian 61%, Asian 38%, others 1%; ROSI8, Caucasian 59%, Asian 38%, other 3%; PLACEBO, Caucasian 61%, Asian 39%, other 0% COMORBIDITIES: 59% hypertension, 42% hyperlididaemia/dyslipidaemia COMEDICATIONS: Not reported PHARMACONAIVE: N/A |
INTERVENTION: SIT 100 mg once daily INTERVENTION: ROS 8 mg once daily CONTROL: Placebo once daily OTHER TREATMENT: All participants continued current regimen of MET. All patients received counselling on exercise and a weight-maintaining diet |
PRIMARY: 1. HbA1c *Mean HbA1c change from baseline 2. Beta-cell function Proinsulin–insulin ratio and HOMA-beta 3. Meal tolerance test SECONDARY: |
Appendix 4 Characteristics of included reviews – long-acting insulin analogues
| Review | Inclusion criteria and methodology | Included studies | Quality |
|---|---|---|---|
|
Duckworth (2007) 140 Focus: Clinical evidence for insulin glargine vs NPH insulin Funding: Industrial (Sanofi-aventis USA) |
INCLUSION CRITERIA: Study design: Not specified Participants: Patients with type 2 diabetes Interventions: Insulin glargine vs NPH insulin Outcomes: HbA1c, FPG, incidence of hypoglycaemia, other safety assessments METHODOLOGY: Search strategy: PubMed 1996–2005; search terms reported; English language only Study selection: Not described Quality assessment: Not described Data extraction: Not described Meta-analysis: No Data analysis: Not described Subgroups/sensitivity analyses: None |
Number of included trials: eight Number of participants: 3379 (range 100–756) TRIALS: Design: All open-label RCTs Duration: 4 weeks to 1 year Quality: Not reported Origin: Not reported Funding: Many of the included trials supported by Sanofi-aventis (no further details) PARTICIPANTS: Age: Not reported Gender: Not reported BMI: Not reported Diabetes duration: Not reported HbA1c: Mean 8.5–9.7% Previous medication: See below, some limited details given INTERVENTIONS: Two trials in patients with previous insulin therapy; five trials in insulin-naive patients on oral therapy; one trial included patients on oral therapy plus insulin; dose titration targets 80–140 mg/dl (4.5–7.8 mmol/l) in two trials, 72–126 mg/dl (4–7 mmol/l) in one trial, 120 mg/dl (6.7 mmol/l) in two trials, ≤ 100 mg/dl (5.6 mmol/l) in three trials; in trials with previous oral agents – four trials continued existing oral therapy, in one trial existing oral therapy was replaced by 3 mg glimepiride, in one trial fixed dose of 2 g MET OUTCOMES: HbA1c, FPG, hypoglycaemia, safety, percentage reaching target HbA1c/FBG |
Appropriate and clearly focused question: Adequately addressed Inclusion/exclusion criteria described: Poorly addressed Literature search sufficiently rigorous to identify all relevant studies: Poorly addressed Study selection described: Not reported Data extraction described: Not reported Study quality assessed and taken into account: Not reported Study flow shown: Not reported Study characteristics of individual studies described: Adequately addressed Quality of individual studies given: Not reported Results of individual studies shown: Adequately addressed Enough similarities between studies selected to make combining them reasonable: Not applicable How well was study done to minimise bias: (–) What is the likely direction in which bias might affect study results? Less effect than reported |
|
Horvath (2007) 141 Focus: Effects of long-term treatment with long-acting insulin analogues (insulin glargine and insulin detemir) compared with NPH insulin in patients with type 2 diabetes Funding: Non-industrial |
INCLUSION CRITERIA: Study design: RCTs with parallel or crossover design, blinded or open-label, with a duration of 24 weeks or longer Participants: Patients with type 2 diabetes Interventions: Long-acting insulin analogues (glargine or detemir) vs NPH insulin; in case of combination with oral agents, the antihyperglycaemic agent had to be part of each treatment arm; s.c. applications for insulin only Outcomes: Primary: overall, severe and nocturnal hypoglycaemia; glycaemic control (HbA1c); secondary: mortality, cardiovascular morbidity, diabetic late complications, QoL, adverse events, costs METHODOLOGY: Search strategy: databases searched: Cochrane Library, MEDLINE, EMBASE, CRD databases; electronic search strategy shown; citation searches of included trials and reviews; additional internet searches listed; information on unpublished trials sought from Sanofi-aventis and Novo Nordisk Study selection: Two reviewers independently screened titles and abstracts; full articles obtained for citations that appeared to fulfil the inclusion criteria (or in case of disagreement); if disagreement persisted, resolved by a third party Quality assessment: Independent assessment of quality by two reviewers; differences in opinion resolved by discussion with a third reviewer; quality parameters assessed: randomisation, allocation concealment, blinding, description of withdrawals and dropouts, ITT analysis, blinding of outcome assessors Data extraction: Done independently by two reviewers using data extraction sheets; differences in data extraction resolved by consensus; information extracted listed Meta-analysis: Yes Data analysis: WMDs or odd ratios calculated, random effects model used; heterogeneity assessed using chi-squared test Subgroups/sensitivity analyses: Planned but not carried out |
Number of included trials: Seven RCTs insulin glargine vs NPH (six analysed, see below), two RCTs insulin detemir vs NPH Number of participants (in analysed trials): 3151 for glargine trials (range 110–764), 980 for detemir trials (505 and 475) TRIALS: Design: All studies were parallel trials; two had a superiority design, one and equivalence and two a non-inferiority design; in none of the trials were participants or caregivers blinded Duration: 6–12 months Quality: All studies rated as being of insufficient methodological quality (rating C); reporting of randomisation poor in most trials, adequate allocation concealment in five trials; discontinuation rates 1.6–10.2%; all main analyses used ITT approach Origin: Four trials Europe, two North America, one Europe and South Africa, one Latin America Funding: Five trials were commercially funded, unclear for the rest PARTICIPANTS: Age: Mean age 55–62 years Gender: Numbers given but partially unclear if they refer to men or women, distribution looks balanced BMI: Mean 27–33 kg/m2 Diabetes duration: Mean 8–14 years HbA1c: Mean 7.9–9.5% Previous medication: No details, none of the trials was performed with pharmaco-naive patients (i.e. controlled on diet/exercise only) INTERVENTIONS: Six studies used combinations with oral antidiabetic drugs (five glargine and one detemir), two with a short-acting insulin (one glargine and one detemir), and one with both (detemir); one study required an upward titration of insulin glargine with a target of a fraction of 50% of the basal insulin requirement while the fraction of NPH on the total insulin requirement was left unchanged, thus introducing a difference in the treatments, and the study was therefore not considered further; one study compared morning or evening glargine with evening NPH, in all other studies glargine or NPH were injected at bedtime (one study choice of bedtime or twice daily); two studies (glargine) changed from previous oral antihyperglycaemic treatment to glimepiride during run-in OUTCOMES: Glycaemic control (HbA1c), hypoglycaemia, FBG, BG profiles, percentage reaching target HbA1c, insulin doses, weight change, adverse events |
Appropriate and clearly focused question: Well covered Inclusion/exclusion criteria described: Well covered Literature search sufficiently rigorous to identify all relevant studies: Well covered Study selection described: Well covered Data extraction described: Well covered Study quality assessed and taken into account: Well covered Study flow shown: Well covered Study characteristics of individual studies described: Well covered Quality of individual studies given: Well covered Results of individual studies shown: Well covered Enough similarities between studies selected to make combining them reasonable: Well covered How well was study done to minimise bias: (++) What is the likely direction in which bias might affect study results? No likely bias |
|
Tran (2007) 142 Focus: Clinical and cost-effectiveness of long-acting insulin analogues (insulin glargine and insulin detemir) for the treatment of diabetes (both type 1 and type 2 diabetes) Funding: Canadian Agency for Drugs and Technology in Health |
INCLUSION CRITERIA: Study design: RCTs Participants: Patients with diabetes (type 1, type 2 or gestational – only type 2 considered here) Interventions: Long-acting insulin analogues (insulin glargine or detemir) vs conventional human insulin or OAD agents Outcomes: Glycaemic control (BG, HbA1c), QoL, hypoglycaemic episodes, adverse events, complications of diabetes, mortality METHODOLOGY: Search strategy: Databases searched – MEDLINE, BIOSIS Previews, PASCAL, EMBASE, PubMed, Cochrane Database of Systematic Reviews from 1990 onwards; electronic search strategy given; alert searches; grey literature obtained by searching listed websites; manufacturers were asked to provide relevant information Study selection: Two reviewers independently selected trials for inclusion; differences in decision resolved by consensus Quality assessment: Jadad scale; allocation concealment, blinding of assessors, ITT analysis Data extraction: One reviewer extracted data into a structured form, another reviewer checked the extraction Meta-analysis: Yes Data analysis: Fixed and random effects models; heterogeneity assessed using Higgins’ I2-value; WMDs, relative risks and risk differences computed Subgroups/sensitivity analyses: None |
Number of included trials: Nine RCTs insulin glargine, two RCTs insulin detemir (type 2 diabetes) Number of participants: 4729 (range 110–756) TRIALS: Design: All open-label parallel trials; 10 full publications, two abstracts/posters; most studies described as multicentre Duration: 4–52 weeks Quality: For full reports, mean Jadad score 2.4 (SD 0.7), allocation concealment adequate in four studies (unclear in remainder), 90% reported ITT analysis Origin: Four trials Europe, four trials North America, two trials Europe and South Africa, one trial international Funding: Industrial (where reported) PARTICIPANTS: Age: Mean 53–61 years (where reported) Gender: 36–49% female (where reported) BMI: Mean 27–35 kg/m2 Diabetes duration: Mean 8.5–13.8 years (where reported) HbA1c: Mean 8.4–9.8% Previous medication: See below INTERVENTIONS: Seven studies including various combinations of oral antihyperglycaemic medications, one study morning vs evening glargine vs evening NPH, one study combination with insulin aspart OUTCOMES: No specific details given – results reported for: glycaemic control, 8-point glucose profiles, hypoglycaemia, adverse events, mortality, QoL |
Appropriate and clearly focused question: Well covered Inclusion/exclusion criteria described: Well covered Literature search sufficiently rigorous to identify all relevant studies: Well covered Study selection described: Well covered Data extraction described: Adequately addressed Study quality assessed and taken into account: Well covered Study flow shown: Well covered Study characteristics of individual studies described: Well covered Quality of individual studies given: Well covered Results of individual studies shown: Well covered Enough similarities between studies selected to make combining them reasonable: Yes How well was study done to minimise bias: (++) What is the likely direction in which bias might affect study results? No likely bias |
|
Warren (2004) 144 Focus: Clinical and cost-effectiveness of insulin glargine in its licensed basal bolus indication (both type 1 and type 2 diabetes) Funding: NICE, UK |
INCLUSION CRITERIA: Study design: Methodology including at least one of: (1) systematic review, (2) RCT, (3) economic evaluations; study duration at least 4 weeks Participants: Patients with type 1 or type 2 diabetes, requiring insulin for glycaemic control (only type 2 considered here) Interventions: Insulin glargine vs other long-acting basal insulin Outcomes: Glycaemic control (BG, HbA1c); incidence and severity of hypoglycaemic episodes METHODOLOGY: Search strategy: Databases searched: Biological Abstracts, CINAHL, Cochrane Controlled Trials Register, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effectiveness, EBM Reviews, EMBASE, HTA Database, MEDLINE, NHS Economic Evaluations Database, OHE Health Economic Evaluations Database, PREMEDLINE, Science Citation Index, Social Sciences Citation Index; electronic search strategies given; searching of reference lists of relevant publications; 45 health services research related resources searched via the internet (list given); citation searches of key papers; no date, language, study or publication type restrictions; list provided by Aventis of peer-reviewed articles of glargine primary research Study selection: Titles and abstracts screened; full copies of primary research reports, reviews and abstracts obtained; no further details Quality assessment: Jadad scale; blinding of outcome assessment Data extraction: Done by one reviewer using customised data extraction sheets Meta-analysis: No Data analysis: Text and tables Subgroups/sensitivity analyses: None |
Number of included trials: Five RCTs for type 2 diabetes Number of participants: 1399 (range 100–518) TRIALS: Design: All prospective, three clearly described as RCTs, none double-blind, design not clearly documented for two trials; two full publications, three abstracts; most studies described as multicentre Duration: 4 to 52 weeks Quality: Assessment only possible for two articles reported in full; both scored 2 (of 3) on Jadad scale; blinding of patients not possible; none of the studies specified blinded outcome assessment Origin: One trial Europe, four trials USA Funding: Not reported PARTICIPANTS: Age: ∼ 59 years (where reported) Gender: 47–38% female (where reported) BMI: Mean 29 to 31 kg/m2 (where reported) Diabetes duration: 10–14 years (where reported) HbA1c: Mean 8.5–9.1% (where reported) Previous medication: See below, no details INTERVENTIONS: Two studies of two formulations of insulin glargine compared with each other and to NPH, three studies of glargine compared with NPH; two studies of patients previously on insulin; three studies of patients previously on oral medication (and continuing oral medication); insulin doses individually titrated to achieve target FBG levels; titration periods of varying durations OUTCOMES: Glycaemic control, hypoglycaemia, FBG, diurnal BG, percentage reaching target FBG |
Appropriate and clearly focused question: Well covered Inclusion/exclusion criteria described: Well covered Literature search sufficiently rigorous to identify all relevant studies: Well covered Study selection described: Adequately addressed Data extraction described: Not adequately addressed Study quality assessed and taken into account: Well covered Study flow shown: Poorly addressed Study characteristics of individual studies described: Well covered Quality of individual studies given: Well covered Results of individual studies shown: Well covered Enough similarities between studies selected to make combining them reasonable: Not applicable How well was study done to minimise bias: (+) What is the likely direction in which bias might affect study results? No likely bias |
|
Wang (2003) 143 Focus: Efficacy and tolerability of insulin glargine Funding: Not reported |
INCLUSION CRITERIA: Study design: Clinical trials, ≥ 100 participants; includes pharmacodynamic studies, only clinical efficacy trials considered here Participants: Type 1 or type 2 diabetes, only type 2 diabetes considered here Interventions: Insulin glargine (no details) Outcomes: HbA1c, FPG, FBG, incidence of hypoglycaemia, measures of tolerability METHODOLOGY: Search strategy: MEDLINE/PubMed, EMBASE (1966–2002), Premedline (November 2002); search words given; searching of reference lists of relevant publications Study selection: Not described Quality assessment: Not described Data extraction: Not described Meta-analysis: No Data analysis: Not described Subgroups/sensitivity analyses: None |
Number of included trials: Seven RCTs for efficacy, one RCT for QoL Number of participants: 2856 (range 100 to 756) TRIALS: Design: All trials multicentre, open-label, randomised trials Duration: 4–52 weeks Quality: Inconsistent reporting of mean or adjusted mean changes in primary and secondary efficacy end points within and between treatment groups; studies were typically statistically underpowered (only three studies included power analysis); five studies only available in abstract form Origin: Europe and USA Funding: Unclear, some industrial, indicated that for most studies authors may have had conflicts of interest PARTICIPANTS: Age: ∼ 59 years Gender: Not reported BMI: Reported for only two studies, mean 29 to 32 kg/m2 Diabetes duration: Not reported HbA1c: Mean 8.4–9.0% (where reported) Previous medication: See below, no details INTERVENTIONS: Insulin doses individually titrated to achieve target FBG level of ≤ 120 mg/dl (6.7 mmol/l) (≤ 100 mg/dl in Fritsche 2003 and Riddle 2003); two trials comparing two formulations of insulin glargine (containing 30 or 80 µg/ml of zinc); three trials of patients not receiving OADs with previous once- or twice-daily NPH insulin with or without short-acting insulin for postprandial control; four studies comparing once-daily insulin glargine with once-daily NPH insulin in previously insulin-naive patients also taking OAD agents OUTCOMES: HbA1c, FPG, self-monitored FBG levels, incidence of hypoglycaemia |
Appropriate and clearly focused question: Adequately addressed Inclusion/exclusion criteria described: Poorly addressed Literature search sufficiently rigorous to identify all relevant studies: Adequately addressed Study selection described: Not reported Data extraction described: Not reported Study quality assessed and taken into account: Poorly addressed Study flow shown: Not reported Study characteristics of individual studies described: Adequately addressed Quality of individual studies given: Poorly addressed Results of individual studies shown: Adequately addressed Enough similarities between studies selected to make combining them reasonable: Not applicable How well was study done to minimise bias: (–) What is the likely direction in which bias might affect study results? Less effect than reported |
Appendix 5 Characteristics of included trials – long-acting insulin analogues
| Study | Design | Participants | Interventions | Outcome measures |
|---|---|---|---|---|
| Insulin-naive, oral antihyperglycaemics – glargine vs NPH insulin | ||||
|
Pan (2007) (LEAD study) 179 China, France, Korea |
Focus: Effect of insulin glargine vs NPH insulin on metabolic control and safety in Asian patients with type 2 diabetes, inadequately controlled on OHAs Design: Non-inferiority study; open-label, parallel group randomised trial, multicentre Duration: 24 weeks Follow-up: No postintervention follow-up Funding: Sanofi-aventis, Korea |
Total number: 443 N glargine: 220; 198 completed the trial N NPH: 223; 201 completed the trial Inclusion criteria: Insulin-naive – Asian; aged ≥ 40 and ≤ 80 years; type 2 diabetes according to WHO criteria plus specified BG criteria; poorly controlled on oral hypoglycaemic agents for ≥ 3 months before study entry; BMI 20–35 kg/m2; HbA1c ≥ 7.5 and ≤ 10.5%, FBG levels > 120 mg/dl (> 6.7 mmol/l) Exclusion criteria: Pregnancy; history of ketoacidosis; likelihood of requiring treatment with drugs prohibited by the protocol (e.g. non-selective beta-blockers, systemic corticosteroids) Age: Glargine, 55.6 (SD 8.4 years); NPH, 56.6 (SD 8.7 years) Gender: Glargine 59.6% female, NPH 55.6% female BMI: Glargine, 24.8 (SD 3.1) kg/m2; NPH, 25.1 (SD 3.3 kg/m2) Ethnicity: n = 126 China, 26 Hong Kong, 19 Indonesia, 112 South Korea, 16 Malaysia, 36 Pakistan, 24 Philippines, 32 Taiwan, 48 Thailand, 4 Singapore Diabetes duration: Glargine, 10.3 (SD 6.3 years); NPH, 10.0 (SD 5.4 years) Previous medication: Not reported, duration of treatment with OHAs: glargine, 9.1 (SD 6.0 years); NPH, 8.6 (SD 5.2 years) Comorbidities: Not reported Subgroups: None |
Glargine: Insulin glargine once daily at bedtime (21.00–23.00 hours), once-daily glimepiride (3 mg) in the morning (07.00–09.00 hours) NPH: NPH insulin once daily at bedtime (21.00–23.00 hours), once-daily glimepiride (3 mg) in the morning (07.00–09.00 hours) Both: Insulin glargine/NPH insulin titrated to a target FBG ≤120 mg/dl (≤6.7 mmol/l), starting at insulin dose of 0.15 U/kg/day Cointerventions: None Adherence assessment: No Screening phase: 3–4 weeks, oral treatments standardised to 3 mg glimepiride, patients were given training in self-administration of insulin and SMBG |
Primary: Change in HbA1c level from baseline to end point HbA1c: HbA1c, proportion of patients with HbA1c < 7.5%, proportion of combined responders (both HbA1c < 7.5% and FBG levels ≤ 120 mg/dl) Hypoglycaemia: Proportion of patients with hypoglycaemia; severe hypoglycaemia (symptoms consistent with hypoglycaemia, BG < 50 mg/dl or prompt recovery after oral carbohydrate, intravenous glucose or glucagons administration and the requirement of third-party assistance); nocturnal hypoglycaemia (while patient was asleep) Glycaemic excursions: Yes, blood glucose profiles Total daily dose: Yes Weight change: BMI Complication rates: No Adverse events: Yes Health-related QoL: No Other: None Timing of assessment: Baseline, 2, 4, 6, 8, 12, 16, 20 and 24 weeks after randomisation |
|
Wang (2007) 185 China |
Focus: Effect of insulin glargine as basal insulin replacement vs NPH insulin in patients with type 2 diabetes, in whom BG was not well controlled with SFUs Design: RCT, single centre Duration: 12 weeks Follow-up: No postintervention follow-up Setting: Unclear Funding: Not reported |
Total number: 24 N glargine: 16 N NPH: 8 Inclusion criteria: Type 2 diabetes for 6 months; age 30–70 years; BG not well controlled (FBG ≥ 7.0 mmol/l and < 13.0 mmol/l); treatment with SFU (equivalent to 7.5 mg/day glibenclamide) or combination treatment with oral agents for > 3 months Exclusion criteria: Obvious renal, liver or heart disease Age: Glargine 57 years (SD 6), NPH 56 years (SD 8) Gender: Glargine 43.8% female, NPH 50% female BMI: Glargine: 24.2 (SD 2.8 kg/m2); NPH: 24.6 (SD 2.5 kg/m2) Ethnicity: Not reported, presumably all Chinese Diabetes duration: Glargine 10.4 (SD 4.3 years); NPH 9.5 (SD 4.9 years) Previous medication: Not reported Comorbidities: Not reported Subgroups: None |
Glargine: Insulin glargine plus extended-release glipizide (glucotrol XL) NPH: NPH insulin plus glucotrol XL Both: Extended-release glipizide (glucotrol XL) 5 mg/day before breakfast; glargine or NPH injected at bedtime, initial dose 0.15 IU/kg/day; dose titrated every 3 days by the patient with instructions from researchers until FBG was < 6.7 mmol/l Cointerventions: None Adherence assessment: No Screening phase: Diabetes education; previous oral antihyperglycaemic therapy stopped and patients treated with glipizide 5 mg/day before breakfast for 2 weeks |
Primary: Unclear HbA1c: HbA1c Hypoglycaemia: Yes; hypoglycaemic event defined as a sensor glucose value of < 3.5 mmol/l for > 15 minutes Glycaemic excursions: Yes, continuous glucose-monitoring system Total daily dose: Yes Weight change: Yes; weight and BMI Complication rates: No Adverse events: No Health-related QoL: No Other: None Timing of assessment: Baseline and week 12 |
| Previous insulin – detemir vs NPH insulin | ||||
|
Montanana (2007)178 (PREDICTIVE-BMI trial) Spain |
Focus: Weight change caused by detemir or NPH used as part of basal bolus regimen in already overweight type 2 diabetes patients Design: Open parallel-group RCT, multicentre Duration: 26 weeks Follow-up: No postintervention follow-up Setting: Unclear Funding: Novo Nordisk |
Total number: 271 N detemir: 126; 125 completed the trial N NPH: 151; 146 completed the trial Inclusion criteria: Men or women ≥ 18 years, type 2 diabetes, had been receiving two daily doses (at least one premix) for ≥ 3 months; HbA1c between 7.5% and 11%; BMI between 25 and 40 kg/m2 Exclusion criteria: Patients receiving oral glucose-lowering drugs (other than MET); daily insulin dose ≥ 2 IU/kg; any condition rendering the patient unsuitable to participate; anticipated changes in concomitant medications known to interfere with glucose metabolism; proliferative retinopathy or maculopathy requiring acute treatment in the preceding 6 months; uncontrolled hypertension; pregnancy and breastfeeding Age: Detemir, 62.1 years (SD 9.3); C, 61.8 years (SD 8.3) Gender: Detemir 62.4% female, C, 56.8% female BMI/weight: Detemir, 31.6 kg/m2 (SD 4.3) / 79.5 kg (SD 11.9); C, 32.0 kg/m2 (SD 4.2) / 82.2 kg (SD 12.2) Ethnicity: 99% white Diabetes duration: Detemir, 16.2 years (SD 8.7); C, 16.4 years (SD 7.4) Previous medication: Detemir, 50.4% MET use; C, 57.5% MET use Comorbidities: Not reported Subgroups: None |
Detemir: Once daily (evening) NPH: Once daily (evening) Both: Basal insulin continually and individually titrated, aiming for pre-breakfast PG of ≤ 6.1 mmol/l without levels of hypoglycaemia considered unacceptable to the patient Cointerventions: All patients received insulin aspart at main meals (individually titrated aiming for postprandial glucose levels of ≤ 10.0 mmol/l); concomitant treatment with MET also allowed Adherence assessment: Not reported |
Primary: Weight change HbA1c: Yes Hypoglycaemia: Yes; all, major (third-party assistance required), minor (self-managed, PG confirmed ≤ 3.0 mmol/l), nocturnal hypoglycaemic events Glycaemic excursions: No Total daily dose: Yes Weight change: Yes Complication rates: No Adverse events: Yes Health-related QoL: No Other: None Timing of assessment: Five clinic visits after randomisation |
| Insulin-naive – detemir vs NPH insulin | ||||
|
Philis-Tsimikas (2006) 180 Denmark, France, Italy, Netherlands, Norway, Spain, USA |
Focus: Effectiveness and tolerability of detemir vs NPH once daily with one or more oral antidiabetic in people with poorly controlled type 2 diabetes Design: Multicentre, randomised, open-label, three-arm parallel trial |
Total number: 504 enrolled, 498 in ITT analysis N morning detemir: 165, 149 completed the trial N evening detemir: 169, 154 completed the trial N evening NPH: 164, 149 completed the trial Inclusion criteria: Age ≥ 18 years, BMI ≤ 40 kg/m2, diagnosis of type 2 diabetes since at least 12 months, insulin naive, HbA1c between 7.5% and 11% after at least 3 months’ treatment with one or more OAD agents; OAD therapy was therapy with MET or an insulin secretagogue or a combination of the two, at least half the recommended maximum dose; at US centres, concomitant treatment with TZDs was permitted throughout study period, at |
N morning detemir: Insulin detemir once daily before breakfast N evening detemir: Insulin detemir once daily in the evening (= interval 1 hour before last meal until bedtime) N evening NPH: Human NPH insulin once daily in the evening |
Primary: HbA1c HbA1c: Yes Hypoglycaemia: Yes; major episodes (requiring third-party assistance), confirmed episodes (PG reading < 3.1 mmol/l, patients able to self-manage the event), nocturnal hypoglycaemia (between 23.00 and 06.00 hours) |
|
Duration: 20 weeks Follow-up: No postintervention follow-up Setting: Outpatient clinic Funding: Novo Nordisk |
European centres TZD was to be discontinued before initiation of insulin treatment; use of alpha-glucosidase inhibitor was permitted but only in combination with another OAD agent Exclusion criteria: Proliferative retinopathy/maculopathy requiring treatment, hypoglycaemia unawareness or recurrent major hypoglycaemia, use or anticipated use of ≥ one drug likely to affect BG regulation (e.g. systemic steroids, non-selective beta-blockers, monoamine oxidase inhibitors), OAD treatment not adhering to approved labelling in the respective country; any disease or condition that would make patient unsuitable for participation (e.g. renal, hepatic, cardiac disease), uncontrolled hypertension, any psychological incapacity or language barrier precluding adequate understanding or cooperation Age: Morning detemir, 58.3 years (SD 10.4); evening detemir, 58.7 years (SD 10.2); NPH insulin, 58.4 years (SD 11.0) Gender: Morning detemir, 40.6% female; evening detemir, 46.2% female; NPH insulin, 42.7% female BMI: Morning detemir, 29.8 kg/m2 (SD 5.0); evening detemir, 29.7 kg/m2 (SD 5.1); NPH insulin, 30.4 kg/m2 (SD 4.8) Ethnicity: Not reported Diabetes duration: Morning detemir, 10.5 years (SD 7.6); evening detemir, 10.5 years (SD 7.0); NPH insulin, 10.0 years (SD 6.9) Previous medication: Morning detemir, 26.1% OAD monotherapy (9.7% MET, 16.4% secretagogue), 73.9% combination therapy (56.4% MET + 1 or 2 secretagogues, 5.5% MET + secretagogue + TZD, 6.7% 2 secretagogues, 1.8% secretagogue + TZD); evening detemir, 21.3% OAD monotherapy (8.3% MET, 13.0% secretagogue), 78.7% combination therapy (53.8% MET + 1 or 2 secretagogues, 8.9% MET + secretagogue + TZD, 7.7% 2 secretagogues, 1.2% secretagogue + TZD); NPH insulin, 24.4% OAD monotherapy (9.8% MET, 14.6% secretagogue), 75.6% combination therapy (53.0% MET + 1 or 2 secretagogues, 6.1% MET + secretagogue + TZD, 9.1% 2 secretagogues, 1.2% secretagogue + TZD) Comorbidities: ∼ 56% hypertension, ∼ 29% hypercholesterolaemia, ∼ 12% dyslipidaemia, ∼ 11% diabetic retinopathy; similar occurrence in treatment groups Subgroups: None |
All groups: insulin injected via pen device, participants advised to keep time of injection constant and to inject insulin subcutaneously, preferably in the thigh, but to rotate sites; initial dose of treatment was 10 IU (U), doses were titrated at clinic visits or by telephone at least once every 4 weeks, based on the mean of three PG levels measured on 3 consecutive days; in patients receiving detemir in the morning, the dose was titrated to aim for pre-dinner PG concentration of ≤ 6.0 mmol/l; in patients receiving detemir or NPH in the evening, titration was aimed to achieve pre-breakfast PG concentration of ≤ 6.0 mmol/l Cointerventions: OAD therapy and dose was to remain unchanged; other cointerventions (similar between groups): ∼ 21% used acetylsalicylic acid, ∼ 19% simvastatin, ∼ 15% atorvastatin Adherence assessment: Not reported |
Glycaemic excursions: 9-point self-measured PG profiles (using capillary blood and plasma-calibrated monitor): immediately before and 90 minutes after main meals, bedtime, 03.00 hours; additional measurements when patients experienced symptoms indicative of hypoglycaemia Total daily dose: Yes Weight change: Yes (calibrated scales) Complication rates: No Adverse events: Adverse events, standard laboratory analyses, fundoscopy, physical examination Health-related QoL: No Other: None Timing of assessment: At least nine telephone contacts and six clinic visits (including screening and randomisation) |
|
| Insulin-naive – glargine vs detemir | ||||
|
Rosenstock (2008) 177 Europe, USA |
Focus: Comparison of clinical outcomes following supplementation of oral glucose-lowering drugs with basal insulin analogues detemir and glargine in patients with type 2 diabetes Design: Open-label, parallel group randomised controlled non-inferiority trial, multicentre Duration: 52 weeks Follow-up: No postintervention follow-up Setting: Unclear Funding: Novo Nordisk |
Total number: 582 N detemir: 291, 231 completed the trial N NPH: 291, 252 completed the trial Inclusion criteria: Insulin-naive men or women ≥ 18 years, type 2 diabetes with ≥ 12 months’ disease duration; HbA1c between 7.5% and 10%; BMI ≤ 40 kg/m2; had been receiving one or two oral agents (MET, insulin secretagogues, alpha-glucosidase inhibitors) ≥ 4 months on at least half of maximum recommended dose Exclusion criteria: Treatment with TZDs; use of more than two oral agents within 6 months; hypoglycaemic unawareness; other medical conditions likely to interfere with trial conduct; withdrawal criteria included pregnancy, HbA1c > 11% after the first 12 weeks of treatment, initiation of medication interfering with glucose metabolism Age: Detemir, 58.4 years (SD 10.2); glargine, 59.4 years (SD 9.6) Gender: Detemir 43% female, glargine 41.2% female BMI/weight: Detemir, 30.6 kg/m2 (SD 4.8) / 87.4 kg (SD 16.6); glargine, 30.5 kg/m2 (SD 4.6) / 87.4 kg (SD 17.4) Ethnicity: Detemir, 86% white, 7.6% black, 2.4% Asian-Pacific Islanders, 4% other; glargine, 90.4% white, 4.1% black, 2.4% Asian-Pacific Islanders, 3.1% other Diabetes duration: Detemir, 9.1 years (SD 6.1); glargine: 9.1 years (SD 6.4) Previous medication: Detemir – monotherapy 25% (11% MET, 14% insulin secretagogues), combination therapy 75% (97% MET + secretagogue); glargine – monotherapy 24% (11% MET, 13% insulin secretagogues), combination therapy 76% (97% MET + secretagogue) Comorbidities: Not reported Subgroups: None |
Detemir: Once daily (evening) detemir or twice daily (morning and evening) (55% used twice-daily injections) Glargine: Once daily (evening) Both: Basal insulin initiated at once daily (evening) 12 U and titrated according to a structured treatment algorithm; people on detemir were allowed to receive an additional morning dose is pre-dinner PG was > 7.0 mmol/l, but only if pre-breakfast PG was < 7.0 mmol/l or nocturnal hypoglycaemia (major episode or PG ≤ 4.0 mmol/l) precluded the achievement of the FPG target; injection of insulin using pen injector; FPG target ≤ 6.0 mmol/l in the absence of hypoglycaemia Cointerventions: Oral glucose-lowering therapy, diet and physical activity recommended to remain stable during the study; no mealtime insulin allowed Adherence assessment: Not reported |
Primary: HbA1c HbA1c: Yes; proportion of participants achieving HbA1c ≤ 7.0% with and without hypoglycaemia Hypoglycaemia: Yes; major (assistance from another person required), minor (confirmed by PG < 3.1 mmol/l) symptoms only (PG ≥ 3.1 mmol/l or no measurement made), nocturnal Glycaemic excursions: Within-participant variation in PG; 10-point self-measured PG profiles Total daily dose: Yes Weight change: Yes Complication rates: No Adverse events: Yes Health-related QoL: No Other: FPG Timing of assessment: 16 scheduled visits, during first 12 weeks contact with weekly investigator |
Appendix 6 Characteristics of included trials – insulin + pioglitazone vs insulin
| Study | Design | Participants | Interventions | Outcome measures |
|---|---|---|---|---|
|
Asnani (2006) 238 USA |
Focus: Effect of PIO on vascular reactivity in patients with insulin-treated type 2 diabetes Design: Randomised, double-blind, placebo-controlled trial, single centre Duration: 4 months Follow-up: No postintervention follow-up Funding: Takeda, NIH |
Total number: 20 N PIO + Ins: 10; 8 completed the trial N P + Ins: 10; 8 completed the trial Inclusion criteria: Age 18–75 years, insulin-treated type 2 diabetes (with or without OAD agents), poor glycaemic control (HbA1c > 7.5%) Exclusion criteria: Active liver disease, pregnant or breastfeeding women, history or recent MI within last 6 months, recent major surgery within last 6 months Age: PIO + Ins: 59 years (SD 6); P + Ins: 57 years (SD 5) Gender: Not reported BMI: Not reported Ethnicity: Not reported Diabetes duration: Not reported Previous medication: Not reported Comorbidities: Not reported Subgroups: None |
PIO + Ins: PIO 30 mg at breakfast, insulin continued as before P + Ins: Placebo, insulin continued as before Cointerventions: Stable lipid-lowering (statins) and antihypertensive therapy (including ACE inhibitors in all); not changed during therapy Adherence assessment: Not reported Screening/titration phase: Unclear |
Primary: Flow-mediated dilatation HbA1c: Yes Hypoglycaemia: No Glycaemic excursions: No Total daily dose: No Weight change: No Complication rates: No Adverse events: No Health-related QoL: No Other: Brachial artery reactivity; laboratory assessments, lipid profile Timing of assessment: Baseline, 4 months |
|
Berhanu (2007) 231 USA |
Focus: Safety and efficacy of PIO administered alone or in combination with MET in reducing insulin dosage requirements for improved glycaemic control in patients with type 2 diabetes Design: Randomised, double-blind, placebo-controlled trial, multicentre Duration: 20 weeks Follow-up: No postintervention follow-up Funding: Takeda Global R&D Centre |
Total number: 222 N PIO + Ins: 110; 96 completed the trial N P + Ins: 112; 102 completed the trial Inclusion criteria: Patients with documented type 2 diabetes; age 18–80 years; could self-monitor BG; previous combination therapy failed (HbA1c ≥ 8.0%) ≤ 3 months before screening combination therapy = SFU plus MET, insulin plus MET after failed SFU, or insulin alone after failed combination therapy with MET and SFU (> 50% maximum SFU and ≥ 2000 mg/day MET required); C-peptide ≥ 0.7 ng/ml; FPG > 120 mg/dl Exclusion criteria: TZDs use < 30 days or insulin treatment > 30 months before screening; BMI < 20 or > 45 kg/m2; history of MI, acute cardiovascular event, or cerebrovascular accident < 6 months before screening; cardiac rhythm disturbance; significant cardiovascular disease including NYHA class III or IV; uncontrolled hypertension; LDL ≥ 175 mg/dl, triglycerides > 500 mg/dl; ALT > 1.5 times upper limit of normal; diabetic nephropathy or anaemia Age: PIO + Ins, 52.9 years (SD11.33); P + Ins, 52.5 years (SD11.07) Gender: PIO + Ins, 56.4% female; P + Ins, 58.9% female BMI: PIO + Ins, 30.7 kg/m2 (SD 6.09); P + Ins, 31.8 kg/m2 (SD 6.2) Ethnicity: PIO + Ins, Hispanic 50.0%, non-Hispanic white 34.9%, non-Hispanic black 12.7%, other 2.7%; P + Ins, Hispanic 58.9%, non-Hispanic white 25.9%, non-Hispanic black 11.6%, other 3.6% Diabetes duration: PIO + Ins, 7.7 years (SD 6.15); P + Ins: 8.5 years (SD 5.43) Previous medication: PIO + Ins, SFUs plus MET 90.0%, insulin plus MET 8.2%, insulin only 1.8%; P + Ins, SFUs plus MET 92.9%, insulin plus MET 5.4%, insulin only 1.8% Comorbidities: Not reported Subgroups: None |
PIO + Ins: PIO titrated to 45 mg/day during first 4 weeks of treatment, plus insulin as below P + Ins: Identical placebo plus insulin as below Both groups: All patients received one or multiple daily injections of Humalog, Humulin 70/30 or Humulin N; insulin adjusted to achieve FPG < 140 mg/dl while avoiding hypoglycaemia Cointerventions: Excluded medications before and during study; hydrochlorothiazide (at doses > 25 mg/day), glucocorticoids, steroid injections for joints, niacin; concurrent use of weight-loss agents and antidiabetic medications not included in the study were not permitted; patients maintained stable MET and, as applicable, previous statin use for duration of study; 98.2% in both groups used MET; 30.9% in PIO group and 28.6% in placebo group used statins Adherence assessment: Pill counts (99.1–99.4% adherence) Screening/titration phase: 1 week screening; instructions on insulin use and up to 1 week SFU discontinuation as applicable; insulin initiated and titrated to achieve FPG < 140 and > 70 mg/dl for 4 additional weeks; after titration period, insulin type, dose and administration schedule were left to the discretion of the clinical investigator; during titration period, instructions regarding diabetes, hypoglycaemia, nutrition, exercise; patients were randomised if FPG < 140 mg/dl achieved during titration |
Primary: Change in insulin dosage from baseline to study end HbA1c: Yes Hypoglycaemia: Hypoglycaemic events (SMBG < 60 mg/dl or laboratory value < 70 mg/dl, more than two simultaneous hypoglycaemia symptoms relieved by oral glucose-containing substance, or resulting in needing assistance for simple tasks) Glycaemic excursions: No Total daily dose: Yes Weight change: Weight Complication rates: No Adverse events: Yes; clinical examinations; ECG; ALT Health-related QoL: No Other: Lipid parameters, C-peptide Timing of assessment: Visits every 2 weeks for the first month, once per month thereafter |
|
Fernandez (2008) 232 USA |
Focus: Relationship between glycaemic control, vascular reactivity and inflammation in type 2 diabetes Design: Double-blind, placebo-controlled RCT, single centre Duration: 36 weeks Follow-up: No postintervention follow-up Funding: ADA, Takeda Pharmaceuticals |
Total number: 30 N PIO + Ins: 10 N P + Ins: 10 N ramipril + Ins: 10 (not considered here) Inclusion criteria: Adult Mexican-Americans with type 2 diabetes requiring insulin therapy (HbA1c > 8.0% despite optimised oral therapy); patients on insulin combination therapy with MET, SFUs or meglitinides included Exclusion criteria: Insulin combination therapy with TZDs Age: Mean age ∼46 years (no details) Gender: Overall ∼60% female (no details) BMI: Overall ∼31–33 kg/m2 (no details) Ethnicity: Mexican-American Diabetes duration: 6.2–8.4 years Previous medication: Use of OAD medications similar between groups Comorbidities: Not reported Subgroups: None |
PIO + Ins: PIO 45 mg/day; started at 15 mg daily and then increased to 30 mg daily in week 2, and to 45 mg daily in week 4 P + Ins: Placebo Ramipril + Ins: Ramipril 10 mg/day (not considered here) All groups: Three-day comprehensive diabetes education and nutritional programme; patients could select between insulin therapy using multiple daily injections (basal bolus therapy using combination of insulin glargine at bedtime plus premeal insulin aspart) or continuous s.c. infusion (Meditronic/Minimed or Animas pump using basal infusion and premeal boluses of insulin aspart); insulin dose adjusted to achieve the following glycaemic goals: fasting and pre-meal capillary BG 80–120 mg/dl, 2-hour postmeal glucose < 160 mg/dl, bedtime glucose < 140 mg/dl Cointerventions: Patients on ACE-inhibitors or angiotensin II receptor blockade were switched to alpha-methyl dopa (at least 2 months before study) and the dose adjusted to re-establish blood pressure control (< 130/80 mmHg) before enrolment; other medication allowed if stable for at least 3 months; nearly half the patients were using a statin and one-third were on antihypertensive therapy Adherence assessment: Compliance with treatment ascertained during each visit (no details) Screening phase: No |
Primary: Vascular analyses HbA1c: Yes Hypoglycaemia: Yes (symptomatic hypoglycaemia requiring glucose ingestion) Glycaemic excursions: No Total daily dose: Yes Weight change: Yes Complication rates: No Adverse events: Yes Health-related QoL: No Other: Euglycaemic-hyperinsulinaemic clamp; vascular studies; lipid parameters Timing of assessment: Clinic visits at 2- to 4-week intervals during first 3 months, every 2 months thereafter |
|
Mattoo (2005) 233 Worldwide |
Focus: Effect of PIO plus insulin vs placebo plus insulin on glycaemic control, serum lipid profile, and selected cardiovascular risk factors in patients with type 2 diabetes whose disease was inadequately controlled with insulin therapy alone, despite efforts to intensify the treatment Design: Randomised double-blind, placebo-controlled parallel group trial, multicentre Duration: 6 months Follow-up: No postintervention follow-up Funding: Eli Lilly, Takeda Europe |
Total number: 289 N PIO + Ins: 142; 128 completed the trial N P + Ins: 147; 135 completed the trial Inclusion criteria: Type 2 diabetes diagnosed according to WHO criteria, use of insulin therapy (with or without oral antihyperglycaemic medication) for ≥ 3 months, HbA1c ≥ 7.5% at screening, ≥ 30 years at diagnosis Exclusion criteria: Type 1 diabetes, clinical signs or symptoms of any chronic systemic condition (defined), signs or symptoms of drug or alcohol abuse; previous therapy with TZDs, systemic glucocorticoid therapy, nicotinic acid at > 500 mg/day, or therapy for malignancy other than basal cell or squamous skin cancer; women breastfeeding or pregnant, women of childbearing potential without active birth control Age: PIO + Ins, 58.8 years (SD 7.4); P + Ins, 58.9 years (SD 6.9) Gender: PIO + Ins, 56.3% female; P + Ins, 57.1% female BMI: PIO + Ins, 32.5 kg/m2 (SD 4.8); P + Ins: 31.8 kg/m2 (SD 5.0) Ethnicity: Not reported Diabetes duration: PIO + Ins, 163.4 months (SD 81.0); P + Ins, 160.9 months (SD 73.7) Previous medication: 149 patients previously on oral agents (MET n = 109, SFU n = 19, MET plus SFU n = 17, other n = 4) Comorbidities: Not reported Subgroups: None |
PIO + Ins: 30 mg PIO plus insulin P + Ins: Identical placebo plus insulin Both: All patients received diabetes education, including dietary and exercise guidelines, and were instructed to maintain their individual diet and exercise regimens throughout the study; patient diaries for SMBG; insulin dose reduced by 10% at randomisation to avoid hypoglycaemia and adjusted thereafter based on SMGB levels Cointerventions: Patients were allowed to use other medication as required, except another OAD agent, systemic glucocorticoid therapy, or nicotinic acid (> 500 mg/day) Adherence assessment: Capsule count (compliance rate ≥ 97.2%) Screening phase: Up to 14 days lead-in phase, patients remained on prescribed insulin therapy regimen, as monotherapy or with OHA; patients with HbA1c ≥ 7.5% then proceeded to insulin intensification period (3 months): insulin dose and number of injections adjusted to achieve fasting and preprandial BG < 5.5. mmol/l and 2-hour postprandial BG < 7.5 mmol/l; patients with HbA1c ≥ 7.0% after insulin intensification were randomised to PIO plus insulin or placebo plus insulin |
Primary: Change in HbA1c level from baseline to end point HbA1c: HbA1c Hypoglycaemia: Yes (1. subjective symptoms only, 2. subjective symptoms with SMBG ≥ 2.8 mmol/l, 3. subjective symptoms with SMBG < 2.8 mmol/l, 4. SMBG < 2.8 mmol/l without symptoms) Glycaemic excursions: No Total daily dose: Yes Weight change: Yes Complication rates: No Adverse events: Yes; adverse events, laboratory testing, physical examination Health-related QoL: No Other: Lipid parameters Timing of assessment: Five visits between randomisation and end of study |
|
Raz (2005) 234 Worldwide |
Focus: Efficacy and safety of biphasic insulin aspart 30/70 (BIAsp 30) plus PIO vs glibenclamide plus PIO and BIAsp 30 monotherapy in type 2 diabetes Design: Randomised, open-label, parallel group trial, multicentre Duration: 18 weeks Follow-up: No postintervention follow-up Funding: Novo Nordisk |
Total number: 283 N PIO + Ins: 93; 73 completed the trial N PIO + glibenclamide: 93; 56 completed the trial (not considered here) N Ins mono: 97; 75 completed the trial Inclusion criteria: Male and female patients with type 2 diabetes; age ≥ 18 years; BMI ≤ 40 kg/m2; treatment with SFU (monotherapy or combination therapy) ≥ 3 months before screening; insufficient glycaemic control (HbA1c 7.4–14.7%) Exclusion criteria: Significant disease or conditions likely to affect trial or health outcomes (including history of drug or alcohol dependence, impaired hepatic function, cardiac disease) Age: PIO + Ins, 56.7 years (SD10.5); Ins mono, 55.2 years (SD 9.1) Gender: PIO + Ins, 47% female; Ins mono, 35% female BMI: PIO + Ins, 29.4 kg/m2 (SD 4.6); Ins mono, 29.5 kg/m2 (SD 4.9) Ethnicity: Not reported Diabetes duration: PIO + Ins, 9.2 years (SD 5.3); Ins mono, 10.0 years (SD 5.8) Previous medication: Patients taking other oral agents with SFU: PIO + Ins – none 14.0%, acarbose 9.7%, meglitinides 3.2%, MET 83.9%, TZDs 7.5%; ins mono – none 13.4%, acarbose 12.4%, meglitinides 1.0%, MET 80.4%, TZDs 4.1% Comorbidities: Not reported Subgroups: None |
PIO + Ins: 30 mg PIO once daily after breakfast plus biphasic insulin aspart 30/70 (BIAsp 30). BIAsp 30 initiated at a dose of 0.2 U/kg/day PIO + glibenclamide: 30 mg PIO once daily after breakfast plus glibenclamide (starting dose 5 mg in patients already on glibenclamide, equivalent dose not exceeding 10 mg in patients previously on other SFUs) (not considered here) Ins mono: BIAsp 30 initiated at a dose of 0.3 U/kg/day Insulin therapy: Biphasic insulin aspart 30/70 (30% rapid-acting soluble insulin aspart, 70% intermediate-acting protamine-crystallised insulin aspart); BIAsp 30 injected immediately (within 5 minutes) before breakfast (50% of dose) and before dinner (50% of dose); BIAsp 30 titrated individually by patients using SMBG to achieve target BG values of 5–8 mmol/l for fasting, preprandial and night-time measurements, and 5–10 mmol/l for postprandial readings; BIAsp 30 injections with NovoPen 3; all dose titrations completed within 8 weeks of treatment Cointerventions: Any patient treated with insulin sensitiser other than PIO was told to stop treatment 14 days before randomisation; no manipulation of lipid-lowering regimens Adherence assessment: Checking patient diaries Screening phase: None |
Primary: End of trial HbA1c HbA1c: Yes Hypoglycaemia: Major hypoglycaemic episodes (patient unable to self-treat, BG < 50 mg/dl, or when symptoms remitted after administration of intravenous glucose or intramuscular glucagons after food intake); minor hypoglycaemic episodes (BG < 50 mg/dl, patient handled the event without assistance from others); symptomatic episodes (hypoglycaemic symptoms present but not confirmed by BG measurement, assistance from others not required) Glycaemic excursions: Yes, BG profiles (7 and 8 point) Total daily dose: Yes Weight change: Weight Complication rates: No Adverse events: Yes Health-related QoL: No Other: Lipid profiles Timing of assessment: Screening, 8 weeks, end of trial (HbA1c); baseline, 4, 8, 12, 18 weeks (lipids) |
|
Rosenstock (2002)235 (PIO 014 study group) USA |
Focus: Effect of two doses of PIO (15 or 30 mg) in combination with a stable insulin regimen to improve glycaemic control in patients whose type 2 diabetes is poorly controlled despite current insulin therapy Design: Double-blind, placebo-controlled RCT, multicentre Duration: 16 weeks Follow-up: No postintervention follow-up Funding: Takeda Pharmaceuticals |
Total number: 566 N PIO15 + Ins: 191; 161 completed the trial N PIO30 + Ins: 188; 172 completed the trial N P + Ins: 187; 164 completed the trial Inclusion criteria: 30–75 years, type 2 diabetes; insulin treatment for ≥ 30 units/day for ≥ 4 months, with stable dosage for at least 30 days; at screening HbA1c ≥ 8.0%, fasting C-peptide > 0.7 µg/L Exclusion criteria: History of ketoacidosis, unstable or rapidly progressive diabetic retinopathy, nephropathy or neuropathy; impaired hepatic function (AST, ALT, total bilirubin or alkaline phosphatase > 2.5 times upper limit of normal); impaired kidney function (serum creatinine > 1.8 mg/dl); anaemia; unstable or symptomatic cardiovascular or cerebrovascular conditions (defined) Age: PIO15 + Ins, 56.9 years (SE 10.4); PIO30 + Ins, 57.5 years (SE 9.9); P + Ins, 56.7 years (SE 9.4) Gender: PIO15 + Ins, 53.9% female; PIO30 + Ins, 49.5% female; P + Ins, 54.5% female BMI: PIO15 + Ins, 33.2 kg/m2 (SE 5.4 ); PIO30 + Ins, 34.3 kg/m2 (SE 6.2); P + Ins, 33.2 kg/m2 (SE 5.2) Ethnicity: PIO15 + Ins, 74.9% Caucasian; PIO30 + Ins, 73.4% Caucasian; P + Ins: 71.1% Caucasian Diabetes duration: Not reported Previous medication: 88% insulin monotherapy; 12% combination with oral agents (8% MET, 2% glyburide, 2% glipizide); 134 patients receiving serum lipid-reducing agent (classes approximately evenly distributed across groups) Comorbidities: Not reported Subgroups: None |
N PIO15 + Ins: 15 mg PIO plus usual insulin regimen N PIO30 + Ins: 30 mg PIO plus usual insulin regimen N P + Ins: Placebo plus usual insulin regimen All: Insulin dose could be decreased in response to hypoglycaemia; maximum permitted decrease in insulin dose at any one time: 10% of patient’s current total daily dosage; reduced dose remained fixed unless new occurrences of hypoglycaemia warranted another 10% decrease Cointerventions: Lipid-lowering medications allowed, provided patient had been taking stable dose for > 60 days and regimen was continued without alteration throughout the study; no dietary intervention/modification Adherence assessment: No Screening phase: 2 weeks – patients on OHA in addition to insulin discontinued oral agent at beginning of screening period; screening followed by one week (for patients on stable insulin monotherapy) or 4 weeks (for patients previously on insulin plus oral agents) single-blind placebo treatment period (stable insulin regimen in combination with placebo) |
Primary: Unclear, presumably HbA1c at study end point HbA1c: Yes Hypoglycaemia: Yes; defined as FPG ≤ 100 mg/dl (5.6 mmol/l) on two occasions symptoms of hypoglycaemia not explained by other conditions Glycaemic excursions: No Total daily dose: Yes Weight change: Yes Complication rates: No Adverse events: Yes; laboratory values, vital signs, ECGs, any adverse events Health-related QoL: No Other: Serum lipid measurements (triglycerides and cholesterol) Timing of assessment: Patients seen every 4 weeks |
|
Scheen (2006) 236 19 European countries Part of PROactive trial (investigating only patients concomitantly treated with insulin) Abstract only |
Focus: Effects of PIO on the secondary prevention of macrovascular events in type 2 diabetes Design: Randomised double-blind outcome study, multicentre Duration: Mean 34.5 months Follow-up: No postintervention follow-up Funding: Takeda Europe, Eli Lilly |
Total number: 1760 N PIO + Ins: 864 N P + Ins: 896 Inclusion criteria: Male or female with type 2 diabetes; age 35–75 years; HbA1c level above the upper limit of normal (local equivalent of 6.5% for a DCCT-traceable assay), despite management of diabetes with diet alone or with oral BG-lowering agents; increased risk of macrovascular disease as defined in the trial; insulin allowed if given in combination with oral agents Exclusion criteria: Current use of PIO or any other TZDs; signs of type 1 diabetes; insulin as sole therapy for diabetes; planned revascularisation; symptomatic heart failure; leg ulcers, gangrene, or pain at rest; haemodialysis; significantly impaired hepatic function (serum ALT > 2.5 times upper limit of normal) Age: Not reported for subgroup on insulin therapy Gender: Not reported for subgroup on insulin therapy BMI: Not reported for subgroup on insulin therapy Ethnicity: Not reported for subgroup on insulin therapy Diabetes duration: Not reported for subgroup on insulin therapy Previous medication: At baseline, insulin combined with MET monotherapy in 53%, SFU monotherapy in 24%, dual therapy with MET and SFU 12% Comorbidities: Not reported Subgroups: Abstract reports subgroup of larger trial – in the main trial only about one-third of patients received concomitant insulin therapy |
PIO + Ins: PIO plus previous treatment; forced titration phase in the first 2 months of treatment, with stepwise increase of PIO dose from 15 to 30 mg and then up to 45 mg, to maintain patients at maximum tolerated dose; dose could be adjusted at any time within 15 to 45 mg range, based on tolerability P + Ins: Placebo plus previous treatment Both: Investigators encouraged to maintain glycaemia at < 6.5% Cointerventions: Proportion of concomitant oral therapy remained similar: PIO + Ins, MET alone 47%, SFU alone 16%, MET plus SFU 10%; P + Ins, MET alone 52%, SFU alone 16%, MET plus SFU 11% Adherence assessment: No Screening phase: Not reported |
Primary: (of PROactive trial) Time from randomisation to any of (composite end point): all-cause mortality, non-fatal MI, acute coronary syndrome, cardiac intervention (including coronary artery bypass graft or percutaneous coronary intervention), stroke, major leg amputation (above ankle), bypass surgery; or revascularisation in the leg HbA1c: Yes Hypoglycaemia: Yes (but undefined) Glycaemic excursions: No Total daily dose: Yes Weight change: No Complication rates: Not reported here Adverse events: Yes Health-related QoL: No Other: None (in this abstract) Timing of assessment: Unclear |
|
Shah (2007) 237 USA Abstract only |
Focus: Effects of a PIO and insulin combination vs insulin therapy alone on body fat distribution Design: Randomised double-blind placebo-controlled trial, single centre Duration: 12–16 weeks Follow-up: No postintervention follow-up Setting: Unclear Funding: Not stated |
Total number: 25 N PIO + Ins: 12 N P + Ins: 13 Inclusion criteria: Insulin-treated, obese type 2 diabetes patients Exclusion criteria: Not reported Age: Not reported Gender: Not reported BMI: 36.5 kg/m2 Ethnicity: Not reported Diabetes duration: Not reported Previous medication: Not reported Comorbidities: Not reported Subgroups: None |
PIO + Ins: PIO (30 mg titrated to 45 mg) and insulin P + Ins: Placebo and insulin Cointerventions: Not reported Adherence assessment: Not reported |
Primary: Body fat distribution HbA1c: HbA1c Hypoglycaemia: No Glycaemic excursions: No Total daily dose: No Weight change: Yes Complication rates: No Adverse events: No Health-related QoL: No Other: Subcutaneous adipose tissue, visceral adipose tissue (abdominal CT scans) Timing of assessment: Not reported |
Appendix 7 Characteristics of included trials – pioglitazone + insulin vs pioglitazone
| Study | Design | Participants | Interventions | Outcome measures |
|---|---|---|---|---|
|
USA Abstract only |
Focus: Safety and efficacy of BIAsp 30 (30% soluble and 70% protaminated insulin aspart) in insulin-naive type 2 diabetes patients taking any two OAD agents Design: Randomised, parallel group trial, single/multicentre unclear Duration: 34 weeks Follow-up: No postintervention follow-up Funding: Novo Nordisk |
Total number: 181 N BIAsp 30 + MET + PIO: 93 N MET + PIO: 88 Inclusion criteria: Insulin naive, type 2 diabetes; HbA1c 7.5–12%, taking any two OAD agents Exclusion criteria: Not reported Age: Not reported Gender: Not reported BMI: Not reported Ethnicity: Not reported Diabetes duration: Not reported Previous medication: Not reported Comorbidities: Not reported Subgroups: None |
BIAsp 30 + MET + PIO: BIAsp 30 (30% soluble and 70% protaminated insulin aspart) added to an optimised treatment of MET and PIO; BIAsp 30 initiated at 6 U twice a day (pre-breakfast and pre-supper) and titrated to target BG (4.4–6.1 mmol/l) by an algorithm-directed forced titration MET + PIO: Optimised treatment of MET and PIO without insulin Cointerventions: Not reported Adherence assessment: Not reported Run-in phase: 8-week run-in – treatment changed to MET (2500 mg/day) and PIO (30 or 45 mg/day) |
Primary: HbA1c (presumably) HbA1c: Yes Hypoglycaemia: Minor hypoglycaemia (BG < 3.1 mmol/l) Glycaemic excursions: No Total daily dose: No Weight change: Weight Complication rates: No Adverse events: Yes Health-related QoL: No Other: None Timing of assessment: Not reported |
Appendix 8 Pair-wise comparisons
Male BMI 30
| Comparison 1: EXE_GLA vs GLA | No comparison | With comparison | ||||
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.607 | 8.538 | 0.069 | 8.394 | 8.331 | 0.063 |
| Total QALYs | 8.567 | 8.464 | 0.103 | 8.354 | 8.258 | 0.096 |
| Direct drug cost (£) | 8813 | 7939 | 875 | 8592 | 7727 | 865 |
| Total cost (£) | 18,953 | 18,258 | 696 | 19,469 | 18,778 | 691 |
| ICER | 6755 | 7180 | ||||
| Comparison 2: SIT vs ROSI | No comparison | With comparison | ||||
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 8.566 | 8.549 | 0.017 | 8.347 | 8.342 | 0.005 |
| Total QALYs | 8.479 | 8.447 | 0.032 | 8.263 | 8.242 | 0.021 |
| Direct drug cost (£) | 5793 | 5938 | –145 | 5628 | 5779 | –151 |
| Total cost (£) | 16,083 | 16,277 | –194 | 16,650 | 16,853 | –203 |
| ICER | –6055 | –9849 | ||||
| Comparison 3: VIL vs PIO | No comparison | With comparison | ||||
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 8.561 | 8.590 | –0.029 | 8.353 | 8.378 | –0.025 |
| Total QALYs | 8.468 | 8.479 | –0.011 | 8.262 | 8.269 | –0.007 |
| Direct drug cost (£) | 5371 | 5824 | –453 | 5220 | 5665 | –445 |
| Total cost (£) | 15,731 | 16,180 | –449 | 16,309 | 16,756 | –446 |
| ICER | 39,846 | 66,799 | ||||
| Comparison 4: GLA vs NPH | No comparison | With comparison | ||||
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 8.538 | 8.540 | –0.002 | 8.331 | 8.333 | –0.003 |
| Total QALYs | 8.464 | 8.457 | 0.007 | 8.258 | 8.253 | 0.006 |
| Direct drug cost (£) | 7939 | 6111 | 1828 | 7727 | 5946 | 1780 |
| Total cost (£) | 18,258 | 16,402 | 1855 | 18,778 | 16,980 | 1798 |
| ICER | 281,349 | 320,029 | ||||
| Comparison 5: DET vs NPH | No comparison | With comparison | ||||
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 8.530 | 8.540 | –0.010 | 8.316 | 8.333 | –0.018 |
| Total QALYs | 8.472 | 8.457 | 0.015 | 8.259 | 8.253 | 0.006 |
| Direct drug cost (£) | 8826 | 6111 | 2715 | 8585 | 5946 | 2638 |
| Total cost (£) | 19,128 | 16,402 | 2726 | 19,621 | 16,980 | 2641 |
| ICER | 187,726 | 417,625 | ||||
Male BMI 30 but no weight changes within UKPDS Outcomes Model
| Comparison 1: EXE_GLA vs GLA | No comparison | With comparison | ||||
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.599 | 8.547 | 0.053 | 8.386 | 8.338 | 0.048 |
| Total QALYs | 8.559 | 8.472 | 0.087 | 8.347 | 8.265 | 0.082 |
| Direct drug cost (£) | 8808 | 7945 | 863 | 8587 | 7732 | 856 |
| Total cost (£) | 18,999 | 18,222 | 777 | 19,513 | 18,740 | 773 |
| ICER | 8967 | 9449 | ||||
| Comparison 2: SIT vs ROSI | No comparison | With comparison | ||||
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 8.562 | 8.562 | 0.000 | 8.354 | 8.353 | 0.001 |
| Total QALYs | 8.476 | 8.460 | 0.015 | 8.269 | 8.253 | 0.016 |
| Direct drug cost (£) | 5790 | 5947 | –157 | 5632 | 5787 | –154 |
| Total cost (£) | 16,089 | 16,272 | –183 | 16,670 | 16,848 | –178 |
| ICER | –11,878 | –11,011 | ||||
| Comparison 3: VIL vs PIO | No comparison | With comparison | ||||
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 8.562 | 8.603 | –0.041 | 8.354 | 8.389 | –0.035 |
| Total QALYs | 8.469 | 8.492 | –0.023 | 8.263 | 8.279 | –0.017 |
| Direct drug cost (£) | 5371 | 5833 | –461 | 5221 | 5672 | –451 |
| Total cost (£) | 15,745 | 16,191 | –446 | 16,325 | 16,763 | –438 |
| ICER | 19,477 | 26,270 | ||||
| Comparison 4: GLA vs NPH | No comparison | With comparison | ||||
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 8.547 | 8.550 | –0.004 | 8.338 | 8.341 | –0.003 |
| Total QALYs | 8.472 | 8.468 | 0.005 | 8.265 | 8.261 | 0.005 |
| Direct drug cost (£) | 7945 | 6118 | 1826 | 7732 | 5952 | 1780 |
| Total cost (£) | 18,222 | 16,389 | 1833 | 18,740 | 16,958 | 1782 |
| ICER | 387,629 | 379,631 | ||||
| Comparison 5: DET vs NPH | No comparison | With comparison | ||||
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 8.535 | 8.550 | –0.015 | 8.329 | 8.341 | –0.012 |
| Total QALYs | 8.477 | 8.468 | 0.009 | 8.272 | 8.261 | 0.012 |
| Direct drug cost (£) | 8831 | 6118 | 2713 | 8598 | 5952 | 2646 |
| Total cost (£) | 19,132 | 16,389 | 2743 | 19,638 | 16,958 | 2680 |
| ICER | 303,770 | 226,163 | ||||
Female BMI 30
| Comparison 1: EXE_GLA vs GLA | No comparison | With comparison | ||||
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 9.468 | 9.397 | 0.071 | 9.210 | 9.148 | 0.062 |
| Total QALYs | 9.423 | 9.318 | 0.105 | 9.167 | 9.071 | 0.096 |
| Direct drug cost (£) | 9394 | 8385 | 1010 | 9140 | 8143 | 997 |
| Total cost (£) | 19,436 | 18,598 | 838 | 19,969 | 19,138 | 831 |
| ICER | 7970 | 8653 | ||||
| Comparison 2: SIT vs ROSI | No comparison | With comparison | ||||
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 9.436 | 9.402 | 0.034 | 9.175 | 9.153 | 0.022 |
| Total QALYs | 9.344 | 9.294 | 0.050 | 9.085 | 9.047 | 0.038 |
| Direct drug cost (£) | 6244 | 6379 | –135 | 6053 | 6195 | –142 |
| Total cost (£) | 16,415 | 16,568 | –153 | 17,003 | 17,178 | –175 |
| ICER | –3079 | –4604 | ||||
| Comparison 3: VIL vs PIO | No comparison | With comparison | ||||
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 9.428 | 9.427 | 0.000 | 9.175 | 9.176 | –0.001 |
| Total QALYs | 9.328 | 9.310 | 0.019 | 9.078 | 9.061 | 0.017 |
| Direct drug cost (£) | 5824 | 6265 | –441 | 5646 | 6082 | –437 |
| Total cost (£) | 15,959 | 16,502 | –543 | 16,581 | 17,112 | –531 |
| ICER | –29,027 | –30,976 | ||||
| Comparison 4: GLA vs NPH | No comparison | With comparison | ||||
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 9.397 | 9.395 | 0.002 | 9.148 | 9.147 | 0.002 |
| Total QALYs | 9.318 | 9.308 | 0.010 | 9.071 | 9.061 | 0.010 |
| Direct drug cost (£) | 8385 | 6497 | 1887 | 8143 | 6308 | 1835 |
| Total cost (£) | 18,598 | 16,742 | 1856 | 19,138 | 17,341 | 1797 |
| ICER | 177,940 | 179,074 | ||||
| Comparison 5: DET vs NPH | No comparison | With comparison | ||||
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 9.398 | 9.395 | 0.002 | 9.146 | 9.147 | –0.001 |
| Total QALYs | 9.335 | 9.308 | 0.027 | 9.085 | 9.061 | 0.024 |
| Direct drug cost (£) | 9310 | 6497 | 2812 | 9039 | 6308 | 2732 |
| Total cost (£) | 19,538 | 16,742 | 2796 | 20,048 | 17,341 | 2706 |
| ICER | 102,007 | 113,988 | ||||
Male BMI 35
| Comparison 1: EXE_GLA vs GLA | No comparison | With comparison | ||||
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 8.533 | 8.448 | 0.085 | 8.328 | 8.252 | 0.076 |
| Total QALYs | 8.493 | 8.375 | 0.118 | 8.289 | 8.180 | 0.109 |
| Direct drug cost (£) | 9958 | 9863 | 96 | 9703 | 9612 | 91 |
| Total cost (£) | 20,311 | 20,360 | –49 | 20,787 | 20,844 | –57 |
| ICER | –413 | –522 | ||||
| Comparison 2: SIT vs ROSI | No comparison | With comparison | ||||
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 8.485 | 8.473 | 0.012 | 8.285 | 8.274 | 0.011 |
| Total QALYs | 8.399 | 8.371 | 0.028 | 8.201 | 8.174 | 0.027 |
| Direct drug cost (£) | 6619 | 6767 | –148 | 6438 | 6586 | –147 |
| Total cost (£) | 17,165 | 17,363 | –198 | 17,712 | 17,906 | –194 |
| ICER | –7090 | –7254 | ||||
| Comparison 3: VIL vs PIO | No comparison | With comparison | ||||
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 8.490 | 8.504 | –0.014 | 8.288 | 8.302 | –0.014 |
| Total QALYs | 8.397 | 8.393 | 0.004 | 8.198 | 8.194 | 0.004 |
| Direct drug cost (£) | 6111 | 6552 | –441 | 5937 | 6374 | –436 |
| Total cost (£) | 16,717 | 17,095 | –378 | 17,264 | 17,656 | –392 |
| ICER | –100,734 | –98,356 | ||||
| Comparison 4: GLA vs NPH | No comparison | With comparison | ||||
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 8.448 | 8.443 | 0.005 | 8.252 | 8.250 | 0.002 |
| Total QALYs | 8.375 | 8.361 | 0.013 | 8.180 | 8.169 | 0.010 |
| Direct drug cost (£) | 9863 | 7349 | 2514 | 9612 | 7162 | 2450 |
| Total cost (£) | 20,360 | 17,857 | 2503 | 20,844 | 18,415 | 2429 |
| ICER | 189,400 | 233,187 | ||||
| Comparison 5: DET vs NPH | No comparison | With comparison | ||||
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 8.445 | 8.443 | 0.001 | 8.249 | 8.250 | –0.001 |
| Total QALYs | 8.387 | 8.361 | 0.025 | 8.192 | 8.169 | 0.023 |
| Direct drug cost (£) | 11,084 | 7349 | 3734 | 10,803 | 7162 | 3641 |
| Total cost (£) | 21,579 | 17,857 | 3722 | 22,043 | 18,415 | 3627 |
| ICER | 146,632 | 157,478 | ||||
Female BMI 35
| Comparison 1: EXE_GLA vs GLA | No comparison | With comparison | ||||
| Exenatide | Glargine | Net | Exenatide | Glargine | Net | |
| UKPDS QALYs | 9.391 | 9.306 | 0.085 | 9.143 | 9.069 | 0.074 |
| Total QALYs | 9.346 | 9.227 | 0.119 | 9.099 | 8.991 | 0.108 |
| Direct drug cost (£) | 10,645 | 10,388 | 257 | 10,350 | 10,100 | 249 |
| Total cost (£) | 20,907 | 20,781 | 126 | 21,396 | 21,289 | 107 |
| ICER | 1058 | 988 | ||||
| Comparison 2: SIT vs ROSI | No comparison | With comparison | ||||
| Sitagliptin | Rosiglitazone | Net | Sitagliptin | Rosiglitazone | Net | |
| UKPDS QALYs | 9.350 | 9.329 | 0.021 | 9.105 | 9.087 | 0.018 |
| Total QALYs | 9.258 | 9.222 | 0.037 | 9.015 | 8.981 | 0.034 |
| Direct drug cost (£) | 7138 | 7282 | –144 | 6925 | 7069 | –144 |
| Total cost (£) | 17,542 | 17,769 | –227 | 18,121 | 18,335 | –214 |
| ICER | –6205 | –6315 | ||||
| Comparison 3: VIL vs PIO | No comparison | With comparison | ||||
| Vildagliptin | Pioglitazone | Net | Vildagliptin | Pioglitazone | Net | |
| UKPDS QALYs | 9.347 | 9.343 | 0.003 | 9.103 | 9.100 | 0.004 |
| Total QALYs | 9.248 | 9.226 | 0.021 | 9.007 | 8.985 | 0.022 |
| Direct drug cost (£) | 6627 | 7065 | –439 | 6424 | 6856 | –433 |
| Total cost (£) | 16,988 | 17,458 | –470 | 17,598 | 18,047 | –449 |
| ICER | –21,965 | –20,618 | ||||
| Comparison 4: GLA vs NPH | No comparison | With comparison | ||||
| Glargine | NPH | Net | Glargine | NPH | Net | |
| UKPDS QALYs | 9.306 | 9.303 | 0.003 | 9.069 | 9.065 | 0.003 |
| Total QALYs | 9.227 | 9.216 | 0.012 | 8.991 | 8.980 | 0.012 |
| Direct drug cost (£) | 10,388 | 7796 | 2592 | 10,100 | 7576 | 2524 |
| Total cost (£) | 20,781 | 18,208 | 2572 | 21,289 | 18,792 | 2497 |
| ICER | 219,805 | 212,009 | ||||
| Comparison 5: DET vs NPH | No comparison | With comparison | ||||
| Detemir | NPH | Net | Detemir | NPH | Net | |
| UKPDS QALYs | 9.313 | 9.303 | 0.010 | 9.071 | 9.065 | 0.006 |
| Total QALYs | 9.250 | 9.216 | 0.034 | 9.010 | 8.980 | 0.030 |
| Direct drug cost (£) | 11,663 | 7796 | 3867 | 11,336 | 7576 | 3760 |
| Total cost (£) | 22,135 | 18,208 | 3926 | 22,592 | 18,792 | 3800 |
| ICER | 114,229 | 125,938 | ||||
List of abbreviations
- ADA
- American Diabetes Association
- ADOPT
- A Diabetes Outcome Progression Trial
- BIAsp 30
- biphasic insulin aspart 30
- BMI
- body mass index
- BNF
- British National Formulary
- CADTH
- Canadian Agency for Drugs and Technologies in Health
- CG
- clinical guideline
- CHF
- chronic heart failure
- CI
- confidence interval
- CORE
- Center for Outcomes Research
- CSII
- continuous subcutaneous insulin infusion
- DAFNE
- Dose Adjustment For Normal Eating
- DAWN
- Diabetes Attitude Wishes and Need
- DCCT
- Diabetes Control and Complications Trial
- DPP-4
- dipeptidyl peptidase-4
- DSC-R
- Diabetes Symptom Checklist-Revised
- EASD
- European Association for the Study of Diabetes
- EMEA
- European Medicines Evaluation Agency
- EQ-5D
- European Quality of Life-5 Dimensions
- FBG
- fasting blood glucose
- FDA
- Food and Drug Administration
- FPG
- fasting plasma glucose
- GDG
- Guideline Development Group
- GLP-1
- glucagon-like peptide-1
- HbA1c
- glycated haemoglobin
- HDL
- high-density lipoprotein
- HFS
- Hypoglycaemia Fear Survey
- HOMA-beta
- homeostasis model assessment beta
- HR
- hazard ratio
- ICER
- incremental cost-effectiveness ratio
- IDF
- International Diabetes Federation
- IFG
- impaired fasting glucose
- IGT
- impaired glucose tolerance
- ISPOR
- International Society For Pharmacoeconomics and Outcomes Research
- ITT
- intention to treat
- IU
- International Unit
- LAR
- long-acting release
- LDL
- low-density lipoprotein
- LEAD
- Liraglutide Effect and Action in Diabetes
- MDI
- multiple daily injection
- MHRA
- Medicines and Healthcare Products Regulatory Agency
- MI
- myocardial infarction
- MTRAC
- The Midlands Therapeutics Reviews and Advisory Committee
- NICE
- National Institute for Health and Clinical Excellence
- NPH
- Neutral Protamine Hagedorn
- OAD
- oral antidiabetic
- OGLA
- oral glucose-lowering agent
- OHA
- oral antihyperglycaemic agent
- OR
- odds ratio
- PG
- plasma glucose
- PGWB
- Psychological General Well-Being Index
- PPAR-g
- peroxisome proliferator-activated receptor-g
- PSSRU
- Personal Social Services Research Unit
- PSU
- Prescribing Support Unit
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCPE
- Royal College of Physicians of Edinburgh
- RCT
- randomised controlled trial
- RR
- relative risk
- SBP
- systolic blood pressure
- SD
- standard deviation
- SE
- standard error
- SF-36
- Short Form questionnaire-36 items
- SMC
- Scottish Medicines Consortium
- TA
- technology appraisal
- TAR
- technology assessment report
- TFS
- Treatment Flexibility Scale
- THIN
- The Health Improvement Network
- TZD
- thiazolidinedione
- UKPDS
- United Kingdom Prospective Diabetes Study
- UTI
- urinary tract infection
- VAS
- visual analogue scale
- VLDL
- very-low-density lipoprotein
- WMD
- weighted mean difference
- YHPHO
- York and Humber Public Health Observatory
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Riemsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
-
Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review.
By McDaid C, Maund E, Rice S, Wright K, Jenkins B, Woolacott N.
-
A systematic review of outcome measures used in forensic mental health research with consensus panel opinion.
By Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al.
-
The clinical effectiveness and cost-effectiveness of topotecan for small cell lung cancer: a systematic review and economic evaluation.
By Loveman E, Jones J, Hartwell D, Bird A, Harris P, Welch K, et al.
-
Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The Screening for Haemoglobinopathies in First Trimester (SHIFT) trial.
By Dormandy E, Bryan S, Gulliford MC, Roberts T, Ades T, Calnan M, et al.
-
Early referral strategies for management of people with markers of renal disease: a systematic review of the evidence of clinical effectiveness, cost-effectiveness and economic analysis.
By Black C, Sharma P, Scotland G, McCullough K, McGurn D, Robertson L, et al.
-
A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with Type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and Psychological Therapies (ADaPT) study.
By Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al.
-
A randomised controlled equivalence trial to determine the effectiveness and cost–utility of manual chest physiotherapy techniques in the management of exacerbations of chronic obstructive pulmonary disease (MATREX).
By Cross J, Elender F, Barton G, Clark A, Shepstone L, Blyth A, et al.
-
A systematic review and economic evaluation of the clinical effectiveness and cost-effectiveness of aldosterone antagonists for postmyocardial infarction heart failure.
By McKenna C, Burch J, Suekarran S, Walker S, Bakhai A, Witte K, et al.
-
Avoiding and identifying errors in health technology assessment models: qualitative study and methodological review.
By Chilcott JB, Tappenden P, Rawdin A, Johnson M, Kaltenthaler E, Paisley S, et al.
-
BoTULS: a multicentre randomised controlled trial to evaluate the clinical effectiveness and cost-effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A.
By Shaw L, Rodgers H, Price C, van Wijck F, Shackley P, Steen N, et al. , on behalf of the BoTULS investigators.
-
Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project.
By Baker R, Bateman I, Donaldson C, Jones-Lee M, Lancsar E, Loomes G, et al.
-
Cetuximab for the first-line treatment of metastatic colorectal cancer.
By Meads C, Round J, Tubeuf S, Moore D, Pennant M and Bayliss S.
-
Infliximab for the treatment of acute exacerbations of ulcerative colitis.
By Bryan S, Andronis L, Hyde C, Connock M, Fry-Smith A and Wang D.
-
Sorafenib for the treatment of advanced hepatocellular carcinoma.
By Connock M, Round J, Bayliss S, Tubeuf S, Greenheld W and Moore D.
-
Tenofovir disoproxil fumarate for the treatment of chronic hepatitis B infection.
By Jones J, Colquitt J, Shepherd J, Harris P and Cooper K.
-
Prasugrel for the treatment of acute coronary artery syndromes with percutaneous coronary intervention.
By Greenhalgh J, Bagust A, Boland A, Saborido CM, Fleeman N, McLeod C, et al.
-
Alitretinoin for the treatment of severe chronic hand eczema.
By Paulden M, Rodgers M, Griffin S, Slack R, Duffy S, Ingram JR, et al.
-
Pemetrexed for the first-line treatment of locally advanced or metastatic non-small cell lung cancer.
By Fleeman N, Bagust A, McLeod C, Greenhalgh J, Boland A, Dundar Y, et al.
-
Topotecan for the treatment of recurrent and stage IVB carcinoma of the cervix.
By Paton F, Paulden M, Saramago P, Manca A, Misso K, Palmer S, et al.
-
Trabectedin for the treatment of advanced metastatic soft tissue sarcoma.
By Simpson EL, Rafia R, Stevenson MD, Papaioannou D.
-
Azacitidine for the treatment of myelodysplastic syndrome, chronic myelomonocytic leukaemia and acute myeloid leukaemia.
By Edlin R, Connock M, Tubeuf S, Round J, Fry-Smith A, Hyde C, et al.
-
The safety and effectiveness of different methods of earwax removal: a systematic review and economic evaluation.
By Clegg AJ, Loveman E, Gospodarevskaya E, Harris P, Bird A, Bryant J, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection in women and men.
By Hislop J, Quayyum Z, Flett G, Boachie C, Fraser C, Mowatt G.
-
School-linked sexual health services for young people (SSHYP): a survey and systematic review concerning current models, effectiveness, cost-effectiveness and research opportunities.
By Owen J, Carroll C, Cooke J, Formby E, Hayter M, Hirst J, et al.
-
Systematic review and cost-effectiveness evaluation of ‘pill-in-the-pocket’ strategy for paroxysmal atrial fibrillation compared to episodic in-hospital treatment or continuous antiarrhythmic drug therapy.
By Martin Saborido C, Hockenhull J, Bagust A, Boland A, Dickson R, Todd D.
-
Chemoprevention of colorectal cancer: systematic review and economic evaluation.
By Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, et al.
-
Cross-trimester repeated measures testing for Down’s syndrome screening: an assessment.
By Wright D, Bradbury I, Malone F, D’Alton M, Summers A, Huang T, et al.
-
Exploring the needs, concerns and behaviours of people with existing respiratory conditions in relation to the H1N1 ‘swine influenza’ pandemic: a multicentre survey and qualitative study.
By Caress A-L, Duxbury P, Woodcock A, Luker KA, Ward D, Campbell M, et al.
-
Influenza A/H1N1v in pregnancy: an investigation of the characteristics and management of affected women and the relationship to pregnancy outcomes for mother and infant.
By Yates L, Pierce M, Stephens S, Mill AC, Spark P, Kurinczuk JJ, et al.
-
The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK.
By Rubin GJ, Potts HWW, Michie S.
-
The impact of illness and the impact of school closure on social contact patterns.
By Eames KTD, Tilston NL, White PJ, Adams E, Edmunds WJ.
-
Vaccine effectiveness in pandemic influenza – primary care reporting (VIPER): an observational study to assess the effectiveness of the pandemic influenza A (H1N1)v vaccine.
By Simpson CR, Ritchie LD, Robertson C, Sheikh A, McMenamin J.
-
Physical interventions to interrupt or reduce the spread of respiratory viruses: a Cochrane review.
By Jefferson T, Del Mar C , Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al.
-
Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR).
By Peek GJ, Elbourne D, Mugford M, Tiruvoipati R, Wilson A, Allen E, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Consultant Adviser, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of NETSCC External Relations
-
Ms Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Warwick Clinical Trials Unit
-
Director, Nottingham Clinical Trials Unit
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Ms Kay Pattison, NHS R&D Programme/DH, Leeds
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Mr A S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital
-
Dr Dianne Baralle, Consultant & Senior Lecturer in Clinical Genetics, Human Genetics Division & Wessex Clinical Genetics Service, Southampton, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Service User Representative
-
Professor Anthony Robert Kendrick, Professor of Primary Medical Care, University of Southampton
-
Dr Susanne M Ludgate, Director, Medical Devices Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr David Mathew Service User Representative
-
Dr Michael Millar, Lead Consultant in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, University College London
-
Mrs Una Rennard, Service User Representative
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr W Stuart A Smellie, Consultant, Bishop Auckland General Hospital
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Alan J Williams, Consultant in General Medicine, Department of Thoracic Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist Commissioning Advisory Group (NSCAG), Department of Health
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook Clinical Programmes Director, Bazian Ltd, London
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr Colin Greaves Senior Research Fellow, Peninsular Medical School (Primary Care)
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Miss Nicky Mullany, Service User Representative
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Service User Representative
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust, Bristol
-
Reader in Wound Healing and Director of Research, University of Leeds, Leeds
-
Professor Bipin Bhakta Charterhouse Professor in Rehabilitation Medicine, University of Leeds, Leeds
-
Mrs Penny Calder Service User Representative
-
Professor Paul Carding, Professor of Voice Pathology, Newcastle Hospital NHS Trust, Newcastle
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry, London
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol, Bristol
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and the London School of Medicine and Dentistry, London
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester, Manchester
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham, Nottingham
-
Dr Kate Radford, Division of Rehabilitation and Ageing, School of Community Health Sciences. University of Nottingham, Nottingham
-
Mr Jim Reece, Service User Representative
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton, Southampton
-
Dr Pippa Tyrrell, Stroke Medicine, Senior Lecturer/Consultant Stroke Physician, Salford Royal Foundation Hospitals’ Trust, Salford
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford, Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University, Cardiff
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health , London
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Dr Ursula Wells PRP, DH, London
Interventional Procedures Panel
-
Consultant Surgeon & Honorary Clinical Lecturer, University of Sheffield
-
Mr David P Britt, Service User Representative, Cheshire
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Nadim Malik, Consultant Cardiologist/ Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Mr Michael Thomas, Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Mrs Isabel Boyer, Service User Representative, London
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Professor Robin Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Service User Representative, Gloucestershire
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician & Cardiologist, County Durham & Darlington Foundation Trust
-
Mr John Needham, Service User, Buckingmashire
-
Ms Mary Nettle, Mental Health User Consultant, Gloucestershire
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Howard Ring, Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry & Warwickshire Partnership Trust
-
Dr Alastair Sutcliffe, Senior Lecturer, University College London
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Professor Tom Walley, HTA Programme Director, Liverpool
-
Dr Ursula Wells, Policy Research Programme, DH, London
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington