Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 03/39/13. The contractual start date was in June 2005. The draft report began editorial review in January 2010 and was accepted for publication in September 2010. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© 2011 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2011 Queen’s Printer and Controller of HMSO
Chapter 1 Background and rationale
Children with cancer
The study took place under the auspices of the UK Children’s Cancer Study Group [UKCCSG, now the Children’s Cancer and Leukaemia Group (CCLG)]. Approximately 1500 children (up to the age of 15 years) are diagnosed with cancer in the UK every year, and leukaemia accounts for around 30% of these diagnoses. Approximately 90% of children with a cancer diagnosis in the UK are treated in a CCLG centre (www.cclg.org.uk).
The duration of treatment for cancer varies but is usually < 2 years. The majority of children are able to spend a large proportion of this time outside hospital in the community. Most children have a central venous catheter (CVC) inserted into a large vein, which remains in place for many months. This allows treatment to be given at home, or in hospital for more intensive treatment, while minimising interference with daily life. These devices are usually either tunnelled catheters (e.g. the Hickman catheter) or subcutaneous ports. After treatment, > 70% will eventually be cured of cancer (www.cclg.org.uk). However, infection is a major hazard for children undergoing treatment for cancer. Most will be admitted to hospital at least once for infection during their treatment for cancer. The dilemma facing clinicians is to distinguish between infections due to the CVC and other sources.
Diagnosis of central venous catheter-associated infection
Widespread use of CVCs has led to these devices becoming recognised as a major risk factor for hospital-acquired bloodstream infection in adults and children. 1–4 The rate of infection associated with CVCs varies from < 1 to 15 episodes per 1000 days of central line use, depending upon the patient population and a range of other factors. 5 The rate of CVC-associated infection in children undergoing treatment for cancer varies from 1.7 to > 5 per 1000 CVC days. 3,6,7 Complications include septic thrombophlebitis, endocarditis, septic shock and the dissemination of septic emboli. Studies in adults have reported an attributable mortality for CVC-associated infection of up to 25%, but rates for children have not been reported. 8 The cost of CVC-associated infection can be many thousands of pounds per episode, depending on the virulence of the infecting agent. 9
The CVC has been considered the source of nearly half of the episodes of bloodstream infection in some studies involving immunocompromised patients. 10,11 Discrimination between the CVC and other sources of bloodstream infection is important because treatment strategies differ. In addition to systemic antibiotics, CVC-associated infection requires either antibiotic treatment that is targeted at microbial colonisation of the CVC lumen by being left in the CVC lumen, or instilled slowly, or removal of the CVC. In children with cancer who have long-term surgically implanted CVCs, removal and reinsertion of a CVC carries operative and anaesthetic risks as well as costs, and risks using up venous access sites. It is this group of patients that particularly needs improved diagnostic methods. There is a variety of clinical and microbiological techniques for diagnosing CVC-associated infection.
CVC-associated infection is most apparent clinically when a patient with few other risk factors for infection develops signs and symptoms of infection associated with inflammation at the site of the device, or has fever, rigors, chills and/or hypotension associated with CVC manipulation (FRC), or develops septic shock. 12 A clinical diagnosis is more difficult in immunocompromised patients, in whom clinical presentation may be non-specific and there are other potential sources of infection. 13 Isolation of staphylococci or other skin bacteria from multiple blood cultures, Bacillus spp. or fungi raises the probability that the CVC is the source of infection.
In adults, a variety of culture methods are used to identify the CVC as the source of infection. These techniques include:
-
Comparison of blood cultures taken simultaneously from the CVC and a peripheral vein. Numerous studies have shown quantitative differences in the concentration of micro-organisms in blood collected through a CVC compared with blood collected from a peripheral vein when there is a CVC-associated infection. 14–16 A relatively cost-effective way of estimating the differences in microbial numbers between blood collected from a CVC and peripheral blood is to use the differential time to positivity. 17 When a blood culture bottle is continuously monitored using an automated microbial growth detection device (as is widely used in diagnostic laboratories), the time to detection of positivity is a function of microbial numbers in the inoculated blood. Assuming that the blood volumes are similar, detection of positivity in the blood drawn from the intravascular device > 2 hours before positivity in the blood drawn from the peripheral site is highly predictive of a CVC-associated infection. Other studies have shown a link between time to positivity (a marker of bacterial load) and outcome for both Staphylococcus aureus18 and Streptococcus pneumoniae19 bloodstream infections. An alternative method for quantifying organisms when there are large numbers of bacteria in blood drawn through a CVC is to use visualisation techniques such as acridine orange leucocyte cytospin staining, and this technique can provide a rapid diagnosis. 10,20 All these techniques for assessing the differential organism load are appropriate for CVCs that have been inserted for several weeks, in which CVC-associated infection is likely to be intraluminal, but less effective for detecting CVC-associated infection soon after insertion, when organisms may be colonising the outside of the catheter.
-
Comparison of blood culture samples from the CVC and CVC tip: semi-quantitative culture methods can be used to identify colonisation of a CVC once it has been removed [> 15 colony-forming units (CFUs)/ml from a 5-cm segment of the catheter tip]. 21,22 When indistinguishable isolates are cultured from blood cultures and from the device, that is strong evidence implicating the intravascular device in the aetiology of bacteraemia. 23–25
-
Other methods that have been used to diagnose intravascular device-associated infection include luminal brushing. 26,27
Rationale for the study
Many of the diagnostic techniques used in adults are not routinely feasible in children. Reliance on paired blood samples is problematic in children with cancer because of resistance by staff, patients and parents to the routine collection of peripheral blood samples. An additional problem is that children undergoing treatment for cancer frequently receive antibiotics both for prophylaxis and for treatment of infection, which reduces the reliability of diagnostic methods based on laboratory culture. CVC tip culture is not feasible because the CVC would not be removed early on in children with cancer unless the child was extremely ill. Finally, intraluminal brushing is not possible in children because of the narrow catheter gauge and the risk of dislodging thrombi. These problems have led to the development of a molecular method for the diagnosis of CVC-associated infection in children with cancer. 28
The principle underlying the molecular method is based on evidence that the concentration of bacteria and associated bacterial DNA (deoxyribonucleic acid) is high in blood drawn through a colonised CVC. The technique measures DNA that is common to all bacteria, from the 16S rDNA (ribosomal DNA) region. An advantage of the technique is that it can detect infection in patients in whom antibiotics have rendered bacteria non-viable and therefore undetectable by culture. The method has a relatively high detection level of around 10 genome copies per µl of blood (equivalent to 1000 CFUs/ml). The number of bacteria in the peripheral blood of a patient with bloodstream infection rarely exceeds 100 CFUs/ml. Previous studies have shown that a level of bacteria of 1000 CFUs/ml in blood drawn through the CVC discriminates between CVC-associated infection and infection associated with sources other than the CVC. 15 It also reduces the chances of a positive bacterial DNA test result arising as a consequence of sample contamination.
The method described in this study avoids the need for paired blood cultures from the CVC and a peripheral vein, and uses a small volume (< 2 ml) of blood that is normally discarded when the CVC is accessed. 28 The method can be automated and results can be generated within 2 hours, rather than the 48 hours required for blood culture. DNA testing therefore has the potential to lead to earlier initiation of appropriate treatment than is currently possible with reliance on blood cultures.
Overview of the study
The overall aim of our study was to improve the detection and treatment of CVC-associated bloodstream infection in children with cancer who are admitted with fever. In Chapter 2 we report the first step in this process: determination of the accuracy of bacterial DNA testing for detecting CVC-associated infection. Knowing the accuracy of the test allows us to estimate a child’s risk of CVC-associated bloodstream infection. However, to be useful, the test needs to help clinicians decide which children are most likely to benefit from different treatment options. The original plan for the study was to conduct a randomised controlled trial (RCT) comparing DNA testing with standard testing followed by treatment conditional on the test results. However, the accuracy study, and other studies, revealed no consensus about what treatment should be given. 29 We found wide variation in the types of CVC-targeted treatment offered and which children were treated. For example, the duration of ‘CVC-targeted’ treatment (e.g. antibiotic lock treatment or slow infusion) varied from 5 days in one centre to 2 weeks in another. Moreover, several centres did not offer CVC-targeted treatment at all, and none routinely removed CVCs for infection. Partly the reason for this lack of consensus relates to clinicians’ uncertainty about the evidence of what works for CVC-associated infection and whether the evidence applies to children with cancer. Information is also lacking on the prognosis, given standard care, of serious adverse events such as eventual CVC removal for infection, recurrent infection or complications of infection. In summary, it was not possible to proceed immediately to a trial. It was agreed that an evidence synthesis was required to determine how tests on admission predict adverse prognosis for children admitted with fever, what interventions are effective and which groups of patients stand to benefit most from improved detection and treatment.
The three components of the evidence synthesis are:
-
An analysis of the prognosis of serious adverse events, given standard practice (i.e. no targeted treatment for CVC-associated infection), for children admitted with suspected CVC-associated bloodstream infection. This section uses follow-up data for children included in the accuracy study (see Chapter 2) to determine the prognosis for CVC removal or recurrent infection. Our premise was that clinicians would use information from DNA results, in combination with information from the clinical history and examination and the blood culture taken on admission, to decide on whether bloodstream infection is sufficiently likely to warrant immediate treatment, and what treatment should be given.
-
An overview of the effectiveness of different treatment options for CVC-associated infection in children with cancer. This section reports systematic reviews of three intervention options and the findings of a survey of practice regarding use of antimicrobial lock solutions for preventing or treating CVC-associated infection.
-
An analysis of the clinical effectiveness of different test–treatment strategies. In this section, we compile a balance sheet of outcomes to illustrate the consequences of different test–treatment strategies.
The detailed objectives, methods and results of each of these analyses are reported in the ensuing chapters. The final chapter includes a discussion of the implications of our findings for practice and the priorities for further research.
Chapter 2 Accuracy of DNA testing for central venous catheter-associated infection in children with cancer
Introduction
In this section, we report findings from a prospective study to determine the accuracy of bacterial DNA for discriminating between children with and without a CVC-associated bloodstream infection. CVC-associated infection was measured by a composite reference standard based on blood culture results, clinical findings and clinicians’ judgement. The results of this evaluation were published in 2008. 30
Methods
The accuracy study involved eight UK paediatric oncology centres [Belfast, Bristol, Great Ormond Street (London), Liverpool, Newcastle upon Tyne, Nottingham, Royal Marsden (London) and University College Hospital (London)] and was co-ordinated by the Supportive Care Group of the CCLG. The protocol for the study was agreed by the CCLG (following a national meeting) and received ethical approval through the Trent Multicentre Research Ethics Committee (reference number 05/MRE04/23). A summary of the protocol for the study is in Appendix 1. A copy of the full protocol and ethics approval is available from the CCLG website (www.cclg.org.uk) or from the principal investigator, Mike Millar.
Participants
Eligible patients were children, adolescents or young adults aged 0–18 years who were undergoing treatment for cancer/leukaemia, or who were immunosuppressed with a severe haematological disorder. Participants had to have a tunnelled single-, double- or triple-lumen CVC or an implanted CVC port in situ, which would be required for a minimum of 3 months. Patients who failed to meet these criteria and those with untunnelled short-term CVCs were excluded. Eligible patients were invited to participate soon after insertion of a CVC or port, or at a later outpatient visit or inpatient stay (in the case of patients with existing devices).
Recruitment
Eligible patients were enrolled into the study whenever they presented with a febrile episode, defined by an axillary or ear temperature of > 38 °C for > 4 hours, or > 38 °C on two occasions > 4 hours apart within a 24-hour period, or > 38.5 °C on one occasion, or based on the oncology centre’s definition of fever. We excluded patients admitted who had received intravenous (i.v.) antimicrobial therapy during the preceding 2 weeks. Written informed consent was taken at the time of recruitment to the study from the parent/guardian or from the patient where appropriate.
Data collection
Data were collected prospectively and before the molecular tests were carried out.
Clinical data collection
Clinical data were collected at baseline (within 72 hours of fever presentation) and at 4 weeks after presentation, using standard questionnaires (see data collection sheets in Appendix 2). The baseline data sheet at 72 hours requested information concerning diagnoses, samples collected for laboratory analyses, CVC details (e.g. number of lumens), antibiotics administered, and symptoms and signs at presentation (including FRC).
The data sheet completed at 4 weeks requested the results of laboratory investigations, details of antibiotics prescribed, duration of fever, clinical response to treatment, details of CVC management (including whether the CVC was removed as part of the management of suspected CVC-associated infection), other sources of infection, specific agents of infection identified and classification, by the clinician responsible for the patient’s care, of whether the infection episode was probably, possibly or unlikely to be due to CVC-associated infection.
Clinical data sheets were returned to the CCLG data centre in Leicester, where the data were extracted and entered into an excel database (Microsoft Corporation, Redmond, WA, USA). The molecular test results and clinical databases were merged for the analysis of test performance.
Reference standard – definitions of central venous catheter-associated infection
See the protocol in Appendix 1. Febrile episodes were classified as probable, possible, unlikely or unclassifiable bacterial CVC-associated infections. The classification of the fever episodes was carried out at the CCLG data centre by staff who were unaware of the results of the 16S rDNA analyses. The definitions were agreed by clinical collaborators in CCLG centres, and broadly reflected the criteria used in the CCLG centres for defining CVC-associated infection.
Episodes were classified as probable if any of the following criteria were met:
-
two or more blood cultures collected within 72 hours of presentation that were culture-positive for a skin commensal, e.g. a coagulase-negative staphylococcus (including positive blood cultures from different lumens of the same CVC on the same or different occasions of sampling)
-
a positive blood culture from a patient with signs or symptoms of infection, and an isolate with the same identification and antibiotic susceptibility profile as that of an isolate from the CVC tip culture
-
FRC, together with a response to CVC-targeted treatment (see below*)
-
inflammation extending at least 2 cm along the tunnel from the CVC exit site in a patient with systemic signs or symptoms of infection.
Note Using these criteria, an episode of fever could be classified as probable CVC infection in the absence of a positive blood culture.
Episodes were defined as possible if:
-
a child’s clinical condition resolved in response to appropriate i.v. antibiotic treatment (according to blood culture isolate) and CVC-targeted treatment.
*CVC-targeted treatment required that all of the lumens were exposed to antibiotic treatment and/or the CVC was removed within 7 days of fever presentation. In practice, adherence to these criteria was not documented at the time, and data collection at 28 days revealed that few patients (n = 24, see Table 5) were recorded as receiving CVC-targeted therapy. These classifications may have been interpreted as a response to i.v. antibiotic therapy. A complete response to treatment was defined as resolution of fever within 5 days of the initiation of treatment, and no recurrence of fever within 5 days of discontinuing CVC-targeted treatment.
Episodes were classified as unlikely to be due to bacterial CVC-associated infection if:
-
the child showed a complete resolution of symptoms without CVC-targeted treatment for bacterial CVC-associated infection – this classification could include episodes with a positive blood culture or where the CVC was removed for a fungal CVC-associated infection (i.e. not a bacterial CVC-associated infection).
Unclassifiable episodes were defined as those that did not fit the definition of probable, possible or unlikely bacterial CVC-associated infection. These included episodes for which there was insufficient information to classify an episode, episodes in which a patient remained febrile with or without specific treatment of CVC-associated infection for > 2 weeks, and episodes in which there was recurrence of fever within 5 days of discontinuing systemic antibiotic therapy.
Episodes that were unclassifiable using the above definitions were reclassified using the classifications probable, possible, unlikely and unclassifiable, recorded by the clinician responsible for patient care at 4 weeks after episode presentation (see proforma in Appendix 2). Only those episodes unclassifiable according to the predefined criteria and clinician’s judgement were considered to be unclassifiable in the final analyses. Clinicians had access to the definitions used in the formal classification.
Collection and processing of routine samples for microbiological analyses
Routine samples were collected at the time of presentation, including blood for culture. These samples were processed in the local laboratory according to local protocols. Centres were encouraged to send CVC tips for quantitative culture, particularly if a CVC was removed for suspected CVC-associated infection. The results of these routine analyses were used to support the classification of episodes (see above).
Analysis of microbial 16S rDNA in blood samples
The laboratory analyses were carried out in a purpose-built molecular diagnostic laboratory at Barts and the London NHS Trust by staff with both training and relevant experience in performing molecular diagnostic tests. Staff were blind to the blood culture results and vice versa.
Collection of samples for quantitative 16S rDNA and other microbiological analyses
Venous blood was collected in 2-ml vacutainer tubes (Vacuette™ K3E; Becton Dickinson, Oxford, UK) from each lumen of the CVC when patients presented with fever. It is routine practice in many CCLG centres to withdraw and discard a small volume of blood before collecting blood for culture or other analyses. This ‘discard’ blood was accepted as a suitable sample for 16S rDNA analyses. Samples were stored at participating centres at ≤ –20 °C until collected in batches for transport on dry ice to the laboratory at Barts and the London NHS Trust. Routine samples were also collected at the time of presentation, including blood for culture. Centres were encouraged to send CVC tips for quantitative culture, particularly if a CVC was removed for suspected CVC-associated infection. Samples were analysed for bacterial 16S rDNA when they had been collected at fever presentation and within 72 hours of the start of i.v. antibiotic treatment. The date of sampling was recorded so that delays in sampling could be taken into account in the analysis. When the bacterial DNA concentration was > 0.5 pg/µl, the 16S rDNA region in the sample was amplified followed by sequencing of the amplified product to identify specific bacteria.
Molecular methods
The methods for the 16S rDNA assay have been described previously by Warwick et al. 28 For the purposes of this study, all extractions were performed as described below, although subsequent work is now performed using automated DNA extraction methods.
DNA extraction from clinical and control samples
DNA was extracted from 200-µl aliquots of ethylenediaminetetra-acetic acid (EDTA)-anticoagulated whole blood. Each sample was mixed with 1200 µl of freshly prepared 0.17 M ammonium chloride and incubated at room temperature for 30 minutes. Following centrifugation at 11,600 g for 10 minutes, the pellet was washed twice with 500 µl of sterile saline (0.9% w/v) and then extracted using a QIAamp™ DNA minikit (Qiagen, Hilden, Germany). The pellet was resuspended in 180 µl of Qiagen ATL (animal tissue lysis) buffer [containing EDTA and SDS (sodium dodecyl sulphate)] and exposed to six freeze–thaw cycles (cycling between –70 and +50 °C), with vortexing between cycles, before being heated in a boiling water bath for 10 minutes. The remainder of the extraction procedure was performed according to the manufacturer’s protocol. DNA was eluted in 50 µl of buffer and stored at –20 °C until analysis.
Several controls were run routinely with each batch of tests. These included blood samples from a healthy individual with and without spiking with bacteria. An extraction control of blood spiked with 103 CFUs of Staphylococcus epidermidis/µl was found to yield DNA levels close to the lower limit of detection. Bacterial DNA controls containing known amounts of bacterial DNA extracted from Enterococcus faecalis (100 pg to 100 fg) and a negative control (with no DNA in the reaction) to detect reagent contamination), were also included in each run.
Polymerase chain reaction conditions (TaqMan assay)
Real-time polymerase chain reactions (PCRs) were performed using the ABI Prism™ 7900HT sequence detection system (Applied Biosystems, Warrington, UK) in optical 384-well plates. Reaction mixtures contained (1 × dilution) TaqMan universal PCR mastermix (Applied Biosystems), 300 nM each of the forward and reverse primers, 100 nM fluorescent probe, 2 µl of template DNA and water to a final volume of 20 µl. The cycling conditions comprised 50 °C for 2 minutes and 95 °C for 10 minutes, followed by 40 cycles of 95 °C for 125 seconds and 60 °C for 1 minute. The primer sequences were forward primer, 5′-TCCT ACGGGAGGCAGCAGT-3′; reverse primer, 5′-GGACTACCA GGGTATCTAATCCTGTT-3′; and probe sequence, 5′-CGTATTA CCGCGGCTGCTGGCAC-3′. 28
The threshold cycle (Ct) value, which is inversely proportional to the log of the amount of target DNA initially present, was calculated using sds software v.2.0 (Applied Biosystems). All samples were run in triplicate. The median cycle result was used to calculate bacterial DNA concentrations by comparison with a DNA reference curve constructed from the results obtained using DNA standards.
Identification using DNA sequencing
When a sample contained > 0.5 pg of bacterial DNA/µl of blood, it was possible to amplify a 1300-bp (base pair) 16S rRNA gene fragment directly from the DNA extracts using oligonucleotide primers 5′-TCAGATTGAACGCTGGCGGC-3′ (forward) and 5′-CCCGGGAACGTATTCACCG-3′ (reverse). Each PCR assay was performed in a total volume of 25 µl containing 0.2 µM of each primer, 2 mM MgCl2, 1 U of Taq DNA polymerase (Promega, Southampton, UK) and 2 µl of DNA extract prepared in Reaction Buffer A (Promega). PCR cycle conditions comprised 95 °C for 3 minutes, followed by 30 cycles of 95 °C for 10 seconds, 58 °C for 20 seconds and 72 °C for 30 seconds using a Palm Cycler (Corbett Research, Sydney, Australia). PCR products were sequenced, using the forward primer and the internal primer 5′-TGCCAGCAGCCGCGGTAATA-3′, on an ABI Prism 3700 DNA Analyzer (PE Biosystems, Warrington, UK). The sequences were aligned using the Clustal W algorithm to produce a consensus sequence. This was analysed using the BLAST algorithm at the National Center for Biotechnology Information site. 31
Results for samples containing > 0.125 to 0.5 pg of bacterial DNA per µl of extracted whole blood were reported as positive only when the concentration was > 0.125 pg/µl on repeat testing. All the results of the molecular tests were entered into an excel spreadsheet for statistical analysis.
Statistical methods
The designation of episodes into probable, possible, unlikely or unclassifiable categories was based on the prospective data collected from the time of episode recruitment up to 28 days post recruitment. This classification was carried out at the UKCCSG (now CCLG) centre in Leicester and independently from the laboratory carrying out the molecular tests.
Sensitivity, specificity and positive and negative predictive values were calculated, together with exact binomial 95% confidence limits. stata v.9 software (StataCorp, College Station, TX, USA) was used for the analyses. When multiple lumens were present, the highest bacterial DNA concentration detected at that sampling time was used for each episode.
Test reproducibility
The volumes of blood available from this patient group precluded re-extraction of DNA from the majority of samples. Although we requested 0.5 ml, which would have allowed two separate extractions, in practice we frequently received < 0.4 ml. Each DNA extraction was tested in triplicate and the median result was used in the final analyses.
Results
Children admitted to hospital with fever were recruited into the study between 7 November 2005 and 6 November 2006. Samples and clinical data sheets were collected from 301 episodes of fever in 207 children. The numbers recruited by each centre were Belfast 15, Bristol 51, Great Ormond Street 2, Liverpool 63, Newcastle upon Tyne 63, Nottingham 19, Royal Marsden 19 and University College Hospital 31. We were unable to accurately estimate the number of eligible patients who were not recruited.
Exclusions from the analyses
Forty-one episodes were excluded from analysis.
The reasons for exclusion in 10 episodes were no written consent form, inappropriate sample storage or loss of sample, or antibiotics given intravenously during a 14- to 3-day period before the onset of fever. A further 26 episodes were excluded because of failure to collect samples from all lumens.
Five episodes were excluded because CVC-associated infection was considered to have been acquired post admission to hospital (diagnosed 5–23 days after initial presentation). Four of these five episodes were associated with positive blood cultures, and one episode was a tunnel infection. In one of these episodes, a sample was collected for 16S rDNA analysis at the time of fever recurrence (5 days after initial presentation), and this sample gave a bacterial DNA concentration of 0.34 pg/µl blood, while blood cultures taken at the same time grew Stenotrophomonas maltophilia.
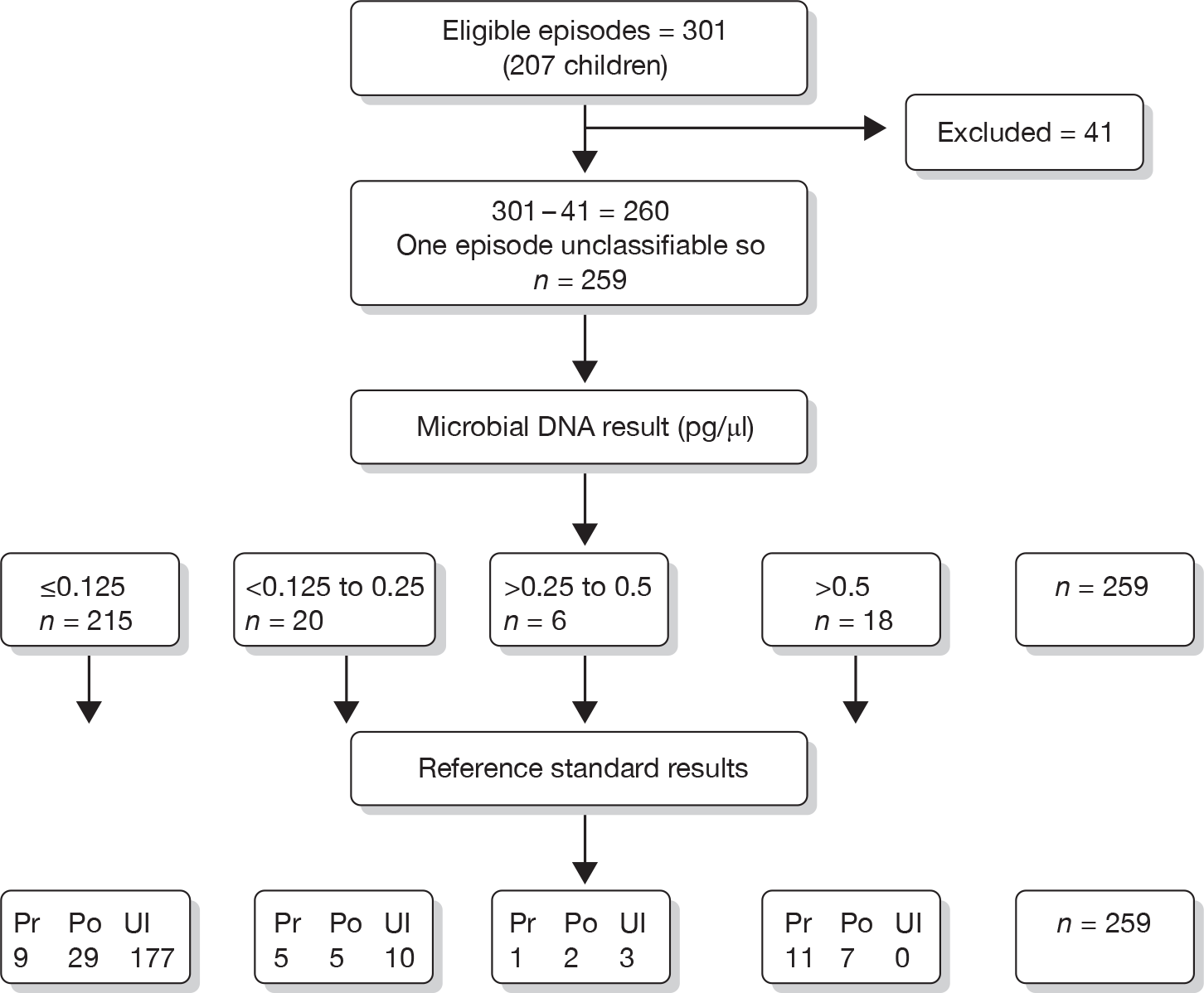
The proportion of eligible episodes excluded from analysis ranged from 0% to 33.3% for each centre. CVC tips were sent for culture from 16 (84%) of 19 episodes in which the CVC was removed. The numbers of episodes overall, the number with different microbial DNA results and the numbers within each reference group are shown in Figure 1.
FIGURE 1.
Eligible episodes, exclusions and numbers with different microbial DNA results and in each reference group. Pr, probable; Po, possible; Ul, unlikely.
Exposure to antibiotics
The patient had received oral antimicrobial agents in the previous 2 weeks in 133 (51.1%) of the 260 evaluable fever episodes, with 125 (48.1%) receiving an antibacterial agent and eight receiving antifungal or antiviral prophylaxis. In 117 episodes, these antibacterial agents were prophylactic (trimethoprim–sulfamethoxazole in 110 episodes and ciprofloxacin in seven episodes). In 17 episodes, oral antibacterial agents were being administered for treatment at the time of fever presentation (with or without prophylactic agents). Nine patients were receiving both prophylactic and therapeutic oral antibacterial agents.
Timing of sample collection relative to episode presentation
The date on which the blood for 16S rDNA was collected was the date of fever presentation (day 0) in 189, day 1 after fever presentation in 46, day 2 in 21 and day 3 in 4 of the 260 episodes. Of those episodes in which the date of collection was on day 0 or 1 of fever, 67 patients had been started on i.v. antibiotics before the DNA sample was collected.
The classification of fever episodes according to the reference standard for central venous catheter-associated infection
The classification of fever episodes according to the reference standard for CVC-associated infection and the timing of sampling is shown in Table 1, which shows the results from 259 episodes that were classified as probable, possible or unlikely. A single episode was classified as unclassifiable and is not included in the table.
| CVC infection (bacterial DNA level, pg/µl) | Category A | Category B | Category C |
|---|---|---|---|
| Probable | |||
| > 0.5 | 11 | 11 | 10 |
| > 0.25 to 0.5 | 1 | 1 | 1 |
| > 0.125 to 0.25 | 5 | 4 | 2 |
| ≤ 0.125 | 9 | 4 | 2 |
| n | 26 | 20 | 15 |
| Possible | |||
| > 0.5 | 7 | 7 | 6 |
| > 0.25 to 0.5 | 2 | 2 | 1 |
| > 0.125 to 0.25 | 5 | 4 | 2 |
| ≤ 0.125 | 29 | 27 | 20 |
| n | 43 | 40 | 29 |
| Unlikely | |||
| > 0.5 | 0 | 0 | 0 |
| > 0.25 to 0.5 | 3 | 3 | 3 |
| > 0.125 to 0.25 | 10 | 9 | 7 |
| ≤ 0.125 | 177 | 160 | 137 |
| n | 190 | 172 | 147 |
The number of episodes for different levels of microbial DNA is shown according to the reference standard criteria for probable, possible and unlikely CVC-associated infection in Table 1. Table 2 shows further details in terms of DNA test result, blood culture result and classification of CVC-associated infection. A positive blood culture was recorded for 47 episodes, of which 24 were classified as probable CVC-associated infection (Table 2). There were five episodes with a positive blood culture that were classified as unlikely to be CVC-associated infection. All of the 18 episodes with DNA levels > 0.5 pg/µl had a positive blood culture. Sequencing of the bacterial DNA in these samples was performed following amplification of 16S rDNA from DNA extracts. The sequence identifications obtained are summarised in Table 3.
| Bacterial DNA level (pg/µl) | Classification of CVC infection status | ||||||
|---|---|---|---|---|---|---|---|
| Counts | Post-test probability (%) | ||||||
| Probable or possible vs unlikely | Probable vs possible or unlikely | ||||||
| Probable | Possible | Unlikely | Probable or possible | Unlikely | Probable | Possible or unlikely | |
| Pathogens for which early removal recommendeda | 4 | 7 | 0 | 100 | 0 | 36 | 64 |
| > 0.5 | 3 | 4 | 0 | 100 | 0 | 43 | 57 |
| > 0.125 to 0.5 | 0 | 1 | 0 | 100 | 0 | 0 | 100 |
| ≤ 0.125 | 1 | 2 | 0 | 100 | 0 | 33 | 67 |
| Skin commensals onlyb | 12 | 9 | 0 | 100 | 0 | 57 | 43 |
| > 0.5 | 5 | 0 | 0 | 100 | 0 | 100 | 0 |
| > 0.125 to 0.5 | 5 | 2 | 0 | 100 | 0 | 71 | 29 |
| ≤ 0.125 | 2 | 7 | 0 | 100 | 0 | 22 | 78 |
| Other bacteria | 8 | 7 | 5 | 75 | 25 | 40 | 60 |
| > 0.5 | 3 | 3 | 0 | 100 | 0 | 50 | 50 |
| > 0.125 to 0.5 | 1 | 2 | 1 | 75 | 25 | 25 | 75 |
| ≤ 0.125 | 4 | 2 | 4 | 60 | 40 | 40 | 60 |
| Negative culture | 2 | 20 | 185 | 11 | 89 | 1 | 99 |
| > 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| > 0.125 to 0.5 | 0 | 2 | 12 | 14 | 86 | 0 | 100 |
| ≤ 0.125 | 2 | 18 | 173 | 10 | 90 | 1 | 99 |
| Total | 26 | 43 | 190 | 27 | 73 | 10 | 90 |
| Bacterial DNA (pg/μl blood) | Bacterial identification by sequencing | Blood culture identification |
|---|---|---|
| 0.7 | Staphylococcus spp. | Coagulase-negative staphylococcus |
| 0.7 | S. epidermidis | Coagulase-negative staphylococcus |
| 1.1 | Acinetobacter spp. | Acinetobacter spp. |
| 1.1 | S. aureus | S. aureus |
| 1.4 | Enterobacter spp. | Enterobacter cloacae |
| 1.6 | S. epidermidis | Coagulase-negative staphylococci |
| 1.6 | Klebsiella oxytoca | K. oxytoca |
| 2.9 | Acinetobacter baumannii | Acinetobacter spp./P. aeruginosa |
| 5.6 | S. aureus | S. aureus |
| 9.7 | S. epidermidis | Coagulase-negative staphylococci |
| 11.25 | Vibrio harveyi | V. harveyi |
| 12.8 | A. baumannii | A. baumannii |
| 13.1 | Bacillus cereus | Bacillus spp. |
| 13.1 | K. oxytoca | K. ocytoca |
| 21.3 | Escherichia coli | Enterobacter spp. |
| 21.6 | Corynebacterium tuberculostericum | Coagulase-negative staphylococci |
| 160 | Unreadable sequence | Mixed Staphylococcus spp. |
| 425 | P. aeruginosa | P. aeruginosa |
Table 4 shows likelihood ratios, sensitivity and specificity, and the post-test probability for each level of DNA and according to the timing of DNA sampling. Category C represents samples taken on the same day as or day after fever presentation, whereas category A represents results for the whole study group and is likely to reflect results achievable in practice. The receiver operating characteristic curve shows greater test accuracy the sooner DNA sampling was performed after fever presentation (category C).
| Bacterial DNA (pg/μl blood) | Eligible, all lumens sampled (%) | |||
|---|---|---|---|---|
| Sensitivity, % (95% CI) | Specificity, % (95% CI) | LR (95% CI) | Post-test probability, % | |
| Reference standard grouped as probable vs possible or unlikely | ||||
| > 0.5a | 42 (23 to 63) | 97 (94 to 99) | 14.08 (5.98 to 33.17) | 61 |
| > 0.25 to 0.5 | 46 (27 to 67) | 95 (91 to 97) | 1.79 (0.22 to 14.76) | 17 |
| > 0.125 to 0.25 | 65 (44 to 83) | 88 (84 to 92) | 2.99 (1.18 to 7.55) | 25 |
| ≤ 0.125 | 0.39 (0.23 to 0.67) | 4 | ||
| Reference standard grouped as probable or possible vs unlikely | ||||
| > 0.5 | 26 (16 to 38) | 100 (97 to 100) | NA | 100 |
| > 0.25 to 0.5 | 30 (20 to 43) | 98 (95 to 100) | 2.75 (0.57 to 13.32) | 50 |
| > 0.125 to 0.25 | 45 (33 to 57) | 93 (89 to 96) | 2.75 (1.2 to 6.33) | 50 |
| ≤ 0.125 | 0.59 (0.48 to 0.73) | 18 | ||
| Bacterial DNA (pg/μl blood) | Sampled within 48 hours of admission with fever (%) | |||
|---|---|---|---|---|
| Sensitivity, % (95% CI) | Specificity, % (95% CI) | LR (95% CI) | Post-test probability, % | |
| Reference standard grouped as probable vs possible or unlikely | ||||
| > 0.5 a | 55 (32 to 77) | 97 (93 to 99) | 16.66 (7.27 to 38.18) | 61 |
| > 0.25 to 0.5 | 60 (36 to 81) | 94 (90 to 97) | 2.12 (0.26 to 17.27) | 17 |
| > 0.125 to 0.25 | 80 (56 to 94) | 88 (83 to 92) | 3.26 (1.17 to 9.07) | 24 |
| ≤ 0.125 | 0.23 (0.09 to 0.55) | 2 | ||
| Reference standard grouped as probable or possible vs unlikely | ||||
| > 0.5 | 30 (19 to 43) | 100 (97 to 100) | NA | 100 |
| > 0.25 to 0.5 | 35 (23 to 48) | 98 (95 to 100) | 2.87 (0.59 to 13.82) | 50 |
| > 0.125 to 0.25 | 48 (35 to 62) | 93 (88 to 96) | 2.55 (1.03 to 6.3) | 47 |
| ≤ 0.125 | 0.56 (0.43 to 0.71) | 16 | ||
| Bacterial DNA (pg/μl blood) | Category B, plus i.v. antibiotics not given on days before DNA sample (%) | |||
|---|---|---|---|---|
| Sensitivity, % (95% CI) | Specificity, % (95% CI) | LR (95% CI) | Post-test probability, % | |
| Reference standard grouped as probable vs possible or unlikely | ||||
| > 0.5 a | 67 (38 to 88) | 97 (93 to 99) | 19.56 (8.24 to 46.4) | 63 |
| > 0.25 to 0.5 | 73 (45 to 92) | 94 (90 to 97) | 2.93 (0.35 to 24.61) | 20 |
| > 0.125 to 0.25 | 87 (60 to 98) | 89 (84 to 93) | 2.61 (0.62 to 10.99) | 18 |
| ≤ 0.125 | 0.15 (0.04 to 0.54) | 1 | ||
| Reference standard grouped as probable or possible vs unlikely | ||||
| > 0.5 | 36 (22 to 52) | 100 (96 to 100) | NA | 100 |
| > 0.25 to 0.5 | 41 (26 to 57) | 98 (94 to 100) | 2.23 (0.38 to 12.91) | 40 |
| > 0.125 to 0.25 | 50 (35 to 65) | 93 (88 to 97) | 1.91 (0.59 to 6.22) | 36 |
| ≤ 0.125 | 0.54 (0.4 to 0.72) | 14 | ||
Specificity was 100% for high levels of DNA (> 0.5 pg/µl), provided that the reference standard was grouped as probable and possible CVC-associated infection versus unlikely. Sensitivity was 36% at this cut-off. This dichotomy is most likely to be relevant to clinical practice, as clinicians have a low threshold for admitting and treating any child with a possible CVC-associated infection with i.v. antibiotics. In this context, a highly sensitive test would be most useful to rule out children not requiring admission. Given a cut-off of ≥ 0.125 pg/µl, the sensitivity was 65% for the whole study population, rising to 80% for those sampled on day 0 or day 1 of fever presentation and not given any antibiotics before sampling. The likelihood ratios (LRs) show that intermediate levels of DNA are associated with only a small increase in the risk of CVC-associated infection, whereas DNA > 0.5 pg/µl is highly predictive (LRs 14–19). Low levels of DNA (≤ 0.125 pg/µl) did not substantially diminish the risk of CVC-associated infection (LRs 0.39–0.15). If the reference standard of CVC-associated infection was classified as probable or possible versus unlikely, high levels of DNA (> 0.5 pg/µl) were highly specific (LRs infinity), but low levels of DNA (≤ 0.125 pg/µl) did not rule out CVC-associated infection (LRs 0.59–0.54).
We conducted subgroup analyses according to how long the CVC had been in situ prior to the febrile episode. We found a doubling in the risk of raised DNA (> 0.125 pg/µl compared with ≤ 0.125 pg/µl) in children with a CVC in situ for ≥ 4 weeks compared with those with one in situ for < 4 weeks, which was not significant at the 5% level [odds ratio 1.97, 95% confidence interval (CI) 0.92 to 3.01; 255 children had CVC duration recorded, 32 of whom had a CVC for < 4 weeks]. Sensitivity and specificity for children with a CVC in situ for ≥ 4 weeks did not differ appreciably from the overall results (LRs ranged from 0.3 to 14.9).
Table 5 shows the distribution of DNA and blood culture results according to CVC removal or CVC-targeted antibiotic treatment. In 17 (6.5%) of the 260 evaluable episodes, CVCs were removed during the 28-day follow-up period. All but one CVC (a damaged CVC) were removed for suspected CVC-associated infection. The proportion of CVCs removed within 4 weeks of fever presentation increased as the bacterial DNA concentration increased (Table 5). The CVC was removed in 6 (2.8%) of 216 episodes with DNA ≤ 0.125 pg/µl, 1 (5%) of 20 episodes with > 0.125 to 0.25 pg/µl, one (16.7%) of six episodes with > 0.25 to 0.5 pg/µl and 9 (50%) of 18 episodes with > 0.5 pg/µl.
| Bacterial DNA level (pg/µl) | CVC removal for infectiona | Targeted treatmentb | ||||
|---|---|---|---|---|---|---|
| Yes | No | Days to removal | Yes | No | Missingc | |
| Pathogens for which early removal is recommended | 6 | 5 | 5 | 6 | 0 | |
| > 0.5 | 6 | 1 | 2, 4, 4, 6, 8, 11 | 4 | 3 | 0 |
| > 0.125 to ≤ 0.5 | 0 | 1 | 0 | 1 | 0 | |
| ≤ 0.125 | 0 | 3 | 1 | 2 | 0 | |
| Skin commensal only | 3 | 18 | 6 | 12 | 3 | |
| > 0.5 | 1 | 4 | 21 | 3 | 2 | 0 |
| > 0.125 to ≤ 0.5 | 2 | 5 | 2, 9 | 2 | 3 | 2 |
| ≤ 0.125 | 0 | 9 | 1 | 7 | 1 | |
| Other bacteria | 4 | 16 | 6 | 13 | 1 | |
| > 0.5 | 2 | 4 | 2, 8 | 3 | 3 | 0 |
| > 0.125 to ≤ 0.5 | 0 | 4 | 1 | 2 | 1 | |
| ≤ 0.125 | 2 | 8 | 3, 11 | 2 | 8 | 0 |
| Negative culture | 4 | 204 | 7 | 169 | 31 | |
| > 0.5 | 0 | 0 | 0 | 0 | 0 | |
| > 0.125 to ≤ 0.5 | 0 | 15 | 0 | 10 | 4 | |
| ≤ 0.125 | 4 | 189 | 10, 16, 17, 19 | 7 | 159 | 27 |
| Total | 17 | 243 | 24 | 200 | 35 | |
Discussion
The 16S rDNA test yielded sensitivity for episodes defined as probable CVC-associated infection, specificity and positive predictive values similar to those reported for paired quantitative blood cultures. 32 Unlike many reported evaluations, this study was performed by laboratory staff working at a distant site unaware of the clinical details of individual patients, and the results were achieved despite the frequent exposure of patients to oral antibiotics in the 2-week period preceding fever presentation.
The method reported here has a relatively high minimum detection level of c. 10 genome copies/µl of blood. This relatively high minimum detection level probably explains the episodes with positive blood culture and undetectable bacterial DNA (although the possibility of blood culture contamination cannot be excluded). This high detection level also reduces the chances of a positive bacterial DNA test result arising as a consequence of sample contamination. A limitation of the methodology used in this study was the use of the discard sample. The implicit assumption was that this sample would represent microbial colonisation throughout the CVC lumen. This assumption may not be correct. We would recommend the collection of a sufficient sample volume to ensure that the whole volume of the CVC lumen is sampled. Extraction of microbial DNA from a larger volume would also potentially increase test sensitivity.
The manual DNA extraction method described in this study is time-consuming, but subsequent evaluations have obtained comparable results using automated DNA extraction systems, with considerable savings in technicians’ time (results not shown). The quantitative bacterial DNA method used in the present study does not generate a product that is sufficiently informative to allow bacterial identification. When the bacterial DNA concentration was > 0.5 pg/µl, it was possible to identify bacteria by amplification of a discriminatory 16S rDNA region, followed by sequencing of the amplified product. The majority of identifications according to molecular and conventional laboratory methods were consistent. Discrepant identifications probably reflect the limitations of routine laboratory standard operating procedures.
Previous reports have suggested a link between time to positivity (a marker of bacterial load) and outcome for both S. aureus18 and S. pneumoniae19 bloodstream infections. In the present study, increasing bacterial DNA load in blood samples drawn through the CVC was associated with an increasing risk of CVC removal for suspected infection. Information was collected for only 4 weeks after fever presentation. Prolonging the period of data collection might allow a better assessment of the implications for outcomes in patients with high bacterial load CVC-associated infection (see Chapter 3). Bacterial load is an important determinant of the efficiency of sterilisation and disinfection processes, so it is perhaps not surprising to find a relationship between the effectiveness of antimicrobial treatment of CVC-associated infection and bacterial load.
Whether measurement of high or low levels of DNA is most useful depends on how the test will be used in practice. In the original proposal for this study we envisaged the main benefit of using a molecular test for CVC-associated infection to be a reduction in unnecessary CVC removal – based on estimates that 60% of CVCs removed for suspected infection were removed unnecessarily (see background to study in trial protocol, Appendix 1, and Farr33). However, the results showed that removal of a CVC for suspected infection without FRC or a DNA result of < 0.125 pg/µl was uncommon, so the number of ‘unnecessary’ CVC removals defined by clinical criteria or DNA level was small. Hence, the potential benefit of the DNA test in reducing unnecessary CVC removal is also small. This finding concurs with the stated current practice in paediatric oncology in the UK and much of Europe,34 which is to retain CVCs if removal can be avoided. On the other hand, the bacterial DNA test does identify children with episodes of probable CVC-associated infection in whom improved treatment strategies for CVC-associated infection could be targeted. The test was not sufficiently sensitive to rule out patients at low risk of CVC-associated infection.
The main limitation of the accuracy study was the lack of an adequate reference standard. We used criteria for a CVC-associated bloodstream infection that combined blood culture results with clinical signs of CVC-associated infection and response to treatment, based on clinicians’ judgement. These judgements may have been strongly influenced by the blood culture result, which could have biased results in favour of underestimating the accuracy of bacterial DNA testing. This means that we were unable to determine whether DNA testing is more accurate than blood culture, and whether DNA testing would improve the prediction of outcomes over and above information currently available from clinical signs and blood culture. In Chapter 3, we aim to address this question by comparing the prediction of DNA and other tests for prognostic outcomes, including CVC removal and recurrence of bloodstream infection.
Chapter 3 Prognostic markers for sequelae of central venous catheter-associated bloodstream infection
Background
To decide on the introduction of a new test, clinicians need to know the added value of bacterial DNA testing over and above information that would be available from other tests that would usually be performed. Clinicians can opt to add a new test to an existing set of tests, use the new test instead of an existing test, or not use the new test at all. In Chapter 2, we compared bacterial DNA testing with a clinical reference standard for CVC-associated bloodstream infection. However, this reference standard is imperfect and, because it includes one of the existing tests used on admission (blood culture), the accuracy study does not provide information on whether DNA testing is more effective than blood culture. To address this question, we compared DNA testing and blood culture as predictors of the consequences of CVC-associated infection. This makes sense clinically as the usual intervention for children admitted with fever is at least 5 days of i.v. antibiotics. Many children with a bloodstream infection from any source (CVC or other sites) will be adequately treated by this regimen. Clinicians particularly want to identify children who are unlikely to respond to such treatment and need additional interventions targeted at CVC-associated infection, or even need their CVC removed. Clinicians also need to be able to identify children who do not need the 5 days of antibiotics at all, and could be discharged early on. This last question cannot be addressed by this study as no centre routinely discharged children early.
To predict the children likely to need additional targeted interventions, we analysed outcomes for a cohort of children derived from the accuracy study reported in Chapter 2. We determined the prognosis for outcomes at 28 days and 6 months after admission, according to tests and markers assessed on all children at admission. The primary outcomes were days of i.v. antibiotic treatment and CVC removal.
In addition to these secondary analyses of existing data, we searched the literature for studies on prognostic outcomes in children with cancer who had suspected CVC-associated infection (see Chapter 5, Figure 5 and search strategy in Appendix 5). As we found no relevant studies, we explored using other data sets for secondary analysis.
We obtained a data set from a longitudinal study of children with cancer conducted in the 1990s by Tweddle et al. 35 The study, UKCCSG SC 9403, was instituted jointly by the UKCCSG (now CCLG) and the Paediatric Oncology Nurses’ Forum (PONF) of the Royal College of Nursing. The design was a prospective observational study examining both mechanical and infective complications of CVCs in children being treated for cancer.
Eligible participants were all patients requiring central venous access for cancer therapy administered by a UKCCSG centre over a 20-month period from 1994 to 1996. Infection episodes requiring i.v. antibiotic treatment were recorded in the data set and we assumed that children were admitted to hospital for these episodes. To reproduce the cohort derived from the accuracy study reported in Chapter 2, we randomly selected one i.v. treatment period for each child, provided treatment started > 2 weeks after a previous treatment period. The cohort comprised 1069 patients, of whom 339 had at least one admission meeting our criteria. During these analyses we were notified of concerns about data errors by the Clinical Trials Unit (CTU) in Leicester, where the data were held. As the CTU was in the process of closing, no further data checking was possible. In view of the lack of confidence in the data expressed by the custodians, we have not used these analyses. Characteristics of the cohort are summarised in Appendix 8.
Methods for prognostic analyses of the accuracy study cohort
The aim of the secondary analyses of the accuracy cohort (described in Chapter 2) was to determine how clinical signs or test characteristics recorded at admission discriminate between children with and without sequelae of CVC-associated bloodstream infection. We assumed that this cohort represents the baseline prognosis in patients treated with standard care rather than targeted treatment for CVC-associated infection. This assumption is based on practice reported by collaborating centres and the fact that CVC-targeted treatment was recorded for only 24/260 infection episodes in the accuracy study (see Table 2).
The study was co-ordinated through the Supportive Care Group of the CCLG and involved eight UK centres. They were Belfast, Bristol, Great Ormond Street (London), Liverpool, Newcastle upon Tyne, Nottingham, Royal Marsden (London) and University College Hospital (London).
Population
We defined the population using the same eligibility criteria as the original accuracy study (in Chapter 2): children with cancer and a CVC expected to remain in situ for 3 months who were admitted from the community with fever and had not received i.v. antibiotics within the previous 2 weeks. As the accuracy study data set included multiple admissions with fever for the same child, often within a few months of the first admission, we confined our prognostic analyses to the first admission. For this reason, the results differ from the accuracy study. We found 181 eligible children who had 181 index admissions and 87 recurrent admissions (total of 268 admissions). This differs from the 260 admissions analysed in the accuracy study, as our definition of recurrent admission included children admitted for i.v. antibiotics regardless of whether they met the entry criteria for the accuracy study (e.g. fever and no i.v. treatment within previous 2 weeks).
Data collection
We used the clinical data as recorded on the data collection proforma for the accuracy study (see Appendix 2). We approached all centres for further data on outcomes up to 6 months after the index admission and for any relevant missing data for the 28-day follow-up. Research nurses in each centre were sent a spreadsheet of included patient admissions, showing the data available for key variables (e.g. date of admission, date of death, and dates for end of initial i.v. treatment, CVC removal, and start and end of recurrent treatment periods). They were asked to check the results and add information where this was highlighted as missing or inconsistent. Mike Millar repeatedly contacted non-responders and visited two centres (Newcastle upon Tyne and Royal Marsden) to undertake data extraction himself. Data returns were checked and further queries were sent if necessary. This process began in December 2008 and was stopped in October 2009 when the data set was closed for final analyses.
Prognostic markers
The markers examined were test results or clinical characteristics recorded in the data set that would be available to clinicians on admission or within 72 hours of admission. These are described in detail in Table 6. Two test results were considered in all analyses in addition to DNA results, blood culture and clinical signs (FRC) recorded on admission, as these are routinely performed on all children with suspected CVC-associated infection. A positive blood culture can be due to different sources of infection. The accuracy study found that half the bloodstream infections were classified as probably owing to CVC-associated infection and half as possibly CVC-associated infection (see Table 5).
| Name | Description |
|---|---|
| Population | Child had at least one admission that was included in the analyses for the accuracy study. The first admission was selected as the index admission |
| Prognostic markers | |
| Age | Number of years from date of birth to date at index admission |
| Type of cancer | Classified according to International Classification of Diseases for Oncology as non-haematological or haematological |
| Number of lumens | Single; multiple (two or three lumens) |
| Type of CVC | External vs implanted port or other type of CVC (see Glossary) |
| Duration of CVC insertion before treatment episode | Number of months from date of insertion of CVC in situ at index admission and date of index admission |
| Oral antibiotics received in 2 weeks before infection episode | Yes or no |
| FRC | Recorded at admission: a sign of CVC-associated infection (yes/no) |
| Superficial signs of tunnel/exit site infection | Recorded at admission (yes/no) |
| Quantitative bacterial DNA results | Based on sample at admission: > 0.5 pg/µl; > 0.125 to ≤ 0.5 pg/µl; and ≤ 0.125 pg/µl |
| Blood culture results |
Positive blood cultures were classified into three groups based on current best practice recommendations for treating bacterial CVC-associated bloodstream infection according to the type of organism isolated:13 Pathogens refer to bacterial isolates that should lead to prompt CVC removal – examples include S. aureus and P. aeruginosa Other refers to isolates for which antimicrobial lock treatment is recommended instead of prompt CVC removal – examples include the Enterobacteriaceae (such as Klebsiella spp.) One child with candidaemia was included in this category Skin bacteria refers to blood culture isolates for which antimicrobial lock treatment is recommended. Prompt CVC removal is not recommended unless special circumstances apply – examples include coagulase-negative staphylococci Other and skin bacteria were grouped together in the prognostic analyses as ‘other’ because of sparse data. Children with a positive blood culture may or may not have a CVC-associated infection Negative blood cultures |
| Outcomes | |
| Time to end of initial i.v. antibiotic treatment during index infection episode | Number of days from start of first treatment period to end of initial i.v. treatment period. Any gaps of ≤ 5 days between IV treatment episodes were considered to be part of the same treatment period. Initial i.v. treatment period was defined as any i.v. treatment started ≤ 5 days after admission or after stopping oral treatment started on the day of admission |
| Recurrent episode of infection requiring i.v. treatment | Any admission for i.v. antibiotics that started > 5 days after stopping initial i.v. treatment or after stopping oral treatment started on the day of admission. The duration of the recurrent i.v. treatment episode was from the start of recurrent i.v. treatment until the end of the last i.v. treatment. Treatments given < 5 days after the stop date of the last i.v. treatment were regarded as part of the same i.v. treatment episode |
| Duration of i.v. treatment | Actual days of i.v. treatment given from admission with suspected infection until 28 days later. Includes initial and subsequent i.v. treatment periods. Gaps of < 5 days between stopping and starting different i.v. treatment regimens are not included in this total |
| Time to recurrent episode of infection | Number of days from end of initial treatment episode to start of first recurrent i.v. treatment episode |
| Rate of recurrent i.v. treatment episodes | Number of recurrent i.v. treatment episodes per 1000 CVC days at risk. Time at risk was defined as the interval between the end of the index i.v. treatment episode (or 48 hours after admission if oral antibiotics given) to 28 days or 6 months after index admission |
| Reason CVC removed during follow-up period | Classified as infection; death; CVC damage or accidental removal; reason not stated; not removed |
| Time to CVC removal | Number of days from index admission to CVC removal within 28 days or 6 months after index admission |
| Incidence of CVC removal | Calculated as CVC removal for any reason divided by time at risk for CVC removal. Time at risk is from date of index admission until CVC removal or 28 days or 6 months |
Outcomes
The primary outcomes were (1) total duration of any i.v. treatment episodes during the 28-day follow-up period (even if the CVC was removed before 28 days) and (2) removal of the CVC, measured by survival analyses of time to removal within 28 days. These outcomes were reanalysed for the 6-month follow-up, as a study by Rijnders et al. 36 showed that the rate of recurrent infections following CVC-associated bloodstream infection in patients given standard care compared with antibiotic locks starts to diverge from 6–8 weeks after the start of treatment. Unfortunately, the 6-month follow-up data were not complete for the whole cohort, and were therefore regarded as secondary outcomes. Death was too rare to be included in the analyses, and serious complications of infection were not reported. Other secondary outcomes were (3) recurrence of bloodstream infection requiring i.v. antibiotics, measured using survival analyses of time to recurrence and, to take account of multiple recurrences, the rate of recurrence during the 28-day follow-up period originally used for the accuracy study; and (4) duration of initial i.v. antibiotic treatment, a proxy marker for the severity of the initial infection. This outcome was measured by survival analyses of time to stopping initial antibiotic therapy (see Table 6).
Categorical variables were reported as counts and proportions, and continuous variables as means with the standard error and/or medians with interquartile range (IQR); incidence rates were reported as events per 1000 CVC days.
Missing data
Missing data arose mainly in the start and end dates of antibiotic treatment periods. Dates were imputed using the mean duration of treatment in patients with complete data. We excluded cases with both dates missing (2/181 children from the 28-day analyses and 82/181 from the 6-month follow-up; Table 7).
| Variable | Duration of follow-up | |
|---|---|---|
| 28 days | 6 months | |
| Total number of patients | 181 | 181 |
| Patients excluded owing to missing data | 2 | 82 |
| Number of patients with index admission included in analysis | 179 | 99 |
| Characteristics before admission | ||
| Age at admission with suspected infection | ||
| Overall n (%) | 179 (100) | 99 (100) |
| Median (IQR) | 7 (3 to 11) | 7 (3 to 11) |
| Mean (SEM) | 7 (0.4) | 7 (0.5) |
| < 3 years n (%) | 35 (20) | 20 (20) |
| Median (IQR) | 2 (1 to 2) | 2 (2 to 3) |
| Mean (SEM) | 2 (0.1) | 2 (0.2) |
| ≥ 3 years n (%) | 144 (80) | 79 (80) |
| Median (IQR) | 8 (5 to 12) | 8 (5 to 12) |
| Mean (SEM) | 9 (0.4) | 9 (0.5) |
| Cancer type | ||
| Non-haematological, n (%) | 62 (35) | 35 (35) |
| Haematological, n (%) | 116 (65) | 64 (65) |
| Number of lumens in the CVC | ||
| Single, n (%) | 80 (45) | 39 (39) |
| Multiple, n (%) | 99 (55) | 60 (61) |
| Type of CVC | ||
| External, n (%) | 135 (75) | 90 (91) |
| Implanted port, n (%) | 44 (25) | 9 (9) |
| Duration of CVC insertion before admission for fever, months | ||
| Median (IQR) | 4 (1 to 8) | 4 (1 to 8) |
| Oral antibiotics in 2 weeks before infection admission | ||
| Yes, n (%) | 85 (47) | 35 (35) |
| No, n (%) | 91 (51) | 62 (63) |
| Missing | 3 | 0 |
| Characteristics on admission for infection episode | ||
| FRC | ||
| Yes, n (%) | 13 (7) | 10 (10) |
| No, n (%) | 166 (93) | 89 (90) |
| Superficial signs of tunnel/exit site infection within 3 days of admission | ||
| Tunnel or exit site, n (%) | 10 (6) | 4 (4) |
| No superficial signs, n (%) | 169 (94) | 95 (96) |
| Bacterial DNA result based on sample at admission | ||
| > 0.5 pg/µl, n (%) | 13 (7) | 11 (11) |
| > 0.125 to 0.5 pg/µl, n (%) | 15 (8) | 7 (7) |
| ≤ 0.125 pg/µl, n (%) | 151 (84) | 81 (82) |
| Characteristics at 48 hours after admission | ||
| Blood culture result (see definitions in Table 6) | ||
| Pathogens, n (%) | 5 (3) | 3 (3) |
| Other positive result, n (%) | 31 (17) | 19 (19) |
| Negative culture, n (%) | 143 (80) | 77 (78) |
| Outcomes | ||
| Follow-up period | ||
| Duration of follow-up after admission (in days) | ||
| Mean (median) | 28 (28) | 183 (183) |
| Recurrent infection episode | ||
| Number of patients with recurrent periods of i.v. treatment after index episode | ||
| n (%) | 34 (19) | 66 (67) |
| Time to second period of i.v. treatment | ||
| Median (IQR) | 21 (15 to 22) | 48 (29 to 97) |
| Mean (SEM) | 19 (0.9) | 66 (5.8) |
| Incidence of recurrent admission for i.v. treatment (per 1000 days)a | ||
| Mean | 8.817 | 3.829 |
| Days of i.v. treatment | ||
| Days of i.v. treatment during index infection episode | ||
| Median (IQR) | 4 (3 to 7) | 5 (2 to 8) |
| Mean (SEM) | 6 (0.4) | 8 (1.4) |
| Days of i.v. treatment after discharge following index admission | ||
| Median (IQR) | 0 (0 to 0) | 7 (4 to 12) |
| Mean (SEM) | 1 (0.2) | 9 (0.9) |
| CVC removal | ||
| Reason CVC removed during follow-up period | ||
| Total, n (%) | 10 (6) | 47 (47) |
| Infection, n (%) | 10 (6) | 24 (24) |
| Death, n (%) | 0 (0) | 1 (1) |
| CVC damage/accidental removal, n (%) | 0 (0) | 0 (0) |
| Reason not stated, n (%) | 0 (0) | 22 (22) |
| Not removed, n (%) | 169 (94) | 52 (53) |
| Incidence of CVC removal/1000 days' follow-upb | ||
| Mean | 1.995 | 2.6 |
Statistical analysis
Survival analysis was used for time-to-event outcomes associated with each prognostic variable, and hazard ratios (HRs), CIs and p-values were calculated. Survival curves were plotted using Kaplan–Meier estimates for time-to-event outcomes for each of the three tests (DNA, blood culture and clinical signs of FRC). Poisson regression was used to calculate rate ratios for recurrent i.v. treatment periods, taking into account multiple recurrences in some patients. Linear regression analysis was used to determine the effect of prognostic markers on the total duration of i.v. treatment.
The multivariable analyses were confined to two primary outcomes: time to CVC removal and the total duration of i.v. treatment during follow-up. We did not undertake multivariable analyses for recurrent treatment episodes owing to lack of power. To determine the added predictive value of DNA status, we analysed multivariable models that included blood culture and clinical signs, with and without DNA status. We compared the goodness of fit of these models using the Akaike’s information criterion (AIC) statistic. We included additional variables that were associated with time to CVC removal or the total duration of i.v. treatment, provided that they were not strongly correlated with other variables in the model. Statistical analysis was performed using r v.2.9.2 (R Foundation for Statistical Computing, Vienna, Austria). 37 We carried out a sensitivity analysis restricted to prognostic markers available on the day of admission and excluding blood culture results.
Results
The distribution of prognostic markers and outcome variables are shown in Table 7 for 179 children with sufficient data for inclusion in the 28-day follow-up and for 99 children included in the 6-month follow-up. The age distribution between the two data sets was similar, with 20% of children aged < 3 years and 65% with haematological cancer. The median duration of CVC insertion before the index admission was 4 months. Few children (7%) had FRC. However, one-fifth had a positive blood culture, although few of these contained pathogens, as defined in Table 2.
The relationship between clinical signs, DNA test and blood culture results is shown in Table 8. All test results are negative for 73% of children (131/179). The univariate analyses for follow-up to 28 days show relatively few associations at a 5% level of significance. Implanted CVCs and those with a single lumen were associated with earlier stopping of initial i.v. antibiotic treatment than external ports or CVCs with multiple lumens (i.e. HR for stopping treatment was > 1.0; Table 9). Children with FRC or with a positive blood culture were less likely to stop initial treatment early (HR < 1.0) and had a longer overall duration of i.v. treatment. They were also more likely to have their CVC removed. These findings are not surprising as duration of treatment and the decision to remove the CVC will be partly determined by the blood culture result and by the presence of clinical signs of CVC-associated infection. The effect of high levels of bacterial DNA varied according to whether the CVC was removed or not. Subgroup analyses in the lower part of Table 9 and Appendix 3 show that a high level of DNA was associated with increased days of i.v. treatment in patients in whom the CVC was not removed, but this relationship was not observed for patients with the CVC removed, partly because so few patients were studied.
| FRC | BC | DNA (pg/µl) | |||||
|---|---|---|---|---|---|---|---|
| 28-day follow-up period | 6-month follow-up period | ||||||
| > 0.5 | > 0.125 to ≤ 0.5 | ≤ 0.125 | > 0.5 | > 0.125 to ≤ 0.5 | ≤ 0.125 | ||
| Yes | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 |
| Yes | Others | 5 | 1 | 2 | 4 | 1 | 1 |
| Yes | None | 0 | 0 | 5 | 0 | 0 | 4 |
| No | Pathogen | 3 | 0 | 2 | 2 | 0 | 1 |
| No | Others | 5 | 7 | 11 | 5 | 3 | 5 |
| No | None | 0 | 7 | 131 | 0 | 3 | 70 |
| Coding | No. of patients | Time to end of index episode | Time to recurrence | Recurrence (yes/no) | Time to CVC removal | Total duration of i.v. treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Rem. | Rec. | HR (95% CI) | p-value | HR (95% CI) | p-value | Rate ratio (95% CI) | p-value | HR (95% CI) | p-value | Estimated coefficient (95% CI) | p-value | ||
| Characteristics before index admission | ||||||||||||||
| Age at admission with suspected infection | ||||||||||||||
| < 3 years | 1 | 35 | 0 | 7 | 1.13 (0.78 to 1.63) | 0.535 | 1.11 (0.48 to 2.55) | 0.805 | 1.06 (0.46 to 2.43) | 0.894 | 0.00 (0 to ∞) | 0.998 | –0.06 (–2.09 to 1.97) | 0.954 |
| ≥ 3 years (ref.) | 0 | 144 | 10 | 27 | ||||||||||
| Cancer type | ||||||||||||||
| Non-haematological | 1 | 62 | 3 | 12 | 1.01 (0.74 to 1.38) | 0.966 | 1.10 (0.54 to 2.24) | 0.785 | 1.05 (0.52 to 2.14) | 0.883 | 0.80 (0.21 to 3.09) | 0.746 | 0.60 (–1.08 to 2.29) | 0.482 |
| Haematological (ref.) | 0 | 116 | 7 | 21 | ||||||||||
| Number of lumens | ||||||||||||||
| Single | 1 | 80 | 1 | 16 | 1.95 (1.43 to 2.66) | < 0.0005 | 1.11 (0.56 to 2.17) | 0.769 | 0.96 (0.49 to 1.89) | 0.917 | 0.13 (0.02 to 1.06) | 0.056 | –3.16 (–4.71 to –1.61) | <0.0005 |
| Multiple (ref.) | 0 | 99 | 9 | 18 | ||||||||||
| Type of VAD | ||||||||||||||
| Implanted port | 2 | 44 | 2 | 8 | 1.65 (1.16 to 2.33) | 0.005 | 0.96 (0.44 to 2.12) | 0.922 | 0.86 (0.39 to 1.90) | 0.712 | 0.77 (0.16 to 3.63) | 0.741 | –1.94 (–3.80 to –0.09) | 0.041 |
| External (ref.) | 1 | 135 | 8 | 26 | ||||||||||
| Duration of CVC insertion before treatment episode (per month) | ||||||||||||||
| 1.00 (0.99 to 1.02) | 0.642 | 0.97 (0.91 to 1.02) | 0.228 | 0.96 (0.91 to 1.02) | 0.222 | 1.03 (0.98 to 1.08) | 0.273 | 1.00 (–14.85 to 16.85) | 0.902 | |||||
| Oral antibiotics in 2 weeks before infection episode | ||||||||||||||
| Yes | 1 | 85 | 5 | 13 | 1.03 (0.76 to 1.40) | 0.826 | 0.64 (0.32 to 1.28) | 0.208 | 0.66 (0.33 to 1.32) | 0.239 | 1.05 (0.30 to 3.64) | 0.936 | 0.04 (–1.60 to 1.67) | 0.965 |
| No (ref.) | 0 | 91 | 5 | 21 | ||||||||||
| Characteristics at index admission | ||||||||||||||
| FRC | ||||||||||||||
| Yes | 1 | 13 | 5 | 1 | 0.49 (0.27 to 0.88) | 0.017 | 0.37 (0.05 to 2.74) | 0.333 | 0.47 (0.06 to 3.46) | 0.461 | 16.39 (4.73 to 56.79) | < 0.0005 | 3.61 (0.55 to 6.68) | 0.022 |
| No (ref.) | 0 | 166 | 5 | 33 | ||||||||||
| Blood culture | ||||||||||||||
| Pathogens | 2 | 5 | 2 | 1 | 0.48 (0.19 to 1.17) | 0.105 | 0.97 (0.13 to 7.12) | 0.976 | 1.17 (0.16 to 8.62) | 0.875 | 25.71 (4.27 to 154.7) | <0.0005 | 4.39 (–0.39 to 9.18) | 0.074 |
| Other | 1 | 31 | 5 | 4 | 0.57 (0.38 to 0.84) | 0.005 | 0.61 (0.21 to 1.74) | 0.355 | 0.73 (0.26 to 2.08) | 0.560 | 8.40 (2.01 to 35.14) | 0.004 | 2.99 (0.91 to 5.08) | 0.005 |
| None (ref.) | 0 | 143 | 3 | 29 | ||||||||||
| Bacterial DNA result (pg/µl), all patients | ||||||||||||||
| > 0.5 | 4 | 13 | 5 | 1 | 0.53 (0.30 to 0.94) | 0.029 | 0.35 (0.05 to 2.60) | 0.307 | 0.44 (0.06 to 3.25) | 0.424 | 14.57 (4.20 to 50.47) | < 0.0005 | 3.38 (0.30 to 6.45) | 0.033 |
| > 0.125 to ≤ 0.5 | 1 | 15 | 0 | 2 | 0.66 (0.39 to 1.12) | 0.124 | 0.64 (0.15 to 2.69) | 0.545 | 0.72 (0.17 to 3.00) | 0.650 | 0.00 (0 to ∞) | 0.998 | 1.96 (–0.92 to 4.84) | 0.184 |
| ≤ 0.125 (ref.) | 0 | 151 | 5 | 31 | ||||||||||
| Bacterial DNA result (pg/µl), patients with CVC removed before 28-day follow-up period | ||||||||||||||
| > 0.5 | 4 | 5 | 5 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| > 0.125 to ≤ 0.5 | 1 | 0 | 0 | 0 | 1.86 (0.44 to 7.09) | 0.400 | 0.39 (0.03 to 4.34) | 0.443 | 0.44 (0.30 to 0.63) | < 0.0005 | 1.25 (0.32 to 4.82) | 0.750 | –4.80 (–14.36 to 4.76) | 0.354 |
| ≤ 0.125 (ref.) | 0 | 5 | 5 | 2 | ||||||||||
| Bacterial DNA result (pg/µl), patients without CVC removed before 28-day follow-up period | ||||||||||||||
| > 0.5 | 4 | 8 | 0 | 0 | 0.44 (0.21 to 0.90) | 0.025 | 0.00 (0 to ∞) | 0.997 | 0.00 (0 to 5.30e + 225) | 0.950 | NA | NA | 4.73 (1.03 to 8.43) | 0.013 |
| > 0.125 to ≤ 0.5 | 1 | 15 | 0 | 2 | 0.59 (0.34 to 1.01) | 0.054 | 0.67 (0.16 to 2.81) | 0.583 | 0.62 (0.49 to 0.79) | < 0.0005 | NA | NA | 2.18 (–0.58 to 4.94) | 0.124 |
| ≤ 0.125 (ref.) | 0 | 146 | 0 | 29 | ||||||||||
Similar patterns were observed for follow-up at 6 months, although associations were weaker and fewer were significant at the 5% level (see Appendix 3). In the 6-month follow-up, use of oral antibiotics in the 2 weeks prior to index admission appeared to be protective for recurrent i.v. treatment and CVC removal, and children younger than 3 years appeared to have a reduced risk of recurrent infection. These results should be regarded with caution because the cohort represents just over 50% of those eligible for inclusion. In addition, the large number of comparisons also increases the chance of associations being statistically significant by chance.
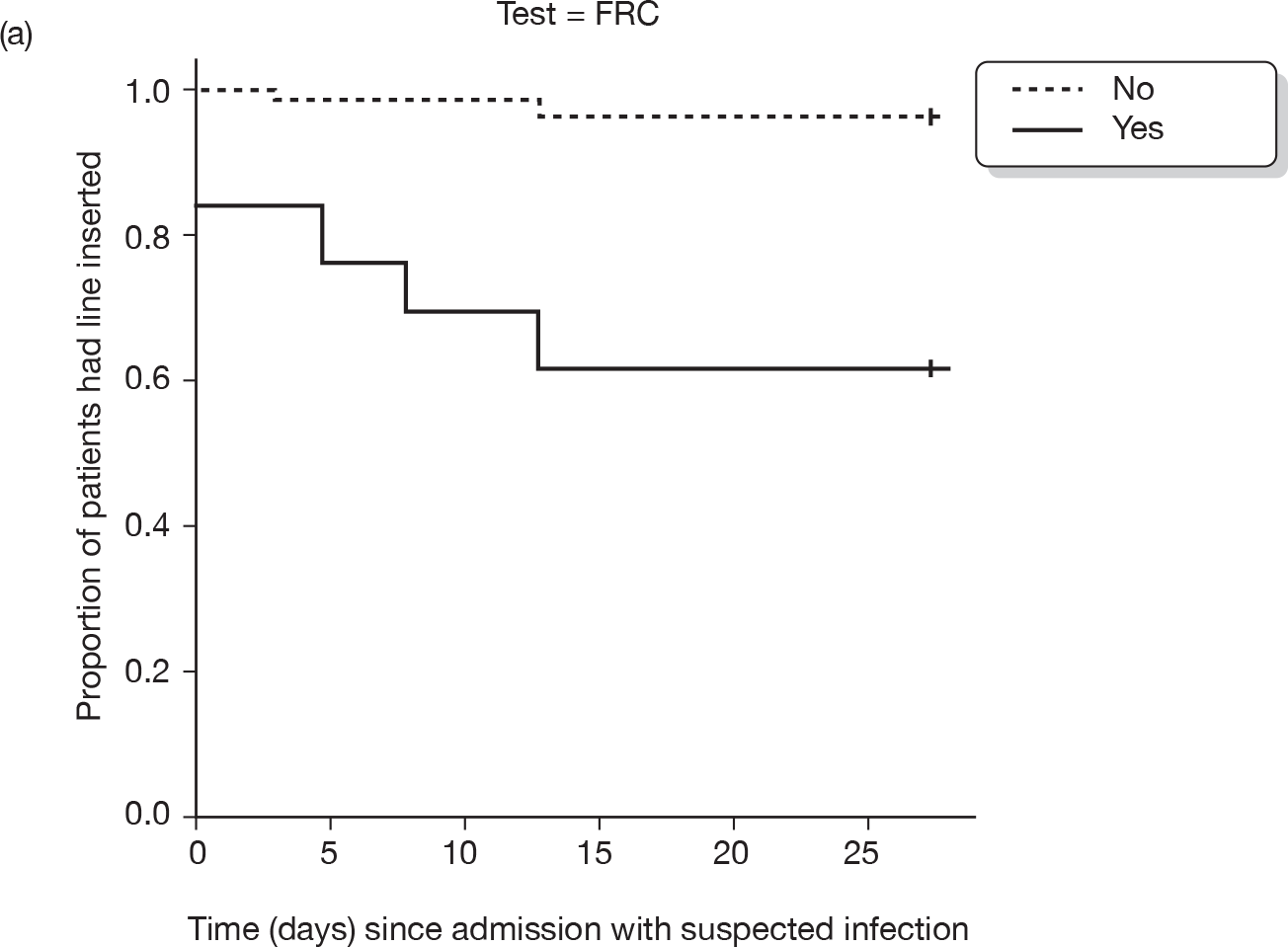
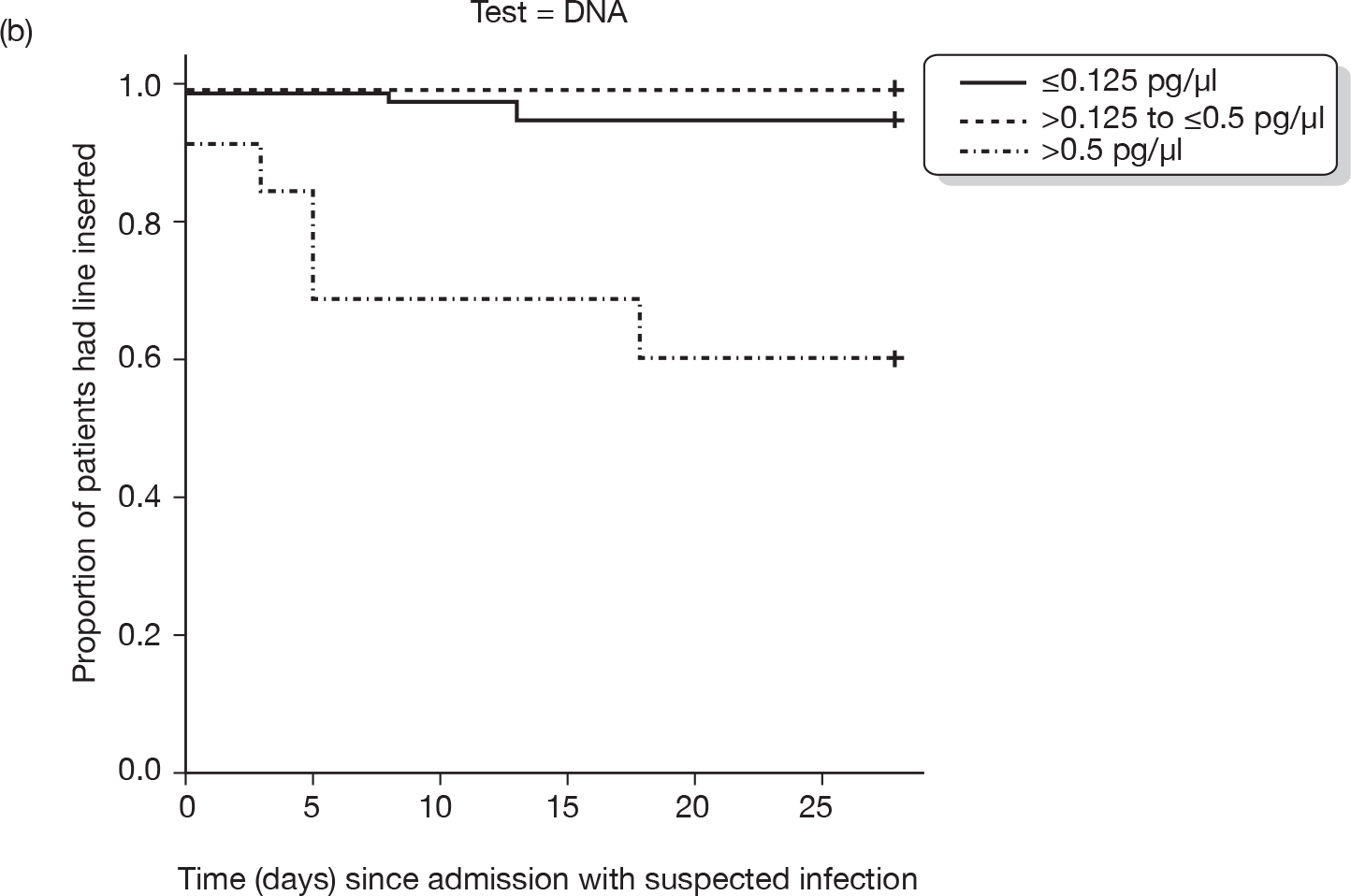
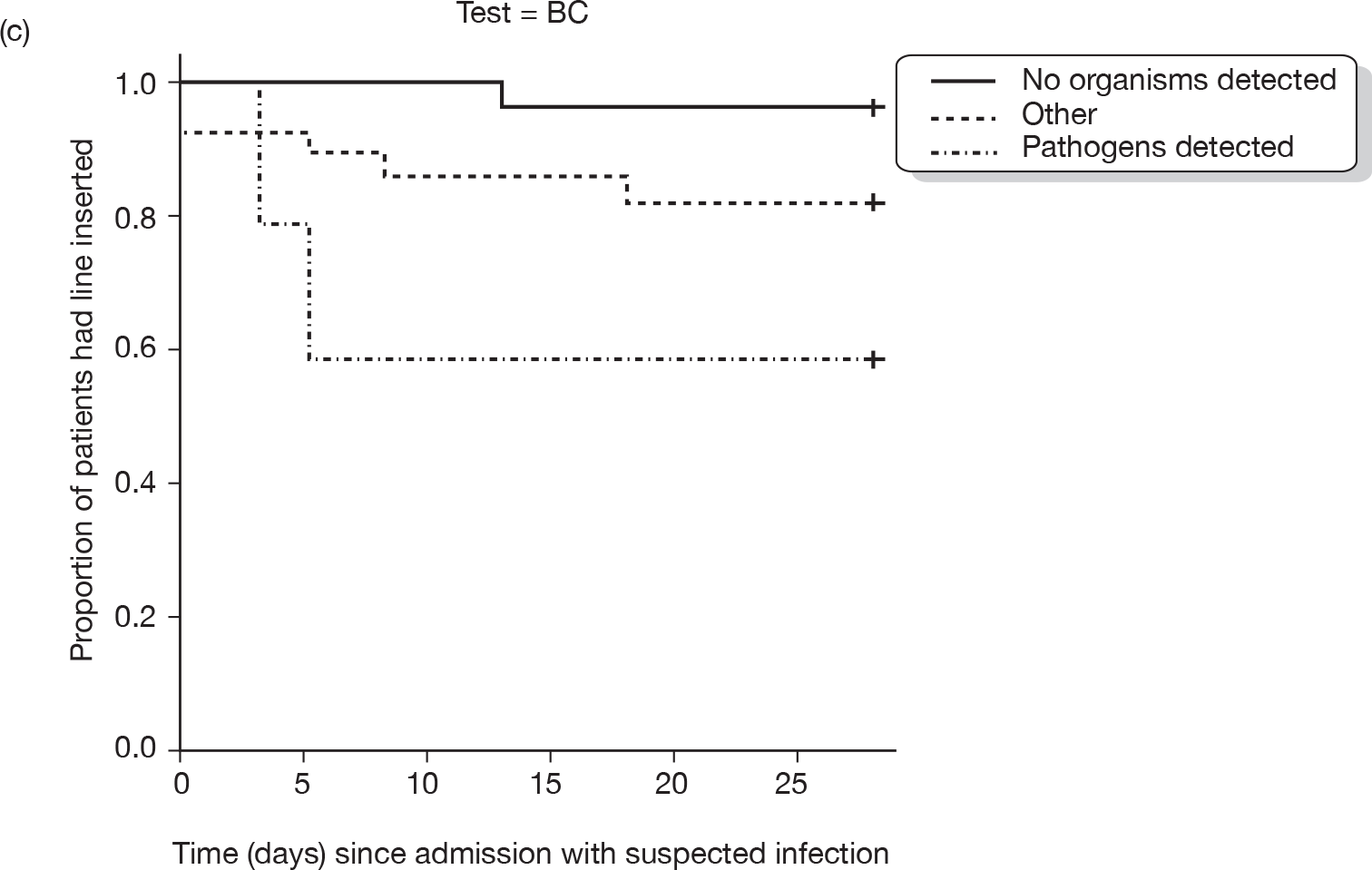
Figures 2 and 3 show survival plots for the three tests of clinical signs (FRC), bacterial DNA and blood culture for two outcomes: recurrent i.v. treatment episode and CVC removal. Consistent with the effects shown in Table 9 for the 28-day outcomes, these tests do not discriminate between children with recent infection, but show a clear effect for CVC removal. Similar patterns are seen for the cohort followed up for 6 months (see Appendix 3).
FIGURE 2.
Kaplan–Meier plots of time to recurrent infection requiring i.v. treatment in cohort followed up for 28 days according to three test results: (a) FRC; (b) bacterial DNA concentration; (c) blood culture (BC) result.
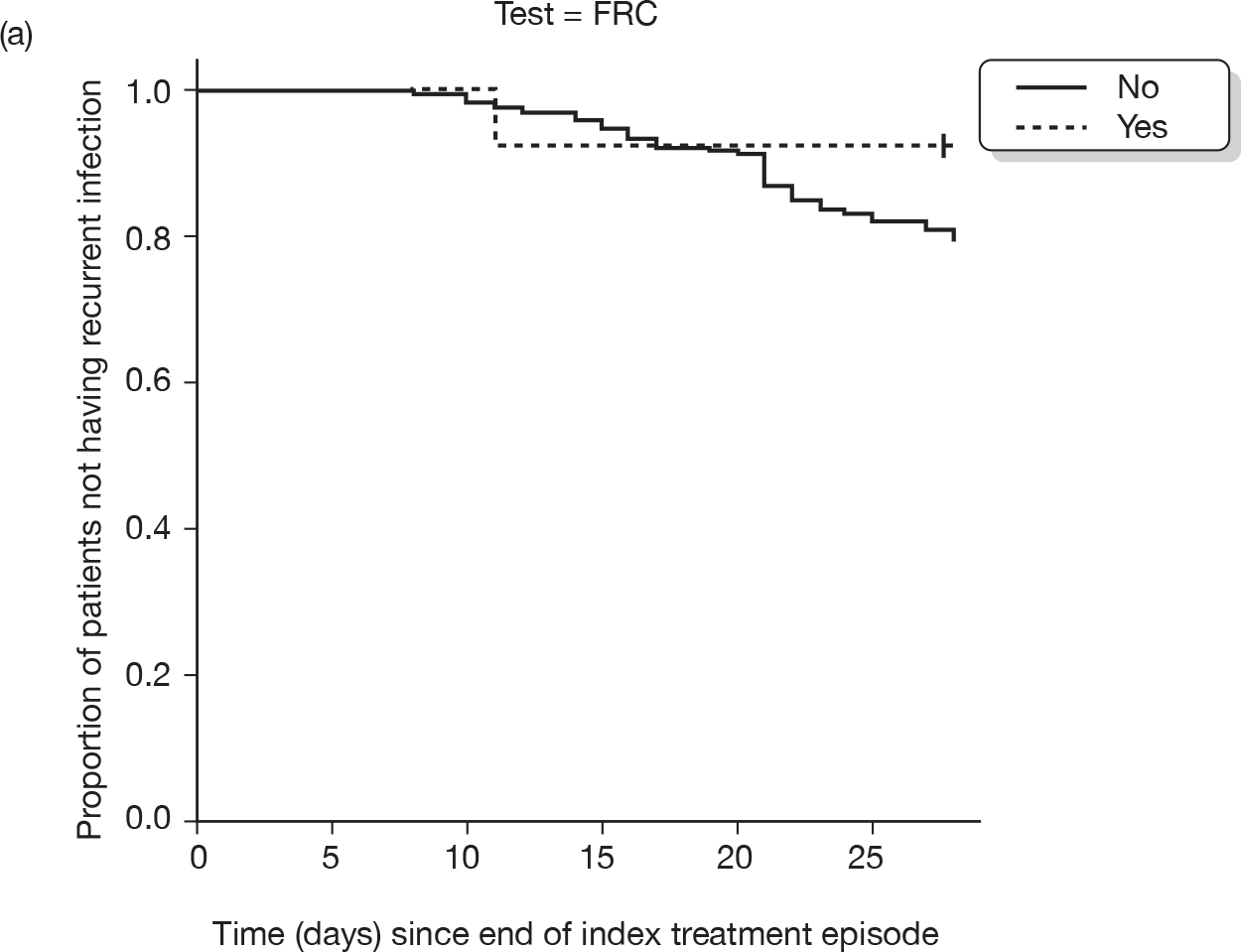
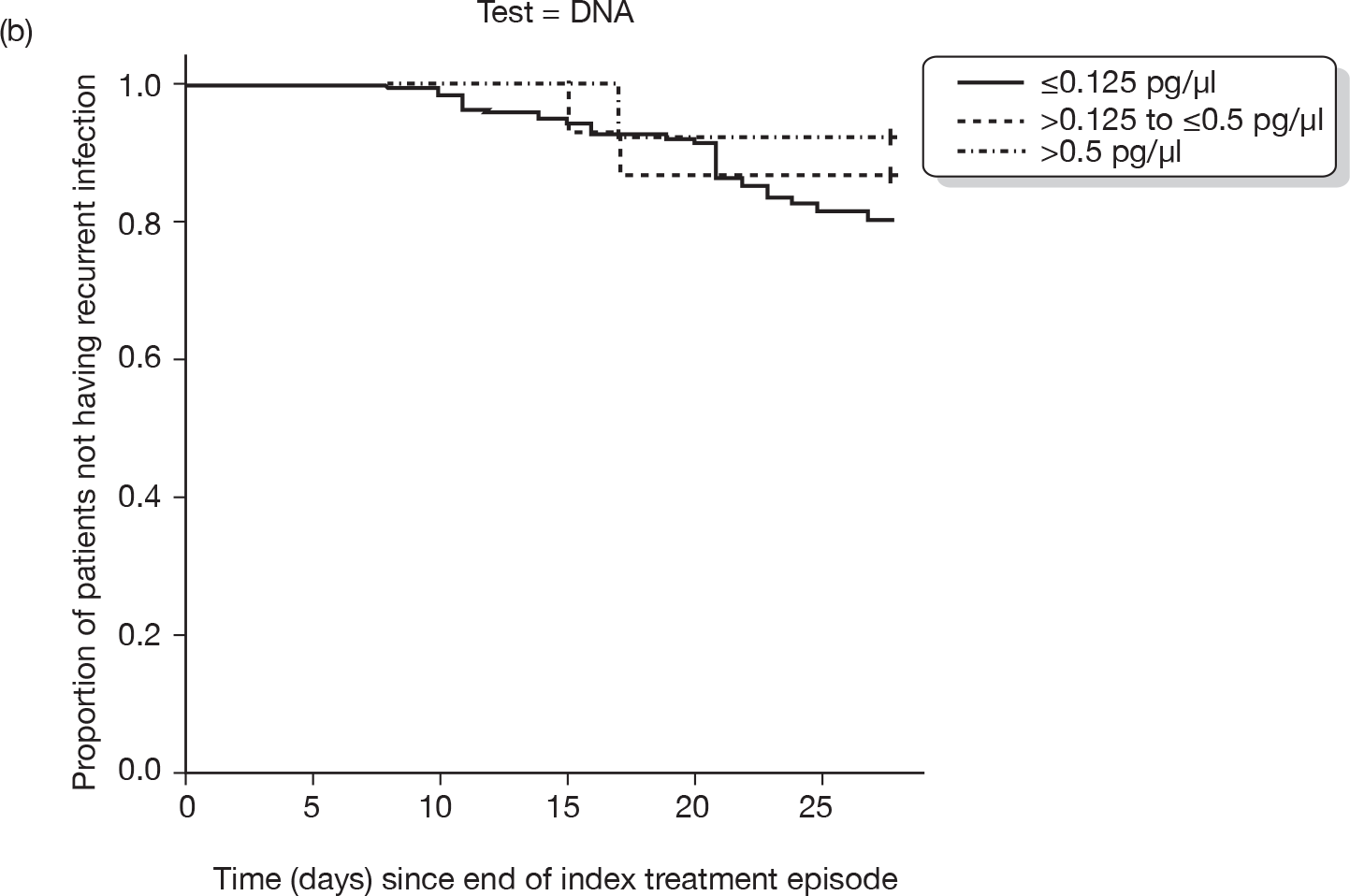
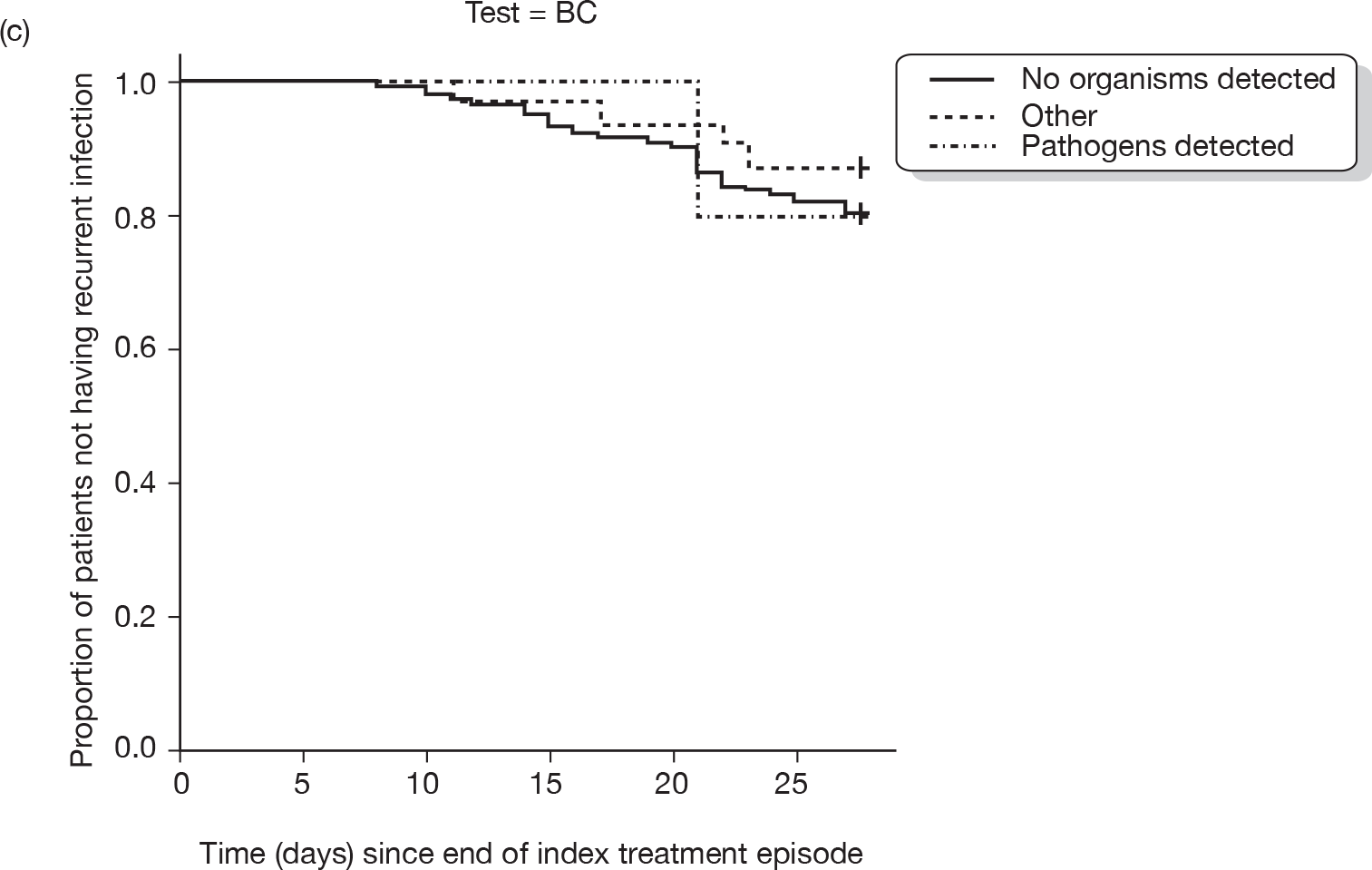
FIGURE 3.
Kaplan–Meier plots of time to CVC removal in cohort followed up for 28 days according to three test results: (a) FRC; (b) bacterial DNA; (c) blood culture (BC).
Multivariable analyses
The strong associations between clinical signs of FRC and pathogens isolated on blood culture and an increased risk of CVC removal persisted in the multivariable analyses. The addition of bacterial DNA to the model attenuated this relationship slightly. Single-lumen CVCs were associated with a reduced overall duration of i.v. treatment: this effect was not altered by inclusion of DNA level in the model. DNA level was not significantly predictive of any outcome and did not significantly improve the fit of the model, as measured by the AIC. Similar results were found for the cohort followed up for 6 months (see Appendix 3, Table 22).
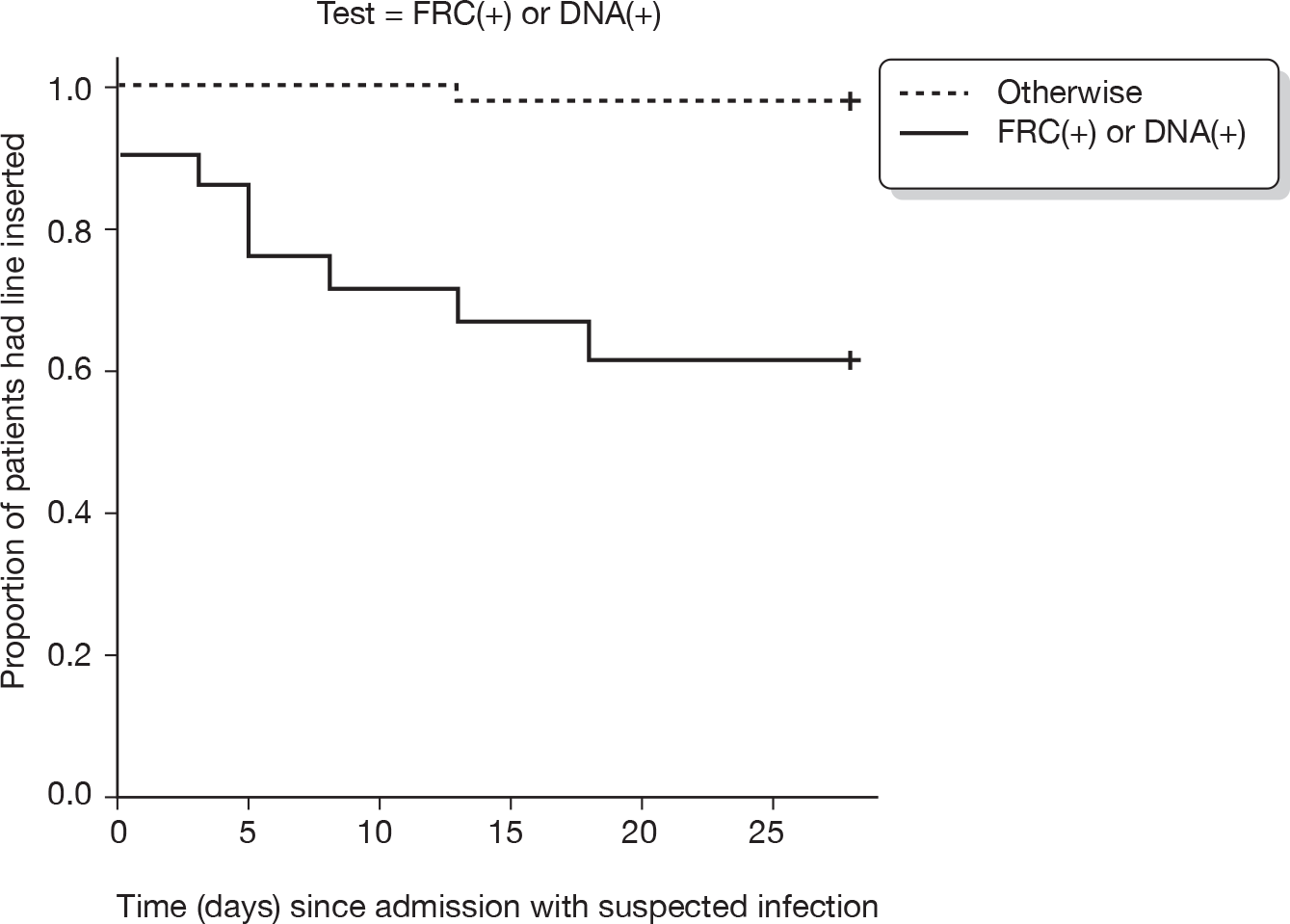
The sensitivity analyses showed that if only markers available on the day of admission were considered, bacterial DNA did contribute significantly to the prediction of CVC removal and duration of i.v. treatment (Table 10 and Figure 4). If high DNA (> 0.5 pg/µl) or clinical signs of FRC were considered as a combined marker (vs any other result for FRC or DNA), a positive result was highly predictive of CVC removal and i.v. treatment duration.
FIGURE 4.
Sensitivity analysis showing survival analysis for time to CVC removal at 28 days given FRC-positive or DNA level > 0.5 pg/µl (vs FRC-negative or DNA ≤ 0.5 pg/µl).
| Explanatory variables | Time to CVC removal | Total duration of i.v. treatment [adjusted for indicator variable: CVC removal with follow-up period (yes/no)] | ||||||
|---|---|---|---|---|---|---|---|---|
| Model without DNA | Model with DNA | Model without DNA | Model with DNA | |||||
| HR (95% CI) | p-value | HR (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | |
| Single lumen | 0.17 (0.02 to 1.37) | 0.096 | 0.17 (0.02 to 1.37) | 0.096 | –2.94 (–4.50 to –1.37) | 0.000 | –2.79 (–4.42 to –1.17) | 0.001 |
| With FRC | 13.50 (3.87 to 47.08) | < 0.0005 | 6.93 (1.63 to 29.33) | 0.009 | 2.65 (–0.57 to 5.87) | 0.109 | 2.33 (–0.98 to 5.64) | 0.170 |
| DNA (> 0.5 pg/µl) | 4.51 (1.06 to 19.20) | 0.042 | 1.44 (–1.88 to 4.77) | 0.395 | ||||
| DNA (0.125–0.5 pg/µl) | 0.00 (0 to ∝) | 0.998 | 0.73 (–2.15 to 3.61) | 0.620 | ||||
| AIC | 87.55 | 84.60 | 596.21 | 599.28 | ||||
| Explanatory variables | Time to CVC removal | Total duration of i.v. treatment (Adjusted for indicator variable: CVC removal with follow up period (Yes/No)) | ||||||
|---|---|---|---|---|---|---|---|---|
| Model without DNA | Model with DNA | Model without DNA | Model with DNA | |||||
| HR (95% CI) | p-value | HR (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | |
| DNA as independent variable | ||||||||
| Single lumen | 0.17 (0.02 to 1.37) | 0.096 | 0.17 (0.02 to 1.37) | 0.096 | –2.94 (–4.50 to –1.37) | 0.000 | –2.79 (–4.42 to –1.17) | 0.001 |
| With FRC | 13.50 (3.87 to 47.08) | <0.0005 | 6.93 (1.63 to 29.33) | 0.009 | 2.65 (–0.57 to 5.87) | 0.109 | 2.33 (–0.98 to 5.64) | 0.170 |
| DNA (> 0.5 pg/µl) | 4.51 (1.06 to 19.20) | 0.042 | 1.44 (–1.88 to 4.77) | 0.395 | ||||
| DNA (0.125–0.5 pg/µl) | 0.00 (0 to ∝) | 0.998 | 0.73 (–2.15 to 3.61) | 0.620 | ||||
| AIC | 87.55 | 84.60 | 596.21 | 599.28 | ||||
| Model DNA + FRC | Model DNA + FRC | |||||||
| Single lumen | 0.26 (0.03 to 2.07) | 0.202 | –2.82 (–4.38 to –1.26) | 0.001 | ||||
| FRC (+) or DNA > 0.5 pg/µl | 29.63 (6.17 to 142.23) | 0.000 | 2.97 (0.20 to 5.75) | 0.037 | ||||
| AIC | 87.55 | 596.21 | ||||||
Discussion
These findings provide no evidence that bacterial DNA, used as a single test on admission in this patient population, improved the prediction of outcomes at 28 days related to CVC-associated bloodstream infection. Analyses based on follow-up to 6 months did not change these conclusions but were underpowered to detect potentially important effects. Limitations of the study are discussed in Chapter 6.
Chapter 4 Systematic reviews of interventions
Overview of the systematic reviews
Scope of the reviews: rationale
We conducted systematic reviews for three treatment comparisons. These were selected based on clinical opinion (Mike Millar in discussion with the CCLG) and the available research literature. 38 The clinically important outcomes were resolution of infection, removal of the CVC owing to infection and recurrence of infection. The intervention options reviewed are outlined in brief below.
-
Early CVC removal compared with retaining the CVC and treatment in situ Central venous catheter access is particularly important in children not only for the administration of cytotoxic drugs but also to avoid the trauma of repeated venepuncture. In paediatric oncology practice, removal of the CVC for suspected CVC-associated infection is seen as a last resort reserved for children with complicated or unresolving CVC-associated infection. This is because, compared with adults, CVC reinsertion carries a greater anaesthetic and operative risk, involves greater technical difficulties and is more likely to ‘use up’ venous access sites that might be needed in future.
-
Treat the suspected CVC-associated infection with an antimicrobial lock solution compared with a standard heparin lock Antibiotic or antiseptic lock solution (together referred to as antimicrobial) can be used to treat suspected CVC-associated infection, and in children might be used to ‘salvage’ the line – avoiding removal.
-
Antimicrobial locks to prevent CVC-associated infection We conducted a review of the effectiveness of locks to prevent CVC-associated infection, as this option might reduce the overall incidence of admission of children with suspected CVC-associated infection.
The section on locks includes a survey of paediatric oncology units in the UK: on the use of antimicrobial locks in practice, and on the formulation of locks used.
The inclusion criteria for these reviews distinguished between interventions affecting infection within the CVC and interventions involving the whole patient. We reasoned that antimicrobial locks are interventions that act on infection within the CVC and should therefore have a similar effect across patient groups. We included any studies in adults or children in these reviews (2 and 3). On the other hand, the criteria for CVC removal are related to problems with venous access, as well as the underlying clinical problem, and are likely to vary between children and adults. We therefore restricted the review of CVC removal to studies in children and adolescents with cancer.
One further strategy, used by some clinicians for children with suspected CVC-associated bloodstream infection, is to administer systemic antibiotics by slow infusion instead of bolus i.v. injection. The rationale, to increase the duration of exposure of organisms colonising the CVC to antibiotics, is based on evidence that bactericidal action is time dependent. 39 We did not conduct a systematic review of this option for two reasons. First, we found no relevant studies for slow infusion compared with bolus administration of antibiotics (see Figure 5). Second, our searches highlighted difficulties in the definition of slow and bolus. For example, we found one systematic review of 17 RCTs that compared continuous infusion with intermittent administration of antibiotics. 40 Clinical failure was lower, albeit with equivocal statistical significance, in patients randomised to continuous infusion. We also found one study protocol (see Appendix 4) that randomised patients either to bolus injection with teicoplanin or to prolonged teicoplanin exposure, which could involve slow infusion (over 1–2 hours) or a teicoplanin lock (either given at the clinician’s discretion). There is a need for further research using clearly defined criteria for the duration and dosage of antibiotic administration.
FIGURE 5.
Flow diagram of searches.
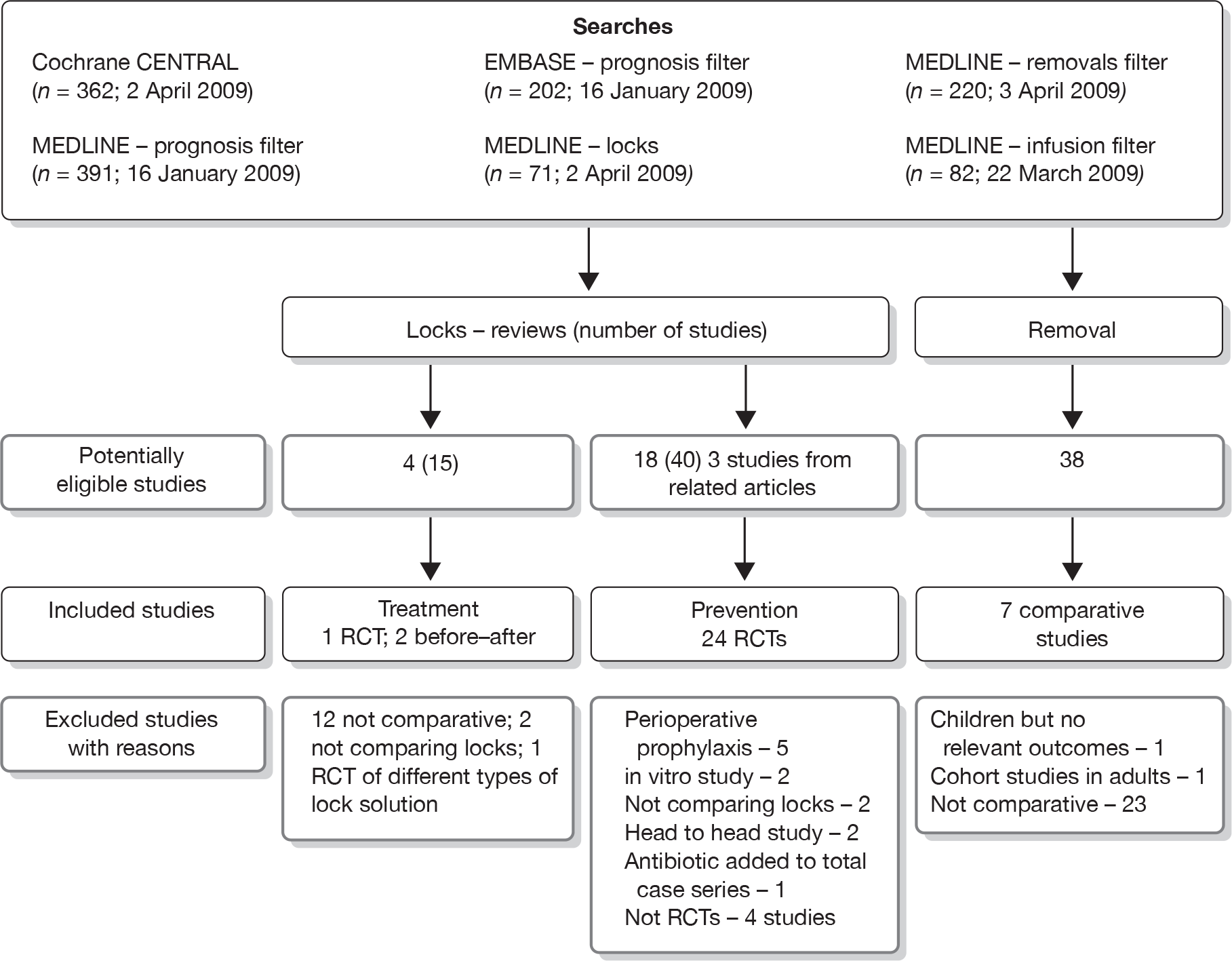
No protocol for any of these reviews has been published elsewhere and there is no registration number for these reviews.
Search strategy, selection of studies and data extraction
The results of the searches are summarised in Figure 5. Search terms are given in Appendix 5. First, we conducted a broad search of the Cochrane Central Register of Controlled Trials (CENTRAL) to identify any RCTs that included terms relating to CVC and infection. Second, we conducted a sensitive search for prognostic studies, using terms related to follow-up or prognosis combined with terms for CVC and infection or removal, and restricted to children or adolescents. Third, we devised searches for comparisons involving locks and removal of the CVC. Fourth, we carried out a search for infusion versus bolus treatment, prior to aborting this review (reasons given above). Because of changes in the quality of supportive care for patients with CVCs during the last 15 years, we restricted studies to those published after 1994. We did not impose any language restrictions.
Mike Millar and Ruth Gilbert scanned all the abstracts from the two broad-based searches to identify potentially eligible studies for any of the reviews. Mike Millar scanned all abstracts from all of the searches and Ruth Gilbert scanned all the searches labelled as ‘prognosis’ and those from CENTRAL.
Full copies of potentially eligible studies were reviewed by one author (RG, MM or WZ) and included and excluded studies were decided by discussion within the group. Data extraction was initially carried out by Weiwei Zhou and checked by Ruth Gilbert. No additional data were sought directly from investigators.
Systematic review of early central venous catheter removal compared with retention and treatment in situ
Structured summary
Context In patients with suspected CVC-associated infection, early removal of the CVC may reduce the risk of infection complications but at the cost of further procedures to insert a new CVC.
Objective To determine the effectiveness of early CVC removal compared with retention and treatment of CVC-associated infection on the duration of infection, complications arising from infection and recurrence of CVC-associated infection in children with cancer.
Data sources We searched MEDLINE, EMBASE and CENTRAL from 1995 until April 2009. Search terms included synonyms for CVC, infection and removal. We also included any studies identified in searches for other questions included in this report.
Study selection We included any comparative studies in children with cancer who had a CVC inserted, and compared removal with treatment in situ.
Data extraction Weiwei Zhou extracted the data, which were checked by Ruth Gilbert.
Data synthesis We could not conduct a meta-analysis as the intervention, comparator and outcomes were variable and presentation of results was not consistent. We found seven retrospective cohort studies but no RCTs. All were poor quality. Timing of CVC removal was confounded by the patient’s condition, with sicker patients more likely to retain their CVC and more likely to die.
Conclusions The increased risk of death or infection complications associated with CVC retention compared with early removal could be explained by retention of the CVC in the sickest patients. RCTs are needed to quantify any potential benefits of early versus deferred CVC removal.
Rationale
Standard clinical teaching and a priori reasoning indicates that CVC removal is an effective intervention for CVC-associated infection, as it removes the source of infection. The decision is difficult however. First, only a proportion of bloodstream infections are due to the CVC. Second, CVC-associated infection may resolve with treatment and not require removal of the CVC. Nevertheless, clinical experience and studies based on case series and cohort studies suggest that CVC removal reduces the duration of systemic antibiotic treatment and the risk of serious complications of infection. 41–43 The clinical dilemma is therefore when to remove the CVC, and in which patients. Early removal could potentially avoid prolonged efforts to treat a CVC-associated infection with the CVC in situ, and could avoid potentially serious complications, such as sepsis and end-organ damage, which can be fatal. On the other hand, CVC removal necessitates reinsertion, which involves operative trauma and complications of insertion, including bleeding or pneumothorax, and potentially reduces the availability of venous access in the longer term. 5 A further question is whether early removal reduces the risk of recurrent CVC-associated infection. Recurrence is a particular concern in patients with low-grade CVC-associated infection due to commensal bacteria, such as coagulase-negative staphylococci. In such patients, symptoms may subside with systemic antibiotic treatment but may recur several weeks after cessation of antibiotic treatment. 36
Review question
In children with cancer and suspected CVC-associated infection, does early removal of the CVC, compared with retention of the CVC and treatment, reduce adverse outcomes related to the duration of treatment for infection, infection-related complications or recurrence of CVC-associated infection?
Inclusion criteria
We included any comparative studies published after 1994, whether randomised, other parallel group comparisons, or before–after comparisons. The population included any children with a CVC inserted for any length of time. We accepted any type of CVC and any type of removal, whether complete removal and replacement through a new site, or replacement over a guide wire using the same venous access site. 44 We excluded studies in adults or in children without cancer.
Data extraction
We extracted characteristics of the study, participants, interventions and outcomes, as shown in Table 11. Where possible, we recorded for each study arm, the number of participants, the duration of infection, the number with complications (including death) and the number of recurrent CVC-associated infections. Because of the varied reporting of results, we were unable to conduct a meta-analysis.
| Primary author and reference | Year published | Country | Population | Study design | Participants | Comparison | Findings |
|---|---|---|---|---|---|---|---|
| Pasqualotto45 | 2007 | Brazil | Children and neonates | Retrospective cohort | 61 children with candidaemia and CVC | Removal timing not specified | Failure to remove CVC was associated with early death, but not late death, after adjustment for PRISIM score. Sicker patients had CVC retained |
| Buckley46 | 2007 | USA | Children, tertiary referral hospital, with CVC and positive blood cultures for E. coli or Klebsiella | Retrospective cohort | 118 children with BSI | CVC removed in cancer patients (69% of 31 children) more often than others (38%) | 14% had infection recurrence or died; these outcomes were not related to CVC removal |
| Nazemi47 | 2003 | USA | Neonates with CVC | Retrospective cohort | 53 neonates with Enterobacteriaceae BSI | Early removal within 2 days of first BSI vs later | 15 CVCs removed early and 38 removed late (similar baseline characteristics in both groups): no difference in recurrence or duration of BSI; 17/38 CVCs in late group retained. In late removal group, CVC retained in 88% (of 13) with BSI lasting 1 day, 24% (of 25) lasting > 1 day. Decreased risk of retention if severe thrombocytopenia was present |
| Karlowicz48 | 2000 | USA | Neonates with CVC | Retrospective cohort | 113 neonates with Candida spp. BSI | Early removal within 3 days of first BSI vs later | 50 CVCs were removed early and 63 removed later (similar baseline characteristics). Early removal was associated with reduced duration of candidaemia and reduced mortality (1/50 in early group vs 10/54 with late removal) |
| Karlowicz49 | 2002 | USA | Neonates with CVC | Retrospective cohort | 113 neonates with CoNS BSI | Early removal within 3 days of first BSI vs later | 56 CVCs were removed early and 63 late (similar characteristics): similar risk of recurrent CoNS BSI [8/56 (14%) vs 6/63 (10%)]; but persistent CoNS > 3 days more in late removal group [7/56 (13%) vs 27/63 (43%)]. In late removal group, CVC retained in 79% (of 28) with BSI lasting 1–2 days, 44% (of 16) lasting 3–4 days, and none (n = 19) lasting > 4 days |
| Benjamin50 | 2001 | USA | Neonates with CVC | Retrospective cohort | 153 episodes of BSI | Removal within 24 hours of positive culture vs treatment to sterilise line | Persistent bacteraemia and/or end-organ damage after immediate removal in 2/25 vs 59/128 without removal [odds ratio 17.3 (95% CI 2.2 to 139.4]; in group not removed, adverse outcome in 9/10 with S. aureus BSI, 32/42 with Gram-negative BSI, 47/84 with coagulase-negative staphylococcal BSI |
| Stamos51 | 1995 | USA | Children with CVC, preterm (n = 16), cancer (n = 10) | Retrospective cohort | 70 episodes of candidaemia in 65 children | Removal within 2 days of candidaemia detection | Results given for only 30 patients: 4/19 with early removal died vs 9/11 with late or no removal. No adjustment for differences in illness severity |
Results
We found no randomised studies and no controlled studies that used an explicit method for allocating patients to CVC removal or retention. From the 38 potentially eligible studies (see Figure 5), we found one systematic review43 and eight retrospective cohort studies in children. 45–52 We excluded seven retrospective cohort studies in adults. 41,42,53–57 We excluded one further study in children with cancer,52 as none of the required outcomes was reported in children with CVC removal and retention.
The systematic review by Nucci and Anaissie43 reported 14 cohort studies, four of which were in children,48,51,58,59 that compared CVC removal with retention in patients with candidaemia. We included only two studies48,51 that were discussed in that review43 as they involved children and were published after 1994. However, their review elucidates the critical source of bias inherent in observation studies of CVC removal: the timing of removal depends on the patient’s condition. Among patients with candidaemia, sicker patients were less likely to have their CVC removed and were more likely to die. Because of this problem, Nucci and Anaissie43 separately analysed seven studies,60–66 six published after 1994,60–65 that reported multivariable analyses with adjustment for severity of illness, but none of these included children. Most studies (5/7) reported a significant reduction in mortality with CVC removal in the multivariable analyses. 60,61,63–65 Similar results were found in the seven studies48,51,58,59,67–69 (three published after 1994)48,51,69 that did not adequately adjust for severity of illness. One subsequent study,45 of 61 children in Brazil, provided further evidence of this bias by showing that CVC removal was associated with early death, but not with later death, supporting the explanation that CVCs are least likely to be removed from the sickest patients. A recent commentary by Pasqualotto and Severo70 called for an RCT of CVC removal compared with retention in patients with candidaemia to address these serious biases in observational studies. 71
We included seven retrospective cohort studies that reported the association between CVC removal and risk of death, complications or recurrent infection in children (see Table 11). 45–51 The studies involved different patient groups (four studies were confined to neonates)47–50 and different types of bloodstream infection (five studies were restricted to specific organisms),45,47–49,51 making it difficult to assess consistency of results. None of the studies presented results adjusted for severity of illness, but three studies, one of bloodstream infection due to Enterobacteriaceae,47 one in neonates with coagulase-negative staphylococcal bloodstream infection49 and one in neonates with candidaemia,48 were from the same team of investigators and reported similar baseline characteristics in babies according to CVC removal or retention. 47–49 In the three studies involving bacteria, the risk of recurrent bloodstream infection was similar in the groups with and without CVC removal. In the group with the CVC retained, the risks of recurrent bloodstream infection and eventual CVC removal were strongly related to the number of days with positive blood cultures. These findings suggest that markers of persistent bacteraemia, such as daily repeated blood cultures, could provide a useful test to identify children most likely to benefit from CVC removal. A further study in neonates showed that persistent bacteraemia was associated with end-organ damage and was markedly increased in babies with CVC removal delayed for > 24 hours after the first positive blood culture result. The worst outcomes were associated with infection with S. aureus and Gram-negative organisms. 50
The excluded studies in adults reported a strong association between CVC removal and a reduced risk of complications of infection, consistent with the review findings of Nucci and Anaissie,43 but none of these studies took into account severity of illness. Overall, the included and excluded studies support the well-established clinical practice of removing the CVC in the presence of CVC-associated bloodstream infection. However, they also indicate that there is a significant minority of patients in whom CVC-associated bloodstream infection was successfully treated, and in whom CVC removal could be avoided.
Conclusions
The research evidence underpinning removal or retention of a CVC in patients with a CVC-associated bloodstream infection is of poor quality and there are no RCTs. The evidence suggests that retention of the CVC is strongly associated with complications of infection, particularly for candidaemia, S. aureus and some Gram-negative organisms. The evidence for removal or retention is far from certain for children at low to moderate risk of serious consequences, particularly those with coagulase-negative staphylococcal infection. The risks of infection associated with CVC retention need to be balanced against the problems of venous access and complications associated with CVC reinsertion in children. There is an urgent need for RCTs to evaluate the timing of CVC removal compared with treatment in situ in patient groups for whom removal is recommended. 13
Elsewhere in this report (see Chapters 3 and 5), we analyse bacterial DNA testing, in conjunction with clinical signs of CVC-related infection and blood culture, for identifying children who could benefit from CVC removal. However, findings from two studies in neonates, reported in this review,47,49 suggest that serial tests measuring bacteraemia persistence in response to treatment, rather than tests solely at presentation with suspected CVC-related infection, may be more useful than a single test on admission for predicting which children require CVC removal.
Background to reviews of antimicrobial locks for treatment or prevention
Injection of lock solution to fill the CVC lumens is standard practice to maintain CVC patency when not in use for infusion of fluids or administration of drugs. The standard lock solution is heparinised saline. The amount injected is typically 1–2 ml in children (0.4 ml in neonates). 72 Antimicrobial and antiseptic agents have been added to heparinised saline and other solutions to prevent adherence and multiplication of bacteria in the lumen and to eradicate bacteria that adhere to the CVC tubing. Antibiotic lock solutions can achieve much higher levels of antibiotic within the CVC lumen than could be safely achieved within the bloodstream. 34,73–75 The lock solution is left in the CVC until the next time the lumen needs to be used for fluid or drug administration to the patient, usually for at least 2 hours, though dwell times from 20–60 minutes up to several days have been reported. 76 Recommended practice is to withdraw and discard the lock solution before using the CVC again for infusion or administration of drugs in order to avoid adverse effects due to excessive blood levels of antibiotics or antiseptic solution.
Advantages of antibiotic or antiseptic locks include their low cost and the simple substitution of a different type of lock solution. Disadvantages include selection pressure, either for antibiotic-resistant organisms or for particular pathogens. 5 A further disadvantage is the need to allow a minimum dwell time, when the CVC lumen cannot be accessed, which can be associated with adverse effects, such as hypoglycaemia in neonates. 77 When used for treatment, antibiotic or antiseptic locks are almost always given in addition to systemic i.v. therapy. The type of antibiotic depends on the infecting organism and the dwell time is usually hours (e.g. 8–12 hours per day36) rather than days. The primary aim is to treat the current episode of infection and to reduce the risk of infection recurrence and complications. When used for prevention, antibiotic or antiseptic locks are given without other systemic treatment and the dwell time can be several days (e.g. between treatments or dialysis episodes). The primary aim is to reduce the risk of a CVC-associated infection developing. In view of these differences, we have reviewed the use of locks for treatment and prevention separately.
Systematic review of antibiotic locks for treating central venous catheter-associated infection
Structured summary
Context In patients with suspected CVC-associated infection, instillation of antibiotic lock solution into the CVC lumen, in addition to systematic i.v. antibiotic treatment, may be more likely to eradicate infecting organisms, thereby reducing the need for CVC removal owing to treatment failure and reducing the risk of recurrent infection.
Objective To determine the effectiveness of antibiotic lock treatment compared with no lock treatment or placebo on recovery from CVC-associated bloodstream infection or the risk of recurrent infection (composite outcome termed treatment failure).
Data sources We searched MEDLINE, EMBASE and CENTRAL from 1995 until April 2009. Search terms included synonyms for CVC, infection and lock.
Study selection We included any comparative studies in any patients with a suspected CVC-associated bloodstream infection who were treated with any type of antibiotic lock solution compared with those not treated with antibiotic lock solution.
Data extraction Weiwei Zhou extracted the data, which were checked by Ruth Gilbert.
Data synthesis We calculated the relative risk for any measure of treatment failure, and pooled results using a random effects model. We found one good-quality RCT36 comparing antibiotic lock treatment with placebo and two historical comparative studies,78,79 one comparing antibiotic lock treatment with routine replacement of the CVC. The other historical comparative study did not describe practice before introduction of lock treatment. The pooled relative risk showed no evidence of a significant reduction in the risk of treatment failure (relative risk 0.70, 95% CI 0.47 to 1.05).
Conclusions There is weak evidence for a reduced risk of treatment failure in patients undergoing antibiotic lock treatment compared with no lock treatment. Further RCTs are needed.
Review question
In patients with suspected CVC-associated infection, does antibiotic lock solution, compared with a standard heparin lock solution, reduce treatment failure?
Inclusion criteria
We included any comparative study published after 1994, including studies that were randomised, observational parallel group comparisons and before–after studies. We accepted any type or age of patient, any type of CVC and any type of antimicrobial lock solution compared with a non-antimicrobial solution. The outcome of treatment failure could be defined by any measure reflecting persistence of bloodstream infection or complications of bloodstream infection. We excluded studies without a comparison group.
Data extraction
We extracted characteristics of the study, participants, interventions and outcomes, as shown in Table 12, and the number of participants and CVCs randomised and outcomes recorded (Table 13). We calculated a relative risk for treatment failure based on the number of treatment failures reported using a denominator based on the number of CVCs with the outcome measured.
| Study details | Type of locks | Clinical problem | Age group | Mean age (years) | Number of subjects | Number of CVCs | Type of CVCs | Intervention group | Control group | Mean duration of CVC after randomisation (days) | Lock dwell time | Treatment failure |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Description of included trials (treatment) | ||||||||||||
| Rijnders,36 2005, Belgium | AB | Haematology or oncology or gastroenterology or haemodialysis | Adults/children | 48 | 46 | 46 | M | Vancomycin + heparin or ceftazidime + heparin | Placebo + heparin | 180 | BD | (1) CVC removal for any reason except not needed; (2) relapse of BSI with the same phenotypic strain; (3) death during initial AB lock treatment phase; (4) death due to CRBSI during the 6-month follow-up |
| Fortun,78 2006, Spain | AB | Chemotherapy or parenteral nutrition | Adults | 52–58 | 39 | 48 | NT | Vancomycin + heparin (if G+), or ciproflaxacin or gentamicin + heparin (if G–) | Not stated | NS | 8–12 hours | (1) CVC removal within 1 month; (2) relapse of BSI with the same phenotypic strain |
| Poole,79 2004, USA | AB | Haemodialysis | Adults | 52–54 | 137 | 137 | T | Vancomycin + heparin; ceftazidime + heparin; cefazolin + heparin (in both lumens) | Routine CVC removal | 154, 71 (median) | BD | (1) Persistent fever or haemodynamic instability > 48 hours after initiation of AB lock; (2) post-treatment BSI for any organism |
| Description of excluded trials (treatment) | ||||||||||||
| Onders82 2008, USA | AB | Haemodialysis | Children | 15 | 42 | 59 | T | TPA + tobramycin (G–) or vancomycin (G–) | Heparin + tobramycin (G–) or vancomycin (G+) | 262 | 48–72 hours | Positive blood culture after end of treatment |
| Primary author and reference | Number of CVCs randomised | Number of CVCs with outcome measured | Number of CVC days of follow-up | Treatment failure (primary) | Baseline risk of treatment failure in control | Treatment failure [relative risk (95% CI)] | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | |||
| Rijnders36 | 22 | 24 | 21 | 23 | NA | NA | 7 | 13 | 0.57 | 0.59 (0.29 to 1.19) |
| Fortun78 | 19 | 29 | 19 | 29 | NA | NA | 3 | 10 | 0.34 | 0.46 (0.14 to 1.45) |
| Poole79 | 68 | 69 | 47 | 69 | 154 | 71 | 14 | 24 | 0.35 | 0.86 (0.50 to 1.48) |
Results
We found four systematic reviews,73,75,80,81 one other review,34 and four comparative studies (see Table 12). 36,78,79,82 One of these was excluded as the authors compared different types of antimicrobial lock solutions. 82 Of the remaining three studies, only one was an RCT. 36 Rijnders et al. 36 compared vancomycin or ceftazidime and heparin lock with heparin alone, in children and adults with proven or suspected CVC-related bloodstream infection (see Table 12). This was a good-quality trial in which treatment and placebo were randomised by the hospital pharmacist and allocation was concealed from clinicians entering patients into the trial. In practice, the study population was selected to favour patients with coagulase-negative staphylococcal infection (29/46) or unproven CVC-related infection. A large number of potentially eligible patients were excluded from the trial because their physician requested removal of the CVC (e.g. all CVC-associated bloodstream infections due to S. aureus, fungal or Gram-negative infections). These recruitment problems, in addition to failing to recruit the planned sample size, led to the study being stopped.
The remaining two studies78,79 compared cohorts of adult patients in whom antibiotic locks were used with a historical cohort of patients in the same centre before antibiotics locks were introduced. The main weakness of these before–after comparisons is that other practices may have changed, apart from the use of antibiotic locks. For example, the US study by Poole et al. 79 excluded patients with enterococcal bloodstream infection in the phase when antibiotic locks were used, but did not specify this exclusion for the historical cohort.
Patients, interventions and outcomes differed between the three studies. In the study by Rijnders et al. 36 patients included a mix of adults and children who required a CVC, Poole et al. 79 studied adults undergoing haemodialysis, and Fortun et al. 78 studied adults receiving chemotherapy or parenteral nutrition. Most patients in both intervention and control groups had CVC-associated bloodstream infection due to coagulase-negative staphylococci. However, all three studies had an imbalance between the comparison groups, with fewer patients with Gram-positive bloodstream infection in the control group than in the group treated with antibiotic locks.
Interventions also differed. In the study by Poole et al.,79 patients did not receive concomitant systemic antibiotic therapy, but patients in the control group underwent CVC exchange. Finally, the criteria for the outcome – treatment failure – differed, ranging from follow-up of 1 month78 to 24 weeks. 36 The baseline risk of treatment failure ranged from 34% to 57% (see Table 13). As none of the studies reported sufficient information to allow a pooled analysis of the time to treatment failure, we calculated a relative risk and pooled relative risk for treatment failure. In view of the differences between the studies, we used a random effects model.
The relative risk of treatment failure reported in the RCT by Rijnders et al. 36 was 0.59 with a 95% CI that included 1.0 (0.29 to 1.19; Table 13). The pooled relative risk, based on all three included studies, did not provide evidence of a significant benefit of antibiotic lock solution at the 5% level (pooled relative risk 0.70, 95% CI 0.47 to 1.05; Figure 6). The results were moderately heterogenous (I2-value 0, 95% CI 0 to 90).
FIGURE 6.
Forest plot and pooled relative risk (random effects model).
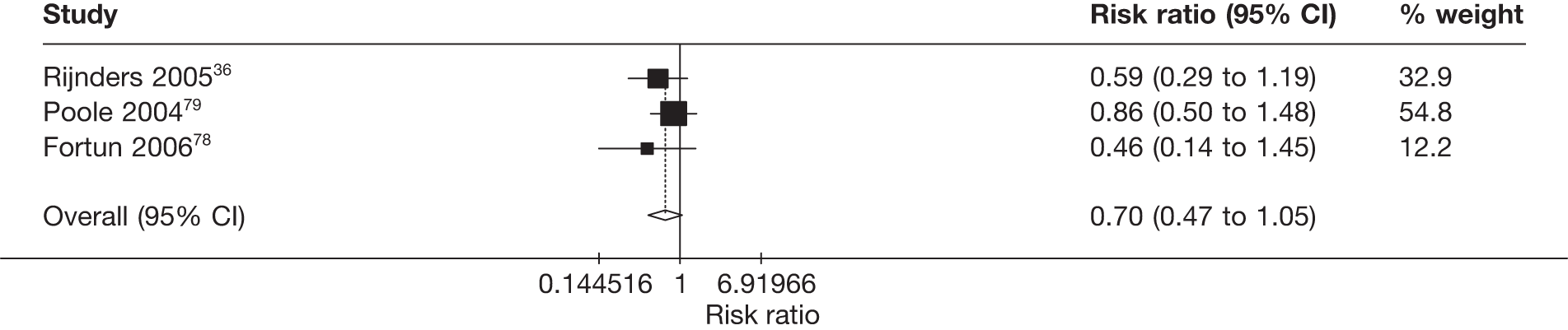
Conclusions
There is no clear evidence that treatment of CVC-associated bloodstream infection with locks reduces the risks of CVC removal, recurrent infection or ongoing symptoms. Information is lacking on how treatment effectiveness varies according to the type of infecting organism. RCTs are needed in children, for whom the pressure to ‘save the line’ may lead to inclusion of patients with infection due to a greater diversity of pathogens than seen in studies involving adults.
Systematic review of antimicrobial locks for prevention
Structured summary
Context Antibiotic or antiseptic lock solution may reduce the risk of CVC-associated infection.
Objective To determine the effectiveness of antibiotic or antiseptic lock solution compared with heparin lock solution for preventing CVC-associated bloodstream infection.
Data sources We searched MEDLINE, EMBASE and CENTRAL from 1995 until April 2009. Search terms included synonyms for CVC, infection and lock. We searched for reviews, in order to identify trials, and for RCTs. We also included any studies identified in searches for other questions included in this report.
Study selection We included any RCTs of antibiotic or antiseptic lock solutions compared with non-antimicrobial solutions in any patients with a CVC, provided bloodstream infection was reported.
Data extraction Weiwei Zhou extracted the data, which were checked by Ruth Gilbert.
Data synthesis We included 24 trials. All were included in the meta-analysis. Under half of the studies (n = 10) reported adequate allocation concealment and nine were placebo controlled. Studies included adults and children with cancer or requiring haemodialysis or intensive care. The pooled incidence rate ratio was 0.46 (95% CI 0.39 to 0.53).
Conclusions Despite moderate heterogeneity (I2-value 34, 95% CI 0 to 60) and weak evidence of funnel plot asymmetry, all but one trial had a central estimate consistent with a beneficial effect of lock solution, particularly antibiotic locks, compared with heparinised saline. This strongly beneficial effect of antimicrobial locks appeared to be consistent across different subgroups and is unlikely to be explained by failure to publish negative trials.
Review question
In patients with a CVC, does an antimicrobial lock solution (antibiotic or antiseptic), compared with a standard heparin lock solution, reduce the risk of CVC-associated bloodstream infection?
Inclusion criteria
We included studies in which either the patient or the CVC was randomised to any type of antimicrobial lock solution or a standard non-antimicrobial solution (such as heparinised saline). Urokinase was excluded as this is not an antimicrobial solution. Studies could be conducted in any setting or patient group, provided the patient was not known to have a CVC-associated bloodstream infection at the time of randomisation. The primary outcome was bloodstream infection requiring systemic antibiotics. We favoured bloodstream infection, as this requires admission and treatment regardless of the source of infection. If this was not reported, we accepted CVC-associated bloodstream infection. Our search strategy sought any type of systematic review, overview or meta-analysis that reported an RCT of antimicrobial lock solution in patients with a CVC (see Search strategy, selection of studies and data extraction, above, and Appendix 5). We retrieved the full copy of any potentially eligible study published after 1994.
Data extraction and analysis
We extracted characteristics of the study, participants, interventions and outcomes, as shown in Table 12, and the number of participants and CVCs randomised, total days of follow-up and bloodstream infection events (Tables 14 and 15). We calculated an incidence rate ratio for bloodstream infection in each study and used the Mantel–Haenszel method to calculate a pooled incidence rate ratio. This method is appropriate for pooled analyses when event rates are low or zero rates occur in one arm of the trial. However, the method does not allow a random effects analysis. One trial101 had no events in either treatment group and was excluded from the meta-analysis. To generate a funnel plot using stata would have required excluding four studies with zero events in the intervention arm,84,88,89,92 thereby underestimating asymmetry. Instead, we added 0.5 events to the intervention and control arm for these four studies, solely for the funnel plot and Egger test of asymmetry.
| Study details | Type of locks | Condition | Age group | Mean age (years) | Number of subjects | Number of CVCs | Type of CVCs | Intervention group | Control group | Mean duration of follow-up (days) | Explicit lock (vs flush) | Lock dwell time | Outcome measure | Allocation concealment | Placebo control |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Daghistani,83 1996, USA | AB | Cancer | Adults | 10 | 61 | 64 | NT | Vancomycin + amikacin | Heparin | 320 | No | NS | CRBSI | Yes | Yes |
| Carratala,84 1999, Spain | AB | Cancer | Adults | 43 | 120 | NT | Vancomycin (25 µg/ml) + heparin | Heparin | 11 | Yes | 1 hour, every 2 days, then aspirated | CRBSI | Yes | Yes | |
| Rackoff,85 1995, USA | AB | Cancer | Children | 8 | 63 | T | Vancomycin + heparin | Heparin | 145 | No | NS | BSI | NS | Yes | |
| Barriga,86 1997, Chile | AB | Cancer | Children | 83 | T | Vancomycin + heparin | Heparin | 201 | No | NS | BSI | Yes | Yes | ||
| Henrickson,87 2000, USA | AB | Cancer | Children | 126 | 154 | T | Vancomycin + heparin + ciprofloxaxin or vancomycin + heparin | Heparin | 241 | No | NS | BSI | Yes | Yes | |
| Cooper,88 1999, USA | AB | Haemodialysis | Adults | 36 | T | Gentamicin | Heparin | 86 | Yes | BD | CRBSI | NS | NS | ||
| Dogra,89 2002, Australia | AB | Haemodialysis | Adults | 57 | 83 | 112 | T | Gentamicin + citrate | Heparin | 71 | Yes | BD | BSI | Yes | Yes |
| Pervez,90 2002, USA | AB | Haemodialysis | Adults | 50 | 55 | 55 | T | Gentamicin + Tricitrasol + bag over CVC hub | Heparin + bag | 81 | Yes | BD | CRBSI | NS | OL |
| McIntyre,91 2004, UK | AB | Haemodialysis | Adults | 61 | 50 | T | Gentamicin + heparin | Heparin | 114 | Yes | NS | CRBSI | Yes | OL | |
| Bleyer,92 2005, USA | AB | Haemodialysis | Adults | 54 | 60 | M | Minocycline–EDTA | Heparin | 78 | Yes | BD | CRBSI | NS | Yes | |
| Saxena,93 2005, Saudi Arabia | AB | Haemodialysis | Adults | 48 | 208 | 208 | NT | Cefotaxime + heparin | Heparin | 365 | Yes | BD | CRBSI | Yes | Yes |
| Kim,94 2006, Korea | AB | Haemodialysis | Adults | 55 | 120 | Cefazolin + gentamicin + heparin | Heparin | 38 | Yes | BD | CRBSI | NS | Yes | ||
| Nori,95 2006, USA | AB | Haemodialysis | Adults | 58 | 62 | T | Gentamicin + tricitrate, minocycline–EDTA | Heparin | 100 | Yes | BD | CRBSI | NS | OL | |
| Saxena,96 2006, Saudi Arabia | AB | Haemodialysis | Adults | 77 | 118 | 124 | T | Cefotaxime + heparin | Heparin | 368 | Yes | BD | CRBSI | Yes | Yes |
| Zhang,97 2006, China | AB | Haemodialysis | Adults | NS | 101 | T | Gentamicin + heparin | Heparin | 92 | NS | NS | NS | NS | OL | |
| Al-Hwiesh,98 2007, Saudi Arabia | AB | Haemodialysis | Adults | 47 | 63 | 81 | T | Vancomycin + gentamicin + heparin | Heparin | 256 | Yes | BD | BSI | NS | OL |
| Zhang,99 2009, China | AB | Haemodialysis | Adults | 52 | 140 | T | Gentamicin + heparin | Heparin | 243 | No | NS | CRBSI | NS | OL | |
| Garland,72 2005, USA | AB | Intensive care | Children | 2 | 85 | NT | Vancomycin | Heparin | 20 | Yes | ≥ 20 minutes | BSI | Yes | Yes | |
| Simon,100 2008, Germany | AS | Cancer | Children | 179 | T | TauroLock | Heparin | 71 | Yes | One to two times a week | BSI | NS | NS | ||
| Hendrickx,101 2001, Belgium | AS | Haemodialysis | Adults | 70 | 19 | T | Citrate | Heparin | 168 | Yes | BD | CRBSI | NS | OL | |
| Betjes,102 2004, Netherlands | AS | Haemodialysis | Adults | 54 | 58 | 76 | NT | Citrate + taurolidine | Heparin | 59 | Yes | BD | CRBSI | NS | OL |
| Weijmer,103 2005, Netherlands | AS | Haemodialysis | Adults | 62 | 291 | 291 | M | Citrate | Heparin | 57 | No | NS | CRBSI | Yes | Yes |
| Macrae,104 2008, Canada | AS | Haemodialysis | Adults | 66 | 61 | T | Citrate | Heparin | 67 | No | BD | CRBSI | NS | OL | |
| Power,105 2009, UK | AS | Haemodialysis | Adults | 63 | 232 | T | Citrate (46.7%) | Heparin | 146 | Yes | NS | CRBSI | NS | OL |
| Primary author and reference | Condition | Age group | Year published | Number of CVCs with outcome measured | Number of CVC days of follow-up | Number of BSI events | BSI rate (per 1000 CVC days) in control | Rate ratio (95% CI) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | ||||||
| Antibiotic lock | |||||||||||
| Garland72 | Intensive care | Children | 2005 | 42 | 43 | 853 | 843 | 7 | 18 | 21.35 | 0.38 (0.14 to 0.96) |
| Zhang99 | Haemodialysis | Adults | 2009 | 71 | 69 | 17,781 | 16,299 | 1 | 11 | 0.67 | 0.08 (0 to 0.57) |
| Daghistani83 | Cancer | Adults | 1996 | 30 | 34 | 9814 | 10,033 | 2 | 3 | 0.30 | 0.68 (0.06 to 5.95) |
| Carratala84 | Cancer | Adults | 1999 | 60 | 57 | 600 | 627 | 0 | 4 | 6.38 | 0 (0 to 1.58) |
| Rackoff85 | Cancer | Children | 1995 | 32 | 31 | 4378 | 4780 | 10 | 10 | 2.09 | 1.09 (0.41 to 2.92) |
| Barriga86 | Cancer | Children | 1997 | 39 | 44 | 8666 | 8011 | 18 | 26 | 3.25 | 0.64 (0.33 to 1.21) |
| Henrickson87 | Cancer | Children | 2000 | 73 | 80 | 18,899 | 18,045 | 11 | 31 | 1.72 | 0.34 (0.15 to 0.69) |
| Cooper88 | Haemodialysis | Adults | 1999 | 19 | 17 | 1485 | 1610 | 0 | 3 | 1.86 | 0 (0 to 2.62) |
| Dogra89 | Haemodialysis | Adults | 2002 | 53 | 55 | 3280 | 2643 | 0 | 7 | 2.65 | 0 (0 to 0.56) |
| Pervez90 | Haemodialysis | Adults | 2002 | 14 | 41 | 1613 | 3207 | 1 | 8 | 2.49 | 0.25 (0.01 to 1.85) |
| McIntyre91 | Haemodialysis | Adults | 2004 | 25 | 25 | 3252 | 2470 | 1 | 10 | 4.05 | 0.08 (0 to 0.53) |
| Bleyer92 | Haemodialysis | Adults | 2005 | 30 | 27 | 2336 | 2118 | 0 | 1 | 0.47 | 0 (0 to 35.36) |
| Saxena93 | Haemodialysis | Adults | 2005 | 159 | 49 | 58,035 | 17,885 | 96 | 56 | 3.13 | 0.53 (0.38 to 0.75) |
| Kim94 | Haemodialysis | Adults | 2006 | 60 | 60 | 2261 | 2242 | 1 | 7 | 3.12 | 0.14 (0 to 1.10) |
| Nori95 | Haemodialysis | Adults | 2006 | 41 | 20 | 4455 | 1734 | 1 | 7 | 4.04 | 0.06 (0 to 0.43) |
| Saxena96 | Haemodialysis | Adults | 2006 | 59 | 60 | 21,535 | 21,900 | 36 | 79 | 3.61 | 0.46 (0.30 to 0.70) |
| Zhang97 | Haemodialysis | Adults | 2006 | 49 | 52 | 5635 | 3665 | 0 | 3 | 0.82 | 0 (0 to 1.57) |
| Al-Hwiesh98 | Haemodialysis | Adults | 2007 | 37 | 44 | 7179 | 7650 | 4 | 30 | 3.92 | 0.14 (0.04 to 0.40) |
| Antiseptic lock | |||||||||||
| Hendrickx101 | Haemodialysis | Adults | 2001 | 10 | 9 | 1703 | 1493 | 0 | 0 | 0.00 | |
| Simon100 | Cancer | Children | 2008 | 95 | 98 | 6705 | 6086 | 25 | 30 | 4.93 | 0.76 (0.43 to 1.33) |
| Betjes102 | Haemodialysis | Adults | 2004 | 37 | 39 | 1519 | 1885 | 0 | 4 | 2.12 | 0 (0 to 1.88) |
| Weijmer103 | Haemodialysis | Adults | 2005 | 148 | 143 | 8182 | 8049 | 9 | 33 | 4.10 | 0.27 (0.11 to 0.57) |
| Macrae104 | Haemodialysis | Adults | 2008 | 25 | 21 | 3182 | 2121 | 5 | 6 | 2.83 | 0.56 (0.13 to 2.18) |
| Power105 | Haemodialysis | Adults | 2009 | 132 | 100 | 19,285 | 17,349 | 13 | 12 | 0.69 | 0.97 (0.41 to 2.34) |
We assessed heterogeneity by calculating the Q statistics and I2-value for all studies combined. We also performed subgroup analyses to explore variation in the incidence rate ratio and I2-value, according to allocation concealment and characteristics of the population (e.g. cancer, children, type of CVC), intervention (antibiotic lock or not) and outcome measure (bloodstream infection or CVC-associated bloodstream infection). We also generated a funnel plot to explore variation in the incidence rate ratio according to study precision.
Results
We found 17 reviews. 5,73,74,77,106–116 Two of these reviews77,106 contained 21 of 24 RCTs included in our review. Scrutiny of published guidelines did not yield additional studies. 13,38,117,118 One further systematic review119 was published after the searches were complete, and contained four further studies. 99,120–122 Only one of these, involving gentamicin (total 140 patients),99 was an RCT and contained data that could be used in the meta-analysis. In total, we found eight systematic reviews. 5,77,106,108–111,115,119 We excluded a further 17 studies because they were not trials, did not compare antimicrobial locks or compared a single perioperative administration of lock solution (see Table 23, Appendix 6). We found one trial in progress using TauroLock in children with cancer (NCTs 00735813, 00545831, 0074916).
Of the 245 included trials, 18 compared various antibiotic lock solutions with heparinised saline (see Table 14). 72,83–99 The remaining six studies included citrate or taurolidine. 100–105,123 Most studies were conducted in patients undergoing haemodialysis (n = 17), but there were four studies in children with cancer. 85–87,100 No studies compared locks in adults or children receiving parenteral nutrition.
Under half of the studies (n = 10) reported adequate allocation concealment, and nine of these were placebo controlled (see Table 14). At least five studies randomised more CVCs than there were patients, so that the same patient was included in the trial more than once. 87,89,96,98 In other studies, poor reporting made it hard to assess repeated inclusion of the same patient. Similarly, loss to follow-up was hard to assess because of poor reporting but was ≤ 10% where numbers randomised and assessed for outcome were reported. 84,92,96,105 The duration of follow-up ranged from 20 to 368 days (see Table 14). There was substantial variation in the baseline rate of bloodstream infection in the control group. The rate was lowest (< 1/1000 CVC days) in adults undergoing haemodialysis and highest (up to 21/1000 CVC days) in children in intensive care (Figure 7).
FIGURE 7.
Baseline rate of bloodstream infection by age and condition.
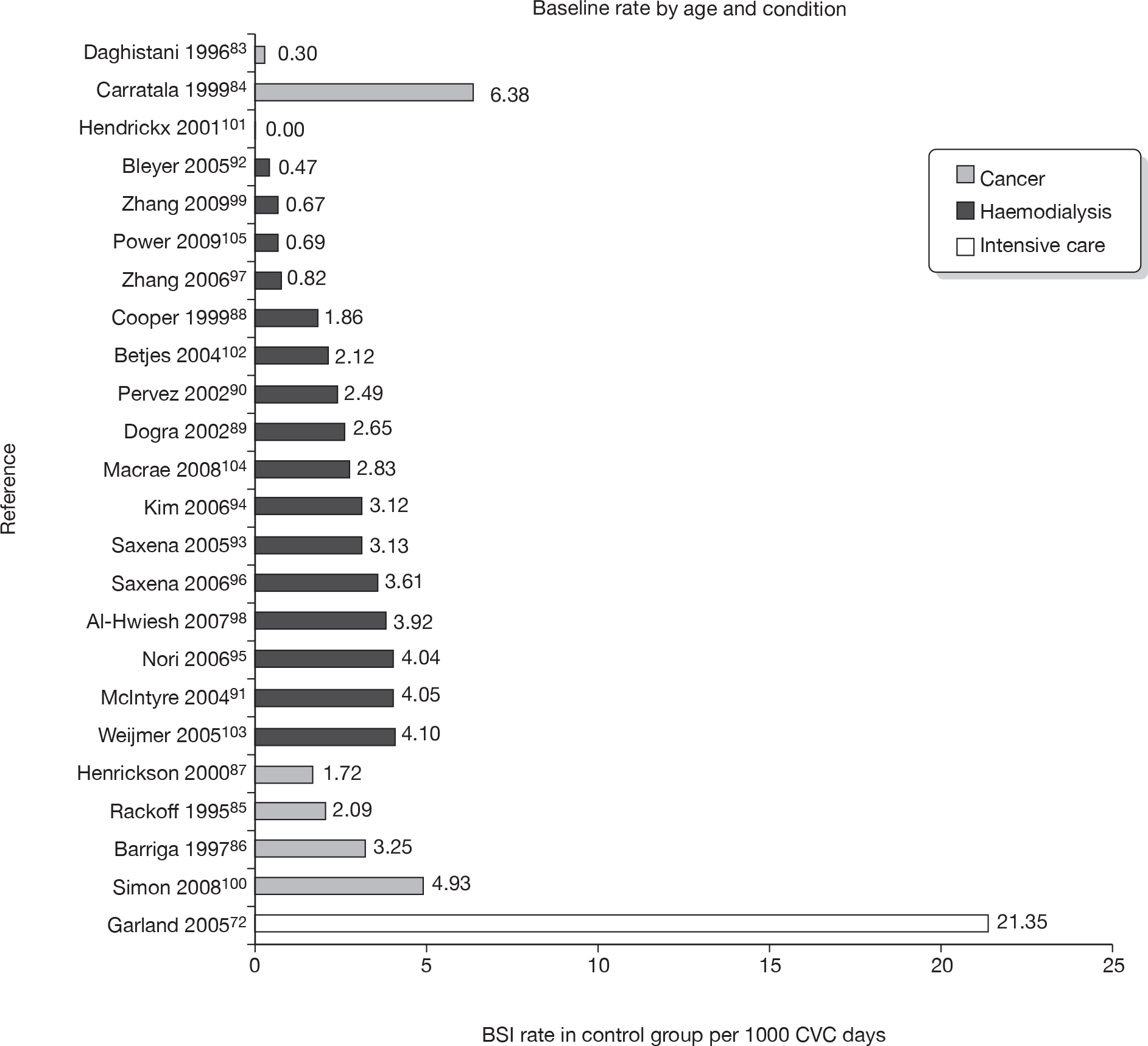
Despite the large number of studies and 3043 patients studied (see Table 14), this review lacked the power to detect CVC-associated bloodstream infection due to resistant organisms because of the low rate of bloodstream infection (see Table 15). Fourteen studies followed up patients for ≥ 3 months, three of these followed patients for > 10 months (see Table 14). 83,93,96 Very large studies with long-term follow-up would be required to provide clear evidence to support or refute widespread concerns about rare but serious infections with resistant organisms due to the use of antimicrobial locks. However, other studies have reported selection of antibiotic-resistant strains. Guerraoui et al. 124 reported resistant strains of S. epidermidis after prolonged use of gentamicin locks for prophylaxis in permanent haemodialysis catheters. Finally, in a before–after study comparing taurolidine with heparin saline locks in children with cancer, Simon et al. 100 reported a reduction in CVC-associated infection with staphylococci and an increase in CVC-associated infection with E. coli (10/27 in the taurolodine group vs 4/31 in the control group; odds ratio for E. coli occurrence 3.97, 95% CI 1.12 to 13.93).
The pooled incidence rate ratio for all 23 studies included in the meta-analysis (one excluded because of zero events) was 0.46 with narrow confidence limits (95% CI 0.39 to 0.53; Figure 8). There was moderate heterogeneity across studies (I2-value 34; see Table 15), but the chi-squared test for heterogeneity was not significant at the 5% level (p = 0.0579). All except one trial had a central estimate consistent with a beneficial effect of lock solution compared with heparinised saline (see Figure 8 and Table 15).
FIGURE 8.
Forest plot and pooled incidence rate ratio for bloodstream infection in patients randomised to antimicrobial lock prophylaxis or standard heparin lock. IRR, incidence rate ratio; M–H, weighting for Mantel–Haenszel model.
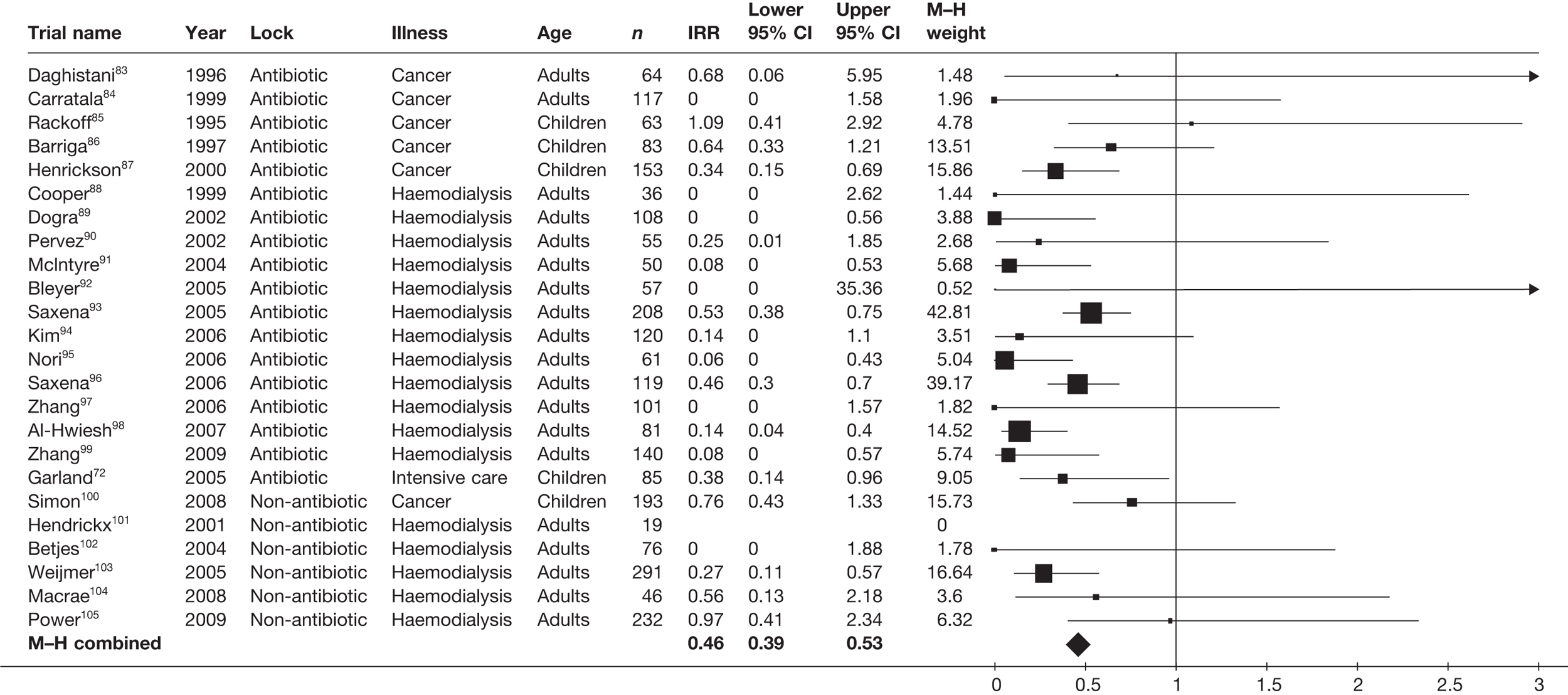
We explored sources of heterogeneity using subgroup analyses (Table 16). The pooled incidence rate ratio was similar in studies regardless of the quality of allocation concealment, but was lower in studies using antibiotic rather than antiseptic solution (see Table 16). There was moderate heterogeneity within subgroups according to condition and child or adult populations, and the pooled incidence rate ratio was closer to 1.0 in studies of children than in those of adults (see Table 16). Nevertheless, the effect of antimicrobial lock solution was substantial and significant at the 5% level for subgroups of children with cancer and for babies in intensive care (see Table 16 and Figure 8). There was evidence that rate ratios were lower for patients with a tunnelled CVC than for those with other forms, and where the lock solution had been explicitly administered as a flush (see Table 16).
| n | IRR (95% CI) | Q-statistic | p-value (chi-squared test) | I2-value (95% CI) | |
|---|---|---|---|---|---|
| All studies | 23 | 0.43 (0.36 to 0.51) | 33.29 | 0.0579 | 34 (0 to 60) |
| Allocation concealment | |||||
| Yes | 10 | 0.43 (0.35 to 0.62) | 8.48 | 0.4869 | 0 (0 to 62) |
| Not stated | 13 | 0.43 (0.32 to 0.59) | 24.7 | 0.0163 | 51 (8 to 74) |
| Type of lock | |||||
| Antibiotic | 18 | 0.40 (0.33 to 0.48) | 24.51 | 0.1061 | 31 (0 to 61) |
| Non-antibiotic | 5 | 0.56 (0.39 to 0.79) | 7.01 | 0.1354 | 43 (0 to 79) |
| Age group | |||||
| Adults | 18 | 0.37 (0.30 to 0.46) | 24.79 | 0.0994 | 31 (0 to 61) |
| Children | 5 | 0.59 (0.44 to 0.79) | 6.24 | 0.1821 | 36 (0 to 76) |
| Type of lock, age group, condition | |||||
| Antibiotic_Adults_Cancer | 2 | 0.29 (0.06 to 1.42) | 0.85 | 0.3569 | |
| Antibiotic_Adults_Haemodialysis | 12 | 0.36 (0.28 to 0.45) | 18.16 | 0.0778 | 39 (0 to 69) |
| Antibiotic_Children_Cancer | 3 | 0.56 (0.38 to 0.83) | 4.46 | 0.1075 | 55 (0 to 87) |
| Antibiotic_Children_Intensive | 1 | 0.38 (0.14 to 0.96) | |||
| Antiseptic_Adults_Haemodialysis | 4 | 0.45 (0.28 to 0.71) | 5.78 | 0.123 | 48 (0 to 83) |
| Antiseptic_Children_Cancer | 1 | 0.76 (0.43 to 1.33) | |||
| Type of CVC | |||||
| Tunnel-cuffeda | 15 | 0.44 (0.36 to 0.54) | 28.28 | 0.0131 | 50 (10 to 73) |
| Non-tunnelled | 5 | 0.47 (0.35 to 0.64) | 0.78 | 0.9405 | 0 (0 to 79) |
| Mixed | 2 | 0.26 (0.12 to 0.54) | 0.01 | 0.9342 | |
| Explicit lock | |||||
| Yesb | 15 | 0.43 (0.35 to 0.52) | 22.31 | 0.0726 | 37 (0 to 66) |
| No | 7 | 0.44 (0.32 to 0.61) | 10.81 | 0.0945 | 44 (0 to 77) |
| Outcome measured | |||||
| BSIc | 7 | 0.47 (0.36 to 0.63) | 13.67 | 0.0335 | 53 (0 to 79) |
| CRBSI | 15 | 0.41 (0.33 to 0.51) | 18.76 | 0.1742 | 25 (0 to 60) |
The funnel plot showed weak evidence of asymmetry (Figure 9). The Egger test for asymmetry was of equivocal significance (Egger test p = 0.073). A L’Abbé plot did not indicate a strong relationship between the baseline event rate and the incidence rate ratio (plot not shown).
FIGURE 9.
Funnel plot for studies of antimicrobial lock prophylaxis compared with standard heparin solution for preventing CVC-associated infection. For five studies with at least one arm with zero events, we added 0.5 to each arm.
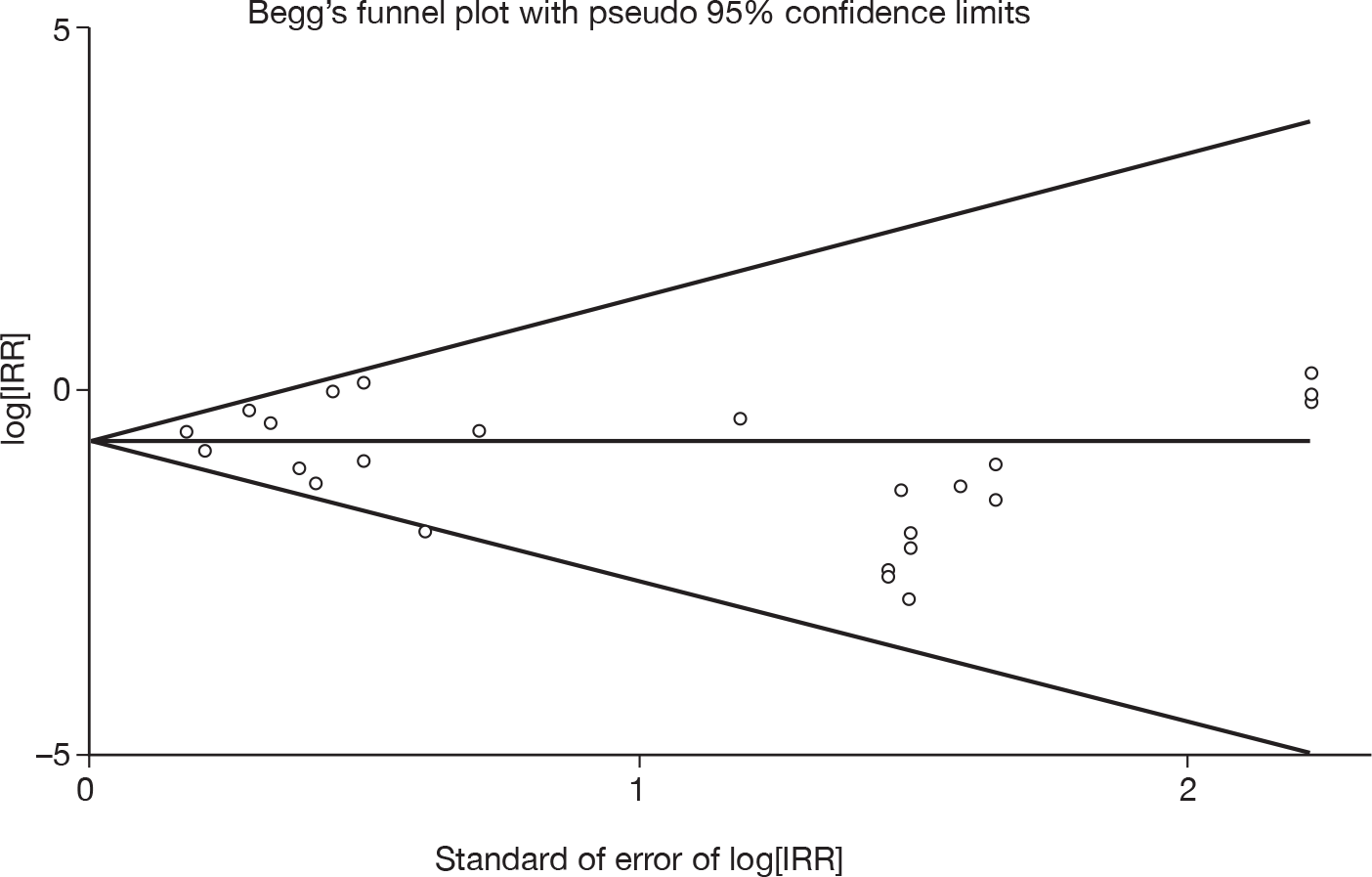
Conclusions
This review provides strong evidence that antimicrobial locks, and particularly antibiotic locks, reduce the risk of bloodstream infection. Although the magnitude of effect appears to be less for antiseptic lock solution and for children with cancer than for adults with cancer, the effects are nevertheless marked and likely to be clinically important in all patient groups studied. Although these findings are consistent across all patient groups, there is weak evidence of funnel plot asymmetry, which could be explained by failure to publish negative trials. Such publication bias would reduce the magnitude of effect but, unless very large negative trials remain unpublished, would be unlikely to reverse the evidence of benefit.
Survey of practice
Evidence for the effectiveness of antimicrobial lock solution for preventing CVC-associated bloodstream infection has now been summarised in nine systematic reviews (including our own). 5,77,106–111 These reviews consistently report a reduced rate of CVC-associated infection in patients given antimicrobial lock prophylaxis compared with heparin lock solution. According to our review (based on 24 RCTs), the rate of infection was halved in patients given antimicrobial lock prophylaxis. The evidence that antibiotic solutions are effective for treating CVC-associated infection is much weaker. There have been five systematic reviews including our own,73,75,80,112 but only one RCT36 and two before–after studies. 78,79 Our systematic review found no clear evidence for the effectiveness of antibiotic lock treatment for CVC-associated bloodstream infection.
These findings from systematic reviews contrast with recommendations for practice in national and international guidelines. Most recently, the Infectious Disease Society of America recommended using lock treatment rather than CVC removal for CVC-associated bloodstream infection due to pathogens other than S. aureus, P. aeruginosa, Bacillus spp., Micrococcus spp., propionibacteria, fungi or mycobacteria in patients with long-term CVCs. 13 Despite the acknowledged weak evidence base, antibiotic lock treatment has been recommended for nearly a decade in patients with CVC-associated infection. 116 In contrast, national guidelines in the UK and USA, and international guidelines for specific disease groups, recommend against routine use of antimicrobial locks to prevent infection except for patients with recurrent CVC-associated bloodstream infection. 38,125–127 Reasons against using antimicrobial locks for preventing infection include the theoretical risk of antibiotic resistance and the potential for systemic toxicity from leakage of the lock solution into the bloodstream. 76 Some guidelines state that antimicrobial lock works only for preventing CVC-associated infection in neutropenic patients,125,126 a perception disproved by the consistent finding of benefit in patients receiving haemodialysis in our review. Views may be beginning to change, however. The British Society for Haematology guidelines do not explicitly recommend use of antimicrobial locks for prevention or treatment, but mention both applications,128 and the most recent guidelines from the USA advocate antimicrobial lock prophylaxis for patients with limited venous access. 13,76
The disparity in the literature between evidence for effectiveness of antimicrobial locks and recommended practice was mirrored in our discussions with paediatric oncologists. We therefore undertook a national survey of paediatric oncology centres to determine the extent to which antimicrobial locks were used for prevention or treatment of CVC-associated bloodstream infection, any experiences of adverse effects, and what were the perceived disadvantages that discouraged their use. In centres that reported using locks, we sent a questionnaire to the hospital pharmacist requesting details of the formulation of lock solutions used.
Methods
We developed a questionnaire in collaboration with the clinical experts involved in the CCLG Supportive Care Group. The questionnaire included a brief letter summarising the available evidence on the effectiveness of antimicrobial locks for prevention and treatment of CVC-associated bloodstream infection (see Appendix 7). We asked about current use of antimicrobial locks for prevention or treatment, adverse effects, factors that might discourage their use, and the proportion of children for whom locks could be used in their centre. We sent the questionnaire to the CCLG co-ordinating clinician at each of the 21 CCLG centres in the UK in July 2009.
Results
Questionnaire responses were received from 18 (86%) of the 21 UK centres (Aberdeen, Belfast, Birmingham, Bristol, Cambridge, Cardiff, Dublin, Glasgow, Great Ormond Street, Leeds, Leicester, Liverpool, Manchester, Newcastle upon Tyne, Nottingham, Oxford, Southampton and University College London). The responses are shown in Table 17. Of those who replied 12 (67%) used locks for treatment and only four (22%) used locks for prevention (14 used antibiotic locks for prevention or treatment).
| Currently used? | Could be used for? (%) | Adverse effects | Factors discouraging use of antimicrobial lock solutions | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antibiotic resistance | Doubts over efficacy | Safety profile | Costs | Lumen time | Inconvenience | ||||||||||||
| P | T | P | T | P | T | P | T | P | T | P | T | P | T | P | T | ||
| 1 | No | No | 0 | < 5 | 1 | 1 | 1 | 1 | 1 | ||||||||
| 2 | No | No | 0 | ||||||||||||||
| 3 | No | No | No | 1 | |||||||||||||
| 4 | No | No | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| 5 | No | Yes | 0 | 20 | No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 6 | No | Yes | 20 | 50 | No | 1 | 1 | 1 | 1 | 1 | |||||||
| 7 | No | Yes | 100 | No | 1 | 1 | |||||||||||
| 7 | No | Yes | 60 | 10 | No | 1 | 1 | 1 | |||||||||
| 8 | No | Yes | 70 | 70 | Yes | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 9 | No | Yes | 90 | 50 | No | 1 | 1 | 1 | 1 | 1 | 1 | ||||||
| 10 | No | Yes | No | 1 | 1 | 1 | |||||||||||
| 11 | No | Yes | 60 | No | 1 | 1 | 1 | 1 | |||||||||
| 12 | No | Yes | 75 | No | 1 | 1 | 1 | ||||||||||
| 13 | No | Yes | 100 | No | |||||||||||||
| 14 | Yes | No | 95 | 80 | Yes | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||
| 15 | Yes | No | No | ||||||||||||||
| 16 | Yes | Yes | 60–80 | 60–80 | No | 1 | 1 | 1 | 1 | 1 | |||||||
| 17 | Yes | Yes | Yes | 1 | |||||||||||||
| 18 | No | No | 20–30 | > 80 | No | 1 | 1 | 1 | 1 | 1 | |||||||
| Total | 4 | 12 | 3 | 11 | 1 | 13 | 3 | 3 | 0 | 7 | 1 | 8 | 8 | 10 | 2 | ||
Responses from CCLG clinicians
A substantial proportion raised concerns about the use of antimicrobial locks particularly for the prevention of CVC-associated infection (see Table 17 and Appendix 7). Thirteen (72%) of the 18 centres expressed doubts about the efficacy of locks for prevention (despite the evidence summarised in the letter accompanying the questionnaire) and 10 (56%) centres expressed concerns about the potential for antimicrobial locks used for prevention to select for antibiotic-resistant microbes. Estimates of the proportions of children for whom antimicrobial locks would be feasible ranged from 0% to 100% for prevention and for treatment.
Survey of formulation of locks for treatment
An issue that became apparent following informal discussion with local pharmacists is the paucity of commercially available antibiotic lock solutions. In the UK, commercially available antimicrobial locks are limited to TauroLock (taurolidine citrate; Kimal, TauroPharm GmbH, Waldbuttelbrunn, Germany) and Citra-Lock (trisodium citrate; Dirinco, Eindhoven, Holland), which are used only for prevention. There are no commercially available antibiotic lock solutions for prevention or treatment so that, in practice, using antimicrobial locks requires either the use of a commercially available product or considerable support from local hospital pharmacies. For example, the provision of antimicrobial lock solution for prevention would require the manufacture of > 200 ampoules/pre-packed syringes of lock solution per child per year with a CVC or port. For a centre with 100 children undergoing active treatment for cancer this would be a significant undertaking (even for a large hospital pharmacy).
An additional problem is the limited data on stability of antibiotic solutions, particularly if stored in pre-filled plastic syringes. These uncertainties are further compounded when antibiotic solutions are prepared and stored in the presence of heparin, which interacts with some antibiotics. One option is not to use heparin and use saline instead, and some CVC manufacturers specify the use of heparin flushes or locks and some do not. However, a recent RCT with 203 children undergoing treatment for cancer randomised to either heparin or saline flush solutions showed a significantly higher rate of complications (CVC occlusion or bacteraemia) in the children in whom saline was used (as opposed to heparin),129 although there was no difference in the retention of CVCs between the two groups.
Concerns with respect to stability, the potential for interactions with heparin, plastics and combinations of antimicrobials, and the lack of standardisation or accepted best practice guidelines for the use of antimicrobial locks are reflected in recent literature. 130 In the small number of limited studies that have reported antimicrobial stability and activity in candidate lock solutions there is considerable variation in the concentrations, conditions and methodologies used. 131–136
In summary, uncertainties remain concerning:
-
selection of antibiotic according to microbial aetiology
-
interactions between antibiotics and other drugs, including heparin, and with plastics
-
shelf life of pre-prepared solutions
-
requirement for heparin
-
antibiotic concentration
-
optimum diluent
-
frequency of use of locks, and dwell times.
In the light of discussions with local hospital pharmacists, we asked the 14 clinicians who had replied to the initial questionnaire and who reported the use of antimicrobial locks for prevention or treatment for details of the formulation of lock solutions used. To respond, clinicians usually referred to the hospital pharmacists for further details. We received replies from seven centres (Table 18).
| Antimicrobial | Concentrations used | Diluent |
|---|---|---|
| Vancomycin | 2, 5 or 10 mg/ml | 0.9% sodium chloride |
| 2 mg/ml | 0.9% sodium chloride + heparin 90 U/ml in final volume | |
| Gentamicin | 2 or 10 mg/ml | 0.9% sodium chloride |
| 10 mg/ml | Vial solution + heparin 90 U/ml in final volume | |
| 1 mg/ml | Water for injection | |
| Amikacin | 2 or 5 mg/ml | Water for injection |
| Amphotericin | 1 mg/ml | Water for injection |
| Ciprofloxacin | 2 mg/ml | Water for injection |
| Piperacillin and tazobactam | 90 mg/ml | |
| Teicoplanin | 67–133 mg/ml | Water for injection + heparin 90 U/ml in final volume |
| 67–133 mg/ml | Diluent provided by manufacturer + 0.9% sodium chloride to make up CVC volume | |
| Alcohol | 75% ethanol | water |
The information from the seven centres that replied showed four different vancomycin preparations and four different gentamicin preparations. Teicoplanin was used instead of vancomycin in two centres (two different preparations) and amikacin was used as an alternative to gentamicin in two centres (two different preparations).
Discussion
Antimicrobial locks are used by two-thirds of the paediatric oncology units in the UK for treating suspected CVC-associated bloodstream infection, but by only one-fifth of units reported using locks for prevention. In practice, the description of prevention reflects prolonged use in patients who had been treated with antibiotic locks and does not represent prophylactic use in patients without an infection. These patterns of use contrast strongly with the available evidence. Despite this lack of evidence, clinicians are under enormous pressure to use any means that might save a ‘precious’ line and avoid the trauma of removal and CVC reinsertion. Yet interventions that delay removal of the line can increase the risk of serious complications or death owing to CVC-related infection. There is an urgent need for an RCT of lock treatment compared with standard therapy to guide practice. There is also a need to develop strategies to allow sufficient lock dwell time but minimise competition for access to CVC lumens for infusion of fluids and drug administration.
Clinicians’ reluctance to substitute antimicrobial locks for the current heparin locks in order to prevent CVC-associated infection, despite strong evidence of effectiveness, partly reflects the practical difficulties of accessing ready-mixed lock solution. Although seven units expressed concerns about costs, in practice these are small compared with the costs of admission for CVC-associated infection. Further short-term efficacy studies of antibiotic locks for prevention are not required, but there is a need to ensure ready access to lock solution for prevention and to minimise the potential for drug errors. There may still be a need for longer-term studies that focus on the potential for use of antimicrobial locks to select for antimicrobial-resistant microbes and the clinical consequences of selection of antimicrobial resistance. The evidence for efficacy of antimicrobial locks is strongest for antibiotic locks that are not commercially available in pre-filled syringes (e.g. gentamicin 10 mg/ml is available in a glass vial). The use of antimicrobial locks for prevention would require that antimicrobials for which there are efficacy data be made available in pre-filled syringes.
Chapter 5 Clinical effectiveness of strategies combining test results with interventions
Rationale
The multivariable analyses indicated that the addition of bacterial DNA results did not improve the prediction of these outcomes, over and above the information provided by clinical signs and blood culture results (see Chapter 3). However, these analyses did not take into account the potential value of the earlier timing offered by DNA testing. Blood culture results are usually available 48 hours after sampling, whereas bacterial DNA results can be available within 2 hours, and, in combination with clinical signs on admission, could lead to early intervention. For example, early CVC removal in patients with a high DNA level and clinical signs of CVC infection, or early stopping of i.v. antibiotics in patients with negative results, could potentially avoid unnecessary days of admission for i.v. treatment, although the disadvantages could include unnecessary CVC removal or worsening of infection after stopping treatment.
The best way to assess the potential consequences of different test–treatment strategies is to undertake a cost-effectiveness analysis in which the various outcome states are measured in terms of quality-adjusted life-years (QALYs) and the entire health-care costs associated with each test–treatment strategy and its consequences are calculated. The cost/QALY gained from moving from one strategy to a more effective one can then be calculated and compared with costs that the health-care system is usually willing to pay (around £30,000/QALY).
We did not consider these complex analyses to be justified, given the quality of the available data. First, data on prognosis were limited in terms of sample size and duration of follow-up. Second, we lacked robust data from the systematic reviews on treatment effectiveness for removal of the CVC, antibiotic locks for treatment and early stopping of treatment.
Instead, we present simple balance sheet tabulations to illustrate the potential consequences of alternative treatment strategies for different clinical subgroups. The purpose is to show which strategies yield the greatest potential gains in order to guide further research. These illustrative analyses are based on optimistic assumptions about the effectiveness of different interventions, and take no account of the uncertainty in the parameters, which is particularly problematic given the number of zero cells (see Tables 19 and 20). The data used in the analyses are shown for outcome at 28 days in Table 19 and for outcomes at 6 months in Table 25 in Appendix 9. Our inferences are based on outcomes at 28 days because of potential selection biases and the scarcity of data in the 6-month follow-up.
| Clinical subgroup | Test results | Number of patients | Outcomes (days during 2-day follow-up) | Strategies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FRC | DNA (pg/µl) | Blood culture | Total | Recurrent i.v. treatment episode | CVC removed by 28 days | Initial treatment | Recurrent i.v. treatment | Total i.v. treatment | DNA + FRC: early removal | DNA + FRC early stop | BC + FRC remove @ 48 hours | BC + FRC stop @ 48 hours | BC + FRC + DNA remove @ 48 hours | BC + FRC + DNA stop @ 48 hours | |
| All | 179 | 34 | 10 | 1047 | 143 | 1190 | |||||||||
| A | FRC+ | > 0.5 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R0 | R48 | R48 | |||
| B | FRC+ | > 0.5 | Other | 5 | 0 | 2 | 44 | 0 | 44 | R0 | |||||
| C | FRC+ | > 0.5 | None | 0 | 0 | 0 | 0 | 0 | 0 | R0 | |||||
| D | FRC+ | 0.125–0.5 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R48 | |||||
| E | FRC+ | 0.125–0.5 | Other | 1 | 0 | 0 | 11 | 0 | 11 | ||||||
| F | FRC+ | 0.125–0.5 | None | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| G | FRC+ | < 0.125 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R48 | |||||
| H | FRC+ | < 0.125 | Other | 2 | 1 | 2 | 9 | 2 | 11 | ||||||
| I | FRC+ | < 0.125 | None | 5 | 0 | 1 | 64 | 0 | 64 | ||||||
| J | FRC- | > 0.5 | Pathogen | 3 | 0 | 2 | 29 | 0 | 29 | ||||||
| K | FRC- | > 0.5 | Other | 5 | 1 | 1 | 45 | 7 | 52 | ||||||
| L | FRC- | > 0.5 | None | 0 | 0 | 0 | 0 | 0 | 0 | S48 | |||||
| M | FRC– | 0.125–0.5 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| N | FRC– | 0.125–0.5 | Other | 7 | 0 | 0 | 55 | 0 | 55 | ||||||
| O | FRC– | 0.125–0.5 | None | 7 | 2 | 0 | 53 | 4 | 57 | S48 | |||||
| P | FRC– | < 0.125 | Pathogen | 2 | 1 | 0 | 17 | 6 | 23 | S48 | |||||
| Q | FRC– | < 0.125 | Other | 11 | 2 | 0 | 99 | 7 | 106 | S48 | |||||
| R | FRC– | < 0.125 | None | 131 | 27 | 2 | 621 | 117 | 738 | S48 | S48 | S48 | |||
| Strategy | Total number of events | Difference compared with standard care | ||||||
|---|---|---|---|---|---|---|---|---|
| Recurrence | CVCs removed | Unnecessary removal | i.v. days | Recurrence | CVCs removed | Unnecessary removal | i.v. days | |
| Balance sheet for 179 patients | ||||||||
| Standard | 34 | 10 | 0 | 1190 | ||||
| DNA + FRC: early removal | 34 | 13 | 3 | 1121 | 0 | 3 | 3 | –69 |
| DNA + FRC early stop | 34 | 10 | 0 | 453 | 0 | 0 | 0 | –737 |
| BC + FRC remove @ 48 hours | 34 | 10 | 0 | 1190 | 0 | 0 | 0 | 0 |
| BC + FRC stop @ 48 hours | 34 | 10 | 0 | 516 | 0 | 0 | 0 | –674 |
| BC + FRC + DNA remove @ 48 hours | 34 | 10 | 0 | 1190 | 0 | 0 | 0 | 0 |
| BC + FRC+DNA stop @ 48 hours | 34 | 10 | 0 | 569 | 0 | 0 | 0 | –621 |
| i.v. treatment of any FRC/DNA/BC+ | 31.9 | 7.6 | 0 | 1054 | –2 | –2 | 0 | –136 |
| Balance sheet for 1000 patients | ||||||||
| Standard | 190 | 56 | 0 | 6648 | 0 | 0 | 0 | 0 |
| DNA + FRC: early removal | 190 | 73 | 17 | 6263 | 0 | 17 | 17 | –385 |
| DNA + FRC early stop | 190 | 56 | 0 | 2531 | 0 | 0 | 0 | –4117 |
| BC + FRC remove @ 48 hours | 190 | 56 | 0 | 6648 | 0 | 0 | 0 | 0 |
| BC + FRC stop @ 48 hours | 190 | 56 | 0 | 2883 | 0 | 0 | 0 | –3765 |
| BC + FRC + DNA remove @ 48 hours | 190 | 56 | 0 | 6648 | 0 | 0 | 0 | 0 |
| BC + FRC+DNA stop @ 48 hours | 190 | 56 | 0 | 3179 | 0 | 0 | 0 | –3469 |
| i.v. treatment of any FRC/DNA/BC+ | 178 | 42 | 0 | 5891 | –12 | –13 | 0 | –758 |
Methods
Clinical subgroups
First, we devised clinical subgroups of patients based on combinations of the three tests on admission that are used by clinicians to predict CVC-associated infection and its sequelae:
-
Clinical signs of FRC [defined as FRC-positive (+) if any sign present, and FRC-negative (–) if not].
-
Bacterial DNA level (three levels, negative ≤ 0.125 pg/µl; intermediate > 1.25 to 0.5 pg/µl; and high > 0.5 pg/µl, referred to as positive in Tables 19 and 20).
-
Blood culture [positive for bacterial species (pathogens) for which prompt CVC removal is recommended, other or skin bacteria such as coagulase-negative staphylococci, other (including Enterobacteriaceae), or negative culture]. We grouped skin bacteria and other bacteria because of small numbers of patients (see Table 6 for further details).
Treatment options
Second, we specified three alternative treatment options (to standard care):
-
Removal of the CVC for suspected CVC-associated bloodstream infection This could be done early, on the day of admission after the results of the clinical assessment and DNA test. Alternatively, the CVC could be removed on day 3 of admission, when the blood culture result would be available 48 hours after admission. We assumed that CVC removal for infection would be followed by 5 days of i.v. antibiotics. As the systematic review of the effectiveness of CVC removal did not provide a quantitative measure of the effectiveness of this manoeuvre, we assumed that removal would be 100% effective at stopping any recurrent infection requiring i.v. treatment during the follow-up period. The results therefore provide the most optimistic assessment of the outcomes of this option.
-
Early stopping of i.v. treatment for children at very low risk of bloodstream infection Treatment could be stopped early on the day of admission or on day 3, when the blood culture results were available. As we found no relevant studies to include in a review of this intervention option, we assumed that stopping treatment would have no adverse effects in terms of additional recurrences of infection requiring i.v. treatment. This option therefore illustrates the maximum potential benefit from early stopping of treatment.
-
Lock treatment Our systematic review and meta-analysis showed no evidence of a statistically significant benefit of lock treatment on treatment failure, defined by CVC removal or recurrent infection (pooled relative risk 0.70, 95% CI 0.47 to 1.05). However, to illustrate the potential benefits of lock treatment, we assumed a 30% reduction in the risk of CVC removal and recurrent i.v. treatment episode.
-
Standard care We considered that the data set derived from the prognostic analyses (see Chapter 3) reflected outcomes given standard care without early CVC removal or early stopping of treatment for any patient group. This assumption was based on discussions with clinicians in the CCLG and on the results for timing of CVC removal and duration of initial i.v. treatment. The prognostic data set also reflects outcomes in the absence of any routine targeted treatment for CVC-associated bloodstream infection. We base this assumption on responses to questions about slow infusion of antibiotics or whether antibiotics were locked into all lumens of the CVC (see Table 5). There was no evidence that this practice related to specific clinical groups.
Treatment strategies
Third, we generated treatment strategies by specifying which treatments would be used for specific clinical groups. This judgement was based on discussions with clinicians in the CCLG.
Results
The distribution of outcomes according to clinical subgroup is shown in Table 19 for the cohort followed up to 28 days. The outcomes for the whole cohort, given different treatment strategies, and differences compared with standard care are summarised in the clinical balance sheet in Table 20. Tables for the 6-month follow-up are shown in Appendix 11.
The differences in outcomes between the test–treatment strategies and standard care show that the largest potential gains are associated with early stopping of i.v. treatment in low-risk children (see Table 20). These analyses are only illustrative and cannot distinguish between strategies when the differences are small. For example, we have no measure of the uncertainty around the 352 days per 1000 children admitted (see Table 20) saved by stopping after a negative DNA test compared with 2 days later after a negative blood culture result, and cannot therefore infer whether these savings would justify the additional cost of DNA testing for all admitted children. The strategy of lock treatment for any child with a positive test would result in a moderate reduction in i.v. treatment days. The benefits would vary only marginally with or without the inclusion of DNA testing.
Least benefits are to be gained from strategies involving early removal of the CVC, in terms of i.v. treatment days saved. These estimates are limited by a low event rate for recurrent i.v. treatment and CVC removal in high-risk children, and do not take into account the very high values placed by parents, children and clinicians on avoiding complications of CVC infection. There is some evidence that early CVC removal on day 1 would save more i.v. treatment days than removal on day 3, but at a cost of unnecessary CVC removal. Clinicians and patients would need to decide whether benefits in the order of 23 additional i.v. treatment days saved per additional CVC removed unnecessarily (385/17) would be an acceptable trade-off.
Conclusions
These crude analyses suggest that the largest reduction in adverse outcomes would result from a strategy of early discharge (≤ 48 hours post admission) for low-risk children. Moderate potential benefits would result from antibiotic lock treatment for all children with a positive test result, and least benefit would be derived from a strategy of early CVC removal. Bacterial DNA testing would add marginal benefits to these strategies that might not justify the costs of testing. These analyses are based on sparse data and on assumptions of treatment effectiveness that need to be evaluated in RCTs.
Chapter 6 Discussion
Main findings
The diagnostic accuracy study (see Chapter 2) showed that bacterial DNA testing had limited accuracy for predicting CVC-associated bloodstream infection. Raised DNA values (> 0.125 pg/µl) detected two-thirds (66%) of probable CVC-associated infections but were not specific (88%). These results are comparable with other diagnostic tests for CVC-associated infection. 15
In the prognostic analyses (see Chapter 3), we found that high bacterial DNA was associated with CVC removal and with an increased duration of i.v. antibiotic treatment (i.v. days). However, DNA levels did not improve the prediction of these outcomes over and above other characteristics that would be available to clinicians, such as clinical signs of CVC-associated infection and blood culture results. However, DNA was predictive of CVC removal and duration of i.v. treatment, in combination with clinical signs, when we assumed that blood culture results were not yet available. These findings suggest that DNA testing should not be added to the baseline test work-up for children with cancer who are admitted with suspected infection.
To determine which treatments would be most effective for children at different levels of risk of CVC-associated infection, we undertook a series of systematic reviews (see Chapter 5):
-
We found no trials that evaluated early removal of the CVC compared with treating infection with the CVC in situ. Findings from observational studies that compared removal with retention and treatment were confounded by deferred removal in the sickest patients.
-
We found only one trial and two before–after studies, which provided no clear evidence that antibiotic lock treatment reduced the risk of recurrent infection or CVC removal. However, we could not exclude a small to moderate benefit.
-
We found 24 trials published since 1994 on prophylactic use of antibiotic or antiseptic locks. Overall, antimicrobial locks halved the risk of bloodstream infection in a variety of patient groups, and we found weak evidence to suggest that antibiotic locks were more effective than antiseptic locks. Contrary to the available evidence, our national survey of paediatric oncology centres found that locks are being used for treatment rather than prevention and that problems related to formulation of lock solutions currently impede a shift to prophylactic use in children.
-
We found no relevant studies for slow infusion compared with bolus administration of antibiotics. However, we found one systematic review of 17 RCTs that compared continuous infusion with intermittent administration of antibiotics. 40 Clinical failure was lower, albeit with equivocal statistical significance, in patients randomised to continuous infusion,40 and the length of time with drug concentration above the minimum inhibitory concentration was higher with continuous infusion. 137
-
We found no studies that compared early stopping of antibiotics with a standard duration of i.v. therapy of at least 5 days in children with cancer.
In the clinical effectiveness analysis (see Chapter 5), we made optimistic assumptions about the effectiveness of interventions to illustrate where the greatest potential benefits (measured by i.v. treatment days avoided) might be gained from changes to standard care. Most i.v. treatment days would be saved by early stopping of treatment for children at low risk of infection who had no positive baseline tests for CVC-associated bloodstream infection. We assumed that stopping treatment had no adverse effects. Further i.v. treatment days could be saved by using lock treatment for children with any positive result at baseline, assuming a 30% reduction in i.v. treatment days associated with recurrent infection. Relatively few i.v. treatment days would be saved by early removal of the CVC, and this could incur a penalty of unnecessary removal of the CVC. The analyses did not take into account the uncertainty in any of the estimates used, and were not designed to distinguish between the marginal benefits of different test–treatment strategies. There have been few studies of the economic and other costs of the various CVC-associated infection management strategies. A formal economic analysis would be required to quantify the relative effectiveness of alternative test–treatment strategies, taking into account the uncertainty of the parameter estimates and the severity of the various outcomes (see Recommendations for research).
Study limitations
The accuracy study was limited primarily by the lack of an adequate reference standard. We used criteria for a CVC-associated bloodstream infection that combined blood culture results with clinical signs of CVC-associated infection and response to treatment, based on the judgement of the clinician. These judgements may have been strongly influenced by the blood culture result, which could have biased results in favour of underestimating the accuracy of bacterial DNA testing. In addition, the type of treatment and treatment response were poorly documented. This may have led to overinclusion of patients in the probable and possible categories of CVC-associated infection, thereby underestimating the sensitivity of DNA testing.
A second problem arose because the reference standard was not related to the type of treatment required. We endeavoured to address this issue in the clinical effectiveness analysis (see Chapter 5), by using clinical opinion to determine which treatments would be offered to patients with different combinations of clinical signs and test results. A third issue is that 79 patients were counted more than once (there were 260 admissions and CVCs for 181 children). Such clustering of patients would mean that the reported CIs overestimate the certainty of the estimates of sensitivity and specificity. Accuracy also changed slightly owing to clustering of patients with repeated admissions when we restricted analyses to the first admission only. Strengths of the study were the clearly defined and clinically relevant criteria for inclusion of patients in the study and prospective collection of data on clinical signs, blood culture, bacterial DNA and clinician opinion, in all patients.
The prognostic study provided information on the risks of outcomes related to CVC-associated infection, such as recurrent bloodstream infection requiring i.v. antibiotics and CVC removal, according to clinical signs and test results at admission. These analyses allowed us to determine the effectiveness of bacterial DNA testing over and above other test results that would be available to the clinician. However, there were several limitations. First, when we restricted analyses to one infection event per child, there were few outcome events (e.g. only 10 children had their CVC removed in the 28 days after admission with fever). Using the outcome total i.v. treatment days improved the power to detect an effect. We sought further follow-up data to 6 months post admission, but these data were complete for only 99 of the 181 children in the cohort. Second, the clinically important outcomes, CVC removal and i.v. treatment days, were affected by local practice and are partly conditional on the clinical signs and blood culture results at admission. More objective measures of signs and symptoms reflecting resolution and recurrence of infection would be ideal, but are complex to record and analyse. Parents contributing to the CCLG have highlighted the need for research into repeated measures of patient-reported quality of life in order to capture subtle morbidity associated with persistent CVC infection and its management.
A third limitation was that treatments given in response to baseline characteristics altered prognostic outcomes. We assumed that the cohort represented ‘standard care’, as no centres routinely used targeted treatment for CVC infection, and only 24 of 260 infection episodes had any record of such a targeted intervention (see Table 2, Chapter 2). However, we did not attempt to analyse details of the type, intensity and changes in treatment that would have been given to patients who failed to respond to the initial treatment. As a result, the prognostic analyses probably underestimate the discrimination of baseline characteristics for patients who could benefit from interventions for CVC-associated infection. This bias increases with length of follow-up (from 28 days to 6 months). Fourth, our focus was on baseline test characteristics that can be used to inform early decisions about treatment. In practice, clinicians also use repeated observations to determine changes in signs, symptoms or test results, in response to treatment. These may be more accurate than baseline characteristics, especially for patients at high risk of complications who may benefit from CVC removal. Repeated measures were not recorded in our data and are more complex to analyse. Despite these limitations, these prognostic analyses provide useful information on outcomes in a setting where targeted interventions for CVC-associated infection were rarely used.
A fifth limitation of this study was the requirement to limit blood sampling and additional manipulations in this vulnerable population. A larger blood volume could potentially give improved test sensitivity (through extraction of bacterial DNA from a larger volume of blood). A series of blood samples from each CVC lumen would have allowed us to investigate the hypothesis that microbial colonisation is not homogenous along the intra luminal pathway.
The main limitation of the series of systematic reviews was the poor quality of included studies and lack of RCTs. An exception was the review of antimicrobial locks for preventing CVC-associated infection, which included 24 RCTs. Using the incidence rate ratio as the effect measure, we were unable to use standard metaregression techniques to explore sources of heterogeneity between these trials, but instead presented results for subgroups. A key question for future studies is to quantify the effectiveness of antibiotic compared with antiseptic lock solution for preventing CVC-associated infection.
Implications for practice
The bacterial DNA test reported in this study is recommended for diagnosing CVC-associated infection by the most recent guidelines from the Infectious Disease Society of America. 13 This recommendation is based on a small accuracy study of patients receiving total parenteral nutrition. 28 Our findings do not support routine use of DNA testing in children with cancer who are admitted from the community. However, we recommend that repeated DNA testing be evaluated (as a marker of microbial load and response to treatment) to identify children who might benefit from CVC removal. This approach is analogous to the use of viral load to assist in the assessment of treatment efficacy in patients with cytomegalovirus or human immunodeficiency virus (HIV) infection.
We found strong evidence to support prophylactic use of locks for prevention of CVC-associated infection in children with cancer, and weak evidence to suggest that antibiotic locks are more effective than antiseptic locks. We found no RCTs that evaluated the effectiveness of ethanol locks. Further research is urgently needed to address issues related to formulation and administration of antibiotic locks to facilitate implementation.
As reported by others, our study highlighted variation in the management of children with cancer and fever who are admitted from home. 29 In view of the lack of evidence to support the treatment options considered in this study, there is no evidence to recommend approaches to management other than the use of antibiotic locks for prophylaxis.
Recommendations for research
We list the research priorities in order of the number of patients likely to benefit from changes in practice:
-
The option of stopping i.v. treatment early compared with the standard duration of i.v. treatment (5–7 days) requires evaluation for children at low risk of systemic infection, for example those with no signs or test results indicative of CVC-associated infection (approximately 77% of children with cancer and a CVC who are admitted with fever; see Table 20, Chapter 5). Bacterial DNA testing would only marginally improve the identification of this low-risk group and may not justify the costs of testing. Further work is required to define the comparator arms. For example, should ‘early stopping’ mean no i.v. treatment at all and no admission, or discharge after 48 hours of i.v. antibiotics once blood culture results are known? What additional monitoring should be included for the early discharge arm to ensure readmission if symptoms persist? Similarly, what type, dosage and duration of i.v. treatment should define the standard treatment arm, before and after blood culture results are known? The fever and neutropenia study group of the CCLG is currently seeking funding to evaluate strategies for early discharge. 138
-
We have concluded that there is strong evidence in favour of the use of antibiotic locks for the prevention of CVC-associated bloodstream infection. On the other hand, the systematic review found relatively few studies in children with cancer (four studies). 85–87,100 None of the trials involved children undergoing care in a UK cancer centre. A large proportion of the trials of use of antimicrobial locks for prevention have involved renal patients:
-
There are significant differences in treatment and preventive practices both between specialty groups and across national boundaries, so it can be argued that a UK trial of the use of antimicrobial locks is still required to provide evidence relevant to UK paediatric oncology practice. This type of trial should include a cost-effectiveness analysis. It should also include methods that would detect the emergence of antibiotic resistance and drug toxicities associated with long-term exposure to antimicrobial lock solutions.
-
In addition, laboratory studies are required to determine the optimal formulation (e.g. concentration and diluent) of lock solutions for home use and storage conditions.
-
When locks are expected to be used for longer than 18 months, for example in patients with total parenteral nutrition, surveillance studies are needed to evaluate the emergence of antimicrobial resistance.
-
There is a need for head-to-head clinical trials to determine the optimum type of antibiotic, lock dwell time and frequency of administration. Important potential adverse effects include the impact of antibiotic lock prophylaxis on organism selection and resistance and on antibiotic use for treating symptomatic infections.
-
-
Antibiotic lock treatment should be evaluated for children with cancer who are admitted with one or more positive signs of CVC-associated infection (e.g. FRC, positive blood culture, or, if available, raised levels of bacterial DNA). Our analyses (see Chapter 6) suggest that this group comprises 23% of children admitted with fever and suspected CVC-associated infection. A placebo-controlled randomised trial is required to determine the effectiveness and cost-effectiveness of early i.v. antibiotic lock therapy compared with deferred antibiotic lock treatment in children with cancer. Follow-up should be continued for at least 3 months to detect late recurrence of bloodstream infection. 36,139 The study should determine the effect of lock treatment on clinical outcome measures reflecting signs and symptoms of persisting or recurrent infection and on patient-reported measures of quality of life. Reliance on microbiological outcomes (i.e. blood culture), or CVC removal, which is strongly influenced by blood culture results, may not adequately distinguish the effect of lock treatment on morbidity.
-
Prior to a trial of locks for treatment, preliminary research is required to define the type of antibiotics and the appropriate formulation, according to blood culture results. There is also a need to determine how long the lock solution should dwell in the CVC before the lumen is aspirated and used for other treatments. Currently dwell time is very variable. The recent Infectious Diseases Society of America guidelines recommend that antibiotic locks be left in each of the venous access device lumens for a minimum of 1 hour in any 24-hour period and a maximum of 24 hours. 13
-
There is controversy about the benefits of early CVC removal compared with in situ treatment of CVC infection in children with proven and persistent CVC-associated bloodstream infection. Paediatric oncologists in the CCLG reference group reported that CVC removal is not routine for any children with CVC-associated infection. On the other hand, recent international guidelines recommend CVC removal if CVC-associated infection is due to S. aureus, P. aeruginosa, fungi or mycobacteria. 13 An observational study by Raad et al. 139 showed that, in adults with cancer and CVC-associated infection due to coagulase-negative staphylococci, the rate of recurrent infection was 6.6 times higher with continued treatment with the CVC in situ than with CVC removal. Further uncertainties remain with respect to a number of other CVC-associated infections (both Gram-positive and -negative). 42,47,53,140 An RCT is needed to compare early CVC removal with treatment in situ of specific CVC-associated bloodstream infections, but should be confined to children with repeatedly positive tests for CVC-associated bloodstream infection. A diagnostic accuracy study could be integrated into this trial to determine whether repeated DNA testing improves the prediction of children likely to benefit from early CVC removal. This trial would involve around 5% of children admitted to hospital with cancer and fever (estimate based on 10/179 patients requiring CVC removal within 28 days), but would also be suitable for a much larger number of hospitalised children with suspected CVC infection. An additional element to a prospective study could be to compare bacterial DNA results in febrile and non-febrile children. This might allow determination of the natural history of DNA levels in children with and without CVC-associated infection. However, this type of study would raise ethical issues about sampling in children without a clinical indication.
-
We do not recommend an RCT involving DNA testing as a single test on admission for children with cancer admitted from the community with fever. DNA testing may add more information for inpatients on i.v. antibiotics, in whom blood cultures are unreliable. In addition, DNA testing is a developing area, and it is likely that test performance will improve. There is also a need for further evaluation of sampling strategies, for example to determine the optimal blood volume required and whether the discard sample can be used.
-
Variation in practice between centres could be defined more clearly, systematised, and then examined in observational studies to provide information on the effectiveness of alternative practices. 29,138 Specification of management protocols, and linkage of routine data on individual patient admissions and blood culture results over time are now feasible and should be considered as a potentially efficient approach to evaluating the impact of variation in practice.
Acknowledgements
This study could not have been carried out without the help and support of research nurses and medical staff at CCLG paediatric oncology centres. We are also grateful to others who contributed in various ways to the project. We have listed below particular individuals and their contributions. Named authors of the report are not included in the acknowledgements list.
Those who predominantly contributed to recruitment and data collection:
Selena Peters, United Bristol Healthcare Trust, Bristol
Judith Armstrong, United Bristol Healthcare Trust, Bristol
Louise Soanes, Royal Marsden Hospital, Sutton
Mary Taj, Royal Marsden Hospital, Sutton
Annabel Foot, United Bristol Healthcare Trust, Bristol
Colin Steward, University of Bristol, Bristol
Anthony McCarthy, Royal Victoria Hospital, Belfast
Sara Stoneham, University College Hospital, London
Margaret Parr, Queen’s Medical Centre, Nottingham
Julie Evans, Queen’s Medical Centre, Nottingham
Elisabeth Whiles, Queen’s Medical Centre, Nottingham
Diane Strauther, Queen’s Medical Centre, Nottingham
Annie Parry, Royal Victoria Infirmary, Newcastle upon Tyne
Lisa Price, Royal Victoria Infirmary, Newcastle upon Tyne
Kevin Windebank, Royal Victoria Infirmary, Newcastle upon Tyne
Yvonne Wright, Royal Marsden Hospital, Sutton
Sue Hemsworth, Alder Hey Children’s Hospital, Liverpool
Sheila Fox, United Bristol Healthcare Trust, Bristol
Julia Chisholm, Great Ormond Street Hospital, London
Barney Reeves, London School of Tropical Medicine and Hygiene, London
Joanne Coast, University of Birmingham, Birmingham.
Julia Chisholm also provided access to the Paediatric Infections in Febrile Neutropenia audit database.
Those who contributed to laboratory analysis:
Simon Warwick, Barts and The London NHS Trust, London
Gemma Johnson, Barts and The London NHS Trust, London.
Those who have contributed to the Trial Steering and Data Monitoring Committees:
David Dunn, Medical Research Council Clinical Trials Unit, London
Steve Pedler, Royal Victoria Infirmary, Newcastle upon Tyne
Gary Nicolin, Southampton General Hospital, Southampton
Mathew Sydes, Medical Research Council Clinical Trials Unit, London
Ruth Gilbert chaired the Trial Steering Committee and Mathew Sydes chaired the Data Monitoring Committee.
Kevin Windebank provided access to data collected on complications associated with CVCs in children undergoing treatment for cancer in UK paediatric cancer centres during the 1990s. We are grateful to Tony Ades for discussions about methods for evaluating prognostic outcomes and determining the clinical effectiveness of DNA testing.
Contribution of authors
Mike Millar conceived, designed and co-ordinated the overall study, and co-ordinated the accuracy study. He is also guarantor for the report. He developed the design for the synthesis of evidence together with Ruth Gilbert. Enid Hennessy carried out the statistical analyses for the accuracy study. Weiwei Zhou carried out all statistical analyses in this report and wrote the methods sections. Mark Wilks, Roderick Skinner and Barry Pizer contributed to the overall design of the study and Mark Wilks contributed to the laboratory analyses. Ruth Gilbert designed and carried out the synthesis of evidence following on from the accuracy study and wrote the report together with Mike Millar. All authors contributed to the drafting of the report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Brun-Buisson C, Doyon F, Carlet J. Bacteremia and severe sepsis in adults: a multicenter prospective survey in ICUs and wards of 24 hospitals. French Bacteremia Sepsis Study Group. Am J Respir Crit Care Med 1996;154:617-24.
- Waghorn DJ. Intravascular device-associated systemic infections: a 2 year analysis of cases in a district general hospital. J Hosp Infect 1994;28:91-101.
- Fletcher SJ, Bodenham AR. Catheter-related sepsis: an overview, Part 1. BMJ 1999;9:46-53.
- Nosocomial Infection National Surveillance Scheme . Surveillance of Hospital-Acquired Bacteraemia in English Hospitals 1997–2002 2009.
- Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc 2006;81:1159-71.
- Cesaro S, Corro R, Pelosin A, Gamba P, Zadra N, Fusaro F, et al. A prospective survey on incidence and outcome of Broviac/Hickman catheter-related complications in pediatric patients affected by hematological and oncological diseases. Ann Hematol 2004;83:183-8.
- Abbas AA, Fryer CJ, Paltiel C, Chedid F, Felimban SK, Yousef AA, et al. Factors influencing central line infections in children with acute lymphoblastic leukemia: results of a single institutional study. Pediatr Blood Cancer 2004;42:325-31.
- Veenstra DL, Saint S, Sullivan SD. Cost-effectiveness of antiseptic-impregnated central venous catheters for the prevention of catheter-related bloodstream infection. JAMA 1999;282:554-60.
- Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al. The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation. Health Technol Assess 2008;12.
- Gowardman JR, Montgomery C, Thirlwell S, Shewan J, Idema A, Larsen PD, et al. Central venous catheter-related bloodstream infections: an analysis of incidence and risk factors in a cohort of 400 patients. Intensive Care Med 1998;24:1034-9.
- Tacconelli E, Tumbarello M, Pittiruti M, Leone F, Lucia MB, Cauda R, et al. Central venous catheter-related sepsis in a cohort of 366 hospitalised patients. Eur J Clin Microbiol Infect Dis 1997;16:203-9.
- O’Grady NP, Barie PS, Bartlett J, Bleck T, Garvey G, Jacobi J, et al. Practice parameters for evaluating new fever in critically ill adult patients. Task Force of the American College of Critical Care Medicine of the Society of Critical Care Medicine in collaboration with the Infectious Disease Society of America. Crit Care Med 1998;26:392-408.
- Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O’Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 2009;49:1-45.
- Telenti A, Steckelberg JM, Stockman L, Edson RS, Roberts GD. Quantitative blood cultures in candidemia. Mayo Clin Proc 1991;66:1120-3.
- Siegman-Igra Y, Anglim AM, Shapiro DE, Adal KA, Strain BA, Farr BM. Diagnosis of vascular catheter-related bloodstream infection: a meta-analysis. J Clin Microbiol 1997;35:928-36.
- Sherertz RJ, Raad II, Belani A, Koo LC, Rand KH, Pickett DL, et al. Three-year experience with sonicated vascular catheter cultures in a clinical microbiology laboratory. J Clin Microbiol 1990;28:76-82.
- Blot F, Nitenberg G, Chachaty E, Raynard B, Germann N, Antoun S, et al. Diagnosis of catheter-related bacteraemia: a prospective comparison of the time to positivity of hub-blood versus peripheral-blood cultures. Lancet 1999;354:1071-7.
- Marra AR, Edmond MB, Forbes BA, Wenzel RP, Bearman GM. Time to blood culture positivity as a predictor of clinical outcome of Staphylococcus aureus bloodstream infection. J Clin Microbiol 2006;44:1342-6.
- Peralta G, Rodriguez-Lera MJ, Garrido JC, Ansorena L, Roiz MP. Time to positivity in blood cultures of adults with Streptococcus pneumoniae bacteremia. BMC Infect Dis 2006;6.
- Kite P, Dobbins BM, Wilcox MH, McMahon MJ. Rapid diagnosis of central-venous-catheter-related bloodstream infection without catheter removal. Lancet 1999;354:1504-7.
- Maki DG, Jarrett F, Sarafin HW. A semiquantitative culture method for identification of catheter-related infection in the burn patient. J Surg Res 1977;22:513-20.
- Brun-Buisson C, Abrouk F, Legrand P, Huet Y, Larabi S, Rapin M. Diagnosis of central venous catheter-related sepsis. Critical level of quantitative tip cultures. Arch Intern Med 1987;147:873-7.
- Maki DG, Stolz SS, Wheeler S, Mermel LA. A prospective, randomized trial of gauze and two polyurethane dressings for site care of pulmonary artery catheters: implications for catheter management. Crit Care Med 1994;22:1729-37.
- Maki DG, Stolz SM, Wheeler S, Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter. A randomized, controlled trial. Ann Intern Med 1997;127:257-66.
- Raad I, Darouiche R, Dupuis J, Abi S, Gabrielli A, Hachem R, et al. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections: a randomized, double-blind trial. Ann Intern Med 1997;127:267-74.
- Kite P, Dobbins BM, Wilcox MH, Fawley WN, Kindon AJ, Thomas D, et al. Evaluation of a novel endoluminal brush method for in situ diagnosis of catheter related sepsis. J Clin Pathol 1997;50:278-82.
- Van H, Webb SAR, Fong S, Golledge CL, Roberts BL, Thompson WR. Central venous catheters revisited – infection rates and an assessment of the new fibrin analysing system brush. Anaesth Intensive Care 1996;24:330-3.
- Warwick S, Wilks M, Hennessy E, Powell-Tuck J, Small M, Sharp J, et al. Use of quantitative 16S ribosomal DNA detection for diagnosis of central vascular catheter-associated bacterial infection. J Clin Microbiol 2004;42:1402-8.
- Phillips B, Selwood K, Lane SM, Skinner R, Gibson F, Chisholm JC. Variation in policies for the management of febrile neutropenia in United Kingdom Children’s Cancer Study Group centres. Arch Dis Child 2007;92:495-8.
- Millar MR, Johnson G, Wilks M, Skinner R, Stoneham S, Pizer B, et al. Molecular diagnosis of vascular access device-associated infection in children being treated for cancer or leukaemia. Clin Microbiol Infect 2008;14:213-20.
- Altschul SF, Madden TL, Schaffer AA, Zhang J, Zhang Z, Miller W, et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res 1997;25:3389-402.
- Safdar N, Fine JP, Maki DG. Meta-analysis: methods for diagnosing intravascular device-related bloodstream infection. Ann Intern Med 2005;142:451-66.
- Farr BM. Accuracy and cost-effectiveness of new tests for diagnosis of catheter-related bloodstream infections. Lancet 1999;354:1487-8.
- Simon A, Bode U, Beutel K. Diagnosis and treatment of catheter-related infections in paediatric oncology: an update. Clin Microbiol Infect 2006;12:606-20.
- Tweddle DA, Windebank KP, Barrett AM, Leese DC, Gowing R. Central venous catheter use in UKCCSG oncology centres. United Kingdom Children’s Cancer Study Group and the Paediatric Oncology Nursing Forum. Arch Dis Child 1997;77:58-9.
- Rijnders BJ, Van WE, Vandecasteele SJ, Stas M, Peetermans WE. Treatment of long-term intravascular catheter-related bacteraemia with antibiotic lock: randomized, placebo-controlled trial. J Antimicrob Chemother 2005;55:90-4.
- R Development Core Team . R: a Language and Environment for Statistical Computing 2009. www.R-project.org.
- O’Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, et al. Guidelines for the prevention of intravascular catheter-related infections. The Hospital Infection Control Practices Advisory Committee, Center for Disese Control and Prevention, USA. Pediatrics 2002;110.
- Ley BE, Jalil N, McIntosh J, Smart A, Wilson M, Foot AB, et al. Bolus or infusion teicoplanin for intravascular catheter associated infections in immunocompromised patients?. J Antimicrob Chemother 1996;38:1091-5.
- Kasiakou SK, Sermaides GJ, Michalopoulos A, Soteriades ES, Falagas ME. Continuous versus intermittent i.v. administration of antibiotics: a meta-analysis of randomised controlled trials. Lancet Infect Dis 2005;5:581-9.
- Cherifi S, Jacobs F, Strale H, Struelens M, Byl B. Outcome of totally implantable venous access device-related bacteraemia without device removal. Clin Microbiol Infect 2007;13:592-8.
- Coyle VM, McMullan R, Morris TC, Rooney PJ, Hedderwick S. Catheter-related bloodstream infection in adult haematology patients: catheter removal practice and outcome. J Hosp Infect 2004;57:325-31.
- Nucci M, Anaissie E. Should vascular catheters be removed from all patients with candidemia? An evidence-based review. Clin Infect Dis 2002;34:591-9.
- Onder AM, Chandar J, Coakley S, Abitbol C, Montane B, Zilleruelo G. Predictors and outcome of catheter-related bacteremia in children on chronic hemodialysis. Pediatr Nephrol 2006;21:1452-8.
- Pasqualotto AC, de Moraes AB, Zanini RR, Severo LC. Analysis of independent risk factors for death among pediatric patients with candidemia and a central venous catheter in place. Infect Control Hosp Epidemiol 2007;28:799-804.
- Buckley J, Coffin SE, Lautenbach E, Prasad P, Chu J, Goyal M, et al. Outcome of Escherichia coli and/or Klebsiella bloodstream infection in children with central venous catheters. Infect Control Hosp Epidemiol 2007;28:1308-10.
- Nazemi KJ, Buescher ES, Kelly RE, Karlowicz MG. Central venous catheter removal versus in situ treatment in neonates with enterobacteriaceae bacteremia. Pediatrics 2003;111:e269-74.
- Karlowicz MG, Hashimoto LN, Kelly RE, Buescher ES. Should central venous catheters be removed as soon as candidemia is detected in neonates?. Pediatrics 2000;106.
- Karlowicz MG, Furigay PJ, Croitoru DP, Buescher ES. Central venous catheter removal versus in situ treatment in neonates with coagulase-negative staphylococcal bacteremia. Pediatr Infect Dis J 2002;21:22-7.
- Benjamin DK, Miller W, Garges H, Benjamin DK, McKinney RE, Cotton M, et al. Bacteremia, central catheters, and neonates: when to pull the line. Pediatrics 2001;107:1272-6.
- Stamos JK, Rowley AH. Candidemia in a pediatric population. Clin Infect Dis 1995;20:571-5.
- Adler A, Yaniv I, Solter E, Freud E, Samra Z, Stein J, et al. Catheter-associated bloodstream infections in pediatric hematology–oncology patients: factors associated with catheter removal and recurrence. J Pediatr Hematol Oncol 2006;28:23-8.
- Hanna H, Afif C, Alakech B, Boktour M, Tarrand J, Hachem R, et al. Central venous catheter-related bacteremia due to gram-negative bacilli: significance of catheter removal in preventing relapse. Infect Control Hosp Epidemiol 2004;25:646-9.
- Lai CH, Wong WW, Chin C, Huang CK, Lin HH, Chen WF, et al. Central venous catheter-related Stenotrophomonas maltophilia bacteraemia and associated relapsing bacteraemia in haematology and oncology patients. Clin Microbiol Infect 2006;12:986-91.
- Sandoe JA, Witherden IR, Au-Yeung HK, Kite P, Kerr KG, Wilcox MH. Enterococcal intravascular catheter-related bloodstream infection: management and outcome of 61 consecutive cases. J Antimicrob Chemother 2002;50:577-82.
- Chee L, Brown M, Sasadeusz J, MacGregor L, Grigg AP. Gram-negative organisms predominate in Hickman line-related infections in non-neutropenic patients with hematological malignancies. J Infect 2008;56:227-33.
- Rodriguez D, Park BJ, Almirante B, Cuenca-Estrella M, Planes AM, Mensa J, et al. Impact of early central venous catheter removal on outcome in patients with candidaemia. Clin Microbiol Infect 2007;13:788-93.
- Eppes SC, Troutman JL, Gutman LT. Outcome of treatment of candidemia in children whose central catheters were removed or retained. Pediatr Infect Dis J 1989;8:99-104.
- Dato VM, Dajani AS. Candidemia in children with central venous catheters: role of catheter removal and amphotericin B therapy. Pediatr Infect Dis J 1990;9:309-14.
- Nucci M, Colombo AL, Silveira F, Richtmann R, Salomao R, Branchini ML, et al. Risk factors for death in patients with candidemia. Infect Control Hosp Epidemiol 1998;19:846-50.
- Anaissie EJ, Rex JH, Uzun O, Vartivarian S. Predictors of adverse outcome in cancer patients with candidemia. Am J Med 1998;104:238-45.
- Nucci M, Silveira MI, Spector N, Silveira F, Velasco E, Akiti T, et al. Risk factors for death among cancer patients with fungemia. Clin Infect Dis 1998;27:107-11.
- Nguyen MH, Peacock JE, Tanner DC, Morris AJ, Nguyen ML, Snydman DR, et al. Therapeutic approaches in patients with candidemia. Evaluation in a multicenter, prospective, observational study. Arch Intern Med 1995;155:2429-35.
- Hung CC, Chen YC, Chang SC, Luh KT, Hsieh WC. Nosocomial candidemia in a university hospital in Taiwan. J Formos Med Assoc 1996;95:19-28.
- Luzzati R, Amalfitano G, Lazzarini L, Soldani F, Bellino S, Solbiati M, et al. Nosocomial candidemia in non-neutropenic patients at an Italian tertiary care hospital. Eur J Clin Microbiol Infect Dis 2000;19:602-7.
- Goodrich JM, Reed EC, Mori M, Fisher LD, Skerrett S, Dandliker PS, et al. Clinical features and analysis of risk factors for invasive candidal infection after marrow transplantation. J Infect Dis 1991;164:731-40.
- Rex JH, Bennett JE, Sugar AM, Pappas PG, Serody J, Edwards JE, et al. Intravascular catheter exchange and duration of candidemia. NIAID Mycoses Study Group and the Candidemia Study Group. Clin Infect Dis 1995;21:994-6.
- Lecciones JA, Lee JW, Navarro EE, Witebsky FG, Marshall D, Steinberg SM, et al. Vascular catheter-associated fungemia in patients with cancer: analysis of 155 episodes. Clin Infect Dis 1992;14:875-83.
- Girmenia C, Martino P, De BF, Gentile G, Boccanera M, Monaco M, et al. Rising incidence of Candida parapsilosis fungemia in patients with hematologic malignancies: clinical aspects, predisposing factors, and differential pathogenicity of the causative strains. Clin Infect Dis 1996;23:506-14.
- Pasqualotto AC, Severo LC. The importance of central venous catheter removal in patients with candidaemia: time to rethink our practice?. Clin Microbiol Infect 2008;14:2-4.
- Buckler BS, Sams RN, Goei VL, Krishnan KR, Bemis MJ, Parker DP, et al. Treatment of central venous catheter fungal infection using liposomal amphotericin-B lock therapy. Pediatr Infect Dis J 2008;27:762-4.
- Garland JS, Alex CP, Henrickson KJ, McAuliffe TL, Maki DG. A vancomycin–heparin lock solution for prevention of nosocomial bloodstream infection in critically ill neonates with peripherally inserted central venous catheters: a prospective, randomized trial. Pediatrics 2005;116:e198-205.
- Bestul MB, Vandenbussche HL. Antibiotic lock technique: review of the literature. Pharmacotherapy 2005;25:211-27.
- Carratala J. The antibiotic-lock technique for therapy of ‘highly needed’ infected catheters. Clin Microbiol Infect 2002;8:282-9.
- Korbila IP, Bliziotis IA, Lawrence KR, Falagas ME. Antibiotic-lock therapy for long-term catheter-related bacteremia: a review of the current evidence. Expert Rev Anti Infect Ther 2007;5:639-52.
- Marschall J, Mermel LA, Classen D, Arias KM, Podgorny K, Anderson DJ, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol 2008;29:S22-30.
- Safdar N, Maki DG. Use of vancomycin-containing lock or flush solutions for prevention of bloodstream infection associated with central venous access devices: a meta-analysis of prospective, randomized trials. Clin Infect Dis 2006;43:474-84.
- Fortun J, Grill F, Martin-Davila P, Blazquez J, Tato M, Sanchez-Corral J, et al. Treatment of long-term intravascular catheter-related bacteraemia with antibiotic-lock therapy. J Antimicrob Chemother 2006;58:816-21.
- Poole CV, Carlton D, Bimbo L, Allon M. Treatment of catheter-related bacteraemia with an antibiotic lock protocol: effect of bacterial pathogen. Nephrol Dial Transplant 2004;19:1237-44.
- Anoop P, Anjay M. Towards evidence based medicine for paediatricians. Role of antibiotic line locks in the treatment of infected central venous access devices. Arch Dis Child 2009;94:556-9.
- Capdevila JA, Segarra A, Planes AM, Ramirez-Arellano M, Pahissa A, Piera L, et al. Successful treatment of haemodialysis catheter-related sepsis without catheter removal. Nephrol Dial Transplant 1993;8:231-4.
- Onder AM, Chandar J, Simon N, Diaz R, Nwobi O, Abitbol CL, et al. Comparison of tissue plasminogen activator-antibiotic locks with heparin-antibiotic locks in children with catheter-related bacteraemia. Nephrol Dial Transplant 2008;23:2604-10.
- Daghistani D, Horn M, Rodriguez Z, Schoenike S, Toledano S. Prevention of indwelling central venous catheter sepsis. Med Pediatr Oncol 1996;26:405-8.
- Carratala J, Niubo J, Fernandez-Sevilla A, Juve E, Castellsague X, Berlanga J, et al. Randomized, double-blind trial of an antibiotic-lock technique for prevention of gram-positive central venous catheter-related infection in neutropenic patients with cancer. Antimicrob Agents Chemother 1999;43:2200-4.
- Rackoff WR, Weiman M, Jakobowski D, Hirschl R, Stallings V, Bilodeau J, et al. A randomized, controlled trial of the efficacy of a heparin and vancomycin solution in preventing central venous catheter infections in children. J Pediatr 1995;127:147-51.
- Barriga FJ, Varas M, Potin M, Sapunar F, Rojo H, Martinez A, et al. Efficacy of a vancomycin solution to prevent bacteremia associated with an indwelling central venous catheter in neutropenic and non-neutropenic cancer patients. Med Pediatr Oncol 1997;28:196-200.
- Henrickson KJ, Axtell RA, Hoover SM, Kuhn SM, Pritchett J, Kehl SC, et al. Prevention of central venous catheter-related infections and thrombotic events in immunocompromised children by the use of vancomycin/ciprofloxacin/heparin flush solution: a randomized, multicenter, double-blind trial. J Clin Oncol 2000;18:1269-78.
- Cooper R, Raad T. Prevention of bacteraemia in patients with tunneled cuffed ‘permanent’ hemodialysis catheters (PCs) using gentamicin catheter packing. J Am Soc Nephrol 1999;10.
- Dogra GK, Herson H, Hutchison B, Irish AB, Heath CH, Golledge C, et al. Prevention of tunneled hemodialysis catheter-related infections using catheter-restricted filling with gentamicin and citrate: a randomized controlled study. J Am Soc Nephrol 2002;13:2133-9.
- Pervez A, Ahmed M, Ram S, Torres C, Work J, Zaman F, et al. Antibiotic lock technique for prevention of cuffed tunnel catheter associated bacteremia. J Vasc Access 2002;3:108-13.
- McIntyre CW, Hulme LJ, Taal M, Fluck RJ. Locking of tunneled hemodialysis catheters with gentamicin and heparin. Kidney Int 2004;66:801-5.
- Bleyer AJ, Mason L, Russell G, Raad II, Sherertz RJ. A randomized, controlled trial of a new vascular catheter flush solution (minocycline-EDTA) in temporary hemodialysis access. Infect Control Hosp Epidemiol 2005;26:520-4.
- Saxena AK, Panhotra BR. The impact of catheter-restricted filling with cefotaxime and heparin on the lifespan of temporary hemodialysis catheters: a case controlled study. J Nephrol 2005;18:755-63.
- Kim SH, Song KI, Chang JW, Kim SB, Sung SA, Jo SK, et al. Prevention of uncuffed hemodialysis catheter-related bacteremia using an antibiotic lock technique: a prospective, randomized clinical trial. Kidney Int 2006;69:161-4.
- Nori US, Manoharan A, Yee J, Besarab A. Comparison of low-dose gentamicin with minocycline as catheter lock solutions in the prevention of catheter-related bacteremia. Am J Kidney Dis 2006;48:596-605.
- Saxena AK, Panhotra BR, Sundaram DS, Morsy MN, Al-Ghamdi AM. Enhancing the survival of tunneled haemodialysis catheters using an antibiotic lock in the elderly: a randomised, double-blind clinical trial. Nephrology (Carlton) 2006;11:299-305.
- Zhang P, Zhang W, He Q, Yuan J, Xie W, Jiang W, et al. A randomized controlled study on prevention of cuff-tunneled catheter related bacteremia with gentamicinheparin lock solution: The metaphase result. J Am Soc Nephrol 2006;17.
- Al-Hwiesh AK, Abdul-Rahman IS. Successful prevention of tunneled, central catheter infection by antibiotic lock therapy using vancomycin and gentamycin. Saudi J Kidney Dis Transpl 2007;18:239-47.
- Zhang P, Yuan J, Tan H, Lv R, Chen J. Successful prevention of cuffed hemodialysis catheter-related infection using an antibiotic lock technique by strictly catheter-restricted antibiotic lock solution method. Blood Purif 2009;27:206-11.
- Simon A, Ammann RA, Wiszniewsky G, Bode U, Fleischhack G, Besuden MM. Taurolidine-citrate lock solution (TauroLock) significantly reduces CVAD-associated grampositive infections in pediatric cancer patients. BMC Infect Dis 2008;8.
- Hendrickx L, Kuypers D, Evenepoel P, Maes B, Messiaen T, Vanrenterghem Y. A comparative prospective study on the use of low concentrate citrate lock versus heparin lock in permanent dialysis catheters. Int J Artif Organs 2001;24:208-11.
- Betjes MG, van AM. Prevention of dialysis catheter-related sepsis with a citrate-taurolidine-containing lock solution. Nephrol Dial Transplant 2004;19:1546-51.
- Weijmer MC, van den Dorpel MA, Van de Ven PJ, ter Wee PM, van Geelen JA, Groeneveld JO, et al. Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol 2005;16:2769-77.
- Macrae JM, Dojcinovic I, Djurdjev O, Jung B, Shalansky S, Levin A, et al. Citrate 4% versus heparin and the reduction of thrombosis study (CHARTS). Clin J Am Soc Nephrol 2008;3:369-74.
- Power A, Duncan N, Singh SK, Brown W, Dalby E, Edwards C, et al. Sodium citrate versus heparin catheter locks for cuffed central venous catheters: a single-center randomized controlled trial. Am J Kidney Dis 2009;53:1034-41.
- Yahav D, Rozen-Zvi B, Gafter-Gvili A, Leibovici L, Gafter U, Paul M. Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: systematic review and meta-analysis of randomized, controlled trials. Clin Infect Dis 2008;47:83-9.
- van de Wetering MD, van Woensel JB. Prophylactic antibiotics for preventing early central venous catheter Gram positive infections in oncology patients. Cochrane Database Syst Rev 2007;1.
- James MT, Conley J, Tonelli M, Manns BJ, MacRae J, Hemmelgarn BR. Meta-analysis: antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann Intern Med 2008;148:596-605.
- Labriola L, Crott R, Jadoul M. Preventing haemodialysis catheter-related bacteraemia with an antimicrobial lock solution: a meta-analysis of prospective randomized trials. Nephrol Dial Transplant 2008;23:1666-72.
- Jaffer Y, Selby NM, Taal MW, Fluck RJ, McIntyre CW. A meta-analysis of hemodialysis catheter locking solutions in the prevention of catheter-related infection. Am J Kidney Dis 2008;51:233-41.
- Bradshaw JH, Puntis JW. Taurolidine and catheter-related bloodstream infection: a systematic review of the literature. J Pediatr Gastroenterol Nutr 2008;47:179-86.
- Simon A, Bode U, Lieber K, Beutel K, Fleischhack G. Review and update of the use of urokinase in the prevention and management of CVAD-related complications in pediatric oncology patients. Am J Infect Control 2008;36:54-8.
- Raad I. Intravascular-catheter-related infections. Lancet 1998;351:893-8.
- Sitges-Serra A, Girvent M. Catheter-related bloodstream infections. World J Surg 1999;23:589-95.
- Kethireddy S, Safdar N. Urokinase lock or flush solution for prevention of bloodstream infections associated with central venous catheters for chemotherapy: a meta-analysis of prospective randomized trials. J Vasc Access 2008;9:51-7.
- Berrington A, Gould FK. Use of antibiotic locks to treat colonized central venous catheters. J Antimicrob Chemother 2001;48:597-603.
- Mermel LA, Farr BM, Sherertz RJ, Raad II, O’Grady N, Harris JS, et al. Guidelines for the management of intravascular catheter-related infections. Clin Infect Dis 2001;32:1249-72.
- Wolf HH, Leithauser M, Maschmeyer G, Salwender H, Klein U, Chaberny I, et al. Central venous catheter-related infections in hematology and oncology: guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2008;87:863-76.
- Rabindranath KS, Bansal T, Adams J, Das R, Shail R, MacLeod AM, et al. Systematic review of antimicrobials for the prevention of haemodialysis catheter-related infections. Nephrol Dial Transplant 2009;24:3763-74.
- Meeus G, Kuypers DR, Claes K, Evenepoel P, Maes B, Vanrenterghem Y. A prospective, randomized, double–blind crossover study on the use of 5% citrate lock versus 10% citrate lock in permanent hemodialysis catheters. Blood Purif 2005;23:101-5.
- Buturovic J, Ponikvar R, Kandus A, Boh M, Klinkmann J, Ivanovich P. Filling hemodialysis catheters in the interdialytic period: heparin versus citrate versus polygeline: a prospective randomized study. Artif Organs 1998;22:945-7.
- Saxena AK, Panhotra BR, Sundaram DS, Al-Hafiz A, Naguib M, Venkateshappa CK, et al. Tunneled catheters’ outcome optimization among diabetics on dialysis through antibiotic-lock placement. Kidney Int 2006;70:1629-35.
- Dillon PW, Jones GR, Bagnall-Reeb HA, Buckley JD, Wiener ES, Haase GM. Prophylactic urokinase in the management of long-term venous access devices in children: a Children’s Oncology Group study. J Clin Oncol 2004;22:2718-23.
- Guerraoui AA, Dacosta EE, Roche BB. Emergence of multiresistant Staphylococcus epidermidis (MRSE) after lock antibiotic regimen by gentamicin in permanent hemodialysis catheters. Prospective study, 1999–2003. J Am Soc Nephrol 2004;15.
- Pratt RJ, Pellowe C, Loveday HP, Robinson N, Smith GW, Barrett S, et al. The epic project: developing national evidence-based guidelines for preventing healthcare associated infections. Phase I: guidelines for preventing hospital-acquired infections. Department of Health (England). J Hosp Infect 2001;47:S3-82.
- Pittiruti M, Hamilton H, Biffi R, MacFie J, Pertkiewicz M. ESPEN Guidelines on Parenteral Nutrition: central venous catheters (access, care, diagnosis and therapy of complications). Clin Nutr 2009;28:365-77.
- Members of the Central Venous Access Device Guideline Panel . Managing Central Venous Access Devices in Cancer Patients: A Clinical Practice Guideline 2006.
- Bishop L, Dougherty L, Bodenham A, Mansi J, Crowe P, Kibbler C, et al. Guidelines on the insertion and management of central venous access devices in adults. Int J Lab Hematol 2007;29:261-78.
- Cesaro S, Tridello G, Cavaliere M, Magagna L, Gavin P, Cusinato R, et al. Prospective, randomized trial of two different modalities of flushing central venous catheters in pediatric patients with cancer. J Clin Oncol 2009;27:2059-65.
- Del Pozo JL. Role of antibiotic lock therapy for the treatment of catheter-related bloodstream infections. Int J Artif Organs 2009;32:678-88.
- Bookstaver PB, Williamson JC, Tucker BK, Raad II, Sherertz RJ. Activity of novel antibiotic lock solutions in a model against isolates of catheter-related bloodstream infections. Ann Pharmacother 2009;43:210-19.
- Droste JC, Jeraj HA, MacDonald A, Farrington K. Stability and in vitro efficacy of antibiotic-heparin lock solutions potentially useful for treatment of central venous catheter-related sepsis. J Antimicrob Chemother 2003;51:849-55.
- Lee JY, Ko KS, Peck KR, Oh WS, Song JH. In vitro evaluation of the antibiotic lock technique (ALT) for the treatment of catheter-related infections caused by staphylococci. J Antimicrob Chemother 2006;57:1110-15.
- Robinson JL, Tawfik G, Saxinger L, Stang L, Etches W, Lee B. Stability of heparin and physical compatibility of heparin/antibiotic solutions in concentrations appropriate for antibiotic lock therapy. J Antimicrob Chemother 2005;56:951-3.
- Saxinger LM, Williams KE, Lyon M, Mochoruk M. Stability of Antibiotics in Heparin at 37°C: Toward Antibiotic Locks for Central Venous Catheter Infections [abstract 626] n.d.
- Vercaigne LM, Sitar DS, Penner SB, Bernstein K, Wang GQ, Burczynski FJ. Antibiotic-heparin lock: in vitro antibiotic stability combined with heparin in a central venous catheter. Pharmacotherapy 2000;20:394-9.
- Kasiakou SK, Lawrence KR, Choulis N, Falagas ME. Continuous versus intermittent i.v. administration of antibacterials with time-dependent action: a systematic review of pharmacokinetic and pharmacodynamic parameters. Drugs 2005;65:2499-511.
- Dommett R, Geary J, Freeman S, Hartley J, Sharland M, Davidson A, et al. Successful introduction and audit of a step-down oral antibiotic strategy for low risk paediatric febrile neutropaenia in a UK, multicentre, shared care setting. Eur J Cancer 2009;45:2843-9.
- Raad I, Kassar R, Ghannam D, Chaftari AM, Hachem R, Jiang Y. Management of the catheter in documented catheter-related coagulase-negative staphylococcal bacteremia: remove or retain?. Clin Infect Dis 2009;49:1187-94.
- Boktour M, Hanna H, Ansari S, Bahna B, Hachem R, Tarrand J, et al. Central venous catheter and Stenotrophomonas maltophilia bacteremia in cancer patients. Cancer 2006;106:1967-73.
Appendix 1 Protocol for the accuracy study (Chapter 2)
Synopsis
A complete copy is available from the CCLG website (www.cclg.org.uk) or from the principal investigator, Mike Millar.
The diagnosis or exclusion of a central venous catheter (CVC)-associated infection may carry considerable importance in the management of a child with cancer or leukaemia but is frequently difficult. Improvement in diagnostic techniques may allow genuine CVC-associated infections to be treated earlier and more effectively, and may reduce the rate of unnecessary CVC removal in patients who do not have CVC-associated infection.
There are two parts to this study and it is expected to run for a total of 3 years and 6 months. Patients will be recruited and informed consent obtained separately for each part of the study.
The aim of Part One is to determine the optimum threshold values for a molecular test for the diagnosis or exclusion of CVC-associated infection in children and adolescents (0–18 years inclusive) undergoing treatment at a collaborating UKCCSG centre. Part One simply requires observation of all febrile episodes in recruited patients, with blood samples being taken on one occasion at the time of fever from all CVC lumens for the quantitative 16S rDNA test method (1 ml EDTA anticoagulated) as well as for the standard culture method. Simple clinical information will be collected concerning the febrile episode and its treatment and outcome. Patients will be followed for 4 weeks from its presentation.
It is anticipated that any UKCCSG centre will be able to enter patients into Part One, even though some may not take part subsequently in Part Two (see below). The optimum threshold values will be derived from the results of Part One before patient recruitment commences for Part Two of the study. Part One requires 1000 febrile episodes and should be completed in the first year of the study. It is anticipated that there will be a hold on the study in between Part One and Part Two while the data from Part One are analysed. This may be up to 2 months.
The aim of Part Two of the study is to test the hypothesis that a test for CVC-associated infection based on quantitative bacterial 16S rDNA analysis will improve the management of suspected CVC-associated infections in patients being treated for cancer. For logistical reasons, Part Two may be performed on a limited centre basis. Patients (0–18 years inclusive) will be eligible whether or not they have previously participated in Part One, and patients will be randomised to availability of the 16S rDNA test (Arm A) or not (Arm B). All other aspects of management, including investigation by standard culture techniques, will remain unaltered in both randomisation groups. The 16S rDNA result should be made available to the doctor with responsibility for patient care within 48 hours, and will incorporate the likelihood ratios (both negative and positive) of probable CVC-associated infection for a known test value. A repeat sample(s) can be tested during the same episode if the clinician considers that it/they will help patient management. Simple clinical information will be collected, as in Part One. The primary outcome measure is CVC survival; secondary outcome measures include duration of antibiotic treatment and hospitalisation for fever, mortality and an economic analysis. Part Two requires randomisation of 330 patients and should be completed within 24 months. This allows 18 months for patient recruitment and a minimum of 6 months’ follow-up after each episode.
Appendix 2 Data collection sheets (accuracy study, Chapter 2)
Appendix 3 Prognostic markers for sequelae of central venous catheter-associated bloodstream infection: 6-month follow-up period (Chapter 3)
| Coding | No. of patients | Time to end of index episode | Time to next i.v. treatment period | Recurrence (yes/no) | Time to CVC removal | Total duration of i.v. treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Rem. | Rec. | HR (95% CI) | p-value | HR (95% CI) | p-value | Rate ratio (95% CI) | p-value | HR (95% CI) | p-value | Estimated coefficient (95% CI) | p-value | ||
| Characteristics before index admission | ||||||||||||||
| Age at start of treatment period (or at the time of presentation of a recruited episode of fever) | ||||||||||||||
| < 3 years | 1 | 20 | 11 | 18 | 1.25 (0.76 to 2.06) | 0.378 | 2.12 (1.23 to 3.67) | 0.007 | 1.59 (1.04 to 2.41) | 0.030 | 1.26 (0.64 to 2.48) | 0.504 | –1.23 (–8.73 to 6.28) | 0.750 |
| ≥ 3 years (ref.) | 0 | 79 | 36 | 48 | ||||||||||
| Cancer type | ||||||||||||||
| Non-haematological | 1 | 35 | 19 | 26 | 1.16 (0.76 to 1.76) | 0.493 | 1.33 (0.81 to 2.18) | 0.261 | 1.25 (0.85 to 1.84) | 0.251 | 1.32 (0.74 to 2.37) | 0.350 | –0.75 (–7.06 to 5.55) | 0.816 |
| Haematological (ref.) | 0 | 64 | 28 | 40 | ||||||||||
| Number of lumens | ||||||||||||||
| Single | 1 | 39 | 17 | 24 | 1.39 (0.92 to 2.10) | 0.120 | 0.79 (0.48 to 1.31) | 0.366 | 0.83 (0.56 to 1.23) | 0.351 | 0.78 (0.43 to 1.42) | 0.421 | –6.27 (–12.32 to –0.23) | 0.045 |
| Multiple (ref.) | 0 | 60 | 30 | 42 | ||||||||||
| Type of vascular access device | ||||||||||||||
| Implanted port | 2 | 9 | 4 | 5 | 1.51 (0.75 to 3.02) | 0.247 | 0.67 (0.27 to 1.68) | 0.397 | 0.79 (0.39 to 1.63) | 0.526 | 0.89 (0.32 to 2.47) | 0.818 | –4.70 (–15.15 to 5.75) | 0.380 |
| External (ref.) | 1 | 90 | 43 | 61 | ||||||||||
| Duration of CVC insertion before treatment episode | ||||||||||||||
| 1.02 (0.99 to 1.05) | 0.178 | 0.99 (0.95 to 1.03) | 0.497 | 0.98 (0.94 to 1.01) | 0.127 | 0.99 (0.95 to 1.03) | 0.635 | –7.50 (–37.39 to 22.39) | 0.640 | |||||
| Oral antibiotics in 2 weeks before infection episode | ||||||||||||||
| Yes | 1 | 35 | 21 | 16 | 0.78 (0.51 to 1.21) | 0.267 | 0.43 (0.24 to 0.76) | 0.004 | 0.67 (0.44 to 1.04) | 0.074 | 1.79 (1.01 to 3.19) | 0.047 | 3.45 (–2.91 to 9.82) | 0.290 |
| No (ref.) | 0 | 62 | 26 | 48 | ||||||||||
| Characteristics at index admission | ||||||||||||||
| FRC | ||||||||||||||
| Yes | 1 | 10 | 8 | 5 | 0.53 (0.27 to 1.06) | 0.074 | 0.65 (0.26 to 1.61) | 0.351 | 0.66 (0.31 to 1.42) | 0.291 | 3.73 (1.73 to 8.03) | 0.001 | 10.42 (0.64 to 20.21) | 0.039 |
| No (ref.) | 0 | 89 | 39 | 61 | ||||||||||
| Blood culture | ||||||||||||||
| Pathogens | 2 | 3 | 1 | 1 | 0.54 (0.17 to 1.71) | 0.293 | 0.35 (0.05 to 2.51) | 0.294 | 0.62 (0.15 to 2.50) | 0.498 | 0.86 (0.12 to 6.28) | 0.881 | –1.25 (–18.93 to 16.43) | 0.890 |
| Other | 1 | 19 | 12 | 13 | 0.53 (0.32 to 0.89) | 0.016 | 1.01 (0.55 to 1.86) | 0.970 | 1.03 (0.64 to 1.65) | 0.918 | 1.78 (0.92 to 3.44) | 0.086 | 3.23 (–4.47 to 10.92) | 0.413 |
| None (ref.) | 0 | 77 | 34 | 52 | ||||||||||
| Bacterial DNA result (pg/µl), all patients | ||||||||||||||
| ≥ 0.5 | 4 | 11 | 8 | 5 | 0.61 (0.32 to 1.15) | 0.127 | 0.51 (0.20 to 1.28) | 0.151 | 0.48 (0.21 to 1.10) | 0.084 | 2.61 (1.21 to 5.64) | 0.014 | –1.16 (–10.84 to 8.53) | 0.815 |
| ≥ 0.125 to < 0.5 | 1 | 7 | 3 | 5 | 0.84 (0.39 to 1.83) | 0.661 | 1.22 (0.49 to 3.04) | 0.673 | 1.12 (0.57 to 2.23) | 0.737 | 0.99 (0.30 to 3.21) | 0.983 | –0.26 (–12.14 to 11.61) | 0.966 |
| < 0.125 (ref.) | 0 | 81 | 36 | 56 | ||||||||||
| Bacterial DNA result (pg/µl) to patients with CVC removed before 28-day follow-up period | ||||||||||||||
| ≥ 0.5 | 4 | 8 | 8 | 3 | 0.74 (0.34 to 1.63) | 0.460 | 0.39 (0.12 to 1.30) | 0.125 | 0.44 (0.29 to 0.68) | < 0.0005 | 2.23 (1.01 to 4.95) | 0.048 | –4.61 (–17.60 to 8.38) | 0.490 |
| ≥ 0.125 to < 0.5 | 1 | 3 | 3 | 2 | 1.22 (0.37 to 4.01) | 0.746 | 1.06 (0.25 to 4.49) | 0.933 | 0.62 (0.35 to1.10) | 0.100 | 1.29 (0.39 to 4.23) | 0.679 | –4.53 (–24.5 to 15.45) | 0.659 |
| < 0.125 (ref.) | 0 | 36 | 36 | 26 | ||||||||||
| Bacterial DNA result (pg/µl), patients without CVC removed before 28-day follow-up period | ||||||||||||||
| ≥ 0.5 | 4 | 3 | 0 | 2 | 0.45 (0.14 to 1.47) | 0.185 | 0.84 (0.20 to 3.52) | 0.813 | 0.61 (0.34 to 1.08) | 0.090 | NA | NA | 4.53 (–11.93 to 21.00) | 0.592 |
| ≥ 0.125 to < 0.5 | 1 | 4 | 0 | 3 | 0.62 (0.22 to 1.75) | 0.367 | 1.41 (0.43 to 4.63) | 0.571 | 1.60 (1.16 to 2.21) | < 0.0005 | NA | NA | 3.03 (–11.37 to 17.44) | 0.682 |
| < 0.125 (ref.) | 0 | 45 | 0 | 30 | ||||||||||
FIGURE 10.
Kaplan–Meier plots of time to recurrent infection requiring i.v. treatment in cohort followed up for 6 months according to three test results. (a) FRC; (b) bacterial DNA; (c) blood culture (BC).
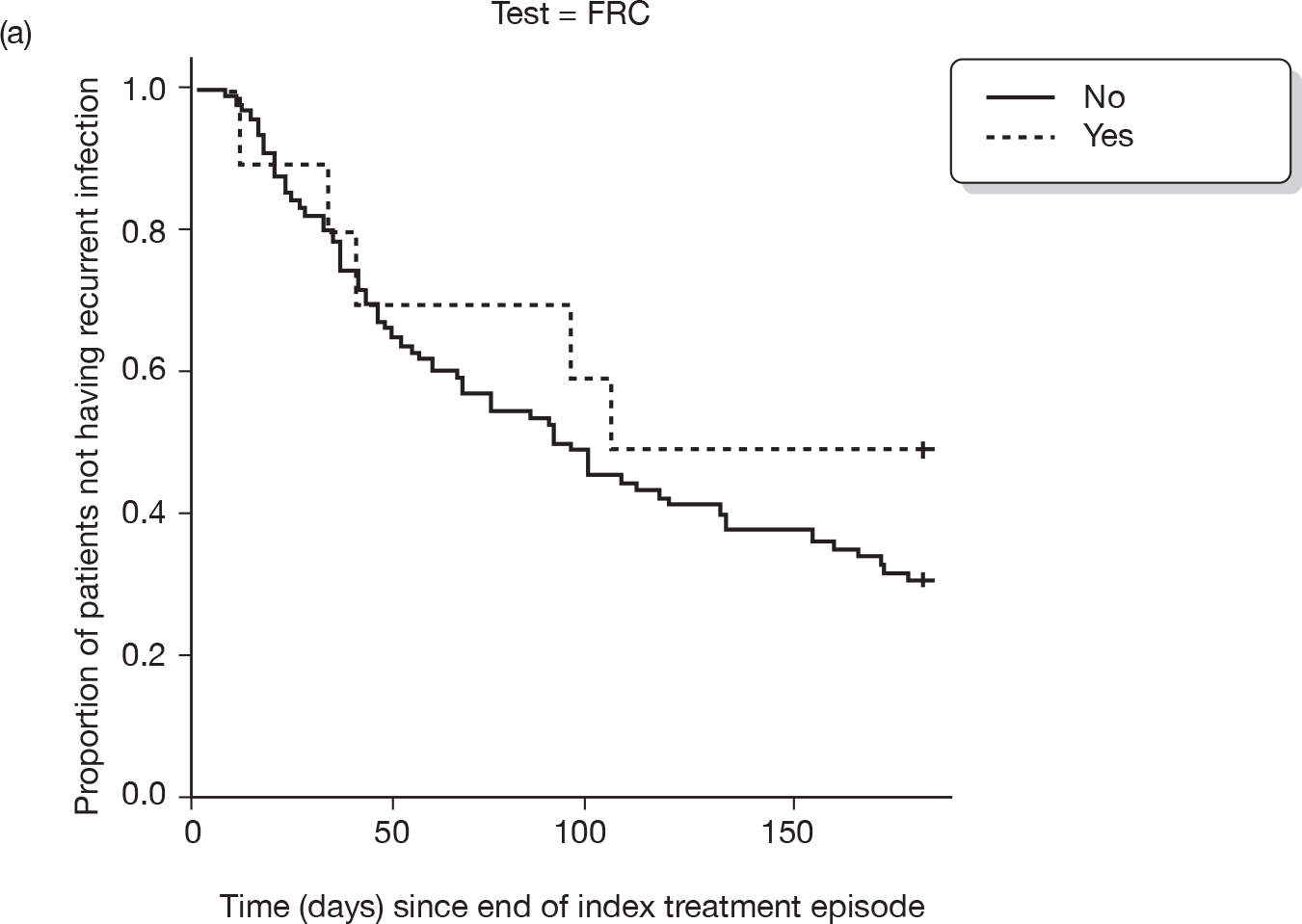
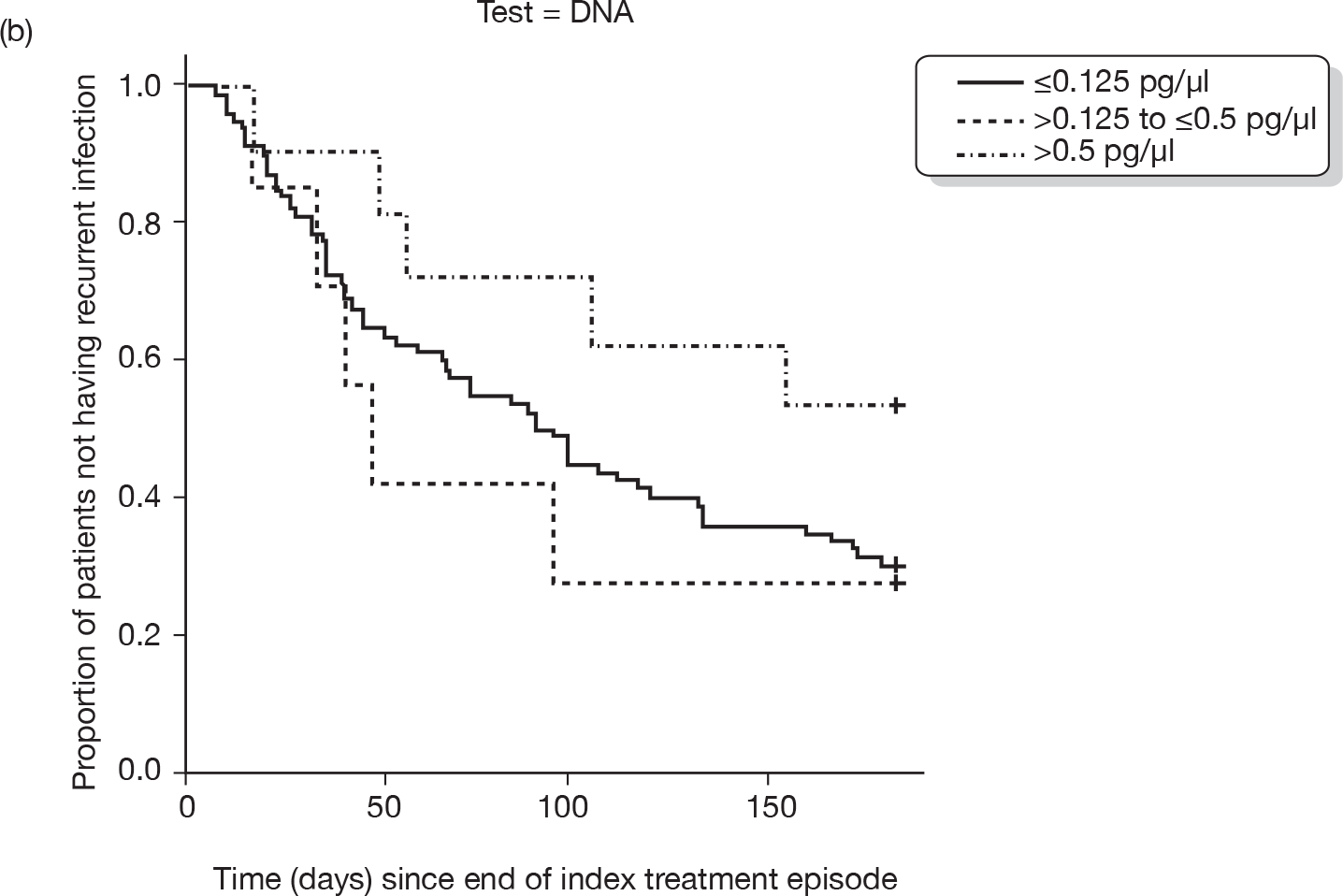
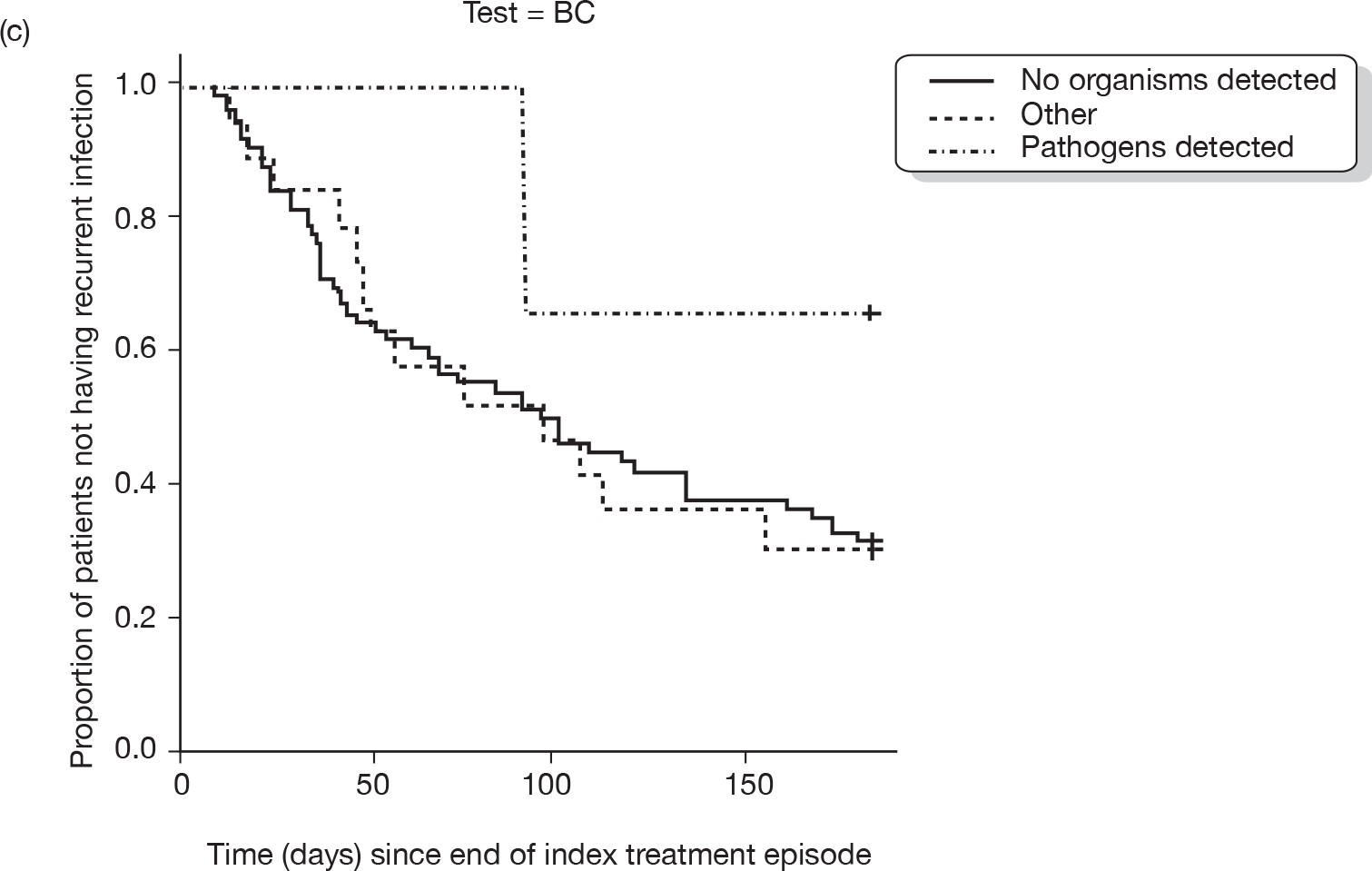
FIGURE 11.
Kaplan Meier–plots of time to CVC removal in cohort followed up for 6 months according to three test results (a) FRC; (b) bacterial DNA; (c) blood culture (BC).
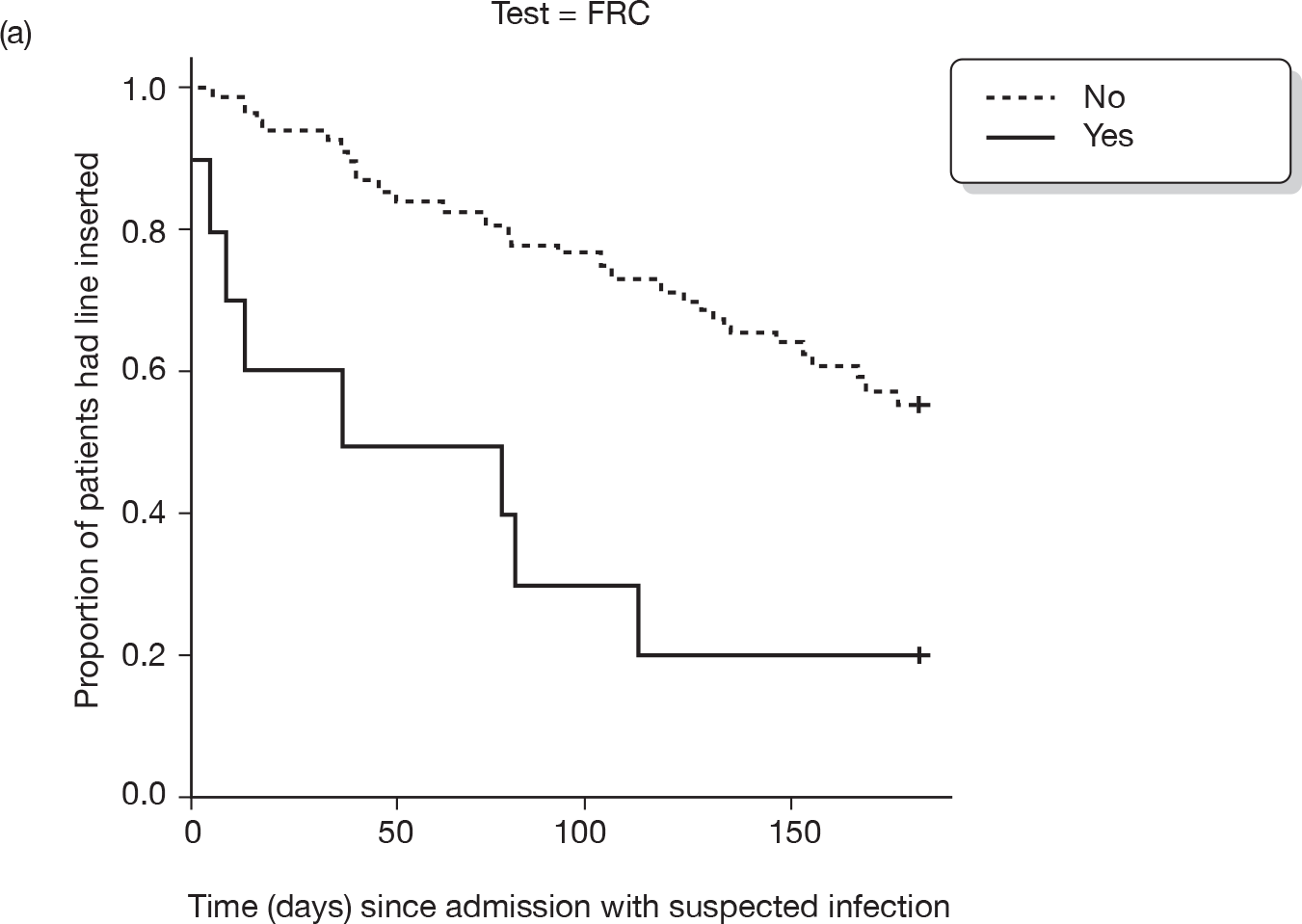
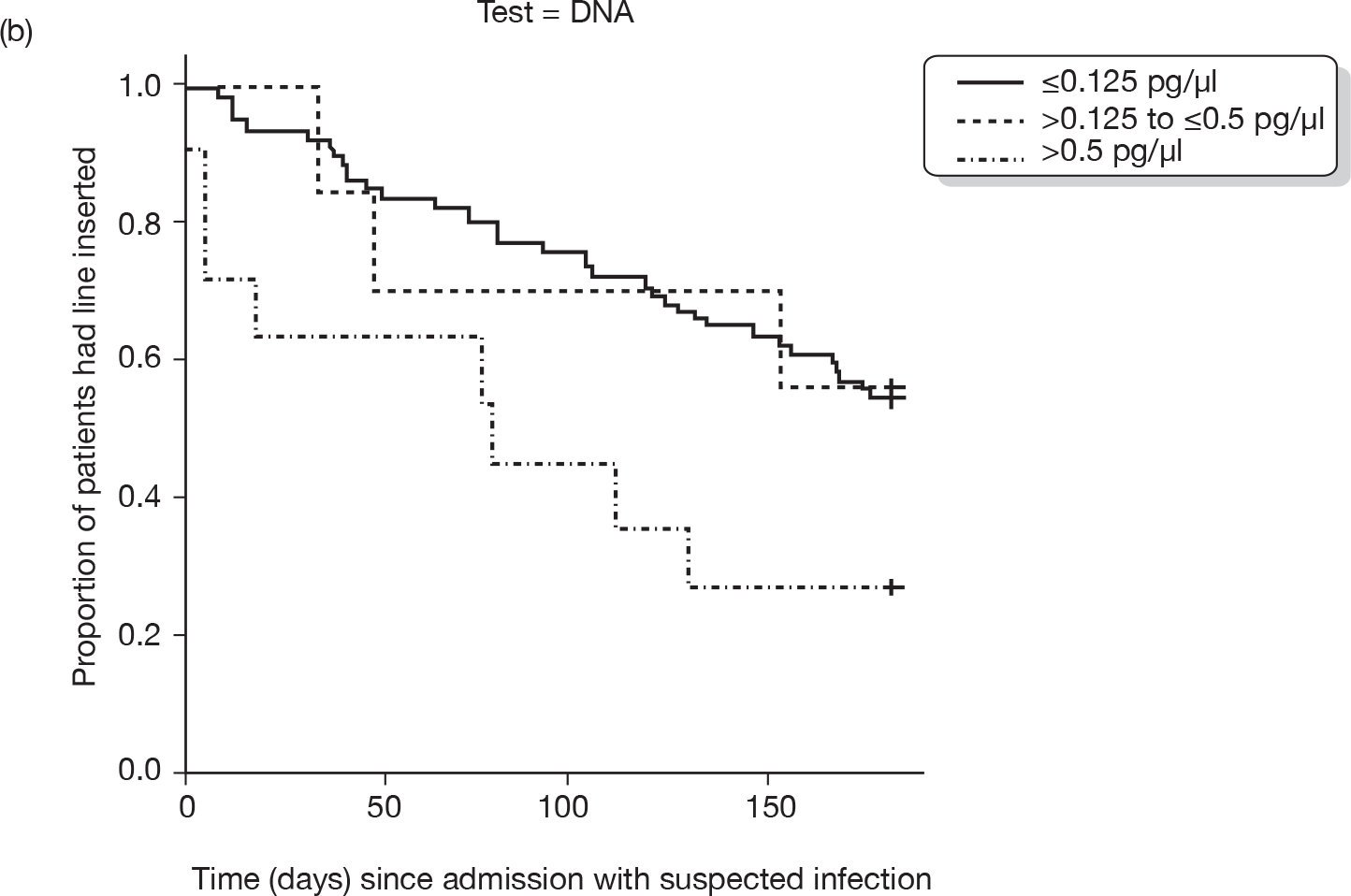
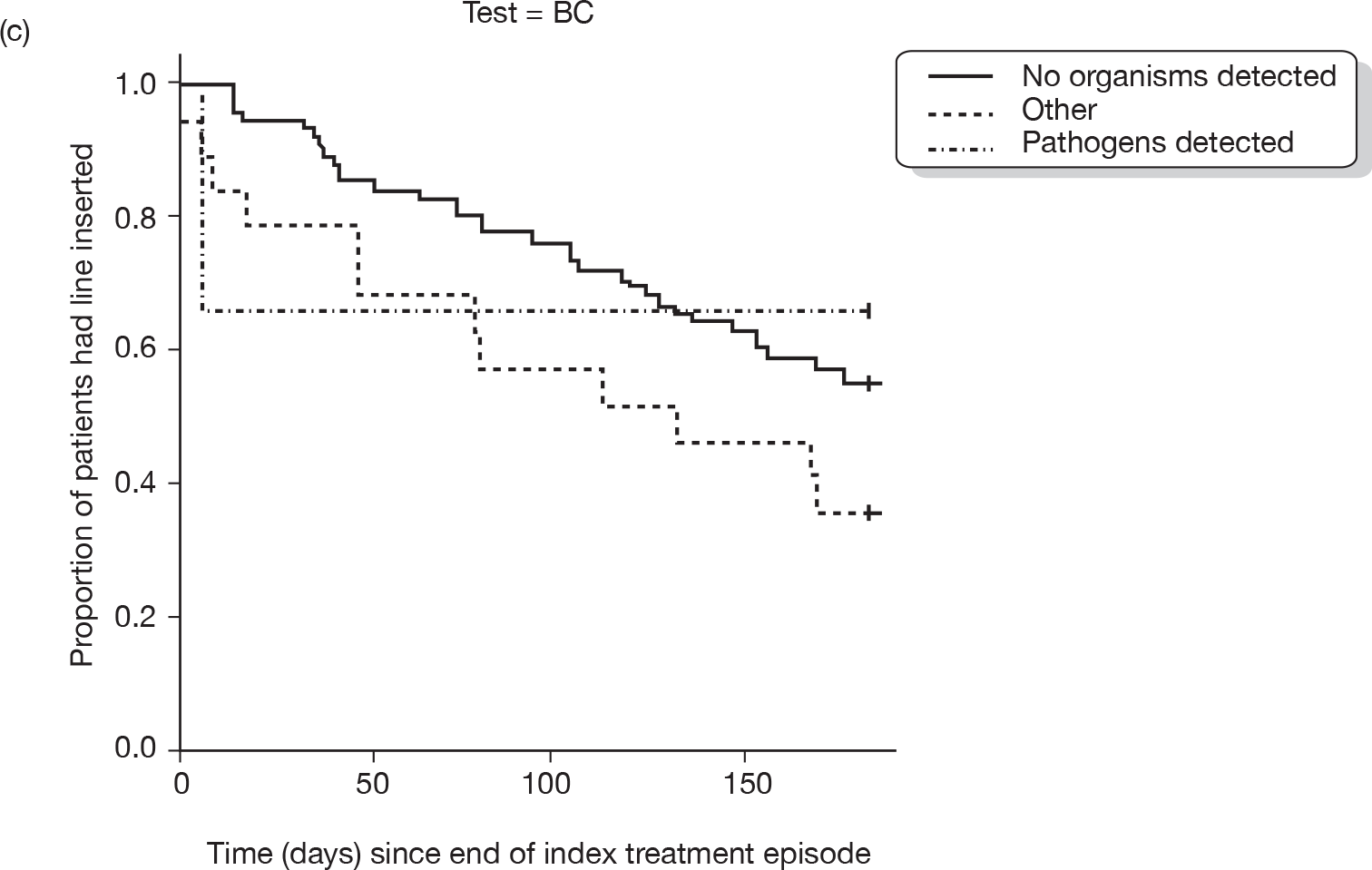
| Explanatory variables | Time to CVC removal | |||||
|---|---|---|---|---|---|---|
| Model without DNA | Model with DNA | |||||
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Oral antibiotics in 2 weeks before infection episode | 1.68 | (0.94 to 2.99) | 0.081 | 1.64 | (0.92 to 2.95) | 0.096 |
| With FRC | 3.36 | (1.55 to 7.27) | 0.002 | 2.98 | (1.30 to 6.79) | 0.010 |
| DNA (> 0.5 pg/µl) | 1.93 | (0.86 to 4.35) | 0.111 | |||
| DNA (0.125–0.5 pg/µl) | 0.81 | (0.24 to 2.71) | 0.730 | |||
| AIC | 395.84 | 397.24 | ||||
| Explanatory variables | Total duration of i.v. treatment adjusted for indicator variable: CVC removal with follow-up period (yes/no) | |||||
|---|---|---|---|---|---|---|
| Model without DNA | Model with DNA | |||||
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Single lumen | –6.30 | (–12.28 to –0.32) | 0.042 | –7.15 | (–13.34 to –0.97) | 0.026 |
| With FRC | 10.44 | (0.53 to 20.36) | 0.042 | 12.49 | (2.11 to 22.88) | 0.020 |
| DNA (> 0.5 pg/µl) | –6.27 | (–16.22 to 3.69) | 0.221 | |||
| DNA (0.125–0.5 pg/µl) | –4.45 | (–16.25 to 7.36) | 0.462 | |||
| AIC | 537.44 | 539.49 | ||||
Appendix 4 Slow infusion versus bolus infection for treating suspected central venous catheter-associated infection (Chapter 4)
Summary of ‘A randomised study comparing bolus injection with infused and/or line-locked teicoplanin’ [SC (Supportive Care) 1999 010].
Full protocol available from the CCLG website, www.cclg.org.uk.
Principal investigator: Dr Barry Pizer, Consultant Paediatric Oncologist, Alder Hey Children’s Hospital, Liverpool, UK.
This protocol is for a randomised study comparing teicoplanin given by bolus injection with prolonged (i.e. 2 hours) infusion and/or antibiotic lock for treating septicaemia due to coagulase-negative staphylococci in children with CVCs. The hypothesis is that prolonged exposure of bacteria to teicoplanin, as afforded by infused or ‘line-locked’ antibiotic, will result in an increased success rate from therapy for CVC-related septicaemia as compared with treatment with bolus teicoplanin. The study is confined to the investigation of the treatment of coagulase-negative staphylococci infections as these are the most common group of organisms causing CVC-related septicaemia. Inclusion of other Gram-positive organisms may affect the results of the study pertaining to coagulase-negative staphylococci septicaemia. Recruitment started in 1999 and finished in 2009. Results have not yet been published.
Appendix 5 Search terms for the systematic review (Chapter 4)
Search for papers on prognosis
An initial search was carried out for papers reporting prognosis for subsequent infection, infection complications or death in children with CVC-associated infection.
We searched MEDLINE using PubMed and the following terms. The search was repeated for EMBASE (see Figure 5, Chapter 4).
Our search included synonyms for text words in all fields and MeSH terms for: central venous, intravascular, port, or indwelling AND catheter or device AND removal.
CVC terms
((central[All Fields] AND (“veins”[MeSH Terms] OR “veins”[All Fields] OR “venous”[All Fields]) AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])) OR (intravascular[All Fields] AND (“equipment and supplies”[MeSH Terms] OR (“equipment”[All Fields] AND “supplies”[All Fields]) OR “equipment and supplies”[All Fields] OR “device”[All Fields])) OR (intravascular[All Fields] AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])) OR (PICC[All Fields] AND line[All Fields]) OR (PICC[All Fields] AND port[All Fields]) OR (“catheters, indwelling”[MeSH Terms] OR (“catheters”[All Fields] AND “indwelling”[All Fields]) OR “indwelling catheters”[All Fields] OR (“indwelling”[All Fields] AND “catheter”[All Fields]) OR “indwelling catheter”[All Fields]) OR (tunneled[All Fields] AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])))
AND
Date restriction
((“1995”[EDAT]: “3000”[EDAT])
AND
Age restriction
(“infant”[MeSH Terms] OR “child”[MeSH Terms] OR “adolescent”[MeSH Terms]))
AND
Prognosis terms
(“incidence”[MeSH Terms:noexp] OR “mortality”[MeSH Terms] OR “follow-up studies”[MeSH Terms:noexp] OR (prognos[Text Word] OR prognose[Text Word] OR prognosed[Text Word] OR prognoses[Text Word] OR prognosi[Text Word] OR prognosic[Text Word] OR prognosies[Text Word] OR prognosing[Text Word] OR prognosis[Text Word] OR prognosis/clinical[Text Word] OR prognosis/course[Text Word] OR prognosis/diagnosis[Text Word] OR prognosis/favorable[Text Word] OR prognosis/good[Text Word] OR prognosis/invasion[Text Word] OR prognosis/metastasis[Text Word] OR prognosis/outcome[Text Word] OR prognosis/outcomes[Text Word] OR prognosis/prevention[Text Word] OR prognosis/prognostic[Text Word] OR prognosis/survival[Text Word] OR prognosis/wish[Text Word] OR prognosis’[Text Word] OR prognosisa[Text Word] OR prognosisand[Text Word] OR prognosised[Text Word] OR prognosiss[Text Word] OR prognosistic[Text Word] OR prognositc[Text Word] OR prognositcally[Text Word] OR prognosite[Text Word] OR prognositic[Text Word] OR prognosits[Text Word] OR prognosls[Text Word] OR prognosonis[Text Word] OR prognosprognosis[Text Word] OR prognossis[Text Word] OR prognostc[Text Word] OR prognostiating[Text Word] OR prognostic[Text Word] OR prognostic/diagnostic[Text Word] OR prognostic/experimental[Text Word] OR prognostic/metastatic[Text Word] OR prognostic/pharmacogenetic[Text Word] OR prognostic/predicting[Text Word] OR prognostic/predictive[Text Word] OR prognostic/progression[Text Word] OR prognostic/proliferative[Text Word] OR prognostic/risk[Text Word] OR prognostic/severity[Text Word] OR prognostic/staging[Text Word] OR prognostic/survival[Text Word] OR prognostic/therapeutic[Text Word] OR prognostic/treatment[Text Word] OR prognostic’[Text Word] OR prognostic’s[Text Word] OR prognostica[Text Word] OR prognosticable[Text Word] OR prognosticably[Text Word] OR prognosticaion[Text Word] OR prognostical[Text Word] OR prognostically[Text Word] OR prognosticaly[Text Word] OR prognosticantly[Text Word] OR prognosticants[Text Word] OR prognosticate[Text Word] OR prognosticated[Text Word] OR prognosticates[Text Word] OR prognosticating[Text Word] OR prognostication[Text Word] OR prognostications[Text Word] OR prognosticative[Text Word] OR prognosticator[Text Word] OR prognosticator’s[Text Word] OR prognosticators[Text Word] OR prognosticatory[Text Word] OR prognosticfactors[Text Word] OR prognosticfeature[Text Word] OR prognostician[Text Word] OR prognosticians[Text Word] OR prognosticity[Text Word] OR prognosticks[Text Word] OR prognosticly[Text Word] OR prognostico[Text Word] OR prognosticon[Text Word] OR prognostics[Text Word] OR prognostification[Text Word] OR prognostigate[Text Word] OR prognostigram[Text Word] OR prognostikon[Text Word] OR prognostis[Text Word] OR prognostisity[Text Word] OR prognostive[Text Word] OR prognostix[Text Word] OR prognostk[Text Word] OR prognostocrit[Text Word] OR prognosys[Text Word]) OR (predict[Text Word] OR predict/affect[Text Word] OR predict/assess[Text Word] OR predict/classify[Text Word] OR predict/estimate[Text Word] OR predict/evaluate[Text Word] OR predict/exclude[Text Word] OR predict/interpret[Text Word] OR predict/monitor[Text Word] OR predict/prognosticate[Text Word] OR predict/rank[Text Word] OR predict/refine[Text Word] OR predict/rule[Text Word] OR predict’[Text Word] OR predict’’[Text Word] OR predict7[Text Word] OR predicta[Text Word] OR predictab[Text Word] OR predictabe[Text Word] OR predictabilities[Text Word] OR predictability[Text Word] OR predictability/rhythm[Text Word] OR predictability’[Text Word] OR predictabilty[Text Word] OR predictable[Text Word] OR predictable/controlled[Text Word] OR predictable/unpredictable[Text Word] OR predictable/variable[Text Word] OR predictable’[Text Word] OR predictables[Text Word] OR predictablity[Text Word] OR predictably[Text Word] OR predictabuity[Text Word] OR predictal[Text Word] OR predictalbe[Text Word] OR predictand[Text Word] OR predictands[Text Word] OR predictaquatic[Text Word] OR predictated[Text Word] OR predictative[Text Word] OR predictbias[Text Word] OR predictd[Text Word] OR predicte[Text Word] OR predicted[Text Word] OR predicted/100[Text Word] OR predicted/30[Text Word] OR predicted/actual[Text Word] OR predicted/assumed[Text Word] OR predicted/baseline[Text Word] OR predicted/dlco[Text Word] OR predicted/established[Text Word] OR predicted/expected[Text Word] OR predicted/have[Text Word] OR predicted/hypothesized[Text Word] OR predicted/hypothetical[Text Word] OR predicted/measured[Text Word] OR predicted/observed[Text Word] OR predicted/predicted[Text Word] OR predicted/recommended[Text Word] OR predicted/sd[Text Word] OR predicted/se[Text Word] OR predicted/uncharacterized[Text Word] OR predicted/unit[Text Word] OR predicted/y[Text Word] OR predicted/year[Text Word] OR predicted/yr[Text Word] OR predicted’[Text Word] OR predictedfrom[Text Word] OR predictedl[Text Word] OR predictedl/e[Text Word] OR predictedmore[Text Word] OR predictedness[Text Word] OR predictee[Text Word] OR predictees[Text Word] OR predicter[Text Word] OR predicters[Text Word] OR predictet[Text Word] OR predictibility[Text Word] OR predictible[Text Word] OR predictically[Text Word] OR predictice[Text Word] OR predictie[Text Word] OR predictied[Text Word] OR predictif[Text Word] OR predictifs[Text Word] OR predictim[Text Word] OR predictin[Text Word] OR predictinf[Text Word] OR predicting[Text Word] OR predicting/assembling[Text Word] OR predicting/assessing[Text Word] OR predicting/estimating[Text Word] OR predicting/evaluating[Text Word] OR predicting/optimizing[Text Word] OR predicting/preventing[Text Word] OR predicting’[Text Word] OR predictinginteractions[Text Word] OR predictingpostoperative[Text Word] OR predictingprognosis[Text Word] OR predictingthe[Text Word] OR predictintegral[Text Word] OR predictiom[Text Word] OR prediction[Text Word] OR prediction/analysis[Text Word] OR prediction/annotation[Text Word] OR prediction/assessment[Text Word] OR prediction/confirmation[Text Word] OR prediction/detection[Text Word] OR prediction/estimation[Text Word] OR prediction/experimental[Text Word] OR prediction/explanation[Text Word] OR prediction/feedback[Text Word] OR prediction/histology[Text Word] OR prediction/integration[Text Word] OR prediction/national[Text Word] OR prediction/parameter[Text Word] OR prediction/postdiction[Text Word] OR prediction/ppfinder[Text Word] OR prediction/precipitation/prevention[Text Word] OR prediction/prevention[Text Word] OR prediction/prognosis[Text Word] OR prediction/recognition[Text Word] OR prediction/reproducibility[Text Word] OR prediction/sensitivity[Text Word] OR prediction/sensitivity/specificity[Text Word] OR prediction/singular[Text Word] OR prediction/treatment[Text Word] OR prediction/verification[Text Word] OR prediction’[Text Word] OR prediction’s[Text Word] OR prediction36[Text Word] OR predictional[Text Word] OR predictionalgorithms[Text Word] OR predictioncapacity[Text Word] OR predictioncenter[Text Word] OR predictioncenter/casp6/org[Text Word] OR predictioning[Text Word] OR predictions[Text Word] OR predictions/estimates[Text Word] OR predictions/h[Text Word] OR predictions/impressions[Text Word] OR predictions/number[Text Word] OR predictions/total[Text Word] OR predictions’[Text Word] OR predictionst[Text Word] OR predictit[Text Word] OR predictition[Text Word] OR predictitive[Text Word] OR predictiv[Text Word] OR predictive[Text Word] OR predictive/confounding[Text Word] OR predictive/data[Text Word] OR predictive/descriptive[Text Word] OR predictive/diagnostic[Text Word] OR predictive/face/construct[Text Word] OR predictive/proactive[Text Word] OR predictive/prognostic[Text Word] OR predictive/protective[Text Word] OR predictive/risk[Text Word] OR predictive/surrogate[Text Word] OR predictive/validation[Text Word] OR predictive/vector[Text Word] OR predictive’[Text Word] OR predictivefactors[Text Word] OR predictively[Text Word] OR predictively’[Text Word] OR predictiveness[Text Word] OR predictiveof[Text Word] OR predictives[Text Word] OR predictivetrade[Text Word] OR predictivites[Text Word] OR predictivities[Text Word] OR predictivity[Text Word] OR predictivo[Text Word] OR predictivy[Text Word] OR predictly[Text Word] OR predictment[Text Word] OR predictmorbidity[Text Word] OR predictnls[Text Word] OR predictol[Text Word] OR predictome[Text Word] OR predicton[Text Word] OR predictons[Text Word] OR predictor[Text Word] OR predictor/correlate[Text Word] OR predictor/criterion[Text Word] OR predictor/happiness[Text Word] OR predictor/independent[Text Word] OR predictor/mediator[Text Word] OR predictor/outcome[Text Word] OR predictor/training[Text Word] OR predictor’[Text Word] OR predictor’’[Text Word] OR predictor’s[Text Word] OR predictora[Text Word] OR predictore[Text Word] OR predictores[Text Word] OR predictorfor[Text Word] OR predictorof[Text Word] OR predictorr[Text Word] OR predictors[Text Word] OR predictors/conditions[Text Word] OR predictors/correlates[Text Word] OR predictors/formulas[Text Word] OR predictors/indicators[Text Word] OR predictors/institutionalization[Text Word] OR predictors/markers[Text Word] OR predictors/mediators[Text Word] OR predictors/other[Text Word] OR predictors/risk[Text Word] OR predictors/svmtm[Text Word] OR predictors’[Text Word] OR predictorsof[Text Word] OR predictorvsl2[Text Word] OR predictory[Text Word] OR predictpatientevents[Text Word] OR predictprotein[Text Word] OR predictprotein’[Text Word] OR predictregulon[Text Word] OR predictrive[Text Word] OR predicts[Text Word] OR predictt[Text Word] OR predictthe[Text Word] OR predicttive[Text Word] OR predicttoxicity[Text Word] OR predictve[Text Word] OR predictyate[Text Word]) OR (course[Text Word] OR course/6[Text Word] OR course/activity[Text Word] OR course/aging[Text Word] OR course/best[Text Word] OR course/clerkship[Text Word] OR course/clerkships[Text Word] OR course/curriculum[Text Word] OR course/donor[Text Word] OR course/dose[Text Word] OR course/effectiveness[Text Word] OR course/faculty[Text Word] OR course/immunologic[Text Word] OR course/laboratory[Text Word] OR course/materials[Text Word] OR course/module[Text Word] OR course/nil[Text Word] OR course/open[Text Word] OR course/outcome[Text Word] OR course/outcome/treatment[Text Word] OR course/patient[Text Word] OR course/period[Text Word] OR course/prognosis[Text Word] OR course/program[Text Word] OR course/residency[Text Word] OR course/severity[Text Word] OR course/social[Text Word] OR course/theory[Text Word] OR course/training[Text Word] OR course/treatment[Text Word] OR course/tumor[Text Word] OR course/tutorial[Text Word] OR course/workshop[Text Word] OR course’[Text Word] OR course’’[Text Word] OR course’s[Text Word] OR course95[Text Word] OR coursebook[Text Word] OR coursebooks[Text Word] OR coursebuilder[Text Word] OR coursed[Text Word] OR coursefor[Text Word] OR courseille[Text Word] OR coursely[Text Word] OR coursemaster[Text Word] OR coursemates[Text Word] OR coursemodifying[Text Word] OR coursen[Text Word] OR courseof[Text Word] OR courseofacute[Text Word] OR courser[Text Word] OR coursers[Text Word] OR coursersef[Text Word] OR courses[Text Word] OR courses/1[Text Word] OR courses/1,000[Text Word] OR courses/100[Text Word] OR courses/165[Text Word] OR courses/33[Text Word] OR courses/advanced[Text Word] OR courses/areas[Text Word] OR courses/awards[Text Word] OR courses/child[Text Word] OR courses/classes[Text Word] OR courses/clerkships[Text Word] OR courses/congresses[Text Word] OR courses/course[Text Word] OR courses/disciplines[Text Word] OR courses/individual[Text Word] OR courses/lectures[Text Word] OR courses/materials[Text Word] OR courses/nt/is[Text Word] OR courses/patient[Text Word] OR courses/person[Text Word] OR courses/person/year[Text Word] OR courses/programs[Text Word] OR courses/pt[Text Word] OR courses/schools[Text Word] OR courses/seminars[Text Word] OR courses/themes/topics[Text Word] OR courses/workshops[Text Word] OR courses/year[Text Word] OR courses’[Text Word] OR coursesabout[Text Word] OR coursesteaching[Text Word] OR courseware[Text Word] OR coursewares[Text Word] OR coursewise[Text Word] OR coursework[Text Word] OR coursework/continuing[Text Word] OR coursey[Text Word])
Cochrane Central Register of Controlled Trials
We searched CENTRAL for any RCTs that included text words or MeSH terms relating to CVC and infection for patients of any age.
(central ven* cathe*):ti,ab,kw OR MeSH descriptor Catheterization, Central Venous
AND
(infec*):ti,ab,kw OR MeSH descriptor Infection
Early central venous catheter removal versus treatment in situ to reduce infection complications
We considered any potentially eligible studies found from scanning the abstracts generated by the searches above. In addition, we conducted specific searches of PubMed for comparative studies of CVC removal versus treatment in situ.
The search terms used were: terms for CVC, removal included as a text word, date limit for articles published from 1995 onwards.
Terms for CVC
((central[All Fields] AND (“veins”[MeSH Terms] OR “veins”[All Fields] OR “venous”[All Fields]) AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])) OR (intravascular[All Fields] AND (“equipment and supplies”[MeSH Terms] OR (“equipment”[All Fields] AND “supplies”[All Fields]) OR “equipment and supplies”[All Fields] OR “device”[All Fields])) OR (PICC[All Fields] AND line[All Fields]) OR port[All Fields] OR (“catheters, indwelling”[MeSH Terms] OR (“catheters”[All Fields] AND “indwelling”[All Fields]) OR “indwelling catheters”[All Fields] OR (“indwelling”[All Fields] AND “catheter”[All Fields]) OR “indwelling catheter”[All Fields]) OR (tunnelled[All Fields] AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])))
Antimicrobial locks for treatment or prevention (any age group)
We considered any potentially eligible studies found from scanning the abstracts generated by the searches above. In addition, we conducted specific searches of PubMed for reviews, meta-analyses or RCTs of antimicrobial locks.
Terms for CVCs
((central[All Fields] AND (“veins”[MeSH Terms] OR “veins”[All Fields] OR “venous”[All Fields]) AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])) OR (intravascular[All Fields] AND (“equipment and supplies”[MeSH Terms] OR (“equipment”[All Fields] AND “supplies”[All Fields]) OR “equipment and supplies”[All Fields] OR “device”[All Fields])) OR (PICC[All Fields] AND line[All Fields]) OR port[All Fields] OR (“catheters, indwelling”[MeSH Terms] OR (“catheters”[All Fields] AND “indwelling”[All Fields]) OR “indwelling catheters”[All Fields] OR (“indwelling”[All Fields] AND “catheter”[All Fields]) OR “indwelling catheter”[All Fields]) OR (tunnelled[All Fields] AND (“catheterization”[MeSH Terms] OR “catheterization”[All Fields] OR “catheter”[All Fields])))
Limits were publication date from 1995, meta-analysis, RCT, review.
Locks (for treatment or prevention): lock was included as a text word.
Slow infusion versus bolus injection of antibiotics
This search considered any potentially eligible studies found from scanning the abstracts generated by the searches above. In addition, we conducted specific searches using terms for CVC AND RCTs (as above) AND synonyms for infusion, parenteral, intravenous or bolus.
Appendix 6 Studies excluded from the systematic review (Chapter 4)
| Author | Year published | Country | Journal | Study design | Population | Reason for exclusion |
|---|---|---|---|---|---|---|
| Bernardini | 1996 | USA | Am J Kidney Dis | RCT | Peritoneal dialysis | Mupirocin vs oral rifampicin |
| Bernardini | 2005 | USA | J Am Soc Nephrol | RCT | Peritoneal dialysis | Oral gentamicin vs muciprocin |
| De Sio | 2004 | Italy | Pediatr Infect Dis J | Case series | Oncology | Vancomycin + urokinase |
| Dillon | 2004 | USA | J Clin Oncol | RCT | Children on haemodialysis | Urokinase vs heparin |
| Duncan | 2005 | UK | J Am Soc Nephrol | RCT | Haemodialysis | Citrate vs heparin |
| Haimi-Cohen | 2001 | USA | Antimicrob Agents Chemother | Experimental | Paediatric oncology | In vitro study |
| Johnson | 2002 | Australia | Nephrol Dial Transplant | RCT | Haemodialysis | Mupirocin vs no treatment |
| Kacica | 1994 | USA | J Pediatr | RCT | Neonatal ICU | Vancomycin added to TPN vs none |
| Kethireddy | 2008 | USA | J Vasc Access | Systematic review of RCTs | Oncology | Urokinase vs heparin, five RCTs |
| Ljungman | 1997 | Sweden | Support Care Cancer | RCT | Adult oncology | Perioperative prophylaxis |
| Mouw | 2008 | USA | J Pediatr Surg | Historical case series | Children with short gut syndrome | Ethanol – no comparison |
| Ranson | 1990 | UK | J Hosp Infect | RCT | Adult oncology | Perioperative prophylaxis |
| van Rooden | 2008 | Netherlands | J Clin Oncol | RCT | Chemotherapy | Urokinase vs saline |
| Sesso | 1998 | Brazil | J Am Soc Neprhol | RCT | Haemodialysis | Muciprocin ointment vs none |
| Smith | 1989 | UK | Antimicrob Agents Chemother | Case–control study | Paediatric oncology | Vancomycin vs teicoplanin |
| Spafford | 1994 | USA | J Pediatr | RCT | Neonatal ICU | Vancomycin added to TPN vs none |
| Vassilomaniakis | 1995 | Greece | Bone Marrow Transplant | RCT | Bone marrow transplant patients | Prophylactic systemic vancomycin vs none |
| Vazquez | 1999 | Spain | Haematologica | RCT | Neutropenic oncology | Vancomycin vs teicoplanin systemic treatment |
Appendix 7 Antimicrobial lock questionnaire
Antimicrobial locks used for the treatment or prevention of central venous catheter-associated infections in children with cancer
Questionnaire objective To identify concerns with respect to the use of antimicrobial locks for the treatment or prevention of CVC-associated infections in children undergoing treatment for cancer.
An antimicrobial lock is defined as the ‘locking’ of a solution containing an antimicrobial substance into the lumen of a central vascular access device in order to treat or prevent infection associated with that device. These antimicrobial locks can be used for variable periods but usually in excess of 2 hours. Antimicrobial substances that have been reported for prevention or treatment can be any one or more of a wide range of chemicals (including chelating agents, alcohols and acids), antibiotics, enzymes and disinfectants. Antimicrobial locks used for prevention are almost always both antimicrobial and anticoagulant. An example of antimicrobial locks for prevention is the use of vancomycin with heparin. In this case the vancomycin/heparin solution is used as a direct replacement for heparin and may be left in the line for variable durations depending upon the requirements for line usage.
Nine systematic reviews have shown that lock solutions prevent CVC infection (see, for example, Yahav et al. 106 and Safdar and Maki77). Most of the RCTs were of adult patients undergoing haemodialysis through a CVC: the pooled relative risk of CVC-associated infection found in the meta-analyses is 0.3–0.6 in patients in whom antimicrobial locks were used as a routine locking solution compared with patients given placebo or heparin locks. To understand what this means, imagine that the relative risk is 0.5. This means that the frequency of infection would be halved, for example from a rate of 10/1000 CVC days with heparin to 5/1000 CVC days with a lock solution.
There are limited published data on the use of locks for treatment, but a major potential benefit is prevention of recurrent infection (see Rijnders et al. 36). In the only RCT that has examined treatment of CVC infection using antibiotic locking solutions (heparin with vancomycin or ceftazidine), probably because of the small sample size the study found no significant difference (HR 0.55, p = 0.10). 36 It might be that further studies will show that locks can be used to treat CVC-associated infections that respond poorly to current treatment regimes such as those caused by fungi, S. aureus and resistant Gram-negative bacteria, but there are insufficient data to answer this question at the moment.
In summary, there is evidence for the effectiveness of locks for prevention of CVC infection, particularly in patients undergoing haemodialysis.
We are trying to find out whether locks are being used in paediatric oncology practice and what are the concerns and perceived disadvantages, including feasibility issues, disadvantages, contraindications and potential costs.
Could you please answer the following questions in as much detail as possible.
Questions
| 1) | Are antimicrobial locks used in your centre for children with cancer? | |||
| a) to prevent CVC infection | Yes ☐ | No ☐ | ||
| b) to treat suspected CVC infection | Yes ☐ | No ☐ | ||
| (for example in a child presenting with fever and with coagulase negative staphylococci isolated from both lumens of a central line) | ||||
| 2) | If yes – have you any experience of side-effects or adverse events attributable to the use of antimicrobial locks? | |||
| Yes ☐ | No ☐ | |||
| If yes – please specify | ||||
| 3) | Please could you list below anything that might discourage you from using antimicrobial locks | |||
| For prevention | For treatment | |||
| Selection of antibiotic resistance | N/A | |||
| Doubts about efficacy | ||||
| Safety profile | ||||
| Costs | ||||
| Availability of lumen time | ||||
| Inconvenience | ||||
| Other | ||||
| If other, please specify | ||||
| Comments | ||||
| 4) | Please can you give an indication of the proportion of children undergoing treatment for cancer in your centre in whom you think it would be feasible to use antimicrobial locks – assuming that this will require a minimum of 2 hours of antimicrobial lock time in each lumen for treatment, and there will be no problems with availability of lock solutions in shared care or the community for continuing preventive use and where the locking solution is a direct replacement for heparin flushes and locks. | |||
| For treatment | % | For prevention | % | |
Appendix 8 Secondary analyses of unpublished study by Windebank et al. to determine prognostic markers for infection recurrence and central venous catheter removal (Chapter 3)
This was a prospective, multicentre, multidisciplinary study of CVCs in paediatric oncology patients, which analysed factors involved in early failure.
| Number of patients included for analysis | 334 |
| Duration of follow-up | 6 months |
| Number with infection episode | 334 |
| Excluded owing to missing data | 0 |
| Total number of patients | 334 |
| Characteristics before admission | |
|---|---|
| Age at start of treatment period | |
| Overall n (%) | 313 (94) |
| Median (IQR) | 6 (3 to 11) |
| Mean (SEM) | 7 (0.3) |
| < 3 years n (%) | 74 (22) |
| Median (IQR) | 2 (1 to 2) |
| Mean (SEM) | 2 (0.1) |
| ≥ 3 years n (%) | 239 (72) |
| Median (IQR) | 7 (5 to 12) |
| Mean (SEM) | 8 (0.3) |
| Cancer type | |
| Non-haematological, n (%) | 117 (35) |
| Haematological, n (%) | 217 (65) |
| Number of lumens | |
| Single, n (%) | 104 (31) |
| Multiple, n (%) | 214 (64) |
| Type of venous access device | |
| External, n (%) | 188 (56) |
| Implanted port, n (%) | 24 (7) |
| Missing, n (%) | 122 (37) |
| Duration of CVC insertion before treatment episode in months | |
| Median (IQR) | 2 (1 to 4) |
| Characteristics on admission for infection episode | |
| FRC [with line flushing (WB) detail to footnote] | |
| Yes, n (%) | 12 (4) |
| No, n (%) | 278 (83) |
| Superficial signs of tunnel/exit site infection within 3 days of treatment period or within 3 days after if on admission | |
| Tunnel or exit site, n (%) | 15 (4) |
| No signs recorded, n (%) | 319 (96) |
| At 48 hours after admission | |
| Blood culture group | |
| Pathogens (excluding skin commensals), n (%) | 18 (5) |
| Other, n (%) | 30 (9) |
| None recorded, n (%) | 286 (86) |
| Outcomes | |
| Follow-up period | |
| Duration of follow-up (show lines for mean and median)a | |
| Median (IQR) | 128 (55 to 183) |
| Mean (SEM) | 116 (3.6) |
| Recurrent infection episode | |
| Number of patients with recurrent i.v. treatment periods after index episode | |
| n (%) | 199 (60) |
| Time to second period of i.v. treatment | |
| Median (IQR) | 52 (26 to 104) |
| Mean (SEM) | 64 (3.1) |
| Incidence of recurrence (per 1000 days)b | |
| Mean | 7.449 |
| Days of i.v. treatment | |
| Days of i.v. treatment during index infection episode | |
| Median (IQR) | 6 (4 to 9) |
| Mean (SEM) | 8 (0.4) |
| Days of i.v. treatment after initial infection episode | |
| Median (IQR) | 4 (0 to 10) |
| Mean (SEM) | 7 (0.6) |
| CVC removal | |
| Reason CVC removed during follow-up period | |
| Total, n (%) | 225 (67) |
| Infection, n (%) | 65 (19) |
| Death (not during treatment episode), n (%) | 19 (6) |
| CVC damage, n (%) | 0 (0) |
| Reason not stated, n (%) | 141 (42) |
| Not removed, n (%) | 109 (33) |
| Incidence of CVC removal/1000 days’ follow-upa (A, B, C + from day of admission) | |
| Mean | 5.813 |
| Rate of death/1000 days’ follow-up (n)a (A, B, C + from day of admission) | |
| Mean | 0.672 |
Appendix 9 Clinical effectiveness at 6-month follow-up
| Clinical subgroup | Test results | Number of patients | Outcomes (days during 6-month follow-up) | Strategies | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FRC | DNA (pg/µl) | Blood culture | Total | Recurrent i.v. treatment episode | CVC removed by 28 days | Initial treatment | Recurrent i.v. treatment | Total i.v. treatment | DNA + FRC early removal | DNA + FRC early stop | BC + FRC remove @ 48 hours | BC + FRC stop @ 48 hours | BC + FRC + DNA remove @ 48 hours | BC + FRC + DNA stop @ 48 hours | |
| All | 99 | 66 | 47 | 756 | 613 | 1369 | |||||||||
| A | FRC+ | > 0.5 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R0 | R48 | R48 | |||
| B | FRC+ | > 0.5 | Other | 4 | 1 | 4 | 34 | 9 | 43 | R0 | |||||
| C | FRC+ | > 0.5 | None | 0 | 0 | 0 | 0 | 0 | 0 | R0 | |||||
| D | FRC+ | 0.125–0.5 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R48 | |||||
| E | FRC+ | 0.125–0.5 | Other | 1 | 1 | 0 | 11 | 10 | 21 | ||||||
| F | FRC+ | 0.125–0.5 | None | 0 | 0 | 0 | 0 | 0 | 0 | ||||||
| G | FRC+ | < 0.125 | Pathogen | 0 | 0 | 0 | 0 | 0 | 0 | R48 | |||||
| H | FRC+ | < 0.125 | Other | 1 | 1 | 1 | 4 | 2 | 6 | ||||||
| I | FRC+ | < 0.125 | None | 4 | 2 | 3 | 128 | 34 | 162 | ||||||
| J | FRC– | > 0.5 | Pathogen | 2 | 0 | 1 | 21 | 0 | 21 | ||||||
| K | FRC– | > 0.5 | Other | 5 | 4 | 3 | 45 | 32 | 77 | ||||||
| L | FRC– | > 0.5 | None | 0 | 0 | 0 | 0 | 0.00 | 0 | S48 | |||||
| M | FRC– | 0.125–0.5 | Pathogen | 0 | 0 | 0 | 0 | 0.00 | 0 | ||||||
| N | FRC– | 0.125–0.5 | Other | 3 | 2 | 1 | 29 | 27 | 56 | ||||||
| O | FRC– | 0.125–0.5 | None | 3 | 2 | 2 | 9 | 10 | 19 | S48 | |||||
| P | FRC– | < 0.125 | Pathogen | 1 | 1 | 0 | 6 | 9 | 15 | S48 | |||||
| Q | FRC– | < 0.125 | Other | 5 | 4 | 3 | 61 | 49 | 110 | S48 | |||||
| R | FRC– | < 0.125 | None | 70 | 48 | 29 | 408 | 431 | 839 | S48 | S48 | S48 | |||
| Strategy | Total number of events | Difference compared with standard care | ||||||
|---|---|---|---|---|---|---|---|---|
| Recurrence | CVCs removed | Unnecessary removal | i.v. days | Recurrence | CVCs removed | Unnecessary removal | i.v. days | |
| Balance sheet for 99 patients | ||||||||
| Standard | 66 | 47 | 0 | 1369 | ||||
| DNA + FRC early removal | 65 | 47 | 0 | 1306 | –1 | 0 | 0 | –63 |
| DNA + FRC early stop | 66 | 47 | 0 | 894 | 0 | 0 | 0 | –475 |
| BC + FRC remove @ 48 hours | 66 | 47 | 0 | 1369 | 0 | 0 | 0 | 0 |
| BC + FRC stop @ 48 hours | 66 | 47 | 0 | 952 | 0 | 0 | 0 | –417 |
| BC + FRC+DNA remove @ 48 hours | 66 | 47 | 0 | 1369 | 0 | 0 | 0 | 0 |
| BC + FRC+DNA stop @ 48 hours | 66 | 47 | 0 | 961 | 0 | 0 | 0 | –408 |
| i.v. treatment if any FRC/DNA/BC+ | 60.6 | 41.6 | 0 | 1210 | –5 | –5 | 0 | –159 |
| Balance sheet per 1000 patients | ||||||||
| Standard | 667 | 475 | 0 | 13,828 | 0 | 0 | 0 | 0 |
| DNA + FRC early removal | 657 | 475 | 0 | 13,192 | –10 | 0 | 0 | –636 |
| DNA + FRC early stop | 667 | 475 | 0 | 9030 | 0 | 0 | 0 | –4798 |
| BC + FRC remove @ 48 hours | 667 | 475 | 0 | 13,828 | 0 | 0 | 0 | 0 |
| BC + FRC stop @ 48 hours | 667 | 475 | 0 | 9616 | 0 | 0 | 0 | –4212 |
| BC + FRC+DNA remove @ 48 hours | 667 | 475 | 0 | 13,828 | 0 | 0 | 0 | 0 |
| BC + FRC+DNA stop @ 48 hours | 667 | 475 | 0 | 9707 | 0 | 0 | 0 | –4121 |
| i.v. treatment if any FRC/DNA/BC+ | 612 | 420 | 0 | 12,222 | –55 | –55 | 0 | –1606 |
Glossary
- Antimicrobial lock
- An antimicrobial solution placed in the lumen of a CVC for a period exceeding 2 hours. This may be an antibiotic (used in patients for the treatment of infection) or an antiseptic solution (not generally used for systemic treatment).
- Central venous catheter (CVC)
- A flexible tube with the tip placed in a large vein, most commonly in the thorax.
- CVC-associated infection
- Bloodstream infection associated with microbial colonisation of a CVC. Infection may be diagnosed by clinical signs and does not always require a positive blood culture.
- Implanted port
- Vascular access port placed under the skin and connected to a large blood vessel – accessed through the skin.
- Intraluminal
- Inside the lumen of a CVC.
- Long-term CVC
- These can remain in place for many months and are usually tunnelled CVCs or implanted ports.
- Tunnelled CVC
- A surgically implanted CVC with a cuff that lies in a subcutaneous tunnel and anchors the catheter and inhibits microbial migration from the skin surface along the catheter (may also be called Hickman or Broviac catheter).
List of abbreviations
- AIC
- Akaike’s information criterion
- CCLG
- Children’s Cancer and Leukaemia Group
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CFU
- colony-forming unit (measure of bacterial numbers)
- CI
- confidence interval
- CVC
- central venous catheter
- DNA
- deoxyribonucleic acid
- EDTA
- ethylenediaminetetra-acetic acid
- FRC
- fever, rigors, chills and/or hypotension associated with CVC manipulation
- HR
- hazard ratio
- IQR
- interquartile range
- i.v.
- intravenous
- LR
- likelihood ratio
- PCR
- polymerase chain reaction; method of amplifying a single or a few copies of a molecule of DNA by many orders of magnitude to enable quantitative or qualitative detection
- RCT
- randomised controlled trial
- rDNA
- ribosomal deoxyribonucleic acid
- UKCCSG
- United Kingdom Children’s Cancer Study Group (now CCLG)
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Professor of General Practice, Department of Primary Health Care, University of Oxford Programme Director,
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics and Clinical Trials, Queen Mary, Department of Epidemiology and Public Health, Imperial College London
-
Professor Peter Brocklehurst, Director, National Perinatal Epidemiology Unit, University of Oxford
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Jonathan Green, Professor and Acting Head of Department, Child and Adolescent Psychiatry, University of Manchester Medical School
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, Head of Nuffield Department of Surgery, University of Oxford
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norris, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor James Raftery, Chair of NETSCC and Director of the Wessex Institute, University of Southampton
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norris Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor James Raftery, Chair of NETSCC and Director of the Wessex Institute, University of Southampton
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire Country Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr David P Britt, Public contributor
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Professor Nicholas James, Professor of Clinical Oncology, School of Cancer Sciences, University of Birmingham
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/ Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Mr John Chapman, Public contributor
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Ms Kylie Gyertson, Oncology and Haematology Clinical Trials Manager, Guy’s and St Thomas’ NHS Foundation Trust London
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Martin Shelly, General Practitioner, Silver Lane Surgery, Leeds
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation of Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Professor Bruce Campbell, Consultant Vascular & General Surgeon, Royal Devon & Exeter Hospital, Wonford
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Neill McIntosh, Edward Clark Professor of Child Life and Health, University of Edinburgh
-
Professor Rajan Madhok, Consultant in Public Health, South Manchester Primary Care Trust
-
Professor Sir Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, Director, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Philip Shackley, Senior Lecturer in Health Economics, Sheffield Vascular Institute, University of Sheffield
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Dr Nick Summerton, GP Appraiser and Codirector, Research Network, Yorkshire Clinical Consultant, Primary Care and Public Health, University of Oxford
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Dr Ross Taylor, Senior Lecturer, University of Aberdeen
-
Dr Richard Tiner, Medical Director, Medical Department, Association of the British Pharmaceutical Industry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington