Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 05/46/01. The contractual start date was in February 2007. The draft report began editorial review in October 2011 and was accepted for publication in March 2012. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design.The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2012. This work was produced by Pickard et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to NETSCC.
2012 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
In 2005, the UK government National Institute for Health Research Health Technology Assessment (NIHR HTA) programme called for a randomised controlled trial (RCT) to give a definitive answer to the question ‘Is there a benefit to using antimicrobial-coated urethral catheters over catheters without antimicrobial coatings in adults requiring catheterisation expected to be of limited duration, and what are the costs?’ This report describes the research (the CATHETER trial) that was subsequently commissioned.
The CATHETER trial was a large pragmatic UK-based multicentre RCT. It aimed to establish whether or not the short-term use of either of two commercially available antimicrobial catheters – an antimicrobial-impregnated urethral catheter (nitrofurazone) or an antiseptic-coated urethral catheter (silver alloy) – in comparison with the use of a standard urethral catheter reduced the incidence of symptomatic catheter-associated urinary tract infection (CAUTI) up to 6 weeks after catheter insertion, and whether or not these catheters are cost-effective in the context of the UK NHS.
Background
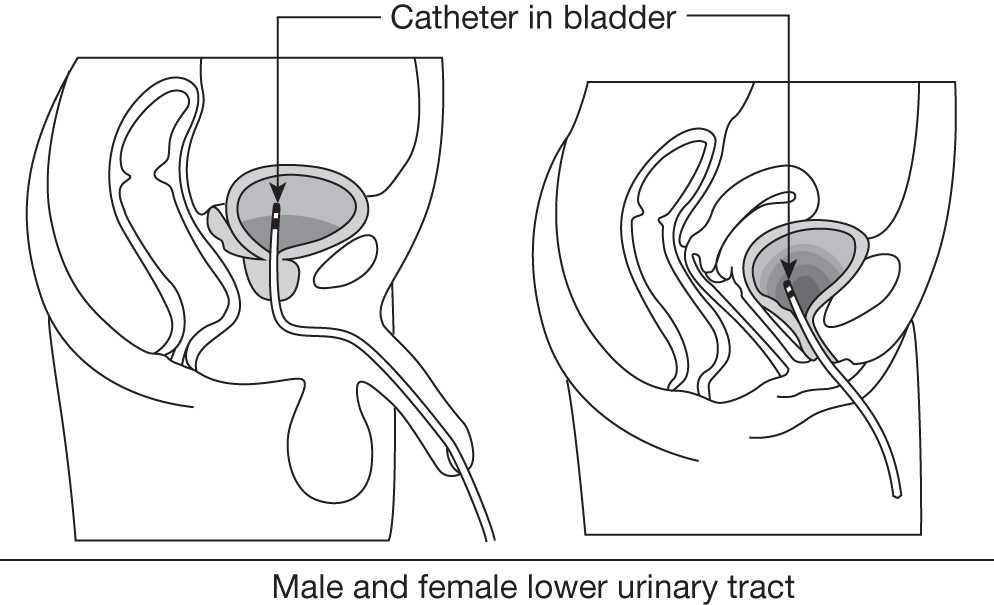
Urethral catheter design
Tubes that can be inserted through the urethra to drain the urinary bladder have been used for centuries. The current standard single-use indwelling catheter design was developed by a urologist, Frederic Foley, in the mid-1930s and marketed by the American company CR Bard Inc. The catheter consists of a drainage channel, open both at the tip positioned in the bladder and at the other end outside the body, which can be connected to a drainage bag. 1 A second channel allows inflation, through a port with a non-return valve next to the drainage outlet, of a 10-ml retention balloon, which is positioned in the bladder and prevents the catheter coming out (Figure 1). The catheter is inserted into the urethra by a trained health professional, using an aseptic technique and lubricating anaesthetic gel, and is left indwelling for as long as is necessary; removal requires deflation of the balloon and simple withdrawal of the catheter. 2
FIGURE 1.
A urethral catheter positioned in the female and male bladder.
The calibre, length, number of channels and material of manufacture of the catheter can all be varied. 3 Natural extruded rubber (latex) continues to be used as the standard material of manufacture, although usually with an added internal and external water-resistant coating of polytetrafluoroethylene (PTFE) to ensure that smoother surfaces are in contact with the urethral mucosa and urine. In 2011, these standard catheters in the UK NHS cost approximately £0.914 (US$1.48; €1.03) each. More recently, catheters made out of moulded plastics, such as silicone, have become available. These have the advantage of consistent smooth surfaces and hypoallergenicity but with higher costs of material and manufacture with a unit cost to the UK NHS in 2011 of £2.074 (US$3.41; €2.37).
Use of urethral catheters in hospitals
Urethral catheters are one of the most commonly applied medical devices, with an estimated 96 million used worldwide in 1999. 5 Within the UK, approximately 15–25% of the 14.5 million patients admitted to NHS hospitals each year will receive catheterisation at some stage during their stay. 6–9 The most common usage is for short term (which we have arbitrarily defined as up to and including 14 days) perioperative bladder drainage during and immediately after surgical or other interventional procedures. This patient group is the primary focus for our trial. 10 Other reasons for urethral catheterisation include prolonged unconsciousness or immobility, monitoring of urine output for management of fluid balance in critically ill patients, acute urinary retention and longer-term care of urinary incontinence. For patients undergoing interventions that require temporary catheterisation, the catheter is generally inserted just prior to starting the procedure and is removed when the patient is sufficiently recovered in terms of bladder function and mobility to safely re-establish normal micturition. The duration of catheterisation for these purposes is highly variable, with a recent study recording a mean [standard deviation (SD)/median] of 3.5 (4.8/2) days. 11 The type of catheter used depends on local purchasing policies and indication for use; for example, a recent audit in a large north-east England acute care hospital, which is likely to be typical of current NHS practice, showed that of the 15% of inpatients with an indwelling catheter, 50% were fitted with a silicone catheter and 36% a PTFE-coated latex catheter; in 14% the catheter type was unknown. 12
Definition of catheter-associated urinary tract infection
Normally, the urethral antimicrobial barrier is closed, preventing infection. The presence of an indwelling urinary catheter disrupts this barrier and allows colonisation of the urethra and subsequently the bladder with commensal and externally acquired organisms. These may result in bacteriuria, symptomatic urinary tract infection (UTI), and, rarely, bloodstream infection; these are collectively referred to as CAUTI. 13,14 For epidemiological and health protection purposes, CAUTI continues to be predominantly defined worldwide through consensus policy documents produced by the US government Centers for Disease Control and Prevention (CDC).
The CDC definition of symptomatic UTI associated with urethral catheterisation at the time of trial inception (2007)15 required the presence of appropriate symptoms together with either microbiological confirmation of significant bacteriuria or that a clinical diagnosis of UTI had been made and treatment instituted (Box 1).
Patient has an indwelling urethral catheter or has had one in the last 7 days before the urine culture
and
patient has at least one of the following signs or symptoms with no other recognised cause: fever (> 38°C), urgency, frequency, dysuria, or suprapubic tenderness
and
patient has a positive urine culture, that is, ≥ 105 microorganisms per cm3 of urine with no more than two species of microorganisms
Criterion 2Patient has an indwelling urethral catheter or has had one in the last 7 days before the urine culture
and
patient has at least two of the following signs or symptoms with no other recognised cause: fever (> 38 °C), urgency, frequency, dysuria or suprapubic tenderness
and
at least one of the following:
-
(a) positive dipstick for leucocyte esterase and/or nitrite
-
(b) pyuria (urine specimen with ≥ 10 WBC/mm3 or ≥ 3 WBC/high-power field of unspun urine)
-
(c) organisms seen on Gram stain of unspun urine
-
(d) at least two urine cultures with repeated isolation of the same uropathogen (Gram-negative bacteria or Staphylococcus saprophyticus) with ≥ 102 colonies/ml in non-voided specimens
-
(e) < 105 colonies/ml of a single uropathogen (Gram-negative bacteria or S. saprophyticus) in a patient being treated with an effective antimicrobial agent for a urinary tract infection
-
(f) physician diagnosis of a urinary tract infection
-
(g) physician institutes appropriate therapy for a urinary tract infection
WBC, white blood cell.
The CDC definitions were updated in 2009 while our trial was in progress. 16 The 2009 specification states that symptomatic infection can be deemed catheter-related only if an indwelling urinary catheter had been present within 48 hours of diagnosis. In addition, there must be evidence of concurrent symptoms and urinary abnormality – either pyuria or bacteriuria. Criteria 2f and 2g concerning physician diagnosis and treatment initiation have been removed in the updated 2009 version. This more restricted definition was designed for reporting of CAUTI from US hospitals as part of national surveillance of health-care-associated infections. It is less appropriate for our pragmatic trial design where we wished to additionally capture the community impact of CAUTI following discharge from hospital and avoid reliance on submission and microbiological analysis of urine specimens. For the primary outcome of the trial we therefore based definition of CAUTI on criterion 2g of the 2004 CDC definition. We do recognise, however, that other definitions of CAUTI have been used in previous trials. We therefore defined microbiologically proven antibiotic-treated UTI and the presence of bacteriuria irrespective of symptoms or treatment as tertiary outcomes.
The impact of catheter-associated urinary tract infection on hospital-based care
It is estimated that individuals with an indwelling catheter are faced with a daily risk of 5% of developing bacteriuria,6 with the proportion affected after 7 and 14 days of indwelling catheterisation being approximately 35% and 70%, respectively. It has been estimated that symptomatic UTI occurs in 20% of patients with bacteriuria,17,18 and while bloodstream infection occurs in < 1%,19,20 it is associated with a high (30%) mortality rate. An important possible consequence of development of CAUTI in an individual is the prolonging of hospital stay. Estimates of the average duration of this extra stay vary from 0.55 to 5 days. 21 CAUTI can also adversely affect health-related quality of life (QoL). 5,22 Both of these factors are important in health economic terms, as they impact on both QoL reduction and additional treatment costs, which, for the UK in 1995, were estimated to amount to a mean [95% confidence interval (CI)] of £1327 (£1140–1465) per episode, which extrapolates to a cost of £125M per annum to the NHS. 21 The presence of bacteriuria in hospital patients with an indwelling catheter is also a potential source of cross-infection, particularly in critical care units, with an estimated risk per episode of 15%. 23 In addition to CAUTI risk, short-term indwelling urethral catheters, although useful to avoid the need for voluntary bladder emptying, also contribute to postoperative discomfort, loss of dignity and delayed discharge from hospital.
The increasing realisation that hospital-acquired infections account for significant morbidity and mortality, together with associated financial and personal costs, led health-care providers to develop strategies to reduce the burden of these events. UTI, in general, is one of the two most common hospital-acquired infections, accounting for between 20% and 40% of cases. 24–26 Between 56% and 80% of these cases can be attributed to the use of indwelling urethral catheters. 20,26,27 CAUTI is therefore a major focus of these preventative strategies. The UK government Department of Health set up the Saving Lives initiative in 2007 and, subsequently, the High Impact Actions for Nursing and Midwifery initiative in 2009, which made reduction in CAUTI a key aim for the NHS through High Impact Action number 6. 28 This was based on guidelines for urethral catheter insertion and subsequent care developed from a systematic review of the evidence. 29
Pathogenesis of catheter-associated urinary tract infections
The development of bacteriuria associated with an indwelling catheter is thought to occur in stages. Microbes gain entry to the normally sterile upper urethra and bladder either by physical introduction during catheter insertion or by migration along the interface between the outer catheter surface and the urethral mucosa, or by upward migration through the internal catheter channel lumen following colonisation of the drainage system. 30 The disruption of the normal filling and emptying cycle of the bladder, and the position of the catheter drainage channel inlet above the catheter balloon resulting in a urine residue in the bladder, prevent physical removal of invading bacteria and so facilitate urinary colonisation. 31 Bacteria then adhere to the urinary tract epithelium or the catheter surface and excite an inflammatory reaction resulting in local and systemic symptoms. 32–34 Bacteria expressing more aggressive virulence factors can migrate further into the upper urinary tract or bloodstream, resulting in worsening sepsis. 35 As the duration of catheterisation increases, bacteria begin to attach to the catheter surfaces, where they multiply and produce polysaccharides, forming a biofilm. 36 Subsequently, mineral precipitation due to increased urinary pH causes catheter blockage and urinary stagnation, further facilitating bacterial growth. 37
Microbiology
Urinary tract infection associated with short-term catheterisation typically involves a single organism, in contrast with long-term catheterisation, where polymicrobial infection is frequent (Table 1). 38 Although a variety of microorganisms may be associated with CAUTI, enteric Gram-negative bacilli are the most frequently isolated. 40 Escherichia coli is the most frequently isolated single species, but other species such as Klebsiella spp., Proteus spp. and Enterobacter spp. are also commonly identified. Enterococci, Pseudomonas aeruginosa and Candida spp. are also important causes of CAUTI, particularly in patients within critical care settings. 40 Staphylococci and other Gram-negative bacilli are isolated less frequently. 38
| Pathogen | % CAUTI |
|---|---|
| E. coli | 13 |
| Other Gram-negative bacilli, such as Proteus spp. | 26 |
| Enterococcus spp. and Streptococcus spp. | 26 |
| Candida spp. | 30 |
| Polymicrobial | 5 |
Risk factors for catheter-associated urinary tract infection
A number of patient characteristics are associated with increased risk of CAUTI, including female sex, older age, impaired immunity and illness severity. Care process factors include lack of antibiotic use, longer duration of catheterisation, insertion by poorly trained personnel, and deviation from catheter care protocols. 38
Measures and strategies aimed at reducing catheter-associated urinary tract infections
There are a number of existing recommendations that can reduce the risk of CAUTI (Box 2) and the evidence for each of these has been summarised in recent reviews. 29,38,41–44
-
Reduction in prevalence of catheterisation
-
Reduction in duration of catheterisation
-
Maintenance of closed drainage system
-
On insertion
-
Throughout duration of catheterisation
-
On removal
-
Closed drainage systems
-
Antimicrobial catheters
-
Sealed catheter and drainage systems
-
Catheter valves
A range of UK guideline and best practice documents have encouraged implementation of some of these measures into the NHS with performance monitoring of individual NHS organisations to ensure compliance. These can be broadly divided into eight distinct actions. 29,45–48
-
education of patients, their care-givers and health-care personnel, in terms of hand hygiene and steps in preventing spread of infection
-
assessing the need for catheterisation – to avoid or consider alternatives
-
selection of appropriate type of catheter for individual and clinical context
-
use of strict aseptic technique for catheter insertion
-
use of antibiotic prophylaxis in selected high-risk groups at insertion
-
use of a closed drainage system or catheter valve
-
maintenance of a sterile closed drainage system by obtaining urine specimens from the sampling port, positioning of drainage bag above floor level and below bladder level; frequent emptying of drainage bag to maintain urine flow and prevent reflux; daily washing of meatus
-
reduction in duration of catheterisation: regular review of need for catheterisation and aim for early removal of catheter.
Development of urethral catheters containing antimicrobials
The most researched technical innovation in catheter design over the past 10 years has been the introduction of antimicrobial coatings applied to catheter surfaces or impregnated into the catheter material. Several manufactures have marketed either antimicrobial-impregnated or silver-coated catheters as representing a technology to reduce CAUTI risk and it is this development that is the focus of this trial. 23
Silver
Silver has long been recognised as an antimicrobial agent with demonstrated activity against uropathogens through multiple mechanisms of action. 49 Silver exposure results in limited toxicity to mammalian cells50 and does not appear to induce microbial resistance. 51 Two silver-containing compounds have been used for urethral catheters: silver oxide and silver alloy. Silver oxide-coated catheters showed lack of clinical efficacy in early clinical studies and were superseded by silver alloy-coated urethral catheters, which showed more promise in reducing bacteriuria during catheterisation. 42 The current most widely used device is a hydrogel silver alloy-coated latex catheter marketed by CR Bard Inc., New Jersey, USA, with a 2007 UK NHS cost of £6.46. 52 This catheter has metallic silver in a gold and platinum coating, linked to a latex base on the external surface of the catheter and on the inner luminal surfaces. Silver ions are released into the periurethral space to exert antibacterial activity. The outer hydrogel layer gives the catheter its self-lubricating properties. 53
Antimicrobials
A potentially more direct method of inhibiting CAUTI is to coat or impregnate catheters with antimicrobials active against expected uropathogens. Two antimicrobial agents have been used in clinical studies. Initially, a minocycline/rifampicin mixture was used. 54 Despite promising preliminary results, this specific catheter was not pursued by the development company (Cook Urological). The second antimicrobial agent used for catheter impregnation was nitrofurazone, a topical nitrofuran related to nitrofurantoin, which has a spectrum of activity against many potential uropathogens. Nitrofurazone-impregnated urethral catheters are commercially available and marketed by Rochester Medical Corp in 2007 at a UK NHS cost of £5.29. 4 For this catheter design, nitrofurazone is impregnated into the external and internal luminal surfaces to give an effective concentration of 10.2 µg/mm3. The drug then elutes over time into the external surface–urethral mucosa and internal lumen–urinary boundaries. 55
Evidence for clinical and bacteriological effectiveness
Several systematic reviews have investigated the effectiveness of antimicrobial catheters in reducing CAUTI, including pooled data from up to 13,000 patients. The results of five systematic reviews23,42,56–58 suggest that silver alloy-coated catheters reduce the incidence of bacteriuria in hospitalised patients catheterised for < 2 weeks in comparison with standard catheters. The magnitude of relative risk reduction varied in each of the analyses due to different inclusion criteria, ranging from 16% (95% CI 6% to 47%; absolute risk reduction of 2.0%)58 to 46% (95% CI 33% to 57%; absolute risk reduction of 11.3%). 42 The pooled results for nitrofurazone-impregnated catheters showed a relative risk reduction of up to 48% (95% CI 32% to 66%; absolute risk reduction 8.6%);42 however, the benefit of this type of catheter appeared to be limited to the initial 7 days of catheterisation. It should be noted that these event rates and associated risk reductions apply to CAUTI diagnosis based solely on microbiological identification of bacteriuria without any patient-driven or clinician-defined contribution to the primary outcomes used. Overall, the methodological quality of these reviews was poor to moderate according to the AMSTAR quality assessment tool,59 with the exception of that by Schumm et al. ,42 which was methodologically more robust. [K Schumm (now K Gillies) and T Lam, authors of the updated Cochrane review, were both members of the trial steering and project management groups and are named authors of this monograph.]
In summary, these systematic reviews have concluded that silver alloy-coated and nitrofurazone-impregnated catheters do show promise for the reduction of CAUTI. The reviews did, however, highlight a number of uncertainties regarding the evidence base, in particular the clinical and health economic relevance of the outcome measures used.
Problems with current evidence
Clinical effectiveness
The majority of studies used the presence of bacteriuria on microbiological examination as the outcome measure for a diagnosis of CAUTI without specifying as to whether or not it was symptomatic and without linking to clinical decision to treat with antibiotics. 23,42,58 The lack of use of an outcome explicitly measuring patient benefit hampers interpretation of these data to guide change in practice. In addition, the majority of the individual trials were small and of poor to moderate methodological quality, with wide variations in study design, population studied, and outcome definitions, together with failure to account for confounding factors. 23,42 These aspects may account for the heterogeneity in effect size between individual studies and between meta-analyses. Given these uncertainties, the authors of systematic reviews and clinical practice guidelines emphasised the urgent need for well-designed, adequately powered RCTs using outcome measures of relevance to patients and health-care systems to determine the clinical effectiveness of antimicrobial-coated catheters. 42
Cost-effectiveness
For the background to our planned economic evaluation we performed a systematic literature search that identified 400 economic studies, of which six reports5,60–64 and two systematic reviews65,66 were deemed relevant, although only one was from the perspective of the UK NHS. 61 All reports concerned the comparison between silver alloy-coated and standard catheters, with no data on nitrofurazone-impregnated catheters. The design of the studies varied with two being model-based,5,61 two trial-based,60,62 and two surveillance-based studies. 63,64 These studies were summarised and critically evaluated (see Appendix 1).
A study using a decision model based on a simulated cohort of 1000 hospitalised patients from various specialties in the USA5 found that, based on an assumption that silver alloy-coated catheter use would result in a 47% relative reduction in CAUTI rate, there was a probability of 0.84 that cost savings would accrue with change in practice. A UK NHS-based study61 reported that if routine use of silver alloy-coated catheters was adopted, and assuming an additional cost of £9 per catheter, lower costs of extra hospital stay in medical patients, and a baseline risk for CAUTI of 7.3%, relative risk reductions in CAUTI of 14.6% in catheterised medical patients, and of 11.4% in catheterised surgical patients were required before cost savings could be made.
An economic analysis performed within a large cluster randomised trial involving 28,000 patients62 reported that use of silver alloy-coated catheters could lead to cost reduction of between 3.3% (US$14,456) and 35.5% (US$537,293) in annual institutional CAUTI costs, depending on whether low (US$840) or high (US$4693) estimates of the cost of an individual episode of CAUTI were used. A masked prospective study from a single institution calculated that the annual cost saving from the 41 episodes of CAUTI saved by routine use of silver alloy-coated catheters was US$98,021. 60 A study using surveillance data estimated that use of silver alloy-coated catheters resulted in a decrease in CAUTI incidence from 6.13/1000 catheter-days to 2.16/1000 catheter-days. 63 It was calculated that this would result in annual cost savings for the institution of either US$5811 or US$484,070, depending on whether low (US$700) or high (US$5682) estimates of the cost of an individual episode of CAUTI were used. Finally, estimates of annual, single institutional cost savings associated with routine use of silver alloy-coated catheters ranged from US$12,564 to US$142,315 based on mean (median) cost of a single episode of CAUTI of US$1214 (US$614). 64
The methodological quality of the studies varied and it is difficult to draw general conclusions from them. For example, in the model-based analyses, assumptions concerning baseline rate of CAUTI, the relative risk reduction associated with the intervention, and calculation of cost of CAUTI varied. Overall, these results do illustrate the high degree of uncertainty regarding the cost implications following introduction of antimicrobial catheters, and this predominantly reflects imprecision of the parameter estimates included in the specific models.
Need for a trial
The current frequency of indwelling urethral catheterisation in UK NHS acute hospitals suggests that more than 2 million people are at risk of CAUTI each year. The subsequent costs in terms of patient morbidity and extra care mean that CAUTI continues to be an important health-care problem. Current evidence from meta-analyses of predominantly small explanatory trials shows that antimicrobial catheters do reduce the risk of developing bacteriuria during periods of short-term urethral catheterisation. The logical next step is to demonstrate that this antimicrobial effect translates into clinical benefit for patients in terms of reducing the risk of symptomatic UTI requiring antibiotic treatment, and that it achieves this at an acceptable cost to the NHS. The current evidence base suggested that a pragmatic trial design was required which would be able to provide a definitive result generalisable across the population at risk. From a clinical effectiveness perspective, any trial would also need to measure discomfort and urinary symptom burden suffered by individuals within a specific health-care system, the UK NHS in this instance.
Trial objectives
The following questions were addressed: in hospitalised adults requiring short-term catheterisation what is the clinical benefit and cost-effectiveness of using antimicrobial-impregnated or antiseptic-coated urethral catheters over standard urethral catheters? Two pragmatic comparisons of equal importance were made:
-
antimicrobial-impregnated silicone catheter (nitrofurazone) compared with standard PTFE-coated latex catheter
-
antiseptic-coated hydrogel latex catheter (silver alloy) compared with standard PTFE-coated latex catheter.
The systematic review and meta-analysis of available randomised studies current at the time of inception of the trial suggested that the use of silver alloy catheters resulted in a 40% reduction in risk of catheter-associated symptomatic UTI against standard comparators [RR 0.60 (95% CI 0.50 to 0.73)]. 41 A previous epidemiological review estimated that for people catheterised for up to 10 days the absolute risk (95% CI) of developing bacteriuria was 26% (95% CI 23% to 29%) and of these, around a quarter (6.5% of the total) would develop a symptomatic infection. 67
These summarised data were used to generate the hypothesis to be tested by this trial: use of either silver alloy-coated or nitrofurazone-impregnated catheters reduces the incidence of CAUTI during short-term use by 40% relative to the standard catheter, with an absolute reduction of at least 2.8% (from 7.0% to 4.2%).
Chapter 2 Trial design
The CATHETER trial was a RCT testing three types of short-term urinary catheters in a range of clinical settings in the UK.
Participants
Potential participants were identified according to the inclusion and exclusion criteria detailed below.
Inclusion criteria
Adults (≥ 16 years of age) requiring urethral catheterisation (which was expected to be required for a maximum of 14 days), from selected hospital wards with a high volume of short-term catheterisation.
Exclusion criteria
-
Patients for whom urinary catheterisation was expected to be longer-term (defined as > 14 days).
-
Patients who had urological intervention or instrumentation within the 7 days preceding recruitment (e.g. catheterisation, cystoscopy, prostatic biopsy and nephrostomy insertion).
-
Patients who required non-urethral catheterisation (e.g. suprapubic catheterisation).
-
Patients who had a known allergy to any of the following: latex, silver salts, hydrogel, silicone or nitrofurazone.
-
Any patient who had a microbiologically confirmed symptomatic UTI, at time of randomisation.
-
Patients who were unable to give informed consent or retrospective informed consent.
Participants were equally allocated to one of the three trial interventions using a web- or telephone-based system managed by the Centre for Healthcare Randomised Trials (CHaRT), University of Aberdeen. The inclusion criterion for participation of centres was a high volume of short-term catheterisations, principally as part of elective surgical activity. Twenty-four centres took part in the trial: Aberdeen Royal Infirmary; Royal Blackburn Hospital & Burnley General Hospital; Blackpool Victoria Hospital; Bristol Royal Infirmary; Edinburgh Royal Infirmary; Guy’s Hospital; Harrogate District Hospital; Hillingdon Hospital; Hinchingbrooke Hospital; Raigmore Hospital, Inverness; Liverpool Women’s Hospital; Newcastle upon Tyne Hospitals (Newcastle General Hospital, Freeman Hospital, and Royal Victoria Infirmary); Norfolk and Norwich University Hospital; North Tyneside General Hospital; Nottingham City Hospital; Royal Preston Hospital; Queen Alexandra Hospital, Portsmouth; Southampton General Hospital; Sunderland Royal Hospital; Musgrove Park Hospital, Taunton; Torbay Hospital and Yeovil District Hospital. The trial recruited from a wide range of clinical settings including cardiovascular, obstetrics and gynaecology, orthopaedics and neurosurgery as detailed in Chapter 4.
Planned trial interventions
There were two experimental groups of equal importance:
-
nitrofurazone-impregnated silicone urethral catheter (N), sourced from Rochester Medical, UK (product reference number 95214)
-
silver alloy-coated latex hydrogel urethral catheter (S), sourced from CR Bard Ltd, UK (product reference number 236514UKS).
The control group was managed with a PTFE-coated latex urethral catheter (P), sourced from CR Bard Ltd, UK (product reference number 1254S14UK).
All catheters used in the trial had an external circumference of 14 mm, termed 14 French (Fr) or 14 Charrière (Ch), with equivalent luminal calibre, length, recommended balloon volume (10 ml), drainage ports and external connection fittings. The silver alloy-coated and control catheters were manufactured from latex, whereas the nitrofurazone catheters were made from silicone. The choice of a PTFE catheter as the ‘standard’ control was based on the results of an audit of short-term catheter use in all secondary care wards in Newcastle upon Tyne Hospitals and Aberdeen Royal Infirmary, which confirmed that the PTFE-coated latex urethral catheter was the most commonly used in both hospitals (> 70%).
Proposed duration of intervention
The period of urethral catheterisation was expected to be between 1 and 14 days.
Comparisons
The outcomes were compared with:
-
nitrofurazone-impregnated catheters and standard PTFE catheters
-
silver alloy-coated catheters and standard PTFE catheters.
Outcome measures
Primary outcome measure
Incidence of symptomatic UTI treated with antibiotics at any time up to 6 weeks post randomisation (number of participants with at least one occurrence). This was defined as any symptom reported up to 3 days after catheter removal, at 1 or 2 weeks post catheter removal, or at 6 weeks post randomisation combined with a prescription of antibiotics, at any of these times (see Table 4).
Subgroup analyses of the primary outcome examined possible interaction with participant age, sex, comorbidity, duration of catheterisation, indication for catheterisation and antibiotic use prior to trial enrolment.
Details of which data contributed to the primary outcome are shown later in this chapter (see Table 4), and Chapter 3 (see Important changes to methods after trial commencement) details how the attributes of the primary outcome were strengthened during the course of the trial.
Secondary outcome measures
Clinical
Microbiological confirmation of bacteriuria in addition to primary outcome: this was defined as those who fulfilled the criteria for the primary outcome and in addition had any microbiologically positive result where there were ≥ 104 colony-forming units (CFUs)/ml of no more than two different species of uropathogen. This was assessed by a protocol-mandated urine sample at 3 days after catheter removal.
Economic
-
Incremental cost per infection averted and quality-adjusted life-years (QALYs) gained.
-
QALYs estimated from European Quality of Life-5 Dimensions (EQ-5D) responses.
-
Cost to the NHS and patient of the different catheters.
Tertiary outcome measures
Individual analysis of the components of the definition of the primary and secondary outcomes is shown below.
Patient self-reported symptoms
-
Bacteriuria: any microbiologically positive result (≥ 104 CFU/ml of no more than two different species of uropathogen 3 days after catheter removal).
Other significant clinical events: septicaemia and mortality
-
Adverse effects of catheterisation apart from symptomatic UTI (e.g. urethral discomfort and pain on removal).
-
Antibiotic use following randomisation and indication.
Chapter 3 Methods
Ethics and regulatory approvals
The CATHETER trial and subsequent amendments were reviewed and given a favourable opinion by the North of Scotland Research Ethics Service, Grampian Research Ethics Committee 1 (reference 06/S0801/110) and local Research and Development Departments as appropriate prior to commencement. The trial was conducted according to the principles of Good Clinical Practice (GCP) and was registered and assigned an International Standard Randomised Clinical Trial Number (ISRCTN75198618). The CATHETER trial was not classed as a trial involving an Investigational Medicinal Product or Medical Device and therefore did not come under the EU Clinical Trials Directive.
Participants
Trial flow
The trial process is detailed in Figure 2.
FIGURE 2.
The CATHETER trial recruitment processes and procedures.
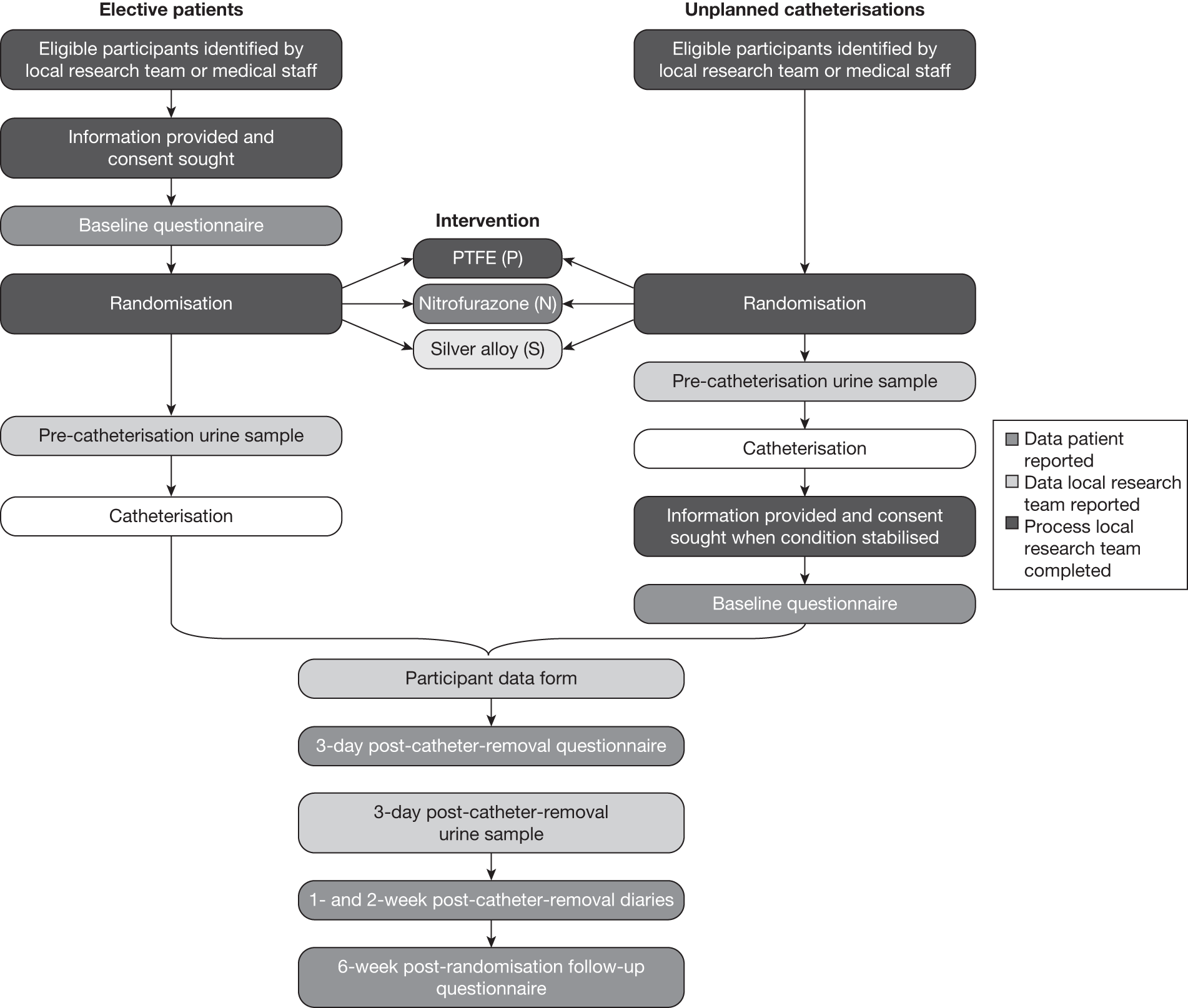
Identification of patients
Patients were identified either by a member of the local research team or by ward staff. In order to publicise the trial to ward staff and patients, laminated recruitment posters were placed at prominent locations at each site as appropriate.
Recruitment process
Once a patient was identified as being eligible for the trial, he/she was approached by a member of the local research team and given the trial patient information sheet (see Appendix 2). Once the patient had been given time to consider and understand the implications and requirements of the trial, and was happy to take part, he/she was asked to sign the trial consent form (see Appendix 2).
The only exception to this was for patients in unplanned situations (e.g. non-elective admissions and catheterisations). The local research team was made aware of this and, once the patient’s condition had stabilised, he/she was provided with the patient information sheet and given an opportunity to consent retrospectively to take part in the trial; this methodology for recruitment was approved as part of our ethics submission. The decision to catheterise such patients was based solely on clinical need by the local clinical care team. As the antiseptic/antimicrobial-impregnated catheters have previously been reported to lessen the risk of infection compared with the usual standard catheter, the inclusion of these patients in the trial prior to informed consent did not pose a clinical risk, did not lessen their standard of care and was not thought to be otherwise disadvantageous to the participant. Patients who subsequently gave informed consent then completed the normal trial processes. Patients who declined to give informed consent retained the trial catheter as appropriate but no trial data were collected.
Randomisation and allocation to intervention
Eligible participants were randomly allocated 1 : 1 : 1 to one of the three interventions using a computer-generated system that was concealed and remote from the users. The local research team or ward staff performed randomisation using either the automated interactive voice recognition (IVR) telephone randomisation application or the CATHETER trial website (www.charttrials.abdn.ac.uk/catheter), both managed by CHaRT, University of Aberdeen. Both methods of randomisation were available 24 hours a day, 7 days a week. Compliance with the allocated intervention was recorded. No stratification or minimisation was used.
Blinding of trial interventions
The nitrofurazone catheter was easily identifiable because of its bright-yellow colour. To guard against bias in this respect, although the recruiter knew the allocated intervention, as far as was practicable participants and clinicians making decisions regarding the participant’s catheter care were not told. General practitioners (GPs) were also not informed by trial staff of the catheter type the participant received and therefore were unlikely to be influenced by knowledge of the catheter type. Urine samples taken at baseline and 3 days after catheterisation were analysed by staff at a local laboratory, who were blind to the intervention.
Interventions
The calibre of urinary catheters is measured as the external circumference in millimetres, Fr or Ch gauge, and they can be supplied in differing lengths to suit the male (38–46 cm) or female (24–28 cm) urethra. The uniform calibre and length of the three catheters tested in this trial was specified as 14 Fr and 40 cm, respectively. 68 This was chosen as 14 Fr is the standard calibre for short-term monitoring use. A longer urethral catheter does not cause problems when used in women, but it is not possible to use a shorter catheter in men. They were purchased direct from the manufacturers (CR Bard Ltd UK, Rochester Medical, UK) by the trial office at a unit price fixed in 2007 for the duration of the trial and distributed by the trial office in Aberdeen to the sites as needed. Each catheter had a detachable sticker attached to the outer packaging. This sticker displayed the ‘CATHETER’ logo and either ‘N’, ‘S’ or ‘P’ to denote catheter type (N = nitrofurazone, S = silver, P = PTFE). These stickers were then placed directly on to the participants’ consent forms to permit verification that they were given the catheter to which they were randomised.
Data collection
Questionnaires and diaries were designed to obtain information on symptomatic UTIs as well as other catheter-associated problems (e.g. urethral discomfort), QoL, and any health economic implications, such as costs to the participants and the NHS (see Appendix 3). Clinical data at baseline and throughout the participant’s hospital stay were collected by the local research team (see Appendix 4). An amended version of the UTI Symptom Assessment Questionnaire69 was used to assess UTI symptoms 3 days post catheterisation.
Following informed consent, the participants were asked to complete a baseline questionnaire before randomisation (for participants undergoing unplanned catheterisation, randomisation occurred before informed consent and the baseline questionnaire was then collected after consent was obtained). At baseline, a sterile mid-stream specimen of urine (MSSU) was collected and sent for microbiological analysis, in an accredited laboratory [Clinical Pathology Accreditation UK (CPA)] according to local diagnostic protocols, immediately prior to catheterisation (if one had not been sent within the preceding 48 hours). In situations where this was not possible, a specimen of urine was obtained during the process of catheter insertion, i.e. catheter specimen of urine (CSU) using standard aseptic techniques.
Three days post catheter removal, participant-reported outcome data were recorded by a questionnaire given to the participant by the local research team. When possible, these data were collected while the participant was hospitalised, but in situations where the participant was discharged before this time point, they were asked to complete this at home and return it to the trial office. An MSSU was collected for culture within or at 3 days of catheter removal (analysed in CPA-accredited laboratories according to local diagnostic protocols). For the purposes of the trial we defined a positive urine culture as the presence of at least 104 (CFUs)/ml.
If a clinical diagnosis of symptomatic UTI was made at any stage, including during the period of catheterisation, either a CSU or MSSU was obtained according to normal clinical practice.
Participants were asked to complete diaries at 1 and 2 weeks post catheter removal and at 6 weeks post randomisation. Table 2 describes the outcome data collected.
| Outcome data | Collected by | Baseline | Time post catheter removal | Time post randomisation | ||
|---|---|---|---|---|---|---|
| 3 days | 1 week | 2 week | 6 weeks | |||
| Urinary tract symptoms | Participant | ✓ | ✓ | ✓ | ✓ | ✓ |
| EQ-5D | Participant | ✓ | ✓ | ✓ | ✓ | ✓ |
| Antibiotic use | Clinical | ✓ | ✓ | |||
| Antibiotic use | Participant | ✓ | ✓ | ✓ | ||
| Antibiotic use | GP | ✓ | ✓ | ✓ | ||
| Use of health services | Participant | ✓ | ||||
Diaries and questionnaires completed prior to hospital discharge were collected by the local recruitment co-ordinator. On discharge, patients were supplied with a pack containing the relevant 1- and 2-week diaries and pre-paid addressed envelopes to return the diaries to the trial office. At 6 weeks post catheterisation, participants were sent the follow-up questionnaire from the trial office and asked to return it using the pre-paid addressed envelope provided. Where necessary, participants who did not return their diaries or questionnaires were telephoned either by the local research co-ordinator or a member of the trial office and asked to return their paperwork. If possible, primary outcome data were collected by phone at this point.
Where the period of catheterisation was longer than initially anticipated (i.e. the catheter was still in place after day 14), trial data were collected as if the catheter had been removed on day 14 (e.g. the 3-day post removal questionnaire was completed 17 days post catheterisation). The date of catheter removal was subsequently recorded. The rationale for this was that it would not be appropriate to exclude data from these participants but it also would not be justified to prolong follow-up for any participant beyond the planned 6 weeks after randomisation. Given the likely small numbers of participants affected, we chose to use the same documentation but we instructed local trial staff to aid participant completion, as the majority of patients affected were likely to remain in hospital during the extended period of catheterisation. This ensured that we captured any UTI event during the 6-week period and ensured effective use of limited resources.
Collection of information to describe urinary tract infections
The primary outcome was derived using information collected from the sources at the time points described in Table 3 and was determined using the algorithm described in Appendix 5.
| 1. | During catheterisation | Ward-based diagnosis from symptoms and observations (supported by microbiology where appropriate) and clinician-directed use of antibiotics for UTI. Data recorded by local research team |
| 2. | Three days post catheter removal | Ward-based diagnosis from symptoms and observations and clinician directed use of antibiotics for UTI. Urine specimen for microbiological confirmation of bacteriuria |
| Data recorded by local research team and participant | ||
| 3. | One and two weeks post catheter removal | Participant diary collected data on symptoms, clinician contact and antibiotic usage for UTI. Where antibiotic use was documented this was confirmed as being for UTI by the participant’s GP |
| 4. | Six weeks post randomisation | Symptoms, clinician contact, antibiotic usage for UTI and hospital readmissions were reported by the participants. Where antibiotic use was documented this was confirmed as being for UTI by the participant’s GP |
Participants met the definition of the primary outcome if they fulfilled the criteria described in Table 4. This is expanded in Appendix 5.
| Outcome measurement | Method of collection |
|---|---|
| Received antibiotics for UTI during catheterisation with associated symptoms | Recorded from clinical records |
| Participants given an antibiotic for a symptomatic UTI | Recorded at 3 days post catheterisation from clinical records and participant report |
| Participant-reported symptomatic UTI at 1 or 2 weeks post catheter removal or 6 weeks post randomisation with GP confirmation of antibiotic prescription for UTI | Recorded up to 6 weeks post randomisation from participant diaries and questionnaires and GP records |
General practitioner confirmation of antibiotic prescription
Where participants reported antibiotic use at 1, 2 or 6 weeks or failed to return any trial paperwork at these time points, confirmation of these details, or a request for this information, was sent to the participant’s GP. This included a brief letter explaining the need for this information and a table for the GP to complete asking whether or not the participant had presented to them with a UTI during the period of their participation in the trial, and if so whether or not they had given the participant a prescription for antibiotics for UTI (see Appendix 4).
Change of status/withdrawal
The status of some participants changed during the trial for a number of reasons. These included post-randomisation exclusions; participants deciding they no longer wished to be a part of the trial; and decisions by medical staff that it was not appropriate for the participant to remain in the trial.
Participants were free to decline further follow-up from the trial at any point without giving a reason. Participants could also be withdrawn for medical reasons. In such cases, primary outcome data were still collected if the participant consented to the use of their relevant hospital and general practice records.
In addition, some patients were classed as post-randomisation exclusions for one of the following reasons:
-
patients who were randomised but received a suprapubic catheter
-
patients who were randomised but did not have any catheter inserted
-
emergency patients who were randomised but subsequently declined to participate in the trial.
The justification for excluding participants who did not receive a urethral catheter from the analysis was that they did not fulfil intention-to-treat criteria, as the ultimate decision-maker, the responsible clinician in the operating suite, determined that an alternative urine drainage option was preferred.
Data management
Data collected at site were input into the electronic CATHETER database through the trial web portal (www.charttrials.abdn.ac.uk/catheter) by the local research team; those received by the trial office were entered by the trial office staff.
At the end of the trial, a random 10% sample of all of the trial data were re-entered by the trial office to verify correct data input. Any discrepancies between originally entered data and re-entered data were reviewed and checked against the original paper copy by an individual who was not involved in entering either data set. Incorrectly entered data were corrected at the time of checking. An initial data entry error rate of > 5% would have triggered a requirement to re-enter the entire data set from that questionnaire. This was not found to be necessary.
Trial oversight committees
A Trial Steering Committee (TSC), consisting of an independent chairperson, two further independent members and the grant holders, provided oversight of the trial. The TSC met six times over the course of the trial (at least annually).
The independent Data Monitoring Committee (DMC) met early in the trial and agreed its terms of reference and other procedures. They then met six times over the course of the trial (at least annually). The DMC reported any recommendations to the chairperson of the TSC.
Important changes to methods after trial commencement
Primary outcome
In response to recommendations from the DMC in June 2008, the TSC reviewed the method of recording the definition of the primary outcome to ensure that the trial was reliably capturing all events that determined catheter-associated symptomatic UTI. Over the course of the third and fourth meetings (dates 8 June 2009 and 23 November 2009) the DMC commented on a higher than anticipated proportion of trial participants with a positive primary outcome. Further investigation showed that this was due to high levels of urinary tract symptoms reported by the trial participants at 3 days, perhaps due to irritation from the recently removed urethral catheter, together with uncertainty regarding the purpose of prescribed antibiotics. As a result, at this time point (3 days post catheter removal) description and recording of the events needed to qualify as symptomatic UTI were strengthened in the case report form to explicitly include a record of appropriate antibiotic treatment for patient reported symptomatic UTI. Although it was felt that this had been implicit in the original wording, an amendment was made stating this to clearly qualify which events define the primary outcome.
Sample size calculation
The original sample size calculation for the trial was revised upwards. Given that the primary outcome for the trial was patient-reported symptomatic UTI supported by antibiotic treatment rather than bacteriuria or microbiology confirmed UTI, it became evident during the trial that the actual incidence of symptomatic UTIs without the requirement for microbiologically proven bacteriuria was greater than originally anticipated. This prompted a reassessment of the initial sample size calculation. Both the original and revised calculations are outlined below.
Original proposed size of the trial
Based on the Cochrane review and other data,5,41,67 the anticipated incidence of UTI in the standard control group was 7.0% and a reasonable estimate of the effect of the intervention catheters would reduce this to 4.2% [absolute risk reduction 2.8%, relative risk (RR) 0.60, odds ratio (OR) 0.58]. We estimated that based on a stricter alpha error rate of 0.025 (to correct for the two principal comparisons) and 90% power, 1750 participants were required for each arm of the trial. We inflated this to adjust for an anticipated 8.0% post-randomisation exclusion rate resulting in 1900 per arm, or 5700 total randomised.
Revised sample size calculation
Ongoing monitoring of the overall rate of the primary outcome in the trial indicated that the original estimate of the incidence of symptomatic UTI supported by antibiotic treatment was an underestimate and consequently this was revised upwards from 7% to 11% in the PTFE control group. The effect size was revised in light of this to reduce the primary outcome to 7.7% in the primary catheter groups (absolute risk reduction 3.3%, RR 0.7, OR 0.67). Recalculating the sample size based on these new parameters resulted in approximately 2000 required for each arm of the trial. Furthermore, the empirical rate of post-randomisation exclusion was also higher than originally estimated and therefore the final number required was inflated to compensate for an estimated 15% post-randomisation exclusion rate, resulting in a total required sample size of approximately 7035.
Recruitment from specific clinical areas
As described in the trial protocol, we originally intended to have a wider recruitment area encompassing patients admitted to hospital for both elective and emergency reasons, including those admitted to or transferred to critical care areas who required unplanned catheterisation. Early in the trial it was established that recruitment and pre-consent randomisation of participants undergoing unplanned catheterisation was resource intensive in terms of NHS clinical and research staff activity, and that there was a high rate of subsequent refusal of consent, which raised ethical concerns. In discussion with the trial management committees, it was decided to concentrate our finite resources on recruitment of patients admitted for elective interventions associated with planned urethral catheterisation. To ensure generalisability we proceeded to establish a large number of sites including all of the relevant clinical specialties.
Statistical methods/trial analysis
All analyses were carried out using SAS software version 9.2 for Windows (SAS Institute, Cary, NC, USA), unless otherwise stated. The principal comparisons within the trial were between those allocated to (1) the nitrofurazone and PTFE catheters and (2) silver alloy and PTFE catheters. All UTI outcomes were also summarised as the absolute risk difference expressed as a percentage. The primary and secondary outcomes were analysed using generalised linear models. All estimates are presented with 97.5% CIs (to reflect the stricter level of alpha due to multiple comparisons used in sample size calculations). Estimates from marginal models (unadjusted) and conditional models are presented adjusted for:
-
age (< 60 years, ≥ 60 years)
-
sex
-
comorbidity (pre-existing urological disease, diabetes, immune suppression)
-
indication for catheterisation (incontinence, urinary retention and monitoring purpose)
-
antibiotic use prior to enrolment.
All outcomes related to UTI were based on the intention-to-treat principle, with all included participants analysed as randomised, regardless of the catheter received. All participants were assumed to have not had a UTI unless indicated otherwise (see algorithm for primary outcome).
Quality-of-life data were analysed in a repeated measures framework using SAS PROC MIXED. An AR(1) autoregressive correlation structure was used. QoL data are presented as means and SDs at each time point, and presented in a graph for ease of comparison over time. Analysis was by complete case intention to treat; sensitivity to missing data was explored using PROC MI under the missing-at-random assumption.
All outcomes related to symptoms and catheter-associated discomfort were analysed using ordered logit models (also called proportional odds or ordered logistic regression) that were suitable for ordinal outcome data implemented in Stata 11.2 (StataCorp LP, College Station, TX, USA). Results are presented as ORs (and 97.5% CIs). To aid interpretation the difference in predicted probabilities (and 97.5% CIs) of being in a particular category between intervention and control catheters are also presented. 70 Analysis was complete case intention-to-treat and a sensitivity analysis using multiple imputations (under the assumption of missing at random) was carried out for each of these outcomes.
Timing and frequency of analyses
The data monitoring committee considered confidential interim inspection of the data on five occasions. At the first meeting, the DMC recommended refining the definition of algorithm used to define the primary outcome; this was due to a higher than anticipated rate of UTI (for further details, see Chapter 3, Important changes to methods after trial commencement).
Planned secondary subgroup analyses and sensitivity analyses
Subgroup analyses of the primary outcome examined possible effect modification of the following:
-
age (< 60 years, ≥ 60 years)
-
sex
-
comorbidity (pre-existing urological disease, diabetes, immune suppression)
-
indication for catheterisation (incontinence, urine retention and monitoring purpose)
-
antibiotic use prior to randomisation
-
duration of catheterisation.
Modification of the treatment effect was explored using tests for interaction (all at stricter levels of significance; p < 0.01), and results are presented as forest plots with 99% CIs to reflect the exploratory nature of these analyses. Two further post hoc effect modification sensitivity analyses were carried out treating (1) age and (2) duration of catheterisation as continuous variable interactions with treatment allocation to explore any potential differential effects across catheters. All subgroup and treatment effect modification analyses were analysed using the same generalised linear modelling framework as the main analyses. A further sensitivity analysis was carried out to assess any potential impact of centre on the precision of estimates of treatment effects by including a random effect for centre in the model for the primary outcome.
Economics methods
Introduction
Two types of economic analyses were planned. The first was a ‘within-trial’, economic evaluation undertaken using data collected as part of the trial, and the second was based on a modelling exercise aiming to address the uncertainty (background noise) introduced by the heterogeneity in terms of underlying illness and type of operative procedure undergone by trial participants. The question addressed by both economic evaluations was: what is the cost-effectiveness of antimicrobial-impregnated (nitrofurazone) or antiseptic-coated (silver alloy) catheter versus standard PTFE-coated catheter? The methods and analysis for both the within-trial analysis and the modelling analysis are described below. The perspective of study was that of the UK’s NHS.
Within-trial analysis
Measurement of resource utilisation
The use of health services was recorded prospectively for each participant. Resource utilisation data were collected using the questionnaires at baseline, 3 days after catheter removal, 1 week and 2 weeks after catheter removal, and at 6 weeks post randomisation. As noted earlier the questionnaires were targeted at identifying symptomatic antibiotic-treated UTI as well as other catheter-associated problems (e.g. urethral discomfort), QoL, and any health economic implications such as costs to the NHS. The areas of resource considered are outlined in Table 5 and are grouped into four broad areas:
-
intervention resource use
-
other secondary care resource use
-
primary care resource use
-
resource use incurred by the patient.
| Area of resource use | Source | Reported outcome |
|---|---|---|
| Intervention | ||
| Antimicrobial impregnated (nitrofurazone) | CRF | No. used |
| Antiseptic coated (silver alloy) | CRF | No. used |
| PTFE | CRF | No. used |
| Days in hospital (by level of care) | ||
| Medical ward | CRF | No. of days |
| Urology | CRF | No. of days |
| Cardiothoracic | CRF | No. of days |
| General surgery | CRF | No. of days |
| Obstetrics and gynaecology | CRF | No. of days |
| Ear, nose and throat | CRF | No. of days |
| Orthopaedics | CRF | No. of days |
| Vascular | CRF | No. of days |
| Gastroenterology | CRF | No. of days |
| Other costs | ||
| Antibiotics prescribed after discharge | PQ | No. and type |
| Outpatient visits | PQ | No. |
| Practice nurse home and surgery visits | PQ | No. |
| Practice doctor home and surgery visits | PQ | No. |
| Other health-care professional visits | PQ | No. and type |
The number and type of catheter used were collected from the case report form. Use of secondary care services following the period of catheterisation was collected using the 6-week participant follow-up questionnaire. This recorded information on outpatient visits and readmissions to hospital for a UTI during the 6-week period after randomisation. The use of primary care services including contacts with primary care practitioners (e.g. GPs and practice nurses) and prescription medications were collected using the health-care utilisation questionnaires administered at 1 and 2 weeks after catheter removal and at 6 weeks after randomisation.
Derivation of costs
Unit costs were based on study-specific estimates and data from standard sources. A summary of unit costs is presented in Table 6. Unit costs for the interventions were obtained from the manufacturers of the products through personal communication or from published price lists. The unit cost per day in hospital for each level of care was obtained from Information Services Division (ISD) of NHS Scotland. 71 This source does not give a cost per inpatient-day for all hospital services but rather presents data as a total cost per average case for each clinical specialty along with an average length of stay. We used these data to calculate ‘cost per day’ for each level of care. The total cost per case for each specialty provided by ISD includes both theatre costs and allocated costs (representing the costs of running the hospital). The former were omitted from our analyses, as we were not concerned with the costs of surgery undergone by trial participants (apart from the catheter unit cost) and we omitted the infrastructure costs, as they represent a fixed cost that will not vary with length of stay. The unit cost per case with these two elements removed was divided by the trial estimate of average length of stay for each specialty to give a cost per day. For example, the total gross cost per case in urology given by ISD was £2019 and the direct theatre cost per case was £479 (22%). We estimated the unit cost per stay by taking the theatre cost per case away from the unit cost per stay and then removing the allocated costs. This figure was then divided by the trial estimate of average length of stay for this specialty (3.3 days) to give the trial estimate of cost per day of £321 for participants treated under this specialty group.
| Area of resource use | Unit cost (£ sterling) | Notes |
|---|---|---|
| Intervention | ||
| Antimicrobial impregnated (nitrofurazone) | 5.29 | Personal communication with manufacturer (cost includes VAT). This was the price to the NHS of the catheter at trial commencement (2007) |
| Antiseptic impregnated (silver alloy) | 6.46 | Personal communication with manufacturer (cost includes VAT). This was the price to the NHS of the catheter at trial commencement (2007) |
| PTFE | 0.86 | This was the price to the NHS of the catheter at trial commencement (2007) |
| Cost per day in hospital (by level of care) | ||
| Medical ward | 265 | Based on specialty group costs, inpatients in medical ward (excluding long stay) (ISD) |
| Neurology | 498 | Based on specialty group costs, inpatients in neurology department (excluding long stay) (ISD) |
| Urology | 321 | Based on specialty group costs, inpatients in urology department (excluding long stay) (ISD) |
| Cardiothoracic department | 530 | Based on specialty group costs, inpatients in cardiothoracic department (excluding long stay) (ISD) |
| General surgery | 331 | Based on specialty group costs, inpatients in general surgery department (excluding long stay) (ISD) |
| Obstetrics and gynaecology | 337 | Based on specialty group costs, inpatients in obstetrics and gynaecology department (excluding long stay) (ISD) |
| ENT | 492 | Based on specialty group costs, inpatients in ENT department (excluding long stay) (ISD) |
| Orthopaedics department | 321 | Based on specialty group costs, inpatients in orthopaedics department (excluding long stay) (ISD) |
| Vascular | 305 | Based on specialty group costs, inpatients in vascular department (excluding long stay) (ISD) |
| Gastroenterology | 341 | Based on specialty group costs, inpatients in gastroenterology department (excluding long stay) (ISD) |
| Other costs | ||
| Antibiotics | 5.41 | Cost of antibiotic based on the average cost of UTI prescriptions in Scotland (ISD) |
| Outpatient visit | 94 | Based on the total average total direct cost per attendance of all specialties outpatient consultant-led clinics (ISD) |
| Practice nurse visit | 10 | Based on cost per consultation (PSSRU) |
| GP visit | 36 | Based on per surgery consultation lasting average of 11.7 minutes (PSSRU) |
| Personal costs incurred by participants for visits to other health-care professionals | Various | As provided by the participants |
Total patient NHS costs were derived by combining information on resource use with information on the unit costs of those resources. For each area of resource use, estimates of resource utilisation were combined with unit costs to derive total costs for each item of resource use for each patient. Averages were then calculated to give estimates for each item of resource use. The patient-level costs for each item of resource were summed to produce a total cost for each patient and allow an estimate of average total cost per patient to be calculated.
Effectiveness outcomes for cost-effectiveness analysis
Effectiveness was measured in terms of number of catheter-associated symptomatic UTIs treated with antibiotics up to 6 weeks after randomisation (trial primary outcome) and QALYs at 6 weeks.
Quality-adjusted life-years were derived using data from participant completion of the EQ-5D, a generic health status measurement tool, at baseline, 3 days after catheter removal, 1 and 2 weeks after catheter removal and at 6 weeks post randomisation as part of the main study questionnaires. The EQ-5D measure divides health status into five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each of these dimensions can have three levels, giving 243 possible health states. 72 These responses were converted into health–state utilities using UK population tariffs. 73 The utility scores were used to estimate the mean QALY score for each of the three trial groups. The estimation of QALYs took into account the death of any study participants with allocation of a utility score of zero from date of death to the date of 6 weeks after randomisation for participants who died during their involvement in the trial. QALYs were estimated using linear extrapolation between the QALY scores at baseline and all available EQ-5D data.
Incremental cost per infection avoided and quality-adjusted life-year gained
Average costs per patient for each intervention were calculated and the described comparisons were made. Similarly, the average number of QALYs were calculated for each intervention and compared with the control. Data collected on costs and effects of the interventions were combined to obtain an incremental cost-effectiveness ratio (ICER). This was performed by dividing the mean difference in costs by the difference in effect between the interventions and control group. This provides the incremental cost per infection avoided or incremental cost per additional QALY gained for the new interventions relative to standard practice, i.e. ΔC/ΔE = ICER (where C = cumulative costs at 6 weeks and E = cumulative effects over 6 weeks).
Measures of variance for these costs, infections and QALYs were derived using bootstrapping. 74 From the results of the bootstrapping, cost-effectiveness acceptability curves (CEACs) were created. CEACs are used to represent whether or not the two novel interventions are cost-effective at various threshold values for society’s willingness to pay for an infection avoided or additional QALY. CEACs present results when the analysis follows a net benefit approach. This approach utilises a straightforward rearrangement of the cost-effectiveness decision rule used when calculating ICERs (see below) to create the net monetary benefit (NMB). The NMB of the interventions in question is as shown below:
where λ represents the decision-maker’s willingness to pay for an infection avoided or for a QALY gained. If the above expression holds true, the intervention is considered cost-effective. As society’s willingness to pay is unknown, the NMB will be calculated for a number of possible λ values, including the threshold value of £20,000–30,000 for a QALY that is often adopted by policy-makers within the NHS. 75 The estimates of NMB at various threshold values for society’s willingness to pay for a unit of outcome are used to produce graphical and tabular representations of the CEAC.
Data analysis
As trial data were collected over a 6-week period no discounting was carried out. The number of missing data for variables used in the cost analysis was low, and data that were missing were therefore considered to be missing completely at random.
Subgroup analyses
Subgroup analyses similar to those described in Statistical methods/trial analysis examined possible modification of the cost-effectiveness results by the following characteristics:
-
age (< 60 years, ≥ 60 years)
-
sex
-
comorbidity (pre-existing urological disease, diabetes, immunosuppression)
-
duration of catheterisation (< 4 days, ≥ 4 days)
-
indication for catheterisation (incontinence, urine retention and monitoring purpose)
-
use of antibiotics in the last 7 days
-
use of antibiotics at catheterisation.
Effect modification was explored using tests for interaction (all at stricter levels of significance; p < 0.01), and results are cost differences with 99% CIs to reflect the exploratory nature of these analyses.
Sensitivity analysis
Sensitivity analysis was performed to gauge the impact of varying key assumptions and/or parameter values in the base-case analysis.
-
Sensitivity analysis around cost per day of hospital treatment. This analysis explored the impact of using an alternative source of unit cost data for the cost per day in hospital. Sensitivity analysis was performed using unit costs from other published sources, for example NHS reference costs. 76
-
The base-case analysis was conducted using data that were adjusted for the characteristics mentioned above for the subgroup analyses. To indicate the importance of adjusting for these baseline factors a further analysis has been conducted using cost data that were not adjusted for any potential imbalance at baseline.
Model-based analysis
A decision-analytic model was developed to compare the different catheters in terms of the loss of QoL (based on the responses to the EQ-5D collected as part of the trial) and change in cost caused by a symptomatic catheter-associated UTI (Figure 3). In this modelling exercise, a comparison was drawn between the three different types of catheter (as shown in Figure 3). The trial-based analysis was expected to be characterised by considerable variation between patients in terms of both costs and QALYs. This was because, as noted above, participants within the trial were being treated for a variety of different conditions and the effect of these underlying conditions may have obscured or distorted the effect of the different catheters. Therefore, a modelling exercise was conducted which made the assumption that differences between the randomised arms are solely the result of differences in the risk of infections occurring.
FIGURE 3.
Simple decision tree.
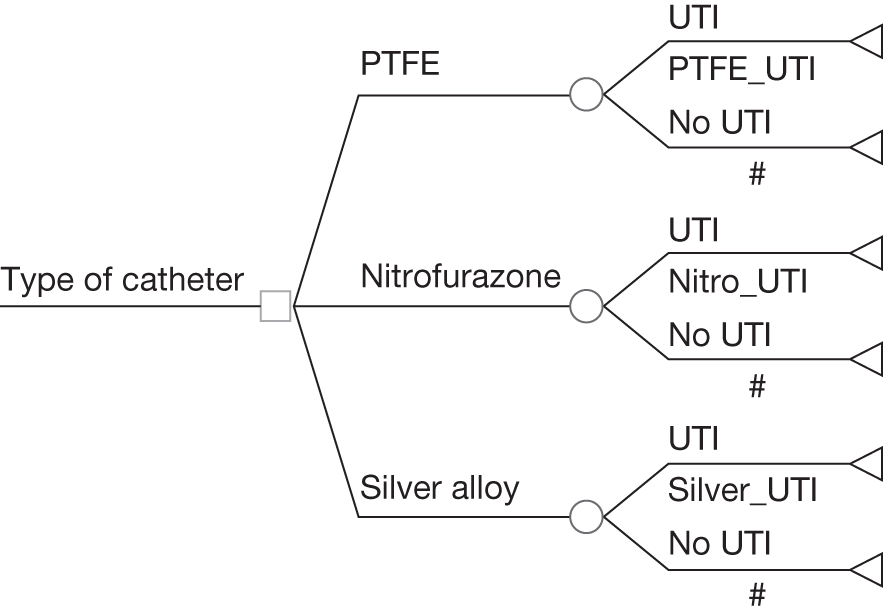
Model-based analysis was performed from the perspective of the UK NHS. In this analysis it was assumed that the only difference in QoL was caused only by a symptomatic UTI and that the type of catheter did not affect QoL except by changing the risk of a symptomatic UTI occurring. Parameters used in the model included the costs of participants’ care, QALYs and the probability of having a symptomatic UTI. The costs and QALYs data required were derived from the within-trial analysis and were estimated based on whether or not a participant had a symptomatic UTI.
Regression methods were used to estimate the QALYs for those with and without a symptomatic UTI. A similar approach was used to estimate costs associated with developing a symptomatic UTI compared with costs for those without an infection. The parameters required for the model were the risk of infection, the utilities associated with participants experiencing or not experiencing an infection, and management costs. Data to inform the model were derived from the within-trial analysis.
Data collected on costs and effects of the interventions were combined to obtain an ICER. This was performed by calculating the mean difference in costs between each intervention group and control, and dividing by the difference in effect between each intervention group and control. This generated the cost per QALY gained for the new interventions relative to standard practice, i.e. ΔC/ΔE = incremental cost-effectiveness ratio (where C = cumulative costs at 6 weeks and E = cumulative effects over the same period). Measures of variance for these outcomes were estimated by bootstrapping estimates of costs and QALYs, and incremental cost per participant with UTI and per QALY. Incremental cost-effectiveness data are presented in terms of CEACs.
Sensitivity analysis
Parameter uncertainty was integrated by the incorporation of probability distributions into the model and using the Monte Carlo simulation. Other forms of uncertainty, such as that associated with cost estimates detailed in the within-trial analysis, were addressed by using the cost results of different samples from the study population, such as those who had an EQ-5D score of ‘1’ (full health) at 3 days and those participants treated on the obstetrics and gynaecology ward who were hypothesised to have experienced a homogeneous pathway of care. Other analyses considered the impact of basing costs and QALYs on whether or not a participant had experienced a symptomatic UTI at 3 days after catheter removal together with the impact of excluding inpatient costs.
Chapter 4 Participant baseline characteristics
Trial recruitment
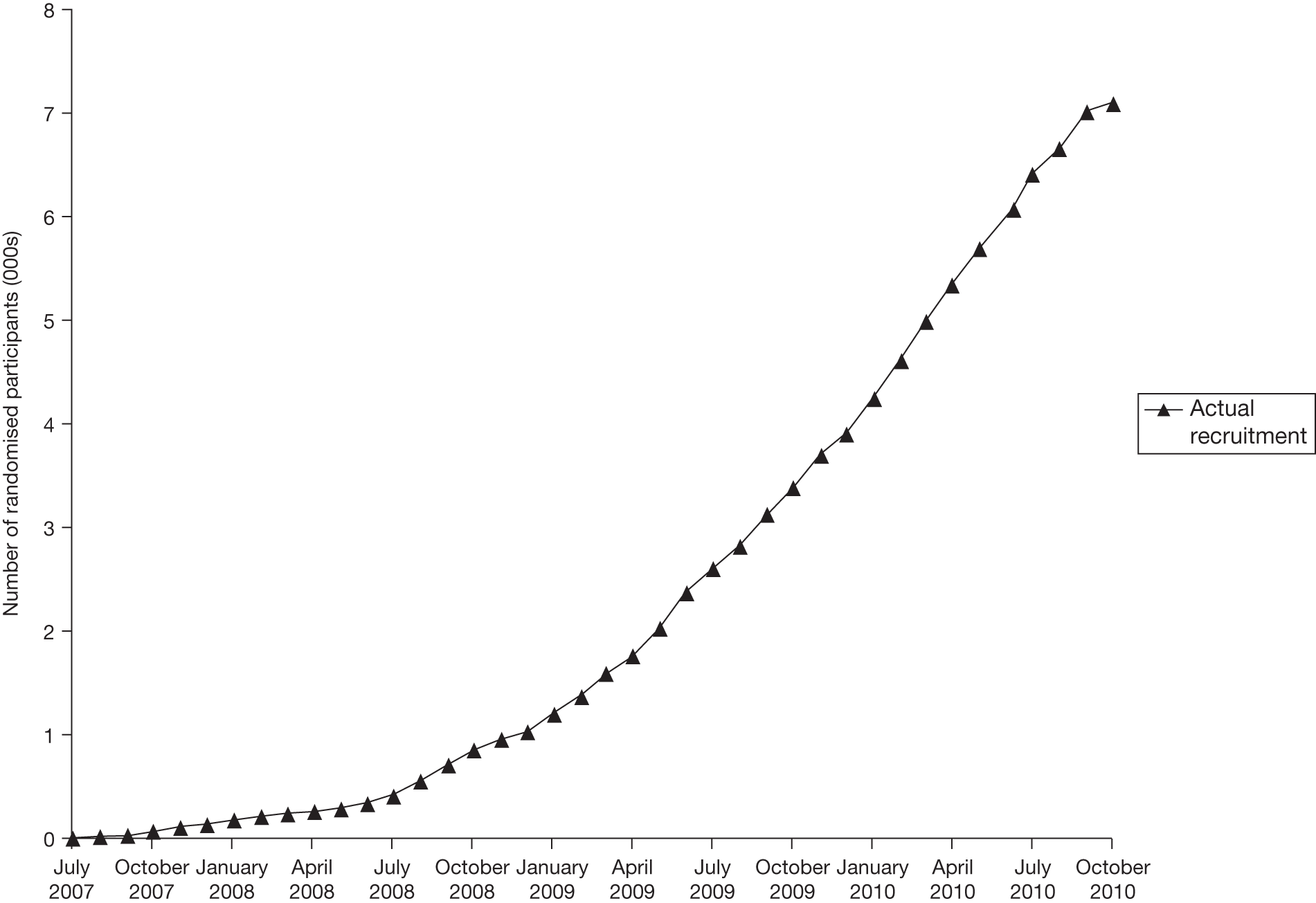
In total, 7102 patients anticipated to require short-term catheterisation as part of their standard care were randomised from 24 hospitals over 40 months between July 2007 and October 2010. Figure 4 shows total recruitment from all sites over time and Table 7 shows the numbers recruited at each site and the number of months over which that site recruited.
| Site | Ward specialties recruited | No. randomised | Percentage of total recruitment (7102) | Months recruiting |
|---|---|---|---|---|
| Aberdeen Royal Infirmary | Cardiothoracic, general surgery, vascular, obstetrics and gynaecology | 1421 | 20.0 | 40 |
| Royal Blackburn Hospital & Burnley General Hospital | Obstetrics and gynaecology | 109 | 1.5 | 7 |
| Blackpool Victoria Hospital | Cardiothoracic, obstetrics and gynaecology | 203 | 2.9 | 16 |
| Bristol Royal Infirmary | Cardiothoracic, general surgery | 6 | 0.1 | 5 |
| Edinburgh Royal Infirmary | Obstetrics and gynaecology | 114 | 1.6 | 25 |
| Guy’s Hospital, London | Renal transplant | 234 | 3.3 | 17 |
| Harrogate District Hospital | Obstetrics and gynaecology | 4 | 0.1 | 5 |
| Hillingdon Hospital | General surgery, obstetrics and gynaecology | 201 | 2.8 | 29 |
| Hinchingbrooke Hospital | Orthopaedics | 64 | 0.9 | 10 |
| Raigmore Hospital, Inverness | Orthopaedics, general surgery | 971 | 13.7 | 34 |
| Liverpool Women’s Hospital | Obstetrics and gynaecology | 149 | 2.1 | 8 |
| Newcastle General Hospital | Neurosurgery, general surgery | 869 | 12.2 | 29 |
| Freeman Hospital, Newcastle | Cardiothoracic | 486 | 6.8 | 17 |
| Royal Victoria Infirmary, Newcastle | Obstetrics and gynaecology | 312 | 4.4 | 10 |
| Norfolk and Norwich University Hospital | Orthopaedics, obstetrics and gynaecology | 42 | 0.6 | 8 |
| North Tyneside General Hospital | General surgery, urology, obstetrics and gynaecology, medical ward, orthopaedics | 619 | 8.7 | 20 |
| Nottingham City Hospital | Orthopaedics, obstetrics and gynaecology | 158 | 2.2 | 12 |
| Queen Alexandra Hospital, Portsmouth | Obstetrics and gynaecology | 151 | 2.1 | 7 |
| Royal Preston Hospital | Obstetrics and gynaecology | 109 | 1.5 | 16 |
| Southampton General Hospital | Cardiothoracic | 575 | 8.1 | 26 |
| Sunderland Royal Hospital | Obstetrics and gynaecology | 64 | 0.9 | 24 |
| Musgrove Park Hospital, Taunton | General surgery, orthopaedics | 33 | 0.5 | 14 |
| Torbay Hospital | General surgery, medical ward | 90 | 1.3 | 9 |
| Yeovil District Hospital | General surgery, obstetrics and gynaecology | 118 | 1.7 | 11 |
| Total | 7102 | 100 | 399 | |
FIGURE 4.
The CATHETER trial: recruitment over time.
Patient flow
The flow of participants through the trial is summarised in Figure 5, in line with recommendations of the Consolidated Standards of Reporting Trials (CONSORT) statement. 77 Included in the total of 7102 randomised participants were 905 participants randomised following unplanned catheterisations, of whom 385 subsequently refused consent to be involved in the trial and were thereby excluded. A further 45 participants withdrew consent before catheterisation and were excluded from the trial. In total, there were 708 post-randomisation exclusions, equally distributed throughout the groups, for reasons such as use of a suprapubic catheter or no catheterisation (e.g. due to cancellation of procedures or catheterisation not being deemed necessary by treating clinical staff), as well as the 385 who refused consent following unplanned catheterisation (Table 8); this reduced the number of participants included in the trial to 6394 – 90% of those randomised.
| Reason for post-randomisation exclusion (n) | Nitrofurazone (n = 258) | Silver alloy (n = 225) | PTFE (n = 225) |
|---|---|---|---|
| Consent not givena or withdrawn | 160 | 138 | 132 |
| Suprapubic catheter | 10 | 15 | 9 |
| Not catheterised | 77 | 60 | 72 |
| Missed | 1 | 4 | 1 |
| Other reason | 5 | 1 | 4 |
| Patient died | 1 | 0 | 0 |
| No reason | 4 | 7 | 7 |
FIGURE 5.
Consort diagram. a, Generally participants underwent catheterisation in the operating suite. In 272 (4.3%) of cases an alternative catheter to that allocated by randomisation was inserted mainly due to error by clinical staff. b, We achieved verification of the primary outcome for all participants. A total of 907 (14%) participants did not complete the planned 6-week post-randomisation follow-up (see Table 12).
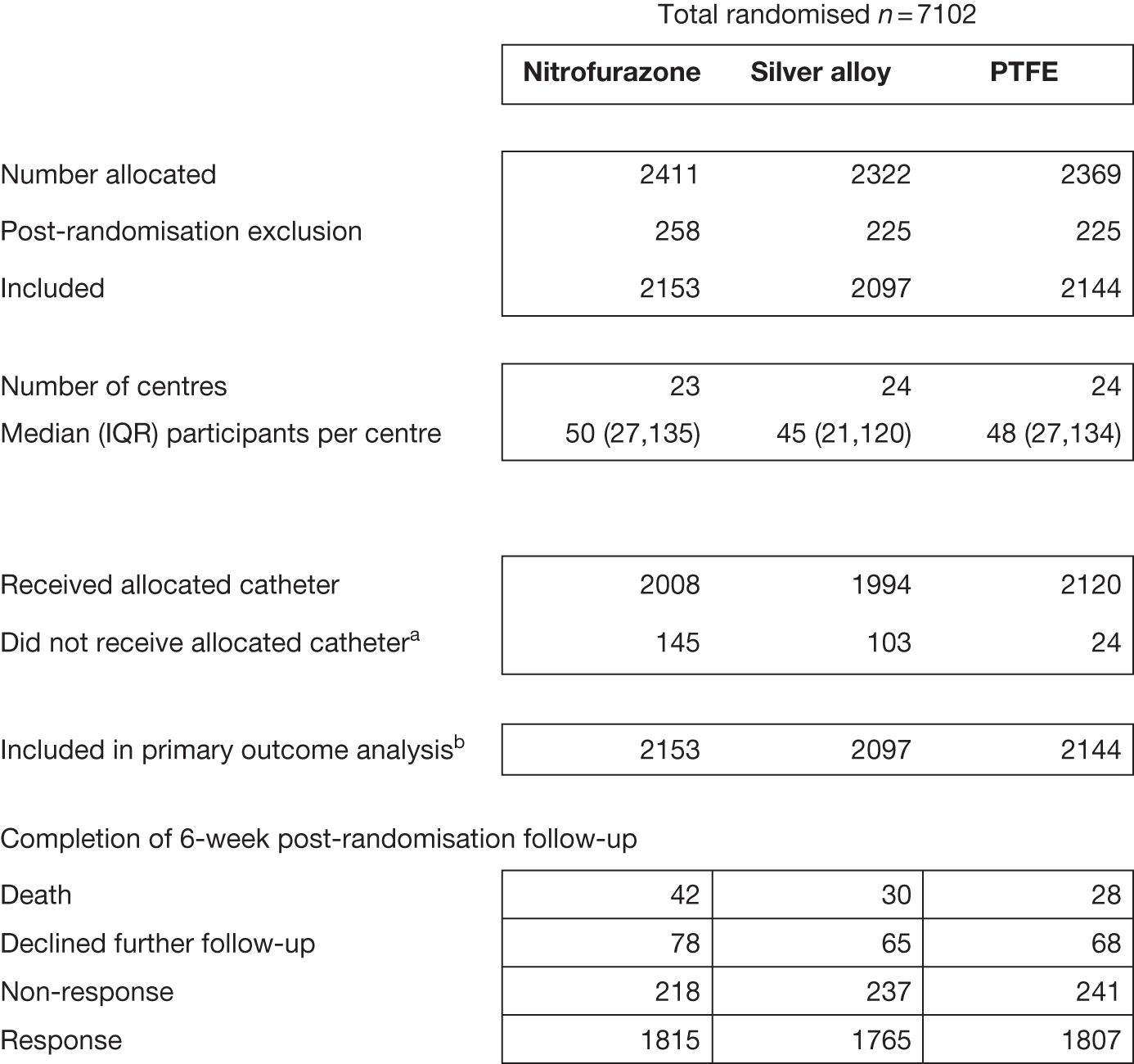
Baseline characteristics
As one would expect with a large sample size, the randomised groups were well balanced at baseline across all measured covariates (Table 9). Participants were drawn from a wide age range (17–92 years) with a median of 61 years. Women accounted for 62% of the trial population. Subgroups were pre-specified to identify those at a greater risk of developing a UTI. A total of 10% of participants had pre-existing urological disease or diabetes and 7% were receiving immunosuppressive therapy. In the baseline urine sample taken prior to catheterisation (MSSU 84%) or at the time of catheterisation (CSU 16%), 8% of participants had ≥ 104 CFU/ml and 27% had a pyuria with white blood cell (WBC) count of > 10/mm3 but were asymptomatic; 18% of participants had received antibiotics in the 7 days prior to randomisation for a variety of indications (Table 10).
| Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) | |
|---|---|---|---|
| Age (n) | 2152 | 2096 | 2143 |
| Mean (SD) | 58.46 (16.15) | 58.95 (15.82) | 58.84 (15.97) |
| Median (IQR) | 61 (47 to 71) | 61 (47 to 72) | 61 (47 to 72) |
| (min., max.) | (17, 91) | (17, 92) | (18, 91) |
| Sex (n) | 2152 | 2097 | 2143 |
| Female | 1333 (61.9) | 1319 (62.9) | 1325 (61.8) |
| Pre-existing urological disease (n) | 2138 | 2084 | 2136 |
| Yes | 214 (10.0) | 196 (9.4) | 214 (10.0) |
| Diabetes (n) | 2138 | 2083 | 2136 |
| Yes | 197 (9.2) | 207 (9.9) | 216 (10.1) |
| Immune suppression (n) | 2137 | 2079 | 2132 |
| Yes | 135 (6.3) | 144 (6.9) | 151 (7.1) |
| Urine sample: n | 2074 | 2002 | 2057 |
| MSSU | 1735 (83.7) | 1709 (85.4) | 1721 (83.7) |
| CSU | 339 (16.3) | 293 (14.6) | 336 (16.3) |
| No. of CFU/ml: n | 2071 | 1998 | 2054 |
| < 104 | 1923 (92.9) | 1830 (91.6) | 1901 (92.6) |
| 104 | 64 (3.1) | 71 (3.6) | 69 (3.4) |
| ≥ 105 | 84 (4.1) | 97 (4.9) | 84 (4.1) |
| Pyuria (n) | 2074 | 2002 | 2057 |
| < 10 WBC/mm | 1521 (73.3) | 1446 (72.2) | 1499 (72.9) |
| > 10 WBC/mm | 553 (26.7) | 556 (27.8) | 558 (27.1) |
| EQ-5D (n) | 2127 | 2076 | 2123 |
| Mean (SD) | 0.717 (0.292) | 0.723 (0.291) | 0.722 (0.299) |
| Median (IQR) | 0.796 (0.689 to 0.883) | 0.796 (0.656 to 1) | 0.812 (0.689 to 1.00) |
| (min., max.) | (–0.594, 1) | (–0.594, 1) | (–0.594, 1) |
| EQ-5D VAS (n) | 2132 | 2076 | 2118 |
| Mean (SD) | 70.4 (21.1) | 71.0 (20.2) | 70.6 (21.4) |
| Median (IQR) | 75 (60 to 88) | 75.00 (60 to 90) | 75.00 (55 to 90) |
| (min., max.) | (0, 100) | (0, 100) | (0, 100) |
| Symptom severity (n) | 2143 | 2088 | 2136 |
| Mean (SD) | 1.98 (2.64) | 1.88 (2.50) | 1.83 (2.49) |
| Median (IQR) | 1 (0 to 3) | 1.00 (0 to 3) | 1.00 (0 to 3) |
| (min., max.) | (0, 16) | (0, 21) | (0, 16) |
| Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) | |
|---|---|---|---|
| Reason for catheterisation (n) | 2095 | 2057 | 2091 |
| Unplanned emergency | 94 (4.5) | 94 (4.6) | 89 (4.3) |
| Elective monitoring | 2001 (95.5) | 1963 (95.4) | 2002 (95.7) |
| Antibiotics in 7 days prior to randomisation (n) | 2153 | 2097 | 2144 |
| Yes | 396 (18.4) | 370 (17.6) | 385 (18.0) |
| Antibiotic at the time of catheterisation (n) | 2153 | 2097 | 2144 |
| Yes | 1537 (71.4) | 1529 (72.9) | 1547 (72.2) |
| Type of catheter used (n) | 2153 | 2097 | 2144 |
| Nitrofurazone | 2008 (93.3) | 11 (0.5) | 8 (0.4) |
| Silver alloy | 22 (1.0) | 1994 (95.1) | 16 (0.7) |
| PTFE | 123 (5.7) | 92 (4.4) | 2120 (98.9) |
| Duration of catheterisation (days) (n) | 2100 | 2048 | 2100 |
| Mean (SD) | 2.78 (3.3) | 2.95 (3.6) | 2.85 (3.3) |
| Median (IQR) | 2 (1 to 3) | 2 (1 to 3) | 2 (1 to 3) |
| (min., max.) | (1, 42) | (1, 65) | (1, 45) |
| Duration of hospitalisation (days) (n) | 2105 | 2046 | 2102 |
| Mean (SD) | 7.43 (8.0) | 8.03 (9.3) | 7.76 (8.3) |
| Median (IQR) | 6 (3 to 8) | 6 (3 to 9) | 6 (3 to 9) |
| (min., max.) | (1, 159) | (1, 154) | (1, 105) |
Intervention received and descriptors of care
Table 10 contains details on the intervention received and aspects of in-hospital care. The main reason for catheterisation was for monitoring purposes during and after surgery. Duration of catheterisation and length of hospital stay were similar across all three groups, as was the proportion of participants receiving antibiotics for surgical prophylaxis.
Over 93% of participants in each arm received the catheter to which they were allocated. In the majority of cases where the allocated catheter was not used, this was due to theatre staff inserting a standard PTFE catheter in error. Analyses were by catheter allocated (intention to treat).
Descriptive data for duration of catheterisation showed a mean of 2.78 days in the nitrofurazone group, 2.95 days in the silver alloy group and 2.85 days in the PTFE control group, whereas the median was the same in all groups at 2 days. A total of 219 (3.43%) participants experienced a duration of catheterisation of > 14 days with 79 (3.67%) in the nitrofurazone group, 73 (3.48%) in the silver alloy group and 67 (3.13%) in the control group. Hospital stay varied widely, with a markedly skewed distribution; the median was 6 days in each group, but the upper extreme of the range varied, with the longest stay being 159 days (see Table 10).
Allocation of participants to the three trial groups was equal across all centres (Table 11).
| Centre | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Aberdeen Royal Infirmary | 430 (20.0) | 459 (21.9) | 434 (20.2) |
| Royal Blackburn Hospital & Burnley General Hospital | 40 (1.9) | 33 (1.6) | 36 (1.7) |
| Blackpool Victoria Hospital | 64 (3.0) | 69 (3.3) | 69 (3.2) |
| Bristol Royal Infirmary | 3 (0.1) | 1 (0.0) | 2 (0.1) |
| Edinburgh Royal Infirmary | 42 (2.0) | 36 (1.7) | 28 (1.3) |
| Guy’s Hospital, London | 75 (3.5) | 72 (3.4) | 81 (3.8) |
| Harrogate District Hospital | 0 (0.0) | 3 (0.1) | 1 (0.0) |
| Hillingdon Hospital | 72 (3.3) | 60 (2.9) | 66 (3.1) |
| Hinchingbrooke Hospital | 22 (1.0) | 20 (1.0) | 14 (0.7) |
| Raigmore Hospital, Inverness | 270 (12.5) | 269 (12.8) | 243 (11.3) |
| Liverpool Women’s Hospital | 57 (2.6) | 46 (2.2) | 45 (2.1) |
| Newcastle General Hospital | 250 (11.6) | 240 (11.4) | 264 (12.3) |
| Freeman Hospital, Newcastle | 155 (7.2) | 147 (7.0) | 165 (7.7) |
| Royal Victoria Infirmary, Newcastle | 95 (4.4) | 95 (4.5) | 113 (5.3) |
| Norfolk and Norwich University Hospital | 14 (0.7) | 5 (0.2) | 9 (0.4) |
| North Tyneside General Hospital | 156 (7.2) | 144 (6.9) | 155 (7.2) |
| Nottingham City Hospital | 46 (2.1) | 47 (2.2) | 51 (2.4) |
| Queen Alexandra Hospital, Portsmouth | 50 (2.3) | 43 (2.1) | 51 (2.4) |
| Royal Preston Hospital | 34 (1.6) | 37 (1.8) | 36 (1.7) |
| Southampton General Hospital | 189 (8.8) | 187 (8.9) | 178 (8.3) |
| Sunderland Royal Hospital | 18 (0.8) | 16 (0.8) | 29 (1.4) |
| Musgrove Park Hospital, Taunton | 8 (0.4) | 10 (0.5) | 6 (0.3) |
| Torbay Hospital | 27 (1.3) | 22 (1.0) | 26 (1.2) |
| Yeovil District Hospital | 36 (1.7) | 36 (1.7) | 42 (2.0) |
Response rates
Participant response rates are shown in Table 12. Response rates were similar across the three trial arms, with overall response rates of 88% for the 3 days post catheter removal questionnaire, 72% and 71% for the 1 and 2 weeks post catheter removal diaries and 84% for the questionnaire at 6 weeks post randomisation.
| Time point | Nitrofurazone: n = 2153 | Silver alloy: n = 2097 | PTFE: n = 2144 |
|---|---|---|---|
| Three days | |||
| Death | 12 (0.6) | 9 (0.4) | 11 (0.5) |
| Declined further follow-up | 59 (2.7) | 39 (1.9) | 50 (2.3) |
| Non-response | 188 (8.7) | 209 (10.0) | 177 (8.3) |
| Response | 1894 (88.0) | 1840 (87.7) | 1906 (88.9) |
| One week | |||
| Death | 26 (1.2) | 23 (1.1) | 22 (1.0) |
| Declined further follow-up | 75 (3.5) | 57 (2.7) | 64 (3.0) |
| Non-response | 488 (22.7) | 526 (25.1) | 491 (22.9) |
| Response | 1564 (72.6) | 1491 (71.1) | 1567 (73.1) |
| Two weeks | |||
| Death | 27 (1.3) | 23 (1.1) | 23 (1.1) |
| Declined further follow-up | 75 (3.5) | 57 (2.7) | 64 (3.0) |
| Non-response | 503 (23.4) | 556 (26.5) | 505 (23.6) |
| Response | 1548 (71.9) | 1461 (69.7) | 1552 (72.4) |
| Six weeks | |||
| Death | 42 (2.0) | 30 (1.4) | 28 (1.3) |
| Declined further follow-up | 78 (3.6) | 65 (3.1) | 68 (3.2) |
| Non-response | 218 (10.1) | 237 (11.3) | 241 (11.2) |
| Response | 1815 (84.3) | 1765 (84.2) | 1807 (84.3) |
Denominators reflect the number of participants that were included in the analysis for specific aspects of the data and reflect the response to the individual question.
Chapter 5 Outcomes and results
Primary outcome
The incidence of the primary outcome at any time up to 6 weeks post randomisation (number of participants with at least one occurrence of symptomatic UTI treated with antibiotics) was 10.6% (228/2153) and 12.5% (263/2097) in the nitrofurazone and silver alloy groups, respectively. The rate of symptomatic UTI in the PTFE control catheter group was 12.6% (271/2144). Table 13 contains the estimated ORs and 97.5% CIs, for both the raw data and those adjusted using logistic regression models. The estimated absolute risk reduction between nitrofurazone and PTFE was 2.1% (97.5% CI –0.1% to 4.2%). Between the silver alloy and PTFE this was estimated as 0.1% (97.5% CI –2.2% to 2.4%). Table 13 contains the estimated ORs and 97.5% CIs from unadjusted and adjusted logistic regression models. The full logistic regression model for the primary outcome can be found in Appendix 6.
| Estimate | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Incidence n (%) | 228 (10.6) | 263 (12.5) | 271 (12.6) |
| Absolute risk difference (97.5% CI) compared with PTFE, expressed as a percentage | –2.1 (–4.2 to 0.1) | –0.1 (–2.4 to 2.2) | |
| Comparison | |||
| OR (97.5% CI); p-value | |||
| Nitrofurazone vs PTFE | |||
| Unadjusted | 0.82 (0.66 to 1.01); 0.037 | ||
| Adjusted | 0.81 (0.65 to 1.01); 0.031 | ||
| Silver alloy vs PTFE | |||
| Unadjusted | 0.99 (0.81 to 1.22); 0.92 | ||
| Adjusted | 0.96 (0.78 to 1.19); 0.69 | ||
Secondary outcomes
The incidence of a symptomatic UTI with a prescription of antibiotics within 6 weeks of randomisation (primary outcome), together with the additional criterion of an associated microbiologically positive urine result (≥ 104 CFU/ml) during the 6 weeks post randomisation was 3.2% in the nitrofurazone group, 5.0% in the silver alloy group and 4.6% in the PTFE control catheter group. ORs and CIs are presented in Table 14.
| Estimate | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Incidence n (%) | 69 (3.2) | 105 (5.0) | 99 (4.6) |
| Absolute risk difference (97.5% CI) compared with PTFE, expressed as a percentage | –1.4 (–2.7 to –0.1) | 0.4 (–1.2 to 1.9) | |
| Comparison | |||
| OR (97.5% CI); p-value | |||
| Nitrofurazone vs PTFE | |||
| Unadjusted | 0.68 (0.48 to 0.99); 0.017 | ||
| Adjusted | 0.68 (0.47 to 0.98); 0.019 | ||
| Silver alloy vs PTFE | |||
| Unadjusted | 1.08 (0.78 to 1.52); 0.55 | ||
| Adjusted | 1.09 (0.78 to 1.51); 0.58 | ||
The incidence of antibiotic-treated symptomatic UTI within 3 days post catheter removal, together with a positive urinary microbiology result, was 0.7% in the nitrofurazone group, 1.7% in the silver alloy group and 1.3% in the PTFE group. ORs and CIs are presented in Table 15.
| Estimate | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Incidence n (%) | 15 (0.7) | 35 (1.7) | 28 (1.3) |
| Absolute risk difference (97.5% CI) compared with PTFE, expressed as a percentage | –0.6 (–1.3 to 0.1) | 0.3 (–0.4 to 1.2) | |
| Comparison | |||
| OR (97.5%CI); p-value | |||
| Nitrofurazone vs PTFE | |||
| Unadjusted | 0.53 (0.24 to 1.12); 0.049 | ||
| Silver alloy vs PTFE | |||
| Unadjusted | 1.28 (0.70 to 2.36); 0.33 | ||
Tertiary clinical outcomes
Incidence of bacteriuria at, or within, 3 days of catheter removal
The rate of bacteriuria at 3 days post catheterisation was 13.5% (249/1846) in the nitrofurazone group, 17.4% (310/1785) in the silver alloy group and 17.5% (321/1839) in the PTFE control catheter group. Estimates of ORs and CIs from adjusted and unadjusted logistic regression models are presented in Table 16. The estimated absolute risk reduction between the nitrofurazone and PTFE catheters was 3.5% (97.5% CI 0.8 to 6.1). Between the silver alloy and PTFE this was estimated as an increase of 0.4% (97.5% CI –3.2 to 2.4).
| Estimate | Nitrofurazone (n = 1846) | Silver alloy (n = 1785) | PTFE (n = 1839) |
|---|---|---|---|
| Incidence n (%) | 249 (13.5) | 310 (17.4) | 321(17.5) |
| Absolute risk difference (97.5% CI) compared with PTFE, expressed as a percentage | –3.5% (–6.1 to –0.8) | 0.4% (–2.4 to 3.2) | – |
| Comparison | |||
| OR (97.5% CI); p-value | |||
| Nitrofurazone vs PTFE | |||
| Unadjusted | 0.74 (0.60 to 0.91); 0.001 | ||
| Adjusted | 0.73 (0.59 to 0.90); 0.001 | ||
| Silver alloy vs PTFE | |||
| Unadjusted | 0.99 (0.82 to 1.21); 0.944 | ||
| Adjusted | 0.99 (0.81 to 1.21); 0.887 | ||
Symptomatic urinary tract infection at 3 days of catheter removal
The rate of symptomatic UTI with a prescription of antibiotics at 3 days post catheter removal was 4.9% (106/2153) in the nitrofurazone group, 6.6% (137/2079) in the silver alloy group and 5.9% (127/2144) in the PTFE control catheter group. Estimates of ORs and CIs from adjusted and unadjusted logistic regression models are presented in Table 17 below. The estimated absolute risk reduction between the nitrofurazone and PTFE catheters was 1.0% (97.5% CI –0.6 to 2.5). Between the silver alloy and PTFE this was estimated as an increase of 0.6% (97.5% CI 1.1 to –2.3). Table 17 contains the estimated ORs and 97.5% CIs from unadjusted and adjusted logistic regression models.
| Estimate | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Incidence n (%) | 106 (4.9) | 137 (6.6) | 127 (5.9) |
| Absolute risk difference (97.5% CI) compared with PTFE, expressed as a percentage | 1.0 (–2.5 to 0.6) | 0.6 (–2.3 to 1.1) | |
| Comparison | |||
| OR (97.5% CI); p-value | |||
| Nitrofurazone vs PTFE | |||
| Unadjusted | 0.82 (0.61 to 1.11); 0.144 | ||
| Adjusted | 0.81 (0.59 to 1.10); 0.123 | ||
| Silver alloy vs PTFE | |||
| Unadjusted | 1.12 (0.84 to 1.49); 0.369 | ||
| Adjusted | 1.09 (0.82 to 1.46); 0.502 | ||
Three-day symptom score
The three-day symptom score was the sum of ratings from ‘0’ (no symptoms) to ‘3’ (severe symptoms) for seven symptoms of UTI. The minimum score was therefore ‘0’ and the highest score was ‘21’, with a higher score indicating more severe symptoms. The proportion of participants within each study group who completed this score was similar, averaging 87%.
There was no statistically significant difference between either nitrofurazone or silver alloy catheters compared with control in terms of self-reported symptoms at 3 days (Table 18). A sensitivity analysis using multiple imputations did not change these results.
| Category | Nitrofurazone (n = 1857) | Silver (n = 1794) | PTFE (n = 1859) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| No discomfort | 1257 | 67.7 | 1231 | 68.6 | 1306 | 70.3 |
| Mild | 423 | 22.8 | 419 | 23.4 | 412 | 22.2 |
| Moderate | 145 | 7.8 | 111 | 6.2 | 113 | 6.1 |
| Severe | 32 | 1.7 | 33 | 1.8 | 28 | 1.5 |
| ORs from proportional odds model | ||||||
| OR (97.5% CI) | 1.14 (0.98 to 1.35) | 1.08 (0.93 to 1.28) | ||||
| Difference in estimated percentage in each category and 97.5% CI compared with PTFE | ||||||
| No discomfort | –3.0 (–6.4 to 0.5) | –1.8 (–5.3 to 1.7) | ||||
| Mild | 1.9 (–0.4 to 4.2) | 1.2 (–1.1 to 3.5) | ||||
| Moderate | 0.8 (–0.2 to 1.7) | 0.5 (–0.5 to 1.4) | ||||
| Severe | 0.2 (0.0 to 5.0) | 0.1 (–0.1 to 0.4) | ||||
Catheter discomfort
There were no significant differences in self-reported discomfort between each of the interventional catheters and the control catheter reported at the stage of catheter insertion (Table 19).
| Category | Nitrofurazone (n = 1834) | Silver (n = 1794) | PTFE (n = 1865) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| No discomfort | 1729 | 94.3 | 1710 | 95.3 | 1773 | 95.1 |
| Mild | 80 | 4.4 | 58 | 3.2 | 78 | 4.2 |
| Moderate | 16 | 0.9 | 16 | 0.9 | 10 | 0.5 |
| Severe | 9 | 0.5 | 10 | 0.6 | 4 | 0.2 |
| ORs from proportional odds model | ||||||
| OR (97.5% CI) | 1.18 (0.84 to 1.65) | 0.97 (0.68 to 1.39) | ||||
| Difference in estimated percentage in each category and 97.5% CI compared with PTFE | ||||||
| No discomfort | –0.7 (–2.1 to 0.8) | 0.1 (–1.3 to 1.5) | ||||
| Mild | 0.5 (–0.6 to 1.7) | –0.1 (–2.1 to 1.0) | ||||
| Moderate | 0.1 (–0.1 to 0.3) | 0 (–0.2 to 0.2) | ||||
| Severe | 0.1 (0.1 to 0.2) | 0 (–0.1 to 0.1) | ||||
Participants randomised to nitrofurazone catheters were 5.3% (97.5% CI 2.1% to 8.4%) less likely to report no discomfort during the period of catheterisation (Table 20). Those randomised to silver catheters were more likely to report no discomfort: 3.3% (97.5% CI 0.3% to 6.3%).
| Category | Nitrofurazone (n = 1879) | Silver (n = 1829) | PTFE (n = 1889) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| No discomfort | 1383 | 73.6 | 1507 | 82.4 | 1493 | 79.0 |
| Mild | 384 | 20.4 | 252 | 13.8 | 307 | 16.3 |
| Moderate | 77 | 4.1 | 44 | 2.4 | 66 | 3.5 |
| Severe | 35 | 1.9 | 26 | 1.4 | 23 | 1.2 |
| ORs from proportional odds model | ||||||
| OR (97.5% CI) | 1.34 (1.13 to 1.6) | 0.81 (0.67 to 0.97) | ||||
| Difference in estimated percentage in each category and 97.5% CI compared with PTFE | ||||||
| No discomfort | –5.3 (–8.4 to –2.1) | 3.3 (0.3 to 6.3) | ||||
| Mild | 3.8 (1.5 to 6.1) | –2.5 (–4.7 to –0.2) | ||||
| Moderate | 1.0 (0.4 to 1.6) | –0.6 (–1.1 to –0.1) | ||||
| Severe | 0.5 (0.2 to 0.8) | –0.3 (–0.5 to 0.0) | ||||
At catheter removal, participants in the nitrofurazone group were 12.3% (8.8% to 15.8%) less likely than participants in the PTFE group to report having no discomfort (Table 21). They were more likely to rate discomfort during catheter removal as mild, moderate or severe. There was no significant difference in discomfort during catheter removal between the silver alloy and PTFE catheters, 2.3% (97.5% CI –1.1% to 5.6%).
| Category | Nitrofurazone (n = 1867) | Silver (n = 1817) | PTFE (n = 1881) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| No discomfort | 1160 | 62.1 | 1296 | 71.3 | 1382 | 73.5 |
| Mild | 530 | 28.4 | 442 | 24.3 | 431 | 22.9 |
| Moderate | 126 | 6.7 | 65 | 3.6 | 56 | 3.0 |
| Severe | 51 | 2.7 | 14 | 0.8 | 12 | 0.6 |
| ORs from proportional odds model | ||||||
| OR (97.5% CI) | 1.77 (1.51 to 2.07) | 1.12 (0.95 to 1.32) | ||||
| Difference in estimated percentage in each category and 97.5% CI compared with PTFE | ||||||
| No discomfort | –12.3 (–15.8 to –8.8) | –2.3 (–5.6 to 1.1) | ||||
| Mild | 9.2 (6.6 to 11.9) | 1.8 (–0.9 to 4.4) | ||||
| Moderate | 2.3 (1.6 to 3.1) | 0.4 (–0.2 to 1.0) | ||||
| Severe | 0.8 (0.5 to 1.2) | 0.1 (–0.1 to 0.3) | ||||
There were no significant differences between interventional and control catheter groups in self-reported discomfort in the period after the catheter was removed (Table 22). Multiple imputation of missing responses did not change any results of analyses of self-reported discomfort data.
| Category | Nitrofurazone (n = 1866) | Silver (n = 1810) | PTFE (n = 1881) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| None | 1659 | 88.9 | 1620 | 89.5 | 1696 | 90.2 |
| Mild | 143 | 7.7 | 139 | 7.7 | 146 | 7.8 |
| Moderate | 54 | 2.9 | 35 | 1.9 | 24 | 1.3 |
| Severe | 10 | 0.5 | 16 | 0.9 | 15 | 0.8 |
| ORs from proportional odds model | ||||||
| OR (97.5% CI) | 1.15 (0.90 to 1.46) | 1.08 (0.85 to 1.39) | ||||
| Difference in estimated percentage in each category and 97.5% CI compared with PTFE | ||||||
| None | –1.3 (–3.5 to 1.0) | –0.7 (–3.0 to 1.5) | ||||
| Mild | 0.9 (–0.7 to 2.5) | 0.5 (–1.1 to 2.1) | ||||
| Moderate | 0.3 (–0.2 to 0.7) | 0.2 (–0.3 to 0.6) | ||||
| Severe | 0.1 (–0.1 to 0.3) | 0.1 (–0.1 to 0.2) | ||||
Secondary economic outcome measures
Quality of life
Health-related QoL was measured using the EQ-5D. Response rates were low, at 63%, for diaries completed 1 week after catheter removal, which participants took home from hospital to return by post. However, response rates improved at the 6-week post-randomisation time point, at which 80% of trial participants returned the questionnaire containing the EQ-5D questions.
Table 23 and Figure 6 show that EQ-5D scores followed the same pattern in each group, with no evidence of a difference between the groups. Incorporating a time by treatment interaction showed that treatment effects were not different over time and these terms were dropped from the model for ease of interpretation. The mean (97.5% CI; p-value) difference in EQ-5D score between the nitrofurazone and PTFE groups was –0.001 (97.5% CI –0.022 to 0.003; 0.15), and for the silver alloy group compared with the PTFE group was –0.012 (97.5% CI –0.025 to 0.001; 0.07).
| Follow-up time point | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Baseline | 2127, 0.717 (0.292) | 2076, 0.723 (0.291) | 2123, 0.722 (0.299) |
| 3 days | 1860, 0.592 (0.274) | 1801, 0.579 (0.281) | 1871, 0.593 (0.271) |
| 1 week | 1363, 0.619 (0.272) | 1308, 0.602 (0.292) | 1366, 0.614 (0.270) |
| 2 weeks | 1405, 0.696 (0.259) | 1328, 0.687 (0.270) | 1398, 0.695 (0.248) |
| 6 weeks | 1705, 0.777 (0.243) | 1665, 0.783 (0.240) | 1721, 0.795 (0.234) |
FIGURE 6.
Plot of EQ-5D scores over time. Bars are mean ± 1 SD. Note that the relative timing of responses compared with baseline varied for the 3-day, and 1- and 2-week time points and labels are notional only, for illustration.
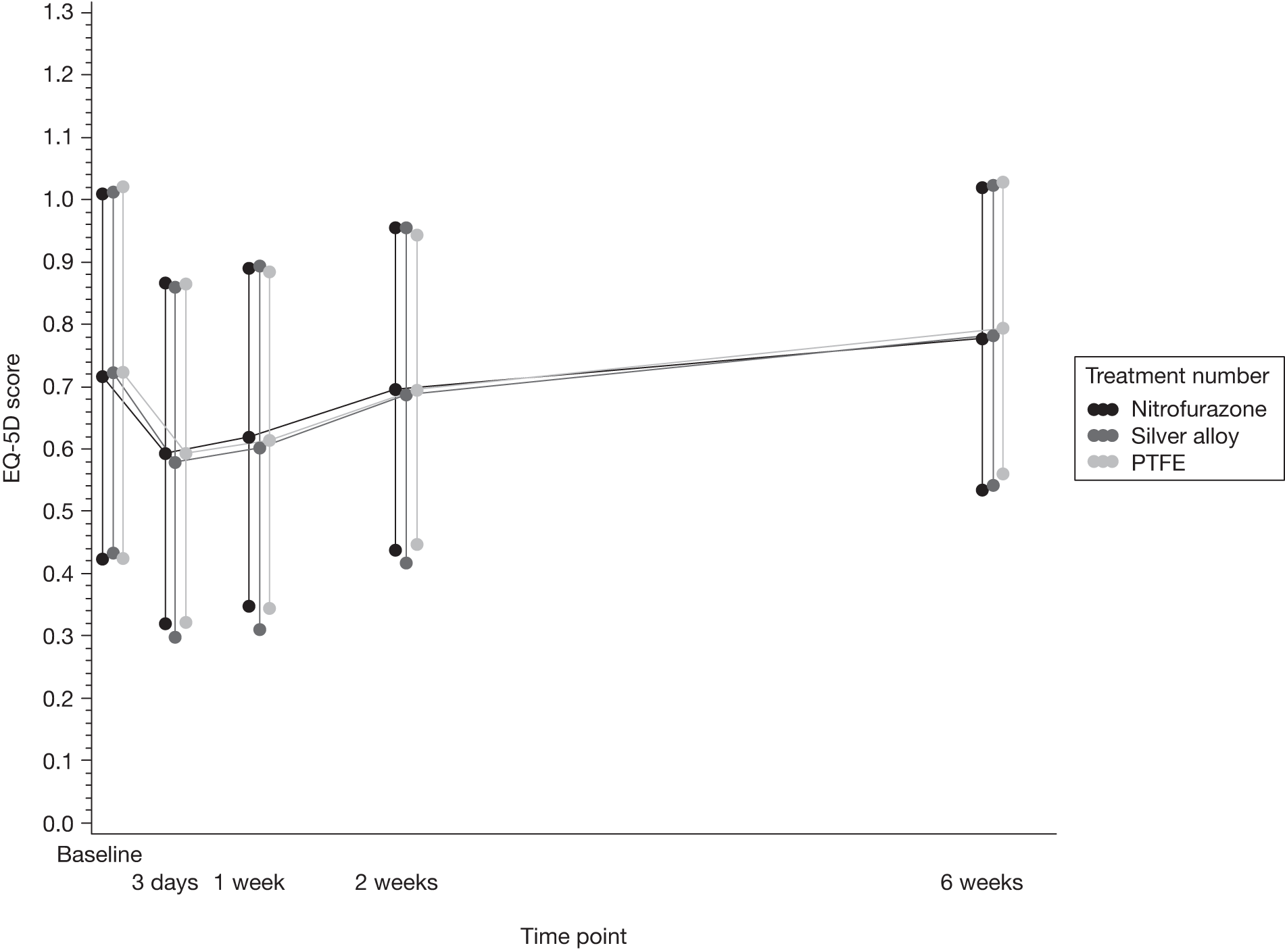
The EQ-5D visual analogue scale (VAS) followed an almost identical pattern (Table 24 and Figure 7).
| Follow-up time point | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Baseline | 2132, 70.46 (21.00) | 2118, 70.94 (20.15) | 2076, 70.61 (21.30) |
| 3 days | 1866, 65.09 (18.59) | 1881, 65.20 (18.40) | 1810, 64.94 (18.60) |
| 1 week | 1389, 68.80 (17.48) | 1366, 68.06 (18.26) | 1317, 68.21 (18.20) |
| 2 weeks | 1416, 75.01 (17.12) | 1403, 74.53 (18.05) | 1338, 74.62 (17.40) |
| 6 weeks | 1761, 78.47 (17.37) | 1768, 78.30 (16.95) | 1717, 78.53 (17.25) |
FIGURE 7.
Plot of EQ-5D-VAS over time. Bars are mean ± 1 SD. Note that relative timing of responses compared with baseline varied for the 3-day, and 1- and 2-week time points and labels are notional only, for illustration.
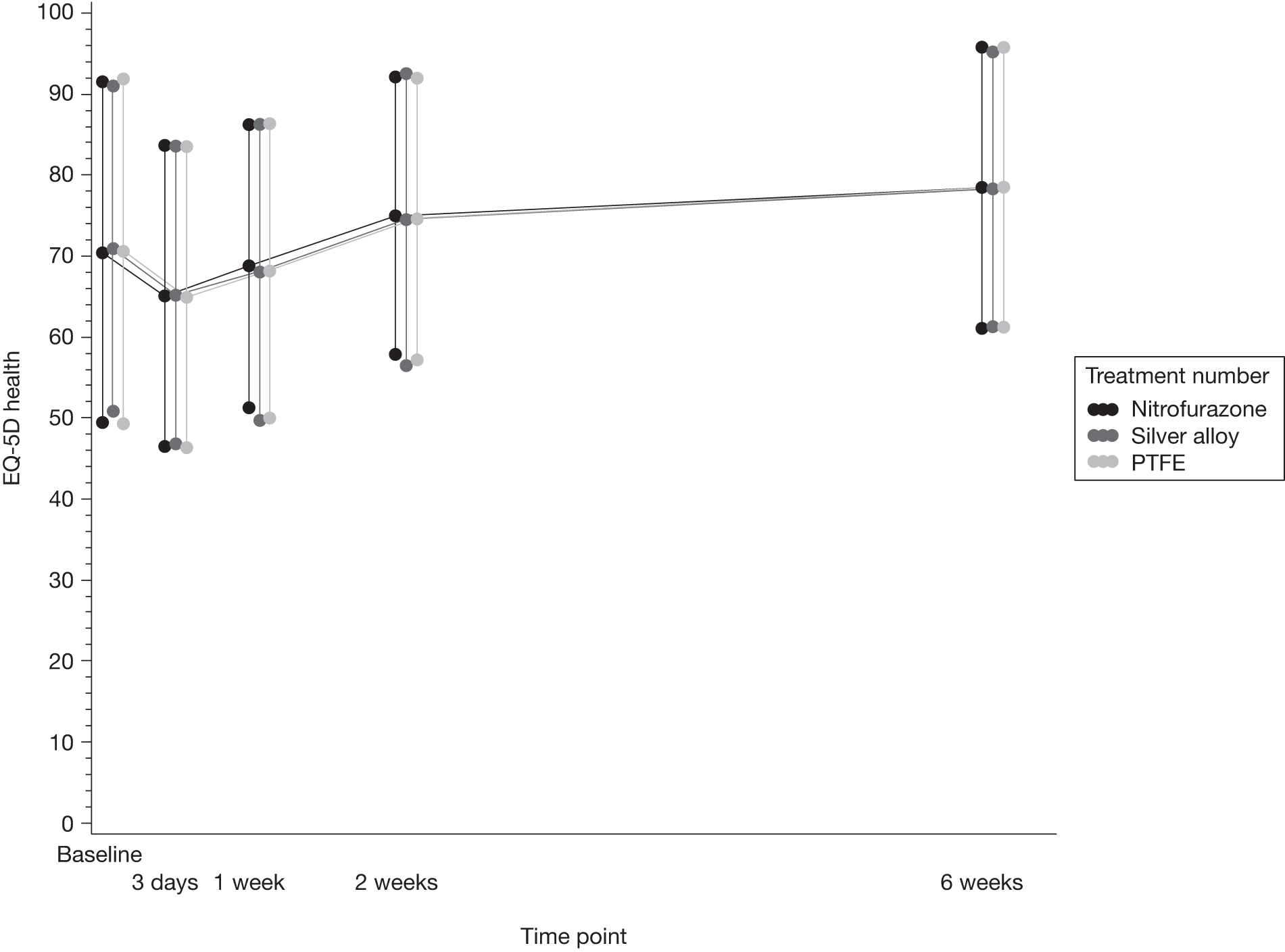
Significant clinical events
Significant clinical events are presented in Table 25. There were two cases of septicaemia in the trial; neither was due to catheterisation, with both being due to infections acquired from the participants’ intravenous line.
| Significant clinical events n (%) | Nitrofurazone (n = 2153) | Silver alloy (n = 2097) | PTFE (n = 2144) |
|---|---|---|---|
| Haematuria | 38 (1.8) | 21 (1.0) | 32 (1.5) |
| Septicaemiaa | – | 1 (< 0.1) | 1 (< 0.1) |
Subgroup analysis
The following subgroups analyses were performed to establish whether or not any risk or protective factors influenced rates of UTI in the trial groups:
-
sex
-
older age
-
comorbidity (immune suppression)
-
indication for catheterisation
-
antibiotic use prior to randomisation.
For most outcomes there was no apparent differential treatment effect between subgroups (Figures 8 and 9). The only potential exception to this was antibiotic use in the 7 days prior to randomisation, where there was marginal evidence that participants subsequently randomised to nitrofurazone who had received antibiotics in the previous 7 days had a greater incidence of UTI at any time up to 6 weeks after randomisation.
FIGURE 8.
Forest plot of subgroup analyses, UTI at any point up to 6 weeks post randomisation for nitrofurazone vs PTFE comparison.
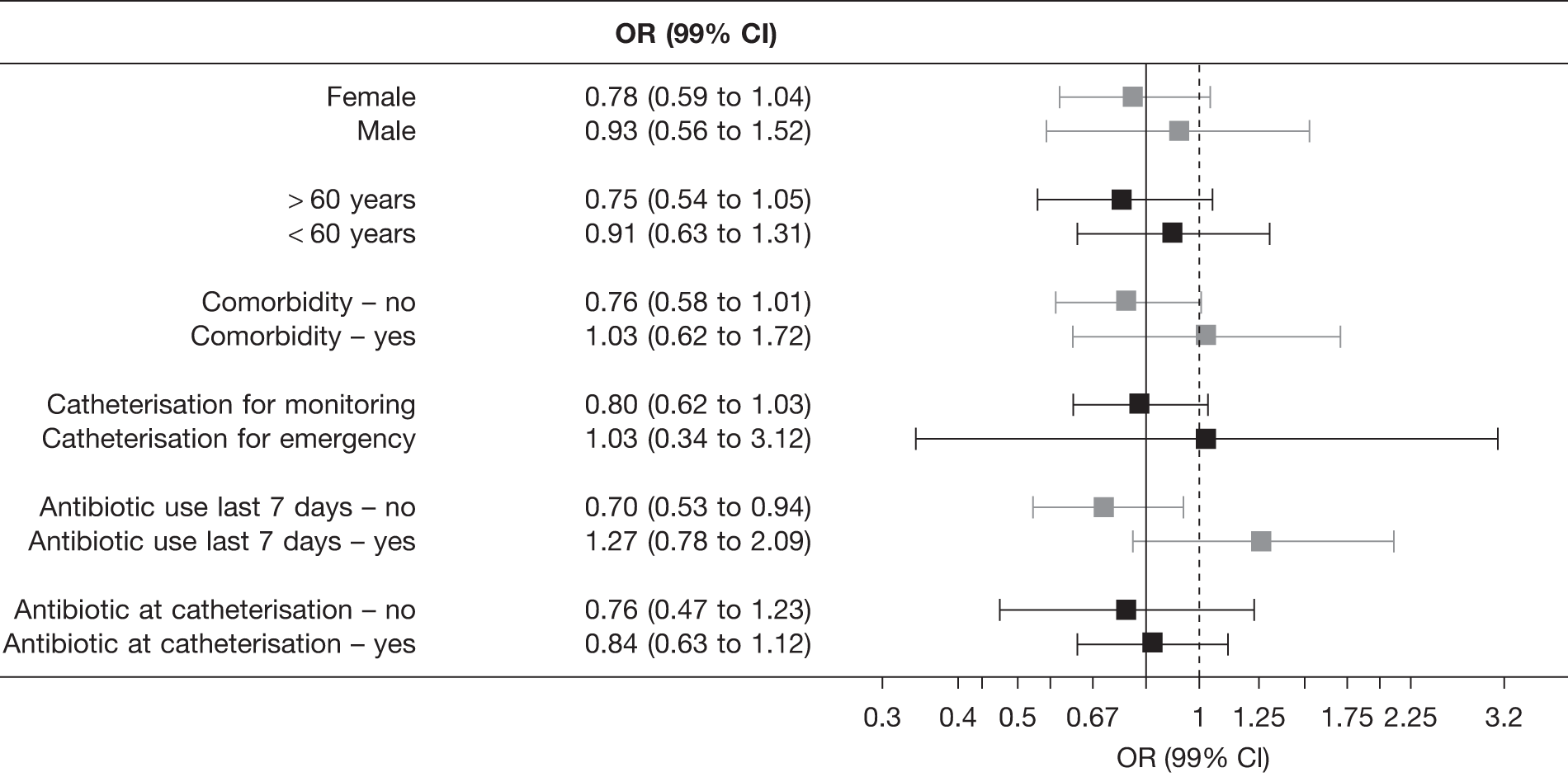
FIGURE 9.
Forest plot of subgroup analyses, UTI at any point up to 6 weeks post randomisation for silver alloy vs PTFE comparison.
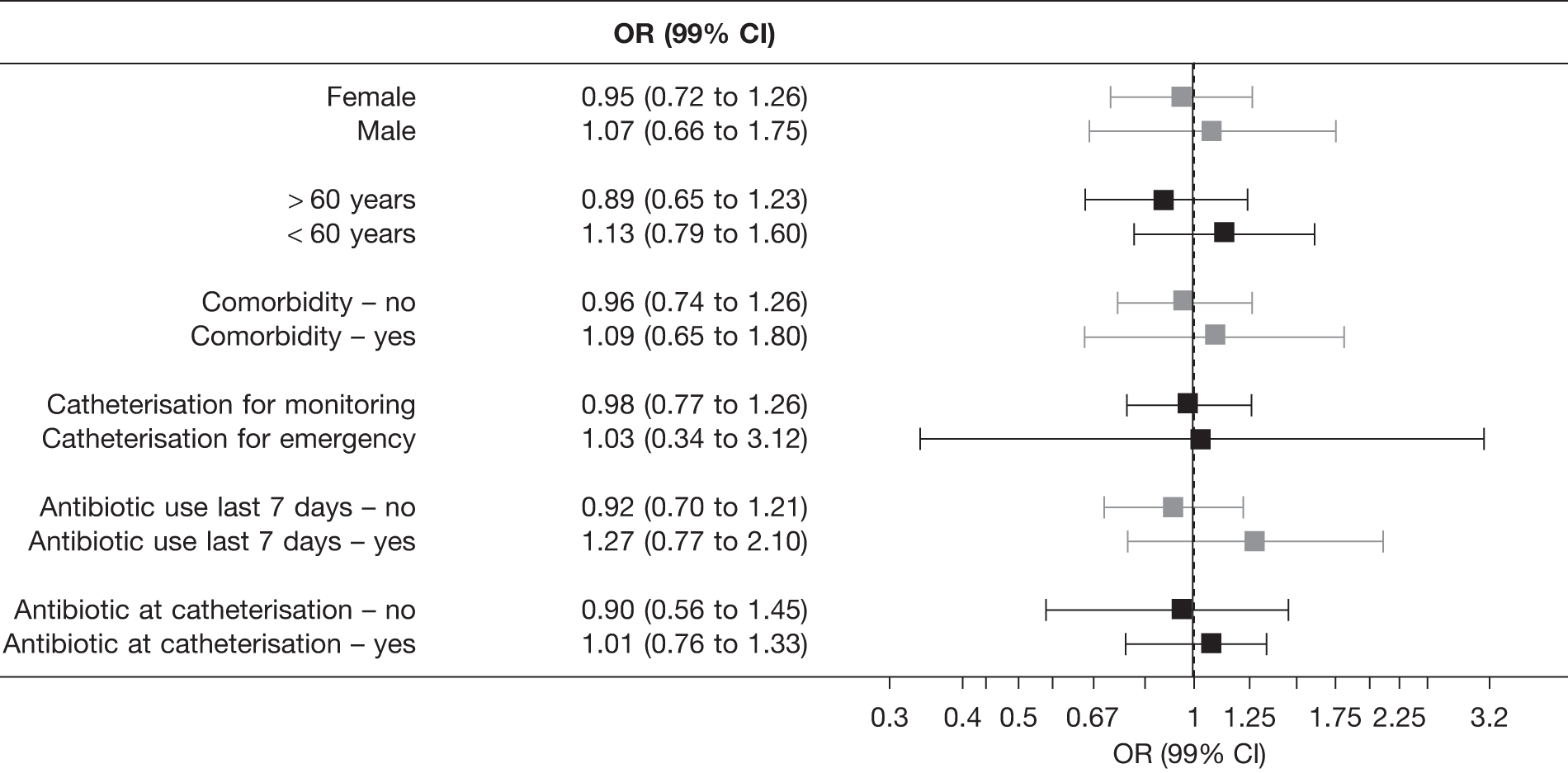
It is clear from Figure 10 the probability of suffering a catheter-associated UTI increased with age. The interaction between age and catheter type was not significant; there was no evidence that treatment effects were modified by age. The p-value for age-by-nitrofurazone and age-by-silver was 0.53 and 0.65, respectively.
FIGURE 10.
Plot of predicted probability of UTI at any point up to 6 weeks post randomisation by age (in years) and allocated catheter.
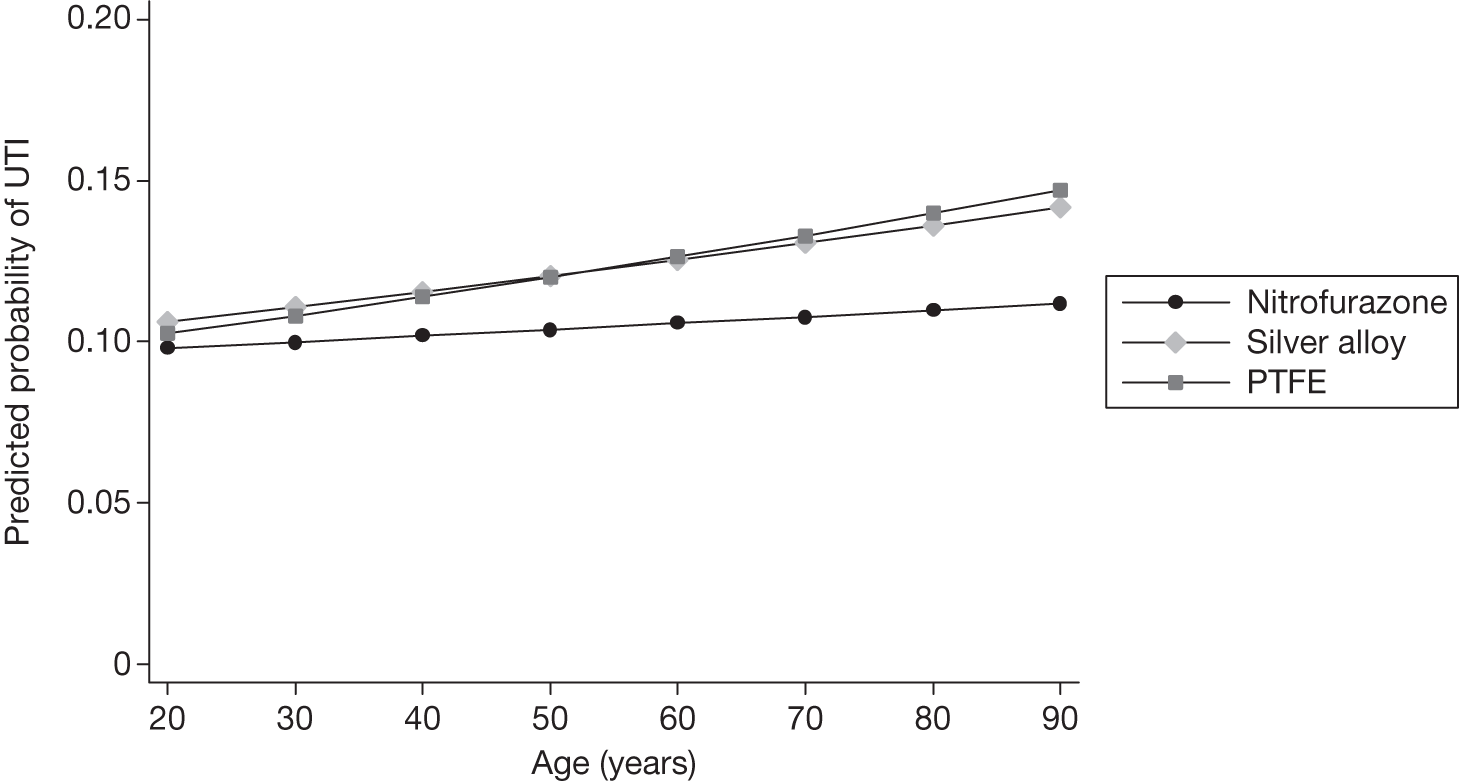
As expected the probability of UTI increased with duration of catheterisation (Figure 11). The interaction between duration and catheter type was not significant; there was no evidence that treatment effects were modified by duration of catheter. The p-value for duration-by-nitrofurazone and duration-by-silver was 0.19 and 0.87, respectively.
FIGURE 11.
Plot of predicted probability of UTI at any point up to 6 weeks post randomisation by duration of catheterisation (in days) and allocated catheter.
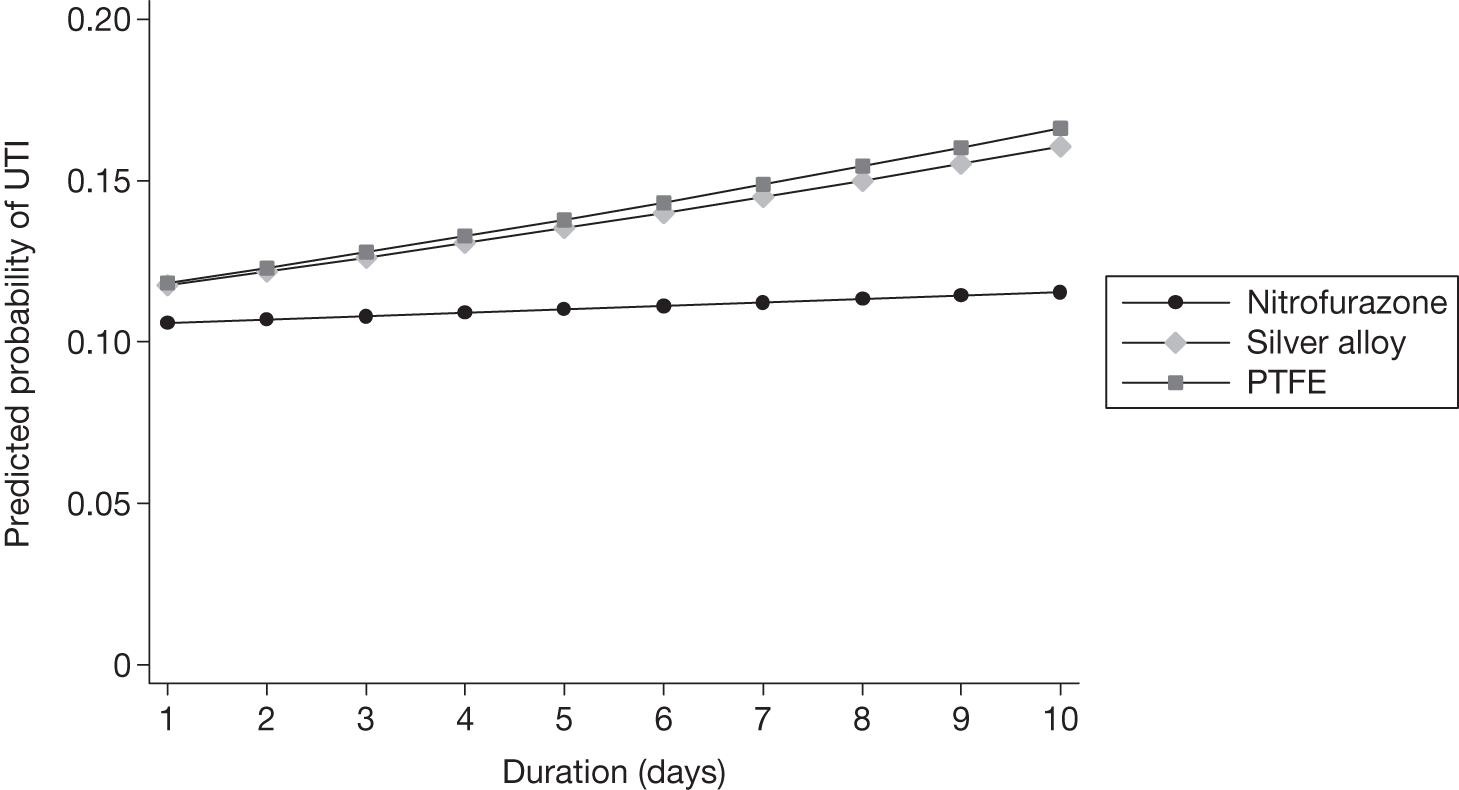
Centre effect
Adjusting for centre by including a random effect for centre (Table 26, third column) had negligible effect on fixed-treatment-effect estimates (see Table 26, second column) and CIs for both the marginal adjusted and unadjusted models.
| Comparison | OR (97.5% CI); p-value | |
|---|---|---|
| Fixed effects | Random effects | |
| Nitrofurazone vs PTFE | ||
| Unadjusted | 0.82 (0.66 to 1.01); 0.037 | 0.83 (0.69 to 1.02); 0.039 |
| Adjusted | 0.81 (0.65 to 1.01); 0.031 | 0.83 (0.68 to 1.02); 0.045 |
| Silver alloy vs PTFE | ||
| Unadjusted | 0.99 (0.81 to 1.22); 0.92 | 1.00 (0.84 to 1.22); 0.88 |
| Adjusted | 0.96 (0.78 to 1.19); 0.69 | 0.99 (0.81 to 1.20); 0.88 |
Chapter 6 Resource use, costs and cost-effectiveness
Within-trial analysis
It was planned to conduct a within-trial analysis to estimate the incremental cost per infection averted and incremental cost per QALY gained for the two randomised comparisons: nitrofurazone compared with PTFE and silver alloy compared with PTFE. As is described below, these analyses are not reported in the main body of the report because of concerns that the estimates of costs and to a lesser extent effectiveness as measured by participant response to the EQ-5D derived from within the trial comparison were unreliable. The planned ‘within-trial’ analyses are therefore not reported in the main body of the report but are included as Appendix 7. In this section we report the within-trial data describing resource use, costs and QALYs. We have refrained from reporting comparisons between randomised groups, except to illustrate the reasoning behind our decision that such comparisons are surrounded by sufficient uncertainty to make any interpretation hazardous.
Analysis of resource use and costs
Table 27 details the average resource use for the three randomised groups. As this table shows, the use of health services was generally similar. The exception to this is differences in length of stay where mean differences between nitrofurazone and PTFE groups may be economically important (see Appendix 7, Table 44).
| Resource type | Nitrofurazone: n, mean (SD) | Silver alloy: n, mean (SD) | PTFE: n, mean (SD) |
|---|---|---|---|
| Intervention | |||
| No. of catheters used | 2153, 1.03 (0.21) | 2097, 1.04 (0.29) | 2144, 1.03 (0.21) |
| Secondary care resource use | |||
| Length of stay (days) | 2104, 7.27 (6.58) | 2047, 7.72 (6.87) | 2102, 7.57 (7.00) |
| No. of outpatient visits | 1668, 0.02 (0.28) | 1614, 0.02 (0.17) | 1671, 0.02 (0.19) |
| No. of visits to other providers | 1656, 0.02 (0.41) | 1605, 0.01 (0.14) | 1662, 0.01 (0.20) |
| No. of inpatient readmissions | 1669, 0.08 (1.26) | 1605, 0.01 (0.24) | 1673, 0.02 (0.54) |
| Primary care resource use | |||
| Primary care doctor visit | 1661, 0.11 (0.44) | 1605, 0.13 (0.47) | 1659, 0.12 (0.45) |
| Primary care nurse visit | 1667, 0.03 (0.27) | 1606, 0.04 (0.34) | 1669, 0.05 (1.05) |
| Medications | |||
| Treatment course of antibiotics for UTIa | 1160, 0.18 (0.38) | 1130, 0.18 (0.39) | 1154, 0.20 (0.40) |
Estimation of NHS costs
Table 28 is a conversion of Table 27 into costs to the NHS. As indicated by the SD, the cost data were highly skewed to the right; while most of the participants incurred low costs, some of them incurred very high costs. In terms of NHS costs incurred after trial participants were catheterised, the mean total cost per patient was £3259 (SD £3152) in the nitrofurazone group, £3438 (SD £3270) in the silver alloy group and £3390 (SD £3405) in the PTFE group. The main driver of total costs was length of stay. The cost of catheters themselves did differ (although the use of catheters was very similar) but the magnitude of differences was comparatively small. The reason for this was that the unit costs were higher for nitrofurazone and silver alloy catheters than for PTFE catheters.
| Resource type | Nitrofurazone (n), mean £ (SD) | Silver alloy (n), mean £ (SD) | PTFE (n), mean £ (SD) |
|---|---|---|---|
| Intervention | |||
| Catheter | 2153, 5.15 (1.19) | 2097, 6.34 (1.86) | 2144, 0.96 (0.65) |
| Secondary care resource use | |||
| Length of stay | 2104, 3302.98 (3107.74) | 2047, 3505.72 (3266.80) | 2102, 3444.63 (3397.18) |
| Outpatient visit | 1668, 1.63 (26.10) | 1614, 1.81 (16.28) | 1671, 1.91 (18.30) |
| Visit to other providers | 1661, 0.87 (12.13) | 1606, 1.04 (13.05) | 1664, 1.16 (18.70) |
| Inpatient readmissions | 1669, 26.53 (412.18) | 1605, 3.88 (77.16) | 1673, 6.67 (177.44) |
| Primary care resource use | |||
| GP doctor visit | 1661, 3.88 (15.80) | 1605, 4.67 (17.08) | 1659, 4.32 (16.33) |
| GP nurse visit | 1667, 0.35 (2.68) | 1606, 0.45 (3.43) | 1669, 0.51 (10.49) |
| Medications | |||
| Antibiotics for UTIa | 1160, 0.96 (2.06) | 1130, 0.98 (2.09) | 1154, 1.07 (2.16) |
| Total | 2153, 3259.24 (3151.69) | 2097, 3438.08 (3269.61) | 2144, 3390.02 (3405.13) |
Quality-adjusted life-years
Table 29 reports the within-trial EQ-5D scores for groups randomised at baseline, 3 days after catheter removal, 1 and 2 weeks after catheter removal, and 6 weeks after randomisation. QALYs were estimated from these data. The results were very similar between each of the intervention groups and control: the mean (SD) QALYs were 0.081 (0.02) for the nitrofurazone group, 0.079 (0.02) for the silver alloy group, and 0.081 (0.02) for the PTFE group.
| EQ-5D | Nitrofurazone (n), mean (SD) | Silver alloy (n), mean (SD) | PTFE (n), mean (SD) |
|---|---|---|---|
| Baseline | 2126, 0.717 (0.29) | 2076, 0.722 (0.29) | 2123, 0.722 (0.30) |
| 3 days | 1859, 0.592 (0.27) | 1801, 0.578 (0.28) | 1871, 0.593 (0.27) |
| 1 week | 1363, 0.618 (0.27) | 1308, 0.601 (0.29) | 1366, 0.614 (0.27) |
| 2 weeks | 1405, 0.696 (0.26) | 1328, 0.686 (0.27) | 1398, 0.694 (0.25) |
| 6 weeks | 1704, 0.776 (0.24) | 1665, 0.782 (0.24) | 1721, 0.794 (0.23) |
| QALYsa | 1116, 0.081 (0.02) | 1077, 0.079 (0.02) | 1123, 0.081 (0.02) |
Interpretation of cost and effects data
As noted above, a within-trial economic evaluation is not reported in the main body of the text. The reason for this is that there are concerns that chance differences between participants in each of the randomised groups in terms of their overall medical care are likely to be influencing the estimates of differences in costs (and effects) derived from the trial data.
From the data reported in Tables 27 and 28, above, it can be seen that the estimates of total cost for each catheter and difference in cost between nitrofurazone and silver alloy groups compared with PTFE are driven by length of stay. The length of stay was on average 0.30 days less for nitrofurazone than for PTFE (Appendix 7, Table 44, reports the 97.5% CI as –0.77 to 0.17 days). The length of stay was on average 0.15 day longer for silver alloy than for PTFE (Appendix 7, Table 44, reports the 97.5% CI as I –0.34 to 0.63 days). These differences are not statistically significant at the 2.5% level but will be reflected in the CEACs, which describe the probability that an intervention is cost-effective. Our concern was that the mean difference in length of stay recorded between randomised groups was clinically implausible, and was being driven by imbalances between groups unrelated to the type of catheter to which they were randomised, such as the treatment course of their underlying health problem. For example, if nitrofurazone catheters prevent 2 infections per 100 people receiving this type of catheter compared with PTFE catheters, then, assuming that the only driver of differences in length of stay was the difference in infection rate, this means that each episode of infection was accompanied by a reduction in length of stay of 15 days [(0.3 days × 100)/2]. Although it is possible that there may be other mechanisms apart from catheter-associated UTI by which the catheter choice may influence length of stay other than a UTI, we made the judgement that a within-trial economic evaluation based on these data would be misleading.
Modelling results
A second pre-planned analysis was to base the economic evaluation on a simple decision-analytic model. Within this exercise an analysis has been performed that is centred on the cost and QALY implications caused by differences in UTI rates. For the base-case analysis the risk of infection is based on the risk of infection associated with PTFE catheters, and the separate absolute risk differences for each of nitrofurazone or silver alloy catheters compared with PTFE (these data are reported in Chapter 5).
This analysis makes the assumption that differences between the catheters in terms of costs and QALYs are driven by the difference in the risk of suffering a UTI for participants allocated to differing catheters and the cost of the catheter. One concern with this analysis is that those who suffer an infection may be more likely to incur extra costs or suffer worse QoL for reasons that are unconnected to having an infection, such as a more severe underlying illness or worse general health. In an attempt to explore the importance of this issue, a series of alternative analyses were defined that were believed to represent a more homogeneous population.
In this section we report on the base-case model analysis, the analyses based on potentially homogeneous subpopulations, and additional sensitivity analyses conducted to explore the impact of excluding data on the main driver of the results – length of stay.
Base-case analysis based on risk of infection as defined for the primary trial outcome
For the model-based analysis data inputs to the model relate to:
-
The absolute risk of infection for participants randomised to PTFE (control).
-
The absolute risk difference for infection for nitrofurazone compared with PTFE and silver alloy compared with PTFE.
-
The cost of care over the 6-week study period for those participants who did not suffer a UTI.
-
The difference in costs over the 6-week study period for those who suffered an infection compared with those who did not.
-
The number of catheters used per participant and the unit cost of each type of catheter.
-
The estimate of QALYs for the 6-week study period for those who did not suffer an infection.
-
The difference in QALYs for the 6-week study period for those who suffered an infection compared with those who did not.
Data on the risk of infection for PTFE and the absolute risk differences were based on trial primary outcomes results reported in Chapter 5. Tables 30 and 31 report the NHS resource use and NHS costs for those who have a UTI and those who did not. As expected, the results of the comparison showed that participants who suffered a UTI had statistically significantly higher resource use (see Table 30) and hence costs (see Table 31). The main driver of the difference in total costs (excluding the unit cost of the catheter) appeared to be differences in length of stay. The total costs when the cost of the catheter was excluded for those both with and without a UTI were used to populate the economic model. It was also assumed that for each arm of the model (each arm representing one of the three catheters) one catheter per person would be used.
| Resource type | UTI (n), mean (SD) | No UTI (n), mean (SD) | Difference, mean (97.5% CI) |
|---|---|---|---|
| Intervention | |||
| Catheter (no. used) | 762, 1.07 (0.31) | 5630, 1.03 (0.22) | 0.04 (0.02 to 0.06) |
| Primary care | |||
| GP doctor visit | 598, 0.66 (0.95) | 4325, 0.04 (0.26) | 0.62 (0.58 to 0.66) |
| GP nurse visit | 611, 0.22 (1.79) | 4329, 0.02 (0.19) | 0.20 (0.15 to 0.26) |
| Secondary care | |||
| Length of stay (days) | 759, 8.08 (7.73) | 5492, 7.44 (6.68) | 0.63 (0.04 to 1.23) |
| Outpatient visit | 614, 0.07 (0.33) | 4337, 0.01 (0.20) | 0.06 (0.04 to 0.08) |
| Visit to other providers | 607, 0.05 (0.26) | 4314, 0.01 (0.28) | 0.04 (0.02 to 0.07) |
| Inpatient readmissions | 618, 0.17 (1.66) | 4327, 0.02 (0.59) | 0.15 (0.07 to 0.22) |
| Medications | |||
| Antibiotic prescriptions for UTIb | 637, 0.62 (0.49) | 2805, 0.08 (0.28) | 0.54 (0.50 to 0.57) |
| Resource type | UTI (n), mean (SD) | No UTI (n), mean (SD | Adjusted difference,a mean (97.5% CI) | Unadjusted difference, mean (97.5% CI) |
|---|---|---|---|---|
| Intervention | ||||
| Catheter | 762, 4.11 (2.79) | 5630, 4.14 (2.65) | –0.07 (–0.32 to 0.19) | 0.03 (–0.20 to 0.27) |
| Primary care | ||||
| GP doctor visit | 598, 23.90 (34.16) | 4325, 1.56 (9.19) | 22.26 (18.99 to 25.54) | 22.33 (20.90 to 23.77) |
| GP nurse visit | 611, 2.21 (17.94) | 4329, 0.18 (1.91) | 2.13 (0.32 to 3.95) | 2.02 (1.39 to 2.66) |
| Secondary care | ||||
| Length of stay | 759, 3652.60 (3538.76) | 5492, 3385.18 (3218.75) | 471.85 (178.05 to 765.67) | 267.42 (15.54 to 550.38) |
| Outpatient visit | 614, 6.58 (31.31) | 4337, 1.08 (18.58) | 5.62 (2.55 to 8.69) | 5.50 (3.51 to 7.49) |
| Visit to other providers | 611, 4.12 (23.58) | 4318, 0.58 (13.21) | 3.57 (1.38 to 5.76) | 3.54 (2.10 to 4.98) |
| Inpatient readmissions | 618, 54.14 (543.35) | 4327, 6.52 (193.93) | 46.77 (–8.50 to 102.06) | 47.62 (22.15 to 73.08) |
| Medications | ||||
| Antibiotics | 637, 3.36 (2.63) | 2805, 0.46 (1.52) | 2.85 (2.60 to 3.10) | 2.90 (2.72 to 3.07) |
| Total (excluding catheter cost) | 762, 3779.42 (3573.4) | 5630, 3375.42 (3232.91) | 547.63 (288.55 to 860.71) | 403.97 (120.53 to 687.41) |
Table 32 reports the EQ-5D scores for those who suffered a UTI and those who did not. From these data it was estimated that the mean QALYs were 0.075 (SD 0.03) for the group that suffered a UTI and 0.081 (SD 0.02) for the group that did not. The mean difference in QALYs after adjusting for baseline EQ-5D and other characteristics was 0.006 (97.5% CI –0.009 to –0.003) lower for the participants who suffered a UTI.
| EQ-5D | UTI (n), mean (SD) | No UTI (n), mean (SD) | Difference |
|---|---|---|---|
| Baseline | 751, 0.734 (0.29) | 5573, 0.719 (0.29) | |
| 3 days | 671, 0.555 (0.28) | 4858, 0.593 (0.27) | |
| 1 week | 516, 0.565 (0.29) | 3519, 0.619 (0.27) | |
| 2 weeks | 524, 0.645(0.28) | 3605, 0.700 (0.26) | |
| 6 weeks | 652, 0.750 (0.27) | 4436, 0.790 (0.23) | |
| QALYsa | 424, 0.075 (0.02) | 2891, 0.081 (0.02) | –0.006 (–0.009 to –0.003)b |
A summary of the parameters, their values, source and the distribution used in the probabilistic sensitivity analysis is reported in Table 33.
| Variable name | Value | Source and distributiona |
|---|---|---|
| Risk of infection for PTFE | 0.126 | Based on the value from the trial analysis (see Table 13). Beta distribution; α = number of events in group = 271; β = number of people without the event in the group = 1873 |
| Relative risk of infection for nitrofurazone | –0.021 | Based on the estimated absolute risk difference between nitrofurazone and PFTE (see Chapter 5, Primary outcome). Normal distribution: SD = 0.01 |
| Relative risk of infection for silver alloy | –0.001 | Based on the estimated absolute risk difference between nitrofurazone and PTFE (see Chapter 5, Primary outcome). Normal distribution: SD = 0.01 |
| Utility associated with a catheter infection | 0.075 | Based on data reported in Table 32. Beta distribution: α and β derived from mean (0.075369) and SD (0.02454) of QALYs for a UTI |
| Additional utility associated with not suffering a UTI | +0.006 | Based on the adjusted analysis difference in QALYs reported in Table 32. Normal distribution: SD = 0.001 |
| Health-care costs for those without UTI | £3375.42 | Based on cost estimate reported in Table 31. Log-normal distribution: Derived from mean = 3375.42 and median costs = 2359 derived from trial data |
| Additional health-care costs for those suffering a UTI | £547.63 | Based on the adjusted analysis results cost difference estimate in Table 31. Normal distribution: mean = 547.63, SD = 425.62 |
| Cost of nitrofurazone catheter | £5.29 | Personal communication with the manufacturer (Rochester). Point estimate, no distribution attached |
| Cost of silver alloy catheter | £6.46 | Personal communication with the manufacturer (CR Bard). Point estimate, no distribution attached |
| Cost of PTFE catheter | £0.86 | NHS Supplies. Point estimate, no distribution attached |
The results of the model using the absolute risk reduction recorded as the primary outcome for trial data suggest that nitrofurazone is, on average, the least costly trial intervention, followed by PTFE and then silver alloy (Table 34). It is also, on average, the most effective catheter, with PTFE and silver alloy having similar effectiveness. This latter finding was expected, given the very small mean difference in risk of an infection between silver alloy and PTFE catheters. Overall, there is a 70% chance that nitrofurazone would be the least costly option and over an 80% probability that it would be considered cost-effective when society is willing to pay a maximum of £30,000 per QALY. Silver alloy has virtually no chance of being considered cost-effective when compared with the other two catheters. For nitrofurazone the reduction in the subsequent cost of care caused by a likely reduction in the risk of infections more than compensates for the increased cost of the catheter. However, the same is not true for silver alloy.
| Intervention | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER | Probability (%) of being cost-effective at different threshold values for society’s willingness to pay for an additional QALY: | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| £0 | £10,000 | £20,000 | £30,000 | £50,000 | ||||||
| Nitrofurazone | 3438.43 | 0.08232 | 73 | 77 | 81 | 84 | 89 | |||
| PTFE | 3445.50 | 7.10 | 0.08218 | –0.0001 | Dominated | 27 | 23 | 19 | 16 | 11 |
| Silver alloy | 3450.55 | 12.10 | 0.08219 | 0 | Dominated | 0 | 0 | 0 | 0 | 0 |
What the probabilistic analysis reported in Table 34 does not portray is the magnitude and variation in cost. The difference in cost between nitrofurazone and PTFE is graphically illustrated in Figure 12 and that for silver alloy and PTFE in Figure 13. For the comparison of nitrofurazone against PTFE, the 97.5% CI was –£36.19 to £11.45 and for the comparison of silver alloy against PTFE the 97.5% CI was £4.13 to £5.92.
FIGURE 12.
Distribution of health-care cost differences for participants randomised to nitrofurazone compared with PTFE. Based on 1000 Monte Carlo simulations.
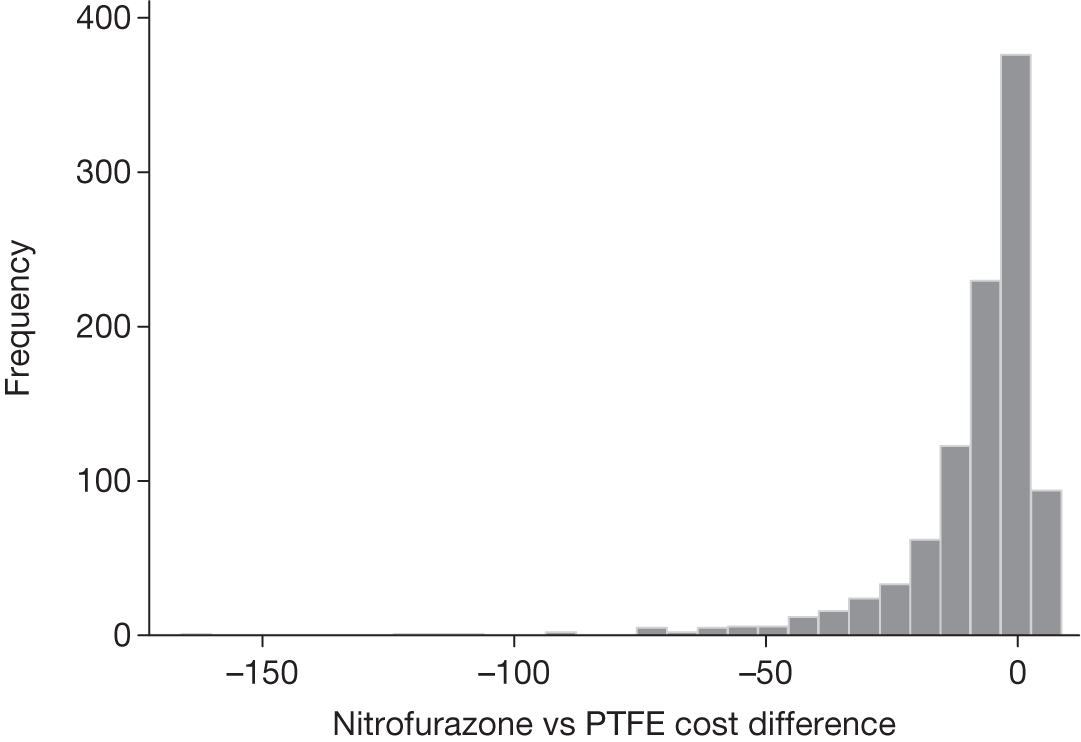
FIGURE 13.
Distribution of health-care cost differences for participants randomised to silver alloy compared with PTFE. Based on 1000 Monte Carlo simulations.
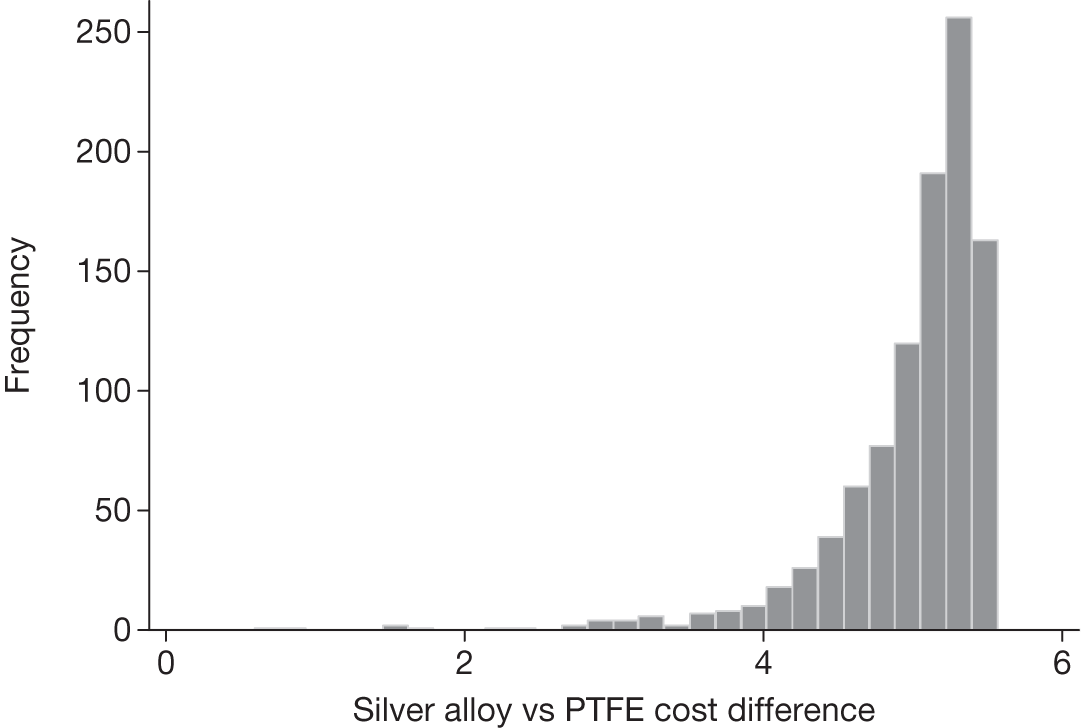
Analyses for more ‘homogeneous’ patient groups
Three participant groups believed to represent more homogeneous patient populations were defined. These were:
-
Those admitted to an obstetrics and gynaecology specialty ward only. For this analysis the costs and QALY for those with and without a UTI were based on this subgroup. We used the same risk of a UTI as in the base case, as these data were assumed to be robust and precise.
-
Those with an EQ-5D score of 1 at 3 days after catheter removal. Again the costs and QALY for those with and without a UTI were based on this subgroup and the risk of a UTI was taken to be the same as the base case.
-
Those participants who were recorded as having a symptomatic CAUTI treated with antibiotics at 3 days post catheter removal. Costs and QALY risks were defined in the same way as for the two previous subgroup analyses.
Tables 35–37 describe the costs and QALYs for each of these analyses. The first subgroup considered consisted of women who were admitted to an obstetrics and gynaecology specialty ward (n = 1736; UTI 336; no UTI 1400). For this subgroup, the adjusted difference in total costs between those who had an infection and those who did not was £141 (97.5% CI –117 to 400) and the QALY difference was –0.007 (97.5% CI –0.011 to –0.003) (see Table 35). The second subgroup we analysed, based on data from participants who reported that they had an EQ-5D score of ‘1’ (full health) at 3 days post catheter removal (n = 436; UTI 33; no UTI 403), resulted in a £988 (97.5% CI –64 to 2052) difference in costs and –0.002 (97.5% CI –0.012 to 0.007) difference in QALYs (see Table 36). Finally, Table 37 describes costs and QALYs for all trial participants, based on their infection status using the secondary trial outcome of symptomatic antibiotic-treated UTI at 3 days post catheter removal (n = 6394; UTI 370; no UTI 6023). Participants who suffered a UTI had, on average, £1417 higher cost (97.5% CI 982 to 1925) and –0.004 fewer QALYs (97.5% CI –0.009 to 0.000) compared with those who did not suffer a UTI.
| Resource type | UTI (n), mean (SD) | No UTI (n), mean (SD) | Adjusted difference,a mean (97.5% CI) | Unadjusted difference, mean (97.5% CI) |
|---|---|---|---|---|
| Intervention | ||||
| Catheter | 336, 4.21 (3.03) | 1400, 4.15 (3.01) | –0.01 (–0.43 to 0.41) | 0.06 (–0.34 to 0.48 ) |
| Primary care | ||||
| GP doctor visit | 273, 31.78 (4.81) | 1077, 3.07(12.81) | 29.31 (24.28 to 34.35 ) | 28.71 (25.76 to 31.65 ) |
| GP nurse visit | 285, 1.37 (4.81) | 1085, 0.14 (1.89) | 1.24 (0.55 to 1.94 ) | 1.23 (0.82 to 1.64 ) |
| Secondary care | ||||
| Length of stay | 335, 1958.21 (2003.18) | 1370, 1805.98 (1870.84) | 57.49 (–190.71 to 305.68 ) | 152.24 (–107.18 to 411.66) |
| Outpatient visit | 287, 8.18 (33.73) | 1088, 1.55 (14.45) | 6.79 (2.20 to 11.37 ) | 6.63 (3.65 to 9.62 ) |
| Visit to other providers | 288, 5.07 (24.41) | 1078, 0.30 (8.66) | 4.91 (1.56 to 8.25 ) | 4.77 (2.75 to 6.79 ) |
| Inpatient readmissions | 286, 41.28 (78.50) | 1082, 2.12 (51.79) | 40.43 (4.10 to 76.75 ) | 39.16 (18.98 to 59.35 ) |
| Medications | ||||
| Antibiotics | 311, 3.58 (2.56) | 765, 0.63 (1.74) | 2.95 (2.59 to 3.31 ) | 2.95 (2.65 to 3.26 ) |
| Total | 336, 2033.38 (2084.74) | 1400, 1777.32 (1871.29) | 141.46 (–116.76 to 399.68) | 256.06 (–4.83 to 516.96) |
| Total without cost of catheter (used in model) | 336, 2029.17 (2084.76) | 1375, 1805.41 (1872.72) | 127.93 (–136.78 to 392.64) | 233.76 (–37.3 to 485.36) |
| QALYs | 219, 0.080 (0.02) | 832, 0.086 (0.02) | –0.007 (–0.011 to –0.003 ) | –0.006 (–0.010 to –0.003) |
| Resource type | UTI (n), mean (SD) | No UTI (n), mean (SD) | Adjusted difference,a mean (97.5% CI) | Unadjusted difference, mean (97.5% CI) |
|---|---|---|---|---|
| Intervention | ||||
| Catheter | 33, 4.20 (2.61) | 403, 4.20 (2.43) | –0.30 (–1.40 to 0.80) | 0.01 (–0.99 to 1.00) |
| Primary care | ||||
| GP doctor visit | 27, 20 (23.06) | 333, 1.08 (6.15) | 18.63 (8.41 to 8.85) | 19.92 (15.05 to 22.79) |
| GP nurse visit | 28, 2.14 (5.68) | 332, 0.27 (3.05) | 1.96 (–0.51 to 4.44) | 1.87 (0.40 to 3.34) |
| Secondary care | ||||
| Length of stay | 33, 3154.36 (2946.53) | 400, 2468.29 (2341.09) | 912.73 (–164.41 to 1989.87) | 686.07 (–288.09 to 1660.24) |
| Outpatient visit | 30, 0 (0) | 334, 0.844 (8.88) | 1.00 (–2.40 to 0.39) | –0.84 (–4.50 to 2.81) |
| Visit to other providers | 28, 0.10 (0.57) | 333, 0.61 (6.76) | –0.26 (–0.99 to 0.48) | 0.50 (–3.38 to 2.38) |
| Inpatient readmissions | 30, 54.67 (299.42) | 332, 0 (0) | 57.19 (–38.88 to 153.25) | 54.67 (18.20 to 91.13) |
| Medications | ||||
| Antibiotics | 31, 3.32 (2.68) | 239, 0.14 (0.85) | 3.14 (2.07 to 4.21) | 3.18 (2.66 to 3.70) |
| Total | 33, 3229.65 (2944.67) | 403, 2456.51 (2342.01) | 988.45 (–64.47 to 2051.50) | 773.14 (–200.85 to 1747.14) |
| Total without cost of catheter (used in model) | 33, 3225.45 (2944.27) | 403, 2452.31 (2342.01) | 988.75 (–64.01 to 2051.74) | 773.15 (–200.86 to 1747.15) |
| QALYs | 25, 0.099 (0.02) | 252, 0.102 (0.02) | –0.002 (–0.012 to 0.007) | –0.003 (–0.011 to 0.004) |
| Type of sensitivity | UTI (n), mean (£) | No UTI (n), mean(£) | Differencea |
|---|---|---|---|
| Costs using 3-day post-catheter removal UTI outcomea | 370, 4748.72 | 6023, 3331.24 | 1417.48 (981.60 to 1925.18) |
| QALYs | 184, 0.076 | 3132, 0.081 | –0.004 (–0.009 to 0.000) |
Table 38 summarises the data used for each subgroup analysis, along with details of the distribution and the data used to define that distribution.
| Variable name | Value | Source |
|---|---|---|
| Maternity specialty participants | ||
| Health-care costs for participants without reported UTI | £1805.41 | Based on cost estimate reported in Table 35. Log-normal distribution: derived from adjusted mean = 1805.41 and median costs = 1383 derived from trial data |
| Cost difference between UTI and no UTI | £127.93 | Based on the adjusted analysis results cost difference estimate in Table 35. Normal distribution: mean = 127.93, SD = 116.55 |
| QALYs for participants who experienced UTI over 6-week trial period | 0.080 | Based on data reported in Table 35. Beta distribution: α and β derived from mean (0.07961) and SD (0.02061) of QALYs for a UTI |
| QALY difference UTI and no UTI | 0.007 | Based on the adjusted analysis difference in QALYs reported in Table 35. Normal distribution: SD = 0.0015 |
| All other parameters | Same as base case | |
| EQ-5D score at 3 days = 1 | ||
| Health-care costs for participants without reported UTI | £2452.31 | Based on cost estimate reported in Table 36. Log-normal distribution: derived from adjusted mean = 2452.31 and median costs = 1844 derived from trial data |
| Cost difference between UTI and no UTI | £988.75 | Based on the adjusted analysis results cost difference estimate in Table 36. Normal distribution: mean = 988.75, SD = 471.97 |
| QALYs for participants who experienced UTI over 6-week trial period | 0.099 | Based on data reported in Table 36. Beta distribution: α and β derived from mean (0.09909) and SD (0.01904) of QALYs for a UTI |
| QALY difference UTI and no UTI | 0.002 | Based on the adjusted analysis difference in QALYs reported in Table 36. Normal distribution: SD = 0.0050 |
| All other parameters | Same as base case | |
| At 3 days post catheterisation | ||
| Health-care costs for participants without reported UTI | £3331.25 | Based on cost estimate reported in Table 37. Log-normal distribution: derived from adjusted mean = 3331.25 and median costs = 2317 derived from trial data |
| Cost difference between UTI and no UTI | £1417.48 | Based on the adjusted analysis results cost difference estimate Table 37. Normal distribution: mean = 1417.48, SD = 209.10 |
| QALYs for participants who experienced UTI over 6-week trial period | 0.076 | Based on data reported in Table 37. Beta distribution: α and β derived from mean (0.07553) and SD (0.02553) of QALYs for a UTI |
| QALY difference UTI and no UTI | 0.004 | Based on the adjusted analysis difference in QALYs reported in Table 36. Normal distribution: SD = 0.0021 |
| All other parameters | Same as base case | |
Table 39 describes the results of each of these three subgroup analyses. Also shown in this table are the results of the base-case analysis to facilitate comparison. In the first subgroup analysis, considering those admitted to the obstetrics and gynaecology specialty ward, the cost associated with PTFE was on average the lowest and silver alloy catheters were on average the most costly (£5.47 more costly than PTFE). The most effective catheter was nitrofurazone. When society was unwilling to pay any price for additional QALYs, PTFE had almost an 80% chance of being considered cost-effective. This likelihood fell to 30% when the threshold value for society’s willingness to pay was £30,000. When society’s willingness to pay was £30,000, nitrofurazone had a 70% chance of being considered cost-effective; however, this result is driven by the small difference in QALYs gained over PTFE, which may not be of clinical significance.
| Intervention | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER | Probability (%) of being cost-effective at different threshold values for society’s willingness to pay for an additional QALY: | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| £0 | £10,000 | £20,000 | £30,000 | £50,000 | ||||||
| Base-case analysis | ||||||||||
| Nitrofurazone | 3438.4 | 0.08232 | 73 | 77 | 80 | 84 | 89 | |||
| PTFE | 3445.5 | 7.1 | 0.08218 | –0.0001 | Dominated | 27 | 23 | 20 | 16 | 11 |
| Silver alloy | 3450.55 | 12.1 | 0.08219 | 0 | Dominated | 0 | 0 | 0 | 0 | 0 |
| Participants admitted into the obstetric and gynaecology specialty ward | ||||||||||
| PTFE | 1918.27 | 0.08712 | 77 | 60 | 41 | 29 | 15 | |||
| Nitrofurazone | 1920.01 | 1.74 | 0.08726 | 0.00015 | £11,497 | 23 | 40 | 59 | 71 | 85 |
| Silver alloy | 1923.74 | 3.73 | 0.08712 | –0.00014 | Dominated | 0 | 0 | 0 | 0 | 0 |
| EQ-5D score at 3 days = 1 (full health) | ||||||||||
| Nitrofurazone | 2561.8 | 0.10106 | 91 | 91 | 91 | 91 | 92 | |||
| PTFE | 2578.2 | 16.3 | 0.10098 | –0.00008 | Dominated | 9 | 9 | 9 | 9 | 8 |
| Silver alloy | 2582.8 | 20.9 | 0.10098 | –0.00007 | Dominated | 0 | 0 | 0 | 0 | 0 |
| Three-day symptomatic antibiotic-treated UTI outcome | ||||||||||
| Nitrofurazone | 3485.9 | 0.08118 | 97 | 97 | 97 | 97 | 97 | |||
| PTFE | 3511.3 | 25.3 | 0.08108 | –0.00010 | Dominated | 3 | 3 | 3 | 3 | 3 |
| Silver alloy | 3515.5 | 29.5 | 0.08109 | –0.00009 | Dominated | 0 | 0 | 0 | 0 | 0 |
When the analysis was restricted to those with an EQ-5D score of ‘1’ at 3 days, or based on UTI status at 3 days post catheter removal, the nitrofurazone-impregnated catheter was least costly and the silver alloy-coated catheter was most costly. Nitrofurazone was also associated with more QALYs gained on average. In both of these analyses, nitrofurazone had a greater than 90% chance of being considered cost-effective when society was unwilling to pay any price for additional QALYs (willingness-to-pay value = 0). The likelihood of nitrofurazone being cost-effective increased as society’s threshold value for a QALY increased, although it should be noted that any QALY gains from the use of nitrofurazone over standard catheters were small and may not be clinically important.
For illustrative clarity, Figures 14 and 15 show the cost difference for nitrofurazone compared with PTFE and silver alloy compared with PTFE for those participants admitted to obstetrics and gynaecology ward. For this subgroup the 97.5% CI for nitrofurazone versus PTFE was –£6.65 to 7.59, and for silver alloy compared with PTFE it was £5.21 to £5.73.
FIGURE 14.
Distribution of health-care cost differences for participants from the obstetrics and gynaecology specialty subgroup randomised to nitrofurazone compared with PTFE. Based on 1000 Monte Carlo simulations.
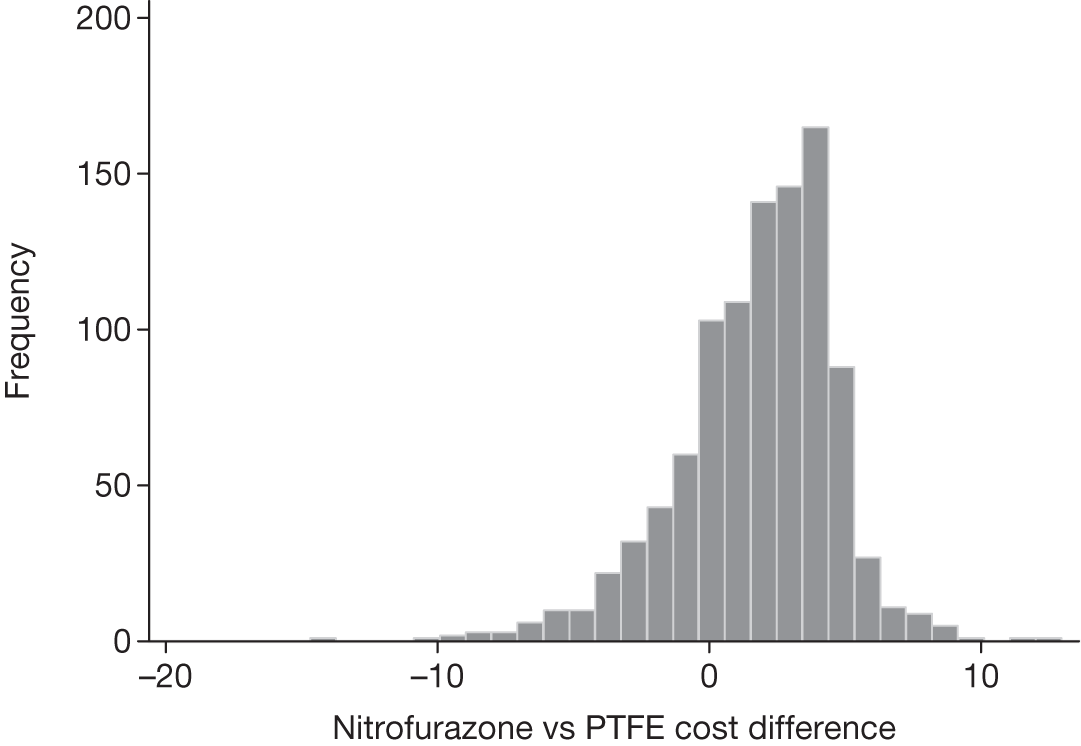
FIGURE 15.
Distribution of health-care cost differences for participants from the obstetrics and gynaecology specialty subgroup randomised to silver alloy compared with PTFE. Based on 1000 Monte Carlo simulations.
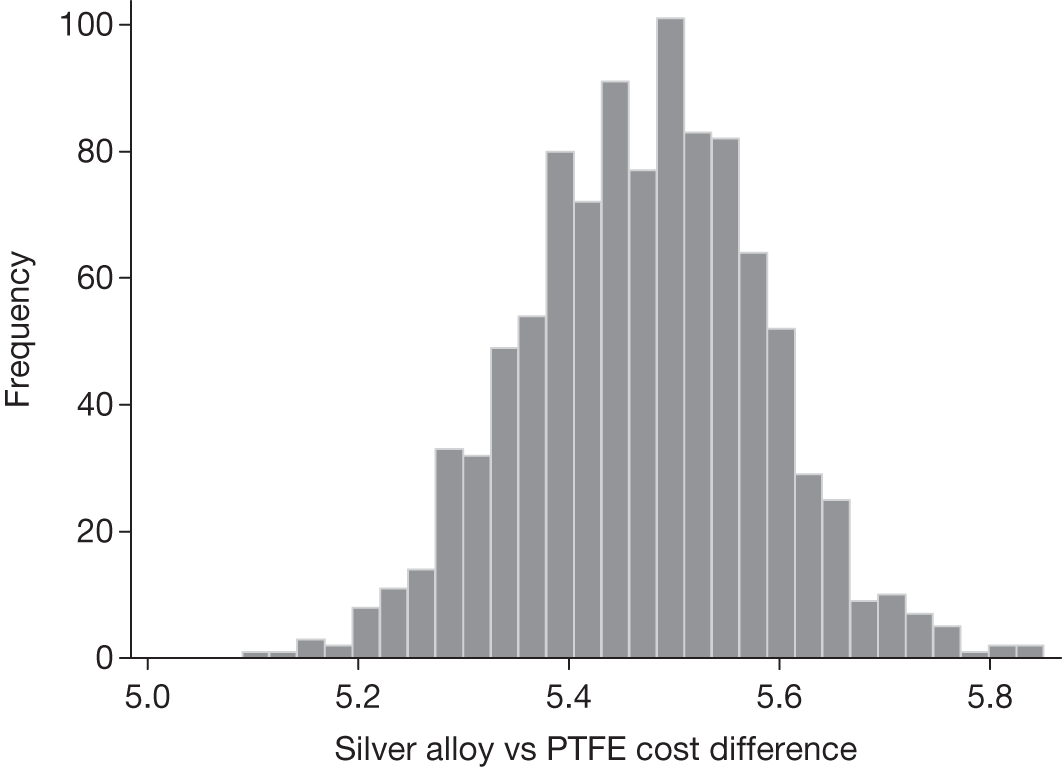
Figures 16 and 17 show the cost differences for the subgroup of participants who had an EQ-5D score of ‘1’ at 3 days. For this subgroup the 97.5% CI for nitrofurazone compared with PTFE was –£61.42 to 7.09, and for silver alloy compared with PTFE it was £3.53 to £5.62.
FIGURE 16.
Distribution of health-care cost differences for participants from the subgroup with perfect health (EQ-5D score = 1) at 3 days post catheter removal randomised to nitrofurazone compared with PTFE. Based on 1000 Monte Carlo simulations.
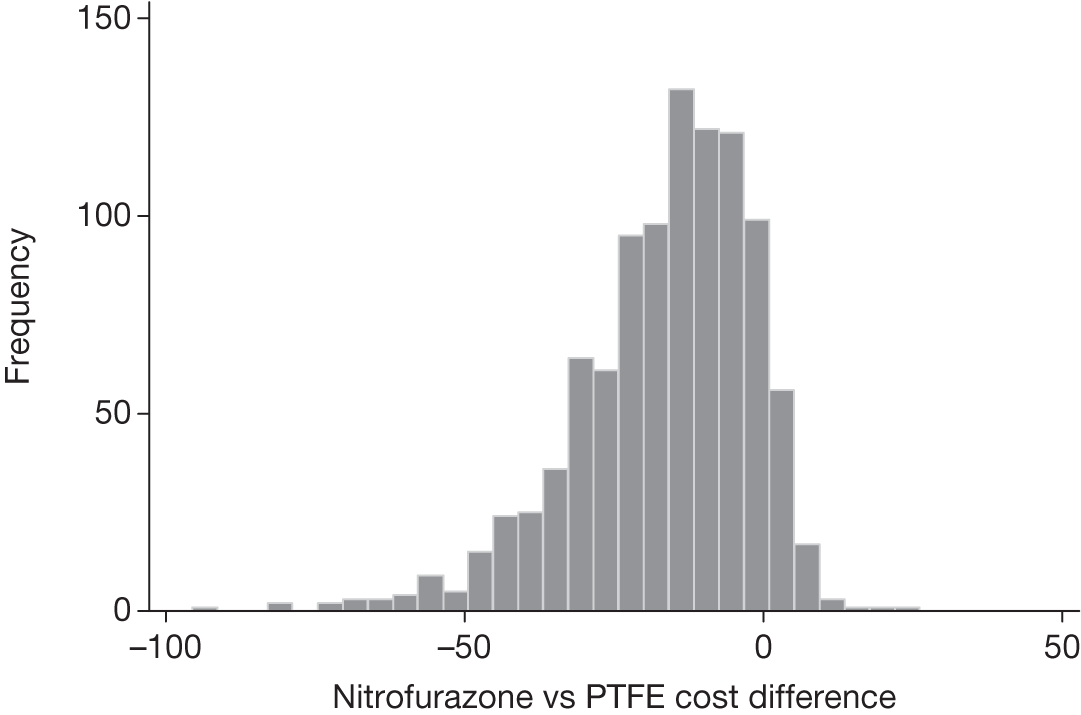
FIGURE 17.
Distribution of health-care cost differences for participants from the subgroup with perfect health (EQ-5D score = 1) at 3 days post catheter removal randomised to silver alloy compared with PTFE. Based on 1000 Monte Carlo simulations.
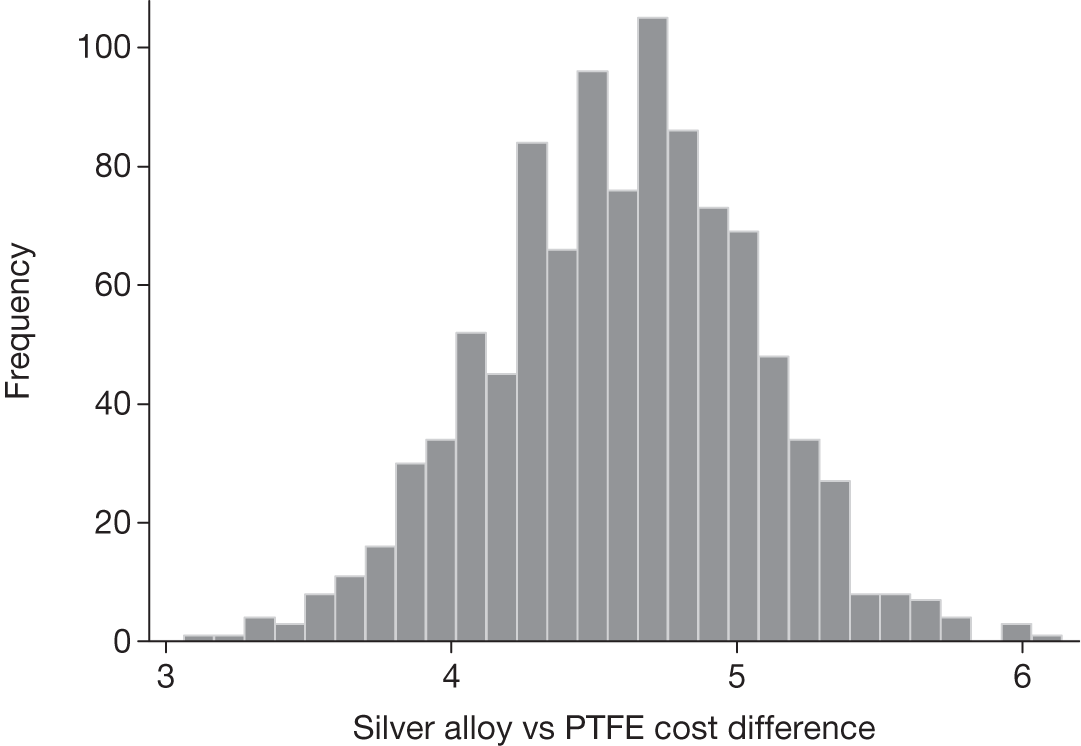
Figures 18 and 19 show the cost differences when costs and QALYs are based on those with and without a UTI at 3 days post catheter removal. For this analysis, the 97.5% CI for nitrofurazone compared with PTFE was –£62.62 to £3.78, and for silver alloy compared with PTFE it was £3.71 to £4.66.
FIGURE 18.
Distribution of health-care cost differences for participants with the outcome of UTI at 3 days post catheter removal randomised to nitrofurazone compared with PTFE. Based on 1000 Monte Carlo simulations.
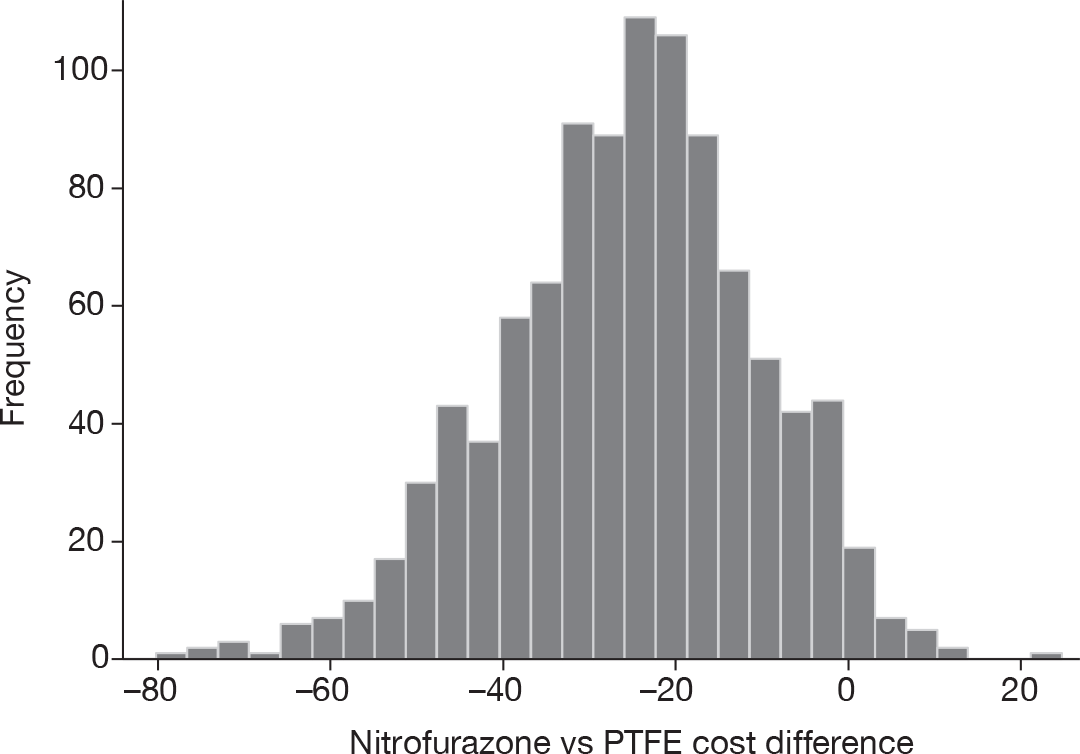
FIGURE 19.
Distribution of health-care cost differences for participants with the outcome of UTI at 3 days post catheter removal randomised to silver alloy compared with PTFE. Based on 1000 Monte Carlo simulations.
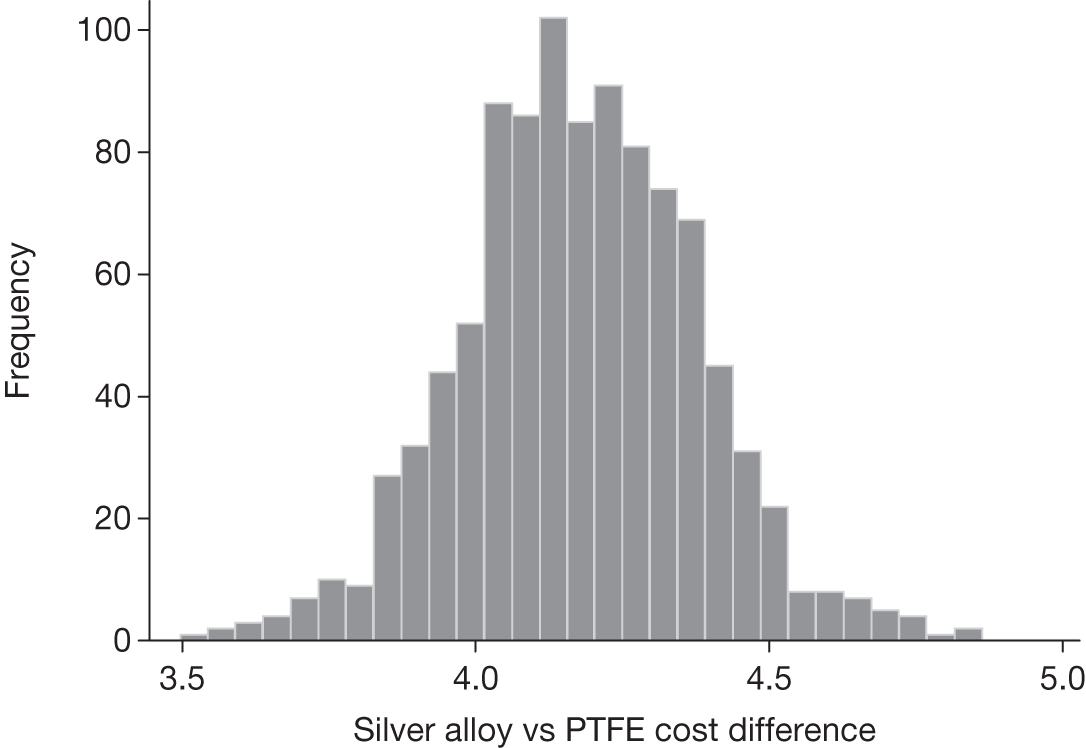
Other sensitivity analysis
As already noted, one driver of the cost differences between trial intervention groups and between participants who did or did not report UTI was the differences in length of stay, which may have been influenced by imbalances in care and illness factors between groups. In this sensitivity analysis the base-case analysis is repeated but with inpatient costs excluded in an attempt to neutralise the influence of initial inpatient treatment costs incurred during the period of catheterisation.
Table 40 describes the differences in costs and QALYs between those with and without a UTI once inpatient costs are excluded. Details of parameter values used in the model are described in Appendix 9, Tables 56–58, and the results of the analysis are shown in Table 41, below.
| Type of sensitivity | UTI (n), mean (£) | No UTI (n), mean (£) | Differencea |
|---|---|---|---|
| Costs excluding the length of stay | 762, 81.54 | 5629, 13.30 | 67.41 (21.88 to 112.87) |
| QALYs | 424, 0.077 | 2891, 0.083 | –0.006 (–0.009 to –0.003) |
| Intervention | Cost (£) | Incremental cost (£) | QALY | Incremental QALY | ICER | Probability (%) of being cost-effective at different threshold values for society’s willingness to pay for an additional QALY: | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| £0 | £10,000 | £20,000 | £30,000 | £50,000 | ||||||
| Base-case analysis | ||||||||||
| Nitrofurazone | 3438.4 | 0.08232 | 73 | 77 | 80 | 84 | 89 | |||
| PTFE | 3445.5 | 7.1 | 0.08218 | –0.0001 | Dominated | 27 | 23 | 20 | 16 | 15 |
| Silver alloy | 3450.55 | 12.1 | 0.08219 | 0 | Dominated | 0 | 0 | 0 | 0 | 0 |
| No inpatient costs | ||||||||||
| PTFE | 23.0 | 0.08102 | 100 | 93 | 69 | 47 | 23 | |||
| Nitrofurazone | 26.0 | 3.0 | 0.08113 | 0.00011 | 28,602 | 0 | 7 | 31 | 53 | 77 |
| Silver alloy | 28.6 | 2.5 | 0.08103 | –0.00010 | Dominated | 0 | 0 | 0 | 0 | 0 |
The results of the analysis described in Table 41 show that when inpatient costs are excluded then the savings in health-care costs incurred after discharge from hospital are not large enough to compensate for the higher unit price of the nitrofurazone or silver alloy catheter. On average the nitrofurazone catheters are marginally more effective than the PTFE or silver alloy catheters but the difference in QALYs may not be of clinical significance. When society is unwilling to pay anything for an additional QALY then PTFE would have a probability of being considered cost-effective that approaches 100%. When society’s willingness to pay for a QALY approaches £30,000 then the likelihood that nitrofurazone would be considered cost-effective increases to 50%. It should be noted that this result arises from the assumption made in the analysis that any difference in QALYs, no matter how small, is important.
Figures 20 and 21 display the differences in costs more clearly. For this analysis the 97.5% CI for nitrofurazone compared with PTFE is £0.82 to £4.53 and for silver alloy compared with PTFE it is £5.49 to £5.57.
FIGURE 20.
Distribution of health-care cost (£ sterling) differences for participants randomised to nitrofurazone compared with PTFE and excluding costs of the initial episode of hospital stay. Based on 1000 Monte Carlo simulations.
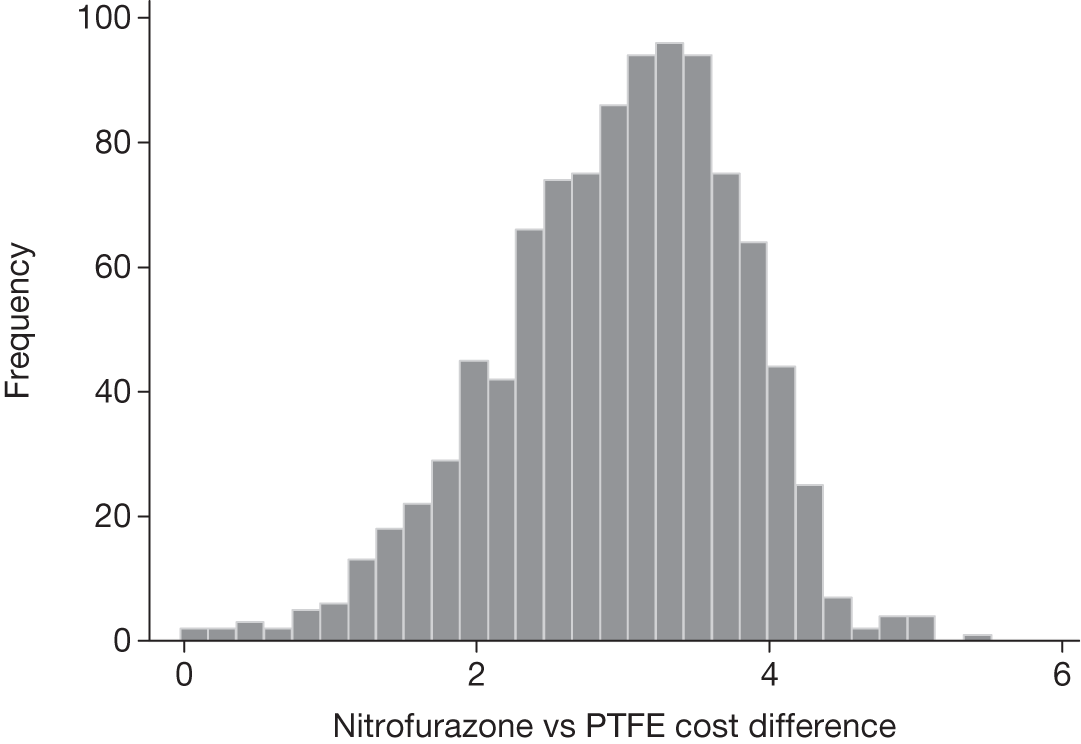
FIGURE 21.
Distribution of health-care cost (£ sterling) differences for participants randomised to silver alloy compared with PTFE and excluding costs of the initial episode of hospital stay. Based on 1000 Monte Carlo simulations.
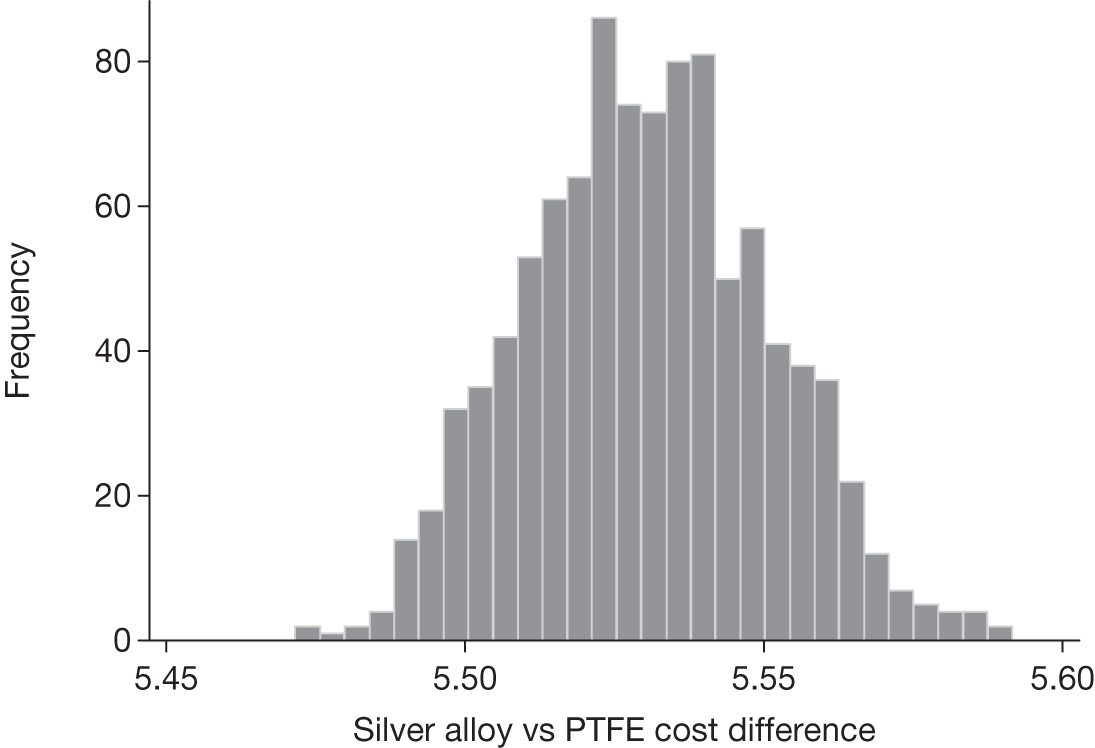
Chapter 7 Discussion
The UK government NIHR HTA programme commissioned this research in order to answer the question: ‘Is there a benefit to using antimicrobial-coated urethral catheters over catheters without antimicrobial coatings in adults requiring catheterisation expected to be of limited duration, and what are the costs?’ from the perspective of the UK NHS.
Minimum important difference
Interpretation of the findings of the CATHETER trial depends on the level of benefit that would justify changes in policy and/or practice. We judged that if 1 in around 30 people having short-term urethral catheterisation in hospital avoided a UTI as a consequence of using an antimicrobial- or antiseptic-impregnated catheter, this would offset the known extra ‘upfront’ costs of these catheters. This was the basis of the sample size calculations described in Chapter 3: an absolute effect of this size was equivalent to an OR of 0.67, and the trial had 90% power to detect this difference at an adjusted alpha error rate of 0.025 [set at this level to reflect the two principal comparisons being made: (1) nitrofurazone-impregnated catheters compared with PTFE catheters and (2) silver alloy-coated catheters compared with PTFE catheters].
The collection of resource use data allowed us subsequently to compare the costs of those participants who had a UTI with those who did not, and hence estimate the extra costs of a UTI. As can be seen in Table 31, the estimates based on all participants were around £400–500 per infection, although the figure did vary more widely in subgroup comparisons. A saving of £400–500 for each UTI avoided does, however, suggest that the ‘break-even’ point in terms of costs would be a smaller benefit. The antimicrobial catheters cost about £4 and £5 more than the standard, suggesting that avoiding just one UTI every 100 times the more expensive catheters were used would offset the extra costs. Comparison of those who had a UTI with those who did not also allowed estimation of the health-related QoL gained by avoiding a UTI (0.006; CI 0.003 to 0.009) (see Table 32). The figures for costs avoided and QALYs gained were then used in an economic model to derive estimates of cost–utility. As discussed in Chapter 5, there are substantial uncertainties in deriving the estimates of the cost of a UTI and QALYs lost as a consequence of a UTI and this should not be forgotten. Nevertheless, a tension between what is considered to constitute a ‘minimum important difference’ clinically, or indeed from an individual patient point of view, and what is the minimum difference economically lies at the heart of interpretation of the trial’s results.
Principal findings of the trial
Nitrofurazone-impregnated catheter
The primary end point results of the trial are summarised in Table 13. The adjusted OR when comparing nitrofurazone with PTFE was 0.81, with 97.5% CI of 0.65 to 1.01. The best estimate of effect (0.81) is thus less than the clinical effect that was the basis of the sample size calculation (OR 0.67). The CI just includes the OR sought (lower boundary 0.65) and just crosses the point of ‘no difference’ (1.0). Our conclusion, therefore, is that nitrofurazone catheters do not provide the protective effect that we prespecified as clinically important. Putting this another way, the best estimate is that the use of a nitrofurazone catheter would prevent 1 UTI in every 48 people catheterised but that the ‘true’ figure lies anywhere between 1 in 24 people and no protective effect at all. Reflecting the considerations about costs above, the cost–utility analysis was more encouraging, suggesting that there was a 70% chance that the nitrofurazone catheter would be the least costly option, with an 80% chance of cost-effectiveness at a threshold of £20,000 per QALY.
Silver alloy-coated catheter
The primary end point results are again summarised in Table 13. The adjusted OR for the comparison of the silver alloy catheters compared with PTFE catheters was 0.96, with 97.5% CI of 0.78 to 1.19. The best estimate of effect 0.96 is thus close to no difference (1.0). The lower end of the CI (0.78) is well short of the pre-set difference considered to be clinically important (0.67) and hence can be said to rule out such a difference. Furthermore, the other end of the CI (1.19) is consistent with a substantially increased risk of UTI. To put this in terms of numbers needed to treat, the best estimate is that 1000 people would need to receive a silver alloy catheter to prevent one UTI, but that the true effect may be anywhere between 1 infection prevented in 42 people and 1 infection caused in 45 people. In the economic analysis, when compared with the other catheters, it was very unlikely that the silver alloy catheter could be cost-effective.
Strengths and weaknesses of the trial
Effectiveness
The trial was designed at the outset to provide primary outcome information that could be directly used by NHS policy-makers to help decide whether or not antimicrobial catheters should be implemented as the standard for short-term catheterisation, predominantly following surgery or other interventional procedures. The resultant pragmatic trial design encompassed recruitment of a large sample of the relevant population across a representative spectrum of NHS hospitals and services. The only additional interventions to routine care for trial participants were random allocation of type of catheter, a urine sample at 3 days after catheter removal and trial questionnaires. The primary outcome, symptomatic UTI, defined as the presence of symptoms suggestive of UTI together with physician prescription of an antibiotic to treat UTI within 6 weeks of randomisation, was recorded by completion of case report forms during hospital stay, participant questionnaire after discharge and review of primary care records. These methods were highly effective in that all participant-reported prescriptions of antibiotic for UTI were confirmed from clinician record and that primary outcome data were obtained for all except one non-responder (for whom we assumed no UTI). We therefore believe that the results of this trial are indicative of the clinical effectiveness of the different antimicrobial catheters in preventing UTI. Estimates of QoL changes and, in the context of a large RCT, costs should also be representative. However, given the wide variety of health problems and interventions experienced by participants, some parameters, such as length of hospital stay, show such variability that chance differences in illness trajectory are likely to obscure any impact of urethral catheterisation.
A key criticism of previous studies has been the use of outcomes that are not directly relevant to patient experience or health-care costs, such as a microbiological finding of bacteriuria alone without taking account of patient-reported symptoms or prescription of antibiotic for UTI. 42 Indeed, the lack of clinically meaningful end points in all previous clinical trials of antimicrobial-coated catheters has hindered the assessment of clinical effectiveness and cost-effectiveness of such catheters. 23,42,58 There is some evidence that clinician-defined CAUTI may not align well with the presence of bacteriuria on microbiological culture. 10 To address this, we chose a definition of CAUTI that included both patient-reported symptoms and clinician action in terms of prescription of an appropriate antibiotic. This did conform to criterion 2g of the 2004 CDC definition of CAUTI, and was more relevant to both patient experience and the requirement for additional health-care resource use. 38 We chose a 6-week period of trial observation following randomisation, as this would generally encompass at least a 4-week period following catheter removal and capture events occurring following discharge from hospital; lack of community follow-up being a further criticism of previous trials. 42 Reassuringly, we found agreement in direction of effect between bacteriuria and clinical diagnosis of CAUTI with 13.5% of the nitrofurazone group and 17.4% in the silver alloy group having urinary bacterial counts of 104 CFU/ml within 3 days of catheter removal compared with 17.5% of those receiving the standard catheter (see Table 16). In addition, when a concurrent finding of bacteriuria was used as an additional criterion to the primary outcome of symptomatic UTI, the relative risk reduction was maintained with rates of 3.2%, 5.0% and 4.6% seen in the nitrofurazone, silver alloy, and control groups, respectively (see Table 14). These additional data provide some evidence that microbiological and symptomatic infection were linked in the present trial. In summary, we feel that our primary outcome did successfully address the aim of this pragmatic trial and our use of other definitions of UTI allows comparison with previous studies. The differing overall incidence rates found for these outcomes suggest that they are capturing distinct diagnostic constructs that do, however, have considerable overlap in terms of attribution of each outcome to individual trial participants.
As expected for a RCT of this size, all groups were well balanced at baseline on predicted risk factors of CAUTI (female sex, older age, diabetes and pre-existing lower urinary tract dysfunction). Furthermore, clinician-driven variables (e.g. antibiotic use prior to catheterisation, duration of catheterisation29,35,78) were also balanced between groups. Regarding patient factors thought to confer increased risk, we did find higher CAUTI rates among women, older participants, and those who experienced longer duration of catheterisation, but not among those with comorbidities such as diabetes, urinary tract dysfunction or immune suppression. Our analyses for interaction did not provide any evidence that these risk factors differentially affected the incidence of UTI within the three trial groups. We acknowledge that there were many possibly relevant characteristics of participant care that we did not capture. The wide variety of surgical interventions received by participants for disparate conditions may have resulted in imbalance of uncollected characteristics, which may have particularly affected the small effect sizes recorded and may also have influenced the magnitude and distribution of key economic parameters such as length of stay.
For the purposes of this trial a key eligibility criterion was an intended duration of catheterisation of between 1 and 14 days. Recruitment was therefore concentrated on clinical areas admitting men and women for elective surgical or interventional procedures where temporary indwelling catheterisation was part of the standard care pathway, with few participants recruited from patients primarily admitted to medical or critical care areas. Similarly, we deliberately avoided recruiting patients from the urology wards, as such patients represent a group at high risk of developing CAUTI, and they are not representative of the majority of patients receiving short-term catheters in NHS hospitals. The problems associated with using urology patients in antimicrobial catheter trials have been well documented, the most important of which is the higher background bacteriuria rate, which may lead to an overestimation of the effect size of the catheters. 23,58 The prevalence of short-term catheterisation in different clinical areas is uncertain but a previous study did document that elective surgical areas predominate, accounting for 78% of cases. 10 In addition an increased rate of CAUTI has been documented in patients treated in medical areas, although it was unclear if this was adjusted for duration of catheterisation, which is likely to be longer for medical patients who are generally admitted as emergencies. 39
We were unable to carry out a planned subanalysis concerning participants who were catheterised as part of their admission to a critical care area. Many of our trial participants did have part of their hospital stay on a critical care ward, particularly those undergoing neurosurgery or cardiothoracic surgery. The duration of such stays was difficult to measure within the logistical constraints of such a large trial, as they varied from a few hours to a number of days. We therefore decided against capturing this information. Recruitment of patients undergoing unplanned catheterisation as part of urgent care of critical illness or trauma proved logistically difficult and resource intensive and therefore was not prioritised. In addition, the need for randomisation prior to obtaining participant consent, although approved by our Ethics Committee, was associated with a relatively high rate of subsequent refusal of consent.
Given the recruitment policy for our trial, the results may therefore not be generalisable to patients admitted as emergencies to medical, trauma or critical care areas, or to urology patients, as the baseline bacteriuria rate is likely to be higher owing to underlying disease, the average duration of catheterisation is likely to be longer and the range of infecting organisms may differ. In line with the recruitment policy, the average duration of catheterisation was short, being ≤ 3 days for 75% of participants, which is similar to that found in a large cohort study from the USA. 11 As expected, we found CAUTI rates to be higher in those catheterised for at least 4 days but the three trial groups were well balanced for duration of catheterisation, with all showing a median [interquartile range (IQR)] of 2 (1–3) days.
In theoretical terms, the clinical and bacteriological effectiveness of both technologies involves a balance between the duration of their antimicrobial effect in terms of profile of antimicrobial activity and the underlying risk of infection in each individual. All studies, including ours, document that the risk of infection increases with increasing duration of catheterisation. Previous reviews have suggested that the key potential benefit of such catheters will occur during short periods of catheterisation of up to 2–3 weeks. 30 This recommendation is in line with in vitro findings suggesting that the antimicrobial activity of nitrofurazone-impregnated catheters was limited to 5 days’ exposure and that for silver alloy hydrogel-coated catheters was limited to 1 day of exposure to common bacterial strains causing CAUTI. 79 Given that the antimicrobial activity for both devices would be predicted to be maximal within the first 2 weeks of catheterisation and that for the majority of hospitalised patients any planned urinary catheterisation is of short duration,11 our decision to restrict trial participation to those patients predicted to have a period of catheterisation of between 1 and 14 days appears appropriate and does not restrict valid conclusions to be drawn concerning the clinical effectiveness of either technology. A test subanalysis adjusting for interaction catheterisation confirmed that the incidence of UTI did increase with increasing duration but did not provide any evidence that either antimicrobial catheter had greater or lesser effectiveness with its continued use up to 14 days compared with control.
Another key possible confounding variable was the use of prophylactic antibiotics at the time of catheterisation, given principally to reduce infective complications of the particular surgery being carried out. Again, all groups were well balanced for this variable, with approximately 72% receiving prophylactic antibiotic, and CAUTI rates were similar irrespective of prophylactic antibiotic use. These findings were not altered when only participants receiving antibiotics active against common uropathogens were separately considered (data not shown).
In contrast to the majority of previous randomised trials concerning this technology, allocation concealment was managed using a computerised system that was remote from the users, thereby protecting against selection bias. 42 The slightly higher rates of participants receiving a different catheter to the one allocated seen among those randomised to nitrofurazone catheters (6.7%) and those randomised to silver alloy catheters (4.9%) compared with control (1.1%) are most likely to be related to PTFE being the standard widely available control catheter and hence this was more likely to be chosen as an alternative if there were difficulties inserting one or other of the antimicrobial catheters. All analyses were based on the intention-to-treat principle to guard against any bias that this might have introduced. The lack of difference in duration of catheterisation across the groups also suggests the inability to blind participants and clinicians to the allocated intervention did not result in a systematic bias in terms of one type tending to be removed earlier than another. In addition, the median (IQR) length of hospital stay was similar in all three groups at 6 (3–9) days. Follow-up was high across the groups, especially in terms of the primary outcome where antibiotic use was confirmed by the participant’s GP, who was likely to be unaware of the intervention received. Attrition throughout the trial (due to participants declining further follow-up or not responding to requests or due to intervening death) was low and there was no apparent differential loss to follow-up in the trial arms. In all other respects there was no evidence of bias. The pragmatic nature of our trial did have drawbacks. We did not monitor any other interventions that may have influenced CAUTI rates, such as methods of catheter insertion and catheter care violations,48 although efforts were made at all participating centres to emphasise the need for adherence to established best practice guidelines throughout the duration of the trial. To assess whether or not catheter care differed between centres, we did carry out a subanalysis adjusting for centre and found no difference in rates of infection between trial groups. There was variation in overall infection rates between centres, the reasons for which are likely to be multifactorial. Possible factors include differing specialties from which participants were recruited, variation in duration of catheterisation and variation in use of surgical antibiotic prophylaxis. Our pragmatic approach to trial design was intended to ensure that it was representative of current practice across the NHS, which enhances the generalisability of the trial results. It is also possible that adherence to emerging NHS-wide standards for catheter care may have increased over the relatively long duration of the trial as a consequence of the High Impact Actions initiative in NHS England. 28
We decided on the 6-week period of trial participation after review of the literature, internal discussion and consultation with external clinical and microbiologist experts. Our rationale was that we aimed to have outcome data collected for at least 4 weeks after catheter removal for all participants and therefore allowed for a 14-day duration of catheterisation and ensured that we had a certain starting time and date for each participant. This was longer than previous trials because, in line with the pragmatic design and anticipating the short hospital stay experienced by most participants, we captured all relevant events and included an ongoing patient and community health-care perspective. It is likely that a small number of participants suffered a community-acquired UTI at some time during the 6-week period of trial participation, although their recent catheterisation will have remained a risk factor. Given the large sample size and consequently well-matched baseline participant characteristics we cannot envisage that the rate of occurrence of community-acquired UTI subsequent to catheter removal differed between the trial groups.
Cost-effectiveness
Within-trial analysis
The trial was not powered to detect a difference in QoL score or any health economic outcome and it was anticipated that it would be difficult to identify any differential effect on QoL between the three study groups given that the catheterisation episode itself was a minor part of the participants’ overall care. Despite this caveat, the economic analysis envisaged as part of this trial is important as it was the first opportunity to evaluate the cost-effectiveness of current commercially available antimicrobial catheters in a pragmatic setting and, in particular, using data from a large RCT. The methods of the economic analysis were rigorous and reproducible and efforts were made to assess the importance of uncertainty surrounding the estimates of costs, effects and cost-effectiveness.
The underlying assumption for the pre-planned within-trial economic evaluation was that the data produced by the trial would represent the best available evidence. The lack of statistical significance for key secondary outcomes is predominantly a reflection of lack of power within the trial for these outcomes but it is still likely that underlying distributions are reflective of reality. In the within-trial analysis (see Appendix 7) the main driver of likely cost-effectiveness was cost and, more specifically, for both nitrofurazone and silver alloy catheters, relative differences in length of stay. As noted above, these data require careful interpretation. The cost differences were not in themselves statistically significant at the 2.5% level but they drive the results of the within-trial analysis owing to the lack of apparent effect on QoL. A judgement is required as to whether or not the estimated difference in length of stay between groups is clinically plausible. In the base-case trial analysis the difference in length of stay is, on average, 0.3 days shorter in the nitrofurazone group than in the PTFE group. If the only determinant of differences in length of stay was whether or not an infection was suffered then this would equate to each infection avoided, resulting in 15 fewer days in hospital, a clearly implausible result. It is possible that there are other mechanisms by which the use of different catheters might influence length of stay, such as the bright colour of the nitrofurazone device and its association with more discomfort in use but the study team made a judgement that such differences were unlikely to be having such a sizeable effect and hence any results of an economic evaluation based on such data would also be unsound.
Model-based analysis
As an alternative to a within-trial analysis, a model-based analysis was also planned primarily to focus more closely on the costs and QALY differences between those who suffered an infection and those who did not. The model assumed that differences in costs and QALYs between randomised groups were solely a consequence of potential differences in the incidence of UTI. The base-case analysis did not account for unobserved heterogeneity in uncontrolled characteristics between those who suffered an infection and those who did not. The implication of this is that the analysis may be confounded by the scenario that those participants who suffered an infection were more likely to (1) suffer an infection because of underlying ill health; (2) incur extra costs not only because they have an infection but also because of the increased severity of their underlying condition; and (3) lose QoL again not just because they have an infection but because of the increased severity of their underlying condition. In order to explore these possibilities, a number of sensitivity analyses were performed, considering comparisons between those who had a UTI and those who did not in a number of subgroups that were hypothesised post hoc to be more homogeneous than the whole trial population.
For the model-based analysis, the mean health-care cost differences between the different trial groups were considerably less than the mean cost differences estimated in the within-trial analysis, although the direction of the differences was unaltered. This was primarily because the costs in the model were determined by the modest differences in infection rates and the difference in costs between those participants who did or did not suffer a UTI. Again, differences in QALYs were very small and not statistically significant.
The sensitivity analyses were conducted using more homogeneous patient subsets defined post hoc. These included considering only patients admitted to obstetric and gynaecology specialty wards; using infection rates at 3 days after catheter removal; and including only those patients who had an EQ-5D score of ‘1’ at 3 days. For each of these three sensitivity analyses, differences in QALYs were very small, but for two analyses (infection rate at 3 days and EQ-5D = 1) the magnitude of the estimated cost of a UTI was greater than that observed in the analysis based on all participants and hence the cost saving for the nitrofurazone group was greater. For the third sensitivity analysis, both nitrofurazone and silver alloy catheters were, on average, slightly more costly than PTFE and there was a < 25% probability that nitrofurazone would be less costly than PTFE (the probability for silver alloy was approximately 0%). However, given the distributions associated with catheter infections, cost and QALYs there was an approximately 70% chance that nitrofurazone would be the most likely option to be considered cost-effective when the threshold value for society’s willingness to pay for a QALY was £30,000.
As already noted, one of the main components of cost was the inpatient stay. These data were highly skewed to the right, as they are naturally bounded by zero, but they have no logical upper bound and with such a large sample size there was likely to be a number of outliers with long stay and hence high cost. Hospital stay was truncated in line with the duration of trial participation at maximum of 6 weeks. This has the impact of omitting very long stays. A recent review of difficulties faced in handling skewed data concluded that most of the methods identified had undergone limited testing in different situations and their use in practice was very restricted; therefore, no detailed guidance could be provided. 80 The authors outlined three groups of methods, termed orbits, which had been previously used but all related to studies with small sample size. The simple truncation method we applied seems a credible option for the data produced by our trial.
During planning of the trial we elected to measure QoL changes by participant completion of a relevant questionnaire (EQ-5D) at baseline, 3 days after catheter removal, at 1 and 2 weeks after catheter removal, and at 6 weeks after randomisation. The collection of QoL measures at these time points would reflect the global changes incurred by each individual as a consequence of undergoing and recovering from specific health-care interventions. However, the number of different factors influencing each participant’s score makes determining the impact of a particular catheter on the risk of UTI and on QoL difficult to identify. Our sensitivity analyses, using homogeneous participant subsets defined post hoc, suggest that there would be a trend in favour of nitrofurazone because, based on the primary trial outcome, there was a trend towards reduced infections and lower QALYs among those who suffered a UTI. For the subgroup with a UTI 3 days post catheter removal the mean (97.5% CI) loss of QALYs was –0.004 (–0.009 to 0), for those who suffered a UTI but had a EQ-5D score of ‘1’ at 3 days post catheter removal it was –0.002 (–0.012 to 0.007) and for those admitted to obstetrics and gynaecology it was –0.007 (–0.011 to –0.003). It is likely that the pain and discomfort associated with catheter insertion or removal was not captured by the EQ-5D, as the EQ-5D elicits QoL on the day it is completed, potentially missing the impact of preceding events of short duration.
Alternative approaches to capture short but severe effects on QoL would have been to increase the frequency of QoL measurement or to ask respondents to complete QoL measures when events occurred. The practicalities of this in terms of administrative and respondent burden make it unfeasible. Furthermore, even if it were possible to ask those suffering a UTI or discomfort to complete a QoL measure, we would need some form of control to know what the QoL decrement should be compared with those who are not suffering a UTI or discomfort. An alternative approach would be to use some of the stated preference techniques used in economics, such as a time trade-off, standard gamble or contingent valuation method to elicit valuations for the different states of health that might exist. These approaches might value the profile of outcomes expected following the use of each of the different types of catheter or elicit the valuations of the presence or absence of specific events, such as UTI or discomfort of use. Such data could then be used in either a within-trial or a model-based analysis.
Nitrofurazone catheters
In the first section of this chapter we summarised the main findings. 81 Some evidence from our trial for possible modest bacteriological effectiveness of the nitrofurazone catheter is provided by the results using differing definitions of CAUTI reported as secondary outcomes, which show a consistent direction of effect. The rate of symptomatic CAUTI at 3 days following catheter removal, an outcome particularly relevant to the control of health-care-related infection in hospitals, showed a modest trend from 5.9% to 4.9% (p = 0.14). The rate of the more stringent CDC criterion outcome of microbiologically proven symptomatic UTI at 3 days was reduced from 1.3% to 0.7% (p = 0.05) and at 6 weeks from 4.6% to 3.2% (p = 0.02), the latter representing a 30% relative risk reduction. None of these results was changed by adjustment for pre-set confounding factors. The suggestion that, in this trial, the findings related to nitrofurazone-impregnated catheters for secondary bacteriological outcomes have borderline statistical significance would be in line with those reported from the most recent meta-analysis of previous RCTs. 42 The study given most weight in this meta-analysis was that by Stensballe et al. ,82 which is also methodologically closest to the present trial. They used treatment for CAUTI with antibiotics as a secondary outcome, finding a RR of 0.27 (a reduction in incidence from 17.5% to 4.8%) in favour of nitrofurazone catheters among 200 patients admitted with trauma. The difference in our results is likely to reflect a lower risk profile in our sample together with a shorter catheter duration and lower intensity of care.
Our trial was not designed to explain any superiority in clinical effectiveness found for the technology under study and, given the lack of evidence for overall effectiveness of the nitrofurazone catheters, the results of any subgroup analysis should be interpreted with great caution. None of the tests for interaction was significant. It is plausible that participants randomised to use of nitrofurazone-impregnated catheters who had used antibiotics in the 7 days prior to catheterisation would be less likely to benefit in terms of reduction in CAUTI rate compared with those with no previous antibiotic use, and there is some suggestion of this. This might reflect alteration of urogenital flora that protect against UTI. 83 There is also some in vitro data to suggest that nitrofurazone-impregnated catheters inhibit the growth of a wider range of uropathogens and for a longer period compared with silver alloy-coated catheters. 79 This in vitro superiority may not be relevant to day-to-day use for short-term catheterisation and also may be affected by differing release mechanisms for the antimicrobial agents in the two catheter designs.
The nitrofurazone catheters were made from silicone impregnated with the active agent, unlike the latex-based coated construction of the silver alloy and standard catheters. They might therefore be expected to have different physical characteristics that may impact on their use. We did find evidence that participants allocated to nitrofurazone catheters found the presence and removal of the catheter more uncomfortable than the standard group. The cause of these differences are not known but, given that the Cochrane review found that silicone catheters tended to result in fewer urethral side effects than latex catheters, then the material of manufacture is unlikely to be the problem. 42 It is possible that surface changes resulting from the impregnation technique may be at fault or that the catheter was more rigid or had subtle differences in retention balloon or drainage eyelet configuration. We understand that the manufacturer has recently changed the manufacturing process with the aim of greater comfort of use (Rochester Medical, personal communication, 2010).
Evidence from previous studies comparing nitrofurazone catheters with standard silicone controls suggest that it is unlikely that the possible lower rate of CAUTI seen in the nitrofurazone group was due to its latex-free construction rather than the antibiotic content. 42,82 In addition, we found no evidence of unsuspected latex allergy among randomised participants, although we did not collect data concerning the number of participants deemed ineligible because of known or suspected latex allergy.
Previous studies have suggested that the antimicrobial activity of the nitrofurazone coating has reduced effectiveness beyond 7 days of catheterisation. 42 In the present trial, the effect size in terms of reduction in rate of symptomatic UTI in comparison with the control group did reduce by a further statistically non-significant degree among participants catheterised for 4 days or longer, although the study lacked power to specifically address this question with any certainty. Overall we did not find any evidence of interaction between duration of catheterisation and relative clinical effectiveness in terms of reduction in UTI risk.
Although our model-based health economic analysis suggested that nitrofurazone-impregnated catheters may be cost-effective, the principal driver of these results was that, based on the balance of data, the cost savings from avoiding an infection would compensate for the increased unit cost of the nitrofurazone catheter compared with PTFE. The 97.5% CI for cost savings per patient includes £0 but even at the upper end are relatively modest (mean difference –£7.07; 97.5% CI –£36.19 to £11.45). Nevertheless, given the volume of catheterisation within the NHS, even this small difference may lead to substantial savings overall. This finding should be treated cautiously given the limitations of the analysis and the considerable uncertainty particularly regarding estimates of key parameters, such as length of stay.
Silver alloy catheters
Following the positive findings of recent meta-analyses of the results of previous trials and the success of ‘fast-track’ implementation to the UK NHS in ‘Showcase Hospitals’ under the UK government’s Healthcare Associated Infections (HCAI) Technology Innovation Programme,52 silver alloy-coated catheters have already been adopted by some NHS organisations as the preferred catheter for routine, short-term use. This was supported by uncontrolled audit data from the UK and USA suggesting benefit in terms of reduction in health-care-associated infections,63,84 although other such studies have found no beneficial effect over standard catheters. 85 Current guidance documents from the USA and the UK still consider that although there is low-quality evidence in favour of the use of silver alloy antimicrobial catheters, more evidence of benefit, in particular in combating symptomatic UTI, is needed. 29,38,86 It is therefore crucial that the findings of the present pragmatic trial, which failed to provide evidence that this technology would reduce CAUTI, are considered in the context of previous more explanatory trials that did find benefit.
As discussed at the start of this chapter, CIs for the present trial results were wide enough to include what some people would consider clinically important reductions in CAUTI {absolute risk reduction [mean (97.5% CI)] for silver compared with standard –0.1% (–2.4 to 2.2)}, but not to the extent considered important in the design of this trial. It is worth noting that this trial population was recruited from a range of different clinical areas and across multiple NHS hospital sites. This heterogeneity in population provides generalisability of our findings. Furthermore, the OR for the primary outcome and secondary outcomes using alternative definitions for CAUTI was consistently close to 1. We were also unable to identify, on post hoc analysis, a subgroup where use of silver alloy catheters resulted in a reduction in CAUTI compared with standard PTFE catheters. The recently updated meta-analysis42 found that silver alloy catheters resulted in a relative risk reduction for the outcome of bacteriuria (asymptomatic and symptomatic) of between 0.54 and 0.64 dependent on catheter duration. By far the largest study for this review with an associated high weighting was that by Maki et al. ,87 which was published only in abstract form and showed a risk ratio of 0.74 (95% CI 0.56 to 0.99). The other smaller included studies did, however, have the same direction of effect. There are few published details of the Maki et al. 87 study, although it does appear to have used microbiological bacteriuria found by multiple sampling during the period of catheterisation as the primary outcome rather than symptomatic UTI occurring during, or for a specified period after, catheterisation. From our trial design we are unable to comment whether or not bacteriuria rates during catheterisation were reduced in participants allocated to the silver alloy groups. Urine samples were purposefully only sampled at or within 3 days following catheter removal, when both bacteriuria and microbiologically proven CAUTI rates in the silver alloy group were similar to control group. What we can say is that if such a difference existed it did not translate to a definite reduction in the rate of symptomatic UTI either at 3 days or at 6 weeks. Although asymptomatic to the host, bacteria can be implicated in cross-infection in the clinical area. We did not collect any data concerning this possibility but for most surgical units with predominantly short stay and short catheter duration it may not be a major problem.
The study by Maki et al. 87 also found no apparent correlation between bacteriuria with either symptoms or antibiotic use; indeed a further published report using the same patient sample reported no relationship between documented bacteriuria and symptomatic UTI. 10 The Maki et al. trial87 therefore used an explanatory trial design that may not have necessarily been appropriate to capture information regarding relative clinical effectiveness and cost-effectiveness. The other large trial finding fewer cases of UTI in the silver alloy catheter group was that by Karchmer et al. 62 This had a very different design being a cluster randomised trial involving clinical areas and included a crossover to the alternative intervention, the analysis of which prevented inclusion in the Cochrane meta-analysis. The trial objective appeared pragmatic but the differing trial design makes comparison with our findings difficult. In this trial, although clinical areas using silver alloy catheters experienced lower rates of CAUTI than areas using standard catheters, the actual number of patients catheterised – and of those, the number suffering UTI – was not stated. It appears from the report that the absolute rate of CAUTI among patients in the participating clinical areas was low with a difference of 3.1% compared with 2.1% in favour of silver alloy-coated catheters. Our more straightforward randomisation of individual participants led to a much lower contamination of trial arms and more explicit balancing of baseline characteristics to limit confounding. The trial by Karchmer et al. 62 also included critical care areas for which the incidence was higher but no reduction in CAUTI was seen on subgroup analysis.
Other systematic reviews23,58 attempted to account for the apparent disparity in effect estimates between different trials of silver alloy catheters by stratifying studies into those published pre 1995 and those published post 1995. This categorisation revealed that studies prior to 1995 resulted in median relative risk reductions of bacteriuria of 56–76% (absolute risk reduction 13–32%), whereas those from after 1995 found lower relative risk reductions of 6–47% with a median of 16% (absolute risk reduction 0.5–6%). One review noted that the older studies tended to be methodologically weaker and suggested that the earlier higher estimates of significant efficacy may have been unreliable. Our study finding no evidence of a benefit does fit with this trend of decreasing beneficial effect size for the use of silver alloy catheters in later studies that seem likely to have been methodologically more robust. Lack of agreement between a large, robustly designed, pragmatic trial and smaller initial explanatory trials has been observed previously where an initially promising intervention has subsequently been found to lack clinical effectiveness and cost-effectiveness. 88 Indeed, up to one-third of meta-analyses purporting successful therapy are later discredited after a large-scale, well-done RCT is completed. 88
Our economic model predicted that silver alloy-coated catheters were highly unlikely to be considered cost-effective for the UK NHS. The main driver for this was that it was unlikely that any reduction in cost consequent on the observed reduction in risk of CAUTI would compensate for the higher unit cost of the catheter. Furthermore, any gain in QALYs consequent on the observed reduction in CAUTI rate was unlikely to be large enough to justify any increased expenditure. Reflecting this, the estimated mean (97.5% CI) net additional NHS cost of silver alloy catheters per patient compared with PTFE was £5.00 (£4.13 to £5.92), which is about £1 less than the current price of a silver alloy-coated catheter currently charged to the NHS. This is an important conclusion given that some NHS organisations have deployed this catheter for routine use. The conclusion is grounded in a trial encompassing a large representative sample of the NHS patient population that would be expected to receive the silver alloy catheter if routinely used. The population studied was also consistent with that targeted in the commissioning outline for the trial which reflected the information needs of the NHS.
Implications for clinical practice and the NHS
Health-care policy initiatives in both the UK and US seek to reduce health-care-associated infection in general, and catheter-associated in particular, by providing support for health-care providers to follow best practice, by monitoring the incidence of health-care-associated infection and, in the future, by introducing financial penalties for event occurrence. 89,90 Current strategies include primary prevention by reducing use and duration of catheterisation, secondary prevention by correct catheter care, and tertiary prevention by antimicrobial use. 38,48 The use of catheters that incorporate antimicrobial agents potentially fulfils the last objective but requires development and successful testing of appropriate technology. Clinicians and health-care organisations will therefore be attentive to the findings of this trial, particularly as the volume of catheter usage remains high at 2.1 million people (14.5%12 of the 14.5 million people admitted to hospitals in the NHS in England during 2010)91 and the numbers suffering CAUTI are substantial – approximately 49,000 in Scotland in 2004 (Scottish CAUTI report14) and 562,000 in the USA in 2002. 92
Antiseptics such as silver are attractive as the preventive antimicrobial component because they are not generally associated with bacterial ecological changes such as resistance patterns that may result in community harm. 63 This trial was designed to fill the evidence gap identified by a number of literature reviews concerning the clinical effectiveness of the currently available silver alloy-coated catheter. Unfortunately, the findings provide no evidence that this catheter gives any benefit to patients or the NHS for general short-term use over the standard option. Individual clinicians and NHS organisations will need to consider this lack of evidence of benefit and the substantial current cost difference (£7.45 vs £0.91 in 2011 NHS prices4) in deciding whether to invest or disinvest in this technology.
As summarised at the start of this chapter, the results for nitrofurazone catheters are more difficult to interpret. Most importantly, we found no evidence that these catheters achieved our defined minimum clinically important level of effectiveness. The secondary results do suggest a modest bacteriological effect, which was statistically significant. The economic analysis suggests that this more modest reduction in UTIs could be cost-effective but with considerable uncertainty around the model parameter estimates. The health economic analysis suggested that, although any improvement in QoL as measured by QALYs is likely to be very modest at best and was not significant at the 97.5% level, the use of nitrofurazone catheters is likely to reduce net NHS costs (97.5% CI), based on model-based analysis with a reduction of £7.07 (–£36.19 to £11.45). Caution is required in interpreting the estimates of cost differences obtained from the model, as, despite the attempts to consider more homogeneous groups, the patient population within the trial were heterogeneous and differences in infection rates, costs and QALYs may be influenced by subtle but unknown imbalance between groups. These provisos to our conclusions should result in a cautious approach towards consideration of any policy change by clinicians or NHS organisations. Other more generic factors also encourage a cautious approach. Indiscriminate use of antimicrobials, particularly in hospitals, is actively discouraged because of higher risk of phenotypic changes to both infecting and commensal bacteria, resulting in increased virulence and widening of antimicrobial resistance. 93 It remains unclear whether or not this would be a problem if nitrofurazone-containing catheters were more widely used, this not being a chosen outcome to be explored in the present trial. The evidence we do have, predominantly for the closely related agent, nitrofurantoin, is somewhat reassuring, as surveillance studies show a very low and stable resistant pattern amongst urinary pathogens. 55 The slight, but statistically significant, increase in catheter discomfort during and immediately after catheterisation may also influence views of change in practice to their wider use. It is unclear whether these observed differences are related to nitrofurazone release or the catheter material itself. It may also be the case that patients would be willing to trade off a minor degree of increased discomfort during catheterisation against a lower risk of UTI.
In summary, the lack of evidence found in this trial supportive of use of silver alloy catheters for short-term catheterisation at their current unit price will influence decisions regarding their continued use for this indication. Decisions regarding nitrofurazone catheters are more complex. At present, they appear little used in the NHS and this may be due to a number of factors including limited evidence, cost (£3.63, 2011 NHS price4), appearance, concerns regarding indiscriminate antibiotic use and commercial marketing. Clinicians and managers will have to weigh up the lack of improvement in rates of CAUTI shown in the present trial together with these wider considerations to plan any change in practice.
Catheter-associated urinary tract infection (CAUTI) remains a problem for the NHS, although the results from the present trial are somewhat reassuring that life-threatening consequences are very uncommon. There is morbidity, however, which is associated with moderate but significantly increased cost to the patient and to the NHS through requirement for antibiotic and further, potentially avoidable, use of primary and secondary care services.
Implications for research
This trial has provided evidence that silver alloy-coated catheters are not likely to be cost-effective for general short-term use in hospitals but a number of questions remain and there are concerns that chance imbalance in subtle confounders may have introduced bias against demonstrating potential benefit of the use of silver alloy. There has been much investment in the study of silver as an antimicrobial agent with both in vitro experiments and early clinical trials providing evidence for its bacteriological effectiveness when used as an adjunct to a number of invasive devices such as wound dressings, central venous lines and urinary catheters. The extent of the antimicrobial activity, however, does not seem so far to have been translated to pragmatic benefit when more clinically based outcome measures are used. 94 The reasons for these conflicting results remain uncertain. The difference in methodology between smaller explanatory trials and larger pragmatic trials embedded in day-to-day clinical practice is likely to be one reason for the marked reduction in estimates of effect. Other reasons could be insufficient activity or release of the active silver agent and technological design issues concerning the coating or embedding of the agent in the carrier device. One solution being explored is the use of silver nanoparticles as an alternative drug delivery mechanism. There is no doubt that antiseptics have a number of advantages over antibiotics for this use and it is interesting that other well-established agents such as triclosan, and emerging agents such as elemental carbon and copper, are under investigation. In summary, research priorities regarding silver alloy catheters are to (1) establish why they are not effective from a clinical rather than microbiologically point of view and (2) identify newer agents or delivery systems/materials that increase clinical effectiveness.
The uptake of antimicrobial-containing devices is necessarily cautious given the higher risks of individual sensitivity and encouragement of increased bacterial virulence. Nitrofurazone is commonly chosen as an agent because of its wide spectrum of activity and low rates of resistance. The widespread use of impregnated catheters in the NHS would raise substantial concerns regarding possible detrimental long-term effects related to changes in the virulence and resistance patterns of organisms found in hospitals and in the community. Further research may be beneficial to demonstrate whether or not these concerns are likely to be realised. The other main issue raised by this trial is the higher rates of discomfort seen with the nitrofurazone catheters. Further work to (1) identify the cause and (2) determine whether or not it could be engineered out by further device development may be warranted. We understand that the manufacturer of the nitrofurazone catheters used in our study has made progress on this issue and the current nitrofurazone-impregnated catheter available to the NHS is considered to have less risk of discomfort than that used for the trial (Rochester Medical, personal communication). It may also be important to determine the impact of any discomfort for an individual’s overall experience during an episode in hospital. It may be that patients would be happy to accept a mild degree of increased discomfort in return for a smaller risk reduction for CAUTI than that sought in our trial. These aspects could be explored in QoL studies among recipients and potential recipients of the different types of catheter.
Chapter 8 Recommendations and further research
Implications for the NHS and patients
Catheter-associated urinary tract infection remains an important cause of health-care-related morbidity worldwide and therefore a target for development of effective preventative strategies. This trial examined the clinical effectiveness and cost-effectiveness of the short-term use of two widely available antimicrobial catheters and found that neither reached our prestated levels of clinical or statistical significance. Our health economics model predicted that the silver alloy-coated catheter tested was unlikely to be cost-effective for use in the NHS at its unit price. Although the results of the economic analysis for the nitrofurazone-impregnated catheter were more favourable there was a high degree of uncertainty. For NHS organisations in which these interventions are already in use there may be an opportunity to reallocate resources without loss of benefit, whereas those organisations considering implementation may wish to await further evidence of benefit or the emergence of alternatives.
At present it seems appropriate for patients, clinicians and the NHS to persist with simple strategies to prevent CAUTI, such as avoidance of catheter use, aseptic catheter insertion and limitation of duration of catheterisation, as emphasised in recent guidance documents.
Unanswered questions and further research
Minimum clinically important difference
It remains difficult for researchers and trial designers to determine the necessary level of clinical effectiveness required as a basis for decisions about policy and practice. Standardisation of methods of setting the prestated minimum clinically important difference is required.
Core outcomes
In common with many areas of research, there is a lack of consensus of what outcome measures should be used, which leads to difficulty in systematically summarising results of different trials and in performing statistical meta-analysis. We suggest that definition of a core outcome set for trials of interventions for UTI would be beneficial and the COMET initiative95 would be useful in planning such research.
Valuation of benefit
Assessment of both the costs and consequences in terms of health-related QoL of interventions, such as urethral catheterisation, which are a subsidiary part of the care of people undergoing a more major intervention, such as elective surgery, is problematic. Accurate but feasible methods of capturing any changes in well-being specific to the subsidiary intervention and the costs associated purely with the benefits and harms of the subsidiary intervention are required.
Further exploration of antimicrobial devices
The concept of antimicrobial catheters as a device to reduce risk of CAUTI remains attractive but exploration of different antimicrobial agents and methods of retention in materials used for catheter manufacture is required.
Alternatives to a very short duration catheterisation
Many participants in our trial had catheter duration of less than 2 days but remained at high risk of suffering CAUTI. Alternatives to very short periods of indwelling catheterisation should be sought.
Other interventions to reduce catheter-associated urinary tract infection
Much progress has been made in providing training and monitoring of techniques of catheter insertion and catheter care. More recently, monitoring of CAUTI has been mandated for Medicare providers in the USA and included as a voluntary option for NHS provider organisations. One less researched possibility is to reduce catheter duration. Current guidance suggests that duration of < 24 hours should be the norm (USA) or that duration should be minimised (UK). Catheter duration is often part of entrenched care pathways and altering these requires behavioural change. Research to establish mechanisms to drive behavioural change and empower patients would be useful to find out whether or not ‘bottom-up’ approaches are more effective than ‘top-down’ initiatives such as guidelines and policy documents.
Alternative uses of antimicrobial catheters
There is no evidence concerning the effectiveness of antimicrobial catheter devices for longer-term catheterisation, intermittent catheterisation or suprapubic catheterisation. Further early-phase evidence of efficacy is first required.
Acknowledgements
Thanks
We thank the NIHR HTA for funding the CATHETER trial. We also thank the staff of the NIHR HTA for their helpful administrative support. We express special thanks to all of the CATHETER trial participants and staff at each of our recruiting centres for taking part in this trial.
The CATHETER trial would not have been possible without the dedication of the CATHETER trial study office staff (Kath Starr, Karen McIntosh, Anne Duncan and Christiane Pflanz-Sinclair) based in the CHaRT within the Health Services Research Unit, University of Aberdeen. The trial received invaluable statistical support from Charles Boachie and Graeme MacLennan, and invaluable economics input from Mary Kilonzo and Luke Vale. Gladys McPherson and her team provided excellent IT and database support, and Alison McDonald was always available to support the trial manager.
We also thank the independent members of the Trial Steering Committee [Professor Mike Bishop (Chairperson), Professor Suzanne Hagen and Professor Peter Davey] and the Data Monitoring Committee [Professor Lelia Duley (Chairperson), Dr Steff Lewis, Mr Marcus Drake and Mr Kurt Naber], whose voluntary support and advice were essential to the success of the CATHETER trial.
Sincere thanks are due to the staff of the North of Scotland Research Ethics Committee for dealing with our substantive amendments during the course of the trial. The CATHETER study team acknowledges the support of the NIHR, through the Comprehensive Local Research Networks and the Primary Care Research Network.
We acknowledge, with thanks, Bayer Healthcare Pharmaceuticals (West Haven, CT, USA) for giving us permission to use their UTI Symptom Assessment Questionnaire.
In addition, we are grateful to Katie Gillies, the first CATHETER trial manager; John Norrie, the Director of ChaRT; Jennifer Burr, ex-Director of CHaRT; and the staff of the Health Services Research Unit, University of Aberdeen.
Special thanks are extended to Adrian Grant, who was Director of the Health Services Research Unit when the CATHETER trial was mounted, and, since stepping down as Director, has maintained the same level of intellectual input and enthusiasm to the successful completion of the trial.
Contribution of authors
Professor James N’Dow (Professor of Urology) was the Chief Investigator of the study; he had complete involvement and oversight of the study design, execution and data collection, and was responsible for the final report.
Professor Robert Pickard (Professor of Urology) contributed his clinical expertise to the design of the study, interpretation of the trial findings and to the final report writing.
Mr Thomas Lam (Senior Clinical Lecturer in Urology) contributed his clinical expertise to the design of the study, day-to-day clinical support of the trial and the final report writing.
Mr Graeme MacLennan (Senior Statistician) contributed to the statistical analysis of the study, and writing of the results and discussion chapters.
Ms Kath Starr (Trial Manager) was responsible for the day-to-day management of the study and also contributed to the final report writing.
Ms Mary Kilonzo (Research Fellow, Health Economics) contributed to the analysis of the health economics component of the study and also to the writing of the health economics chapters.
Mrs Gladys McPherson (Senior IT Manager) designed the programming of the study database, data analysis and writing of the final report.
Dr Katie Gillies (previous CATHETER trial manager) was responsible for the establishment of the trial, the initial day-to-day management of the study and also contributed to the final report writing.
Mrs Alison McDonald (Senior Trial Manager) contributed to the design of the study, provided support to the trial staff and contributed to the writing of the final report.
Dr Kathy Walton (Consultant Microbiologist) contributed to the design of the study, provided day-to-day microbiological support as necessary and contributed to the writing of the final report.
Dr Brian Buckley (Chairperson, Bladder and Bowel Foundation) contributed to the consumer aspect of the study and writing of the final report.
Professor Cathryn Glazener (Professor of Health Services Research) contributed to the design of the study and the writing of the final report.
Mr Charles Boachie (Statistician) contributed to the statistical analysis of the study.
Dr Jennifer Burr (ex-Director of CHaRT) contributed to the delivery of the trial and the writing up of the final report.
Professor John Norrie (Director of CHaRT), contributed to the design of the study and contributed to the writing of the final report.
Professor Luke Vale (Professor of Health Economics) contributed to the writing of the health economics chapters and the interpretation of the health economics findings.
Professor Adrian Grant (Trialist) contributed to the overall study design and gave expert guidance on the final report writing.
Trial Steering Committee
Professor Michael Bishop (Chairperson), Professor Suzanne Hagen and Professor Peter Davey.
Data Monitoring Committee
Professor Lelia Duley (Chairperson), Dr Steff Lewis, Mr Marcus Drake and Mr Kurt Naber.
Project Management Group
James N’Dow, Adrian Grant, Thomas Lam, John Norrie, Graeme MacLennan, Luke Vale, Mary Kilonzo, Cathryn Glazener, Robert Pickard, Kathy Walton, Kathryn Getliffe, Brian Buckley, Jennifer Burr, Alison McDonald, Gladys McPherson, Katie Gillies and Kath Starr.
Principal investigators
James N’Dow, Steven Bramwell, Raj Persad, Ed Babu, Robert Pickard, Prasad Bollina, Roland Koerner, Mandy Fader, Ruaridh MacDonagh, Jonathon Olsburgh, Augustine Tang, Sanjeev Prashar, Richard Parkinson, Arpit Patel, Mohammad Khawaja, Stuart Irving, Rob Mason, Karen Ward, Simon Hill, Adrian Barnett and Anoop Chauhan.
Research nurses/fellows
Minimol Paulose, Gladys Makuta, Kathleen Macleod, Katrina Hurley, Mariam Nasseri, Rashmi Bhardwaj, Jean Antonelli, Sam Donaldson, Lynne Palmer, Amy King, Philandra Costello, Lesley Naik, Hannah Routley, Faith McMeekin, Christine Brewer, Golda-Grace Azanu, Charlotte Bramhall, Jane Brooks, Judith Saba, Jackie Purcell, Rosario Hannigan, Pete Johnson, Amanda Banks, Helen Bowyer, Barbara Williams-Yesson, Clare Buckley, Jenny Jagger, Melissa Cambell-Kelly, Tracy Ord, Andrew Hall, Pauline Mercer, Lesley Harris, Margaret Brunton, Gerry Geraghty, Allan Fairclough, Rachel Worton, Lynn Watkins and Francis Williams.
NHS trusts and health boards
NHS Grampian, NHS Highland, University Hospitals Bristol NHS Trust, Hillingdon Hospitals NHS Trust, Newcastle upon Tyne Hospitals NHS Foundation Trust, NHS Lothian, City Hospitals Sunderland NHS Foundation Trust, Southampton University Hospitals NHS Trust, Northumbria Healthcare NHS Trust, Taunton and Somerset NHS Foundation Trust, Guy’s and St Thomas’ NHS Foundation Trust, Blackpool, Fylde and Wyre Hospitals NHS Foundation Trust, Lancashire Teaching Hospitals NHS Foundation Trust, Nottingham University Hospitals NHS Trust, Hinchingbrooke Health Centre NHS Trust, Yeovil District Hospital NHS Foundation Trust, Norfolk and Norwich University Hospitals NHS Foundation Trust, South Devon Healthcare NHS Foundation Trust, Liverpool Women’s Hospital NHS Foundation Trust, Lancashire Care NHS Foundation Trust, Harrogate and District NHS Foundation Trust, and Portsmouth Hospitals NHS Trust.
Publication
Pickard R, Lam T, MacLennan G, Starr K, Kilonzo M, McPherson G, et al. Antimicrobial catheters for reduction of symptomatic urinary tract infection in adults requiring short-term catheterisation in hospital: a multicentre randomised controlled trial [published online ahead of print 5 November, 2012]. Lancet 2012. URL: www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)61380-4/fulltext.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Foley FE. A haemostatic bag catheter: one piece latex rubber structure for control of bleeding and constant drainage following prostatic resection. J Urol 1937;38:134-9.
- Thomsen TW, Setnik GS. Videos in clinical medicine. Male urethral catheterization. N Engl J Med 2006;354.
- Lawrence EL, Turner IG. Materials for urinary catheters: a review of their history and development in the UK. Med Eng Phys 2005;27:443-53.
- NHS . NHS Cat Product Categories 2011. my.supplychain.nhs.uk/catalogue (accessed August 2011).
- Saint S, Veenstra DL, Sullivan SD, Chenoweth C, Fendrick AM. The potential clinical and economic benefits of silver alloy urinary catheters in preventing urinary tract infection. Arch Intern Med 2000;160:2670-5.
- Haley RW, Hooton TM, Culver DH, Stanley RC, Emori TG, Hardison CD, et al. Nosocomial infections in US hospitals, 1975–1976: estimated frequency by selected characteristics of patients. Am J Med 1981;70:947-59.
- Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol 2010;31:319-26.
- Weinstein JW, Mazon D, Pantelick E, Reagan-Cirincione P, Dembry LM, Hierholzer WJ. A decade of prevalence surveys in a tertiary-care center: trends in nosocomial infection rates, device utilization, and patient acuity. Infect Control Hosp Epidemiol 1999;20:543-8.
- Glynn A, Ward V, Wilson J. Socio-economic burden of healthcare associated infection. London: PHLS; 1997.
- Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med 2000;160:678-82.
- Wald HL, Ma A, Bratzler DW, Kramer AM. Indwelling urinary catheter use in the postoperative period: analysis of the national surgical infection prevention project data. Arch Surg 2008;143:551-7.
- Bhardwaj R, Pickard R, Rees J. Documented adherence to standards and guidelines: an audit. Br J Nurs 2010;19:S26-30.
- Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. Infection Control and Applied Epidemiology: Principles and Practice. Association for Professionals in Infection Control and Epidemiology. St Louis, MO: Mosby; 1996.
- Scottish Surveillance of Healthcare Associated Infection Programme . Surveillance of Catheter Associated Urinary Tract Infections: Annual Report. 2005. www.documents.hps.scot.nhs.uk/hai/sshaip/publications/cauti/cauti-annual-report-2005–06.pdf (accessed July 2011).
- Horan TC, Gaynes RP, Mayhall CG. Hospital epidemiology and infection control. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.
- Centers for Disease Control and Prevention (CDC) . Catheter-Associated Urinary Tract Infection (CAUTI) Event 2011. www.cdc.gov/nhsn/PDFs/pscManual/7pscCAUTIcurrent.pdf (accessed August 2011).
- Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control 1981;2:380-6.
- Garibaldi RA, Mooney BR, Epstein BJ, Britt MR. An evaluation of daily bacteriologic monitoring to identify preventable episodes of catheter-associated urinary tract infection. Infect Control 1982;3:466-70.
- Krieger JN, Kaiser DL, Wenzel RP. Urinary tract etiology of bloodstream infections in hospitalized patients. J Infect Dis 1983;148:57-62.
- Bryan CS, Reynolds KL. Hospital-acquired bacteremic urinary tract infection: epidemiology and outcome. J Urol 1984;132:494-8.
- Plowman R, Graves N, Griffin M, Roberts JA, Swan AV, Cookson BD, et al. The socioeconomic burden of hospital acquired infection. London: Pubic Health Laboratory Service; 1999.
- Tambyah PA, Knasinski V, Maki DG. The direct costs of nosocomial catheter-associated urinary tract infection in the era of managed care. Infect Control Hosp Epidemiol 2002;23:27-31.
- Johnson JR, Kuskowski MA, Wilt TJ. Systematic review: antimicrobial urinary catheters to prevent catheter-associated urinary tract infection in hospitalized patients. Ann Intern Med 2006;144:116-26.
- Haley RW, Culver DH, White JW, Morgan WM, Emori TG. The nationwide nosocomial infection rate. A new need for vital statistics. Am J Epidemiol 1985;121:159-67.
- Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ET. The Second National Prevalence Survey of infection in hospitals – overview of the results. J Hosp Infect 1996;32:175-90.
- Smyth ET, McIlvenny G, Enstone JE, Emmerson AM, Humphreys H, Fitzpatrick F, et al. Four country healthcare associated infection prevalence survey 2006: overview of the results. J Hosp Infect 2008;69:230-48.
- Turck M, Stamm W. Nosocomial infection of the urinary tract. Am J Med 1981;70:651-4.
- High Impact Actions: Protection from Infection. Coventry: NHS Institute for Innovation and Improvement; 2011.
- Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, et al. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2007;65:1-64.
- Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis 2001;7:342-7.
- Rubino SM, Scialabba MA. A clinical evaluation of a modified Foley catheter. Am J Obstet Gynecol 1983;146:103-4.
- Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol 1987;25:2216-17.
- Daifuku R, Stamm WE. Bacterial adherence to bladder uroepithelial cells in catheter-associated urinary tract infection. N Engl J Med 1986;314:1208-13.
- Schaeffer AJ, Rajan N, Cao Q, Anderson BE, Pruden DL, Sensibar J, et al. Host pathogenesis in urinary tract infections. Int J Antimicrob Agents 2001;17:245-51.
- Lo E, Nicolle L, Classen D, Arias KM, Podgorny K, Anderson DJ, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol 2008;29:41-50.
- Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 2002;15:167-93.
- Stickler DJ, Jones GL, Russell AD. Control of encrustation and blockage of Foley catheters. Lancet 2003;361:1435-7.
- Guideline for Prevention of Catheter-Associated Urinary Tract Infections. Atlanta, GA: CDA; 2009.
- Tambyah PA, Maki DG. The relationship between pyuria and infection in patients with indwelling urinary catheters: a prospective study of 761 patients. Arch Intern Med 2000;160:673-7.
- Shuman EK, Chenoweth CE. Recognition and prevention of healthcare-associated urinary tract infections in the intensive care unit. Crit Care Med 2010;38:S373-9.
- Brosnahan J, Jull A, Tracy C. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database Syst Rev 2004;1.
- Schumm K, Lam TB. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database Syst Rev 2008;2.
- Willson M, Wilde M, Webb ML, Thompson D, Parker D, Harwood J, et al. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: part 2: staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs 2009;36:137-54.
- Parker D, Callan L, Harwood J, Thompson DL, Wilde M, Gray M. Nursing interventions to reduce the risk of catheter-associated urinary tract infection. Part 1: Catheter selection. J Wound Ostomy Continence Nurs 2009;36:23-34.
- National Institute for Health and Clinical Excellence (NICE) . CG2: Infection Control: Prevention of Healthcare-Associated Infections in Primary and Community Care 2003. www.nice.org.uk/nicemedia/live/10922/29117/29117.pdf (accessed July 2011).
- Royal College of Nursing . Catheter Care: RCN Guidance for Nurses 2008. www.rcn.org.uk/__data/assets/pdf_file/0018/157410/003237.pdf (accessed July 2011).
- Department of Health (DoH) . Essential Steps to Safe, Clean Care: Reducing Healthcare-Associated Infections in Primary Care Trusts; Mental Health Trusts; Learning Disability Organisations; Independent Healthcare; Care Homes; Hospices; GP Practices and Ambulance Services. Urinary Catheter Care 2007. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4136277.pdf (accessed July 2011).
- Best Practice Statement: urinary catheterisation and catheter care. Edinburgh: NHS Quality Improvement Scotland; 2004.
- Franken A, van den Bosch EEM, Crespo-Biel O, Loontjens JA, Dias AA. Anti-microbial coatings for urological applications. Eur Cell Mater 2007;14.
- Gosheger G, Hardes J, Ahrens H, Streitburger A, Buerger H, Erren M, et al. Silver-coated megaendoprostheses in a rabbit model – an analysis of the infection rate and toxicological side effects. Biomaterials 2004;25:5547-56.
- Percival SL, Bowler PG, Russell D. Bacterial resistance to silver in wound care. J Hosp Infect 2005;60:1-7.
- HCAI Technology Innovation Programme . Showcase Hospitals Report Number 1: Bardex I.C. Silver Alloy and Hydrogel-Coated Catheter 2009. hcai.dh.gov.uk/files/2011/03/090616_HCAI_Technology_Innovation_Programme_Showcase_Hospitals_Report_1_Bardex_IC.pdf (accessed July 2011).
- Jacobsen SM, Stickler DJ, Mobley HL, Shirtliff ME. Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin Microbiol Rev 2008;21:26-59.
- Darouiche RO, Smith JA, Hanna H, Dhabuwala CB, Steiner MS, Babaian RJ, et al. Efficacy of antimicrobial-impregnated bladder catheters in reducing catheter-associated bacteriuria: a prospective, randomized, multicenter clinical trial. Urology 1999;54:976-81.
- Guay DR. An update on the role of nitrofurans in the management of urinary tract infections. Drugs 2001;61:353-64.
- Saint S, Elmore JG, Sullivan SD, Emerson SS, Koepsell TD. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infection: a meta-analysis. Am J Med 1998;105:236-41.
- Dunn S, Pretty L, Reid H. Management of short term indwelling urethral catheters to prevent urinary tract infections. Best Practice 2000;4:1-6.
- Drekonja DM, Kuskowski MA, Wilt TJ, Johnson JR. Antimicrobial urinary catheters: a systematic review. Exp Rev Med Dev 2008;5:495-506.
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7.
- Bologna RA, Tu LM, Polansky M, Fraimow HD, Gordon DA, Whitmore KE. Hydrogel/silver ion-coated urinary catheter reduces nosocomial urinary tract infection rates in intensive care unit patients: a multicenter study. Urology 1999;54:982-7.
- Plowman R, Graves N, Esquivel J, Roberts JA. An economic model to assess the cost and benefits of the routine use of silver alloy coated urinary catheters to reduce the risk of urinary tract infections in catheterized patients. J Hosp Infect 2001;48:33-42.
- Karchmer TB, Giannetta ET, Muto CA, Strain BA, Farr BM. A randomized crossover study of silver-coated urinary catheters in hospitalized patients. Arch Intern Med 2000;160:3294-8.
- Rupp ME, Fitzgerald T, Marion N, Helget V, Puumala S, Anderson JR, et al. Effect of silver-coated urinary catheters: efficacy, cost-effectiveness, and antimicrobial resistance. Am J Infect Control 2004;32:445-50.
- Lai KK, Fontecchio SA. Use of silver-hydrogel urinary catheters on the incidence of catheter-associated urinary tract infections in hospitalized patients. Am J Infect Control 2002;30:221-5.
- Halton KA, Cook DA, Whitby M, Paterson DL, Graves N. Cost effectiveness of antimicrobial catheters in the intensive care unit: Addressing uncertainty in the decision. Crit Care 2009;13.
- Scott BM. Clinical and cost effectiveness of urethral catheterisation: a review. J Perioperat Pract 2010;20:235-40.
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control 2000;28:68-75.
- Carr HA. A short history of the Foley catheter: from handmade instrument to infection-prevention device. J Endourol 2000;14:5-8.
- Clayson D, Wild D, Doll H, Keating K, Gondek K. Validation of a patient-administered questionnaire to measure the severity and bothersomeness of lower urinary tract symptoms in uncomplicated urinary tract infection (UTI): The UTI Symptom Assessment questionnaire. BJU Int 2005;96:350-9.
- Long JS. Regression models for categorical dependent variables using Stata. College Station, TX: Stata Press; 2003.
- Information and Statistics Division (ISD) . Scottish Health Service Costs 2008. 2009. www.isdscotlandarchive.scot.nhs.uk/isd/797.html (accessed March 2011).
- The EuroQol Group . EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208.
- Kind P, Hardman G, Macran S. UK population norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40.
- National Institute for Health and Clinical Excellence (NICE) . Guide to the Methods of Technology Appraisal. 2008. www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf (accessed February 2011).
- Department of Health (DoH) . NHS Reference Costs 2009–2010 2011. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_123459 (accessed July 2011).
- Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340.
- Saint S, Lipsky BA. Preventing catheter-related bacteriuria: should we? Can we? How?. Arch Intern Med 1999;159:800-8.
- Johnson JR, Delavari P, Azar M. Activities of a nitrofurazone-containing urinary catheter and a silver hydrogel catheter against multidrug-resistant bacteria characteristic of catheter-associated urinary tract infection. Antimicrob Agents Chemother 1999;43:2990-5.
- Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ 2011;20:897-916.
- Hackshaw A, Kirkwood A. Interpreting and reporting clinical trials with results of borderline significance. BMJ 2011;343.
- Stensballe J, Tvede M, Looms D, Lippert FK, Dahl B, Tonnesen E, et al. Infection risk with nitrofurazone-impregnated urinary catheters in trauma patients: a randomized trial. Ann Intern Med 2007;147:285-93.
- Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med 1987;83:27-33.
- Seymour C. Audit of catheter-associated UTI using silver alloy-coated Foley catheters. Br J Nurs 2006;15:598-603.
- Madeo M, Davies D, Johnson G, Owen E, Wadsworth P, Martin CR. The impact of using silver alloy urinary catheters in reducing the incidence of urinary tract infections in the critical care setting. Br J Infect Contr 2004;5:21-4.
- Curtis J, Perry K. CEP06001: Evidence review: Bardex IC Foley Catheter. London: NHS Centre for Evidence Based Purchasing; 2006.
- Maki DG, Knasinski V, Halvorson K, Tambyah PA. A novel silver hydrogel-impregnated indwelling urinary catheter reduces CAUTIs: a prospective double-blind trial. Infect Control Hosp Epidemiol 1998;19.
- LeLorier J, Gregoire G, Benhaddad A, Lapierre J, Derderian F. Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med 1997;337:536-42.
- Health Protection Agency (HPA) . HCAI and Antimicrobial Point Prevalence Survey – England 2011. www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/HCAI/HCAIPointPrevalenceSurvey (accessed October 2011).
- Centers for Disease Control and Prevention (CDP) . National Healthcare Safety Network. 2011. www.cdc.gov/nhsn (accessed October 2011).
- Hospital Episode Statistics . NHS Health and Social Care Information Centre 2011. www.hesonline.nhs.uk (accessed August 2011).
- Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol 2011;32:101-14.
- Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst Rev 2005;4.
- Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al. A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: The VULCAN trial. Health Technol Assess 2009;13.
- Core Outcome Measures in Effectiveness Trials (COMET) Initiative . www.comet-initiative.org (accessed September 2012).
- Drummond MF. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
Appendix 1 Critical appraisal of the economic studies using a checklist for assessing economic evaluations
Economic studies were appraised as described in Drummond 2005. 96
Study 1
Plowman R, Graves N, Esquivel J, Roberts JA. An economic model to assess the cost and benefits of the routine use of silver alloy coated urinary catheters to reduce the risk of UTIs in catheterized patients. J Hosp Infect 2001;48:33–42.
| Yes/partly/no/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Yes | The authors considered both the costs and the effects (number of NUTIs) of silver alloy-coated catheters. The viewpoint for the analysis was explicitly stated as that of the NHS |
| 2. | Was a comprehensive description of the competing alternatives given? | No | No comparator was used, as the study objective was to assess the number of NUTIs occurring in catheterised patients admitted to specialties of interest at one or more hospitals; the economic burden those infections impose on the hospital sector in terms of number of extra days patients remain in hospital and their associated value; and the potential benefits of an intervention that aims to reduce the incidence of this type of infection |
| 3. | Was the effectiveness of the programmes or services established? | Yes | The authors stated that literature on the incidence of NUTIs, risk factors for them, their impact on the mortality and the economic burden imposed was reviewed. The authors also identified the costs of an additional day in hospital and the cost of the intervention |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | Yes | The relevant costs and consequences were identified |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Yes | The parameters used to populate the model included the number of admissions to the specialties of interest, the number (or proportion) of patients within the group of interest, the number of patients catheterised, the estimated incidence of NUTIs occurring in catheterised patients, the average number of additional days that catheterised patients with a NUTI stayed in hospital, and the cost of an additional day in hospital |
| 6. | Were the costs and consequences valued credibly? | Yes | Data on number of admissions and specialties were obtained from the Hospital Episode Statistics database and number of patients catheterised were obtained from an audit carried out in England and Wales. Estimates of costs per bed-day were retrieved from the Chartered Institute of Public Finance Accountants health service data base. The additional cost of the silver alloy catheter was based on personal communication with the manufacturer |
| 7. | Were costs and consequences adjusted for differential timing? | No | Not relevant |
| 8. | Was incremental analysis of costs and consequences performed? | No | The model was not set up to compare different interventions, although it could be adapted to do so, therefore no incremental analysis was performed although the results suggest the reduction in incidence of NUTIs that would be required to cover the cost of the intervention |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences? | Yes | One-way sensitivity analysis was performed using the following parameters: incidence of NUTI additional bed-days and the value of extra bed-days |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Partly | The author highlighted the issues that the users should consider if they were to use results of the analysis. The model was set up to so that it could be adapted to the particular needs of the user |
Study 2
Rupp ME, Fitzgerald T, Marion Mario N, Helget V, Puumala S, Anderson JR, et al. Effect of silver-coated urinary catheters: efficacy, cost-effectiveness, and antimicrobial resistance. Am J InfectControl 2004;32:445–50.
| Yes/no/partly/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Yes | The authors have considered both the costs and the effects (UTIs avoided) of two comparators. The viewpoint for the analysis has not been explicitly stated, although it appears to be that of the health service provider |
| 2. | Was a comprehensive description or the competing alternatives given? | Partly | The competing alternatives have been cited as uncoated catheter and no further details have been provided. The information on the types of catheters is included under the cost-effectiveness heading and therefore not obvious to the reader |
| 3. | Was the effectiveness of the programmes of services established? | Yes | The rate of infection expressed as UTI/1000 was collected prospectively in 2001 and 2002 (when coated urinary catheters were in use) and compared with historical controls for the same units for 1999 and 2000 (when uncoated urinary catheters were used) |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | Yes | The relevant costs and consequences were identified from various sources. The number and cost of catheters and costs associated with NUTI were identified |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Yes | The measure of UTI was based on the number of UTI per 1000 catheter-days, which appears to be the most widely used method of measuring the rate of infection. The number of catheters used was obtained from hospital purchasing department records |
| 6. | Were the costs and consequences valued credibly? | Yes | The purchase cost of the catheters was provided by the manufacturer and the costs associated with NUTIs were derived from the medical literature and ranged from US$589 to $3805. No details were provided on how the costs associated with NUTI were arrived at |
| 7. | Were costs and consequences adjusted for differential timing? | No | The costs and consequences were not adjusted for differential timing. However, it was not necessary as the analysis was conducted at one time point in time and the analytic horizon, from the beginning of the interventions to the resolutions in outcomes of interest, was well inside 1 year |
| 8. | Was incremental analysis of costs and consequences performed? | Yes | The results are presented explicitly in the text as well as the relevant tables. The analysis does not provide the cost-effectiveness ratios for the comparator, as it mainly focuses on the incremental effectiveness and the cost savings associated with silver alloy catheter |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences? | No | Uncertainty was not explicitly handled, although the authors presented some low and high range estimates in the cost analysis. There was also some analysis on the percentage reduction break-even efficacy threshold (37–57%) |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Yes | The results are compared with published papers. Although data were also collected on the UTI/1000 patient-days the authors did not perform any cost analysis using this data, which had lower differences in the overall rates. The authors indicated the need for decision-makers to use caution when accepting the cost figures and that they should examine the data carefully in the context of their experience |
Study 3
Saint S, Veenstra DLD, Sullivan SDS, Chenoweth C, Fendrick AM. The potential clinical and economic benefits of silver alloy urinary catheters in preventing urinary tract infection. Arch Intern Med 2000;160:2670–5.
| Yes/no/partly/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Yes | The authors considered both the costs and effects (incidence of symptomatic UTI and bacteraemia). The costs and consequences of two types (silver and standard) of catheters were compared. The perspective of the analysis was stated as that of the health-care payer |
| 2. | Was a comprehensive description of the competing alternatives given? | Yes | The competing alternatives were described |
| 3. | Was the effectiveness of the programmes or services established? | Yes | The authors addressed the clinical evidence using evidence from published studies including a meta-analysis they had performed. They used a decision-analytic model to inform decision-makers on the clinical and economic impact of using urinary catheters coated with silver alloy |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | Yes | All of the relevant costs and consequences were addressed |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Yes | The measurement of consequences was derived from several published sources and was also based on assumptions that the authors made. The consequences were measured in terms of likelihood of clinical events. Details were also provided on how the authors arrived at the estimates for the protective effect of systemic antimicrobial agents and silver catheters. The measurement of costs of the interventions and the consequential resource use costs were straightforward |
| 6. | Were the costs and consequences valued credibly? | Yes | As the effects are measured in natural units it was not appropriate to value them in monetary terms. The reporting of the valuation of costs was handled adequately from the stated perspective |
| 7. | Were costs and consequences adjusted for differential timing? | No | Costs and consequences were not discounted to present values as it was inappropriate as they all appeared in the present |
| 8. | Was incremental analysis of costs and consequences performed? | Yes | The study could have benefited from a results table as the results were reported in the text |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences? | Yes | The authors performed threshold and sensitivity analysis on several variables as reported in tables 1 and 2 to handle the uncertainty in their analysis |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Partly | The analysis does not provide cost-effectiveness ratios for the alternatives. It focuses on the percentage relative decrease in the incidence of symptomatic UTI and estimated cost saving per patient. The authors highlighted the limitations of their analysis |
Study 4
Karchmer TBT, Giannetta ET, Muto CA, Strain BA, Farr BM. A randomized crossover study of silver-coated urinary catheters in hospitalized patients. Arch Intern Med 2000;160:3294–8.
| Yes/no/partly/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Yes | The authors considered the costs and benefits (reduction in UTIs) of two interventions. The viewpoint for the analysis has not been explicitly stated although it appears to be that of the health service provider |
| 2. | Was a comprehensive description or the competing alternatives given? | Partly | Uncoated catheters were explicitly stated as the comparator although no justification was provided for this choice |
| 3. | Was the effectiveness of the programmes of services established? | Yes | The authors collected data over 1 year. During the first 6 months, wards randomised to group 1 were stocked with silver-coated catheters, whereas those in group 2 used uncoated catheters, and after a 1-month washout period the catheters were changed. Hospital-wide surveillance for nosocomial infections was conducted |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | Yes | The authors collected data on costs associated with catheters, type of infection and the hospital where the data were collected |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Yes | The costs of the catheters and components used were obtained from the manufacturer. The rates of infection were calculated in similar methods used by other studies, i.e. number of infections per 100 patients, per 1000 patient-days and per 100 catheters |
| 6. | Were the costs and consequences valued credibly? | Yes | The costs and consequences were reported separately and adequate details of methods of cost estimation were provided but the constituents of the costs were not fully reported. It was not clear if the cost data were based on true costs or charges |
| 7. | Were costs and consequences adjusted for differential timing? | No | The costs and consequences were not adjusted for differential timing. However, it was not necessary as the analysis was conducted at one time point in time and the analytic horizon, from the beginning of the interventions to the resolutions in outcomes of interest, was well inside 1 year |
| 8. | Was incremental analysis of costs and consequences performed? | Yes | Costs and benefits were not combined, as the use of the silver-coated catheters was the dominant strategy |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences? | No | No sensitivity analysis was conducted |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Partly | The results of the study should be interpreted cautiously owing to the limitations of the study design, lack of sensitivity analysis and the lack of statistical analysis of the cost data |
Study 5
Lai KK, Fontecchio SA. Use of silver-hydrogel urinary catheters on the incidence of catheter-associated urinary tract infections in hospitalized patients. Am J Infect Control 2002;30:221–5.
| Yes/no/partly/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Yes | The authors considered the costs of CAUTI by comparing coated and non-coated catheters. The perspective of the study was not explicitly stated but it appears to be that of the health service provider |
| 2. | Was a comprehensive description of the competing alternatives given? | Partly | The authors did not provide much detail about the non-coated catheters but stated that they were non-coated, standard urinary catheters. More details were provided on the type and manufacturer of the coated silver hydrogel catheter |
| 3. | Was the effectiveness of the programmes or services established? | Yes | The primary clinical outcome was CAUTI rate per 1000 patient-days and was derived by dividing the number of UTIs with the patient-days of all hospitalised patients. The rate for the non-coated catheters was estimated historically by using the two months’ data (January 1996 and January 1997), whereas the rate for the coated catheter was estimated in the month of January 1997 |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | Yes | Medical records were reviewed closely for resource utilisation, such as laboratory tests and antibiotics among others that were related to CAUTI |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Partly | Although the study reported that all patients with CAUTI were identified along with the costs and consequences of CAUTIs, the cost analysis was performed on a randomly selected group of patients and no justification was provided for this decision. Also the costs were estimated using assumptions on the number of UTI that would be observed monthly using different number of data points for the two different groups. It is therefore hard to establish how reliable and generalisable the results are |
| 6. | Were the costs and consequences valued credibly? | Yes | Charges for the resources used for CAUTI were obtained and tallied to obtain the average cost of CAUTI at the medical centre |
| 7. | Were costs and consequences adjusted for differential timing? | No | The costs and consequences were not adjusted for differential timing. However it was not necessary as the analysis was conducted at one time point in time and the analytic horizon, from the beginning of the interventions to the resolutions in outcomes of interest, was well inside 1 year |
| 8. | Was incremental analysis of costs and consequences performed? | Yes | Based on the assumptions on the number of catheters per year the centre would have 216 fewer CAUTI when they used the coated catheters. This translated into a net saving of US$142,315 per year as a reduction in the rate of CAUTI |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences? | No | No sensitivity analysis was conducted |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Partly | The authors indicate that their results were not statistically significantly different between the same groups and compared their findings with some of the published studies. They also highlighted the limitations of their study that included the fact that it was not a randomised controlled study but relied on a historical control and that demographic data and risk factor data were not gathered for the two groups of patients to see whether or not they were comparable. There were also issues relating to bias that had not been addressed and it is therefore difficult to determine how generalisable these results are to other users |
Study 6
Bologna RA, Tu LM, Polansky M, Fraimow HD, Gordon DA, Whitmore KE. Hydrogel/silver ion-coated urinary catheter reduces nosocomial urinary tract infection rates in intensive care unit patients: a multicenter study. Urology 1999;54:982–7.
| Yes/no/partly/unclear | Comments | ||
|---|---|---|---|
| 1. | Was a well-defined question posed in an answerable form? | Unclear | The authors stated that they investigated the Bardex IC catheter for its ability to reduce NUTI |
| 2. | Was a comprehensive description of the competing alternatives given? | Yes | Although a description of the coated catheter was provided it was implied that the catheters were similar and the difference was that one was coated and the other was not. The alternative used in the standard catheter group was the standard type of catheter in use |
| 3. | Was the effectiveness of the programmes of services established? | Yes | Five institutions participated in the study. Infections were identified in three ways: prospective review of microbiology reports of patients, review of antimicrobial usage and through formal chart reviews during daily rounds. CAUTIs were determined by the number of infections per 1000 days the patients had an indwelling catheter. A baseline period using a standard latex catheter was selected at each hospital during which time usage rate and NUTI rate were monitored. A blind switch was made to Bardex IC catheter |
| 4. | Were all the important and relevant cost and consequences for each alternative identified? | No | Only the cost of the catheters was reported. The authors stated that it was difficult to estimate the cost of hospitalisation, extent of patient evaluation and increased duration of hospitalisation if any that a NUTI induced |
| 5. | Were costs and consequences measured accurately in appropriate physical units? | Partly | The outcome NUTI was measured in a similar to that in other studies. Although the study was performed in five hospitals the costs analysis was performed in the only centre that reported statistically significantly different results in NUTIs. The cost of the catheters was stated as cost per catheter although it was not clear where the costs came from |
| 6. | Were the costs and consequences valued credibly? | Partly | See above |
| 7. | Were costs and consequences adjusted for differential timing? | No | The costs and consequences were not adjusted for differential timing. However, it was not necessary, as the analysis was conducted at one point in time and the analytic horizon, from the beginning of the interventions to the resolutions in outcomes of interest, was well inside 1 year |
| 8. | Was incremental analysis of costs and consequences performed? | Partly | Incremental analysis was performed for the NUTI but none was carried out for the costs |
| 9. | Was allowance made for uncertainty in the estimates of cost and consequences | No | No sensitivity analysis was performed |
| 10. | Did the presentation and discussion of study results include all issues of concern to users? | Partly | The authors had some discussion of their results and highlighted two issues that needed to be considered. They also compared their findings with those of other studies. The authors did not explore how their findings were generalisable beyond the trial but identified a need for further research. One of the limitations of the study was that there was some variability number of months for which the catheters were used. This was in the hospitals themselves, as well as between the hospitals. The adjusted analysis did not take into account this variability |
Appendix 2 Patient information sheets
Patient information booklet
Consent form
Appendix 3 CATHETER patient questionnaires
Baseline questionnaire
Three days post CATHETER removal questionnaire
Week 1 diary
Week 2 diary
Follow-up questionnaire
General practitioner urinary tract infection confirmation letter
General practitioner urinary tract infection confirmation table
Appendix 4 CATHETER case report forms
Participant data form
Three-day post catheter removal urine results
Change of status form
Serious adverse event report
Appendix 5 Algorithm to determine primary outcome
Consenting participants that reached week 6 of the trial (excluding any deaths within 7 days of randomisation) were checked to see if they had a confirmed UTI at 3 days (‘given antibiotics for a UTI since removal of the catheter’ from the 3-day urine results form or ‘given antibiotics for UTI during catheterisation’ from participant data form). If they had a UTI at 3 days then they were logged as having a confirmed UTI during the study.
All participants without a confirmed UTI at 3 days were checked to see if they had a symptom or antibiotics reported in any returned diary or 6-week questionnaire. For example, in the diaries if the answer was ‘yes’ to any of the following questions ‘In the past 7 days have you had a urine infection?’ or ‘Did you see a doctor in relation to a urine infection?’ or ‘Did you see a nurse in relation to a urine infection?’ or ‘Did you receive antibiotics for a urine infection?’ or text was present in the box ‘If yes to Question 4, which antibiotics did you receive?’ and they had not already had a confirmed UTI and their GP had not been previously contacted then a letter would be sent requesting GP confirmation of antibiotic prescription between the date of recruitment and end date (42 days after randomisation). The same process was repeated for the 2-week diary and the 6-week questionnaire.
If a participant had no UTI at 3 days and had not returned any symptom data in the diaries or questionnaire then they were followed up by a letter to their GP asking if the participant had been diagnosed with a UTI and whether or not antibiotics had been prescribed between the date of recruitment and end date (42 days after randomisation).
Participants who had not had a confirmed UTI at 3 days and did not meet the criteria for having a letter sent out to GP were recorded as having no UTI during the study.
Appendix 6 Full logistic regression model for the primary outcome
| Covariate | OR | 95% CI | p-value |
|---|---|---|---|
| Nitrofurazone | 0.81 | 0.67 to 0.98 | 0.031 |
| Silver | 0.96 | 0.80 to 1.16 | 0.686 |
| Female | 2.21 | 1.83 to 2.67 | < 0.001 |
| Age > 60 years | 1.39 | 1.18 to 1.63 | < 0.001 |
| Comorbidity | 0.97 | 0.81 to 1.17 | 0.742 |
| Emergency catheterisation | 1.27 | 0.88 to 1.85 | 0.207 |
| Antibiotic use last 7 days | 0.68 | 0.56 to 0.82 | < 0.001 |
| Antibiotic use at catheterisation | 0.91 | 0.76 to 1.10 | 0.332 |
Appendix 7 Within-trial cost-effectiveness analysis
Introduction
This appendix describes the results of the prestated within-trial cost-effectiveness analysis. As described elsewhere, concerns that imbalances between trial groups could not be adequately adjusted for, particularly with respect to length of stay, led to a judgement that the within-trial analysis might be potentially misleading. Nevertheless, as this judgement could be questioned, this analysis is provided here for completeness. In the main analysis presented, the data are taken at face value.
Analysis of resource use and costs
Table 43 (a replication of Table 27) and Table 44 detail the average resource use and the mean differences both for the catheters used, and for subsequent use of health services. For the comparisons of the PTFE group with nitrofurazone, and PTFE with silver alloy, there was no use of health services that was statistically significantly different between the groups. For both comparisons the CIs for most areas of resource use were sufficiently narrow to rule out any economically important differences (although this is a subjective judgement). The exception to this is differences in length of stay, for which the CIs could potentially include economically important differences.
| Resource type | Nitrofurazone (n), mean (SD) | Silver alloy (n), mean (SD) | PTFE (n), mean (SD) |
|---|---|---|---|
| Intervention | |||
| Catheter allocation and no. of catheters used | 2153, 1.03 (0.21) | 2097, 1.04 (0.29) | 2144, 1.03 (0.21) |
| Secondary care resource use | |||
| Length of stay | 2104, 7.27 (6.58) | 2047, 7.72 (6.87) | 2102, 7.57 (7.00) |
| Outpatient visit | 1668, 0.02 (0.28) | 1614, 0.02 (0.17) | 1671, 0.02 (0.19) |
| Visit to other providers | 1656, 0.02 (0.41) | 1605, 0.01 (0.14) | 1662, 0.01 (0.20) |
| Inpatient readmissions | 1669, 0.08 (1.26) | 1605, 0.01 (0.24) | 1673, 0.02 (0.54) |
| Primary care resource use | |||
| GP doctor visit | 1661, 0.11 (0.44) | 1605, 0.13 (0.47) | 1659, 0.12 (0.45) |
| GP nurse visit | 1667, 0.03 (0.27) | 1606, 0.04 (0.34) | 1669, 0.05 (1.05) |
| Medications | |||
| Antibioticsa | 1160, 0.18 (0.38) | 1130, 0.18 (0.39) | 1154, 0.20 (0.40) |
| Resource type | Antimicrobial-impregnated (nitrofurazone) vs PTFE: mean difference (97.5% CI) | Antiseptic-impregnated (silver alloy) vs PTFE: mean difference (97.5% CI) |
|---|---|---|
| Intervention | ||
| Catheter | 0.005 (–0.01 to 0.02) | 0.007 (–0.01 to 0.02) |
| Secondary care resource use | ||
| Length of stay | –0.30 (–0.77 to 0.17) | 0.15 (–0.34 to 0.63) |
| Outpatient visit | –0.003 (–0.02 to 0.02) | –0.001 (–0.02 to 0.01) |
| Visit to other providers | 0.008 (–0.02 to 0.03) | –0.0002 (–0.01 to 0.01) |
| Inpatient readmissions | 0.06 (–0.01 to 0.14) | –0.008 (–0.04 to 0.02) |
| Primary care resource use | ||
| GP doctor visit | –0.01 (–0.05 to 0.02) | 0.010 (–0.03 to 0.05) |
| GP nurse visit | –0.02 (–0.08 to 0.04) | –0.006 (–0.07 to 0.06) |
| Medications | ||
| Antibioticsa | –0.02 (–0.06 to 0.01) | –0.017 (–0.05 to 0.02) |
Estimation of NHS costs
Tables 45 and 46 are conversions of Tables 43 and 44 into costs to the NHS. As indicated by the SD, the cost data were highly skewed to the right; while most of the patients had low costs, some of them had very high costs. In terms of NHS costs (see Tables 45 and 46) incurred after the patients received the catheters, the mean total cost per patient in the nitrofurazone group was £3259 (SD £3152), the mean cost in the silver alloy group was £3438 (SD £3270) and the mean cost of the PTFE group was £3390 (SD £3405). There was, however, no evidence of statistically significant differences in the total mean costs or other costs, although the CIs are sufficiently wide to include economically important differences that may favour any of the catheters. The mean difference in costs per patient of catheters for the intervention groups compared with PTFE was higher for both: nitrofurazone (£4.19, 97.5% CI 4.11 to 4.26) and silver alloy (£5.39, 97.5% CI 5.30 to 5.49). Reflecting the findings described above, other costs tended to be lower in the nitrofurazone group, particularly differences in length of stay, which was the main driver of differences in mean costs between groups. The implications of differences in length of stay are explored later as part of the sensitivity analysis.
| Resource type | Nitrofurazone (n), mean £ (SD) | Silver alloy (n), mean £ (SD) | PTFE (n), mean £ (SD) |
|---|---|---|---|
| Intervention | |||
| Catheter | 2153, 5.15 (1.19) | 2097, 6.34 (1.86) | 2144, 0.96 (0.65) |
| Secondary care resource use | |||
| Length of stay | 2104, 3302.98 (3107.74) | 2047, 3505.72 (3266.80) | 2102, 3444.63 (3397.18) |
| Outpatient visit | 1668, 1.63 (26.10) | 1614, 1.81 (16.28) | 1671, 1.91 (18.30) |
| Visit to other providers | 1661, 0.87 (12.13) | 1606, 1.04 (13.05) | 1664, 1.16 (18.70) |
| Inpatient readmissions | 1669, 26.53 (412.18) | 1605, 3.88 (77.16) | 1673, 6.67 (177.44) |
| Primary care resource use | |||
| GP doctor visit | 1661, 3.88 (15.80) | 1605, 4.67 (17.08) | 1659, 4.32 (16.33) |
| GP nurse visit | 1667, 0.35 (2.68) | 1606, 0.45 (3.43) | 1669, 0.51 (10.49) |
| Medications | |||
| Antibiotics | 1160, 0.96 (2.06) | 1130, 0.98 (2.09) | 1154, 1.07 (2.16) |
| Total | 2153, 3259 (3152) | 2097, 3438 (3270) | 2144, 3390 (3405) |
| Resource type | Nitrofurazone (A), mean difference (97.5% CI)a | Silver alloy (B), mean difference (97.5% CI)a |
|---|---|---|
| Intervention | ||
| Catheter | 4.19 (4.12 to 4.26) | 5.39 (5.30 to 5.49) |
| Secondary care resource use | ||
| Length of stay | –127.81 (–338.98 to 83.35) | 101.16 (–112.22 to 314.54) |
| Outpatient visit | –0.26 (–2.08 to 1.55) | –0.10 (–1.51 to 1.30) |
| Other health-care providers | –0.29 (–1.60 to 1.01) | –0.15 (–1.42 to 1.13) |
| Inpatient readmissions | 21.00 (–4.73 to 46.73) | –4.03 (–15.34 to 7.27) |
| Primary care resource use | ||
| GP doctor visit | –0.44 (–1.75 to 0.87) | 0.20 (–1.15 to 1. 56) |
| GP nurse visit | –0.16 (–0.76 to 0.44) | –0.08 (–0.71 to 0.54) |
| Medications | ||
| Antibiotics | –0.13 (–0.33 to 0.07) | –0.12 (–0.33 to 0.08) |
| Total | –108.49 (–319.09 to 102.10) | 81.37 (–131.07 to 293.81) |
Quality-adjusted life-years
Table 47 reports the EQ-5D scores for trial groups at baseline, 3 days, 1 and 2 weeks after catheter removal and 6 weeks after randomisation. Also reported is the mean difference between the groups in EQ-5D score at these time points (Table 48). From these data it was estimated that the mean QALYs were 0.081 (SD 0.02) for the nitrofurazone group, 0.079 (SD 0.02) for the silver alloy group and 0.081 (SD 0.02) for the PTFE group. The mean difference in QALYs after adjusting for minimisation and baseline EQ-5D scores was 0.0002 (97.5% CI –0.002 to 0.002) higher QALY value for nitrofurazone group compared with PTFE, which was not statistically significant. For the silver alloy group QALYs were, on average, –0.001 (97.5% –0.003 to 0.001) lower for the PTFE group, and, again, this difference was not statistically significant. Although it is a matter of judgement, the difference in QALYs as described by the CIs is small and may not include a meaningful difference.
| EQ-5D | Nitrofurazone (n), mean (SD) | Silver alloy (n), mean (SD) | PTFE (n), mean (SD) |
|---|---|---|---|
| Baseline | 2126, 0.717 (0.29) | 2076, 0.722 (0.29) | 2123, 0.722 (0.30) |
| 3 days | 1859, 0.592 (0.27) | 1801, 0.578 (0.28) | 1871, 0.593 (0.27) |
| 1 week | 1363, 0.618 (0.27) | 1308, 0.601 (0.29) | 1366, 0.614 (0.27) |
| 2 weeks | 1405, 0.696 (0.26) | 1328, 0.686 (0.27) | 1398, 0.694 (0.25) |
| 6 weeks | 1704, 0.776 (0.24) | 1665, 0.782 (0.24) | 1721, 0.794 (0.23) |
| QALYsa | 1116, 0.081 (0.02) | 1077, 0.079 (0.02) | 1123, 0.081 (0.02) |
| EQ-5D | Nitrofurazone, mean (97.5% CI) | Silver alloy, mean (97.5% CI) |
|---|---|---|
| Baseline | ||
| 3 days | –0.001 (–0.021 to 0.019) | –0.015 (–0.035 to 0.006) |
| 1 week | 0.004 (–0.019 to 0.027) | –0.012 (–0.037 to 0.012) |
| 2 weeks | 0.002 (–0.020 to 0.023) | –0.008 (–0.030 to 0.014) |
| 6 weeks | –0.018 (–0.036 to 0.001) | –0.012 (–0.030 to 0.006) |
| QALYsa | 0.0002 (–0.002 to 0.002) | –0.001 (–0.003 to 0.001) |
Estimation of cost-effectiveness
Incremental cost per infection averted
Taking the results of the primary outcome reported in detail in Table 13 in Chapter 5 and the differences in cost reported in Table 46, a three-way comparison of the different catheter groups was made (Table 49). On average, nitrofurazone was associated with lower costs, with a cost reduction of £108, and was more effective, being associated, on average, with 0.021 UTIs compared with PTFE. An incremental cost per infection avoided is not calculated in this circumstance, as, on average, nitrofurazone is less costly and more effective. On average, the care of participants in the silver alloy group cost £81 more than PTFE but the patients suffered 0.001 fewer UTIs. Therefore, the incremental cost per number of infections was £81,370 for silver alloy compared with PTFE.
| Catheter type | Deterministic results | Probability (%) of being cost-effective for different threshold values for society’s willingness to pay for a life-year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Average cost (£) | Incremental cost (£)a | No. of infections | Incremental no. of infections averted | ICER | £0 | £10,000 | £20,000 | £30,000 | £40,000 | £50,000 | |
| Nitrofurazone | 3259.24 | 0.106 | 88 | 89 | 89 | 90 | 90 | 90 | |||
| PTFE | 3390.02 | 108.49 | 0.126 | 0.021 | Dominated by NFa | 9 | 9 | 9 | 9 | 9 | 9 |
| Silver alloy | 3438.08 | 81.37 | 0.125 | –0.001 | Dominated by NFa | 3 | 2 | 2 | 1 | 1 | 1 |
The data presented above do not reflect the statistical imprecision surrounding estimates of costs and infections. Therefore, Tables 49 and 50 also show the probability that an intervention would be considered cost-effective at different threshold values for society’s willingness to pay to avoid an infection. These data show that nitrofurazone had an approximately 90% chance of being considered cost-effective at all willingness-to-pay thresholds considered. The main driver of these data is the trend towards lower costs in the nitrofurazone group compared with control (which, in turn, are driven by the trend towards a shorter length of stay). The probability of either silver alloy or PTFE being cost-effective over the range of threshold values considered was low (approximately 9% for PTFE and between 1% and 3% for silver alloy).
| Nitrofurazone vs PTFE: mean (97.5% CI) | Silver alloy vs PTFE: mean (97.5% CI) | |
|---|---|---|
| Difference in mean costs | –108.49 (–319.09 to 102.10) | 81.37 (–131.07 to 293.81) |
| Differences in QALYs | 0.0002 (–0.002 to 0.002) | –0.001 (–0.003 to 0.001) |
| ICER (£/QALY) | Nitrofurazone is dominant | PTFE is dominant |
| Probability (%) intervention is cost-effective at | ||
| £0 per QALY | 88 | 19 |
| £20,000 per QALY | 88 | 15 |
| £30,000 per QALY | 88 | 13 |
| £50,000 per QALY | 86 | 11 |
Sensitivity analysis on the cost and risk reduction differences
Incremental cost-effectiveness ratio results of two-way sensitivity analyses using the 2.5th and 97.5th percentile values for both costs and absolute risk reduction reported in Table 46 and below (see Table 54)for nitrofurazone compared with PTFE ranged from £2431 to £319,090. The ICERS for silver alloy compared with PTFE ranged from £5958 to £12,242.
Incremental cost per quality-adjusted life-years gained
The cost-effectiveness results for nitrofurazone indicate that, on average, it is less costly and more effective than PTFE (although the CIs surrounding costs in particular are very wide). The results for the silver alloy catheter group indicate that, on average, silver alloy is more costly and less effective than PTFE (i.e. again CIs surrounding costs in particular are wide). Also included in Table 50 are the results of the probabilistic sensitivity analysis (described in more detail below). These results show the likelihood for each pair-wise comparison that an intervention would be considered cost-effective at different illustrative thresholds for society’s willingness to pay for a QALY ranging from £0 to £50,000. When the willingness to pay for a QALY is £0, this means that society is not willing to pay for any additional QALYs. However, in the context of this evaluation, one interpretation of differences in QALYs reported in Table 48 is that there is no meaningful difference in QALYs. In such a circumstance the decision is made on cost alone which is equivalent to data presented when the willingness to pay for a QALY is £0.
Figure 22 shows that nitrofurazone catheters have over 85% chance of being cost-effective compared with PTFE catheters over the threshold values for willingness to pay for a QALY considered. Compared with PTFE, silver alloy has less than a 20% chance of being considered cost-effective at the same thresholds.
FIGURE 22.
Cost-effectiveness acceptability curve for nitrofurazone, silver alloy and PTFE.
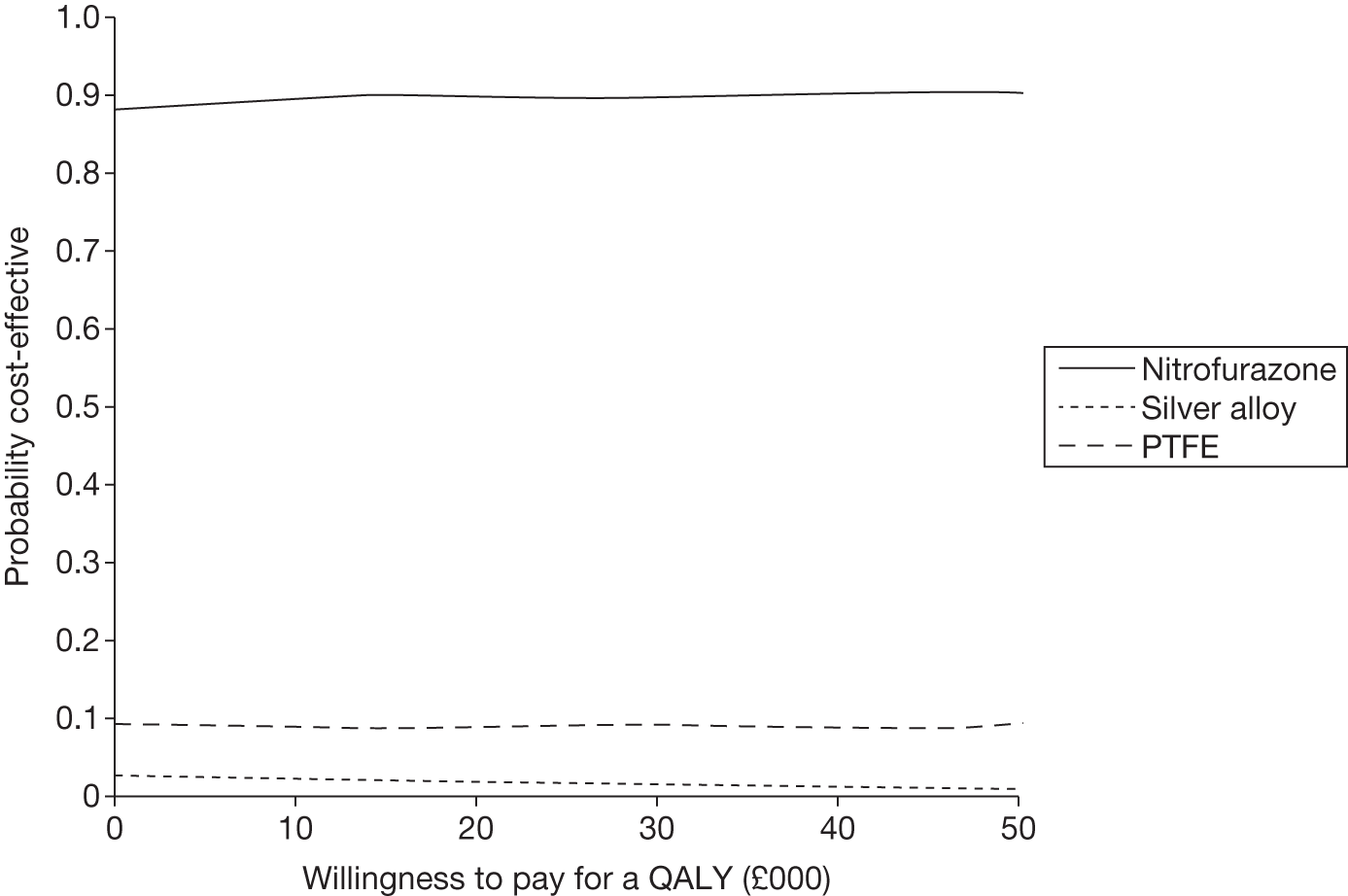
Figures 23 and 24 show the results of the non-parametric bootstrapping that was undertaken to handle the uncertainty around the QALY and cost estimates for both pair-wise comparisons. For the comparison of nitrofurazone with PTFE the results of 1000 bootstrap simulations (see Figure 23 and 24) indicate that for the majority of the bootstrap estimates the nitrofurazone group had lower costs and slightly higher QALYs.
FIGURE 23.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone vs PTFE.
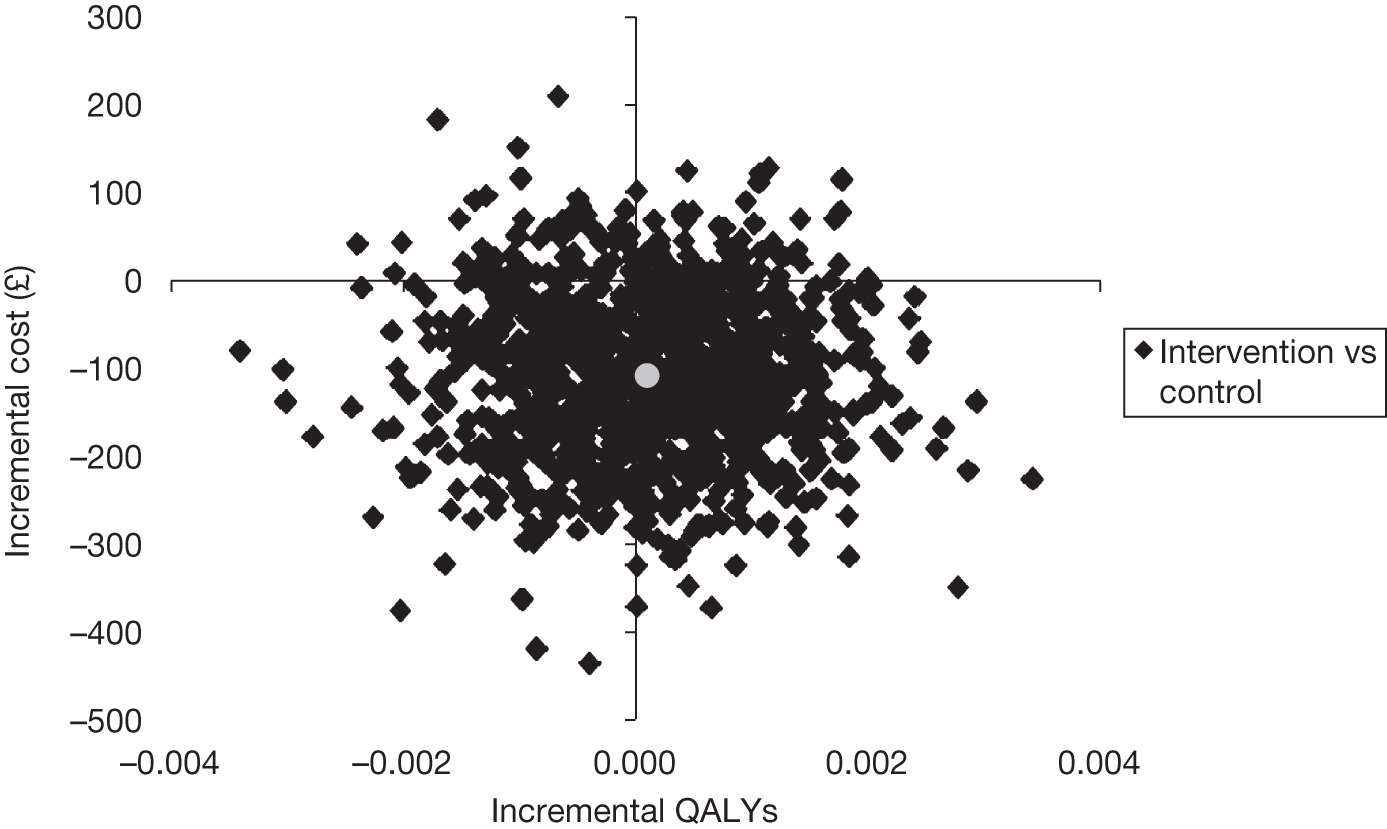
FIGURE 24.
Cost-effectiveness acceptability curve for nitrofurazone vs PTFE.
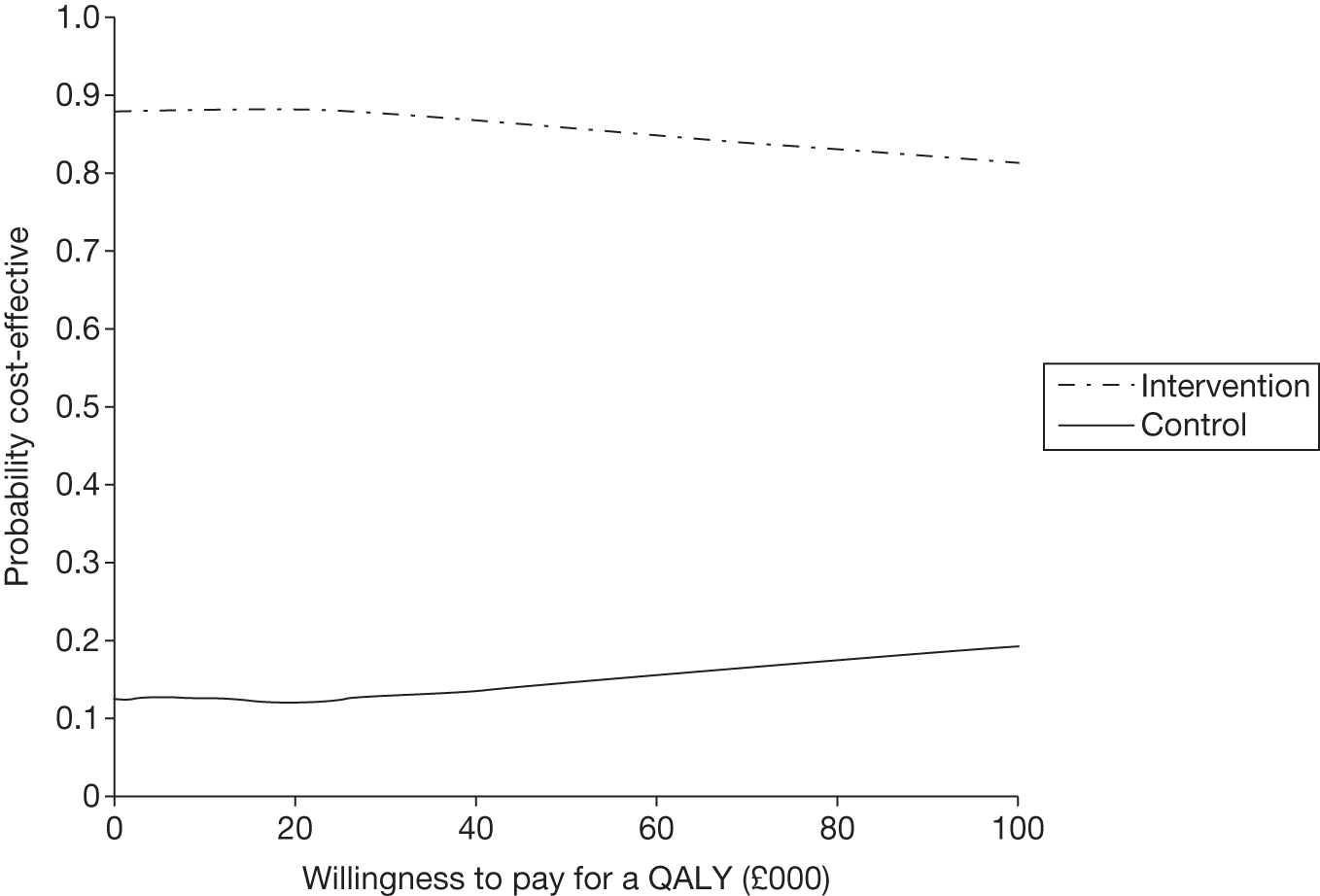
For the comparison of silver alloy with PTFE the results of 1000 bootstrap simulations (Figures 25 and 26) show that for the majority of bootstrap estimates the PTFE group had lower costs and slightly higher QALYs than the silver alloy catheters. Hence, in Figure 25 the PTFE group (control) was much more likely to be considered cost-effective at all threshold values for society’s willingness to pay for a QALY considered.
FIGURE 25.
Representation of the uncertainty in differential mean costs and QALYs for silver alloy vs PTFE.
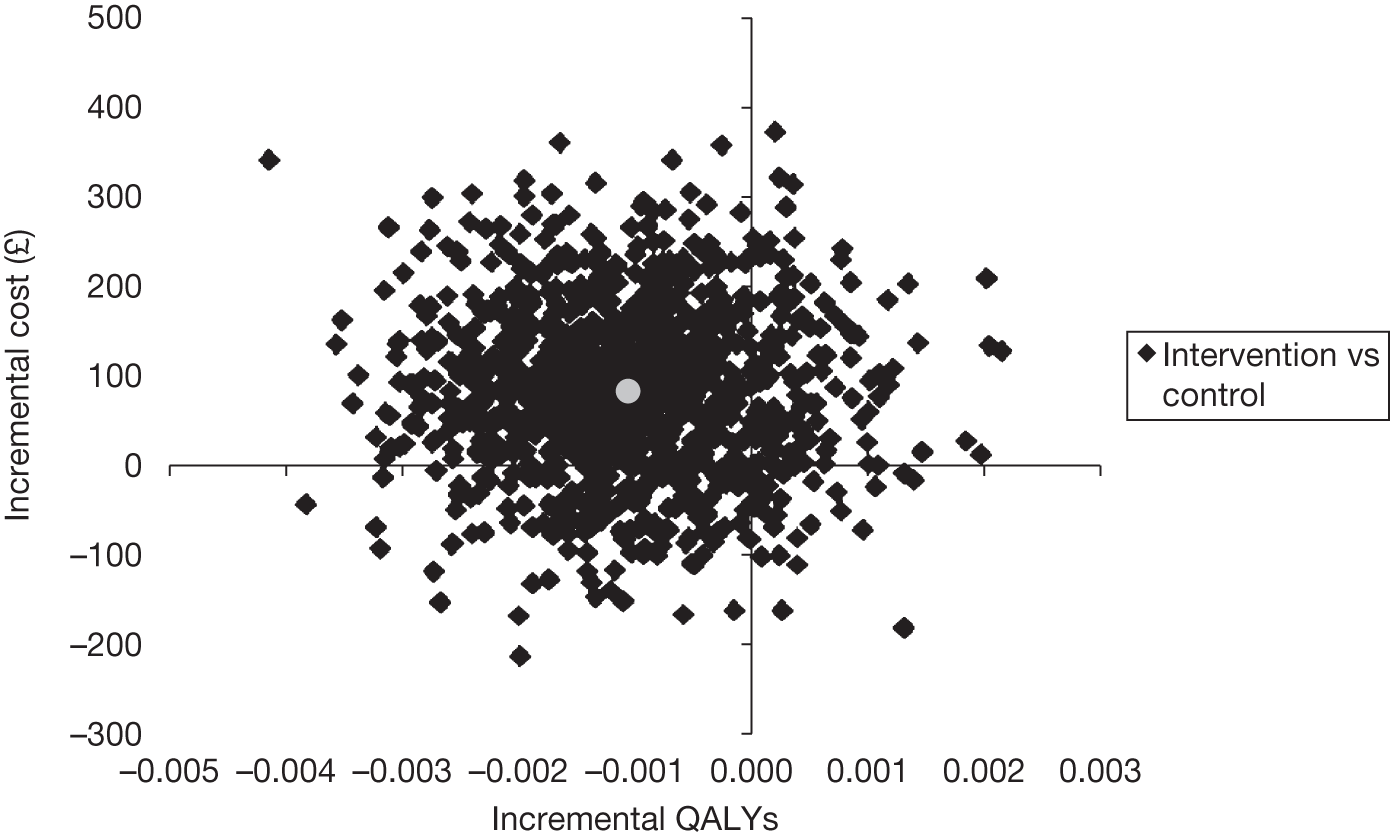
FIGURE 26.
Cost-effectiveness acceptability curve for silver alloy vs PTFE.
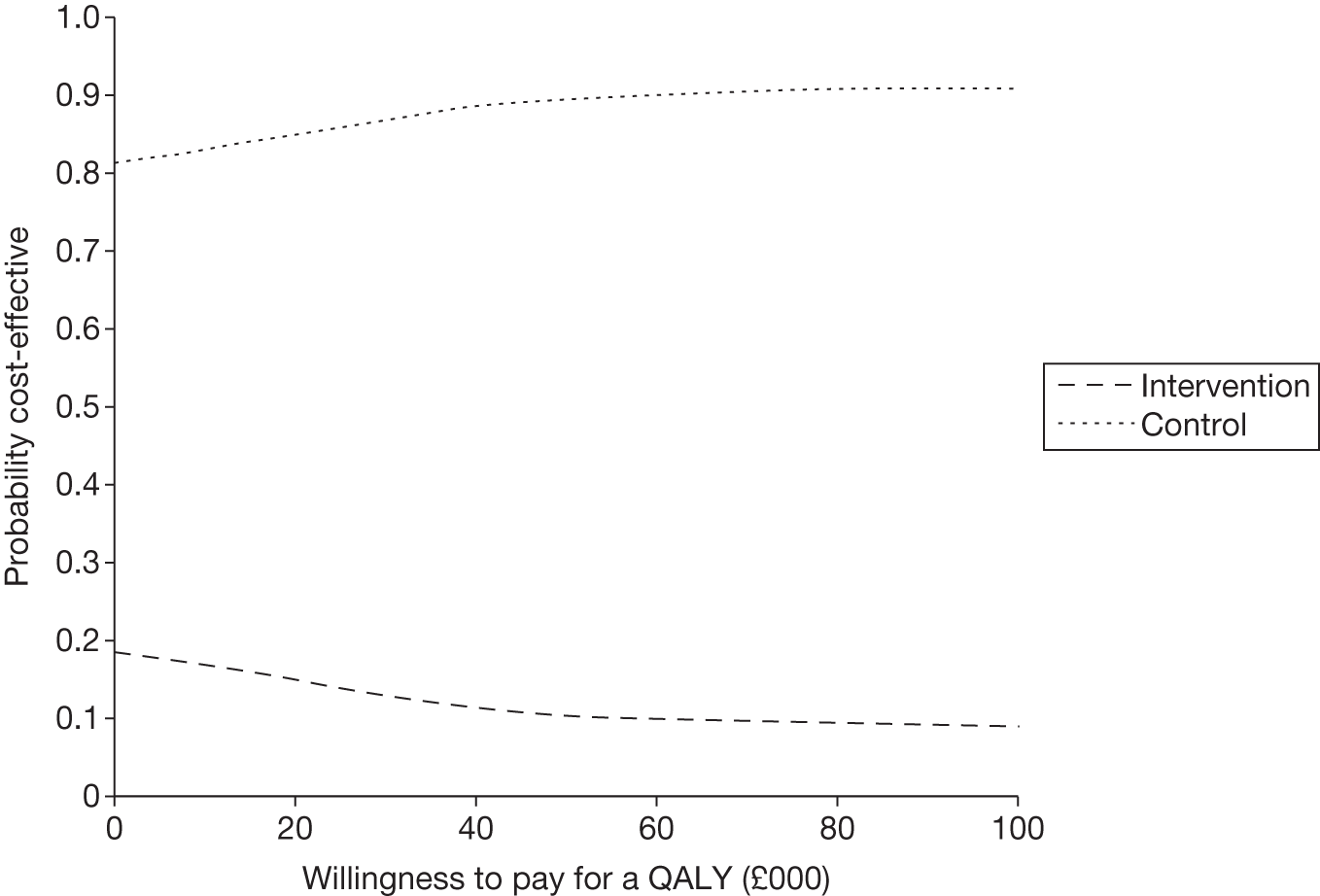
Subgroup analysis
The results of the subgroup analyses of the primary outcome examining possible effect modification of age (< 60 years, ≥ 60 years), sex, comorbidity (pre-existing urological disease, diabetes, immunosuppression), duration of catheterisation (< 4 days, ≥ 4 days), indication for catheterisation (incontinence, urinary retention and monitoring purpose) and antibiotic use prior to enrolment for the nitrofurazone group were similar to those reported in the base-case analysis in that none of the differences was statistically significant (Table 51). The subgroup that had the highest difference in costs for the comparison of nitrofurazone group with PTFE was the subgroup that had a catheter for > 4 days (£–275), followed by that of patients ≥ 65 years old (£–222). None of the results of the interaction terms included in the regression model was statistically significant. (The product of the variables of interest, e.g. the interaction term for the female group in patients that got nitrofurazone was a product of female and the treatment that was received, i.e. nitrofurazone. The presence of an interaction effect implies that the effect of sex on costs varies as a function of the type of catheter received). Three of the subgroups (those participants who were < 60 years old, had antibiotic use in the last 7 days, and had antibiotics at catheterisation) within the nitrofurazone group had higher costs than PTFE but they were not statistically significantly different.
| Subgroup | Mean cost difference (£), (99% CI) |
|---|---|
| Female | –156.07 (–472.67 to 160.53) |
| Male | –84.65 (–488.07 to 318.78) |
| ≥ 60 years | –221.88 (–567.41 to 123.64) |
| < 60 years | 0.30 (–358.61 to 359.21) |
| Comorbidity: no | –152.30 (–445.94 to 141.33) |
| Comorbidity: yes | –17.55 (–549.54 to 514.43) |
| Catheterisation for: monitoring | –138.39 (–405.78 to 129.00) |
| Catheterisation for: emergency | –98.26 (–1349.32 to 1152.79) |
| Antibiotic use last 7 days: no | –171.09 (–457.15 to 114.96) |
| Antibiotic use last 7 days: yes | 77.16 (–524.45 to 678.78) |
| Antibiotic at catheterisation: no | –114.41 (–616.04 to 387.21) |
| Antibiotic at catheterisation: yes | 134.46 (–434.59 to 165.67) |
| Catheter duration ≥ 4 days | –275.46 (–897.72 to 346.81) |
| Catheter duration < 4 days | –19.35 (–261.75 to 223.04) |
The results of the subgroup analysis for silver alloy compared with PTFE followed a similar pattern to those of the base-case analysis with the exception of females, those who had no comorbidities and those who had catheters for ≥ 4 days. These groups had lower costs for the silver alloy catheters than PTFE (Table 52). The highest difference in costs was in the group that were catheterised for emergency purposes in which the cost in the silver alloy group was £612 higher than the PTFE group. However, none of the results was statistically significantly different and none of the results of the interaction terms was statistically significant.
| Subgroup | Mean cost difference (£), (99% CI) |
|---|---|
| Female | –11.60 (–334.24 to 311.04) |
| Male | 194.90 (–220.50 to 610.29) |
| ≥ 60 years | 64.11 (–287.78 to 416.01) |
| < 60 years | 47.6 (–319.56 to 414.89) |
| Comorbidity: no | –55.87 (–356.68 to 244.93) |
| Comorbidity: yes | 410.27 (–129.35 to 949.89) |
| Catheterisation for: monitoring | 21.67 (–252.10 to 295.43) |
| Catheterisation for: emergency | 612.18 (–662.54 to 1886.91) |
| Antibiotic use last 7 days: no | 52.56 (–239.37 to 344.49) |
| Antibiotic use last 7 days: yes | 75.79 (–547.08 to 698.65) |
| Antibiotic at catheterisation: no | 146.92 (–374.04 to 667.89) |
| Antibiotic at catheterisation: yes | 31.33 (–275.01 to 337.67) |
| Catheter duration ≥ 4 days | –214.96 (–828.55 to 398.63) |
| Catheter duration < 4 days | 78.31 (–170.84 to 327.46) |
Sensitivity analysis
Sensitivity around cost per day
A sensitivity analysis around length of stay considered the use of alternative unit cost data. In this sensitivity analysis, elective inpatient excess bed-days based on Health Resource Group (HRG) data from the National Schedule of Reference Costs 2009–10 for NHS Trusts76 were used instead of the data from ISD. 71 As Table 53 illustrates, the direction of cost results was similar to that of the base-case analysis using NHS Scotland ISD data, although the magnitude in the differences was lower.
| Nitrofurazone vs PTFE: mean (97.5% CI) | Silver alloy vs PTFE: mean (97.5% CI) | |
|---|---|---|
| Difference in mean costs | –88.00 (–241.98 to 65.97) | 41.58 (–113.43 to 196.58) |
| Differences in QALYs | 0.0002 (–0.002 to 0.002) | –0.001(–0.003 to 0.001) |
| ICER (£/QALY) | Nitrofurazone is dominant | Silver alloy is dominated |
| Probability (%) intervention is cost-effective at | ||
| £0 per QALY | 90 | 27 |
| £20,000 per QALY | 91 | 17 |
| £30,000 per QALY | 90 | 14 |
| £50,000 per QALY | 88 | 12 |
Use of unadjusted differences in costs and quality-adjusted life-years instead of the adjusted differences used in the base-case analysis
The base-case analysis was based on differences between different groups that were adjusted for age (< 60 years, ≥ 60 years), sex, comorbidity (pre-existing urological disease, diabetes, immunosuppression), duration of catheterisation (< 4 days, ≥ 4 days), indication for catheterisation (incontinence, urinary retention and monitoring purpose) and antibiotic use prior to enrolment. The results of the sensitivity analysis using unadjusted cost and QALY differences are presented in Table 54.
The unadjusted results of nitrofurazone compared with PTFE were similar to those obtained from the adjusted analysis. The mean difference in QALY was similar to that of the base case and again this difference was not statistically significant. Similarly, the cost difference was slightly higher than estimated in the base case; again, this difference was not statistically significant. The net effect of this was a small increase in the probability of nitrofurazone being considered cost-effective over the threshold values for society’s willingness to pay for an additional QALY considered (Figures 27 and 28).
| Nitrofurazone vs PTFE: mean (97.5% CI) | Silver alloy vs PTFE: mean (97.5% CI) | |
|---|---|---|
| Difference in mean costs | –130.78 (–355.20 to 103.87) | 48.07 (–180.73 to 276.86) |
| Differences in QALYs | 0.0002 (–0.002 to 0.002) | –0.001 (–0.003 to 0.001) |
| ICER (£/QALY) | Nitrofurazone is dominant | Silver alloy is dominated |
| Probability (%) intervention is cost-effective at | ||
| £0 per QALY | 91 | 30 |
| £20,000 per QALY | 91 | 24 |
| £30,000 per QALY | 91 | 20 |
| £50,000 per QALY | 90 | 15 |
FIGURE 27.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone vs PTFE.
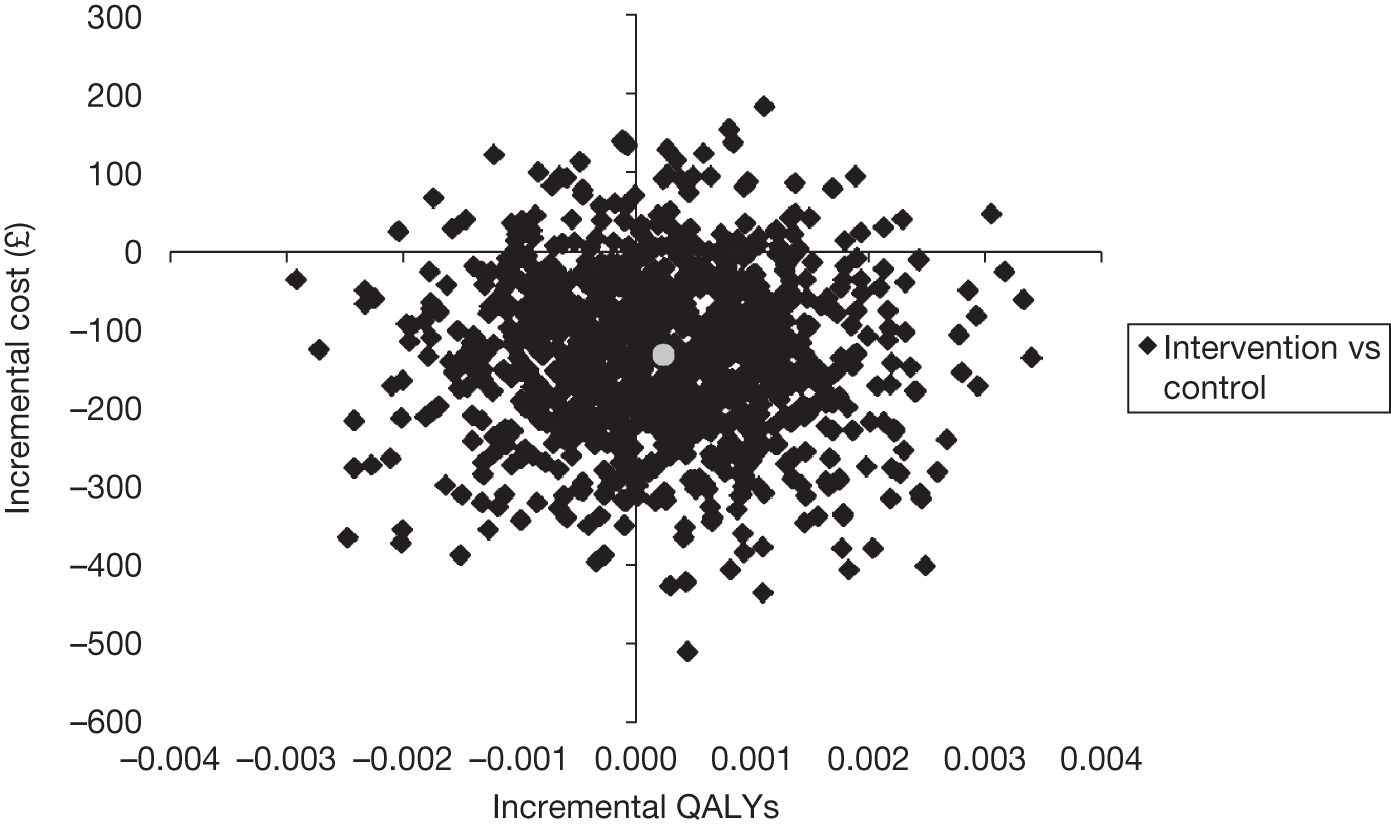
FIGURE 28.
Cost-effectiveness acceptability curve for nitrofurazone vs PTFE.
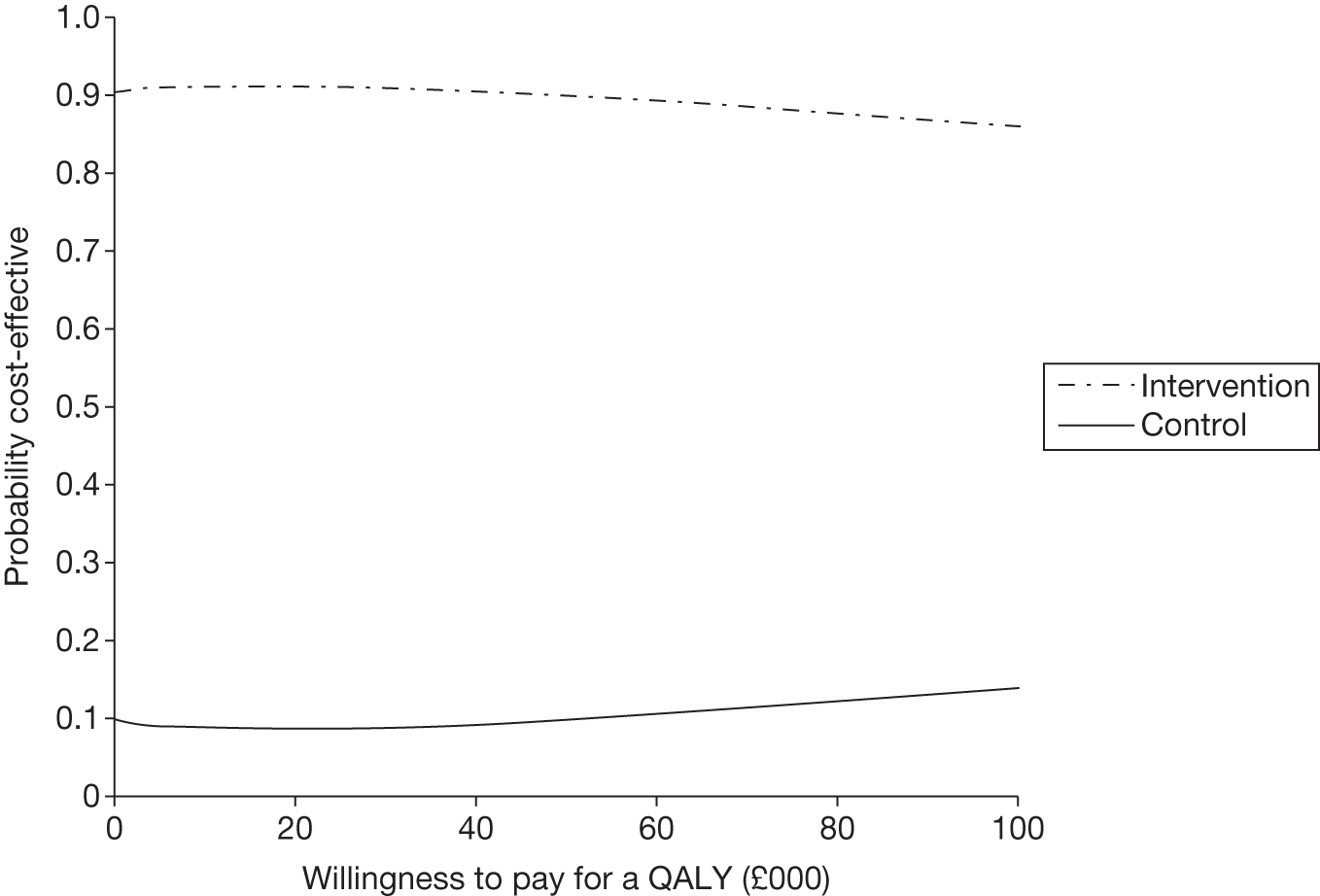
The unadjusted results of the silver alloy group compared with PTFE were similar to those of the adjusted analysis as the differences in QALYs and cost were smaller than reported for the base-case analysis. As a consequence this slightly increased the probability of silver alloy being considered cost-effective at all threshold values for society’s willingness to pay for a QALY considered (Figures 29 and 30).
FIGURE 29.
Representation of the uncertainty in differential mean costs and QALYs for silver alloy vs PTFE.

FIGURE 30.
Cost-effectiveness acceptability curve for silver alloy vs PTFE.
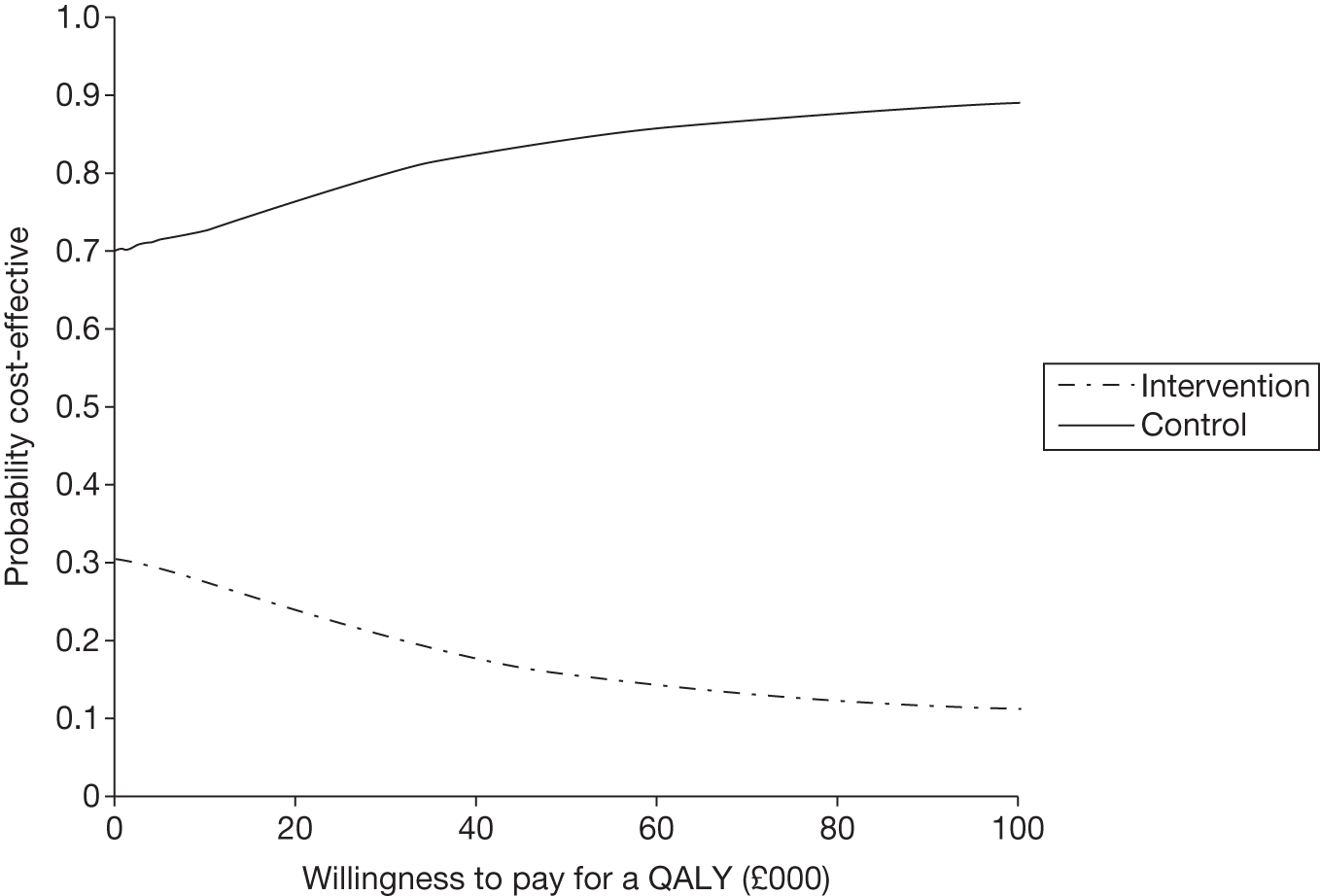
Appendix 8 The CATHETER trial protocol
The CATHETER trial
Types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation.
Protocol
The CATHETER trial
Title of trial: types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation.
This protocol describes a major multicentre UK trial to establish whether using different types of urethral catheters, coated with antibiotic or antiseptic, in adults requiring short-term catheterisation can reduce symptomatic urinary tract infections. The study is designed to be as simple as possible for those participating and those involved in clinical care.
Recruitment officers in each centre will identify and recruit patients who require short-term catheterisation and collect patient information and urine samples. Patients will be followed up at 3 days and 1 and 2 weeks post catheter removal, and at 6 weeks following randomisation.
Trial basics
Full title of study
Types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation: multicentre randomised controlled trial of antibiotic and antiseptic impregnated urethral catheters (the CATHETER trial).
(Keywords: short-term urethral catheter, anti-microbial, silver alloy, nitrofurazone, silicone, randomised controlled trial, catheter-associated symptomatic urinary tract infection, bacteriuria, bacteraemia, cost–benefit analysis)
Acronym
None.
Contact trialist
| Position | Chief Investigator | Trial manager |
| Name | James N’Dow | Kath Starr |
| Address | Academic Urology Unit, Health Sciences Building, University of Aberdeen, AB25 5ZD | Academic Urology Unit/HSRU, Health Sciences Building, University of Aberdeen, AB25 5ZD |
| Telephone | 01224 554963 | 01224 559644 |
| Fax | 01224 554580 | 01224 554580 |
| j.ndow@abdn.ac.uk | k.starr@abdn.ac.uk |
The need for a trial
What is the problem to be addressed?
Development of symptomatic urinary tract infection in adults following short-term urethral catheterisation in hospitalised adults.
What are the principal research questions to be addressed?
What is the clinical benefit and cost-effectiveness of using antibiotic- or antiseptic-impregnated urethral catheters over standard urethral catheters in hospitalised adults requiring short-term catheterisation? Two pragmatic comparisons will be made comparing catheters, as they would be used in the NHS:
-
antibiotic-impregnated (nitrofurazone) catheter versus ‘standard’ PTFE (PolyTetraFluoro-Ethylene)-coated latex catheter
-
antiseptic-impregnated (silver alloy) catheter versus ‘standard’ PTFE (PolyTetraFluoro-Ethylene)-coated latex catheter.
The hypothesis being tested is that use of either of the impregnated catheters will reduce the incidence of catheter-associated symptomatic urinary tract infection by 40% relative to the standard PTFE coated latex catheter (an absolute reduction of around 3%).
Why is a trial required now and what is the available evidence?
25% of patients admitted to hospital will require urethral catheterisation at some stage during their stay1, and the risk of developing bacteriuria, the presence of bacteria in the urine, in catheterised patients is approximately 5% per day increase1. It has been estimated that symptomatic urinary tract infection occurs in approximately 20% of patients with bacteriuria2,3 whilst bacteraemia, the presence of bacteria in the blood, occurs in up to 4% of these patients4,5. Catheter-associated symptomatic urinary tract infections (CASUTI) are the leading cause of hospital acquired infections, accounting for between 23% and 40% of all cases6,7, and such infections result in additional morbidity3,5 and mortality8 and represent a considerable economic burden to the health-care sector, patients and their carers9,10. Consequently, any intervention that reduces the incidence of CASUTI may have wide-ranging repercussions. A wide variety of preventive approaches have been investigated, including mental care measures, pre-connected catheter-collection systems, antiseptic drainage bags, routine bladder irrigation, and prophylactic antibiotics, but the evidence in support of these measures is weak at best11. However, coating of urinary catheters with antibiotic or antiseptic compounds is thought to be a potentially effective preventative measure. Both, however, are more expensive than standard uncoated catheters.
A recent Cochrane review of randomised controlled trials12 concluded that the silver alloy impregnated catheter (an antiseptic impregnated catheter) has the most evidence of benefit out of the antibiotic/antiseptic impregnated urethral catheters available. However, the included trials were small and of poor or moderate quality. A reduction in risk of catheter-associated urinary tract infections by up to 40% was reported in hospitalised adults having a short-term catheter. The evidence for antibiotic-impregnated urethral catheters was even weaker, with only one type of catheter (i.e. minocycline and rifampicin impregnated catheter) from one trial being considered in the review12. However, minocycline and rifampicin impregnated catheters are no longer available (oral communication with Cook Urological, 03/10/05). Another recent small trial investigating a different type of antibiotic-impregnated catheter (nitrofurazone impregnated urethral catheter, marketed by Rochester Medical) revealed no evidence of a difference in the incidence of bacteriuria between the nitrofurazone impregnated and standard silicone catheters in patients catheterised for up to 1 week13, although confidence intervals were wide.
In summary, the majority of clinical trials conducted thus far have been small and of poor to moderate quality in terms of trial methodology and design, outcome measures (such as reporting of bacteriuria rather than symptomatic urinary tract infection) and the lack of a comprehensive evaluation.
How will the results of this trial be used?
The trial results will have implications for the management of patients requiring short-term urethral catheterisation in hospital and rationalise catheter-purchasing policies for large organisations like the NHS. If the use of an antibiotic or antiseptic impregnated urethral catheter leads to a significant reduction in CASUTI compared with a standard catheter and proves to be cost-effective, it will inform future short-term catheter policies in secondary care. In addition, the trial will also explore whether in high-risk sub groups more expensive catheters might be more likely to be cost-effective. The trial will clarify amongst currently available catheters, which should be used in the NHS.
Research methods (including feasibility study results)
Results of audit of short-term catheter policies
A one week audit was conducted in Aberdeen Royal Infirmary and Freeman Hospital (Newcastle) in October 2005. The purpose of the audit was to determine current short-term catheter policies across specialities and to identify high volume users. Elements of practice reviewed included the number of catheterisations performed, types of catheters used, indication for catheterisation, estimated duration of catheterisation, and use of prophylactic and concurrent antibiotic therapy. Data from hospital purchasing department records for each individual ward was also reviewed to determine general trends in number and type of catheters used over a 12-month period and to provide further supporting evidence of high volume users. There were 148 short-term urethral catheterisations reported during that week. PTFE-coated latex catheters were most commonly used (74%). Antibiotic prophylaxis was used in 39%, and 20% of patients were already on concurrent antibiotics at the time of catheterisation. Catheter-related urinary sepsis was documented in 29 cases (20%), of which 17 (11%) had culture-positive urinary infections.
Results of feasibility study of short-term catheter in secondary care
Following on from the audit we undertook a feasibility study. The aim of the 2 week feasibility study was to devise and test recruitment methods, baseline questionnaires, and to provide estimates of numbers likely to be eligible for the trial. The feasibility study aimed to replicate the main study protocol including randomisation and was undertaken in Aberdeen Royal Infirmary in four different clinical specialities. These specialities were identified as high volume users of short-term catheters from the audit (Results of audit of short-term catheter policies above), namely General Surgery, Acute Medical Assessment Unit, the Stroke Unit and Gynaecology. The first week of the two-week feasibility study was dedicated to fine-tuning the practicalities of the study in the Urology ward because of the experience of the medical and nursing staff and then rolled out to the other specialities towards the end of the first week. A dedicated researcher visited the four wards daily. Of 14 patients identified during their hospital admission requiring a short-term catheter, nine were approached and five were missed. All nine approached agreed and consented to take part in the feasibility study. Thus our estimate of 60% of those approached likely to want to participate (Table 1) is conservative, though based on a small sample.
| Participants with a short-term catheter | |
|---|---|
| Participants needed per arm (minimum) | 1970 |
| Allowing for 17% dropout | 2362 |
| Total number of participants needed in 3 arms | 7086 |
Design
A ten-centre randomised controlled trial testing three short-term urinary catheter policies in a range of high-volume clinical settings. Participants will be randomised either by using a telephone system or a web-based system. The Centre for Healthcare Randomised Trials (CHaRT), Health Services Research Unit, University of Aberdeen, as the Trial Data Centre, will manage the randomisation process. As at June 2008, ten centres have agreed to participate: Newcastle upon Tyne Hospitals NHS Trust, City Hospitals Sunderland NHS Foundation Trust, Gateshead Healthcare NHS Foundation Trust, Aberdeen Royal Infirmary NHS Grampian, Raigmore Hospital NHS Highland, Southampton University Hospitals NHS Trust, Northumbria Healthcare NHS Foundation Trust, Western General and Royal Infirmary of Edinburgh Hospital NHS Lothian, Bristol Royal Infirmary United Bristol Healthcare NHS Trust and Hillingdon Hospital NHS Trust.
Setting
Secondary care units with a high volume of short-term catheterisation. In October 2005, an audit of catheter use in Newcastle and Aberdeen identified high volume units including: surgical specialities, general medical wards, care of the elderly wards, high dependency and intensive care units. These are the specialities that will be targeted in the main trial.
Inclusion/exclusion criteria
-
Inclusion:
-
– Adult patients (≥16 years of age) requiring urethral catheterisation (expected to be required for a maximum of 14 days), in pre-selected units with a high volume of short-term catheterisation.
-
-
Exclusion:
-
– Patients for whom urinary catheterisation is expected to be long-term (i.e. > 14 days).
-
– Urological intervention or instrumentation within preceding 7 days (e.g. catheterisation, cystoscopy, prostatic biopsy and nephrostomy insertion).
-
– Non-urethral catheterisation (e.g. suprapubic catheterisation).
-
– Known allergy to any of the following: latex, silver salts, hydrogel, silicone or nitrofurazone
-
– Any patient who has a microbiologically confirmed symptomatic urinary tract infection, at time of randomisation.
-
– Unable to give informed consent.
-
The planned trial interventions
-
Experimental groups: There will be two experimental groups managed with:
-
silver alloy impregnated hydrogel urethral catheter (S).
-
nitrofurazone impregnated silicone urethral catheter (N).
-
-
Control group
There will be one control group managed with a PTFE coated latex urethral catheter – the ‘standard’ control (P).
Participants will be randomised 1:1:1 to the three groups. Size 14 Ch catheters will be used for all three arms. The choice of catheter as ‘standard’ control was based on the results of the audit of short-term catheter use in all secondary care wards in Newcastle and Aberdeen (see Results of audit of short-term catheter policies), which confirmed that the PTFE-coated latex urethral catheter was the most commonly used in both hospitals (over 70%); it is also relatively inexpensive compared with the coated catheters (at approximately £0.86 each for the PTFE-coated catheter vs £5.50 for the antiseptic coated and £4.50 for the antibiotic coated, 2007 prices).
Each catheter will have a detachable sticker attached to the outer packaging. This sticker will display the ‘CATHETER’ logo and either ‘N’, ‘S’ or ‘P’ to denote catheter type (N, Nitrofurazone; S, Silver; P, PTFE). These stickers will then be stuck directly onto Patient Consent Forms so as to determine that the patient was given the catheter they were randomised to.
Proposed outcome measures
Primary clinical outcome measure
Incidence of symptomatic urinary tract infection at any time up to 6 weeks post randomisation (number of participants with at least one occurrence). This will be defined as any symptom reported at 3 days or 1 or 2 weeks post catheter removal or 6 weeks post-randomisation combined with a prescription of antibiotics, at any of these times, for presumed symptomatic UTI.
Subgroup analyses of the primary outcome will examine possible effect modification of age, gender, co-morbidity, duration of catheterisation, indication for catheterisation, and antibiotic use prior to enrolment.
Secondary clinical outcome measures
Microbiological support of the primary outcome. Defined as those who fulfil the criteria for the primary outcome and in addition have any microbiologically positive result where there is ≥ 104 CFU/mL of no more than two different species of uropathogen.
Tertiary clinical outcomes
Early symptomatic urinary tract infection, defined as any self reported symptom with a prescription of antibiotics and a positive microbiological test (≥ 104 CFU/mL of no more than two different species of uropathogen) between randomisation and 3 days post catheter removal.
Individually analyse the components of the definition of the primary and secondary outcome:
-
Any self-reported symptoms.
-
Any antibiotic prescription for presumed symptomatic UTI.
-
Any microbiologically positive result (≥ 104 CFU/mL of no more than two different species of uropathogen).
Health-related quality of life measured by the EQ-5D up to 6 weeks.
Other significant clinical events: septicaemia and mortality.
Adverse effects of catheterisation apart from symptomatic UTI (e.g. urethral discomfort and pain on removal).
Antibiotic use following randomisation and indication.
Assessment of the risk of anti-microbial resistance towards silver and nitrofurazone using urine specimens from patients, or catheter tips, diagnosed with symptomatic UTI and bacteriuria14.
Secondary economic outcome measures
-
Incremental cost per infection averted and QALYs gained.
-
Cost to the NHS and patient of the different catheters.
-
Quality-adjusted life-years (QALYs) estimated from EQ-5D responses.
Proposed duration of intervention
The mean period of urethral catheterisation is expected to be between 1 and 14 days.
What is the proposed frequency and duration of follow-up and how will outcome measures be measured?
Following enrolment in the trial, a mid-stream specimen of urine will be sent for microbiological analysis (i.e. microscopy, culture and sensitivity) immediately prior to catheterisation, if one has not been sent within the preceding 48 hours (baseline sample). Where this is not possible, a specimen of urine will be obtained during catheterisation (i.e. catheter-specimen of urine) using standard aseptic techniques. Urine will also be collected again for microbiological analysis within, or at, 3 days after catheter removal. If patients are discharged home prior to the third post-catheter removal day a sample will be taken as close to the 3 day after removal time point as possible. However, patients will also be provided with sterile urine collection bottles to be filled and submitted by post, or local NHS courier service, on the third post-catheter removal day if the sample taken in hospital is before the 3 day removal time point. If a clinical diagnosis of symptomatic UTI is made at any stage, including during the period of catheterisation, either a catheter-specimen or mid-stream specimen of urine will be obtained by ward staff or the patient’s GP according to normal clinical practice.
Participants will complete the following questionnaires at the specified time points:
-
baseline questionnaire (EQ-5D and a urinary symptom questionnaire) around the time of recruitment
-
a 3 days after catheter removal questionnaire (Urinary Symptoms and EQ-5D)
-
patient diary to be completed at 1 and 2 weeks after catheter removal (will contain specific UTI questions and EQ-5D)
-
final set of questionnaires (i.e. EQ-5D and specific Health Economic questionnaires) 6 weeks after randomisation.
The questionnaires will be targeted at identifying symptomatic UTI as well as other catheter-associated problems (e.g. urethral discomfort), quality of life, and any health economic implications such as costs to the patients and the NHS. Questionnaires completed prior to hospital discharge will be collected by the Recruitment Co-ordinator. Questionnaires completed after hospital discharge will be posted back to the Data Centre (CHaRT, University of Aberdeen); patients will be supplied with a discharge pack containing the relevant questionnaires and stamped addressed envelopes. The Recruitment Co-ordinator will telephone participants when at home to remind and help them to complete Trial questionnaires and submit urine samples. This will also provide another opportunity to answer any questions the participants may have about the Trial and the associated paperwork. This phone call system will not be standard practice and will only be used when participants fail to send back questionnaires or urine samples once they have been discharged from hospital.
Collection of information to describe UTIs
Information will be collected in five phases to contribute data to identify UTIs.
| 1. | During catheterisation | Ward-based diagnosis from symptoms, observations and microbiology or clinician directed use of antibiotics for UTI – data recorded by trial co-ordinator |
| 2. | 3 days post catheter removal | Urine specimen and symptoms will give symptomatic UTI, asymptomatic UTI and symptomatic sterile urine – data recorded by participant |
| 3. | 1 and 2 weeks post catheter removal | Patient diary will record symptoms and clinician contact together with antibiotic usage – data recorded by patient; this will give evidence of symptoms, clinician diagnosis but no microbiology unless patient/GP requests urine sample |
| 4. | 6 weeks post randomisation | Clinician contact, antibiotic usage and hospital readmissions will be gathered |
Proposed sample size
Based on the Cochrane review and other data12,15,16, the anticipated incidence of UTI in the standard control group is 7%. Given that this trial is assessing patient reported outcomes rather than microbiology or clinician reported symptoms, the predicted incidence rate of UTIs is 11% and it is reasonable to hypothesise that the impregnated catheters will reduce this to about 8%. The increased cost associated with use of the silver alloy and nitrofurazone catheters is further justification for aiming to identify an effect of this size. With 90% power and alpha set at 2.5% rather than 5% (to adjust for the two comparisons of antibiotic impregnated catheter and control catheter, and antiseptic impregnated catheter and control catheter), and using chi-square tests of association to compare the incidence of CASUTI in an intervention group and the control group, the trial would require an estimated 1970 fully followed up participants per group, inflated to 2362 per group to allow for an observed loss to follow up of 17%, giving a total of 7086.
Statistical analysis
All primary analyses will be according to the intention-to-treat principle, and will be governed by a Statistical Analysis Plan, which will be agreed by the Trial Steering Committee (TSC). The outcomes listed in Proposed outcome measures will be compared with (a) antibiotic impregnated and control and (b) antiseptic impregnated and control using generalised linear models (for example, for the primary outcome of proportion of participants with symptomatic catheter associated infection, a logistic regression model will be used, adjusting for any covariates felt to be of prognostic importance). Nominal 95% confidence intervals will be calculated. Subgroup analyses will examine possible effect modification of age, gender, co-morbidity, duration of catheterisation, indication for catheterisation, and antibiotic use prior to enrolment using tests for interaction (all at stricter levels of significance P< 0.01). We will also explore the comparison of antibiotic and antiseptic groups. A single main analysis will be performed at the end of the trial when all follow up has been completed. An independent Data Monitoring Committee (DMC, see below) will review confidential interim analyses as frequently as requested (see Independent supervision) of accumulating data but at least annually.
Economic evaluation
The economic evaluation will be integrated into the trial. Outcomes and costs will be assessed from the perspective of the NHS and patients for a 6-week time horizon. The alternatives compared are described in The planned trial interventions.
Effectiveness will be measured in terms of number of symptomatic urinary tract infections up to 6 weeks after randomisation and quality-adjusted life-years (QALYs) at six weeks. QALYs will be derived using data from EQ-5D administered at baseline, 3 days, 1 week, 2 weeks and at 6 weeks post randomisation as part of the main study questionnaires. These responses will be converted into health state utilities using UK population tariffs. The estimation of QALYs will take account of the mortality of study participants. Participants who die within the study follow-up will be assigned a zero utility weight from their death until the end of the study follow up. QALYs will be estimated using linear extrapolation between the QALY scores at baseline and all available EQ-5D.
Costs for the six week follow-up will be assessed from the trial. The number of infections will be collected using the baseline questionnaire, the UTI questionnaire completed 3 days after catheter removal, the patient diary at 1 and 2 weeks after catheter removal and from the final questionnaire at 6 weeks. Other cost generating events of the interventions such as the use of primary care services including contacts with primary care practitioners (e.g. GPs and practice nurses) and prescription medications, will be collected using the health-care utilisation questionnaires administered at 1, 2 and 6 weeks follow-up. Use of secondary care services following the period of catheterisation will be collected using the 6 week follow up questionnaire. If patients are identified as having been re-admitted following their discharge, within the 6 weeks post randomisation, they will be further investigated using the NHS Patient Administration System (PAS). This will record information on non-protocol outpatient visits, readmissions relating to the use and consequences of urinary catheters. This approach will ensure that information on the use of secondary care services that could be main determinants of incremental costs can be identified without overburdening the participants.
Estimates of resource utilisation will be combined with unit costs to derive total costs. Unit costs will be based on study-specific estimates and data from standard sources. Participant costs will be based on self-purchased health care (e.g. prescription costs, over the counter medications), will be collected as part of the health-care utilisation questions (see above). The results of these analyses will be presented as point estimates of mean incremental costs, QALYs and cost per QALY. Measures of variance for these outcomes will be derived using bootstrapping and deterministic sensitivity analysis will be used to explore other forms of uncertainty (e.g. the exploration of the implication of extrapolating outcomes beyond the 6 weeks time horizon). Similar sub-group analysis to that described in Statistical analysis will also be undertaken.
A simple decision model will be developed to compare the different catheters in terms of the loss of quality of life (based on the responses to the EQ-5D collected as part of the trial) and change in cost caused by a symptomatic catheter-associated infection. In this analysis it will be assumed that the only loss of quality of life will be caused by a symptomatic catheter-associated infection and that the type of catheter does not affect quality of life except by changing the risk of a symptomatic catheter-associated infection occurring. Regression methods will be used to estimate the loss of quality of life for those with a symptomatic catheter-associated infection compared with those without a symptomatic catheter-associated infection. A similar approach will be used to estimate costs associated with developing a symptomatic catheter-associated infection compared with costs for those without a symptomatic catheter-associated infection. Estimates of cost for each arm of the decision model (i.e. each type of catheter) will be adjusted to reflect the cost of using the catheter. Probabilistic sensitivity analysis will be performed along with deterministic analysis to reflect other forms of uncertainty within the model.
Practical arrangements for identifying and allocating participants to trial groups
(a) Identifying potentially eligible participants: A potentially eligible participant will be identified by either ward staff, operating theatre staff, or by the local recruitment co-ordinator. The recruitment co-ordinator will visit the wards daily to check on possible activity that day and by doing so, also promote the trial. Laminated recruitment sheets will be placed prominently at the nurses station/doctors room on the wards. Participants will be identified according to the pre-stated inclusion and exclusion criteria from pre-determined high volume units. The local recruitment co-ordinator will obtain informed consent (see below) and ensure completion of in-hospital questionnaires and other data collection.
(b) Informed consent: Participants will be provided with written information and will sign a consent form once they have had enough time to understand the implications and requirements of the trial. The only exception to this will be for adults in an emergency situation.
In emergency situations common reasons for short-term catheterisation are acute urinary retention or for monitoring purposes in an unwell patient. These patients will be provisionally included in the trial according to a protocol which will respect both their right to best quality care and the ethical requirement of informed consent. As the decision to catheterise is based solely on clinical need by the caring physician, we propose that a randomised catheter is used in an emergency situation. Once the patient’s condition has settled, they will be provided with an information sheet and an opportunity to opt out of the trial if they wish, with assurances that such a decision will not affect the level of care they receive. As the antiseptic/antibiotic-impregnated catheters are reported to lessen the risk of infection compared with the usual standard catheter, we feel this proposed protocol for including adults in emergency situations is justified. Ethics Committee approval was secured from the all Research Ethics Committees involved in the trial to include such patients in the study using the above arrangements for post-procedure consent or withdrawal.
Although unlikely, we have anticipated a situation whereby a patient may have been randomised and is discharged before the recruitment co-ordinator can obtain informed consent (e.g. if over the weekend). Therefore, we propose to send a letter to any patient that may have been randomised to the trial and ‘missed’ by the recruiter. This letter will describe the trial, a patient information sheet will also be sent, and will invite them to participate in the trial. They will be asked to contact the recruitment co-ordinator if they are interested in taking part in the trial. A copy of the letter that will be sent to the patient is enclosed.
(c) Recruitment: The feasibility study and audit indicated that although the ‘office hours’ are busy periods for the flow of potentially eligible participants, it will be necessary to be able to recruit throughout the 24 hour period. The telephone randomisation system is the easiest way to effectively recruit throughout this period.
(d) Randomisation: Eligible participants will be randomised centrally by simple randomisation to the three groups using either by telephone to the automated IVR telephone randomisation application at CHaRT in Aberdeen.
(e) Data Management. The recruitment co-ordinator, during the daily round, will input the last session’s data via the study web portal to the Study Data Centre in Aberdeen on a daily basis.
(f) Use of Posters. The inclusion of posters to be displayed in the treatment rooms of wards taking part in the trial as reminders of:
-
the trial and
-
the catheters to be used in the trial.
Posters are also to be included in admission lounges and ward areas to highlight the trial to eligible patients. It is hoped that this will alert patients to the trial so that when they are approached to take part, they have some familiarity with the research. Each site will have posters than contain site specific contact details.
(g) Withdrawal: Any patient who is withdrawn from the study for personal or medical reasons will be recorded appropriately using a specific Withdrawal Form. The form will record what the patient has withdrawn from e.g. questionnaires being sent, their hospital and GP records being accessed (for the results of medically indicated urine samples and antibiotics prescribed for UTIs) and contact by the CATHETER team.
Some patients will be classed as post-randomisation exclusions as opposed to withdrawals. Patients who will be categorised as post-randomisation exclusions are as follows:
-
emergency patients who retrospectively refuse consent
-
those patients who are randomised due to medical intention to catheterise but are never catheterised
-
those patients who are randomised but receive a suprapubic catheter in theatre.
In line with this a notice (a CATHETER compliments slip, see enclosed) documenting that the patient was never catheterised or received a suprapubic catheter will be placed in the patients notes. The recruiter will explain to the patient that they are no longer in the trial.
Methods for protecting against other sources of bias
As indicated, the study will be open, with at least the antibiotic catheter easily identifiable by its unavoidably bright yellow colour. The concern about ‘open’ use of catheters is that knowing which catheter has been used might influence clinical decisions, such as about sending a urine specimen for culture or removing a catheter. To guard against bias introduced in this way, we shall standardise clinical policies in these respects. Further protection comes from the fact that the person inserting the catheter is unlikely to be the same person making later clinical decisions specifically regarding timing of catheter removal. All urine samples will be tested ‘blind’ to the catheter allocation. Outcome assessment in terms of symptoms of UTI will be made by patient self-completed questionnaires. Participants will not be told until the end of the study which catheter has been used to protect against the influence of preconceptions on the participants’ side in respect of self-reported outcomes. While researchers will be blinded to type of catheter, clinical staff performing the catheterisation will not be.
To attempt to standardise catheter insertion technique, catheter care, catheter urine sampling and catheter removal policies, a protocol has been developed and tested in the feasibility study and will be implemented in all centres involved in the trial. This protocol incorporates principles of ‘Best Practice’ based on published guidelines17. In addition, the protocol also advocates that patients with asymptomatic bacteriuria should not routinely be treated with antibiotics18. Catheter care violations, such as inappropriate collection of urine (e.g. from catheter bag rather than from the sampling port or accidental disconnection of the closed-drainage system) will be recorded to attempt to explain false-positive diagnosis of bacteriuria12. Every attempt will also be made to record any catheter changes or reinsertion of a catheter during the trial period.
Ethical arrangements
This project has been approved by the Grampian MREC. We believe this is a very low risk study, with a correspondingly favourable risk: benefit ratio, since both patients and society (through efficient allocation of resources within NHS) will benefit from the results of the research. We do not anticipate that there will be risks to participants, and they may benefit from participation in the trial. Society will benefit from the conclusions of the research, which will be used to inform future short-term catheter policies in secondary care. An information leaflet will be given to each potential participant to inform them of the benefits and known drawbacks that may apply. Informed signed consent will be obtained from the participants in all centres. Participants who cannot give informed consent (e.g. due to their mental state) will be excluded. The trial will be co-ordinated from a centre with considerable experience of multicentre trials (CHaRT), cognisant of the implications of research governance and other legal frameworks for the conduct of trials. This is not classed as a trial of any investigational medicinal products or Medical Devices, and so does not come under the EU Clinical Trials Directive. Nevertheless we will conduct the study to the standards required by ICH GCP, and the NHS and Universities Research Governance as well as all other applicable legal, ethical and regulatory requirements.
The risk of adverse events associated with catheterisation is minimal. Please see appendix 1 for further information on SAE reporting.
Arrangements for independent supervision are described below.
Independent supervision
A Trial Steering Committee that will include an independent Chairperson and other independent members and a consumer representative will oversee the trial. The Steering Committee will meet at least three times over the course of the study, and at least annually. The DMC will meet early in the trial to agree its terms of reference and other procedures. While its deliberations will take into account the full implications of any recommendations it may choose to make (such as whether or not any interim findings are sufficiently convincing to change clinical practice), the statistical guidelines adopted are likely to be those suggested by Peto19 based on a difference in a main outcome measure of at least three standard deviations. The DMC will report any recommendations to the Chairperson of the TSC.
Source of funding for study
The study is funded by the UK NHS Health Technology Assessment Programme.
Participating centres
The following centres have agreed in principle to take part in the trial:
Aberdeen Royal Infirmary NHS Grampian
Newcastle upon Tyne Hospitals NHS Trust
City Hospitals Sunderland NHS Foundation Trust
Gateshead Healthcare NHS Foundation Trust
Raigmore Hospital NHS Highland
Southampton University Hospitals NHS Trust
Northumbria Healthcare NHS Foundation Trust
Royal Infirmary of Edinburgh NHS Lothian
Bristol Royal Infirmary United Bristol Healthcare NHS Trust.
Project timetable and milestones
Duration 33 months
1–6 months: set up office, assemble team, secure ethical approval
7–12 months: establish eight centres
7–24 months: identify and recruit 5700 participants requiring short-term catheterisation (an average of 720 is feasible in each of the eight centres based on the Newcastle and Aberdeen audits)
10–25.5 months: follow up at 6 weeks
25.5–33 months: complete data collection, analysis and dissemination.
Figure 1 shows the projected recruitment of centres and participants, and projected number who would be approached. Our plan is to establish two centres relatively early in the project (by seven months) and to roll out to the others over the subsequent five months. We recognise that this will need prior preparation. An application to MREC will be submitted between funding decision and the start date.
FIGURE 1.
Projected recruitment chart.
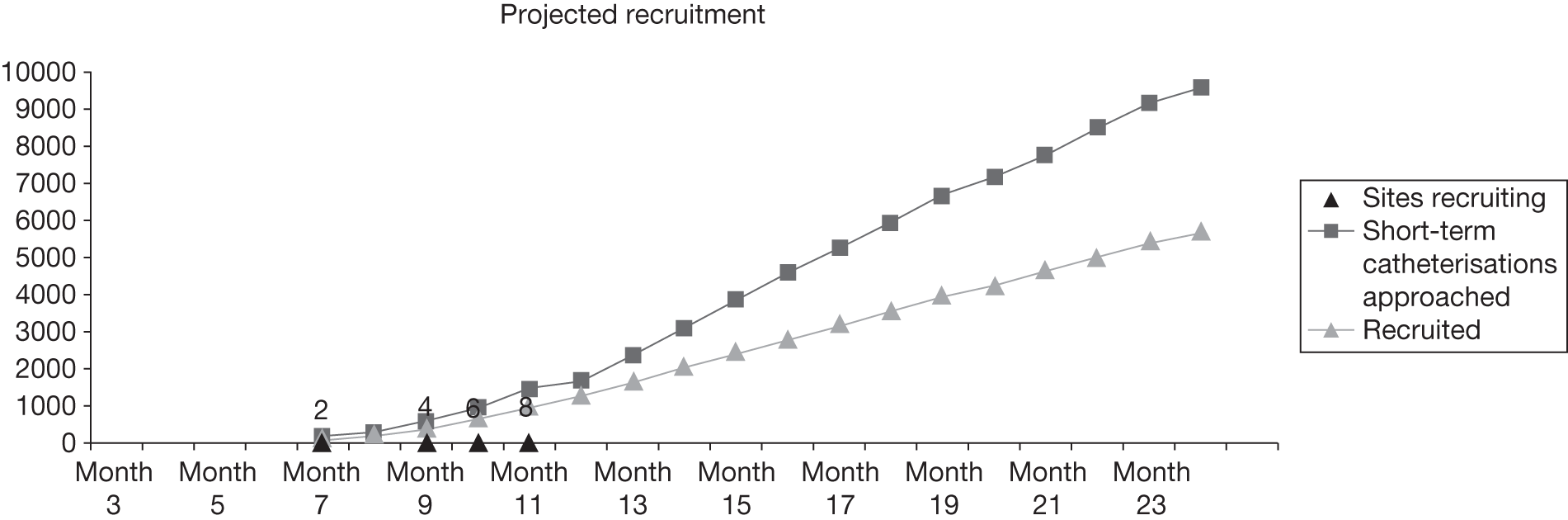
The participant recruitment graph in Figure 1 has been modelled to take into account: the rollout to the centres over the first 5 months and that there are likely to be slightly fewer short-term catheters inserted around August and over Christmas due to a reduction in elective surgical throughput.
Milestones
Based on the groundwork that has already been done, particularly the feasibility study and audit of short-term catheter policies, we believe that we are ready to mount the full trial. However, specific, time-related milestones have been listed in Table 2, to allow close monitoring of progress.
| Year one | |
|---|---|
| By month 2 | MREC approval |
| By month 7 | Set up office and administrative base |
| Construct access database, including randomisation program | |
| Establish first two centres | |
| (LREC approval, R&D negotiations, appoint local recruitment co-ordinator) | |
| By month 9 | First Steering Committee Meeting |
| Establish third and fourth centres | |
| By month 12 | First Data Monitoring Committee meeting. Roll out to further four centres |
| 1285 participants recruited | |
| Year two | |
| By month 18 | 3595 participants recruited |
| By month 24 | Second Steering Committee meeting. Second Data Monitoring Committee meeting |
| 5700 participants recruited | |
| Year three | |
| By month 25.5 | Follow up of participants at 6 weeks after randomisation completed |
| By month 32 | Data analysis completed |
| By month 33 | Final Steering Committee meeting |
| Submit Final Report and main papers describing the trials | |
Expertise
The applicants are a multidisciplinary team that includes clinical experts, a consumer representative, experienced trialists, statisticians and health economists. They will form a Trial Management Group. James N’Dow (the Lead Applicant), Rob Pickard and Thomas Lam are academic urologists with a special interest in incontinence and members of the Cochrane Incontinence Group. James N’Dow and Cathryn Glazener are editors of the Cochrane Incontinence Group responsible for delivering the Cochrane review that prompted the call for this trial. Adrian Grant is the Co-Chairperson of the Cochrane Collaboration and has many years experience of multicentre trials. John Norrie is an experienced trialist and medical statistician and is Director of the Aberdeen Centre for Healthcare Randomised Trials (CHaRT). Luke Vale is Professor in Health Technology Assessment with a joint appointment between the Health Economics Research Unit and the Health Services Research Unit in Aberdeen. All have extensive experience in the design, conduct, analysis and reporting of multicentre trials. Brian Buckley has an academic interest in patient/carer representation, and is the current chairperson of Incontact, a charitable organisation advocating consumer issues in incontinence. Kathy Orr is a consultant microbiologist with a special interest in UTIs. Mary Kilonzo is a Research Fellow in Health Economics. Graeme MacLennan is an experienced statistician in the Health Services Research Unit in Aberdeen. Kathy Getliffe brings expertise from a nursing perspective.
Consumers
One of the applicants, Brian Buckley, is chairperson of Incontact, a consumer group for people with continence problems. Dr Buckley will be a member of both the Trial Management Group and Trial Steering Committee. He has contributed to the development of the design of the proposed study and to this application. We have sought, and will continue to seek, Dr Buckley’s advice (and through him, the advice of other members of Incontact) to ensuring that we take into account patient and carer views of the acceptability and relevance of the trial. We shall (through Brian Buckley) involve Incontact in the dissemination of the study findings.
Appendix 1: Reporting of serious adverse events
The CATHETER trial involves conservative interventions which are well established in clinical practice, we do not anticipate any adverse effects which are related to the catheter. However, due to the nature of the trial (e.g. hospital setting, patients undergoing surgery) some patients are at risk of any of the events listed below. We will monitor all of these events but will only report those which are believed to have a causal relationship to the intervention which the patient was randomised to.
Collaborators and participants may contact the chairperson of the Steering Committee through the Study Office about any concerns they may have about the study. If concerns arise about procedures, participants or clinical or research staff (including risks to staff) these will be relayed to the Chairperson of the Data Monitoring Committee.
All of the following are defined as serious adverse events
-
Resulted in death.
-
Life-threatening.
-
Required inpatient hospitalisation or prolongation of existing hospitalisation.
-
Septicaemia.
-
Persistent or significant disability/incapacity.
- Haley RW, Hooton TM, Culver DH, Stanley RC, Emori TG, Hardison CD, et al. Nosocomial infections in US hospitals, 1975–1976: estimated frequency by selected characteristics of patients. Am J Med 1981;70:947-59.
- Hartstein AI, Garber SB, Ward TT, Jones SR, Morthland VH. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control 1981;2:380-6.
- Garibaldi RA, Mooney BR, Epstein BJ, Britt MR. An evaluation of daily bacteriologic monitoring to identify preventable episodes of catheter-associated urinary tract infection. Infect Control 1982;3:466-70.
- Krieger JN, Kaiser DL, Wenzel RP. Urinary tract etiology of bloodstream infections in hospitalised patients. J Infect Dis 1983;148:57-62.
- Bryan CS, Reynolds KL. Hospital-acquired bacteremic urinary tract infection: epidemiology and outcome. J Urol 1984;132:494-8.
- Haley RW, Culver DH, White JW, Morgan WM, Emori TG. The nationwide nosocomial infection rate. A new need for vital statistics. Am J Epidemiol 1985;121:159-67.
- Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ET. Second National Prevalence Survey of infection in hospitals: overview of the results. J Hosp Infect 1996;32:175-90.
- Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary-tract infection. N Engl J Med 1982;307:637-42.
- Haley RW, Schaberg DR, Crossley KB, Von Allmen SD, McGowan JE. Extra charges and prolongation of stay attributable to nosocomial infections: a prospective interhospital comparison. Am J Med 1981;70:51-8.
- Plowman RM, Graves N, Roberts JA. Hospital Acquired Infection 1997.
- Dunn S, Pretty L, Reid H. Management of short-term indwelling urethral catheters to prevent urinary tract infections. Best Practice 2000;4:1-6. URL: www.joannabriggs.edu.au.
- Brosnahan J, Jull A, Tracy C. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database Syst Rev 2004;1.
- Lee SJ, Kim SW, Cho YH, Shin WS, Lee SE, Kim CS, et al. A comparative multicentre study on the incidence of catheter-associated urinary tract infection between nitrofurazone-coated and silicone catheters. Int J Antimicrob Agents 2004;24:65-9.
- Rupp ME, Fitzgerald T, Marion N, Helget V, Puumala S, Anderson JR, et al. Effect of silver-coated urinary catheters: efficacy, cost-effectiveness and anti-microbial resistance. Am J Infect Control 2004;32:445-50.
- Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control 2000;28:68-75.
- Saint S, Veenstra DL, Sullivan SD, Chenoweth C, Fendrick AM. The potential clinical and economic benefits of silver alloy urinary catheters in preventing urinary tract infection. Arch Intern Med 2000;160:2670-5.
- Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, et al. Epic2: National Evidence-Based Guidelines for Preventing Healthcare-Associated Infections in NHS Hospitals in England. J Hosp Infect 2007;65:1-59.
- Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society . Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis 2005;40:643-54.
- Whitehead J. The Design and Analysis of Sequential Clinical Trials 1997.
- Horan TC, Gaynes RP, Mayhall CG. Hospital Epidemiology and Infection Control. Philadelphia, PA: Lippincott Williams amp; Wilkins; 2004.
Appendix 2: CATHETER trial patient questionnaires and case report forms
Appendix 9 Details of methods used to estimate distributions for model parameters
| Variable name | Parameters/information |
|---|---|
| Cost of no UTI | Log normal, u (mean of logs) = ln(2359), sigma (SD of logs) = sqrt[ln(3375.42/2359) × 2]; expected value: 3375.42 |
| Cost difference | Normal, mean = 547.6296, SD = 425.6165; expected value: 547.6296 |
| PTFE risk | Beta, real-numbered parameters, alpha = 271, beta = 1873; expected value: 0.126399254 |
| Cost difference | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| QALY difference | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| No UTI QALY | Beta, real-numbered parameters, alpha = [(0.07536942) × (1-0.0753694)/(0.02454172)], beta = [0.0753694 × (1 – 0.0753694)/(0.02454172)] – [(0.07536942) × (1 – 0.0753694)/(0.02454172)]; expected value: 0753694 |
| Nitrofurazone risk reduction | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| Silver alloy risk reduction | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| Variable name | Parameters/information |
|---|---|
| Cost no UTI | Log normal, u (mean of logs) = ln(1383), sigma (SD of logs) = sqrt[ln(1805.411/1383) × 2]; expected value: 1805.411 |
| PTFE risk | Beta, real-numbered parameters, alpha = 271, beta = 1873; expected value: 0.126399254 |
| QALY difference | Normal, mean = 0.0069204, SD = 0.0015331; expected value: 0.0069204 |
| Cost difference | Normal, mean = 127.93, SD = 116.55; expected value: 127.93 |
| Nitrofurazone risk reduction | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| Silver risk reduction | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| QALY with a UTI | Beta, real-numbered parameters, alpha = [(0.07961892) × (1 – 0. 0796189)/(0.02061812)], beta = [0.0796189 × (1 – 0.0796189)/(0.02061812)] – [(0.07961892) × (1 – 0.0796189)/(0.02061812)]; expected value: 0.0796189 |
| Variable name | Parameters/information |
|---|---|
| Cost no UTI | Log normal, u (mean of logs) = ln(1844), sigma (SD of logs) = sqrt[ln(2452.314/1844) × 2]; expected value: 2452.314 |
| PTFE risk | Beta, real-numbered parameters, alpha = 271, beta = 1873; expected value: 0.126399254 |
| QALY difference | Normal, mean = 0.0024116, SD = 0.0050177; expected value: 0.0024116 |
| Cost difference | Normal, mean = 988.7469, SD = 471.9682; expected value: 988.7469 |
| Nitrofurazone risk reduction | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| Silver alloy risk reduction | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| QALY with a UTI | Beta, real-numbered parameters, alpha = [(0.09909562) × (1 – 0.0990956)/(0.01904892)], beta = [0.0990956 × (1 – 0.0990956)/(0.01904892)] – [(0.09909562) × (1 – 0.0990956)/(0.01904892)]; expected value: 0.0990956 |
| Variable name | Parameters/information |
|---|---|
| Cost no UTI | Log normal, u (mean of logs) = ln(2317), sigma (SD of logs) = sqrt[ln(3331.245/2317) × 2]; expected value: 3331.245 |
| PTFE risk | Beta, real-numbered parameters, alpha = 271, beta = 1873; expected value: 0.126399254 |
| QALY difference | Normal, mean = 0.0044876, SD = 0.0020633; expected value: 0.0044876 |
| Cost difference | Normal, mean = 1417.482, SD = 209.0975; expected value: 1417.482 |
| Nitrofurazone risk reduction | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| Silver risk reduction | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| QALY with a UTI | Beta, real-numbered parameters, alpha = [(0.07553412) × (1 – 0.075534)/(0.02553342)], beta = [0.075534 × (1 – 0.075534)/(0.02553342)] – [(0. 0755342) × (1 – 0.075534)/(0.02553342)]; expected value: 0.075534 |
| Variable name | Parameters/information |
|---|---|
| Cost no UTI | Log normal, u (mean of logs) = ln(5.29), sigma (SD of logs) = sqrt[ln(13.29876/5.29) × 2]; expected value: 13.29876 |
| PTFE risk | Beta, real-numbered parameters, alpha = 271, beta = 1873; expected value: 0.126399254 |
| QALY difference | Normal, mean = 0.0063294, SD = 0.0013823; expected value: 0.0063294 |
| Cost difference | Normal, mean = 67.94424, SD = 20.29843; expected value: 67.94424 |
| Nitrofurazone risk reduction | Normal, mean = –0.021, SD = 0.01; expected value: –0.021 |
| Silver risk reduction | Normal, mean = 0.001, SD = 0.01; expected value: 0.001 |
| QALY with a UTI | Beta, real-numbered parameters, alpha = [(0.07665482) × (1 – 0.0766548)/(0.02561182)], beta = [0.0766548 × (1 – 0.0766548)/(0.02561182)] – [(0.07665482) × (1 – 0.0766548)/(0.02561182)]; expected value: 0.0766548 |
Appendix 10 Cost/quality-adjusted life-year plots and cost-effectiveness acceptability curves for the base-case and sensitivity analyses
FIGURE 31.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone, PTFE and silver alloy for base-case analysis.
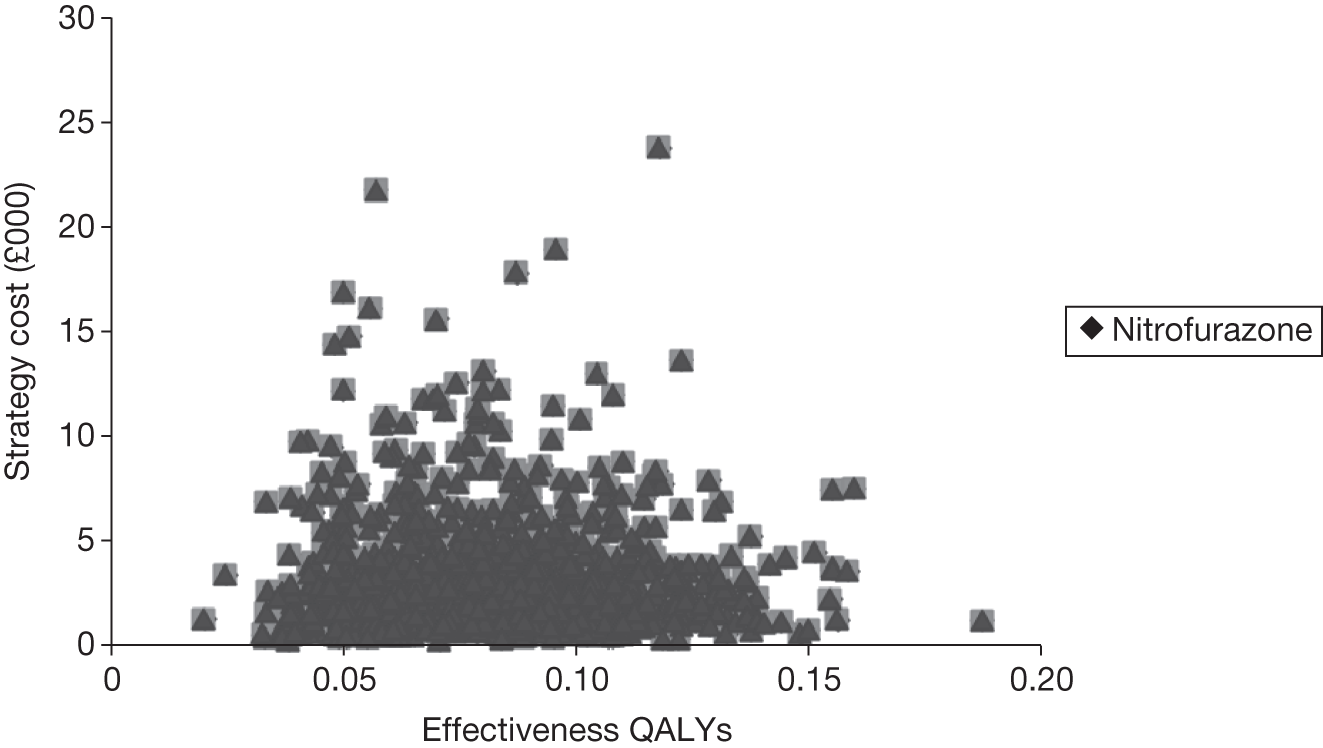
FIGURE 32.
Cost-effectiveness acceptability curve for nitrofurazone, PTFE and silver alloy for base-case analysis.
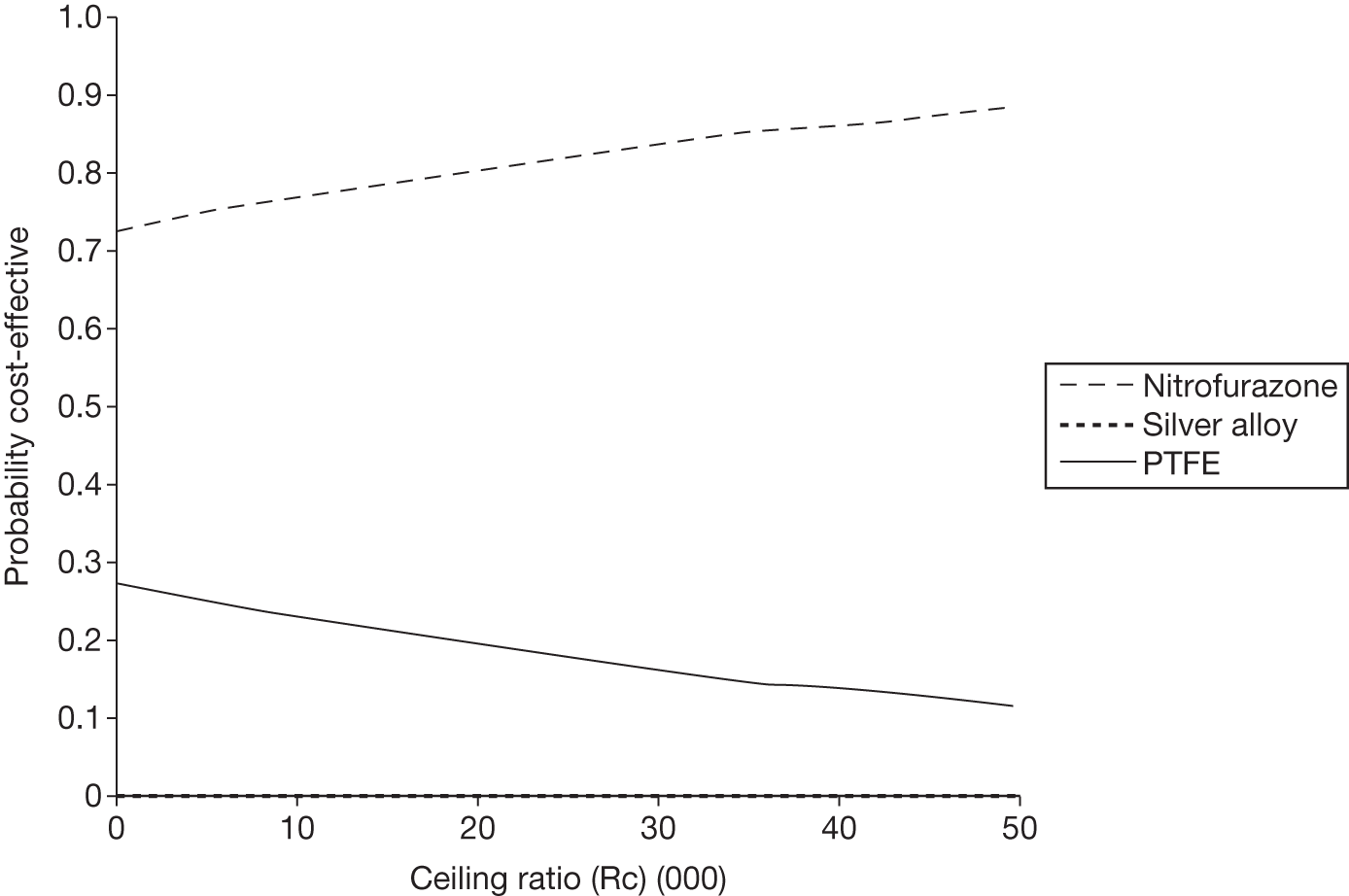
FIGURE 33.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone, PTFE and silver alloy for analysis on patients admitted to maternity specialty.
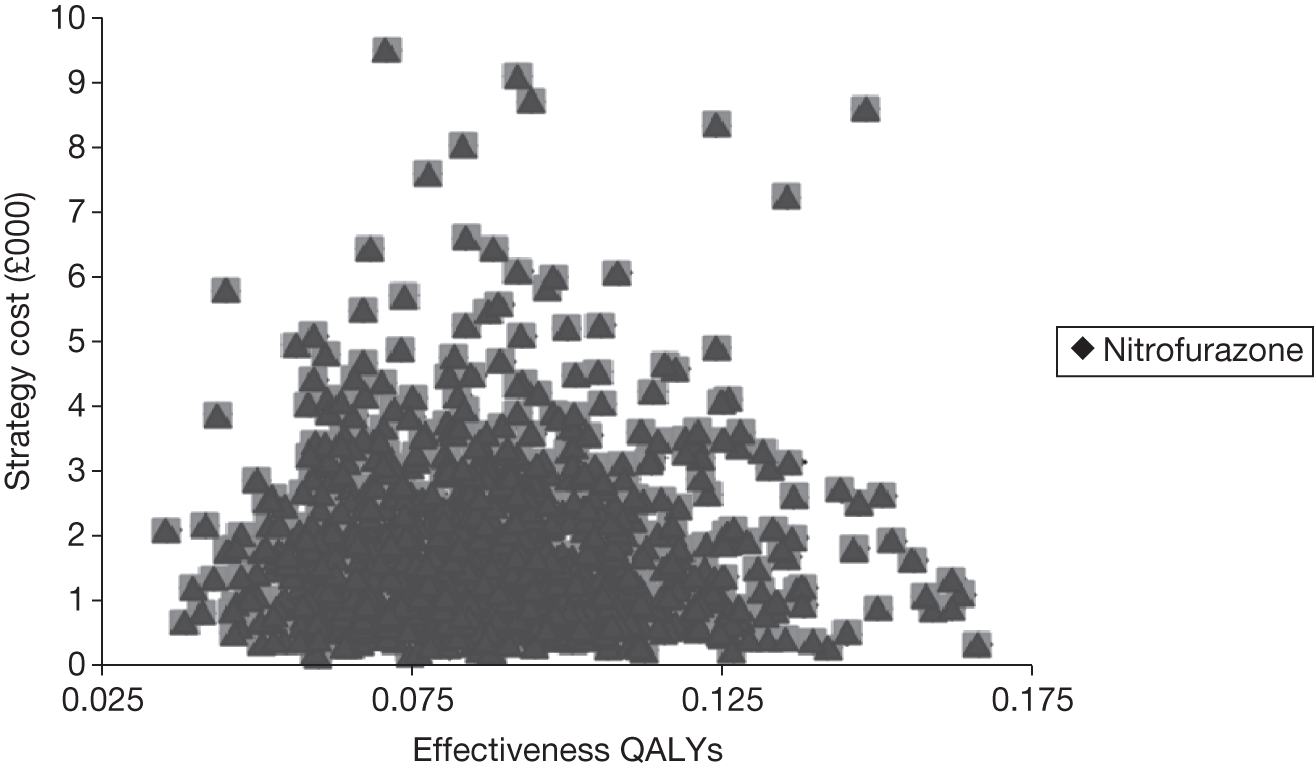
FIGURE 34.
Cost-effectiveness acceptability curve for nitrofurazone, PTFE and silver alloy for patients admitted into obstetric specialty.
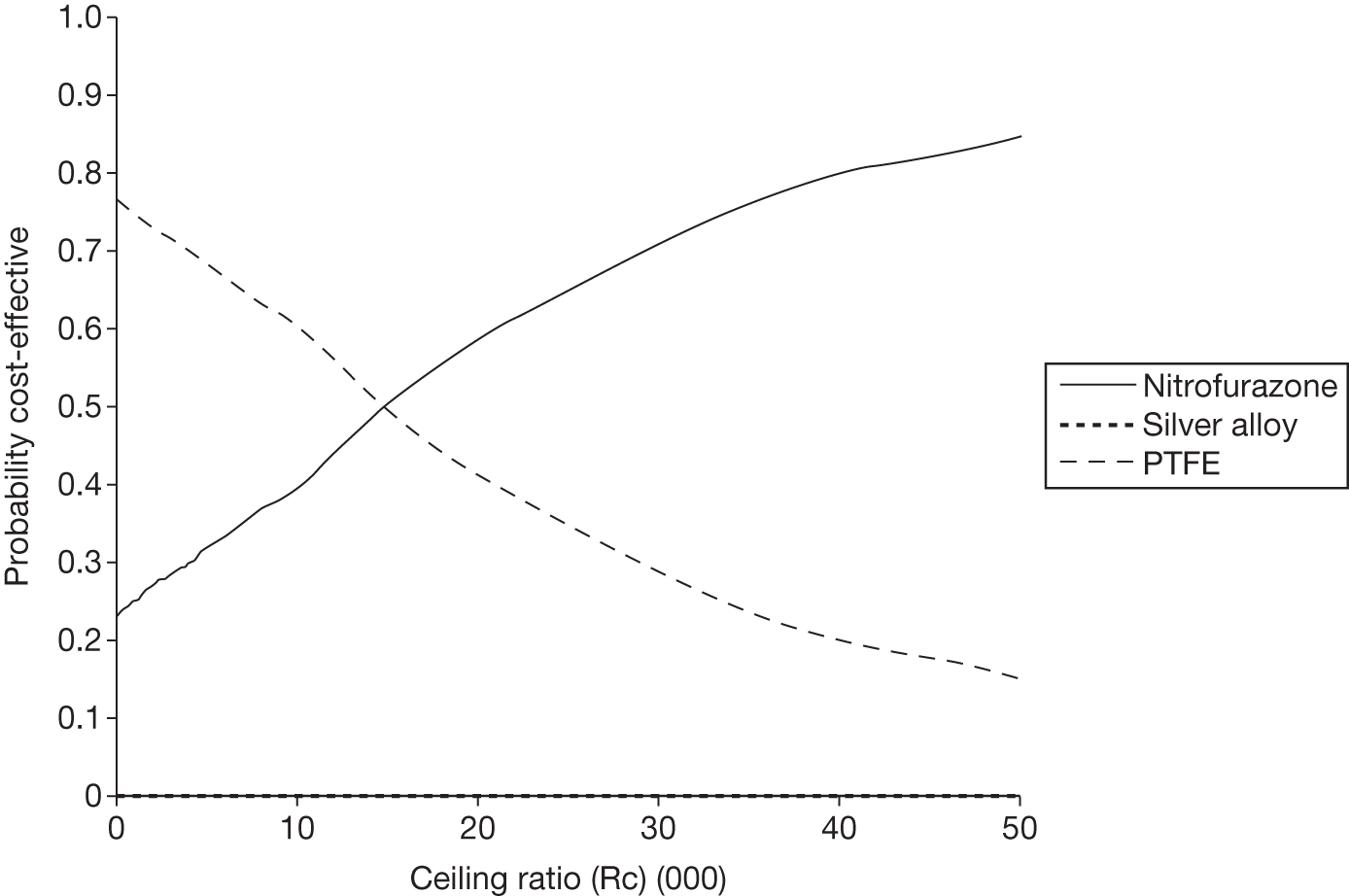
FIGURE 35.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone, PTFE and silver alloy for EQ-5D = 1 (full health) score analysis.
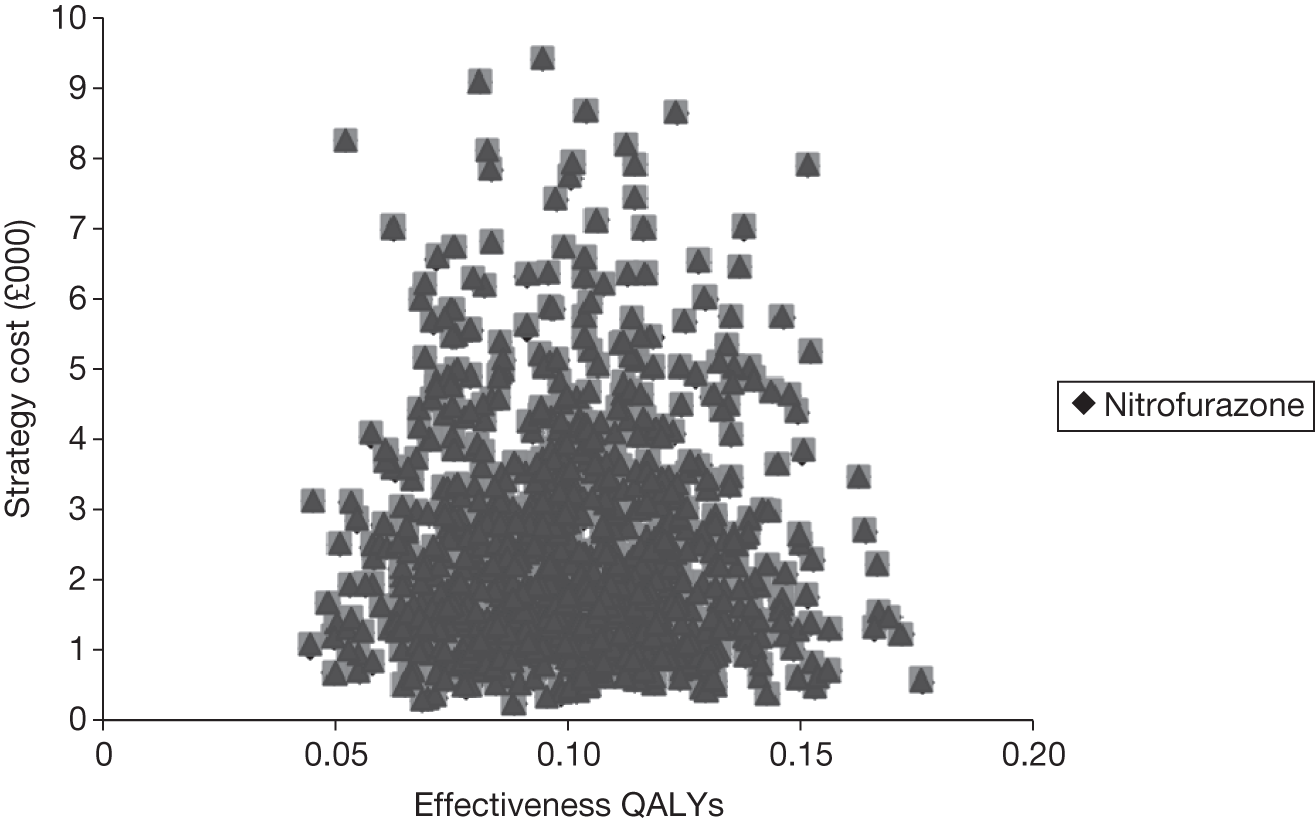
FIGURE 36.
Cost-effectiveness acceptability curve for nitrofurazone, PTFE and silver alloy for EQ-5D = 1 (full health) score.
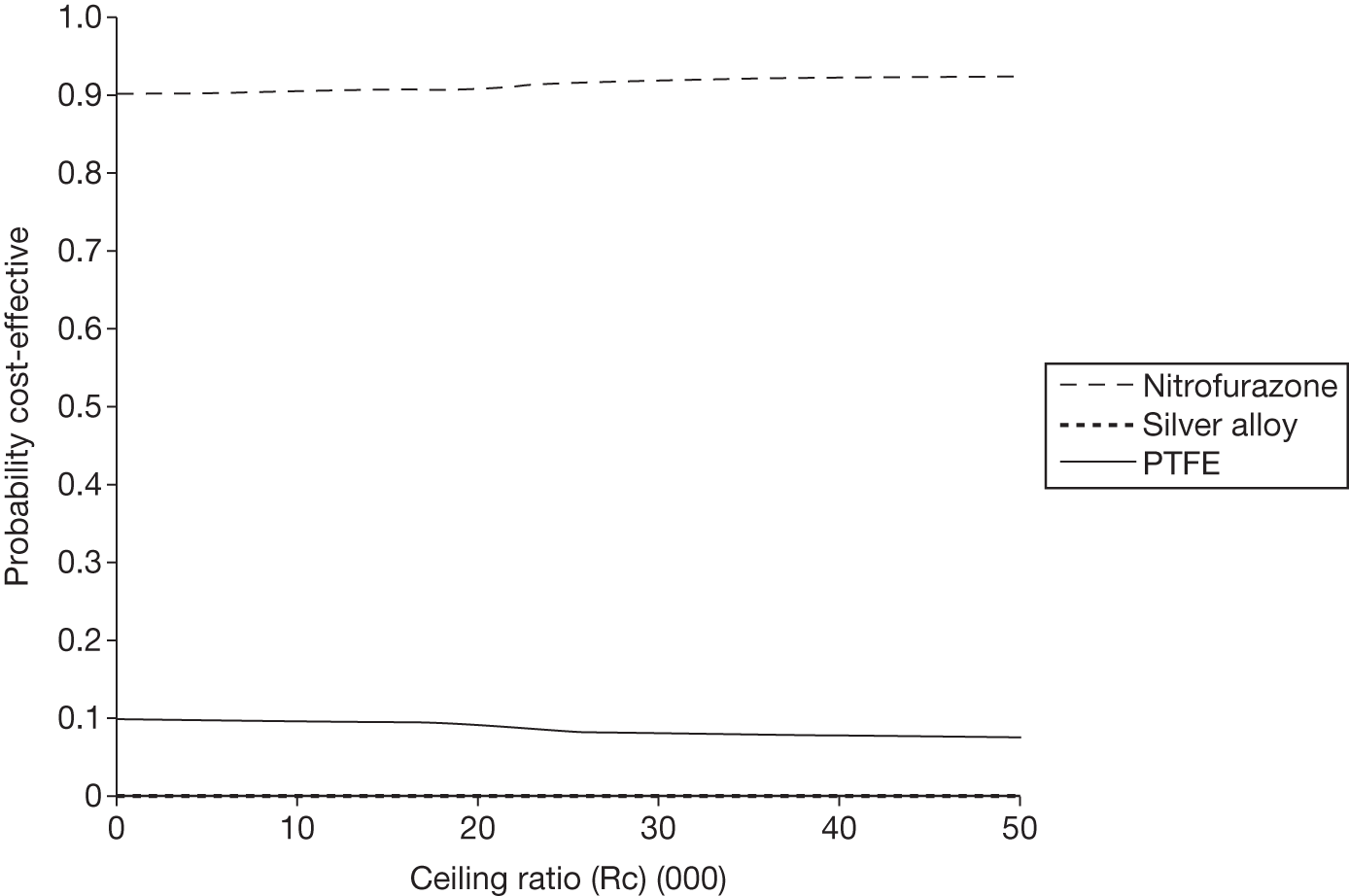
FIGURE 37.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone, PTFE and silver alloy for 3 days’ outcome analysis.
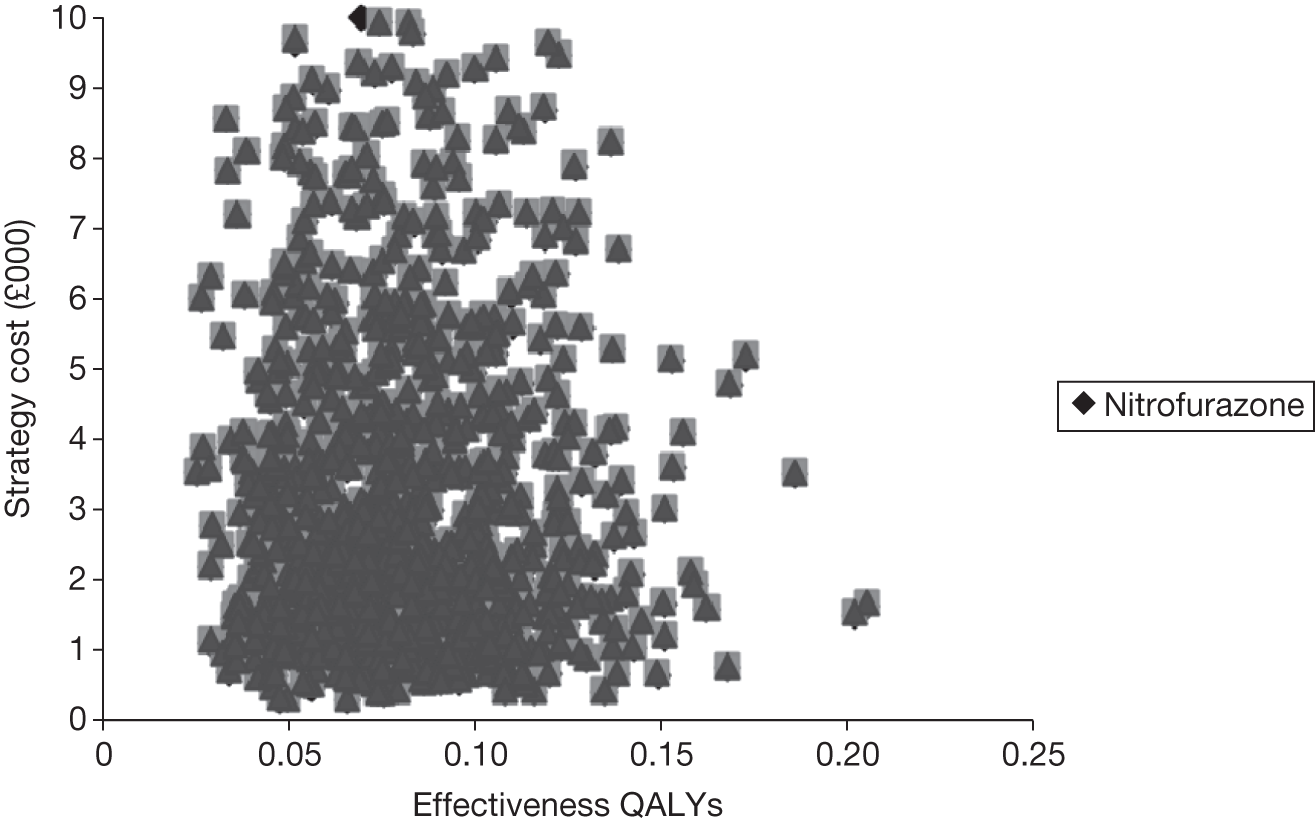
FIGURE 38.
Cost-effectiveness acceptability curve for nitrofurazone, PTFE and silver alloy for 3 days’ outcome analysis.
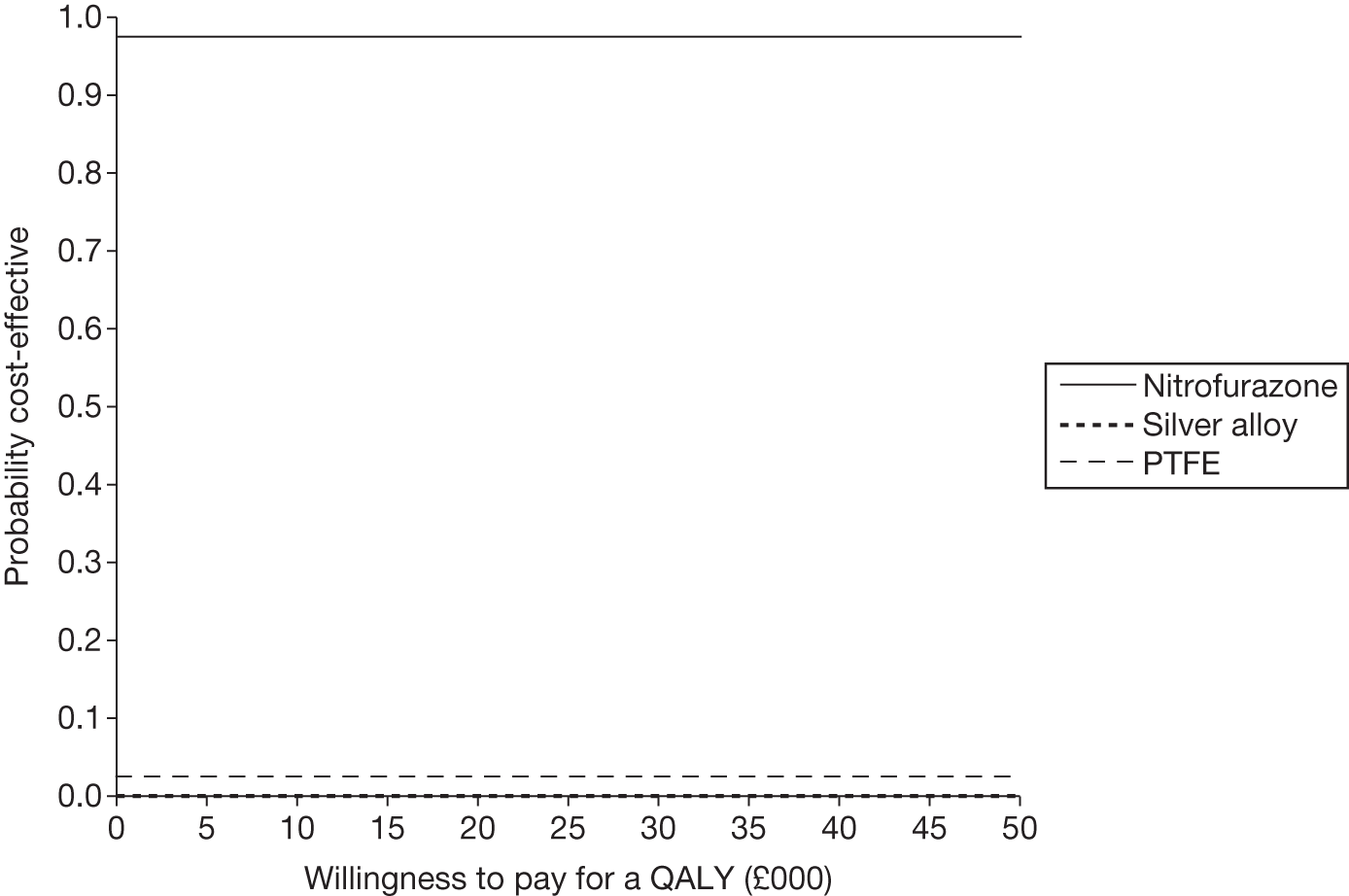
FIGURE 39.
Representation of the uncertainty in differential mean costs and QALYs for nitrofurazone, PTFE and silver alloy for analysis excluding inpatient cost data.
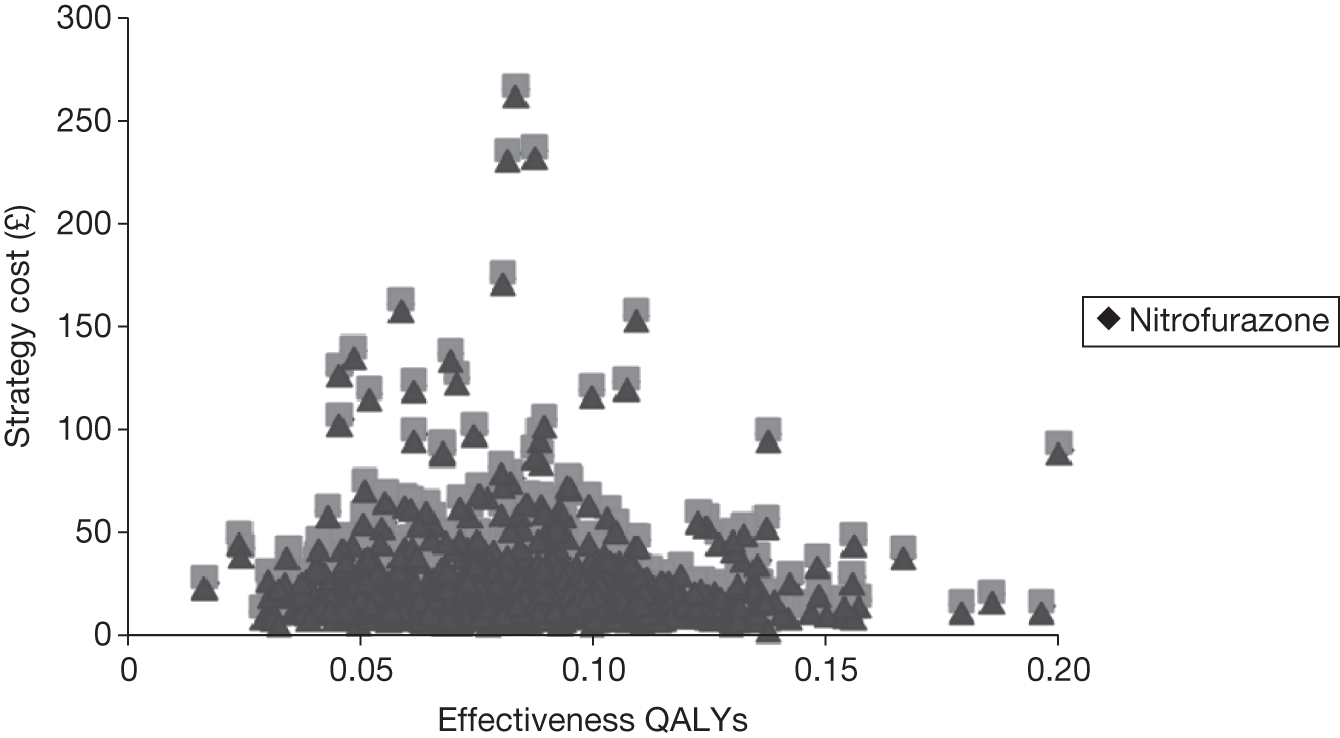
FIGURE 40.
Cost-effectiveness acceptability curve for nitrofurazone, PTFE and silver alloy for analysis excluding inpatient cost data.
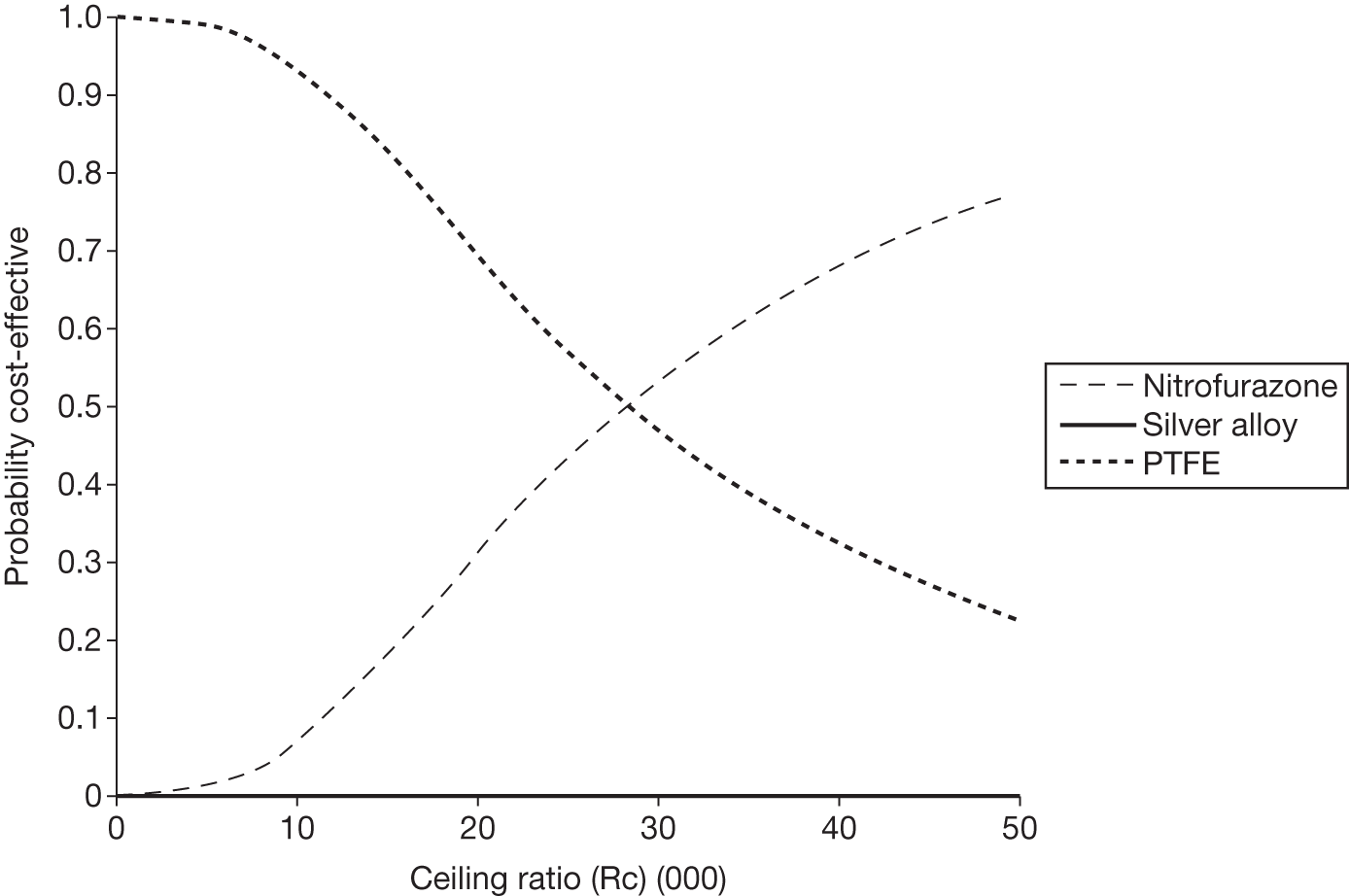
List of abbreviations
- CAUTI
- catheter-associated urinary tract infection
- CDC
- Centers for Disease Control and Prevention
- CEAC
- cost-effectiveness acceptability curve
- CFU
- colony-forming unit
- CHaRT
- Centre for Healthcare and Randomised Trials
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CPA
- Clinical Pathology Accreditation (UK)
- CSU
- catheter specimen of urine
- DMC
- Data Monitoring Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- GCP
- Good Clinical Practice
- GP
- general practitioner
- HCAI
- Healthcare Assisted Infection
- HRG
- Health Resource Group
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- IQR
- interquartile range
- ISD
- Information Services Division
- ISRCTN
- International Standard Randomised Clinical Trial Number
- IVR
- interactive voice recognition
- MSSU
- mid-stream specimen of urine
- NICE
- National Institute for Health and Clinical Excellence
- NIHR
- National Institute for Health Research
- NMB
- net monetary benefit
- OR
- odds ratio
- PSSRU
- Personal Social Services Research Unit
- PTFE
- polytetrafluoroethylene
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- RR
- relative risk
- SD
- standard deviation
- TSC
- Trial Steering Committee
- UTI
- urinary tract infection
- VAS
- visual analogue scale
- WBC
- white blood cell
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Professor of Bio-Statistics, Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Zarko Alfirevic, Head of Department for Women’s and Children’s Health, Institute of Translational Medicine, University of Liverpool
-
Professor Judith Bliss, Director of ICR-Clinical Trials and Statistics Unit, The Institute of Cancer Research
-
Professor David Fitzmaurice, Professor of Primary Care Research, Department of Primary Care Clinical Sciences, University of Birmingham
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, Department of Specialist Radiology, University College Hospital, London
-
Professor Angela Harden, Professor of Community and Family Health, Institute for Health and Human Development, University of East London
-
Dr Joanne Lord, Reader, Health Economics Research Group, Brunel University
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Dion Morton, Professor of Surgery, Academic Department of Surgery, University of Birmingham
-
Professor Gail Mountain, Professor of Health Services Research, Rehabilitation and Assistive Technologies Group, University of Sheffield
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Director, Centre for Healthcare Randomised Trials, Health Services Research Unit, University of Aberdeen
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Peter Tyrer, Professor of Community Psychiatry, Centre for Mental Health, Imperial College London
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Caroline Watkins, Professor of Stroke and Older People’s Care, Chair of UK Forum for Stroke Training, Stroke Practice Research Unit, University of Central Lancashire
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health