Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 98/34/05. The contractual start date was in October 2001. The draft report began editorial review in May 2007 and was accepted for publication in October 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
see Acknowledgements
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2011. This work was produced by Price et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2011 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Scientific background
Asthma is a condition of the bronchial airways, characterised by airway hyper-responsiveness (or airway irritability) and reversible airway obstruction. In 2002, an estimated 3 million people, or 5% of the UK population, had asthma. 1,2 Asthma is caused by chronic inflammation of the small, or bronchial, airways. This inflammation causes the production of mucus, oedema formation, and nerve end exposure, and leads to an increase in airway hyper-responsiveness. Increased airway hyper-responsiveness causes narrowing of the airways (or bronchoconstriction), which may lead to coughing, wheezing, chest tightness and shortness of breath. In asthma, airway bronchoconstriction can be substantially reversed with a short-acting β2-agonist or reliever medication.
Untreated chronic inflammation in the airways may lead, in some individuals, to structural changes (or airway remodelling), irreversible bronchoconstriction and persistent symptoms. The recognition that airway inflammation is present even in patients with mild asthma has led to a shift towards introducing anti-inflammatory therapy earlier in the management of asthma,2,3 with increased prescribing of inhaled corticosteroids4,5 in patients requiring daily use of a short-acting β2-agonist [step 2 of British Thoracic Society (BTS) Asthma Guidelines]. 4,5 However, while there is some evidence of reduced morbidity, many patients with asthma still have considerable symptoms and lifestyle limitation. 6 Possible reasons for this include lack of disease recognition, poor adherence to inhaled steroids, poor inhaler technique, untreated rhinitis, smoking, and an inability of inhaled steroids alone to fully control asthma, with an increasing emphasis on the role of adding additional therapy to inhaled steroids rather than routinely increasing inhaled steroid dose. As a result these patients end up being treated at step 3 of the BTS Asthma Guidelines. 4
Efficacy studies of antiasthma therapies have traditionally used measures of airways function, such as spirometry [forced expiratory volume in 1 second (FEV1)]7,8 and domiciliary peak expiratory flow (PEF),7 or measures of airway hyper-reactivity, such as methacholine bronchial challenge testing,9–12 to demonstrate therapeutic effectiveness. While these measures provide objective information on airway function, they provide no information on patient perceived effectiveness of an asthma treatment or asthma control. Indeed, the ‘real-life’ control of asthma is now regularly assessed in terms of changes in patient-reported quality of life (QOL), symptoms, exacerbations and rescue medication use. As the correlation is often poor between objective measures of airway function (e.g. domiciliary PEF) and measures of asthma control, international guidelines encourage the collection of measures of both airway function and disease control. 5
Anti-inflammatory treatments with the potential to treat mild to moderate asthma are inhaled corticosteroids and leukotriene receptor antagonists. Corticosteroids work by suppressing the production of inflammatory mediators by airway epithelial and smooth muscle cells, endothelial cells and fibroblasts. 13 However, inhaled steroids have been shown to have limited impact on suppressing the production or release of the cysteinyl leukotrienes LTC4, LTD4 and LTE4, biologically active mediators derived from arachidonic acid, which collectively account for the biological activity known as slow-reacting substance of anaphylaxis. 14,15 These leukotrienes mediate many responses that are associated with asthma, including mucus production, decreased mucociliary clearance, changes in vascular permeability, inflammatory cell influx and smooth muscle contraction. 16 Thus, leukotriene receptor antagonists that act to reduce the production or block the action of leukotrienes may be important in asthma management and complementary to inhaled corticosteroids.
Leukotriene receptor antagonists
Montelukast and zafirlukast are orally active, potent selective leukotriene CysLT1 receptor antagonists. The safety and tolerability of both of these leukotriene antagonists are well established. 17,18 Compared with placebo they have been shown to improve airway function and symptoms, and decrease short-acting β2-agonist use. 19–21 They also inhibit early- and late-phase bronchoconstriction that is induced by inhaled allergen,22,23 and attenuate exercise-induced bronchoconstriction at a level at least comparable to long-acting β2-agonist. 24 Montelukast has also been shown to decrease sputum and peripheral blood eosinophil levels. 25 Results from adult Phase III clinical studies demonstrate that, compared with placebo, montelukast21 and zafirlukast19 improve FEV1, daytime symptoms, total daily β2-agonist use, nocturnal asthma, morning and evening PEF, asthma-specific QOL, patient and investigator global evaluations, and asthma exacerbation rate in patients using short-acting β2-agonist only. Other studies have demonstrated the additive effects of montelukast in patients taking inhaled steroids. 26 Additionally, results from a chronic exercise study demonstrate the ability of montelukast to attenuate exercise-induced bronchoconstriction at the end of the dosing interval over a 12-week period without loss of effect27 and a comparable effect to long-acting β2-agonist. 24 Montelukast also reduces blood21 and sputum eosinophils. 25
Leukotriene antagonists could potentially be used at step 2 or step 3 of the asthma guidelines. At step 2, leukotriene antagonists would be used as an alternative to inhaled steroids, while at step 3 leukotriene antagonists would be used as an alternative to long-acting β2-agonists as add-on therapy to inhaled steroids in patients who are not controlled on inhaled steroids alone.
Recent studies evaluating the use of montelukast or zafirlukast against inhaled steroids at step 2 suggest that leukotriene antagonists are inferior to inhaled steroids in short-term double-blind double-dummy studies and in patients with significant asthma severity. In a meta-analysis, Ducharme28 reported that patients randomised to a leukotriene antagonist had a 60% increased risk of exacerbation compared with a patient receiving 400 µg of the inhaled steroid beclometasone dipropionate. Those randomised to inhaled steroid had a significantly increased FEV1 compared with leukotriene antagonist. However, Israel et al. 29 reported that although 400 µg beclometasone significantly improved FEV1 compared with montelukast, they found no significant difference in the number of exacerbations, possibly indicating that leukotriene antagonists may confer benefits in asthma control which are equivalent to those of inhaled steroids.
In patients with unstable asthma currently receiving an inhaled steroid, the addition of montelukast or zafirlukast leads to clinically important improvements in airway function, asthma exacerbations, attacks and symptoms, as reviewed by Currie and McLaughlin. 30 All inhaled steroids have debilitating side effects; although these are largely associated with high doses, local side effects appear to be more common at lower doses than previously recognised. 31 Indeed guidelines advocate tapering inhaled steroids to the minimum effective dose. 4,5 Although neither montelukast nor zafirlukast is licensed for steroid sparing (i.e. minimising the dose of inhaled steroid), Lofdahl et al. ,32 Price et al. 33 and Riccioni et al. 34 have reported some evidence that this may be possible.
Two recent meta-analyses have examined the effects of leukotriene antagonists as add-on therapy to inhaled steroids. 35,36 Ducharme et al. ,35 compared the effects of adding leukotriene antagonist versus long-acting β2-agonist to inhaled steroid therapy in trials of 28 days or longer, and found a 17% lower risk of asthma exacerbation with add-on long-acting β2-agonist: 38 patients receiving inhaled steroid had to be treated for 48 weeks with add-on long-acting β2-agonist rather than add-on leukotriene antagonist to prevent one exacerbation. Lung function, symptoms and the use of rescue short-acting β2-agonist were also better with long-acting β2-agonist. The authors note that while the internal validity of their findings is supported by the homogeneity of studied patients and trials, the external validity or generalisability of their findings is an issue. 35 Indeed, a limitation of the majority of the studies performed to date is that they are not ‘real world’, and do not necessarily reflect the issues of poorer compliance and adherence to inhaled medications compared with oral medications observed in primary care. They also rarely take a true intention-to-treat approach with patients who cease study therapies and drop out of the study at that point. 37
The second systematic review (pooling of data by meta-analyses performed when feasible) looked only at studies of ≥ 12 weeks’ duration that compared montelukast as add-on to inhaled steroid with inhaled steroid monotherapy or with salmeterol as add-on to inhaled steroid. 36 Compared with inhaled steroid monotherapy, add-on montelukast to inhaled steroid improved control of mild to moderate asthma. Compared with add-on salmeterol, add-on montelukast to inhaled steroid was less effective with regard to most clinical outcomes in the medium term; however, over 48 weeks the proportions of patients with ≥ 1 exacerbation were similar, as were hospitalisation and emergency treatment rates. The rate of serious adverse events over 48 weeks was significantly higher with add-on salmeterol; thus, montelukast may have a better long-term safety profile. 36
At the time of commissioning this study, the data regarding the cost-effectiveness of leukotriene antagonists in primary care were limited. In one primary care centre, a prospective audit of outcomes and cost associated with montelukast suggested that as an add-on option in patients at step 3, there might be significant clinical benefits at little additional cost. 38 Recent studies have suggested that, at step 2 of the asthma guidelines, use of a leukotriene antagonist compared with an inhaled steroid is associated with higher health-care resource utilisation. 39 However, this study did not evaluate clinical outcomes or patient reported measures of disease control.
Hypotheses
In older children and adult patients with chronic asthma, initiation of a leukotriene receptor antagonist will provide, at no greater cost to the National Health Service (NHS) and patients, clinical improvements in QOL and other important asthma parameters that are at least equal to the alternative treatment options of inhaled corticosteroid at step 2 and adding a long-acting β2-agonist at step 3. This study was designed as two separate, but concurrent, equivalence trials to determine whether a leukotriene antagonist is an equal choice to inhaled steroid as monotherapy, and to long-acting β2-agonist as add-on therapy, for a real-world population of patients with perhaps milder asthma and who are less likely to adhere to therapy than those enrolled in classical clinical trials.
Rationale for this study
Need for cost-effectiveness data
In response to growing pressure on health-care budgets, and the availability of a choice of different therapeutic interventions for many diseases, evidence on the relative value for money of new or different therapeutic interventions is becoming increasingly important. In recognition of this, the UK Department of Health has provided guidelines to encourage the evaluation of therapeutic interventions from an economic perspective, in parallel with traditional investigations into efficacy and safety. 40 Indeed the UK National Institute for Health and Clinical Excellence (NICE), established in 1999, evaluates medicines (new and current) for use within the NHS by reviewing both clinical and economic evidence.
Asthma is a condition for which economic evaluation of therapeutic interventions is particularly relevant; the prevalence is high, with reported treatment prevalence rates for the UK ranging from 2% to 5% for adults and up to 10% for school-aged children,1 and a range of different therapeutic interventions are available. 4 The high-prevalence chronic nature of the disease, along with the range of therapeutic interventions, make the management of asthma a considerable financial burden on the NHS. 41 However, published investigations into the costs of asthma management either have focused on isolated components of treatment, such as specific medications, or have used limited retrospective data for estimates of health-care utilisation. 41–45 Only minimal information is available on the ‘real-world’ cost of asthma management, including costs to primary and secondary care, the patient, and the indirect cost of lost productivity to the economy.
Leukotriene receptor antagonists could potentially be used at both steps 2 and 3 of the asthma guidelines. 4,5 Although leukotriene antagonists are more expensive to prescribe, in terms of drug acquisition costs, than low-dose inhaled steroids (∼£24 per 28 days versus ∼£8 per 28 days, respectively46), and although less effective in terms of objective measures of lung function, they appear to produce comparable overall asthma control29 and are associated with superior adherence. 37,47 Leukotriene antagonists may therefore result in significant health gain and savings in other areas of health and patient costs, which might justify additional prescribing costs. There is some evidence from long-term trials that this may be the case. 48 However, markers of cost-effectiveness in asthma clinical trials have included cost per asthma-free day or cost to achieve a given improvement in lung function. 49 Outcomes such as asthma-free days and improvement in lung function are good clinical measures. However, the latter is not necessarily correlated with meaningful changes in overall QOL for the patient, and the former does not cover all aspects of health-related QOL that may be of relevance to the patient. More appropriate markers are required.
The purpose of this study was to compare the long-term effectiveness and total cost of asthma management to the NHS, patients and society in two groups of patients – one group receiving leukotriene antagonist and the other group receiving the most effective evidence-based alternatives at step 2 (inhaled steroid) and step 3 (long-acting β2-agonist). It is important to provide a convincing investigation of the cost-effectiveness of prescribing leukotriene antagonists. To this end, we proposed a long-term study, taking the wider costs of asthma management into account, to be conducted in a manner reflecting real clinical practice. The primary efficacy variable for this study was the validated Juniper disease-specific asthma QOL scale – the Mini Asthma Quality of Life Questionnaire (MiniAQLQ). 50 This was chosen because it captures outcomes of relevance to patients and their primary caregivers, thus reflecting ‘real life’. We regarded a difference of > 0.3 in MiniAQLQ score as a meaningful difference because although 0.5 has been regarded in individuals as a minimum clinically important difference,51 many studies, even versus placebo, have found smaller differences of 0.3–0.421 to be associated with clinical benefit. Therefore, we have opted for this more conservative figure for a population difference.
Evaluation of effectiveness at step 2 of asthma guidelines
Many patients are not fully controlled by inhaled steroids, due to a mixture of lack of complete clinical effectiveness and poor adherence with regular treatment. Alternative treatments for inhaled steroids, such as the leukotriene receptor antagonists zafirlukast and montelukast, may have a role, with some studies suggesting fairly similar overall asthma control and proportion of responders to inhaled steroids,52,53 greater patient preference54 and higher adherence rates. 55
At the time of designing and commissioning of this study, UK guidelines for the management of asthma in older children and adults (written in 1995) did not propose a clear role for leukotriene antagonists. 56 However, the latest Global Initiative For Asthma (GINA)/World Health Organization and UK guidelines suggest they may be used at step 2 as an alternative to inhaled steroids. 4,5
Evaluation of effectiveness at step 3 of asthma guidelines
Many patients taking inhaled steroids continue to have symptoms, reduced asthma-specific QOL and excessive relief treatment use, and thus require additional treatment. 57 BTS and GINA guidelines suggest two options: increasing the dose of inhaled steroid or adding a long-acting β2-agonist. 4,5 However, some view the safety, tolerability and compliance with high doses of inhaled steroids with some concern,5,58,59 and most studies suggest that adding a long-acting β2-agonist may be most likely to be clinically effective. 60,61
Adding in a leukotriene antagonist may be useful at this step for two reasons (1) steroids do not appear to suppress leukotriene production14,15 and (2) montelukast and zafirlukast have both been shown to give add-on benefit to inhaled steroid. 26,30 Leukotriene antagonists may enable inhaled steroid tapering and thus maintenance on a lower dose of inhaled steroid. 32
Chapter 2 Methods
This study comprised two separate randomisations, thus two pragmatic randomised controlled trials, powered for equivalence, comparing leukotriene antagonists with (1) inhaled steroids for patients initiating controller therapy at step 2 and (2) long-acting β2-agonists on a background of inhaled steroids for patients at step 3 of the asthma guidelines with regard to disease-specific QOL and resource use in the short term (2 months) and the long term (2 years) on an intention-to-treat basis. The trials were conducted with minimal interference with routine clinical care to evaluate real-life outcomes for patients with asthma in general practice. Patients and health-care providers were not blinded to treatment allocations; however, data collection and statistical analyses were blinded.
The study was reviewed and approved by the Eastern Multi Centre Research Ethics Committee (Ref. 00/5/13) and local (research consortia and primary care trust) ethical and research governance committees, and was conducted in accordance with appropriate research guidelines.
Participants
In the BTS British Guideline on the Management of Asthma4 the therapy of patients from the age of 6 years upwards follows the same strategy as for adults, except for alterations in dosage ranges to adjust for differences in body mass. Since exactly the same strategy is used across the age range of older children and adults, the findings of studies will have greater generalisability if they enrol patients from that entire range. Owing to limitations of validity of the MiniAQLQ and the Asthma Control Questionnaire (ACQ),62 we were unable to study children below the age of 12 but did allow children over this age, as well as adults of all ages, to be included to maximise generalisability of the study findings.
In the initial design of the study, participant recruitment was to be by primary care practice staff, as they conducted acute and routine respiratory care visits, identifying patients who met the entry criteria, informing them of the study and, if appropriate, consenting and enrolling them into the study. However, recruitment by this strategy was slower than originally anticipated owing to changes in clinical practice resulting from delays in study funding and changes in national asthma guidelines. The protocol and the process of identification of eligible patients were therefore modified, as described below, to allow prospective identification of possible study participants. All patients entering the study met the same eligibility criteria and follow-up was identical.
Further recruitment into the study was via a three-stage process.
Recruitment stage 1
Patients aged 12–80 years, attending 53 participating primary care (or general) practices in Norfolk, Suffolk, Essex, Cambridgeshire, Bedfordshire, Hampshire and Dorset, in the UK, who had received a prescription of short-acting β2-agonist in the previous 2 years, were invited, by letter, to provide data allowing eligibility for the studies to be determined. Patients were asked to provide information on their current asthma status and inhaler usage. The case notes of patients whose asthma status was consistent with eligibility in the study were reviewed by practice and study staff against the following eligibility criteria.
Inclusion criteria
-
Capable of understanding the study and study procedures (and parent/guardian’s capability of understanding the study and study procedures for patients aged under 16 years).
-
Patient had a diagnosis of asthma [defined as (1) documented reversibility after inhaled short-acting β2-agonist and/or (2) PEF variability on PEF diary and/or (3) physician-diagnosed asthma and/or (4) physician diagnosis of asthma plus history of response to treatment].
-
Step 2 trial Patient was not currently receiving, and had not received, inhaled steroid or leukotriene antagonist within the previous 12 weeks.
-
Step 3 trial (1) Patient had received inhaled steroid for at least the last 12 weeks, as ascertained from prescribing records and patient self-report and (2) had not received a long-acting β2-agonist or leukotriene antagonist in the previous 12 weeks.
Exclusion criteria
-
Patient had participated in a clinical trial involving an investigational or marketed drug within 90 days.
-
Patients had received a substantial change in antiasthma medication within the previous 12 weeks.
-
Patient was a current, or recent past, abuser (within past 3 years) of alcohol or illicit drugs.
-
Patient had any other active, acute or chronic pulmonary disorder or unresolved respiratory infection within previous 12 weeks.
-
Patient had a history of any illness that was considered to be immediately life threatening, would pose restriction on participation or successful completion of the study or would be put at risk by any study drugs (e.g. allergy to leukotriene antagonist).
-
Patient had received systemic, intramuscular or intra-articular corticosteroids within the previous 2 weeks (artificial baseline).
Patients who met those entry criteria that could be assessed by a records review in their general practice were invited for a screening visit (visit 1 – see Figure 1 and Table 1). All patients had at least 24 hours to review the patient information sheet prior to attending the visit. Patients attending for at least visit 1 will, from here on, be referred to as ‘participants’.
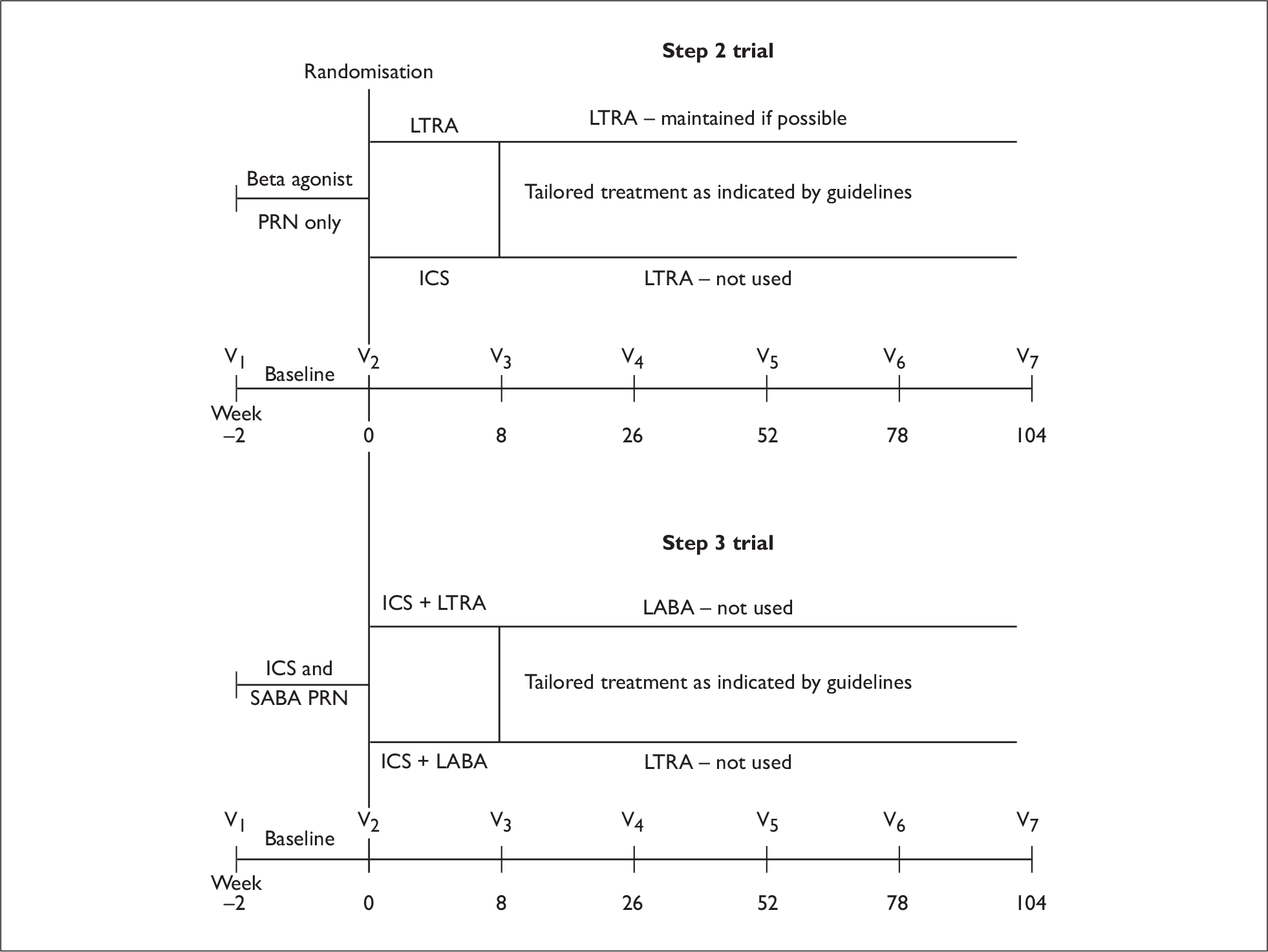
FIGURE 1.
Study flow charts, Patients at step 2 received initial controller therapy with leukotriene antagonist or inhaled steroid, Patients at step 3 received leukotriene antagonist or long-acting β2-agonist as add-on to inhaled steroid, ICS, inhaled corticosteroids; LTRA, leukotriene receptor antagonist; LABA, long-acting β2-agonist; PRN, ‘pro re nata’ – as needed; SABA, short-acting β2-agonist.
| Visit | Baseline | Trial period | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
| Study timescale (weeks) | –2 | 0 | 8 | 26 | 52 | 78 | 104 |
| Leeway allowed (days)a | ± 7 | ± 21 | ± 21 | ± 21 | ± 21 | ± 21 | |
| GP and/or practice asthma nurse procedures | |||||||
| Assess inclusion/exclusion criteria | ✓ | ||||||
| Informed consent | ✓ | ||||||
| Record clinical/asthma history and prior medications | ✓ | ||||||
| Review clinical data and asthma therapy (per clinical need) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Check patient has/can adequately use PEF meter | ✓ | ||||||
| Treatment arm randomisation by dial-up centre | ✓ | ||||||
| Review action plan for worsening asthma | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Review any adverse experiences | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Record PEF (no inhaled β2-agonist for 4 hours if possible) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Confirm patient resource utilisation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Blinded research assistant/study office | |||||||
| Collect completed patient symptom diary card | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Collect data on patient costs | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Asthma QOL and EQ-5D (quality of life) questionnaries | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Rhinitis questionnaires | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Dispense patient diary card for subsequent visit | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Collect resource use data from practice records | ✓ | ||||||
Recruitment stage 2
At visit 1, participants (and parent or guardian if appropriate) gave written informed consent and were allocated a unique study number. Participants were reviewed for the following additional entry criteria:
-
Peak expiratory flow, while withholding β2-agonist for at least 4 hours, of > 50% predicted.
-
Females of child-bearing potential agreed to use adequate contraception throughout the study.
Participants meeting the above criteria completed a 2-week PEF diary,63 ACQ,64 and asthma-specific QOL questionnaire (MiniAQLQ)50 prior to returning for visit 2.
Recruitment stage 3
At visit 2, participants scoring ≥ 1 on the ACQ (range 0–6, with ≤ 0.75 being optimal65) and/or ≤ 6 (out of a maximum best score of 7) on the MiniAQLQ were registered and randomised within the step 2 or step 3 study by an automated ‘dial-up’ centre at the University of East Anglia, Norwich, UK. A computer responded to the telephone calls from practices by recording identification information. It then used input from the practice about the step at which the patient was to enter the study to perform a look-up into predefined tables of randomisation allocations (see Randomisation, below) and then inform the caller of the allocation for that participant.
Interventions
Using a pragmatic, randomised controlled trial design, leukotriene antagonist prescription was compared with (1) inhaled steroid prescription at step 2 of the guidelines and (2) long-acting β2-agonist against a background of inhaled steroid at step 3 (Figure 1). Patients and health-care providers were aware of treatment allocations, while study data collection and statistical analyses were blinded.
-
Leukotriene receptor antagonist montelukast 10 mg, once daily (as Singulair®; Merck, Sharp & Dohme Ltd, Hoddesden, UK) or zafirlukast 20 mg, twice daily (as Accolate™, AstraZeneca Ltd, Kings Langley, UK).
-
Inhaled corticosteroid – step 2 study inhaled beclometasone dipropionate, budesonide or fluticasone propionate.
-
Long-acting β2-agonist – step 3 study salmeterol (as Serevent®, GlaxoSmithKline, Uxbridge, UK) or formoterol (as Foradil®, Novartis Pharmaceuticals UK Ltd, Camberley, UK; or Oxis®, AstraZeneca Ltd, Kings Langley, UK); these are also available in fixed dose combinations with inhaled steroid (as Seretide™, GlaxoSmithKline, Uxbridge, UK and Symbicort®, AstraZeneca Ltd, Kings Langley, UK).
All individual drug and device choices within treatment allocations were made according to normal clinical practice by the health professional involved (and bearing in mind BTS guidelines), subject to the restrictions outlined below.
Other asthma medications
-
Inhaled short-acting β2-agonist was permitted throughout the study ‘as needed’.
-
Theophylline, cromoglycate, nedocromil and ipratropium were permitted if clinically appropriate.
-
Inhaled steroids were permitted after randomisation in both arms in the step 2 trial. However, if clinically acceptable, participants within the leukotriene antagonist arm were to be given every chance to manage without inhaled steroid.
-
In step 2 and step 3 trials, practices were asked to use leukotriene antagonists only within that treatment arm assigned to them.
-
Long-acting β2-agonists were permitted in both arms of the step 2 trial. Practices were asked not to use them in the leukotriene antagonist step 3 arm.
-
If participants required a disallowed asthma medication, this fact was noted, the medication was given and the patient was continued in the study. As the planned analysis was on an intention-to-treat basis, participants were not discontinued for receiving a disallowed medication.
Allowed allergic rhinitis and conjunctivitis medications
-
Topical treatment or antihistamines were preferred.
Excluded therapy
-
β-Receptor blocking agents (including ocular preparations).
-
Non-steroidal anti-inflammatory agents, when a patient had a known or suggestive history of aspirin-sensitive asthma.
Objectives
Primary objective
To compare QOL with leukotriene receptor antagonist against alternative treatments at steps 2 (inhaled corticosteroid) and 3 (long-acting β2-agonist) of the guidelines, comparing resource use in the short term (over 2 months) and the long term (2 years) to the NHS and society (on an intention-to-treat basis), using cost–utility and cost-effectiveness approaches.
Secondary objectives
To compare two markers of asthma control: (1) the validated ACQ, which evaluates symptoms of asthma and reliever treatment usage, and (2) asthma exacerbations requiring oral steroid therapy or hospitalisation. Other outcomes compared between the two treatment groups at 2 months and throughout the 2-year study period included respiratory tract infections, consultations for respiratory tract infection, short-acting β2-agonist prescriptions, daily inhaled steroid dose (step 3 study only), per cent predicted PEF (%PPEF) at clinic visits, secondary QOL measures, 2-week domiciliary diary cards of symptoms and PEF, and time off work because of asthma. As the design was pragmatic in nature, and to ensure minimal dropouts, the major focus in terms of data collection were the primary study end points and the markers of asthma control (ACQ and exacerbations).
Outcome measures
-
Primary outcome measure: The primary outcome was a between-group comparison of disease-specific QOL (described in Health status measures, below) and cost to achieve this to the NHS and patient at 2 months (the primary time point) and 2 years (described in section Resource use assessment, below).
-
Secondary outcome measures:
-
– ACQ score
-
– number of asthma exacerbations – defined as requiring at least one course of oral corticosteroids or hospitalisation for asthma; when a patient received more than one course of oral steroid during the course of the study, any two courses of oral steroid prescribed within a 14-day period were considered as a single exacerbation, irrespective of the fact the patient required ≥ 2 courses of oral steroid.
-
– attendance at primary care practice for upper and/or lower respiratory tract infections (number of total respiratory tract infections and number of primary care practice attendances for those respiratory tract infections)
-
– short-acting β2-agonist prescriptions
-
– change in inhaled steroid dose (for step 3 participants only)
-
– clinic PEF, percentage of predicted normal values calculated using the Roberts equation66
-
– Mini Rhinitis Quality of Life Questionnaire (mRQLQ) scores67
-
– Royal College of Physicians – three (RCP3) asthma questions scores68,69
-
– personal objectives scores
-
– changes in treatment after randomisation
-
– adherence with prescribed therapy.
-
Safety was evaluated by the analysis of the overall incidence of adverse experiences.
Health status measures
Participants completed the following self-administered questionnaires at visit 2, and prior to attending visits 3–7. Participants were asked to return completed questionnaires to the study office.
-
Mini Asthma Quality of Life Questionnaire (age-specific version50) The MiniAQLQ is a validated 15-item asthma-specific QOL questionnaire, which is a self-administered shortened version of the 32-item AQLQ,51,70 used to evaluate the impact of asthma on QOL. Eleven questions assess the presence of asthma-related symptoms rated from 1 (all of the time) to 7 (none of the time); and four questions assess specific activity limitations as a result of asthma, rated from 1 (totally limited) to 7 (not at all limited). The final score is a mean of the responses ranging from 1 (worst) to 7 (best), and the minimum clinically important difference in MiniAQLQ score is 0.5. 51
-
Asthma Control Questionnaire The validated ACQ assesses five asthma-related symptoms, judged by international consensus to be the most important in evaluating asthma control. 62 These are night-time awakenings by asthma, severity of asthma symptoms on awakening, daily activity limitations because of asthma, shortness of breath and wheezing; patients score each question on a 7-point scale from 0 (best) to 6 (worst). A sixth question categorises daily number of puffs of short-acting bronchodilator from 0 (none) to 6 (more than 16 puffs most days). The overall score is the mean of the responses from 0 (totally controlled) to 6 (severely uncontrolled). A shortened version of the ACQ, excluding airway calibre, was used in this study. 64 An ACQ score of ≤ 0.75 is considered to represent well-controlled asthma, whereas a score of ≥ 1.5 respresents asthma that is not well controlled. 65 The minimum clinically important difference in ACQ score is 0.5. 64
-
– In addition, as mentioned under Participants, above, the ACQ and MiniAQLQ were completed by patients prior to, or at, visit 1 as part of the screening process.
-
-
European Quality of life-5 Dimensions (EQ-5D) questionnaire The EQ-5D comprises five questions (dimensions) on aspects of overall health (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) and a visual analogue scale, recording the respondents’ self-rated health status on a vertical graduated (0–100) ‘thermometer’. 71 The five questions are converted into a single utility index representing overall health, using equations relevant to the UK population. 72 Alternatively, direct measurements from the visual analogue scale can be used.
-
Mini Rhinoconjunctivitis Quality of Life Questionnaire The Mini Rhinoconjunctivitis Quality of Life Questionnaire is a shortened 14-item version of the 28-item Rhinoconjunctivitis Quality of Life Questionnaire that assesses how troubled the patient has been by rhinoconjunctivitis – from 0 (not troubled) to 6 (extremely troubled) – with regard to five domains: activity limitations, practical problems, nose symptoms, eye symptoms and other symptoms. 73,74
-
RCP3 questions The RCP recommends three questions to use to evaluate the impact of disease severity on quality of life in asthma patients (RCP3). 68,69 The questions are (1) Do you have difficulty sleeping because of asthma symptoms (including cough)? (2) Have you had usual asthma symptoms (cough, wheeze, chest tightness, shortness of breath) during the day? and (3) Has your asthma interfered with your usual activities (housework, work/school, etc. )?
-
Personal objectives At visit 2, participants were asked to identify three activities that occurred regularly (not seasonally) in their life, and which they found difficult to do because of their asthma. These activities were events (e.g. cleaning, walking to work, aerobics), and not things or places avoided (e.g. cats, smoky rooms), as these do not count as activities. At each visit, participants graded their ability to undertake their chosen activities on a visual analogue scale of 0–100.
Resource use assessment
Resource use was divided into four groups: prescribed medications and devices, over-the-counter medications, primary and secondary care activity, and lost productivity. Data were extracted from primary care practice databases using miquest (www.connectingforhealth.nhs.uk/miquest) and apollo sql suite (www.apollo-medical.com/products/sql.htm). Where it was not practical to use automated extraction, a researcher transposed the data from the practice record system to the project database manually. Extraction was by the miquest query system at 34 practices and apollo sql suite at seven practices; manual retrieval was performed at 17 practices. At four practices, data were collected using both manual and miquest systems during the development of the data extraction and collection tools. Duplicate data were removed. Data were extracted manually for 97 participants, and from miquest or apollo data systems for 586. For all participants, 100% of the records were reviewed by a research associate to ensure that the records represented a cost attributable to asthma or asthma-related care as described in the section Prescribed medications, below. Data were also obtained from patient-completed diary cards, as detailed below. The price year for this analysis was 2005, and all costs incurred in the second year post randomisation were discounted by 3.5%.
Prescribed medications
Prescribed medications data were extracted from primary care practice records for the following conditions:
-
asthma
-
chest infections and/or bronchitis
-
other respiratory tract infections
-
eczema, hay fever, rhinitis and allergic conjunctivitis
-
any adverse events considered to be related to asthma medication, for example oral thrush treatment.
Details recorded were:
-
name of medication (brand name if branded medication prescribed) or device
-
dosage
-
formulation
-
amount prescribed
-
indication
-
date prescribed.
After confirmation of the data in the practice, records were mapped from the various coding systems used by each of the primary care practice software systems (including Read codes), using further information about the product description as given in the miquest ‘Rubric’ field, to a single table of unit costs indexed using the British National Formulary46 code with unique extensions for each distinct product found [P. Richmond, prescribing data analyst, Broadland Primary Care Trust (PCT): List of unique product descriptions and codes; modified from the ePACT (Electronic Prescribing Analysis and CosT) codes from the Prescription Pricing Authority, 7 July 2005, personal communication]. From this a total quantity and cost were calculated.
Over-the-counter medications
Over-the-counter medication use data were extracted from patient diary cards. Prices were taken as stated by the patient (88%), or, if not stated (12%), from retail pharmacy websites (www.boots.com and www.sainsburys.com). All prices were adjusted to 2005 values using the Retail Prices Index (www.statistics.gov.uk).
NHS activity
All consultations with health-care professionals for conditions listed in Prescribed medications, above, were extracted from primary care records. Consultations initiated for another indication in which these problems were addressed (e.g. a regular consultation for contraception at which asthma problems were reported) were assigned 50% of the time of the consultation. Consultations were divided into the following categories:
-
Primary care regular attendance at asthma clinic with nurse or GP.
-
Primary care – patient initiated GP and nurse clinic/home visits, out-of-hours visits and telephone consultations.
-
Secondary care outpatient, inpatient, day case, emergency medicine and diagnostic procedures.
Study visits were timed to coincide with routine patient follow-up as per normal clinical practice for the management of asthma. Study visits (e.g. those clinical consultations that occurred for routine patient follow-up and therefore study data collection) were excluded from the analysis, as stated in the study protocol. However, where part of the study visit was used for non-routine patient follow-up, for example treatment of an exacerbation, 50% of the visit time was allocated to acute management of asthma rather than routine care. Unit costs and sources for the consultation scenarios are detailed in Appendix 1 (Unit costs table).
Indirect costs
Data on lost productivity were extracted from patient diaries where participants had noted the number of hours or days taken off work due to hospitalisation, primary care visits or other (asthma exacerbations, etc.). A day was counted as 8 hours.
Secondary outcome measures
At visit 1, and prior to visits 3–7, patients were given a validated diary card containing questions on asthma, to be completed in the 2 weeks immediately prior to the next visit. 63 As the duration between study visits was usually longer than 2 weeks, participants were contacted 2 weeks before study visits by the study office to remind them to complete the diary. The diary captured daytime and overnight symptoms, β2-agonist use and resource utilisation. Diary cards were explained to study participants at visit 1 and reviewed by their practice nurse at each study visit. Diary cards were inspected by the GP to ensure that (1) the patient demonstrated proper use of the diary card in the baseline period at visit 2 and (2) the participant’s symptoms were severe/mild enough to justify a treatment change when the patient reported unstable/stable asthma. Outcome measures collected in the diary were as follows.
Peak expiratory flow
Peak expiratory flow was measured prior to medication in the morning and evening during the 2-week baseline assessment and for 2 weeks before study visits. The best of three blows was recorded. Participants were asked to refrain from using short-acting β2-agonist during the 4 hours immediately prior to PEF measurement.
Daytime asthma symptoms
Prior to going to bed, participants scored his/her asthma symptoms against a validated four-question daytime symptom score (marked on a 6-point scale of 0–5):
-
How often did you experience asthma symptoms today? (‘none’ to ‘all of the time’).
-
How much did your asthma symptoms bother you today? (‘not at all’ to ‘severely bothered’).
-
How much activity could you do today? (‘more’ to ‘less than usual’).
-
How often did your asthma affect your activities today? (‘none’ to ‘all of the time’).
Overnight asthma symptom score
Upon arising, and before taking any medications, participants answered the following question:
-
Did you wake-up with asthma during the night or on arising at normal time? (yes or no)
‘As needed’ short-acting β2-agonist use
Participants recorded the total number of ‘puffs’ of ‘as needed’ short-acting β2-agonist used during the day (from waking to time of going to bed) and at night. Salbutamol that was used during study visits to assess airway reversibility was excluded. If nebulised β2-agonist was used then this was recorded as six puffs.
Change in treatment
Numbers of patients with treatment changes, and reasons for change, were tabulated for all patients who were not lost to follow-up, who did not use a self-management treatment plan, and who had 18-month or 2-year treatment data. In addition, the days to treatment change were recorded.
Perception of therapy and adherence
Comparisons between objective measures of adherence and perceptions of oral therapy post-randomisation provide important complementary data to the cost-effectiveness analysis. Detailed patient interviews were conducted at intervals of between 3 and 6 months on 28 participants within the study time period to elucidate information on participants’ perceptions of inhaled and oral therapy and adherence to long-term therapy.
Adherence to treatment was further analysed for patients who had at least 6 months of treatment without any change. Actual prescriptions issued versus prescribing instructions for periods in which they were valid were examined.
Safety monitoring and measurements
Action plan for treatment of worsening of asthma (self-management plan)
All participants had a personal asthma action plan provided, which adhered to asthma management guidelines and included information on self-treatment, when to seek help and how urgently to do so.
Evaluating and recording adverse experiences
Adverse experiences were monitored throughout the study and during the 14 days after completion of the study, and were recorded at each examination according to Good Clinical Practice guidelines. Adverse experiences were defined as any unfavourable and unintended change in structure, function or chemistry of the body temporally associated with any study medication, whether or not considered related. Clinically significant worsening of any pre-existing condition is also included. Serious adverse experiences were reported within 24 hours to the sponsor, the Health Technology Assessment (HTA) programme Coordinating Centre and Multi Centre Research Ethics Committee.
Discontinuation
Criteria for patient discontinuation during the study
Participants could discontinue study medication or participation at any time. Participants were discontinued from the study medication or participation if any of the following criteria were met:
-
An adverse event occurred that suggested the patient’s health could have been in jeopardy from continued study participation or that the patient was unable to complete study procedures successfully.
-
The patient became pregnant.
Withdrawal of participants from the study
Participants who were withdrawn post randomisation from the study due to procedural errors (but were not discontinuations) continued to receive normal routine clinical care from their GP following withdrawal from the study.
Sample size and power calculation
This was based on the published literature50,75 regarding sample sizes for assessing treatment differences in QOL. Treating this as an equivalence study, and assuming no true difference between the treatments in QOL for a two-tailed alpha of 0.05 and an upper limit of 0.3 for the 95% confidence interval (CI) for the difference between arms, a sample size of 142 participants was required. To allow for a 20% dropout rate, we aimed to recruit 178 participants to each study arm, resulting in a total of 356 participants at each of steps 2 and 3 (totalling 712 participants).
Randomisation
Participants were registered for entry into the study after giving written informed consent and returning completed QOL questionnaires. At visit 2, participants eligible for entry into step 2 or step 3 studies were randomised into the study. Randomisation into the study was stratified by practice, with a block size of 6. Practice nurses were informed of the randomised treatment to be given to their patient via an automated telephone centre (see Participants, above).
Blinding
This was a single-blind randomised controlled trial. General practitioners (GPs)/practice asthma nurses and participants were aware of the randomisation, while study research assistants were blinded to the randomisation. The role of the GPs/practice asthma nurses and research assistants in the conduct of the study is described below:
-
General practitioners/practice asthma nurses GPs/practice asthma nurses had minimal involvement in data collection except baseline prior to randomisation, implementing the randomisation allocation and thereafter in administering the resource data collection sheet with participants. This allowed clinical freedom to change treatment as per normal management. Randomisation allocation was given directly to the GPs/practice asthma nurses by an independent automated telephone answering system.
-
Research assistants Research assistants were non-clinical personnel who worked with practice staff to ensure proper completion of the diaries and self-completed QOL and disease-related questionnaires. They collected resource use information from participants, data from prescribing records, and clinical resource utilisation data for the participants at the end of the study period. When collecting resource data the research assistants were blind to the randomised allocation of the participants.
Data and statistical analysis
All analyses were performed blind to study arm allocation. This section outlines the statistical analysis procedures that were performed.
Effectiveness analysis
Baseline comparability between treatment groups
Baseline comparability between the treatment groups was evaluated by summarising and comparing the following parameters:
-
Demographics age, sex, race, education, employment, disease history, weight, height, PEF, %PPEF, and PEF reversibility after salbutamol.
-
Efficacy outcome measures primary and secondary outcome measures.
For the outcomes recorded on patient diary cards (nocturnal awakenings, symptom score, diurnal variation, etc.), the baseline was defined as the average of all values obtained during the 14 days between visits 1 and 2. For the other continuous efficacy end points, baseline was defined as the last value obtained before the start of randomised therapy. For binary outcomes, the baseline value was the sum of events occurring within the baseline period. For outcome measures obtained from the patient diary card, the baseline period was defined as the 14 days (or, if < 14 days, as many days of data as were available). For data obtained from the electronic patient record, the baseline period was defined as the 12 months prior to randomisation.
Primary outcomes
The primary outcome analysis was an intention-to-treat analysis of the MiniAQLQ score using multiple imputation where data were missing and including all patients with data at baseline and one post-randomisation time point. Analysis of covariance was used, with treatment as a fixed effect, and baseline value as covariate, to analyse MiniAQLQ scores at 2 months (the primary time point) and 2 years. A 95% CI for the difference between treatment mean scores was derived. The treatments were deemed to be equivalent if the 95% CI excluded a mean difference > 0.3 on the MiniAQLQ score (thus, 95% CI between –0.3 and 0.3), a difference chosen using an a priori conservative approach, based on 0.3 being substantially less than the 0.5 minimum clinically important difference for the MiniAQLQ.
This study was designed as two equivalence trials to determine whether leukotriene receptor antagonist is an equal choice to inhaled corticosteroid as monotherapy, and to long-acting β2-agonist as add-on therapy, for a real-world population of patients with perhaps milder asthma and less likely to adhere to therapy than those enrolled in classical clinical trials.
In addition, a one-sided 95% CI (i.e. the lower bound from a 90% CI) was constructed for the difference in MiniAQLQ score. This was a secondary analysis to examine non-inferiority (rather than equivalence) of leukotriene antagonist versus control.
Secondary outcomes
The ACQ score analysis, like that for MiniAQLQ score, was an intention-to-treat analysis using multiple imputation for missing data, including all patients with data at baseline and one post-randomisation time point. The PEF values as percentage of predicted normal values were calculated using the Roberts equation and were compared between treatment groups at 2 months and 2 years using the Mann–Whitney test. Rates of asthma exacerbations, respiratory tract infections, and consultations for respiratory tract infections were compared using the Wald chi-squared test from the Poisson model. For other secondary end points, the last-observation-carried-forward approach was used for patients with missing follow-up data, again including only those with data for at least one post-randomisation time point; and an analysis of covariance was used, including treatment arm and baseline value as covariate.
-
Frequency of exacerbations requiring hospitalisation, GP attendances and oral steroid courses The count of exacerbations included all events where data indicated that the participant had a prescription for oral corticosteroids and/or a hospital admission for asthma. Issues of oral steroids related to asthma exacerbations were identified from primary care practice records. Where two or more consecutive courses of oral steroids were issued within 3 days of one course completing and a second being issued, this was regarded as a single exacerbation.
-
Frequency of consultations for respiratory tract infections The count of respiratory tract infections included all events where the Read code (or the rubric in the case of manually entered items) was for any diagnosed infection or combination of symptoms that strongly suggested an acute infection of either viral or bacterial aetiology. The combination of symptoms included ‘productive cough with green sputum’, and ‘fever, cough, sore throat’. Events with descriptions such as ‘allergic…’ or ‘chronic…’ were excluded. All free text associated with the records was searched for the same phrases. In the case of entries where a single less specific symptom was recorded, such as ‘cough’, the database was searched for other records that could provide further clarification, for example the acute prescription of an antibiotic on that date. For both exacerbations and respiratory tract infections, when all such records were flagged, multiple records (e.g. clinic visits or courses of oral steroids) for a patient within a period of 14 days were considered to be a single event. Participants were considered to have multiple separate events if the duration between events was > 14 days.
-
Short-acting β2-agonist consumption (prescribing records) Number of inhalers of short-acting β2-agonist over the 2-year duration of the study was determined by totalling the number of issues requested, adjusting where appropriate for multiple inhalers of short-acting β2-agonist being prescribed within a single issue.
-
Daily inhaled corticosteroid dose for step 3 trial only Daily dose of inhaled steroid was calculated from prescription records for the year prior to randomisation and the following 2 years. Daily dose of inhaled steroid was normalised to the efficacy of beclometasone dipropionate by multiplying daily dose of fluticasone propionate and beclometasone delivered as QVAR® (Ivax Laboratories, Aylesbury, UK) by 2. Budesonide was considered to have equivalent efficacy to beclometasone on a microgram per microgram basis.
-
Asthma symptoms from diary card (for 2 weeks before each study visit) Data for the 14 days immediately prior to each visit (or as much as was available if less than 14 days) were averaged or, for binary variables, the percentage of days with a positive response was taken.
-
Clinic and diary PEF records (for 2 weeks before each study visit).
-
Diurnal variation in PEF Diurnal variability was calculated according to the BTS Guidelines:4 [(highest PEF–lowest PEF)/highest PEF].
-
mRQLQ.
-
Need for further treatment intervention beyond initial treatment.
The record of any participant whose medication dosage or device was changed after randomisation was reviewed by research assistants to determine the recorded reason for the change. Reasons for change were categorised as: associated with an asthma exacerbation (a change within 14 days of the use of or written reference to a use of short course of oral steroids or symptoms requiring use of secondary care services); to address poor symptom control (notes of respiratory symptoms); a report or suspicion of a side effect; after an adverse event; patient preference: to decrease the dosage; because of practice-based administrative policies; and/or reason unknown.
To confirm the results of the intention-to-treat analysis, we repeated the analyses after limiting to those participants who completed the study as per protocol and who were on an entirely fixed treatment regime. The population included in these analyses strictly included only participants whose prescribed therapy at randomisation was a fixed dose (not a prescribed range to be adjusted) and who did not have any change in either the initial drug prescribed at randomisation or the prescribed daily dose of that drug, or the addition of any other preventive asthma therapy at any time during the study, including the study final visit.
Planned secondary analysis
Planned subgroup analyses identified in the study protocol and in the minutes of study steering committee meetings are listed in Appendix 2.
Economic analyses
The protocol stated that where equivalence was demonstrated, a cost-minimisation analysis would be performed. As the results suggested ‘near-equivalence’ and, furthermore, as the study was powered to detect a difference in MiniAQLQ only (and not costs or other outcome measures), we present both comparisons of cost and cost-effectiveness analyses on MiniAQLQ, ACQ and quality-adjusted life-years (QALYs) gained, showing which of the treatments has the highest probability of being cost-effective.
Three cost-effectiveness analyses were performed: (1) comparison of incremental cost with incremental point improvement in MiniAQLQ score; (2) comparison of incremental cost and incremental point improvement in ACQ score; and (3) comparison of incremental cost and incremental QALYs gained (i.e. cost–utility analysis). Each analysis was conducted at 2 months’ and 2 years’ follow-up, from the NHS and societal perspectives.
Analyses were undertaken, based on complete case analysis, an imputed dataset, and imputed dataset adjusted for baseline MiniAQLQ, ACQ, or utility as appropriate. The imputed data comprised the complete case analysis plus imputed values for missing observations using Rubin’s Multiple Imputation approach. This is preferable to single imputation approaches, as it takes account of uncertainty in the missing values themselves, and therefore better characterises the associated uncertainty. 76
Multiple imputation was carried out on variables at an aggregate level (Appendix 1, Table 55) using solas software (Statistical Solutions, Cork, Republic of Ireland). In each case, data were imputed with five iterations using the propensity score method, with all other variables used as potential covariates as well as age, education, employment and gender. The imputed variables were visually reviewed to ensure that predicted values were within logical limits. Summary statistics were generated from the five imputed datasets using Rubin’s rule76 (this is simply the mean of the estimates for each of the imputed data sets). See Appendix 1 (Imputation approach for economic analyses) for a more detailed summary of the imputation technique.
Results are presented as total cost per patient, mean MiniAQLQ, ACQ or total QALYs per patient, increments, and incremental cost-effectiveness ratio (ICER) defined as the difference in cost divided by the difference in outcome:
If this is below a threshold of ‘willingness to pay’ for a point improvement in outcome score (λ), the intervention is deemed cost-effective in relation to the comparator.
Incremental net benefit (INB) was calculated by rearranging the ICER equation:
(Note that λ is now on the right-hand side, and thus INB depends on the value of λ being known. We therefore present charts plotting INB for a variety of plausible values of λ.)
A non-parametric bootstrap approach was used to generate CIs around INB and to generate cost-effectiveness acceptability curves (CEACs), showing the probability that leukotriene receptor antagonists are cost-effective compared with inhaled corticosteroid/long-acting β2-agonist, given varying thresholds of willingness to pay for a point improvement in outcome (MiniAQLQ, ACQ or QALY gained).
Resource use
All items of resource use in the four areas (prescribed medications, over-the-counter medications, NHS activity, and indirect costs) were allocated to one of three time points: 0–2 months post randomisation, > 2 months to 1 year and > 1 year to 2 years. Where primary care record data were truncated, the patient’s follow-up was counted as missing for that and subsequent periods (for example, where a patient’s record was truncated after 36 weeks of follow-up, period 1 data were counted as present, but periods 2 and 3 were counted as missing).
Unit costs were assigned for each scenario from a variety of relevant sources (Appendix 1, Unit costs table), with prices taken from 2005 sources or adjusted to 2005 values using the Retail Price Index as appropriate. Quantities were multiplied by unit costs to calculate the total and per-patient cost. All costs incurred in the third time period (> 1 year to 2 years) were discounted by 3.5%.
Indirect costs were valued by multiplying the number of hours off work by a unit cost of £13.13, the national average gross wage in 2005. 77 For many of the indirect cost observations, the date the event took place was not reported. For these events, the date of the activity was taken as the date the patient diary was completed.
Cost-effectiveness analysis
Two cost-effectiveness analyses were performed comparing incremental cost with incremental point improvement in (1) MiniAQLQ score and (2) ACQ score. For both analyses, the primary analyses were based on complete case analysis. Secondary analyses were performed, based on an imputed data set, and the imputed data set adjusted for baseline MiniAQLQ and ACQ, respectively. Results are presented as total cost per patient, mean ACQ/MiniAQLQ score at visits 3 (2 months) and 7 (2 years), increments (95% CIs) and ICER.
Cost–utility analysis
The EQ-5D health profiles were converted into utilities using standard conversion algorithms that were relevant to the UK population. 72 QALYs were calculated from utilities by computing the area under the curve. Where 2-month and 2-year follow-up dates varied from target date, straight-line imputation was used to estimate the utility on the appropriate day. QALYs gained during the second year post randomisation were discounted at 3.5%.
Analyses were based on complete case analysis, the imputed data set and imputed data set adjusted for baseline utility. Observations were included in the complete case analysis for the 2-month follow-up if there was at minimum a valid EQ-5D reading at visit 2 (baseline) and visit 3 (2 months). Missing values for the interim visits (visits 4–6) were estimated using straight-line imputation.
Safety analyses
All randomised participants were included in the safety analyses. The primary variables for the safety analysis were the overall incidence of adverse experiences and incidences of common adverse experiences reported by participants.
Chapter 3 Results
Recruitment
All patients with any evidence of asthma from 53 participating practices were sent a postal asthma symptom questionnaire (adapted from the ACQ), which was used to evaluate initial eligibility. For patients meeting these initial criteria, a review of the their notes was undertaken to confirm eligibility. A further 80 patients from the practices were identified as meeting study entry criteria at the time of clinical visits by general practice staff. Of those patients considered potentially eligible, 449 (step 2) and 482 (step 3) responded positively to an invitation and were booked to attend a screening visit (Figures 2 and 3).
FIGURE 2.
Step 2, the Consolidated Standards of Reporting Trials (CONSORT) e-flowchart for primary end point.
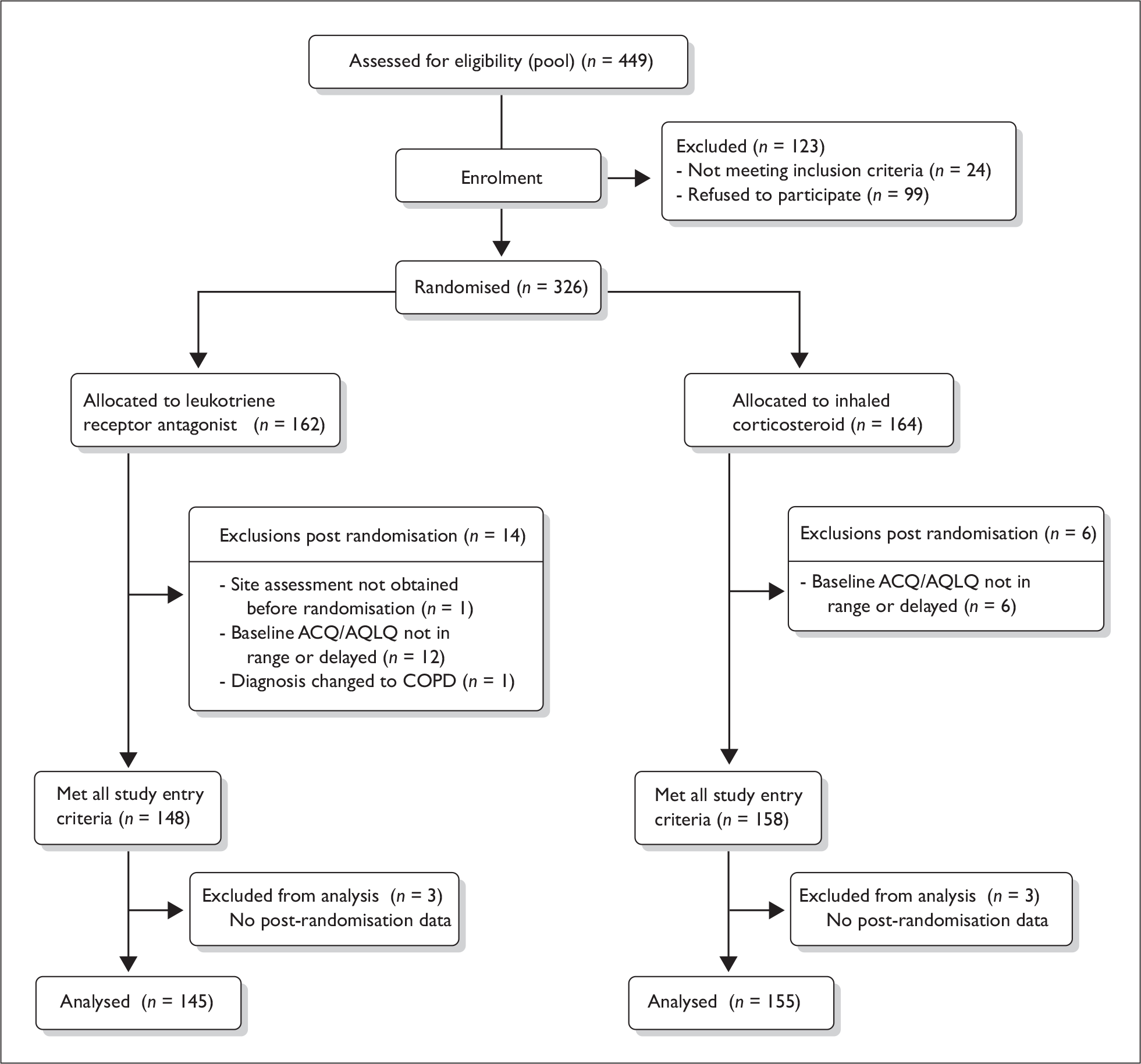
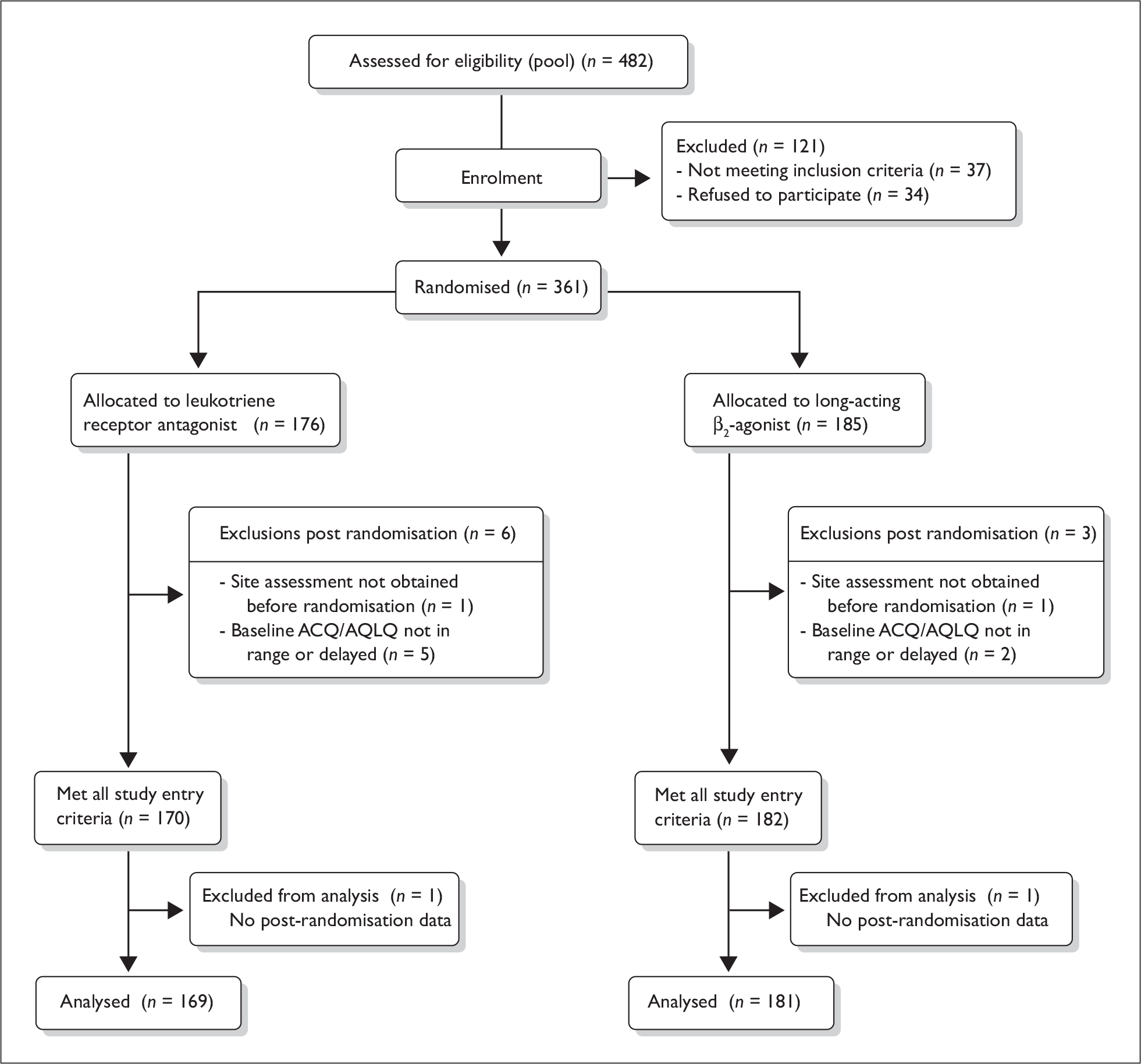
FIGURE 3.
Step 3, the CONSORT e-flowchart for primary end point.
Work began on the study in October 2001, with initial piloting in one practice of study procedures completed by May 2002. Further practices were recruited from October 2001 through to September 2004. The first patient was enrolled on 3 May 2002 with the last step 3 patient being enrolled on 18 February 2004. The last step 2 patient was enrolled on 4 February 2005. The last clinical and QOL follow-up data were collected on 8 January 2007. The last resource data collection was in the same week.
Numbers analysed versus screened
For the step 2 trial, of the 449 screened, 123 participants were excluded (99 declined to participate and 24 were identified prior to randomisation as ineligible) and 326 participants were randomised (compared with the target of 356). No significant difference was found in mean age between excluded and analysed populations. There were more females among those excluded than those analysed (Table 2). For the step 3 trial, of the 482 screened, 121 participants were excluded (84 declined to participate and 37 were identified prior to randomisation as ineligible) and 361 participants were randomised (compared with the target of 356). No significant difference was found in either the sex distribution or mean age between excluded and analysed populations (Table 2).
| Total n with sex available | Males (%) | Total n with age at screening available | Mean (SD), age (years) | |
|---|---|---|---|---|
| Step 2 patients screened = 449 | ||||
| Excluded | 114 | 40 (35.1) | 96 | 47.30 (17.34) |
| Analysed | 326 | 162 (49.7) | 326 | 44.74 (16.49) |
| Total | 440 | 202 (45.9) | 422 | 45.32 (16.70) |
| Step 3 patients screened = 482 | ||||
| Excluded | 119 | 52 (43.7) | 115 | 49.74 (17.34) |
| Analysed | 361 | 136 (37.7) | 361 | 50.02 (15.93) |
| Total | 480 | 188 (39.2) | 476 | 49.95 (16.84) |
Duration of follow-up in the study for analysed groups
No significant differences were observed in the duration of follow-up in the study between analysed groups in the step 2 or step 3 studies (Table 3).
| Mean days (SD) | Median days | Maximum days | Minimum days | |
|---|---|---|---|---|
| Step 2 trial | ||||
| LTRA | 746 (75) | 743 | 1260 | 447 |
| ICS | 748 (64) | 740 | 1092 | 526 |
| Step 3 trial | ||||
| LTRA | 753 (76) | 739 | 1201 | 611 |
| LABA | 748 (76) | 733 | 1308 | 573 |
Numbers analysed
At step 2, 20 patients were excluded post-randomisation (Figure 2), and 13 of the remaining 306 patients (4.2%) were lost to follow-up. Post-randomisation data were available for 7 out of the 13 lost to follow-up; thus, 300/306 patients (98%) had post-randomisation data and were included in the primary intention-to-treat analyses. The per-protocol population, who received an entirely fixed treatment regime throughout the study, included 65/145 (45%) patients in the leukotriene antagonist group and 82/155 (53%) patients in the inhaled steroid group.
In the step 3 trial, nine patients were excluded post randomisation (Figure 3). Twelve of the remaining 352 patients (3.4%) were lost to follow-up; however, post-randomisation data were available for 10 out of these 12 and thus a total of 350 patients were included in the primary intention-to-treat analysis, including 169 and 181 in leukotriene antagonist and long-acting β2-agonist groups, respectively. Patients who met the per-protocol definition of a fixed treatment regime and no therapeutic change of any kind and were included in the MiniAQLQ analyses numbered 60/169 (36%) and 80/181 (44%), respectively.
Randomisation data
For the step 2 trial, this process resulted in an almost equal distribution of participants between leukotriene antagonist and inhaled steroid arms (162 and 164 participants, respectively). However, for the step 3 study, 9 fewer participants were randomised to leukotriene antagonist than to long-acting β2-agonist (176 and 185 participants, respectively). This difference is likely to have arisen for two reasons. Firstly, a small number of practices had one or two more participants randomised to long-acting β2-agonist than leukotriene antagonist. Secondly, because of an error in the way that the randomisation telephone calls were performed, practice 12 had four more participants randomised to long-acting β2-agonist than to leukotriene antagonist (13 and 9 participants, respectively). There was never any prior or biasing knowledge of the allocation on the part of the nurse performing the randomisation, but the result was an excess of four participants receiving long-acting β2-agonist at that practice.
Step 2 trial
Demographics and baseline characteristics
Characteristics of participants screened and found eligible for the step 2 trial are shown in Tables 4 and 5.
| Leukotriene antagonist (N = 148) | Inhaled steroid (N = 158) | ||
|---|---|---|---|
| Sex | Female | 73 (49%) | 83 (53%) |
| Male | 75 (51%) | 75 (47%) | |
| Age | Mean (SD) | 47.6 (16.5) | 44.1 (16.4) |
| Race | Caucasian | 144 (97%) | 153 (97%) |
| Non-Caucasian | 0 | 1 (1%) | |
| Not known | 4 (3%) | 4 (3%) | |
| Height (cm) | Mean (SD) |
n = 138 169.6 (9.2) |
n = 153 169.1 (9.6) |
| PEF (l/min) | Mean (SD) |
n = 147 438 (139) |
434 (127) |
| %PPEF (%) | Median (IQR) |
n = 134 85.97 (77.43 to 94.16) |
n = 150 85.07 (73.92 to 95.42) |
| Salbutamol PEF reversibility (%) | Mean (SD) |
n = 128 9.20 (10.7) |
n = 142 8.74 (9.17) |
| SABA puffs/day | Mean (SD) |
n = 140 3.0 (3.2) |
n = 145 2.9 (3.1) |
| Asthma exacerbations in last year | Mean (SD) | 0.13 (0.036) | 0.10 (0.029) |
| Asthma Control Questionnaire | Mean (SD) | 1.99 (0.70) | 2.06 (0.84) |
| MiniAQLQ | Mean (SD) | 4.75 (0.92) | 4.72 (0.95) |
| mRQLQ | Mean (SD) |
n = 113 1.58 (1.29) |
n = 131 1.78 (1.35) |
| EQ-5D utility | Mean (SD) |
n = 118 0.795 (0.245) |
n = 131 0.830 (0.195) |
| Personal objectives (0–100 VAS) | Mean (SD) |
n = 99 42.59 (18.03) |
n = 118 38.89 (18.15) |
| RCP3 | Mean (SD) |
n = 133 2.07 (0.81) |
n = 146 2.06 (0.79) |
| Sleep difficulty | Yes | 79 (58%) | 86 (56%) |
| No | 58 (42%) | 67 (44%) | |
| Missing | 11 | 5 | |
| Day symptoms | Yes | 125 (93%) | 142 (94%) |
| No | 10 (7%) | 9 (6%) | |
| Missing | 13 | 7 | |
| Interferes with activities | Yes | 65 (49%) | 74 (49%) |
| No | 69 (51%) | 76 (51%) | |
| Missing | 14 | 8 | |
| LTRA (N = 148) | ICS (N = 158) | ||
|---|---|---|---|
| Continued education > 16 | Yes | 72 (50%) | 81 (53%) |
| No | 70 (49%) | 67 (44%) | |
| Student | 2 (1%) | 4 (7%) | |
| Not known | 4 | 6 | |
| Professional qualification | Yes | 45 (33%) | 50 (35%) |
| No | 88 (64%) | 84 (59%) | |
| Student | 4 (3%) | 8 (6%) | |
| Not known | 11 | 16 | |
| Employment position | Employer | 5 (5%) | 8 (7%) |
| Employee | 74 (73%) | 90 (84%) | |
| Self-employed | 21 (21%) | 9 (8%) | |
| Disabled | 1 (1%) | 0 | |
| Not known | 47 | 51 | |
| Smoking habit | Current smoker | 37 (25%) | 30 (19%) |
| Ex-smoker | 54 (37%) | 54 (35%) | |
| Never smoked | 56 (38%) | 71 (46%) | |
| Not known | 1 | 3 | |
| Current smoker over age 45 | 15 (10%) | 11 (7%) | |
No substantial differences were identified between the arms. A small female preponderance was noted in the inhaled steroid arm, but not in the leukotriene antagonist arm of the study. Most participants were Caucasian. Mean %PPEF was indicative of airflow obstruction consistent with untreated asthma of mild to moderate severity. Most participants had daytime asthma symptoms, with half having additional night-time symptoms. Half of participants felt that their asthma symptoms interfered with their daily activities. Education and occupation status of participants is shown in Table 5.
Most participants were in employment. Only 40% of participants had never smoked. Approximately 20% of participants were active smokers at randomisation into the study, including 26 (9%) who were over the age of 45 (Table 5). Baseline diary card data for these participants are shown in Table 6.
| LTRA (N = 148) | ICS (N = 158) | |
|---|---|---|
| Mean (SD) morning waking with symptoms |
0.48 (0.36) n = 129 |
0.48 (0.34) n = 147 |
| Mean (SD) puffs of reliever at night |
0.78 (0.88) n = 125 |
0.99 (1.37) n = 141 |
| Mean (SD) morning PEF |
408.9 (99.1) n = 127 |
402.5 (100.2) n = 146 |
| Mean (SD) daytime asthma symptom score (0–6)a |
1.88 (1.18) n = 129 |
1.81 (1.29) n = 145 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’ (0–6)a |
1.63 (1.18) n = 128 |
1.48 (1.23) n = 145 |
| Mean (SD) daily activity score (0–6)b |
2.68 (1.12) n = 126 |
2.38 (1.27) n = 145 |
| Mean (SD) score for interference on activities from asthma (0–6)a |
1.38 (1.24) n = 128 |
1.28 (1.33) n = 147 |
| Mean (SD) puffs of reliever during the day |
2.26 (1.67) n = 126 |
2.18 (1.99) n = 145 |
| Mean (SD) evening PEF |
420.6 (101.1) n = 127 |
413.9 (103.0) n = 147 |
| Mean (SD) diurnal variation in PEF (%) |
7.1 (4.8) n = 127 |
7.7 (5.4) n = 147 |
Primary analyses
Change in QOL
Mini asthma quality of life questionnaire
Mean MiniAQLQ score increased (improved) from baseline in both leukotriene antagonist and inhaled steroid randomised groups (Table 7 and Figure 4).
| Treatment duration | Outcome measure | LTRA | ICS | Difference (95% CI) LTRA–ICS | Adjusted differencea (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) | n | 122 | 132 | 0.0 (–0.25 to 0.26) | –0.02 (–0.24 to 0.20) |
| Mean | 5.25 | 5.28 | |||
| SD | 1.03 | 1.10 | |||
| 2 yearsb | n | 145 | 155 | –0.10 (–0.35 to 0.17) | –0.11 (–0.35 to 0.13) |
| Mean | 5.52 | 5.63 | |||
| SD | 1.07 | 1.16 |
FIGURE 4.
Step 2: ACQ, MiniAQLQ and %PPEF over 2 years of treatment. Mean (standard deviation) ACQ (from 0 ‘best’ to 6 ‘worst’) and MiniAQLQ (from 1 ‘worst’ to 7 ‘best’) scores and median (interquartile range) %PPEF at baseline and over 2 years of treatment with leukotriene antagonist or inhaled steroid.
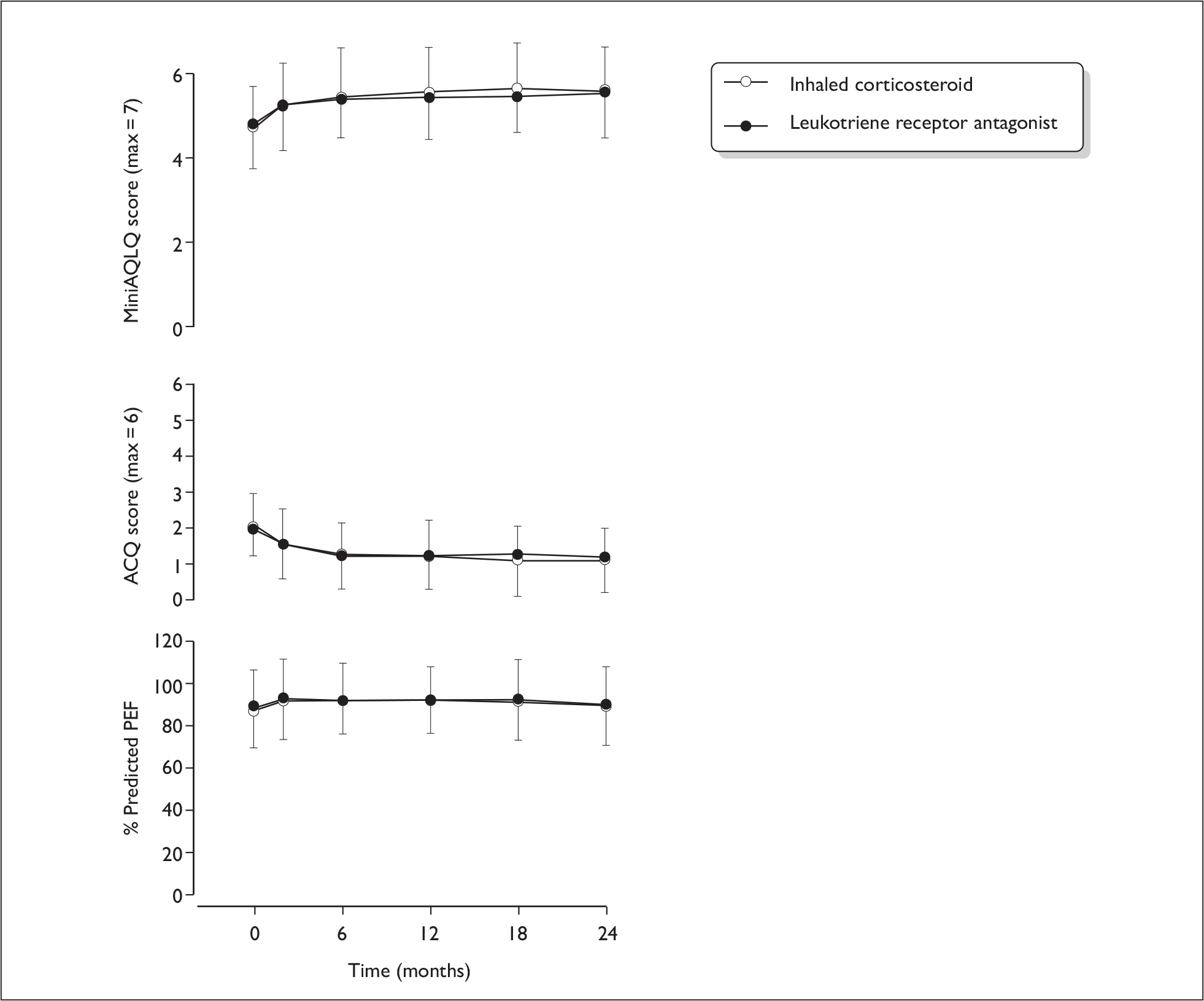
No statistically significant between-group differences in MiniAQLQ score were found at the 2-month time point, either unadjusted or adjusted for baseline values. At 2 months, the 95% CIs for both the unadjusted and adjusted differences in MiniAQLQ score were within the limits for equivalence: (–0.25 to 0.26) and –0.02 (–0.24 to 0.20), respectively, i.e. excluding 0.3. The limit of the one-sided 95% CI for the unadjusted difference was –0.25, and –0.18 for the adjusted difference.
At the 2-year visit, while the difference was again not statistically significant, and the estimated difference between groups was small, the 95% CI did include the equivalence value of 0.3, favouring inhaled steroid [imputed results, unadjusted difference (95% CI) –0.10 (–0.35 to 0.17), adjusted difference (95% CI) –0.11 (–0.35 to 0.13)]. The limit of the one-sided 95% CI for the unadjusted difference was –0.32 and was –0.31 for the adjusted difference, i.e. inferiority could not be excluded.
Asthma Control Questionnaire
Mean ACQ score decreased (improved) substantially from baseline in both leukotriene antagonist and inhaled steroid randomised groups (Table 8 and Figure 4). Again, no significant between-group differences in ACQ score were found at either the 2-month or 2-year time points, whether unadjusted or adjusted for baseline values. At 2 years (imputed results), the adjusted difference (95% CI) was 0.13 (–0.07 to 0.33). The CI is well within the minimum clinically important difference of 0.5.
| Treatment duration | LTRA | ICS | Difference (95% CI) LTRA–ICS | Adjusted differencea (95% CI) | |
|---|---|---|---|---|---|
| 2 months (visit 3) | n | 123 | 132 | –0.02 (–0.24 to 0.21) | 0.01 (–0.20 to 0.22) |
| Mean | 1.54 | 1.53 | |||
| SD | 0.93 | 1.00 | |||
| 2 yearsb | n | 145 | 155 | 0.10 (–0.11 to 0.32) | 0.13 (–0.07 to 0.33) |
| Mean | 1.23 | 1.15 | |||
| SD | 0.95 | 0.92 |
Quality-adjusted life-years
Leukotriene antagonist participants experienced a mean of 0.122 QALYs over the 2-month period, compared with 0.132 in inhaled steroid participants, a mean (95% CI) difference of approximately 0.01 (–0.019 to 0.001) QALYs, falling to 0.001 (–0.005 to 0.002) QALYs after adjustment for baseline utility (Table 9). Over 2 years, leukotriene antagonist participants experienced 0.153 (–0.274 to –0.032) fewer QALYs than inhaled steroid participants. However, after adjusting for baseline utility, the difference falls to 0.050 (–0.126 to 0.026) QALYs, equivalent to 2.5 weeks of perfect health.
| LTRA | ICS | Difference (95% CI) LTRA–ICS | Adjusted differencea (95% CI) | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| EQ-5D utility | ||||||
| Baseline | 118 | 0.795 (0.245) | 131 | 0.830 (0.195) | – | – |
| 2 months | 118 | 0.819 (0.261) | 124 | 0.856 (0.212) | – | – |
| 2 years | 132 | 0.826 (0.261) | 143 | 0.881 (0.218) | – | – |
| QALYs gained | ||||||
| 2 months | 95 | 0.122 (0.036) | 106 | 0.132 (0.025) | –0.010 (–0.019 to 0.001) | –0.001 (–0.005 to 0.002) |
| 2 years (discounted) | 81 | 1.569 (0.458) | 94 | 1.722 (0.327) | –0.153 (–0.274 to –0.032) | –0.050 (–0.126 to 0.026) |
Resource use and cost
Point estimate costs and quantities of prescription medicines, over-the-counter medicines, NHS activity and indirect costs are reported in Tables 10–13. Total NHS costs are the sum of prescriptions and NHS activity. Total societal costs are NHS costs plus over-the-counter medications and indirect costs.
| Treatment duration | LTRA | ICS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total items | Mean (SD) items | Total cost (£) | Mean (SD) cost (£) | n | Total items | Mean items (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | 159 | 463 | 2.88 (1.87) | 10,055.61 | 62.46 (31.30) | 164 | 330 | 2.01 (1.38) | 2969.78 | 18.11 (14.92) |
| 2 years (discounted) | 154 | 3489 | 22.7 (16.1) | 60,509.00 | 393 (299) | 157 | 2797 | 17.8 (15.2) | 28,882.00 | 184 (237) |
| Treatment duration | LTRA | ICS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total items | Mean (SD) items | Total cost (£) | Mean (SD) cost (£) | n | Total items | Mean items (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | 109 | 49 | 0.45 (0.73) | 211.26 | 1.94 (6.96) | 108 | 79 | 0.73 (1.16) | 1041.07 | 9.64 (46.97) |
| 2 years (discounted) | 109 | 225 | 2.06 (1.52) | 756.39 | 6.94 (11.83) | 108 | 268 | 2.48 (2.33) | 1637.09 | 15.16 (49.66) |
| Treatment | LTRA | ICS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total contacts | Mean (SD) contacts | Total cost (£) | Mean (SD) cost (£) | n | Total contacts | Mean (SD) contacts | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | ||||||||||
| Total routine care | 156 | 41 | 0.26 (0.63) | 331.67 | 2.13 (5.52) | 158 | 25 | 0.16 (0.56) | 255.00 | 1.61 (5.98) |
| Total patient initiated | 156 | 50 | 0.32 (0.75) | 1153.05 | 7.39 (22.79) | 158 | 22 | 0.14 (0.46) | 371.00 | 2.35 (8.08) |
| Total secondary care | 156 | 4 | 0.03 (0.25) | 635.95 | 4.08 (41.93) | 158 | 3 | 0.02 (0.18) | 381.00 | 2.41 (22.53) |
| Total NHS activity | 156 | 95 | 0.61 (1.09) | 2120.67 | 13.59 (61.00) | 158 | 50 | 0.32 (0.71) | 1007.00 | 6.37 (24.16) |
| 2 years (discounted) | ||||||||||
| Total routine care | 151 | 474 | 3.14 (2.53) | 4055.67 | 26.86 (24.92) | 151 | 420 | 2.78 (2.32) | 3827.35 | 25.35 (22.92) |
| Total patient initiated | 151 | 397 | 2.63 (3.19) | 8761.64 | 58.02 (78.46) | 151 | 416 | 2.75 (3.46) | 9181.14 | 60.80 (81.95) |
| Total secondary care | 151 | 40 | 0.26 (0.87) | 12,045.23 | 79.77 (601.74) | 151 | 55 | 0.36 (1.06) | 8446.08 | 55.93 (268.62) |
| Total NHS activity | 151 | 911 | 6.03 (4.89) | 24,862.54 | 164.65 (633.99) | 151 | 891 | 5.90 (5.25) | 21,454.57 | 142.08 (310.13) |
| Treatment duration | LTRA | ICS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total hours | Mean (SD) hours | Total cost (£) | Mean (SD) cost (£) | n | Total hours | Mean hours (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | 80 | 335 | 4.19 (18.54) | 4398.55 | 54.98 (243.43) | 71 | 142 | 2.00 (10.37) | 1864.46 | 26.26 (136.16) |
| 2 years (discounted) | 80 | 1309.5 | 16.37 (62.61) | 14,938.39 | 186.73 (740.80) | 71 | 1075 | 15.14 (86.24) | 14,114.75 | 198.80 (1132.29) |
Over 2 months and 2 years, patients who were prescribed leukotriene antagonists were significantly more expensive than patients who were prescribed inhaled steroid participants in terms of both NHS (NHS activity plus prescription medicines) and societal costs (all costs – Table 14). At 2 months, leukotriene antagonist participants cost on average £70 more, or 2.5 times the cost, of inhaled steroid participants (95% CI £29 to £111), and at 2 years, £294 more, or 1.8 times the cost of inhaled steroid participants (95% CI £107 to £481). This may be driven principally by higher prescription costs and possibly compliance (including leukotriene antagonists themselves) and/or higher NHS activity in the leukotriene antagonist group.
| Treatment duration | LTRA | ICS | Cost (£) difference (95% CI) |
||||
|---|---|---|---|---|---|---|---|
| n | Total cost (£) | Mean (SD) cost (£) | n | Total cost (£) | Mean (SD) cost (£) | ||
| Total NHS costs (prescription medicines and NHS activity combined) | |||||||
| 2 months | 156 | 12,029.60 | 77.11 (66.38) | 158 | 3839.82 | 24.30 (30.56) | 52.81 (41.29 to 64.33) |
| 2 years (discounted) | 147 | 84,309.00 | 573.00 (764) | 148 | 49,090.00 | 332.00 (435) | 242.00 (100 to 384) |
| Societal costs (prescription and over-the-counter medicines – NHS activity and indirect costs combined) | |||||||
| 2 months | 74 | 8704.96 | 117.63 (152.94) | 65 | 3097.17 | 47.65 (81.52) | 69. 99 (29.47 to 110.50) |
| 2 years (discounted) | 70 | 46,628.00 | 666.00 (664) | 60 | 22,341.00 | 372.00 (374) | 294.00 (107 to 481) |
Cost-effectiveness analyses
Mini Asthma Quality of Life Questionnaire
At both 2 months (Table 15) and 2 years (Table 16), inhaled steroid is, on average, a dominant strategy over leukotriene antagonist. Mean INB is negative, irrespective of willingness to pay for a point improvement in MiniAQLQ.
| n | Cost (£) | MiniAQLQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline MiniAQLQ) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | |
| NHS | 120 | 127 | 80 | 25 | 5.242 | 5.278 | 55 | –0.036 | (ICS dominant) | 52 | –0.019 | (ICS dominant) | 53 | –0.081 | (ICS dominant) |
| Societal | 63 | 57 | 117 | 52 | 5.257 | 5.410 | 65 | –0.153 | (ICS dominant) | 37 | –0.019 | (ICS dominant) | 38 | –0.081 | (ICS dominant) |
| n | Cost (£) | MiniAQLQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline MiniAQLQ) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | |
| NHS | 133 | 140 | 587 | 327 | 5.529 | 5.633 | 260 | –0.104 | (ICS dominant) | 233 | –0.086 | (ICS dominant) | 242 | –0.151 | (ICS dominant) |
| Societal | 64 | 60 | 666 | 372 | 5.549 | 5.681 | 294 | –0.132 | (ICS dominant) | 209 | –0.086 | (ICS dominant) | 217 | –0.151 | (ICS dominant) |
Incremental net benefit details (± 95% CI) are shown in Figure 5a–d. Note, however, that there is a great deal of uncertainty around these estimates (95% CI in Figure 5).
FIGURE 5.
Step 2: INB, MiniAQLQ, INB and 95% CI are shown for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d), results based on imputed data adjusted for baseline MiniAQLQ.
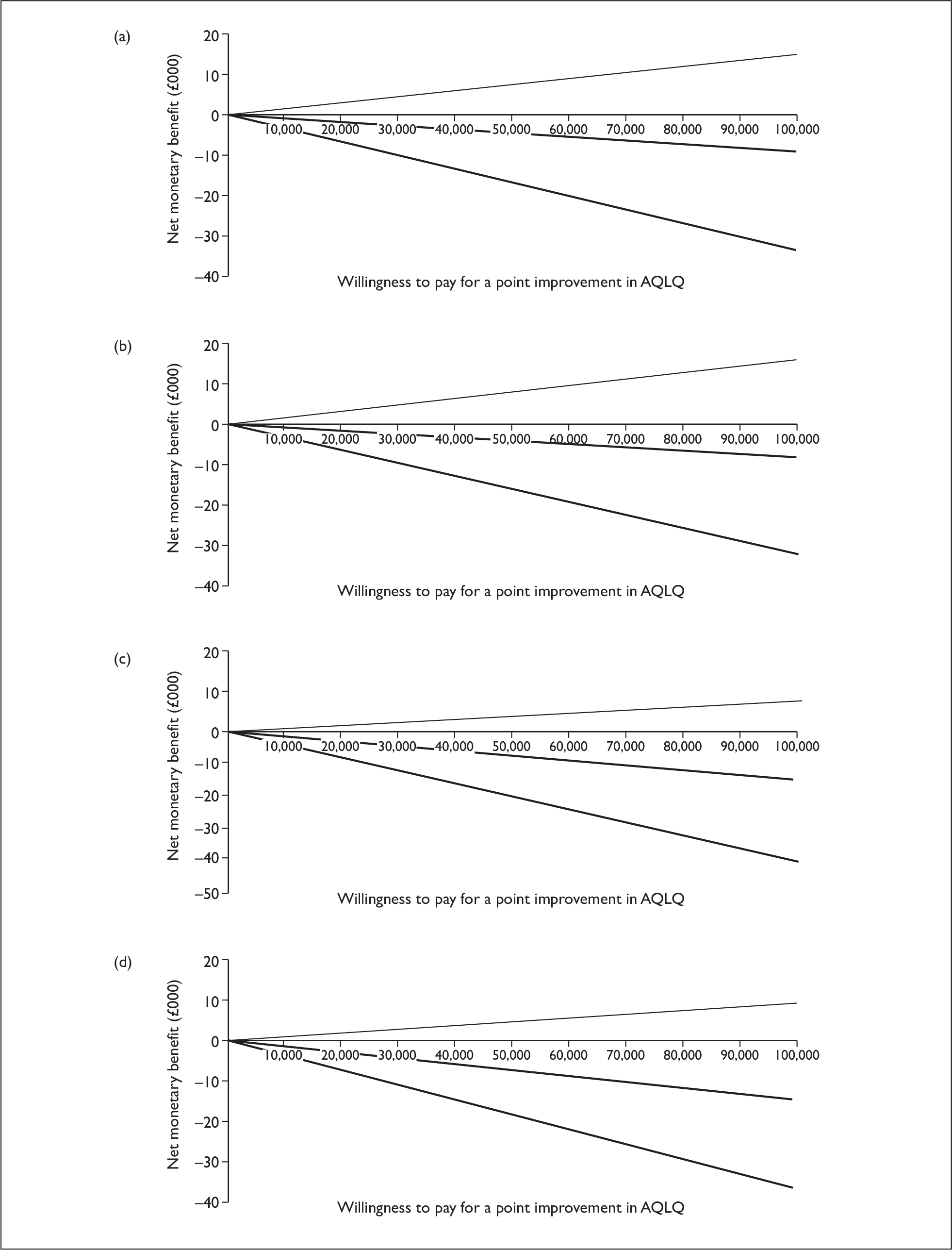
Even with a very high willingness to pay for a point improvement in MiniAQLQ, there is, at most, only a 25% probability of leukotriene antagonist being cost-effective compared with inhaled steroid in step 2 patients (Figure 6).
FIGURE 6.
Step 2: MiniAQLQ CEACs. Based on imputed, adjusted results of MiniAQLQ, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and these outcomes took place at 2 months or 2 years. This figure indicates that in all cases the probability of leukotriene antagonist being cost-effective compared with inhaled steroid is < 50%, irrespective of the willingness to pay for a point improvement in MiniAQLQ.
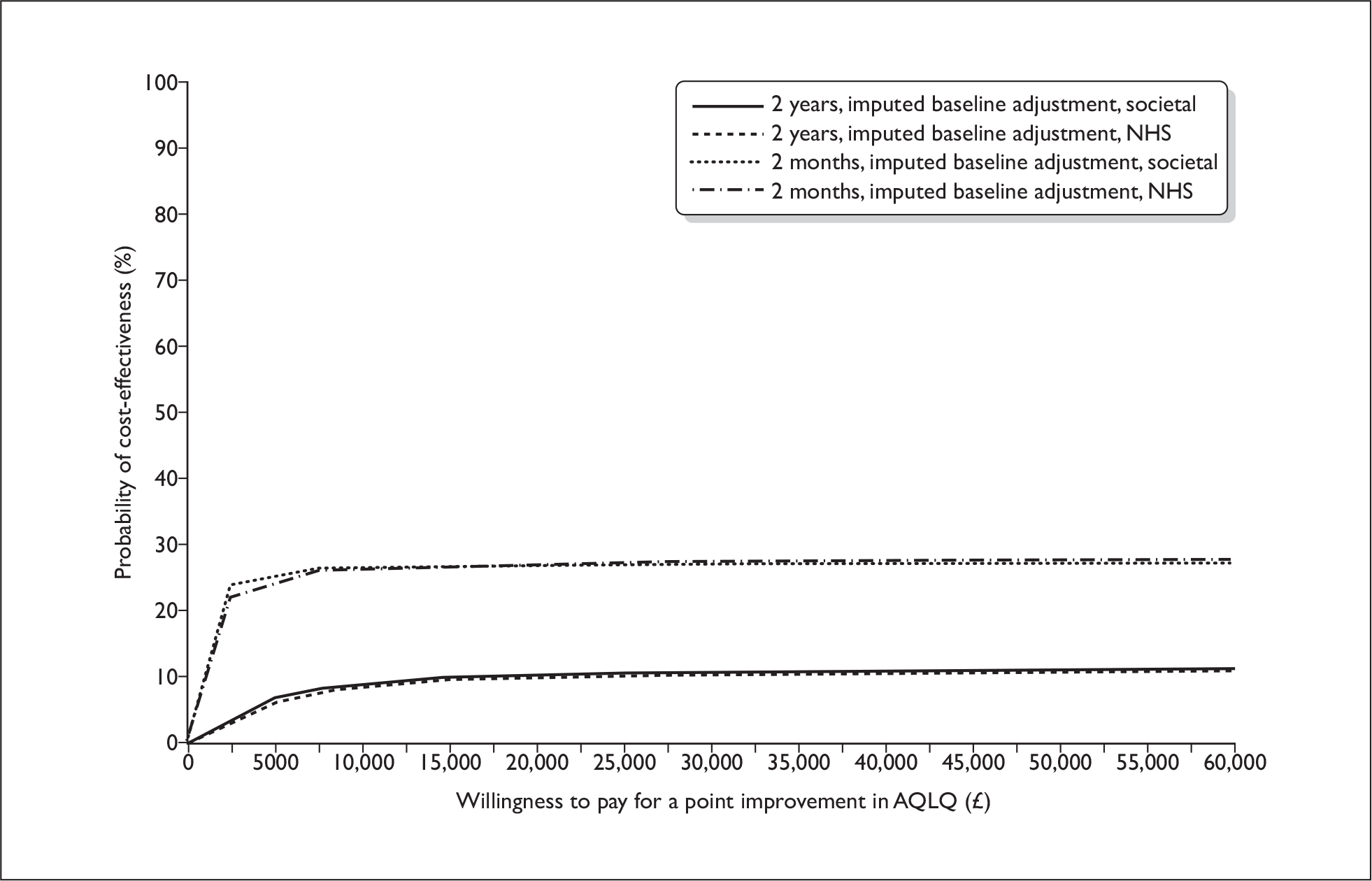
Asthma Control Questionnaire
At both 2 months (Table 17) and 2 years (Table 18), inhaled steroid is on average, a dominant strategy over leukotriene antagonist. Mean INB is negative, irrespective of willingness to pay for a point improvement in ACQ. However, there is great deal of uncertainty around this estimate (95% CIs in Figure 7).
| n | Cost (£) | ACQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline ACQ) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | |
| NHS | 121 | 127 | 80 | 25 | 1.550 | 1.541 | 55 | –0.009 | (ICS dominant) | 52 | –0.015 | (ICS dominant) | 53 | –0.083 | (ICS dominant) |
| Societal | 64 | 57 | 116 | 52 | 1.544 | 1.489 | 64 | –0.055 | (ICS dominant) | 37 | –0.015 | (ICS dominant) | 38 | –0.083 | (ICS dominant) |
| n | Cost (£) | ACQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline ACQ) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | |
| NHS | 133 | 140 | 587 | 327 | 1.223 | 1.142 | 260 | –0.081 | (ICS dominant) | 233 | –0.062 | (ICS dominant) | 249 | –0.116 | (ICS dominant) |
| Societal | 64 | 60 | 666 | 372 | 1.086 | 1.094 | 294 | 0.009 | 34546 | 209 | –0.062 | (ICS dominant) | 220 | –0.116 | (ICS dominant) |
FIGURE 7.
Step 2: INB, ACQ, INB and 95% CI are shown for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d) 2-year societal perspectives. Results based on imputed data adjusted for baseline ACQ.
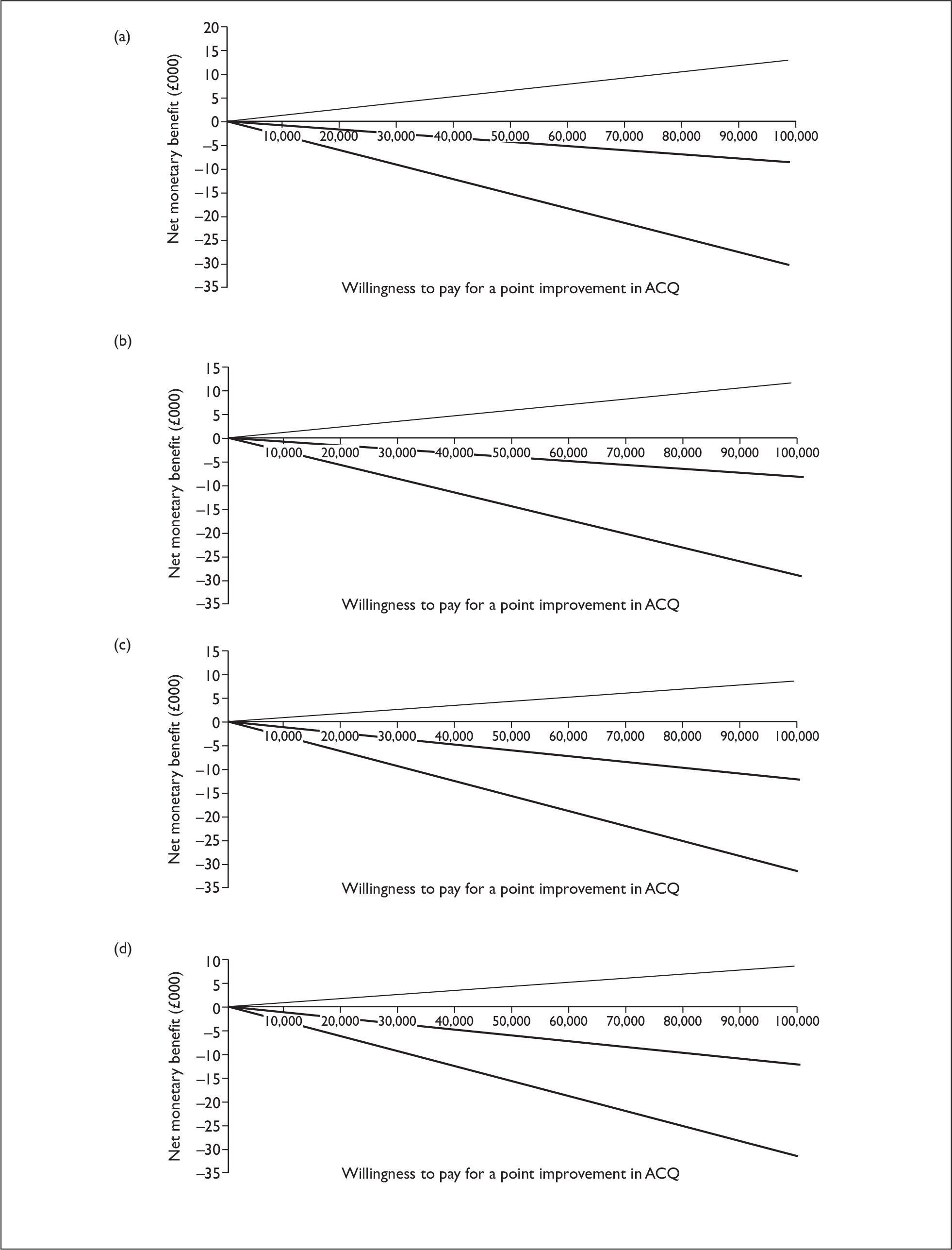
Incremental net benefit (± 95% CI) is shown in Figure 7a–d. A higher ACQ score indicates worsening of asthma control, and negative incremental ACQ indicates that leukotriene antagonist is less effective than inhaled steroid.
Even with a very high willingness to pay for a point improvement in ACQ, there is only at most a 22% probability of leukotriene antagonist being cost-effective compared with inhaled steroid in step 2 patients (Figure 8).
FIGURE 8.
Step 2: ACQ CEACs. Based on imputed, adjusted results of ACQ, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and these outcomes took place at 2 months or 2 years. This figure indicates that in all cases the probability of leukotriene antagonist being cost-effective compared with inhaled steroid is < 50%, irrespective of the willingness to pay for a point improvement in ACQ.
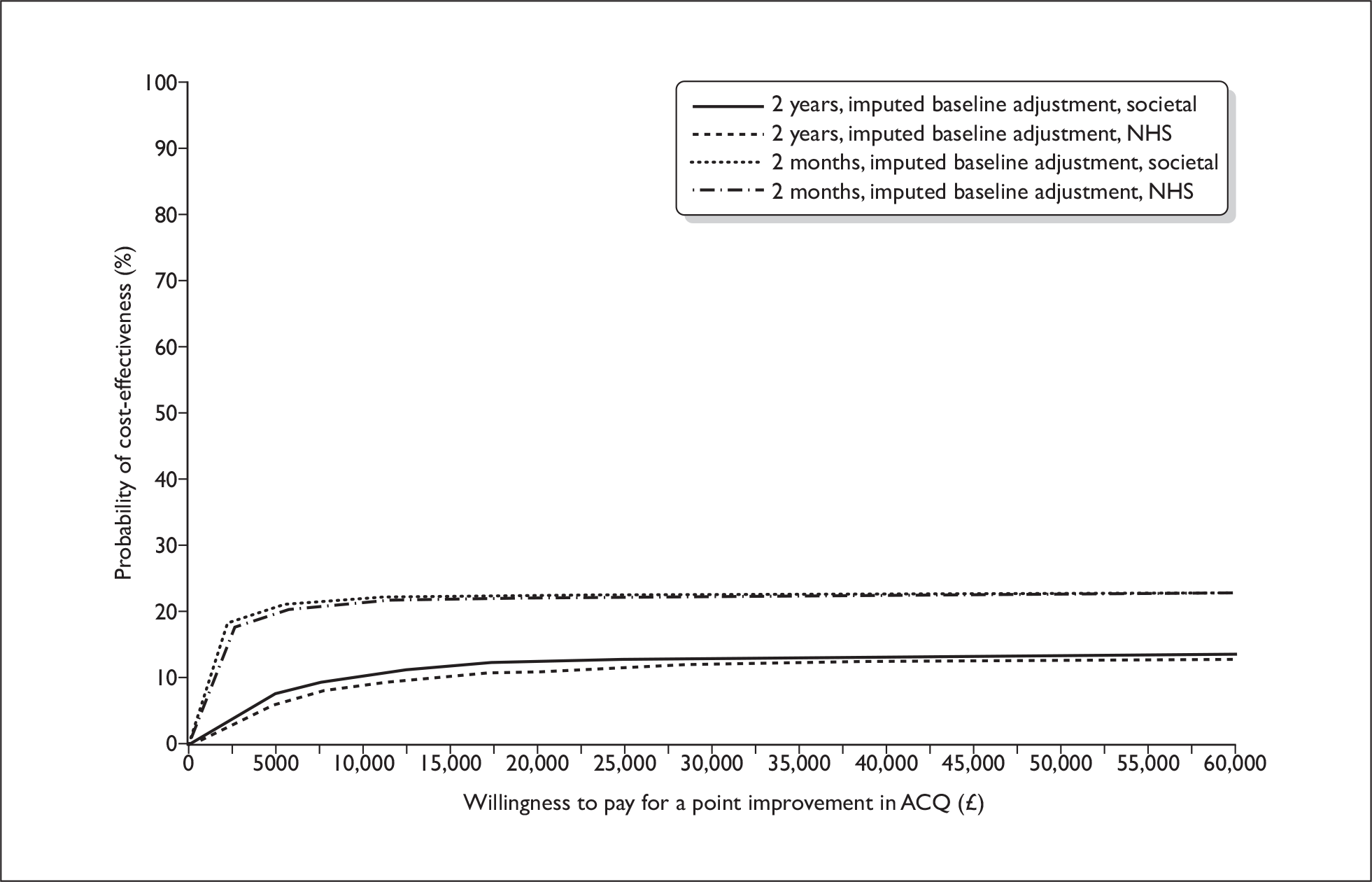
Quality-adjusted life-years (cost–utility analysis)
At both 2 months (Table 19) and 2 years (Table 20) inhaled steroid is, on average, a dominant strategy over leukotriene antagonist. Mean INB is negative, irrespective of willingness to pay for QALY (Figure 9).
| n | Cost (£) | QALYs | Source data only | Including imputed data | Including imputed data (adjusted for baseline utility) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB/£30 k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB/£30 k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB/£30 k (95% CI) | |
| NHS | 94 | 102 | 85 | 27 | 0.122 | 0.133 | 58 | –0.011 | (ICS dominant) | 0.10 | –277 (–454 to 97) | 52 | –0.006 | (ICS dominant) | 1.24 | –177(–151 to 112) | 52 | –0.004 | (ICS dominant) | 2.82 |
–155 (–305 to 0) |
| Societal | 52 | 45 | 115 | 59 | 0.118 | 0.135 | 56 | –0.017 | (ICS dominant) | 0.20 | –406 (–677 to 159) | 37 | –0.006 | (ICS dominant) | 2.12 | –128 (–212 to 142) | 36 | –0.004 | (ICS dominant) | 3.50 |
–145 (–305 to 8) |
| n | Cost (£) | QALYs | Source data only | Including imputed data | Including imputed data (adjusted for baseline utility) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | ICS | LTRA | ICS | LTRA | ICS | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB/£30 k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB|£30 k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30 k (%) | INB/£30 k (95% CI) | |
| NHS | 78 | 89 | 616 | 369 | 1.571 | 1.736 | 247 | –0.165 | (ICS dominant) | 0.00 | –3551(–5986 to 1270) | 233 | –0.091 | (ICS dominant) | 0.98 | –698 | 228 | –0.073 | (ICS dominant) | 3.30 |
–2255 (–4550 to 211) |
| Societal | 43 | 39 | 711 | 433 | 1.524 | 1.731 | 278 | –0.207 | (ICS dominant) | 1.00 | –4349(–8157 to 762) | 209 | –0.091 | (ICS dominant) | 1.26 | –87 | 204 | –0.073 | (ICS dominant) | 3.14 |
–2241 (–4542 to 118) |
FIGURE 9.
Step 2: INB, QALYs, INB and 95% CI are shown for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d) 2-year societal perspectives. Results based on imputed data adjusted for baseline utility.
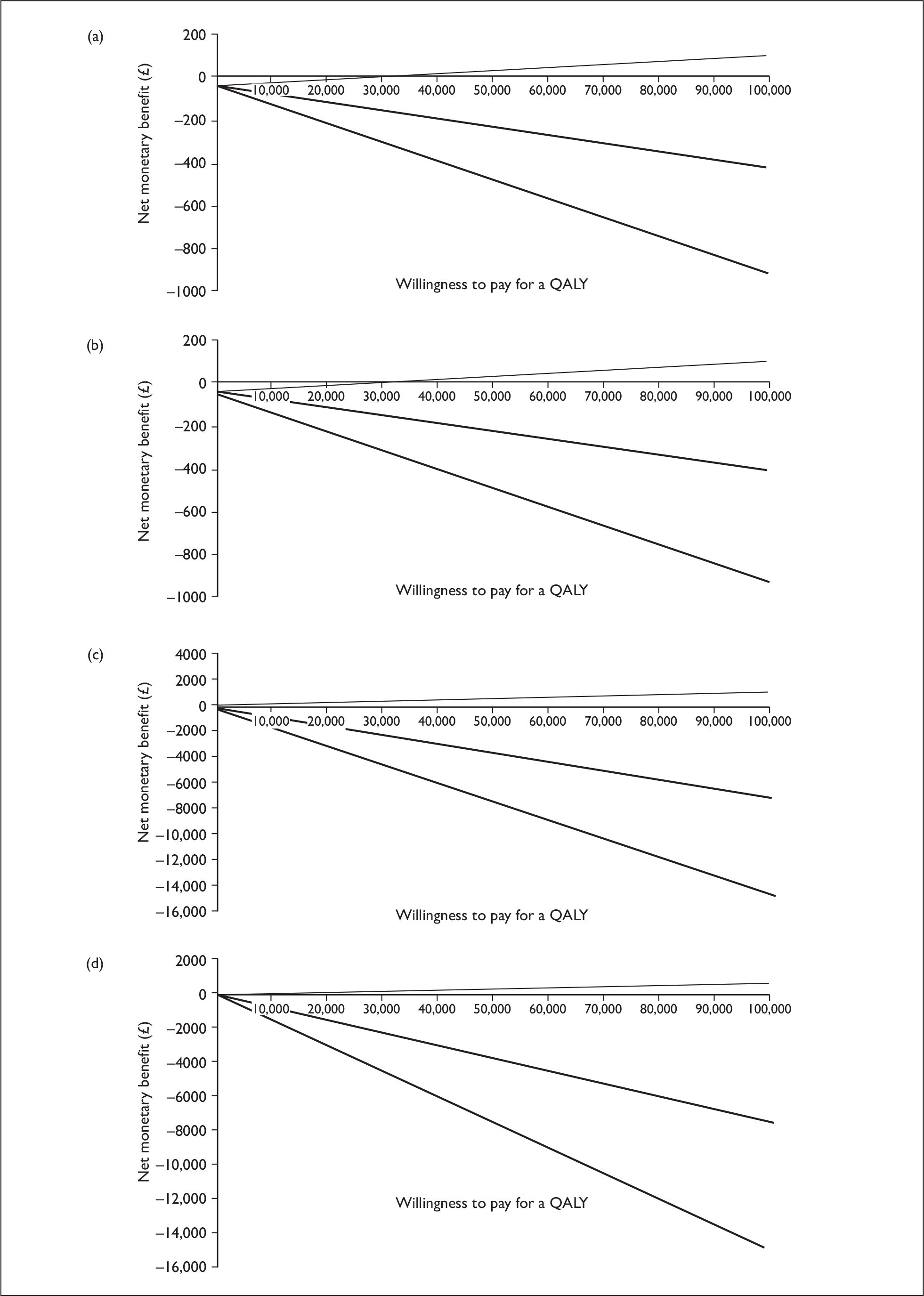
At a typical willingness to pay of £30,000 per QALY gained, mean (95% CI) INB at 2 months is –£155 (–£305 to £0) or –£145 (–£305 to £8) from the NHS and societal perspectives, respectively, deteriorating to –£2255 (–£4450 to £211) and –£2241 (–£4542 to £118) at 2 years. At the £30,000 threshold, there is a very low probability (2.8% to 3.5%) of leukotriene antagonist being cost-effective compared with inhaled steroid in patients at step 2 of the national asthma guidelines (Tables 19 and 20, and Figure 10).
FIGURE 10.
Step 2: Cost–utility analysis – CEACs. Based on imputed, adjusted results of cost–utility analysis, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and these outcomes took place at 2 months or 2 years. This figure indicates that the probability of leukotriene antagonist being cost-effective compared with inhaled corticosteroid is approximately 2.8–3.5%, given a typical willingness to pay of £30,000 per QALY gained.
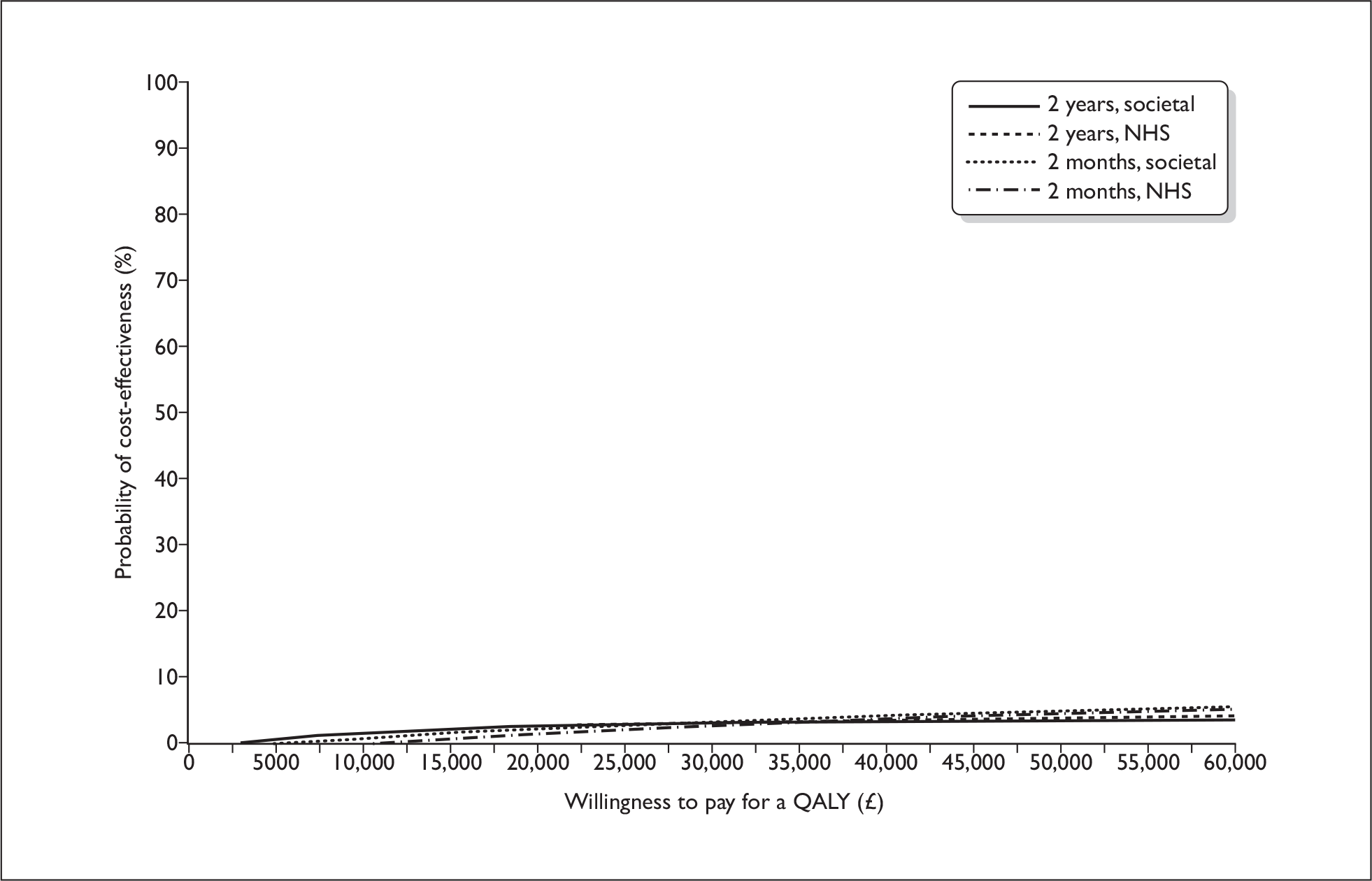
Figure 10 indicates that in all cases the probability of leukotriene antagonist being cost-effective compared with inhaled steroid is below 50%, irrespective of the willingness to pay for a QALY.
Summary of cost-effectiveness analyses
The results of the cost-effectiveness analyses suggest that leukotriene antagonists are both more expensive and less, although not statistically significantly, effective than inhaled steroids, with a very low probability of cost-effectiveness compared with inhaled steroids for patients initiating controller therapy at step 2 of the national asthma guidelines.
Whether an intervention is deemed cost-effective is dependent upon the willingness-to-pay threshold for a unit of outcome. For QALYs, a ‘reasonable’ willingness to pay is thought to be in the order of £30,000. The threshold for a point improvement in MiniAQLQ or ACQ is less well established. However, even given an infinite willingness to pay for a point improvement in MiniAQLQ or ACQ, there is at best a 22–25% probability that leukotriene antagonists are a cost-effective alternative to inhaled steroids in patients at step 2 of the national asthma guidelines (depending on time horizon and perspective).
Secondary analyses
Asthma exacerbations, hospitalisations and respiratory tract infections
No significant differences were found in the number of exacerbations or respiratory tract infections experienced by participants receiving leukotriene antagonist or inhaled steroid (Table 21). (Number of exacerbations included hospitalisations as well as courses of oral steroids.) Similarly, no significant difference was found in the number of consultations associated with respiratory tract infections.
| LTRA (n = 148) | ICS (n = 158) | Rate ratio (95% CI) | |
|---|---|---|---|
| Mean (SD) exacerbations over 2 years | 0.44 (0.94) | 0.35 (0.95) | 1.27 (0.83 to 1.92), p = 0.230 |
| Mean (SD) respiratory tract infections over 2 years | 1.01 (1.68) | 1.06 (1.57) | 0.95 (0.70 to 1.30), p = 0.764 |
| Mean (SD) consultations for respiratory tract infections over 2 years | 1.23 (2.12) | 1.20 (1.82) | 1.02 (0.74 to 1.41), p = 0.891 |
| Adjusted differencea (95% CI) LTRA–ICS | |||
| Mean (SD) SABA inhalers prescribed over 2 years (inhalers/day) |
n = 138 0.014 (0.015) |
n = 140 0.013 (0.014) |
0.001 (–0.001 to 0.004), p = 0.260 |
There were no hospital admissions during the first 2 months of the study. Subsequently, over the remainder of the 2 years, there were four hospital admissions for seven nights in total in the leukotriene antagonist group and two hospital admissions for six nights in total in the inhaled steroid group.
Prescribed short-acting β2-agonist
No significant difference was found in the use of short-acting β2-agonist (Table 21). On average, participants randomised to leukotriene antagonist received 1.28 short-acting β2-agonist inhalers every 3 months, whereas those randomised to inhaled steroid received 1.19 short-acting β2-agonist inhalers every 3 months. Over the 2-year study period, on average 10.22 compared with 9.49 short-acting β2-agonist inhalers were issued to participants who were randomised to leukotriene antagonist and inhaled steroid, respectively.
Clinic %PPEF and domiciliary data
For clinic %PPEF, minor improvement was observed in both leukotriene antagonist and inhaled steroid treated groups, and no significant differences were found between the groups at either the 2-month or 2-year time points (Table 22 and Figure 4).
| Measure | LTRA | ICS | p-value |
|---|---|---|---|
| Baseline |
n = 134 85.97 (77.43 to 94.16) |
n = 150 85.07 (73.92 to 95.42) |
|
| 2 months |
n = 98 88.15 (80.09 to 97.90) |
n = 106 86.56 (75.38 to 97.18) |
p = 0.228 |
| 2 years |
n = 100 88.84 (81.93 to 99.96) |
n = 112 87.62 (76.13 to 99.56) |
p = 0.197 |
Diary cards were completed by approximately one-half of participants at 2 months and one-third at 2 years. No significant differences were observed in the diary card data at either 2 months (Table 23) or 2 years (Table 24).
| LTRA (N = 148) | ICS (N = 158) | Difference (95% CI) LTRA–ICS, p-value | Adjusted differencea (95% CI) | |
|---|---|---|---|---|
| Mean (SD) morning waking with symptoms |
n = 76 0.29 (0.33) |
n = 81 0.29 (0.32) |
–0.01 (–0.11 to 0.09) p = 0.873 |
0.01 (–0.08 to 0.10) p = 0.866 |
| Mean (SD) puffs of reliever at night – original scale |
n = 69 0.67 (0.90) |
n = 73 0.77 (1.19) |
–0.11 | |
| Mean (SD) puffs of reliever at night – logged scale |
n = 69 0.39 (0.47) |
n = 73 0.42 (0.51) |
–0.03 (–0.19 to 0.14) p = 0.729 |
–0.01 (–0.16 to 0.13) p = 0.857 |
| Mean (SD) morning PEF |
n = 74 417.0 (99.1) |
n = 81 419.4 (111.2) |
–2.4 (–35.9 to 31.2) p = 0.889 |
–3.4 (–14.8 to 8.0) p = 0.558 |
| Mean (SD) daytime asthma symptom score |
n = 75 1.26 (1.12) |
n = 80 1.34 (1.14) |
–0.08 (–0.44 to 0.28) p = 0.663 |
–0.08 (–0.40 to 0.25) p = 0.632 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’ |
n = 75 1.10 (1.08) |
n = 80 1.14 (1.08) |
–0.04 (–0.39 to 0.30) p = 0.801 |
–0.09 (–0.39 to 0.21) p = 0.556 |
| Mean (SD) daily activity score |
n = 74 2.38 (1.21) |
n = 79 2.26 (1.32) |
0.12 (–0.28 to 0.53) p = 0.555 |
0.02 (–0.35 to 0.38) p = 0.930 |
| Mean (SD) score for interference on activities from asthma |
n = 75 0.96 (1.11) |
n = 80 1.08 (1.13) |
–0.13 (–0.48 to 0.23) p = 0.482 |
–0.20 (–0.52 to 0.11) p = 0.203 |
| Mean (SD) puffs of reliever during the day – original scale |
n = 70 1.57 (1.67) |
n = 78 1.42 (1.49) |
0.15 | |
| Mean (SD) puffs of reliever during the day – logged scale |
n = 70 0.76 (0.60) |
n = 78 0.72 (0.56) |
0.04 (–0.15 to 0.23) p = 0.669 |
0.03 (–0.14 to 0.20) p = 0.703 |
| Mean (SD) evening PEF |
n = 74 426.9 (100.3) |
n = 81 423.7 (112.0) |
3.3 (–30.6 to 37.1) p = 0.848 |
–2.4 (–13.0 to 8.2) p = 0.654 |
| Mean (SD) PEF diurnal variability (%) |
n = 74 5.8 (4.3) |
n = 81 6.2 (4.4) |
–0.4 (–1.8 to 0.9) p = 0.529 |
–0.3 (–1.7 to 1.0) p = 0.621 |
| LTRA (N = 148) | ICS (N = 158) | Difference (95% CI) LTRA–ICS, p-value | Adjusted differencea (95% CI), p-value | |
|---|---|---|---|---|
| Mean (SD) morning waking with symptoms |
n = 47 0.31 (0.34) |
n = 57 0.21 (0.29) |
0.10 (–0.02 to 0.23) p = 0.105 | 0.11 (–0.01 to 0.23) p = 0.063 |
| Mean (SD) puffs of reliever at night – original scale |
n = 45 0.52 (0.79) |
n = 52 0.48 (0.96) |
0.05 | |
| Mean (SD) puffs of reliever at night – logged scale |
n = 45 0.33 (0.41) |
n = 52 0.28 (0.42) |
0.05 (–0.12 to 0.22) p = 0.546 | 0.03 (–0.14 to 0.21) p = 0.717 |
| Mean (SD) morning PEF |
n = 47 412.4 (102.6) |
n = 54 419.2 (137.8) |
–6.77 (–55.3 to 41.8) p = 0.783 | –21.5 (–50.5 to 7.6) p = 0.146 |
| Mean (SD) daytime asthma symptom score |
n = 47 1.43 (1.15) |
n = 55 1.16 (1.21) |
0.27 (–0.20 to 0.73) p = 0.259 | 0.12 (–0.31 to 0.55) p = 0.577 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’ |
n = 47 1.24 (1.15) |
n = 56 1.14 (1.39) |
0.11 (–0.37 to 0.61) p = 0.673 | –0.01(–0.43 to 0.41) p = 0.957 |
| Mean (SD) daily activity score |
n = 47 2.22 (1.37) |
n = 56 2.07 (1.44) |
0.15 (–0.40 to 0.71) p = 0.581 | 0.02 (–0.57 to 0.62) p = 0.934 |
| Mean (SD) score for interference on activities from asthma |
n = 47 1.08 (1.16) |
n = 55 0.88 (1.26) |
0.19 (–0.29 to 0.67) p = 0.427 | 0.01 (–0.41 to 0.43) p = 0.959 |
| Mean (SD) puffs of reliever during the day – original scale |
n = 45 1.67 (1.70) |
n = 56 1.24 (1.42) |
0.43 | |
| Mean (SD) puffs of reliever during the day – logged scale |
n = 45 0.80 (0.60) |
n = 56 0.64 (0.57) |
0.16 (–0.07 to 0.39) p = 0.172 | 0.16 (–0.07 to 0.38) p = 0.170 |
| Mean (SD) evening PEF |
n = 46 419.6 (104.7) |
n = 57 408.8 (129.8) |
10.8 (–36.1 to 57.7) p = 0.649 | –12.5 (–37.6 to 12.5) p = 0.322 |
| Mean (SD) PEF diurnal variability (%) |
n = 37 4.4 (3.4) |
n = 44 4.6 (3.0) |
–0.1 (–1.6 to 1.3) p = 0.852 | –0.2 (–1.7 to 1.2) p = 0.742 |
Secondary QOL scores and rhinitis scores
No significant differences were observed in the mRQLQ, RCP3 questions or personal objectives scores after 2 months or 2 years (Table 25). However, at both time points all measures showed a substantial improvement from baseline.
| Measure | LTRA | ICS | Difference (95% CI) LTRA–ICS, p-value | Adjusted differencea (95% CI), p-value |
|---|---|---|---|---|
| 2-month outcomes | ||||
| mRQLQ |
n = 114 1.48 (1.15) |
n = 124 1.55 (1.20) |
–0.07 (–0.37 to 0.23), p = 0.638 | 0.07 (–0.35 to 0.21), p = 0.639 |
| RCP3 |
n = 123 1.21 (0.96) |
n = 139 1.37 (1.06) |
–0.16 (–0.40 to 0.09), p = 0.216 | –0.13 (–0.38 to 0.12), p = 0.322 |
|
Personal objectives (0–100 VAS) |
n = 82 54.7 (22.4) |
n = 90 50.3 (22.6) |
4.44 (–11.21 to 2.33), p = 0.197 | 2.40(–4.53 to 9.32), p = 0.495 |
| 2-year outcomes | ||||
| mRQLQ |
n = 145 1.26 (1.23) |
n = 152 1.26 (1.28) |
0.00 (–0.29 to 0.28), p = 0.355 | 0.02 (–0.27 to 0.31), p = 0.900 |
| RCP3 |
n = 147 1.23 (0.99) |
n = 155 1.14 (0.98) |
0.10 (–0.13 to 0.31), p = 0.432 | 0.11 (–0.12 to 0.34), p = 0.360 |
|
Personal objectives (0–100 VAS) |
n = 97 66.5 (20.9) |
n = 107 69.1 (18.9) |
–2.58 (–8.07 to 2.91), p = 0.355 | –4.62 (–10.75 to 1.51), p = 0.139 |
Changes in treatment after randomisation
At 2 months, eight patients (6%) and five patients (3%) in the leukotriene antagonist and inhaled steroid groups, respectively, had a change in treatment from initial randomised therapy class. By the end of the study 45 (31%) and 32 (21%), respectively, patients had a change in treatment. The changes in treatment by 2 months and 2 years are tabulated in Table 26.
| Treatment change by 2 months, n (%) | |
|---|---|
| Participants in ICS arm | N = 155 |
| Add LABA | 3 (2) |
| Change to LTRA | 2 (1) |
| Total | 5 (3) |
| Participants in LTRA arm | N = 145 |
| Change to ICS | 6 (4) |
| Change to ICS and LABA | 1 (1) |
| Multiple changes | 1 (1) |
| Total | 8 (6) |
| Treatment change by 2 years, n (%) | |
| Participants in ICS arm | N = 155 |
| Add LABA | 28 (18) |
| Change to LTRA | 4 (3) |
| Total | 32 (21) |
| Participants in LTRA arm | N = 145 |
| Add ICS | 4 (3) |
| Add ICS and LABA | 2 (1) |
| Change to ICS | 27 (19) |
| Change to ICS and LABA | 8 (6) |
| Change to ICS and then add LABA | 3 (2) |
| Multiple changes | 1 (1) |
| Total | 45 (31) |
Per-protocol population (fixed treatment regime and no changes within or from randomised therapy class) analyses
Our per-protocol population was defined as those patients who were prescribed a fixed treatment regime at randomisation (i.e. no self-management plan) and who had no change in that fixed regime at any time including the final study visit, i.e. no change in device, dose or therapeutic class. After restricting the groups to only those who had completed the entire study intervention period as per this definition of per-protocol and who had analysable data, 65 leukotriene antagonist and 82 inhaled steroid participants were identified. There was a preponderance of male participants in both treatment groups (56–57% – Appendix 5, Table 59). Randomised therapy was changed or varied during the study for the remaining 83 and 76 participants in leukotriene antagonist and inhaled steroid groups, respectively.
Results for these per-protocol participants are reported in Appendix 5, Tables 59–66. There was no significant difference (unadjusted or adjusted) between treatment groups in either MiniAQLQ or ACQ score at any time point. For MiniAQLQ scores, the adjusted differences between treatment groups at 2 months and 2 years favoured leukotriene antagonist, with 95% CI outside the limits of equivalence at both time points [adjusted difference for imputed results at 2 years, 0.05 (–0.28 to 0.37)]. Similarly, all ACQ differences favoured leukotriene antagonist.
Results for the secondary analyses were similar to those for the intention-to-treat analyses. There were no significant differences between treatment groups other than a marginally better result for clinic %PPEF in the leukotriene antagonist group at 2 years (p = 0.058).
Adherence to therapy
Adherence data were analysable for 217 participants overall. In the leukotriene antagonist group (n = 121, or 82%), median adherence (interquartile range) to leukotriene antagonist therapy was 61.4% (17.5–92.1%). In the inhaled steroid group (n = 96, or 61%), median adherence to inhaled steroid therapy was 41.1% (13.7–65.4%).
Step 3 trial
Demographics and baseline characteristics
Characteristics of participants screened and found eligible for the step 3 trial are shown in Tables 27 and 28. No substantial differences were identified between the arms. A female preponderance was noted in both arms of the trial. Most participants were Caucasian. Mean %PPEF was indicative of airflow obstruction consistent with asthma of mild to moderate severity (with ongoing treatment with inhaled steroid).
| LTRA (N = 170) | LABA (N = 182) | ||
|---|---|---|---|
| Sex | Female | 109 (64%) | 111 (61%) |
| Male | 61 (36%) | 71 (39%) | |
| Age | Mean (SD) |
n = 169 51.0 (16.0) |
49.7 (16.1) |
| Race | Caucasian | 168 | 178 |
| Non-Caucasian | 0 | 2 | |
| Not known | 2 | 2 | |
| Height (cm) | Mean (SD) |
n = 156 167.0 (10.0) |
n = 171 167.0 (9.3) |
| PEF (l/min) | Mean (SD) |
n = 166 416 (125) |
n = 178 419 (125) |
| %PPEF | Median (IQR) |
n = 152 90.46 (80.24 to 99.67) |
n = 167 88.64 (76.67 to 99.89) |
| Salbutamol PEF reversibility (%) | Mean (SD) |
n = 163 9.01 (10.1) |
n = 170 8.26 (9.63) |
| ICS dose (µg/day)a | Mean (SD) | 425 (351) | 451 (390) |
| SABA puffs/day, prior year | Mean (SD) |
n = 162 4.3 (4.0) |
n = 175 4.4 (3.5) |
| Asthma exacerbations in last year | Mean (SD) | 0.18 (0.44) | 0.24 (0.56) |
| ACQ | Mean (SD) | 2.01 (0.85) | 2.19 (0.87) |
| MiniAQLQ | Mean (SD) | 4.63 (1.03) | 4.41 (1.04) |
| mRQLQ | Mean (SD) |
n = 139 1.95 (1.27) |
n = 159 2.02 (1.31) |
| EQ-5D utility | Mean (SD) |
n = 148 0.780 (0.237) |
n = 159 0.772 (0.234) |
| Personal Objectives (0–100 VAS) | Mean (SD) |
n = 130 38.12 (19.24) |
n = 142 36.35 (19.05) |
| RCP3 | Mean (SD) |
n = 159 1.98 (0.86) |
n = 177 2.03 (0.81) |
| Sleep difficulty | Yes | 91 (54%) | 85 (49%) |
| No | 76 (46%) | 89 (51%) | |
| Missing | 3 | 8 | |
| Day symptoms | Yes | 155 (94%) | 162 (94%) |
| No | 11 (6%) | 12 (6%) | |
| Missing | 4 | 8 | |
| Interferes with activities | Yes | 82 (50%) | 79 (46%) |
| No | 83 (50%) | 92 (54%) | |
| Missing | 5 | 11 | |
| LTRA (N = 170) | LABA (N = 182) | ||
|---|---|---|---|
| Continued education > 16 years | Yes | 78 (47%) | 87 (48%) |
| No | 89 (53%) | 93 (52%) | |
| Not known | 3 | 2 | |
| Professional qualification | Yes | 39 (23%) | 46 (26%) |
| No | 127 (77%) | 133 (74%) | |
| Not known | 4 | 3 | |
| Employment position | Employer | 9 (8%) | 4 (3%) |
| Employee | 91 (78%) | 95 (77%) | |
| Self-employed | 17 (15%) | 25 (20%) | |
| Not known | 53 | 58 | |
| Smoking habit | Current smoker | 29 (17%) | 31 (17%) |
| Ex-smoker | 63 (38%) | 75 (42%) | |
| Never smoked | 76 (45%) | 74 (41%) | |
| Not known | 2 | 2 | |
| Current smoker and over age 45 | 16 (10%) | 16 (9%) | |
Most participants had daytime asthma symptoms, with half having additional night-time symptoms. Half of participants felt that their asthma symptoms interfered with their daily activities. Education and occupation status of participants are shown in Table 28. Most participants were in employment. Only 40% of patients had never smoked; 17% of participants were active smokers, including 26 (9%) who were over the age of 45 (Table 28). Baseline diary card data for these participants are shown in Table 29.
| LTRA (N = 170) | LABA (N = 182) | |
|---|---|---|
| Mean (SD) morning waking with symptoms | 0.47 (0.35) n = 159 | 0.46 (0.36) n = 176 |
| Mean (SD) puffs of reliever at night | 0.95 (1.42) n = 153 | 0.91 (1.01) n = 168 |
| Mean (SD) morning PEF | 391.1 (101.5) n = 158 | 393.7 (104.7) n = 175 |
| Mean (SD) daytime asthma symptom scorea | 1.91 (1.23) n = 159 | 1.91 (1.13) n = 176 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’a | 1.65 (1.24) n = 159 | 1.68 (1.10) n = 174 |
| Mean (SD) daily activity scoreb | 2.58 (1.21) n = 156 | 2.45 (1.10) n = 173 |
| Mean (SD) score for interference on activities from asthmaa | 1.38 (1.32) n = 157 | 1.52 (1.18) n = 174 |
| Mean (SD) puffs of reliever during the day | 2.73 (2.59) n = 154 | 2.74 (2.01) n = 175 |
| Mean (SD) evening PEF | 397.3 (100.0) n = 156 | 405.4 (101.5) n = 173 |
| Mean (SD) diurnal variation in PEF (%) | 6.5 (4.4) n = 158 | 6.5 (4.4) n = 175 |
Primary analyses
Change in QOL
Mini Asthma Quality of Life Questionnaire
Mean MiniAQLQ score increased from baseline in both leukotriene antagonist and long-acting β2-agonist randomised groups (Table 30 and Figure 11). No statistically significant between-group differences in MiniAQLQ score were found at the 2-month time point either unadjusted or adjusted for baseline values. In each case, the point estimate of the mean difference between groups was small. The 95% CIs for the unadjusted difference in MiniAQLQ score was just at the limits for equivalence: (–0.18 to 0.30). However, the 95% CI for the adjusted difference was within the value of 0.3, i.e. (–0.29 to 0.10). The limit of the one-sided 95% CI for the unadjusted difference was –0.16 and was –0.28 for the adjusted difference.
| Treatment duration | Outcome measure | LTRA | LABA | Difference (95% CI) LTRA–LABA | Adjusted differenceb (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
153 5.09 (1.15) |
156 5.04 (1.11) |
0.06 (–0.18 to 0.30) | –0.10 (–0.29 to 0.10) |
| 2 yearsc (visit 7) |
n Mean (SD) |
169 5.43 (1.14) |
181 5.42 (1.08) |
0.01 (–0.22 to 0.25) | –0.11 (–0.32 to 0.11) |
FIGURE 11.
Step 3: ACQ, MiniAQLQ and %PPEF over 2 years of treatment. Mean (standard deviation) ACQ (from 0 ‘best’ to 6 ‘worst’) and MiniAQLQ (from 1 ‘worst’ to 7 ‘best’) scores and median (interquartile range) %PPEF at baseline and over 2 years of treatment with leukotriene receptor antagonist or long-acting β2-agonist as add-on to ICS.
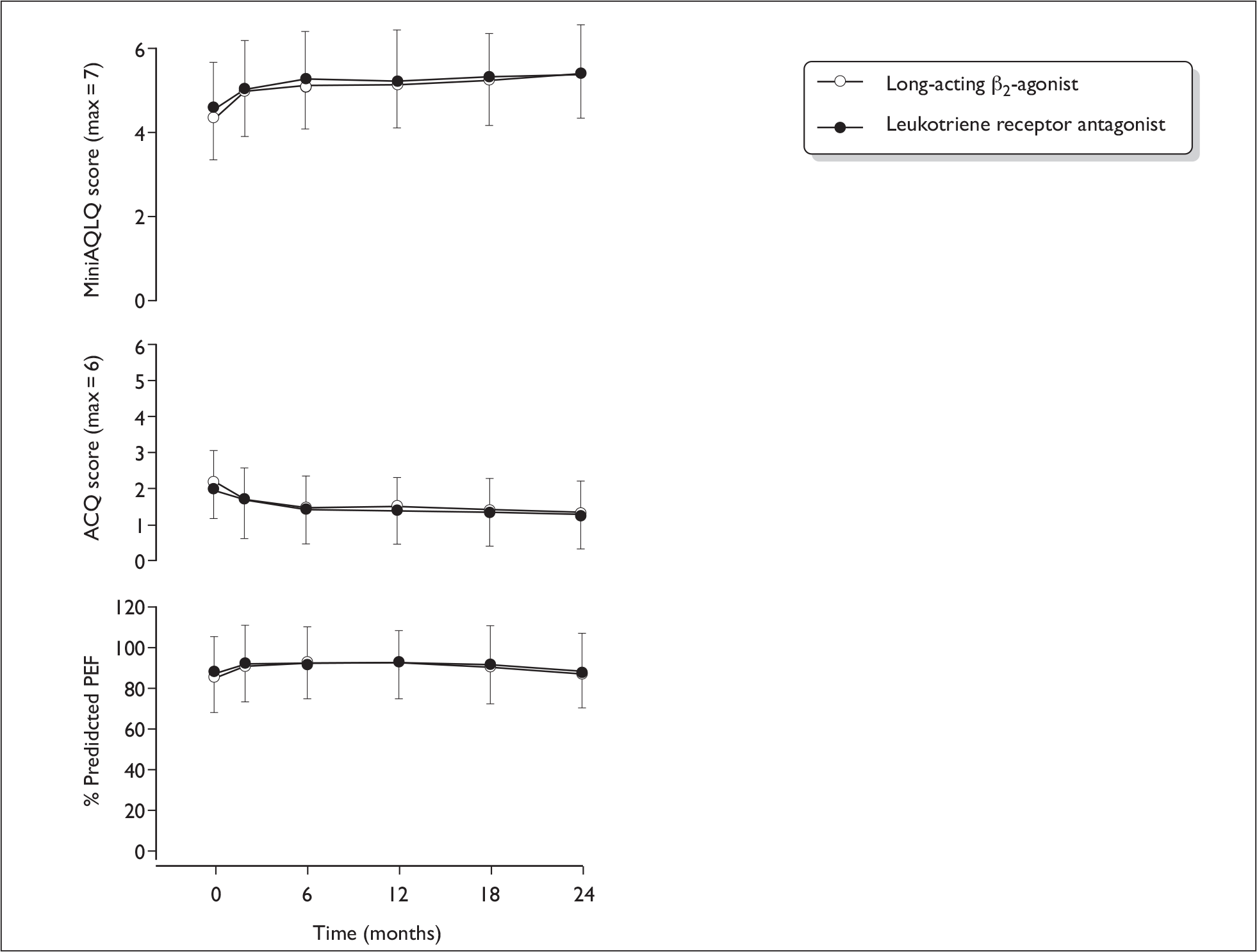
At the 2-year visit, the estimated between-group mean difference was again small and not statistically significant. The 95% CI for the unadjusted difference did not include 0.3 (–0.22 to 0.25). The 95% CI for the adjusted difference did, although marginally, include 0.3 in favour of long-acting β2-agonist (–0.32 to 0.11). The limit of the one-sided 95% CI for the unadjusted difference was –0.30 and was –0.28 for the adjusted difference, i.e. inferiority of leukotriene antagonist could be excluded.
Asthma Control Questionnaire
Mean ACQ score decreased (improved) from baseline in both leukotriene antagonist and long-acting β2-agonist randomised groups (Table 31 and Figure 11). No significant differences in ACQ score were found at either the 2-month or 2-year time points. At 2 years, the adjusted difference (95% CI) was 0.04 (–0.15 to 0.22). The CI is well within the minimum clinically important difference of 0.5.
| Treatment duration | LTRA | LABA | Difference (95% CI) LTRA–LABA | Adjusted differencea (95% CI) | |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
153 1.62 (1.00) |
156 1.60 (0.98) |
0.01 (–0.20 to 0.22) | 0.12 (–0.06 to 0.30) |
| 2 yearsb (visit 7) |
n Mean (SD) |
169 1.31 (0.96) |
181 1.34 (0.92) |
–0.04 (–0.24 to 0.16) | 0.04 (–0.15 to 0.22) |
Quality-adjusted life-years
Leukotriene antagonist patients experienced a mean 0.122 QALYs over the 2-month period, compared with 0.120 in long-acting β2-agonist patients, a mean (95% CI) difference of +0.002 (–0.007 to 0.010) QALYs, falling to –0.001 (–0.004 to 0.002) QALYs after adjustment for baseline utility (Table 32). Over 2 years, leukotriene antagonist patients gained 0.041 (–0.072 to 0.156) more QALYs than long-acting β2-agonist patients. However, after adjusting for baseline utility, the difference drops to 0.012 (–0.064 to 0.088) QALYs, equivalent to 4.4 days of perfect health gained.
| LTRA | LABA | Difference (95% CI) LTRA–LABA | Adjusted differencea (95% CI) | |||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| EQ-5D utility | ||||||
| Baseline | 148 | 0.780 (0.237) | 159 | 0.772 (0.234) | – | – |
| 2 months | 127 | 0.796 (0.267) | 130 | 0.794 (0.225) | – | – |
| 2 years | 160 | 0.807 (0.255) | 170 | 0.798 (0.268) | – | – |
| QALYs gained | ||||||
| 2 months | 120 | 0.122 (0.35) | 120 | 0.120 (0.032) |
0.002 (–0.007 to 0.010) |
–0.001 (–0.004 to 0.002) |
| 2 years (discounted) | 112 | 1.597 (0.418) | 115 | 1.556 (0.451) |
0.041 (–0.072 to 0.156) |
0.012 (–0.064 to 0.088) |
Resource use and cost
Point estimate costs and quantities of prescription medicines, over-the-counter medicines, NHS activity and indirect costs are reported in Tables 33–36.
| Treatment duration | LTRA | LABA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total items | Mean (SD) items | Total cost (£) | Mean (SD) cost (£) | n | Total items | Mean items (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | 175 | 707 | 4.02 (2.30) | 12,984 | 73.77 (33.22) | 184 | 682 | 3.69 (2.61) | 13,403 | 73 (38) |
| 2 years (discounted) | 169 | 7129 | 42.2 (27.3) | 116,477 | 689 (404) | 177 | 6262 | 35.4 (31.1) | 103,599 | 585 (437) |
| Treatment duration | LTRA | LABA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Total items | Mean (SD) items | Total cost (£) | Mean (SD) cost (£) | n | Total items | Mean items (SD) | Total cost (£) | Mean (SD) cost (£) | Cost (£) difference | |
| 2 months | 131 | 130 | 0.99 (0.96) | 453.34 | 3.46 (11.32) | 142 | 133 | 0.94 (0.88) | 362.80 | 2.55 (7.02) | 0.91 |
| 2 years (discounted) | 131 | 293 | 2.24 (2.11) | 1024.69 | 7.82 (18.82) | 142 | 311 | 2.19 (1.46) | 850.38 | 5.99 (10.54) | 1.83 |
| Treatment | LTRA | LABA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total items | Mean (SD) items | Total cost (£) | Mean (SD) cost (£) | n | Total items | Mean items (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | ||||||||||
| Total routine care | 175 | 38 | 0.22 (0.59) | 403.34 | 2.30 (6.32) | 182 | 47 | 0.26 (0.73) | 398.34 | 2.19 (6.61) |
| Total patient initiated | 175 | 59 | 0.34 (0.79) | 1154 | 6.59 (17.17) | 182 | 56 | 0.31 (0.75) | 1129 | 6.20 (15.54) |
| Total secondary care | 175 | 1 | 0.01 (0.08) | 191 | 1.09 (17.44) | 182 | 4 | 0.02 (0.18) | 76 | 0.42 (3.43) |
| Total NHS activity | 175 | 98 | 0.56 (0.99) | 1748.34 | 9.99 (25.00) | 182 | 107 | 0.59 (1.05) | 1603.34 | 8.81 (17.64) |
| 2 years (discounted) | ||||||||||
| Total routine care | 169 | 646 | 3.82 (2.63) | 5710.33 | 33.79 (26.53) | 176 | 699 | 3.97 (2.56) | 5934.30 | 33.72 (24.49) |
| Total patient initiated | 169 | 654 | 3.87 (4.20) | 13,333.99 | 78.90 (89.75) | 176 | 561 | 3.19 (2.94) | 12,187.43 | 69.25 (71.42) |
| Total secondary care | 169 | 74 | 0.44 (1.16) | 12,873.62 | 76.18 (370.05) | 176 | 47 | 0.27 (0.91) | 13,091.82 | 74.39 (511.48) |
| Total NHS activity | 169 | 1374 | 8.13 (5.94) | 31,917.94 | 188.86 (398.89) | 176 | 1307 | 7.43 (4.19) | 31,213.56 | 177.35 (541.93) |
| Treatment duration | LTRA | LABA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Total hours | Mean (SD) hours | Total cost (£) | Mean (SD) cost (£) | n | Total hours | Mean hours (SD) | Total cost (£) | Mean (SD) cost (£) | |
| 2 months | 110 | 292 | 2.65 (13.94) | 3833.96 | 34.85 (183.08) | 115 | 295 | 2.57 (13.57) | 3873.35 | 33.68 (178.14) |
| 2 years (discounted) | 110 | 1468 | 13.35 (51.96) | 19,274.84 | 175.23 (682.17) | 115 | 1077 | 9.37 (53.84) | 13,368.11 | 116.24 (702.80) |
Total NHS costs are the sum of prescriptions and NHS activity. Total societal costs are NHS costs plus over-the-counter medications and indirect costs. At 2 months, costs were similar between the two groups, although point estimate was higher in leukotriene antagonist patients [+£2 (95% CI –£7 to +£11 from NHS perspective), +£15 (95% CI –£35 to +£65 from societal perspective – Table 37)]. At 2 years, leukotriene antagonist patients cost £115 (–£46 to £276) or £263 (–£3 to £529) more than long-acting β2-agonist patients from the NHS or societal perspectives, respectively.
| Treatment | LTRA | LABA | |||||
|---|---|---|---|---|---|---|---|
| n | Total cost (£) | Mean (SD) cost (£) | n | Total cost (£) | Mean (SD) cost (£) | Cost (£) difference (95% CI) |
|
| Total NHS costs (prescription medicines and NHS activity combined) | |||||||
| 2 months | 175 | 14,732.57 | 84.19 (41.71) |
262.83 (–3 to 529) |
14,911.91 | 81.93 (45.84) | 2.25 (–6.88 to 11.39) |
| 2 years (discounted) | 166 | 147,299.54 | 887.35 (617.05) | 132,052.97 | 772.24 (862.96) | 115.11 (–46 to 276) | |
| Societal costs (prescription and over-the-counter medicines – NHS activity and indirect costs combined) | |||||||
| 2 months | 101 | 12,818.31 | 126.91 (202.11) | 11,655.96 | 112.08 (158.73) | 14.84 (–35.13 to 64.80) | |
| 2 years (discounted) | 97 | 111,196.77 | 1146.36 (965.55) | 87,469.45 | 883.53 (923.89) | 262.83 (–3 to 529) | |
Cost-effectiveness analyses
MiniAQLQ
The incremental cost per point improvement in MiniAQLQ is £48 and £115, respectively, from the NHS and societal perspectives at 2 months (Table 38). At 2 years this has deteriorated to £3366 and £6267 (Table 39). Mean INB is positive so long as the willingness to pay for a point improvement in MiniAQLQ is greater than these mean estimates. However, we did not detect a statistically significant result at any threshold (Figure 12).
| n | Cost (£) | MiniAQLQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline MiniAQLQ) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | |
| NHS | 153 | 155 | 84 | 82 | 5.092 | 5.038 | 3 | 0.055 | 47 | 3 | 0.040 | 67 | 3 | 0.058 | 48 |
| Societal | 95 | 90 | 129 | 115 | 5.110 | 4.978 | 14 | 0.132 | 109 | 6 | 0.040 | 162 | 7 | 0.058 | 115 |
| n | Cost (£) | MiniAQLQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline MiniAQLQ) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | Inc. cost (£) | Inc. AQLQ | ICER (£) | |
| NHS | 155 | 164 | 891 | 791 | 5.452 | 5.416 | 100 | 0.037 | 2734 | 111 | 0.016 | 6886 | 114 | 0.034 | 3366 |
| Societal | 94 | 96 | 1152 | 893 | 5.352 | 5.438 | 259 | –0.086 | (LABA dominant) | 213 | 0.016 | 13,235 | 215 | 0.034 | 6367 |
FIGURE 12.
Step 3: INB, MiniAQLQ, INB and 95% CI for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d) 2-year societal perspectives. Results based on imputed data adjusted for baseline MiniAQLQ.
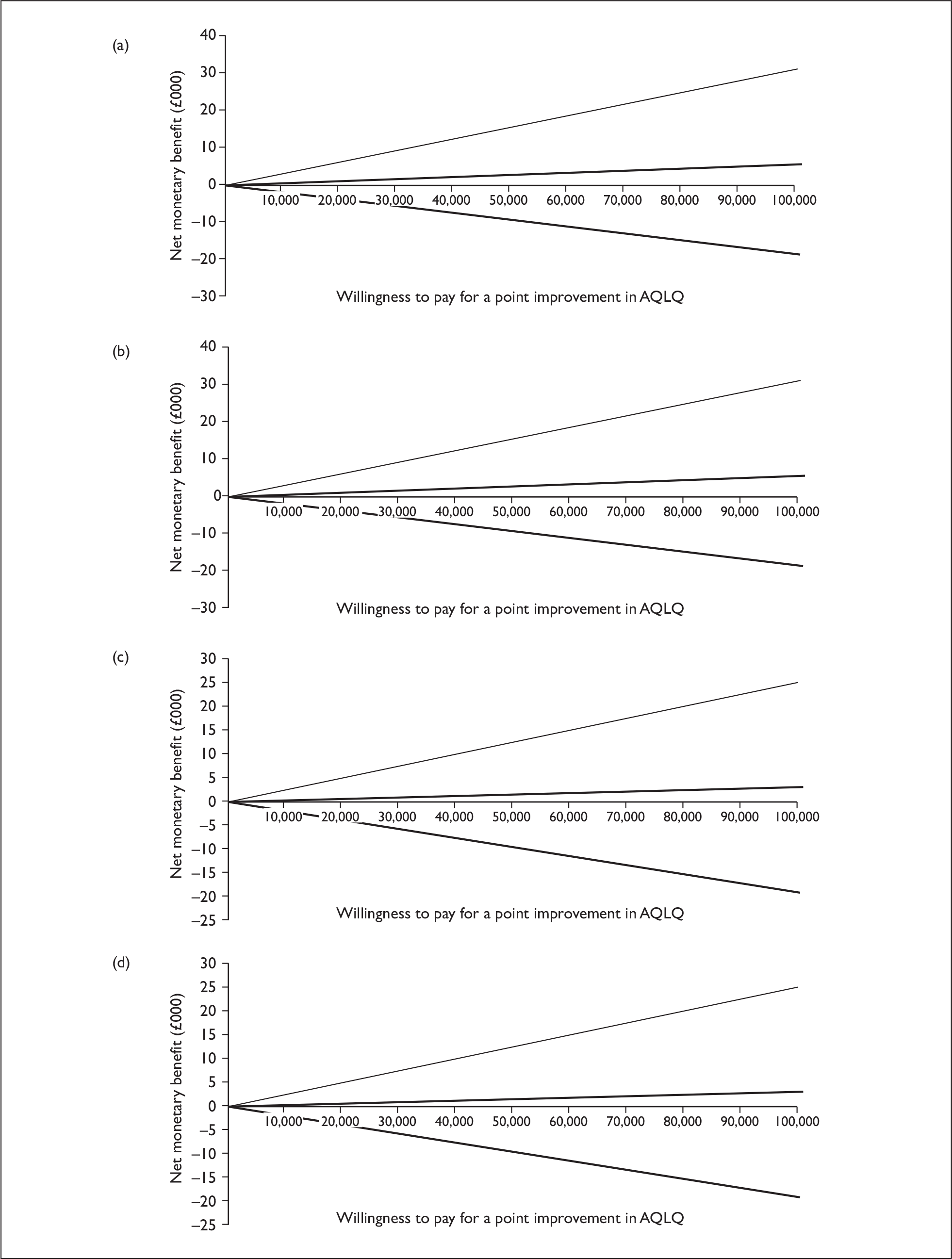
At higher thresholds, there is between a 61% and 68% probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist in step 3 patients (Figure 13). However, from a societal perspective over 2 years, there is a 50% or greater probability of leukotriene antagonists being cost-effective only when the threshold is above £385 per point improvement in MiniAQLQ.
FIGURE 13.
Step 3: MiniAQLQ CEACs. Based on imputed, adjusted results of MiniAQLQ, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and that these outcomes took place at 2 months or 2 years. The figure indicates that in all cases the probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist is above 50%, irrespective of the willingness to pay for a point improvement in MiniAQLQ. The exception is the 2-year analysis from a societal perspective, where the probability is above 50% as long as the willingness to pay for a point improvement in MiniAQLQ is > £432.
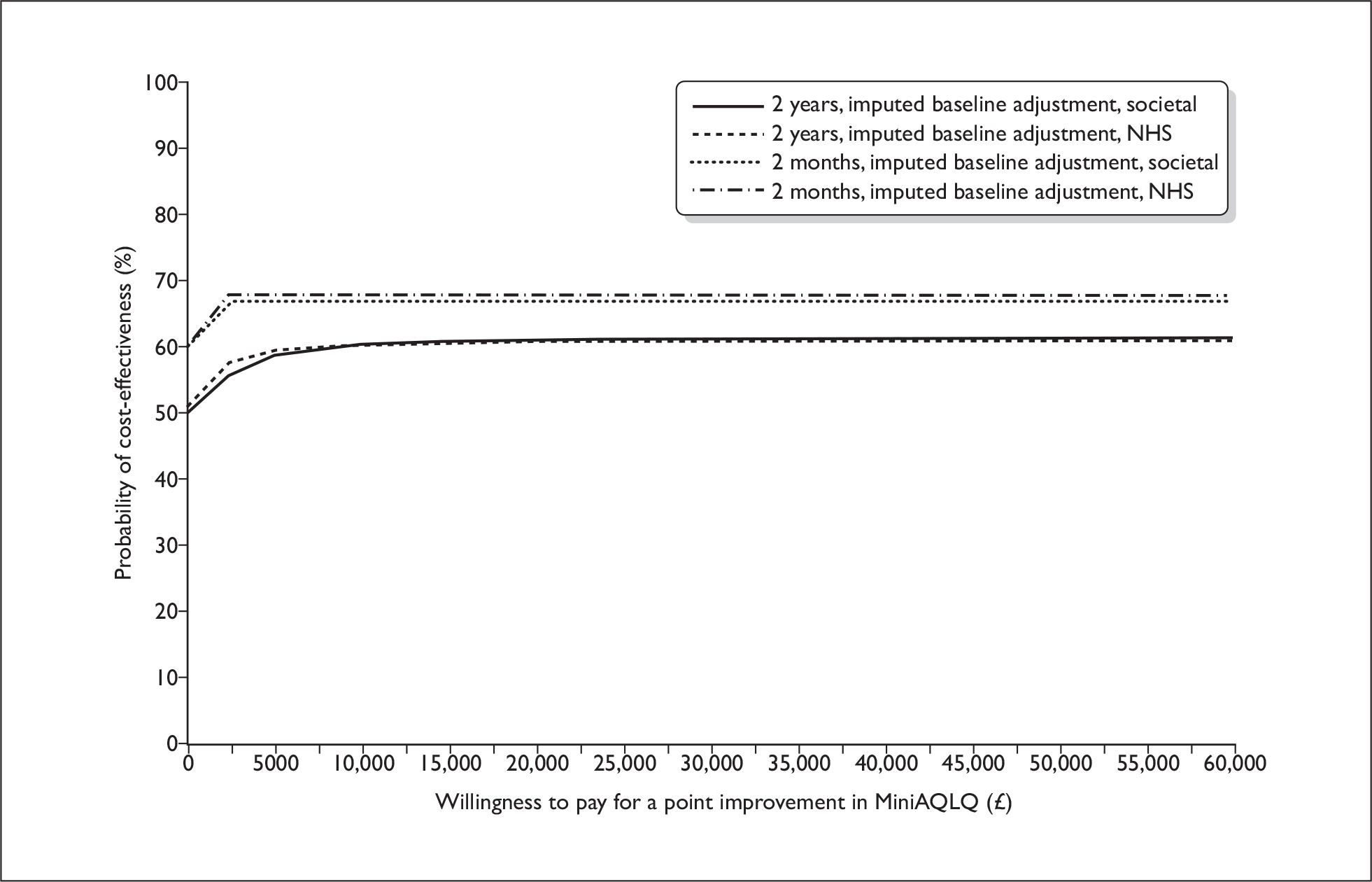
Asthma Control Questionnaire
Over 2 months (Table 40) and 2 years (Table 41), long-acting β2-agonist is, on average, a dominant strategy over leukotriene antagonist. Mean INB is negative, irrespective of willingness to pay for a point improvement in ACQ. However, there is great deal of uncertainty around this estimate (Figure 14).
| n | Cost (£) | ACQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline ACQ) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | |
| NHS | 153 | 155 | 84 | 82 | 1.616 | 1.606 | 3 | 0.010 | (LABA dominant) | 3 | 0.020 | (LABA dominant) | 4 | 0.106 | (LABA dominant) |
| Societal | 95 | 90 | 129 | 115 | 1.642 | 1.619 | 14 | 0.024 | (LABA dominant) | 6 | 0.020 | (LABA dominant) | 7 | 0.106 | (LABA dominant) |
| n | Cost (£) | ACQ | Source data only | Including imputed data | Including imputed data (adjusted for baseline ACQ) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | Inc. cost (£) | Inc. ACQ | ICER (£) | |
| NHS | 154 | 164 | 886 | 791 | 1.272 | 1.350 | 96 | –0.077 | 1241 | 111 | –0.063 | 1768 | 133 | 0.002 | (LABA dominant) |
| Societal | 94 | 96 | 1152 | 893 | 1.349 | 1.306 | 259 | 0.044 | (LABA dominant) | 213 | –0.063 | 3398 | 226 | 0.002 | (LABA dominant) |
FIGURE 14.
Step 3: INB, ACQ, INB and 95% CI are shown for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d) 2-year societal perspectives. Results based on imputed data adjusted for baseline ACQ.
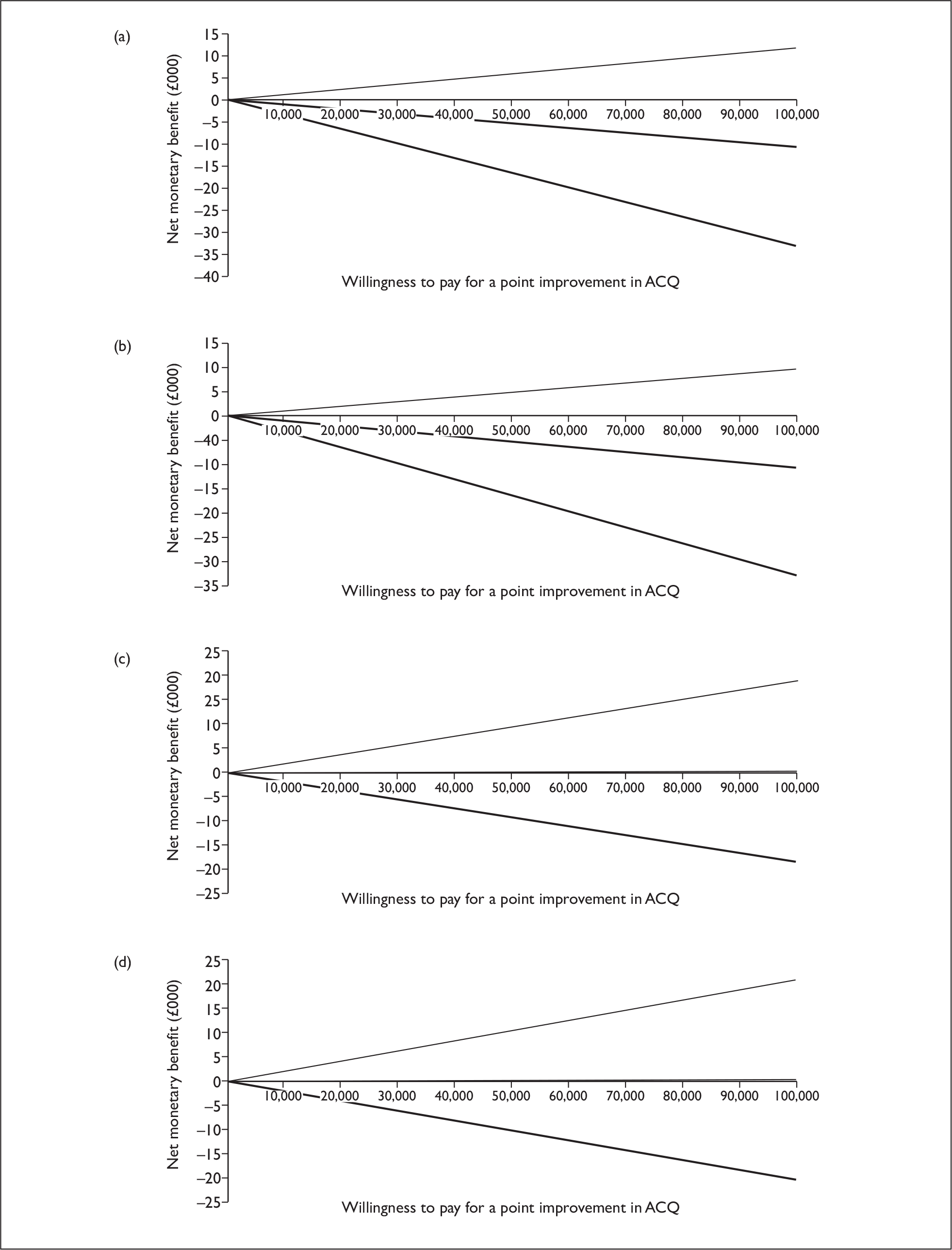
Even with a very high willingness to pay for a point improvement in ACQ, there is up to a 49% probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist in step 3 patients (depending on perspective and time horizon – Figure 15).
FIGURE 15.
Step 3: ACQ CEACs. Based on imputed, adjusted results of ACQ, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and that these outcomes took place at 2 months or 2 years. This figure indicates that over a 2-year time horizon the probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist approaches 50% as the willingness to pay for a point improvement in ACQ rises.
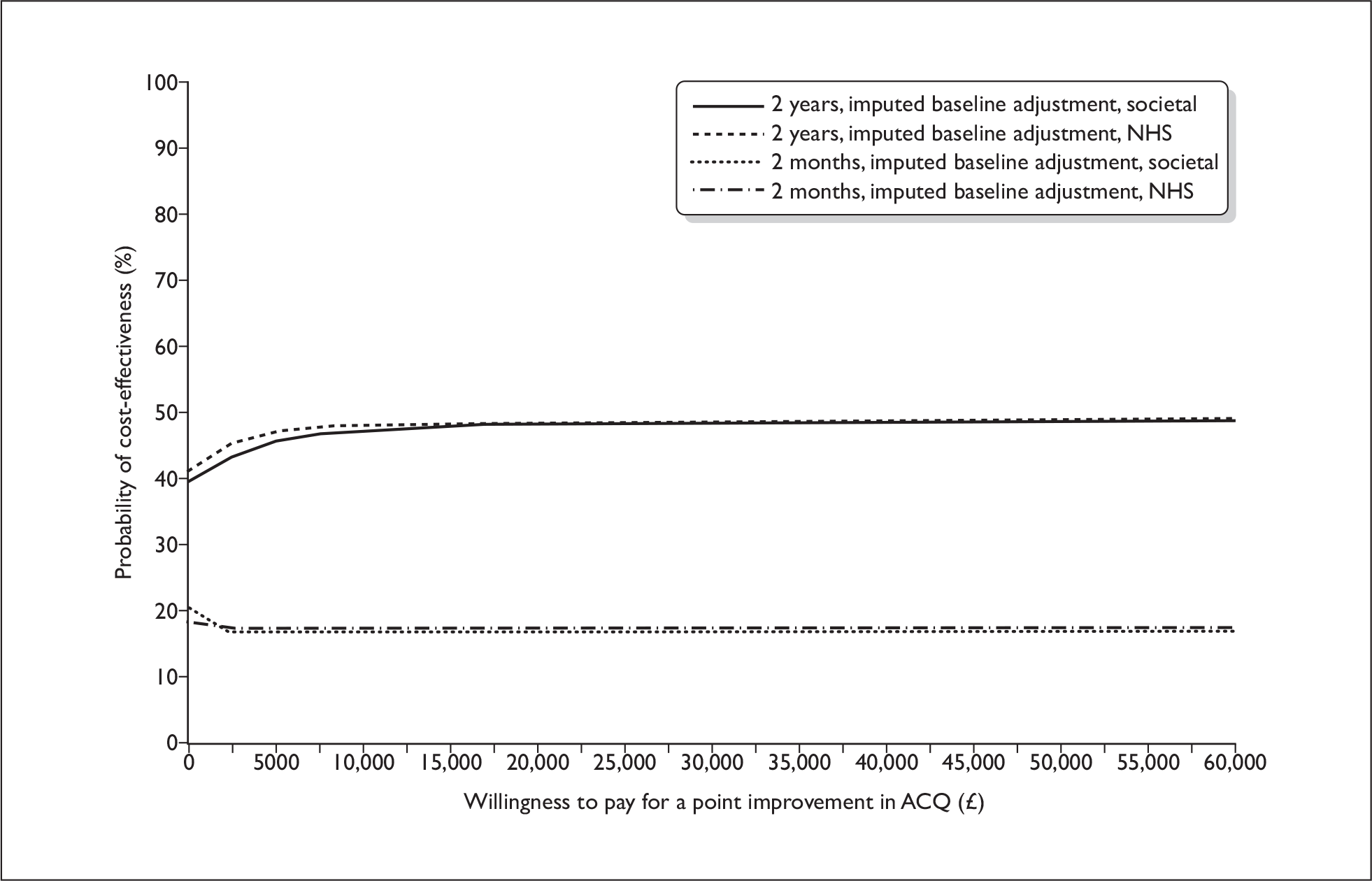
Quality-adjusted life-years (cost–utility analysis)
The incremental cost per QALY gained is between £5521 and £22,589, dependent upon perspective and time horizon (Tables 42 and 43).
| n | Cost (£) | QALYs | Source data only | Including imputed data | Including imputed data (adjusted for BL utility) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | |
| NHS | 119 | 119 | 87 | 87 | 0.122 | 0.120 | 0 | 0.001 | (LTRA dominant) | 60.00 | 24 (–143 to 204) | 3 | 0.001 | 2470 | 60.00 |
57 (–15 to –44) |
3 | 0.001 | 5521 | 54.64 |
14 (–161 to 194) |
| Societal | 77 | 74 | 117 | 126 | 0.122 | 0.119 | –9 | 0.002 | (LTRA dominant) | 67.80 | 54 (–181 to 276) | 6 | 0.001 | 6018 | 58.56 |
36 (7 to –36) |
6 | 0.001 | 12,290 | 54.10 |
9 (–155 to 191) |
| n | Cost (£) | QALYs | Source data only | Including imputed data | Including imputed data (adjusted for BL utility) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LTRA | LABA | LTRA | LABA | LTRA | LABA | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | Inc. cost (£) | Inc. QALYs | ICER (£) | P£30k (%) | INB/£30k (95% CI) | |
| NHS | 108 | 109 | 956 | 869 | 1.601 | 1.548 | 88 | 0.053 | 1643 | 81.60 |
983 (–1429 to 3449) |
111 | 0.015 | 7164 | 57.76 |
–378 (1673 to 1896) |
113 | 0.009 | 11919 | 53.16 |
154 (–2443 to 2893) |
| Societal | 72 | 70 | 1157 | 952 | 1.610 | 1.566 | 205 | 0.044 | 4668 | 68.60 |
680 (–2308 to 3547) |
213 | 0.015 | 13,769 | 54.34 |
168 (327 to 1369) |
214 | 0.009 | 22,589 | 51.56 |
142 (–2567 to 2825) |
At a typical willingness to pay of £30,000 per QALY gained, mean (95% CI) INB at 2 months is £14 (–£161 to £194) or £9 (–£155 to £191) from the NHS and societal perspectives, and £154 (–£2443 to £2893) and £142 (–£2567 to £2825) at 2 years (Tables 42 and 43, and Figure 16).
FIGURE 16.
Step 3: INB, QALYs. INB and 95% CI are shown for (a) 2-month NHS; (b) 2-month societal; (c) 2-year NHS; and (d) 2-year societal perspectives. Results based on imputed data adjusted for baseline utility.
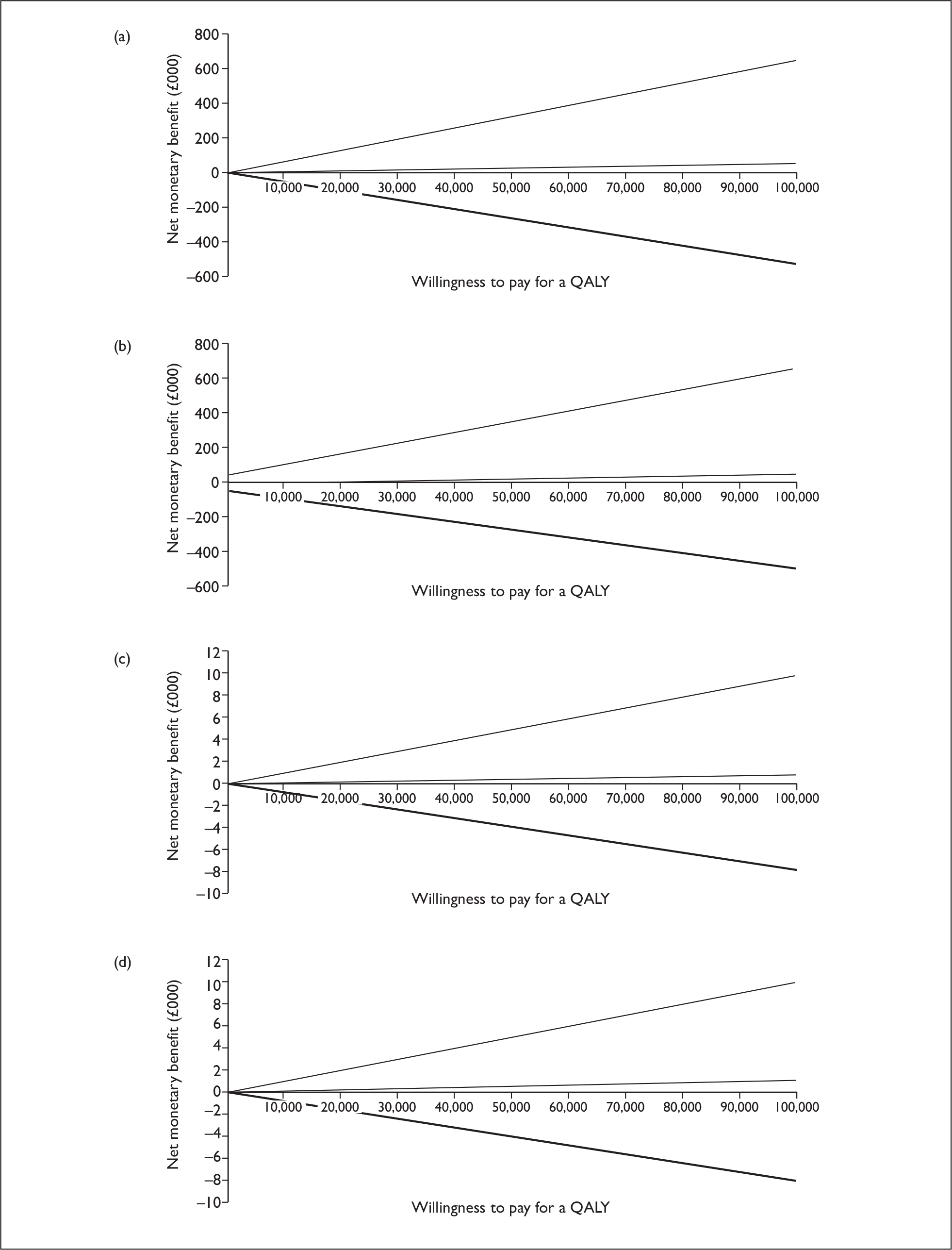
At the £30,000 threshold, there is between a 51.6% and 54.6% probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist in patients at step 3 of the national asthma guidelines (dependent on time horizon and perspective – Tables 42 and 43, and Figure 17).
FIGURE 17.
Step 3: cost–utility analysis: CEACs. Based on imputed, adjusted results of cost–utility analysis, societal/NHS indicates that results were from a societal or NHS cost perspective, respectively, and these outcomes took place at 2 months or 2 years. This figure indicates that in all cases the probability of leukotriene antagonist being cost-effective compared with long-acting β2-agonist is marginally above 50%, given a typical willingness to pay of £30,000 per QALY gained. At a willingness to pay of £20,000, the probability is between 48.5% and 54.0%, depending upon time horizon and perspective.
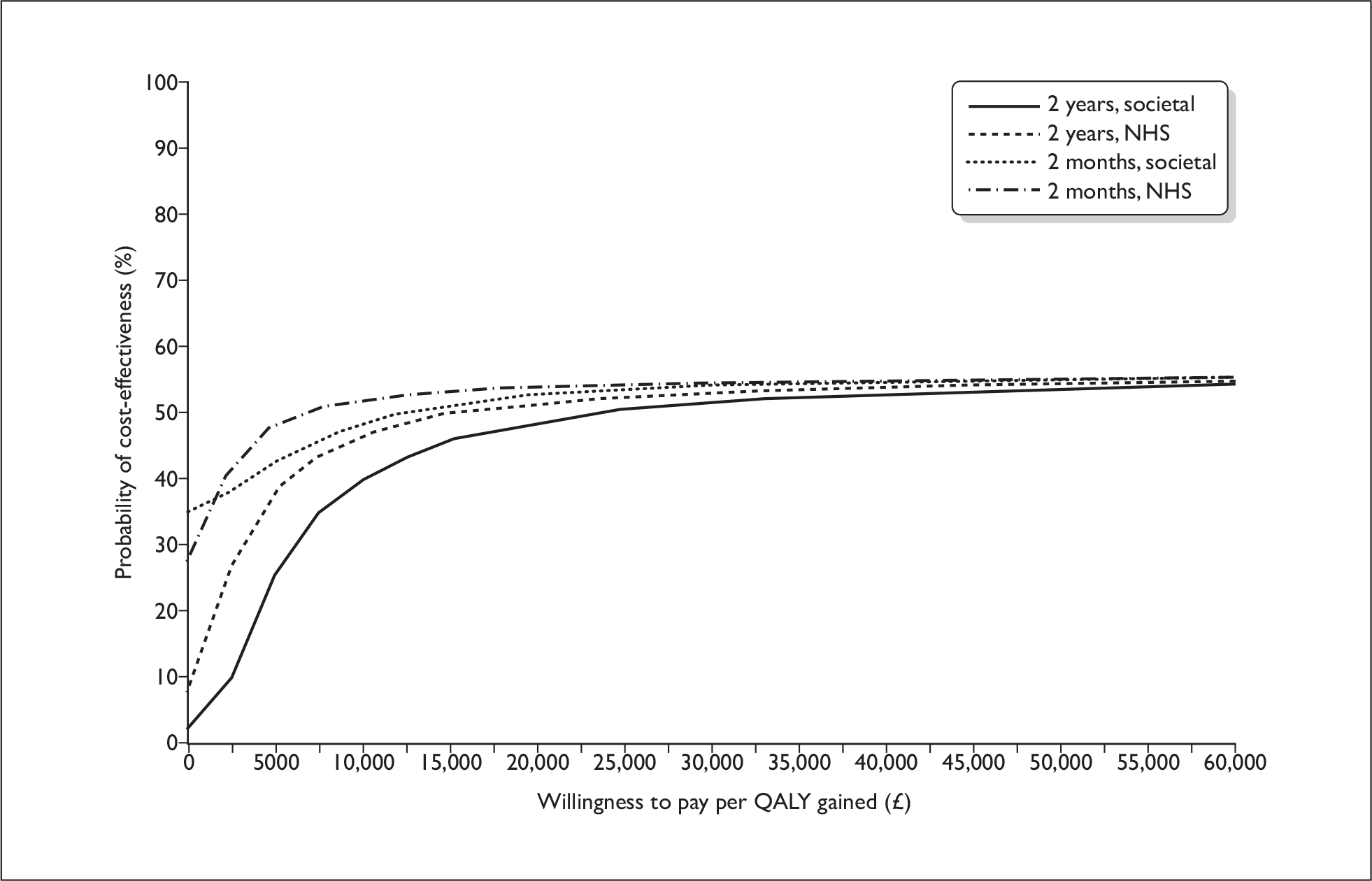
Summary of cost-effectiveness analyses
The results of the cost-effectiveness analyses are somewhat equivocal: mean INB is positive when considering MiniAQLQ, as long as the willingness to pay for a point improvement in MiniAQLQ is > £6267 (2-year time horizon, societal analysis). However, when considering ACQ as the outcome measure, mean INB is always negative, yet the point estimate of the ICER is £22,589 (which would yield a positive mean INB at a ‘typical’ £30,000 threshold). The results are therefore contradictory, depending on the outcome measure.
There is at least a 50% probability of leukotriene antagonist being cost-effective, so long as the willingness to pay for a point improvement in MiniAQLQ is, at worst, £6200, and, at best, £47 (depending upon perspective and time horizon), and for a QALY, at least £6180–£23,600.
Whether an intervention is deemed cost-effective is dependent upon this willingness-to-pay threshold. A ‘reasonable’ threshold for QALYs is thought to be in the order of £30,000. The threshold for a point improvement in MiniAQLQ or ACQ is less well established. However, the results of the cost–utility analysis suggest a 51.6–54.6% probability of cost-effectiveness at a willingness to pay of £30,000 per QALY gained.
Secondary analyses
Asthma exacerbations, hospitalisations and respiratory tract infections
No significant differences were found in the number of exacerbations or respiratory tract infections experienced by participants receiving leukotriene antagonist or long-acting β2-agonist (Table 44). Similarly, no significant difference was found in the number of consultations associated with respiratory tract infections.
| LTRA (n = 170) | LABA (n = 182) | Rate ratio (95% CI) | |
|---|---|---|---|
| Mean (SD) exacerbations over 2 years | 0.62 (1.13) | 0.61 (1.03) | 1.02 (0.74 to 1.41), p = 0.895 |
| Mean (SD) respiratory tract infections over 2 years | 1.23 (2.01) | 1.33 (1.72) | 0.93 (0.70 to 1.22), p = 0.581 |
| Mean (SD) consultations for respiratory tract infections over 2 years | 1.49 (2.62) | 1.52 (2.07) | 0.98 (0.74 to 1.30), p = 0.897 |
| Adjusted differencea (95% CI) LTRA–LABA |
|||
| Mean (SD) SABA inhalers prescribed over 2 years (inhalers/day) | 0.022 (0.020) | 0.017 (0.017) | 0.004 (0.002 to 0.006), p = 0.001 |
| Mean (SD) ICS dose (µg/day) for year 1 | 445 (20.4) | 467 (19.7) | –7.87 (–63.4 to 47.6), p = 0.780 |
| Mean (SD) ICS dose (µg/day) for year 2 | 466 (24.8) | 438 (23.9) | 42.8 (–24.0 to 109.6), p = 0.208 |
There were no hospital admissions during the first 2 months of the study. Subsequently, over the remainder of the 2 years there were three hospital admissions for four nights total in the leukotriene antagonist group, and five hospital admissions for six nights in total in the long-acting β2-agonist group.
Prescribed short-acting β2-agonist and inhaled corticosteroid
Participants receiving leukotriene antagonist were prescribed significantly more short-acting β2-agonist inhalers than participants receiving long-acting β2-agonist (Table 44). On average, participants randomised to leukotriene antagonist received 2.01 short-acting β2-agonist inhalers every 3 months compared with 1.55 short-acting β2-agonist inhalers every 3 months for those receiving long-acting β2-agonist. Over the 2-year study period an average of 16.06 versus 12.41 short-acting β2-agonist inhalers were issued to participants randomised to leukotriene antagonist and long-acting β2-agonist, respectively.
No significant change in inhaled steroid dose/day was observed from baseline to 12 or 24 months following randomisation for leukotriene antagonist or long-acting β2-agonist {leukotriene antagonist: difference at 12 months and 24 months = –15.0 [standard deviation (SD) 243] and –36.2 (SD 324) µg/day; long-acting β2-agonist: difference at 12 months and 24 months = –17.4 (SD 306) and 10.4 (SD 331) µg/day}. Similarly, no significant difference was found between the groups receiving leukotriene antagonist or long-acting β2-agonist at either time point (Table 44).
Clinic per cent predicted peak expiratory flow and domiciliary data
For clinic %PPEF, slight improvement was observed in both leukotriene antagonist and long-acting β2-agonist-treated groups at 2 months, followed by a slight decrease at 2 years. However, no significant differences between the groups were found at either the 2-month or 2-year time points (Table 45 and Figure 11).
| Measure | LTRA | LABA | p-value |
|---|---|---|---|
| Baseline |
n = 152 90.46 (80.24 to 99.67) |
n = 167 88.64 (76.67 to 99.89) |
|
| 2 months |
n = 131 93.22 (84.02 to 105.04) |
n = 142 92.78 (80.19 to 102.87) |
p = 0.451 |
| 2 years |
n = 120 91.43 (80.94 to 99.36) |
n = 136 89.68 (77.31 to 100.41) |
p = 0.563 |
Diary cards were completed by approximately two-thirds of participants at 2 months and half at 2 years. As recorded on the diary cards at 2 months, participants receiving long-acting β2-agonist had significantly higher morning and evening domiciliary PEF than participants receiving leukotriene antagonist (Table 46).
| LTRA (n = 170) | LABA (n = 182) | Difference (95% CI) LTRA–LABA, p-value | Adjusted differencea (95% CI), p-value | |
|---|---|---|---|---|
| Mean (SD) morning waking with symptoms |
n = 113 0.31 (0.34) |
n = 123 0.25 (0.32) |
0.06 (–0.02 to 0.15), p = 0.144 | 0.03 (–0.04 to 0.10), p = 0.402 |
| Mean (SD) puffs of reliever at night – original scale |
n = 101 0.91 (1.38) |
n = 110 0.60 (0.99) |
0.30 | |
| Mean (SD) puffs of reliever at night – logged scale |
n = 101 0.48 (0.53) |
n = 110 0.35 (0.47) |
0.14 (0.00 to 0.27), p = 0.050 | 0.12 (0.01 to 0.24), p = 0.036 |
| Mean (SD) morning PEF |
n = 112 399.0 (108.3) |
n = 121 419.1 (102.3) |
–20.2 (–47.4 to 7.0), p = 0.145 | –17.9 (–26.8 to –8.9), p < 0.001 |
| Mean (SD) daytime asthma symptom score |
n = 113 1.63 (1.37) |
n = 122 1.53 (1.37) |
0.10 (–0.25 to 0.46), p = 0.562 | 0.04 (–0.25 to 0.34), p = 0.778 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’ |
n = 112 1.46 (1.39) |
n = 122 1.39 (1.41) |
0.07 (–0.29 to 0.43), p = 0.709 | 0.05 (–0.26 to 0.36), p = 0.751 |
| Mean (SD) daily activity score |
n = 110 2.42 (1.28) |
n = 122 2.27 (1.37) |
0.15 (–0.19 to 0.50), p = 0.390 | 0.08 (–0.23 to 0.39), p = 0.622 |
| Mean (SD) score for interference on activities from asthma |
n = 111 1.41 (1.42) |
n = 121 1.32 (1.37) |
0.09 (–0.27 to 0.46), p = 0.607 | 0.12 (–0.19 to 0.43), p = 0.439 |
| Mean (SD) puffs of reliever during the day – original scale |
n = 108 2.45 (2.75) |
n = 118 1.67 (1.96) |
0.78 | |
| Mean (SD) puffs of reliever during the day – logged scale |
n = 108 0.98 (0.70) |
n = 118 0.77 (0.63) |
0.21 (0.04 to 0.39), p = 0.018 | 0.19 (–0.04 to 0.33), p = 0.011 |
| Mean (SD) evening PEF |
n = 112 402.0 (107.5) |
n = 122 425.2 (99.4) |
–23.2 (–49.9 to 3.5), p = 0.089 | –10.8 (–19.4 to –2.2), p = 0.014 |
| Mean (SD) PEF diurnal variability (%) |
n = 112 5.8 (4.4) |
n = 122 4.9 (3.6) |
–0.9 (–0.1 to 1.9), p = 0.085 | 0.8 (–0.05 to 1.7), p = 0.064 |
By 2 years, morning PEF was still significantly higher in participants receiving long-acting β2-agonist, although the mean difference was unlikely to be clinically significant (396 versus 420 l/minute in leukotriene antagonist and long-acting β2-agonist groups, respectively); no significant difference was found in the evening PEF (Table 47). At 2 months, participants receiving leukotriene antagonist had higher diurnal variability than participants receiving long-acting β2-agonist, although this difference did not reach significance (p = 0.064). No significant difference was found after 2 years. At 2 months, participants receiving long-acting β2-agonist required significantly fewer daytime and night-time puffs of short-acting β2-agonist than participants receiving leukotriene antagonist, although by 2 years this difference was no longer apparent. No significant differences in symptom scores were found.
| LTRA (n = 170) | LABA (n = 182) | Difference (95% CI) LTRA–LABA, p-value | Adjusted differencea (95% CI), p-value | |
|---|---|---|---|---|
| Mean (SD) morning waking with symptoms |
n = 85 0.29 (0.35) |
n = 98 0.24 (0.33) |
0.05 (–0.05 to 0.15), p = 0.288 | 0.01 (–0.07 to 0.10), p = 0.723 |
| Mean (SD) puffs of reliever at night – original scale |
n = 75 0.69 (1.04) |
n = 87 0.63 (0.87) |
0.07 | |
| Mean (SD) puffs of reliever at night – logged scale |
n = 75 0.38 (0.50) |
n = 87 0.37 (0.45) |
0.01 (–0.14 to 0.15), p = 0.897 | 0.00 (–0.14 to 0.14), p = 0.950 |
| Mean (SD) morning PEF |
n = 83 395.6 (105.9) |
n = 98 419.8 (97.0) |
–24.2 (–54.0 to 5.6), p = 0.111 | –13.7 (–25.6 to –1.8), p = 0.024 |
| Mean (SD) daytime asthma symptom score |
n = 85 1.40 (1.28) |
n = 97 1.44 (1.24) |
–0.04 (–0.41 to 0.33), p = 0.849 | –0.08 (–0.40 to 0.23), p = 0.606 |
| Mean (SD) score for daytime ‘bother from asthma symptoms’ |
n = 85 1.12 (1.19) |
n = 97 1.26 (1.27) |
–0.14 (–0.50 to 0.23), p = 0.454 | –0.06 (–0.37 to 0.26), p = 0.721 |
| Mean (SD) daily activity score |
n = 83 2.23 (1.22) |
n = 97 2.32 (1.39) |
–0.09 (–0.47 to 0.30), p = 0.666 | –0.06 (–0.41 to 0.27), p = 0.697 |
| Mean (SD) score for interference on activities from asthma |
n = 85 1.13 (1.25) |
n = 97 1.25 (1.39) |
–0.12 (–0.51 to 0.27), p = 0.551 | 0.01 (–0.31 to 0.34), p = 0.920 |
| Mean (SD) puffs of reliever during the day – original scale |
n = 84 1.89 (2.31) |
n = 95 1.49 (1.65) |
0.40 | |
| Mean (SD) puffs of reliever during the day – logged scale |
n = 84 0.80 (0.70) |
n = 95 0.73 (0.60) |
0.07 (–0.18 to 0.27), p = 0.447 | 0.08 (–0.09 to 0.25), p = 0.336 |
| Mean (SD) evening PEF |
n = 83 401.7 (106.0) |
n = 98 425.8 (96.8) |
–24.1 (–53.8 to 5.7), p = 0.112 | –5.7 (–17.8 to 6.3), p = 0.349 |
| Mean (SD) PEF diurnal variability (%) | 5.7 (4.7) | 5.2 (4.3) | 0.6 (–0.9 to 2.0), p = 0.443 | 0.2 (–1.1 to 1.5), p = 0.718 |
Secondary QOL scores and rhinitis scores
No significant differences were observed in RCP3 questions or personal objectives scores after 2 months or 2 years (Table 48). However, at both time points, these two measures showed a substantial improvement from baseline. A trend towards significance was observed in the personal objectives, with participants receiving long-acting β2-agonist achieving a higher score at 2 months. However, this benefit was lost after 2 years. The mRQLQ score was significantly better (p = 0.01) in the leukotriene antagonist than the long-acting β2-agonist group at 2 months, but was comparable in the two groups at 2 years.
| Measure | LTRA | LABA | Difference (95% CI) LTRA–LABA, p-value | Adjusted differencea (95% CI), p-value |
|---|---|---|---|---|
| 2-month outcomes | ||||
| mRQLQ |
n = 125 1.50 (1.06) |
n = 131 1.89 (1.28) |
–0.39 (–0.68 to –0.10), p = 0.01 | –0.26 (–0.50 to –0.03), p = 0.029 |
| RCP3 |
n = 150 1.40 (1.00) |
n = 154 1.25 (0.96) |
0.15 (–0.07 to 0.37), p = 0.194 | 0.15 (–0.07 to 0.37), p = 0.181 |
| Personal objectives |
n = 106 52.4 (23.6) |
n = 115 55.4 (24.5) |
–2.96 (–9.34 to 3.43), p = 0.362 | –4.64 (–10.3 to 1.04), p = 0.109 |
| 2-year outcomes | ||||
| mRQLQ |
n = 162 1.32 (1.22) |
n = 178 1.55 (1.29) |
–0.23 (–0.50 to 0.04), p = 0.10 | –0.13 (–0.38 to 0.11), p = 0.273 |
| RCP3 |
n = 167 1.01 (0.94) |
n = 181 1.14 (0.93) |
–1.01 (–1.16 to 0.87), p = 0.190 | –0.11 (–0.31 to 0.08), p = 0.255 |
| Personal objectives |
n = 120 65.9 (22.6) |
n = 146 67.4 (20.3) |
–1.51 (–6.70 to 3.68), p = 0.568 | –3.68 (–8.98 to 1.62), p = 0.173 |
Changes in treatment after randomisation
Overall, by 2 months, seven patients (4%) in the leukotriene antagonist group and none (0%) in the long-acting β2-agonist group had a change in treatment from initial randomised therapy class.Over the course of the study, 43 patients (27%) in the leukotriene antagonist group and none (0%) in the long-acting β2-agonist group had a change in treatment. The changes in treatment by 2 months and 2 years are tabulated in Table 49.
| Treatment change by 2 months, n (%) | |
|---|---|
| Participants in LABA arm | N = 181 |
| 0 (0) | |
| Participants in LTRA arm | N = 161 |
| Add LABA | 1 (1) |
| Change to LABA | 6 (4) |
| Total | 7 (4) |
| Treatment change by 2 years, n (%) | |
| Participants in ICS arm | N = 181 |
| 0 (0) | |
| Participants in LTRA arm | N = 161 |
| Add LABA | 18 (11) |
| Change to LABA | 25 (16) |
| Total | 43 (27) |
Per-protocol population (fixed treatment regime and no changes within or from randomised therapy class) analyses
Our per-protocol population was defined as those patients who were prescribed a fixed treatment regime at randomisation (i.e. no self-management plan) and who had no change in that fixed regime at any time including the final study visit, i.e. no change in device, dose or therapeutic class. After restricting the participant groups to only those meeting that definition and who had analysable data, 60 leukotriene antagonist and 80 long-acting β2-agonist participants were identified (Appendix 5). Conversely, 110 and 102 patients, respectively, received a different treatment or variable course of treatment during the 2 years. Results for the per-protocol participant groups are summarised in Appendix 5, Tables 67–74.
There were no significant differences between treatment groups in MiniAQLQ or ACQ scores for these participants (Appendix 5, Tables 69 and 70). Adjusted differences at 2 months and 2 years favoured long-acting β2-agonist with 95% CI outside the limits of equivalence [MiniAQLQ adjusted difference (95% CI) at 2 years = –0.05 (–0.36 to 0.26)].
In contrast to the intention-to-treat results, these results did not show significant differences between groups for short-acting β2-agonist prescriptions, equivalent to 12.4 versus 11 inhalers over 2 years in leukotriene antagonist and long-acting β2-agonist groups, respectively (Appendix 5, Table 72). Consistent with the intention-to-treat analyses, at 2 months the leukotriene antagonist group had significantly lower (i.e. better) mRQLQ scores than the long-acting β2-agonist group (Appendix 5, Table 74). Although the mRQLQ score was still lower at 2 years for the leukotriene antagonist than the long-acting β2-agonist group, this difference was no longer significant (Appendix 5, Table 74).
Adherence to treatment
Adherence data were analysable for 220 patients, overall, who had at least 6 months of unchanged therapy. In the leukotriene antagonist group (n = 99, or 60%), median adherence (interquartile range) to inhaled steroid was 82.1% (34.2–116.3%) and to leukotriene antagonist 90.1% (23.2–99.6%). In the long-acting β2-agonist group (n = 121, or 69%), median adherence to inhaled steroid was 64.9% (36.7–93.6%) and to long-acting β2-agonist 49.3% (20–73.9%).
Adverse events
Adverse reactions to study medications
Twenty-six adverse reactions to study medication were reported by practices participating in the study. Fifteen patients (four at step 2 and 11 at step 3) had a total of 19 adverse reactions to the leukotriene antagonist montelukast, of which one was considered by the site nurse practitioner or GP to be a ‘serious adverse reaction’ (Table 50).
| Randomised treatment | Study medication | SAR | Discontinued medication | Continued medication | Total | Recovered |
|---|---|---|---|---|---|---|
| LTRA | Montelukast | Increase in epileptic fits | 1 | – | 1 | 1 |
Two patients (both at step 2) reported a total of three adverse reactions (non-serious) to the inhaled steroid beclometasone dipropionate and a further two patients (both at step 3) reported a total of four adverse reactions (non-serious) to the long-acting β2-agonist salmeterol (Table 51). All other adverse reactions reported were consistent with the manufacturer’s product information. All patients recovered from the adverse reactions.
| Randomised treatment | Study medication | Adverse reactions | Discontinued medication | Continued medication | Total | Recovered |
|---|---|---|---|---|---|---|
| LTRA | Montelukast | Headache | 1 | – | 1 | 1 |
| Disturbed sleep | – | 1 | 1 | 1 | ||
| Not known | – | 1 | 1 | 1 | ||
| Increase in epileptic fits | 1 | – | 1 | 1 | ||
| ICS | Beclometasone dipropionate | Cough | – | 1 | 1 | 1 |
| Breathlessness | – | 1 | 1 | 1 | ||
| Symptoms of oesophagitis | 1 | – | 1 | 1 |
| Randomised treatment | Study medication | Adverse reaction | Discontinued medication | Continued medication | Total | Recovered |
|---|---|---|---|---|---|---|
| LTRA | Montelukast | Headache | 2a | – | 2 | 2 |
| Disturbed sleep | 1 | 2 | 3 | 3 | ||
| Lethargy | 2 | – | 2 | 2 | ||
| Bloating | 1 | – | 1 | 1 | ||
| Swollen fingers | 1 | – | 1 | 1 | ||
| Dry cough | 1 | – | 1 | 1 | ||
| Altered (mild) mental status | 1 | – | 1 | 1 | ||
| Not known | 2 | – | 2 | 2 | ||
| LABA | Salmeterol | Palpitations | – | 1 (half dose) | 1 | 1 |
| Tingling in arms | – | 1 (half dose) | 1 | 1 | ||
| Not known | 2 | – | 2 | 2 |
Adverse events unrelated to study medication
One patient reported an adverse reaction to Tylex (Table 52). The medication was stopped and the patient recovered. No change was made to the study medication as a result of this adverse event.
| Adverse event | Drug involved | Action | Outcome | Randomised treatment |
|---|---|---|---|---|
| Allergic reaction | Tylex | Discontinued Tylex | Recovered | Step 2, LTRA (montelukast) |
Serious adverse events unrelated to study medication
One patient, randomised to inhaled steroid in the step 2 study, died as a result of a bronchogenic carcinoma (Table 53). This was considered to be unrelated to the medication.
| Adverse event | Cause | Randomised treatment |
|---|---|---|
| Death | Bronchogenic carcinoma | Step 2, ICS (beclometasone) |
Chapter 4 Discussion
Interpretation
The results of this study provide no evidence of superiority of inhaled steroid or long-acting β2-agonist over leukotriene antagonist, nor vice versa, in patients at either step 2 or step 3, in terms of the primary end point of asthma-specific QOL (MiniAQLQ score). For initial controller therapy at step 2, the results were equivalent at 2 months. After adjusting for baseline characteristics at 2 years, the 95% CIs did include the threshold for equivalence of 0.3 in favour of inhaled steroid. This was true of the one-sided 95% CI, i.e. inferiority of leukotriene antagonist could not be excluded. Conversely, the per-protocol population (fixed treatment regime and no changes within randomised therapy class at any stage) results also included the threshold for equivalence of 0.3, but this time in favour of leukotriene antagonist. Therefore, the results were inconsistent between the intention to treat and per-protocol analyses and equivalence could not be excluded. However, any possible advantage of one over the other looks clinically insignificant.
For add-on therapy at step 3, at 2 months results were equivalent, and at 2 years the intention-to-treat analysis resulted in near equivalence of leukotriene antagonist and long-acting β2-agonist (the lower bounds marginally missing the equivalence value) with the possibility of a minor advantage for long-acting β2-agonist. The per-protocol results were consistent with this, but, again, any advantage of long-acting β2-agonist appears clinically insignificant.
We chose a conservative approach in selecting 0.3 as the threshold for equivalence or non-inferiority, because the minimum clinically important difference for MiniAQLQ is 0.5. 51 Therefore, although a difference from 0.3 to 0.5 does not meet our study definition of equivalence, the outer bounds of the CIs for the differences are less than the minimum that is clinically important difference for this parameter.
There were no significant differences between treatment groups in results for most of the secondary end points, including, most importantly, the two markers of asthma control, ACQ score and exacerbation rate. The 95% CIs for differences in ACQ score were well within the 0.5 minimum clinically important difference for both step 2 and 3 trials at both time points and in both intention-to-treat and per-protocol analyses. In addition, there were no significant differences in secondary health-related QOL measures, asthma symptoms as measured by diary card, the RCP3 questions and respiratory tract infections. Hospitalisations were infrequent in both step 2 and 3 trials.
At step 2, no significant differences were found in short-acting β2-agonist prescriptions between arms. At step 3, short-acting β2-agonist prescriptions over 2 years were significantly greater in the leukotriene antagonist arm than the long-acting β2-agonist arm of the intention-to-treat population but not the per-protocol population. Calculations of short-acting β2-agonist prescriptions in this study were based on the numbers of inhalers prescribed and do not reliably represent actual short-acting β2-agonist use, because prescribed inhalers may not have been dispensed or used. Instead, ACQ scores, which incorporate a question on actual short-acting β2-agonist use (puffs/day) during the prior 7 days, were not significantly different between leukotriene antagonist and long-acting β2-agonist groups. Composite measures, such as the ACQ, are recommended for evaluating asthma control by the current European Respiratory Society (ERS)/American Thoracic Society (ATS) task force, which notes the challenges in measuring and comparing short-acting β2-agonist use in clinical trials, suggesting that this outcome be derived from a diary or visit-based questionnaire. 78 Statistically significant differences in diary-recorded lung function between treatment groups in the step 3 trial were small and unlikely to be of clinical significance.
The number of participants included in the per-protocol analysis for both study arms was small [in the step 2 study 65/145 (45%) and 82/155 (53%) of the LTRA and ICS arms respectively, and 60/169 (36%) and 80/181 (44%) of the LTRA and LABA arms respectively in the step 3 study] because of substantial use of self-management plans with prescription instructions permitting adjustments to dosage, prescriptions which were technically changes (often within randomised class) but which were the result of a change of practice prescription policy, or prescriptions from an encounter with a non-study aware provider who made a change as allowed as per normal asthma management, often only for a single prescription issue, and which thus did not truly represent a substantial change in therapy. Nonetheless, these changes resulted in participants being excluded from the per-protocol group. While large and clinically as well as statistically comparable improvements from baseline were seen in all treatment groups investigated in this study, final mean outcomes are still not optimal and suggest that further intervention is required for many of the patients studied.
From a health economic perspective, mean results indicate that in a primary care setting, at step 2, inhaled steroids are more cost-effective than leukotriene antagonists due, principally, to the greater acquisition costs of leukotriene antagonists than inhaled steroids. At step 3 of the guidelines, results are somewhat inconsistent. Whilst leukotriene antagonists were slightly more expensive than long-acting β2-agonists, patients receiving leukotriene antagonists had marginally better overall health-related QOL (as measured in QALYs), and hence we estimate a mean incremental cost per QALY gained of £22,589 (societal perspective, 2-year time horizon), with a probability of between 51.6% and 54.6% of leukotriene antagonists being cost-effective compared with long-acting β2-agonist at a willingness to pay of £30,000 per QALY gained. There was no statistically significant difference in INB at any threshold willingness to pay for a point improvement in MiniAQLQ or ACQ, or at a threshold of £30,000 per QALY gained (the exception being at low thresholds for QALYs in step 2 patients, for which the upper bound for the 95% CI for INB is negative – see Figures 6, 8, 10, 13, 15 and 17). Mean results based on ACQ also suggested that long-acting β2-agonist dominated leukotriene antagonist.
In the step 2 trial, we observed that, by 2 months, patients receiving leukotriene antagonist had received approximately twice as many NHS contacts as their inhaled steroid counterparts, and that the majority of the contacts were in primary care. Whether this was related to the issuing of prescriptions for leukotriene antagonist and a greater perceived need to follow the patient, given that leukotriene antagonists are rarely used in the UK as first-line anti-inflammatory therapy, is unknown. However, given that leukotriene antagonists are available only in 28-day packs, compared with a 200-dose inhaler that could sustain a patient for up to 3 months, the likelihood of greater follow-up in the leukotriene antagonist group to reissue prescriptions is to be expected due to repeat prescriptions being used as a trigger for review in many practices. This explanation is further supported by the lack of difference in ACQ score and exacerbations. If lack of familiarity with this class of therapy contributed to consultations this would be likely to be a smaller factor in the future and reduce the cost of treatment to the NHS of using a leukotriene antagonist.
Indirect costs are costs attributable to lost productivity and/or time off work due to ill health. Our results indicate that over the longer time horizon mean indirect costs are lower for leukotriene antagonist versus inhaled steroid patients at step 2 but higher for leukotriene antagonist versus long-acting β2-agonist at step 3. Although we cannot exclude chance in explaining these findings (and response rate to time off work questions was poor), it should be noted that in step 2 patients at 2 years the hours of work lost per patient randomised to inhaled steroid were lower than those lost per patient randomised to leukotriene antagonist, yet the cost is slightly higher. This apparent contradiction is due to the differential timing of costs and the effect of discounting: a greater proportion of the time off work was reported for the inhaled steroid group in the first year.
A key driver of the cost-effectiveness of one drug compared with another is usually the acquisition cost. At current prices, we estimate a mean ICER of £22,589 in step 3 patients. If the price of leukotriene antagonists falls following patent expiry, the ICER will also fall and the probability of their being cost-effective compared with long-acting β2-agonists in these patients (step 3) will rise.
Study strengths and limitations
Conducting a pragmatic randomised control trial in a primary care setting has advantages and disadvantages over conducting a randomised controlled trial as a clinical and explanatory clinical trial.
Generalisability
Conducting this study in a ‘real-life’ setting has enabled this project to collect valuable information about outcomes and the costs associated with the management of asthma. To ensure that we maintained scientific validity while minimising the impact of the study on the day-to-day management of asthma, we used a concealed randomised allocation of participants to the two treatment arms, using a telephone automated dial-up centre, standardised procedures for the recording and collection of outcomes data (by non-clinicians blinded to the randomisation) and blinded data analysis.
There is a substantial body of evidence that suggests that outcomes in a clinical trial setting may not be matched in real life, in particular because patients in clinical trials are highly selected and < 10% of outpatients with asthma meet trial selection criteria. 79,80 Indeed, as depicted in Table 54, the baseline characteristics of patients in this study differed in several respects from those of patients in the Gaining Optimal Asthma controL (GOAL),81 one of the largest, long-term asthma studies undertaken in adults in the last few years. Patients in the present study had similar health-related QOL impairment, but less lung function impairment and were more likely to be smokers.
| Current study, step 2 (n = 306) | GOAL, stratum 1 (n = 1098) | Current study, step 3 (n = 352) | GOAL, stratum 2 (n = 1163) | |
|---|---|---|---|---|
| Sex (% female) | 51 | 57 | 63 | 59 |
| Age, mean (SD) | 45.8 (16.4) | 36.3 (15.6) | 50.4 (16.0) | 40.4 (16.5) |
| MiniAQLQ/AQLQ score | 4.7 (0.9) | 4.4 (1.0) | 4.5 (1.0) | 4.6 (1.1) |
| Lung function, %PPEF | 86 | 77 | 90 | 78 |
| Per cent reversibility | 8.9 (9.8) | Median = 22a | 8.7 (9.8) | Median = 22a |
| Current smoking (%) | 22 | 9b | 17 | 6b |
| Dropout rate (%) | 4.2 | 15.4 | 3.4 | 15.4 |
We are confident that the generalisability (external validity) of this multipractice trial is high. The conduct of this study in a patient’s own primary care practice by their normal GP and practice nurse retained the ‘real-life’ setting, thereby enabling the generalisability of our results to primary care. Conversely, the fact that therapy was administered in open-label fashion, and provision of asthma care was not dictated by study design, could reduce the internal validity of the study, as the risk of error or bias increases.
Our choice of primary outcome measure was made because the asthma-specific QOL is a patient-centred outcome, which is increasingly recognised as reflecting the impact of asthma. Our secondary outcomes focused on asthma control as measured by the ACQ and exacerbations of asthma, this being in line with the latest ERS/ATS task force on outcome measures for studies of asthma. 78
The broad inclusion criteria for this study meant that active smokers, who are typically excluded from clinical trials, were included in our study population in proportions similar to reported asthma population norms for the UK. This exclusion criterion is usually included in clinical trials, as increasing evidence suggests that active smokers may not respond to asthma treatments to the same extent or in the same way as non-smokers. 82–84 Also, we did not use as an entry criterion a minimum of a 15% increase in FEV1 above baseline following 400 µg salbutamol, which is one that is conventionally used in clinical trials designed to evaluate asthma therapies. Due to time constraints in general practice, the minimum of 20 minutes required to perform this test often prohibits its use in ‘real life’. The omission of this criterion means that a small proportion of participants included in our study population may have had a mix of asthma and chronic obstructive pulmonary disease. Again, this reflects real life more closely and therefore increases the external validity of this study.
To reflect real-life management, active monitoring (e.g. dose or pill counting) was not included in the design of this study. Instead, the rate at which prescriptions are refilled for asthma therapy is used in primary care to monitor disease stability and adherence to treatment. This indirect measure of adherence was included in the design of the study resulting in our results being highly generalisable to real-life primary care management of asthma. In an explanatory clinical trial, adherence to treatment is often much higher than in primary care, typically because of intensive monitoring. This often generates disparities between the apparent outcomes of a clinical trial and the benefits afforded by the same treatment in real life.
A limitation of this study was that by 2 years many patients were switched from initial randomised therapy to alternative therapy due to a range of factors including practice protocols for inhalers and chlorofluorocarbon transition (6 out of 126 at step 2; 31 out of 132 at step 3). However, few patients had changed therapy before 2 months and thus results at 2 months can be considered to represent the efficacy of assigned therapy.
Some patients randomised to leukotriene antagonist, on being reviewed by a GP at their practice who was unfamiliar with the study, were changed to inhaled steroid or long-acting β2-agonist, as per normal clinical protocol depending on their study arm. In addition, because of shorter durations of drug supplies in those provided with a leukotriene antagonist, greater review resulted, providing greater opportunities to change therapy. Whilst no difference in exacerbations or objective markers of asthma control was found, clinical records suggested that many patients had a change in therapy due to current symptoms. It is difficult to interpret whether this is due simply to the variable nature of asthma or ongoing poor asthma control.
Poor adherence to the completion of PEF diary cards was found in both studies, but was most pronounced in the step 2 trial in which only one-third of patients completed the diary cards throughout the study. Whether poor adherence to the completion of symptom diary cards is a reflection of poor adherence in general, is unknown. While symptom diary cards for predicting subsequent episodes of poor asthma control85 and asthma control questionnaires for predicting health-care utilisation86 have been suggested as useful tools, they are useful only when patients are willing to complete them. Further work is required to improve the uptake of symptom diary cards as a means of monitoring disease severity in patients with mild to moderate asthma.
Ideally, we would have determined expenditure on prescription medications other than the randomised treatments. However, the wide use during the study of combination devices that codeliver an inhaled steroid and long-acting β2-agonist (for example Seretide contains fluticasone and salmeterol, and Symbicort contains budesonide and formoterol) prevented the isolation of the cost of a long-acting β2-agonist from the cost of inhaled steroid. Indeed the pragmatic nature of the study design placed no restriction on the antiasthma medications that could be prescribed. However, it is reasonable to conclude that for the step 2 trial, the significantly higher cost of prescribed medications received by the leukotriene antagonist randomised group compared with the inhaled steroid control group could at least, in part, be due to the higher relative cost of a leukotriene antagonist (∼£25 per 28-day course) compared with low-dose inhaled steroid (typically £8 per 28-day course). For the step 3 trial, the combination of fluticasone or budesonide (at 800 µg beclometasone dipropionate equivalent dose) with a leukotriene antagonist amounts to ∼£47 for a 28-day course, compared with ∼£38 for an equivalent 28-day course of either Seretide or Symbicort. This difference may at least, in part, be responsible for the significantly higher cost of prescription medications for the leukotriene antagonist group than the long-acting β2-agonist group.
Smoking and response to asthma therapies
Active smoking has been shown to reduce the anti-inflammatory efficacy of inhaled steroids. 82,83 As the anti-inflammatory action of long-acting β2-agonist reported in vitro has not been confirmed in vivo, leukotriene antagonists may provide an alternative anti-inflammatory treatment for asthma in smokers. Indeed Lazarus and colleagues84 recently reported that mild asthmatics who were also active smokers had a significantly lower response to inhaled steroid than non-smoking mild asthmatics. However, the active smokers had a significantly greater response to the leukotriene antagonist montelukast than the non-smoking patients, suggesting that in contrast with inhaled steroid, smoking does not significantly affect the action of the leukotriene antagonist montelukast. Whether this difference reflects changes in the mediation of airway inflammation in smokers or not, is not known. Furthermore, as Lazarus and colleagues84 conducted their study under clinical trial conditions, whether comparable results would be found under ‘real-life’ primary care conditions is unknown.
Comparison with prior studies
To our knowledge, there have been no other published pragmatic, head-to-head studies comparing leukotriene antagonist and inhaled steroid at step 2 or leukotriene antagonist and long-acting β2-agonist as add-on to inhaled steroid at step 3 for patients with asthma in primary care. Specifically, prior studies have enrolled selective patient populations, requiring evidence of airway reversibility, substantially impaired lung function and/or excluding patients with concomitant conditions or who smoke. They have also suffered from relatively high dropout rates, which may influence intention-to-treat approaches to analysis. Nonetheless, results of longer-term studies could be of relevance in comparison with the present study.
At step 2, open-label treatment for 36 weeks with fluticasone or montelukast gave comparable results for some patients with mild asthma, whereas fluticasone improved asthma control more than montelukast for patients who had decreased lung function and greater albuterol use at baseline. 87 In another study, the effectiveness of montelukast and inhaled beclometasone was similar over 2+ years of open-label treatment, and the authors speculated that the initially greater mean effect of beclometasone on lung function was offset over time by better adherence to orally administered montelukast. 48 We found that adherence to treatment with leukotriene antagonist was substantially better than that to inhaled therapy by patients in this study who had at least 6 months of unchanged therapy. At step 2, median adherence was 61% and 41% to leukotriene antagonist and inhaled steroid, respectively. At step 3, median adherence was substantially higher in the leukotriene antagonist arm than in the long-acting β2-agonist arm, both to inhaled steroid (82% versus 65%) and to add-on therapy (90% with montelukast versus 49% with long-acting β2-agonist).
With regard to step 3, a recent systematic review looking only at studies of ≥ 12 weeks’ duration comparing montelukast with salmeterol as add-on to inhaled steroid found that while salmeterol may be more effective with regard to most clinical outcomes in the medium term, over 48 weeks, the proportions of patients with ≥ 1 exacerbation were similar, as were hospitalisation and emergency treatment rates. 36 The rate of serious adverse events over 48 weeks was significantly higher with add-on salmeterol; thus, montelukast may have a better long-term safety profile.
Prior reviews of health economic studies in asthma have pointed out the need for longer-term studies using a pragmatic trial design and outcome measures that reflect asthma control and are clinically meaningful and relevant to patients. 88,89 We believe that the design of this study addresses that need and provides results meaningful for decision-makers.
Statistical issues
Missing data are a limitation in any clinical trial. This is a particular issue in economic evaluations, where, typically, not only are multidimensional QOL and other outcome measures collected, but complex resource use questionnaires may also be required. Indeed, in this study, we collected data on the costs associated with prescription and over-the-counter medications, NHS resources and time off work. The number of observations for which both outcome and cost data were available is therefore less than the number of observations for either outcomes or cost data alone.
We used Rubin’s multiple imputation technique76 to handle missing data. Imputation of missing values is feasible in this study and desirable as while there were a large number of observations with incomplete data, the actual number of data elements missing from each individual observation was small [218/683 patients (32%) had complete data, yet 514/683 (75%) had only four or fewer of the 13 data items missing]. The complete case analysis therefore excludes a lot of valid data. The particular strength of Rubin’s multiple imputation approach is that it acknowledges that missing values are uncertain, and therefore estimates several possible values for each (five imputations are usually considered sufficient76). It therefore provides a better characterisation of uncertainty than single-imputation techniques.
Nevertheless, the use of multiple imputation rests on a number of assumptions. Firstly, that the data are at least missing at random (that is, the probability that an observation is missing can depend on the observed variables, but not on the missing variable itself), and, secondly, that the data follow a multivariate normal distribution.
If data are not missing at random then, in principle, the missingness process could be modelled. However, this adds to the (already substantial) complexity of the model and studies have shown that even when ‘missing at random’ is violated, multiple imputation may still be superior to other approaches. 90 Furthermore, multiple imputation may provide a sufficient approximation of missing data with appropriately transformed variables, and it is suggested that even binary variables may be approximated by estimating under a normal assumption and rounding the continuous values. 91
We presented results of the economic evaluation in terms of the ICER. Whether or not an intervention is deemed cost-effective depends on whether or not the ICER is below some threshold of willingness to pay for that unit of outcome. Where the unit of outcome is QALYs gained, a threshold of approximately £30,000 is considered a de facto standard. However, such a threshold for point improvement in MiniAQLQ and ACQ is currently undefined. This has implications for representing uncertainty in the estimate of cost-effectiveness because a standard 95% CI is not necessarily defined for the ICER due to its ratio properties. We therefore calculated CEACs as well as the INB and its associated CI. However, to estimate a meaningful value of the INB requires knowledge of the threshold, which for MiniAQLQ and ACQ is unknown. Therefore we presented INB based on MiniAQLQ and ACQ plotted for an arbitrarily wide range of values (see Figures 6, 8, 13 and 15), rather than stating a point estimate (with CI) in Tables 14–17 and 37–40.
Further study
There are several validated assessment tools that are currently used for different aspects of asthma compliance and control. In addition to the Juniper ACQ,62,64 MiniAQLQ,50 EQ-5D71 and RCP3 questions68,69 that we used here, additional measures that have been used to evaluate asthma compliance and control include the Beliefs about Medicines Questionnaire,92 the Illness Perception Questionnaire,93 the Medication Adherence Report Scale (R. Horne, University of London, 2004, personal communication), and the Satisfaction with Information about Medicines Scale. 94 However, a limitation of these tools is that no one single measure allows the evaluation of patient perceptions about their illness and therapy, and current symptoms, adherence, side effects and control. In addition, the RCP3 questions is a set of questions that has not been validated. The development of a unified and yet easily performed test that would aid in the assessment of all of these areas would provide a valuable tool for both research use as well as clinical management of patients. A Minimal Asthma Assessment Tool was developed alongside these trials, partially utilising data collected from the patient-reported outcome measures. 95
Twenty-eight in-depth interviews have also been conducted and are currently being analysed to understand patients’ perceptions of preventative therapies. This substudy has been described in a PhD thesis96 and is being analysed for potential further publication.
Chapter 5 Conclusions
Results of this pragmatic trial in UK primary care were equivalent with regard to asthma-specific QOL (MiniAQLQ) at 2 months after commencing controller therapy with leukotriene antagonist or inhaled steroid (step 2 of the BTS guidelines). Our equivalence criterion for MiniAQLQ was not met at 2 years; however, there were no statistically significant differences between treatment groups at this time. There were no differences in asthma control measures (ACQ score and exacerbations) at 2 months or 2 years; thus, any possible advantage of one over the other appears to be clinically unimportant. All treatments were associated with substantial mean improvements which may at least in part have been due to regression to the mean or treatment effects. At 2005 UK prices of leukotriene antagonist and inhaled steroid, leukotriene antagonist was not a cost-effective alternative to inhaled steroid at step 2.
Results of add-on therapy with leukotriene antagonist or long-acting β2-agonist for patients with uncontrolled asthma already receiving inhaled steroid (step 3) were equivalent at 2 months (step 3 of the BTS guidelines), and at 2 years almost met our equivalence criterion. There were no significant differences between treatment groups in ACQ score or exacerbations. Leukotriene antagonist was of borderline cost-effectiveness compared with long-acting β2-agonist.
Implications for health care
The evidence suggests that while any advantage of one treatment over the other appears to be clinically unimportant, leukotriene receptor antagonists are unlikely to be a cost-effective alternative to inhaled corticosteroids, at 2005 prices, as initial asthma controller therapy at step 2. In addition, the evidence suggests that leukotriene antagonists may be clinically equivalent to long-acting β2-agonists as add-on to inhaled steroids in terms of QOL as well as secondary measures, and, furthermore, suggests that leukotriene antagonists could be repositioned as an equal alternative to long-acting β2-agonists at step 3 of the BTS guidelines. When generic leukotriene antagonist formulations become available in the next few years their cost-effectiveness as an alternative to ICS may justify further evaluation, particularly in the subgroup of patients with limited impairment of lung function, those newly diagnosed with asthma to minimise inhaler education and those with fears about inhalers or inhaled steroids.
Recommendations for research
-
Establish in primary care, whether leukotriene antagonists will be more or less beneficial than inhaled steroids alone or as an add-on to inhaled steroids in treating patients with asthma who are also active smokers.
-
Determine why the ACQ correlates more poorly with economic outcomes of asthma than the MiniAQLQ and EQ-5D.
-
Understand further the reasons why patients were switched from study medication when there was no real clinical indication to do so, and examine ways to minimise this happening in future pragmatic primary care-based clinical trials.
Acknowledgements
We gratefully acknowledge the support and assistance of many who have helped this study, including:
-
The participants, who were willing to share their experiences to extend our knowledge in this area.
-
The GPs, nurses and administrative staff in the participating practices (as listed below), with particular thanks to: Leslie Hand, Pauline Hughes, Val Newall, Jackie Rooks-Maynard, Anne Sibley, Lisa Tighe, Jenny Triegaardt and Jenny Willington.
-
Data management and research staff: Philip Archer, Kate Ashton, Wayne Bolt, Tony Dyer, Kimberly Garrison, Julie Houghton, Emma Koro, Heather Leishman, Georgina Munzer, Quynh Nguyen, Sasha Rust-Andrews, Anna Seaton, Fletcher Sewall, Heather Tuddenham and Xiaohong Zheng. Special thanks go to Carole Bull and Linda Kemp.
-
Individuals from other organisations whose ideas and support have been important in the design and implementation of the study include: Jon Bell, Don Haynes, Mark Levy, Helen Macdonald, Peter Richmond, Clare Symms and Liz Wakerly.
-
We appreciate the practical support for research in general practice provided by the Suffolk and Norfolk Research Network (SAND) and the Norfolk PCT Research Office, and other PCTs and the participating GP practices, listed below.
-
Editorial support: Elizabeth V. Hillyer and Martha Joseph.
We gratefully acknowledge support for the implementation of the study from Clement-Clarke International, and unrestricted educational grants from Merck Sharp & Dohme Ltd, AstraZeneca Ltd, and Respiratory Research Ltd, who contributed to excess NHS costs incurred in undertaking the study.
Participating practices
Thorpewood Surgery, Norwich; Bacon Road Medical Centre, Norwich; Drayton and St Faith Medical Practice, Drayton; Botesdale Health Centre, Botesdale; Fakenham Medical Practice, Fakenham; Beccles Medical Centre, Beccles; Siam Surgery, Sudbury; Beach Road Surgery, Lowestoft; Grimston Medical Centre, Grimston; Cutlers Hill Surgery, Halesworth; Mattishall Surgery, Mattishall; Aldborough Surgery, Norwich; Needham Market Country Practice, Needham Market; Costessey Medical Centre, Old Costessey, Norwich; Attleborough Surgeries, Attleborough; Coltishall Surgery, Coltishall; Bungay Medical Practice, Bungay; South Quay Surgery, Great Yarmouth; Millwood Surgery, Bradwell, Great Yarmouth; Lattice Barn Surgery, Ipswich; Leiston Surgery, Leiston; Harleston Medical Centre, Harleston; East Thurrock Medical Centre, Grays; Stowmarket Health Centre, Stowmarket; Orchard Medical Centre, Ipswich; Church Plain Surgery, Loddon; Holt Medical Practice, Holt; Mersea Road Surgery, Colchester; Birchwood Surgery, North Walsham; Leighton Road Surgery, Linslade; Kingswood Medical Centre, Basildon; Parish Fields Practice, Diss; Barrow Hill Surgery, Bury St Edmunds; Little Waltham Surgery, Chelmsford; John Tasker House, Great Dunmow; Yaxley Group Practice, Yaxley, Peterborough; James Fisher Medical Centre, Bournemouth; Neera Medical Centre, Stanford-le-Hope; Hethersett Surgery, Hethersett; The White House Surgery, Weston, Southampton; West Pottergate Health Centre, Norwich; Grays Surgery, Grays; Laindon Health Centre, Basildon; Rigg-Milner Medical Centre, East Tilbury; Sheringham Health Centre, Sheringham; The Barn Surgery, Gillingham; Lynwood Health Centre, Romford; The Burnhams Surgery, King’s Lynn; Angel Hill Surgery, Bury St Edmunds; Framfield House, Woodbridge; Hoveton & Wroxham Medical Centre, Hoveton; The Woottons Surgery, King’s Lynn; Rookery Medical Partnership, Newmarket; Wells Health Centre, Wells Next The Sea; Wood Lane Surgery, Hornchurch; Capital Road Surgery, Higher Openshaw, Manchester; The Witham Health Centre, Witham.
Contribution of authors
David Price (Professor, Primary Care Medicine) was involved in original design and grant submission, management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication. Stanley Musgrave (Research Associate, Norwich Medical School) was involved in study implementation, management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication. Ed Wilson (Lecturer, Health Economics), was involved in data validation, analysis plan production, interpretation of data, study report and final publication. Erika Sims (Research Fellow, Health Economics) was involved in management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication. Lee Shepstone (Professor, Medical Statistics) was involved in original design and grant submission, management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication. Annie Blyth (Research Associate, Norwich Medical School) was involved in study implementation, management and steering committee activity, data validation, study report and final publication. Jamie Murdoch (Research Associate, School of Nursing and Midwifery) was involved in study implementation, management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication. Miranda Mugford (Professor, Health Economics) was involved in original design and grant submission, management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Elizabeth Juniper (Professor Emeritus, Clinical Epidemiology and Biostatistics) was involved in original design and grant submission, management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Jon Ayres (Professor, Environmental and Respiratory Medicine) was involved in original design and grant submission, management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Stephanie Wolfe (Respiratory and Research Nurse) was involved in original design and grant submission, management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Daryl Freeman (General Practitioner) was involved in study management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Alistair Lipp (Director, Public Health) was involved in study management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Richard Gilbert (General Practitioner) was involved in study management and steering committee activity, analysis plan production, interpretation of data, study report and final publication. Ian Harvey (Professor and Dean, Faculty of Health) was involved in original design and grant submission, management and steering committee activity, data validation, analysis plan production, interpretation of data, study report and final publication.
Conflicts of interest
David Price has consultant arrangements with Astra Zeneca, GlaxoSmithKline, Merck, Sharpe and Dohme, Schering Ploughm and Teva; has grants/research support from AstraZeneca, GlaxoSmithKline, Merck, Sharpe and Dohme, Mundipharma, Novartis, Schering Plough and Teva; and is a member of the speakers’ bureau fgor GlaxoSmithKline, Merck, Sharpe and Dohme, Mundipharma, Novartis, Schering Plough and Teva.
Stanley Musgrave owned stock in Merck Sharpe and Dohme (MSD) within 3 years of beginning this work. He disposed of that stock prior to beginning this work and has had no further financial interest in MSD. During the time that he owned MSD stock he had no role in the preparation of this study. He has grants/research support from MSD and AstraZeneca, and Altana Pharma.
Ed Wilson has received a consultancy fee from a manufacturer of a budesonide inhaler (Meda Pharmaceuticals, 2006).
Erika Sims has received funding from MSD and AstraZeneca to attend international conferences. She has previously undertaken research studies sponsored by MSD, although the funding for these trials did not support her salary.
Elizabeth Juniper has consultant arrangements with GlaxoSmithKline and Astra Zeneca. She also has stock/other equity ownership in GlaxoSmithKline and Pfizer; and is a copyright holder of the MiniAQLQ, ACQ and MiniRQLQ. During the last 5 years she has had financial support from Johnson & Johnson, Schering Plough, Medpointe Pharma, CMP Therapeutics, Alterhealth, Pierre Fabre, GlaxoSmithKline, Munipharma, Ception Therapeutics, Sunten Phytotech, UCB Pharma, Activus Pharma, Novartis, Wyeth, Allergopharma, Airsonett, Embria Health Sciences, CV Technologies, Kalobios, Stallergens, AstraZeneca, Alk Abello, Medicinova, Artu Biologicals, Curalogic, IFE Europe, Genentech, Epigenesis, Merck, Cipla, Amgen, Rottapharma, Allergy Therapeutics, NovoNordisk, Inflazyme, Allergy Choices, Abbott Laboratories, Mitsubishi, Boehringher Ingelheim, Cytos Technologies, Wellpoint/Healthcore, Altanapharma, Capnia, Ivax Laboratories, Critical Therapeutics, Kyowa Hakko, Asthmatx, Neolab, Protein Design Laboratories, ClinPhone, Arriva, Schulman Ronca Bucuvals, Laboratories SMB, Vista Health Plan, Hal Allergy BV, Suburban Lung Associates, Galephar MF SA, Mannkind Corp, Prognostix, Formix Biosciences, Oxagen, SC Ellen Fast Comimpex SRL, Medimmune, Quintiles, PDL Biopharma, Bencard, Efficas, Pfizer, Alcon Lab, Aventis, Pahrmaxis, Assist Tech, Hoffmann LaRoche, Aerocrine, Dynavax, Medtap, Pharmaengine, Topigen, ClineDavis & Mann, Teikoku Pharma, NeoLab, KGK Synergise, and AB Science.
Stephanie Wolfe is on the advisory boards of Teva, Novartis, Astra Zeneca and GSK. She also attends speaker meetings for: Pfizer, Boehringer, Astra Zeneca, Altana Pharma (a Nycomed company), GSK and MSD.
Publications
Murdoch J, Musgrave S, Price D, Rust-Andrews S, Juniper E. Profiles of asthma control in 12488 patients in 30 practices in East Anglia. Prim Care Resp J 2003;12:70.
Wilson ECF, Sims EJ, Musgrave SD, Shepstone L, Blyth A, Murdoch J, et al. The cost-effectiveness of leukotriene receptor antagonists versus inhaled corticosteroids for initial asthma controller therapy: a pragmatic trial. Pharmacoeconomics 2010;28:585–95.
Wilson ECF, Price D, Musgrave SD, Sims EJ, Shepstone L, Murdoch J, et al. The cost-effectiveness of leukotriene receptor antagonists versus long acting beta-2 agonists as add-on therapy to inhaled corticosteroids for asthma: a pragmatic trial. Pharmacoeconomics 2010;28:597–608.
Price D, Musgrave SD, Shepstone L, Hillyer EV, Sims EJ, Gilbert RFT, et al. Leukotriene antagonists as first-line or add-on asthma-controller therapy. N Engl J Med 2011;364:1695–707.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Chung F, Barnes N, Allen M, Angus R, Corris P, Knox A, et al. Assessing the burden of respiratory disease in the UK. Respir Med 2002;96:963-75.
- Selroos O, Pietinalho A, Lofroos AB, Riska H. Effect of early vs late intervention with inhaled corticosteroids in asthma. Chest 1995;108:1228-34.
- Long-term effects of budesonide or nedocromil in children with asthma . The Childhood Asthma Management Program Research Group. N Engl J Med 2000;343:1054-63.
- British Thoracic Society, Scottish Intercollegiate Guidelines Network . British Guideline on the Management of Asthma 2008. www.sign.ac.uk/guidelines/fulltext/101/index.html.
- Global Initiative for Asthma . GINA Report, Global Strategy for Asthma Management and Prevention 2008. www.ginasthma.org.
- Price D. The Air Study: asthma in real life. Asthma 1999;4:74-8.
- Pauwels RA, Lofdahl CG, Postma DS, Tattersfield AE, O’Byrne P, Barnes PJ, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. Formoterol and Corticosteroids Establishing Therapy (FACET) International Study Group. N Engl J Med 1997;337:1405-11.
- Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet 2003;361:1071-6.
- Davis BE, Cockcroft DW. Effect of a single dose of montelukast sodium on methacholine chloride PC20. Can Respir J 2005;12:26-8.
- Riccioni G, Ballone E, D’Orazio N, Sensi S, Di Nicola M, Di Mascio R, et al. Effectiveness of montelukast versus budesonide on quality of life and bronchial reactivity in subjects with mild-persistent asthma. Int J Immunopathol Pharmacol 2002;15:149-55.
- Sont JK, Willems LN, Bel EH, van Krieken JH, Vandenbroucke JP, Sterk PJ. Clinical control and histopathologic outcome of asthma when using airway hyperresponsiveness as an additional guide to long-term treatment. The AMPUL Study Group. Am J Respir Crit Care Med 1999;159:1043-51.
- van der Woude HJ, Boorsma M, Bergqvist PB, Winter TH, Aalbers R. Budesonide/formoterol in a single inhaler rapidly relieves methacholine-induced moderate-to-severe bronchoconstriction. Pulm Pharmacol Ther 2004;17:89-95.
- Barnes PJ, Adcock IM. How do corticosteroids work in asthma?. Ann Intern Med 2003;139:359-70.
- Dworski R, Fitzgerald GA, Oates JA, Sheller JR. Effect of oral prednisone on airway inflammatory mediators in atopic asthma. Am J Respir Crit Care Med 1994;149:953-9.
- O’Shaughnessy KM, Wellings R, Gillies B, Fuller RW. Differential effects of fluticasone propionate on allergen-evoked bronchoconstriction and increased urinary leukotriene E4 excretion. Am Rev Respir Dis 1993;147:1472-6.
- Dahlen S-E, Page C, Gardiner P. Airway hyperresponsiveness: is it really important for asthma?. Oxford: Blackwell Scientific; 1993.
- Spector SL. Safety of antileukotriene agents in asthma management. Ann Allergy Asthma Immunol 2001;86:18-23.
- Storms W, Michele TM, Knorr B, Noonan G, Shapiro G, Zhang J, et al. Clinical safety and tolerability of montelukast, a leukotriene receptor antagonist, in controlled clinical trials in patients aged > or = 6 years. Clin Exp Allergy 2001;31:77-8.
- Fish JE, Kemp JP, Lockey RF, Glass M, Hanby LA, Bonuccelli CM. Zafirlukast for symptomatic mild-to-moderate asthma: a 13-week multicenter study. The Zafirlukast Trialists Group. Clin Ther 1997;19:675-90.
- Nathan RA, Bernstein JA, Bielory L, Bonuccelli CM, Calhoun WJ, Galant SP, et al. Zafirlukast improves asthma symptoms and quality of life in patients with moderate reversible airflow obstruction. J Allergy Clin Immunol 1998;102:935-42.
- Reiss TF, Chervinsky P, Dockhorn RJ, Shingo S, Seidenberg B, Edwards TB. Montelukast, a once-daily leukotriene receptor antagonist, in the treatment of chronic asthma: a multicenter, randomized, double-blind trial. Montelukast Clinical Research Study Group. Arch Intern Med 1998;158:1213-20.
- Diamant Z, Grootendorst DC, Veselic-Charvat M, Timmers MC, De Smet M, Leff JA, et al. The effect of montelukast (MK-0476), a cysteinyl leukotriene receptor antagonist, on allergen-induced airway responses and sputum cell counts in asthma. Clin Exp Allergy 1999;29:42-51.
- Taylor IK, O’Shaughnessy KM, Fuller RW, Dollery CT. Effect of cysteinyl-leukotriene receptor antagonist ICI 204.219 on allergen-induced bronchoconstriction and airway hyperreactivity in atopic subjects. Lancet 1991;337:690-4.
- Edelman JM, Turpin JA, Bronsky EA, Grossman J, Kemp JP, Ghannam AF, et al. Oral montelukast compared with inhaled salmeterol to prevent exercise-induced bronchoconstriction. A randomized, double-blind trial. Exercise Study Group. Ann Intern Med 2000;132:97-104.
- Pizzichini E, Leff JA, Reiss TF, Hendeles L, Boulet LP, Wei LX, et al. Montelukast reduces airway eosinophilic inflammation in asthma: a randomized, controlled trial. Eur Respir J 1999;14:12-8.
- Laviolette M, Malmstrom K, Lu S, Chervinsky P, Pujet JC, Peszek I, et al. Montelukast added to inhaled beclomethasone in treatment of asthma. Montelukast/Beclomethasone Additivity Group. Am J Respir Crit Care Med 1999;160:1862-8.
- Leff JA, Busse WW, Pearlman D, Bronsky EA, Kemp J, Hendeles L, et al. Montelukast, a leukotriene-receptor antagonist, for the treatment of mild asthma and exercise-induced bronchoconstriction. N Engl J Med 1998;339:147-52.
- Ducharme FM. Inhaled glucocorticoids versus leukotriene receptor antagonists as single agent asthma treatment: systematic review of current evidence. BMJ 2003;326.
- Israel E, Chervinsky PS, Friedman B, Van Bavel J, Skalky CS, Ghannam AF, et al. Effects of montelukast and beclomethasone on airway function and asthma control. J Allergy Clin Immunol 2002;110:847-54.
- Currie GP, McLaughlin K. The expanding role of leukotriene receptor antagonists in chronic asthma. Ann Allergy Asthma Immunol 2006;97:731-41.
- Foster JM, van Sonderen E, Lee AJ, Sanderman R, Dijkstra A, Postma DS, et al. A self-rating scale for patient-perceived side effects of inhaled corticosteroids. Respir Res 2006;7.
- Lofdahl CG, Reiss TF, Leff JA, Israel E, Noonan MJ, Finn AF, et al. Randomised, placebo controlled trial of effect of a leukotriene receptor antagonist, montelukast, on tapering inhaled corticosteroids in asthmatic patients. BMJ 1999;319:87-90.
- Price DB, Rouleau MY, Fletcher CP, Patel P, Olivenstein R, Myhr L, et al. Use of montelukast in tapering inhaled corticosteroid therapy: an open-label, 48-week trial. Curr Ther Res 2001;62:743-55.
- Riccioni G, Vecchia RD, Castronuovo M, Ilio CD, D’Orazio N. Tapering dose of inhaled budesonide in subjects with mild-to-moderate persistent asthma treated with montelukast: a 16-week single-blind randomized study. Ann Clin Lab Sci 2005;35:285-9.
- Ducharme FM, Lasserson TJ, Cates CJ. Long-acting beta2-agonists versus anti-leukotrienes as add-on therapy to inhaled corticosteroids for chronic asthma. Cochrane Database Syst Rev 2006.
- Joos S, Miksch A, Szecsenyi J, Wieseler B, Grouven U, Kaiser T, et al. Montelukast as add-on therapy to inhaled corticosteroids in the treatment of mild to moderate asthma: a systematic review. Thorax 2008;63:453-62.
- Kelloway JS, Wyatt RA, Adlis SA. Comparison of patients’ compliance with prescribed oral and inhaled asthma medications. Arch Intern Med 1994;154:1349-52.
- Price DB. Montelukast: real life effectiveness and cost-effectiveness in primary care. Am J Respir Crit Care Med 1999;158.
- O’Connor RD, Parasuraman B, Roberts C, Leibman C. Inhaled corticosteroids vs leukotriene receptor antagonists: health care costs across varying asthma severities. Ann Allergy Asthma Immunol 2006;97:236-43.
- Drummond M. Economic analysis alongside clinical trials. Research and Development Directorate of the NHS 1994:F51030-D031.
- Clark THJ. Action asthma: the occurrence and cost of asthma. Worthing: Cambridge Medical Publications; 1990.
- Price DB, Appleby JL. Fluticasone propionate: an audit of outcomes and cost-effectiveness in primary care. Respir Med 1998;92:351-3.
- Price DB, Cargill K, Wolfe S, Darby H. Salmeterol xinafoate: an analysis of outcomes and cost-effectiveness using a primary care database. Respir Med 1998;92:1302-4.
- Weiss KB, Sullivan SD. The economic costs of asthma: a review and conceptual model. Pharmacoeconomics 1993;4:14-30.
- Whiteman IA. The management of mild-to-moderate asthmatics in general practice; a retrospective analysis. Br J Med Econ 1993;6:25-3.
- British national formulary. London: Pharmaceutical Press; 2006.
- Jones C, Santanello NC, Boccuzzi SJ, Wogen J, Strub P, Nelsen LM. Adherence to prescribed treatment for asthma: evidence from pharmacy benefits data. J Asthma 2003;40:93-101.
- Williams B, Noonan G, Reiss TF, Knorr B, Guerra J, White R, et al. Long-term asthma control with oral montelukast and inhaled beclomethasone for adults and children 6 years and older. Clin Exp Allergy 2001;31:845-54.
- Booth PC. A comparison of the cost-effectiveness of alternative prophylactic therapies in the treatment of adult asthma. Br J Med Econ 1995;8:65-72.
- Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J 1999;14:32-8.
- Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol 1994;47:81-7.
- Laitinen LA. Comparative efficacy of zafirukast & low dose steroids in asthmatics on prn beta-agonists. Eur Respir J 1997;10:419S-20S.
- Malmstrom K, Rodriguez-Gomez G, Guerra J, Villaran C, Pineiro A, Wei LX, et al. Oral montelukast, inhaled beclomethasone, and placebo for chronic asthma. A randomized, controlled trial. Montelukast/Beclomethasone Study Group. Ann Intern Med 1999;130:487-95.
- Ringdal N. A comparison of patient preference for treatment with oral zafirlukast or inhaled beclomethasone [abstract P2806]. Eur Respir J 1997;10.
- Chung KF, Naya I. Compliance with an oral asthma medication: a pilot study using an electronic monitoring device. Respir Med 2000;94:852-8.
- The British Guidelines on asthma management . 1995 review and position statement. Thorax 1997;52:S1-2.
- Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med 2006;6.
- Barnes PJ, Pedersen S, Busse WW. Efficacy and safety of inhaled corticosteroids. New developments. Am J Respir Crit Care Med 1998;157:S1-53.
- Kelly HW. Asthma pharmacotherapy: current practices and outlook. Pharmacotherapy 1997;17:13-21S.
- Greening AP, Ind PW, Northfield M, Shaw G. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Allen & Hanburys Limited UK Study Group. Lancet 1994;344:219-24.
- Ind PW, Dal Negro R, Colman NC, Fletcher CP, Browning D, James MH. Addition of salmeterol to fluticasone propionate treatment in moderate-to-severe asthma. Respir Med 2003;97:555-62.
- Juniper EF, O’Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902-7.
- Santanello NC, Barber BL, Reiss TF, Friedman BS, Juniper EF, Zhang J. Measurement characteristics of two asthma symptom diary scales for use in clinical trials. Eur Respir J 1997;10:646-51.
- Juniper EF, Svensson K, Mork AC, Stahl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med 2005;99:553-8.
- Juniper EF, Bousquet J, Abetz L, Bateman ED. Identifying ‘well-controlled’ and ‘not well-controlled’ asthma using the Asthma Control Questionnaire. Respir Med 2006;100:616-21.
- Roberts CM, MacRae KD, Winning AJ, Adams L, Seed WA. Reference values and prediction equations for normal lung function in a non-smoking white urban population. Thorax 1991;46:643-50.
- Juniper EF, Thompson AK, Ferrie PJ, Roberts JN. Development and validation of the mini Rhinoconjunctivitis Quality of Life Questionnaire. Clin Exp Allergy 2000;30:132-40.
- Clinical Effectiveness and Evaluation Unit . Measuring Clinical Outcome in Asthma: A Patient Focused Approach 1999.
- Pearson MG, Bucknall CE. Asthma care. Thorax 2000;55.
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47:76-83.
- EuroQol Group . EuroQol – a new facility for the management of health related quality of life. Health Policy 1990;16:199-208.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108.
- Juniper EF, Guyatt GH. Development and testing of a new measure of health status for clinical trials in rhinoconjunctivitis. Clin Exp Allergy 1991;21:77-83.
- Juniper EF, Thompson AK, Ferrie PJ, Roberts JN. Development and validation of the mini Rhinoconjuctivitis Quality of Life Questionnaire. Clin Exp Allergy 2000;30:132-40.
- Juniper EF, Guyatt GH, Ferrie PJ, Griffith LE. Measuring quality of life in asthma. Am Rev Respir Dis 1993;147:832-8.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 1987.
- Office for National Statistics . Annual Survey of Hours and Earnings (ASHE) 2005.
- Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009;180:59-9.
- Herland K, Akselsen JP, Skjonsberg OH, Bjermer L. How representative are clinical study patients with asthma or COPD for a larger “real life” population of patients with obstructive lung disease?. Respir Med 2005;99:11-9.
- Travers J, Marsh S, Williams M, Weatherall M, Caldwell B, Shirtcliffe P, et al. External validity of randomised controlled trials in asthma: to whom do the results of the trials apply?. Thorax 2007;62:219-23.
- Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med 2004;170:836-44.
- Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC. Influence of cigarette smoking on inhaled corticosteroid treatment in mild asthma. Thorax 2002;57:226-30.
- Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med 2003;168:1308-11.
- Lazarus SC, Chinchilli VM, Rollings NJ, Boushey HA, Cherniack R, Craig TJ, et al. Smoking affects response to inhaled corticosteroids or leukotriene receptor antagonists in asthma. Am J Respir Crit Care Med 2007;175:783-90.
- McCoy K, Shade DM, Irvin CG, Mastronarde JG, Hanania NA, Castro M, et al. Predicting episodes of poor asthma control in treated patients with asthma. J Allergy Clin Immunol 2006;118:1226-33.
- Vollmer WM, Markson LE, O’Connor E, Frazier EA, Berger M, Buist AS. Association of asthma control with health care utilization: a prospective evaluation. Am J Respir Crit Care Med 2002;165:195-9.
- Zeiger RS, Bird SR, Kaplan MS, Schatz M, Pearlman DS, Orav EJ, et al. Short-term and long-term asthma control in patients with mild persistent asthma receiving montelukast or fluticasone: a randomized controlled trial. Am J Med 2005;118:649-57.
- Campbell JD, Spackman DE, Sullivan SD. Health economics of asthma: assessing the value of asthma interventions. Allergy 2008;63:1581-92.
- Heaton PC. Cost effectiveness of leukotriene modifiers in adults with asthma. Pharmacoeconomics 2006;24:727-42.
- Greenland S, Finkle W. D. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol 1995;142:1255-64.
- Schafer J. The Multiple Imputation FAQ Page 2009. www.stat.psu.edu/∼jls/mifaq.html.
- Horne R, Weinman J, Hankins M. The Beliefs about Medicines Questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 1999;14:1-24.
- Weinman J, Petrie KJ, Moss-Morris R, Horne R. The Illness Perception Questionnaire: a new method for assessing the cognitive representations of illness. Psychol Health 1996;11:431-45.
- Horne R, Hankins M, Jenkins R. The Satisfaction with Information about Medicines Scale (SIMS): a new measurement tool for audit and research. Qual Health Care 2001;10:135-40.
- Horne R, Musgrave S, Lee A, Price D. The Minimal Asthma Assessment Tool (MAAT): a new method for prioritising patients for primary care review by identifying poor asthma control and the causes of poor control. General Practice Airways Group Annual Conference 2005.
- Murdoch J. The Discursive Construction of Prophylactic Medicine-Taking for People With Asthma: Interactional Issues and Moral Discourses 2010.
Appendix 1 Background information for economic analysis
Read codes for asthma-related medications
The following Read codes were used to search for relevant asthma-related prescriptions in the miquest searches. In cases where the GP practice software system used other codes, the analogous codes were used.
| Clinical use | Read code(s) | BNF codes | Description related to Read codes |
|---|---|---|---|
| Respiratory | c.. | 3a | All respiratory medications |
| p4.. | 3.1.5 | Respiratory devices – spacers, peak flow meters | |
| Oral steroids | fe6.. | 6.3.2 | Prednisolone |
| Antibiotic and antifungal | ey.. | 5.4.8 | Pneumocystitis drugs |
| eh.. | 5.2 | Antifungal drugs | |
| lc.. | 12.3.2 | Oropharyngeal anti-infective drugs | |
| ec-ed | 5.1.8–5.1.9 | Sulphonamides, trimethoprim, antituberculosis drugs | |
| e1-ea | 5.1.1–5.1.6 | Penicillinase-sensitive penicillins, penicillinase-resistant penicillins, broad-spectrum penicillins, antipseudomonal penicillins, other penicillins, cephalosporins and cephalomycins, tetracyclines systemic, aminoglycosides, macrolides, clindamycin and lincomycin | |
| eb2.. | 5.1.7 | Chloramphenicol (systemic) | |
| eb7.. | Vancomycin | ||
| Conjunctivitis | k6.. | 11.4.2 | Corticosteroids and anti-inflammatory preps – eye |
| k3.. | 11.3 | Topical preparations eye | |
| Skin | m1-m5 | 13.1 – 13.5 | Vehicles and diluents, emollients and barrier preparations, local anaesthetic and antipruritic preparations, topical corticosteroids, psoriasis and eczema preparations |
| mb.. | 13.9 | Scalp preparations | |
| mc-me mh-mi mn.. | 13.10.1 13.10.2 13.11 | Antibacterial, antifungal topical preparations, disinfecting cleansing agents, wound ulcer preparations | |
| Rhinitis | l8.. | 12.2.1 | Nasal allergy drugs |
| l9.. | 12.2.2 | Topical nasal decongestants |
Details of respiratory prescriptions
| Read codes | BNF subchapter | Medication |
|---|---|---|
| c1.. | 3. 1. 1. 1 | Selective β2-agonists |
| 3. 1. 1. 1 | Formoterol | |
| 3. 1. 1. 1 | Salbutamol inhaler | |
| 3. 1. 1. 1 | Salbutamol – other forms | |
| 3. 1. 1. 1 | Salmeterol | |
| 3. 1. 1. 1 | Terbutaline | |
| c3.. and c5.. | 3.1.2 and 3.1.4 | Antimuscarinic |
| c4.. | 3. 1. 3 | Xanthine |
| c1D.. and c67 | 3. 2 | Compound ICS/LABA |
| c6.. | 3. 2 | Inhaled corticosteroids |
| c7.. | 3. 3. 1 | Cromolyn |
| cA.. | 3. 3. 2 | LTRA |
| c8.. | 3. 4. 1 | Antihistamines |
| bp1.. | 3. 4. 3 | Allergic emergencies |
| cd..-ce.. | 3. 7 | Mucolytics |
| cf.. | 3. 8 | Aromatics |
| cg.. – ch.. | 3. 9 | Cough preparations |
| ci.. | 3. 10 | Systemic nasal decongestants |
Unit costs
| Description of scenarios | Cost (£) | Source |
|---|---|---|
| Acute condition appointment (therefore 10 min), non-study visit, seen by nurse, respiratory-related reason is primary reason for consultation, seen in surgery | 10.00 | Nurse consultation including qualification costs (PSSRU 2005, p. 130)a |
| Routine clinic appointment (therefore 30 min), non study visit, seen by nurse, primary reason for consultation, seen in surgery | 15.00 | Nurse consultation per hour in clinic including qualification costs/2 (PSSRU 2005, p. 130)a |
| Acute condition appointment, non-study visit, seen by nurse, secondary reason for consultation (therefore 5? min), seen in surgery | 5.00 | Nurse consultation including qualification costs/2 (PSSRU 2005, p. 130)a |
| Routine clinic appointment, non study visit, seen by nurse, secondary reason for consultation (therefore 5? min), seen in surgery | 5.00 | Nurse consultation including qualification costs/2 (PSSRU 2005, p. 130)a |
| Routine appointment, study visit , seen by nurse, primary reason for consultation, seen in surgery | 15.00 | Nurse consultation per hour in clinic including qualification costs/2 (PSSRU 2005, p. 130)a |
| Acute condition, study visit, seen by nurse, primary reason for consultation, seen in surgery | 15.00 | Nurse consultation per hour in clinic including qualification costs/2 (PSSRU 2005, p. 130)a |
| Acute condition, study visit, seen by nurse, secondary reason for consultation, seen in surgery | 5.00 | Nurse consultation including qualification costs/2 (PSSRU 2005, p. 130)a |
| Routine appointment, study visit, seen by nurse, secondary reason for consultation, seen in surgery | 5.00 | Nurse consultation including qualification costs/2 (PSSRU 2005, p. 130)a |
| Acute condition, non-study visit, GP consultation, primary reason for consultation (therefore 10 min), seen in surgery | 24.00 | GP surgery consultation of 10 minutes including qualification costs and direct care staff costs (PSSRU 2005, p. 133)a |
| Acute condition, non-study visit, GP consultation-secondary reason for consultation (therefore 5? min), seen in surgery | 12.00 | GP surgery consultation of 10 minutes including qualification costs and direct care staff costs/2 (PSSRU 2005, p. 133)a |
| GP home visit | 69.00 | GP home visit of 13.2 minutes, including 12 minutes’ travel time, direct care staff and qualification costs (PSSRU 2005, p. 133)a |
| Paramedic home visit | 311.00 | Average cost per patient journey, paramedic unit (PSSRU 2005, p. 108)a |
| Ambulance run | 311.00 | Note: Unit cost data cannot distinguish between these – data should indicate one or the other, not both or else this is double counting |
| Nurse telephone consultation | 10.00 | No data available. Assumed same cost as 10-minute nurse appointment |
| GP telephone consultation | 25.00 | GP telephone consultation lasting 10.8 minutes, including direct care staff costs and qualification costs (PSSRU 2005, p. 133)a |
| Out-of-hours GP consultation, not at night | 49.61 | Scott et al. (2003)b |
| Out-of-hours GP consultation, at night | 49.61 | Scott et al. (2003)b |
| Out-of-hours GP telephone consultation | 51.68 | OOH GP visit costs 2.067 as much as a routine GP visit. Therefore, assume OOHT costs 2.067 × daytime GP telephone consultation |
| ‘Walk-in-clinic’ visit | 26.06 | NHS Reference Costs 2005. PCT and trust combined data, TA&EMIS, weighted average of walk-in centre unit costs (HRGs V100WIFA and V100WIFU). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Call to NHS Direct | 15.00 | Approximation of average cost per call across three sites in 2001. Is crude average so spurious precision to adjust to 2005 price. URL: www.shef.ac.uk/content/1/c6/02/40/50/nhsd3.pdf |
| Saw a consultant – first visit | 191.00 | NHS Reference Costs 2005. PCT and trust combined data, outpatient, first attendance, adult (TOPS FAA), Thoracic medicine (specialty code 340). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Saw a consultant – repeat visit | 127.00 | NHS Reference Costs 2005. PCT and trust combined data, outpatient, follow-up attendance, adult (TOPS FUA), thoracic medicine (specialty code 340). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Saw private consultant | 127.00 | Some patients saw private consultant. For external validity purposes, these cost the same as NHS and accrued to NHS |
| Hospital service/appointment | 127.00 | NHS Reference Costs 2005. PCT and trust combined data, outpatient, follow-up attendance, adult (TOPS FUA), thoracic medicine (specialty code 340). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Chest X-ray | 19.00 | NHS Reference Costs 2005. PCT and trust combined data, (TRADIO), Band A – (no further details provided) (code RBA1). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| CT scan – chest | 69.00 | NHS Reference Costs 2005. PCT and trust combined data, (TRADIO), Band C5 – CT other (code RBC5). URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Labs – RAST tests | 7.15 | NHS Reference Costs 2005. PCT and trust combined data, (TPATH), immunology. URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Labs – skin prick allergen sensitivity test | 127.00 | Assumed is same as consultant repeat visit |
| Microbiology diagnostics | 6.31 | NHS Reference Costs 2005. PCT and trust combined data, (TPATH), microbiology/immunology cost URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Day-case admission | 394.73 | NHS Reference Costs 2005. PCT and trust combined data, (TDC), weighted average asthma admission with and without complications (HRG D21 and D22) URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| General ward – further nights | ||
| Inpatient admission for asthma | 1979.88 | NHS Reference Costs 2005. PCT and trust combined data, (TELIP), weighted average asthma admission with or without complications (HRG D21 and D22) URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Admission to specialist thoracic care ward | 1979.88 | Assumed equal to inpatient admission for asthma |
| Admission to intensive care unit | Note: reference costs should include ICU costs – danger of double counting | |
| A&E attendance | 70.95 | NHS Reference Costs 2005. PCT and trust combined data, (TA&E, weighted average HRGs V07 and V08). No investigation died/admitted and referred/discharged. URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
| Influenza vaccine | 5.00 | £5 for ‘flu vaccine alone (price range £3.98–6.59, BNF 49, March 2005). Note: excludes nurse visit |
| Pneumococcal vaccine | 21.67 | £21.67 (means price of pneumococcal vaccine, BNF 49, March 2005). Note: excludes nurse visit |
| Nebulisation (with short-acting beta/salbutamol) in surgery, for acute symptoms | 30.00 | Nurse hour in clinic including qualification costs (PSSRU 2005, p. 130) |
| MRI scan | 312.00 | NHS Reference Costs 2005. PCT and trust combined data, (TRADIO RBF1, Band F1 – MRI) URL: www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4133221%26chk=TxHkqo |
Imputation approach for economic analyses
| Variable | Description |
|---|---|
| AQLQV2 | Baseline miniAQLQ score |
| ACQV2 | Baseline ACQ score |
| V2Utility | Baseline EQ-5D utility score |
| QALY8wk | QALYs gained at 8 weeks |
| NHS8wk | NHS costs at 8 weeks |
| Societal8wk | Societal costs at 8 weeks |
| AQLQv3 | MiniAQLQ score at visit 3 (8 weeks) |
| ACQv3 | ACQ score at visit 3 (8 weeks) |
| AQLQv7 | MiniAQLQ score at visit 7 (2 years) |
| ACQv7 | ACQ score at visit 7 (2 years) |
| QALY104wkDisc | QALYs gained at 2 years (discounted at 3.5%) |
| NHS104wkDisc | NHS costs at 2 years (discounted at 3.5%) |
| Societal104wkDisc | Societal costs at 2 years (discounted at 3.5%) |
Summary of missing data
In total, 687 patients were enrolled in the study (steps 2 and 3). Four patients were excluded from the analysis due to their ineligibility (one due to incorrect diagnosis, three due to site not approved).
Overall, across all patients enrolled in the study (both steps 2 and 3), 7065 out of 8879 data points (80%) were present. Societal costs and QALY scores were variables with the highest proportion of missing data. These are the most complex compound variables, therefore, in any analysis, are most likely to have missing values (Table 56). Analysed by observation, 218 out of 683 patients (32%) had compete data at all time points; however, 75% of patients had at most four of the 13 variables missing (Table 57 and Figure 18).
| Variable | Present | Missing | Missing (%) | Sum |
|---|---|---|---|---|
| AQLQV2 | 614 | 69 | 10 | 683 |
| ACQV2 | 617 | 66 | 10 | 683 |
| V2Utility | 554 | 129 | 19 | 683 |
| QALY8wk | 439 | 244 | 36 | 683 |
| NHS8wk | 671 | 12 | 2 | 683 |
| Societal8wk | 344 | 339 | 50 | 683 |
| AQLQv3 | 582 | 101 | 15 | 683 |
| ACQv3 | 583 | 100 | 15 | 683 |
| AQLQv7 | 653 | 30 | 4 | 683 |
| ACQv7 | 650 | 33 | 5 | 683 |
| QALY104wkDisc | 400 | 283 | 41 | 683 |
| NHS104wkDisc | 632 | 51 | 7 | 683 |
| Societal104wkDisc | 326 | 357 | 52 | 683 |
| Complete data | 218 (32%) |
|---|---|
| ≤ 1 missing item | 234 (34%) |
| ≤ 2 missing items | 416 (61%) |
| ≤ 3 missing items | 463 (68%) |
| ≤ 4 missing items | 514 (75%) |
| ≤ 5 missing items | 575 (84%) |
| ≤ 10 missing items | 676 (99%) |
| ≤ 13 missing items | 683 (100%) |
FIGURE 18.
Summary of missingness by observation.
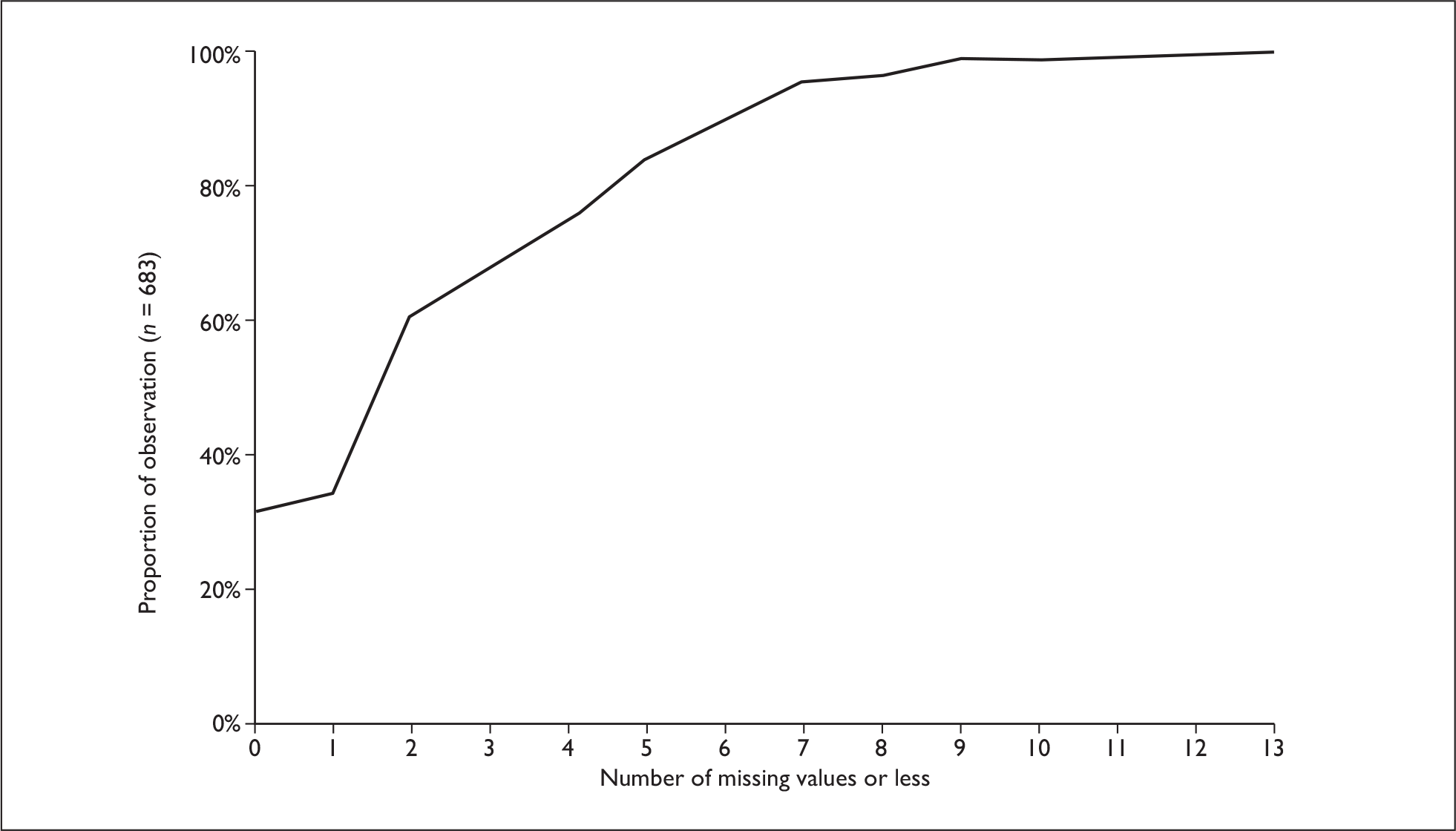
Interpretation 5% of observations had four or less missing values out of 13 variables.
Missing data were imputed as follows. Firstly, distributions of data were visualised to check for normality. Skewed data were transformed to improve their approximation to a normal distribution. Table 58 summarises transformations performed.
| Variable | Skewed | Transformation | Transformed variable name |
|---|---|---|---|
| AQLQV2 | Left | Square | sqAQLQv2 |
| ACQV2 | Symmetric | – | – |
| V2Utility | Left | Square | sqV2Utility |
| QALY8wk | Left | Square | sqQALY8wk |
| NHS8wk | Right | Natural Log | lnNHS8Wk |
| Societal8wk | Right | Natural Log | lnSocietal8Wk |
| AQLQv3 | Left | Square | sqAQLQv3 |
| ACQv3 | Right | Natural Log | lnACQv3 |
| AQLQv7 | Left | Square | sqAQLQv7 |
| ACQv7 | Right | Natural Log | lnACQv7 |
| QALY104wkDisc | Left | Square | sqQALY8wkDisc |
| NHS104wkDisc | Right | Natural Log | lnNHS104WkDisc |
| Societal104wkDisc | Right | Natural Log | lnSocietal104WkDisc |
The variables ACQv2, AQLQv2, QALY8Wk and QALY104WkDisc exhibited bimodal distributions, with a number of observations recorded at full health. Therefore additional binary variables were defined: ‘ACQ_V2_zero’, ‘AQLQ_v2_zero’, ‘Healthy0’, ‘Healthy8’ and ‘Healthy104’ with a value of 1 where the patient reported full health at each of these time points. Resulting QALYs were then estimated using a two-part model.
Due to computational constraints, it was not possible to impute missing values for all variables simultaneously. Therefore. they were split into groups (Table 59). In each case, data were imputed with five iterations using the propensity score method, with all other variables employed as potential covariates as well as age, education, employment and gender. The imputed variables were re-transformed to natural units and visually reviewed to ensure predicted values were within logical limits.
| 1. Costs | lnNHS8wklnSocietal8WklnNHS104WkDisclnSocietal104WkDisc |
| 2. Baseline utility/QALYs | Healthy0SqV2Utility |
| 3. EQ-5D utility < 1 at 8 or 104 weeks | Healthy8Healthy104 |
| 4. 8-week QALY scores | sqQALY8wk |
| 5. 2-year QALY scores | sqQALY104wkDisc |
| 6. Baseline ACQ and MiniAQLQ scores | ACQv2sqAQLQv2ACQ_V2_zeroAQLQ_V2_zero |
| 7. MiniAQLQ and ACQ scores | AQLQv3ACQv3AQLQv7ACQv7 |
Appendix 2 Planned secondary analysis
The following items have been collated from several sources, including the study protocol and the study steering committee meeting minutes.
-
A per-protocol analysis will also be performed for the primary and the key secondary end points. It will be used to corroborate the conclusions drawn from the intention-to-treat analyses. The per-protocol analysis population will exclude patients and/or data points with clinically important protocol deviations based on a set of prespecified criteria.
-
A per-treatment maintained analysis will be performed to look at the impact of clinical decisions about discontinuing perceived ineffective treatments.
-
A repeated measures analysis of variance will be used to examine changes in life quality over time using scores from each visit. A comparison of profiles over time will be made between treatment groups.
-
Treatment differences for secondary end points will be examined using appropriate statistical tests and expressed together with 95% CIs.
-
The time course of the treatment effect will be studied using the morning PEF measurements obtained from the patient-recorded diary cards. The daily morning PEF measurements will be expressed as changes from baseline and analysed using a repeated measures analysis of variance.
-
A sensitivity analysis will be undertaken, including those patients with either missing or out of range baseline MiniAQLQ or ACQ scores as their clinician had determined that they should have an increase in asthma therapy.
-
The analysis should be repeated in the following subgroups:
-
– by age stratification
-
– those with the presence or absence of any evidence for a mixture of chronic and reactive obstructive pulmonary disease
-
– the sub group who would meet European Medicines Evaluation Agency inclusion criteria (compare with observational data publications comparing with randomised controlled trials)
-
– the subgroups of those with rhinitis versus those without rhinitis – and, subdividing those with rhinitis by how the information was obtained: clinical history of rhinitis (from GP practice data), versus use of rhinitis medications, versus response on questionnaire (RQLQ)
-
– those with reversibility versus non reversibility
-
– those staying with assigned randomised therapy versus those going off that therapy/those going to other therapy
-
– smokers/non-smokers
-
– analysis of population defined with higher ACQ cut points (1.25 suggested by LJ)
-
– duration since diagnosis versus response
-
– diagnostic and prescribing standards versus outcomes (by practice)
-
– comparative analysis of QOL measures (e.g. ACQ/AQLQ, RCP3 and 21, patient-defined targets, symptom diary card, etc).
-
Validation of tools: RCP3 & 21 questions, EQ-5D, oral steroid use (as an independent measure of asthma control).
Appendix 3 Details of NHS activity costs
Step 2 study: NHS activity costs at 2 months
Quantities and costs of asthma-related NHS resources during the first 2 months of treatment.
| Treatment | LTRA | ICS | p-value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | ||
| Routine nurse visits | 156 | 25 | 0.16 | 0.40 | 235 | 1.51 | 4.66 | 158 | 19 | 0.12 | 0.41 | 225 | 1.42 | 5.47 | |
| Vaccinations | 156 | 16 | 0.10 | 0.30 | 97 | 0.62 | 2.25 | 158 | 6 | 0.04 | 0.19 | 30 | 0.19 | 0.96 | |
| Total routine care | 156 | 41 | 0.26 | 0.63 | 332 | 2.13 | 5.52 | 158 | 25 | 0.16 | 0.56 | 255 | 1.61 | 5.98 | |
| GP in clinic | 156 | 31 | 0.20 | 0.54 | 720 | 4.62 | 12.75 | 158 | 14 | 0.09 | 0.38 | 276 | 1.75 | 7.40 | |
| GP home visit | 156 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| GP out of hours at night | 156 | 5 | 0.03 | 0.33 | 248 | 1.59 | 16.35 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| GP telephone consultationa | 156 | 3 | 0.02 | 0.14 | 75 | 0.48 | 3.44 | 158 | 1 | 0.01 | 0.08 | 25 | 0.16 | 1.99 | |
| Nurse in clinic | 156 | 5 | 0.03 | 0.18 | 50 | 0.32 | 1.77 | 158 | 5 | 0.03 | 0.18 | 50 | 0.32 | 1.76 | |
| Nurse telephone consultation | 156 | 6 | 0.04 | 0.19 | 60 | 0.38 | 1.93 | 158 | 2 | 0.01 | 0.11 | 20 | 0.13 | 1.12 | |
| Other | 156 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Total patient initiated | 156 | 50 | 0.32 | 0.75 | 1153 | 7.39 | 22.79 | 158 | 22 | 0.14 | 0.46 | 371 | 2.35 | 8.08 | |
| Outpatient | 156 | 2 | 0.01 | 0.11 | 254 | 1.63 | 14.33 | 158 | 3 | 0.02 | 0.18 | 381 | 2.41 | 22.53 | |
| Inpatient admission | 156 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Day-case admission | 156 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Accident and emergency | 156 | 2 | 0.01 | 0.16 | 382 | 2.45 | 30.58 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Diagnostics | 156 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 158 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Total secondary care | 156 | 4 | 0.03 | 0.25 | 636 | 4.08 | 41.93 | 158 | 3 | 0.02 | 0.18 | 381 | 2.41 | 22.53 | |
| Total NHS resources used | 156 | 95 | 0.61 | 1.09 | 2121 | 13.59 | 61.00 | 158 | 50 | 0.32 | 0.71 | 1007 | 6.37 | 24.16 | 0.008 |
Step 3 study: NHS activity costs at 2 months
Quantities and costs of asthma related NHS resources during the first 2 months of treatment.
| Treatment | LTRA | LABA | p-value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | ||
| Routine nurse visits | 175 | 26 | 0.15 | 0.39 | 310 | 1.77 | 4.97 | 182 | 31 | 0.17 | 0.47 | 285 | 1.57 | 4.80 | |
| Vaccinations | 175 | 12 | 0.07 | 0.30 | 93 | 0.53 | 3.01 | 182 | 16 | 0.09 | 0.30 | 113 | 0.62 | 2.82 | |
| Total routine care | 175 | 38 | 0.22 | 0.59 | 403 | 2.30 | 6.32 | 182 | 47 | 0.26 | 0.73 | 398 | 2.19 | 6.61 | |
| GP in clinic | 175 | 32 | 0.18 | 0.55 | 756 | 4.32 | 13.07 | 182 | 42 | 0.23 | 0.61 | 984 | 5.41 | 14.52 | |
| GP home visit | 175 | 2 | 0.01 | 0.11 | 138 | 0.79 | 7.36 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| GP out of hours at night | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| GP telephone consultationa | 175 | 1 | 0.01 | 0.08 | 25 | 0.14 | 1.89 | 182 | 1 | 0.01 | 0.07 | 25 | 0.14 | 1.85 | |
| Nurse in clinic | 175 | 16 | 0.09 | 0.38 | 155 | 0.89 | 3.70 | 182 | 8 | 0.04 | 0.23 | 70 | 0.38 | 2.13 | |
| Nurse telephone consultation | 175 | 8 | 0.05 | 0.24 | 80 | 0.46 | 2.35 | 182 | 5 | 0.03 | 0.16 | 50 | 0.27 | 1.64 | |
| Other | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Total patient initiated | 175 | 59 | 0.34 | 0.79 | 1154 | 6.59 | 17.17 | 182 | 56 | 0.31 | 0.75 | 1129 | 6.20 | 15.54 | |
| Outpatient | 175 | 1 | 0.01 | 0.08 | 191 | 1.09 | 14.44 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Inpatient admission | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Day-case admission | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Accident and emergency | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Diagnostics | 175 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 182 | 4 | 0.02 | 0.18 | 76 | 0.42 | 3.43 | |
| Total secondary care | 175 | 1 | 0.01 | 0.08 | 191 | 1.09 | 14.44 | 182 | 4 | 0.02 | 0.18 | 76 | 0.42 | 3.43 | |
| Total NHS resources used | 175 | 98 | 0.56 | 0.99 | 1748 | 9.99 | 25.00 | 182 | 107 | 0.59 | 1.05 | 1603 | 8.81 | 17.64 | 0.900 |
Step 2 study: NHS activity costs at 104 weeks
Quantities and costs of asthma related NHS resources during 104 weeks of treatment.
| Treatment | LTRA | ICS | p-value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | ||
| Routine nurse visits | 151 | 300 | 1.99 | 1.70 | 2858 | 18.93 | 20.15 | 151 | 272 | 1.80 | 1.54 | 2807 | 18.59 | 18.19 | |
| Vaccinations | 151 | 174 | 1.15 | 1.08 | 1198 | 7.93 | 9.88 | 151 | 148 | 0.98 | 0.98 | 1020 | 6.75 | 8.95 | |
| Total routine care | 151 | 474 | 3.14 | 2.53 | 4056 | 26.86 | 24.92 | 151 | 420 | 2.78 | 2.32 | 3827 | 25.35 | 22.92 | |
| GP in clinic | 151 | 301 | 1.99 | 2.77 | 6787 | 44.95 | 64.89 | 151 | 308 | 2.04 | 2.50 | 6947 | 46.01 | 57.20 | |
| GP home visit | 151 | 5 | 0.03 | 0.21 | 336 | 2.22 | 14.37 | 151 | 5 | 0.03 | 0.34 | 333 | 2.21 | 22.33 | |
| GP out of hours at night | 151 | 11 | 0.07 | 0.40 | 544 | 3.60 | 19.90 | 151 | 15 | 0.10 | 0.41 | 731 | 4.84 | 20.13 | |
| GP telephone consultationa | 151 | 17 | 0.11 | 0.41 | 495 | 3.28 | 14.55 | 151 | 21 | 0.14 | 0.69 | 515 | 3.41 | 16.92 | |
| Nurse in clinic | 151 | 46 | 0.30 | 0.84 | 432 | 2.86 | 7.97 | 151 | 44 | 0.29 | 0.84 | 413 | 2.73 | 8.09 | |
| Nurse telephone consultation | 151 | 17 | 0.11 | 0.42 | 168 | 1.11 | 4.19 | 151 | 21 | 0.14 | 0.37 | 207 | 1.37 | 3.60 | |
| Other | 151 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | 151 | 2 | 0.01 | 0.11 | 35 | 0.23 | 2.41 | |
| Total patient initiated | 151 | 397 | 2.63 | 3.19 | 8762 | 58.02 | 78.46 | 151 | 416 | 2.75 | 3.46 | 9181 | 60.80 | 81.95 | |
| Outpatient | 151 | 14 | 0.09 | 0.41 | 1752 | 11.60 | 50.66 | 151 | 30 | 0.20 | 0.71 | 3795 | 25.13 | 90.33 | |
| Inpatient admission | 151 | 4 | 0.03 | 0.26 | 7853 | 52.00 | 503.32 | 151 | 2 | 0.01 | 0.11 | 3826 | 25.34 | 219.42 | |
| Day-case admission | 151 | 1 | 0.01 | 0.08 | 395 | 2.61 | 32.12 | 151 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Accident and emergency | 151 | 9 | 0.06 | 0.33 | 1823 | 12.08 | 85.60 | 151 | 8 | 0.05 | 0.30 | 548 | 3.63 | 20.62 | |
| Diagnostics | 151 | 12 | 0.08 | 0.32 | 222 | 1.47 | 5.88 | 151 | 15 | 0.10 | 0.36 | 277 | 1.84 | 6.65 | |
| Total secondary care | 151 | 40 | 0.26 | 0.87 | 12,045 | 79.77 | 601.74 | 151 | 55 | 0.36 | 1.06 | 8446 | 55.93 | 268.62 | |
| Total NHS resources used | 151 | 911 | 6.03 | 4.89 | 24,863 | 164.65 | 633.99 | 151 | 891 | 5.90 | 5.25 | 21,455 | 142.08 | 310.13 | 0.635 |
Step 3 study: NHS activity costs at 104 weeks
Quantities and costs of asthma-related NHS resources during 104 weeks of treatment.
| Treatment | LTRA | LABA | p-value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | n | Total quantity | Mean quantity | SD | Total cost (£) | Mean cost (£) | SD (£) | ||
| Routine nurse visits | 169 | 414 | 2.45 | 1.82 | 4129 | 24.43 | 21.54 | 176 | 437 | 2.48 | 1.69 | 4106 | 23.33 | 18.86 | |
| Vaccinations | 169 | 232 | 1.37 | 1.02 | 1581 | 9.36 | 9.69 | 176 | 262 | 1.49 | 1.08 | 1828 | 10.39 | 10.57 | |
| Total routine care | 169 | 646 | 3.82 | 2.63 | 5710 | 33.79 | 26.53 | 176 | 699 | 3.97 | 2.56 | 5934 | 33.72 | 24.49 | |
| GP in clinic | 169 | 452 | 2.67 | 3.17 | 10,152 | 60.07 | 72.71 | 176 | 417 | 2.37 | 2.29 | 9253 | 52.57 | 51.22 | |
| GP home visit | 169 | 9 | 0.05 | 0.23 | 612 | 3.62 | 15.31 | 176 | 13 | 0.07 | 0.40 | 874 | 4.96 | 26.91 | |
| GP out of hours at night | 169 | 4 | 0.02 | 0.15 | 195 | 1.15 | 7.44 | 176 | 8 | 0.05 | 0.21 | 390 | 2.22 | 10.19 | |
| GP telephone consultationa | 169 | 32 | 0.19 | 0.66 | 814 | 4.82 | 16.63 | 176 | 24 | 0.14 | 0.48 | 641 | 3.64 | 12.62 | |
| Nurse in clinic | 169 | 118 | 0.70 | 1.17 | 1123 | 6.65 | 11.26 | 176 | 68 | 0.39 | 0.87 | 628 | 3.57 | 8.39 | |
| Nurse telephone consultation | 169 | 34 | 0.20 | 0.52 | 336 | 1.99 | 5.13 | 176 | 26 | 0.15 | 0.52 | 257 | 1.46 | 5.16 | |
| Other | 169 | 5 | 0.03 | 0.17 | 101 | 0.60 | 3.97 | 176 | 5 | 0.03 | 0.20 | 146 | 0.83 | 5.77 | |
| Total patient initiated | 169 | 654 | 3.87 | 4.20 | 13,334 | 78.90 | 89.75 | 176 | 561 | 3.19 | 2.94 | 12,187 | 69.25 | 71.42 | |
| Outpatient | 169 | 40 | 0.24 | 0.83 | 5668 | 33.54 | 120.42 | 176 | 19 | 0.11 | 0.54 | 2500 | 14.21 | 72.09 | |
| Inpatient admission | 169 | 3 | 0.02 | 0.17 | 5806 | 34.35 | 330.56 | 176 | 5 | 0.03 | 0.25 | 9766 | 55.49 | 484.06 | |
| Day-case admission | 169 | 1 | 0.01 | 0.08 | 395 | 2.34 | 30.36 | 176 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Accident and emergency | 169 | 3 | 0.02 | 0.23 | 453 | 2.68 | 34.84 | 176 | 0 | 0.00 | 0.00 | 0 | 0.00 | 0.00 | |
| Diagnostics | 169 | 27 | 0.16 | 0.49 | 552 | 3.27 | 11.29 | 176 | 23 | 0.13 | 0.40 | 826 | 4.69 | 27.02 | |
| Total secondary care | 169 | 74 | 0.44 | 1.16 | 12,874 | 76.18 | 370.05 | 176 | 47 | 0.27 | 0.91 | 13,092 | 74.39 | 511.48 | |
| Total NHS resources used | 169 | 1374 | 8.13 | 5.94 | 31,918 | 188.86 | 398.89 | 176 | 1307 | 7.43 | 4.19 | 31,214 | 177.35 | 541.93 | 0.920 |
Appendix 4 Study data collection instruments
Study visit form
The form presented here is the version of the form used at study visit 2. A slight variant of this form was used at visits 3 to 7 which had fewer instructions on the first page, since the text of the Personal Objectives were only specified by the participants at V2, thereafter they were pre-filled by study staff. Therefore, the response was only marking a score, and the instructions were modified accordingly.
Clinical record form
The form presented here is the version of the form used for step 3 participants in the study. The form for step 2 participants differed solely in the page headers, which labelled it as step 2; the text regarding identification of eligible patients based on medication taken before enrolment; and the instructions for the medication at randomisation.
Symptom diary card
The form presented here is the version of the form used for all participants at the baseline visit. At study visits 3 to 7, the form for each of the four study arms was modified appropriately for that arm, differing slightly in the labelling on the instruction side of the form (printed on the reverse of the form), but are other wise identical.
ELEVATE study
Patient symptom diary card – baseline visit
INSTRUCTIONS TO THE PATIENT
Please complete the asthma diary in the following manner:
Each day fill in the date and then:
OVERNIGHT ASTHMA SYMPTOMS
Complete in the morning upon arising and before taking any medication.
-
Overnight asthma symptoms.
-
Total number of puffs of reliever (blue inhaler) taken since you went to bed.
-
Peak Flow Measurement.
DAYTIME ASTHMA SYMPTOMS
Complete in the evening before going to bed just before taking your asthma treatment:
-
Peak Flow Measurement.
-
Daytime asthma symptoms. Asthma symptoms may include: chest discomfort (tightness), cough, wheezing and shortness of breath (breathlessness). Choose a number from 0 to 6 which best describes your answer to each of the first four questions.
-
Total number of puffs of reliever (blue inhaler) taken since arising. Do NOT count any puffs taken at the clinic.
Resource data collection sheet
The form presented here is the version of the form used at study visits 3–7. A variant of this form was used at visit 2, which had a slight difference in the wording of the prompting phrase about the time period that applied to the questions. On the visit 2 version, the phrase ‘In the last year’ is used instead of ‘Since your last visit for this study (state that date):__ / __ / __ …’
Resource diary
Appendix 5 Details of findings for per-protocol (fixed treatment regime and no changes within or from randomised therapy class) participants
| LTRA (n = 65) | ICS (n = 82) | ||
|---|---|---|---|
| Sex |
Female Male |
28 (43%) 37 (57%) |
36 (44%) 46 (56%) |
| Age, years | Mean (SD) | 45.7 (17.1) | 41.8 (16.0) |
| Height, cm | Mean (SD) |
n = 60 170.9 (8.4) |
n = 80 170.1 (9.7) |
| %PPEF | Median (IQR) |
n = 58 82.99 (74.97 to 90.54) |
n = 78 83.61 (73.06 to 92.12) |
| SABA in last year, puffs/day | Mean (SD) |
n = 58 3.24 (3.52) |
n = 74 2.57 (2.71) |
| MiniAQLQ | Mean (SD) | 4.78 (0.86) | 4.65 (0.97) |
| ACQ | Mean (SD) | 1.92 (0.68) | 2.07 (0.85) |
| mRQLQ | Mean (SD) |
n = 51 1.71 (1.14) |
n = 62 1.92 (0.165) |
| Personal objectives (0–100 VAS) | Mean (SD) |
n = 28 41.6 (19.1) |
n = 57 38.04 (2.19) |
| EQ-5D utility | Mean (SD) |
n = 53 0.821 (0.22) |
n = 62 0.843 (0.17) |
| RCP3 questions | Mean (SD) |
n = 59 1.83 (0.83) |
n = 76 2.11 (0.79) |
| Sleep difficulty |
Yes No Missing |
31 (53%) 28 (47%) 6 |
55 (67%) 27 (33%) 0 |
| Day symptoms |
Yes No Missing |
54 (92%) 5 (9%) 6 |
75 (94%) 5 (6%) 2 |
| Interferes with activities |
Yes No Missing |
31 (53%) 28 (47%) 6 |
36 (45%) 44 (55%) 2 |
| LTRA (n = 65) | ICS (n = 82) | ||
|---|---|---|---|
| Continued education > 16 |
Yes No Not known |
32 (52%) 30 (48%) 3 |
43 (56%) 34 (44%) 5 |
| Professional qualification |
Yes No Not known |
21 (36%) 37 (64%) 7 |
27 (37%) 46 (63%) 9 |
| Employment position |
Employer Manager Employee Self-employed Not known |
4 (9%) 0 31 (67%) 11 (24%) 19 |
5 (9%) 0 44 (80%) 6 (11%) 27 |
| Smoking habit |
Current smoker Ex-smoker Non-smoker Not known |
17 (26%) 20 (31%) 28 (43%) – |
17 (21%) 21 (26%) 43 (53%) 1 |
| Treatment duration | Outcome measure | LTRA (n = 65) | ICS (n = 82) | Difference (95% CI) LTRA–ICS | Adjusted differenceb (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 57 5.47 (0.98) |
n = 66 5.35 (1.03) |
0.12 (–0.24 to 0.48) |
0.14 (–0.15 to 0.44) |
| 2 yearsc |
n Mean (SD) |
n = 64 5.80 (1.04) |
n = 79 5.70 (1.18) |
0.10 (–0.27 to 0.47) |
0.05 (–0.28 to 0.37) |
| Treatment duration | Outcome measure | LTRA (n = 65) | ICS (n = 82) | Difference (95% CI) LTRA–ICS | Adjusted differencea (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 57 1.34 (0.85) |
n = 66 1.45 (0.99) |
–0.12 (–0.45 to 0.21) |
–0.10 (–0.38 to 0.19) |
| 2 yearsb |
n Mean (SD) |
n = 64 0.97 (0.85) |
n = 79 1.12 (0.93) |
–0.15 (–0.45 to 0.15) |
–0.08 (–0.35 to 0.19) |
| Treatment duration | Outcome measure | LTRA (n = 65) | ICS (n = 82) | Difference (p-value) LTRA–ICS | Adjusted differenceb (p-value) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 41 0.12 (0.04) |
n = 46 0.14 (0.02) |
–0.02 (p = 0.06) | –0.003 (p = 0.117) |
| 2 years (visit 7) |
n Mean (SD) |
n = 35 1.61 (0.43) |
n = 43 1.79 (0.21) |
–0.18 (p = 0.03) | –0.077 (p = 0.151) |
| LTRA (n = 65) | ICS (n = 82) | Rate ratio (95% CI) | |
|---|---|---|---|
| Mean (SD) exacerbations over 2 years | 0.20 (0.47) | 0.15 (0.45) | 1.37 (0.71 to 2.63), p = 0.352 |
| Mean (SD) respiratory tract infections over 2 years | 0.91 (1.66) | 0.91 (1.22) | 0.99 (0.62 to 1.56), p = 0.975 |
| Mean (SD) consultations for respiratory tract infections over 2 years | 1.18 (2.28) | 1.05 (1.53) | 1.12 (0.69 to 1.82), p = 0.621 |
| Adjusted differencea (95% CI) LTRA–ICS |
|||
| Mean (SD) SABA inhalers prescribed over 2 years (inhalers/day) |
n = 57 0.011 (0.012) |
n = 71 0.011 (0.012) |
–0.001 (–0.004 to 0.002) p = 0.356 |
| Measure | LTRA | ICS | p-value |
|---|---|---|---|
| Baseline |
n = 58 82.99 (74.97 to 90.54) |
n = 78 83.61 (73.06 to 92.12) |
|
| 2 months |
n = 46 88.25 (77.81 to 95.69) |
n = 51 87.58 (80.19 to 97.58) |
p = 0.942 |
| 2 years (imputed) |
n = 42 91.28 (83.37 to 100.40) |
n = 55 85.79 (77.53 to 96.93) |
p = 0.058 |
| Measure | LTRA | ICS | Difference (95% CI)a LTRA–ICS | Adjusted differencea (95% CI) LTRA–ICS |
|---|---|---|---|---|
| 8-week outcomes | ||||
| mRQLQ |
n = 50 1.31 (1.03) |
n = 60 1.53 (1.14) |
–0.222 (–0.636 to 0.191), p = 0.284 | –0.194 (–0.562 to 0.173), p = 0.297 |
| RCP3 |
n = 62 1.02 (0.95) |
n = 67 1.22 (0.92) |
–0.207 (–0.533 to 0.118), p = 0.209 | –0.183 (–0.564 to 0.199), p = 0.345 |
| Personal objectives (0–100 VAS) |
n = 45 61.42 (21.46) |
n = 30 53.65 (22.04) |
7.77 (–2.47 to –18.01), p = 0.134 | 6.31 (–5.25 to 17.87), p = 0.279 |
| 2-year outcomes | ||||
| mRQLQ |
n = 64 1.09 (1.15) |
n = 76 1.22 (1.26) |
–0.130 (–0.538 to 0.277), p = 0.528 | 0.00 (–0.446 to 0.441), p = 0.991 |
| RCP3 |
n = 64 0.42 (0.69) |
n = 78 0.42 (0.71) |
–0.112 (–0.421 to 0.197), p = 0.763 | –0.139 (–0.456 to 0.177), p = 0.386 |
| Personal objectives (0–100 VAS) |
n = 36 74.74 (16.35) |
n = 56 71.79 (18.15) |
2.95 (–4.47 to 10.36), p = 0.421 | 2.75 (–6.48 to 11.98), p = 0.395 |
| LTRA (N = 60) | LABA (N = 80) | ||
|---|---|---|---|
| Sex |
Female Male |
35 (58%) 25 (42%) |
42 (53%) 38 (47%) |
| Age, years | Mean (SD) | 50.7 (15.5) | 48.2 (16.9) |
| Height, cm |
Mean (SD) Missing |
168.6 (12.1) 4 |
167.9 (9.9) 5 |
| %PPEF | Median (IQR) |
n = 56 92.31 (82.10 to 101.94) |
n = 74 88.65 (76.67 to 99.89) |
| SABA in last year, puffs/day | Mean (SD) |
n = 57 4.23 (3.35) |
n = 77 4.04 (2.91) |
| MiniAQLQ | Mean (SD) | 4.78 (1.01) | 4.30 (1.06) |
| ACQ | Mean (SD) | 1.91 (0.84) | 2.25 (0.92) |
| mRQLQ | Mean (SD) |
n = 53 1.73 (1.24) |
n = 73 2.09 (1.23) |
| Personal objectives (0–100 VAS) | Mean (SD) |
n = 44 39.86 (18.55) |
n = 61 35.80 (16.43) |
| EQ-5D utility | Mean (SD) |
n = 56 0.80 (0.25) |
n = 73 0.78 (0.24) |
| RCP3 questions | Mean (SD) |
n = 59 1.81 (0.88) |
n = 80 2.13 (0.82) |
| Sleep difficulty |
Yes No Missing |
25 (43%) 33 (57%) 2 |
41 (54%) 35 (46%) 4 |
| Day symptoms |
Yes No Missing |
55 (95%) 3 (5%) 2 |
72 (95%) 4 (5%) 4 |
| Interferes with activities |
Yes No Missing |
23 (40%) 34 (60%) 3 |
35 (47%) 40 (53%) 5 |
| LTRA (n = 60) | LABA (n = 80) | ||
|---|---|---|---|
| Continued education > 16 |
Yes No Not known |
29 (49%) 30 (51%) 1 |
40 (51%) 39 (49%) 1 |
| Professional qualification |
Yes No Not known |
14 (24%) 44 (76%) 2 |
21 (27%) 58 (73%) 1 |
| Employment position |
Employer Employee Self-employed Not known |
5 (12%) 26 (63%) 10 (24%) 19 |
3 (5%) 41 (71%) 14 (24%) 22 |
| Smoking habit |
Current smoker Ex-smoker Non-smoker Not known |
7 (12%) 27 (45%) 26 (43%) – |
15 (19%) 32 (41%) 32 (41%) 1 |
| Treatment duration | Outcome measure | LTRA (n = 60) | LABA (n = 80) | Difference (95% CI) LTRA–LABA | Adjusted differenceb (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 56 5.38 (1.10) |
n = 67 5.06 (1.22) |
0.32 (–0.10 to 0.74) | –0.02 (–0.36 to 0.31) |
| 2 yearsc |
n Mean (SD) |
n = 60 5.65 (0.92) |
n = 80 5.49 (1.08) |
0.16 (–0.36 to 0.50) | –0.05 (–0.36 to 0.26) |
| Treatment duration | Outcome measure | LTRA (n = 60) | LABA (n = 80) | Difference (95% CI) (LTRA–LABA) | Adjusted differenceb (95% CI) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 56 1.37 (0.98) |
n = 67 1.47 (1.01) |
–0.09 (–0.45 to 0.27) | 0.11 (–0.22 to 0.44) |
| 2 yearsc |
n Mean (SD) |
n = 60 1.07 (0.73) |
n = 80 1.20 (0.85) |
–0.13 (–0.40 to 0.13) | –0.01 (–0.27 to 0.24) |
| Treatment duration | Outcome measure | LTRA (n = 60) | LABA (n = 80) | Difference (p-value) LTRA–LABA | Adjusted differenceb (p-value) |
|---|---|---|---|---|---|
| 2 months (visit 3) |
n Mean (SD) |
n = 47 0.13 (0.03) |
n = 50 0.12 (0.04) |
0.01 (p = 0.329) | 0.000 (p = 0.938) |
| 2 years (visit 7) |
n Mean (SD) |
n = 41 1.66 (0.42) |
n = 48 1.54 (0.51) |
0.12 (p = 0.221) | 0.038 (p = 0.519) |
| LTRA (n = 60) | LABA (n = 80) | Rate ratio (95% CI) | |
|---|---|---|---|
| Mean (SD) exacerbations over 2 years | 0.33 (0.84) | 0.43 (0.91) | 0.79 (0.42 to 1.45), p = 0.441 |
| Mean (SD) respiratory tract infections over 2 years | 1.07 (2.11) | 1.25 (1.87) | 0.85 (0.52 to 1.41), p = 0.534 |
| Mean (SD) consultations for respiratory tract infections over 2 years | 1.43 (3.00) | 1.40 (2.14) | 1.02 (0.62 to 1.69), p = 0.927 |
| Adjusted differencea (95% CI) LTRA–LABA | |||
| Mean (SD) SABA inhalers prescribed over 2 years (inhalers/day) |
n = 60 0.017 (0.017) |
n = 73 0.015 (0.013) |
0.002 (–0.002 to 0.006), p = 0.307 |
| Measure | LTRA | LABA | p-value |
|---|---|---|---|
| Baseline |
n = 56 92.31 (82.10 to 101.94) |
n = 74 88.65 (76.67 to 99.89) |
|
| 2 months |
n = 50 96.04 (86.58 to 106.09) |
n = 61 92.37 (80.01 to 101.63) |
p = 0.243 |
| 2 years (imputed) |
n = 44 90.21 (79.56 to 100.44) |
n = 55 89.84 (79.46 to 102.87) |
p = 0.949 |
| Measure | LTRA | LABA | Difference (95% CI) LTRA–LABA | Adjusted differencea (95% CI) LTRA–LABA |
|---|---|---|---|---|
| 8-week outcomes | ||||
| mRQLQ |
n = 47 1.26 (1.00) |
n = 55 1.79 (1.15) |
–0.530 (–0.957 to –0.103), p = 0.016 | –0.404 (–0.772 to –0.036), p = 0.032 |
| RCP3 questions |
n = 55 1.16 (0.92) |
n = 69 1.19 (0.96) |
–0.025 (–0.362 to 0.312), p = 0.884 | 0.036 (–0.310 to 0.381), p = 0.839 |
| Personal objectives (0–100 VAS) |
n = 38 58.22 (21.23) |
n = 54 55.89 (22.97) |
2.33 (–11.70 to 7.04), p = 0.618 | 0.95 (–7.43 to 9.32), p = 0.823 |
| 2-year outcomes | ||||
| mRQLQ |
n = 59 1.10 (1.11) |
n = 78 1.24 (1.11) |
–0.141 (–0.520 to 0.238), p = 0.463 | 0.079 (–0.275 to 0.433), p = 0.659 |
| RCP3 questions |
n = 59 0.83 (0.77) |
n = 80 1.18 (0.92) |
–0.345 (–0.637 to –0.052), p = 0.021 | –0.276 (–0.571 to 0.019), p = 0.066 |
| Personal objectives (0–100 VAS) |
n = 46 64.57 (24.56) |
n = 69 66.03 (19.39) |
–1.46 (–9.61 to 6.68), p = 0.735 | –5.02 (–13.09 to 3.05), p = 0.220 |
List of abbreviations
- %PPEF
- per cent predicted peak expiratory flow
- ACQ
- Asthma Control Questionnaire
- ATS
- American Thoracic Society
- BNF
- British National Formulary
- BTS
- British Thoracic Society
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- EQ-5D
- European Quality of life-5 Dimensions questionnaire
- ERS
- European Respiratory Society
- FEV1
- forced expiratory volume in 1 second
- GINA
- Global Initiative For Asthma
- GP
- general practitioner
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ICS
- inhaled corticosteroid
- INB
- incremental net benefit
- LABA
- long-acting β2-agonist
- LTRA
- leukotriene receptor antagonist
- MiniAQLQ
- Mini Asthma Quality of Life Questionnaire
- mRQLQ
- Mini Rhinitis Quality of Life Questionnaire
- NHS
- National Health Service
- PCT
- primary care trust
- PEF
- peak expiratory flow
- PRN
- pro re nata – as needed
- RCP3
- Royal College of Physicians three questions
- QALY
- quality-adjusted life-year
- QOL
- quality of life
- SABA
- short-acting β2-agonist
- SD
- standard deviation
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Professor of General Practice, Department of Primary Health Care, University of Oxford Programme Director,
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics and Clinical Trials, Queen Mary, Department of Epidemiology and Public Health, Imperial College London
-
Professor Peter Brocklehurst, Director, National Perinatal Epidemiology Unit, University of Oxford
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Jonathan Green, Professor and Acting Head of Department, Child and Adolescent Psychiatry, University of Manchester Medical School
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, Head of Nuffield Department of Surgery, University of Oxford
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norris, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor James Raftery, Chair of NETSCC and Director of the Wessex Institute, University of Southampton
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire Country Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr David P Britt, Public contributor
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Professor Nicholas James, Professor of Clinical Oncology, School of Cancer Sciences, University of Birmingham
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Mr John Chapman, Public contributor
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Ms Kylie Gyertson, Oncology and Haematology Clinical Trials Manager, Guy’s and St Thomas’ NHS Foundation Trust London
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Martin Shelly, General Practitioner, Silver Lane Surgery, Leeds
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation of Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Professor Bruce Campbell, Consultant Vascular & General Surgeon, Royal Devon & Exeter Hospital, Wonford
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Neill McIntosh, Edward Clark Professor of Child Life and Health, University of Edinburgh
-
Professor Rajan Madhok, Consultant in Public Health, South Manchester Primary Care Trust
-
Professor Sir Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, Director, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Philip Shackley, Senior Lecturer in Health Economics, Sheffield Vascular Institute, University of Sheffield
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Dr Nick Summerton, GP Appraiser and Codirector, Research Network, Yorkshire Clinical Consultant, Primary Care and Public Health, University of Oxford
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Dr Ross Taylor, Senior Lecturer, University of Aberdeen
-
Dr Richard Tiner, Medical Director, Medical Department, Association of the British Pharmaceutical Industry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington